REVIEW article
Combating the covid-19 pandemic: experiences of the first wave from nepal.

- 1 Faculty of Science, Nepal Academy of Science and Technology, Lalitpur, Nepal
- 2 Nepal Environment and Development Consultant Pvt. Ltd., Kathmandu, Nepal
- 3 Central Department of Environmental Science, Institute of Science and Technology, Tribhuvan University, Kathmandu, Nepal
- 4 Nepal Development Society, Bharatpur, Nepal
- 5 Kantipur Dental College Teaching Hospital and Research Center, Kathmandu University, Kathmandu, Nepal
- 6 National Disaster Risk Reduction Centre, Kathmandu, Nepal
- 7 Little Buddha College of Health Sciences, Kathmandu, Nepal
Unprecedented and unforeseen highly infectious Coronavirus Disease 2019 (COVID-19) has become a significant public health concern for most of the countries worldwide, including Nepal, and it is spreading rapidly. Undoubtedly, every nation has taken maximum initiative measures to break the transmission chain of the virus. This review presents a retrospective analysis of the COVID-19 pandemic in Nepal, analyzing the actions taken by the Government of Nepal (GoN) to inform future decisions. Data used in this article were extracted from relevant reports and websites of the Ministry of Health and Population (MoHP) of Nepal and the WHO. As of January 22, 2021, the highest numbers of cases were reported in the megacity of the hilly region, Kathmandu district (population = 1,744,240), and Bagmati province. The cured and death rates of the disease among the tested population are ~98.00 and ~0.74%, respectively. Higher numbers of infected cases were observed in the age group 21–30, with an overall male to female death ratio of 2.33. With suggestions and recommendations from high-level coordination committees and experts, GoN has enacted several measures: promoting universal personal protection, physical distancing, localized lockdowns, travel restrictions, isolation, and selective quarantine. In addition, GoN formulated and distributed several guidelines/protocols for managing COVID-19 patients and vaccination programs. Despite robust preventive efforts by GoN, pandemic scenario in Nepal is, yet, to be controlled completely. This review could be helpful for the current and future effective outbreak preparedness, responses, and management of the pandemic situations and prepare necessary strategies, especially in countries with similar socio-cultural and economic status.

