
Research Topics & Ideas: Healthcare
100+ Healthcare Research Topic Ideas To Fast-Track Your Project

Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a healthcare-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the healthcare domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Healthcare Research Topics
- Allopathic medicine
- Alternative /complementary medicine
- Veterinary medicine
- Physical therapy/ rehab
- Optometry and ophthalmology
- Pharmacy and pharmacology
- Public health
- Examples of healthcare-related dissertations
Allopathic (Conventional) Medicine
- The effectiveness of telemedicine in remote elderly patient care
- The impact of stress on the immune system of cancer patients
- The effects of a plant-based diet on chronic diseases such as diabetes
- The use of AI in early cancer diagnosis and treatment
- The role of the gut microbiome in mental health conditions such as depression and anxiety
- The efficacy of mindfulness meditation in reducing chronic pain: A systematic review
- The benefits and drawbacks of electronic health records in a developing country
- The effects of environmental pollution on breast milk quality
- The use of personalized medicine in treating genetic disorders
- The impact of social determinants of health on chronic diseases in Asia
- The role of high-intensity interval training in improving cardiovascular health
- The efficacy of using probiotics for gut health in pregnant women
- The impact of poor sleep on the treatment of chronic illnesses
- The role of inflammation in the development of chronic diseases such as lupus
- The effectiveness of physiotherapy in pain control post-surgery
Topics & Ideas: Alternative Medicine
- The benefits of herbal medicine in treating young asthma patients
- The use of acupuncture in treating infertility in women over 40 years of age
- The effectiveness of homoeopathy in treating mental health disorders: A systematic review
- The role of aromatherapy in reducing stress and anxiety post-surgery
- The impact of mindfulness meditation on reducing high blood pressure
- The use of chiropractic therapy in treating back pain of pregnant women
- The efficacy of traditional Chinese medicine such as Shun-Qi-Tong-Xie (SQTX) in treating digestive disorders in China
- The impact of yoga on physical and mental health in adolescents
- The benefits of hydrotherapy in treating musculoskeletal disorders such as tendinitis
- The role of Reiki in promoting healing and relaxation post birth
- The effectiveness of naturopathy in treating skin conditions such as eczema
- The use of deep tissue massage therapy in reducing chronic pain in amputees
- The impact of tai chi on the treatment of anxiety and depression
- The benefits of reflexology in treating stress, anxiety and chronic fatigue
- The role of acupuncture in the prophylactic management of headaches and migraines
Topics & Ideas: Dentistry
- The impact of sugar consumption on the oral health of infants
- The use of digital dentistry in improving patient care: A systematic review
- The efficacy of orthodontic treatments in correcting bite problems in adults
- The role of dental hygiene in preventing gum disease in patients with dental bridges
- The impact of smoking on oral health and tobacco cessation support from UK dentists
- The benefits of dental implants in restoring missing teeth in adolescents
- The use of lasers in dental procedures such as root canals
- The efficacy of root canal treatment using high-frequency electric pulses in saving infected teeth
- The role of fluoride in promoting remineralization and slowing down demineralization
- The impact of stress-induced reflux on oral health
- The benefits of dental crowns in restoring damaged teeth in elderly patients
- The use of sedation dentistry in managing dental anxiety in children
- The efficacy of teeth whitening treatments in improving dental aesthetics in patients with braces
- The role of orthodontic appliances in improving well-being
- The impact of periodontal disease on overall health and chronic illnesses
Tops & Ideas: Veterinary Medicine
- The impact of nutrition on broiler chicken production
- The role of vaccines in disease prevention in horses
- The importance of parasite control in animal health in piggeries
- The impact of animal behaviour on welfare in the dairy industry
- The effects of environmental pollution on the health of cattle
- The role of veterinary technology such as MRI in animal care
- The importance of pain management in post-surgery health outcomes
- The impact of genetics on animal health and disease in layer chickens
- The effectiveness of alternative therapies in veterinary medicine: A systematic review
- The role of veterinary medicine in public health: A case study of the COVID-19 pandemic
- The impact of climate change on animal health and infectious diseases in animals
- The importance of animal welfare in veterinary medicine and sustainable agriculture
- The effects of the human-animal bond on canine health
- The role of veterinary medicine in conservation efforts: A case study of Rhinoceros poaching in Africa
- The impact of veterinary research of new vaccines on animal health
Topics & Ideas: Physical Therapy/Rehab
- The efficacy of aquatic therapy in improving joint mobility and strength in polio patients
- The impact of telerehabilitation on patient outcomes in Germany
- The effect of kinesiotaping on reducing knee pain and improving function in individuals with chronic pain
- A comparison of manual therapy and yoga exercise therapy in the management of low back pain
- The use of wearable technology in physical rehabilitation and the impact on patient adherence to a rehabilitation plan
- The impact of mindfulness-based interventions in physical therapy in adolescents
- The effects of resistance training on individuals with Parkinson’s disease
- The role of hydrotherapy in the management of fibromyalgia
- The impact of cognitive-behavioural therapy in physical rehabilitation for individuals with chronic pain
- The use of virtual reality in physical rehabilitation of sports injuries
- The effects of electrical stimulation on muscle function and strength in athletes
- The role of physical therapy in the management of stroke recovery: A systematic review
- The impact of pilates on mental health in individuals with depression
- The use of thermal modalities in physical therapy and its effectiveness in reducing pain and inflammation
- The effect of strength training on balance and gait in elderly patients
Topics & Ideas: Optometry & Opthalmology
- The impact of screen time on the vision and ocular health of children under the age of 5
- The effects of blue light exposure from digital devices on ocular health
- The role of dietary interventions, such as the intake of whole grains, in the management of age-related macular degeneration
- The use of telemedicine in optometry and ophthalmology in the UK
- The impact of myopia control interventions on African American children’s vision
- The use of contact lenses in the management of dry eye syndrome: different treatment options
- The effects of visual rehabilitation in individuals with traumatic brain injury
- The role of low vision rehabilitation in individuals with age-related vision loss: challenges and solutions
- The impact of environmental air pollution on ocular health
- The effectiveness of orthokeratology in myopia control compared to contact lenses
- The role of dietary supplements, such as omega-3 fatty acids, in ocular health
- The effects of ultraviolet radiation exposure from tanning beds on ocular health
- The impact of computer vision syndrome on long-term visual function
- The use of novel diagnostic tools in optometry and ophthalmology in developing countries
- The effects of virtual reality on visual perception and ocular health: an examination of dry eye syndrome and neurologic symptoms
Topics & Ideas: Pharmacy & Pharmacology
- The impact of medication adherence on patient outcomes in cystic fibrosis
- The use of personalized medicine in the management of chronic diseases such as Alzheimer’s disease
- The effects of pharmacogenomics on drug response and toxicity in cancer patients
- The role of pharmacists in the management of chronic pain in primary care
- The impact of drug-drug interactions on patient mental health outcomes
- The use of telepharmacy in healthcare: Present status and future potential
- The effects of herbal and dietary supplements on drug efficacy and toxicity
- The role of pharmacists in the management of type 1 diabetes
- The impact of medication errors on patient outcomes and satisfaction
- The use of technology in medication management in the USA
- The effects of smoking on drug metabolism and pharmacokinetics: A case study of clozapine
- Leveraging the role of pharmacists in preventing and managing opioid use disorder
- The impact of the opioid epidemic on public health in a developing country
- The use of biosimilars in the management of the skin condition psoriasis
- The effects of the Affordable Care Act on medication utilization and patient outcomes in African Americans
Topics & Ideas: Public Health
- The impact of the built environment and urbanisation on physical activity and obesity
- The effects of food insecurity on health outcomes in Zimbabwe
- The role of community-based participatory research in addressing health disparities
- The impact of social determinants of health, such as racism, on population health
- The effects of heat waves on public health
- The role of telehealth in addressing healthcare access and equity in South America
- The impact of gun violence on public health in South Africa
- The effects of chlorofluorocarbons air pollution on respiratory health
- The role of public health interventions in reducing health disparities in the USA
- The impact of the United States Affordable Care Act on access to healthcare and health outcomes
- The effects of water insecurity on health outcomes in the Middle East
- The role of community health workers in addressing healthcare access and equity in low-income countries
- The impact of mass incarceration on public health and behavioural health of a community
- The effects of floods on public health and healthcare systems
- The role of social media in public health communication and behaviour change in adolescents
Examples: Healthcare Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a healthcare-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various healthcare-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Improving Follow-Up Care for Homeless Populations in North County San Diego (Sanchez, 2021)
- On the Incentives of Medicare’s Hospital Reimbursement and an Examination of Exchangeability (Elzinga, 2016)
- Managing the healthcare crisis: the career narratives of nurses (Krueger, 2021)
- Methods for preventing central line-associated bloodstream infection in pediatric haematology-oncology patients: A systematic literature review (Balkan, 2020)
- Farms in Healthcare: Enhancing Knowledge, Sharing, and Collaboration (Garramone, 2019)
- When machine learning meets healthcare: towards knowledge incorporation in multimodal healthcare analytics (Yuan, 2020)
- Integrated behavioural healthcare: The future of rural mental health (Fox, 2019)
- Healthcare service use patterns among autistic adults: A systematic review with narrative synthesis (Gilmore, 2021)
- Mindfulness-Based Interventions: Combatting Burnout and Compassionate Fatigue among Mental Health Caregivers (Lundquist, 2022)
- Transgender and gender-diverse people’s perceptions of gender-inclusive healthcare access and associated hope for the future (Wille, 2021)
- Efficient Neural Network Synthesis and Its Application in Smart Healthcare (Hassantabar, 2022)
- The Experience of Female Veterans and Health-Seeking Behaviors (Switzer, 2022)
- Machine learning applications towards risk prediction and cost forecasting in healthcare (Singh, 2022)
- Does Variation in the Nursing Home Inspection Process Explain Disparity in Regulatory Outcomes? (Fox, 2020)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Need more help?
If you’re still feeling a bit unsure about how to find a research topic for your healthcare dissertation or thesis, check out Topic Kickstarter service below.

You Might Also Like:

