

Dr. Alter’s Before and After IMAGE GALLERY
Female procedures.

LABIAPLASTY (Labia Minora Reduction)

CLITORAL HOOD REDUCTION WITH/WITHOUT CLITOROPEXY

LABIA MAJORA REMODELING

COMBINATION FEMALE GENITAL SURGERIES

REVISION OF BOTCHED LABIAPLASTIES

CLITORIS REDUCTION

PUBIC LIPOSUCTION

PUBIC MONS LIFT

INTERSEX & COMPLEX FEMALE RECONSTRUCTION
Male procedures.

BURIED/HIDDEN PENIS CORRECTIVE SURGERY – ADULT
Buried/hidden penis corrective surgery – child, penoscrotal webbing, scrotum reduction, male genital reconstruction, penis enlargement reconstruction, congenital penile curvature, gender confirmation procedures.

MALE TO FEMALE GENDER CONFIRMATION SURGERY

MALE-TO-FEMALE SEX REASSIGNMENT REVISIONS
Female-to-male chest contouring, female to male metaidoioplasty, gender confirmation breast augmentations, cosmetic procedures.

ABDOMINOPLASTY
Breast augmentation, breast reconstruction & breast reduction, liposuction, patient-first policy.
Dr. Alter and the entire team are dedicated to providing every patient with exceptional individualized care—from consultation to recovery. We take the time to learn about your concerns, goals, and desires, so we can build a plan that addresses your concerns and gets you the results you deserve.
Thoughts & Insights

Your Ultimate Guide to Labiaplasty Recovery

Botched Labiaplasty? There’s Still Hope
A botched labiaplasty can be a devastating experience, and for some women, it can cause them to lose confidence in themselves and feel uncomfortable in their bodies. But it doesn’t have to…

Why You Should Choose a Specialist for your Labiaplasty

5 Labiaplasty Benefits You Should Know About
Our locations.
BEVERLY HILLS

NEW YORK CITY
- Reconstructive Procedures
Transfeminine Bottom Surgery
Feminizing genital surgery.
The goal of transfeminine bottom surgery, or feminizing genital surgery, is to reconstruct the male genitalia into female genitalia.
Table of Contents
- Introduction
- Consultation
- Questions to Ask
- Risks and Safety
- Preparation
- Procedure Steps
- Glossary of Terms
- Choosing a Plastic Surgeon
What results should I expect after transfeminine bottom surgery?
The final results of transfeminine bottom surgery can help alleviate the feelings of gender dysphoria that some individuals may experience.
Over time, the new vagina will settle into position and the scar lines will improve, although they'll never disappear completely. There are trade-offs, but most transwomen feel these are small compared to the large improvement in their quality of life and the ability to look and feel like a woman.
The prostate gland is not removed from your body during the procedure. Although the amount of prostate growth as a result of estrogen therapy is small, the risk of developing prostate cancer is not zero. Careful monitoring of prostate health through exam is essential to your long-term health.
When you go home, if you experience shortness of breath, chest pains, or unusual heartbeats, seek medical attention immediately. Should any of these complications occur, you may require hospitalization and additional treatment.
The practice of medicine and surgery is not an exact science. Although good results are expected, there is no guarantee. In some situations, it may not be possible to achieve optimal results with a single surgical procedure and another surgery may be necessary.
Following your physician's instructions is key to the success of your surgery. It is important that the surgical incisions are not subjected to excessive force, abrasion, or motion during the time of healing. Your doctor will give you specific instructions on how to care for yourself.
Find Your Surgeon
On the blog.

Facial feminization surgery is a combination of procedures designed to soften the facial features and feminize the face. There are many procedures that are available to feminize the face.
- Boosted by positive cultural changes, gender affirmation procedures are soaring Kaitlin Clark
- American Society of Plastic Surgeons releases first-ever facial, breast/chest and genital data for gender affirmation procedures Kaitlin Clark
On The Vlog
Patient care center, before & after photos.

Video Gallery
3d animations, patient safety.
- Reference Manager
- Simple TEXT file
People also looked at
Original research article, male-to-female gender-affirming surgery: 20-year review of technique and surgical results.

- 1 Serviço de Urologia, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 2 Serviço de Psiquiatria, Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil
- 3 Serviço de Psiquiatria, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Purpose: Gender dysphoria (GD) is an incompatibility between biological sex and personal gender identity; individuals harbor an unalterable conviction that they were born in the wrong body, which causes personal suffering. In this context, surgery is imperative to achieve a successful gender transition and plays a key role in alleviating the associated psychological discomfort. In the current study, a retrospective cohort, we report the 20-years outcomes of the gender-affirming surgery performed at a single Brazilian university center, examining demographic data, intra and postoperative complications. During this period, 214 patients underwent penile inversion vaginoplasty.
Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18–61 years); the average of operative time was 3.3 h (range 2–5 h); the average duration of hormone therapy before surgery was 12 years (range 1–39). The most commons minor postoperative complications were granulation tissue (20.5 percent) and introital stricture of the neovagina (15.4 percent) and the major complications included urethral meatus stenosis (20.5 percent) and hematoma/excessive bleeding (8.9 percent). A total of 36 patients (16.8 percent) underwent some form of reoperation. One hundred eighty-one (85 percent) patients in our series were able to have regular sexual intercourse, and no individual regretted having undergone GAS.
Conclusions: Findings confirm that it is a safety procedure, with a low incidence of serious complications. Otherwise, in our series, there were a high level of functionality of the neovagina, as well as subjective personal satisfaction.
Introduction
Transsexualism (ICD-10) or Gender Dysphoria (GD) (DSM-5) is characterized by intense and persistent cross-gender identification which influences several aspects of behavior ( 1 ). The terms describe a situation where an individual's gender identity differs from external sexual anatomy at birth ( 1 ). Gender identity-affirming care, for those who desire, can include hormone therapy and affirming surgeries, as well as other procedures such as hair removal or speech therapy ( 1 ).
Since 1998, the Gender Identity Program (PROTIG) of the Hospital de Clínicas de Porto Alegre (HCPA), Universidade Federal do Rio Grande do Sul, Brazil has provided public assistance to transsexual people, is the first one in Brazil and one of the pioneers in South America. Our program offers psychosocial support, health care, and guidance to families, and refers individuals for gender-affirming surgery (GAS) when indicated. To be eligible for this surgery, transsexual individuals must have been adherent to multidisciplinary follow-up for at least 2 years, have a minimum age of 21 years (required for surgical procedures of this nature), have a positive psychiatric or psychological report, and have a diagnosis of GD.
Gender-affirming surgery (GAS) is increasingly recognized as a therapeutic intervention and a medical necessity, with growing societal acceptance ( 2 ). At our institution, we perform the classic penile inversion vaginoplasty (PIV), with an inverted penis skin flap used as the lining for the neovagina. Studies have demonstrated that GAS for the management of GD can promote improvements in mental health and social relationships for these patients ( 2 – 5 ). It is therefore imperative to understand and establish best practice techniques for this patient population ( 2 ). Although there are several studies reporting the safety and efficacy of gender-affirming surgery by penile inversion vaginoplasty, we present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
Patients and Methods
Subjects and study setup.
This is a retrospective cohort study of Brazilian transgender women who underwent penile inversion vaginoplasty between January of 2000 and March of 2020 at the Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil. The study was approved by our institutional medical and research ethics committee.
At our institution, gender-affirming surgery is indicated for transgender women who are under assistance by our program for transsexual individuals. All transsexual women included in this study had at least 2 years of experience as a woman and met WPATH standards for GAS ( 1 ). Patients were submitted to biweekly group meetings and monthly individual therapy.
Between January of 2000 and March of 2020, a total of 214 patients underwent penile inversion vaginoplasty. The surgical procedures were performed by two separate staff members, mostly assisted by residents. A retrospective chart review was conducted recording patient demographics, intraoperative and postoperative complications, reoperations, and secondary surgical procedures. Informed consent was obtained from all individual participants included in the study.
Hormonal Therapy
The goal of feminizing hormone therapy is the development of female secondary sex characteristics, and suppression/minimization of male secondary sex characteristics.
Our general therapy approach is to combine an estrogen with an androgen blocker. The usual estrogen is the oral preparation of estradiol (17-beta estradiol), starting at a dose of 2 mg/day until the maximum dosage of 8 mg/day. The preferred androgen blocker is spironolactone at a dose of 200 mg twice a day.
Operative Technique
At our institution, we perform the classic penile inversion vaginoplasty, with an inverted penis skin flap used as the lining for the neovagina. For more details, we have previously published our technique with a step-by-step procedure video ( 6 ). All individuals underwent intestinal cleansing the evening before the surgery. A first-generation cephalosporin was used as preoperative prophylaxis. The procedure was performed with the patient in a dorsal lithotomy position. A Foley catheter was placed for bladder catheterization. A inverted-V incision was made 4 cm above the anus and a flap was created. A neovaginal cavity was created between the prostate and the rectum with blunt dissection, in the Denonvilliers space, until the peritoneal fold, usually measuring 12 cm in extension and 6 cm in width. The incision was then extended vertically to expose the testicles and the spermatic cords, which were removed at the level of the external inguinal rings. A circumferential subcoronal incision was made ( Figure 1 ), the penis was de-gloved and a skin flap was created, with the de-gloved penis being passed through the scrotal opening ( Figure 2 ). The dorsal part of the glans and its neurovascular bundle were bluntly dissected away from the penile shaft ( Figure 3 ) as well as the urethra, which included a portion of the bulbospongious muscle ( Figure 4 ). The corpora cavernosa was excised up to their attachments at the symphysis pubis and ligated. The neoclitoris was shaped and positioned in the midline at the level of the symphysis pubis and sutured using interrupted 5-0 absorbable suture. The corpus spongiosum was reduced and the urethra was shortened, spatulated, and placed 1 cm below the neoclitoris in the midline and sutured using interrupted 4-0 absorbable suture. The penile skin flap was inverted and pulled into the neovaginal cavity to become its walls ( Figure 5 ). The excess of skin was then removed, and the subcutaneous tissue and the skin were closed using continuous 3-0 non-absorbable suture ( Figure 6 ). A neo mons pubis was created using a 0 absorbable suture between the skin and the pubic bone. The skin flap was fixed to the pubic bone using a 0 absorbable suture. A gauze impregnated with Vaseline and antibiotic ointment was left inside the neovagina, and a customized compressive bandage was applied ( Figure 7 —shows the final appearance after the completion of the procedures).

Figure 1 . The initial circumferential subcoronal incision.

Figure 2 . The de-gloved penis being passed through the scrotal opening.

Figure 3 . The dorsal part of the glans and its neurovascular bundle dissected away from the penile shaft.
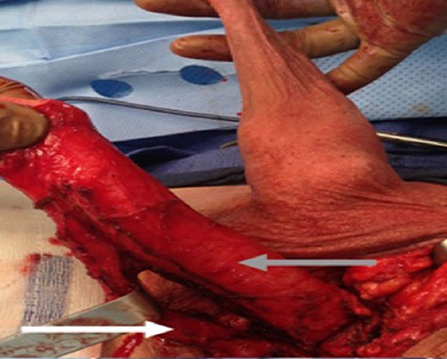
Figure 4 . The urethra dissected including a portion of the bulbospongious muscle. The grey arrow shows the penile shaft and the white arrow shows the dissected urethra.

Figure 5 . The inverted penile skin flap.
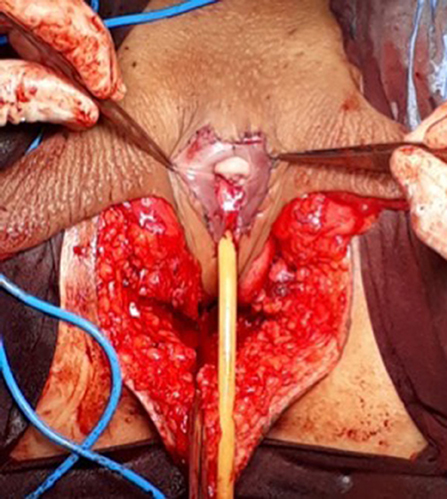
Figure 6 . The neoclitoris and the urethra sutured in the midline and the neovaginal cavity.
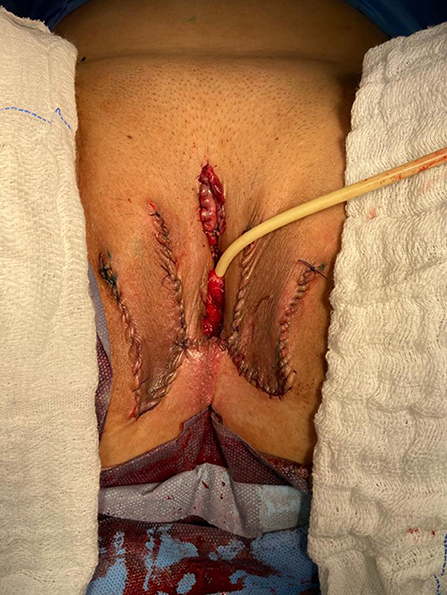
Figure 7 . The final appearance after the completion of the procedures.
Postoperative Care and Follow-Up
The patients were usually discharged within 2 days after surgery with the Foley catheter and vaginal gauze packing in place, which were removed after 7 days in an ambulatorial attendance.
Our vaginal dilation protocol starts seven days after surgery: a kit of 6 silicone dilators with progressive diameter (1.1–4 cm) and length (6.5–14.5 cm) is used; dilation is done progressively from the smallest dilator; each size should be kept in place for 5 min until the largest possible size, which is kept for 3 h during the day and during the night (sleep), if possible. The process is performed daily for the first 3 months and continued until the patient has regular sexual intercourse.
The follow-up visits were performed 7 days, 1, 2, 3, 6, and 12 months after surgery ( Figure 8 ), and included physical examination and a quality-of-life questionnaire.