Introduction
The unanticipated outbreak of the novel coronavirus was first reported in Wuhan, China, in December 2019; it transmits from human to human via droplets and aerosol ( 1 ). The WHO declared Coronavirus Disease 2019 (COVID-19) as a Public Health Emergency of International Concern (PHEIC) on January 30, 2020, and a pandemic on March 11, 2020 ( 2 ). As a result, countries worldwide adopted various mitigative measures ( 3 , 4 ) and eradication strategies ( 5 ), aiming to reduce potentially enormous damage and reach zero cases, respectively. However, significant gaps in advance preparedness and the implementation of response plans resulted in the rapid spread of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) globally with 219 nations reporting it as of January 22, 2021 1 ( 6 ).
The Federal Democratic Republic of Nepal is a landlocked country in South Asia bordered by India in the south, east, and west, and China in the north. Its population, gross domestic product (GDP), and human development index (HDI) are 29.24 million 2 , 30.64 billion 3 , and 0.579 4 , respectively. The constitution of Nepal (2015) consists of a three-tier (federal, province, and local) governmental system. Each tier has the constitutional power to enact laws and mobilize its resources. In Nepal, the first case of COVID-19 was reported on January 23, 2020, in a 32-year-old Nepalese man who returned from Wuhan, China. Two months after the first case, the second case was diagnosed through domestic testing on March 23 in a returnee from France ( 7 ). Subsequently, the Government of Nepal (GoN) imposed early interventions approved by the WHO, including a travel ban and the Indo-Nepal and China-Nepal borders closure 5 . ( 8 ) to delay the possible onset of the detrimental effects of the outbreak across the country.
This review presents a 1-year (up to January 22, 2021) scenario of COVID-19 in Nepal, reviews the strategies employed by the GoN to control COVID-19, and provides suggestions for the prevention and control of current and future pandemics. Federal, provincial, and district-level daily cases of COVID-19 [confirmed by real-time PCR (qRT-PCR), cured, and death] in Nepal from January 23, 2020, to January 22, 2021, were obtained from the Ministry of Health and Population (MoHP), GoN 6 . Searches using the website of MoHP of Nepal, PubMed, the WHO, the worldometer official website, and Google were conducted to gather the information on the number of deaths, cured, and confirmed cases of COVID-19 and reports describing the approach taken by the government to contain COVID-19 in Nepal. The search terms included “COVID-19 in Nepal” and “Prevention and management of COVID-19 in Nepal.” Data used in this article were extracted from relevant documents and websites. The figures were constructed by using Origin 2016 and GIS 10.4.1. We did not consult any databases that are privately owned or inaccessible to the public.
Epidemic Status of COVID-19 in Nepal
The MoHP of Nepal confirmed the first and second cases of COVID-19, respectively, in January and March, in an interval of 2 months 1 ( 9 ). As of January 22, 2021, 268,948 COVID-19 positive cases were reported, with 263,546 recovered, and 1,986 death cases 6 . This data showed nearly 0.74% death and about 98% recovery rate in Nepal. The case fatality rate (CFR) was 0.5% up to March 30 in Nepal ( 9 ). The CFR in the USA, Brazil, and Russia is similar (~2%), whereas in the South Asian Association of Regional Cooperation (SAARC) countries, the CFR varied from ~0.09 to ~4.7 % ( Table 1 ). In total, 2,035,301 qRT-PCR tests were performed in Nepal, indicating about 13.47% current prevalence of COVID-19 among the qRT-PCR tested population as compared with 2.5% as of March 31, 2020 2 . As of reviewing, the prevalence of COVID-19 among the qRT-PCR tested population is higher than the neighboring countries, China (~0.055%) and India (~0.099%) ( Table 1 ). In addition, up to the third quarter of 2020, <1% of the confirmed COVID-19 cases were symptomatic across all age groups, while the proportion of symptomatic cases progressively increased beyond 55 years of age from 1.3 to 9% 7 , 8 . Unlike Nepal, higher symptomatic cases were reported from other parts of the world during the same period ( 10 ). Understandably, the scenario of the proportion of symptomatic to asymptomatic cases remains to vary between countries and care facilities. Few possible reasons for low symptomatic cases reported in the Nepalese population may be poor health-seeking behavior and utilization of tertiary health care services ( 11 ) for mild symptomatic cases, home isolation without a diagnosis, and a high rate of self-medication practices ( 12 ).
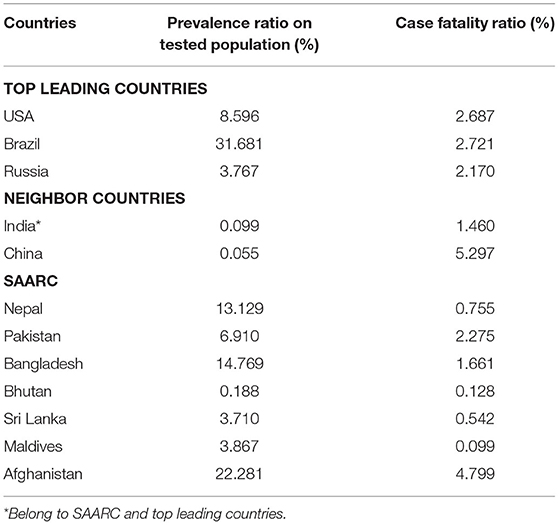
Table 1 . Prevalence and case fatality ratio (CFR) of COVID-19 of top leading countries, neighbor countries of Nepal, and SAARC as of Jan 28, 2021.
Among the provinces, Bagmati province ( n = 144,278) has the highest number of confirmed cases in Nepal, followed by province no. 1 ( n = 30,422) and Lumbini ( n = 30,308) ( Figure 1A ). As depicted in Table 2 , the confirmed cases of COVID-19 are distributed throughout the country in all the administrative districts. The total number of confirmed cases is highest in the Kathmandu district ( n = 103,523) followed by Lalitpur ( n = 16,106), Morang ( n = 13,236), and Rupandehi ( n = 9,708) districts and lowest in Manang ( n = 20), Mugu ( n = 37), Mustang ( n = 43), and Humla ( n = 44) districts ( Table 2 ).
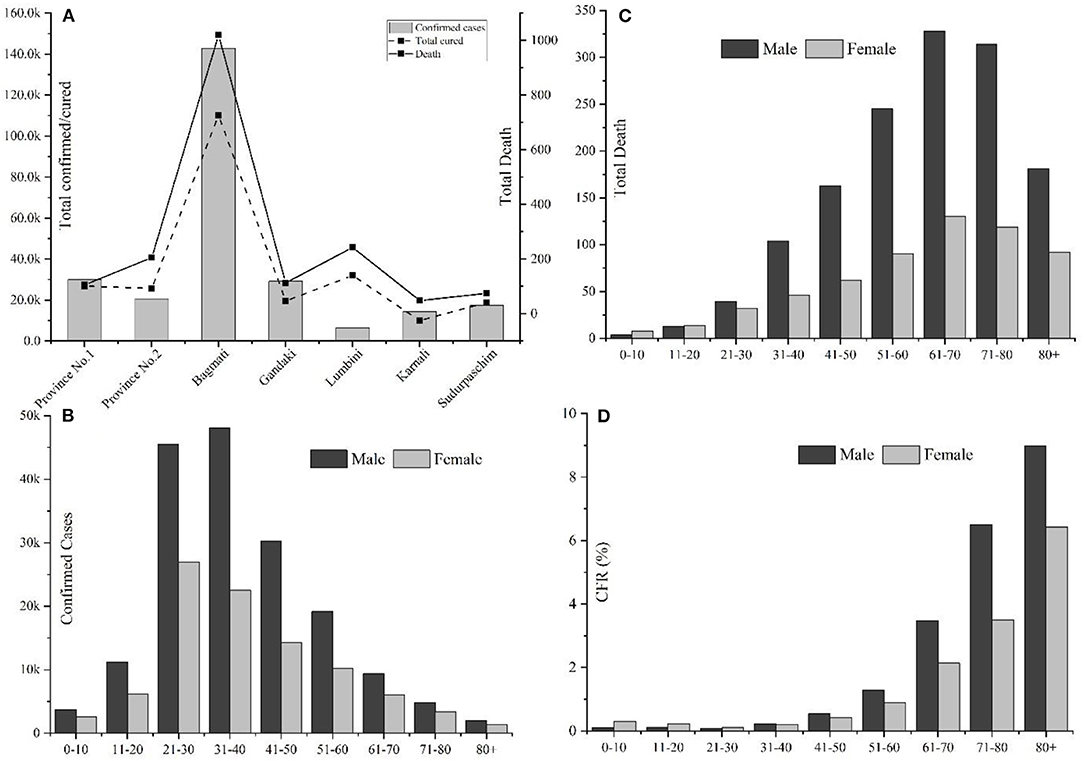
Figure 1 . Overview of COVID-19 cases in Nepal up to January 22, 2021. (A) Province-wise distribution of total confirmed cases, recovery, and deaths; (B) Gender, age-wise distribution of COVID-19 confirmed cases; (C) Gender-age wise distribution of COVID-19 death cases; and (D) Age and gender-wise case fatality rate (CFR) in Nepal.
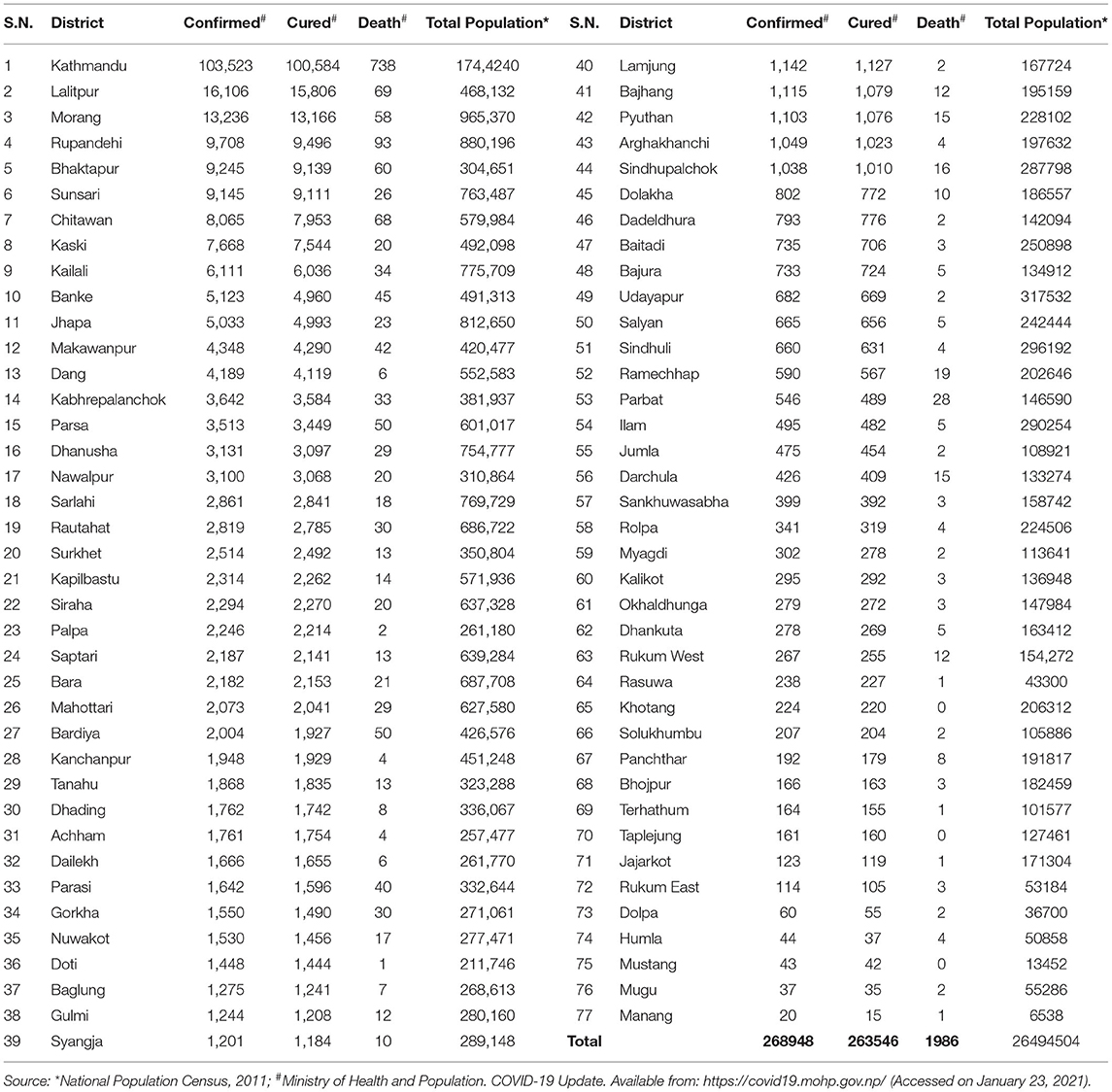
Table 2 . District wise distribution of confirmed cases, recoveries, and deaths due to COVID-19 and total population in Nepal.
Among 268,948 confirmed cases, 174,193 were males, and 94,755 were females, with a male-to-female sex ratio of 1.85. The largest number of infected cases was reported in the age group 21–30 years (26.92%, n = 72,396), followed by the age group of 31–40 years (26.26%, n = 70,648) ( Figure 1B ); however, the number of death cases was higher in the age group 61–70 (23%, n = 458) ( Figure 1C ). A higher death trend in old age is also observed in Europe, America, and Asian countries ( 13 , 14 ). Overall, male death was ~2.33 times the death rate of females. Reports have indicated that men are at greater risk of around two time of acquiring severe outcomes of COVID-19, including hospitalizations, intensive care unit (ICU) admissions, and deaths ( 15 ). The enhanced susceptibility of males for COVID-19 associated adverse events may be correlated with the hormonal and immunological differences between males and females ( 15 , 16 ). Among a total of 1,986 fatal cases (Male: n = 1,391; female: n = 595), over half ( n = 1,166) were observed in senior adults (≥60 years). One early study among the Nepalese children suggested that male children were more commonly infected than female children ( 17 ).
Among 1,986 fatal cases (mean age: 66.15 years), 623 (31.37%), 721 (36.30%), and 642 (32.32%) were with no report of comorbidities, with single comorbidities, and with multiple comorbidities, respectively. In cases with single comorbidities, the highest incidence was reported in respiratory disease ( n = 184) followed by hypertension ( n = 117), renal disease ( n = 107), diabetes ( n = 77), liver disease ( n = 44), and cardiovascular disease ( n = 36) ( Figure 2 ). Similar results are reported from other parts of the world ( 18 ). The detailed epidemiological trend analysis of COVID-19 in Nepal is shown in Figure 3 .
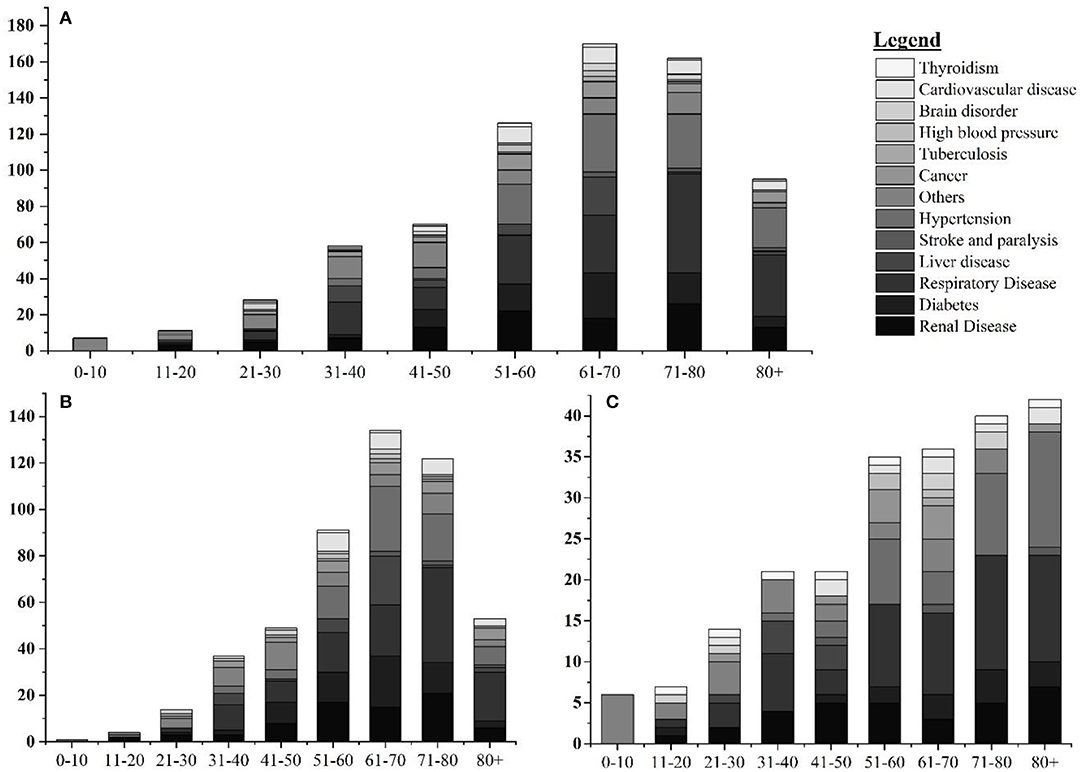
Figure 2 . Age and gender-wise distribution fatal cases with single comorbidities. (A) Age-wise distribution of leading single comorbidities among COVID-19 deaths; (B) age-wise distribution of leading single comorbidities among COVID-19 deaths in Nepal in male; and (C) age-wise distribution of leading single comorbidities among COVID-19 deaths in Nepal in female.
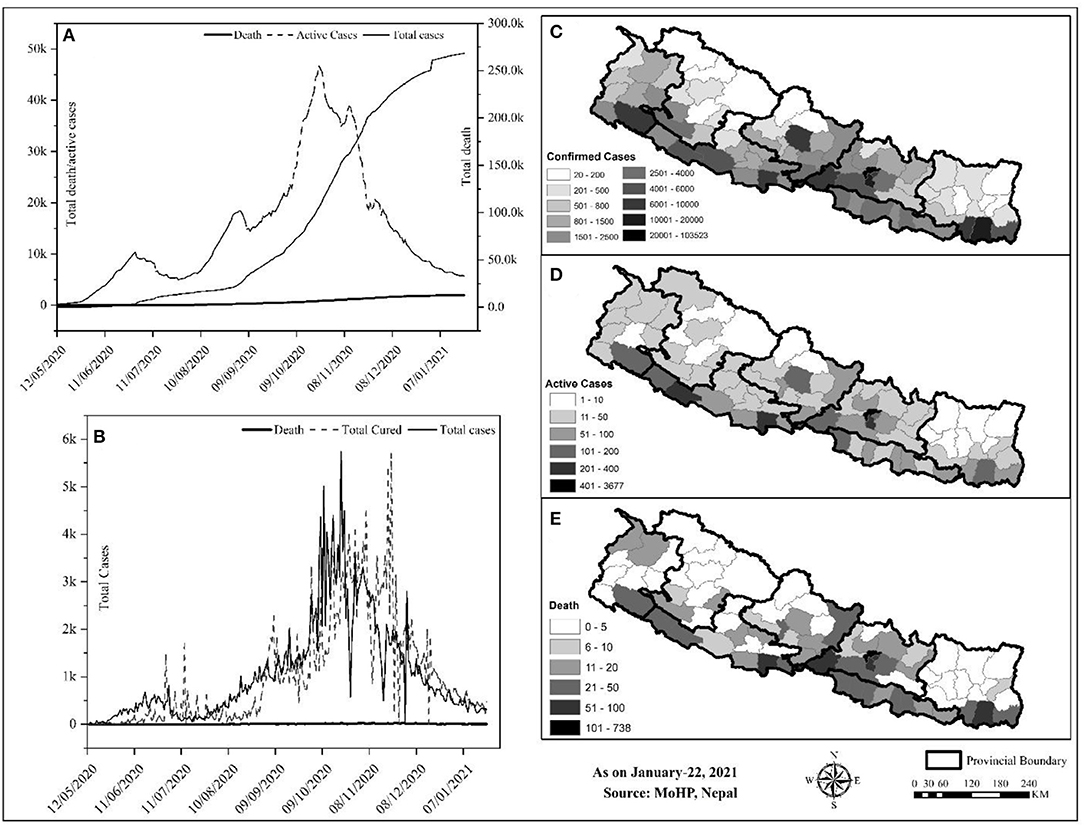
Figure 3 . Trend and spatial distribution of COVID-19 cases in Nepal. (A) Cumulative trend analysis of COVID-19 cases, (B) daily case wise trend analysis of COVID-19, (C–E) spatial distribution of infected, recovered, and death cases.
Geographically, Nepal is divided into three distinct ecological zones, mountain, hilly, and low-plain land from north to south. Politically, Nepal is divided into 7 provinces, 77 districts, and 753 local bodies. There were multiple peaks of active cases of COVID-19 in Nepal: active cases rapidly increased from early May to early July 2020, then increased slowly up to late July and increased at a higher rate again up to the end of December, and then decreased sharply ( Figure 3A ). The spatial distribution of COVID-19 confirmed cases, recovery, and deaths were compared ( Figures 3B–D ). Approximately, 64.84% of the total confirmed cases were reported from the hill regions, with single megacity Kathmandu contributing nearly half, 33.31% of lowland-plain areas, and 1.85% of Himalayan regions. The reported cases in the megacities are relatively higher than in the other regions. The higher number of cases in megacities may be correlated with dense populations in these areas ( 8 ). In the earlier months, the testing facilities and contact tracing were limited only to few districts, including the capital, Kathmandu, which gradually became available in other parts of the country. However, the testing frequency and testing facilities are still not homogeneous due to the lack of required technical resources and professional workforces ( 19 ) 9 .
The Response of Nepal Government to COVID-19
Nepal has adopted many readiness and response-related initiatives at the federal, provincial, and local government levels to fight against COVID-19. Initially, the government had set health desks and allocated spaces for quarantine purposes at the international airport and at the borders, crossing points of entry (PoE) with India and China 10 , to withstand the influx of many possible infected individuals from India and other countries. The open border and the politico-religious relationship with India and migrant workers returning from the Middle East, and other countries were a source of rapid transmission to Nepal 10 , 11 . The Nepal-China official border crossing points have remained closed since January 21, 2020. On March 24, 2020, the GoN imposed a complete “lockdown” of the country up to July 21, 2020. As part of the lockdown, businesses were closed, the restriction was imposed on movement within the country, workplaces were closed, travel was banned, and air transportation was halted 11 , 12 . In addition, for COVID-19 preparedness and response, the GoN developed a quarantine procedure and issued an international travel advisory notice. Closing the border was critical as Nepal and India share open borders across which citizens travel freely for business and work.
The GoN underestimated both the short and long-term impacts of border closure 11 . Around 2.8 million Nepali migrant workers work in India. Though the GoN discussed holding these workers in India with its Indian counterpart 13 , this plan did not materialize. Nepal has 1,690 km-long open borders with India, which could not keep migrant workers long despite the restrictions implemented by both governments 12 . As a consequence, the majority of COVID-19 cases were in the districts along the Indo-Nepal border. The decision of the government to lockdown the country from March 10, 2020, without sufficient preparation pushed daily wage laborers in urban areas to lose their jobs, and, hence, they were trapped without food or money. Ultimately, after a couple of days of lockdown, both migrant workers and daily wage laborers started walking the long way home due to the economic crisis.
As per the cabinet decision on March 25, 2020, Nepal established a COVID-19 response fund, developed a relief package 13 , and distributed relief to families in need through a “one door policy” 13 designed to reduce the COVID-19 impact; however, there were several gaps: the selection of families was unfair, GoN delayed the procurement of relief, relief packages did not include cash, and relief materials were inadequate and substandard 14 , 15 . The government has not adequately taken into account the impact of COVID-19 on the socio-economic sector. For instance, people participated in meetings, rallies, political demonstrations, and protests, where the virus could quickly spread among a large group of people. The government has, yet, to develop a stimulus package for social and economic recovery at the micro and macro levels. As the government has allocated $788 million for the health sector for the fiscal year (July–June 2020), a budget of 32% larger than the previous fiscal year, it should address the COVID-19 impact on the socio-economic front 16 . There is an opportunity to integrate all fragmented social protection schemes to strengthen socio-economic conditions and to emphasize more tremendous efforts, capacities, and resources to cope with the likely impacts of the COVID-19 pandemic 16 .
In addition, a minimal standard of quarantine as per the “Quarantine Operation and Management Protocol” (2076 B.S.) and “Standards for Home Quarantine” were imposed for all provinces 16 , 17 . The Sukraraj Infectious and Tropical Disease Hospital (SITDH) in Teku, Kathmandu, was designated by GoN as the primary hospital for COVID-19 cases along with Patan Hospital, the Armed Police Forces Hospital, in the Kathmandu Valley, followed by twenty-four hubs, and four satellite hospitals across the country 18 . Similarly, MoHP updated the National Public Health Laboratory (NPHL) capacity for confirmatory laboratory diagnosis of the COVID-19 from January 27, 2020, followed by the regional laboratory. The interim guideline for the establishing and operating of molecular laboratories for COVID-19 testing in Nepal was imposed to make uniformity in the test results 14 . Furthermore, the NPHL organized the training of trainers for laboratory staff in collaboration with the Medical Laboratory Association of Nepal 19 Ministry of Health and Population established two hotline numbers (1115 and 1133) to address public concerns, and prepared and disseminated regular press briefings, and improved its websites to channel appropriate information to the public. Besides, MoHP also conveyed decisions, notices, and situation updates periodically through its websites. Further, the Health Emergency Operation Centre (HEOC) of MoHP launched a “Viber communication group” to circulate updates on COVID-19 11, 13 . Early testing and timely contact tracing are crucial restrictive policies to control the spreading of the SARS-CoV-2 virus ( 20 , 21 ); however, in the earlier days of the pandemic, Nepal could not perform enough diagnostic tests and timely contact tracing; it resulted in a crucial time lag in identifying and isolating COVID-19 patients and caused delays in the ability of government to respond to the pandemic adequately. To alert and improve the testing and tracing response of the government, youth-led protests were carried out in different parts of the country 20 . Health Sector Emergency Response Plan was implemented in May 2020, focusing on the COVID-19 pandemic. This plan intends to prepare and strengthen the health system response capable of minimizing the adverse impact of the COVID-19 pandemic. Government of Nepal devised a comprehensive plan on March 27, 2020, for quarantining people who arrived in Nepal from COVID-19 affected countries. The GoN had initially airlifted 175 Nepalese from six cities across Hubei Province of China on February 15, 2020, followed by Middle East countries, Australia, and so on 13 .
Ministry of Health and Population engaged in developing, endorsing, improving, and disseminating contextualized technical guidelines, standard operating procedures (SOPs), tools, and training in all other critical aspects of the response to COVID-19, for instance, surveillance, case investigation, laboratory testing, contact tracing, case detection, isolation and management, infection prevention and control, empowering health and community volunteers, media communication and community engagement, rational use of personal protective equipment (PPE), requirements of drugs and equipment for case management and public health interventions, and continuity of essentials services 13 ( 15 ). The major contextualized technical guidelines, SOPs, tools, and training materials developed by GoN to respond to COVID-19 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 were listed in Table 3 .
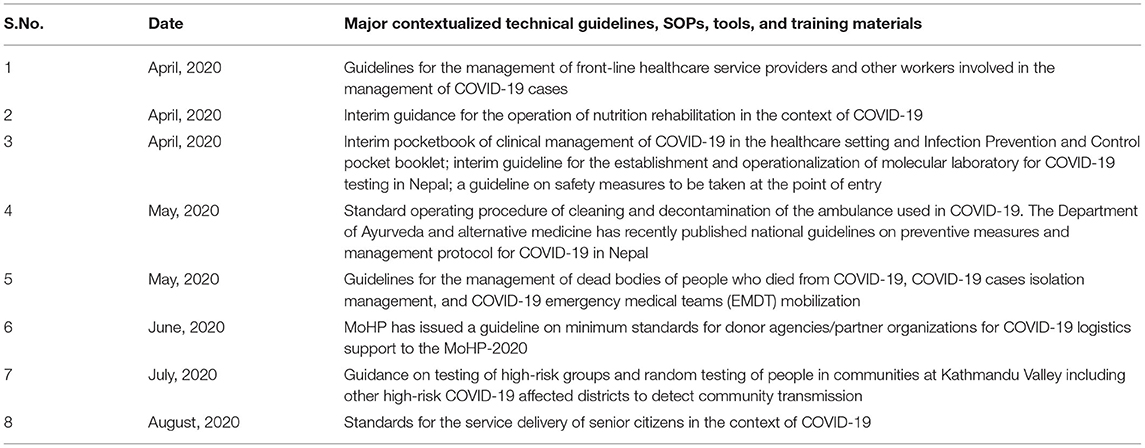
Table 3 . Major contextualized technical guidelines, standard operating protocols, tools, and training materials developed by the Government of Nepal (GoN) to respond to COVID-19.
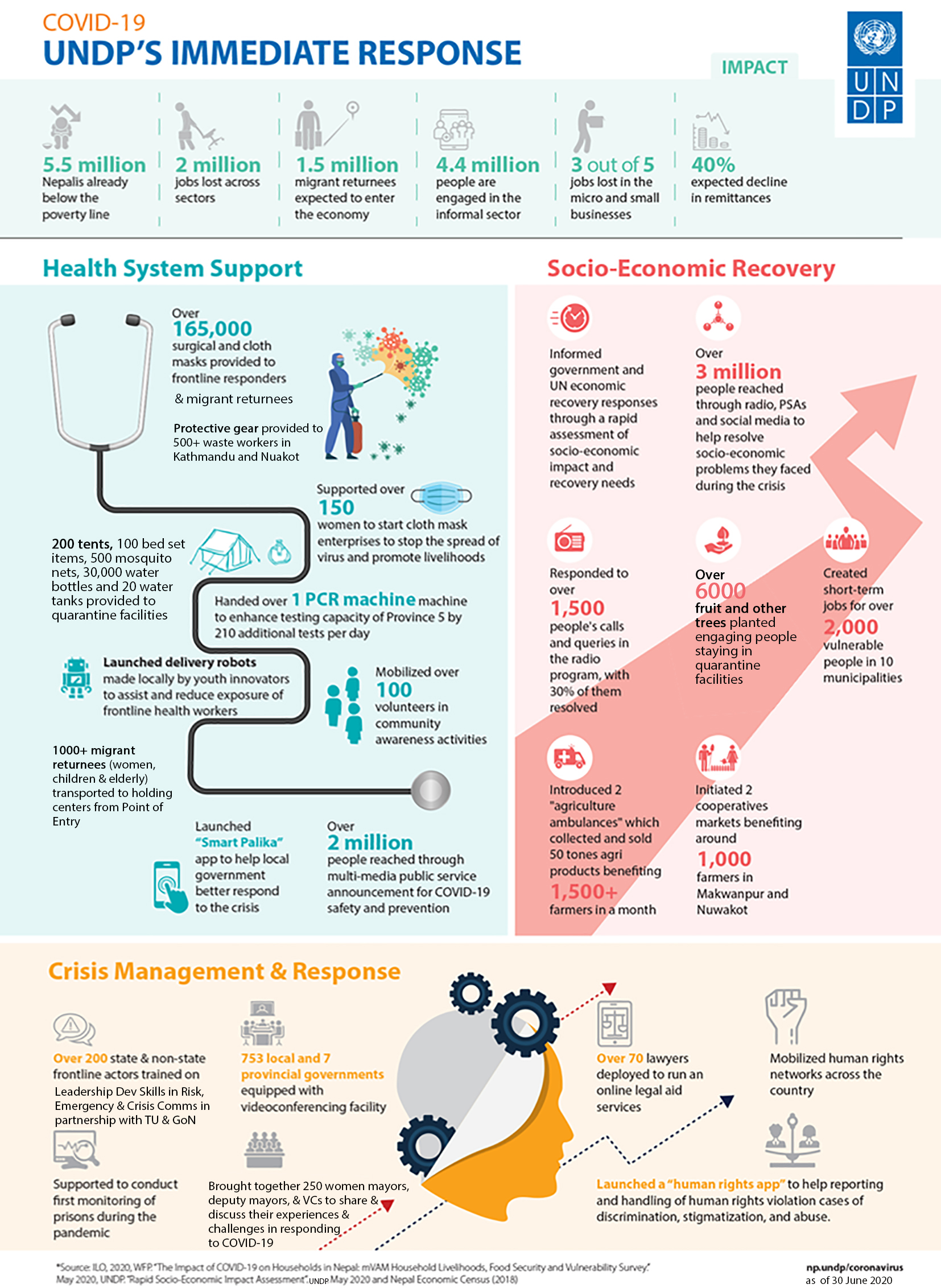
Ministry of Health and Population and supporting organizations, such as United Nations Development Program (UNDP), UNICEF, and World Vision managed crucial supplies of PPE, facemasks, gloves, and sanitizers to ensure the protection of frontline workers and supporting staffs 13 , 30 , 31 , 32 . The frontline media of the nation increased online awareness programs via the involvement of celebrities, doctors, and experts of microbiology and infectious diseases on physical distancing and the importance and use of masks and sanitizers to prevent the COVID-19 contagion. In addition, camping programs were launched by the involvement of youth volunteers of the community in central Nepal 33 .
Government of Nepal received funds from the World Bank ($29 million), the United States of America ($1.8 million), and Germany ($1.22 million) to keep people protected from COVID-19 through health systems preparedness, emergency response, and research. In addition, support from UNICEF and countries, including China, India, and the USA, in the form of emergency medical supplies and equipment were received within January 2020 to March 2020. Private companies, corporate houses, business organizations, and individuals have also contributed to the prevention, control, and treatment fund of coronavirus ($13.8 million), established by GoN to cope with COVID-19. The Prime Minister Relief Fund is also expected to be utilized. The GoN allowed international NGOs to divert 20% of their program budget to COVID-19 preparedness and response; for instance, the Social Welfare Council has allocated $226 million 31 , 33 , 34 , 35 , 36 , 37 .
The GoN has formed a committee to coordinate the preparedness and response efforts, including the MoHP, Ministry of Home Affairs, Ministry of Foreign Affairs, Ministry of Finance, Ministry of Culture, Tourism and Civil Aviation, Ministry of Urban Development, Nepal Army, Nepal Police, and Armed Police Force. The Humanitarian Country Team (HCT) includes the Red Cross Movement and civil society organizations (national and international NGOs). Under the joint leadership of the office of Resident Coordinator and the WHO, the HCT has initiated contingency planning and preparedness interventions, including the dissemination of communications materials to raise community-level awareness across the country 21 . The clusters led by the GoN and co-led by the International Astronomical Search Collaboration (IASC) cluster leads and partners are working on finalizing contingency plans, which will be consolidated into an overall joint approach with the Government and its international partners. The UN activated the provincial focal point agency system to support coordination between the international community and the GoN at the provincial level 21 .
However, despite these robust efforts implemented by GoN, few lapses existed. Examples are the following: issues of inconsistent implementation of immigration policies usually at Indo-Nepal borders 38 , 39 , 40 , shortage and misuse of crucial protective suits and other supplies in hospitals, the ease and the end of lockdown, lack of poor infrastructure facilities, and continuous spread of COVID-19 across the country ( 19 ). The GoN decided to lift the lockdown effective from July 22, 2020, completely; however, the socio-administrative and health measures with the potential for high-intensity transmission (colleges, seminars, training, workshops, cinema halls, party palaces, dance bars, swimming pools, religious places, etc.) remained closed until the following directive as of September 1, 2020. Long route bus services and domestic and international passenger flights were halted until August 1, 2020 41 . A high-level committee at the MoHP has requested all satellite hospitals (public, private, and others) to allocate 20% of their beds for COVID-19 cases. The respective hub hospitals coordinate with the HEOC and satellite hospitals to manage COVID-19 cases 42 . After lifting lockdown for 3 weeks, the federal government has given authority to local administrations to decide on restrictions and lockdown measures as COVID-19 cases continue to rise. In addition, the authority to impose necessary restrictions if COVID-19 active cases surpass the threshold of 200 was given to the Chief District Officer (CDO) 43 . Since March 2020, all the central hospitals, provincial hospitals, medical colleges, academic institutions, and hub-hospitals were designated to provide treatment care for COVID-19 cases. At this stage of operation, the major challenges for the COVID-19 response were managing quarantine facilities, lack of enough human resources, having limited laboratories for testing, and availability of limited stock of medical supplies, including PPEs 14 . To the best of our knowledge, this pandemic is the most extensive public health emergency the GoN faced in its recent history.
There is no doubt that GoN has taken major initiatives to fight the COVID-19 pandemic. The MoHP, together with associated national and international organizations are closely monitoring and evaluating the signs of outbreaks, challenges, and enforcing the plan and strategies to mitigate the possible impact; however, many challenges and difficulties, such as management of testing, hospital beds, and ventilators, quarantine centers, frontline staffs, movement of people during the lockdown, are yet to be solved 18 , 30 , 38 , 44 , 45 , 46 , 47 . Therefore, in the opinion of the authors, we recommend some steps to be implemented as soon as possible to mitigate and lessen the impacts of COVID-19 ( Table 4 ).
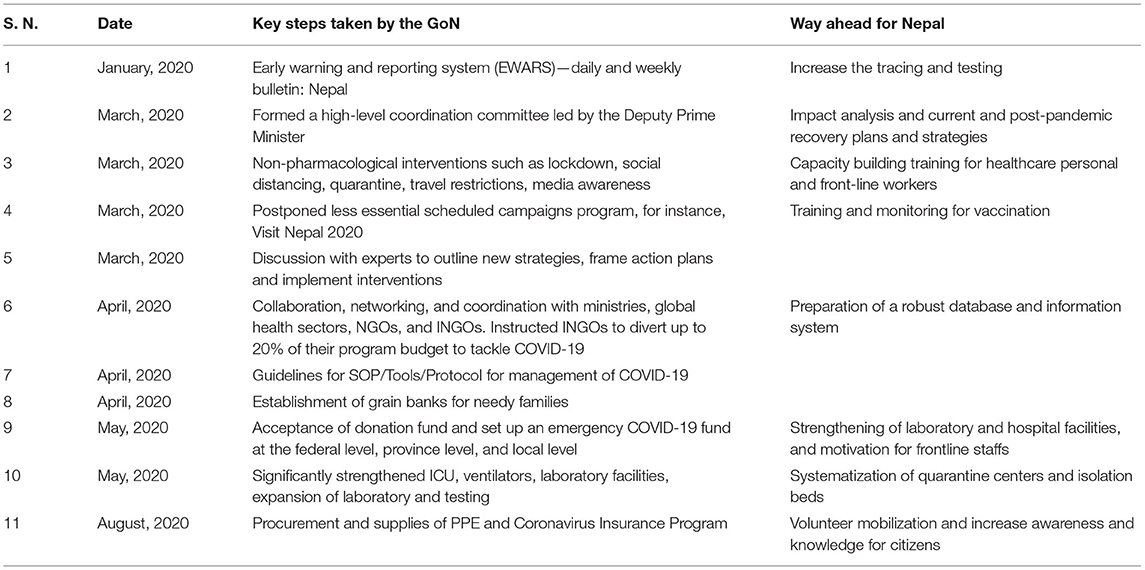
Table 4 . Major steps taken by GoN and way forward in the response to COVID-19 outbreak.
To strengthen its coordination mechanism, the government formed a team to monitor conditions and measures applied to control the outbreak; a COVID-19 coordination committee 11 to coordinate the overall response, and a COVID-19 crisis management center 14 to coordinate daily operations; however, these teams and committees did not function efficiently because roles and authorities were not delegated to ministries and government. A new institution was created, instead of using the National Disaster Risk Reduction and Management Authority (NDRRMA) 48 , which enhanced additional confusion. The MoHP is responsible for overall policy formulation, planning, organization, and coordination of the health sector at federal, provincial, district, and community levels during the COVID-19 pandemic situation. Allegedly, there is an opportunity to strengthen coordination among the tiers of governments by following protocols and guidance for effective preparedness and response. For example, some quarantine centers were so poorly run that, in turn, could potentially develop into breeding grounds for the COVID-19 transmission 15 .
