
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
Theme 5: How Do We Control Our Fertility?

5.1 Human Reproductive Anatomy
Human reproductive anatomy.
In general, the reproductive structures in humans can be divided into three main categories: gonads, internal genitalia and external genitalia. The gonads are the organs in which gametes , the cells that fuse in fertilization to form new individuals, develop and mature. All other reproductive structures are called genitalia, or genitals. Internal genitalia are found inside of the body, while external genitalia are visible from the outside. The structures seen in adult males and females actually come from the same precursors in embryos, so there are many similarities in both structure and function between males and females. There is also a wide spectrum of structures present in any one individual; many people have structures that resemble a combination of male and female structures, or that resemble neither. In this textbook, we will define “male” and “female” based on individuals who have the most typical structures characteristic of those two sexes; other types of structures are also normal and common. We will describe the functions of these structures during vaginal sexual intercourse, since that is the sexual act used in reproduction; keep in mind that other types of sexual activity are also common and normal.
Male Reproductive Anatomy
In the male reproductive system, the scrotum houses the testicles or testes (singular: testis), including providing passage for blood vessels, nerves, and muscles related to testicular function. The testes are gonads, and they produce sperm (the male gametes) and some reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 in) in size and divided into wedge-shaped lobules by connective tissue called septa.
Sperm are immobile at body temperature; therefore, the scrotum and penis are external to the body, as illustrated in Figure 1 so that a proper temperature is maintained for motility.
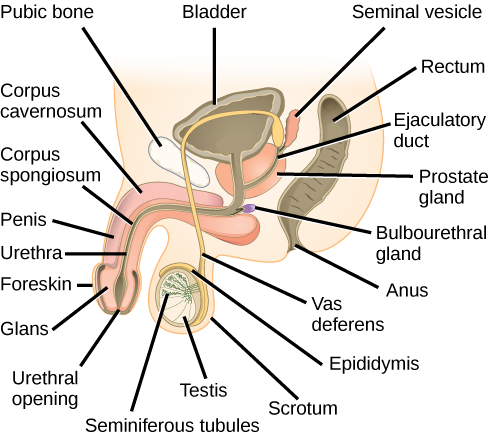
The internal genitalia in males are important for the production of sperm, and of other components of . the semen. Sperm mature in seminiferous tubules that are coiled inside the testes, as illustrated in Figure 1 . The walls of the seminiferous tubules are made up of the developing sperm cells, with the least developed sperm at the periphery of the tubule and the fully developed sperm in the lumen. The sperm cells are mixed with “nursemaid” cells called Sertoli cells which protect the germ cells and promote their development. Other cells mixed in the wall of the tubules are the interstitial cells of Leydig . These cells produce high levels of testosterone once the male reaches adolescence.
When the sperm have developed flagella and are nearly mature, they leave the testicles and enter the epididymis, shown in Figure 1 . This structure resembles a comma and lies along the top and posterior portion of the testes; it is the site of sperm maturation. The sperm leave the epididymis and enter the vas deferens (or ductus deferens), which carries the sperm, behind the bladder, and forms the ejaculatory duct with the duct from the seminal vesicles. During a vasectomy, a section of the vas deferens is removed, preventing sperm from being passed out of the body during ejaculation and preventing fertilization.
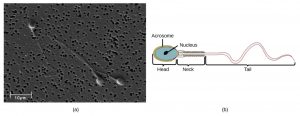
Semen is a mixture of sperm and spermatic duct secretions (about 10 percent of the total) and fluids from accessory glands that contribute most of the semen’s volume. Sperm are haploid cells, consisting of a flagellum as a tail, a neck that contains the cell’s energy-producing mitochondria, and a head that contains the genetic material. Figure 2 shows a micrograph of human sperm as well as a diagram of the parts of the sperm. An acrosome is found at the top of the head of the sperm. This structure contains enzymes that can digest the protective coverings that surround the egg to help the sperm penetrate and fertilize the egg. An ejaculate (a single emission of sperm) will contain from two to five milliliters of fluid with from 50–120 million sperm per milliliter.
The bulk of the semen comes from the accessory glands associated with the male reproductive system. These are the seminal vesicles, the prostate gland, and the bulbourethral gland, all of which are illustrated in Figure 1 . The seminal vesicles are a pair of glands that lie along the posterior border of the urinary bladder. The glands make a solution that is thick, yellowish, and alkaline. As sperm are only motile in an alkaline environment, a basic pH is important to reverse the acidity of the vaginal environment. The solution also contains mucus, fructose (a sperm mitochondrial nutrient), a coagulating enzyme, ascorbic acid, and local-acting hormones called prostaglandins. The seminal vesicle glands account for 60 percent of the bulk of semen.
The penis , illustrated in Figure 1 , is an organ that drains urine from the renal bladder and functions as a copulatory organ during intercourse. The penis contains three tubes of erectile tissue running through the length of the organ. These consist of a pair of tubes on the dorsal side, called the corpus cavernosum, and a single tube of tissue on the ventral side, called the corpus spongiosum. This tissue will become engorged with blood, becoming erect and hard, in preparation for sexual intercourse. The organ is inserted into the vagina culminating with an ejaculation. During intercourse, the smooth muscle sphincters at the opening to the renal bladder close and prevent urine from entering the penis. An orgasm is a two-stage process: first, glands and accessory organs connected to the testes contract, then semen (containing sperm) is expelled through the urethra during ejaculation. After intercourse, the blood drains from the erectile tissue and the penis becomes flaccid.
The walnut-shaped prostate gland surrounds the urethra, the connection to the urinary bladder. It has a series of short ducts that directly connect to the urethra. The gland is a mixture of smooth muscle and glandular tissue. The muscle provides much of the force needed for ejaculation to occur. The glandular tissue makes a thin, milky fluid that contains citrate (a nutrient), enzymes, and prostate specific antigen (PSA). PSA is a proteolytic enzyme that helps to liquefy the ejaculate several minutes after release from the male. Prostate gland secretions account for about 30 percent of the bulk of semen.
The bulbourethral gland , or Cowper’s gland, releases its secretion prior to the release of the bulk of the semen. It neutralizes any acid residue in the urethra left over from urine. This usually accounts for a couple of drops of fluid in the total ejaculate and may contain a few sperm. Withdrawal of the penis from the vagina before ejaculation to prevent pregnancy may not work if sperm are present in the bulbourethral gland secretions. The location and functions of the male reproductive organs are summarized in Table 1 .
Female Reproductive Anatomy
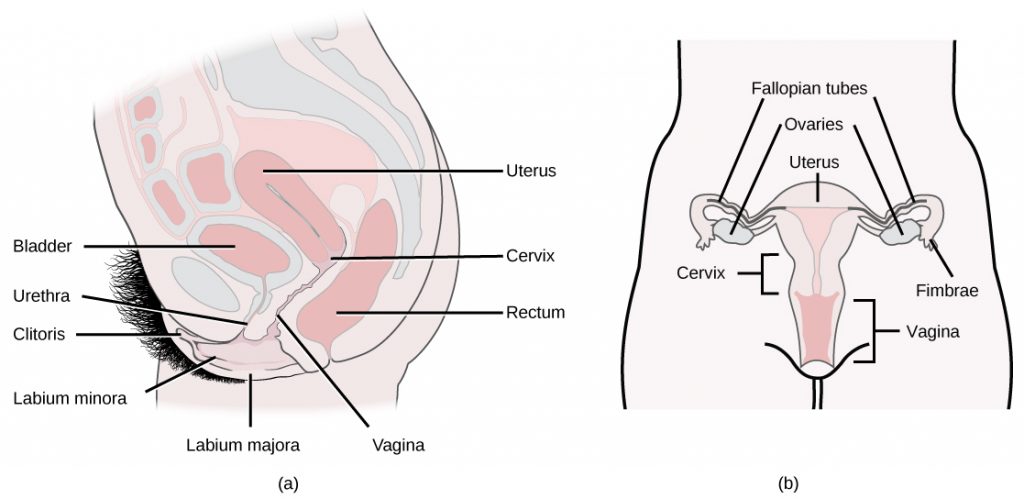
A number of reproductive structures are exterior to the female’s body. These include the breasts and the vulva, which consists of the mons pubis, clitoris, labia majora, labia minora, and the vestibular glands, all illustrated in Figure 3 . The location and functions of the female reproductive organs are summarized in Table 2 . The mons pubis is a round, fatty area that overlies the pubic bone. The clitoris is a structure with erectile tissue that contains a large number of sensory nerves and serves as a source of stimulation during intercourse. The labia majora are a pair of elongated folds of tissue that run posterior from the mons pubis and enclose the other components of the vulva. The labia majora derive from the same tissue that produces the scrotum in a male. The labia minora are thin folds of tissue centrally located within the labia majora. These labia protect the openings to the vagina and urethra. The mons pubis and the anterior portion of the labia majora become covered with hair during adolescence; the labia minora is hairless. The greater vestibular glands are found at the sides of the vaginal opening and provide lubrication during intercourse. The vulva is the name for the entire set of external genitalia in the inguinal (groin) area of females; in common language this is sometimes referred to as the vagina, but that is not anatomically accurate; the vagina is an entirely internal structure.
The breasts consist of mammary glands and fat. The size of the breast is determined by the amount of fat deposited behind the gland. Each gland consists of 15 to 25 lobes that have ducts that empty at the nipple and that supply the nursing child with nutrient- and antibody-rich milk to aid development and protect the child.
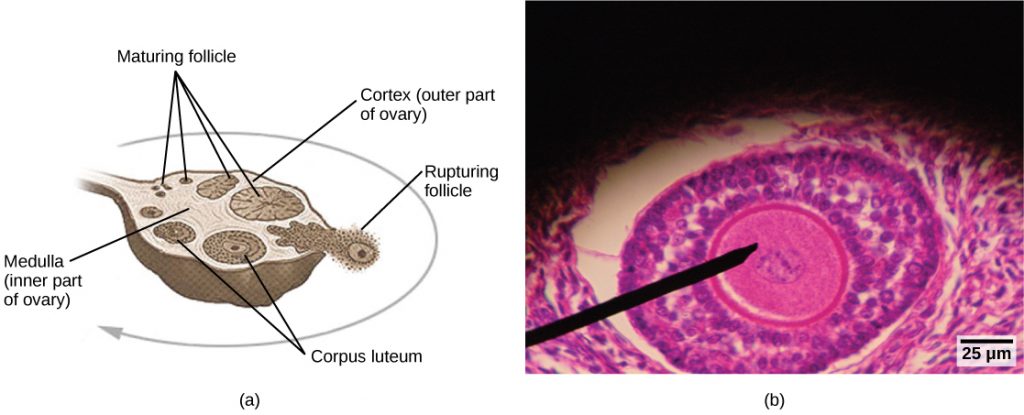
Internal female reproductive structures include ovaries, oviducts, the uterus , and the vagina, shown in Figure 3 . The two ovaries (the female gonads) are held in place in the abdominal cavity by a system of ligaments. Ovaries consist of a medulla and cortex: the medulla contains nerves and blood vessels to supply the cortex with nutrients and remove waste. The outer layers of cells of the cortex are the functional parts of the ovaries. The cortex is made up of follicular cells that surround eggs that develop during fetal development in utero . During the menstrual period, a batch of follicular cells develops and prepares the eggs for release. At ovulation, one follicle ruptures and one egg is released, as illustrated in Figure 4a .
The oviducts , or fallopian tubes, extend from the uterus in the lower abdominal cavity to the ovaries, but they are not in contact with the ovaries. The lateral ends of the oviducts flare out into a trumpet-like structure and have a fringe of finger-like projections called fimbriae, illustrated in Figure 4b . When an egg is released at ovulation, the fimbrae help the non-motile egg enter into the tube and passage to the uterus. The walls of the oviducts are ciliated and are made up mostly of smooth muscle. The cilia beat toward the middle, and the smooth muscle contracts in the same direction, moving the egg toward the uterus. Fertilization usually takes place within the oviducts and the developing embryo is moved toward the uterus for development. It usually takes the egg or embryo a week to travel through the oviduct. Sterilization in females is called a tubal ligation; it is analogous to a vasectomy in males in that the oviducts are severed and sealed.
The uterus is a structure about the size of a females’s fist. This is lined with an endometrium rich in blood vessels and mucus glands. The uterus supports the developing embryo and fetus during gestation. The thickest portion of the wall of the uterus is made of smooth muscle. Contractions of the smooth muscle in the uterus aid in passing the baby through the vagina during labor. A portion of the lining of the uterus sloughs off during each menstrual period, and then builds up again in preparation for an implantation. Part of the uterus, called the cervix, protrudes into the top of the vagina. A small opening called the cervical orifice allows menstrual fluid out of the cervix into the vagina, and sperm into the uterus. During childbirth the cervical orifice is greatly enlarged.
The vagina is a muscular tube that serves several purposes. It allows menstrual flow to leave the body. It is the receptacle for the penis during intercourse and the vessel for the delivery of offspring. It is lined cells that produce acidic secretions that limit the growth of microbes that could potentially travel into the uterus.
Development of Reproductive Organs in Humans.
The reproductive tissues of male and female humans develop similarly in utero (in a fetus developing in the mother’s uterus) for the first several weeks of gestation. The hormone testosterone is typically only released in embryos that have a male sex chromosome (the Y chromosome, discussed in the next chapter), and this hormone controls the generation of reproductive structures. A low level of the hormone testosterone is released from male gonads in the developing embryos, starting at around the second month of gestation. Testosterone causes the undeveloped tissues to differentiate into male sexual organs. When testosterone is absent, the tissues develop into female sexual tissues. Primitive gonads become testes or ovaries. Tissues that produce a penis in males produce a clitoris in females. The tissue that will become the scrotum in a male becomes the labia in a female; that is, they are homologous structures. Because of this, there are often variations in development resulting in structures that may have characteristics of both sexes, or of neither sex, depending on hormonal levels and other factors present during embryogenesis. These variations in sexual structures are quite common and normal.
Sexual Response During Intercourse
The sexual response in humans is both psychological and physiological. Both sexes experience sexual arousal through psychological and physical stimulation. There are four phases of the sexual response. During phase one, called excitement, vasodilation leads to vasocongestion in erectile tissues in both males and females. The nipples, clitoris, labia, and penis engorge with blood and become enlarged. Vaginal secretions are released to lubricate the vagina to facilitate intercourse. During the second phase, called the plateau, stimulation continues, the outer third of the vaginal wall enlarges with blood, and breathing and heart rate increase.
During phase three, or orgasm, rhythmic, involuntary contractions of muscles occur in both sexes. In the male, the reproductive accessory glands and tubules constrict placing semen in the urethra, then the urethra contracts expelling the semen through the penis. In females, the uterus and vaginal muscles contract in waves that may last slightly less than a second each. During phase four, or resolution, the processes described in the first three phases reverse themselves and return to their normal state. Males experience a refractory period in which they cannot maintain an erection or ejaculate for a period of time ranging from minutes to hours.
Section Summary
The reproductive structures that evolved in humans allow males and females to mate, fertilize internally, and support the growth and development of offspring. Reproductive structures include gonads, internal and external genitalia. Some male and female reproductive structures have analogous functions and are derived from common precursor structures. Both males and females have four stages of the sexual response.
Human Biology Copyright © by Sarah Malmquist and Kristina Prescott is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book
If you're seeing this message, it means we're having trouble loading external resources on our website.
If you're behind a web filter, please make sure that the domains *.kastatic.org and *.kasandbox.org are unblocked.
To log in and use all the features of Khan Academy, please enable JavaScript in your browser.
High school biology
Course: high school biology > unit 8.
- Welcome to the reproductive system
- Egg, sperm, and fertilization
- The reproductive system review
The reproductive system
- (Choice A) Uterus A Uterus
- (Choice B) Ovary B Ovary
- (Choice C) Oviduct (fallopian tube) C Oviduct (fallopian tube)
- (Choice D) Vagina D Vagina
The website is not compatible for the version of the browser you are using. Not all the functionality may be available. Please upgrade your browser to the latest version.
- Social Media
- Access Points
- Print/Export Standards
- Standards Books
- Coding Scheme
- Standards Viewer App
- Course Descriptions
- Graduation Requirements
- Course Reports
- Gifted Coursework
- Career and Technical Education (CTE) Programs
- Browse/Search
- Original Student Tutorials
- MEAs - STEM Lessons
- Perspectives STEM Videos
- STEM Reading Resources
- Math Formative Assessments
- CTE Related Resources
- Our Review Process
- Professional Development Programs
- iCPALMS Tools
- Resource Development Programs
- Partnership Programs
- User Testimonials
- iCPALMS Account
![assignment on the topic reproductive system Cpalms [Logo]](https://www.cpalms.org/images/cpalms_color.png)
- Not a member yet? SIGN UP
- Home of CPALMS
- Standards Info. & Resources
- Course Descriptions & Directory
- Resources Vetted by Peers & Experts
- PD Programs Self-paced Training
- About CPALMS Initiatives & Partnerships
- iCPALMS Florida's Platform
The Human Reproductive System, Part 1
Explore the genetic advantage of sexual reproduction, describe the basic anatomy and physiology of both the male and female human reproductive systems, describe the process of human development leading up to birth, and identify major changes associated with each trimester of pregnancy.
This interactive tutorial is part 1 in a two-part series. Click here to