Figure 8 . Appearance after 1 month of the procedure.
Statistical Analysis
The statistical analysis was conducted using Statistical Product and Service Solutions Version 18.0 (SPSS). Outcome measures were intra-operative and postoperative complications, re-operations. Descriptive statistics were used to evaluate the study outcomes. Mean values and standard deviations or median values and ranges are presented as continuous variables. Frequencies and percentages are reported for dichotomous and ordinal variables.
Patient Demographics
During the period of the study, 214 patients underwent penile inversion vaginoplasty, performed by two staff surgeons, mostly assisted by residents ( Table 1 ). The average age at the time of surgery was 32.2 years (range 18–61 years). There was no significant increase or decrease in the ages of patients who underwent SRS over the study period (Fisher's exact test: P = 0.065; chi-square test: X 2 = 5.15; GL = 6; P = 0.525). The average of operative time was 3.3 h (range 2–5 h). The average duration of hormone therapy before surgery was 12 years (range 1–39). The majority of patients were white (88.3 percent). The most prevalent patient comorbidities were history of tobacco use (15 percent), human immunodeficiency virus infection (13 percent) and hypertension (10.7 percent). Other comorbidities are listed in Table 1 .
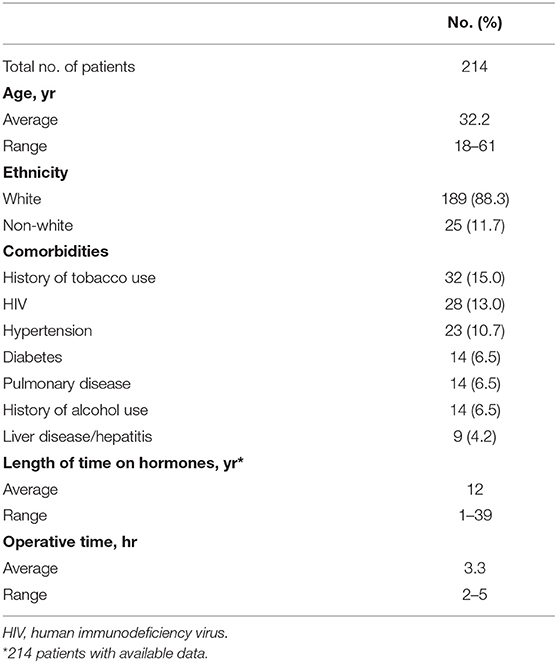
Table 1 . Patient demographics.
Multidisciplinary follow-up was comprised of 93.45% of patients following up with a urologist and 59.06% of patients continuing psychiatric follow-up, median follow-up time of 16 and 9.3 months after surgery, respectively.
Postoperative Results
The complications were classified according to the Clavien-Dindo score ( Table 2 ). The most common minor postoperative complications (Grade I) were granulation tissue (20.5 percent), introital stricture of the neovagina (15.4 percent) and wound dehiscence (12.6 percent). The major complications (Grade III-IV) included urethral stenosis (20.5 percent), urethral fistula (1.9 percent), intraoperative rectal injury (1.9 percent), necrosis (primarily along the wound edges) (1.4 percent), and rectovaginal fistula (0.9 percent). A total of 17 patients required blood transfusion (7.9 percent).
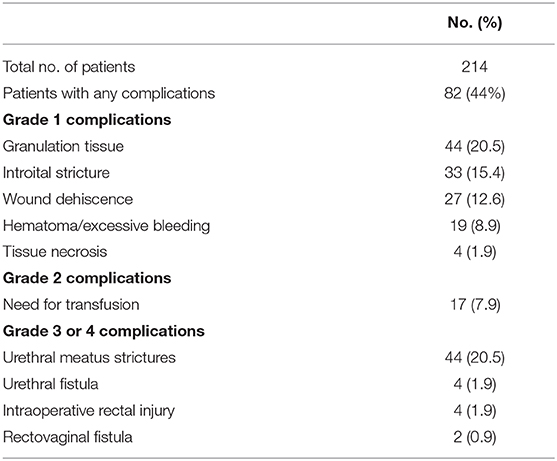
Table 2 . Complications after penile inversion vaginoplasty.
A total of 36 patients (16.8 percent) underwent some form of reoperation.
One hundred eighty-one (85 percent) patients in our series were able to have regular sexual vaginal intercourse, and no individual regretted having undergone GAS.
Penile inversion vaginoplasty is the gold-standard in gender-affirming surgery. It has good functional outcomes, and studies have demonstrated adequate vaginal depths ( 3 ). It is recognized not only as a cosmetic procedure, but as a therapeutic intervention and a medical necessity ( 2 ). We present the largest South-American cohort to date, examining demographic data, intra and postoperative complications.
The mean age of transsexual women who underwent GAS in our study was 32.2 years (range 18–61 years), which is lower than the mean age of patients in studies found in the literature. Two studies indicated that the mean ages of patients at time of GAS were 36.7 years and 41 years, respectively ( 4 , 5 ). Another study reported a mean age at time of GAS of 36 years and found there was a significant decrease in age at the time of GAS from 41 years in 1994 to 35 years in 2015 ( 7 ). According to the authors, this decrease in age is associated with greater tolerance and societal approval regarding individuals with GD ( 7 ).
There was no grade IV or grade V complications. Excessive bleeding noticed postoperatively occurred in 19 patients (8.9 percent) and blood transfusion was required in 17 cases (7.9 percent); all patients who required blood transfusions were operated until July 2011, and the reason for this rate of blood transfusion was not identified.
The most common intraoperative complication was rectal injury, occurring in 4 patients (1.9 percent); in all patients the lesion was promptly identified and corrected in 2 layers absorbable sutures. In 2 of these patients, a rectovaginal fistula became evident, requiring fistulectomy and colonic transit deviation. This is consistent with current literature, in which rectal injury is reported in 0.4–4.5 percent of patients ( 4 , 5 , 8 – 13 ). Goddard et al. suggested carefully checking for enterotomy after prostate and bladder mobilization by digital rectal examination ( 4 ). Gaither et al. ( 14 ) commented that careful dissection that closely follows the urethra along its track from the central tendon of the perineum up through the lower pole of the prostate is critical and only blunt dissection is encouraged after Denonvilliers' fascia is reached. Alternatively, a robotic-assisted approach to penile inversion vaginoplasty may aid in minimizing these complications. The proposed advantages of a robotic-assisted vaginoplasty include safer dissection to minimize the risk of rectal injury and better proximal vaginal fixation. Dy et al. ( 15 ) has had no rectal injuries or fistulae to date in his series of 15 patients, with a mean follow-up of 12 months.
In our series, we observed 44 cases (20.5 percent) of urethral meatus strictures. We credit this complication to the technique used in the initial 5 years of our experience, in which the urethra was shortened and sutured in a circular fashion without spatulation. All cases were treated with meatal dilatation and 11 patients required surgical correction, being performed a Y-V plastic reconstruction of the urethral meatus. In the literature, meatal strictures are relatively rare in male-to-female (MtF) GAS due to the spatulation of the urethra and a simple anastomosis to the external genitalia. Recent systematic reviews show an incidence of five percent in this complication ( 16 , 17 ). Other studies report a wide incidence of meatal stenosis ranging from 1.1 to 39.8 percent ( 4 , 8 , 11 ).
Neovagina introital stricture was observed in 33 patients (15.4 percent) in our study and impedes the possibility of neovaginal penetration and/or adversely affects sexual life quality. In the literature, the reported incidence of introital stenosis range from 6.7 to 14.5 percent ( 4 , 5 , 8 , 9 , 11 – 13 ). According to Hadj-Moussa et al. ( 18 ) a regimen of postoperative prophylactic dilation is crucial to minimize the development of this outcome. At our institution, our protocol for vaginal dilation started seven days after surgery and was performed three to four times a day during the first 3 months and was continued until the individual had regular sexual intercourse. We treated stenosis initially with dilation. In case of no response, we propose a surgical revision with diamond-shaped introitoplasty with relaxing incisions. In recalcitrant cases, we proposed to the patient a secondary vaginoplasty using a full-thickness skin graft of the lower abdomen.
One hundred eighty-one (85 percent) patients were classified as having a “functional vagina,” characterized as the capacity to maintain satisfactory sexual vaginal intercourse, since the mean neovaginal depth was not measured. In a review article, the mean neovaginal depth ranged from 10 to 13.5 cm, with the shallowest neovagina depth at 2.5 cm and the deepest at 18 cm ( 17 ). According to Salim et al. ( 19 ), in terms of postoperative functional outcomes after penile inversion vaginoplasty, a mean percentage of 75 percent (range from 33 to 87 percent) patients were having vaginal intercourse. Hess et al. found that 91.4% of patients who responded to a questionnaire were very satisfied (34.4%), satisfied (37.6%), or mostly satisfied (19.4%) with their sexual function after penile inversion vaginoplasty ( 20 ).
Poor cosmetic appearance of the vulva is common. Amend et al. reported that the most common reason for reoperation was cosmetic correction in the form of mons pubis and mucosa reduction in 50% of patients ( 16 ). We had no patient regrets about performing GAS, although 36 patients (16.8 percent) were reoperated due to cosmetic issues. Gaither et al. propose in order to minimize scarring to use a one-stage surgical approach and the lateralization of surgical scars to the groin ( 14 ). Frequently, cosmetic issues outcomes are often patient driven and preoperative patient education is necessary ( 14 ).
Analyzing the quality of life, in 2016, our health care group (PROTIG) published a study assessing quality of life before and after gender-affirming surgery in 47 patients using the diagnostic tool 100-item WHO Quality of Life Assessment (WHOQOL-100) ( 21 ). The authors found that GAS promotes the improvement of psychological aspects and social relations. However, even 1 year after GAS, MtF persons continue to report problems in physical and difficulty in recovering their independence. In a systematic review and meta-analysis of QOL and psychosocial outcomes in transsexual people, researchers verified that sex reassignment with hormonal interventions more likely corrects gender dysphoria, psychological functioning and comorbidities, sexual function, and overall QOL compared with sex reassignment without hormonal interventions, although there is a low level of evidence for this ( 22 ). Recently, Castellano et al. assessed QOL in 60 Italian transsexuals (46 transwomen and 14 transmen) at least 2 years after SRS using the WHOQOL-100 (general QOL score and quality of sexual life and quality of body image scores) to focus on the effects of hormonal therapy. Overall satisfaction improved after SRS, and QOL was similar to the controls ( 23 ). Bartolucci et al. evaluated the perception of quality of sexual life using four questions evaluating the sexual facet in individuals with gender dysphoria before SRS and the possible factors associated with this perception. The study showed that approximately half the subjects with gender dysphoria perceived their sexual life as “poor/dissatisfied” or “very poor/very dissatisfied” before SRS ( 24 ).
Our study has some limitations. The total number of operated patients is restricted within the long follow-up period. This is due to a limitation in our health system, which allows only 1 sexual reassignment surgery to be performed per month at our institution. Neovagin depth measurement was not performed routinely in the follow-up of operated patients.
Conclusions
The definitive treatment for patients with gender dysphoria is gender-affirming surgery. Our series demonstrates that GAS is a feasible surgery with low rates of serious complications. We emphasize the high level of functionality of the vagina after the procedure, as well as subjective personal satisfaction. Complications, especially minor ones, are probably underestimated due to the nature of the study, and since this is a surgical population, the results may not be generalizable for all transgender MTF individuals.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Hospital de Clínicas de Porto Alegre. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
GM: conception and design, data acquisition, data analysis, interpretation, drafting the manuscript, review of the literature, critical revision of the manuscript and factual content, and statistical analysis. ML and TR: conception and design, data interpretation, drafting the manuscript, critical revision of the manuscript and factual content, and statistical analysis. DS, KS, AF, AC, PT, AG, and RC: conception and design, data acquisition and data analysis, interpretation, drafting the manuscript, and review of the literature. All authors contributed to the article and approved the submitted version.
This study was supported by the Fundo de Incentivo à Pesquisa e Eventos (FIPE - Fundo de Incentivo à Pesquisa e Eventos) of Hospital de Clínicas de Porto Alegre.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. Coleman E, Bockting W, Botzer M, Cohen-Kettenis P, DeCuypere G, Feldman J, et al. Standards of care for the health of transsexual, transgender, and gender-non-conforming people, version 7. Int J Transgend. (2012) 13:165–232. doi: 10.1080/15532739.2011.700873
CrossRef Full Text | Google Scholar
2. Massie JP, Morrison SD, Maasdam JV, Satterwhite T. Predictors of patient satisfaction and postoperative complications in penile inversion vaginoplasty. Plast Reconstruct Surg. (2018) 141:911–921. doi: 10.1097/PRS.0000000000004427
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Pan S, Honig SC. Gender-affirming surgery: current concepts. Curr Urol Rep . (2018) 19:62. doi: 10.1007/s11934-018-0809-9
4. Goddard JC, Vickery RM, Qureshi A, Summerton DJ, Khoosal D, Terry TR. Feminizing genitoplasty in adult transsexuals: early and long-term surgical results. BJU Int . (2007) 100:607–13. doi: 10.1111/j.1464-410X.2007.07017.x
5. Rossi NR, Hintz F, Krege S, Rübben H, Vom DF, Hess J. Gender reassignment surgery – a 13 year review of surgical outcomes. Eur Urol Suppl . (2013) 12:e559. doi: 10.1016/S1569-9056(13)61042-8
6. Silva RUM, Abreu FJS, Silva GMV, Santos JVQV, Batezini NSS, Silva Neto B, et al. Step by step male to female transsexual surgery. Int Braz J Urol. (2018) 44:407–8. doi: 10.1590/s1677-5538.ibju.2017.0044
7. Aydin D, Buk LJ, Partoft S, Bonde C, Thomsen MV, Tos T. Transgender surgery in Denmark from 1994 to 2015: 20-year follow-up study. J Sex Med. (2016) 13:720–5. doi: 10.1016/j.jsxm.2016.01.012
8. Perovic SV, Stanojevic DS, Djordjevic MLJ. Vaginoplasty in male transsexuals using penile skin and a urethral flap. BJU Int. (2001) 86:843–50. doi: 10.1046/j.1464-410x.2000.00934.x
9. Krege S, Bex A, Lümmen G, Rübben H. Male-to-female transsexualism: a technique, results and long-term follow-up in 66 patients. BJU Int. (2001) 88:396–402. doi: 10.1046/j.1464-410X.2001.02323.x
10. Wagner S, Greco F, Hoda MR, Inferrera A, Lupo A, Hamza A, et al. Male-to-female transsexualism: technique, results and 3-year follow-up in 50 patients. Urol International. (2010) 84:330–3. doi: 10.1159/000288238
11. Reed H. Aesthetic and functional male to female genital and perineal surgery: feminizing vaginoplasty. Semin PlasticSurg. (2011) 25:163–74. doi: 10.1055/s-0031-1281486
12. Raigosa M, Avvedimento S, Yoon TS, Cruz-Gimeno J, Rodriguez G, Fontdevila J. Male-to-female genital reassignment surgery: a retrospective review of surgical technique and complications in 60 patients. J Sex Med. (2015) 12:1837–45. doi: 10.1111/jsm.12936
13. Sigurjonsson H, Rinder J, Möllermark C, Farnebo F, Lundgren TK. Male to female gender reassignment surgery: surgical outcomes of consecutive patients during 14 years. JPRAS Open. (2015) 6:69–73. doi: 10.1016/j.jpra.2015.09.003
14. Gaither TW, Awad MA, Osterberg EC, Murphy GP, Romero A, Bowers ML, et al. Postoperative complications following primary penile inversion vaginoplasty among 330 male-to-female transgender patients. J Urol. (2018) 199:760–5. doi: 10.1016/j.juro.2017.10.013
15. Dy GW, Sun J, Granieri MA, Zhao LC. Reconstructive management pearls for the transgender patient. Curr. Urol. Rep. (2018) 19:36. doi: 10.1007/s11934-018-0795-y
16. Amend B, Seibold J, Toomey P, Stenzl A, Sievert KD. Surgical reconstruction for male-to-female sex reassignment. Eur Urol. (2013) 64:141–9. doi: 10.1016/j.eururo.2012.12.030
17. Horbach SER, Bouman MB, Smit JM, Özer M, Buncamper ME, Mullender MG. Outcome of vaginoplasty in male-to-female transgenders: a systematic review of surgical techniques. J Sex Med . (2015) 12:1499–512. doi: 10.1111/jsm.12868
18. Hadj-Moussa M, Ohl DA, Kuzon WM. Feminizing genital gender-confirmation surgery. Sex Med Rev. (2018) 6:457–68.e2. doi: 10.1016/j.sxmr.2017.11.005
19. Salim A, Poh M. Gender-affirming penile inversion vaginoplasty. Clin Plast Surg. (2018) 45:343–50. doi: 10.1016/j.cps.2018.04.001
20. Hess J, Rossi NR, Panic L, Rubben H, Senf W. Satisfaction with male-to-female gender reassignment surgery. DtschArztebl Int. (2014) 111:795–801. doi: 10.3238/arztebl.2014.0795
21. Silva DC, Schwarz K, Fontanari AMV, Costa AB, Massuda R, Henriques AA, et al. WHOQOL-100 before and after sex reassignment surgery in brazilian male-to-female transsexual individuals. J Sex Med. (2016) 13:988–93. doi: 10.1016/j.jsxm.2016.03.370
22. Murad MH, Elamin MB, Garcia MZ, Mullan RJ, Murad A, Erwin PJ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol . (2010) 72:214–31. doi: 10.1111/j.1365-2265.2009.03625.x
23. Castellano E, Crespi C, Dell'Aquila C, Rosato R, Catalano C, Mineccia V, et al. Quality of life and hormones after sex reassignment surgery. J Endocrinol Invest . (2015) 38:1373–81. doi: 10.1007/s40618-015-0398-0
24. Bartolucci C, Gómez-Gil E, Salamero M, Esteva I, Guillamón A, Zubiaurre L, et al. Sexual quality of life in gender-dysphoric adults before genital sex reassignment surgery. J Sex Med . (2015) 12:180–8. doi: 10.1111/jsm.12758
Keywords: transsexualism, gender dysphoria, gender-affirming genital surgery, penile inversion vaginoplasty, surgical outcome
Citation: Moisés da Silva GV, Lobato MIR, Silva DC, Schwarz K, Fontanari AMV, Costa AB, Tavares PM, Gorgen ARH, Cabral RD and Rosito TE (2021) Male-to-Female Gender-Affirming Surgery: 20-Year Review of Technique and Surgical Results. Front. Surg. 8:639430. doi: 10.3389/fsurg.2021.639430
Received: 17 December 2020; Accepted: 22 March 2021; Published: 05 May 2021.
Reviewed by:
Copyright © 2021 Moisés da Silva, Lobato, Silva, Schwarz, Fontanari, Costa, Tavares, Gorgen, Cabral and Rosito. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gabriel Veber Moisés da Silva, veber.gabriel@gmail.com
This article is part of the Research Topic
Gender Dysphoria: Diagnostic Issues, Clinical Aspects and Health Promotion
Long-term Outcomes After Gender-Affirming Surgery: 40-Year Follow-up Study
Affiliations.
- 1 From the Department of Plastic and Reconstructive Surgery.
- 2 School of Medicine.
- 3 Department of Obstetrics and Gynecology.
- 4 Department of Urology.
- 5 Department of Psychiatry and Neurobehavioral Sciences, University of Virginia, Charlottesville, VA.
- PMID: 36149983
- DOI: 10.1097/SAP.0000000000003233
Background: Gender dysphoria is a condition that often leads to significant patient morbidity and mortality. Although gender-affirming surgery (GAS) has been offered for more than half a century with clear significant short-term improvement in patient well-being, few studies have evaluated the long-term durability of these outcomes.
Methods: Chart review identified 97 patients who were seen for gender dysphoria at a tertiary care center from 1970 to 1990 with comprehensive preoperative evaluations. These evaluations were used to generate a matched follow-up survey regarding their GAS, appearance, and mental/social health for standardized outcome measures. Of 97 patients, 15 agreed to participate in the phone interview and survey. Preoperative and postoperative body congruency score, mental health status, surgical outcomes, and patient satisfaction were compared.
Results: Both transmasculine and transfeminine groups were more satisfied with their body postoperatively with significantly less dysphoria. Body congruency score for chest, body hair, and voice improved significantly in 40 years' postoperative settings, with average scores ranging from 84.2 to 96.2. Body congruency scores for genitals ranged from 67.5 to 79 with free flap phalloplasty showing highest scores. Long-term overall body congruency score was 89.6. Improved mental health outcomes persisted following surgery with significantly reduced suicidal ideation and reported resolution of any mental health comorbidity secondary to gender dysphoria.
Conclusion: Gender-affirming surgery is a durable treatment that improves overall patient well-being. High patient satisfaction, improved dysphoria, and reduced mental health comorbidities persist decades after GAS without any reported patient regret.
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
- Follow-Up Studies
- Gender Dysphoria* / surgery
- Sex Reassignment Surgery*
- Transgender Persons* / psychology
- Transsexualism* / psychology
- Type 2 Diabetes
- Heart Disease
- Digestive Health
- Multiple Sclerosis
- Diet & Nutrition
- Supplements
- Health Insurance
- Public Health
- Patient Rights
- Caregivers & Loved Ones
- End of Life Concerns
- Health News
- Thyroid Test Analyzer
- Doctor Discussion Guides
- Hemoglobin A1c Test Analyzer
- Lipid Test Analyzer
- Complete Blood Count (CBC) Analyzer
- What to Buy
- Editorial Process
- Meet Our Medical Expert Board
What to Know About Metoidioplasty (Bottom Surgery)
- Who Qualifies?
- Surgical Techniques
- Neophallus Function
- Surgery Follow-Up
- Where to Have Surgery
Metoidioplasty , or "bottom surgery," is a gender-affirming surgical procedure that involves creating a neophallus (new penis) from a hormonally enlarged clitoris . Transgender men and transmasculine people assigned female at birth (AFAB) may elect for a metoidioplasty if they want their genital appearance to align with their gender identity.
In contrast to the more complex phalloplasty that involves several surgeries, metoidioplasty offers a more straightforward phallic reconstruction in one procedure.
During a metoidioplasty, a surgeon cuts the ligaments that connect the clitoris to the pubic bone to release the clitoris and create a penis with erogenous (sexual) sensations. It may also include additional steps, such as urethral lengthening and scrotoplasty (forming a scrotum), to enhance the appearance and functionality of the neophallus.
This article explores metoidioplasty surgical techniques, the recovery process, and what to expect post-surgery.
CarlosDavid.org / Getty Images
Who Qualifies for Metoidioplasty Surgery?
Metoidioplasty is a gender-affirming (sex-reassignment) surgery for transgender men assigned female at birth. According to the 2015 U.S. Transgender Survey, about 4% of trans men have undergone the procedure, while another 53% expressed a desire to undergo metoidioplasty in the future.
The World Professional Association for Transgender Health (WPATH) developed the criteria for gender reaffirmation surgeries to ensure optimal physical and psychological outcomes for those pursuing bottom (genital) surgeries. The eligibility criteria for metoidioplasty include the following:
- Ongoing and well-documented gender dysphoria
- The ability to make informed decisions and provide consent for treatment
- Being 18 years of age or older
- Medical or mental health concerns are well-managed (if applicable)
- At least 12 consecutive months of gender-affirming testosterone therapy
- Living as a male or masculine-presenting person for at least one year in all settings (e.g., work, school, with family members and community)
Though it is not required, regular visits with a mental health or other medical professional are highly recommended before undergoing a metoidioplasty.
Metoidioplasty Surgical Techniques
People can choose a few different metoidioplasty surgical techniques depending on their preferences. Other procedures can occur simultaneously (e.g., hysterectomy) if desired.
Simple Release Metoidioplasty
In the simple release procedure, ligaments attached to the pubic bone are cut and released, and the clitoris is separated from surrounding tissue to enhance the position and visibility of the clitoris. The labia minora are wrapped around the clitoris to create the glans (head) of the newly formed penis.
Ring Metoidioplasty
Similar to the simple release, this technique involves releasing the clitoral ligaments to lengthen the clitoris. This procedure also involves lengthening the urethra using a flap of tissue from the vaginal wall and labia minora. This procedure gives trans men a micropenis with more girth and the ability to stand while urinating.
Belgrade (Full) Metoidioplasty
The Belgrade technique, or full metoidioplasty, involves the removal of the vagina (vaginectomy) and releasing the clitoris to lengthen and straighten the clitoris. The urethra is lengthened using vaginal tissue and buccal mucosa (inner cheek) skin grafts. The penis is reconstructed with the remaining clitoral and labial skin to give it more girth.
Then, the labia minor flaps are joined to create a scrotum (scrotoplasty), and testicular implants may be inserted into the newly created scrotum. A penile pump or vacuum is recommended three weeks post-surgery to lengthen the neophallus and prevent retraction.
Simultaneous Procedures
In addition to metoidioplasty, some trans men may opt for additional procedures performed at the same time to achieve their desired outcomes. These procedures may include:
- Hysterectomy : Removal of the uterus
- Bilateral salpingo-oophorectomy : Removal of the ovaries and fallopian tubes
- Vaginectomy : Removal of the vagina and surrounding tissues
- Scrotoplasty : Forms a new scrotum; testicular implants may be placed to give the appearance of natural testicles
- Erectile implant : A device is placed inside the neophallus to help achieve erections
Metoidioplasty vs. Phalloplasty
Metoidioplasty and phalloplasty are surgical options for transgender men seeking gender-affirming genital reconstruction. Metoidioplasty involves using existing genital tissue, such as the hormonally enlarged clitoris, to create a neophallus. It usually results in a smaller but functional neophallus.
Phalloplasty involves constructing a neophallus using various techniques, including grafting tissue from other body parts. This procedure can provide a larger and more visually realistic phallus but is more complex and may require multiple stages. The choice between metoidioplasty and phalloplasty depends on individual preferences, desired outcomes, and considerations such as surgical risk, recovery time, and aesthetic goals.
Risks to Understand Before Metoidioplasty
While metoidioplasty is generally considered safe, like any surgical intervention, it carries certain risks. Before undergoing metoidioplasty, discuss the risks with a healthcare provider to gain a comprehensive understanding and make an informed decision.
Potential risks include:
- Urethral stricture or stenosis : Narrowing of the urethral passage, leading to difficulty with urination and potential obstruction of urine flow. Sometimes, urine flow may be blocked entirely, requiring surgery to correct the problem.
- Urethral fistula : An abnormal connection or passageway between the urethra and the skin or surrounding tissues. This can result in urine leakage or an abnormal opening along the neophallus.
- Sensation changes : The newly formed penis may have decreased or loss of sensation or feel hypersensitive and tender.
Function of Neophallus Post-Bottom Surgery
Trans men who have undergone metoidioplasty report high levels of satisfaction with the procedure's results, both in appearance and function.
While a neophallus created through metoidioplasty is usually considered a micropenis (1–4 inches), erections and orgasms are achieved by nearly all who have undergone the procedure. Penetrative sex may or may not be possible. Urinating while standing is possible for most men after metoidioplasty.
Metoidioplasty Recovery Period
The recovery period following metoidioplasty depends on the specific surgical technique and can vary from person to person. Most people can expect one week of bed rest immediately following the procedure and gradually resume their activities within about six weeks.
Initially, there will be discomfort, swelling, and bleeding in the genital region, which will gradually subside over time. You may also experience:
- Bruising in the genital area that spreads from the belly down to the legs
- Itching and short, sharp, shooting sensations as the area heals
- Numbness at or near the incision sites, which can persist for months
- Scarring on the genitals that will first appear red or pink and fade over time
Metoidioplasty Follow-Up (and Asking for Help)
You will need assistance and support during the follow-up period after metoidioplasty, as the recovery process can involve discomfort, limited mobility, and restricted activity. You will need a caretaker for at least a week or two after the procedure—someone who can help with daily tasks such as meal preparation, household chores, and running errands.
Your surgeon may restrict certain activities, such as driving, sex, and heavy lifting. You may need help with transportation to follow-up appointments for about six weeks. Most people can resume their normal activities within six weeks post-surgery. Still, getting the OK from a healthcare provider is important to ensure you are properly healed and to lower the risk of complications.
Where to Have Metoidioplasty Surgery
Specialized surgeons with experience in transgender healthcare often perform metoidioplasty surgery. The procedure is usually carried out in a hospital or surgical center with the necessary tools and equipment for the surgery. It is essential to choose a reputable medical facility that is experienced in transgender surgeries and maintains a supportive and inclusive environment.
When considering where to have metoidioplasty surgery, start by asking a mental health professional or another healthcare provider for referrals and recommendations of surgeons who specialize in the procedure. They can provide information and guidance on the options available to you.
Researching and gathering information about the surgeon's qualifications, experience, and success rates, as well as reading reviews or testimonials from other people who have undergone metoidioplasty at the facility, can also help you select the most suitable location for the surgery. Open communication with healthcare providers can ensure that all your questions and concerns are addressed before deciding where to have metoidioplasty surgery.
Metoidioplasty is a gender-affirming surgery for trans-male people assigned female at birth (AFAB). The procedure involves releasing the clitoral ligaments and utilizing the hormonally enlarged clitoris to create a neophallus (new penis).
There are a few different metoidioplasty techniques. Sometimes, people undergo simultaneous procedures, such as hysterectomy and vaginectomy. Metoidioplasty is considered a safe, effective procedure that results in a 1–4 inch functional penis that gives trans men the opportunity to align their physical characteristics with their gender identity.
Djordjevic ML, Stojanovic B, Bizic M. Metoidioplasty: Techniques and outcomes . Transl Androl Urol . 2019;8(3):248-253. doi:10.21037/tau.2019.06.12
Kjölhede A, Cornelius F, Huss F, Kratz G. Metoidioplasty and groin flap phalloplasty as two surgical methods for the creation of a neophallus in female-to-male gender-confirming surgery: A retrospective study comprising 123 operated patients . JPRAS Open . 2019;22:1-8. doi:10.1016/j.jpra.2019.07.003
Stojanovic B, Bencic M, Bizic M, Djordjevic ML. Metoidioplasty in gender affirmation: A review . Indian J Plast Surg . 2022;55(2):156-161. doi:10.1055/s-0041-1740081
National Center for Transgender Equality. Injustice at every turn: a report of the national transgender discrimination survey .
The World Professional Association for Transgender Health. Standards of care for the health of transsexual, transgender, and gender nonconforming people .
Heston AL, Esmonde NO, Dugi DD 3rd, Berli JU. Phalloplasty: techniques and outcomes . Transl Androl Urol . 2019;8(3):254-265. doi:10.21037/tau.2019.05.05
Alberta Medical Association. Metoidioplasty .
Bordas N, Stojanovic B, Bizic M, et al. Metoidioplasty: Surgical options and outcomes in 813 cases . Front Endocrinol (Lausanne) . 2021;12:760284. doi:10.3389/fendo.2021.760284
TransCare BC. Provincial Health Services Authority. Metoidioplasty .
Michigan Medicine: University of Michigan. What to expect: Metoidioplasty at Michigan Medicine .
TransHealthCare. Metoidioplasty - list of surgeons in the USA .
By Lindsay Curtis Curtis is a writer with over 20 years of experience focused on mental health, sexual health, cancer care, and spinal health.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines

