An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection


An Introduction to COVID-19
Simon james fong.
4 Department of Computer and Information Science, University of Macau, Taipa, Macau, China
Nilanjan Dey
5 Department of Information Technology, Techno International New Town, Kolkata, West Bengal India
Jyotismita Chaki
6 School of Information Technology and Engineering, Vellore Institute of Technology, Vellore, Tamil Nadu India
A novel coronavirus (CoV) named ‘2019-nCoV’ or ‘2019 novel coronavirus’ or ‘COVID-19’ by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [1–4]. COVID-19 is a pathogenic virus. From the phylogenetic analysis carried out with obtainable full genome sequences, bats occur to be the COVID-19 virus reservoir, but the intermediate host(s) has not been detected till now.
A Brief History of the Coronavirus Outbreak
A novel coronavirus (CoV) named ‘2019-nCoV’ or ‘2019 novel coronavirus’ or ‘COVID-19’ by the World Health Organization (WHO) is in charge of the current outbreak of pneumonia that began at the beginning of December 2019 near in Wuhan City, Hubei Province, China [ 1 – 4 ]. COVID-19 is a pathogenic virus. From the phylogenetic analysis carried out with obtainable full genome sequences, bats occur to be the COVID-19 virus reservoir, but the intermediate host(s) has not been detected till now. Though three major areas of work already are ongoing in China to advise our awareness of the pathogenic origin of the outbreak. These include early inquiries of cases with symptoms occurring near in Wuhan during December 2019, ecological sampling from the Huanan Wholesale Seafood Market as well as other area markets, and the collection of detailed reports of the point of origin and type of wildlife species marketed on the Huanan market and the destination of those animals after the market has been closed [ 5 – 8 ].
Coronaviruses mostly cause gastrointestinal and respiratory tract infections and are inherently categorized into four major types: Gammacoronavirus, Deltacoronavirus, Betacoronavirus and Alphacoronavirus [ 9 – 11 ]. The first two types mainly infect birds, while the last two mostly infect mammals. Six types of human CoVs have been formally recognized. These comprise HCoVHKU1, HCoV-OC43, Middle East Respiratory Syndrome coronavirus (MERS-CoV), Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) which is the type of the Betacoronavirus, HCoV229E and HCoV-NL63, which are the member of the Alphacoronavirus. Coronaviruses did not draw global concern until the 2003 SARS pandemic [ 12 – 14 ], preceded by the 2012 MERS [ 15 – 17 ] and most recently by the COVID-19 outbreaks. SARS-CoV and MERS-CoV are known to be extremely pathogenic and spread from bats to palm civets or dromedary camels and eventually to humans.
COVID-19 is spread by dust particles and fomites while close unsafe touch between the infector and the infected individual. Airborne distribution has not been recorded for COVID-19 and is not known to be a significant transmission engine based on empirical evidence; although it can be imagined if such aerosol-generating practices are carried out in medical facilities. Faecal spreading has been seen in certain patients, and the active virus has been reported in a small number of clinical studies [ 18 – 20 ]. Furthermore, the faecal-oral route does not seem to be a COVID-19 transmission engine; its function and relevance for COVID-19 need to be identified.
For about 18,738,58 laboratory-confirmed cases recorded as of 2nd week of April 2020, the maximum number of cases (77.8%) was between 30 and 69 years of age. Among the recorded cases, 21.6% are farmers or employees by profession, 51.1% are male and 77.0% are Hubei.
However, there are already many concerns regarding the latest coronavirus. Although it seems to be transferred to humans by animals, it is important to recognize individual animals and other sources, the path of transmission, the incubation cycle, and the features of the susceptible community and the survival rate. Nonetheless, very little clinical knowledge on COVID-19 disease is currently accessible and details on age span, the animal origin of the virus, incubation time, outbreak curve, viral spectroscopy, dissemination pathogenesis, autopsy observations, and any clinical responses to antivirals are lacking among the serious cases.
How Different and Deadly COVID-19 is Compared to Plagues in History
COVID-19 has reached to more than 150 nations, including China, and has caused WHO to call the disease a worldwide pandemic. By the time of 2nd week of April 2020, this COVID-19 cases exceeded 18,738,58, although more than 1,160,45 deaths were recorded worldwide and United States of America became the global epicentre of coronavirus. More than one-third of the COVID-19 instances are outside of China. Past pandemics that have existed in the past decade or so, like bird flu, swine flu, and SARS, it is hard to find out the comparison between those pandemics and this coronavirus. Following is a guide to compare coronavirus with such diseases and recent pandemics that have reformed the world community.
Coronavirus Versus Seasonal Influenza
Influenza, or seasonal flu, occurs globally every year–usually between December and February. It is impossible to determine the number of reports per year because it is not a reportable infection (so no need to be recorded to municipality), so often patients with minor symptoms do not go to a physician. Recent figures placed the Rate of Case Fatality at 0.1% [ 21 – 23 ].
There are approximately 3–5 million reports of serious influenza a year, and about 250,000–500,000 deaths globally. In most developed nations, the majority of deaths arise in persons over 65 years of age. Moreover, it is unsafe for pregnant mothers, children under 59 months of age and individuals with serious illnesses.
The annual vaccination eliminates infection and severe risks in most developing countries but is nevertheless a recognized yet uncomfortable aspect of the season.
In contrast to the seasonal influenza, coronavirus is not so common, has led to fewer cases till now, has a higher rate of case fatality and has no antidote.
Coronavirus Versus Bird Flu (H5N1 and H7N9)
Several cases of bird flu have existed over the years, with the most severe in 2013 and 2016. This is usually from two separate strains—H5N1 and H7N9 [ 24 – 26 ].
The H7N9 outbreak in 2016 accounted for one-third of all confirmed human cases but remained confined relative to both coronavirus and other pandemics/outbreak cases. After the first outbreak, about 1,233 laboratory-confirmed reports of bird flu have occurred. The disease has a Rate of Case Fatality of 20–40%.
Although the percentage is very high, the blowout from individual to individual is restricted, which, in effect, has minimized the number of related deaths. It is also impossible to monitor as birds do not necessarily expire from sickness.
In contrast to the bird flu, coronavirus becomes more common, travels more quickly through human to human interaction, has an inferior cardiothoracic ratio, resulting in further total fatalities and spread from the initial source.
Coronavirus Versus Ebola Epidemic
The Ebola epidemic of 2013 was primarily centred in 10 nations, including Sierra Leone, Guinea and Liberia have the greatest effects, but the extremely high Case Fatality Rate of 40% has created this as a significant problem for health professionals nationwide [ 27 – 29 ].
Around 2013 and 2016, there were about 28,646 suspicious incidents and about 11,323 fatalities, although these are expected to be overlooked. Those who survived from the original epidemic may still become sick months or even years later, because the infection may stay inactive for prolonged periods. Thankfully, a vaccination was launched in December 2016 and is perceived to be effective.
In contrast to the Ebola, coronavirus is more common globally, has caused in fewer fatalities, has a lesser case fatality rate, has no reported problems during treatment and after recovery, does not have an appropriate vaccination.
Coronavirus Versus Camel Flu (MERS)
Camel flu is a misnomer–though camels have MERS antibodies and may have been included in the transmission of the disease; it was originally transmitted to humans through bats [ 30 – 32 ]. Like Ebola, it infected only a limited number of nations, i.e. about 27, but about 858 fatalities from about 2,494 laboratory-confirmed reports suggested that it was a significant threat if no steps were taken in place to control it.
In contrast to the camel flu, coronavirus is more common globally, has occurred more fatalities, has a lesser case fatality rate, and spreads more easily among humans.
Coronavirus Versus Swine Flu (H1N1)
Swine flu is the same form of influenza that wiped 1.7% of the world population in 1918. This was deemed a pandemic again in June 2009 an approximately-21% of the global population infected by this [ 33 – 35 ].
Thankfully, the case fatality rate is substantially lower than in the last pandemic, with 0.1%–0.5% of events ending in death. About 18,500 of these fatalities have been laboratory-confirmed, but statistics range as high as 151,700–575,400 worldwide. 50–80% of severe occurrences have been reported in individuals with chronic illnesses like asthma, obesity, cardiovascular diseases and diabetes.
In contrast to the swine flu, coronavirus is not so common, has caused fewer fatalities, has more case fatality rate, has a longer growth time and less impact on young people.
Coronavirus Versus Severe Acute Respiratory Syndrome (SARS)
SARS was discovered in 2003 as it spread from bats to humans resulted in about 774 fatalities. By May there were eventually about 8,100 reports across 17 countries, with a 15% case fatality rate. The number is estimated to be closer to 9.6% as confirmed cases are counted, with 0.9% cardiothoracic ratio for people aged 20–29, rising to 28% for people aged 70–79. Similar to coronavirus, SARS had bad results for males than females in all age categories [ 36 – 38 ].
Coronavirus is more common relative to SARS, which ended in more overall fatalities, lower case fatality rate, the even higher case fatality rate in older ages, and poorer results for males.
Coronavirus Versus Hong Kong Flu (H3N2)
The Hong Kong flu pandemic erupted on 13 July 1968, with 1–4 million deaths globally by 1969. It was one of the greatest flu pandemics of the twentieth century, but thankfully the case fatality rate was smaller than the epidemic of 1918, resulting in fewer fatalities overall. That may have been attributed to the fact that citizens had generated immunity owing to a previous epidemic in 1957 and to better medical treatment [ 39 ].
In contrast to the Hong Kong flu, coronavirus is not so common, has caused in fewer fatalities and has a higher case fatality rate.
Coronavirus Versus Spanish Flu (H1N1)
The 1918 Spanish flu pandemic was one of the greatest occurrences of recorded history. During the first year of the pandemic, lifespan in the US dropped by 12 years, with more civilians killed than HIV/AIDS in 24 h [ 40 – 42 ].
Regardless of the name, the epidemic did not necessarily arise in Spain; wartime censors in Germany, the United States, the United Kingdom and France blocked news of the disease, but Spain did not, creating the misleading perception that more cases and fatalities had occurred relative to its neighbours
This strain of H1N1 eventually affected more than 500 million men, or 27% of the world’s population at the moment, and had deaths of between 40 and 50 million. At the end of 1920, 1.7% of the world’s people had expired of this illness, including an exceptionally high death rate for young adults aged between 20 and 40 years.
In contrast to the Spanish flu, coronavirus is not so common, has caused in fewer fatalities, has a higher case fatality rate, is more harmful to older ages and is less risky for individuals aged 20–40 years.
Coronavirus Versus Common Cold (Typically Rhinovirus)
Common cold is the most common illness impacting people—Typically, a person suffers from 2–3 colds each year and the average kid will catch 6–8 during the similar time span. Although there are more than 200 cold-associated virus types, infections are uncommon and fatalities are very rare and typically arise mainly in extremely old, extremely young or immunosuppressed cases [ 43 , 44 ].
In contrast to the common cold, coronavirus is not so prevalent, causes more fatalities, has more case fatality rate, is less infectious and is less likely to impact small children.
Reviews of Online Portals and Social Media for Epidemic Information Dissemination
As COVID-19 started to propagate across the globe, the outbreak contributed to a significant change in the broad technology platforms. Where they once declined to engage in the affairs of their systems, except though the possible danger to public safety became obvious, the advent of a novel coronavirus placed them in a different interventionist way of thought. Big tech firms and social media are taking concrete steps to guide users to relevant, credible details on the virus [ 45 – 48 ]. And some of the measures they’re doing proactively. Below are a few of them.
Facebook started adding a box in the news feed that led users to the Centers for Disease Control website regarding COVID-19. It reflects a significant departure from the company’s normal strategy of placing items in the News Feed. The purpose of the update, after all, is personalization—Facebook tries to give the posts you’re going to care about, whether it is because you’re connected with a person or like a post. In the virus package, Facebook has placed a remarkable algorithmic thumb on the scale, potentially pushing millions of people to accurate, authenticated knowledge from a reputable source.
Similar initiatives have been adopted by Twitter. Searching for COVID-19 will carry you to a page highlighting the latest reports from public health groups and credible national news outlets. The search also allows for common misspellings. Twitter has stated that although Russian-style initiatives to cause discontent by large-scale intelligence operations have not yet been observed, a zero-tolerance approach to network exploitation and all other attempts to exploit their service at this crucial juncture will be expected. The problem has the attention of the organization. It also offers promotional support to public service agencies and other non-profit groups.
Google has made a step in making it better for those who choose to operate or research from home, offering specialized streaming services to all paying G Suite customers. Google also confirmed that free access to ‘advanced’ Hangouts Meet apps will be rolled out to both G Suite and G Suite for Education clients worldwide through 1st July. It ensures that companies can hold meetings of up to 250 people, broadcast live to up to about 100,000 users within a single network, and archive and export meetings to Google Drive. Usually, Google pays an additional $13 per person per month for these services in comparison to G Suite’s ‘enterprise’ membership, which adds up to a total of about $25 per client each month.
Microsoft took a similar move, introducing the software ‘Chat Device’ to help public health and protection in the coronavirus epidemic, which enables collaborative collaboration via video and text messaging. There’s an aspect of self-interest in this. Tech firms are offering out their goods free of charge during periods of emergency for the same purpose as newspapers are reducing their paywalls: it’s nice to draw more paying consumers.
Pinterest, which has introduced much of the anti-misinformation strategies that Facebook and Twitter are already embracing, is now restricting the search results for ‘coronavirus’, ‘COVID-19’ and similar words for ‘internationally recognized health organizations’.
Google-owned YouTube, traditionally the most conspiratorial website, has recently introduced a connection to the World Health Organization virus epidemic page to the top of the search results. In the early days of the epidemic, BuzzFeed found famous coronavirus conspiratorial videos on YouTube—especially in India, where one ‘explain’ with a false interpretation of the sources of the disease racketeered 13 million views before YouTube deleted it. Yet in the United States, conspiratorial posts regarding the illness have failed to gain only 1 million views.
That’s not to suggest that misinformation doesn’t propagate on digital platforms—just as it travels through the broader Internet, even though interaction with friends and relatives. When there’s a site that appears to be under-performing in the global epidemic, it’s Facebook-owned WhatsApp, where the Washington Post reported ‘a torrent of disinformation’ in places like Nigeria, Indonesia, Peru, Pakistan and Ireland. Given the encrypted existence of the app, it is difficult to measure the severity of the problem. Misinformation is also spread in WhatsApp communities, where participation is restricted to about 250 individuals. Knowledge of one category may be readily exchanged with another; however, there is a considerable amount of complexity of rotating several groups to peddle affected healing remedies or propagate false rumours.
Preventative Measures and Policies Enforced by the World Health Organization (WHO) and Different Countries
Coronavirus is already an ongoing epidemic, so it is necessary to take precautions to minimize both the risk of being sick and the transmission of the disease.
WHO Advice [ 49 ]
- Wash hands regularly with alcohol-based hand wash or soap and water.
- Preserve contact space (at least 1 m/3 feet between you and someone who sneezes or coughs).
- Don’t touch your nose, head and ears.
- Cover your nose and mouth as you sneeze or cough, preferably with your bent elbow or tissue.
- Try to find early medical attention if you have fatigue, cough and trouble breathing.
- Take preventive precautions if you are in or have recently go to places where coronavirus spreads.
The first person believed to have become sick because of the latest virus was near in Wuhan on 1 December 2019. A formal warning of the epidemic was released on 31 December. The World Health Organization was informed of the epidemic on the same day. Through 7 January, the Chinese Government addressed the avoidance and regulation of COVID-19. A curfew was declared on 23 January to prohibit flying in and out of Wuhan. Private usage of cars has been banned in the region. Chinese New Year (25 January) festivities have been cancelled in many locations [ 50 ].
On 26 January, the Communist Party and the Government adopted more steps to contain the COVID-19 epidemic, including safety warnings for travellers and improvements to national holidays. The leading party has agreed to prolong the Spring Festival holiday to control the outbreak. Universities and schools across the world have already been locked down. Many steps have been taken by the Hong Kong and Macau governments, in particular concerning schools and colleges. Remote job initiatives have been placed in effect in many regions of China. Several immigration limits have been enforced.
Certain counties and cities outside Hubei also implemented travel limits. Public transit has been changed and museums in China have been partially removed. Some experts challenged the quality of the number of cases announced by the Chinese Government, which constantly modified the way coronavirus cases were recorded.
Italy, a member state of the European Union and a popular tourist attraction, entered the list of coronavirus-affected nations on 30 January, when two positive cases in COVID-19 were identified among Chinese tourists. Italy has the largest number of coronavirus infections both in Europe and outside of China [ 51 ].
Infections, originally limited to northern Italy, gradually spread to all other areas. Many other nations in Asia, Europe and the Americas have tracked their local cases to Italy. Several Italian travellers were even infected with coronavirus-positive in foreign nations.
Late in Italy, the most impacted coronavirus cities and counties are Lombardia, accompanied by Veneto, Emilia-Romagna, Marche and Piedmonte. Milan, the second most populated city in Italy, is situated in Lombardy. Other regions in Italy with coronavirus comprised Campania, Toscana, Liguria, Lazio, Sicilia, Friuli Venezia Giulia, Umbria, Puglia, Trento, Abruzzo, Calabria, Molise, Valle d’Aosta, Sardegna, Bolzano and Basilicata.
Italy ranks 19th of the top 30 nations getting high-risk coronavirus airline passengers in China, as per WorldPop’s provisional study of the spread of COVID-19.
The Italian State has taken steps like the inspection and termination of large cultural activities during the early days of the coronavirus epidemic and has gradually declared the closing of educational establishments and airport hygiene/disinfection initiatives.
The Italian National Institute of Health suggested social distancing and agreed that the broader community of the country’s elderly is a problem. In the meantime, several other nations, including the US, have recommended that travel to Italy should be avoided temporarily, unless necessary.
The Italian government has declared the closing (quarantine) of the impacted areas in the northern region of the nation so as not to spread to the rest of the world. Italy has declared the immediate suspension of all to-and-fro air travel with China following coronavirus discovery by a Chinese tourist to Italy. Italian airlines, like Ryan Air, have begun introducing protective steps and have begun calling for the declaration forms to be submitted by passengers flying to Poland, Slovakia and Lithuania.
The Italian government first declined to permit fans to compete in sporting activities until early April to prevent the potential transmission of coronavirus. The step ensured players of health and stopped event cancellations because of coronavirus fears. Two days of the declaration, the government cancelled all athletic activities owing to the emergence of the outbreak asking for an emergency. Sports activities in Veneto, Lombardy and Emilia-Romagna, which recorded coronavirus-positive infections, were confirmed to be temporarily suspended. Schools and colleges in Italy have also been forced to shut down.
Iran announced the first recorded cases of SARS-CoV-2 infection on 19 February when, as per the Medical Education and Ministry of Health, two persons died later that day. The Ministry of Islamic Culture and Guidance has declared the cancellation of all concerts and other cultural activities for one week. The Medical Education and Ministry of Health has also declared the closing of universities, higher education colleges and schools in many cities and regions. The Department of Sports and Culture has taken action to suspend athletic activities, including football matches [ 52 ].
On 2 March 2020, the government revealed plans to train about 300,000 troops and volunteers to fight the outbreak of the epidemic, and also send robots and water cannons to clean the cities. The State also developed an initiative and a webpage to counter the epidemic. On 9 March 2020, nearly 70,000 inmates were immediately released from jail owing to the epidemic, presumably to prevent the further dissemination of the disease inside jails. The Revolutionary Guards declared a campaign on 13 March 2020 to clear highways, stores and public areas in Iran. President Hassan Rouhani stated on 26 February 2020 that there were no arrangements to quarantine areas impacted by the epidemic and only persons should be quarantined. The temples of Shia in Qom stayed open to pilgrims.
South Korea
On 20 January, South Korea announced its first occurrence. There was a large rise in cases on 20 February, possibly due to the meeting in Daegu of a progressive faith community recognized as the Shincheonji Church of Christ. Any citizens believed that the hospital was propagating the disease. As of 22 February, 1,261 of the 9,336 members of the church registered symptoms. A petition was distributed calling for the abolition of the church. More than 2,000 verified cases were registered on 28 February, increasing to 3,150 on 29 February [ 53 ].
Several educational establishments have been partially closing down, including hundreds of kindergartens in Daegu and many primary schools in Seoul. As of 18 February, several South Korean colleges had confirmed intentions to delay the launch of the spring semester. That included 155 institutions deciding to postpone the start of the semester by two weeks until 16 March, and 22 institutions deciding to delay the start of the semester by one week until 9 March. Also, on 23 February 2020, all primary schools, kindergartens, middle schools and secondary schools were declared to postpone the start of the semester from 2 March to 9 March.
South Korea’s economy is expected to expand by 1.9%, down from 2.1%. The State has given 136.7 billion won funding to local councils. The State has also coordinated the purchase of masks and other sanitary supplies. Entertainment Company SM Entertainment is confirmed to have contributed five hundred million won in attempts to fight the disease.
In the kpop industry, the widespread dissemination of coronavirus within South Korea has contributed to the cancellation or postponement of concerts and other programmes for kpop activities inside and outside South Korea. For instance, circumstances such as the cancellation of the remaining Asian dates and the European leg for the Seventeen’s Ode To You Tour on 9 February 2020 and the cancellation of all Seoul dates for the BTS Soul Tour Map. As of 15 March, a maximum of 136 countries and regions provided entry restrictions and/or expired visas for passengers from South Korea.
The overall reported cases of coronavirus rose significantly in France on 12 March. The areas with reported cases include Paris, Amiens, Bordeaux and Eastern Haute-Savoie. The first coronaviral death happened in France on 15 February, marking it the first death in Europe. The second death of a 60-year-old French national in Paris was announced on 26 February [ 54 ].
On February 28, fashion designer Agnès B. (not to be mistaken with Agnès Buzyn) cancelled fashion shows at the Paris Fashion Week, expected to continue until 3 March. On a subsequent day, the Paris half-marathon, planned for Sunday 1 March with 44,000 entrants, was postponed as one of a series of steps declared by Health Minister Olivier Véran.
On 13 March, the Ligue de Football Professional disbanded Ligue 1 and Ligue 2 (France’s tier two professional divisions) permanently due to safety threats.
Germany has a popular Regional Pandemic Strategy detailing the roles and activities of the health care system participants in the case of a significant outbreak. Epidemic surveillance is carried out by the federal government, like the Robert Koch Center, and by the German governments. The German States have their preparations for an outbreak. The regional strategy for the treatment of the current coronavirus epidemic was expanded by March 2020. Four primary goals are contained in this plan: (1) to minimize mortality and morbidity; (2) to guarantee the safety of sick persons; (3) to protect vital health services and (4) to offer concise and reliable reports to decision-makers, the media and the public [ 55 ].
The programme has three phases that may potentially overlap: (1) isolation (situation of individual cases and clusters), (2) safety (situation of further dissemination of pathogens and suspected causes of infection), (3) prevention (situation of widespread infection). So far, Germany has not set up border controls or common health condition tests at airports. Instead, while at the isolation stage-health officials are concentrating on recognizing contact individuals that are subject to specific quarantine and are tracked and checked. Specific quarantine is regulated by municipal health authorities. By doing so, the officials are seeking to hold the chains of infection small, contributing to decreased clusters. At the safety stage, the policy should shift to prevent susceptible individuals from being harmed by direct action. By the end of the day, the prevention process should aim to prevent cycles of acute treatment to retain emergency facilities.
United States
The very first case of coronavirus in the United States was identified in Washington on 21 January 2020 by an individual who flew to Wuhan and returned to the United States. The second case was recorded in Illinois by another individual who had travelled to Wuhan. Some of the regions with reported novel coronavirus infections in the US are California, Arizona, Connecticut, Illinois, Texas, Wisconsin and Washington [ 56 ].
As the epidemic increased, requests for domestic air travel decreased dramatically. By 4 March, U.S. carriers, like United Airlines and JetBlue Airways, started growing their domestic flight schedules, providing generous unpaid leave to workers and suspending recruits.
A significant number of universities and colleges cancelled classes and reopened dormitories in response to the epidemic, like Cornell University, Harvard University and the University of South Carolina.
On 3 March 2020, the Federal Reserve reduced its goal interest rate from 1.75% to 1.25%, the biggest emergency rate cut following the 2008 global financial crash, in combat the effect of the recession on the American economy. In February 2020, US businesses, including Apple Inc. and Microsoft, started to reduce sales projections due to supply chain delays in China caused by the COVID-19.
The pandemic, together with the subsequent financial market collapse, also contributed to greater criticism of the crisis in the United States. Researchers disagree about when a recession is likely to take effect, with others suggesting that it is not unavoidable, while some claim that the world might already be in recession. On 3 March, Federal Reserve Chairman Jerome Powell reported a 0.5% (50 basis point) interest rate cut from the coronavirus in the context of the evolving threats to economic growth.
When ‘social distance’ penetrated the national lexicon, disaster response officials promoted the cancellation of broad events to slow down the risk of infection. Technical conferences like E3 2020, Apple Inc.’s Worldwide Developers Conference (WWDC), Google I/O, Facebook F8, and Cloud Next and Microsoft’s MVP Conference have been either having replaced or cancelled in-person events with internet streaming events.
On February 29, the American Physical Society postponed its annual March gathering, planned for March 2–6 in Denver, Colorado, even though most of the more than 11,000 physicist attendees already had arrived and engaged in the pre-conference day activities. On March 6, the annual South to Southwest (SXSW) seminar and festival planned to take place from March 13–22 in Austin, Texas, was postponed after the city council announced a local disaster and forced conferences to be shut down for the first time in 34 years.
Four of North America’s major professional sports leagues—the National Hockey League (NHL), National Basketball Association (NBA), Major League Soccer (MLS) and Major League Baseball (MLB) —jointly declared on March 9 that they would all limit the media access to player accommodations (such as locker rooms) to control probable exposure.
Emergency Funding to Fight the COVID-19
COVID-19 pandemic has become a common international concern. Different countries are donating funds to fight against it [ 57 – 60 ]. Some of them are mentioned here.
China has allocated about 110.48 billion yuan ($15.93 billion) in coronavirus-related funding.
Foreign Minister Mohammad Javad Zarif said that Iran has requested the International Monetary Fund (IMF) of about $5 billion in emergency funding to help to tackle the coronavirus epidemic that has struck the Islamic Republic hard.
President Donald Trump approved the Emergency Supplementary Budget Bill to support the US response to a novel coronavirus epidemic. The budget plan would include about $8.3 billion in discretionary funding to local health authorities to promote vaccine research for production. Trump originally requested just about $2 billion to combat the epidemic, but Congress quadrupled the number in its version of the bill. Mr. Trump formally announced a national emergency that he claimed it will give states and territories access to up to about $50 billion in federal funding to tackle the spread of the coronavirus outbreak.
California politicians approved a plan to donate about $1 billion on the state’s emergency medical responses as it readies hospitals to fight an expected attack of patients because of the COVID-19 pandemic. The plans, drawn up rapidly in reaction to the dramatic rise in reported cases of the virus, would include the requisite funds to establish two new hospitals in California, with the assumption that the state may not have the resources to take care of the rise in patients. The bill calls for an immediate response of about $500 million from the State General Fund, with an additional about $500 million possible if requested.
India committed about $10 million to the COVID-19 Emergency Fund and said it was setting up a rapid response team of physicians for the South Asian Association for Regional Cooperation (Saarc) countries.
South Korea unveiled an economic stimulus package of about 11.7 trillion won ($9.8 billion) to soften the effects of the biggest coronavirus epidemic outside China as attempts to curb the disease exacerbate supply shortages and drain demand. Of the 11,7 trillion won expected, about 3.2 trillion won would cover up the budget shortfall, while an additional fiscal infusion of about 8.5 trillion won. An estimated 10.3 trillion won in government bonds will be sold this year to fund the extra expenditure. About 2.3 trillion won will be distributed to medical establishments and would support quarantine operations, with another 3.0 trillion won heading to small and medium-sized companies unable to pay salaries to their employees and child care supports.
The Swedish Parliament announced a set of initiatives costing more than 300 billion Swedish crowns ($30.94 billion) to help the economy in the view of the coronavirus pandemic. The plan contained steps like the central government paying the entire expense of the company’s sick leave during April and May, and also the high cost of compulsory redundancies owing to the crisis.
In consideration of the developing scenario, an updating of this strategy is planned to take place before the end of March and will recognize considerably greater funding demands for the country response, R&D and WHO itself.
Artificial Intelligence, Data Science and Technological Solutions Against COVID-19
These days, Artificial Intelligence (AI) takes a major role in health care. Throughout a worldwide pandemic such as the COVID-19, technology, artificial intelligence and data analytics have been crucial in helping communities cope successfully with the epidemic [ 61 – 65 ]. Through the aid of data mining and analytical modelling, medical practitioners are willing to learn more about several diseases.
Public Health Surveillance
The biggest risk of coronavirus is the level of spreading. That’s why policymakers are introducing steps like quarantines around the world because they can’t adequately monitor local outbreaks. One of the simplest measures to identify ill patients through the study of CCTV images that are still around us and to locate and separate individuals that have serious signs of the disease and who have touched and disinfected the related surfaces. Smartphone applications are often used to keep a watch on people’s activities and to assess whether or not they have come in touch with an infected human.
Remote Biosignal Measurement
Many of the signs such as temperature or heartbeat are very essential to overlook and rely entirely on the visual image that may be misleading. However, of course, we can’t prevent someone from checking their blood pressure, heart or temperature. Also, several advances in computer vision can predict pulse and blood pressure based on facial skin examination. Besides, there are several advances in computer vision that can predict pulse and blood pressure based on facial skin examination.
Access to public records has contributed to the development of dashboards that constantly track the virus. Several companies are designing large data dashboards. Face recognition and infrared temperature monitoring technologies have been mounted in all major cities. Chinese AI companies including Hanwang Technology and SenseTime have reported having established a special facial recognition system that can correctly identify people even though they are covered.
IoT and Wearables
Measurements like pulse are much more natural and easier to obtain from tracking gadgets like activity trackers and smartwatches that nearly everybody has already. Some work suggests that the study of cardiac activity and its variations from the standard will reveal early signs of influenza and, in this case, coronavirus.
Chatbots and Communication
Apart from public screening, people’s knowledge and self-assessment may also be used to track their health. If you can check your temperature and pulse every day and monitor your coughs time-to-time, you can even submit that to your record. If the symptoms are too serious, either an algorithm or a doctor remotely may prescribe a person to stay home, take several other preventive measures, or recommend a visit from the doctor.
Al Jazeera announced that China Mobile had sent text messages to state media departments, telling them about the citizens who had been affected. The communications contained all the specifics of the person’s travel history.
Tencent runs WeChat, and via it, citizens can use free online health consultation services. Chatbots have already become important connectivity platforms for transport and tourism service providers to keep passengers up-to-date with the current transport protocols and disturbances.
Social Media and Open Data
There are several people who post their health diary with total strangers via Facebook or Twitter. Such data becomes helpful for more general research about how far the epidemic has progressed. For consumer knowledge, we may even evaluate the social network group to attempt to predict what specific networks are at risk of being viral.
Canadian company BlueDot analyses far more than just social network data: for instance, global activities of more than four billion passengers on international flights per year; animal, human and insect population data; satellite environment data and relevant knowledge from health professionals and journalists, across 100,000 news posts per day covering 65 languages. This strategy was so successful that the corporation was able to alert clients about coronavirus until the World Health Organization and the Centers for Disease Control and Prevention notified the public.
Automated Diagnostics
COVID-19 has brought up another healthcare issue today: it will not scale when the number of patients increases exponentially (actually stressed doctors are always doing worse) and the rate of false-negative diagnosis remains very high. Machine learning therapies don’t get bored and scale simply by growing computing forces.
Baidu, the Chinese Internet company, has made the Lineatrfold algorithm accessible to the outbreak-fighting teams, according to the MIT Technology Review. Unlike HIV, Ebola and Influenza, COVID-19 has just one strand of RNA and it can mutate easily. The algorithm is also simpler than other algorithms that help to determine the nature of the virus. Baidu has also developed software to efficiently track large populations. It has also developed an Ai-powered infrared device that can detect a difference in the body temperature of a human. This is currently being used in Beijing’s Qinghe Railway Station to classify possibly contaminated travellers where up to 200 individuals may be checked in one minute without affecting traffic movement, reports the MIT Review.
Singapore-based Veredus Laboratories, a supplier of revolutionary molecular diagnostic tools, has currently announced the launch of the VereCoV detector package, a compact Lab-on-Chip device able to detect MERS-CoV, SARS-CoV and COVID-19, i.e. Wuhan Coronavirus, in a single study.
The VereCoV identification package is focused on VereChip technology, a Lab-on-Chip device that incorporates two important molecular biological systems, Polymerase Chain Reaction (PCR) and a microarray, which will be able to classify and distinguish within 2 h MERS-CoV, SARS-CoV and COVID-19 with high precision and responsiveness.
This is not just the medical activities of healthcare facilities that are being charged, but also the corporate and financial departments when they cope with the increase in patients. Ant Financials’ blockchain technology helps speed-up the collection of reports and decreases the number of face-to-face encounters with patients and medical personnel.
Companies like the Israeli company Sonovia are aiming to provide healthcare systems and others with face masks manufactured from their anti-pathogenic, anti-bacterial cloth that depends on metal-oxide nanoparticles.
Drug Development Research
Aside from identifying and stopping the transmission of pathogens, the need to develop vaccinations on a scale is also needed. One of the crucial things to make that possible is to consider the origin and essence of the virus. Google’s DeepMind, with their expertise in protein folding research, has rendered a jump in identifying the protein structure of the virus and making it open-source.
BenevolentAI uses AI technologies to develop medicines that will combat the most dangerous diseases in the world and is also working to promote attempts to cure coronavirus, the first time the organization has based its product on infectious diseases. Within weeks of the epidemic, it used its analytical capability to recommend new medicines that might be beneficial.
Robots are not vulnerable to the infection, and they are used to conduct other activities, like cooking meals in hospitals, doubling up as waiters in hotels, spraying disinfectants and washing, selling rice and hand sanitizers, robots are on the front lines all over to deter coronavirus spread. Robots also conduct diagnostics and thermal imaging in several hospitals. Shenzhen-based firm Multicopter uses robotics to move surgical samples. UVD robots from Blue Ocean Robotics use ultraviolet light to destroy viruses and bacteria separately. In China, Pudu Technology has introduced its robots, which are usually used in the cooking industry, to more than 40 hospitals throughout the region. According to the Reuters article, a tiny robot named Little Peanut is distributing food to passengers who have been on a flight from Singapore to Hangzhou, China, and are presently being quarantined in a hotel.
Colour Coding
Using its advanced and vast public service monitoring network, the Chinese government has collaborated with software companies Alibaba and Tencent to establish a colour-coded health ranking scheme that monitors millions of citizens every day. The mobile device was first introduced in Hangzhou with the cooperation of Alibaba. This applies three colours to people—red, green or yellow—based on their transportation and medical records. Tencent also developed related applications in the manufacturing centre of Shenzhen.
The decision of whether an individual will be quarantined or permitted in public spaces is dependent on the colour code. Citizens will sign into the system using pay wallet systems such as Alibaba’s Alipay and Ant’s wallet. Just those citizens who have been issued a green colour code will be permitted to use the QR code in public spaces at metro stations, workplaces, and other public areas. Checkpoints are in most public areas where the body temperature and the code of individual are tested. This programme is being used by more than 200 Chinese communities and will eventually be expanded nationwide.
In some of the seriously infected regions where people remain at risk of contracting the infection, drones are used to rescue. One of the easiest and quickest ways to bring emergency supplies where they need to go while on an epidemic of disease is by drone transportation. Drones carry all surgical instruments and patient samples. This saves time, improves the pace of distribution and reduces the chance of contamination of medical samples. Drones often operate QR code placards that can be checked to record health records. There are also agricultural drones distributing disinfectants in the farmland. Drones, operated by facial recognition, are often used to warn people not to leave their homes and to chide them for not using face masks. Terra Drone uses its unmanned drones to move patient samples and vaccination content at reduced risk between the Xinchang County Disease Control Center and the People’s Hospital. Drones are often used to monitor public areas, document non-compliance with quarantine laws and thermal imaging.
Autonomous Vehicles
At a period of considerable uncertainty to medical professionals and the danger to people-to-people communication, automated vehicles are proving to be of tremendous benefit in the transport of vital products, such as medications and foodstuffs. Apollo, the Baidu Autonomous Vehicle Project, has joined hands with the Neolix self-driving company to distribute food and supplies to a big hospital in Beijing. Baidu Apollo has also provided its micro-car packages and automated cloud driving systems accessible free of charge to virus-fighting organizations.
Idriverplus, a Chinese self-driving organization that runs electrical street cleaning vehicles, is also part of the project. The company’s signature trucks are used to clean hospitals.
This chapter provides an introduction to the coronavirus outbreak (COVID-19). A brief history of this virus along with the symptoms are reported in this chapter. Then the comparison between COVID-19 and other plagues like seasonal influenza, bird flu (H5N1 and H7N9), Ebola epidemic, camel flu (MERS), swine flu (H1N1), severe acute respiratory syndrome, Hong Kong flu (H3N2), Spanish flu and the common cold are included in this chapter. Reviews of online portal and social media like Facebook, Twitter, Google, Microsoft, Pinterest, YouTube and WhatsApp concerning COVID-19 are reported in this chapter. Also, the preventive measures and policies enforced by WHO and different countries such as China, Italy, Iran, South Korea, France, Germany and the United States for COVID-19 are included in this chapter. Emergency funding provided by different countries to fight the COVID-19 is mentioned in this chapter. Lastly, artificial intelligence, data science and technological solutions like public health surveillance, remote biosignal measurement, IoT and wearables, chatbots and communication, social media and open data, automated diagnostics, drug development research, robotics, colour coding, drones and autonomous vehicles are included in this chapter.
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Online education and its effect on teachers during COVID-19—A case study from India
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Area of Humanities and Social Sciences, Indian Institute of Management Indore, Indore, Madhya Pradesh, India
- Surbhi Dayal

