
- Previous Article

Presentation
Clinical pearls, article information, case study: diabetic ketoacidosis in type 2 diabetes: “look under the sheets”.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- Open the PDF for in another window
- Cite Icon Cite
- Get Permissions
Brian J. Welch , Ivana Zib; Case Study: Diabetic Ketoacidosis in Type 2 Diabetes: “Look Under the Sheets”. Clin Diabetes 1 October 2004; 22 (4): 198–200. https://doi.org/10.2337/diaclin.22.4.198
Download citation file:
- Ris (Zotero)
- Reference Manager
Diabetic ketoacidosis (DKA) is a cardinal feature of type 1 diabetes. However, there is a strong, almost dogmatic, errant perception by physicians that DKA is a complication that only occurs in patients with type 1 diabetes. This is not true. DKA does occur in type 2 diabetes; however, it rarely occurs in the absence of a precipitating event.
R.T., a 25-year-old African-American man with type 2 diabetes presented with a 5-day history of nausea and vomiting. He also reported a 2-week history of polyuria and polydipsia and a 10-lb weight loss. A review of symptoms was pertinent for a 5-day history of persistent lower back pain.
The patient was diagnosed with type 2 diabetes 5 years ago when he presented to a different hospital with symptoms of polyuria, polydipsia, and weight loss. He was given a prescription for a sulfonylurea, which he says he took until his initial prescription ran out 1 month later. He had not taken any other medication since that time.
Physical examination revealed an afebrile, obese man (BMI 40 kg/m 2 ) with prominent acanthosis nigricans, no retinopathy by direct funduscopic exam, and a normal neurological exam, including motor function and sensation. The patient had no tenderness to palpation over the lumbrosacral spine or paraspinous muscles despite his complaint of lower back pain.
The laboratory data showed an anion gap, metabolic acidosis, and hyperglycemia (pH of 7.14, anion gap of 24, bicarbonate 6 mmol/l, urinary ketones 150 mg/dl, glucose 314 mg/dl) consistent with the diagnosis of DKA. His white blood count was 20,400/μl. Urinalysis demonstrated no evidence of infection. The patient's hemoglobin A 1c (A1C) was 13.5%.
The patient was admitted and treated aggressively with intravenous fluid and an insulin-glucose infusion. A non-contrast magnetic resonance imaging(MRI) of the lumbosacral spine (L-spine) was obtained because of the patient's persistent complaint of lower back pain. The L-spine MRI results were negative for pathology. However, R.T. reported increasing discomfort and now noted weakness and numbness in his bilateral lower extremities.
Neurology was consulted, and during their assessment, the patient became incontinent and was found to have 0/5 strength in the lower extremities,severely compromised sensation, and decreased rectal tone. A contrast MRI of both the thoracic and lumbar spine was ordered, and the patient was found to have a T10-T12 epidural abscess ( Figure 1 ).

Epidural abscess precipitating DKA in a type 2 diabetic patient.
The patient's antibiotic coverage was broadly expanded, high-dose intravenous steroids were initiated, and neurosurgery was urgently consulted. Emergent evacuation of the epidural abscess with laminectomies of T10-T12 was performed without complication.
R.T.'s neurogenic bladder resolved without further intervention. After intensive inpatient rehabilitation, he had 3/5 strength in bilateral lower extremities and was still unable to ambulate.
S.D., a 39-year-old white man with type 2 diabetes and mild mental retardation, presented with a 3-week history of polyuria and polydipsia, as well as dysuria, left hip pain, and a feeling of incomplete bladder emptying. Because of the severity of his left hip discomfort, the patient required a cane to ambulate.
The patient was diagnosed with type 2 diabetes 4 years ago on the basis of an elevated fasting blood glucose level during a routine medical examination. He was started on oral hypoglycemic agents, but he discontinued them after 1 month because he was unable to pay for them.
On physical exam, S.D. was afebrile but tachycardic (heart rate 131 bpm)and hypertensive (blood pressure 192/118 mmHg). General examination revealed a wasted, severely volume-depleted man. Thrush was observed on oropharyngeal exam. Cardiopulmonary and abdominal examinations were unremarkable. The patient had point tenderness on the anterior aspect of his left hip. Rectal examination revealed a non-tender prostate.
The laboratory data showed an anion gap, metabolic acidosis, and hyperglycemia (pH 7.24, bicarbonate 9 mmol/l, anion gap 24, urinary ketones 150 mg/dl, and glucose 322 mg/dl) consistent with the diagnosis of DKA. Urinalysis was remarkable for large blood, 4+ bacteria, and > 400 white blood cells. S.D.'s serum white blood count was 22,200, and his erythrocyte sedimentation rate was 109 mm/hour. His A1C result was 12.6%.
The patient was admitted and treated with intravenous fluids and an insulin-glucose infusion. Cultures were obtained. S.D. was started empirically on ticarcillin/clavulanic acid because of concern for left hip osteomyelitis and complicated urinary tract infection. An MRI of the left hip was ordered to evaluate for suspected osteomyelitis. Unexpectedly, it revealed left hip myonecrosis and a large loculated prostatic abscess( Figure 2 ).

Prostatic abscess precipitating DKA in a type 2 diabetic patient.
Urology was consulted, and the patient underwent transurethral drainage of the prostatic abscess. Methicillin-sensitive Staphylococcus aureus grew from both blood and urine cultures. S.D. was treated with intravenous antibiotics per culture sensitivities. The myonecrosis was treated conservatively.
The patient recovered well. He was started on subcutaneous insulin and discharged home to complete a 2-week course of intravenous antibiotics.
What is the mechanism of DKA?
Why does DKA occur in type 2 diabetes?
DKA is a cardinal feature of type 1 diabetes, which has led to the widespread errant perception that it is a complication unique to type 1 diabetes. However, it has been repeatedly reported that DKA does occur in patients with type 2 diabetes. 1 - 5 Moreover, as the cases presented here illustrate, it can occur even in patients who were previously insulinindependent.
A recent study evaluating 138 consecutive admissions for DKA at a large academic center observed that 21.7% had type 2 diabetes. 6 Nearly 70% of the admissions involved discontinuation of medications, and almost half had an identifiable infection when an intensive search was undertaken.
A review of the mechanism of DKA is important. Ketoacidosis occurs as a function not only of severe insulin deficiency, but also of elevated glucagon levels. Insulin is an anabolic hormone. Severe insulin deficiency results in decreased glucose utilization by muscle and an unregulated increase in lipolysis. This leads to an enhanced delivery of gluconeogenetic precursors(glycerol and alanine) to the liver. Furthermore, removal of the normal suppressive effect of insulin causes glucagon elevation. 7 , 8 Glucagon is a catabolic hormone. Glucagon promotes gluconeogenesis, decreases oxidation of free fatty acids to triglycerides, and promotes hepatic ketogenesis. 9
Importantly, the concentration of insulin required to suppress lipolysis is only one-tenth of that required to promote glucose utilization. 10 Typically, moderate insulin deficiency (as observed in patients with type 2 diabetes) is associated with sufficient insulin to block lipolysis (and therefore ketoacid formation), but not enough to promote glucose utilization. This leads to hyperglycemia without formation of the ketoacids.
When DKA occurs in patients with type 2 diabetes, the presumed mechanism of ketoacidosis is the combination of relative insulin deficiency and increased secretion of glucagon (as well as other counteregulatory hormones such as cortisol, catecholamines, and growth hormone) in response to stress from 1 ) overwhelming infection, 2 ) infarction of tissue, or 3 ) other severe illness. The elevated catecholamines further suppress insulin secretion to perpetuate a downward spiral. The increased glucagons-to-insulin ratio causes a mismatch that promotes unregulated lipolysis and proteolysis with subsequent uninterrupted formation of ketoacids.