Finally, this study only focuses on analyzing COVID-19 data extracted from the MoHP database for 1 year. Furthermore, we did not quantify the effectiveness of the strategies of GoN and the role of non-governmental organizations and authorities to combat COVID-19 in Nepal.
This study provides an insight into the impacts of the COVID-19 pandemic from the Nepalese context for the period of first-wave from January 2020 to January 2021. Despite the several initiatives taken by the GoN, the current scenario of COVID-19 in Nepal is yet to be controlled in terms of infections and mortality. A total of 268,948 confirmed cases and 1,986 deaths were reported in one year period. The maximum number of cases were reported from Bagmati province ( n = 144,278), all of the 77 districts were affected. The cases showing highly COVID-specific symptoms were low (<1%) in comparison with the reports across the globe ( 10 ), which may be because the average age of the Nepalese population is younger than many of the highly affected European countries. The other reasons may be differences in demographic characteristics, sampling bias, healthcare coverage, testing availability, and inconsistencies relating to the reporting of the data included in the current study. Both the number of infections and deaths are higher in males than in females. Despite the age, testing and positivity, hospital capacity and hospital admission criterion, demographics, and HDI index, the overall case fatality was reported to be less than in some other developed countries ( Table 1 ). Consistent with reports from other countries ( 22 , 23 ), the death rate is higher in the old age group ( Figure 1 ). Spatial distribution displayed the cases, which are majorly distributed in megacities compared with the other regions of the country.
Based on this assessment, in addition to the WHO COVID-19 infection prevention and control guidance 49 , some recommendations, such as massive contact tracing, improving bed capacity in health care settings and rapid test, proper management of isolation and quarantine facilities, and advocacy for vaccines, may be helpful for planning strategies and address the gaps to combat against the COVID-19. Notably, the recommendations provided could benefit the governmental bodies and concerned authorities to take the appropriate decisions and comprehensively assess the further spread of the virus and effective public health measures in the different provinces and districts in Nepal. In this review, we have summarized the ongoing experiences in reducing the spread of COVID-19 in Nepal. The Nepalese response is characterized by nationwide lockdown, social distancing, rapid response, a multi-sectoral approach in testing and tracing, and supported by a public health response. Overall, the broader applicability of these experiences is subject to combat the COVID-19 impacts in different socio-political environments within and across the country in the days to come.
Author Contributions
BB: Conceptualization, writing, and original draft preparation. KB, BB, and AG: data curation. BB, RP, TB, SD, NP, and DG: writing, review, and editing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
KB and AG were employed by Nepal Environment and Development Consultant Pvt. Ltd., in Kathmandu, Nepal.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors are grateful to the Ministry of Health and Population (MoHP), Government of Nepal, for supporting data in this research. We are thankful to the reviewers for their meticulous comments and suggestions, which helped to improve the manuscript.
1. ^ Worldometer. COVID-19 Coronavirus Pandemic . (2020). Available online at: https://www.worldometers.info/coronavirus/ (accessed January 15, 2021).
2. ^ Worldometer. Nepal Population . (2020). Available online at: https://www.worldometers.info/world-population/nepal-population/ (accessed January 15, 2021).
3. ^ Trading Economics. Nepal GDP . (2020). Available online at: https://tradingeconomics.com/nepal/gdp (accessed January 15, 2021).
4. ^ UNDP. Human Development Reports . (2020). Available online at: http://hdr.undp.org/en/countries/profiles/NPL (accessed January 15, 2021).
5. ^ World Health Organization. COVID-19 Nepal: Preparedness and Response Plan (NPRP) . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/covid-19-nepal-preparedness-and-response-plan-(nprp)-draft-april-9.pdf?sfvrsn=808a970a_2 (accessed January 15, 2021).
6. ^ Ministry of Health and Population. COVID-19 Update . (2020). Available online at: https://covid19.mohp.gov.np/ (accessed January 15, 2021).
7. ^ World Health Organization. WHO Nepal Situation Updates-19 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/19-who-nepal-sitrep-covid-19.pdf?sfvrsn=c9fe7309_2 (accessed January 15, 2021).
8. ^ World Health Organization. WHO Nepal Situation Updates-22 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/22-who-nepal-sitrep-covid-19.pdf?sfvrsn=df7c946a_2 (accessed January 15, 2021).
9. ^ World Health Organization. (2020). WHO Nepal Situation Updates-16 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/16–who-nepal–sitrep-covid-19-07082020-final.pdf?sfvrsn=53c5360f_2 (accessed January 15, 2021).
10. ^ Bhattarai, KD. South Asian Voices: COVID-19 and Nepal's Migration Crisis . Available online at: https://southasianvoices.org/covid-19-and-nepals-migration-crisis/ (accessed January 15, 2021).
11. ^ GRADA WORLD Nepal: Government announces nationwide lockdown from March 24–31/update . Available online at: https://www.garda.com/crisis24/news-alerts/326601/nepal-government-announces-nationwide-lockdown-from-march-24-31-update-4 (accessed January 15, 2021).
12. ^ Gautam D. NDRC. Nepal's Readiness and Response to COVID-19 . (2020). Available online at: https://www.preventionweb.net/files/71274_71274nepalsreadinessandresponsetopa.pdf (accessed January 15, 2021).
13. ^ Building Back Better (BBB) from COVID-19: World Vision Policy Brief on Building Back Better from COVID-19 . (2020). Available online at: https://www.wvi.org/sites/default/files/202005/World%20Vision%20Policy%20Brief%20on%20Building%20Back%20Better_25%20May%202020.pdf (accessed January 15, 2021).
14. ^ World Health Organization. WHO Nepal Situation Updates-1 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/who-nepal–sitrep-covid-19-20apr2020.pdf?sfvrsn=c788bf96_2 (accessed January 15, 2021).
15. ^ GoN MoHP. Health Sector Emergency Response Plan COVID-19 Pandemic 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/health-sector-emergency-response-plan-covid-19-endorsed-may-2020.pdf?sfvrsn=ef831f44_2 (accessed January 15, 2021).
16. ^ Gautam, D. The COVID-19 Crisis in Nepal: Coping Crackdown Challenges. National Disaster Risk Reduction Centre, Kathmandu, Nepal. Issue 3, 2020 . Available online at: https://www.alnap.org/help-library/the-covid-19-crisis-in-nepal-coping-crackdown-challenges (accessed January 30, 2021).
17. ^ Gautam, D. Fear of COVID-19 Overshadowing Climate-Induced Disaster Risk Management . Available online at: https://www.spotlightnepal.com/2020/05/08/fear-covid-19-overshadowing-climate-induced-disaster-risk-management/ (accessed January 30, 2021).
18. ^ Pradhan TR. The Kathmandu Post. Nepal Goes Under Lockdown for a Week Starting 6am Tuesday . Available online at: https://kathmandupost.com/national/2020/03/23/nepal-goes-under-lockdown-for-a-week-starting-6am-tuesday (accessed January 30, 2021).
19. ^ World Health Organization. WHO Nepal Situation Updates-3 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/who-nepal–situpdate-3-covid-19-06052020.pdf?sfvrsn=714d14c4_2 (accessed January 30, 2021).
20. ^ Jha IC. The Rising Nepal. MoHP Sets Forth Standards for Home Quarantine . Available online at: https://risingnepaldaily.com/featured/mohp-sets-forth-standards-for-home-quarantine (accessed January 30, 2021).
21. ^ The Kathmandu Post. Youth-Led Protests Against the Government's Handling of Covid-19 Spread to Major Cities . (2020). Available online at: https://kathmandupost.com/national/2020/06/12/youth-led-protests-against-the-government-s-handling-of-covid-19-spread-to-major-cities (accessed January 30, 2021).
22. ^ World Health Organization. WHO Nepal Situation Updates-2 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/who-nepal–sitrep-covid-19-29apr2020.pdf?sfvrsn=dac001bf_2 (accessed January 30, 2021).
23. ^ World Health Organization. WHO Nepal Situation Updates-4 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/who-nepal–situpdate-4-13052020.pdf?sfvrsn=630b68ea_6 (accessed January 30, 2021).
24. ^ World Health Organization. WHO Nepal Situation Updates-18 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/18-who-nepal-sitrep-covid-19-23082020.pdf?sfvrsn=6fb20500_2 (accessed February 5, 2021).
25. ^ World Health Organization. WHO Nepal Situation Updates-5 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/5-who-nepal–situpdate-covid-19-20052020-final.pdf?sfvrsn=7552c8ba_4 (accessed February 5, 2021).
26. ^ World Health Organization. WHO Nepal Situation Updates-7 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/7-who-nepal–situpdate-covid-19-03062020-final.pdf?sfvrsn=87f582d6_2 (accessed February 5, 2021).
27. ^ World Health Organization. WHO Nepal Situation Updates-8 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/8-who-nepal–situpdate-covid-19.pdf?sfvrsn=ce5ecb07_2 (accessed February 5, 2021).
28. ^ World Health Organization. WHO Nepal Situation Updates-10 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/10-who-nepal–situpdate-covid-19-24062020.pdf?sfvrsn=c7f99a61_8 (accessed February 5, 2021).
29. ^ World Health Organization. WHO Nepal Situation Updates-13 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/13–who-nepal–situpdate-covid-19-17072020-v4.pdf?sfvrsn=fc0f19cc_2 (accessed February 5, 2021).
30. ^ World Health Organization. WHO Nepal Situation Updates-17 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/17-who-nepal-sitrep-covid-19-15082020.pdf?sfvrsn=68a53b32_2 (accessed February 10, 2021).
31. ^ UN. Nepal Information Platform, COVID-19 Nepal: Preparedness and Response Plan . Available online at: http://un.org.np/reports/covid-19-nepal-preparedness-and-response-plan (accessed February 10, 2021).
32. ^ UNICEF for Every Child, Supporting COVID-19 Readiness and Response in the West of Nepal . Available online at: https://www.unicef.org/nepal/stories/supporting-covid-19-readiness-and-response-west-nepal (accessed February 10, 2021).
33. ^ UNDP. Enhancing Public Awareness on COVID-19 Through Communications . Available online at: https://www.np.undp.org/content/nepal/en/home/presscenter/articles/2020/Enhancing-public-awareness-of-COVID-19-through-communications.html (accessed February 10, 2021).
34. ^ The World Bank. The Government of Nepal and the World Bank sign $29 Million Financing Agreement for Nepal's COVID-19 (Coronavirus) Response . Available online at: https://www.worldbank.org/en/news/press-release/2020/04/03/world-bank-fast-tracks-29-million-for-nepal-covid-19-coronavirus-response (accessed February 10, 2021).
35. ^ Khatri PP. The Rising Nepal. Govt Receives Over Rs 1.59 Bln In Anti-COVID-19 Fund . Available online at: https://risingnepaldaily.com/main-news/govt-receives-over-rs-159-bln-in-anti-covid-19-fund (accessed February 10, 2021).
36. ^ Dahal A. Govt Does U-Turn to Let NGOs Hand Out Medical Supplies, Food, Cash directly . Available online at: https://myrepublica.nagariknetwork.com/news/govt-does-u-turn-to-let-ingos-hand-out-medical-supplies-food-cash-directly/ (accessed February 10, 2021).
37. ^ Rijal A. The Rising Nepal. China Gives Anti-Corona Medical Aid . Available online at: https://risingnepaldaily.com/main-news/china-gives-anti-corona-medical-aid (accessed February 10, 2021).
38. ^ Nepali Sansar. Nepal Receives 23 Tons ‘COVID-19 Medical Equip' As Gifts from India . (2020). Available online at: https://www.nepalisansar.com/coronavirus/nepal-receives-23-tons-covid-19-medical-equip-as-gifts-from-india/ (accessed February 10, 2021).
39. ^ Koirala S, Bhattarai, S. My Republica. Protect Frontline Healthcare Workers . Available online at: https://myrepublica.nagariknetwork.com/news/protect-frontline-healthcare-workers/ (accessed February 10, 2021).
40. ^ Halder R. Lockdowns and national borders: How to manage the Nepal-India border crossing during COVID-19 . Available online at: https://blogs.lse.ac.uk/southasia/2020/05/19/lockdowns-and-national-borders-how-to-manage-the-nepal-india-border-crossing-during-covid-19/ (accessed February 10, 2021).
41. ^ Raturi K. How Is Nepal Tackling COVID Crisis & Reverse Migration of Workers? Available online at: https://www.thequint.com/voices/opinion/india-nepal-border-coronavirus-pandemic-migrant-workers-exodus-reverse-migration-unemployment (accessed February 10, 2021).
42. ^ World Health Organization. WHO Nepal Situation Updates-14 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/14–who-nepal–sitrep-covid-19-26072020.pdf?sfvrsn=65868c9e_2 (accessed February 10, 2021).
43. ^ World Health Organization. WHO Nepal Situation Updates-19 on COVID-19, 2020 . (2020). Available online at: https://www.who.int/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/19-who-nepal-sitrep-covid-19.pdf?sfvrsn=c9fe7309_2 (accessed February 10, 2021).
44. ^ Prasain S, Pradhan TR. The Kathmandu Post . Available online at: https://kathmandupost.com/politics/2020/08/12/nepal-braces-for-a-return-to-locked-down-life-as-rise-in-covid-19-cases-rings-alarm-bells (accessed February 10, 2021).
45. ^ NHPL. Information regarding Novel Corona Virus . (2020). Available online at: https://www.nphl.gov.np/page/ncov-related-lab-information (accessed February 10, 2021).
46. ^ NHRC. Assessment of Health-related Country Preparedness and Readiness of Nepal for Responding to COVID-19 Pandemic Preparedness and Readiness of Government of Nepal Designated COVID Hospitals . (2020). Available online at: http://nhrc.gov.np/wp-content/uploads/2020/06/Fact-sheet-Preparedness-and-Readiness-of-Government-of-Nepal-Designated-COVID-Hospitals.pdf (accessed February 10, 2021).
47. ^ Koirala S. Comprehensive response to COVID 19 in Nepal . Available online at: https://en.setopati.com/blog/152612 (accessed February 10, 2021).
48. ^ National Disaster Risk Reduction and Management Authority, Ministry of Home Affairs, Government of Nepal . Available online at: https://covid19.ndrrma.gov.np/ (accessed February 10, 2021).
49. ^ World Health Organization. Infection Prevention and Control Guidance - (COVID-19) . (2021). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed February 10, 2021).
1. Jayaweera M, Perera H, Gunawardana B, Manatunge J. Transmission of COVID-19 virus by droplets and aerosols: a critical review on the unresolved dichotomy. Environ Res. (2020) 188:109819. doi: 10.1016/j.envres.2020.109819
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Zheng J. SARS-CoV-2: an emerging coronavirus that causes a global threat. Int J Biol Sci. (2020) 16:1678–85. doi: 10.7150/ijbs.45053
3. Islam N, Sharp SJ, Chowell G. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. (2020) 370:27–43. doi: 10.1136/bmj.m2743
4. Gupta A, Singla M, Bhatia H, Sharma V. Lockdown-the only solution to defeat COVID-19. Int J Diabetes Dev Ctries. (2020) 6:1–2. doi: 10.1007/s13410-020-00826-3
CrossRef Full Text | Google Scholar
5. Lu G, Razum O, Jahn A, Zhang Y, Sutton B, Sridhar D, et al. COVID-19 in Germany and China: mitigation versus elimination strategy. Glob. Health Action . (2021). 14:1875601. doi: 10.1080/16549716.2021.1875601
6. The Lancet. COVID-19: too little, too late. Lancet . (2020) 395:P755. doi: 10.1016/S0140-6736(20)30522-5
7. Bastola A, Sah R, Rodriguez-Morales AJ, Lal BK, Jha R, Ojha HC, et al. The first 2019 novel coronavirus case in Nepal. Lancet Infect Dis. (2020) 20:279–80. doi: 10.1016/s1473-3099(20)30067-0
8. Dhakal S, Karki S. Early epidemiological features of COVID-19 in Nepal and public health response. Front. Med. (2020) 7:524. doi: 10.3389/fmed.2020.00524
9. Panthee B, Dhungana S, Panthee N, Paudel A, Gyawali S, Panthee S. COVID-19: the current situation in Nepal. New Microbes New Infect. (2020) 37:100737. doi: 10.1016/j.nmni.2020.100737
10. Oran DP, Topol EJ. The proportion of SARS-CoV-2 infections that are asymptomatic: a systematic review. Ann Intern Med. (2021) 174:655–62. doi: 10.7326/M20-6976
11. Bhattarai S, Parajuli SB, Rayamajhi RB, Paudel IS, Jha N. Clinical health seeking behavior and utilization of health care services in eastern hilly region of Nepal. J Coll Med. Sci Nepal . (2015). 11:8–16. doi: 10.3126/jcmsn.v11i2.13669
12. Paudel S, Aryal B. Exploration of self-medication practice in Pokhara valley of Nepal. BMC Public Health. (2020) 20:714. doi: 10.1186/s12889-020-08860-w
13. Ioannidis JPA, Axfors C. Contopoulos-Ioannidis DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res . (2020) 188:109890. doi: 10.1016/j.envres.2020.109890
14. Cortis D. On determining the age distribution of COVID-19 pandemic. Front. Publ. Health. (2020) 8:202. doi: 10.3389/fpubh.2020.00202
15. Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. (2020) 11:29. doi: 10.1186/s13293-020-00304-9
16. Sharma G, Volgman AS, Michos ED. Sex differences in mortality from COVID-19 pandemic: are men vulnerable and women protected? JACC Case Rep. (2020) 2:1407–10. doi: 10.1016/j.jaccas.2020.04.027
17. Sharma AK, Chapagain RH, Bista KP, Bohara R, Chand B, Chaudhary NK, et al. Epidemiological and clinical profile of COVID-19 in Nepali children: an initial experience. J Nepal Paediatr Soc. (2020) 40:202–9. doi: 10.3126/jnps.v40i3.32438
18. Piryani RM, Piryani S, Shah JN. Nepal's response to contain COVID-19 infection. J Nepal Health Res Counc. (2020) 18:128–34. doi: 10.33314/jnhrc.v18i1.2608
19. Rayamajhee B, Pokhrel A, Syangtan G. How well the government of nepal is responding to COVID-19? An experience from a resource-limited country to confront unprecedented pandemic. Front Public Health. (2021) 9:597808. doi: 10.3389/fpubh.2021.597808
20. Kretzschmar ME, Rozhnova G, Bootsma MC, van Boven M, van de Wijgert JH, Bonten MJ. Impact of delays on effectiveness of contact tracing strategies for COVID-19: a modelling study. Lancet Public Health. (2020) 5:e452–9. doi: 10.1016/S2468-2667(20)30157-221
21. Contreras S, Biron-Lattes JP, Villavicencio HA, Medina-Ortiz D, Llanovarced-Kawles N, Olivera-Nappa Á. Statistically-based methodology for revealing real contagion trends and correcting delay-induced errors in the assessment of COVID-19 pandemic. Chaos Solit Fract . (2020). 139:110087. doi: 10.1016/j.chaos.2020.110087
22. Levin AT, Hanage WP, Owusu-Boaitey N, Cochran KB, Walsh SP, Meyerowitz-Katz G. Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. (2020) 35:1123–38. doi: 10.1007/s10654-020-00698-1
23. O'Driscoll M, Dos Santos GR, Wang L, Cummings DA, Azman AS, Paireau J, et al. Age-specific mortality and immunity patterns of SARS-CoV-2. Nature . (2021). 590:140–5. doi: 10.1038/s41586-020-2918-0
Keywords: COVID-19, pandemic, preparedness, response, spatial distribution, public health, Nepal
Citation: Basnet BB, Bishwakarma K, Pant RR, Dhakal S, Pandey N, Gautam D, Ghimire A and Basnet TB (2021) Combating the COVID-19 Pandemic: Experiences of the First Wave From Nepal. Front. Public Health 9:613402. doi: 10.3389/fpubh.2021.613402
Received: 05 October 2020; Accepted: 11 June 2021; Published: 12 July 2021.
Reviewed by:
Copyright © 2021 Basnet, Bishwakarma, Pant, Dhakal, Pandey, Gautam, Ghimire and Basnet. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Til Bahadur Basnet, ddst19basnet@hotmail.com
† These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- GET INVOLVED
COVID-19 pandemic
Covid-19 pandemic response.
Humanity needs leadership and solidarity to defeat the coronavirus
The coronavirus COVID-19 pandemic is the defining global health crisis of our time and the greatest challenge we have faced since World War Two. Since its emergence in Asia late last year, the virus has spread to most of the countries.
Nepal, a landlocked country aspiring to graduate from a Least Developed Country status, stands highly vulnerable to the unfolding COVID-19 pandemic. Heedful of its vulnerabilities, the Government of Nepal has enforced a nationwide lockdown and activated its federal, provincial and local level mechanisms to respond to the crisis. While there is an urgent need to strengthen the existing health system to handle the situation in case of any sudden surge of outbreak, standardize the quarantine facilities and provide immediate relief to the most-affected, equally important is to help the country mitigate the socio-economic impacts and prepare for a longer-term recovery.
The secondary impact of the global pandemic is huge and it is already taking a serious toll on an economy that relies heavily on remittances, imports fueled by remittances, informal labor, and tourism revenues.
UNDP is working with the Government of Nepal and the UN Country Team to support the country's preparedness to face the mounting public health emergency, respond to the socio-economic impact of the protracted lockdown on the most vulnerable, and support longer-term recovery measures.
The fact that Nepal’s economy is largely dependent on remittance (25% of GDP), tourism (8% of GDP), agriculture (26% of GDP) and imports of essential items and supplies from outside has made the poor households and the often unskilled workers, including returnee migrants, particularly vulnerable to income losses.
Given that most of these people are outside the official social safety net, they are likely to bear the brunt of the sudden halt or slowdown of economic activities in Nepal.
UNDP response
As part of the UN family and in close coordination with the World Health Organization (WHO), UNDP is responding to requests from national and sub-national governments to help them prepare for, respond to and recover from the COVID-19 pandemic, focusing particularly on the most vulnerable and where they are found. While needs assessments are being drawn, our short and medium-term response will mainly translate in activities that focus on the three major areas: Health System Suppor, Socio-economic Recovery and Crisis Management and Response .
“We are already hard at work, together with our UN family and other partners, on three immediate priorities : supporting the health response including the procurement and supply of essential health products, under WHO’s leadership, strengthening crisis management and response, and addressing critical social and economic impacts.” UNDP Administrator, Achim Steiner
Health system support
Complementing the work of the specialized agencies to bolster health systems management and capacity, UNDP is supporting the provincial and local governments to strengthen their health systems , including by providing much-needed medical supplies, assessment of quarantine facilities and public awareness on COVID-19. The major activites are as follows:
- Enhancing public awareness on COVID19 thorugh communications (PSAs , Community level activities)
- Management of quarantine facilities through monitoring and assessment and logistics support
- Strengthening health support system
- Launched delivery robots to help frontline healthworkers