Phalloplasty for Gender Affirmation
Featured Expert:

Fan Liang, M.D.
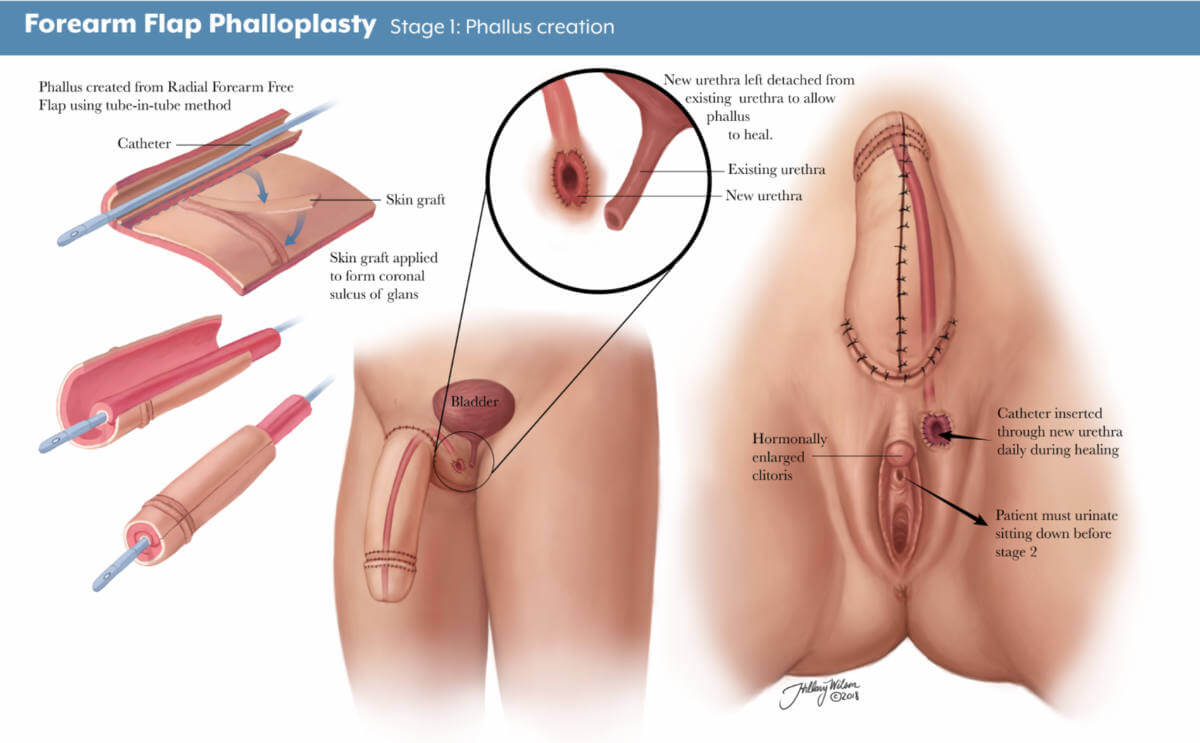
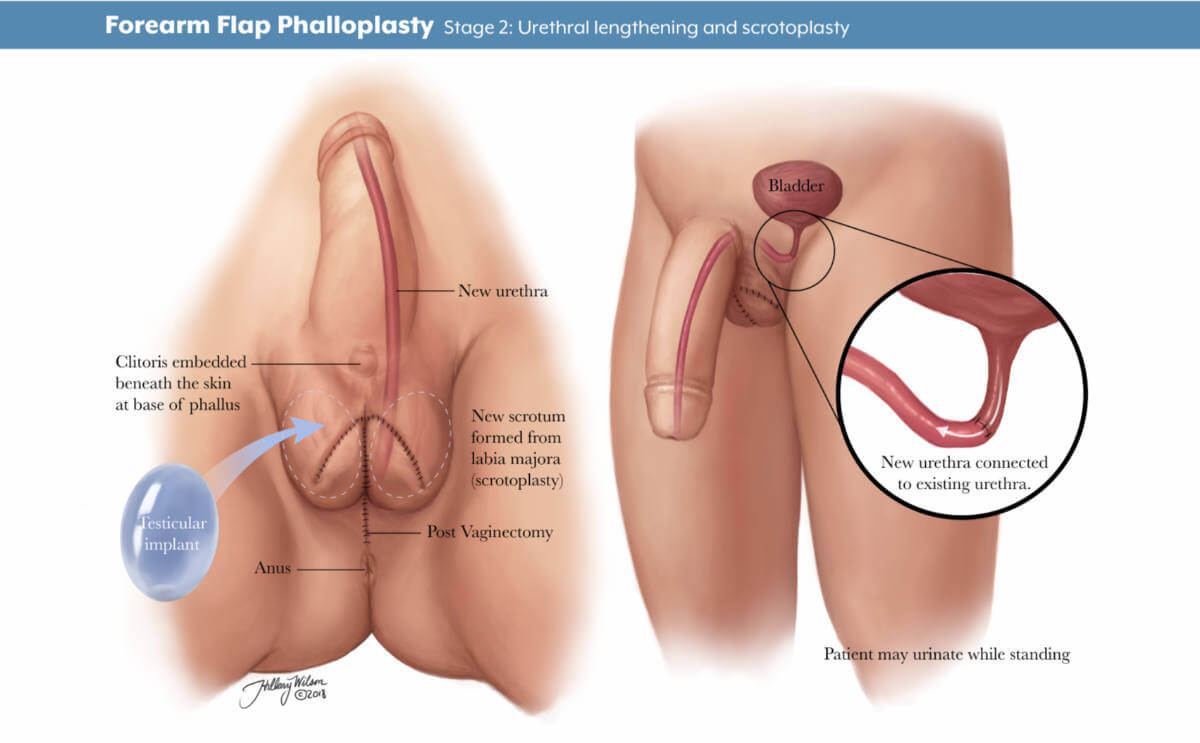
Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including:
- Creating the penis
- Lengthening the urethra so you are able to stand to urinate
- Creating the tip (glans) of the penis
- Creating the scrotum
- Removing the vagina, uterus and ovaries
- Placing erectile and testicular implants
- Skin grafting from the donor tissue site
Gender affirmation surgery is customized to each individual. Your surgical plan may include more or fewer of these steps and procedures. Fan Liang, M.D. , medical director of the Center for Transgender and Gender Expansive Health at Johns Hopkins, explains what you should know.
Are there different types of phalloplasty?
Phalloplasty involves using skin flaps, which are areas of skin moved from one area of the body to another. The skin flap is then reshaped, contoured and reattached to the groin to create the penis. There are three approaches the surgeon may use to construct the penis, using skin from the arm (radial forearm free flap), leg (anterolateral thigh flap) or side (latissimus dorsi flap).
There are pros and cons to each approach. Factors for choosing skin flap locations include the patient’s health and fat distribution, nerve function, blood flow and desired surgical outcomes.
What is a radial forearm free flap?
A radial forearm free flap (RFFF) involves taking the skin, fat, nerves, arteries and veins from your wrist to about halfway up your forearm to create the penis. Typically, the surgeon will use your nondominant hand so it is easier for you to recover and return to your day-to-day activities.
During your surgical consultation, the doctor will check the blood flow to your arm and hand noninvasively. This involves temporarily putting pressure on arteries then releasing the pressure to test blood distribution in the arm and hand.
There are three stages to this procedure.
- Stage 1: The first stage of an RFFF approach is creating the penis using tissue from the forearm. The area where the forearm tissue is taken will require a skin graft. This may occur at the time of the initial phalloplasty surgery, or it may occur three to five weeks afterward. If it occurs later, patients will have a temporary skin covering over the forearm to help it heal.
- Stage 2: The second stage, scheduled about five to six months later, may include lengthening the urethra to allow for urination out of the tip of the penis, creating the scrotum and removing the vagina, and other procedures depending on the patient’s individualized plan.
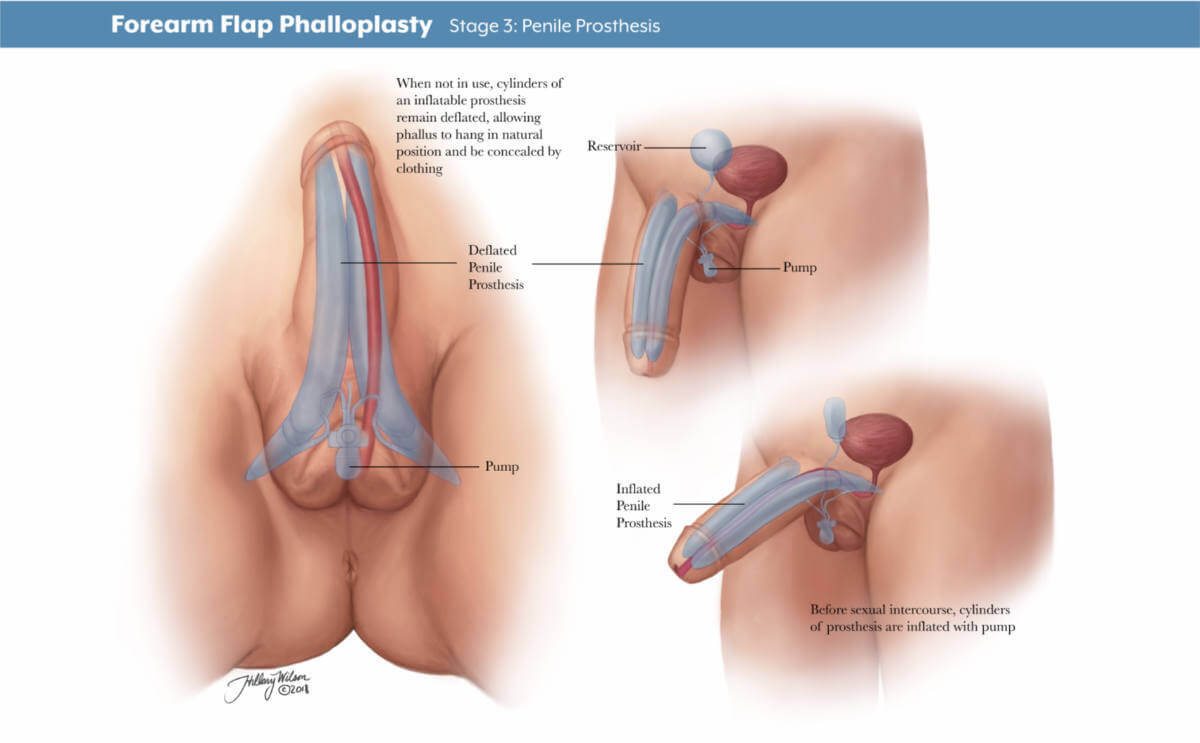
- Stage 3: The third stage of surgery involves putting in place testicle implants and an erectile device to help the patient achieve an erection. The third stage typically takes place 12 months after the second.
Will I have a say in how the phalloplasty is staged and the surgical plan?
Your gender affirmation surgery is highly personalized. Depending on what is most important to you, your surgery team will work with you on a customized plan beforehand. You and your surgeon will discuss your priorities and decide which procedures are right for you. Each stage will be scheduled to ensure your health and safety and provide the best chance of good results.
How long will I be in the hospital?
After your stage 1 surgery, you will stay as an inpatient for four to five days. Your surgical team will frequently monitor the blood supply to the tissue that has been used to create your new penis and ensure you are able to use the bathroom and walk around after surgery. Procedures for stages 2 and 3 do not require a hospital stay.
Will I need a catheter?
During your inpatient stay for stage 1 surgery, you will have a suprapubic tube that goes directly into your bladder and another catheter in your native urethra for at least five days. It is typically removed in the hospital before you go home.
If you decide not to have urethral lengthening as part of stage 2, you will have a Foley catheter placed in the operating room and removed before you leave the hospital. If you decide to have urethral lengthening, you will go home with a Foley catheter in the new urethra and a suprapubic tube. A clamp ensures that the urethra does not leak urine.
What is a suprapubic tube?
A suprapubic tube (SPT) allows urine to drain from your bladder. It is placed in the lower part of your abdomen, below the belly button. The SPT stays in for four to five weeks, depending on your healing and recovery.
When will my SPT be removed?
Before the SPT is removed, around four weeks after surgery, a urologist will perform a retrograde urethrogram. This involves putting dye into the bladder through the new urethra. An X-ray tracks the dye to see if the new urethra is open and ready for urination. If so, the doctor will clamp the SPT and you will be allowed to urinate from your new urethra. If everything looks good after a few days, the SPT is removed.
Forearm Flap Phalloplasty
Stage 1: phallus creation. Enlarged image .
Stage 2: urethral lengthening and scrotoplasty. Enlarged image .
Stage 3: penile prosthesis. Enlarged image .
Other Skin Flaps Used in Phalloplasty
What is an anterolateral thigh flap.
An anterolateral thigh flap (ALT) uses skin, fat, nerves, arteries and veins from the leg to create a penis. A special vascular CT scan can help the surgeon examine the blood supply of each leg to determine which leg will be better for creating the skin flap.
The stage of the ALT phalloplasty are similar to the RFFF. The area where the thigh tissue is taken will also require a skin graft. The resulting scar on the thigh can be covered with shorts.
What is a musculocutaneous latissimus dorsi flap?
A musculocutaneous latissimus dorsi skin flap (MLD) involves the skin, fat, nerves, arteries and veins from the side of your back to create a penis. The surgeon may order a special CT scan to look at the blood flow throughout the donor site area.
The stages of the MLD phalloplasty are similar to the RFFF and ALT. However, the area from which the back tissue is taken usually does not require a skin graft and can be closed in a straight line. The scar can be covered with a shirt. Patients may experience some initial weakness raising their arm, but this improves with time.
How is penis size determined?
Penis size depends on patient preferences and the skin flap harvested from your body. Thinner patients with less fat on the skin flap will have a penis with less girth. Alternatively, patients with a greater amount of fat will have a thicker penis.
The length of the penis depends on the patient’s donor site, but typically it is about 5–6 inches. After the first stage, the penis may decrease in size as postoperative swelling decreases and the tissue settles into its new location.
What determines scrotum size?
Scrotum size is specific to the patient and depends on the amount of skin that is present in the genital area before phalloplasty. The more genital tissue there is, the larger the scrotum and the testicular implants can be.
There are different ways to create the scrotum, including a procedure called V-Y scrotoplasty, a technique that creates a pouch to hold testicular implants. AART silicone round carving blocks have been approved by the FDA to be used as implants.
Procedures to Discuss with Your Physician Before Phalloplasty
Each individual undergoing gender confirmation surgery is different. Your surgeon will work with you to discuss which procedures, and their timing, are best for you and your goals.

Should I have a hysterectomy before phalloplasty surgery?
For those interested in this procedure, hysterectomies are typically done before phalloplasty and do not require a vaginectomy.
Urethral Lengthening Before Phalloplasty
If you choose to have urethral lengthening, this procedure involves lengthening your existing urethra so that you are able to urinate out of the tip of the penis. It involves connecting your current urethra to the new urethra created in the shaft of the penis.
Not all patients choose to have urethral lengthening; however, this will be a necessary step if you want to stand when you urinate. It is also important to know that if you decide not to have urethral lengthening in stage 1 of your phalloplasty, it will not be possible to have the lengthening procedure later.
Complications of Urethral Lengthening
The most common complications for urethral lengthening include urethral strictures (narrowed areas of the urethra), fistula (creation of a passageway between the urethra and another location) and diverticula (formation of a pouch in the urethra). This may require an additional surgical procedure to fix.
What is a metoidioplasty?
A metoidioplasty is a surgical procedure to achieve masculine-appearing genitalia with fewer steps than a phalloplasty. The skin of the labia and around the clitoris is lengthened to achieve the appearance of a penis. Some people prefer to undergo a metoidioplasty if they do not want to use tissue from their arms or legs to create a penis or if they prefer a shorter, more straightforward surgery.
A metoidioplasty procedure has a quicker recovery and fewer complications. Surgeons can discuss metoidioplasty with patients and help them decide if this option is right for them.
Will I need to have hair removal?
Yes, before surgery, after you consult with the surgical team and choose a skin flap site, you will get a template for hair removal that you can give to your hair removal professional.
What if I have a tattoo on my preferred donor site?
As long as there is good blood flow and nerve function, donor sites — even those with a tattoo — can be used.
Penile Function and Sensation After Phalloplasty
What can i do with a reconstructed penis.
Penis function is determined by what you and your surgery team agree on for your surgical plan. If it is important for you to urinate out of the tip of your penis, then urethral lengthening may be a good choice for you. If sensation is most important, your team will focus on a donor site with good nerve innervation. If penetrative sex is most important, and you would like to maintain an erection, then implanting an erectile prosthetic can be part of your surgery plan.
Can I get an erection after phalloplasty?
In stage 3 phalloplasty, a urologist can place a prosthetic erectile device which will allow you to maintain an erection. As of September 2022, no implantable prosthetic devices have been FDA-approved for phalloplasty. Instead, the surgeon can use a device intended for patients with erectile dysfunction to allow transmasculine patients to achieve an erection. There is a risk of infection and implant rejection with an erectile implant . If this happens, it may take six months before another device can be placed into the penis.
What kind of sensation and feeling can I expect?
Sensation recovery varies by patient. Nerve regeneration can begin as early as three weeks after surgery, but it can take longer in some patients. Sometimes sensation can take up to a year or longer. Return of nerve sensation is not guaranteed. As nerves regenerate and strengthen connections, you might experience shooting pain, tingling or electrical sensations. As time goes on, the tingling feeling begins to subside.
What is nerve hookup during phalloplasty?
Nerve hookup involves taking existing nerves from the donor site, such as the arm, and connecting them to nerves located in the pelvis. This allows you to have sensation in the reconstructed penis.
What is clitoral burying during phalloplasty surgery?
Clitoral burying involves moving the clitoris into the base of the penis to increase sensation. This is typically done at stage 2.
Is orgasm possible after phalloplasty?
Orgasm is possible after phalloplasty, especially if your surgery plan emphasizes preserving sensation. It is important to note that your penis will not ejaculate with semen at the time of orgasm.
Find a Doctor
Specializing In:
- Gender Affirmation Surgery
- Transgender Health
At Another Johns Hopkins Member Hospital:
- Howard County Medical Center
- Sibley Memorial Hospital
- Suburban Hospital
Find a Treatment Center
- Center for Transgender and Gender Expansive Health
- Plastic and Reconstructive Surgery
Find Additional Treatment Centers at:

Request an Appointment

Vaginoplasty for Gender Affirmation

Top Surgery

Facial Feminization Surgery (FFS)
Related Topics
Keelee MacPhee, M.D.
Transgender Surgery & Plastic Surgery
TRANSGENDER SURGERY COSMETIC PLASTIC SURGERY BOARD CERTIFIED
MTF Vaginoplasty
In male-to-female sex reassignment, the trans woman may choose to undergo vaginoplasty – the inversion of the penis to create a vagina – as part of her physical transition. This procedure can result in a fully sensate neovagina.
Dr. MacPhee performs this reconstructive procedure by disassembling the penis and utilizing the inverted penile and scrotal skin flap and urethral flap to construct a new vulva, clitoris and vagina. The blood and nerve supplies are preserved to provide sensation, and the urethra is used to create the mucosal part of the vagina that provides additional sensitivity and wetting. The remaining penile and scrotal tissue are used to form the clitoral hood and labia.
The depth and diameter of the neovagina may be limited due the narrowness of the male pelvis. At the time of surgery, a stent is put in place to form vaginal dimensions, and the patient will need to dilate the vagina following surgery, frequently at first and tapering over time. A typical post-op protocol will involve dilating three times a day for 50 minutes each time for the first year. After that, maintenance dilation will be necessary for life. View MTF genital reconstruction results in our Photo Gallery.
Dr. MacPhee also performs orchiectomy, scrotal skin removal and limit-depth vaginoplasty procedures as alternatives to full MTF genital reconstruction .
PHOTO GALLERY

We are grateful for our many patients who are willing to share their experiences and results. Click … Read More >
MEET DR. MACPHEE

A highly skilled Plastic & Reconstructive surgeon in practice for more than 17 years, Dr. Keelee … Read More >
TRANSGENDER SURGERY

Dr. Keelee MacPhee has been performing gender affirming surgery since 2005 and is grateful for the … Read More >
READ OUR BLOG

Tune into our blog for recent news about GRS and the latest trends in cosmetic surgery procedures … Read More >
- About Dr. MacPhee
- Office Environment
- Surgery Hospitals
- Blog / News
- Photo Gallery
- Patient Forms
- Price Transparency
- Referring Therapists
- Referring Physicians

