

Oppositional Defiant Disorder Treatment

Fig 1 : Oppositional Defiant Disorder Treatment Relational Model. Download Media
In this post, I will cover the various oppositional defiant disorder treatment strategies and a real-life ODD Case Study . For details on what is ODD and get an insight on some of the common ODD prevalence statistics, click here .
Table of Contents
- 1 What Exactly is Oppositional Defiant Disorder?
- 2 Common Oppositional Defiant Disorder Symptoms
- 3.1.1 Parent-Child Interaction Therapy:
- 3.1.2 Family Therapy
- 3.1.3 Problem Solving Training
- 3.1.4 Social Skills Therapy
- 3.1.5 Parent Training
- 3.2 For Teachers
- 4 The Need for Praise
- 5.1 Meet Arthur – A Child with ODD
- 5.2 My First Day observing ODD traits in Arthur
- 5.3 Our First Conversation
- 5.4 Getting to Know Each Other
- 5.5 The Brunch at Arthur’s
- 5.6 Alas, Yet another case of Domestic Violence
- 5.7 Giving Him What He Likes, or Not Quite
- 5.8 It’s Time for Action!
- 5.9 And the ODD Therapy Begins Fig 6: Some of these Architectural Sketched from Arthur were my crucial inlet points for ODD Therapy. Still, pretty neat stuff for a 12 year old!
- 5.10 The Bonding has Already Begun…
- 5.11 Using a Journal as a Private Gateway
- 5.12 And the Breakthrough!
- 5.13 Meeting the Grannies
- 5.14 Fast-forward 4 years..
What Exactly is Oppositional Defiant Disorder?
Oppositional Defiant Disorder or ODD is one of the many diagnoses under the umbrella of autism spectrum disorders . This disorder manifests itself as a pattern of angry, irritable, defiant, nonaggressive yet vindictive behavior. Teens especially tend to refuse to comply with rules and restrictions.
They are nonaggressive, yet spend time planning vindictive reactions to things that annoy them. They deliberately annoy others and blame everything on someone else. For more details, please refer to the article on what is ODD .
Common Oppositional Defiant Disorder Symptoms
Here are some common symptoms of Oppositional Defiant Disorder:
- Failing to Accept Responsibility
- Verbal (or physical) hostility towards others
- Persistent refusal to comply with instructions or rules
- Easily annoyed, angered or agitated
- Deliberately trying to push the limits (in a bad way)
- Stubbornness to compromise with adults or peers
- Being deliberately aggravating towards others
- No respect for authority
- Lack of empathy, treating others with disdain
- Often co-exists with other disorders like ADHD or ADD
For a complete list of Oppositional Defiant Disorder Symptoms, please refer to the article on signs of ODD
Oppositional Defiant Disorder Treatment Strategies
For parents.
Treating oppositional defiant disorder involves several types of psychotherapy and training. Parents are often asked to be involved in the psychotherapy and training to assist the entire family in coping with this disorder. Treatment can last several months to years. Treatment for oppositional defiant disorder includes the following:
Parent-Child Interaction Therapy:
Family Therapy
Counseling for the entire family to improve communication and relationships

Fig 2 : How ODD Family Therapy works
Problem Solving Training
This will help your child identify and change their way of thinking which is leading to their behavior issues. Both parent and child will work together to brainstorm ideas on how to solve an issue in a way that works for everyone. Refer to the guidelines below:

Fig 3 : Problem-solving therapy for Oppositional Defiant Disorder. Download Media
Social Skills Therapy
Learning to interact positively with family and peers. Consult the OT (Occupational Therapist) on how you can achieve the following objectives:
- Teach your child how to relieve anger and control temper
- Keep an eye out for any passive-aggressive behavior traits, evaluate its effects on others and design eliminating strategies
- Stress on problem-solving and communication skills. ODD often exists with ADHD which results in learning difficulties
- Encourage role-playing opportunities so that your child can become comfortable and confident while using newly acquired skills
- Strive for positive reinforcements
- Work with your child and rest of your family to address conflict, set clear expectations and set overall focus on improvement
Parent Training
There are mental health therapists trained to help parents develop their skills to handle problems that arise. You will learn how to avoid struggles, give time outs offer your child choices, establish schedules, routines and be consistent with your praise and consequences. The therapist would guide you on how to determine appropriate consequences that will not overwhelm your child. You will also learn how to keep calm, take time for yourself and most importantly, about positive reinforcement .
Positive Reinforcement will:
- Allow the child to acquire new skills, become independent and increase self-esteem
- Provide a motivational boost to your child, thereby allowing the child to progress further
- Keep the child focused on the task
There are primarily 4 types of Reinforcement:
- Social praise and recognition, such as high 5, clapping, hugs and kisses, cuddle and smile
- Tangible rewards like toys, games
- Favorite food such as chocolates, ice-cream, etc. for children who do not respond verbally
- Token economy (works best for teenagers) such as allowance or money
For Teachers
As teachers, use the following BFPF (Belong – Freedom – Power – Fun) formula. As parents, you also can apply the same cheat sheet while educating your child.

Table 1 : Oppositional Defiant Disorder Teaching Strategies
The Need for Praise

As a parent, you must recognize and praise you child for positive behaviors. This should be an immediate praise such as “I really liked the way you helped your brother with the puzzle”. Be specific when you praise your child so they are aware of what you are praising them for. Be a good role model, and avoid power struggles. Set consistent schedules and stick to them! Children love routines and knowing what comes next. Use this to your advantage in setting limits and boundaries.
Make time for your child and you to interact. Even better, make time for the entire family to interact. Make sure that conversations revolve around consistency, praises, how to spend time together, routines and discipline. Nothing can pull the rug out from under you faster than inconsistency!
What is Oppositional Defiant Disorder solution? Make sure everyone in the household gets the same praises and consequences for their actions. Do not focus only on one child, for then, the child with ODD will start believing that they are in control of the situation. Initially, this involves a lot of hard work, however it will pay off with improved behavior and positivity towards your relationship with your child. Let me repeat one more time because its importance couldn’t be stressed enough: Routine, praise and consequences are key ingredients that you need to help your child with oppositional defiant disorder.
Oppositional Defiant Disorder Case Study
In this part of the post, I will talk about a real-life ODD case study.
Note: This is a real-life ODD case study of Arthur (real name hidden for privacy concerns) whose case was handed to me from an international school in Caribbean Islands. This oppositional defiant disorder case study has been drafted from my personal experience as a behavior therapist. It is important to bear in mind that oppositional defiant disorder in children is different for each subject and hence the strategy adopted to treat ODD in children must be tailored to individual subjects.
Meet Arthur – A Child with ODD

My First Day observing ODD traits in Arthur
I decided to attend his class as an observer. The teacher introduced me as a senior teacher looking for a class to place a teaching assistant. The class was pretty evenly split, girls and boys with a total of eighteen 12-13 year olds. Arthur’s desk was situated between a very cute blonde girl and a boy, a little smaller than he was.
The morning was uneventful until lunch break. The class was asked to complete their work and hand it in on their way out of the classroom for lunch. I had noticed Arthur appeared to be working diligently on his paper. On his way out the door he ripped his paper, crumpled it and told the teacher that the girl next to him had written on his paper so he could not do his work. The teacher began to uncrumple the paper. Arthur snatched it off and began to eat the paper!
The rest of the class was dismissed, yet Arthur remained steadfast in his spot in front of the teacher explaining over and over how the girl had ruined his work as he continued to chew the paper. Unfortunately, the teacher dismissed him for lunch as I sat there in utter amazement. His teacher indicated that this was quite common with Arthur. I picked up a piece of the torn paper that had fallen to the ground and on it was a quite detailed architectural drawing.
Our First Conversation
Later that day I spoke individually with several students asking questions about how they liked school etc. I also talked to Arthur. I asked him how he liked school – no answer and no eye contact. I tried again and he shied away muttering “what does it matter”. He did not know that I had seen his drawing so I asked him if he liked art and drawing.
Wow, his eyes lit up, he raised his head, made eye contact and began explaining to me in detail the principles of architecture and how he was going to be an architect. It was a pleasant conversation and I let him take the lead with the conversation.
Getting to Know Each Other
For a week, I returned to observe his class. For Arthur, every day something occurred that was someone else’s fault. And, every day he came to me and showed me drawings he had done and how he was using a Google program called Sketch up to design a house for me. I was a bit surprised that he said he was designing a house for me. However; I did not let him know that. I told him I was honored that he would want to design a house for me. He was all smiles. Yet, when his classmates were around, his head was down and he was drawing, constantly drawing. Every notebook and book had architecturally detailed inscriptions.
I met with the director again and we reviewed his records with a “fine tooth comb” and still found no mention of any behavior problems, no mention whatsoever of ant oppositional defiant disorder symptoms! This struck me very odd. One does not exhibit the type of behavior Arthur did without notice. I asked if the family would meet with me to discuss Arthur and they readily agreed. In fact, they made a big celebration out of a teacher coming to their home. My husband was also invited; this was to be a nice morning brunch with a discussion about Arthur and school.
The Brunch at Arthur’s
When we arrived the maid greeted us at the door. The house was immaculate. Arthur had a younger brother that was six years old. His mother was from Chile yet spoke impeccable English as well as German. I asked if dad was from Germany and the answer was no. He just liked the German culture and wanted his children to learn German customs and traditions. Both children and his wife were fluent in English, Spanish and German. When dad addressed me or my husband he spoke in English. When he talked to his wife or the maid he spoke Spanish. When he spoke to his sons he spoke German.
I was beginning to get an odd uncomfortable feeling. The therapist in me was now in full mode. The boys stood at the table until everyone was seated and dad gave a “command” in German and the boys sat. The boys were not allowed to speak, that was made very clear. Mom did not speak, other than to welcome us. I noticed the younger brother had a bruise on his leg and was acting quite normal for a 6 year old. Mom reached across the table to pass a dish and I also noticed a bruise on her upper arm that was supposed to be covered with her blouse.
The father did all the talking. He looked directly at Arthur and told him that I was there because he was tired of his misbehavior and defiance and that I would be hired to “fix the situation” or he would be sent to military school. Arthur did not respond, he kept eating as if nothing had been said. Dad said something in German, Arthur jumped up said yes dad and left the room. You could feel the fear in the air.
Alas, Yet another case of Domestic Violence

Fig 4 : Oppositional Defiant Disorder and Domestic Violence
Instability, neglect, abuse, violence often accompanies ODD. Often children diagnosed with Oppositional Defiant Disorder have been or are in an abusive situation. The child becomes more aggressive and blames everyone else for whatever happens in their lives. This was what I believed to be causing Arthur’s problems at school. Of course, if you have an abusive situation where you feel any intervention would put the child in danger you must be very careful. It was very apparent to me there was going to be no help from the parents.
I agreed to work with Arthur and his father made a “deal” with Arthur. If Arthur behaved at school and home, did his work, stopped complaining then dad would hire someone with architectural experience to mentor Arthur to see if architectural design was in Arthur’s future? Arthur had little reaction to what his father said other than “yes dad”, again leaving the room.
The school year was almost over by the time I met Arthur and there was very little time for me to implement any therapy for Arthur, other than being a support system. Dad agreed to have me tutor Arthur during the summer. Arthur came to my home several days a week and the other days I went to his house. He was more at ease at my home. He was very polite, never made eye contact and often offered to help with things that were unrelated to schoolwork. Once he offered to do my dishes so I did not have to work so hard. This was coming from a teenage boy!
Giving Him What He Likes, or Not Quite
I incorporated architecture into his studies. His reading and grammar work was all related to architecture. He was not doing well with math and often expressed the attitude that he was going to be an architect, design and build me a house and he did not need math. I was prepared for this response. I asked him how he would figure out how many supplies were needed to build my house. His response was to delete the computer file and tear up the drawings he had done in his sketchbook while running out the door. He threw himself into the swimming pool and purposely beat his head against the side of the pool until I jumped in and held him as tightly as I could.
Arthur calmed down and we sat on the side of the pool silently for quite some time. Arthur would not make eye contact nor would he say a word. I got up and told him I was going to go change my clothes and would meet him back at his home to continue our work. He said nothing other than I will still make you a house.
About a half hour later I returned to Arthur’s house to find him telling his mother that I threw him in the pool and made him hit his head and that his brother had deleted all his computer work. I was not surprised. What surprised me was his mother’s reaction. She sent him to the kitchen to have some ice cream, sent his younger brother to his room after reprimanding him for touching his brother’s computer and then she turned to me, eyes down and said “I am sorry Ms. Mary this is just the way it is, I know you didn’t push Arthur into the pool but this is how he acts when his brother upsets him” I had to take a deep breath as I looked into the kitchen to see Arthur laughing and pointing at me.

Fig 5 : Blaming it on younger sibling is a common symptom of Oppositional Defiant Disorder in Children
Mom disappeared into the younger brother’s bedroom and I could hear her admonishing the young boy. Arthur laughed even louder. I walked over to Arthur kissed him on the cheek and left. I called mom later and set up a time where we could talk. Dad is only home on the weekends as his job takes him out of town weekly. Mom wanted to wait and have me talk to his Dad “because it would cause trouble if she interfered with anything to do with Arthur”.
I am sure you can all see what was happening here. A fearful mom, beaten and abused children. Arthur with definite symptoms of oppositional defiant disorder and possibly other co-existing autism spectrum disorders all left undiagnosed. Abusive family life does not cause autism or oppositional deficit disorder, however it does enhance its effects.
It’s Time for Action!
I spoke to the principal at Arthur’s previous school. I told him what I thought was going on with Arthur. He stopped me in mid sentence and said “we know about the abuse”. Dad was a powerful man in town so it was never mentioned in public or school records, nor was the family approached about the signs and symptoms Arthur was showing off several autism spectrum disorders. “It would have made the family’s life worse if we had even suggested that Arthur was anything but perfect”.
When you have an abusive situation it becomes a matter of safety for all involved. In the United States, an anonymous phone call to Child Protective Services would have prompted an immediate investigation. However, this was not in the United States, it was in a small Caribbean Island community. The culture and the fact that I, along with this family, was a foreigner in another country also made this case difficult.
I could not walk away from this situation. I needed to find a way through therapy to help Arthur. The family was always respectful to me and encouraged me working with Arthur. For that, I am thankful as it allowed me the opportunity to work with him every day for over six months.
Arthur was old enough to understand that things were not right. However, he believed the abuse was his fault and he had no way to cope with his own feelings. His lack of eye contact, aggression, lying, hiding, not caring about anything but drawing his architectural sketches was what I had to work with (and without any support from the family). It amazes me till this day how they even entertained the idea of having someone work with their son, especially when they cared so little.
And the ODD Therapy Begins Fig 6 : Some of these Architectural Sketched from Arthur were my crucial inlet points for ODD Therapy. Still, pretty neat stuff for a 12 year old!
The first week we did very little scholastic work. I let him talk, he was still not making eye contact, and if he would not talk I would ask him something related to architecture that he could explain to me. Hours were spent looking at his drawings that were hidden under his mattress – sketches of buildings on fire, monsters and children being eaten alive. The more I asked, the more he talked. It was a little over a week before he started to make eye contact. I brought him a book I had with Greek and Roman Architecture in it. That was the breakthrough moment.
He made eye contact and touched the book ever so carefully turning each page gently as he ran his hands over the drawings. The journey had begun, a door had been opened. Not only did I have to work on behavioral therapy I also had to worry about the parental response. Arthur began to look forward to my visits and waited daily at the door. He always had a new sketch to show me. We began opening up his circles of communication. He could tell me all about his drawing if I could teach him something new first.
The Bonding has Already Begun…
I lived within a few blocks of Arthurs home and he would now walk their dog past my house daily. He walked with his head down very quickly passed the house until I would yell out the door “Hello”. Every day I would see him in the morning and we would work on schoolwork and only then it would be time for him to draw or tell me about his thoughts or drawings.
I decided to add in game-playing to see how he reacts to winning and losing. It was a simple game of ‘Sorry’ and he won the first two which excited him to want to play a third round. When he lost the third game, destroyed the board, ripped the cards and threw the pieces at his younger brother while running to his mom pointing at the mess and telling her that his brother had done it. Mom knew the truth however her reaction was much the same as it was months ago. Younger brother punished, Arthur unpunished and Arthur smiling at what he had “accomplished”.
Arthur had come out of his shell, let me in to work with him, however because of his undiagnosed condition and lack of behavioral therapy at a young age, the rage would come through. Over this time span his outbursts were less and less, in fact, when this incident occurred he had been doing very well and expressing his feelings in his notebook and discussing them with me.
Using a Journal as a Private Gateway

Fig 7 : Using a Private Journal – Great Tool to treat a Child with Oppositional Defiant Disorder
The use of a private notebook or journal, allowing a child to draw or write how they honestly feel without the fear of being judged is a great tool. It opens an avenue for the child to express what is bothering him/her and provides an inlet for the therapist to take on a role of positive reinforcement, never criticize, always agree with the thoughts behind the sketches and enter into an ice-breaking conversation like, “I see, now let’s think what would happen if we did this”. The journals, notes, and drawings are their true feelings that are trapped without a way out. You, as a parent must find a way to incorporate positive into the negative.
Arthur came to my house later that day, without his dog, and apologized for what he had done; he made eye contact and was truly apologetic, more so with a slight hug. “I don’t know what to do because everything seems to be my fault”. I called his mom, told her where Arthur was and that he was going to have a snack with my husband and I before getting back home.
And the Breakthrough!
I had two pamphlets on my desk on spousal and child abuse. Arthur saw them and asked if he could look through them. He studied them carefully, silently reading, looking at the pictures and scanning through my desk top to see what else was there. I had (on purpose) a page open in a therapy book about ODD. He held the brochures tightly in his left hand as he read the article in the book. He turned to me and said “All of this is me, isn’t it Ms Mary?” He had put two and two together to realize that he had an undiagnosed condition AND a horribly abusive life. He cried, the first tears I saw! He hugged me tight, the first real genuine expression of his feelings. You could feel his relief leaving his body and soul.
“I am not a bad, terrible, crazy person as my dad says”! It was an astonishing moment and a great breakthrough for Arthur. Yet he knew as well as I did that he had to return to that environment. I decided he should come to my house for his tutoring and therapy where he could express himself freely. Mom agreed. Dad was hesitant however he finally agreed; that man needs a therapy, I tell you!
Meeting the Grannies
Grandma and Grandpa came to visit late in the summer, very nice fellows. These were Arthur’s maternal grandparents and they live in Chile. I continued to work with Arthur, had several interactions with the grandparents and things were progressing. I found out that his grandfather actually owned a contracting business that built homes and schools. This explained where Arthur has inherited this obsession with architecture and I was delighted to see how close he was with his grandparents.
One evening my doorbell rang and it was Arthur’s grandparents. Grandpa did all the talking. Grandma was in tears as he spoke. Grandpa said he knew that his son in law was abusive and that he, Arthur’s dad, was diagnosed with autism when he was young. Grandpa was very open and expressed his sorrow at how his daughter stays with him and how the children were treated. He asked if I knew something that would help. You see, Arthur’s dad had approached grandpa and demanded he provide the income for Arthur to study architecture or he would send him alone to attend a military school which he also wanted the grandpa to pay for.
I was very moved with the grandparents concern and the true regret that they were feeling for not having spoken up sooner or been more forceful in removing their daughter and grandchildren from the situation. It is unfortunate that things like this happen all too often in life.
It indeed was a time for law to intervene. Thankfully, Arthur’s grandparents were affluent and I was able to persuade them to demand custody of the 12-year-old boy. I testified, in the capacity of a qualified medical practitioner, that Arthurs was a child with special needs and the presence of his (abusive) family is detrimental to his formative development. His father didn’t seem to complain much, nice riddance he must have thought!
Undiagnosed, abuse, no one caring or daring to get involved, For Arthur this was the start of a new life. The grandparents were given custody, took Arthur back to Chile with them.
Fast-forward 4 years..
Arthur is now 16 years old and has already graduated high school. He is on a medication for his disorder and is working with his grandfather in their construction business. He designed a new house for his grandparents and is overseeing the project management along with his grandfather.
Arthur and I Skype and email often which allows me to monitor his progress and he is always so excited to tell me how great he feels. Arthur has not seen his parents since he went to live with his grandparents, nor have I been able to have any contact with the family (for obvious reasons). His grandparents and I are very proud of him. He finished high school early with good grades and is doing something that he has a passion for. He continues with therapy to handle anger management issues, but all in all he is functioning and performing so well that I am encouraged that someday it will be Grandpa and Grandson’s business!

