Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Perspective
- Open access
- Published: 22 October 2022

Automated clinical coding: what, why, and where we are?
- Hang Dong ORCID: orcid.org/0000-0001-6828-6891 1 , 2 ,
- Matúš Falis 3 ,
- William Whiteley ORCID: orcid.org/0000-0002-4816-8991 4 ,
- Beatrice Alex 3 , 5 ,
- Joshua Matterson ORCID: orcid.org/0000-0002-7085-0153 6 , 7 ,
- Shaoxiong Ji ORCID: orcid.org/0000-0003-3281-8002 8 ,
- Jiaoyan Chen ORCID: orcid.org/0000-0003-4643-6750 2 &
- Honghan Wu ORCID: orcid.org/0000-0002-0213-5668 9
npj Digital Medicine volume 5 , Article number: 159 ( 2022 ) Cite this article
19k Accesses
16 Citations
34 Altmetric
Metrics details
- Health care
- Information technology
Clinical coding is the task of transforming medical information in a patient’s health records into structured codes so that they can be used for statistical analysis. This is a cognitive and time-consuming task that follows a standard process in order to achieve a high level of consistency. Clinical coding could potentially be supported by an automated system to improve the efficiency and accuracy of the process. We introduce the idea of automated clinical coding and summarise its challenges from the perspective of Artificial Intelligence (AI) and Natural Language Processing (NLP), based on the literature, our project experience over the past two and half years (late 2019–early 2022), and discussions with clinical coding experts in Scotland and the UK. Our research reveals the gaps between the current deep learning-based approach applied to clinical coding and the need for explainability and consistency in real-world practice. Knowledge-based methods that represent and reason the standard, explainable process of a task may need to be incorporated into deep learning-based methods for clinical coding. Automated clinical coding is a promising task for AI, despite the technical and organisational challenges. Coders are needed to be involved in the development process. There is much to achieve to develop and deploy an AI-based automated system to support coding in the next five years and beyond.
Similar content being viewed by others

Highly accurate protein structure prediction with AlphaFold

OpenFold: retraining AlphaFold2 yields new insights into its learning mechanisms and capacity for generalization

Artificial intelligence in surgery
Introduction: what is (automated) clinical coding.
Clinical coding is the task of transforming medical records, usually presented as free texts written by clinicians, into structured codes in a classification system like ICD-10 (International Classification of Diseases, Tenth Revision). For example, in Scotland, this means to apply a standard process to classify information about patients into appropriate diagnosis and procedure codes in ICD and OPCS (OPCS Classification of Interventions and Procedures), finally contributing to the Scottish Morbidity Records (SMR01) national data set 1 . The purpose of clinical coding is to provide consistent and comparable clinical information across units of care and over time. The resulting national data are used to support areas, such as health improvement, inform healthcare planning and policy and add to the epidemiological understanding of a wide variety of conditions, so confidence in the data is essential. Also, codes are mainly used for billing purposes in the US 2 . For introductory slides about clinical coding in the UK provided by NHS Digital, see Clinical coding for non coders 3 .
Clinical coding is a non-trivial task for humans. The process of coding usually includes data abstraction or summarisation 4 . More specifically, an expert clinical coder is expected to decipher a large number of documents about a patient’s episode of care, and to select the most accurate codes from a large classification system (or an ontology), according to the contexts in the various documents and the regularly updated coding guidelines. For example, coding in the US adopts the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM), which has around 68,000 diagnosis codes 5 ; ICD-10 is also the main classification for coding in the UK. There is a standard process for manual coding to ensure data consistency: textual analysis, summarisation, and clearly defined steps to classification into codes (or the four steps of analyse, locate, assign, and verify as suggested by the NHS digital in the coding standard of 2021 [6, p.11]). The process minimises the risk of introducing variations caused by artefacts (potentially leading to wrong decision making), thus collecting and analysing data and applying the standard is important. There are regularly updated guidelines and standards for coding (e.g., in Public Health Scotland 6 ). Usually, it can take months or longer to train an expert clinical coder in the NHS (National Health Service) in the UK, and worldwide 7 .
Automated clinical coding is the idea that clinical coding may be automated by computers using AI techniques, e.g., NLP and machine learning 8 . It is a branch of computer-assisted coding (CAC) 9 . In recent years, AI has been considered a promising approach to transforming healthcare by intelligently processing the increasing amount of data with machine learning and NLP techniques 10 . Automated clinical coding is a potential AI application to facilitate the administration and management of clinical records in the hospital and medical research. There has been a surge of articles for automated clinical coding with deep learning (as the current mainstream approach of AI) in the last few years, as reviewed in recent surveys 11 , 12 , 13 .
However, while there is some progress for automated clinical coding, the task is far from solved. For the last two years and more, we have been working on the task and discussing it with practitioners of clinical coding and clinicians from Scotland and the UK. We illustrate the manual and automated clinical coding process, and their potential interactions, in Fig. 1 . In this paper, we aim to summarise the technical challenges of clinical coding, mainly related to deep learning, and propose directions for future research in this area.
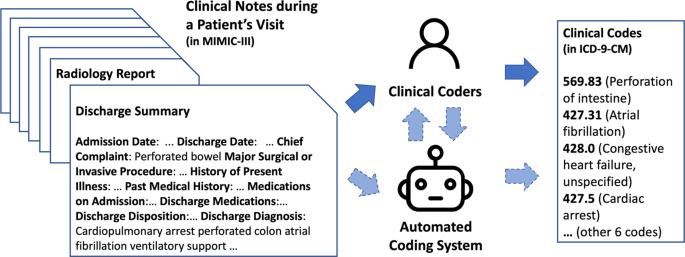
Dashed arrows between clinical coders and the automated coding system suggest potential interactions between them, while this is yet to be considered in many clinical coding systems. Note that the format of data and clinical codes does not reflect the situation of other regions in the world—for example, in the UK, where data may be less structured and there is no universal discharge summary format available.
Why do we need automated clinical coding?
There are some major reasons that automated clinical coding can be helpful. First, manual coding is time-consuming. A clinical coder in NHS Scotland usually codes about 60 cases a day (equivalent to 7–8 min for each case) and an NHS coding department of around 25–30 coders usually codes over 20,000 cases per month. Even so, there is usually a backlog of cases to be coded, which can take several months or more (e.g., over a year 14 ). Second, manual coding may be prone to errors. This may be due to incompleteness in a patient’s data, subjectivity in choosing the diagnosis codes, lack of coding expertise, or data entry errors 4 . The average accuracy of coding in the UK was around 83% with a large variance among studies (50-98%) 15 . In Scotland, the accuracy of coding is very high 16 (e.g., in the assessment during 2019–2020, achieved 92.5% for 3-digit code accuracy and 88.8% for 4-digit code accuracy of main conditions), yet still not perfect and under-coding occurs (for around 20% of the common conditions). On the other hand, computer-assisted coding could improve the accuracy, quality, and efficiency of manual coding, according to a recent, qualitative literature review 9 . We believe that with recent AI technologies (e.g., NLP), automated coding has the potential to better support clinical coders. We mostly focus on the case that AI directly contributes to assigning clinical codes.
Why is automated coding a complex problem to solve?
While humans can achieve high accuracy in clinical coding, the standard procedure, text analysis, text summarisation, and classification into codes, poses immense challenges for computer-based systems. This requires Natural Language Understanding (NLU), one of the classical but largely unsolved areas of AI 17 , 18 , and the linking of natural language to knowledge representations like the ICD-10 classification system. Also, this clinical task poses more specific challenges compared to common NLU tasks. From our experience, these relate mainly to the following difficulties:
Clinical documents are variously structured, notational, lengthy, and incomplete. Clinical coding requires the understanding of texts in clinical documents, which is usually different from other types of documents like publications or texts from social media. They have variable document structures, they can be lengthy (on average around 1500 words 19 in only the discharge summaries in a US intensive care data set, MIMIC-III 20 ), and use terse abbreviations and symbols 8 , 21 (e.g., “a [xx] y/o M w/ Hep C, HTN, CKD, a/w HTN emergency” in a discharge summary and the use of “?” to denote uncertainty and “+” to denote a positive test in MIMIC-III). Coding also requires the understanding of the entirety of a patient’s records, which includes multiple types of documents (e.g., discharge summaries, radiology reports, pathology reports, etc.). These documents are not always in a structured format and are sometimes incomplete or missing.
Classification systems used for coding are complex and dynamic. The ICD-10-CM system (implemented in the US in 2015) has around 68,000 diagnosis codes in a large hierarchy, 5 times more than the previous ICD-9-CM (used in MIMIC-III) 5 . The ICD-11 system 22 (or ICD-11-MMS, ICD-11 for Mortality and Morbidity Statistics, came into effect in early 2022, but is yet to be used in practice in the US or the UK at the time of writing) “contains around 17,000 unique codes for injuries, diseases and causes of death, underpinned by more than 120,000 codable terms” and can code “more than 1.6 million clinical situations” using code combinations 23 . ICD-11 also introduces significant changes in chapter structure, diagnostic categories, diagnostic criteria, etc., for example, in psychiatric classification 24 . ICD-11-MMS has a similar structure as in ICD-10 with more chapters, but distinct from previous versions, ICD-11-MMS has its backbone as a semantic network (“Foundation Component”), a large and deep polyhierarchy (i.e. children can have more than one parents) of medical concepts, where ICD-11-MMS is derived from; coding with ICD-11-MMS also allows “post-coordination” that uses code combinations to express complex phenotypes of a patient 25 and more details and examples are in the ICD-11 reference guide 26 . Besides, to support the localisation of ICD systems, classification standards are updated regularly (e.g., usually every few months in Public Health Scotland 6 ). Automated clinical coding needs to work with dynamic and complex classification systems.
The social-technical issues with automated clinical coding systems are still to be explored. From the perspective of information systems, transitioning to a (semi-)automated coding environment in a national healthcare system is more challenging than the technical issues themselves. How do coders interact with an AI-based CAC system (as modelled in Fig. 1 )? How to present the information in an automated coding system so that coders will easily ignore errors and make the most use of the correct automatic codes? Will coders trust such a system? How will the role of coders change (e.g., from coders to coding editors or coding analysts)? What new skills will coders need 9 ?
How to solve automated clinical coding: symbolic or neural AI?
The two main schools of thought of AI have been either a symbolic, knowledge-based approach or a neural network (which further developed into deep learning) based approach 17 . Putting them into the task of clinical coding, the symbolic AI approach aims at making the use of symbols and rules to represent and model the standard practice that clinical coders apply in their work. The neural network and deep learning approach aims at learning a complex function to match a patient’s information to the appropriate set of medical codes. This function is learned from the training data. From the historical perspective, symbolic AI, as the mainstream approach from 1950 to the early 1980s, did not scale up to complex real-world scenarios, for example, to model the natural language that people use in their daily life 17 , 18 . Neural networks returned in the mid-1980s with machine learning in general. Deep learning methods became the mainstream of AI after 2011 18 , continuing to evolve today 27 .
Coming back to automated clinical coding, while the task has been studied for around 50 years (with the earliest studies around 1970 28 ), the current deep learning-based methods have a short history. Prior to deep learning, most studies use rules (regular expressions, logic expressions, and keywords) with feature engineering methods for text classification 8 , 13 . The issue with pure rule-based methods is that it is not straightforward and it can be time-consuming to extend rules to tens of thousands of codes and their varieties, and inter-relations among codes; this thus needs the support of machine learning with textual features for classification, and historically, some of the classifiers were Decision Trees, Support Vector Machine (SVM), etc 8 , 13 , 29 . Still, rule-based methods like using regular expressions to match various textual descriptions can result in high precision in coding (yet low recall), and have been used to support human coding to largely improve coding efficiency 30 .