Graphic Medical Content
Content May be Inappropriate for Younger Audiences
Are you over 18 years of age?
- Patient Care & Health Information
- Tests & Procedures
- Feminizing surgery
Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation. Bottom surgery can involve removal of the testicles, or removal of the testicles and penis and the creation of a vagina, labia and clitoris. Facial procedures or body-contouring procedures can be used as well.
Not everybody chooses to have feminizing surgery. These surgeries can be expensive, carry risks and complications, and involve follow-up medical care and procedures. Certain surgeries change fertility and sexual sensations. They also may change how you feel about your body.
Your health care team can talk with you about your options and help you weigh the risks and benefits.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Available Sexual Health Solutions at Mayo Clinic Store
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
Many people seek feminizing surgery as a step in the process of treating discomfort or distress because their gender identity differs from their sex assigned at birth. The medical term for this is gender dysphoria.
For some people, having feminizing surgery feels like a natural step. It's important to their sense of self. Others choose not to have surgery. All people relate to their bodies differently and should make individual choices that best suit their needs.
Feminizing surgery may include:
- Removal of the testicles alone. This is called orchiectomy.
- Removal of the penis, called penectomy.
- Removal of the testicles.
- Creation of a vagina, called vaginoplasty.
- Creation of a clitoris, called clitoroplasty.
- Creation of labia, called labioplasty.
- Breast surgery. Surgery to increase breast size is called top surgery or breast augmentation. It can be done through implants, the placement of tissue expanders under breast tissue, or the transplantation of fat from other parts of the body into the breast.
- Plastic surgery on the face. This is called facial feminization surgery. It involves plastic surgery techniques in which the jaw, chin, cheeks, forehead, nose, and areas surrounding the eyes, ears or lips are changed to create a more feminine appearance.
- Tummy tuck, called abdominoplasty.
- Buttock lift, called gluteal augmentation.
- Liposuction, a surgical procedure that uses a suction technique to remove fat from specific areas of the body.
- Voice feminizing therapy and surgery. These are techniques used to raise voice pitch.
- Tracheal shave. This surgery reduces the thyroid cartilage, also called the Adam's apple.
- Scalp hair transplant. This procedure removes hair follicles from the back and side of the head and transplants them to balding areas.
- Hair removal. A laser can be used to remove unwanted hair. Another option is electrolysis, a procedure that involves inserting a tiny needle into each hair follicle. The needle emits a pulse of electric current that damages and eventually destroys the follicle.
Your health care provider might advise against these surgeries if you have:
- Significant medical conditions that haven't been addressed.
- Behavioral health conditions that haven't been addressed.
- Any condition that limits your ability to give your informed consent.
Like any other type of major surgery, many types of feminizing surgery pose a risk of bleeding, infection and a reaction to anesthesia. Other complications might include:
- Delayed wound healing
- Fluid buildup beneath the skin, called seroma
- Bruising, also called hematoma
- Changes in skin sensation such as pain that doesn't go away, tingling, reduced sensation or numbness
- Damaged or dead body tissue — a condition known as tissue necrosis — such as in the vagina or labia
- A blood clot in a deep vein, called deep vein thrombosis, or a blood clot in the lung, called pulmonary embolism
- Development of an irregular connection between two body parts, called a fistula, such as between the bladder or bowel into the vagina
- Urinary problems, such as incontinence
- Pelvic floor problems
- Permanent scarring
- Loss of sexual pleasure or function
- Worsening of a behavioral health problem
Certain types of feminizing surgery may limit or end fertility. If you want to have biological children and you're having surgery that involves your reproductive organs, talk to your health care provider before surgery. You may be able to freeze sperm with a technique called sperm cryopreservation.
How you prepare
Before surgery, you meet with your surgeon. Work with a surgeon who is board certified and experienced in the procedures you want. Your surgeon talks with you about your options and the potential results. The surgeon also may provide information on details such as the type of anesthesia that will be used during surgery and the kind of follow-up care that you may need.
Follow your health care team's directions on preparing for your procedures. This may include guidelines on eating and drinking. You may need to make changes in the medicine you take and stop using nicotine, including vaping, smoking and chewing tobacco.
Because feminizing surgery might cause physical changes that cannot be reversed, you must give informed consent after thoroughly discussing:
- Risks and benefits
- Alternatives to surgery
- Expectations and goals
- Social and legal implications
- Potential complications
- Impact on sexual function and fertility
Evaluation for surgery
Before surgery, a health care provider evaluates your health to address any medical conditions that might prevent you from having surgery or that could affect the procedure. This evaluation may be done by a provider with expertise in transgender medicine. The evaluation might include:
- A review of your personal and family medical history
- A physical exam
- A review of your vaccinations
- Screening tests for some conditions and diseases
- Identification and management, if needed, of tobacco use, drug use, alcohol use disorder, HIV or other sexually transmitted infections
- Discussion about birth control, fertility and sexual function
You also may have a behavioral health evaluation by a health care provider with expertise in transgender health. That evaluation might assess:
- Gender identity
- Gender dysphoria
- Mental health concerns
- Sexual health concerns
- The impact of gender identity at work, at school, at home and in social settings
- The role of social transitioning and hormone therapy before surgery
- Risky behaviors, such as substance use or use of unapproved hormone therapy or supplements
- Support from family, friends and caregivers
- Your goals and expectations of treatment
- Care planning and follow-up after surgery
Other considerations
Health insurance coverage for feminizing surgery varies widely. Before you have surgery, check with your insurance provider to see what will be covered.
Before surgery, you might consider talking to others who have had feminizing surgery. If you don't know someone, ask your health care provider about support groups in your area or online resources you can trust. People who have gone through the process may be able to help you set your expectations and offer a point of comparison for your own goals of the surgery.
What you can expect
Facial feminization surgery.
Facial feminization surgery may involve a range of procedures to change facial features, including:
- Moving the hairline to create a smaller forehead
- Enlarging the lips and cheekbones with implants
- Reshaping the jaw and chin
- Undergoing skin-tightening surgery after bone reduction
These surgeries are typically done on an outpatient basis, requiring no hospital stay. Recovery time for most of them is several weeks. Recovering from jaw procedures takes longer.
Tracheal shave
A tracheal shave minimizes the thyroid cartilage, also called the Adam's apple. During this procedure, a small cut is made under the chin, in the shadow of the neck or in a skin fold to conceal the scar. The surgeon then reduces and reshapes the cartilage. This is typically an outpatient procedure, requiring no hospital stay.
Top surgery
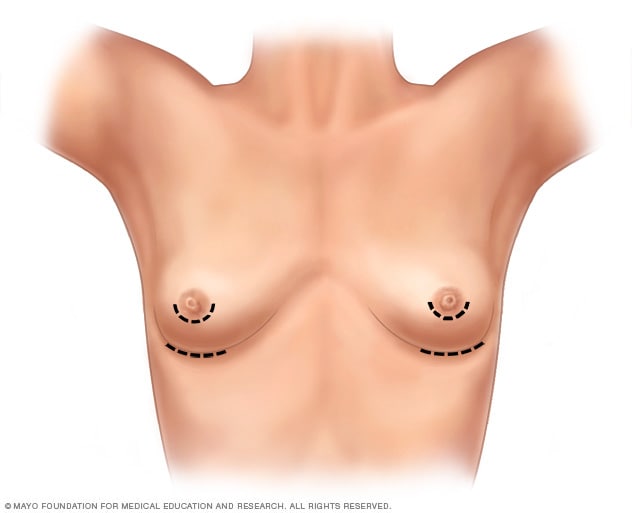
- Breast augmentation incisions
As part of top surgery, the surgeon makes cuts around the areola, near the armpit or in the crease under the breast.
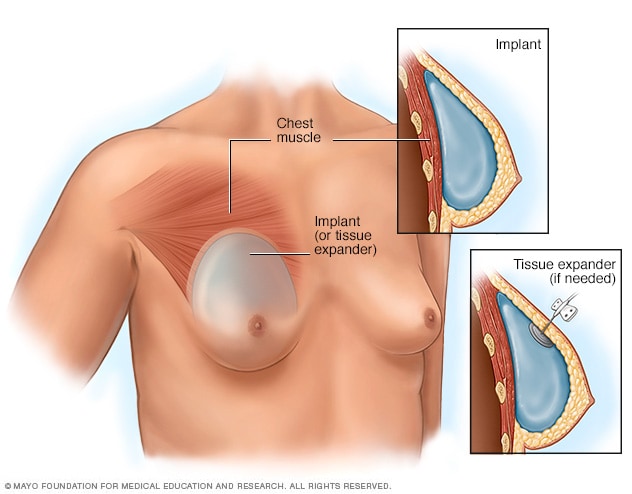
- Placement of breast implants or tissue expanders
During top surgery, the surgeon places the implants under the breast tissue. If feminizing hormones haven't made the breasts large enough, an initial surgery might be needed to have devices called tissue expanders placed in front of the chest muscles.
Hormone therapy with estrogen stimulates breast growth, but many people aren't satisfied with that growth alone. Top surgery is a surgical procedure to increase breast size that may involve implants, fat grafting or both.
During this surgery, a surgeon makes cuts around the areola, near the armpit or in the crease under the breast. Next, silicone or saline implants are placed under the breast tissue. Another option is to transplant fat, muscles or tissue from other parts of the body into the breasts.
If feminizing hormones haven't made the breasts large enough for top surgery, an initial surgery may be needed to place devices called tissue expanders in front of the chest muscles. After that surgery, visits to a health care provider are needed every few weeks to have a small amount of saline injected into the tissue expanders. This slowly stretches the chest skin and other tissues to make room for the implants. When the skin has been stretched enough, another surgery is done to remove the expanders and place the implants.
Genital surgery
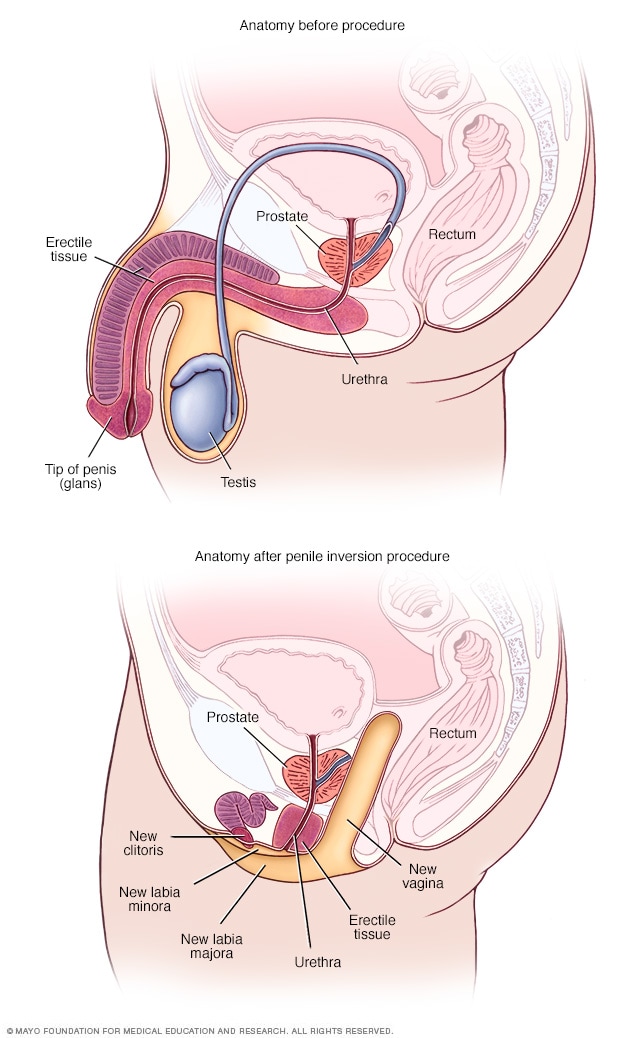
- Anatomy before and after penile inversion
During penile inversion, the surgeon makes a cut in the area between the rectum and the urethra and prostate. This forms a tunnel that becomes the new vagina. The surgeon lines the inside of the tunnel with skin from the scrotum, the penis or both. If there's not enough penile or scrotal skin, the surgeon might take skin from another area of the body and use it for the new vagina as well.
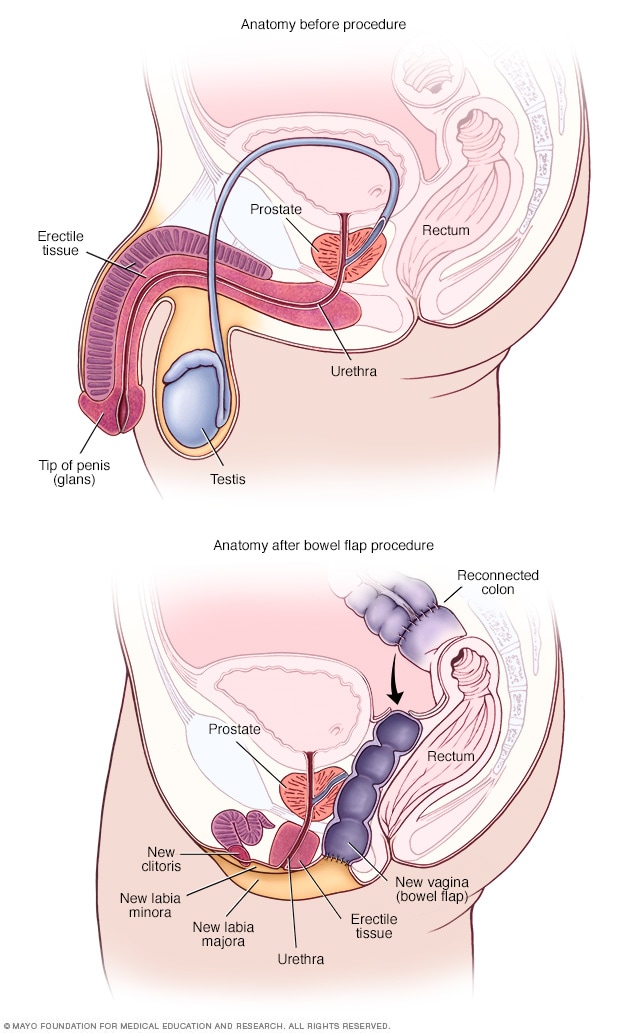
- Anatomy before and after bowel flap procedure
A bowel flap procedure might be done if there's not enough tissue or skin in the penis or scrotum. The surgeon moves a segment of the colon or small bowel to form a new vagina. That segment is called a bowel flap or conduit. The surgeon reconnects the remaining parts of the colon.
Orchiectomy
Orchiectomy is a surgery to remove the testicles. Because testicles produce sperm and the hormone testosterone, an orchiectomy might eliminate the need to use testosterone blockers. It also may lower the amount of estrogen needed to achieve and maintain the appearance you want.
This type of surgery is typically done on an outpatient basis. A local anesthetic may be used, so only the testicular area is numbed. Or the surgery may be done using general anesthesia. This means you are in a sleep-like state during the procedure.
To remove the testicles, a surgeon makes a cut in the scrotum and removes the testicles through the opening. Orchiectomy is typically done as part of the surgery for vaginoplasty. But some people prefer to have it done alone without other genital surgery.
Vaginoplasty
Vaginoplasty is the surgical creation of a vagina. During vaginoplasty, skin from the shaft of the penis and the scrotum is used to create a vaginal canal. This surgical approach is called penile inversion. In some techniques, the skin also is used to create the labia. That procedure is called labiaplasty. To surgically create a clitoris, the tip of the penis and the nerves that supply it are used. This procedure is called a clitoroplasty. In some cases, skin can be taken from another area of the body or tissue from the colon may be used to create the vagina. This approach is called a bowel flap procedure. During vaginoplasty, the testicles are removed if that has not been done previously.
Some surgeons use a technique that requires laser hair removal in the area of the penis and scrotum to provide hair-free tissue for the procedure. That process can take several months. Other techniques don't require hair removal prior to surgery because the hair follicles are destroyed during the procedure.
After vaginoplasty, a tube called a catheter is placed in the urethra to collect urine for several days. You need to be closely watched for about a week after surgery. Recovery can take up to two months. Your health care provider gives you instructions about when you may begin sexual activity with your new vagina.
After surgery, you're given a set of vaginal dilators of increasing sizes. You insert the dilators in your vagina to maintain, lengthen and stretch it. Follow your health care provider's directions on how often to use the dilators. To keep the vagina open, dilation needs to continue long term.
Because the prostate gland isn't removed during surgery, you need to follow age-appropriate recommendations for prostate cancer screening. Following surgery, it is possible to develop urinary symptoms from enlargement of the prostate.
Dilation after gender-affirming surgery
This material is for your education and information only. This content does not replace medical advice, diagnosis and treatment. If you have questions about a medical condition, always talk with your health care provider.
Narrator: Vaginal dilation is important to your recovery and ongoing care. You have to dilate to maintain the size and shape of your vaginal canal and to keep it open.
Jessi: I think for many trans women, including myself, but especially myself, I looked forward to one day having surgery for a long time. So that meant looking up on the internet what the routines would be, what the surgery entailed. So I knew going into it that dilation was going to be a very big part of my routine post-op, but just going forward, permanently.
Narrator: Vaginal dilation is part of your self-care. You will need to do vaginal dilation for the rest of your life.
Alissa (nurse): If you do not do dilation, your vagina may shrink or close. If that happens, these changes might not be able to be reversed.
Narrator: For the first year after surgery, you will dilate many times a day. After the first year, you may only need to dilate once a week. Most people dilate for the rest of their life.
Jessi: The dilation became easier mostly because I healed the scars, the stitches held up a little bit better, and I knew how to do it better. Each transgender woman's vagina is going to be a little bit different based on anatomy, and I grew to learn mine. I understand, you know, what position I needed to put the dilator in, how much force I needed to use, and once I learned how far I needed to put it in and I didn't force it and I didn't worry so much on oh, did I put it in too far, am I not putting it in far enough, and I have all these worries and then I stress out and then my body tenses up. Once I stopped having those thoughts, I relaxed more and it was a lot easier.
Narrator: You will have dilators of different sizes. Your health care provider will determine which sizes are best for you. Dilation will most likely be painful at first. It's important to dilate even if you have pain.
Alissa (nurse): Learning how to relax the muscles and breathe as you dilate will help. If you wish, you can take the pain medication recommended by your health care team before you dilate.
Narrator: Dilation requires time and privacy. Plan ahead so you have a private area at home or at work. Be sure to have your dilators, a mirror, water-based lubricant and towels available. Wash your hands and the dilators with warm soapy water, rinse well and dry on a clean towel. Use a water-based lubricant to moisten the rounded end of the dilators. Water-based lubricants are available over-the-counter. Do not use oil-based lubricants, such as petroleum jelly or baby oil. These can irritate the vagina. Find a comfortable position in bed or elsewhere. Use pillows to support your back and thighs as you lean back to a 45-degree angle. Start your dilation session with the smallest dilator. Hold a mirror in one hand. Use the other hand to find the opening of your vagina. Separate the skin. Relax through your hips, abdomen and pelvic floor. Take slow, deep breaths. Position the rounded end of the dilator with the lubricant at the opening to your vaginal canal. The rounded end should point toward your back. Insert the dilator. Go slowly and gently. Think of its path as a gentle curving swoop. The dilator doesn't go straight in. It follows the natural curve of the vaginal canal. Keep gentle down and inward pressure on the dilator as you insert it. Stop when the dilator's rounded end reaches the end of your vaginal canal. The dilators have dots or markers that measure depth. Hold the dilator in place in your vaginal canal. Use gentle but constant inward pressure for the correct amount of time at the right depth for you. If you're feeling pain, breathe and relax the muscles. When time is up, slowly remove the dilator, then repeat with the other dilators you need to use. Wash the dilators and your hands. If you have increased discharge following dilation, you may want to wear a pad to protect your clothing.