To summarize, DKA is not a unique feature of type 1 diabetes. Though much more common in type 1 diabetes, it does occur in patients with type 2 diabetes, as illustrated by these case reports. However, it is rare for DKA to occur in type 2 diabetes in the absence of some precipitating event. When DKA occurs in an individual with type 2 diabetes, the clinician should “look under the sheets” and initiate an intensive search for the precipitating factor. Once identified, the trigger should be treated promptly and appropriately.
DKA does occur in type 2 diabetes.
DKA in type 2 diabetes rarely occurs without a trigger.
When it does, an intensive search for the precipitating factor should be undertaken.
Brian J. Welch, MD, and Ivana Zib, MD, are fellows in the Division of Endocrinology and Metabolism at the University of Texas Southwestern Medical Center in Dallas.
The authors thank Philip Raskin, MD, for his support and guidance.
Email alerts
- Online ISSN 1945-4953
- Print ISSN 0891-8929
- Diabetes Care
- Clinical Diabetes
- Diabetes Spectrum
- Standards of Medical Care in Diabetes
- Scientific Sessions Abstracts
- BMJ Open Diabetes Research & Care
- ShopDiabetes.org
- ADA Professional Books
Clinical Compendia
- Clinical Compendia Home
- Latest News
- DiabetesPro SmartBrief
- Special Collections
- DiabetesPro®
- Diabetes Food Hub™
- Insulin Affordability
- Know Diabetes By Heart™
- About the ADA
- Journal Policies
- For Reviewers
- Advertising in ADA Journals
- Reprints and Permission for Reuse
- Copyright Notice/Public Access Policy
- ADA Professional Membership
- ADA Member Directory
- Diabetes.org
- X (Twitter)
- Cookie Policy
- Accessibility
- Terms & Conditions
- Get Adobe Acrobat Reader
- © Copyright American Diabetes Association
This Feature Is Available To Subscribers Only
Sign In or Create an Account
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria’s vital signs were as follows: BP 87/50, HR 118, RR 28, O2 95% on room air, diffuse abdominal pain at a level of 5, on a verbal numeric 1-10 scale, with non-radiating pain beginning that morning. She was A&O x3, oriented to self, place, and situation, but sluggish. Upon assessment it is revealed that she is experiencing blurry vision, Kussmaul respirations, dry, flushed skin, poor skin turgor, weakness, and a fruity breath smell. Labs were drawn. During the first hour of admission, Maria requested water four times and urinated three times.
Code status: Full code
Medical hx : Type 1 Diabetes
Insurance : None
Allergies : NKA
Significant Lab Values
- Blood glucose 388
- ABGs: pH 7.25, Bicarb 12 mEq/L, paCO2 30 mm Hg, anion gap 20 mEq/L, paO2 94%
- Urinalysis: Ketones and acetone present, BUN 25 mL/dL, Cr 2.1 ml/dL
- Chemistry: sodium 111 mEq/L, potassium 5.5 mEq/L, chloride 90 mEq/L, phosphorus 2.5 mg/dL, Magnesium 2.0 mg/dL
- CBC: WBC 13,000 mcL, RBC 4.7 mcL, Hgb 12.6 g/dL , Hct 37% (Wolters Kluwer, 2018).
Diagnosis: Diabetes Ketoacidosis
- Oxygen administration by nasal cannula on 2L and airway management
- Establish IV access
- IV fluid administration with 0.9% NS; prepare to titrate to 0.45% normal saline as needed
- Monitor blood glucose levels
- Administer 0.1-0.15 unit/kg IV bolus of regular insulin
- IV drip infusion at 0.1 unit/kg/hr of regular insulin to hyperglycemia after bolus,
- Addition of Dextrose to 0.9% NS as glucose levels decreases to 250 mg/dL
- Monitor potassium levels
- Potassium replacement via IV when the potassium level is 5.0 mg/dL or less and urine output is adequate
- Assess for signs of hypokalemia or hyperkalemia
- Monitor vital signs and cardiac rhythm
- Q1-2hr fingerstick blood glucose checks initially, then q4-6hr once stabilized
- Monitor blood pH, I&O
- Assess level of consciousness; provide seizure and safety precautions (Henry et al., 2016)
- Notify MD of any critical changes
Maria Fernandez was then transferred to the ICU unit for close observation, maintenance of IV insulin drip, cardiac monitoring, fluid resuscitation, and correction for metabolic acidosis.
Upon discharge, Maria was reeducated on Type 1 Diabetes Mellitus through the use of preferred learning materials.
- What is the priority assessment data that supports DKA diagnosis?
- What education strategies would you consider implementing to improve treatment adherence after discharge?
- What considerations, services, or resources would you anticipate to be offered by case management or social services?
Henry, N.J., McMichael, M., Johnson, J., DiStasi, A., Ball, B.S., Holman, H.C., Elkins, C.B., Janowski, M.J., Hertel, R.A., Barlow, M.S., Leehy, P., & Lemon, T. (2016). RN adult medical surgical nursing: Review module (10 th ed.). Leawood, KS: Assessment Technologies Institute.
Wolters Kluwer. (2018). Lippincott Nursing Advisor (Version 4.1.0) [Mobile application software]. Retrieved from http://itunes.apple.com
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

- Blood gases/acid-base
- Cardiac markers
- Coagulation/fibrinolysis
- Infection/sepsis
- Information management
- Kidneys/fluids
- Neonatology
- Point-of-care testing
- Process optimization
- Quality assurance
- Preanalytical phase
- Creatinine/urea
- Electrolytes
- Hemoglobins
- Natriuretic peptide
- About this site
- Journal scanner Explore selected articles curated by biochemist and journalist Chris Higgins
Sign up for our quarterly newsletter and get the newest articles from acutecaretesting.org

- Journal scans >
Printed from acutecaretesting.org
Severe diabetic ketoacidosis – a remarkable case study

Summarized from Van de Vyver C, Damen J, Haentjens C et al . An exceptional case of diabetic ketoacidosis. Case Reports in Emergency Medicine 2017.
Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of type 1 diabetes caused by insulin deficiency. It is characterized by raised blood glucose (hyperglycemia), metabolic acidosis, and increased blood/urine ketones. Dehydration and electrolyte disturbance are common and affected patients may develop some degree of acute kidney injury (AKI) consequent on fluid loss (hypovolemia) due to osmotic diuresis associated with severe hyperglycemia. DKA evolves rapidly over a short time frame (hours rather than days) and can occur (rarely) in those with type 2 diabetes. This DKA case study is particularly noteworthy because of the severity of the hyperglycemia and acid-base disturbance, and the fact that the patient survived such profound metabolic disturbance and associated life-threatening hemodynamic changes. The case concerns a 33-year-old woman with ”brittle” type 1 diabetes treated with continuous subcutaneous insulin infusion (insulin pump). She had, in common with many brittle diabetics, a history of gastroparesis (delayed stomach emptying). Some 36 hours prior to emergency hospital admission she complained of abdominal pain and vomiting after attending a party. Her condition deteriorated before transfer to hospital. The ambulance team reported a rapid decline in Glasgow Coma Score (GCS) from 13 to 3 in only 10 minutes, sinus tachycardia, undetectable peripheral pulse, and hypotension (BP 99/52 mmHg).
Clinical examination revealed severe dehydration and respiratory distress (respiration rate 40 breaths/min). Urgent intubation was necessary and systolic blood pressure dropped further to 55 mmHg. Initial (fingerstick) blood glucose was above the upper detection limit of the analyzer and blood ketones were >8.0 mmol/L. Blood gas analysis revealed severe metabolic acidosis (pH 6.74, bicarbonate 5 mmol/L, p CO 2 39.9 mmHg (5.3 kPa) and hypoxemia ( p O 2 50.2 mmHg, 6.7 kPa). Among other abnormal laboratory test results, perhaps the most remarkable was serum glucose 107 mmol/L (1924 mg/dL). (Serum glucose >33 mmol/L (600 mg/dL) is rarely seen in patients with DKA.) White blood count (32.8x10 9 /L), C-reactive protein (789 nmol/L) and lactate (4.6 mmol/L) were also grossly elevated. Other laboratory testing revealed severe hyponatremia (sodium 113 mmol/L), severe hyperkalemia (6.7 mmol/L) and acute kidney failure (serum creatinine 332 µmol/L). Following presumptive diagnosis of DKA, sepsis and acute renal failure, the patient was treated with aggressive IV fluids, norepinephrine, bicarbonate, and insulin, IV bolus and drip. Intensive investigation for evidence of infection proved fruitless. With treatment, the patient’s condition improved over the following days and she was extubated. Normal renal function was restored after 2 days. In discussion of this case history, the authors briefly review the pathogenesis and treatment of DKA in general terms. They also highlight some interesting features of this case. One aspect discussed relates to the blood gas results on admission, in particular the curiously normal p CO 2 (39.9 mmHg, 5.3kPa).