15 Comments
I need topics that will match the Msc program am running in healthcare research please
Hello Mabel,
I can help you with a good topic, kindly provide your email let’s have a good discussion on this.
Can you provide some research topics and ideas on Immunology?
Thank you to create new knowledge on research problem verse research topic
Help on problem statement on teen pregnancy
This post might be useful: https://gradcoach.com/research-problem-statement/
can you provide me with a research topic on healthcare related topics to a qqi level 5 student
Please can someone help me with research topics in public health ?
Hello I have requirement of Health related latest research issue/topics for my social media speeches. If possible pls share health issues , diagnosis, treatment.
I would like a topic thought around first-line support for Gender-Based Violence for survivors or one related to prevention of Gender-Based Violence
Please can I be helped with a master’s research topic in either chemical pathology or hematology or immunology? thanks
Can u please provide me with a research topic on occupational health and safety at the health sector
Good day kindly help provide me with Ph.D. Public health topics on Reproductive and Maternal Health, interventional studies on Health Education
may you assist me with a good easy healthcare administration study topic
May you assist me in finding a research topic on nutrition,physical activity and obesity. On the impact on children
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 06 May 2021
Co-producing knowledge in health and social care research: reflections on the challenges and ways to enable more equal relationships
- Michelle Farr ORCID: orcid.org/0000-0001-8773-846X 1 , 2 ,
- Philippa Davies ORCID: orcid.org/0000-0002-2678-7126 1 , 2 ,
- Heidi Andrews 1 , 2 ,
- Darren Bagnall 1 , 2 ,
- Emer Brangan ORCID: orcid.org/0000-0002-1288-0960 1 , 2 , 3 &
- Rosemary Davies ORCID: orcid.org/0000-0001-9969-1902 1 , 4
Humanities and Social Sciences Communications volume 8 , Article number: 105 ( 2021 ) Cite this article
6222 Accesses
22 Citations
32 Altmetric
Metrics details
- Health humanities
- Medical humanities
Researchers are increasingly encouraged to co-produce research, involving members of the public, service users, policy makers and practitioners in more equal relationships throughout a research project. The sharing of power is often highlighted as a key principle when co-producing research. However, health and social care research, as with many other academic disciplines, is carried out within embedded hierarchies and structural inequalities in universities, public service institutions, and research funding systems—as well as in society more broadly. This poses significant challenges to ambitions for co-production. This article explores the difficulties that are faced when trying to put ideal co-production principles into practice. A reflective account is provided of an interdisciplinary project that aimed to better understand how to reduce power differentials within co-produced research. The project facilitated five workshops, involving researchers from different disciplines, health, social care and community development staff and public contributors, who all had experience in co-production within research. In the workshops, people discussed how they had attempted to enable more equal relationships and shared ideas that supported more effective and equitable co-produced research. Shared interdisciplinary learning helped the project team to iteratively develop a training course, a map of resources and reflective questions to support co-produced research. The gap between co-production principles and practice is challenging. The article examines the constraints that exist when trying to share power, informed by multidisciplinary theories of power. To bring co-production principles into practice, changes are needed within research practices, cultures and structures; in understandings of what knowledge is and how different forms of knowledge are valued. The article outlines challenges and tensions when co-producing research and describes potential ideas and resources that may help to put co-production principles into practice. We highlight that trying to maintain all principles of co-production within the real-world of structural inequalities and uneven distribution of resources is a constant challenge, often remaining for now in the realm of aspiration.
Introduction
Co-production of research—where researchers, practitioners and members of the public collaborate to develop research together—is promoted as a way to strengthen public involvement, and create and implement more relevant and applicable knowledge, that is used in practice (Staniszewska et al., 2018 ; Hickey et al., 2018 ). Academic disciplines and funding bodies define the concept of co-production differently, using divergent methods and theories (Facer and Enright, 2016 ), with subsequent debate about what co-production is and who may be doing it ‘properly’. We use the INVOLVE definition and principles of co-producing research (Box 1 ) (Hickey et al., 2018 ), which includes the often-agreed principle to share power more equally between partners. However, the extent to which this is achievable within structural inequalities and institutional hierarchies is debatable (Flinders et al., 2016 ).
This commentary article reflects on a project that aimed to:
share interdisciplinary learning about co-produced research
understand how to enable more equal relationships with co-production partners, particularly public contributors—defined as members of the public including patients, potential patients, carers and people who use health and social care services (in contrast to people who have a professional role in health and social care services or research) (NIHR CED, 2020 ).
develop training and resources to support co-produced research.
The project was developed by a team of three applied health researchers, a public involvement lead and three public contributors (with in-depth experiences of co-produced research) undertaken within the National Institute for Health Research (NIHR) Applied Research Collaboration (ARC) West, an organisation that develops applied health and social care research. Through facilitating five project workshops, we engaged with eleven researchers from five disciplines; six practitioners; and eleven public contributors with involvement and co-produced research experiences. We shared practical lessons across disciplinary boundaries about how to do co-produced research more equitably (Oliver and Boaz, 2019 ). These workshops helped the project team progressively and iteratively develop a training course, a map of resources (Farr et al., 2020 ) and reflective questions (Davies et al., 2020 ), freely available to support co-produced research.
This article explores the extent to which these multidisciplinary lessons can help us transform knowledge production in more equitable ways, outlining our learning from this project. First, we overview some conceptual issues with the use of the word ‘co-production’. We then discuss key matters raised in our interdisciplinary workshops: ‘Who is involved and when in co-produced research?’; ‘Power dynamics within health and social care research’; and ‘Communication and relationships’. We conclude by highlighting that bringing co-production principles into the real research world is fraught with difficult and messy compromises. Researchers (often lower in the academic hierarchy) may be caught up in battling systems and policies to enable co-production to happen, especially where they attempt to address issues of power and control within the research process.
Box 1: INVOLVE a Definitions and principles of co-produced research (Hickey et al., 2018 )
‘ Co-producing a research project is an approach in which researchers, practitioners and the public work together, sharing power and responsibility from the start to the end of the project, including the generation of knowledge ’ (p. 4).
Principles include:
Sharing power where research is owned by everyone and people are working together in more equal relationships
Including all perspectives and skills to ensure that everyone who wants to make a contribution can do so, with diversity, inclusiveness and accessibility being key
Respecting and valuing the knowledge of everyone , with everyone being of equal importance, and benefitting from the collaboration
Reciprocity and mutuality , building and maintaining relationships and sharing learning
Understanding each other with clarity over people’s roles and responsibilities.
a INVOLVE supported active public involvement in NHS, public health and social care research, with a new NIHR Centre for Engagement and Dissemination (CED) launched in April 2020.
The concept of co-production
The NVOLVE co-production principles (Box 1 ) (Hickey et al., 2018 ) build on public policy co-production literature (Boyle and Harris, 2009 ; Staniszewska et al., 2018 ), which explores how service users can take an active role within the provision of public services (Brudney and England, 1983 ; Ostrom, 1996 ). A key premise is that service users have a fundamental role in producing services and outcomes that are important to them (Brandsen and Honingh, 2016 ). While in our project we particularly wanted to focus on ways of sharing power with service users and public contributors, defining who is involved in co-produced research varies across disciplines. The active involvement of service users/members of the public has sometimes been lost in research that is labelled as co-produced. UK funding councils such as the Economic and Social Research Council (ESRC) talk of co-produced research as developed between academic and non-academic organisations or communities (Campbell and Vanderhoven, 2016 ; ESRC, 2019 ). In health services research, authors have used the non-specific language of ‘stakeholders’ (Oliver et al., 2019 ). Sometimes the main research co-production partner has been practitioners (Heaton et al., 2016 ) and service users have been relegated to ‘context’ (Marshall et al., 2018 ), rather than being active agents and partners. This obfuscation of the role of service users/ members of the public in co-production is detrimental to the drive for inclusivity, democratisation and equity within co-produced research, which addresses the needs of service users/ marginalised citizens (Williams et al., 2020 ), overlooking the long political history of demands from service users to be more democratically involved in health and social care services and research (Beresford, 2019 ).
In our project, we particularly wanted to focus on how to equalise relationships with service users and public contributors (defined above) within co-produced research. The egalitarian and democratic principles of co-production means that service users, who may have been marginalised and are on the receiving end of professional ‘expertise’, now become equal partners in research (Williams et al., 2020 ). Best practice in co-produced research remains contested, with a significant theory-practice gap (Lambert and Carr, 2018 ). We wanted to understand what practices and resources could help bring principles into practice, when we are working within a context of structural inequalities.
Who is involved and when in co-produced research?
INVOLVE states that co-production should ‘occur from the start to the end of the project’ (Hickey et al., 2018 ) (p. 4). The principle to ‘include all perspectives and skills—make sure the research team includes all those who can make a contribution’ (Hickey et al., 2018 ) (p. 4) can be highly aspirational.
In our interdisciplinary workshops we discussed how there is often a lack of funding to pay public contributors to help develop a funding application. Formative ideas about research priorities and design can often be made by researchers before other people are involved. Our workshop discussions noted that involving all stakeholders who potentially have an interest in a project could be a very large and diverse group. It would be difficult to involve everyone, and this could be in tension with the idea that smaller groups can work better together. There are usually practical constraints on team numbers, budgets to pay for public contributors’ time and project scale and size. A tension can exist between the number of people you can viably include, and the diversity of the group you are working with. More generally, workshop participants highlighted problematic issues of claims to representation, where people within a co-production group need to be aware that they don’t speak for everyone—not even everyone in a group they are there to ‘represent’—and there was a need to look for opportunities to draw other perspectives in.
Workshop discussions included that when public contributors join a project there is a need to support people to take on different roles, and for people to also have choice and work from their strengths, rather than assuming that everyone has to do everything. Some group members may feel they lack skills or expertise in particular areas, and so may need training, support and mentoring. There may also be assumptions about who is going to do what work, which may need to be explicitly discussed and agreed. Ensuring proper payment of public contributors is an essential element of co-production. If public contributors are going to collect research data, they need appropriate payment, contracts and to follow all research governance processes. Within UK National Health Service (NHS) research that may mean having Research Passports, Good Clinical Practice training and Disclosure and Barring Service checks, if they are working with vulnerable people or children. Not all these processes are designed for public contributors, they can be potentially problematic to navigate, and researchers may need to support public contributors through this process. Table 1 summarises some of the challenges around who is involved, and when in co-produced research, and potential practices and resources that may help.
Power dynamics within health and social care research
Theoretical perspectives on power.
Critical and interdisciplinary perspectives on power can help us understand how to facilitate more equitable partnerships within research and co-produced work (Farr, 2018 ; Oliver and Boaz, 2019 ). The first principle of co-production is to share power through ‘an equal and reciprocal relationship’ between professionals and people using services (Boyle and Harris, 2009 ) (p. 11). However, several authors highlight how co-production can be a rhetorical device to hide power and social inequities (Flinders et al., 2016 ; Thomas-Hughes, 2018 ). Using Lukes ( 2005 ) dimensions of power, Gaventa ( 2007 ) conceives that power can be visible (institutions, structures, resources, rules), hidden (agenda-setting, some voices more dominant within decision-making), or invisible (embedded in beliefs and language).
Focussing first on visible aspects, structural and resource issues can impinge on people’s ability to co-produce, for example funders’ top-down control of research priorities and funding streams, alongside NHS and government political priorities. University research environments can be competitive, ‘unkind and aggressive’, which can crowd out ‘collegiality and collaboration’ (WellcomeTrust, 2020 ), exactly the kind of principles that academics are being encouraged to adopt through co-production. Traditional research frameworks are ill-fitted to the challenges of transforming power and control that are needed for co-productive practice (Lambert and Carr, 2018 ). Power hierarchies are intrinsic to research processes, with people experiencing competing expectations (from public contributors and communities, co-researchers, colleagues and institutions) when working in this way (Lenette et al., 2019 ). How do researchers create co-production circles of equality, reciprocity and share power with public contributors, when often researchers themselves are on temporary contracts and subject to the pressures of publishing, funding, impact and self-promotion within ‘toxic’ (Wellcome Trust, 2020 ) competitive structures? Understanding who is involved and how in decision-making processes (hidden aspects of power) is essential to understand how power is exercised. However, political scientists have long ago illustrated that ‘even the most internally democratic small collectives cannot in fact achieve equality of power in their decisions’ (Mansbridge, 1996 , p. 54).
Scrutinising invisible aspects of power, power can be seen to operate through knowledge, social relations and the language we use (Foucault, 1977 ). The principle of respecting and valuing the knowledge of all (Hickey et al., 2018 ) can be challenging in a healthcare context where a knowledge hierarchy with traditional positivist epistemological assumptions values an ‘unbiased, objective’ position. Co-productive approaches can be grounded in critical theory (Bell and Pahl, 2018 ; Facer and Enright, 2016 ), as opposed to traditional scientific paradigms. The experiential contextualised and tacit knowledge of people who use services, and related qualitative and participatory action methods, can be valued less than knowledge derived from randomised controlled trials (RCTs). This increases the challenge of co-production, as the values and methods of health and social care research may align less with co-production principles. Indeed the very idea that co-production and the sharing of power can actually happen within mainstream University spaces has been contested, with Rose and Kalathil ( 2019 ) arguing that Eurocentric hierarchical institutions that privilege rationality and reason will never be coming from a place where different knowledges are valued equally.
Understanding power in practice
In our project it was difficult to maintain a focus on power relations in the face of a strong tendency to emphasise practicalities, highlighting the difficulties of bringing these issues into clearer focus. An analysis of power dynamics may be an important aspect of a sociological study, but not one considered of such importance within health and social care research.
Focussing first on visible, structural aspects of power, workshop participants discussed their experience that within research that is formally ‘owned’ by a University (i.e., the Principal Investigator (PI) legally responsible for the project is situated within a University) there are associated issues of accountability and formal responsibility for delivering a funded research project. This creates constraints where projects have to deliver what is described rather than what emerges from the co-production process. How a PI works to develop a collaborative leadership style is an under-researched area. Within our own project we all held some unspoken assumptions about leadership and ensuring progress toward our project objectives. Workshop participants highlighted that organisational systems may not support co-production (e.g., finance, human resources and funding systems) so researchers may have to be tenacious to advocate for system changes in order to achieve things, which can be frustrating and time-consuming. For these myriad reasons, realistic resourcing of researcher time for co-production is needed, and many researchers may still end up putting discretionary time into projects to make co-production a success. There are few tools to help researchers avoid or alleviate risks to themselves and their stakeholders, such risks including practical costs, personal and professional costs to researchers, and costs to stakeholders (Oliver et al., 2019 ).
In relation to decision-making, workshop participants noted that in a pragmatic sense, doing everything by committee and consensus can impede project progress, as no decisions can be made until everyone is present at meetings. Even if decisions are made with everyone present, the power dynamics between people does not necessarily ensure that decisions are shared and agreed by everyone. Within our own project, where we were trying to stick to the principles of co-production, we found that we often had discussions between paid staff members outside of team meetings where thinking was developed and decisions taken. If public contributors are without employment contracts and are not working alongside other staff, there is potential for them to be excluded from informal discussions and decisions in day-to-day tasks. In our workshops there were discussions about whether researchers needed to ‘get out of the way’ and ‘sit on their hands’ in order to make space for others. We discussed how to practically create space for diverse knowledge and skills to be shared and considered whether it is possible to identify shared interests or if there is always a political struggle for power.
Through our project, we reflected as a team how assumptions and practices of how we do healthcare research may be deeply embedded within academic cultures. This links with Foucault’s perspectives on power dynamics (Foucault, 1977 ), every act and assumption we make is imbued with power, which makes power particularly hard to observe, grasp, critique, challenge and transform. We all have subconscious beliefs and work within cultural assumptions, thus continual critical reflective practice, and constant attention to fluctuating power relations is needed (Farr, 2018 ; Bell and Pahl, 2018 ). In workshops, suggested ways to address cultural issues included harnessing the current trends for co-production and using this to start challenging engrained cultures and accepted ways of doing things. Current funder prioritisation of co-production can enable senior researcher support for co-production, as organisational leaders recognise the cultural capital of the word and practices of ‘co-production’. Raising awareness of NIHR and other policy commitments to co-production may be a useful influencing strategy to engage more senior staff, as organisational support can be crucial to facilitate co-production. However, there is always the risk of tokenism and rhetoric (Flinders et al., 2016 ; Thomas-Hughes, 2018 ).
We considered within our project that the relationships between personal experiential knowledge, practice-based knowledge of healthcare staff, and dominant healthcare research need to be better understood if we are to co-produce knowledge together. We reflected on whether the aim of co-production projects is to modify the knowledge hierarchy completely, or to bring in experiential expertise/lived experience to influence the knowledge production process so the knowledge produced is more practical/effective/implementable. This second, more limited aim of making evidence more co-productively, so that it is more useful in practice may be more achievable, whereas modifying the dominant knowledge hierarchy was beyond our scope and influence.
Communication and relationships
The above dimensions of power (Lukes, 2005 ) have been augmented and brought together into a broader theoretical framework (Haugaard, 2012 ), which also incorporates ‘power with’ (Arendt, 1970 ), where emancipatory power can be harnessed through our ‘capacity to act in concert’. Arendt’s work highlights how we can collectively use our power together in more empowering ways. This links with a key principle of co-production, reciprocity, where everyone benefits from working together.
Consideration of what different team members want from working together, and therefore what reciprocity means within a project is needed. We discussed in the interdisciplinary workshops how the kind of benefits wanted by public contributors might include developing skills, confidence and work experience, and meeting such expectations may not usually be considered as research aims. Through our project we saw how co-production is strongly reliant on good communication and relationships. Strong facilitation and chairing skills are needed within meetings, to encourage everyone to contribute and challenge unhelpful behaviours, e.g., using jargon, or one person speaking a lot to the exclusion of others. People in our workshops discussed how some public contributors might need additional support to get more involved, e.g., having pre-meetings to help people get to grips with some information and/or issues, or the provision of materials in different accessible formats. If a co-production project includes people with specific communication needs, the group may need additional time and skills to be able to offer ways of working that are suitable for all. The NIHR is encouraging researchers to involve communities and groups that are often excluded. This means more outreach work to go out and meet with people in the places that they find accessible and comfortable, which can include project meetings in community locations, which may require additional resources.
Developing relationships and trust between team members may take time and requires emotional work. In our workshops we discussed how if the public contributor role includes sharing personal experiences for the benefit of the project, then researchers may also need to drop the ‘professional’ mask and share more personally and expose their own vulnerabilities (Batalden, 2018 ) to support more equal relationships. The challenges of university structural hierarchies were also discussed, including how it was often the responsibility of more ‘junior’ (i.e., lower in the hierarchy) researchers, and often women, to do the relational work (Lenette et al., 2019 ). Senior researchers do not necessarily understand the implications of co-production, for example one person shared how their Principal Investigator assumed that having a public contributor on the team would increase capacity and speed work up, unappreciative of the extra time needed for support, training and communication, including at the weekends, when public contributors could be carrying out work. Meeting the support and learning needs of team members can be challenging, both for researchers and public contributors, as co-produced research may take researchers outside the skills and knowledge usually expected in their professional environment. Even when these needs within a co-production project are recognised, research funders may not understand the resource and capacity implications.
A key element of running a co-production project identified within our work was the ongoing need for time to reflect on group processes to support and maintain different ways of working. Finding time for reflection can be challenging alongside creating an environment where everyone can honestly reflect on what it’s like to be in the group. This requires strong facilitation skills, particularly if there are tensions and conflicts. Addressing communication and relationship challenges are key to developing and sustaining a sense of shared ownership, and we outline some helpful practices in Table 2 .
Reflections on our own attempts at co-production
The conception of our project came initially from conversations between a researcher and public involvement specialist with previous experience as a service user and user-controlled research, wanting to create a space to share interdisciplinary learning between everyone about co-production. It could be argued that as the generation of the idea did not include public members in this first discussion it was not truly co-produced. We acknowledged that there were gaps between the lessons our project produced, and how the project itself had been carried out. It was very challenging to implement all INVOLVE principles (Hickey et al. 2018 ), and we question the extent to which they can ever be fully realised within our current contexts. Practically, we found that we should have allocated more resources to payment of our public contributors to take on additional roles. A focus on relationships and reflection was hard to maintain in the face of a small group trying to deliver an ambitious project to time, alongside other competing commitments. However, in our own reflective discussions we acknowledged that a sense of ongoing commitment to the project from everyone felt key to our group process and successfully getting the project done. In writing this article we met together several times to plan and develop sections, tables and points we wanted to get across. However, the actual writing tended to fall to the academics and public involvement specialist, who had more of the technical knowledge of what was expected. Demands of time, the juggling of commitments, and lack of resources meant that writing the article was not truly ‘co-produced’. Indeed, through the process, a public contributor co-author said they found the reviewers’ comments ‘a bit overwhelming’, with uncertainty of how to approach this. Another public contributor co-author expressed similar experiences with reviewers comments on another paper they had previously co-authored. The publication process can be a challenge to researchers as well, who are more familiar with these traditional academic practices.
Sharing power in the face of embedded hierarchies and inequalities is an obvious challenge for co-production. The gap between co-production principles and practice is a tricky territory. Working with everyone who is interested in an issue, having a focus on meeting the priorities of communities and people we work with, and co-producing all aspects of a project from beginning to end will be difficult to deliver in many projects in health and social care research. Working directly with members of the public is likely to require more adaptation of research project processes and to ‘usual ways of doing things’, alongside additional time and resources. People have different skills and uneven access to resources, and people may need considerable training and support to work together more equally. However, our experience is that funders do not necessarily understand this and doing co-production on a small budget can be particularly challenging. Time investment and the emotional work required to build relationships necessary for successful co-production is both under-appreciated and under-resourced. This reflects disparities in power between those who do this work and those who hold most power in universities. Recognising, recording, documenting and consistently budgeting for this work may help to make it more visible. Timing of funding is also crucial as many research teams do not have access to institutional ‘core’ funding, or seed funding grants, for public contributor involvement at the research development stage. As it is unlikely that most co-production projects will be able to include people with all the relevant perspectives and skills it is important to actively discuss and agree who can be involved and to be open about and discuss restrictions, which can be an act of power in itself.
Oliver and Boaz ( 2019 ) want to ‘open the door’ to more critical multidisciplinary accounts of evidence production and use, highlighting that some people want to direct energies to democratise knowledge for all. Interdisciplinary lessons from this project question the extent to which co-production processes can enable this, given the challenges we have highlighted. We consider that the jury is still out on the viability of co-production in the context of health and social care research. While some (Rose and Kalathil, 2019 ) find the promise of co-production untenable in mental health, we hope we can find a meaningful way forward. However, ‘putting what we already know [about co-production] into practice’ (Oliver and Boaz, 2019 ) can be very challenging. Our own experiences led us to reflect that to be working toward co-production principles means that you have to consistently be challenging ‘business as usual’—we consider a key point here is how to maintain sufficient self and team support to keep trying to do this in practice. Establishing reflective processes that encourage consideration of power issues are likely to be essential. Our approach to help ourselves and others navigate the challenges of co-production has been to identify ways in which groups can start to address power issues as highlighted in Tables 1 and 2 , and to develop practical freely available outputs including a map of resources and reflective questions (Farr et al., 2020 ; Davies et al., 2020 ). We need to understand more about how effective these strategies are, and whether co-production really does make a difference to the use of research. We need to encourage honest reporting of projects, their outcomes and the balance between the benefits and challenges of trying to implement the principles. However, power structures may mitigate against reporting of challenges and problems in research. Other research gaps include understanding what projects will benefit most from a co-production approach. Can co-production deliver more practical and implementable research findings, and if so how? How do we best challenge and change some of the structural inequalities within academia that impede co-production (Williams et al., 2020 )? How do we integrate experiential, practice and research-based knowledge to improve health and social care?
Our experiences on this project highlight the ongoing challenges to truly put the principles of co-production into practice. During this project we used the phrase ‘I am always doing what I can’t do yet in order to learn how to do it’ (van Gogh, 1885 ), to illustrate our limitations, yet continual striving toward an ideal. The quote continues ‘…I’ll end by saying that the work is difficult, and that, instead of quarrelling, the fellows who paint peasants and the common people would do wisely to join hands as much as possible. Union is strength…’ (van Gogh, 1885 ). Forgiving the dated language and connotations of this quote, the principles of joining hands and facilitating union are important co-production ideals that we continually need to remember, relearn and put our hearts into practising.
Arendt H (1970) On violence. Allen Lane, Penguin, London
Google Scholar
Batalden P (2018) Getting more health from healthcare: quality improvement must acknowledge patient coproduction—an essay by Paul Batalden. BMJ 362:k3617. https://doi.org/10.1136/bmj.k3617
Article PubMed Central Google Scholar
Bell DM, Pahl K (2018) Co-production: towards a utopian approach. Int J Soc Res Methodol 21(1):105–117. https://doi.org/10.1080/13645579.2017.1348581
Article Google Scholar
Beresford P (2019) Public participation in health and social care: exploring the co-production of knowledge. Front Sociol 3(41). https://doi.org/10.3389/fsoc.2018.00041
Boyle D, Harris M (2009) The challenge of co-production. New Economics Foundation, London
Brandsen T, Honingh M (2016) Distinguishing different types of coproduction: a conceptual analysis based on the classical definitions. Publ Admin Rev 76(3):427–435. https://doi.org/10.1111/puar.12465
Brudney JL, England RE (1983) Toward a definition of the coproduction concept. Publ Admin Rev 43(1):59–65. https://doi.org/10.2307/975300
Campbell HJ, Vanderhoven D (2016) N8/ESRC research programme. Knowledge that matters: realising the potential of co-production. N8 Research Partnership, Manchester, https://www.n8research.org.uk/media/Final-Report-Co-Production-2016-01-20.pdf . Accessed 23 Mar 2021
Davies R, Andrews H, Farr M, Davies P, Brangan E, Bagnall D (2020) Reflective questions to support co-produced research. National Institute for Health Research (NIHR) ARC West and People in Health West of England, University of Bristol and University of West of England. http://bit.ly/CoProResources . Accessed 23 Mar 2021
ESRC (2019) Guidance for collaboration. Economic and Social Research Council. https://esrc.ukri.org/collaboration/guidance-for-collaboration/ . Accessed 29 Nov 2020
Facer K, Enright B (2016) Creating Living knowledge: the connected communities programme, community-university relationships and the participatory turn in the production of knowledge. University of Bristol/ AHRC Connected Communities, Bristol
Farr M (2018) ‘Power dynamics and collaborative mechanisms in co-production and co-design processes’. Crit Social Policy 38(4):623–644. https://doi.org/10.1177/0261018317747444
Farr M, Davies R, Davies P, Bagnall D, Brangan E, Andrews H (2020) A map of resources for co-producing research in health and social care. University of Bristol and University of West of England, National Institute for Health Research (NIHR) ARC West and People in Health West of England http://bit.ly/CoProResources . Accessed 23 Mar 2021
Flinders M, Wood M, Cunningham M (2016) The politics of co-production: risks, limits and pollution. Evid Policy 12(2):261–279. https://doi.org/10.1332/174426415X14412037949967
Foucault M (1977) Discipline and punish: the birth of the prison. Allen Lane, London
Gaventa J (2007) Levels, spaces and forms of power: analysing opportunities for change. In: Berenskoetter F, Williams MJ (eds) Power in world politics. Routledge, Abingdon, pp. 204–224
Haugaard M (2012) Rethinking the four dimensions of power: domination and empowerment. J Polit Power 5(1):33–54. https://doi.org/10.1080/2158379X.2012.660810
Heaton J, Day J, Britten N (2016) Collaborative research and the co-production of knowledge for practice: an illustrative case study. Implement Sci 11(1):20. https://doi.org/10.1186/s13012-016-0383-9
Article PubMed PubMed Central Google Scholar
Hickey G, Brearley S, Coldham T, Denegri S, Green G, Staniszewska S, Tembo D, Torok K, Turner K (2018) Guidance on co-producing a research project. INVOLVE, Southampton
INVOLVE (2019) Co-production in action: number one. INVOLVE, Southampton
Lambert N, Carr S (2018) ‘Outside the Original Remit’: Co-production in UK mental health research, lessons from the field. Int J Ment Health Nurs. 27(4):1273–1281
Lenette C, Stavropoulou N, Nunn C, Kong ST, Cook T, Coddington K, Banks S (2019) Brushed under the carpet: examining the complexities of participatory research. Res All 3(2):161–179. https://doi.org/10.18546/RFA.03.2.04
Lukes S (2005) Power: a radical view. Macmillan, London
Book Google Scholar
Mansbridge J (1996) Using power/ fighting power: the polity. In: Benhabib S (ed.) Democracy and Difference. Princeton University Press, Princeton, pp. 46–66
Marshall M, Mear L, Ward V, O’Brien B, Davies H, Waring J, Fulop N (2018) Optimising the impact of health services research on the organisation and delivery of health services: a study of embedded models of knowledge co-production in the NHS (Embedded). NIHR. https://www.journalslibrary.nihr.ac.uk/programmes/hsdr/165221/#/ . Accessed 23 Mar 2021
NIHR CED (2020) Centre for engagement and dissemination recognition payments for public contributors. https://www.nihr.ac.uk/documents/centre-for-engagement-and-dissemination-recognition-payments-for-public-contributors/24979#1 . Accessed 23 Mar 2021
Oliver K, Boaz A (2019) Transforming evidence for policy and practice: creating space for new conversations. Pal Commun 5(1):60. https://doi.org/10.1057/s41599-019-0266-1
Oliver K, Kothari A, Mays N (2019) The dark side of coproduction: do the costs outweigh the benefits for health research? J Health Res Policy Syst 17(1):33. https://doi.org/10.1186/s12961-019-0432-3
Ostrom E (1996) Crossing the great divide: coproduction, synergy, and development. World Dev 24(6):1073–1087. https://doi.org/10.1016/0305-750X(96)00023-X
Rose D, Kalathil J (2019) Power, privilege and knowledge: the untenable promise of co-production in mental “health”. Front Sociol 4:57. https://doi.org/10.3389/fsoc.2019.00057
Staniszewska S, Denegri S, Matthews R, Minogue V (2018) Reviewing progress in public involvement in NIHR research: developing and implementing a new vision for the future. BMJ Open 8(7):e017124. https://doi.org/10.1136/bmjopen-2017-017124
Thomas-Hughes H (2018) Ethical ‘mess’ in co-produced research: reflections from a U.K.-based case study. Int J Soc Res Methodol 21(2):231–242. https://doi.org/10.1080/13645579.2017.1364065
van Gogh V (1885) RE: Letter from Vincent van Gogh to Anthon Van Rappard
WellcomeTrust (2020) What researchers think about the culture they work in. Wellcome Trust, London, https://wellcome.org/sites/default/files/what-researchers-think-about-the-culture-they-work-in.pdf . Accessed 23 Mar 2021
Williams O, Sarre S, Papoulias SC, Knowles S, Robert G, Beresford P, Rose D, Carr S, Kaur M, Palmer VJ (2020) Lost in the shadows: reflections on the dark side of co-production. Health Research Policy and Systems 18 (1)
Download references
Acknowledgements
This project was funded by the University of Bristol Public Engagement Seed Funding and Research Staff Development fund. It was supported by the National Institute for Health Research (NIHR) Applied Research Collaboration West (NIHR ARC West). The views expressed in this article are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. Many thanks to everyone who attended our workshops, got involved in and supported the project to help us develop our resources and training. We couldn’t have done this with you!
Author information
Authors and affiliations.
The National Institute for Health Research Applied Research Collaboration West (NIHR ARC West) at University Hospitals Bristol and Weston NHS Foundation Trust, Bristol, UK
Michelle Farr, Philippa Davies, Heidi Andrews, Darren Bagnall, Emer Brangan & Rosemary Davies
Population Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK
Michelle Farr, Philippa Davies, Heidi Andrews, Darren Bagnall & Emer Brangan
School of Health and Social Wellbeing, University of the West of England, Bristol, UK
Emer Brangan
Faculty of Health and Applied Sciences, University of the West of England, Bristol, UK
Rosemary Davies
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Michelle Farr .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Farr, M., Davies, P., Andrews, H. et al. Co-producing knowledge in health and social care research: reflections on the challenges and ways to enable more equal relationships. Humanit Soc Sci Commun 8 , 105 (2021). https://doi.org/10.1057/s41599-021-00782-1
Download citation
Received : 28 February 2020
Accepted : 31 March 2021
Published : 06 May 2021
DOI : https://doi.org/10.1057/s41599-021-00782-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Ready, set, co(produce): a co-operative inquiry into co-producing research to explore adolescent health and wellbeing in the born in bradford age of wonder project.
- Hannah Nutting
- Rosemary R. C. McEachan
Research Involvement and Engagement (2024)
Create to Collaborate: using creative activity and participatory performance in online workshops to build collaborative research relationships
- Alice Malpass
- Astrid Breel
- Michelle Farr
Research Involvement and Engagement (2023)
Coproducing health research with Indigenous peoples
- Chris Cunningham
- Monica Mercury
Nature Medicine (2023)
Patient and public involvement in an international rheumatology translational research project: an evaluation
- Savia de Souza
- Eva C. Johansson
- Ruth Williams
BMC Rheumatology (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

