'I Lost 190 Pounds Using Therapy To Manage My Binge-Eating Disorder'
“I’d eat until I felt sick, go to bed, and wakeup for a midnight snack.”

I grew up overweight, but I didn't really become aware of it until third grade. It hit me one day in gym class when a boy I had a crush on told me I looked like I was pregnant—I was devastated.
Then, my weight started to yo-yo. In high school, I tried out LA Weight Loss and lost 85 pounds, but gained it all back (and then some) so that by my sophomore year in college, I weighed 353 pounds. But it didn't end there: I had gastric bypass surgery as a 19-year-old college student and lost 154 pounds. But, 10 years later, my weight crept back up 305 pounds.

Once I hit 325 pounds again—my second highest weight—I knew I needed to make some changes.
In January 2017, I made a New Year's resolution to lose weight once and for all—and my first step was getting treatment for binge-eating disorder, depression, and anxiety. I realized I needed help when I found myself living the same dismal day over and over again—and food was my only oasis.
It took therapy to make me realize how awful my eating habits had become: I ate from the moment I woke up to the moment I went to bed. I'd often eat until I felt sick, go to bed, then wake up and do it all again the next day—and sometimes I'd even wake up in the middle of the night and snack. I also had physical symptoms: I always felt lethargic, sluggish, and bloated.
In therapy, we worked on developing normalized eating habits—but absolutely no crash or fad dieting.
I did still revamp my diet though, and I chose to keep it as simple as possible for myself. I ate 1,200 calories per day, which meant I had to drastically reduce my portion sizes. Because of that, I began eating foods that were already portioned out for me, like cans of soup or 100-calorie packs of popcorn. I also cut way back on fast food. Here's what I typically eat in a day:
- Breakfast: Coffee and a vanilla protein shake
- Lunch: Progresso Light Chicken and Vegetable Rotini Soup, an orange
- Snacks: 100-calorie bag Orville Redenbacher popcorn sprayed with I Can't Believe It's Not Butter Spray and sprinkled with Truvia, a sugar-free gelatin cup, or a low-fat cheese stick
- Dinner: Steak Portobello Lean Cuisine, with sautéed mushrooms and half of a light English muffin
- Dessert: Halo Top Ice Cream (rotating flavors, but Peanut Butter Cup is my favorite)
I also started to exercise regularly, committing to 45 minutes of movement daily.
Before therapy and dieting, I was constantly in pain and out of shape—even hoisting myself out of bed every morning was super-painful.
After I saw some progress with dieting, I added in exercise and chose to do essentially all cardio: primarily walking on the treadmill and increasing the incline gradually. I used the elliptical machine for some variety. Finally, after several months and feeling more fit, I mounted the stair-stepper machine and it became my go-to for an intense workout.
Two years after I decided to make a change, I've lost 190 pounds.
I always tell people that small, daily efforts really add up—all of my progress was achieved one day at a time. On really difficult days—which I still have—I take things one meal or one moment at a time.
And while I'm proud of my weight loss, I want other women to know that they should never put their lives on hold while they're waiting to lose weight, like I did in the past. If there's no weight or size limit on your interests, then get out there and pursue them now. It makes the journey the much more enjoyable.

Weight-Loss Success Stories

This Mom Lost 95 Lbs. With WW And Walking

This Mom Lost 95 Lbs. With Keto And IF

This Mom Lost 75 Lbs. With The 80/20 Rule

'I Lost 135 Pounds By Counting Macros'

How 8 Women Crushed Their Resolutions In 2022

'What Finally Made Weight Loss Click For Me'

The 30-Day Fitness Challenge You Need To Try

‘I Lost 190 Lbs. By Eating Healthy And Running’

This Mom Lost 90 Lbs. By Counting Calories

‘I Lost 90 Pounds With Portion Control, Lifting’

'I Lost 100 Lbs. With WW And Jazzercise'
Binge eating linked to weight-loss challenges
Someone who binge eats consumes an objectively large amount of food while feeling a loss of control over eating. When episodes occur weekly for several months, the action moves into the realm of binge-eating disorder. So how does this type of eating affect people with Type 2 diabetes and obesity who are actively working to lose weight?
According to new findings from the University of Pennsylvania published in the journal Obesity , it presents a significant obstacle: Those who continue to binge eat while trying to lose weight drop about half as much as those who don't or those who do and then subsequently stop.
"Continued binge eating can act as a barrier to achieving success," said Ariana Chao, an assistant professor in the Penn School of Nursing.
Chao studies how addictive-like eating behaviors influence treatment effectiveness for different populations. To better understand the role of binge eating in weight loss, she and colleagues from Penn's Perelman School of Medicine, the Children's Hospital of Philadelphia, the University of Connecticut and the National Institute of Diabetes and Digestive and Kidney Diseases assessed data from a study called Action for Health in Diabetes, or Look AHEAD. This multi-center randomized, controlled trial included more than 5,000 participants ages 45 to 76, all with a body mass index above 25 (or 27 for those using insulin) and Type 2 diabetes.
Look AHEAD's original aim was to compare the effects on cardiovascular morbidity and mortality of two treatment options: an intensive lifestyle intervention designed to induce weight loss and diabetes support and education. The former included dietary recommendations, physical activity and behavior modifications; those in the latter group were encouraged to attend three sessions per year, one each about physical activity, social support and eating.
In addition, Look AHEAD annually assessed binge eating. Via a questionnaire, participants noted any instances in the past six months during which they consumed excess food and felt a lack of control over that consumption.
For this study, Chao and her team, which included Thomas Wadden, the Albert J. Stunkard Professor of Psychology in Psychiatry and director of Penn's Center for Weight and Eating Disorders, analyzed the impact of binge eating on weight loss. The researchers found that at four years, participants who reported no binge eating or a reduced tendency to do so lost more weight than those who continued to binge eat. Participants lost 4.6 percent of initial body weight compared to 1.9 percent.
"Previously, it was unclear whether people who binge eat need to be treated for that behavior before attempting behavioral weight loss or whether they'll do OK in behavioral weight loss without it," said Chao, who has a secondary appointment in the Department of Psychiatry. "Our findings suggest that people who continue to binge eat after they start a behavioral weight-loss program need an additional treatment like cognitive behavioral therapy, which is one of the most effective for this condition."
Such treatment includes work to recognize the interconnectedness of thoughts, feelings and behaviors, Chao said. For instance, if someone eats to cope with stress, CBT could aim to untangle why and how to change the behavior.
Though this study looked at a particular subset of people, two-thirds of the adult population in the United States is either overweight or obese. For that reason, Wadden said it's important for clinicians to screen for these behaviors and, if found, refer those patients for additional care.
"Individuals with a history of binge eating shouldn't be excluded or discouraged from engaging in behavioral weight loss," he said. "But binge eating should be monitored regularly during weight loss. Participants who continue to report this may benefit from additional or more targeted treatment to ensure success."
- Diet and Weight Loss
- Eating Disorder Research
- Eating Disorders
- Dieting and Weight Control
- Nutrition Research
- Bulimia nervosa
- Weight Watchers
- Cardiac arrest
- Hyperthyroidism
- Deadly nightshade and related plants
Story Source:
Materials provided by University of Pennsylvania . Note: Content may be edited for style and length.
Journal Reference :
- Ariana M. Chao, Thomas A. Wadden, Amy A. Gorin, Jena Shaw Tronieri, Rebecca L. Pearl, Zayna M. Bakizada, Susan Z. Yanovski, Robert I. Berkowitz. Binge Eating and Weight Loss Outcomes in Individuals with Type 2 Diabetes: 4-Year Results from the Look AHEAD Study . Obesity , 2017; 25 (11): 1830 DOI: 10.1002/oby.21975
Cite This Page :
Explore More
- Stopping Flu Before It Takes Hold
- Cosmic Rays Illuminate the Past
- Star Suddenly Vanish from the Night Sky
- Dinosaur Feather Evolution
- Warming Climate: Flash Droughts Worldwide
- Record Low Antarctic Sea Ice: Climate Change
- Brain 'Assembloids' Mimic Blood-Brain Barrier
- 'Doomsday' Glacier: Catastrophic Melting
- Blueprints of Self-Assembly
- Meerkat Chit-Chat
Trending Topics
Strange & offbeat.

Healthy weight loss: a how-to guide
- Top 10 tips
- What to eat
- High protein
- Intermittent fasting
- Other diets
- Metabolic health
- Measuring success
- Breaking a plateau
- The long term

Everyone knows that to lose weight, you’re supposed to eat fewer calories and burn more. The problem is, eating less than you’d like is often easier said than done.
You might be able to deal with hunger for a few weeks or even months, but at some point, hunger wins. And then, the weight tends to come back.
What’s the best way to achieve weight loss in a healthy, sustainable way, without hunger or “white-knuckle” willpower?
The approaches that work tend to follow the same basic principles: eat the lowest calorie foods that fill you up, eliminate high-processed foods that don’t, and make sure you get essential nutrition.
It sounds easy. But why do so many of us struggle with healthy weight loss?
This guide will tell you the best ways to achieve healthy weight loss. It has our top weight loss tips, what to eat and what to avoid, the common mistakes you might be making, how to eat fewer calories, and much more.
But first, what is “healthy weight loss?”
Healthy weight loss starts with setting realistic goals . After that, we define healthy weight loss as mainly losing fat mass instead of lean body mass, improving your metabolic health, having a minimal decline in your resting metabolic rate, and making sure you can maintain your dietary lifestyle long-term.
If you’re struggling with your weight, it may not be your fault. The industrial food environment is stacked against you. The good news is that there are effective approaches to reach your best weight and improve your metabolic health long term! Here’s how.
Key takeaways
Top 10 weight loss tips
- Avoid eating carbs and fat together. This combination provides excessive calories with little to no nutritional value — think pizza, cookies, chips, donuts, etc. — and may increase cravings.
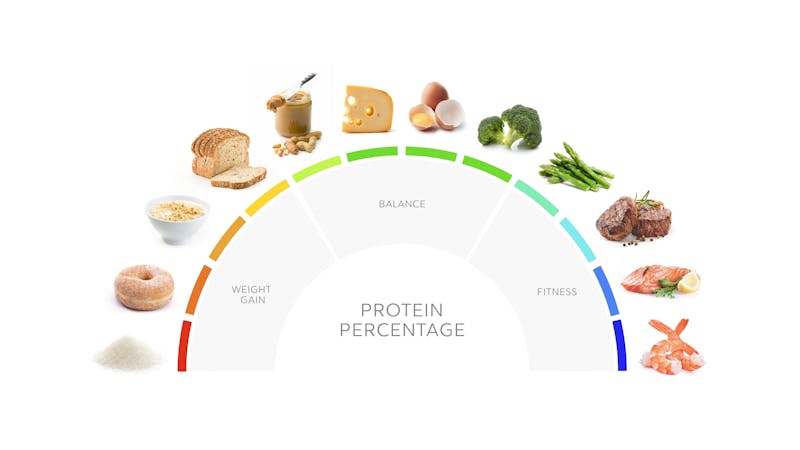
- Eat at least 30 grams of protein at most meals. Protein foods are the most satiating and nutrient-dense type of food.
- On a low carb approach, which is often a successful weight loss strategy, limit net carbs to less than 100 grams (or keep them as low as 20 grams per day, if you want to try a keto diet).
- Fill your plate with fibrous veggies. These provide abundant nutrients, high food volume, and relatively few calories.
- Add enough fat for taste and to enjoy your food, but not more than you need. Let’s be honest, fat tastes great! Taste is an essential part of long-term nutritional success. But too much fat can add calories you don’t need.
- If you’re hungry, start with adding more protein and vegetables. Again, these are the most satiating and nutritious food for the fewest calories.
- Find foods you enjoy that fit the above criteria. Check out our recipes here .
- Stay physically active. You don’t have to run marathons, but physical activity added to a healthy diet can help maintain fat loss while preserving muscle mass.
- Get adequate restorative sleep. Sleep like your health depends on it, because it does!
- Create an environment to promote your success. It isn’t just about knowing what to do. It’s also about creating the environment that will help you succeed. For example, removing tempting foods from your kitchen is just one great way to get started.
What foods to eat and what foods to avoid for healthy weight loss

For healthy weight loss, you want to make every calorie count.
But that doesn’t mean you have to count calories.
How is that possible? By focusing on the foods in the list below, you’ll ensure you are getting adequate nutrition, eating filling foods, and naturally decreasing your caloric intake.
We recommend focusing the bulk of your nutrition on “foods with the most nutrition per calorie”, consider portion control of foods with “moderate nutrition”, and reduce or eliminate foods with the least nutrition per calorie. Give it a try!
Foods with the most nutrition per calorie:
- Meat and poultry
- Non-starchy vegetables
- Dairy products like yogurt and cottage cheese
- Soy, beans, and lentils
Foods with moderate nutrition per calorie:
- Nuts and seeds
- Fatty processed meats like bacon
- Starchy vegetables
- Low-sugar fruits like berries, olives, and avocados
- Whole grains
Foods with the least nutrition per calorie
- Foods with high amounts of sugar and refined starches
- Sugar-sweetened beverages and fruit juice
- Beer and sweetened alcoholic beverages
- Pure added fats like oil and butter
Are you still hungry between meals, or are you looking for ways to add more protein to your diet? Take a look at our guide on high-protein snacks for weight loss. You can choose from hard-boiled eggs, a can of tuna, beef jerky, lupini beans, black soybeans, and more.