Metabolic acidosis usually provokes compensatory hyperventilation and reduced p CO 2 . The authors propose plausible theories to explain the much higher than expected p CO 2 in this case. They also propose that the remarkably high blood glucose in this case is the result of the combined effect of reduced glucose elimination consequent on renal failure and the presence of gastroparesis.
May contain information that is not supported by performance and intended use claims of Radiometer's products. See also Legal info .

has a master's degree in medical biochemistry and he has twenty years experience of work in clinical laboratories.

Acute care testing handbook
Get the acute care testing handbook.
Your practical guide to critical parameters in acute care testing.

Scientific webinars
Check out the list of webinars.
Radiometer and acutecaretesting.org present free educational webinars on topics surrounding acute care testing presented by international experts.
Sign up for the Acute Care Testing newsletter
Management of diabetic ketoacidosis: a case study
- Isabelle Cristina Krasniak Ferregato Hospital Universitário do Oeste do Paraná https://orcid.org/0000-0002-6118-8604
- Brennda Enis Gasques Almeida UPA Tancredo - Consórcio Intermunicipal Samu Oeste – CONSAMU https://orcid.org/0000-0003-0104-3208
- Juliana Pieri de Oliveira Hospital municipal 19 de março https://orcid.org/0000-0002-5083-7226
- Brena Marques Sbardelotto UPA Tancredo - Consórcio Intermunicipal Samu Oeste – CONSAMU https://orcid.org/0000-0002-6263-1639
- Marise Vilas Boas Pescador Centro Universitário FAG https://orcid.org/0000-0003-3718-1063
Objective: To report the clinical management of a patient with Diabetic Ketoacidosis (DKA), from the a literature review about the theme. Methods: Case study, analyzing treatment protocols about the correlation of the effectiveness of the correction of Ketoacidosis with the incidence of complications secondary to the respective treatment in a patient hospitalized in Pediatric Unit. Results: The patient presented DKA in first decompensation. The reduction speed of blood glucose in the first hour was superior to 100 mg/dL/hour, and the HGT data from the subsequent hours up to the eighth hour of treatment in the medical records were not found. Variable concentrations of glucose and potassium in the plan for basic water and electrolyte needs were utilized within the first 24 hours. The infusion of intermediate NPH began 36 hours after the start of the treatment. Regarding data complications, it was observed that the patient presented hypoglycemia, hypopotassemia, persistence of metabolic acidosis by early withdrawal of regular insulin infusion, with subsequent alkalosis due to the use of bicarbonate in the correction of acidosis. Conclusion: After data collection and analysis in the light of the theoretical reference framework, it was observed the non-existence of a specific protocol to the DKA treatment in the studied service, being that the use of these protocols help in the adequate treatment of the acute complication of diabetes, which avoids a greater risk of complications and reduces morbimortality.
American Diabetes Association (2005). Diagnosis and classification of diabetes mellitus. - Diabetes Care. http://www.diabetes.org .
Arieff, A. I., Kleeman, C. R., Kerian, A., & Bagdoyan, H. (1974). Cerebral edema in diabetic comas. II. Effects of hyperosmolality, hyperglycemia and insulin in diabetic rabbits. The Journal of Clinical Endocrinology & Metabolism, 38(6), 1057-1067.
Bureau, M. A., Bégin, R., Berthiaume, Y., Shapcott, D., Khoury, K., & Gagnon, N. (1980). Cerebral hypoxia from bicarbonate infusion in diabetic acidosis. The Journal of Pediatrics, 96(6), 968-973.
Bratton, S. L., & Krane, E. J. (1992). Diabetic ketoacidosis: Pathophysiology, management and complications. Journal of Intensive Care Medicine, 7(4), 199-211.
Carlotti, A. P. C. P., Bohn, D., & Halperin, M. L. (2003). Importance of timing of risk factors for cerebral oedema during therapy for diabetic ketoacidosis. Archives of disease in childhood, 88(2), 170-173.
Chiasson, J. L., Aris-Jilwan, N., Bélanger, R., Bertrand, S., Beauregard, H., Ékoé, J. M., ... & Havrankova, J. (2003). Diagnosis and treatment of diabetic ketoacidosis and the hyperglycemic hyperosmolar state. Cmaj, 168(7), 859-866.
Dunger, D. B., Sperling, M. A., Acerini, C. L., Bohn, D. J., Daneman, D., Danne, T. P. A., ... & Wolfsdorf, J. I. (2004). ESPE/LWPES consensus statement on diabetic ketoacidosis in children and adolescents. Archives of disease in childhood, 89(2), 188-194.
Felner, E. I., & White, P. C. (2001). Improving management of diabetic ketoacidosis in children. Pediatrics, 108(3), 735-740.
Hoffman, W. H., Steinhart, C. M., el Gammal, T. A. H. E. R., Steele, S., Cuadrado, A. R., & Morse, P. K. (1988). Cranial CT in children and adolescents with diabetic ketoacidosis. American journal of neuroradiology, 9(4), 733-739.
Lantry, J., Dezman, Z., & Hirshon, J. M. (2012). Pathophysiology, management and complications of hypothermia. British Journal of Hospital Medicine, 73(1), 31-37.
Lopes, C. L., Pinheiro, P. P., Barberena, L. S., & Eckert, G. U. (2017). Cetoacidose diabética em uma unidade de terapia intensiva pediátrica☆. Jornal de Pediatria, 93, 179-184.
Sociedade Brasileira de Diabetes (2018). Diretrizes Sociedade Brasileira de Diabetes 2017-2018. https://www.diabetes.org.br/profissionais/images/2017/diretrizes/diretrizes-sbd-2017-2018.pdf

- PDF (Português (Brasil))
How to Cite
- Endnote/Zotero/Mendeley (RIS)
Copyright (c) 2022 Isabelle Cristina Krasniak Ferregato; Brennda Enis Gasques Almeida; Juliana Pieri de Oliveira; Brena Marques Sbardelotto; Marise Vilas Boas Pescador

This work is licensed under a Creative Commons Attribution 4.0 International License .
Authors who publish with this journal agree to the following terms:
1) Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share the work with an acknowledgement of the work's authorship and initial publication in this journal.
2) Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
3) Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their website) prior to and during the submission process, as it can lead to productive exchanges, as well as earlier and greater citation of published work.
JOURNAL METRICS
Índice H5 (Google Metrics): 28 (2023)
Score CiteFactor: 1.78 (2020-21)
- Español (España)
- Português (Brasil)
Make a Submission
Base de Dados e Indexadores: Base , Diadorim , Sumarios.org , DOI Crossref , Dialnet , Scholar Google , Redib , Latindex
Research, Society and Development - ISSN 2525-3409

CDRR Editors. Avenida Sulim Abramovitc, 100 - Centro, Vargem Grande Paulista - SP, 06730-000 E-mail: [email protected] |

Advertisement
Diabetic ketoacidosis in acromegaly: a case study—somatostatin analogs adverse event or disease complication?
