

A Step-by-Step Guide To Case Discussion
By ashi jain.

Join InsideIIM GOLD
Webinars & Workshops
- Compare B-Schools
- Free CAT Course
Take Free Mock Tests
Upskill With AltUni
CAT Study Planner

Are you comfortable in Decision Making in a given situation How aptly you analyze the situation with a logical approach How much time do you take in arriving at a decision How good are you in taking the rightful course of action
Solved Example:
Hari, the only working member of the family has been working an organization for 25 years. His job required long standing hours. One day, while working, he lost his leg in an accident. The company paid for his medical reimbursement.
Since he was a hardworking employee; the company offered him another compensatory job. He refused by saying, ‘Once a Lion, always a Lion’. As an HR, what solution would you suggest?
Identification of the Problem:
Obvious: accident, refusal of job, only earning member, his attitude, and inability to do his current job Hidden: the reputation of the company at stake, the course of action might influence other employees
Action Plan:
As an HR, you are first expected to check the company records and find out how a similar case has been dealt with in the past. Second, you need to take cognizance of the track record of the employee highlighted by the keyword ‘hardworking’.
Given the situation at hand, he is deemed unfit for his current role. However, the problem arises because of his attitude towards the compensatory job. Hence, in such a case, counselling is required.

Here, three levels of Counselling is required: 1. Ist level is with Hari 2. IInd level of counselling is required with the Union Leader (if any) to keep the collective interest and the reputation of the company in mind 3. IIIrd level of counselling is required with his family members as they constitute of the afflicted party
If the counselling does not work, one should also identify a contingency plan or Plan B. In this case, the Contingency Plan would be – hire someone from his family for a compensatory role.
Note that the following options are out of scope and should be avoided: 1. Increase Hari’s salary so that he gives in and agrees to do the compensatory job 2. Status Quo – do not bother as long as the Company is making a profit 3. Replace Hari with someone else
1. Pinpoint the key issues to be solved and identify their cause and effects
2. Start broad and try to work through a range of issues methodically
3. Connect the facts and evidence and focus on the big picture
4. Discuss any trade-offs or implications of your proposed solution
5. Relate your conclusion back to the problem statement and make sure you have answered all the questions
1. Do not be anxious if you are not able to understand the situation well or unable to justify the problem. Read again, a little slowly, it will help you understand better.
2. Do not jump to conclusions; try to move systematically and gradually.
3. Do not panic if you are unable to analyze the situation. Listen carefully to others as the discussion starts, it will help you gauge the problem at hand.
All the best! Ace the GDPI season.

Related Tags

FMS Delhi Summer Placements 2024: Median Stipend at 3 Lakhs
Mini Mock Test
CUET-PG Mini Mock 2 (By TISS Mumbai HRM&LR)
CUET-PG Mini Mock 3 (By TISS Mumbai HRM&LR)

CUET-PG Mini Mock 1 (By TISS Mumbai HRM&LR)
MBA Admissions 2024 - WAT 1
SNAP Quantitative Skills
SNAP Quant - 1
SNAP VARC Mini Mock - 1
SNAP Quant Mini Mock - 2
SNAP DILR Mini Mock - 4
SNAP VARC Mini Mock - 2
SNAP Quant Mini Mock - 4
SNAP LR Mini Mock - 3
SNAP Quant Mini Mock - 3
SNAP VARC Mini Mock - 3
SNAP - Quant Mini Mock 5
XAT Decision Making 2020
XAT Decision Making 2019
XAT Decision Making 2018
XAT Decision Making -10
XAT Decision Making -11
XAT Decision Making - 12
XAT Decision Making - 13
XAT Decision Making - 14
XAT Decision Making - 15
XAT Decision Making - 16
XAT Decision Making - 17
XAT Decision Making 2021
LR Topic Test
DI Topic Test
ParaSummary Topic Test
Take Free Test Here
Life of indian mba students in milan, italy - what’s next.
By InsideIIM Career Services
IMI Delhi: Worth It? | MBA ROI, Fees, Selection Process, Campus Life & More | KYC
How to calculate the real cost of an mba in 2024 ft. imt nagpur professors, mahindra university mba: worth it | campus life, academics, courses, placement | know your campus, how to uncover the reality of b-schools before joining, ft. masters' union, gmat focus edition: syllabus, exam pattern, scoring system, selection & more | new gmat exam, how to crack the jsw challenge 2023: insider tips and live q&a with industry leaders, why an xlri jamshedpur & fms delhi graduate decided to join the pharma industry, subscribe to our newsletter.
For a daily dose of the hottest, most insightful content created just for you! And don't worry - we won't spam you.
Who Are You?
Top B-Schools
Write a Story
InsideIIM Gold

InsideIIM.com is India's largest community of India's top talent that pursues or aspires to pursue a career in Management.

Follow Us Here
Konversations By InsideIIM
TestPrep By InsideIIM
- NMAT by GMAC
- Score Vs Percentile
- Exam Preparation
- Explainer Concepts
- Free Mock Tests
- RTI Data Analysis
- Selection Criteria
- CAT Toppers Interview
- Study Planner
- Admission Statistics
- Interview Experiences
- Explore B-Schools
- B-School Rankings
- Life In A B-School
- B-School Placements
- Certificate Programs
- Katalyst Programs
Placement Preparation
- Summer Placements Guide
- Final Placements Guide
Career Guide
- Career Explorer
- The Top 0.5% League
- Konversations Cafe
- The AltUni Career Show
- Employer Rankings
- Alumni Reports
- Salary Reports
Copyright 2024 - Kira9 Edumedia Pvt Ltd. All rights reserved.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
What the Case Study Method Really Teaches
- Nitin Nohria

Seven meta-skills that stick even if the cases fade from memory.
It’s been 100 years since Harvard Business School began using the case study method. Beyond teaching specific subject matter, the case study method excels in instilling meta-skills in students. This article explains the importance of seven such skills: preparation, discernment, bias recognition, judgement, collaboration, curiosity, and self-confidence.
During my decade as dean of Harvard Business School, I spent hundreds of hours talking with our alumni. To enliven these conversations, I relied on a favorite question: “What was the most important thing you learned from your time in our MBA program?”
- Nitin Nohria is the George F. Baker Jr. and Distinguished Service University Professor. He served as the 10th dean of Harvard Business School, from 2010 to 2020.
Partner Center
This Is What You Need to Know to Pass Your Group Case Interview
- Last Updated January, 2024
If you’re on this page, chances are you’ve been told you’re scheduled for a group interview.
After practicing for weeks to get good at cracking a normal case interview, hearing you have a group interview might make you feel like you’ve scaled a huge mountain only to find that there’s an even higher peak beyond it that you need to climb.
Group case interviews present some different challenges than individual cases, but if you know what those challenges are, you can overcome them.
We’ll tell you how.
In this article, we’ll cover what a group case interview is, why consulting firms use them, the key to passing your group interview, and tell you the 6 tips on group interviews you need to know.
If this is your first time to MyConsultingOffer.org, you may want to start with this page on Case Interview Prep . But if you’re ready to learn everything you need to know to pass a group case, you’re in the right place.
Let’s get started!
What is a Group Case Interview?
The group needs to come to a collective point of view on what the client’s problem is, how to structure their analysis, and what the final recommendation should be.
The group should also agree on how the analysis of the case will be conducted at a high level, but the actual number-crunching will need to be divided between group members in order to complete the work in the allotted time.
The group’s analysis and recommendation will be presented to one or more interviewers.
Why Do Consulting Firms Use Group Case Interviews?
It can feel difficult to trust your team members when you know that you’re all competing for the same job, but that’s what the group case is about — it tests teamwork skills in a high-stakes environment.
Management consultants are hired to solve big, thorny business problems, ones that require the work of multiple people to solve.
While there is a hierarchy on consulting teams with a partner leading the work, consulting partners simultaneously manage multiple clients or multiple studies at one large client.
They won’t work with your team every day and in their absence, the team still needs to be able to work together effectively.
Even if a partner is leading a team’s problem-solving discussion, each consultant has a responsibility to make sure the team’s best thinking is being put forward to help the client.
Ideas are both expected from each member of the team and valued.
Even the newest analyst has a contribution to make.
T he analyst may have been the person to analyze the data and therefore be closest to the information that will drive the solution to the problem.
The flat power-structure of the team makes it critical that each consultant works well with others on teams.
In assessing each member of a group case team, interviewers will ask themselves:
Does each of the recruits listen as well as lead?
Are they open to other peoples’ ideas?
Can they perform independent analysis and interpret what impact their work has on the overall problem the team is trying to solve?
Can they persuade team members of their points of view?
The Key to Passing the Group Case: Make Sure Your Group Is Organized
A group case must be solved by going through the same 4 steps as individual cases : the opening, structuring the problem, the analysis, and the recommendation.
Your team should break down the time you have to solve the case into time allotted to each of these steps to ensure you don’t spend too long in one area and not reach a recommendation.
Make sure the team agrees on a single statement of the client’s problem.
Take the time for everyone to read the materials, take notes, and suggest what they think is the key question(s) that need to be solved in this case.
Write it on a whiteboard or somewhere else to ensure there’s agreement. You can’t solve the problem together if you don’t agree on what the problem is.
Usually, someone in the group will take the lead on organizing the group.
If no one does, this is your opportunity to demonstrate your leadership and teamwork skills, but if there are people fighting over the leadership position (unlikely since everyone is on their “best behavior”), then contribute and don’t worry that you aren’t “leading” the discussion just yet.
Create a clear, MECE structure to analyze the problem.
This is even more important to solving a group case than an individual one because you need to make sure that when the group breaks up so each member can perform part of the analysis, all the issues are covered and there’s not duplicated effort between team members.
After your group structures the problem, split up the analysis that needs to be done between members of the group.
If no one suggests breaking up the analysis, then volunteer the idea. Be sure to explain how each person’s piece fits into the team effort.
Each person should do their analysis independently to ensure there is sufficient time to complete all the required tasks, though the team should regroup briefly if someone has a problem they need help with or comes up with an insight that could influence the work other group members are doing.
While you do your own analysis, you’ll need to demonstrate you understand the bigger picture by involving your teammates, sharing how your findings impacts their work, and articulating how all the insights lead to an answer to the client’s problem.
After everyone has completed their analysis, the group should come back together so everyone can report their results and the group can collectively come to a recommendation to present to interviewers.
In addition to the normal 4 parts of the case, group cases usually require you to present your recommendation to the interviewer(s).
Be sure to build time into your schedule for creating slides, deciding who presents what, and practicing your delivery.
Many groups fail because they begin their presentation without deciding who has which role.
In consulting, this is like going into a client meeting without knowing who is presenting which slide to the client and makes your team look unprofessional.
Presentation
Start with your recommendation and then provide the key pieces of analysis and/or reasoning that support it.
Again, the work will need to be divided between team members to ensure you get slides written in the allotted time.
For more information on writing good slide presentations, see Written Case Interview page.
6 Tips to Pass Your Group Case Interview
Tip 1: organize your team.
A disorganized team will not be able to complete their analysis and develop a strong recommendation in the time allotted.
See the previous section for the steps the group needs to complete to solve the case.
If someone else does take charge, don’t fight for control.
Show leadership by making points that help to move the team’s problem solving forward, not fighting so that it goes backwards.
Tip 2: Move the Problem-Solving Forward
With multiple team members trying to contribute and express their point of view, it’s possible to have a lot of discussion without getting closer to a solution to the client’s business problem. You can overcome this by:
- Summing up what the team has agreed on so far,
- Providing insight into how the team’s discussion impacts the problem you’re tasked with solving, and/or
- Steering the team to discuss the next steps.
If it feels like the team is rehashing the same topics, use these options to move the problem solving forward.
Tip 3: Make Fact-Based Decisions
It’s okay to disagree with team members but always disagree like a consultant. Challenge teammates’ ideas with data, not opinions.
If there is analysis that needs to be done to determine which point of view is correct, table the discussion until the analysis has been completed.
Tip 4: Don't Steamroll Teammates
As mentioned earlier, consulting teams value the ideas and input of every team member.
Because of this, cutting off, interrupting or talking over other team members is more likely to get you turned down for a consulting job than hired.
The quality of your contribution to group discussions is more important than the quantity (or air time) you consume.
Demonstrate your collaboration and interpersonal skills.
Tip 5: Remain Confident When the Team Presents
Keep your poker face on even if your teammates don’t make every point the way you would have made it.
Like steamrolling teammates in discussions, frowning or shaking your head as they present will make it look like you’re not a team player.
Tip 6: Remember, Everyone Can Get Offers
In many jobs, there is only one position open.
At consulting firms, a class of new analysts and associates is hired each year.
There aren’t quotas regarding hiring only one person from a group interview team, so working cooperatively to solve the problem is a better strategy than undermining other members of your group to appear smarter than they are.
We’ve seen group interviews where no one gets a job offer and that can be because teammates undermine each other.
Don’t Over-Invest in Prepping for a Group Case Study Interview
Like the written case interview , group cases come up infrequently.
The 2 most common types of case interviews are individual interviews: the candidate-led interview or the interviewer-led interview.
In the candidate-led interview , the recruit is responsible for moving the problem solving forward. After they ensure they understand the problem and structure how they’d approach solving it, they pick one piece of the problem to start drilling down on first. Candidate-led cases are commonly used by Bain and BCG.
In the interviewer-led interview , the interviewer will suggest the first part of the case a recruit should probe after they have presented their opening and structured the problem. Interviewer-led interviews are commonly used by McKinsey .
Because individual cases are much more common than group cases, don’t spend time preparing for a group case unless you’re sure you’ll have one.
If you’re invited to take part in a group case interview, your preparation on individual cases will ensure you have a good approach cracking the case.
At this point, we hope you feel confident you can pass your group case interview.
In this article, we’ve covered what a group case interview is, why consulting firms use them, the key to passing your group interview, and the 6 tips on group interviews you need to know.
Still have questions?
If you have more questions about group interviews, leave them in the comments below. One of My Consulting Offer’s case coaches will answer them.
People prepping for a group case interview have also found the following other pages helpful:
- Case Interview Math ,
- Written Case Interview , and
- Bain One Way Interview .
Help with Case Study Interview Preparation
Thanks for turning to My Consulting Offer for advice on case study interview prep. My Consulting Offer has helped almost 85% of the people we’ve worked with get a job in management consulting. We want you to be successful in your consulting interviews too.
If you want a step-by-step solution to land more offers from consulting firms, then grab the free video training series below. It’s been created by former Bain, BCG, and McKinsey Consultants, Managers and Recruiters.
It contains the EXACT solution used by over 500 of our clients to land offers.
The best part?
It’s absolutely free. Just put your name and email address in and you’ll have instant access to the training series.
© My CONSULTING Offer
3 Top Strategies to Master the Case Interview in Under a Week
We are sharing our powerful strategies to pass the case interview even if you have no business background, zero casing experience, or only have a week to prepare.
No thanks, I don't want free strategies to get into consulting.
We are excited to invite you to the online event., where should we send you the calendar invite and login information.
Organizing Your Social Sciences Research Assignments
- Annotated Bibliography
- Analyzing a Scholarly Journal Article
- Group Presentations
- Dealing with Nervousness
- Using Visual Aids
- Grading Someone Else's Paper
- Types of Structured Group Activities
- Group Project Survival Skills
- Leading a Class Discussion
- Multiple Book Review Essay
- Reviewing Collected Works
- Writing a Case Analysis Paper
- Writing a Case Study
- About Informed Consent
- Writing Field Notes
- Writing a Policy Memo
- Writing a Reflective Paper
- Writing a Research Proposal
- Generative AI and Writing
- Acknowledgments
A case study research paper examines a person, place, event, condition, phenomenon, or other type of subject of analysis in order to extrapolate key themes and results that help predict future trends, illuminate previously hidden issues that can be applied to practice, and/or provide a means for understanding an important research problem with greater clarity. A case study research paper usually examines a single subject of analysis, but case study papers can also be designed as a comparative investigation that shows relationships between two or more subjects. The methods used to study a case can rest within a quantitative, qualitative, or mixed-method investigative paradigm.
Case Studies. Writing@CSU. Colorado State University; Mills, Albert J. , Gabrielle Durepos, and Eiden Wiebe, editors. Encyclopedia of Case Study Research . Thousand Oaks, CA: SAGE Publications, 2010 ; “What is a Case Study?” In Swanborn, Peter G. Case Study Research: What, Why and How? London: SAGE, 2010.
How to Approach Writing a Case Study Research Paper
General information about how to choose a topic to investigate can be found under the " Choosing a Research Problem " tab in the Organizing Your Social Sciences Research Paper writing guide. Review this page because it may help you identify a subject of analysis that can be investigated using a case study design.
However, identifying a case to investigate involves more than choosing the research problem . A case study encompasses a problem contextualized around the application of in-depth analysis, interpretation, and discussion, often resulting in specific recommendations for action or for improving existing conditions. As Seawright and Gerring note, practical considerations such as time and access to information can influence case selection, but these issues should not be the sole factors used in describing the methodological justification for identifying a particular case to study. Given this, selecting a case includes considering the following:
- The case represents an unusual or atypical example of a research problem that requires more in-depth analysis? Cases often represent a topic that rests on the fringes of prior investigations because the case may provide new ways of understanding the research problem. For example, if the research problem is to identify strategies to improve policies that support girl's access to secondary education in predominantly Muslim nations, you could consider using Azerbaijan as a case study rather than selecting a more obvious nation in the Middle East. Doing so may reveal important new insights into recommending how governments in other predominantly Muslim nations can formulate policies that support improved access to education for girls.
- The case provides important insight or illuminate a previously hidden problem? In-depth analysis of a case can be based on the hypothesis that the case study will reveal trends or issues that have not been exposed in prior research or will reveal new and important implications for practice. For example, anecdotal evidence may suggest drug use among homeless veterans is related to their patterns of travel throughout the day. Assuming prior studies have not looked at individual travel choices as a way to study access to illicit drug use, a case study that observes a homeless veteran could reveal how issues of personal mobility choices facilitate regular access to illicit drugs. Note that it is important to conduct a thorough literature review to ensure that your assumption about the need to reveal new insights or previously hidden problems is valid and evidence-based.
- The case challenges and offers a counter-point to prevailing assumptions? Over time, research on any given topic can fall into a trap of developing assumptions based on outdated studies that are still applied to new or changing conditions or the idea that something should simply be accepted as "common sense," even though the issue has not been thoroughly tested in current practice. A case study analysis may offer an opportunity to gather evidence that challenges prevailing assumptions about a research problem and provide a new set of recommendations applied to practice that have not been tested previously. For example, perhaps there has been a long practice among scholars to apply a particular theory in explaining the relationship between two subjects of analysis. Your case could challenge this assumption by applying an innovative theoretical framework [perhaps borrowed from another discipline] to explore whether this approach offers new ways of understanding the research problem. Taking a contrarian stance is one of the most important ways that new knowledge and understanding develops from existing literature.
- The case provides an opportunity to pursue action leading to the resolution of a problem? Another way to think about choosing a case to study is to consider how the results from investigating a particular case may result in findings that reveal ways in which to resolve an existing or emerging problem. For example, studying the case of an unforeseen incident, such as a fatal accident at a railroad crossing, can reveal hidden issues that could be applied to preventative measures that contribute to reducing the chance of accidents in the future. In this example, a case study investigating the accident could lead to a better understanding of where to strategically locate additional signals at other railroad crossings so as to better warn drivers of an approaching train, particularly when visibility is hindered by heavy rain, fog, or at night.
- The case offers a new direction in future research? A case study can be used as a tool for an exploratory investigation that highlights the need for further research about the problem. A case can be used when there are few studies that help predict an outcome or that establish a clear understanding about how best to proceed in addressing a problem. For example, after conducting a thorough literature review [very important!], you discover that little research exists showing the ways in which women contribute to promoting water conservation in rural communities of east central Africa. A case study of how women contribute to saving water in a rural village of Uganda can lay the foundation for understanding the need for more thorough research that documents how women in their roles as cooks and family caregivers think about water as a valuable resource within their community. This example of a case study could also point to the need for scholars to build new theoretical frameworks around the topic [e.g., applying feminist theories of work and family to the issue of water conservation].
Eisenhardt, Kathleen M. “Building Theories from Case Study Research.” Academy of Management Review 14 (October 1989): 532-550; Emmel, Nick. Sampling and Choosing Cases in Qualitative Research: A Realist Approach . Thousand Oaks, CA: SAGE Publications, 2013; Gerring, John. “What Is a Case Study and What Is It Good for?” American Political Science Review 98 (May 2004): 341-354; Mills, Albert J. , Gabrielle Durepos, and Eiden Wiebe, editors. Encyclopedia of Case Study Research . Thousand Oaks, CA: SAGE Publications, 2010; Seawright, Jason and John Gerring. "Case Selection Techniques in Case Study Research." Political Research Quarterly 61 (June 2008): 294-308.
Structure and Writing Style
The purpose of a paper in the social sciences designed around a case study is to thoroughly investigate a subject of analysis in order to reveal a new understanding about the research problem and, in so doing, contributing new knowledge to what is already known from previous studies. In applied social sciences disciplines [e.g., education, social work, public administration, etc.], case studies may also be used to reveal best practices, highlight key programs, or investigate interesting aspects of professional work.
In general, the structure of a case study research paper is not all that different from a standard college-level research paper. However, there are subtle differences you should be aware of. Here are the key elements to organizing and writing a case study research paper.
I. Introduction
As with any research paper, your introduction should serve as a roadmap for your readers to ascertain the scope and purpose of your study . The introduction to a case study research paper, however, should not only describe the research problem and its significance, but you should also succinctly describe why the case is being used and how it relates to addressing the problem. The two elements should be linked. With this in mind, a good introduction answers these four questions:
- What is being studied? Describe the research problem and describe the subject of analysis [the case] you have chosen to address the problem. Explain how they are linked and what elements of the case will help to expand knowledge and understanding about the problem.
- Why is this topic important to investigate? Describe the significance of the research problem and state why a case study design and the subject of analysis that the paper is designed around is appropriate in addressing the problem.
- What did we know about this topic before I did this study? Provide background that helps lead the reader into the more in-depth literature review to follow. If applicable, summarize prior case study research applied to the research problem and why it fails to adequately address the problem. Describe why your case will be useful. If no prior case studies have been used to address the research problem, explain why you have selected this subject of analysis.
- How will this study advance new knowledge or new ways of understanding? Explain why your case study will be suitable in helping to expand knowledge and understanding about the research problem.
Each of these questions should be addressed in no more than a few paragraphs. Exceptions to this can be when you are addressing a complex research problem or subject of analysis that requires more in-depth background information.
II. Literature Review
The literature review for a case study research paper is generally structured the same as it is for any college-level research paper. The difference, however, is that the literature review is focused on providing background information and enabling historical interpretation of the subject of analysis in relation to the research problem the case is intended to address . This includes synthesizing studies that help to:
- Place relevant works in the context of their contribution to understanding the case study being investigated . This would involve summarizing studies that have used a similar subject of analysis to investigate the research problem. If there is literature using the same or a very similar case to study, you need to explain why duplicating past research is important [e.g., conditions have changed; prior studies were conducted long ago, etc.].
- Describe the relationship each work has to the others under consideration that informs the reader why this case is applicable . Your literature review should include a description of any works that support using the case to investigate the research problem and the underlying research questions.
- Identify new ways to interpret prior research using the case study . If applicable, review any research that has examined the research problem using a different research design. Explain how your use of a case study design may reveal new knowledge or a new perspective or that can redirect research in an important new direction.
- Resolve conflicts amongst seemingly contradictory previous studies . This refers to synthesizing any literature that points to unresolved issues of concern about the research problem and describing how the subject of analysis that forms the case study can help resolve these existing contradictions.
- Point the way in fulfilling a need for additional research . Your review should examine any literature that lays a foundation for understanding why your case study design and the subject of analysis around which you have designed your study may reveal a new way of approaching the research problem or offer a perspective that points to the need for additional research.
- Expose any gaps that exist in the literature that the case study could help to fill . Summarize any literature that not only shows how your subject of analysis contributes to understanding the research problem, but how your case contributes to a new way of understanding the problem that prior research has failed to do.
- Locate your own research within the context of existing literature [very important!] . Collectively, your literature review should always place your case study within the larger domain of prior research about the problem. The overarching purpose of reviewing pertinent literature in a case study paper is to demonstrate that you have thoroughly identified and synthesized prior studies in relation to explaining the relevance of the case in addressing the research problem.
III. Method
In this section, you explain why you selected a particular case [i.e., subject of analysis] and the strategy you used to identify and ultimately decide that your case was appropriate in addressing the research problem. The way you describe the methods used varies depending on the type of subject of analysis that constitutes your case study.
If your subject of analysis is an incident or event . In the social and behavioral sciences, the event or incident that represents the case to be studied is usually bounded by time and place, with a clear beginning and end and with an identifiable location or position relative to its surroundings. The subject of analysis can be a rare or critical event or it can focus on a typical or regular event. The purpose of studying a rare event is to illuminate new ways of thinking about the broader research problem or to test a hypothesis. Critical incident case studies must describe the method by which you identified the event and explain the process by which you determined the validity of this case to inform broader perspectives about the research problem or to reveal new findings. However, the event does not have to be a rare or uniquely significant to support new thinking about the research problem or to challenge an existing hypothesis. For example, Walo, Bull, and Breen conducted a case study to identify and evaluate the direct and indirect economic benefits and costs of a local sports event in the City of Lismore, New South Wales, Australia. The purpose of their study was to provide new insights from measuring the impact of a typical local sports event that prior studies could not measure well because they focused on large "mega-events." Whether the event is rare or not, the methods section should include an explanation of the following characteristics of the event: a) when did it take place; b) what were the underlying circumstances leading to the event; and, c) what were the consequences of the event in relation to the research problem.
If your subject of analysis is a person. Explain why you selected this particular individual to be studied and describe what experiences they have had that provide an opportunity to advance new understandings about the research problem. Mention any background about this person which might help the reader understand the significance of their experiences that make them worthy of study. This includes describing the relationships this person has had with other people, institutions, and/or events that support using them as the subject for a case study research paper. It is particularly important to differentiate the person as the subject of analysis from others and to succinctly explain how the person relates to examining the research problem [e.g., why is one politician in a particular local election used to show an increase in voter turnout from any other candidate running in the election]. Note that these issues apply to a specific group of people used as a case study unit of analysis [e.g., a classroom of students].
If your subject of analysis is a place. In general, a case study that investigates a place suggests a subject of analysis that is unique or special in some way and that this uniqueness can be used to build new understanding or knowledge about the research problem. A case study of a place must not only describe its various attributes relevant to the research problem [e.g., physical, social, historical, cultural, economic, political], but you must state the method by which you determined that this place will illuminate new understandings about the research problem. It is also important to articulate why a particular place as the case for study is being used if similar places also exist [i.e., if you are studying patterns of homeless encampments of veterans in open spaces, explain why you are studying Echo Park in Los Angeles rather than Griffith Park?]. If applicable, describe what type of human activity involving this place makes it a good choice to study [e.g., prior research suggests Echo Park has more homeless veterans].
If your subject of analysis is a phenomenon. A phenomenon refers to a fact, occurrence, or circumstance that can be studied or observed but with the cause or explanation to be in question. In this sense, a phenomenon that forms your subject of analysis can encompass anything that can be observed or presumed to exist but is not fully understood. In the social and behavioral sciences, the case usually focuses on human interaction within a complex physical, social, economic, cultural, or political system. For example, the phenomenon could be the observation that many vehicles used by ISIS fighters are small trucks with English language advertisements on them. The research problem could be that ISIS fighters are difficult to combat because they are highly mobile. The research questions could be how and by what means are these vehicles used by ISIS being supplied to the militants and how might supply lines to these vehicles be cut off? How might knowing the suppliers of these trucks reveal larger networks of collaborators and financial support? A case study of a phenomenon most often encompasses an in-depth analysis of a cause and effect that is grounded in an interactive relationship between people and their environment in some way.
NOTE: The choice of the case or set of cases to study cannot appear random. Evidence that supports the method by which you identified and chose your subject of analysis should clearly support investigation of the research problem and linked to key findings from your literature review. Be sure to cite any studies that helped you determine that the case you chose was appropriate for examining the problem.
IV. Discussion
The main elements of your discussion section are generally the same as any research paper, but centered around interpreting and drawing conclusions about the key findings from your analysis of the case study. Note that a general social sciences research paper may contain a separate section to report findings. However, in a paper designed around a case study, it is common to combine a description of the results with the discussion about their implications. The objectives of your discussion section should include the following:
Reiterate the Research Problem/State the Major Findings Briefly reiterate the research problem you are investigating and explain why the subject of analysis around which you designed the case study were used. You should then describe the findings revealed from your study of the case using direct, declarative, and succinct proclamation of the study results. Highlight any findings that were unexpected or especially profound.
Explain the Meaning of the Findings and Why They are Important Systematically explain the meaning of your case study findings and why you believe they are important. Begin this part of the section by repeating what you consider to be your most important or surprising finding first, then systematically review each finding. Be sure to thoroughly extrapolate what your analysis of the case can tell the reader about situations or conditions beyond the actual case that was studied while, at the same time, being careful not to misconstrue or conflate a finding that undermines the external validity of your conclusions.
Relate the Findings to Similar Studies No study in the social sciences is so novel or possesses such a restricted focus that it has absolutely no relation to previously published research. The discussion section should relate your case study results to those found in other studies, particularly if questions raised from prior studies served as the motivation for choosing your subject of analysis. This is important because comparing and contrasting the findings of other studies helps support the overall importance of your results and it highlights how and in what ways your case study design and the subject of analysis differs from prior research about the topic.
Consider Alternative Explanations of the Findings Remember that the purpose of social science research is to discover and not to prove. When writing the discussion section, you should carefully consider all possible explanations revealed by the case study results, rather than just those that fit your hypothesis or prior assumptions and biases. Be alert to what the in-depth analysis of the case may reveal about the research problem, including offering a contrarian perspective to what scholars have stated in prior research if that is how the findings can be interpreted from your case.
Acknowledge the Study's Limitations You can state the study's limitations in the conclusion section of your paper but describing the limitations of your subject of analysis in the discussion section provides an opportunity to identify the limitations and explain why they are not significant. This part of the discussion section should also note any unanswered questions or issues your case study could not address. More detailed information about how to document any limitations to your research can be found here .
Suggest Areas for Further Research Although your case study may offer important insights about the research problem, there are likely additional questions related to the problem that remain unanswered or findings that unexpectedly revealed themselves as a result of your in-depth analysis of the case. Be sure that the recommendations for further research are linked to the research problem and that you explain why your recommendations are valid in other contexts and based on the original assumptions of your study.
V. Conclusion
As with any research paper, you should summarize your conclusion in clear, simple language; emphasize how the findings from your case study differs from or supports prior research and why. Do not simply reiterate the discussion section. Provide a synthesis of key findings presented in the paper to show how these converge to address the research problem. If you haven't already done so in the discussion section, be sure to document the limitations of your case study and any need for further research.
The function of your paper's conclusion is to: 1) reiterate the main argument supported by the findings from your case study; 2) state clearly the context, background, and necessity of pursuing the research problem using a case study design in relation to an issue, controversy, or a gap found from reviewing the literature; and, 3) provide a place to persuasively and succinctly restate the significance of your research problem, given that the reader has now been presented with in-depth information about the topic.
Consider the following points to help ensure your conclusion is appropriate:
- If the argument or purpose of your paper is complex, you may need to summarize these points for your reader.
- If prior to your conclusion, you have not yet explained the significance of your findings or if you are proceeding inductively, use the conclusion of your paper to describe your main points and explain their significance.
- Move from a detailed to a general level of consideration of the case study's findings that returns the topic to the context provided by the introduction or within a new context that emerges from your case study findings.
Note that, depending on the discipline you are writing in or the preferences of your professor, the concluding paragraph may contain your final reflections on the evidence presented as it applies to practice or on the essay's central research problem. However, the nature of being introspective about the subject of analysis you have investigated will depend on whether you are explicitly asked to express your observations in this way.
Problems to Avoid
Overgeneralization One of the goals of a case study is to lay a foundation for understanding broader trends and issues applied to similar circumstances. However, be careful when drawing conclusions from your case study. They must be evidence-based and grounded in the results of the study; otherwise, it is merely speculation. Looking at a prior example, it would be incorrect to state that a factor in improving girls access to education in Azerbaijan and the policy implications this may have for improving access in other Muslim nations is due to girls access to social media if there is no documentary evidence from your case study to indicate this. There may be anecdotal evidence that retention rates were better for girls who were engaged with social media, but this observation would only point to the need for further research and would not be a definitive finding if this was not a part of your original research agenda.
Failure to Document Limitations No case is going to reveal all that needs to be understood about a research problem. Therefore, just as you have to clearly state the limitations of a general research study , you must describe the specific limitations inherent in the subject of analysis. For example, the case of studying how women conceptualize the need for water conservation in a village in Uganda could have limited application in other cultural contexts or in areas where fresh water from rivers or lakes is plentiful and, therefore, conservation is understood more in terms of managing access rather than preserving access to a scarce resource.
Failure to Extrapolate All Possible Implications Just as you don't want to over-generalize from your case study findings, you also have to be thorough in the consideration of all possible outcomes or recommendations derived from your findings. If you do not, your reader may question the validity of your analysis, particularly if you failed to document an obvious outcome from your case study research. For example, in the case of studying the accident at the railroad crossing to evaluate where and what types of warning signals should be located, you failed to take into consideration speed limit signage as well as warning signals. When designing your case study, be sure you have thoroughly addressed all aspects of the problem and do not leave gaps in your analysis that leave the reader questioning the results.
Case Studies. Writing@CSU. Colorado State University; Gerring, John. Case Study Research: Principles and Practices . New York: Cambridge University Press, 2007; Merriam, Sharan B. Qualitative Research and Case Study Applications in Education . Rev. ed. San Francisco, CA: Jossey-Bass, 1998; Miller, Lisa L. “The Use of Case Studies in Law and Social Science Research.” Annual Review of Law and Social Science 14 (2018): TBD; Mills, Albert J., Gabrielle Durepos, and Eiden Wiebe, editors. Encyclopedia of Case Study Research . Thousand Oaks, CA: SAGE Publications, 2010; Putney, LeAnn Grogan. "Case Study." In Encyclopedia of Research Design , Neil J. Salkind, editor. (Thousand Oaks, CA: SAGE Publications, 2010), pp. 116-120; Simons, Helen. Case Study Research in Practice . London: SAGE Publications, 2009; Kratochwill, Thomas R. and Joel R. Levin, editors. Single-Case Research Design and Analysis: New Development for Psychology and Education . Hilldsale, NJ: Lawrence Erlbaum Associates, 1992; Swanborn, Peter G. Case Study Research: What, Why and How? London : SAGE, 2010; Yin, Robert K. Case Study Research: Design and Methods . 6th edition. Los Angeles, CA, SAGE Publications, 2014; Walo, Maree, Adrian Bull, and Helen Breen. “Achieving Economic Benefits at Local Events: A Case Study of a Local Sports Event.” Festival Management and Event Tourism 4 (1996): 95-106.
Writing Tip
At Least Five Misconceptions about Case Study Research
Social science case studies are often perceived as limited in their ability to create new knowledge because they are not randomly selected and findings cannot be generalized to larger populations. Flyvbjerg examines five misunderstandings about case study research and systematically "corrects" each one. To quote, these are:
Misunderstanding 1 : General, theoretical [context-independent] knowledge is more valuable than concrete, practical [context-dependent] knowledge. Misunderstanding 2 : One cannot generalize on the basis of an individual case; therefore, the case study cannot contribute to scientific development. Misunderstanding 3 : The case study is most useful for generating hypotheses; that is, in the first stage of a total research process, whereas other methods are more suitable for hypotheses testing and theory building. Misunderstanding 4 : The case study contains a bias toward verification, that is, a tendency to confirm the researcher’s preconceived notions. Misunderstanding 5 : It is often difficult to summarize and develop general propositions and theories on the basis of specific case studies [p. 221].
While writing your paper, think introspectively about how you addressed these misconceptions because to do so can help you strengthen the validity and reliability of your research by clarifying issues of case selection, the testing and challenging of existing assumptions, the interpretation of key findings, and the summation of case outcomes. Think of a case study research paper as a complete, in-depth narrative about the specific properties and key characteristics of your subject of analysis applied to the research problem.
Flyvbjerg, Bent. “Five Misunderstandings About Case-Study Research.” Qualitative Inquiry 12 (April 2006): 219-245.
- << Previous: Writing a Case Analysis Paper
- Next: Writing a Field Report >>
- Last Updated: Jun 3, 2024 9:44 AM
- URL: https://libguides.usc.edu/writingguide/assignments
The Discussion Group Experience
Leadership Insights Blog
Overview dropdown up, overview dropdown down, benefits expand all collapse all, gain a better understanding of the case materials gain a better understanding of the case materials dropdown down, practice teaching and learning from others practice teaching and learning from others dropdown down, "test-market" ideas and opinions before class "test-market" ideas and opinions before class dropdown down, get to know a handful of people more deeply get to know a handful of people more deeply dropdown down, benefits dropdown up, benefits dropdown down, gain a better understanding of the case materials, practice teaching and learning from others, "test-market" ideas and opinions before class, get to know a handful of people more deeply, best practices expand all collapse all, designate one discussion leader designate one discussion leader dropdown down, ensure 100 percent attendance ensure 100 percent attendance dropdown down, expect 100 percent participation expect 100 percent participation dropdown down, encourage challenging viewpoints encourage challenging viewpoints dropdown down, stay focused and use time wisely stay focused and use time wisely dropdown down, accept responsibility to learn and teach accept responsibility to learn and teach dropdown down, best practices dropdown up, best practices dropdown down, designate one discussion leader, ensure 100 percent attendance, expect 100 percent participation, encourage challenging viewpoints, stay focused and use time wisely, accept responsibility to learn and teach, what can i expect on the first day dropdown down.
Most programs begin with registration, followed by an opening session and a dinner. If your travel plans necessitate late arrival, please be sure to notify us so that alternate registration arrangements can be made for you. Please note the following about registration:
HBS campus programs – Registration takes place in the Chao Center.
India programs – Registration takes place outside the classroom.
Other off-campus programs – Registration takes place in the designated facility.
What happens in class if nobody talks? Dropdown down
Professors are here to push everyone to learn, but not to embarrass anyone. If the class is quiet, they'll often ask a participant with experience in the industry in which the case is set to speak first. This is done well in advance so that person can come to class prepared to share. Trust the process. The more open you are, the more willing you’ll be to engage, and the more alive the classroom will become.
Does everyone take part in "role-playing"? Dropdown down
Professors often encourage participants to take opposing sides and then debate the issues, often taking the perspective of the case protagonists or key decision makers in the case.
View Frequently Asked Questions
Subscribe to Our Emails
- Utility Menu
GA4 tagging code