- Published: March 2, 2023
- https://doi.org/10.1371/journal.pone.0282287
- Reader Comments
COVID pandemic resulted in an initially temporary and then long term closure of educational institutions, creating a need for adapting to online and remote learning. The transition to online education platforms presented unprecedented challenges for the teachers. The aim of this research was to investigate the effects of the transition to online education on teachers’ wellbeing in India.
The research was conducted on 1812 teachers working in schools, colleges, and coaching institutions from six different Indian states. Quantitative and qualitative data was collected via online survey and telephone interviews.
The results show that COVID pandemic exacerbated the existing widespread inequality in access to internet connectivity, smart devices, and teacher training required for an effective transition to an online mode of education. Teachers nonetheless adapted quickly to online teaching with the help of institutional training as well as self-learning tools. However, respondents expressed dissatisfaction with the effectiveness of online teaching and assessment methods, and exhibited a strong desire to return to traditional modes of learning. 82% respondents reported physical issues like neck pain, back pain, headache, and eyestrain. Additionally, 92% respondents faced mental issues like stress, anxiety, and loneliness due to online teaching.
As the effectiveness of online learning perforce taps on the existing infrastructure, not only has it widened the learning gap between the rich and the poor, it has also compromised the quality of education being imparted in general. Teachers faced increased physical and mental health issues due to long working hours and uncertainty associated with COVID lockdowns. There is a need to develop a sound strategy to address the gaps in access to digital learning and teachers’ training to improve both the quality of education and the mental health of teachers.
Citation: Dayal S (2023) Online education and its effect on teachers during COVID-19—A case study from India. PLoS ONE 18(3): e0282287. https://doi.org/10.1371/journal.pone.0282287
Editor: Lütfullah Türkmen, Usak University College of Education, TURKEY
Received: November 13, 2021; Accepted: January 27, 2023; Published: March 2, 2023
Copyright: © 2023 Surbhi Dayal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: Data apart from manuscript has been submitted as supporting information .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
As of November 4, 2021, the spread of novel coronavirus had reached 219 countries and territories of the world, infecting a total of 248 million people and resulting in five million deaths [ 1 ]. In March 2020, several countries including India declared a mandatory lockdown, resulting in the temporary closure of many institutions, not least educational ones. Since then, various restrictions and strategies have been implemented to counter the spread of the virus. These include wearing masks, washing hands frequently, maintaining social and physical distance, and avoiding public gatherings. The pandemic has greatly disrupted all aspects of human life and forced new ways of functioning, notably in work and education, much of which has been restricted to the household environment. The closure for over a year of many schools and colleges across the world has shaken the foundations of the traditional structures of education. Due to widespread restrictions, employees have been forced to carve out working spaces in the family home; likewise, students and teachers have been compelled to bring classes into homes [ 2 ]. Nearly 1.6 billion learners in more than 190 countries have been physically out of school due to the pandemic. In total, 94 percent of the world’s student population has been affected by school closures, and up to 99 percent of this student population come from low-to middle-income countries [ 3 ].
According to the World Economic Forum, the pandemic has changed how people receive and impart education [ 4 ]. Physical interaction between students and teachers in traditional classrooms has been replaced by exchanges on digital learning platforms, such as online teaching and virtual education systems, characterized by an absence of face-to-face connection [ 5 ]. Online education has thus emerged as a viable option for education from preschool to university level, and governments have used tools such as radio, television, and social media to support online teaching and training [ 6 ]. Various stakeholders, including government and private institutions, have collaborated to provide teachers with resources and training to teach effectively on digital platforms. New digital learning platforms like Zoom, Google Classroom, Canvas, and Blackboard have been used extensively to create learning material and deliver online classes; they have also allowed teachers to devise training and skill development programs [ 7 ]. Many teachers and students were initially hesitant to adopt online education. However indefinite closure of institutions required educational facilities to find new methods to impart education and forced teachers to learn new digital skills. Individuals have experienced different levels of difficulty in doing this; for some, “it has resulted in tears, and for some, it is a cup of tea” [ 8 ].
Teachers have reported finding it difficult to use online teaching as a daily mode of communication, and enabling students’ cognitive activation has presented a significant challenge in the use of distance modes of teaching and learning. Teachers have also expressed concerns about administering tests with minimal student interaction [ 9 ]. Lack of availability of smart devices, combined with unreliable internet access, has led to dissatisfaction with teacher-student interaction. Under pressure to select the appropriate tools and media to reach their students, some teachers have relied on pre-recorded videos, which further discouraged interaction. In locations where most teaching is done online, teachers in tier 2 and tier 3 cities (i.e., semi-urban areas) have had to pay extra to secure access to high-speed internet, digital devices, and reliable power sources [ 10 ]. Teachers in India, in particular, have a huge gap in digital literacy caused by a lack of training and access to reliable electricity supply, and internet services. In rural or remote areas, access to smart devices, the internet, and technology is limited and inconsistent [ 6 ]. In cities, including the Indian capital Delhi, even teachers who are familiar with the required technology do not necessarily have the pedagogical skills to meet the demands of online education. The absence of training, along with local factors (for example, stakeholders’ infrastructure and socio-economic standing), contributes to difficulties in imparting digital education successfully [ 10 ]. The gap in digital education across Indian schools is striking. For example, only 32.5% of school children are in a position to pursue online classes. Only 11% of children can take online classes in private and public schools, and more than half can only view videos or other recorded content. Only 8.1% of children in government schools have access to online classes in the event of a pandemic-related restrictions [ 11 ].
The adverse effects of COVID-19 on education must therefore be investigated and understood, particularly the struggles of students and teachers to adapt to new technologies. Significant societal effects of the pandemic include not only serious disruption of education but also isolation caused by social distancing. Various studies [ 7 , 12 , 13 ] have suggested that online education has caused significant stress and health problems for students and teachers alike; health issues have also been exacerbated by the extensive use of digital devices. Several studies [ 6 , 11 , 14 ] have been conducted to understand the effects of the COVID lockdown on digital access to education, students’ physical and emotional well-being, and the effectiveness of online education. However, only a few studies [ 13 , 15 – 17 ] have touched the issues that teachers faced due to COVID lockdown.
In this context, this study is trying to fill existing gaps and focuses on the upheavals that teachers went through to accommodate COVID restrictions and still impart education. It also provides an in-depth analysis of consequences for the quality of education imparted from the teachers’ perspective. It discusses geographical inequalities in access to the infrastructure required for successful implementation of online education. In particular, it addresses the following important questions: (1) how effectively have teachers adapted to the new virtual system? (2) How has online education affected the quality of teaching? (3) How has online education affected teachers’ overall health?
Because of lockdown restrictions, data collection for this study involved a combination of qualitative and quantitative methods in the form of online surveys and telephonic interviews. A questionnaire for teachers was developed consisting of 41 items covering a variety of subjects: teaching styles, life-work balance, and how working online influences the mental and physical well-being of teachers. In the interviews, participants were asked about their experiences of online teaching during the pandemic, particularly in relation to physical and mental health issues. A pilot study was conducted with thirty respondents, and necessary changes to the items were made before the data collection. The survey tool was created using google forms and disseminated via email, Facebook, and WhatsApp. A total of 145 telephonic interviews were also conducted to obtain in-depth information from the respondents.
The data were collected between December 2020 and June 2021. The Research Advisory Committee on Codes of Ethics for Research of Aggrawal College, Ballabhgarh, Haryana, reviewed and approved this study. A statement included in the google survey form as a means of acquiring written consent from the participants. Information was gathered from 1,812 Indian teachers in six Indian states (Assam, Haryana, Karnataka, Madhya Pradesh, New Delhi, and Rajasthan) working in universities, schools, and coaching institutions. Nearly three-quarters of the total sample population was women. All participants were between the ages of 18 and 60, with an average age of 34 and a clear majority being 35 or younger. Nearly three-quarters of participants work in private institutions (25% in semi-government entities and the remainder in government entities). In terms of education, 52% of participants have a graduate degree, 34% a postgraduate degree, and 14% a doctorate. Table 1 summarizes the demographic characteristics of the participants.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0282287.t001
Results & discussion
Upon analyzing the survey responses, three crucial areas were identified for a better understanding of the effect of COVID-19 on the Indian education system and its teachers: how effectively teachers have adapted, how effective teaching has been, and how teachers’ health has been affected.
1. How effectively have teachers adapted to the new virtual system?
The first research question concerns how willing teachers were to embrace the changes brought about by the online teaching system and how quickly they were able to adapt to online modes of instruction. This information was gathered from December 2020 to June 2021, at which point teachers had been dealing with school lockdowns for months and therefore had some time to become conversant with online teaching.
While 93.82% of respondents were involved in online teaching during the pandemic, only 16% had previously taught online. These results were typically different from the results of a similar study conducted in Jordon where most of the faculty (60%) had previous experience with online teaching and 68% of faculty had also received formal training [ 16 ]. Since the spread of COVID-19 was rapid and the implementation of the lockdown was sudden, government and educational institutions were not prepared for alternative modes of learning, and teachers needed some time for adjustment. Several other factors also affected the effectiveness of the transition to online education, namely access to different types of resources and training [ 18 ].
a. Access to smart devices.
Online teaching requires access to smart devices. A surprising number of teachers stated that they had internet access at home via laptops, smartphones, or tablets. A more pertinent question, however, was whether they had sole access to the smart device, or it was shared with family members. Only 37.25% of those surveyed had a device for their exclusive use while others shared a device with family members, due to lack of access to additional devices and affordability of new devices. During the lockdown, an increase in demand led to a scarcity of smart devices, so that even people who could afford to buy a device could not necessarily find one available for purchase. With children attending online classes, and family members working from home, households found it difficult to manage with only a few devices, and access to a personal digital device became an urgent matter for many. Respondents admitted to relying on their smartphones to teach courses since they lacked access to other devices. Teachers on independent-school rosters were significantly better equipped to access smart devices than those employed at other types of schools. The data also indicates that teachers in higher education and at coaching centers had relatively better access to laptops and desktop computers through their institutions, whereas teachers in elementary and secondary schools had to scramble for securing devices for their own use.
b. Internet access.
Internet access is crucial for effective delivery of online education. However, our survey shows that teachers often struggled to stay connected because of substantial differences between states in the availability of internet. Of the respondents, 52% reported that their internet was stable and reliable, 32% reported it to be satisfactory and the rest reported it to be poor. Internet connectivity was better in the states of Karnataka, New Delhi, and Rajasthan than in Assam, Haryana, and Madhya Pradesh. Internet connectivity in Assam was particularly poor. Consequently, many teachers with access to advanced devices were unable to use them due to inadequate internet connection.
The following comments from a teacher in Assam capture relevant situational challenges: “I do not have an internet modem at home, and teaching over the phone is difficult. My internet connection is exhausted, and I am unable to see or hear the students.” Another teacher from Haryana reported similar difficulties: “During the lockdown, I moved to my hometown, and I do not have internet access here, so I go to a nearby village and send videos to students every three days.” Another teacher from Madhya Pradesh working at a premier institution reported experiencing somewhat different concerns: “I am teaching in one of the institute’s semi-smart classrooms, and while I have access to the internet, my students do not, making it difficult to hear what they are saying.”
These responses indicates clearly that it is not only teachers living in states where connectivity was poor who experienced difficulties in imparting education to students; even those who had good internet connectivity experiences problems caused by the poor internet connections of their students.
c. Tools for remote learning.
Teachers made use of a variety of remote learning tools, but access to these tools varied depending on the educator’s affiliation. Teachers at premier institutions and coaching centers routinely used the Zoom and Google Meet apps to conduct synchronous lessons. Teachers at state colleges used pre-recorded videos that were freely available on YouTube. Teachers in government schools used various platforms, including WhatsApp for prepared material and YouTube for pre-recorded videos. To deliver the content, private school teachers used pre-recorded lectures and Google Meet. In addition to curriculum classes, school teachers offered life skill classes (for example, cooking, gardening, and organizing) to help students become more independent and responsible in these difficult circumstances. In addition to online instruction, 16% of teachers visited their students’ homes to distribute books and other materials. Furthermore, of this 36% visited students’ homes once a week, 29% visited twice a week, 18% once every two weeks, and the rest once a month. Additionally, a survey done on 6435 respondents across six states in India reported that 21% teachers in schools conducted home visits for teaching children [ 19 ].
d. Knowledge and training for the use of information and communication technologies.
With the onset of the pandemic, information and communication technology (ICT) became a pivotal point for the viability of online education. The use of ICT can facilitate curriculum coverage, application of pedagogical practices and assessment, teacher’s professional development, and streamlining school organization [ 20 ]. However, the effective adoption and implementation of ICT necessitated delivery of appropriate training and prolonged practice. Also the manner in which teachers use ICT is crucial to successful implementation of online education [ 21 ]. While countries such as Germany, Japan, Turkey, the United Kingdom, and the United States recognized the importance of ICT by integrating it into their respective teacher training programmes [ 22 ], this has not been case in India. However, there are some training programmes available to teachers once they commence working. In accordance with our survey results, the vast majority of respondents (94%) lacked any ICT training or experience. In the absence of appropriate tools and support, these teachers self-experimented with online platforms, with equal chances of success and failure.
The transition from offline to online or remote learning was abrupt, and teachers had to adapt quickly to the new systems. Our data indicate that teachers in professional colleges and coaching centers received some training to help them adapt to the new online system, whereas teachers in urban areas primarily learned on their own from YouTube videos, and school teachers in rural areas received no support at all. Overall, teachers had insufficient training and support to adjust to this completely new situation. Policy research conducted on online and remote learning systems following COVID-19 has found similar results, namely that teachers implemented distance learning modalities from the start of the pandemic, often without adequate guidance, training, or resources [ 23 ]. Similar trends have been found in the Caribbean, where the unavailability of smart learning devices, lack of or poor internet access, and lack of prior training for teachers and students hampered online learning greatly. Furthermore, in many cases the curriculum was not designed for online teaching, which was a key concern for teachers [ 24 ]. Preparing online lectures as well as monitoring, supervising and providing remote support to students also led to stress and anxiety. Self-imposed perfectionism further exacerbated these issues while delivering online education [ 15 ]. A study conducted on 288 teachers from private and government schools in Delhi and National Capital Region area, also found that transition to online education has further widened the gap between pupils from government and private schools. It was more difficult to reach students from economically weaker sections of the society due to the digital divide in terms of access, usage, and skills gap. The study also found that even when teachers were digitally savvy, it did not mean that they know how to prepare for and take online classes [ 10 ].
2. How has online education affected the quality of teaching?
Once teachers had acquired some familiarity with the online system, new questions arose concerning how online education affected the quality of teaching in terms of learning and assessment, and how satisfied teachers were with this new mode of imparting education. To address these questions, specific questionnaire items about assessment and effectiveness of teaching has been included.
a. Effectiveness of online education.
Respondents agreed unanimously that online education impeded student-teacher bonding. They reported several concerns, including the inattentiveness of the majority of the students in the class, the physical absence of students (who at times logged in but then went elsewhere), the inability to engage students online, and the difficulty of carrying out any productive discussion given that only a few students were participating. Another significant concern was the difficulty in administrating online tests in light of widespread cheating. In the words of one teacher: “I was teaching a new class of students with whom I had never interacted in person. It was not easy because I could not remember the names of the students or relate to them. Students were irritated when I called out their names. It had a significant impact on my feedback. I would like us to return to class so I do not have to manage four screens and can focus on my students and on solving their problems.”
For these reasons, 85.65% of respondents stated that the quality of education had been significantly compromised in the online mode. As a result, only 33% reported being interested in continuing with online teaching after COVID-19. The results show slightly higher dissatisfaction in comparison to another study conducted in India that reported 67% of teachers feeling dissatisfied with online teaching [ 25 ]. Findings of this study were similar to the findings of a survey of lecturers in Ukraine assessing the effectiveness of online education. Lower quality student work was cited as the third most mentioned problem among the problems cited by instructors in their experience with online teaching, right behind unreliable internet connectivity and the issues related with software and hardware. Primary reasons for lower quality student work were drop in the number of assignments and work quality as well as cheating. Almost half (48.7%) of the participants expressed their disapproval of online work and would not like to teach online [ 26 ].
Due to the nature of the online mode, teachers were also unable to use creative methods to teach students. Some were accustomed to using physical objects and role-playing to engage students in the classroom, but they found it extremely difficult to make learning exciting and to engage their students in virtual space. Similar trends have been reported in Australia, where schoolteachers in outback areas did not find online education helpful or practical for children, a majority of whom came from low-income families. The teachers were used to employing innovative methods to keep the students engaged in the classroom. However, in online teaching, they could not connect with their students using those methods, which significantly hampered their students’ progress. Some teachers mentioned difficulties with online teaching caused by not being able to use physical and concrete objects to improve their instructions [ 27 ].
b. Online evaluation.
Of our respondents, 81% said that they had conducted online assessments of their students. Teachers used various online assessment methods, including proctored closed/open book exams and quizzes, assignment submissions, class exercises, and presentations. Teachers who chose not to administer online assessments graded their students’ performance based on participation in class and previous results.
Almost two-thirds of teachers who had administered online assessments were dissatisfied with the effectiveness and transparency of those assessments, given the high rates of cheating and internet connectivity issues. They also reported that family members had been helping students to cheat in exams because they wanted their children to get higher grades by any means necessary. In response, the teachers had tried to devise methods to discourage students and their families from cheating, but they still felt powerless to prevent widespread cheating.
As one respondent stated: “We are taking many precautions to stop cheating, such as asking to install a mirror behind the student and doing online proctoring, but students have their ways out for every matter. They disconnect the internet cable or turn it off and reconnect it later. When we question them, they have a connectivity reason ready”.
Teachers are also concerned about the effects of the digital skills gap on their creation of worksheets, assessments, and other teaching materials. As a result, some private companies have been putting together teacher training programs. The main challenge pertains to be implementation of a type of specialized education that many teachers are unfamiliar with and unwilling to adopt [ 28 ]. Because of the lack of effective and transparent online assessments, school teachers have reported that students were promoted to the next level regardless of their performance. Thus, only time will tell how successful online education has been in terms of its effects on the lives of learners.
3. How has online education affected teacher’s overall health?
The onset of the COVID-19 pandemic brought about a situation that few people had experienced or even imagined living through. Governments and individuals tried their best to adjust to the new circumstances, but sudden lockdown, confinement to the household periphery, and working from home had adverse effects on the mental and physical health of many people, including educators and students. To clarify the effects of online education on teachers’ overall health, a number of questionnaire items were focused on respondents’ feelings during the lockdown, the physical and mental health issues they experienced, and their concerns about the future given the uncertainty of the present situation.
a. Physical health issues.
COVID-19 brought a multitude of changes to the lives of educators. Confinement to the household, working from home, and an increased burden of household and caregiving tasks due to the absence of paid domestic assistants increased physical workload and had corresponding adverse effects on the physical health of educators.
Of the study participants, 82% reported an increase in physical health issues since the lockdown ( Fig 1 ). Notably, 47% of those who were involved in digital mode of learning for less than 3 hours per day reported experiencing some physical discomfort daily, rising to 51% of teachers who worked online for 4–6 hours per day and 55% of teachers who worked more than 6 hours per day. Respondents reported a variety of physical health issues, including headaches, eye strain, back pain, and neck pain.
https://doi.org/10.1371/journal.pone.0282287.g001
The number of hours worked showed a positive correlation with the physical discomfort or health issues experienced. A chi-square test was applied to determine the relationship between the number of online working hours and the frequency of physical issues experienced by the participants and found it to be significant at the 0.05 level ( Table 2 ).
https://doi.org/10.1371/journal.pone.0282287.t002
As Fig 2 shows, 28% respondents’ complaint about experiencing giddiness, headaches; 59% complain of having neck and back pain. The majority of the participants had eye-strain problems most of the time; 32% faced eye problems sometimes, and 18% reported never having any eye issue. In addition, 49% had experienced two issues at the same time and 20% reported experiencing more than 2 physical issues at the same time.
https://doi.org/10.1371/journal.pone.0282287.g002
The data in this study indicates a link between bodily distresses and hours worked. As working hours increased, so did reports of back and neck pain. 47% respondents reported back and neck pain after working for 3 hours or less, 60% after working for 3–6 hours, and nearly 70% after working for 6 hours or more.
The analysis also indicates link between physical issues experienced and the educator’s gender. Women experienced more physical discomfort than men, with 51% reporting frequent discomfort, compared to only 46% of men. Only 14% of female educators reported never experiencing physical discomfort, against 30% of male educators.
In terms of types of discomfort, 76% of female teachers and 51% of male teachers reported eye strain; 62% of female teacher and 43% of male teachers reported back and neck pain; 30% of female teachers and 18% of male teachers said they had experienced dizziness and headaches. The gender differences may be caused by the increase in household and childcare responsibilities falling disproportionately on female educators compared to their male counterparts. Several studies [ 17 , 29 – 31 ] have reported similar results, indicating that the gender gap widened during the pandemic period. The social expectations of women to take care of children increased the gender gap during the pandemic by putting greater responsibilities on women in comparison to men [ 29 ]. Women in academics were affected more in comparison to the men. Working from home burdened female educators with additional household duties and childcare responsibilities. A study done [ 32 ] in France, Germany, Italy, Norway, Sweden, the United States and the United Kingdom discovered that women were immensely affected by lockdown in comparison to men. On top of this, women with children are affected more than women without children.
No effect of age on physical discomfort was observed in this study but increasing use of online tools (such as class websites) for content creation and delivery and extended working periods were major contributors to health problems.
b. Mental health issues.
The psychological effects of the COVID-19 pandemics have also proved difficult to manage. Being at home all day with limited social interaction, not to mention other pandemic-related sources of stress, affected the mental health of many people. The majority of the participants in this study admitted experiencing mental health issues including anxious feelings, low mood, restlessness, hopelessness, and loneliness. According to UNESCO [ 33 ], due to the sudden closure of schools and adaptability to new systems, teachers across the world are suffering from stress. Studies conducted in various parts of the world confirmed similar trends [ 34 , 35 ]. In Israel, teachers reported psychological stress due to online teaching. 30.4% teachers reported being stressed in comparison to 6.1% teachers in traditional classroom settings [ 34 ]. In Spain, teachers experienced various kinds of mental health issues like anxiety, stress, and depression [ 36 ]. An Arabian study found an increased number of cases related to anxiety, depression, and violence during the pandemic [ 37 ]. In New Zealand teachers in Higher education reported being overwhelmed due to the online teaching [ 15 ].
Online teaching appears to have negatively affected the mental health of all the study participants. Women (94%) reported more mental health issues than men (91%), as shown in Fig 3 . Nearly two-thirds of participants said they had been dealing with mental health issues regularly and a third occasionally; only 7% said they never dealt with them. Findings of this study are in line with other studies which found that female teachers had higher levels of stress and anxiety in comparison to men [ 36 ]. Studies conducted in China reported that teachers developed mental health issues due to online classes [ 37 , 38 ].
https://doi.org/10.1371/journal.pone.0282287.g003
Our analysis indicated a positive relationship between the number of working hours and the frequency of mental health issues. Of the respondents who worked online for less than 3 hours, 55% experienced some kind of mental health issue; this rose to 60% of participants who worked online for 3–6 hours, and 66% of those who worked more than 6 hours every day. A chi-square test was applied to determine the relationship between the number of online working hours and the frequency of mental issues experienced by the participants and found it to be significant at the 0.05 level ( Table 3 ).
https://doi.org/10.1371/journal.pone.0282287.t003
In terms of types of mental health issues, respondents reported restlessness, anxious feelings, and a sense of powerlessness, along with feelings of hopelessness, low mood, and loneliness as shown in Fig 4 . The stress of adapting to a new online working environment, the extended hours of work required to prepare content in new formats, the trial-and-error nature of learning and adopting new practices, uncertainty caused by lockdown, and an overall feeling of having no control were some of the contributing factors.
https://doi.org/10.1371/journal.pone.0282287.g004
