
34th Annual
Ethnographic & qualitative research conference (eqrc), march 21-22 , 2022.
Proposal Submission extended deadline is FEBRUARY 28, 2022.
Registration extended deadline is Monday, MARCH 1 4 , 2022.
Virtual Conference
Due to the c ontinuing Covid-19 pandemic circumstances, EQRC will be held again as a " virtual conference ," during March 21-2 2, 2022 .
Both pre-recorded lecture sessions as well as poster sessions will be posted on the conference website in an open-view format. These will remain available through the link for registered participants through August 1, 2022.
Call for Papers
W e invite scholars to participate in the conference by presenting research projects among a broad spectrum of topics. Employment of traditional ethnographic and qualitative research projects provides the common thread for conference papers.
Proposals will be peer-reviewed among three strands: Results of qualitative and ethnographic research studies , qualitative research methods , and pedagogical issues in qualitative research.
Formats include lecture and poster presentations. The lectures will be 15-minute video presentations by authors and posters will be posted via PDF documents (see details HERE ) . Authors may request respective formats and all presentations (videos/posters) will be posted on the conference web page.
Submit a proposal that includes a title, an abstract of not more than 150 words, and a summary that does not exceed more than 600 words. If the proposal is accepted for presentation, then the title, abstract and a URL to your lecture or poster will all be included in the conference program.
Registration extended deadline is Monday, MARCH 14, 2022.
The EQRC conference has a long tradition of reputable quality, including previous hosting institutions being University of Massachusetts, Columbia University, Duquesne University, SUNY at Albany, Cedarville University, and University of Nevada at Las Vegas.
Presenters of both lecture and poster session presentations may submit their written papers for journal publication consideration. After a peer-review proc ess (different from conference review) these submitted papers, if selected, will be published in the quarterly issued Journal of Ethnographic & Qualitative Research (JEQR). To learn more about JEQR, please go to the website at www.jeqr.org .
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Practical thematic...
Practical thematic analysis: a guide for multidisciplinary health services research teams engaging in qualitative analysis
- Related content
- Peer review
- Catherine H Saunders , scientist and assistant professor 1 2 ,
- Ailyn Sierpe , research project coordinator 2 ,
- Christian von Plessen , senior physician 3 ,
- Alice M Kennedy , research project manager 2 4 ,
- Laura C Leviton , senior adviser 5 ,
- Steven L Bernstein , chief research officer 1 ,
- Jenaya Goldwag , resident physician 1 ,
- Joel R King , research assistant 2 ,
- Christine M Marx , patient associate 6 ,
- Jacqueline A Pogue , research project manager 2 ,
- Richard K Saunders , staff physician 1 ,
- Aricca Van Citters , senior research scientist 2 ,
- Renata W Yen , doctoral student 2 ,
- Glyn Elwyn , professor 2 ,
- JoAnna K Leyenaar , associate professor 1 2
- on behalf of the Coproduction Laboratory
- 1 Dartmouth Health, Lebanon, NH, USA
- 2 Dartmouth Institute for Health Policy and Clinical Practice, Geisel School of Medicine at Dartmouth College, Lebanon, NH, USA
- 3 Center for Primary Care and Public Health (Unisanté), Lausanne, Switzerland
- 4 Jönköping Academy for Improvement of Health and Welfare, School of Health and Welfare, Jönköping University, Jönköping, Sweden
- 5 Highland Park, NJ, USA
- 6 Division of Public Health Sciences, Department of Surgery, Washington University School of Medicine, St Louis, MO, USA
- Correspondence to: C H Saunders catherine.hylas.saunders{at}dartmouth.edu
- Accepted 26 April 2023
Qualitative research methods explore and provide deep contextual understanding of real world issues, including people’s beliefs, perspectives, and experiences. Whether through analysis of interviews, focus groups, structured observation, or multimedia data, qualitative methods offer unique insights in applied health services research that other approaches cannot deliver. However, many clinicians and researchers hesitate to use these methods, or might not use them effectively, which can leave relevant areas of inquiry inadequately explored. Thematic analysis is one of the most common and flexible methods to examine qualitative data collected in health services research. This article offers practical thematic analysis as a step-by-step approach to qualitative analysis for health services researchers, with a focus on accessibility for patients, care partners, clinicians, and others new to thematic analysis. Along with detailed instructions covering three steps of reading, coding, and theming, the article includes additional novel and practical guidance on how to draft effective codes, conduct a thematic analysis session, and develop meaningful themes. This approach aims to improve consistency and rigor in thematic analysis, while also making this method more accessible for multidisciplinary research teams.
Through qualitative methods, researchers can provide deep contextual understanding of real world issues, and generate new knowledge to inform hypotheses, theories, research, and clinical care. Approaches to data collection are varied, including interviews, focus groups, structured observation, and analysis of multimedia data, with qualitative research questions aimed at understanding the how and why of human experience. 1 2 Qualitative methods produce unique insights in applied health services research that other approaches cannot deliver. In particular, researchers acknowledge that thematic analysis is a flexible and powerful method of systematically generating robust qualitative research findings by identifying, analysing, and reporting patterns (themes) within data. 3 4 5 6 Although qualitative methods are increasingly valued for answering clinical research questions, many researchers are unsure how to apply them or consider them too time consuming to be useful in responding to practical challenges 7 or pressing situations such as public health emergencies. 8 Consequently, researchers might hesitate to use them, or use them improperly. 9 10 11
Although much has been written about how to perform thematic analysis, practical guidance for non-specialists is sparse. 3 5 6 12 13 In the multidisciplinary field of health services research, qualitative data analysis can confound experienced researchers and novices alike, which can stoke concerns about rigor, particularly for those more familiar with quantitative approaches. 14 Since qualitative methods are an area of specialisation, support from experts is beneficial. However, because non-specialist perspectives can enhance data interpretation and enrich findings, there is a case for making thematic analysis easier, more rapid, and more efficient, 8 particularly for patients, care partners, clinicians, and other stakeholders. A practical guide to thematic analysis might encourage those on the ground to use these methods in their work, unearthing insights that would otherwise remain undiscovered.
Given the need for more accessible qualitative analysis approaches, we present a simple, rigorous, and efficient three step guide for practical thematic analysis. We include new guidance on the mechanics of thematic analysis, including developing codes, constructing meaningful themes, and hosting a thematic analysis session. We also discuss common pitfalls in thematic analysis and how to avoid them.
Summary points
Qualitative methods are increasingly valued in applied health services research, but multidisciplinary research teams often lack accessible step-by-step guidance and might struggle to use these approaches
A newly developed approach, practical thematic analysis, uses three simple steps: reading, coding, and theming
Based on Braun and Clarke’s reflexive thematic analysis, our streamlined yet rigorous approach is designed for multidisciplinary health services research teams, including patients, care partners, and clinicians
This article also provides companion materials including a slide presentation for teaching practical thematic analysis to research teams, a sample thematic analysis session agenda, a theme coproduction template for use during the session, and guidance on using standardised reporting criteria for qualitative research
In their seminal work, Braun and Clarke developed a six phase approach to reflexive thematic analysis. 4 12 We built on their method to develop practical thematic analysis ( box 1 , fig 1 ), which is a simplified and instructive approach that retains the substantive elements of their six phases. Braun and Clarke’s phase 1 (familiarising yourself with the dataset) is represented in our first step of reading. Phase 2 (coding) remains as our second step of coding. Phases 3 (generating initial themes), 4 (developing and reviewing themes), and 5 (refining, defining, and naming themes) are represented in our third step of theming. Phase 6 (writing up) also occurs during this third step of theming, but after a thematic analysis session. 4 12
Key features and applications of practical thematic analysis
Step 1: reading.
All manuscript authors read the data
All manuscript authors write summary memos
Step 2: Coding
Coders perform both data management and early data analysis
Codes are complete thoughts or sentences, not categories
Step 3: Theming
Researchers host a thematic analysis session and share different perspectives
Themes are complete thoughts or sentences, not categories
Applications
For use by practicing clinicians, patients and care partners, students, interdisciplinary teams, and those new to qualitative research
When important insights from healthcare professionals are inaccessible because they do not have qualitative methods training
When time and resources are limited

Steps in practical thematic analysis
- Download figure
- Open in new tab
- Download powerpoint
We present linear steps, but as qualitative research is usually iterative, so too is thematic analysis. 15 Qualitative researchers circle back to earlier work to check whether their interpretations still make sense in the light of additional insights, adapting as necessary. While we focus here on the practical application of thematic analysis in health services research, we recognise our approach exists in the context of the broader literature on thematic analysis and the theoretical underpinnings of qualitative methods as a whole. For a more detailed discussion of these theoretical points, as well as other methods widely used in health services research, we recommend reviewing the sources outlined in supplemental material 1. A strong and nuanced understanding of the context and underlying principles of thematic analysis will allow for higher quality research. 16
Practical thematic analysis is a highly flexible approach that can draw out valuable findings and generate new hypotheses, including in cases with a lack of previous research to build on. The approach can also be used with a variety of data, such as transcripts from interviews or focus groups, patient encounter transcripts, professional publications, observational field notes, and online activity logs. Importantly, successful practical thematic analysis is predicated on having high quality data collected with rigorous methods. We do not describe qualitative research design or data collection here. 11 17
In supplemental material 1, we summarise the foundational methods, concepts, and terminology in qualitative research. Along with our guide below, we include a companion slide presentation for teaching practical thematic analysis to research teams in supplemental material 2. We provide a theme coproduction template for teams to use during thematic analysis sessions in supplemental material 3. Our method aligns with the major qualitative reporting frameworks, including the Consolidated Criteria for Reporting Qualitative Research (COREQ). 18 We indicate the corresponding step in practical thematic analysis for each COREQ item in supplemental material 4.
Familiarisation and memoing
We encourage all manuscript authors to review the full dataset (eg, interview transcripts) to familiarise themselves with it. This task is most critical for those who will later be engaged in the coding and theming steps. Although time consuming, it is the best way to involve team members in the intellectual work of data interpretation, so that they can contribute to the analysis and contextualise the results. If this task is not feasible given time limitations or large quantities of data, the data can be divided across team members. In this case, each piece of data should be read by at least two individuals who ideally represent different professional roles or perspectives.
We recommend that researchers reflect on the data and independently write memos, defined as brief notes on thoughts and questions that arise during reading, and a summary of their impressions of the dataset. 2 19 Memoing is an opportunity to gain insights from varying perspectives, particularly from patients, care partners, clinicians, and others. It also gives researchers the opportunity to begin to scope which elements of and concepts in the dataset are relevant to the research question.
Data saturation
The concept of data saturation ( box 2 ) is a foundation of qualitative research. It is defined as the point in analysis at which new data tend to be redundant of data already collected. 21 Qualitative researchers are expected to report their approach to data saturation. 18 Because thematic analysis is iterative, the team should discuss saturation throughout the entire process, beginning with data collection and continuing through all steps of the analysis. 22 During step 1 (reading), team members might discuss data saturation in the context of summary memos. Conversations about saturation continue during step 2 (coding), with confirmation that saturation has been achieved during step 3 (theming). As a rule of thumb, researchers can often achieve saturation in 9-17 interviews or 4-8 focus groups, but this will vary depending on the specific characteristics of the study. 23
Data saturation in context
Braun and Clarke discourage the use of data saturation to determine sample size (eg, number of interviews), because it assumes that there is an objective truth to be captured in the data (sometimes known as a positivist perspective). 20 Qualitative researchers often try to avoid positivist approaches, arguing that there is no one true way of seeing the world, and will instead aim to gather multiple perspectives. 5 Although this theoretical debate with qualitative methods is important, we recognise that a priori estimates of saturation are often needed, particularly for investigators newer to qualitative research who might want a more pragmatic and applied approach. In addition, saturation based, sample size estimation can be particularly helpful in grant proposals. However, researchers should still follow a priori sample size estimation with a discussion to confirm saturation has been achieved.
Definition of coding
We describe codes as labels for concepts in the data that are directly relevant to the study objective. Historically, the purpose of coding was to distil the large amount of data collected into conceptually similar buckets so that researchers could review it in aggregate and identify key themes. 5 24 We advocate for a more analytical approach than is typical with thematic analysis. With our method, coding is both the foundation for and the beginning of thematic analysis—that is, early data analysis, management, and reduction occur simultaneously rather than as different steps. This approach moves the team more efficiently towards being able to describe themes.
Building the coding team
Coders are the research team members who directly assign codes to the data, reading all material and systematically labelling relevant data with appropriate codes. Ideally, at least two researchers would code every discrete data document, such as one interview transcript. 25 If this task is not possible, individual coders can each code a subset of the data that is carefully selected for key characteristics (sometimes known as purposive selection). 26 When using this approach, we recommend that at least 10% of data be coded by two or more coders to ensure consistency in codebook application. We also recommend coding teams of no more than four to five people, for practical reasons concerning maintaining consistency.
Clinicians, patients, and care partners bring unique perspectives to coding and enrich the analytical process. 27 Therefore, we recommend choosing coders with a mix of relevant experiences so that they can challenge and contextualise each other’s interpretations based on their own perspectives and opinions ( box 3 ). We recommend including both coders who collected the data and those who are naive to it, if possible, given their different perspectives. We also recommend all coders review the summary memos from the reading step so that key concepts identified by those not involved in coding can be integrated into the analytical process. In practice, this review means coding the memos themselves and discussing them during the code development process. This approach ensures that the team considers a diversity of perspectives.
Coding teams in context
The recommendation to use multiple coders is a departure from Braun and Clarke. 28 29 When the views, experiences, and training of each coder (sometimes known as positionality) 30 are carefully considered, having multiple coders can enhance interpretation and enrich findings. When these perspectives are combined in a team setting, researchers can create shared meaning from the data. Along with the practical consideration of distributing the workload, 31 inclusion of these multiple perspectives increases the overall quality of the analysis by mitigating the impact of any one coder’s perspective. 30
Coding tools
Qualitative analysis software facilitates coding and managing large datasets but does not perform the analytical work. The researchers must perform the analysis themselves. Most programs support queries and collaborative coding by multiple users. 32 Important factors to consider when choosing software can include accessibility, cost, interoperability, the look and feel of code reports, and the ease of colour coding and merging codes. Coders can also use low tech solutions, including highlighters, word processors, or spreadsheets.
Drafting effective codes
To draft effective codes, we recommend that the coders review each document line by line. 33 As they progress, they can assign codes to segments of data representing passages of interest. 34 Coders can also assign multiple codes to the same passage. Consensus among coders on what constitutes a minimum or maximum amount of text for assigning a code is helpful. As a general rule, meaningful segments of text for coding are shorter than one paragraph, but longer than a few words. Coders should keep the study objective in mind when determining which data are relevant ( box 4 ).
Code types in context
Similar to Braun and Clarke’s approach, practical thematic analysis does not specify whether codes are based on what is evident from the data (sometimes known as semantic) or whether they are based on what can be inferred at a deeper level from the data (sometimes known as latent). 4 12 35 It also does not specify whether they are derived from the data (sometimes known as inductive) or determined ahead of time (sometimes known as deductive). 11 35 Instead, it should be noted that health services researchers conducting qualitative studies often adopt all these approaches to coding (sometimes known as hybrid analysis). 3
In practical thematic analysis, codes should be more descriptive than general categorical labels that simply group data with shared characteristics. At a minimum, codes should form a complete (or full) thought. An easy way to conceptualise full thought codes is as complete sentences with subjects and verbs ( table 1 ), although full sentence coding is not always necessary. With full thought codes, researchers think about the data more deeply and capture this insight in the codes. This coding facilitates the entire analytical process and is especially valuable when moving from codes to broader themes. Experienced qualitative researchers often intuitively use full thought or sentence codes, but this practice has not been explicitly articulated as a path to higher quality coding elsewhere in the literature. 6
Example transcript with codes used in practical thematic analysis 36
- View inline
Depending on the nature of the data, codes might either fall into flat categories or be arranged hierarchically. Flat categories are most common when the data deal with topics on the same conceptual level. In other words, one topic is not a subset of another topic. By contrast, hierarchical codes are more appropriate for concepts that naturally fall above or below each other. Hierarchical coding can also be a useful form of data management and might be necessary when working with a large or complex dataset. 5 Codes grouped into these categories can also make it easier to naturally transition into generating themes from the initial codes. 5 These decisions between flat versus hierarchical coding are part of the work of the coding team. In both cases, coders should ensure that their code structures are guided by their research questions.