- Demonstrating Moves Live
- Raw Clips Library
- Facilitation Guide
Structuring the Case Discussion
Well-designed cases are intentionally complex. Therefore, presenting an entire case to students all at once has the potential to overwhelm student groups and lead them to overlook key details or analytic steps. Accordingly, Barbara Cockrill asks students to review key case concepts the night before, and then presents the case in digestible “chunks” during a CBCL session. Structuring the case discussion around key in-depth questions, Cockrill creates a thoughtful interplay between small group work and whole group discussion that makes for more systematic forays into the case at hand.
Barbara Cockrill , Harold Amos Academy Associate Professor of Medicine
Student Group
Harvard Medical School
Homeostasis I
40 students
Additional Details
First-year requisite
- Classroom Considerations
- Relevant Research
- Related Resources
- CBCL provides students the opportunity to apply course material in new ways. For this reason, you might consider not sharing the case with students beforehand and having them experience it in class with fresh eyes.
- Chunk cases so students can focus on case specifics and gradually build-up to greater complexity and understanding.
- Introduce variety into case-based discussions. Integrate a mix of independent work, small group discussion, and whole group share outs to keep students engaged and provide multiple junctures for students to get feedback on their understanding.
- Instructor scaffolding is critical for effective case-based learning ( Ramaekers et al., 2011 )
- This resource from the Harvard Business School provides suggestions for questioning, listening, and responding during a case discussion .
- This comprehensive resource on “The ABCs of Case Teaching” provides helpful tips for planning and “running” your case .
Related Moves