Only since around 2017 31 , 32 , deep learning has been applied to automated coding and there are abundant studies in this area (reflected in recent surveys 11 , 12 , 13 and curation of papers in automated medical coding 33 ). Unlike rule-based and traditional machine learning methods, pure deep learning methods do not require expert rules and hand-crafted textual features, thus easily applicable, while achieving better overall performance by learning from a sufficient amount of data 32 . Most of the studies formulate the task as a multi-label classification problem 34 , while some studies formulate the task as a concept extraction or a Named Entity Recognition and Linking (NER + L) problem 35 , 36 . Though it seems that deep learning is the main method applied to automated clinical coding, we argue that there is still an important need for knowledge-based approaches in this area, and a better solution is to combine both schools of thought in the design of an automated clinical coding system. A recent trend is knowledge-augmented deep learning methods, where several studies used various embedding -based approaches to incorporate knowledge graphs into deep learning (to name a few 37 , 38 , 39 , 40 ) or directly integrated the subsumption relations of codes into the model 41 and the evaluation 42 ; however, the knowledge used is usually limited to the definition and hierarchies in the target ontology ICD-9 (except Freebase in Teng et al. 38 ), while the other vast number of clinical ontologies (e.g., UMLS, SNOMED-CT, and others) are not leveraged with the multi-label classification approach; also other information in the ontologies like axioms, logical expressions, and class attributes have not been leveraged. Coding standard and guidelines have also not been leveraged to enhance deep learning, where a challenge would be the need to extract and represent the knowledge from them, which varies by locations and requires input from coding experts.
How do state-of-the-art deep learning models work so far?
Coding tasks involving complex reasoning, such as those in which disparate pieces of information must be connected, are a difficult challenge for current NLP systems .—Kukafka et al. 43 , and also quoted in Stanfill et al. 8 .
Clinical coding is a complex testbed for contemporary AI, especially for machine learning and deep learning applied to NLP. During the last few years, the problem itself elicits applied and theoretical research on text representation learning 19 , 44 , multi-task learning 41 , 45 , zero-shot learning 37 , 46 , meta-learning 47 , multi-modal learning 48 , etc. The pursuit of a full-fledged deep learning-based clinical coding system, however, is far from being achieved: at the time of writing, the best Micro-F1 score (a harmonic mean of precision and recall evaluated based on pairs of a patient’s information and a code) on the full 8932 ICD-9 codes for the MIMIC-III data was under 60% (between 58–60%) 45 , 49 , 50 , 51 , 52 . MIMIC-III discharge summaries 20 , although coded with the older and obsolete version of ICD (ICD-9-CM, the ninth version, Clinical Modification), are the main data sets used for benchmarking 19 . This data set is also now older (collected over 10 years ago, from 2001 to 2012), and only represents an intensive care data set in the US, thus not representative of the documents available in the UK or other regions.
The main principle of the current deep learning approach is to find a complex function (non-linear and constructed by multiple layers) to match a clinical note of a patient’s visit to a set of codes. As we introduced earlier, this is the multi-label classification setting. This approach, however, has several major limitations when applied to clinical coding:
Handling unseen, infrequent, and imbalanced labels: In the MIMIC-III data set, around 5000 codes appear fewer than 10 times in the training data and over 50% of codes never appear 37 . Vanilla deep learning models rely on large amounts of data for training and fail completely for new or unseen labels. Multi-label classification is also very challenging, especially when there are many labels or when the labels are imbalanced.
Lack of symbolic reasoning capabilities: Manual coding involves reasoning beyond just locating concepts in the notes. The coders sometimes need to connect different pieces of information together 8 , 43 . The information from different sources may even be contradictory to each other for the same patient. Their decisions are based on a standard coding process, aided by coding guidelines 53 . Deep learning, on the other hand, tries to simply learn from the labelled data the association between texts and codes in different (pre-trained) embedding spaces, without explicitly modelling the reasoning process. Human-like reasoning may be supported by knowledge-based techniques, which can potentially boost the performance and explainability of coding of deep learning methods. The reasoning may include formalising coding guidelines into logical expressions 29 and creating regular expressions to capture various diagnosis descriptions of a code 30 , and leveraging various semantics in knowledge graphs constructed from several linked ontologies including the target ICD hierarchy.
Handling long documents: Looking for the relevant information of a code from a long document poses a “needle-in-the-haystack” problem. The recent Transformer-based pre-trained language models (e.g., BERT, Bi-directional Encoding Representations from Transformers 54 ) usually require a limited length of up to 512 sub-word tokens (where a word can be tokenised into several sub-words) as input due to the memory-demanding self-attention mechanism, while discharge summaries alone in MIMIC-III have on average around 1500 tokens or words 19 and up to over 10,000 tokens, not counting other types of clinical notes. More recent studies applied Longformer 55 , TransformerXL 56 , BigBird 57 to clinical coding to process documents of up to 4,096 tokens, but this is still insufficient for the clinical notes. On the other hand, text redundancy (or “Note Bloat” problem 58 ) is prevalent in clinical note creation, as measured in recent studies 58 , 59 . This may impede the performance of deep learning models for code prediction, which may be alleviated through text de-duplication based on text similarity measures 58 .
What are the potential challenges to address for automated clinical coding?
An empirical fact is that the current BERT-based approaches still do not achieve better performance than CNN-based methods for multi-label classification applied to clinical coding 44 , 60 , 61 , except for the study 52 . The limitation of BERT may be due to its inefficiency in modelling concept-level information (usually represented in a few keywords or phrases instead of complex relations of tokens in the context) and long documents 60 .
Besides, as we stated previously, manual coding is largely based on a standard and implied process with rules applied to the healthcare system, e.g., priority of certain codes, hypothetical mentions, code definitions, mutual exclusion, etc. Future deep learning-based systems need to integrate knowledge reasoning with rules and ontologies to achieve improved and more explainable results.
We list the technical challenges from our work in clinical coding and suggest relevant references below. Some of the challenges are also presented in a different way in a recent, concurrent review in Teng et al. 13 . The challenges of explainability and few- and zero-shot learning are more relevant to the multi-label classification approach but may be alleviated by the NER + L approach.
Creating gold standard coding data sets—the current widely used benchmark data set MIMIC-III may have been significantly under-coded 62 . There is a lack of large, openly available, and expert-labelled data sets from Electronic Health Records in this area, and models trained on MIMIC-III may not simply generalise to other data sets due to the difference in length, style, and language (for example, clinical notes in China, Spain, or even the UK). Various expert-labelled coding data sets are also needed for different purposes of using clinical codes (for decision making, diagnosis, epidemiology, etc.), for example, for epidemiology studies to identify deep phenotypes (potentially link to nuanced terminologies like SNOMED CT) from multimodal and multi-source clinical data. Ensuring accurate and publicly available data sets from more healthcare systems for various purposes will better support the clinical NLP community.
Coding from heterogeneous, incomplete, and noisy sources—Clinical coding should be based on all the relevant documents of a patient, rather than just discharge summaries as in the majority of recent studies, as discussed in Alonso et al. 14 . This brings the challenges of long documents as discussed previously. Structured data , such as laboratory results, can also be included as a source for coding 48 . Radiographs can be useful for coding as well. Besides, real-world data for clinical coders are usually incomplete and noisy , even for the same type of document (e.g., discharge summary), there is no guarantee that the document is available for all cases and presented in a unified format (i.e. can be hand-written or typed, with various levels of completeness).
Explainability of clinical coding—coders need to understand how the decisions are made by the system. The challenge is more related to the deep learning based multi-label classification approach. Work in this area so far uses label-wise attention mechanisms to highlight key n -grams 19 , words, and sentences 61 , 63 . However, the highlighted texts mostly indicate associations instead of causality. Further studies are needed to evaluate the usefulness of highlights for clinical coders and also to integrate more inherently explainable methods, for example, integrating symbolic representations of the coding steps with deep learning.
Human-in-the-loop learning with coders’ feedback—to better deploy an automated coding tool into practice, it is essential to involve coders’ feedback in the system 9 . The feedback may take different forms, for example, manual corrections, highlights, and rules. The feedback may need to be incorporated into a deep learning system for coding. There may be many rounds of updating the system based on coders’ feedback. There were examples in NER + L tools, which are yet to be deployed for clinical coding: in MedCATTrainer 64 , a dedicated interface is deployed for users to add new concepts, new synonyms and abbreviations, corrections of concepts (of samples selected using active learning), and binary annotations of temporality and phenotyping, then the model is re-run with the feedback; an interface is also designed in SemEHR 65 to allows users to add labels for mentions, which is used to either train a confidence model or to form post-processing rules to refine the results; manually added rules may also be integrated with weak supervision to generate coded data for training 66 , 67 . A relevant area to human-in-the-loop learning is active learning, with is about selecting the minimum set of most important data for humans to provide annotation feedback; active learning is deployed in NER + L in MedCATTrainer 64 , and evaluated in automated coding to potentially reduce human annotations 68 .
Few-shot and zero-shot learning—many codes have a low frequency or even no occurrence (or “unseen”) in the training data, this is a key problem for multi-label classification with many labels (e.g., 68,000 codes in ICD-10) 37 . The best systems so far to work with low-frequent (<5 times) codes on the MIMIC-III data set are still below or around 40% recall at K (or the percentage of correct codes in top- K predictions, K = 10 or 15) 37 , 46 , 47 . Better support for few-shot and zero-shot learning will improve the overall coding performance and usage. Knowledge (e.g., descriptions, properties, relations from multiple linked sources, and coding rules) can bridge the gap between the seen and unseen codes, as reviewed in the general domain 69 .
Adaptation to terminology changes—how a trained model can be adapted to modified standards for coding or a completely new ontology (for example from ICD-10 to ICD-11 24 )? As we described earlier, ICD-11 is semantically more complex than ICD-10 with a poly-hierarchical backbone structure and the post-coordination of codes. The transition of terminologies may require novel paradigms in deep learning (e.g., self-supervised learning, transfer learning, and meta-learning), accurate ontology matching, concept drift handling, and the above-mentioned robust few-shot and zero-shot learning for new codes with no or few training data.
Knowledge representation and reasoning in coding—finally and most fundamentally, many of the above technical directions suggest to integrate knowledge or semantic information in coding classification systems and ontologies. ICD code descriptions 19 , 55 and hierarchies 41 , 42 have been considered in recent studies (and see the blog about hierarchical evaluation 70 for ref. 41 ). Other ontologies, such as CCS 71 and code synonyms in UMLS, have been adopted recently to achieve state-of-the-art performance 45 , 51 . Also, manual coding is mainly based on a standard process and coding guidelines, potentially formalised as a set of rules and terminologies deployed in the healthcare system, for example, the priority of certain codes, the number of codes for each case, the mutual exclusion among certain codes, the rules to code hypothetical cases (e.g., possible and probable), the locally defined specific codes, etc. An example of formalising and integrating rules regarding the mutual exclusion of codes and hypothetical cases with machine learning is presented in the study 29 . These guidelines need to be formally represented in a machine-readable way and to be iteratively integrated into the deep learning-based automated coding system.