Mental health issues were more common among those under the age of 35, with 64% reporting a problem most of the time compared to 53% of those over 35. It has been found that job uncertainty is one of the primary causes of a higher prevalence of mental health concerns among younger respondents than among older respondents. These findings are in line with other studies which found higher levels of stress among the young people in comparison to older one [ 36 , 39 ]. Feelings of loneliness and a sense of no control were reported by 30% of respondents under the age of 35, with these feelings occurring constantly or most of the time; only 12% of respondent over the age of 35 reported experiencing these feelings always or most of the time. Of respondents under 35 years of age 61% felt lonely at some point during the COVID-19 pandemic, compared to only 40% of those age 35 or older.
This study also found gender-based differences in the frequency of mental health issues experienced, with 62% of male respondents and 52% of female respondents reporting that they had always experienced mental health issues. The types of issues also differed by gender, with men more likely to report restlessness and loneliness and women more likely to report feeling anxious or helpless. More female respondents reported feelings of hopelessness than male respondents (76% compared to 69%), and they were also more anxious (66%).
The uncertainty of the pandemic seems to have caused helplessness and anxious feelings for female teachers in particular, perhaps because a lack of paid domestic help increased the burden of household and caregiving tasks disproportionately for women at a time when the pressure to adapt to new online platforms was particularly acute. In some cases, respondents left their jobs to accommodate new family dynamics, since private employers offered no assistance or flexibility. Deterioration of mental health also led to the increased number of suicides in Japan during COVID-19 [ 39 ].
However, female teachers fared better than their male counterparts on some measures of mental health. Although half of the respondents (men and women equally) reported low mood during the pandemic, the men reported more restlessness (53%) and loneliness (59%) than the women (50% and 49%, respectively). Restrictions on eating and drinking outside the household may have had a disproportionate effect on male respondents, making them more likely to feel restless or lonely than their female counterparts, who may have handled COVID-related isolation better by being more involved in household work and caregiving.
Number of hours worked online was also a factor contributing to mental health issues. Just as respondents had more physical complaints (including eye strain, back and neck pain, and headaches) the more hours they worked online, respondents who worked longer hours online reported more mental health issues.
One of the major drawbacks of online education is the widespread occurrence of physical and mental health issues, and the results of this study corroborate concerns on this point. This study found that online teaching causes more mental and physical problems for teachers than another study, which only found that 52.7% of respondents had these problems [ 12 ].
A report by the University of Melbourne has also indicated that online teaching and learning have a negative effect on the physical and mental well-being of individuals. Teachers working from home, in particular, have reported isolation, excessive screen time, inability to cope with additional stress, and exhaustion due to increased workload; despite being wary of the risks of exposure to COVID-19, they were eager to return to the campus [ 27 ].
c. Support mechanisms.
In general, teachers experienced good support from family and colleagues during the pandemic, with 45.64% of teachers reported receiving strong support, 29.64 percent moderate support (although the remainder claimed to have received no or only occasional support from family and colleagues). 9.39% of male respondents reported that they have never received any support in comparison to 4.36% females. Female respondents reported receiving more support than male respondents perhaps because they have access to a more extensive network of family members and coworkers. Children, parents, and siblings were cited as the provider of a robust support system by most female respondents. For example, maternal relatives called or texted children to keep them engaged and helped them with homework, and female participants said their peers helped them to prepare lectures and materials. A link was also found between age and support; the older the respondent, the stronger the support system. A possible explanation for this difference is that older people have had time to develop stronger and longer-lasting professional and personal ties than younger people.
This study explored the effects of the COVID-19 pandemic on the Indian education system and teachers working across six Indian states. The effectiveness of online education methods varied significantly by geographical location and demographics based on internet connectivity, access to smart devices, and teachers’ training. While premier higher education institutions and some private institutions had provided teachers with the necessary infrastructure and training to implement effective successful online learning with relatively few challenges, teachers at schools and community colleges have more often been left to adopt a trial-and-error approach to the transition to an online system. Further, it indicates that online education has had a significant effect on the quality of education imparted and the lives and wellbeing of teachers. While online learning has enabled teachers to reach out to students and maintain some normalcy during a time of uncertainty, it has also had negative consequences. Owing to the lack of in-person interaction with and among students in digital classes, the absence of creative learning tools in the online environment, glitches and interruptions in internet services, widespread cheating in exams, and lack of access to digital devices, online learning adversely affected the quality of education. Teachers experienced mounting physical and mental health issues due to stress of adjusting to online platforms without any or minimal ICT training and longer working hours to meet the demands of shifting responsibilities. A positive correlation was found between working hours and mental and physical health problems.
The long-term impact of COVID-19 pandemic on both the education system and the teachers would become clear only with time. Meanwhile, this study sheds light on some of the issues that teachers are facing and needs to be addressed without further ado. These findings will provide direction to the policy makers to develop sound strategies to address existing gaps for the successful implementation of digital learning. However, researchers should continue to investigate the longer-term effects of COVID pandemic on online education.
Supporting information
S1 file. supplementary material..
https://doi.org/10.1371/journal.pone.0282287.s001
- 1. WHO Coronavirus (COVID-19) Dashboard. [cited 14 Jan 2022]. Available: https://covid19.who.int
- View Article
- Google Scholar
- 3. unesco_covid-19_response_in_cambodia.pdf. Available: https://en.unesco.org/sites/default/files/unesco_covid-19_response_in_cambodia.pdf
- PubMed/NCBI
- 11. aser2020wave1report_feb1.pdf. Available: https://img.asercentre.org/docs/ASER%202021/ASER%202020%20wave%201%20-%20v2/aser2020wave1report_feb1.pdf
- 19. India Case Study.pdf. Available: https://www.unicef.org/rosa/media/16511/file/India%20Case%20Study.pdf
- 23. UNSDG | Policy Brief: Education during COVID-19 and beyond. [cited 21 Jan 2022]. Available: https://unsdg.un.org/resources/policy-brief-education-during-covid-19-and-beyond , https://unsdg.un.org/resources/policy-brief-education-during-covid-19-and-beyond
- 25. Report on rapid assessment of learning during school closures in context of COVID-19.pdf. Available: https://www.unicef.org/india/media/6121/file/Report%20on%20rapid%20assessment%20of%20learning%20during%20school%20closures%20in%20context%20of%20COVID-19.pdf
- 31. Reflections on motherhood and the impact of COVID 19 pandemic on women’s scientific careers—Guatimosim—2020—Journal of Neurochemistry—Wiley Online Library. [cited 30 Jun 2022]. Available: https://onlinelibrary.wiley.com/doi/10.1111/jnc.15158
- 33. https://plus.google.com/+UNESCO . Adverse consequences of school closures. In: UNESCO [Internet]. 10 Mar 2020 [cited 30 Jun 2022]. Available: https://en.unesco.org/covid19/educationresponse/consequences
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 11
- The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA study): a protocol study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5621-1833 Adrian I Espiritu 1 , 2 ,
- http://orcid.org/0000-0003-1135-6400 Marie Charmaine C Sy 1 ,
- http://orcid.org/0000-0002-1241-8805 Veeda Michelle M Anlacan 1 ,
- http://orcid.org/0000-0001-5317-7369 Roland Dominic G Jamora 1
- 1 Department of Neurosciences , College of Medicine and Philippine General Hospital, University of the Philippines Manila , Manila , Philippines
- 2 Department of Clinical Epidemiology, College of Medicine , University of the Philippines Manila , Manila , Philippines
- Correspondence to Dr Adrian I Espiritu; aiespiritu{at}up.edu.ph
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes.
Objectives The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA) study investigators will conduct a nationwide, multicentre study involving 37 institutions that aims to determine the neurological manifestations and factors associated with clinical outcomes in COVID-19 infection.
Methodology and analysis This is a retrospective cohort study (comparative between patients with and without neurological manifestations) via medical chart review involving adult patients with COVID-19 infection. Sample size was determined at 1342 patients. Demographic, clinical and neurological profiles will be obtained and summarised using descriptive statistics. Student’s t-test for two independent samples and χ 2 test will be used to determine differences between distributions. HRs and 95% CI will be used as an outcome measure. Kaplan-Meier curves will be constructed to plot the time to onset of mortality (survival), respiratory failure, intensive care unit (ICU) admission, duration of ventilator dependence, length of ICU stay and length of hospital stay. The log-rank test will be employed to compare the Kaplan-Meier curves. Stratified analysis will be performed to identify confounders and effects modifiers. To compute for adjusted HR with 95% CI, crude HR of outcomes will be adjusted according to the prespecified possible confounders. Cox proportional regression models will be used to determine significant factors of outcomes. Testing for goodness of fit will also be done using Hosmer-Lemeshow test. Subgroup analysis will be performed for proven prespecified effect modifiers. The effects of missing data and outliers will also be evaluated in this study.
Ethics and dissemination This protocol was approved by the Single Joint Research Ethics Board of the Philippine Department of Health (SJREB-2020–24) and the institutional review board of the different study sites. The dissemination of results will be conducted through scientific/medical conferences and through journal publication. The lay versions of the results may be provided on request.
Trial registration number NCT04386083 .
- adult neurology
- epidemiology
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-040944
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms Study is a nationwide, multicentre, retrospective, cohort study with 37 Philippine sites.
Full spectrum of neurological manifestations of COVID-19 will be collected.
Retrospective gathering of data offers virtually no risk of COVID-19 infection to data collectors.
Data from COVID-19 patients who did not go to the hospital are unobtainable.
Recoding bias is inherent due to the retrospective nature of the study.
Introduction
The COVID-19 has been identified as the cause of an outbreak of respiratory illness in Wuhan, Hubei Province, China, in December 2019. 1 The COVID-19 pandemic has reached the Philippines with most of its cases found in the National Capital Region (NCR). 2 The major clinical features of COVID-19 include fever, cough, shortness of breath, myalgia, headache and diarrhoea. 3 The outcomes of this disease lead to prolonged hospital stay, intensive care unit (ICU) admission, dependence on invasive mechanical ventilation, respiratory failure and mortality. 4 The specific pathogen that causes this clinical syndrome has been named SARS-CoV-2, which is phylogenetically similar to SARS-CoV. 4 Like the SARS-CoV strain, SARS-CoV-2 may possess a similar neuroinvasive potential. 5
A study on cases with COVID-19 found that about 36.4% of patients displayed neurological manifestations of the central nervous system (CNS) and peripheral nervous system (PNS). 6 The associated spectrum of symptoms and signs were substantially broad such as altered mental status, headache, cognitive impairment, agitation, dysexecutive syndrome, seizures, corticospinal tract signs, dysgeusia, extraocular movement abnormalities and myalgia. 7–12 Several reports were published on neurological disorders associated with patients with COVID-19, including cerebrovascular disorders, encephalopathy, hypoxic brain injury, frequent convulsive seizures and inflammatory CNS syndromes like encephalitis, meningitis, acute disseminated encephalomyelitis and Guillain-Barre syndrome. 7–16 However, the estimates of the occurrences of these manifestations were based on studies with a relatively small sample size. Furthermore, the current description of COVID-19 neurological features are hampered to some extent by exceedingly variable reporting; thus, defining causality between this infection and certain neurological manifestations is crucial since this may lead to considerable complications. 17 An Italian observational study protocol on neurological manifestations has also been published to further document and corroborate these findings. 18
Epidemiological data on the proportions and spectrum of non-respiratory symptoms and complications may be essential to increase the recognition of clinicians of the possibility of COVID-19 infection in the presence of other symptoms, particularly neurological manifestations. With this information, the probabilities of diagnosing COVID-19 disease may be strengthened depending on the presence of certain neurological manifestations. Furthermore, knowledge of other unrecognised symptoms and complications may allow early diagnosis that may permit early institution of personal protective equipment and proper contact precautions. Lastly, the presence of neurological manifestations may be used for estimating the risk of certain important clinical outcomes for better and well-informed clinical decisions in patients with COVID-19 disease.
To address this lack of important information in the overall management of patients with COVID-19, we organised a research study entitled ‘The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA Study)’.
This quantitative, retrospective cohort, multicentre study aims: (1) to determine the demographic, clinical and neurological profile of patients with COVID-19 disease in the Philippines; (2) to determine the frequency of neurological symptoms and new-onset neurological disorders/complications in patients with COVID-19 disease; (3) to determine the neurological manifestations that are significant factors of mortality, respiratory failure, duration of ventilator dependence, ICU admission, length of ICU stay and length of hospital stay among patients with COVID-19 disease; (4) to determine if there is significant difference between COVID-19 patients with neurological manifestations compared with those COVID-19 patients without neurological manifestations in terms of mortality, respiratory failure, duration of ventilator dependence, ICU admission, length of ICU stay and length of hospital stay; and (5) to determine the likelihood of mortality, respiratory failure and ICU admission, including the likelihood of longer duration of ventilator dependence and length of ICU and hospital stay in COVID-19 patients with neurological manifestations compared with those without neurological manifestations.
Scope, limitations and delimitations
The study will include confirmed cases of COVID-19 from the 37 participating institutions in the Philippines. Every country has its own healthcare system, whose level of development and strategies ultimately affect patient outcomes. Thus, the results of this study cannot be accurately generalised to other settings. In addition, patients with ages ≤18 years will be excluded in from this study. These younger patients may have different characteristics and outcomes; therefore, yielded estimates for adults in this study may not be applicable to this population subgroup. Moreover, this study will collect data from the patient records of patients with COVID-19; thus, data from patients with mild symptoms who did not go to the hospital and those who had spontaneous resolution of symptoms despite true infection with COVID-19 are unobtainable.
Methodology
To improve the quality of reporting of this study, the guidelines issued by the Strengthening the Reporting of Observational Studies in Epidemiology Initiative will be followed. 19
Study design
The study will be conducted using a retrospective cohort (comparative) design (see figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Schematic diagram of the study flow.
Study sites and duration
We will conduct a nationwide, multicentre study involving 37 institutions in the Philippines (see figure 2 ). Most of these study sites can be found in the NCR, which remains to be the epicentre of the COVID-19 pandemic. 2 We will collect data for 6 months after institutional review board approval for every site.
Location of 37 study sites of the Philippine CORONA study.
Patient selection and cohort description
The cases will be identified using the designated COVID-19 censuses of all the participating centres. A total enumeration of patients with confirmed COVID-19 disease will be done in this study.
The cases identified should satisfy the following inclusion criteria: (A) adult patients at least 19 years of age; (B) cases confirmed by testing approved patient samples (ie, nasal swab, sputum and bronchoalveolar lavage fluid) employing real-time reverse transcription PCR (rRT-PCR) 20 from COVID-19 testing centres accredited by the Department of Health (DOH) of the Philippines, with clinical symptoms and signs attributable to COVID-19 disease (ie, respiratory as well as non-respiratory clinical signs and symptoms) 21 ; and (C) cases with disposition (ie, discharged stable/recovered, home/discharged against medical advice, transferred to other hospital or died) at the end of the study period. Cases with conditions or diseases caused by other organisms (ie, bacteria, other viruses, fungi and so on) or caused by other pathologies unrelated to COVID-19 disease (ie, trauma) will be excluded.
The first cohort will involve patients with confirmed COVID-19 infection who presented with any neurological manifestation/s (ie, symptoms or complications/disorder). The comparator cohort will compose of patients with confirmed COVID-19 infection without neurological manifestation/s.
Sample size calculation
We looked into the mortality outcome measure for the purposes of sample size computation. Following the cohort study of Khaledifar et al , 22 the sample size was calculated using the following parameters: two-sided 95% significance level (1 – α); 80% power (1 – β); unexposed/exposed ratio of 1; 5% of unexposed with outcome (case fatality rate from COVID19-Philippines Dashboard Tracker (PH) 23 as of 8 April 2020); and assumed risk ratio 2 (to see a two-fold increase in risk of mortality when neurological symptoms are present).
When these values were plugged in to the formula for cohort studies, 24 a minimum sample size of 1118 is required. To account for possible incomplete data, the sample was adjusted for 20% more. This means that the total sample size required is 1342 patients, which will be gathered from the participating centres.
Data collection
We formulated an electronic data collection form using Epi Info Software (V.7.2.2.16). The forms will be pilot-tested, and a formal data collection workshop will be conducted to ensure collection accuracy. The data will be obtained from the review of the medical records.
The following pertinent data will be obtained: (A) demographic data; (B) other clinical profile data/comorbidities; (C) neurological history; (D) date of illness onset; (E) respiratory and constitutional symptoms associated with COVID-19; (F) COVID-19 disease severity 25 at nadir; (G) data if neurological manifestation/s were present at onset prior to respiratory symptoms and the specific neurological manifestation/s present at onset; (H) neurological symptoms; (i) date of neurological symptom onset; (J) new-onset neurological disorders or complications; (K) date of new neurological disorder or complication onset; (L) imaging done; (M) cerebrospinal fluid analysis; (N) electrophysiological studies; (O) treatment given; (P) antibiotics given; (Q) neurological interventions given; (R) date of mortality and cause/s of mortality; (S) date of respiratory failure onset, date of mechanical ventilator cessation and cause/s of respiratory failure; (T) date of first day of ICU admission, date of discharge from ICU and indication/s for ICU admission; (U) other neurological outcomes at discharge; (V) date of hospital discharge; and (W) final disposition. See table 1 for the summary of the data to be collected for this study.
- View inline
Data to be collected in this study
Main outcomes considered
The following patient outcomes will be considered for this study:
Mortality (binary outcome): defined as the patients with confirmed COVID-19 who died.
Respiratory failure (binary outcome): defined as the patients with confirmed COVID-19 who experienced clinical symptoms and signs of respiratory insufficiency. Clinically, this condition may manifest as tachypnoea/sign of increased work of breathing (ie, respiratory rate of ≥22), abnormal blood gases (ie, hypoxaemia as evidenced by partial pressure of oxygen (PaO 2 ) <60 or hypercapnia by partial pressure of carbon dioxide of >45), or requiring oxygen supplementation (ie, PaO 2 <60 or ratio of PaO 2 /fraction of inspired oxygen (P/F ratio)) <300).
Duration of ventilator dependence (continuous outcome): defined as the number of days from initiation of assisted ventilation to cessation of mechanical ventilator use.
ICU admission (binary outcome): defined as the patients with confirmed COVID-19 admitted to an ICU or ICU-comparable setting.
Length of ICU stay (continuous outcome): defined as the number of days admitted in the ICU or ICU-comparable setting.
Length of hospital stay (continuous outcome): defined as the number of days from admission to discharge.
Data analysis plan
Statistical analysis will be performed using Stata V.7.2.2.16.
Demographic, clinical and neurological profiles will be summarised using descriptive statistics, in which categorical variables will be expressed as frequencies with corresponding percentages, and continuous variables will be pooled using means (SD).
Student’s t-test for two independent samples and χ 2 test will be used to determine differences between distributions.
HRs and 95% CI will be used as an outcome measure. Kaplan-Meier curves will be constructed to plot the time to onset of mortality (survival), respiratory failure, ICU admission, duration of ventilator dependence (recategorised binary form), length of ICU stay (recategorised binary form) and length of hospital stay (recategorised binary form). Log-rank test will be employed to compare the Kaplan-Meier curves. Stratified analysis will be performed to identify confounders and effects modifiers. To compute for adjusted HR with 95% CI, crude HR of outcomes at discrete time points will be adjusted for prespecified possible confounders such as age, history of cardiovascular or cerebrovascular disease, hypertension, diabetes mellitus, and respiratory disease, COVID-19 disease severity at nadir, and other significant confounding factors.
Cox proportional regression models will be used to determine significant factors of outcomes. Testing for goodness of fit will be done using Hosmer-Lemeshow test. Likelihood ratio tests and other information criteria (Akaike Information Criterion or Bayesian Information Criterion) will be used to refine the final model. Statistical significance will be considered if the 95% CI of HR or adjusted HR did not include the number one. A p value <0.05 (two tailed) is set for other analyses.
Subgroup analyses will be performed for proven prespecified effect modifiers. The following variables will be considered for subgroup analyses: age (19–64 years vs ≥65 years), sex, body mass index (<18.5 vs 18.5–22.9 vs ≥23 kg/m 2 ), with history of cardiovascular or cerebrovascular disease (presence or absence), hypertension (presence or absence), diabetes mellitus (presence or absence), respiratory disease (presence or absence), smoking status (smoker or non-smoker) and COVID-19 disease severity (mild, severe or critical disease).
The effects of missing data will be explored. All efforts will be exerted to minimise missing and spurious data. Validity of the submitted electronic data collection will be monitored and reviewed weekly to prevent missing or inaccurate input of data. Multiple imputations will be performed for missing data when possible. To check for robustness of results, analysis done for patients with complete data will be compared with the analysis with the imputed data.
The effects of outliers will also be assessed. Outliers will be assessed by z-score or boxplot. A cut-off of 3 SD from the mean can also be used. To check for robustness of results, analysis done with outliers will be compared with the analysis without the outliers.
Study organisational structure
A steering committee (AIE, MCCS, VMMA and RDGJ) was formed to direct and provide appropriate scientific, technical and methodological assistance to study site investigators and collaborators (see figure 3 ). Central administrative coordination, data management, administrative support, documentation of progress reports, data analyses and interpretation and journal publication are the main responsibilities of the steering committee. Study site investigators and collaborators are responsible for the proper collection and recording of data including the duty to maintain the confidentiality of information and the privacy of all identified patients for all the phases of the research processes.
Organisational structure of oversight of the Philippine CORONA Study.
This section is highlighted as part of the required formatting amendments by the Journal.
Ethics and dissemination
This research will adhere to the Philippine National Ethical Guidelines for Health and Health-related Research 2017. 26 This study is an observational, cohort study and will not allocate any type of intervention. The medical records of the identified patients will be reviewed retrospectively. To protect the privacy of the participant, the data collection forms will not contain any information (ie, names and institutional patient number) that could determine the identity of the patients. A sequential code will be recorded for each patient in the following format: AAA-BBB where AAA will pertain to the three-digit code randomly assigned to each study site; BBB will pertain to the sequential case number assigned by each study site. Each participating centre will designate a password-protected laptop for data collection; the password is known only to the study site.
This protocol was approved by the following institutional review boards: Single Joint Research Ethics Board of the DOH, Philippines (SJREB-2020-24); Asian Hospital and Medical Center, Muntinlupa City (2020- 010-A); Baguio General Hospital and Medical Center (BGHMC), Baguio City (BGHMC-ERC-2020-13); Cagayan Valley Medical Center (CVMC), Tuguegarao City; Capitol Medical Center, Quezon City; Cardinal Santos Medical Center (CSMC), San Juan City (CSMC REC 2020-020); Chong Hua Hospital, Cebu City (IRB 2420–04); De La Salle Medical and Health Sciences Institute (DLSMHSI), Cavite (2020-23-02-A); East Avenue Medical Center (EAMC), Quezon City (EAMC IERB 2020-38); Jose R. Reyes Memorial Medical Center, Manila; Jose B. Lingad Memorial Regional Hospital, San Fernando, Pampanga; Dr. Jose N. Rodriguez Memorial Hospital, Caloocan City; Lung Center of the Philippines (LCP), Quezon City (LCP-CT-010–2020); Manila Doctors Hospital, Manila (MDH IRB 2020-006); Makati Medical Center, Makati City (MMC IRB 2020–054); Manila Medical Center, Manila (MMERC 2020-09); Northern Mindanao Medical Center, Cagayan de Oro City (025-2020); Quirino Memorial Medical Center (QMMC), Quezon City (QMMC REB GCS 2020-28); Ospital ng Makati, Makati City; University of the Philippines – Philippine General Hospital (UP-PGH), Manila (2020-314-01 SJREB); Philippine Heart Center, Quezon City; Research Institute for Tropical Medicine, Muntinlupa City (RITM IRB 2020-16); San Lazaro Hospital, Manila; San Juan De Dios Educational Foundation Inc – Hospital, Pasay City (SJRIB 2020-0006); Southern Isabela Medical Center, Santiago City (2020-03); Southern Philippines Medical Center (SPMC), Davao City (P20062001); St. Luke’s Medical Center, Quezon City (SL-20116); St. Luke’s Medical Center, Bonifacio Global City, Taguig City (SL-20116); Southern Philippines Medical Center, Davao City; The Medical City, Pasig City; University of Santo Tomas Hospital, Manila (UST-REC-2020-04-071-MD); University of the East Ramon Magsaysay Memorial Medical Center, Inc, Quezon City (0835/E/2020/063); Veterans Memorial Medical Center (VMMC), Quezon City (VMMC-2020-025) and Vicente Sotto Memorial Medical Center, Cebu City (VSMMC-REC-O-2020–048).
The dissemination of results will be conducted through scientific/medical conferences and through journal publication. Only the aggregate results of the study shall be disseminated. The lay versions of the results may be provided on request.
Protocol registration and technical review approval
This protocol was registered in the ClinicalTrials.gov website. It has received technical review board approvals from the Department of Neurosciences, Philippine General Hospital and College of Medicine, University of the Philippines Manila, from the Cardinal Santos Medical Center (San Juan City) and from the Research Center for Clinical Epidemiology and Biostatistics, De La Salle Medical and Health Sciences Institute (Dasmariñas, Cavite).
Acknowledgments
We would like to thank Almira Abigail Doreen O Apor, MD, of the Department of Neurosciences, Philippine General Hospital, Philippines, for illustrating figure 2 for this publication.
- Adhikari SP ,
- Wu Y-J , et al
- Department of Health
- Philippine Society for Microbiology and Infectious Diseases
- Hu Y , et al
- Li Yan‐Chao ,
- Bai Wan‐Zhu ,
- Hashikawa T ,
- Wang M , et al
- Paterson RW ,
- Benjamin L , et al
- Hall JP , et al
- Varatharaj A ,
- Ellul MA , et al
- Mahammedi A ,
- Vagal A , et al
- Collantes MEV ,
- Espiritu AI ,
- Sy MCC , et al
- Merdji H , et al
- Sharifi Razavi A ,
- Poyiadji N ,
- Noujaim D , et al
- Zhou H , et al
- Moriguchi T ,
- Goto J , et al
- Nicholson TR , et al
- Ferrarese C ,
- Priori A , et al
- von Elm E ,
- Altman DG ,
- Egger M , et al
- Li J , et al
- Centers for Disease Control and Prevention
- Khaledifar A ,
- Hashemzadeh M ,
- Solati K , et al
- McGoogan JM
- Philippine Research Ethics Board
VMMA and RDGJ are joint senior authors.
AIE and MCCS are joint first authors.
Twitter @neuroaidz, @JamoraRoland
Collaborators The Philippine CORONA Study Group Collaborators: Maritoni C Abbariao, Joshua Emmanuel E Abejero, Ryndell G Alava, Robert A Barja, Dante P Bornales, Maria Teresa A Cañete, Ma. Alma E Carandang-Concepcion, Joseree-Ann S Catindig, Maria Epifania V Collantes, Evram V Corral, Ma. Lourdes P Corrales-Joson, Romulus Emmanuel H Cruz, Marita B Dantes, Ma. Caridad V Desquitado, Cid Czarina E Diesta, Carissa Paz C Dioquino, Maritzie R Eribal, Romulo U Esagunde, Rosalina B Espiritu-Picar, Valmarie S Estrada, Manolo Kristoffer C Flores, Dan Neftalie A Juangco, Muktader A Kalbi, Annabelle Y Lao-Reyes, Lina C Laxamana, Corina Maria Socorro A Macalintal, Maria Victoria G Manuel, Jennifer Justice F Manzano, Ma. Socorro C Martinez, Generaldo D Maylem, Marc Conrad C Molina, Marietta C Olaivar, Marissa T Ong, Arnold Angelo M Pineda, Joanne B Robles, Artemio A Roxas Jr, Jo Ann R Soliven, Arturo F Surdilla, Noreen Jhoanna C Tangcuangco-Trinidad, Rosalia A Teleg, Jarungchai Anton S Vatanagul and Maricar P Yumul.
Contributors All authors conceived the idea and wrote the initial drafts and revisions of the protocol. All authors made substantial contributions in this protocol for intellectual content.
Funding Philippine Neurological Association (Grant/Award Number: N/A). Expanded Hospital Research Office, Philippine General Hospital (Grant/Award Number: N/A).
Disclaimer Our funding sources had no role in the design of the protocol, and will not be involved during the methodological execution, data analyses and interpretation and decision to submit or to publish the study results.
Map disclaimer The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
- Browse All Articles
- Newsletter Sign-Up