Experiencing the Case as a Student Team

Regulating the Flow of Energy in the Classroom

Designing Focused Discussions for Relevance and Transfer of Knowledge

Search form

- Table of Contents
- Troubleshooting Guide
- A Model for Getting Started
- Justice Action Toolkit
- Best Change Processes
- Databases of Best Practices
- Online Courses
- Ask an Advisor
- Subscribe to eNewsletter
- Community Stories
- YouTube Channel
- About the Tool Box
- How to Use the Tool Box
- Privacy Statement
- Workstation/Check Box Sign-In
- Online Training Courses
- Capacity Building Training
- Training Curriculum - Order Now
- Community Check Box Evaluation System
- Build Your Toolbox
- Facilitation of Community Processes
- Community Health Assessment and Planning
- Section 4. Techniques for Leading Group Discussions
Chapter 16 Sections
- Section 1. Conducting Effective Meetings
- Section 2. Developing Facilitation Skills
- Section 3. Capturing What People Say: Tips for Recording a Meeting
- Main Section
A local coalition forms a task force to address the rising HIV rate among teens in the community. A group of parents meets to wrestle with their feeling that their school district is shortchanging its students. A college class in human services approaches the topic of dealing with reluctant participants. Members of an environmental group attend a workshop on the effects of global warming. A politician convenes a “town hall meeting” of constituents to brainstorm ideas for the economic development of the region. A community health educator facilitates a smoking cessation support group.
All of these might be examples of group discussions, although they have different purposes, take place in different locations, and probably run in different ways. Group discussions are common in a democratic society, and, as a community builder, it’s more than likely that you have been and will continue to be involved in many of them. You also may be in a position to lead one, and that’s what this section is about. In this last section of a chapter on group facilitation, we’ll examine what it takes to lead a discussion group well, and how you can go about doing it.
What is an effective group discussion?
The literal definition of a group discussion is obvious: a critical conversation about a particular topic, or perhaps a range of topics, conducted in a group of a size that allows participation by all members. A group of two or three generally doesn’t need a leader to have a good discussion, but once the number reaches five or six, a leader or facilitator can often be helpful. When the group numbers eight or more, a leader or facilitator, whether formal or informal, is almost always helpful in ensuring an effective discussion.
A group discussion is a type of meeting, but it differs from the formal meetings in a number of ways: It may not have a specific goal – many group discussions are just that: a group kicking around ideas on a particular topic. That may lead to a goal ultimately...but it may not. It’s less formal, and may have no time constraints, or structured order, or agenda. Its leadership is usually less directive than that of a meeting. It emphasizes process (the consideration of ideas) over product (specific tasks to be accomplished within the confines of the meeting itself. Leading a discussion group is not the same as running a meeting. It’s much closer to acting as a facilitator, but not exactly the same as that either.
An effective group discussion generally has a number of elements:
- All members of the group have a chance to speak, expressing their own ideas and feelings freely, and to pursue and finish out their thoughts
- All members of the group can hear others’ ideas and feelings stated openly
- Group members can safely test out ideas that are not yet fully formed
- Group members can receive and respond to respectful but honest and constructive feedback. Feedback could be positive, negative, or merely clarifying or correcting factual questions or errors, but is in all cases delivered respectfully.
- A variety of points of view are put forward and discussed
- The discussion is not dominated by any one person
- Arguments, while they may be spirited, are based on the content of ideas and opinions, not on personalities
- Even in disagreement, there’s an understanding that the group is working together to resolve a dispute, solve a problem, create a plan, make a decision, find principles all can agree on, or come to a conclusion from which it can move on to further discussion
Many group discussions have no specific purpose except the exchange of ideas and opinions. Ultimately, an effective group discussion is one in which many different ideas and viewpoints are heard and considered. This allows the group to accomplish its purpose if it has one, or to establish a basis either for ongoing discussion or for further contact and collaboration among its members.
There are many possible purposes for a group discussion, such as:
- Create a new situation – form a coalition, start an initiative, etc.
- Explore cooperative or collaborative arrangements among groups or organizations
- Discuss and/or analyze an issue, with no specific goal in mind but understanding
- Create a strategic plan – for an initiative, an advocacy campaign, an intervention, etc.
- Discuss policy and policy change
- Air concerns and differences among individuals or groups
- Hold public hearings on proposed laws or regulations, development, etc.
- Decide on an action
- Provide mutual support
- Solve a problem
- Resolve a conflict
- Plan your work or an event
Possible leadership styles of a group discussion also vary. A group leader or facilitator might be directive or non-directive; that is, she might try to control what goes on to a large extent; or she might assume that the group should be in control, and that her job is to facilitate the process. In most group discussions, leaders who are relatively non-directive make for a more broad-ranging outlay of ideas, and a more satisfying experience for participants.
Directive leaders can be necessary in some situations. If a goal must be reached in a short time period, a directive leader might help to keep the group focused. If the situation is particularly difficult, a directive leader might be needed to keep control of the discussion and make
Why would you lead a group discussion?
There are two ways to look at this question: “What’s the point of group discussion?” and “Why would you, as opposed to someone else, lead a group discussion?” Let’s examine both.
What’s the point of group discussion?
As explained in the opening paragraphs of this section, group discussions are common in a democratic society. There are a number of reasons for this, some practical and some philosophical.
A group discussion:
- G ives everyone involved a voice . Whether the discussion is meant to form a basis for action, or just to play with ideas, it gives all members of the group a chance to speak their opinions, to agree or disagree with others, and to have their thoughts heard. In many community-building situations, the members of the group might be chosen specifically because they represent a cross-section of the community, or a diversity of points of view.
- Allows for a variety of ideas to be expressed and discussed . A group is much more likely to come to a good conclusion if a mix of ideas is on the table, and if all members have the opportunity to think about and respond to them.
- Is generally a democratic, egalitarian process . It reflects the ideals of most grassroots and community groups, and encourages a diversity of views.
- Leads to group ownership of whatever conclusions, plans, or action the group decides upon . Because everyone has a chance to contribute to the discussion and to be heard, the final result feels like it was arrived at by and belongs to everyone.
- Encourages those who might normally be reluctant to speak their minds . Often, quiet people have important things to contribute, but aren’t assertive enough to make themselves heard. A good group discussion will bring them out and support them.
- Can often open communication channels among people who might not communicate in any other way . People from very different backgrounds, from opposite ends of the political spectrum, from different cultures, who may, under most circumstances, either never make contact or never trust one another enough to try to communicate, might, in a group discussion, find more common ground than they expected.
- Is sometimes simply the obvious, or even the only, way to proceed. Several of the examples given at the beginning of the section – the group of parents concerned about their school system, for instance, or the college class – fall into this category, as do public hearings and similar gatherings.
Why would you specifically lead a group discussion?
You might choose to lead a group discussion, or you might find yourself drafted for the task. Some of the most common reasons that you might be in that situation:
- It’s part of your job . As a mental health counselor, a youth worker, a coalition coordinator, a teacher, the president of a board of directors, etc. you might be expected to lead group discussions regularly.
- You’ve been asked to . Because of your reputation for objectivity or integrity, because of your position in the community, or because of your skill at leading group discussions, you might be the obvious choice to lead a particular discussion.
- A discussion is necessary, and you’re the logical choice to lead it . If you’re the chair of a task force to address substance use in the community, for instance, it’s likely that you’ll be expected to conduct that task force’s meetings, and to lead discussion of the issue.
- It was your idea in the first place . The group discussion, or its purpose, was your idea, and the organization of the process falls to you.
You might find yourself in one of these situations if you fall into one of the categories of people who are often tapped to lead group discussions. These categories include (but aren’t limited to):
- Directors of organizations
- Public officials
- Coalition coordinators
- Professionals with group-leading skills – counselors, social workers, therapists, etc.
- Health professionals and health educators
- Respected community members. These folks may be respected for their leadership – president of the Rotary Club, spokesperson for an environmental movement – for their positions in the community – bank president, clergyman – or simply for their personal qualities – integrity, fairness, ability to communicate with all sectors of the community.
- Community activists. This category could include anyone from “professional” community organizers to average citizens who care about an issue or have an idea they want to pursue.
When might you lead a group discussion?
The need or desire for a group discussion might of course arise anytime, but there are some times when it’s particularly necessary.
- At the start of something new . Whether you’re designing an intervention, starting an initiative, creating a new program, building a coalition, or embarking on an advocacy or other campaign, inclusive discussion is likely to be crucial in generating the best possible plan, and creating community support for and ownership of it.
- When an issue can no longer be ignored . When youth violence reaches a critical point, when the community’s drinking water is declared unsafe, when the HIV infection rate climbs – these are times when groups need to convene to discuss the issue and develop action plans to swing the pendulum in the other direction.
- When groups need to be brought together . One way to deal with racial or ethnic hostility, for instance, is to convene groups made up of representatives of all the factions involved. The resulting discussions – and the opportunity for people from different backgrounds to make personal connections with one another – can go far to address everyone’s concerns, and to reduce tensions.
- When an existing group is considering its next step or seeking to address an issue of importance to it . The staff of a community service organization, for instance, may want to plan its work for the next few months, or to work out how to deal with people with particular quirks or problems.
How do you lead a group discussion?
In some cases, the opportunity to lead a group discussion can arise on the spur of the moment; in others, it’s a more formal arrangement, planned and expected. In the latter case, you may have the chance to choose a space and otherwise structure the situation. In less formal circumstances, you’ll have to make the best of existing conditions.
We’ll begin by looking at what you might consider if you have time to prepare. Then we’ll examine what it takes to make an effective discussion leader or facilitator, regardless of external circumstances.
Set the stage
If you have time to prepare beforehand, there are a number of things you may be able to do to make the participants more comfortable, and thus to make discussion easier.
Choose the space
If you have the luxury of choosing your space, you might look for someplace that’s comfortable and informal. Usually, that means comfortable furniture that can be moved around (so that, for instance, the group can form a circle, allowing everyone to see and hear everyone else easily). It may also mean a space away from the ordinary.
One organization often held discussions on the terrace of an old mill that had been turned into a bookstore and café. The sound of water from the mill stream rushing by put everyone at ease, and encouraged creative thought.
Provide food and drink
The ultimate comfort, and one that breaks down barriers among people, is that of eating and drinking.
Bring materials to help the discussion along
Most discussions are aided by the use of newsprint and markers to record ideas, for example.
Become familiar with the purpose and content of the discussion
If you have the opportunity, learn as much as possible about the topic under discussion. This is not meant to make you the expert, but rather to allow you to ask good questions that will help the group generate ideas.
Make sure everyone gets any necessary information, readings, or other material beforehand
If participants are asked to read something, consider questions, complete a task, or otherwise prepare for the discussion, make sure that the assignment is attended to and used. Don’t ask people to do something, and then ignore it.
Lead the discussion
Think about leadership style
The first thing you need to think about is leadership style, which we mentioned briefly earlier in the section. Are you a directive or non-directive leader? The chances are that, like most of us, you fall somewhere in between the extremes of the leader who sets the agenda and dominates the group completely, and the leader who essentially leads not at all. The point is made that many good group or meeting leaders are, in fact, facilitators, whose main concern is supporting and maintaining the process of the group’s work. This is particularly true when it comes to group discussion, where the process is, in fact, the purpose of the group’s coming together.
A good facilitator helps the group set rules for itself, makes sure that everyone participates and that no one dominates, encourages the development and expression of all ideas, including “odd” ones, and safeguards an open process, where there are no foregone conclusions and everyone’s ideas are respected. Facilitators are non-directive, and try to keep themselves out of the discussion, except to ask questions or make statements that advance it. For most group discussions, the facilitator role is probably a good ideal to strive for.
It’s important to think about what you’re most comfortable with philosophically, and how that fits what you’re comfortable with personally. If you’re committed to a non-directive style, but you tend to want to control everything in a situation, you may have to learn some new behaviors in order to act on your beliefs.
Put people at ease
Especially if most people in the group don’t know one another, it’s your job as leader to establish a comfortable atmosphere and set the tone for the discussion.
Help the group establish ground rules
The ground rules of a group discussion are the guidelines that help to keep the discussion on track, and prevent it from deteriorating into namecalling or simply argument. Some you might suggest, if the group has trouble coming up with the first one or two:
- Everyone should treat everyone else with respect : no name-calling, no emotional outbursts, no accusations.
- No arguments directed at people – only at ideas and opinions . Disagreement should be respectful – no ridicule.
- Don’t interrupt . Listen to the whole of others’ thoughts – actually listen, rather than just running over your own response in your head.
- Respect the group’s time . Try to keep your comments reasonably short and to the point, so that others have a chance to respond.
- Consider all comments seriously, and try to evaluate them fairly . Others’ ideas and comments may change your mind, or vice versa: it’s important to be open to that.
- Don’t be defensive if someone disagrees with you . Evaluate both positions, and only continue to argue for yours if you continue to believe it’s right.
- Everyone is responsible for following and upholding the ground rules .
Ground rules may also be a place to discuss recording the session. Who will take notes, record important points, questions for further discussion, areas of agreement or disagreement? If the recorder is a group member, the group and/or leader should come up with a strategy that allows her to participate fully in the discussion.
Generate an agenda or goals for the session
You might present an agenda for approval, and change it as the group requires, or you and the group can create one together. There may actually be no need for one, in that the goal may simply be to discuss an issue or idea. If that’s the case, it should be agreed upon at the outset.
How active you are might depend on your leadership style, but you definitely have some responsibilities here. They include setting, or helping the group to set the discussion topic; fostering the open process; involving all participants; asking questions or offering ideas to advance the discussion; summarizing or clarifying important points, arguments, and ideas; and wrapping up the session. Let’s look at these, as well as some do’s and don’t’s for discussion group leaders.
- Setting the topic . If the group is meeting to discuss a specific issue or to plan something, the discussion topic is already set. If the topic is unclear, then someone needs to help the group define it. The leader – through asking the right questions, defining the problem, and encouraging ideas from the group – can play that role.
- Fostering the open process . Nurturing the open process means paying attention to the process, content, and interpersonal dynamics of the discussion all at the same time – not a simple matter. As leader, your task is not to tell the group what to do, or to force particular conclusions, but rather to make sure that the group chooses an appropriate topic that meets its needs, that there are no “right” answers to start with (no foregone conclusions), that no one person or small group dominates the discussion, that everyone follows the ground rules, that discussion is civil and organized, and that all ideas are subjected to careful critical analysis. You might comment on the process of the discussion or on interpersonal issues when it seems helpful (“We all seem to be picking on John here – what’s going on?”), or make reference to the open process itself (“We seem to be assuming that we’re supposed to believe X – is that true?”). Most of your actions as leader should be in the service of modeling or furthering the open process.
Part of your job here is to protect “minority rights,” i.e., unpopular or unusual ideas. That doesn’t mean you have to agree with them, but that you have to make sure that they can be expressed, and that discussion of them is respectful, even in disagreement. (The exceptions are opinions or ideas that are discriminatory or downright false.) Odd ideas often turn out to be correct, and shouldn’t be stifled.
- Involving all participants . This is part of fostering the open process, but is important enough to deserve its own mention. To involve those who are less assertive or shy, or who simply can’t speak up quickly enough, you might ask directly for their opinion, encourage them with body language (smile when they say anything, lean and look toward them often), and be aware of when they want to speak and can’t break in. It’s important both for process and for the exchange of ideas that everyone have plenty of opportunity to communicate their thoughts.
- Asking questions or offering ideas to advance the discussion . The leader should be aware of the progress of the discussion, and should be able to ask questions or provide information or arguments that stimulate thinking or take the discussion to the next step when necessary. If participants are having trouble grappling with the topic, getting sidetracked by trivial issues, or simply running out of steam, it’s the leader’s job to carry the discussion forward.
This is especially true when the group is stuck, either because two opposing ideas or factions are at an impasse, or because no one is able or willing to say anything. In these circumstances, the leader’s ability to identify points of agreement, or to ask the question that will get discussion moving again is crucial to the group’s effectiveness.
- Summarizing or clarifying important points, arguments, or ideas . This task entails making sure that everyone understands a point that was just made, or the two sides of an argument. It can include restating a conclusion the group has reached, or clarifying a particular idea or point made by an individual (“What I think I heard you say was…”). The point is to make sure that everyone understands what the individual or group actually meant.
- Wrapping up the session . As the session ends, the leader should help the group review the discussion and make plans for next steps (more discussion sessions, action, involving other people or groups, etc.). He should also go over any assignments or tasks that were agreed to, make sure that every member knows what her responsibilities are, and review the deadlines for those responsibilities. Other wrap-up steps include getting feedback on the session – including suggestions for making it better – pointing out the group’s accomplishments, and thanking it for its work.
Even after you’ve wrapped up the discussion, you’re not necessarily through. If you’ve been the recorder, you might want to put the notes from the session in order, type them up, and send them to participants. The notes might also include a summary of conclusions that were reached, as well as any assignments or follow-up activities that were agreed on.
If the session was one-time, or was the last of a series, your job may now be done. If it was the beginning, however, or part of an ongoing discussion, you may have a lot to do before the next session, including contacting people to make sure they’ve done what they promised, and preparing the newsprint notes to be posted at the next session so everyone can remember the discussion.
Leading an effective group discussion takes preparation (if you have the opportunity for it), an understanding of and commitment to an open process, and a willingness to let go of your ego and biases. If you can do these things, the chances are you can become a discussion leader that can help groups achieve the results they want.
Do’s and don’ts for discussion leaders
- Model the behavior and attitudes you want group members to employ . That includes respecting all group members equally; advancing the open process; demonstrating what it means to be a learner (admitting when you’re wrong, or don’t know a fact or an answer, and suggesting ways to find out); asking questions based on others’ statements; focusing on positions rather than on the speaker; listening carefully; restating others’ points; supporting your arguments with fact or logic; acceding when someone else has a good point; accepting criticism; thinking critically; giving up the floor when appropriate; being inclusive and culturally sensitive, etc.
- Use encouraging body language and tone of voice, as well as words . Lean forward when people are talking, for example, keep your body position open and approachable, smile when appropriate, and attend carefully to everyone, not just to those who are most articulate.
- Give positive feedback for joining the discussion . Smile, repeat group members’ points, and otherwise show that you value participation.
- Be aware of people’s reactions and feelings, and try to respond appropriately . If a group member is hurt by others’ comments, seems puzzled or confused, is becoming angry or defensive, it’s up to you as discussion leader to use the ground rules or your own sensitivity to deal with the situation. If someone’s hurt, for instance, it may be important to point that out and discuss how to make arguments without getting personal. If group members are confused, revisiting the comments or points that caused the confusion, or restating them more clearly, may be helpful. Being aware of the reactions of individuals and of the group as a whole can make it possible to expose and use conflict, or to head off unnecessary emotional situations and misunderstandings.
- Ask open-ended questions . In advancing the discussion, use questions that can’t be answered with a simple yes or no. Instead, questions should require some thought from group members, and should ask for answers that include reasons or analysis. The difference between “Do you think the President’s decision was right?” and “Why do you think the President’s decision was or wasn’t right?” is huge. Where the first question can be answered with a yes or no, the second requires an analysis supporting the speaker’s opinion, as well as discussion of the context and reasons for the decision.
- Control your own biases . While you should point out factual errors or ideas that are inaccurate and disrespectful of others, an open process demands that you not impose your views on the group, and that you keep others from doing the same. Group members should be asked to make rational decisions about the positions or views they want to agree with, and ultimately the ideas that the group agrees on should be those that make the most sense to them – whether they coincide with yours or not. Pointing out bias – including your own – and discussing it helps both you and group members try to be objective.
A constant question that leaders – and members – of any group have is what to do about racist, sexist, or homophobic remarks, especially in a homogeneous group where most or all of the members except the leader may agree with them. There is no clear-cut answer, although if they pass unchallenged, it may appear you condone the attitude expressed. How you challenge prejudice is the real question. The ideal here is that other members of the group do the challenging, and it may be worth waiting long enough before you jump in to see if that’s going to happen. If it doesn’t, you can essentially say, “That’s wrong, and I won’t allow that kind of talk here,” which may well put an end to the remarks, but isn’t likely to change anyone’s mind. You can express your strong disagreement or discomfort with such remarks and leave it at that, or follow up with “Let’s talk about it after the group,” which could generate some real discussion about prejudice and stereotypes, and actually change some thinking over time. Your ground rules – the issue of respecting everyone – should address this issue, and it probably won’t come up…but there are no guarantees. It won’t hurt to think beforehand about how you want to handle it.
- Encourage disagreement, and help the group use it creatively . Disagreement is not to be smoothed over, but rather to be analyzed and used. When there are conflicting opinions – especially when both can be backed up by reasonable arguments – the real discussion starts. If everyone agrees on every point, there’s really no discussion at all. Disagreement makes people think. It may not be resolved in one session, or at all, but it’s the key to discussion that means something.
All too often, conflict – whether conflicting opinions, conflicting world views, or conflicting personalities – is so frightening to people that they do their best to ignore it or gloss it over. That reaction not only leaves the conflict unresolved – and therefore growing, so that it will be much stronger when it surfaces later– but fails to examine the issues that it raises. If those are brought out in the open and discussed reasonably, the two sides often find that they have as much agreement as disagreement, and can resolve their differences by putting their ideas together. Even where that’s not the case, facing the conflict reasonably, and looking at the roots of the ideas on each side, can help to focus on the issue at hand and provide solutions far better than if one side or the other simply operated alone.
- Keep your mouth shut as much as possible . By and large, discussion groups are for the group members. You may be a member of the group and have been asked by the others to act as leader, in which case you certainly have a right to be part of the discussion (although not to dominate). If you’re an outside facilitator, or leader by position, it’s best to confine your contributions to observations on process, statements of fact, questions to help propel the discussion, and clarification and summarization. The simple fact that you’re identified as leader or facilitator gives your comments more force than those of other group members. If you’re in a position of authority or seen as an expert, that force becomes even greater. The more active you are in the discussion, the more the group will take your positions and ideas as “right,” and the less it will come to its own conclusions.
- Don’t let one or a small group of individuals dominate the discussion . People who are particularly articulate or assertive, who have strong feelings that they urgently want to express, or who simply feel the need – and have the ability – to dominate can take up far more than their fair share of a discussion. This often means that quieter people have little or no chance to speak, and that those who disagree with the dominant individual(s) are shouted down and cease trying to make points. It’s up to the leader to cut off individuals who take far more than their share of time, or who try to limit discussion. This can be done in a relatively non-threatening way (“This is an interesting point, and it’s certainly worth the time we’ve spent on it, but there are other points of view that need to be heard as well. I think Alice has been waiting to speak…”), but it’s crucial to the open process and to the comfort and effectiveness of the group.
- Don’t let one point of view override others , unless it’s based on facts and logic, and is actually convincing group members to change their minds. If a point of view dominates because of its merits, its appeal to participants’ intellectual and ethical sensibilities, that’s fine. It’s in fact what you hope will happen in a good group discussion. If a point of view dominates because of the aggressiveness of its supporters, or because it’s presented as something it’s wrong to oppose (“People who disagree with the President are unpatriotic and hate their country”), that’s intellectual bullying or blackmail, and is the opposite of an open discussion. As leader, you should point it out when that’s happening, and make sure other points of view are aired and examined.
Sometimes individuals or factions that are trying to dominate can disrupt the process of the group. Both Sections 1 and 2 of this chapter contain some guidelines for dealing with this type of situation.
- Don’t assume that anyone holds particular opinions or positions because of his culture, background, race, personal style, etc . People are individuals, and can’t be judged by their exteriors. You can find out what someone thinks by asking, or by listening when he speaks.
- Don’t assume that someone from a particular culture, race, or background speaks for everyone else from that situation . She may or may not represent the general opinion of people from situations similar to hers…or there may not be a general opinion among them. In a group discussion, no one should be asked or assumed to represent anything more than herself.
The exception here is when someone has been chosen by her community or group to represent its point of view in a multi-sector discussion. Even in that situation, the individual may find herself swayed by others’ arguments, or may have ideas of her own. She may have agreed to sponsor particular ideas that are important to her group, but she may still have her own opinions as well, especially in other areas.
- Don’t be the font of all wisdom . Even if you know more about the discussion topic than most others in the group (if you’re the teacher of a class, for instance), presenting yourself as the intellectual authority denies group members the chance to discuss the topic freely and without pressure. Furthermore, some of them may have ideas you haven’t considered, or experiences that give them insights into the topic that you’re never likely to have. Model learning behavior, not teaching behavior.
If you’re asked your opinion directly, you should answer honestly. You have some choices about how you do that, however. One is to state your opinion, but make very clear that it’s an opinion, not a fact, and that other people believe differently. Another is to ask to hold your opinion until the end of the discussion, so as not to influence anyone’s thinking while it’s going on. Yet another is to give your opinion after all other members of the group have stated theirs, and then discuss the similarities and differences among all the opinions and people’s reasons for holding them. If you’re asked a direct question, you might want to answer it if it’s a question of fact and you know the answer, and if it’s relevant to the discussion. If the question is less clear-cut, you might want to throw it back to the group, and use it as a spur to discussion.
Group discussions are common in our society, and have a variety of purposes, from planning an intervention or initiative to mutual support to problem-solving to addressing an issue of local concern. An effective discussion group depends on a leader or facilitator who can guide it through an open process – the group chooses what it’s discussing, if not already determined, discusses it with no expectation of particular conclusions, encourages civil disagreement and argument, and makes sure that every member is included and no one dominates. It helps greatly if the leader comes to the task with a democratic or, especially, a collaborative style, and with an understanding of how a group functions.
A good group discussion leader has to pay attention to the process and content of the discussion as well as to the people who make up the group. She has to prepare the space and the setting to the extent possible; help the group establish ground rules that will keep it moving civilly and comfortably; provide whatever materials are necessary; familiarize herself with the topic; and make sure that any pre-discussion readings or assignments get to participants in plenty of time. Then she has to guide the discussion, being careful to promote an open process; involve everyone and let no one dominate; attend to the personal issues and needs of individual group members when they affect the group; summarize or clarify when appropriate; ask questions to keep the discussion moving, and put aside her own agenda, ego, and biases.
It’s not an easy task, but it can be extremely rewarding. An effective group discussion can lay the groundwork for action and real community change.
Online resources
Everyday-Democracy . Study Circles Resource Center. Information and publications related to study circles, participatory discussion groups meant to address community issues.
Facilitating Political Discussions from the Institute for Democracy and Higher Education at Tufts University is designed to assist experienced facilitators in training others to facilitate politically charged conversations. The materials are broken down into "modules" and facilitation trainers can use some or all of them to suit their needs.
Project on Civic Reflection provides information about leading study circles on civic reflection.
“ Suggestions for Leading Small-Group Discussions ,” prepared by Lee Haugen, Center for Teaching Excellence, Iowa State University, 1998. Tips on university teaching, but much of the information is useful in other circumstances as well.
“ Tips for Leading Discussions ,” by Felisa Tibbits, Human Rights Education Associates.
Print resources
Forsyth, D . Group Dynamics . (2006). (4th edition). Belmont, CA: Thomson Wadsworth.
Johnson, D., & Frank P. (2002). Joining Together: Group theory and group skills . (8th edition). Boston: Allyn & Bacon.
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
Research Methods at SCS
- Basic Strategies
- Literature Reviews & Annotated Bibliographies
- Qualitative & Quantitative Methods
Case Studies
Focus groups.
- White Papers
- << Previous: Qualitative & Quantitative Methods
- Next: Surveys >>
- Last Updated: Jan 26, 2024 10:52 AM
- URL: https://guides.library.georgetown.edu/research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Patient Exp
Focus Group Discussion as a Tool to Assess Patient-Based Outcomes, Practical Tips for Conducting Focus Group Discussion for Medical Students—Learning With an Example
Balaji zacharia.
1 Department of Orthopedics, Government Medical College, Kozhikode, Kerala, India
Puneeth Katapadi Pai
2 Government Medical College, Kozhikode, Kerala, India
3 Department of Surgical Oncology, Regional Cancer Center, Trivandrum, Kerala, India
Patient-based outcomes (patient-reported outcomes) of any intervention can change according to factors like age, gender, region, culture, education, and socioeconomic status. Most of the available outcome measuring tools have a surgeon-related bias. Focus group discussion (FGD) is a simple and effective way to assess the outcome of an intervention. In FGD, people from similar backgrounds and experiences discuss a specific topic of interest. Our objective is to discuss the problems of common outcome measuring tools for patient satisfaction and to understand the method of conducting an FGD. We have set our own published article on patient-based outcomes after total knee arthroplasty (TKA) as an example for explaining the method of conducting an FGD. The planning, advantages, disadvantages, practicalities, and problems of conducting an FGD are explained. In conclusion, many of the tools used for assessing patient satisfaction is surgeon-centered. Focus group discussion is simple, cost-effective, requiring a small number of participants, and can be completed in a short period. It is an effective tool for assessing patient-based outcomes in TKA.
Introduction
The patient satisfaction assessment is very important in medical practice. It helps to improve medical care and make the patient happier ( 1 ). A patient’s expectation after a procedure is defined as the anticipation of certain events happening during or after surgery ( 2 ). Patient dissatisfaction can result either from inappropriate expectations or from a lack of proper information regarding the outcomes. The surgeon gives importance to procedural success. They are usually unaware of patient dissatisfaction. Regional, social, cultural, and economic factors have a bearing on the outcomes of any treatment ( 3 ).
Surgical outcomes refer to data regarding operation results, including information about mortality and morbidity, recovery time, operative numbers, and repeat rates ( 4 ). This is different from the surgeon’s expectations about the outcome which vary with the type of surgery, the seriousness of the condition, the age and fitness of the patient, the experience of the surgeon, and the volume of surgery done. Most of the tools used to find out the outcomes and measure the ability of the surgeon to produce statistically significant data using certain prescribed parameters ( 5 ). The surgeon judges the success of surgery based on the anatomical, radiological, and functional outcomes. The majority of the tools used for measuring the outcomes of surgery are based on the fact that the patient and the clinician have a common viewpoint about the outcome. This is not always true as the patient and the doctor have different perceptions about all domains of outcomes. This is true in subjective quality-of-life domains like emotional and social functioning ( 6 ). This may be probably due to the differing priorities of the 2 groups. This discrepancy between patient and clinician in the validation of health-related outcomes has guided the development of many validated patient-related outcome measures like Short Form 36 (SF 36), Eating disorder Quality of life (ED-QOL), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Oxford Knee Score, and so on. These tools allow patients to rate their health and they are the center of outcome assessment ( 7 ).
Total knee replacement (TKR) is a common surgery done for osteoarthritis (OA) of the knee worldwide. It has a major effect on the activities of daily living. The geographical, social, cultural, economic, and many factors of a population can influence the outcomes of TKR. Expectations after the knee replacement will differ entirely among different populations ( 8 ). A successful TKR may not be a satisfactory one for the patient due to differences in factors determining the outcome measures ( Table 1 ). Many previous studies have looked into the patient-reported outcomes of TKR ( Table 2 ).
A Comparison Between the Factors Affecting the Outcomes in a Successful Total Knee Replacement and Patient Satisfaction After a Total Knee Replacement.
Abbreviation: TKR, total knee replacement.
The List of Few Previous studies to Assess Patient-Reported Outcomes After Total Knee Replacement With the Methods Used for Assessment and Their Conclusions.
Abbreviations: FGD, focus group discussion; HOOS, Hip disability and Osteoarthritis Outcome Score; KOOS, Knee injury and Osteoarthritis Outcome Score; ODI, Oswestry Disability Index; RAND, RAND-36 scales; TKA, total knee arthroplasty; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
Focus group discussion (FGD) is a qualitative research method. It can be used for evaluating the outcomes of health care interventions ( 9 ). A focused group discussion is an effective way to bring people from similar backgrounds and experiences to discuss a specific topic of interest. This group is guided by a moderator/leader. The moderator introduces the topic for discussion and helps the group to participate in a lively and natural way. The participants should stay on the topic and not wander ( 10 – 12 ).
There are many advantages to FGD. It can be used to explore the outcomes that cannot be explained statistically. Responses in FGD are spoken open-ended, relatively broad, and qualitative ( 13 ). They have more depth and variety. There can be nonverbal communication and group interactions. They can give an idea closer to what people are thinking and feeling. Focus group discussion is a good way to gather in-depth information about the community’s thoughts and opinions on a topic ( 14 , 15 ). Focus group discussion can yield a lot of information about a topic in a relatively short time. All these pieces of information may not be relevant. Observations and the opinions we get from FGD have to be mentioned in their own words. It can cause difficulties during translation ( 16 , 17 ). Thematic analysis and constant comparison techniques are used for data analysis ( 18 ).
Our objective is to discuss FGD as a tool to assess patient satisfaction. We also want to give some general guidelines for conducting FGD. This is based on our article published in the Journal of Medical Devices : Evidence and Research “Patient-based outcome analysis is important to determine the success of total knee arthroplasty: the result of a focus group discussion” ( 19 ) (We have taken permission from the publisher).
Materials and Methods
Fifty patients were selected for FGD. Among them, 42 patients participated in FGD. The remaining 8 did not participated. We included persons who had completed 2 years after primary TKR. Six FGD sessions was conducted. We included participants who were homogeneous in terms of age, status, class, occupation, and follow-up characteristics. Patients with inflammatory arthritis, secondary OA, posttraumatic arthritis, old high tibial osteotomy, and revision TKR were excluded from our study. Since we aimed to find out the patient-reported outcomes, we used a purposive sampling method. We collected the patient details from our hospital records. We selected a moderator who had no relationship with the patients. The participants were divided into 8 groups, each having 6 members. The allocation was done by simple randomization. After each FGD, we went through the discussions and created new domains and subdomains. Based on this, we prepared new questions for the next sessions. It helped us to discuss a bit deeper into the new domains ( 19 ). Proper planning is needed before the conduct of FGD ( Appendix A ).
The group’s composition and the discussion should be carefully planned to create a nonthreatening environment. All participants feel free to talk openly and give honest opinions. There is freedom for the participants to agree or disagree with each other. We have to support them to come out with their own opinions. They are free to express their thoughts and feelings, although their responses are hard or impossible to record on a scale.
The demographic data of the participants were collected. We also checked the knee society score of all the participants before FGD. The FGD sessions were started with a self-introduction session. We gave some time for the participants for getting to know each other. This helped them to alleviate their fear of open discussion. Then the moderator introduced himself and his team. The moderator explained the objective of this discussion and the procedure. Then he initiated the FGD by putting an open general question. Group members were free to talk openly. The groups took more time to respond than individuals. Some group members felt hesitant to speak openly. Participants were actively encouraged to express their own opinions and to respond to other members and questions posed by the leader. The moderator made sure that the discussions revolved around the topic. The group members could often stimulate thought for each other which might not have occurred otherwise. We stopped the sessions when no fresh domains emerged ( 20 , 21 ).
During our FGD, most of the participants were discussing the problems they had before the knee arthroplasty and about various treatment methods used by them to overcome these difficulties. They discussed about why they were reluctant to come for operative treatment, how they felt after surgery, and their satisfaction after TKR. We created new domains and subdomains after each FGD by making a transcript of the discussions in the patient’s own words and carefully analyzing them. No fresh domains or subdomains emerged after the fourth FGD.
During each FGD, the opinions of the participants in their own words were taken down by a person. We used both written and voice recordings of our FGD. The data obtained are analyzed by 2 different individuals who are not part of the FGD. This was to ensure the naturality and credibility of the findings. A thematic analysis of the findings was done. Thematic analysis is a qualitative descriptive method to identify and analyze the narrative materials to report patterns or themes. This method has the flexibility for analysis. These interpretations and observations were combined and a conclusion was made.
We had obtained institutional research committee approval for this study. The patients were informed about the study and that data from the FGD would be submitted for publication and their consent was taken.
We have taken the results from 4 FGD because the opinions plateaued thereafter. There were 24 participants between the ages of 50 to 65 years. Among the 24 participants, 15 were males and 9 females. The average knee society score was 1.18 with a standard deviation of 0.50. Five major domains were evolved after our FGD. From the major domains, many minor domains were also developed ( Table 3 ). From the FGD conducted, we found that the socioeconomic impact of OA of the knee is worse than the clinical and radiological severity of the disease. Patients with high preoperative expectations have low satisfaction levels. Surgeon–patient communication has a major impact on patient-reported outcomes. The patient satisfaction level is different from those measured using objective scoring systems. Patient satisfaction levels are high for pain relief, pain-free movements, and social independence. But they are not satisfied because of their inability to returning to their original occupation and performing activities that require knee flexion.
The Major and Minor Domains Emerged From our Focus Group Discussion to Assess Patient Satisfaction After Total Knee Replacement.
From our analysis, we found that loss of function was a major concern before surgery. The pain and deformity were the next. One patient told us, “Walking caused severe pain that I was restricted to my home. I was unable to squat in the toilet.” Some of them even converted their squat toilets to western type of toilets.
The social disabilities due to OA of the knee were far more than we thought. The majority of patients were restricted to their homes. They avoided attending family functions. The majority said they needed help from their children or others in climbing upstairs or for walking long distances. The difficulty to use squat toilets was another social issue. These issues were causing mental stress and depression in some patients. Loss of income due to inability to go to work was another problem. Some stopped going to work while others went to work but were less efficient. They had to take more leaves which led to reduced pay. Most of these patients were belonging to a low- or middle-income group. This affected their daily livelihood. There was a delay of 2 to 3 years before surgery for most of the patients. The affordability of total knee arthroplasty (TKA) was the major issue. They tried different modalities like Ayurveda, massaging, and acupuncture in-between. The majority were unaware of the results of TKR. Some were reluctant to do a TKR due to the fear of undergoing surgery.
Most of them were happy after TKR as they could walk and climb stairs independently. They had minimum pain compared to the preoperative level. Some patients thought they could go for manual work and use the squat toilet after TKR. They opined low satisfaction levels because they couldn’t do it after TKR. But some patients were aware of these problems before surgery and their satisfaction level was high. Proper preoperative education and expectations have a bearing on postoperative outcomes. We also came to know that most of the patients were not getting proper postoperative rehabilitation. They were taught about the rehabilitation protocol postoperatively but were not doing it properly. Some said that they were hesitant to flex the knee because they feared something might happen to the implant. Some blamed the doctors for not explaining these things.
There are some reasons behind selecting patients after TKR for assessing their satisfaction. The number of patients opting for TKR is increasing in our population. We are working in a government medical college in a developing country. Most of our patients for TKR hail from low socioeconomic status. Most of them are manual laborers and living in rural areas having limited road connectivity to their houses. They have to walk or climb hilly terrains. They have to work on farms or fields to earn their livelihood. They use squat toilets. After TKR, most of them want to return to their prior occupation. They can’t change their living conditions. Most patients become aware of the postoperative limitations only after TKR. Many of our patients were unhappy after TKR even when they are clinically and radiologically fine. This prompted us to find out the patient-reported outcome of our patients after TKR. We used FGD as a tool for knowing our patient’s satisfaction and opinions regarding TKR. The usually used measuring tools are surgeon-dependent and originate from developed countries.
Practical Problems in Conducting an FGD
As in any research method, finding a representative sample is very important in FGD. Make sure that all the participants are similar in their regional, cultural, educational, language, and socioeconomic status. Otherwise, there can be disparities in their opinions regarding the same issues. For example, if we are conducting an FGD about strengthening public transport and participants from rural and urban areas are included, their perceptions and opinion may vary. The city dwellers may be using their vehicles for travel they may be worried about traffic blocks or pathetic situations on the road, whereas the rural dwellers will be more worried about the number of buses and the making of new roads. In our case, all patients belonged to the same region, similar age-group, same diagnosis, and similar socioeconomic status ( 22 , 23 ).
Focus group discussion can be a powerful tool for gathering data on experiences, beliefs, attitudes, and perceptions. Asking sensitive questions is not at all a problem in the FGD. As all the participants belong to the same cohort, hence the topic of discussion becomes very simple for them ( 24 ). Usually, 1 or 2 questions for the starting of the discussion are needed. Usually, they are simple and general questions. Sometimes, new questions will be added which are emerging from the analysis of previous FGD. The questions are formed by the participants and the answers of which come from themselves. We have not come across any difficult situations where we have a problem with asking a sensitive question. We have prepared a set of questions for our FGD ( Table 4 ).
The Main Questions and the Probes Prepared for Our Focus Group Discussion.
Abbreviation: TKA, total knee arthroplasty.
Recruiting participants is not a difficult task in FGD. In most cases, we can find out the participants from the cohort. We can collect the details of the participants from the outpatient clinic, from community nurses, hospital records, or from registries ( 25 ). We have obtained the details about our participants from the hospital records. We contacted them over telephones. One of our residents was given the charge of contacting the participants before each session.
Language barrier can be a problem. The participants and the moderator need to be well-versed in the language in which they are conducting FGD. Analysis of data and their interpretations also becomes difficult if they are not using the same language. We conducted the FGD in our mother tongue Malayalam. We did have some difficulty in translating certain colloquial terms into the English language during the publication of our results.
Maintaining quality and consistency during each session is very important ( 26 ). The audio or video recording of the FGD sessions helps to maintain the quality of the procedure. Quality control is the responsibility of the moderator. We had an audio recording of all our proceedings. And the moderator had full control of the whole team during the entire session.
Our Experiences
Our journey started by searching the literature for a simple but practical method for assessing patient satisfaction after TKA. After deciding to conduct FGD, we collected patients from the hospital records. They were randomly allocated to 6 groups. The date, time, and place of each session were decided. There was a delay of 10 days between each FGD. The moderator, a person for writing, and another one for recording were identified. Two senior doctors from our department were assigned for data analysis. A table with 7 chairs was arranged for the moderator and team members. All the data collected were handed over to the team leader after the end of each session. Each session lasted for about 1.5 to 3 hours. We can surely say that the success of our project is the result of teamwork not only among the persons involved in the conduct of the FGD but also among all the participants. Since there are no interventions involved in this research, there is little to worry about the safety aspect of the researcher and participants. But great care was taken to protect the identity of the participants. Our greatest difficulty was in translating the data during publication.
Assessment of patient-reported outcomes is important in any health care intervention. This helps the treating doctor to make necessary modifications in their practices which will ultimately help the community. The regional, cultural, social, and economic status of the patients have a bearing on their level of satisfaction. It is better to develop tools that can be used for various populations. From our experience, we think that FGD is a very effective tool for measuring patient-reported outcomes/satisfaction. It can be conducted with a minimum number of participants. Planning and preparations are less cumbersome. As we are ensuring the homogeneity of the participants, we can get an emic perspective about the subject. Even information about certain sensitive issues can be obtained during FGD. As there are no interventions involved, it is well accepted and cost-effective. We found that patient-based outcomes of TKR differ from the Knee Society Score. Focus group discussion is a simple and surgeon-friendly tool for measuring patient-reported outcomes after TKR.
Patient-based outcome measurements are important for the evaluation of any intervention. Focus group discussion is a simple and effective way to find out the patient-based outcomes. Focus group discussion is a simple and surgeon-friendly tool for measuring patient-reported outcomes after TKR.
Important Points to Be Noted While Planning a Focus Group Discussion
- Decide the number of groups*
- Make sure all participants are homogenous
- Assign the place, date, time of each focus group discussion (FGD)
- Inform the participants early regarding the FGD**
- Find out a moderator who is knowledgeable in the topic and knows the vernacular language
- Ask the moderator to prepare some leading questions***
- Arrange a person for writing and arrange an audiovisual team.
*Better to create small groups and 5 to 6 groups are enough. Too many participants make it difficult to control them during FGD, also the discussion can get going out of context.
**So that they can come on time.
***These questions should be based on the experiences of the moderator and also from the previously published literature about the topic.
Authors’ Note: The corresponding author Balaji Zacharia contributed to conceptualize the idea, helped in collecting data, analyzing, statistics, writing, and editing the manuscript. The coauthors helped in collecting data, analysis, statistics, writing, and editing the manuscript.
We have no conflict of interest for this manuscript and we have not accepted any financial assistance from within or outside of our institution for collecting data, writing the manuscript, and for its publications. This study was approved by the institutional ethics committee of Government Medical College, Kozhikode, Kerala, India. Written informed consent was obtained from the patients for their anonymised information to be published in this article. This article does not contain any studies with human subjects.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.

Case Study Research Method in Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews).
The case study research method originated in clinical medicine (the case history, i.e., the patient’s personal history). In psychology, case studies are often confined to the study of a particular individual.
The information is mainly biographical and relates to events in the individual’s past (i.e., retrospective), as well as to significant events that are currently occurring in his or her everyday life.
The case study is not a research method, but researchers select methods of data collection and analysis that will generate material suitable for case studies.
Freud (1909a, 1909b) conducted very detailed investigations into the private lives of his patients in an attempt to both understand and help them overcome their illnesses.
This makes it clear that the case study is a method that should only be used by a psychologist, therapist, or psychiatrist, i.e., someone with a professional qualification.
There is an ethical issue of competence. Only someone qualified to diagnose and treat a person can conduct a formal case study relating to atypical (i.e., abnormal) behavior or atypical development.
Famous Case Studies
- Anna O – One of the most famous case studies, documenting psychoanalyst Josef Breuer’s treatment of “Anna O” (real name Bertha Pappenheim) for hysteria in the late 1800s using early psychoanalytic theory.
- Little Hans – A child psychoanalysis case study published by Sigmund Freud in 1909 analyzing his five-year-old patient Herbert Graf’s house phobia as related to the Oedipus complex.
- Bruce/Brenda – Gender identity case of the boy (Bruce) whose botched circumcision led psychologist John Money to advise gender reassignment and raise him as a girl (Brenda) in the 1960s.
- Genie Wiley – Linguistics/psychological development case of the victim of extreme isolation abuse who was studied in 1970s California for effects of early language deprivation on acquiring speech later in life.
- Phineas Gage – One of the most famous neuropsychology case studies analyzes personality changes in railroad worker Phineas Gage after an 1848 brain injury involving a tamping iron piercing his skull.
Clinical Case Studies
- Studying the effectiveness of psychotherapy approaches with an individual patient
- Assessing and treating mental illnesses like depression, anxiety disorders, PTSD
- Neuropsychological cases investigating brain injuries or disorders
Child Psychology Case Studies
- Studying psychological development from birth through adolescence
- Cases of learning disabilities, autism spectrum disorders, ADHD
- Effects of trauma, abuse, deprivation on development
Types of Case Studies
- Explanatory case studies : Used to explore causation in order to find underlying principles. Helpful for doing qualitative analysis to explain presumed causal links.
- Exploratory case studies : Used to explore situations where an intervention being evaluated has no clear set of outcomes. It helps define questions and hypotheses for future research.
- Descriptive case studies : Describe an intervention or phenomenon and the real-life context in which it occurred. It is helpful for illustrating certain topics within an evaluation.
- Multiple-case studies : Used to explore differences between cases and replicate findings across cases. Helpful for comparing and contrasting specific cases.
- Intrinsic : Used to gain a better understanding of a particular case. Helpful for capturing the complexity of a single case.
- Collective : Used to explore a general phenomenon using multiple case studies. Helpful for jointly studying a group of cases in order to inquire into the phenomenon.
Where Do You Find Data for a Case Study?
There are several places to find data for a case study. The key is to gather data from multiple sources to get a complete picture of the case and corroborate facts or findings through triangulation of evidence. Most of this information is likely qualitative (i.e., verbal description rather than measurement), but the psychologist might also collect numerical data.
1. Primary sources
- Interviews – Interviewing key people related to the case to get their perspectives and insights. The interview is an extremely effective procedure for obtaining information about an individual, and it may be used to collect comments from the person’s friends, parents, employer, workmates, and others who have a good knowledge of the person, as well as to obtain facts from the person him or herself.
- Observations – Observing behaviors, interactions, processes, etc., related to the case as they unfold in real-time.
- Documents & Records – Reviewing private documents, diaries, public records, correspondence, meeting minutes, etc., relevant to the case.
2. Secondary sources
- News/Media – News coverage of events related to the case study.
- Academic articles – Journal articles, dissertations etc. that discuss the case.
- Government reports – Official data and records related to the case context.
- Books/films – Books, documentaries or films discussing the case.
3. Archival records
Searching historical archives, museum collections and databases to find relevant documents, visual/audio records related to the case history and context.
Public archives like newspapers, organizational records, photographic collections could all include potentially relevant pieces of information to shed light on attitudes, cultural perspectives, common practices and historical contexts related to psychology.
4. Organizational records
Organizational records offer the advantage of often having large datasets collected over time that can reveal or confirm psychological insights.
Of course, privacy and ethical concerns regarding confidential data must be navigated carefully.
However, with proper protocols, organizational records can provide invaluable context and empirical depth to qualitative case studies exploring the intersection of psychology and organizations.
- Organizational/industrial psychology research : Organizational records like employee surveys, turnover/retention data, policies, incident reports etc. may provide insight into topics like job satisfaction, workplace culture and dynamics, leadership issues, employee behaviors etc.
- Clinical psychology : Therapists/hospitals may grant access to anonymized medical records to study aspects like assessments, diagnoses, treatment plans etc. This could shed light on clinical practices.
- School psychology : Studies could utilize anonymized student records like test scores, grades, disciplinary issues, and counseling referrals to study child development, learning barriers, effectiveness of support programs, and more.
How do I Write a Case Study in Psychology?
Follow specified case study guidelines provided by a journal or your psychology tutor. General components of clinical case studies include: background, symptoms, assessments, diagnosis, treatment, and outcomes. Interpreting the information means the researcher decides what to include or leave out. A good case study should always clarify which information is the factual description and which is an inference or the researcher’s opinion.
1. Introduction
- Provide background on the case context and why it is of interest, presenting background information like demographics, relevant history, and presenting problem.
- Compare briefly to similar published cases if applicable. Clearly state the focus/importance of the case.
2. Case Presentation
- Describe the presenting problem in detail, including symptoms, duration,and impact on daily life.
- Include client demographics like age and gender, information about social relationships, and mental health history.
- Describe all physical, emotional, and/or sensory symptoms reported by the client.
- Use patient quotes to describe the initial complaint verbatim. Follow with full-sentence summaries of relevant history details gathered, including key components that led to a working diagnosis.
- Summarize clinical exam results, namely orthopedic/neurological tests, imaging, lab tests, etc. Note actual results rather than subjective conclusions. Provide images if clearly reproducible/anonymized.
- Clearly state the working diagnosis or clinical impression before transitioning to management.
3. Management and Outcome
- Indicate the total duration of care and number of treatments given over what timeframe. Use specific names/descriptions for any therapies/interventions applied.
- Present the results of the intervention,including any quantitative or qualitative data collected.
- For outcomes, utilize visual analog scales for pain, medication usage logs, etc., if possible. Include patient self-reports of improvement/worsening of symptoms. Note the reason for discharge/end of care.
4. Discussion
- Analyze the case, exploring contributing factors, limitations of the study, and connections to existing research.
- Analyze the effectiveness of the intervention,considering factors like participant adherence, limitations of the study, and potential alternative explanations for the results.
- Identify any questions raised in the case analysis and relate insights to established theories and current research if applicable. Avoid definitive claims about physiological explanations.
- Offer clinical implications, and suggest future research directions.
5. Additional Items
- Thank specific assistants for writing support only. No patient acknowledgments.
- References should directly support any key claims or quotes included.
- Use tables/figures/images only if substantially informative. Include permissions and legends/explanatory notes.
- Provides detailed (rich qualitative) information.
- Provides insight for further research.
- Permitting investigation of otherwise impractical (or unethical) situations.
Case studies allow a researcher to investigate a topic in far more detail than might be possible if they were trying to deal with a large number of research participants (nomothetic approach) with the aim of ‘averaging’.
Because of their in-depth, multi-sided approach, case studies often shed light on aspects of human thinking and behavior that would be unethical or impractical to study in other ways.
Research that only looks into the measurable aspects of human behavior is not likely to give us insights into the subjective dimension of experience, which is important to psychoanalytic and humanistic psychologists.
Case studies are often used in exploratory research. They can help us generate new ideas (that might be tested by other methods). They are an important way of illustrating theories and can help show how different aspects of a person’s life are related to each other.
The method is, therefore, important for psychologists who adopt a holistic point of view (i.e., humanistic psychologists ).
Limitations
- Lacking scientific rigor and providing little basis for generalization of results to the wider population.
- Researchers’ own subjective feelings may influence the case study (researcher bias).
- Difficult to replicate.
- Time-consuming and expensive.
- The volume of data, together with the time restrictions in place, impacted the depth of analysis that was possible within the available resources.
Because a case study deals with only one person/event/group, we can never be sure if the case study investigated is representative of the wider body of “similar” instances. This means the conclusions drawn from a particular case may not be transferable to other settings.
Because case studies are based on the analysis of qualitative (i.e., descriptive) data , a lot depends on the psychologist’s interpretation of the information she has acquired.
This means that there is a lot of scope for Anna O , and it could be that the subjective opinions of the psychologist intrude in the assessment of what the data means.
For example, Freud has been criticized for producing case studies in which the information was sometimes distorted to fit particular behavioral theories (e.g., Little Hans ).
This is also true of Money’s interpretation of the Bruce/Brenda case study (Diamond, 1997) when he ignored evidence that went against his theory.
Breuer, J., & Freud, S. (1895). Studies on hysteria . Standard Edition 2: London.
Curtiss, S. (1981). Genie: The case of a modern wild child .
Diamond, M., & Sigmundson, K. (1997). Sex Reassignment at Birth: Long-term Review and Clinical Implications. Archives of Pediatrics & Adolescent Medicine , 151(3), 298-304
Freud, S. (1909a). Analysis of a phobia of a five year old boy. In The Pelican Freud Library (1977), Vol 8, Case Histories 1, pages 169-306
Freud, S. (1909b). Bemerkungen über einen Fall von Zwangsneurose (Der “Rattenmann”). Jb. psychoanal. psychopathol. Forsch ., I, p. 357-421; GW, VII, p. 379-463; Notes upon a case of obsessional neurosis, SE , 10: 151-318.
Harlow J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39 , 389–393.
Harlow, J. M. (1868). Recovery from the Passage of an Iron Bar through the Head . Publications of the Massachusetts Medical Society. 2 (3), 327-347.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Further Information
- Case Study Approach
- Case Study Method
- Enhancing the Quality of Case Studies in Health Services Research
- “We do things together” A case study of “couplehood” in dementia
- Using mixed methods for evaluating an integrative approach to cancer care: a case study
Related Articles
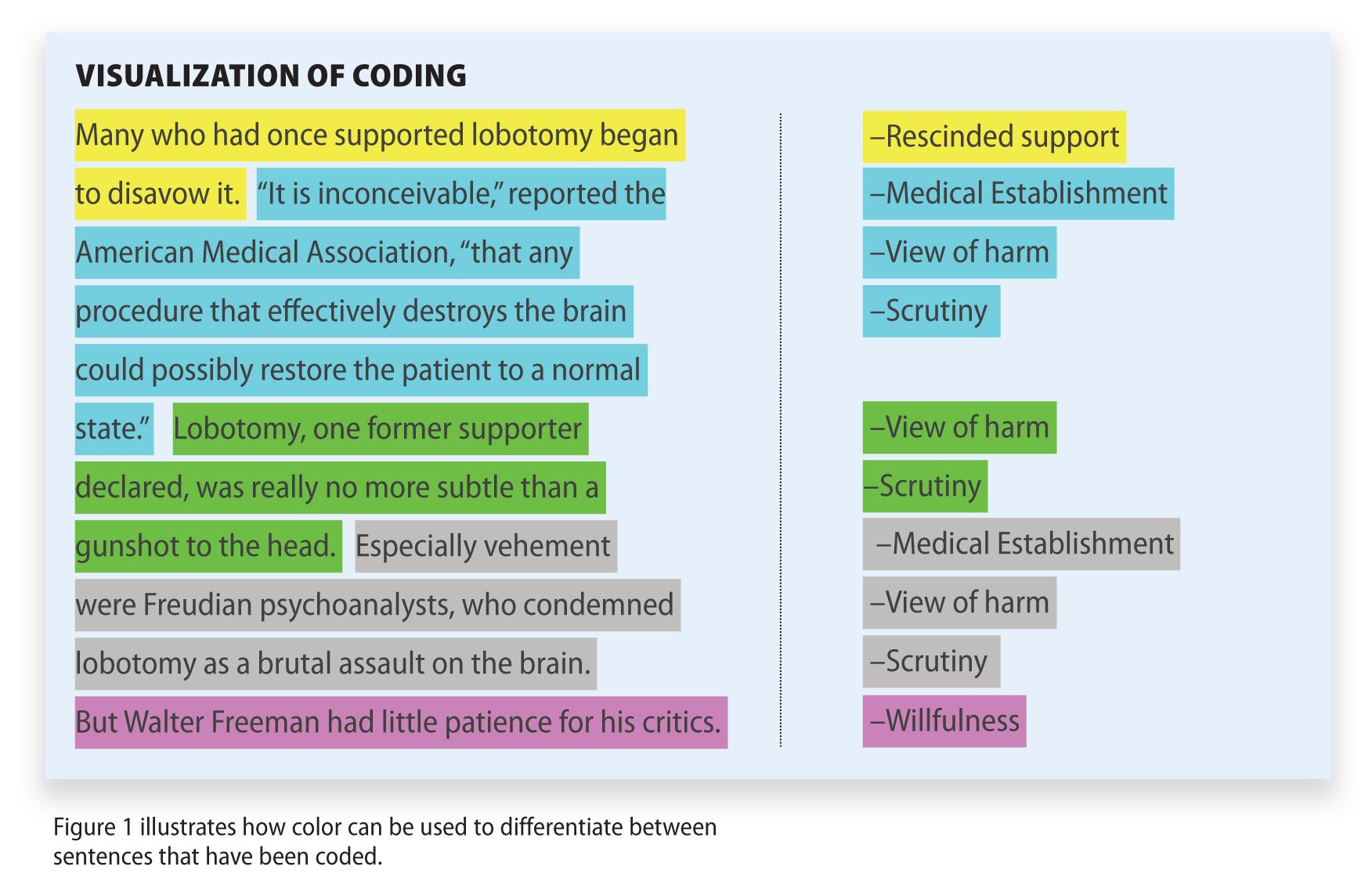
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
DSpace JSPUI
Egyankosh preserves and enables easy and open access to all types of digital content including text, images, moving images, mpegs and data sets.
- IGNOU Self Learning Material (SLM)
- 14. School of Gender and Development Studies (SOGDS)
- Master's Degree Programmes
- MA in Gender and Development Studies (MAGD)
- MGS-003 Gender Analysis
- Block-2 Tools of Gender Analysis
Items in eGyanKosh are protected by copyright, with all rights reserved, unless otherwise indicated.