Attachments
General information, source and access information, aligned standards, suggested tutorials.
Explore the process of human development leading up to birth, and identify major changes associated with each trimester of pregnancy.
This interactive tutorial is part 2 in a two-part series. Click here to launch .
Related Resources
Congratulations, you have successfully created an account..
A verifications link was sent to your email at . Please check your email and click on the link to confirm your email address and fully activate your iCPALMS account. Please check your spam folder.
Did you enter an incorrect email address?
Did not receive an email, you have not completed your profile information. please take a few moments to complete the section below so we can customize your cpalms experience., there was an error creating your account. please contact support [email protected] for assistance., modal header, feedback form.
Please fill the following form and click "Submit" to send the feedback.
Your Email Address: *
Your comment : *, teacher rating, leave cpalms.
You are leaving the CPALMS website and will no longer be covered by our Terms and Conditions.

Stay in touch with CPALMS

Loading....
This website is trying to open a CPALMS page using an iFrame, which is against our terms of use . Click the link below to view the resource on CPALMS.org.
Module 11: The Reproductive System
Anatomy and physiology of the female reproductive system, learning objectives.
By the end of this section, you will be able to:
- Describe the structure and function of the organs of the female reproductive system
- List the steps of oogenesis
- Describe the hormonal changes that occur during the ovarian and menstrual cycles
- Trace the path of an oocyte from ovary to fertilization
The female reproductive system functions to produce gametes and reproductive hormones, just like the male reproductive system; however, it also has the additional task of supporting the developing fetus and delivering it to the outside world. Unlike its male counterpart, the female reproductive system is located primarily inside the pelvic cavity. Recall that the ovaries are the female gonads. The gamete they produce is called an oocyte . We’ll discuss the production of oocytes in detail shortly. First, let’s look at some of the structures of the female reproductive system.
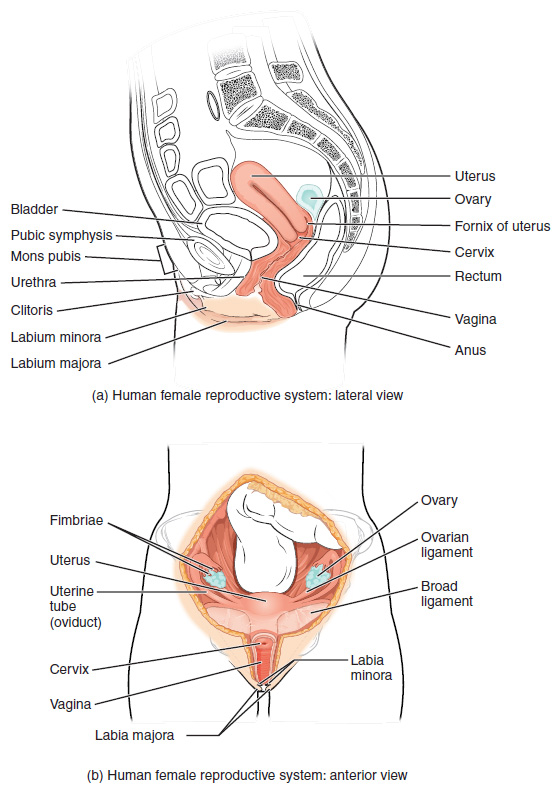
Figure 1. The major organs of the female reproductive system are located inside the pelvic cavity.
External Female Genitals
The external female reproductive structures are referred to collectively as the vulva . The mons pubis is a pad of fat that is located at the anterior, over the pubic bone. After puberty, it becomes covered in pubic hair. The labia majora (labia = “lips”; majora = “larger”) are folds of hair-covered skin that begin just posterior to the mons pubis. The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) extend medial to the labia majora. Although they naturally vary in shape and size from woman to woman, the labia minora serve to protect the female urethra and the entrance to the female reproductive tract.
The superior, anterior portions of the labia minora come together to encircle the clitoris (or glans clitoris), an organ that originates from the same cells as the glans penis and has abundant nerves that make it important in sexual sensation and orgasm. The hymen is a thin membrane that sometimes partially covers the entrance to the vagina. An intact hymen cannot be used as an indication of “virginity”; even at birth, this is only a partial membrane, as menstrual fluid and other secretions must be able to exit the body, regardless of penile–vaginal intercourse. The vaginal opening is located between the opening of the urethra and the anus. It is flanked by outlets to the Bartholin’s glands (or greater vestibular glands).

Figure 2. The external female genitalia are referred to collectively as the vulva.
The vagina is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract. It also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called the fornix—meets the protruding uterine cervix. The walls of the vagina are lined with an outer, fibrous adventitia; a middle layer of smooth muscle; and an inner mucous membrane with transverse folds called rugae . Together, the middle and inner layers allow the expansion of the vagina to accommodate intercourse and childbirth. The thin, perforated hymen can partially surround the opening to the vaginal orifice. The hymen can be ruptured with strenuous physical exercise, penile–vaginal intercourse, and childbirth. The Bartholin’s glands and the lesser vestibular glands (located near the clitoris) secrete mucus, which keeps the vestibular area moist.
The vagina is home to a normal population of microorganisms that help to protect against infection by pathogenic bacteria, yeast, or other organisms that can enter the vagina. In a healthy woman, the most predominant type of vaginal bacteria is from the genus Lactobacillus . This family of beneficial bacterial flora secretes lactic acid, and thus protects the vagina by maintaining an acidic pH (below 4.5). Potential pathogens are less likely to survive in these acidic conditions. Lactic acid, in combination with other vaginal secretions, makes the vagina a self-cleansing organ. However, douching—or washing out the vagina with fluid—can disrupt the normal balance of healthy microorganisms, and actually increase a woman’s risk for infections and irritation. Indeed, the American College of Obstetricians and Gynecologists recommend that women do not douche, and that they allow the vagina to maintain its normal healthy population of protective microbial flora.
The ovaries are the female gonads. Paired ovals, they are each about 2 to 3 cm in length, about the size of an almond. The ovaries are located within the pelvic cavity, and are supported by the mesovarium, an extension of the peritoneum that connects the ovaries to the broad ligament . Extending from the mesovarium itself is the suspensory ligament that contains the ovarian blood and lymph vessels. Finally, the ovary itself is attached to the uterus via the ovarian ligament.
The ovary comprises an outer covering of cuboidal epithelium called the ovarian surface epithelium that is superficial to a dense connective tissue covering called the tunica albuginea. Beneath the tunica albuginea is the cortex, or outer portion, of the organ. The cortex is composed of a tissue framework called the ovarian stroma that forms the bulk of the adult ovary. Oocytes develop within the outer layer of this stroma, each surrounded by supporting cells. This grouping of an oocyte and its supporting cells is called a follicle . The growth and development of ovarian follicles will be described shortly. Beneath the cortex lies the inner ovarian medulla, the site of blood vessels, lymph vessels, and the nerves of the ovary. You will learn more about the overall anatomy of the female reproductive system at the end of this section.
The Ovarian Cycle
The ovarian cycle is a set of predictable changes in a female’s oocytes and ovarian follicles. During a woman’s reproductive years, it is a roughly 28-day cycle that can be correlated with, but is not the same as, the menstrual cycle (discussed shortly). The cycle includes two interrelated processes: oogenesis (the production of female gametes) and folliculogenesis (the growth and development of ovarian follicles).
Gametogenesis in females is called oogenesis . The process begins with the ovarian stem cells, or oogonia . Oogonia are formed during fetal development, and divide via mitosis, much like spermatogonia in the testis. Unlike spermatogonia, however, oogonia form primary oocytes in the fetal ovary prior to birth. These primary oocytes are then arrested in this stage of meiosis I, only to resume it years later, beginning at puberty and continuing until the woman is near menopause (the cessation of a woman’s reproductive functions). The number of primary oocytes present in the ovaries declines from one to two million in an infant, to approximately 400,000 at puberty, to zero by the end of menopause.
The initiation of ovulation —the release of an oocyte from the ovary—marks the transition from puberty into reproductive maturity for women. From then on, throughout a woman’s reproductive years, ovulation occurs approximately once every 28 days. Just prior to ovulation, a surge of luteinizing hormone triggers the resumption of meiosis in a primary oocyte. This initiates the transition from primary to secondary oocyte. However, as you can see in Figure 3, this cell division does not result in two identical cells. Instead, the cytoplasm is divided unequally, and one daughter cell is much larger than the other. This larger cell, the secondary oocyte, eventually leaves the ovary during ovulation. The smaller cell, called the first polar body , may or may not complete meiosis and produce second polar bodies; in either case, it eventually disintegrates. Therefore, even though oogenesis produces up to four cells, only one survives.

Figure 3. Click for a larger image. The unequal cell division of oogenesis produces one to three polar bodies that later degrade, as well as a single haploid ovum, which is produced only if there is penetration of the secondary oocyte by a sperm cell.
How does the diploid secondary oocyte become an ovum —the haploid female gamete? Meiosis of a secondary oocyte is completed only if a sperm succeeds in penetrating its barriers. Meiosis II then resumes, producing one haploid ovum that, at the instant of fertilization by a (haploid) sperm, becomes the first diploid cell of the new offspring (a zygote). Thus, the ovum can be thought of as a brief, transitional, haploid stage between the diploid oocyte and diploid zygote.
The larger amount of cytoplasm contained in the female gamete is used to supply the developing zygote with nutrients during the period between fertilization and implantation into the uterus. Interestingly, sperm contribute only DNA at fertilization —not cytoplasm. Therefore, the cytoplasm and all of the cytoplasmic organelles in the developing embryo are of maternal origin. This includes mitochondria, which contain their own DNA. Scientific research in the 1980s determined that mitochondrial DNA was maternally inherited, meaning that you can trace your mitochondrial DNA directly to your mother, her mother, and so on back through your female ancestors.
Everyday Connections: Mapping Human History with Mitochondrial DNA
When we talk about human DNA, we’re usually referring to nuclear DNA; that is, the DNA coiled into chromosomal bundles in the nucleus of our cells. We inherit half of our nuclear DNA from our father, and half from our mother. However, mitochondrial DNA (mtDNA) comes only from the mitochondria in the cytoplasm of the fat ovum we inherit from our mother. She received her mtDNA from her mother, who got it from her mother, and so on. Each of our cells contains approximately 1700 mitochondria, with each mitochondrion packed with mtDNA containing approximately 37 genes.
Mutations (changes) in mtDNA occur spontaneously in a somewhat organized pattern at regular intervals in human history. By analyzing these mutational relationships, researchers have been able to determine that we can all trace our ancestry back to one woman who lived in Africa about 200,000 years ago. Scientists have given this woman the biblical name Eve, although she is not, of course, the first Homo sapiens female. More precisely, she is our most recent common ancestor through matrilineal descent.
This doesn’t mean that everyone’s mtDNA today looks exactly like that of our ancestral Eve. Because of the spontaneous mutations in mtDNA that have occurred over the centuries, researchers can map different “branches” off of the “main trunk” of our mtDNA family tree. Your mtDNA might have a pattern of mutations that aligns more closely with one branch, and your neighbor’s may align with another branch. Still, all branches eventually lead back to Eve.
But what happened to the mtDNA of all of the other Homo sapiens females who were living at the time of Eve? Researchers explain that, over the centuries, their female descendants died childless or with only male children, and thus, their maternal line—and its mtDNA—ended.
Folliculogenesis
Again, ovarian follicles are oocytes and their supporting cells. They grow and develop in a process called folliculogenesis , which typically leads to ovulation of one follicle approximately every 28 days, along with death to multiple other follicles. The death of ovarian follicles is called atresia, and can occur at any point during follicular development. Recall that, a female infant at birth will have one to two million oocytes within her ovarian follicles, and that this number declines throughout life until menopause, when no follicles remain. As you’ll see next, follicles progress from primordial, to primary, to secondary and tertiary stages prior to ovulation—with the oocyte inside the follicle remaining as a primary oocyte until right before ovulation.
Folliculogenesis begins with follicles in a resting state. These small primordial follicles are present in newborn females and are the prevailing follicle type in the adult ovary. Primordial follicles have only a single flat layer of support cells, called granulosa cells , that surround the oocyte, and they can stay in this resting state for years—some until right before menopause.
After puberty, a few primordial follicles will respond to a recruitment signal each day, and will join a pool of immature growing follicles called primary follicles . Primary follicles start with a single layer of granulosa cells, but the granulosa cells then become active and transition from a flat or squamous shape to a rounded, cuboidal shape as they increase in size and proliferate. As the granulosa cells divide, the follicles—now called secondary follicles —increase in diameter, adding a new outer layer of connective tissue, blood vessels, and theca cells —cells that work with the granulosa cells to produce estrogens.
Within the growing secondary follicle, the primary oocyte now secretes a thin acellular membrane called the zona pellucida that will play a critical role in fertilization. A thick fluid, called follicular fluid, that has formed between the granulosa cells also begins to collect into one large pool, or antrum . Follicles in which the antrum has become large and fully formed are considered tertiary follicles (or antral follicles). Several follicles reach the tertiary stage at the same time, and most of these will undergo atresia. The one that does not die will continue to grow and develop until ovulation, when it will expel its secondary oocyte surrounded by several layers of granulosa cells from the ovary. Keep in mind that most follicles don’t make it to this point. In fact, roughly 99 percent of the follicles in the ovary will undergo atresia, which can occur at any stage of folliculogenesis.