- 12 Dec 2023
- Research & Ideas
- 15 Aug 2023
- Cold Call Podcast

- 10 Feb 2023

- 01 Feb 2023
- What Do You Think?

- 12 Oct 2022

- 04 Oct 2022

- 06 Sep 2022

- 21 Jul 2022

- 12 Jul 2022

- 09 Jun 2022

- 14 Apr 2022

- 14 Mar 2022

- 24 Feb 2022

- 10 Feb 2022

- 08 Feb 2022

- 20 Jan 2022
.jpg)
- 11 Jan 2022

- 02 Nov 2021

- 22 Oct 2021
- 19 Oct 2021
Official websites use .gov
A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.

About COVID-19
What is covid-19.
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States.
COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs and respiratory system. Other parts of your body may also be affected by the disease. Most people with COVID-19 have mild symptoms, but some people become severely ill.
Some people including those with minor or no symptoms will develop Post-COVID Conditions – also called “Long COVID.”
How does COVID-19 spread?
COVID-19 spreads when an infected person breathes out droplets and very small particles that contain the virus. Other people can breathe in these droplets and particles, or these droplets and particles can land on their eyes, nose, or mouth. In some circumstances, these droplets may contaminate surfaces they touch.
Anyone infected with COVID-19 can spread it, even if they do NOT have symptoms.
The risk of animals spreading the virus that causes COVID-19 to people is low. The virus can spread from people to animals during close contact. People with suspected or confirmed COVID-19 should avoid contact with animals.
What are antibodies and how do they help protect me?
Antibodies are proteins your immune system makes to help fight infection and protect you from getting sick in the future. A positive antibody test result can help identify someone who has had COVID-19 in the past or has been vaccinated against COVID-19. Studies show that people who have antibodies from an infection with the virus that causes COVID-19 can improve their level of protection by getting vaccinated.
Who is at risk of severe illness from COVID-19?
Some people are more likely than others to get very sick if they get COVID-19. This includes people who are older , are immunocompromised (have a weakened immune system), have certain disabilities , or have underlying health conditions . Understanding your COVID-19 risk and the risks that might affect others can help you make decisions to protect yourself and others .
What are ways to prevent COVID-19?
There are many actions you can take to help protect you, your household, and your community from COVID-19. CDC’s Respiratory Virus Guidance provides actions you can take to help protect yourself and others from health risks caused by respiratory viruses, including COVID-19. These actions include steps you can take to lower the risk of COVID-19 transmission (catching and spreading COVID-19) and lower the risk of severe illness if you get sick.
CDC recommends that you
- Stay up to date with COVID-19 vaccines
- Practice good hygiene (practices that improve cleanliness)
- Take steps for cleaner air
- Stay home when sick
- Seek health care promptly for testing and treatment when you are sick if you have risk factors for severe illness . Treatment may help lower your risk of severe illness.
Masks , physical distancing , and tests can provide additional layers of protection.
What are variants of COVID-19?
Viruses are constantly changing, including the virus that causes COVID-19. These changes occur over time and can lead to new strains of the virus or variants of COVID-19 . Slowing the spread of the virus, by protecting yourself and others , can help slow new variants from developing. CDC is working with state and local public health officials to monitor the spread of all variants, including Omicron.
- COVID-19 Testing
- COVID-19 Vaccines
- Preventing Respiratory Viruses
- Reinfection
- Difference Between Flu and COVID-19
- COVID Data Tracker
Search for and find historical COVID-19 pages and files. Please note the content on these pages and files is no longer being updated and may be out of date.
- Visit archive.cdc.gov for a historical snapshot of the COVID-19 website, capturing the end of the Federal Public Health Emergency on June 28, 2023.
- Visit the dynamic COVID-19 collection to search the COVID-19 website as far back as July 30, 2021.
To receive email updates about COVID-19, enter your email address:
Exit Notification / Disclaimer Policy
- The Centers for Disease Control and Prevention (CDC) cannot attest to the accuracy of a non-federal website.
- Linking to a non-federal website does not constitute an endorsement by CDC or any of its employees of the sponsors or the information and products presented on the website.
- You will be subject to the destination website's privacy policy when you follow the link.
- CDC is not responsible for Section 508 compliance (accessibility) on other federal or private website.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 29 May 2024
Examining the impact of the COVID-19 pandemic on homecare services among individuals with traumatic and non-traumatic spinal cord injuries
- Arrani Senthinathan ORCID: orcid.org/0000-0002-9304-3039 1 ,
- Mina Tadrous 1 , 2 ,
- Swaleh Hussain 1 , 3 ,
- Sandra McKay 4 , 5 , 6 , 7 ,
- Rahim Moineddin 3 , 8 ,
- Cherry Chu ORCID: orcid.org/0000-0002-4072-0083 2 ,
- Susan B. Jaglal 3 , 5 , 6 , 9 ,
- John Shepherd 9 , 10 ,
- Lauren Cadel ORCID: orcid.org/0000-0001-6925-8163 1 ,
- Vanessa K. Noonan ORCID: orcid.org/0000-0003-3226-9218 11 , 12 ,
- B. Catharine Craven ORCID: orcid.org/0000-0001-8234-6803 5 , 10 , 13 , 14 ,
- Karen Tu 8 , 15 , 16 &
- Sara J. T. Guilcher ORCID: orcid.org/0000-0002-9552-9139 1 , 3 , 5 , 6
Spinal Cord ( 2024 ) Cite this article
20 Accesses
3 Altmetric
Metrics details
- Health care
- Health services
Study design
Descriptive repeated-cross sectional retrospective longitudinal cohort study.
To investigate the impact of the COVID-19 pandemic on homecare services in individuals with traumatic or non-traumatic Spinal Cord Injury (SCI).
Health administrative database in Ontario, Canada.
A repeated cross-sectional study using linked health administrative databases from March 2015 to June 2022. Monthly homecare utilization was assessed in 3381 adults with SCI using Autoregressive Integrated Moving Average (ARIMA) models.
Compared to pre-pandemic levels, between March 2020 to June 2022, the traumatic group experienced a decrease in personal and/or homemaking services, as well as an increase in nursing visits from April 2020–March 2022 and June 2022. Case management increased at various times for the traumatic group, however therapies decreased in May 2020 only. The non-traumatic group experienced a decrease in personal and/or homemaking services in July 2020, as well as an increase in nursing visits from March 2020 to February 2021 and sporadically throughout 2020. Case management also increased at certain points for the non-traumatic group, but therapies decreased in April 2020, July 2020, and September 2021.
The traumatic group had decreases in personal and/or homemaking services. Both groups had increases in nursing services, increases in case management, and minimal decreases in therapies at varying times during the pandemic. Investigation is warranted to understand the root cause of these changes, and if they resulted in adverse outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
251,40 € per year
only 20,95 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Examining the impact of COVID-19 on health care utilization among persons with chronic spinal cord injury/dysfunction: a population study
The impact of COVID-19 and associated lockdowns on traumatic spinal cord injury incidence: a population based study

