Vasectomy and Vasectomy Reversals—a Review of the Current Literature
- Published: 01 June 2023
- Volume 15 , pages 138–147, ( 2023 )

Cite this article

- Alison E. Schulz 1 ,
- Mustufa Babar 1 ,
- Ari P. Bernstein 2 ,
- Justin Loloi 3 &
- Valary Raup ORCID: orcid.org/0000-0001-6014-8785 2
240 Accesses
Explore all metrics
Purpose of review
Vasectomy is a commonly performed outpatient procedure for male contraception with high success and low failure rates. Vasectomy reversal permits couples desiring the ability to conceive naturally after vasectomy to avoid assisted reproductive technology in many cases. Our review discusses current and emerging vasectomy and vasectomy reversal practices, techniques, and outcomes.
Recent Findings
Various vasectomy techniques have been utilized for vas isolation and occlusion, most notably the no-scalpel vasectomy with intraluminal cauterization and fascial interposition. There are few comparative studies between vasectomy techniques, making it difficult to determine the optimal operative approach. Overall compliance rates with post-vasectomy semen analyses are low, complicating study of vasectomy success rates. The most common methods for reversal include vasovasostomy and vasoepididymostomy, each with their own range of techniques. With recent technological advancements, many novel approaches and tools have been employed to improve patency and pregnancy success such as robotic techniques and anti-fibrotic agents. In addition, there are many patient and partner factors that can affect vasectomy and vasectomy reversal outcomes. Vasectomy reversals need to be approached algorithmically with outcomes assessed based on technique and time since vasectomy.
Further research across multiple institutions is needed comparing outcomes of novel vasectomy and vasectomy reversal to traditional approaches. Emerging non-surgical options for male contraception will play an important role in the practice of urologists in future years.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
The evolution of vasectomy reversal.
Vasectomy Reversal
Robot-assisted vasovasostomy using a single layer anastomosis, papers of particular interest, published recently, have been highlighted as: • of importance •• of major importance.
Schwingl PJ, Guess HA. Safety and effectiveness of vasectomy. Fertil Steril. 2000;73(5):923–36.
Article CAS PubMed Google Scholar
Ostrowski KA, Holt SK, Haynes B, Davies BJ, Fuchs EF, Walsh TJ. Evaluation of vasectomy trends in the United States. Urology. 2018;118:76–9.
Article PubMed Google Scholar
Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost effectiveness of contraceptives in the United States. Contraception. 2009;79(1):5–14.
Patel RD, Loloi J, Labagnara K, Watts KL. Search trends signal increased vasectomy interest in states with sparsity of urologists after overrule of Roe vs. Wade J Urol. 2022;208(4):759–61.
Hendry WF. Vasectomy and vasectomy reversal. Br J Urol. 1994;73(4):337–44.
Sharlip ID. What is the best pregnancy rate that may be expected from vasectomy reversal? J Urol. 1993;149(6):1469–71.
Haws JM, Morgan GT, Pollack AE, Koonin LM, Magnani RJ, Gargiullo PM. Clinical aspects of vasectomies performed in the United States in 1995. Urology. 1998;52(4):685–91.
Holt BA, Higgins AF. Minimally invasive vasectomy. Br J Urol. 1996;77(4):585–6.
Auyeung AB, Almejally A, Alsaggar F, Doyle F. Incidence of post-vasectomy pain: systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(5)1788. This study compares the non-scalpel vasectomy technique to the traditional scalpel approach for vasectomy. They found that the incidence of post-vasectomy pain was three times higher following the traditional approach, suggesting that non-scalpel vasectomy has a lower pain burden for the patient.
Labrecque M, Dufresne C, Barone MA, St-Hilaire K. Vasectomy surgical techniques: a systematic review. BMC Med. 2004;2:21.
Article PubMed PubMed Central Google Scholar
Castillo Jimeno JM, Santiago González A, Rodríguez Pérez MJ, QuelAlzueta N, Ruiz Rubio JL, Antón López MJ, et al. Unique incision vasectomy: review of 1,800 cases. Arch Esp Urol. 1992;45(1):63–4.
CAS PubMed Google Scholar
Barone MA, Irsula B, Chen-Mok M, Sokal DC. Effectiveness of vasectomy using cautery. BMC Urol. 2004;4:10.
Sokal D, Irsula B, Chen-Mok M, Labrecque M, Barone MA. A comparison of vas occlusion techniques: cautery more effective than ligation and excision with fascial interposition. BMC Urol. 2004;4(1):12.
Sokal D, Irsula B, Hays M, Chen-Mok M, Barone MA. Vasectomy by ligation and excision, with or without fascial interposition: a randomized controlled trial [ISRCTN77781689]. BMC Med. 2004;2:6.
Altok M, Şahin AF, Divrik RT, Yildirim U, Zorlu F. Prospective comparison of ligation and bipolar cautery technique in non-scalpel vasectomy. Int Braz J Urol. 2015;41(6):1172–7.
Munro NP, Kotwal S, Gogoi NK, Weston PM, Browning AJ, Harrison SC, et al. Fulguration of the lumen does not improve vasectomy sterilization rates. BJU Int. 2009;104(3):371–5.
Sharlip ID, Belker AM, Honig S, Labrecque M, Marmar JL, Ross LS, et al. Vasectomy: AUA guideline. J Urol. 2012;188(6 Suppl):2482–91.
Dohle GR, Diemer T, Kopa Z, Krausz C, Giwercman A, Jungwirth A. European Association of Urology guidelines on vasectomy. Actas Urol Esp. 2012;36(5):276–81.
Sivardeen KA, Budhoo M. Post vasectomy analysis: call for a uniform evidence-based protocol. Ann R Coll Surg Engl. 2001;83(3):177–9.
CAS PubMed PubMed Central Google Scholar
Dhar NB, Bhatt A, Jones JS. Determining the success of vasectomy. BJU Int. 2006;97(4):773–6.
McMartin C, Lehouillier P, Cloutier J, Singbo N, Labrecque M. Can a low sperm concentration without assessing motility confirm vasectomy success? A retrospective descriptive study. J Urol. 2021;206(1):109–14.
Labrecque M, Hays M, Chen-Mok M, Barone MA, Sokal D. Frequency and patterns of early recanalization after vasectomy. BMC Urol. 2006;6:25.
Jamieson DJ, Costello C, Trussell J, Hillis SD, Marchbanks PA, Peterson HB. The risk of pregnancy after vasectomy. Obstet Gynecol. 2004;103(5 Pt 1):848–50.
Labrecque M, Hoang DQ, Turcot L. Association between the length of the vas deferens excised during vasectomy and the risk of postvasectomy recanalization. Fertil Steril. 2003;79(4):1003–7.
Jee SH, Hong YK. One-layer vasovasostomy: microsurgical versus loupe-assisted. Fertil Steril. 2010;94(6):2308–11.
Lipshultz LI, Rumohr JA, Bennett RC. Techniques for vasectomy reversal. Urol Clin North Am. 2009;36(3):375–82.
Dickey RM, Pastuszak AW, Hakky TS, Chandrashekar A, Ramasamy R, Lipshultz LI. The evolution of vasectomy reversal. Curr Urol Rep. 2015;16(6):40.
Herrel LA, Goodman M, Goldstein M, Hsiao W. Outcomes of microsurgical vasovasostomy for vasectomy reversal: a meta-analysis and systematic review. Urology. 2015;85(4):819–25.
Yahyazadeh SR, Sadighi Gilani MA, Karimi A. Vasectomy reversal: unilateral versus bilateral vasovasostomy. Andrologia. 2021;53(9):e14178.
Fuchs ME, Anderson RE, Ostrowski KA, Brant WO, Fuchs EF. Pre-operative risk factors associated with need for vasoepididymostomy at the time of vasectomy reversal. Andrology. 2016;4(1):160–2.
Silber SJ. Microscopic vasoepididymostomy: specific microanastomosis to the epididymal tubule. Fertil Steril. 1978;30(5):565–71.
Thomas AJ Jr. Vasoepididymostomy. Urol Clin North Am. 1987;14(3):527–38.
Chan PT. The evolution and refinement of vasoepididymostomy techniques. Asian J Androl. 2013;15(1):49–55.
Grober ED, Jarvi K, Lo KC, Shin EJ. Mini-incision vasectomy reversal using no-scalpel vasectomy principles: efficacy and postoperative pain compared with traditional approaches to vasectomy reversal. Urology. 2011;77(3):602–6.
Savage J, Manka M, Rindels T, Alom M, Sharma KL, Trost L. Reinforcing vasal suture technique improves sperm concentration and pregnancy rates in men undergoing vasovasostomy for vasectomy reversal. Transl Androl Urol. 2020;9(1):73–81. This study demonstrates a novel vasovasostomy technique which led to significantly higher sperm concentrations and pregnancy rates compared to traditional approach. In addition, it was a significant predictor of success, even after controlling for preoperative and intraoperative variables .
Kavoussi PK. Validation of robot-assisted vasectomy reversal. Asian J Androl. 2015;17(2):245–7.
Li P, Zhi EL, Yao CC, Xia SJ, Li Z. A novel approach: successful management of vasectomy reversal with a three-dimensional digital image microscope system. Asian J Androl. 2021;23(1):118–9.
Allameh F, Hosseini J, Qashqai H, Mazaherylaghab H. Efficacy of intraoperative Mitomycin-C in vasovasostomy procedure: a randomized clinical trial. Int J Fertil Steril. 2019;13(3):240–4.
Deck AJ, Berger RE. Should vasectomy reversal be performed in men with older female partners? J Urol. 2000;163(1):105–6.
Hinz S, Rais-Bahrami S, Kempkensteffen C, Weiske WH, Schrader M, Magheli A. Fertility rates following vasectomy reversal: importance of age of the female partner. Urol Int. 2008;81(4):416–20.
Kapadia AA, Anthony M, Martinez Acevedo A, Fuchs EF, Hedges JC, Ostrowski KA. Reconsidering vasectomy reversal over assisted reproduction in older couples. Fertil Steril. 2018;109(6):1020–4.
Fuchs EF, Burt RA. Vasectomy reversal performed 15 years or more after vasectomy: correlation of pregnancy outcome with partner age and with pregnancy results of in vitro fertilization with intracytoplasmic sperm injection. Fertil Steril. 2002;77(3):516–9.
Nusbaum DJ, Marks SF, Marks MBF, Burrows PJ, Zollman R, Samplaski MK. The effect of male age over 50 years on vasectomy reversal outcomes. Urology. 2020;145:134–40.
Boorjian S, Lipkin M, Goldstein M. The impact of obstructive interval and sperm granuloma on outcome of vasectomy reversal. J Urol. 2004;171(1):304–6.
Kolettis PN, Sabanegh ES, D’Amico AM, Box L, Sebesta M, Burns JR. Outcomes for vasectomy reversal performed after obstructive intervals of at least 10 years. Urology. 2002;60(5):885–8.
Grober ED, Karpman E, Fanipour M. Vasectomy reversal outcomes among patients with vasal obstructive intervals greater than 10 years. Urology. 2014;83(2):320–3.
Ostrowski KA, Polackwich AS, Kent J, Conlin MJ, Hedges JC, Fuchs EF. Higher outcomes of vasectomy reversal in men with the same female partner as before vasectomy. J Urol. 2015;193(1):245–7.
Chan PT, Goldstein M. Superior outcomes of microsurgical vasectomy reversal in men with the same female partners. Fertil Steril. 2004;81(5):1371–4.
Uvin V, De Brucker S, De Brucker M, Vloeberghs V, Drakopoulos P, Santos-Ribeiro S, et al. Pregnancy after vasectomy: surgical reversal or assisted reproduction? Hum Reprod. 2018;33(7):1218–27.
van Dongen J, Tekle FB, van Roijen JH. Pregnancy rate after vasectomy reversal in a contemporary series: influence of smoking, semen quality and post-surgical use of assisted reproductive techniques. BJU Int. 2012;110(4):562–7.
Farber NJ, Flannigan R, Srivastava A, Wang H, Goldstein M. Vasovasostomy: kinetics and predictors of patency. Fertil Steril. 2020;113(4):774-80.e3. This article analyzed various factors that affect patency following a vasovasostomy . As patency is a desired outcome of vasovasostomy , this article identified ways to improve outcomes by finding any sperm intraoperatively .
Scovell JM, Mata DA, Ramasamy R, Herrel LA, Hsiao W, Lipshultz LI. Association between the presence of sperm in the vasal fluid during vasectomy reversal and postoperative patency: a systematic review and meta-analysis. Urology. 2015;85(4):809–13.
Farber NJ, Flannigan R, Li P, Li PS, Goldstein M. The kinetics of sperm return and late failure following vasovasostomy or vasoepididymostomy: a systematic review. J Urol. 2019;201(2):241–50. There are few studies that study late re-canalization failure following vasovasostomy . This is one study that found late failure to be relatively common following vasectomy reversal and identified factors that may be predictive of recanalization .
Hollingsworth MR, Sandlow JI, Schrepferman CG, Brannigan RE, Kolettis PN. Repeat vasectomy reversal yields high success rates. Fertil Steril. 2007;88(1):217–9.
Lorenzini MS, Lorenzini F, Bezerra CA. Vasectomy re-reversal: effectiveness and parameters associated with its success. Int Braz J Urol. 2021;47(3):544–8.
Benger JR, Swami SK, Gingell JC. Persistent spermatozoa after vasectomy: a survey of British urologists. Br J Urol. 1995;76(3):376–9.
Kendrick JS, Gonzales B, Huber DH, Grubb GS, Rubin GL. Complications of vasectomies in the United States. J Fam Pract. 1987;25(3):245–8.
Awsare NS, Krishnan J, Boustead GB, Hanbury DC, McNicholas TA. Complications of vasectomy. Ann R Coll Surg Engl. 2005;87(6):406–10.
Sokal D, McMullen S, Gates D, Dominik R. A comparative study of the no scalpel and standard incision approaches to vasectomy in 5 countries. The Male Sterilization Investigator Team. J Urol. 1999;162(5):1621–5.
Yang F, Li J, Dong L, Tan K, Huang X, Zhang P, et al. Review of vasectomy complications and safety concerns. World J Mens Health. 2021;39(3):406–18.
Seenu V, Hafiz A. Routine antibiotic prophylaxis is not necessary for no scalpel vasectomy. Int Urol Nephrol. 2005;37(4):763–5.
Chantarasak ND, Basu PK. Fournier’s gangrene following vasectomy. Br J Urol. 1988;61(6):538–9.
Kessler RB, Kimbrough RC 3rd, Jones SR. Infective endocarditis caused by Staphylococcus hominis after vasectomy. Clin Infect Dis. 1998;27(1):216–7.
Viddeleer AC, Lycklama à Nijeholt GA. Lethal Fournier’s gangrene following vasectomy. J Urol. 1992;147:1613–4.
Appell RA, Evans PR. Vasectomy: etiology of infectious complications. Fertil Steril. 1980;33(1):52–3.
Rayala BZ, Viera AJ. Common questions about vasectomy. Am Fam Physician. 2013;88(11):757–61.
PubMed Google Scholar
Tan WP, Levine LA. An overview of the management of post-vasectomy pain syndrome. Asian J Androl. 2016;18(3):332–7.
Article CAS PubMed PubMed Central Google Scholar
Tandon S, Sabanegh E Jr. Chronic pain after vasectomy: a diagnostic and treatment dilemma. BJU Int. 2008;102(2):166–9.
Reynolds-Wright JJ, Anderson R. Male contraception: where are we going and where have we been? BMJ Sex Reprod Health. 2019;45(4):236–42.
Download references
Author information
Authors and affiliations.
Albert Einstein College of Medicine, New York, NY, USA
Alison E. Schulz & Mustufa Babar
Department of Urology, New York University Langone Health, 555 Madison Avenue, Floor 2, New York, NY, 10022, USA
Ari P. Bernstein & Valary Raup
Department of Urology, Montefiore Medical Center, New York, USA
Justin Loloi
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the literature review, organization, and writing of the primary text of the manuscript. Valary Raup, MD contributed to the organization and editing of the final manuscript text.
Corresponding author
Correspondence to Valary Raup .
Ethics declarations
Human and animal rights and informed consent.
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Male Sexual Dysfunction and Disorders
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Schulz, A.E., Babar, M., Bernstein, A.P. et al. Vasectomy and Vasectomy Reversals—a Review of the Current Literature. Curr Sex Health Rep 15 , 138–147 (2023). https://doi.org/10.1007/s11930-023-00364-z
Download citation
Accepted : 08 May 2023
Published : 01 June 2023
Issue Date : September 2023
DOI : https://doi.org/10.1007/s11930-023-00364-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Vasectomy reversal
- Vasovasostomy
- Vasoepididymostomy
- Male contraception
Advertisement
- Find a journal
- Publish with us
- Track your research

- Copy/Paste Link Link Copied
NICHD Vasectomy Research Information
Vasectomy is a safe, inexpensive, and highly effective method of male sterilization. Surgical advances have reduced healing time and postsurgical complications, making it a more acceptable choice now for many men seeking permanent birth control.
NICHD research activities on vasectomy have focused mainly on the procedure’s long-term safety and effectiveness as well as on the development and evaluation of acceptable and less-invasive surgical techniques.
These activities fall under the Institute’s broad and long-standing objective of developing safe, effective, easy-to-use, and long-lasting contraceptive methods in order to prevent and reduce unintended pregnancies.
NICHD Research Goals
NICHD research efforts on vasectomy fall within the Institute’s broad and long-standing goal of developing safe, effective, easy-to-use, and long-lasting contraceptive methods to prevent and reduce unintended pregnancies.
To this end, NICHD continues to refine, improve, and evaluate vasectomy and other established contraceptive methods. Notably, increasing efforts to develop acceptable male contraceptives beyond the vasectomy and condom is among NICHD’s scientific goals for reproductive health (PDF 2 MB).
Presently, NICHD research activity on male contraception is largely focused on developing new contraceptive methods that employ hormonal and nonhormonal agents as well as on supporting research and development that may lead to new methods for reversibly inhibiting sperm production or function.
Research Activities and Advances
The development of effective, safe, and acceptable contraceptive methods for men is an important part of preventing and reducing unintended pregnancies. NICHD invests in male contraceptive research and development, including studies of vasectomy.
Institute Activities and Advances
Other activities and advances.
Most NICHD research on vasectomy is supported through the institute's Contraceptive Research Branch (CRB), formerly the Contraceptive Discovery and Development Branch (CDDB). Branch-supported vasectomy research has focused on the procedure's long-term safety and effectiveness as well as on the development and evaluation of less-invasive surgical techniques. For example:
- CRB supported a large, national population-based case-control study in response to some studies published in the early 1990s suggesting that vasectomy might increase the risk of prostate cancer. Several other studies found no increased risk of prostate cancer among vasectomized men. Despite this conflicting evidence, urologists had been concerned enough to increase screening for prostate cancer among vasectomized men and to discourage vasectomies in men with a family history of prostate cancer. The results of the branch-supported national case-control study, published in 2002 in the Journal of the American Medical Association , were considered definitive evidence that prostate cancer was not linked with vasectomy 1 ( PMID: 12069674 ).
- CRB provided support through Family Health International for Cochrane Reviews of scalpel versus no-scalpel incision for vasectomy.
Vasectomy research is one piece of CRB’s portfolio in male contraception research and development. In addition, the branch leads the Preclinical Contraceptive Development Program to encourage and support basic, applied, and clinical studies on topics such as mechanisms that regulate sperm maturation and motility and identification of new therapeutic targets for male contraception. A group of scientists also supported by CRB are building on the promising results of their work from 2004, when they demonstrated complete and reversible contraception in male monkeys immunized with Eppin, a protein found only in the testes and epididymis ( PMID: 15539605 ).
Additionally, CRB funds the Biological Testing Facility and Chemical Synthesis Facility through contract mechanisms. These facilities support research on the identification and development of male and female contraceptive agents.
A study supported by the Fertility and Infertility Branch (FIB) evaluated the role of epididymal dendritic cells in male reproductive function. The study could have implications for both contraceptive development and treating male infertility ( Project number: 1R01HD069623-01 ).
NICHD was actively involved in the 2001 and 2003 Expert Consultations on Vasectomy , interagency workshops that included more than 50 experts from 24 organizations, institutions, and universities. The 3-day workshops prioritized future research related to vasectomy techniques and developed guidelines for techniques in diverse healthcare settings. Attendees reviewed recent clinical research findings and discussed their programmatic implications. Participants also reviewed key steps needed to improve vasectomy services in Africa, Latin America, Asia, and other areas of the world.
- Eunice Kennedy Shriver National Institute of Child Health and Human Development. (2006). New study finds vasectomy does not increase prostate cancer risk . Retrieved May 24, 2012, from https://www.nichd.nih.gov/newsroom/releases/vasectomy
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Intention to use vasectomy and its associated factors among married men in Debre Tabor Town, North West Ethiopia, 2019
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Writing – review & editing
Affiliation Department of Midwifery, College of Medicine and Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
Affiliation Department of Midwifery, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Roles Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Resources, Software, Supervision
Roles Conceptualization, Formal analysis, Investigation, Writing – review & editing
Roles Formal analysis, Project administration, Resources
Roles Formal analysis, Funding acquisition, Supervision, Validation, Visualization, Writing – original draft
- Alemu Degu Ayele,
- Fentahun Yenealem Beyene,
- Kihinetu Gelaye Wudineh,
- Bekalu Getnet Kassa,
- Yitayal Ayalew Goshu,
- Gedefaye Nibret Mihretie