Figure 4. Click for a larger image. (a) The maturation of a follicle is shown in a clockwise direction proceeding from the primordial follicles. FSH stimulates the growth of a tertiary follicle, and LH stimulates the production of estrogen by granulosa and theca cells. Once the follicle is mature, it ruptures and releases the oocyte. Cells remaining in the follicle then develop into the corpus luteum. (b) In this electron micrograph of a secondary follicle, the oocyte, theca cells (thecae folliculi), and developing antrum are clearly visible. EM × 1100. (Micrograph provided by the Regents of University of Michigan Medical School © 2012)
Hormonal Control of the Ovarian Cycle
The process of development that we have just described, from primordial follicle to early tertiary follicle, takes approximately two months in humans. The final stages of development of a small cohort of tertiary follicles, ending with ovulation of a secondary oocyte, occur over a course of approximately 28 days. These changes are regulated by many of the same hormones that regulate the male reproductive system, including GnRH, LH, and FSH.
As in men, the hypothalamus produces GnRH, a hormone that signals the anterior pituitary gland to produce the gonadotropins FSH and LH. These gonadotropins leave the pituitary and travel through the bloodstream to the ovaries, where they bind to receptors on the granulosa and theca cells of the follicles. FSH stimulates the follicles to grow (hence its name of follicle-stimulating hormone), and the five or six tertiary follicles expand in diameter. The release of LH also stimulates the granulosa and theca cells of the follicles to produce the sex steroid hormone estradiol, a type of estrogen. This phase of the ovarian cycle, when the tertiary follicles are growing and secreting estrogen, is known as the follicular phase.
The more granulosa and theca cells a follicle has (that is, the larger and more developed it is), the more estrogen it will produce in response to LH stimulation. As a result of these large follicles producing large amounts of estrogen, systemic plasma estrogen concentrations increase. Following a classic negative feedback loop, the high concentrations of estrogen will stimulate the hypothalamus and pituitary to reduce the production of GnRH, LH, and FSH. Because the large tertiary follicles require FSH to grow and survive at this point, this decline in FSH caused by negative feedback leads most of them to die (atresia). Typically only one follicle, now called the dominant follicle, will survive this reduction in FSH, and this follicle will be the one that releases an oocyte. Scientists have studied many factors that lead to a particular follicle becoming dominant: size, the number of granulosa cells, and the number of FSH receptors on those granulosa cells all contribute to a follicle becoming the one surviving dominant follicle.

Figure 5. Click for a larger image. The hypothalamus and pituitary gland regulate the ovarian cycle and ovulation. GnRH activates the anterior pituitary to produce LH and FSH, which stimulate the production of estrogen and progesterone by the ovaries.
When only the one dominant follicle remains in the ovary, it again begins to secrete estrogen. It produces more estrogen than all of the developing follicles did together before the negative feedback occurred. It produces so much estrogen that the normal negative feedback doesn’t occur. Instead, these extremely high concentrations of systemic plasma estrogen trigger a regulatory switch in the anterior pituitary that responds by secreting large amounts of LH and FSH into the bloodstream. The positive feedback loop by which more estrogen triggers release of more LH and FSH only occurs at this point in the cycle.
It is this large burst of LH (called the LH surge) that leads to ovulation of the dominant follicle. The LH surge induces many changes in the dominant follicle, including stimulating the resumption of meiosis of the primary oocyte to a secondary oocyte. As noted earlier, the polar body that results from unequal cell division simply degrades. The LH surge also triggers proteases (enzymes that cleave proteins) to break down structural proteins in the ovary wall on the surface of the bulging dominant follicle. This degradation of the wall, combined with pressure from the large, fluid-filled antrum, results in the expulsion of the oocyte surrounded by granulosa cells into the peritoneal cavity. This release is ovulation.
In the next section, you will follow the ovulated oocyte as it travels toward the uterus, but there is one more important event that occurs in the ovarian cycle. The surge of LH also stimulates a change in the granulosa and theca cells that remain in the follicle after the oocyte has been ovulated. This change is called luteinization (recall that the full name of LH is luteinizing hormone), and it transforms the collapsed follicle into a new endocrine structure called the corpus luteum , a term meaning “yellowish body”. Instead of estrogen, the luteinized granulosa and theca cells of the corpus luteum begin to produce large amounts of the sex steroid hormone progesterone, a hormone that is critical for the establishment and maintenance of pregnancy. Progesterone triggers negative feedback at the hypothalamus and pituitary, which keeps GnRH, LH, and FSH secretions low, so no new dominant follicles develop at this time.
The post-ovulatory phase of progesterone secretion is known as the luteal phase of the ovarian cycle. If pregnancy does not occur within 10 to 12 days, the corpus luteum will stop secreting progesterone and degrade into the corpus albicans , a nonfunctional “whitish body” that will disintegrate in the ovary over a period of several months. During this time of reduced progesterone secretion, FSH and LH are once again stimulated, and the follicular phase begins again with a new cohort of early tertiary follicles beginning to grow and secrete estrogen.
The Uterine Tubes
The uterine tubes (also called fallopian tubes or oviducts) serve as the conduit of the oocyte from the ovary to the uterus. Each of the two uterine tubes is close to, but not directly connected to, the ovary and divided into sections. The isthmus is the narrow medial end of each uterine tube that is connected to the uterus. The wide distal infundibulum flares out with slender, finger-like projections called fimbriae . The middle region of the tube, called the ampulla , is where fertilization often occurs. The uterine tubes also have three layers: an outer serosa, a middle smooth muscle layer, and an inner mucosal layer. In addition to its mucus-secreting cells, the inner mucosa contains ciliated cells that beat in the direction of the uterus, producing a current that will be critical to move the oocyte.
Following ovulation, the secondary oocyte surrounded by a few granulosa cells is released into the peritoneal cavity. The nearby uterine tube, either left or right, receives the oocyte. Unlike sperm, oocytes lack flagella, and therefore cannot move on their own. So how do they travel into the uterine tube and toward the uterus? High concentrations of estrogen that occur around the time of ovulation induce contractions of the smooth muscle along the length of the uterine tube. These contractions occur every 4 to 8 seconds, and the result is a coordinated movement that sweeps the surface of the ovary and the pelvic cavity. Current flowing toward the uterus is generated by coordinated beating of the cilia that line the outside and lumen of the length of the uterine tube. These cilia beat more strongly in response to the high estrogen concentrations that occur around the time of ovulation. As a result of these mechanisms, the oocyte–granulosa cell complex is pulled into the interior of the tube. Once inside, the muscular contractions and beating cilia move the oocyte slowly toward the uterus. When fertilization does occur, sperm typically meet the egg while it is still moving through the ampulla.
Practice Question
Watch this video to observe ovulation and its initiation in response to the release of FSH and LH from the pituitary gland. What specialized structures help guide the oocyte from the ovary into the uterine tube?
If the oocyte is successfully fertilized, the resulting zygote will begin to divide into two cells, then four, and so on, as it makes its way through the uterine tube and into the uterus. There, it will implant and continue to grow. If the egg is not fertilized, it will simply degrade—either in the uterine tube or in the uterus, where it may be shed with the next menstrual period.

Figure 6. This anterior view shows the relationship of the ovaries, uterine tubes (oviducts), and uterus. Sperm enter through the vagina, and fertilization of an ovulated oocyte usually occurs in the distal uterine tube. From left to right, LM × 400, LM × 20. (Micrographs provided by the Regents of University of Michigan Medical School © 2012)
The open-ended structure of the uterine tubes can have significant health consequences if bacteria or other contagions enter through the vagina and move through the uterus, into the tubes, and then into the pelvic cavity. If this is left unchecked, a bacterial infection (sepsis) could quickly become life-threatening. The spread of an infection in this manner is of special concern when unskilled practitioners perform abortions in non-sterile conditions. Sepsis is also associated with sexually transmitted bacterial infections, especially gonorrhea and chlamydia. These increase a woman’s risk for pelvic inflammatory disease (PID), infection of the uterine tubes or other reproductive organs. Even when resolved, PID can leave scar tissue in the tubes, leading to infertility.
Watch this series of videos to look at the movement of the oocyte through the ovary. The cilia in the uterine tube promote movement of the oocyte. What would likely occur if the cilia were paralyzed at the time of ovulation?
The Uterus and Cervix
The uterus is the muscular organ that nourishes and supports the growing embryo. Its average size is approximately 5 cm wide by 7 cm long (approximately 2 in by 3 in) when a female is not pregnant. It has three sections. The portion of the uterus superior to the opening of the uterine tubes is called the fundus . The middle section of the uterus is called the body of uterus (or corpus). The cervix is the narrow inferior portion of the uterus that projects into the vagina. The cervix produces mucus secretions that become thin and stringy under the influence of high systemic plasma estrogen concentrations, and these secretions can facilitate sperm movement through the reproductive tract.
Several ligaments maintain the position of the uterus within the abdominopelvic cavity. The broad ligament is a fold of peritoneum that serves as a primary support for the uterus, extending laterally from both sides of the uterus and attaching it to the pelvic wall. The round ligament attaches to the uterus near the uterine tubes, and extends to the labia majora. Finally, the uterosacral ligament stabilizes the uterus posteriorly by its connection from the cervix to the pelvic wall.
The wall of the uterus is made up of three layers. The most superficial layer is the serous membrane, or perimetrium , which consists of epithelial tissue that covers the exterior portion of the uterus. The middle layer, or myometrium , is a thick layer of smooth muscle responsible for uterine contractions. Most of the uterus is myometrial tissue, and the muscle fibers run horizontally, vertically, and diagonally, allowing the powerful contractions that occur during labor and the less powerful contractions (or cramps) that help to expel menstrual blood during a woman’s period. Anteriorly directed myometrial contractions also occur near the time of ovulation, and are thought to possibly facilitate the transport of sperm through the female reproductive tract.
The innermost layer of the uterus is called the endometrium . The endometrium contains a connective tissue lining, the lamina propria, which is covered by epithelial tissue that lines the lumen. Structurally, the endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers). The stratum basalis layer is part of the lamina propria and is adjacent to the myometrium; this layer does not shed during menses. In contrast, the thicker stratum functionalis layer contains the glandular portion of the lamina propria and the endothelial tissue that lines the uterine lumen. It is the stratum functionalis that grows and thickens in response to increased levels of estrogen and progesterone. In the luteal phase of the menstrual cycle, special branches off of the uterine artery called spiral arteries supply the thickened stratum functionalis. This inner functional layer provides the proper site of implantation for the fertilized egg, and—should fertilization not occur—it is only the stratum functionalis layer of the endometrium that sheds during menstruation.
Recall that during the follicular phase of the ovarian cycle, the tertiary follicles are growing and secreting estrogen. At the same time, the stratum functionalis of the endometrium is thickening to prepare for a potential implantation. The post-ovulatory increase in progesterone, which characterizes the luteal phase, is key for maintaining a thick stratum functionalis. As long as a functional corpus luteum is present in the ovary, the endometrial lining is prepared for implantation. Indeed, if an embryo implants, signals are sent to the corpus luteum to continue secreting progesterone to maintain the endometrium, and thus maintain the pregnancy. If an embryo does not implant, no signal is sent to the corpus luteum and it degrades, ceasing progesterone production and ending the luteal phase. Without progesterone, the endometrium thins and, under the influence of prostaglandins, the spiral arteries of the endometrium constrict and rupture, preventing oxygenated blood from reaching the endometrial tissue. As a result, endometrial tissue dies and blood, pieces of the endometrial tissue, and white blood cells are shed through the vagina during menstruation, or the menses . The first menses after puberty, called menarche , can occur either before or after the first ovulation.
The Menstrual Cycle
Now that we have discussed the maturation of the cohort of tertiary follicles in the ovary, the build-up and then shedding of the endometrial lining in the uterus, and the function of the uterine tubes and vagina, we can put everything together to talk about the three phases of the menstrual cycle —the series of changes in which the uterine lining is shed, rebuilds, and prepares for implantation.
The timing of the menstrual cycle starts with the first day of menses, referred to as day one of a woman’s period. Cycle length is determined by counting the days between the onset of bleeding in two subsequent cycles. Because the average length of a woman’s menstrual cycle is 28 days, this is the time period used to identify the timing of events in the cycle. However, the length of the menstrual cycle varies among women, and even in the same woman from one cycle to the next, typically from 21 to 32 days.
Just as the hormones produced by the granulosa and theca cells of the ovary “drive” the follicular and luteal phases of the ovarian cycle, they also control the three distinct phases of the menstrual cycle. These are the menses phase, the proliferative phase, and the secretory phase.
Menses Phase
The menses phase of the menstrual cycle is the phase during which the lining is shed; that is, the days that the woman menstruates. Although it averages approximately five days, the menses phase can last from 2 to 7 days, or longer. As shown in Figure 7, the menses phase occurs during the early days of the follicular phase of the ovarian cycle, when progesterone, FSH, and LH levels are low. Recall that progesterone concentrations decline as a result of the degradation of the corpus luteum, marking the end of the luteal phase. This decline in progesterone triggers the shedding of the stratum functionalis of the endometrium.