Why we recommend high protein for weight loss

Refined carbohydrates (sugar, bread, pasta, etc.) and refined fats (mostly oils) are high in energy density but lack nutritional value and are easier to overeat.
That’s why, for high nutrition eating, we recommend:
- Reduce your carbohydrate intake.
- Prioritize your protein and fibrous vegetables intake.
- Add just enough fat for taste and, if needed, extra calories.
How to get all essential nutrients
Fortunately, when you focus on whole-food proteins, the fatty acids and micronutrients are naturally present. And when you eat above-ground veggies, you automatically get fiber and additional micronutrients.
Based on calculations of the liver and kidney’s ability to safely handle protein, a 176-pound (80-kilo) person can theoretically consume a maximum of 365 grams of protein per day safely. 7 That’s 73% of a 2,000 calorie diet! It’s safe to say that most people won’t have to worry about eating too much protein.
Why we recommend low carb for weight loss
Low carb and keto diets also allow for adequate protein intake, plenty of above-ground fibrous veggies, and added fat for a complete, delicious, and sustainable healthy weight loss plan.
Based on the above data, plus practical considerations, we think carbohydrate reduction can play an essential role in healthy weight loss.
You can learn more about getting started eating low carb in our guides on a keto diet and a low carb diet for beginners.
Why we recommend intermittent fasting for weight loss
Intermittent fasting is an intentional avoidance of caloric intake for a set period. It can be as short as 12 hours (also called time-restricted eating) or as long as five or more days.
One reason that improved results were not seen in the time-restricted eating group may be that subjects ended up eating more calories during their eating window.
Fasting is not an excuse to binge eat or “make up for lost calories.”
Instead, fasting is meant to purposefully reduce caloric intake to preserve resting metabolic rate (the amount of energy you burn at rest), maintain lean muscle mass, and improve metabolic health. 15 In other words, intermittent fasting doesn’t just help with weight loss, but with healthy weight loss.
You can learn more about intermittent fasting in our intermittent fasting for beginners guide .
What other diets work for weight loss?
High-protein, low carb diets, which might also include short-term intermittent fasting, may be the best choice for many people to succeed with healthy weight loss.
Which diet is right for you? Only you can answer this question. The key is to find a pattern of eating that:
- Focuses on foods you like to eat
- Feels sustainable and enjoyable
- Helps you reduce your caloric intake
- Prevents excessive hunger
- Provides adequate nutrition
You may want to experiment with different diets to find the right one for you. And remember that it’s OK to change up your dietary approach as you age — and as your health, eating preferences, and lifestyle change.
How to eat fewer calories
That’s not what we are promoting.
Instead, we promote eating better. That means eating in a way that naturally allows you to reduce your calories without hunger. Does it sound too good to be true?
It doesn’t have to be.
These are all hyperpalatable foods that can make it difficult to control the amount you eat. 28 Overeating may have nothing to do with willpower or “being strong.” Instead, your brain may be telling you: This tastes great and has lots of calories for survival, I want more!
How to achieve metabolic health

However, you shouldn’t define health as merely avoiding disease. While that may be a great starting point, you don’t have to stop there!
Take waist circumference, for example. If you go by the definition used for metabolic syndrome, a normal waist circumference for a male is 39 inches (99 cm). Does that mean 39 inches is your end goal?
Maybe not! A waist size of 35 inches (88 cm) is likely much healthier for a 5’ 8” male than 39 inches. 31 Even though this may be your “end goal,” don’t expect to get there overnight. Continue to strive for slow and steady improvements over time, heading toward a more desirable result.
Just because medicine defines certain metrics as “normal” doesn’t mean they are your goal. Instead, focus on the lifestyles that get to the root cause of metabolic disease.
How can you achieve the goal of metabolic health? Here are our top eight tips.
8 tips to improve metabolic health
- Limit carbs — especially refined starches and sugars. Refined starches and sugars are the foods most likely to cause you to overeat calories and raise your blood sugar, insulin, blood pressure, and triglycerides. 32 A low carb approach may be the most effective diet for improving metabolic syndrome. 33 Low carb diets also successfully reduce hunger for most people. 34
- Eat adequate protein. Numerous studies demonstrate that, despite a slight temporary increase in insulin, higher protein diets improve insulin sensitivity over the long run and contribute to metabolic health. 35
- Moderate your fat intake. Excessive fat intake can raise triglycerides and worsen insulin resistance, especially if fat is combined with carbs or contributes to eating too many calories overall. 36 Eat enough fat to enjoy your meals, and eat fat that naturally comes with your food, such as the skin on your chicken or a naturally fatty rib eye. But don’t go out of your way to add unneeded fat to your foods.
- Don’t smoke. This should go without saying due to the strong connection of smoking to cancer and heart disease risk, but it also contributes to metabolic disease. 37
- Drink minimal to moderate amounts of alcohol. Alcohol provides empty calories that can affect liver health and undermine metabolic health. 38
- Manage stress and sleep well. Poorly controlled chronic stress and poor sleep can increase the likelihood of insulin resistance. 39
- Get regular physical activity. Muscles burn glucose. Building and using your muscles help promote insulin sensitivity and efficient energy utilization. 40
- Practice time-restricted eating or intermittent fasting. 41 Giving your body time without ingesting nutrients allows your insulin levels to decrease, improves insulin sensitivity, allows your body to learn to efficiently use fat for energy, and may even tap into autophagy. 42 The net result is improved metabolic health.
How to measure weight loss

The scale may tell you if your weight is going up or down. But healthy weight loss involves much more than the number on the scale.
Consider trying any of these three techniques in addition to using the scale:
- Follow your waist measurement and your waist-to-height ratio. All you need is a tape measure. If your weight is the same on the scale, but your waist is getting smaller, that is still a fantastic healthy fat loss victory! As we detail in our guide on losing belly fat , waist circumference is one of the best measurements to predict metabolic health and track healthy weight loss. 44
- How do your clothes fit? If you don’t have a tape measure, all you have to do is put on your (non-stretchy) pants. It doesn’t get much easier than that. Are your pants looser? That means your waist is getting smaller. If you are doing resistance training, you might also find that your arms and legs look more toned. That is a good sign that you are building muscle mass.
- Test your body composition. This requires additional tools — either a bioimpedance scale or a more detailed assessment with a DEXA scan or equivalent measuring device. A DEXA scan will not only tell you if your weight is changing, but it will also quantify how much weight loss was fat mass, lean body mass, and visceral fat. As a bonus, you also can follow your bone density to ensure maintaining strong bones is part of your healthy weight loss progress.
How to break weight loss plateaus

But it helps to have a plan for when the plateaus come. Here are the eight best tips for helping you to overcome a plateau and get back on track with healthy weight loss.
Top 8 tips for breaking a weight loss plateau 45
- Are you eating enough protein? Take a couple of days to measure all of the protein you eat and count every gram. Yes, it can be a hassle, but it can also be illuminating. You may think you are eating “plenty of protein,” only to find out you’re actually getting just 15% of your calories from protein. If that’s the case, the best tip for breaking your stall is to increase your protein intake.
- Are you eating enough fibrous vegetables? Fibrous vegetables are one of the best ways to increase nutrients for the minimum number of calories, increase stomach fullness, and slow gastric emptying. 46 Again, keeping track of your intake for a couple of days can help guide you in increasing your consumption of fiber-filled veggies. Aim for at least four cups per day.
- Are you limiting your non-nutrient calories? After increasing your protein and fiber-filled vegetables, what’s left? It’s usually non-nutrient calories — the extra dose of cream or butter, the rice that “comes with” your meal, the sugary salad dressing that seems so innocent. Or maybe it’s the ritual glass of wine with dinner. Experiencing a plateau is the perfect time to take stock of your non-nutrient calories and cut them in half or cut them out completely if you can.
- Are you struggling with cravings or snacking? Usually, addressing protein and fibrous vegetables can help cut down on snacking and cravings. However, if you still find yourself snacking, first make sure you are eating high-protein snacks . Next, make sure you’re snacking for real hunger and not boredom or routine. Finally, try eliminating non-nutritive sweeteners that can stimulate cravings, such as erythritol, stevia, and other sweet additives. 47
- How are you sleeping? Plateaus aren’t always about what you eat. Not only can poor sleep negatively affect your food choices during the day, but lack of sleep can also change your hormonal environment, making it nearly impossible to lose weight. 48 Make sure you prioritize good sleep hygiene. It’s easy to talk about but harder to do. Eliminate screens an hour before bed. Keep a steady sleep-wake routine. Make sure your bedroom is cool, dark, and quiet. Kick the kids and dogs out of your bed. You can keep your spouse, but only if their snoring doesn’t keep you up!
- Are you exercising? Exercise by itself is not great for weight loss. However, regular physical activity can help maintain weight loss and break plateaus when combined with healthy eating. Just make sure your exercise helps build muscle and doesn’t leave you hungry and craving food. For instance, you may find 20 minutes of resistance training more effective than 45 minutes on a treadmill.
- Have you tried time-restricted eating or intermittent fasting? For some, spacing out the timing between meals can naturally reduce caloric intake and allow for lower insulin levels. The combination may be enough to break a weight loss plateau.
Read even more in our detailed guide on tips to break a weight loss stall .

Maintaining weight loss long term
Authors have written hundreds of books on tips to maintain beneficial behavior change, and most of the tips aren’t a secret. The problem is when the recommendations become more items on your “to-do” list, adding chores to your routine that take time and energy you don’t have to give.
If that’s the case, don’t let yourself get overwhelmed. Pick one or two tips that resonate most with you, and stop there. Just because a tip made the list doesn’t mean you have to do it. The list is merely a collection of suggestions to try and see what works best for you.
Top tips for long-term success
- Connect with your why, to keep your motivation for maintaining your weight loss front and center.
- Create accountability with a partner, a coach, an app, or a calendar.
- Control your environment. Don’t allow temptations in your house or workplace.
- See your new way of eating as a lifestyle, not a diet. It isn’t something you “do.” It’s something you “are.” The language you use can make all the difference.
- Keep it enjoyable. Find recipes you love that fit within your eating pattern.
- Celebrate small successes on your way to bigger successes.
- Realize that you won’t be perfect, and that’s OK. Minor detours don’t have to derail you. Anticipate roadblocks and have a plan to get past them.
- Incorporate smart strategies for optimizing your sleep, stress management, and physical activity. Better habits in these areas can help with long-term, healthy weight maintenance.
Sample meals and meal plans

Keto for beginners
Guide A keto diet is a very low-carb, high-fat diet. You eat fewer carbs and replace it with fat, resulting in a state called ketosis. Get started on keto with delicious recipes, amazing meal plans, health advice, and inspiring videos to help you succeed.

Low carb for beginners
Guide Want to try a low carb diet for weight loss or health? In this top low carb guide, we show you what you need to get started: what to eat, what to avoid and how to avoid side effects. Get delicious low carb recipes and meal plans.
High-protein diet
Guide Our guide helps you understand what a high-protein diet is and why it might help you lose weight and improve your health.
Weight loss

4. Enjoy healthier foods
Adopting a new eating style that promotes weight loss must include lowering your total calorie intake. But decreasing calories need not mean giving up taste, satisfaction or even ease of meal preparation.
One way you can lower your calorie intake is by eating more plant-based foods — fruits, vegetables and whole grains. Strive for variety to help you achieve your goals without giving up taste or nutrition.
Get your weight loss started with these tips:
- Eat at least four servings of vegetables and three servings of fruits daily.
- Replace refined grains with whole grains.
- Use modest amounts of healthy fats, such as olive oil, vegetable oils, avocados, nuts, nut butters and nut oils.
- Cut back on sugar as much as possible, except the natural sugar in fruit.
- Choose low-fat dairy products and lean meat and poultry in limited amounts.
5. Get active, stay active
While you can lose weight without exercise, regular physical activity plus calorie restriction can help give you the weight-loss edge. Exercise can help burn off the excess calories you can't cut through diet alone.
Exercise also offers numerous health benefits, including boosting your mood, strengthening your cardiovascular system and reducing your blood pressure. Exercise can also help in maintaining weight loss. Studies show that people who maintain their weight loss over the long term get regular physical activity.
How many calories you burn depends on the frequency, duration and intensity of your activities. One of the best ways to lose body fat is through steady aerobic exercise — such as brisk walking — for at least 30 minutes most days of the week. Some people may require more physical activity than this to lose weight and maintain that weight loss.
Any extra movement helps burn calories. Think about ways you can increase your physical activity throughout the day if you can't fit in formal exercise on a given day. For example, make several trips up and down stairs instead of using the elevator, or park at the far end of the lot when shopping.
6. Change your perspective
It's not enough to eat healthy foods and exercise for only a few weeks or even months if you want long-term, successful weight management. These habits must become a way of life. Lifestyle changes start with taking an honest look at your eating patterns and daily routine.
After assessing your personal challenges to weight loss, try working out a strategy to gradually change habits and attitudes that have sabotaged your past efforts. Then move beyond simply recognizing your challenges — plan for how you'll deal with them if you're going to succeed in losing weight once and for all.
You likely will have an occasional setback. But instead of giving up entirely after a setback, simply start fresh the next day. Remember that you're planning to change your life. It won't happen all at once. Stick to your healthy lifestyle and the results will be worth it.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
- Hensrud DD, et al. Ready, set, go. In: The Mayo Clinic Diet. 2nd ed. Mayo Clinic; 2017.
- Duyff RL. Reach and maintain your healthy weight. In: Academy of Nutrition and Dietetics Complete Food and Nutrition Guide. 5th ed. John Wiley & Sons; 2017.
- Losing weight: Getting started. Centers for Disease Control and Prevention. http://www.cdc.gov/healthyweight/losing_weight/getting_started.html. Accessed Nov. 15, 2019.
- Do you know some of the health risks of being overweight? National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/health-topics/weight-control/health_risks_being_overweight/Pages/health-risks-being-overweight.aspx. Accessed Nov. 15, 2019.
- 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Journal of the American College of Cardiology. 2014; doi:10.1016/j.jacc.2013.11.004.
- 2015-2020 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. http://health.gov/dietaryguidelines/2015/guidelines. Accessed Nov. 15, 2019.
- Physical activity for a healthy weight. Centers for Disease Control and Prevention. http://www.cdc.gov/healthyweight/physical_activity/index.html. Accessed Nov. 15, 2019.
Products and Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- The Mayo Clinic Diet Online
- A Book: The Mayo Clinic Diet Bundle
- A Book: Live Younger Longer
- Calorie calculator
- Carbohydrates
- Counting calories
- Weight-loss plateau
- Hidradenitis suppurativa: Tips for weight-loss success
- Keep the focus on your long-term vision
- Maintain a healthy weight with psoriatic arthritis
- BMI and waist circumference calculator
- Metabolism and weight loss
- Weight gain during menopause
- Weight Loss After Breast Cancer
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
- Healthy Lifestyle
- Weight loss 6 strategies for success
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Berkman ND, Brownley KA, Peat CM, et al. Management and Outcomes of Binge-Eating Disorder [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2015 Dec. (Comparative Effectiveness Reviews, No. 160.)