Jessi: I mean, it's such a strange, unfamiliar feeling to dilate and to have a dilator, you know to insert a dilator into your own vagina. Because it's not a pleasurable experience, and it's quite painful at first when you start to dilate. It feels much like a foreign body entering and it doesn't feel familiar and your body kind of wants to get it out of there. It's really tough at the beginning, but if you can get through the first month, couple months, it's going to be a lot easier and it's not going to be so much of an emotional and uncomfortable experience.
Narrator: You need to stay on schedule even when traveling. Bring your dilators with you. If your schedule at work creates challenges, ask your health care team if some of your dilation sessions can be done overnight.
Alissa (nurse): You can't skip days now and do more dilation later. You must do dilation on schedule to keep vaginal depth and width. It is important to dilate even if you have pain. Dilation should cause less pain over time.
Jessi: I hear that from a lot of other women that it's an overwhelming experience. There's lots of emotions that are coming through all at once. But at the end of the day for me, it was a very happy experience. I was glad to have the opportunity because that meant that while I have a vagina now, at the end of the day I had a vagina. Yes, it hurts, and it's not pleasant to dilate, but I have the vagina and it's worth it. It's a long process and it's not going to be easy. But you can do it.
Narrator: If you feel dilation may not be working or you have any questions about dilation, please talk with a member of your health care team.
Research has found that gender-affirming surgery can have a positive impact on well-being and sexual function. It's important to follow your health care provider's advice for long-term care and follow-up after surgery. Continued care after surgery is associated with good outcomes for long-term health.
Before you have surgery, talk to members of your health care team about what to expect after surgery and the ongoing care you may need.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
Feminizing surgery care at Mayo Clinic
- Tangpricha V, et al. Transgender women: Evaluation and management. https://www.uptodate.com/ contents/search. Accessed Aug. 16, 2022.
- Erickson-Schroth L, ed. Surgical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Coleman E, et al. Standards of care for the health of transgender and gender diverse people, version 8. International Journal of Transgender Health. 2022; doi:10.1080/26895269.2022.2100644.
- AskMayoExpert. Gender-affirming procedures (adult). Mayo Clinic; 2022.
- Nahabedian, M. Implant-based breast reconstruction and augmentation. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Erickson-Schroth L, ed. Medical transition. In: Trans Bodies, Trans Selves: A Resource by and for Transgender Communities. 2nd ed. Kindle edition. Oxford University Press; 2022. Accessed Aug. 17, 2022.
- Ferrando C, et al. Gender-affirming surgery: Male to female. https://www.uptodate.com/contents/search. Accessed Aug. 17, 2022.
- Doctors & Departments
- Care at Mayo Clinic
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Dtsch Arztebl Int
- v.111(47); 2014 Nov
Satisfaction With Male-to-Female Gender Reassignment Surgery
Jochen hess.
1 Department of Urology at the University Hospital Essen
Roberto Rossi Neto
2 Clinica Urologia, General Hospital Ernesto Simoes Filho, Salvador, Brasilien
Herbert Rübben
Wolfgang senf.
3 Department of Psychosomatic Medicine and Psychotherapy, University of Essen
The frequency of gender identity disorder is hard to determine; the number of gender reassignment operations and of court proceedings in accordance with the German Law on Transsexuality almost certainly do not fully reflect the underlying reality. There have been only a few studies on patient satisfaction with male-to-female gender reassignment surgery.
254 consecutive patients who had undergone male-to-female gender reassignment surgery at Essen University Hospital’s Department of Urology retrospectively filled out a questionnaire about their subjective postoperative satisfaction.
119 (46.9%) of the patients filled out and returned the questionnaires, at a mean of 5.05 years after surgery (standard deviation 1.61 years, range 1–7 years). 90.2% said their expectations for life as a woman were fulfilled postoperatively. 85.4% saw themselves as women. 61.2% were satisfied, and 26.2% very satisfied, with their outward appearance as a woman; 37.6% were satisfied, and 34.4% very satisfied, with the functional outcome. 65.7% said they were satisfied with their life as it is now.
The very high rates of subjective satisfaction and the surgical outcomes indicate that gender reassignment surgery is beneficial. These findings must be interpreted with caution, however, because fewer than half of the questionnaires were returned.
Culturally, gender is considered an obvious, unambiguous dichotomy. The term “gender identity” denotes the consistency of one’s emotional and cognitive experience of one’s own gender and the objective manifestations of a particular gender. In gender identity disorder, one’s own anatomical sex is objectively perceived but is felt to be alien, whereas the term “gender incongruence” refers to a difference between an individual’s gender identity and prevailing cultural norms. Finally, gender dysphoria is the suffering that results. The treatment guidelines of the World Professional Association of Transgender Health (WPATH) state that gender identity need not coincide with anatomical sex as determined at birth. Transgender identity should therefore be considered neither negative nor pathological ( 1 ). Unfortunately, gender incongruence often leads to discrimination against the affected individual, which can favor the development of psychological complaints such as anxiety disorders and depression ( 2 – 4 ). While some transgender individuals are able to realize their gender identity without surgery, for many gender reassignment surgery is an essential, medically necessary step in the treatment of their gender dysphoria ( 5 ). Research conducted to date has shown that gender reassignment surgery has a positive effect on subjective wellbeing and sexual function ( 2 , 6 , 7 ). The surgical procedure (penile inversion with sensitive clitoroplasty) is described in eBox 1 .
Surgical procedure for penile inversion vaginoplasty
- Open the scrotum.
- Remove both testicles, including the spermatic cord, from the superficial inguinal ring.
- Make a circular cut around the skin of the shaft of the penis under the glans and prepare the skin of the shaft of the penis as far as the base of the penis.
- Separate the urethra from the erectile tissue.
- Separate the neurovascular bundle from the erectile tissue.
- Perform bilateral resection of the erectile tissue.
- Create a space for the neovagina between the rectum and urethra or prostate (the prostate is left intact).
- Invert the skin of the shaft of the penis and close the distal end.
- Insert a placeholder into the neovagina (= the inverted skin of the shaft of the penis).
- Create passages for the neoclitoris (former glans penis) and urethra and then fix in place.
- Inject fibrin glue into the neovagina.
- Position the neovagina, including the placeholder.
- Adjust the labia majora.
- During a second operation six to eight weeks after the first, the vaginal entrance is constructed and minor plastic corrections are made if necessary.
Surgery lasts an average of approximately 3.5 hours. Preservation of the neurovascular bundle results in a sensitive clitoroplasty. The most common complications in short-term postoperative recovery include superficial wound healing problems around the external sutures. In the medium and long term there is a risk of loss of depth ( 23 , 24 , 30 , e15 , e23 , e25 ) or breadth ( 24 , 30 , e11 , e19 , e25 ) of the neovagina in particular. These problems usually result from inconsistent dilatation ( e27 ).
No official figures are available on the prevalence of transgender or gender-nonconforming individuals, and it is very difficult to arrive at a realistic estimate. There is no central reporting register in Germany. Furthermore, figures for those who seek medical help for gender dysphoria would in any case give only an imprecise idea of the true prevalence. The global prevalence of transgender individuals has been estimated at approximately 1 per 11 900 to 1 per 45 000 for male-to-female individuals and approximately 1 per 30 400 to 1 per 200 000 for female-to-male individuals ( 1 ). Weitze and Osburg estimate prevalence in Germany at 1 per 42 000 ( 8 ). In contrast, De Cuypere et al. ( 9 ) suppose a prevalence of 1 per 12 900 for Belgium. Biosnich et al. ( 10 ) estimate prevalence among US veterans at 1 per 4366. This compares to an estimated prevalence of 1 per 23 255 in the general population. Even if percentages of transgender individuals in different parts of the world are comparable, it is highly likely that cultural differences will lead to differing behavior and expression of gender identity, resulting in differing levels of gender dysphoria ( 1 ). The ratio of male-to-female to female-to-male transgender individuals varies greatly. Although it was given as approximately 3:1 by van Kesteren ( 11 ), it is 2.3:1 according to Weitze and Osburg ( 8 ) and 1.4:1 according to Dhejne ( 3 ). Garrels ( 12 ) found a gradual decrease in the difference between the two figures in Germany, with the ratio decreasing from 3.5:1 (in the 1950s and 60s) to 1.2:1 (1995 to 1998) ( Table 1 ).
MTF: male-to-female; FTM: female-to-male
Criteria for diagnosis
Transsexualism is primarily a problem of gender identity (transidentity) or gender role (transgenderism) rather than of sexuality ( 13 ). In Germany, it is diagnosed according to ICD-10 (10 th revision of the International Statistical Classification of Diseases and Related Health Problems).
Criteria for diagnosis include the following:
- Feeling of unease or not belonging to biological gender
- Desire to live and be accepted as a member of the opposite sex
- Presence of this desire for at least two years persistently
- Wish for hormonal treatment and surgery
- Not a symptom of another mental disorder
- Not associated with intersex, genetic, or gender chromosomal abnormalities.
Psychological aspects of transsexualism
According to Senf, no disruption to an individual’s identity is comparable in scale to the development of transsexualism ( 14 ). Transsexualism is a dynamic, biopsychosocial process which those affected cannot escape. An affected individual gradually becomes aware that he or she is living in the wrong body. The feeling of belonging to the opposite sex is experienced as an unchangeable, unequivocal identity ( 14 , 15 ). The individual therefore strives to change his or her inner identity. This change is associated with a change in psychosocial role, and in most cases with hormonal and/or surgical reassignment of the body to the desired gender ( 14 ). Coping with the development of transsexualism poses enormous challenges to those affected and often leads to a considerable psychological burden. In some cases this results in mental illness. Transsexualism itself need not lead to a mental disorder ( 14 ). Psychotherapeutic support is beneficial and is a major part of standard treatment and the examination of transsexual individuals in Germany ( 15 ).
This study aimed to evaluate the effect of male-to-female gender reassignment surgery on the satisfaction of transgender patients.
Data collection
Retrospective inquiry involved consecutive inclusion of 254 patients who had undergone male-to-female gender reassignment surgery involving penile inversion vaginoplasty at Essen University Hospital’s Department of Urology between 2004 and 2010. All patients received a questionnaire ( eBox 2 ) by post, with a franked return envelope. The questions were contained within a follow-up questionnaire developed by Essen University Hospital’s Department of Urology ( 16 ). Because the process was anonymized, patients who had not sent back the questionnaire could not be contacted. The diagnosis of “transidentity” had been made previously following specialized medical examination and in accordance with ICD-10.
Questionnaire
1. How satisfied are you with your outward appearance?
A) Very satisfied
B) Satisfied
C) Dissatisfied
D) Very dissatisfied
2. How satisfied were you with the gender reassignment surgery process?
C) Mostly satisfied
D) Dissatisfied
E) Very dissatisfied
3. How satisfied are you with the aesthetic outcome of your surgery?
4. How satisfied are you with the functional outcome of your surgery?
5. How satisfied are you with your life now, on a scale from 1 (very dissatisfied) to 10 (very satisfied)?
6. How do you see yourself today?
A) As a woman
B) More female than male
C) More male than female
D) As a man
7. Do you feel accepted as a woman by society?
A) Yes, completely
D) No/Not sure
8. Has your life become easier since surgery?
B) Somewhat easier
C) Somewhat harder
9. Have your expectations of life as a woman been fulfilled?
C) Mostly not
D) Not at all
10. How easy is it for you to achieve orgasm?
A) Very easy
B) Usually easy
C) Rarely easy
D) Never achieve orgasm
11. If you compare your orgasm earlier as a man and now as a woman, what is your orgasm like now?
A) More intense
B) Equally/Roughly equally intense
C) Less intense
Statistical evaluation was performed using SPSS (Statistical Package for the Social Sciences, 17.0). Correlation analyses were performed using SAS (Statistical Analysis System, 9.1 for Windows). The distribution of categorical and ordinal data was described using absolute and relative frequencies. Fisher’s exact test was used to compare categorical and ordinal variables in independent samples. The Mann–Whitney U-test was used to compare satisfaction scale distribution of two independent samples. This nonparametric test was used in preference to the t -test because the Shapiro–Wilk test indicated that distribution was not normal. Spearman’s correlation analysis was performed.
A total of 119 completed questionnaires were returned, all of which were included in the evaluation. This represents a response rate of 46.9%. Because the questionnaires were anonymous, no data on patients’ ages could be obtained. The average age of a comparable cohort of patients at Essen University Hospital’s Department of Urology between 1995 and 2008 ( 17 ) was 36.7 years (16 to 68 years). The median time since surgery was 5.05 years (standard deviation: 1.6 years; range: 1 to 7 years). Not all patients had completed the questionnaire in full, so for some questions the total number of responses is not 119.
Following surgery, 63 of 103 patients (61.2%) were satisfied with their outward appearance as women, and a further 27 (26.2%) were very satisfied ( Figure 1 ). 45.5% ( n = 50) were very satisfied with the gender reassignment surgery process, 30% ( n = 33) satisfied, 22.7% ( n = 25) mostly satisfied, and 1.8% ( n = 2) dissatisfied. Figure 2 shows the high rates of subjective satisfaction with the aesthetic outcome of surgery. Overall, approximately three-quarters (70 of 94 responses) reported that they were satisfied or very satisfied. A further 21 (22.3%) were mostly satisfied. Figures for satisfaction with the functional outcome of surgery were similar ( Figure 3 ). A total of 67 of 93 respondents (72%) were satisfied or very satisfied. A further 18 patients (19.4%) were mostly satisfied. Table 2 compares the rates of subjective satisfaction with aesthetic and functional outcome with other studies.