- Case Report
- Published: 17 October 2019
- Volume 57 , pages 491–493, ( 2020 )
Cite this article
- Nunzia Prencipe ORCID: orcid.org/0000-0002-9951-1796 1 ,
- Fabio Bioletto 1 ,
- Chiara Bona 1 ,
- Filippo Gatti 1 &
- Silvia Grottoli 1
294 Accesses
3 Citations
Explore all metrics
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Ferraù F, Albani A, Ciresi A, Giordano C, Cannavò S (2018) Diabetes secondary to acromegaly: physiopathology, clinical features and effects of treatment. Front Endocrinol. https://doi.org/10.3389/fendo.2018.00358
Article Google Scholar
Vergès B (2017) Effects of anti-somatostatin agents on glucose metabolism. Diabetes Metab 43(5):411–415. https://doi.org/10.1016/j.diabet.2017.05.003
Article CAS PubMed Google Scholar
Shimon I, Adnan Z, Gorshtein A et al (2018) Efficacy and safety of long-acting pasireotide in patients with somatostatin-resistant acromegaly: a multicenter study. Endocrine. https://doi.org/10.1007/s12020-018-1690-5
Article PubMed Google Scholar
Colao A, Bronstein MD, Freda P et al (2014) Pasireotide versus octreotide in acromegaly: a head-to-head superiority study. J Clin Endocrinol Metab 99(3):791–799. https://doi.org/10.1210/jc.2013-2480
Article CAS PubMed PubMed Central Google Scholar
Samson SL (2016) Management of hyperglycemia in patients with acromegaly treated with pasireotide LAR. Drugs 76(13):1235–1243. https://doi.org/10.1007/s40265-016-0615-y
Download references

Acknowledgements
The authors would like to thank their patient for giving the consent to the publication of her medical history.
Author information
Authors and affiliations.
Division of Endocrinology, Diabetology and Metabolism, Department of Medical Science, University Hospital “Città della Salute e della Scienza di Torino”, Corso Dogliotti 14, 10126, Turin, Italy
Nunzia Prencipe, Fabio Bioletto, Chiara Bona, Filippo Gatti & Silvia Grottoli
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Nunzia Prencipe .
Ethics declarations
Conflict of interest.
All the authors declare that they have nothing to disclose and no conflict of interest.
Ethical approval
The case-study has been reported in accordance with the Principles of Declaration of Helsinki.
Informed consent
The person involved in this case-study gave informed consent prior to her inclusion. Details that might disclose the identity of the subject have been omitted.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Prencipe, N., Bioletto, F., Bona, C. et al. Diabetic ketoacidosis in acromegaly: a case study—somatostatin analogs adverse event or disease complication?. Acta Diabetol 57 , 491–493 (2020). https://doi.org/10.1007/s00592-019-01437-z
Download citation
Received : 10 September 2019
Accepted : 10 October 2019
Published : 17 October 2019
Issue Date : April 2020
DOI : https://doi.org/10.1007/s00592-019-01437-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Adult diabetic ketoacidosis.
Jenna M. Lizzo ; Amandeep Goyal ; Vikas Gupta .
Affiliations
Last Update: July 10, 2023 .
- Continuing Education Activity
Diabetic ketoacidosis (DKA) is characterized by uncontrolled hyperglycemia, metabolic acidosis, and increased body ketone concentration. It is a life-threatening complication of diabetes and is usually seen in patients with type-1 diabetes mellitus. Rarely it may also occur in patients with type-2 diabetes mellitus. DKA is a state of a relative or absolute insulin deficiency that is worsened by hyperglycemia, dehydration, and acidosis. In most cases, the trigger is an infection, new-onset diabetes, or lack of compliance with treatment. This activity highlights the role of the interprofessional team in evaluating and managing patients suffering from this disorder in order to achieve the best outcomes.
- Review the etiology of diabetic ketoacidosis.
- Describe the management of a patient with diabetic ketoacidosis.
- Summarize the abnormal laboratory parameters in a patient with diabetic ketoacidosis.
- Explain the importance of improving care coordination among an interprofessional team to improve outcomes for patients affected by diabetic ketoacidosis.
- Introduction
Diabetic ketoacidosis (DKA) is characterized by hyperglycemia, acidosis, and ketonemia. It is a life-threatening complication of diabetes and typically seen in patients with type-1 diabetes mellitus, though it may also occur in patients with type-2 diabetes mellitus. In most cases, the trigger is new-onset diabetes, an infection, or a lack of compliance with treatment.
Diabetic ketoacidosis more commonly occurs in patients with type 1 diabetes, though it can also occur in patients with type 2 diabetes. Patients with type 2 diabetes are also at risk. In both populations, catabolic stress of acute illness or injuries such as trauma, surgery, or infections may be a trigger. Common precipitating factors for DKA are non-compliance, new-onset diabetes, and other acute medical illness. The most common types of infections are pneumonia and urinary tract infections. Other conditions like alcohol abuse, trauma, pulmonary embolism, and myocardial infarction can also precipitate DKA. Drugs that affect carbohydrate metabolisms, such as corticosteroids, thiazides, sympathomimetic agents, and pentamidine, may precipitate DKA. Conventional, as well as atypical antipsychotic drugs, may also cause hyperglycemia and rarely DKA. [1]
SGLT2 inhibitors can predispose to diabetic ketoacidosis via multiple mechanisms. When SGLT2 inhibitors are used together with insulin, insulin doses are often decreased to avoid hypoglycemia. A lower dose of insulin may not be sufficient to suppress lipolysis and ketogenesis. SGLT2 is also expressed in pancreatic α-cells. SGLT2 inhibitors promote glucagon secretion and may decrease urinary excretion of ketone bodies, leading to an increase in plasma ketone body levels as well as hyperglycemia and DKA. [2] While hyperglycemia is typically the hallmark of DKA, a small subset of patients may experience euglycemic DKA. Euglycemic DKA results in a high anion gap metabolic acidosis with positive serum and urine ketones when serum glycemic levels are less than 250 mg/dL. SGLT-2 inhibitors may precipitate euglycemic DKA. [3]
One of the major causes of recurrent DKA in the inner-city population in the United States is non-compliance with insulin. Socioeconomic and educational factors play a significant role in poor adhesion to medications, including insulin. A recent report suggests that cocaine abuse is an independent risk factor associated with DKA recurrence. [4]
- Epidemiology
Diabetic ketoacidosis incidence ranges from 0 to 56 per 1000 person-years, shown in different studies from different geographic areas. DKA has a higher prevalence rate among women and non-Whites. Incidence is higher among patients using injectable insulin compared to the subcutaneous insulin infusion pumps. [5]
Rates of DKA among children varies widely from country to country. The lowest incidence was found in Nigeria (2.9 cases per 100,000). The highest incidence rate was found in Sweden and Finland, with 41.0 and 37.4 per 100,000. [6] In the United States, one study reported nursing home residents accounted for 0.7% of DKA. Increased mortality was associated with nursing home residence among patients with DKA. [7] Mortality rate greater than 5% has been reported in the elderly and patients with concomitant life-threatening illnesses. Death in these conditions is rarely because of the metabolic complications of hyperglycemia or ketoacidosis alone.