I am Ash and I celebrate Neurodiversity! Growing up with an elder brother with severe Autism was tough – but it has also taught me essential life lessons. I don’t believe that people with Autism are necessarily or have any disorder (except in extreme cases). They are just different! And that is something to be proud of! I am passionate about helping other families who may have Autism conditions in their family. So please reach out and drop me a note. I will be glad to help 🙂
Previous Post Is Autism a Psychological Disorder
Next post homeopathy for autism, you may also like.

You took the effort and time to change one’s life. Hope the several other Arthurs out there find the care they need.
oh my. so beautiful. we will never meet, Ms. Mary, but, as a stranger who thinks my family may have this and other issues going on in terms of ODD and ADD and Autism and such, thank you. thank you for wakening little Arthur to the joy of self knowledge. there is no greater gift you can give a person, than to lead them to themselves. thank you. thank you.
Leave a Reply Cancel Reply
Save my name, email, and website in this browser for the next time I comment.
Autism 360™ is a Parent led intervention program where you work one-on-one with our inter-disciplinary team of clinicians to focus on your child's development. We provide you with all the tools, strategies and resources needed to achieve that transformation.
USA | Canada | UK | Australia
Email : [email protected]
Phone USA : (513) 647-4748
Phone AU : 1300 771 869
- Privacy Policy, Data Collection & Terms of Service
- Privacy Policy
All Rights Reserved
- Online Assessments
- Download App
Connection denied by Geolocation Setting.
Reason: Blocked country: Russia
The connection was denied because this country is blocked in the Geolocation settings.
Please contact your administrator for assistance.
- Patient Care & Health Information
- Diseases & Conditions
- Oppositional defiant disorder (ODD)
Even the best-behaved children can be difficult and challenging at times. But oppositional defiant disorder (ODD) includes a frequent and ongoing pattern of anger, irritability, arguing and defiance toward parents and other authority figures. ODD also includes being spiteful and seeking revenge, a behavior called vindictiveness.
These emotional and behavioral issues cause serious problems with family life, social activities, school and work. But as a parent, you don't have to try to manage a child with ODD alone. Your health care provider, a mental health professional and a child development expert can help.
Treatment of ODD involves learning skills to help build positive family interactions and to manage problem behaviors. Other therapy, and possibly medicines, may be needed to treat related mental health conditions.
Sometimes it's difficult to recognize the difference between a strong-willed or emotional child and one with oppositional defiant disorder. It's common for children to show oppositional behavior at certain stages of development.
Symptoms of ODD generally begin during preschool years. Sometimes ODD may develop later, but almost always before the early teen years. Oppositional and defiant behaviors are frequent and ongoing. They cause severe problems with relationships, social activities, school and work, for both the child and the family.
Emotional and behavioral symptoms of ODD generally last at least six months. They include angry and irritable mood, argumentative and defiant behavior, and hurtful and revengeful behavior.
Angry and irritable mood
- Often and easily loses temper.
- Is frequently touchy and easily annoyed by others.
- Is often angry and resentful.
Argumentative and defiant behavior
- Often argues with adults or people in authority.
- Often actively defies or refuses to follow adults' requests or rules.
- Often annoys or upsets people on purpose.
- Often blames others for their own mistakes or misbehavior.
Hurtful and revengeful behavior
- Says mean and hateful things when upset.
- Tries to hurt the feelings of others and seeks revenge, also called being vindictive.
- Has shown vindictive behavior at least twice in the past six months.
ODD can be mild, moderate or severe:
- Mild. Symptoms occur only in one setting, such as only at home, school, work or with peers.
- Moderate. Some symptoms occur in at least two settings.
- Severe. Some symptoms occur in three or more settings.
For some children, symptoms may first be seen only at home. But with time, problem behavior also may happen in other settings, such as school, social activities and with friends.
When to see a doctor
Your child isn't likely to see their own behavior as a problem. Instead, your child will probably complain about unreasonable demands or blame others for problems.
If you think your child may have ODD or other problem behavior, or you're concerned about your ability to parent a challenging child, seek help from a child psychologist or a child psychiatrist with expertise in behavior problems. Ask your child's pediatrician or other health care provider for a referral to a mental health provider.
There is a problem with information submitted for this request. Review/update the information highlighted below and resubmit the form.
From Mayo Clinic to your inbox
Sign up for free and stay up to date on research advancements, health tips, current health topics, and expertise on managing health. Click here for an email preview.
Error Email field is required
Error Include a valid email address
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Thank you for subscribing!
You'll soon start receiving the latest Mayo Clinic health information you requested in your inbox.
Sorry something went wrong with your subscription
Please, try again in a couple of minutes
There's no known clear cause of oppositional defiant disorder. Causes may include a combination of genetic and environmental factors:
- Genetics. A child's natural personality or character — also called temperament — may contribute to developing ODD . Differences in the way nerves and the brain function also may play a role.
- Environment. Problems with parenting that may involve a lack of supervision, inconsistent or harsh discipline, or abuse or neglect may contribute to developing ODD .
Risk factors
Oppositional defiant disorder is a complex problem. Possible risk factors for ODD include:
- Temperament — a child who has a temperament that includes difficulty managing emotions, such as reacting with strong emotions to situations or having trouble tolerating frustration.
- Parenting issues — a child who experiences abuse or neglect, harsh or inconsistent discipline, or a lack of proper supervision.
- Other family issues — a child who lives with parent or family relationships that are unstable or has a parent with a mental health condition or substance use disorder.
- Environment — problem behaviors that are reinforced through attention from peers and inconsistent discipline from other authority figures, such as teachers.
Complications
Children and teenagers with oppositional defiant disorder may have trouble at home with parents and siblings, in school with teachers, and at work with supervisors and other authority figures. Children and teens with ODD may struggle to make and keep friends and relationships.
ODD also may lead to other problems, such as:
- Poor school and work performance.
- Antisocial behavior.
- Legal problems.
- Impulse control problems.
- Substance use disorder.
Many children and teens with ODD also have other mental health conditions, such as:
- Attention-deficit/hyperactivity disorder (ADHD).
- Conduct disorder.
- Depression.
- Anxiety disorders.
- Learning and communication disorders.
Treating these other mental health conditions may help reduce ODD symptoms. It may be difficult to treat ODD if these other conditions are not evaluated and treated appropriately.
There's no sure way to prevent oppositional defiant disorder. But positive parenting and early treatment can help improve behavior and prevent the situation from getting worse. The earlier that ODD can be managed, the better.
Treatment can help restore your child's self-esteem and rebuild a positive relationship between you and your child. Your child's relationships with other important adults in their life — such as teachers and care providers — also will benefit from early treatment.
- Oppositional defiant disorder. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed Oct. 11, 2022.
- Oppositional defiant disorder. American Academy of Child and Adolescent Psychiatry. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-With-Oppositional-Defiant-Disorder-072.aspx. Accessed Oct. 12, 2022.
- Oppositional defiant disorder (ODD). Merck Manual Professional Version. https://www.merckmanuals.com/professional/pediatrics/mental-disorders-in-children-and-adolescents/oppositional-defiant-disorder-odd. Accessed Oct. 12, 2022.
- Ferri FF. Oppositional defiant disorder (ODD). In: Ferri's Clinical Advisor 2023. Elsevier; 2023. https://www.clinicalkey.com. Accessed Oct. 12, 2022.
- Kliegman RM, et al. Disruptive, impulse control, and conduct disorders. In: Nelson Textbook of Pediatrics. 21st ed. Elsevier; 2020. https://www.clinicalkey.com. Accessed Oct. 12, 2022.
- Oppositional defiant disorder. American Association for Marriage and Family Therapy. https://www.aamft.org/Consumer_Updates/Oppositional_Defiant_Disorder.aspx. Accessed Oct. 12, 2022.
- Dulcan MK, ed. Oppositional defiant disorder and conduct disorder. In: Dulcan's Textbook of Child and Adolescent Psychiatry. 3rd ed. American Psychiatric Association Publishing; 2021. https://psychiatryonline.org. Accessed Oct. 12, 2022.
- Kaur M, et al. Oppositional defiant disorder: Evidence-based review of behavioral treatment programs. Annals of Clinical Psychiatry. 2022; doi:10.12788/acp.0056.
- Sawchuk CN (expert opinion). Mayo Clinic. Nov. 25, 2022.
- Symptoms & causes
- Diagnosis & treatment
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 22 June 2023
Oppositional defiant disorder
- David J. Hawes ORCID: orcid.org/0000-0003-3260-1225 1 ,
- Frances Gardner 2 ,
- Mark R. Dadds 1 ,
- Paul J. Frick 3 ,
- Eva R. Kimonis 4 ,
- Jeffrey D. Burke 5 &
- Graeme Fairchild 6
Nature Reviews Disease Primers volume 9 , Article number: 31 ( 2023 ) Cite this article
2526 Accesses
8 Citations
28 Altmetric
Metrics details
- Social behaviour
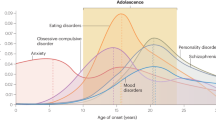
Oppositional defiant disorder (ODD) is a disruptive behaviour disorder involving an ongoing pattern of angry/irritable mood, argumentative/defiant behaviour and vindictiveness. Onset is typically before 8 years of age, although ODD can be diagnosed in both children and adults. This disorder is associated with substantial social and economic burden, and childhood ODD is one of the most common precursors of other mental health problems that can arise across the lifespan. The population prevalence of ODD is ~3 to 5%. A higher prevalence in males than females has been reported, particularly before adolescence. No single risk factor accounts for ODD. The development of this disorder seems to arise from the interaction of genetic and environmental factors, and mechanisms embedded in social relationships are understood to contribute to its maintenance. The treatment of ODD is often successful, and relatively brief parenting interventions produce large sized treatment effects in early childhood. Accordingly, ODD represents an important focus for research, practice and policy concerning early intervention and prevention in mental health.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
92,52 € per year
only 92,52 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others

Adults who microdose psychedelics report health related motivations and lower levels of anxiety and depression compared to non-microdosers