How satisfied are you with your outward appearance? (103 responses)

How satisfied are you with the aesthetic outcome of your surgery? (94 responses)

How satisfied are you with the functional outcome of your surgery? (93 responses)
*1 Functional satisfaction includes satisfaction with depth and breadth of the neovagina and satisfaction with penetration or intercourse
*2 Aesthetic satisfaction includes satisfaction with appearance of external genitalia
In order to gather information on patients’ general satisfaction with their lives, they were asked to place themselves on a Likert scale ranging from 1 (“very dissatisfied”) to 10 (“very satisfied”). Of the total of 102 respondents, 7 (6.9 percent) selected scores from 1 to 3 (2 × 1, 1 × 2, 4 × 3) and 39 (38.2%) scores from 4 to 7 (4 × 4, 16 × 5, 8 × 6, 11 × 7). 56 patients (54.9%) placed themselves in the top third (32 × 8, 13 × 9, 11 × 10). 88 of 103 participants (85.4%) felt completely female following surgery, and 11 (10.7%) mostly female ( Figure 4 ). 69 of 102 women (67.6%) saw themselves as fully accepted as women by society, 25 (24.5%) mostly, and 6 (5.9%) rarely. Two women (2.0%) were not sure of their answer to this question. Of 95 respondents, 65 (68.4%) answered with a clear “Yes” that their life had become easier since surgery. 14 (14.7%) found life somewhat easier, 9 (9.5%) somewhat harder, and 7 (7.4%) harder. Expectations of life as a woman were completely fulfilled for 51 of 102 (50.0%) women, and mostly for 41 (40.2%). The expectations of 6 (5.9%) patients were mostly not fulfilled, and those of 4 (3.9%) were not fulfilled at all.