Figure 7. Click for a larger image. The correlation of the hormone levels and their effects on the female reproductive system is shown in this timeline of the ovarian and menstrual cycles. The menstrual cycle begins at day one with the start of menses. Ovulation occurs around day 14 of a 28-day cycle, triggered by the LH surge.
Proliferative Phase
Once menstrual flow ceases, the endometrium begins to proliferate again, marking the beginning of the proliferative phase of the menstrual cycle. It occurs when the granulosa and theca cells of the tertiary follicles begin to produce increased amounts of estrogen. These rising estrogen concentrations stimulate the endometrial lining to rebuild.
Recall that the high estrogen concentrations will eventually lead to a decrease in FSH as a result of negative feedback, resulting in atresia of all but one of the developing tertiary follicles. The switch to positive feedback—which occurs with the elevated estrogen production from the dominant follicle—then stimulates the LH surge that will trigger ovulation. In a typical 28-day menstrual cycle, ovulation occurs on day 14. Ovulation marks the end of the proliferative phase as well as the end of the follicular phase.
Secretory Phase
In addition to prompting the LH surge, high estrogen levels increase the uterine tube contractions that facilitate the pick-up and transfer of the ovulated oocyte. High estrogen levels also slightly decrease the acidity of the vagina, making it more hospitable to sperm. In the ovary, the luteinization of the granulosa cells of the collapsed follicle forms the progesterone-producing corpus luteum, marking the beginning of the luteal phase of the ovarian cycle. In the uterus, progesterone from the corpus luteum begins the secretory phase of the menstrual cycle, in which the endometrial lining prepares for implantation. Over the next 10 to 12 days, the endometrial glands secrete a fluid rich in glycogen. If fertilization has occurred, this fluid will nourish the ball of cells now developing from the zygote. At the same time, the spiral arteries develop to provide blood to the thickened stratum functionalis.
If no pregnancy occurs within approximately 10 to 12 days, the corpus luteum will degrade into the corpus albicans. Levels of both estrogen and progesterone will fall, and the endometrium will grow thinner. Prostaglandins will be secreted that cause constriction of the spiral arteries, reducing oxygen supply. The endometrial tissue will die, resulting in menses—or the first day of the next cycle.
Disorders of the Female Reproductive System
Research over many years has confirmed that cervical cancer is most often caused by a sexually transmitted infection with human papillomavirus (HPV). There are over 100 related viruses in the HPV family, and the characteristics of each strain determine the outcome of the infection. In all cases, the virus enters body cells and uses its own genetic material to take over the host cell’s metabolic machinery and produce more virus particles.
HPV infections are common in both men and women. Indeed, a recent study determined that 42.5 percent of females had HPV at the time of testing. These women ranged in age from 14 to 59 years and differed in race, ethnicity, and number of sexual partners. Of note, the prevalence of HPV infection was 53.8 percent among women aged 20 to 24 years, the age group with the highest infection rate.
HPV strains are classified as high or low risk according to their potential to cause cancer. Though most HPV infections do not cause disease, the disruption of normal cellular functions in the low-risk forms of HPV can cause the male or female human host to develop genital warts. Often, the body is able to clear an HPV infection by normal immune responses within 2 years. However, the more serious, high-risk infection by certain types of HPV can result in cancer of the cervix. Infection with either of the cancer-causing variants HPV 16 or HPV 18 has been linked to more than 70 percent of all cervical cancer diagnoses. Although even these high-risk HPV strains can be cleared from the body over time, infections persist in some individuals. If this happens, the HPV infection can influence the cells of the cervix to develop precancerous changes.
Risk factors for cervical cancer include having unprotected sex; having multiple sexual partners; a first sexual experience at a younger age, when the cells of the cervix are not fully mature; failure to receive the HPV vaccine; a compromised immune system; and smoking. The risk of developing cervical cancer is doubled with cigarette smoking.

Figure 8. In most cases, cells infected with the HPV virus heal on their own. In some cases, however, the virus continues to spread and becomes an invasive cancer.
When the high-risk types of HPV enter a cell, two viral proteins are used to neutralize proteins that the host cells use as checkpoints in the cell cycle. The best studied of these proteins is p53. In a normal cell, p53 detects DNA damage in the cell’s genome and either halts the progression of the cell cycle—allowing time for DNA repair to occur—or initiates apoptosis. Both of these processes prevent the accumulation of mutations in a cell’s genome. High-risk HPV can neutralize p53, keeping the cell in a state in which fast growth is possible and impairing apoptosis, allowing mutations to accumulate in the cellular DNA.
The prevalence of cervical cancer in the United States is very low because of regular screening exams called pap smears. Pap smears sample cells of the cervix, allowing the detection of abnormal cells. If pre-cancerous cells are detected, there are several highly effective techniques that are currently in use to remove them before they pose a danger. However, women in developing countries often do not have access to regular pap smears. As a result, these women account for as many as 80 percent of the cases of cervical cancer worldwide.
In 2006, the first vaccine against the high-risk types of HPV was approved. There are now two HPV vaccines available: Gardasil ® and Cervarix ® . Whereas these vaccines were initially only targeted for women, because HPV is sexually transmitted, both men and women require vaccination for this approach to achieve its maximum efficacy. A recent study suggests that the HPV vaccine has cut the rates of HPV infection by the four targeted strains at least in half. Unfortunately, the high cost of manufacturing the vaccine is currently limiting access to many women worldwide.
The Breasts
Whereas the breasts are located far from the other female reproductive organs, they are considered accessory organs of the female reproductive system. The function of the breasts is to supply milk to an infant in a process called lactation. The external features of the breast include a nipple surrounded by a pigmented areola , whose coloration may deepen during pregnancy. The areola is typically circular and can vary in size from 25 to 100 mm in diameter. The areolar region is characterized by small, raised areolar glands that secrete lubricating fluid during lactation to protect the nipple from chafing. When a baby nurses, or draws milk from the breast, the entire areolar region is taken into the mouth.
Breast milk is produced by the mammary glands , which are modified sweat glands. The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple. These lactiferous ducts each extend to a lactiferous sinus that connects to a glandular lobe within the breast itself that contains groups of milk-secreting cells in clusters called alveoli . The clusters can change in size depending on the amount of milk in the alveolar lumen. Once milk is made in the alveoli, stimulated myoepithelial cells that surround the alveoli contract to push the milk to the lactiferous sinuses. From here, the baby can draw milk through the lactiferous ducts by suckling. The lobes themselves are surrounded by fat tissue, which determines the size of the breast; breast size differs between individuals and does not affect the amount of milk produced. Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.

Figure 9. During lactation, milk moves from the alveoli through the lactiferous ducts to the nipple.
During the normal hormonal fluctuations in the menstrual cycle, breast tissue responds to changing levels of estrogen and progesterone, which can lead to swelling and breast tenderness in some individuals, especially during the secretory phase. If pregnancy occurs, the increase in hormones leads to further development of the mammary tissue and enlargement of the breasts.
Hormonal Birth Control
Birth control pills take advantage of the negative feedback system that regulates the ovarian and menstrual cycles to stop ovulation and prevent pregnancy. Typically they work by providing a constant level of both estrogen and progesterone, which negatively feeds back onto the hypothalamus and pituitary, thus preventing the release of FSH and LH. Without FSH, the follicles do not mature, and without the LH surge, ovulation does not occur. Although the estrogen in birth control pills does stimulate some thickening of the endometrial wall, it is reduced compared with a normal cycle and is less likely to support implantation.
Some birth control pills contain 21 active pills containing hormones, and 7 inactive pills (placebos). The decline in hormones during the week that the woman takes the placebo pills triggers menses, although it is typically lighter than a normal menstrual flow because of the reduced endometrial thickening. Newer types of birth control pills have been developed that deliver low-dose estrogens and progesterone for the entire cycle (these are meant to be taken 365 days a year), and menses never occurs. While some women prefer to have the proof of a lack of pregnancy that a monthly period provides, menstruation every 28 days is not required for health reasons, and there are no reported adverse effects of not having a menstrual period in an otherwise healthy individual.
Because birth control pills function by providing constant estrogen and progesterone levels and disrupting negative feedback, skipping even just one or two pills at certain points of the cycle (or even being several hours late taking the pill) can lead to an increase in FSH and LH and result in ovulation. It is important, therefore, that the woman follow the directions on the birth control pill package to successfully prevent pregnancy.
Aging and the Female Reproductive System
Female fertility (the ability to conceive) peaks when women are in their twenties, and is slowly reduced until a women reaches 35 years of age. After that time, fertility declines more rapidly, until it ends completely at the end of menopause. Menopause is the cessation of the menstrual cycle that occurs as a result of the loss of ovarian follicles and the hormones that they produce. A woman is considered to have completed menopause if she has not menstruated in a full year. After that point, she is considered postmenopausal. The average age for this change is consistent worldwide at between 50 and 52 years of age, but it can normally occur in a woman’s forties, or later in her fifties. Poor health, including smoking, can lead to earlier loss of fertility and earlier menopause.
As a woman reaches the age of menopause, depletion of the number of viable follicles in the ovaries due to atresia affects the hormonal regulation of the menstrual cycle. During the years leading up to menopause, there is a decrease in the levels of the hormone inhibin, which normally participates in a negative feedback loop to the pituitary to control the production of FSH. The menopausal decrease in inhibin leads to an increase in FSH. The presence of FSH stimulates more follicles to grow and secrete estrogen. Because small, secondary follicles also respond to increases in FSH levels, larger numbers of follicles are stimulated to grow; however, most undergo atresia and die. Eventually, this process leads to the depletion of all follicles in the ovaries, and the production of estrogen falls off dramatically. It is primarily the lack of estrogens that leads to the symptoms of menopause.
The earliest changes occur during the menopausal transition, often referred to as peri-menopause, when a women’s cycle becomes irregular but does not stop entirely. Although the levels of estrogen are still nearly the same as before the transition, the level of progesterone produced by the corpus luteum is reduced. This decline in progesterone can lead to abnormal growth, or hyperplasia, of the endometrium. This condition is a concern because it increases the risk of developing endometrial cancer. Two harmless conditions that can develop during the transition are uterine fibroids, which are benign masses of cells, and irregular bleeding. As estrogen levels change, other symptoms that occur are hot flashes and night sweats, trouble sleeping, vaginal dryness, mood swings, difficulty focusing, and thinning of hair on the head along with the growth of more hair on the face. Depending on the individual, these symptoms can be entirely absent, moderate, or severe.
After menopause, lower amounts of estrogens can lead to other changes. Cardiovascular disease becomes as prevalent in women as in men, possibly because estrogens reduce the amount of cholesterol in the blood vessels. When estrogen is lacking, many women find that they suddenly have problems with high cholesterol and the cardiovascular issues that accompany it. Osteoporosis is another problem because bone density decreases rapidly in the first years after menopause. The reduction in bone density leads to a higher incidence of fractures.
Hormone therapy (HT), which employs medication (synthetic estrogens and progestins) to increase estrogen and progestin levels, can alleviate some of the symptoms of menopause. In 2002, the Women’s Health Initiative began a study to observe women for the long-term outcomes of hormone replacement therapy over 8.5 years. However, the study was prematurely terminated after 5.2 years because of evidence of a higher than normal risk of breast cancer in patients taking estrogen-only HT. The potential positive effects on cardiovascular disease were also not realized in the estrogen-only patients. The results of other hormone replacement studies over the last 50 years, including a 2012 study that followed over 1,000 menopausal women for 10 years, have shown cardiovascular benefits from estrogen and no increased risk for cancer. Some researchers believe that the age group tested in the 2002 trial may have been too old to benefit from the therapy, thus skewing the results. In the meantime, intense debate and study of the benefits and risks of replacement therapy is ongoing. Current guidelines approve HT for the reduction of hot flashes or flushes, but this treatment is generally only considered when women first start showing signs of menopausal changes, is used in the lowest dose possible for the shortest time possible (5 years or less), and it is suggested that women on HT have regular pelvic and breast exams.
Chapter Review
The external female genitalia are collectively called the vulva. The vagina is the pathway into and out of the uterus. The man’s penis is inserted into the vagina to deliver sperm, and the baby exits the uterus through the vagina during childbirth.
The ovaries produce oocytes, the female gametes, in a process called oogenesis. As with spermatogenesis, meiosis produces the haploid gamete (in this case, an ovum); however, it is completed only in an oocyte that has been penetrated by a sperm. In the ovary, an oocyte surrounded by supporting cells is called a follicle. In folliculogenesis, primordial follicles develop into primary, secondary, and tertiary follicles. Early tertiary follicles with their fluid-filled antrum will be stimulated by an increase in FSH, a gonadotropin produced by the anterior pituitary, to grow in the 28-day ovarian cycle. Supporting granulosa and theca cells in the growing follicles produce estrogens, until the level of estrogen in the bloodstream is high enough that it triggers negative feedback at the hypothalamus and pituitary. This results in a reduction of FSH and LH, and most tertiary follicles in the ovary undergo atresia (they die). One follicle, usually the one with the most FSH receptors, survives this period and is now called the dominant follicle. The dominant follicle produces more estrogen, triggering positive feedback and the LH surge that will induce ovulation. Following ovulation, the granulosa cells of the empty follicle luteinize and transform into the progesterone-producing corpus luteum. The ovulated oocyte with its surrounding granulosa cells is picked up by the infundibulum of the uterine tube, and beating cilia help to transport it through the tube toward the uterus. Fertilization occurs within the uterine tube, and the final stage of meiosis is completed.
The uterus has three regions: the fundus, the body, and the cervix. It has three layers: the outer perimetrium, the muscular myometrium, and the inner endometrium. The endometrium responds to estrogen released by the follicles during the menstrual cycle and grows thicker with an increase in blood vessels in preparation for pregnancy. If the egg is not fertilized, no signal is sent to extend the life of the corpus luteum, and it degrades, stopping progesterone production. This decline in progesterone results in the sloughing of the inner portion of the endometrium in a process called menses, or menstruation.
The breasts are accessory sexual organs that are utilized after the birth of a child to produce milk in a process called lactation. Birth control pills provide constant levels of estrogen and progesterone to negatively feed back on the hypothalamus and pituitary, and suppress the release of FSH and LH, which inhibits ovulation and prevents pregnancy.