Mechanisms linking social media use to adolescent mental health vulnerability

Investigating child sexual abuse material availability, searches, and users on the anonymous Tor network for a public health intervention strategy
Lavigne, J. V., LeBailly, S. A., Hopkins, J., Gouze, K. R. & Binns, H. J. The prevalence of ADHD, ODD, depression, and anxiety in a community sample of 4-year-olds. J. Clin. Child Adolesc. Psychol. 38 , 315–328 (2009).
Article PubMed Google Scholar
Rissanen, E. et al. The long‐term cost of childhood conduct problems: Finnish Nationwide 1981 Birth Cohort Study. J. Child Psychol. Psychiatry 63 , 683–692 (2022).
França, M. H. et al. Individual and population level estimates of work loss and related economic costs due to mental and substance use disorders in Metropolitan São Paulo, Brazil. J. Affect. Disord. 296 , 198–207 (2022).
Copeland, W. E., Shanahan, L., Costello, E. J. & Angold, A. Childhood and adolescent psychiatric disorders as predictors of young adult disorders. Arch. Gen. Psychiatry 66 , 764–772 (2009).
Article PubMed PubMed Central Google Scholar
Comer, J. S., Chow, C., Chan, P. T., Cooper-Vince, C. & Wilson, L. A. S. Psychosocial treatment efficacy for disruptive behavior problems in very young children: a meta-analytic examination. J. Am. Acad. Child Adolesc. Psychiatry 52 , 26–36 (2013).
Krueger, R. F. et al. Etiologic connections among substance dependence, antisocial behavior, and personality: modeling the externalizing spectrum. J. Abnorm. Psychol. 111 , 411–424 (2002).
Lahey, B. B., Van Hulle, C. A., Singh, A. L., Waldman, I. D. & Rathouz, P. J. Higher-order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Arch. Gen. Psychiatry 68 , 181–189 (2011).
Beauchaine, T. P., Zisner, A. R. & Sauder, C. L. Trait impulsivity and the externalizing spectrum. Annu. Rev. Clin. Psychol. 13 , 343–368 (2017).
Bornovalova, M. A., Hicks, B. M., Iacono, W. G. & McGue, M. Familial transmission and heritability of childhood disruptive disorders. Am. J. Psychiatry 167 , 1066–1074 (2010).
Burke, J. D., Evans, S. C. & Carlson, G. A. Debate: oppositional defiant disorder is a real disorder. Child Adolesc. Ment. Health 27 , 297–299 (2022).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn (American Psychiatric Association, 2013).
Waldman, I. D., Rowe, R., Boylan, K. & Burke, J. D. External validation of a bifactor model of oppositional defiant disorder. Mol. Psychiatry 26 , 682–693 (2021).
Burke, J. D. et al. Identifying the irritability dimension of ODD: application of a modified bifactor model across five large community samples of children. J. Abnorm. Psychol. 123 , 841–851 (2014).
World Health Organization. The ICD-11 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines (WHO, 2018).
Boylan, K., Vaillancourt, T., Boyle, M. & Szatmari, P. Comorbidity of internalizing disorders in children with oppositional defiant disorder. Eur. Child Adolesc. Psychiatry 16 , 484–494 (2007).
Burke, J. D., Mulvey, E. P. & Schubert, C. A. Prevalence of mental health problems and service use among first-time juvenile offenders. J. Child Fam. Stud. 24 , 3774–3781 (2015).
Aebi, M. et al. Oppositional defiant disorder dimensions and subtypes among detained male adolescent offenders. J. Child Psychol. Psychiatry 57 , 729–736 (2016).
Teplin, L. A., Abram, K. M., McClelland, G. M., Dulcan, M. K. & Mericle, A. A. Psychiatric disorders in youth in juvenile detention. Arch. Gen. Psychiatry 59 , 1133–1143 (2002).
Canino, G., Polanczyk, G., Bauermeister, J. J., Rohde, L. A. & Frick, P. J. Does the prevalence of CD and ODD vary across cultures. Soc. Psychiatry Psychiatr. Epidemiol. 45 , 695–704 (2010).
Vasileva, M., Graf, R. K., Reinelt, T., Petermann, U. & Petermann, F. Research review: a meta‐analysis of the international prevalence and comorbidity of mental disorders in children between 1 and 7 years. J. Child Psychol. Psychiatry 62 , 372–381 (2021).
Li, F. et al. Prevalence of mental disorders in school children and adolescents in China: diagnostic data from detailed clinical assessments of 17,524 individuals. J. Child Psychol. Psychiatry 63 , 34–46 (2022).
Mohammadi, M. R. et al. Lifetime prevalence, sociodemographic predictors, and comorbidities of oppositional defiant disorder: the National Epidemiology of Iranian Child and Adolescent Psychiatric disorders (IRCAP). Braz. J. Psychiatry 42 , 162–167 (2020).
Demmer, D. H., Hooley, M., Sheen, J., McGillivray, J. A. & Lum, J. A. G. Sex differences in the prevalence of oppositional defiant disorder during middle childhood: a meta-analysis. J. Abnorm. Child Psychol. 45 , 313–325 (2017). This meta-analytic review reports on male to female prevalence ratios of ODD during middle childhood in community samples, as well as sex differences in prevalence across cultures and over time.
Maughan, B., Rowe, R., Messer, J., Goodman, R. & Meltzer, H. Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J. Child Psychol. Psychiatry 45 , 609–621 (2004).
Johnston, O. G., Derella, O. J. & Burke, J. D. Identification of oppositional defiant disorder in young adult college students. J. Psychopathol. Behav. Assess. 40 , 563–572 (2018).
Article Google Scholar
Nock, M. K., Kazdin, A. E., Hiripi, E. & Kessler, R. C. Lifetime prevalence, correlates, and persistence of oppositional defiant disorder: results from the National Comorbidity Survey Replication. J. Child Psychol. Psychiatry 48 , 703–713 (2007).
Merikangas, K. R. et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 49 , 980–989 (2010).
Bunting, B. P., Murphy, S. D., O’Neill, S. M. & Ferry, F. R. Lifetime prevalence of mental health disorders and delay in treatment following initial onset: evidence from the Northern Ireland Study of Health and Stress. Psychol. Med. 42 , 1727–1739 (2012).
Article CAS PubMed Google Scholar
Anderson, N. P., Feldman, J. A., Kolko, D. J., Pilkonis, P. A. & Lindhiem, O. National norms for the Vanderbilt ADHD diagnostic parent rating scale in children. J. Pediatr. Psychol. 47 , 652–661 (2022).
Rowe, R., Costello, E. J., Angold, A., Copeland, W. E. & Maughan, B. Developmental pathways in oppositional defiant disorder and conduct disorder. J. Abnorm. Psychol. 119 , 726–738 (2010).
Diamantopoulou, S., Verhulst, F. C. & Van Der Ende, J. Gender differences in the development and adult outcome of co-occurring depression and delinquency in adolescence. J. Abnorm. Psychol. 120 , 644–655 (2011).
Burke, J. D., Johnston, O. G. & Perkins, A. G. Where should psychopathic traits be placed in a diagnostic framework? Evidence for a grandiose-manipulative specifier for ODD. Res. Child Adolesc. Psychopathol. 50 , 1289–1298 (2022).
Copeland, W. E., Shanahan, L., Erkanli, A., Costello, E. J. & Angold, A. Indirect comorbidity in childhood and adolescence. Front. Psychiatry 4 , 144 (2013).
Burke, J. D., Johnston, O. G. & Butler, E. J. The irritable and oppositional dimensions of oppositional defiant disorder: integral factors in the explanation of affective and behavioral psychopathology. Child Adolesc. Psychiatr. Clin. N. Am. 30 , 637–647 (2021).
Evans, S. C. et al. Irritability in child and adolescent psychopathology: an integrative review for ICD-11. Clin. Psychol. Rev. 53 , 29–45 (2017).
Stringaris, A., Zavos, H., Leibenluft, E., Maughan, B. & Eley, T. C. Adolescent irritability: phenotypic associations and genetic links with depressed mood. Am. J. Psychiatry 169 , 47–54 (2012).
Hudziak, J. J., Derks, E. M., Althoff, R. R., Copeland, W. & Boomsma, D. I. The genetic and environmental contributions to oppositional defiant behavior: a multi-informant twin study. J. Am. Acad. Child Adolesc. Psychiatry 44 , 907–914 (2005).
Tuvblad, C., Zheng, M., Raine, A. & Baker, L. A. A common genetic factor explains the covariation among ADHD ODD and CD symptoms in 9-10 year old boys and girls. J. Abnorm. Child Psychol. 37 , 153–167 (2009).
Anckarsater, H. et al. The child and adolescent twin study in Sweden (CATSS). Twin Res. Hum. Genet. 14 , 495–508 (2011).
Mikolajewski, A. J., Taylor, J. & Iacono, W. G. Oppositional defiant disorder dimensions: genetic influences and risk for later psychopathology. J. Child Psychol. Psychiatry 58 , 702–710 (2017). This large twin study found that common genetic influences underlie the covariance between irritable symptoms of ODD in childhood and internalizing problems in late adolescence, whereas headstrong/hurtful symptoms of ODD share genetic influences with substance use disorder symptoms.
Stringaris, A., Cohen, P., Pine, D. S. & Leibenluft, E. Adult outcomes of youth irritability: a 20-year prospective community-based study. Am. J. Psychiatry 166 , 1048–1054 (2009).
Veroude, K. et al. Genetics of aggressive behavior: an overview. Am. J. Med. Genet. B Neuropsychiatr. Genet. 171B , 3–43 (2016).
Aebi, M. et al. Gene-set and multivariate genome-wide association analysis of oppositional defiant behavior subtypes in attention-deficit/hyperactivity disorder. Am. J. Med. Genet. B Neuropsychiatr. Genet. 171 , 573–588 (2016).
Barker, E. D. et al. A methylome-wide association study of trajectories of oppositional defiant behaviors and biological overlap with attention deficit hyperactivity disorder. Child Dev. 89 , 1839–1855 (2018).
Boden, J. M., Fergusson, D. M. & Horwood, L. J. Risk factors for conduct disorder and oppositional/defiant disorder: evidence from a New Zealand birth cohort. J. Am. Acad. Child Adolesc. Psychiatry 49 , 1125–1133 (2010).
PubMed Google Scholar
Afifi, T. O., Boman, J., Fleisher, W. & Sareen, J. The relationship between child abuse, parental divorce, and lifetime mental disorders and suicidality in a nationally representative adult sample. Child Abus. Negl. 33 , 139–147 (2009).
Patterson, G. R. & Reid, J. B. Social interactional processes within the family: the study of the moment-by-moment family transactions in which human social development is imbedded. J. Appl. Dev. Psychol. 5 , 237–262 (1984).
Snyder, J., Schrepferman, L. & St. Peter, C. Origins of antisocial behavior: negative reinforcement and affect dysregulation of behavior as socialization mechanisms in family interaction. Behav. Modif. 21 , 187–215 (1997).
Dadds, M. & Hawes, D. Integrated Family Intervention for Child Conduct Problems: a Behaviour-Attachment-Systems Intervention for Parents (Australian Academic Press, 2006).
Smith, J. D. et al. Coercive family process and early-onset conduct problems from age 2 to school entry. Dev. Psychopathol. 26 , 917–932 (2014). Using data from a multisite randomized prevention trial, this sophisticated study examined reciprocal influences between coercive interactions between children and care-givers, oppositional and aggressive behaviour, and growth in early childhood (ages 2–5 years) and school-age conduct problems (ages 7.5 and 8.5 years).
Scaramella, L. V. & Leve, L. D. Clarifying parent–child reciprocities during early childhood: the early childhood coercion model. Clin. Child Fam. Psychol. Rev. 7 , 89–107 (2004).
Burke, J. D., Pardini, D. A. & Loeber, R. Reciprocal relationships between parenting behavior and disruptive psychopathology from childhood through adolescence. J. Abnorm. Child Psychol. 36 , 679–692 (2008).
Stormshak, E. A., Bierman, K. L., McMahon, R. J. & Lengua, L. J. Parenting practices and child disruptive behavior problems in early elementary school. Conduct Problems Prevention Research Group. J. Clin. Child Psychol. 29 , 17–29 (2000).
Article CAS PubMed PubMed Central Google Scholar
Waddell, C., Schwartz, C., Andres, C., Barican, J. L. & Yung, D. Fifty years of preventing and treating childhood behaviour disorders: a systematic review to inform policy and practice. Evid. Based Ment. Health 21 , 45–52 (2018).
Costello, E. J., Compton, S. N., Keeler, G. & Angold, A. Relationships between poverty and psychopathology: a natural experiment. J. Am. Med. Assoc. 290 , 2023–2029 (2003).
Article CAS Google Scholar
Greene, R. W. et al. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am. J. Psychiatry 159 , 1214–1224 (2002).
Conger, R. D. et al. Economic pressure in African American families: a replication and extension of the family stress model. Dev. Psychol. 38 , 179–193 (2002).
van Goozen, S. H. et al. Salivary cortisol and cardiovascular activity during stress in oppositional-defiant disorder boys and normal controls. Biol. Psychiatry 43 , 531–539 (1998).
van Goozen, S. H., Matthys, W., Cohen-Kettenis, P. T., Buitelaar, J. K. & van Engeland, H. Hypothalamic-pituitary-adrenal axis and autonomic nervous system activity in disruptive children and matched controls. J. Am. Acad. Child Adolesc. Psychiatry 39 , 1438–1445 (2000).
Snoek, H., Van Goozen, S. H., Matthys, W., Buitelaar, J. K. & van Engeland, H. Stress responsivity in children with externalizing behavior disorders. Dev. Psychopathol. 16 , 389–406 (2004).
van de Wiel, N. M., van Goozen, S. H., Matthys, W., Snoek, H. & van Engeland, H. Cortisol and treatment effect in children with disruptive behavior disorders: a preliminary study. J. Am. Acad. Child Adolesc. Psychiatry 43 , 1011–1018 (2004).
Schoorl, J., van Rijn, S., de Wied, M., van Goozen, S. H. M. & Swaab, H. Neurobiological stress responses predict aggression in boys with oppositional defiant disorder/conduct disorder: a 1-year follow-up intervention study. Eur. Child Adolesc. Psychiatry 26 , 805–813 (2017).
Dorn, L. D. et al. Salivary gonadal and adrenal hormone differences in boys and girls with and without disruptive behavior disorders: contextual variants. Biol. Psychol. 81 , 31–39 (2009).
Pauli-Pott, U. et al. Long-term cortisol secretion in attention deficit hyperactivity disorder: roles of sex, comorbidity, and symptom presentation. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-023-02180-1 (2023).
Scassellati, C., Bonvicini, C., Faraone, S. V. & Gennarelli, M. Biomarkers and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. J. Am. Acad. Child Adolesc. Psychiatry 51 , 1003–1019.e20 (2012).
Fairchild, G., Baker, E. & Eaton, S. Hypothalamic-pituitary-adrenal axis function in children and adults with severe antisocial behavior and the impact of early adversity. Curr. Psychiatry Rep. 20 , 84 (2018).
Lorber, M. F. Psychophysiology of aggression, psychopathy, and conduct problems: a meta-analysis. Psychol. Bull. 130 , 531–552 (2004).
van Goozen, S. H., Snoek, H., Matthys, W., van Rossum, I. & van Engeland, H. Evidence of fearlessness in behaviourally disordered children: a study on startle reflex modulation. J. Child Psychol. Psychiatry 45 , 884–892 (2004).
De Wied, M., Boxtel, A. V., Posthumus, J. A., Goudena, P. P. & Matthys, W. Facial EMG and heart rate responses to emotion-inducing film clips in boys with disruptive behavior disorders. Psychophysiology 46 , 996–1004 (2009).
de Wied, M., van Boxtel, A., Matthys, W. & Meeus, W. Verbal, facial and autonomic responses to empathy-eliciting film clips by disruptive male adolescents with high versus low callous-unemotional traits. J. Abnorm. Child Psychol. 40 , 211–223 (2012).
Kimonis, E. R. et al. Facial reactions to emotional films in young children with conduct problems and varying levels of callous‐unemotional traits. J. Child Psychol. Psychiatry 64 , 357–366 (2023).
Matthys, W., Vanderschuren, L. J. & Schutter, D. J. The neurobiology of oppositional defiant disorder and conduct disorder: altered functioning in three mental domains. Dev. Psychopathol. 25 , 193–207 (2013). The review examines evidence from neurobiological studies of ODD and CD within the conceptual framework of three interrelated mental domains: punishment processing, reward processing and cognitive control.
Matthys, W., van Goozen, S. H., de Vries, H., Cohen-Kettenis, P. T. & van Engeland, H. The dominance of behavioural activation over behavioural inhibition in conduct disordered boys with or without attention deficit hyperactivity disorder. J. Child Psychol. Psychiatry 39 , 643–651 (1998).
van Goozen, S. H. et al. Executive functioning in children: a comparison of hospitalised ODD and ODD/ADHD children and normal controls. J. Child Psychol. Psychiatry 45 , 284–292 (2004).
Luman, M., Sergeant, J. A., Knol, D. L. & Oosterlaan, J. Impaired decision making in oppositional defiant disorder related to altered psychophysiological responses to reinforcement. Biol. Psychiatry 68 , 337–344 (2010).
Schutter, D. J., van Bokhoven, I., Vanderschuren, L. J., Lochman, J. E. & Matthys, W. Risky decision making in substance dependent adolescents with a disruptive behavior disorder. J. Abnorm. Child Psychol. 39 , 333–339 (2011).
Kleine Deters, R. et al. Executive functioning and emotion recognition in youth with oppositional defiant disorder and/or conduct disorder. World J. Biol. Psychiatry 21 , 539–551 (2020).
Noordermeer, S. D. et al. Neurocognitive deficits in attention-deficit/hyperactivity disorder with and without comorbid oppositional defiant disorder. J. Atten. Disord. 24 , 1317–1329 (2020).
Oosterlaan, J., Logan, G. D. & Sergeant, J. A. Response inhibition in AD/HD, CD, comorbid AD/HD + CD, anxious, and control children: a meta-analysis of studies with the stop task. J. Child Psychol. Psychiatry 39 , 411–425 (1998).
Scheres, A., Oosterlaan, J. & Sergeant, J. A. Response execution and inhibition in children with AD/HD and other disruptive disorders: the role of behavioural activation. J. Child Psychol. Psychiatry 42 , 347–357 (2001).
Lipszyc, J. & Schachar, R. Inhibitory control and psychopathology: a meta-analysis of studies using the stop signal task. J. Int. Neuropsychol. Soc. 16 , 1064–1076 (2010).
Hobson, C. W., Scott, S. & Rubia, K. Investigation of cool and hot executive function in ODD/CD independently of ADHD. J. Child Psychol. Psychiatry 52 , 1035–1043 (2011).
Noordermeer, S. D., Luman, M. & Oosterlaan, J. A systematic review and meta-analysis of neuroimaging in oppositional defiant disorder (ODD) and conduct disorder (CD) taking attention-deficit hyperactivity disorder (ADHD) into account. Neuropsychol. Rev. 26 , 44–72 (2016).
Fahim, C. et al. Neuroanatomy of childhood disruptive behavior disorders. Aggress. Behav. 37 , 326–337 (2011).
Wang, Y. et al. White matter abnormalities associated with disruptive behavior disorder in adolescents with and without attention-deficit/hyperactivity disorder. Psychiatry Res. 202 , 245–251 (2012).
Finger, E. C. et al. Impaired functional but preserved structural connectivity in limbic white matter tracts in youth with conduct disorder or oppositional defiant disorder plus psychopathic traits. Psychiatry Res. 202 , 239–244 (2012).
Rogers, J. C. et al. White matter microstructure in youths with conduct disorder: effects of sex and variation in callous traits. J. Am. Acad. Child Adolesc. Psychiatry 58 , 1184–1196 (2019).
Marsh, A. A. et al. Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders. Am. J. Psychiatry 165 , 712–720 (2008).
Marsh, A. A. et al. Empathic responsiveness in amygdala and anterior cingulate cortex in youths with psychopathic traits. J. Child Psychol. Psychiatry 54 , 900–910 (2013).
Marsh, A. A. et al. Reduced amygdala-orbitofrontal connectivity during moral judgments in youths with disruptive behavior disorders and psychopathic traits. Psychiatry Res. 194 , 279–286 (2011).
Bjork, J. M., Chen, G., Smith, A. R. & Hommer, D. W. Incentive-elicited mesolimbic activation and externalizing symptomatology in adolescents. J. Child Psychol. Psychiatry 51 , 827–837 (2010).
Cohn, M. D. et al. Incentive processing in persistent disruptive behavior and psychopathic traits: a functional magnetic resonance imaging study in adolescents. Biol. Psychiatry 78 , 615–624 (2015).
Zhu, Y. et al. Differences in functional activity between boys with pure oppositional defiant disorder and controls during a response inhibition task: a preliminary study. Brain Imaging Behav. 8 , 588–597 (2014).
Rubia, K., Smith, A. B., Brammer, M. J., Toone, B. & Taylor, E. Abnormal brain activation during inhibition and error detection in medication-naive adolescents with ADHD. Am. J. Psychiatry 162 , 1067–1075 (2005).
Rubia, K. et al. Dissociated functional brain abnormalities of inhibition in boys with pure conduct disorder and in boys with pure attention deficit hyperactivity disorder. Am. J. Psychiatry 165 , 889–897 (2008).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 3rd edn (American Psychiatric Association, 1980).
Moffitt, T. E. et al. Research review: DSM-V conduct disorder: research needs for an evidence base. J. Child Psychol. Psychiatry 49 , 3–33 (2008).
Frick, P. J. & Nigg, J. T. Current issues in the diagnosis of attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder. Annu. Rev. Clin. Psychol. 8 , 77–107 (2012). This review addresses the major issues and evidence that informed the evaluation of diagnostic criteria for the externalizing disorders (ODD, CD and ADHD) during the development of DSM-5.
Stringaris, A. & Goodman, R. Longitudinal outcome of youth oppositionality: irritable, headstrong, and hurtful behaviors have distinctive predictions. J. Am. Acad. Child Adolesc. Psychiatry 48 , 404–412 (2009).
Egger, H. L. & Angold, A. Common emotional and behavioral disorders in preschool children: presentation, nosology, and epidemiology. J. Child Psychol. Psychiatry 47 , 313–337 (2006).
Wakschlag, L. S. et al. Defining the developmental parameters of temper loss in early childhood: implications for developmental psychopathology: early childhood parameters of temper loss. J. Child Psychol. Psychiatry 53 , 1099–1108 (2012).
Frick, P. J., Ray, J. V., Thornton, L. C. & Kahn, R. E. Can callous-unemotional traits enhance the understanding, diagnosis, and treatment of serious conduct problems in children and adolescents? A comprehensive review. Psychol. Bull. 140 , 1–57 (2014).
McMahon, R. J., Witkiewitz, K. & Kotler, J. S. Predictive validity of callous–unemotional traits measured in early adolescence with respect to multiple antisocial outcomes. J. Abnorm. Psychol. 119 , 752–763 (2010).
De Brito, S. A. et al. Psychopathy. Nat. Rev. Dis. Primers 7 , 49 (2021).
Lochman, J. E. et al. An empirically based alternative to DSM-5’s disruptive mood dysregulation disorder for ICD-11. World Psychiatry 14 , 30–33 (2015).
Frick, P. J. Developmental pathways to conduct disorder: implications for future directions in research, assessment, and treatment. J. Clin. Child Adolesc. Psychol. 41 , 378–389 (2012).
Walker, T. M., Frick, P. J. & McMahon, R. J. in Assessment of Disorders in Childhood and Adolescence 5th edn Vol. 132 (Guild Publications, 2020).
Achenbach, T. & Rescorla, L. Manual for the ASEBA school-age forms and profiles: child behavior checklist for ages 6–18 (University of Vermont, 2001).
Reynolds, C. & Kamphaus, R. Behavior Assessment System for Children 3rd edn (Pearson, 2015).