While multi-label classification is a straightforward formulation of clinical coding, another approach is through named entity extraction and linking or NER + L (for example in the work of MedCAT 35 and the study of rare disease identification 66 , 67 with SemEHR 65 ), although less adopted in the recent literature. NER + L is based on the general approach of clinical information extraction, which is also more recently enhanced by deep learning 72 . NER + L is explainable and feasible, as it inherently links the code to the piece of text in the document and helps handle the long document problem, but the extracted codes still need to be summarised to the final set of codes, and abide by the standard process and guidelines of coding. NER + L methods may help alleviate the coding of few-shot and zero-shot codes by extracting the concepts in the target ontology from clinical notes. A downside of NER + L-based coding is that it requires contextual understanding, i.e., the negation, temporality, and experiencer of the extracted concept or code 35 , 65 , which are not needed using the multi-label classification approach. These two formulations (multi-label classification and NER + L) may be combined in the design of a clinical coding system. A recent attempt is to use either text enrichment or multi-task learning to integrate NER + L identified concepts 36 , which however does not improve over the multi-label classification approach, and warrants future studies for alternative methods. The study 73 uses NER + L and ontologies to help synthesise clinical notes by replacing words with synonyms or with names of sibling codes (thus to predict the sibling codes) to potentially improve few- and zero-shot coding. Also, the study 62 used NER + L to explore the under-coded problem of clinical coding. The study 74 proposes to rank ICD-10 codes extracted from an off-the-shelf NER + L system for billing code prediction, which better addresses the few- and zero- shot problem than multi-label classification. More benchmarking results for NER + L enhanced methods are needed for comparison.
Automated clinical coding systems also need to be tailored for different purposes (e.g., billing vs. health-related research) and contexts (e.g., countries). For billing purposes, automated coding systems aim at predicting Diagnosis-Related Groups (DRGs) in the US (and Healthcare Resource Groups, HRGs in the UK), which have a smaller number of codes, usually grouped from the full set of ICD codes but can potentially be predicted prior to the ICD coding 75 . For health-related research, automated coding task needs a variety of classification systems (usually with high granularity) for use in case detection or phenotyping, thus other terminologies (e.g., SNOMED CT 76 , ORDO 67 , 77 , and ICD-11 in the near future 25 ) and customised terminologies (e.g., for sub-stroke phenotyping 78 ), and also see the surveys 8 , 79 . NER + L systems with rule-based inference can help improve the phenotyping when data are scarce to be used for supervised learning 67 , 80 . Automated coding systems can also be jointly designed with clinical outcome predictions (e.g., readmission and mortality) using deep learning in an end-to-end manner 81 . Also, case detection in some health-related research may favour precision (PPV) than recall (sensitivity) for evaluation 82 , which needs to be considered in building and tuning the automated coding system. In terms of other country-related factors, a known issue mentioned earlier in the US is “Note Bloat”, where content-importing shortcuts like copy-and-paste are used, which may reduce the time of documentation 58 . The “Note Bloat” phenomenon exacerbates the redundant entry of data in notes that is pulled in or copy-and-pasted from discrete places (e.g., various charts) in the Electronic Health Record (EHR). Training a model to fill codes to the charts needs to remove information from the notes (e.g., ICD codes) that is already present in the charts in the EHR. Also, it is shown that de-duplication of clinical notes improves the performance of prediction tasks, including predicting codes in the DRGs for billing 58 . More country related factors, e.g., billing and insurance, may also affect the system design and would warrant future studies.
Besides, industry organisations, beyond healthcare institutions and academia, play a key role related to automated clinical coding. There are also increasing collaborations between industry and academia. The Epic EHR system is deployed in the University College London Hospital (UCLH) for the management of EHRs. Recently, the CogStack team (including King’s College Hospital (KCH), NIHR Mausley Biomedical Research Centre, and UCLH) is collaborating with the UCLH Epic team to integrate an NLP component into the NoteReader interface in the Epic system. The NER + L tool MedCAT is planned to be deployed to populate structured information (by extracting concepts including diagnosis, symptoms, medications, etc.) from newly-created clinical notes to reduce documentation time and verify and complement structured information 83 . Working with five NHS Trusts in England, the CogStack team has also received an AI award from the National Institute of Health Research for developing AI-based clinical coding of medical records (see news from KCH 84 ). The project aims to enable more efficient and accurate analysis, free up staff time, and improve research. Industry NER + L APIs (e.g., Amazon Comprehend Medical InferICD10CM 85 , Microsoft Text Analytics for health 86 and Google Healthcare Natural Language API 87 ) have been released during the last two to three years 88 , 89 to support clinical concept extraction from texts with price charges. Many technology companies in the industry also provide proprietary solutions and paid services for (semi-)automated clinical coding including Deloitte 90 , Optum 91 , Capita 92 and CHKS 93 . However, the research access and inner working of the systems are usually not available, leaving it hard to contrast and compare technically. Due to its promising potentials both clinically and financially, the automated coding also attracts great attentions from start-up companies. For example, AKASA in the US is developing a deep-learning based solution, aiming to tackle automated clinical coding adapting a multi-label classification approach. They reported performances with the state-of-the-art results on MIMIC-III full codes, better than human coding in the experiments 50 (also see news 94 ). These contribute to the overall picture of the promising potential of automated clinical coding.
In this paper, we reviewed the task of automated clinical coding from the perspectives of AI researchers and clinical coding professionals, what it is and why it is an important task, and summarised the challenges of the recent deep learning methods for the task. We then position several key directions for future studies.
While we summarised the technical challenges, there are many organisational challenges to be addressed to deploy an AI-based coding tool into the clinical coding environment, as reviewed in Campbell and Giadresco 9 , where an essential idea is that coders need to be involved in the model development and deployment stage. Coders are usually occupied with their coding work and it may not be easy to engage them for system testing. Further research support on projects in medical informatics and computer science is needed to address these challenges.
How far are we from automated clinical coding that is human-centred, explainable, intelligent, and robust to complex real-world scenarios? We cannot give a concrete estimation, but it seems we now have a clearer path and a list of challenges to address. With the growing number of studies and projects in academia and the industry, we look forward to seeing more advances in AI-assisted clinical coding in the next five years and beyond and its application into practice in the near future.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
The authors declare that all data supporting the findings of this perspective article are available within the paper.
Public Health Scotland. National Data Catalogue. General acute inpatient and day case - Scottish Morbidity Record (SMR01). https://www.ndc.scot.nhs.uk/National-Datasets/data.asp?SubID=5 (2020).
American Academy of Professional Coders (AAPC). What is medical coding? https://www.aapc.com/medical-coding/medical-coding.aspx (2022).
NHS Digital. Clinical coding for non coders. https://hscic.kahootz.com/gf2.ti/f/762498/30719205.1/PPSX/-/Coding_for_non_coders_automaticnew.ppsx (2017).
Enrico, C. In Guide to Health Informatics Ch. 24 (Taylor & Francis Group, 2015).
National Center for Health Statistics. International Classification of Diseases, (ICD-10-CM/PCS) transition – background. https://www.cdc.gov/nchs/icd/icd10cm_pcs_background.htm (2015).
Public Health Scotland. Terminology Services. Scottish Clinical Coding Standards. https://www.isdscotland.org/Products-and-services/Terminology-services/Clinical-coding-guidelines/ (2022).
Otero Varela, L. et al. International Classification of Diseases clinical coding training: an international survey. Health Inf. Manag. https://doi.org/10.1177/18333583221106509 (2022)
Stanfill, M. H., Williams, M., Fenton, S. H., Jenders, R. A. & Hersh, W. R. A systematic literature review of automated clinical coding and classification systems. J. Am. Med Inf. Assoc. 17 , 646–651 (2010).
Article Google Scholar
Campbell, S. & Giadresco, K. Computer-assisted clinical coding: a narrative review of the literature on its benefits, limitations, implementation and impact on clinical coding professionals. HIM J. 49 , 5–18 (2020).
Jiang, F. et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc. Neurol . https://doi.org/10.1136/svn-2017-000101 (2017)
Kaur, R., Ginige, J. A. & Obst, O. AI-based ICD coding and classification approaches using discharge summaries: A systematic literature review. Expert Syst. Appl . 118997 https://doi.org/10.1016/j.eswa.2022.118997 (2022).
Ji, S., Sun, W., Dong, H., Wu, H. & Marttinen, P. A unified review of deep learning for automated medical coding. Preprint at arXiv http://arxiv.org/abs/2201.02797 (2022).
Teng, F. et al. A review on deep neural networks for ICD coding. In IEEE Transactions on Knowledge and Data Engineering 1–19 (IEEE, 2022)
Alonso, V. et al. Problems and barriers during the process of clinical coding: a Focus Group Study of coders’ perceptions. J. Med. Syst. 44 , 62 (2020).
Burns, E. M. et al. Systematic review of discharge coding accuracy. J. Public Health 34 , 138–148 (2012).
Article CAS Google Scholar
Public Health Scotland. Data quality assurance. Assessment of SMR01 Data Scotland Report 2019 V1. https://beta.isdscotland.org/media/7465/assessment-of-smr01-data-scotland-report-2019-v1.pdf (2019).
Wooldridge, M. The Road to Conscious Machines: The Story of AI (Penguin UK, 2020).
Russell, S. J. & Norvig, P. Artificial Intelligence: A Modern Approach, Global Edition (Pearson, 2021).
Mullenbach, J., Wiegreffe, S., Duke, J., Sun, J. & Eisenstein, J. Explainable prediction of medical codes from clinical text. In Proc. 2018 Conference of the North American Chapter of the Association for Computational Linguistics: Human Language Technologies, Volume 1 (Long Papers) 1101–1111 (Association for Computational Linguistics, 2018).
Johnson, A. E. W. et al. MIMIC-III, a freely accessible critical care database. Sci. Data 3 , 1–9 (2016).
Barrows Jr, R. C., Busuioc, M. & Friedman, C. Limited parsing of notational text visit notes: ad-hoc vs. NLP approaches. In Proc. AMIA Symposium 51 (American Medical Informatics Association, 2000).
World Health Organization. ICD-11 for Mortality and Morbidity Statistics (WHO, 2022).
World Health Organization. WHO’s new International Classification of Diseases (ICD-11) comes into effect. https://www.who.int/news/item/11-02-2022-who-s-new-international-classification-of-diseases-(icd-11)-comes-into-effect (2022).
Gaebel, W., Stricker, J. & Kerst, A. Changes from ICD-10 to ICD-11 and future directions in psychiatric classification. Dialogues Clin. Neurosci. 22 , 7–15 (2020).
Chute, C. G. The rendering of human phenotype and rare diseases in ICD-11. J. Inherit. Metab. Dis. 41 , 563–569 (2018).
World Health Organization. ICD-11 Reference Guide. 2.10 Precoordination and postcoordination. https://icdcdn.who.int/icd11referenceguide/en/html/index.html#precoordination-and-postcoordination (2022).
Bengio, Y., Lecun, Y. & Hinton, G. Deep learning for AI. Commun. ACM 64 , 58–65 (2021).
Dinwoodie, H. P. & Howell, R. W. Automatic disease coding: the ‘fruit-machine’ method in general practice. Br. J. Prev. Soc. Med. 27 , 59–62 (1973).
CAS PubMed PubMed Central Google Scholar
Farkas, R., & Szarvas, G. Automatic construction of rule-based ICD-9-CM coding systems. BMC Bioinformatics 9 , 1–9 (2008).