UNDP provides 400 oxygen concentrators to Nepal on June 11 2021
Socio-Economic Recovery
UNDP is using its extensive experience of working on early recovery, livelihood support and job creation by mobilizing cooperatives, developing enterprises and community infrastructures. Some of the key activites are as follows:
- Rapid assessment of socio-economic impact and recovery needs
- Short-term employment programme and livelihood recovery for the most vulnerable
- Support to local farmers for supply and delivery of their produces
- Green initiatives supporting livelihood
- Promoting women entreprenuers in local mask making

Women in Pokhara are on the frontline of mask production during the COVID-19 pandemic. This has helped address the problems of shortage and possible black marketing of masks, while also giving them a decent living amidst the crisis.
Crisis management and response
UNDP will also focus on enhancing crisis response and management capacities at the sub-national level, which include communication support and skill transfer to provincial governments and municipalities. Here are some of the key activites:
- Support the overall UN wide Preparedness and Response Plan and co-lead the Socio-Economic Recovery Cluster
- Communications support to provincial and local governments
- Live phone-in radio program aimed at helping connect people with government authorities and inform policies
- Crisis Communications training to representatives of local governments and other actors

Radio journalists at work. The Association of Community Radio Broadcasters (ACORAB) in Nepal and Community Information Network (CIN), with the support of UNDP, have launched a live phone-in radio program, which aims to help local governments address socio-economic issues/problems faced by the vulnerable people during the COVID-19 lockdown. Photo: CIN
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Twin crises in Nepal:...
Twin crises in Nepal: covid-19 and climate change
- Related content
- Peer review
- Basu Dev Pandey , doctor and professor 1 2 ,
- Kouichi Morita , professor 3 ,
- Anthony Costello , professor of global health and sustainable development 4
- 1 Everest International Clinic and Research Center, Kathmandu, Nepal,
- 2 Department of Molecular Epidemiology, Institute of Tropical Medicine, Nagasaki University, Japan
- 3 Department of Virology, Institute of Tropical Medicine, Nagasaki University, Japan
- 4 University College London, UK
Nepal has been on the frontline of both the covid-19 pandemic and climate change, and in both crises the response by the international community and Nepal’s government has been marked by a failure to prepare or to invest proactively in strong prevention measures.
The first case of covid-19 in Nepal was reported in January 2020 and the country’s modest first wave peaked in late October 2020 with a case fatality rate of less than 1%. 1 2 As cases fell steadily in January 2021, the government relaxed—a response that would turn out to be premature.
Throughout spring 2021, hundreds of thousands of people assembled on the streets in party political activities to prepare for the May election, adding to the number of people already joining gatherings for seasonal weddings and religious festivals. Meanwhile, in March 2021 the new delta variant, considered more infectious and virulent by the World Health Organization (WHO), was contributing to surging case numbers in India. 3 In April, at a time when cases in India were steadily rising, an estimated 50 000 Nepali pilgrims went to northern India for Kumbh Mela, a Hindu festival participated in by millions of people. 4 While there, many of the pilgrims caught covid-19.
Thousands of migrant workers also crossed over into Nepal from India, bringing the Delta strain with them, where it spread rapidly through the populous Kathmandu valley. 5 In Kathmandu, the hallways and courtyards of hospitals became crowded with patients competing to get a bed linked to an oxygen supply. Many patients were turned away due to lack of oxygen, ICU beds, and ventilators. Nepal’s president called a state of health emergency and 75 out of 77 districts had imposed a lockdown by 23 May. Nepal’s Ministry of Health and Population (MoHP) reported the country’s highest number of daily deaths (246) so far on 19 May 2021. 6
Restrictions were lifted as cases fell in July 2021 but the number of deaths surged again in August with a test positivity rate of 24% and more than 2500 cases recorded per day. 7 Many people in Nepal’s scattered rural population lack access to tests and deaths go unrecorded—a situation that is little different from India, where estimates suggest there were as many as 3.4-4.9 million excess deaths from the pandemic’s start to June 2021, numbers that are around 10-fold higher than official reports. 8 Hospitals and ICUs were full again during this period, including many severe cases in children. This wave hit the country so hard because communities were unprepared, the government had a false sense of security, residents relaxed social distancing, and authorities allowed religious festivals and political gatherings to go ahead as normal. The country still faces shortages of oxygen, ventilators, and other intensive care equipment.
Vaccines could have helped to relieve this pressure on Nepal’s hospitals, but the country has been beset by difficulties in obtaining them. At the end of March 2021, at a crucial point in the pandemic, India banned exports of AstraZeneca jabs until 2022. 9 This included one million doses already purchased by Nepal. By 11 December 2021, just 30% of the population had received two doses of the vaccine. 10 Nepal was not in a strong position then as the new omicron variant emerged and began to spread globally. First reported in Nepal by its MoHP in late December 2021, the omicron variant peaked with more than 10 000 daily cases on 18 January 2022. 11 12 More than 600 healthcare workers at the five biggest public hospitals in Kathmandu were infected and their absence added to the strain on the health system. 12 The number of daily deaths was much lower in the third wave (32 at its peak compared with 246 in the second wave) and cases dropped quickly to 2.9 per 100 000 population at the national level by the first week of March. 13 14 15 As before, the India-Nepal border was without strict screening, social distancing restrictions were relaxed, and compliance with public health protocols was often poor, all contributing to this third wave. But the introduction of covid-19 vaccination undoubtedly helped to reduce hospitalisations and mortality.
Against the backdrop of the covid-19 pandemic, another crisis unfolded. The annual monsoon season beginning in June 2021 brought flooding and landslides like never before across many of Nepal’s districts. Major rivers and streams swelled dangerously, and people lost their lives. After 200 mm of rain fell in six days up to 14 June, floods from the Melamchi river alone swept away 13 suspension bridges, seven motor bridges, and numerous stretches of road, destroying 337 houses, 259 enterprises, and thousands of acres of rice paddies. 16 The risk of flooding grows as glaciers in the Himalayas melt as a result of both rising temperatures and the proliferation of black carbon deposits from industry, vehicles, and cooking. 17
The government was overwhelmed, lacking as they do comprehensive plans for monsoon flooding. They mobilised the army and the Red Cross to assist communities, and arranged safe areas, drinking water, and food supplies. But they have no early warning systems, no anticipatory plans in place, and poor communication with many officials in local municipalities. A flood warning via Twitter was only sent out on 16 June—two days after dangerous flooding was first reported. 18 The country’s disaster budgets are tiny and procurement law does not allow relief materials and equipment to be bought in advance—only after disaster strikes subject to government approval. 19 Policies that build resilience against climate related disasters should be a top priority for the government because, while the pandemic may recede, the impacts of climate change will only worsen.
The latest reports from the Intergovernmental Panel on Climate Change have been red alerts for the world, describing climate change as widespread, rapid, and intensifying. 20 The mountain ranges of South Asia contain almost 55 000 glaciers that store more freshwater than anywhere but the North and South Poles. A World Bank report estimates that global black carbon emissions could be cut in half with policies that are currently economically and technically feasible, allied with the cuts in carbon emissions set out in the Paris Agreement. 21 Without urgent action, glacier melt will threaten hundreds of millions of people in Nepal, Afghanistan, India, Pakistan, China, and beyond.
As a low income country, Nepal deserves much greater international support through the Covax scheme to provide vaccines, diagnostics, and treatments, and for climate resilience through the “loss and damage” funds agreed at the COP26 summit in Glasgow. At the same time, Nepal’s government could have done far more to mobilise preventive and responsive measures for these twin crises; making sure the country is better prepared for the next one must be a priority.
Competing interests: None declared.
Provenance and peer review: Not commissioned; not peer reviewed.
- ↵ Bastola A, Sah R, Rodriguez-Morales A J, Kumar Lal B, et al. The first 2019 novel coronavirus case in Nepal. Lancet Infectious Diseases. 20:3:279 - 280. doi: 10.1016/S1473-3099(20)30067-0 OpenUrl CrossRef PubMed
- ↵ Ministry of Health and Population, Government of Nepal. Nepal: Covid 19 Response Situation Report No.XXXVI. Dec 14 2020. https://reliefweb.int/report/nepal/nepal-covid-19-response-situation-report-noxxxvi-14-december-2020
- ↵ Sharma G. Covid infections surge in Nepal fuelled by mutant strains in India. Reuters. 26 Apr 2021. https://www.reuters.com/world/china/covid-19-infections-surge-nepal-fueled-by-mutant-strains-india-2021-04-26/
- ↵ Pandey g. India Covid: Kumbh Mela pilgrims turn into super-spreaders. BBC News. 10 May 2021. https://www.bbc.com/news/world-asia-india-57005563
- Weissenbach B
- ↵ Nepal reports 242 new COVID cases, 1 death on Sunday. Nepal News Nationwide. 12 Dec 2021. https://www.nepalnews.com/s/nation/nepal-reports-242-new-covid-cases-1-death-on-sunday
- ↵ Update S. #68: Coronavirus Disease 2019 (COVID-19). WHO Country Office for Nepal. Reporting Date: 27 July – 2 August 2021. https://cdn.who.int/media/docs/default-source/nepal-documents/novel-coronavirus/who-nepal-sitrep/-68_weekly-who-nepal-situation-updates.pdf?sfvrsn=bb521cc0_5
- ↵ Anand A, Sandefur J, Subramanian A. Three New Estimates of India’s All-Cause Excess Mortality during the COVID-19 Pandemic. Centre for Global Development Working Paper. 20 Jul 2021. https://www.cgdev.org/publication/three-new-estimates-indias-all-cause-excess-mortality-during-covid-19-pandemic
- ↵ Gettleman J, Schmall E, Mashal M. India Cuts Back on Vaccine Exports as Infections Surge at Home. The New York Times. 25 Mar 2021. https://www.nytimes.com/2021/03/25/world/asia/india-covid-vaccine-astrazeneca.html
- ↵ Poudel A. Nepal receives 1 965 600 doses of Moderna vaccine from COVAX. The Kathmandu Post. 12 Dec 2021. https://kathmandupost.com/health/2021/12/12/nepal-receives-1-965-600-doses-of-moderna-vaccine-from-covax
- ↵ Poudel A. Nepal reports new Omicron case. The Kathmandu Post. 22 Dec 2021. https://kathmandupost.com/health/2021/12/22/nepal-reports-new-omicron-case-third-to-date
- ↵ Nepal faces new omicron-fueled coronavirus surge. Deutsche Welle. 19 Jan 2022. https://www.dw.com/en/nepal-faces-new-omicron-fueled-coronavirus-surge/a-60481393
- ↵ Omicron: Nepal makes quarantine mandatory for travellers arriving from 67 countries. The Times of India. 18 Dec 2021. https://timesofindia.indiatimes.com/articleshow/88352043.cms?utm_source=contentofinterest&utm_medium=text&utm_campaign=cppst
- ↵ Nepal Covid-19 tally: 3,540 new cases, 6,359 recoveries, 32 deaths in 24 hours. Onlinekhabar. 30 Jan 2022. https://english.onlinekhabar.com/nepal-covid-19-tally-3540-new-cases-6359-recoveries-32-deaths-in-24-hours.html
- ↵ World Health Organization Regional Office for South East Asia. COVID-19 Weekly Situation Report: Week #09 (03 March – 09 March 2022). 11 Mar 2022. https://cdn.who.int/media/docs/default-source/searo/whe/coronavirus19/sear-weekly-reports/searo-weekly-situation-report-9-2022.pdf?sfvrsn=f712043a_7
- ↵ Maharjan SB, Steiner JF, Bhakta Shrestha A, et al. The Melamchi flood disaster: Cascading hazard and the need for multihazard risk management. Disaster Task Force, ICIMOD. 4 Aug 2021. https://www.icimod.org/article/the-melamchi-flood-disaster/
- ↵ Mandal CK. Black carbon speeding up melting of glaciers, posing water scarcity threat to millions, report finds. The Kathmandu Post. 5 Jun 2021. https://kathmandupost.com/climate-environment/2021/06/05/black-carbon-speeding-up-melting-of-glaciers-posing-water-scarcity-threat-to-millions-report-finds
- ↵ Nepal Flood Alert. Twitter. 16 Jun 2021. https://twitter.com/DHM_FloodEWS/status/1405005910997540864
- ↵ Public Procurement Monitoring Office, Government Of Nepal. The Public Procurement Act, 2063 (2007). para 66 https://ppmo.gov.np/image/data/files/acts_and_regulations/public_procurement_act_2063.pdf
- ↵ Intergovernmental Panel on Climate Change (IPCC). Climate change widespread, rapid, and intensifying. IPCC Report. 9 Aug 2021 https://www.ipcc.ch/2021/08/09/ar6-wg1-20210809-pr/
An Overview of the Impact of COVID-19 on Nepal’s International Tourism Industry
- First Online: 01 November 2022
Cite this chapter