Management and Outcomes of Binge-Eating Disorder [Internet].
Executive summary, definition of binge-eating disorder and loss-of-control eating.
Binge-eating disorder (BED) is characterized by recurrent episodes of binge eating—i.e., eating episodes that occur in a discrete period of time (≤2 hours) and involve the consumption of an amount of food that is definitely larger than most people would consume under similar circumstances. Other core features of BED are a sense of lack of control over eating during binge episodes, significant psychological distress (e.g., shame, guilt) about binge eating, and the absence of regular use of inappropriate compensatory behaviors, such as purging, fasting, and excessive exercise.
In May 2013, the American Psychiatric Association (APA) recognized BED as a distinct eating disorder in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5). 1 Previously (in the DSM-IV), BED had been designated as a provisional diagnosis.
Table A presents the DSM-IV and DSM-5 diagnostic criteria for BED. In the shift from provisional to formal diagnosis for BED, APA experts changed the criterion for frequency of BED from twice per week to once per week and the duration criterion from 6 months to 3 months, in line with those for bulimia nervosa.
DSM-IV and DSM-5 diagnostic criteria for binge-eating disorder.
A sense of loss of control (LOC) during binge episodes is a core feature of BED. The term “LOC eating” is used to describe these episodes, but it is also used more broadly throughout the literature to describe binge-like eating behavior accompanied by a sense of LOC that occurs across a wide spectrum of individuals. That spectrum includes, among others, individuals who exhibit some features of BED but do not meet full diagnostic criteria for the disorder (i.e., subthreshold BED) and individuals with other eating disorders (bulimia nervosa, anorexia nervosa binge-eating/purge subtype).
The spectrum of those described as exhibiting LOC eating also includes individuals for whom diagnosis of threshold BED is challenging for unique reasons, such as postbariatric surgery patients and children. Bariatric surgery significantly reduces the stomach size and capacity, effectively rendering it physically impossible for a patient to meet BED criterion 1a ( Table A ; i.e., to consume a definitely large amount of food). In the bariatric surgery literature, LOC eating is used not only to describe binge-like behavior that falls short of meeting criterion 1a, but also to describe eating behavior that is contraindicated based on meal size and meal content. Children, especially young children, may not meet BED criterion 1a because their parents or others limit the quantity of food they consume or because they are unable to provide accurate quantification of the amount they eat. For the purposes of our review, LOC eating treatment and outcomes are limited to postbariatric surgery patients and children, and do not include individuals in other groups who may meet subclinical diagnosis of BED.
Prevalence of Binge-Eating Disorder and Loss-of-Control Eating
Prevalence estimates (and citations) are covered in more detail in the full report. In the United States, the prevalence of BED among adults is about 3.5 percent in women and about 2 percent in men based on DSM-IV criteria and slightly higher based on DSM-5 criteria. 2 , 3 BED is more common among obese individuals 4 , 5 and slightly lower among Latino- and Asian-Americans (1.9% and 2.0%, respectively) than among the general population. 6 , 7 BED is typically first diagnosed in young adulthood (early to mid-20s); 8 , 9 symptoms often persist well beyond midlife. 10 – 12
The prevalence of LOC eating is unknown. In postbariatric surgery patients, it may be as high as 25 percent. 13 , 14 In children at risk for adult obesity because of either their own overweight or that of their parents, prevalence may be as high as 32 percent. 15
- Current Challenges and Controversies in Diagnosing These Disorders
In diagnosing BED, assessing whether a patient is eating an atypically large amount of food is not wholly quantitative; it requires the clinician’s evaluation of the patient’s self-report. Assessment by a structured clinical interview is considered the gold standard. We included only studies in which participants were identified as meeting DSM-IV or DSM-5 criteria for BED as determined through a structured interview.
Assessing BED and LOC in children poses unique challenges, in part because neither the DSM-IV nor the DSM-5 established a minimum age for a BED diagnosis. As a result, when diagnosing adolescents, some clinicians consider BED criteria and others consider LOC eating criteria. We included studies of LOC eating in children ages 6–17 years.
In the postbariatric surgery circumstance, defining LOC eating is not straightforward; assessment methods are not standardized. Patients may report their disordered eating behaviors as a general subjective sense of lack of control over their eating rather than in terms of specific overconsumption based on the amount of food. Also, LOC eating may manifest in the consumption of food types and patterns of intake that are contraindicated after surgery.
- Current Challenges and Controversies in Treating These Disorders
Treating patients with BED targets the core behavioral features (binge eating) and psychological features (i.e., eating, weight, and shape concerns, and distress) of this condition. Other important targets of treatment include metabolic health (in patients who are obese, have diabetes, or both) and mood regulation (e.g., in patients with coexisting depression or anxiety). Table B describes commonly used approaches. Treatments for LOC eating for postbariatric surgery patients and children reflect BED treatment options; treatment of children may include a role for parents.
Treatments commonly used for binge-eating disorder.
- Scope and Key Questions
This review addresses the efficacy and effectiveness of interventions for individuals meeting DSM-IV or DSM-5 criteria for BED, for postbariatric surgery patients with LOC eating, and for children with LOC eating. (Hereafter, the term “effectiveness” refers to both efficacy and effectiveness, including comparative effectiveness.) We also attempted to examine whether treatment effectiveness differed in subgroups based on sex, race, ethnicity, sexual orientation, body mass index (BMI), duration of illness, or coexisting conditions.
Broadly, we included pharmacological, psychological, behavioral, and combination interventions. We considered physical and psychological health outcomes in four major categories: (1) binge behavior (binge eating or LOC eating); (2) binge-eating–related psychopathology (e.g., weight and shape concerns, dietary restraint); (3) physical health functioning (i.e., weight and other indexes of metabolic health—e.g., diabetes); and (4) general psychopathology (e.g., depression, anxiety). Additional outcomes of interest included social and occupational functioning and harms of treatment.
We also examined the course of illness of BED and of LOC eating, particularly given their relatively high comorbidity with other medical and psychiatric conditions. In addition, clinical interest in understanding whether LOC eating reliably predicts poorer weight outcomes and new-onset BED over time is considerable. Little is known about the temporal stability of BED in the community generally, and of LOC in postbariatric surgery patients and children specifically.
Ultimately, the information produced in this review is intended to contribute to improved care for patients, better decisionmaking capacity for clinicians, and more sophisticated policies from those responsible for establishing treatment guidelines or making various insurance and related decisions.
Key Questions
We addressed 15 Key Questions (KQs). Nine are about effectiveness of treatment (benefits and harms overall and benefits for various patient subgroups)—three for BED, three for LOC eating among bariatric surgery patients, and three for LOC eating among children. The other six KQs deal with course of illness, overall and for various subgroups, for BED or LOC eating.
What is the evidence for the effectiveness of treatments or combinations of treatments for binge-eating disorder?
What is the evidence for harms associated with treatments for binge-eating disorder?
Does the effectiveness of treatments for binge-eating disorder differ by age, sex, race, ethnicity, initial body mass index, duration of illness, or coexisting conditions?
What is the course of illness of binge-eating disorder?
Does the course of illness of binge-eating disorder differ by age, sex, race, ethnicity, sexual orientation, body mass index, duration of illness, or coexisting conditions?
What is the evidence for the effectiveness of treatments or combinations of treatments for loss-of-control eating among bariatric surgery patients?
What is the evidence for harms associated with treatments for loss-of-control eating among bariatric surgery patients?
Does the effectiveness of treatments for loss-of-control eating among bariatric surgery patients differ by age, sex, race, ethnicity, initial body mass index, duration of illness, or coexisting conditions?
What is the course of illness of loss-of-control eating among bariatric surgery patients?
Does the course of illness of loss-of-control eating among bariatric surgery patients differ by age, sex, race, ethnicity, sexual orientation, initial body mass index, duration of illness, or coexisting conditions?
What is the evidence for the effectiveness of treatments or combinations of treatments for loss-of-control eating among children?
What is the evidence for harms associated with treatments for loss-of-control eating among children?
Does the effectiveness of treatments for loss-of-control eating among children differ by age, sex, race, ethnicity, initial body mass index, duration of illness, or coexisting conditions?
What is the course of illness of loss-of-control eating among children?
Does the course of illness of loss-of-control eating among children differ by age, sex, race, ethnicity, initial body mass index, duration of illness, or coexisting conditions?
Analytic Frameworks
The relationships among the patient populations, interventions, comparators, and outcomes are depicted for each treatment KQ in Figure A and for each course-of-illness KQ in Figure B .
Analytic framework for binge-eating disorder and loss-of-control eating: effectiveness and harms of interventions. BMI = body mass index; GERD = gastroesophageal reflux disease; KQ = Key Question
Analytic framework for binge-eating disorder and loss-of-control eating: course of illness (outcomes of the disorders). BMI = body mass index; GERD = gastroesophageal reflux disease; KQ = Key Question
Topic Refinement and Protocol Review
This topic and its KQs were developed through a public process. The Binge-Eating Disorder Association nominated the topic. The RTI International–University of North Carolina Evidence-based Practice Center (EPC) further developed and refined the topic with input from Key Informants in the field. The Agency for Healthcare Research and Quality (AHRQ) posted provisional KQs for public comment on January 13, 2014. We incorporated public comments and guidance from a Technical Expert Panel into the final research protocol (posted on the AHRQ Web site on April 4, 2014).
Literature Search Strategy
Search strategy.
We conducted focused searches of MEDLINE ® (via PubMed ® ), Embase ® , CINAHL (nursing and allied health database), Academic OneFile, and the Cochrane Library. An experienced research librarian used a predefined list of search terms and medical subject headings. The librarian completed the searches for the draft report on June 23, 2014; she conducted a second (update) search on January 19, 2015, during peer review.
We searched for relevant unpublished and gray literature, including trial registries, specifically ClinicalTrials.gov and Health Services Research Projects in Progress. AHRQ requested Scientific Information Packets (SIPs) from the developers and distributors of interventions identified in the literature review. We also requested Technical Expert Panel members’ and Peer Reviewers’ recommendations of additional published, unpublished, and gray literature not identified by the review team. We included unpublished studies that met all inclusion criteria and contained enough information on their research methods to permit us to make a standard risk-of-bias assessment of individual studies. This could include, but was not limited to, conference posters and proceedings, studies posted on the Web site ClinicalTrials.gov, and U.S. Food and Drug Administration (FDA) medication approval packages. We included unpublished studies that met all inclusion criteria and contained enough information to permit us to make a standard risk-of-bias assessment. We searched reference lists of pertinent review articles for studies that we should consider for inclusion in this review, including our earlier review on this topic. 16 – 18
Inclusion and Exclusion Criteria
We developed inclusion and exclusion criteria with a framework in mind that considered the relationship among the patient populations, interventions, comparators, outcomes, timing of outcome assessments, and settings (PICOTS). We considered only trials or studies written in English; additional evidence possibly available in non–English-language studies that had an abstract in English is also discussed.
The populations of interest are (1) individuals meeting DSM-IV or DSM-5 criteria for BED, (2) postbariatric surgery patients with LOC eating, and (3) children with LOC eating. We excluded studies of individuals with co-occurring anorexia nervosa or bulimia nervosa and studies of children younger than 6 years of age. We excluded trials with fewer than 10 participants and nonrandomized studies with fewer than 50 participants.
Treatments of interest include pharmacological interventions (e.g., antidepressants, anticonvulsants, attention-deficit hyperactivity disorder [ADHD] medications, and weight loss medications) and interventions that combine various psychological and behavioral techniques and principles to varying degrees (e.g., cognitive behavioral therapy [CBT], interpersonal psychotherapy [IPT], behavioral weight loss [BWL], dialectical behavioral therapy [DBT], and psychodynamic interpersonal therapy [PIPT]). We sought evidence on complementary and alternative medicine treatments but did not find any, and such interventions are not further discussed. Treatment combinations could involve psychological and behavioral interventions or psychological and behavioral with pharmacological interventions. Included studies had to have at least two groups. Acceptable comparisons included one of the other treatment comparisons, placebo, nonintervention, wait-list controls, or treatment as usual.
For psychological and behavioral interventions, we evaluated evidence by modality separately: individual and group therapy, and therapist-led and self-help approaches. The modalities involve a different therapist-patient relationship and level of health care resources; and only group therapy includes the influence of other patients suffering from the condition in the therapeutic process.
We specified a broad range of outcomes—intermediate and final health benefit outcomes and treatment harms ( Figures A and B ). We analyzed five groups of treatment effectiveness and course-of-illness outcomes: binge-eating outcomes, eating-related psychopathology outcomes, weight-related outcomes, general psychological outcomes (e.g., depression), and other (e.g., quality of life). Potential harms (also a broad range of minor to severe side effects or adverse events) varied across intervention types. Outcome differences for subgroups were evaluated for both treatment effectiveness and course of illness. We reported treatment outcomes at the end of treatment or later, but course-of-illness studies had a 1-year minimum followup from the diagnosis.
We included studies with inpatient or outpatient settings. We did not exclude studies based on geography.
Study designs included meta-analyses, systematic reviews, randomized controlled trials (RCTs), nonrandomized controlled trials, prospective and retrospective cohort studies, and case-control studies. We counted systematic reviews only if they provided information used in the evidence synthesis.
Study Selection
Trained members of the research team reviewed article abstracts and full-text articles. Two members independently reviewed each title and abstract using the predefined inclusion and exclusion criteria. Studies marked for possible inclusion by either reviewer underwent a full-text review. Two members of the team independently reviewed each full-text article. If both reviewers agreed that a study did not meet the eligibility criteria, it was excluded; each reviewer recorded the primary reason for exclusion. If reviewers disagreed, they resolved conflicts by discussion and consensus or by consulting a third member of the review team. We screened unpublished studies and reviewed SIPs using the same title/abstract and full-text review processes. The project coordinator tracked abstract and full-text reviews in an EndNote database (EndNote ® X4).
Data Abstraction
We developed a template for evidence tables using the PICOTS framework and abstracted relevant information into the tables using Microsoft Excel. We recorded characteristics of study populations, interventions, comparators, settings, study designs, methods, and results. Six trained members of the team participated in the data abstraction. One reviewer initially abstracted the relevant data from each included article; a second more senior member of the team reviewed each data abstraction against the original article for completeness and accuracy.
Risk-of-Bias Assessment
We assessed risk of bias with three appropriate tools, described in more detail in the full report: (1) one for judging trials based on the Cochrane risk-of-bias tool for RCTs and summary judgments corresponding with EPC guidance; (2) one for evaluating risk of bias in non-RCTs and observational studies (modified from 2 existing tools); and (3) AMSTAR (A Measurement Tool To Assess Systematic Reviews) for assessing the quality of a systematic review. Two independent reviewers rated the risk of bias for each study. Disagreements between the two reviewers were resolved by discussion and consensus or by consulting a third member of the team.
Risk of bias is reported as a rating of low, medium, or high. RCTs with a high risk of bias are those with at least one major issue that has the potential to cause significant bias and thus might invalidate its results; such flaws include different application of inclusion/exclusion criteria between arms, substantial differences in arms at baseline, high overall attrition, differential attrition across arms that is not adequately addressed through analytic methods, or lack of control for concurrent treatment. An RCT may be evaluated as medium risk of bias, in contrast to low risk of bias, if the study does not have an obvious source of significant bias but, while it is unlikely that the study is biased because of the reported conduct in relation to other aspects of the trial, information on multiple bias criteria is unclear because of gaps in reporting. A key consideration in evaluating the risk of bias of cohort and case-control studies (only for our course-of-illness analyses) was control for critical potential confounding through design or statistical analyses. If critical information for making that assessment was not reported or was unclear, or if the conduct or analysis was severely flawed, we rated the study as high risk of bias.
To maintain a focus on interpretable evidence, we opted generally not to use trials with a high risk of bias in synthesizing treatment benefits. However, we did consider studies with high risk of bias in sensitivity analyses of our meta-analyses of treatment benefits and as allowable evidence for both treatment harms and course of illness.