Zhou, L., Cheng, C., Ou, D. & Huang, H. Construction of a semi-automatic ICD-10 coding system. BMC Med. Inform. Decis. Mak. 20 , 1–12 (2020).
Shi, H., Xie, P., Hu, Z., Zhang, M. & Xing, E. P. Towards automated ICD coding using deep learning. Preprint at arXiv https://arxiv.org/abs/1711.04075 (2017).
Karimi, S., Dai, X., Hassanzadeh, H. & Nguyen, A. Automatic diagnosis coding of radiology reports: a comparison of deep learning and conventional classification methods. in BioNLP 2017 328–332 (Association for Computational Linguistics, 2017).
acadTags. Awesome-medical-coding-NLP. https://github.com/acadTags/Awesome-medical-coding-NLP (2022).
Nam, J., Kim, J., Loza Mencía, E., Gurevych, I. & Fürnkranz, J. In Machine Learning and Knowledge Discovery in Databases (eds. Calders, T., Esposito, F., Hüllermeier, E. & Meo, R.) 437–452 (Springer, 2014).
Kraljevic, Z. et al. Multi-domain clinical natural language processing with MedCAT: the medical concept annotation toolkit. Artif. Intelligence Med . 117 , 102083 (2021).
Wiegreffe, S., Choi, E., Yan, S., Sun, J. & Eisenstein, J. Clinical concept extraction for document-level coding. In Proc. 18th BioNLP Workshop and Shared Task 261–272 (Association for Computational Linguistics, 2019)
Rios, A. & Kavuluru, R. Few-shot and zero-shot multi-label learning for structured label spaces. In Proc. 2018 Conference on Empirical Methods in Natural Language Processing 3132–3142 (Association for Computational Linguistics, 2018).
Teng, F., Yang, W., Chen, L., Huang, L. & Xu, Q. Explainable prediction of medical codes with knowledge graphs. Front. Bioeng. Biotechnol. 8 , 867 (2020).
Xie, X., Xiong, Y., Yu, P. S. & Zhu, Y. EHR coding with multi-scale feature attention and structured knowledge graph propagation. In Proc. 28th ACM International Conference on Information and Knowledge Management 649–658 (ACM, 2019).
Cao, P. et al. Hypercore: hyperbolic and co-graph representation for automatic ICD coding. In Proc. 58th Annual Meeting of the Association for Computational Linguistics 3105–3114 (Association for Computational Linguistics, 2020).
Falis, M. et al. Ontological attention ensembles for capturing semantic concepts in ICD code prediction from clinical text. In Proc. Tenth International Workshop on Health Text Mining and Information Analysis (LOUHI 2019) 168–177 (Association for Computational Linguistics, 2019).
Falis, M., Dong, H., Birch, A. & Alex, B. CoPHE: a count-preserving hierarchical evaluation metric in large-scale multi-label text classification. In Proc. 2021 Conference on Empirical Methods in Natural Language Processing 907–912 (Association for Computational Linguistics, 2021).
Kukafka, R., Bales, M. E., Burkhardt, A. & Friedman, C. Human and automated coding of rehabilitation discharge summaries according to the international classification of functioning, disability, and health. J. Am. Med. Inform. Assoc. 13 , 508–515 (2006).
Ji, S., Hölttä, M. & Marttinen, P. Does the magic of BERT apply to medical code assignment? A quantitative study. Computers Biol. Med. 139 , 104998 (2021).
Sun, W., Ji, S., Cambria, E. & Marttinen, P. Multitask balanced and recalibrated network for medical code prediction. ACM Trans. Intelligent Syst. Technol . https://doi.org/10.1145/3563041 (2022)
Chalkidis, I. et al. An empirical study on large-scale multi-label text classification including few and zero-shot labels. In Proc. 2020 Conference on Empirical Methods in Natural Language Processing (EMNLP) 7503–7515 (Association for Computational Linguistics, 2020).
Wang, R. et al. Meta-LMTC: meta-learning for large-scale multi-label text classification. In Proc. 2021 Conference on Empirical Methods in Natural Language Processing 8633–8646 (Association for Computational Linguistics, 2021).
Xu, K. et al. Multimodal machine learning for automated ICD coding. In Machine Learning for Healthcare Conference 197–215 (PMLR, 2019).
Liu, Y., Cheng, H., Klopfer, R., Gormley, M. R. & Schaaf, T. Effective convolutional attention network for multi-label clinical document classification. In Proc. 2021 Conference on Empirical Methods in Natural Language Processing 5941–5953 (Association for Computational Linguistics, 2021).
Kim, B. H., & Ganapathi, V. Read, attend, and code: pushing the limits of medical codes prediction from clinical notes by machines. In Machine Learning for Healthcare Conference 196–208 (PMLR, 2021).
Yuan, Z., Tan, C., & Huang, S. Code synonyms do matter: multiple synonyms matching network for automatic ICD coding. In Proc. 60th Annual Meeting of the Association for Computational Linguistics (Volume 2: Short Papers) 808–814 (Association for Computational Linguistics, 2022).
Huang, C. W., Tsai, S. C., & Chen, Y. N. PLM-ICD: automatic ICD coding with pretrained language models. In Proc. 4th Clinical Natural Language Processing Workshop 10–20 (Association for Computational Linguistics, 2022).
Terminology and Classifications Delivery Service, National Health Service Digital. National Clinical Coding Standards ICD-10 5th Edition. https://classbrowser.nhs.uk/ref_books/ICD-10_2021_5th_Ed_NCCS.pdf (2021).
Devlin, J., Chang, M.-W., Lee, K. & Toutanova, K. BERT: pre-training of deep bidirectional transformers for language understanding. In Proc. 2019 Conference of the North American Chapter of the Association for Computational Linguistics: Human Language Technologies, Volume 1 (Long and Short Papers) 4171–4186 (Association for Computational Linguistics, 2019).
Feucht, M., Wu, Z., Althammer, S. & Tresp, V. Description-based label attention classifier for explainable ICD-9 classification. In Proc. Seventh Workshop on Noisy User-generated Text (W-NUT 2021) 62–66 (Association for Computational Linguistics, 2021).
Yogarajan, V., Pfahringer, B., Smith, T., & Montiel, J. In Artificial Neural Networks and Machine Learning – ICANN 2022 (eds. Pimenidis, E., Angelov, P., Jayne, C., Papaleonidas, A. & Aydin, M.) 209–221 (Springer Nature Switzerland, 2022).
Michalopoulos, G., Malyska, M., Sahar, N., Wong, A. & Chen, H. ICDBigBird: a contextual embedding model for ICD code classification. In Proc. 21st Workshop on Biomedical Language Processing 330–336 (Association for Computational Linguistics, 2022).
Liu, J., Capurro, D., Nguyen, A. & Verspoor, K. “Note Bloat” impacts deep learning-based NLP models for clinical prediction tasks. J. Biomed. Inform . 133 , 104149 (2022)
Searle, T., Ibrahim, Z., Teo, J. & Dobson, R. Estimating redundancy in clinical text. J. Biomed. Inform. 124 , 103938 (2021).
Gao, S. et al. Limitations of transformers on clinical text classification. IEEE J. Biomed. Health Inform . 25 , 3596–3607 (2021).
Dong, H., Suárez-Paniagua, V., Whiteley, W. & Wu, H. Explainable automated coding of clinical notes using hierarchical label-wise attention networks and label embedding initialisation. J. Biomed. Inform. 116 , 103728 (2021).
Searle, T., Ibrahim, Z. & Dobson, R. Experimental evaluation and development of a silver-standard for the MIMIC-III clinical coding dataset. In Proc. 19th SIGBioMed Workshop on Biomedical Language Processing 76–85 (Association for Computational Linguistics, 2020).
Baumel, T., Nassour-Kassis, J., Cohen, R., Elhadad, M. & Elhadad, N. In Workshops at the Thirty-Second AAAI Conference on Artificial Intelligence . 409-416 (2018).
Searle, T., Kraljevic, Z., Bendayan, R., Bean, D. & Dobson, R. MedCATTrainer: a biomedical free text annotation interface with active learning and research use case specific customisation. In Proc. 2019 Conference on Empirical Methods in Natural Language Processing and the 9th International Joint Conference on Natural Language Processing (EMNLP-IJCNLP): System Demonstrations 139–144 (Association for Computational Linguistics, 2019).
Wu, H. et al. SemEHR: a general-purpose semantic search system to surface semantic data from clinical notes for tailored care, trial recruitment, and clinical research. J. Am. Med. Inform. Assoc. 25 , 530–537 (2018).
Dong, H. et al. Rare disease identification from clinical notes with ontologies and weak supervision. In 2021 43rd Annual International Conference of the IEEE Engineering in Medicine Biology Society (EMBC) 2294–2298 (EMBC, 2021).
Dong, H. et al. Ontology-based and weakly supervised rare disease phenotyping from clinical notes. Preprint at http://arxiv.org/abs/2205.05656 (2022).
Ferreira, M. D. et al. Active learning for medical code assignment. In Workshops from ACM Conference on Health, Inference, and Learning (CHIL) 2021. Preprint at arXiv http://arxiv.org/abs/2104.05741 (2021).
Chen, J. et al. Knowledge-aware zero-shot learning: survey and perspective. In Proc. Thirtieth International Joint Conference on Artificial Intelligence, IJCAI 2021 4366–4373 (IJCAI, 2021).
Falis, M. Blood is thicker than water, a hierarchical evaluation metric for document classification. https://www.ltg.ed.ac.uk/blood-is-thicker-than-water/ (2021).
Healthcare Cost and Utilization Project (HCUP). Clinical classifications software (CCS) for ICD-9-CM. https://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp (2017).
Hahn, U. & Oleynik, M. Medical information extraction in the age of deep learning. Yearb. Med. Inform. 29 , 208–220 (2020).
Falis, M., Dong, H., Birch, A. & Alex, B. Horses to zebras: ontology-guided data augmentation and synthesis for ICD-9 coding. In Proc. 21st Workshop on Biomedical Language Processing 389–401 (Association for Computational Linguistics, 2022).
DeYoung, J., Shing, H.-C., Kong, L., Winestock, C. & Shivade, C. Entity anchored ICD coding. Accepted to American Medical Informatics Association (AMIA) 2022 Annual Symposium. Preprint at arXiv http://arxiv.org/abs/2208.07444 (2022).
Liu, J., Capurro, D., Nguyen, A. & Verspoor, K. Early prediction of diagnostic-related groups and estimation of hospital cost by processing clinical notes. NPJ Digital Med. 4 , 1–8 (2021).
Donnelly, K. SNOMED-CT: The advanced terminology and coding system for eHealth. Stud. Health Technol. Inform. 121 , 279 (2006).
PubMed Google Scholar
Vasant, D. et al. ORDO: an ontology connecting rare disease, epidemiology and genetic data. In Bio-Ontology @ ISMB 2014 . 1-4. https://www.researchgate.net/publication/281824026_ORDO_An_Ontology_Connecting_Rare_Disease_Epidemiology_and_Genetic_Data (2014).
Alex, B. et al. Text mining brain imaging reports. J. Biomed. Semant. 10 , 1–11 (2019).
Ford, E., Carroll, J. A., Smith, H. E., Scott, D. & Cassell, J. A. Extracting information from the text of electronic medical records to improve case detection: a systematic review. J. Am. Med. Inform. Assoc. 23 , 1007–1015 (2016).