- Asmod Karki ORCID: orcid.org/0000-0003-2270-0545 5 ,
- Nama Raj Budhathoki ORCID: orcid.org/0000-0002-2041-4986 6 , 7 &
- Deepak Raj Joshi ORCID: orcid.org/0000-0001-5620-7025 8
Part of the book series: Global Perspectives on Health Geography ((GPHG))
378 Accesses
COVID-19 severely impacted Nepal’s economy. The tourism industry, a major contributor to Nepal’s gross domestic product (GDP), has been one of the major sectors to bear the secondary impact due to COVID-19. This chapter provides an overview of the economic and non-economic impact of COVID-19 on the tourism sector. The discussion centers around two major stakeholders: businesses and workers. It also elaborates on the major stakeholders’ expectations on the government to withstand and recover from the economic shock.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
The portal can be accessed here: http://tourismincovid.klldev.org/
The business and workforce survey questionnaires can be downloaded from the landing page of http://tourismincovid.klldev.org/
Based on conversations with labor union leaders on January 10, 2021.
A long list of major tourism projects could be found in the Investment Board Nepal’s site: https://ibn.gov.np/project-bank/
Business Standard India. (2021, August 3). Covid-19 lockdown extended in kathmandu valley . Retrieved from https://www.business-standard.com/article/international/nepal-covid-19-lockdown-extended-in-kathmandu-valley-till-aug-11-121080301817_1.html
C2M2 Kathmandu Portal. (2021). COVID-19 and its impacts on nepalese tourism . Retrieved from http://tourismincovid.klldev.org/
CCMC. (2020). CCMC’s 11th board meeting . Crisis Management Coordination Center. Retrieved from https://ccmc.gov.np/key_decisions/key%20decision%202077.05.29.pdf
Google Scholar
COVID19-Dashboard. (2021). Retrieved from https://covid19.mohp.gov.np/
Department of Immigration. (2021). Arrival departure data from January to December 2020 . Retrieved from https://www.immigration.gov.np/public/upload/e66443e81e8cc9c4fa5c099a1fb1bb87/files/Data_jan_Dec_2020(1).pdf
Department of Immigration. (2022). Arrival and departure record of 2021 . Retrieved from https://www.immigration.gov.np/page/arrival-departure-report?page=1
ILO. (2021). Informal economy in Nepal . Retrieved from https://www.ilo.org/kathmandu/areasofwork/informal-economy/lang%2D%2Den/index.htm
Lal, A. (2017, August 28). From the shangri-la to a hippie paradise. The Record . Retrieved from https://www.recordnepal.com/from-the-shangri-la-to-a-hippie-paradise
Mali, D. S. (2020, January 7). Making visit Nepal 2020 a success. The Himalayan Times . Retrieved from https://thehimalayantimes.com/opinion/making-visit-nepal-2020-a-success
Ministry of Culture, Tourism and Civil Aviation. (2020). Press Release . Retrieved from https://www.tourism.gov.np/files/Press%20RELEASE%20FILE%20PDF/Covid_19_WorkProgress_77_3_19.pdf
Ministry of Foreign Affairs. (2021, June 23). Guidelines to be followed by Nepali and foreign nationals travelling to Nepal . Retrieved from https://mofa.gov.np/wp-content/uploads/2021/06/Guidelines-to-be-followed-by-Nepali-and-foreign-nationals-travelling-to-Nepal-2021.pdf
Nepali Sansar. (2020). COVID-19 threat: Nepal government cancels ‘visit Nepal 2020 . Retrieved from https://www.nepalisansar.com/tourism/covid-19-threat-nepal-cancels-visit-nepal-2020/
Nepali Times. (2020). Nepal ends COVID-19 lockdown . Retrieved from https://www.nepalitimes.com/latest/nepal-ends-covid-19-lockdown/
NRB News. (2021). A publication of central bank of Nepal. NRB Monetary Policy for 2020–21 . 41 (1).
Online Khabar. (2021, December 28). Government announcement to give staff 10-day travel leave yet to be implemented . Retrieved from https://english.onlinekhabar.com/travel-leave-not-yet.html
Prasain, S. (2021, June 17). Tourism is Nepal’s fourth largest industry by employment study. The Kathmandu Post . Retrieved from https://kathmandupost.com/money/2021/06/17/tourism-is-nepal-s-fourth-largest-industry-by-employment-study
RSS. (2021). Tourism entrepreneurs demand COVID vaccine within 30 days . Rastriya Samachar Samiti. Retrieved from https://thehimalayantimes.com/nepal/tourism-entrepreneurs-demand-covid-vaccine-within-30-days
Shakya, A. (2017, October 11). A vision for visit Nepal 2020. New Business Age . Retrieved from http://www.newbusinessage.com/MagazineArticles/view/1943
Shivakoti, A. (2021). Impact of COVID-19 on tourism in Nepal. The Gaze: Journal of Tourism and Hospitality, 12 (1), 1–22.
Shrestha, P. M. (2020, December 20). Covid-19 affected businesses to protest demanding relief and rehabilitation package . Retrieved from https://kathmandupost.com/money/2020/12/20/covid-19-affected-businesses-to-protest-demanding-relief-and-rehabilitation-package
The World Bank. (2022). International tourism and number of arrivals . The World Bank Group. Retrieved from https://data.worldbank.org/indicator/ST.INT.ARVL?locations=NP
Ulak, N. (2021). COVID-19 pandemic and its impact on tourism industry in Nepal. Journal of Tourism & Adventure, 3 (1), 50–75. https://doi.org/10.3126/jota.v3i1.31356
Article Google Scholar
UNDP. (2021). Nepal multidimensional poverty index 2021. UNDP in Nepal . Retrieved from https://www.np.undp.org/content/nepal/en/home/library/poverty/Nepal-MPI-2021.html
WTTC. (2020). Economic impact report . World Travel and Tourism Council. Retrieved from https://wttc.org/Research/Economic-Impact
Download references
Acknowledgements
This book chapter would not have been possible without the exceptional work by a number of people at Kathmandu Living Labs (KLL). We are grateful, in particular, to:
Sazal Sthapit
Arogya Koirala
Aishworya Shrestha
Roshan Poudel
Manoj Thapa
Our special thanks to Dr. Melinda Laituri for her constant encouragement to write this chapter as well as for her constructive feedback on our earlier draft. This research was possible thanks to the Cities’ COVID Mitigation Mapping (C2M2) Program, developed by the U.S. Department of State’s Humanitarian Information Unit and the American Association of Geographers (AAG).
Author information
Authors and affiliations.
Kathmandu Living Labs, Chundevi, Nepal
Asmod Karki
Nama Raj Budhathoki
Humanitarian OpenStreetMap Team (HOT), Washington DC, USA
World Tourism Network, Honolulu, HI, USA
Deepak Raj Joshi
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nama Raj Budhathoki .
Editor information
Editors and affiliations.
Colorado State University, Fort Collins, CO, USA
Melinda Laituri
Michigan State University, East Lansing, MI, USA
Robert B. Richardson
Virginia Tech, Blacksburg, VA, USA
Junghwan Kim
Rights and permissions
Reprints and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Karki, A., Budhathoki, N.R., Joshi, D.R. (2022). An Overview of the Impact of COVID-19 on Nepal’s International Tourism Industry. In: Laituri, M., Richardson, R.B., Kim, J. (eds) The Geographies of COVID-19. Global Perspectives on Health Geography. Springer, Cham. https://doi.org/10.1007/978-3-031-11775-6_10
Download citation
DOI : https://doi.org/10.1007/978-3-031-11775-6_10
Published : 01 November 2022
Publisher Name : Springer, Cham
Print ISBN : 978-3-031-11774-9
Online ISBN : 978-3-031-11775-6
eBook Packages : Earth and Environmental Science Earth and Environmental Science (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Understanding COVID-19 in Nepal
Affiliation.
- 1 Sukraraj Tropical and Infectious Disease Hospital, Teku, Kathmandu, Nepal.
- PMID: 32335607
- DOI: 10.33314/jnhrc.v18i1.2629
The novel coronavirus COVID-19 (SARS-CoV-2) was first reported in 31 December 2019 in Wuhan City, China. The first case of COVID-19 was officially announced on 24 January, 2020, in Nepal. Nine COVID-19 cases have been reported in Nepal. We aim to describe our experiences of COVID-19 patients in Nepal. Keywords: COVID-19; experience; Nepal.
- Asymptomatic Diseases
- Betacoronavirus
- Coronavirus Infections / epidemiology*
- Coronavirus Infections / transmission
- Coronavirus*
- Disease Outbreaks
- Health Knowledge, Attitudes, Practice
- Middle Aged
- Nepal / epidemiology
- Pneumonia, Viral / epidemiology*
- Pneumonia, Viral / transmission
- Young Adult

- High contrast
- Children in Nepal
- How and where we work
- Invest in every child
- Our Partners
- Press centre
Search UNICEF
Covid-19 in nepal: assessing impact and opportunities for a child and family-friendly response, a national e-conference on 10 december 2020.

About a year ago , at the International Social Protection Conference (18-19 th November 2019,) the government of Nepal and key members of civil society and development community came together to put together a vison for resilient social protection for all Underlying this vision was the commitment to protect the children, marginalized and the vulnerable from attenuating impacts of a disaster and enable them to access basic services to help then reach their potential. This was before COVID 19, a crisis inflicting hitherto unprecedented impact on lives, economy, jobs livelihoods and childhood. The lessons from this conference are ever more relevant today.
COVID is a crisis of child rights as much a crisis of health and economics. While for adults, the hardship lasting for months and possibly years will be over with slow though inevitable recovery of economies and regeneration of jobs and livelihoods, a large section of children particularly 0-6-year-old, face a future bleaker than before. According to UNICEF’s Child and Family Tracker (CFT), an estimated 6 million children are now in poverty, including multidimensional poverty- a fourfold increase over the pre-COVID stats. Though for many this will be a transitory experience, many more would suffer irreversible loss of their potential of cognitive and physical growth and development, decelerating Nepal’s accumulation of human capital, productivity of labour and the potential for economic growth.
In response to the threat of COVID, Nepal responded with alacrity, imposing a strict lockdown on 23 March which lasted well into July. As a result, economic activity and growth slowed down with millions losing jobs/ earnings. Families with children were especially hit. According to UNICEF’s CFT, about 61 per cent of the respondents of this national 7000 HHs monthly, longitudinal survey have had no earnings in the last three months.
Putting a child’s face on this crisis is important because children have borne the brunt of poverty in Nepal disproportionately. It is also because the transmission loss of income (through loss of jobs, income or remittances) means reduction in quantity and quality of food and a risk of increased undernutrition with possible results in stunting and wasting. Children form about 40 per cent of Nepal’s population. And about 50 per cent of then live in the bottom two quintiles, the two groups most vulnerable to shocks. Since lockdown 8 million children have been out of school and though an increasing proportion of children have started learning at home, the access of modern, digital platforms of learning is accessible mostly to children attending private schools in urban (metro and sub-metropolitan) municipalities. Confined to homes that are under extreme economic stress, devoid of the normal avenues of socialization, children are also exhibiting signs of deteriorating mental health. Domestic violence has increased, which is bad news for any context, but especially for Nepal, where Violence against Children was high even pre-COVID. Though data is hard to glean on sensitive protection issues like forced/child marriage trafficking and Gender Based Violence, evidence from disasters, less extreme than that of COVID, indicate these crises often result in aggravation of such practices, as families struggle to ensure basic survival, literally.
Amidst growing distress, Government of Nepal has responded with a slew of relief measures, a mix of macro, meso and micro responses within the National Relief, Recovery and Rehabilitation Programme. rolled out to provide relief and to shore up the businesses including small and medium enterprises The National Planning Commission has assessed the socio-economic impact of COVID to guide the implementation and detailing of this national response. While COVID continues to perplex global planners and researchers, with the full impact still unfurling and responses being crafted, NPC and UNICEF believe it is prudent to take stock and examine the evidence about the impact of COVID in Nepal and reflect on the ongoing and planned response, with inputs and inspirations gathered from some of the global responses in child relevant sectors- social protection , education , health and nutrition and child protection.
Against the backdrop of the recent anniversary of Child Right Convention and the Human Rights Day, an e-conference is planned on 10 December to gather key policy makers and practitioners to stimulate this reflection and inform national policy response.
Click HERE for a summary of the conference
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dialogues Health
- v.3; 2023 Dec
- PMC10257514
A critical analysis of health system in Nepal: Perspectives based on COVID-19 response
Bihari sharan kuikel.
a Department of Public Health and Community Programs, Kathmandu University School of Medical Sciences, Dhulikhel, Nepal
Archana Shrestha
b Institute for Implementation Science and Health, Kathmandu, Nepal
c Center of Methods for Implementation and Prevention Science, Yale School of Public Health, New Haven, CT, USA
Dong Roman Xu
d Southern Medical University, Guangzhou, China
Brish Bahadur Shahi
e Ministry of Social Development, Karnali Province, Nepal
Bakhat Bhandari
Ravi kanta mishra.
f Ministry of Health and Population, Kathmandu, Nepal
Navaraj Bhattrai
g Nepal Public Health Foundation, Kathmandu, Nepal
Kiran Acharya
h New ERA, Kathmandu, Nepal
Ashish Timalsina
i Family Welfare Division, Department of Health Services, Kathmandu, Nepal
Nripa Raj Dangaura
Bikram adhikari.
j HERD International, Lalitpur, Nepal