- Published: September 3, 2020
- https://doi.org/10.1371/journal.pone.0238293
- Peer Review
- Reader Comments
Vasectomy is one of the most effective and permanent male contraceptive methods, and involves cutting and ligating the vas deferens to make the semen free of sperm during ejaculation. Although it is effective, simple, and safe, it is not well known and practiced in the majority of our community. This study assessed the intention to use vasectomy and its associated factors among married men in Debre Tabor Town, North West Ethiopia, 2019.
A community- based cross-sectional study was conducted among 402 married men from March 05 to April 15, 2019. A simple random sampling technique was employed to select the study participants. Data was collected by face to face interview using a structured and pre-tested questionnaire. Questions concerned socio-demographic and reproductive variables and views on vasectomy. The association between variables was analyzed using a bivariable and multivariable logistic regression model.
A total of 402 participants were included with a response rate of 98.75%. The mean participant age was 37.12(SD ± 6.553) years with the age range of 20–56 years. The prevalence of intention to use vasectomy was 19.6% with 95%CI (15.6%-23.4%). Multivariable logistic regression showed that age from 30–39 years (AOR = 3.2(95% CI: 1.19–8.86)), having more than three living children (AOR = 2.5(95% CI: 1.41–4.68)), good knowledge (AOR = 3.4(95%CI: 1.88–6.40)) and positive attitude (AOR = 4.8(95% CI: 2.61–8.80)) of married men were significantly associated with intention to use vasectomy.
Conclusion and recommendation
Intention to use vasectomy was comparable with findings in four regions of Ethiopia (Amhara, Oromia, SNNP, and Tigray). Age, the number of living children, knowledge, and attitude were significantly associated with the intention to use vasectomy. Improving the level of knowledge and attitude towards vasectomy is an essential strategy to scale up the intention of men to use vasectomy.
Citation: Ayele AD, Beyene FY, Wudineh KG, Kassa BG, Goshu YA, Mihretie GN (2020) Intention to use vasectomy and its associated factors among married men in Debre Tabor Town, North West Ethiopia, 2019. PLoS ONE 15(9): e0238293. https://doi.org/10.1371/journal.pone.0238293
Editor: Wen-Jun Tu, Chinese Academy of Medical Sciences and Peking Union Medical College, CHINA
Received: October 21, 2019; Accepted: August 14, 2020; Published: September 3, 2020
Copyright: © 2020 Ayele et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the manuscript and its Supporting Information files.
Funding: Yes, Bahirdar University.
Competing interests: The authors have declared that no competing interests exist
In mid-2016, the estimated population of Ethiopia was 101.7 million which is the second fast population growth in Africa next to Nigeria [ 1 ]. It is also affected by high maternal morbidity and mortality related to unintended and unwanted pregnancies [ 1 , 2 ]. The goal of family planning all over the world has attracted attention due to its importance in decision making about population growth and development issues [ 3 ]. Worldwide, using contraceptives potentially reduced maternal mortality by 44% [ 4 ].
Even though the 1994 International Conference on Population and Development (ICPD) in Cairo emphasized that men’s involvement in sexual and reproductive health issues is very important for a better outcome and set clear directions to increase men’s participation in family planning, male involvement in family planning is still very low in Africa [ 5 – 7 ].
Vasectomy is a male method of contraceptive which is known and acceptable only in some developed countries of the world. Although it is safe and easy to perform, only 45 million couples worldwide rely on it [ 8 , 9 ].
International health organizations in recent years have suggested that the involvement of men on the utilization and promotion of contraceptive methods is very crucial to provide couples with more male-oriented contraceptive choices, such as vasectomy. Even though its procedure is simple and easy with a high success rate (>99%) and minimal complications, it is underutilized around the world, especially in developing countries including Ethiopia [ 10 – 12 ]
Couples who complete their family or no want more children, vasectomy is the option than tubal ligation, due to it poses fewer surgical risks. Although it’s a higher effective, simple process and fewer complications, currently vasectomy users in the United States only 8% [ 13 ].
Ethiopia has a target plan to increase the contraceptive prevalence to 55% by the year 2020 [ 14 ]. To achieve this goal, the government in collaboration with other stack holders focuses on different FP methods by increasing demand and access to long-acting and permanent methods [ 15 ]. Due to this effort, the Contraceptive Prevalence Rate (CPR) with currently married women were reached 36%, with 35% using modern methods and 1% using traditional methods. Of 35%, injectable (23%), implant (8%), IUD(2%), pills(2%), male condom and tubal ligation <1% Ethiopia Demographic Health Survey (EDHS 2016) [ 16 ].
Different reviewed literature reports showed that the intention to use vasectomy was associated with different variables [ 11 , 15 , 17 , 18 ]. Age, educational status, occupation, religion, Cultural beliefs, societal norms, lack of knowledge about the procedure for a vasectomy, and misconceptions were found to be predictors of intention to use vasectomy. In addition, the duration of married time, number of living children, complete family size, the future desire of more children, accessibility of service, level of knowledge, and attitude of men towards vasectomy have an influence on intention to use vasectomy [ 18 – 22 ].
According to EDHS 2016, the national demand for family planning is 58%. However, vasectomy utilization is almost negligible [ 16 ]. There are very few studies on the intention of married men to use vasectomy in Ethiopia. Therefore, this study was designed to determine the intention of men to use vasectomy and identify factors associated with the intention to use vasectomy among married men in Debre Tabor Town, Northwest Ethiopia.
Study design and setting
A community- based cross-sectional study design was conducted in Debre Tabor Town from March 05 to April 15, 2019. The Town is found in the Amhara region, and it is a capital city of South Gondar Zone, North West Ethiopia. It is located 665 kilometers from the capital city of Ethiopia and 103 kilometers North West of Bahir Dar Town. The Town was divided into six small administrative units called kebeles with a total population of 92, 530 based on the 2018 report of Town administration [ 23 ]. The Town had one general hospital, three health centers, and four health posts that provide family planning and other health services in the study area. All married men whose wives were in the reproductive age group living in all six kebeles of Debre Tabor Town were the study population. All married men whose wives were in the reproductive age group in the town within the study period were included. Whereas married men whose wife were in the reproductive age group who were critically ill (bed reddened), had already done vasectomy, had infertile wife, and had a wife with a hysterectomy and married men women who live less than 6 months during data collection period in Debre Tabor town were excluded.
Sample size calculation and sampling procedures
Epi-Info version 7 statistical software was used to calculate the sample size assuming that 39% of men had the intention to use vasectomy [ 21 ], 95% confidence interval with a 5% margin of error. By adding a 10% non-response rate the final sample size was 402. A simple random sampling technique was applied to select 402 married men. A total of 14,088 households and 14,614 married men were living in the town [ 23 ]. A household was sampling unit in each kebeles and samples were allocated proportionally to each kebeles based on their total household number. Household numbers with married men in each kebeles were found from the kebeles registration book. Study households were selected from each kebeles through a simple random sampling technique by using a table of random numbers starting from kebele one from a random start point. The first household was selected in each kebele by using the lottery method. One married man per household was interviewed. When two or more eligible men were found in one household, only one was interviewed by lottery method and if no eligible men were identified in the selected household, the next eligible household located in the clockwise direction was visited and included until we got the desired sample size ( Fig 1 ).
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0238293.g001
Measurement and data collection procedure
Data were collected via face to face interview techniques using a structured, validated, and pre-tested questionnaire. The tool was first prepared in English then translated to Amharic and back to English by language experts to maintain the consistency of the instrument. Three diploma holder male midwives conducted the face to face interview and one BSc degree midwife supervised the data collection process. The information was collected on participants socio-demographic characteristics (age, religion, educational status, wife education, occupation and wife occupation), Reproductive characteristics (duration of married life, number of living children, the desire of more children, discussion with a partner, support from a partner), knowledge- related, and attitude- related questions ( S1 File ). Intention to use vasectomy means the planning of respondents to use vasectomy as a contraceptive method for a future time [ 24 ]. In this study knowledge about vasectomy was determined by using nine knowledge’s related questions. A value of one and zero was given for each correct and incorrect answer respectively and labeled as good knowledge; those individuals who answered at least five knowledge related questions and poor knowledge; those answered less than five knowledge’s related questions. In this study attitude about vasectomy was determined by using nine attitudes related questions and labeled as a positive attitude; those participants who scored greater than or equals to the mean score and negative attitude; those individuals who scored less than the mean score [ 25 , 26 ].
Data quality assurance
The data collection tool was prepared after an intensive review of relevant literature. Pretest of the questionnaire was done on 20 married men in Wereta Town and adjustments were made accordingly. Any error, ambiguity or incompleteness identified was corrected immediately. Data collectors and supervisors were trained for one day about the contents of the questionnaire, the aim of the study, method of data collection, confidentiality, responders’ right, and informed consent. The completeness of the data was checked by data collectors during data collection and also immediately after data collection by the supervisor and principal investigator.
Data processing, analysis, and interpretation
Data were cleaned, coded, and entered by using Epi-Data version 3.1 and then exported to SPSS version 23 for analysis. Descriptive statistics like frequencies and percentages were used to present the categorical independent variables and mean/standard deviation was used to describe a continuous variable. Frequency tables and graphs were used to present descriptive results. Bivariable logistic regression analysis was executed by computing odds ratio (OR) with a 95% confidence interval to see the association between each independent and dependent variable. Finally, all independent variables associated with dependent variables with p<0.2 were entered into multivariable logistic regression for further analysis by controlling confounding factors and significant association was identified based on p<0.05 and adjusted odds ratio (AOR) with 95% CI. Model adequacy was checked using the Hosmer and Lemeshow goodness of fit test (p-value = 0.41).
Ethics approval and consent to participate
Ethical clearance was obtained from the institutional review board of Bahir Dar University. A support letter was written to the Debre Tabor town administration and consent was obtained. Participants of the study were informed about the purpose, objectives, and their right to participate or not participate in the study. Privacy and confidentiality of the study participant were ensured by keeping all information anonymous. Written informed consent was obtained from each participant.
Socio-demographic characteristics of participants
A total of 402 married men participated in this study with a response rate of 98.75%. Half of the respondents 200(50.3%) were belonged to the age group of 30–39 years with the mean age and standard deviation of 37.12 (±6.553) years and with the age range of 20–56 years. The majority of the participants, 387(96.7%) were Amhara by ethnicity and orthodox Christian followers, 355(89.4%). More than half of the participants, 252(63.4%) were their educational status was college and above and one hundred eight two (45.8%) participants wives have attained college and above in their educational status. One hundred seventy-three (43.6%) participants and one hundred thirteen was a civil servant by occupation ( Table 1 ).
https://doi.org/10.1371/journal.pone.0238293.t001
Reproductive characteristics of participants
Among the respondents, 157(39.5%) were living with their wives from 6–10 years with the average duration of marriage 9.85 years. Two hundred forty-three (61.2%) of participants had three living children. The majority of the study participants, 355(89.4%) were discussed about FP with their partner. One hundred two (25.7%) participants got emotional support from their partner to use vasectomy. Two hundred eighty-one (70.8%) participants were completed their family size. Among 116(29.2%) participants who had not completed their family size, 83(72%) participants were their number of children desire was three and less than three for their future life ( Table 2 ).
https://doi.org/10.1371/journal.pone.0238293.t002
Knowledge of participants towards vasectomy
Two third of the study participants 247(62.2) had poor knowledge about vasectomywhile150 (37.8%) of them had good knowledge ( Table 3 ).
https://doi.org/10.1371/journal.pone.0238293.t003
The attitude of participants towards vasectomy
The majority of participants 245(61.7%) had a negative attitude while 152(38.3%) had a positive attitude towards vasectomy ( Table 4 ).
https://doi.org/10.1371/journal.pone.0238293.t004
Intention to use vasectomy and reason not to use vasectomy among study participants
This study identified that 19.6% with 95% CI (15.6–23.4) participants had the intention to use vasectomy as a contraceptive method for their future life.
In this study, 80.4% of the participants had no intention to use vasectomy as a contraceptive method for their future life due to many reasons. Among this, lack of awareness (74%) was the major reason followed by religious prohibition (70.5%) ( Fig 2 ).
https://doi.org/10.1371/journal.pone.0238293.g002
Factors affecting intention to use vasectomy among study participants
In binary logistic regression; age, participant wife occupation, duration of the married year, number of living children, and level of knowledge and attitude of participants had an association with intention to use vasectomy. In multivariable binary logistic regression analysis, after adjusting other co-variables by using backward likelihood stepwise method; age, number of living children, level of knowledge, and attitude had a significant association with intention of married men to use vasectomy.
Participants whose age group between 30–39 years were 3.2 times more likely to have the intention to use vasectomy [AOR = 3.2, (95% CI: 1.19–8.86)] as compared to Participants whose age lies below 30 years. Married men who had more than 3 alive children were 2.5 times higher the odds of intention to use vasectomy [AOR = 2.5(95% CI: 1.41–4.68)] as compared to men who had less than or equals to three alive children.
Moreover, study participants who had good knowledge about vasectomy were 3.4 times the odds of intention to use vasectomy [AOR = 3.4(95% CI: 1.88–6.40)] as compared with study participants who had poor knowledge about vasectomy. Participants who had a positive attitude towards vasectomy were 4.8 times more likely to use vasectomy as compared with their counterparts [AOR = 4.8(95%CI: 2.61–8.80)] ( Table 5 )
https://doi.org/10.1371/journal.pone.0238293.t005
Within the sphere of family planning, vasectomy is very often ignored, despite being one of the safest, simplest, and highly effective and least expensive contraceptive methods [ 5 ]. The descriptive report of this study revealed that around 37.8% and 38.3% of participants had good knowledge and positive attitude towards vasectomy respectively. This implied that there was poor knowledge and attitude towards vasectomy in the study area; to improve this; the country should design and implement the following strategies in its program;—Provision of Information and Services for Men in clinic setup, Outreach Male Motivators, and Peer Educators; Community Engagement; design community communication program; comprehensive Sexuality Education should be design and design community campaign. When compared to studies done in Malaysian private medical college which is (60.9%and 76%) of the respondents had a positive attitude and showed good acceptance towards vasectomy [ 27 ] which is significantly higher than from our studies. This might be due to the difference in study participants since the previous study was conducted on the medical students they might be hade a better view and attitude towards vasectomy than the general population.
Another surprising descriptive report of this study was participants educational level, college and above (63.4%) and participants occupation, civil servant (43.6%). This implies that as participants more educated and becoming civil servants; they might have easy access to information regarding to their fertility desire and might have more awareness and easily decide to use it. When compare to the finding in EDHS 2016 report which was (5%) and not more than 5% of respondents attained secondary school and above and their occupation is civil servant [ 16 ] respectively. This might be due to difference in study population, study area and time. The previous study was conducted at large country level which included both urban and remote rural areas that might be results lower educational level and civil servants whereas the current study was conducted at single town the educational characteristics might be more educated and also as they more educated the more being civil servant also since they are nearby information and access to education. And the other hypothesis might be the previous study participants marital status were both married and un married respondents were considered whereas current study only on married respondents considered; this also might be reason of the difference.
This study showed that 19.6% of participants had the intention to use vasectomy for their future life. This finding was in lined with the studies done in India showed that 21.4% and 21% of the participants had the intention to use vasectomy [ 28 , 29 ] respectively.
The intention of married men to use vasectomy in this study was also in agreement with study conducted in Bangalore rural population (17%) [ 30 ], Indonesia (16.6%) [ 20 ] and four regions of Ethiopia (Oromia, Amhara, SNNP and Tigray) (18.1%) [ 15 ].
But the finding of this study was lower than studies conducted in Kenya and Rwanda (27.5%, 26.6%) [ 18 , 19 ] respectively. The discrepancy may be due to differences in the number of children the participants had since only 38.8% of participants in this study had more than three children but in the comparable studies (76.6% and 63.3%) of the participant had more than three children respectively. In addition, only 38.3% of the participant in this study had a positive attitude but in Rwanda, 60% of the participant had a positive attitude towards vasectomy which had a direct relationship with their intention.
According to our study, the intention to use vasectomy as a FP method was also lower than study conducted in the East Wollega zone of the Oromia region (30%) [ 22 ]. The discrepancy may be due to difference in study setting and participants. The current study was community- based but the previous study was done in a health institution and the participants were men who were visiting health institutions together with their partner for FP service, maternity and child health unit, which has a positive impact on their intention by increasing their awareness about the method.
The finding of our study was higher than the study conducted in India (11%) and Turkey(11.4%) [ 17 ] and [ 10 ] respectively. The variation may be due to difference in the marital status of study participants, in the current study only married men participated but in the previous study, the participants were both married and unmarried men who had a significant difference in their intention since thinking about vasectomy without being married is not ideal and visible. And also the difference is might be difference in socio-demographic characteristics, study area, and participants.
The result of this study revealed that being in the age category of 30–39 years had an increased intention to use vasectomy as a contraceptive method as compared to the age category of 20–29 years. This finding is supported by studies conducted in India and Nepal [ 17 , 31 ]. Another study conducted in Indonesia also showed that the age of the respondent which was found between 30–39 had a significant relationship with intention to vasectomy [ 32 ].
The possible explanation for this finding might be participants in this age category (30–39) might have easy access to information and educated from the younger once, as the educational status increase, the knowledge might also scale up in the same fashion which had a positive impact on intention. The other reason might be men in the age category of 30–39 may have steady jobs, a greater number of living children, and stable family life from younger once. Another explanation those mens, whose aged 40 and above years might be thought that their wives near to menopause and no more have children at more.
According to our study finding, having more than three living children was the other predictor variable as it stated that having more than three children increase the intention of participants to use vasectomy. Similar studies conducted in Indonesia stated that as the number of alive children increases the intention to use vasectomy was also increased [ 20 , 32 ]. Likewise, research conducted in India also concluded that the number of living children was a significant predictor for intention to use vasectomy [ 33 ]. The finding of this result was also supported by studies performed in Kenya and Rwanda [ 18 , 19 ]. The possible reason may be men who had a smaller number of children might have a high future fertility desire and their intention to use the contraceptive methods might be low. In other words, since vasectomy is permanent and irreversible, it is a choice of contraceptive method for those men who had more children and for those who want to limit their family.
The result of this study also showed that there was a positive relationship between knowledge of vasectomy and its acceptance by married men; it revealed that participants who had good knowledge about vasectomy had a higher intention to use it. The finding was also in line with a study conducted in Nigeria and the Kingdom of Eswatini [ 34 ] and [ 11 ] respectively. This might imply that knowledge plays an important role in the intention of vasectomy by increasing the awareness of individuals, having good knowledge about vasectomy used to helps men to know the importance of it from other methods avoids different misconceptions, changes the behavior and positively affects the attitude of men towards vasectomy.
Men who had a positive attitude towards vasectomy had increased intention to use it from that of men who had a negative attitude. The finding of this study was in agreement with the study finding from Nepal and Indonesia [ 21 ] and [ 20 ].
This might be attitude is a key factor that influence the intention, men with positive attitude towards vasectomy are better able to use it and share responsibilities in FP practice with their partner. The other reason may be individual who had positive attitude, they can break myths and misconception that was negatively affects intention to use vasectomy.
Generally, even though the health policy of Ethiopia puts or states different strategies to decrease maternal mortality like optimum utilization of family planning, but no practical change in attitudinal, behavioral, cultural and reliogional change is showed in men’s family planning utilization like vasectomy; therefore, the countries policy should work for practical change rather theoretical report. In addition, for researcher community based, qualitative studies should run, that can find out more explorative factors.
In conclusion, the prevalence of intention of married men to use vasectomy for future life was inlined with a study done in four regions of Ethiopia (Amhara, Oromia, SNNP and Tigray). Age (30–39) years, having more than three living children, having good knowledge, and a positive attitude towards vasectomy were significantly associated with the intention to use vasectomy for future life as a contraceptive method. As per finding, improving level of knowledge and attitude towards vasectomy is an essential strategy to scale up the intention of men to use vasectomy. We also recommend further researchers to come up with additional and detailed findings especially on qualitative aspect.
Supporting information
S1 file. english version questionnaires..
https://doi.org/10.1371/journal.pone.0238293.s001
Acknowledgments
The authors would like to acknowledge College of Medicine and Health Sciences, Bahir Dar University, for sponsoring this research project. We would also like to extend our heart full gratitude to Debre Tabor town Administration for permitting to conduct the study and providing the necessary preliminary information. The last but not the list we would like to extend our appreciation to the study participants, supervisor and data collectors.
- View Article
- Google Scholar
- PubMed/NCBI
- 5. United Nation Population Information Network. Report of the international conference on Population and development. Cairo. Available at www.un.org/popin/icpd/conference/offeng/poahtml 1994.
- 9. Ajuwon. A, Desmenuu A. Men’s awareness of, Barriers to, and Intention to adopt VasectomyamongMarriedMeninIbadan, Nigeria. https:/wwwresearchgatenet/peblication/313512381 . 2014.
- 15. Marie Stopes International Ethiopia Addis Ababa. Knowledge, Attitudes and Practices (KAP) Survey, Permanent Methods of Family Planning in four regions of Ethiopia. USAID. 2017.
- 26. Burian P., Catherine P. Quee C. et al. Recent experience and lessons learned in vasectomy programming in low-resource settings: a document review. Durham, NC: FHI 360 and Washington, DC: Population Council, the Evidence Project. 2016.
Impact of vasectomy on the sexual satisfaction of couples: experience from a specialized clinic
Affiliations.
- 1 UROGATE Associates Frankfurt, in cooperation with Frankfurt University Medical Center, Germany.
- 2 Department of Urology, Frankfurt University Medical Center, Frankfurt, Germany.
- PMID: 29104791
- PMCID: PMC5656365
- DOI: 10.5173/ceju.2017.1294
Introduction: Vasectomy is the simplest, safest, and most effective form of definitive fertility control in men [1]. Vasectomy is used for 10% of contraception worldwide but only for 2% in Germany [2]. The aim of this study was to investigate the impact of vasectomy on the sexual satisfaction of sterilized men and their partners.
Material and methods: Vasectomized men and their partners were surveyed by means of the IIEF (International Index for Erectile Function) and the FSFI (Female Sexual Function Index) questionnaires. A total of 294 couples were surveyed; 90 men answered the IIEF, and 74 women answered the FSFI. The results of the questionnaires were compared to a historical comparison group. The men were also surveyed with a not validated questionnaire, which was returned by 95 men. The two-sample t-test for independent samples, the chi-squared test, and the Wilcoxon-Mann-Whitney test were carried out.
Results: The vasectomized men had significantly better results than the healthy historical comparison group in the IIEF domains of erectile function, orgasm, sexual desire, and intercourse satisfaction. For the female partners of the sterilized men, there were almost no significant differences in any questions of the FSFI in comparison to the control group. A significant difference was observed only in the domain 'arousal'.
Conclusions: Vasectomy does not have a negative impact on the sexual satisfaction of the affected couples. In fact, sexual satisfaction improved for the sterilized men, while the satisfaction of the women was not reduced by the vasectomy.
Keywords: FSF; IIEF; sexual satisfaction; vasectomy.