Rannikmäe, K. et al. Developing automated methods for disease subtyping in UK Biobank: an exemplar study on stroke. BMC Med. Inform. Decis. Mak. 21 , 1–9 (2021).
Lovelace, J., Hurley, N. C., Haimovich, A. D. & Mortazavi, B. J. Dynamically extracting outcome-specific problem lists from clinical notes with guided multi-headed attention. In Machine Learning for Healthcare Conference 245–270 (PMLR, 2020).
Rannikmäe, K. et al. Accuracy of identifying incident stroke cases from linked health care data in UK Biobank. Neurology 95 , e697–e707 (2020).
Noor, K. et al. Deployment of a free-text analytics platform at a UK National Health Service Research Hospital: CogStack at University College London Hospitals. JMIR Med. Inform. 10 , e38122 (2022).
King’s College Hospital NHS Foundation Trust. CogStack wins an artificial intelligence in health and care. https://www.kch.nhs.uk/news/public/news/view/34965 (2021).
Amazon Web Services. ICD-10-CM linking. https://docs.aws.amazon.com/comprehend-medical/latest/dev/ontology-icd10.html (2022).
Azure. What is text analytics for health in Azure Cognitive Service for Language? https://docs.microsoft.com/en-us/azure/cognitive-services/language-service/text-analytics-for-health/overview?tabs=ner (2022).
Google Cloud. Healthcare natural language API. https://cloud.google.com/healthcare-api/docs/concepts/nlp (2022).
Bodnari, A. Healthcare gets more productive with new industry-specific AI tools. https://cloud.google.com/blog/topics/healthcare-life-sciences/now-in-preview-healthcare-natural-language-api-and-automl-entity-extraction-for-healthcare (2020).
Amazon Web Services. Announcing ICD-10-CM and RxNorm ontology linking for Amazon Comprehend Medical. https://aws.amazon.com/about-aws/whats-new/2019/12/announcing-icd-10-cm-rxnorm-ontology-linking-amazon-comprehend-medical/ (2019).
Miranda, M. Automated clinical coding. The AI-based solution to address the critical shortage of clinical coders. https://www2.deloitte.com/au/en/blog/consulting-blog/2020/automated-clinical-coding.html (2020).
Optum Inc. Enterprise computer-assisted coding (CAC). https://www.optum360.com/solutions/coding-and-documentation/coding-and-cdi-technology/enterprise-cac.html (2022).
Capita plc. Creating better health outcomes with automated clinical coding. https://www.capita.com/expertise/industry-specific-services/health-services/healthcare-business-operations/clinical-coding/automated-clinical-coding (2022).
CHKS. Automated clinical coding. https://www.chks.co.uk/Clinical-coding (2022).
Mace, S. Making medical coding better and faster with artificial intelligence. Medical Technology Schools. https://www.medicaltechnologyschools.com/health-information-technology/medical-coding-and-artificial-intelligence (2021).
Download references
Acknowledgements
The work is supported by WellCome Trust iTPA Awards (PIII009, PIII032), Health Data Research UK National Phenomics and Text Analytics Implementation Projects, and the United Kingdom Research and Innovation (grant EP/S02431X/1), UKRI Centre for Doctoral Training in Biomedical AI at the University of Edinburgh, School of Informatics. H.D. and J.C. are supported by the Engineering and Physical Sciences Research Council (EP/V050869/1) on “ConCur: Knowledge Base Construction and Curation”. HW was supported by Medical Research Council and Health Data Research UK (MR/S004149/1, MR/S004149/2); British Council (UCL-NMU-SEU international collaboration on Artificial Intelligence in Medicine: tackling challenges of low generalisability and health inequality); National Institute for Health Research (NIHR202639); Advanced Care Research Centre at the University of Edinburgh. We thank constructive comments from Murray Bell and Janice Watson in Terminology Service in Public Health Scotland, and information provided by Allison Reid in the coding department in NHS Lothian, Paul Mitchell, Nicola Symmers, and Barry Hewit in Edinburgh Cancer Informatics, and staff in Epic Systems Corporation. Thanks for the suggestions from Dr. Emma Davidson regarding clinical research. Thanks to the discussions with Dr. Kristiina Rannikmäe regarding the research on clinical coding and with Ruohua Han regarding the social and qualitative aspects of this research. In Fig. 1 , the icon of “Clinical Coders” was from Freepik in Flaticon, https://www.flaticon.com/free-icon/user_747376 ; the icon of “Automated Coding System” was from Free Icon Library, https://icon-library.com/png/272370.html .
Author information
Authors and affiliations.
Centre for Medical Informatics, Usher Institute, University of Edinburgh, Edinburgh, UK
Department of Computer Science, University of Oxford, Oxford, UK
Hang Dong & Jiaoyan Chen
School of Informatics, University of Edinburgh, Edinburgh, UK
Matúš Falis & Beatrice Alex
Centre for Clinical Brain Sciences, University of Edinburgh, Edinburgh, UK
William Whiteley
Edinburgh Futures Institute, University of Edinburgh, Edinburgh, UK
Beatrice Alex
Epic Systems Corporation, Verona, WI, USA
Joshua Matterson
University College London Hospitals NHS Foundation Trust, Clinical Research Informatics Unit, London, UK
Department of Computer Science, Aalto University, Espoo, Finland
Shaoxiong Ji
Institute of Health Informatics, University College London, London, UK
You can also search for this author in PubMed Google Scholar
Contributions
H.D. and H.W. conceived the research on automated clinical coding. H.D., H.W., W.W., B.A., and F.M. discussed the research regularly. H.D., H.W., B.A., and W.W. initiated the writing of this paper. H.D. and F.M. discussed the research with practitioners in clinical coding and received their feedback, with support from H.W. and W.W. S.J. and J.C. provided comments on AI for clinical coding as researchers in the field of AI. J.M. provided comments on the contexts and the design of clinical coding systems from the perspective of the industry. H.D. drafted the manuscript. All authors edited and revised the manuscript and approved the final version of the manuscript.
Corresponding authors
Correspondence to Hang Dong or Honghan Wu .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Reporting summary, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Dong, H., Falis, M., Whiteley, W. et al. Automated clinical coding: what, why, and where we are?. npj Digit. Med. 5 , 159 (2022). https://doi.org/10.1038/s41746-022-00705-7
Download citation
Received : 30 March 2022
Accepted : 07 October 2022
Published : 22 October 2022
DOI : https://doi.org/10.1038/s41746-022-00705-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: AI and Robotics newsletter — what matters in AI and robotics research, free to your inbox weekly.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Lippincott Open Access
Hospital-Wide Intervention in Billing and Coding to Capture Complexity of Care at an Academic Referral Center
Danielle decicco.
West Virginia University School of Medicine, Morgantown, West Virginia, and J. W. Ruby Memorial Hospital Department of Medicine, Morgantown, West Virginia
Troy M. Krupica
West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine and Section of Hospital Medicine

Ronald Pellegrino
West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine
Ziad O. Dimachkie
Associated data.
Downcoding at nonprofit healthcare institutions can account for significant revenue losses that, in turn, can affect the amount and quality of care they provide. Using the inpatient medical note to assess the complexity of care, we wanted to quantify the visit coding distribution at the largest tertiary care center in West Virginia and to improve the documentation and coding if found to be below national benchmarks.
We measured the number of encounters and associated documentation of level 1, 2, and 3 visits among hospitalists. We compared our data to national benchmark data. We then implemented a multifaceted, multidisciplinary intervention to improve documentation and coding.
Principal Findings:
We found a significant average increase of level 3 admission history and physical visits of 76% ( p < .0001) and 112% ( p < .001) for subsequent encounters compared with baseline preintervention visit types. With team-based coding interventions in place, documentation accurately now reflects the complexity of care delivered. Based on Medicare reimbursement rates, this new accuracy has led to an increase in revenue of $233, 988.79 per 10,000 encounters.
Applications to Practice:
Provider knowledge of medical billing and coding guidelines is essential. In particular, large academic institutions typically operate on small margins, so even simple adjustments and quality improvement efforts in billing and coding can help immensely by accurately representing the amount and quality of medical services. An institution can markedly improve revenues by coding notes to reflect the true complexity of care that is delivered.
INTRODUCTION
In healthcare, accurate billing and coding are both essential and problematic. Physician providers, medical institutions, and insurers alike widely recognize upcoding as a detriment to healthcare because it leads to fraud and overbilling ( Kesselheim & Brennan, 2005 ; McKinnon, 2004 ). On the other hand, downcoding accounts for significant revenue losses, especially at nonprofit institutions that provide complex care for large volumes of patients ( Fleishon et al., 2017 ; Kesselheim & Brennan, 2005 ; Terry, 2006 ) when it misrepresents the services rendered ( McKinnon, 2004 ).
The heavy burden of documentation can lead to errors of omission in the medical records, and studies have shown that overly cautious physicians tend to downcode ( Powell et al., 2012 ; Weiner et al., 2020 ). Downcoding can be related to time constraints, which are associated with less thorough documentation and more errors of omission and commission ( Powell et al., 2012 ; Weiner et al., 2020 ). This practice has an impact on the amount and quality of care when physicians increase the number of patients seen in a day to meet productivity targets.
In inpatient medicine, the medical note is the primary indicator of decision-making and care complexity of patient encounters. Visit demarcations range from levels 1 (reflecting low-complexity medical decision-making) to 3 (reflecting comprehensive, high-complexity medical decision-making; American Medical Association, 2021 ; Centers for Medicare & Medicaid Services, 1995 , 1997 ).
Many hospitals use hospitalist teams to provide care for most patients ( Wachter et al., 1999 ). Reimbursement depends on the note type for inpatient medicine for the initial and follow-up visits that hospitalists document during a patient's admission. Academic centers typically encounter patients who are sicker than those at other facilities ( Fleishon et al., 2017 ). Therefore, we evaluated our large academic tertiary care center—the only one in the state—for appropriateness of inpatient note coding. We hypothesized that the billing levels would be on par or higher than averages across the United States, given the country's complex patient population. The objective of our retrospective cohort study was twofold: to quantify the number of encounter types and then to improve their quality if they were below national quality benchmarks.
We analyzed data from 26 hospitalists providing care over a 2 1 / 2 -year period (see Supplementary Table 1, published as Supplemental Digital Content at http://links.lww.com/JHM/A86 ). The data included 7,987 admission encounters and 51,583 subsequent encounters; they were obtained using Tableau Analytics, which is used for systems-level accounting at the institution. The analysis was completed in two phases.
First, we analyzed the total number of visit types for the 26 hospitalists for 1 year. We used statistical models such as the Student t test and analysis of variance to evaluate level 1, 2, and 3 visits (Figure (Figure1). 1 ). We compared that data to benchmarks provided by the Society of Hospital Medicine ( White et al., 2018 ). We then implemented a multidisciplinary response including education, collaboration, and system optimization, which we based on plan–do–study–act (PDSA) quality improvement principles. After our initial analysis, we iterated small interventions and studied their systemwide effects ( Taylor et al., 2014 ).

Research Design
Among the interventions was education in the basic tenets of inpatient billing and coding, notably time-based billing. To address department barriers across the organization, we included providers, coders, compliance team members, and information technologists. We had found that coders, for example, hesitated to reach out to providers and confirm that their notes were appropriately coded. To help coders overcome this barrier and clarify diagnoses when necessary, we used the direct chat feature in the electronic health record (EHR) system and electronic messaging to facilitate communication between the coders and providers.
