Endocrine System Disorders NCLEX Practice Questions (50 Questions)
Welcome to your NCLEX practice questions quiz for endocrine system disorders. In this nursing test bank , test your nursing competence and knowledge on the nursing care of different endocrine system disorders.

Endocrine System Disorders Nursing Test Bank
In this section are the NCLEX practice questions for endocrine system disorders. This nursing test bank set includes 50 questions divided into two parts. All questions on this set are updated to give you the most challenging questions, along with insightful rationales to reinforce learning .
Quiz Guidelines
Before you start, here are some examination guidelines and reminders you must read:
- Practice Exams : Engage with our Practice Exams to hone your skills in a supportive, low-pressure environment. These exams provide immediate feedback and explanations, helping you grasp core concepts, identify improvement areas, and build confidence in your knowledge and abilities.
- You’re given 2 minutes per item.
- For Challenge Exams, click on the “Start Quiz” button to start the quiz.
- Complete the quiz : Ensure that you answer the entire quiz. Only after you’ve answered every item will the score and rationales be shown.
- Learn from the rationales : After each quiz, click on the “View Questions” button to understand the explanation for each answer.
- Free access : Guess what? Our test banks are 100% FREE. Skip the hassle – no sign-ups or registrations here. A sincere promise from Nurseslabs: we have not and won’t ever request your credit card details or personal info for our practice questions. We’re dedicated to keeping this service accessible and cost-free, especially for our amazing students and nurses. So, take the leap and elevate your career hassle-free!
- Share your thoughts : We’d love your feedback, scores, and questions! Please share them in the comments below.
Quizzes included in this guide are:
Recommended Resources
Recommended books and resources for your NCLEX success:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Saunders Comprehensive Review for the NCLEX-RN Saunders Comprehensive Review for the NCLEX-RN Examination is often referred to as the best nursing exam review book ever. More than 5,700 practice questions are available in the text. Detailed test-taking strategies are provided for each question, with hints for analyzing and uncovering the correct answer option.

Strategies for Student Success on the Next Generation NCLEX® (NGN) Test Items Next Generation NCLEX®-style practice questions of all types are illustrated through stand-alone case studies and unfolding case studies. NCSBN Clinical Judgment Measurement Model (NCJMM) is included throughout with case scenarios that integrate the six clinical judgment cognitive skills.

Saunders Q & A Review for the NCLEX-RN® Examination This edition contains over 6,000 practice questions with each question containing a test-taking strategy and justifications for correct and incorrect answers to enhance review. Questions are organized according to the most recent NCLEX-RN test blueprint Client Needs and Integrated Processes. Questions are written at higher cognitive levels (applying, analyzing, synthesizing, evaluating, and creating) than those on the test itself.

NCLEX-RN Prep Plus by Kaplan The NCLEX-RN Prep Plus from Kaplan employs expert critical thinking techniques and targeted sample questions. This edition identifies seven types of NGN questions and explains in detail how to approach and answer each type. In addition, it provides 10 critical thinking pathways for analyzing exam questions.

Illustrated Study Guide for the NCLEX-RN® Exam The 10th edition of the Illustrated Study Guide for the NCLEX-RN Exam, 10th Edition. This study guide gives you a robust, visual, less-intimidating way to remember key facts. 2,500 review questions are now included on the Evolve companion website. 25 additional illustrations and mnemonics make the book more appealing than ever.

NCLEX RN Examination Prep Flashcards (2023 Edition) NCLEX RN Exam Review FlashCards Study Guide with Practice Test Questions [Full-Color Cards] from Test Prep Books. These flashcards are ready for use, allowing you to begin studying immediately. Each flash card is color-coded for easy subject identification.

Recommended Links
An investment in knowledge pays the best interest. Keep up the pace and continue learning with these practice quizzes:
- Nursing Test Bank: Free Practice Questions UPDATED ! Our most comprehenisve and updated nursing test bank that includes over 3,500 practice questions covering a wide range of nursing topics that are absolutely free!
- NCLEX Questions Nursing Test Bank and Review UPDATED! Over 1,000+ comprehensive NCLEX practice questions covering different nursing topics. We’ve made a significant effort to provide you with the most challenging questions along with insightful rationales for each question to reinforce learning.
9 thoughts on “Endocrine System Disorders NCLEX Practice Questions (50 Questions)”
This is great. I wish i could get a class for learning nclex rn
I like your assistance in questions and answers they have helped alot
Really do appreciate, attempting this questions has really helped
7. Question A 67-year-old MALE client has been complaining of sleeping more, increased urination, anorexia, weakness, irritability, depression, and bone pain that interferes with HER going outdoors. Based on these assessment findings, nurse Richard would suspect which of the following disorders?
MESSY question. Someone fix it pls.
Thanks for letting us know. I have fixed the question.
Excellent resource
this is so good, a lot of knowledge feed here, may God bless you guys
Alot of knowledge here. Thank you for the access .
Leave a Comment Cancel reply
This website is intended for healthcare professionals

- { $refs.search.focus(); })" aria-controls="searchpanel" :aria-expanded="open" class="hidden lg:inline-flex justify-end text-gray-800 hover:text-primary py-2 px-4 lg:px-0 items-center text-base font-medium"> Search
Search menu
Al Halteet S, Abdel-Hadi A, Hassan M, Awad M. Prevalence and antifungal susceptibility profile of clinically relevant Candida Species in postmenopausal women with diabetes. Biomed Res Int. 2020; 2020 https://doi.org/10.1155/2020/7042490
Andrade M, Bayram-Weston Z, Knight J. Endocrine system 4: adrenal glands. Nursing Times. 2021; 117:(8)54-58
Arima H, Azuma Y, Morishita Y, Hagiwara D. Central diabetes insipidus. Nagoya J Med Sci. 2016; 78:(4)349-358 https://doi.org/10.18999/nagjms.78.4.349
Caron P, Brue T, Raverot G Signs and symptoms of acromegaly at diagnosis: the physician's and the patient's perspectives in the ACRO-POLIS study. Endocrine. 2019; 63:(1)120-129 https://doi.org/10.1007/s12020-018-1764-4
Escobar-Morreale HF. Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment. Nat Rev Endocrinol. 2018; 14:(5)270-284 https://doi.org/10.1038/nrendo.2018.24
Fox T, Brooke A, Vaidya B. Eureka Endocrinology, 1st edn. London: JP Medical Ltd; 2015
Goff LM. Ethnicity and type 2 diabetes in the UK. Diabet Med. 2019; 36:(8)927-938 https://doi.org/10.1111/dme.13895
Khan S, Fitch S, Knox S, Arora R. Exocrine gland structure-function relationships. Development. 2022; 149:(1) https://doi.org/10.1242/dev.197657
Knight J. Endocrine system 1: overview of the endocrine system and hormones. Nursing Times. 2021; 117:(5)38-42
Knight J, Andrade M, Bayram-Weston Z. Endocrine system 3: thyroid and parathyroid glands. Nursing Times. 2021; 117:(7)46-50
Kumar and Clark's clinical medicine, 9th edn. In: Kumar PJ, Clark ML (eds). Elsevier: Edinburgh; 2017
Liu Y, Zhi X. Advances in genetic diagnosis of Kallmann syndrome and genetic interruption. Reproductive Sciences. 2021; https://doi.org/10.1007/s43032-021-00638-8
National Institute for Health and Care Excellence. Thyroid disease: assessment and management. NICE Guidance NG145. 2019. https://www.nice.org.uk/guidance/ng145 (accessed 9 March 2022)
National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. NICE Guidance NG28. 2022. https://www.nice.org.uk/guidance/ng28 (accessed 14 March 2022)
Hypoparathyroidism: too little parathyroid hormone production. 2018. https://www.endocrineweb.com/conditions/hypoparathyroidism/hypoparathyroidism (accessed 9 March 2022)
Current diagnosis and management of Graves' disease. 2018. https://pubmed.ncbi.nlm.nih.gov/29950539
Tan DX, Xu B, Zhou X, Reiter RJ. Pineal calcification, melatonin production, aging associated health consequences and rejuvenation of the pineal gland. Molecules. 2018; 23:(2) https://doi.org/10.3390/molecules23020301
Taylor PN, Albrecht D, Scholz A Global epidemiology of hyperthyroidism and hypothyroidism. Nature Reviews Endocrinology. 2018; 14:(5)301-316 https://doi.org/10.1038/nrendo.2018.18
van den Beld A, Kaufman J, Zillikens M, Lamberts S, Egan J, van der Lely A. The physiology of endocrine systems with ageing. Lancet Diabetes Endocrinol. 2018; 6:(8)647-658 https://doi.org/10.1016/S2213-8587(18)30026-3
Walter MH, Abele H, Plappert CF. The role of oxytocin and the effect of stress during childbirth: neurobiological basics and implications for mother and child. Front Endocrinol (Lausanne). 2021; 12 https://doi.org/10.3389/fendo.2021.742236
Wémeau J, Klein M, Sadoul J, Briet C, Vélayoudom-Céphise F. Graves' disease: Introduction, epidemiology, endogenous and environmental pathogenic factors. Ann Endocrinol (Paris). 2018; 79:(6)599-607 https://doi.org/10.1016/j.ando.2018.09.002
World Health Organization. Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. Abbreviated report of a WHO consultation. 2011. https://apps.who.int/iris/handle/10665/70523 (accessed 9 March 2022)
World Health Organization. Endocrine disrupters and child health: Possible developmental early effects of endocrine disrupters on child health. 2012. https://www.who.int/publications/i/item/9789241503761 (accessed 9 March 2022)
The endocrine system and associated disorders
Emily Ashwell
Community Caseload Manager Nurse, Buckinghamshire Healthcare NHS Trust
View articles