Data Synthesis
For quantitative synthesis (meta-analyses to estimate overall effect sizes using Comprehensive Meta-Analysis, version 3.2), we had sufficiently similar evidence for placebo-controlled trials of second-generation antidepressants and lisdexamfetamine and for wait-list–controlled trials of therapist-led CBT. We did all other analyses qualitatively, based on our reasoned judgment of similarities in measurement of interventions and outcomes, and homogeneity of patient populations.
Strength of the Body of Evidence
We graded the strength of evidence based on the “Methods Guide for Effectiveness and Comparative Effectiveness Reviews.” 19 This EPC approach incorporates five key domains: study limitations, directness, consistency, precision of the evidence, and reporting bias. Reviewers may also consider three optional domains if relevant to the evidence: increasing dose response, large magnitude of effect, and an effect that would have been larger if confounding variables had not been controlled for in the analysis.
Grades reflect the strength of the body of evidence to answer each KQ. A grade of high strength of evidence indicates that we have high confidence that the evidence reflects the true effect. Moderate strength of evidence indicates that we have moderate confidence that the evidence reflects the true effect. Low strength of evidence suggests that we have low confidence that the evidence reflects the true effect. Insufficient evidence signifies that the evidence is not available, that we are unable to estimate an effect, or that we have no confidence in the estimate of the effect.
Two reviewers assessed each domain independently and also assigned an overall grade for comparisons for each key outcome; they resolved any conflicts through consensus discussion. If they did not reach consensus, the team brought in a third party to settle the conflict.
Applicability
We assessed the applicability both of individual studies and of the body of evidence. For individual studies, we examined factors that may limit applicability (e.g., characteristics of populations, interventions, or comparators). Such factors may lessen our ability to generalize the effectiveness of an intervention for use in everyday practice. We abstracted key characteristics of applicability into evidence tables. During data synthesis, we assessed the applicability of the body of evidence using the abstracted characteristics.
Peer Review and Public Commentary
Experts in BED and LOC eating, specifically clinicians and researchers specializing in pharmacotherapy treatment, psychotherapy and behavioral treatment, pediatrics, and evidence-based interventions, were invited to provide external peer review of the draft review. AHRQ staff (Task Order Officer and EPC Program Director) and an Associate Editor also provided comments. Associate Editors are leaders in their fields who are also actively involved as directors or leaders at their EPC. The draft report was posted on the AHRQ Web site for 4 weeks to elicit public comment. We responded to all reviewer comments and noted any resulting revisions to the text in the Disposition of Comments Report. This disposition report will be made available 3 months after AHRQ posts the final review on its Web site.
We report results by KQ, grouped basically by intervention comparison (for treatment effectiveness and harms). We cover BED, LOC eating, and then course-of-illness findings in that order. Tables C–E summarize key findings and strength-of-evidence grades. The full report contains summary tables for results. Appendix D of the full report documents risk-of-bias assessments; Appendix E presents evidence tables for all included studies.
Literature Searches
Figure C , a PRISMA [Preferred Reporting Items for Systematic Reviews and Meta-Analyses] diagram, depicts our literature search results. We identified a total of 4,395 unduplicated citations and determined that 918 met criteria for full-text review. We excluded 809 full-text articles based on our inclusion criteria and retained 105 articles reporting on a total of 83 trials or studies and 1 systematic review. Because we used some abstractions from our 2006 systematic review on eating disorders to develop some BED treatment and course-of-illness results, we consider that review as included evidence. 16 – 18 However, we reevaluated the risk of bias for all earlier included studies because we updated our assessment tools.
PRISMA diagram for binge-eating disorder treatment and course of illness. AHRQ = Agency for Healthcare Research and Quality; KQ = Key Question; PRISMA = Preferred Reporting Items for Systematic Reviews and Meta-Analyses a Three studies (3 articles) also (more...)
We did not use 19 studies in our main analyses of treatment benefits because of their high risk of bias. In keeping with standard approaches, however, we included one of these studies, which compared an antidepressant medication with placebo, in sensitivity analysis of our meta-analysis findings. 20 This was the only study with high risk of bias that reported on a treatment comparison that we evaluated through meta-analysis. We also used seven of the studies with high risk of bias in our assessment of treatment harms. 20 – 26
We used 52 studies (67 articles) in our main analysis of treatment benefits (both BED and LOC eating). Fifteen studies (23 articles) met inclusion criteria for course-of-illness KQs. We used all 15 studies in that evidence synthesis, regardless of our risk-of-bias rating for the study.
Of the 20 fair- or good-quality studies on treatment for BED from our previous systematic review, 19 trials met the inclusion criteria for this review. One study was excluded because it used sibutramine, a treatment method no longer available in the United States. 27 Four studies 20 , 24 , 28 , 29 that we had rated as good or fair quality for the earlier review were newly rated as high risk of bias; we omitted them, therefore, from our main analyses. The earlier review also included three studies on BED course of illness that we have used here. 30 – 32
Key Question 1. Effectiveness of Interventions for Binge-Eating Disorder
For treatment effectiveness for BED, we address three broad categories of treatment: pharmacological, psychological or behavioral, and combination treatments.
For medications, the 18 included trials involved second-generation antidepressants, anticonvulsants, ADHD medications, an antiobesity drug, and a variety of other agents, including one dietary supplement. Among the antidepressants were several selective serotonin reuptake inhibitors (SSRIs) and several agents that primarily inhibit norepinephrine reuptake (i.e., norepinephrine-dopamine reuptake inhibitor [NDRI] or selective serotonin-norepinephrine reuptake inhibitor [SNRI]). Among the ADHD medications were lisdexamfetamine and atomoxetine.
In the category of psychological and behavioral treatments, the 23 included trials involved CBT, DBT, IPT, BWL, PIPT, and inpatient treatment.
Seven trials provided data on combination treatments, including pairings of CBT, BWL, hypocaloric diet, and diet counseling with either an antidepressant or an antiobesity medication. Two of the seven trials paired compound nonpharmacotherapy treatments (i.e., CBT plus BWL, CBT plus diet counseling) with an antidepressant. All trials testing a combination psychological plus pharmacological treatment arm also included a comparable combination placebo-controlled treatment arm (e.g., CBT plus antidepressant compared with CBT plus placebo).
Given the variability in outcome reporting and treatment comparisons, we were able to conduct meta-analyses only to measure the effectiveness on several outcomes of antidepressant treatments, as a class, compared with placebo; lisdexamfetamine compared with placebo; and therapist-led CBT compared with wait-list.
Pharmacological Interventions: Antidepressants Compared With Placebo
Eight RCTs (all placebo controlled) examined the effectiveness of antidepressants for treating BED patients. Of these, six involved an SSRI, 33 – 38 and one each involved an NDRI 39 or an SNRI. 40 In the six SSRI trials, two studied fluoxetine, 33 , 34 and one each studied citalopram, 38 escitalopram, 35 fluvoxamine, 36 and sertraline. 37 Assessments were conducted at the end of treatment.
As a class, antidepressants were associated with better binge-eating outcomes than placebo: abstinence (high strength of evidence for benefit), reduction in frequency of binge episodes per week (high strength of evidence for benefit), and reduction in binge days per week (moderate strength of evidence for benefit). Antidepressants were also associated with greater reductions in eating-related obsessions and compulsions (moderate strength of evidence for benefit). Weight reductions and BMI reductions were no greater with antidepressants (for both outcomes, low strength of evidence for no difference). Lastly, antidepressants were associated with greater reductions in symptoms of depression (low strength of evidence for benefit). The evidence was insufficient to evaluate outcomes for any specific antidepressant medication.
Pharmacological Interventions: Antidepressants Compared With Other Active Interventions
One trial involved a head-to-head comparison of two second-generation antidepressants (fluoxetine and sertraline). 41 The evidence was insufficient for concluding anything about treatment superiority.
Pharmacological Interventions: Anticonvulsants Compared With Placebo
Three placebo-controlled RCTs provided evidence about treating BED patients with anticonvulsants; two involved topiramate 42 , 43 and one lamotrigine. 44 Topiramate was associated with abstinence among a greater percentage of participants and with greater reductions in binge eating, obsessions and compulsions related to binge-eating, and weight (moderate strength of evidence for benefit); it also produced greater increases in cognitive restraint and reductions in hunger, disinhibition, and impulsivity (low strength of evidence for benefit). The evidence on the efficacy of lamotrigine was limited to one small trial (insufficient strength of evidence).
Pharmacological Interventions: Attention-Deficit Hyperactivity Disorder Medications Compared With Placebo
The included evidence consisted of four placebo-controlled RCTs of pharmacological interventions that were originally formulated for ADHD and were now being tested for treating patients with BED. One trial investigated the norepinephrine reuptake inhibitor atomoxetine, 45 which has been associated with weight loss; the other three studied the stimulant lisdexamfetamine. 46 The effectiveness of atomoxetine was examined in one small RCT (insufficient strength of evidence). Based on evidence from three RCTs, lisdexamfetamine was associated with abstinence among a greater percentage of participants, greater reductions in binge episodes per week, decreased eating-related obsessions and compulsions, and greater reductions in weight (high strength of evidence for all of these outcomes). Depression measures were not consistently reported across the three studies; one of the studies found no difference from placebo (insufficient strength of evidence). Recently, lisdexamfetamine became the first medication approved by the FDA for treating BED patients. 47
Pharmacological Interventions: Other Medications Compared With Placebo
Three placebo-controlled RCTs dealt with other pharmacological interventions. One trial each investigated the following: the sulfonic acid acamprosate, which is a mixed GABA A receptor agonist/NMDA receptor antagonist; 48 the μ-opioid antagonist ALKS-33 (also known as samidorphan); 49 and the dietary supplement chromium picolinate. 50 The strength of evidence is insufficient to determine effectiveness of any of these treatments because each was studied in a single, small sample trial.
Behavioral Interventions: Cognitive Behavioral Therapy Compared With No or Limited Intervention
CBT can be delivered in various formats; approaches include therapist-led, partially therapist-led, and self-help strategies (i.e., structured, guided, and pure). The two therapist-led approaches can involve either individual sessions (one-on-one) or group sessions.
Nine trials compared CBT with limited or no intervention. 51 – 59 Of 12 comparisons (in 7 separate trials) involving CBT and wait-list controls, 5 involved therapist-led CBT, 51 – 55 2 involved partially therapist-led CBT, 54 , 55 2 used structured self-help CBT, 54 , 55 2 used guided self-help CBT including one Internet-based guide 56 and one in-person guide, 57 and 1 used pure self-help CBT. 57 Two wait-list trials delivered CBT in an individual format 56 , 57 and five delivered CBT in a group format. 51 – 55
Therapist-led CBT was related to various improved outcomes, including abstinence, binge frequency, and eating-related psychopathology (high strength of evidence for all outcomes). In contrast, reductions in BMI and symptoms of depression were not greater (both moderate strength of evidence for no difference). Similarly, partially therapist-led CBT was related to a greater likelihood of abstinence and reduced binge frequency (both low strength of evidence), but reductions in BMI and symptoms of depression were not greater (both low strength of evidence for no difference). Structured self-help was associated with reduced binge frequency (low strength of evidence) but no greater reduction in BMI or symptoms of depression (low strength of evidence for no difference).
Five small RCTs examined the effectiveness of guided or pure self-help CBT, but they differed in delivery format or comparator, and therefore evidence was insufficient for all comparisons and outcomes.
Behavioral Interventions: Cognitive Behavioral Therapy Compared With Cognitive Behavioral Therapy Variants
Seven trials compared CBT delivered in one format with CBT delivered in a different format. 54 , 55 , 57 , 60 – 63 Variations across trials resulted in four therapist-led comparisons: exposure versus cognitive restructuring, 60 CBT alone versus CBT plus ecological momentary assessment, 61 individual versus group, 62 and fully therapist-led versus partially therapist-led interventions. 54 , 55 , 63 Several self-help comparisons were also tested: one for guided self-help versus pure self-help 57 and two for therapist-led versus structured self-help. 54 , 63
Only three of these comparisons were replicated in more than one trial. Binge-eating outcomes did not differ across comparisons of variations in therapist-led CBT, with one exception favoring therapist-led over structured self-help in one trial (low strength of evidence for no difference). BMI and depression outcomes did not differ across types of CBT (both moderate strength of evidence for no difference).
Behavioral Interventions: Cognitive Behavioral Therapy Compared With Behavioral Weight Loss
Four trials compared CBT with BWL approaches; 59 , 64 – 66 one also compared CBT and BWL (separately) with CBT plus BWL. 65 The CBT format varied across trials and included both therapist-led 64 , 65 and guided self-help. 59 , 66 For comparisons with therapist-led CBT, results were mixed. Binge frequency was lower in the therapist-led CBT arm (low strength of evidence), and BMI reduction was greater in the BWL arm at the end of treatment (moderate strength of evidence); the groups did not differ with respect to abstinence, eating-related psychopathology, or depression outcomes (low strength of evidence for no difference). Evidence on comparisons with guided self-help was insufficient because all comparisons were limited to single, small trials.
Behavioral Interventions: Cognitive Behavioral Therapy Compared With Interpersonal Therapy
Three trials compared CBT with interpersonal therapy strategies in treating patients with BED. 51 , 66 , 67 Two trials compared therapist-led IPT with either therapist-led CBT 68 or guided self-help CBT. 66 Another trial compared therapist-led CBT with therapist-led PIPT. 51 Because trials differed in the intervention types that were compared, we could not synthesize results across trials (insufficient strength of evidence for all outcomes).
Behavioral Interventions: Cognitive Behavioral Therapy Combined With Diet or Weight-Loss Interventions
Three trials examined the use of CBT plus additional interventions involving either diet or weight-loss strategies (or both) in treating patients with BED. These involved two trials comparing CBT alone with CBT plus a diet or weight-loss intervention 65 , 69 and a single trial comparing CBT plus a low-energy dense diet with CBT plus general nutritional counseling. No significant differences were found for virtually any outcomes (insufficient strength of evidence in all cases).
Behavioral Interventions: Behavioral Weight Loss
Two trials tested BWL interventions for BED patients. These compared guided self-help BWL with an active control 59 and therapist-led BWL with therapist-led IPT. 66 Strength of evidence was insufficient because each comparison was limited to one small trial.
Behavioral Interventions: Psychodynamic Interpersonal Therapy Versus Wait-List
One small trial examined the effectiveness of therapist-led group PIPT. 51 Strength of evidence was insufficient for all outcomes.
Behavioral Interventions: Dialectical Behavioral Therapy
One trial evaluated therapist-led DBT against therapist-led active comparison-group therapy (insufficient strength of evidence for all outcomes). 70 – 72
Behavioral Interventions: Inpatient Treatment Versus Inpatient Treatment Plus Active Therapies
Three trials examined treatment in an inpatient setting. 73 – 75 In each trial, patients received a standard inpatient care program and were randomized to additional active therapies. Two trials used virtual reality treatments that aimed to reduce body image distortions and food-related anxiety. However, these trials differed in several ways, so results were all based on single, small studies (insufficient strength of evidence for all outcomes).
Pharmacological Interventions: Combination Treatments Compared With Placebo and With Other Treatments
Evidence about combination interventions came from seven placebo-controlled RCTs. In all seven trials, investigators combined a medication with a psychological treatment; in two, they combined a medication with two psychological treatments. 34 , 76 Three trials used an antidepressant; 34 , 76 , 77 one, an anticonvulsant; 78 and three, an antiobesity agent. 79 – 81 The psychological interventions included CBT in three trials, 34 , 78 , 80 BWL in one trial, 80 CBT plus BWL in one trial, 77 hypocaloric diet in one trial, 81 and group psychological support plus diet counseling in one trial. 76 The strength of evidence was insufficient to reach a conclusion concerning the effectiveness of any specific combination treatment because each combination was studied only in a single, small trial.
Key Question 2. Harms Associated With Treatments or Combinations of Treatments for Binge-Eating Disorder
Virtually all harms were limited to pharmacotherapy intervention trials (reported in 33 trials). Harms associated with treating BED patients and discontinuations from studies attributable to harms occurred approximately twice as often in patients receiving pharmacotherapy as in those receiving placebo. The number of serious adverse events was extremely low. Topiramate was associated with a significantly higher number of events involving sympathetic nervous system arousal (e.g., sweating, dry mouth, rapid heart rate) and “other” events (moderate strength of evidence), as well as a higher number of events related to sleep disturbance (low strength of evidence). Fluvoxamine was associated with greater gastrointestinal (GI) upset and sleep disturbances (low strength of evidence). Lisdexamfetamine was associated with a significantly higher likelihood of insomnia and headache (high strength of evidence), as well as greater GI upset, central nervous system arousal, and decreased appetite (moderate strength of evidence).
Key Questions 6 and 7. Effectiveness of Interventions (and Harms From Interventions) for Loss-of-Control Eating in Bariatric Surgery Patients
We found no evidence meeting our inclusion criteria that examined treatments or combinations of treatments for LOC eating among bariatric surgery patients.
Key Questions 11 and 12. Effectiveness of Interventions (and Harms From Interventions) for Loss-of-Control Eating in Children
Four small trials examined behavioral interventions for children with LOC eating. 82 – 85 One trial was a pilot for a larger trial by the same investigator group. The trials differed in the age range of participants (adolescents only or both adolescents and younger children), the definition of LOC eating that the investigators used to determine participant eligibility, treatment comparisons, and measures used to evaluate binge outcomes. With the exception of weight (low strength of evidence for no difference), strength of evidence was insufficient across all outcomes.
Key Questions 3, 8, and 13. Differences in the Effectiveness of Treatments or Combinations of Treatments for Subgroups
We found no evidence on differences by age, sex, race, ethnicity, sexual orientation, initial BMI, duration of illness, or coexisting conditions in any of our three populations of interest: patients with binge-eating disorder, bariatric surgery patients with LOC eating, and children with LOC eating.
Key Question 4. Course of Illness Among Individuals With Binge-Eating Disorder
Our evidence included 10 studies; all followed patients who had been identified through their earlier participation in a treatment study. 30 , 31 , 62 , 66 , 67 , 86 – 93 Factors that individual studies identified as being related to better outcomes included more rapid response to treatment, improvement in eating-related psychopathology, and improvement in non–eating-related psychopathology. Studies differed in the characteristics that the investigators had hypothesized might be related to better outcomes (insufficient strength of evidence). Binge outcomes were the most commonly reported outcomes across studies. Four studies reported weight outcomes (BMI), but results were mixed (insufficient strength of evidence). One study found an increased risk of miscarriage among women with BED (insufficient strength of evidence). 94 Finally, one study (of attempted suicides) 93 and a review article of three studies (of suicides) 92 found no evidence of increased risk of suicide among BED patients 5 years after treatment (moderate strength of evidence for no effect).
Key Question 9. Course of Illness Among Bariatric Surgery Patients With Loss-of-Control Eating
Two studies met our inclusion criteria but differed in the criteria they used for defining LOC eating before surgery. 32 , 95 One study found that LOC eating before surgery was related to LOC eating following surgery but not to weight loss or weight regain (insufficient strength of evidence across all outcomes because of a lack of clear and consistent findings in more than 1 study.)
Key Question 14. Course of Illness Among Children With Loss-of-Control Eating
Evidence concerning the course of illness among children with LOC eating behavior came from three longitudinal cohort studies. 96 – 102 Early adolescent binge or LOC eating predicted similar behavior in later adolescence in two studies (low strength of evidence). Evidence of additional outcomes was limited or inconsistent across studies (insufficient strength of evidence).
Key Questions 5, 10, and 15. Differences in Course of Illness for Subgroups
We found no evidence examining differences in the course of illness based on differences in sociodemographic or health characteristics (age, sex, race, ethnicity, sexual orientation, initial BMI, duration of illness, or coexisting conditions) in any of our three populations of interest: individuals with binge-eating disorder, bariatric surgery patients with LOC eating, and children with LOC eating.
Key Findings and Strength of Evidence
We limit our discussion to key findings, chiefly on effectiveness ( KQ 1 ) and harms ( KQ 2 ) of common therapies for BED patients. Tables document main findings and strength-of-evidence grades (arrived at following AHRQ guidance). Other treatment results for BED and all treatment results for LOC eating can be found in the previous results section and in more detail in the full report. We comment briefly on course of illness in this section.
Key Question 1. Effectiveness of Treatments or Combinations of Treatments for Binge-Eating Disorder
Commonly studied treatments for BED patients are pharmacological agents and therapies that combine psychological and behavioral approaches. For outcomes of pharmaceuticals (compared with placebo) and psychological and behavioral treatments (compared with wait-list or inactive controls), findings are limited to outcomes measured at the end of treatment. In contrast, patients enrolled in comparative effectiveness trials comparing two or more psychological and behavioral treatments or two or more formats of the same intervention tended to be assessed beyond the end of treatment, most commonly less than 1 year but in some instances 2 years or more.
Pharmacological Interventions
Table C summarizes the pharmacological interventions on which we had low, moderate, or high strength of evidence for clinical outcomes. Evidence based on meta-analyses pertains to second-generation antidepressants and lisdexamfetamine; evidence based on qualitative synthesis pertains to topiramate and lisdexamfetamine.
Strength of evidence for pharmacological interventions to improve outcomes in binge-eating disorder.
As a class, second-generation antidepressants were superior to placebo for achieving BED-specific and related clinical outcomes; the magnitude of the benefits generally was modest. Evidence was insufficient to demonstrate the effectiveness or comparative effectiveness of specific second-generation antidepressants for treating BED patients. Antidepressants were 1.67 times as likely as placebo to help patients achieve abstinence from binge eating (high strength of evidence). They reduced the weekly frequency of binge-eating episodes by approximately two-thirds of a binge episode per week (high strength of evidence) and approximately one binge-eating day (moderate strength of evidence). Even though patients improved, many did not achieve abstinence with antidepressants; 41 percent of those receiving antidepressants and 23 percent of those receiving placebo achieved abstinence.
For treating psychological aspects and correlates of BED, antidepressants helped reduce obsessive thoughts and compulsions related to binge eating and modestly improved symptoms of depression (low strength of evidence for benefit).
Overweight and obese patients treated with antidepressants did not lose significantly more weight during treatment than those who did not receive an antidepressant; BMI did not differ between groups (low strength of evidence for no difference in both cases). Given the limited impact on weight and the short length of treatment (6 to 12 weeks), finding no difference in the change in BMI at the end of treatment is not surprising.
Topiramate reduced the frequency of binge eating by approximately 1 binge day per week more than placebo; it helped more patients (BED, 58%; placebo, 28%) achieve abstinence from binge eating (moderate strength of evidence for benefit). Topiramate helped lower obsessive thoughts and compulsions related to binge eating by approximately 30 percent more than placebo and reduce greater general psychological distress symptoms by approximately 23 percent more than placebo (moderate strength of evidence for benefit). Among overweight and obese patients, those treated with topiramate lost, on average, approximately 10 pounds more (equivalent to ~4% more total body weight) than those who received placebo (moderate strength of evidence for benefit). Compared with placebo, topiramate also decreased patients’ susceptibility to hunger as a trigger for binge eating, improved their general tendency to act less impulsively, increased their sense of cognitive control over their binge eating, and decreased disruptions in their social and family life (low strength of evidence for benefit).
Lisdexamfetamine improved binge-eating outcomes. Patients treated with lisdexamfetamine were 2.61 times as likely to achieve abstinence from binge eating as those who received placebo (high strength of evidence for benefit): across all study participants, 40 percent in the treatment arm, compared with 15 percent in the placebo arm, achieved abstinence. Patients treated with lisdexamfetamine also experienced a greater reduction in binge-eating days per week than those receiving placebo: point estimates of the differences in two Phase 3 trials were 1.3 and 1.7 fewer days, respectively (high strength of evidence for benefit). Lisdexamfetamine was associated with superior eating-related psychopathology outcomes, as measured through the Yale-Brown Obsessive Compulsive Scale Modified for Binge Eating (YBOCS-BE) (high strength of evidence for benefit), and with weight reduction (high strength of evidence). However, data on depression and other psychological outcomes were too limited to be evaluated (insufficient strength of evidence).
Psychological and Behavioral Interventions
Table D summarizes the psychological and behavioral interventions for which we had low, moderate, or high strength of evidence for treatment benefits. We found evidence for all outcomes at the end of treatment and for some outcomes over periods as long as 6 years after treatment ended.
Strength of evidence for psychological or behavioral interventions to improve outcomes in binge-eating disorder.
CBT reduced outcomes related to BED, measured as binge frequency and achieved abstinence, compared with those on wait-list. These benefits were apparent for four forms of CBT (therapist led, high strength of evidence; partially therapist led, structured self-help CBT, and guided self-help CBT, all low strength of evidence). Evidence of the benefits of therapist-led CBT was particularly compelling; meta-analyses estimated a 4.95 times greater likelihood of abstinence (59% CBT; 11% wait-list) and a reduction of 2.3 binge episodes per week. For reducing general and eating-related psychological symptoms, therapist-led CBT reduced patients’ susceptibility to hunger and eating concerns and improved their sense of control over eating (high strength of evidence); guided self-help CBT helped patients reduce global eating-related psychopathology (low strength of evidence). However, across the various forms of CBT, treatment was generally no better than wait-list for reducing weight or symptoms of depression (low strength of evidence for no difference). Collectively, this body of evidence suggests that some forms of CBT help patients with BED improve in several key behavioral and eating-specific psychological domains.
We examined the comparative effectiveness of three different forms of CBT with each other: therapist-led CBT, partially therapist-led CBT, and structured self-help CBT. These comparisons are of interest, as they provide insight about the relative importance of therapist involvement in the effectiveness of CBT. Across comparisons, we found virtually no differences in binge-eating, BMI, or depression outcomes (low strength of evidence for no difference). All three of the CBT approaches were generally effective at helping patients both achieve binge abstinence and reduce binge frequency, most notably at end of treatment but throughout both short-term (6 month) and long-term (12 month) followup. Thus, although CBT variations generally did not differ in their ability to improve outcomes related to binge eating, they produced significant improvements in core outcome domains (regardless of treatment arm) over time.
We compared therapist-led CBT with therapist-led BWL treatment on outcomes assessed at the end of treatment and, in limited studies, for up to 6 years after treatment ended. CBT was superior to BWL for decreasing binge frequency at end of treatment and up to 12-month followup (low strength of evidence for benefit). BWL produced better BMI outcomes than CBT at end of treatment (moderate strength of evidence), but BWL patients tended to regain the weight they had lost during treatment. However, groups did not differ in abstinence, eating-related psychopathology, or symptoms of depression at end of treatment or at 12-month or 6-year followup.
Key Question 2. Evidence for Harms Associated With Treatments for Binge-Eating Disorder