The prognosis substantially worsens at the extremes of age in the presence of coma, hypotension, and severe comorbidities. [1] In urban Black patients, poor compliance with insulin was the leading precipitating cause of DKA. Substance abuse is a major contributing factor for non-adherence to therapies. Obesity is common in Blacks with DKA; it is found in more than half of those with newly diagnosed diabetes mellitus. Enhanced patient education and better access to medical care help in reducing the development of these hyperglycemic emergencies. [8]
Diabetic ketoacidosis (DKA) is one of the life-threatening but preventable complications of diabetes. CDC's United States Diabetes Surveillance System (USDSS) indicated an increase in hospitalization rates for DKA from 2009 to 2014, most notably in persons aged less than 45 years. [9] However, overall mortality due to hyperglycemic crisis among adults with diabetes has declined in the U.S. Scope for further improvement remains, especially to further reduce death rates among Black men and to prevent deaths occurring at home. [10]
The geriatric population is at particular risk for developing hyperglycemic crises with the development of diabetes. Some of the causes are increased insulin resistance and a decrease in the thirst mechanism. The elderly are particularly vulnerable to hyperglycemia and dehydration, the critical components of hyperglycemic emergencies. With increased diabetes surveillance and aggressive early treatment of hyperglycemia and its complications, morbidity, and mortality from acute diabetic crises in the geriatric population can be significantly reduced. [11]
- Pathophysiology
Diabetes mellitus is characterized by insulin deficiency and increased plasma glucagon levels, which can be normalized by insulin replacement. [12] Normally, once serum glucose concentration increases, it enters pancreatic beta cells and leads to insulin production. Insulin decreases hepatic glucose production by inhibiting glycogenolysis and gluconeogenesis. Glucose uptake by skeletal muscle and adipose tissue is increased by insulin. Both of these mechanisms result in the reduction of blood sugar. In diabetic ketoacidosis, insulin deficiency and increased counter-regulatory hormones can lead to increased gluconeogenesis, accelerated glycogenolysis, and impaired glucose utilization. This will ultimately cause worsening hyperglycemia.
Insulin deficiency and increased counterregulatory hormones also lead to the release of free fatty acids into circulation from adipose tissue (lipolysis), which undergo hepatic fatty acid oxidation to ketone bodies (beta-hydroxybutyrate and acetoacetate), resulting in ketonemia and metabolic acidosis. [1] Glucagon is not crucial for the development of ketoacidosis in diabetes mellitus, as has previously been mentioned; however, it may accelerate the onset of ketonemia and hyperglycemia in situations of insulin deficiency. [13] Patients treated with SGLT2 are at increased risk of developing euglycemic DKA.
Diuresis induced by hyperglycemia, dehydration, hyperosmolarity, and electrolyte imbalance results in a decrease of glomerular filtration. Due to worsening renal function, hyperglycemia/hyperosmolality worsens. Potassium utilization by skeletal muscle is also impaired by hyperosmolality and impaired insulin function. This results in intracellular potassium depletion. Osmotic diuresis also leads to loss of potassium resulting in low total body potassium. The potassium level in patients with DKA varies, and a patient's normal plasma potassium level might indicate low total body potassium. [4] Hyperosmolarity appears to be the main factor responsible for the lowering of consciousness in patients with diabetic ketoacidosis. [14]
New data suggests that hyperglycemia leads to a severe inflammatory state and an increase in proinflammatory cytokines (tumor necrosis factor-alpha and interleukin-beta, -6, and -8), C-reactive protein, lipid peroxidation, and reactive oxygen species, as well as cardiovascular risk factors, plasminogen activator inhibitor-1 and free fatty acids in the absence of apparent infection or cardiovascular pathology. After insulin therapy and IV fluid hydration, the pro-inflammatory cytokines return to normal values within 24 hours. [1]
- History and Physical
The patient with diabetic ketoacidosis may present with a myriad of symptoms and physical exam findings. Patients may have symptoms of hyperglycemia like polyphagia, polyuria, or polydipsia. As patients become more volume-depleted, they may experience decreased urine output, dry mouth, or decreased sweating indicative of dehydration. They may complain of many other symptoms, including anorexia, nausea, vomiting, abdominal pain, and weight loss.
If there is a superimposed infection that triggered the episode of DKA, the patient may have other infectious symptoms like fever, cough, or other urinary symptoms. In patients who may be developing cerebral edema, headache, or confusion may be present. Medication history should also be elicited, including what medications the patient is prescribed and how the patient has been using them. Substance use (drug and alcohol) should be ascertained. [15]
On examination, vital signs typically reveal tachycardia and tachypnea. Due to the possibility of an infectious trigger for DKA, the patient may be febrile or hypothermic. Blood pressure may also vary, though hypotension is possible and indicative of a more severe disease process. Patients are often ill-appearing. Kussmaul breathing, which is labored, deep, and tachypneic, may occur. Some providers may appreciate a fruity scent to the patient's breath, indicative of the presence of acetone. Patients may have signs of dehydration, including poor capillary refill, skin turgor, and dry mucous membranes. Abdominal tenderness is possible. In the most severe cases, altered mental status, general drowsiness, and focal neurologic deficits can be appreciated and are signs of cerebral edema. If found, this needs to be treated immediately. [16]
Commonly accepted criteria for diabetic ketoacidosis are blood glucose greater than 250 mg/dl, arterial pH less than 7.3, serum bicarbonate less than 15 mEq/l, and the presence of ketonemia or ketonuria. The normal anion gap is 12 mEq/l. Anion gap greater than 14-15 mEq/l indicates the presence of an increased anion gap metabolic acidosis. [17] Arterial pH may be normal or even raised if other types of metabolic or respiratory alkalosis coexist. Typical examples are vomiting or diuretic use. [18] Blood glucose may be normal or minimally elevated in patients with DKA (<300 mg/dl), where the underlying risk of hypoglycemia preexists, such as in patients with alcohol use disorder or patients receiving insulin or SGLT2 inhibitors.
The majority of patients with DKA who present to the hospital are found to have leukocytosis. Serum sodium in the lab report is falsely low in DKA and can be corrected by adding 1.6 mEq to the measured serum sodium for each 100 mg/dl of glucose above 100 mg/dl. Serum potassium is usually elevated because of a shift of potassium from the intracellular to the extracellular space caused by acidosis and insulin deficiency. However, total body potassium may be depleted or may quickly become depleted with insulin administration. Magnesium is often low and requires repletion as well. The serum phosphate level in DKA may be elevated despite total-body phosphate depletion. [19]
Other tests like cultures of urine, sputum, and blood, serum lipase, and chest radiograph may need to be performed depending upon the case. Pneumonia and urinary tract infections are the most common infections precipitating DKA. Measurement of glycated hemoglobin (A1C) provides information about glucose trends over months.
In acute DKA, the ketone body ratio (3-beta-hydroxybutyrate:acetoacetate) rises from normal (1:1) to as high as 10:1. In response to insulin therapy, 3-beta-hydroxybutyrate (3-HB) levels commonly decrease long before acetoacetate (AcAc) levels. The frequently employed nitroprusside test only detects acetoacetate in blood and urine. This test provides only a semiquantitative assessment of ketone levels and is associated with false-positive results. Recently, inexpensive quantitative tests of 3-HB levels have become available for common use, and these tests offer options for monitoring and treating diabetes and other states characterized by the abnormal metabolism of ketone bodies. [20]
The serum level of pancreatic enzymes is elevated in DKA due to disorder in carbohydrate metabolism. [21] In DKA, patients presenting with abdominal pain and elevated pancreatic enzymes should not be diagnosed with acute pancreatitis promptly. [22] In the case of a dilemma, imaging like a CT scan would help in distinguishing mild to moderate elevation of enzymes due to DKA from acute pancreatitis. Lipid derangement is commonly seen in patients with DKA. In one study, before insulin treatment, mean plasma triglyceride and cholesterol levels were 574 mg/dl (range 53 to 2355) and 212 mg/dl (range 118 to 416), respectively. Insulin therapy resulted in rapid decreases in plasma triglyceride levels below 150 mg/dl at 24 hours. Plasma apoprotein (apo) B levels were in the normal upper range (101 mg/dl) before treatment and decreased with therapy due to significant decreases in VLDL, but not IDL or LDL apoB. [23]
An ECG will help detect ischemic changes or signs of hypokalemia or hyperkalemia. Peaked T waves can signal hyperkalemia, and low T waves with U wave indicating hypokalemia.
Imaging: A chest X-ray may be done to rule out consolidation. MRI, and to some degree, CT imaging of the head can detect cerebral edema, but imaging should not delay treatment if cerebral edema is suspected.
- Treatment / Management
Fluid resuscitation and maintenance, insulin therapy, electrolyte replacement, and supportive care are the mainstays of management in diabetic ketoacidosis.