The endocrine system and the hormones it produces control a range of processes in the body, as well as helping to maintain homeostasis. When this complex system is disrupted, including by changes associated with ageing, disease may result. This article provides an overview of the endocrine systems, key glands and hormones, and some of the problems that can arise from disruption to the system. A case study is provided to illustrate one possible presentation of endocrine disruption, in the form of diabetes-associated complications.
The endocrine system comprises several distinct glands and tissues, which are made up of specialised cells that synthesise, store, and secrete hormones. Hormones are chemical messengers that can act on nearby cells via interstitial fluid (paracrine effect), on the cell of origin (autocrine effect), at a distant site (endocrine or exocrine effects), or as neurotransmitters ( Knight, 2021 ). Neurotransmitters across synapses contribute to the rapid actions of the nervous system. In contrast, endocrine effects tend to be slow to develop and result in prolonged responses potentially lasting weeks, as hormones travel in the bloodstream from an endocrine gland to another organ. Hormones control a wide range of physiological processes, including growth, metabolism, sleep, immune system response, ‘fight or flight’, reproduction, mood, and behaviour ( Kumar and Clark, 2017 ). They also assist in maintaining homeostasis (a state of physiological equilibrium) by regulating the body's internal environment in response to changes in the external environment. The human body produces more than 100 hormones to carry out these processes, and research is continuing to further our understanding of their functions and interactions as well as identifying more hormones ( Knight, 2021 ).
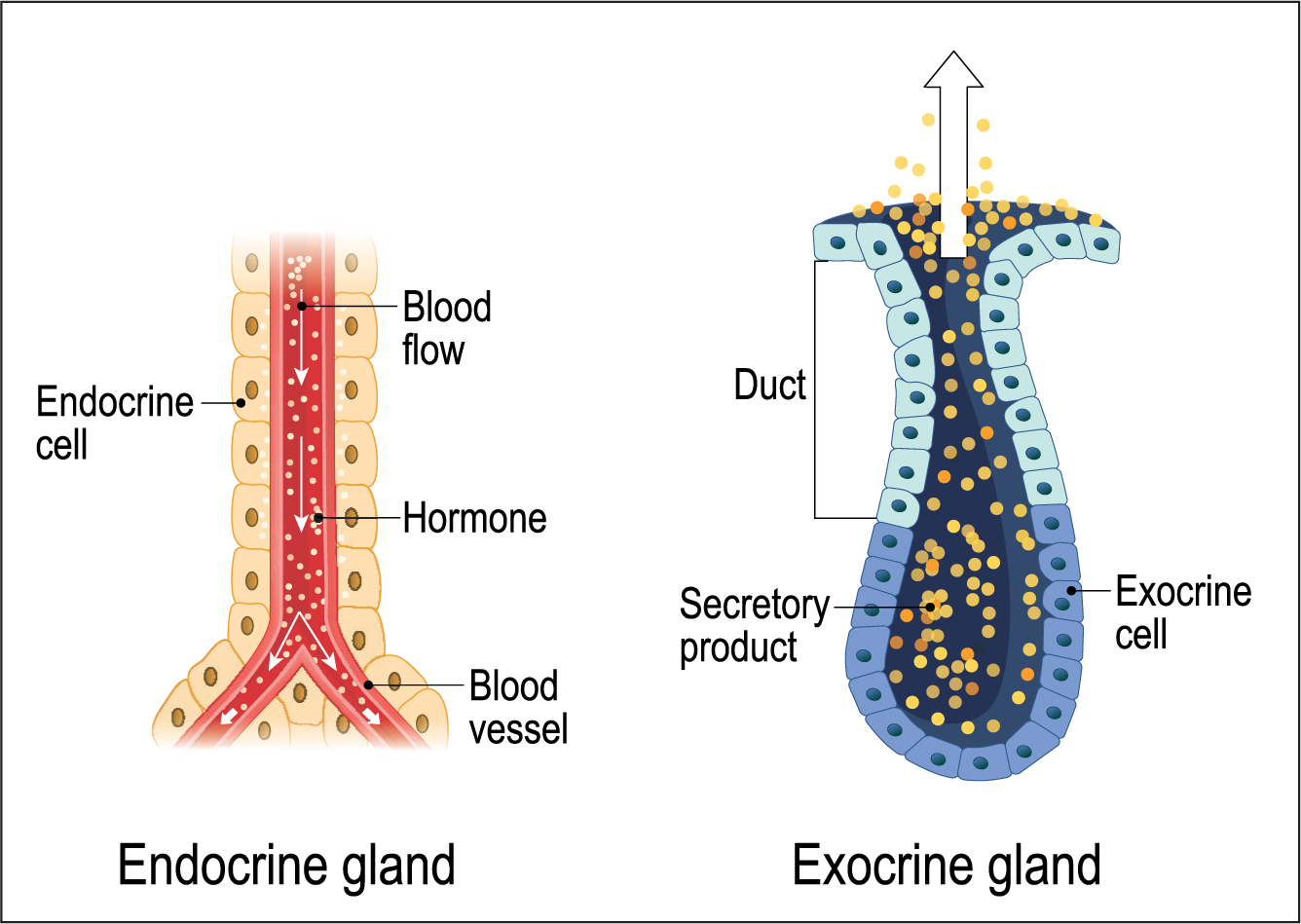
Endocrine and exocrine glands
All glandular tissues produce secretions. Exocrine glands are arranged so they secrete theirs via a central duct, which directs the secretions (hormones) to the desired location, for example sweat from glands in the skin ( Khan et al, 2022 ). In contrast, endocrine glands release their secretions into the bloodstream, as part of their primary function. Therefore, endocrine glands have a rich blood supply to ensure efficient transport of their hormones around the body and enable them to continuously monitor blood for changes that initiate hormone secretion ( Fox et al, 2015 ) ( Figure 1 ).
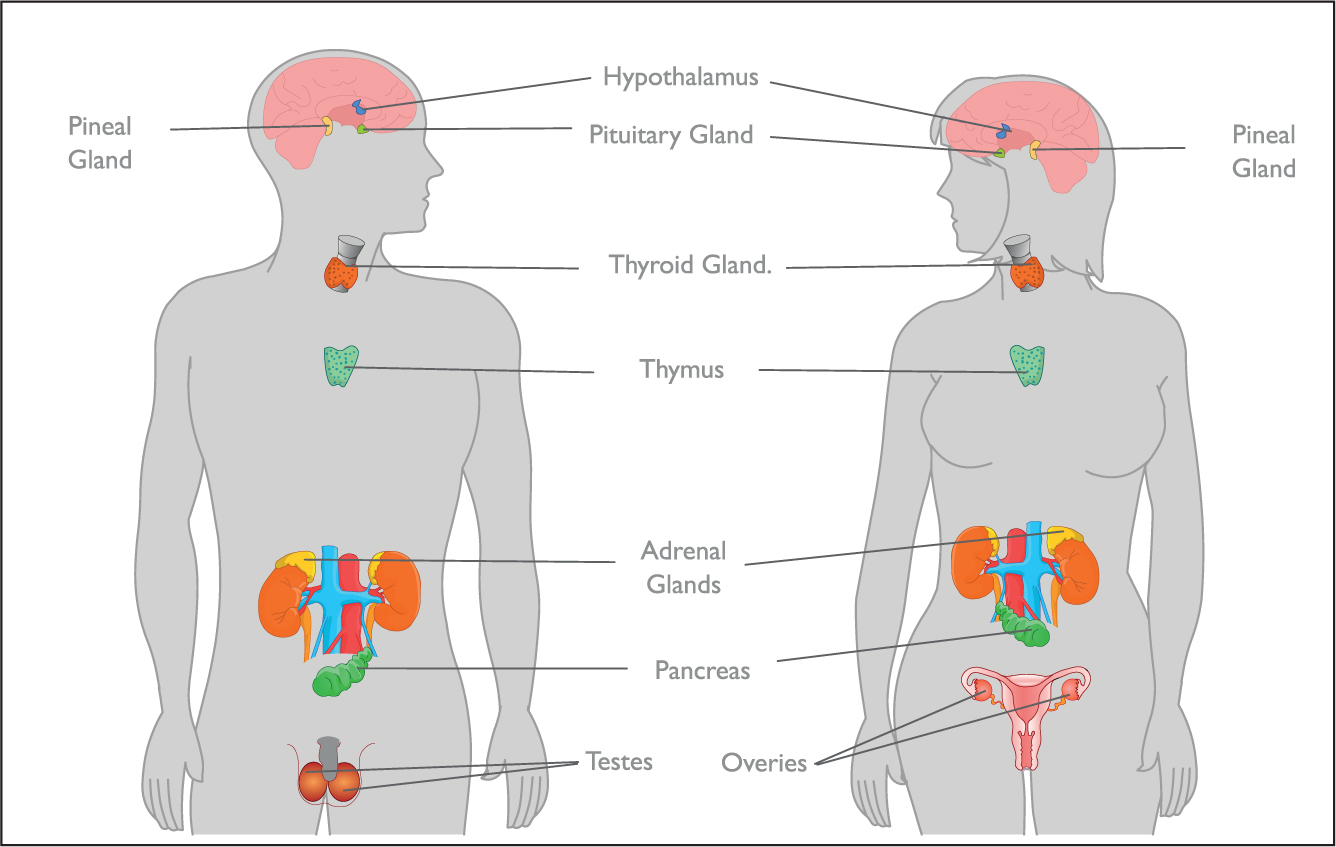
The hypothalamus is a part of the brain that releases several hormones, which affects other endocrine glands' hormone production, acting as the endocrine control centre and linking the nervous system with the endocrine system ( Fox et al, 2015 ). This is connected to the pituitary gland, which produces hormones controlling growth, metabolism, and sexual development. The pineal gland is also located in the brain and produces melatonin, which affects wakefulness ( Tan et al, 2018 ).
Outside of the brain there is the thyroid gland, which sets the body's metabolic rate, the parathyroid glands, which control the absorption and excretion of calcium and phosphate, and the thymus gland, which releases thymosin, stimulating the production of immune T cells ( Fox et al, 2015 ). The adrenal glands, located on top of each kidney, control blood pressure, fluid and electrolyte balance, and the body's response to physiological and psychological stress ( Andrade et al, 2021 ). The endocrine glands of the pancreas secrete insulin and glucagon, which together regulate blood glucose concentration. Reproductive glands (testes in males and ovaries in females) release sex hormones that enable reproduction and sexual maturation ( Figure 2 ). In addition, the intestine and adipose tissue also secrete hormones as part of their primary function, although these are not major endocrine glands. Other organs, such as the liver, kidney, heart, and skin all have secondary endocrine functions ( Fox et al, 2015 ).
Hormone signalling pathways
Hormones are grouped into three chemical classes: peptides, amines, and lipids (mainly steroids) and are synthesised by endocrine glands cells before being stored in preparation for rapid secretion as required ( Fox et al, 2015 ). On release they are transported through the body in the blood, where they then employ their desired physiological effects by binding to specific receptors on the outer membrane or within their target cells. Intracellular binding directly affects the cell's gene expression, whereas extracellular binding changes the cell's metabolism through cascade reactions. Many medications have been created to target these receptor sites by imitating a hormone's action (for example, people with hypothyroidism can be given levothyroxine to mimic the thyroxine they are lacking), or by acting as a competitive antagonist, blocking target receptors to prevent the hormone from binding and employing its effect (for example, beta blockers can be used to treat the adrenaline-related symptoms of hyperthyroidism) ( Knight, 2021 ). Once used, hormones are then released from the target cells either unchanged or inactivated and transported to the liver or kidneys to be broken down and excreted as bile or urine, respectively.
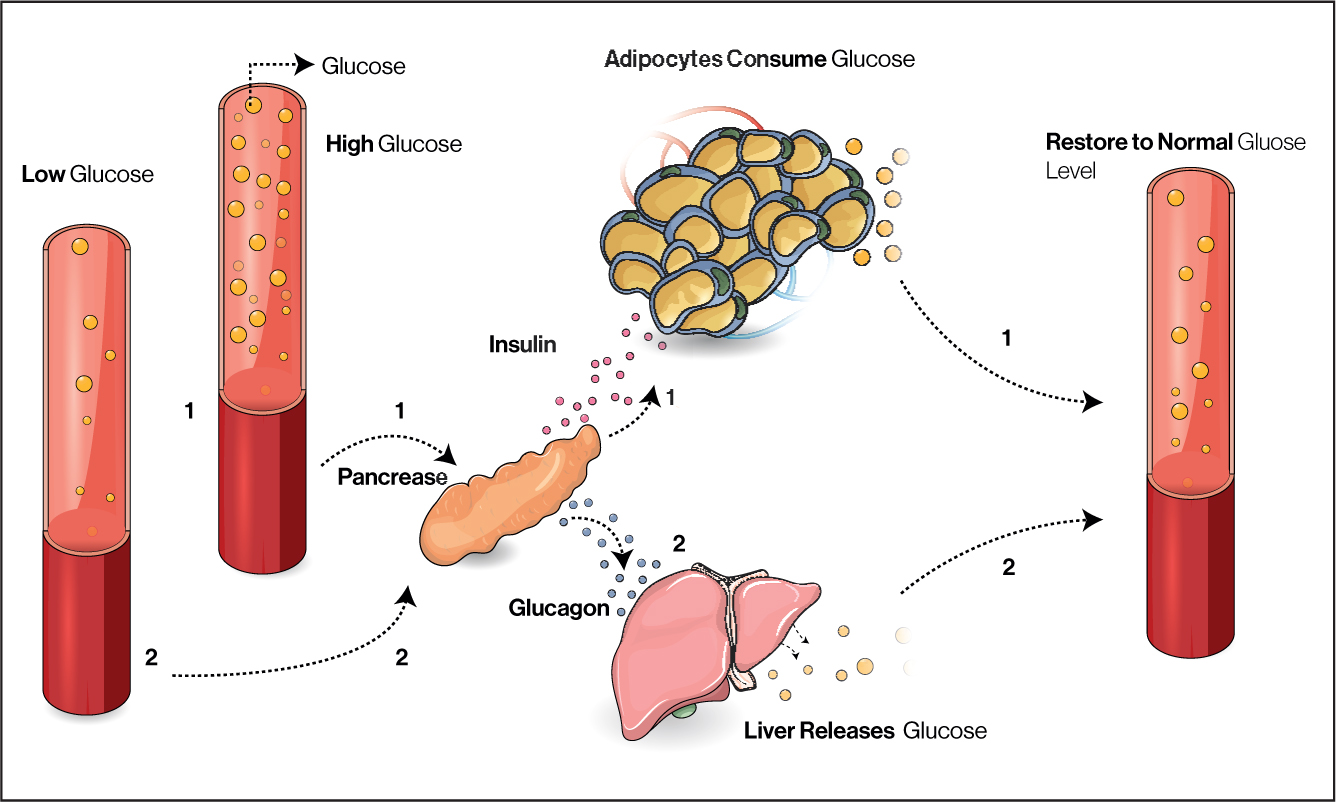
Hormone production is controlled with feedback loops. Most often these involve negative feedback mechanisms, where the effects of a hormone inhibit its release to maintain homeostasis, such as the mechanisms involved in blood glucose regulation ( Figure 3 ). Hypoglycaemia and hyperglycaemia in diabetes mellitus demonstrate deviation from a normal range (in this case blood sugar), which can can be symptomatic and contribute to more severe pathology. In positive feedback mechanisms a hormone's effects stimulate its secretion, for example, in childbirth oxytocin is released, stimulating uterine contractions and pushing the baby towards the cervix, which stimulates the release of more oxytocin ( Walter et al, 2021 ).
Aetiology of endocrine disorders
Disturbance at any point in these complex processes or development of these glands can result in disease. Endocrine disorders largely result from too much or too little hormone secretion. This hormonal imbalance may be due to a problem with the endocrine feedback system, genetic disorder, infection, injury or disease of the endocrine gland, or the growth of nodules or tumours in the glands ( Kumar and Clark, 2017 ). For example, in Cushing's disease the negative feedback loop is disturbed so pituitary hormone ACTH production may become excessive as it is not inhibited by excessive cortisol, resulting in symptoms such as central obesity and high blood pressure. Ageing also lessens the endocrine system's functioning, as the secretion of several hormones is reduced, along with target cells sensitivity to the hormones produced. Examples include falling oestrogen levels triggering menopause, decreasing growth hormone causing loss of muscle mass, declining melatonin levels disturbing sleep, and insulin sensitivity reducing, which increases the risk of diabetes—although these changes fluctuate significantly between individuals ( van den Beld et al, 2018 ). Children are also at risk of endocrine disorders, most commonly thyroidal dysfunctions, diabetes, cryptorchidism, precocious puberty, and pancreatic and thyroid cancers ( World Health Organization (WHO), 2012 ).
Diagnosis of endocrine disorders is based on signs and symptoms, physical examination, medical history, imaging tests to detect tumours, and blood and urine analysis to determine the levels of hormone within them. Once diagnosed treatment can be targeted to the specific disorder and individual, managing their symptoms and maintaining homeostasis with medications, surgery, chemotherapy, or radiation therapy as required ( Knight, 2021 ).
Endocrine disorders
Although not exhaustive, Table 1 gives some examples of hormones and disorders for key glands. Table 2 gives an elaboration of the cause and signs and symptoms for a disorder for each gland.
Hypothyroidism
Thyroid diseases are among the most common of the endocrine disorders and can affect people of all ages. The most common of these disorders is hypothyroidism, where the thyroid gland is underactive, resulting in a deficiency of T3 and T4 in the bloodstream ( Knight et al, 2021 ). Hypothyroidism caused by diseases of the thyroid gland, such as infection, inflammation, or deficiency, is known as primary hypothyroidism and is more likely to affect women. When hypothyroidism results from pituitary or hypothalamic disorders, including benign or malignant growths or following head trauma, it is known as secondary hypothyroidism ( Taylor et al, 2018 ). Autoimmune thyroiditis is the most common cause of primary hypothyroidism in high-income countries, but iodine deficiency remains a major cause in many parts of the world ( Knight et al, 2021 ). Iodine is also vital during pregnancy as thyroid hormones are essential for neurological development and the foetus relies entirely on maternal thyroid hormones until about 14 weeks' gestation when it begins to produce its own ( Taylor et al, 2018 ). Autoimmune thyroiditis with inflammation of the thyroid (goitre) is called Hashimoto's thyroiditis and occurs when the follicular components of the thyroid gland are progressively destroyed by the patient's own immune system, resulting in reduced secretion of T3 and T4, and a reduced metabolic rate. Most individuals with mild hypothyroidism have non-specific symptoms including tiredness, lethargy, weight gain and depression, all of which are common in the general population. Therefore, diagnosis is confirmed with biochemical tests ( Taylor et al, 2018 ).
Once diagnosed treatment for hypothyroidism usually involves taking the drug levothyroxine, a synthetic form of T4. The dose of levothyroxine is calculated based on body weight, except in the case of people with ischaemic heart disease who are given a lower dose as it can precipitate severe angina ( Kumar and Clark, 2017 ).
Hyperthyroidism
Hyperthyroidism is caused when an overactive thyroid gland excretes excessive amounts of hormones. This affects around 2% of women and 0.2% of men, with the incidence increasing with age in both sexes ( National Institute for Health and Care Excellence (NICE), 2019 ). Graves' disease is the most common form of hyperthyroidism. It is an autoimmune disorder, characterised by the signs and symptoms shown in Table 2 , where antibodies are produced that bind to the same receptors as TSH and subsequently increase metabolic rate, raising the body's core temperature, which leads to increased sweating and weight loss ( Knight et al, 2021 ). Graves' disease can also cause a build-up of inflamed, fibrous, fatty tissue behind the eyes, causing them to bulge.
Risk factors for Graves' disease include smoking and being female ( Wémeau et al, 2021 ). Hyperthyroidism can be treated using anti-thyroid drugs or radioactive iodine (radioiodine) therapy that works by damaging and killing some of the follicular cells that secrete hormones, although this is not suitable for pregnant or breastfeeding women ( Subekti and Pramono, 2018 )
Presentation
Ms Singh is 56 years old and attends her GP after a week of severe itching (pruritus) and noticing thick white vaginal discharge.
Initial interpretation
Sexually transmitted diseases should be considered as a potential cause of vaginal discharge. However, in a woman over 50 years old, thrush (Candida albicans) is the most common cause ( Al Halteet et al, 2020 ).
Ms Singh had two previous episodes of thrush in the past few months, which she self-medicated with over-the-counter antifungal pessaries from the pharmacy. These temporarily improved her symptoms, which then reoccurred a few weeks later. She is finding the itching bothersome and was wondering if anything else can be prescribed to clear up the infection for good.
Her husband has no symptoms, and she has had no new sexual contacts in the last 30 years. In the past year she has been feeling increasingly tired and has put on 12 kg. Her older brother was diagnosed with diabetes mellitus and recently died following a stroke aged 64 years and her mother has several lower leg ulcers.
Physical examination
Ms Singh is obese with a body mass index (BMI) of 36.4 kg/m 2 . Her blood pressure is raised at 148/94 mmHg. A sample of her vaginal discharge, which is thick, white, and cottage-cheese like, has been sent for analysis.
Further investigations
Urinalysis identifies the presence of glucose in her urine (glycosuria). A random venous blood glucose reading of 12.8 mmol/litre is above normal range, and later her blood test results show her haemoglobin A1c (HbA1c), a marker of long-term glucose levels, is also high at 68 mmol/mmol. Table 3 shows the WHO reference levels for these tests in diabetes diagnosis.
Source: WHO, 2011
Interpretation of findings
Ms Singh has a strong family history of diabetes mellitus. Her obesity and ethnicity are also predisposing factors for type 2 diabetes mellitus ( Goff, 2019 ). These factors alongside her test results lead to Ms Singh being diagnosed with type 2 diabetes. Her high glucose levels in the urine and blood allows yeasts to flourish and accounts for her recurrent episodes of thrush.
Initially Ms Singh is given diet and lifestyle education to manage her diabetes, this will be reviewed in a few months to see how effective it has been. Her risk of further episodes of thrush will reduce as she improves her glucose control but, in this instance, she will be prescribed another antifungal pessary.
If her type 2 diabetes worsens or is unsuccessfully managed by diet and lifestyle adjustments, she may then be prescribed medications such as metformin and eventually even insulin ( NICE, 2022 ).
- Endocrine glands produce hormones, which maintain homeostasis with feedback loops and control bodily processes
- Hormones travel via the bloodstream and bind with specific receptors to produce their desired effect on target cells
- Endocrine disorders largely result from too much or too little hormone secretion due to disruption in the gland or at any point in the complex feedback pathways
- Medications can be used to mimic hormones or block receptors to attempt to reverse the effects of endocrine disorders
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
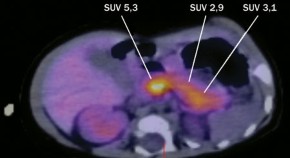
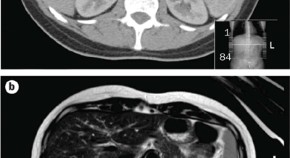
A patient with a large recurrent pheochromocytoma demonstrating the pitfalls of diagnosis
This Case Study illustrates some of the potential pitfalls of diagnosis and demonstrates a combination of problems of follow-up biochemical screening in a patient operated for a large pheochromocytoma at increased risk of malignant disease. The difficulty in assessing the presence of disease after initial surgical resection and reaching a diagnosis of malignancy are highlighted.
- Jörg Singer
- Christian A. Koch
- Ralf Paschke
A premenopausal woman with virilization secondary to an ovarian Leydig cell tumor
Virilizing ovarian tumors are rare neoplasms that may affect both women of reproductive age and postmenopausal women. This Case Study describes a young woman with longstanding amenorrhea and virilization and highlights the challenges and pitfalls in the diagnosis and choice of proper treatment for this uncommon cause of female hyperandrogenism.
- André M. Faria
- Ricardo V. Perez
- Maria A. A. Pereira
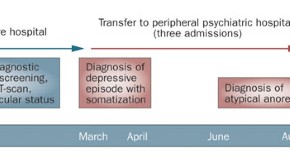
Addisonian crisis in a young man with atypical anorexia nervosa
Despite remarkable progress in the diagnosis and treatment of primary adrenal insufficiency, patients still suffer from delayed diagnosis, impaired well-being and the risk of life-threatening adrenal crisis. This Case Study highlights the need to evaluate individuals with chronic hyponatremia or unexplained weight loss and lack of energy for adrenal insufficiency.
- Bruno Allolio
- Katharina Lang
- Stefanie Hahner
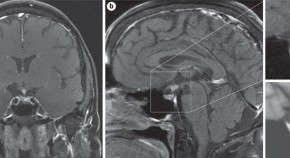
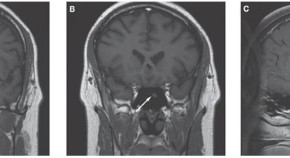
A patient with diabetes insipidus, anterior hypopituitarism and pituitary stalk thickening
Pituitary stalk thickening may occur as a result of diverse causes, including neoplastic, inflammatory and infectious diseases, and may lead to central diabetes insipidus, anterior hypopituitarism and local mass effect. This report discusses the case of a patient with pituitary stalk thickening associated with Langerhans cell histiocytosis, and highlights pertinent diagnostic and management issues.
- Nicholas A. Tritos
- Thomas N. Byrne
- Anne Klibanski
Klinefelter syndrome presenting as behavioral problems in a young adult
This Case Study describes an 18-year-old Somali man who initially presented to medical care with behavioral problems and was later diagnosed as having Klinefelter syndrome. Presented from the perspective of the primary care provider, this case illustrates the challenges in the clinical diagnosis and issues associated with long-term management of this relatively under-recognized condition.
- Alexandra M. Molnar
- Genji S. Terasaki
- John K. Amory
Focal congenital hyperinsulinism in a patient with septo-optic dysplasia
This Case Study describes an infant diagnosed as having focal congenital hyperinsulinism associated with septo-optic dysplasia, highlighting the importance of maintaining a high degree of suspicion in all infants who are investigated for chronic hypoglycemia. The authors report an as yet unidentified genetic etiology that may account for both focal congenital hyperinsulinism and septo-optic dysplasia.
- Raja Padidela
- Ritika R. Kapoor
- Khalid Hussain
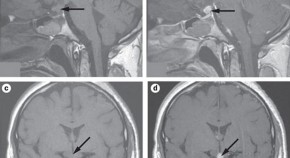
Lymphocytic hypophysitis with diabetes insipidus in a young man
Lymphocytic hypophysitis—an inflammatory condition of presumed autoimmune etiology—is characterized by an enlargement of the pituitary gland, resulting in its dysfunction. Although found generally in peripartum women, this Case Study of a 29-year-old man, who was referred to a neurosurgical clinic for evaluation of a suprasellar mass and diabetes insipidus, illustrates the need to consider this disorder in men.
- Ole-Petter R. Hamnvik
- Anna R. Laury
- Ursula B. Kaiser

Reevaluation of a case of type 1 diabetes mellitus diagnosed before 6 months of age
The authors of this Case Study demonstrate the substantial impact of molecular genetic testing in the improvement of diagnostics and patient treatment on the basis of the case of a 17-year-old patient who was diagnosed as having type 1 diabetes mellitus in early infancy, but after reassessment was found to have neonatal diabetes mellitus owing to a Kir6.2 mutation.
- Angus G. Jones
- Andrew T. Hattersley

Treatment of postmenopausal osteoporosis in a patient with celiac disease
This Case Study describes a patient diagnosed as having celiac disease as a result of examinations for secondary causes of bone loss. As osteoporosis in patients with celiac disease might result from a reduction of nutrient absorption in the small bowel, leading to calcium and/or vitamin D deficiency, the investigators highlight the need to evaluate secondary causes of osteoporosis in patients with persistent decline in BMD, particularly in postmenopausal women after treatment with hormone replacement therapy.
- JoAnn V. Pinkerton
- Alan C. Dalkin
- Edward B. Stelow
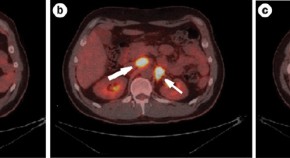
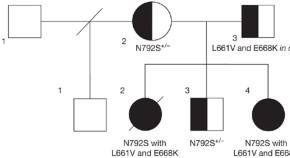
Paraganglioma syndrome type 1 in a patient with Carney–Stratakis syndrome
A thorough understanding of the diagnosis and treatment of familial paraganglioma syndromes is required for optimal therapy and management of patients with mutations of the succinate dehydrogenase complex. In this Case Study, Ayala-Ramirez and colleagues discuss current techniques for the localization of pheochromocytomas, paragangliomas and gastrointestinal stromal tumors and address the controversies of surgical removal of bilateral pheochromocytomas caused by a hereditary syndrome in a patient with Carney-Stratakis syndrome and paraganglioma syndrome type 1.
- Montserrat Ayala-Ramirez
- Glenda G. Callender
- Camilo Jimenez
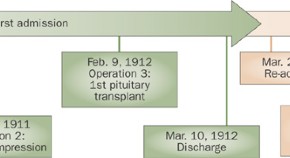
Harvey Cushing's attempt at the first human pituitary transplantation
Advances in organ and tissue transplantation continue to improve the care of patients with multiple diseases. The authors present the case of a patient with hypopituitarism secondary to a suprasellar mass, in whom the first documented pituitary gland transplantation was performed. This case study illustrates Harvey Cushing's pioneering work in pituitary transplantation in the early 20th century and the essential relationship between laboratory research and clinical practice.
- Courtney Pendleton
- Hasan A. Zaidi
- Alfredo Quiñones-Hinojosa
Diagnosis of insulinoma in a patient with hypoglycemia without obvious hyperinsulinemia
Initial diagnosis of insulinoma requires demonstration of inappropriately elevated insulin levels and concurrent hypoglycemia in the absence of administration of exogenous insulin or sulphonylureas. This article presents the case of a patient with insulinoma, who presented with hypoglycemia without coinciding evident hyperinsulinemia according to current guidelines. The article details current diagnostic criteria and highlights the role of clinical judgment in the investigation and management of cases, which do not conform to an expected pattern.
- Catarina Coelho
- Maralyn R. Druce
- Ashley B. Grossman

A case of diabetic Charcot arthropathy of the foot and ankle
Charcot arthropathy of the neuropathic foot and ankle is characterized by bone and joint destruction and deformities that may lead to ulcer, soft tissue infection, osteomyelitis and amputation. This article reviews the evaluation and treatment of this condition, highlighted by a clinical case of a man with type 2 diabetes mellitus who had Charcot collapse of the longitudinal arch, rocker bottom deformity and plantar ulcer.
- John M. Embil
- Elly Trepman

A woman with polycystic ovary syndrome treated for infertility by in vitro fertilization
This case illustrates some of the difficulties in treating anovulatory women with polycystic ovary syndrome, which is the most common cause of anovulatory infertility. Insulin resistance is a contributing factor to the pathogenesis of the syndrome. Assisted conception therapy is an effective treatment for women with polycystic ovary syndrome who are refractory to standard ovulation induction therapies or who have co-existing infertility factors. However, women with polycystic ovaries are particularly sensitive to stimulation with gonadotropins and have an increased risk of developing ovarian hyperstimulation syndrome.
- Thomas Tang
- Adam H. Balen