Developing the codebook
A codebook is a shared document that lists code labels and comprehensive descriptions for each code, as well as examples observed within the data. Good code descriptions are precise and specific so that coders can consistently assign the same codes to relevant data or articulate why another coder would do so. Codebook development is iterative and involves input from the entire coding team. However, as those closest to the data, coders must resist undue influence, real or perceived, from other team members with conflicting opinions—it is important to mitigate the risk that more senior researchers, like principal investigators, exert undue influence on the coders’ perspectives.
In practical thematic analysis, coders begin codebook development by independently coding a small portion of the data, such as two to three transcripts or other units of analysis. Coders then individually produce their initial codebooks. This task will require them to reflect on, organise, and clarify codes. The coders then meet to reconcile the draft codebooks, which can often be difficult, as some coders tend to lump several concepts together while others will split them into more specific codes. Discussing disagreements and negotiating consensus are necessary parts of early data analysis. Once the codebook is relatively stable, we recommend soliciting input on the codes from all manuscript authors. Yet, coders must ultimately be empowered to finalise the details so that they are comfortable working with the codebook across a large quantity of data.
Assigning codes to the data
After developing the codebook, coders will use it to assign codes to the remaining data. While the codebook’s overall structure should remain constant, coders might continue to add codes corresponding to any new concepts observed in the data. If new codes are added, coders should review the data they have already coded and determine whether the new codes apply. Qualitative data analysis software can be useful for editing or merging codes.
We recommend that coders periodically compare their code occurrences ( box 5 ), with more frequent check-ins if substantial disagreements occur. In the event of large discrepancies in the codes assigned, coders should revise the codebook to ensure that code descriptions are sufficiently clear and comprehensive to support coding alignment going forward. Because coding is an iterative process, the team can adjust the codebook as needed. 5 28 29
Quantitative coding in context
Researchers should generally avoid reporting code counts in thematic analysis. However, counts can be a useful proxy in maintaining alignment between coders on key concepts. 26 In practice, therefore, researchers should make sure that all coders working on the same piece of data assign the same codes with a similar pattern and that their memoing and overall assessment of the data are aligned. 37 However, the frequency of a code alone is not an indicator of its importance. It is more important that coders agree on the most salient points in the data; reviewing and discussing summary memos can be helpful here. 5
Researchers might disagree on whether or not to calculate and report inter-rater reliability. We note that quantitative tests for agreement, such as kappa statistics or intraclass correlation coefficients, can be distracting and might not provide meaningful results in qualitative analyses. Similarly, Braun and Clarke argue that expecting perfect alignment on coding is inconsistent with the goal of co-constructing meaning. 28 29 Overall consensus on codes’ salience and contributions to themes is the most important factor.
Definition of themes
Themes are meta-constructs that rise above codes and unite the dataset ( box 6 , fig 2 ). They should be clearly evident, repeated throughout the dataset, and relevant to the research questions. 38 While codes are often explicit descriptions of the content in the dataset, themes are usually more conceptual and knit the codes together. 39 Some researchers hypothesise that theme development is loosely described in the literature because qualitative researchers simply intuit themes during the analytical process. 39 In practical thematic analysis, we offer a concrete process that should make developing meaningful themes straightforward.
Themes in context
According to Braun and Clarke, a theme “captures something important about the data in relation to the research question and represents some level of patterned response or meaning within the data set.” 4 Similarly, Braun and Clarke advise against themes as domain summaries. While different approaches can draw out themes from codes, the process begins by identifying patterns. 28 35 Like Braun and Clarke and others, we recommend that researchers consider the salience of certain themes, their prevalence in the dataset, and their keyness (ie, how relevant the themes are to the overarching research questions). 4 12 34

Use of themes in practical thematic analysis
Constructing meaningful themes
After coding all the data, each coder should independently reflect on the team’s summary memos (step 1), the codebook (step 2), and the coded data itself to develop draft themes (step 3). It can be illuminating for coders to review all excerpts associated with each code, so that they derive themes directly from the data. Researchers should remain focused on the research question during this step, so that themes have a clear relation with the overall project aim. Use of qualitative analysis software will make it easy to view each segment of data tagged with each code. Themes might neatly correspond to groups of codes. Or—more likely—they will unite codes and data in unexpected ways. A whiteboard or presentation slides might be helpful to organise, craft, and revise themes. We also provide a template for coproducing themes (supplemental material 3). As with codebook justification, team members will ideally produce individual drafts of the themes that they have identified in the data. They can then discuss these with the group and reach alignment or consensus on the final themes.
The team should ensure that all themes are salient, meaning that they are: supported by the data, relevant to the study objectives, and important. Similar to codes, themes are framed as complete thoughts or sentences, not categories. While codes and themes might appear to be similar to each other, the key distinction is that the themes represent a broader concept. Table 2 shows examples of codes and their corresponding themes from a previously published project that used practical thematic analysis. 36 Identifying three to four key themes that comprise a broader overarching theme is a useful approach. Themes can also have subthemes, if appropriate. 40 41 42 43 44
Example codes with themes in practical thematic analysis 36
Thematic analysis session
After each coder has independently produced draft themes, a carefully selected subset of the manuscript team meets for a thematic analysis session ( table 3 ). The purpose of this session is to discuss and reach alignment or consensus on the final themes. We recommend a session of three to five hours, either in-person or virtually.
Example agenda of thematic analysis session
The composition of the thematic analysis session team is important, as each person’s perspectives will shape the results. This group is usually a small subset of the broader research team, with three to seven individuals. We recommend that primary and senior authors work together to include people with diverse experiences related to the research topic. They should aim for a range of personalities and professional identities, particularly those of clinicians, trainees, patients, and care partners. At a minimum, all coders and primary and senior authors should participate in the thematic analysis session.
The session begins with each coder presenting their draft themes with supporting quotes from the data. 5 Through respectful and collaborative deliberation, the group will develop a shared set of final themes.
One team member facilitates the session. A firm, confident, and consistent facilitation style with good listening skills is critical. For practical reasons, this person is not usually one of the primary coders. Hierarchies in teams cannot be entirely flattened, but acknowledging them and appointing an external facilitator can reduce their impact. The facilitator can ensure that all voices are heard. For example, they might ask for perspectives from patient partners or more junior researchers, and follow up on comments from senior researchers to say, “We have heard your perspective and it is important; we want to make sure all perspectives in the room are equally considered.” Or, “I hear [senior person] is offering [x] idea, I’d like to hear other perspectives in the room.” The role of the facilitator is critical in the thematic analysis session. The facilitator might also privately discuss with more senior researchers, such as principal investigators and senior authors, the importance of being aware of their influence over others and respecting and eliciting the perspectives of more junior researchers, such as patients, care partners, and students.
To our knowledge, this discrete thematic analysis session is a novel contribution of practical thematic analysis. It helps efficiently incorporate diverse perspectives using the session agenda and theme coproduction template (supplemental material 3) and makes the process of constructing themes transparent to the entire research team.
Writing the report
We recommend beginning the results narrative with a summary of all relevant themes emerging from the analysis, followed by a subheading for each theme. Each subsection begins with a brief description of the theme and is illustrated with relevant quotes, which are contextualised and explained. The write-up should not simply be a list, but should contain meaningful analysis and insight from the researchers, including descriptions of how different stakeholders might have experienced a particular situation differently or unexpectedly.
In addition to weaving quotes into the results narrative, quotes can be presented in a table. This strategy is a particularly helpful when submitting to clinical journals with tight word count limitations. Quote tables might also be effective in illustrating areas of agreement and disagreement across stakeholder groups, with columns representing different groups and rows representing each theme or subtheme. Quotes should include an anonymous label for each participant and any relevant characteristics, such as role or gender. The aim is to produce rich descriptions. 5 We recommend against repeating quotations across multiple themes in the report, so as to avoid confusion. The template for coproducing themes (supplemental material 3) allows documentation of quotes supporting each theme, which might also be useful during report writing.
Visual illustrations such as a thematic map or figure of the findings can help communicate themes efficiently. 4 36 42 44 If a figure is not possible, a simple list can suffice. 36 Both must clearly present the main themes with subthemes. Thematic figures can facilitate confirmation that the researchers’ interpretations reflect the study populations’ perspectives (sometimes known as member checking), because authors can invite discussions about the figure and descriptions of findings and supporting quotes. 46 This process can enhance the validity of the results. 46
In supplemental material 4, we provide additional guidance on reporting thematic analysis consistent with COREQ. 18 Commonly used in health services research, COREQ outlines a standardised list of items to be included in qualitative research reports ( box 7 ).
Reporting in context
We note that use of COREQ or any other reporting guidelines does not in itself produce high quality work and should not be used as a substitute for general methodological rigor. Rather, researchers must consider rigor throughout the entire research process. As the issue of how to conceptualise and achieve rigorous qualitative research continues to be debated, 47 48 we encourage researchers to explicitly discuss how they have looked at methodological rigor in their reports. Specifically, we point researchers to Braun and Clarke’s 2021 tool for evaluating thematic analysis manuscripts for publication (“Twenty questions to guide assessment of TA [thematic analysis] research quality”). 16
Avoiding common pitfalls
Awareness of common mistakes can help researchers avoid improper use of qualitative methods. Improper use can, for example, prevent researchers from developing meaningful themes and can risk drawing inappropriate conclusions from the data. Braun and Clarke also warn of poor quality in qualitative research, noting that “coherence and integrity of published research does not always hold.” 16
Weak themes
An important distinction between high and low quality themes is that high quality themes are descriptive and complete thoughts. As such, they often contain subjects and verbs, and can be expressed as full sentences ( table 2 ). Themes that are simply descriptive categories or topics could fail to impart meaningful knowledge beyond categorisation. 16 49 50
Researchers will often move from coding directly to writing up themes, without performing the work of theming or hosting a thematic analysis session. Skipping concerted theming often results in themes that look more like categories than unifying threads across the data.
Unfocused analysis
Because data collection for qualitative research is often semi-structured (eg, interviews, focus groups), not all data will be directly relevant to the research question at hand. To avoid unfocused analysis and a correspondingly unfocused manuscript, we recommend that all team members keep the research objective in front of them at every stage, from reading to coding to theming. During the thematic analysis session, we recommend that the research question be written on a whiteboard so that all team members can refer back to it, and so that the facilitator can ensure that conversations about themes occur in the context of this question. Consistently focusing on the research question can help to ensure that the final report directly answers it, as opposed to the many other interesting insights that might emerge during the qualitative research process. Such insights can be picked up in a secondary analysis if desired.
Inappropriate quantification
Presenting findings quantitatively (eg, “We found 18 instances of participants mentioning safety concerns about the vaccines”) is generally undesirable in practical thematic analysis reporting. 51 Descriptive terms are more appropriate (eg, “participants had substantial concerns about the vaccines,” or “several participants were concerned about this”). This descriptive presentation is critical because qualitative data might not be consistently elicited across participants, meaning that some individuals might share certain information while others do not, simply based on how conversations evolve. Additionally, qualitative research does not aim to draw inferences outside its specific sample. Emphasising numbers in thematic analysis can lead to readers incorrectly generalising the findings. Although peer reviewers unfamiliar with thematic analysis often request this type of quantification, practitioners of practical thematic analysis can confidently defend their decision to avoid it. If quantification is methodologically important, we recommend simultaneously conducting a survey or incorporating standardised interview techniques into the interview guide. 11
Neglecting group dynamics
Researchers should concertedly consider group dynamics in the research team. Particular attention should be paid to power relations and the personality of team members, which can include aspects such as who most often speaks, who defines concepts, and who resolves disagreements that might arise within the group. 52
The perspectives of patient and care partners are particularly important to cultivate. Ideally, patient partners are meaningfully embedded in studies from start to finish, not just for practical thematic analysis. 53 Meaningful engagement can build trust, which makes it easier for patient partners to ask questions, request clarification, and share their perspectives. Professional team members should actively encourage patient partners by emphasising that their expertise is critically important and valued. Noting when a patient partner might be best positioned to offer their perspective can be particularly powerful.
Insufficient time allocation
Researchers must allocate enough time to complete thematic analysis. Working with qualitative data takes time, especially because it is often not a linear process. As the strength of thematic analysis lies in its ability to make use of the rich details and complexities of the data, we recommend careful planning for the time required to read and code each document.
Estimating the necessary time can be challenging. For step 1 (reading), researchers can roughly calculate the time required based on the time needed to read and reflect on one piece of data. For step 2 (coding), the total amount of time needed can be extrapolated from the time needed to code one document during codebook development. We also recommend three to five hours for the thematic analysis session itself, although coders will need to independently develop their draft themes beforehand. Although the time required for practical thematic analysis is variable, teams should be able to estimate their own required effort with these guidelines.
Practical thematic analysis builds on the foundational work of Braun and Clarke. 4 16 We have reframed their six phase process into three condensed steps of reading, coding, and theming. While we have maintained important elements of Braun and Clarke’s reflexive thematic analysis, we believe that practical thematic analysis is conceptually simpler and easier to teach to less experienced researchers and non-researcher stakeholders. For teams with different levels of familiarity with qualitative methods, this approach presents a clear roadmap to the reading, coding, and theming of qualitative data. Our practical thematic analysis approach promotes efficient learning by doing—experiential learning. 12 29 Practical thematic analysis avoids the risk of relying on complex descriptions of methods and theory and places more emphasis on obtaining meaningful insights from those close to real world clinical environments. Although practical thematic analysis can be used to perform intensive theory based analyses, it lends itself more readily to accelerated, pragmatic approaches.
Strengths and limitations
Our approach is designed to smooth the qualitative analysis process and yield high quality themes. Yet, researchers should note that poorly performed analyses will still produce low quality results. Practical thematic analysis is a qualitative analytical approach; it does not look at study design, data collection, or other important elements of qualitative research. It also might not be the right choice for every qualitative research project. We recommend it for applied health services research questions, where diverse perspectives and simplicity might be valuable.
We also urge researchers to improve internal validity through triangulation methods, such as member checking (supplemental material 1). 46 Member checking could include soliciting input on high level themes, theme definitions, and quotations from participants. This approach might increase rigor.
Implications
We hope that by providing clear and simple instructions for practical thematic analysis, a broader range of researchers will be more inclined to use these methods. Increased transparency and familiarity with qualitative approaches can enhance researchers’ ability to both interpret qualitative studies and offer up new findings themselves. In addition, it can have usefulness in training and reporting. A major strength of this approach is to facilitate meaningful inclusion of patient and care partner perspectives, because their lived experiences can be particularly valuable in data interpretation and the resulting findings. 11 30 As clinicians are especially pressed for time, they might also appreciate a practical set of instructions that can be immediately used to leverage their insights and access to patients and clinical settings, and increase the impact of qualitative research through timely results. 8
Practical thematic analysis is a simplified approach to performing thematic analysis in health services research, a field where the experiences of patients, care partners, and clinicians are of inherent interest. We hope that it will be accessible to those individuals new to qualitative methods, including patients, care partners, clinicians, and other health services researchers. We intend to empower multidisciplinary research teams to explore unanswered questions and make new, important, and rigorous contributions to our understanding of important clinical and health systems research.