Enter the URL below into your favorite RSS reader.
Vasectomy Regret or Lack Thereof
- Citation (BibTeX)
View more stats
Vasectomy is a procedure that results in permanent yet reversible sterility and remains a great contraceptive option for many. Previous research studies have highlighted frequency of vasectomy utilization, defining characteristics of individuals who opt for this method, various surgical techniques, and the risks and benefits associated with the procedure. What remains to be defined is why or why not individuals may experience post-vasectomy regret and whether the previous characteristics correlate.
The objective of this review is to synthesize information regarding reasons individuals may regret their vasectomy and seek reversal, what options exist for accomplishing the reversal, and patients’ fertility prognosis post-vasovasostomy.
This review utilized a combination of secondary and tertiary data analysis across a wide scope of academic databases pertaining to the topic of interest.
Typically, most males who have sought a vasectomy are satisfied with their decision, however, approximately 6% of this population seeks reversal. Key factors influencing vasectomy regret include age at the time of vasectomy, parental status, pre- and post-operative relationship status, unresolved physical and psychosexual problems, and development of chronic scrotal pain following the procedure. Few options exist for vasectomy reversal including microsurgical reconstructive vasectomy reversal (VR) and sperm extraction for in vitro fertilization. There is no guarantee that fertility will be restored in any case but a major predictive factor for success is the time interval prior to reversal.
Vasectomy is intended to be a permanent form of contraception; however, a minor chance remains that individuals may experience post-operative regret due to various factors. This warrants proper comprehensive counseling by the patient’s provider regarding benefits and risks, procedural outcomes, opportunities for reversal, and fertility prognosis.
Introduction
Vasectomy is a widely available, safe, and effective form of male contraception that helps to ease the contraceptive burden on females while simultaneously offering males the opportunity to take a more active role in pregnancy prevention. Vasectomy is the fourth most utilized method of pregnancy prevention preceded by oral contraceptives (30.6%), female sterilization (27.0%), and male condoms (18.0%). 1 , 2 Trends demonstrated dramatic increases in male sterilization between 1965 and 1976 3 and a marked decline in vasectomies between 2002 and 2017 1 , 4 , 5 which could be attributed to a multitude of factors including periods of economic uncertainty. 1 , 4 Despite numbers trending downward, it still appears that approximately half a million men in the United States (US) choose to undergo this procedure annually. 6
Given the permanence and subsequent challenges posed by vasectomy reversal, proper counseling for individuals seeking vasectomies and involved partners is warranted. Critical information to be discussed with patients includes, but is not limited to, other forms of contraception, understanding that the procedure results in permanent sterility, future family intent, risk of pregnancy, and future therapeutic approaches such as sperm extraction for use in in vitro fertilization and vasectomy reversal. 2 , 6–8
Few studies have investigated characteristics of individuals seeking vasectomy reversal along with other predictive factors. One notable factor is age; men seeking vasectomy reversal tended to have undergone the initial procedure earlier than men not seeking reversal. 2 , 9 This article seeks to uncover regret, or lack thereof, in individuals who have chosen vasectomy as a form of contraception and options for those who seek reversal.
Vasectomy Overview
What is a vasectomy.
A vasectomy is a surgical procedure that can be performed in an outpatient setting, typically by a urologist, utilizing local anesthesia. 2 The purpose of this procedure is to divide and occlude the vas deferens which cuts off the supply of sperm to the ejaculate fluid. 7 , 10 Sperm makes up a small fraction of the ejaculate volume, therefore there will generally be no perceivable changes in the amount of ejaculate post-operatively. 10
Vasectomy is a permanent form of contraception relied upon by both males and females as an alternative to other long-acting methods such as tubal sterilization. 11 Studies have demonstrated that three of the most cost-effective contraceptives in the US are the copper-T IUD, vasectomy, and the Levonorgestrel intrauterine system (LNG-20 IUS) when factors such as the cost of unintended pregnancy are accounted for. 12 Other benefits to this method include being a reliable method of contraception with only about a 1/2000 chance of failure, a one-time cost that may be covered by insurance, minimal to no effects on sexual pleasure, and association with shorter operation and recovery time as opposed to tubal ligation. 2 , 7 , 13 Overall, this method persists as a safe, effective option that helps relieve the contraceptive burden on females. 14
Prevalence of vasectomies in the US
Over the last two decades, vasectomy utilization among men aged 18-45 has decreased according to National Survey of Family Growth (NSFG), with the biggest decrease amongst the lowest and highest age groups. 1 , 5 It remains a more common method of contraception in developed Western countries such as the US, Canada, and the United Kingdom as opposed to many Asian and Latin American countries. 1 , 5 Within the US, vasectomies tend to be more highly utilized in Western and North Central regions with no significant difference in rural versus non-rural areas. 5 Additionally, temporal trends have demonstrated increases in the number of vasectomies performed during the month of March (for March Madness) and at the end of the year which correlate to more time off and accumulation of insurance premiums. 5
Demographics and vasectomy utilization
Characteristics have been associated with individuals seeking and opting to undergo vasectomies. From 2002-2017, studies show that the average age of men seeking a vasectomy remained stable around the 31–33-year age range whereas the average age of men at the time of their last child showed a steady increase. 1 Studies have investigated the differences in men who were childless at the time of vasectomy versus men who previously had children in which most demographic information was extremely similar. Factors that set these two groups apart, however, included larger income, less religious affiliation and more geographic mobility amongst the childless group. 3 There was also no difference in styles of psychological adjustment or marital satisfaction following the procedure, and this operation appeared to be not only physically, but also psychologically safe for men with and without children. 3 Over time, however, a growing correlation has appeared between the number of men seeking this form of contraception and the number of offspring that they have. 1
Positive associations found with the use of vasectomy included factors such as increased age, non-Hispanic white race, marital status, higher levels of education, lack of Catholic religious affiliation, and possession of private health insurance. 1 , 5 , 15 Individuals born in the US are also more likely to undergo the procedure as opposed to immigrant populations, and studies demonstrated notable disparities in the number of Hispanic and black men that utilize this option. 1 , 5 , 15 A strong positive correlation exists between vasectomies and higher socioeconomic status, specifically with total household incomes that meet or exceed $50,000 annually. 1 While it is less common for men under the age of 25 to undergo this procedure, any individual with the ability to provide informed consent can opt to do so following proper counseling by a provider. 7
Surgical techniques
While approximately 30 different methods of isolation of the vas deferens and occlusion of the vas exist, there are two main vasectomy surgical techniques that are important to discuss, conventional versus no-scalpel methods. 2 , 7 , 8 , 13 , 14 , 16 The conventional vasectomy technique requires bilateral scrotal incisions which allows for access to and transection of the vas deferens, a less popular technique in the US. 2 , 8 , 14 The no-scalpel method, or minimally invasive vasectomy (MIV) is now more highly recommended due to improved outcomes such as shorter operation times, less bleeding and risk of infection, hematoma, less peri- and post-operative pain, and a quicker resumption to sexual activity. 7 , 16 The MIV consists of a small puncture through the scrotal skin with a sharp forceps-like instrument, externalization of the vas deferens and subsequent transection. 2 , 7 , 8 , 14 A difference in the effectiveness of these two methods has yet to be identified. 16
Once transected, there are multiple methods by which the vas deferens can be occluded. Three of these divisional methods include mucosal cautery (MC) with fascial interposition (FI), MC without FI, and open-ended vasectomy which leaves the testicular end of the vas unoccluded and uses MC with FI on the other end. 2 , 8 , 15 Typically, ligatures and clips are avoided in this procedure. MC appears more effective than electrocautery, and FI is utilized in conjunction with MC in order to make a tissue barrier between the two vas ends thereby decreasing chances of failure. 2 , 8 , 14 , 15 Following a vasectomy, males should continue to use other contraceptive methods until success of the surgery has been proven via post-vasectomy semen analysis (PVSA) . 2 , 8 , 14 , 17 Typically, azoospermia, or lack of sperm in the semen, occurs anywhere from eight to sixteen weeks post-operatively and approximately 20 ejaculations after the procedure, but some patients may never reach this end goal and will instead persist with nonmotile sperm which may still be an indication for procedure success. 2 , 7 , 8 , 14 , 17 , 18
Risks Associated with vasectomies
Complications associated with vasectomies include hematoma formation, infection, post-vasectomy pain syndrome, congestive epididymitis, and sperm granuloma. 2 , 14 , 19 , 20 Incidence rates of infections such as Fournier’s gangrene, sexually transmitted infections (STIs), and endocarditis, as well as hematoma formation are between 0.2-1.5% and 4-22%, respectively. The incidence of post-vasectomy pain syndrome is 1-14%, whereas incidence for sperm granulomas is the highest at 40%. 19 , 20 Vasectomies have been associated with no increased risk for other conditions such as prostate cancer, cardiovascular disease, sexual dysfunction, changes in reproductive hormones or development of antisperm antibodies. 20 A final, and, perhaps, one of the more concerning risks associated with vasectomies is failure of the procedure resulting in an unplanned pregnancy. Failure of this procedure, associated with late re-canalization, unprotected sexual activity before clearance, and technical errors occurs in <1% of all cases, 2 , 7 , 21 however, patients must be aware of this possibility and follow the advice of their provider.
Factors Influencing Vasectomy Regret
Given the global popularity of vasectomy as a means of contraception, there have been no shortage of studies conducted to analyze potential complications and side effects of the procedure. In general, it has been seen that serious side-effects on the patient’s health, whether physical, hormonal, or psychosexual, are uncommon. The procedure is generally regarded as one of the safest and most reliable forms of contraception. 22 , 23 Overall, most men are satisfied with their vasectomy and tend to report either unchanged or increased levels of sexual fulfillment and intimacy with their partner. 24 Despite this, there are a small number of men who regret the procedure and may go on to seek a reversal (for reference the number of men seeking reversal is around 6%). 9 Given the small number of physical complications associated with the procedure, most of the reasons why a patient may regret having a vasectomy tend to center around personal and social factors, such as the age at which they undergo the procedure, whether they have children, or changes in their relationship status.
Young age at the time of vasectomy has been seen to correlate strongly with vasectomy regret. Specifically, those men who elect to undergo vasectomy prior to age 30-35 are much more likely to regret their decision than men who have the procedure done later in life. 25–27 One study demonstrated that men who underwent vasectomy in their 20s are 12.5 times more likely to seek a reversal than older men. 9 It has been observed that some of the regretful men in this age bracket made an impulsive decision to get a vasectomy in a state of emotional turmoil or out of reaction to a stressful situation. Examples of men fitting this profile would include those who experience an initial panic following the news of a pregnancy, those who suffer from a depressive disorder, or those who are experiencing financial difficulties. Once the crisis resolves, these men may regret their sterilization. 27
Parental status
The relationship between the parental status of a man and post-vasectomy regret is multifaceted. It has been seen that, all things being equal, there are negligible differences in post-operative regret between married, voluntarily childless men and married men who fathered children pre-vasectomy. 3 Moreover, recent data analyses have shown that men who were voluntarily childless prior to vasectomy are actually less likely to undergo a vasectomy reversal than men with children (though feelings of regret were not analyzed). 28 , 29 This relationship is likely more complex than it appears at first, however, as there are consistent demographic differences between voluntarily childless men and men with children. For instance, voluntarily childless men tend to be less religious and have a higher income. Among men who have children prior to vasectomy other factors come into play. Of note, there tends to be increased regret among those who have lost a child post-vasectomy. 27 , 30–33 Outside of tragic circumstances such as these, some of these men that experience regret have simply changed their minds about the number of children they wish to have. 33–35 This latter reason for regret was seen to be particularly related to a couple having very young children at the time the man underwent the procedure. 25
Relationship status
The relationship between a man and his partner both pre- and post-vasectomy can play a significant role in post-operative regret. Previously married men are more likely to regret having a vasectomy after they have gone through a divorce. 32 , 33 Some men have reported that they underwent a vasectomy in hopes of saving a failing marriage, only to regret the decision following the ultimate dissolution of the relationship. 27 In one retrospective questionnaire it was found that 94% of men regretting their vasectomy had entered a new relationship following the procedure. 26 Many men experiencing regret post-divorce or breakup have felt that their sterility placed them at a distinct disadvantage in pursuing new, romantic relationships. Among those divorced, post-vasectomy men who do remarry, many may feel a significant desire to father a child with their new partner. 27 , 33
Other factors contributing to vasectomy regret
The characteristics discussed above tend to be the most frequent traits common to men regretting vasectomy. However, the following few are still noteworthy and may commonly overlap with both each other and previously enumerated factors. Among some patients, unrealistic expectations of what they can expect following the procedure lead to regret when these hopes fail to materialize. An example of this would be a man struggling with impotence who believes a vasectomy will cure him. 36 As noted previously, physical and psychosexual problems following vasectomy tend to be rare. However, there are a small number of men who note feelings such as “incompleteness” or inadequacy following vasectomy and believe a reversal will rid them of these feelings. 27 , 33 , 36 Finally, a small number of men can develop chronic scrotal pain, leading to procedural regret. 24 , 37 As is apparent, some characteristics, such as young age and marital disharmony, are identifiable signs that a man may be liable to regret their vasectomy in the future. Others, such as death of a child or chronic pain, are unfortunately unpredictable. In any case, restoral of fertility post-vasectomy is by no means guaranteed. 38 Given this, increased efforts to identify and provide targeted counsel to men at risk for post-vasectomy regret is a worthwhile endeavor.
Vasectomy Regret: Operative Options and Fertility Prognosis
Vasectomy reversal and in-vitro fertilization.
While vasectomy remains an effective and safe method of birth control, about 3-6% of men seek reversal of the procedure due to various circumstances, including remarriage, loss of a child, an altered financial situation, or post-vasectomy pain syndrome. 39 A patient seeking reversal should be counseled on the options for pursuing conception post-vasectomy keeping in mind that the most important prognostic factor for successful reversal is the time interval of obstruction. 40 The first option is a reconstructive vasectomy reversal (VR) procedure. Microsurgical reconstructive VR procedures remain the gold standard of treatment for vasectomy revision. Due to the complexity of the procedure, only a minority of urologists will perform the procedure, and financial barriers exist due to this procedure rarely being covered by insurance. 6 VR is achieved through reattachment of the vas deferens either through vasovasostomy, the reconnection of the two severed ends of vas deferens to each other, or vasoepididymostomy, the connection of the vas deferens directly to the epididymis. The microsurgical approach to vasovasostomy shows an increased likelihood of sperm returning to semen and postoperative pregnancy success when compared to a macrosurgical approach. 41 When evaluating the success rate of unilateral versus bilateral vasovasostomies, there was no statistical difference in the return of sperm to semen or pregnancy rate between the two surgical approaches. 42
The second option for patients with conception-oriented vasectomy regret is sperm extraction for in vitro fertilization (IVF), which might also present a financial burden upon the patient due to the variability of insurance coverage. 6 When comparing conception-directed options, VR is more cost-effective than IVF if neither procedure is covered by insurance. IVF is a more effective option for couples seeking pregnancy post-vasectomy if a female factor of infertility is present in addition to the male’s vasectomy. Lastly, IVF may present a backup option in the event of a failed reconstructive VR in which the patient opted to cryopreserve sperm at the time of the procedure.
Pregnancy success rates are similar for both IVF and VR; therefore, the couple’s decision should involve thorough discussions with a VR experienced urologist and an IVF experienced reproductive endocrinologist. 43 In these discussions, couples should consider the fertility and age of the female partner, the number of children the couple wants, and the relative success of each procedure based on their unique situation, as these factors may alter the prognosis of VR or IVF. A patient seeking VR for psychological or pain-related reasons rather than fertility restoration should consider alternative pain management methods before surgical intervention due to the unknown pathogenesis of post-vasectomy pain syndrome and indefinite postoperative relief of pain with VR. 41 In a study of 31 patients who underwent VR for post-vasectomy pain, only 34% of patients reported complete alleviation, while 82% reported improved pain relief by the 3.2-month follow-up. 44
Fertility prognosis post-vasectomy
Vasectomy is a safe and reliable form of birth control, yet there is no guarantee of the ability to restore fertility in patients who seek reversal of this procedure. Data suggest that in the case of a patient seeking vasectomy reversal, fertility is only restored in about 50% of cases due to changes in the epididymis and vas anastomosis after a vasectomy. The primary causes of failed vasectomy reversal are stenosis of the previous vasovasostomy, epididymal blockage, elevated anti-sperm antibody response, and ceased spermatogenesis. 23 A study of 1469 patients who underwent microsurgical vasectomy reversal found that the interval of time between vasectomy and VR was a highly predictive factor of a patient’s likelihood of successful restoration of sperm within the semen. About 97% of patients successfully restored sperm within the semen if less than three years passed between vasectomy and VR. With an interval of 3 to 8 years between procedures, that number dropped to 88%. At 9 to 14 years between procedures, only 79% of patients experienced restoration of sperm to semen. 45
Even with the successful restoration of sperm count and motility within the semen, natural conception may remain unachievable for a patient and their partner. In a standardized analysis of fertility restoration based on a population of 95 men with healthy postoperative sperm concentration (20 x 10(6)/ml) and motility (50% or greater), only 66.6% of patients achieved pregnancy with their partner. 38 The likelihood of natural conception success post-VR can also be predicted by the time interval between vasectomy and reversal. At an interval of 3 years between vasectomy and VR, 76% of patients achieved pregnancy success. With an interval of 3-8 years between procedures, that number dropped to 53%. At an interval of 9 to 14 years, only 44% of VR patients achieved pregnancy. 45
A viable option for patients who undergo VR, especially those facing an increased time interval between the vasectomy and VR is cryopreservation of sperm at the time of VR. In a study of VR failure followed by IVF of cryopreserved sperm from the VR procedure, 67% of patients succeeded in pregnancy via IVF. 46 In the event of initial VR failure to restore sperm to semen, repeated microsurgical VR procedures are the primary option for patients seeking natural conception success with their partner. Repeated microsurgical VR yields restoration of sperm to semen in 75% of patients and pregnancy success in about 43% of patients. 45 The likelihood of success with repeated VR procedures is positively correlated to the presence of spermatozoa in the vas deferens fluid. 47 Failure to achieve pregnancy with evidence of healthy sperm count and motility may be suggestive of partner infertility. 38
Fertility and pregnancy success highly depends upon the female partner’s age. In a study of men who underwent VR with an obstruction interval of 15 years or more, those with a female partner aged <30 years compared to those with female partners aged 36-40 years resulted in pregnancy success rates of 64% and 32% respectively. With vasectomy reversal sometimes indicated to take six months or more for sperm to return to the patient’s ejaculate, VR is argued as inappropriate for conception-seeking couples facing advanced maternal age at the time of VR. 48
Vasectomy is a rapid, cost-effective, and safe procedure utilized to obtain permanent sterility in males. While this outcome can be achieved through many methods, currently the MIV is the most highly recommended. There are proven benefits associated with vasectomies such as decreased cost as compared to other contraceptives, shorter operation and recovery times versus tubal ligation, quick return to sexual activity, and a high success rate. Factors associated with individuals opting to utilize this form of contraception include, but are not limited to, socioeconomic status, race, increased age and number of offspring, and birth location. Recent trends have demonstrated a marked decrease in the number of vasectomies being performed which can be attributed to a multitude of factors.
Individuals seeking vasectomy reversal may do so due to various factors including changes in relationship status, parental status at the time of procedure, age, and other minor factors. However, males who are above the age of 30 at the time of the procedure and who are childless tend to seek vasectomy reversals less frequently than other males. Reversal of a vasectomy may be accomplished through re-anastomosis of the vas deferens that was previously ligated via microsurgical techniques. Another option for patients with post-vasectomy regret is sperm extraction for IVF. Success of the VR procedure is dependent upon the extent of the damage done at the time of the vasectomy and the duration of vas occlusion. Overall fertility and pregnancy success is also reliant upon factors such as the fertility and age of the patient’s partner. Providers must properly counsel their patients, ensuring that they are aware of the benefits, risks, potential complications and long-term effects of vasectomies, thereby allowing them to make a well-informed decision.
- Subscribe Now (Opens in new window)
- Air Force Times (Opens in new window)
- Marine Corps Times (Opens in new window)
- Navy Times (Opens in new window)
- Pentagon & Congress
- Defense News (Opens in new window)
- Flashpoints
- Benefits Guide (Opens in new window)
- Military Pay Center
- Military Retirement
- Military Benefits
- Discount Depot
- Gear Scout (Opens in new window)
- Military Culture
- Military Fitness
- Military Movies & Video Games
- Military Sports
- Transition Guide (Opens in new window)
- Pay It Forward (Opens in new window)
- Black Military History (Opens in new window)
- Congressional Veterans Caucus (Opens in new window)
- Military Appreciation Month (Opens in new window)
- Military History
- Vietnam Vets & Rolling Thunder (Opens in new window)
- Honor the Fallen (Opens in new window)
- Hall of Valor (Opens in new window)
- Service Members of the Year (Opens in new window)
- Create an Obituary (Opens in new window)
- Medals & Misfires
- Installation Guide (Opens in new window)
- Task Force Violent
- Battle Bracket
- CFC Givers Guide
- Photo Galleries
- Early Bird Brief
- Newsletters (Opens in new window)
- Long-Term Care Partners
- Navy Federal
- Digital Edition (Opens in new window)
Younger troops get more vasectomies after Dobbs decision, study finds
Younger, unmarried troops were more likely to get vasectomies following the 2022 Supreme Court decision that struck down nationwide abortion rights , according to a new study in the International Journal of Impotence Research published on May 18 .
Researchers at the Uniformed Services University of the Health Sciences looked at vasectomies of male active-duty, retirees and dependents across all military branches within the military’s health system. Service members aged 18 to 64 had 96,617 vasectomies covered by the system from 2018 to 2022, including a large increase in the months following to the Supreme Court’s Dobbs v. Jackson Women’s Health Organization decision, which put reproductive healthcare laws in the hands of state lawmakers.
The average number of vasectomies in the months after the Dobbs decision increased 22.1% compared to the averages of the months pre-Dobbs from 2018 to 2021.
“We assess that the reversal of Roe v. Wade was a significant driver of a sizable increase in vasectomy incidence within the [military health system], specifically amongst younger and unmarried men,” according to the study. “State level restrictions on abortion access may have mediated this effect; with more stringent restrictions resulting in higher rates of vasectomy utilization.”
The number of vasectomies before the Dobbs decision remained relatively consistent, minus the first year of the COVID-19 pandemic when the number of vasectomies decreased, according to researchers. In the months following the Dobbs decision beginning in June 2022, though, men receiving vasectomies trended younger, unmarried and of a more junior rank than before the Dobbs decision.
Republicans back abortion ban in $360B VA budget draft for next year
Va would see a 10% boost in funding under a plan advanced by republican appropriators on tuesday, but democrats oppose other parts of the bill..
Men under the age of 30, who weren’t married, were more likely post-Dobbs to have a vasectomy, going against trends before the Supreme Court case, which saw older men at the age of “family completion” having the procedure, researchers wrote.
However, the jump in the procedure’s usage also depended on individual state’s positions on reproductive rights, researchers found.
Researchers compared the increases in two specific states: Texas and Virginia. The states represented a good comparison, researchers said, given their large active-duty service member populations and differences in laws regarding reproductive rights. Texas, which enacted a nearly complete abortion ban after the Dobb’s decision, saw a 29.3% increase in vasectomies among active-duty troops. Virginia, with no similar law, saw a smaller increase in the procedure’s use of 10.6%.
The study pointed to the findings as a sign of a changing reproductive healthcare landscape for service members, given federal law does not allow government dollars to be spent on abortion services, researchers noted.
“These findings demonstrate the robustness of changes in the landscape of vasectomy utilization in a universally insured, geographically representative population,” researchers wrote. “The [military health system] must be cognizant of the profound effect that the Dobbs decision has had on the state of reproductive health care access in America.”
“It must be agile in appropriately allocating reproductive care assets and resources to those areas greatest effected by the reversal of Roe v. Wade to best support the needs of service members and their families,” they added.
Zamone “Z” Perez is a reporter at Military Times. He previously worked at Foreign Policy and Ufahamu Africa. He is a graduate of Northwestern University, where he researched international ethics and atrocity prevention in his thesis. He can be found on Twitter @zamoneperez.
In Other News