Pseudohypoparathyroidism type 1a and insulin resistance in a child
This article presents the case of a child with pseudohypoparathyroidism type 1a and associated endocrinopathies, namely, growth hormone deficiency, hypothyroidism, parathyroid hormone resistance and insulin resistance. The article details the natural history and management of these endocrinopathies, including the controversy over growth-hormone therapy, and potential mechanisms for insulin resistance in pseudohypoparathyroidism type 1a.
- Benjamin U. Nwosu
- Mary M. Lee
A case of severe, refractory diabetic gastroparesis managed by prolonged use of aprepitant
Gastroparesis is a complication of diabetes mellitus that is associated with prolonged periods of suboptimal glycemic control. This article describes a patient who had diabetic gastroparesis that was unresponsive to conventional treatments. Her severe vomiting was successfully controlled by use of the antiemetic drug aprepitant for 4 months before a gastric electrical stimulation device was fitted.
- Kiang Chong
- Ketan Dhatariya

Evaluation of a child for secondary causes of obesity and comorbidities
Childhood obesity is a serious public health concern. This Case Study discusses the evaluation and treatment of a child with obesity. The article details how careful assessment can exclude genetic causes of obesity in most children and outlines how children without genetic causes of the condition can benefit from individualized lifestyle modification programs.
- Robert E. Kramer
- Stephen R. Daniels
Generalized arterial calcification of infancy: treatment with bisphosphonates
Generalized arterial calcification of infancy is a rare and often fatal genetic disorder, for which no formalized treatment approach exists. This article describes a case where treatment with nitrogen-containing bisphosphonates resulted in normalization of the arterial structure.
- Kim A Ramjan
- Tony Roscioli
- Craig FJ Munns
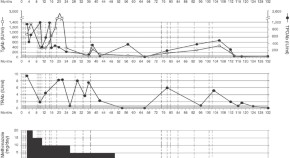
Cyclic Cushing syndrome due to an ectopic pituitary adenoma
Cyclic Cushing syndrome is a rare disorder characterized by periodic fluctuations in adrenal cortisol secretion, with phases of hypercortisolism alternating with periods of normal or low cortisol production. This Case Study discusses diagnostic challenges and treatment options in a patient with cyclic Cushing syndrome due to an ectopic pituitary adenoma.
- Rahfa K Zerikly
- Amir H Hamrahian
A patient with stress-related onset and exacerbations of Graves disease
Emotional stress might affect thyroid function by causing immunological perturbations and also via neural pathways. This article demonstrates a case in which both the onset of Graves disease and later exacerbations of hyperthyroidism were triggered by stressful events, and discusses management strategies for patients with stress-related Graves disease.
- Roberto Vita
- Daniela Lapa
- Salvatore Benvenga
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

12.1: Case Study: Hormones and Health
- Last updated
- Save as PDF
- Page ID 16788

- Suzanne Wakim & Mandeep Grewal
- Butte College
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Case Study: Hormonal Havoc
18-year-old Gabrielle checks her calendar. It has been 42 days since her last menstrual period, two weeks later than the length of the average woman’s menstrual cycle. Although many women would suspect pregnancy if their period was late, Gabrielle has not been sexually active. She is not even sure she is “late” because her period has never been regular. Ever since her first period at 13 years of age, her cycle lengths have varied greatly, and there are months where she does not get a period at all. Her mother told her that a girl’s period is often irregular when it first starts, but Gabrielle’s still has not become regular five years later. She decides to go to the student health center on her college campus to get it checked out.

The doctor asks her about the timing of her menstrual periods and performs a pelvic exam. She also notices that Gabrielle is overweight, has acne, and excess facial hair. As she explains to Gabrielle, while these physical characteristics can be perfectly normal, in combination with an irregular period they can be signs of a disorder of the endocrine, or hormonal, system called polycystic ovary syndrome (PCOS).
In order to check for PCOS, the doctor refers Gabrielle for a pelvic ultrasound and sends her to the lab to get blood work done. When her lab results come back, Gabrielle learns that her levels of androgens (a group of hormones) are high, and so is her blood glucose (sugar). The ultrasound showed that she has multiple fluid-filled sacs known as cysts in her ovaries. Based on Gabrielle’s symptoms and test results, the doctor tells her that she does indeed have PCOS.
PCOS is common in young women. It is estimated that between 1 in 10 to 20 women of childbearing age have PCOS — as many as five million women in the United States. You may know someone with PCOS or may have it yourself.
Read the rest of this chapter to learn about the glands and hormones of the endocrine system, their functions, how they are regulated, and the disorders — such as PCOS — that can arise when hormones are not regulated properly. At the end of the chapter, you will learn more about PCOS, its possible long-term consequences including fertility problems and diabetes, and how these negative outcomes can sometimes be prevented with lifestyle changes and medications.
Chapter Overview: Endocrine System
In this chapter, you will learn about the endocrine system, a system of glands that secrete hormones that regulate many of the body’s functions. Specifically, you will learn about:
- The glands that make up the endocrine system and how hormones act as chemical messengers in the body.
- The general types of endocrine system disorders.
- The types of endocrine hormones, including steroid hormones such as sex hormones, and non-steroid hormones such as insulin; and how they affect the functions of their target cells by binding to different types of receptor proteins.
- How the levels of hormones are regulated mostly through negative, but sometimes through positive, feedback loops.
- The master gland of the endocrine system, the pituitary gland, controls other parts of the endocrine system through the hormones that it secretes; and how the pituitary itself is regulated by hormones secreted from the hypothalamus of the brain.
- The thyroid gland and its hormones, which regulate processes such as metabolism and calcium homeostasis; how the thyroid is regulated; and the disorders that can occur when there are problems in thyroid hormone regulation, such as hyperthyroidism and hypothyroidism.
- The adrenal glands, which secrete hormones that regulate processes such as metabolism, electrolyte balance, responses to stress, and reproductive functions; and the disorders that can occur when there are problems in adrenal hormone regulation, such as Cushing’s syndrome and Addison’s disease.
- The pancreas, which secretes hormones that regulate blood glucose levels such as insulin; and disorders of the pancreas and its hormones including diabetes.
As you read this chapter, think about the following questions:
- Why can hormones have such a broad-range effect on the body, such as is seen in PCOS?
- Which hormones normally regulate blood glucose and how is this related to diabetes?
- What are androgens? How do you think their functions relate to some of the symptoms that Gabrielle is experiencing?
Attributions
- Calendar by Andreanna Moya CC BY 2.0 via flickr.com
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(10); 2023 Oct
- PMC10624418

Advancements in the Management of Endocrine System Disorders and Arrhythmias: A Comprehensive Narrative Review
Yogita kumari.
1 Medicine, Jinnah Postgraduate Medical Centre, Karachi, PAK
2 Internal Medicine, Liaquat University of Medical and Health Sciences, Jamshoro, PAK
Fahad Waqar
3 Medicine, Allama Iqbal Medical College, Lahore, PAK
Ahmad Talal Asif
4 Medicine, King Edward Medical University (KEMU) Lahore, Lahore, PAK
Beena Irshad
5 Medicine, Sharif Medical and Dental College, Lahore, PAK
6 Internal Medicine, Jinnah Sindh Medical University, Karachi, PAK
Vaidheesh Varagantiwar
7 Medicine, Rajiv Gandhi Institute of Medical Sciences, Adilabad, IND
Mahendra Kumar
8 Medicine, Sardar Patel Medical College Bikaner India, Bikaner, IND
9 Medicine, Peoples University of Medical & Health Science for Women, Nawabshah, PAK
Surat Chand
10 Medicine, Ghulam Mohammad Mahar Medical College, Sukkur, PAK
Satesh Kumar
11 Medicine and Surgery, Shaheed Mohtarma Benazir Bhutto Medical College, Karachi, PAK
Giustino Varrassi
12 Pain Medicine, Paolo Procacci Foundation, Rome, ITA
Mahima Khatri
13 Medicine and Surgery, Dow University of Health Sciences, Karachi, Karachi, PAK
Tamam Mohamad
14 Cardiovascular Medicine, Wayne State University, Detroit, USA
In recent years, notable advancements have been made in managing endocrine system disorders and arrhythmias. These advancements have brought about significant changes in healthcare providers' approach towards these complex medical conditions. Endocrine system disorders encompass a diverse range of conditions, including but not limited to diabetes mellitus, thyroid dysfunction, and adrenal disorders. Significant advancements in comprehending the molecular underpinnings of these disorders have laid the foundation for implementing personalized medicine. Advancements in genomic profiling and biomarker identification have facilitated achieving more accurate diagnoses and developing customized treatment plans. Furthermore, the utilization of cutting-edge pharmaceuticals and advanced delivery systems presents a significant advancement in achieving enhanced glycemic control and minimizing adverse effects for individuals afflicted with endocrine disorders. Arrhythmias, characterized by irregular heart rhythms, present a substantial risk to cardiovascular well-being. Innovative strategies for managing arrhythmia encompass catheter-based ablation techniques, wearable cardiac monitoring devices, and predictive algorithms powered by artificial intelligence. These advancements facilitate the early detection, stratification of risks, and implementation of targeted interventions, ultimately leading to improved patient outcomes. Incorporating technology and telemedicine has been instrumental in enhancing the accessibility and continuity of care for individuals diagnosed with endocrine disorders and arrhythmias. The utilization of remote patient monitoring and telehealth consultations enables prompt modifications to treatment regimens and alleviates the need for frequent visits to the clinic. This is particularly significant in light of the current global health crisis. This review highlights the interdisciplinary nature of managing endocrine disorders and arrhythmias, underscoring the significance of collaboration among endocrinologists, cardiologists, electrophysiologists, and other healthcare professionals. Multidisciplinary care teams have enhanced their capabilities to effectively address the intricate relationship between the endocrine and cardiovascular systems. In summary, endocrine system disorders and arrhythmias management have undergone significant advancements due to groundbreaking research, technological advancements, and collaborative healthcare approaches. This narrative review provides a comprehensive overview of the advancements, showcasing their potential to enhance patient care, improve quality of life, and decrease healthcare expenses. Healthcare providers must comprehend and integrate these advancements into their clinical practice to enhance outcomes for individuals with endocrine system disorders and arrhythmias.