Other challenges complicated efforts to get all professionals on board. For example, the compliance team's main concern was to ensure that notes were not upcoded, which could trigger an audit and the clawback of payments. We addressed this concern by demonstrating through a cost analysis based on our random audit of internal notes that downcoding was far more prevalent and resulted in significant revenue loss. Overall, the cost of downcoding throughout the study period was hundreds of thousands of dollars higher than any penalty incurred from sporadic instances of upcoding. We also promised to monitor coding through internal audits to ensure that no systemic upcoding would occur as a result of our interventions.
For the coding department, the primary concerns were related to the associated culture change. Consistent with the compliance team's concerns, coders often erred to the lower of two levels whenever there was room for discretion in coding notes. This resulted in systemic downcoding, particularly for nonprocedural areas such as inpatient internal medicine. We addressed this concern by establishing collaboration between compliance and coding in which appropriate coding rather than downcoding was seen as the goal when applying discretion to avoid penalties.
Unlike outpatient providers, inpatient providers were not accustomed to coding their own notes. This barrier required a significant amount of effort on our part to explain the nuances of inpatient documentation regarding coding, which we did in a series of weekly lunchtime lectures.
We selected members from all groups (providers, coders, compliance team members, and information technologists) together for a pilot program. We expanded EHR access to include a pilot coding module based on the outpatient EHR coding module, so the providers could self-code. After completing a note, each provider coded it for level 1, 2, or 3 and added ancillary codes (such as “advanced care planning”) from a pop-up menu. The coders then independently reviewed each note and coded it as they normally would. When the coders did not agree with a provider's assessment, they entered a brief description of the discrepancy. We optimized this process by implementing a real-time comparative coding module for providers, so they could see their frequency of coding concurrence and disparity with the coders and the reasons for these differences. We later met with the providers and coders to review notes and discuss areas for improvement. Typically, either the medical reasoning documented by the provider did not capture the services accurately or the professional coders did not fully appreciate the complexity of the medical decision-making described in the note. This intervention spanned about 6 months before changes were made and observed in the health system.
In the second, postintervention phase, we formally studied our PDSA cycle. We followed 26 full-time hospitalists for 12 months after the interventions. The hospitalists worked the same number of pre- and postintervention shifts, and because they were compared to their own data preintervention, we could implement a paired t test to evaluate the difference between the number of encounters of each level pre- and postintervention (see Figure Figure1 1 for process flow and timeline of intervention).
The financial analysis was performed using the work relative value units (wRVUs) and percentages of level 1, 2, and 3 visits. We used the following formula for each type of visit:
We multiplied the wRVU total per 10,000 encounters by the $36.09 reimbursement rate determined by Medicare to estimate the cost benefit of the intervention. The reimbursement number is from the study's 2018–2020 time frame.
Preintervention data found 51% of new encounters at level 2, and 42% at level 3. Of repeat encounters, 66% were level 2, and 33% level 3 (Figure (Figure1). 1 ). Our provider post hoc analysis of these notes showed that 58% of level 2 encounters met level 3 criteria.
Postintervention inpatient admission encounters averaged 23% level 2 and 74% level 3 (Figure (Figure1; 1 ; level 2 p < .05, level 3 p < .001), and repeat encounters averaged 29% level 2 and 70% level 3 (level 2 p < .01, level 3 p < .001). Overall, results showed significant average improvement of level 3 admission encounters of 76% (Figure (Figure2A, 2 A, p < .001) and 112% (Figure (Figure2B, 2 B, p < .001) for subsequent encounters compared with baseline preintervention visit types. This reflected an improvement of 13.6% wRVUs per new encounter and 14.3% wRVUs per repeat encounter (Table (Table1). 1 ). Based on Medicare reimbursement rates, this translated to a conservative estimate of revenue increase of $233,988.79 per 10,000 encounters (Table (Table1 1 ).

Improvement of Level 3 Visits, Postintervention
Note. wRVU = work relative value unit.
The results of this study indicate that implementing quality improvement tactics for inpatient note documentation and coding can help a health system generate a significant amount of revenue. The analysis of coding practices resulted in significant improvements to level 3 billing at our hospital, for both initial and follow-up inpatient encounters.
As the primary referral center for West Virginia, the tertiary academic medical center in this study provides the highest level of care. And as such, it should have an inpatient note coding level distribution that is at least near the national average. Prior to our quality improvement project, however, the coding levels were significantly below average—routinely downcoded notes did not accurately capture the complexity of medical care for the many high-acuity patients.
The intervention described here to change documentation and coding practices has led to increased reimbursement because it truly reflects the complexity of care rendered by inpatient providers. This increase in revenue has allowed the expansion of services, which is particularly important for academic centers that care for a disproportionate number of socioeconomically disadvantaged patients.
Study Limitations
Limitations of our work include the lack of a standard control group, as the billing and coding department in this study is shared across all inpatient hospital services. Any change implemented in the coding department affects the entire hospital. Therefore, we used the control data of pre-intervention hospitalist encounter type. Results across the entire health system may be within a margin of error, as our cohort of hospitalists averaged a similar volume across time. As at many hospitals, total volume of visits was affected by the COVID-19 pandemic and thus total revenues may be affected.
Billing and coding may be the parts of medicine that no one likes to discuss. Nevertheless, financing healthcare remains a key issue ( Kesselheim & Brennan, 2005 ; Wachter et al., 1999 ). By using a multipronged, multidisciplinary approach to improve provider documentation and coding practices, an institution can markedly improve revenues by ensuring that coding notes accurately reflect the complexity of care delivered. Future research could extend this study to evaluate groups outside of the hospitalists' pre- and postintervention and evaluate proceduralists using similar approaches.
Supplementary Material
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's website ( www.jhmjournalonline.com ).
Contributor Information
Danielle DeCicco, West Virginia University School of Medicine, Morgantown, West Virginia, and J. W. Ruby Memorial Hospital Department of Medicine, Morgantown, West Virginia.
Troy M. Krupica, West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine and Section of Hospital Medicine.
Ronald Pellegrino, West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine.
Ziad O. Dimachkie, West Virginia University School of Medicine and J. W. Ruby Memorial Hospital Department of Medicine and Section of Hospital Medicine.
- American Medical Association. (2021). CPT evaluation and management (E/M) . https://www.ama-assn.org/practice-management/cpt/cpt-evaluation-and-management
- Centers for Medicare & Medicaid Services. (1995). Documentation guidelines for evaluation and management services . https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnedwebguide/downloads/95docguidelines.pdf
- Centers for Medicare & Medicaid Services. (1997). Documentation guidelines for evaluation and management services . https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
- Fleishon H. B., Itri J. N., Boland G. W., Duszak R., Jr. (2017). Academic medical centers and community hospitals integration: Trends and strategies . Journal of the American College of Radiology , 14 ( 1 ), 45–51. 10.1016/j.jacr.2016.07.006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kesselheim A. S., Brennan T. A. (2005). Overbilling vs. downcoding—the battle between physicians and insurers . New England Journal of Medicine , 352 ( 9 ), 855–857. 10.1056/nejmp058011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McKinnon P. (2004). Stealth downcoding and what you can do about it . Journal of Medical Practice Management , 20 ( 1 ), 28–29. https://pubmed.ncbi.nlm.nih.gov/15500019/ [ PubMed ] [ Google Scholar ]
- Powell A., Savin S., Savva N. (2012). Physician workload and hospital reimbursement: Overworked physicians generate less revenue per patient . Manufacturing and Service Operations Management , 14 ( 4 ), 512–528. 10.1287/msom.1120.0384 [ CrossRef ] [ Google Scholar ]
- Taylor M. J., McNicholas C., Nicolay C., Darzi A., Bell D., Reed J. E. (2014). Systematic review of the application of the plan-do-study-act method to improve quality in healthcare . BMJ Quality and Safety , 23 ( 4 ), 290–298. 10.1136/bmjqs-2013-001862 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Terry K. (2006). Blending: The new downcoding . Medical Economics , 83 ( 9 ), 34–38. https://pubmed.ncbi.nlm.nih.gov/16749632/ [ PubMed ] [ Google Scholar ]
- Wachter R. M., Whitcomb W. F., Nelson J. R. (1999). Financial implications of implementing a hospitalist program . Healthcare Financial Management , 53 ( 3 ), 48–51. https://pubmed.ncbi.nlm.nih.gov/10351056/ [ PubMed ] [ Google Scholar ]
- Weiner S. J., Wang S., Kelly B., Sharma G., Schwartz A. (2020). How accurate is the medical record? A comparison of the physician's note with a concealed audio recording in unannounced standardized patient encounters . Journal of the American Medical Informatics Association , 27 ( 5 ), 770–775. 10.1093/jamia/ocaa027 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- White A. W., Anders J. A., Anoff D. A., Creamer J. C., Flores L. F., George R. G., Huang B. H., Kurian L. K., Merchant M. M., Narreddy K. N., Papetti E. P., Sites C. S., Small S. S., Stephan T. S., Trask A. T., Vuong K. V., Siy J. S. (2018, October). 2018 State of Hospital Medicine Report . Society of Hospital Medicine. https://www.hospitalmedicine.org/practice-management/shms-state-of-hospital-medicine/ [ Google Scholar ]
Advertisement
Problems and Barriers during the Process of Clinical Coding: a Focus Group Study of Coders’ Perceptions
- Systems-Level Quality Improvement
- Published: 08 February 2020
- Volume 44 , article number 62 , ( 2020 )
Cite this article

- Vera Alonso 1 , 2 ,
- João Vasco Santos 1 , 2 , 3 ,
- Marta Pinto 2 , 4 , 5 ,
- Joana Ferreira 1 , 2 ,
- Isabel Lema 1 , 2 ,
- Fernando Lopes 1 , 2 &
- Alberto Freitas ORCID: orcid.org/0000-0003-2113-9653 1 , 2
1439 Accesses
25 Citations
Explore all metrics
Coded data are the basis of information systems in all countries that rely on Diagnosis Related Groups in order to reimburse/finance hospitals, including both administrative and clinical data. To identify the problems and barriers that affect the quality of the coded data is paramount to improve data quality as well as to enhance its usability and outcomes. This study aims to explore problems and possible solutions associated with the clinical coding process. Problems were identified according to the perspective of ten medical coders, as the result of four focus groups sessions. This convenience sample was sourced from four public hospitals in Portugal. Questions relating to problems with the coding process were developed from the literature and authors’ expertise. Focus groups sessions were taped, transcribed and analyzed to elicit themes. Variability in the documents used for coding, illegibility of hand writing when coding on paper, increase of errors due to an extra actor in the coding process when transcribed from paper, difficulties in the diagnoses’ coding, coding delay and unavailability of resources and tools designed to help coders, were some of the problems identified. Some problems were identified and solutions such as the standardization of the documents used for coding an episode, the adoption of the electronic coding, the development of tools to help coding and audits, and the recognition of the importance of coding by the management were described as relevant factors for the improvement of the quality of data.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Problems and Barriers in the Transition to ICD-10-CM/PCS: A Qualitative Study of Medical Coders’ Perceptions
Barriers to data quality resulting from the process of coding health information to administrative data: a qualitative study.

The use of electronic patient records for medical research: conflicts and contradictions
Software application developed by the Serviços Partilhados do Ministério da Saúde (SPMS) – Ministry of Health Shared Services – and distributed to hospitals. SIMH facilitates episode coding directly into the application with the main purpose of collecting, editing and grouping inpatient and outpatient episodes by DRGs and integrating it with administrative data [ 62 ].