Acknowledgments
All members of the Coproduction Laboratory provided input that shaped this manuscript during laboratory meetings. We acknowledge advice from Elizabeth Carpenter-Song, an expert in qualitative methods.
Coproduction Laboratory group contributors: Stephanie C Acquilano ( http://orcid.org/0000-0002-1215-5531 ), Julie Doherty ( http://orcid.org/0000-0002-5279-6536 ), Rachel C Forcino ( http://orcid.org/0000-0001-9938-4830 ), Tina Foster ( http://orcid.org/0000-0001-6239-4031 ), Megan Holthoff, Christopher R Jacobs ( http://orcid.org/0000-0001-5324-8657 ), Lisa C Johnson ( http://orcid.org/0000-0001-7448-4931 ), Elaine T Kiriakopoulos, Kathryn Kirkland ( http://orcid.org/0000-0002-9851-926X ), Meredith A MacMartin ( http://orcid.org/0000-0002-6614-6091 ), Emily A Morgan, Eugene Nelson, Elizabeth O’Donnell, Brant Oliver ( http://orcid.org/0000-0002-7399-622X ), Danielle Schubbe ( http://orcid.org/0000-0002-9858-1805 ), Gabrielle Stevens ( http://orcid.org/0000-0001-9001-178X ), Rachael P Thomeer ( http://orcid.org/0000-0002-5974-3840 ).
Contributors: Practical thematic analysis, an approach designed for multidisciplinary health services teams new to qualitative research, was based on CHS’s experiences teaching thematic analysis to clinical teams and students. We have drawn heavily from qualitative methods literature. CHS is the guarantor of the article. CHS, AS, CvP, AMK, JRK, and JAP contributed to drafting the manuscript. AS, JG, CMM, JAP, and RWY provided feedback on their experiences using practical thematic analysis. CvP, LCL, SLB, AVC, GE, and JKL advised on qualitative methods in health services research, given extensive experience. All authors meaningfully edited the manuscript content, including AVC and RKS. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding: This manuscript did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests: All authors have completed the ICMJE uniform disclosure form at https://www.icmje.org/disclosure-of-interest/ and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Provenance and peer review: Not commissioned; externally peer reviewed.
- Ziebland S ,
- ↵ A Hybrid Approach to Thematic Analysis in Qualitative Research: Using a Practical Example. 2018. https://methods.sagepub.com/case/hybrid-approach-thematic-analysis-qualitative-research-a-practical-example .
- Maguire M ,
- Vindrola-Padros C ,
- Vindrola-Padros B
- ↵ Vindrola-Padros C. Rapid Ethnographies: A Practical Guide . Cambridge University Press 2021. https://play.google.com/store/books/details?id=n80HEAAAQBAJ
- Schroter S ,
- Merino JG ,
- Barbeau A ,
- ↵ Padgett DK. Qualitative and Mixed Methods in Public Health . SAGE Publications 2011. https://play.google.com/store/books/details?id=LcYgAQAAQBAJ
- Scharp KM ,
- Korstjens I
- Barnett-Page E ,
- ↵ Guest G, Namey EE, Mitchell ML. Collecting Qualitative Data: A Field Manual for Applied Research . SAGE 2013. https://play.google.com/store/books/details?id=-3rmWYKtloC
- Sainsbury P ,
- Emerson RM ,
- Saunders B ,
- Kingstone T ,
- Hennink MM ,
- Kaiser BN ,
- Hennink M ,
- O’Connor C ,
- ↵ Yen RW, Schubbe D, Walling L, et al. Patient engagement in the What Matters Most trial: experiences and future implications for research. Poster presented at International Shared Decision Making conference, Quebec City, Canada. July 2019.
- ↵ Got questions about Thematic Analysis? We have prepared some answers to common ones. https://www.thematicanalysis.net/faqs/ (accessed 9 Nov 2022).
- ↵ Braun V, Clarke V. Thematic Analysis. SAGE Publications. 2022. https://uk.sagepub.com/en-gb/eur/thematic-analysis/book248481 .
- Kalpokas N ,
- Radivojevic I
- Campbell KA ,
- Durepos P ,
- ↵ Understanding Thematic Analysis. https://www.thematicanalysis.net/understanding-ta/ .
- Saunders CH ,
- Stevens G ,
- CONFIDENT Study Long-Term Care Partners
- MacQueen K ,
- Vaismoradi M ,
- Turunen H ,
- Schott SL ,
- Berkowitz J ,
- Carpenter-Song EA ,
- Goldwag JL ,
- Durand MA ,
- Goldwag J ,
- Saunders C ,
- Mishra MK ,
- Rodriguez HP ,
- Shortell SM ,
- Verdinelli S ,
- Scagnoli NI
- Campbell C ,
- Sparkes AC ,
- McGannon KR
- Sandelowski M ,
- Connelly LM ,
- O’Malley AJ ,

9th World Conference on Qualitative Research
The World Conference on Qualitative Research (WCQR) is an annual event that brings together researchers, world-renowned authors, and research groups from 40+ countries, sharing their experiences with qualitative methods, making the WCQR one of the most relevant platforms for discussing and disseminating the best scientific production in Qualitative Research.
The 9th World Conference on Qualitative Research (WCQR2025) will be held from 4 to 6 February 2025 at Jagiellonian University, in Kraków, Poland, and from 11 to 13 February 2025 Online.
The growing success over the years is an essential indicator of a multidisciplinary, committed, and involved community in the context of qualitative research. The WCQR encourages the submission of scientific works that focus on several fields of application in Qualitative Research, from Education to Health, Social Sciences, Engineering and Technology, among others, as well as a crosswise and holistic view, with the approach of several themes and dimensions of research..
Kraków (Poland)
4 to 6 February 2025
11 to 13 February 2025
Researchers from 40+ countries
The place for networking
Renowned keynote speakers
The best authors and researchers in the field
Diverse programme
Register now and secure your spot
Meet one of the main worldwide events dedicated to qualitative research
Exchange experiences with researchers from different areas of knowledge
INTERNATIONAL EVENT
Participants from all over the world
PUBLICATION OF WORKS
Partnership with journals of high impact factor
EVALUATION CRITERIA
Thorough review process of submitted papers
DEDICATED ORGANIZATION
Close and personalized support before, during and after the event

- Keynotes & Plenary Sessions
- Norman K. Denzin Memorial Session
- SIG in Arts-Based Research
- SIG in Autoethnography
- A Day In Spanish and Portuguese (ADISP)
- Coalition for Critical Qualitative Inquiry
- Indigenous Inquiries
- Day in Mixed Methods SIG
- New Materialisms
- SIG In Critical and Poststructural Qualitative Psychology
- Social Work Day
- Registration
- Lifetime Achievement Award
- Qualitative Book Award
- Qualitative Dissertation Award
- Past Award Winners
- Past Congresses
- Collaborating Sites
- IAQI Newsletters
- Qualitative Event Calendar
Full Panel Submission
Individual paper/poster/roundtable submission.
In order to submit, you have to create a new account every year.
For panel submissions, please have the primary presenter of each paper create a submission through the Panel Submissions site. In order to be scheduled correctly, please ensure that each submission uses the same title in the Panel Title field.
Prepare your abstract submission using the following guidelines. The more closely you follow these guidelines, the more likely your abstract will be published error-free. Click on the links for Panel or Paper/Poster/Roundtable Submission to submit your abstract. We encourage Panel submissions. Fully formed panels will receive priority in the scheduling process. The difference between Panels and Roundtables is that panelists are authors or co-authors presenting a paper, whereas roundtable participants don’t necessarily have a paper, but discuss a proposed topic.
For submission questions please consult the Submission FAQs . If you still have a question, contact us at: [email protected]
Trouble logging in?
- You are logging into the right site using the links above.
- Next, make sure you’ve created an account. Do you have two accounts? Is there a typo in your email address?
- If you need your username and password, there is a link on the homepage of the submission site that will ask the system to send them an email with this info.
- If you need further assistance, please contact us at [email protected] .
Submission and participation guidelines
- The official language of the Congress and Congress program is English. Abstracts and panel sessions in other languages, including Spanish, Portuguese, and Turkish are considered and encouraged for the Special Interest Group days.
- There are two categories of submissions: General Congress and Special Interest Groups, previously called pre-congress days (eg. SIG in Spanish and Portuguese, SIG in Social Work, SIG in Indigenous Qualitative Inquiries, etc.). Please choose one category to submit your abstract.
- Panel submissions are comprised of at least four (4) but not more than five (5) papers, each paper with full abstract and author information. Proposals with incomplete abstract/author information will not be considered. Panels are guaranteed an 75-minute slot (individual paper presentations are expected to run 12-15 minutes).
- Abstracts for panels, or individual papers, are limited to 150 words.
- Each panel requires a chair, which can be self-nominated (during the submission process) or assigned by Congress organizers.
- We welcome proposals that broadly cover both traditional and experimental approaches to and practices of qualitative research. Our Congress is committed to helping qualitative researchers from all disciplines and all parts of the world participate in an all-inclusive dialogue about the state of the art in qualitative research.
- All congress sessions take place at venues on the University of Illinois campus.
- Please follow for A Guide to Disability Resources and Services offered at the University of Illinois at Urbana Champaign. Learn more.
- If you have a request for ASL interpretation services, please contact us by 15 February. Please make requests to [email protected] with “ASL Interpreter Request” in the subject line.
Instructions for Formatting Your Abstract Titles, the Abstract, and How to Submit
- Prepare your abstract submission using the following guidelines. The more closely you follow these guidelines, the more likely your abstract will be published error-free.
- Click on the links for Panel or Paper, Poster, or Roundtable Submission to submit your abstract, through the links provided above.
- Plain text.
- DO NOT cut and paste text from an e-mail into the text-block field (not following this requirement will mean data corruption).
- 150 words only – this is an absolute limit. The text box space is finite.
- No soft or hard returns.
- No bullets, hyphens, or other non-text characters.
- No footnotes or bibliography.
- Abstract titles should follow the formatting rules found in The Chicago Manual of Style. Here are some general guidelines.
- Capitalize the first, last, and all major words in between (nouns, pronouns, verbs, adjectives, adverbs, and some conjunctions)
- Lowercase prepositions, regardless of length (in, over, between, on, above, through)
- Lowercase the definite and indefinite articles (a, an, the)
- Lowercase conjunctions (and, or, but, for, nor)
- Hyphenated words-always capitalize the first and second word (Part-Time)
- Faculty Learning Community: Experiences with Qualitative Data Analysis Software Melissa Freeman, University of Georgia
- In Search of Mother: Defining a Mother-Centered Theory for Understanding the Mothering Practices of Poor and Working Class Black Women. Amira Millicent Davis, University of Illinois at Urbana-Champaign
- List authors/contributors with first name, middle initial (optional), and last name (i.e., Norman K. Denzin, Jonathan Wyatt, James Salvo)
- Include affiliation for each author — department, university (i.e., Norman K. Denzin, Institute of Communications Research, University of Illinois at Urbana-Champaign)
- Please note that your online submission (abstract) will be used as the text for the final program and abstract e-book (Once the program is ready, all abstracts are published online in our page and downloadable).
Please prepare your abstract submission using the above guidelines. YOU MUST REGISTER IN ORDER TO APPEAR IN THE PROGRAM . Click on the links for Panel or Paper/Poster Submission to submit your abstract. We encourage Panel submissions. Fully formed panels will receive priority in the scheduling process.

International Conference on Qualitative Research in Sport and Exercise

On behalf of the International Society of Qualitative Research in Sport and Exercise , we are delighted to announce that our International Conference (QRSE) returns in 2024 - July 29th (pre-conference workshops), 30th, 31st & August 1st (main conference). The conference is hosted by the Centre for Qualitative Research and the Department of Health, University of Bath, UK.
Monday the 29th of July will host several qualitative workshop sessions. Details of these will be announced at a later date.
All conference announcements will be made via the website and twitter @qrse2024 @qrsesoc
The QRSE 2024 conference organising committee can be contacted at [email protected]
Please be patient regarding a response. All committee members volunteer their time to make the conference happen whilst doing a full time academic job.
CALL FOR PAPERS
Conference committee, key dates & conta ct details, fees & registration, pre-conference w orkshops, qrse edi conference gr ant, accommodati on, travelling to bath, where next.
Would yo u like to host the 2026 conference?
Please contact [email protected] and [email protected] to express an interest.

Proceedings of the 2022 3rd International Conference on Mental Health, Education and Human Development (MHEHD 2022)
Critical Review of Quantitative and Qualitative Research
There are both advantages and disadvantages involved in quantitative and qualitative research which are underpinned by divergent theories and assumptions. It is usually dependent on the nature of research to choose the appropriate research paradigm. In China’s current educational studies, researchers have the tendency to use mixed method design strategy to address research questions more holistically by combining two different data sources in a single study. So critical assessment of quantitative and qualitative research can help researchers better choose the appropriate research method in their studies.
Download article (PDF)
Cite this article
- PROSPECTIVE STUDENTS
- CURRENT STUDENTS
THE 5TH QUALITATIVE RESEARCH CONFERENCE 2022 (QRC 2022)

Qualitative Health Research Network

2024 Qualitative Health Research Network Conference
“Exploring progress: qualitative health research through crisis, disruption and emergence”.
Than you to everyone who presented, attended, sponsored, and organised the 2024 conference that took place on the 28 th and 29 th February 2024 . This was a virtual conference with a pre-conference in-person workshop day held at University College London a few weeks before (16th of February).
Watch recrordings of the conference via the 'on demand' tab (conference attendees only - available for 60 days)
Conference theme
The QHRN organises biennial international conferences to allow emerging and experienced researchers from within and outside the UCL community to present, experiment with, and learn about qualitative theory, methods, and writing.
For our sixth conference, we turned our attention to what we have learned through crisis and continued disruption, and how this has the potential to aid understanding and inform progress in the field of qualitative health research. This conference embraced the learnings that have arisen in response to ongoing significant political, social and societal disruptions and their impact on human relationships, healthcare services, as well as political and ethical based values.
By focusing on emergence as a lens to understand the challenges and uncertainty we are facing in our work, the conference theme was designed to address questions on how we creatively proceed, and how the variety of responses might align on a spectrum between success and failure. In this way we built a platform for critical reflection and discussion on the complexities that impact us as a global research community.
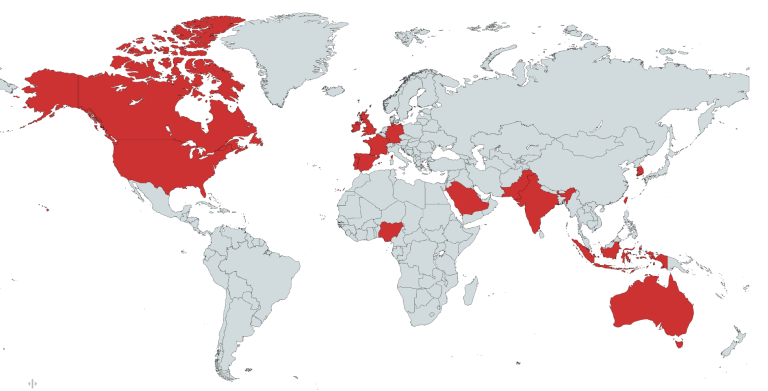
We had just under 200 people register from the conference who came from across 19 countries! See the map below for all the countries where attendees were based.