Introduction and background
The complex orchestration of human physiology depends on the seamless interaction of multiple systems, each playing a distinct role in preserving well-being and equilibrium. Among these, the endocrine system and the cardiac conduction system are recognized as two crucial components that coordinate intricate physiological processes. The former regulates the release of hormones, which play a crucial role in various physiological processes such as metabolism, growth, and reproduction [ 1 ]. The latter governs the rhythmic pulsation of the heart, guaranteeing the uninterrupted flow of blood, oxygen, and nutrients necessary for sustaining life. However, when these intricately balanced systems experience disruptions, they can result in significant medical complications, leading to conditions commonly referred to as endocrine system disorders and arrhythmias [ 2 ]. Endocrine system disorders encompass a wide range of conditions characterized by hormone imbalances. These imbalances can originate from different endocrine glands, including the thyroid, pancreas, adrenal, and pituitary glands. These disorders encompass various conditions, such as diabetes mellitus, thyroid dysfunction, adrenal insufficiency, and polycystic ovary syndrome (PCOS). Although these conditions vary in their presentation and causes, they are connected by a shared factor of hormonal dysregulation that can significantly impact an individual's health and overall well-being [ 1 ]. On the other hand, arrhythmias are a category of cardiac rhythm abnormalities that involve irregularities in the heart's electrical signalling system. These irregularities can vary from harmless palpitations to severe conditions like ventricular fibrillation (VF). Some notable arrhythmias include atrial fibrillation (AF), ventricular tachycardia (VT), and bradycardia. While certain arrhythmias may not exhibit symptoms or have a relatively mild impact, others present substantial risks to individuals, potentially resulting in cardiac arrest and sudden death [ 2 ].
Managing disorders related to the endocrine system and arrhythmias is of significant clinical importance, given the widespread occurrence and impact of these conditions on global healthcare. In recent years, notable advancements have been made in these disorders' comprehension, identification, and management. These advancements have been driven by progress in medical technology, pharmacotherapy, and clinical research. This comprehensive narrative review examines recent advancements, innovations, and breakthroughs in managing disorders related to the endocrine system and arrhythmias. The prevalence of endocrine system disorders has become a significant global health concern. It is worth mentioning that diabetes mellitus has become a global health issue, as indicated by the World Health Organization (WHO) estimate that 422 million adults were affected by diabetes in the year 2014 [ 1 ]. As mentioned above, the figure has consistently increased, imposing a growing strain on healthcare systems and global economies. Diabetes is a medical condition characterized by chronic hyperglycemia caused by impaired insulin secretion or action. This condition is associated with complications, including cardiovascular disease, neuropathy, nephropathy, and retinopathy. The economic implications of diabetes are substantial, as it is estimated that global healthcare spending associated with diabetes will surpass $760 billion by 2045 [ 2 ].
Thyroid disorders have a significant global prevalence, impacting approximately 200 million individuals worldwide [ 3 ]. The thyroid gland is an essential endocrine system component and critical in regulating metabolism and overall homeostasis. Thyroid dysfunctions, including hypothyroidism, hyperthyroidism, and thyroid nodules, pose considerable clinical challenges. These disorders have the potential to result in a wide range of clinical manifestations, such as fluctuations in weight, disturbances in mood, and disruptions in metabolic function. In addition, conditions such as PCOS have received growing recognition for their significant implications on women's health [ 2 , 3 ]. PCOS is a prevalent endocrine disorder that primarily affects women in their reproductive years. It is distinguished by hormone level disruptions, irregular menstrual cycle irregularities, and the possibility of infertility [ 4 ]. In addition to its reproductive implications, PCOS is linked to metabolic disturbances, insulin resistance, and an elevated risk of cardiovascular disease. As a result, PCOS is a complex disorder with substantial clinical and public health implications. Additionally, the domain of arrhythmias poses distinctive challenges within the discipline of cardiology. AF, the most prevalent sustained arrhythmia, has become a notable issue of public health importance. According to estimates, it is projected that by 2030, the United States will experience a prevalence of approximately 14 to 17 million individuals living with AF [ 5 ]. AF presents significant morbidity and mortality risks due to its association with an elevated risk of stroke, heart failure, and overall mortality [ 6 ]. Ventricular arrhythmias, such as VT and VF, are serious medical conditions that can potentially be life-threatening. If not promptly addressed, these conditions can lead to sudden cardiac death. These cardiac arrhythmias frequently manifest in individuals with pre-existing structural heart disease, presenting a notable clinical obstacle. Moreover, bradycardias, characterized by abnormally slow heart rates, can result in syncope, compromised organ perfusion, and a diminished quality of life. The worldwide incidence of arrhythmias is anticipated to increase due to the ageing of populations and the growing prevalence of risk factors like obesity and hypertension [ 7 ]. Therefore, comprehending and effectively managing arrhythmias to prevent cardiovascular events and enhance patient outcomes is paramount.
The interplay between endocrine system disorders and arrhythmias adds complexity to the landscape. Diabetes mellitus, for instance, is not exclusively a metabolic disorder but also a substantial factor in cardiovascular morbidity and mortality [ 8 ]. People diagnosed with diabetes are at an increased risk of developing atherosclerosis, hypertension, and coronary artery disease. These conditions can make individuals more susceptible to experiencing arrhythmias. Thyroid disorders have also been linked to the occurrence of arrhythmias. Both hypothyroidism and hyperthyroidism can potentially disrupt cardiac electrophysiology, impacting the heart's normal rhythm [ 9 , 10 ]. The thyroid hormones significantly impact the electrical properties of the heart, and any disruption in their levels can result in the development of arrhythmias. The complex nature of this relationship highlights the importance of adopting a comprehensive and integrated approach to patient care. Healthcare professionals should be able to identify and effectively address the primary endocrine disorder and its potential cardiovascular implications. In the field of cardiology and electrophysiology, medical professionals need to take into account the hormonal environment when assessing and managing arrhythmias.
This extensive narrative review aims to offer healthcare professionals, researchers, and policymakers a thorough comprehension of the latest developments in managing endocrine system disorders and arrhythmias. This review seeks to provide a comprehensive understanding of the dynamic developments in the medical field by analyzing the most recent research findings, clinical trials, and technological advancements. This narrative review examines the recent advancements in diagnostic tools and techniques utilized to precisely identify endocrine system disorders and arrhythmias. Specifically, it explores the development of customized treatment plans tailored to individual patients, taking into account genomic profiling and the identification of relevant biomarkers. This discussion will focus on the various innovative approaches and therapeutic modalities that have emerged in the field of arrhythmia treatment. These include catheter-based ablation techniques, wearable cardiac monitoring devices, and artificial intelligence-driven predictive algorithms. Highlighting the significance of interdisciplinary collaboration within the healthcare field, it is crucial to recognize the value of cooperation among various healthcare professionals, including endocrinologists, cardiologists, and electrophysiologists. This collaboration is essential in effectively addressing the intricate interplay between the endocrine and cardiovascular systems. Please emphasize the effects of these advancements on patient-centered care, quality of life, and healthcare outcomes. This narrative review is a testament to the unwavering commitment to acquiring knowledge and driving innovation in medicine. This statement highlights the significant impact of research, technology, and collaboration in improving patient care and reducing the impact of endocrine system disorders and arrhythmias on individuals and healthcare systems.
Methodology
This narrative review employs a systematic and comprehensive approach to gather, evaluate, and synthesize relevant literature.
Literature Search Strategy
A comprehensive search of electronic databases was conducted, including PubMed/MEDLINE, Embase, Scopus, and Google Scholar. These databases were chosen for their comprehensive biomedical and clinical research literature coverage. The search queries were constructed using a combination of medical subject headings (MeSH) terms and keywords. Terms related to endocrine system disorders, arrhythmias, and advancements in their management were used in the search strategy. Sample search terms included "endocrine disorders," "thyroid dysfunction," "arrhythmia," "diabetes management," and "atrial fibrillation treatment." Boolean operators such as "AND" and "OR" were used to refine the search and combine relevant search terms effectively. For instance, "endocrine disorders AND arrhythmia" was used to identify articles relevant to both topics.
Inclusion and Exclusion Criteria
Articles were included if they were peer-reviewed, published in English, and contained information on recent advancements in managing endocrine system disorders and arrhythmias. Review articles, original research studies, clinical trials, and expert opinion pieces were considered for inclusion. Articles published before the year 2000 were excluded to focus on recent developments.
Data Collection
The initial database search yielded a broad pool of articles. Titles and abstracts of these articles were screened for relevance. Articles not aligning with the review's scope were excluded at this stage. Full-text versions of potentially relevant articles were obtained and thoroughly reviewed. Additional articles not meeting the inclusion criteria or needing more substantial information on recent advancements were excluded during this stage. Pertinent information from the selected papers, including study design, key findings, methodologies, and references to additional relevant sources, was extracted for incorporation into the review.
Synthesis of Information
The information extracted from the selected articles was categorized into thematic areas, including but not limited to diagnostic advancements, personalized medicine, therapeutic innovations, telemedicine, interdisciplinary collaboration, and patient-centered care. A narrative approach was used to synthesize the information obtained from the selected articles. This involved organizing and presenting the findings in a coherent and logical narrative that follows the review's structure. The selected articles were critically appraised for their quality, relevance, and potential bias. Studies with rigorous methodologies, large sample sizes, and clinical significance were given greater weight in the narrative synthesis.
Data Presentation and Reporting
The review is structured to provide a comprehensive overview of advancements in managing endocrine system disorders and arrhythmias. The information is coherently and organized, following the headings and subheadings outlined in the review's structure.
Limitations
It is acknowledged that the review may be subject to publication bias, as it primarily relies on published peer-reviewed articles. Relevant advancements or studies that have not been published or are in non-English languages may not be included. The review focuses on recent advances, potentially excluding valuable historical context or earlier contributions to the field. The study encompasses a wide range of medical specialties, which may introduce variations in the depth and breadth of information available in different areas.
Ethical Considerations
Ethical approval was not required for this narrative review, as it solely relies on publicly available, peer-reviewed literature analysis.
Historical perspective
The historical evolution of our understanding and management of endocrine disorders and arrhythmias has been a fascinating journey marked by significant milestones and breakthroughs. This section will trace the developments in these domains, shedding light on the fundamental discoveries and innovations that have paved the way for modern advancements in the field.
Understanding and Treatment of Endocrine Disorders
The history of endocrinology can be traced back to ancient civilizations where observations of endocrine-related phenomena were made. In ancient Greece, the term "goiter" was coined to describe the enlargement of the thyroid gland. However, its hormonal basis was not understood at the time [ 11 ]. Ancient Indian texts also documented the clinical manifestations of diabetes-like symptoms and prescribed treatments. However, the endocrine nature of diabetes was not recognized [ 12 ], and the 19th century witnessed significant advancements in understanding endocrine disorders.
In 1850, Thomas Addison described the condition now known as Addison's disease, recognizing the importance of the adrenal glands in maintaining health. Simultaneously, the work of Parry and Graves led to the recognition of Graves' disease and its association with thyroid dysfunction. These discoveries laid the foundation for understanding autoimmune endocrine disorders [ 13 ]. The early 20th century marked a watershed moment in endocrinology with the discovery of hormones. In 1905, Bayliss and Starling introduced the concept of hormone signaling with their description of secretin. This hormone regulates pancreatic secretion [ 14 ]. This laid the groundwork for understanding hormonal regulation in the endocrine system. One of the most significant breakthroughs in endocrinology occurred with the discovery of insulin.
In 1921, Banting and Best successfully isolated insulin, a hormone produced by the pancreas, leading to a life-saving treatment for diabetes. This marked the birth of modern endocrine therapy and the dawn of personalized medicine for diabetes management [ 15 ]. The 20th century saw the development of hormone replacement therapy (HRT) for various endocrine disorders. For instance, the introduction of levothyroxine in the 1950s revolutionized the treatment of hypothyroidism. Additionally, using corticosteroids in the 1940s transformed the management of adrenal insufficiency [ 15 ]. The development of diagnostic imaging techniques, such as ultrasound and scintigraphy, in the 20th century greatly enhanced the diagnosis and management of endocrine disorders. These technologies allowed for non-invasive visualization and assessment of endocrine glands, improving the accuracy of diagnoses [ 16 ].
Understanding and Treatment of Arrhythmias
The history of arrhythmia dates back to ancient times when irregular heartbeats were noted by physicians like Hippocrates in ancient Greece. However, the mechanisms behind arrhythmias remained a mystery. In the late 19th century, we witnessed a pivotal moment with the invention of the electrocardiogram (ECG) by Willem Einthoven in 1903. This groundbreaking technology allowed the recording of electrical activity in the heart. It provided valuable insights into the underlying mechanisms of arrhythmias [ 16 ]. In the 20th century, the role of the atrioventricular (AV) node in cardiac conduction and bradycardia became clearer. The identification of AV block by Wenckebach in 1899 (Wenckebach, 1899) and Mobitz in 1924 (Mobitz, 1924) marked essential milestones in understanding the electrical conduction system of the heart [ 16 ]. The development of cardiac catheterization techniques in the mid-20th century allowed for assessing arrhythmias' structural and electrical causes [ 17 ]. This innovation laid the groundwork for more precise diagnostic and therapeutic interventions. The development of antiarrhythmic drugs, such as quinidine and procainamide, in the 20th century, marked a significant advancement in arrhythmia management [ 18 ]. These medications could suppress arrhythmias and restore normal cardiac rhythm. Catheter ablation, a technique used to treat arrhythmias by selectively destroying abnormal cardiac tissue, was introduced in the late 20th century [ 18 ]. This minimally invasive procedure has revolutionized the treatment of certain arrhythmias. Implantable devices, such as pacemakers and implantable cardioverter-defibrillators (ICDs), became increasingly sophisticated and widely used in the late 20th century [ 19 ]. These devices provided life-saving interventions for individuals with bradyarrhythmia and tachyarrhythmias. The 21st century has seen further refinements in catheter ablation techniques and the development of advanced cardiac mapping systems. These advancements have greatly improved arrhythmia treatments' precision and success rates [ 20 ]. The historical perspective of endocrine disorders and arrhythmias reveals a fascinating journey from ancient observations to modern advancements. Key milestones, such as the discovery of insulin and the invention of the electrocardiogram, have revolutionized our ability to understand, diagnose, and treat these conditions. These historical developments continue to shape the landscape of endocrinology and cardiology, emphasizing the importance of ongoing research and innovation in improving patient care and outcomes.
Advances in diagnostic tools
Medicine is continually evolving, and nowhere is this more evident than in diagnostics. Advances in diagnostic tools have played a pivotal role in early detection, accurate characterization, and personalized treatment of various medical conditions. This comprehensive discussion will explore the latest diagnostic techniques and technologies in endocrine system disorders and arrhythmias. We will specifically delve into the role of genomic profiling, biomarker identification, and cutting-edge imaging modalities in enhancing our understanding and management of these complex medical conditions.
Genomic Profiling: Unlocking the Genetic Code
Genomic profiling has emerged as a transformative tool in diagnosing and managing endocrine disorders and arrhythmias. It involves the comprehensive analysis of an individual's genetic material to identify specific genetic variations, mutations, or alterations that may predispose them to these conditions. Genomic profiling encompasses next-generation sequencing (NGS), whole-genome, and whole-exome sequencing. Genomic studies have identified specific genetic variants associated with PCOS, shedding light on its underlying genetic basis [ 21 ]. These findings offer opportunities for personalized treatment and risk prediction. Genetic markers related to thyroid dysfunction have been identified, allowing for a better understanding of the genetic susceptibility to conditions like Graves' disease and Hashimoto's thyroiditis [ 22 ]. Genomic profiling has been instrumental in identifying mutations in ion channel genes responsible for long QT syndrome (LQTS) [ 23 ]. This knowledge has led to targeted therapies and risk stratification. Genetic testing has revealed mutations in sodium channel genes as a cause of Brugada syndrome, guiding clinical management [ 23 ]. Genomic profiling not only aids in diagnosis but also allows for the development of precision medicine approaches, tailoring treatments to an individual's genetic makeup. Additionally, it enables the identification of at-risk family members, facilitating preventive measures.
Biomarker Identification: Unveiling Disease Signatures
Biomarkers are measurable indicators of normal biological processes, pathogenic processes, or pharmacological responses to therapeutic interventions. In the context of endocrine disorders and arrhythmias, biomarker identification has grown increasingly important as it can enable early disease detection, prognostication, and monitoring of treatment responses. Here, we explore recent advancements in biomarker discovery. Glycated haemoglobin (HbA1c) remains a cornerstone biomarker for diabetes management, but novel biomarkers are being explored. For example, the discovery of specific microRNAs (miRNAs) associated with diabetes has shown promise in early diagnosis and predicting disease progression [ 23 ]. Thyroid-stimulating hormone (TSH) and thyroxine (T4) levels have traditionally been used to diagnose thyroid dysfunction. Recent research has focused on identifying novel biomarkers, including serum thyroglobulin and thyroid peroxidase antibodies, to improve diagnostic accuracy [ 24 ].
Arrhythmias
Biomarkers like brain natriuretic peptide (BNP) and N-terminal pro-BNP have emerged as predictors of AF recurrence and severity [ 22 ]. Additionally, circulating microRNAs have shown potential as diagnostic and prognostic biomarkers in AF. Identifying biomarkers for risk stratification in ventricular arrhythmias is crucial. Biomarkers like C-reactive protein (CRP) and cardiac troponins have been studied for their association with arrhythmic events [ 23 ]. Advancements in high-throughput technologies, such as mass spectrometry and proteomics, have accelerated biomarker discovery by allowing the simultaneous analysis of thousands of molecules in biological samples. These emerging biomarkers promise to improve the precision and timeliness of diagnosis in endocrine disorders and arrhythmias.
Cutting-Edge Imaging Modalities: Visualizing Anatomy and Function
In diagnosing and managing endocrine disorders and arrhythmias, imaging modalities have undergone remarkable advancements, enabling clinicians to visualize anatomical structures and functional aspects of the endocrine and cardiovascular systems with unprecedented detail. High-resolution ultrasound has become the standard for evaluating thyroid nodules, aiding in the characterization of nodules as benign or suspicious for malignancy [ 24 ]. Positron emission tomography (PET) imaging with radiolabeled tracers, such as 18F-fluorodeoxyglucose (FDG), has proven valuable in detecting neuroendocrine tumors [ 25 ]. Advances in ECG technology, including 12-lead Holter monitors and mobile ECG devices, have improved the detection and monitoring of arrhythmias, especially AF [ 26 ]. Cardiac MRI provides exquisite anatomical and functional information, aiding in assessing arrhythmia substrates, myocardial infarctions, and cardiomyopathies. Advances in diagnostic tools have ushered in a new era of precision medicine, revolutionizing the diagnosis and management of endocrine disorders and arrhythmias. Genomic profiling has unveiled the genetic underpinnings of these conditions, paving the way for personalized treatment approaches. Biomarker identification offers promising avenues for early diagnosis and treatment monitoring. Cutting-edge imaging modalities provide clinicians with unprecedented insights into the anatomy and function of the endocrine and cardiovascular systems. These advancements enhance diagnostic accuracy and transform healthcare delivery, allowing for tailored interventions that improve patient outcomes and quality of life. As research evolves, the future promises even more sophisticated and effective diagnostic tools for better healthcare.
Personalized medicine in endocrine disorders
In recent years, personalized medicine has emerged as a groundbreaking paradigm in healthcare, revolutionizing the diagnosis and treatment of various medical conditions, including endocrine disorders. This approach acknowledges the inherent variability among individuals and seeks to tailor medical interventions to a patient's unique genetic makeup, lifestyle, and clinical characteristics. In this comprehensive discussion, we will explore how advancements in personalized medicine are reshaping the management of endocrine disorders. We will delve into the role of genomic data, individualized therapy plans, and the tangible improvements in patient outcomes resulting from this patient-centric approach.
The Era of Genomic Medicine: Unraveling Genetic Complexity
Genomic medicine has been a pivotal driver of personalized treatment in endocrine disorders. The human genome project, completed in 2003, marked a significant milestone by providing a comprehensive map of the human genome's structure and function. This monumental achievement paved the way for a deeper understanding of the genetic underpinnings of endocrine disorders, enabling clinicians to unravel their complexities and devise targeted therapies. PCOS, a common endocrine disorder affecting women, showcases the power of genomic medicine. Recent studies have identified specific genetic variants associated with PCOS, shedding light on its multifactorial aetiology [ 27 ]. This genetic insight allows for tailored treatment approaches based on an individual's genetic predisposition, potentially optimizing therapeutic outcomes. The genetic basis of thyroid disorders, including autoimmune conditions like Graves' disease and Hashimoto's thyroiditis, has been elucidated through genomic research [ 27 ]. Understanding the genetic susceptibility of patients can guide therapeutic choices, such as the selection of antithyroid drugs or the consideration of thyroidectomy.
Tailored Therapy Plans: Precision in Action
Advancements in genomics have paved the way for the development of individualized therapy plans, where treatment decisions are guided by a patient's unique genetic profile, biomarker data, and clinical presentation. These personalized approaches offer tangible benefits, including improved treatment efficacy and minimizing adverse effects. Diabetes management exemplifies the shift toward personalized care. Genetic testing can identify monogenic forms of diabetes, which differ significantly from the more common type 2 diabetes [ 28 ]. Accurate classification of diabetes subtypes informs treatment strategies, such as sulfonylureas for patients with monogenic diabetes. In the realm of adrenal disorders, personalized approaches have gained traction. For instance, patients with primary aldosteronism may undergo adrenal vein sampling to localize the source of excess aldosterone production [ 28 ]. This information guides therapeutic decisions, such as deciding between surgery and medical management.
Genomic Data in Decision-Making: Realizing Improved Outcomes
Integrating genomic data into clinical decision-making has yielded substantial benefits in terms of patient outcomes. By tailoring treatments to an individual's genetic makeup, healthcare providers can optimize therapeutic responses, minimize adverse effects, and enhance overall quality of life. In cancer-related endocrine disorders like thyroid cancer, genomic testing can identify specific genetic mutations (e.g., BRAF, RET) that inform prognosis and guide treatment choices [ 29 ]. Targeted therapies, including tyrosine kinase inhibitors, have emerged as effective treatments for patients with specific genetic alterations. Genomic analysis has revealed the genetic basis of growth hormone deficiency, allowing for the identification of gene mutations responsible for this condition [ 30 ]. This genetic insight enables the precise prescription of growth hormone replacement therapy, leading to improved growth and quality of life for affected individuals.
Challenges and Considerations
The handling of genomic data raises concerns about privacy and ethical implications. Safeguarding patient information and ensuring informed consent are critical considerations in personalized medicine [ 31 ]. Genomic testing can be expensive, and access to these services may be limited in some regions. Efforts to make genomic testing more cost-effective and accessible are ongoing [ 23 ]. Successful implementation of personalized medicine often requires collaboration among healthcare professionals from various specialties, including genetic counsellors, endocrinologists, and pharmacists [ 32 ]. Patients need to be informed about the benefits and limitations of genomic testing. Clear communication and education are essential to ensure patients can make informed decisions about their healthcare [ 33 ]. Personalized medicine has ushered in a new era of patient-centric care, transforming the landscape of endocrine disorder management. Genomic data and individualized therapy plans are at the forefront of this revolution, allowing clinicians to tailor treatments to each patient's unique genetic and clinical characteristics. The result is improved treatment efficacy, minimized adverse effects, and enhanced patient outcomes. As genomic research advances, the potential for personalized medicine to improve the lives of individuals with endocrine disorders remains promising. However, addressing challenges related to data privacy, cost, interdisciplinary collaboration, and patient education will be crucial in realizing the full potential of personalized medicine in endocrinology.
Innovations in arrhythmia management
Arrhythmias, irregular heart rhythms, have long been a challenge in cardiology. Over the years, innovations in arrhythmia management have transformed the landscape of diagnosis and treatment, offering new hope for patients with these conditions. This comprehensive discussion will delve into cutting-edge methods for diagnosing and treating arrhythmias. Specifically, we will explore catheter-based ablation techniques, cardiac monitoring devices, and predictive algorithms, highlighting how these innovations revolutionize arrhythmia management. Catheter-based ablation techniques have emerged as a cornerstone of arrhythmia management, offering precise and effective treatment options for patients with various arrhythmic disorders. These techniques involve using catheters to target and eliminate the abnormal electrical pathways responsible for arrhythmias. AF, the most common sustained arrhythmia, has witnessed significant advancements in ablation strategies. Pulmonary vein isolation (PVI) has become a standard approach, targeting triggers in the pulmonary veins [ 34 ]. Recent innovations include using advanced mapping technologies like contact force sensing catheters, enhancing the accuracy of lesion delivery. Catheter-based ablation has also revolutionized VT management. Substrate mapping, involving identifying scar tissue and abnormal electrograms, plays a crucial role in VT ablation [ 35 ]. Stereotactic body radiation therapy (SBRT) has emerged as a novel non-invasive approach for refractory VT [ 36 ]. SVTs, including atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT), are amenable to catheter ablation. Radiofrequency ablation at specific anatomical sites, such as the slow pathway for AVNRT, has high success rates. These catheter-based approaches have improved the efficacy of arrhythmia treatment and reduced complications, shorter hospital stays, and enhanced patient outcomes.
Cardiac Monitoring Devices: Continuous Vigilance
Cardiac monitoring devices have evolved to provide continuous, real-time arrhythmias surveillance, aiding in diagnosis and treatment. These devices come in various forms, from wearable monitors to implantable devices, enabling healthcare providers to capture crucial data for informed decision-making. ICDs have become a standard of care for patients at risk of sudden cardiac death due to ventricular arrhythmias [ 37 ]. Advanced ICDs provide defibrillation and offer continuous monitoring and remote data transmission to healthcare providers. Devices like pacemakers and implantable loop recorders (ILRs) have seen remarkable advancements. ILRs, in particular, have become powerful tools for diagnosing cryptogenic strokes and unexplained syncope by recording heart rhythm data over extended periods [ 37 ]. The proliferation of wearable technology, including smartwatches and chest patches, has democratized cardiac monitoring. These devices can detect arrhythmias, record ECGs, and provide real-time alerts to users and healthcare professionals [ 38 ].
Predictive Algorithms: Anticipating Arrhythmias
Integrating artificial intelligence (AI) and predictive algorithms into arrhythmia management has ushered in a new era of proactive care. These algorithms leverage vast datasets to predict arrhythmic events, enabling early intervention and prevention. AI-based predictive algorithms analyze patients' ECG data to forecast AF episodes. Such algorithms can aid in the timely initiation of anticoagulation therapy to prevent stroke. Predictive models for VT and VF can identify patients at high risk of sudden cardiac death [ 39 ]. These algorithms inform the selection of appropriate therapies, including ICD implantation. Predictive algorithms can be seamlessly integrated into telehealth platforms, allowing remote monitoring of high-risk patients. This approach ensures timely intervention and reduces healthcare system burden. Using cardiac monitoring devices and predictive algorithms raises data security and privacy concerns. Ensuring the secure transmission and storage of patient data is paramount. Access to advanced arrhythmia management tools should be equitable across diverse populations. Disparities in access to care and technology must be addressed. Predictive algorithms require rigorous validation to ensure their accuracy and clinical utility. Collaboration between clinicians and data scientists is essential in this regard. Balancing the cost of implementing these innovations with their clinical benefits is crucial. Health economic analyses are essential to determine cost-effectiveness. Innovations in arrhythmia management are ushering in a new era of precision and proactive care. Catheter-based ablation techniques are offering effective and less invasive treatment options. Cardiac monitoring devices are providing continuous vigilance, enabling early diagnosis and intervention. Predictive algorithms are helping anticipate arrhythmic events, potentially saving lives. As technology advances and research in this field progresses, arrhythmia management will become even more patient-centric and data-driven. Addressing challenges related to data security, health equity, clinical validation, and cost-effectiveness will be crucial in harnessing the full potential of these innovations to improve the lives of individuals with arrhythmias.
Telemedicine and remote patient monitoring
Telemedicine and remote patient monitoring have revolutionized healthcare by transcending geographical boundaries and enabling patients to access high-quality care from their homes. This transformation has significant implications for the management of endocrine disorders and arrhythmias. In this comprehensive analysis, we will explore the role of telemedicine and remote monitoring in these two medical domains, emphasizing how these technologies enhance access to care, promote patient compliance, and contribute to improved health outcomes.
Telemedicine in Endocrine Management
Endocrine disorders, which encompass conditions affecting the thyroid, adrenal glands, and pancreas, often require ongoing monitoring and medication adjustments. Telemedicine enables endocrinologists to conduct remote consultations with patients, eliminating the need for frequent in-person visits. This is particularly beneficial for individuals with conditions like diabetes, where regular check-ups are essential. Integrated with telemedicine platforms, CGM devices allow patients to transmit real-time glucose data to their healthcare providers. This facilitates timely adjustments to insulin regimens and improves glycemic control [ 40 ]. Patients can receive medication management and dosage adjustments through telemedicine, reducing non-adherence risk. Telehealth visits also enhance patient education about the importance of medication adherence [ 40 ].
Remote Monitoring in Arrhythmia Management
Arrhythmias, including AF and VT, require continuous monitoring and prompt intervention. These portable devices can record cardiac rhythms over extended periods and transmit data remotely. Patients with suspected arrhythmias can wear these devices, and healthcare providers can review the recorded data remotely, leading to early diagnosis and treatment. Implantable devices such as pacemakers and defibrillators have remote monitoring capabilities. These devices automatically transmit data to healthcare providers, allowing them to detect and address arrhythmias promptly [ 24 ]. Specialized arrhythmia clinics offer telehealth appointments for arrhythmia patients. These clinics provide expert consultation and remote monitoring, ensuring patients receive the necessary care and support.
Improving Access to Care
Patients in rural areas often face challenges in accessing specialized endocrine or cardiology care. Telemedicine bridges this gap, enabling remote consultations with specialists. Patients with chronic endocrine disorders or arrhythmias may need frequent follow-up visits. Telemedicine eliminates the need for extensive travel, reducing patients' financial and logistical burdens. Telemedicine allows patients to consult with renowned specialists worldwide, breaking geographical barriers. This is particularly advantageous for individuals with complex or rare conditions [ 41 ].
Enhancing Patient Compliance
Remote patient monitoring encourages patients to adhere to regular check-ups and monitoring. Knowing that their data is being transmitted and reviewed by healthcare providers incentivizes patients to stay engaged in their care. Telehealth visits offer opportunities for healthcare providers to discuss medication adherence with patients. Medication regimens can be adjusted based on patient feedback and monitoring data. Telehealth appointments provide a platform for patient education. Healthcare providers can educate patients about lifestyle modifications, medication compliance, and self-monitoring, leading to better adherence [ 26 ].
Patients may need access to the necessary technology or have limited digital literacy. Efforts are needed to ensure equitable access. Protecting patient data from breaches and ensuring compliance with privacy regulations is paramount. Policies and reimbursement models must evolve to support telehealth and remote monitoring, ensuring financial sustainability. Seamless integration of telemedicine and remote monitoring with electronic health records (EHRs) is essential to streamline care coordination [ 27 ]. Telemedicine and remote patient monitoring have emerged as transformative tools in managing endocrine disorders and arrhythmias. These technologies improve access to specialized care, enhance patient compliance, and improve health outcomes. Healthcare systems can harness the full potential of telemedicine and remote monitoring to deliver patient-centred care by addressing technology access, data security, reimbursement, and interoperability challenges. In a rapidly evolving healthcare landscape, telemedicine and remote monitoring continue to shape the future of healthcare delivery, offering innovative solutions for patients with chronic and complex conditions.
Interdisciplinary collaboration
The demand for comprehensive and patient-centred care has become increasingly imperative in the rapidly evolving healthcare landscape. To meet this demand, interdisciplinary collaboration among healthcare professionals has emerged as a fundamental approach. Collaboration among healthcare specialists enhances the quality of care. It improves patient outcomes, particularly in complex fields such as endocrinology and cardiology. This comprehensive essay emphasizes the importance of interdisciplinary collaboration. It shows how endocrinologists, cardiologists, and other specialists work together to provide holistic care. By exploring how these professionals collaborate and sharing pertinent studies and evidence, this essay will underscore the vital role of interdisciplinary collaboration in modern healthcare.
Importance of Interdisciplinary Collaboration
Interdisciplinary collaboration in healthcare is the practice of healthcare professionals from various fields working together to provide patient-centred care. This collaboration extends beyond the conventional silos of medical specialties and fosters a comprehensive, holistic approach to patient management. Collaboration allows healthcare providers to address all aspects of a patient's health, considering physical and psychological factors. This comprehensive approach leads to a more accurate diagnosis and effective treatment plan. Research consistently demonstrates that interdisciplinary collaboration results in improved patient outcomes. A study published in the Journal of General Internal Medicine found that collaborative care models for chronic diseases led to better clinical outcomes and increased patient satisfaction [ 29 ]. Collaboration can lead to more efficient use of resources, reducing redundancy and unnecessary tests. This, in turn, lowers healthcare costs while maintaining or improving the quality of care. Interdisciplinary teams bring together diverse perspectives, allowing for more creative problem-solving and innovative approaches to patient care [ 31 ]. Collaboration emphasizes patient preferences and values, ensuring the care plan aligns with the patient's goals and needs.
Interdisciplinary Collaboration in Endocrinology
Endocrinology is a medical specialty focused on the endocrine system, encompassing hormone-producing glands and their hormones. Conditions treated by endocrinologists include diabetes, thyroid disorders, and hormonal imbalances. Collaborative care in endocrinology involves working closely with other specialists to address the diverse aspects of patients' health. Diabetic patients often require a multi-faceted approach involving endocrinologists, dietitians, and primary care physicians. For instance, a study in Diabetes Care highlighted the benefits of a team-based care approach involving endocrinologists and pharmacists in managing type 2 diabetes, leading to improved glycemic control [ 32 ]. Patients with thyroid disorders may need the expertise of an endocrinologist in conjunction with a surgeon if surgery is required or a radiologist for thyroid imaging. This collaborative approach ensures a thorough evaluation and tailored treatment. Endocrinologists collaborate with mental health professionals when hormonal imbalances lead to mood disorders. Such collaboration helps address both the physical and psychological aspects of the condition.
Interdisciplinary Collaboration in Cardiology
Cardiology focuses on the heart and circulatory system, addressing conditions like heart disease, arrhythmias, and congestive heart failure. Collaboration in cardiology is crucial for a holistic understanding and management of cardiovascular diseases. Cardiologists work closely with primary care physicians to assess cardiovascular risk factors such as hypertension, high cholesterol, and diabetes. This collaboration enables early intervention and lifestyle modifications. In cases where invasive procedures like angioplasty or stent placement are necessary, cardiologists collaborate with interventional radiologists or cardiovascular surgeons. This multidisciplinary approach ensures that the best course of action is taken. The management of congestive heart failure often involves a team of healthcare professionals, including cardiologists, nurses, pharmacists, and dietitians. Collaboration helps in optimizing medication regimens and educating patients on self-care.
The Collaborative Model
One can examine the Collaborative Care Model, often employed in addressing chronic illnesses, to understand how interdisciplinary collaboration operates in healthcare. This model is particularly relevant in the context of endocrinology and cardiology. Healthcare providers from various disciplines, including physicians, nurses, psychologists, social workers, and pharmacists, work together to provide patient-centered care. A designated care coordinator ensures that information is shared among team members and that the patient's care plan is cohesive and consistent. Team members meet regularly and communicate to discuss patient progress, adjust treatment plans, and address any challenges or concerns. Patients are actively involved in their care and decision-making, with clear communication and education provided to help them manage their condition effectively. A study in JAMA Internal Medicine demonstrated the effectiveness of the Collaborative Care Model in improving outcomes for patients with depression and chronic medical conditions [ 34 ]. This model can easily be adapted to address the complex needs of patients with endocrine and cardiac disorders. Interdisciplinary collaboration among healthcare professionals is paramount in providing holistic and patient-centered care. In endocrinology and cardiology, collaboration between specialists leads to improved patient outcomes, enhanced problem-solving, efficient resource utilization, and better healthcare delivery. The Collaborative Care Model exemplifies how interdisciplinary teams can work together to address complex health conditions effectively. By emphasizing the importance of interdisciplinary collaboration and showcasing its practical application in patient care, healthcare systems can better meet the evolving needs of patients in today's dynamic healthcare landscape.
Patient-centered care
Patient-centred care is a fundamental principle of modern healthcare that places the patient at the forefront of decision-making and treatment. It encompasses the physical aspects of medical treatment and healthcare's emotional, psychological, and social dimensions. Over the years, healthcare delivery and management advancements have significantly transformed the patient experience and quality of life. This essay explores the impact of these advancements on patient experience and quality of life, drawing on patient testimonials and case studies to illustrate the benefits of modern management approaches.
Advancements in Patient-Centered Care
The integration of technology has revolutionized healthcare. EHRs, telemedicine, wearable devices, and mobile health apps have enhanced patient engagement and communication with healthcare providers. Patients can now access their medical records, schedule appointments, and receive real-time health data, empowering them to participate in their care actively [ 36 ]. Advances in genomics and precision medicine have allowed for tailored treatment plans based on an individual's genetic makeup. Personalized medicine ensures that treatments are more effective and have fewer side effects, resulting in a higher quality of life for patients [ 37 ]. Access to reliable health information online has enabled patients to become more informed about their conditions and treatment options. Educational resources, such as online videos and forums, help patients make informed decisions and actively engage in their healthcare journey. Collaborative care models involving multiple healthcare professionals from different disciplines have become more common. This approach ensures that patients receive comprehensive care that addresses their physical, emotional, and social needs. For example, a Journal of General Internal Medicine study found that collaborative care for chronic diseases improved clinical outcomes and patient satisfaction [ 38 ].
Impact on Patient Experience
Patients are now more empowered to engage in their healthcare decisions actively. They can access their medical information and communicate with healthcare providers remotely. This enhanced sense of control and involvement leads to better patient experiences. Telemedicine and online appointment scheduling have significantly reduced wait times for routine consultations. Patients no longer have to endure long waits in waiting rooms, leading to increased convenience and satisfaction. Technology-driven communication tools enable patients to ask questions, seek clarifications, and share concerns with their healthcare providers easily. Timely and effective communication enhances trust and patient-provider relationships. Personalized medicine and access to health information allow patients to make informed decisions about their treatment options. They can actively participate in selecting the most suitable treatment plan, resulting in a sense of empowerment [ 39 ].
Impact on Quality of Life
Personalized medicine minimizes the risk of adverse reactions to medications, improving the quality of life for patients with chronic conditions. For example, targeted therapies are associated with fewer side effects in oncology than traditional chemotherapy. Telemedicine and mobile health apps enable patients to access healthcare services from the comfort of their homes. This convenience is especially valuable for individuals with mobility limitations or those living in remote areas [ 40 ]. Remote monitoring and wearable devices allow healthcare providers to track patients' health parameters continuously. This real-time data helps in early detection and prompt intervention, improving symptom management and overall well-being [ 40 ]. Advancements in patient-centered care, driven by technology, personalized medicine, patient education, and collaborative care models, have transformed the healthcare landscape. These advancements have empowered patients, improved their experiences, and enhanced their quality of life. Patient testimonials and case studies highlight the real-world impact of these innovations, demonstrating how modern management approaches are shaping a more patient-centric healthcare system. As healthcare continues to evolve, it is crucial to prioritize patient-centered care to ensure that patients receive adequate treatment and have a positive and empowering healthcare experience.
Challenges and future directions
Endocrinology and arrhythmia management have significantly improved patient care and outcomes. However, they also face significant challenges and limitations that must be addressed to advance patient care further. This essay will explore the challenges and limitations of endocrine and arrhythmia management and speculate on future trends and research directions. By examining the ongoing issues and emerging possibilities, we can gain insight into the evolving healthcare landscape in these critical areas.
Challenges in Endocrine Management
The intricate regulatory mechanisms of hormones make diagnosing and treating endocrine disorders challenging. Hormonal imbalances may have subtle symptoms and require meticulous evaluation. For some endocrine conditions, such as rare genetic disorders, treatment options are limited, and research into new therapies is scarce. Patients with these conditions often face lifelong management challenges. Access to specialized endocrinologists can be limited, especially in rural areas. This geographical disparity can result in delayed diagnosis and management. Hormone replacement therapies, commonly used in endocrine disorders like hypothyroidism, can be costly and financially burden patients, affecting their treatment adherence.
Challenges in Arrhythmia Management
Arrhythmias, especially asymptomatic ones, often go undiagnosed. Routine screenings and monitoring are not standard, sometimes leading to delayed intervention. Some treatment modalities, like antiarrhythmic medications, can have side effects and may not be effective in all patients. Balancing the benefits and risks of treatment is a complex process. Access to electrophysiologists specializing in arrhythmia management can be limited in certain regions, leading to disparities in care quality. Accurate risk stratification for arrhythmias remains challenging, making it difficult to identify high-risk patients who may benefit from interventions like implantable devices.
Future Directions in Endocrine Management
Advances in genomics are leading to personalized treatment plans for endocrine disorders. Tailored therapies based on an individual's genetic profile can optimize treatment efficacy and minimize side effects. Telemedicine can bridge the gap in access to specialized endocrinologists, enabling remote consultations and monitoring for patients in underserved areas. Continuous remote monitoring can enhance disease management. AI-powered tools can assist in the early detection and diagnosis of endocrine disorders by analyzing large datasets and identifying subtle patterns. These technologies can improve diagnostic accuracy. Empowering patients with knowledge about their condition through digital health resources can promote self-management and adherence to treatment plans, reducing the burden on healthcare systems [ 41 ].
Future Directions in Arrhythmia Management
The development of non-invasive diagnostic tools, such as wearable ECG monitors and implantable loop recorders, can aid in the early detection of arrhythmias and improve diagnostic accuracy. Ongoing research in electrophysiology is exploring new treatments, such as ablation techniques, that target arrhythmia sources more precisely, resulting in better outcomes and fewer side effects. AI-driven algorithms can analyze patient data to predict arrhythmia risk more accurately. This can aid in identifying high-risk patients who may benefit from preventive interventions. Telehealth solutions are becoming increasingly crucial for arrhythmia management. They enable remote consultations, monitoring, and follow-ups, improving access to specialized care [ 42 ]. Endocrine and arrhythmia management are crucial aspects of healthcare, but they face several challenges that impact patient care. These challenges include complex disease mechanisms, limited treatment options, and disparities in access to specialized care. However, the future holds promising developments in both fields. Precision medicine, telemedicine, AI applications, and patient empowerment transform endocrine management. Advanced diagnostic tools, electrophysiology research, AI for risk prediction, and telehealth solutions are shaping the future of arrhythmia management. Healthcare providers and researchers can improve patient outcomes and enhance the quality of care in endocrinology and arrhythmia management by addressing current challenges and focusing on these emerging trends.
Conclusions
From integrating technology and telemedicine to personalized medicine and artificial intelligence, the healthcare field is experiencing rapid transformation. These advancements can significantly improve patient care, outcomes, and overall quality of life. One overarching theme from this discussion is the importance of staying current with these advancements in clinical practice. Healthcare professionals are entrusted with the well-being of their patients, and by embracing these innovations, they can provide more precise, accessible, and patient-centred care. Telemedicine allows for remote consultations and monitoring, ensuring that even patients in underserved areas can access specialized care. Personalized medicine tailors treatments to individual genetic profiles, minimizing side effects and optimizing therapeutic outcomes. Artificial intelligence assists in early diagnosis, risk prediction, and treatment planning, enhancing accuracy and efficiency. In an era of rapid scientific progress, healthcare providers must continually educate themselves and adapt their practices to incorporate these advancements. By doing so, they improve patient care and contribute to the ongoing evolution of healthcare towards a more patient-centric and effective system. In this dynamic landscape, staying informed and embracing innovation is not just a choice but a responsibility for healthcare professionals dedicated to providing the best possible care to their patients.
The authors have declared that no competing interests exist.
Author Contributions
Acquisition, analysis, or interpretation of data: Satesh Kumar, Fahad Waqar, Beena Irshad, Mahendra Kumar, Mahima Khatri
Critical review of the manuscript for important intellectual content: Satesh Kumar, Yogita Kumari, Fahad Waqar, Ahmad Talal Asif, Beena Irshad, Vaidheesh Varagantiwar, Mahendra Kumar, FNU Neha, Giustino Varrassi, Mahima Khatri, Tamam Mohamad
Concept and design: Yogita Kumari, Pooja Bai, Ahmad Talal Asif, Sahil Raj, Vaidheesh Varagantiwar, FNU Neha, Surat Chand, Giustino Varrassi, Tamam Mohamad
Drafting of the manuscript: Pooja Bai, Sahil Raj, Surat Chand
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