Goodman, R. The strengths and difficulties questionnaire: a research note. J. Child Psychol. Psychiatry 38 , 581–586 (1997).
Pelham, W. E., Gnagy, E. M., Greenslade, K. E. & Milich, R. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J. Am. Acad. Child Adolesc. Psychiatry 31 , 210–218 (1992).
Florida International University. Parent/teacher DBD rating scale FIU https://ccf.fiu.edu/research/_assets/dbd-rating-scale.pdf (2023).
Gadow, K. D. & Sprafkin, J. N. Child Symptom Inventory 4: Screening and Norms Manual (Checkmate Plus, 2002).
Shemmassian, S. K. & Lee, S. S. Comparative validity of DSM-IV and alternative empirically derived approaches for the assessment of ADHD. J. Atten. Disord. 21 , 405–415 (2017).
Vaughn, A. J. & Hoza, B. The incremental utility of behavioral rating scales and a structured diagnostic interview in the assessment of attention-deficit/hyperactivity disorder. J. Emot. Behav. Disord. 21 , 227–239 (2013).
Husky, M. M. et al. Psychometric properties of the Strengths and Difficulties Questionnaire in children aged 5–12 years across seven European countries. Eur. J. Psychol. Assess. 36 , 65–76 (2020).
Eyberg, S. M. Eyberg Child Behavior Inventory and Sutter–Eyberg Student Behavior Inventory – Revised: Professional Manual (Psychological Assessment Resources, 1999).
Green, H., McGinnity, A., Meltzer, H., Ford, T. & Goodman, R. Mental Health of Children and Young People in Great Britain, 2004 (American Psychological Association, 2005).
Lawrence, D. et al. The mental health of children and adolescents: report on the second Australian child and adolescent survey of mental health and wellbeing (Commonwealth of Australia, 2015).
Merikangas, K. R. et al. Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 50 , 32–45 (2011).
Hendriks, A. M., Bartels, M., Colins, O. F. & Finkenauer, C. Childhood aggression: a synthesis of reviews and meta-analyses to reveal patterns and opportunities for prevention and intervention strategies. Neurosci. Biobehav. Rev. 91 , 278–291 (2018).
Leijten, P. et al. Meta-analyses: key parenting program components for disruptive child behavior. J. Am. Acad. Child Adolesc. Psychiatry 58 , 180–190 (2019). In this highly informative study, two meta-analyses were conducted to identify which components of evidence-based parenting programmes for conduct problems most account for programme effects, when delivered for the purpose of prevention and treatment.
Durlak, J. A. & Wells, A. M. Evaluation of indicated preventive intervention (secondary prevention) mental health programs for children and adolescents. Am. J. Community Psychol. 26 , 775–802 (1998).
Grove, A. B., Evans, S. W., Pastor, D. A. & Mack, S. D. A meta-analytic examination of follow-up studies of programs designed to prevent the primary symptoms of oppositional defiant and conduct disorders. Aggress. Violent Behav. 13 , 169–184 (2008).
Sawyer, A. M., Borduin, C. M. & Dopp, A. R. Long-term effects of prevention and treatment on youth antisocial behavior: a meta-analysis. Clin. Psychol. Rev. 42 , 130–144 (2015).
Kaminski, J. W. & Claussen, A. H. Evidence base update for psychosocial treatments for disruptive behaviors in children. J. Clin. Child Adolesc. Psychol. 46 , 477–499 (2017).
Patterson, G. R., Dishion, T. J. & Bank, L. Family interaction: a process model of deviancy training. Aggress. Behav. 10 , 253–267 (1984).
Campbell, S. B., Shaw, D. S. & Gilliom, M. Early externalizing behavior problems: toddlers and preschoolers at risk for later maladjustment. Dev. Psychopathol. 12 , 467–488 (2000).
Webster-Stratton, C. & Taylor, T. Nipping early risk factors in the bud: reventing substance abuse, delinquency, and violence in adolescence through interventions targeted at young children (0–8 years). Prev. Sci. 2 , 165–192 (2001).
Conduct Problems Prevention Research Group The effects of the fast track preventive intervention on the development of conduct disorder across childhood: fast track preventive intervention. Child Dev. 82 , 331–345 (2011).
Article PubMed Central Google Scholar
National Institute for Health and Care Excellence. Antisocial Behaviour and Conduct Disorders in Children and Young People: Recognition and Management . Clinical guideline [CG158] (NICE, 2017).
World Health Organization. WHO guidelines on parenting interventions to prevent maltreatment and enhance parent–child relationships in children aged 0–17 years. WHO https://www.who.int/publications/i/item/9789240065505 (2023).
Beelmann, A., Arnold, L. S. & Hercher, J. Parent training programs for preventing and treating antisocial behavior in children and adolescents: a comprehensive meta-analysis of international studies. Aggress. Violent Behav. 68 , 101798 (2023).
Kaehler, L. A., Jacobs, M. & Jones, D. J. Distilling common history and practice elements to inform dissemination: Hanf-model BPT programs as an example. Clin. Child Fam. Psychol. Rev. 19 , 236–258 (2016).
Forehand, R., Lafko, N., Parent, J. & Burt, K. B. Is parenting the mediator of change in behavioral parent training for externalizing problems of youth? Clin. Psychol. Rev. 34 , 608–619 (2014).
Backhaus, S., Gardner, F., Melendez-Torres, G., Jochim, J. & Leijten, P. Social learning theory-based parenting interventions for children aged 2–10 years to prevent child maltreatment and promote positive development: systematic review and meta-analysis for the WHO Guideline. WHO https://cdn.who.int/media/docs/default-source/documents/violence-prevention/systematic_reviews-for-the-who-parenting-guideline-jan-27th-2023.pdf?sfvrsn=158fd424_3 (2023).
Gardner, F., Backhaus, S., Melendez-Torres, G., Knerr, W. & Lachman, J. Parenting interventions in low-and-middle-income countries for reducing child maltreatment and harsh parenting and promoting positive development: systematic review and meta-analysis for the WHO Guideline. WHO https://cdn.who.int/media/docs/default-source/documents/violence-prevention/systematic_reviews-for-the-who-parenting-guideline-jan-27th-2023.pdf?sfvrsn=158fd424_3 (2023).
Overbeek, G. et al. Longer-term outcomes of the Incredible Years parenting intervention. Prev. Sci. 22 , 419–431 (2021).
Van Aar, J., Leijten, P., de Castro, B. O. & Overbeek, G. Sustained, fade-out or sleeper effects? A systematic review and meta-analysis of parenting interventions for disruptive child behavior. Clin. Psychol. Rev. 51 , 153–163 (2017).
Fossum, S., Handegård, B. H., Adolfsen, F., Vis, S. A. & Wynn, R. A meta-analysis of long-term outpatient treatment effects for children and adolescents with conduct problems. J. Child Fam. Stud. 25 , 15–29 (2016).
Spencer, C. M., Topham, G. L. & King, E. L. Do online parenting programs create change?: a meta-analysis. J. Fam. Psychol. 34 , 364–374 (2020).
Leijten, P. et al. Individual participant data meta-analysis: impact of conduct problem severity, comorbid attention-deficit/hyperactivity disorder and emotional problems, and maternal depression on parenting program effects. J. Am. Acad. Child Adolesc. Psychiatry 59 , 933–943 (2020).
Gardner, F. et al. Equity effects of parenting interventions for child conduct problems: a pan-European individual participant data meta-analysis. Lancet Psychiatry 6 , 518–527 (2019). This study found no evidence for differential effects by social disadvantage among children ( n = 1,696; children aged 2–10 years) who received the Incredible Years parenting intervention, and was used to argue that such intervention might be an important tool for reducing social disparities and improving long-term outcomes in disadvantaged families of children with conduct problems.
Gardner, F. et al. Could scale-up of parenting programmes improve child disruptive behaviour and reduce social inequalities? Using individual participant data meta-analysis to establish for whom programmes are effective and cost-effective. Public Health Res. 5 , 1–144 (2017).
Gardner, F. et al. The earlier the better? Individual participant data and traditional meta‐analysis of age effects of parenting interventions. Child Dev. 90 , 7–19 (2019).
Bakker, M. J., Greven, C. U., Buitelaar, J. K. & Glennon, J. C. Practitioner review: psychological treatments for children and adolescents with conduct disorder problems–a systematic review and meta-analysis. J. Child Psychol. Psychiatry 58 , 4–18 (2017).
Nye, E., Melendez‐Torres, G. J. & Gardner, F. Mixed methods systematic review on effectiveness and experiences of the Incredible Years Teacher Classroom Management programme. Rev. Educ. 7 , 631–669 (2019).
Ford, T. et al. The effectiveness and cost-effectiveness of the Incredible Years® Teacher Classroom Management programme in primary school children: results of the STARS cluster randomised controlled trial. Psychol. Med. 49 , 828–842 (2019).
Troncoso, P. & Humphrey, N. Playing the long game: a multivariate multilevel non-linear growth curve model of long-term effects in a randomized trial of the Good Behavior Game. J. Sch. Psychol. 88 , 68–84 (2021).
Webster-Stratton, C., Reid, M. J. & Hammond, M. Treating children with early-onset conduct problems: intervention outcomes for parent, child, and teacher training. J. Clin. Child Adolesc. Psychol. 33 , 105–124 (2004).
Williams, M. E., Bywater, T., Lane, E., Williams, N. C. & Hutchings, J. Building social and emotional competence in school children: a randomised controlled trial. Psychology 10 , 107–121 (2019).
Kuhn, M., Gonzalez, E., Weil, L., Izguttinov, A. & Walker, S. Effectiveness of child-focused interventions for externalizing behavior: a rapid evidence review. Res. Child Adolesc. Psychopathol. 50 , 987–1009 (2022).
McCart, M. R. & Sheidow, A. J. Evidence-based psychosocial treatments for adolescents with disruptive behavior. J. Clin. Child Adolesc. Psychol. 45 , 529–563 (2016).
Battagliese, G. et al. Cognitive-behavioral therapy for externalizing disorders: a meta-analysis of treatment effectiveness. Behav. Res. Ther. 75 , 60–71 (2015).
Muratori, P. et al. Effects of a universal prevention program on externalizing behaviors: exploring the generalizability of findings across school and home settings. J. Sch. Psychol. 77 , 13–23 (2019).
Muratori, P. et al. Six-year outcome for children with ODD or CD treated with the coping power program. Psychiatry Res. 271 , 454–458 (2019).
Helander, M. et al. The effect of adding Coping Power Program–Sweden to Parent Management Training-effects and moderators in a randomized controlled trial. Behav. Res. Ther. 103 , 43–52 (2018).
Mushtaq, A., Lochman, J. E., Tariq, P. N. & Sabih, F. Preliminary effectiveness study of Coping Power program for aggressive children in Pakistan. Prev. Sci. 18 , 762–771 (2017).
American Academy of Child and Adolescent Psychiatry. ODD: a guide for families. American Academy of Child and Adolescent Psychiatry https://www.aacap.org/App_Themes/AACAP/docs/resource_centers/odd/odd_resource_center_odd_guide.pdf (2009).
Scott, S., Knapp, M., Henderson, J. & Maughan, B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. Br. Med. J. 323 , 191 (2001).
Leadbeater, B. J. & Ames, M. E. The longitudinal effects of oppositional defiant disorder symptoms on academic and occupational functioning in the transition to young adulthood. J. Abnorm. Child Psychol. 45 , 749–763 (2017).
Burke, J. D., Rowe, R. & Boylan, K. Functional outcomes of child and adolescent oppositional defiant disorder symptoms in young adult men. J. Child Psychol. Psychiatry 55 , 264–272 (2014). In this unique study of functional outcomes in adulthood (at 24 years of age) associated with ODD, ODD symptoms from childhood through adolescence were found to predict poorer adult functioning with peers, poorer romantic relationships, a poorer paternal relationship and fewer job recommendations.
Shaw, D. S., Sitnick, S. L., Reuben, J., Dishion, T. J. & Wilson, M. N. Transactional effects among maternal depression, neighborhood deprivation, and child conduct problems from early childhood through adolescence: a tale of two low-income samples. Dev. Psychopathol. 28 , 819–836 (2016).
Patterson, G. R., Forgatch, M. S. & DeGarmo, D. S. Cascading effects following intervention. Dev. Psychopathol. 22 , 949–970 (2010).
Woelbert, E., Kirtley, A., Balmer, N. & Dix, S. How much is spent on mental health research: developing a system for categorising grant funding in the UK. Lancet Psychiatry 6 , 445–452 (2019).
Burt, S. A. et al. Commentary: childhood conduct problems are a public health crisis and require resources: a commentary on Rivenbark et al. J. Child Psychol. Psychiatry 59 , 711–713 (2018).
Havighurst, S. S. et al. A review of Australian Government funding of parenting intervention research. Aust. N. Zeal. J. Public Health 46 , 262–268 (2022).
GBD Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Psychiatry 9 , 137–150 (2022).
Rubia, K. “Cool” inferior frontostriatal dysfunction in attention-deficit/hyperactivity disorder versus “hot” ventromedial orbitofrontal-limbic dysfunction in conduct disorder: a review. Biol. Psychiatry 69 , e69–e87 (2011).
Burke, J. D., Loeber, R., Lahey, B. B. & Rathouz, P. J. Developmental transitions among affective and behavioral disorders in adolescent boys. J. Child Psychol. Psychiatry 46 , 1200–1210 (2005).
Rowe, R., Maughan, B., Pickles, A., Costello, E. J. & Angold, A. The relationship between DSM-IV oppositional defiant disorder and conduct disorder: findings from the Great Smoky Mountains Study. J. Child Psychol. Psychiatry 43 , 365–373 (2002).
Chacko, A. et al. Engagement in behavioral parent training: review of the literature and implications for practice. Clin. Child Fam. Psychol. Rev. 19 , 204–215 (2016).
Dadds, M. R. et al. Therapist-assisted online treatment for child conduct problems in rural and urban families: two randomized controlled trials. J. Consult. Clin. Psychol. 87 , 706–719 (2019). Through two RCTs, this paper provides compelling support for the online delivery of evidence-based parenting interventions for conduct problems with families living in urban as well as rural/remote regions.
Prinz, R. J., Metzler, C. W., Sanders, M. R., Rusby, J. C. & Cai, C. Online‐delivered parenting intervention for young children with disruptive behavior problems: a noninferiority trial focused on child and parent outcomes. J. Child Psychol. Psychiatry 63 , 199–209 (2022).
Awah, I. et al. ‘It provides practical tips, practical solutions!’: acceptability, usability, and satisfaction of a digital parenting intervention across African countries. Psychol. Health Med. 27 , 107–123 (2022).
Kazdin, A. E. Annual research review: expanding mental health services through novel models of intervention delivery. J. Child Psychol. Psychiatry 60 , 455–472 (2019).
Tully, L. A., Hawes, D. J., Doyle, F. L., Sawyer, M. G. & Dadds, M. R. A national child mental health literacy initiative is needed to reduce childhood mental health disorders. Aust. N. Zeal. J. Psychiatry 53 , 286–290 (2019).
Bloss, C., Brown, S. & Sawrikar, V. Does behavioural parent training reduce internalising symptoms (or not) among children with externalising problems? Systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry https://doi.org/10.1007/s00787-022-02122-3 (2022).
Wilkinson, S., Waller, R. & Viding, E. Practitioner review: involving young people with callous unemotional traits in treatment–does it work? A systematic review. J. Child Psychol. Psychiatry 57 , 552–565 (2016).
Dadds, M. R., Cauchi, A. J., Wimalaweera, S., Hawes, D. J. & Brennan, J. Outcomes, moderators, and mediators of empathic-emotion recognition training for complex conduct problems in childhood. Psychiatry Res. 199 , 201–207 (2012).
Dadds, M. R., English, T., Wimalaweera, S., Schollar‐Root, O. & Hawes, D. J. Can reciprocated parent–child eye gaze and emotional engagement enhance treatment for children with conduct problems and callous–unemotional traits: a proof‐of‐concept trial. J. Child Psychol. Psychiatry 60 , 676–685 (2019).
Kimonis, E. R. et al. Parent–child interaction therapy adapted for preschoolers with callous–unemotional traits: an open trial pilot study. J. Clin. Child Adolesc. Psychol. 48 , S347–S361 (2019).
Fleming, G. E. et al. Parent training adapted to the needs of children with callous–unemotional traits: a randomized controlled trial. Behav. Ther. 53 , 1265–1281 (2022).
Stringaris, A. & Goodman, R. Three dimensions of oppositionality in youth. J. Child Psychol. Psychiatry 50 , 216–223 (2009).
Lavigne, J. V., Gouze, K. R., Bryant, F. B. & Hopkins, J. Dimensions of oppositional defiant disorder in young children: heterotypic continuity with anxiety and depression. J. Abnorm. Child Psychol. 42 , 937–951 (2014).
Burke, J. D., Hipwell, A. E. & Loeber, R. Dimensions of oppositional defiant disorder as predictors of depression and conduct disorder in preadolescent girls. J. Am. Acad. Child Adolesc. Psychiatry 49 , 484–492 (2010).
PubMed PubMed Central Google Scholar
Herzhoff, K. & Tackett, J. L. Subfactors of oppositional defiant disorder: converging evidence from structural and latent class analyses. J. Child Psychol. Psychiatry 57 , 18–29 (2016). Together with Burke et al. (2010), using mixed gender community and replication samples (combined n = 730) to evaluate the structural models of ODD, this study found that a two-factor model including irritability and oppositionality subfactors best fit the data.
Ezpeleta, L., Granero, R., De La Osa, N., Penelo, E. & Domènech, J. M. Dimensions of oppositional defiant disorder in 3‐year‐old preschoolers. J. Child Psychol. Psychiatry 53 , 1128–1138 (2012).
Ollendick, T. H., Booker, J. A., Ryan, S. & Greene, R. W. Testing multiple conceptualizations of oppositional defiant disorder in youth. J. Clin. Child Adolesc. Psychol. 47 , 620–633 (2018).
Patterson, G. R. Coercive Family Process Vol. 3 (Castalia, 1982).
Noordermeer, S. D. S. et al. Structural brain abnormalities of attention-deficit/hyperactivity disorder with oppositional defiant disorder. Biol. Psychiatry 82 , 642–650 (2017).
Download references
Author information
Authors and affiliations.
School of Psychology, University of Sydney, Sydney, New South Wales, Australia
David J. Hawes & Mark R. Dadds
Centre for Evidence-Based Intervention, Department of Social Policy and Intervention, University of Oxford, Oxford, UK
Frances Gardner
Department of Psychology, Louisiana State University, Baton Rouge, LA, USA
Paul J. Frick
Parent-Child Research Clinic, School of Psychology, University of New South Wales, Sydney, New South Wales, Australia
Eva R. Kimonis
Department of Psychological Sciences, University of Connecticut, Storrs, CT, USA
Jeffrey D. Burke
Department of Psychology, University of Bath, Bath, UK
Graeme Fairchild
You can also search for this author in PubMed Google Scholar
Contributions
Introduction (D.J.H.); Epidemiology (J.D.B.); Mechanisms/pathophysiology (M.R.D. and G.F.); Diagnosis, screening and prevention (P.J.F. and E.R.K.); Management (F.G.); Quality of life (M.R.D.); Outlook (D.J.H.); Overview of Primer (D.J.H.).
Corresponding author
Correspondence to David J. Hawes .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Peer review
Peer review information.
Nature Reviews Disease Primers thanks C. Dose, S. Evans, C. Hautmann, J. Lochman, U. Pauli-Pott and the other, anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Hawes, D.J., Gardner, F., Dadds, M.R. et al. Oppositional defiant disorder. Nat Rev Dis Primers 9 , 31 (2023). https://doi.org/10.1038/s41572-023-00441-6
Download citation
Accepted : 11 May 2023
Published : 22 June 2023
DOI : https://doi.org/10.1038/s41572-023-00441-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Case Report on Oppositional Defiant Disorder
Article sidebar, main article content.
Even the best-behaved children can occasionally act harsh and hard. Oppositional defiant disorder (ODD), on the other hand, may be present in your child or teenager if they consistently act hostile, impatient, argumentative, defiant, or vindictive against you or other adults in positions of authority and trouble in learning and academic outcomes. This is mainly caused by neurobiological imbalance, lack of parenting concern and family issues. This is a complex mental illness which dangerous to child should identifying in initial stage and treat it in appropriate way, otherwise it leads to unexplained psychological disorders like Conduct disorders, anxiety, depression and substance abuse. This can be managed with psychotherapeutic treatment then psychopharmacological agent. In this case study, the 12 year old boy with ODD was assessed in 6 months duration by Rorschach technique, questionnaire and semi interview methods for collect information. Parents and children can benefit significantly from psychological intervention in the short- and long-term results especially on emotional aspect of care because ODD child shows more emotional instability and behaviour abnormalities. The psychotherapy was used to treat the ODD like cognitive behavioural therapy especially positive reinforcement methods, which helped him improve his problem-solving skills, communication, impulse control, anger management. In additionally, he and his parents received family counselling to help with social skills, family interactions, and issue communication. The findings draw attention to improvements in all aspects including child’s interactions with others, adaptive behaviour and measurable academic outcome eventually could saw significant parent behavioural changes towards their child treatment.
Article Details
Ramires VRR, Godinho LBR, Carvalho C, Gastaud M, Goodman G. Child psychoanalytic psychotherapy: a single case study. PsychoanalPsychother [Internet]. 2017;31(1):75–93. Available from: http://dx.doi.org/10.1080/02668734.2017.1280692
Bambery M, Porcerelli JH. Psychodynamic therapy for oppositional defiant disorder: changes in personality, object relations, and adaptive function after six months of treatment. J Am PsychoanalAssoc [Internet]. 2006 Autumn;54(4):1334–9. Available from: http://dx.doi.org/10.1177/00030651060540040108
Oppositional defiant disorder [Internet]. Psychoanalysis.center. [cited 2022 Oct 21]. Available from: http://www.psychoanalysis.center/mental-health-therapy/oppositional-defiant-disorder
Wagner TM. Oppositional defiant disorder handout for professionals [Internet]. 142.34.196. [cited 2022 Oct 26]. Available from: http://136.142.34.196/files/pdf/WagnerODDHandoutForProfessionals [Wiki].pdf
Heflinger CA, Humphreys KL. Identification and treatment of children with oppositional defiant disorder: A case study of one state’s public service system. PsycholServ [Internet]. 2008;5(2):139–52. Available from: http://dx.doi.org/10.1037/1541-1559.5.2.139