Rabin Dhital
k Rural Development and Empowerment Center, Nuwakot, Nepal
Biraj Man Karmacharya
Associated data.
The interview transcripts generated and analyzed during this study are not publicly available to maintain the confidentiality of the participants but are available from the corresponding author on reasonable request.
Nepal moved from a unitary government to a federal system of government in 2015 under its constitution. Nepal is a federal democratic republic governed by three levels of government: a federal, provincial, and local level. The response to COVID-19 in Nepal has been majorly led and controlled by the federal government. All three levels of government are performing their responsibilities; however, they face various challenges in responding to COVID-19. This study aimed to critically analyze Nepal's health system in the context of the COVID-19 response.
We conducted semi-structured in-depth interviews by telephone among the policymakers, health workers, and stakeholders at the federal, provincial, and local levels ( n = 41) between January to July 2021. The interviews were audio recorded, transcribed into English, and coded using inductive-deductive approaches.
COVID-19 considerably impacted routine health care, mainly maternity services and immunization. Inadequate financial resources, inadequate human resources, and the lack of ventilators, ICUs, and X-ray services were the significant challenges in tackling and managing COVID-19 effectively.
The study found that all three levels of government perform their roles and responsibilities and effectively manage the pandemic. The federal and provincial governments focused more on the plans and policy development, while the local government demonstrated greater accountability in implementing those plans and policies. Therefore, all three tiers of government need to coordinate together for preparing and communicating information in times of emergency. Besides, it is imperative to empower local governments to maintain Nepal's federal health system.
1. Background
In December 2019, the first case of COVID-19 caused by the novel coronavirus named as Severe Acute Respiratory syndrome Coronavirus 2 (SARS-CoV-2) was reported by officials in Wuhan, China; with the rapid spread of disease from China to other countries, it was declared as a Public Health Emergency of International Concern (PHEIC) by World Health Organization (WHO) on 30 January 2020 [ 1 ]. As of 30 August,2020 —over 1.8 million new COVID-19 cases and 38,000 new deaths were reported globally; since the start of the outbreak, a cumulative total of nearly 25 million cases and 800,000 deaths have been reported [ 2 ].
COVID-19 has been an unprecedented challenge globally. COVID-19 is a complex challenge for all governments, especially those with limited state capability [ 3 ]. Health systems worldwide are being challenged by the increasing demand for care of people with COVID-19, along with the disruption in health service delivery due to fear of COVID contraction, stigma, misinformation, and limitations on movement [ 4 ]. The alarming speed of the COVID-19 pandemic harms the global economy; the global cost of the pandemic could range from $2.0 trillion to $4.1 trillion, equivalent to a loss of 2.3% to 4.8% of global gross domestic product [ 5 ].
There was a wide variation in the national response to COVID-19 across the states of Latin America. Brazil and Mexico exhibited high heterogeneity in their subnational responses [ [6] , [7] , [8] , [9] ]. There was a lack of uniform federal response and coordination between national and sub-national levels making the health system vulnerable to combat against COVID-19 pandemic. Argentina and Colombia showed consistent national guidelines with subnational variations. Bolivia, Chile, and Peru had homogeneous policies guided by centralized national policies [ 7 ]. The study emphasized that subnational responses cannot replace coordinated national policy and recommended that governments focus on evidence-based national policies while coordinating with subnational governments. The study found that the decentralization of health decision-making before the pandemic influenced the implementation of national policies. The structure of a country's government (federal or unitary) did not explain the stringency of the response. Overall, there was significant cross-national and subnational variation in public health policies across Latin America [ 7 ].
Another study examines the roles of subnational and national governments in Canada and the United States during the early phase of the COVID-19 pandemic. In the United States, state and local governments were first to take action, while in Canada, policy-making was spread out between bureaucratic institutions and provincial or federal governments, with provinces playing a significant role. The study compares the two countries across several dimensions and find that sub-national governments played a more significant role in policy development than national-level policies. However, the study highlights the uncertainty and needs for clarity regarding which level of government should be responsible for implementing policies [ 10 ].
Nepal moved from a unitary government to a federal system of government in 2015 under its constitution [ 11 ]. Nepal is a federal democratic republic governed by three levels of government: a federal, provincial, and local level [ 12 ]. In Nepal, the first case was reported on January 23, 2020, of a 32-year-old Nepali man returning from Wuhan [ 13 ]. Once the first case was identified, Nepal focused mainly on identifying and managing cases [ 14 ]. The response to COVID-19 in Nepal was substantially led and controlled by the federal government [ 15 ]. The decisions related to the pandemic response were very top-down, often patronizing, in the form of directives, guidelines, and requests to provincial and local governments. The provinces established isolation centers, testing labs, and managed medicines and other essential services. Local governments' response concentrated on establishing and managing quarantine facilities and distributing relief packages to needy people. Even though all three levels of government worked together, a systematic, centralized approach was adopted, which compromised the roles of provincial and local governments. Furthermore, the provincial and local level was not provided space to influence the response to the pandemic independently except for carrying out their routine responsibilities [ 15 ].
The World Health Organization's (WHO) Health Systems Building Blocks is a classic framework used in various studies to describe the health system response to the COVID-19 pandemic [ [16] , [17] , [18] ]. As shown in Fig. 1 , the building blocks are leadership and governance, service delivery, health workforce, information, financing and, logistics. The service delivery block emphasizes providing quality healthcare services, while the health workforce block focuses on ensuring a skilled and sufficient healthcare workforce. The information system block highlights the importance of reliable data for effective decision-making, and the access to essential medicines block emphasizes the equitable availability of medicines. The financing block underscores the need for sustainable funding mechanisms, and the leadership/governance block emphasizes effective management and coordination of the health system. By addressing these six building blocks, countries can strengthen their health systems and enhance their ability to respond to health challenges, including pandemics like COVID-19, and improve overall population health outcomes [ 19 ].