We identified potential harms or side effects only for pharmacotherapy trials (comparisons with placebo). Table E summarizes the interventions for which we had low, moderate, or high strength of evidence for harms. Symptoms of sympathetic nervous system arousal were more common among patients who received topiramate than those who received placebo (moderate strength of evidence). Topiramate was also associated with headaches and sleep disturbances (low strength of evidence) and with a collection of other symptoms, including rash, high blood pressure, confusion, and taste aversion (moderate strength of evidence). Patients treated with fluvoxamine reported symptoms of GI upset and sleep disturbances more frequently than patients who received placebo (low strength of evidence). Patients treated with lisdexamfetamine more commonly experienced GI upset (moderate strength of evidence), sympathetic nervous system arousal (moderate strength of evidence), insomnia (high strength of evidence), headache (high strength of evidence) and decreased appetite (moderate strength of evidence).
Strength of evidence for harms of pharmacological interventions to improve outcomes in binge-eating disorder.
Ten studies (trials or observational studies, including 3 rated high risk of bias) provided information on outcomes of BED patients 1 year or longer after their diagnosis; all involved only individuals who had participated in BED treatment studies. Investigators commonly reported binge outcomes, but they tended to offer different hypotheses about what factors might be related to better outcomes; these variables included more rapid response to treatment, improvement in eating-related psychopathology, and improvement in non–eating-related psychopathology. One study found that the odds of miscarriage were higher among women with BED (1 study, insufficient evidence); a review article (3 studies) and an additional study found no evidence of increased risk of suicide among BED patients 5 years after treatment (moderate strength of evidence for no effect.)
Findings in Relation to What Is Already Known
Our 2006 review, “Management of Eating Disorders , ” 16 – 18 included evidence on treatment and course of illness for BED. Based on our qualitative analysis of eight RCTs, we concluded that medications improved clinical outcomes. Two later meta-analyses reached a similar conclusion. Stefano and colleagues 103 included seven (of our 8) RCTs and focused specifically on antidepressant medications; Reas and Grilo 104 included six of those RCTs and two new trials of SSRIs, and focused specifically on SSRIs. Those studies estimated similar effect sizes for abstinence (risk ratio of nonabstinence from binge eating: 0.77 and 0.81, respectively), but they reached different conclusions about weight and depression outcomes.
For the current review, we excluded two of the eight RCTs from our earlier review (one because it was newly rated as high risk of bias and a second because it used a medication no longer available in the United States). Also, we included two newer antidepressant trials, 39 , 40 one anticonvulsant trial, 44 one trial of atomoxetine, 45 and three new trials of lisdexamfetamine 46 , 105 – 107 not included in either the 2008 or 2009 meta-analyses.
Based on this additional evidence, we confirmed our earlier conclusion about the effectiveness of second-generation antidepressants for binge abstinence and binge frequency. We also provided new findings regarding the effectiveness of second-generation antidepressants for eating-related obsessions and compulsions, weight, and depression outcomes. In the current review, we included one additional anticonvulsant RCT but were not able to add new information regarding effect size for anticonvulsant medications because of high variability among studies.
With regard to psychological and behavioral interventions, our previous review concluded that CBT effectively reduces binge frequency and increases binge abstinence, based on a qualitative synthesis of eight RCTs. For the current review, we excluded 2 of the 8 RCTs from our earlier review (newly rated as high risk of bias 28 , 29 ) and added 16 new RCTs. 51 – 53 , 56 , 58 , 59 , 61 , 62 , 64 – 66 , 69 , 70 , 74 , 75 , 108 Based on this newer body of evidence, we confirmed our earlier conclusion establishing CBT as an effective treatment for improving binge abstinence and reducing binge frequency; we also reported its effectiveness at reducing eating-related psychopathology. We provided new findings about the effectiveness of different forms of therapist involvement in CBT interventions and for promising interventions such as IPT and DBT.
For BED course of illness, our earlier review identified only three studies. Although the evidence base is larger for this review, the new studies provide little additional insight. They are mostly case series designs without comparisons or controls for potential confounding factors associated with outcomes, and they are limited to patients followed after treatment.
Our review is the only one that we have identified that has summarized the evidence on treatment and course of illness for bariatric surgery patients and children with LOC eating.
Implications for Clinical and Policy Decisionmaking
We had hoped to comment on the effectiveness and harms of specific pharmacological and psychological or behavioral treatments for BED and on the comparative effectiveness of specific treatments for BED. Unfortunately, the heterogeneity in approaches precluded offering much in the way of implications for clinical practice or policy decisionmaking. Key conclusions with meaningful ramifications for either clinical applications or policymaking follow.
For several key outcomes, we found clear evidence of benefits with second-generation antidepressants; however, we cannot comment on the effectiveness of any specific second-generation antidepressant. We confirmed previous observations of benefit with topiramate and presented new evidence of clear benefit from lisdexamfetamine. We also found strong evidence of benefit with therapist-led CBT for several key outcomes and support for the effectiveness of other forms of CBT (i.e., partially therapist-led CBT and guided self-help CBT).
Harms of psychological and behavioral treatments were rarely reported but commonly known side effects with topiramate, fluvoxamine, and lisdexamfetamine were reported. The FDA has determined that these three drugs are associated with potential risk during pregnancy; in particular, topiramate is associated with increased risk of oral clefts in newborns. 109 No pregnancy-related harms occurred in the included studies, in which women of childbearing age were overrepresented. 8 Nonetheless, clinicians may want to counsel women patients of childbearing age about the pregnancy risks of these medications in determining their long-term treatment plans.
Overall, based on the available evidence for both benefits and harms, clinicians may find second-generation antidepressants, topiramate, medications formulated for ADHD (notably lisdexamfetamine), and a few forms of CBT to be reasonable choices for the treatment of BED.
The superiority of a few CBT formats was determined for efficacy but not for comparative effectiveness; outcomes from CBT interventions were assessed in comparison with no intervention at all (wait-list control). Limited data emerged on the comparative effectiveness of various formats of CBT or comparisons between CBT formats and other approaches. Although virtually none of the available evidence showed superiority of one approach over another, we caution readers not to conclude that this implies that the various behavioral and psychological intervention formats are identical in terms of outcomes; the point is that they are not significantly different. None of the included comparative effectiveness studies was designed to examine the equivalence or noninferiority of approaches. 110 These findings have implications for decisionmakers who may be considering the resources needed for therapist-led interventions relative to those for other, less therapist-intensive forms of CBT or other behavioral interventions. These considerations may be particularly relevant for broader community settings, such as rural areas that may have limited availability of specialized treatment for BED or LOC eating.
Data on other promising treatment options, such as IPT and DBT, were limited to single trials because investigators used a wide array of delivery formats. Clinicians may want to consider these treatments for some patients. The effect of IPT on binge abstinence may be particularly durable; one study found that at 4-year followup, binge abstinence was greater in IPT than CBT patients.
We had wanted to examine the potential impact of the DSM-5 changes to make the BED diagnostic criteria less stringent: the binge frequency criterion was lessened and the duration of illness shortened. Clinicians, patients, and policymakers might have considerable interest in knowing whether effective treatment options may differ in this newly included group of patients. Unfortunately, no study provided separate results for a patient population diagnosed according to DSM-5.
We also sought to provide useful evidence concerning effective treatments for two specific populations of individuals with LOC eating. Given the complete lack of studies for bariatric surgery patients and only inconclusive or inconsistent information about children, we cannot pose any definitive implications for clinicians or policymakers at this time.
Findings about BED treatment interventions are likely to be applicable to all adults age 18 and older with the disorder, but chiefly to overweight or obese women. We cannot comment on the applicability of treatment findings for specific subgroups of adults (even among women) or whether findings extend to BED patients diagnosed based on DSM-5 criteria (which are less stringent than those for DSM-IV). Also unclear is whether our findings apply to adolescents with BED or to various minority groups.
The evidence base about treating LOC eating was small for children and nonexistent for bariatric surgery patients. Thus, generalizing to child patient populations is probably inappropriate, and generalizing to bariatric surgery patients is impossible. A key drawback is that appropriate and consistent diagnostic criteria that clinicians might reliably use to identify LOC eating have not been established.
For BED course of illness, generalizing our findings to an untreated population would be inappropriate. We can, however, offer hypotheses about several ongoing concerns. In particular, untreated BED could likely become a chronic condition that might, in turn, result in deleterious mental and physical health effects. Left untreated, the condition may lead to or worsen other mental health concerns (e.g., depression or anxiety) or physical health conditions (e.g., diabetes or irritable bowel syndrome).
Interventions and Comparators
In general, we believe that the findings about selected second-generation antidepressants, topiramate, ADHD medications, and a few forms of CBT are applicable to the BED patient populations studied. Only lisdexamfetamine has FDA approval for treating BED (presumably taking both benefits and adverse events into account).
For most treatments, tested in only a single study, we cannot draw any clear implications for clinical or policy decisionmaking. This is true for classes of interventions and single agents, such as individual antidepressants. No evidence is available on complementary and alternative medicine approaches for either BED or LOC eating.
Although we cast a wide net for outcomes, our primary focus was on reductions in commonly measured BED symptomatology, including binge frequency, eating-related obsessions and compulsions, restraint, shape and weight concerns, weight, and depression. Investigators used a considerable array of different measures or instruments to assess these outcomes; this heterogeneity constrains our ability to conclude that findings can be generalized with confidence across all outcome categories of interest. We did not find sufficient information to draw any conclusions about treatment effectiveness for more global measures, such as quality of life or lost productivity; neither did we find evidence about treatment effectiveness as it relates to final health outcomes such as diabetes, gastric reflux, and irritable bowel syndrome. Given the scarcity of information about LOC eating, we can conclude little or nothing about the applicability of these trials to proposed or potential outcomes of treatment among bariatric surgery patients or children.
All trials of medications measured outcomes at the end of treatment, but many of these trials were relatively short; only two trials reported followup beyond the end of treatment. 111 , 112 Similar studies examining the efficacy of psychological and behavioral interventions measured outcomes at the end of treatment. Comparative effectiveness studies on different psychological or behavioral interventions or different intervention formats were more likely to include both short- and long-term followup; one trial extended to 6 years after the end of treatment. Generally, the applicability of these trials for understanding the long-term impacts of treatment (benefits or harms) is relatively limited because the long-term efficacy of the individual treatments has not been established; the applicability of these studies (especially the pharmacological trials) for short-term benefits may be somewhat stronger.
The evidence base for both BED and, in children, LOC eating was largely outpatient care, which is the standard of care in the United States. We found very limited evidence about inpatient therapies, and the patient populations in studies of inpatient care (all conducted in Italy) would be unlikely to be eligible to receive inpatient care in the United States. Of all the trials we included for either BED or LOC, most were conducted in clinical settings in North America (mainly United States but also Canada); evidence also came from studies conducted in Scandinavia or elsewhere in Europe.
Generally, apart from considerations relating to health systems and insurance for the few investigations done outside North America, results are applicable to U.S. patient populations. However, most studies were conducted in supervised settings generally associated with academic research and medical centers, where medication treatment was likely managed by a psychiatrist, and psychological and behavioral treatments were likely delivered by highly trained personnel. It is unclear whether our findings apply to the real-world settings in which individuals seek and receive treatment in their local community through contact with their primary care physician or other community-based providers who do not have specific expertise in BED treatment.
Limitations of the Review Process
For this review, we excluded non–English-language studies based largely on limitations of time and resources. However, we examined English-language abstracts of non–English-language studies to assess the potential size of the literature that would be missed through this approach. Based on this exercise, we concluded that by limiting our review to English-language studies only, we may have missed only one systematic review of exercise as treatment for BED patients.
Limitations of the Evidence Base
For all medications except fluoxetine, topiramate, and lisdexamfetamine; many psychological and behavioral studies; and all combination treatment studies, the evidence base for treatment efficacy comprised only single studies. The evidence base was extremely limited in scope and volume for treatment of LOC eating in children and nonexistent for bariatric surgery patients after surgery. Evidence about harms was limited because adverse events, serious adverse events, and study discontinuations clearly attributable to adverse events were not uniformly collected or reported in studies.
We also encountered a nontrivial number of trials or other studies with substantial drawbacks in methods. The problems involved randomization and allocation concealment, masking of outcomes assessors, attrition (or differential attrition), and questionable analytic techniques (e.g., no intention-to-treat analyses). Other issues in the overall evidence base included small sample sizes (and thus lack of power for determining intended effects), lack of clarity in defining the conditions (or not reporting data separately for DSM-IV and DSM-5 patients), short studies (e.g., outcomes measured only at end of treatment, which could be just a matter of weeks), and lack of information on statistical methods (or data on confidence intervals or similar information on statistical tests).
Research Gaps
Subgroups studied.
No study addressed differences in treatment outcomes among important subgroups defined by age, sex, race, ethnicity, or other relevant patient characteristics. Observational and cross-sectional studies have shown that binge eating may be more common among certain racial minorities, yet treatment studies have failed to address whether outcomes differ between groups defined by race. These gaps limit applicability to these important groups.
Secondary analyses of data from treatment studies have shed some light on factors that may be important for future consideration, including age and sex. Nevertheless, the specific analyses that were conducted did not address whether treatment effectiveness was the same or different in these subgroups. For instance, as in our earlier systematic review of eating disorders, we identified very little information about the impact of treatments on either men or boys.
Moreover, despite the high comorbidity between BED and depression and between BED and obesity, no studies specifically compared outcomes in groups of patients defined either by baseline level of depression or by baseline weight status. Second-generation antidepressants have a small but significant impact on symptoms of depression in BED patients with low levels of depressive symptoms. Whether the small benefit of second-generation antidepressants is meaningful, or perhaps amplified, in BED patients with higher levels of depression warrants further study.
In light of growing awareness of LOC eating in children and concerns that LOC eating has negative health effects and predisposes to BED later in life, treatment studies focusing on children are needed.
Outcomes Measured (Benefits or Harms)
The evidence base was deficient for outcomes related to social and occupational functioning or quality of life more generally. It was similarly poor in relation to final health outcomes such as glucose intolerance or dysregulation that may predispose patients to diabetes and other chronic conditions. Also lacking is evidence of harms associated with psychological or behavioral treatments. A fourth critical gap concerns longer term benefits and harms for all single and combination treatment modalities.
Interventions
We found strong evidence that CBT is beneficial for patients with BED; however, that conclusion was limited largely to therapist-led CBT because of insufficient information regarding other CBT formats. At present, the body of evidence for CBT constitutes a collection of disparate studies testing variations in format; furthermore, the rationale for comparing different formats is not consistently grounded in an a priori mechanism of action.
The number of therapists with expertise in CBT for BED is limited. This limitation poses a challenge for implementation of our findings. One useful step might be to compare directly, in adequately powered head-to-head trials, whether therapist-led CBT is superior to other CBT formats. If modified versions that require less therapist involvement can be shown to be as effective as therapist-led CBT through equivalence or noninferiority trials, such information could help make CBT more scalable than it has been to this point. Findings might then guide the next generation of studies that are needed to move the field closer to an individualized approach to treatment. Those future studies should consider other psychological or behavioral interventions that have shown promise (IPT and DBT). In addition, they should be adequately powered to test for differences in outcomes across key subgroups (e.g., groups defined by age, sex, race, ethnicity, mental health comorbidities, and weight), for which a dearth of information still exists.
Second-generation antidepressants were beneficial in reducing symptoms of depression, and topiramate was beneficial for reducing symptoms of impulsivity. A head-to-head comparison of the effectiveness of these two treatment options on mood and impulse regulation outcomes might help clinicians and patients make first-line pharmacotherapy treatment choices based on individual patients’ needs and preferences. Further examination of lamotrigine may also be warranted, despite the negative findings for abstinence in one small trial; in that trial, the lamotrigine response rate (50%) was similar to that of topiramate (58% percent), but the placebo response rate was extremely high (71%). Further examination of lamotrigine may also be justified because, owing to its unique biochemical structure and function relative to topiramate, it may be associated with fewer sympathetic nervous system and other side effects. 113 , 114
Head-to-head comparisons involving pharmacological treatment, psychological treatment, and combination treatments are also needed to determine whether, as one study suggests, 34 gains persist longer following psychological (CBT) or combination (CBT + fluoxetine) treatment than following pharmacological (fluoxetine) treatment alone. This information would help patients and providers optimize their plans to address both short- and long-term goals of treatment.
CBT comparative effectiveness evidence has focused on whether less specialized care can be as effective as more intensive services (e.g., those with substantial involvement of therapists); more studies of these comparisons are needed. In addition, studies of stepped-care models can elucidate whether and when a combination treatment or a shift to higher levels of care (e.g., intensive outpatient, partial hospitalization, residential treatment, or inpatient) is warranted for patients who are not responding adequately to conventional outpatient treatment.
Despite current interest in complementary and alternative medicine, neutraceuticals, and mindfulness-based interventions for regulating appetite, eating behavior, and weight, the literature is deficient regarding these types of interventions for BED. We searched clinical trial registries to determine whether additional evidence was available from newly completed but as-yet unpublished studies. We also checked for evidence of studies that were selectively withheld from publication because of unfavorable outcomes (possible publication bias). Based on these activities, we did not determine that reporting bias was a concern.
We included as evidence a report of a Phase 2 trial of lisdexamfetamine dimesylate (Vyvanse ® ), one of two included medications originally formulated to treat patients with ADHD. In this trial, separate study arms compared dosages of 30 mg/day, 50 mg/day, and 70 mg/day with placebo. The FDA approved this medication for treatment of BED in January 2015, expanding significantly our earlier evidence base. The FDA approval was based on the results of two Phase 3 trials, limited to lisdexamfetamine dimesylate dosages of 50 or 70 mg/day (N = 773). We obtained data on these trials through the gray literature. Peer-reviewed publication of the Phase 3 trials would add to our confidence about the conduct and outcomes of these studies. In addition, the mechanism of action of lisdexamfetamine for treating BED patients is unknown, so whether similar results would emerge for other stimulants or other medications currently used to treat ADHD patients is unknown.
Deficiencies in Methods
Our 2006 review, “Management of Eating Disorders,” 16 – 18 identified several methodological issues within the BED treatment literature and recommended changes for future studies. Some of these deficiencies persist; they include inadequate reporting of randomization and allocation concealment and insufficient attention to treatment group differences in the use of cointerventions. These and other factors led us to change our risk-of-bias ratings (e.g., to high risk of bias) for some studies and, in turn, reduced the strength of the evidence for the current review.
The 2006 review also highlighted several critical needs for advancing the field. Our suggestions included conducting replication studies, doing longer term followup studies, and streamlining and standardizing outcome measures to eliminate reporting of false discoveries. Unfortunately, with few exceptions, 42 , 43 , 54 , 55 replication studies do not exist; thus, the evidence base remains insufficient to address whether gains achieved during short-term treatment persist after treatment ends. This gap is especially critical for pharmacological treatments, as patients and their providers seek to understand the need for ongoing medical management to maintain treatment gains.
The field would benefit from the development of universally accepted definitions of remission and recovery. 115 To reach this goal requires longer term followup periods with periodic reevaluation of a core set of psychological, behavioral, and physiological outcomes. Standard definitions of remission and recovery should consider a continuum approach rather than focus on just a fixed point in time.
We have two recommendations for improved designs. First, studies should implement a minimum 1-year followup period. Even longer periods of followup may be warranted to capture the remissions and improvements in illness that can occur long term. Similarly, longer trials might help clarify what treatments provide better outcomes with fewer side effects and are better for patients who do not fully recover but live with a chronic illness.
Second, future studies should include a reasonably limited set of eating-specific instruments (such as the Eating Disorder Examination questionnaire, the Three-Factor Eating Questionnaire, or the YBOCS-BE) and general psychological symptom (depression, anxiety, negative body image) self-report instruments. Adaptations of existing reliable and valid instruments 40 that are specific to binge eating might help to move the field closer to an understanding of the core determinants of recovery and relapse, but such adaptations should be used only if they are clearly described so that others can replicate their use. Such descriptions should include basic information on the reliability, validity, and reproducibility of these newer instruments.
Additionally, considering the perspective of the patient in defining remission and recovery is crucial. Using such preferences or values in developing consistent definitions of these types of patient-centered outcomes would be a major advance in this clinical area. Interweaving this information with reliable, validated measures would allow researchers and clinicians to generate a comprehensive set of parameters by which remission and recovery could be measured. Consistent and thorough reporting of these outcomes (e.g., fully descriptive data at each major assessment point) would help improve calibration of these instruments against each other, which is ultimately needed for future efforts to use meta-analysis to evaluate treatment effect size.
Further, there are several etiological and treatment considerations that might merit further study to better elucidate the onset, maintenance, and treatment of BED. For example, given the prevalence of underlying metabolic disorders (e.g., diabetes mellitus, polycystic ovary syndrome) in patients with BED, it would be useful to more fully examine the role of these disorders in the development and maintenance of BED. With regard to treatment, there may be utility in evaluating treatment interventions originally developed for post-traumatic stress disorder, given the incidence of BED in those with trauma histories.
Finally, we recommend that studies continue to measure and report binge frequency as both discrete binge episodes and binge days per week. More data are needed to resolve whether one or the other is the better choice for assessing treatment effects.
- Conclusions
Overall, we found the body of evidence to be small; often uneven across treatment types and comparisons; and, in some areas of interest, nonexistent. Nevertheless, we can conclude that antidepressants as a class, lisdexamfetamine, topiramate, and CBT effectively address major characteristics of binge eating, On the other hand, we were able to draw few conclusions regarding the comparative effectiveness of interventions or combinations of interventions. In addition, we found that harms were measured in only pharmacotherapeutic treatments. In light of the timing of this report so soon after publication of the DSM-5, the body of evidence may reasonably be expected to grow over the next few years.
Our meta-analyses provided strong evidence that second-generation antidepressants, lisdexamfetamine, and therapist-led CBT increase the likelihood of achieving abstinence. Meta-analyses also provided strong evidence that CBT and second-generation antidepressants reduce binge frequency and that second-generation antidepressants reduce obsessions and compulsions related to binge eating. Our qualitative assessments provided additional support for lisdexamfetamine (reduced binge frequency and obsessions and compulsions related to binge eating) and topiramate for treating BED patients as well. Overall, treatment benefits outweighed harms; harms were limited to medications and were severe and treatment limiting in very rare cases only.
Additional, adequately powered, multisite RCTs are needed to replicate encouraging findings observed to date only in single trials. Investigators should increase the sample sizes on which they base conclusions about treatment effectiveness; in designing comparative effectiveness studies, they should consider whether the goal is to determine whether treatment options are equivalent or superior.
The possible course of illness of LOC eating in children has been studied in three well-designed cohort studies that followed children through adolescence and into adulthood. Of particular concern in these studies is examining the important clinical and policy aspects of the role of early LOC eating on future risk of obesity and BED. The strength of conclusions that we could draw were limited by the diversity of definitions of LOC eating across both treatment trials and the longitudinal cohort studies. In particular, studies differed in the length of time that the adolescent or preadolescent respondents needed to manifest the behavior, varying from occurrence in the past year, at least once in the past 3 months, or at least weekly during the past year.
Several studies considered the relative role and importance of objective or subjective binge episodes. Distinguishing between these two constructs may be an important step for improving clinical understanding of the course of illness, in part because the frequency of subjective binge-eating behavior can be highly distressing for bariatric surgery and other patients. Furthermore, developing a common core of outcomes and a convention for reporting and analyzing those outcomes would greatly improve the capacity to compile aggregate data, compare findings across trials, and combine data from different treatment trials. These enhancements would in turn improve the ability of clinical and policy decisionmakers to understand risk factors more clearly and to develop treatment guidelines in these patient populations.
- Cite this Page Berkman ND, Brownley KA, Peat CM, et al. Management and Outcomes of Binge-Eating Disorder [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2015 Dec. (Comparative Effectiveness Reviews, No. 160.) Executive Summary.
- PDF version of this title (6.9M)
In this Page
Other titles in these collections.
- AHRQ Comparative Effectiveness Reviews
- Health Services/Technology Assessment Texts (HSTAT)
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Recent Activity
- Executive Summary - Management and Outcomes of Binge-Eating Disorder Executive Summary - Management and Outcomes of Binge-Eating Disorder
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
- Share full article
Advertisement
Supported by
scam or not
Can Dieting Actually Lead to Long-Term Weight Loss?
We asked experts to explain what diets can (and can’t) do for our health.