S. SUTTON HAMILTON, MD, AND JOHN ARMANDO, LCSW
Am Fam Physician. 2008;78(7):861-866
A more recent article on oppositional defiant disorder is available .
Patient information: See related handout on oppositional defiant disorder , written by the authors of this article.
Author disclosure: Nothing to disclose.
Oppositional defiant disorder is defined by the Diagnostic and Statistical Manual of Mental Disorders , 4th ed., as a recurrent pattern of developmentally inappropriate, negativistic, defiant, and disobedient behavior toward authority figures. This behavior often appears in the preschool years, but initially it can be difficult to distinguish from developmentally appropriate, albeit troublesome, behavior. Children who develop a stable pattern of oppositional behavior during their preschool years are likely to go on to have oppositional defiant disorder during their elementary school years. Children with oppositional defiant disorder have substantially strained relationships with their parents, teachers, and peers, and have high rates of coexisting conditions such as attention-deficit/hyperactivity disorder and mood disorders. Children with oppositional defiant disorder are at greater risk of developing conduct disorder and antisocial personality disorder during adulthood. Psychological intervention with both parents and child can substantially improve short- and long-term outcomes. Research supports the effectiveness of parent training and collaborative problem solving. Collaborative problem solving is a psychological intervention that aims to develop a child's skills in tolerating frustration, being flexible, and avoiding emotional overreaction. When oppositional defiant disorder coexists with attention-deficit/hyperactivity disorder, stimulant therapy can reduce the symptoms of both disorders.
Oppositional defiant disorder is among the most commonly diagnosed mental health conditions in childhood. It is defined by a recurrent pattern of developmentally inappropriate levels of negativistic, defiant, disobedient, and hostile behavior toward authority figures. 1 This behavior must be present for more than six months and must not be caused by psychosis or a mood disorder, and the behavior must negatively impact the child's social, academic, or occupational functioning ( Table 1 ). 1
Several large community-based studies have found that approximately 3 percent of children meet criteria for oppositional defiant disorder as described by the Diagnostic and Statistical Manual of Mental Disorders , 4th ed. (DSM-IV). 2 – 4 However, studies show considerable variance associated with differences in the criteria used, age at assessment, and number of informants used, resulting in prevalence estimates of 1 to 16 percent. 5
Children with oppositional defiant disorder have substantially impaired relationships with parents, teachers, and peers. These children are not only impaired in comparison with their peers, scoring more than two standard deviations below the mean on rating scales for social adjustment, but they also show greater social impairment than do children with bipolar disorder, major depression, and multiple anxiety disorders. 6 When compared with oppositional defiant disorder, only conduct disorder and pervasive developmental disorder had nonstatistical differences in social adjustment. 6
Oppositional defiant disorder is more common in boys than girls, but the data are inconsistent. 7 Some researchers propose that different criteria be used with girls, who tend to exhibit aggression more covertly. 5 Girls may use verbal, rather than physical, aggression, often excluding others or spreading rumors about another child. Oppositional defiant disorder is more common among children in low-income households and is typically diagnosed in late preschool to early elementary school with symptoms often appearing two or three years earlier. Cross-sectional epidemiologic studies show a gradually increasing prevalence of oppositional defiant disorder as children age. 4
Researchers agree there is no single cause or even greatest single risk factor for oppositional defiant disorder. Rather, it is best understood in the context of a biopsychosocial model in which a child's biologic vulnerabilities and protective factors interact complexly with the protective and harmful aspects of his or her environment to determine the likelihood of developing this disorder. 5
Recent theories conceptualize children with oppositional defiant disorder as possessing deficits in a discrete skill set that lead to oppositional behavior. 6 An apparently noncompliant child who “explodes” in response to a parental demand may lack the cognitive or emotional skills required to comply with the adult's request. For example, a child may not have developed the skill of affective modulation, and tends to emotionally overreact, losing his or her capacity to reason. A child may possess deficits in his or her executive cognitive skills (e.g., working memory, ability to change tasks, organized problem solving). These deficits undermine the child's ability to comply with adult demands. Such skill deficits are components of the transactional conceptualization of oppositional defiant disorder, which emphasizes the interaction of the children and parents, and the context of the behavior. An important feature of this model is the relative predictability of the context (e.g., bath time, dinnertime) and the parent and child behaviors that precipitate a child's meltdown.
Neurobiologic theories have been explored in the etiology of aggression. Neurotransmitters such as serotonin, norepinephrine, and dopamine have been investigated in their role with aggression. No single neurotransmitter or neurologic pathway has been identified as the root cause. Oppositional defiant disorder is clearly familial, but research has yet to determine what role genetics play because studies on the genetics of the disorder have produced inconsistent results. 5 Smoking during pregnancy and malnutrition during pregnancy have been associated with the development of oppositional defiant disorder, although causality has not been firmly established. 8
Natural History
The natural history of oppositional defiant disorder is not completely understood. The majority of persons who are diagnosed with the disorder in childhood will later develop a stable pattern of oppositional defiant disorder behavior, an affective disorder, or oppositional defiant disorder with coexisting attention-deficit/hyperactivity disorder (ADHD) or affective disorders. Some children persist with oppositional defiant disorder without coexisting conditions. Children who were diagnosed with oppositional defiant disorder at a young age (e.g., preschool, early elementary school) may later transition to a diagnosis of ADHD, anxiety, or depression. 9 In general, earlier and more severe oppositional defiant disorder is associated with a poorer long-term prognosis. 9
Coexisting Conditions
Coexisting conditions are common in children with oppositional defiant disorder, particularly ADHD and mood disorders. The extent and nature of their coexistence is not precisely defined. The most comprehensive study of children with ADHD is the Multimodal Treatment Study of Children with ADHD. In this study, researchers found that 40 percent of children with ADHD also meet diagnostic criteria for oppositional defiant disorder. 10 Children who have both disorders tend to be more aggressive, have more persistent behavioral problems, experience more rejection from peers, and more severely underachieve academically. 5
In one community study of children with oppositional defiant disorder, 14 percent had coexisting ADHD, 14 percent had anxiety, and 9 percent had a depressive disorder. 7 The authors of another study found that children with oppositional defiant disorder were twice as likely to have severe major depression or bipolar disorder compared with a reference group. 6 , 11 Specific data are lacking, but expert consensus is that learning disabilities and language disorders also commonly coexist with oppositional defiant disorder. 5
Oppositional defiant disorder has commonly been regarded as a subset and precursor of the more serious conduct disorder, in part because most children with conduct disorder have a history of oppositional defiant disorder. Approximately one third of children with oppositional defiant disorder subsequently develop conduct disorder, 40 percent of whom will develop antisocial personality disorder in adulthood. 12 Children with coexisting oppositional defiant disorder and ADHD are particularly likely to develop conduct disorder.
Among other features, aggression toward other people and animals, a disregard for the rights of others, and the theft or destruction of others' property characterize conduct disorder. 1 The DSM-IV precludes diagnosing a child with both oppositional defiant disorder and conduct disorder. When a diagnosis of conduct disorder is made, the diagnosis of oppositional defiant disorder must be dropped if strict adherence to the DSM-IV is sought. Some researchers conceptualize conduct disorder and oppositional defiant disorder less as separate disorders, but rather as differing primarily in the severity of their disruptive behavior. Other researchers consider the two as entirely separate disorders. There is little disagreement that conduct disorder is more serious and is a poor outcome for children previously diagnosed with oppositional defiant disorder.
Lisa is a five-year-old girl whose parents asked their family physician to see her because of their increasing concern about her temper tantrums in the home. The parents indicated that Lisa often becomes enraged and argumentative with them, refusing to follow rules or take direction. In particular, they report difficulty getting her to transition from playing with her toys to coming to the dinner table. After Lisa ignored her parents' repeated prompts, her father became frustrated and told her that she had lost her dessert privilege. Lisa became aggressive and destructive, breaking her toys and smashing food and water from the dinner table into the carpet. Her parents described similar scenarios at bedtime, bath time, and when getting dressed in the morning. They described her as irritable in these situations and they felt she was deliberately ignoring or trying to annoy them.
Tools such as the National Initiative for Children's Healthcare Quality (NICHQ) Vanderbilt Assessment Scale, 13 designed for the primary care evaluation of children with suspected or diagnosed ADHD, contain questions that aid in the identification of oppositional defiant disorder. Use of this or similar instruments, such as the SNAP-IV Teacher and Parent Rating Scale for children with ADHD, 14 may allow enhanced detection of oppositional defiant disorder as well as other psychological concerns. Screening tools such as the Pediatric Symptom Checklist are not specific for oppositional defiant disorder, but can screen for cognitive, emotional, or behavioral problems, thereby identifying children who require additional investigation. 15 Table 2 provides more information on how to access these tools online. 13 – 15
Table 3 provides a differential diagnosis for oppositional defiant disorder. 1 A higher index of suspicion should be maintained in children with known risk factors such as ADHD because approximately 40 percent of children with ADHD have coexisting oppositional defiant disorder. 10 It is useful to recognize the role of established environmental risk factors such as living in a single-parent household and having low socioeconomic status. Chronically obese children are also at increased risk for oppositional defiant disorder. 4 Relevant family history includes that of oppositional defiant disorder, conduct disorder, or antisocial personality disorder. 1
Oppositional defiant disorder is most commonly diagnosed during the elementary school years, although most children with the disorder have a history of significant oppositional behavior in preschool.
The initial step in diagnosis is to determine whether or not the behavior is, in fact, abnormal. A certain amount of oppositional behavior is normal in childhood. Oppositional defiant disorder is only distinguishable by the duration and degree of the behavior. Physicians should carefully explore the possibility that the child's oppositional behavior is caused by physical or sexual abuse, or neglect. Given the wide range of normal oppositional behavior during the preschool years, caution should be exercised in diagnosing this disorder in the preschool-age child. 5 Assessment of the child with a potential diagnosis of oppositional defiant disorder depends on establishing a therapeutic alliance with both the child and family. The assessment should include information gathered from multiple sources (e.g., preschool, teachers) as well as history obtained from the child directly.
To satisfy DSM-IV criteria for oppositional defiant disorder, a child must frequently demonstrate behavior from at least four of nine criteria ( Table 1 ). 1 The behavior must be considerably more frequent than is typically observed in persons of comparable age and developmental level and must cause clinically significant impairment in social, academic, or occupational functioning. 1
When the diagnosis is unclear, patients should be referred to a psychologist or psychiatrist trained in the assessment of children with behavioral disorders. For children in elementary school, a physician's written request should facilitate a school-based evaluation by an appropriate professional. Evaluation of preschool children can most often be prompted by a telephone call to a county's Child Find or similar program. When available, a developmental-behavioral pediatrician can be an ideal beginning point of an assessment. Structured psychological interviews (such as the National Institute of Mental Health's Diagnostic Interview Schedule for Children [DISC] version 2.3), typically administered by a psychologist, can be used for formal diagnosis. When these services are unavailable, physicians may wish to use a brief series of questions that researchers have shown to possess 90 percent sensitivity and 94 percent specificity for identifying oppositional defiant disorder ( Table 4 ). 7
Neuroimaging (e.g., functional magnetic resonance imaging, single-photon emission computed tomography, electroencephalography) has a role in the research of aggressive behavior, but it has no clinical role in the evaluation of children with suspected oppositional defiant disorder.
Nonpharmacologic Treatment
Research supports outpatient psychological interventions for children with oppositional defiant disorder. Studies have demonstrated that parent training is an effective means of reducing disruptive behavior. 16 Parents often come to see their child's behavior as deliberate and under the child's control, intentionally hurtful toward the parent, or as an attribute of a disliked family member (e.g., an abusive partner). 17 The difficult behavior and social disruption caused by children with oppositional defiant disorder can have adverse effects on the mental health of their parents. 18 Parent training teaches parents to be more positive and less harsh in their discipline style. Media-based parent training (e.g., watching a video) has been shown to be effective with results continuing one year after the intervention. 19 In a randomized study, investigators found that applying parent training to both the child and parent is superior to training aimed solely at the parent, supporting the generally agreed-upon principle that therapies are more effective when both parent and child are involved. 20
Multisystemic therapy is a term for a community-based intervention that explicitly attempts to intervene in multiple real-life settings (e.g., home, school). Studies support the evidence behind multisystemic therapy, but there are limitations in the ability to generalize findings. 13
Collaborative problem-solving interventions seek to facilitate joint problem solving, rather than to teach and motivate children to comply with parental demands. This model encourages parents and children to identify issues and to use cognitive approaches to resolve the conflict to the mutual satisfaction of both parties. Collaborative problem solving appears to be at least as effective as parent training. 21
Pharmacologic Treatment
Several studies have found that medicines used in the treatment of ADHD, such as methylphenidate (Ritalin), atomoxetine (Strattera), and amphetamine/dextroamphetamine (Adderall), are effective in the treatment of ADHD with coexisting oppositional defiant disorder. 22 – 24 According to these studies, stimulants reduced the symptoms of both ADHD and oppositional defiant disorder symptoms. There are also two small studies that show the effectiveness of clonidine (Catapres) in treating children with ADHD and oppositional defiant disorder, either as monotherapy or as augmentation to medical therapy. 25 , 26 Studies have not demonstrated that stimulants reduce the symptoms of oppositional defiant disorder when ADHD is absent.
There is evidence that programs for preschool children (e.g., Head Start) reduce delinquency and, by inference, oppositional defiant disorder. 13 In elementary school-age children, the greatest evidence on prevention supports parent management strategies. Researched programs include the Triple P-Positive Parenting Program and Incredible Years parenting series. Both of these use self-directed, multimedia, parenting and family support strategies to prevent severe behavioral problems in children by enhancing the knowledge, skills, and confidence of parents. These programs are most appropriate for parents whose children appear to be at risk of developing emotional and/or behavioral problems. School-based programs that focus on anti-bullying, antisocial behavior, or peer groups can also be effective prevention approaches. 27
Family physicians should suspect oppositional defiant disorder when parents report an excessively argumentative, defiant, and hostile school-age child. Oppositional defiant disorder is common in children with ADHD, and use of the validated instruments mentioned in this article for the assessment and diagnosis of ADHD can help physicians to identify oppositional defiant disorder. Suspicion for oppositional defiant disorder should be raised when known risk factors (e.g., family history of oppositional defiant disorder/conduct disorder, ADHD, low socioeconomic status) are present. Formal diagnosis may require referral to a children's psychologist or psychiatrist.
Children with oppositional defiant disorder are best served by referral to a professional who is skilled and knowledgeable in evidence-based therapies for these children, although finding such professionals can be challenging. A physician's ability to locate particular resources for a child will depend on the family's insurance, financial resources, and motivation, as well as the availability of such resources in their community. There is no single best way to connect a child to the best services for him or her, and it is often prudent to explore multiple avenues to find the optimal available services. A physician's knowledge of oppositional defiant disorder, its typical symptoms, and best available treatments can allow the physician to serve as a patient advocate, to connect families with services, and to provide families with educational materials and online resources.
Diagnostic and Statistical Manual of Mental Disorders . 4th ed. rev. Washington, DC: American Psychiatric Association; 1994.
Maughan B, Rowe R, Messer J, Goodman R, Meltzer H. Conduct disorder and oppositional defiant disorder in a national sample: developmental epidemiology. J Child Psychol Psychiatry. 2004;45(3):609-621.
Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111(4 pt 1):851-859.
Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60(8):837-844.
Steiner H, Remsing L for the Work Group on Quality Issues. Practice parameter for the assessment and treatment of children and adolescents with oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(1):126-141.
Greene RW, Biederman J, Zerwas S, Monuteaux MC, Goring JC, Faraone SV. Psychiatric comorbidity, family dysfunction, and social impairment in referred youth with oppositional defiant disorder. Am J Psychiatry. 2002;159(7):1214-1224.
Angold A, Costello EJ. Toward establishing an empirical basis for the diagnosis of oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 1996;35(9):1205-1212.
Raine A. Annotation: the role of prefrontal deficits, low autonomic arousal, and early health factors in the development of antisocial and aggressive behavior in children. J Child Psychol Psychiatry. 2002;43(4):417-434.
Lavigne JV, Cicchetti C, Gibbons RD, Binns HJ, Larsen L, DeVito C. Oppositional defiant disorder with onset in preschool years: longitudinal stability and pathways to other disorders. J Am Acad Child Adolesc Psychiatry. 2001;40(12):1393-1400.
The MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Multimodal Treatment Study of Children with ADHD. Arch Gen Psychiatry. 1999;56(12):1073-1086.
Kadesjö C, Hägglöf B, Kadesjö B, Gillberg C. Attention-deficit-hyperactivity disorder with and without oppositional defiant disorder in 3- to 7-year-old children. Dev Med Child Neurol. 2003;45(10):693-699.
Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: a review of the past 10 years, part I. J Am Acad Child Adolesc Psychiatry. 2000;39(12):1468-1484.
National Iniatitive for Children's Healthcare Quality. Caring for children with ADHD: a resource toolkit for clinicians. http://www.nichq.org/NICHQ/Topics/ChronicConditions/ADHD/Tools/ADHD.htm. (password required). Accessed November 29, 2007.
Swanson JM. The SNAP-IV teacher and parent rating scale. http://www.adhdcanada.com/pdfs/SNAP-IVTeacherParetnRatingScale.pdf . Accessed November 29, 2007.
Massachusetts General Hospital. Pediatric symptom checklist. http://www.massgeneral.org/allpsych/PediatricSymptomChecklist/psc_english.PDF. Accessed November 29, 2007.
Farmer EM, Compton SN, Bums BJ, Robertson E. Review of the evidence base for treatment of childhood psychopathology: externalizing disorders. J Consult Clin Psychol. 2002;70(6):1267-1302.
Dadds MR, Hawes D. Integrated Family Intervention for Child Conduct Problems: A Behaviour-Attachment-Systems Intervention for Parents . Bowen Hills, Queensland, Australia: Australian Academic Press; 2006:1–10.
Kashdan TB, Jacob RG, Pelham WE, et al. Depression and anxiety in parents of children with ADHD and varying levels of oppositional defiant behaviors: modeling relationships with family functioning. J Clin Child Adolesc Psychol. 2004;33(1):169-181.
Montgomery P, Bjornstad G, Dennis J. Media-based behavioural treatments for behavioural problems in children. Cochrane Database Syst Rev. 2006(1):CD002206.
Webster-Stratton C, Hammond M. Treating children with early-onset conduct problems: a comparison of child and parent training interventions. J Consult Clin Psychol. 1997;65(1):93-109.
Greene RW, Ablon JS, Goring JC, et al. Effectiveness of collaborative problem solving in affectively dysregulated children with oppositional-defiant disorder: initial findings. J Consult Clin Psychol. 2004;72(6):1157-1164.
Swanson JM, Kraemer HC, Hinshaw SP, et al. Clinical relevance of the primary findings of the MTA: success rates based on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001;40(2):168-179.
Newcorn JH, Spencer TJ, Biederman J, Milton DR, Michelson D. Atomoxetine treatment in children and adolescents with attention-deficit/hyperactivity disorder and comorbid oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2005;44(3):240-248.
Biederman J, Spencer TJ, Newcorn JH, et al. Effect of comorbid symptoms of oppositional defiant disorder on responses to atomoxetine in children with ADHD: a meta-analysis of controlled clinical trial data. Psychopharmacology (Berl). 2007;190(1):31-41.
Connor DF, Barkley RA, Davis HT. A pilot study of methylphenidate, clonidine, or the combination in ADHD comorbid with aggressive oppositional defiant or conduct disorder. Clin Pediatr (Phila). 2000;39(1):15-25.
Hazell PL, Stuart JE. A randomized controlled trial of clonidine added to psychostimulant medication for hyperactive and aggressive children. J Am Acad Child Adolesc Psychiatry. 2003;42(8):886-894.
Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: a review of the past 10 years, part II. J Am Acad Child Adolesc Psychiatry. 2002;41(11):1275-1293.
Continue Reading
More in afp, more in pubmed.
Copyright © 2008 by the American Academy of Family Physicians.
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference. This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. See permissions for copyright questions and/or permission requests.
Copyright © 2024 American Academy of Family Physicians. All Rights Reserved.
Mary, a 4-year-old with oppositional defiant disorder
Affiliation.
- 1 Walter Reed Army Medical Center, Department of Psychiatry, 6900 Georgia Avenue, NW, Washington, DC 20307, USA.
- PMID: 12053858
Objective: Examine the treatment course of a 4-year-old girl with oppositional defiant disorder, which developed in the context of her father's deployment to Bosnia.
Method: A case report of the interventions made with this patient and her clinical outcomes.
Results: The patient's behavior improved substantially with regular therapy sessions and with a designated playtime with her mother.
Conclusions: One possible cause of oppositional defiant disorder is a parent-child attachment deficit. In this case, the child's parents are both active duty service members and her father was deployed overseas. Young children have difficulty verbalizing feelings of loss and may respond behaviorally by exerting control over their immediate environment. Some children may respond to unstructured play sessions in which they are able to express feelings and gain some control in their interactions with adults.
Publication types
- Case Reports
- Attention Deficit and Disruptive Behavior Disorders / etiology
- Attention Deficit and Disruptive Behavior Disorders / therapy*
- Child Behavior Disorders / etiology
- Child, Preschool
- Constipation / psychology*
- Family Characteristics
- Military Personnel
- Mother-Child Relations