Chapter 15: Pathology of the Endocrine System
Catherine A. Hammett-Stabler; Susan J. Maygarden
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Introduction.
- HYPOTHALAMIC–PITUITARY AXIS
- TROPIC HORMONES OF THE ANTERIOR PITUITARY
- TUMORS AFFECTING PITUITARY FUNCTION
- POSTERIOR PITUITARY
- THE ADRENAL GLANDS AND THEIR HORMONES
- ADRENAL HORMONES
- ADRENAL CORTICAL INSUFFICIENCY
- ADRENAL CORTICAL HYPERFUNCTION
- PARATHYROID
- Full Chapter
- Supplementary Content
Disorders stemming from the endocrine system are among the most frequently encountered patient problems. Currently, diabetes (discussed under Pancreas) and thyroid disorders rank within the top ten most encountered diagnoses. On a broader scale, endocrinopathies cross all ages and genders and often manifest as other clinical entities that make diagnosis challenging. Because multiple organ systems are usually involved, endocrinology can seem daunting in an organ-based approach. However, it can be divided into more manageable sections by approaching the topic first by the gland involved, that is, pituitary, adrenal, or thyroid, and then from the clinical perspective of hyperfunction or hypofunction, based on the concentrations of the respective hormones or peptides secreted into the circulation. This chapter will thus be divided by system or gland and subdivided by functional defect. Diagnosis of endocrine disorders makes heavy use of clinical laboratory testing and that emphasis is reflected in this chapter.
The key glands of the endocrine system include the hypothalamus, pituitary, thyroid, parathyroids, adrenals, pancreas, and gonads. These organs synthesize and secrete specific biochemical messengers, known as hormones, into the blood in a synchronized collaboration with the central nervous system (CNS) and the immune system to regulate metabolism, growth, development, and reproduction ( Figure 15-1 ). Other tissues, such as adipose and gut, are also metabolically active and involved in these activities as well. The term hormone, derived from the Greek hormon meaning to set in motion, was chosen because these compounds act on cells some distance from their site of origin (hence the derivation of the word endocrine , from the Greek krino, to separate). Now we know that many hormones also act locally on neighboring cells at the paracrine level, and even on the very cell from which they originate in an autocrine manner.
Several classification schemes of hormones are recognized, but the simplest consists of three broad groups: peptides, steroids, and amino acid derivatives. The peptide hormones represent the largest and most diverse hormone class and include examples such as growth hormone (GH), adrenocorticotropic hormone (ACTH), and insulin. These are typically synthesized and stored for quick release into the circulation when needed, either as specific gene products or through post-translational modification of precursors and are usually water-soluble. All steroid hormones are derived from cholesterol, and as such, are lipophilic. Compounds in this class are not stored, so the rate of synthesis regulates secretion. Examples of steroid hormones include cortisol, aldosterone, and the androgens. The last group, amines, is derived from the amino acid tyrosine and includes the thyroid hormones (thyroxine (T4) and triiodothyronine (T3)) and the catecholamines (epinephrine, norepinephrine, and dopamine). Each of these compounds is stored as granules in the cytoplasm until needed.
Sign in or create a free Access profile below to access even more exclusive content.
With an Access profile, you can save and manage favorites from your personal dashboard, complete case quizzes, review Q&A, and take these feature on the go with our Access app.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Skip to content