The WHO Health Systems Framework for the health care system [ 20 ].
Two studies were conducted, one in Nigeria [ 16 ] and another in Sub-Saharan Africa (SSA) [ 17 ], using the World Health Organization's (WHO) building blocks of the health system to evaluate the preparedness and response to the COVID-19 pandemic. In Nigeria, the study revealed a sub-optimal response characterized by inadequate funding, a shortage of human resources, and insufficient infrastructure within the health system [ 16 ]. Similarly, the study conducted in SSA highlighted the long-standing challenges of abysmal health system financing and inadequate government investment, which hindered the effective functioning of the health system during the COVID-19 pandemic. These challenges not only impede the health system's ability to address the pandemic's demands but also affect the provision of other essential health services [ 17 ].
Nepal, with a poor health system due to inadequate resources, is more vulnerable. Nepal's existing public health system does not have adequate capacity to address COVID-19 or any other pandemic, for that matter [ 21 ]. Nepal, at its initial stage of the federalization process, needs more precise roles and responsibilities, coordination mechanisms, information channels, and fiscal relations for an effective response to a pandemic of the magnitude of COVID-19 [ 15 ]. Understanding and analyzing the roles and responsibilities of each health system level can play a vital role in future preparedness and response to public health emergencies like COVID-19. However, there needs to be more research analyzing the health system in the context of COVID-19. Thus, the study aims to critically analyze Nepal's health system in the context of COVID-19 response. The study contributes to identifying gaps in the health system and helps address those gaps for better preparedness, response, and management in the future.
2. Methodology
2.1. study design.
A qualitative study was conducted using phenomenological approach [ 22 ] which was involved in-depth interviews to collect the information from policymakers, health workers and stakeholders at the federal, provincial, and local levels. The objective of the study was to examine the perspectives of health workers and policy makers directly engaged in the COVID-19 pandemic response and management. To achieve this objective, a phenomenological approach was utilized, allows to describe of relevant phenomena based on the personal experiences and insights of individuals involved [ 23 ].
2.2. Study setting
The study was conducted in the national capital Kathmandu [ 24 ] and Karnali province of Nepal—Nepalese healthcare system is divided into federal, provincial, and local [ 12 ] governments. For federal COVID-19 preparedness and response, we collected the data under the Ministry of Health and Population, and for provincial and local level COVID-19 response, we selected Karnali province. It is one of the seven self-governed provinces of Nepal, which mainly constitute mountain land of the north and mid hills of Nepal. It is the largest province of Nepal with an area of 27,984 Km 2 , and it is the lowest-population province of Nepal with a total population of 15,70,418. Karnali province is divided into ten districts, and districts are subdivided into 79 local governments (25 municipalities and 54 rural municipalities) [ 25 ].
When the spread of coronavirus began in the country, Karnali Province was far from COVID-19 preparedness. There were only 17 ICU beds with six ventilators in the health facilities of the Jumla and Surkhet districts. The biggest hospital in the province did not have adequate ICU beds and ventilator service. The quarantine facilities in the municipalities do not meet the government's prescribed standards. There were no proper arrangements for the migrant workers returning from India—further, the geographical remoteness and shortage of human resources constraints the COVID-19 containment measures [ [26] , [27] , [28] ].
2.3. Study participants
The study participants in this research encompassed diverse individuals who played crucial roles in managing COVID-19 at the federal, provincial, and local levels. Representatives from institutions such as the Ministry of Health and Population, Epidemiology and Disease Control Division, National Academy of Health Sciences, and Tribhuwan University Teach Hospital were included at the Federal level. Additionally, participants from the provincial level were selected from the Ministry of Social Development, Provincial Health Directorate, Karnali Academy of Health Sciences, and front-line health workers directly involved in COVID-19 management. The involvement of local levels was ensured by the participation of the mayor/chairpersons, Chief Administrative Officer, Health Coordinators, and COVID-19-infected and recovered patients. Furthermore, stakeholders from organizations such as the Lions Club, Rotary Club, and journalists were also included in the study, reflecting the comprehensive nature of the research participants.
2.4. Sample size
A total of 41 interviews were conducted for this study, comprising 10 interviews from the federal level, 13 from the provincial level, and 18 from the local level. The sample size determination was based on reaching code saturation [ 29 ], which signifies the point at which no new or additional information emerged from the interviews.
2.5. Sampling technique
A purposive sampling [ 30 ] method was used for the selection of the participants. The participants shared common characteristics and were actively involved in COVID-19 management. By virtue of their experience, these participants were expected to provide the necessary information required by the study more effectively due to their firsthand experience in the field.
2.6. Data collection
The study utilized semi-structured in-depth interviews to collect the data from 41 study participants. All the interviews were conducted remotely via telephone between January to July 2021 due to the country's pandemic. An interview guideline was developed to collect the data based on the literature review and input from the experts. The tool was validated through pre-testing. Before the data collection, the research assistants were trained on the qualitative method, tools, and how to find the most appropriate and clear language to express technical terms to the team with relevant experience in qualitative methods. All the interviews were audio recorded, and verbatim notes were also taken during the interview. Each interview lasted for about 40–45 min. An iterative process [ 31 ] was used by reviewing each interview shortly after completion and adjusting subsequent interviews probing more deeply into themes emerging in earlier interviews. All the interviews were transcribed verbatim in Nepali and then translated into English. We assessed all transcripts for accuracy by cross-checking the audio recordings.
2.7. Data analysis
The data were analyzed using thematic analysis [ 32 ]. The initial codebook was deductively developed based on the interview guide and revised to include emerging code using an inductive approach. The Consolidated Criteria for Reporting Qualitative Studies (COREQ) guideline [ 33 ] were used in the preparation of this manuscript.
3. Ethical consideration
The study was approved by the ethical review committee at Kathmandu University School of Medical Sciences (Ref: 127/20; KUSMS IRC). The participants were informed about the objectives and methodology of the study. Participants were asked to participate voluntarily. Participants were informed that they had a total right not to participate or discontinue the study at any time during the study.
Among the 41 respondents interviewed, 10 were from the Federal level (4 health workers, 3 policymakers, 3 stakeholders), 13 from the Provincial level (5 health workers, 5 policymakers, 3 stakeholders), and 18 from the local level (6 health workers, 10 policymakers, 2 stakeholders). Most (85.4%) were male, and only 6 (14.6%) were female. The mean age of the respondents was 40.1 years (SD: 10.5). Table 1 shows the demographics of the respondents who participated in the study.
Socio-demographic characteristics of the participants.
Using thematic analysis, the findings from the study were categorized into six themes according to the WHO's building blocks of the health system.
4.1. Leadership and governance
The three tiers of the government had their own roles and responsibilities in response to COVID-19 pandemic with more responsibility to the local governments. The federal and provincial level were more concentrated on formulation of the various plans, policies, guidelines, and directives, and facilitated in their implementation. And the local government was more responsible in the implementation and followed the plans, policies and guidelines provided by the federal and provincial government.
“We developed guidelines for most of the things… We found the active leadership of the provincial government. Likewise, the local government was also active. There was engagement of both provincial and local governments in things like quarantine management, contact tracing, establishment of hospitals. They both led the situation in an effective manner. There was good intention from both the government in managing COVID. The stakeholders were also actively involved under the leadership of the provincial and local government.” (Federal level policy maker; p1; Kathmandu)
“The Federal government is leading COVID-19 management. It has been developing policy and guidelines. Central government is like our parenting body that is why we are following the policies developed by it as much as we can regarding the things as how to make it understandable to people, regarding lockdown…..In the context of COVID management, local government has major roles in implementation rather than central and provincial government. That's why local government is active for implementation.” (Local level policy maker; p6; Salyan)
However, lack of clarity on roles and responsibilities of each level of government has created problems in implementation and management.
“The local government says that it has to be done by the provincial government while the federal government says that since the system has undergone a local level it is to be done by them. So we are in a dilemma regarding our job description.” (Provincial level policymaker; p3; Kalikot)
There is coordination between the local, provincial and federal level of government through different means of communication and information. Regarding the COVID-19 management part federal, provincial and local all of them are fulfilling their responsibility accordingly and with the combination of these bodies the things are proceeding well.
“Now from federal level to province level to local level communication and coordination is being done. Province government communicates every activities of federal government and it communicates that information to the local level trough hard copy or email or soft copy or telephone or by the use of different media they are coordinating with local levels….” (Provincial level policy maker; p2; Dolpa)
However, lacking coordination between federal and provincial governments was expressed by the stakeholder of the Provincial level.
“We see the Nepal government at the central level, provincial level and local level, and what we have found is that there is no proper coordination between the federal government and provincial government.” (Provincial level Stakeholder, p2; Surkhet)
4.2. Service delivery
Most of the health workers in this study agreed that there was a significant impact of COVID- 19 on routine health care with mostly maternity services, immunization as the health facilities were mainly providing COVID related services. Additionally, the health facilities were unable to provide its usual routine health services due to the lockdown. And there was fear of contracting COVID from the health personnel among the people. As a result, pregnant women did not visit the health facilities for ANC checkups and the people with chronic diseases did not get timely checkup, follow-up and medication. Consequently, there was an increase in the number of home deliveries and neonatal deaths. Likely, there was also an increase in immunization drop-out rate among the children. Along with this, due to more number of COVID-19 patients, even non-COVID critically ill patients were not getting ICU and ventilators.
“….. Due to COVID-19, we have postponed the surgery on our regular plan… Due to the pressure of COVID-19 patients, we could not keep non-COVID critically ill patients in ICU and ventilators…”. (Federal level Front line HW; p6; Bhaktapur)
“For the people with chronic diseases, they are not getting timely medication, timely checkup, and timely follow up and it has affected them. In case of pregnant mother, they don't get timely ANC checkup which has added up for the increased neonatal mortality.” (Provincial Level Front Line HW p9; Jumla)
“There has been a big influence on regular health service because of COVID. People stay at home because of fear of getting infected of COVID-19 while visiting health centers. That's why it has created a negative impact. The number of people who are having home delivery has increased because of lockdown which even lead to death of 1/2 newborns along with it people also don't visit for ANC and dropout in routine immunization has also increased.” (Local level, policy makers, p8, Dailekh)
At all three levels, institutional isolation was preferred over home isolation because at institutional isolation, there was an arrangement of food and accommodation. The patients would have better and timely care and treatment from the health workers. Moreover, in the context of inadequate space, home isolation was difficult. So, institutional isolation was better than home isolation.
“In Jumla, the traditional houses have no separate toilet, kitchen, bathroom and almost the entire family lives in 1/2 rooms. Moreover, there is no proper ventilation so home isolation is difficult in the context of Jumla. Initially we encouraged for home isolation but it was not effective and due to this, we decided to keep people in institutional isolation.” (Provincial Level, Hospital Manager; p7, Jumla)
However, the governments have managed the cases of home isolation. Those cases of home isolation were constantly monitored by the health workers. They followed up the cases for their health conditions either through the phone calls or visit to the patient's house on a regular basis. At local level, the health facility also provided the essential medicines and corona prevention, control and treatment kit to home isolation patients. The federal level hospital was providing counselling to the people living in home isolation.
“For home isolation, if a person tests positive then it will be recorded in rural municipality and later on as chief of health center and other health service provider relating to COVID will call them time to time to get informed about their health condition.” (Local level policy maker; p6; Salyan)
At local and provincial level, the contact tracing was not done effectively mainly due to inadequate human resources and lack of orientation and training to the existing human resources. The federal level was also back in the contact tracing process due to various circumstances.
“...The contact tracing is not conducted as per the guidelines. As we look at Salyan, it has not been done effectively because we don't have enough human resources. There is scarcity of human resources and these should be provided. They should be provided with proper training on contact tracing after which the situation could be better.” (Provincial Level Policy Maker, p4, Salyan)
“Under the leadership of a medical officer, we have formulated and mobilized a CICT team and trained the team about it... But the doctor has returned to his/her own sanctioned place and we are not able to provide CICT orientation to the new doctor. So, presently we could not do contact tracing effectively like before.” (Local Level Policy Maker, p8, Dailekh)
4.3. Human resources
The Karnali Province and its local levels had insufficient health personnel. In addition, specialist human resources were inadequate for critical case management. At the local level, though the federal government has provided a certain amount for only three months, there were not enough applicants. This could be due to no secure job. As a result, the local level was unable to afford specialized health personnel. Likely, at provincial level, there was only one doctor available for providing the services to 25/28 patients.
“There is scarcity of doctors and there are hardly 5 doctors out of district and there are no doctors on local level and in each hospital, 25/ 28 patients are admitted daily and for these patients there is one medical officer who can hardly give medicines in sufficient manner.” (Provincial Level Policy Maker, p3, Kalikot)
Additionally, at the provincial level, there was a shortage of skilled human resources. Despite having ventilator and oxygen plants in the hospitals, they were not in function because of lack of human resources with the required skills to operate those equipment.
“The provision for the availability of oxygen plants in every hospital of the district is not complete but still is in process. We have beds, we have ventilators but the human resources who have skills and abilities to operate those available ventilators are still inadequate. For this, proper training should be given and these all are in process”. (Provincial level Policy Makers, p2, Surkhet)
The inadequate number of human resources was due to difficulty in human resource mobilization after the staff adjustment. After the staff adjustment, staff were adjusted at the federal, provincial and local level. The sanctioned posts at provincial and local were vacant and there was no vacancy announcement from the concerned authority. So, the local level, with its own resources, temporarily recruited the health workers for effective service delivery. And for the federal government, it was difficult to mobilize staff in this situation of a pandemic.
“The sanctioned posts are not well fulfilled and because of staff adjustment, health workers who were working here also moved. So as the staff are not coming after additional staff adjustment we are providing service by hiring temporary staff. We do have a great challenge of lack of human resource but still we are managing by hiring temporary staffs….I have been reporting time and again about the vacant post of health workers to concerned authority but still it's not being heard from any places...” (Local level Policy Makers, p8, Dailekh)
For the motivations of the frontline health workers, the Provincial and the local government were providing incentives and allowances such as communication allowance, hazard allowance. However, health workers expressed their opinion on security rather than the 50% hazard allowances.
“Motivation program has been initiated in Karnali provinces. Doctors in Surkhet are provided with 50 % allowance and 135% as in Humla/Dolpa as per their level and for other health service providers and health officers, the money grant of 4000 is made available, which has provided support for motivation…”. (Provincial level policy Makers, p1, Salyan)
“They are receiving hazard allowance as per the decision of our local executive. They are receiving a daily allowance of NPR 650 per day. We are also providing them with PPE sets, masks and sanitizer. Rural municipality will be held accountable if they encounter with any problem and get sick.” (Local level Policy Makers, p9, Dolpa)
4.4. Information system
There was a regular information flow mechanism between the three tiers of government. The local government reported community level COVID data to the provincial level daily via online which is then reported to the federal level. The federal and provincial governments collected different COVID-19 related information on a daily basis. However, the quality of data was a major concern.
“Every district of our local level reports on the number of patients admitted in isolation centers, numbers of patients under treatment, number of patients who have recovered and of the ones who lost their lives during treatment to DCCMC and health service offices. We compile all this information from the district, and report it to the Ministry of Social Development, and in CCMC and Ministry of Health and Department of Health Service...” (Provincial Level; Policy Maker, p5, Dailekh)
“We are reporting our works and its findings daily via online. We collect information regarding health situation, COVID-19 condition from the 7 health service centers of 6 different wards of Thatigadh RM and this report is handed over to health office, Dailekh. DAO is informed about it through HO. Similarly central will get informed through DAO. We exchange this information on time in this way.” (Local Level Policy Makers, p8, Dailekh)
“There are large number of patient in local level and we are having easy access about the data of patient from local level but the reliability of the data is a major concern.” (Federal Level Front Line Health Workers, p3, Kathmandu)
In Karnali province, due to technical issues with the internet and lack of electricity which caused problems with data entry and reporting. However, they reported either by phone call or by using a mobile data pack. And lack of technical competency among the staff has resulted in low quality of data.
“...Lack of electricity facilities has created difficulty in reporting system and sometimes even due the lack of technical knowledge on reporting process among the staffs has also created the problem in reporting.” (Provincial Level Policy Makers, p5, Dailekh)
“Health service providers from the lab are reporting via online but we are facing some problems regarding reporting. Due to internet problems we are not able to report at time. Sometimes we have to send data of 100 people collectively but due to internet problems we are using mobile data. Still the online data entry from computers have stopped completely. Sometimes there is a network problem and even at times of emergency we cannot make a call. It is getting somehow difficult because of it.” (Local Level Policy Maker, p10, Jumla)
4.5. Financing
At the local level, the government has initiated budget allocation for the COVID-19 management. However, the budget was inadequate. As a result, corona crisis funds were established at the municipal level in order to handle and respond to COVID-19 effectively. The budget provided from the federal and provincial government and other financial aids were deposited in the fund and the local government was using those funds for the COVID management and other immediate financial problems.
“For controlling the COVID-19 we have separated one crore as per our capacity so we have been managing from it. But still the budget we are receiving from the central government is still not enough. It is causing us problem for COVID-19 management.” (Local Level Policy Makers, p2, Dolpa)
“The COVID-19 fund has been established at the local level where the budget sent from the central and provincial government along with the fund given by any other parties is deposited but we have quite a low amount in it. Last year, province had sent us 15/20 lakhs amount but we don't have any idea about the amount of budget provincial and central government is sending us this year.” (Local Level Policy Maker, p6, Salyan)
The COVID-19 response fund was primarily managed by local governments. In the context of managing the expenses for the COVID-19 response, the deficit budget was maintained through the fund transfer mechanism. The approved budget for the developmental sector as well as other programs budget which could not be implemented in this year due to COVID-19 was transferred to the corona crisis fund.
“We are receiving a budget from both province and center and along with it the executive body of the rural municipality had decided to deposit and operate those budgets of other different headings which are not being operated due to lockdown also into the disaster management fund for control of COVID-19. …We were given a budget from the province both last year and now. We are using the budget of rural municipality under different headings by diverting those amount into it.” (Local Level Policy Maker, p9, Dolpa)
However, the provincial government faced some challenges like late release of budget and no proper guidelines on budget expenditure. Due to these, it was difficult in timely procurement of the necessary materials for COVID management.
“…….We have the necessary budget but we did not find necessary materials in the market. No medicines were found so it was very difficult to manage COVID-19 this time…”. (Provincial Level Policy Makers, p5, Dailekh)
4.6. Logistics
The Provincial and local government were able to manage the necessary resources. PPEs and other essential equipment were scarce in the early days of COVID-19. Later, the local government was able to obtain the PPEs, oxygen cylinders, and other required equipment using its own resources. And the provincial government was also prepared from the first wave and was having enough stocks. So this was no longer a major concern. However, the federal government was having problems in the supply of the PPE and testing kits due to a shortage of the materials and the need to import from outside.
“We have a shortage of PPE and a test kit for PCR as we need to buy it from outside. As it does have high demand, we are having the condition of untimely supply of these things.” (Federal level Policy Makers, P3, Kathmandu)
“As we were preparing from the first wave and as we were given donations, we did not face much crisis of other equipment as compared to oxygen. We assumed there might be a second wave coming and thus we prepared from the first wave. That's why, we don't face difficulties in PCR, masks and kit till now and we have enough stock as well.” (Provincial Level Health Care Manager, p7, Jumla)
“I have not experienced any sort of deficiency in our municipality because municipality have been easily providing us the materials that we have demanded relating with COVID- 19.” (Local Level Policy Makers, P7, Surkhet)
There was remarkable support from different I /NGO, private sectors, developmental partners working at local, provincial and federal level. They supported the government with necessary logistics, equipment and testing kits.
“During the second wave, there was a shortage of testing kits. So we [Lions Club 325] bought kits of worth $40,000 during this pandemic, and distributed it to the diagnosis centers where needed.” (Federal Level Stakeholder, p5)
“Different organizations working in Karnali Pradesh and different private organizations also helped us by providing oxygen plants, oxygen concentrators, oxygen cylinder management and different health related equipment…”. (Provincial Level Policy Makers, p1, Surkhet)
“USAID AND UNICEF have been helping us. UNICEF had helped us by providing oxygen concentrator, pulse oxymeter whereas USAID had provided us with medicines, masks, sanitizer and PPE set.” (Local Level Front Line HW, p11, Dailekh)
The Karnali Provincial and local government was having difficulty in handling this pandemic situation with the existing physical infrastructures. The existing infrastructure in a remote part of Karnali was inadequate. Due to the lack of ventilators, ICU and X-ray services, health facilities were unable to manage the critical cases in an effective manner.
“Looking at the numbers of diseased patients, we have a sufficient isolation center. We had started off with 15 beds which was later increased to 40 and we faced difficulties then to some extent and in the midway, we placed the severely symptomatic patients which made us easier. We don't have ICU, HDU and they are not in the district as well. It is difficult to bring in Kalikot and yes, ICU, HDU are not enough. This was not made possible by Nepal government or by us as well.” (Provincial Level, Front Line HW, p10, Kalikot)
“We do have 3 health centers in total but we don't have oxygen management in any of them for now. Similarly we also have x-ray and video x-ray machines. Likewise we also don't have bed and test kits. Hence, these things are to be fulfilled.” (Local Level Policy Makers, p5, Dolpa)
4.7. Lesson learnt
Majority of the policy makers learnt that early preparedness is required for better COVID management. The three tiers of government should be prepared in terms of human resources, the infrastructure and other necessary resources.
“The necessity of redefining our approaches and infrastructures, modification of acts is what we learnt from this pandemic along with this we have also learnt about the need of framework for legal provisions and necessity of readiness in order to tackle with similar kind of pandemics…”. (Federal Level Policy Makers, p2, Kathmandu)
“Mainly we weren't properly prepared, our preparedness was not enough. Though we talked about the ratio of health institutions, nurse patient ratio, doctor patient ratio, the human resources and equipment in the first wave, the oxygen preparedness was not done suddenly in the second wave. We were not prepared properly. So, we should develop the health sector by considering equipment, manpower and we must increase the capacity to tackle the disaster. If we have 100 patients in PHCC level, we can handle about 50 patients during a disaster. We should plan thoroughly and we must strengthen our capacity.” (Provincial Level, Health Care Manager, p7, and Jumla)
“It's learnt there should be early preparedness from all tiers of government by targeting the health of individuals as there may be these kinds of problems in the coming future too. If it is not done then it would lead to a fearful situation as loss of people's lives. That's why the major thing is there should be the management of hospitals with beds and specialized doctors even in the lower level…”. (Local Level Policy Makers, p6, Salyan)
4.8. Recommendation
The policymakers and health workers recommended that each level of government should attend the competencies to work independently in their concerned area with major focus on local level. There is a huge responsibility of the local level government in the implementation process during this pandemic. A proper coordination and clarity on the roles and responsibilities in each level of government is needed for the effective COVID-19 management.
“It has come to the point of realization regarding the competency and need of each level of government, how the local level run without the province can and how can federal work without the province. So on the basis of this realization, responsibility, adjustment, human resource and capacity building should be addressed accordingly…”. (Federal Level, Policy Makers, p2, Kathmandu)
“The government should not work through a blanket approach. While formulating a plan, things such as: background of the province, geographical difficulty, provincial capacity and their income and others should be taken into consideration. The matching point or logistic point or the matching point in catchment area, if these all are possible, then all Nepalese or all citizens will have access to health service as mentioned in constitution.” Provincial Level Policy Makers, p2, Surkhet
“Local government would be competent if it is provided with technical support and power/right to manage the health emergency so that it could move forward by deciding their risk on its own.” (Local Level Policy Makers, p5, Dolpa)
“The local government should be very active and technically competent as it has a more significant role in the implementation process. Depending upon the federal level might not always work. So, the local level government should stay active by managing human resources. Along with it there should be adequate development of physical structures. Likewise, there should be coordination between the federal, provincial and local government.” (Local Level, Front Line HW, p13, West Rukum)
5. Discussion
5.1. leadership and governance.
The three tiers of the government had their own roles and responsibilities in response to COVID-19 pandemic. The federal and provincial level were more concentrated on formulation of the various plans, policies, guidelines, and directives, and facilitated in their implementation. And, the local government was more responsible in the implementation and followed the plans, policies and guidelines provided by the federal and provincial government. However, there was poor coordination and unclear roles and responsibilities which led to miscommunication. So, things got overlapped regarding work between the local, provincial and federal level. This finding is also echoed by the previous several studies that found that the poor coordination between the three tiers of the health system (federal, provincial and local) was an important gap in the health service preparedness in COVID-19 management [ 34 ]. Since the functions and responsibilities of the three levels of government were not clearly defined and there was no effective mechanism for coordination and collaboration, there were barriers in COVID-19 management [ 35 ]. The federal and provincial governments passed protocols, guidelines, but their immediate implementation was not satisfactory. The local government complained regarding the circulation of those guidelines, protocols. As per the local government, the federal and provincial governments have not done much to circulate those protocols, and guidelines [ 36 ].
5.2. Service delivery
The COVID pandemic had its impact on routine health care. People avoided going to the health facility because they were afraid of contracting COVID from the health personnel. As a result, home delivery and immunization drop-out rates had increased. This result is supported by the previous study [ 37 ] , where the lockdown has caused disruption in the routine health care services such as maternal health, immunization and chronic diseases. There was an increase in home deliveries and few neonatal deaths.
The study conducted in a joint initiative of the Integrated Health Information Management Section, Management Division, Department of Health Services, Ministry of Health and Population and Nepal Health Sector Support Program (NHSSP) suggested that there was an initial impacts of COVID-19 in all service utilization [ 38 ]. During the initial lockdown, there was a medicine shortage, delivery services were unavailable, and ambulance services too were unavailable for many days. Likely, there was more number of maternal deaths in COVID-19 months. The participants in our study reported that at all the three levels, both institutional, and home isolation services were properly managed. There was an arrangement of food and accommodation as well as timely care and treatment from the health workers. However, a previous study had contrast finding where the participants reported that the isolation and quarantine services were inadequate to provide good care for COVID-19 patients. Particularly, political connections and those in positions of power and affluence used the medical facilities, leaving the poor and underprivileged without care [ 37 ].
In our study, at all level, the contract tracing was not done effectively mainly due to inadequate human resources and lack of orientation and training to the existing human resources. Similarly, a rapid assessment found that it was easy to conduct contact tracing in rural areas since it was simple to diagnose the cases but it was more difficult in urban areas [ 35 ].
5.3. Human resources
In our study, the participants reported that the existing human resources were inadequate which appeared as a major challenge in providing COVID-19 services. These findings have been supported by the previous studies [ 34 , 39 , 40 ] where the existing health workers were divided to provide both COVID-19 and non-COVID health care services. The doctors were insufficient in number and there was no additional health workers for substitution. The government was unable to increase the number of the health workers due to the short term vacancy announcement which went unfilled [ 34 ].
Moreover, there was a shortage of specialized human resources for critical case management in the provincial and local level. After the staff adjustment, staffs were adjusted at the federal, provincial and local level. It was difficult to mobilize staff from one level to another level of government in this situation of a pandemic which posed a significant impact on COVID-19 management. Additionally, there were more vacant posts at provincial and local level. There was no vacancy announcement by the concerned body for the fulfillment of sanctioned posts. This has also caused problems in human resource management.
Most participants in our study expressed that the provincial and the local government were providing incentives and allowances such as communication allowance, hazard allowance as the motivations for the frontline health workers, However, a study conducted in 3 public hospitals of Eastern Nepal had a contrast finding. The participants stated that there was an unfair lack of appreciation and compensation for their efforts, which left them less motivated to work during this difficult period [ 40 ].
5.4. Information system
There was a regular online information flow mechanism between the three tiers of government. The local level reported on the data of new cases, treated cases, recovered cases, and deaths to the provincial level, which was then reported to the federal level. The federal and provincial government also updated the local level on the current situation. There was two-way communication. However, there were some challenges in data entry and reporting from local and provincial level to the federal level such as technical issues with the internet, electricity and inadequate technically competent human resource. The study conducted in a joint initiative of the Integrated Health Information Management Section, Management Division also had similar finding. In the COVID-19 month, there was no discernible difference in the HMIS reporting's timeliness. However, the main factors affecting the performance of Maternal and Perinatal Death Surveillance and Response during the pandemic period were determined to be inadequate institutionalization of systems, limited access to internet resources, and a lack of human resources and monitoring mechanisms [ 38 ].
5.5. Health financing
The COVID-19 response fund was primarily managed by local governments. Budgetary support was also granted by the federal and provincial governments to local governments for COVID19 management. But the budget grant was insufficient. As a result, corona crisis funds were established at the municipal level in order to handle and respond to COVID-19 effectively. The limited financial transfer has been the major challenge to local levels in combating Covid-19.[ 36 ] There were some challenges in budget expenditure such as late budget release and no clear instruction on the budget expenditure process due to which the procurement and the implementation process could not be accomplished on time.
5.6. Logistics
PPEs and other essential equipment were scarce in the early days of COVID-19. Later, the local and the provincial government was able to obtain the PPEs, oxygen cylinders, and other required equipment using its own resources, so this was no longer a major concern. There was remarkable logistics support from I/NGOs, UN agencies, EDPs working at the local, provincial and federal level. This finding is also in accordance with a study done which focused on the rapid assessment of COVID19 related policies, guidelines, and directives issued by MoHP and its agencies and its implementation practices [ 35 ]. During the early stages of COVID-19, it was challenging to manage the cases in Karnali Province because of limited PPEs and other necessary equipment. Later, this was no longer a serious issue due to the support of numerous government and non-governmental organizations.
However, the existing infrastructure in a remote part of Karnali was inadequate. Due to the lack of ventilators, ICU and X-ray services, health facilities were unable to manage the critical cases in an effective manner. These findings are supported by the studies [ 34 , 40 ] where hospitals had to run the services in the limited resources such as isolation beds, ICUs and ventilators, oxygen plant, PPEs etc. The existing buildings, other infrastructure and equipment were reportedly made worse by the COVID-19. Insufficient capacity for lab testing and contact tracking were the major issues as expressed by the health workers [ 34 ].
5.7. Strengths and limitations
The research involved various participants, such as policymakers, healthcare workers, stakeholders, and individuals who have recovered from COVID-19. These participants represent different levels of government, resulting in diverse opinions. The study was conducted in Karnali province and its local levels in Nepal. The region is characterized by various factors, including limited health and transportation infrastructure, a shortage of medical staff, insufficient testing capabilities, and the return of family members from India. Additionally, the area has mountainous and hilly terrain [ 25 , 41 ]. As a result, these study's findings may not be applicable to other regions of Nepal. However, our research findings can be utilized to shape forthcoming policies and programs, specifically focusing on enhancing preparedness and managing disaster and health emergencies in Nepal.
6. Conclusion
The study concludes that all three tiers of government perform their roles and responsibilities in responding and managing COVID-19 pandemic. However, the local level was more significant role in the implementation process. Therefore, it is essential to strengthen the local level government to ensure the sustainability of Nepal's federal health system. Additionally, effective coordination among all three tiers of government is essential for preparedness and communication of the information during the time of emergency.
The study was partially funded by Nepal Health Research Council to implement the study under PG Health Research Grant 2021.
Availability of data and materials
Authors' contributions.
Conceived and designed the study: BSK, BMK and AS.
Tool translation to Nepali: BSK, AT, and BA.
Facilitated data collection in the field: BSK, AT, and RD.
Data transcription and coding: BSK, NRD, RD and KA.
Data analysis: BSK, NB, BA, AT, and KA.
Writing an original draft and editing of the manuscript: BSK, and BA.
Critical revision of the manuscript: BMK, AS, DX, BBS, BB, and RKM.
All authors have read and approved the manuscript.
Declaration of Competing Interest
The authors declare that they have no competing interest.
Acknowledgement
The authors are thankful to all the policymakers, health workers, and stakeholders at federal, provincial, and local levels who participated in this study despite their busy duty schedules. Lastly, the authors would like to thank all who have contributed directly and indirectly to accomplish this study.
Appendix A Supplementary data to this article can be found online at https://doi.org/10.1016/j.dialog.2023.100142 .
Appendix A. Supplementary data
- Contributors
- Mission and Values
- Submissions
- The Regulatory Review In Depth

Lessons Learned From COVID-19
Lee a. fleisher and matthew a. fleisher.