Critical Thinking Questions
- Follow the path of ejaculated sperm from the vagina to the oocyte. Include all structures of the female reproductive tract that the sperm must swim through to reach the egg.
- Identify some differences between meiosis in men and women.
- Explain the hormonal regulation of the phases of the menstrual cycle.
- Endometriosis is a disorder in which endometrial cells implant and proliferate outside of the uterus—in the uterine tubes, on the ovaries, or even in the pelvic cavity. Offer a theory as to why endometriosis increases a woman’s risk of infertility.
- The sperm must swim upward in the vagina, through the cervix, and then through the body of the uterus to one or the other of the two uterine tubes. Fertilization generally occurs in the uterine tube.
- Meiosis in the man results in four viable haploid sperm, whereas meiosis in the woman results in a secondary oocyte and, upon completion following fertilization by a sperm, one viable haploid ovum with abundant cytoplasm and up to three polar bodies with little cytoplasm that are destined to die.
- As a result of the degradation of the corpus luteum, a decline in progesterone concentrations triggers the shedding of the endometrial lining, marking the menses phase of the menstrual cycle. Low progesterone levels also reduce the negative feedback that had been occurring at the hypothalamus and pituitary, and result in the release of GnRH and, subsequently, FSH and LH. FSH stimulates tertiary follicles to grow and granulosa and theca cells begin to produce increased amounts of estrogen. High estrogen concentrations stimulate the endometrial lining to rebuild, marking the proliferative phase of the menstrual cycle. The high estrogen concentrations will eventually lead to a decrease in FSH because of negative feedback, resulting in atresia of all but one of the developing tertiary follicles. The switch to positive feedback that occurs with elevated estrogen production from the dominant follicle stimulates the LH surge that will trigger ovulation. The luteinization of the granulosa cells of the collapsed follicle forms the progesterone-producing corpus luteum. Progesterone from the corpus luteum causes the endometrium to prepare for implantation, in part by secreting nutrient-rich fluid. This marks the secretory phase of the menstrual cycle. Finally, in a non-fertile cycle, the corpus luteum will degrade and menses will occur.
- Endometrial tissue proliferating outside of the endometrium—for example, in the uterine tubes, on the ovaries, or within the pelvic cavity—could block the passage of sperm, ovulated oocytes, or a zygote, thus reducing fertility.
alveoli: (of the breast) milk-secreting cells in the mammary gland
ampulla: (of the uterine tube) middle portion of the uterine tube in which fertilization often occurs
antrum: fluid-filled chamber that characterizes a mature tertiary (antral) follicle
areola: highly pigmented, circular area surrounding the raised nipple and containing areolar glands that secrete fluid important for lubrication during suckling
Bartholin’s glands: (also, greater vestibular glands) glands that produce a thick mucus that maintains moisture in the vulva area; also referred to as the greater vestibular glands
body of uterus: middle section of the uterus
broad ligament: wide ligament that supports the uterus by attaching laterally to both sides of the uterus and pelvic wall
cervix: elongate inferior end of the uterus where it connects to the vagina
clitoris: (also, glans clitoris) nerve-rich area of the vulva that contributes to sexual sensation during intercourse
corpus albicans: nonfunctional structure remaining in the ovarian stroma following structural and functional regression of the corpus luteum
corpus luteum: transformed follicle after ovulation that secretes progesterone
endometrium: inner lining of the uterus, part of which builds up during the secretory phase of the menstrual cycle and then sheds with menses
fimbriae: fingerlike projections on the distal uterine tubes
follicle: ovarian structure of one oocyte and surrounding granulosa (and later theca) cells
folliculogenesis: development of ovarian follicles from primordial to tertiary under the stimulation of gonadotropins
fundus: (of the uterus) domed portion of the uterus that is superior to the uterine tubes
granulosa cells: supportive cells in the ovarian follicle that produce estrogen
hymen: membrane that covers part of the opening of the vagina
infundibulum: (of the uterine tube) wide, distal portion of the uterine tube terminating in fimbriae
isthmus: narrow, medial portion of the uterine tube that joins the uterus
labia majora: hair-covered folds of skin located behind the mons pubis
labia minora: thin, pigmented, hairless flaps of skin located medial and deep to the labia majora
lactiferous ducts: ducts that connect the mammary glands to the nipple and allow for the transport of milk
lactiferous sinus: area of milk collection between alveoli and lactiferous duct
mammary glands: glands inside the breast that secrete milk
menarche: first menstruation in a pubertal female
menses: shedding of the inner portion of the endometrium out though the vagina; also referred to as menstruation
menses phase: phase of the menstrual cycle in which the endometrial lining is shed
menstrual cycle: approximately 28-day cycle of changes in the uterus consisting of a menses phase, a proliferative phase, and a secretory phase
mons pubis: mound of fatty tissue located at the front of the vulva
myometrium: smooth muscle layer of uterus that allows for uterine contractions during labor and expulsion of menstrual blood
oocyte: cell that results from the division of the oogonium and undergoes meiosis I at the LH surge and meiosis II at fertilization to become a haploid ovum
oogenesis: process by which oogonia divide by mitosis to primary oocytes, which undergo meiosis to produce the secondary oocyte and, upon fertilization, the ovum
oogonia: ovarian stem cells that undergo mitosis during female fetal development to form primary oocytes
ovarian cycle: approximately 28-day cycle of changes in the ovary consisting of a follicular phase and a luteal phase
ovaries: female gonads that produce oocytes and sex steroid hormones (notably estrogen and progesterone)
ovulation: release of a secondary oocyte and associated granulosa cells from an ovary
ovum: haploid female gamete resulting from completion of meiosis II at fertilization
perimetrium: outer epithelial layer of uterine wall
polar body: smaller cell produced during the process of meiosis in oogenesis
primary follicles: ovarian follicles with a primary oocyte and one layer of cuboidal granulosa cells
primordial follicles: least developed ovarian follicles that consist of a single oocyte and a single layer of flat (squamous) granulosa cells
proliferative phase: phase of the menstrual cycle in which the endometrium proliferates
rugae: (of the vagina) folds of skin in the vagina that allow it to stretch during intercourse and childbirth
secondary follicles: ovarian follicles with a primary oocyte and multiple layers of granulosa cells
secretory phase: phase of the menstrual cycle in which the endometrium secretes a nutrient-rich fluid in preparation for implantation of an embryo
suspensory ligaments: bands of connective tissue that suspend the breast onto the chest wall by attachment to the overlying dermis
tertiary follicles: (also, antral follicles) ovarian follicles with a primary or secondary oocyte, multiple layers of granulosa cells, and a fully formed antrum
theca cells: estrogen-producing cells in a maturing ovarian follicle
uterine tubes: (also, fallopian tubes or oviducts) ducts that facilitate transport of an ovulated oocyte to the uterus
uterus: muscular hollow organ in which a fertilized egg develops into a fetus
vagina: tunnel-like organ that provides access to the uterus for the insertion of semen and from the uterus for the birth of a baby
vulva: external female genitalia
- Anatomy & Physiology. Provided by : OpenStax CNX. Located at : http://cnx.org/contents/[email protected] . License : CC BY: Attribution . License Terms : Download for free at http://cnx.org/contents/[email protected]
- Biology Article
Female Reproductive System
The female reproductive system consists of the primary as well as accessory sex organs. The primary sex organs in females are a pair of ovaries, which produce ova or egg and they also secrete female sex hormones like progesterone and estrogen. The other accessory sex organs include the uterus, fallopian tubes, cervix and vagina. The external genitalia comprises the labia minora, labia majora and clitoris. The mammary glands are not considered genital organs but are important glands in the female reproductive system.
Let’s learn more about the female reproductive system with a well-labelled diagram.
Table of Contents:
Labelled diagram of female reproductive system.
- Female Reproductive System Anatomy
Menstrual Cycle
Reproduction control, frequently asked questions, female reproductive system anatomy.
The female reproductive system is framed to perform different functions. It creates egg cells that are essential for reproduction known as ova. The system is organized to deliver the ova to the region of fertilization. The egg fertilization takes place in the Fallopian tubes along with the sperm. The implanting in the walls of the uterus and initiating the stages of pregnancy is the next step of fertilized eggs. Apart from the above-mentioned functions, the female reproductive system is also involved in the production of female sex hormones to maintain the reproductive cycle.
The female reproductive system is composed of a pair of ovaries along with oviducts, vagina, cervix, uterus, and the external genitalia that are located in the pelvic region. These parts along with a pair of mammary glands that are integrated both functionally and structurally also support the process of ovulation, fertilization, birth and finally the child care.
Also check: Bartholin Ducts (Glands)
Ovaries act as the main female sex organs that produce the female gamete and various hormones . These organs are situated one on both the side of the lower abdomen. Each ovary measures about 2 to 4 cm in length which is then connected to the uterus and pelvic wall through ligaments. The ovary is surrounded by a thin covering of epithelium, encloses the ovarian stroma and is divided into two zones – outer cortex and the inner medulla. The cortex consists of various ovarian follicles in different stages of development. The ovarian follicle is called the basic unit of the female reproductive system. Each oviduct is divided into three anatomical regions- ampulla, isthmus, and infundibulum.
A uterus is also called the womb. It is a muscular, inverted pear-shaped organ of the female reproductive system. The walls of the uterus consist of three layers- the inner glandular layer, the middle thick layer, and the outer thin layer. These three layers are maintained by ligaments which are attached to the pelvic wall which then opens into the vagina from a narrow cervix. The cervical canal along with the vagina creates the birth canal. The vagina is a muscular tube which starts at the lower end of the uterus to the outside.
Fallopian Tubes
Fallopian tubes are a pair of muscular tubes and funnel-shaped structures, extend from the right and left of the superior corners of the uterus to the edge of the ovaries. These tubes are enclosed in small projections called fimbriae that swipe over the ovaries to pick up released ova and deliver them to the infundibulum for supplying the uterus. Each fallopian tube is covered by cilia that functions by carrying the ovum to the uterus.
Related Video:
The vagina is a muscular and elastic tube that connects the cervix to the external body. It functions as the receptacle for the penis in sexual intercourse and delivers sperm to the fallopian tubes and uterus. It also acts as a birth canal by expanding to allow delivery of the fetus during childbirth.
The external genitalia comprises the labia minora , labia majora and clitoris
Ovulation is the process of releasing the eggs from the ovaries. This process takes place as soon as the follicle is fully grown and reaches its size along with the accumulation of liquid in the follicle without a significant rise in pressure. As the follicle swells out, a small oval-shaped area, the stigma or macula pellucida appears sticking outward as a clear cone area and later undergoes localized changes in colour, integrity, and translucency. The secretion of estrogen hormones reaches the maximum level before the ovulation. After the surge of luteinizing hormone, ovulation occurs at the site of the stigma. This surge is essential for ovulation. Ovulation is the process in which the follicle is separated by releasing of follicular fluid along with the ovum surrounded by the corona radiata. The cells of the corona radiata will separate later in the presence of spermatozoa. In ruminants, the oocytes have already lost their corona at the time of ovulation. The very active fimbriae, end of the oviduct picks up the ovum. If fertilized ovum or zygote undergoes cleavage and makes its way to the uterus for implantation. If not fertilized, it degenerates within 24 hours.
All females, after reaching their puberty produce mature egg cell every month during a process called the menstrual cycle . During this period, an ovary discharges a mature egg, which travels to the uterus. In the uterus, if the egg is not fertilized, the lining in the uterine sheds away and a new cycle begins. Overall a menstrual cycle lasts for 28 days, in some cases, these cycles may either last for 21 days or as long as 35 days in some individuals. The entire process of the menstrual cycle is controlled by the endocrine system and the hormones involved are FSH, LH, estrogen, and progesterone. Both FSH and LH hormones are produced by the pituitary gland, whereas estrogen and progesterone hormones are produced by the ovaries. Alon with the hormonal disorders, there are many other factors, which are responsible for the disturbance in the menstrual cycle. The responsible factors include diet, exercise, stress and weight gain or loss affects the menstrual cycle. The cycle may be irregular at times, especially during puberty. The menstrual cycles occur every month from the time of puberty up to the age of 45 to 55, except during pregnancy. After the age of 55 ovaries slows down their production of hormone and release of mature eggs. Progressively, the menstrual cycle stops, therefore, the woman is no longer able to become pregnant.
Fertilization and Pregnancy
Following implantation, the placenta originates from maternal and fetal tissues, producing human chorionic gonadotropin (HCG) that helps in maintaining the level of corpus luteum in the ovary until the placenta begins synthesizing its own progesterone and estrogen hormones.
Estrogen and Progesterone
Estrogen and progesterone hormones are produced by the ovaries that foster the development of reproductive organs by maintaining the proper uterine cycle and by developing female secondary sex characteristics. During menopause, usually between age 45 and 55, the uterine cycle stops, and the ovaries are no longer produce estrogen and progesterone hormones. Infertility In general, infertility can be defined as the failure in couples of not getting pregnant, despite having carefully timed, unprotected sex for one year. It is estimated to be around 15% of all couples undergo infertility. The reasons behind this infertility in males and females are-
In Females:
- Blocked oviducts.
- Endometriosis.
- Low sperm count.
- Sperm abnormalities.
There are various birth control methods and some of them are as mentioned below.
- Abstinence.
- Birth control pills
- Intrauterine device.
- Male condom.
- Contraceptive implants.
- The morning after pills.
To know more about the female reproductive system and its functions, visit BYJU’S.
Recommended Video:

Further Reading
What are the three layers of the uterus?
The outer thin layer or the serous layer is the covering of the uterus derived from the peritoneum. Then comes the myometrium or the middle muscular layer. It is the thickest layer and is made of smooth muscle fibres. The third layer is the glandular layer called the inner mucus layer or the endometrium.
What is the cervix?
The cervix is the lower constricted part of the uterus that is divided into two portions. The upper supravaginal portion communicates with body of the uterus and the lower vaginal portion projects into the anterior wall of the vagina. The cervical canal along with the vagina creates the birth canal.
What are the functions of the ovary?
Female ovaries have two functions, endocrine and gametogenic functions. The endocrine function is the secretion of female sex hormones like the estrogen and progesterone. The gametogenic function is the production and release of the egg or ovum for reproduction.
Also check:
- External Reproductive System of Women
- Female External Features and Anatomy
- Human External Reproductive Organs
- Genital Openings in Females
- Functions of Vestibule in Female Reproductive System
Put your understanding of this concept to test by answering a few MCQs. Click ‘Start Quiz’ to begin!
Select the correct answer and click on the “Finish” button Check your score and answers at the end of the quiz
Visit BYJU’S for all Biology related queries and study materials
Your result is as below
Request OTP on Voice Call
Leave a Comment Cancel reply
Your Mobile number and Email id will not be published. Required fields are marked *
Post My Comment
Sir please demo classes now
Register with BYJU'S & Download Free PDFs
Register with byju's & watch live videos.
Female Reproductive System Anatomy and Physiology