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

6.119: Oppositional Defiant Disorder
- Last updated
- Save as PDF
- Page ID 64899
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Name : Stewie Griffin
Source : Family Guy (Television series, 1999 – Present)
Background Information Stewie Griffin is a Caucasian male who is presumed to be one years old, although he may be four to five years old because in later episodes he attends preschool. Stewie is unemployed but shows a mastery level of physics and mechanical engineering. He has designed such things as mind control devices, weather control, fighter jets, and teleportation devices. Although there are not any known distinct physical illnesses, abnormalities, or disorders currently within Stewie Griffin, there are observable health concerns. The patient displays unprovoked hostility towards others, constant disobeying of parental rules, is extremely vengeful and vindictive, and easily loses his temper quite frequently. Stewie currently lives with his parents, Peter and Lois Griffin. Stewie’s father, Peter Griffin shows observable symptoms of mild mental retardation. This is evident when he took an IQ test in one of the episodes and scored a 70. It is also observed that Stewie’s parents exhibit a strong sense of control over his life, such as scheduling play dates for him to go on, toys he can/can not play with, and what/when, he can eat. Stewie exhibits strong introversion in social relationships. He does not have close relationships with anyone outside of his immediate family. This is due to the fact that Stewie sees his peers as obstacles in his path toward world domination. Because of this, he frequently kills off the lesser characters with tanks, guns, and other assorted weaponry. There have not been patterns of consistent alcohol usage by Stewie, but he has excessively used alcohol on occasion. This is particularly problematic, as any type of alcohol usage by a one year old can severely inhibit brain development. Stewie’s goal is to attain world domination by first killing his mother, who he fears will stand in his way. All of Stewie’s daily activities are designed to accomplish these two goals by creating weapons such as rocket launchers, engaging in violent criminal activities, carjacking, loan sharking, and forgery. Other weaknesses that Stewie displays are his stresses of infant life, such as teething and eating his vegetables.
Description of the Problem Stewie Griffin currently displays a multitude of symptoms indicative of oppositional defiant disorder. He displays disobedient actions towards authority figures; however, Stewie believes that he is conducting himself in an appropriate manner for his own self-preservation. He also suffers from delusional behaviors such as having conversations with his stuffed teddy bear Rupert. He protects Rupert and will avenge any harm that comes Rupert’s way. Stewie deliberately annoys his peers by picking on them and continuously making rude remarks about their appearance or inabilities as a person. He also shows anger and resentfulness towards his mother because he feels that he is wrongly punished for activities he is supposed to carry out for the betterment of himself and world domination. As a result of this, he is also very spiteful and vindictive. For example, in one episodes Stewie loans Brian some money and they contractually agree that payment would be made on a certain date, but Brian does not repay on that date, so Stewie beats Brian with a bat daily until he receives payment. Stewie often uses a scapegoat for his own mistakes. When his attempts to kill his mother fail, he blames her for being unfair and bitchy.
Diagnosis The diagnosis for Stewie Griffin that fits appropriately is Oppositional Defiant Disorder (313.81) . A. To be diagnosed with Oppositional Defiant Disorder a pattern of negativism, hostile, and defiant behavior lasting at least 6 months during which four (or more) of the following are present: 1. Often loses temper 2. Often argues with adults 3. Often actively defies complying with adults’ requests/rules 4. Often deliberately annoys people 5. Often blames others for his or her mistakes 6. Is often easily annoyed by others 7. Is often angry and resentful 8. Is often spiteful or vindictive
Stewie Griffin undoubtedly shows more than four symptoms of Oppositional Defiant Disorder, as described in the section “Description of the Problem.”
B. Consider a criterion met only if the behavior occurs more frequently than is typically observed in individuals of comparable age and developmental level. Stewie possesses the ability to talk fluently at age one and interact with people at an intimate social level that is not yet observable in the one year old population. Typical one year olds rely heavily on parental care, where Stewie is significantly more independent than his peers (e.g. taking trips to San Francisco and Rhode Island).
C. The disturbance in behavior causes clinically significant impairment in social, academic, or occupational functioning. Stewie is significantly impaired in social functioning because he does not develop and nurture his relationships, instead he sees his peers as obstacles towards his goal that he must defeat at all costs. Because of this, he does not have any significant social relationship with anyone outside his immediate family.
D. The behaviors do not occur exclusively during the course of a Psychotic or Mood Disorder. Characteristics of oppositional defiant disorder can be observed in the patient in all settings and instances throughout his daily activities.
E. If the individual is age 18 years or older, criteria are not met for Antisocial Personality Disorder. The patient is between the ages of 1-4 years old.
F. There is a recurrent pattern of negativistic, defiant, disobedient, and hostile behavior towards authority figures. Stewie is in constant confliction with how he is going to succeed in killing his mother and attaining world domination.
G. Occurs outside of normal developmental levels and leads to impairment in functioning. Stewies behavior is clearly outside of normal development for a one year old, and this leads to impairment in functioning such as developing strategies to kill his mother and take over the world (e.g. making weapons with the purpose of carrying out these goals).
Accuracy of Portrayal The typical person watching Family Guy would be able to reach the conclusion that the character Stewie Griffin is abnormally developing compared to his average peer. A person with an Abnormal Psychology background would be able to further determine that Stewie showed all the symptoms for Oppositional Defiant Disorder. This is a cartoon character created to break the boundaries of normal development for babies, even to represent the general helplessness of an infant through the eyes of an adult. This show helps illustrate Oppositional Defiant Disorder by successfully creating a character that exemplifies every characteristic of the disorder, and not wavering from season to season. Although Stewie is not an accurate portrayal of the average one year old, he still can be related to children suffering from this disorder. Therefore, Stewie Griffin is an accurate illustration of someone with Oppositional Defiant Disorder.
Treatment To treat Stewie Griffin, after a full medical examination, it would be best to teach him problem-solving skills as well as parent management training. Problem solving skills would help Stewie learn to solve problems in a logical and predictable manner. The downfall with this strategy is that is time consuming and on average requires 20 sessions. Another effective way to treat Oppositional Defiant Disorder is parent management training. This allows the parents to develop and implement structured management programs at home. This is designed to improve interactions between child and parent. Parents implementing this strategy should positively reinforce good behaviors. A secondary methodology of treating Oppositional Defiant Disorder is to medicate the child using Ritalin. Research has shown children treated with Ritalin who have Oppositional Defiant Disorder, 75% of the children no longer showed symptoms of ODD.
Name : Walker Bobby and Texas Ranger “TR” Bobby
Source : Talladega Nights: The Ballad of Ricky Bobby (Movie, 2006)
Background Information Walker and Texas Ranger Bobby are pre-pubescent males, with an estimated age of 11 and 7, respectively. Neither boy holds a job because of their young age. The Bobby brothers do not display any specific health issues. Walker and Texas Ranger live with both of their parents and their maternal grandfather, Chip. Their father, Ricky, is a famous racecar driver who displays some symptoms of Narcissistic personality disorder, claiming that he is “the best there is,” and that he “piss[es] excellence.” Their mother, Carley, does not show any observable symptoms of a mental disorder. However, she is very materialistic, markedly aggressive when provoked, and shows extreme devotion to her husband, at least until the promise of better prospect comes along (e.g., she leaves Ricky for Cal when Ricky can no longer race). In other words, their mother is a gold-digger. The family unit is still very much intact – they eat dinner together every night and attend all of Ricky’s races together. While the bonds between the family are obviously very strong, Walker and Texas Ranger display many types of defiant and hostile behaviors toward authority figures. Most likely due to their lack of shock and surprise, these behaviors are not typically directed towards their parents. Rather, the Bobby brothers act out to other close adults like both of their grandfathers, Chip and Reese, and their grandmother, Lucy. In fact, the boys’ mother and father seem to condone this behavior, claiming that they did not raise “sissies”. Walker and Texas Ranger were never portrayed as having done illicit drugs, although they did inquire about a comment that their grandfather Reese had made about possessing marijuana. Besides the problems that they have run into at school due to behavioral issues, the boys do not possess any real life difficulties. They do not have any deeply defined goals either as they are just kids looking to enjoy themselves while they can. Due to their inconsistent and overindulgent lifestyle, Walker and Texas Ranger’s coping skills are not very good. They handle less-than-perfect situations with immaturity and anger, often lashing out at whoever they believe will take it. Their weaknesses are handling new, unwanted situations (such as Sunday school) and being polite to adults.
Description of the Problem Walker and Texas Ranger currently display a multitude of symptoms indicative of oppositional defiant disorder. They are consistently defiant and hostile, spouting out at whomever they believe deserves the criticism or hatred. These two display a constant need to argue and swear, especially to adults. They argue most often with their grandfathers, Chip and Reese, their grandmother, Lucy, and their teachers in school. There is nothing off limits for these boys. Their actions and criticisms are often unnecessary and cruel – usually just for the purpose of upsetting or annoying the adults around them.
Diagnosis The diagnosis for the Bobby brothers that fits most appropriately is Oppositional Defiant Disorder (313.81). To be diagnosed with Oppositional Defiant Disorder the following criteria must be met:
- Often loses temper
- Often argues with adults
- Often actively defies or refuses to comply with adults’ requests or rules
- Often deliberately annoys people
- Often blames others for his or her mistakes or misbehavior
- Is often touchy or easily annoyed by others
- Is often angry or resentful
- Is often spiteful or vindictive
*Note – Consider a criterion met only if the behavior occurs more frequently than is typically observed in individuals of comparable age and developmental level. Walker and Texas Ranger meet all criteria for oppositional defiant disorder except for number 5, blaming others for mistakes or misbehavior. They constantly insulted and swore at adults, threw Chip’s war medals off of a bridge to make him mad, argued with their teachers, and purposefully peed their pants and refused to take them off just to prove a point. These behaviors are more extreme than those of children at similar developmental levels. Where most children their age might only do these sorts of things once, Walker and Texas Ranger do them all of the time.
- The disturbance in behavior causes clinically significant impairment in social, academic, or occupational functioning.
The boys do not know how to function in a social setting, repulsing most adults who come into contact with them. The boys do not seem to care what other people think of them. They say mean things, causing adults to react negatively, creating a viscious cycle of disobedience. Academic functioning, although mentioned briefly, is most likely effected. Texas Ranger, specifically, flaunted his bad behavior in the classroom.
- The behaviors do not occur exclusively during the course of a Psychotic or Mood Disorder.
The characteristics previously described are displayed in many contexts over a lasting period of time. They are not a result of a psychotic or mood disorder.
- Criteria are not met for Conduct Disorder, and, if the individual is age 18 years or older, criteria are not met for Antisocial Personality Disorder.
Walker and Texas Ranger are approximately 11 and 7 years old, respectively. They did not physically aggress towards others and did not commit any serious crimes.
- Recurrent pattern of negativistic, defiant, disobedient, and hostile behavior towards authority figures.
The symptoms are constant – they do not vary from day to day. Their disobedience is only in response to authority figures.
- Occurs outside of normal developmental levels and leads to impairment in functioning.
Most children their ages do not insult, swear, and act out this much. The quality of their interactions are severely inhibited and functioning is impaired.
Accuracy of Portrayal The average person watching these boys would immediately recognize that there is a significant problem. Walker and Texas Ranger are on the extreme side of disobedience. Most parents would probably be able to relate the problems of these characters to those of their own children, only to a much lesser degree. They would learn that Oppositional Defiant Disorder is characterized by defiance, hostility, frequent outbursts of rage, swearing, and disobedience. The portrayal of this disorder is very accurate – the boys’ behavior was consistent throughout the movie and did not waiver. Their depiction, in particular, was very extreme as their behavior was observed both at home and in school. The inaccurate aspects of the boys’ portrayal would be their display of oppositional behaviors in unfamiliar territory, their lack of temper tantrums or clear frustration with difficult situations, and the ease and rapid pace of change in behavior once their grandmother decided it was time to start acting appropriately.
Treatment In the movie, Walker and Texas Ranger’s grandmother, Lucy, took things into her own hands. She established what she called, “Granny Law,” and broke the boys like “wild horses” with community service, yoga, disposal of their weapons, and church attendance.
As a mental health professional, it would be best to first conduct a structured or semi-structured clinical interview to explore fully the family’s history, the symptoms that pertain to ODD, and the possible co-morbid problems that can occur as a result of the disorder. The first measure of treatment that should be implemented are Problem-Solving – Skills-Training programs, which involve teaching children how to solve problems in a logical and predictable manner. The only setback of this training is that it is extremely time-consuming, requiring an average of twenty sessions. Another possible treatment is called Parent Management Training. This training teaches parents how to effectively implement contingency management programs at home, allowing both parent and child to better enjoy their interactions by learning how to praise positive behaviors, establishing schedules and sticking to them, and maintaining effective timeouts. This greatly increases awareness in the child as to what is expected of them as well as what will happen if they misbehave.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Sisli Etfal Hastan Tip Bul
- v.52(4); 2018