Hacking the Case Interview
Consulting group case interviews are given to candidates to assess teamwork in addition to communication skills, quantitative skills, and business acumen. They are used by consulting firms such as Bain, Deloitte, PwC , and EY-Parthenon .
Have an upcoming consulting group case interview? We have you covered. In this article, we'll go through in detail:
- What is a consulting group case interview?
- Different formats of consulting group case interviews
- Why are consulting group case interviews used?
- What do consulting group case interviews assess?
- How to solve consulting group case interviews
- How to stand out in consulting group case interviews
- Consulting group case interview tips
If you’re looking for a step-by-step shortcut to learn case interviews quickly, enroll in our case interview course . These insider strategies from a former Bain interviewer helped 30,000+ land consulting offers while saving hundreds of hours of prep time.
What is a Consulting Group Case Interview?
Consulting group case interviews are a special variant of the traditional case interview. Before preparing for group case interviews, you should first become familiar with how to solve a traditional case interview .
Like a case interview, you’ll still be placed in a hypothetical business situation and asked to develop a recommendation or answer to a business problem. However, for consulting group case interviews, you’ll be put in a group of 3 to 6 people with other candidates that are also interviewing for the same consulting job.
The group will be given materials which contain the case background, objective, and other information needed to solve the case. You’ll initially have some time to read the information independently, but will spend most of the time discussing the case and working together as a group.
During these discussions, the interviewer will be observing and taking notes on each candidate.
For some group case interviews, you will also create a group presentation. As a group, you’ll present your recommendation to the interviewer who will ask follow-up questions on the work and findings.
Consulting group case interviews are much less commonly used than traditional case interviews, but they are as equally as important. They are typically given in second or final round interviews .
For firms and offices that use group case interviews, you will not receive a consulting job offer unless you can pass them.
Different Formats of Consulting Group Case Interviews
There are two different formats of consulting group case interviews:
Discussion only group case interviews
Presentation group case interviews.
A discussion only group case interview has the following structure:

This format of group case interview has no presentation component. The group will be given materials with the case background information and objective.
You’ll have some time to read the information independently, but then the interviewer will bring the group together and ask the group to discuss different questions related to solving the case.
The interviewer will be heavily involved in the discussion by asking questions for the group to answer and steering the direction of the discussion.
The discussion only group case interview is focused on assessing the answers that candidates contribute to the group and how well candidates communicate with each other.
A presentation group case interview has the following structure:

The group will be given materials that not only contain the case background and objective, but contain other information needed to solve the case. There is typically more material given in this format because you will be given more time to prepare and discuss.
The group will be given about an hour to discuss the case and create a group presentation. During this time, the interviewer will be listening in on the conversations that the group will have, but they will not interfere or answer any questions.
It is up to the group how they want to allocate their time, what topics they want to discuss, and how they want to handle creating and giving the group presentation.
Once time is up, the group will present their work and findings to the interviewer, who will ask follow-up questions.
The presentation group case interview is focused on assessing how well each candidate contributes to the group, how well candidates work with each other, and the quality of the final presentation.
Why are Consulting Group Case Interviews Used?
Consulting group case interviews are used because they are another way for consulting firms to predict which candidates would make the best consultants.
Group case interviews simulate the consulting job by placing you in a hypothetical business situation. You will need to work as a team to analyze and discuss information and then give a presentation on your recommendation. This is what consultants do every day .
These types of case interviews are used in addition to traditional case interviews because they assess a set of skills that traditional case interviews cannot assess.
Group case interviews focus on teamwork and collaboration. By putting candidates into groups, interviewers can assess how candidates work with other people and how open candidates are to other people’s ideas.
They can see how effectively candidates communicate and persuade teammates and how candidates can balance listening and leading.
What do Consulting Group Case Interviews Assess?
There are four major qualities that group case interviews assess.
Logical, structured thinking : Consultants need to be organized and methodical to work efficiently.
- Can you structure complex problems in a clear, simple way?
- Can you use logic and reason to make appropriate conclusions?
Interpersonal skills : Relationships are important in consulting. You’ll be working with teammates and clients every day, so fostering strong relationships is imperative.
- Are you easy to work with?
- Can you handle conflict or disagreement with teammates?
Teamwork skills : Consultants work closely in small teams. To be successful, consultants need to know how to work effectively in groups.
- Can you make meaningful contributions while working in a group?
- Do you bring out the best ideas and qualities in other people?
Presentation skills : Consultants need strong communication skills to present their work in a clear, concise, and persuasive way.
- Can you communicate in a clear and concise way?
- Are you articulate and persuasive in what you are saying?