By Alice Callahan
Dieting has long been viewed as the path to smaller bodies and better health. Stick to the right diet, the $75 billion U.S. weight loss industry may have you think, and you, too, can lose weight and keep it off.
The rise of new weight loss drugs like Wegovy and Zepbound has highlighted just how ineffective dieting has been for the millions of people who have tried it. In a 2021 clinical trial of semaglutide (the active ingredient in Wegovy), for example, those taking the medication lost about 15 percent of their body weight in a little over a year, while those relying on just diet and exercise dropped only about 2 percent.
But there are many people who want to lose a few pounds for whom weight loss drugs are not the right choice. For those people, is old-fashioned dieting a good option?
We asked some experts to help explain what dieting can — and can’t — do for you.
Can a diet help you lose weight?
In the short term, diets do seem to help most people lose at least a small amount of weight, whether it’s a low-fat or low-carbohydrate diet or just plain calorie restriction, said Dr. Ellen Schur, the director of the University of Washington Nutrition and Obesity Research Center.
But individual results can vary. In one 2018 clinical trial , for example, researchers asked 600 people to follow either a low-fat or a low-carb diet for one year. While most participants lost weight — on average, 5 to 6 percent of their body weight (or 12 to 13 pounds) — about 15 percent gained weight during the study, and a few lost as many as 50 to 60 pounds.
It’s common, though, for people’s weight loss to plateau at around six to eight months, after which they are at risk of regaining that weight, said Dr. Maria Collazo-Clavell, an endocrinologist at the Mayo Clinic. Research suggests that most people return to their previous weight within about four years .
For those who are successful at keeping their weight off, it’s not clear if it’s because of their genetics, health history or simply their life circumstances, such as having a supportive partner, a stable job or time to cook, said Kevin Hall, a nutrition and metabolism scientist at the National Institutes of Health.
Why doesn’t the weight stay off?
When you lose weight, your body responds by increasing your appetite and reducing the number of calories you burn, Dr. Hall said.
He and others have estimated that for every two pounds of weight you lose, your metabolism slows by about 25 calories per day, and your appetite increases by about 95 calories per day. So in other words, if you lose 20 pounds, your body will burn roughly 250 calories less each day while craving about 950 calories more.
To maintain your weight loss through dieting over time, you’ll have to continue eating less while resisting a rising appetite and slower metabolism, which is “increasingly difficult,” Dr. Schur said.
The drive to eat more is so strong because our brains “sense that our energy stores are being depleted,” she added, and “that’s a threat to our survival.”
The new weight loss drugs prevent weight regain in part by reducing normal appetite signals, Dr. Collazo-Clavell said. But when people stop taking the drugs, the weight returns , probably for the same reasons described above.
Are there health risks associated with dieting for weight loss?
Dieting often results in cycles of weight loss and regain, and some research has suggested that this can be harmful, said Kendrin Sonneville, an associate professor of nutritional sciences at the University of Michigan School of Public Health.
Some, but not all , studies have found that weight fluctuation is associated with earlier death , cardiovascular disease , Type 2 diabetes and depression ; however, these studies sometimes include people who have lost and regained weight because of health problems, not just from dieting.
“There’s not conclusive evidence that it’s harmful to go up and down,” Dr. Schur said, but there is debate about the possibility.
Dr. Sonneville also worries that dieting may put some people at risk of developing an eating disorder. Anecdotally, many people with eating disorders say that their conditions began with dieting, she said. While clinical weight loss trials have not borne this out, those studies have had many limitations and have not fully assessed how dieting affects “people’s relationship with food and their bodies in the long term,” Dr. Sonneville said, so more research is needed.
Most people who diet don’t develop an eating disorder, Dr. Sonneville said, but even then, their relationships with food can deteriorate if they start “prioritizing weight and nutrition over joy and culture and connection.”
If you have a difficult relationship with food and your body, or if you have experienced binge eating or another eating disorder, Dr. Schur said, it is more important to focus on a healthy relationship with food than on your weight.
If dieting doesn’t work, what should we do?
People sometimes think that if they just “grit their teeth and white-knuckle it through” a diet to lose 10 or 20 pounds, “they can start to relax,” Dr. Hall said. “That’s the wrong way to think about it.”
If you want to change the way you eat in order to lose weight, you have to sustain those changes “for the rest of your life,” he said. “Otherwise, you’re going to regain the weight.” Given that, consider making healthy changes that you can stick with, he said.
If you consume a lot of ultraprocessed foods , reducing your intake can be a sustainable approach. Short-term research has shown that those who consume mostly ultraprocessed foods tend to eat more and gain more weight than those who consume minimally processed foods, though Dr. Hall acknowledged that a lack of time, money and access to whole foods are all potential barriers to making this change.
Dr. Collazo-Clavell suggested adopting a Mediterranean eating pattern , which focuses on healthy fats, whole grains, legumes, nuts, fruits and vegetables. Taking time to eat at least two or three square meals each day can help you feel full and be less likely to overeat at the end of the day, she added. And avoid eating within three hours of going to bed , which is associated with weight gain.
Getting regular physical activity can also help with keeping the weight off and has many other benefits, including a longer life and a lower risk of dementia, Dr. Schur said.
Ayana Habtemariam, a dietitian in Arlington, Va., encourages her clients — many of whom have spent decades dieting — to practice intuitive eating . This involves tuning in to your body’s hunger and fullness cues more deeply, and redefining success so that you can feel happy and confident regardless of your size, she said.
All of the experts we spoke with agreed on one point: People will benefit from adopting healthy habits, “even if they don’t lose a pound,” Dr. Collazo-Clavell said.
Alice Callahan is a Times reporter covering nutrition and health. She has a Ph.D. in nutrition from the University of California, Davis. More about Alice Callahan
A Guide to Better Nutrition
Ultraprocessed foods are clearly linked to poor health. But scientists are only beginning to understand why .
Calorie restriction and intermittent fasting both increase longevity in animals, aging experts say. Here’s what that means for you .
A viral TikTok trend touts “Oatzempic,” a half cup of rolled oats with a cup of water and the juice of half a lime, as a weight-loss hack. We asked the experts if there was anything to it .
Sodium is everywhere in our diets. But how much salt is too much ?
Patients were told for years that cutting calories would ease the symptoms of polycystic ovary syndrome. But research suggests dieting may not help at all .
62 Weight Loss Essay Topic Ideas & Examples
🏆 best weight loss topic ideas & essay examples, 🎓 good research topics about weight loss, ⭐ simple & easy weight loss essay titles.
- Dieting: Losing Weight Without Losing Your Mind It is, therefore, important to look for information on the health consequences of diabetes in order to promote determination and perseverance to lose weight.
- Weight Loss in an Elderly Male Polypharmacy becomes a challenge and stress for Roy, which leads to loss of weight. Dysgeusia predisposes Roy to a distorted taste of food, leading to a disorder that emanates from foul, salty, and metallic perceptions.
- Weight Loss in Breastfeeding Babies: Definition of Medical Diagnosis Weight loss may occur in newborns within the first week of their lives to up to 10%, probably because the baby is not getting enough milk, the mother not producing enough milk, or as a […]
- Effects of Diet and Physical Activity on Weight Loss and Cardiometabolic Risk Factors in Severely Obese Adults The study wanted to establish whether the outcomes of the African American people differed from those of white people. In addition, the human ethics committee of the university evaluated and endorsed the study.
- Health Promotion Weight Loss: How to Change People Behaviors and How to Keep Them Motivated to Lose Weight For example, when advising people on losing weight one should try to talk to them to get to details about their eating habits and whether they know how risky those are habits to their lives.
- Marketing Factors in Weight Loss Industry The purpose of this paper is to identify marketing environmental factors that influence products in the weight loss and nutrition industry.
- Biopsychology: Weight Loss Program and Mama Wawa Whatever the reasons are, one requires a program that would be of assistance in the weight reduction and to maintain it as well.
- Weight Loss Program: Behavior Modification Project for a College Class The plan was to adopt a new exercise and diet routine that would assist me in achievement of my desired outcome.
- Weight Loss Program: Losing Part of an Overweight A person should also be emotionally ready to reduce weight and have a continuous commitment to the program of weight loss.
- Reasons for Losing Weight Analysis Losing excessive weight produces several long-term benefits in the body of the individual by reducing the number of potential risks to health and life.
- Oat Chocolate Cookies Recipe for Weight Loss Diet The association of cookies with weight gain and obesity has led to a significant decline in the consumption of cookies over the last few years. The role of oats in the recipe is to enrich […]
- The UAE Population: Xenical and Weight Loss The main variables observed in this study will be the following: the efficiency of Xenical for weight loss in the UAE populations and the preferences linked to the use of Xenical compared to other medications […]
- Xenical and Weight Loss in the UAE Population The hypotheses are the following: The effectiveness of Xenical is seen as sufficient by the population of the UAE. The effectiveness of Xenical is seen as insufficient by the same population.
- The Gulf Cooperation Council: Weight Loss Surgeries The paper carried analysis of descriptive statistics and graphs for the number of weight loss surgeries in the GCC. The results show that there was a significant increase in the number of weight loss surgeries […]
- Exercise vs. Diet for Weight Loss The starting point of their research is formulated in the following hypothesis: insufficient physical activity or lack thereof is not a contributor to the global problem of obesity.
- Psychological Implications of Weight Loss Surgery Most people hardly prepare themselves for the psychological hurdles that may arise as a result of the new body that they acquire soon after the weight loss surgery. Most people who have undergone the weight […]
- Obesity and Weight Loss: Exercising and Dieting However, the reality is that they also had once crossed the threshold of the gym for the first time and managed to overcome anxiety.
- The Weight Loss Science and the Recommended Procedures Weight loss is the act of engaging in a number of activities, including body exercises and dieting, in a bid to reduce body mass.
- Healthy Foods and Obesity: Unhealthy Weight Loss Methods and Media Weight Loss Campaigns This is ironical bearing in mind the amount of information in the media encouraging people to adopt healthy eating habit in effect to contain the increase of obesity.
- Weight Loss Systems: The Dietary Approaches to Weight Loss Although a balance of a check on the causes of obesity is required for a person to lose weight, this paper focuses on the dietary approaches to weight loss.
- Weight Loss Alternatives: Viable Options for Losing That Extra Weight Since the onset of this century, one of the most prevalent problems that has afflicted the society, especially in the developed countries, is that of obesity.
- Diabetic and Elder Patients Experience Superior Cardiovascular Benefits After Gastric Bypass Induced Weight Loss
- Common Fat and Weight Loss Myths
- Family Functioning and Weight Loss in a Sample of African Americans and Whites
- Health and Social Care: Bariatric Surgery Weight Loss Successes
- Dangerous Weight Loss Drugs vs. Safer Alternatives
- Chemistry and Weight Loss Drugs
- Dieting and Weight Loss Drugs
- Fad Diet Programs and Its Effects – Nourishment, Obesity, Weight Loss Plans
- Diet Pills and Weight Loss Supplements
- Essential Weight Loss Guides on How You Lose Poundage Fast
- Cardiovascular Risks and Benefits of Medications Used for Weight Loss
- Herbal Remedies Used for Weight Loss
- Eating Wisely and Exercise Plan For Weight Loss
- Food Cue Reactivity and the Brain-Heart Axis During Cognitive Stress
- Disturbing New Study About Obesity and Weight Loss
- Eating Habits for Effortless Weight Loss
- Body Image and Body Avoidance Nine Years After Bariatric Surgery and Conventional Weight Loss Treatment
- Advertisement for the Weight Loss Product
- Excessive Weight Loss Teenage Girls
- America’s Obsession With Weight Loss and Body Image
- Chinese Diet Green Tea for Weight Loss
- Behavior Modification and Weight Loss
- Cognitive Behavioural Therapy for Weight Loss
- Anorexia Nervosa: Self Starvation and Dramatic Weight Loss
- Calorie Restriction for Weight Loss
- Aged and Weight Loss Surgery
- Diet Soda and Its Effect on Your Weight Loss Program
- Fast and Lasting Weight Loss: Fast Weight Loss for Special Occasions
- Diet and Fitness Winning Tactics for Weight Loss
- Aerobic Exercise for Weight Loss
- Exercise Program for Weight Loss Strength and Vitality
- Distribution and Disavowal: Managing the Parental Stigma of Children’s Weight and Weight Loss
- Encouraging Healthy Living Without the Emphasis on Weight Loss as the Main Purpose of Living Healthy
- Abdominal Exercise and Weight Loss
- Cosmetic and Weight Loss Surgery
- Eating Healthy and Weight Loss While Breastfeeding
- Busy Moms and Weight Loss Challenge
- Exercise and Weight Loss: The Science of Preserving Muscle Mass
- Different Methods for Weight Loss
- Chromium Picolinate and Weight Loss
- Fitness Topics
- Obesity Ideas
- Social Norms Essay Ideas
- Wellness Essay Topics
- Sugar Paper Topics
- Yoga Questions
- Diabetes Questions
- Malnutrition Titles
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, March 2). 62 Weight Loss Essay Topic Ideas & Examples. https://ivypanda.com/essays/topic/weight-loss-essay-topics/
"62 Weight Loss Essay Topic Ideas & Examples." IvyPanda , 2 Mar. 2024, ivypanda.com/essays/topic/weight-loss-essay-topics/.
IvyPanda . (2024) '62 Weight Loss Essay Topic Ideas & Examples'. 2 March.
IvyPanda . 2024. "62 Weight Loss Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/weight-loss-essay-topics/.
1. IvyPanda . "62 Weight Loss Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/weight-loss-essay-topics/.
Bibliography
IvyPanda . "62 Weight Loss Essay Topic Ideas & Examples." March 2, 2024. https://ivypanda.com/essays/topic/weight-loss-essay-topics/.