An official website of the Department of Health & Human Services

- Search All AHRQ Sites
- Email Updates
Informing Improvement in Care Quality, Safety, and Efficiency
- Contact DHR
Funded Projects
Since 2004, the Agency for Healthcare Research and Quality (AHRQ) Digital Healthcare Research Program has funded projects to develop an evidence base for how technology improves healthcare decision making, supports patient-centered care, and improves the quality and safety of medication management.
- Search AHRQ-Funded Projects
Search the entire portfolio of AHRQ-funded digital healthcare research projects. Projects can be identified by technology studied, medical condition, population, status of the project, principal investigator, organization, funding mechanism and location.
- AHRQ-Funded Projects Map
Identify AHRQ-funded digital healthcare research projects by clicking on a state.
- Director's Corner
- Current Priorities
- Executive Summary
- Research Spotlight
- Research Themes and Findings
- Research Dissemination
- Research Overview
- 2020 Year in Review
- 2019 Year in Review
- Engaging and Empowering Patients
- Optimizing Care Delivery for Clinicians
- Supporting Health Systems in Advancing Care Delivery
- Our Experts
- AHRQ Digital Healthcare Research Publications Database
- A Practical Guide for Implementing the Digital Healthcare Equity Framework
- ePROs in Clinical Care
- Guide to Integrate Patient-Generated Digital Health Data into Electronic Health Records in Ambulatory Care Settings
- Health IT Survey Compendium
- Time and Motion Studies Database
- Health Information Security and Privacy Collaboration Toolkit
- Implementation in Independent Pharmacies
- Implementation in Physician Offices
- Children's Electronic Health Record (EHR) Format
- Project Resources Archives
- Archived Tools & Resources
- National Webinars
- Funding Opportunities
- Digital Healthcare Research Home
- 2018 Year in Review Home
- Research Summary
- Research Spotlights
- 2019 Year in Review Home
- Annual Report Home
- Open access
- Published: 30 May 2018
Collaborative and partnership research for improvement of health and social services: researcher’s experiences from 20 projects
- M. E. Nyström 1 , 2 ,
- J. Karltun 3 ,
- C. Keller 4 &
- B. Andersson Gäre 5 , 6
Health Research Policy and Systems volume 16 , Article number: 46 ( 2018 ) Cite this article
45k Accesses
104 Citations
38 Altmetric
Metrics details
Getting research into policy and practice in healthcare is a recognised, world-wide concern. As an attempt to bridge the gap between research and practice, research funders are requesting more interdisciplinary and collaborative research, while actual experiences of such processes have been less studied. Accordingly, the purpose of this study was to gain more knowledge on the interdisciplinary, collaborative and partnership research process by investigating researchers’ experiences of and approaches to the process, based on their participation in an inventive national research programme. The programme aimed to boost collaborative and partnership research and build learning structures, while improving ways to lead, manage and develop practices in Swedish health and social services.
Interviews conducted with project leaders and/or lead researchers and documentation from 20 projects were analysed using directed and conventional content analysis.
Collaborative approaches were achieved by design, e.g. action research, or by involving practitioners from several levels of the healthcare system in various parts of the research process. The use of dual roles as researcher/clinician or practitioner/PhD student or the use of education designed especially for practitioners or ‘student researchers’ were other approaches. The collaborative process constituted the area for the main lessons learned as well as the main problems. Difficulties concerned handling complexity and conflicts between different expectations and demands in the practitioner’s and researcher’s contexts, and dealing with human resource issues and group interactions when forming collaborative and interdisciplinary research teams. The handling of such challenges required time, resources, knowledge, interactive learning and skilled project management.
Conclusions
Collaborative approaches are important in the study of complex phenomena. Results from this study show that allocated time, arenas for interactions and skills in project management and communication are needed during research collaboration to ensure support and build trust and understanding with involved practitioners at several levels in the healthcare system. For researchers, dealing with this complexity takes time and energy from the scientific process. For practitioners, this puts demands on understanding a research process and how it fits with on-going organisational agendas and activities and allocating time. Some of the identified factors may be overlooked by funders and involved stakeholders when designing, performing and evaluating interdisciplinary, collaborative and partnership research.
Peer Review reports
Healthcare organisations are complex and knowledge intensive, with patients often taking for granted that care providers use the best available knowledge on diagnosis and treatment. Evidence-based medicine and practice ensure that the best available knowledge is used systematically in clinical care (e.g. [ 1 ]). Nevertheless, the gap between research and practice in healthcare is well-known and a recognised concern (e.g. [ 2 , 3 ]), where failures to translate research into practical actions contribute to health inequities [ 4 , 5 ]. The process from research-produced knowledge to its use in healthcare practices can take considerable time (e.g. [ 6 ]). The estimated lack of research use in the United States and the Netherlands has suggested that 30–40% of patients do not receive care complying with current research evidence [ 7 ]. The required increase in the speed of uptake of evidence-based clinical practice guidelines has been frequently discussed (e.g. [ 8 ]) and factors influencing their adoption have been extensively studied (e.g. [ 9 , 10 ]). Getting research into policy and practice in healthcare is a recognised, world-wide concern (e.g. [ 11 ]).
Several research areas deal with aspects related to the transfer of knowledge and use of research findings for improving healthcare. The view of research production as separate from the use of research findings initially inspired research on diffusion and implementation processes [ 12 , 13 ], mainly focusing on the later stages of the research process with variable emphasis on a division between knowledge production and its implementation.
The shortcomings of the traditional ‘linear’ model of research-into-practice have become more evident [ 14 ]. Van de Ven and Johnson [ 15 ] suggest that the problem may be one of methods for knowledge production rather than knowledge transfer or knowledge translation. To enhance a faster and more systematic use of knowledge, collaborative and interdisciplinary research approaches have been asked for as well as more useful research [ 15 , 16 , 17 ]. Research collaboration is assumed to enable and enhance both the use of research and increase the amount of research relevant to end users.
Research on knowledge transfer and exchange describes an interactive exchange of knowledge between research users and researcher producers [ 18 , 19 ]. Knowledge transfer and exchange interaction between researchers and practitioners can take place from the on-set of the research process and involve more long-standing relationships. Several approaches to knowledge transfer have been described, focusing, for example, on systematic synthesis and guidelines, social interaction between researchers and decision-makers, contextual features and organisational readiness [ 20 ]. The Canadian Institute of Health Research uses the term ‘integrated knowledge translation’ to describe projects where the knowledge users are involved as equal partners during the entire research process [ 21 , 22 ].
Funding organisations have started to request research proposals to include researcher–decision-maker partnerships in collaborative research teams with representatives of industry, local communities and professional organisations (e.g. [ 23 , 24 ]). The increased focus on research-use is also mirrored in research funders’ strategies (e.g. [ 25 ]). Some examples of collaborative initiatives are the Partnership projects and Centres financed by the National Health and Medical Research Council in Australia, the Dutch Academic Collaborative Centres for Public Health in the Netherlands, and The Collaborations for Leadership in Applied Health Research and Care in the United Kingdom (e.g. [ 26 ]), as well as the practice-based research networks and structured use of practice facilitators [ 27 , 28 ] and the Integrated Delivery Systems Research Network programme to foster public–private collaboration between health service researchers and healthcare delivery systems in the United States [ 29 ]. There are three main strategies that research funding agencies might use to enhance knowledge translation – push, pull, or linkage and exchange. The push–pull strategies distinguish between mechanisms driven by science (push) and those driven by the demands of practitioners or policy-makers (pull) [ 30 ]. The linkage and exchange model is based on co-construction of applied knowledge and the relevance of applied research to both practitioners and researchers [ 31 ]. In a recent review of the ways research funding agencies support science integration into policy and practice in the field of health [ 30 ], most of the 13 agencies investigated used one or two of these strategies. The large heterogeneity of users and how this may affect the use of various mechanisms for research initiation, development and dissemination was highlighted in this review.
Collaboration has been addressed for some time in community-based participatory research regarding public health and social issues in society (e.g. [ 32 , 33 ]), for example, on how to achieve policy level collaboration (e.g. [ 24 , 34 ]) and evidence-informed policy-making (e.g. [ 35 ]). Nevertheless, there is a need for more empirical research on the actual processes, conditions and outcomes of the more recent collaborative and partnership research initiatives in healthcare [ 36 , 37 ] and, to date, there are few empirical studies on researchers’ approaches and experiences of the combination of interdisciplinary and collaborative and partnership research, including the actual effect of such programme or project calls. Less explored is also research partnership aiming to respond to the challenges and priorities of the health system and much research has been based on assumptions of researcher-driven initiatives with newly established collaborations [ 38 ].
Collaborative and partnership research
Approaches, strategies and roles.
Collaboration and partnerships are two concepts used to describe the involvement of people and groups from different contexts and with different experiences, perspectives and agendas in research and development. Accordingly, collaborative research contains social relations and a variation of potential roles for those involved during the research process. In earlier research, means for collaboration were described in the form of ‘linkage mechanisms’ between researcher and user contexts, i.e. the presence of intermediaries (boundary spanners); formal and informal contacts with users during studies; involvement of users during data collection; and interim feedback [ 39 ]. The boundary-spanning role of knowledge brokers has been brought forward as a bridge between research and practice (e.g. [ 40 ]). Knowledge brokering has been defined as “ all the activity that links decision-makers with researchers, facilitating their interaction so that they are able to better understand each other’s goals and professional cultures, influence each other’s work, forge new partnerships, and promote the use of research-based evidence in decision-making ” ([ 40 ], p. 131). Individuals, teams or organisations can all play the role of knowledge brokers [ 41 , 42 ]. Michaels [ 43 ] describes six primary brokering strategies that span from more passive dissemination of information, interaction by seeking and using expert’s advice and linking different actors, to active engagements and close collaborative relations with healthcare actors, and which aim to inform, consult, match-make, engage, collaborate and build capacity. A recent study highlights the importance of effective ‘relationship brokering’ in researcher-health system partnership for establishing a meaningful collaboration [ 38 ].
A detailed road map on research collaboration is offered by Martin [ 44 ] in his description of five approaches to co-production of research. Depending on the chosen approach, stakeholders can be more or less involved in phases of the research process, from study design, data collection and analyses, to dissemination, while the degree of academic independence of the researcher/s and the utilisation of the research results may vary. Consequently, practitioners can play the role of informants, recipients, endorsers, commissioners or co-researchers.
On programme level, King et al. [ 45 ] describe four research programme operating models used in a collaborative approach to enhance research-informed practice in community-based clinical service organisations. The models describe the types of partnership involved such as the ‘clinician-researcher skills development model’, ‘clinician and researcher evaluation model’, ‘researcher-led evaluation model’, and the ‘knowledge-conduit model’. To differentiate research-practice partnerships from other ways of conducting research, Øvretveit et al. [ 46 ] suggest five criteria for partnership research, namely research that contributes to actions taken by actors within a health system; studies intended to produce quick and actionable findings as well as scientific publications; both researchers and practitioners take part in defining the research question and interpret findings; significant time and contributions from both researchers and practitioners; and an extensive formulated description of the partnership approach.
Challenges and enabling features
One challenge for collaborative and partnership research concerns the variation of views on the production and use of knowledge and on the relationship between researcher and practitioner, spanning from top-down to bottom-up or from linear to interactive and multidimensional (e.g. [ 39 , 47 ]). Depending on research tradition and/or experiences, basic assumptions regarding knowledge and learning can vary among researchers, but also among stakeholders (e.g. [ 48 ]). Sibbald et al. [ 49 ] identified challenges such as role clarity, organisational change and cultural differences regarding expectations on research output and (positive) effects on actual practice and found that role ambiguity, multiple roles and role conflicts could hamper social relationships. Factors facilitating collaboration were already established relationships, the alignments of goals/objectives, skilled and experienced researchers, and the use of regular, multi-modal communication.
Another influence on collaboration, mainly from the researcher context, is the variety of research paradigms and areas and related basic assumptions. One approach to be expected is action research, where knowledge creation is combined with practice development. There are a variety of action research approaches depending on, for example, how the collaborative element is organised [ 50 ]. The interactive research approach builds on action research and emphasises the common learning and knowledge creation for both practitioners and researchers during the complete process [ 51 ]. Both approaches involve a number of different roles for the researcher to enact [ 52 ].
Based on a realist evaluation, Rycroft-Malone et al. [ 36 ] list features of research collaboration likely to enhance knowledge use, namely attention to communication mechanisms, setting intermediate/outcome goals, providing time and space for the development and implementation of plans, making the choice of topic with resonance and relevance, close proximity between partners, re-balancing and sharing power, and allowing time to develop mutual trust and respect. These features put other demands on the planning and execution of research than a traditional approach when research has precedence over practice.
Sibbald et al. [ 49 ] present a model describing the research partnership process, with enablers, facilitators, challenges and impact, and identify three partnership types based on an empirical study as token, asymmetric or egalitarian partnerships. In Fig. 1 , features of the research partnership process are presented, grounded on aspects highlighted by Sibbald et al. [ 49 ] and Rycroft Malone et al. [ 36 ].
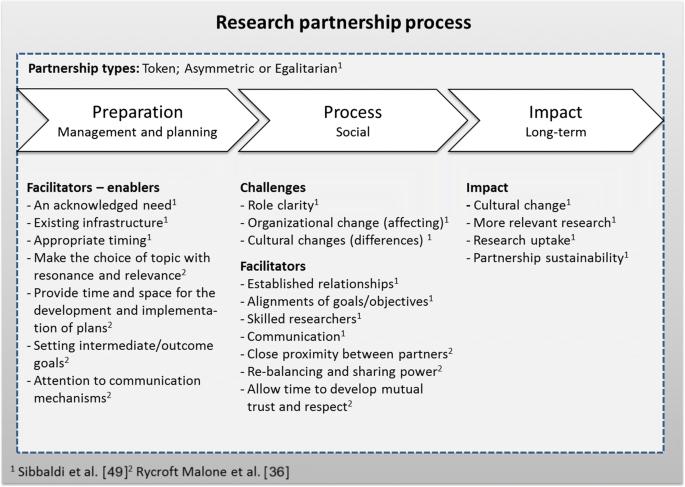
Model over the research partnership process (adopted after Sibbald et al. [ 49 ] and Rycroft Malone et al. [ 36 ])
Collaborative and partnership research poses specific demands regarding project management. According to a review [ 53 ], collaborative research can be characterised by heterogeneity of actors, collective responsibilities, demands for applicability in addition to scientific requirements, and by being funded by public agencies with specific agendas. Project management in collaborative projects usually involves three paradoxes [ 53 ]:
To reach expected results, both freedom and flexibility to handle the uncertainty in research is needed, as well as a tight and managed firm project structure.
The necessary integration of different views of the actors involved may also lead to intercultural, interorganisational and interdisciplinary problems that need to be managed.
The limited formal authority of the project manager is in contrast with the demands for integrative managing of results, commitment and involvement of all parties.
Thus, collaborative and partnership research may have the potential to enhance the use of knowledge in practice and thereby improve healthcare and social services, but also to challenge the practitioners’ and researchers’ views, assumptions and roles.
The empirical base of the present study is an example of a collaborative and interdisciplinary research initiative – a national research programme seeking to boost collaborative and partnership research to improve health and social services in Sweden. The purpose of the study was to gain more knowledge on the interdisciplinary, collaborative and partnership research process by investigating researchers’ experiences based on their participation in this national programme. We have studied the experiences of researchers in all 20 research projects funded by the programme during the period 2008–2014, focusing on three themes – complexity in collaboration, collaborative procedures, and challenges, obstacles and lessons learned. The research questions posed were (1) what types of research approaches, research focus and partners/actors were involved in the projects? (2) How was collaborative and partnership research achieved, according to the researchers? (3) What were the challenges and obstacles to interdisciplinary, collaborative and partnership research encountered, and what main lessons were learned?
This study is based on analyses of interviews and archival data. The interviews were performed during the final stages of the projects and the documents covered the entire project period.
Empirical setting – the national research programme
The Vinnvård research programme was financed by a consortium of research funders, including the Ministry of Health and Social Welfare, Sweden’s innovation agency VINNOVA, Vårdalstiftelsen and the Swedish Association of Local Authorities and Regions. It was the first major attempt by research funders in Sweden to address the challenges of the ‘quality chasm’ in health and social services focusing on organisational aspects, with clear aspirations to bridge research and practice, stimulate interdisciplinary research and enhance research collaboration between universities/research institutions and healthcare/social service organisations. In addition, new research and learning infrastructures were expected to emerge. The requirements and evaluation criteria for the applications reflected these aspirations and documented active cooperation between practitioners, researchers and other public actors was asked for. Moreover, applications had to include an interdisciplinary approach, a common vision for all parties involved and documented approaches for securing participation and dissemination of research and/or development results. Both researchers and practitioners/public institutions could apply for funding. Non-researchers were part of the peer-review panel in both calls. The programme’s broad approach was new, both to the funding agencies and the research community. With a focus on health and social services, the programme aimed to (1) increase the use of research-based knowledge (bridge research and practice), (2) develop innovative ways of organising work, (3) stimulate the development of institutional learning structures with a focus on how to lead, manage and develop practices in organisations, and (4) establish more research on how to lead, manage and develop practices in health and social services organisations at Swedish universities.
The subsequent aims (3 and 4) had a more long-term character than the preceding ones (aims 1 and 2) and can be seen as a means to build long-lasting support for these. During the period studied (2008–2013) there were two calls for projects lasting up to 4 years each. A total of 20 projects were funded, 9 in 2008–2011 and 11 in 2009–2013, all of which are included in the present study. All projects were on-going when the interviews were conducted and all except one had ended when the archival data was gathered in May 2015.
Data collection
Interviews were conducted between September and November 2011, when most projects were in their later stages. In total, 17 respondents with an equal gender distribution were chosen based on their overall project involvement. Four respondents were responsible for two projects each and one project was represented by two respondents. All 20 projects were covered. All respondents held a PhD and were intensely involved in the projects, either as project leaders, principal investigators, or as the most important researcher, as judged by the project leader. The semi-structured interviews had the aim of following up on the main goals and lessons learned within the projects and covered the characters of the projects with its overall contributions, roles taken in projects, collaborations, and participating or studied organisations and institutional levels. Questions followed five themes for each one of the four programme goals, namely interpretations of the goal, the importance it was given, how it was fulfilled, how the project had worked to reach the goal, and results related to the goal. Practical examples of the last two themes were requested. The last part of the interview covered how the four goals were integrated, any expected or unexpected insights, difficulties experienced, and emphasised and miscellaneous findings. In a few cases, interviews were complemented by the respondents with written comments or documents. Interviews lasted 40 to 120 min, with longer interviews with respondents representing two projects. The respondents received the questions a week in advance. Each interview was recorded and transcribed verbatim.
Archival data were gathered in May 2015 and consisted of the projects’ final reports and, for one project not yet finished, a progress report (same structure as the final reports, but without a popular science description and financial report). The report template had the following headings: introduction; short summary on how the project had worked to fulfil the research programme’s goals (with subheadings for each of the four goals); publication list; participation in national and international conferences/workshops; PhD students; description of potential problems encountered; description of the most important lessons learned; popular science description; references; and financial accounting. Reports varied in length from 4 to 42 pages, with an average of 19 pages; yet the four-page report came from the project not yet finished. A total of 386 pages were analysed.
Data analysis
Qualitative data in interviews and documents were scrutinised in several steps, first by using a mix between directed (guided by the research questions) and conventional content analysis [ 54 ]. The entire material was read through to get a sense of the whole and then analysed to identify relevant text related to the research questions. Both data sources were then further used for determining themes, categories and overall patterns. Finally, a summative content analysis [ 54 ] was applied to get a sense of variation by identifying how many projects provided information in the identified categories. Three researchers performed the analyses, first individually and through meetings held to discuss and validate interpretations.
Document analysis focused on information related to the three research questions, namely (1) system level actors involved (care recipient, unit/clinic/ward, organisation, region/county council, and/or national level) and basic project information; (2) descriptions of or activities and strategies for research collaboration, including with which actors; and (3) obstacles/problems encountered and main lessons learnt. A fourth category (Other) was used in order not to miss important aspects. Described collaborations and process reflections (i.e. obstacles/problems and lessons learnt) were the main categories used to sort the material for questions 2 and 3. In a second iterative step for these questions, subcategories were identified, tested, revised and defined. The category definitions were then used in a third step for a final text classification of data.
As the interviews were performed when the projects were still ongoing, they were used to complement, add details, provide examples and validate information found in documents. Moreover, they also added a more personal perspective on the results based on the experience of the main researchers.
Project overviews and the complexity of the collaborations
Of the 20 projects, 14 included three or more stakeholder levels, indicating an elaborated multilevel or system view. Five projects actively involved care recipients (and sometimes their next-of-kin) in design of solutions or interactive co-production. Two projects had a sole clinical focus (screening for atrial fibrillation and improving methods for stroke care), but such foci were present in several projects’ sub-studies. Four projects (three geographical sites) had a deliberate strategy to build learning structures that involved university level education at undergraduate and/or master’s levels, but education was included in several projects, sometimes as distance learning or continuing education for professionals. All projects except two involved PhD students, with a total of 72 for the programme overall. Most projects ( n = 16) clearly stated that their research group was interdisciplinary and some discussed the benefits and obstacles encountered due to this. A total of 203 articles in scientific journals (including submitted manuscripts) were reported to have been produced during the 6-year period. The widespread target groups and involved organisational levels in the projects’ research activities are illustrated in Table 1 . More information on the projects is provided in Additional file 1 .
Descriptions of collaborative procedures
Descriptions of the research collaboration varied – from describing a more or less interactive research design to more explicit descriptions of when and how practitioners were involved during the research process. Practitioner’s and researcher’s boundary-spanning roles served as important bridges between the two contexts. Five main categories were identified to cover the various ways collaborations were described. In Fig. 2 , the number and proportion of the projects providing descriptions in each of these categories is provided.
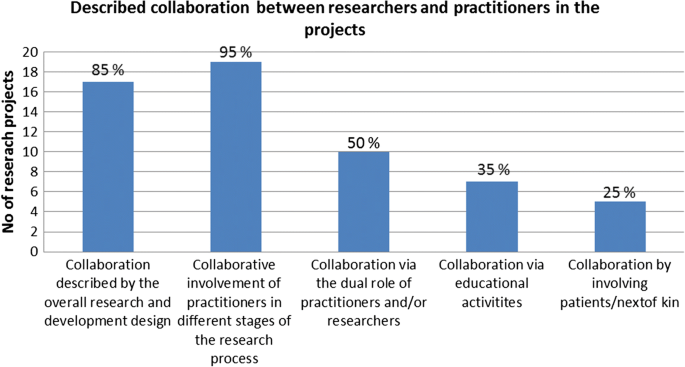
Number and proportion of projects ( n = 20) providing descriptions in the different subcategories of collaboration
Collaboration as described by the overall research and development design
Seventeen projects (85%) clearly described an interactive research design that either involved healthcare practitioners, managers, politicians, patients, next-of-kin or a mixture of those. Seven projects used the term ‘action research’ or ‘action-oriented research’, two used the term ‘interactive research model’, and one used the term ‘participatory design’, all of which imply a close interaction between researchers and practitioners. Examples of statements are “ the project’s action research approach has involved a continuous and iterative collaboration that has both fed into and questioned on-going [change and learning] processes ” and “ we used a participatory design where the young people actively participated in the creation of what to study, that is the effects of using a web-based instrument ”. Four projects developed information and communication technology-based solutions in close collaboration with practitioners. The terms ‘co-design’ or ‘co-creator’ were often used in two projects involving patients and their next-of-kin and in a project focusing on mixed learning networks with researchers, patients and other actors.
Collaborative involvement of practitioners in different stages of the research process
Interactive forms were described as being used during the following stages: (1) mapping of the research problem and its manifestation in practice, and formulation of research questions; (2) planning, creation of interventions and choices of design; (3) investigation, test, follow-up and implementation processes; (4) analyses, reflection and learning; and (5) reporting on and dissemination of results, including further implementation of studied intervention. Nineteen projects (95%) described an interactive approach in at least one of these stages. Collaboration or interaction was most common during follow-ups and feedback processes (Stage 3 and 5), and less interaction was described during the formulation of the research problem and during analyses (Stage 1 and 4). Statements like “ conducting research with practitioners, not on practitioners ” and “ patients have participated in the mapping [of the current situation]” are examples of Stage 1. Stage 2 is exemplified by the statements “ practitioners participated during the construction of the interview [manual]”. Statements such as “ the researchers and contact persons [from the healthcare organisations] have met 1–2 times a year to discuss and reconcile research questions, data collections and results from different sub-projects ” represent several stages (Stage 1, 2, 3 and 5). Involving practitioners directly in analyses (Stage 4) was not explicitly mentioned, but the described interactive sessions could involve the discussion and validation of results. Statements such as “ the researchers regularly fed back their observations and analyses to the hospital management and hospital unit representatives ”; “ we had several formal and informal feedback sessions and this feedback has been further used ”; or “ the feedback and the action research approach have given researchers an opportunity to stimulate reflection and contribute with knowledge on implementation, learning and change ” can represent situations when practitioners participated in the interpretation of results and that this had effects on both research and practice. Thus, if researchers in the research teams holding dual roles are not accounted for, no project involved non-researchers in the entire research process.
Collaboration enhanced by the dual role of practitioners and/or researchers
Ten projects (50%) described a dual, boundary-spanning role held by either the practitioners or the researchers. This dual role of being involved in both practical work and research was more common for clinicians performing research in the area of their expertise, e.g. in projects and sub-cases with a clinical focus. This can be exemplified by statements such as “we are conducting research with actively serving practitioners and clinicians ” or as a statement made by a clinician project leader “ improvement work for increased quality in healthcare is best performed directly in connection to the meeting between patients and professional care-givers ”. In one case, in the Clinical Innovation Fellowship programme, teams of practitioners were trained as action researchers for 2 months (fellows) and spent 6 months working in clinical quality improvement in healthcare, sometimes in collaboration with students working on their masters or bachelor thesis. Examples on practitioners’ dual role were described as “ some healthcare staff became PhD students and thereby gained a double bridge-building role ” (e.g. conducting research within their organisation). The role of translating knowledge as part of the dual role was exemplified as “ we have involved healthcare staff as interpreters ”. No further details on what this actually meant were provided. Three projects described that their research team consisted of both researchers and practitioners.
Collaboration via education
Seven projects (35%) described interactive processes linked to educational activities, either designed for enhancing learning and (sustained) interaction between researchers, practitioners and their organisations, or designed for students to participate in and study development initiatives while learning together with practitioners. Some involved the development of new programmes and courses where “ experience-based education ” was essential or where networks of previous healthcare students (now as practitioners) were established as a resource. Some examples concerned the interaction between students and practitioners exemplified by statements such as “ collaboration with students concerning knowledge on improvement, using a model for learning that involves multi-professional teams with care professionals and students that together reflect on the potential improvements of the care practices ”, or the involvement of students in the development of healthcare practices exemplified by one project’s new master’s programme where conducting an improvement project in practice was a basic requirement for a master’s thesis.
Collaboration by involving patients/next-of-kin
Five projects (25%) described an active involvement of patients in the research process. One project developed mixed learning networks with both patients and their next-of-kin in an active learning process. Another project had “ engaged patients, relatives and care professionals in the work of changing care practices ” describing patients as “ co-creators, co-producers and co-evaluators ”. Two projects had developed information and communication technology solutions together with patients and one project had given patients the opportunity to conduct single randomised controlled trial (RCT) studies using their own measurements.
Challenges, obstacles encountered and the main lessons learned from the research collaborations
Seventeen projects (85%) provided detailed descriptions of problems encountered and a meta-reflection of lessons learned. The others reported no problems or none that could not be dealt with and/or interpreted the question on lessons learned as an opportunity to report on detailed project results. We could not find any patterns for the two projects reporting no problems (19 and 20). Described problems were classified into six categories and similar categories also summarise the lessons learnt, except for ‘staff-related issues’, which was mentioned only as a problem. In Fig. 3 , the number and proportion of the projects providing descriptions in these categories is presented. The most reported problem category concerned the collaborative and partnership research and development process (with practitioners) followed by issues related to the practitioners’ context and the research design and methods used. Thus, most problems described were related to the adaptation to or collaboration with practitioners and their organisations and the different agendas of and demands from the practitioners’ and researchers’ context. It was sometimes difficult to maximise the fit between the project’s agenda, the research process and the dynamic agendas and activities of the organisations and their representatives. A third of the projects reported on problems within a single context or issues related to research staff or designs. Most of the lessons learned also concerned the collaborative and partnership research process. Otherwise, lessons learned were more evenly spread, except for the staff category.
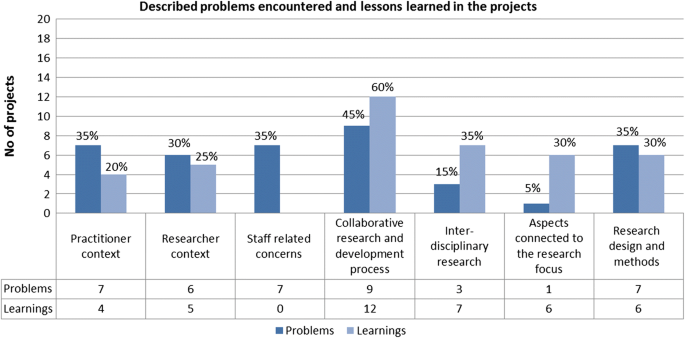
Number and proportion of projects ( n = 20) providing descriptions in the subcategories of problems encountered and lessons learned
Reported problems related to ‘the practitioner context’ concerned partner engagement, competing activities, economy, political decisions and organisational changes. Examples of problems were “ delays, organisational changes and changes in management teams that altered the initial engagement in the project ”; “ other parallel development projects have taken time for our collaborating organisations ” and “ the development unit that was to coordinate interventions within the county council was closed down ”. The major lessons learned mirrored these problems, acknowledging the anchoring, flexibility and time needed to work with the practitioners’ (politically governed) organisations. Examples of statements provided are “ county councils and universities are large organisations where change takes time and anchoring on several levels must be secured ” or “ changes in health and social care occur quickly and are difficult to foresee and improvements have to adjust to this, and to document such periods is both a challenge and an opportunity ”.
Reported problems related to ‘the researcher context’ often concerned the PhD, master or bachelor level students involved, where university demands caused delays, frustration or extra work. Examples of statements were “ writing applications to fully finance participating PhD students have taken a lot of time and energy ”, “ the full student participation was delayed and affected the project ”, and “ the choice to build a school for research studies have delayed publications ”. Learnings included the need to deal with such aspects and the demands this put on the project management and the research group, exemplified by “ the research field is young and it has been central to build networks and cooperation with others ” and “ to build research and education demands active and competent project management, not only an effective administrative management but also an overarching research perspective, and this administration and research overview is time demanding ”.
The category ‘staff-related concerns’ contained human resource management issues related to research group members (mainly researchers and PhD students) and no lessons learned related to these were recorded. Issues concerned interruptions or delays in the project process due to recruitment of staff, leave due to sickness, parental leave or other changes in work situation. Example of statements were, “ one researcher was on leave for a long-time due to sickness and this made us have to start all over again with analyses ”, “ the project leader was assigned a mission by the government ”, and “ two of the project’s PhD students went on parental leave for a total period of 3 years, which delayed the project ”.
Problems related to ‘the collaborative and partnership research and development process’ concerned the time and energy needed for the process, expectations on the practitioner organisation, and differences in focus and pace of the more rigorous scientific process compared to the quicker decision-processes in the practitioners’ contexts. Statements such as “ the interactive research process takes more time to establish ”, “ output data were supposed to be generated and provided by the county council, we had to use whatever we could find when this could not be done ”, and “ our organisational partners’ need for quick results and tendency to change work approaches towards the introduced intervention made it hard to scientifically evaluate the results ”. The lessons learned described were related to insights concerning different views, contexts and efforts to handle dilemmas. Example of statements were, “ research and practice are two systems with a different pace, demands on PhD students delay analyses and cause delays in the feedback to practitioners ”, “ practitioners sometimes have un-realistic expectations on researchers ”, and “ the importance as a researcher to always be prepared to re-evaluate, be flexible and adapt the project focus and time plan after the dynamic situation of the empirical reality studied ”. Some important actors in the researcher context made this process difficult, exemplified by “ the ethical board approving the project has demanded a clear distinction between research and improvement work ”.