US military funeral traditions honor the fallen on land, air and sea
From missing man formation flyovers to taps, here’s how the services pay respect to america's fallen heroes..
Former President Obama surprises volunteers at Memorial Day event
Obama joined local veterans groups and scouts in a volunteer event at a virginia cemetery ahead of memorial day..
World War II ace Richard Bong’s plane found, explorers believe
Searchers announced thursday they’ve discovered what they believe is the wreckage of world war ii ace richard bong’s plane..
Proposal would boost retirement help for military working dogs
Lawmakers want to start a new grant program to cover medical costs for retired military working dogs..
Senator wants answers on DOD’s medical treatment for terror victims
Sen. elizabeth warren, d-mass., wants to know how often military medical facilities have treated victims of terror..

New study finds 12-fold higher risk of suicide attempt for adult transgender patients
A new study found a significantly higher risk of suicide attempts, self-harm, and PTSD for individuals who have undergone gender transition surgeries.
The study , published in April, found that individuals who had undergone gender transition surgery had a 12-fold higher suicide attempt risk than those who had not, a statistic that sparked significant attention online Friday.
The study was conducted using data from 90 million U.S. adult patients between the ages of 18 and 60. It did not include minors .
Researchers examined emergency room treatment data in this age bracket for patients who had undergone previous gender transition surgery, compared to those who had no reproductive surgeries and also patients who had sterilizing surgeries, including vasectomy and tubal ligation.
The de-identified patient data does not clarify at what age the patient surgically transitioned.
The results showed that 3.5% of those who had surgically transitioned were treated for suicide attempts, compared to 0.3% of non-transitioned patients. Medically transitioned patients were also treated for suicide or self-harm at 4.5% and PTSD at 9.2%, compared to 0.5% and 1.2%, respectively, for non-transitioned patients.
The rates of suicide attempt, self-harm, and PTSD are also slightly higher for those who underwent vasectomy or tubal ligation, but they do not reach the levels of transgender patients in any category.
The study was recently uploaded to PubMed, the National Institute of Health database of peer-reviewed studies to inform doctors of the latest research in their fields to better treat patients.
Limitations to the study include a lack of representation as to why transgender patients had higher rates of suicidality, self-harm, and PTSD. It also does not examine whether adverse mental health conditions were present prior to surgery.
Dr. Dietrich Jehle , an author of the study and the Program Director for the Emergency Medicine Department of the University of Texas Medical Branch at Galveston, did not respond to the Washington Examiner’s request for comment.
Although there has been a long-standing debate over whether or not to treat underage patients with gender dysphoria with mental health techniques or physical and anatomical intervention, the discussion has heightened in recent weeks following the publication of a 388-page report from the U.K.’s National Health Services last month.
The report, written by pediatrician and President of the Royal College of Pediatrics Hilary Cass, consisted of a comprehensive review of global evidence and data on gender transition for minors, finding that medically transitioning minors have serious harmful effects.
Cass found that arguments in favor of sex transition for minors in the U.K. were “built on shaky foundations” and supported by “remarkably weak evidence.”
CLICK HERE TO READ MORE FROM THE WASHINGTON EXAMINER
In August, the American Academy of Pediatrics reaffirmed its support of gender transition for minors, promising to undergo a systematic review of scholarship on the topic.
Over 20 states in the U.S. have either outlawed gender transition surgeries for minors or issued restrictions on hormonal gender transition therapies.

- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
How to Thrive as You Age
Like to bike your knees will thank you and you may live longer, too.

Allison Aubrey

A large new study shows people who bike have less knee pain and arthritis than those who do not. PamelaJoeMcFarlane/Getty Images hide caption
A large new study shows people who bike have less knee pain and arthritis than those who do not.
We are in the middle of National Bike Month , and cycling enthusiasts love to talk up the benefits of their favorite activity.
"It's definitely my longevity drug," says Brooks Boliek, 65, an avid cyclist of many decades, who used to commute to his office on a bicycle.
A substantial body of evidence supports the health benefits of cycling, everything from strengthening the immune system to boosting the likelihood of living longer. Now, a new study finds people who are in the habit of riding a bike are significantly less likely to have osteoarthritis and experience pain in their knees by age 65, compared to people who don't bike.
The study, which was funded in part by the National Institutes of Health, and published in the American College of Sports Medicine's flagship peer-reviewed journal, included about 2,600 men and women, with an average age of 64 years old. They were surveyed about their physical activity over their lifetime. As part of the study, researchers took X-ray images to evaluate signs of arthritis in their knee joints. "Bicyclers were 21% less likely to have X-ray evidence and symptoms of osteoarthritis compared to those who did not have a history of bicycling," explains study author Dr. Grace Lo of Baylor College of Medicine.
"I was surprised to see how very strong the benefit was," Lo says given the profile of the participants. The people enrolled in the study were not competitive athletes, but rather "average" people, ranging from their mid-40's up to 80 years old. All of them had elevated risks of developing knee arthritis due to weight, family history or former injuries.
The study can not prove cause and effect, given it was an observational study that assessed osteoarthritis at one point in time. But the findings, which are published in the journal Medicine & Science in Sports & Exercise , validate the advice many health care providers give to patients about the benefits of cycling and other non weight-bearing exercises.
"Cycling is very low impact," says musculoskeletal researcher Matt Harkey , an assistant professor at Michigan State University and a co-author of the study. Cycling also helps to build strength in the muscles around the knee which can help protect the joint. In addition, the rhythmic motion of pedaling on a bicycle can move synovial fluid , the viscous, egg white -like liquid in joints that helps reduce friction and absorb shock. "What it does is help to circulate the synovial fluid throughout the joint to help to kind of lubricate [the joint] and provide nutrient delivery to the cartilage," Harkey says.

Cycling enthusiast Brooks Boliek calls biking his "longevity drug," and the research backs him up on that. Allison Aubrey/NPR hide caption
Cycling enthusiast Brooks Boliek calls biking his "longevity drug," and the research backs him up on that.
Of course, there are many types of exercise that are good for health, though cycling seems to have a leg up when it comes to protecting joints. Oftentimes, people give up contact sports such as basketball, as they age, given the risk of injury.
"It can be expected that physical activity in which there is little weight-bearing on joints will be more beneficial than those that need constant stamping," such as running, says Norman Lazarus, a professor emeritus at King's College London, who is in his late 80's and is still cycling. (NPR profiled his cycling research in 2018.)
Lazarus says the results of the new study – pointing to a benefit – are not surprising, though he points out that biking does bring risk of injury . He says it's important for cyclists to understand the risk of overuse injuries as well as the importance of technique and getting a proper fitting bike. Each year, thousands of bicyclists are injured in motor vehicle crashes, and older adults are at higher risk of serious injury. Research shows it's safer to bike on trails or paths separated from traffic.
Risks, aside, research shows biking is good for longevity. "There's good data to support that people live longer when they bicycle," says Lo. She points to a study that found people who cycled one hour per week were about 22% less likely to die prematurely. This was a study of people with diabetes, so it's possible that the benefits are greater for people without the disease.
"This is an exercise [people] can participate in over a lifetime," Lo says, and it can also be done indoors on a stationary bike. "I think that it is a great preventative strategy for many things, including arthritis," she says.
Biking enthusiast Brooks Boliek says cycling brings him joy and a sense of accomplishment. "I'm very goal oriented," he says, and a daily ride gives him something to focus on. "It gives me something to live for."
A sense of purpose that keeps his heart pumping and his muscles strong. He says he'd love to keep riding until the day he dies.
Find Allison Aubrey on Instagram at @allison.aubrey and on X @AubreyNPR .
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
An Early Look at Black Voters’ Views on Biden, Trump and Election 2024
Black voters are more confident in biden than trump when it comes to having the qualities needed to serve another term, table of contents.
- Black voters consistently align with the Democratic Party
- Black voters prefer Biden in 2024 election, but some would replace both candidates
- Black voters’ views on Biden and Trump as presidents
- Black Americans’ policy priorities
- Acknowledgments
- Methodology