Incidence and mortality of spinal cord injury from 2008 to 2020: a retrospective population-based cohort study in the Piedmont Region, Italy
Data availability.
The dataset from this study is held securely in coded form at ICES. While legal data sharing agreements between ICES and data providers (e.g., healthcare organizations and government) prohibit ICES from making the dataset publicly available, access may be granted to those who meet pre-specified criteria for confidential access, available at www.ices.on.ca/DAS (email: [email protected]). The full dataset creation plan and underlying analytic code are available from the authors upon request, understanding that the computer programs may rely upon coding templates or macros that are unique to ICES and are therefore either inaccessible or may require modification.
Hopwood P, MacEachen E, McAiney C, Tong C. Personal support work and home care in Ontario during the COVID-19 pandemic. Healthc Policy Polit Santé. 2022;18:61–75.
Google Scholar
Sinn C-LJ, Sultan H, Turcotte LA, McArthur C, Hirdes JP. Patterns of home care assessment and service provision before and during the COVID-19 pandemic in Ontario, Canada. PLOS ONE. 2022;17:e0266160.
Article CAS PubMed PubMed Central Google Scholar
Hapsari AP, Ho JW, Meaney C, Avery L, Hassen N, Jetha A, et al. The working conditions for personal support workers in the Greater Toronto Area during the COVID-19 pandemic: a mixed-methods study. Can J Public Health. 2022;113:817–33.
Article PubMed PubMed Central Google Scholar
Biering-Sørensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International Spinal Cord Injury Core Data Set (version 2.0)—including standardization of reporting. Spinal Cord. 2017;55:759–64.
Article PubMed Google Scholar
New PW, Marshall R. International Spinal Cord Injury Data Sets for non-traumatic spinal cord injury. Spinal Cord. 2014;52:123–32.
Article CAS PubMed Google Scholar
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (Revised 2011). J Spinal Cord Med. 2011;34:535–46.
Draganich C, Philippus A, Eagye KJ, Mikolajczyk B, Morse LR, Monden KR. Changes in essential care in individuals with spinal cord injury during the COVID-19 pandemic. Spinal Cord. 2023;61:76–82.
Huang J, Pacheco Barzallo D, Rubinelli S, Münzel N, Brach M, Gemperli A. Professional home care and the objective care burden for family caregivers of persons with spinal cord injury: Cross sectional survey. Int J Nurs Stud Adv. 2021;3:100014.
Chan BC-F, Cronin S, Jaglal SB, Craven BC. Publicly funded home care service use in the first 2 years after spinal cord injury in Ontario, Canada. Home Health Care Serv Q. 2020;39:95–106.
Huang J, Pacheco Barzallo D, Rubinelli S, Münzel N, Brach M, Gemperli A. What influences the use of professional home care for individuals with spinal cord injury? A cross-sectional study on family caregivers. Spinal Cord. 2019;57:924–32.
Jones A, Maclagan LC, Schumacher C, Wang X, Jaakkimainen RL, Guan J, et al. Impact of the COVID-19 pandemic on home care services among community-dwelling adults with dementia. J Am Med Dir Assoc. 2021;22:2258–62.
Hill EJR, L’Hotta AJ, Kennedy CR, James AS, Fox IK. Living with cervical spinal cord injury during the COVID-19 pandemic: A qualitative study. Arch Rehabil Res Clin Transl. 2022;4:100208.
PubMed PubMed Central Google Scholar
Smith EM, Boucher N, Miller WC. Caregiving services in spinal cord injury: A systematic review of the literature. Spinal Cord. 2016;54:562–9.
Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord. 2004;42:513–25.
Senthinathan A, Cimino S, Jaglal SB, Craven BC, Tu K, Guilcher S. The impact of the COVID-19 virus and pandemic on healthcare utilization, access, delivery, experiences, and outcomes in the spinal cord injuries/dysfunction population: A scoping review study. PLOS ONE. 2024;19:e0297384.
Senthinathan A, Tadrous M, Hussain S, Craven BC, Jaglal SB, Moineddin R, et al. Examining the impact of COVID-19 on health care utilization among persons with chronic spinal cord injury/dysfunction: a population study. Spinal Cord. 2023. https://doi.org/10.1038/s41393-023-00930-1 .
Matsuoka M, Sumida M. The effect of the COVID-19 pandemic on the health-related quality of life in home-based patients with spinal cord injuries in Japan. J Spinal Cord Med. 2022;45:760–4.
Rohn EJ, Hearn JH, Philippus AM, Monden KR. “It’s been a double-edged sword”: An online qualitative exploration of the impact of COVID-19 on individuals with spinal cord injury in the US with comparisons to previous UK findings. J Spinal Cord Med 2024;47:51–63.
Vives Alvarado JR, Miranda-Cantellops N, Jackson SN, Felix ER. Access limitations and level of psychological distress during the COVID-19 pandemic in a geographically-limited sample of individuals with spinal cord injury. J Spinal Cord Med. 2022;45:700–9.
Cameron-Blake E, Breton C, Sim P, Tatlow H, Hale T, Wood A, et al. Variation in the Canadian Provincial and Territorial responses to COVID19. Blavatnik Sch Gov Work Pap. 2021. https://doi.org/10.1038/s41562-021-01079-8 .
Article Google Scholar
North American Observatory on Health Systems and Policies. (2020). North American COVID-19 Policy Response Monitor: Ontario. Toronto, Canada: North American Observatory on Health Systems and Policies.
Hearn JH, Rohn EJ, Monden KR. Isolated and anxious: A qualitative exploration of the impact of the COVID-19 pandemic on individuals living with spinal cord injury in the UK. J Spinal Cord Med. 2022;45:691–9.
Bhattarai M, Limbu S, Sherpa PD. Living with spinal cord injury during COVID-19: a qualitative study of impacts of the pandemic in Nepal. Spinal Cord. 2022;60:984–9.
Hatefi M, Borji M, Jamshidbeigi Y. Challenges of Patients with Spinal Cord Injury During the COVID-19 Pandemic: A Qualitative Study. Arch Neurosci. 2021; 8. https://doi.org/10.5812/ans.118744 .
Lakhani A, Dema S, Hose J, Erdem N, Wollersheim D, Grimbeek P, et al. What happens post-lockdown for people with disability? Autonomy, quality of life, service access and health changes for people with spinal cord injury in Victoria, Australia after COVID-19 social distancing restrictions. Health Soc Care Community. 2022;30:e5366–77.
Faleiros F, Alves D, Schoeller SD, Machado WCA, Corbo L, Zuchetto M. What will the post-pandemic world be like? A qualitative study on the perceptions of Brazilians with spinal cord injury. Middle East J Rehabil Health Stud. 2022; 9. https://doi.org/10.5812/mejrh.113705 .
Monden KR, Andrews E, Pilarski C, Hearn J, Wudlick R, Morse LR. COVID-19 and the spinal cord injury community: Concerns about medical rationing and social isolation. Rehabil Psychol. 2021;66:373–9.
Righi G, Baroni E, Righi L, Belloni L, Del Popolo G. Perception of the COVID-19 pandemic among people with spinal cord injury: an Italian survey. Spinal Cord Ser Cases. 2022;8:2.
Sharma Y, Whiting A, Dutta T. A survey of the challenges faced by individuals with disabilities and unpaid caregivers during the COVID-19 pandemic. Int J Environ Res Public Health. 2022;19:10075.
Dicks MA, Clements ND, Gibbons CR, Verduzco-Gutierrez M, Trbovich M. Atypical presentation of Covid-19 in persons with spinal cord injury. Spinal Cord Ser Cases. 2020;6:38.
Gustafson K, Stillman M, Capron M, O’Connell C, Longoni Di Giusto M, Tyagi N, et al. COVID-19 and spinal cord injury and disease: results of an international survey as the pandemic progresses. Spinal Cord Ser Cases. 2021;7:13.
Bronskill SE, Carter MW, Costa AP, Esensoy AV, Gill SS, Gruneir A, et al. Aging in Ontario: An ICES Chartbook of Health Service Use by Older Adults – Technical Report. Toronto: Institute for Clinical Evaluative Sciences; 2010.
Fattah J, Ezzine L, Aman Z, El Moussami H, Lachhab A. Forecasting of demand using ARIMA model. Int J Eng Bus Manag; 2018;10:1–9.
Holroyd-Leduc JM, Laupacis A. Continuing care and COVID-19: a Canadian tragedy that must not be allowed to happen again. Can Med Assoc J. 2020;192:E632–3.
King EC, Zagrodney KA, Rabeenthira P, Van Belle TA, McKay SM. Why did home care personal support service volumes drop during the COVID-19 pandemic? The contributions of client choice and personal support worker availability. Health Serv Insights. 2023;16:11786329231210692.
Download references
Acknowledgements
This study was supported by ICES (formerly named the Institute for Clinical Evaluative Sciences), an independent, non-profit research institute funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). As a prescribed entity under Ontario’s privacy legislation, ICES is authorized to collect and use health care data for the purposes of health system analysis, evaluation, and decision support. Secure access to these data are governed by policies and procedures approved by the Information and Privacy Commissioner of Ontario. This document used data adapted from the Statistics Canada Postal CodeOM Conversion File, which is based on data licensed from Canada Post Corporation, and/or data adapted from the Ontario Ministry of Health Postal Code Conversion File, which contains data copied under license from Canada Post Corporation and Statistics Canada. Parts of this material are based on data and/or information compiled and provided by the Ontario Ministry of Health, and the Canadian Institute for Health Information. The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred. Parts of this material are based on data and information provided by Ontario Health (OH). The opinions, results, view, and conclusions reported in this paper are those of the authors and do not necessarily reflect those of OH. No endorsement by OH is intended or should be inferred. Dr. Guilcher is currently supported by the University of Toronto Centre for the Study of Pain Scientist Salary Award. Dr. Karen Tu is supported by a Chair in Family and Community Medicine Research in Primary Care at UHN and a Research Scholar award from the Department of Family and Community Medicine at the University of Toronto. Dr B. Catharine Craven is supported by UHN Foundation in her role as the University of Toronto/University Health Network COPE Family Chair in SCI Health Services Innovation. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
This study was funded as part of a CIHR operating grant (#478336). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources.
Author information
Authors and affiliations.
Leslie Dan Faculty of Pharmacy, University of Toronto, Toronto, ON, Canada
Arrani Senthinathan, Mina Tadrous, Swaleh Hussain, Lauren Cadel & Sara J. T. Guilcher
Women’s College Hospital Institute for Health Systems Solutions and Virtual Care, Women’s College Hospital, Toronto, ON, Canada
Mina Tadrous & Cherry Chu
ICES, Toronto, ON, Canada
Swaleh Hussain, Rahim Moineddin, Susan B. Jaglal & Sara J. T. Guilcher
VHA Home HealthCare, Toronto, ON, Canada
Sandra McKay
Institute of Health Policy Management and Evaluation, University of Toronto, Toronto, ON, Canada
Sandra McKay, Susan B. Jaglal, B. Catharine Craven & Sara J. T. Guilcher
Department of Physical Therapy, Temerty Faculty of Medicine, University of Toronto, Toronto, ON, Canada
Sandra McKay, Susan B. Jaglal & Sara J. T. Guilcher
Ted Rogers School of Management, Toronto Metropolitan University, Toronto, ON, Canada
Department of Family and Community Medicine, University of Toronto, Toronto, ON, Canada
Rahim Moineddin & Karen Tu
Rehabilitation Sciences Institute, University of Toronto, Toronto, ON, Canada
Susan B. Jaglal & John Shepherd
KITE (Knowledge Innovation Talent Everywhere), Toronto Rehabilitation Institute - University Health Network, Toronto, ON, Canada
John Shepherd & B. Catharine Craven
Praxis Spinal Cord Institute, Vancouver, BC, Canada
Vanessa K. Noonan
International Collaboration on Repair Discoveries, Vancouver, BC, Canada
Department of Medicine, Faculty of Medicine, University of Toronto, Toronto, ON, Canada
B. Catharine Craven
Spinal Cord Rehabilitation Program, Toronto Rehabilitation Institute – University Health Network, Toronto, ON, Canada
North York General Hospital, Toronto, ON, Canada
Toronto Western Family Health Team, University Health Network, Toronto, ON, Canada
You can also search for this author in PubMed Google Scholar
Contributions
SJTG and AS conceptualized the study. SJTG, JS, BCC, KT, SJ, RM, LC, VN, and SM helped acquire the funding for this study. SH abstracted the associated data for this study from databases. AS, SJTG, and MT prepared, coordinated, and guided the data analyses. CC conducted the data analysis. AS, SJTG, and SM interpreted the findings. AS wrote the first draft of the manuscript, as well as, created all associated figures and tables. All authors critically reviewed and approved the manuscript.
Corresponding author
Correspondence to Arrani Senthinathan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethics approval
Section 45 of PHIPA authorizes ICES to collect personal health information, without consent, for the purpose of analysis or compiling statistical information with respect to the management of, evaluation or monitoring of, the allocation of resources to or planning for all or part of the health system. Projects that use data collected by ICES under section 45 of PHIPA, and use no other data, are exempt from REB review. The use of the data in this project is authorized under section 45 and approved by ICES’ Privacy and Legal Office (#2023 0904 527 000).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary material, rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Senthinathan, A., Tadrous, M., Hussain, S. et al. Examining the impact of the COVID-19 pandemic on homecare services among individuals with traumatic and non-traumatic spinal cord injuries. Spinal Cord (2024). https://doi.org/10.1038/s41393-024-00999-2
Download citation
Received : 18 March 2024
Revised : 17 May 2024
Accepted : 22 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1038/s41393-024-00999-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 30 May 2024
“Implementation of intensified COVID-19 vaccination optimization (ICVOPT) campaigns strategy in complex humanitarian emergency settings and hard-to-reach areas; a case of South Sudan”
- Dickens Atwongyeire 1 ,
- Ayesheshem Ademe Tegegne 1 ,
- Fabian Ndenzako 1 ,
- Brendan Dineen 1 ,
- Anson Edu Benjamin 1 ,
- Benz Luo 1 ,
- Ferede Melesachew 1 ,
- Emmanuel George Bachan 1 &
- Andrew Baguma 1
BMC Infectious Diseases volume 24 , Article number: 544 ( 2024 ) Cite this article
Metrics details
Introduction
The COVID-19 pandemic is still a public health concern in South Sudan having caused suffering since the first case of COVID-19 was introduced on 28 th February 2020. COVAX vaccines have since been introduced using a number of strategies including fixed site, temporary mobile, hit and run in flooded and conflict affected areas. We aim to describe the 2 ICVOPT campaigns that were conducted to improve the uptake and document lessons learnt during the initial rollout of the COVID-19 vaccination programin South Sudan between February 2022 and June 2022 each lasting for 7-days.
Methodology
We conducted an operational cross-sectional descriptive epidemiological study of a series of the intensified COVID-19 vaccination Optimization (ICVOPT) campaigns from February 2022 to June 2022. Before the campaign, a bottom up micro-planning was conducted, validated by the County Health Departments (CHDs) and national MOH team. Each of the 2 campaigns lasted for 7 days targeting 30% of the eligible unvaccinated target population who were18 years and above. Each team consisted of 2 vaccinators, 2 recorders and 1 mobilizer. The teams employed both fixed site, temporary mobile, hit and run in flooded and conflict affected areas. The number of teams were calculated based on the daily workload per day (80 persons per team/day) for the duration of the campaigns.
A total of 444,030 individuals were vaccinated with primary series COVID-19 vaccine (J&J) out of the targeted 635,030 persons. This represented 69.9% of target population in the selected 28 counties and 10 states of South Sudan in 7 days’ ICVOPT campaigns. More eligible persons were reached in 7 days campaigns than the 9 months of rollout of the COVID-19 vaccine prior to ICVOPT campaigns using the fixed site strategy at the health facility posts.
Intensified COVID-19 vaccination Optimization (ICVOPT) campaigns were vital and fast in scaling up vaccination coverages as compared to the fixed site vaccination strategies (2022 progress report on the Global Action Plan for Healthy Lives and Well-being for All Stronger collaboration for an equitable and resilient recovery towards the health-related Sustainable Development Goals, incentivizing collaboration, 2022) in complex humanitarian emergency settings and hard-to-reach areas of South Sudan.
Peer Review reports
“Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. The virus was first reported from Wuhan city in China in December, 2019, which in less than three months had spread throughout the globe. It was declared a global pandemic by the World Health Organization (WHO) on 11th of March 2020 [ 1 ].
South Sudan was equally affected by the pandemic with the Ministry of Health declaring the first 29-year old female, a returnee COVID-19 patient from the Netherlands on 28 February 2020 via Addis Ababa. She presented with fever, cough, headache and shortness of breath, subsequently laboratory confirmed on the 4th April 2020. Several activities were undertaken including screening using infra-red thermometers, quarantine and isolation of returnees from the highest risk countries at the time, enforcing total lockdown. In addition, curfews, travel restrictions, simple day-to-day measures like regular hand washing with soap and water; sanitizers, practicing cough hygiene, maintaining a social distance of at least one meter [ 1 ] were also utilized. In Africa, the first deliveries of the COVAX facility vaccines were registered in Ivory Coast and Ghana by February 24th 2021 which marked the start of what would be the largest, most rapid and complex global rollout of COVID-19 vaccines in history [ 2 ]. Thereafter, through the COVAX facility, vaccines were secured and deployed on 7th April 2021 in South Sudan, employing a number of strategies in the rollout of COVID-19 vaccination programme. The country employed fixed site strategy where vaccination activities were localized at the health facility. COVID-19 vaccination had been used like the rest of the world to bring the effects of the COVID-19 pandemic under control, in line with WHO’s 5 core components of COVID-19 preparedness, readiness and response [ 3 ]. The need to scale up COVID-19 vaccine uptake in South Sudan became necessary and of concern to WHO AFRO as it was evident that from April 2021 to December 2021 the cumulative percentage vaccination coverage was less than 2% and therefore failed to hit its WHO global target of 40% by the end of December 2021 [ 4 ]. That situation placed the country amongst the last three poorly performing countries in the continent of Africa [ 5 ]. This had been blamed on low risk perception by the population, lack of trust in government programs, misconceptions against COVID-19 vaccines causing infertility [ 6 ]. The vaccine was also associated with “sign of the beast” mentioned in the bible and number 666, infodemics from social media platforms such as recipients dying after 2 years post vaccination among others [ 6 ]. To make considerable progress, The World Health Organization Regional Office for Africa (WHO AFRO) supported the member states Ministries of Health with financial and human resources in form of technical assistance in driving the COVID-19 response in Africa. This gave South Sudan in particular an opportunity to employ a campaign mode of service delivery, Intensified COVID-19 vaccination Optimization (ICVOPT) with support from WHO South Sudan. The strategy employed multi-stakeholder approach to ensure political, social, community participation which enhanced programme ownership and possible future sustainable programming by integrating it into existing EPI structures and PHC services [ 3 ]. The strategy was able to bring vaccination services close to the most affected population by using mobile outreaches and hit and run modalities- employed in the security compromised states of Unity, Lakes, Upper Nile and Jonglei; due to civil conflict, cattle rustling and “revenge killing” and severe episodes of flooding. A group of vaccination teams would mobilize communities through their leaders to enable them access life saving services in a short period of time and then they would retreat afterwards to safer areas.
It is important to note that these states and counties affected by armed conflict, flooding and severe food shortages suffered from poor COVID-19 vaccination coverage rates.This is consistent with the UN security council report that vaccination rates in conflict-affected countries and areas facing humanitarian crises tended to be particularly low, as they faced additional challenges in planning, delivering critical services and administering the vaccines to the most vulnerable populations that need the jabs [ 7 ]. The report further goes on to highlight that as of 24th March 2022, Burundi and Haiti had received enough doses to cover only 3% of their populations; the Democratic Republic of the Congo and Yemen, 4%; Cameroon, 6% whereas Mali and South Sudan (8%) eight% [ 7 ]. The report emphasized that Syria had received enough doses to vaccinate 35% of its population and Nigeria 17%, slightly better than their humanitarian context affected counterparts. Much as planning, delivery and administering the vaccines seemed to be severely affected equally in these countries, some countries are more affected than others [ 7 ]. The factors responsible for low coverages included limited logistical capacity, humanitarian access challenges, fragmented healthcare systems, low capacity of government to train, recruit and sustain qualified health care workers that are well remunerated, which causes chronic brain drain and consequently shortage of healthcare workers [ 7 , 8 ]. Complicated issues related to poor access to eligible vulnerable populations remained a challenge for such countries such as Syria. Even though countries affected by humanitarian crises are fully supported by the concerted COVID-19 vaccination delivery partnership (CoVDP) and COVAX facility partners, absorption of these vaccines remains low. Issues around hesitancy remain due to difficulties in reaching appropriate information Education and communication (IEC) materials and access to the community leaders and communities in its entirety. Observations have been made that trust in fellow community mobilization members, community members and political leaders from such communities appeared to be low which further exacerbated the low coverage rates [ 7 ]. This affected the quality of COVID-19 vaccination activities offered and also the quality of data captured and eventually reported into the reporting databases. Due to protracted conflicts, there is usually weak governance, mistrust of government programs and eventually mistrust and or distrust of information like this one on COVID-19 and its vaccines [ 6 ]. The lower rates of vaccination may be also explained by skeptical attitudes towards vaccination making them susceptible to vaccine hesitation which can be addressed with clear, accessible and tailored information campaigns way beyond the COVID-19 vaccination campaigns period so that all the myths, misinformation and rumors can be counteracted by well-structured and informed community leadership structures [ 9 , 10 ].