Problems related to conducting ‘inter-disciplinary research’ gave examples of paradigmatic differences in perspectives, assumptions, experiences, methods and ways to report results. Examples of statements were “ PhD students struggled against time and felt fragmented and torn between their own research area and the demand for interdisciplinary research ” and “ to form such group consisting of different disciplines takes a long time and the mixed methods approach demanded a period of interactive learning for the interdisciplinary research group ”. Lessons learned related to conducting interdisciplinary research concerned insights into the process of building interdisciplinary teams and benefits of several perspectives, for example, “ interdisciplinary research is not easily or quickly established, it takes a long time for participants to build trust and understanding of each other’s perspectives and terminology, and to be attentive and responsive towards each other’s contributions ” and “ the importance of a firmly grounded theoretical framework and the creation of instructions for the research activities during an interactive process ”.
Problems connected to ‘the research focus’ were reported by one project and concerned the investigated health economic concept, which was new to the area and demanded a shift in perspective. Six projects reflected on lessons learned connected to the research focus, for example, “ internet-based support and coaching have provided coaches with increased insights into how large a disability individuals with neuropsychiatric disabilities can actually have ” and “ the care structure is a central factor for improvement and the availability of stroke units essential ”.
Problems related to the chosen ‘research design and methods’ concerned demands of specific methods and instruments, for example, “ building a computer model and the inclusion in the RCT study has taken more time than anticipated ”, “ the ethno-methodological observation method is time and resource consuming ”, and “ it was challenging to find data for follow-up studies and a lot of work studying patient journals ”. The reported lessons learned concerned the chosen approach, design or spread of interventions exemplified by the following statements: “ the meta-study has been important for synthesising and extracting knowledge ”, “ action research is an important method for gaining new knowledge and for stimulating participation in improvement initiatives ”, and “ the major lesson learned has been that the work to implement findings does not start or continue by itself, it will demand large efforts and continuing economic resources ”.
Addressing complex research areas in complex systems affects the complexity of the collaboration
The research programme was set out to address problems related to the gap between research and practice in health and social services. Several projects reported putting large efforts on addressing this broad and interdisciplinary content by trying to frame clinical and service activities within general organisational frameworks. Many projects focused on how to organise care to achieve a more research-based practice or to identify hindrances, contradictions or opportunities related to development. To study such complex phenomena over several system levels often requires longitudinal designs, interdisciplinary approaches and a mix of methods [ 55 ], in combination with participatory approaches (e.g. [ 15 ]). A large variation of research and methodological approaches, most of them very demanding, was used in the projects, from action research to quasi-experimental studies and RCT designs. Single or multiple case studies using qualitative and mixed methods were common. The use of a demanding research design and the lack of a research culture on behalf of practitioners and their organisation can act as a strong barrier for research collaboration [ 56 ].
Research use represents a specific form or knowledge utilisation [ 57 , 58 ], where research findings support decisions through a complex process enacted at a practical level. Scott-Findlay and Golden-Biddle [ 59 ] argue that understanding this process only at an individual level is misguiding and should be complemented with an understanding of practitioners’ research use at an organisational level. When making major changes in line with new research knowledge the authors propose strategies involving efforts to change organisational culture and consideration of the organisation’s values and assumptions. This indicates the need for researchers to have an in-depth understanding not only of the involved practitioners as individuals or professional groups but also of their organisations in order to enhance the use of research findings.
A majority of the projects addressed several levels of the involved healthcare organisations (or systems) implying several types of partners and stakeholders to interact with. Demands put on project management and the project group corresponded with these multidimensional views and mixed approaches – providing variable room and energy to support and adhere to demands related to collaboration and research use. The importance to understand and address the interaction and inter-connection between system levels during development efforts has been highlighted by several researchers [ 60 , 61 ]. The types of project management, research design and collaboration across the organisational system that are needed to get access, and to build, co-create and transfer knowledge in order to enhance development in organisations have been less discussed. Recently, the heterogeneity among knowledge users and the need for relationship brokering in collaborative and partnership research has been highlighted [ 38 ].
Different perceptions of interdisciplinary, collaborative and partnership research and on the roles and relationships of involved actors
Any empirical research process is characterised by interaction between the researcher and practitioner context, each one in a constant flux, continuously changing and restructuring. The research process in itself also differs depending on the type of research and focus, for example, if there is an innovative or developmental component involved to be tested and evaluated or if an on-going situation or phenomenon is investigated. Qualified practitioners, sometimes enrolled as PhD students, served as knowledge brokers interpreting results – in both directions – when understanding the practical phenomenon in theoretical terms and when translating theories and models used into practical terms. Educational fora and interactive learning approaches were a significant part of many projects, often combined with active involvement of practitioners. Involvement of patients and their next-of-kin, often during intervention design, was also described.
Based on our findings, using the terms introduced by Sibbald et al. [ 49 ], two projects could be described as having a more researcher-dominant or token partnership, while eight projects involved non-researchers to some extent in an asymmetric partnership and ten projects had features that indicated a more egalitarian partnership.
The role of the researcher varied – from being deeply and practically involved in a development process in the practitioner context, to more distant when studying the effects of different care choice models. Martin [ 44 ] listed the various roles of practitioners in research collaborations, but researchers are also able to enact different roles, depending on opportunities, preferences and the chosen research focus (explorative, descriptive, explanatory, intervention and action oriented). An ability to describe the nature of both the practitioners’ and researchers’ roles may indicate the type of interaction, participation, involvement or influence that can be expected from both parties. In Fig. 4 , the potential roles of practitioners [ 44 ] are displayed together with some suggested potential roles for researchers to enact. Indications of egalitarian partnership were identified in projects that clearly described interactive research approaches, but otherwise our data did not provide much detail on the relationships and roles. For an in-depth study of the enactment of different roles over time, situation and context would provide more information on how the researcher–practitioner relations evolve over time, both initially and in long-term partnerships.
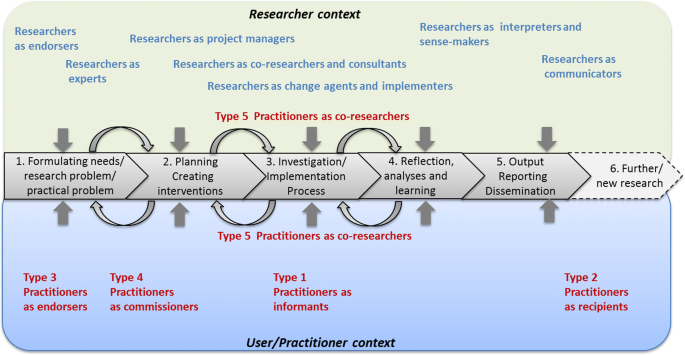
The five types of potential roles of practitioners during a research process according to Martin [ 44 ], and some suggested potential roles for researchers to enact
Interdisciplinary research, often across faculties, was enhanced, further developed and deepened in the majority of the projects. There were several examples of clinical researchers working together with both social scientists and scientists from technical faculties. Building trust and lessons learned concerning different perspectives and ways of conducting research were important. The programme’s goals regarding the expected development of institutional learning structures and establishment of research on how to lead, manage and develop practices in health services organisations might have aided this development, more so than traditional programme calls.
Creating long-term relationships between researchers and decision-makers might be a useful way for bridging research and practice. For such a strategy to become successful it has been argued that it must be complemented with strategies for involving researchers in decision-making around policy and practice and with core funding for building and upholding capacity for knowledge exchange [ 24 ]. Maintaining such relationships for longer periods often requires formal support or structure. The national collaborative examples (e.g. practice-based research networks) described in the introduction can be one way to achieve this. Incentives for supporting and nourishing such relationships are scarce in the research context where funding is often difficult to obtain and outcomes are measured in production of scientific publications. Supporting the costs associated with research involvement (for both parts) can facilitate partnership with managers and decision-makers [ 34 ]. This is an important message to research funders, who despite tasks to increase “ research utilisation and interaction with society ”, often support short-term projects with more limited scopes – a strategy that is seen as insufficient for sustaining practitioner relationships and achieving goals of research utilisation [ 24 ].
Research collaboration between researchers and decision-makers and other types of stakeholders can be ethically challenging, especially when members of the team are insiders or participants in a studied case. The role of insiders needs to be clarified, for example, with regards to access to raw data and ensuring anonymity and confidentiality [ 62 ], but also a sensitivity on how to handle organisational information as a researcher. Hofmeyer et al. [ 62 ] recommend the use of self-reflection and ethical dialogues to enhance shared meanings and understandings among researchers and decision-makers – a practice that requires time, motivation and skills, and which could be highlighted in future programmes aiming for collaborative and partnership research.
Experienced challenges, obstacles and enablers for interdisciplinary collaborative, partnership research
There were indications of the tension between the demands from the practitioner versus the researcher contexts and the role of the researcher. Dilemmas occurred, for example, when adhering to conflicting demands for knowledge translation and the different types of knowledge production [ 63 ], such as a curiosity-driven inquiry based on a positivist epistemology or a problem-solving epistemology with knowledge production in the context of application [ 64 ].
Collaboration in the projects’ research constellations was mentioned both as an asset and a challenge, especially the interdisciplinary aspect where team members might differ in views and ways to handle collaboration. That interdisciplinary research is challenging is not a new insight (e.g. [ 65 , 66 ]) and there are strategies to facilitate such research, i.e. selective collaboration, cross-training, sustained relationships, good humour, participation in peer review, declaring the place of one’s work, and balancing dissemination of research between peer and other audiences [ 67 ]. Past experience of interdisciplinary collaborations and an understanding of different views on epistemology are foundations that can enhance collaborations. There were indications in some projects that participating researchers did gain a deepened appreciation of the need to join several paradigms in order to understand the complexities of the issues at hand. The ‘inside’ clinical PhD students could act as door openers and knowledge brokers [ 68 ] to the world and practice of health and social services for the social or technical sciences PhD students, and vice versa. Clinical researchers and PhD students were invited to new knowledge paradigms by social scientists. Other practitioners involved as co-researchers in the projects could employ various brokering strategies, e.g. to engage, collaborate and build capacity [ 43 ]. The described challenges for these persons to adhere to expectations and demands from several contexts in their in-between role and the conflicts that follow when demands are incompatible or role expectations are ambiguous have also been identified elsewhere (e.g. [ 40 , 68 ]). Previous research has shown that innovative researchers tend to be more engaged in research collaborations, both disciplinary and interdisciplinary, than adaptive researchers who prefer to work with well-established procedures within existing frameworks and in stable groups [ 69 , 70 ]. Female scientists are also more engaged in interdisciplinary research, while years of research experience has been found to be positively correlated with collaboration both within one’s own discipline and with researchers from other scientific disciplines [ 70 , 71 ].
Some of the problems and enablers experienced in the projects correspond to the enabling factors in the research partnership process as described by Sibbald et al. [ 49 ] and Rycroft-Malone et al. [ 36 ]. The described difficulties due to changes occurring in the partner organisation, role problems due to ambiguous or conflicting demands, and different view and paces for knowledge production and use between researcher and partner organisations correspond to the challenges described by Sibbald et al. [ 49 ] (Fig. 1 ). Problems and lessons learned related to time needed for development of mutual trust and respect, power issues, and planning and implementing change are in line with Rycroft-Malone et al.’s [ 36 ] observations (Fig. 1 ). Skilled project leaders and researchers able to handle various perspectives and enhance communication among involved actors and the establishment of infrastructures and long-term relationships, as in the sustainable collaborative structures initiated or strengthened by the projects, are all considered as enablers for research partnership [ 49 ].
Ideally, there is room for a mixture of research approaches in a programme, in line with current debates on mixed methods where Gorard et al. advocate the development of a research community where “ all methods have a role, and a key place in the full research cycle from the generation of ideas to the rigorous testing of theories for amelioration ” ([ 72 ] p. 162, [ 73 ]). Collaborative approaches are amendable to many different research topics, designs and disciplines, and the mixture of projects, research approaches and collaborations in the programme provides an example of this. It also shows the need to consider how to evaluate research applications when broader, complex issues are the topics, as also highlighted by others [ 38 ]. Assessment of the benefits and lessons learned through participating in the research process for individuals and partnership organisations, as well as of the sustainability of partnerships and joint interventions, might be a way forward.
Limitations of the study
The study mainly represents project leaders’ and senior scientists’ views on the research programme and their own project’s efforts to bridge research and practice and initiate collaborative and partnership research. No representatives of the involved practitioners were interviewed and the reporting on impact and collaboration with stakeholders was retrieved via project documents and interviews with representatives of the projects. To expand the understanding of the entire process and all actors’ perspective on the acquired knowledge, the partners’ views will need to be addressed. We also acknowledge that there might be information missing in final reports depending on the amount of text provided and how questions in the report template were interpreted, as well as the potential bias introduced by providing ‘socially accepted’ information to highlight the project’s benefits. We sought to reduce this bias by asking representatives from all projects to read through the results of analyses and comment on any missing information or misunderstandings – all projects provided answers and five of them provided additional information or corrections. Frequencies and proportions were calculated to indicate trends and overall patterns and should otherwise be interpreted with caution. Due to resources, it was no possible, but it would be interesting for future research, to address the actual impact of the collaborative and partnership projects on healthcare practices, on further collaboration, and in terms of cultural change, research use and relevance of the research conducted [ 49 ], despite the potential challenges posed by the projects’ diversity.
Using collaborative efforts to perform research on complex areas in complex systems requires a contextual understanding, longitudinal efforts, collaboration on multiple system levels and often interdisciplinary designs. Described problems, mirrored in the lessons learned, provided an indication on challenges to manage interdisciplinary, collaborative and partnership research, enact different roles and bridge several worlds as a researcher. Staffing, funding PhD students and paying attention to the work environment are some of the duties adhering to the tasks of an employer. Administrating and handling the project budget and monitoring its progress belong to the role of a project leader/administrator. Possessing knowledge on research designs and on the characteristics, demands, etc. of several disciplines is important in interdisciplinary, collaborative and partnership research. Finally, skills in collaboration and communication are needed, including a basic understanding of both the researcher and the practitioner contexts, while not forgetting any ethical concerns. Such demands and the often ambiguous roles and conflicting expectations make the research process challenging.
Funders, as well as managers, practitioners and researchers, might underestimate the complexity induced and efforts needed to collaborate during a research process, especially in multifaceted and complex research areas. Both interdisciplinary research teams and researcher–non-researcher teams can be challenging and time-consuming per se. By mixing these two conditions the situation becomes exponentially complex, as everyone has to learn about each other and adapt in various ways. The development of support from various decision-makers and build trust and understanding with involved practitioners at several levels of a healthcare system/organisation will need both skills in and arenas for communication and interaction. For the researchers, this takes time and energy from actual work with data collection, analyses and scientific writing. For the practitioners, this puts demands on understanding a research process and how it fits with ongoing organisational agendas and activities, and allocating enough time. Nevertheless, ensuring good relations (relationship brokering) is an important precondition for establishing a research process and gaining access to high quality data, especially on complex issues.
Another process that might be overlooked is the formation and building of research teams and the enactment of different roles in research intending to be both interdisciplinary and collaborative. If collaboration is not already established among researchers and involved partners, the experiences show that these processes need significant time and effort on behalf of both researchers and practitioners. Such efforts must not be underestimated if project agendas and schedules are to be realistic. The different roles and skills and the time required by researchers to both conduct research and contribute to the solving of complex problems in society by forming interdisciplinary research collaborations and collaborations with decision-makers and practitioners may be underestimated or simply ignored by involved stakeholders. Many researchers (especially PhD students) are not trained or experienced in working with interdisciplinary research teams or in a collaborative way with practitioners. Practitioners, in turn, may lack experience and skills in research collaboration. Both these aspects may have contributed to the problems encountered in this study. The lessons expressed can thus provide input for future collaborative or partnership research initiatives.
Research funders, as well as researchers and partners, may also benefit from gaining an overall understanding of the different types of research that can aid an understanding of and support changes in health and social services – from explanatory studies and experimental research to explorative studies and case study research, as in this case, which focused on understanding larger systems and more complex phenomena. Moreover, a flexibility regarding content and schedule is necessary to meet the complex demands, particularly concerning the time and resources needed for project management. To avoid exhaustive situations for involved researchers and practitioners, such considerations need to be included in the agenda of the funding body.
There is a need for more empirical studies on the conditions for researchers and practitioners in collaborative partnership and interdisciplinary research processes with the aim to increase the capabilities in addressing complex questions and the ‘usefulness’ of research in practice. An assessment of the efforts made to handle the different contexts and views of all involved actors in interdisciplinary, collaborative and partnership research initiatives in greater detail would provide more information on such processes and on their outcomes. Future studies could also address some remaining questions, including do the efforts to build interdisciplinary, collaborative and partnership research lead to better uptake and use of research outcomes, or provide more useful outcomes for practitioners and patients? Do they lead to deeper learning and understanding for researchers, and does the bilateral learning process and integrated knowledge translation between practice and academia occur?
Comments on the results of the national programme
The programme’s goals can be considered as new and innovative in the Swedish context. Further, the programme chose to fund less traditional research projects such as intervention studies, studies of natural experiments and the building of new infrastructures. This approach may be risky with regards to results evaluation, but the rich variety of projects, foci, new structures and lessons learned provided more types of results than traditional ones (i.e. scientific presentations and publications), which fits rather well with the initial broad aims of the programme. Scientific production, measured through traditional metrics, was substantial. Other presented results were categorised into five areas of innovation (what to develop) – a product/artefact, an approach when meeting patient/next-of-kin, routines and work procedures, administrative systems and structures, and increased organisational learning/competence. All projects reported results in at least two categories, and six projects reported results in all categories. Some of these were tangible, like employment of nurses in new roles, education of hundreds of care providers, new IT systems, web portals, academic courses, and a decision support used yearly in 25,000 patient meetings; some results were also very vulnerable. Quality in care processes can take long time to develop, especially when many actors and interests are involved, but might be destroyed by one major politically decided organisational change.
Sackett DL, Rosenberg WM, Gray JM, Haynes RB, Richardson WS. Evidence-based medicine. BMJ Brit Med J. 1996;313:170.
Article Google Scholar
Glasgow RE, Emmons KM. How can we increase translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–33. https://doi.org/10.1146/annurev.publhealth.28.021406.144145 .
Article PubMed Google Scholar
McIntyre D. Bridging the gap between research and practice. Camb J Educ. 2005;35(3):357–82.
Aita M, Richer MC, Héon M. Illuminating the processes of knowledge transfer in nursing. Worldviews Evid Based Nurs. 2007;4:146–55.
Berwick DM. Disseminating innovations in health care. JAMA. 2003;289:1969–75.
Grol R, Grimshaw J. From best evidence to best practice: effective implementation of change in patients’ care. Lancet. 2003;362:1225–30.
Grol R. Successes and failures in the implementation of evidence-based guidelines for clinical practice. Med Care. 2001;39:8. Suppl. 2, II46–II54
Grimshaw J, Eccles M, Tetroe J. Implementing clinical guidelines: current evidence and future implications. J Contin Educ Health Prof. 2004;24:31–7.
Cabana M, Rand C, Powe N, Wu M, Abbound P, Rubin H. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65.
Article PubMed CAS Google Scholar
Richter-Sundberg L, Kardakis T, Garvare R, Weinehall L, Nyström ME. Addressing implementation challenges when developing evidence based guidelines for health promotion – A case study of the Swedish national guidelines for disease prevention. BMC Health Serv Res. 2015;15:19. https://doi.org/10.1186/s12913-014-0672-4.
Article PubMed PubMed Central Google Scholar
Uzochukwu BC, Onwujekwe OE, Mbachu CO, Okwuosa C, Etiaba E, Nyström ME, Gilson L. The challenge of bridging the gap between researchers and policy makers: Experiences of a Health Policy Research Group in engaging policy makers to support evidence informed policy making in Nigeria. Glob Health. 2016;12:67.
Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature, FMHI Publication. Tampa: Louis de la Parte Florida Mental Health Institute, National Implementation Research Network, University of South Florida; 2005. p. 231.
Google Scholar
Greenhalgh T, Robert G, MacFarlane F, Bate P, Kyriakidou O. Diffusion of innovation in service organisations: systematic review and recommendations. Milbank Q. 2004;82:581–629.
Rycroft-Malone J, Kitson A, Harvey G, McCormack B, Seers K, Titchen A. Ingredients for change: revisiting a conceptual framework. Qual Saf Health Care. 2002;11:174–80.
Article PubMed PubMed Central CAS Google Scholar
Van de Ven AH, Johnson PE. Knowledge for theory and practice. Acad Manag Rev. 2006;31:802–21.
Golden-Biddle K, Reay T, Petz S. Toward a communicative perspective of collaborating in research: the case of the researcher-decision-maker partnership. J Health Serv Res Policy. 2003;8(Suppl 2):20–5.
Straus SE, Tetroe JM, Graham ID. Knowledge translation is the use of knowledge in health care decision making. J Clin Epidemiol. 2011;64:6–10.
Mitton C, Adair CE, McKenzie E, Patten SB, Perry BW. Knowledge transfer and exchange: review and synthesis of the literature. Milbank Q. 2007;85:729–68.
Thompson GN, Estabrooks CA, Degner LF. Clarifying the concepts in knowledge transfer: a literature review. J Adv Nurs. 2006;53:691–701.
Oborn E. Facilitating implementation of the translational research pipeline in neurological rehabilitation. Curr Opin Neurol. 2012;25:676–81.
Bowen S, Graham ID. Integrated knowledge translation. In: Straus SE, Tetroe J, Graham ID, editors. Knowledge Translation in Health Care: Moving from Evidence to Practice, 2nd ed. Chichester: Wiley; 2013. p. 14–23.
Straus SE, Tetroe J, Graham ID. Knowledge translation in healthcare: moving from evidence to practice. 2nd ed. Chichester: Wiley; 2013.
Canadian Institutes of Health Research. Knowledge to Action: A Knowledge Translation Casebook. 2008. http://www.cihr-irsc.gc.ca/e/documents/kt_casebook_e.pdf . Accessed 1 Sep 2015.
Mitchell P, Pirkis J, Hall J, Haas M. Partnerships for knowledge exchange in health services research, policy and practice. J Health Serv Res Policy. 2009;14:104–11.
Boaz A, Fitzpatrick S, Shaw B. Assessing the impact of research on policy: a literature review. Sci Public Policy. 2009;36:255–70.
Rycroft-Malone J, Wilkinson JE, Burton CR, Andrews G, Ariss S, Baker R, Dopson S, Graham I, Harvey G, Martin G, McCormack BG, Staniszewska S, Thompson C. Implementing health research through academic and clinical partnerships: a realistic evaluation of the Collaborations for Leadership in Applied Health Research and Care (CLAHRC). Implement Sci. 2011;6:74. https://doi.org/10.1186/1748-5908-6-74 .
DeVoe JE, Likumahuwa S, Eiff MP, Nelson CA, Carroll JE, Hill CN, Gold R, Kullberg PA. Lessons learned and challenges ahead: report from the OCHIN Safety Net West practice-based research network (PBRN). J Am Board Fam Med. 2012;25:560–4.
Nagykaldi Z, Mold JW, Robinson A, Niebauer L, Ford A. Practice facilitators and practice-based research networks. J Am Board Fam Med. 2006;19:506–10.
Gold M, Taylor EF. Moving research into practice: lessons from the US Agency for Healthcare Research and Quality's IDSRN program. Implement Sci. 2007;2:1–9.
Smits PA, Denis JL. How research funding agencies support science integration into policy and practice: an international overview. Implement Sci. 2014;9:1.
Lomas J. Using ‘linkage and exchange’ to move research into policy at a Canadian foundation. Health Aff. 2000;19:236–40.
Article CAS Google Scholar
Israel BA, Schulz AJ, Parker EA, Becker AB. Community-based participatory research: policy recommendations for promoting a partnership approach in health research. Educ Health. 2001;14:182–97.
Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010;100(Suppl. 1):40–6.
Ross SE, Lavis JN, Rodriguez C, Woodside JM, Denis JL. Partnership experiences: involving decision-makers in the research process. J Health Serv Res Policy. 2003;8(Suppl 2):26–34.
Strehlenert H, Richter-Sundberg L, Nyström ME, Hasson H. Evidence-informed policy formulation and implementation: Comparative case study of two national policies for improving health and social care in Sweden. Implement Sci. 2015;10:169. https://doi.org/10.1186/s13012-015-0359-1 .
Rycroft-Malone J, Burton CR, Wilkinson J, Harvey G, McCormack B, Baker R, Dopson S, Graham ID, Staniszewska S, Thompson C, Ariss S, Melville-Richards L, Williams L. Collective action for implementation: a realist evaluation of organisational collaboration in healthcare. Implement Sci. 2016;11:17. https://doi.org/10.1186/s13012-016-0380-z .
Cordero C, Delino R, Jeyaseelan L, Lansang MA, Lozano JM, Kumar S, Moreno S, Pietersen M, Quirino J, Thamlikitkul V, Welch VA, Tetroe J, ter Kuile A, Graham ID, Grimshaw J, Neufeld V, Wells G, Tugwell P. Funding agencies in low-and middle-income countries: support for knowledge translation. Bull World Health Organ. 2008;86(7):524–34.
Bowen S, Botting I, Graham ID, Huebner LA. Beyond “two cultures”: Guidance for establishing effective researcher/health system partnerships. Int J Health Policy Manag. 2017;6(1):27.
Huberman M. Research utilization: the state of the art. Knowledge Policy. 1994;7:22–42.
Lomas J. The in-between world of knowledge brokering. Br Med J. 2007;334:129–32.
Knight C, Lyall C. Knowledge brokers: the role of intermediaries in producing research impact. Evid Policy. 2013;9:309–16.
Nyström ME, Hansson J, Garvare R, Andersson Bäck M. Locally based research and development units as knowledge brokers and change facilitators in health and social care of older people in Sweden. Evid Policy. 2015;11:57–80.
Michaels S. Matching knowledge brokering strategies to environmental policy problems and settings. Environ Sci Pol. 2009;12:994–1011.
Martin S. Co-production of social research: strategies for engaged scholarship. Public Money Manag. 2010;30:211–8.
King G, Currie M, Smith L, Servais M, McDougall J. A framework of operating models for interdisciplinary research programs in clinical service organisations. Eval Prog Plann. 2008;31:160–73.
Øvretveit J, Hempel S, Magnabosco J, Mittman B, Rubenstein L, Ganz D. Guidance for Research-Practice Partnerships (R-PPs) and Collaborative Research. J Health Organ Manag. 2014;28:115–26.
Svensson L, Ellström PE, Brulin G. Introduction on interactive research. Int J Action Res. 2007;3:233–49.
Nyström ME, Höög E, Garvare R, Weinehall L, Ivarsson A. Change and learning strategies in large scale change programs: describing the variation of strategies used in a health promotion program. J Organ Chang Manag. 2013;26:1020–44.
Sibbald SL, Tetroe J, Graham ID. Research funder required partnerships: a qualitative inquiry. Implement Sci. 2014;9:176. https://doi.org/10.1186/s13012-014-0176-y .
Elden M, Chisholm RF. Emerging varieties of action research: introduction to the special issue. Hum Relat. 1993;46:121–42.
Aagaard Nielsen K, Svensson L. Action and Interactive Research. Maastricht: Shaker Publishing BV; 2006.
Westlander G. Researcher roles in action research. In: Aagaard Nielsen K, Svensson L, editors. Action and Interactive Research. Maastricht: Shaker Publishing BV; 2006.
vom Brocke J, Lippe S. Managing collaborative research projects: A synthesis of project management literature and directives for future research. Int J Proj Manag. 2015;33:1022–39.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88.
Creswell J, Tashakkori A. Differing perspectives on mixed methods research. J Mixed Method Res. 2007;1:303–8.
Richter-Sundberg L, Nyström ME, Krakau I, Sandahl C. Improving treatment of depression in primary health care: A case study of obstacles to perform a clinical trial designed to implement practice guidelines. Prim Health Care Res. 2014;16:188–200. https://doi.org/10.1017/S1463423614000243 .
Estabrooks CA. Research utilization and qualitative research. In: Morse J, Swanson J, Kuzel A, editors. The Nature of Qualitative Evidence. Thousand Oaks: Sage; 2001. p. 275–98.
Loomis M. Knowledge utilization and research utilization in nursing. J Nurs Scholarsh. 1985;17:35–9.
Scott-Findlay S, Golden-Biddle K. Understanding how organisational culture shapes research use. J Nurs Admin. 2005;35:359–65.
Pawson R, Greenhalg J, Brennan C, Glidewell E. Do reviews of healthcare interventions teach us how to improve healthcare systems? Soc Sci Med. 2014;114:129–37. https://doi.org/10.1016/j.socscimed.2014.05.032 .
Willis CD, Best A, Riley B, Herbert CP, Millar J, Howland D. Systems thinking for transformational change in health. Evid Policy. 2014;10:113–26.
Hofmeyer A, Scott C, Lagendyk L. Researcher-decision-maker partnerships in health services research: Practical challenges, guiding principles. BMC Health Serv Res. 2012;12:280. https://doi.org/10.1186/1472-6963-12-280 .
Gibbons M, Limoges C, Nowotny H, Schwartzman S, Scott P. The New Production of Knowledge. London: Sage; 1994.
Estabrooks CA, Norton P, Birdsell JM, Newton MS, Adewale AJ, Thornley R. Knowledge translation and research careers: Mode I and Mode II activity among health researchers. Res Policy. 2008;37:1066–78.
Brewer GD. The challenges of interdisciplinarity. Policy Sci. 1999;32:327–37.
Bromme R. Beyond one’s own perspective: the psychology of cognitive interdisciplinarity. In: Weingart P, Stehr N, editors. Practising Interdisciplinarity. Toronto: University of Toronto Press; 2000. p. 115–33.
Giacomini M. Interdisciplinarity in health services research: dreams and nightmares, maladies and remedies. J Health Serv Res Policy. 2004;9:177–83.
Meyer M. The rise of the knowledge broker. Sci Commun. 2010;32:118–27.
Van Rijnsoever FJ, Hessels LK, Vandeberg RLJ. A resource-based view on the interactions of university researchers. Res Policy. 2008;37:1255–66.
Van Rijnsoever FJ, Hessels LK. Factors associated with disciplinary and interdisciplinary research collaboration. Res Policy. 2011;40:463–72.
Rhoten D, Pfirman S. Women in interdisciplinary science: exploring preferences and consequences. Res Policy. 2007;36:56–75.
Gorard S. Current contexts for research in educational leadership and management. Educ Manag Adm Lead. 2005;33:155–64.
Symonds JE, Gorard S. Death of mixed methods? Or the rebirth of research as a craft. Eval Res Educ. 2010;23:121–36.
Download references
Acknowledgements
We wish to thank the interview respondents for their participation, the research project leaders and representatives for reviewing results for potential biases or misinterpretations, and Professor John Øvretveit who provided helpful comments to improve the manuscript.
This work was mainly supported by the universities where the authors were situated (Karolinska Institutet and Jönköping University), with additional contribution from the Vinnvård research programme in Sweden 2014–15 [no grant no provided]. The Vinnvård research programme management placed no restrictions and had no influence on the research process.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. It consists of transcripts from interviews and project documents (all in Swedish). Excerpts from the data sources are presented in the article as citations (translated to English and checked by multi-lingual persons).
Author information
Authors and affiliations.
Department of Learning, Informatics, Management and Ethics, Medical Management Centre, Karolinska Institutet, SE 171 77, Stockholm, Sweden
M. E. Nyström
Department of Public Health and Clinical Medicine, Epidemiology and Global Health, Umeå University, SE 901 87, Umeå, Sweden
Department of Industrial Engineering and Management, School of Engineering, Jönköping University, P.O. Box 1026, SE 551 11, Jönköping, Sweden
Jönköping International Business School, Jönköping University, P.O. Box 1026, SE 551 11, Jönköping, Sweden
Futurum, Region Jönköping County, Sweden
B. Andersson Gäre
The Jönköping Academy for Improvement of Health and Welfare, School of Health Sciences, Jönköping University, P.O. Box 1026, SE 55111, Jönköping, Sweden
You can also search for this author in PubMed Google Scholar
Contributions
MN, CK, JK and BA-G designed the study, MN collected the archival data, and CK and JK conducted the interviews. MN, CK and JK performed the analyses and MN drafted the manuscript. All authors read, contributed to and approved the final manuscript.
Corresponding author
Correspondence to M. E. Nyström .
Ethics declarations
Ethics approval and consent to participate.
For the 20 investigated projects, regional Ethical Committees approved the studies according to Swedish regulations. The project documents and the Swedish report on the interview study (data used in the study) are openly displayed on the programme’s public website ( http://www.vinnvard.se ). Seeking ethical approval for this type of study is not required according to Swedish regulations. Participation in the original interview study was based on informed consent, also for open publication. For this study, the interviewed project leaders and senior researchers were given an additional opportunity to read and comment on the results of the analyses and to correct or add missing information and provide consent; they all provided answers, information and consent.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Overview of the projects based on information in documents. (DOCX 19 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Nyström, M.E., Karltun, J., Keller, C. et al. Collaborative and partnership research for improvement of health and social services: researcher’s experiences from 20 projects. Health Res Policy Sys 16 , 46 (2018). https://doi.org/10.1186/s12961-018-0322-0
Download citation
Received : 29 August 2017
Accepted : 04 May 2018
Published : 30 May 2018
DOI : https://doi.org/10.1186/s12961-018-0322-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Collaborative research
- co-production
- integrated knowledge translation
- partnership research
- quality improvement
- social services
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]