Conference keynote speakers
We hosted four brilliant keynote speakers including:
- Professor Jennie Popay (Lancaster University) who presented the talk "Critical Qualitative (Public) Health Equity Research: reviewing the present, re-imagining the future".
- Dr Laura Sheard (University of York) who discussed "Telling a story or reporting the facts: Why is descriptive analysis often favoured over interpretative analysis in health research?"
- Dr Sohail Jannesari (Kings College London and Brighton & Sussex Medical School) spoke on "Imaginative Roots: Cultivating Decolonial Methods"
- Dr Alison Thomas (Queen Mary University of London) will discussed "Navigating the tensions of researching patient experience in participatory healthcare design"
Oral presentations
Accepted abstracts were published by BMJ Open. These can be viewed via this link: UCL’s Qualitative Health Research Network Conference Abstracts 2024 .
Conference programme
Click here to view the conference programme
Pre-conference workshops
Our pre-conference workshops was held in-person at University College London on Friday 16th February 2024!
A huge thank you to everyone who organised, hosted, and attended the workshop day! It was a wonderful oppotunity to network, discuss and critically reflect on some of the key elements of qualitative health research, and get involved interactive sessions on innovative approaches.
Clich here to view the QHRN pre-conference workshop programme
Announcements:.
Check out Daniel Turner's (founder and director of Quirkos) blog based on his QHRN pre-conference workshop session!
Titled " NOT Coding Qualitative Data, and Delayed Categorisation"
“ We are proud to announce that our 2024 conference is sponsored by BMJ Open and Quirkos! :
YouTube Widget Placeholder https://www.youtube.com/watch?v=7ALimgN8vv0
YouTube Widget Placeholder https://youtu.be/ojnvEC-lCuI
The QHRN are delighted to be offering bursary places to cover the costs of registration for the QHRN 2024 conference .
The deadline for applying for a bursary place (6th December 2023) has passed and all applicants have now been notified of the outcome of their application. Thank you to eveyone who registered an application.
An amazing day at the QHRN Critical Workshop (3rd of November 2023)

A huge thank you to Yasmin Garcia Sterling and Alma Ionescu for organising this year's QHRN critical workshop, and the wonderful keynote speaker Dr Stephen Roberts (UCL Lecturer in Global Health). This event was part of the lead up to our QHRN international conference ( 28th and 29th February 2024) and gave opportunity to delegates from across England to critically discuss the theme of what we have learned through crisis and continued disruption, and how this has the potential to aid understanding and inform progress in the field of qualitative health research.
Follow @UCL_QHRN
40th Qualitative Analysis Conference "Origin Stories:" Tracing the Origin of Ideas, Selves, and Communities
2024 announcements, the 40th annual qualitative analysis conference: "origin stories:" tracing the origin of ideas, selves, and communities june 26-28, 2024.
Our plenary speakers for 2024 are set! We look forward to welcoming Keynote Speaker Scott Grills (Brandon University), and Featured Speakers Dan Henhawk (University of Manitoba) and Jacqueline Low (Univeristy of New Brunswick)!
We are pleased to announce a return to the Wilfrid Laurier University - Brantford Campus - for the 2024 Qualitatives!
Please follow the links above to find the Call for Papers and instructions to submit an abstract for consideration for the conference.
Emotion impact factors and emotion management strategy among quarantined college students as close contacts during COVID-19 epidemic: a qualitative study
- Published: 16 May 2024
Cite this article

- Lin Zhang ORCID: orcid.org/0000-0002-4051-0772 2 na1 ,
- Yi Mou ORCID: orcid.org/0000-0002-6836-5933 3 na1 &
- Chen Guo ORCID: orcid.org/0000-0003-4291-5412 1 , 4
42 Accesses
Explore all metrics
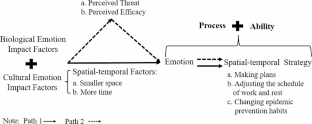
This research aimed to explore the emotion impact factors and emotion management strategies for college students quarantined as close contacts during the COVID-19 outbreak by analyzing data collected in real time (Lee et al. in DARPA information survivability conference and exposition II, DISCEX’01, vol 1, pp 89–100, IEEE, 2001), and built an emotion impact factors—emotion management strategies model. This study was undertaken among colleges in Shanghai Omicron wave in 2022, whose scale exceeded the original outbreak in Wuhan. An exploratory qualitative research design was adopted. From March to April in 2022, in-depth interviews were carried out with 54 Chinese college students with an average age of 19.91 years during the quarantine period, who were identified as close contacts by the local Center for Disease Control and were quarantined at designated quarantine centers away from campus. Data was collected during the quarantine period and was analyzed with grounded theory approach. The results revealed that there were two paths of emotion impact factors and the corresponding emotion management strategies. Participants adopted spatial-temporal, self-care, social support and control strategies to solve emotional issues separately, when they were influenced by different cultural emotion impact factors, including spatial-temporal, personal, interpersonal and informational emotion impact factors. They adopted the same four strategies as well when influenced by the biological emotion impact factors of perceived threat and perceived efficacy (see Figs. 1, 2, 3, 4 in the “Results”). These findings contribute to the framework of Hochschild’s concept of emotion management to understand how college students quarantined as close contacts adapted by combining the cultural and biological emotion impact factors, and combining the process of effort and ability aspects of emotion management during quarantine, and to expand on the concept of emotion management in the context of being in isolation for a period of time, especially in a life-stage vulnerable to emotional issues, and have implications for public health practitioners and policymakers.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Understanding loneliness in the twenty-first century: an update on correlates, risk factors, and potential solutions
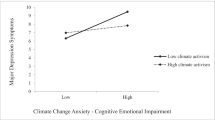
Climate change anxiety and mental health: Environmental activism as buffer

Social Media—The Emotional and Mental Roller-Coaster of Gen Z: An Empirical Study
Data availability.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Aldao, A. (2013). The future of emotion regulation research: Capturing context. Perspectives on Psychological Science , 8 (2), 155–172.
Article PubMed Google Scholar
Arnett, J. J., Žukauskienė, R., & Sugimura, K. (2014). The new life stage of emerging adulthood at ages 18–29 years: Implications for mental health. The Lancet Psychiatry , 1 (7), 569–576.
Bartlett, J. D., Griffin, J., & Thomson, D. (2020). Resources for supporting children’s emotional well-being during the COVID-19 pandemic. Child trends, 12 .
Black, C., Roos, L. L., & Roos, N. P. (2005). From health statistics to health information systems: a new path for the twenty-first century. Health Statistics: Shaping Policy and Practice to Improve the Population’s Health , 443– 61.
Brooks, S. K., Webster, R. K., Smith, L. E., et al. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet , 395 (10227), 912–920.
Article Google Scholar
Buzzi, C., Tucci, M., Ciprandi, R., Brambilla, I., Caimmi, S., Ciprandi, G., & Marseglia, G. L. (2020). The psycho-social effects of COVID-19 on Italian adolescents’ attitudes and behaviors. Italian Journal of Pediatrics , 46 (1), 1–7.
Caplan, G. (1981). Mastery of stress: Psychosocial aspects. The American Journal of Psychiatry .
Chae, J. (2015). Online cancer information seeking increases cancer worry[J]. Computers in Human Behavior , 52 , 144–150.
Changeux, J. P. (1985). Neuronal man: The biology of mind . Oxford University Press.
Charmaz, K. (2006). Constructing grounded theory: A practical guide through qualitative analysis . sage.
China Daily (2022). Dynamic Zero remains best option for China . 27th May,2022. Available: http://hk.ocmfa.gov.cn/eng/zydt_1/202206/t20220604_10698607.htm .
Clabaugh, A., Duque, J. F., & Fields, L. J. (2021). Academic stress and emotional well-being in United States college students following onset of the COVID-19 pandemic. Frontiers in Psychology , 12 , 628787.
Article PubMed PubMed Central Google Scholar
Coan, J. A., & Maresh, E. L. (2014). Social baseline theory and the social regulation of emotion. Handbook of emotion regulation, 2 , 221–236. New York: Guilford Press.
Control, C. C. F. D. (2020). Guidelines for Investigation and Management of Close contacts of COVID-19 cases. China CDC Weekly , 2 (19), 329–331.
Feiz Arefi, M., Babaei-Pouya, A., & Poursadeqiyan, M. (2020). The health effects of quarantine during the COVID-19 pandemic. Work (Reading, Mass.) , 67 (3), 523–527.
PubMed Google Scholar
Fogel, A., Nwokah, E., Dedo, J. Y., Messinger, D., Dickson, K. L., Matusov, E., & Holt, S. A. (1992). Social process theory of emotion: A dynamic systems approach. Social Development , 1 (2), 122–142.
Forte, A., Orri, M., Brandizzi, M., Iannaco, C., Venturini, P., Liberato, D., & Monducci, E. (2021). My life during the Lockdown: Emotional experiences of European adolescents during the COVID-19 Crisis. International Journal of Environmental Research and Public Health , 18 (14), 7638.
Fu, Q., Zhang, X. Y., & Li, S. W. (2020). Strategies for risk management of medical staff’s occupational exposure to COVID-19. Chinese Journal of Nosocomiology , 30 (6), 801–805.
Google Scholar
Gaeta, M. L., Gaeta, L., & Rodriguez, M. A. D. S. (2021). The impact of COVID-19 home confinement on Mexican college students: Emotions, coping strategies, and self-regulated learning. Frontiers in Psychology , 12 , 1323.
Gheorghe, V., & Bouroș, M. (2020). Perceived social support mediates the relationship between emotional intelligence and anxiety levels among adolescents, during the pandemic. Paths of Communication in Postmodernity , 182.
Glaser Barney, G., & Strauss Anselm, L. (1967). The discovery of grounded theory: Strategies for qualitative research. New York Adline De Gruyter , 17 (4), 364.
Gross, J. J. (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology , 2 (3), 271–299.
Gross, J. J. (2014). Emotion regulation: Conceptual and empirical foundations. Handbook of Emotion Regulation , 2 , 3–20.
Han, T., Ma, W. D., Gong, H., et al. (2021). Investigation and analysis of negative emotion among college students during home quarantine of COVID-19. Journal of Xi’an Jiaotong University (Medical Sciences) , 42 (1), 132–136.
Hochschild, A. R. (1979). Emotion work, feeling rules, and social structure. American Journal of Sociology , 85 (3), 551–575.
Jones, K., Mallon, S., & Schnitzler, K. (2021). A scoping review of the psychological and emotional impact of the COVID-19 pandemic on children and young people. Illness Crisis & Loss , 10541373211047191.
Lee, W., Stolfo, S. J., Chan, P. K., Eskin, E., Fan, W., Miller, M., & Zhang, J. (2001, June). Real time data mining-based intrusion detection. In Proceedings DARPA Information Survivability Conference and Exposition II. DISCEX’01 (Vol. 1, pp. 89–100). IEEE.
Levenson, R. W. (1999). The intrapersonal functions of emotion. Cognition & Emotion , 13 (5), 481–504.
Levenson, R. W., Soto, J., & Pole, N. (2007). Emotion, biology, and culture (pp. 780–796). Handbook of cultural psychology.
Levin, L. S., & Idler, E. L. (1983). Self-care in health. Annual Review of Public Health , 4 (1), 181–201.
Levine, L., Kay, A., & Shapiro, E. (2022). The anxiety of not knowing: Diagnosis uncertainty about COVID-19. Current Psychology , 1–8.
Li, R. (2022). Fear of COVID-19: What causes fear and how individuals cope with it. Health Communication , 37 (13), 1563–1572.
Li, Y., & Peng, J. (2020). Coping strategies as predictors of anxiety: Exploring positive experience of Chinese university in health education in COVID-19 pandemic. Creative Education , 11 (5), 735–750.
Liu, X. F. (2013). Study on the connotation and the status of emotion management. Journal of Jiangsu Normal University (Philosophy and Social Sciences Edition) , 39 (6), 141–146.
Liu, S., Lithopoulos, A., Zhang, C. Q., Garcia-Barrera, M. A., & Rhodes, R. E. (2021). Personality and perceived stress during COVID-19 pandemic: Testing the mediating role of perceived threat and efficacy. Personality and Individual Differences , 168 , 110351.
Ma, Z. H., Liu, Z. X., & Xia, Y. W. (2021). Research on the impacts of campus control measures on college students’ mentality and behaviors. Global Journal of Media Studies , 8 (6), 45–68.
Martinelli, N., Gil, S., Belletier, C., Chevalère, J., Dezecache, G., Huguet, P., & Droit-Volet, S. (2021). Time and emotion during lockdown and the COVID-19 epidemic: Determinants of our experience of time? Frontiers in Psychology , 11 , 616169.
Mocan, A. S., Iancu, S. S., & Baban, A. S. (2018). Association of cognitive emotional regulation strategies to depressive symptoms in type 2 diabetes patients. Romanian Journal of Internal Medicine , 56 (1), 34–40. https://doi.org/10.1515/rjim-2017-0037 .
Opitz, P. C., Gross, J. J., & Urry, H. L. (2012). Selection, optimization, and compensation in the domain of emotion regulation: Applications to adolescence, older age, and major depressive disorder. Social and Personality Psychology Compass , 6 (2), 142–155.
Ren, H., He, X., Bian, X., Shang, X., & Liu, J. (2021). The protective roles of exercise and maintenance of daily living routines for Chinese adolescents during the COVID-19 quarantine period. Journal of Adolescent Health , 68 (1), 35–42.
Roberto, A. J., Zhou, X., & Lu, A. H. (2021). The effects of perceived threat and efficacy on college students’ social distancing behavior during the COVID-19 pandemic. Journal of Health Communication , 26 (4), 264–271.
Rogers, A. A., Ha, T., & Ockey, S. (2021). Adolescents’ perceived socio-emotional impact of COVID-19 and implications for mental health: Results from a US-based mixed-methods study. Journal of Adolescent Health , 68 (1), 43–52.
Saarni, C. (1993). Socialization of emotion. In M. Lewis, & J. M. Haviland (Eds.), Handbook of emotions (pp. 435–446). Guilford Press.
Sakakibara, R., & Kitahara, M. (2016). The relationship between cognitive emotion regulation questionnaire (CERQ) and depression, anxiety: Meta-analysis. Shinrigaku Kenkyu: The Japanese Journal of Psychology , 87 (2), 179–185. https://doi.org/10.4992/jjpsy.87.15302 .
Samson, A. C., & Gross, J. J. (2012). Humour as emotion regulation: The differential consequences of negative versus positive humour. Cognition & Emotion , 26 (2), 375–384.
Scherer, K. R. (1994). Emotion serves to decouple stimulus and response. In P. Ekman, & R. J. Davidson (Eds.), The nature of emotion: Fundamental questions (pp. 127–130). Oxford University Press.
Segre, G., Campi, R., Scarpellini, F., Clavenna, A., Zanetti, M., Cartabia, M., & Bonati, M. (2021). Interviewing children: The impact of the COVID-19 quarantine on children’s perceived psychological distress and changes in routine. BMC Pediatrics , 21 (1), 1–11.
Shanahan, L., Steinhoff, A., Bechtiger, L., Murray, A. L., Nivette, A., Hepp, U., & Eisner, M. (2022). Emotional distress in young adults during the COVID-19 pandemic: Evidence of risk and resilience from a longitudinal cohort study. Psychological Medicine , 52 (5), 824–833.
Shanghai Municipal Health Commission (2022). 26th June, 2022. Available: https://wsjkw.sh.gov.cn/xwfb/20220626/3c4144b4ac94405e9a9ceef6987eda61.html .