Comparing Attention-Deficit/Hyperactivity Disorder and Oppositional Defiant Disorder Singly and Together in Terms of Behavioral Problems, Family Conflict, and Cognitive Functions
Arzu Önal sönmez.
1 Department of Child and Adolescent Psychiatry, Acıbadem Mehmet Ali Aydınlar University Faculty of Medicine, İstanbul, Turkey
Mehmet Levent Kayaalp
2 Department of Child and Adolescent Psychiatry, İstanbul University Cerrahpaşa Faculty of Medicine, İstanbul, Turkey
Objectives:
The purpose of this study is to profile three groups of children with attention-deficit/hyperactivity disorder (ADHD), oppositional defiant disorder (ODD), and both ADHD and ODD, through analyzing their cognitive abilities, personality traits, and family characteristics.
The study included 60 patients, with 20 patients in each group. Patients were selected according to the DSM IV criteria. They completed the Wechsler Intelligence Scale for Children–Revised (WISC-R) and the Bender Visual Motor Gestalt Test, and their mothers filled out the Child Behavior Checklist (CBCL) and Marital Conflict Questionnaire.
There were no significant differences in picture completion, block design, and coding, which are the WISC-R subtests, between the three groups. In addition, there was no significant difference in verbal, performance, and WISC-R scores. Finally, there was no significant difference when the subdivisions of the CBCL externalizing and internalizing behaviors were analyzed individually. The Frequency of Marital Conflict Score and Conflict Expansion Score were analyzed, and there were no significant differences found between the three groups. The highest average of the Bender Visual Motor Gestalt Test was in the ODD group, whereas the lowest average was in the ADHD group.
Conclusion:
When comparing ADHD and ODD in terms of cognitive abilities, the observed differences may be because ODD has no genetic or organic component, and ADHD has an organic basis. In ODD, cognitive abilities are intact, which should underline the environmental and family factors.
Attention-deficit/hyperactivity disorder (ADHD) is the most frequently encountered multifactorial neurodevelopmental disorder in childhood. The distinction between differential diagnosis and comorbidity is not always clear. Generally, if the symptoms can be completely explained by another disorder, then the diagnosis is not ADHD.[ 1 ] Oppositional defiant disorder (ODD), conduct disorder (CD), anxiety disorder, mood disorder, and learning disorders are comorbidities seen in children.[ 2 ] ODD is the most frequently seen comorbidity among them.[ 3 , 4 ]
In a study conducted on children with ADHD, aged 6–17 years, Biederman et al. found comorbidities in 46% of children and 31% of adolescents with ODD, and 25% of children and 42% of adolescents with CD.[ 5 ] In a model in which the relationships between ADHD, ODD, and DBD were defined, it was assumed that behavioral disorders show a progressive progression from mild to severe, and it has been suggested that CD develops only in children with ADHD. In other words, it has been suggested that antisocial personality disorder may develop in a subgroup of children who develop CD.[ 6 ]
Although the role of ADHD in the development of disruptive behavior disorders is controversial, it is emphasized that the association between ODD and ADHD may be determinative for the early onset of the ADHD symptoms. In general, the idea that ADHD affects the developmental course and severity of the CD has been reported as a point of consensus in the literature.[ 7 ]
The treatment approach for ADHD and mood and anxiety disorders is different, and the diagnosis of solely ODD and the evaluation of therapeutic approaches are different. It has been thought that the treatment of the symptoms associated with ODD will contribute positively to the treatment of ODD. In a multimodal treatment study related to ADHD, it was found that stimulant therapy showed positive improvements in patients with ADHD-related oppositional behaviors.[ 8 ]
Compared with the general population, comorbidities associated with ODD are frequently seen. When compared with psychiatric and non-psychiatric groups, ODD is an important risk factor when it is evaluated in terms of social incompatibility. Concomitancy between ADHD and ODD is quite common, but in some studies, a significant percentage of ADHD patients did not have comorbid ODD. Childhood mood and anxiety disorders have been also frequently associated with ODD. Comorbidity of CD could not be isolated from studies when investigating the association between ODD and other psychiatric disorders.[ 9 - 13 ]
Disorders in child–family relationship and family functioning have been reported to be an important factor in the development of ODD and CD in ADHD.[ 14 ] The aim of this study was to compare cognitive abilities, personality traits, and family traits in children with ADHD, ODD, and both ADHD and ODD. Utilizing the psychometric evaluation methods and scales, the differences between the groups are discussed, and it has been planned to obtain the information about the profiles of these three groups.
In our study, a total of 60 children aged between 6 and 11 years diagnosed with ADHD, ODD, and ADHD+ODD were enrolled in the study. The groups were based on age and socioeconomic status. To evaluate the behaviors of the subjects in the study, the mothers of the children and adolescents aged 4–18 years filled out the Child Behavior Checklist (CBCL). The Marital Conflict Scale was filled out by parents to evaluate the marital relations between them. The WISC-R and Bender Visual Motor Gestalt Test were applied to all children. A history of neurological, physical, or chronic diseases, the presence of another psychiatric disorder, use of medications, and IQ below 85 based on the WISC-R intelligence test results were determined as exclusion criteria in our study. An ethics committee approval was obtained from the ethics committee of Cerrahpaşa Faculty of Medicine.
Data Collection
Child behavior checklist for ages 4–18.
The CBCL was developed by Achenbach and Edelbrock in 1983 to evaluate the competence areas and problem behaviors of children and adolescents aged 4–18, in accordance with the information obtained from their parents. The Turkish translation of the 1991 form was made by Erol and Kılıç, and the translation was reviewed in 1985 to ensure its applicability in our country (Akçakın, 1985; Erol and Şimşek, 1998). Adaptation and standardization studies of the scale were performed by Erol et al.[ 15 ]
Marital Conflict Scale
This scale was developed by Hatipoglu in 1993 to measure marriage conflicts. The scale consists of 70 items related to highly potential sources of marital conflicts including communication, relationships among friends and relatives, children, business, economic issues, and sexuality. For each item, there are five options available.[ 16 ]
Wechsler Intelligence Scale for Children–R
The Wechsler Intelligence Scale for Children–R (WISC-R) was developed by Wechsler and adapted to Turkish by Savaşır and Şahin in 1995.
It is a verbal and performance test applied to children aged between 6 and 16 years. One of the verbal parts of the test and all of the performance parts should be responded to within a determined time period. It consists of 12 subtests including verbal and performance skills.[ 17 ]
Bender Visual Motor Gestalt Test
This test, which evaluates visual motor perception, consists of nine cards with figures on them. It was designed by Lauretta Bender at the Bellevue Psychiatric Hospital in New York University in 1938. Its standardization for Turkish children was performed by Somer in 1988.[ 18 ]
Statistical Method
Statistical analysis was conducted using the SPSS for Mac v.13. Data were evaluated as the mean±standard deviation. Chi-square test, Fisher’s exact test, Kruskal–Wallis test, and analysis of variance were used to compare demographic features (parental education, class) and evaluate the scores.
The safety level was accepted as 95%, and a p-value of <0.05 was considered to be statistically significant.
A total of 60 patients aged 6–11 years were included in the study. Fifty cases were male (85%) and 9 (15%) were female. The ADHD group consisted of 1 (5%) girl and 19 (95%) boys; the ODD group consisted of 4 (20%) girls and 16 (80%) boys; and the ADHD+ODD group consisted of 4 (20%) girls and 16 (80%) boys. The mean ages of the ADHD (8.8±1.399 years), ODD (9.0±1.29 years), and ADHD+ODD (8.9±1.25 years) groups were calculated as indicated. There was no statistically significant difference between the three groups in terms of the mean age of the groups (p=.926) ( Table 1 ).
General characteristics of the groups
ADHD: Attention-deficit/hyperactivity disorder; ODD: Oppositional defiant disorder. *Chi-square and Fisher’s exact test were used.
The mean values for the picture arrangement, block design, and coding subtests were compared. In the ADHD group, the mean picture arrangement subtest scores were 8.50±1.98 in the ADHD, 9.00±2.07 in the ODD, and 9.70±2.02 in the ADHD + ODD groups. No significant difference was found between the groups. In the ADHD group, the mean subset scores of the block design were 10.10±2.75 in the ADHD, 10.85±2.83 in the ODD, and 11.10±2.55 in the ADHD+ODD groups. There was no significant difference between the groups with respect to the block design subtest. In the ADHD group, the mean scores of coding subtest were 11.10±1.97 in the ADHD, 11.65±3.32 in the ODD, and 10.90±3.21 in the ADHD+ODD groups, respectively. There was no significant difference between the groups regarding the coding subtest ( Table 2 ).
Psychometric assessments *
ADHD: Attention-deficit/hyperactivity disorder; ODD: Oppositional defiant disorder. WISC-R: Wechsler Intelligence Scale for Children–Revised.
The mean scores of the CBCL were compared between the three groups. The mean Social Introversion subset scores were 60.95±8.36 in the ADHD, 60.50±8.41 in the ODD, and 61.15±6.42 in the ADHD+ODD groups. No significant difference was found between the groups in terms of social introversion (p=.912). The mean scores of Somatic Complaints were 60.05±8.28 in the ADHD, 64.35±13.36 in the ODD, and 60.30±9.85 in the ADHD+ODD groups.
There was no significant difference between the groups in terms of somatic complaints (p=.646). In the subset of Anxiety/Depression, mean scores were 63.85±8.02 in the ADHD, 66.45±10.04 in the ODD, and 63.55±10.79 in the ADHD+ODD groups. There was no significant difference between the groups in terms of the anxiety/depression subset scores (p=.601). The mean Social Problems subset scores were 63.80±8.22 in the ADHD, 64.50±11.05 in the ODD, and 62.75±7.58 in the ADHD+ODD groups.
No significant difference was found between the groups in terms of social problems (p=.897). The mean scores in the section of Thought Problems were 64.20±8.38 in the ADHD, 64.95±9.64 in the ODD, and 67.30±8.76 in the ADHD+ODD groups. No significant difference was found between the groups in terms of Thought Problems (p=.441). The mean scores in the section of Attention Problems were 68.70±8.44 in the ADHD, 68.60±9.00 in the ODD, and 68.55±8.50 in the ADHD+ODD groups.
There was no significant difference between the groups in terms of attention problems (p=.761). The mean subset scores in the section of Criminal Behavior were 65.15±9.01 in the ADHD, 62.85±8.80 in the ODD, and 64.15±9.57 in the ADHD+ODD groups. No significant difference was found between the groups in terms of criminal behavior (p=.602). The mean subset scores in the section of Aggressive Behaviors were 68.10±10.80 in the ADHD, 65.65±8.79 in the ODD, and 69.40±8.03 in the ADHD+ODD groups.
A significant difference was not detected between groups (p=.390). The mean subset scores of the section of Internalizing Behaviors were 63.80±11.34 in the ADHD, 67.05±9.55 in the ODD, and 64.20±8.58 in the ADHD+ODD groups. There was no significant difference between the groups in terms of internalizing behaviors (p=.721). The mean subset scores of the Externalizing Behaviors section were 66.50±9.45 in the ADHD, 65.05±8.35 in the ODD, and 68.30±7.20 in the ADHD+ODD groups without significant difference between groups (p=.443). The mean total scores of the Internalizing and Externalizing Behaviors were 67.65±10.35 in the ADHD, 69.20±7.64 in the ODD, and 70.45±6.75 in the ADHD+ODD groups. A significant intergroup difference was not detected (p=.944) ( Table 2 ).
The Marital Conflict Scale was analyzed in two subsets, as the “Conflict Score” and the “Conflict Frequency Score,” and it was compared between groups. The mean Conflict Scores were 6.65±6.49 in the ADHD, 10.20±9.92 in the ODD, and 7.45±6.84 in the ADHD+ODD groups. A significant difference was not found between groups (p=.503). The mean Conflict Frequency Scores were 1.55±1.14 in the ADHD, 2.05±1.27 in the ODD, and 1.81±1.32 in the ADHD+ODD groups. No significant difference was found between groups (p=.443) ( Table 2 ). The mean Bender Visual Motor Gestalt Test scores were compared between three groups. The mean scores were 37.25±8.18 in the ADHD, 58.25±16.64 in the ODD, and 41.00±10.20 in the ADHD+ODD groups. A significant difference was detected between the three groups as for the Bender Motor Visual Gestalt Perception Test. The highest mean score was found in the ODD group and the lowest mean score in the ADHD group ( Table 2 ).
In this study, we aimed to investigate similar and different aspects of cognitive abilities, and personality and family traits, in children with ADHD, ODD, and both ADHD and ODD. Although ODD is a common clinical diagnosis, it is a rare subject of research.[ 19 ] Some researchers have suggested that because of the frequent association of ODD with ADHD, ODD is a different phenotypic appearance of ADHD rather than a separate disorder, while some others have advocated that it is a milder form of CD.[ 20 ] Still others have suggested that it is difficult to distinguish it from normal oppositional behaviors.[ 21 ]
In one research study, it has been shown that ODD comorbidity in ADHD is associated with aggression and negative parent–child rapport.[ 22 ] Social (high crime rates), familial (low socioeconomic level, problematic parenting functions, fragmented families, parental psychopathology), and child-related (temperament, other psychiatric disorders) risk factors are detected in the etiology of disruptive behavior disorders.[ 23 ] In this study, there was no significant difference between the three groups in terms of parental education. In our study, the fact that the families were not fragmented, that they were homogeneous in terms of belonging to the middle socioeconomic level, and that the education level of parents did not differ between the three groups provides homogeneity between the groups and eliminates sociodemographic differences.
The problems experienced by children with ADHD in the field of selective attention disrupt the processing of information in short-term memory.[ 24 ] Children with ADHD are unable to recover their attention in the number sequences subtest of the WISC-R, and as a result, they have difficulty in processing the numbers in short-term memory. Similarly, in the arithmetic subtest, they experience difficulty in keeping their attention on the same subject, and they usually use the right method of solving arithmetic problems they need to solve mentally, but they could not give the right answer.[ 25 - 29 ] Children with ADHD who have a visual perception disorder are often unable to form the required shapes using cubes together with simple errors in the block design test. Rotational errors are often found in the shapes they form correctly. Due to the fact that the cubes are three-dimensional, children are experiencing difficulties in the perception of depth, and they form figures on different surfaces of the cubes. In this study, no significant difference was found between the groups regarding the block design subtest. In the coding subtest, which measures the motor coordination skill and attention-gathering ability with visual perception, it was observed that many symbols are configured wrongly or upside-down, and the subjects could not use their time efficiently.[ 30 ] In this study, no significant difference was found between the groups regarding the coding subtest results. Children with ADHD receive low scores from the WISC-R coding, arithmetic, number sequences, block design, and image-editing subtests.[ 31 , 32 ] The findings of this study were not consistent with the literature. Since IQs of all of the children were over 85, the patients who met the diagnosis of mental retardation were excluded from the study, and because there was a lack of any significant difference between the three groups as well regarding the WISC-R scores, we can conclude that ADHD and/or ODD develop irrespectively of the intelligence quotient.
In another study, it was shown that the verbal score, performance score, and all other scores were lower in the ADHD group than in the control group.[ 33 ] It is assumed that an inadequate development of planning and editing skills, which are shown as the elements of ADHD that make learning difficult and also decrease work performance and lead to carelessness, concentration difficulties, and impatience may be responsible for low school success.[ 34 ] It is thought that ADHD may lead to grade repetition irrespective of the IQ level.[ 35 ] For this reason, it is observed that problems continue through adulthood.[ 36 - 38 ] In this study, no significant difference was found between the three groups in terms of the verbal score, performance score, and all other scores.
It is known that the CBCL subsets of social introversion, somatic problems, and anxiety/depression demonstrate problems-inward orientation.[ 39 ]
In this study, no significant difference was found between the groups in terms of the mean subset scores of social introversion, somatic problems, and total inward orientation problems. Exclusion of additional diagnoses is thought to be a cause of finding no difference between the groups in terms of these subdivisions. It was concluded that untreated adolescents with ADHD had problems of inward orientation more frequently than children with ADHD, and these complaints were seen more often in patients who were not treated with age than in control subjects.[ 40 ] Other mental disorders, mainly anxiety and mood disorders, are frequently associated with ADHD.[ 41 - 43 ] The symptoms of anxiety and depression were more frequently encountered in children with ODD compared to children with ADHD.[ 44 ] In this study, no significant difference was found between the three groups in terms of anxiety/depression based on CBCL.
It was stated that children with ADHD are not wanted by their peers and that they have difficulty in maintaining peer relations.[ 38 ] It was also indicated that children with ADHD have more behavioral problems, experiencing difficulties in socialization and complying with social order in each period of their lives, including the pre-school period.[ 45 ]
The subsets of the CBCL showing externalizing behavior problems include aggressive and criminal behaviors. In our study, there was no significant difference between the groups in these subdivisions. In a study, it was determined that aggression in boys with ADHD started in the early stages of life and was frequently associated with ODD symptoms.[ 46 ]
It has been suggested that children with ADHD more frequently commit delinquent acts and enter correctional facilities, and that they carry a high risk of getting involved in criminal acts.[ 47 , 48 ] As indicated by various authors, if pediatric patients with do ADHD have behavioral problems, then they are more prone to committing crimes in adulthood. Besides, it was also stated that ADHD patients with more severe ODD symptoms are more frequently arrested and commit crimes more ruthlessly.[ 49 , 50 ]
In this study, no significant difference was found between the mean scores of the subdivisions of the crime-related behaviors of the CBCL in the three groups. It was thought that there could be no difference due to the lack of a healthy control group.
There was no significant difference between the groups in the Marriage Conflict Scale.
It has been detected that both male and female children reacted unfavorably to conflicts, while girls were more likely to show their reaction of anger, sadness, and fear more heavily than boys.[ 51 ] In contrast, in a longitudinal study conducted with 1747 families for 5 years, the relationship between the marital conflict and child harmony was investigated, and no difference was observed with respect to gender.[ 52 ]
Similarly, in a study in which the responses of children to interparental conflicts were investigated, no gender differences were found.[ 53 ] The most important result of this study was the statistically significant difference between the three groups in the Bender Motor Visual Gestalt Perception Test. The highest mean score was found in the ODD group. Although it is frequently used to determine the visual impairment of children with ADHD, it is seen that a scarce number of studies have been performed regarding visual impairment in patients with ADHD. In other studies, it was found that children with ADHD had significantly lower scores in CD compared to the healthy control group.[ 54 - 57 ] It has been reported in the literature that the high error score obtained from the Bender Motor Visual Gestalt Perception Test was related to the increase in the severity of ADHD.[ 58 , 59 ] When the characteristics of the participants of these studies are examined, it is noteworthy that these cases received drug treatment. The findings of the Bender Motor Visual Gestalt Perception Test can be considered to be a result of these conditions. It has been thought that these features measured by the Bender Motor Visual Gestalt Perception Test represent various functions of intelligence, and it can be used as an intelligence test.[ 60 ]
The Bender Motor Visual Gestalt Perception Test is also used to evaluate adult patients with brain damage and neurological disorders, and those with schizophrenia and mental disability. It may also be used as a component of the neuropsychological test battery in patients with brain damage.[ 61 ] The tool is used to detect both developmental features and organic disorders.
The low Bender Motor Visual Gestalt Perception Test scores in the ADHD group support the fact that ADHD may be of organic origin.
Numerous studies performed on adults and experimental animals suggest that dysregulation of hyperactivity and motor movements are associated with impairments in the frontostriatal structures. Differences are observed in the frontostriatal pathway, which connects the frontal lobe, suplementary motor area, and parietal cortices in ADHD.[ 62 - 65 ] The fact that an excessive mobility and carelessness are thought to be caused by disturbances in the frontostriatal area is an important finding favoring the argument that ADHD is of organic origin.[ 57 , 66 ]
As a result, the highest and the lowest mean scores of the Bender Visual Motor Gestalt Test were found in the ODD and the ADHD groups, respectively.
Similar studies should be carried out in larger groups to enrich the findings obtained in this study. In addition, it is thought that among the ADHD subtypes, attention deficit is in the forefront, and neuropsychological evaluations should be considered separately in patients with mobility.
Limitations
In our study, the lack of a healthy control group was one of the most important limitations. Increasing the number of samples and adding the control group will help to obtain more meaningful results.
Disclosures
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship contributions: Concept – A.Ö.S.; Design – M.L.K, A.Ö.S.; Supervision – M.L.K; Materials – M.L.K., A.Ö.S.; Data collection &/or processing – A.Ö.S.; Analysis and/or interpretation – A.Ö.S.; Literature search – A.Ö.S.; Writing – A.Ö.S.; Critical review – M.L.K.