- Member Organisations
- Research, Implementation and Impact
- Social Care and Social Work
- Social Care - Kent, Surrey & Sussex Region
- Starting Well: Children's Mental Health
- Primary and Community Health Services
- Living Well with Dementia
- Co-production
- Public Health
- Digital Innovation
- Economics of Health and Social Care
- Implementation
- Rapid Evidence Synthesis
- Public and Community Involvement
- What is PCIE?
- Getting Involved
- Support for researchers
- Introduction
- An overview of ARC KSS
- Who can help you with PCIE?
- Terminology and PCIE
- Why and When to do PCIE
- Why involve members of the public in research?
- Why do members of the public want to get involved in research?
- When to get members of the public involved?
- How to do PCIE
- Communication and Accessibility
- Planning for involvement and engagement
- How to recruit members of the public
- Equality, Diversity and Inclusion (EDI)
- Approaches – different options for undertaking PCIE
- Facilitating meetings and Group dynamics
- Impact and Evaluation
- Examples/Case Studies
- Appendix/Useful tools
- Learning and Development

- Learning and Development Finder
- Researchers Journeys

- Research Week
- Previous Research Weeks

- Resource Library
Your Health and Social Care Research Quick Guide
This guide is designed for those in practice to navigate the world of research.

In this section
Produced by Dr Diana Ramsey , ARC KSS Darzi Fellow (2021-2022) with insights and support from people working to deliver research in the Health and Social Care region, the Your Health and Social Care Research Quick Guide is a resource to help those working in health or social care to start or develop their research journey.
Packed with information, links and personal stories from people working across Kent, Surrey and Sussex, this guide has been designed to answer any questions you might have in regards to getting involved in research, building networks, research training and resources.
Whatever your research experience, this guide is for you.
View guide here


Subscribe to our newsletter
Sign up here
You can unsubscribe at any time by clicking the link in the footer of our emails. For information about our privacy practices, please visit this page . We use e-shot as our marketing platform. Learn more about e-shot's privacy practices here .
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Health Res Policy Syst

Collaborative and partnership research for improvement of health and social services: researcher’s experiences from 20 projects
M. e. nyström.
1 Department of Learning, Informatics, Management and Ethics, Medical Management Centre, Karolinska Institutet, SE 171 77 Stockholm, Sweden
2 Department of Public Health and Clinical Medicine, Epidemiology and Global Health, Umeå University, SE 901 87 Umeå, Sweden
3 Department of Industrial Engineering and Management, School of Engineering, Jönköping University, P.O. Box 1026, SE 551 11 Jönköping, Sweden
4 Jönköping International Business School, Jönköping University, P.O. Box 1026, SE 551 11 Jönköping, Sweden
B. Andersson Gäre
5 Futurum, Region Jönköping County, Sweden
6 The Jönköping Academy for Improvement of Health and Welfare, School of Health Sciences, Jönköping University, P.O. Box 1026, SE 55111 Jönköping, Sweden
Associated Data
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. It consists of transcripts from interviews and project documents (all in Swedish). Excerpts from the data sources are presented in the article as citations (translated to English and checked by multi-lingual persons).
Getting research into policy and practice in healthcare is a recognised, world-wide concern. As an attempt to bridge the gap between research and practice, research funders are requesting more interdisciplinary and collaborative research, while actual experiences of such processes have been less studied. Accordingly, the purpose of this study was to gain more knowledge on the interdisciplinary, collaborative and partnership research process by investigating researchers’ experiences of and approaches to the process, based on their participation in an inventive national research programme. The programme aimed to boost collaborative and partnership research and build learning structures, while improving ways to lead, manage and develop practices in Swedish health and social services.
Interviews conducted with project leaders and/or lead researchers and documentation from 20 projects were analysed using directed and conventional content analysis.
Collaborative approaches were achieved by design, e.g. action research, or by involving practitioners from several levels of the healthcare system in various parts of the research process. The use of dual roles as researcher/clinician or practitioner/PhD student or the use of education designed especially for practitioners or ‘student researchers’ were other approaches. The collaborative process constituted the area for the main lessons learned as well as the main problems. Difficulties concerned handling complexity and conflicts between different expectations and demands in the practitioner’s and researcher’s contexts, and dealing with human resource issues and group interactions when forming collaborative and interdisciplinary research teams. The handling of such challenges required time, resources, knowledge, interactive learning and skilled project management.
Conclusions
Collaborative approaches are important in the study of complex phenomena. Results from this study show that allocated time, arenas for interactions and skills in project management and communication are needed during research collaboration to ensure support and build trust and understanding with involved practitioners at several levels in the healthcare system. For researchers, dealing with this complexity takes time and energy from the scientific process. For practitioners, this puts demands on understanding a research process and how it fits with on-going organisational agendas and activities and allocating time. Some of the identified factors may be overlooked by funders and involved stakeholders when designing, performing and evaluating interdisciplinary, collaborative and partnership research.
Electronic supplementary material
The online version of this article (10.1186/s12961-018-0322-0) contains supplementary material, which is available to authorized users.
Healthcare organisations are complex and knowledge intensive, with patients often taking for granted that care providers use the best available knowledge on diagnosis and treatment. Evidence-based medicine and practice ensure that the best available knowledge is used systematically in clinical care (e.g. [ 1 ]). Nevertheless, the gap between research and practice in healthcare is well-known and a recognised concern (e.g. [ 2 , 3 ]), where failures to translate research into practical actions contribute to health inequities [ 4 , 5 ]. The process from research-produced knowledge to its use in healthcare practices can take considerable time (e.g. [ 6 ]). The estimated lack of research use in the United States and the Netherlands has suggested that 30–40% of patients do not receive care complying with current research evidence [ 7 ]. The required increase in the speed of uptake of evidence-based clinical practice guidelines has been frequently discussed (e.g. [ 8 ]) and factors influencing their adoption have been extensively studied (e.g. [ 9 , 10 ]). Getting research into policy and practice in healthcare is a recognised, world-wide concern (e.g. [ 11 ]).
Several research areas deal with aspects related to the transfer of knowledge and use of research findings for improving healthcare. The view of research production as separate from the use of research findings initially inspired research on diffusion and implementation processes [ 12 , 13 ], mainly focusing on the later stages of the research process with variable emphasis on a division between knowledge production and its implementation.
The shortcomings of the traditional ‘linear’ model of research-into-practice have become more evident [ 14 ]. Van de Ven and Johnson [ 15 ] suggest that the problem may be one of methods for knowledge production rather than knowledge transfer or knowledge translation. To enhance a faster and more systematic use of knowledge, collaborative and interdisciplinary research approaches have been asked for as well as more useful research [ 15 – 17 ]. Research collaboration is assumed to enable and enhance both the use of research and increase the amount of research relevant to end users.
Research on knowledge transfer and exchange describes an interactive exchange of knowledge between research users and researcher producers [ 18 , 19 ]. Knowledge transfer and exchange interaction between researchers and practitioners can take place from the on-set of the research process and involve more long-standing relationships. Several approaches to knowledge transfer have been described, focusing, for example, on systematic synthesis and guidelines, social interaction between researchers and decision-makers, contextual features and organisational readiness [ 20 ]. The Canadian Institute of Health Research uses the term ‘integrated knowledge translation’ to describe projects where the knowledge users are involved as equal partners during the entire research process [ 21 , 22 ].
Funding organisations have started to request research proposals to include researcher–decision-maker partnerships in collaborative research teams with representatives of industry, local communities and professional organisations (e.g. [ 23 , 24 ]). The increased focus on research-use is also mirrored in research funders’ strategies (e.g. [ 25 ]). Some examples of collaborative initiatives are the Partnership projects and Centres financed by the National Health and Medical Research Council in Australia, the Dutch Academic Collaborative Centres for Public Health in the Netherlands, and The Collaborations for Leadership in Applied Health Research and Care in the United Kingdom (e.g. [ 26 ]), as well as the practice-based research networks and structured use of practice facilitators [ 27 , 28 ] and the Integrated Delivery Systems Research Network programme to foster public–private collaboration between health service researchers and healthcare delivery systems in the United States [ 29 ]. There are three main strategies that research funding agencies might use to enhance knowledge translation – push, pull, or linkage and exchange. The push–pull strategies distinguish between mechanisms driven by science (push) and those driven by the demands of practitioners or policy-makers (pull) [ 30 ]. The linkage and exchange model is based on co-construction of applied knowledge and the relevance of applied research to both practitioners and researchers [ 31 ]. In a recent review of the ways research funding agencies support science integration into policy and practice in the field of health [ 30 ], most of the 13 agencies investigated used one or two of these strategies. The large heterogeneity of users and how this may affect the use of various mechanisms for research initiation, development and dissemination was highlighted in this review.
Collaboration has been addressed for some time in community-based participatory research regarding public health and social issues in society (e.g. [ 32 , 33 ]), for example, on how to achieve policy level collaboration (e.g. [ 24 , 34 ]) and evidence-informed policy-making (e.g. [ 35 ]). Nevertheless, there is a need for more empirical research on the actual processes, conditions and outcomes of the more recent collaborative and partnership research initiatives in healthcare [ 36 , 37 ] and, to date, there are few empirical studies on researchers’ approaches and experiences of the combination of interdisciplinary and collaborative and partnership research, including the actual effect of such programme or project calls. Less explored is also research partnership aiming to respond to the challenges and priorities of the health system and much research has been based on assumptions of researcher-driven initiatives with newly established collaborations [ 38 ].
Collaborative and partnership research
Approaches, strategies and roles.
Collaboration and partnerships are two concepts used to describe the involvement of people and groups from different contexts and with different experiences, perspectives and agendas in research and development. Accordingly, collaborative research contains social relations and a variation of potential roles for those involved during the research process. In earlier research, means for collaboration were described in the form of ‘linkage mechanisms’ between researcher and user contexts, i.e. the presence of intermediaries (boundary spanners); formal and informal contacts with users during studies; involvement of users during data collection; and interim feedback [ 39 ]. The boundary-spanning role of knowledge brokers has been brought forward as a bridge between research and practice (e.g. [ 40 ]). Knowledge brokering has been defined as “ all the activity that links decision-makers with researchers, facilitating their interaction so that they are able to better understand each other’s goals and professional cultures, influence each other’s work, forge new partnerships, and promote the use of research-based evidence in decision-making ” ([ 40 ], p. 131). Individuals, teams or organisations can all play the role of knowledge brokers [ 41 , 42 ]. Michaels [ 43 ] describes six primary brokering strategies that span from more passive dissemination of information, interaction by seeking and using expert’s advice and linking different actors, to active engagements and close collaborative relations with healthcare actors, and which aim to inform, consult, match-make, engage, collaborate and build capacity. A recent study highlights the importance of effective ‘relationship brokering’ in researcher-health system partnership for establishing a meaningful collaboration [ 38 ].
A detailed road map on research collaboration is offered by Martin [ 44 ] in his description of five approaches to co-production of research. Depending on the chosen approach, stakeholders can be more or less involved in phases of the research process, from study design, data collection and analyses, to dissemination, while the degree of academic independence of the researcher/s and the utilisation of the research results may vary. Consequently, practitioners can play the role of informants, recipients, endorsers, commissioners or co-researchers.
On programme level, King et al. [ 45 ] describe four research programme operating models used in a collaborative approach to enhance research-informed practice in community-based clinical service organisations. The models describe the types of partnership involved such as the ‘clinician-researcher skills development model’, ‘clinician and researcher evaluation model’, ‘researcher-led evaluation model’, and the ‘knowledge-conduit model’. To differentiate research-practice partnerships from other ways of conducting research, Øvretveit et al. [ 46 ] suggest five criteria for partnership research, namely research that contributes to actions taken by actors within a health system; studies intended to produce quick and actionable findings as well as scientific publications; both researchers and practitioners take part in defining the research question and interpret findings; significant time and contributions from both researchers and practitioners; and an extensive formulated description of the partnership approach.
Challenges and enabling features
One challenge for collaborative and partnership research concerns the variation of views on the production and use of knowledge and on the relationship between researcher and practitioner, spanning from top-down to bottom-up or from linear to interactive and multidimensional (e.g. [ 39 , 47 ]). Depending on research tradition and/or experiences, basic assumptions regarding knowledge and learning can vary among researchers, but also among stakeholders (e.g. [ 48 ]). Sibbald et al. [ 49 ] identified challenges such as role clarity, organisational change and cultural differences regarding expectations on research output and (positive) effects on actual practice and found that role ambiguity, multiple roles and role conflicts could hamper social relationships. Factors facilitating collaboration were already established relationships, the alignments of goals/objectives, skilled and experienced researchers, and the use of regular, multi-modal communication.
Another influence on collaboration, mainly from the researcher context, is the variety of research paradigms and areas and related basic assumptions. One approach to be expected is action research, where knowledge creation is combined with practice development. There are a variety of action research approaches depending on, for example, how the collaborative element is organised [ 50 ]. The interactive research approach builds on action research and emphasises the common learning and knowledge creation for both practitioners and researchers during the complete process [ 51 ]. Both approaches involve a number of different roles for the researcher to enact [ 52 ].
Based on a realist evaluation, Rycroft-Malone et al. [ 36 ] list features of research collaboration likely to enhance knowledge use, namely attention to communication mechanisms, setting intermediate/outcome goals, providing time and space for the development and implementation of plans, making the choice of topic with resonance and relevance, close proximity between partners, re-balancing and sharing power, and allowing time to develop mutual trust and respect. These features put other demands on the planning and execution of research than a traditional approach when research has precedence over practice.
Sibbald et al. [ 49 ] present a model describing the research partnership process, with enablers, facilitators, challenges and impact, and identify three partnership types based on an empirical study as token, asymmetric or egalitarian partnerships. In Fig. 1 , features of the research partnership process are presented, grounded on aspects highlighted by Sibbald et al. [ 49 ] and Rycroft Malone et al. [ 36 ].

Model over the research partnership process (adopted after Sibbald et al. [ 49 ] and Rycroft Malone et al. [ 36 ])
Collaborative and partnership research poses specific demands regarding project management. According to a review [ 53 ], collaborative research can be characterised by heterogeneity of actors, collective responsibilities, demands for applicability in addition to scientific requirements, and by being funded by public agencies with specific agendas. Project management in collaborative projects usually involves three paradoxes [ 53 ]:
- To reach expected results, both freedom and flexibility to handle the uncertainty in research is needed, as well as a tight and managed firm project structure.
- The necessary integration of different views of the actors involved may also lead to intercultural, interorganisational and interdisciplinary problems that need to be managed.
- The limited formal authority of the project manager is in contrast with the demands for integrative managing of results, commitment and involvement of all parties.
Thus, collaborative and partnership research may have the potential to enhance the use of knowledge in practice and thereby improve healthcare and social services, but also to challenge the practitioners’ and researchers’ views, assumptions and roles.
The empirical base of the present study is an example of a collaborative and interdisciplinary research initiative – a national research programme seeking to boost collaborative and partnership research to improve health and social services in Sweden. The purpose of the study was to gain more knowledge on the interdisciplinary, collaborative and partnership research process by investigating researchers’ experiences based on their participation in this national programme. We have studied the experiences of researchers in all 20 research projects funded by the programme during the period 2008–2014, focusing on three themes – complexity in collaboration, collaborative procedures, and challenges, obstacles and lessons learned. The research questions posed were (1) what types of research approaches, research focus and partners/actors were involved in the projects? (2) How was collaborative and partnership research achieved, according to the researchers? (3) What were the challenges and obstacles to interdisciplinary, collaborative and partnership research encountered, and what main lessons were learned?
This study is based on analyses of interviews and archival data. The interviews were performed during the final stages of the projects and the documents covered the entire project period.
Empirical setting – the national research programme
The Vinnvård research programme was financed by a consortium of research funders, including the Ministry of Health and Social Welfare, Sweden’s innovation agency VINNOVA, Vårdalstiftelsen and the Swedish Association of Local Authorities and Regions. It was the first major attempt by research funders in Sweden to address the challenges of the ‘quality chasm’ in health and social services focusing on organisational aspects, with clear aspirations to bridge research and practice, stimulate interdisciplinary research and enhance research collaboration between universities/research institutions and healthcare/social service organisations. In addition, new research and learning infrastructures were expected to emerge. The requirements and evaluation criteria for the applications reflected these aspirations and documented active cooperation between practitioners, researchers and other public actors was asked for. Moreover, applications had to include an interdisciplinary approach, a common vision for all parties involved and documented approaches for securing participation and dissemination of research and/or development results. Both researchers and practitioners/public institutions could apply for funding. Non-researchers were part of the peer-review panel in both calls. The programme’s broad approach was new, both to the funding agencies and the research community. With a focus on health and social services, the programme aimed to (1) increase the use of research-based knowledge (bridge research and practice), (2) develop innovative ways of organising work, (3) stimulate the development of institutional learning structures with a focus on how to lead, manage and develop practices in organisations, and (4) establish more research on how to lead, manage and develop practices in health and social services organisations at Swedish universities.
The subsequent aims (3 and 4) had a more long-term character than the preceding ones (aims 1 and 2) and can be seen as a means to build long-lasting support for these. During the period studied (2008–2013) there were two calls for projects lasting up to 4 years each. A total of 20 projects were funded, 9 in 2008–2011 and 11 in 2009–2013, all of which are included in the present study. All projects were on-going when the interviews were conducted and all except one had ended when the archival data was gathered in May 2015.
Data collection
Interviews were conducted between September and November 2011, when most projects were in their later stages. In total, 17 respondents with an equal gender distribution were chosen based on their overall project involvement. Four respondents were responsible for two projects each and one project was represented by two respondents. All 20 projects were covered. All respondents held a PhD and were intensely involved in the projects, either as project leaders, principal investigators, or as the most important researcher, as judged by the project leader. The semi-structured interviews had the aim of following up on the main goals and lessons learned within the projects and covered the characters of the projects with its overall contributions, roles taken in projects, collaborations, and participating or studied organisations and institutional levels. Questions followed five themes for each one of the four programme goals, namely interpretations of the goal, the importance it was given, how it was fulfilled, how the project had worked to reach the goal, and results related to the goal. Practical examples of the last two themes were requested. The last part of the interview covered how the four goals were integrated, any expected or unexpected insights, difficulties experienced, and emphasised and miscellaneous findings. In a few cases, interviews were complemented by the respondents with written comments or documents. Interviews lasted 40 to 120 min, with longer interviews with respondents representing two projects. The respondents received the questions a week in advance. Each interview was recorded and transcribed verbatim.
Archival data were gathered in May 2015 and consisted of the projects’ final reports and, for one project not yet finished, a progress report (same structure as the final reports, but without a popular science description and financial report). The report template had the following headings: introduction; short summary on how the project had worked to fulfil the research programme’s goals (with subheadings for each of the four goals); publication list; participation in national and international conferences/workshops; PhD students; description of potential problems encountered; description of the most important lessons learned; popular science description; references; and financial accounting. Reports varied in length from 4 to 42 pages, with an average of 19 pages; yet the four-page report came from the project not yet finished. A total of 386 pages were analysed.
Data analysis
Qualitative data in interviews and documents were scrutinised in several steps, first by using a mix between directed (guided by the research questions) and conventional content analysis [ 54 ]. The entire material was read through to get a sense of the whole and then analysed to identify relevant text related to the research questions. Both data sources were then further used for determining themes, categories and overall patterns. Finally, a summative content analysis [ 54 ] was applied to get a sense of variation by identifying how many projects provided information in the identified categories. Three researchers performed the analyses, first individually and through meetings held to discuss and validate interpretations.
Document analysis focused on information related to the three research questions, namely (1) system level actors involved (care recipient, unit/clinic/ward, organisation, region/county council, and/or national level) and basic project information; (2) descriptions of or activities and strategies for research collaboration, including with which actors; and (3) obstacles/problems encountered and main lessons learnt. A fourth category (Other) was used in order not to miss important aspects. Described collaborations and process reflections (i.e. obstacles/problems and lessons learnt) were the main categories used to sort the material for questions 2 and 3. In a second iterative step for these questions, subcategories were identified, tested, revised and defined. The category definitions were then used in a third step for a final text classification of data.
As the interviews were performed when the projects were still ongoing, they were used to complement, add details, provide examples and validate information found in documents. Moreover, they also added a more personal perspective on the results based on the experience of the main researchers.
Project overviews and the complexity of the collaborations
Of the 20 projects, 14 included three or more stakeholder levels, indicating an elaborated multilevel or system view. Five projects actively involved care recipients (and sometimes their next-of-kin) in design of solutions or interactive co-production. Two projects had a sole clinical focus (screening for atrial fibrillation and improving methods for stroke care), but such foci were present in several projects’ sub-studies. Four projects (three geographical sites) had a deliberate strategy to build learning structures that involved university level education at undergraduate and/or master’s levels, but education was included in several projects, sometimes as distance learning or continuing education for professionals. All projects except two involved PhD students, with a total of 72 for the programme overall. Most projects ( n = 16) clearly stated that their research group was interdisciplinary and some discussed the benefits and obstacles encountered due to this. A total of 203 articles in scientific journals (including submitted manuscripts) were reported to have been produced during the 6-year period. The widespread target groups and involved organisational levels in the projects’ research activities are illustrated in Table 1 . More information on the projects is provided in Additional file 1 .
System/organisational levels where research was performed and levels where support was needed in order to establish the projects and keep them going; the summary provides an overview for comparison
dep. Department, Internat. international organisation, Nat. national organisation, Reg. regional organisation, Org. local organisation, Unit clinical department or other organisational unit, Care recipient individual patient (incl. next-of-kin)
Descriptions of collaborative procedures
Descriptions of the research collaboration varied – from describing a more or less interactive research design to more explicit descriptions of when and how practitioners were involved during the research process. Practitioner’s and researcher’s boundary-spanning roles served as important bridges between the two contexts. Five main categories were identified to cover the various ways collaborations were described. In Fig. 2 , the number and proportion of the projects providing descriptions in each of these categories is provided.