The purpose of this paper is to describe the ICVOPT campaigns that were conducted to improve uptake and provide evidence based information that could be used in similar settings to rollout COVID-19 vaccination and other influenza like illnesses vaccinations. We aim to describe the 2 ICVOPT campaigns that have been conducted to improve the uptake and document lessons learnt during the initial rollout of the COVID-19 vaccination program in South Sudan between February 2022 and June 2022 during the 7-days campaigns.
Study setting
South Sudan is a landlocked country located in East Africa covering approximately 640,000km 2 with a projected population of 13,154,416 and a population density of 18 per square kilometer. The country is divided into ten states, 3 administrative units, 80 counties and 507 Payams. The country became independent on 9th July 2011, however, the country has struggled with tribal clashes and armed conflict, undeveloped road infrastructure that is even made worth by rains, causing massive floods, population movements and disruptions during the rainy seasons to the detriment of the health services and health indicators in the country.
Study design
We conducted a retrospective descriptive analysis of ICVOPT campaigns conducted in South Sudan from February 2022 and June 2022 amongst adult persons aged 18 years and above according to the South Sudan Immunization Technical Advisory Group (SSITAG) recommendations on COVID-19 Vaccine policy in the country.
Study description
An operational Cross-sectional descriptive epidemiological analysis of a series of the Intensified COVID-19 Vaccination Optimization (ICVOPT) campaigns was conducted in February 2022 and June 2022 during the 7 days campaigns. A total of 28 counties of the 80 counties were selected based on availability of funds, hard to reach status and low vaccination coverages at the time.
The coordination and planning meetings were held in the selected States and counties based on high number of unvaccinated persons, hard to reach counties as follows: 1st phase of ICVOPT; Northern Bahr El Ghazal (Aweil Centre), Unity (Rubkhona), Eastern Equatoria (Torit, Magwi), Western Bahr El Ghazal (Jur River, Wau) Central Equatoria (Juba). 2nd phase ICVOPT; Upper Nile (Manyo, Fashoda, Maban, Baliet, Akoka), Jonglei (Bor South, Twic East, Duk, Pibor), Lakes (Cueibet, Rumbek East, Awerial, Yirol west), Unity (Guit, Pariang, Mayom, Panyijar), Warrap ( Twic, Gogrial West, Gogrial East). Bottom up planning was facilitated by a robust WHO EPI and state coordination mechanisms (WHO EPI officers, EPI field national supervisors and Health Education and Promotion (HEP) officers were selected by Ministry of Health (MOH), oriented and deployed to support different areas of technical and risk communication and community engagement at state and county levels. Each county was supported by one EPI national supervisor and one HEP officer to support the county health department (CHD) in risk communication and community engagement activities. These campaigns were resourced through WHO direct implementation mechanisms. WHO States Coordination offices were urged to support all preparations. Activities supported included microplanning support, training of the vaccinators, recorders, social mobilizers, community meetings and other advocacy meetings like launch ceremonies for governance and leadership buy-ins, building trust by communities in the vaccine towards uptake of the COVID-19 vaccine. The vaccination sessions consisted of 5 team members: 2 vaccinators, 2 recorders and 1 social mobilizer. The vaccination activities took an average of 7 days at designated vaccination posts but the vaccination teams were allowed to change locations (mobile and temporary vaccination posts) to new areas whenever the primary locations were exhausted of the people in need of the vaccinations. The team supervisor in liaison with the social mobilizer mobilized the communities where they were going next through their community leaders for vaccination. Vaccination teams took advantage of the different humanitarian activities like Insecticide treated nets (ITNs) distribution, food distribution, health camps, cattle camps, market areas, churches and waterpoints to position the vaccination posts. The strategy also used Focus group Discussion (FGD) meetings with women groups, youth leaders, youth groups, religious leaders and community leaders in all the counties reached.
Data sources
All the data compiled was derived from the South Sudan COVID-19 vaccination dashboard at national level and reports provided by the COVID-19 vaccination team. A compilation of data occurred at the vaccination site level using tally sheets, daily summaries and sent it to the team supervisor who oversaw 3 vaccination teams, who in turn summarized daily teams’ summaries, reported it to the data manager at the County Health department (CHD) to be entered into the Open Data Kit (ODK) online tool. This data would then be received at the national level, verified and cleaned accordingly.
We conducted a basic analysis from the available information using excel spreadsheet to conduct descriptive analysis and produce graphs (Figs. 1 and 2 ) and tables (Tables 1 , 2 and 3 ) from the South Sudan COVID-19 vaccination dashboard and reports from the COVID-19 vaccination team of South Sudan.
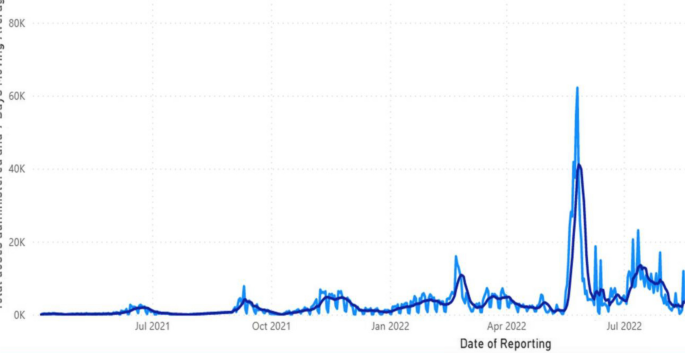
A graph showing the contribution of the 2 phases of ICVOPT campaigns towards scale up of COVID-19 Vaccination between Feb-June 2022, South Sudan
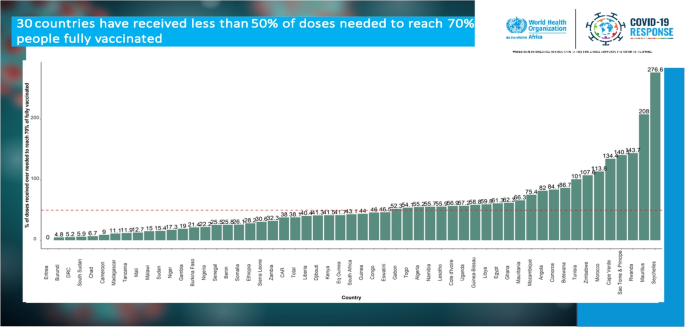
A graph showing South Sudan’s low performance during early rollout of vaccination programme in 2022
In February 2022, 69,553 persons were vaccinated with primary series COVID-19 vaccine (J&J), whereas a total of 374,477 persons were vaccinated after the second ICVOPT campaign in June 2022, making a total of 444,030 individuals who had been reached with COVID-19 vaccine (J&J). This was against the 635,030 persons targeted between the February 2022 and June 2022, representing 69.9% of target population in the selected 28 counties and 10 states, which raised the coverage to 29.1% (Tables 1 and 2 ). It is worth noting that some counties though improved in coverages after the intensified campaigns, some of them were still below the required standards. These were Magwi (25%), Twic East (13%), Jur River (50%), Juba (30%), Duk (25%), Bor South (22%), Awerial (27%), Parieng (53%). It was observed that low risk perceptions, hesitancy among the youth populations through social media, poor coordination from the vaccine hesitant county and states administrators contributed immensely to the low performance. Consideration of the vaccinated persons before and after the ICVOPT campaigns indicated that averagely 29% more persons were vaccinated with the COVID-19 vaccine. Some counties registered better performance than their counterparts as shown in Tables 1 and 2 .
Data as of 27th June 2022 from South Sudan COVID-19 vaccination dashboard
This graph highlights the chronology of events from when vaccination rollout began in April 2021 up to when the Ministry of Health (MOH) in collaboration with WHO and partners initiated the 2 phases of Intensified COVID-19 Vaccination Optimization campaigns to help scale up vaccination coverages between February 2022 and June 2022. This is indicated by sharp spikes in performance.
This graph illustrates the performance of South Sudan in COVID-19 vaccination as compared to other African states during early 2022. South Sudan was one of the lowest performing countries in the rollout of the COVID-19 vaccination services prior to this ICVOPT initiation.
In our study, we found out that some counties had performed above 60% of the target population (Akoka and Maban), while Magwi (25%), Twic East (13%), Jur River (50%), Juba (30%), Duk (25%), Bor South (22%), Awerial (27%), Parieng (53%) performed < 60% of the micro plan target. Good performance in some counties could be attributed to better leadership advocacy, social mobilization and community engagement at all levels, presence of IDPs and refugees in respective counties and presence of enabling health infrastructure and supportive cluster partners. Poor performance in some counties could be associated with some of the highlighted factors. There were numerous instances of insecurity (shooting, vaccinator arrests leading to confiscation of the vaccines and data tools) that led to threats, intimidation, neglecting of vaccination sites, harassments to the communities and the vaccination teams that were observed in many areas leading to lower COVID-19 vaccination coverages in those Payams and counties. The lower the vaccination coverages the lower the community herd immunity attained to protect them from the negative impacts of COVID-19 pandemic like severe illness, hospitalizations and deaths.
It is important to note that various areas had not been reached optimally due to the inaccessibility challenges because of inter-tribal clashes [ 11 , 12 , 13 ]. This was related to other humanitarian challenges like flooding, severe drought associated with severe food insecurities that had devastated some parts of the country putting the COVID-19 vaccination never number one priority. Poor penetration of information into the communities had been attributed to shortage of risk communication and community engagement rendering them hesitant to the vaccine, partly due to shortage of megaphone and batteries where some of them would do social mobilization activities without megaphones. High levels of hesitancy in some communities had been attributed to low risk perception levels to the COVID-19 pandemic itself and hence poor uptake of the vaccines. Some areas however lacked optimal coordination mechanisms, multiple infodemics circulating on series of social media outlets persisted in most counties and Payams [ 14 ]. These infodemics have been associated with saturation of some communities with negative information on COVID-19 vaccine that led to deep rooted anti-COVID-19 vaccination propaganda by some overzealous religious and traditional leaders especially in Jonglei state. These included “Infertility in the reproductively active young persons, “vaccine recipients must die within two years of the receiving the vaccine”, the vaccines cause blood clots, vaccine was connected with the biblical concept of “illuminati” from a misconception related to toll free number ‘6666’ and biblical ‘666’ in the Holy Bible citing Revelations 13: 16–17 verses as confirmation [ 14 , 15 ].
We aim to describe the 2 ICVOPT campaigns that have been conducted to improve the uptake and document lessons learnt during the initial rollout of the COVID-19 vaccination program in South Sudan between February 2022 and June 2022 in each of the 7-days campaigns.
Lessons learned and good practices
The bottom-up microplan development & engagement of counties’ leaderships during planning and implementation motivated teams at respective levels to work harder to perform better than was expected [ 12 , 16 ]. Strong leadership support, commitment & engagement during pre, intra & post campaign activities with States, County, Payam, Bomas provided a platform for reaching out to the communities with COVID-19 vaccination services as witnessed during ICVOPT [ 17 ]. This helped in reaching out to the vulnerable populations like elderly persons, IDPs/Refugees, females by bringing COVID-19 vaccination services ‘’closer to the people” and communities alike [ 17 ] Early initiation of Social mobilization activities including engagement of the churches, mosque and community leaders, youth and women groups at Payams and Bomas improved awareness about COVID-19 vaccination. The RCCE teams also engaged youths, women groups through Focused Group Discussions (FGDs), community dialogue meetings and held one on one advocacy meetings with their leaders to cascade awareness to their community members [ 17 ]. Regular daily coordination meetings (Performance Review meetings) at the different coordination levels like States, Counties, Payams aimed at daily review of the teams performance, identified gaps and devised appropriate corrective actions for improved performance during prospective vaccination campaigns, playing a key role in achieving the objectives of the ICVOPT campaigns. Vaccination teams took advantage of the different humanitarian activities like Insecticide treated nets (ITNs) distribution, food distribution, health camps and other community congregational points like market areas, churches and water points to position the vaccination posts. The strategy also used FGD meetings with women groups, youth leaders, youth groups, religious leaders and community leaders in all the counties reached. These interventions if utilized well in complex humanitarian emergency settings and hard-to-reach areas in collaboration with community leaders lead to improved response to crises and disasters in similar humanitarian settings.
Countries operating in humanitarian settings face a multitude of challenges in rolling out vaccination programmes. Intensified COVID-19 vaccination Optimization (ICVOPT) campaigns were vital and fast in scaling up vaccination coverages as compared to the fixed site vaccination strategies [ 18 ] in complex humanitarian emergency settings and hard-to-reach areas of South Sudan. Several ICVOPT campaigns were necessary to raise the COVID-19 vaccination coverages to build a sustainable community herd immunity against the COVID-19 pandemic in the country.
Limitations of the study
The study analyzed challenges, good practices and lessons learned during implementation of vaccination activities for use by members states experiencing similar humanitarian settings. By virtue of the complex fragile humanitarian context and weakened health systems some information may not be available, hence making it difficult to conclude on the effects of this innovation.
Availability of data and materials
Data is publicly available for information. The datasets generated and/or analyzed during the current study are available in the “Republic of South Sudan Ministry of Health COVID-19 Vaccination dashboard and reports” repository.
Abbreviations
County Health Department
COVID-19 Vaccine Delivery Partnership
Corona Virus Disease 2019
Expanded Programme on Immunization
Focus Group Discussions
Intensified COVID-19 vaccination Optimization
Information Education and Communication
Insecticide Treated Mosquito Nets
Ministry of Health
Risk Communication and Community Engagement
United Nations
Regional Office for Africa
World Health Organization
Lone SA, Ahmad A. COVID-19 pandemic–an African perspective. Emerging Microbes and Infections. Volume 9. Taylor and Francis Ltd; 2020. pp. 1300–8.
Burki TK. Challenges in the rollout of COVID-19 vaccines worldwide. Lancet Respir Med. 2021;9(4):e42–43.
Article CAS PubMed PubMed Central Google Scholar
WHO’s Strategic Preparedness, Readiness and Response Plan to End COVID-19 pandemic.
Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. Lancet Infect Dis. 2022;22(9):1293–302.
Impouma B, Mboussou F, Farham B, Makubalo L, Mwinga K, Onyango A, et al. COVID-19 vaccination rollout in the World Health Organization African region: status at end June 2022 and way forward. Epidemiol Infect. 2022;150:e143.
Lieberman A. Humanitarians plan for COVID-19 vaccinations in conflict zones devex.com/news/humanitarians-plan-for-covid-19-vaccinations-in-conflict-zones-98971. 2021.
What’s In Blue Briefing on COVID-19 Vaccines in Conflict and Humanitarian Settings. Available from: https://www.securitycouncilreport.org/whatsinblue/2022/04/briefing-on-covid-19-vaccines-in-conflict-and-humanitarian-settings.php?print=true .
Warsame A, Fuje M, Checchi F, Blanchet K, Palmer J. Evaluating COVID-19 decision-making in a humanitarian setting: the case study of Somalia. PLOS Global Public Health. 2022;2(3):e0000192.
Article PubMed PubMed Central Google Scholar
Immordino P, Graci D, Casuccio A, Restivo V, Mazzucco W. COVID-19 vaccination in migrants and refugees: lessons learnt and good practices. Vaccines (Basel). 2022;10(11):1965.
Article PubMed Google Scholar
French J, Deshpande S, Evans W, Obregon R. Key guidelines in developing a pre-emptive COVID-19 vaccination uptake promotion strategy. International Journal of Environmental Research and Public Health. 2020;17:1–14 (MDPI AG).
Article Google Scholar
Zard M, Lau LS, Bowser DM, Fouad FM, Lucumí DI, Samari G, et al. Leave no one behind: ensuring access to COVID-19 vaccines for refugee and displaced populations. Nat Med. 2021;27:747–9 (Nature Research).
Ayenigbara IO, Adegboro JS, Ayenigbara GO, Adeleke OR, Olofintuyi OO. The challenges to a successful COVID-19 vaccination programme in Africa. Vol. 11, •GERMS. 2021. Available from: www.germs.ro .
COVID-19 immunization in refugees and migrants: principles and key considerations.
Rapid Review. Vaccine hesitancy and building confidence in COVID-19 vaccination.
Soeters HM, Doshi RH, Fleming M, Adegoke OJ, Ajene U, Aksnes BN, et al. CDC’s COVID-19 international vaccine implementation and evaluation program and lessons from earlier vaccine introductions. Emerg Infect Dis. 2022;28(13):S208–216.
Ekzayez A, al-Khalil M, Jasiem M, Al Saleh R, Alzoubi Z, Meagher K, et al. Perspectives COVID-19 response in Northwest Syria: Innovation and community engagement in a complex conflict. J Public Health (Oxf). 2020;42:504–9 (Oxford University Press).
Considerations. for integrating COVID-19 vaccination tnto immunization programmes and primary health care for 2022 and beyond.
2022 progress report on the Global Action Plan for Healthy Lives and Well-being for All Stronger collaboration for an equitable and resilient recovery towards the health-related Sustainable Development Goals, incentivizing collaboration. 2022. http://apps.who.int/bookorders .
Download references
Acknowledgements
We thank our WHO Country Representative (Dr Fabian Ndenzako), EPR Team lead, Incident Manager, Dr Ademe Ayesheshem Tegegne for repeatedly providing support during authorship of this manuscript and lastly the COVID-19 vaccination team for the cooperation and teamwork during the implementation of the ICVOPT campaigns and during compilation of this paper. Special appreciation goes to my family members and more particularly to my wife (Mpeirwe Winfred) and children (Aaliyah, Azalea, Joel and Anastacia Gracias) for the continuous unlimited love, support and divine prayers that have helped me to succeed in my current and previous works. I thank all the anonymous reviewers for providing comments continuously to improve this manuscript to be ready for final publication.
No funding was available for this study.
Author information
Authors and affiliations.
World Health Organization, Central Equatoria State, Juba, South Sudan
Dickens Atwongyeire, Ayesheshem Ademe Tegegne, Fabian Ndenzako, Brendan Dineen, Anson Edu Benjamin, Benz Luo, Ferede Melesachew, Emmanuel George Bachan & Andrew Baguma
You can also search for this author in PubMed Google Scholar
Contributions
AD, ATA, planned, implemented campaigns, initiated and conceived the authorship of the paper, AEB, DB, FM planned, monitored the campaigns. FN supervised and monitored the campaigns, BA, BA supported data collection during campaigns and review of data presented, supported on referencing software. All authors contributed to the review, revision and approved the final manuscript submitted.
Corresponding author
Correspondence to Dickens Atwongyeire .
Ethics declarations
Ethics approval and consent to participate.
Not applicable as this involved review of reports and dashboards.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Atwongyeire, D., Tegegne, A.A., Ndenzako, F. et al. “Implementation of intensified COVID-19 vaccination optimization (ICVOPT) campaigns strategy in complex humanitarian emergency settings and hard-to-reach areas; a case of South Sudan”. BMC Infect Dis 24 , 544 (2024). https://doi.org/10.1186/s12879-024-09371-4
Download citation
Received : 27 August 2023
Accepted : 01 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12879-024-09371-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- COVID 19 intensification
- Optimization
- Complex humanitarian setting
- South Sudan
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
Exploring the impact of recent COVID-19 infection on perfusion and functional parameters derived from gated myocardial perfusion imaging in patients undergoing evaluation for coronary artery disease
- Original Article
- Published: 28 May 2024
Cite this article