State Resources
National Resources
Nursing Organizations
- MNWC Initiatives
Maryland Nursing Workforce Center
- NextGen NCLEX
NextGen NCLEX Test Bank
The purpose of this project was to develop a repository of nextgen nclex questions that can be accessed by all faculty and students in maryland..
The questions can be used by faculty to prepare students to understand the new format of Next Generation (NextGen) test items that are like those that will be used by the National Council of State Boards of Nursing (NCSBN) licensing exam beginning in April 2023 to test students’ ability to make clinical judgments.
Disclaimer: The items in the test bank are accessible to all through this nonsecure website. The test questions are not recommended to be used for summative assessments.
The test bank is composed of case studies with six questions each that follow the NCSBN Clinical Judgment Measurement Model steps:
- recognize cues
- analyze cues
- prioritize hypotheses
- generate solutions
- take action
- evaluate outcomes.
In addition, seven questions for reviewing bow-tie or trend items are included. All case studies were subjected to rigorous review both by the project team and subject matter experts.
The names of the case studies are provided with hyperlinks to all items.
- Using the Maryland NextGen Test Bank
- Student Instructions for Using the Test Bank
NCLEX Next Gen Test Bank
7.1 Assess and Analyze the Impact of Nutrition on the Endocrine System
Learning outcomes.
By the end of this section, you should be able to:
- 7.1.1 Recognize the normal function of the endocrine system.
- 7.1.2 Recognize cues of nutritional impact on the endocrine system.
- 7.1.3 Analyze cues of nutritional impact on the endocrine system.
Normal Function of the Endocrine System
The endocrine system is a network of cells, tissues, and organs that regulate and control all processes using hormones . Hormones are secretions that help regulate organ function by exerting their effects on certain cells in the organ. They coordinate biological functions like metabolism, sexual reproduction, blood pressure, body temperature, heart rate, growth, development, and sleeping. Related to nutrition, the endocrine system regulates appetite and how nutrients are used.
The hypothalamus is a region in the brain that regulates the endocrine system through its connection and coordination with the nervous system. The pituitary gland , also located in the brain , regulates other glands like the adrenal, thyroid, and testicles. These glands include the thyroid, parathyroid, adrenal, pineal, and pancreas which play critical roles in regulating calcium levels in the body, metabolism, sexual development, and blood pressure, and insulin production, respectively. Figure 7.2 shows the pituitary gland and other key parts of the endocrine system. The goal of regulating hormone levels in the blood is to reach a state of balance or homeostasis . Imbalances can lead to health problems like high blood pressure, changes in mood and behavior, and weight gain (Betts et al., 2022).
Nutrition plays a vital role in maintaining homeostasis and affecting hormone functions. Overall, a balanced diet with limited ultra-processed food, a variety of fruits and vegetables, whole grains, and lean protein sources is important for endocrine health. This diet helps individuals maintain a healthy weight and decrease the risk for hormonal imbalances. Table 7.1 lists the glands that play a key role in secreting and regulating hormones and related nutritional factors.
Alterations in Endocrine System Function
Endocrine disorders develop in one of two ways. Primary endocrine disorders result from problems with the peripheral glands, while secondary endocrine disorders result when the pituitary gland is either overstimulated or understimulated by the hypothalamus causing an alteration in the peripheral gland’s function. The result of all endocrine disorders is either hyper-functioning or hypo-functioning of the affected gland.
Alterations in Endocrine System Function – Diabetes
The most prevalent endocrine disorder is diabetes (Agency for Healthcare Research and Quality, n.d.). It is estimated that 37.3 million Americans have diabetes, with approximately 8.5 million cases (23%) undiagnosed (National Institute of Diabetes and Digestive and Kidney Diseases, 2023). Diabetes develops when the body is not able to maintain adequate blood glucose control (Sapra & Bhandari, 2023). Type 1 diabetes typically develops early in life and occurs when insulin producing cells (beta cells) are destroyed in the pancreas resulting in low to non-existent levels of insulin. Type 2 diabetes results from insulin resistance that develops gradually from obesity and aging. The insufficient amount of insulin (type 1 diabetes) and/or functionally ineffective amounts of insulin (type 2 diabetes) result in elevated blood glucose levels.
Glycemic control , which is the maintenance of optimal blood glucose levels, is essential to manage potential complications of diabetes effectively. Poorly controlled blood glucose levels lead to vascular and neurological complications including myocardial infarctions, cerebral vascular accidents, renal disease, neuropathies, and retinopathy (Sapra & Bhandari, 2023). These complications result from several different mechanisms triggered by elevated blood glucose levels that either cause buildup within vessels that impede blood flow, reduce the ability of the vessels to autoregulate, or trigger altered biochemical processes that hinder the vessel’s functionality (Brutsaert, 2022). The risk for these conditions developing is increased in clients who have co-morbid conditions.
Special Considerations
Differences in insulin sensitivity among diverse populations.
Members of US racial/ethnic minority groups have higher rates of insulin resistance than non-Hispanic White members of the population. This is most likely attributed to both genetic and lifestyle factors (Caballero, 2018).
Alterations in Endocrine System Function – Other Endocrine Disorders
Other endocrine disorders commonly seen are hypo/hyperthyroidism and adrenal disorders. Hypothyroidism results from the decreased levels of thyroid hormones T4 and T3 . Accordingly, thyroid stimulating hormone (TSH) is increased, indicating that the thyroid gland is not functioning properly. It usually results from autoimmune causes, but it could also occur after radioactive iodine therapy or surgery for hyperthyroidism or goiter (Braunstein, 2022). Hyperthyroidism is caused by increased secretion of T4 and T3 caused by Graves’ disease , goiter, or thyroiditis. Adrenal insufficiency is caused by Addison’s disease or a disorder regulating the pituitary gland and results in low cortisol levels in the body (Grossman, 2022). In an effort to stimulate the adrenal glands, adrenocorticotropic hormone (ACTH) is released. Conversely, Cushing’s disease/syndrome develops when corticosteroid levels in the body are high either from taking corticosteroid medications or from overproduction by the adrenal glands.
Assessment of Nutrition and the Function of the Endocrine System
Endocrine disorders can be difficult to diagnose. Frequently these conditions develop over time, and clients present with symptoms that are non-specific. A thorough history and physical is essential.
Health History and Physical Assessment
Taking a client’s health history is the first step when assessing the client’s endocrine system. In addition to general health history questions, it is important to identify conditions for which the client may be at risk and to assess the need for genetic testing (Bickley et al., 2021). When collecting information on the client’s nutritional status for potential effects on the endocrine system, the nurse should ask about changes in appetite, thirst and fluid intake, and bowel function. It is also important to know if the client has experienced any changes in weight or energy levels.
After obtaining a thorough health history, a physical assessment should be performed to look for signs of endocrine dysfunction:
- Inspect the body, looking for abnormal hair growth, skin changes, and abnormal body proportions.
- Auscultate heart sounds for rate and rhythm as some endocrine disorders cause tachydysrhythmias. Also listen over the carotid arteries and directly over the thyroid gland for any bruits.
- Palpate the thyroid gland ( Figure 7.3 ), adrenal glands, and testes for tenderness, size, symmetry, and shape, looking for any nodules, enlargement, or changes in texture.
- Assess weight, height, and body mass index (BMI) for any changes in body composition.
- Assess sexual development, including secondary sex characteristics, and menstrual cycles.
- Evaluate the client’s mood and behavior for any changes.
- Perform point-of-care blood glucose testing (Bickley et al., 2021).
Laboratory Tests for Endocrine Functioning
Laboratory testing for endocrine disorders includes tests measuring hormones, vitamin levels, electrolytes, and kidney function among others. Table 7.2 lists the commonly ordered laboratory tests specific to endocrine disorders.
Analysis of Nutrition and the Endocrine System
The endocrine system requires adequate nutrition to function. Nutritional deficits or imbalances can cause various endocrine abnormalities. For example, the most common cause worldwide for goiter, or an enlarged thyroid ( Figure 7.4 ), is iodine deficiency as iodized salt is not consistently used worldwide (Can & Rehman, 2023). However, in the United States, its use has significantly reduced goiter development (Can & Rehman, 2023). Instead, goiter formation in the United States is usually caused by Hashimoto’s thyroiditis or Graves’ disease. Clients who primarily consume other types of salt (kosher, sea, etc.) need to obtain iodine in their diet through other means.
A thorough analysis of the client’s nutrition status can help identify potential endocrine-related issues. The nurse should review the nutritional assessment to identify any nutrient-related deficiencies. For example, a client with limited fruit and vegetable consumption is at risk for vitamin C deficiency . Vitamin C deficiency is associated with multiple health problems. Specifically related to the endocrine system, vitamin C affects the regulation of several important hormones including insulin growth factor and sex steroids (Shi, Rath, & Niedzwiecki, 2021). Conversely, when evaluating the client’s nutrition status, there is potential to find excessive intake of nutrients. For example, a diet with excessive carbohydrate intake can increase blood glucose levels in individuals contributing to the development of insulin resistance and diabetes. Once nutritional imbalances are identified, the nurse can work with the client to make dietary changes and reduce the risk for developing endocrine disorders (Bickley et al., 2021). Table 7.3 lists signs and symptoms of common endocrine disorders and their corresponding nutritional factors.
Obtaining Adequate Iodine through Diet Sources
Dozens of countries, including the United States, add iodine to table salt. Despite this practice, there are still groups who are at risk for iodine deficiency :
- People who do not use iodized salt including people in Southeast Asia, sub-Saharan Africa, and Eastern Europe
- Pregnant women
- Vegans and people who eat few or no dairy products, seafood, and eggs
- People living in areas with iodine-deficient soils – primarily mountainous areas (Himalayas, Alps, and Andes regions) or river valleys prone to flooding (South and Southeast Asia)
- People who consume foods that interfere with iodine uptake including soy, cassava, and cruciferous vegetables
Alternative sources of dietary iodine for these groups include:
- Seaweed (kelp, nori, kombu, and wakame) (traditionally consumed in China, Japan, and Korea)
- Fish and other seafood
- Dairy products
Fruits and vegetables, although they have a lot of other health benefits, are not a good source of iodine.
(source: NIH, 2023)
Unfolding Case Study
Read the following clinical scenario and then answer the questions that follow. This case study will evolve throughout the chapter.
Meena, a 44-year-old Indian American female was recently diagnosed with hypothyroidism and type 2 diabetes. She has a history of class 1 obesity, with a BMI of 33. Meena lives alone and works as an office administrator. Her hobbies include reading, watching movies, and cooking. Meena presents to the clinic complaining of fatigue and feeling cold even in warm temperatures.
- Have you experienced any changes in your weight or appetite?
- Do you have trouble sleeping?
- Are you able to track what you eat?
- Do you like to cook?
- How much protein do you eat?
- Do you consume a lot of sugar?
- What type of salt do you use on food?
- Do you eat hot meals?
This book may not be used in the training of large language models or otherwise be ingested into large language models or generative AI offerings without OpenStax's permission.
Want to cite, share, or modify this book? This book uses the Creative Commons Attribution License and you must attribute OpenStax.
Access for free at https://openstax.org/books/nutrition/pages/1-introduction
- Authors: Emerald Charity Bilbrew, Jody Vogelzang, Kelli Whittington
- Publisher/website: OpenStax
- Book title: Nutrition for Nurses
- Publication date: Mar 20, 2024
- Location: Houston, Texas
- Book URL: https://openstax.org/books/nutrition/pages/1-introduction
- Section URL: https://openstax.org/books/nutrition/pages/7-1-assess-and-analyze-the-impact-of-nutrition-on-the-endocrine-system
© May 15, 2024 OpenStax. Textbook content produced by OpenStax is licensed under a Creative Commons Attribution License . The OpenStax name, OpenStax logo, OpenStax book covers, OpenStax CNX name, and OpenStax CNX logo are not subject to the Creative Commons license and may not be reproduced without the prior and express written consent of Rice University.

Endocrine System Study Guide With Answers Q&A | NURSING.com

What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
Use this simple Q& A page over the endocrine system to test your knowledge and prepare for upcoming tests. Feel free to print, copy, share, and use this study guide in any way!
Remember: Adrenal HYPO function = Addisons: Adrenal HYPER function=Cushings: Thyroid HYPER function=Graves
The biggest tip I can give with learning endocrine D/Os is to focus on the pituitary hormones.
What does each hormone do?
Once you know this you can quickly determine what the results of HYPER or HYPO function will be. ie. . . ACTH stimulates the adrenal cortex to release cortisol.
What does cortisol do? Think increased GLUCOSE, decreased IMMUNITY, decreased INFLAMMATION. So, with HYPER function of the Adrenals, we will have even more glucose, less immunity, and less inflammation. . . what would someone like this look like? This is Cushing’s .
The opposite will lead to Addison’s . So think of how each gland interrelates, then simply think of what each hormone does. From there it becomes much easier to figure out what the resulting assessment findings will uncover.
.png?width=740&name=stencil.instagram-photo%20(95).png)
Download chart
Endocrine System Q&A Nursing Care
- anterior and posterior
- pituitary, thyroid, parathyroid, adrenal, pancreas, thymus, pineal, gonads
- hypothalamus
- GH (growth hormone), TSH ( thyroid stimulating hormone) , ACTH 9adrenocorticotropic hormone), FSH, LH, Prolactin
- T3, T4 , Thyrocalcitonin
- regulate metabolism
- production and release of TSH when stimulated by the hypothalamus.
- lowers blood calcium by inhibiting bone resorption
- produce PTH (parathyroid hormone) which raises blood Ca levels
- on top of the kidneys
- adrenal medulla and adrenal cortex
- The adrenal medulla secretes two catecholamines: epinephrine, and norepinephrine. Epinephrine prepares the body for the fight or flight response by converting glycogen to glucose and increasing HR. Norepinephrine produces extensive vasoconstriction.
- ACTH adrenocorticotropic hormone from the anterior pituitary gland
- corticosteroids
- mineralcorticoids: aldersteron
- glucocorticoids: cortisol
- adrenal sex hormones: androgens & estrogen
- increase blood glucose by stimulating gluconeogensis, decrease inflammatory response, decrease immune response
- Alpha, Beta, Delta . . . islets of Langerhans
- Alpha . . . glucagon . . . increase glucose via gluconeogensis
- Beta . . . insulin . . . regulate protein, fat, and carbohydrate metabolism
- Delta . . . somatostatin . . . inhibitory hormone
- ACTH, GH, LH, FSH, PRL, TSH
- mainly affects thyroid, adrenal, and gonadal function. Atrophy of all endocrine glands, hair loss, impotence, amenorrhea, hypoglycemia
- coarse features, thick heel pads, thick tongue, decreased libido, amenorrhea, impotence, acromegaly
- ADH (vasopressin) from the posterior pituitary
- ADH promotes resorption of fluid in distal tubules. Without resorption massive amounts of urine are excreted.
- excessive water conservation
- posterior pituitary
- Graves Disease
- responsiveness to catecholimes
- increase metabolism
- increased heat
- weight change
- increased appetite
- nervousness
- bruit heard over thyroid
- warm, sweaty skin
- exopthalmus
- increase systolic BP
- uncontrolled hyperthyroid, surgery, infection
- admin Tylenol, provide cooling blanket
- in can increase thyroid hormone levels
- hypocalcemia
- hypercalcemia due to a decrease in Thyrocalcitonin
- lethargy, weakness, muscle aches, CHF, dry skin, Brady, constipation, weight gain
- persistently low thyroid production
- hypotension, hypotermia, hypoglycemia, brady
- increased Ca and bone demineralization
- fatigue, wt loss, fractures, HTN, joint pain, polyuria, renal calculi . . . think increased Ca
- chvotsek and Trousseaus
- carpopedal spams indicate neuromuscular irritability – sign of decreased Ca levels
- buffalo hump, moon face, fatigue, muscle weakness, hyperglycemia
- adrenal cortex secrets cortisol which increases blood glucose by stimulating gluconeogensis
- Cushings Syndrome
- Addisons Disease
- hypoglycemia, hyponatremia, GI disturbances, hyperpigmentation due to decreased secretion of cortisol
Selected Resource:
Hargrove-Huttel, R. (2000). Lippincott’s review series: Medical-surgical nursing . (3rd ed.). Philadelphia: Lippincott.
Image Credit: ntr23

Nearly half of all nurses are feeling burned out and that’s scary.
Top 10 most embarrassing things nurses have done at work…#9 is hard not to laugh at… | nursing.com, similar blog posts.