Number and proportion of projects ( n = 20) providing descriptions in the different subcategories of collaboration
Collaboration as described by the overall research and development design
Seventeen projects (85%) clearly described an interactive research design that either involved healthcare practitioners, managers, politicians, patients, next-of-kin or a mixture of those. Seven projects used the term ‘action research’ or ‘action-oriented research’, two used the term ‘interactive research model’, and one used the term ‘participatory design’, all of which imply a close interaction between researchers and practitioners. Examples of statements are “ the project’s action research approach has involved a continuous and iterative collaboration that has both fed into and questioned on-going [change and learning] processes ” and “ we used a participatory design where the young people actively participated in the creation of what to study, that is the effects of using a web-based instrument ”. Four projects developed information and communication technology-based solutions in close collaboration with practitioners. The terms ‘co-design’ or ‘co-creator’ were often used in two projects involving patients and their next-of-kin and in a project focusing on mixed learning networks with researchers, patients and other actors.
Collaborative involvement of practitioners in different stages of the research process
Interactive forms were described as being used during the following stages: (1) mapping of the research problem and its manifestation in practice, and formulation of research questions; (2) planning, creation of interventions and choices of design; (3) investigation, test, follow-up and implementation processes; (4) analyses, reflection and learning; and (5) reporting on and dissemination of results, including further implementation of studied intervention. Nineteen projects (95%) described an interactive approach in at least one of these stages. Collaboration or interaction was most common during follow-ups and feedback processes (Stage 3 and 5), and less interaction was described during the formulation of the research problem and during analyses (Stage 1 and 4). Statements like “ conducting research with practitioners, not on practitioners ” and “ patients have participated in the mapping [of the current situation]” are examples of Stage 1. Stage 2 is exemplified by the statements “ practitioners participated during the construction of the interview [manual]”. Statements such as “ the researchers and contact persons [from the healthcare organisations] have met 1–2 times a year to discuss and reconcile research questions, data collections and results from different sub-projects ” represent several stages (Stage 1, 2, 3 and 5). Involving practitioners directly in analyses (Stage 4) was not explicitly mentioned, but the described interactive sessions could involve the discussion and validation of results. Statements such as “ the researchers regularly fed back their observations and analyses to the hospital management and hospital unit representatives ”; “ we had several formal and informal feedback sessions and this feedback has been further used ”; or “ the feedback and the action research approach have given researchers an opportunity to stimulate reflection and contribute with knowledge on implementation, learning and change ” can represent situations when practitioners participated in the interpretation of results and that this had effects on both research and practice. Thus, if researchers in the research teams holding dual roles are not accounted for, no project involved non-researchers in the entire research process.
Collaboration enhanced by the dual role of practitioners and/or researchers
Ten projects (50%) described a dual, boundary-spanning role held by either the practitioners or the researchers. This dual role of being involved in both practical work and research was more common for clinicians performing research in the area of their expertise, e.g. in projects and sub-cases with a clinical focus. This can be exemplified by statements such as “we are conducting research with actively serving practitioners and clinicians ” or as a statement made by a clinician project leader “ improvement work for increased quality in healthcare is best performed directly in connection to the meeting between patients and professional care-givers ”. In one case, in the Clinical Innovation Fellowship programme, teams of practitioners were trained as action researchers for 2 months (fellows) and spent 6 months working in clinical quality improvement in healthcare, sometimes in collaboration with students working on their masters or bachelor thesis. Examples on practitioners’ dual role were described as “ some healthcare staff became PhD students and thereby gained a double bridge-building role ” (e.g. conducting research within their organisation). The role of translating knowledge as part of the dual role was exemplified as “ we have involved healthcare staff as interpreters ”. No further details on what this actually meant were provided. Three projects described that their research team consisted of both researchers and practitioners.
Collaboration via education
Seven projects (35%) described interactive processes linked to educational activities, either designed for enhancing learning and (sustained) interaction between researchers, practitioners and their organisations, or designed for students to participate in and study development initiatives while learning together with practitioners. Some involved the development of new programmes and courses where “ experience-based education ” was essential or where networks of previous healthcare students (now as practitioners) were established as a resource. Some examples concerned the interaction between students and practitioners exemplified by statements such as “ collaboration with students concerning knowledge on improvement, using a model for learning that involves multi-professional teams with care professionals and students that together reflect on the potential improvements of the care practices ”, or the involvement of students in the development of healthcare practices exemplified by one project’s new master’s programme where conducting an improvement project in practice was a basic requirement for a master’s thesis.
Collaboration by involving patients/next-of-kin
Five projects (25%) described an active involvement of patients in the research process. One project developed mixed learning networks with both patients and their next-of-kin in an active learning process. Another project had “ engaged patients, relatives and care professionals in the work of changing care practices ” describing patients as “ co-creators, co-producers and co-evaluators ”. Two projects had developed information and communication technology solutions together with patients and one project had given patients the opportunity to conduct single randomised controlled trial (RCT) studies using their own measurements.
Challenges, obstacles encountered and the main lessons learned from the research collaborations
Seventeen projects (85%) provided detailed descriptions of problems encountered and a meta-reflection of lessons learned. The others reported no problems or none that could not be dealt with and/or interpreted the question on lessons learned as an opportunity to report on detailed project results. We could not find any patterns for the two projects reporting no problems (19 and 20). Described problems were classified into six categories and similar categories also summarise the lessons learnt, except for ‘staff-related issues’, which was mentioned only as a problem. In Fig. 3 , the number and proportion of the projects providing descriptions in these categories is presented. The most reported problem category concerned the collaborative and partnership research and development process (with practitioners) followed by issues related to the practitioners’ context and the research design and methods used. Thus, most problems described were related to the adaptation to or collaboration with practitioners and their organisations and the different agendas of and demands from the practitioners’ and researchers’ context. It was sometimes difficult to maximise the fit between the project’s agenda, the research process and the dynamic agendas and activities of the organisations and their representatives. A third of the projects reported on problems within a single context or issues related to research staff or designs. Most of the lessons learned also concerned the collaborative and partnership research process. Otherwise, lessons learned were more evenly spread, except for the staff category.

Number and proportion of projects ( n = 20) providing descriptions in the subcategories of problems encountered and lessons learned
Reported problems related to ‘the practitioner context’ concerned partner engagement, competing activities, economy, political decisions and organisational changes. Examples of problems were “ delays, organisational changes and changes in management teams that altered the initial engagement in the project ”; “ other parallel development projects have taken time for our collaborating organisations ” and “ the development unit that was to coordinate interventions within the county council was closed down ”. The major lessons learned mirrored these problems, acknowledging the anchoring, flexibility and time needed to work with the practitioners’ (politically governed) organisations. Examples of statements provided are “ county councils and universities are large organisations where change takes time and anchoring on several levels must be secured ” or “ changes in health and social care occur quickly and are difficult to foresee and improvements have to adjust to this, and to document such periods is both a challenge and an opportunity ”.
Reported problems related to ‘the researcher context’ often concerned the PhD, master or bachelor level students involved, where university demands caused delays, frustration or extra work. Examples of statements were “ writing applications to fully finance participating PhD students have taken a lot of time and energy ”, “ the full student participation was delayed and affected the project ”, and “ the choice to build a school for research studies have delayed publications ”. Learnings included the need to deal with such aspects and the demands this put on the project management and the research group, exemplified by “ the research field is young and it has been central to build networks and cooperation with others ” and “ to build research and education demands active and competent project management, not only an effective administrative management but also an overarching research perspective, and this administration and research overview is time demanding ”.
The category ‘staff-related concerns’ contained human resource management issues related to research group members (mainly researchers and PhD students) and no lessons learned related to these were recorded. Issues concerned interruptions or delays in the project process due to recruitment of staff, leave due to sickness, parental leave or other changes in work situation. Example of statements were, “ one researcher was on leave for a long-time due to sickness and this made us have to start all over again with analyses ”, “ the project leader was assigned a mission by the government ”, and “ two of the project’s PhD students went on parental leave for a total period of 3 years, which delayed the project ”.
Problems related to ‘the collaborative and partnership research and development process’ concerned the time and energy needed for the process, expectations on the practitioner organisation, and differences in focus and pace of the more rigorous scientific process compared to the quicker decision-processes in the practitioners’ contexts. Statements such as “ the interactive research process takes more time to establish ”, “ output data were supposed to be generated and provided by the county council, we had to use whatever we could find when this could not be done ”, and “ our organisational partners’ need for quick results and tendency to change work approaches towards the introduced intervention made it hard to scientifically evaluate the results ”. The lessons learned described were related to insights concerning different views, contexts and efforts to handle dilemmas. Example of statements were, “ research and practice are two systems with a different pace, demands on PhD students delay analyses and cause delays in the feedback to practitioners ”, “ practitioners sometimes have un-realistic expectations on researchers ”, and “ the importance as a researcher to always be prepared to re-evaluate, be flexible and adapt the project focus and time plan after the dynamic situation of the empirical reality studied ”. Some important actors in the researcher context made this process difficult, exemplified by “ the ethical board approving the project has demanded a clear distinction between research and improvement work ”.
Problems related to conducting ‘inter-disciplinary research’ gave examples of paradigmatic differences in perspectives, assumptions, experiences, methods and ways to report results. Examples of statements were “ PhD students struggled against time and felt fragmented and torn between their own research area and the demand for interdisciplinary research ” and “ to form such group consisting of different disciplines takes a long time and the mixed methods approach demanded a period of interactive learning for the interdisciplinary research group ”. Lessons learned related to conducting interdisciplinary research concerned insights into the process of building interdisciplinary teams and benefits of several perspectives, for example, “ interdisciplinary research is not easily or quickly established, it takes a long time for participants to build trust and understanding of each other’s perspectives and terminology, and to be attentive and responsive towards each other’s contributions ” and “ the importance of a firmly grounded theoretical framework and the creation of instructions for the research activities during an interactive process ”.
Problems connected to ‘the research focus’ were reported by one project and concerned the investigated health economic concept, which was new to the area and demanded a shift in perspective. Six projects reflected on lessons learned connected to the research focus, for example, “ internet-based support and coaching have provided coaches with increased insights into how large a disability individuals with neuropsychiatric disabilities can actually have ” and “ the care structure is a central factor for improvement and the availability of stroke units essential ”.
Problems related to the chosen ‘research design and methods’ concerned demands of specific methods and instruments, for example, “ building a computer model and the inclusion in the RCT study has taken more time than anticipated ”, “ the ethno-methodological observation method is time and resource consuming ”, and “ it was challenging to find data for follow-up studies and a lot of work studying patient journals ”. The reported lessons learned concerned the chosen approach, design or spread of interventions exemplified by the following statements: “ the meta-study has been important for synthesising and extracting knowledge ”, “ action research is an important method for gaining new knowledge and for stimulating participation in improvement initiatives ”, and “ the major lesson learned has been that the work to implement findings does not start or continue by itself, it will demand large efforts and continuing economic resources ”.
Addressing complex research areas in complex systems affects the complexity of the collaboration
The research programme was set out to address problems related to the gap between research and practice in health and social services. Several projects reported putting large efforts on addressing this broad and interdisciplinary content by trying to frame clinical and service activities within general organisational frameworks. Many projects focused on how to organise care to achieve a more research-based practice or to identify hindrances, contradictions or opportunities related to development. To study such complex phenomena over several system levels often requires longitudinal designs, interdisciplinary approaches and a mix of methods [ 55 ], in combination with participatory approaches (e.g. [ 15 ]). A large variation of research and methodological approaches, most of them very demanding, was used in the projects, from action research to quasi-experimental studies and RCT designs. Single or multiple case studies using qualitative and mixed methods were common. The use of a demanding research design and the lack of a research culture on behalf of practitioners and their organisation can act as a strong barrier for research collaboration [ 56 ].
Research use represents a specific form or knowledge utilisation [ 57 , 58 ], where research findings support decisions through a complex process enacted at a practical level. Scott-Findlay and Golden-Biddle [ 59 ] argue that understanding this process only at an individual level is misguiding and should be complemented with an understanding of practitioners’ research use at an organisational level. When making major changes in line with new research knowledge the authors propose strategies involving efforts to change organisational culture and consideration of the organisation’s values and assumptions. This indicates the need for researchers to have an in-depth understanding not only of the involved practitioners as individuals or professional groups but also of their organisations in order to enhance the use of research findings.
A majority of the projects addressed several levels of the involved healthcare organisations (or systems) implying several types of partners and stakeholders to interact with. Demands put on project management and the project group corresponded with these multidimensional views and mixed approaches – providing variable room and energy to support and adhere to demands related to collaboration and research use. The importance to understand and address the interaction and inter-connection between system levels during development efforts has been highlighted by several researchers [ 60 , 61 ]. The types of project management, research design and collaboration across the organisational system that are needed to get access, and to build, co-create and transfer knowledge in order to enhance development in organisations have been less discussed. Recently, the heterogeneity among knowledge users and the need for relationship brokering in collaborative and partnership research has been highlighted [ 38 ].
Different perceptions of interdisciplinary, collaborative and partnership research and on the roles and relationships of involved actors
Any empirical research process is characterised by interaction between the researcher and practitioner context, each one in a constant flux, continuously changing and restructuring. The research process in itself also differs depending on the type of research and focus, for example, if there is an innovative or developmental component involved to be tested and evaluated or if an on-going situation or phenomenon is investigated. Qualified practitioners, sometimes enrolled as PhD students, served as knowledge brokers interpreting results – in both directions – when understanding the practical phenomenon in theoretical terms and when translating theories and models used into practical terms. Educational fora and interactive learning approaches were a significant part of many projects, often combined with active involvement of practitioners. Involvement of patients and their next-of-kin, often during intervention design, was also described.
Based on our findings, using the terms introduced by Sibbald et al. [ 49 ], two projects could be described as having a more researcher-dominant or token partnership, while eight projects involved non-researchers to some extent in an asymmetric partnership and ten projects had features that indicated a more egalitarian partnership.
The role of the researcher varied – from being deeply and practically involved in a development process in the practitioner context, to more distant when studying the effects of different care choice models. Martin [ 44 ] listed the various roles of practitioners in research collaborations, but researchers are also able to enact different roles, depending on opportunities, preferences and the chosen research focus (explorative, descriptive, explanatory, intervention and action oriented). An ability to describe the nature of both the practitioners’ and researchers’ roles may indicate the type of interaction, participation, involvement or influence that can be expected from both parties. In Fig. 4 , the potential roles of practitioners [ 44 ] are displayed together with some suggested potential roles for researchers to enact. Indications of egalitarian partnership were identified in projects that clearly described interactive research approaches, but otherwise our data did not provide much detail on the relationships and roles. For an in-depth study of the enactment of different roles over time, situation and context would provide more information on how the researcher–practitioner relations evolve over time, both initially and in long-term partnerships.

The five types of potential roles of practitioners during a research process according to Martin [ 44 ], and some suggested potential roles for researchers to enact
Interdisciplinary research, often across faculties, was enhanced, further developed and deepened in the majority of the projects. There were several examples of clinical researchers working together with both social scientists and scientists from technical faculties. Building trust and lessons learned concerning different perspectives and ways of conducting research were important. The programme’s goals regarding the expected development of institutional learning structures and establishment of research on how to lead, manage and develop practices in health services organisations might have aided this development, more so than traditional programme calls.
Creating long-term relationships between researchers and decision-makers might be a useful way for bridging research and practice. For such a strategy to become successful it has been argued that it must be complemented with strategies for involving researchers in decision-making around policy and practice and with core funding for building and upholding capacity for knowledge exchange [ 24 ]. Maintaining such relationships for longer periods often requires formal support or structure. The national collaborative examples (e.g. practice-based research networks) described in the introduction can be one way to achieve this. Incentives for supporting and nourishing such relationships are scarce in the research context where funding is often difficult to obtain and outcomes are measured in production of scientific publications. Supporting the costs associated with research involvement (for both parts) can facilitate partnership with managers and decision-makers [ 34 ]. This is an important message to research funders, who despite tasks to increase “ research utilisation and interaction with society ”, often support short-term projects with more limited scopes – a strategy that is seen as insufficient for sustaining practitioner relationships and achieving goals of research utilisation [ 24 ].
Research collaboration between researchers and decision-makers and other types of stakeholders can be ethically challenging, especially when members of the team are insiders or participants in a studied case. The role of insiders needs to be clarified, for example, with regards to access to raw data and ensuring anonymity and confidentiality [ 62 ], but also a sensitivity on how to handle organisational information as a researcher. Hofmeyer et al. [ 62 ] recommend the use of self-reflection and ethical dialogues to enhance shared meanings and understandings among researchers and decision-makers – a practice that requires time, motivation and skills, and which could be highlighted in future programmes aiming for collaborative and partnership research.
Experienced challenges, obstacles and enablers for interdisciplinary collaborative, partnership research
There were indications of the tension between the demands from the practitioner versus the researcher contexts and the role of the researcher. Dilemmas occurred, for example, when adhering to conflicting demands for knowledge translation and the different types of knowledge production [ 63 ], such as a curiosity-driven inquiry based on a positivist epistemology or a problem-solving epistemology with knowledge production in the context of application [ 64 ].
Collaboration in the projects’ research constellations was mentioned both as an asset and a challenge, especially the interdisciplinary aspect where team members might differ in views and ways to handle collaboration. That interdisciplinary research is challenging is not a new insight (e.g. [ 65 , 66 ]) and there are strategies to facilitate such research, i.e. selective collaboration, cross-training, sustained relationships, good humour, participation in peer review, declaring the place of one’s work, and balancing dissemination of research between peer and other audiences [ 67 ]. Past experience of interdisciplinary collaborations and an understanding of different views on epistemology are foundations that can enhance collaborations. There were indications in some projects that participating researchers did gain a deepened appreciation of the need to join several paradigms in order to understand the complexities of the issues at hand. The ‘inside’ clinical PhD students could act as door openers and knowledge brokers [ 68 ] to the world and practice of health and social services for the social or technical sciences PhD students, and vice versa. Clinical researchers and PhD students were invited to new knowledge paradigms by social scientists. Other practitioners involved as co-researchers in the projects could employ various brokering strategies, e.g. to engage, collaborate and build capacity [ 43 ]. The described challenges for these persons to adhere to expectations and demands from several contexts in their in-between role and the conflicts that follow when demands are incompatible or role expectations are ambiguous have also been identified elsewhere (e.g. [ 40 , 68 ]). Previous research has shown that innovative researchers tend to be more engaged in research collaborations, both disciplinary and interdisciplinary, than adaptive researchers who prefer to work with well-established procedures within existing frameworks and in stable groups [ 69 , 70 ]. Female scientists are also more engaged in interdisciplinary research, while years of research experience has been found to be positively correlated with collaboration both within one’s own discipline and with researchers from other scientific disciplines [ 70 , 71 ].
Some of the problems and enablers experienced in the projects correspond to the enabling factors in the research partnership process as described by Sibbald et al. [ 49 ] and Rycroft-Malone et al. [ 36 ]. The described difficulties due to changes occurring in the partner organisation, role problems due to ambiguous or conflicting demands, and different view and paces for knowledge production and use between researcher and partner organisations correspond to the challenges described by Sibbald et al. [ 49 ] (Fig. (Fig.1). 1 ). Problems and lessons learned related to time needed for development of mutual trust and respect, power issues, and planning and implementing change are in line with Rycroft-Malone et al.’s [ 36 ] observations (Fig. (Fig.1). 1 ). Skilled project leaders and researchers able to handle various perspectives and enhance communication among involved actors and the establishment of infrastructures and long-term relationships, as in the sustainable collaborative structures initiated or strengthened by the projects, are all considered as enablers for research partnership [ 49 ].
Ideally, there is room for a mixture of research approaches in a programme, in line with current debates on mixed methods where Gorard et al. advocate the development of a research community where “ all methods have a role, and a key place in the full research cycle from the generation of ideas to the rigorous testing of theories for amelioration ” ([ 72 ] p. 162, [ 73 ]). Collaborative approaches are amendable to many different research topics, designs and disciplines, and the mixture of projects, research approaches and collaborations in the programme provides an example of this. It also shows the need to consider how to evaluate research applications when broader, complex issues are the topics, as also highlighted by others [ 38 ]. Assessment of the benefits and lessons learned through participating in the research process for individuals and partnership organisations, as well as of the sustainability of partnerships and joint interventions, might be a way forward.
Limitations of the study
The study mainly represents project leaders’ and senior scientists’ views on the research programme and their own project’s efforts to bridge research and practice and initiate collaborative and partnership research. No representatives of the involved practitioners were interviewed and the reporting on impact and collaboration with stakeholders was retrieved via project documents and interviews with representatives of the projects. To expand the understanding of the entire process and all actors’ perspective on the acquired knowledge, the partners’ views will need to be addressed. We also acknowledge that there might be information missing in final reports depending on the amount of text provided and how questions in the report template were interpreted, as well as the potential bias introduced by providing ‘socially accepted’ information to highlight the project’s benefits. We sought to reduce this bias by asking representatives from all projects to read through the results of analyses and comment on any missing information or misunderstandings – all projects provided answers and five of them provided additional information or corrections. Frequencies and proportions were calculated to indicate trends and overall patterns and should otherwise be interpreted with caution. Due to resources, it was no possible, but it would be interesting for future research, to address the actual impact of the collaborative and partnership projects on healthcare practices, on further collaboration, and in terms of cultural change, research use and relevance of the research conducted [ 49 ], despite the potential challenges posed by the projects’ diversity.
Using collaborative efforts to perform research on complex areas in complex systems requires a contextual understanding, longitudinal efforts, collaboration on multiple system levels and often interdisciplinary designs. Described problems, mirrored in the lessons learned, provided an indication on challenges to manage interdisciplinary, collaborative and partnership research, enact different roles and bridge several worlds as a researcher. Staffing, funding PhD students and paying attention to the work environment are some of the duties adhering to the tasks of an employer. Administrating and handling the project budget and monitoring its progress belong to the role of a project leader/administrator. Possessing knowledge on research designs and on the characteristics, demands, etc. of several disciplines is important in interdisciplinary, collaborative and partnership research. Finally, skills in collaboration and communication are needed, including a basic understanding of both the researcher and the practitioner contexts, while not forgetting any ethical concerns. Such demands and the often ambiguous roles and conflicting expectations make the research process challenging.
Funders, as well as managers, practitioners and researchers, might underestimate the complexity induced and efforts needed to collaborate during a research process, especially in multifaceted and complex research areas. Both interdisciplinary research teams and researcher–non-researcher teams can be challenging and time-consuming per se. By mixing these two conditions the situation becomes exponentially complex, as everyone has to learn about each other and adapt in various ways. The development of support from various decision-makers and build trust and understanding with involved practitioners at several levels of a healthcare system/organisation will need both skills in and arenas for communication and interaction. For the researchers, this takes time and energy from actual work with data collection, analyses and scientific writing. For the practitioners, this puts demands on understanding a research process and how it fits with ongoing organisational agendas and activities, and allocating enough time. Nevertheless, ensuring good relations (relationship brokering) is an important precondition for establishing a research process and gaining access to high quality data, especially on complex issues.
Another process that might be overlooked is the formation and building of research teams and the enactment of different roles in research intending to be both interdisciplinary and collaborative. If collaboration is not already established among researchers and involved partners, the experiences show that these processes need significant time and effort on behalf of both researchers and practitioners. Such efforts must not be underestimated if project agendas and schedules are to be realistic. The different roles and skills and the time required by researchers to both conduct research and contribute to the solving of complex problems in society by forming interdisciplinary research collaborations and collaborations with decision-makers and practitioners may be underestimated or simply ignored by involved stakeholders. Many researchers (especially PhD students) are not trained or experienced in working with interdisciplinary research teams or in a collaborative way with practitioners. Practitioners, in turn, may lack experience and skills in research collaboration. Both these aspects may have contributed to the problems encountered in this study. The lessons expressed can thus provide input for future collaborative or partnership research initiatives.
Research funders, as well as researchers and partners, may also benefit from gaining an overall understanding of the different types of research that can aid an understanding of and support changes in health and social services – from explanatory studies and experimental research to explorative studies and case study research, as in this case, which focused on understanding larger systems and more complex phenomena. Moreover, a flexibility regarding content and schedule is necessary to meet the complex demands, particularly concerning the time and resources needed for project management. To avoid exhaustive situations for involved researchers and practitioners, such considerations need to be included in the agenda of the funding body.
There is a need for more empirical studies on the conditions for researchers and practitioners in collaborative partnership and interdisciplinary research processes with the aim to increase the capabilities in addressing complex questions and the ‘usefulness’ of research in practice. An assessment of the efforts made to handle the different contexts and views of all involved actors in interdisciplinary, collaborative and partnership research initiatives in greater detail would provide more information on such processes and on their outcomes. Future studies could also address some remaining questions, including do the efforts to build interdisciplinary, collaborative and partnership research lead to better uptake and use of research outcomes, or provide more useful outcomes for practitioners and patients? Do they lead to deeper learning and understanding for researchers, and does the bilateral learning process and integrated knowledge translation between practice and academia occur?
Comments on the results of the national programme
The programme’s goals can be considered as new and innovative in the Swedish context. Further, the programme chose to fund less traditional research projects such as intervention studies, studies of natural experiments and the building of new infrastructures. This approach may be risky with regards to results evaluation, but the rich variety of projects, foci, new structures and lessons learned provided more types of results than traditional ones (i.e. scientific presentations and publications), which fits rather well with the initial broad aims of the programme. Scientific production, measured through traditional metrics, was substantial. Other presented results were categorised into five areas of innovation (what to develop) – a product/artefact, an approach when meeting patient/next-of-kin, routines and work procedures, administrative systems and structures, and increased organisational learning/competence. All projects reported results in at least two categories, and six projects reported results in all categories. Some of these were tangible, like employment of nurses in new roles, education of hundreds of care providers, new IT systems, web portals, academic courses, and a decision support used yearly in 25,000 patient meetings; some results were also very vulnerable. Quality in care processes can take long time to develop, especially when many actors and interests are involved, but might be destroyed by one major politically decided organisational change.
Additional file
Overview of the projects based on information in documents. (DOCX 19 kb)
Acknowledgements
We wish to thank the interview respondents for their participation, the research project leaders and representatives for reviewing results for potential biases or misinterpretations, and Professor John Øvretveit who provided helpful comments to improve the manuscript.
This work was mainly supported by the universities where the authors were situated (Karolinska Institutet and Jönköping University), with additional contribution from the Vinnvård research programme in Sweden 2014–15 [no grant no provided]. The Vinnvård research programme management placed no restrictions and had no influence on the research process.
Availability of data and materials
Authors’ contributions.
MN, CK, JK and BA-G designed the study, MN collected the archival data, and CK and JK conducted the interviews. MN, CK and JK performed the analyses and MN drafted the manuscript. All authors read, contributed to and approved the final manuscript.
Ethics approval and consent to participate
For the 20 investigated projects, regional Ethical Committees approved the studies according to Swedish regulations. The project documents and the Swedish report on the interview study (data used in the study) are openly displayed on the programme’s public website ( http://www.vinnvard.se ). Seeking ethical approval for this type of study is not required according to Swedish regulations. Participation in the original interview study was based on informed consent, also for open publication. For this study, the interviewed project leaders and senior researchers were given an additional opportunity to read and comment on the results of the analyses and to correct or add missing information and provide consent; they all provided answers, information and consent.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
M. E. Nyström, Email: [email protected] .
J. Karltun, Email: [email protected] .
C. Keller, Email: [email protected] .
B. Andersson Gäre, Email: [email protected] , Email: [email protected] .