Pew Research Center has a long history of conducting surveys that examine the views of American voters. This analysis of Black voters’ views on political party affiliation, policy priorities and 2024 presidential candidates relies on data from four of these studies.
The first of these studies was conducted among 5,140 adults from Jan. 16 to 21, 2024, on Pew Research Center’s American Trends Panel (ATP). There were 759 Black adults in the sample, which included an oversample of non-Hispanic Black men. This survey provided the data on Black voters’ views on domestic policy priorities discussed in this report. For more information on this study, see its methodology and questionnaire .
The second was conducted among 3,600 adults from April 1 to 7, 2024, on the Center’s ATP. There were 611 Black adults in the sample, which included an oversample of non-Hispanic Black men. This survey provided the data on Black voters’ views on foreign policy priorities discussed in this report. For more information on this study, see its methodology and questionnaire .
The third used annual totals of data from Pew Research Center telephone surveys (1994-2018) and online surveys (2019-2023) among registered voters. All telephone survey data was adjusted to account for differences in how people respond to surveys on the telephone compared with online surveys. All online survey data was drawn from the Center’s ATP. This combination of surveys provided the data for Black voters’ political party affiliation trends. For more information on this study, see its methodology and the full report . Read more on how we adjusted for mode effects when combining telephone and online surveys .
The fourth was conducted among 8,709 adults from April 8 to 14, 2024, on the Center’s ATP. There was an oversample of non-Hispanic Black adults, for a total of 1,372 Black adults in the sample. This survey provided the data on Black voters’ views on Joe Biden, Donald Trump and the 2024 presidential election discussed in this report. For more information on this study, see its methodology and questionnaire .
The terms Black Americans and Black adults are used interchangeably throughout this report to refer to U.S. adults who self-identify as single-race Black and say they have no Hispanic background.
Black Americans include those who are registered to vote, not registered or are unsure. Discussions and charts limited to registered voters will be labeled as such and they will be referred to as Black voters .
Democrats and Democratic leaners are respondents who identify politically with the Democratic Party or who identify politically as independent or with some other party but lean toward the Democratic Party.
Republicans and Republican leaners are respondents who identify politically with the Republican Party or who identify politically as independent or with some other party but lean toward the Republican Party.
(In later uses, the terms Democrat and Republican are inclusive of those who lean to each party.)
Black voters will play a key role in determining the outcome of the 2024 presidential election. And while Black voters remain overwhelmingly Democratic and support Joe Biden over Donald Trump by a wide margin, Biden’s advantage among this group is not as wide as it was four years ago.
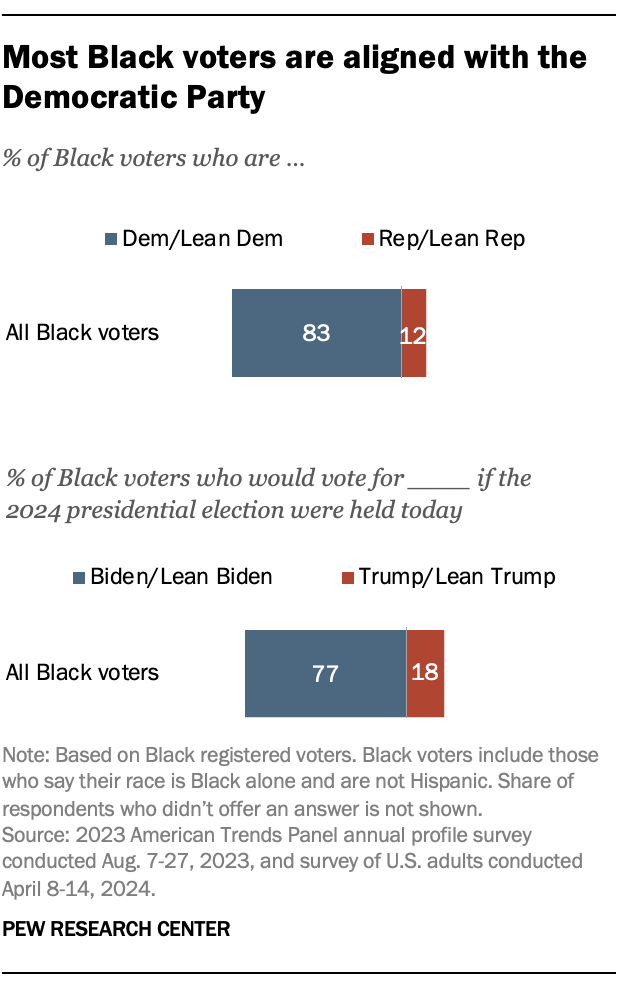
Today, American voters are about evenly split between the two major political coalitions, both in their partisan identification and in their presidential vote preference .
But Black voters remain largely aligned with the Democratic Party (83% identify with or lean to the Democrats), and 77% of Black registered voters say they would prefer to vote for Biden over Trump in the 2024 presidential election .
At the same time, Black voters are very critical of Trump . Most say he was a poor or terrible president (72%). And many Black adults think he broke the law in his alleged efforts to change the outcome of the 2020 election (65%).
Despite their support for Biden and criticism of Trump, about half of Black voters (49%) say they would replace both Biden and Trump with different candidates if they had the ability to decide. This is similar to the share of all voters who say this.
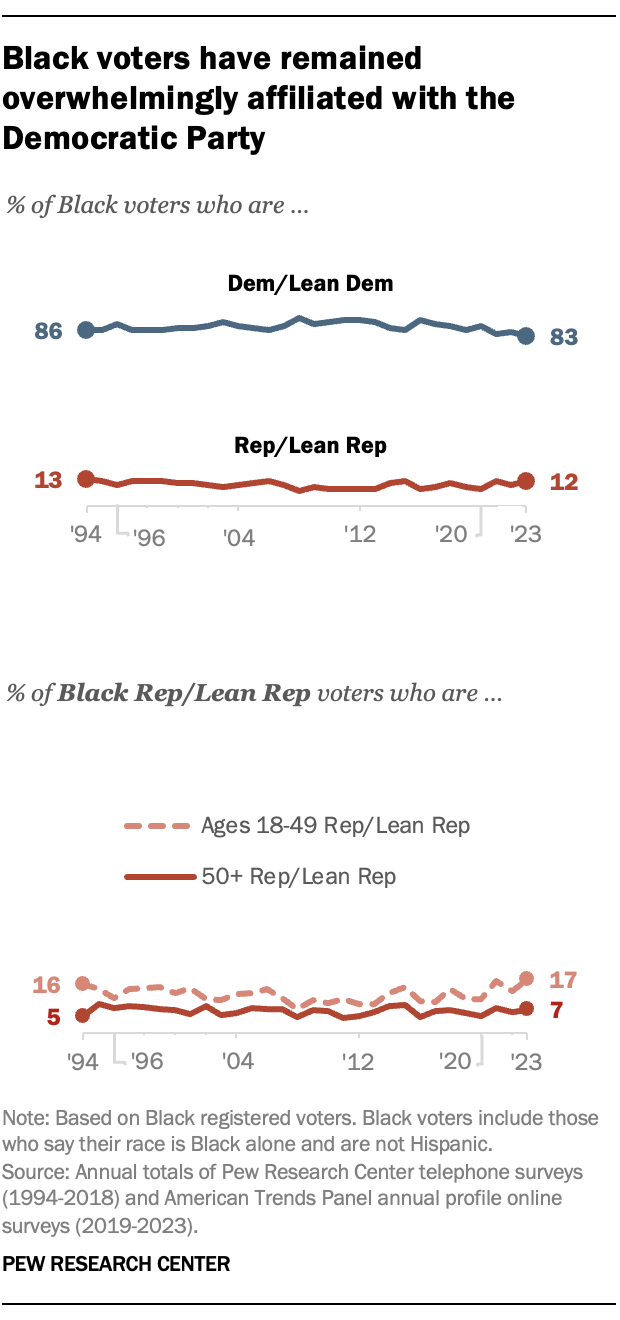
Currently, 83% of Black registered voters identify as or lean Democratic, while 12% are Republican or lean Republican. This share is slightly smaller than the 88% who associated with the Democratic Party in 2020. Still, the vast majority of Black voters have consistently identified with or leaned toward the Democratic Party over the last 30 years .
Similar shares of Black men (81%) and Black women (84%) are affiliated with or lean toward the Democratic Party. Roughly eight-in-ten or more Black men and women have consistently identified with or leaned toward the Democratic Party since 1994.
Although the majority of Black voters across education levels are Democrats, there has been a slight decrease in affiliation with the Democratic Party among those with college degrees in recent years. While 93% of Black voters with college degrees identified with or leaned toward the Democratic Party in 2012, that number had decreased to 85% in 2020 and then 79% in 2023.
Overall, older voters have tended to be more Republican than younger voters in recent decades, but this is not true for Black voters. While 7% of Black voters 50 and older currently identify as or lean Republican, 17% of Black voters under 50 are aligned with the Republican Party. This is not new, as younger Black voters have tended to be more Republican than older Black voters over the last 25 years.
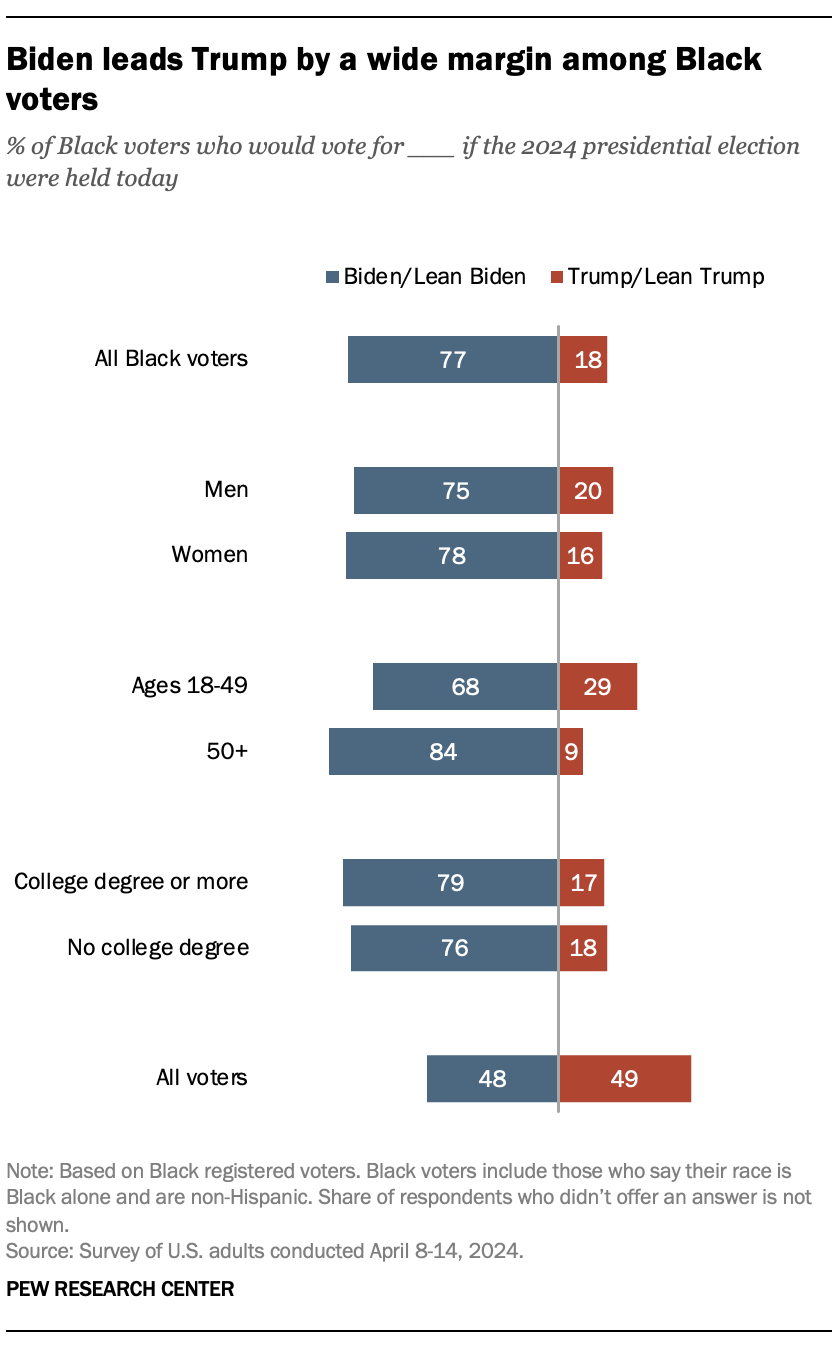
When it comes to the significance of the 2024 presidential election’s outcome, 55% of Black voters say it really matters who wins. Fewer say it does not matter (17%) or are somewhere in between (28%) in their views of the upcoming election’s importance.
Black voters’ preferences
As of April 2024, the majority of Black voters say they would vote for or lean toward Joe Biden (77%). Fewer say they would vote for or lean toward Donald Trump (18%).
Among all registered voters, 49% favor Trump while 48% support Biden.
The wide margin between Black voters’ preference for Democratic candidates over Republican candidates is nothing new. In 2016, there was an 85 percentage point difference in the share of Black voters who voted for Hilary Clinton (91%) over Trump (6%). And in 2020, Biden (92%) had a wide advantage over Trump (8%) among Black voters.
The current margin of support for Biden (59 points – 77% to 18%) is lower than it was in 2020 or for Hillary Clinton in 2016, according to Pew Research Center validated voter studies .
Younger Black voters are more likely than older Black voters to say they would vote for Trump. While about two-thirds of Black voters under 50 favor Biden (68%), 29% support Trump. Black voters 50 and older favor Biden by a wider margin (84% vs. 9%).
However, this pattern is reversed among all registered voters: Older voters are slightly more likely than younger voters to prefer Trump (51% vs. 46%), while younger voters prefer Biden (52% vs. 46%).
Many Black voters are dissatisfied with the Biden-Trump matchup
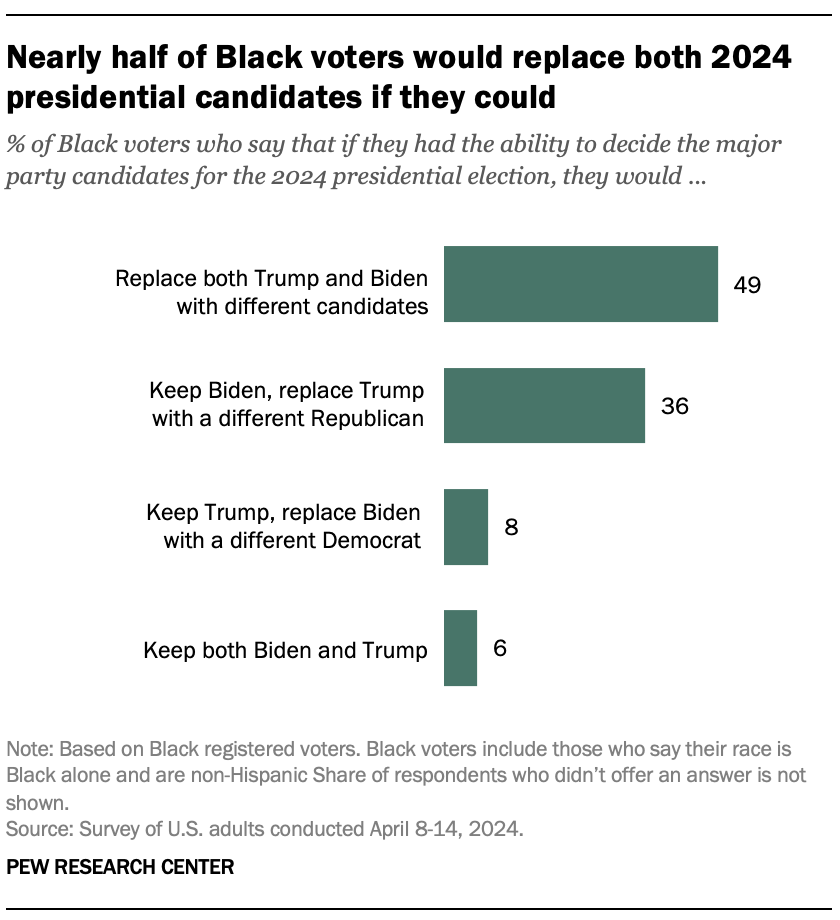
About half of Black voters (49%) say they would replace both Trump and Biden with different candidates if they had the ability to do so. An identical share of all registered voters say this.
Fewer Black voters say they would keep Biden and replace Trump with a different Republican (36%). Even fewer say they would keep Trump and replace Biden with a different Democrat (8%). And only 6% say they would keep both candidates.
Like the rest of U.S. voters, Black voters differ on this question by age and education . Younger Black voters (57%) are more likely than older voters (37%) to say both candidates should be replaced. And a larger share of older than younger Black voters say they would keep Biden and replace Trump (42% vs. 22%).
Nearly 60% of Black voters with a college degree say they would replace both candidates if they had the ability, while 45% of those without a degree say the same.
A majority of Black Americans (55%) approve of the way Joe Biden is handling his job as president .
This is a shift from a January 2024 Pew Research Center survey , when Black adults were evenly split in their ratings of Biden’s job performance (49% disapproved, 48% approved).
Biden’s ratings among Black Americans were far more positive earlier in his term. For instance, in a March 2021 Center survey , 87% approved of his job performance.
Despite shifts among Black Americans in their ratings of Biden, they are still more likely than other racial and ethnic groups and the U.S. public overall (35%) to approve of Biden’s job performance.
Black voters are more confident in Biden than Trump
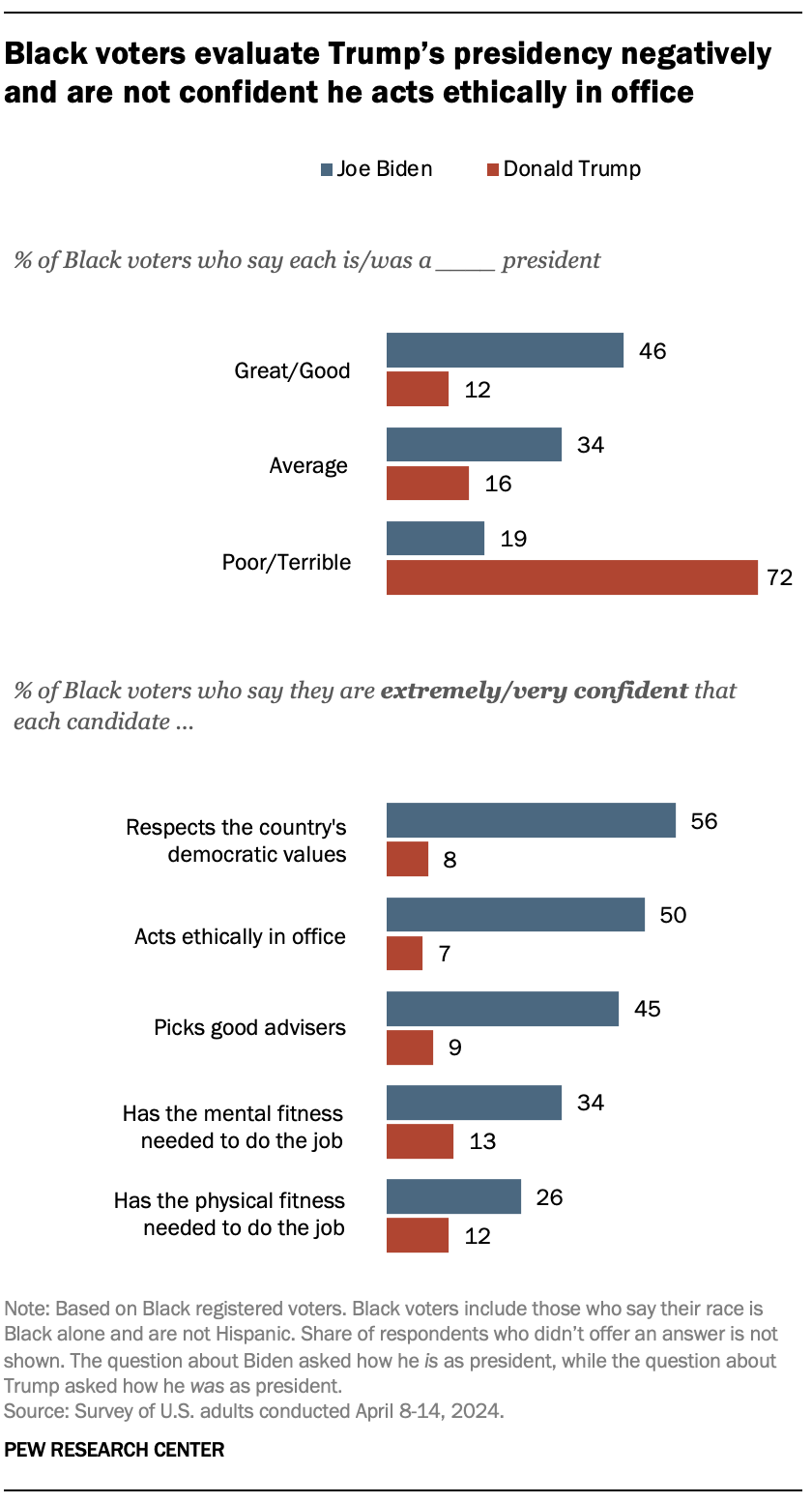
In further assessments of his presidency, 46% of Black voters say Biden is a great or good president. Far fewer say Trump was great or good during his time in office (12%). And a large majority of Black voters say Trump was a poor or terrible president (72%). Only 19% say the same about Biden.
Black voters are also much more confident that Biden has the qualities to effectively serve another term as president. A majority of Black voters (56%) are extremely or very confident that Biden respects the country’s democratic values, and half are confident that he acts ethically as president. No more than 8% of Black voters say Trump has either of these qualities .
Although most Black voters don’t express much confidence about the mental and physical fitness of either Trump or Biden, they are more confident in Biden. About a third of Black voters (34%) say Biden has the mental fitness needed to serve another term as president, and 26% say the same about his physical fitness. Only about one-in-ten say this about Trump.
Black voters are more likely than other racial and ethnic groups and the general public overall to say Biden has the mental and physical fitness to serve another term.
Trump’s election-related criminal charges
Beyond their critical views about Trump as president, the majority of Black Americans (65%) also believe he broke the law in an effort to change the outcome of the 2020 election. They are more likely than other racial and ethnic groups – and the U.S. public overall (45%) – to hold this view.
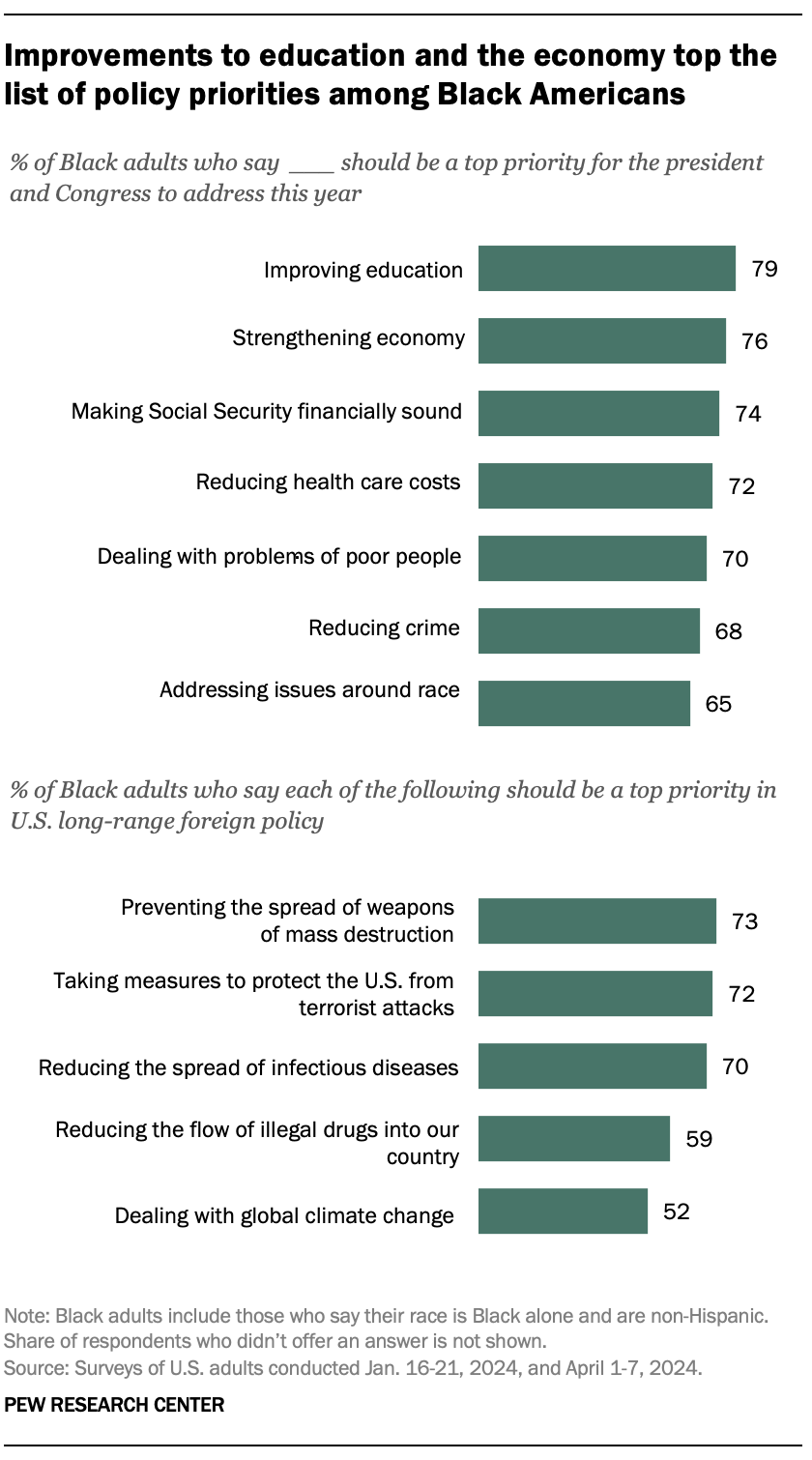
For Americans overall, the economy (73%) sits at the top of the list of policy priorities for the president and Congress in 2024.
However, for Black Americans, improving the education system (79%) and ensuring Social Security is financially sound (74%) are just as important as strengthening the economy (76%).
Clear majorities of Black Americans also say reducing health care costs (72%), dealing with the problems of poor people (70%), reducing crime (68%) and addressing issues around race (65%) should be top priorities.
Foreign policy priorities
When it comes to international issues , most Black Americans (82%) say it is more important for President Biden to focus on domestic policy than on foreign policy (13%). Most adults in the U.S. share this view, with 83% saying domestic policy is more important.
However, when it comes to long-range foreign policy goals , Black adults are more likely than the general public to say that preventing the spread of weapons of mass destruction (73% vs. 63%), reducing the spread of infectious diseases (70% vs. 52%) and dealing with global climate change (52% vs. 44%) should be top priorities.
CORRECTION (May 20, 2024): Due to an editorial error, a previous version of the report overstated the share of Black adults who say Trump broke the law in seeking to change the outcome of the 2020 election. It was 65%.
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Black Americans
- Donald Trump
- Election 2024
- Race, Ethnicity & Politics
- U.S. Elections & Voters
- Voter Demographics
- Voters & Voting
Americans have mixed views about how the news media cover Biden’s, Trump’s ages
More than 80% of americans believe elected officials don’t care what people like them think, voters’ views of trump and biden differ sharply by religion, in tight presidential race, voters are broadly critical of both biden and trump, changing partisan coalitions in a politically divided nation, most popular, report materials.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
Research puts dollar figure on climate savings from electric school buses
A substantial portion of the half-million school buses in the United States are “highly polluting old diesel vehicles,” the researchers write.
Switching to electric school buses could yield significant health and climate benefits, researchers suggest in a new analysis that seeks to quantify those gains in dollar terms.
Published in the journal PNAS, the study estimated the per-mile benefits of replacing diesel buses with electric ones in 3,108 U.S. counties. Researchers combined data about average diesel bus pollution with statistical estimates of the cost of maintenance and repair, the environmental impact of diesel emissions, and the dollar value of new childhood asthma cases and deaths that could be attributed to such pollution.
A substantial portion of the half-million school buses in the United States are “highly polluting old diesel vehicles,” the researchers write. Though emissions have fallen over time thanks to increased regulation, they add, older, more polluting diesel models are still common. As of June 2023, they write, just 2,277 electric school buses had been ordered or delivered, or were operating nationwide.
Replacing the average diesel bus would generate a benefit of $84,200 per bus, split nearly evenly between health and climate effects. Such a replacement would cut 181 metric tons of carbon dioxide emissions per bus and reduce childhood deaths and asthma cases from diesel emissions, the researchers conclude.
The benefits would vary depending on the location, with buses generating as much as $247,600 in benefits in dense metropolitan areas. Impacts would be smaller in rural areas because diesel emissions affect smaller populations there.
The benefits would come at a cost, the researchers acknowledge; they estimate an unsubsidized electric school bus costs an average of $156,000 more than a new diesel school bus over the vehicle’s lifetime. But in large metropolitan areas, they write, “replacing a relatively small number of miles driven by [diesel buses] could lead to substantial public health benefits.”
“In a dense urban setting where old diesel buses still comprise most school bus fleets, the savings incurred from electrifying these buses outweigh the costs of replacement,” Kari Nadeau, a professor of climate and population studies and environmental health at the Harvard T.H. Chan School of Public Health and the study’s senior author, said in a news release . “Not to mention how the tangible benefits of electric school buses can improve lives — especially for racial minorities and those living in low-income communities who are disproportionately impacted by the everyday health risks of air pollution.”
Black, Hispanic and low-income Americans would probably experience the greatest health benefits of large metropolitan areas electrifying their school bus fleet, the researchers write. They call for more research on the exposure of the children riding the buses to particulate pollution, because data on in-cabin pollution generated by newer buses is still unclear.