- Writing Correction
- Online Prep Platform
- Online Course
- Speaking Assessment
- Ace The IELTS
- Target Band 7
- Practice Tests Downloads
- IELTS Success Formula
- Essays Band 9 IELTS Writing Task 2 samples – IELTS Band 9 essays
- Essays Band 8 IELTS Writing – samples of IELTS essays of Band 8
- Essays Band 7 IELTS Writing – samples of IELTS essays of Band 7
- Essays Band 6 IELTS Writing – samples of IELTS essays of Band 6
- Essays Band 5 IELTS Writing – samples of IELTS essays of Band 5
- Reports Band 9 IELTS Writing – samples of IELTS reports of Band 9 (Academic Writing Task 1)
- Reports Band 8 IELTS Writing – samples of IELTS reports of Band 8
- Reports Band 7 IELTS Writing – samples of IELTS reports of Band 7
- Letters Band 9 IELTS Writing Task 1 – samples of IELTS letters of Band 9
- Letters Band 8 IELTS Writing – samples of IELTS letters of Band 8
- Letters Band 7 IELTS Writing – samples of IELTS letters of Band 7
- Speaking Samples
- Tests Samples
- 2023, 2024 IELTS questions
- 2022 IELTS questions
- 2021 IELTS questions
- 2020 IELTS questions
- High Scorer’s Advice IELTS high achievers share their secrets
- IELTS Results Competition
- IELTS-Blog App
IELTS Band 9 essay, topic: Some say that people should diet and exercise to lose weight, while others think they should eat better and change their lifestyle (opinion)
- IELTS Essays - Band 9
This is a model response to a Writing Task 2 topic from High Scorer’s Choice IELTS Practice Tests book series (reprinted with permission). This answer is likely to score IELTS Band 9.
Set 1 General Training book, Practice Test 4
Writing Task 2
You should spend about 40 minutes on this task.
Write about the following topic:
Today’s society provides people with various ways to lose weight, such as special diets or exercise regimes. Many people believe though that poor food and today’s lifestyle should be addressed first. What is your opinion?
Give reasons for your answer and include any relevant examples from your knowledge or experience.
You should write at least 250 words.
In modern day western society one can easily become obese, as the availability of cheap and unhealthy food is high. Nonetheless, many people desire to be healthy and slim and therefore have chosen to follow special diets or exercise regimes so as to not become obese. Others believe, however, that people should be better informed about today’s unhealthy lifestyles and the poor food they are consuming before such diets and regimes are taken into consideration. Personally, I agree that the unhealthy lifestyle of many people must be addressed before thinking about ways of losing weight through special diets.
It has become habitual for people to cook using ingredients that have been pre-cooked or to which chemicals have been added. Additionally, several people consume a lot of microwave and fast food, which are both easy to purchase and prepare, but are often fairly unhealthy. Due to the fact that it has become less popular to cook meals using fresh ingredients, people consume chemicals, taste intensifiers, salt and sugar without realising. By consuming food that has been made by mass production, one no longer has to think largely about how a meal is prepared and can simply consume it without thinking about the ingredients.
It seems logical that in order to lose weight effectively and over a long period of time, one has to learn to eat in a healthy way and to carry out sport on a regular basis. Learning how to cook with fresh ingredients is an important aspect of eating in a healthy way, and, by doing so, people can avoid eating food that has been pre-made. If people do not understand this concept, they will fall back into unhealthily habits after their diet is over.
In conclusion, today’s unhealthy lifestyles as well as the poor quality food consumed by people on a regular basis must be addressed before thinking about diets or exercise regimes. If people can combine exercise with wholesome eating habits, they will be happier and healthier.
Go here for more IELTS Band 9 Essays
Related posts:
- IELTS essay, topic: Many people do not exercise enough and eat an unhealthy diet (reasons and solutions) This essay topic was seen in a recent IELTS tests...
- IELTS essay, topic: Unemployment payments encourage people not to seek work (opinion) This is a model response to a Writing Task 2...
4 thoughts on “IELTS Band 9 essay, topic: Some say that people should diet and exercise to lose weight, while others think they should eat better and change their lifestyle (opinion)”
Is it okay if we give our opinion in first para like this. And also mention again same in last para?
Hi Varsha, yes you can write your opinion in the intro paragraph.
what do you mean \”consume a lot of microwave\” ?
This sentence is referring to microwave food, ‘consume a lot of microwave food’ – which is food cooked in the microwave.
Leave a Reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.