- Maryam Alvandi ORCID: orcid.org/0000-0002-1829-5068 1 , 2 ,
- Zahra Shaghaghi ORCID: orcid.org/0000-0002-7467-4820 3 ,
- Zhino Fatehi 4 ,
- Behshad Naghshtabrizi 5 ,
- Tayeb Mohammadi 7 , 8 &
- Safoora Nikzad 6
Explore all metrics
This study seeks to evaluate how recent COVID-19 infection affects myocardial perfusion and functional parameters derived from gated myocardial perfusion imaging in patients undergoing evaluation for coronary artery disease. The goal is to enhance our understanding of COVID-19’s influence on the cardiovascular system.
Conducted at Farshchian Heart Hospital from 2022 to 2023, this case–control study enrolled patients suspected of coronary artery disease, stratified into two groups: those with confirmed COVID-19 infection within the past 6 months (study group) and those without prior COVID-19 infection (control group). Employing a 2-day protocol, stress testing and gated SPECT MPI were performed. Statistical analysis included descriptive statistics, Chi-square test, Student’s t test, and Mann–Whitney U test.
Among the 86 patients included, 43 were in each group. Significantly higher summed stress core and summed difference score values were observed in the study group compared to the control group ( p < 0.05). In addition, the study group exhibited significantly altered global left ventricular ejection fraction, end-diastolic volume, and end-systolic volume ( p < 0.05). Non-perfusion findings, including transient ischemic dilation and transient right ventricular visualization, were more prevalent in the study group.
Recent COVID-19 infection is associated with impaired myocardial perfusion and altered functional parameters as detected by MPI. These findings underscore the intricate interplay between COVID-19 and cardiovascular health, emphasizing the importance of comprehensive evaluation and management strategies to address cardiac complications in affected individuals. Further research is warranted to elucidate the underlying mechanisms and optimize patient care in the context of COVID-19-associated cardiovascular manifestations.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
The Role of Multimodality Imaging in Cardiomyopathy
Prognostic relevance of global work index and global constructive work in patients with non-ischemic dilated cardiomyopathy
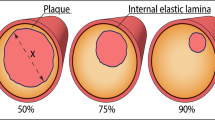
Diagnosis of myocardial infarction at autopsy: AECVP reappraisal in the light of the current clinical classification
Data availability.
The data used in this study are available upon request. Interested researchers can obtain the data by contacting the first author.
Abbreviations
- Coronary artery disease
- Myocardial perfusion imaging
Single-photon emission computed tomography
Summed stress score
Summed difference score
Summed rest score
Left ventricular ejection fraction
End-diastolic volume
End-systolic volume
Acute respiratory distress syndrome
Necrosis factor-alpha
Myocardial perfusion scan
Angiotensin-converting enzyme 2
Transient ischemic dilation
Transient right ventricular visualization
Neuropilin 1
Cathepsin B/L
Computed tomography
Ejection fraction
Cardiovascular magnetic resonance imaging
Transmembrane serine protease 2
Hawkins RB, Charles EJ, Mehaffey JH. Socio-economic status and COVID-19-related cases and fatalities. Public Health. 2020;189:129–34.
Article CAS PubMed Google Scholar
Pan F, Yang L, Li Y, Liang B, Li L, Ye T, et al. Factors associated with death outcome in patients with severe coronavirus disease-19 (COVID-19): a case-control study. Int J Med Sci. 2020;17(9):1281–92.
Article CAS PubMed PubMed Central Google Scholar
Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, et al. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666–87.
Ji T, Liu Z, Wang G, Guo X, Lai C, Chen H, et al. Detection of COVID-19: a review of the current literature and future perspectives. Biosens Bioelectron. 2020;166: 112455.
Yazdi A, Alvandi M, Shaghaghi Z, Hashemi SH, Inanloo SO, Hashemi S, et al. Coronavirus disease in cardiovascular patients: clinical characteristics and final prognosis. Avicenna J Clin Microbiol Infect. 2023;10(1):20–6.
Article CAS Google Scholar
Xie Y, You Q, Wu C, Cao S, Qu G, Yan X, et al. Impact of cardiovascular disease on clinical characteristics and outcomes of coronavirus disease 2019 (COVID-19). Circ J. 2020;84(8):1277–83.
Nishiga M, Wang DW, Han Y, Lewis DB, Wu JC. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17(9):543–58.
Oliveira RKF, Nyasulu PS, Iqbal AA, Hamdan Gul M, Ferreira EVM, Leclair JW, et al. Cardiopulmonary disease as sequelae of long-term COVID-19: current perspectives and challenges. Front Med (Lausanne). 2022;9:1041236.
Article PubMed Google Scholar
Naghshtabrizi B, Alvandi M, Shaghaghi Z, Hadei SK, Fariba F, Moradi M, et al. Transient ischemic dilation or transient RV visualization in patients with normal SPECT stress myocardial perfusion imaging: correlation with CT coronary artery calcium scoring and coronary angiography. J Nucl Cardiol. 2022;29(5):2149–56.
Alvandi M, Shaghaghi Z, Aryafar V, Fariba F, Sanaei Z. The evaluation of left ventricular dyssynchrony in hypertensive patients with a preserved systolic function undergoing gated SPECT myocardial perfusion imaging. Ann Nucl Med. 2019;33(12):899–906.
Hadei SK, Alvandi M, Ramezani M, Aloosh O, Shaghaghi Z, Moradi A. Applying Wells score to inconclusive perfusion only modified PIOPED II (Prospective Investigation of Pulmonary Embolism Diagnosis II) readings in order to optimize the lung scintigraphy diagnostic yield in acute pulmonary embolism detection. Ann Nucl Med. 2020;34(8):521–6.
Hassanzadeh S, Neshat S, Heidari A, Moslehi M. Myocardial perfusion imaging in the era of COVID-19: a systematic review. Clin Transl Imaging. 2023;11(2):165–97.
Shu H, Wen Z, Li N, Zhang Z, Ceesay BM, Peng Y, et al. COVID-19 and cardiovascular diseases: from cellular mechanisms to clinical manifestations. Aging Dis. 2023;14(6):2071–88.
Article PubMed PubMed Central Google Scholar
Nappi C, Megna R, Acampa W, Assante R, Zampella E, Gaudieri V, et al. Effects of the COVID-19 pandemic on myocardial perfusion imaging for ischemic heart disease. Eur J Nucl Med Mol Imaging. 2021;48(2):421–7.
Assante R, D’Antonio A, Mannarino T, Gaudieri V, Zampella E, Mainolfi CG, et al. Impact of COVID-19 infection on short-term outcome in patients referred to stress myocardial perfusion imaging. Eur J Nucl Med Mol Imaging. 2022;49(5):1544–52.
Thornton GD, Shetye A, Knight DS, Knott K, Artico J, Kurdi H, et al. Myocardial perfusion imaging after severe COVID-19 infection demonstrates regional ischemia rather than global blood flow reduction. Front Cardiovasc Med. 2021;8: 764599.
Kotecha T, Knight DS, Razvi Y, Kumar K, Vimalesvaran K, Thornton G, et al. Patterns of myocardial injury in recovered troponin-positive COVID-19 patients assessed by cardiovascular magnetic resonance. Eur Heart J. 2021;42(19):1866–78.
Escher F, Pietsch H, Aleshcheva G, Bock T, Baumeier C, Elsaesser A, et al. Detection of viral SARS-CoV-2 genomes and histopathological changes in endomyocardial biopsies. ESC Heart Fail. 2020;7:2440–7.
Bailey AL, Dmytrenko O, Greenberg L, Bredemeyer AL, Ma P, Liu J, et al. SARS-CoV-2 infects human engineered heart tissues and models COVID-19 myocarditis. JACC Basic Transl Sci. 2021;6(4):331–45.
Bojkova D, Wagner J, Shumliakivska M, Aslan G, Saleem U, Hansen A, et al. SARS-CoV-2 infects and induces cytotoxic effects in human cardiomyocytes. Cardiovasc Res. 2020;116:2207–15.
Chen S, Yang L, Nilsson-Payant B, Han Y, Jaffré F, Zhu J, et al. SARS-CoV-2 infected cardiomyocytes recruit monocytes by secreting CCL2. Res Sq. 2020. https://doi.org/10.21203/rs.3.rs-94634/v1 .
Abdi A, AlOtaiby S, Badarin FA, Khraibi A, Hamdan H, Nader M. Interaction of SARS-CoV-2 with cardiomyocytes: insight into the underlying molecular mechanisms of cardiac injury and pharmacotherapy. Biomed Pharmacother. 2022;146: 112518. https://doi.org/10.1016/j.biopha.2021 .
Ceasovschih A, Sorodoc V, Shor A, Haliga RE, Roth L, Lionte C, et al. Distinct features of vascular diseases in COVID-19. J Inflamm Res. 2023;16:2783–800.
Vacanti G, Bramlage P, Schymik G, Schmitt C, Luik A, Swojanowsky P, et al. Reduced rate of admissions for acute coronary syndromes during the COVID-19 pandemic: an observational analysis from a tertiary hospital in Germany. Herz. 2020;45(7):663–7.
Nappi F, Avtaar Singh SS. Endothelial dysfunction in SARS-CoV-2 infection. Biomedicines. 2022;10(3):654.
Einstein AJ, Hirschfeld C, Williams MC, Vitola JV, Better N, Villines TC, et al. Worldwide disparities in recovery of cardiac testing 1 year into COVID-19. J Am Coll Cardiol. 2022;79(20):2001–17.
Pelle MC, Zaffina I, Lucà S, Forte V, Trapanese V, Melina M, et al. Endothelial dysfunction in COVID-19: potential mechanisms and possible therapeutic options. Life (Basel). 2022;12(10):1605.
CAS PubMed Google Scholar
Zhang C. The role of inflammatory cytokines in endothelial dysfunction. Basic Res Cardiol. 2008;103(5):398–406.
Araz M, Soydal Ç, Sütçü G, Demir B, Özkan E. Myocardial perfusion SPECT findings in postCOVID period. Eur J Nucl Med Mol Imaging. 2022;49(3):889–94.
Hasnie UA, Bhambhvani P, Iskandrian AE, Hage FG. Prevalence of abnormal SPECT myocardial perfusion imaging during the COVID-19 pandemic. Eur J Nucl Med Mol Imaging. 2021;48(8):2447–54.
Çap M, Bilge Ö, Gündoğan C, Tatlı İ, Öztürk C, Taştan E, et al. SPECT myocardial perfusion imaging identifies myocardial ischemia in patients with a history of COVID-19 without coronary artery disease. Int J Cardiovasc Imaging. 2022;38(2):447–56.
Hasnie UA, Hawi R, Andrikopoulou E, Iskandrian AE, Hage FG. Stress testing and myocardial perfusion imaging for patients after recovery from severe COVID-19 infection requiring hospitalization: a single-center experience. J Nucl Cardiol. 2021;28(5):2167–73.
Drakos S, Chatzantonis G, Bietenbeck M, Evers G, Schulze AB, Mohr M, et al. A cardiovascular magnetic resonance imaging-based pilot study to assess coronary microvascular disease in COVID-19 patients. Sci Rep. 2021;11(1):15667.
Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, et al. Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging. 2020;13(11):2330–9.
Al-Ani F, Chehade S, Lazo-Langner A. Thrombosis risk associated with COVID-19 infection. A scoping review. Thromb Res. 2020;192:152–60.
Download references
Acknowledgements
The authors would like to thank the Clinical Research Development Unit of Farshchian Heart Hospital, Hamadan University of Medical Sciences, Hamadan, Iran, for their assistance throughout the period of study.
Author information
Authors and affiliations.
Cardiovascular Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Maryam Alvandi
Department of Nuclear Medicine and Molecular Imaging, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
Cancer Research Center, Hamadan University of Medical Sciences, Hamadan, Iran
Zahra Shaghaghi
Student Research Committee, Hamadan University of Medical Sciences, Hamadan, Iran
Zhino Fatehi
Clinical Research Development Unit of Farshchian Heart Hospital, Hamadan University of Medical Sciences, Hamadan, Iran
Behshad Naghshtabrizi
Department of Medical Physics, Faculty of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran
Safoora Nikzad
Department of Biostatistics, School of Public Health, Hamadan University of Medical Sciences, Hamadan, Iran
Tayeb Mohammadi
Research Center for Health Sciences, Hamadan University of Medical Sciences, Hamadan, Iran
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Zahra Shaghaghi .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Alvandi, M., Shaghaghi, Z., Fatehi, Z. et al. Exploring the impact of recent COVID-19 infection on perfusion and functional parameters derived from gated myocardial perfusion imaging in patients undergoing evaluation for coronary artery disease. Ann Nucl Med (2024). https://doi.org/10.1007/s12149-024-01946-0
Download citation
Received : 19 February 2024
Accepted : 19 May 2024
Published : 28 May 2024
DOI : https://doi.org/10.1007/s12149-024-01946-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research