Step into the powerful realm of the female reproductive system anatomy and physiology. Nursing students, discover the miraculous cycles and stages that cradle and nurture life.
Table of Contents
Fallopian tubes, mons veneris, labia minora, labia majora, skene’s glands, bartholin’s gland, perineal body, internal structures.
- The ovaries are the ultimate life-maker for the females.
- For its physical structure, it has an estimated length of 4 cm and width of 2 cm and is 1.5 cm thick. It appears to be shaped like an almond. It looks pitted, like a raisin, but is grayish white in color.
- It is located proximal to both sides of the uterus at the lower abdomen.
- For its function, the ovaries produce, mature, and discharge the egg cells or ova.
- Ovarian function is for the maturation and maintenance of the secondary sex characteristics in females.
- It also has three divisions: the protective layer of epithelium, the cortex, and the central medulla.
- The fallopian tubes serve as the pathway of the egg cells towards the uterus.
- It is a smooth, hollow tunnel that is divided into four parts: the interstitial, which is 1 cm in length; the isthmus, which is2 cm in length; the ampulla, which is 5 cm in length; and the infundibular, which is 2 cm long and shaped like a funnel.
- The funnel has small hairs called the fimbria that propel the ovum into the fallopian tube.
- The fallopian tube is lined with mucous membrane, and underneath is the connective tissue and the muscle layer.
- The muscle layer is responsible for the peristaltic movements that propel the ovum forward.
- The distal ends of the fallopian tubes are open, making a pathway for conception to occur.
- The uterus is described as a hollow, muscular, pear-shaped organ.
- It is located at the lower pelvis, which is posterior to the bladder and anterior to the rectum.
- The uterus has an estimated length of 5 to 7 cm and width of 5 cm. it is 2.5 cm deep in its widest part.
- For non-pregnant women, it is approximately 60g in weight.
- Its function is to receive the ovum from the fallopian tube and provide a place for implantation and nourishment.
- It also gives protection for the growing fetus.
- It is divided into three: the body, the isthmus, and the cervix. f
- The body forms the bulk of the uterus, being the uppermost part. This is also the part that expands to accommodate the growing fetus.
- The isthmus is just a short connection between the body and the cervix. This is the portion that is cut during a cesarean section .
- The cervix lies halfway above the vagina, and the other half extends into the vagina. It has an internal and external cervical os, which is the opening into the cervical canal.
External Structures
- The mons veneris is a pad of fat tissues over the symphysis pubis.
- It has a covering of coarse, curly hairs, the pubic hair .
- It protects the pubic bone from trauma .
- The labia minora is a spread of two connective tissue folds that are pinkish in color.
- The internal surface is composed of mucous membrane and the external surface is skin.
- It contains sebaceous glands all over the area.
- Lateral to the labia minora are two folds of fat tissue covered by loose connective tissue and epithelium, the labia majora.
- Its function is to protect the external genitalia and the distal urethra and vagina from trauma .
- It is covered in pubic hair that serves as additional protection against harmful bacteria that may enter the structure.
- It is a smooth, flattened surface inside the labia wherein the openings to the urethra and the vagina arise.
- The clitoris is a small, circular organ of erectile tissue at the front of the labia minora.
- The prepuce, a fold of skin, serves as its covering.
- This is the center for sexual arousal and pleasure for females because it is highly sensitive to touch and temperature.
- Also called as paraurethral glands, they are found lateral to the urethral meatus and have ducts that open into the urethra.
- The secretions from this gland lubricate the external genitalia during coitus.
- Also called bulbovaginal gland, this is another gland responsible for the lubrication of the external genitalia during coitus.
- It has ducts that open into the distal vagina.
- Both of these glands secretions are alkaline to help the sperm survive in the vagina.
- This is a ridge of tissue which is formed by the posterior joining of the labia minora and majora.
- During episiotomy , this is the tissue that is cut to enlarge the vaginal opening.
- This is a muscular area that stretches easily during childbirth.
- Most pregnancy exercises such as Kegel’s and squatting are done to strengthen the perineal body to allow easier expansion during childbirth and avoid tearing the tissue.
- This covers the opening of the vagina.
- It is tough, elastic, semicircle tissue torn during the first sexual intercourse.
Craving more insights? Dive into these related materials to enhance your study journey!
- Anatomy and Physiology Nursing Test Banks . This nursing test bank includes questions about Anatomy and Physiology and its related concepts such as: structure and functions of the human body, nursing care management of patients with conditions related to the different body systems.
1 thought on “Female Reproductive System Anatomy and Physiology”
Leave a comment cancel reply.

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

23.5: Practice Practical- the Reproductive System
- Last updated
- Save as PDF
- Page ID 65175
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Fill in the blank with the correct word or words.
Query \(\PageIndex{1}\)

- school Campus Bookshelves
- menu_book Bookshelves
- perm_media Learning Objects
- login Login
- how_to_reg Request Instructor Account
- hub Instructor Commons
Margin Size
- Download Page (PDF)
- Download Full Book (PDF)
- Periodic Table
- Physics Constants
- Scientific Calculator
- Reference & Cite
- Tools expand_more
- Readability
selected template will load here
This action is not available.

22.5: Laboratory Activities and Assignment
- Last updated
- Save as PDF
- Page ID 53848