How do you see yourself today? (103 responses)
There was a correlation between self-perception as a woman (“How do you see yourself today?”) and perceived acceptance by society ( r = 0.495; p <0.01). There was also a correlation between self-perception and answers to whether life had become easier since surgery ( r = 0.375; p <0.01) and whether expectations of life as a woman had been fulfilled ( r = 0.419; p <0.01). Patients who saw themselves completely as women reported higher scores for current satisfaction with their lives than patients who only saw themselves as more female than male ( r = 0.347; p <0.01).
Patients were asked how easy they found it to achieve orgasm. A total of 91 participants answered this question: 75 (82.4%) reported that they could achieve orgasm. Of these, 19 (20.9%) still achieved orgasm very easily, 39 (42.9%) usually easily, and 17 (18.7%) rarely easily. Participants were also asked to compare their experience of orgasm before and after surgery (more intense/the same/less intense). Over half of those who answered this question (43 of 77, 55.8%) experienced more intense orgasm postoperatively, and 16 patients (20.8%) experienced the same intensity.
According to Sohn et al. ( 18 ), subjective satisfaction rates of 80% can be expected following gender reassignment surgery. Löwenberg ( 19 ) reported 92% general satisfaction with the outcome of gender reassignment surgery. The study by Imbimbo et al. ( 20 ) found a similarly high satisfaction rate (94%); however, subjective assessment of general satisfaction and the question of whether or not patients regretted the decision to undergo gender reassignment surgery were queried in one combined question. It is likely that most patients do not actually regret their decision to undergo surgery, even though general postoperative satisfaction is limited. Löwenberg’s figures also show this ( 19 ): 69% of those asked were satisfied with their overall life situation, but 96% would opt for surgery again. In the authors’ own study population, general satisfaction with surgery was achieved in 87.4% of patients. Regardless of surgical results, over half of patients (54.9%) were in the top third (“completely satisfied”) and a further 38.2% in the middle third (“fairly satisfied”) of the general life satisfaction scale.
A retrospective survey performed by Happich ( 21 ) found more than 90% satisfaction with gender reassignment. Sexual experience following surgery is a very important factor in satisfaction with gender reassignment. It depends essentially on the functionality of the neovagina. Figures for satisfaction with functional outcome range from 56% to 84% ( 16 , 19 , 20 , 22 , 23 ). In the authors’ population, satisfaction with function was 72% (“very satisfied” and “satisfied”) or 91.4% (including also “mostly satisfied”). According to Happich ( 21 ), satisfaction with sexual experience is positively correlated with satisfaction with outcome of surgery. Other studies ( 16 , 23 – 25 ) have also found surgical outcome to be one of the essential factors in postoperative satisfaction. Löwenberg ( 19 ) also found a correlation between satisfaction with surgery and satisfaction with aesthetic appearance of the external genitalia. In our study, almost all patients (98.2%) were satisfied with the gender reassignment surgery process ( n = 50, 45.5% “very satisfied”; n = 33, 30% “satisfied”; n = 25, 22.7% “mostly satisfied”).
The Imbimbo et al. working group ( 20 ) reported 78% satisfaction with aesthetic appearance of the neogenitalia (36% “very satisfied,” 32% “satisfied,” 10% “mostly satisfied”). Happich found 82.1% satisfaction with outcome of surgery (46 of 56 patients). Of these, 33.9% of patients reported high satisfaction and 48.2% good to medium satisfaction ( 21 ). A similar value was obtained in the survey by Hepp et al. ( 22 ). Löwenberg ( 19 ) found higher values (94%) for satisfaction with aesthetic outcome of surgery. This population included 106 male-to-female transgender individuals who underwent surgery at Essen University Hospital’s Department of Urology between 1997 and 2003. In the population described here (254 patients, 2004 to 2010) satisfaction with aesthetic outcome was still higher (96.8%).
Orgasm was possible for 82.4% of study participants. The ability to achieve orgasm was lower than in an earlier study population ( 16 ). Figures in the literature vary widely (29% to 100%) and sometimes include small case numbers ( Table 3 ). Overall, the figures for this study match those of comparable studies of a similar size. Finally, it is not clear why more than half the participants experienced orgasm more intensely following surgery than preoperatively. One possible explanation is that postoperatively patients were able to experience orgasm in a body that matched their perception.
Limitations
The response rate of less than 50% must be mentioned as a shortcoming of this study. This may have led to a bias in the results. If all patients who did not take part in the survey were dissatisfied, up to 50.1% and 54.6% would be dissatisfied with aesthetic or functional outcome respectively. According to Eicher, the suicide rate in transgender individuals following successful surgery is no higher than in the general population ( 26 ), so suicide is a very unlikely reason for nonparticipation. Contacting transfemale patients for long-term follow-up after successful surgery is generally difficult (2, 3, 22, 23, 25, 27, 28). This may be because a patient has moved since successful surgery, for example, ( 21 ). Postoperative contact is particularly difficult in countries such as Germany which have no central registers. Response rates to surveys in retrospective research are between 19% ( 28 ) and 79% ( 29 ). Goddard et al. obtained a response rate of 30% in a retrospective survey following gender reassignment surgery ( 30 ). A follow-up survey performed by Löwenberg et al. had a similar response rate, 49% ( 19 ). It is also possible that the positive results of our survey represent patients’ wish for social desirability rather than the real situation. However, this cannot be verified retrospectively.
Taking into account the limitations mentioned above, the high rates of subjective satisfaction with outward female appearance and with aesthetic and functional outcome of surgery indicate that the study participants benefited from gender reassignment surgery.
Key Messages
- At the core of the transsexual experience lies the awareness that one is a member of a realistically perceived anatomical sex (matching of genotype and phenotype), but a subjective feeling of belonging to the other gender.
- Change to the gender inwardly identified with is associated with a change in psychosocial role and in most cases with hormonal and surgical reassignment of the body to the desired gender.
- Although transsexualism itself is not a mental disorder, it can favor the development of mental problems.
- Transsexualism is a dynamic, biopsychosocial process which affected individuals cannot escape.
- The high rates of subjective satisfaction with outward female appearance and with aesthetic and functional outcome of surgery indicate that study participants benefited from gender reassignment surgery.
Acknowledgments
Translated from the original German by Caroline Devitt, M.A.
Conflict of interest statement
Dr. Hess has received reimbursement of conference fees and travel expenses from AMS American Medical Systems.
The other authors declare that no conflict of interest exists.

Results of gender reassignment surgery
Vaginoplasty

Buttock augmentation

Facial feminiZation
BREAST AUGMENTATION

Phalloplasty

Post-phalloplasty aesthetics

Metaidoioplasty
Do you need more information about gender affirmation surgery ? Do you have questions about a sex reassignment surgery ?
(18 years in Spain)
Are you 18 years or older?
Blog The Education Hub
https://educationhub.blog.gov.uk/2024/05/16/new-rshe-guidance-what-it-means-for-sex-education-lessons-in-schools/
New RSHE guidance: What it means for sex education lessons in schools
R elationships, Sex and Health Education (RSHE) is a subject taught at both primary and secondary school.
In 2020, Relationships and Sex Education was made compulsory for all secondary school pupils in England and Health Education compulsory for all pupils in state-funded schools.
Last year, the Prime Minister and Education Secretary brought forward the first review of the curriculum following reports of pupils being taught inappropriate content in RSHE in some schools.
The review was informed by the advice of an independent panel of experts. The results of the review and updated guidance for consultation has now been published.
We are now asking for views from parents, schools and others before the guidance is finalised. You can find the consultation here .
What is new in the updated curriculum?
Following the panel’s advice, w e’re introducing age limits, to ensure children aren’t being taught about sensitive and complex subjects before they are ready to fully understand them.
We are also making clear that the concept of gender identity – the sense a person may have of their own gender, whether male, female or a number of other categories – is highly contested and should not be taught. This is in line with the cautious approach taken in our gu idance on gender questioning children.
Along with other factors, teaching this theory in the classroom could prompt some children to start to question their gender when they may not have done so otherwise, and is a complex theory for children to understand.
The facts about biological sex and gender reassignment will still be taught.
The guidance for schools also contains a new section on transparency with parents, making it absolutely clear that parents have a legal right to know what their children are being taught in RSHE and can request to see teaching materials.
In addition, we’re seeking views on adding several new subjects to the curriculum, and more detail on others. These include:
- Suicide prevention
- Sexual harassment and sexual violence
- L oneliness
- The prevalence of 'deepfakes’
- Healthy behaviours during pregnancy, as well as miscarriage
- Illegal online behaviours including drug and knife supply
- The dangers of vaping
- Menstrual and gynaecological health including endometriosis, polycystic ovary syndrome (PCOS) and heavy menstrual bleeding.
What are the age limits?
In primary school, we’ve set out that subjects such as the risks about online gaming, social media and scams should not be taught before year 3.
Puberty shouldn’t be taught before year 4, whilst sex education shouldn’t be taught before year 5, in line with what pupils learn about conception and birth as part of the national curriculum for science.
In secondary school, issues regarding sexual harassment shouldn’t be taught before year 7, direct references to suicide before year 8 and any explicit discussion of sexual activity before year 9.
Do schools have to follow the guidance?
Following the consultation, the guidance will be statutory, which means schools must follow it unless there are exceptional circumstances.
There is some flexibility w ithin the age ratings, as schools will sometimes need to respond to questions from pupils about age-restricted content, if they come up earlier within their school community.
In these circumstances, schools are instructed to make sure that teaching is limited to the essential facts without going into unnecessary details, and parents should be informed.
When will schools start teaching this?
School s will be able to use the guidance as soon as we publish the final version later this year.
However, schools will need time to make changes to their curriculum, so we will allow an implementation period before the guidance comes into force.
What can parents do with these resources once they have been shared?
This guidance has openness with parents at its heart. Parents are not able to veto curriculum content, but they should be able to see what their children are being taught, which gives them the opportunity to raise issues or concerns through the school’s own processes, if they want to.
Parents can also share copyrighted materials they have received from their school more widely under certain circumstances.
If they are not able to understand materials without assistance, parents can share the materials with translators to help them understand the content, on the basis that the material is not shared further.
Copyrighted material can also be shared under the law for so-called ‘fair dealing’ - for the purposes of quotation, criticism or review, which could include sharing for the purpose of making a complaint about the material.
This could consist of sharing with friends, families, faith leaders, lawyers, school organisations, governing bodies and trustees, local authorities, Ofsted and the media. In each case, the sharing of the material must be proportionate and accompanied by an acknowledgment of the author and its ownership.
Under the same principle, parents can also share relevant extracts of materials with the general public, but except in cases where the material is very small, it is unlikely that it would be lawful to share the entirety of the material.
These principles would apply to any material which is being made available for teaching in schools, even if that material was provided subject to confidentiality restrictions.
Do all children have to learn RSHE?
Parents still have the right to withdraw their child from sex education, but not from the essential content covered in relationships educatio n.
You may also be interested in:
- Education Secretary's letter to parents: You have the right to see RSHE lesson material
- Sex education: What is RSHE and can parents access curriculum materials?
- What do children and young people learn in relationship, sex and health education
Tags: age ratings , Gender , Relationships and Sex Education , RSHE , sex ed , Sex education
Sharing and comments
Share this page, related content and links, about the education hub.
The Education Hub is a site for parents, pupils, education professionals and the media that captures all you need to know about the education system. You’ll find accessible, straightforward information on popular topics, Q&As, interviews, case studies, and more.
Please note that for media enquiries, journalists should call our central Newsdesk on 020 7783 8300. This media-only line operates from Monday to Friday, 8am to 7pm. Outside of these hours the number will divert to the duty media officer.
Members of the public should call our general enquiries line on 0370 000 2288.
Sign up and manage updates
Follow us on social media, search by date, comments and moderation policy.
- My View My View
- Following Following
- Saved Saved
The impact of gender identity issues on custody proceedings
- Medium Text

- Company Klehr Harrison Harvey Branzburg LLP Follow
Parental disagreement
What is best for the child, expert testimony and evaluation, legal protections, mediation and alternative dispute resolution.
Sign up here.

David J. Steerman is chair of the family law group at Klehr Harrison Harvey Branzburg LLP. His legal career is dedicated to helping individuals and families resolve all forms of legal issues including, but not limited to, divorce (negotiated and litigated), custody, all forms of support, prenuptial and post nuptial agreements in Pennsylvania and New Jersey. He is based in Philadelphia and can be reached at [email protected].
Read Next / Editor's Picks
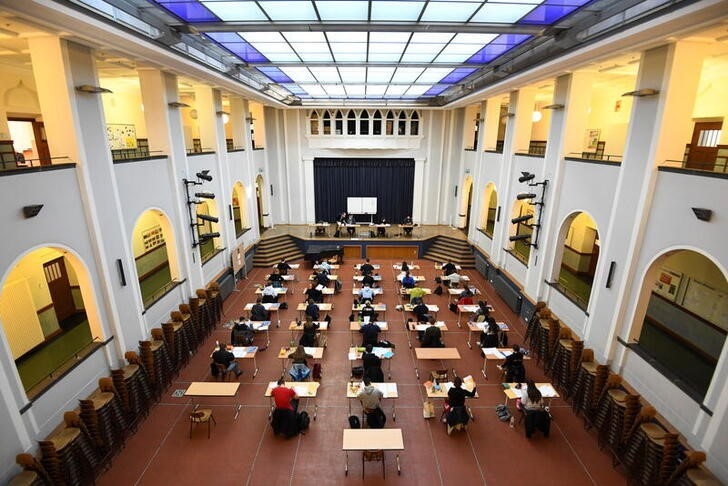
Industry Insight Chevron

David Thomas
Mike Scarcella, David Thomas

Karen Sloan

Henry Engler
- Share full article
Advertisement
Supported by
Guest Essay
The Gender Gap Is Now a Gender Gulf