IMAGES
COMMENTS
An Introduction to COVID-19. Simon James Fong, 4 Nilanjan Dey, 5 and Jyotismita Chaki 6 ... as per WorldPop's provisional study of the spread of COVID-19. ... The very first case of coronavirus in the United States was identified in Washington on 21 January 2020 by an individual who flew to Wuhan and returned to the United States. The second ...
The spread of the "Severe Acute Respiratory Coronavirus 2" (SARS-CoV-2), the causal agent of COVID-19, was characterized as a pandemic by the World Health Organization (WHO) in March 2020 and has triggered an international public health emergency [].The numbers of confirmed cases and deaths due to COVID-19 are rapidly escalating, counting in millions [], causing massive economic strain ...
The United States' Response to COVID-19: A Case Study, Synopsis | Introduction | 1 Despite the United States' enormous wealth and unparalleled medical and scientific capacity, the country's epidemic dwarfs that of any other country. The U.S. reports more than 28 million cases and 500,000 deaths, accounting for 25%
As reported by the CDC, from February 12 to April 2, 2020, of 149,760 cases of confirmed COVID-19 in the United States, 2572 (1.7%) were children aged <18 years, similar to published rates in ...
Introduction. The coronavirus disease (COVID-19), discovered in December 2019 in China, has reached the level of a pandemic and, till June 2021, it has affected more than 171 million people worldwide and caused more than 3.5 million deaths all over the world [].The COVID-19 pandemic as a major health crisis has caught the attention of many researchers, which has led to the creation of a broad ...
The COVID-19 pandemic has meant that young university students have had to adapt their learning and have a reduced relational context. Adversity contexts build models of human behaviour based on ...
NATIONAL CENTER FOR CASE STUDY TEACHING IN SCIENCE Introduction As one of the leading virologists in the Epidemic Intelligence Service (EIS) branch of the Centers for Disease Control (CDC), you have been tapped to lead a team of scientists in tracking the spread of the novel coronavirus (COVID-19) pandemic in the United States.
An introduction to the CFR Task Force Report on pandemic preparedness and the lessons of COVID-19. ... being prepared for the worst-case scenario of a severe pandemic and ready to execute on that ...
2.2.1 Introduction. A year after the declaration of the global pandemic status by the World Health Organization (WHO), coronavirus disease (COVID-19) remains a major threat in many parts of the world. ... Case Study—COVID-19. In: Kanbara, S., Miyagawa, S., Miyazaki, H. (eds) Disaster Nursing, Primary Health Care and Communication in ...
Executive summary. This report examines primary health care (PHC) in Jordan in the context of the COVID-19 pandemic between early 2020 and August 2022. PHC, as outlined in the 1978 Declaration of Alma-Ata and further emphasized in the Astana Declaration in 2018 (1), is a comprehensive approach to health that combines governmental and society ...
Coronavirus disease (COVID-19) is an infectious disease caused by the SARS-CoV-2 virus. Most people infected with the virus will experience mild to moderate respiratory illness and recover without requiring special treatment. However, some will become seriously ill and require medical attention. Older people and those with underlying medical ...
An overview of the COVID-19 pandemic The first COVID-19 case in Georgia was detected on 26 February 2020, almost two months after the novel virus was identified. Through its multisectoral response and its appropriate and coordinated activities, the GoG managed to delay the arrival of the first COVID-19 case entrance in the country (Government
Approximately 6% of patients with Covid-19 have a critical illness that is characterized by respiratory failure, shock, or multiorgan dysfunction. 1 Data from China show an incidence of acute ...
Training & Exercises. COVID-19 vaccines. 12 May 2021. How lessons learned from the Ebola virus helped Liberia respond to the COVID-19 pandemic. 22 March 2021. El Salvador's President takes the lead in promoting a stringent lockdown against COVID-19 with support from all levels, including the PAHO/WHO country office.
Results from these studies are essential to preventing further zoonotic introductions of SARS-CoV-2 into the human population. WHO continues to collaborate with animal health and human health experts, Member States, and other partners to identify gaps and research priorities for the control of COVID-19, including the eventual identification of
Introduction. As of November 4, 2021, the spread of novel coronavirus had reached 219 countries and territories of the world, infecting a total of 248 million people and resulting in five million deaths [].In March 2020, several countries including India declared a mandatory lockdown, resulting in the temporary closure of many institutions, not least educational ones.
Introduction:The coronavirus disease of 2019 (COVID-19) pandemic has resulted in a great deal of morbidity and mortality worldwide. ... Overall, our office performed 5 autopsies during the study period where COVID-19 was considered the primary cause of death, 4 cases where COVID-19 was considered a contributory cause of death, and 28 cases ...
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes. Objectives The ...
COVID-19. 127 Results. 12 Dec 2023. Research & Ideas. COVID Tested Global Supply Chains. Here's How They've Adapted. by Scott Van Voorhis. 15 Aug 2023. Cold Call Podcast.
COVID-19 (coronavirus disease 2019) is a disease caused by a virus named SARS-CoV-2. It can be very contagious and spreads quickly. Over one million people have died from COVID-19 in the United States. COVID-19 most often causes respiratory symptoms that can feel much like a cold, the flu, or pneumonia. COVID-19 may attack more than your lungs ...
Descriptive repeated-cross sectional retrospective longitudinal cohort study. To investigate the impact of the COVID-19 pandemic on homecare services in individuals with traumatic or non-traumatic ...
In this systematic review and meta-analysis, we identified, reviewed, and extracted from the scientific literature retrospective and prospective cohort studies and test-negative case-control studies published from inception up to Sept 31, 2022, that estimated the reduction in risk of COVID-19 among individuals with a past SARS-CoV-2 infection in comparison to those without a previous infection.
The concept of pandemic fatigue has been invoked by governments and health authorities as a political strategy to delay the introduction of or loosen COVID-19 protections and frame COVID-19 safety as a matter of personal responsibility and choice, though a review of empirical studies suggests that such fatigue is less of an issue than is often ...
Introduction The COVID-19 pandemic is still a public health concern in South Sudan having caused suffering since the first case of COVID-19 was introduced on 28th February 2020. COVAX vaccines have since been introduced using a number of strategies including fixed site, temporary mobile, hit and run in flooded and conflict affected areas. We aim to describe the 2 ICVOPT campaigns that were ...
Based on studies using the Oxford COVID-19 Government Response Tracker panel database and its lockdown stringency index (Hale et al., Citation 2021), they found that the average lockdown in Europe and the United States to have reduced deaths attributed to COVID-19 by merely 3.2% in the first half of 2020 (Herby et al., Citation 2023).
Objective This study seeks to evaluate how recent COVID-19 infection affects myocardial perfusion and functional parameters derived from gated myocardial perfusion imaging in patients undergoing evaluation for coronary artery disease. The goal is to enhance our understanding of COVID-19's influence on the cardiovascular system. Method Conducted at Farshchian Heart Hospital from 2022 to 2023 ...