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Health Sci Pract
- v.4(4); 2016 Dec 23
A Review of 10 Years of Vasectomy Programming and Research in Low-Resource Settings
Dominick shattuck.
a Georgetown University's Institute for Reproductive Health, Washington, DC, USA.
Brian Perry
b Duke Clinical Research Institute, Durham, NC, USA.
Catherine Packer
c FHI 360, Durham, NC, USA.
Dawn Chin Quee
Associated data.
Reviewed areas included misconceptions and lack of knowledge among men, women, and providers; approaches to demand generation including community-based and mass media communications; service delivery innovations consisting of the no-scalpel vasectomy technique, whole-site training, cascade training, task shifting, and mobile outreach; and engagement of religious and community leaders to create an enabling environment.
Vasectomy is a highly effective and safe contraceptive method for couples who want to stop childbearing, but only 2.4% of men around the world use this method. We conducted an extensive review of the vasectomy research literature and programmatic reports, published between April 2005 and April 2015, to synthesize barriers and facilitators to vasectomy adoption. Of the more than 230 documents initially retrieved in our search, we ultimately included 75 documents in our review and synthesized the findings according to the Supply–Enabling Environment–Demand (SEED) Programming Model. Regarding promoting demand for vasectomy services, we found there was a general lack of awareness about the method among both men and women, which often fueled erroneous assumptions about how vasectomy affects men. Several types of programmatic activities directly addressed knowledge gaps and negative misperceptions, including community-based and mass media communications, employer-based promotion, and group counseling. For supply of services, the lack of or inaccurate knowledge about vasectomy was also prevalent among providers, particularly among community-based health workers. Programmatic activities to improve service delivery included the use of evidence-based vasectomy techniques such as no-scalpel vasectomy, whole-site trainings, task shifting, cascade training, and mobile outreach. Finally, programmatic approaches to building a more enabling environment included engagement of governments and other community and religious leaders as well as campaigns with gender transformative messaging that countered common myths and encouraged men's positive engagement in family planning and reproductive health. In summary, a successful vasectomy program is comprised of the mutually reinforcing components of continual demand for services and access to and supply of well-trained providers. In addition, there is an underlying need for enabling policies within the cultural and gender environments that extend beyond vasectomy and include men not just as default partners of female family planning clients but as equal beneficiaries of family planning and reproductive health programs in their own right. Accelerating progress toward meaningful integration of vasectomy into a comprehensive contraceptive method mix is only possible when political and financial will are aligned and support the logistical and promotional activities of a male reproductive health agenda.
Over the last several decades, national family planning initiatives have led to significant gains in many developing countries as exemplified through improvements in key Family Planning 2020 (FP2020) indicators. 1 The initiatives continue to expand the quality of and access to family planning services, predominantly for women. More recently, research and programs that engage men in family planning and that combat inequitable gender norms have also increased in effectiveness and scope. A search of the abstracts accepted to the 2015 International Conference on Family Planning with the term “male involvement” resulted in 49 presentations across a variety of aspects that included improving couple communication, improving service delivery for men, and looking for new ways to increase male involvement in family planning. 2 With this growing support and refinement of gender and male involvement programming, now is an opportune time to incorporate voluntary vasectomy services into national family planning strategies.
Research suggests that demand for permanent methods may increase over time as the age when women desire to limit family size (that is, to stop childbearing) continues to decrease. 3 Analysis of Demographic and Health Survey data from 18 countries between 2004 and 2010 found that the demand to limit births began to exceed the demand for spacing births, on average, at 33 years old. In some countries, however, the desire to limit births predominated at an age as low as 23 years. 3
When a couple desires to limit their family size, the most effective methods with the least side effects should be available. Vasectomy is one of these methods but is used little around the world. On the other hand, female sterilization (tubal ligation) is the most commonly used form of contraception worldwide: 19% of women in union are sterilized versus 2.4% of men globally. 4 This is despite the fact that vasectomy has no side effects and, compared with female sterilization, is less risky of a procedure, provides a quicker recovery period, and costs the health system less per client. The correlation between the use of female sterilization and vasectomy is complex, as less developed countries contribute to the highest use of female sterilization but have the lowest prevalence of vasectomy.
Vasectomy is one of the most effective contraceptive methods with no side effects but is little used around the world.
Many other couples depend on short-acting methods (e.g., condoms, pills, injectables) to limit their births, which, when compared with long-acting or permanent methods (LAPMs), have greater costs for both governments and clients (time and money), are less effective due to potential product failure, and have higher rates of discontinuation and/or incorrect use. 5
Vasectomy, however, could be a viable option for many couples. Providers across the globe have been trained to perform no-scalpel vasectomies (NSV). This method requires only a small puncture in a man's scrotum to access the vas deferens, with the client under local anesthesia. NSV has been found to be the preferred technique by physicians for isolating and accessing the vas deferens. 6 – 9 Cauterization of the lumen of the vas deferens combined with fascial interposition results in the lowest risk of occlusive failure (well below 1%, according to post-vasectomy semen analysis). 7 , 8 This technique is already widely used in North America. 10 Recently, it was integrated within all district hospitals across Rwanda, 11 suggesting that providers in low-resource settings can be trained in this method and that training in supplemental NSV with advanced occlusion (e.g., fascial interposition and thermal cautery) can maximize the effectiveness of ongoing vasectomy programs in low-resource settings. 12
In this article, we review recent literature related to voluntary vasectomy programs in low-resource settings to synthesize common barriers and facilitators to vasectomy uptake and identify recommendations to strengthen future vasectomy promotion efforts.
In April 2015, we conducted a search of both the peer-reviewed and gray literature using 8 search engines: POPLINE, PubMed, Global Health, Cumulative Index to Nursing and Allied Health Literature (CINAHL), Africa-Wide Information, Academic Search Premier, Google Scholar, and the United States Agency for International Development's (USAID's) Development Experience Clearinghouse. Keywords used in the search were as follows: vasectomy OR “male sterilization” AND accept* OR “communication strategy” OR “contraceptive methods chosen” OR counsel* OR “delivery of health care” OR demand OR evaluat* OR “health services” OR implement* OR intervention* OR introduce* OR messaging OR program* OR promot* OR “scale up” OR “scaling up” OR “social marketing” OR success OR uptake. To limit our search to the most current and relevant literature, our inclusion criteria included documents published in English within the last 10 years (April 2005 to April 2015). We excluded documents describing vasectomy programs from Australia, Canada, the United Kingdom, or the United States. It is possible that some important resources published prior to April 2005 may not be reflected in this current review.
Our search retrieved more than 230 documents, of which approximately two-thirds were excluded because they were duplicates or did not meet our criteria. Two analysts categorized the remaining 75 documents according to their subject matter. We created matrices in Microsoft Excel to summarize and synthesize the content of the documents in each category, to highlight important barriers to and facilitators of vasectomy uptake, and to highlight key recommendations for future vasectomy programs. Finally, we applied the Supply–Enabling Environment–Demand (SEED) Programming Model to present the key findings from the 75 documents we reviewed. (See the supplementary material for a table of all 75 documents organized by region of the vasectomy program or research.) The SEED model has been established as a useful global framework for sexual and reproductive health programming. 13 It is based on the principle that programs will be more successful and sustainable if they address the multifaceted determinants of health and if they include interventions that simultaneously (1) address the availability and quality of services and other supply -related issues, (2) strengthen the health system and foster an enabling environment for healthy sexual and re-productive health behavior, and (3) improve knowledge of sexual and reproductive health and promote demand for services. The SEED domains are—by design—overlapping and interrelated, as programmatic activities designed to address deficiencies in one domain can often improve conditions in other domains as well.
We reviewed 75 documents from the peer-reviewed and gray literature on vasectomy programs.
Information gathered from this review has been published in a final report for USAID and has been used to inform the development of 8 country-specific advocacy briefs ( https://www.fhi360.org/resource/promoting-evidence-based-vasectomy-programming ).
Demand for Vasectomy Services
To be motivated to use vasectomy services, an individual or couple first needs accurate knowledge of and positive attitudes toward vasectomy. Potential vasectomy clients must also know where services are available, understand details about the procedure (e.g., side effects, recovery time, and time required for back-up contraception), and believe that services are confidential. Below, we outline barriers and facilitators related to demand for vasectomy services.
Barriers to Promoting Demand for Vasectomy
Lack of knowledge. Much of the literature we reviewed indicated there was a general lack of awareness about vasectomy and lack of basic knowledge about the procedure among prospective clients (both men and women), posing a major initial demand-promotion barrier. In 5 studies from Ethiopia, Nigeria, and Turkey, 14 – 18 awareness of vasectomy as a family planning method ranged from 15.6% of Ethiopian women 14 to 39.6% of unmarried Turkish men. 16 However, awareness of vasectomy was high in India (97.4%) 2 and Nepal (77%). 19 Still, basic knowledge of how the procedure is conducted, requirements related to follow-up, or side effects from the procedure was still lacking across sites and studies. 19 – 23 Disparities between men's and women's knowledge of vasectomy were rarely discussed in the literature. Among the few exceptions were two qualitative studies, from Malawi 24 and Nigeria, 25 that found that men were less knowledgeable than women about family planning methods in general and about LAPMs specifically.
Men and women generally lack knowledge about vasectomy, posing a major demand-promotion barrier.
Negative attitudes. Inaccurate knowledge often fueled erroneous assumptions about how vasectomy affects men physiologically and psychologically. 17 , 18 , 20 – 33 In some studies, participants perceived that vasectomy hurt a man's pride 34 or caused a man to lose his “masculinity.” 35 Men worried that others would view them negatively if knowledge of their vasectomy was public. 22 , 36 In Ghana 23 and India, 22 participants felt that if a man got a vasectomy he would be viewed as “under the control of” or a “slave to” his wife. Another Indian study found that women preferred female sterilization over vasectomy because they felt it was better for a woman (than a man) to be “debilitated” since the economic contributions of men were more highly valued than those of women. 32 A number of studies mentioned negative attitudes about the method because people thought vasectomy would lead to male infidelity 23 , 29 , 30 or an inability to perform sexually, 36 and some women feared men would retaliate or reject the possibility of method failure, resulting in negative consequences for women. 22
Inaccurate knowledge often fuels erroneous assumptions about how vasectomy affects men physiologically and psychologically.
Low intention to use. In most of the documents reviewed, prospective clients' willingness to use vasectomy was very low, due in large part to limited knowledge and negative attitudes. A Nigerian study found that only a small percentage of men reported even considering a vasectomy. 37 Similarly, few Nigerian or Indian women viewed vasectomy as acceptable, 17 , 32 or something their husband would choose. 32 This is partially exemplified in an Indian study where 68% of men found vasectomy acceptable, but only 34% suggested they would adopt it. 20
We should note that acceptability and use of contraception is not solely dependent upon client (or provider) knowledge and attitudes toward the method. Behavioral theories abound describing the multitude of factors that contribute to client acceptance (e.g., opportunity and financial costs, social norms, perceived need, etc.), but accurate knowledge and positive attitudes are fundamental to ensuring informed and voluntary use of any method or health care procedure.
Facilitators to Promoting Demand for Vasectomy
Although documentation of knowledge and attitudinal barriers abounded in the literature, references to important facilitating factors were also present, including perceived benefits of the procedure among men and women as well as demographic information about the expected va-sectomy client base. Programmatic activities that directly addressed knowledge gaps and rampant negative misperceptions toward vasectomy included community-based and mass media communications, an employer-based promotion intervention, and a group counseling approach.
Perceived benefits. Positive attitudes toward and perceived benefits of vasectomy—although mentioned in fewer than half of the articles reviewed—are important building blocks for increasing demand for services. Frequently cited benefits were related to the high contraceptive effectiveness of the method, clients' quick recovery time, and the comparative safety and lower costs associated with the vasectomy procedure versus tubal ligation. 18 , 20 – 22 , 24 , 25 , 29 , 30 , 37 Men and women in Cambodia and Malawi reported the benefits of sharing family planning responsibilities. 24 , 36 Tanzanian women suggested that vasectomy would eliminate the possibility of having a child out of wedlock. 29 , 30 In addition, Brazilian, 38 Indian, 22 Rwandan, 39 – 41 and Tanzanian 29 , 30 men described how vasectomy was beneficial to preserving the health of women (e.g., by avoiding frequent pregnancies and negative impacts of other forms of contraception) and that it was considered a minor procedure compared with female sterilization. Hearing positive testimonials was one of the main drivers of positive attitudes toward vasectomy in India—women felt encouraged and men were more open to the procedure. 22
Frequently cited benefits of vasectomy included high contraceptive effectiveness, quick recovery time, and comparative safety and lower costs compared with tubal ligation.
Overall, in articles related to vasectomy client perspectives, couples using vasectomy were satisfied with the fast recovery time and the maintenance of sexual function. 39 , 42 – 44 Motivations leading to vasectomy uptake included the desire to limit births, limited financial resources (not being able to afford more children), concern for women's health (desire to avoid pregnancies, births, and contraceptive side effects), and dissatisfaction with other contraceptive methods. 29 , 30 , 33 , 39 – 42 , 45 , 46 Persuasive sources of vasectomy information for men included health workers, peers, and satisfied clients. 31 , 32 , 39 , 43 , 45 , 47 , 48 Men in Ghana, 49 Rwanda, 41 and Turkey 50 typically reported having heard about vasectomy through the media or from health care workers, which helped them learn how to access services.
Expected vasectomy clientele. Vasectomy—and sterilization in general—is not an appropriate family planning option for everyone. Therefore, it may be valuable for vasectomy programs to understand who their expected client base is. Based on our review, couples using vasectomy were generally older (over 30 years old), were married or in union, had multiple children (often 4 or more) and more children than couples using reversible methods, and had a history of prior contraceptive use. 29 , 30 , 33 , 41 , 43 , 45 , 47 , 49 , 51 However, socioeconomic levels, education levels, and numbers of children of vasectomy clients varied within and between regions. 45 – 47 , 50 – 52 Previous contraceptive use among wives of vasectomy clients varied from a low of 37% in Pakistan 46 to 59.2% in Turkey 50 and 87% in Rwanda. 41 It is important to note that the range of potential vasectomy clients is likely more diverse than current users and that there may be a growing demand for limiting births (and resulting unmet need) among other demographics. Van Lith et al., 4 for example, describe a landscape in which younger couples in sub-Saharan Africa are increasingly interested in limiting births.
Couples using vasectomy are generally older (over 30), are married or in union, have multiple children, and have a history of prior contraceptive use.
Community-based and mass media communications. Community-based and mass media communications can increase awareness and drive demand for vasectomy. The Capacity Project's pilot program in Rwanda developed robust communication materials to increase general knowledge and positive attitudes toward vasectomy. Communications strategies included outreach by community health workers (CHWs), 47 formation of 12 va-sectomy support cooperatives for male clients, video testimonials of clients that were used in education and communication campaigns, 40 , 41 , 47 and dissemination of strategic messaging through various media outlets, including radio, which informed potential clients of upcoming service days. 53
The ACQUIRE Project led a vasectomy communication campaign called “Get a Permanent Smile” in several low-resource settings. 54 The campaign countered pervasive myths and rumors about vasectomy using various media outlets such as posters and television broadcasts staggered to coincide with seasonal periods of high media attention (in Bangladesh) and television and radio ads complemented by an information “hotline” and community outreach (in Ghana). 55 Spikes in demand for vasectomy were tied to the communication activities, 55 which highlights the important link between mass media promotion and uptake of vasectomy services.
The “Get a Permanent Smile” campaign conducted in many low-resource settings resulted in spikes in demand for vasectomy.
Employer-based promotion. The RESPOND Project engaged men and promoted male involvement in reproductive health, including vasectomy, in 10 Indian workplaces. The companies involved in this 18-month employer-based health promotional campaign ranged from waste management to manufacturing to beverage bottling. Through the program, employees were allowed to attend health-related activities during normal working hours. Educational materials focused on LAPMs, and strategies included training industry-related health coordinators on LAPMs and interpersonal communication, positioning health desks in well-trafficked areas of the company, establishing health (including family planning) referral systems, and establishing a hotline for family planning referrals. 56 Employees who participated in the campaign reported a stronger intent to use family planning and were more likely to have discussed family planning with their partners than employees who did not participate. 57 Additionally, many existing family planning users switched from short-acting or traditional methods to LAPMs after participating in the intervention.
Group counseling. In the Philippines, a group counseling intervention promoted open discussion with couples about NSV, which resulted in increased knowledge and acceptability of vasectomy among potential users. 58 The authors suggested that as participants interacted, argued, and agreed or disagreed about certain issues, they encouraged each other to try particular contraceptive methods. They noted that the advantage of having couples together in the session was that after being exposed to the same information about contraceptive methods, members of the couple were then able to discuss their own plans and make a decision together. 59
Supply of Vasectomy Services
Provision of high-quality vasectomy services must include adequate infrastructure, supplies, and equipment as well as well-trained, skilled, motivated, and supported staff. It is also important to have administrative, financial, and management systems in place that are accountable to the communities they serve.
Barriers to Vasectomy Service Delivery
Lack of provider knowledge. Lack of provider knowledge of vasectomy or inaccurate knowledge was a major service delivery barrier identified in the literature. In one publication, Nigerian physicians were reported to have good general knowledge of vasectomy as a permanent method, but some thought that it would impair a man's ability to ejaculate or would increase his risk for prostate cancer. 60 Another study in Nigeria found that 90% of male health workers interviewed were aware of vasectomy, but they had varying degrees of knowledge as to whether local, general, or no anesthesia was used during the procedure. 26 A qualitative study from Cambodia found that, in general, village-level providers had little or incorrect knowledge about LAPMs, including vasectomy. 36 Two surveys conducted in India explored vasectomy knowledge of CHWs and found that there was a great deal of knowledge around a person's eligibility for vasectomy as well as how long the procedure typically takes, but little knowledge of the details of the procedure (i.e., whether NSV requires stitches, the amount of time a man would need to take away from work, and post-vasectomy contraceptive requirements). In addition, some CHWs erroneously believed that after vasectomy a man would lose physical strength, become weak or get sick often, would not be able to have an erection or ejaculate, and would have reduced libido 61 , 62 —many of the same misconceptions held by men and women in general. It is evident from these studies that more needs to be done to improve provider knowledge about vasectomy, particularly among community-based health workers on the front lines of the health system. Community-level staff often provide people with their first exposure to new services that are available in health centers; their clear understanding and buy-in of methods such as sterilization are essential to shaping the public knowledge and perceptions of vasectomy.
Lack of knowledge about vasectomy is also prevalent among providers.
Negative attitudes among providers. Two studies that we reviewed explored how family planning providers' negative attitudes toward vasectomy influenced their willingness to provide the method. 42 , 60 Both studies described how some providers acknowledged counseling biases toward female sterilization and avoided counseling on vasectomy. Provider attitudes and individual perceptions of appropriate family planning methods for their culture (Nigeria) 60 were juxtaposed against their fear of complications and limited financial gains from providing vasectomies (China). 42
Acceptability of vasectomy among providers was split between professional acceptability (i.e., willingness to refer clients for vasectomy) and personal willingness to use the method themselves. For example, in 2 Nigerian studies, a minority of providers (19.2%) accepted vasectomy as a contraceptive method and less than half of those would consider using the method themselves (41.3%) 26 ; none of the doctors (or their partners) in either study actually had had a vasectomy.
Facilitators of Vasectomy Service Delivery
Programmatic activities geared toward creating or improving vasectomy service delivery included the use of evidence-based vasectomy techniques, whole-site trainings, task shifting, cascade training, mobile outreach, and tools to assist in program planning.
Evidence-based vasectomy techniques. Each of the programs in our review trained providers in NSV, highlighting the practicality of using this method to access the vas deferens in low-resource settings. Various methods were used by the different programs for occluding the vas once exposed, but Labrecque et al.'s 63 review and evaluation of Asian vasectomy programs noted that most vasectomies were performed with NSV and simple ligation and excision technique for vas occlusion. This may be true in many low-resource countries due to the paucity of vasectomy services; however, to date no thorough review has been conducted.
Most vasectomy programs in Asia use the no-scalpel vasectomy technique with simple ligation and excision for vas occlusion.
From 2003 to 2004, the ACQUIRE Project visited vasectomy centers in Bangladesh, Cambodia, India, Nepal, and Thailand to observe vasectomy techniques and to demonstrate the novel occlusion techniques using handheld, battery-powered cautery devices and fascial interposition. 9 ACQUIRE also conducted interviews with key informants in each country to gauge interest in the use of thermal cautery and/or fascial interposition techniques. The fascial interposition technique was largely known and even taught in the Asian countries visited but was seldom performed in Bangladesh, India, or Nepal. Barriers cited for not adopting fascial interposition included insufficient surgical skills, the additional time needed to perform the technique, and that it was not mandatory by country standards. Providers in these countries showed interest in the use of thermal cautery for vas occlusion. 9
Whole-site training. Beginning in 2005, FRONTIERS and local partners in Guatemala developed a systemic vasectomy introduction model for Ministry of Health hospitals and maternity clinics. 64 The model involved training the entire health team—surgeons, nurses, receptionists, and others who might provide referrals—on the benefits, procedures, and side effects of vasectomy. This whole-site approach increased general knowledge about vasectomy for the site teams. However, in a post-training survey, knowledge gaps remained around post-procedure counseling guidelines and characteristics of potential vasectomy clients. 65 , 66 After the end of this project, the ministry used the whole-site model to introduce services in 10 additional hospitals and maternities. 65 – 67
Likewise, the ACQUIRE Project in Ghana offered whole-site trainings to establish “male-friendly” services, in which all health staff were trained in NSV counseling and services. 55 , 62 The whole-site training resulted in staff being more receptive to offering men's health services, a better understanding of male anatomy, fewer misconceptions about vasectomy, and more comfort in talking to men about vasectomy. 55 Other related research from Jharkhand, India, also found that training CHWs in NSV and male anatomy increased knowledge about the procedure and reduced misconceptions, which improved counseling for potential clients. 61
Task shifting. Vasectomy is considered a quick and routine procedure in most instances, which can be a benefit to physicians in low-resource settings who are extremely busy. For this reason, the discussion of task shifting vasectomy responsibilities to lower-level providers is common. In our search, we found some examples of this discussion and changes in policies. For example, Trollip et al. (2009) studied the safety and efficacy of vasectomy provision by junior-level doctors in South Africa. 68 Procedure times and complication rates for 479 vasectomies were analyzed to assess the capacity of the physicians to perform the procedure, although they were not compared with those of more senior staff. Average operating times decreased significantly over time, but complication rates did not increase. This study suggests that with training and experience even junior-level medical staff may be able to efficiently provide vasectomy services without compromising the safety and efficacy of the procedure.
With training and experience, junior-level medical staff may be able to efficiently provide vasectomy services without compromising safety and efficacy.
The low rate of complications in general for vasectomy clients suggests that more investigation is necessary to determine the appropriateness of task shifting this procedure. Alternatively, an indirect approach to increasing services is being implemented in Malawi, where long-acting methods, comprising intrauterine devices (IUDs) and implants, are provided by outreach staff. 69 This task shifting allows CHWs to provide a wider array of services that, in turn, may afford more technically skilled providers greater availability to offer more permanent methods to clients who have reached their desired family size. 24 , 25 , 28
Cascade training. To systematically and cost-effectively build the capacity of clinics and service providers, many of the vasectomy programs we reviewed relied on a cascade approach to training. 53 , 54 , 70 With the cascade approach, a small group of motivated providers and health staff are identified and trained to provide vasectomy service training. Once trained, this cadre is then trained as trainers. Over time, opportunities are provided for them to diffuse the knowledge and training to other providers and staff during the life of the program and after it ends ( Figure ).