How to Solve Consulting Group Case Interviews
Solving consulting group case interviews follows the same steps as solving traditional case interviews. There are four main steps:
- Understand the problem
- Create a framework
- Answer quantitative and qualitative questions
- Develop a recommendation
1. Understand the problem
The first step to solving a consulting group case interview is to fully understand the problem or objective. What is the overall business question that the group is trying to answer?
Answering or solving the wrong business problem is the quickest way to fail a group case interview.
2. Create a framework
Next, as a group, you’ll want to create some kind of framework to help you solve the case. A framework is a tool that helps you structure and break down complex problems into simpler, smaller components.
For group case interviews, your framework will help guide the group discussion. The framework collects and organizes all of the topics that the group needs to discuss and all of the questions the group needs to answer.
3. Discuss and answer quantitative and qualitative questions
Once your group has aligned on a framework to use, you can move onto the discussion. During the discussion, you will answer many of the questions that were raised in the framework that was created.
Some of these questions will be qualitative, requiring only business knowledge and judgment to answer. Other questions may be more quantitative, requiring some calculations or estimations from the case information provided.
It is up to the group what order they want to answer and discuss the questions. It is also up to the group whether they want to tackle these questions as an entire group or if they want to split up into smaller groups.
Discussion will continue until the group has reached an answer or conclusion that is accepted by everyone.
4. Develop a recommendation
Once you have finished discussing and answering all of the important questions, you will need to align on an overall recommendation.
To do this, review all of the answers and conclusions that the group has drawn. Identify which recommendation they collectively support.
If the group case interview has a presentation component, you will also need to decide how to split up the presentation across the different members of the group.
How to Stand Out in Consulting Group Case Interviews
The best way to stand out and distinguish yourself in a group case interview is to focus on adding as much value as you can to the group.
There are six different ways you can add value to the group.
Lead or facilitate the discussion
If the interviewer is not leading the discussion and just observing the group, one way to add value is to lead or facilitate the discussion.
You can propose what topics to discuss, the order they should be discussed in, and how much time should be allocated to each topic. When the group gets off track or goes on a tangent, you can bring the group’s focus back together.
Leading or facilitating the discussion establishes you as a group leader, which will leave a positive impression on the interviewer. However, because this role has so much responsibility and visibility, many people will try to take on this role.
Therefore, a group may have multiple leaders or facilitators. When trying to lead the group, make sure you remain respectful and do not interrupt other people when they are speaking.
Expand upon other people’s ideas
Another way to add value is to expand upon other people’s ideas. If a group member suggests a great idea or raises a good point, you can build upon it.
Wait until the group member has finished speaking and then jump in and compliment that person’s idea. Add more details or give more examples to make the idea more concrete.
Synthesize information
Another easy way to add value to the group is to synthesize information that other people have said. A synthesis is simply a reconciliation of different viewpoints and ideas together. This requires minimal effort, but adds tremendous value to the group.
What is the best way to synthesize information?
First, concisely summarize the major ideas that group members have made. Then, state what you like about each idea. Finally, propose an idea that consolidates the best points of each idea.
Synthesizing information does not require much thinking because you are simply repurposing the ideas of other people. This makes it an easy way to contribute to the group.
Keep track of time
Time goes by very quickly in a consulting group case interview. Therefore, a simple way to add value is to be a time keeper and make sure that the team is on track.
In the beginning of the discussion, you can propose a schedule or plan to make the most of the limited time that the group has. You can then volunteer to keep track of the time so that the group can finish discussing and deciding on everything that it needs to.
Play devil’s advocate
Another way to add value to the group is by playing devil’s advocate. You can help the team develop strong points and ideas by testing the team’s thinking and considering potential risks or downsides.
When the team has decided on an idea, bring up potential risks or downsides that the team should consider. This helps the team develop a more fully thought out answer or recommendation.
Be careful when playing devil’s advocate. You do not want to be attacking ideas or bringing them down. Instead, you want to be offering constructive feedback to test the idea and make it stronger.
The final way to add value to the group is to take notes for the team. By taking notes and keeping track of what other people are saying, you’ll be able to recall what has been discussed if any group members have questions.
This way of adding value to the group is not as recommended as the other strategies to add value.
Taking notes deprives you of opportunities to speak. Therefore, it is better to focus on understanding what other people are saying to identify opportunities to speak up rather than to focus on taking the best notes.
Consulting Group Case Interview Tips
Below are the seven biggest group case interview tips. Follow these tips to give yourself an edge over other candidates.
1. Treat your group members as teammates, not competition
While you may feel like you are competing against members of your group for a job offer, this is not the case. Multiple people or even all people in your group can receive job offers.
Rather than treating your group members like competition and trying to make yourself look better than them, treat your group members as teammates. You should think about the group case interview as your team versus the case, not you versus your teammates.
If you work well as a group and deliver an outstanding discussion or presentation, that increases the likelihood that members of the group will receive offers. If the group spends all of their time attacking each other’s comments and fighting for speaking time, the group will likely deliver a poor discussion or presentation, which makes everyone in the group look bad.
The key is to focus on delivering an outstanding result and not to focus on competing with other teammates.
2. Don’t speak too much and don’t speak too little
How much should you speak in a group case interview?
The problem with speaking too little during a group case interview is that you won’t have many opportunities to demonstrate your interpersonal, teamwork, and presentation skills. Interviewers may also think that you are shy and afraid of speaking in a group, qualities that are not ideal for a consultant.
The problem with speaking too much during a group case interview is that you may be seen as too aggressive and controlling. Speaking too much reflects poorly on you because you are taking away opportunities from other teammates to speak and contribute. You may come off as rude and disruptive if you interrupt people and talk over them.
If you were to rank order all of the members in your group by how much each person spoke, you would want to fall right in the middle. That is the perfect balance of speaking and listening.
3. Speak only if you are adding value to the group
Just because you speak a lot during a group case interview does not mean that you are doing well. The quality of what you are saying is much more important than the quantity.
If you are speaking a lot, but not adding that much value to the group, you will be seen as a poor teammate. A great teammate knows when to speak and when to listen.
Therefore, you should only speak if you are adding value to the group. Do not speak just to reach your participation quota.
4. Don’t interrupt or talk over people
The most common way to fail a group case interview is to come off as a jerk. Consultants work closely in small teams and no one wants to work with someone that is a jerk.
How do you avoid this?
First, don’t interrupt or talk over people. If someone is speaking, allow them to finish what they are saying before jumping in with your own thoughts. Second, don’t attack other people’s ideas. You may bring up your concerns and disagreements, but you should never blatantly tell someone that their idea is bad.
As long as you are a nice and respectful teammate, you will be miles ahead of anyone that is overly aggressive, pushy, or rude.
5. Involve other people
An easy way to demonstrate that you are a great teammate is to involve other people.
If you notice that someone has not spoken in a long time, ask them what their thoughts are on the discussion. If you notice that someone was cut off when speaking, ask them to finish their thoughts after the person interrupting them finishes what they are saying.
All of these actions require minimal effort, but add tremendous value to the group while making you look like a great teammate.
6. Don’t spend too much time reading independently
In the beginning of the group case interview, your group will be given materials on the case background, objective, and other information needed to solve the case. Your group members will likely spend the beginning of the group case interview reading the materials by themselves.
Do not spend too much time reading the material independently.
The purpose of the group case interview is to have discussions and work together as a group. The more time your group spends reading the material independently, the less time the group has to demonstrate interpersonal and teamwork skills.
7. You don’t need to have your idea or recommendation chosen
Remember that multiple or even all people in your group can receive job offers. Therefore, you do not need to have your own ideas or recommendations chosen in order to receive an offer.
Fighting or pushing too hard for your own ideas and recommendations may actually harm you. It may suggest that you are not open to other people’s ideas and not willing to support your teammates.
Learn Case Interviews 10x Faster
Here are the resources we recommend to learn the most robust, effective case interview strategies in the least time-consuming way:
- Comprehensive Case Interview Course (our #1 recommendation): The only resource you need. Whether you have no business background, rusty math skills, or are short on time, this step-by-step course will transform you into a top 1% caser that lands multiple consulting offers.
- Hacking the Case Interview Book (available on Amazon): Perfect for beginners that are short on time. Transform yourself from a stressed-out case interview newbie to a confident intermediate in under a week. Some readers finish this book in a day and can already tackle tough cases.
- The Ultimate Case Interview Workbook (available on Amazon): Perfect for intermediates struggling with frameworks, case math, or generating business insights. No need to find a case partner – these drills, practice problems, and full-length cases can all be done by yourself.
- Case Interview Coaching : Personalized, one-on-one coaching with former consulting interviewers
- Behavioral & Fit Interview Course : Be prepared for 98% of behavioral and fit questions in just a few hours. We'll teach you exactly how to draft answers that will impress your interviewer
- Resume Review & Editing : Transform your resume into one that will get you multiple interviews
Land Multiple Consulting Offers
Complete, step-by-step case interview course. 30,000+ happy customers.
- Open access
- Published: 03 June 2024
The use of evidence to guide decision-making during the COVID-19 pandemic: divergent perspectives from a qualitative case study in British Columbia, Canada
- Laura Jane Brubacher ORCID: orcid.org/0000-0003-2806-9539 1 , 2 ,
- Chris Y. Lovato 1 ,
- Veena Sriram 1 , 3 ,
- Michael Cheng 1 &
- Peter Berman 1
Health Research Policy and Systems volume 22 , Article number: 66 ( 2024 ) Cite this article
Metrics details
The challenges of evidence-informed decision-making in a public health emergency have never been so notable as during the COVID-19 pandemic. Questions about the decision-making process, including what forms of evidence were used, and how evidence informed—or did not inform—policy have been debated.
We examined decision-makers' observations on evidence-use in early COVID-19 policy-making in British Columbia (BC), Canada through a qualitative case study. From July 2021- January 2022, we conducted 18 semi-structured key informant interviews with BC elected officials, provincial and regional-level health officials, and civil society actors involved in the public health response. The questions focused on: (1) the use of evidence in policy-making; (2) the interface between researchers and policy-makers; and (3) key challenges perceived by respondents as barriers to applying evidence to COVID-19 policy decisions. Data were analyzed thematically, using a constant comparative method. Framework analysis was also employed to generate analytic insights across stakeholder perspectives.
Overall, while many actors’ impressions were that BC's early COVID-19 policy response was evidence-informed, an overarching theme was a lack of clarity and uncertainty as to what evidence was used and how it flowed into decision-making processes. Perspectives diverged on the relationship between 'government' and public health expertise, and whether or not public health actors had an independent voice in articulating evidence to inform pandemic governance. Respondents perceived a lack of coordination and continuity across data sources, and a lack of explicit guidelines on evidence-use in the decision-making process, which resulted in a sense of fragmentation. The tension between the processes involved in research and the need for rapid decision-making was perceived as a barrier to using evidence to inform policy.
Conclusions
Areas to be considered in planning for future emergencies include: information flow between policy-makers and researchers, coordination of data collection and use, and transparency as to how decisions are made—all of which reflect a need to improve communication. Based on our findings, clear mechanisms and processes for channeling varied forms of evidence into decision-making need to be identified, and doing so will strengthen preparedness for future public health crises.
Peer Review reports
The challenges of evidence-informed decision-making Footnote 1 in a public health emergency have never been so salient as during the COVID-19 pandemic, given its unprecedented scale, rapidly evolving virology, and multitude of global information systems to gather, synthesize, and disseminate evidence on the SARS-CoV-2 virus and associated public health and social measures [ 1 , 2 , 3 ]. Early in the COVID-19 pandemic, rapid decision-making became central for governments globally as they grappled with crucial decisions for which there was limited evidence. Critical questions exist, in looking retrospectively at these decision-making processes and with an eye to strengthening future preparedness: Were decisions informed by 'evidence'? What forms of evidence were used, and how, by decision-makers? [ 4 , 5 , 6 ].
Scientific evidence, including primary research, epidemiologic research, and knowledge synthesis, is one among multiple competing influences that inform decision-making processes in an outbreak such as COVID-19 [ 7 ]. Indeed, the use of multiple forms of evidence has been particularly notable as it applies to COVID-19 policy-making. Emerging research has also documented the important influence of ‘non-scientific’ evidence such as specialized expertise and experience, contextual information, and level of available resources [ 8 , 9 , 10 ]. The COVID-19 pandemic has underscored the politics of evidence-use in policy-making [ 11 ]; what evidence is used and how can be unclear, and shaped by political bias [ 4 , 5 ]. Moreover, while many governments have established scientific advisory boards, the perspectives of these advisors were reportedly largely absent from COVID-19 policy processes [ 6 ]. How evidence and public health policy interface—and intersect—is a complex question, particularly in the dynamic context of a public health emergency.
Within Canada, a hallmark of the public health system and endorsed by government is evidence-informed decision-making [ 12 ]. In British Columbia (BC), Canada, during the early phases of COVID-19 (March—June 2020), provincial public health communication focused primarily on voluntary compliance with recommended public health and social measures, and on supporting those most affected by the pandemic. Later, the response shifted from voluntary compliance to mandatory enforceable government orders [ 13 ]. Like many other jurisdictions, the government’s public messaging in BC asserted that the province took an approach to managing the COVID-19 pandemic and developing related policy that was based on scientific evidence, specifically. For example, in March 2021, in announcing changes to vaccination plans, Dr. Bonnie Henry, the Provincial Health Officer, stated, " This is science in action " [ 14 ]. As a public health expert with scientific voice, the Provincial Health Officer has been empowered to speak on behalf of the BC government across the COVID-19 pandemic progression. While this suggests BC is a jurisdiction which has institutionalized scientifically-informed decision-making as a core tenet of effective public health crisis response, it remains unclear as to whether BC’s COVID-19 response could, in fact, be considered evidence-informed—particularly from the perspectives of those involved in pandemic decision-making and action. Moreover, if evidence-informed, what types of evidence were utilized and through what mechanisms, how did this evidence shape decision-making, and what challenges existed in moving evidence to policy and praxis in BC’s COVID-19 response?
The objectives of this study were: (1) to explore and characterize the perspectives of BC actors involved in the COVID-19 response with respect to evidence-use in COVID-19 decision-making; and (2) to identify opportunities for and barriers to evidence-informed decision-making in BC’s COVID-19 response, and more broadly. This inquiry may contribute to identifying opportunities for further strengthening the synthesis and application of evidence (considered broadly) to public health policy and decision-making, particularly in the context of future public health emergencies, both in British Columbia and other jurisdictions.
Study context
This qualitative study was conducted in the province of British Columbia (BC), Canada, a jurisdiction with a population of approximately five million people [ 15 ]. Within BC’s health sector, key actors involved in the policy response to COVID-19 included: elected officials, the BC Government’s Ministry of Health (MOH), the Provincial Health Services Authority (PHSA), Footnote 2 the Office of the Provincial Health Officer (PHO), Footnote 3 the BC Centre for Disease Control (BCCDC), Footnote 4 and Medical Health Officers (MHOs) and Chief MHOs at regional and local levels.
Health research infrastructure within the province includes Michael Smith Health Research BC [ 16 ] and multiple post-secondary research and education institutions (e.g., The University of British Columbia). Unlike other provincial (e.g., Ontario) and international (e.g., UK) jurisdictions, BC did not establish an independent, formal scientific advisory panel or separate organizational structure for public health intelligence in COVID-19. That said, a Strategic Research Advisory Council was established, reporting to the MOH and PHO, to identify COVID-19 research gaps and commission needed research for use within the COVID-19 response [ 17 ].
This research was part of a multidisciplinary UBC case study investigating the upstream determinants of the COVID-19 response in British Columbia, particularly related to institutions, politics, and organizations and how these interfaced with, and affected, pandemic governance [ 18 ]. Ethics approval for this study was provided by the University of British Columbia (UBC)’s Institutional Research Ethics Board (Certificate #: H20-02136).
Data collection
From July 2021 to January 2022, 18 semi-structured key informant interviews were conducted with BC elected officials, provincial and regional-level health officials, and civil society actors (e.g., within non-profit research organizations, unions) (Table 1 ). Initially, respondents were purposively sampled, based on their involvement in the COVID-19 response and their positioning within the health system organizational structure. Snowball sampling was used to identify additional respondents, with the intent of representing a range of organizational roles and actor perspectives. Participants were recruited via email invitation and provided written informed consent to participate.
Interviews were conducted virtually using Zoom® videoconferencing, with the exception of one hybrid in-person/Zoom® interview. Each interview was approximately one hour in duration. One to two research team members led each interview. The full interview protocol focused on actors’ descriptions of decision-making processes across the COVID-19 pandemic progression, from January 2020 to the date of the interviews, and they were asked to identify key decision points (e.g., emergency declaration, business closures) [see Additional File 1 for the full semi-structured interview guide]. For this study, we used a subset of interview questions focused on evidence-use in the decision-making process, and the organizational structures or actors involved, in BC's early COVID-19 pandemic response (March–August 2020). Questions were adapted to be relevant to a respondent’s expertise and particular involvement in the response. ‘Evidence’ was left undefined and considered broadly by the research team (i.e., both ‘scientific’/research-based and ‘non-scientific’ inputs) within interview questions, and therefore at the discretion of the participant as to what inputs they perceived and described as ‘evidence’ that informed or did not inform pandemic decision-making. Interviews were audio-recorded over Zoom® with permission and transcribed using NVivo Release 1.5© software. Each transcript was then manually verified for accuracy by 1–2 members of the research team.
Data analysis
An inductive thematic analysis was conducted, using a constant comparative method, to explore points of divergence and convergence across interviews and stakeholder perspectives [ 19 ]. Transcripts were inductively coded in NVivo Release 1.5© software, which was used to further organize and consolidate codes, generate a parsimonious codebook to fit the data, and retrieve interview excerpts [ 20 ]. Framework analysis was also employed as an additional method for generating analytic insights across stakeholder perspectives and contributed to refining the overall coding [ 21 ]. Triangulation across respondents and analytic methods, as well as team collaboration in reviewing and refining the codebook, contributed to validity of the analysis [ 22 ].
How did evidence inform early COVID-19 policy-making in BC?
Decision-makers described their perceptions on the use of evidence in policy-making; the interface between researchers and policy-makers; and specific barriers to evidence-use in policy-making within BC’s COVID-19 response. In discussing the use of evidence, respondents focused on ‘scientific’ evidence; however, they noted a lack of clarity as to how and what evidence flowed into decision-making. They also acknowledged that ‘scientific’ evidence was one of multiple factors influencing decisions. The themes described below reflect the narrative underlying their perspectives.
Perceptions of evidence-use
Multiple provincial actors generally expressed confidence or had an overall impression that decisions were evidence-based (IDI5,9), stating definitively that, "I don’t think there was a decision we made that wasn’t evidence-informed" (IDI9) and that "the science became a driver of decisions that were made" (IDI5). However, at the regional health authority level, one actor voiced skepticism that policy decisions were consistently informed by scientific evidence specifically, stating, "a lot of decisions [the PHO] made were in contrast to science and then shifted to be by the science" ( IDI6). The evolving nature of the available evidence and scientific understanding of the virus throughout the pandemic was acknowledged. For instance, one actor stated that, "I’ll say the response has been driven by the science; the science has been changing…from what I’ve seen, [it] has been a very science-based response" (IDI3).
Some actors narrowed in on certain policy decisions they believed were or were not evidence-informed. Policy decisions in 2020 that actors believed were directly informed by scientific data included the early decision to restrict informal, household gatherings; to keep schools open for in-person learning; to implement a business safety plan requirement across the province; and to delay the second vaccine dose for maximum efficacy. One provincial public health actor noted that an early 2020 decision made, within local jurisdictions, to close playgrounds was not based on scientific evidence. Further, the decision prompted public health decision-makers to centralize some decision-making to the provincial level, to address decisions being made 'on the ground' that were not based on scientific evidence (IDI16). Similarly, they added that the policy decision to require masking in schools was not based on scientific evidence; rather, "it's policy informed by the noise of your community." As parents and other groups within the community pushed for masking, this was "a policy decision to help schools stay open."
Early in the pandemic response, case data in local jurisdictions were reportedly used for monitoring and planning. These "numerator data" (IDI1), for instance case or hospitalization counts, were identified as being the primary mode of evidence used to inform decisions related to the implementation or easing of public health and social measures. The ability to generate epidemiological count data early in the pandemic due to efficient scaling up of PCR testing for COVID-19 was noted as a key advantage (IDI16). As the pandemic evolved in 2020, however, perspectives diverged in relation to the type of data that decision-makers relied on. For example, it was noted that BCCDC administered an online, voluntary survey to monitor unintended consequences of public health and social measures and inform targeted interventions. Opinions varied on whether this evidence was successfully applied in decision-making. One respondent emphasized this lack of application of evidence and perceived that public health orders were not informed by the level and type of evidence available, beyond case counts: "[In] a communicable disease crisis like a pandemic, the collateral impact slash damage is important and if you're going to be a public health institute, you actually have to bring those to the front, not just count cases" (IDI1).
There also existed some uncertainty and a perceived lack of transparency or clarity as to how or whether data analytic ‘entities’, such as BCCDC or research institutions, fed directly into decision-making. As a research actor shared, "I’m not sure that I know quite what all those channels really look like…I’m sure that there’s a lot of improvement that could be driven in terms of how we bring strong evidence to actual policy and practice" (IDI14). Another actor explicitly named the way information flowed into decision-making in the province as "organic" (IDI7). They also noted the lack of a formal, independent science advisory panel for BC’s COVID-19 response, which existed in other provincial and international jurisdictions. Relatedly, one regional health authority actor perceived that the committee that was convened to advise the province on research, and established for the purpose of applying research to the COVID-19 response, "should have focused more on knowledge translation, but too much time was spent commissioning research and asking what kinds of questions we needed to ask rather than looking at what was happening in other jurisdictions" (IDI6). Overall, multiple actors noted a lack of clarity around application of evidence and who is responsible for ensuring evidence is applied. As a BCCDC actor expressed, in relation to how to prevent transmission of COVID-19:
We probably knew most of the things that we needed to know about May of last year [2020]. So, to me, it’s not even what evidence you need to know about, but who’s responsible for making sure that you actually apply the evidence to the intervention? Because so many of our interventions have been driven by peer pressure and public expectation rather than what we know to be the case [scientifically] (IDI1).
Some described the significance of predictive disease modelling to understand the COVID-19 trajectory and inform decisions, as well as to demonstrate to the public the effectiveness of particular measures, which "help[ed] sustain our response" (IDI2). Others, however, perceived that "mathematical models were vastly overused [and] overvalued in decision-making around this pandemic" (IDI1) and that modellers stepped outside their realm of expertise in providing models and policy recommendations through the public media.
Overall, while many actors’ impressions were that the response was evidence-informed, an overarching theme was a lack of clarity and uncertainty with respect to how evidence actually flowed into decision-making processes, as well as what specific evidence was used and how. Participants noted various mechanisms created or already in place prior to COVID-19 that fed data into, and facilitated, decision-making. There was an acknowledgement that multiple forms of evidence—including scientific data, data on public perceptions, as well as public pressure—appeared to have influenced decision-making.
Interface between researchers and policy-makers
There was a general sense that the Ministry supported the use of scientific and research-based evidence specifically. Some actors identified particular Ministry personnel as being especially amenable to research and focused on data to inform decisions and implementation. More broadly, the government-research interface was characterized by one actor as an amicable one, a "research-friendly government", and that the Ministry of Health (MOH), specifically, has a research strategy whereby, "it’s literally within their bureaucracy to become a more evidence-informed organization" (IDI11). The MOH was noted to have funded a research network intended to channel evidence into health policy and practice, and which reported to the research side of the MOH.
Other actors perceived relatively limited engagement with the broader scientific community. Some perceived an overreliance on 'in-house expertise' or a "we can do that [ourselves] mentality" within government that precluded academic researchers’ involvement, as well as a sense of "not really always wanting to engage with academics to answer policy questions because they don’t necessarily see the value that comes" (IDI14). With respect to the role of research, an actor stated:
There needs to be a provincial dialogue around what evidence is and how it gets situated, because there’s been some tension around evidence being produced and not used or at least not used in the way that researchers think that it should be (IDI11).
Those involved in data analytics within the MOH acknowledged a challenge in making epidemiological data available to academic researchers, because "at the time, you’re just trying to get decisions made" (IDI7). Relatedly, a research actor described the rapid instigation of COVID-19 research and pivoting of academic research programs to respond to the pandemic, but perceived a slow uptake of these research efforts from the MOH and PHSA for decision-making and action. Nevertheless, they too acknowledged the challenge of using research evidence, specifically, in an evolving and dynamic pandemic:
I think we’ve got to be realistic about what research in a pandemic situation can realistically contribute within very short timelines. I mean, some of these decisions have to be made very quickly...they were intuitive decisions, I think some of them, rather than necessarily evidence-based decisions (IDI14).
Relatedly, perspectives diverged on the relationship between 'government' and public health expertise, and whether or not public health actors had an independent voice in articulating evidence to inform governance during the pandemic. Largely from Ministry stakeholders, and those within the PHSA, the impressions were that Ministry actors were relying on public health advice and scientific expertise. As one actor articulated, "[the] government actually respected and acknowledged and supported public health expertise" (IDI9). Others emphasized a "trust of the people who understood the problem" (IDI3)—namely, those within public health—and perceived that public health experts were enabled "to take a lead role in the health system, over politics" (IDI12). This perspective was not as widely held by those in the public health sector, as one public health actor expressed, "politicians and bureaucrats waded into public health practice in a way that I don't think was appropriate" and that, "in the context of a pandemic, it’s actually relatively challenging to bring true expert advice because there’s too many right now. Suddenly, everybody’s a public health expert, but especially bureaucrats and politicians." They went on to share that the independence of public health to speak and act—and for politicians to accept independent public health advice—needs to be protected and institutionalized as "core to good governance" (IDI1). Relatedly, an elected official linked this to the absence of a formal, independent science table to advise government and stated that, "I think we should have one established permanently. I think we need to recognize that politicians aren't always the best at discerning scientific evidence and how that should play into decision-making" (IDI15).
These results highlight the divergent perspectives participants had as to the interface between research and policy-making and a lack of understanding regarding process and roles.
Challenges in applying evidence to policy decisions
Perspectives converged with respect to the existence of numerous challenges with and barriers to applying evidence to health policy and decision-making. These related to the quality and breadth of available data, both in terms of absence and abundance. For instance, as one public health actor noted in relation to health policy-making, "you never have enough information. You always have an information shortage, so you're trying to make the best decisions you can in the absence of usually really clear information" (IDI8). On the other hand, as evidence emerged en masse across jurisdictions in the pandemic, there were challenges with synthesizing evidence in a timely fashion for 'real-time' decision-making. A regional health authority actor highlighted this challenge early in the COVID-19 pandemic and perceived that there was not a provincial group bringing new synthesized information to decision-makers on a daily basis (IDI6). Other challenges related to the complexity of the political-public health interface with respect to data and scientific expertise, which "gets debated and needs to be digested by the political process. And then decisions are made" (IDI5). This actor further expressed that debate among experts needs to be balanced with efficient crisis response, that one has to "cut the debate short. For the sake of expediency, you need to react."
It was observed that, in BC’s COVID-19 response, data was gathered from multiple sources with differing data collection procedures, and sometimes with conflicting results—for instance, 'health system data' analyzed by the PHSA and 'public health data' analyzed by the BCCDC. This was observed to present challenges from a political perspective in discerning "who’s actually getting the 'right' answers" (IDI7). An added layer of complexity was reportedly rooted in how to communicate such evidence to the public and "public trust in the numbers" (IDI7), particularly as public understanding of what evidence is, how it is developed, and why it changes, can influence public perceptions of governance.
Finally, as one actor from within the research sector noted, organizationally and governance-wise, the system was "not very well set up to actually use research evidence…if we need to do better at using evidence in practice, we need to fix some of those things. And we actually know what a lot of those things are." For example , "there’s no science framework for how organizations work within that" and " governments shy away from setting science policy " (IDI11). This challenge was framed as having a macro-level dimension, as higher-level leadership structures were observed to not incentivize the development and effective use of research among constituent organizations, and also micro-level implications. From their perspective, researchers will struggle without such policy frameworks to obtain necessary data-sharing agreements with health authorities, nor will they be able to successfully navigate other barriers to conducting action-oriented research that informs policy and practice.
Similarly, a research actor perceived that the COVID-19 pandemic highlighted pre-existing fragmentation, "a pretty disjointed sort of enterprise" in how research is organized in the province:
I think pandemics need strong leadership and I think pandemic research response needed probably stronger leadership than it had. And I think that’s to do with [how] no one really knew who was in charge because no one really was given the role of being truly in charge of the research response (IDI14).
This individual underscored that, at the time of the interview, there were nearly 600 separate research projects being conducted in BC that focused on COVID-19. From their perspective, this reflected the need for more centralized direction to provide leadership, coordinate research efforts, and catalyze collaborations.
Overall, respondents perceived a lack of coordination and continuity across data sources, and a lack of explicit guidelines on evidence-use in the decision-making process, which resulted in a sense of fragmentation. The tension between the processes involved in research and the need for rapid decision-making was perceived as a barrier to using evidence to inform policy.
This study explored the use of evidence to inform early COVID-19 decision-making within British Columbia, Canada, from the perspectives of decision-makers themselves. Findings underscore the complexity of synthesizing and applying evidence (i.e., ‘scientific’ or research-based evidence most commonly discussed) to support public health policy in 'real-time', particularly in the context of public health crisis response. Despite a substantial and long-established literature on evidence-based clinical decision-making [ 23 , 24 ], understanding is more limited as to how public health crisis decision-making can be evidence-informed or evidence-based. By contributing to a growing global scholarship of retrospective examinations of COVID-19 decision-making processes [ 25 , 26 , 27 , 28 ], our study aimed to broaden this understanding and, thus, support the strengthening of public health emergency preparedness in Canada, and globally.
Specifically, based on our findings on evidence-based public health practice, we found that decision-makers clearly emphasized ‘evidence-based’ or ‘evidence-informed’ as meaning ‘scientific’ evidence. They acknowledged other forms of evidence such as professional expertise and contextual information as influencing factors. We identified four key points related to the process of evidence-use in BC's COVID-19 decision-making, with broader implications as well:
Role Differences: The tensions we observed primarily related to a lack of clarity among the various agencies involved as to their respective roles and responsibilities in a public health emergency, a finding that aligns with research on evidence-use in prior pandemics in Canada [ 29 ]. Relatedly, scientists and policy-makers experienced challenges with communication and information-flow between one another and the public, which may reflect their different values and standards, framing of issues and goals, and language [ 30 ].
Barriers to Evidence-Use: Coordination and consistency in how data are collected across jurisdictions reportedly impeded efficiency and timeliness of decision-making. Lancaster and Rhodes (2020) suggest that evidence itself should be treated as a process, rather than a commodity, in evidence-based practice [ 31 ]. Thus, shifting the dialogue from 'barriers to evidence use' to an approach that fosters dialogue across different forms of evidence and different actors in the process may be beneficial.
Use of Evidence in Public Health versus Medicine: Evidence-based public health can be conflated with the concept of evidence-based medicine, though these are distinct in the type of information that needs to be considered. While ‘research evidence’ was the primary type of evidence used, other important types of evidence informed policy decisions in the COVID-19 public health emergency—for example, previous experience, public values, and preferences. This concurs with Brownson’s (2009) framework of factors driving decision-making in evidence-based public health [ 32 ]. Namely, that a balance between multiple factors, situated in particular environmental and organizational context, shapes decision-making: 1) best available research evidence; 2) clients'/population characteristics, state, needs, values, and preferences; and 3) resources, including a practitioner’s expertise. Thus, any evaluation of evidence-use in public health policy must take into consideration this multiplicity of factors at play, and draw on frameworks specific to public health [ 33 ]. Moreover, public health decision-making requires much more attention to behavioural factors and non-clinical impacts, which is distinct from the largely biology-focused lens of evidence-based medicine.
Transparency: Many participants emphasized a lack of explanation about why certain decisions were made and a lack of understanding about who was involved in decisions and how those decisions were made. This point was confirmed by a recent report on lessons learned in BC during the COVID-19 pandemic in which the authors describe " the desire to know more about the reasons why decisions were taken " as a " recurring theme " (13:66). These findings point to a need for clear and transparent mechanisms for channeling evidence, irrespective of the form used, into public health crisis decision-making.
Our findings also pointed to challenges associated with the infrastructure for utilizing research evidence in BC policy-making, specifically a need for more centralized authority on the research side of the public health emergency response to avoid duplication of efforts and more effectively synthesize findings for efficient use. Yet, as a participant questioned, what is the realistic role of research in a public health crisis response? Generally, most evidence used to inform crisis response measures is local epidemiological data or modelling data [ 7 ]. As corroborated by our findings, challenges exist in coordinating data collection and synthesis of these local data across jurisdictions to inform 'real-time' decision-making, let alone to feed into primary research studies [ 34 ].
On the other hand, as was the case in the COVID-19 pandemic, a 'high noise' research environment soon became another challenge as data became available to researchers. Various mechanisms have been established to try and address these challenges amid the COVID-19 pandemic, both to synthesize scientific evidence globally and to create channels for research evidence to support timely decision-making. For instance: 1) research networks and collaborations are working to coordinate research efforts (e.g., COVID-END network [ 35 ]); 2) independent research panels or committees within jurisdictions provide scientific advice to inform decision-making; and 3) research foundations, funding agencies, and platforms for knowledge mobilization (e.g., academic journals) continue to streamline funding through targeted calls for COVID-19 research grant proposals, or for publication of COVID-19 research articles. While our findings describe the varied forms of evidence used in COVID-19 policy-making—beyond scientific evidence—they also point to the opportunity for further investments in infrastructure that coordinates, streamlines, and strengthens collaborations between health researchers and decision-makers that results in timely uptake of results into policy decisions.
Finally, in considering these findings, it is important to note the study's scope and limitations: We focused on evidence use in a single public health emergency, in a single province. Future research could expand this inquiry to a multi-site analysis of evidence-use in pandemic policy-making, with an eye to synthesizing lessons learned and best practices. Additionally, our sample of participants included only one elected official, so perspectives were limited from this type of role. The majority of participants were health officials who primarily referred to and discussed evidence as ‘scientific’ or research-based evidence. Further work could explore the facilitators and barriers to evidence-use from the perspectives of elected officials and Ministry personnel, particularly with respect to the forms of evidence—considered broadly—and other varied inputs, that shape decision-making in the public sphere. This could include a more in-depth examination of policy implementation and how the potential societal consequences of implementation factor into public health decision-making.
We found that the policy decisions made during the initial stages of the COVID-19 pandemic were perceived by actors in BC's response as informed by—not always based on—scientific evidence, specifically; however, decision-makers also considered other contextual factors and drew on prior pandemic-related experience to inform decision-making, as is common in evidence-based public health practice [ 32 ]. The respondents' experiences point to specific areas that need to be considered in planning for future public health emergencies, including information flow between policy-makers and researchers, coordination in how data are collected, and transparency in how decisions are made—all of which reflect a need to improve communication. Furthermore, shifting the discourse from evidence as a commodity to evidence-use as a process will be helpful in addressing barriers to evidence-use, as well as increasing understanding about the public health decision-making process as distinct from clinical medicine. Finally, there is a critical need for clear mechanisms that channel evidence (whether ‘scientific’, research-based, or otherwise) into health crisis decision-making, including identifying and communicating the decision-making process to those producing and synthesizing evidence. The COVID-19 pandemic experience is an opportunity to reflect on what needs to be done to guild our public health systems for the future [ 36 , 37 ]. Understanding and responding to the complexities of decision-making as we move forward, particularly with respect to the synthesis and use of evidence, can contribute to strengthening preparedness for future public health emergencies.
Availability of data and materials
The data that support the findings of this study are not publicly available to maintain the confidentiality of research participants.
The terms 'evidence-informed' and 'evidence-based' decision-making are used throughout this paper, though are distinct. The term 'evidence-informed' suggests that evidence is used and considered, though not necessarily solely determinative in decision-making [ 38 ].
The Provincial Health Services Authority (PHSA) works with the Ministry of Health (MOH) and regional health authorities to oversee the coordination and delivery of programs.
The Office of the Provincial Health Officer (PHO) has binding legal authority in the case of an emergency, and responsibility to monitor the health of BC’s population and provide independent advice to Ministers and public offices on public health issues.
The British Columbia Centre for Disease Control (BCCDC) is a program of the PHSA and provides provincial and national disease surveillance, detection, treatment, prevention, and consultation.
Abbreviations
British Columbia
British Columbia Centre for Disease Control
Coronavirus Disease 2019
Medical Health Officer
Ministry of Health
Provincial Health Officer
Provincial Health Services Authority
Severe Acute Respiratory Syndrome Coronavirus—2
University of British Columbia
Rubin O, Errett NA, Upshur R, Baekkeskov E. The challenges facing evidence-based decision making in the initial response to COVID-19. Scand J Public Health. 2021;49(7):790–6.
Article PubMed Google Scholar
Williams GA, Ulla Díez SM, Figueras J, Lessof S, Ulla SM. Translating evidence into policy during the COVID-19 pandemic: bridging science and policy (and politics). Eurohealth (Lond). 2020;26(2):29–48.
Google Scholar
Vickery J, Atkinson P, Lin L, Rubin O, Upshur R, Yeoh EK, et al. Challenges to evidence-informed decision-making in the context of pandemics: qualitative study of COVID-19 policy advisor perspectives. BMJ Glob Heal. 2022;7(4):1–10.
Piper J, Gomis B, Lee K. “Guided by science and evidence”? The politics of border management in Canada’s response to the COVID-19 pandemic. Front Polit Sci. 2022;4
Cairney P. The UK government’s COVID-19 policy: what does “Guided by the science” mean in practice? Front Polit Sci. 2021;3(March):1–14.
Colman E, Wanat M, Goossens H, Tonkin-Crine S, Anthierens S. Following the science? Views from scientists on government advisory boards during the COVID-19 pandemic: a qualitative interview study in five European countries. BMJ Glob Heal. 2021;6(9):1–11.
Salajan A, Tsolova S, Ciotti M, Suk JE. To what extent does evidence support decision making during infectious disease outbreaks? A scoping literature review. Evid Policy. 2020;16(3):453–75.
Article Google Scholar
Cairney P. The UK government’s COVID-19 policy: assessing evidence-informed policy analysis in real time. Br Polit. 2021;16(1):90–116.
Lancaster K, Rhodes T, Rosengarten M. Making evidence and policy in public health emergencies: lessons from COVID-19 for adaptive evidence-making and intervention. Evid Policy. 2020;16(3):477–90.
Yang K. What can COVID-19 tell us about evidence-based management? Am Rev Public Adm. 2020;50(6–7):706–12.
Parkhurst J. The politics of evidence: from evidence-based policy to the good governance of evidence. Abingdon: Routledge; 2017.
Office of the Prime Minister. Minister of Health Mandate Letter [Internet]. 2021. https://pm.gc.ca/en/mandate-letters/2021/12/16/minister-health-mandate-letter
de Faye B, Perrin D, Trumpy C. COVID-19 lessons learned review: Final report. Victoria, BC; 2022.
First Nations Health Authority. Evolving vaccination plans is science in action: Dr. Bonnie Henry. First Nations Health Authority. 2021.
BC Stats. 2021 Sub-provincial population estimates highlights. Vol. 2021. Victoria, BC; 2022.
Michael Smith Health Research BC [Internet]. 2023. healthresearchbc.ca. Accessed 25 Jan 2023.
Michael Smith Health Research BC. SRAC [Internet]. 2023. https://healthresearchbc.ca/strategic-provincial-advisory-committee-srac/ . Accessed 25 Jan 2023.
Brubacher LJ, Hasan MZ, Sriram V, Keidar S, Wu A, Cheng M, et al. Investigating the influence of institutions, politics, organizations, and governance on the COVID-19 response in British Columbia, Canada: a jurisdictional case study protocol. Heal Res Policy Syst. 2022;20(1):1–10.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
DeCuir-Gunby JT, Marshall PL, McCulloch AW. Developing and using a codebook for the analysis of interview data: an example from a professional development research project. Field Methods. 2011;23(2):136–55.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(117):1–8.
Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;39(3):124–30.
Sackett D. How to read clinical journals: I. Why to read them and how to start reading them critically. Can Med Assoc J. 1981;1245:555–8.
Evidence Based Medicine Working Group. Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA Netw. 1992;268(17):2420–5.
Allin S, Fitzpatrick T, Marchildon GP, Quesnel-Vallée A. The federal government and Canada’s COVID-19 responses: from “we’re ready, we’re prepared” to “fires are burning.” Heal Econ Policy Law. 2022;17(1):76–94.
Bollyky TJ, Hulland EN, Barber RM, Collins JK, Kiernan S, Moses M, et al. Pandemic preparedness and COVID-19: an exploratory analysis of infection and fatality rates, and contextual factors associated with preparedness in 177 countries, from Jan 1, 2020, to Sept 30, 2021. Lancet. 2022;6736(22):1–24.
Kuhlmann S, Hellström M, Ramberg U, Reiter R. Tracing divergence in crisis governance: responses to the COVID-19 pandemic in France, Germany and Sweden compared. Int Rev Adm Sci. 2021;87(3):556–75.
Haldane V, De Foo C, Abdalla SM, Jung AS, Tan M, Wu S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80.
Article CAS PubMed Google Scholar
Rosella LC, Wilson K, Crowcroft NS, Chu A, Upshur R, Willison D, et al. Pandemic H1N1 in Canada and the use of evidence in developing public health policies—a policy analysis. Soc Sci Med. 2013;83:1–9.
Article PubMed PubMed Central Google Scholar
Saner M. A map of the interface between science & policy. Ottawa, Ontario; 2007. Report No.: January 1.
Lancaster K, Rhodes T. What prevents health policy being “evidence-based”? New ways to think about evidence, policy and interventions in health. Br Med Bull. 2020;135(1):38–49.
Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health. 2009;30:175–201.
Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health. 2002;56:119–27.
Article CAS PubMed PubMed Central Google Scholar
Khan Y, Brown A, Shannon T, Gibson J, Généreux M, Henry B, et al. Public health emergency preparedness: a framework to promote resilience. BMC Public Health. 2018;18(1):1–16.
COVID-19 Evidence Network to Support Decision-Making. COVID-END [Internet]. 2023. https://www.mcmasterforum.org/networks/covid-end . Accessed 25 Jan 2023.
Canadian Institutes of Health Research. Moving forward from the COVID-19 pandemic: 10 opportunities for strengthening Canada’s public health systems. 2022.
Di Ruggiero E, Bhatia D, Umar I, Arpin E, Champagne C, Clavier C, et al. Governing for the public’s health: Governance options for a strengthened and renewed public health system in Canada. 2022.
Adjoa Kumah E, McSherry R, Bettany-Saltikov J, Hamilton S, Hogg J, Whittaker V, et al. Evidence-informed practice versus evidence-based practice educational interventions for improving knowledge, attitudes, understanding, and behavior toward the application of evidence into practice: a comprehensive systematic review of undergraduate studen. Campbell Syst Rev. 2019;15(e1015):1–19.
Download references
Acknowledgements
We would like to extend our gratitude to current and former members of the University of British Columbia Working Group on Health Systems Response to COVID-19 who contributed to various aspects of this study, including Shelly Keidar, Kristina Jenei, Sydney Whiteford, Dr. Md Zabir Hasan, Dr. David M. Patrick, Dr. Maxwell Cameron, Mahrukh Zahid, Dr. Yoel Kornreich, Dr. Tammi Whelan, Austin Wu, Shivangi Khanna, and Candice Ruck.
Financial support for this work was generously provided by the University of British Columbia's Faculty of Medicine (Grant No. GR004683) and Peter Wall Institute for Advanced Studies (Grant No. GR016648), as well as a Canadian Institutes of Health Research Operating Grant (Grant No. GR019157). These funding bodies were not involved in the design of the study, the collection, analysis or interpretation of data, or in the writing of this manuscript.
Author information
Authors and affiliations.
School of Population and Public Health, University of British Columbia, Vancouver, Canada
Laura Jane Brubacher, Chris Y. Lovato, Veena Sriram, Michael Cheng & Peter Berman
School of Public Health Sciences, University of Waterloo, Waterloo, Canada
Laura Jane Brubacher
School of Public Policy and Global Affairs, University of British Columbia, Vancouver, Canada
Veena Sriram
You can also search for this author in PubMed Google Scholar
Contributions
CYL, PB, and VS obtained funding for and designed the study. LJB, MC, and PB conducted data collection. LJB and VS analyzed the qualitative data. CYL and LJB collaboratively wrote the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Laura Jane Brubacher .
Ethics declarations
Ethics approval and consent to participate.
This case study received the approval of the UBC Behavioural Research Ethics Board (Certificate # H20-02136). Participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Semi-structured interview guide [* = questions used for this specific study]
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Brubacher, L.J., Lovato, C.Y., Sriram, V. et al. The use of evidence to guide decision-making during the COVID-19 pandemic: divergent perspectives from a qualitative case study in British Columbia, Canada. Health Res Policy Sys 22 , 66 (2024). https://doi.org/10.1186/s12961-024-01146-2
Download citation
Received : 08 February 2023
Accepted : 29 April 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s12961-024-01146-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Decision-making
- Public health
- Policy-making
- Qualitative
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Work & Careers
- Life & Arts
- Currently reading: Case study: joining up skills and health support in Wales
- Will AI revolutionise education for the better?
- Tech and generational changes increase urgency of upskilling
- Retraining workers for the AI world
- What are organisations doing to ensure staff have the right skills?
- Employers look to rip the ‘paper ceiling’ for non-graduates
- The challenges of upskilling for marginalised workers
Case study: joining up skills and health support in Wales

- Case study: joining up skills and health support in Wales on x (opens in a new window)
- Case study: joining up skills and health support in Wales on facebook (opens in a new window)
- Case study: joining up skills and health support in Wales on linkedin (opens in a new window)
- Case study: joining up skills and health support in Wales on whatsapp (opens in a new window)
Georgina Quach
Roula Khalaf, Editor of the FT, selects her favourite stories in this weekly newsletter.
In remote areas of Wales, people are often forced to travel long distances for minimum wage jobs. In the town of Caerphilly, near Cardiff, one man was even “bought trainers” by the council for his commute.
“Because of poor bus links, it was faster for him to walk over the mountain to work,” explains Tammy Boyce, senior consultant at the Institute of Health Equity. “These are not conditions for people who are on the edge of good mental or poor physical health.”
In Wales, this is a growing problem. Since the Covid pandemic, it has been an outlier within the UK in experiencing increased levels of sickness absence and economic inactivity. This has prompted local authorities and training providers to join up their skills and health support.
Just north of Caerphilly is Blaenau Gwent, the former coal-mining borough once represented by Aneurin Bevan, a minister in the postwar Labour government and the main architect of the UK’s NHS. Now, 40 years after its deindustrialisation, the area is at the sharp end of a broader labour market malaise in Wales, where the proportion of people neither working nor seeking work remains stubbornly above 2019 levels.
About 44 per cent of Blaenau Gwent’s economically inactive population cite long-term sickness as their reason for leaving the workforce, compared with the 33.4 per cent average in Wales and 27.5 per cent in the UK, according to the latest annual population survey. “Residents are — and should be — angry there hasn’t been more done,” says Boyce.

This is particularly concerning because people who are inactive due to sickness tend to have extended periods of worklessness, according to research by the Resolution Foundation — hampering the Wales’ attempts to boost productivity after decades of lagging the wider UK employment rate. One of the Welsh government’s targets is to close the 1.7 percentage point gap by 2050.
Victoria Winckler, director of the Welsh think-tank Bevan Foundation, says: “This is not about people’s behaviour or individual choices, this is about the structural problems in Wales’s economy. There isn’t a range of well-paid jobs suitable for people with health conditions. The alternative to being ‘on the sick’ is a very physically demanding job,” she says. Two of her staff members work a four-day week in order to care for their fathers, both former miners who had contracted industrial diseases.
“Coming up with a way to motivate and support people is a real policy conundrum,” says Nick Smith, the Labour MP for Blaenau Gwent. “Access to local employment can be challenging in somewhere like Gwent, which is geographically distant from other employment markets.” There are only two trains an hour from Ebbw Vale to Newport and Cardiff.
“Some people move into other sectors or retrain,” notes Smith. “But it’s a hard thing to do if you’ve been working down the pit or in the steelworks for a long time, it’s a big change.”
So, in recent years, skills programmes have sprung up locally that are geared towards both helping people navigate these barriers and fulfilling skills shortages.
For example, Smith helped launch a new cyber security course at Ebbw Vale college Coleg Gwent. “The cyber sector is more permeable to residents just getting started in it, because you don’t need to have a degree,” Smith says. “The course has gone from success to success.” Companies including Welsh Water and Admiral, the insurer, have hired people straight from this course.
Other initiatives are combining wellbeing and employment support, in a bid to reverse the rising levels of economic inactivity, particularly among young people.

About a quarter of the customers of ITEC Training, which supports school leavers in 15 sites across Wales into work, have some kind of disability.
“Post-Covid, we are now seeing very low levels of maturity, low confidence, and a high prevalence of mental health issues,” says Gareth Matthews, director of ITEC, which is one of the providers contracted to deliver Jobs Growth Wales+, a Welsh government skills programme for 16-19 year olds. “An average 16 year old is presenting as a 13 year old,” he says.
ITEC seeks to move them from being “locked away in their bedrooms” to work placements, by teaching numeracy, digital, and presentation skills, through exercises similar to those in TV show Dragons’ Den .
“The economically inactive cohort used to be predominantly older workers but, increasingly, we are seeing this among younger people,” explains Matthews.
He says ITEC completely “overhauled” its delivery model during Covid to adjust to the pandemic-related decline in confidence and maturity. It co-designed a wellbeing assessment tool, which fed back data about the learners’ biggest social or health barriers, and introduced new staff roles in counselling. ITEC also negotiated with the government to add wraparound wellbeing support to the existing programme.
Julie Dyer, ITEC’s head of operations, says: “It is absolutely pointless looking just at academic employability skills when their wellbeing is so, so bad.” Since April 2022, Jobs Growth Wales+ has helped 10,000 learners, 60 per cent of whom leave with employment or an apprenticeship, or go into higher education.
“You can just sense the increase in confidence and self-belief and pride in what they’re doing,” says Matthews. “. Given the background they came from, it’s remarkable.” But the government funding for these projects is being outpaced by soaring demand.
Training providers emphasise that engaging out-of-work people and benefits claimants can be challenging — and requires the Department for Work and Pensions to promote such opportunities. According to the Learning and Work Institute (LWI), a think-tank, only one in 10 out-of-work disabled people in the UK are currently getting help to find work through support programmes run by the DWP and other agencies.
“Those problems are massively compounded in Wales, where you have a higher disability rate and higher disability employment gap than the UK average,” says Joshua Miles, LWI’s director of Wales. This year, LWI partnered with Merthyr Valley Homes, in another deprived part of south Wales, to upskill tenants on one of their housing estates.
“In Wales the big levers to address economic inactivity are reserved to Westminster,” points out Miles, adding that regional policy in Denmark and Germany — with some industry similarities to Wales — better reflects local needs. After Brexit, EU funding for Wales’ employability schemes was replaced by the Shared Prosperity Fund, which Westminster administers.

Boosting Wales’ employment rate (74.1 per cent) to that of Denmark’s (80.1 per cent, its record high in 2022) would require an extra 115,000 people to find work.
And the benefits of achieving this are clear to Boyce, at the Institute of Health Equity: “Helping people into jobs is what changes someone’s life — getting out of the house, having that regular contact with people, a regular income.”
Promoted Content
Explore the series.

Follow the topics in this article
- Future of work Add to myFT
- UK employment Add to myFT
- Flexible working Add to myFT
- Georgina Quach Add to myFT
International Edition
575.744.81 - Environmental Chemistry
Description.
This course focuses on the environmental behavior and fate of anthropogenic contaminants in aquatic environments. Students learn to predict contaminant properties influencing contaminant transfers between hydrophobic phases, air, water, sediments, and biota, based on a fundamental understanding of physico-chemical properties, intermolecular interactions, and basic thermodynamic principles. Mechanisms of important transformation reactions and techniques and quantitative models for predicting the environmental fate or human exposure potential of contaminants are discussed.