In patients with DKA, the fluid deficit could be up to 10-15% of the body weight. [1] Immediate fluid resuscitation is vital to correct hypovolemia, restore tissue perfusion, and to clear ketones. Hydration improves glycemic control independent of insulin.
Choice of Fluids
Isotonic fluids have been well established for more than 50 years as preferred fluids. Colloids vs. crystalloids were compared for critically ill patients, in a 2013 meta-analysis, and crystalloid was found to be non-inferior. [24] Traditionally, 0.9% normal saline has been used. There has been a concern that normal saline may contribute to hyperchloremia and hyperchloremic metabolic acidosis; however, this typically occurs when it is used for large volumes. There have been small studies comparing normal saline with other solutions like Ringer lactate. These studies did not show differences in clinical outcomes. [25] [26] [27] Normal saline continues to be used for initial hydration.
Infusion Rate
Infusion of 15-20 ml per Kg body weight in the first 1 hour is typically appropriate. Aggressive hydration with 1 liter/hour for 4 hours has been compared in a study to a slower rate of hydration at half the rate. Slower hydration was found to be equally effective. [28] However, in critically ill patients, including those with hypotension, aggressive fluid therapy is preferred. There has been extensive debate regarding the risk of cerebral edema in patients with aggressive early volume resuscitation. There are studies that have demonstrated rates of increased cerebral edema with aggressive volume, particularly in the pediatric population. Yet other studies show no difference in outcome and theorize that patients at greatest risk from cerebral edema present at a later stage and are the most severe volume depleted. [29]
Maintainance:
The subsequent choice for fluid replacement depends on hemodynamics, the state of hydration, serum electrolyte levels, and urinary output. [1] In patients who have high serum sodium level, 0.45% NaCl infused at 4–14 ml/kg/hour or 250–500 mL/hr is appropriate, and for patients with hyponatremia, 0.9% NaCl at a similar rate is preferred. [30] Maintenance fluids may need to be adjusted if hyperchloremic metabolic acidosis becomes a concern, then you can switch to the Ringer lactate solution.
Insulin Therapy
The discovery of insulin, along with the antibiotics, has led to a drastic decrease in mortality with DKA, down to 1%. Intravenous insulin by continuous infusion is the standard of care. Previous treatment protocols have recommended the administration of an initial bolus of 0.1 U/kg, followed by the infusion of 0.1 U/kg/h. A more recent prospective randomized trial demonstrated that a bolus is not necessary if patients are given hourly insulin infusion at 0.14 U/kg/hr. [31] When the plasma glucose reaches 200-250 mg/dl, and if the patient still has an anion gap, then dextrose containing fluids should be initiated, and the insulin infusion rate may need to be reduced.
Treatment of adult patients who have uncomplicated, mild diabetic ketoacidosis can be treated with subcutaneous insulin lispro hourly in a non-intensive care setting may be safe and cost-effective as opposed to treatment with intravenous regular insulin in the intensive care setting as shown in many studies. [32] In one of these studies, the patients received subcutaneous insulin lispro at a dose of 0.3 U/kg initially, followed by 0.1 U/kg every hour until blood glucose was less than 250 mg/dl. Then insulin dose was decreased to 0.05 or 0.1 U/kg given every hour until the resolution of DKA. [32] Similarly, insulin aspart has been used and found to be similar in efficacy. [33]
Patients with DKA should be treated with insulin until resolution. Criteria for resolution of ketoacidosis include blood glucose less than 200 mg/dl and two of the following criteria: a serum bicarbonate level >=more than 15 mEq/l, a venous pH more than 7.3, or a calculated anion gap equal or less than 12 mEq/l. Patients can be transitioned to subcutaneously administered insulin when DKA has resolved, and they are able to eat. Those previously treated with insulin might be recommended on their home dose if they had been well controlled.
Insulin-naive patients should receive a multi-dose insulin regimen beginning at a dose of 0.5 to 0.8 U/kg/day. To prevent the recurrence of ketoacidosis in the transition period, insulin infusion should be continued for 2 hrs after the starting of subcutaneous insulin and check blood sugar and complete metabolic profile again before stopping the insulin drip. If the patient cannot tolerate oral intake, intravenous insulin, and fluids may be continued. The use of long-acting insulin analogs during the initial management of DKA may facilitate the transition from intravenous to subcutaneous insulin therapy. [34]
Electrolyte Replacement
Patients with DKA are often found to initially have mild to moderate hyperkalemia, despite a total body deficit of potassium. The initiation of insulin causes an intracellular shift of potassium and lowers the potassium concentration, potentially resulting in severe hypokalemia. [35] [36] Hence patients with serum potassium levels of less than 3.3 mmol/L need initial management with fluid resuscitation and potassium replacement while delaying commencement of insulin until after potassium levels are above 3.3 mmol/L, to avoid cardiac arrhythmias, arrest, and respiratory muscle weakness. [34] In other patients, potassium replacement should be started when the serum concentration is less than 5.2 mEq/L to maintain a level of 4 to 5 mEq/L. The administration of 20 to 30 mEq of potassium per liter of fluids is sufficient for most patients; however, lower doses are required for patients with acute or chronic renal failure. [37]
Hypokalemia is commonly associated with hypomagnesemia. Repletion of both potassium and magnesium may need to be done, and it may be difficult to improve potassium levels until magnesium levels are repleted.
Bicarbonate
Bicarbonate replacement does not appear to be beneficial. In one study, the difference in time to resolution of acidosis (8 hours vs. 8 hours; p = 0.7) and time to hospital discharge (68 hours vs. 61 hours; p = 0.3) was found to be statistically insignificant between patients who received intravenous bicarbonate (n = 44) compared with those who did not (n = 42). [38] In another pediatric study, children with diabetic ketoacidosis who have low PaCO2 and high BUN concentrations at presentation and those treated with bicarbonate were at increased risk for cerebral edema. [39] Proposed pitfalls of the use of sodium bicarbonate therapy in DKA may include paradoxical CSF acidosis, hypokalemia, large sodium bolus, and cerebral edema. However, it may be used in patients with severe acidemia. The most recent ADA guidelines do recommend the use of sodium bicarbonate therapy in patients with pH less than 7.1. [38]
The role of phosphate replacement in DKA has been looked at in different studies. In one randomized study with 44 patients, phosphate therapy did not alter the duration of DKA, insulin dosage required to correct the acidosis, abnormal muscle enzyme levels, glucose disappearance, or morbidity and mortality. Although theoretically appealing, phosphate therapy is not an essential part of the treatment for DKA in most patients, an unusual case of severe hypophosphatemia (1.0 mg/dl) related seizure in a child with diabetic ketoacidosis (DKA) has been described in the literature. [40]
Laboratory Monitoring
- Hourly point-of-care testing (POCT) glucose should be performed
- Serum glucose and electrolyte levels may need to be done every 2 hours until the patient is stable, then every 4 hours
- Initial blood urea nitrogen (BUN)
- Initial VBG or ABG monitoring, followed by as-needed precipitating events
There are multiple risks associated with intubation in patients with DKA. Intubation should be avoided if at all possible. Treating as above with a focus on administering fluids and insulin will almost always lead to an improvement in acidosis and overall clinical presentation. Patients attempt to compensate for severe acidosis by creating a compensatory respiratory alkalosis that manifests via tachypnea and Kussmaul breathing. If patients are no longer able to generate respiratory alkalosis due to comatose state or severe fatigue, intubation should be considered. However, the risks of intubation in DKA include a rise in PaCO2 during sedation and/or paralysis, which can decrease pH further, increasing the risk of aspiration due to gastroparesis, and difficulty matching the degree of respiratory compensation once the patient is on a ventilator. If a patient is intubated and placed on a ventilator, it is essential to attempt to match the patient's minute ventilation such that respiratory alkalosis is created to compensate for the metabolic acidosis of DKA. If not, there will be worsening acidosis, which can ultimately lead to cardiac arrest. It is reasonable to start with a tidal volume of 8 ml/kg based on ideal body weight and respiratory rate, similar to the patient's compensating respiratory rate. However, care should be taken that auto-PEEP is not occurring due to the rapid respiratory rate. [41]
Cerebral Edema
Mental status and neurologic exam should be monitored in all patients with DKA. In any patient who is severely obtunded or comatose or who has declining mental status despite treatment or focal neurologic deficits, there should be a very low threshold to treat for cerebral edema. Mannitol is typically the first-line agent, though there are also studies in both TBI literature and DKA literature regarding the use of 3% saline.