- Free Case Studies
- Business Essays
Write My Case Study
Buy Case Study
Case Study Help
- Case Study For Sale
- Case Study Service
- Hire Writer
Oppositional Defiant Disorder
As defined by ICD-10, mental disorder is a general term which implies the existence of clinically recognizable set of symptoms or behaviors associated with the interference of a person’s functioning (First et al, 2004). It includes a range of cognitive, emotional and behavioral disorders that interferes with both the life and productivity of an individual. According to DSM-IV-TR, for any disease or condition to be regarded as a metal disorder, it must have a manifestation of behavioral, psychological or biological dysfunction in the said individual. This paper will look at Opposition Defiant Disorder as an example of a mental disorder. The Opposition Defiant Disorder Opposition Defiant Disorder (ODD) is a recurrent pattern of negativistic, defiant, disobedient and hostile behavior by children or adolescents towards adults or authority figures.
In order to be diagnosed as suffering from the disorder, such behaviors must occur for a period not less than six months. According to DSMIV-TR, the behavior qualifying the disorder should not have as a result of a change in one’s mood or any psychotic disorder. This disorder is common among children especially from the age of eight years old. However, studies have shown that the disorder is increasingly becoming common among the adolescent teens. The disorder is characterized by angry and hostile behaviors that exceed the normal level of misbehavior. Though it may be challenging to differentiate such behaviors from the normal misbehavior, the fact that the sufferers of the disorder display a consistent pattern of uncooperative, defiant, hostile, and annoying behaviors toward people in authority makes it easily noticed.
We Will Write a Custom Case Study Specifically For You For Only $13.90/page!
It can also be noticed by observing any form of disruption of the child’s normal daily activities both at home and at school. Causes/etiology of Oppositional Defiant Disorder Though there is no definite cause of underpinning the disorder, its etiology is believed to be multi-factorial. That is to say that the disorder results from a number of causes related to developmental, biological, genetics and psychological factors. Biological causes More researches done in the recent years have linked the disorder to biological processes. By April 2008, a study published by BMC Psychiatry found an association between chemicals in the Brain and ODD.
They also found out that there is genetic link in the causal factors. The study found a reasonable ground to link the disease to some given chemicals in the brain. The same findings were supported by another group of researchers from the University of Southern California. They equally found out a strong link between genetics and the disorder. These studies revealed that many children and teens with the disorder also have close family members with the same disorder or certain other mental illnesses. This suggests that the vulnerability to develop ODD may be inherited.
Some studies have also suggested that the disorder may be caused by defects or injuries of the specific parts of the brain. Still another group of scientists have argued that there is enough evidence to link ODD to abnormal amounts of neurotransmitters. These cells enable communication between the brain nerve cells. Whenever the chemicals have defects or are out of balance, the communication in the brain may be adversely affected. This can be a potential cause of ODD.
Developmental causes The developmental theorists have linked the occurrence of the disorder to incomplete emotional and psychological development by the sufferers. This means that the sufferers may suffer limitations or developmental delays in their ability to process thoughts and feelings. They are therefore faced with challenges during the latter stages of their lives when they are faced with much difficult situations. Their ability to cope with the stresses of life may be very low leading to serious problems like depression and anxiety which later develop into ODD. Psychological causes Psychological theorists have hypothesized that such factors as temperament have a strong relationship to the disorder.
According to research, the occurrence is rampant during the early childhood stages especially when parents put unduly restrictiveness or pressure on their children. The information released by AACAP has shown that the sufferer’s brain especially the part enabling them to reason, and control the impulse is always affected. According to various psycologists, this is why children with the disorder are not finding it easy identifying social cues from peers. The result is misinterpretation of interactions which fuels their temperament and blame game. The sufferers thus often see hostile intent even where none exists.
This in turn affects their ability to manage stressors and to socialize. Environmental causes A link has also been found between the kind of environment in which one is brought up and the possibility of the occurrence of the ODD. Such factors include dysfunctional family life, a family history of mental illness and substance abuse. Another factor which is of great importance here is inconsistent discipline by parents. Noting that the defiant behaviors relating to the disorder can be learnt and that the child looks to those around him/her as the models, a child in such an environment can easily slowly contact the disorder. AACAP has stated that lack of structure, inconsistent discipline practices, and exposure to abuse or violence are potential causes of the disorder.
Symptoms of the Disorder It is usually challenging to identify the difference between a strong willed or emotional child and one with the disorder. This is because to an extent, the oppositional behaviors are expected at certain stages of a child’s development. However, it is argued that if such oppositional behaviors goes beyond six months and are clearly disruptive to the family or school environment then the child would possible be suffering from the disorder. Generally ODD is characterized by behaviors such as negativity, defiance, disobedience and often hostile behavior towards adults and authority figures. Such behaviors might cause the child to regularly and consistently show symptoms which are useful indicators of the disorder.
The symptoms include losing one’s temper, involving oneself in argument with adults with an ill motive and actively defying the rules set by adults. The sufferers of the disorder also deliberately do things that will annoy other people as well as blaming others for the mistakes they have done. The negativistic and defiant behaviors are expressed by such behaviors as consistent stubbornness and unwillingness to compromise.Manifestations of the disorder are best expressed when the patient is at home. It is therefore better to observe the progress of the suspected individuals’ behavior in the home setting and not at school or in the larger community.
It is also advisable for the researches to study the victims during their interaction with adults or their peers especially those who are well known to them. Apart from these usual symptoms, the disorder often occurs along with other behavioral and mental health problems. These include the Attention-Deficit/Hyperactive Disorder (ADHD), Anxiety Disorder and the Depression Disorder. Others like the Learning Disorder and Substance Abuse Disorders may also be common with the sufferer. The Prevalence of Oppositional Defiant Disorder Generally it is believed that sixteen percent of any given population suffers from the disorder. Studies have shown that around one in every ten children under the age of 12 years are thought to have ODD.
The probability is always higher for boys than for girls by two to one. As stated above, it is common for the sufferers of the disorder to also be diagnosed with ADHD. Studies have shown that between 35 and 50 percent of those with ADHD also has Oppositional Defiance Disorder. Studies have also shown that the disease is common among the school age children affecting around 20 percent. However, such percentages differ depending on a person’s definition of what a normal childhood behavior and a defiant behavior is. Such definitions vary across races, cultures, and even gender.
The behaviors related to the disorder usually starts to manifest at the age of 8 though sometimes it may start even much earlier during the preschool years. The Current Theories/Approaches to the Treatment of Oppositional Defiant Disorder Treatment for ODD majorly focuses on therapy and training because medications are not the primary treatment. The types of therapy that are normally used to prevent or treat the disorder include parent training, individual and family therapy, cognitive behavioral therapy, and social skills training. It must however be noted that any successful treatment requires the cooperation of those close to the patient. Early intervention and treatment is recommended to avoid the situation of the childrenn from getting worse especially in their later stages of life (Matthys & Lochman, 2010).
Parenting Training Programs Formal training programs have been designed to equip the parents with necessary strategies of managing their children and adolescents’ behavior. Parents are taught more positive and less frustrating ways of parenting to ensure that they do not frustrate the patients further. The training specifically focuses on the useful approaches to dealing with both the children and the adolescents with ODD. Parents are also taught how to negotiate with their children while also improving their children’s behavior through such techniques as positive reinforcement. The trainings enable the parents to establish more effective and consistent discipline methods. The first approach includes the individual and family therapy.
The individual therapy seeks to provide the victims of the disorder with forums in which they can explore their feelings and behaviors with a neutral therapist. The individual therapy also seeks to equip the sufferers with the necessary anger management skills. This enables the defiant individual to slowly correct their defying behavior. The patients are also equipped with skills that are useful in finding solutions to the usual problems facing them as well as enabling them to improve on their interpersonal relations. During the therapy, medications for depression and anxiety may also be given if deemed fit by the therapist.
Family therapy is recommended to help address the problems related to family interactions. The therapy specifically seek to modify the way the family is structured, the strategies employed by the family in handling difficulties and the ways in which parents reward mistakes. The program may also address stress related issues affecting children and adolescents with ODD. In case of a child, the therapist may recommend Parent Child Interaction Therapy (PCIT). This approach equips the parents with more effective parenting techniques which help improves the quality of the parent child relationship.
The second approach is the cognitive-behavioral training which is also called cognitive problem solving training. The main goal of the therapist here is to help patients control their aggression. This enable them change their social behavior. The patients are rewarded for any transformation in behavior to encourage them to change further. Studies have shown that cognitive therapy can help the patients of the disorder to improve on their level of self control, self guidance and problem solving strategies.
The approach utilizes collaborative problem solving in which the parent works together with the child to come up with the solutions that work for both of them.The third approach is the social skills training. It is usually done together with therapy to make the process more effective in helping the sufferers change their behaviors. It also involves the use reinforcement strategies such as behavior rewards to help a teenager to learn and maintain positive behaviors. Such trainings should be provided in the sufferers’ natural environment to help them apply what they learn directly to their lives. A part from these trainings, parents have also been advised to: give effective time-outs with their children, avoid power struggles with them, they should also remain calm and unemotional even in the face of opposition by the sufferers.
Parents should also offer acceptable choices to their children by giving them certain amount autonomy. It is also recommended for parents to have certain activities that they do together with their children. Parents must live knowing that they are their children’s role model. The last approach to the treatment of the disorder is medication. This approach is only recommended when the symptoms of the disorder occur alongside other conditions. The conditions that may warrant treatment approach include the presence of ADHD, anxiety and/or depression.
This is because there is no medication for treating symptoms of ODD. Medication can therefore only be ministered when there is another emotional or behavioral disorder accompanying the ODD. Conclusion In conclusion, it is clear that more research need to be done to establish the causes, prevention and treatment of the disorder. As things stand an individual may develop to a worse condition without the knowledge of the people around him or her. With the current increase of those contacting the disease, the situation should never be allowed to remain the same.
Related posts:
- Case Study on Acute Stress Disorder
- Post-Traumatic Stress Disorder
- Bipolar Disorder
- The Mind of an Eating Disorder Patient
- To Stand Defiant: The Sophie Scholl Story
- Colony Collapse Disorder
- Psychological Disorder Analysis
Quick Links
Privacy Policy
Terms and Conditions
Testimonials
Our Services
Case Study Writing Service
Case Studies For Sale
Our Company
Welcome to the world of case studies that can bring you high grades! Here, at ACaseStudy.com, we deliver professionally written papers, and the best grades for you from your professors are guaranteed!
[email protected] 804-506-0782 350 5th Ave, New York, NY 10118, USA
Acasestudy.com © 2007-2019 All rights reserved.

Hi! I'm Anna
Would you like to get a custom case study? How about receiving a customized one?
Haven't Found The Case Study You Want?
For Only $13.90/page

Oppositional Defiant Disorder Warning Signs: What To Look Out For
If you're experiencing new, severe, or persistent symptoms, contact a health care provider..
Some of the common symptoms associated with ODD are:
- Frequent temper tantrums
- Excessive arguing with adults
- Never obeys adults requests and question rules
- Attempting to annoy adults or upset people
- Easy provocation to anger/annoyance
- Frequent anger/irritation
- Spiteful attitude and revenge seeking
→ Common treatment options
→ Questions to ask your doctor
- The cause of ODD is not known. It is believed that genetics and environmental factors play key role in developing the disease. There are few other biological causes which might be the cause of ODD.
- Genetics: Genetically determined neurobiological factors could be the key for natural predisposition or temperament
- Environment: Problems with parenting that may involve a lack of supervision, inconsistent or harsh discipline , or abuse or neglect
- Biological: Defects or injuries in certain parts of the brain also lead to serious behavioral problems in kids
→ Do you have a health question on your mind for oppositional defiant disorder? Ask professionals from across the world
→ Interested to know more? Check out the full article here
Disclaimer: For informational purposes only. Consult a medical professional for advice. Source: Focus Medica.


IMAGES
VIDEO
COMMENTS
Oppositional Defiant Disorder Case Study. In this part of the post, I will talk about a real-life ODD case study. Note: This is a real-life ODD case study of Arthur (real name hidden for privacy concerns) whose case was handed to me from an international school in Caribbean Islands. This oppositional defiant disorder case study has been drafted ...
Introduction. The diagnosis of oppositional defiant disorder (ODD) is broadly based on frequent and persistent angry or irritable mood, argumentativeness/defiance, and vindictiveness. 1 It is "qualitatively" different from conduct disorder (CD), which talks about impingement of others' rights and violation of age-appropriate social norms.
Oppositional defiant disorder (ODD) is a type of childhood disruptive behavior disorder that primarily involves problems with the self-control of emotions and behaviors. According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the main feature of ODD is a persistent pattern of angry or irritable mood, argumentative or defiant behavior, or vindictiveness ...
Oppositional defiant disorder (ODD) ... Also in this case it would be recommendable to considerably lower the cut-off to provide sufficient sensitivity for the detection of ODD symptoms in youth with DS. ... age of onset outcomes and risk factors of onset of DSM-5 oppositional defiant disorder: a cohort study of Spanish children from ages 3 to ...
Background: Oppositional defiant disorder (ODD) is a common clinical condition seen among children and adolescents in behavioral health settings. In this article, we review behavioral treatment programs and their clinical use in managing ODD. ... We found 1,665 articles, including clinical trials, review articles, and case control studies of ...
at oppositional defiant disorder, or ODD, with a case study. Listen to the story of Jason. Think about the behaviors Jason exhibits. Later in the program we will reveal just which of these behaviors are typical of an eight year old like Jason, and which may characterize a more serious mental health disorder. "Get out of my face.
oDD: a guide for Families n 1 Oppositional Defiant Disorder: A Guide for Families is adapted from the American Academy of Child and Adolescent Psychiatry's Practice Parameter for the Assessment and Treatment of Children and Adolescents with Oppositional Defiant Disorder. The AACAP Practice Parameter was written to aid clinicians, child and adolescent
The current case study extends the use of individual CBT to a preschool aged girl with oppositional defiant disorder (ODD), and is the first to investigate its efficacy in combination with behaviorally-based parent training and classroom teacher consultation.
Oppositional defiant disorder (ODD) is diagnosed broadly on the basis of frequent and persistent angry or irritable mood, argumentativeness/defiance, and vindictiveness. Since its inception in the third Diagnostic and Statistical Manual of Mental Disorders, epidemiological and longitudinal studies have strongly suggested a distinct existence of ODD that is different from other closely related ...
Oppositional and defiant behaviors are frequent and ongoing. They cause severe problems with relationships, social activities, school and work, for both the child and the family. Emotional and behavioral symptoms of ODD generally last at least six months. They include angry and irritable mood, argumentative and defiant behavior, and hurtful and ...
The following case study is presented to highlight the importance of consistency in identifying and treating oppositional defiant disorder in a pediatric patient with a life-threatening medical illness. A pediatric transplant patient's oppositional behaviors are described, as well as the educational behavioral training program provided to the ...
Abstract. Oppositional defiant disorder (ODD) is a disruptive behaviour disorder involving an ongoing pattern of angry/irritable mood, argumentative/defiant behaviour and vindictiveness. Onset is ...
Introduction. The diagnosis of oppositional defiant disorder (ODD) is broadly based on frequent and persistent angry or irritable mood, argumentativeness/defiance, and vindictiveness. 1 It is "qualitatively" different from conduct disorder (CD), which talks about impingement of others' rights and violation of age-appropriate social norms.
Oppositional defiant disorder (ODD), on the other hand, may be present in your child or teenager if they consistently act hostile, impatient, argumentative, defiant, or vindictive against you or other adults in positions of authority and trouble in learning and academic outcomes. ... In this case study, the 12 year old boy with ODD was assessed ...
Oppositional Defiant Disorder [DSM-4, ©1994; DSM-4-TR, ©2000; DSM-5, ©2013; 313.81 (F91.3)] is a relatively. new addition to the diagnostic armamentum of psychology and psychiatry. Criteria for this diagnosis include a. pattern of angry/irritable mood, argumentative/defiant behavior, and vindictiveness lasting at least 6 months.
The following case study is presented to highlight the importance of consistency in identifying and treating oppositional defiant disorder in a pediatric patient with a life-threatening medical illness. A pediatric transplant patient's oppositional behaviors are described, as well as the educational behavioral training program provided to the ...
Oppositional defiant disorder (ODD) is a mental disorder characterized by disruptive behavior, a pattern of angry and irritable mood, argumentative, and vindictive behavior. ... (SUD) and personality disorders such as antisocial personality disorder . Neuroimaging studies in children with CD revealed a smaller size of the amygdala, the insula ...
Oppositional defiant disorder is defined by the Diagnostic and Statistical Manual of Mental Disorders, 4th ed., as a recurrent pattern of developmentally inappropriate, negativistic, defiant, and ...
Objective: Examine the treatment course of a 4-year-old girl with oppositional defiant disorder, which developed in the context of her father's deployment to Bosnia. Method: A case report of the interventions made with this patient and her clinical outcomes. Results: The patient's behavior improved substantially with regular therapy sessions ...
The diagnosis for Stewie Griffin that fits appropriately is Oppositional Defiant Disorder (313.81). A. To be diagnosed with Oppositional Defiant Disorder a pattern of negativism, hostile, and defiant behavior lasting at least 6 months during which four (or more) of the following are present: 1. Often loses temper. 2.
Oppositional defiant disorder (ODD), conduct disorder (CD), anxiety disorder, mood disorder, ... Garland EJ, Weiss M. Case study: obsessive difficult temperament and its response to serotonergic medication. J Am Acad Child Adolesc Psychiatry. 1996; 35:916-20. [Google Scholar]
January 2019. DOI: 10.1007/978-3-319-45635-5_5. In book: Clinician's Guide to ADHD Comorbidities in Children and Adolescents (pp.37-45) Authors: Joseph Sadek. Dalhousie University. To read the ...
Oppositional Defiant Disorder. As defined by ICD-10, mental disorder is a general term which implies the existence of clinically recognizable set of symptoms or behaviors associated with the interference of a person's functioning (First et al, 2004). It includes a range of cognitive, emotional and behavioral disorders that interferes with ...
Symptoms. If you're experiencing new, severe, or persistent symptoms, contact a health care provider. Some of the common symptoms associated with ODD are: Frequent temper tantrums. Excessive ...