Institute of Epidemiology & Health Care

Research projects
All students undertake an independent research project which culminates in a dissertation written up as a mock paper submission to the British Journal of Health Psychology . This has led to a number of projects being published. See below for further information.
Recently Published Research Projects
The following peer-reviewed publications began life as UCL MSc Health Psychology student projects:
Roche, C.; Fisher, A.; Fancourt, D.; Burton, A. Exploring Barriers and Facilitators to Physical Activity during the COVID-19 Pandemic: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19 , 9169.
McKinlay, A.R., Simon, Y.R., May, T., Fancourt, D., Burton, A. How did UK social distancing restrictions affect the lives of women experiencing intimate partner violence during the COVID-19 pandemic? A qualitative exploration of survivor views. BMC Public Health 23, 123 (2023).
Ooi L, Paul E, Burton A, Fancourt D, McKinlay AR (2023) A qualitative study of positive psychological experiences and helpful coping behaviours among young people and older adults in the UK during the COVID-19 pandemic. PLoS ONE 18(1): e0279205.
Lally, P., Miller, N., Roberts, A., Beeken, R. J., Greenfield, D. M., Potts, H. W. W., . . . Fisher, A. (2022). An app with brief behavioural support to promote physical activity after a cancer diagnosis (APPROACH): study protocol for a pilot randomised controlled trial . Pilot Feasibility Stud, 8 (1) , 74-?. doi:10.1186/s40814-022-01028-w
Gilchrist, K., & Vindrola-Padros, C. (2022). Advocating for carers: a qualitative study exploring the needs of UK carers of patients with an acoustic neuroma . International Journal of Care and Caring . doi:10.1332/239788221x16432145729095
Manby, L., Dowrick, A., Karia, A., Maio, L., Buck, C., Singleton, G., . . . Vindrola-Padros, C. (2022). Healthcare workers' perceptions and attitudes towards the UK's COVID-19 vaccination programme: A rapid qualitative appraisal . BMJ Open, 12 (2) . doi:10.1136/bmjopen-2021-051775
Vera San Juan, N., Clark, S. E., Camilleri, M., Jeans, J. P., Monkhouse, A., Chisnall, G., & Vindrola-Padros, C. (2022). Training and redeployment of healthcare workers to intensive care units (ICUs) during the COVID-19 pandemic: a systematic review . BMJ OPEN, 12 (1) , ARTN e050038. doi:10.1136/bmjopen-2021-050038
Clark, S. E., Chisnall, G., & Vindrola-Padros, C. (2022). A systematic review of de-escalation strategies for redeployed staff and repurposed facilities in COVID-19 intensive care units (ICUs) during the pandemic . eClinicalMedicine, 44 , 101286. doi:10.1016/j.eclinm.2022.101286
Perski, O., Stevens, C., West, R., Shahab, L. (2021). Pilot randomised controlled trial of the Risk Acceptance Ladder (RAL) as a tool for targeting health communications. Plos One, 16: e0259949.
Aronsen, S., Conway, R., Lally, P., Roberts, A., Croker, H., Beeken, R. J., & Fisher, A. (2021). Determinants of sleep quality in 5835 individuals living with and beyond breast, prostate, and colorectal cancer: a cross-sectional survey . Journal of Cancer Survivorship . doi:10.1007/s11764-021-01127-2
Conway, R. E., Rigler, F., Croker, H. A., Lally, P. J., Beeken, R. J., & Fisher, A. (2021). Dietary supplement use by individuals living with and beyond breast, prostate, and colorectal cancer: A cross-sectional survey . CANCER, 128 (6) , 1331-1338. doi:10.1002/cncr.34055
Taak, K., Brown, J., & Perski, O. (2021). Exploring views on alcohol consumption and digital support for alcohol reduction in UK‐based Punjabi‐Sikh men: A think aloud and interview study. Drug and alcohol review , 40 (2), 231-238.
Almeida-Meza P, Steptoe A, Cadar D. (2021). Markers of cognitive reserve and dementia incidence in the English Longitudinal Study of Ageing. Br J Psychiatry, 218 , 243-251. doi: 10.1192/bjp.2020.54.
Loeffler A, Steptoe A. (2021). Bidirectional longitudinal associations between loneliness and pain, and the role of inflammation. Pain, 162 , 930-937. doi : 10.1097/j.pain.0000000000002082.
Fortmann, J., Fisher, A., Hough, R., Gregory, A., & Pugh, G. (2021). Sleep Quality Among Teenagers and Young Adults With Canc er . Cancer Nursing . 44(1):13-19
Jackson, S.E., Farrow, E., Brown, J., Shahab, L. (2020). Is dual use of nicotine products and cigarettes associated with smoking reduction and cessation behaviours: A prospective study in England. BMJ Open, 10, e036055.
Elpers A-L, Steptoe A. (2020). Associations between dehydroepiandrosterone sulphate (DHEAS) and cognitive function in 5,061 older men and women in the English Longitudinal Study of Ageing. Psychoneuroendocrinology, 117 , 104702
Kaushal, A., Waller, J., von Wagner, C., Kummer, S., Whitaker, K., Puri, A., . . . Renzi, C. (2020). The role of chronic conditions in influencing symptom attribution and anticipated help-seeking for potential lung cancer symptoms: a vignette-based study. BJGP Open. doi:10.3399/bjgpopen20X101086
Kaushal, A., Stoffel, S. T., Kerrison, R., & von Wagner, C. (2020). Preferences for different diagnostic modalities to follow up abnormal colorectal cancer screening results: a hypothetical vignette study. BMJ Open, 10 (7), e035264. doi:10.1136/bmjopen-2019-035264
Pugh, G., Petrella, A., Pabary, A., Cross, A., Hough, R., Soanes, L., Sabiston C, Fisher, A. (2020). Health Professionals' Views on Lifestyle Advice Delivery to Teenage and Young Adult Cancer Patients: A Qualitative Study . Cancer Nursing . 45(1):e238-e245
McMichael, L., Faric, N., Newby, K., Potts, H. W. W., Hon, A., Smith, L., Steptoe A, Fisher, A. (2020). Parents of Adolescents Perspectives of Physical Activity, Gaming and Virtual Reality: Qualitative Study . JMIR Serious Games . 25;8(3):e14920 doi:10.2196/14920
Sarah E Jackson , Emily Hill , Lion Shahab , Emma Beard , Susan Michie , Jamie Brown (2019), Prevalence and correlates of long-term e-cigarette and nicotine replacement therapy use: a prospective study in England
Faric, N., Yorke, E., Varnes, L., Newby, K., Potts, H., Smith, L., Steptoe A, Fisher, A. (2019). Adolescents' perceptions and attitudes about physical activity, exergaming and virtual reality: A qualitative intervention development study . JMIR Serious Games . 7(2): e11960 doi:10.2196/11960
Newby, K., Varnes, L., Yorke, E., Meisel, S. F., & Fisher, A. (2019). Illness Risk Representation beliefs underlying adolescents' cardiovascular disease risk appraisals and the preventative role of physical activity . British Journal of Health Psychology , e12400. doi:10.1111/bjhp.12400
Smith S.G., Beard E., McGowan J.A., Fox E., Cook C., Pal R., Waller, J., Shahab, L. (2018). The development of a tool to assess beliefs about mythical causes of cancer: the Cancer Awareness Measure Mythical Causes Scale. BMJ Open 8: e022825.
Fortmann, J., Fisher, A., Hough, R., Gregory, A., & Pugh, G. (2018). Sleep Quality, Fatigue, and Quality of Life Among Teenage and Young Adult Cancer Survivors . Journal of Adolescent and Young Adult Oncology, 7 (4), 465-471. doi:10.1089/jayao.2018.0004
Smith L, Sawyer A, Gardner B, Seppala K, Ucci M, Marmot A, Lally P, Fisher A Occupational Physical Activity Habits of UK Office Workers: Cross-Sectional Data from the Active Buildings Study . International journal of environmental research and public health 15(6):09
Hackett RA, Moore, C., Steptoe A, Lassale C. (2018). Health behaviour changes after diabetes diagnosis: Findings from the English Longitudinal Study of Ageing . Scientific Reports. 8 (1), 16938
Wu J, Tombor I, Shahab L, & West R (2017) Usability testing of a smoking cessation smartphone application ('SmokeFree Baby'): A think-aloud study with pregnant smokers Digital Health Volume 3: 1-9
Agustina E, Dodd R, Waller J, & Vrinten C (2017) Understanding middle ‐ aged and older adults'first associationswith the word"cancer": A mixed methods study in England Journal of the Psychological, Social & Behavioural Dimensions of Cancer 1-7
Shahab, L., Mortimer, E., Bauld, L., McGowan, J.A., McNeill, A., Tyndale, R.F. (2017). Characterising the nicotine metabolite ratio and its association with treatment choice: A cross sectional analysis of Stop Smoking Services in England . Scientific Reports 7: 17613.
Landowska K, Waller J, Bedford H, et al (2017) Influences on university students' intention to receive recommended vaccines: a cross-sectional survey BMJ Open 2017;7:e016544. doi: 10.1136/bmjopen-2017-016544
Hollamby A, Davelaar EJ, Cadar D (2017). Increased Physical Fitness Is Associated with Higher Executive Functioning in People with Dementia. Frontiers in Public Health, doi.org/10.3389/fpubh.2017.00346
Tang MY, Shahab L, Robb KA, Gardner B (2016) Are parents more willing to vaccinate their children than themselves? Journal of Health Psychology
Jawad M, Choaie E, Brose L, Dogar O, Grant A, Jenkinson E, McEwen A, Millet C, Shahab L (2016) Waterpipe Tobacco Use in the United Kingdom: A Cross-Sectional Study among University Students and Stop Smoking Practitioners PLoS ONE 11
Puszkiewicz, P, Roberts, A L, Smith, L, Wardle, J, & Fisher, A (2016) Assessment of Cancer Survivors' Experiences of Using a Publicly Available Physical Activity Mobile Application . JMIR Cancer, 2 (1), e7
Rolfe C. & Gardner B. (2016) Experiences of hearing loss and views towards interventions to promote uptake of rehabilitation support among UK adults International Journal of Audiology 55, p. 666-673
Mansfield L, Hall J, Smith L, Rasch M, Reeves E, Dewitt S, Gardner B (2018) "Could you sit down please?" A qualitative analysis of employees' experiences of standing in normally-seated workplace meetings PLoS ONE 11
https://doi.org/10.1371/journal.pone.0198483
Gardner B, Corbridge S, McGowan L (2015) Do habits always override intentions? Pitting unhealthy snacking habits against snack-avoidance intentions BMC Psychology; 3:8
Toma A, Hamer M, Shankar A (2015) Associations between neighborhood perceptions and mental well-being among older adults Health & Place; 34: 46-53
Nelson V, Goniewiczb ML, Beard E, Brown J, Sheals K, West R, Shahab L(2015) Comparison of the characteristics of long-term users of electronic cigarettes versus nicotine replacement therapy: A cross-sectional survey of English ex-smokers and current smokers Drug and Alcohol Dependence; 153: 300-305
Bennet KF, Wagner VC, Robb KA (2015) Supplementing factual informaiton with patient narratives in the cancer screening context: A qualitative study of acceptability and preferences. Health Expectations 18 (6):2032-41
Silla K, Beard E, Shahab L (2014) Characterization of Long-Term Users of Nicotine Replacement Therapy: Evidence From a National Survey Nicotine & Tobacco Research; 16: 1050-1055
Steinmo S, Hagger-Johnson G, Shahab L (2014) Bi-directional association between mental health and physical activity in older adults: Whitehall II prospective cohort study Preventive Medicine; 66: 74-79
Gardner B, Sheals K, Wardle J, McGowan L (2014) Putting habit into practice, and practice into habit: a process evaluation and exploration of the acceptability of a habit-based dietary behaviour change intervention International Journal of Behavioral Nutrition and Physical Activity; 11:135
Richards B, McNeill A, Croghan E, Percival J, Ritchie D, McEwen A (2014) Smoking cessation education and training in UK nursing schools: A national survey Journal of Nursing Education and Practice; 4:188-198
Farič N, Potts HWW (2014) Motivations for contributing to health-related articles on Wikipedia: An interview study Journal of Medical Internet Research; 16: e260
Silla K, Beard E, Shahab L (2014). Nicotine Replacement Therapy use among smokers and ex-smokers: associated attitudes and beliefs: A qualitative study BMC Public Health; 14: 1311
Norris E, Myers L (2013) Determinants of Personal Protective Equipment (PPE) use in UK motorcyclists: Exploratory research applying an extended Theory of Planned Behaviour Accident Analysis & Prevention; 60: 219-30.
Wahlich C, Gardner B, McGowan L (2013) How, when and why do young women use nutrition information on food labels? A qualitative analysis Psychology & Health; 28: 202-216
Nadarzynski T, Waller J, Robb K.A, Marlow L.A.V (2012) Perceived risk of cervical cancer among pre-screening age women (18-24 years): the impact of information about cervical cancer risk factors and the causal role of HPV Sexually Transmitted Infections; 88: 400-6
Ghanouni A, Smith S, Halligan S, Plumb A, Boone D, Magee M, Wardle J, Von Wagner C (2011) P ublic Perceptions and preferences for CT colonography or colonoscopy in colorectal cancer screening Patient Education and Counseling; 89: 116-121
Some project titles from 2014/15:
- Randomized Controlled Trial of a smartphone App for smoking cessation, with focus on craving management - BupaQuit (Won DHP Outstanding Thesis Award)
- Parents and children's experiences of IV epoprostenol as treatment for pulmonary hypertension
- The impact of time perspective on sexual health behaviours in college students
- Testing the risk acceptance ladder (RAL) in a student population: An online evaluation
- Reducing sedentary behaviour in older adults
Some project titles from 2013/14:
- The long-term effects of e-cigarette and nicotine replacement therapy use
- Examining the links between quality of life, work productivity, physical activity and sitting time in an occupational setting
- Pre-existing cognitive dysfunction in patients with colo-rectal cancer
- Perceptions of obesity: unhealthy or just unattractive
- Can Being Mindful Help You Change Your Smoking Behaviour?
Some project titles from 2012/13:
- Why do people eat what they eat?
- Age and Time trends in Multiple Health Behaviours
- Health professionals' attitudes as a predictor of intention to recommend cervical screenings and the HPV vaccine - a questionnaire based study.
- Is inflammation driven mainly by somatic symptoms of depression in patients with heart disease?
- The impact of midlife tea and coffee consumption on cognitive decline in early old age in the Whitehall II cohort
Cookies on Be Part of Research
We use some essential cookies to make this service work.
We would like to use additional cookies to remember your settings, understand how you use Be Part of Research and improve the service.
We also use cookies set by other sites to help us deliver content via their services.
Keep up to date
Sign up for news and information about taking part and shaping research.
I'm looking for research about
- Myths about health and care research
- How research is regulated
- Frequently asked questions
- Why taking part matters
- Who can take part
- What to expect on a study
- Consenting to a study
- Supporting research without taking part in a study
Search for a study
- Register with Be Part of Research
- Information for health and care professionals
- Information for researchers
- Resources and materials
- Web developer resources
- Get in touch
What is health and care research?

Health and care research plays an important role in all our lives. It seeks to find answers about the best options to improve health and care for all of us. It is key to finding new and better ways of preventing, diagnosing, and treating disease and other health conditions.
What getting involved in research helps to achieve
Health and care research enables health professionals to find answers to important questions.
By getting involved in research, you’ll be helping make new discoveries which could one day save lives.
Health and care research allows us to:
- diagnose diseases earlier or more accurately
- provide life-changing treatments
- prevent people from developing conditions
- improve health and care for generations to come
- ensure everyone has a better quality of life
The different types of health and care research
Health research.
Sometimes health research studies may be referred to as ‘clinical trials’.
They usually compare the effects of a treatment with another to see which works best. They may involve patients (people with particular health conditions), people who are unaffected by the condition, or both.
Health research can also involve research on samples of blood or other tissues, or tests such as scans or x-rays. Researchers can also analyse information in patient records, or the data from health and lifestyle surveys.
Public health research
Public health research tackles some of the bigger health issues that affect society as a whole. For example, the impact of eating less junk food or how many steps a day are needed for good health. It also looks at the benefits, costs, acceptability and wider impact of treatments.
You can learn more by listening to our public health research podcast .
Social care research
Social care research is about improving the lives of people who receive care and support from social care services. It focuses on the evidence needed to improve people’s wellbeing and independence, protect human rights and promote equality.
Studies could be about exploring the impact of new technology in care environments. Or changing social care policies and practice.
Watch the video below to learn more about the different types of research you can take part in. Read the video transcript for different ways to take part in health and care research .
Explaining common myths about research

We want you to understand all the facts before deciding to take part in research. On our myths about research page , we correct some common misconceptions about health and care research.
Why health and care research matters
Learn more about why taking part in research matters and how your participation helps support the NHS.
The history and key achievements of health and care research
You can learn about the impact health and care research has already had on so many people’s lives by reading our history of research blog post .
We look at the first clinical trial and research’s role in the discovery of the first contraceptive pill, penicillin and aspirin.
Interested in learning more about research?
There are some key pages across this site which can help you understand more about health and care research.
Visit the links below to find out how we’re regulated, common questions, and our glossary for research jargon so that everything is easy to understand.
- How our research is regulated
Writing a research proposal
The format of a research proposal varies depending on what or who it is required by. They can vary in length, ie. be very concise or quite long and detailed. Also the headings for the different sections can vary. Therefore, this guide deals with the research proposal in its most generic form, which should be easily modifiable to fit the criteria for any research body.
The ultimate aim of any research proposal is to convince people that your research is important, has not been done before, is worthwhile and is feasible. Hence you have to make a strong argument for your research. The language used should be clear and easy to understand, as often non-experts will assess it. Some funders may, and the Research Ethics Committee application form will, want a ‘lay’ summary in addition to your basic proposal document. It is usually only in the background and methodology sections that writers tend to assume that the intended audience has a particular knowledge of their research area.
Additionally, it is crucial that different sections of your research proposal should link or follow on from each other, eg. the research question should link with the methodology. This may sound obvious, but revisions of one section can lead to mis-matches. Check this before submitting your proposal!
Typical stages in a research proposal
1. The purpose of a research proposal is:
- To help to focus on a relevant and current topic.
- To identify a gap or inadequacy in the research literature.
- To make sure that these are your ideas, and to help you to focus and crystallise your ideas.
- To help you to focus on what the actual stages involved in the research process will be, eg. the exact methodology and data analysis that will be adopted.
- To justify a proposed research project to a particular audience, eg. supervisor, departmental or faculty committee, external funding body etc.
2. Some strategies before you start:
- Search through literature for topic related articles and books, ie. search through databases/catalogues/journals etc.
- Look at what is already being done in the area i.e. existing data and research.
- Read critically, ie. look for interesting and suitable gaps – areas for research.
- Talk to your employer for approval – there is no point in starting research that you will not be allowed to complete.
- Talk to your local research and development teams. They will be able to tell you the specific criteria for any research proposal and may highlight some issues that you have overlooked.
- Talk to experts or supervisors in the field – in person, phone, letters, e-mail.
- If it is helpful, use concept maps to link ideas, and or formulate questions that the literature review should address.
3. Identifying your research question:
Any research proposal needs to have a clear research question for it to succeed. Without a clear question research will become confused and lack direction. Subsequent analysis will be difficult because the research question is key to forming your hypothesis or aims, and later analysis.
Do start by writing a question, not a statement. This will help clarify exactly what the issue is that you are trying to find a solution to. Hypotheses, aims etc can then follow from this.
Your research question should:
- Be as clear and concise as you can make it. Don’t use multi-barrelled questions if you can avoid them.
- Be informative – state your population of interest, locality etc.
- Avoid technical jargon – this is the golden rule in most areas of research proposals. Remember that your research question is what will capture the interest of the reader / assessor.
- Relate to the proposal title – often the research question is quoted as the title of the proposal.
- Relate to the aim of the research – again, the research question is often quoted as the research aim.
It should be obvious from your question alone what the project will aim to do, and on who.
4. Project title:
The title should be brief but informative. It is important that it is clear and easy to understand, and describes what your proposed research is. As previously stated, this is often the research question.
5. Abstract or summary:
This is a very important section which bears a disproportionate share of responsibility for success or failure of a proposal, as it may act as the initial ‘hook’.
It needs to be written for a wider audience, so technical vocabulary has to be limited. The abstract also needs to come quickly to the proposed research. Abstracts for grant proposals usually begin with the objective or purpose of the study, move on to methodology (procedures and design), and close with a modest but precise statement of the projects’ significance.
The significance should:
- Be about one paragraph – if it needs any longer it is advisable to rethink your research or break it down into more manageable chunks.
- Explain to the reader why the study is “significant”, in the sense of advancing general knowledge.
- Explain what the benefits to the patient / health community are.
- Encourage funding.
Although you present this first in the document, write it last so that its content accurately reflects the whole proposal.
6. Introduction:
The introduction is also written so that a more general audience can easily obtain a general idea of what the project is about, and the major concepts involved. It will also typically begin with the purpose of the proposed research. The introduction will typically be quite short, leaving the detail to the background and methodology sections.
7. Background:
It is only in the background and methodology sections that writers tend to assume that their intended audience is a specialist in their research area, and so use more technical language.
This section will include the literature review.
The purpose of a literature review is as follows:
- To become familiar with the research area and keep up to date with the current research in your area of interest.
- Identify an appropriate research question.
- Establish a theoretical framework for the research.
- Justify the need for the research.
Through the actual process of writing the literature review you, the researcher, can explore the relevant literature, formulate a problem, defend the value of the research, and compare the findings and ideas with your own. The literature review establishes a context and orientates the reader to your research topic.
The common structure of the literature review is likened to a “funnel effect”, which goes from general to more specific studies etc directly relating your intended project, ending with your research question, problem or objective.
In summary the stages of a literature review are as follows:
- General statement(s) about the field of research – the setting.
- More specific statements about the previous research.
- Statements that indicate the need for more investigation.
- Very specific statement(s) of the research question, problem or objective.
Your Trust librarians will be able to help with appropriate literature searching techniques if required.
8. Methodology:
The method or methodology section describes the steps you will follow in conducting your research. It is a very important section as assessors will scrutinise it to evaluate the feasibility and likelihood of successful completion of your proposed research.
Examine methodology sections of research articles in your research area. Arrange to discuss your research with a statistical and/or methodological specialist (Trust and other local research clinics / groups). Discuss with other researchers in your discipline the methodologies they have adopted. Consult methodology texts and statistical packages.
Overview of research:
Population/sample to be studied, including:
- How you have arrived at the sample size.
- How they will be recruited.
- Location of the research.
- Restrictions/limiting conditions.
- Sampling technique.
- Procedures.
- Analysis tools and methods.
9. Timescale:
10. Budget:
11. Ethical considerations:
- Benefits vs risks of the involvement in the project.
- Receipt of informed consent.
- Protection of participants (including data protection and storage issues).
- Privacy, minimising discomfort etc.
- Community values.
12. Dissemination strategy:
- The targets of your research eg. staff, patients, service users or carers,
- services locally and/or nationally,
- policies that drive the above services.
13. Bibliography and references:
Good luck with your project!
Useful reading: Bowling A (2002), Research Methods in Health: Investigating Health and Health Services 2Rev Ed edition, Open University Press Polgar S and Thomas SA. (4 th Edition 2004) Introduction to Research in the Health Sciences. Churchill Livingstone. MRC Good Research Practice Guidance
Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.