Shalini Jayasundera
Course Structure
The course content is divided into modules. Clicking Course Modules on the left navigation menu can access course modules. A module will have several sections including the overview, content, readings, discussions, and assignments. Students are encouraged to preview all sections of the module before starting. Most modules run for a period of seven (7) days, exceptions are noted on the Course Outline page under Syllabus and Couse Information . Students should regularly check the Calendar and Announcements for assignment due dates.
Course Topics
- Rationale and make up of organic compounds
- Molecular Interactions, Thermodynamics and Organic Acids & Bases
- Vapor Pressure
- Solubility in Water
- Air-water partitioning
- Organic liquid-water partitioning
- Sorption – solid/liquid exchange
- Transformation Processes –Overview
- Air-water exchange
- Modeling Tools: Fugacity Model
- Modeling Tools: Box Models
Course Goals
To understand the basic principles of the behavior of organic compounds in the environment using their chemical structure and to apply that knowledge to quantitatively asses the dynamics of anthropogenic chemicals in natural environments using the necessary conceptual tools and information.
Course Learning Outcomes (CLOs)
Schwarzenbach, R. P., Gschwend, P. M., & Imboden, D. M. (2017). Environmental Organic Chemistry (3rd ed.). Hoboken, N.J.: John Wiley & Sons.
ISBN-13: 978-1-118-76723-8
Textbook information for this course is available online through the appropriate bookstore website: For online courses, search the BNC website .
Student Coursework Requirements
It is expected that each module will take approximately 4–7 hours per week to complete. Here is an approximate breakdown: reading the assigned sections of the texts (approximately 2–3 hours per week) as well as some outside reading, reading the content documents (approximately 1–2 hours per week), and assignments (approximately 1–2 hours per week).
This course will consist of the following basic student requirements:
Preparation and Participation – Weekly Module Discussion Topics (11% of Final Grade Calculation)
You are responsible for carefully reading all assigned material and being prepared for discussion. The majority of readings are from the assigned and researched material on the weekly topic. Additional reading may be assigned to supplement text readings.
Post your initial response to the discussion questions by the evening of day 4 for that module week. Posting a response to the discussion question is part one of your grade for module discussions (i.e., Timeliness).
Part two of your grade for module discussion is your interaction (i.e., responding to classmate postings with thoughtful responses) with at least two classmates (i.e., Critical Thinking). Just posting your response to a discussion question is not sufficient; we want you to interact with your classmates. Be detailed in your postings and in your responses to your classmates' postings. Feel free to agree or disagree with your classmates. Please ensure that your postings are civil and constructive.
I will monitor module discussions and will respond to some of the discussions as discussions are posted. In some instances, I will summarize the overall discussions and post the summary for the module.
Evaluation of preparation and participation is based on contribution to discussions.
In Module 12 each student is expected to submit a Discussion Portfolio of his or her best discussion responses throughout the course. This will consist of the following:
- Cover sheet with name.
- 3 Responses to discussion questions from Dr. Jayasundera.
- 3 responses to other students’ postings of Dr. Jayasundera’s discussion questions.
Please specify which question you are including in your discussion post portfolio.
Post your initial response to the discussion questions by the evening of Day 4 for that module week. For example, if the module week starts on a Tuesday, the discussion posting will be due by 12:00am (midnight) on Friday. Post your follow-up response to other students’ postings by midnight of Day 7 of that module week (e.g. Monday at 12:00am). Posting a response to the discussion question is part one of your grade for module discussions (i.e., Timeliness).
Preparation and participation is evaluated by the following grading elements:
- Timeliness (50%)
- Critical Thinking (50%)
Preparation and participation is graded as follows:
- 100–90 = A—Timeliness [regularly participates; all required postings; early in discussion; throughout the discussion]; Critical Thinking [rich in content; full of thoughts, insight, and analysis].
- 89–80 = B—Timeliness [frequently participates; all required postings; some not in time for others to read and respond]; Critical Thinking [substantial information; thought, insight, and analysis has taken place].
- 79–70 = C—Timeliness [infrequently participates; all required postings; most at the last minute without allowing for response time]; Critical Thinking [generally competent; information is thin and commonplace].
- <70 = F—Timeliness [rarely participates; some, or all required postings missing]; Critical Thinking [rudimentary and superficial; no analysis or insight is displayed].
Assignments – Weekly Case Study Assignments (24% of Final Grade Calculation)
Assignments include a mix of qualitative and quantitative module weekly assignments related to the “pet” chemical selected by the student in Module 1 for their Final Course Project (case study). The students will be developing estimates of compound properties and environmental fate using the capabilities learned in each module in support of the final Case Study Paper – use the list of compounds provided by the instructor or a student selected chemical - confirm with the Instructor (e.g. calculations, estimations, literature reviews, and model summaries).
All assignments are due according to the dates in the Calendar.
Assignments will be graded on a weekly basis and each submission should include the following:
- Cover sheet with name and assignment identifier.
- Name & page number indicator (i.e., Frank Smith, page x of y) on each page.
- All Figures and Tables captioned and labeled appropriately.
- Problem statement.
- Assumptions.
- Computations.
- Conclusions/discussion delineated.
Each Assignment is worth 2.4% of the overall grade. There are 12 Assignments throughout the course of which the top 10 graded assignments will be selected towards 24% of the course grade.
The course also includes Questions and Problems that are quantitative problem sets that are questions derived at the end of each assigned chapter in the textbook. The Questions and Problems will not be submitted and therefore will not be graded however completion of these problem sets will greatly improve the quality of the Assignments.
Note: All Assignments will be attached as work products to the final student submission of the Case Study Paper.
If, after submitting a written assignment you are not satisfied with the grade received, you are encouraged to redo the assignment and resubmit it. If the resubmission results in a better grade, that grade will be substituted for the previous grade.
Course Project - Case Study (35% of Final Grade Calculation)
Students will start working on the assigned course project from Module 2. The last week will be devoted to the course project.
The Final Course Project will consist of two items:
An individual Case Study topic will be assigned to each student during Module 2. The topic will be determined based on Module 1 Assignment. The chosen topic will be used for developing estimates of compound properties and environmental fate throughout the duration of the course and the final Case Study Paper.
Dr. Jayasundera will correspond and decide a day and time for the entire class to present in Module 14. Once a date and time has been selected you will present your Case Study Paper to your group and Dr.
Jayasundera. The presentation will be 15 minutes (8 -10 minutes for presentation of material and 5 minutes for questions and answers).
The Final Course Project is evaluated by the following grading elements:
Case Study Paper (as related to the student’s technical understanding of concepts learned in the Course, substantial information; thought, insight, and analysis; weekly work products in attachments, preparation and presentation of material, clarity of presented material as described in Course Project Description) (20%)
Student Presentation (as related to the student’s technical understanding, preparation and presentation of material, clarity of presented material, responses to questions asked during the presentation by other students and instructor as described in the Final Course Project Description) (15%)
Course Project is graded as follows:
- 100–90 = A— Student Preparation and Participation [completion of case study paper well written for a scientific audience in a journal publication; well prepared and available during presentation; student well versed in use of Zoom]; Student Understanding [rich in content related to concepts learned in the course; full of thought, insight, and analysis].
- 89–80 = B— Student Preparation and Participation [case study paper written for a scientific audience in a journal publication, prepared and available during presentation; student generally versed in use of Zoom] Student Understanding [information presented on concepts learned in the course is well defined and understood; substantial information; thought, insight, and analysis has taken place].
- 79–70 = C—Student Preparation and Participation [paper not necessarily written for a scientifically literate audience in a journal publication; generally prepared and available during presentation; individual generally versed in use of Zoom]; Student Understanding [generally competent on concepts learned in the course; information is thin and commonplace].
- <70 = F—Student Preparation and Participation [ paper not written for a scientifically literate audience in a journal publication, material included in paper is not well understood; individual has difficulty with use of Zoom]; Student Understanding [rudimentary and superficial understanding of concepts learned in the course; no analysis or insight displayed].
Exams (30% of Final Grade Calculation, combined from 10% for Midterm and 20% for Final)
The midterm exam will be available in Module 5 and the final exam will be available in Module 12. You will have one week to complete the exams and they will be due by 5PM exactly one week from their release. You may use the course text and Module Content to complete the exams.
Students must submit examinations as Word documents or as scanned PDF documents. Both must include all calculations (using Excel spreadsheets, where necessary), assumptions, and answers.
The exams are evaluated by the following grading elements:
- Each part of question is answered (20%)
- Writing quality and technical accuracy (30%) (Writing is expected to meet or exceed accepted graduate- level English and scholarship standards. That is, all assignments will be graded on grammar and style as well as content.)
- Rationale for answer is provided (20%)
- Examples are included to illustrate rationale (15%) (If a student does not have direct experience related to a particular question, then the student is to provide analogies versus examples.)
- Outside references are included (15%) Exams are graded as follows:
- 100–90 = A—All parts of question are addressed; Writing Quality/ Rationale/ Examples/ Outside References [rich in content; full of thought, insight, and analysis].
- 89–80 = B—All parts of the question are addressed; Writing Quality/ Rationale/ Examples/ Outside References [substantial information; thought, insight, and analysis has taken place].
- 79–70 = C—Majority of parts of the question are addressed; Writing Quality/ Rationale/ Examples/ Outside References [generally competent; information is thin and commonplace].
- <70 = F—Some parts of the question are addressed; Writing Quality/ Rationale/ Examples/ Outside References [rudimentary and superficial; no analysis or insight displayed].
Grading Policy
Assignments are due according to the dates posted in your Blackboard course site. You may also check these due dates in the Course Outline or the Assignments in the corresponding modules. I will post grades one week after assignment due dates.
A grade of A indicates achievement of consistent excellence and distinction throughout the course—that is, conspicuous excellence in all aspects of assignments and discussion in every week.
A grade of B indicates work that meets all course requirements on a level appropriate for graduate academic work. These criteria apply to both undergraduates and graduate students taking the course.
EP uses a +/- grading system (see “Grading System”, Graduate Programs catalog, p. 10).
100-98 = A+
Final grades will be determined by the following weighting:
Academic Policies
Students may add a course up to one week after the start of the term for that particular course. Students may drop courses according to the drop deadlines outlined in the EP academic calendar ( https://ep.jhu.edu/student-services/academic-calendar/ ). Between the 6th week of the class and prior to the final withdrawal deadline, a student may withdraw from a course with a W on their academic record. A record of the course will remain on the academic record with a W appearing in the grade column to indicate that the student registered and withdrew from the course.
All students are required to read, know, and comply with the Johns Hopkins University Krieger School of Arts and Sciences (KSAS) / Whiting School of Engineering (WSE) Procedures for Handling Allegations of Misconduct by Full-Time and Part-Time Graduate Students.
This policy prohibits academic misconduct, including but not limited to the following: cheating or facilitating cheating; plagiarism; reuse of assignments; unauthorized collaboration; alteration of graded assignments; and unfair competition. Course materials (old assignments, texts, or examinations, etc.) should not be shared unless authorized by the course instructor. Any questions related to this policy should be directed to EP’s academic integrity officer at [email protected] .
Johns Hopkins University values diversity and inclusion. We are committed to providing welcoming, equitable, and accessible educational experiences for all students. Students with disabilities (including those with psychological conditions, medical conditions and temporary disabilities) can request accommodations for this course by providing an Accommodation Letter issued by Student Disability Services (SDS). Please request accommodations for this course as early as possible to provide time for effective communication and arrangements.
For further information or to start the process of requesting accommodations, please contact Student Disability Services at Engineering for Professionals, [email protected] .
The fundamental purpose of the JHU regulation of student conduct is to promote and to protect the health, safety, welfare, property, and rights of all members of the University community as well as to promote the orderly operation of the University and to safeguard its property and facilities. As members of the University community, students accept certain responsibilities which support the educational mission and create an environment in which all students are afforded the same opportunity to succeed academically.
For a full description of the code please visit the following website: https://studentaffairs.jhu.edu/policies-guidelines/student-code/
JHU is committed to creating a classroom environment that values the diversity of experiences and perspectives that all students bring. Everyone has the right to be treated with dignity and respect. Fostering an inclusive climate is important. Research and experience show that students who interact with peers who are different from themselves learn new things and experience tangible educational outcomes. At no time in this learning process should someone be singled out or treated unequally on the basis of any seen or unseen part of their identity. If you have concerns in this course about harassment, discrimination, or any unequal treatment, or if you seek accommodations or resources, please reach out to the course instructor directly. Reporting will never impact your course grade. You may also share concerns with your program chair, the Assistant Dean for Diversity and Inclusion, or the Office of Institutional Equity . In handling reports, people will protect your privacy as much as possible, but faculty and staff are required to officially report information for some cases (e.g. sexual harassment).
When a student enrolls in an EP course with “audit” status, the student must reach an understanding with the instructor as to what is required to earn the “audit.” If the student does not meet those expectations, the instructor must notify the EP Registration Team [ [email protected] ] in order for the student to be retroactively dropped or withdrawn from the course (depending on when the "audit" was requested and in accordance with EP registration deadlines). All lecture content will remain accessible to auditing students, but access to all other course material is left to the discretion of the instructor.

A Case Study Investigating the Utilization of ChatGPT in Online Discussions
- Xi Lin East Carolina University https://orcid.org/0000-0003-2387-4117
- Ken Luterbach East Carolina University https://orcid.org/0000-0003-1545-5000
- Kristen H. Gregory East Carolina University https://orcid.org/0000-0002-4879-0991
- Sarah E. Sconyers East Carolina University https://orcid.org/0009-0006-8136-5125
This study explored the impact of integrating ChatGPT into asynchronous online discussions. The analysis encompassed students’ log data from Canvas and their perspectives on using ChatGPT. Results revealed a significant enhancement in overall discussion participation when ChatGPT is encouraged, emphasizing its potential as a catalyst for constructive conversations and the development of generic skills. Students also acknowledge ChatGPT’s positive influence on critical thinking and knowledge exploration. In summary, integrating ChatGPT not only enhances participation and engagement but also fosters a sense of community, promotes online interaction, and cultivates essential skills. This study concluded by discussing issues associated with using ChatGPT for online discussions and highlighting implications for its appropriate integration into online discussion boards.
Author Biographies
Xi lin, east carolina university.
Xi Lin is an associate professor in the Department of Interdisciplinary Professions at East Carolina University. Her research focuses on student engagement and interaction in online and distance learning and international students and faculty in the US higher education. More information about her can be found at http://whoisxilin.weebly.com/
Ken Luterbach, East Carolina University
Ken Luterbach is an associate professor of Instructional Technology in the College of Education at East Carolina University. His professional interests focus primarily on creative use of computers for learning and productivity, which involves work in computational thinking, CS for All, AI for All, and educational robotics. In teaching, he favors the development of lessons that challenge students to innovate through design and development.
Kristen H. Gregory, East Carolina University
Kristen H. Gregory is an associate professor of elementary education in the College of Education at East Carolina University. Previously, she worked as an elementary classroom teacher, K12 reading specialist, community college faculty, and faculty professional development manager. She currently teaches courses on classroom assessment, curriculum development, and educational research for undergraduate and graduate students. Her research focuses on the relationship between professional learning and in-service and pre-service teachers’ pedagogical decisions, professional identity, and use of reflective practice.
Sarah E. Sconyers, East Carolina University
Sarah Sconyers is the Director of Assessment, Data Management, and Digital Learning for East Carolina University’s College of Education. She previously served as the edTPA Coordinator and as an Instructional Consultant for the college. Before coming to ECU, Sarah spent twelve years as a secondary social studies teacher with Chapel Hill-Carrboro City Schools.
Copyright (c) 2024 Xi Lin, Ken Luterbach, Kristen H. Gregory, Sarah E. Sconyers

This work is licensed under a Creative Commons Attribution 4.0 International License .
As a condition of publication, the author agrees to apply the Creative Commons – Attribution International 4.0 (CC-BY) License to OLJ articles. See: https://creativecommons.org/licenses/by/4.0/ .
This licence allows anyone to reproduce OLJ articles at no cost and without further permission as long as they attribute the author and the journal. This permission includes printing, sharing and other forms of distribution.
Author(s) hold copyright in their work, and retain publishing rights without restrictions

The DOAJ Seal is awarded to journals that demonstrate best practice in open access publishing
OLC Membership

OLC Research Center

Information
- For Readers
- For Authors
- For Librarians
- Open access
- Published: 03 June 2024
Factors leading to lapses in professional behaviour of Gynae residents in Pakistan: a study reflecting through the lenses of patients and family, consultants and residents
- Humera Noreen 1 ,
- Rahila Yasmeen 2 &
- Shabana Ali Mohammad 2
BMC Medical Education volume 24 , Article number: 611 ( 2024 ) Cite this article
Metrics details
Introduction
Professional behaviour is the first manifestation of professionalism. In teaching hospitals, the residents can be considered vulnerable to lapses in professional behaviour when they fail to meet the set standards of professionalism. Residents of some specialties are more at risk of lapses in professional behaviour due to the demanding nature of work. Research focusing on the behaviour of residents in the field of Gynae and the underlying factors contributing to such behaviour is notably lacking in the literature. Additionally, there is a gap in understanding the perspectives of patients from Pakistan on this matter, as it remains unexplored thus far, which constitutes the central focus of this study.
An increase in complaints lodged against Gynae resident’s professional behaviour in Pakistan Citizen Portal (PCP) was observed. Therefore, an exploratory qualitative study was conducted to investigate the factors and rationales contributing to the lapses in resident’s professional behaviour.
The study collected the viewpoints of three stakeholder groups: patients and their families, consultants and residents. The study was conducted in three phases. First, the document analysis of written complaints was conducted, followed by face-to-face interviews (11 per group) conducted by trained researchers from an independent 3rd party. Finally, the interview data was transcribed, coded and analysed.
In total 15 themes were identified from the interviews with 3 stakeholders, which were then categorized and resulted in 6 overlapping themes. The most prevalent lapse reported by all 3 stakeholders was poor verbal behaviour of residents.
The highly ranked factors contributing to triggering the situation were associated with workplace challenges, well-being of residents, limited resources, patients and family characteristics, patients’ expectations, lack of administrative and paramedic support, cultural factors and challenges specific to Gynae specialty .
Another intriguing and emerging theme was related to the characteristics of patients and attendants which helped in understanding the causes and implications of conflicting environments. The value of competency also emphasized that can be accomplished by training and mentoring systems. The thorough examination of these factors by key stakeholders aided in accurately analysing the issue, its causes, and possible solutions. The study's findings will assist higher authorities in implementing corrective actions and offering evidence-based guidance to policymakers to improve healthcare system.
Peer Review reports
Understanding human behaviour is very important to comprehend how people see, interpret and adapt to various environments and to have an insight about the reasons people change their behaviour [ 1 ]. The same principle applies to professional behaviour (PB) in workplace environments including healthcare. The professional behaviour in a healthcare system could be defined as placing the best interests of patients at the center of everything you do [ 2 ].
Lapses in professional behaviour lack a unified definition, one could say that any behaviour that impairs the ability of the medical team to achieve desired outcomes is considered as lapse in PB or when someone is not following the standards expected from a person in their profession and behaving against them. Lapses could also be taken as a behaviour characterized by actions that a reasonable person would view as humiliating, rude, disrespectful, abusive language, demeaning, and bullying [ 3 ]. Lapses in professional conduct not only impact patient-doctor relationships, patient safety, and the quality of care but also the doctor's career [ 4 ].
According to Accreditation Council for Graduate Medical Education (ACGME) guidelines, residents must acquire professional behaviour as a core competency. The expected domains of professional behaviour projected by the residents include empathy, honesty, and respect for others [ 5 ] . Residents are susceptible to engaging in a variety of lapses in professional behaviour throughout their residency, which is a crucial time for doctors to build their ethical norms. It is essential to have a complete awareness of the relevant causes or events in order to prevent resident misbehaviour [ 6 ].
There is a scarcity of literature specifically examining the assessment of trainees' reasons and varieties of professional conduct lapses [ 7 ]. In the existing body of literature, the behavioural deficiencies observed among residents encompass various misconduct aspects, including disruptive practices involving patient care neglect, absence of empathy, and disrespect toward patients, as well as verbal or nonverbal misuse of authority and unwelcoming demeanor [ 8 , 9 , 10 ].
However, it's been acknowledged that addressing lapses in professional behaviour poses one of the most difficult challenges for medical educators. Understanding the underlying reasons behind such lapses is intricate, with the context in which the behaviour manifests playing a pivotal role [ 7 ].
Research indicates a connection between unprofessional conduct during undergraduate and postgraduate training and similar behaviour in later practice [ 11 ]. A conceptual framework has been proposed for evaluating and addressing lapses in PB [ 3 ]. To identify the root causes of PB lapses, it is crucial to determine whether residents understand professional expectations and are willing to adhere to them, or if there are barriers or distractions hindering their ability to exhibit professional behaviour [ 12 ]. The problem of lapses in PB is not specific to any specialty and appears to be occurring in various demographic groups/countries [ 13 , 14 , 15 ].
In teaching hospitals tasked with training new physicians, the diverse background of patients and their attendants often leads to an overwhelming environment. This diversity breeds a behavioural gap, primarily driven by the varying interests of individuals involved. Patients and their attendants bring different levels of understanding, influenced by educational exposure, personal values, and background, which can disrupt interactions and impact patient-doctor relationships [ 16 ].
Furthermore, residents face additional pressures that contribute to their susceptibility to unprofessional behaviour. The urgency to quickly acquire clinical knowledge during their residency often supersedes their focus on professional conduct, leading to a lack of understanding in this regard [ 17 , 18 ]. Additionally, residents may feel compelled to remain silent about professional challenges they encounter during their training to uphold the hospital's public image [ 14 ]. Therefore, it becomes a difficult task for medical tutors to unfold the truth and deal with it in the best interest of doctors and patients.
Several studies reported by developed countries have explored various facets of professionalism in alignment with their respective healthcare systems and policies [ 13 , 15 , 18 ]. However, it is crucial to recognise that the findings of these studies may not be directly applicable to developing countries without appropriate contextual adaptation.
As a developing country, Pakistan presents a unique set of factors that differ from those observed in developed nations, including government policies, patient awareness, medical practices, doctor workload, and cultural influences. Furthermore, there is a scarcity of data regarding patient perceptions of PB lapses, the underlying reasons for inappropriate resident behaviour, and the specific contextual factors within the local environment that influence resident conduct.
Research indicates that certain medical specialties, such as OB-GYN and Surgery, face increased risks of specific unprofessional behaviours due to their distinct stressors [ 14 ]. Therefore, it is suggested to conduct context-specific assessments to identify and mitigate these stressors effectively [ 19 ]. A narrative study conducted in King Edward, Lahore Pakistan aimed to explore conflicts in Obs and Gynae, revealing organizational, interpersonal, and individual conflicts [ 20 ]. Further investigation is required to understand the underlying factors and triggers of these conflicts. While various factors influencing professionalism in junior medical professionals have been identified, there is a notable gap in research focusing specifically on Gynae residents. A recent study has reported high rates of unprofessional behaviour among dismissed General Practice residents (90%), with a significant proportion displaying disrespect towards patients or staff (27%) [ 21 ]. Unprofessional behaviour among doctors is regulated by disciplinary bodies of respective country which have extensive effects on doctors health and career. A higher incidence of disciplinary actions noted in Obstetrics and Gynaecology [ 22 ]. Majeed et al. reported in the narrative review that issues related to poor ethical behaviour by trainees are usually presented as patient’s complaints. Disrespectful behaviour (worrisome communication, reluctant to talk, behavioural change affecting patients and family) was one of the most reported unprofessional behaviour in the narrative review [ 23 ].
The study's context revolves around a non-profit public sector medical university situated in Rawalpindi (population range of 1,000,000–5,000,000 inhabitants), Punjab, recognized by the Higher Education Commission of Pakistan [ 24 ]. The medical university operates as a small-sized coeducational university (uniRank enrollment range: 3,000–3,999 students) with significant Obstetrics and Gynae patient workload across three allied hospitals [ 25 ]. Due to the overwhelming patient load and resource constraints, unresolved complaints and conflicts have arisen. To address this, Prime Minister's Performance Delivery Unit (PMDU) [ 26 ] initiated a national complaints and grievance redressal mechanism called Pakistan Citizen Portal (PCP) [ 27 ]. ( https://citizenportal.gov.pk/ ), aiming to provide citizens with a streamlined platform for resolving complaints efficiently. A substantial number of complaints were filed against Obs and Gynae residents, prompting the need to investigate the underlying reasons for such grievances. Existing literature highlights the importance of professional behaviour in residents, yet studies specifically targeting Gynae residents' conduct and the reasons behind lapses are lacking. Moreover, the perceptions of Pakistani patients, the primary stakeholders affected, remain unexplored, along with the comparative analysis of opinions among the three main stakeholders (patients, residents and consultants) to unveil the true circumstances surrounding the issue.
Study aims and research questions/objectives
⊳ Research questions
What are the lapses in professional behaviour of Gynae residents?
What are the factors and reasons leading to the lapses in professional behaviour of Gynae residents from the perspectives of patients and family, Gynae consultants and residents in Pakistani context?
⊳ Objectives
To determine the frequency of identified lapses in professional behaviour among the Gynae residents by analysing PCP complaints
To explore the factors and reasons leading to the lapses in professional behaviour of Gynae residents from the perspectives of patients & families, Gynae consultants and residents.
A comprehensive analysis was done which aided in accurately diagnosing the problem, identifying its root causes, and devising effective remedies. The findings of this study are considered key enablers for the higher authorities to implement corrective measures and offer evidence-based guidance to policymakers, thereby enhancing the overall healthcare system.
Study design
The conceptual framework of this study is illustrated in (Fig. 1 ) and represents an exploratory qualitative approach, commonly employed in education and social sciences research [ 28 ]. This qualitative study spanned a duration of 6 months, commencing from Dec 2021 till June 2022, and was conducted within two Obs and Gynae departments within the public healthcare sector in Rawalpindi, Pakistan.

The Conceptual framework of our study. Note: OB1 (Objective 1), OB2 (Objective 2)
Two research methodologies were utilized: document analysis of PCP complaints to identify and confirm the frequency of lapses in professional behaviour among Gynae residents,
(Phase 1) , and in-depth interviews designed on the basis of findings of the document analysis (Phase 2) . The in-depth interviews, conducted with the written consent of the participants, aimed to delve deeper into the perspectives of various stakeholders regarding lapses in professional behaviour and their underlying causes, providing contextual meaning [ 29 ]. Document analysis inform the design of the interview schedule. The study was approved by the institutional review committee of Islamic International Medical College (Ref No Riphah/IIMC/IRC/22/2003; approval date: 27/01/2022).
Participants
The study population consisted of three groups.
- Patients and family
- Consultants
The recruitment of study participants employed purposive sampling, aiming to select individuals or groups highly knowledgeable or experienced in the phenomenon under investigation. Criteria included availability, willingness to participate, and the ability to articulate experiences and opinions effectively [ 30 ]. Participants were chosen from two public sector hospitals in Rawalpindi, Pakistan, comprising stable patients and family members with a minimum one-week hospital stay, residents with over six months of training in the Obs & Gynae department, and consultants engaged in residential calls alongside residents. To ensure the comfort and security of female patients during interviews, both the patient and her husband were included in the first group. Exclusions included patients with less than one-week hospital stay, those deemed unstable or unwilling to engage, newly inducted residents with less than six months of training, and senior medical officers not involved in residential calls. A total of 33 semi-structured interviews were conducted, 11 per group, to explore factors contributing to lapses in professional behaviour. Saturation was achieved by the 10th interview, with one additional interview conducted for confirmation.
Data collection
The data collection was done in a structured manner in two phases.
Phase 1: (The complaints data and document analysis)
In phase 1, complaints uploaded to the PCP portal were examined to address the first objective of this study. Access was granted to a nominated Deputy Medical Superintendent (DMS), who regularly logged in to the Citizen Portal website to review complaints. Specific complaints against residents involve prompt notification of the focal persons in the concerned department, who immediately addressed the issue by investigating the resident and their consultant. Following fact-gathering, complainants were invited for scheduled meetings to evaluate allegations and attempt resolution; unresolved complaints were escalated to higher authorities.
This study's initial step involved confirming the number of complaints against Gynae residents regarding their behaviour. Formal permission was obtained to access all complaints, facilitating the review to determine complaint frequency and comprehend complainants' messages for administrative authorities. Complaint phrases were consolidated into themes, supplemented by additional themes identified in the literature, laying the groundwork for designing a semi-structured interview questionnaire. Complaints lodged by patients and families were documented in Table 1 , highlighting lapses in professional behaviour as a primary concern.
Phase 2: (Interview data)
Interview structure.
In the second phase of data collection, in-depth interviews were conducted for two primary objectives. Firstly, to reconfirm the nature of complaints against Gynae residents, and secondly, to delve deeper into the underlying issues from three distinct perspectives.
Semi-structured one-to-one interviews were chosen as the research instrument due to the sensitive nature of the topic. Three separate interview guides were developed for patients and their families, as well as residents and consultants, following the structure of the AMEE guide 87 [ 31 ].
Special attention was paid to ensuring that the language used in the interview guides was clear and understandable. The guide for patients was prepared in Urdu, while those for consultants and residents were in English. All interviews were conducted in Urdu to accommodate the participants' comfort in expressing their views and were later translated as needed.
Expert validation and pilot testing
The questionnaire used in the interview guide underwent expert validation by four Medical Educationists, who possessed a minimum of 5 years of experience. This validation aimed to assess the clarity and relevance of the questionnaire items in relation to the construct being measured. Feedback provided by the experts led to modifications in some items and adjustments in their sequence.
Following this, pilot testing was conducted, involving one participant from each stakeholder group. The results of the pilot interviews prompted further refinements in the interview guides and probes.
The interview guide consisted of two parts : the first part focused on gathering demographic information, while the second part addressed the study objectives. The demographic section collected details such as age, education, profession, duration of marriage, and family structure. Patients and their families were asked seven questions, while residents and consultants were presented with ten questions, aiming to capture information relevant to the research objectives.
Through this investigation, not only were the specific instances of lapses in professional behaviour among residents examined, but also the broader spectrum of issues that patients raised in their complaints.
Bias control
Considering the sensitivity of the study topic and the senior position of the researcher within the organizational hierarchy, third-party researchers were engaged to conduct the interviews. Each of the three stakeholder groups was interviewed separately. These face-to-face interviews were conducted following rigorous protocols to ensure accuracy and reliability. To mitigate social desirability bias [ 32 ], which could skew responses, the interviews were conducted by a separate team of psychologists who were not affiliated with the organization being studied. This team comprised three members, with each member assigned to interview one of the stakeholder groups, allowing them to develop a better rapport with respondents over time.
Logistics for the interviews were managed by a liaison person from the hospital, ensuring smooth coordination. Participants were provided with information sheets detailing the study aims, interview process, and assurances of data confidentiality and anonymity. The interviews were conducted in a designated space within the hospital premises and began after obtaining written informed consent from each participant. Audio recordings of the interviews were made, with an average duration of 45 min per session.
Challenges encountered during the interviews were addressed through daily online meetings, allowing the interviewers to discuss and overcome any issues faced. Patients and their families initially exhibited reluctance to participate, but counseling and assurances of confidentiality helped alleviate their concerns. For residents, anonymity was assured by assigning specific IDs and group codes to the transcribed interviews.
Each interview was transcribed verbatim and provided to the main researcher for analysis. Similar sets of questions were posed to all three stakeholder groups, aiming to elicit their perspectives on the factors influencing lapses in professional behaviour.
Phase 3: (Data analysis—theme extractions)
In phase 3, the framework method of thematic analysis was employed, known for its structured approach facilitating systematic comparison of data across cases [ 33 ]. This method involves several steps, as depicted in Fig. 2 .