Tatham, A., The increasing importance of clinical coding. Br J Hosp Med 69(7):372–373, 2008. https://doi.org/10.12968/hmed.2008.69.7.30409 .
Article Google Scholar
Cheng, P., Gilchrist, A., Robinson, K. M., and Paul, L., The risk and consequences of clinical miscoding due to inadequate medical documentation: A case study of the impact on health services funding. Health Inf Manag 38(1):35–46, 2009. https://doi.org/10.1177/183335830903800105 .
Article PubMed Google Scholar
Busse R, Geissler A, Quentin W, Wiley M (eds) (2011) Diagnosis-Related Groups in Europe
Averill RF, Goldfield N, Hughes JS, Bonazelli J, McCullough EC, Steinbeck BA, Mullin R, Tang AM (2003) All Patient Refined Diagnosis Related Groups (APR-DRGs). https://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf . Accessed 20 February 2018
Santos, S., Murphy, G., Baxter, K., and Robinson, K. M., Organisational factors affecting the quality of hospital clinical coding. Health Inf Manag 37(1):25–37, 2008. https://doi.org/10.1177/183335830803700103 .
Freitas JA, Silva-Costa T, Marques B, Costa-Pereira A (2010) Implications of data quality problems within hospital administrative databases, in: P.D. Bamidis, N. Pallikarakis (eds), XII Mediterranean Conference on Medical and Biological Engineering and Computing 2010. IFMBE proceedings, vol 29. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-13039-7_208
Chapter Google Scholar
Butz, J., Brick, D., Rinehart-Thompson, L. A., Brodnik, M., Agnew, A. M., and Patterson, E. S., Differences in coder and physician perspectives on the transition to ICD-10-CM/PCS: A survey study. Health Policy Technol 5:251–259, 2016. https://doi.org/10.1016/j.hlpt.2016.03.001 .
Miller, R. H., and Sim, I., Physicians’ use of electronic medical records: Barriers and solutions. Health Aff (Millwood) 23(2):116–126, 2004. https://doi.org/10.1377/hlthaff.23.2.116 .
Sanders TB, Bowens FM, Pierce W, Stasher-Booker B, Thompson EQ, Jones WA (2012) The road to ICD-10-CM/PCS implementation: Forecasting the transition for providers, payers, and other healthcare organizations, Perspect. Health Inf Manag 9: 1f. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3329203/pdf/phim0009-0001f.pdf . Accessed 31 July 2017
Stanfill MH, Kang L, Hsieh K, Beal R, Fenton SH (2014) Preparing for ICD-10-CM/PCS implementation: Impact on productivity and quality. Perspect health Inf Manag 11: 1f. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4142514/pdf/phim0011-0001f.pdf . Accessed 4 July 2017
Pongpirul, K., Walker, D. G., Rahman, H., and Robinson, C., DRG coding practice: A nationwide hospital survey in Thailand. BMC Health Serv Res 11:290, 2011. https://doi.org/10.1186/1472-6963-11-290 .
Article PubMed PubMed Central Google Scholar
Farzandipour, M., Sheikhtaheri, A., and Sadoughi, F., Effective factors on accuracy of principal diagnosis coding based on international classification of diseases, the 10th revision (ICD-10). Int J Inf Manag 30:78–84, 2010. https://doi.org/10.1016/j.ijinfomgt.2009.07.002 .
Southern, D. A., Hall, M., White, D. E., Romano, P. S., Sundararajan, V., Droesler, S. E., Pincus, H. A., and Ghali, W. A., Opportunities and challenges for quality and safety applications in ICD-11: An international survey of users of coded health data. Int J Qual Health Care 28(1):129–135, 2016. https://doi.org/10.1093/intqhc/mzv096 .
Haghighi, M. H. H., Dehghani, M., Teshizi, S. H., and Mahmoodi, H., Impact of documentation errors on accuracy of cause of death coding in an educational hospital in Southern Iran. Health Inf Manag 43(2):35–42, 2014. https://doi.org/10.1177/183335831404300205 .
O’Malley, K. J., Cook, K. F., Price, M. D., Wildes, K. R., Hurdle, J. F., and Ashton, C. M., Measuring diagnoses: ICD code accuracy. Health Serv Res 40(5 Pt 2):1620–1639, 2005. https://doi.org/10.1111/j.1475-6773.2005.00444.x .
Tang, K. L., Lucyk, K., and Quan, H., Coder perspectives on physician-related barriers to producing high-quality administrative data: A qualitative study. CMAJ Open 5(3):E617–E622, 2017. https://doi.org/10.9778/cmajo.20170036 .
McKenzie K, Walker S, Dixon-Lee C, Dear G, Moran-Fuke J (2004) Clinical coding internationally: a comparison of the coding workforce in Australia, America, Canada and England, in: 14th International Federation of Health Records Congress, Washington. https://eprints.qut.edu.au/575/1/575.pdf . Accessed 15 September 2017
Doktorchik, C., Lu, M., and Quan, H., A qualitative evaluation of clinically coded data quality from health information manager perspectives. Health Inf Manag 49(1):19–27, 2019. https://doi.org/10.1177/1833358319855031 .
Santana, R., Financiamento hospitalar e a definição de preços. Revista Portuguesa de Saúde Pública 5:93–118, 2005.
Google Scholar
Lopes F (2010) Médico codificador - Portal da Codificação Clínica e dos GDH. http://portalcodgdh.min-saude.pt/index.php/Médico_codificador . Accessed 17 July 2017
ACSS (2016) Implementação do Sistema de Codificação Clínica ICD-10-CM/PCS em Portugal, em substituição da atual ICD-9-CM. http://www.acss.min-saude.pt//wp-content/uploads/2016/07/Perguntas-Frequentes_-ICD10CMPCS.pdf . Accessed 28 July 2017
Alonso, V., Santos, J. V., Pinto, M., Ferreira, J., Lema, I., Lopes, F., and Freitas, A., Health records as the basis of clinical coding: Is the quality adequate? A qualitative study of medical coders' perceptions. Health Inf Manag 11:1833358319826351, 2019. https://doi.org/10.1177/1833358319826351 .
Alonso V, Santos JV, Pinto M, Ferreira J, Lema I, Lopes F, Freitas A (2019) Problems and Barriers in the Transition to ICD-10-CM/PCS: A Qualitative Study of Medical Coders’ Perceptions, in: Rocha Á, Adeli H, Reis L, Costanzo S (eds) New Knowledge in Information Systems and Technologies. WorldCIST'19 2019. Advances in intelligent systems and computing, vol 932. Springer, Cham. https://doi.org/10.1007/978-3-030-16187-3_8
INE, Statistics Portugal (2017) https://www.ine.pt/xportal/xmain?xpid=INE&xpgid=ine_indicadores&indOcorrCod=0008121&contexto=bd&selTab=tab2&xlang=en . Accessed 4 October 2018
Bardin L (2011) Análise de Conteúdo. 4ª edicao, EDICOES 70, Lisboa
Tong, A., Sainsbury, P., and Craig, J., Consolidated criterio for reporting qualitative research (COREQ): A 32- item checklist for interviews and focus group. Int J Qual Health Care 19(6):349–357, 2007. https://doi.org/10.1093/intqhc/mzm042 .
Cassidy BS (2012) Defining the Core Clinical Documentation Set for Coding Compliance. https://bok.ahima.org/PdfView?oid=105782 . Accessed 9 May 2018
Government of Western Australia (2015) Nursing and Midwifery guide to clinical coding and documentation. http://ww2.health.wa.gov.au/~/media/Files/Corporate/general documents/Clinical coding/Guides and summaries/guid-nursmiddocn.pdf. Accessed 15 May 2018
The Royal Children’s Hospital Melbourne (2017) Health Information Services : Coding. https://www.rch.org.au/rchhis/coding_casemix/Coding/ . Accessed 15 May 2018
ACSS (2014) Circular Normativa N. 23/2014/DPS/ACSS. http://www2.acss.min-saude.pt/Portals/0/CN23.pdf
Robertson, A. R. R., Fernando, B., Morrison, Z., Kalra, D., and Sheikh, A., Structuring and coding in health care records: A qualitative analysis using diabetes as a case study. J Innov Health Inform 22(2):275–283, 2015. https://doi.org/10.14236/jhi.v22i2.90 .
Mckenzie, K., Enraght-Moony, E., Harding, L., Walker, S., Waller, G., and Chen, L., Coding external causes of injuries: Problems and solutions. Accid Anal Prev 40(2):714–718, 2008. https://doi.org/10.1016/j.aap.2007.09.008 .
Naran, S., Hudovsky, A., Antscherl, J., Howells, S., and Nouraei, S. A. R., Audit of accuracy of clinical coding in oral surgery. Br J Oral Maxillofac Surg 52(8):735–739, 2014. https://doi.org/10.1016/j.bjoms.2014.01.026 .
Article CAS PubMed Google Scholar
Tsopra, R., Peckham, D., Beirne, P., Rodger, K., Callister, M., White, H., Jais, J. P., Ghosh, D., Whitaker, P., Clifton, I. J., and Wyatt, J. C., The impact of three discharge coding methods on the accuracy of diagnostic coding and hospital reimbursement for inpatient medical care. Int J Med Inform 115:35–42, 2018. https://doi.org/10.1016/j.ijmedinf.2018.03.015 .
3M (2018) CAC | Computer-Assisted Coding. https://www.3m.com/3M/en_US/360-encompass-system-us/computer-assisted-coding/ . Accessed 29 May 2018
Haefner M (2017) 3 findings on the computer-assisted coding market. https://www.beckershospitalreview.com/finance/3-findings-on-the-computer-assisted-coding-market.html . Accessed 4 June 2018
Benson S (2006) Computer Assisted Coding Software Improves Documentation, Coding, Compliance, and Revenue, in: CAC Proceedings, Perspect Health Inf Manag. https://bok.ahima.org/PdfView?oid=85288 . Accessed 4 June 2018
Crawford, M., Truth about computer-assisted coding: A consultant, HIM professional, and vendor weigh in on the real CAC impact. J AHIMA 84:24–27, 2013.
PubMed Google Scholar
Tully, M., and Carmichael, A., Computer-assisted coding and clinical documentation: First things first. Healthc Financ Manage 66(10):46–49. https://www.ncbi.nlm.nih.gov/pubmed/23088053 . , 2012.
Rudman WJ, Eberhardt JS, Pierce W, Hart-Hester S (2009) Healthcare fraud and abuse. Perspect health Inf Manag 6:1g. http://www.ncbi.nlm.nih.gov/pubmed/20169019 . Accessed 28 May 2018
Dougherty, M., Seabold, S., and White, S. E., Study reveals hard facts on CAC. Journal of AHIMA 84(7):54–56, 2013.
Campell, S., and Giadresco, K., Computer-assisted clinical coding: A narrative review of the literature on its benefits, limitations, implementation and impact on clinical coding professionals. Health Inf Manag 49(1):5–18, 2019. https://doi.org/10.1177/1833358319851305 .
Sand JN, Elison-Bowers P (2013) ICD-10-CM/PCS: Transferring Knowledge from ICD-9-CM. Perspect health Inf Manag 10:1g. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3709880/ . Accessed 15 January 2018
Centers for Medicare and Medicaid Services, National Center for Health Statistics (2017) ICD-10-CM Official Guidelines for Coding and Reporting FY2018. https://www.cms.gov/medicare/coding/icd10/downloads/icd10cm-guidelines-2015.pdf . Accessed 6 June 2018
Lucyk, K., Tang, K., and Quan, H., Barriers to data quality resulting from the process of coding health information to administrative data: A qualitative study. BMC Health Serv Res 17(1):766, 2017. https://doi.org/10.1186/s12913-017-2697-y .