Research Programme for Social Care

The NIHR Research Programme for Social Care (RPSC) call is a bi-annual competition specifically for social care proposals.
The aim of RPSC is to fund research that generates evidence to increase the effectiveness of social care services, provides value for money and benefits people who need or use social care services, and carers. Research will cover both adults and children's social care.
RPSC replaced NIHR's Research for Social Care call (RfSC) in September 2023. The final RfSC call was Call 7. For further information about this, please see the relevant call documents .
Latest funding opportunities for Research Programme for Social Care
Research Programme for Social Care - Call 2
All social care funding opportunities
The Research Programme for Social Care encourages applications from researchers from all stages of their careers, and includes a sub stream for early career researchers as well as funding for capacity building.
Proposals should demonstrate appropriate research expertise, and teams should have a track record of relevant published research.
RPSC invites applications from higher education institutions, charities, local authorities/governments and relevant third sector organisations in all four nations of the UK.
What do we fund?
RPSC funds research that generates evidence to improve, expand and strengthen the way social care is provided for users of care services, carers, the social care workforce, and the public across the UK. Please read the full scope for further details.
How long and how much?
The amount awarded and the length of the funding period depends on the nature of the proposed work. Strong justification for the research duration and funding requested is required and will be considered by the reviewing committee.
RPSC also offers opportunities for early career researchers to apply for applications up to £250,000, providing they are supported by an appropriate team which is suitably resourced. These applications will be reviewed by the assessing committee but will not be in direct competition with larger awards or those from non-early career researchers.
As part of NIHR's drive to develop research capacity, RPSC is offering the opportunity to develop and advance social care research capacity building. Applicants to RPSC can include funding for research capacity development, across all stages of the academic career pathway (i.e., from internships to Masters to PhD to post-doctoral), As a general rule, it is anticipated that 10% to 20% of the overall project programme grant budget should be spent on capacity building within the grant, however each request will be reviewed on its merits. More information can be found in the capacity building guidance .
For more information, see the stage 1 finance guidance .
When is funding available?
RPSC has two researcher-led calls per year and also operates commissioned calls on priority highlight topics. See the dates for our funding competitions .
How to apply
All RPSC calls typically use a two stage application process. Please see the applicant guidance for stage 1 and application guidance for stage 2 to find out more.
Applicants considering submitting a stage 1 application may wish to submit an outline of their proposal for guidance before official submission. This can be done using the pre-submission form . This is not mandatory and purely aimed at helping potential applicants to engage with the requirements of the call (e.g. eligibility and remit).
Research proposals are submitted to RPSC online through the Research Management System. We supply Word document versions of the online application Stage 1 form and Stage 2 form , to help researchers prepare their proposal ahead of submission.
Advice and support is available from the NIHR Research Support Service to develop your research proposal.
If you are applying as a Local Authority, you can find out more information on our Local Authorities page .
If you are applying as a Charity, you can find out more information on our Charities page.
What we fund
Applications through the Research Programme for Social Care should have:
- A clear pathway to social care benefit that could be immediate or over a longer-term
- A strong link with people who need or use social care, carers and organisations which provide social care services or other relevant groups
- An appropriate team, likely consisting of social care researchers, members of the social care workforce, carers, methodologists and people who use social care, reflecting the nature of the application
We are aware that social care is broad. If you are unsure as to whether a topic is within scope for the programme, please see the call specification , contact the team or submit a pre-submission form . We also suggest consulting our logic model, to understand the intended outcomes of the programme, and consider how your topic links to this.
Our programme director
Professor Martin Knapp is Director of the Research Programme for Social Care.
Our funding committee
RPSC is a UK-wide programme open to applicants in England, Wales, Scotland and Northern Ireland. Applications are reviewed by a committee comprising social care experts, methodologists, public and practitioner members.
Committee members review all stage 1 and stage 2 applications and make funding recommendations based on the quality of applications, with support from expert peer reviewers.
The committee recommends projects for funding to the Department of Health and Social Care, which approves the projects to be funded.
Members of NIHR committees are required to declare any interests which conflict, or may be considered to conflict, with NIHR business, or may be perceived as influencing decisions made in the course of their work within NIHR programmes. All members are asked to complete the Register of Interest form (annually), which is intended to capture long term predictable interests that could be perceived to lead to conflicts of interest. These and other interests are judged on a case by case basis at individual meetings.
View our current funding committee A and funding committee B .
NIHR registry of interests
Interested in joining one of our committees? View our committee vacancies .
We offer a wide variety of assistance during all stages of the research process. If in doubt, please get in touch.
If you would like the team to comment briefly on your research plan please complete the presubmission form . If you have a query not answered in the above documents, please check the FAQs ,
Tel: 020 8843 8057 Email: [email protected] Our operating hours are 9am to 5pm.
For support to develop your research proposal contact the NIHR RSS Specialist Centre for Social Care. The RSS Specialist Centre works nationally to provide free and tailored advice to social care researchers of all levels and experience, offering a broad range of methods expertise and research support, including expert advice on public involvement and developing and delivering inclusive research that incorporates the voice of service users, carers and practitioners.
Latest news about Social Care

NIHR-funded calculator uses NHS data to predict patients’ risk of falling

Digital training programme improves quality of life for care residents with dementia

NIHR launches £10m funding programme for social care research

Health Foundation selects 23 innovative projects to improve health and social care through supporting the workforce
22 January 2019
- Quality improvement
- Innovating for Improvement
- Share on Twitter
- Share on LinkedIn
- Share on Facebook
- Share on WhatsApp
- Share by email
- Link Copy link
Twenty-three projects have been selected to receive a total of £1.65 million in funding from the Health Foundation’s Innovating for Improvement programme .
The projects address pressing issues, from staff fatigue in the NHS to meeting the needs of people addicted to non-prescription medicines bought online and prescription medicines. All aim to improve health and social care delivery and gather evidence about how their innovation leads to better outcomes for patients and staff.
This round of Innovating for Improvement reflects the Health Foundation’s commitment to supporting the health and social care workforce. Many of the projects focus on improving the physical and mental wellbeing of frontline staff, team working and relationships.
The innovative ideas will be tested across the UK, with a strong focus on primary care, community and mental health settings.
The programme will run for 15 months from January 2019. Each team will receive up to £75,000 of funding, alongside coaching and peer learning.
The selection of these projects is currently subject to contracts being finalised with the lead organisation of each project.
The 23 projects are:
1. Improving health and wellbeing using a preventative multidisciplinary approach in targeted community settings Abertawe Medical Partnership
2. Introducing telepsychiatry in Child and Adolescent Mental Health Services Aneurin Bevan University Health Board
3. Development and evaluation of an immersive, experiential learning model for re-connecting health care staff to deeper value-based work motivations Birmingham Women’s and Children’s NHS Foundation Trust
4. Changing the conversation: developing an alliancing approach to whole system transformation of health and care Cardiff and Vale University Health Board
5. ATOMIC: Addiction TO Medication: Improving Care Central and North West London NHS Foundation Trust
6. West End Wellbeing: a place-based multidisciplinary approach to meeting needs in Newcastle’s West End Changing Lives
7. Postnatal care: Developing a living library to promote a human-centred model of care Chelsea and Westminster Hospital NHS Foundation Trust
8. Shared Medical Appointments for patients with chronic pain Devon Doctors Ltd
9. A clinically designed stratification tool to develop a tier-based approach to delivery of care in general practice Dickens Place Group
10. Developing Innovative clinical pathway for women with Autism spectrum features and Eating Disorders (DIAED) King’s College London, Psychological Medicine
11. Professional wellbeing: Effective management of staff fatigue during the night shift Newcastle upon Tyne NHS Foundation Trust
12. Implementation of virtual reality preparation for anxious patients in MRI NHS Highland
13. Antenatal Care Education (ACE): improving patient and staff experience through better birth preparedness North Bristol NHS Trust
14. Creative activities to improve staff wellbeing, quality of care and the way people living with dementia and their carers support their own health Northumberland, Tyne and Wear NHS Foundation Trust
15. Engaging the workforce in real time: listening, understanding and responding to what matters most to our staff Northumbria Healthcare NHS Foundation Trust
16. Using cognitive behavioural therapy techniques to improve medicines-related consultations in cardiac health Oxford University Hospitals NHS Foundation Trust
17. Improving children’s social care staff wellbeing through reflexive peer group supervision and critical incident debrief Southampton Children and Families Social Care
18. Empowering prescribers to empower patients and fellow professionals: a novel approach to safe, person-centred practice South Eastern Health and Social Care Trust
19. Fit Families for the Future: Improving our recognition and response to children and families struggling with obesity South Eastern Health and Social Care Trust
20. Reducing opioids through supportive education Stockport NHS Foundation Trust
21. Mental Health Recovery: Supporting staff to deliver rights-respect services Tees, Esk and Wear Valley NHS Trust
22. Developing home-based Parkinson’s care University Hospitals Plymouth NHS Trust
23. Addressing the frequent use of urgent care in the paediatric population of West Kent West Kent Clinical Commissioning Group
Contact at the Health Foundation
Bryony Hirsch Marketing and Communications Officer 020 7257 2069 [email protected]
About this programme
Share this page:
You might also like...
Health Foundation @HealthFdn
- Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
The Q community
Q is an initiative connecting people with improvement expertise across the UK.
Quick links
- News and media
- Events and webinars
Hear from us
Receive the latest news and updates from the Health Foundation
- 020 7257 8000
- [email protected]
- The Health Foundation Twitter account
- The Health Foundation LinkedIn account
- The Health Foundation Facebook account
Copyright The Health Foundation 2024. Registered charity number 286967.
- Accessibility
- Anti-slavery statement
- Terms and conditions
- Privacy policy

This site uses session cookies and persistent cookies to improve the content and structure of the site.
By clicking “ Accept All Cookies ”, you agree to the storing of cookies on this device to enhance site navigation and content, analyse site usage, and assist in our marketing efforts.
By clicking ' See cookie policy ' you can review and change your cookie preferences and enable the ones you agree to.
By dismissing this banner , you are rejecting all cookies and therefore we will not store any cookies on this device.
UK Policy Framework for Health and Social Care Research
This policy framework sets out principles of good practice in the management and conduct of health and social care research in the UK.
These principles protect and promote the interests of patients, service users and the public in health and social care research, by describing ethical conduct and proportionate, assurance-based management of health and social care research, so as to support and facilitate high-quality research in the UK that has the confidence of patients, service users and the public.
It is for organisations and individuals that have responsibilities for health and social care research. This includes funders, sponsors, researchers and their employers, research sites and care providers.
The policy framework applies to health and social care research involving patients, service users or their relatives or carers. This includes research involving them indirectly, for example using information that the NHS or social care services have collected about them.
The Health Research Authority and the health departments in Northern Ireland, Scotland and Wales have developed the policy framework following public consultation . It replaces the separate Research Governance Frameworks in each UK country with a single, modern set of principles for the whole UK.
Read the policy framework
You can read the UK Framework for Health and Social Care Research in full on our website or download the UK Framework for Health and Social Care Research (PDF) .
We welcome your comments on the framework, which will help us improve future versions; and any examples of where you have used the framework as part of your work.

"I welcome publication of the UK Policy Framework for Health and Social Care Research which sets out the principles of good practice in the management and conduct of health and social care research across the UK. The Framework will ensure that the public will continue to feel safe when they take part in research and it will enable researchers to develop innovations which will help to improve the quality of health and care in the UK."
Related links
- Replacing the Research Governance Framework
- New framework for UK health and social care research launched
- UK Policy Framework for Health and Social Care Research: consultation
- Privacy notice
- Terms & conditions
- Accessibility statement
- Feedback or concerns
- Login / Register

‘These three individuals will leave very big shoes to fill’
STEVE FORD, EDITOR
- You are here: Social care
New role to boost research and education in social care nursing
28 May, 2024 By Steve Ford

A nurse has become the first to be appointed to a new academic role created to support the development of nursing in social care settings, which those behind the move have called a “milestone” for the sector.
The University of Salford and the RCN Foundation have jointly announced that Dr Claire Pryor will become the inaugural RCN Foundation chair in adult social care nursing.
“There is an absolute need to ensure our nurses working in social care settings are recognised, supported, and developed” Claire Pryor
The university said the new role had been created to take a “strategic lead in shaping research and education in adult social care nursing at a local, national and international level”.
Dr Pryor will “translate research into professional practice” to improve nursing care and develop the evidence-base to support the “current and next generation of nurses” in adult social care, it added.
She will be based at Salford’s nursing and midwifery directorate in the School of Health and Society, which is the largest specialist provider of nursing and midwifery education in the North West region.
The university noted that it was a UK focused role and Dr Pryor would work closely with England’s chief nurse for adult social care, Professor Deborah Sturdy.
Dr Pryor’s appointment represents the latest in a series of developments in recent weeks that aim to support social care nursing and raise its profile in the profession.
Earlier this month, Northumbria University launched the UK’s first new specialist practice qualification in community adult social care nursing.
In addition, guidelines were launched to encourage and support the development nationally of placements for student nurses and nursing associates in social care settings.
The government arms’-length body Skills for Care published the guidance in collaboration with Professor Sturdy and the Department of Health and Social Care.
Meanwhile, a nurse from a Bristol-based charity carried the ceremonial lamp at the annual Florence Nightingale Commemorative Service, the first to do so from the adult social care sector.
Emily Pimm, who qualified as a nurse in 2006, works as a social care deputy manager at John Wills House Care Home in Westbury-on-Trym, which is run by the St Monica Trust .
“This appointment marks a significant milestone for the nursing profession and the wider social care sector” Deepa Korea
The appointment also follows the government earlier this year embarking on a campaign to boost the domestic pipeline into adult social care nursing.
The DHSC unveiled a package of measures, backed by £75m funding, to recruit new talent to the sector , including investment in adult social care nursing apprenticeships.
Separately, higher education institutions were encouraged to expand placement opportunities in social care to encourage more nurses into such settings.
Dr Pryor will start her new role on 31 July. She is currently assistant professor of adult nursing at Northumbria, where she specialises in frailty, social care nursing and non-medical prescribing.
She began her career as a nursing assistant in care homes prior to becoming a staff nurse in medical assessment and critical care, and then a nurse practitioner for older people in mental health settings.
Commenting on her appointment, Dr Pryor said: “I am excited and passionate about the new role, and the significant impact the focus on adult social care will bring.
“There is an absolute need to ensure our nurses working in social care settings are recognised, supported, and developed throughout their careers,” she said.
“We need to work toward recognition of social care nurses as a highly skilled, autonomous clinicians, and empower them to use specialist and advanced skills, leading and shaping high quality care across the sector.”
Professor Margaret Rowe, dean of the school of health at Salford, said: “The chair role will drive changes to adult social care across the UK in terms of education, professional practice and research.
“We look forward to the benefits her role will no doubt bring to our students as we continue to develop and educate the next generation of nurses in adult social care,” she said.
The RCN Foundation said it chose the University of Salford to host the role following a competitive process.

Dr Claire Pryor
Deepa Korea, RCN Foundation director, said “We are delighted that the inaugural RCN Foundation chair in adult social care nursing has been appointed at the University of Salford.
“This appointment marks a significant milestone for the nursing profession and the wider social care sector,” she said.
“Having a dedicated chair will not only further advance the academic and practical knowledge in adult social care nursing that it so vitally needed, but also ensure that the important work of this part of the nursing workforce is highlighted.
“The role will also develop further the clinical expertise and leadership needed across the sector to meet the complex needs of those accessing social care,” she added.
The RCN Foundation, chaired by former chief nursing officer for England Professor Jane Cummings, is an independent charity whose purpose is to support and strengthen nursing and midwifery.
It does this by providing grants to nurses and midwives facing hardship or who want to enhance their skills and develop their practice, and by funding nursing and midwifery-led projects.
More stories on social care
- Social care nurse carries the Nightingale lamp at Westminster Abbey
- First specialist social care nursing qualification launched
- Next government needs to elevate social care, nurses urge
- Senior Filipino nurse championing social care nursing
- Government unveils plans to boost domestic social care workforce
- Universities urged to expand nurse placements in social care
- New guidance promotes student nurse placements in social care
- Study reveals benefits of multidisciplinary social care placements
- Add to Bookmarks
Related articles
Have your say.
Sign in or Register a new account to join the discussion.

IMAGES
VIDEO
COMMENTS
Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you've landed on this post, chances are you're looking for a healthcare-related research topic, but aren't sure where to start. Here, we'll explore a variety of healthcare-related research ideas and topic thought-starters across a ...
Browse all our research projects by topic We have funded more than 150 external research projects across a range of themes over the last five years. Browse all our research projects by topic. Copy link. Please click below to see the research projects we've funded on the following topics.
While research on integrating health and social care in the US has focused on small interventions implemented in individual clinics and hospitals and is limited by poor study quality and a focus on process measures [51,52], efforts from these broader policy initiatives have reached millions of Americans. Comprehensive evaluation, with a focus ...
Advanced Research Projects Agency for Health. From COVID-19 vaccines to cancer treatments based on immunotherapy, the U.S. has witnessed astounding medical breakthroughs in recent years. To accelerate the pace of innovation and achieve breakthroughs in treatments for diseases such as cancer, diabetes and Alzheimer's, U.S. President Joe Biden ...
The project facilitated five workshops, involving researchers from different disciplines, health, social care and community development staff and public contributors, who all had experience in co ...
Funded Projects. Since 2004, the Agency for Healthcare Research and Quality (AHRQ) Digital Healthcare Research Program has funded projects to develop an evidence base for how technology improves healthcare decision making, supports patient-centered care, and improves the quality and safety of medication management.
Health research entails systematic collection or analysis of data with the intent to develop generalizable knowledge to understand health challenges and mount an improved response to them. The full spectrum of health research spans five generic areas of activity: measuring the health problem; understanding its cause(s); elaborating solutions; translating the solutions or evidence into policy ...
Some examples of collaborative initiatives are the Partnership projects and Centres financed by the National Health and Medical Research Council in Australia, the Dutch Academic Collaborative Centres for Public Health in the Netherlands, and The Collaborations for Leadership in Applied Health Research and Care in the United Kingdom (e.g. ), as ...
The Health Foundation has selected six research projects to take part in its new £2 million Social and Economic Value of Health programme, designed to develop understanding of how people's health makes a vital contribution to society and the economy. ... This project will expand understanding of the impact that a person's physical and ...
Produced by Dr Diana Ramsey, ARC KSS Darzi Fellow (2021-2022) with insights and support from people working to deliver research in the Health and Social Care region, the Your Health and Social Care Research Quick Guide is a resource to help those working in health or social care to start or develop their research journey.. Packed with information, links and personal stories from people working ...
Some examples of collaborative initiatives are the Partnership projects and Centres financed by the National Health and Medical Research Council in Australia, the Dutch Academic Collaborative Centres for Public Health in the Netherlands, and The Collaborations for Leadership in Applied Health Research and Care in the United Kingdom (e.g. ), as ...
Health and social care research projects for educational purposes. Last updated on 3 Sep 2020. As the lockdown eases, we want to update students, supervisors and higher education institutions (HEIs) on our current position on student research and ethics review. Back in March the HRA and devolved administrations announced we had decided to stop ...
Some project titles from 2013/14: The long-term effects of e-cigarette and nicotine replacement therapy use. Examining the links between quality of life, work productivity, physical activity and sitting time in an occupational setting. Pre-existing cognitive dysfunction in patients with colo-rectal cancer. Perceptions of obesity: unhealthy or ...
The projects are focused on specific problems that have been identified: improving the quality of social care for cohorts of people that experience the worst outcomes; building a resilient, safe workforce; and understanding the lived experience of people needing social care. The project teams will help to catalyse further change in the social ...
Health and Care Research Wales has a mission to support and develop excellent research which has a positive impact on the health, wellbeing and prosperity of the people in Wales. To support this mission, excellent public involvement and engagement is necessary, and it is our intention to: improve the ways in which public involvement is embedded ...
Evidence from trials without randomisation or from single before-and-after studies, cohort, time series or matched case-controlled studies or observational studies. Evidence from well-designed descriptive studies or qualitative research. Opinions from expert committees or formal consensus methods. Expert opinion.
The authors based the design of the structured survey of activities on a review of recent reports on programs that integrated health and social care in high-income countries. 3, 6 - 8 This led ...
Health and care research enables health professionals to find answers to important questions. By getting involved in research, you'll be helping make new discoveries which could one day save lives. Health and care research allows us to: diagnose diseases earlier or more accurately. provide life-changing treatments.
Typical stages in a research proposal. 1. The purpose of a research proposal is: To help to focus on a relevant and current topic. To identify a gap or inadequacy in the research literature. To make sure that these are your ideas, and to help you to focus and crystallise your ideas.
Email: [email protected]. Our operating hours are 9am to 5pm. For support to develop your research proposal contact the NIHR RSS Specialist Centre for Social Care. The RSS Specialist Centre works nationally to provide free and tailored advice to social care researchers of all levels and experience, offering a broad range of methods expertise and ...
9.19. The HRA has a specific role to ensure the following: a) The regulation of health and social care research is proportionate, so that research that is clearly lower-risk gets processed accordingly. b) Guidance for researchers is provided by the HRA on behalf of the Devolved Administrations for UK-wide use.
Improving children's social care staff wellbeing through reflexive peer group supervision and critical incident debrief Southampton Children and Families Social Care. 18. Empowering prescribers to empower patients and fellow professionals: a novel approach to safe, person-centred practice South Eastern Health and Social Care Trust. 19.
This includes research involving them indirectly, for example using information that the NHS or social care services have collected about them. The Health Research Authority and the health departments in Northern Ireland, Scotland and Wales have developed the policy framework following public consultation. It replaces the separate Research ...
The government arms'-length body Skills for Care published the guidance in collaboration with Professor Sturdy and the Department of Health and Social Care. Meanwhile, a nurse from a Bristol-based charity carried the ceremonial lamp at the annual Florence Nightingale Commemorative Service, the first to do so from the adult social care sector.
The Health.mil is the official website of the Military Health System. The Military Health System is one of America's largest and most complex health care institutions, and the world's preeminent military health care delivery operation. Our MHS saves lives on the battlefield, combats infectious disease around the world, and is responsible for providing health services to approximately 9.6 ...