IMAGES
VIDEO
COMMENTS
1. Introduction . In the United States, 34% of adults aged 20 and over are considered overweight, 34% obese, and 6% extremely obese [].It is estimated that approximately two-thirds of overweight and obese individuals are currently trying to lose weight [2, 3].Despite the fact that losing weight and maintaining weight loss can be difficult, research shows that 17-20% of overweight or obese ...
This document discusses binge dieting to lose weight excessively. The author's instructor told them they looked too big and needed to lose weight. They saw their large reflection in the mirror and realized they needed to indulge in excessive weight loss. The instructor instructed them to eat only green, leafy foods with low calories and do high-energy activities. Though the journey is hard ...
About the author. Amy Pershing, LMSW, ACSW, CCTP-II, is the founding director of the Bodywise binge eating disorder (BED) treatment program, vice president of the Center for Eating Disorders, and creator of Hungerwise, an online program for ending chronic dieting and weight cycling.Based on 35 years of clinical experience, she has pioneered a treatment approach for binge eating that ...
Get custom essay. After that, the person should drink a lot of water, which will help in the reduction of the amount of food consumed. Healthy eating is crucial to weight loss, and this step should be done in order to promote weight loss and good health. Finally, the person should engage in some physical exercise.
Amber Neal grew up overweight, but when she hit 325 pounds after years of yo-yo dieting (and even gastric bypass surgery), she decided to lose weight for good, and dropped 190 pounds.
Binge Eating and Weight Loss Outcomes in Individuals with Type 2 Diabetes: 4-Year Results from the Look AHEAD Study. Obesity , 2017; 25 (11): 1830 DOI: 10.1002/oby.21975 Cite This Page :
A large percentage of students reported exercising to lose weight, consistent with reports that indicate high levels of exercise in college age populations (Nelson, et al., 2007). Interestingly, binge eating students were more likely to report exercise use than their non-binge eating classmates, which may suggest a healthy approach to weight loss.
The Pritikin Center offers a proven, medically-focused, healthy living program, in a retreat setting, which specializes in weight, heart health, and diabetes. 6 Ways to Recover from Binge Eating and Lose Weight. Discovering why you're binge eating can help you recover from it and develop a healthy lifestyle that promotes weight loss.
Ketogenic diet. Consumption of carbohydrates as < 10% of daily calories or < 50 mg/day 41. May decrease appetite, but long-term safety is unknown. High-protein diet. Increase protein intake to 30% of total daily calories or 1-1.2 g/kg of ideal body weight 43. Useful in maintaining weight loss and increasing satiety 47.
8. Water Really Is Your BFF. 9. The Mental Transformation Is Just as Important as the Physical. 10. If You Want Lasting, Permanent Change—It's about Your Lifestyle. From a young age growing up in the Connecticut suburbs, the number on the scale ebbed and flowed as my relationship with sport did as well. At age 14, I was a soccer whiz, running ...
Diet and exercise. By Mayo Clinic Staff. The key to weight loss is building new habits that lead to eating better and moving more. Eating better means eating healthy, lower calorie meals. Moving more means adding more physical activity, not just exercise, into your life. Being active is vital to losing weight and keeping if off.
1. Recovery and weight loss are mutually exclusive. They're just incompatible. If you're focusing on weight loss then your effort isn't 100% focused on recovery. Actively trying to lose weight during the recovery process might hinder it. Eating disorders and disordered eating put your body in a state of deprivation.
"But by losing weight, they're increasing their level of weight suppression, which makes binge eating and weight regain more likely." Lowe and his colleagues describe this cycle as "a biobehavioral bind." They stress that health-care providers should inquire about a patient's weight history in any clinical evaluation, be it medical or ...
On a low carb approach, which is often a successful weight loss strategy, limit net carbs to less than 100 grams (or keep them as low as 20 grams per day, if you want to try a keto diet). Fill your plate with fibrous veggies. These provide abundant nutrients, high food volume, and relatively few calories. Add enough fat for taste and to enjoy ...
Choose low-fat dairy products and lean meat and poultry in limited amounts. 5. Get active, stay active. While you can lose weight without exercise, regular physical activity plus calorie restriction can help give you the weight-loss edge. Exercise can help burn off the excess calories you can't cut through diet alone.
Amen, Daniel. The Amen Solution: The Brain Healthy Way to Lose Weight and Keep It Off. New York: Crown Publishing Group, 2011. Print. Levine, Judith and Linda, Bine. Helping Your Child Lose Weight the Healthy Way: A Family Approach to Weight Control. London: Citadel Press, 2001. Print. Thomson Medical Company. Lose weight the healthy way: bran ...
Binge-eating disorder (BED) is characterized by recurrent episodes of binge eating—i.e., eating episodes that occur in a discrete period of time (≤2 hours) and involve the consumption of an amount of food that is definitely larger than most people would consume under similar circumstances. Other core features of BED are a sense of lack of control over eating during binge episodes ...
The Bottom Line. If you can't seem to lose the weight for good, check your self-talk. Work on reframing the negative thoughts that hold you back and remember slow and steady wins the race (of keeping off the weight you lost!). "When it comes to weight loss, it's important to focus on what we can control," says Larsen.
So in other words, if you lose 20 pounds, your body will burn roughly 250 calories less each day while craving about 950 calories more. To maintain your weight loss through dieting over time, you ...
Weight Loss in an Elderly Male. Polypharmacy becomes a challenge and stress for Roy, which leads to loss of weight. Dysgeusia predisposes Roy to a distorted taste of food, leading to a disorder that emanates from foul, salty, and metallic perceptions. Weight Loss in Breastfeeding Babies: Definition of Medical Diagnosis.
THESIS STATEMENT: When it comes to successful and lasting weight loss, eating well is only part of the battle, physical activity is an important resource in reducing weight. STRONG ARGUMENT: T here are many ways to lose weight, from diet and exercise to extremes measures such as surgery. The physical exercise helps you prevent many health conditions, stress, and also it makes you feel better.
It seems logical that in order to lose weight effectively and over a long period of time, one has to learn to eat in a healthy way and to carry out sport on a regular basis. Learning how to cook with fresh ingredients is an important aspect of eating in a healthy way, and, by doing so, people can avoid eating food that has been pre-made.