Hyperthyroidism NCLEX Review for Nursing Students + Free Download
Hypothyroidism NCLEX Review for Nursing Students + Free Download
Cushings Syndrome NCLEX Review for Nursing Students + Free Download
- Open access
- Published: 06 June 2024
Multi-stage optimization strategy based on contextual analysis to create M-health components for case management model in breast cancer transitional care: the CMBM study as an example
- Hong Chengang 1 ,
- Wang Liping 1 ,
- Wang Shujin 1 ,
- Chen Chen 1 ,
- Yang Jiayue 1 ,
- Lu Jingjing 1 ,
- Hua Shujie 1 ,
- Wu Jieming 1 ,
- Yao Liyan 1 ,
- Zeng Ni 1 ,
- Chu Jinhui 1 &
- Sun Jiaqi 1
BMC Nursing volume 23 , Article number: 385 ( 2024 ) Cite this article
Metrics details
None of the early M-Health applications are designed for case management care services. This study aims to describe the process of developing a M-health component for the case management model in breast cancer transitional care and to highlight methods for solving the common obstacles faced during the application of M-health nursing service.
We followed a four-step process: (a) Forming a cross-functional interdisciplinary development team containing two sub-teams, one for content development and the other for software development. (b) Applying self-management theory as the theoretical framework to develop the M-health application, using contextual analysis to gain a comprehensive understanding of the case management needs of oncology nursing specialists and the supportive care needs of out-of-hospital breast cancer patients. We validated the preliminary concepts of the framework and functionality of the M-health application through multiple interdisciplinary team discussions. (c) Adopting a multi-stage optimization strategy consisting of three progressive stages: screening, refining, and confirmation to develop and continually improve the WeChat mini-programs. (d) Following the user-centered principle throughout the development process and involving oncology nursing specialists and breast cancer patients at every stage.
Through a continuous, iterative development process and rigorous testing, we have developed patient-end and nurse-end program for breast cancer case management. The patient-end program contains four functional modules: “Information”, “Interaction”, “Management”, and “My”, while the nurse-end program includes three functional modules: “Consultation”, “Management”, and “My”. The patient-end program scored 78.75 on the System Usability Scale and showed a 100% task passing rate, indicating that the programs were easy to use.
Conclusions
Based on the contextual analysis, multi-stage optimization strategy, and interdisciplinary team work, a WeChat mini-program has been developed tailored to the requirements of the nurses and patients. This approach leverages the expertise of professionals from multiple disciplines to create effective and evidence-based solutions that can improve patient outcomes and quality of care.
Peer Review reports
Female breast cancer is the second leading cause of global cancer incidence in 2022, with an estimated 2.3 million new cases, representing 11.6% of all cancer cases [ 1 ]. Due to surgical trauma, side effects of drugs, fear of the recurrence or metastasis of breast cancer, changes in female characteristics, and lack of knowledge, patients with breast cancer frequently experience a series of physical and psychological health problems [ 2 , 3 , 4 , 5 , 6 ]. These health problems seriously affected patients’ life and work [ 7 , 8 ]. At present, community nursing in China is still in the developing stage, and the oncology specialty nursing service capacity of community nurses is not enough to deal with the health problems of breast cancer patients. It made continuous care for out-of-hospital breast cancer patients a weak link in the Chinese oncology nursing service system.
Nowadays, case management is employed to manage health problems for out-of-hospital breast cancer patients worldwide [ 9 , 10 , 11 , 12 , 13 , 14 , 15 ]. Case management involves regular telephone follow-ups and home visits by case management nurses to provide educational support to patients, thereby ensuring uninterrupted continuity of care [ 16 , 17 ]. The home visits and organization of patient information required for case management tasks consume a significant amount of time, manpower, and material resources [ 17 ]. In China, case management services are primarily undertaken by oncology nursing specialists from tertiary hospitals in their spare time [ 18 ]. However, the shortage of nurses has consistently been one of the major challenges facing the nursing industry in China, especially in tertiary hospitals [ 19 ]. Consequently, the implementation and promotion of case management in China also face great difficulties in reality [ 20 ].
The Global Observatory for eHealth (GOe) of the World Health Organization (WHO) defines mobile health (M-Health) as “medical and public health practice supported by mobile devices, such as mobile phones, patient monitoring devices, personal digital assistants (PDAs), and other wireless devices” [ 21 , 22 ]. With the development of digital technology and the COVID-19 pandemic in 2019, M-Health applications were further integrated into healthcare services, which increased the demand for M-Health applications in turn [ 23 , 24 ]. Compared with the traditional health service model, M-Health service model has the advantages of high-level informatization, fast response speed, freedom from time and location constraints, and resource-saving, etc. In the context of limited nursing human resources, M-Health service provides a new solution for the case management of out-of-hospital breast cancer patients [ 23 , 25 , 26 ].
Researchers have developed a range of M-Health applications targeting breast cancer patients. To our knowledge, none of these developed M-Health applications are designed for case management nursing services.
Early M-Health applications were mostly designed for single interventional goals, such as health education, medication compliance, self-monitoring, etc. Larsen et al. applied a M-Health application to monitor and adjust the dosage of oral chemotherapy drugs in breast cancer patients, and the results suggested that the treatment adherence was effectively improved [ 27 ]. Heo and his team successfully promoted self-breast-examination behavior in women under 30 years old using a M-Health application [ 28 ]. Mccarrol carried out a M-Health diet and exercise intervention in overweight breast cancer patients and found that the weight, BMI, and waist circumference of the intervention group decreased after one month [ 29 ]. Smith’s team found that their application promoted the adoption of healthy diet and exercise behaviors among breast cancer patients [ 30 ]. The application designed by Eden et al. enhanced the ability of breast cancer patients receiving chemotherapy to recognize adverse drug reactions [ 31 ]. Keohane and colleagues designed a health educational application based on the best practices and it proved effective in improving breast cancer-related knowledge [ 32 ]. The guideline-based M-Health application developed by Eden et al. optimized breast cancer patients’ individualized health decision-making regarding mammography [ 33 ].
With the progress of computer technology and the emphasis on physical and mental rehabilitation of breast cancer patients, some universities [ 34 , 35 ] in China have separately developed M-Health applications for comprehensive health management, which provide access to online communication, health education, and expert consultation.
Analyzing these developed applications deeply, three factors could be found that hindered the promotion of applications in real life. Firstly, the developing procedure usually lacks contextual analysis based on the actual usage context during the design phase. Secondly, there is a lack of consistent and long-term monitoring and operation staff in the subsequent program implementation. These factors may be the main reasons why many M-Health applications face difficulties in promotion and continuous operation after the research phase. Furthermore, as applications need to be installed on patients’ smartphones, certain hardware requirements, such as memory, may also pose restrict the adoption of M-Health applications to some extent.
In order to meet the needs of supportive care for out-of-hospital breast cancer patients and the needs of case management for oncology nurse specialists, we formed a multidisciplinary research team and collaboratively developed a WeChat mini-program for breast cancer case management in the CMBM (M-health for case management model in breast cancer transitional care) project. WeChat is chosen as the program development platform based on the following considerations. Firstly, WeChat is the most popular and widely used social software in China. As of December 31, 2020, the monthly active users of WeChat have exceeded 1.2 billion, and the daily active users of WeChat mini-programs exceeded 450 million [ 36 ]. Secondly, users can access and use the services of the mini-program directly within the WeChat platform, without the need to download or install additional mobile applications. This reduces the hardware requirements for software applications. The above two factors allow for a positive user experience and a realistic foundation for software promotion.
The purpose of this study is to describe the process of developing a tailored M-health component for the case management model in breast cancer transitional care and to highlight methods for solving the common obstacles faced during the application of M-health nursing service.
Methods and results
The development process was conducted in four steps: (a) An interdisciplinary development team was formed, consisting of two sub-teams dedicated to content and software development. (b) Using the self-management theory as the theoretical framework, contextual analysis was used to understand the case management needs of oncology nursing specialists and the supportive care needs of out-of-hospital breast cancer patients. Through iterative discussion within the interdisciplinary team, the preliminary conception of the application framework and function was formed. (c) A multi-stage optimization strategy was adopted to develop and regularly update the WeChat mini-programs, including three stages (screening, refining, and confirming). (d) During the entire development process, a user-centered principle was followed with the involvement of oncology nursing specialists and breast cancer patients, including development, testing, and iterative development phases.
The interdisciplinary team
An important prerequisite for developing M-health applications is the formation of an interdisciplinary development team. We built a multidisciplinary team consisting of researchers, oncology nursing specialists, and software developers. Each team member brought their expertise from their respective fields, and all individuals were considered members of the same team rather than separate participants with a common goal.
Two sub-teams were established, one responsible for content development, and the other for software development. The content development team consisted of researchers and six senior breast oncology nursing specialists with bachelor’s degrees and over 10 years of clinical experience. Their work included contextual analysis, functional framework design, and content review of the “Information” module. The software development team included researchers and experienced software developers. Their tasks involved developing the mini-program based on the functional framework and requirements designed by the content development team.
The development team used contextual analysis to identify the actual usage needs of two target groups for the mini-program: oncologist nurse specialists and out-of-hospital breast cancer patients.
Involvement of oncology nursing specialists and breast cancer patients following user-centered design principle
Since the oncology nursing specialists and breast cancer patients are targeted users of the mini-program, the two groups fully participated in the development according to the user-centered principle. Nursing specialists who in charge of case management were interviewed about the preliminary functional framework of the mini-program. The interview results are presented in the section “Driving the Development Process via the Contextual Analysis Findings.” Semi-structured in-depth interviews were conducted in the testing and iteration stage to gain user feedback from nursing specialists to improve the applicability and usability of the mini-program. The interview guide can be found in the supplementary material.
Breast cancer patients fully engaged in the three developing phases (Screening, Refining, and Confirming). In the Screening Phase, since the self-management theory was selected as the theoretical framework, the supportive care needs of out-of-hospital breast cancer patients were explored, and the functional framework of the mini-program was constructed accordingly. In the Refining Phase, patients were invited to evaluate the usability and practicality of the mini-program through system tests and semi-structured in-depth interviews. The results of the system test are presented in the Results of System Test section. The feedback from interviews and corresponding iterative updates are listed in Table 1 . In the Confirming Phase, our research team is conducting clinical trials in out-of-hospital breast cancer patients to find out the actual effect of the mini-program on recovery.
The theory framework of the mini-program
This study applied the self-management theory [ 37 ] as the theoretical framework. The self-management theory explains how individual factors and environmental factors influence an individual’s self-efficacy, which ultimately affects the generation and development of individual behaviors. Self-efficacy is influenced by direct experience, indirect learning, verbal persuasion, and psychological arousal. By providing individuals with sufficient knowledge, healthy beliefs, skills, and support, their self-efficacy is increased, and they are likely to engage in beneficial health behaviors and self-management. Individuals who are confident in their abilities to apply self-management behaviors and overcome obstacles by improving their self-management skills and persevere in their efforts to manage their health [ 37 ]. Self-efficacy is directly and linearly positively related to the active adoption of health management behaviors [ 38 ]. The functions of the various parts of the mini-program designed using self-management theory can broaden the pathways and levels of efficacy information generation in four ways: direct experience, indirect learning, verbal persuasion, and mental arousal. Patients with high self-efficacy will take positive steps to achieve desired goals and possess disease-adapted behaviors. The form of the mini-application function block diagram is shown in Fig. 1 .
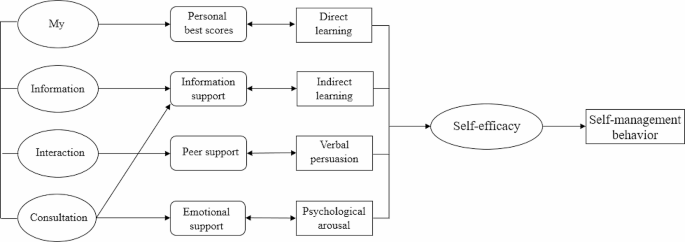
Driving the development process via the contextual analysis findings
Contextual analysis [ 39 ] is a method of discerning the profound significance and influence of language, behavior, events, and so forth, by examining them within a particular environment or background. Rather than being an afterthought, contextual analysis sheds light on the meaning and inner dynamics of our primary subject of interest. Through contextual analysis, we can gain a deeper understanding of the user’s usage scenarios, including their motivations, goals, environment, and behavior. This helps us better understand user needs, as well as the problems and challenges they may encounter when using the software.
In this paper, we adopted contextual analysis to gain a detailed understanding of the needs of oncology nurse specialists and out-of-hospital breast cancer patients. The research team adopted a mixed research strategy to achieve contextual analysis of the target users. A cross-sectional study was conducted among 286 patients and qualitative semi-structured in-depth interviews were applied in 12 patients to find out the supportive care needs of out-of-hospital breast cancer patients. According to the contextual analysis results from patients, the functional framework of the mini-program was constructed. See Fig. 2 for details.
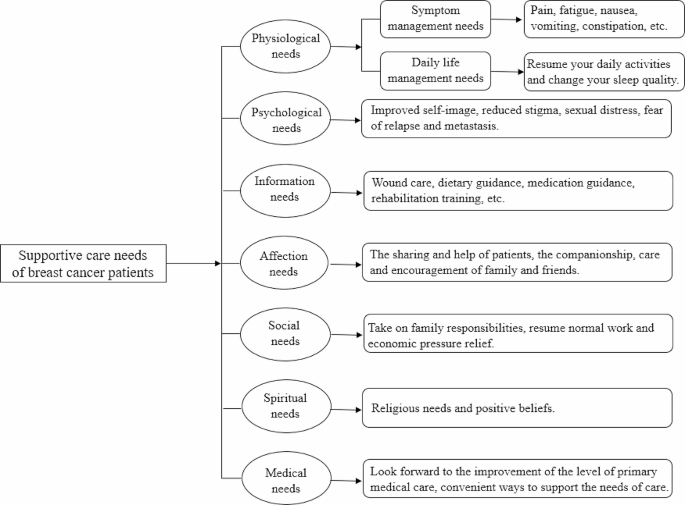
Supportive care needs of out-of-hospital breast cancer patients
Contextual analysis of breast cancer case management nurses was conducted through focus group interview. The interview results were listed as three themes: health information, personal self-management, and case management needs. Health information included breast cancer-related knowledge, the side effects of chemotherapy drugs, and symptom management measures. The key task of personal self-management contained temperature monitoring, weight management, functional exercise, and symptom management. Case management needs involved storage and management of patients’ medical records and development of a nurse-end program.
Based on the contextual analysis results of out-of-hospital breast cancer patients and the oncology case management nurses, the framework and functional block of the mini-program were formed. An overview of the CMBM Software development process is listed in Fig. 3 .
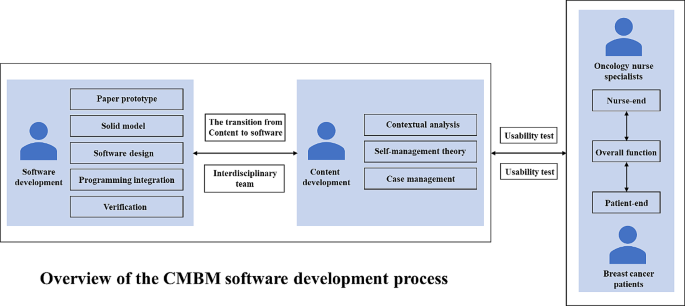
Overview of the CMBM software development process
Patient-end program functional modules
Using the results of the contextual analysis, we design the functional modules of the patient-end program based on the patient’s supportive care needs. For example, the “Information” section is designed to meet the “Information need” of breast cancer patients; the “social needs” and “spiritual needs” of patients suggest that breast cancer patients lack peer support, and for this reason, the"Interaction” section for patients has been added to the app to provide a communication platform for patients.
The patient-end program include four functional modules: “Information”, “Interaction”, “Management” and “My”. In the “Information” module, information about breast cancer treatment and health management are compiled based on clinical guildlines. The “Interaction” module allows patients to interact with fellow patients and consult an case management nurse. In the “Management” module, patients can record and review their self-management-related health status, including three medical parameters (temperature, blood pressure, weight) and three behavioral parameters (daily steps, medication, mindfulness excersice). The “My” module enables patients to input and edit their basic personal information and medical history. The main structure and information support module contents are listed in Fig. 4 .
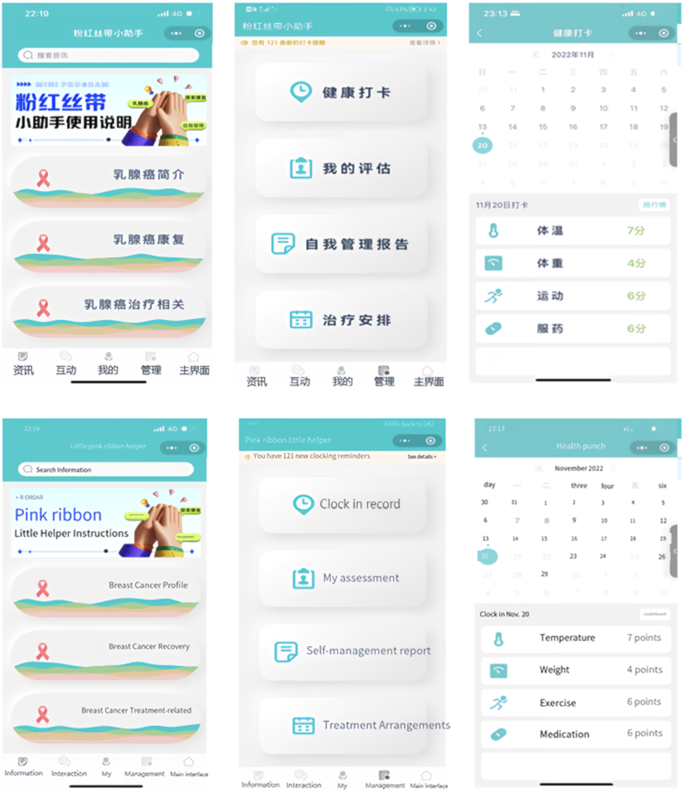
The main menu of patient-end program
Nurse-end program functional modules
The design of the functional modules of the nurse-end program was also derived from the results of contextual analyses. The nurse-end program includes three functional modules: “Consultation”, “Management”, and “My”. The “Consultation” module is mainly used for online communication between case management nurses and patients. Nurses can enter the patient’s name in the search box to open a dialog box, and communicate with each other by sending text, voice and pictures. In the “Management” module, nurses can effortlessly search for patients by entering their name, WeChat nickname, or mobile phone number in the search box. This initiates a seamless dialogue, and with a simple click of the “+” button, patients can be promptly added to the “My Concerns” list. They can view the medical record information on its homepage, and add the postoperative treatment plan for the patient. The “self-management report” feature empowers nurses to stay up-to-date with patients’ recent well-being. By monitoring vital indicators like temperature, weight, and incidents of nausea or vomiting following chemotherapy, nurses can proactively ensure patients’ safety. The “clock in record” feature meticulously logs various patient activities including weight variations, exercise regimens, and medication adherence, providing a holistic view of their health journey. “Treatment monitoring Schedule” enables nurses to create customized chemotherapy schedules. With the first postoperative chemotherapy session scheduled in the calendar, the system seamlessly computes subsequent chemotherapy sessions and associated assessments. This transition to an online system marks a significant advancement from the traditional paper-based chemotherapy planning. Its automated scheduling and data tracking functions serve to alleviate the clinical nursing workload, enhancing efficiency and freeing up valuable time for focused patient care. The “My” module offers nurses the convenience of adding patients of interest or relevant content to their “My Favorites” section, enabling streamlined one-click access for viewing and management. The core structure and informational components of this module are outlined in Fig. 5 .
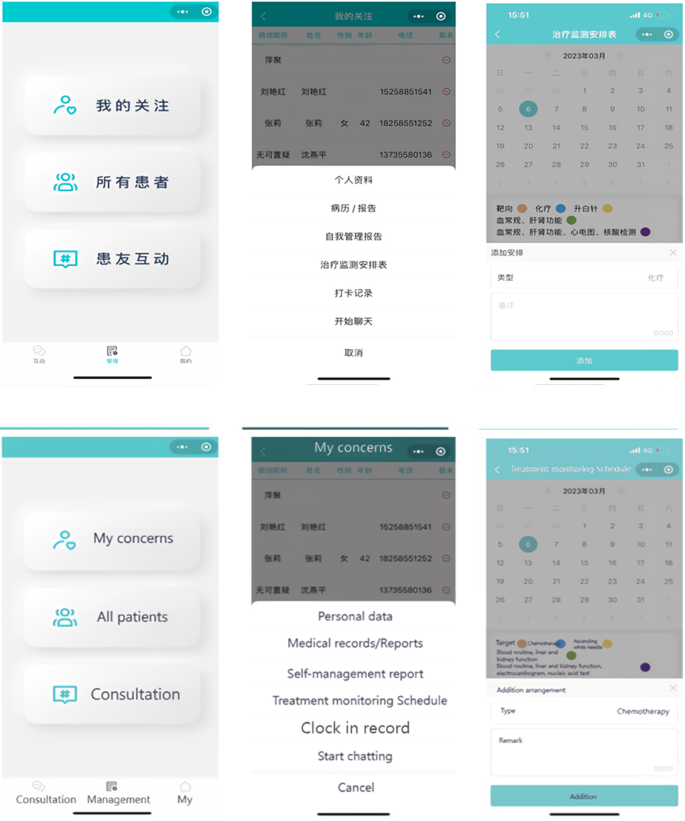
The main menu of nurse-end program
Driving the development process via the multi-stage optimization strategy
We adopted a multi-phase optimization strategy to drive the software development process. This strategy was proposed by Collins in 2005 and has become an important guiding theory for the development and evaluation of M-health interventions in recent years [ 40 ]. The strategy consists of three phases: Screening Phase, Refining Phase, and Confirming Phase. The Screening Phase need theories to identify and incorporate intervention elements. In this study, the initial version (1.0) development was based on self-management theory. Focusing on self-management, the results of contextual analysis, literature review and expert consultation were combined to design the mini-program version (1.0). The Refining Phase involves iterative adjustments to the previously version. In this study, the development team iteratively adjusted the mini-program version (1.0) according to users’ suggestions and test results. The Confirming Phase includes planning for clinical trials to test effect of the mini-program version (2.0) on self-management and recovery outcomes in out-of-hospital breast cancer patients.
Results of system test
Eight out-of-hospital breast cancer patients were recruited for system tests. The patient’s general information is listed in Table 2 .
The 10-item System Availability Scale (SUS)developed by Brooke was used [ 41 ]. The scale is a widely used method for quantitatively assessing user satisfaction with software systems. SUS is a Likert-5 and 10-item questionnaire (4 = strongly agree, 0 = strongly disagree), with Cronbach Alpha of 0.91. Generally, a system score above 60 on the SUS scale could be considered to be easy and simple to use, and the average score of SUS in our research is 78.75. The SUS scores of the mini-program system are presented in Fig. 6 .
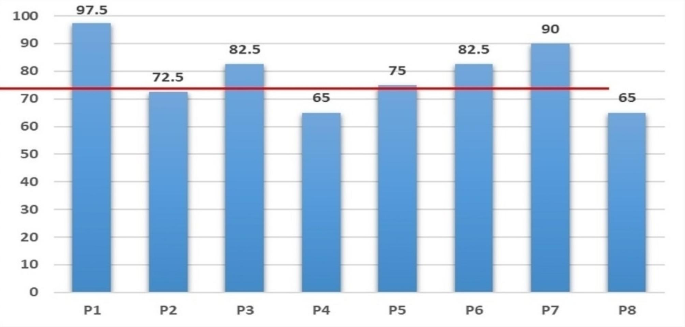
System availability scale (SUS) score of patients
The research team designed the core task tests based on the typical and necessary self-management tasks of out-of-hospital patients. The core task of the “Information” module was listed as an example (Table 3 ). Functional tests include the passing rate for each task, and performance tests include the completion time of each task. More details can be found in Table 4 .
In this article, we demonstrated how to create a customized software solution for breast cancer case management practices based on a multi-stage optimization strategy, applied the contextual analysis method, and followed the user-centered principle. Preliminary test results showed satisfaction and acceptance of the WeChat mini-program among both out-of-hospital breast cancer patients and oncology nursing specialists.
Team effort
There were two typical patterns for developing M-health applications in the past. One was led by software developers, while the other was led by medical professionals. Each of these patterns has its own advantages and disadvantages. To overcome these shortcomings, some projects [ 42 ] developing M-health applications are now utilizing interdisciplinary team collaborations. This approach not only ensures the quality of the software but also makes sure that applications meet the actual needs.
In order to develop a customized software solution, our research team consisted of researchers, oncology nursing specialists, and software developers. The interdisciplinary team work dedicated to customizing software solutions together. Our team members each played to their strengths and held regular meetings to discuss and enhance our understanding and resolution of issues encountered during the software development process. Our team also included informal members: breast cancer patients, whose suggestions contributed to the practicality of the program.
Contextual analysis and user-centered design