Cascade Training Model for Building Capacity in Vasectomy
Cascade training was implemented by the Capacity Project and PROGRESS in Rwanda. In both instances, the projects identified or developed curricula based on established procedures 11 , 71 , 72 and created a skills checklist. This approach facilitated outreach visits by vasectomy teams from district-level hospitals to remote health centers to provide vasectomies and train other providers. Training under the PROGRESS Project took place over 5 days and included thermal cautery and fascial interposition. At the end of the training, the physicians successfully mastered the new occlusion technique. 11 By 2012, the cascade training approach under the PROGRESS Project resulted in more than 64 physicians and 103 nurses trained in 42 hospitals, and 2,523 vasectomies were performed.
Mobile outreach. Mobile outreach services are often provided at static structures, in portable mobile health tents, or in vans. 73 Our review identified several programs that used mobile outreach teams to expand the reach of vasectomy service provision. A key contribution to the success of the NSV program in Rwanda was the extension of service from hospitals to health centers. For example, 56% of vasectomies performed in a sample from one district were conducted at a rural health center as opposed to a district-level hospital. 40
Padmadas et al. (2014) found that vasectomies were significantly more likely to be offered in a mobile clinic rather than a government hospital, particularly in remote locations. 73 The Government of Nepal has mobilized outreach services for voluntary surgical contraception to rural areas of Nepal. Trained surgical teams travel to remote areas from a central location with necessary supplies. In locations where health facilities are not available, temporary settings such as schools and community centers are used. 69 Wickstrom and colleagues from the RESPOND Project noted that community mobilization engages communities in discussing family planning; informs clients about all methods, including LAPMs; and ensures enough of a caseload of LAPM clients to make the outreach visit worthwhile. 69
Tools to assist in program planning. We identified a handful of tools created to assist vasectomy program planners when integrating vasectomy services. 71 – 76 (This is not a comprehensive list of all available tools and training curricula related to vasectomy due to the search criteria used in our study.) The ACQUIRE Project developed 2 training curricula that were designed to instruct physicians and vasectomy assistants to provide safe and effective NSV services. 71 , 72 One document includes curricula on counseling clients; verifying informed decision making and consent; preventing infection and managing complications, as well as supplemental materials on developing, maintaining, and publicizing a vasectomy service. 76 The second document provides guidance for organizing and conducting training in NSV. In many areas, NSV services are provided as part of a team effort; thus, this course included instructions for training vasectomy assistants as well as physicians. 72
EngenderHealth published a checklist of the minimum number and types of medical instruments and supplies needed for provision of hormonal implants, IUDs, female sterilization, and vasectomy, 75 which could be informative in future vasectomy programs and family planning/reproductive health costing studies.
The Johns Hopkins Information and Knowledge for Optimal Health (INFO) Project created a set of tools, checklists, and tables for program implementers and family planning providers to (1) counsel men about vasectomy, (2) identify men with conditions that require a delay or special consideration before vasectomy provision, and (3) explain to men what they should do before and after the vasectomy. 74
Our search did not identify any tools or guidelines to provide couples' counseling, but one article previously discussed referenced use of a group counseling technique involving couples. 61 Another INFO Project toolkit informs family planning/reproductive health program managers about the benefits of vasectomy and considerations for vasectomy integration. 76
Enabling Environment
Sociocultural, economic, and policy factors influence health services as well as social norms related to family planning in general and to va-sectomy in particular. An enabling environment for vasectomy requires engagement of governments, communities, and civil societies to support and advocate gender-equitable norms, accountability, evidence-based policies, and high-quality vasectomy services.
Barriers to Vasectomy Adoption
Social norms against vasectomy. In many studies, vasectomy was viewed by people as the least preferred contraceptive method and was often used only as a “last resort” for women who have experienced side effects from hormonal methods or who might have potential health risks with another pregnancy, or for a couple who has reached or exceeded their desired family size. 22 , 24 , 25 , 36 Across studies, the most commonly mentioned misperceptions about vasectomy among both men and women were (1) a man would become physically weaker after having a vasectomy; (2) a man would be unable to function sexually after having a vasectomy (e.g., would be unable to have an erection or would be impotent, would have reduced sexual desire, would be incapable of enjoying sex or satisfying a woman, or would have impaired ejaculation); and (3) vasectomy was the same as castration.
Many people view vasectomy as a “last resort” for women who have experienced side effects with hormonal methods or other problems.
As mentioned earlier, the literature frequently cited prospective patient and provider reluctance to adopt vasectomy. This lack of acceptance among prospective clients and trusted health care providers perpetuates the intransigent social norm that family planning is a woman's duty. 15 , 16 , 18 , 31
Facilitators for Vasectomy Services
Identifying appropriate areas in national and regional family planning strategies to highlight and support vasectomy integration is essential in formalizing support for the method. The literature we reviewed did not include effective messaging around economic benefits or direct links between programmatic activities and resulting policies. But the literature did include several program documents that described activities that were implemented with the goal of creating a more enabling environment for vasectomy adoption. Below, we combine different program activities around this goal.
Multi-level engagement. Gaining the support of governments and religious and community leaders and institutions can influence public attitudes toward public health campaigns, including vasectomy uptake. As an example, Simbar attributes Iran's increased religious and political support of family planning programming over the last decade as a fundamental component to increased contraceptive uptake in the country. 77 Currently, Iran's vasectomy program is moderately robust with about 30,000 vasectomies provided annually 78 and may provide a model for other countries in the region. Unfortunately, media reports from 2014 suggest that there was legislation passed by the government to ban vasectomy as a means to increase population. 79 We are unaware of the current availability of the method in the country.
In Tanzania, the ACQUIRE Project identified Seventh-Day Adventists as advocates of all forms of contraception, including vasectomy, who even included information on contraception in their sermons. 29 The Heri Seventh Day Adventist Mission Hospital in Tanzania, a focal point of the project's vasectomy promotion and training activities, provided vasectomy services and educational seminars about the benefits of contraception. 29 , 30 This hospital became a regional center of excellence in NSV and provided the majority of vasectomies over a 6-year period in the Kigoma region.
In Bangladesh, the ACQUIRE Project produced a book entitled Family Planning in the Eyes of Islam, designed to engage influential imams (Muslim religious leaders) in family planning, with a focus on LAPMs. This book situated the role of family planning in Islam and the stance taken on family planning in the Qur'an and Hadith, Islam's 2 foremost sacred texts. In addition, the ACQUIRE Project sponsored interactive community forums, largely held in rural areas of Bangladesh, that brought together imams , teachers, businessmen, local politicians, and local family planning service providers to discuss family planning and the important role of LAPMs. 78
Gender transformative messaging. The “Get a Permanent Smile” campaign in Bangladesh and Ghana (as previously described) addressed the myths associated with vasectomy, particularly related to men's interest in and knowledge of family planning. 78 The program created posters and television commercials that contained the message “My husband is best,” which was highly regarded in the community. Men liked the fact that the materials clearly illustrated their role in family planning decision making and the notion that a wife would value the husband's involvement. The materials challenged frequently cited concerns about vasectomy, promoted vasectomy in the communities, and highlighted couples' shared decision making. 81
In Honduras, the “Permanent Smiles” campaign aimed to reposition vasectomy as a simple and effective male method of family planning. 78 Key messages emphasized that vasectomy would have no negative effects on couples' relationships and that vasectomy does not affect a man's sexual performance.
In Ghana, the ACQUIRE Project's vasectomy promotion included an emphasis on the benefits of vasectomy and promoted “satisfied users” through testimonials. Vasectomy was promoted as a contraceptive method that gives a man the ability to care for his partner and children while offering the freedom to enjoy life. 54
DISCUSSION AND RECOMMENDATIONS
This review identified factors that facilitate va-sectomy integration into national family planning agendas from the experiences and evidence of recent vasectomy programs in low-resource settings. Vasectomy, like other contraceptive methods, benefits from well-integrated demand generation activities and adequately trained providers. Supportive policies are directly linked to the potential for va-sectomy uptake. Government health agencies (if they have not done so already) must establish policies and political infrastructure that strategically engage and include men in a comprehensive reproductive health agenda, without undermining the gains made in improving access to family planning for women. Policies that empower women and men to be supportive partners, continual family planning users, and reproductive health advocates lay a solid foundation for future vasectomy programs.
Vasectomy, like other contraceptive methods, benefits from well-integrated demand generation activities and adequately trained providers.
Unfortunately, current approaches to vasectomy integration are focused on the “quick win.” These approaches advocate the benefits of vasectomy to men and couples ready for a vasectomy right now. We suggest that vasectomy can be used to address the fundamental gap between reproductive health programming and men, a gap that exists in both high- and low-resource settings. 81 These approaches would include educating men, including young men, on the range of methods available in their communities, their potential side effects, and their effectiveness. Research has shown that engaging men in family planning and reproductive health increases couple communication, facilitates male involvement in child care, and improves relationships. 82 – 85 Maintaining the status quo of male exclusion from reproductive health services stagnates development and reinforces negative gender norms (i.e., use of contraception is a woman's responsibility). Therefore, increasing men's reproductive health lexicon and addressing existing gender normative barriers can help both families to achieve their reproductive goals and countries to achieve their national family planning goals.
Engaging men in family planning increases couple communication, facilitates male involvement in child care, and improves relationships.
Limited human resources continually limit the service provision, quality of care, and accuracy of clinical data. When considering vasectomy integration, governments should investigate the appropriateness of using health facility staff that are not physicians. It has been suggested that countries where nurses are already performing adult male circumcisions would be skilled enough to take on vasectomy provision. 86 This is not to suggest that vasectomy clients would necessarily be the same men at the same time as circumcision clients, because circumcision clients 87 may not be in the same life stage as vasectomy clients. 41 Also, this would require clear delineation in counseling and promotion of the 2 methods.
Three reasons make a case for exploring this task-shifting option:
- The 2 procedures are similar in surgical complexity.
- Nurses who are already performing adult circumcisions have demonstrated the necessary surgical talent.
- These nurses are accustomed to dealing with men in a reproductive health context.
The benefits of strong intake counseling cannot be understated for vasectomy services. Vasectomy's global history 88 and the mandate of informed choice should be considered when training health facility staff to counsel clients. Clear articulation of vasectomy as a permanent method should be included in counseling. Rates of dissatisfaction and/or regret with vasectomy range between 1% and 2%, 89 and between 3% and 6% of men request reversals. 90 In most low-resource countries, opportunities for a vasectomy reversal is not likely an option. Vasectomy counseling should also address emotional issues associated with the loss of fertility and the end of a couple's reproductive life. The “maturational loss” associated with this change is well documented but seldom investigated in vasectomy research. 91
Universally, the studies and programmatic reports included in this review reflect positive and proactive approaches to vasectomy service provision. Unfortunately, there are also examples of misuse and abusive implementation in the past. 88 Reflecting upon this history is key for program implementers, funders, and policy makers. It should also reinforce the principle of informed choice of family planning methods. Informed choice is one aspect of the growing “rights-based approach” that is currently being integrated into program planning that is being championed by global funders and initiatives including FP2020. 92
The program literature provides examples of channels and activities that changed perceptions of vasectomy and integration of men into reproductive health services. Countering misperceptions across multiple media channels was found to be effective at increasing vasectomy demand. Examples and materials to support vasectomy integration are well established. Use of testimonials, media campaigns, and strategic timing of service delivery was found to facilitate uptake, while training tools have been well established and easily available. At the grassroots level, cadres of existing vasectomy providers are linking themselves with physicians in low-resource settings. 93 Training these providers in low-resource settings and providing them with the necessary equipment is important, but their small scale has limited impact on national contraceptive prevalence rates or on the associated benefits of integrating vasectomy into a national family planning agenda.
Countering misperceptions across multiple media channels has been effective at increasing vasectomy demand.
In conjunction with these somewhat grassroots efforts, World Vasectomy Day—the global campaign that fosters discussions about men's role in reproductive health—held its fourth annual event on Friday, November 18, 2016, in Kenya. 93 Momentum for vasectomy integration is rising and now the challenge is to appropriately pivot the focus of family planning and reproductive health services to include men in meaningful and impactful ways.
Supplementary Material
Acknowledgments.
We are grateful for feedback and resources shared by vasectomy providers and advocates from around the globe. Funding for this review was provided under the USAID-funded Evidence Project, implemented by the Population Council and partners (AID-OAA-A-13-00087).
Competing Interests: None declared.
Peer Reviewed
Cite this article as: Shattuck D, Perry B, Packer C, Quee DC. A review of 10 years of vasectomy programming and research in low-resource settings. Glob Health Sci Pract. 2016;4(4):647–660. http://dx.doi.org/10.9745/GHSP-D-16-00235
Advertisement
Supported by
Raw Milk Containing Bird-Flu Virus Can Sicken Mice, Study Finds
The results bolster evidence that virus-laden raw milk may be unsafe for humans.
- Share full article

By Apoorva Mandavilli
Unpasteurized milk contaminated with H5N1, the bird-flu virus that has turned up in dairy herds in nine states, has been found to rapidly make mice sick, affecting multiple organs, according to a study published on Friday .
The findings are not entirely surprising: At least a half-dozen cats have died after consuming raw milk containing the virus. But the new data add to evidence that virus-laden raw milk may be unsafe for other mammals, including humans.
“Don’t drink raw milk — that’s the message,” said Yoshihiro Kawaoka, a virologist at the University of Wisconsin, Madison, who led the study.
Most commercial milk in the United States is pasteurized. The Food and Drug Administration has found traces of the virus in 20 percent of dairy products sampled from grocery shelves nationwide. Officials have not found signs of infectious virus in those samples and have said that pasteurized milk is safe to consume.
But the findings have global implications, said Dr. Nahid Bhadelia, director of the Boston University Center on Emerging Infectious Diseases, who was not involved in the work.
“If this becomes a more widespread outbreak in cows, there are other places where there isn’t central pasteurization,” she cautioned, “and there are a lot more rural communities that drink milk.”
In the study, Dr. Kawaoka and his colleagues analyzed virus from milk samples from an affected dairy herd in New Mexico. The researchers found that levels of the virus declined slowly in a sample of milk stored at 4 degrees Celsius, suggesting that H5N1 in refrigerated raw milk may remain infectious for several weeks. The findings were published in the New England Journal of Medicine.
Flu viruses survive well at refrigerator temperatures, and the protein in milk also helps to stabilize them, said Richard Webby, an influenza expert at St. Jude Children’s Research Hospital in Memphis, who was not involved in the work.
If people who drink raw milk believe that refrigeration kills the virus, “this clearly shows that’s not the case,” Dr. Webby said.
Mice that were fed the contaminated milk quickly became ill, displaying ruffled fur and lethargy. On the fourth day, the mice were euthanized, and researchers found high levels of the virus in the respiratory system and moderate levels in several other organs. Like infected cows, the mice also harbored the virus in their mammary glands — an unexpected finding.
“These mice are not lactating mice; still the virus can be found in mammary glands,” Dr. Kawaoka said. “It’s very interesting.”
It is unclear whether the presence of virus in mammary glands is a feature of this particular virus or of bird-flu viruses in general, Dr. Webby said: “We’re learning new things every single day.” Mice are common pests in farms, providing yet another potential host for the virus, and cats and birds that feed on infected mice could also become ill.
The cats that died after drinking contaminated milk showed striking neurological symptoms , including stiff body movements, blindness, a tendency to walk in circles and a weak blink response. If the mice had been allowed to live longer, they might have developed similar symptoms, Dr. Webby said.
Also unclear is what the findings mean for the course of infection in people. On Wednesday, federal officials announced that a second dairy worker had tested positive for the H5N1 virus; a nasal swab from that person had tested negative for the virus, but an eye swab tested positive.
Pasteurization kills germs by heating milk to high temperatures. In the new study, when researchers heated the milk at the temperatures and time periods typically used for pasteurization, the virus was either undetectable or greatly diminished, but it was not completely inactivated.
Dr. Kawaoka cautioned that the laboratory conditions were different from those used in commercial pasteurization, so the results did not mean that the milk on grocery shelves contains active virus.
By contrast, the findings that raw milk contains large amounts of virus is “solid,” he said.
Raw milk has become popular in recent years as wellness gurus and right-wing commentators have extolled its alleged virtues , even more so since the bird flu outbreak in dairy cows began. Some argue that it tastes better and is more nutritious than pasteurized milk. Others contend that it boosts immunity.
On the contrary, pasteurization preserves calcium, the key nutrient in milk, and adds vitamin D to help absorb it. Consuming raw milk can lead to serious complications or even death from a variety of pathogens, especially in people with weakened immune systems, according to the Centers for Disease Control and Prevention.
From 1998 to 2018, outbreaks traced to raw milk consumption led to 228 hospitalizations, three deaths and illness in more than 2,600 people.
Apoorva Mandavilli is a reporter focused on science and global health. She was a part of the team that won the 2021 Pulitzer Prize for Public Service for coverage of the pandemic. More about Apoorva Mandavilli
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 14 February 2023
Rising vasectomy volume following reversal of federal protections for abortion rights in the United States
- Raevti Bole 1 ,
- Scott D. Lundy 1 ,
- Evonne Pei 2 ,
- Petar Bajic 1 ,
- Neel Parekh ORCID: orcid.org/0000-0002-6218-9254 1 &
- Sarah C. Vij ORCID: orcid.org/0000-0001-8282-2339 1
International Journal of Impotence Research volume 36 , pages 265–268 ( 2024 ) Cite this article
7013 Accesses
7 Citations
444 Altmetric
Metrics details
- Urogenital reproductive disorders
In June 2022 the United States Supreme Court issued a ruling in the case Dobbs v. Jackson that overturned Roe v. Wade , the 1973 ruling establishing a federally protected right to abortion in the United States. Anecdotal reports suggested increased vasectomy volume following this event; however, no published data exist. We sought to describe trends in vasectomy consultation before and after the Dobbs v. Jackson ruling (referred to as pre- and post- Dobbs herein). Following IRB approval, we reviewed charts of all adults seeking vasectomy consultation in July–August 2021 and July–August 2022 at a large healthcare organization. We then aggregated vasectomy procedural billing data from 2018 to present. The primary outcome was volume of vasectomy consultation appointments and the secondary outcome was number of vasectomies performed. In July–August 2021 (Pre- Dobbs ), 116 men attended vasectomy consultation versus 142 men in July–August 2022 (Post- Dobbs ). Median age Post- Dobbs was significantly younger than Pre- Dobbs (35 vs 38 years, respectively, p = 0.01) with a significant increase in Post- Dobbs men under 30 seeking vasectomy ( p = 0.005). A total of 16.9% (24/142) of Post- Dobbs men were childless, compared to 8.6% (10/116) of Pre- Dobbs men ( p = 0.05). Of those with children, median number of offspring was unchanged at 2. Billing data showed a significant increase in vasectomy procedural volumes Post- Dobbs . While overturning Roe v Wade directly impacted female reproductive rights, number of vasectomy consultations and procedures increased significantly following this decision. Younger men, especially those under 30, as well as childless men were significantly more likely to seek consultation Post- Dobbs compared to the prior reproductive legal climate. While longer-term data are needed, findings indicate that men are invested in maintaining reproductive autonomy for themselves and their partners.
Similar content being viewed by others
Vasectomy incidence in the military health system after the reversal of Roe v. Wade
The percentage of men counseled by urologists who received a vasectomy mildly increased after the publication of the AUA vasectomy guideline