Steps of framework method of thematic analysis
Firstly, the interview data was transcribed (Step 1), followed by familiarization with the transcriptions (Step 2). Initial codes were then generated to capture key concepts and ideas (Step 3), which were subsequently organized into themes, which aligned with the themes identified in the literature (Step 4). Additionally, new themes emerged during this process, enriching the analysis.
A working analytical framework was developed based on these themes (Step 5), and the final step involved interpreting the data within this framework to derive meaningful insights.
Quality and transparency
The study's expenses, which involved hiring third-party researchers, were solely supported by personal finances, without any contribution from public funds. Each researcher dedicated six days to conduct interviews with a total of 33 participants.
To ensure the quality of this study, several triangulation strategies were employed [ 34 ]. Credibility was enhanced through data triangulation by gathering information from three different stakeholder groups. Investigator triangulation involved the participation of multiple researchers, while method triangulation utilized both document analysis and semi-structured interviews.
To establish trustworthiness , transcripts were reviewed by additional researchers, and consultations were held with peers, study supervisors, and co-supervisors throughout the data processing stages. Thick descriptions were provided to elucidate behaviours, experiences, and contextual factors, increasing the study's transferability while acknowledging potential contextual differences.
The study's methodology was transparent, with each research step meticulously described from inception to reporting, ensuring dependability . Detailed records were maintained throughout the study, contributing to the transparency and reliability of the findings.
Team reflexivity
Semi-structured interview guide prepared by HN, main researcher and Gynaecologist by profession. Reviewed by RY, who is Dean of medical education department. Interviews were conducted and transcribed by US, AT and BM who are psychologists. Thematic analysis done by HN (Gynaecologist) and AG (who is also psychologist). Results were reviewed by LE (medical educationist) and FS (PhD and trained in qualitative research). The reflexivity was ensured by critical self-reflection about oneself as researcher and making the position of the researcher and the participants clear. The methodology explained in detail.
The results are described in 2 parts . The 1st part is the complaint data from document analysis of complaints on Pakistan Citizen Portal (PCP). The 2nd part explains the findings from the interview data sets.
Part 1-Complaint data
Participant characteristics for document analysis.
All the complaints are anonymised and can't be tracked back—no demographic data available which lead us to re-verification of these complaints.
The literature shows that complaints provide an opportunity to understand the problems and the ways these can be resolved [ 27 ]. In PCP document, the range of complaints were diverse, 26% ( n = 10/38) were against resident’s professional behaviour which is the core investigation of this study. The rest were related to lack of facilities, infrastructure, and lack of facilities for attendants and huge workload. (Table 1 ).
Part 2- Interview data
Participants characteristics for the interviews.
The following Table 2 shows the demographic of all 3 stakeholders.
Reinforcing evaluation of the identified themes in PCP Document
The first question of interview was asked to re confirm the identified themes in PCP document. This part of the investigation provides a wider perspective of all three stakeholders related to the frequently observed/faced complaints (Table 3 ). Interestingly, the poor verbal communication and behaviour has been listed at the top with the highest value which reinforces the importance of this study. Other issues highlighted were lack of attention and insufficient communication by doctor and the complaints related to labour room. Few of the complaints were against paramedical and lower staff (Table 4 ).
Complaints other than lapses of professional behaviour includes prolonged waiting time, poor infrastructure and limited resources. (Table 4 ).
The interviews provided the researcher with rich insights into the factors and associated reasons for lapses in professional behaviour. Detailed findings are presented in the form of extracted themes and sub-themes for each stakeholder along with associated reasons.
Grouped classification of themes
The analysis was initiated by employing thematic analysis framework, as described in section of data analysis to examine data from three distinct stakeholder groups. Just to clarify, in this context, the term "themes" refers to the factors that each stakeholder perceived as potential contributors to professional lapses. Total; 15 themes extracted on analysis of data from 3 stakeholders (Fig. 3 ).

Total themes, subthemes and codes extracted on analysis of data from 3 stakeholders
The identified themes and sub-themes from the perspectives of the three stakeholders revealed some commonalities. There are a total of six overlapping themes (these are the themes with common consensus and similar perspective). These are discussed in detail later in this section and presented in (Fig. 4 ), indicating the stakeholders with whom these themes overlap. These overlapping themes help in shedding the light on the issue from 3 different angels. A graphical representation of the overlapping themes is depicted as a mesh in Fig. 5 .

Six overlapping themes from 3 stakeholders
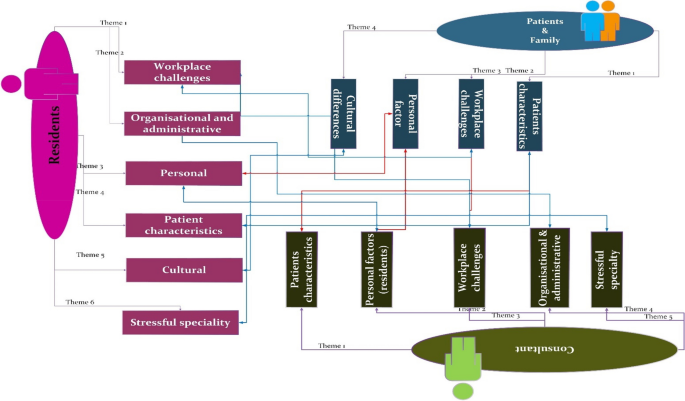
Mesh of overlapping themes (grouped classification of common themes)
In this section, we delve into the six overlapping themes, exploring the analysis results by comparing the perspectives of the three stakeholders. This comprehensive approach provides insights into each theme from various angles, shedding light on the factors influencing lapses in professional behaviour among residents. Additionally, notable quotes are incorporated to offer a vivid and relatable depiction of these findings, enhancing understanding and authenticity.
Theme 1: Personal
The first overlapping theme, depicted in Fig. 6 , illustrates the sub-themes and perspectives of stakeholders regarding this common theme. It showcases stakeholders' viewpoints on potential issues contributing to lapses, closely linked with their ‘personal needs and concerns’. These encompass family concerns, caring responsibilities, individual personality traits, basic human needs, quality of life considerations, competency levels, and overall well-being.

Presenting the reasons associated with the common theme ‘Personal’
For majority residents, balancing caring responsibilities for young children without sufficient family support poses a significant challenge, adding to the stress of professional obligations. Additionally, residents experience frustration and disappointment when they are unable to meet their child's or their own health-related needs adequately.
[Resident] "Family support is very big factor. For example, there is a female doctor and she has children, so if there is a problem at home, it obviously affects the doctor."ID_03
The residents interviewed expressed concerns about their heavy workload, which has adverse effects on their emotional and physical well-being. This indicates the importance for hospital management and administration to devise strategies to address the specific needs of residents and provide them with adequate support for their unavoidable personal responsibilities.
[Resident] “We have mother residents who have to breastfeed their babies and sometime they did not even get time to pump milk for their babies” ID_01
[Resident] “As a Gynae resident we cannot spend proper time with our family. We have 30 to 32 hours so whatever time we have in our house we have to sleep at that time. ID_09
Personal factors such as childcare and household responsibilities have also been emphasised by both patients and consultants as potential triggers for behavioural issues.
[Patient & Attendant] “doc is also human she has to perform all her professional duties along with home responsibilities of taking care of kids and home.” ID_10
[Consultant] "Some of our doctors are very good, counsel the patient properly, talk comfortably and some doctors are in a bad mood in the morning, they may have their own problems that affect them, so they get tired."ID_1.
Many females in Gynae face challenges in securing support from their in-laws and family to manage their households. When in-laws fail to understand the demands of the profession or are not present in the same city, and hiring domestic help is difficult and costly, these stressors can significantly affect their performance and attitude towards their professional responsibilities.
[C] “Doctors mostly have their own tension going on. They may already be suffering from some tension that is affecting them”ID_3
Well-being serves as a vital metric in fostering a positive workplace environment. In the context of this study, we focus on the well-being of residents tasked with serving in the healthcare sector, particularly in the demanding field of Gynae. Recognized as a central aspect across various themes within this study, well-being emerges as a shared concern among all stakeholders, potentially contributing to lapses in professional behaviour.
[C] “if the resident is not feeling well that will also influence her behaviour with patients “ID_5”
The interview findings have outlined several influential factors impacting residents' well-being, with the most prominent being the long working hours, stringent duty schedules, and sacrifices made regarding basic human needs.
[R] There should be any stress relieving activities or vacations for us to spend time with our family. ID_07
[P] Residents are human and they are working a lot so they can get tired by working so much.” ID_09
[R] You cannot take off because it is a big issue and because of that you cannot have mental break from this entire situation. ID_0
There is a pressing need for institutional-level interventions to address various associated factors and support the well-being of residents. This will create a more conducive working environment that positively influences professional behaviour.
[R] “"it’s on the institutional level, patient load and tough routine. We are here for almost thirty six hour; we do not get short breaks for lunch and sleep. We are not machines we are humans, even then we try to give our 100%" ID_04.
Competency is pivotal in managing workload and meeting patients' needs. Notably, patients have never complained about treatment, reflecting positively on professional competency of residents. However, deficiencies in counseling skills, multitasking, and handling conflicts are observed. Consultants discern differences in attitude between senior and junior residents, highlighting the need for tailored training to equip residents for diverse situations.
[Consultant] “Experienced resident will stay cool and calm, and she knows that how to deal with things or how to answer about issues”ID_5
The management should implement a mentoring scheme to train junior members, offering them opportunities to shadow their seniors. Analysis of interview data strongly suggests that the interpersonal theme is closely linked with competency, the demands of the Gynae specialty, and administrative/management factors.
Theme 2: Workplace challenges
This theme delves into workplace challenges as perceived by stakeholders, shedding light on potential factors contributing to lapses in professional behaviour, as shown in Fig. 7 . Sub-themes include interpersonal dynamics, environmental factors, managing multiple responsibilities, workload issues, the role of senior staff, challenges with untrained paramedical personnel, labor room dynamics, basic human needs, and insufficient support from colleagues and superiors.
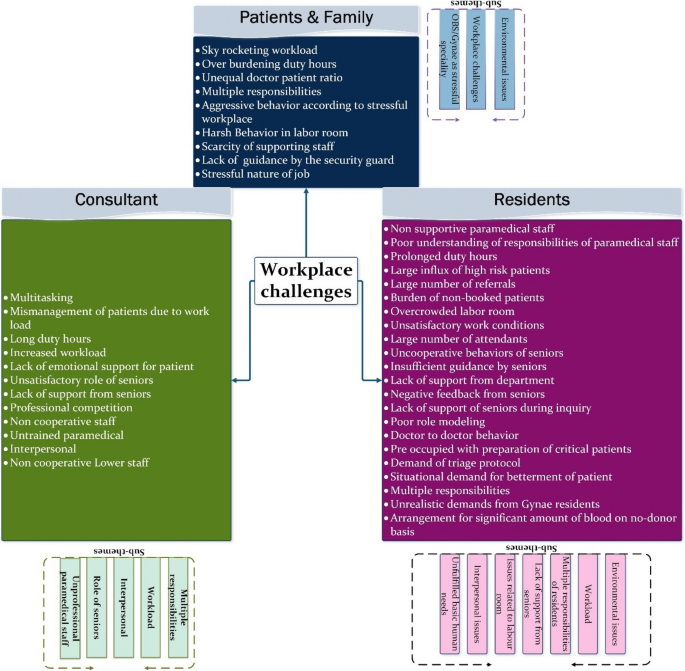
Presenting ‘Workplace challenges’ as a common theme across stakeholders
Interpersonal challenges are frequently highlighted by both residents and consultants. Novice residents struggle with managing conflicts with patients, leading to a tense and stressful environment for all parties involved. This situation is compounded when there is inadequate support from fellow doctors and paramedical staff members.
[Consultant] “Residents and nursing staff did not have good interpersonal relationships and if residents not have nice behaviour with nursing staff they will not get that support from them “ID_6.
Furthermore, the absence of respectful collaboration from other related departments exacerbates the stress and disappointment experienced by residents, ultimately leading to personal frustration that can influence behavioural lapses.
[Resident] In Gynae department our personalities get suppress that even other departments do not respect us. ID_09
Consultants have stressed the importance of training for paramedical staff to offer timely and supportive assistance. They have highlighted the need for paramedical staff to be attentive and responsive, especially during critical emergency situations. Consultants noted that doctors often have to repeatedly request assistance from paramedical staff and may need to raise their voices to convey the urgency of following instructions during critical situations.
[C] “If your paramedical staff is not cooperative then obviously you will get stressed (the doctor not only has to deliver the baby but also send the attendants outside and shout for aya to help her) ID_4.
The physical environment and its related factors significantly impact the satisfaction levels of staff members. Analysis of the data has identified the "environmental factor" as a common theme from both resident and patient/family interviews, as depicted in Fig. 7 . The findings indicate that patients and their attendants recognize the workload of doctors and acknowledge that excessive burden is a primary cause of stress for residents, ultimately affecting their behaviour and well-being.
[P] Duty hours should be reduced and they should get some time for rest and food. There is lot of pressure on them. They start their round at 9am and finish at 2pm because there are 3, 3 patients on each bed. ID_5.
[P] If there are 2 patients on one bed than this will increase anxiety of doc as well. Too many patients are talking simultaneously so this will make her angry. ID_07
[P] On operation day doc is more stressed because she has to manage all the patients and she is alone and feels pressured.” ID_02
The patients have also expressed concern that working hours should be reduced, or the management should consider increasing human resources to cope with the workload. This highlights the interconnection of this theme with other relevant themes.
[P] We should increase the number of doc. The doctor only gets angry when she gets tired and loses her patience level.” ID_07
[P] Patients are coming to doc after 2pm and then they expect their doc to make file but they don’t understand that doc have many other responsibilities.” ID_02
Similarly, from the residents' perspective, it is evident that they are struggling with their workload, and inappropriate physical surroundings further exacerbate their frustrations. Additionally, residents have expressed concerns about issues related to management and counseling of attendants, which adds to their responsibilities. This aligns with the theme discussing various characteristics of attendants, considered significant in creating a conflicting environment.
[R] Unsatisfactory work conditions and patient doctor ratio are among few highlighted by the residents. This can greatly influence the working conditions in support of appropriate environmental factors. A large number of attendants can cause additional management and communication burden for residents to deal with. ID_6.
[R] “Every patient is accompanied by 2 to 3 attendants and you are dealing with patient so every attendant individually comes to us and ask you about the information”. ID_09
Workload emerged as a prevalent theme in both residents' and consultants' data as shown in Fig. 7 . It is consistently highlighted as a significant issue by both groups in their interviews. Patients and their attendants also expressed concerns about the high workload on doctors. Excessive workload is considered one of the most influential factors contributing to observed lapses in professional behaviour.
[R] “doctors get exhaust because of long 36 h duty, at times we did not eat anything or we could not have proper sleep” ID_01
[R] We are not allowed to refuse any referral even if we do they come back again with the reference of DMS. ID_02 "The biggest problem in this is that we are working in the government sector and there is a human capacity of a doctor, if a doctor has a capacity to check of 5 to 6 patients, but in the government sector, a doctor has to check 20 patients. So the doctor feels overburdened." ID_03.
[R] We have one doctor who is deal 130 to 140 patients from 8 to 2 AM. ID_09 “in other countries they have better working conditions and increase number of doctors because of that they have less work load” ID_09.
The findings discussed above highlight a strong association between the environmental factor and well-being, as well as unmet human needs.
There are labor room-related issues highlighted by residents, which can escalate misunderstandings for patients' attendants. Cultural norms often dictate that only female family members accompany the patient during the delivery process. Men are typically not permitted to enter the labor room, especially when female attendants are present or when maintaining the privacy of other patients is a concern. However, this practice can be perceived negatively by patients' male attendants, although it may not reflect the true intent in all cases.
[R] Patients want to have their husbands with them in labour room and in our culture it is not possible. ID_05
[R] “Not allowing male attendants in labor make them think that their patient is in danger”. ID_07
The two overlapping themes identified from residents and consultant data are 'Lack of support from seniors' and 'Role of seniors' , respectively as shown in Fig. 7 . Junior residents have raised concerns regarding the lack of support from senior members. Similarly, consultants have echoed these sentiments, suggesting that seniors are not fulfilling their roles in providing adequate support to junior residents.
[R] " Seniors also pressurize us; they say that you are not examining patients properly or too slowly, because of their responsibility of finishing OPD in given time”. ID_06
Both residents and consultants have emphasized that residents are burdened with multiple tasks , some of which consume significant additional time as shown in Fig. 7 . For instance, residents often find themselves tasked with arranging blood for seriously ill patients by making excessive calls to relevant blood banks and maintaining patient records. Consequently, they struggle to allocate sufficient time to meet every patient's expectations.
[R] “Residents are always concerned about the patients and they tried to arrange things as soon as they can”. ID_09
[C] “doctor has to be a multitasker, for example if we are short on medicine or blood we send our PGT(post graduate trainee) to blood bank in the middle of the night”ID_1
The findings indicate a lack of support from management in sharing additional responsibilities, while simultaneously expecting doctors to multitask . This theme is closely linked to the 'workload' and 'Demand of Gynae specialty' , contributing to a stressful and demanding environment for residents. Another recurring theme identified from resident and consultant data is the 'Unfulfilled basic human needs' . Patients and their attendants have also noted the exhausting routines of residents, who often lack time for relaxation or sleep.
[P] “They are human and they are working a lot so they can get tired by working so much” ID_9
[P] “These doctors are so busy with patients that they don’t have time for self” ID_4
Residents have highlighted long duty hours as a significant factor, leaving them with insufficient time and energy to spend quality time with their families. These extended shifts often involve an excessive workload of patients, leading residents to compromise even on their meal times.
[R] “Because of long duty hours and huge number of patients we do not have time to get proper sleep” ID_01
[R] As a Gynae resident we cannot spend proper time with our family we have 30 to 32 h so whatever time we have in our house we have to sleep at that time. ID_09
Theme 3: Stressful specialty
This theme, prominently observed in the data collected from both residents and consultants as depicted in Fig. 8 , encompasses the sub-themes of 'demand of Gynae specialty', 'nature of profession', and 'unpredictable outcomes related to this profession'. Notably, patients' data only minimally reflects this theme, with only one in 11 patients commenting on the stressful nature of the profession.
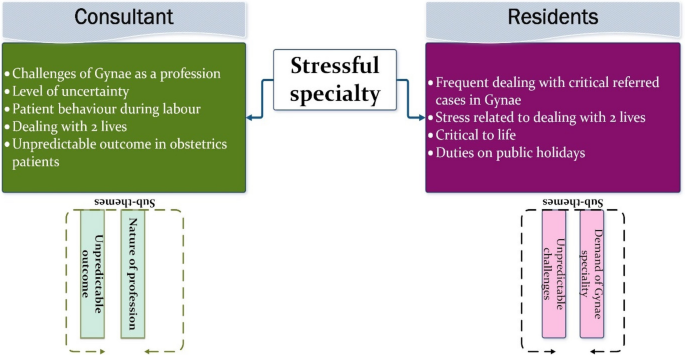
Presenting ‘Stressful specialty’ as a common theme from two stakeholders
Both consultants and residents commonly perceive Gynae as the most stressful domain within the healthcare system, largely due to the simultaneous involvement in the lives of more than one individual. Consequently, this stress may manifest in various ways, potentially leading to lapses in professional behaviour or misinterpretations thereof. The data highlights several specific reasons inherent to the Gynae field, contributing to an overwhelming environment for residents, which can at times be challenging to navigate smoothly.
The unpredictable outcomes associated with Gynae further compound its demanding and challenging nature for those serving within this discipline.
[C] “We have to take care of two lives which is an additional stress for us “ID_6
[R] Residents have high level of tension when patients are non-cooperative, because we have to bear stress of both mother and fetus. ID_07
The interviewed residents have expressed the considerable stress they experience while working in a Gynae department with limited facilities. They highlighted the extra efforts required to arrange supporting resources, such as blood for seriously ill patients. Additionally, residents face the added stress of justifying their efforts and treatments in the unfortunate event of a patient casualty.
[R] “We are aware of our facilities and we have this pressure that even if we examine these excessive number of patients it would be difficult for us to manage them with compromised services, and later we have to justify if the patient expires”. ID_02.
[R] “In our department, our senior PGT herself rushes for the blood of serious patients”. ID_09
The field of Gynae presents unique challenges that are distinct from other areas of the healthcare system. The labor room environment, in particular, poses significant challenges for residents, especially when decisions and treatments are critical to more than one life. Dealing with patients with diverse needs requires patience and experience, as their behaviour can vary greatly during labor, depending on factors such as physical capability, pain tolerance, and cooperation.
Unfavorable workplace conditions can exacerbate the already demanding nature of the work, increasing the likelihood of professional lapses. However, organizational and management interventions can help mitigate these challenges. Improving workplace conditions, adjusting working hours, prioritizing resident well-being, and providing appropriate training are measures that can assist residents in handling such situations more effectively.
Multitasking, another significant challenge, should be minimized by involving support staff and experts at the right time. Residents should not bear sole responsibility for negative outcomes; trained staff should be available to assist them through challenging situations.
Overall, the discussion highlights the interconnectedness of various themes and sub-themes, highlighting the importance of organizational and management decisions in addressing workplace challenges and promoting resident well-being to reduce the occurrence of professional lapses.
Theme 4: Cultural
This theme is consistently identified across all three stakeholders, although residents and patients & families place greater emphasis on associated concerns, as depicted in Fig. 9 . Notably, the top concerns contributing to lapses in professional behaviour and poor understanding of cultural concerns and communication are highlighted.

Presenting sub-themes for ‘Cultural differences’ as a common theme across stakeholders’ data
Cultural differences can create a discriminatory environment across various aspects, while a lack of understanding of diverse needs can lead to significant misunderstandings between patients and residents. Language barriers, in particular, emerge as a critical cultural factor identified by all stakeholders. Communicating with individuals with different language needs, especially when they adhere to distinctive cultural norms, poses considerable challenges. Consultants also raised this issue during their interviews, although it is merged with 'Patients' characteristics' as a matter of importance.
[C] “Language barrier is a big problem. We also have Pathan (Pakhtoon) population who do not understand”ID-1
[R] “Most of the time Pakhtoon community is very difficult to deal. They do not take your opinion even if they are high risk patients, they force for normal delivery”ID_02
[P] “Doctor in labour room are harsh. they move Pathan attendant out of the labour room and say that we will call you when needed but they don’t call anyone anytime” ID_08
In developed countries, the healthcare system is well-equipped with chaperones who assist healthcare professionals in communicating important information to patients and their attendants. However, in Pakistan, such a system is not in place, making it difficult to expect residents to understand a variety of regional languages. This lack of linguistic diversity among residents can exacerbate feelings of being 'left out' among many patients and their attendants, sometimes leading to arguments with residents.
[R] “We have language barrier with Pakhtoon patients and they are mostly aggressive and thought that we do not understand their issues”. 1D_01
[P] “Nobody allow us in ward if we have to discuss something with doc. Our patient is not educated; she can’t explain her concern in Urdu so how will the treatment proceed.” ID_4
[R] “Most of the Pakhtoon community thought that we are biased and most of the time when they are going back they often say that “we are Pathan that’s why you are not paying attention to us” ID_07.
Furthermore, the language barrier or poor understanding of cultural and regional norms can create a biased environment or negatively influence the thoughts of minorities. This theme is reasonably associated with residents' characteristics and management factors. We believe that the administration should carefully address these important issues and consider providing chaperones to assist residents and patients.
Another challenge for residents arises when dealing with patients whose rigid cultural beliefs influence their mindset. Sometimes, residents must follow recommended treatments to save patients' lives, but attendants may challenge these treatments, leading to conflicting arguments.
Residents also encounter situations where they must take actions to ensure privacy for other patients, especially when multiple patients share a room. However, these actions can be misinterpreted and biased against certain communities. While this issue is partly related to patients' and families' understanding of privacy concerns, it is also the responsibility of the administration and supporting staff to educate them about these sensitive aspects. This burden should not solely fall on residents.
Theme 5: Patients’ characteristics
This theme stands out as one of the most discussed, offering rich information about the specific characteristics of patients and their attendants seeking Gynae treatment, as depicted in Fig. 10 . It delves into associated factors attributed to the educational, economic, and cultural backgrounds of patients and their attendants, which significantly influence their behaviour and expectations. Additionally, it addresses contextual causes that may lead to lapses in professional behaviour.

Presenting sub-themes for ‘Patient characteristics’ as a common theme across stakeholders’ data
Pakistan, a developing country, with a literacy rate of 50% and a current birth rate of 3.6 per patient according to PDH 2018 survey, it is a common cultural practice to send senior female members to assist pregnant mothers. This practice is rooted in the belief that experienced females can provide valuable support to new mothers, which is often true. However, it's important not to overlook the fact that patients' attendants are typically the ones who maintain constant contact with residents and serve as the primary point of contact for treatment and critical decisions.
In order to ensure smooth provision of care, it is essential for attendants to cooperate with residents and be capable of interpreting important decisions and communicating needs from both ends. Patients and attendants with lower educational backgrounds often find it challenging to interpret complex information or navigate to the correct physical location when seeking assistance.
[R] “In government sectors literacy rate of patients are low which creates issue” ID_05
Lack of understanding about the sensitivity of the issue and unrealistic expectations from residents are frequent reasons that initiate arguments from patients and their attendants. For instance, they may argue if a resident is giving attention to a patient they don't consider to be serious. This behaviour is often perceived as neglectful by patients and attendants, though it may not accurately reflect the resident's intentions.
[R] “suppose we have emergency and I am checking that patient first so all other patients will start shouting, they will not understand the emergency, being a doctor we know that we have to see the emergency patients first but every patient thinks that their problem is the biggest one” ID_01.
In some cases, the unprofessional behaviour exhibited by residents may be a response to disrespectful acts from patients or attendants . Residents have reported instances of disrespect from patients and attendants who fail to grasp the sensitivity of certain treatments and the necessary preliminary measures before administering them. Additionally, the time taken for preoperative preparations may be misinterpreted as a 'delay' in treatment by patients and their attendants.
[R] "The patient complains that the doctor told us that we will have an operation, why don't you operate, if something happens to our child, you will be responsible, patient says" main tumain dekh lounga"( I will see you). They threaten us and misbehave with us".ID_06.
Residents frequently encounter unrealistic expectations from patients and their families regarding infrastructure and facilities, despite these not being within the residents' purview. Patients and their families may expect residents to provide beds and medication, leading to disappointment when residents are unable to fulfill these needs. Arguments where residents are unjustly blamed are unlikely to be accepted by residents and can escalate into conflicts. However, residents and supporting staff should undergo training to effectively communicate any limitations to patients in a more acceptable and understandable manner.
[R] “"When a patient enters the hospital. She doesn't get a bed and medicine. So it is no longer the doctor's responsibility, but because the doctor is in front of them, they feel that the doctor is responsible for these things" ID_06.
It is crucial for residents to recognize the various needs and support required by patients and their families, irrespective of their educational or economic backgrounds. This necessitates appropriate assistance provided to residents from various aspects such as staff, administration, and management support.
Trust is a fundamental element of the patient-doctor relationship, yet it is another concern highlighted by interviewed residents. Patients and their attendants may not fully trust the treatment provided by doctors, possibly due to limited exposure to the healthcare system in rural areas, where self-trained people (called Dai) are preferred over experienced doctors.
[R]”Even if doctor is thinking positive about the patient, patients have this trust issue that might be this doctor will not do my operation properly, or she will make my delivery difficult.” ID_07.
[R] “Patients with low literacy rate go to Dai. ID_09 Daiyon ka jo counselling level ha wo itna acha hota ha k patient kharab kr k bhi bhai jdain to attendant kuch bhi nahi kahe gain unki nazar ma Dai is very good”(counseling skills of Dai are so convincing that even if the patient encountered the complication they thought that Dai is competent). ID_09.
Patients seeking care at public hospitals are often economically deprived individuals, burdened with family responsibilities. Many rely on daily earnings, and prolonged absence from work can lead to financial strain. Additionally, they may have caregiving responsibilities that necessitate a swift return home, prompting them to insist on expedited treatment. While these unavoidable circumstances add stress to the situation, appropriate counseling can help patients understand the importance of receiving necessary treatment and alleviate the impact of missing appointments or procedures.
[R] “Patients in Gynae wards are in hurry because they have their family responsibilities and they have small kids at home” ID_07
Both residents and consultants have shared their experiences of navigating conflicting environments , which can sometimes lead residents to adopt a harsh tone when communicating with patients and attendants. For instance, in urgent situations requiring aggressive treatment critical to a patient's life, sudden behavioural changes may occur to emphasize the importance of the treatment. This behaviour has a strong link to the attendants' level of understanding and literacy regarding the healthcare system, particularly in the context of Gynae treatment where 2 or more lives may be at risk simultaneously.
[R] “Residents become harsh when attendants or patients do not understand the situation, for example they do not arrange the blood so we have to tell them harshly about it” ID_02
Some senior consultants have provided visionary statements, noting a cultural shift in how the public interacts with medical practitioners. Consequently, there has been a recent increase in aggressive behaviour observed from patients and attendants.
[C] “In past patients and attendants were not so violent but now a days they are violent “ID_6
Privacy is a fundamental concern for individuals worldwide, and developed countries have stringent policies and regulations in place to safeguard individual rights. Any breach of these rights can understandably trigger anxiety and concern. Therefore, it is crucial to communicate with patients and attendants about actions that may lead to security breaches involving residents, in order to prevent unpleasant situations.
[C] “Now a days people used to make our videos “ID_6 “people were aware in past as well but now they have got easy access to the portal for complaints”ID_6
This theme is closely linked with the understanding of patients and attendants regarding the healthcare environment, rules, regulations, and treatment specifics that can potentially trigger professional behavioural issues. Management or administration can play a crucial role in providing upfront information to patients and attendants regarding important regulations related to the Gynae specialty.
Theme 6: Organisational & administrative
Organizational and administrative authorities are integral in developing effective policies to ensure the smooth operation of healthcare systems. In the context of this study, we believe that the hospital administration can significantly contribute to mitigating the issues discussed thus far. They can take the lead in informing policymakers to design policies relevant to the sensitivity of this field.
This theme presents the perspectives of both residents and consultants on organizational and administrative issues that can lead to conflicts and lapses in professional behaviour, as depicted in Fig. 11 . Sub-themes include the lack of support from administration and management issues.