Bajaj, Y., Crabtree, J., and Tucker, A. G., Clinical coding: How accurately is it done? Clin Gov An Int J. 12:159–169, 2007. https://doi.org/10.1108/14777270710775873 .
Alakrawi, Z. M., Nemchik, S., and Sheridan, P. T., New study illuminates the ongoing road to ICD-10 productivity and optimization. J AHIMA 88(3):40–45. http://www.mahima.org/wp-content/uploads/New-Study-Illuminates-the-Ongoing-Road-to-ICD_2016.pdf . , 2017.
Weems S, Heller P, Fenton SH (2015) Results from the veterans health administration ICD-10-CM/PCS coding pilot study. Perspect health Inf Manag 12:1b. https://www.ncbi.nlm.nih.gov/pubmed/26396553 . Accessed 15 January 2018
Barta, A., McNeill, G. C., Meli, P. L., Wall, K. E., and Zeisset, A. M., ICD-10-CM primer. J AHIMA 79:64–66, 2008.
Chute, C. G., Huff, S. M., Ferguson, J. A., Walker, J. M., and Halamka, J. D., There are important reasons for delaying implementation of the new ICD-10 coding system. Health Aff (Millwood) 31(4):836–842, 2012. https://doi.org/10.1377/hlthaff.2011.1258 .
Hazlewood A (2003) ICD-9 CM to ICD-10 CM: Implementation issues and challenges, in: AHIMA’s 75th anniversary National Convention Exhibit Procedings.
Watzlaf VJ, Hornung Garvin J (2007) The Effectiveness of ICD-10-CM in Capturing Public Health Diseases. Perspect Health Inf Manag 4:6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2047296/ . Accessed 7 August 2017
Clark JM, Utter GH, Nuño M, Romano PS, Brown LM, Cooke DT (2019) ICD-10-CM/PCS: Potential methodologic strengths and challenges for thoracic surgery researchers and reviewers. J Thorac dis 11 (Suppl 4):S585-S595. Doi: https://doi.org/10.21037/jtd.2019.01.86 .
ACSS (2017) Circular Normativa N o 19/2017/DPS/ACSS. http://www.acss.min-saude.pt/wp-content/uploads/2016/11/Circular_Normativa_192017_DPS_ACSS.pdf
Manchikanti, L., Falco, F. J. E., and Hirsch, J. A., Necessity and implications of ICD-10: Facts and fallacies. Pain Physician 14(5):E405–E425. https://www.ncbi.nlm.nih.gov/pubmed/21927055 . , 2011.
Top Medical Coding Schools (2018) Medical Coding & Billing Salary Comparisons. https://www.topmedicalcodingschools.com/medical-coding-billing-salary-comparisons/ . Accessed 4 June 2018
Carpentier, P. J., The risk of getting paid: Why ICD-10-CM may increase physician liability under the false claims act. Quinnipiac Health Law 16:117–148, 2013.
Pine, M., Kowlessar, N. M., Salemi, J. L., Miyamura, J., Zingmond, D. S., Katz, N. E., Schindler, J., and Kowlessar, M., Enhancing clinical content and race/ ethnicity data in statewide hospital administrative databases: Obstacles encountered, strategies adopted, and lessons learned health services research. Health Serv Res 50(Suppl 1):1300–1321, 2015. https://doi.org/10.1111/1475-6773.12330 .
Mathauer, I., and Wittenbecher, F., Hospital payment systems based on diagnosis-related groups: Experiences in low-and middle-income countries. Bull World Health Organ 91(10):746–756, 2013. https://doi.org/10.2471/BLT.12.115931 .
Stewart DW, Shamdasani PN (2015) Focus groups: Theory and practice. SAGE publications, 3 edition.
Morgan, D. L., FOCUS GROUPS. Annu. Rev. Sociol 22:129–152, 1996.
SPMS (2017) SIMH – Sistema de Informação Para a Morbilidade Hospitalar. http://spms.min-saude.pt/2017/02/simh-sistema-informacao-morbilidadehospitalar/ . Accessed 25 July 2017
Download references
Acknowledgments
The authors would like to thank the focus group participants and the Project NanoSTIMA (NORTE-01-0145-FEDER-000016).
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The project is financed by the North Portugal Regional Operational Programme (NORTE 2020), under the PORTUGAL 2020 Partnership Agreement, and through the European Regional Development Fund (ERDF).
Author information
Authors and affiliations.
Department of Community Medicine, Information and Health Decision Sciences (MEDCIDS), Faculty of Medicine, University of Porto, Porto, Portugal
Vera Alonso, João Vasco Santos, Joana Ferreira, Isabel Lema, Fernando Lopes & Alberto Freitas
CINTESIS – Center for Health Technology and Services Research, Porto, Portugal
Vera Alonso, João Vasco Santos, Marta Pinto, Joana Ferreira, Isabel Lema, Fernando Lopes & Alberto Freitas
Public Health Unit, ACES Grande Porto VIII Espinho-Gaia, ARS Norte, Espinho, Portugal
João Vasco Santos
Faculty of Psychology and Education Sciences, University of Porto, Porto, Portugal
Marta Pinto
Subgroup of terrorism and security of the crime and justice group of Campbell collaboration, Porto, Portugal
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Vera Alonso .
Ethics declarations
Conflict of interest.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Systems-Level Quality Improvement
Electronic supplementary material
(DOCX 20.1 kb)
Rights and permissions
Reprints and permissions
About this article
Alonso, V., Santos, J.V., Pinto, M. et al. Problems and Barriers during the Process of Clinical Coding: a Focus Group Study of Coders’ Perceptions. J Med Syst 44 , 62 (2020). https://doi.org/10.1007/s10916-020-1532-x
Download citation
Received : 02 July 2019
Accepted : 24 January 2020
Published : 08 February 2020
DOI : https://doi.org/10.1007/s10916-020-1532-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Clinical coding
- International classification of diseases
- Health information management
- Data quality
- Qualitative research
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
However, barriers exist to achieving quality clinical coding outcomes. Canadian authors, Doktorchik et al. (2020), discussed these barriers in their article 'A Qualitative Evaluation of Clinically Coded Data Quality From Health Information Manager Perspectives'.Their interviews with health information managers and clinical coding managers revealed that expectations were increasing for high ...
Automated clinical coding is a potential AI application to facilitate the administration and management of clinical records in the hospital and medical research. There has been a surge of articles for automated clinical coding with deep learning (as the current mainstream approach of AI) in the last few years, as reviewed in recent surveys 11 ...
The use of EHRs can enhance coordinated care, reduce medical errors, and improve quality and patient safety 1 - 4. Moreover, EHRs can enhance the accuracy of coding and the efficiency of reimbursement mechanisms 5. EHRs may better document comorbid conditions to justify higher reimbursement rates from insurers to providers.
Medical coding is a crucial process in clinical trials, as it ensures the consistency and validity of the data collected. This article from the PMC (PubMed Central) database reviews the current standards and challenges of medical coding, and provides some recommendations for improving its quality and efficiency.
The US clinical coding market was valued at $18 billion in 2021, and is expected to grow 8.0% annually until 2030 16. This sizable market has stimulated the race to create the first widely adopted ...
Methods: A systematic review was conducted to identify recently published studies that report on improvements in medical coding and billing accuracy, clinical documentation, and reimbursement rate. A search of three databases yielded a total of 5754 records.
Summary. Clinical coding is the process of converting free text entry into a formal language that may be recognized computationally. There are many different systems in use, such as the well-known ICD-10 and SNOMED CT systems, each with their own use cases, advantages and disadvantages. The design of an ideal coding system is challenging as ...
It is widely believed that health records and their quality have great importance, not only for the medical coding activity but also for further uses of the databases generated by the coded data (e.g. research). However, in order to achieve these purposes fully, complete health records with high data quality is essential.
Automated medical coding, an essential task for healthcare operation and delivery, makes unstructured data manageable by predicting medical codes from clinical documents. Recent advances in deep learning and natural language processing have been widely applied to this task. However, deep learning-based medical coding lacks a unified view of the design of neural network architectures. This ...
This paper proposes an encoder-decoder framework (Fig. 2) to unify existing advanced medical coding models. It dis-cusses the effect of different building blocks to resolve the challenges of medical coding. We provide a complete guide-line for researchers or practitioners to develop efficient neural
U.S. DEPARTMENT OF HEALTH & HUMAN SERVICES. Centers for Disease Control and Prevention National Center for Health Statistics 3311 Toledo Road, Room 4551, MS P08 Hyattsville, MD 20782-2064. FIRST CLASS MAIL POSTAGE & FEES PAID CDC/NCHS PERMIT NO. G-284. OFFICIAL BUSINESS PENALTY FOR PRIVATE USE, $300.
Richard J. B. Dobson. npj Digital Medicine (2022) Clinical coding is the task of transforming medical information in a patient's health records into structured codes so that they can be used for ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on MEDICAL CODING. Find methods information, sources, references or conduct a literature review on ...
Applications to Practice: Provider knowledge of medical billing and coding guidelines is essential. In particular, large academic institutions typically operate on small margins, so even simple adjustments and quality improvement efforts in billing and coding can help immensely by accurately representing the amount and quality of medical services.
Coded data are the basis of information systems in all countries that rely on Diagnosis Related Groups in order to reimburse/finance hospitals, including both administrative and clinical data. To identify the problems and barriers that affect the quality of the coded data is paramount to improve data quality as well as to enhance its usability and outcomes. This study aims to explore problems ...
These full-text databases are meant specifically for those looking up articles in the realm of health, medical coding, medicine, and nursing. Database focuses on complementary, holistic and integrated approaches to health care and wellness. Includes full-text and peer-reviewed articles. (Full text)
Medical coding standardizes the language and presentation of all these elements so they can be more easily understood, tracked, and modified. This common language, mandated by the Health Information Portability and Accountability Act (HIPAA), allows hospitals, providers, and payers to communicate easily and consistently.
Guidelines for coding and billing using the International Classification of Disease, Tenth Revision, Clinical Modification (ICD-10-CM) are set forth by the Centers for Medicare and Medicaid Services (CMS) and the National Center for Health Statistics (NCHS). 2 The current process of coding and billing set forth by CMS relies on evaluation and management (E&M) codes which permit insurance ...
Resources for medical coding professional with news and articles, events, publications, coding help, coding forums, salary surveys, and discounts on products.
Medical Coding Research Paper. Decent Essays. 594 Words. 3 Pages. Open Document. Medical Coding and the Importance of Anatomy & Physiology Those in the medical profession understand that medical coding and billing go hand in hand with the understanding of human anatomy and physiology.
The definition for Medical coding, is the process of converting diagnosis codes to ICD-9/10 codes and procedure codes into CPT codes. A Medical Biller and Coder may specialize in different areas. One area is in-patient facilities, and another area is in and out-patient facilities. An In-patient Coder works in an in-patient facility such as a ...
The Healthcare Common Procedure Coding System (HCPCS) are codes that are for reporting professional services, procedures and supplies. Included in that is medical equipment , ambulance services, orthotics, supplies, medication and dental procedures. The HCPCS was developed by the Health Care Financing Administration in 1983.