The COVID-19 response illustrates steps officials should take to ensure the effectiveness of vaccine mandates.
The COVID-19 pandemic was the worst public health emergency of the last century. Despite aggressive attempts to contain the virus by social isolation, masking, and medical management, over 1.1 million Americans died between January 31, 2020, when the U.S. Department of Health and Human Services (HHS) declared COVID-19 a public health emergency, and March 11, 2023, when HHS declared the public health emergency over. Of those that perished, there was a particularly tremendous loss among the elderly, immunocompromised, and those in nursing homes.
In December 2020, the U.S. Food and Drug Administration issued emergency use authorizations for the Pfizer-BioNTech and Moderna COVID-19 vaccines . Despite the widespread availability of the vaccines at no cost, their adoption varied considerably. For this reason, physicians and public health officials soon called for a COVID-19 vaccine mandate.
In August 2021, President Joseph R. Biden directed the Centers for Medicare and Medicaid Services (CMS) to require nursing homes to ensure their workers were fully vaccinated against COVID-19 as a condition of participating in the Medicare and Medicaid programs. The Social Security Act provides that facilities participating in Medicare must meet certain requirements and that the HHS Secretary may impose additional requirements deemed necessary to protect the health and safety of patients in hospitals, nursing homes, and other CMS-certified facilities.
HHS’s emergency declarations authorized its component agencies, such as CMS, to issue new health and safety regulations. In addition, outside of public health emergencies, CMS has the authority to oversee healthcare delivery systems. CMS issued its vaccine mandate based on substantial evidence demonstrating that the prevalence of nursing home COVID-19 cases was related to low levels of vaccination among care staff. Furthermore, evidence that many nursing homes were not implementing standard infection control practices accelerated vaccine mandate drafting and execution.
The Administrative Procedure Act requires that agencies that wish to forgo notice-and-comment rulemaking during a public health emergency must demonstrate that undergoing notice-and-comment would be “impracticable, unnecessary, or contrary to the public interest.” The Biden Administration concluded on this basis that it could create an emergency regulation to require vaccines in nursing homes. Nevertheless, as CMS was developing its emergency regulation, nursing homes expressed concern that the mandate could trigger widespread staff shortages because workers would refuse to receive the vaccine. The industry feared that a staffing shortage could lead to worse health outcomes for residents.
While developing the vaccine mandate, the CMS Center for Clinical Standards and Quality convened several listening sessions from all corners of the healthcare industry. During this feedback period, several states issued their own vaccine mandates in both nursing homes and hospitals, and individual nursing home chains and hospital systems also proposed vaccine mandates. This patchwork approach further complicated efforts to limit the spread of COVID-19.
Hospitals and nursing homes were concerned that the variation between states’ rules could lead staff to move to different states to avoid a vaccine mandate. Several providers pushed for a national mandate. A marked increase in the proportion of nurses who sought employment through traveling services during the public health emergency validated this concern. Several national leaders suggested that a national mandate would be useful to manage interstate variability.
Because of these concerns, CMS and HHS began to explore the medical benefits of a national mandate for all healthcare facilities that receive Medicare funding. Data from the National Healthcare Safety Network demonstrated that COVID-19 rates among long-term care facilities were higher in facilities with lower vaccination coverage among staff. The agencies also explored the legal basis for a mandate. Critically, they determined that systems for documenting medical and religious exemptions to the vaccine mandate would be needed.
Ultimately, CMS issued its regulation in November 2021. Shortly thereafter, 14 states challenged the regulation and argued that CMS had exceeded its statutory authority under the Social Security Act. In January 2022, the U.S. Supreme Court, in a 5–4 decision, upheld the mandate, explaining that:
The Secretary of Health and Human Services determined that a COVID-19 vaccine mandate will substantially reduce the likelihood that healthcare workers will contract the virus and transmit it to their patients. He accordingly concluded that a vaccine mandate is “necessary to promote and protect patient health and safety” in the face of the ongoing pandemic. The rule thus fits neatly within the language of the statute.
Importantly, the Court found that the HHS Secretary had examined sufficient evidence justifying the decision to “(1) impose the vaccine mandate instead of a testing mandate; (2) require vaccination of employees with ‘natural immunity’ from prior COVID-19 illness; and (3) depart from the agency’s prior approach of merely encouraging vaccination.”
After the Biden Administration declared the public health emergency over in March 2023, CMS ended its vaccine mandate in August. In the end, the mandate did not substantially disrupt the healthcare ecosystem, and staff resignations due to the mandate did not produce national adverse health outcomes.
It is difficult to analyze the precise effects of the vaccine mandate because there were many states and local facilities that had already mandated the vaccine. Nonetheless, there are at least three important lessons public health officials can learn for the future from CMS’s experience in imposing a COVID-19 vaccine mandate.
First, it will be important to address the non-uniform manner in which states and local healthcare facilities adopt a mandatory vaccination policy during any future pandemic. There should be a national vaccine for healthcare facilities as soon as a safe and effective vaccine is approved. Early adoption can ensure national uniformity, which can in turn help prevent localized staffing shortages. The federal government should also monitor and evaluate the impact of any such mandate and adjust the manner of implementation as needed.
Second, public health officials should proactively collect evidence to demonstrate the health and safety implications of unvaccinated staff in Medicare-certified facilities to justify the need to forgo notice and comment rulemaking. This evidence can also help justify a national vaccine mandate if challenged in the courts.
Finally, public health officials should develop and implement rigorous standards for determining who is exempt from the vaccine mandate by balancing civil rights with healthcare concerns. Rigorous standards will help ensure vaccines succeed in cutting community transmission.
The political debate around vaccination continues to this day but these three lessons can help public health officials prepare for future public health emergencies.

Lee A. Fleisher is an emeritus professor of anesthesiology and critical care at the University of Pennsylvania Perelman School of Medicine . From July 2020 to July 2023, he served as the Chief Medical Officer and Director of the Center for Clinical Standards and Quality at the Centers for Medicare & Medicaid Services .

Matthew A. Fleisher is the chief operating officer and managing director of Rubrum Advising .
Related Essays

Regulating the Great Indoors
Scholar argues that environmental law and policy should expand its scope to inside areas.

Cutting Corners on COVID-19 Treatments?
Scholars analyze FDA’s emergency use authorizations during the COVID-19 pandemic.

How Fixing the Past May Create Future Regulatory Problems
Scholar argues that generational amnesia may lead to ineffective regulatory solutions in the future.

The COVID-19 Vaccines Shouldn't Have Been Free
I n a recent essay in the journal Monash Bioethics Review , oncologist Vinay Prasad and health researcher Alyson Haslam provide a comprehensive after-the-fact assessment of the federal government's rollout of the COVID-19 vaccines.
Their basic takeaway is that the vaccines were a "scientific success"tarnished by flawed federal vaccine policy.
The two argue the tremendous benefits of the COVID-19 vaccines for the elderly were undercut by government guidance and messaging that pushed vaccines on the young, healthy, and previously infected when data suggested that wasn't worthwhile (and was in some cases counterproductive).
Worse still, the government even pushed vaccine mandates when it was increasingly clear the vaccines did not stop COVID-19 transmission, they argue.
To correct these errors for future pandemic responses, Prasad and Haslam recommend performing larger vaccine trials and collecting better data on vaccine performance in lower-risk populations. They also urge policy makers to be more willing to acknowledge the tradeoffs of vaccination.
That's sound advice. We'll have to wait and see if the government adopts it come the next pandemic.
There is one policy that they don't mention and doesn't totally depend on the government getting better at judging the risks of new vaccines: Charge people for them.
Had the government not provided COVID-19 vaccines for free and shielded vaccine makers and administrators from any liability for adverse reactions, prices could have better rationed vaccine supply and better informed people about their risks and benefits.
Without prices, people were instead left with flawed government recommendations, incentives, and rationing schemes.
Those who recall early 2021 will remember the complex , often transparently silly eligibility criteria state governments set up to ration scarce vaccine supplies. This often involved prioritizing younger, healthier, often politically connected "essential workers" over elderly people.
Prasad and Haslam criticize this as a government failure to prioritize groups at most risk of dying from COVID-19.
"While the UK prioritized nursing home residents and older individuals…the US included essential workers, including young, resident physicians," write Prasad and Haslam. "Health care workers face higher risks of acquiring the virus due to occupation (though this was and is offset by available personal protective equipment), but this was less than the elevated risk of death faced by older individuals."
Yet if the government hadn't assigned itself the role of distributing vaccines for free, it wouldn't have been forced into this position of rationing scarce vaccine supplies.
Demand for the vaccine is a function of the vaccine's price. Since the vaccine's price was $0, people who stood to gain comparatively less from vaccination and people for whom a vaccine would be lifesaving were equally incentivized to receive it.
Consequently, everyone rushed to get in line at the same time. The government then had to decide who got it first and predictably made flawed decisions.
Had vaccine makers been left to sell their product on an open market (instead of selling doses in bulk to the federal government to distribute for free), the elderly and those most at risk of COVID-19 would have been able to outbid people who could afford to wait longer. Perhaps more lives could have been saved.
Over the course of 2021, the supply of vaccines outgrew demand.
At the same time, as Prasad and Haslam recount, an increasing number of people (particularly young men) were developing myocarditis as a result of vaccination. Nevertheless, the government downplayed this risk, continued to urge younger populations to get vaccinated, and failed to collect data about the potential risks of vaccination.
That's all a failure of the government policy. Even if the government was slow to adjust its recommendations, prices could have played a constructive role in informing people about their own risk-reward tradeoff of getting vaccinated.
If a 20-year-old man who'd already had COVID-19 had to spend something to get vaccinated, instead of nothing, fewer would have. Prasad and Haslam argue that would have been the right call healthwise.
Without prices, that hypothetical 20-year-old's decision was informed mostly by government guidance, and, later, government mandates.
The government compounded this lack of prices by giving liability shields to vaccine makers. As it stands right now, no one is able to sue the maker of a COVID-19 vaccine should they have an adverse reaction. (Unlike standard, non-COVID vaccines, people are also not allowed to sue the government for compensation for the vaccine injuries.)
If pharmaceutical companies had to charge individual consumers to make money off their vaccines, and if those prices had to reflect the liability risks of the side effects some number of people would inevitably have, consumers would have been even better informed about the risks and rewards of vaccination.
One might counter that individual consumers aren't in a position to perform this risk-reward calculation on their own.
That ignores the ways that other intermediaries in a better position to evaluate the costs and benefits of vaccination could contribute to the price signals individuals would use to make their own decisions.
One could imagine an insurance company declining to cover COVID-19 vaccines for the aforementioned healthy 20-year-old while subsidizing their elderly customers to get the shot. (This is, of course, illegal right now. The Affordable Care Act requires most insurance plans to cover the costs of vaccination for everyone.)
Instead, the financial incentives that were attached to vaccination were another part of the federally subsidized vaccination campaign.
State Medicaid programs paid providers bonuses for the number of patients they vaccinated (regardless of how at risk of COVID-19 those patients were). State governments gave out gift cards to those who got vaccinated and entered them in lotteries to win even bigger prizes.
Leaving it up to private companies to produce and charge for vaccines would have one added benefit: It would make it much more difficult for the government to mandate vaccines or otherwise coerce people into getting them.
One of the things that made it easy for local and state governments to bar the unvaccinated from restaurants and schools was that they also had a lot of free, federally subsidized doses to give away. People didn't have a real "excuse" not to get a shot.
Had people been required to pay for vaccines, it would have been more awkward and much harder (politically and practically) to mandate that they do so.
Economist Alex Tabarrok likes to say that a "price is a signal wrapped up in an incentive." They signal crucial information and then incentivize people to act on that information in a rational, efficient way.
By divorcing COVID-19 vaccines from real price signals, we were left with an earnest, government-led vaccination effort. That effort got a lot of lifesaving vaccines to a lot of people.
But it also encouraged and subsidized people to get vaccinated when it was probably not a necessary or even good idea. When not enough people got vaccinated, governments turned to coercive mandates.
The post The COVID-19 Vaccines Shouldn't Have Been Free appeared first on Reason.com .


IMAGES
COMMENTS
The COVID-19 pandemic in Nepal is part of the worldwide pandemic of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first case in Nepal was confirmed on 23 January 2020 when a 31-year-old student, who had returned to Kathmandu from Wuhan on 9 January, tested positive for the disease.
This paper looks at the economic condition of Nepal before the COVID-19 spread, impact of the pandemic on its economy and measures taken to deal with the situation. Nepal's Economic Health before COVID-19 . Nepal's total economy is around US$32 billion (S$44.73 billion) annually. Since 2016, the country has been rebuilding its economy.
Nepal confirmed its first COVID-19 case in a returnee student from Wuhan, China, on Jan 23, 2020, after the throat swabs sent to the WHO laboratory in Hong Kong identified SARS-CoV-2. Even though this was an isolated event with no further identifiable transmission, it set into motion some of the early responses by the Government of Nepal, including setting up screening at the airport ...
By April 6, 2021, the total confirmed cases worldwide are 132.28 million cases and 2.87 million deaths with more than 200 countries affected, and in Nepal alone, there are 278,470 cases confirmed and 3,036 deaths. [ 1] Nepal had its first COVID-19 case on January 13, 2020. The index case was a student studying in Wuhan and had returned to Nepal ...
The MoHP of Nepal confirmed the first and second cases of COVID-19, respectively, in January and March, in an interval of 2 months 1 ( 9 ). As of January 22, 2021, 268,948 COVID-19 positive cases were reported, with 263,546 recovered, and 1,986 death cases 6. This data showed nearly 0.74% death and about 98% recovery rate in Nepal.
In January, 2020, the outbreak of the 2019 novel coronavirus (2019-nCoV) in China spread progressively to other countries,1,2 with WHO declaring it a Public Health Emergency of International Concern.3 Among the affected countries beyond China (where 12 307 cases and 259 deaths were reported as of Feb 1, 2020) are others in Asia, including Nepal.4
The search terms included "COVID-19 in Nepal" and "Prevention and management of COVID-19 in Nepal." Data used in this article were extracted from relevant documents and websites. The figures were constructed by using Origin 2016 and GIS 10.4.1. We did not consult any databases that are privately owned or inaccessible to the public.
On 24 th January 2020, the first case of COVID-19 was reported in a Nepalese student, who had recently returned from China to Nepal, and the second case was identified about 2 months later in a person returning from France. 7 A complete genome sequence of SARS-CoV-2 strain from a Nepalese patient with COVID-19 showed 99.6% identity with SARS ...
The first COVID-19 case in Nepal was recorded on 23 January 2020. The number of cases started increasing from the third week of March 2020 and by the end of 2020 there were 260 593 cases, with 1 856 recorded fatalities.. In early 2021, Nepal's Ministry of Health and Population (MoHP) submitted the National Deployment and Vaccination Plan (NDVP), which was developed with technical support ...
COVID-19 Pandemic Response. The coronavirus COVID-19 pandemic is the defining global health crisis of our time and the greatest challenge we have faced since World War Two. Since its emergence in Asia late last year, the virus has spread to most of the countries. Nepal, a landlocked country aspiring to graduate from a Least Developed Country ...
Nepal has been on the frontline of both the covid-19 pandemic and climate change, and in both crises the response by the international community and Nepal's government has been marked by a failure to prepare or to invest proactively in strong prevention measures. The first case of covid-19 in Nepal was reported in January 2020 and the country's modest first wave peaked in late October 2020 ...
KATHMANDU, 21 May 2021- As Nepal faces breaking point amidst its worst COVID-19 outbreak, the United Nations and partners are today launching the Nepal Covid-19 Response Plan calling for US$ 83.7 million to mobilize an emergency response over the next three months to assist 750,000 of the most vulnerable people affected by the pandemic.
The tourism industry, a major contributor to Nepal's gross domestic product (GDP), has been one of the major sectors to bear the secondary impact due to COVID-19. This chapter provides an overview of the economic and non-economic impact of COVID-19 on the tourism sector. The discussion centers around two major stakeholders: businesses and ...
The recent global pandemic of novel coronavirus disease 2019 (COVID-19) is increasingly alarming. As of 21 June 2020, there are more than 8.7 million cases worldwide, with 460 000 deaths. Nepal is not an exception to COVID-19 and is currently facing a challenge to prevent the spread of infection. The analysis of the detected cases, severity and ...
Preparedness and Response Plans. Nepal Preparedness and Response Plan (Updated on April 2020) Health Sector Emergency Response Plan for COVID-19. South-East Asia Region Preparedness and Response Plan.
The Nepal Preparedness and Response Plan (NPRP) lays out the preparedness actions and key response activities to be undertaken in Nepal, based on the trends and developments of the global COVID-19 pandemic. The plan outlines two levels of interventions; one that is the preparedness that should take
After several months of relatively low daily cases in Nepal, COVID-19 cases began to rapidly spike in mid-April, increasing consistently from 152 on 1 April to over 8,000 per day since 5 May. Despite its relatively small population of 29.5 million, Nepal currently finds itself among the countries with the highest daily number of cases in absolute terms. Over 45% of COVID-19 RT-PCR tests are ...
Study design. A qualitative research methodology was used 21 to assess the perspective of people towards the management of COVID‐19 and vaccination in rural and urban areas of Nepal. The study was guided and presented in accordance with the Consolidated Criteria for Reporting Qualitative research Checklist. 22. 2.2.
COVID-19 as a Challenge to Nepal's Newly Federalized Health System: Capacities, Responsibilities, and Mindsets Asia Pac J Public Health . 2024 Apr 28:10105395241250123. doi: 10.1177/10105395241250123.
The COVID-19 vaccines delivered by COVAX will contribute to the Government of Nepal's efforts to vaccinate some of the most vulnerable people across Nepal. Today, Nepal received its first consignment of COVID-19 vaccine doses shipped through the COVAX Facility, a partnership between CEPI, Gavi, UNICEF and WHO, made possible through generous ...
The novel coronavirus COVID-19 (SARS-CoV-2) was first reported in 31 December 2019 in Wuhan City, China. The first case of COVID-19 was officially announced on 24 January, 2020, in Nepal. Nine COVID-19 cases have been reported in Nepal. We aim to describe our experiences of COVID-19 patients in Nepa …
About a year ago , at the International Social Protection Conference (18-19 th November 2019,) the government of Nepal and key members of civil society and development community came together to put together a vison for resilient social protection for all Underlying this vision was the commitment to protect the children, marginalized and the vulnerable from attenuating impacts of a disaster ...
The response to COVID-19 in Nepal has been majorly led and controlled by the federal government. All three levels of government are performing their responsibilities; however, they face various challenges in responding to COVID-19. This study aimed to critically analyze Nepal's health system in the context of the COVID-19 response.
The COVID-19 pandemic was the worst public health emergency of the last century. Despite aggressive attempts to contain the virus by social isolation, masking, and medical management, over 1.1 million Americans died between January 31, 2020, when the U.S. Department of Health and Human Services (HHS) declared COVID-19 a public health emergency, and March 11, 2023, when HHS declared the public ...
The best Covid-19 travel insurance plans offer "cancel for any reason" upgrades so you can change your mind about your trip if you have concerns about Covid. They also have at least $100,000 ...
The COVID-19 Vaccines Shouldn't Have Been Free. In a recent essay in the journal Monash Bioethics Review, oncologist Vinay Prasad and health researcher Alyson Haslam provide a comprehensive after ...