Southern Weekly (2022, April 2). Expert: The scale of the epidemic in Shanghai is even larger than that in Wuhan, but the severity is lower . Retrieved July 28, 2023, from http://www.infzm.com/contents/225983?source=131 .
Strauss, A., & Corbin, J. (1990). Basics of qualitative research . Sage.
Suls, J. E., & Wills, T. A. E. (1991). Social comparison: Contemporary theory and research . Lawrence Erlbaum Associates, Inc.
Thiruchselvam, R., Hajcak, G., & Gross, J. J. (2012). Looking inward: Shifting attention within working memory representations alters emotional responses. Psychological Science , 23 (12), 1461–1466.
Tian, H., Liu, Y., Li, Y., Wu, C. H., Chen, B., Kraemer, M. U., & Dye, C. (2020). An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science , 368 (6491), 638–642.
Van Maanen, J. (1979). The fact of fiction in organizational ethnography. Administrative Science Quarterly , 24 (4), 539–550.
von Moeller, J., Spengler, K. L., M., et al. (2022). Risk and protective factors of college students’ psychological well-being during the COVID-19 pandemic: Emotional stability, mental health, and household resources. AERA Open , 8 (1), 1–26.
Wang, H., & Wang, Z. Y. (2021). Effects of exercise intervention on anxiety symptoms of isolated college students during the epidemic. Bulletin of Sport Science & Technology , 29 (9), 155.
Wang, Y. H., Chen, D. J., Chen, Y. W., et al. (2022). College students’ generalized anxiety disorder and its relation with meaning in life and boredom during the epidemic. Journal of Guangdong Polytechnic Normal University , 43 (1), 43–50.
Weissman, D. G., Rodman, A. M., Rosen, M. L., Kasparek, S., Mayes, M., Sheridan, M. A., & McLaughlin, K. A. (2021). Contributions of emotion regulation and brain structure and function to adolescent internalizing problems and stress vulnerability during the COVID-19 pandemic: A longitudinal study. Biological Psychiatry Global open Science , 1 (4), 272–282.
WHO (2020, February 11). Key considerations for repatriation and quarantine of travelers in relation to the outbreak of novel coronavirus 2019-nCoV . Retrieved July 28, 2023, from https://www.who.int/news-room/articles-detail/key-considerations-for-repatriation-and-quarantine-of-travellers-in-relation-to-the-outbreak-of-novel-coronavirus-2019-ncov .
Witte, K. (1992). Putting the fear back into fear appeals: The extended parallel process model. Communications Monographs , 59 (4), 329–349.
Witte, K., & Allen, M. (2000). A meta-analysis of fear appeals: Implications for effective public health campaigns. Health Education & Behavior , 27 (5), 591–615.
Xiao, S., & Yang Desen. (1987). &. Effects of social support on physical and mental health[J]. Chinese Mental Health Journal , (4): 183–187.
Xin, M., Luo, S., She, R., et al. (2020). Negative cognitive and psychological correlates of mandatory quarantine during the initial COVID-19 outbreak in China. American Psychologist , 75 (5), 607.
Yin, Q. X., & Zhao, Q. (2021). The relationship between self-efficacy and post-traumatic growth of college students during home quarantine under the COVID-19 epidemic: The mediating role of ruminative meditation . Health Vocational Education.
Zhao, B., Cai, T. J., & Zhang, Z. H. (2020). Presentation and adjustment of college students’ emotional state under COVID-19 Epidemic — based on the perspective of self-care. China Youth Study , (4), 49–54.
Download references
This study was funded by the Philosophy and Social Science Planning Project of Shanghai “Intervention Research on the Internet anxious emotion contagion among College Students from the Perspective of Human-Computer Communication” [grant number:2023BXW004].
Author information
Lin Zhang and Yi Mou are considered as co-first authors.

Authors and Affiliations
Kexue Road NO.100, 450000, Zhengzhou City, Henan Province, China
School of Journalism and Communication, Shanghai University, Shanghai, China
School of Media and Communication, Shanghai Jiao Tong University, Shanghai, China
School of Journalism and Communication, Zhengzhou University, Zhengzhou, China
You can also search for this author in PubMed Google Scholar
Contributions
Design, concepts, interviews, data acquisition, data analysis, and original draft: Lin Zhang. Concepts, manuscript revision and review: Yi Mou and Chen Guo. All authors contributed to the article and approved the submitted version.
Corresponding author
Correspondence to Chen Guo .
Ethics declarations
Conflict of interest.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Zhang, L., Mou, Y. & Guo, C. Emotion impact factors and emotion management strategy among quarantined college students as close contacts during COVID-19 epidemic: a qualitative study. Curr Psychol (2024). https://doi.org/10.1007/s12144-024-06076-4
Download citation
Accepted : 30 April 2024
Published : 16 May 2024
DOI : https://doi.org/10.1007/s12144-024-06076-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emotion impact factors
- Emotion management strategy
- Quarantined college students as close contacts
- COVID-19 quarantine
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 09 May 2024
Overlooked by the obstetric gaze – how women with persistent health problems due to severe perineal trauma experience encounters with healthcare services: a qualitative study
- Katharina Tjernström 1 ,
- Inger Lindberg 1 ,
- Maria Wiklund 2 &
- Margareta Persson 1
BMC Health Services Research volume 24 , Article number: 610 ( 2024 ) Cite this article
184 Accesses
1 Altmetric
Metrics details
During the first year postpartum, about 25 per cent of Swedish women with severe perineal trauma (SPT), i.e., a third- or fourth-degree perineal laceration at childbirth, are unsatisfied with their healthcare contacts. Further, there is a lack of research on the more long-term experiences of healthcare encounters among women with persistent SPT-related health problems. This study explores how women with self-reported persistent SPT-related health problems experience their contact with healthcare services 18 months to five years after childbirth when the SPT occurred.
In this descriptive qualitative study, a purposive sample of twelve women with self-reported persistent health problems after SPT were individually interviewed from November 2020 – February 2022. The data was analysed using inductive qualitative content analysis.
Our results showed a paradoxical situation for women with persistent health problems due to SPT. They struggled with their traumatised body, but healthcare professionals rejected their health problems as postpartum normalities. This paradox highlighted the women’s difficulties in accessing postpartum healthcare, rehabilitation, and sick leave, which left them with neglected healthcare needs, diminished emotional well-being, and loss of financial and social status. Our results indicated that these health problems did not diminish over time. Consequently, the women had to search relentlessly for a ‘key person’ in healthcare who acknowledged their persistent problems as legitimate to access needed care, rehabilitation, and sick leave, thus feeling empowered.
Conclusions
Our study revealed that women with persistent SPT-related health problems experienced complex health challenges. Additionally, their needs for medical care, rehabilitation, and sick leave were largely neglected. Thus, the study highlights an inequitable provision of SPT-related healthcare services in Sweden, including regional disparities in access to care. Hence, the authors suggest that Swedish national guidelines for SPT-related care need to be developed and implemented, applying a woman-centered approach, to ensure equitable, effective, and accessible healthcare.
Peer Review reports
Intrapartum and postpartum healthcare should ideally be high-quality, evidence-based, and a positive experience stemming from woman-centred care with a holistic approach based on human rights [ 1 ]. This approach acknowledges each woman’s articulated needs and expectations in her social, emotional, physical, spiritual, and cultural context [ 2 ]. Nevertheless, during the first year postpartum, about one in four Swedish women with severe perineal trauma (SPT) [ 3 ], i.e., a third- or fourth-degree perineal laceration involving the anal sphincter muscle and anorectal mucosa at vaginal childbirth [ 4 ], are dissatisfied with their care and one in three women report ongoing health problems related to their SPT. Women with SPT may suffer from various physiological and psychological consequences such as pain [ 5 , 6 ] , incontinence [ 7 ], defecation problems [ 8 ], vaginal prolapse [ 5 ], sexual dysfunction [ 9 ] or depression and anxiety [ 10 , 11 , 12 ].
Reducing physical symptoms is essential to support emotional and social recovery after any perineal trauma [ 13 , 14 ]. Women with SPT emphasise that professional, competent, and respectful attitudes from healthcare professionals (HCPs), including individual and adapted information, facilitate, and promote their postpartum recovery. Thus, the HCPs’ competence and knowledge of treatment options is a prerequisite for women to access needed care [ 15 ]. An additional problem in the Swedish context is the lack of national recommendations or guidelines, which enables each of the 21 regions to develop own regional and local guidelines. An audit of the existing regional and local guidelines for prevention and care of SPT shows an unexpected diversity or lack of evidence-based recommendations [ 16 ]. However, dissatisfaction with access to healthcare has been expressed by women with persistent, i.e., beyond one year postpartum, SPT-related health problems [ 6 , 17 ]. Furthermore, women criticise inadequate or absent support [ 6 , 18 ], poor information and education [ 6 , 10 , 18 ], and lack of follow-up care regarding SPT and its potential psychological and social consequences [ 6 , 10 ]. Postpartum care focuses more on the baby than the mother’s well-being [ 18 , 19 ]. Also, the available treatment options are perceived as limited and outdated by those with access to needed care [ 17 , 18 ]. Moreover, women with SPT describe that some HCPs tend to normalise their SPT-related problems [ 10 , 17 , 18 , 19 , 20 , 21 , 22 ], and women are met in unprofessional and disrespectful ways [ 17 , 23 ], where HCPs are perceived as ignorant, nonchalant, and questioning women’s symptoms [ 10 , 17 ]. Previous research [ 24 ] indicates an institutional objectification of women with SPT by Swedish healthcare providers hindering access to healthcare, sick leave, and occupational rehabilitation after SPT. In contrast, women also report being acknowledged and liberated when HCPs have a professional and empathic approach and provide continuity of care that enables access to care for persistent SPT-related health problems [ 17 , 18 , 19 , 25 ]. Thus, several women who sustained an SPT during childbirth do not experience access to needed and necessary care, a fact that needs further exploration.
Globally, sexual and reproductive health and rights (SRHR) are crucial for individual health and gender equality [ 26 ]. Current issues within SRHR and midwifery are controlled by the institutional power in health institutions, i.e., medical power [ 27 ], connected to the still-existing economic and educational disadvantages of women globally, which are also feminist issues [ 26 , 28 ]. As midwife stands for ‘with woman’ [ 28 ], gender or feminist approaches are used in advancing midwifery theory [ 27 , 29 ] and various aspects of SRHR topics such as breastfeeding promotion [ 30 ], birth plans [ 31 ] and attitudes towards contraceptives [ 32 ]. In midwifery and feminist approaches, the biological material body and the socially constructed gendered body are viewed as intertwined [ 33 ]. Moreover, midwifery care is recommended to be woman-centred [ 1 , 2 ], focusing on the individual woman’s needs and transferring control from the institution to the woman herself. However, despite the different organisations of sexual and reproductive healthcare between countries, international research shows similar results regarding women’s diverging experiences with postpartum SPT-related healthcare [ 6 , 15 , 17 , 18 ].
In sum, there is growing evidence showing that many women with persisting health problems caused by SPT are often, but not always, met with mistrust and ignorance when seeking care for their problems. Even though there may be national, regional, or local protocols or guidelines for care after SPT, women with persistent SPT-related problems still raise their voices about the difficulty of getting access to competent quality care. This indicates a potential gender bias [ 34 ] and a need for gender theoretical perspectives in midwifery [ 28 ], as utilized in this study. Additionally, few studies explore the care-seeking experience among this group of women in a longer time perspective after childbirth when the SPT occurred.
The aim of this study is to explore how women with self-reported persistent SPT-related health problems experience their contact with healthcare services 18 months to five years after childbirth when the SPT occurred.
Study design and context
The present study is part of a larger research project investigating the long-term consequences of SPT on quality of life, working life, and healthcare contacts. This study had an inductive qualitative interview study design applying qualitative content analysis to analyse data [ 35 , 36 , 37 ]. This method searches for patterns, e.g., by identifying similarities and differences in the data. The researchers obtain an in-depth understanding of the studied phenomenon through abstraction and interpretation [ 36 ]; thus, an appropriate method to apply to capture women’s experiences of their healthcare encounters when seeking medical help and support. Throughout the research process, the recommendations for qualitative research according to ‘Consolidated criteria for reporting qualitative research’ (COREQ) were followed [ 38 ].
Sweden has 21 partly independent regions primarily responsible for providing healthcare services to the population. Healthcare services are tax-funded, and the regions have extensive autonomy to decide upon the healthcare services within each region based on the frameworks of the Health and Medical Service Act [ 39 ]. Additionally, within the Swedish social security system, 480 days of paid parental leave are allocated to each child in Sweden and can be utilised by their legal guardian(s) until the child is twelve years old. Of these 480 days, 60 days are specifically assigned to each parent, and the remaining days are split between parents as desired. The financial compensation is based on the parent’s income and is financed by taxes [ 40 ].
In Sweden, midwives are the primary care providers to women with normal pregnancies, births, and postpartum care. In case of complications to pregnancy and childbirth, midwives collaborate with other medical professionals, especially obstetricians. For example, midwives suture first- and second-degree perineal lacerations, while obstetricians are responsible for all SPT repairs [ 41 ]. Generally, in Sweden, women who sustain an SPT during childbirth are offered a check-up with the obstetrician responsible for the repair before discharge and should also have a follow-up with an obstetrician or sometimes a physiotherapist within the postnatal period. Thereafter, women with no mayor initial healing problems are advised to contact relevant healthcare services if any health issues related to the SPT should arise in the future. Women presenting with complicated healing are treated accordingly. Additionally, women with second- to fourth-degree perineal lacerations are assessed with questionnaires three times during the first year postpartum by the National Perineal Laceration Register. However, there are no recommendations in Sweden for prolonged check-ups for women with SPT after the postnatal period and no guidelines on organised check-ups for women with prolonged symptoms due to SPT exist [ 42 , 43 ].
Women with persistent SPT-related health problems and characteristics were purposively recruited to achieve a heterogeneous sample reflecting multiple experiences. An overview of inclusion and exclusion criteria can be found in Table 1 .
The closed Swedish Facebook community ‘Förlossningsskadad? Du är inte ensam!’ [‘Injured at childbirth? You are not alone!’] functioned as a recruitment platform for a national sample of women reporting persistent SPT-related health problems. The Facebook community is secluded to women with SPT and started in 2014. During the data collection period (Nov 2020 – Feb 2022), the group had over 7,600 members; today, the community has grown to include over 9,500 members [ 44 ].
In late November 2020, the administrators of the Facebook community pinned a digital poster with study information and a link to the study homepage in the group feed. The study homepage contained written information on the research project and contact details for the research group if any women wanted additional information about the study. Interested potential participants contacted the research group via a contact form on the homepage, and the first author (KT) confirmed that the potential participants met the inclusion criteria via telephone. Thirteen participants from different parts of Sweden showed interest in participating and left their contact information. One woman never responded to our efforts to reach her. The remaining twelve women fulfilled the inclusion criteria and were invited to an interview. Before the interview, the women answered a digital survey on background data (such as demographic data, education, employment, sick leave, and childbirth history) distributed via REDCap ® , a web-based application to create secure online questionnaires and research databases [ 45 ]. The interviews were finalised in February 2022.
Data collection
We collected data via individual open-ended interviews [ 46 ], supported by a semi-structured interview guide [see Additional file 1 ]. The interview guide, developed by KT and MP with input from MW and IL, was based on literature reviews, our awareness of gender as a social construct [ 33 ], and the clinical pre-understanding within the research group. After a pilot interview conducted by KT (not included in the data), minor adjustments were made to the interview guide. The final interview guide covered the topics of everyday life experiences, work, and general functioning. However, despite the mentioned interview topics, the emergent study design and the ability to speak freely about what was perceived as important for their daily functioning, the contacts with healthcare services was brought up in vivid and extensive narratives by all participants as part of their descriptions of their challenges in everyday life and their ability to function at work. Hence, the experiences the women made of the healthcare services played an important role for the women in their daily management of SPT-related health problems.