Presenting sub-themes for ‘Organisational& administrative’ as a common theme across stakeholders’data
An important point to note is the understanding and expectations of patients regarding the provision of facilities and resources necessary for their treatment. During interviews, all patients and families expressed a lack of clarity regarding the roles of hospital administration and doctors.
Both consultants and residents have highlighted challenges including lack of support from administration, limited resources, and excessive workload . A high influx of patients can significantly impact working conditions and hinder the ability to provide maximum satisfaction to all patients.
[C] “We do not have anybody who controls the influx of patients outside the rooms or OPD “ID_6
[C] “Also there is the factor that the workload is very high, already you have many patients and doctors are less, sometimes the government does not give you enough resources to facilitate the patients.”ID_3.
[R] “We have two operation theaters and over there we have one anesthesiologist” ID_02
Administrative support is crucial in ensuring a secure and pleasant working environment for residents. One concern raised by consultants is the management of patient flow within the hospital. A system should be implemented to queue patients and prioritize them based on their order of arrival for check-ups.
[C] “doctor should be given security, they should be given support, one by one the patient should be sent to the doctor so that the resident also gets time to see the patient”ID_3
The doctor-to-patient ratio varies as per the workload and patient intake. A heavy workload can significantly impact the quality of patient care provided. Most importantly, it can adversely affect the well-being of residents, who are already vulnerable due to the high number of patients they must manage.
[R] “we have huge number of patients and ratio of doctors are much less” ID_01
[R] “we only have one guard for security and we have huge number of patients and every patient have 2 attendants along with her so there is almost 150 people in one room so obviously I will get aggressive”. ID_01.
All of the issues discussed above are likely to influence the professional behaviour of residents making them susceptible to react aggressively which is not a pleasant experience for patients and their family.
The findings from interviews involving three main stakeholders, shed light on potential triggers for unprofessional behaviour discussed in previous sections. The synthesis in the discussion session highlights the key insights gleaned from the interviews, emphasizing the importance of understanding and addressing the challenges faced by residents in their professional journey.
“Being a resident is not a crime” (ID_C7).
“Residency is just like War in battlefield” (ID_C7).
The quotes from the interviewed consultant underscore the struggles and efforts inherent in the professional life of residents, emphasizing the pivotal role of residency as a preparation for frontline healthcare responsibilities. As residents navigate hierarchical structures within hospitals, they confront diverse challenges and ethical dilemmas, often without adequate training or support. These circumstances can negatively impact their professional behaviour, contributing to a conflicting healthcare environment. It is imperative to comprehensively explore the realities faced by residents to understand and address inappropriate behaviour effectively.
Demographic inference
The demographic observations from the interviewed stakeholders provide valuable insights into personal issues and patient characteristics that may influence lapses in professional behaviour. For instance, all interviewed patients are housewives with a Matriculation education level, and 45% of them reside in a nuclear family system despite low socioeconomic backgrounds, contrary to societal norms. Consultants, despite higher education and financial independence, are bound to stay in joint families, likely due to the need for familial support in caring for their children amidst demanding work hours. Similarly, a majority of residents reside in a nuclear family system, possibly driven by being unmarried or already established in such living arrangements. These findings highlight a preference for joint family living among Gynae residents and consultants, largely driven by the need for support in childcare due to demanding and long work schedules. However, such living arrangements may also introduce additional stressors related to cultural expectations from family members, as discussed under the 'Personal factors' theme, where stakeholders reflected on their experiences and challenges regarding professional responsibilities and expectations from in-laws.
Role of competency and communication skills
The interview findings regarding personal factors also examined communication skills and patient expectations. Our study revealed that a lack of communication skills when dealing with challenging situations often led to conflicts. Therefore, we recommend enhancing competency in this area to avoid such situations. This finding aligns with the research by Alipour et al., which also underscores the importance of good communication skills in managing challenging patients [ 35 ].
Furthermore, our study found that patients expect physicians to prioritize their needs, respond respectfully to their inquiries and concerns, and uphold their dignity, particularly during sensitive procedures such as those in the delivery room. Patients also value empathy towards their health condition. Similar sentiments were echoed in patient complaints (PCPs), where lack of care or attention from doctors was highlighted. These findings are consistent with prior research emphasizing the importance of communication in maintaining good professional behaviour, with patients specifically emphasizing the significance of being listened to attentively and having medical information explained in understandable terms [ 17 ].
Indeed, previous studies have highlighted the impact of inappropriate practices on patients' satisfaction. For instance, practices like insufficient preparation before patient encounters and failure to provide accurate and relevant information have been associated with decreased patient satisfaction [ 36 , 37 ] Additionally, a common complaint in PCP is the lack of an appropriate number of doctors, which is closely linked to these issues. Addressing these concerns is essential for improving patient care and overall satisfaction levels within healthcare settings.
Contextual understanding and its influence
The study reveals context-specific challenges faced by residents, particularly concerning the involvement of in-laws during residency, a phenomenon unique to the cultural context of Pakistani society. Another pertinent issue is the scarcity of affordable housemaids or child-minders. Unlike many developed countries where joint family structures are less prevalent and childcare support is provided by organizations and governments, there are limited initiatives in Pakistan to offer such support. Developed countries have recognized the value of professional child-minders and after-school clubs, providing safe and reliable childcare services to working parents. Unfortunately, Pakistan lacks such reliable facilities, leaving working parents, including residents, with limited options for childcare. While there is a common perception that grandparents can provide adequate care, those without such support often experience stress and uncertainty regarding the safety and care of their children. These stressors are unavoidable for residents and can significantly impact their performance and attitude towards professional responsibilities.
Addressing these context-specific challenges is crucial for supporting residents and ensuring their well-being amidst the demands of their professional roles.
The interview data highlights residents' multitude of responsibilities , contributing to complaints about long working hours and patient burden, particularly unique to our healthcare system. Unrealistic demands placed on Gynae residents, extending beyond medical care, negatively affect their behaviour due to added burdens. Labour room issues arise from societal norms, with family members often leading to miscommunication between doctors and husbands outside the room. Public distrust in doctors and teaching hospitals, fueled by negative media portrayal, prompts family intervention and threatening behaviour in the labour room, forcing Gynae residents into defensive positions and hindering treatment decisions.
Workplace challenges and their impact
The second major complaint in the PCP document, lack of facilities, aligns well with interview data, which highlights various workplace challenges as possible causes of lapses in professional behaviour. These challenges encompass interpersonal, environmental, and workload-related factors, as well as issues with labor room conditions and support from seniors and paramedical staff.
Junior residents' difficulties in handling conflicts with patients are highlighted in our study, reflecting findings from another study in a Gyane department in Pakistan, emphasizing the need for training in interpersonal skills [ 20 ]. Additionally, our study emphasizes the negative impact of poor working conditions on residents, a finding consistent with previous research linking organizational and environmental factors to professional behaviour [ 38 ].
Excessive workload emerges as a significant factor contributing to observed lapses in professional behaviour, supported by complaints of a huge patient burden in the document analysis. Our results resonate with research from Iran, indicating that high workload and time constraints lead to declining empathy and unprofessional behaviour [ 39 ]. Moreover, a narrative review on physician behaviour underscores the role of increased workload in affecting doctor-patient communication and fostering aggressive behaviour [ 23 ]. Excessive working hours can also lead to unfulfilled basic human needs and burnout among physicians, as highlighted by stakeholders in our interviews.
Our study identifies workplace issues such as lack of staff support, leading to frustration among residents when instructions are not followed, resulting in perceived lapses in professional behaviour. Patient outbursts often stem from staff not meeting requirements, compounded by language barriers and patient illiteracy hindering communication about triage and treatment priorities. Junior residents' concerns about insufficient support from seniors underscore the importance of role modeling in professionalism, as emphasized by previous research highlighting the impact of role modeling on empathy and professional behaviour [ 38 ].
Distinctive stresses associated with this specialty
The study acknowledges existing literature linking high-pressure specialties like surgery and Obs and Gynae with violent behaviours due to unique stresses [ 14 ]. Gynae residents, consultants, and even patients and their families described the profession as inherently stressful and unpredictable. This study highlights how professional behaviour is influenced by the stress of managing the lives of both mother and baby. Additionally, factors such as a high influx of non-booked patients, complicated referrals, unrealistic patient expectations, limited resources, non-cooperative attendants, and unmet human needs contribute to the already stressful environment in our healthcare setup.
Cultural differences and their importance
In developed countries, the healthcare system provides chaperones to assist healthcare experts in communicating vital information to patients and attendants. However, in Pakistan, such a system is absent, making it difficult to expect residents to understand various regional languages like Pashtoo and Gilgiti. This language barrier can exacerbate feelings of exclusion among patients and attendants, leading to conflicts with residents. This finding underscores the complexity of professionalism as a social construct, emphasizing the need to consider context, geographic location, and culture when addressing lapses in professional behaviour [ 40 ].
Why it is important to consider patients characteristics
This study delves into the specific characteristics of patients and attendants, extracted from interviews and unique to this contextual study. Their educational, economic, and cultural backgrounds vary significantly, posing challenges for residents in their interactions. Patients typically have limited education and come from low socioeconomic backgrounds, with predetermined expectations and a sense of entitlement to care due to taxes paid. Accompanied by numerous attendants, they often hold fixed views about doctors' duties. This perception, evident in PCP complaints, contributes to conflicts with doctors, exacerbated by varying tolerance levels. Notably, literature lacks data on patients' perspectives regarding residents' professional behaviour. Remarkably, patients and families do not attribute lapses in professional behaviour to organizational/administrative issues but instead fault residents for perceived deficiencies in hospital facilities and medication availability, likely due to a lack of awareness about administrative roles—a finding specific to impoverished patients in public sector hospitals.
The patient holds a central role in the healthcare system and is a significant stakeholder whose perception of lapses in professional behaviour is explored in this study. This encompasses actions such as imposing additional financial burdens (e.g., recommending costly tests, requiring the purchase of operation accessories) and unnecessarily prolonging hospital stays. Particularly poignant is a patient's observation regarding class-based social discrimination among patients, where "the rich were preferred over the poor," highlighting disparities in access to facilities and guidance for attendants.
Role of organisational & administrative support
Organizational and administrative authorities are pivotal in providing effective hospital facilities, a theme emphasized by residents and consultants in this study. Issues such as limited infrastructure, uncooperative senior behaviour, absence of casual leaves, and inadequate salary packages relative to workload are identified as factors negatively influencing professional behaviour. This underscores the insufficient support provided by the administration, training systems, and external factors, which are perceived as more influential than personal factors. These findings align with other studies that highlight deficiencies in training hospital systems as contributing to lapses in professional conduct among residents [ 41 ]. Additionally, organizational deficits, such as inadequate facilities and poor security, along with a gap between administration and clinical departments, are identified as sources of conflicts [ 20 ]. Overall, these results support the notion that professionalism is situation-sensitive, and the training environment may contribute to the deprofessionalization of residents, as observed in literature [ 42 , 43 , 44 ].
Uniqueness and importance of this study
To the best of our knowledge, this study represents a pioneering effort in thoroughly evaluating the perspectives of patients, consultants, and residents regarding lapses in professional behaviour among Gynae residents in teaching hospitals in Pakistan. Existing literature underscores the significance of complaints in uncovering underlying issues and guiding solutions. Studies by Rogers et al. and Hoffmann et al. have highlighted the prevalence of complaints related to medical professional behaviour in various contexts [ 45 ]. Our research complements these studies by providing deeper insights from multiple perspectives. While professionalism is influenced by environmental and personal factors, literature lacks sufficient data on patients' expectations of doctors. Our study fills this gap by exploring Pakistani patients' perspectives on the factors contributing to lapses in professional behaviour among residents, thereby enriching understanding in this area. Additionally, our study integrates document analysis with interview data to provide a comprehensive analysis.
Contribution of the study
The paradigm shift in understanding professionalism lapses highlights the increasing importance of incorporating patients' perspectives. Our research offers valuable insights from key stakeholders, which can serve as a benchmark for addressing identified issues in healthcare. It emphasizes the need for training residents in professionalism, with educators leveraging the findings of patient complaints to inform their approach.
Traditionally, resident misbehaviour has been attributed to character flaws [ 46 , 47 ] but our study reframes this interpretation within the context of training systems and environments. This nuanced approach enables a deeper understanding of the phenomenon and opens avenues for incident prevention through educational and organizational interventions. While some findings may not be universally applicable, our approach to addressing trainee professional lapses holds implications for diverse educational settings.
The findings of our study disclose several perceptions as a possible influential cause of unprofessional behaviour of residents. Excessive workload, workplace challenges is the residents' most frequently mentioned contributing factors. Another interesting finding of this research is an emerging theme related to the characteristics of patients and attendants which has been attributed by both consultant and resident. These characteristics can be considered useful in understand the causes and implications of conflicting environment. Opinion from administration or higher authorities regarding issues faced by residents and patients offer insight for future work.
Implication for educational practice
This section highlights key lessons learned from the comprehensive interview datasets involving three stakeholders, accompanied by recommendations derived from the research.
Balancing professional commitments with family responsibilities is crucial, as it varies among individuals and can significantly impact professional behaviour.
Management's attention to residents' well-being is paramount, as an unsupportive working environment can negatively affect professional conduct.
Implementing a mentoring scheme for junior members, allowing them to shadow seniors, can enhance their ability to handle complex situations effectively.
Providing trained paramedical staff to assist residents can alleviate their workload, allowing them to focus on critical tasks and improve patient care.
Ensuring supportive working conditions, including physical environment and workload management, can enhance resident well-being and positively influence professional behaviour.
Recognizing the unique challenges of the Gynae specialty is essential for developing policies that support stakeholders in this field.
The specific characteristics of patients and families identified in this study underscore the need for further exploration of their beliefs, understanding, and expectations to address diverse cultural and social needs.
Addressing the specific needs of all stakeholders, including privacy, language comprehension, socio-economic factors, and personal well-being, can foster a harmonious environment and mitigate conflicts.
Strengths and methodological challenges
Major limitation rather challenge of my study was the difficulty in understanding the construct by patients and family. Although all are matriculation by education but they unable to comprehend that there are always some factors behind the some behaviour. It might be a reason of less rich data as compared to consultants and residents. Another limitation might be some element of social desirability bias in patients because we collected data from admitted patients. Although researchers were unbiased but there might be some fear that telling the truth might affect their treatment procedures or behaviour of resident in charge of their ward. Only 2 public sector hospitals were targeted which restrict the scope of the study. Moreover, almost all the participants were female except for 1 male resident (subject to availability) pose g ender-related limitation.
Implications for further research
The research on professionalism in healthcare departments in Pakistan has been limited, leaving several aspects unexplored regarding the reasons behind poor behaviour exhibited by both doctors and patients. A multicenter study involving Gynae departments across various public and private sectors in different cities of Pakistan would provide a more comprehensive understanding of the prevalence, risk factors, significance, and consequences of lapses in professional behaviour.
Future research should also consider including perspectives from paramedical staff, hospital administration, and senior consultants within the Gynae unit to gain a holistic view of the issue.
Given the limited presence of male residents in Gynae obstetrics training, reaching out to them for their perspectives and comparing them with female residents could provide valuable insights.
Additionally, further research focused on remedying the issues identified in this study would be beneficial for the medical education community in addressing professional behaviour concerns effectively.
Availability of data and materials
All datasets used and/or analysed during current study available from corresponding author on reasonable request.
Coffey S. The Cambridge international dictionary of English - Procter, P. APPLIED LINGUISTICS. 1996;17(3):383–7. https://doi.org/10.1093/applin/17.3.383 .
Barnhoorn PC, Nierkens V, Mak-van der Vossen MC, Numans ME, van Mook WN, Kramer AW. Unprofessional behaviour of GP residents and its remediation: a qualitative study among supervisors and faculty. BMC Fam Pract. 2021;22:1–1.
Article Google Scholar
Williams BW, Williams MV. Understanding and remediating lapses in professionalism: lessons from the island of last resort. Ann Thorac Surg. 2020;109(2):317–24.
Barnhoorn PC, Houtlosser M, Ottenhoff-de Jonge MW, Essers GT, Numans ME, Kramer AW. A practical framework for remediating unprofessional behaviour and for developing professionalism competencies and a professional identity. Med Teach. 2019;41(3):303–8.
(Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements(Residency). https://www.acgme.org/globalassets/pfassets/programrequirements/cprresidency_2022v3.pdf ).
Chang HJ, Lee YM, Lee YH, Kwon HJ. Causes of resident lapses in professional conduct during the training: a qualitative study on the perspectives of residents. Med Teach. 2017;39(3):278–84.
Fargen KM, Drolet BC, Philibert I. Unprofessional behaviours among tomorrow’s physicians: Review of the literature with a focus on risk factors, temporal trends, and future directions. Acad Med. 2016;91(6):858–64.
Nittur N, Kibble J. Current practices in assessing professionalism in United States and Canadian allopathic medical students and residents. Cureus. 2017;9(5):e1267.
Google Scholar
Brotherton S, Kao A, Crigger BJ. Professing the values of medicine: the modernized AMA code of medical ethics. JAMA. 2016;316(10):1041–2.
Tricco AC, Rios P, Zarin W, Cardoso R, Diaz S, Nincic V, Mascarenhas A, Jassemi S, Straus SE. Prevention and management of unprofessional behaviour among adults in the workplace: a scoping review. PLoS ONE. 2018;13(7):e0201187.
Krupat E, Dienstag JL, Padrino SL, Mayer JE Jr, Shore MF, Young A, Chaudhry HJ, Pelletier SR, Reis BY. Do professionalism lapses in medical school predict problems in residency and clinical practice? Acad Med. 2020;95(6):888–95.
Seehusen DA. Understanding unprofessionalism in residents. J Grad Med Educ. 2020;12(3):243–6.
Lackritz K, Braverman A, Rana M, Gaspari B, Wolf A. Examining unprofessional behaviour in the OBGYN Clerkship: A Qualitative study of essays written by students. Obstet Gynecol. 2017;1(130):47S.
Roberts NK, Dorsey JK, Wold B. Unprofessional behaviour by specialty: A qualitative analysis of six years of student perceptions of medical school faculty. Med Teach. 2014;36(7):621–5.
Worly B. Professionalism education of OB/GYN resident physicians: What makes a difference?.
Rogers R, Drogin EY. Conducting Miranda evaluations: Applications of psychological expertise and science within the forensic context. Springer Nature; 2019. https://doi.org/10.1007/978-3-030-13511-9 .
Bulk LY, Drynan D, Murphy S, Gerber P, Bezati R, Trivett S, Jarus T. Patient perspectives: four pillars of professionalism. Patient Exp J. 2019;6(3):74–81.
Chandratilake M, McAleer S, Gibson J, Roff S. Medical professionalism: what does the public think? Clin Med. 2010;10(4):364.
Mak-van der Vossen M, Teherani A, van Mook W, Croiset G, Kusurkar RA. How to identify, address and report students’ unprofessional behaviour in medical school. Med Teach. 2020;42(4):372–9.
Waheed K, Al-Eraky M, Naeem NI, Ejaz S, Khanum A. A narrative study on work place based conflicts in Obstetrics and Gynaecology Department. JPMA The Journal of the Pakistan Medical Association. 2021;71(2 (A)):514–7.
Godschalx-Dekker JA, Sijbom CA, Barnhoorn PC, van Mook WN. Unprofessional behaviour of GP residents leading to a dismissal dispute: characteristics and outcomes of those who appeal. BMC Primary Care. 2024;25(1):61.
Norman NB, Soo JM, Lam MY, Thirumoorthy T. Unprofessional behaviour of junior doctors: a retrospective analysis of outcomes by the Singapore medical council disciplinary tribunals. Singapore Med J. 2021;62(3):120.
Majeed N. A narrative review of the unprofessional behaviours of physicians at workplace. Health Prof Educ J. 2021;4(1):26–32.
Javed Y, Ahmad S, Khahro SH. Evaluating the research performance of Islamabad-based higher education institutes. SAGE Open. 2020J;10(1):2158244020902085.
University Overview of Rawalpindi Medical University on uniRank (Australian website) retrieved on 13 March 2024.
"PM Imran Khan launches 'Pakistan Citizen Portal'". www.thenews.com.pk . Retrieved 13.03.24.
Pakistan Citizens' Portal to redress public grievances and improve governance: PM Imran Khan". http://www.radio.gov.pk . Retrieved 13.03.24.
Merriam SB, Tisdell EJ. Qualitative Research: A Guide to Design and Implementation, 4th Edition. Jossey-Bass; 2015. ISBN: 978-1-119-00361-8.
Caelli K, Ray L, Mill J. ‘Clear as mud’: toward greater clarity in generic qualitative research. Int J Qual Methods. 2003;2(2):1–3.
Duan N, Bhaumik DK, Palinkas LA, Hoagwood K. Optimal design and purposeful sampling: complementary methodologies for implementation research. Adm Policy Ment Health Ment Health Serv Res. 2015;42:524–32.
Artino AR Jr, La Rochelle JS, Dezee KJ, Gehlbach H. Developing questionnaires for educational research: AMEE Guide No. 87. Medical Teacher. 2014;36(6):463–74. https://doi.org/10.3109/0142159X.2014.889814 .
Latkin CA, Edwards C, Davey-Rothwell MA, Tobin KE. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in Baltimore, Maryland. Addict Behav. 2017;1(73):133–6.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:1–8.
Creswell JW. Educational research: Planning, conducting, and evaluating quantitative and qualitative research. pearson; 2015.
Alipour F, Shahvari Z, Asghari F, Samadi S, Amini H. Personal factors affecting medical professionalism: a qualitative study in Iran. J Med Ethics Hist Med. 2020;13:3.
Bell BS, Kozlowski SW. A typology of virtual teams: implications for effective leadership. Group Org Manag. 2002;27(1):14–49.
Siu AL, Kravitz RL, Keeler E, Hemmerling K, Kington R, Davis JW, Mitchell A, Burton TM, Morgenstern H, Beers MH, Reuben DB. Postdischarge geriatric assessment of hospitalized frail elderly patients. Arch Intern Med. 1996;156(1):76–81.
West CP, Shanafelt TD. The influence of personal and environmental factors on professionalism in medical education. BMC Med Educ. 2007D;7:1–9.
Yavari N, Asghari F, Shahvari Z, Nedjat S, Larijani B. Obstacles of professional behaviour among medical trainees: A qualitative study from Iran (2018). Journal of Education and Health Promotion. 2019;8(1):193.
Fredrikson M, Jha S, Ristenpart T. Model inversion attacks that exploit confidence information and basic countermeasures. In: Proceedings of the 22nd ACM SIGSAC conference on computer and communications security. 2015. p. 1322–33.
Chang HJ, Lee YM, Lee YH, Kwon HJ. Investigation of unethical and unprofessional behaviour in Korean residency training. Teach Learn Med. 2015;27(4):370–8.
Collier P, Hoeffler A. Aid, policy and peace: Reducing the risks of civil conflict. Defence and Peace Economics. 2002;13(6):435–50.
Coulehan J. Today’s professionalism: engaging the mind but not the heart. Acad Med. 2005;80(10):892–8.
Lopez L, Katz JT. Perspective: creating an ethical workplace: reverberations of resident work hours reform. Acad Med. 2009;84(3):315–9.
Hoffmann WA, Nortjé N. Patterns of unprofessional conduct by medical practitioners in South Africa (2007–2013). SAFP. 2016;58(3):108–13.
Levey RE. Sources of stress for residents and recommendations for programs to assist them. Acad Med. 2001;76(2):142–50.
Sanfey H, DaRosa DA, Hickson GB, Williams B, Sudan R, Boehler ML, Klingensmith ME, Klamen D, Mellinger JD, Hebert JC, Richard KM. Pursuing professional accountability: an evidence-based approach to addressing residents with behavioural problems. Arch Surg. 2012;147(7):642–7.
Download references
Acknowledgements
The authors would like to thank the participants for their involvement and time spent in the study. Special thanks to Dr Faiza Samreen for providing continuous support and guidance throughout the study. Authors would like to acknowledge the Professor Dr Luna Ejaz Kahloon (Dean of Department of Obs/Gynae Rawalpindi Medical University), and Dr Usman Hamdani (Global Institute of Human Development ) Zille e Huma, Ayella Gillani , Aabsha Tasawar, Bushra Mahjabeen, Ambreen Sadaf , MahNoor Urosa Safdar for their feedback and guidance.
Not applicable.
Author information
Authors and affiliations.
Department of Obstetrics &Gynaecology, Rawalpindi Medical University, Rawalpindi, Pakistan
Humera Noreen
Department of Medical Education, Riphah International University, Islamabad, Pakistan
Rahila Yasmeen & Shabana Ali Mohammad
You can also search for this author in PubMed Google Scholar
Contributions
I Dr Humera Noreen as main author design the work, wrote the main Manuscript and prepared figures. Prof Dr Rahila Yasmeen and Dr Shabana Ali helped in interpretation and analysis of data. we all reviewed the manuscript.
Corresponding author
Correspondence to Humera Noreen .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the institutional review committee of Islamic International Medical College (Ref No Riphah/IIMC/IRC/22/2003; approval date: 27/01/2022).
A written informed consent to participate in the study was obtained from all the participants.
The authors confirm that all methods were carried out in accordance with relevant guidelines and regulations in the Declaration of Helsinki.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Noreen, H., Yasmeen, R. & Mohammad, S.A. Factors leading to lapses in professional behaviour of Gynae residents in Pakistan: a study reflecting through the lenses of patients and family, consultants and residents. BMC Med Educ 24 , 611 (2024). https://doi.org/10.1186/s12909-024-05509-9
Download citation
Received : 12 July 2023
Accepted : 02 May 2024
Published : 03 June 2024
DOI : https://doi.org/10.1186/s12909-024-05509-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lapses in professional behaviour
- Professionalism
- Gynae residents
- Factors and reasons
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

COMMENTS
Case Study is a type of Group Discussion exercise. A given case (issue/business problem) is discussed in a group to bring out the best solution to the given problem. The problem is given in the form of text (typically 250-300 words) Crack Your Dream Summer Placements With InsideIIM's MBA Placements Bootcamp S04!
It's been 100 years since Harvard Business School began using the case study method. Beyond teaching specific subject matter, the case study method excels in instilling meta-skills in students.
Although case studies have been discussed extensively in the literature, little has been written about the specific steps one may use to conduct case study research effectively (Gagnon, 2010; Hancock & Algozzine, 2016).Baskarada (2014) also emphasized the need to have a succinct guideline that can be practically followed as it is actually tough to execute a case study well in practice.
Think of yourself as a discussion facilitator. Your goal is to keep the group focused on moving through the case questions. Don't feel that you need to master all the content more thoroughly than the other group members do. Guide the group through the study questions for each assignment. Keep track of time so that your group can discuss all the ...
Revised on November 20, 2023. A case study is a detailed study of a specific subject, such as a person, group, place, event, organization, or phenomenon. Case studies are commonly used in social, educational, clinical, and business research. A case study research design usually involves qualitative methods, but quantitative methods are ...
Abstract. Recently, qua litative studies have been widespread in various areas such as. psychology, business, and soc iology. In this review, the process of qualitative. study has been clar ified ...
Tip 1: Organize Your Team. If no one else takes charge, take on this role. A disorganized team will not be able to complete their analysis and develop a strong recommendation in the time allotted. See the previous section for the steps the group needs to complete to solve the case.
A case study is a research method that involves an in-depth analysis of a real-life phenomenon or situation. Learn how to write a case study for your social sciences research assignments with this helpful guide from USC Library. Find out how to define the case, select the data sources, analyze the evidence, and report the results.
Case Study Method Discussion Groups ... Exploring the case with your discussion group beforehand will increase your comfort level when sharing in the classroom. Get to know a handful of people more deeply. Bonding with the members of your discussion group can lead to personal and professional relationships that last a lifetime. ...
Introduce variety into case-based discussions. Integrate a mix of independent work, small group discussion, and whole group share outs to keep students engaged and provide multiple junctures for students to get feedback on their understanding. Instructor scaffolding is critical for effective case-based learning ( Ramaekers et al., 2011 )
In the latter case, you may have the chance to choose a space and otherwise structure the situation. In less formal circumstances, you'll have to make the best of existing conditions. ... Group discussions are common in our society, and have a variety of purposes, from planning an intervention or initiative to mutual support to problem ...
This Tutorial is an easy direction on how to approach a casebased group discussion. It's highly helpful for the Job aspirants in Management Consulting Firms ...
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The case study was published in Studies in Higher Education (Breen et al., Citation 2001) and has been selected as an example for several reasons. Not only does it demonstrate the use of a very detailed focus-group schedule but it also used recordings of the discussions for a thematic analysis that followed.
Let's look at an example of a group case study interview and how it might play out. Our client is a company suffering from declining profitability. The prompt is presented to a group of 3-6 eager candidates. ... Once the discussion is over, the interviewer may take charge and ask the group a set of questions to move the case ahead. At this ...
ISBN: 9781446248645. Publication Date: 2015-10-01. This sharp, stimulating title provides a structure for thinking about, analysing and designing case study. It explores the historical, theoretical and practical bones of modern case study research, offering to social scientists a framework for understanding and working with this form of inquiry.
Focus group discussion is a good way to gather in-depth information about the community's thoughts and opinions on a topic (14,15). Focus group discussion can yield a lot of information about a topic in a relatively short time. ... a case study reflective paper using an analytical framework. BMC Med Res Methodol. 2009; 9:65. doi:10.1186/1471 ...
Appearance, design and layout of case study. Discussion activities linked to the case study. Relevance to the subject/module being taught. Relevance to you as an individual. ... and further demonstrated through the way the group engaged with case study teaching in tutorials. Awareness of these preferences may help staff to select appropriate ...
A Case Study One case study will be used as an example of focus-group research throughout this ... The key difference between one-to-one interviews and focus-group discussions is that the latter is far more appropriate for the generation of new ideas formed within a social context. In contrast, one-to-one interviews ought to probe individual ...
A focus group discussion is a qualitative research tool ori ginated in sociology and. popular in business, marketing, and education (Sagoe, 2012). Focus group discussion is used. to gather data ...
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews). The case study research method originated in clinical medicine (the case history, i.e., the patient's personal history). In psychology, case studies are ...
DSpace JSPUI eGyanKosh preserves and enables easy and open access to all types of digital content including text, images, moving images, mpegs and data sets
The purpose of the group case interview is to have discussions and work together as a group. The more time your group spends reading the material independently, the less time the group has to demonstrate interpersonal and teamwork skills. 7. You don't need to have your idea or recommendation chosen.
Unilever has 'lost the plot' by fixating on sustainability, says Terry Smith. Companies take step back from making climate target promises. The real impact of the ESG backlash. Unilever's ...
Study context. This qualitative study was conducted in the province of British Columbia (BC), Canada, a jurisdiction with a population of approximately five million people [].Within BC's health sector, key actors involved in the policy response to COVID-19 included: elected officials, the BC Government's Ministry of Health (MOH), the Provincial Health Services Authority (PHSA), Footnote 2 ...
Since April 2022, Jobs Growth Wales+ has helped 10,000 learners, 60 per cent of whom leave with employment or an apprenticeship, or go into higher education. "You can just sense the increase in ...
Once a date and time has been selected you will present your Case Study Paper to your group and Dr. Jayasundera. The presentation will be 15 minutes (8 -10 minutes for presentation of material and 5 minutes for questions and answers). ... (Module Discussions) 11%. Assignments (Case Study Assignments) 24%. Course Project (Case Study Paper ...
This study explored the impact of integrating ChatGPT into asynchronous online discussions. The analysis encompassed students' log data from Canvas and their perspectives on using ChatGPT. Results revealed a significant enhancement in overall discussion participation when ChatGPT is encouraged, emphasizing its potential as a catalyst for constructive conversations and the development of ...
The study collected the viewpoints of three stakeholder groups: patients and their families, consultants and residents. The study was conducted in three phases. First, the document analysis of written complaints was conducted, followed by face-to-face interviews (11 per group) conducted by trained researchers from an independent 3rd party.
This paper focuses on the use of group discussions (GD), as a very open and flexible method of data generation, to learn about organisational characteristics of schools. ... They were conducted as part of a case study to learn about the influence of schools' organisational characteristics on the implementation of health promotion ...