- Rosanna Hartline
- West Hills College Lemoore
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
Laboratory Activities and Assignment
Part 1: review of the reproductive systems.
1. Label the structures listed below on the diagram of the female genitalia below.
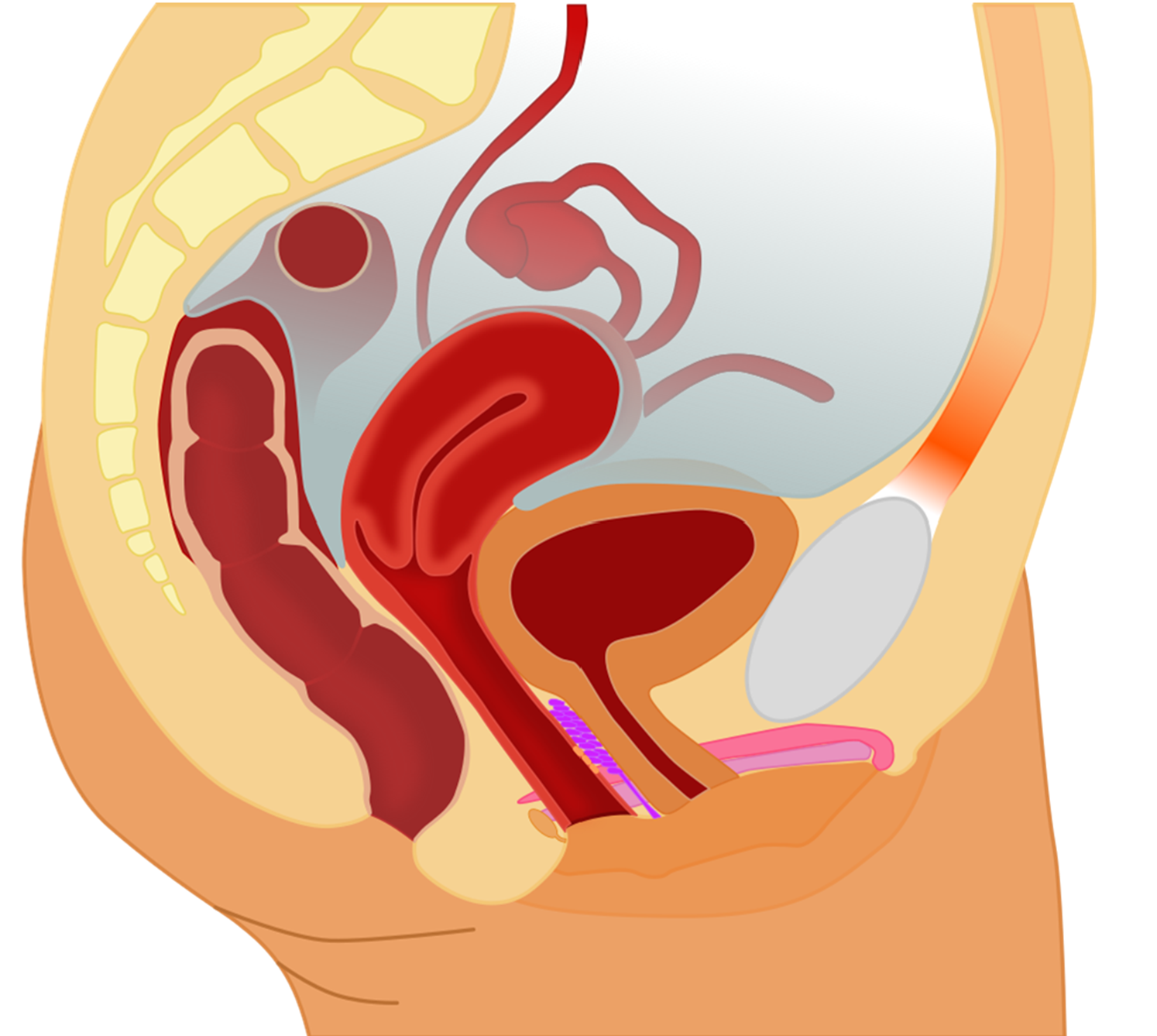
2. Label the structures listed below on the diagram of internal female genitalia below.
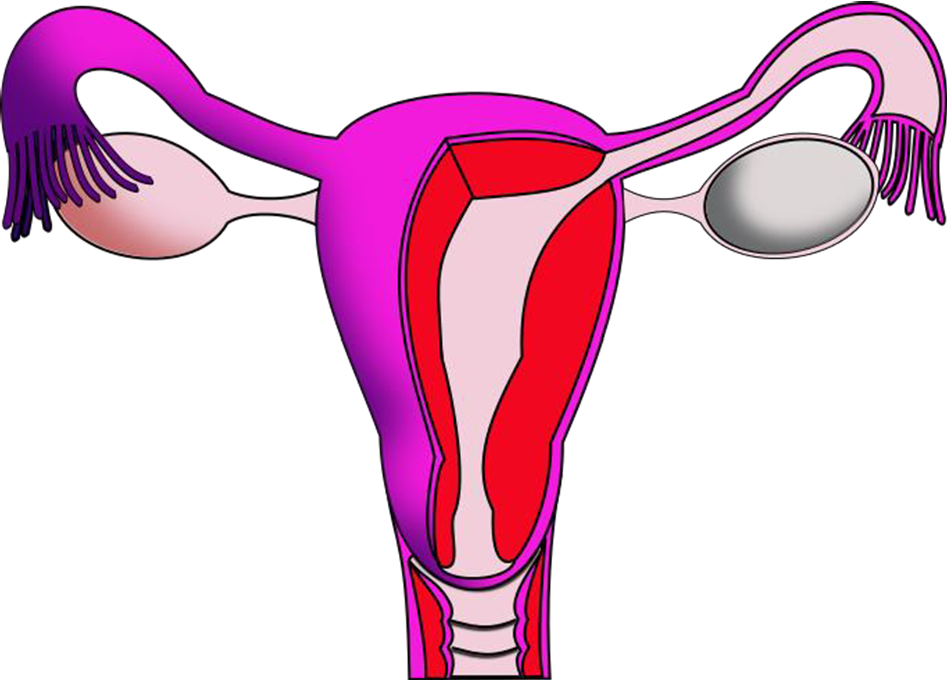
3. Label the structures listed below on the diagram of the external female genitalia.
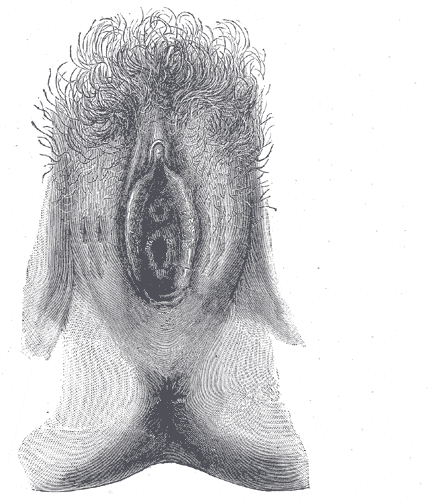
4. Label the structures listed below on the diagram of the male genitalia below.
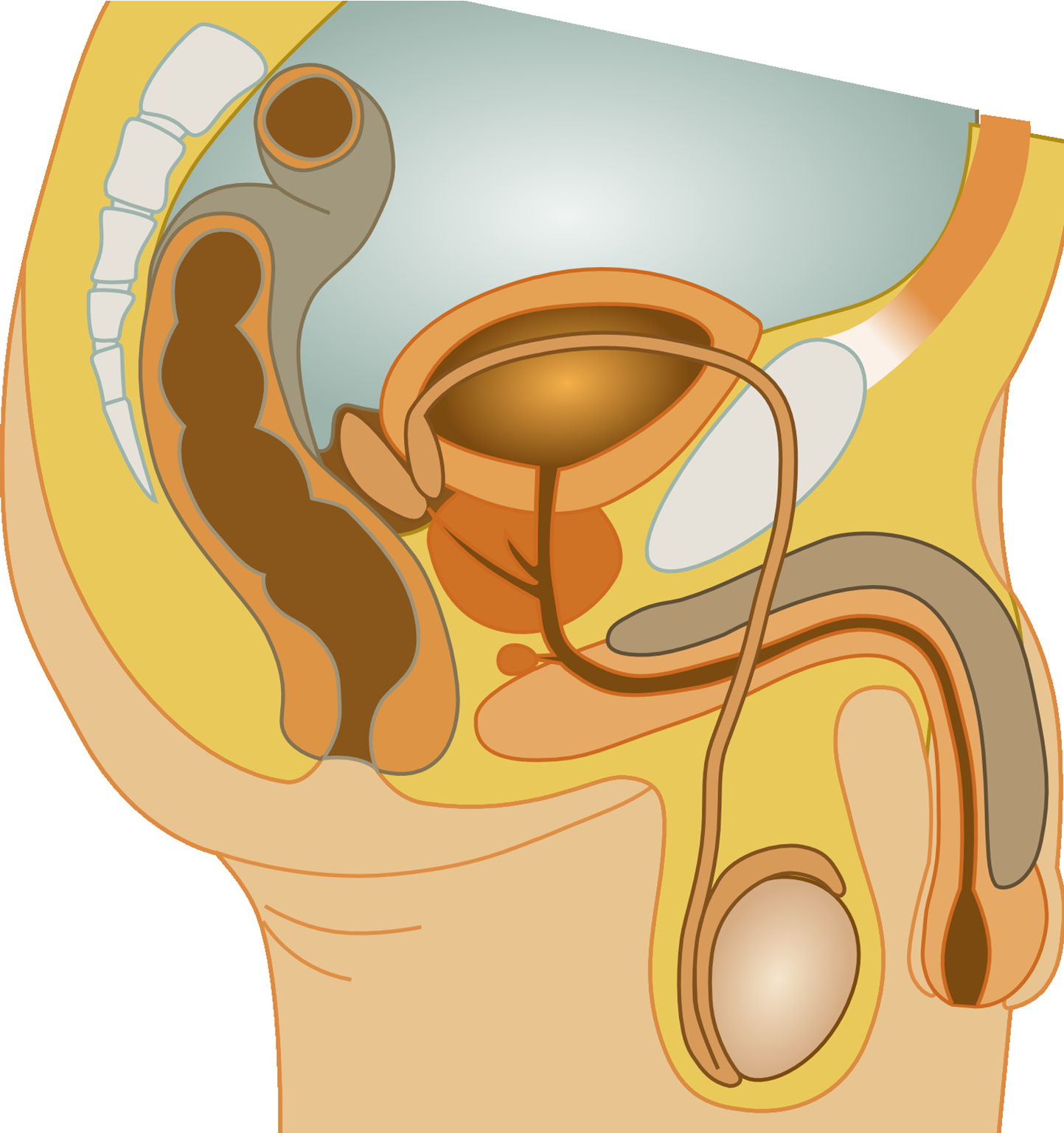
5. Label the structures listed below on the diagram of the male genitalia below.
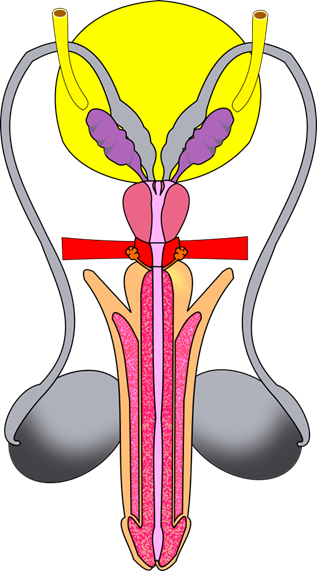
7. On the figure above, number the structures spermatozoa pass through to exit the male reproductive system from where spermatids are created (#1) to the point where they exit the body.
8. On the figure above, add a star (*) next to the name of each structure that contributes to semen.
9. Label the structures listed below on the diagram of the male genitalia below.
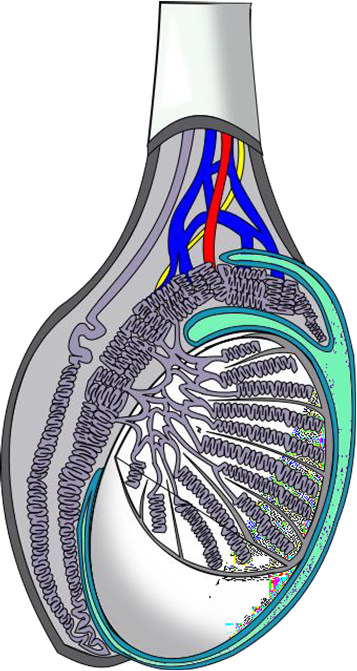
10.Match the structure listed in the table below with its corresponding description.
Part 2: Histology of the Reproductive Systems
- Obtain the slides listed below that are available for today’s lab.
- Focus on each sample and identify the structures listed for each type of tissue.
- Indicate the total magnification you make each illustration at in the space provided.
- Illustrate each tissue you observe with the microscope at the magnification you listed.
- Label each illustration with the structures listed for each.
More than one illustration at more than one magnification will be required to illustrate and label all structures
Label the tissue with: serosa, medulla, cortex, tunica albuginea, follicles, primordial follicles, primary follicles, secondary follicles, antral spaces, primary oocytes, corpus luteum, atretic follicles
More than one illustration at different magnifications and possibly of different slides will be necessary to illustrate and label all structures listed.
Label the tissue with: testis, epididymis, vas deferens, tunica albuginea, tunica vaginalis, seminiferous tubules, lumen of seminiferous tubule, spermatogonia, primary spermatocyte, secondary spermatocyte, spermatid
Part 3: Reproductive Systems Laboratory Activities
Labeling male reproductive anatomical model(s).
- Use the anatomical model(s) provided to your group.
- As a group, identify the structures listed below.
- Write each of the following structures on masking tape or labeling tape (with correct spelling) and stick onto the model to label each structure.
4. When you are done, ask your instructor to verify the labeling is correct.
Instructor Signature Confirming Correct Labeling: ___________________
5. Take a photo of your anatomical model for future reference for studying.
Labeling Female Reproductive Anatomical Model(s)
Attributions, part 1: review of reproductive systems.
- "Anatomy and Physiology Lab Homework" by Laird C Sheldahl is licensed under CC BY-SA 4.0
- "Female anatomy with g-spot-nb.svg" by Tsaitgaist is licensed under CC BY-SA 3.0
- "Gray's Anatomy plates" by Henry Vandyke Carte is in the Public Domain
- "Human Anatomy Lab Manual" by Malgosia Wilk-Blaszczak , Mavs Open Press , University of Texas at Arlington is licensed under CC BY 4.0
- "Male reproductive system.png" by User:Ningyou is licensed under CC BY-SA 3.0
- "Male reproductive tract.png" by Sheldahl is licensed under CC BY-SA 4.0
- "BIOL 250 Human Anatomy Lab Manual SU 19" by Yancy Aquino , Skyline College is licensed under CC BY-NC-SA 4.0
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Physiology, male reproductive system.
Purnima Gurung ; Ekrem Yetiskul ; Ishwarlal Jialal .
Affiliations
Last Update: May 1, 2023 .
- Introduction
The male reproductive system consists of the internal structures: the testes, epididymis, vas deferens, prostate, and the external structures: the scrotum and penis. These structures are well-vascularized with many glands and ducts to promote the formation, storage, and ejaculation of sperm for fertilization, and to produce important androgens for male development. [1] The major male androgen is testosterone, which is produced from Leydig cells in the testes. Testosterone can be converted in the periphery to a more active form, dihydrotestosterone via 5-alpha-reductase, or estradiol via aromatase. Other key hormones include inhibin B and Mullerian inhibiting substance (MIS) hormone, both produced by the Sertoli cells in the testes. Important hormones that modulate these include follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are released from the anterior pituitary gland and are regulated by gonadotropin-releasing hormone (GnRH), produced by the hypothalamus. Together, these hormones form the hypothalamic-pituitary-gonadal axis that promotes and maintains sexual development and function in the male. [2]
- Issues of Concern
It is important to note that testosterone can be converted peripherally to estradiol via aromatase from adipose tissue. Estradiol can go on to be converted to estrogen peripherally. Estradiol/estrogen can play a role in bone resorption, epiphyseal closure, gynecomastia, and vascular effects, and exert an inhibitory effect on the hypothalamus and anterior pituitary similar to testosterone. When levels of estradiol increase in males, this can lead to pathological changes such as weak bones, development of breasts and loss of libido or infertility.
- Cellular Level
Functional cells of the male reproductive system primarily consist of Leydig and Sertoli cells found in the testes. Leydig cells are found in the interstitium of the testes adjacent to the seminiferous tubules. On histology, they have pink cytoplasm and can be identified by pink crystals of Reinke. They produce testosterone, a steroid hormone that exerts its effects by binding intracellular receptors of different tissues and regulating protein expression. [3] Sertoli cells are found in the periphery of the seminiferous tubules. They promote spermatogenesis, which begins at the periphery of the tubules. They bind together to form a blood-testis barrier to keep germ cells contained in the seminiferous tubules and connect with each other through tight junctions. These cells are characterized by their relation to germ cells or primitive spermatogonia. Sertoli cells are much larger than germ cells, which are found nearby, and have less prominent nuclei. Germ cells line the interior of the seminiferous tubules and progress toward the lumen as they mature. These cells feature prominent, dark and dense nuclei. [4]
- Development
In human embryos, the default sexual differentiation is female. However, having the Y chromosome defines differentiation into the male phenotype and the male reproductive system. The Y chromosome contains the sex-determining region (SRY) gene, which encodes for development of the testes. The testes descend from the posterior abdominal wall during development to lie in the scrotum at maturity. The testes develop Sertoli cells, which produce MIS to induce regression of the Mullerian ducts, which form the female reproductive tract. The testes also develop Leydig cells that produce testosterone, the major driver of male reproductive development.
Testosterone plays an important role in stimulating the development of the Wolffian ducts in the male fetus, which become the testes, epididymis, vas deferens and seminal vesicles. Testosterone is also responsible for erythropoiesis, pubertal growth spurt, bone density, closure of epiphyseal plates, deepening of the voice, increase in muscle mass, male physique development and libido. Additionally, testosterone can be converted to dihydrotestosterone (DHT) via 5-alpha-reductase, an enzyme produced by the prostate peripherally. Both DHT and testosterone bind to the same androgen receptors intracellularly, but DHT has a higher affinity. DHT stimulates the development of the prostate, scrotum, and penis. DHT is also responsible for male hair pattern (facial, axial, and pubic hair), including the pathology of male pattern balding, increased sebaceous gland secretion and acne. Together, these hormones promote puberty and subsequent maintenance of the male reproductive system. [5]
Typically, the growth of the testes marks the beginning of puberty in males, which occur between 11 to 13 years of age. This is stimulated by a sudden rise in GnRH from the hypothalamus, which stimulates FSH and LH release from the anterior pituitary. LH stimulates Leydig cells to increase testosterone, which causes growth and pigmentation of the scrotum and penis. Secondary sexual characteristics such as facial, axillary, chest and pubic hair growth, deepening of the voice and growth spurt occur next. At this stage, first fertile ejaculations appear, marking mature reproductive function. Eventually, the epiphyseal growth plates close, marking the end of pubertal development. Pubertal development can continue into a male's 20s.
- Organ Systems Involved
The hypothalamic-pituitary-gonadal axis plays a major role in promoting sexual maturity, sperm production and the development of secondary sex characteristics. It maintains spermatogenesis and sexual function throughout the male’s lifetime. The hypothalamus secretes GnRH into the hypothalamo-hypophyseal portal system to stimulate the anterior pituitary. GnRH is a peptide hormone released by hypothalamic neurons in a pulsatile fashion. It acts on the gonadotrophs of the anterior pituitary via the binding and activation of a G protein receptor, which stimulates the anterior pituitary through inositol 1,4,5-triphosphate (IP3) activation (which increases intracellular calcium) to release FSH and LH. GnRH is inhibited by testosterone, estrogen, estradiol, and prolactin. [2]
In response, the anterior pituitary secretes LH and FSH into the blood. These gonadotropic hormones act on membrane receptors in the Leydig and Sertoli cells of the testes respectively. Both hormones come from the same glycoprotein family and consist of identical alpha subunits, but their different beta-subunit differentiates their functions. Both exert their physiologic effects by binding and activating a G protein receptor, which activates adenylyl cyclase and increases cellular cAMP levels, to stimulate Sertoli and Leydig cells. LH stimulates Leydig cells in the interstitium of the testes to produce testosterone from cholesterol. LH promotes desmolase, which is the initial rate-limiting enzyme that converts cholesterol into pregnenolone. This goes on to produce two key weak androgen intermediates: dehydroepiandrosterone (DHEA) and androstenedione. The enzyme 17-beta-hydroxysteroid dehydrogenase completes the conversion of androstenedione to testosterone. Testosterone acts on the hypothalamus and anterior pituitary via negative feedback to decrease the secretion of LH and FSH. Testosterone can also exert some effect on Sertoli cells, found in the periphery of the seminiferous tubules of testes. FSH and testosterone can stimulate Sertoli cells to release androgen-binding protein (ABP), which provides testosterone to germ cells during spermatogenesis. FSH stimulates Sertoli cells to promote sperm production and release inhibin B and MIS. Inhibin serves as the negative feedback control that Sertoli cells exert on the hypothalamic-pituitary system to decrease FSH release. [6]
Before puberty, the levels of androgens and gonadotropins typically remain low and constant. Once puberty occurs, the hypothalamus releases GnRH in a pulsatile fashion every one to two hours to maintain amounts of FSH, LH and plasma testosterone, all of which regulate each other to maintain hormonal balance. In the third decade of life, testosterone levels are found to decline. [2] [5] [7]
Although a majority of testosterone production in men come from the Leydig cells in testes, the adrenal cortex contributes some androgen production. Similar to the hypothalamic-pituitary-gonadal axis, the adrenal glands are also controlled by the hypothalamus and anterior pituitary to form the hypothalamic-pituitary-adrenal axis. The hypothalamus release corticotrophin-releasing hormone (CRH), which stimulates the release of adrenocorticotropic hormone (ACTH) from the anterior pituitary. ACTH stimulates the enzyme desmolase to convert cholesterol into pregnenolone in the adrenals, similar to testosterone synthesis in the testes. Specifically, the zona reticularis of the adrenal medulla is responsible for generating the weak androgens DHEA and androstenedione, which go on to be converted to testosterone or estradiol peripherally. [2]
The function of the male reproductive system is to produce androgens such as testosterone that maintain male reproductive function and to promote spermatogenesis and transport into the female reproductive system for fertilization. The testes act as both endocrine and exocrine organs in that they are responsible for androgen production and sperm production and transport.
Spermatogenesis starts at puberty with the germ cells found in the basement membrane of the seminiferous tubules of the testes. Sertoli cells stimulated by FSH help regulate spermatogenesis. One cycle of spermatogenesis begins approximately every 13 days; however, spermatogenesis is not consistently synchronous throughout all seminiferous tubules. The first stage of spermatogenesis begins with mitosis of diploid spermatogonia into primary spermatocytes. These spermatocytes undergo meiosis I to produce haploid secondary spermatocytes, which undergo meiosis II to form haploid spermatids. The most primitive spermatocytes are found peripherally in the seminiferous tubules and mature by migrating towards the lumen. Spermatids transform into spermatozoa by reducing cytoplasm. These spermatozoa are still immotile and are released into the tubules to travel to the epididymis for maturation. The epididymis is a coiled structure consisting of a head, body, and tail. The tail eventually joins with the vas deferens, providing an outlet for mature sperms to ejaculate. In the epididymis, the sperm takes about twelve days to mature and develop motility. They are then stored in the tail of the epididymis until ejaculation occurs. A mature sperm consists of a head, midpiece, and tail. The head contains the nucleus with very little cytoplasm. An acrosome or cap covers the head and is filled with lysosomes, which aids with fertilization. The midpiece contains abundant mitochondria to provide energy for the flagellum or tail of the sperm.
During sexual arousal (physical or psychological), vasodilation brings blood to the penis. The penis contains corpora cavernosa and a corpus spongiosum where blood flows along to enlarge and erect the penis. As sexual stimulation continues, blood continues to flow to the genitals, and the testes enlarge in preparation of ejaculation.