As data collection occurred during the COVID-19 pandemic, all participants were interviewed digitally via Zoom ® [ 47 , 48 ]. With the participant’s consent, the interviews were audio-recorded via Zoom ® and a separate digital recorder (as backup). Any Zoom video files automatically generated were deleted directly after the termination of the interview to protect participants’ identities. The first author interviewed all women; in two interviews, co-authors (IL or MW) also attended. The authors had no professional or personal affiliation with the enrolled participants . Detailed interviews ranging from 29 – 112 minutes (median: 61.5 minutes) gave extensive data. All interviews were performed in Swedish and transcribed verbatim. After that, the first author validated the transcripts for accuracy by reviewing the text while listening to the recordings.
Authors’ pre-understanding and theoretical positionality
The research group comprises three midwives (KT, IL, MP) and one physiotherapist (MW). We all have extensive professional experiences from clinical practice in primary and in-patient care, where three authors (KT, IL, MP) have specific professional experiences of caring for women with SPT. Additionally, we are women, feminists, and mothers with various birth experiences. Further, the group holds expertise in gender studies and qualitative research within midwifery science, such as perineal trauma and medical sociology. Hence, we stem from a social constructivist research standpoint and utilise ourselves as co-constructors in the analysis process. As feminist researchers, we apply a gender theoretical lens to the data.
Data analysis
The interviews were analysed using qualitative content analysis with an inductive and stepwise approach focusing on the manifest and latent content [ 35 , 36 , 37 ]. The interviews, transcripts, and analysis steps were performed in Swedish.
The analytical procedure started with reading the transcripts multiple times while highlighting text, meaning units, with content relevant to the aim of this study. Then, identified meaning units were condensed, focusing on preserving their core meaning and labelled with manifest codes [ 35 , 36 , 37 ]. Initially, KT coded one interview and triangulated those codes with the principal investigator (MP). KT then coded the rest of the interviews. In the next step, similar codes were clustered, forming subcategories based on the manifest content. Moving towards an interpretation of the content, categories were created by the abstraction of subcategories. This was done by KT and MP separately and then triangulated to identify significant concepts. Next, the preliminary categories and subcategories were triangulated with the whole research group until a consensus was obtained. To answer the question of ‘what?’ and ‘how?’ within the data, the latent content and thread of meaning were identified by clustering and abstracting the emerging findings to form subthemes and a theme [ 36 , 37 ]. The emerging findings were also peer-reviewed and discussed at a research seminar. The finalisation of the analysis resulted in an overarching theme and four subthemes. The translation of categories, subthemes, theme and inserted citations from Swedish into English was performed as a last step. The translation and choice of words were discussed between authors (all knowledgeable in English) to reach a consensus and minimise translation bias.
During the coding process, the researchers used MAXQDA ® [ 49 ], a software for organising, transcribing, analysing, and visualising qualitative research data, and Microsoft Excel ® [ 50 ] as aids to organise the codes.
Demographics of included participants
The background characteristics of the twelve participants in the final sample are presented in Table 2 .
The participants identified themselves as cis women, i.e., their gender identity matched their sex assigned at birth [ 51 ], and are thus referred to as ‘women’ in this paper. All women were in a partner relationship. The women reported a broad spectrum of physical and phycological health problems following the SPT at childbirth, e.g., urine or anal incontinence, pain in the lower abdomen, sexual dysfunction, and depression. Thirty per cent of the women had full-time employment, and the proportion of parental leave varied from 12% to 100% (three women had an ongoing parental leave with subsequent children at the interview). Further, 60% of the women had a sedentary occupation. Five women had been on sick leave after reconstructive surgery, and five reported sick leave for other reasons than their SPT.
The analysis resulted in one theme, ‘Overlooked by the obstetric gaze – living the paradox of a normalised but traumatised postpartum body’, with related subthemes ‘Questioning whether it’s all in my head’, ‘Fighting persistently for access and legitimacy in no (wo)man's-land’, ‘Facing multidimensional losses when no help in sight’, and ‘Depending on other’s advocacy to navigate an arbitrary system’. An overview of the findings is presented in Table 3 . The findings are presented as an overarching theme and thereafter, the related subthemes and categories. Citations from the participants illustrate the findings. All women have been allocated pseudonyms in the result presentation.
Overlooked by the obstetric gaze – living the paradox of a normalised but traumatised postpartum body
The latent theme ‘Overlooked by the obstetric gaze – living the paradox of a normalised but traumatised postpartum body’ represented the women’s experiences of healthcare encounters covering HCPs’ diminishing attitudes towards women’s persistent SPT-related health problems and the women’s difficulties accessing healthcare and sick leave. We interpreted that the women were assessed by the HCPs’ ‘obstetric gaze’, i.e., a medical gaze in postpartum healthcare normalising their persistent health problems and judging the women’s lower abdomen as ‘fine’ by their looks. The obstetric gaze put the women in a paradoxical situation where HCPs normalised tangible symptoms to be a natural part of childbirth. With no medical legitimacy of the health problems, the women also felt labelled as ‘hysterical’ (exaggerating health problems) by the HCPs. As a result, on the one hand, they had to continue facing persistent and tangible health problems such as incontinence, pain or prolapses. On the other hand, no acknowledgement by HCPs of their health problems led them to question whether their problems were merely a product of their imagination and, thus, only existed ‘in their head’. The theme also comprised women’s struggle for legitimacy in a gendered healthcare system - a no-(wo)man's land. They experienced that healthcare services and social insurance systems were challenging to access and demanded a tenacious and extensive fight to obtain legitimacy for their health problems. Consequently, the women had to put up with neglected healthcare needs, negatively impacting their physical and emotional well-being, and financial and social status when no medical help or rehabilitation was available. However, some women had encountered an HCP who was empathic and understanding, hence not guided by the obstetric gaze. Such encounters legitimised persistent problems and were crucial for accessing needed care, sick leave, and rehabilitation.
Questioning whether it’s all in my head
The subtheme ‘Questioning whether it’s all in my head’ focused on the women’s experiences of facing ignoration and no confirmation of perceived health problems and thus being labelled as a hysterical woman. The related categories referred to a normalisation process that the women experienced in their encounters with HCPs, which made them question their bodily perceptions. Furthermore, the women felt accused of exaggerating symptoms because their persistent SPT-related health problems did not match HPCs’ views of acceptable postpartum symptoms. Thus, it could be understood that the women found themselves in a paradox of suffering from tangible physical consequences after SPT, which were normalised by HCPs and their ‘obstetric gaze’.
Facing HCP's ignoration of perceived problems
The women experienced the HCPs defining their persistent health problems after the SPT as ‘normal’. The HCPs assured the women that their problems would disappear with time or that transient motherhood-related aspects, such as breastfeeding or fragile vaginal mucosa, were the cause of the problem. One woman expressed:
“Then I felt, ‘It should not feel like this; this is something wrong’, and I sought medical attention and was seen by multiple physicians […] They thought my vaginal mucous membrane was not ready for intercourse. I was still breastfeeding, so they thought I should stop breastfeeding. Then maybe the mucous membrane would be restored, which was causing me the pain. I was not listened to at all. I was treated very poorly by one physician in particular, and despite second opinions and so on, nobody… nobody took me seriously.” (Linda)
Consequently, the women perceived that their concerns were ignored. They also learned that the HCPs saw their prolonged physical problems after SPT as an inevitable part of childbirth, which the women should accept. One woman resigned:
“But then [the physician] says something like this: ’Well, that's completely normal’, but I felt like, ‘Yes, but it doesn't feel normal'.” (Emma)
After the genital and pelvic floor examinations, the HCPs often guaranteed the women that ‘everything looked fine’, i.e., reinforcing the normality of the genital area. Although the women described to the HCPs that they struggled with SPT-related problems, their concerns were met with a comment on the physical appearance rather than a comprehensive examination of the pelvic floor's functionality.
One woman responded:
“They think ‘everything looks fine’ and ‘everything looks good and repaired’. I still have problems. I was also referred to a surgeon, who did a rectoscopy, and ‘it looked so nice’. Then, I was referred to a urotherapist to learn how to pinch my muscles because ‘everything would be so good’. She helped me get a second opinion in XX [town], where they discovered that there was still damage." (Jin)
Another woman expressed:
”I couldn’t care less what it [genital area] looks like. Nobody will be down there watching. I only need it [genital area] to function as intended.” (Anna)
Consequently, the women felt ignored and unheard in their contact with healthcare services. They perceived that HCPs did not listen to them, leaving them feeling invisible, sometimes even having severe health problems.
“I was hospitalised with sepsis before someone listened to me.” (Josefin)
Being labelled as a hysterical woman
The women also experienced being labelled as the ‘hysterical woman’ who exaggerated their persistent symptoms and had mental health problems. The women described how the HCPs accused them of imagining their SPT-related health problems. One woman indignantly revealed that the HCP she encountered said, 'These problems only exist in your head’ (Joanna), i.e., suggesting that the perceived symptoms did not exist and rejecting the health concerns. Hence, this attitude made some women believe their problems were a product of their imagination and sometimes made them even question their sanity.
Moreover, the HCPs’ condescending attitudes towards the women made them feel dismissed and devalued. For example, the women shared that HCPs laughed at them or were rough or cold during the examination. Moreover, HCPs expressed that they had ‘seen worse’ (Amanda). Some women also conveyed that they were advised ‘to drink some wine to feel better’ (Elin) when discussing painful intercourses due to their SPT-related health problems.
“You are constantly dismissed, ‘No, but everything looks fine, you have no problems’. Then you start to think you’re imagining things. And then you may not dare to talk about the injuries.” (Jin)
Fighting persistently for access and legitimacy in no (wo)man's-land
The subtheme ‘Fighting persistently for access and legitimacy in no (wo)man's-land’ referred to the women’s experience of gender constructs related to inaccessible healthcare services and their often year-long struggles to access this gendered healthcare and linked social insurance systems. The difficulties in accessing care created negative attitudes towards the healthcare services, making the women wish for general improvements in women’s healthcare.
Struggling to access the gendered healthcare and social insurance systems
The women pointed out that after giving birth, they needed more extensive information on their injury, precautions, available help (follow-up care or re-operation), and sick leave. To overcome the lack of required information, they had to request or actively search for it on their own, which also led to uncertainty about where and when to seek further help if needed.
“I was sent home with a brochure and a pat on the shoulder.” (Amanda)
The women also experienced a lack of adequate healthcare services targeted at their SPT-related health problems. For example, many women did not have access to a pelvic floor clinic or had to travel long distances to see specialists. Hence, their place of residence decided the quality of care the women received. Moreover, some women problematised the organisation of postpartum care as they missed out on follow-up care and even, in some cases, were denied follow-up care or referrals to specialised care were lost. As a result, some women had no opportunity to talk to the operating physician or experienced no follow-up care, although they requested it.
“They said it can take up to a year to get better. So, when that year had passed, and before starting to work again, I called different places in the hospital and asked: What should I do now? […] It took several months before I got an appointment with the surgeon for an assessment. And then I had to get a second opinion. So, it took like seven months before I got an appointment at [a specialist clinic].” (Hawa)
For the women, access to healthcare services, sick leave certificates, and HCPs’ dismissive attitudes were perceived as gender-related, i.e., difficulties in obtaining help from women’s healthcare services would not exist if the services were more women-oriented. One woman illustrated this by expressing: ‘If men gave birth to babies, the situation would not be like this’ (Joanna). Moreover, they perceived that women’s healthcare services were not prioritised. They explicitly stated that the absence of sick leave certificates and benefits was related to their gender. The women were expected to cope without sick leave benefits because vaginal and perineal lacerations of any scope were viewed as a natural part of childbirth, a normal process of a woman’s body. Thus, sequelae thereof did not exist or were taboo in society.
“Everything that happens during and after childbirth and related injuries has been a taboo discussion topic, so it has been completely ‘normal’ to suffer from persistent pain.” (Anna)
“I have applied for compensation from the national patient insurance. I got rejection after rejection; nothing has gone wrong. I was told: 'You simply must expect these things in childbirth. And a caesarean section is not less risky'.” (Hawa)
Thus, the women argued that society and the government did not invest needed resources in women’s healthcare. In addition, those few women receiving a short period of sick cash benefits had it immediately after giving birth or after re-operation, but not for prolonged problems. Further, the women noted that they were not offered sick leave certificates due to persistent physical SPT-related health problems but instead due to mental issues, such as depression or anxiety.
“I've heard about women who have been mentally unwell and have hurt their children. So maybe physicians get cautious and put women on sick leave if they say, ‘I'm not feeling mentally well’. Then they act quickly because they think it's so important. But they don't think about the physical injuries because that's part of [childbirth].” (Jenny)
However, the women shared how they fought long and hard for acknowledgement and care and made demands; for many, this process had covered years. They had to repeatedly insist that something was wrong and felt pressure to prove their health problems to the HCPs. In some women, this led to their persistent problems being diagnosed and acknowledged after several years of delay. The struggle for care involved countless visits and referrals to different HCPs, demanding much strength and persistence, which exhausted them. Sometimes, the sequelae had to develop into an acute health situation, or some women decided to pay for private care to access the proper treatment and rehabilitation. Further, with time, they also became explicit about their demands for sick leave certificates and benefits.
“Well, it [short sick leave period because of birth traumas] just feels like scorn. To me, it is not a sufficient length of sick leave.” (Elin)
Wishing for improvement in women's healthcare
The perceived lack of adequate care and rehabilitation, access to sick leave benefits, and HCPs’ attitude negatively influenced the women’s opinions on healthcare services, especially postpartum healthcare. In addition, the women perceived many HCPs as unprofessional, indifferent, and unstructured. As a result, the women mistrusted the HCPs and lost hope in healthcare services. Thus, they were reluctant to seek further care and were anxious about receiving proper treatment or that HCPs would miss important things.
“I am not being listened to in women's healthcare. This is partly why I feel so disappointed.” (Linda) “You just don't trust the healthcare system. […] Some people have been struggling with their injuries for like 18 years. But the [specialist clinic] – I finally received fantastic treatment, and what if it could be available everywhere [in Sweden]?” (Hawa)
Moreover, the women described a struggle for their rights when deciding whether to report the HCPs to the authorities and pointed out the need to improve women’s healthcare. Reporting HCPs was perceived as complicated as the women did not want to blame specific individuals. The women saw that the major problem lay within the healthcare system and with individual HCPs.
“In the end, I met a fantastic person [healthcare professional]. She wanted me to report the mistreatment when I eventually had the strength. Because no one listened when I said I was ill. So, she has offered to help me if I want to, but I don't know if I have the strength to file a complaint.” (Josefin)
A wish to improve women’s healthcare services was articulated, especially regarding personal follow-up care beyond one year postpartum and the possibility of full-time or part-time sick leave certificates and benefits for persistent problems on equal terms. This wish also strengthened their decision not to give up searching for help and to raise their voices to help themselves and other women.
“I received physiotherapy and the follow-up surveys [the Perineal Laceration Register] during the first year, but thereafter I would have liked to have an annual follow-up for the next years to ensure the status and potential re-operations. […] I can google, but I want to have that information in dialog with a living person, but you do not get that.” (Jenny)
Partaking in developing educational material for HCPs or starting a career within women’s healthcare were some women’s ways to contribute and increase competency in persistent SPT-related health problems.