First trimester abortion protocols by facility type in Switzerland and potential barriers to accessing the service
Introduction.
On June 24, 2022, the United States Supreme Court issued a 6–3 ruling in Dobbs vs. Jackson Women’s Health Organization , with Justice Alito writing the majority opinion that “procuring an abortion is not a fundamental constitutional right because such a right has no basis in the Constitution’s text or in our Nation’s history” [ 1 ]. The ruling, which was leaked in draft form 2 months prior, overturned the landmark 1973 Roe v. Wade decision that established a federally protected right to abortion during the first two trimesters of pregnancy and gave each state the power to set its own abortion laws [ 2 ]. A review of Gallup polls dating back to 1989 found that almost 60% of Americans have consistently supported federal protection for abortion rights across three decades and through multiple generations [ 3 ]. Until June 2022, reproductive autonomy protections had been the law of the land for all reproductive-age women living in the United States.
While this legal decision directly impacted the reproductive rights of females and their bodily autonomy, the decision appears to have exerted profound effects on men too. There have been multiple media outlets reporting on anecdotal increases in the number of men seeking permanent contraception following this event [ 4 , 5 , 6 ]. Despite these assertions, no peer-reviewed published data yet exist on this phenomenon.
We sought to describe for the first time the trends in vasectomy consultation and completion at a large healthcare organization by comparing men presenting for vasectomy consultation in the Pre- Dobbs era compared to the Post- Dobbs era. Because there is a delay in completing the procedures due to provider availability and insurance restrictions, our primary outcome of interest was the number of vasectomy consultations and our secondary outcome included the number of vasectomy procedures performed.
Following institutional IRB approval, we performed a retrospective review of all adult patients seeking consultation for vasectomy in July–August 2021 compared to July–August 2022 at a large midwestern academic healthcare system including 13 community hospitals. The follow-up period for patients seen in July–August 2022 (the “Post- Dobbs ” cohort) was 3 months, while the July 2021 (the “Pre- Dobbs cohort”) was 16 months but was truncated to 3 months for the purposes of statistical analysis. In parallel, we also obtained the billing data for all patients at our institution who underwent vasectomy (Current Procedural Terminology code 55250) between 2018 and 2022.
Demographic data including age, ethnicity, marital status and number of children were extracted from the medical record, aggregated, and analyzed using descriptive statistics. Comparisons were performed between patients attending consultation in July–August 2021 versus July–August 2022 with regard to age, race, number of children, marital status and vasectomy completion with t -test and χ 2 tests where appropriate. The average vasectomy procedural volume for July to September 2018–2021 was compared to the average vasectomy procedural volume for July to September 2022. Threshold for statistical significance was set a priori at p ≤ 0.05. Statistical analyses were performed using IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp.
The primary analysis of vasectomy consultation volume focused on the July–August 2021 (Pre- Dobbs ) and July–August 2022 (Post- Dobbs ) cohorts. In the Pre- Dobbs cohort, 123 men initiated requests for vasectomy consultation and 116 men actually attended the appointment with a urology provider. In the Post- Dobbs cohort, 166 men initiated requests for vasectomy consultation and 142 men actually attended an appointment. The visit attendance rate in 2021 was higher than in 2022 (94.3% vs 85.5%, p = 0.02), although 17 Post- Dobbs appointments were scheduled 3 or more months out and had not taken place at the time of data collection. Overall, there was a 35.0% increase in vasectomy consultation requests and a 22.4% increase in vasectomy consultations from Pre- Dobbs to Post- Dobbs .
The median age of the Post- Dobbs cohort was significantly younger at 35 years old (IQR 10) compared to 38 years old (IQR 9) in the Pre- Dobbs cohort ( p = 0.01) and there was a significant increase in Post- Dobbs men under 30 seeking vasectomy versus pre- Dobbs (23.9% vs 10.3%, p = 0.005). The self-reported race of men seeking vasectomy in 2022 versus 2021 is shown in Table 1 . The proportion of white men seeking consultation significantly increased in July 2022 (83.8% vs 70.7%, p = 0.01).
Seventy-two percent of men in the Post- Dobbs cohort were married compared to 78% in the prior year ( p = 0.29). There was also a significant increase in childless men seeking vasectomy Post- Dobbs at 16.9% (24/142) vs 8.6% (10/116) men ( p = 0.05). The median number of offspring for each patient seeking vasectomy consultation was 2 in both groups (IQR 1).
At 3-month follow-up, 58.6% (68/116 consultations) of Pre- Dobbs men had completed their vasectomy versus 66.2% (94/142 consultations) of Post- Dobbs men ( p = 0.21). At 16-month follow-up, the vasectomy completion rate for men initially seen in July–August 2021 was 79.3% (92/116).
In order to further examine our secondary endpoint, billing data for all patients who underwent vasectomy within our healthcare system from 2018 to August 2022 was extracted. Our results showed a significant increase in median (IQR) vasectomy procedural volume following the 2022 Dobbs decision, increasing from 104 (24) vasectomies per month to 218 (35) vasectomies per month ( p = 0.03, Fig. 1 ).
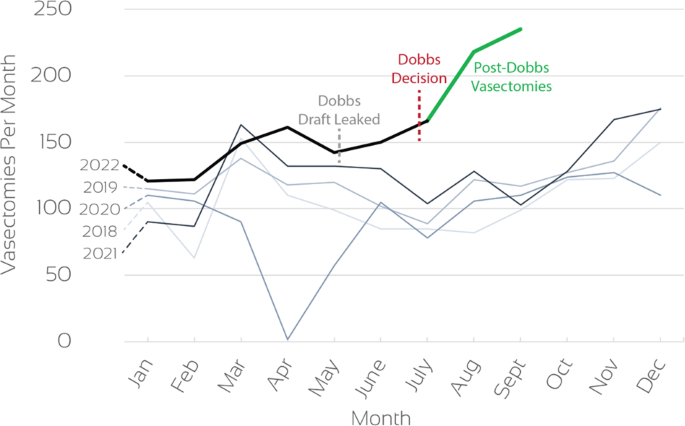
Dobbs decision leak is noted in gray, and the final Dobbs decision is highlighted in red. The green line delineates the 2022 Post- Dobbs cohort.
Permanent contraception for premenopausal women typically involves abdominal surgery to ligate or occlude the fallopian tubes. While overall safe, this is still a procedure with inherent risks such as pain, transfusion risk, infection, damage to abdominal strictures and risks of general anesthesia [ 7 ].
In contrast, permanent contraception for men via vasectomy involves a straightforward minimally invasive procedure in the scrotum [ 8 ]. Despite the fact that vasectomy is less invasive and safer, tubal ligation has historically accounted for the majority of surgeries performed for permanent contraception in the United States [ 8 , 9 ]. Approximately 16% of women undergo tubal ligation as a sterilization technique compared with only 6% of men who undergo vasectomy [ 10 ]. In fact, one study even demonstrated a decrease in the number of vasectomies performed from 2007 to 2015 in the United States across all ages and geographic locations [ 11 ].
While women appear to have historically taken on more responsibility regarding the decision to avoid future offspring, the overturning of Roe v. Wade in June 2022 has changed the landscape of family planning for male partners as well. Multiple news organizations covered stories about non-published reports of more men seeking vasectomies all across the country [ 4 , 5 , 6 ]. We hypothesized that increased discussion around reproductive rights and a strong desire by some couples to avoid legal jeopardy may have contributed to assertive decision making among single and partnered individuals, some of whom may have already considered pursuing elective sterilization but had not yet found the impetus to do so.
In this manuscript, we report clinical data from a high-volume academic medical institution showing a significant increase in vasectomy procedural volumes following Dobbs (Fig. 1 ). While the overall increase in procedural volume includes patients who had initiated consultation prior to the ruling, the legal decision may have prompted many to actually schedule vasectomy rather than putting it off. Within the short interval after this decision, our hospital network also experienced a rise in new vasectomy consultation requests of 35.0% and vasectomy consultation visits of 22.4% compared to the same time period the year prior. Interestingly the rate of men who actually attended their appointment was lower in 2022, showing that some men ultimately did not feel compelled to pursue vasectomy after initial fact-searching. However, when examining the preliminary 3-month follow-up period after consultation in the July–August cohorts, we found that men were proceeding with the vasectomy procedure at a similar rate, indicating that patients who came to appointments were truly interested in acting.
There were multiple other notable findings in our analysis. After Roe v Wade was overturned in June 2022, men seeking vasectomy were significantly younger (35 vs 38 years, p = 0.01) and far more likely to be under the age of 30 (23.9% vs 10.3%, p = 0.005). The median age of men undergoing vasectomy has previously been described at approximately 37 or 36 years of age depending on urban versus rural location [ 12 ]. This surge of younger men choosing to undergo permanent contraception half a decade earlier than historical rates should not be dismissed as expected change over time. The immediacy with which this change was seen indicates that the Post- Dobbs generation has already been significantly affected by the legal climate and the population-based consequences of this decision will continue to be seen in multiple ways for decades to come.
Interestingly there was no change in the proportion of single or married men pursuing vasectomy pre and post Roe v Wade overturning. However, there was a significant increase in childless men pursuing vasectomy after the legal ruling. We hypothesize that both single and partnered men who have decided not to have further offspring now feel it necessary to take reproductive autonomy into their own hands. The invasiveness of female permanent contraception may have some bearing on this decision, but changes in the rates of tubal ligation for women Post- Dobbs have yet to be described.
Prior studies have described racial and ethnic differences in men seeking vasectomy in the United States [ 10 ]. Consistent with the published literature, we also found that the majority of men in our study self-identified as white for both years. There was a significantly higher percentage of white men seeking vasectomy after Roe v Wad e was overturned, and a significant decrease in African American men (Table 1 ). The reasons for this are likely multifactorial in nature, and could include uneven access to healthcare, and differing perceptions of the reproductive legal climate. However, larger numbers would be needed in order to accurately assess for these factors.
One limitation of our study is the short duration of follow-up for the July/August 2022 cohort. In order to minimize the risk of bias in interpreting results such as surgical scheduling, we compared the 3-month vasectomy completion rate in both the 2021 and 2022 cohorts and found these to be similar. In addition, our procedural volume also reflects the increase in consultation, which further strengthens the conclusion that vasectomy interest rose post- Dobbs . Another limitation is the single-institutional nature of our study. However, as our institution is a large quaternary referral center including a network of 13 community hospitals serving our racially diverse region in both urban and rural settings, the database used is likely representative of the greater population. It is also important to note that this study was carried out in Ohio, a state that activated a “heartbeat bill” (Ohio Revised Code, 2919.195) very soon after Roe v Wade was overturned. At the time of writing this manuscript, an Ohio state judge temporarily blocked this law from taking effect based on a challenge from the Ohio American Civil Liberties Union and further deliberations are pending. A strength of our study is that comparison of the same months (July–August) in two different years limits the inherent variability in surgery consultation and scheduling, as patients consider multiple factors when making medical appointments that are unrelated to the legal landscape [ 4 ]. One unique factor that has affected elective medical appointment scheduling over recent years is the COVID-19 pandemic, and it is important to note that during the July–August 2021 time period compared, there was no active national or Ohio-wide surge in cases which would have decreased our volumes. Further study regarding vasectomy consultation and scheduling across the country should be encouraged and is ongoing at our institution.
While the loss of the federally protected right to abortion directly impacted the reproductive rights of women, we demonstrate for the first time that biological males with the potential to cause pregnancy have also been deeply affected as reflected by their reproductive healthcare decisions. An increase in vasectomy consultation visits was seen post- Dobbs , especially among younger men and childless men. Our overall vasectomy procedural volume also demonstrated a significant rise after July 2022 as compared to past years.
While longer-term and multi-institutional data are needed to study this phenomenon, it is clear from our findings that men remain engaged with reproductive autonomy for themselves and for their partners and are capable of rapidly acting when prompted by external stimulus. Legal rulings on reproductive health can have an impact far beyond the boundaries of gender. Policymakers should keep this in mind when discussing issues concerning healthcare and medical decision making.
Data availability
The original data can be made available via the corresponding author upon reasonable request.
United States Reports. Dobbs, State Health Officer of the Mississippi Department of Health et al. v. Jackson Women’s Health Organization et al. Vol. 597. 2022.
United States Reports. Roe et al. v. Wade, District Attorney of Dallas County. Vol. 410. 1973. p. 113.
Saad L. Where Do Americans Stand on Abortion? The Gallup Organization; June 15, 2022.
Dzhanova Y. “I just don’t want children”: some American men are turning to vasectomies after the Supreme Court’s decision to overturn Roe. Business Insider. 2022. https://www.businessinsider.com/how-roe-v-wade-affects-men-american-vasectomies-abortion-2022-8 . Accessed 9 Jan 2023.
Taylor S. Why men as young as 23 are choosing vasectomies in post-Roe America. Bloomberg. 2022. https://www.bloomberg.com/news/articles/2022-07-08/vasectomy-interest-surges-among-men-after-roe-v-wade-decision?leadSource=uverify wall . Accessed 9 Jan 2023.
Ducharme J. Vasectomies are going viral after the Roe v. Wade leak, but they aren’t a solution to abortion bans. Time Magazine. 2022. https://time.com/6178287/vasectomy-sterilization-roe-v-wade/ . Accessed 9 Jan 2023.
Huber AW, Mueller MD, Ghezzi F, Cromi A, Dreher E, Raio L. Tubal sterilization: complications of laparoscopy and minilaparotomy. Eur J Obstet Gynecol Reprod Biol. 2007;134:105–9.
Article PubMed Google Scholar
Velez D, Pagani R, Mima M, Ohlander S. Vasectomy: a guidelines-based approach to male surgical contraception. Fertil Steril. 2021;115:1365–8.
American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology. ACOG Practice Bulletin No. 208: benefits and risks of sterilization. Obstet Gynecol. 2019;133:194–207.
Article Google Scholar
Eisenberg ML, Henderson JT, Amory JK, Smith JF, Walsh TJ. Racial differences in vasectomy utilization in the United States: data from the national survey of family growth. Urology. 2009;74:1020–4.
Ostrowski KA, Holt SK, Haynes B, Davies BJ, Fuchs EF, Walsh TJ. Evaluation of vasectomy trends in the United States. Urology. 2018;118:76–9.
Machen GL, Bird ET, Kavoussi PK. Analysis of urban vs. rural vasectomy demographics: a multi-institutional, retrospective comparison. Transl Androl Urol. 2018;7:931–4.
Article PubMed PubMed Central Google Scholar
Download references
Author information
Authors and affiliations.
Department of Urology, Glickman Urological and Kidney Institute, Cleveland Clinic Foundation, Cleveland, OH, USA
Raevti Bole, Scott D. Lundy, Petar Bajic, Neel Parekh & Sarah C. Vij
Case Western School of Medicine, Cleveland, OH, USA
You can also search for this author in PubMed Google Scholar
Contributions
RB, SDL, EP, PB, NP and SCV conceived and designed the work, acquired data and interpreted results. RB, SDL, EP, PB, NP and SCV drafted or revised the manuscript. RB, SDL, EP, PB, NP and SCV approved the final version and RB, SDL, EP, PB, NP and SCV agreed to be accountable for all aspects of the work.
Corresponding author
Correspondence to Sarah C. Vij .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Bole, R., Lundy, S.D., Pei, E. et al. Rising vasectomy volume following reversal of federal protections for abortion rights in the United States. Int J Impot Res 36 , 265–268 (2024). https://doi.org/10.1038/s41443-023-00672-x
Download citation
Received : 15 December 2022
Revised : 24 January 2023
Accepted : 30 January 2023
Published : 14 February 2023
Issue Date : May 2024
DOI : https://doi.org/10.1038/s41443-023-00672-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
- Max J. Hyman
- Zhong Huang
- Omer A. Raheem
International Journal of Impotence Research (2024)
Uncovering the interhospital price variations for vasectomies in the United States
- Sherry Mortach
- Nicholas Sellke
- Nannan Thirumavalavan
- Benjamin C. Pierson
- Amanda Banaag
- Tracey Pérez Koehlmoos
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

COMMENTS
Research in New Zealand, England, and Mexico reports that there is a social element in talking about vasectomy and that peers could be a source of social support and inclusion when it came to men's vasectomy decision-making (Amor et al., 2008; Gutmann, 2005; Terry & Braun, 2013). Future research might examine peer-to-peer interactions to ...
However, these studies are limited. Therefore, it is thus timely to study the long-term safety and mental consequences and to recommend further research on this method of contraception. The aim of this study was to understand the effects of vasectomy over a long-term postoperative period by analyzing of the laboratory parameters and questionnaires.
Bhatia et al reported substantial increases in serum levels of cholesterol and triglycerides in rabbits that had undergone a vasectomy. However, a large number of studies have confirmed (including Clarkson's research) that there is no association between vasectomy and cardiovascular disease or related factors (even if the time after surgery ...
The results showed that vasectomy will significantly affect the SF-36 score in Model 4. "Role emotional" −6.28 (−10.34, −2.22) and "Mental health" −1.55 (−3.08, −0.02) were ...
2. Review objectives. The purpose of this study is to research the effect of vasectomy on male sexual function. The evaluation of sexual function is mainly conducted by the International erectile function questionnaire-5 (IIEF-5) and general information questionnaire, collecting the data of sexual desire, erectile function, frequency, and duration of sexual intercourse were collected.
Vasectomy is the most commonly performed urologic procedure in the United States and is a highly effective form of male contraception. The introduction of guidelines by urological societies has standardized vasectomy care. ... Recent studies suggest that this is a rare occurrence. 9 The EAA/ASA guidelines, ... Open Research.
Male reproduction and male contraception form an important spectrum within men's health. In this issue's Views and Reviews, four author groups detail important new developments in vasectomy clinical practice guidelines, emerging and investigational techniques in the fields of hormonal and nonhormonal male contraception, useful paradigms for patient care when deciding between sperm extraction ...
Studies were selected based on the following inclusion criteria: (1) study types were cohort, case-control, and cross-sectional studies; (2) studies that compared men with and without vasectomy ...
Controversy regarding trends in vasectomy use is ongoing, which is especially interesting given a clear trend to delay starting a family for both men and women 5.In the recent study by Zhang and ...
Purpose of review Vasectomy is a commonly performed outpatient procedure for male contraception with high success and low failure rates. Vasectomy reversal permits couples desiring the ability to conceive naturally after vasectomy to avoid assisted reproductive technology in many cases. Our review discusses current and emerging vasectomy and vasectomy reversal practices, techniques, and ...
1 INTRODUCTION. Vasectomy is the fourth most common contraceptive method and remains a safe, simple, and effective contraceptive option, with approximately half a million of men in the United States choosing to undergo vasectomy each year. 1, 2 The prevalence of vasectomy had been stable in the 1980s and 1990s in the United States. 3 More recently, a few studies using insurance claims data ...
Vasectomy research is one piece of CRB's portfolio in male contraception research and development. In addition, the branch leads the Preclinical Contraceptive Development Program to encourage and support basic, applied, and clinical studies on topics such as mechanisms that regulate sperm maturation and motility and identification of new ...
Background Vasectomy is one of the most effective and permanent male contraceptive methods, and involves cutting and ligating the vas deferens to make the semen free of sperm during ejaculation. Although it is effective, simple, and safe, it is not well known and practiced in the majority of our community. This study assessed the intention to use vasectomy and its associated factors among ...
Introduction: Vasectomy is the simplest, safest, and most effective form of definitive fertility control in men [1]. Vasectomy is used for 10% of contraception worldwide but only for 2% in Germany [2]. The aim of this study was to investigate the impact of vasectomy on the sexual satisfaction of sterilized men and their partners.
Mortality. Among men with a vasectomy who were free of cancer at the start of the study, 487 died (193 of cardiovascular disease and 173 of cancer) in 184,862 man-years of follow-up, whereas among ...
Vasectomy is a procedure that results in permanent yet reversible sterility and remains a great contraceptive option for many. Previous research studies have highlighted frequency of vasectomy utilization, defining characteristics of individuals who opt for this method, various surgical techniques, and the risks and benefits associated with the ...
At any point during the study, there was an opportunity for participants to opt out. The study was ethically cleared by the Research and Innovation Center of the Valley View University, Ghana, under exempted review. ... Recently, a Ghanaian study examining vasectomy from a female perspective unearthed that in a religiosociocultural society like ...
According to our study the number of children has an inverse relation with level of knowledge. Men who had four or more children are inversely associated with good knowledge about vasectomy. Likewise, research conducted in Gondar Northwest Ethiopia also concluded that the number of children was inversely correlated with knowledge of vasectomy.
The vasectomy study looked at male active-duty, retired and dependents in the military health system. ... according to a new study in the International Journal of Impotence Research published on ...
This study was conducted with the aim of describing the experiences of the men who underwent vasectomy. Materials and Methods: This qualitative study was performed by using a phenomenological research design. The sample consisted of 14 vasectomized men selected through purposive sampling method.
A preclinical study supports the positive association of vasectomy and clinically significant prostate cancer, where vasectomized mice had increased incidence of poorly differentiated, increased ...
The purpose of this study is to research the effect of vasectomy on male sexual function. The evaluation of sexual function is mainly conducted by the International erectile function questionnaire-5 (IIEF-5) and general information questionnaire, collecting the data of sexual desire, erectile function, frequency, and duration of sexual ...
A new study found a significantly higher risk of suicide attempts, self-harm, and PTSD for individuals who have undergone gender transition surgeries. The study, published in April, found that ...
A large new study shows people who bike have less knee pain and arthritis than those who do not. We are in the middle of National Bike Month, and cycling enthusiasts love to talk up the benefits ...
The research was presented at a European Renal Association meeting in Stockholm on Friday and simultaneously published in The ... The study included 3,533 people with kidney disease and Type 2 ...
This survey provided the data on Black voters' views on foreign policy priorities discussed in this report. For more information on this study, see its methodology and questionnaire. The third used annual totals of data from Pew Research Center telephone surveys (1994-2018) and online surveys (2019-2023) among registered voters.
Published in the journal PNAS, the study estimated the per-mile benefits of replacing diesel buses with electric ones in 3,108 U.S. counties. Researchers combined data about average diesel bus ...
Vasectomy is a highly effective and safe contraceptive method for couples who want to stop childbearing, but only 2.4% of men around the world use this method. We conducted an extensive review of the vasectomy research literature and programmatic reports, published between April 2005 and April 2015, to synthesize barriers and facilitators to ...
"Don't drink raw milk — that's the message," said Yoshihiro Kawaoka, a virologist at the University of Wisconsin, Madison, who led the study. Most commercial milk in the United States is ...
Further study regarding vasectomy consultation and scheduling across the country should be encouraged and is ongoing at our institution. ... International Journal of Impotence Research (2024)