Precipitating Events
Infection is a very common trigger for DKA in patients who have new-onset diabetes and previously established diabetes. If there is any suspicion of infection, antibiotics should be administered promptly. As discussed, there can be other events that trigger DKA as well. Treating both DKA and any other underlying etiologies should be done.
- Differential Diagnosis
Diabetic ketoacidosis has a diverse presentation, and this is why several other common pathologies may mimic this diagnosis. It is imperative for the providers to consider the following differential diagnoses when the diagnosis of DKA is suspected:
- Hyperosmolar hyperglycemic nonketotic syndrome
- Starvation ketosis
- Myocardial infarction
- Pancreatitis
- Alcoholic ketoacidosis
- Lactic acidosis
- Sepsis
- Toxicologic exposure (ethylene glycol, methanol, paraldehyde, salicylate)
- Diabetic medication overdose
Diabetic ketoacidosis still carries a mortality rate of 0.2 to 2.5% in developing countries. Patients who present in a comatose state, hypothermia, and oliguria tend to have the worst outcomes. For most patients treated promptly, the outcomes are good, especially if the trigger is not an infection. Elderly patients with concurrent illnesses such as myocardial infarction, pneumonia, or sepsis tend to have long hospital stays and high mortality.
The most important cause of mortality is cerebral edema, usually seen in younger patients. The cerebral edema is primarily due to the intracellular shifts. Another important cause of morbidity is renal dysfunction. A recent study has noted that among patients with type-2 diabetes mellitus who develop DKA, there is a high risk of stroke within the first six months after the event.
- Complications
Hypoglycemia is the most common complication of diabetic ketoacidosis while being treated, occurring in an estimated 5–25% of patients with DKA. [37] Acute adverse outcomes of hypoglycemia include seizures, arrhythmias, and cardiovascular events. Hourly blood sugar monitoring is needed in the acute phase of treatment.
Hypokalemia is common. Severe hypokalemia can cause muscle weakness, cardiac arrhythmias, and cardiac arrest. [8] Monitoring and management are described in this article under the DKA management section in detail. Other possible electrolyte disturbances are hyperchloremia, which can occur in up to 1/3rd of patients, and hypomagnesemia, and hyponatremia. [42]
Cerebral edema is less common in adults than in children. Risk factors include younger age, new-onset diabetes, longer duration of symptoms, the lower partial pressure of carbon dioxide, severe acidosis, low initial bicarbonate level, low sodium level, high glucose level at presentation, rapid hydration, and retained fluid in the stomach. [39]
Rhabdomyolysis may occur in patients with DKA though it occurs more commonly with HHS. It may result in acute kidney failure. Severe hypophosphatemia in relation to DKA can also cause rhabdomyolysis. [43]
Acute respiratory failure could be associated with DKA. Causes could be pneumonia, ARDS, or pulmonary edema. Two varieties of pulmonary edema in DKA have been recognized, secondary to elevated pulmonary venous pressure, and because of increased pulmonary capillary permeability. [44]
TTP and myocarditis have also been described with DKA.
- Deterrence and Patient Education
Education on the disease process of diabetes, including short and long term complications, should be given to all patients. Patients should be taught how and when to check their glucose. Patients should receive education about how to use oral hypoglycemic meds and/or insulin, their side effects, and the importance of compliance. Dietitians, nurses, and multi-disciplinary home health can be important members of the team in assisting with this education.
- Enhancing Healthcare Team Outcomes
Diabetic ketoacidosis is a life-threatening complication of diabetes, and any delay in treatment can lead to death. The disorder can present with varied signs and symptoms and affects many organs; thus, it is best managed by an interprofessional team dedicated to the management of patients with diabetes mellitus. The majority of patients first present to the emergency department, and it is here that the treatment usually starts.
The triage nurse has to be familiar with the signs and symptoms of DKA and immediately admit the patient and notify the emergency department physician. While the patient is being resuscitated, placed on a monitor, and having blood drawn, the intensivist and an endocrinologist should be consulted.
Immediate blood work is necessary to determine the state of ketoacidosis, and imaging may be necessary to rule out pneumonia. If the mental status is altered, a CT scan may be required, and thus the radiologist must be notified about the patient's hemodynamic status. No patient with DKA should go unmonitored to a radiology suite.
The infectious disease expert and cardiologist should be consulted if there is suspicion of infection or MI as the trigger.
The pharmacist and nurses should determine if the patient was compliant with insulin treatment. Following discharge, the social workers should be involved in the care since recurrent DKA admissions are common, especially in inner-city hospitals. Socioeconomic status, education status, access to insulin, the presence of health care coverage, and the presence of mental illness, etc. play a big role in these patients.
An interprofessional team, including social workers, are often needed to address these particular situations. Meticulous discharge planning, involving social workers for patients with socioeconomic needs, and hospital initiated follow up clinics for discharged patients are some of the factors important to reduce the recurrences of DKA in the same individual. Finally, patient education is highly recommended, as in many cases, the cause of DKA is failing to comply with treatment.
In developed countries, the morbidity and mortality rates are low chiefly because of a streamlined interprofessional approach to the management of these patients. However, in developing countries, mortality rates of 0.3 to 2.5% are still reported. The major cause of death in most young patients is cerebral edema.
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jenna Lizzo declares no relevant financial relationships with ineligible companies.
Disclosure: Amandeep Goyal declares no relevant financial relationships with ineligible companies.
Disclosure: Vikas Gupta declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Lizzo JM, Goyal A, Gupta V. Adult Diabetic Ketoacidosis. [Updated 2023 Jul 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Euglycemic diabetic ketoacidosis: A missed diagnosis. [World J Diabetes. 2021] Review Euglycemic diabetic ketoacidosis: A missed diagnosis. Nasa P, Chaudhary S, Shrivastava PK, Singh A. World J Diabetes. 2021 May 15; 12(5):514-523.
- Review Diabetic ketoacidosis: risk factors and management strategies. [Treat Endocrinol. 2003] Review Diabetic ketoacidosis: risk factors and management strategies. Umpierrez GE, Kitabchi AE. Treat Endocrinol. 2003; 2(2):95-108.
- Brentuximab vedotin-associated diabetic ketoacidosis: a case report. [Int J Diabetes Dev Ctries. 2023] Brentuximab vedotin-associated diabetic ketoacidosis: a case report. Köksalan D, Sözen M, Selek A, Gezer E, Cantürk Z, Çetinarslan B. Int J Diabetes Dev Ctries. 2023 Feb; 43(1):120-124. Epub 2022 Jul 16.
- Euglycemic Diabetic Ketoacidosis, a Misleading Presentation of Diabetic Ketoacidosis. [N Am J Med Sci. 2015] Euglycemic Diabetic Ketoacidosis, a Misleading Presentation of Diabetic Ketoacidosis. Thawabi M, Studyvin S. N Am J Med Sci. 2015 Jun; 7(6):291-4.
- A Rare Case of Empagliflozin-Induced Euglycemic Diabetic Ketoacidosis Obscured by Alkalosis. [Cureus. 2022] A Rare Case of Empagliflozin-Induced Euglycemic Diabetic Ketoacidosis Obscured by Alkalosis. Fernandez Felix DA, Madrigal Loria G, Sharma S, Sharma S, Arias Morales CE. Cureus. 2022 Jun; 14(6):e25818. Epub 2022 Jun 10.