“One of my strategies since I got the injury is also to try to influence. Being able to be involved and influence what postpartum care should consist of.” (Jin)
Facing multidimensional losses when no help in sight
The subtheme ‘Facing multidimensional losses when no help in sight’ covered physical and mental health consequences and the financial and social losses the participating women faced when no support or access to needed care and rehabilitation was provided.
Being physically victimised by HCP's malpractice
The women’s experiences covered either being misdiagnosed during the suturing after birth or in the following years when seeking help for persistent SPT-related health problems. Further, they shared how physicians had incorrectly sutured vaginal and perineal muscles after childbirth, leading the women to live with incontinence, pain, prolapses, or sexual dysfunction if their vaginas were sutured too tight. They also described how they endured infections, wound ruptures, sepsis, necrosis, and re-operations. Additionally, the women perceived a general lack of competency regarding communication and persistent SPT-related health problems, including problems related to sex life and sexual functioning, besides a more specific lack regarding suturing techniques and ultrasound examinations.
“I was referred to a specialist clinic. And they found out that all the muscles were separated, the internal and external sphincters were torn, and my pinching ability was kind of weak. So, it was quite the opposite, really, quite the opposite. None of what the other physician had said was true [laughs]. Absolutely incredible. And she is supposed to be a specialist.” (Hawa)
Aching inside
Living with troubled postpartum bodies and the absence of HCPs’ legitimation of the women´s problems made them struggle mentally, feeling speechless and silenced. This neglect reinforced irritation, anger, distress, bitterness, and disappointment towards the HCPs and the healthcare services. One woman illustrated the emotional struggle in this way:
“It's just that the health services don’t believe you, which makes you feel terrible. It's a big deal that no one listens.” (Josefin)
Moreover, the women felt uncertain about their health status due to a default medical diagnosis with concerns for their future and which staff to trust. Consequently, some had to bite the bullet, put up with their situation, and try to think positively. Other women were denying or diminishing their SPT-related health problems, accepting that their symptoms would improve, even disappear or that their condition was ‘normal’ as they had been told. Further, the women described despair because their neglected health problems caused by their SPT made them feel exposed, unsure, and hopeless. In some, this desperation resulted in a mental breakdown, a fear of losing custody of their child due to mental illness or suicidal thoughts.
“Something broke inside of me that day. I felt entirely omitted; I was close to leaving my son and committing suicide. Nobody understood how bad everything was.” (Elin)
Additionally, the women suffered emotionally when motherhood was crushed. Their partner had to take the primary responsibility for the family, and the children had to come in second place as the mothers suffered from various physical and mental health problems. As a result, the women felt they missed their children’s development and could not use their parental social security benefits as desired.
“I feel devasted because people tell me, ‘You are on maternity leave’. I’m not on maternity leave; I’m sick. I should be on sick leave.” (Jaanika)
Suffering financial and societal losses
Moreover, the women suffered financially and societally due to persistent health problems. Some women were denied financial compensation from Patient Insurance (a national insurance system where patients can seek compensation for care injuries). The Social Security Agency and the HCPs were perceived as obstacles to receiving sick cash benefits. They noted that ‘extensive’ health problems were required to receive sick cash benefits and that their health problems paradoxically were not seen as extensive or even a problem per se by the HCPs; hence, no sick leave certificates were issued.
“He [the physician] tried to argue and clarify my pain situation in the sick leave certificate to meet the requirements for a sick leave benefit at the Social Security Agency. I was in so much pain and had to lie down to breastfeed. But, no, ‘If you can manage to hold the baby when breastfeeding, then you are on maternity leave, not sick leave benefit’ [mimicking the official at the Social Security Agency who rejected the certificate and consequently also the sick cash benefit]”. (Jaanika)
Furthermore, the women were set back financially and societally because they could not work full-time due to their persistent health problems. Therefore, some women chose to compensate for their work absence with part-time parental benefits to diminish their working hours and cover their inability to work due to persistent SPT-related health problems. Without a sick leave certificate, i.e., the physicians or the officials at the Social Security Agency’s acknowledgement of a ‘true’ health problem, partners or other relatives were obliged to adjust their work schedules to support or unburden the woman’s suffering and inability to work full-time. This reduction in working hours for the SPT-affected women and, in some cases, their partners was expressed to potentially negatively affect their upcoming careers and pensions. As a result, the women experienced being caught between stools in the social insurance systems:
“[…] You end up in a position where you are neither on sick leave nor unemployment benefits and at the same time cannot perform any offered work [due to persistent problems]. But multiple societal bodies demand and expect you to be a part of the working force, and nobody really listens.” (Elin)
Depending on other’s advocacy to navigate an arbitrary system
The last subtheme, ‘Depending on other’s advocacy to navigate an arbitrary system’, highlights the women’s experiences of, often by chance, finding a single devoted professional, i.e., a ‘key person’, to access needed care and rehabilitation. Such a ‘key person’ was vital to recognising persistent problems, legitimating symptoms, and enabling access to needed care, sick leave, and rehabilitation. The women who finally had legitimation for their health problems described that the medical diagnosis also came with a feeling of sanity and empowerment, relieving them of their paradoxical situation.
Encountering a ‘key person’ to receive needed care
A support system was a prerequisite for enduring their health problems and finding the strength to fight for access to care. This system could be a partner, other family members, or friends who gave the women power and courage, but most importantly – encountering a professional who saw their problems and provided referrals or other options to obtain the needed help and support. In most cases, women would search for years for competent HCPs, such as midwives, physicians, or physiotherapists, who would listen and acknowledge persistent problems. This ‘key person’ showed empathy and trustworthiness, creating relief and security. Further, the ‘key person’ was portrayed as competent, attentive, professional, and respectful. The ‘key persons’ also shared women’s outrage at the mistreatment and default healthcare they endured. Additionally, these ‘key persons’ were surprised that the women were not on sick cash benefits due to their symptoms and that they had to compensate for their financial situation with parental benefits or reduced working hours and lower salaries. Consequently, finding this ‘key person’, often by chance or word of mouth, was crucial for accessing care and marked a significant turning point in the women’s recovery.
“I sought help from another midwife, as I felt something was wrong. This midwife referred me to the physiotherapist, who referred me to a specialist, who then referred me to surgery and rehabilitation.” (Malin)
Some women received follow-up care for their persistent SPT-related health problems during the first year postpartum. If persistent problems occurred and were acknowledged, the women were offered different surgical approaches with various outcomes, consultations by colon specialists, physiotherapy, and psychiatric care. They were grateful for the help they received but felt more comprehensive care was needed.
Feeling sane and empowered
Confirmation of persistent SPT-related health problems was expressed as liberating, strengthening and, as one woman put it, a ‘win’ (Elin). Receiving a medical diagnosis and appurtenant treatment was relieving because the medical confirmation of the symptoms released a considerable burden. These women described being acknowledged, and the diagnosis proved that health problems existed, and the struggles were not in vain. Furthermore, it explicitly stated to everyone, including themselves, that they were not ‘crazy’, ‘imagining things’ or ‘hysterical’.
“So, my laceration has been classified as an injury caused by the healthcare services. This was somehow a confirmation. It's not just that it's in my head, but it has been established that it is a medical injury, and it could have been avoided.” (Jin)
Alongside feelings of sanity and being legitimised, the women experienced empowerment. The women felt supported and confident. Thus, finding an agency to address the taboo of their SPT by talking openly about it and helping others in the same situation was also seen as therapeutic. Further, the legitimation of the sequelae and access to appropriate care gave them time to heal and process their trauma. Receiving sick leave certificates and benefits was seen as a part of the empowerment and legitimacy of their persistent SPT-related health problems, reducing stress, and easing the financial burden. Furthermore, access to occupational rehabilitation and understanding at work became available. Thus, the women who had received the help they needed after a struggle to obtain it were hopeful about the future and possible recovery.
“I have regained my authority to speak up. It [SPT-related health problems] should be out in the open, not withheld.” (Jaanika)
Our main finding was that women with persistent health problems due to SPT at childbirth were caught in a paradox of living in a normalised but traumatised body, and their health problems were rejected as postpartum normalities. Furthermore, our results elucidated the difficulties in accessing postpartum healthcare, rehabilitation, and sick leave benefits. Therefore, the women struggled with neglected healthcare needs, diminished emotional well-being, and loss of financial and social status. Our study highlighted experiences up to 5 years after sustaining SPT, which showed that some women’s SPT-related health problems do not diminish with time. They faced challenges functioning in daily life, at work, and in society. In contrast, finding a ‘key person’, i.e., a professional who acknowledged the women’s persistent problems as legitimate, was a prerequisite for accessing all the needed care and sick leave and enhancing empowerment for the women. Thus, this ‘key person’ was not blinded by the obstetric gaze and instead used their agency and advocacy as support.
In the following, we will discuss our findings related to other empirical studies and problematise them with theoretical reflections.
The paradox of normalising the postpartum body
In our findings, the paradox arose when the HCPs dismissed physical health problems after SPT despite women’s perceived symptoms. Central in this context was a normalisation process where health problems were regarded as ‘normal’ by HCPs, a phenomenon also found in prior research on SPT [ 17 , 18 , 19 , 20 , 21 , 22 ]. The HCPs’ normalisation of women’s health problems can also be found regarding other medical conditions affecting women, such as pelvic organ prolapse [ 52 ], menstrual pain [ 53 ], endometriosis [ 54 ] or nausea and vomiting during pregnancy [ 55 ]. In light of the medicalisation of women’s healthcare, where the medical field has sought to pathologise natural bodily processes such as pregnancy and childbirth [ 33 ], actual medical conditions such as persistent SPT-related health problems are paradoxically normalised. Our findings, therefore, highlight the need to challenge HCPs’ views of what constitutes a ‘normal postpartum body’ or ‘normal postpartum symptoms’ after sustaining SPT.
The key to healthcare
In the context of denied legitimacy of health problems and neglected needs, it appeared that the women became dependent on the goodwill of a ‘key person’, personified as the respectful, competent, and empathetic HCP. Prior research on SPT has also found women struggling with accessing healthcare [ 6 , 17 ] and specific HCPs as enablers of care [ 12 ]. The dependency on a ‘key person’ to access adequate care might highlight a structural problem within the provision of postpartum SPT-related healthcare. Globally, there are a few national guidelines on SPT management and prevention [ 56 ]. Additionally, no national guidelines regarding postpartum care of SPT exist in Sweden, and pelvic floor teams are only available in some Swedish regions [ 16 ]. In our study, the women lacked information, and competent HCPs were hard to find or located far away. Other studies have shown poor patient information and education as a postpartum problem [ 6 , 10 , 18 ], indicating a need to develop targeted oral and written information on wound healing and recovery. Further, women in Australia describe similar challenges to accessing SPT-related healthcare when having persistent SPT-related health problems [ 18 ]. The absence of national Australian guidelines may have led to inconsistent care, failing to meet women’s healthcare needs. Further, women from rural areas have had additional difficulties accessing needed care. In 2021, a clinical standard for SPT was implemented in Australia, comprising care standards for follow-up [ 57 ]. Thus, to improve the national situation in Sweden, more research and resources must be allocated to develop evidence-based recommendations, preferably internationally accepted guidelines [ 56 ]. Moreover, the accessibility of SPT-related healthcare, such as pelvic floor clinics, needs to be expanded so that women can easily meet their ‘key person’ if required.
Woman-(de)centred care?
We found that HCPs were obstructed by their obstetric gaze when assessing women with persistent SPT-related health problems. Obstetric gaze derives from the medical gaze notions [ 58 ], suggesting a gaze that splits the individual from the body, constructing the care-seeker as a medical object or condition instead of an individual with a social context. This gaze blinded HCPs who normalised obvious health problems. Recent advances in women’s healthcare in industrial countries and midwifery research show development towards continuity of care models with a woman-centred approach in different caseload-midwifery projects and informed choice regarding place of childbirth [ 28 , 59 , 60 , 61 ]. Wom e n-centred care [ 2 ] is a widespread care philosophy within midwifery that advocates for providing individualised care to women. Further, wom a n-centred care emphasises the individual woman’s healthcare needs and situation, incorporating the concepts of choice, control, continuity of caregiver, and self-determination. It can be argued that the obstetric gaze obstructed HCPs in providing wom a n-centred care because they did not acknowledge the women’s healthcare needs. Consequently, the women did not have control over their health situation. Making women feel empowered [ 2 , 62 ] is crucial in woman-centred care. Hence, the ‘key persons’ in our study managed to provide wom a n-centred care where acknowledgement of problems as real medical problems and access to care made the women experience empowerment. Therefore, we argue that guidelines regarding follow-up care after SPT should ideally be developed with wom a n-centred care as its core.
Everything looks fine
The biomedical model has traditionally focused on normality and abnormality rather than health [ 63 ]. Theoretically, the ‘obstetric gaze’ is closely tied to the ‘medical gaze’ and the ‘male gaze’, referring to the biomedical paradigm and its power [ 27 , 58 ]. In our study, the obstetric gaze judged the women’s persistent health problems due to SPT as ‘normal’ and the appearance of their genital area as ‘fine’, which created a paradoxical situation regarding the legitimacy of their ongoing health problems after SPT. Generally, the healthcare sector is critiqued for reducing the body to only incorporating organs and tissue, i.e., focusing on physical symptoms [ 27 ].
The women in our study, of which most showed more than one significant symptom after SPT, noted that HCPs would comment on the physical appearance of the perineal area rather than its functionality by telling them that ‘everything looked fine’. The focus on looks rather than functionality regarding SPT-related health problems aligns with the findings presented by others [ 17 ]. Having women describe how their persistent physical pelvic floor problems after SPT during childbirth are trivialised, normalised, questioned, and labelled as mental health issues is of utmost concern. This implies the need for rapid improvements in HCPs’ knowledge and organisation of care but also raises the question of what is considered a normal status and recovery after any perineal laceration in the short- and long-term perspective. A similar discursive focus on women’s appearance instead of their health problems has also been found among HCPs when women seek care for chronic pain [ 64 ]. The sentence ‘Everything looks fine’ can be interpreted as an objectifying, gendered discourse in an obstetric context. This discourse may reinforce the obstetric gaze and, in the broader sense, the medical gaze [ 58 ]. The Swedish Health and Medical Care Act [ 39 ] advocates for the respectful treatment of patients. Hence, it is noteworthy that the women experienced being judged by the looks of their genital area in their medical encounters rather than HCPs addressing the functionality. Such treatment does not align with the legislation and calls for a discourse analysis of the attitudes of HCPs towards women with persistent SPT-related health problems and their experiences of providing care for affected women.
Being subjected to obstetric gaslighting
In light of the women’s perception of their dismissal as dramatic, illegitimate, and irrational patients, we argue that they faced so-called ‘gaslighting’ in an obstetric context [ 65 , 66 ]. Thus, the women experienced being offered sick leave for mental problems instead of their perceived physical health problems, depicting them as hysterical women who exaggerated their condition. Gaslighting is a concept used in medicine in general [ 66 ] and in obstetrics regarding traumatic childbirth experiences [ 65 ]. The concept of hysteria, i.e., a prior medical diagnosis and historical concept theoretically linked to femininity [ 67 , 68 ] and ‘obstetric gaslighting’ [ 65 ], has also been found in research on women’s chronic pain [ 64 ] and endometriosis [ 69 ]. Men with chronic pain are perceived as brave, and women in pain are hysterical, emotional, whining, malingering, or imagining pain [ 64 ]. Further, women with endometriosis are viewed as ‘reproductive bodies’ with a proneness for hysteria [ 69 ]. Obstetric gaslighting, enforced by the normalisation of SPT-related health problems and the gendered stereotype of women as hysterical patients, puts women with SPT in an inferior position towards HCPs and can, therefore, be interpreted as a demonstration of institutional power [ 65 ]. Hence, being overlooked by the obstetric gaze might constitute a form of obstetric gaslighting, a concept that has not been applied to SPT before.