When ejaculation occurs, smooth muscle contractions of the epididymis pushes sperm into the ductus deferens (vas deferens), which sits in the spermatic cord. The ductus deferens delivers the sperm to ejaculatory duct by joining with the seminal vesicle duct near the prostate. The seminal vesicles produce fructose, which provides the energy for sperm motility. It is released within a fluid that mixes with the sperm to form semen. Once in the ejaculatory duct, the semen passes through the prostate, which secretes an alkaline fluid that helps thicken the semen so sperm can better stay within the female reproductive system. The semen then passes the bulbourethral glands or Cowper’s glands, which release a thick fluid that lubricates the urethral opening and clears the urethra of any urine residue. The semen then can enter the female vaginal canal, allowing the sperm to travel to and fertilize a potential egg within the female reproductive system. [2] [6] [8]
- Related Testing
Common tests of male reproductive function include a blood test to measure testosterone levels. A majority of testosterone is bound to plasma proteins, particularly sex-hormone-binding globulins (SHBGs), which serve as storage. Some testosterone is also bound to albumin, which serves as a transporter. Only a small amount of testosterone circulates freely in plasma (normal range: 50 to 210 pg/mL). Total testosterone ranges from 300 to 1000 ng/mL. [9] Other tests include semen analysis, which establishes fertility status and function of the seminiferous tubules, epididymis, and accessory sex glands. [10] A sperm sample is collected and examined microscopically for count, motility, and shape. It can be useful in diagnosing cases of infertility or success of a vasectomy. Normal sperm counts are typically greater than 15 million/mL and motility greater than 40%. Other tests include blood prostate-specific antigen test (PSA), which screens for prostate cancer. The prostate produces PSA typically, and levels can rise in prostatic carcinoma. [11] Recommendations for screening vary but typically screening should start around 50 years of age. A PSA greater than 4 ng/mL may prompt prostatic biopsy to rule out prostatic carcinoma. Physical exams include the digital rectal examination, which helps identify structural changes in prostate size such as benign prostatic hyperplasia, which is common in older men and can lead to urinary difficulties.
- Pathophysiology
An imbalance in the hypothalamic-pituitary-gonadal axis can result in infertility and hypogonadism. Primary hypogonadism (also referred to as hypergonadotropic hypogonadism) results from a gonadal failure to produce adequate testosterone or spermatogenesis despite high LH and FSH levels. Congenital causes of primary hypogonadism include Klinefelter syndrome, androgen synthesis disorder, or cryptorchidism. Acquired causes include hepatic cirrhosis, renal failure, drugs, autoimmune disease, irradiation, infections, trauma or commonly, age. These result in failure of the testes to develop properly, injury to the testes or impaired function. Hence, loss of testicular function results in damaged or underdeveloped Leydig or Sertoli cells that cannot respond to stimuli to maintain reproductive function.
Secondary hypogonadism results from a disruption in the hypothalamic-pituitary axis where low GnRH, LH or FSH leads to low testosterone and spermatogenesis. These disorders can arise from congenital isolated GnRH, LH or FSH deficiency (such as in Kallmann’s, Prader-Willi, Lawrence-Moon, GnRH receptor mutations, beta-subunit mutations in LH or FSH, or the kisspeptin/G protein-coupled receptor fifty-four mutations, which play a role in GnRH release). Acquired causes notably include hyperprolactinemia, panhypopituitarism, drugs (i.e., steroid use or opiates), systemic diseases, tumors, infection, trauma or irradiation. Notably, hyperprolactinemia can suppress GnRH release and is commonly due to prolactinomas, but can also result from hypothalamic-pituitary stalk lesions, drugs (dopamine antagonists, psychotropic agents, etc.) or systemic diseases. [8] [12] [13] [14] These diseases result in loss of the primary stimuli to the testes. Without the proper stimuli (GnRH, LH, or FSH), the Leydig and Sertoli cells, which are functional and intact, cannot exert their effects. This results in low testosterone levels or loss of spermatogenesis.
Other causes of infertility in men include defects in androgen action, hyper/hypothyroidism, adrenal insufficiency, congenital adrenal hyperplasia, disordered sperm transport (i.e., ductal obstruction), and systemic disease. Defects in androgen action, such as androgen insensitivity syndrome, result in a female phenotype despite male genotype due to an inability of the body's tissues to respond to testosterone. Hence, despite high testosterone levels in circulation, the clinical presentation is that of a patient with low testosterone and typically female as the disorder arises from birth.
- Clinical Significance
Disorders of the male reproductive system typically result from decreased testosterone levels or insensitivity to testosterone, which lead to low libido, failure to ejaculate, decrease in bone density, muscle loss, infertility, loss of body hair and, importantly, incomplete sexual development if the disorder is congenital or acquired before puberty. Other less specific symptoms of low testosterone include low energy/depressed mood, anemia or increased body fat. Other comorbidities associated with low testosterone include metabolic syndrome, insulin resistance, and atherosclerosis, [14] [9]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Purnima Gurung declares no relevant financial relationships with ineligible companies.
Disclosure: Ekrem Yetiskul declares no relevant financial relationships with ineligible companies.
Disclosure: Ishwarlal Jialal declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Gurung P, Yetiskul E, Jialal I. Physiology, Male Reproductive System. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Gonadotropins. [LiverTox: Clinical and Researc...] Review Gonadotropins. . LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Physiology, Ovulation. [StatPearls. 2024] Physiology, Ovulation. Holesh JE, Bass AN, Lord M. StatPearls. 2024 Jan
- Review Developments in the control of testicular function. [Baillieres Clin Endocrinol Met...] Review Developments in the control of testicular function. Swerdloff RS, Wang C, Bhasin S. Baillieres Clin Endocrinol Metab. 1992 Apr; 6(2):451-83.
- Hypothalamic-pituitary-gonadal axis in two men with aromatase deficiency: evidence that circulating estrogens are required at the hypothalamic level for the integrity of gonadotropin negative feedback. [Eur J Endocrinol. 2006] Hypothalamic-pituitary-gonadal axis in two men with aromatase deficiency: evidence that circulating estrogens are required at the hypothalamic level for the integrity of gonadotropin negative feedback. Rochira V, Zirilli L, Genazzani AD, Balestrieri A, Aranda C, Fabre B, Antunez P, Diazzi C, Carani C, Maffei L. Eur J Endocrinol. 2006 Oct; 155(4):513-22.
- Effects of castration and chronic steroid treatments on hypothalamic gonadotropin-releasing hormone content and pituitary gonadotropins in male wild-type and estrogen receptor-alpha knockout mice. [Endocrinology. 1998] Effects of castration and chronic steroid treatments on hypothalamic gonadotropin-releasing hormone content and pituitary gonadotropins in male wild-type and estrogen receptor-alpha knockout mice. Lindzey J, Wetsel WC, Couse JF, Stoker T, Cooper R, Korach KS. Endocrinology. 1998 Oct; 139(10):4092-101.
Recent Activity
- Physiology, Male Reproductive System - StatPearls Physiology, Male Reproductive System - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
zygote. gonad. gamete. male reproductive system. female reproductive system. human reproductive system, organ system by which humans reproduce and bear live offspring. Provided all organs are present, normally constructed, and functioning properly, the essential features of human reproduction are (1) liberation of an ovum, or egg, at a specific ...
The main structures of the female reproductive system are internal to the body and shown in Figure 22.2.4 22.2. 4. They include the paired ovaries, which are small, oval structures that produce eggs and secrete estrogen. The two Fallopian tubes (aka uterine tubes) start near the ovaries and end at the uterus.
Male reproductive gland that produces sperm and male hormones. Ovaries. Female reproductive gland that produces eggs and female hormones. Menstrual cycle. Pattern of events in females involving the development and release of an egg. Fertilization. The process in sexual reproduction in which a male gamete and female gamete fuse to form a new cell.
Human reproduction is an example of sexual reproduction. In human beings, both males and females have different reproductive systems; hence, they are known to exhibit sexual dimorphism. Males have testes- also called testicles, while the females have a pair of ovaries. Also read: Sexual Reproduction.
In the male reproductive system, the scrotum houses the testicles or testes (singular: testis), including providing passage for blood vessels, nerves, and muscles related to testicular function. The testes are gonads, and they produce sperm (the male gametes) and some reproductive hormones. Each testis is approximately 2.5 by 3.8 cm (1.5 by 1 ...
Peripheral Nervous System. 62 terms. wsl722. Preview. Study with Quizlet and memorize flashcards containing terms like Meiosis; divide chromosomes in half, Testes, epididymis, vas defrens, seminal vesicles, ejaculatory duct, prostrate gland, urethra, bulbourethral gland, Seminal vesicles, prostrate gland, bulbourethral gland and more.
The reproductive tissues of male and female humans develop similarly in utero until a low level of the hormone testosterone is released from male gonads. Testosterone causes the undeveloped tissues to differentiate into male sexual organs. When testosterone is absent, the tissues develop into female sexual tissues.
The male reproductive system consists of external organs. The testes in the scrotum produce the male gamete, sperm, which is ejaculated in seminal fluid by the penis. The female reproductive system primarily consists of internal organs. The female gamete, ovum, is produced in the ovaries and is released monthly to travel to the uterus via the ...
The LibreTexts libraries are Powered by NICE CXone Expert and are supported by the Department of Education Open Textbook Pilot Project, the UC Davis Office of the Provost, the UC Davis Library, the California State University Affordable Learning Solutions Program, and Merlot. We also acknowledge previous National Science Foundation support under grant numbers 1246120, 1525057, and 1413739.
Other topics in health and medicine. Science; Health and medicine; Unit 12: Reproductive system and pregnancy. Female reproductive system. Learn. Welcome to the reproductive system (Opens a modal) Basics of egg development (Opens a modal) The ovarian cycle (Opens a modal) Reproductive cycle graph - Follicular phase (Opens a modal)
Learn for free about math, art, computer programming, economics, physics, chemistry, biology, medicine, finance, history, and more. Khan Academy is a nonprofit with the mission of providing a free, world-class education for anyone, anywhere.
The function of the male reproductive system (Figure 27.1.1 27.1. 1) is to produce sperm and transfer them to the female reproductive tract. The paired testes are a crucial component in this process, as they produce both sperm and androgens, the hormones that support male reproductive physiology.
Explore the genetic advantage of sexual reproduction, describe the basic anatomy and physiology of both the male and female human reproductive systems, describe the process of human development leading up to birth, and identify major changes associated with each trimester of pregnancy. This interactive tutorial is part 1 in a two-part series.
Vagina. The vagina is a muscular canal (approximately 10 cm long) that serves as the entrance to the reproductive tract.It also serves as the exit from the uterus during menses and childbirth. The outer walls of the anterior and posterior vagina are formed into longitudinal columns, or ridges, and the superior portion of the vagina—called the fornix—meets the protruding uterine cervix.
The female reproductive system has several functions: producing eggs, which are female gametes. secreting female sex hormones. receiving sperm during sexual intercourse. supporting the development of a fetus. delivering a baby during birth. breastfeeding a baby after birth. During puberty, a girl develops into a sexually mature woman capable of ...
the process of sperm & egg coming together, & ending up with a diploid cell which contains half the genetic info from Mom & half from Dad; after this mitotic division occurs to form the baby. diploid cell. a cell containing both sets of chromosomes (46) reproductive. this system functions to procreate/keep species alive, produce/nourish ...
The female reproductive system is framed to perform different functions. It creates egg cells that are essential for reproduction known as ova. The system is organized to deliver the ova to the region of fertilization. The egg fertilization takes place in the Fallopian tubes along with the sperm. The implanting in the walls of the uterus and ...
This nursing test bank includes questions about Anatomy and Physiology and its related concepts such as: structure and functions of the human body, nursing care management of patients with conditions related to the different body systems. Step into the powerful realm of the female reproductive system anatomy and physiology.
Study with Quizlet and memorize flashcards containing terms like Gr. Sperma, Spermatos, Gr. Sperma, Spermatis, Gymnis, Gymnasium and more.
The male reproductive organs include the penis, testes, epididymis, vas deferens, and prostate gland. These organs are shown in the Figure below. The figure also shows some other parts of the male reproductive system. Male reproductive system as viewed from the side. The penis is an external, cylinder-shaped organ that contains the urethra.
Query 23.5.1 23.5. 1. This page titled 23.5: Practice Practical- the Reproductive System is shared under a CC BY-NC-SA 4.0 license and was authored, remixed, and/or curated by Jennifer Lange et al.. Practice Exam Problems.
Part 3: Reproductive Systems Laboratory Activities "Human Anatomy Lab Manual" by Malgosia Wilk-Blaszczak , Mavs Open Press , University of Texas at Arlington is licensed under CC BY 4.0 This page titled 22.5: Laboratory Activities and Assignment is shared under a CC BY-NC-SA 4.0 license and was authored, remixed, and/or curated by Rosanna ...
The male reproductive system consists of the internal structures: the testes, epididymis, vas deferens, prostate, and the external structures: the scrotum and penis. These structures are well-vascularized with many glands and ducts to promote the formation, storage, and ejaculation of sperm for fertilization, and to produce important androgens for male development.[1] The major male androgen ...
Study with Quizlet and memorize flashcards containing terms like Pregnancy tests look for _____ in the urine or the blood, Testosterone _____., Discharge from the vagina and more.