By Thomas B. Edsall
Mr. Edsall contributes a weekly column from Washington, D.C., on politics, demographics and inequality.
Regardless of who wins the presidential election, the coalitions supporting President Biden and Donald Trump on Nov. 5, 2024, will be significantly different from those on Nov. 3, 2020.
On May 22, Split Ticket , a self-described “group of political and election enthusiasts” who created a “website for their mapping, modeling and political forecasting,” published “ Cross Tabs at a Crossroads : Six Months Out.”
Split Ticket aggregated “subgroup data from the cross tabs of 12 reputable national 2024 general election polls” and compared them with 2020 election results compiled by Pew, Catalist and A.P.
Combining data from multiple surveys allowed Split Ticket to analyze large sample sizes and reduce margins of error for key demographic groups.
The Split Ticket report identified the groups in which Trump and Biden are gaining or losing ground.
In Biden’s case, the analysis shows the president falling behind his 2020 margins among Black voters (down 23 percentage points); urban voters (down 15 points); independents, including so-called partisan leaners (down 14); Latinos (down 13); moderates (down 13); and voters ages 18 to 29 (down 12).
“These losses,” the report noted, “reflect withheld support for Biden, as Trump has gained less than what Biden has lost to voters declaring for undecided/other. In other words, they’re unhappy with Biden, but have not realigned with Trump.”
Biden did not fully make up for his losses with gains in other groups: Republicans (plus 3 percentage points); rural voters (plus 3); voters 65 and over (plus 2); voters 50 to 64 (plus 1) and white, non-college voters (plus 1).
Even though April was one of Trump’s worst months in terms of Black support, the study found that
among Black voters, in aggregate Trump is outperforming his 2020 margin by a whopping 23 points. Relative to 2020, Biden has lost more support (–16 points) than Trump has gained (+7 points), with the remaining 9 percent moving to undecided/other. If Trump matches his April polling vote share (15 percent) among Black voters, it would be nearly double what he received in 2020, and would be the strongest performance by a Republican presidential nominee in nearly 50 years.
Among Latino voters, according to Split Ticket,
Trump is outperforming his 2020 margin by 13 points. Once again, compared to 2020, Biden has lost more support (–9 points) than Trump has gained (+3 points). If Trump ends up winning 40 percent of Latino voters, it would match the highest performance by a Republican presidential candidate in the last 50+ years, George W. Bush in 2004.
White voters were far less volatile, according to Split Ticket:
Biden has dropped by 4 points, and Trump has dropped by 3 points, with the balance moving to undecided/other. Among white college grads, Biden’s vote share has dropped by five points since 2020, while Trump’s has dropped by 1.5 points. Among white non-college grads, Biden’s vote share has dropped by three points since 2020, while Trump’s has dropped by four points.
Much of the focus this year has been on young male voters, who are one of the critical wild cards of 2024.
“Young men have repeatedly been found in recent years to be apathetic toward voting , with young women in recent election cycles constantly turning out to vote at higher rates than young men,” Elaine Kamarck and Jordan Muchnick , both of the Brookings Institution, wrote in a recent essay, “ The Growing Gender Gap Among Young People .”
Kamarck and Muchnick noted the conflicting possibilities: “There are more women than men in the country; they make up a larger portion of the electorate; they are more motivated to vote, and vote blue.”
But, they added, the disaffection of young men has potentially significant implications:
We may be in the opening stages of a social backlash to the progressive social movements of the past decades. When significant societal change occurs, some may feel left behind or cheated. Right now, young men fall into that camp.
They added, “If the aim is to build a fairer equitable future where all feel they have a role and are respected, the polling of Gen Z appears to show we are moving in the opposite direction.”
Two years ago, the Survey Center on American Life , a project of the American Enterprise Institute, conducted a poll, the results of which provide insight into the defection of young men of all races and ethnicities from the Democratic Party.
The survey, Politics, Sex and Sexuality : The Growing Gender Divide in American Life, asked 2007 adults 18 and over a series of questions about masculinity and femininity. Men were asked to define themselves as “very masculine,” “somewhat masculine” or “not too or not at all masculine.”
Among Republican men, a majority, 54 percent, described themselves as “very masculine,” 39 percent as “somewhat masculine” and 7 percent as “not too or not at all masculine.”
Among Democratic men, 33 percent said they were “very masculine,” 53 percent “somewhat masculine” and 12 percent “not too or not at all masculine.”
The authors of an analysis of the survey, Daniel A. Cox , Beatrice Lee and Dana Popky , all of the American Enterprise Institute, found that in the case of women and self-defined femininity, there was only a modest partisan division: “Women across the political spectrum are roughly as likely to identify as feminine. Roughly four in 10 Democratic women (42 percent) and Republican women (39 percent) say they are traditionally feminine.”
In other words, self-defined femininity does not differentiate Republican and Democratic women, but self-defined masculinity reflects a key partisan division among men.
Where do two crucial Democratic constituencies, Black and Hispanic men, fit in? It turns out that in terms of self-defined masculinity, they are far closer to Republican men than to Democratic men, according to Cox, Lee and Popky: “A majority of Black men (55 percent) and Hispanic men (52 percent) say they are very manly or masculine.” On this measure, there is statistically virtually no difference between Republican men, Hispanic men and Black men.
In a June 2023 essay, Cox asks in the headline, “ Are Young Men Becoming Conservative? ” He points out that the trends among young men are less easily explained than the trends among young women.
Young men, Cox wrote, “have not had the same type of formative experiences as young women.” Dobbs v. Jackson Women’s Health Organization, which ended the constitutional right to abortion,
was a political accelerant for young women. The #MeToo movement and Donald Trump’s election were seminal political events in the lives of many young women. These experiences continue to shape the outlook of young women who increasingly perceive society as hostile to women and believe that the experiences of other women in the U.S. are connected to what happens in their own lives.
There were, in Cox’s view, no “comparable experiences for young men.”
Without formative political experiences, Cox argued,
what emerges is a type of political apathy. Young men are less engaged on key political issues. For young women, three issues are uniquely salient: climate change, gun policy and abortion. Young men express far less interest in these issues. Young men seem to care more about economic issues — inflation is high on their list of priorities — but they appear less invested in culture war topics or issues that do not affect them directly. Despite being generally supportive of abortion rights, it is hardly a priority for young men. In a poll we released late last year, young men were approximately 30 points less likely than young women to say abortion was a critical concern (32 percent versus 61 percent, respectively).
All of this led Cox to ask:
Are young men adversaries or allies when it comes to issues such as gender equality? Young men appear to be quiescent when it comes to ceding the historic advantages men have enjoyed in American society. Whether this is due to the fact they believe these changes are just and fair or simply inevitable is unclear.
At the same time, “nearly half of young men believe that American society has become ‘too soft and feminine.’”
The growing gender divide between young men and women in the United States is part of a decade-long international trend, according to a survey of 300,000 men and women in 20 mostly advanced nations.
In “ Polarization Extends Into Gender via Young Adults Who Lose Hope ,” Glocalities , a marketing firm based in the Netherlands, found that
young women have significantly strengthened their embrace of liberal and anti-patriarchal values over the last decade while young men increasingly are lagging behind in this trend. In 2014 older men (aged 55 to 65) were the most conservative and younger men (18 to 24) were significantly more liberal; almost 10 years later, young men have become even less liberal than older men.
Both here and abroad, Glocalities reported:
Feelings of hopelessness, societal disillusionment and rebelling against cosmopolitan values partly explain the rise of radical right anti-establishment parties. Now young men are stagnating in their progress toward liberal values. The radical right in many countries increasingly resonates with disillusioned conservative segments among them, who do not feel that establishment parties are serving their interests. This trend has already impacted elections in Poland, Portugal, Germany, Netherlands and South Korea. If policy priorities and electoral strategies remain unchanged, this trend will likely impact the European elections in June, the U.S. presidential elections in November and more to come.
While feelings of hopelessness are common among young people of both sexes, the sense of despair is pushing males and females in opposing directions. Glocalities survey determined that there is a growing “anti-authoritarian trend among young women” who
are more worried about sexual harassment, domestic violence, child abuse and neglect and mental health problems. These worries explain the increasing anti-patriarchal trend among young women and, for example also the rise of the #MeToo movement since it went viral in 2017. Young women demand better prospects in combination with social justice and equality at home, in the workplace and beyond. Globally, young women are likely the most liberal group in human history.
Young men, in contrast, are “more focused on competition, bravery and honor” and “are more patriarchal in their orientations overall when compared with women and even when compared with older men.” The radical right “increasingly resonates with conservative segments among young men.”
One section of the Glocalities study focused on the United States. The study measured trends from 2014 to 2023 among age cohorts of men and women on two scales — one on hope versus despair, the other on control and patriarchy versus freedom and autonomy.
The despair-versus-hope dimension was based on questions “about feeling let down by society and feelings of pessimism and disillusionment about the future.” The control-versus-freedom dimension was “based on a set of strongly differentiating values regarding support for patriarchy versus support for emancipative values including gender role flexibility, gay marriage and unmarried couples cohabitating.”
The survey found that over the past decade, men over the age of 55 became happier and their values moved from controlling and patriarchal toward freedom and autonomy. Men ages 34 to 54 basically stayed in place. Men 18 to 34 moved decisively toward despair and modestly toward patriarchal values (and away from emancipatory values).
Women of all ages became stronger in their belief in freedom and autonomy. Young women, however, stood out, moving almost as much as young men from hope to despair.
I asked Martijn Lampert , the research director of Glocalities, to elaborate on developments over the past 10 years in the United States, including the influence of the #MeToo movement. He replied in an email, “The #MeToo movement globally was a strong driver for young women to become more liberal and emancipated, but we do not consider the #MeToo movement specifically as a driver for young men to shift to the right.”
Instead, in the case of young men,
we interpret the stagnating progress of men on the control-freedom axis to be caused by factors that affect their ambitions first and foremost. Given that their values focus a lot on success, status, recognition et cetera, the current situation does not facilitate this ambition. Because of this they not only become more pessimistic (as we see happening in the United States even more than in Europe), but also become more susceptible to populist forces and a “politics of bravery.’’
Young men, Lampert continued, “are not necessarily conservative in a traditional sense (and in the United States, young men are still more freedom oriented than older men) but are more geared toward ambition, bravery, honor, innovation, loyalty, success, wealth and luxury.”
While young men, in Lampert’s view, are not “a prime target for Trump or the MAGA movement, because Trump positions himself as culturally conservative while young men are still more emancipated and liberal, there certainly are young men who resonate with Trump’s bravery, ambition and his emphasis on success, honor and loyalty.”
What does the future hold?
“Based on the research outcomes, we expect the conflict between emancipatory/feminist values and patriarchal beliefs among young men and women to become more intense.”
Melissa Deckman , the chief executive of P.R.R.I. and author of the forthcoming book “ The Politics of Generation Z : How the Youngest Voters Will Shape Our Democracy,” described by email what she found in her research: First and foremost, “Gen Z women are unique from older generations of women in that they are more engaged in politics than their male counterparts.”
But, Deckman added, “while Gen Z women are fiercely feminist and progressive, Gen Z men are more ideologically diverse. P.R.R.I.’s study on Gen Z shows a gender gap, certainly, on ideology, but Gen Z men are still slightly more likely to self-identify as liberal than conservative.”
Deckman provided The Times with P.R.R.I. poll data showing that among young voters ages 18 to 25, women identify themselves as decisively Democratic (41 percent, compared with 18 percent Republican) and firmly liberal (47 percent, compared with 24 conservative).
Men ages 18 to 25 are Democratic by a much smaller margin (30 percent, compared with 24 percent) and much less liberal (38 percent, compared with 31 percent).
More ominous for Democrats are P.R.R.I.’s data on 13-to-17-year-olds, who will soon become eligible to vote.
Self-described partisanship among girls ages 13 to 17 was 31 percent Democratic to 20 percent Republican, an 11-point Democratic advantage, compared with a 23-point Democratic advantage among women 18 to 25.
Among boys ages 13 to 17, 24 percent said they were Democrats, and 23 percent said they were Republican, a one-point Democratic advantage, compared with the eight-point Democratic edge among men 18 to 25.
In their 2020 paper “ Personality and Social Psychology Bulletin ,” Sarah H. DiMuccio , a consultant with the Danish firm Mannaz , and Eric D. Knowles , a professor of psychology at N.Y.U., suggested another set of reasons for Trump’s appeal to some men:
Perhaps more than any politician in recent history, Donald Trump has rooted his political persona in traditional notions of masculinity. As a candidate and as president, Trump presents himself as dominant, unyielding and virile. From threatening foreign nations with attack to alluding favorably to the size of his penis and testosterone levels, the president’s behavior suggests a desire to place his manhood beyond reproach.
In this light, DiMuccio and Knowles wrote,
we argue that support for harsh political policies, Trump and the present-day Grand Old Party reflects (in part) the psychology of precarious manhood. On this account, some men harbor doubts about their masculinity, which they, in turn, seek to reaffirm through voting behavior and policy preferences that can be characterized as “politically aggressive.”
The authors cited research showing that
laypeople tend to associate the Republican Party with masculinity and the Democratic Party with femininity. Moreover, a content analysis of primary debates in 2012 and 2016 found that Republican candidates utilized more aggressive discourse against their intraparty opponents than did Democrats — with Donald Trump proving to be the most rhetorically aggressive candidate in the history of American presidential debates.
To test their argument, DiMuccio and Knowles conducted a detailed geographic analysis of internet searches for subjects they determined signal anxiety over masculinity or precarious masculinity. The searches included hair loss, steroids, Viagra and more salacious subjects.
They then correlated the data with presidential voting in 2008, 2012 and 2016. In the case of the two earlier contests, Obama-McCain and Obama-Romney, there was no strong linkage between presidential voting and the level of precarious masculinity internet searches.
In the 2016 contest between Trump and Hillary Clinton, however, DiMuccio and Knowles found that “Trump received a higher share of votes in media markets where precarious masculinity-related searches were particularly popular and that this relationship held after adjusting for a range of search-based and demographic covariates.”
Why did the linkage between presidential voting and precarious masculinity emerge with Trump but not in the previous elections?
The authors’ answer:
Trump and the Republican Party he leads appear more consistently aggressive than high-profile G.O.P. politicians of the recent past — including Mitt Romney and John McCain.
“While the recent ideological evolution of the Republican Party may not have occurred without Trump,” the authors went on to say, it is “likely that these changes will far outlast Trump as a political force. Thus, we believe the link between precarious masculinity and Republican voting will generalize to future elections.”
Biden’s struggles with young men, however, have far deeper roots than precarious masculinity.
In 1949 the chemist Carl Djerassi and his co-workers synthesized norethisterone , a potent available progestin that eventually led to the emergence of oral contraceptives . For his obituary, The Guardian used the headline “ How the Inventor of the Pill Changed the World for Women .”
With the backing of two liberal Supreme Court decisions — Griswold v. Connecticut in 1965, overturning a state law prohibiting the sale of contraceptives, and Roe v. Wade in 1973, legalizing abortion nationwide — the birth control pill set in motion the slow but steady emancipation of women and the erosion of men’s dominance in politics and in society writ large.
In this context, the struggle over the 2024 election is the latest chapter in a long saga.
The Times is committed to publishing a diversity of letters to the editor. We’d like to hear what you think about this or any of our articles. Here are some tips . And here's our email: [email protected] .
Follow the New York Times Opinion section on Facebook , Instagram , TikTok , WhatsApp , X and Threads .
An earlier version of this article misstated a year and the degrees of difference in an analysis comparing previous and recent support for President Biden. The previous data is from 2020, not 2000, and the differences are in percentage points, not percentages.
How we handle corrections
Thomas B. Edsall has been a contributor to the Times Opinion section since 2011. His column on strategic and demographic trends in American politics appears every Wednesday. He previously covered politics for The Washington Post. @ edsall

IMAGES
VIDEO
COMMENTS
MALE-TO-FEMALE SEX REASSIGNMENT REVISIONS. by altermd. altermd March 2, 2020. BEFORE & AFTER Gender Confirmation. FEMALE-TO-MALE CHEST CONTOURING. by altermd. ... results you deserve. Schedule Your Consultation Today. Thoughts & Insights. Labiaplasty March 22, 2024. Your Ultimate Guide to Labiaplasty Recovery.
Breast augmentation is often performed as an outpatient procedure but some patients may require one night stay in the hospital. 1 of 7. See before and after photos of patients who have undergone gender-affirming surgeries at Cleveland Clinic, including breast augmentations, facial feminizations, mastectomies and vaginoplasty.
Research consistently shows that people who choose gender affirmation surgery experience reduced gender incongruence and improved quality of life. Depending on the procedure, 94% to 100% of people report satisfaction with their surgery results. Gender-affirming surgery provides long-term mental health benefits, too.
The final results of transfeminine bottom surgery can help alleviate the feelings of gender dysphoria that some individuals may experience. Over time, the new vagina will settle into position and the scar lines will improve, although they'll never disappear completely. There are trade-offs, but most transwomen feel these are small compared to ...
Results: results demonstrate that the average age at the time of surgery was 32.2 years (range, 18 to 61 years); the average of operative time was 3.3 hours (range, 2 to 5 hours); the average duration of hormone therapy before surgery was 12 years (range, 1-39). ... sexual function, and overall QOL compared with sex reassignment without ...
Body congruency score for chest, body hair, and voice improved significantly in 40 years' postoperative settings, with average scores ranging from 84.2 to 96.2. Body congruency scores for genitals ranged from 67.5 to 79 with free flap phalloplasty showing highest scores. Long-term overall body congruency score was 89.6.
Gender affirming surgery can be used to create a vulva and vagina. It involves removing the penis, testicles and scrotum. During a vaginoplasty procedure, tissue in the genital area is rearranged to create a vaginal canal (or opening) and vulva (external genitalia), including the labia. A version of vaginoplasty called vulvoplasty can create a ...
Metoidioplasty is a gender-affirming (sex-reassignment) surgery for transgender men assigned female at birth. According to the 2015 U.S. Transgender Survey, about 4% of trans men have undergone the procedure, while another 53% expressed a desire to undergo metoidioplasty in the future.
Gender-affirming surgery for male-to-female transgender women or transfeminine non-binary people describes a variety of surgical procedures that alter the body to provide physical traits more comfortable and affirming to an individual's gender identity and overall functioning.. Often used to refer to vaginoplasty, sex reassignment surgery can also more broadly refer to other gender-affirming ...
A 2018 study found that 94-100% of participants who had undergone gender-affirming surgery reported satisfaction with the surgical results, with the variance depending on the type of procedure.
Feminizing bottom surgery is a procedure that allows your physical body to match your gender identity. It reconstructs organs in the male reproductive system into parts of a vulva and possibly a vagina. Recovery can take up to several months. Contents Overview Procedure Details Risks / Benefits Recovery and Outlook When To Call the Doctor ...
Featured Expert: Fan Liang, M.D. Phalloplasty is surgery for masculinizing gender affirmation. Phalloplasty is a multistaged process that may include a variety of procedures, including: Creating the penis. Lengthening the urethra so you are able to stand to urinate. Creating the tip (glans) of the penis. Creating the scrotum.
MTF Vaginoplasty. In male-to-female sex reassignment, the trans woman may choose to undergo vaginoplasty - the inversion of the penis to create a vagina - as part of her physical transition. This procedure can result in a fully sensate neovagina. Dr. MacPhee performs this reconstructive procedure by disassembling the penis and utilizing the ...
Overview. Feminizing surgery, also called gender-affirming surgery or gender-confirmation surgery, involves procedures that help better align the body with a person's gender identity. Feminizing surgery includes several options, such as top surgery to increase the size of the breasts. That procedure also is called breast augmentation.
During this period, 214 patients underwent penile inversion vaginoplasty. Results: Results demonstrate that the average age at the time of surgery was 32.2 years (range, 18-61 years); the average of operative time was 3.3 h (range 2-5 h); the average duration of hormone therapy before surgery was 12 years (range 1-39).
Results from studies imply that sex reassignment surgery on the one hand has positive effects in terms of partial aspects of quality of life, such as mental health, sexuality, and life satisfaction, and, on the other hand, on quality of life overall. Because of the studies' high dropout rates (12-77%; median 56%), the results should be ...
Gender-affirming surgery is a surgical procedure, or series of procedures, that alters a person's physical appearance and sexual characteristics to resemble those associated with their identified gender.The phrase is most often associated with transgender health care and intersex medical interventions, although many such treatments are also pursued by cisgender and non-intersex individuals.
In addition to cross-sex hormone therapy, gender-affirming surgery (GAS)—formerly known as sex-reassignment surgery (SRS)—aims to surgically align physical characteristics with one's identity. These surgical interventions target sex-specific physical characteristics such as genitals (e.g., vaginoplasty), chest (e.g., mastectomy), face ...
Löwenberg ( 19) also found a correlation between satisfaction with surgery and satisfaction with aesthetic appearance of the external genitalia. In our study, almost all patients (98.2%) were satisfied with the gender reassignment surgery process ( n = 50, 45.5% "very satisfied"; n = 33, 30% "satisfied"; n = 25, 22.7% "mostly ...
Gender-affirming surgery for female-to-male transgender people includes a variety of surgical procedures that alter anatomical traits to provide physical traits more comfortable to the trans man's male identity and functioning.. Often used to refer to phalloplasty, metoidoplasty, or vaginectomy, sex reassignment surgery can also more broadly refer to many procedures an individual may have ...
Results of gender reassignment surgery. Knowing the before and after of a surgery or treatment performed by the IM GENDER team is important so as to have a clear idea of the results. Vaginoplasty. Buttock augmentation . Facial feminiZation. MASTECTOMY. BREAST AUGMENTATION . Phalloplasty .
The facts about biological sex and gender reassignment will still be taught. The guidance for schools also contains a new section on transparency with parents, making it absolutely clear that parents have a legal right to know what their children are being taught in RSHE and can request to see teaching materials.
, opens new tab from the Williams Institute at the UCLA School of Law shows that as of 2022, approximately 1.6 million people ages 13 and older identified as transgender in the United States. This ...
The Gender Gap Is Now a Gender Gulf. Mr. Edsall contributes a weekly column from Washington, D.C., on politics, demographics and inequality. Regardless of who wins the presidential election, the ...