Contextual analysis is a valuable tool that enables developers to design systems that are more relevant and user-friendly. And it allows us to understand any context-specific characteristics, practice patterns, and the openness of the target setting’s nurses and patients towards technology [ 42 ]. User-centered design can significantly reduce the cost of program iteration. More importantly, it has a profound influence on various aspects of a program including its design, functionality, information architecture, and interactive elements [ 43 ]. By analyzing different contexts, not only did we design features that better meet user needs, but we also predicted and addressed potential issues that users may encounter when using the mini-program in advance, thereby enhancing the user experience. In the iterative development stage, we discovered and improved some deficiencies in the design through core task testing and usability testing. Notably, the completion rate of the core task test reached 100%, indicating that our application is user-friendly and easy to operate.
- Multi-stage optimization strategy
In several priority areas of public health, researchers have successfully applied multi-stage optimization strategies to enhance their work, including software development and intervention programs [ 44 , 45 , 46 ]. In this study, we also apply this strategy to software development. While the multi-stage optimization strategy provides an optimization framework, it is important to note that our optimization objectives (such as software functionality and content requirements) are determined by key users involved in the research (out-of-hospital breast cancer patients and oncology nurse spescialists). This project adopts a multi-stage optimization strategy, iteratively improving the development of the mini-program through screening, refinement, and confirmation stages. Each stage aims to optimize our program.
The research team plans to explore the feasibility of mini program development program through preliminary experiment, and verify the intervention effect of mini program on self-management behavior, self-efficacy and quality of life and other indicators through formal experiment. A randomized controlled trial (IRB-2020-408) was initiated in August 2022 at a Class III hospital in Zhejiang, China, and is currently in the data collection phase.
There is no doubt that M-health will play a core role in the future of health care. However, to successfully implement and promote M-health applications in clinical setting, it is essential to analyze the needs of the target population. Additionally, it is crucial to determine who will be the driving force behind the implementation of the entire M-health project. This study demonstrates how to integrate M-health components into existing breast cancer case management care practices. In addition to providing a reference for other teams interested in developing and integrating M-health components into case management care models, this study also provides a reference for building M-health-featured care work models in practices.
In this study, the collaborative work of an interdisciplinary team with backgrounds in nursing and computer science, along with the active involvement of patients, not only facilitated the planning, developing, updating, and testing of M-health components based on the actual needs of the target population, but also increased the chances of acceptance and long-term implementation of the M-health program in practice.
This study demonstrates how to integrate M-health components into existing breast cancer case management practices. It provides insights for other reserch teams interested in developing and integrating M-health components into daily nursingt practice.
In the context of the digital age, M-health applications are rapidly becoming information sources and decision support tools for healthcare professionals and patients. However, it is crucial not to overlook the issues of information security and digital barriers for older adults.
Through interviews with outpatients with breast cancer and oncology nurses, we have gained insights into their concerns regarding information security. Some interviewees expressed concerns about information security and were worried about the risk of their personal information being leaked during app usage. Such concerns, to some extent, hinder the widespread adoption of M-health applications. Additionally, some interviewees mentioned that older patients, in general, find it challenging to learn and use the various functions of WeChat mini-programs, making it difficult to promote and apply M-health applications among the elderly population.
Solving these issues effectively is not only vital for the patients’ rights and interests but also crucial for the comprehensive implementation of M-health in practice. It is a matter that requires careful consideration in future development of M-health applications.
Data availability
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Bray F, Laversanne M, Sung H et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2024: 1–35.
Wu J, Zeng N, Wang L, Yao L. The stigma in patients with breast cancer: a concept analysis. Asia Pac J Oncol Nurs. 2023;10(10):100293.
Article PubMed PubMed Central Google Scholar
Heidkamp P, Hiltrop K, Breidenbach C, Kowalski C, Pfaff H, Geiser F, Ernstmann N. Coping with breast cancer during medical and occupational rehabilitation: a qualitative study of strategies and contextual factors. BMC Womens Health. 2024;24(1):183.
Zhao H, Li X, Zhou C, Wu Y, Li W, Chen L. Psychological distress among Chinese patients with breast cancer undergoing chemotherapy: concordance between patient and family caregiver reports. J Adv Nurs. 2022;78(3):750–64.
Article PubMed Google Scholar
Jang Y, Seong M, Sok S. Influence of body image on quality of life in breast cancer patients undergoing breast reconstruction: Mediating of self-esteem. J Clin Nurs. 2023;32(17–18):6366–73.
Oh PJ, Cho JR. Changes in fatigue, psychological distress, and Quality of Life after Chemotherapy in women with breast Cancer: a prospective study. Cancer Nurs. 2020 Jan/Feb;43(1):E54–60.
Maass SWMC, Boerman LM, Verhaak PFM, Du J, de Bock GH, Berendsen AJ. Long-term psychological distress in breast cancer survivors and their matched controls: a cross-sectional study. Maturitas. 2019;130:6–12.
Article CAS PubMed Google Scholar
De Vrieze T, Nevelsteen I, Thomis S, De Groef A, Tjalma WAA, Gebruers N, Devoogdt N. What are the economic burden and costs associated with the treatment of breast cancer-related lymphoedema? A systematic review. Support Care Cancer. 2020;28(2):439–49.
Liang Y, Gao Y, Yin G, Chen W, Gan X. Development of a breast cancer case management information platform (BC-CMIP) module based on patient-perceived value. Front Oncol. 2022;12:1034171.
Jin L, Zhao Y, Wang P, Zhu R, Bai J, Li J, Jia X, Wang Z. Efficacy of the whole-course case management model on compliance and satisfaction of breast Cancer patients with whole-course standardized treatment. J Oncol. 2022;2022:2003324.
Scherz N, Bachmann-Mettler I, Chmiel C, Senn O, Boss N, Bardheci K, Rosemann T. Case management to increase quality of life after cancer treatment: a randomized controlled trial. BMC Cancer. 2017;17(1):223.
Yamei Y, Yongfang Zh J, Sh, Xixi C, Dehong Z, Chuner J, Jianfen N. The influence of the whole course professional nursing case management model on the disease uncertainty for breast cancer patients with chemotherapy. J Nur Train. 2018;(02), 99–111.
Cuie P. The whole case management model for breast cancer patients to study the effect of quality of life and psychological society. Hunan Normal University; 2015.
Bleich C, Büscher C, Melchior H, Grochocka A, Thorenz A, Schulz H, Koch U, Watzke B. Effectiveness of case management as a cross-sectoral healthcare provision for women with breast cancer. Psycho Oncol. 2017;26(3):354–60.
Article Google Scholar
Huiting Zh J, Zh, Xiaodan W, Lijuan Zh, Wenhao H, Huiying Q. Exploration of case management model for breast cancer patients. J Nurs Sci. 2017;(14), 19–21.
Woodward J, Rice E. Case management. Nurs Clin North Am. 2015;50(1):109–21.
Luo X, Chen Y, Chen J, Zhang Y, Li M, Xiong C, Yan J. Effectiveness of mobile health-based self-management interventions in breast cancer patients: a meta-analysis. Support Care Cancer. 2022;30(3):2853–76.
Meiqin X, Lingjuan Z. The delivery and inspiration of case management model in China. Chin J Nurs. 2014;(03), 367–71.
Huanhuan L, Zhuangjie X, Yuan L, Ying L, ShouQi W, MeiLing Z, Jie Y, Pengcheng L, Huanhuan Zh, Jiao S. A review of the interventions of nurses’ intent to stay. Chin J Nurs. 2017;(08), 1007–9.
Dan W, Shanling L, Yulin X. Research status of continuous nursing at home and abroad. Nurs Res 2016;(20), 2436–8.
Mariani AW, Pêgo-Fernandes PM. Telemedicine: a technological revolution. Sao Paulo Med J. 2012;130(5):277–8.
Hamine S, Gerth-Guyette E, Faulx D, Green BB, Ginsburg AS. Impact of mHealth chronic disease management on treatment adherence and patient outcomes: a systematic review. J Med Internet Res. 2015;17(2):e52.
Mahmood S, Hasan K, Colder Carras M, Labrique A. Global preparedness against COVID-19: we must leverage the Power of Digital Health. JMIR Public Health Surveill. 2020;6(2):e18980.
Petracca F, Ciani O, Cucciniello M, Tarricone R. Harnessing Digital Health Technologies during and after the COVID-19 pandemic: context matters. J Med Internet Res. 2020;22(12):e21815.
Cong H, Yongyi C, Xiangyu C, Xuying L. Rehabilitation Effect of Chemotherapy-based adverse reactions to breast Cancer patients based on continuous care platform. Oncol Pharma. 2020;(02), 244–51.
Cong A, Liping W. Application progress of mobile health in transitional care of patients with hypertension. Chin J Mod Nurs. 2021;27(4):539–42.
Google Scholar
Larsen ME, Farmer A, Weaver A, Young A, Tarassenko L. Mobile health for drug dose optimisation. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:1540–3.
PubMed Google Scholar
Heo J, Chun M, Lee KY, Oh YT, Noh OK, Park RW. Effects of a smartphone application on breast self-examination: a feasibility study. Healthc Inf Res. 2013;19(4):250–60.
McCarroll ML, Armbruster S, Pohle-Krauza RJ, Lyzen AM, Min S, Nash DW, Roulette GD, Andrews SJ, von Gruenigen VE. Feasibility of a lifestyle intervention for overweight/obese endometrial and breast cancer survivors using an interactive mobile application. Gynecol Oncol. 2015;137(3):508–15.
Smith SA, Whitehead MS, Sheats J, Mastromonico J, Yoo W, Coughlin SS. A Community-Engaged Approach to developing a Mobile Cancer Prevention App: the mCPA Study Protocol. JMIR Res Protoc. 2016;5(1):e34.
Eden KB, Ivlev I, Bensching KL, Franta G, Hersh AR, Case J, Fu R, Nelson HD. Use of an online breast Cancer Risk Assessment and patient decision aid in Primary Care practices. J Womens Health (Larchmt). 2020;29(6):763–9.
Keohane D, Lehane E, Rutherford E, Livingstone V, Kelly L, Kaimkhani S, O’Connell F, Redmond HP, Corrigan MA. Can an educational application increase risk perception accuracy amongst patients attending a high-risk breast cancer clinic? Breast. 2017;32:192–8.
Eden KB, Scariati P, Klein K, Watson L, Remiker M, Hribar M, Forro V, Michaels L, Nelson HD. Mammography decision aid reduces Decisional Conflict for women in their forties considering screening. J Womens Health (Larchmt). 2015;24(12):1013–20.
Zhu J, Ebert L, Liu X, Chan SW. A mobile application of breast cancer e-support program versus routine care in the treatment of Chinese women with breast cancer undergoing chemotherapy: study protocol for a randomized controlled trial. BMC Cancer. 2017;17(1):291.
Ying L. Construction of an M-Health based information support program for women with breast Cancer during diagnosis and treatment process. The Second Military Medical University; 2017.
Pengfei X, Bo Y, Yue H, Jingyun H. An empirical research on the interactive behavior of WeChat subscription number users from the perspective of the theory of interactive ritual chain. Chin J Inf Syst. 2023;(01), 69–83.
Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191Y215.
Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143Y164.
George A, Scott K, Garimella S, Mondal S, Ved R, Sheikh K. Anchoring contextual analysis in health policy and systems research: a narrative review of contextual factors influencing health committees in low and middle income countries. Soc Sci Med. 2015;133:159–67.
Collins LM, Murphy SA, Strecher V. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007;32(5 Suppl):S112–8.
Brooke JB. SUS: a quick and dirty usability scale. Usability Evaluation Ind. 1996;189(194):4–7.
Leppla L, Hobelsberger S, Rockstein D, Werlitz V, Pschenitza S, Heidegger P, De Geest S, Valenta S, Teynor A. SMILe study team. Implementation Science meets Software Development to create eHealth Components for an Integrated Care Model for allogeneic stem cell transplantation facilitated by eHealth: the SMILe Study as an Example. J Nurs Scholarsh. 2021;53(1):35–45.
Luna D, Quispe M, Gonzalez Z, Alemrares A, Risk M, Garcia Aurelio M, Otero C. User-centered design to develop clinical applications. Literature review. Stud Health Technol Inf. 2015;216:967.
Piper ME, Fiore MC, Smith SS, Fraser D, Bolt DM, Collins LM, Mermelstein R, Schlam TR, Cook JW, Jorenby DE, Loh WY, Baker TB. Identifying effective intervention components for smoking cessation: a factorial screening experiment. Addiction. 2016;111(1):129–41.
Spring B, Pfammatter AF, Marchese SH, Stump T, Pellegrini C, McFadden HG, Hedeker D, Siddique J, Jordan N, Collins LM. A factorial experiment to optimize remotely delivered behavioral treatment for obesity: results of the Opt-IN Study. Obes (Silver Spring). 2020;28(9):1652–62.
O’Hara KL, Knowles LM, Guastaferro K, Lyon AR. Human-centered design methods to achieve preparation phase goals in the multiphase optimization strategy framework. Implement Res Pract. 2022;3:26334895221131052.
PubMed PubMed Central Google Scholar
Download references
Acknowledgements
The authors would like to express our sincere gratitude to all the breast cancer patients who participated in this research.
This study was supported by the Zhejiang Provincial Natural Science Foundation of China (LY18H160061) and Funding for innovation and entrepreneurship of high-level overseas students in Hangzhou.
Author information
Authors and affiliations.
School of Nursing, Hangzhou Normal University, Hangzhou City, Zhejiang Province, 311100, China
Hong Chengang, Wang Liping, Wang Shujin, Chen Chen, Yang Jiayue, Lu Jingjing, Hua Shujie, Wu Jieming, Yao Liyan, Zeng Ni, Chu Jinhui & Sun Jiaqi
You can also search for this author in PubMed Google Scholar
Contributions
HCG conceived the entire paper framework and was responsible for writing the paper. WSJ and CC conducted all interviews and managed the mini-programs. YJY, LJJ and HSJ were responsible for the collection of clinical nurse data. CJH and SJQ were responsible for patient data collection. Data analysis was conducted by WJM, YLY and ZN. WLP was responsible for the revision, editing and approval of manuscripts. All authors have rigorously revised and edited successive drafts of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Wang Liping .
Ethics declarations
Ethics approval and consent to participate.
The study was reviewed and approved by the Ethics Committee of ZheJiang Cancer Hospital (Ethic ID: ZJZLYY IRB-2020-408). All the participants signed written informed consent forms. This study was conducted in accordance with the 1964 Declaration of Helsinki guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Chengang, H., Liping, W., Shujin, W. et al. Multi-stage optimization strategy based on contextual analysis to create M-health components for case management model in breast cancer transitional care: the CMBM study as an example. BMC Nurs 23 , 385 (2024). https://doi.org/10.1186/s12912-024-02049-x
Download citation
Received : 22 November 2023
Accepted : 29 May 2024
Published : 06 June 2024
DOI : https://doi.org/10.1186/s12912-024-02049-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- User-centered design
- Contextual analysis
- Breast cancer patients
- Case management
- Transitional care
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
Nicole Whitworth. Nicole is a Professional Nursing Tutor with over 15 years experience, and the founder of Your Nursing Tutor. She has a BSN, and an MA in Clinical Psychology. Nicole specializes in providing easy-to-follow, proven study methods (like the Silver Bullet Study System) that transform frustrated nursing students into calm, confident ...
Introduction. This resource is a collection of four case-based exercises intended to provide medical students with structured and focused opportunities to link basic science with clinical application. The cases are designed to help students self-evaluate their knowledge and develop a robust and well- integrated understanding of endocrine ...
The major endocrine organs of the body include the pituitary, thyroid, parathyroid, adrenal, pineal, and thymus glands, the pancreas, and the gonads. Hypothalamus. The hypothalamus, which is part of the nervous system, is also considered a major endocrine organ because it produces several hormones.
Endocrine System Disorders Nursing Test Bank. In this section are the NCLEX practice questions for endocrine system disorders. This nursing test bank set includes 50 questions divided into two parts. All questions on this set are updated to give you the most challenging questions, along with insightful rationales to reinforce learning.
The endocrine system is always working behind the scenes, regulating various organs by releasing hormones and using feedback loops. This chapter will discuss medications that affect three of the major endocrine glands: the adrenal glands, the pancreas, and the thyroid. ... Case Study 1. Ms. J.S. is a 45-year-old woman who was admitted to the ...
The doctor sketched a quick diagram on the whiteboard in his office. "First, your pituitary senses the level of thyroid hormone in your blood, if the amount is low, then it releases Thyroid Stimulating Hormone to stimulate the thyroid to release more thyroid hormone. Basically, the pituitary is attempting to return the system to a normal ...
Endocrine Case Study The endocrine system secretes different types of hormones directly into the bloodstream. Some of these hormones are transported on carrier proteins and some are dissolved directly in the plasma. Our hormones regulate a large range of physiological functions. If a person experiences hormonal dysfunction, physiological
A case study is provided to illustrate one possible presentation of endocrine disruption, in the form of diabetes-associated complications. The endocrine system comprises several distinct glands and tissues, which are made up of specialised cells that synthesise, store, and secrete hormones.
This Case Study describes a young woman with longstanding amenorrhea and virilization and highlights the challenges and pitfalls in the diagnosis and choice of proper treatment for this uncommon ...
This page titled 12.1: Case Study: Hormones and Health is shared under a CK-12 license and was authored, remixed, and/or curated by Suzanne Wakim & Mandeep Grewal via source content that was edited to the style and standards of the LibreTexts platform; a detailed edit history is available upon request. 18 year-old Gabrielle checks her calendar.
Patient testimonials and case studies highlight the real-world impact of these innovations, demonstrating how modern management approaches are shaping a more patient-centric healthcare system. As healthcare continues to evolve, it is crucial to prioritize patient-centered care to ensure that patients receive adequate treatment and have a ...
Endocrine System Overview Endocrinology is the study of endocrine cells/organs, the hormones secreted, regulation of hormone secretion and the effects of hormones on their target cells/organs. Endocrine vs. Exocrine tissues Endocrine secretes hormones, while exocrine secretes all the other stuff (mucus, enzymes, sweat).
Endocrine Practice Questions with Answers and NCLEX. Review. The endocrine system is a complex pathway that plays a role in the function of a variety of organ and blood systems. Its headquarters are located in the brain where the hypothalamus and the pituitary gland release a variety of hormones that can lead to profound effects systemically.
The endocrine system is a meticulously organized network of glands, each producing specific hormones that act as messengers, regulating bodily processes. Unlike the rapid transmission of the nervous system, hormones travel through the bloodstream, reaching target cells across the body to maintain equilibrium. Crucial Players: Glands and Hormones.
The key glands of the endocrine system include the hypothalamus, pituitary, thyroid, parathyroids, adrenals, pancreas, and gonads. These organs synthesize and secrete specific biochemical messengers, known as hormones, into the blood in a synchronized collaboration with the central nervous system (CNS) and the immune system to regulate ...
The test bank is composed of case studies with six questions each that follow the NCSBN Clinical Judgment Measurement Model steps: recognize cues. analyze cues. prioritize hypotheses. generate solutions. take action. evaluate outcomes. In addition, seven questions for reviewing bow-tie or trend items are included.
Chapter 28 - Endocrine Emergencies. Published online by Cambridge University Press: 04 May 2017. By. Aylwin J. Chick. Edited by. Daniele Bryden and. Andrew Temple. Chapter. Get access.
This is an endocrine disorder characterized by chronic anovulation, polycystic ovaries, and hyperandrogenism. 3 It results in a presentation similar to our patient's case with irregular menses, obesity, insulin resistance, and can also lead to depression.
Learning Outcomes. By the end of this section, you should be able to: 7.1.1 Recognize the normal function of the endocrine system.; 7.1.2 Recognize cues of nutritional impact on the endocrine system.; 7.1.3 Analyze cues of nutritional impact on the endocrine system.; Normal Function of the Endocrine System. The endocrine system is a network of cells, tissues, and organs that regulate and ...
Typically a result of chromaffin cell tumor called pheochromocytoma -uncontrolled sympathetic nervous system activity, hyperglycemia, increased metabolic rate, rapid heartbeat and palpitations, hypertension, intense nervousness, and sweating. Study with Quizlet and memorize flashcards containing terms like Growth Hormone Hypo-secretion ...
Use this simple Q& A page over the endocrine system to test your knowledge and prepare for upcoming tests. Feel free to print, copy, share, and use this study guide in any way! Remember: Adrenal HYPO function = Addisons: Adrenal HYPER function=Cushings: Thyroid HYPER function=Graves. The biggest tip I can give with learning endocrine D/Os is to ...
Introduction: This resource is a collection of four case-based exercises intended to provide medical students with structured and focused opportunities to link basic science with clinical application. The cases are designed to help students self-evaluate their knowledge and develop a robust and well-integrated understanding of endocrine ...
Type 1 diabetes mellitus is an endocrine AE oftentimes associated with PD-1/PD-L1 blockade. 54,55 In our study, the addition of ICB was associated with a higher incidence of type 1 diabetes, particularly with the addition of PD-1 blockade, consistent with previous research in the advanced disease setting. 55,56 The finding of our study supports ...
Endocrine Society is a global community of 18,000-plus endocrine investigators and clinicians more than 100 countries. Members focus on improving patient care, advancing research, shaping effective policy, and ensuring the future of endocrinology.
None of the early M-Health applications are designed for case management care services. This study aims to describe the process of developing a M-health component for the case management model in breast cancer transitional care and to highlight methods for solving the common obstacles faced during the application of M-health nursing service. We followed a four-step process: (a) Forming a cross ...
Introduction: This resource is a collection of four case-based exercises intended to provide medical students with structured and focused opportunities to link basic science with clinical application. The cases are designed to help students self-evaluate their knowledge and develop a robust and well- integrated understanding of endocrine physiology and pathophysiology in the context of a ...
Endocrine disruptors (EDs) pose a serious threat to human health and the environment and require a comprehensive evaluation to be identified. The identification of EDs require a substantial amount of data, both in vitro and in vivo, due to the current scientific criteria in the EU. At the same time, the EU strives to reduce animal testing due to concerns regarding animal welfare and ...