Recent Activity
- Adult Diabetic Ketoacidosis - StatPearls Adult Diabetic Ketoacidosis - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
Diabetic ketoacidosis (DKA) is a cardinal feature of type 1 diabetes. ... Open the PDF for in another window; Share Icon Share. Facebook; Twitter; LinkedIn; Email; Cite Icon Cite. Get Permissions. Citation. Brian J. Welch, Ivana Zib; Case Study: Diabetic Ketoacidosis in Type 2 Diabetes: "Look Under the Sheets". Clin Diabetes 1 October 2004 ...
** The data in Tables 1 and 2 (following page) and the description of the patient's condition and treatment have been modified from a case reported by A.N. Cebeci and A. G. Üven ("Delirium in Diabetic Ketoacidosis: A Case Report," The Journal of Clinical Research in Pediatric Endo-crinology . 4(1): 39-41, 2012).
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria's vital signs were as follows: BP 87/50, HR 118, RR 28 ...
Diabetic ketoacidosis (DKA) is the leading cause of death before the age of 30 in people with type 1 diabetes, therefore prompt diagnosis and treatment is vital. This article provides some clinical case studies to illustrate how the presentation of DKA can
Case Reports in Emergency Medicine 2017. Diabetic ketoacidosis (DKA) is a potentially life-threatening acute complication of type 1 diabetes caused by insulin deficiency. It is characterized by raised blood glucose (hyperglycemia), metabolic acidosis, and increased blood/urine ketones. Dehydration and electrolyte disturbance are common and ...
Diabetic ketoacidosis is characterized by a serum glucose level greater than 250 mg per dL, a pH less than 7.3, a serum bicarbonate level less than 18 mEq per L, an elevated serum ketone level ...
Diabetic Ketoacidosis Upon Diagnosis: A Biochemistry Case Study. Diabetes mellitus is a metabolic disorder characterised by hyperglycemia. The two main types of diabetes mellitus are type 1 diabetes mellitus (T1DM) and type 2 (T2DM), which exhibit similar symptoms while having two very difer-ent pathophysiologies (Alam et al., 2014).
Abstract and Figures. We present a case of diabetic ketoacidosis, known as one of the most serious metabolic complications of diabetes. We were confronted with rapid neurological deterioration and ...
Severe hypertriglyceridemia (HTG) is a rare complication of insulin resistance. Its presentation with diabetic ketoacidosis (DKA) has been reported in a few cases, where most patients have type-1 diabetes mellitus (DM). Our case represents a unique presentation of DKA associated with severe HTG above 10,000 mg/dL in an adult with type-2 DM.
We present a case of diabetic ketoacidosis in a child with type 1 diabetic mellitus. It is a life threatening complications if timely intervention is not done. Timely management with fluid therapy along with insulin should be done. Regular monitoring and neurological observation are equally important to prevent complications like cerebral edema.
Diabetic Ketoacidosis commonly presents with hyponatremia, but hypernatremia is a rare entity. We report a unique case of a 50-year-old woman admitted with altered sensorium with blood glucose 979 milligrams/deciliter, serum osmolarity 363 mOsm/kilograms, and serum sodium 144 milliequivalents/liter.
In this article, we provide a narrative review of management of DKA in adults along with discussion of the various professional guidelines and propose evidence-based recommendations on the topic. We conducted a literature search through PubMed and Google Scholar using the following search terms: "diabetic ketoacidosis," "DKA ...
KEYWORDS: diabetic ketoacidosis, inpatient, complications DOI: 10.7861/clinmed.2022-0300 Background The prevalence of diabetes in the UK continues to increase at an alarming rate, with almost 4 million people diagnosed with diabetes and 1 million people are estimated to remain undiagnosed.1 In hospital, the prevalence is greater still with
Background: Diabetic ketoacidosis (DKA) is a common consequence of electrolyte and dehydration abnormalities that affect individuals with type-1 diabetes. DKA is a major diabetic complication ...
Diabetic ketoacidosis (DKA) is an acute complication of diabetes mellitus that can be associated with increased morbidity and mortality, particularly if it is diagnosed late and not treated appropriately. The management of DKA includes careful clinical evaluation, correction of metabolic abnormalities with intravenous fluids, insulin and electrolyte replacement with frequent monitoring of the ...
Objective: To report the clinical management of a patient with Diabetic Ketoacidosis (DKA), from the a literature review about the theme. Methods: Case study, analyzing treatment protocols about the correlation of the effectiveness of the correction of Ketoacidosis with the incidence of complications secondary to the respective treatment in a patient hospitalized in Pediatric Unit.
Abstract and Figures. Diabetic ketoacidosis (DKA) is the most common hyperglycemic emergency and causes the greatest risk for death that could be prevented in patients with diabetes mellitus. DKA ...
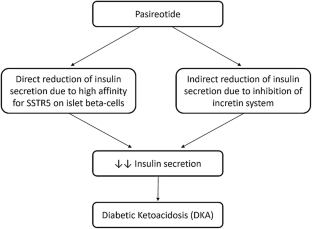
To our knowledge, this is the first reported case of diabetic ketoacidosis surely caused by pasireotide treatment. One case of DKA was previously reported, but with a few limits, as it was described in a patient with McCune-Albright syndrome with poor biochemical control of acromegaly disease and in which DKA appeared 2 months after pasireotide last administration; furthermore, no remarks were ...
Abstract. Diabetic ketoacidosis (DKA) is an acute complication of diabetes mellitus, both type I and type II, as well as other types with diabetes such gestacional diabetes mellitus. It is characterized by blood glucose levels greater than 250 mg/dL and metabolic acidosis (pH < 7.3 and serum bicarbonate < 15 mEq/dL) with an increased anion gap ...
Diabetic ketoacidosis (DKA) is a serious and potentially life-threatening complication of Type 1 and rarely Type 2 diabetes. It remains a significant cause of morbidity in children with diabetes and has an estimated mortality rate of 0.15-0.5%. Prompt recognition and management of DKA and its complications are vital.
1 INTRODUCTION. Type 1 diabetes mellitus (T1DM) is children's most frequent endocrine disease. Globally, 542,000 children are diagnosed with T1DM, with an estimated 86,000 new cases yearly. 1, 2 Diabetic ketoacidosis (DKA) is one of its main complications, and its incidence varies from 1 to 12 cases per 100 individuals/year. 3-5 DKA is defined as the presence of serum glucose > 200 mg/dL (> 11 ...
Diabetic ketoacidosis is considered one of the most common causes of death in a patient with type 1 diabetes. Diabetic ketoacidosis is characterized by hyperglycemia, hyperosmolarity, ketosis, and ...
RAPID Reasoning Case Study: STUDENT Diabetic Ketoacidosis (DKA) History of Present Problem: Diana Humphries is a 45-year-old woman with chronic kidney disease stage III and diabetes mellitus type1 who checks her blood sugar daily, or whenever she feels like it. She has been feeling increasingly nauseated the past 12 hours.
Diabetic ketoacidosis (DKA) is characterized by hyperglycemia, acidosis, and ketonemia. It is a life-threatening complication of diabetes and typically seen in patients with type-1 diabetes mellitus, though it may also occur in patients with type-2 diabetes mellitus. In most cases, the trigger is new-onset diabetes, an infection, or a lack of compliance with treatment.
Aims: We evaluated attainment of the hemoglobin A1c (HbA1c) target of ≤7.0%, its temporal trends, and associated factors among adults with type 1 diabetes in Ontario, Canada, using administrative data. Methods: We conducted a retrospective cohort study, including Ontarians with type 1 diabetes ≥18 years old with ≥1 HbA1c test between April 1, 2012 (fiscal year 2013), and March 31, 2023 ...
Fluid, electrolyte and acid-base balance case study. Uploaded by yukaterada30 on coursehero.com. Ann is 28-year-old woman with a history of type 1 diabetes mellitus diagnosed when she was 5- year-old. She has been brought into the emergency department this morning by her partner, Greg as she is lethargic and unable to make any sense.