Implications and significance
Our study indicated that women continue to have problems accessing healthcare for persistent SPT-related health problems several years postpartum. Additionally, women with persistent SPT-related health problems often depended on a ‘key person’ with the competence to open the doors to comprehensive care, as shown in our findings. The Swedish Government launched a multi-million project from 2015 to 2022 to improve and promote women’s health [ 70 ]. Despite this investment, the depicted experiences of the included women reflect upon remaining structural and clinical problems within Swedish healthcare, which need further attention, investigation, and actions. Additionally, there are considerable differences in reported satisfaction and prevalence of complications at the one-year follow-up between the regions [ 3 ], indicating that there are suboptimal healthcare services. With a significant variation in satisfaction and recovery at one year, there are reasons to believe that women with prolonged problems may experience problems getting access to needed care.
Our study also showed that SPT-related healthcare services are not available on equal terms to women with persistent SPT-related health problems. In general, many women within this group had problems accessing care and sick leave for years. However, depending on where the women reside, not all women have access to specialised care. This inequity may be explained by Sweden having 21 self-governing health regions, and in the absence of national guidelines regarding SPT care and follow-up, the healthcare provision for affected women varies. To secure access to postpartum care for women with SPT in general and those with different prerequisites within this group, implementation studies are needed to develop and evaluate the effect of national guidelines for follow-up care regarding SPT.
Strengths and limitations
This study has strengths and limitations that need to be addressed. A significant strength, enhancing credibility and transferability, was providing a clear context and thick descriptions of our results, where we thoroughly portrayed the women’s voices using quotations [ 35 ]. Further, our detailed account of the study context, data collection, and data analysis process facilitated the transferability of our study. Including three women born outside of Sweden added to the variety of the sample and thus improved credibility because qualitative research often overlooks immigrants' experiences. However, the migrant women spoke Swedish well enough to participate in an interview, indicating that they have been living in Sweden for some time and might be familiar with the healthcare system. Finally, the credibility and dependability of this study were also strengthened by the frequent use of interdisciplinary triangulation between the authors throughout data analysis and the writing process, as well as peer review at a research seminar.
A potential limitation was that this study may not have fully explored the situation of women with fourth-degree lacerations or those with lower education, as most participants had third-degree perineal lacerations and higher education. Further, we could not include non-binary persons and same-sex or single parents, which may be a weakness; consequently, future studies should focus on the under-represented participant groups and migrant women needing an interpreter. Additionally, all women responded voluntarily to the study invitation. Thus, our participants might be particularly outspoken about their problems or interested in raising their voices or experiences. However, they represented a variety of persistent SPT-related health problems of various severity, and some had been able to get access to medical help, whereas others had not. Additionally, our findings cohered to similar studies [ 12 , 17 ] covering shorter periods after the SPT, which may indicate that the experiences of the challenging search for needed help remain over time. Therefore, our findings may reflect other women’s experiences seeking care for SPT-related health problems and may be transferable to other women’s experiences with persistent health problems of a rare condition.
The data for this study was comprehensive and rich. Information power in qualitative research is an ongoing discussion, and the number of participants and their representativity can be seen as a limitation of credibility and transferability [ 71 , 72 ]. Graneheim, Lindgren and Lundman [ 36 ] argue that sample size should be determined by the study’s aim and the data’s quality so that variations in experiences can be captured. They do, therefore, not recommend a specific number of participants, but others do [ 71 ]. With this in mind, the authors believe that the women’s detailed descriptions of the included concepts and the extensive length of the conducted interviews enabled us to achieve sufficient information power based on the richness of the data [ 72 ].
By qualitatively exploring how women with persistent SPT-related health problems experienced their healthcare encounters, we interpreted that they faced a paradox of being reassured of normality by HCPs despite reporting sequelae symptoms. Thus, women’s needs for medical care, rehabilitation, and sick leave were largely neglected. Further, our study might indicate a structural problem within women’s postpartum healthcare, indicating that access to care depended on encountering a ‘key person’, a professional who acknowledged persistent problems as real symptoms. Access to quality care provided with a professional attitude was essential for the future well-being of women with persistent SPT-related health problems. Thus, it should not depend on meeting a single ‘key person’. Therefore, national guidelines for long-term postpartum care of persistent SPT-related health problems must be developed in Sweden. Additionally, to ensure that healthcare services meet the individual needs of women with persistent SPT-related health problems, it is crucial to consider arranging the organisation and availability of quality care for these women from a woman-centred perspective.
Availability of data and materials
The original recordings and transcripts from the current study are not publicly available due to securing the individual privacy and confidentiality of the participants. Data are available from the corresponding author upon reasonable request.
Abbreviations
Healthcare professionals
Interquartile range
Strategic Research Area Health Care Science
- Severe perineal trauma
Sexual and reproductive health and rights
World Health Organisation
World Health Organization (WHO). WHO recommendations: Intrapartum care for a positive childbirth experience. Geneva: WHO; 2018. Cited 2024 Feb 14. Available from: https://www.who.int/publications/i/item/9789241550215 .
Leap N. Woman-centred or women-centred care: does it matter? Br J Midwifery. 2009;17(1):12–6.
Article Google Scholar
Uustal E. Bristning vid förlossning grad 3 - 4. Årsrapport från GynOp-registret avseende operationer utförda år 2022. [Laceration at childbirth, grade 3 - 4, Annual Report of surgeries 2022]. Umeå: The Swedish National Quality Register of Gynecological Surgery; 2023. Cited 2024 Maj 8. Available from: https://www.gynop.se/rapporter/arsrapporter/ .
World Health Organization (WHO). International statistical classification of diseases and related health problems (ICD) 10th revision. Geneva: WHO; 2019. Cited 2024 Maj 8. Available from: https://icd.who.int/browse10/2019/en .
d’Almeida I. Women’s experiences following obstetric anal sphincter injury. J Pelvic Obstet Gynaecol Physiother. 2020;127:39–50.
Google Scholar
Darmody E, Bradshaw C, Atkinson S. Women’s experience of obstetric anal sphincter injury following childbirth: An integrated review. Midwifery. 2020;91:102820.
Article PubMed Google Scholar
LaCross A, Groff M, Smaldone A. Obstetric anal sphincter injury and anal incontinence following vaginal birth: a systematic review and meta-analysis. J Midwifery Women’s Health. 2015;60(1):37–47.
Samarasekera DN, Bekhit MT, Wright Y, Lowndes RH, Stanley KP, Preston JP, et al. Long-term anal continence and quality of life following postpartum anal sphincter injury. Colorectal Dis. 2008;10(8):793–9.
Article CAS PubMed Google Scholar
Andreucci CB, Bussadori JC, Pacagnella RC, Chou D, Filippi V, Say L, et al. Sexual life and dysfunction after maternal morbidity: a systematic review. BMC Pregnancy Childbirth. 2015;15:307.
Article PubMed PubMed Central Google Scholar
Beck CT. Effects of fourth-degree perineal lacerations on women’s physical and mental health. J Obstet Gynecol Neonatal Nurs. 2021;50(2):133–42.
Keighley MR, Perston Y, Bradshaw E, Hayes J, Keighley DM, Webb S. The social, psychological, emotional morbidity and adjustment techniques for women with anal incontinence following Obstetric Anal Sphincter Injury: use of a word picture to identify a hidden syndrome. BMC Pregnancy Childbirth. 2016;16(1):275.
Article CAS PubMed PubMed Central Google Scholar
Lindqvist M, Lindberg I, Nilsson M, Uustal E, Persson M. “Struggling to settle with a damaged body” - A Swedish qualitative study of women’s experiences one year after obstetric anal sphincter muscle injury (OASIS) at childbirth. Sex Reprod Healthc. 2019;19:36–41.
Shoorab NJ, Taghipour A, Mirteimouri M, Roudsari RL. Social recovery: a neglected dimension of caring for women with perineal trauma in Iran. Iran J Nurs Midwifery Res. 2020;25(4):333–40.
Jahani Shoorab N, Mirteimouri M, Taghipour A, Latifnejad Roudsari R. Women’s experiences of emotional recovery from childbirth-related perineal trauma: a qualitative content analysis. Int J Community Based Nurs Midwifery. 2019;7(3):181–91.
PubMed Google Scholar
Swedish Agency for Health Technology Assessment and Assessment of Social Services. Practices to improve detection of perineal tears and women’s views and experiences of healthcare providers following sustained perineal tear. A systematic review. 2021. Report No.: 323.
Persson M, Lindberg I, Ohman A. Regional and clinical guidelines for prevention and care of obstetric anal sphincter injuries - A critical frame analysis. Midwifery. 2023;119:103608.
Huber M, Tunon K, Lindqvist M. “From hell to healed” - A qualitative study on women’s experience of recovery, relationships and sexuality after severe obstetric perineal injury. Sex Reprod Healthc. 2022;33:100736.
Priddis HS, Schmied V, Kettle C, Sneddon A, Dahlen HG. “A patchwork of services”–caring for women who sustain severe perineal trauma in New South Wales–from the perspective of women and midwives. BMC Pregnancy Childbirth. 2014;14:236.
Priddis H, Schmied V, Dahlen H. Women’s experiences following severe perineal trauma: a qualitative study. BMC Womens Health. 2014;14(1):32.
Williams A, Lavender T, Richmond DH, Tincello DG. Women’s experiences after a third-degree obstetric anal sphincter tear: a qualitative study. Birth. 2005;32(2):129–36.
Herron-Marx S, Williams A, Hicks C. A Q methodology study of women’s experience of enduring postnatal perineal and pelvic floor morbidity. Midwifery. 2007;23(3):322–34.
Crookall R, Fowler G, Wood C, Slade P. A systematic mixed studies review of women’s experiences of perineal trauma sustained during childbirth. J Adv Nurs. 2018;74(9):2038–52.
Priddis H, Dahlen H, Schmied V. Women’s experiences following severe perineal trauma: a meta-ethnographic synthesis. J Adv Nurs. 2013;69(4):748–59.
Tjernström K, Lindberg I, Wiklund M, Persson M. Negotiating the ambiguity of an (in)authentic working life: a grounded theory study into severe perineal trauma. BMC Women’s Health. 2023;23(1):47.
Lindqvist M, Persson M, Nilsson M, Uustal E, Lindberg I. “A worse nightmare than expected” - a Swedish qualitative study of women’s experiences two months after obstetric anal sphincter muscle injury. Midwifery. 2018;61:22–8.
United Nations. The Sustainable Development Goals Report 2022. New York City: United Nations; 2022. Cited 2024 Feb 24. Available from: https://unstats.un.org/sdgs/report/2022/ .
Fahy K, Foureur M, Hastie C. Birth territory and midwifery guardianship : theory for practice, education, and research. Edinburgh: Books for Midwives; 2008.
Walsh D, Christianson M, Stewart M. Why midwives should be feminists. Midirs Midwifery Digest. 2015;25(2):154–60.
Buchanan K, Newnham E, Geraghty S, Whitehead L. Navigating midwifery solidarity: a feminist participatory action research framework. Women Birth. 2023;36(1):e169–74.
Benoit B, Goldberg L, Campbell-Yeo M. Infant feeding and maternal guilt: The application of a feminist phenomenological framework to guide clinician practices in breast feeding promotion. Midwifery. 2016;34:58–65.
Westergren A, Edin K, Walsh D, Christianson M. Autonomous and dependent-The dichotomy of birth: a feminist analysis of birth plans in Sweden. Midwifery. 2019;68:56–64.
Alspaugh A, Barroso J, Reibel M, Phillips S. Women’s contraceptive perceptions, beliefs, and attitudes: an integrative review of qualitative research. J Midwifery Womens Health. 2020;65(1):64–84.
Davis DL, Walker K. Re-discovering the material body in midwifery through an exploration of theories of embodiment. Midwifery. 2010;26(4):457–62.
Govender V, Penn-Kekana L. Gender biases and discrimination: a review of health care interpersonal interactions. Global Public Health. 2008;3(sup1):90–103.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: a discussion paper. Nurse Educ Today. 2017;56:29–34.
Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108:103632.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Ministry of Health and Social Affairs. Hälso- och sjukvårdslag (2017:30) [Health and Medical Care Act]. Stockholm: The Swedish Riksdag; 2017. Cited 2024 Maj 8. Available from: https://www.riksdagen.se/sv/dokument-och-lagar/dokument/svensk-forfattningssamling/halso-och-sjukvardslag-201730_sfs-2017-30/ .
The Swedish Social Insurance Agency. Parental benefits. 2023. Cited 2024 Feb 20. Available from: https://www.forsakringskassan.se/english/parents/when-the-child-is-born/parental-benefit .
The Swedish Association of Midwives. Kompetensbeskrivning för legitimerad barnmorska [Description of competences for registered midwives]. Stockholm: The Swedish Association of Midwives; 2018. Updated 2019 Jan. Cited 2024 Feb 20. Available from: https://storage.googleapis.com/barnmorskeforbundet-se/uploads/2020/04/Kompetensbeskrivning-for-legitimerad-barnmorska.pdf .
Bäckenbottenutbildning [Pelvic floor education]. Utbildningsmaterial: Uppföljning [Educational material: Follow-up]. 2022. Cited 2024 Maj 8. Available from: https://backenbottenutbildning.se/index.php/utbildningsmaterial/uppfoljning .
GynOp [The Swedish National Quality Register of Gynecological Surgery]. About GynOp. 2023. Cited 2024 Feb 20. Available from: https://www.gynop.se/home/about-gynop/ .
Öhman H, Schesny S, Bearth L, Löwendahl J. Förlossningsskadad? Du är inte ensam! [Injured at childbirth? You are not alone!’]. 2014. Cited 2024 Feb 20. Available from: https://www.facebook.com/groups/forlossningsskadad/ .
Vanderbilt University. About REDCap. Nashville: Vanderbilt; 2023. Updated 2023. Cited 2024 Feb 20. Available from: https://projectredcap.org/about/ .
Kvale S, Brinkmann S. Interviews: learning the craft of qualitative research interviewing. 2nd ed. Los Angeles: Sage Publications; 2009.
Keen S, Lomeli-Rodriguez M, Joffe H. From challenge to opportunity: virtual qualitative research during COVID-19 and beyond. Int J Qual Methods. 2022;21:16094069221105076.
Thunberg S, Arnell L. Pioneering the use of technologies in qualitative research - A research review of the use of digital interviews. Int J Soc Res Methodol. 2022;25(6):757–68.
MAXQDA. Why MAXQDA? Berlin: VERBI Software GmbH; 2024. Cited 2024 Maj 8. Available from: https://www.maxqda.com/why-maxqda .
Microsoft. Microsoft Excel. Redmond: Microsoft; 2024. Cited 2024 Maj 8. Available from: https://www.microsoft.com/sv-se/microsoft-365/excel?market=se .
Griffin GA. Dictionary of Gender Studies. Oxford: Oxford University Press; 2017.
Book Google Scholar
Abhyankar P, Uny I, Semple K, Wane S, Hagen S, Wilkinson J, et al. Women’s experiences of receiving care for pelvic organ prolapse: a qualitative study. BMC Womens Health. 2019;19(1):45.
Scott KD, Hintz EA, Harris TM. “Having pain is normal”: How talk about chronic pelvic and genital pain reflects messages from menarche. Health Commun. 2022;37(3):296–306.
Pettersson A, Bertero CM. How women with endometriosis experience health care encounters. Womens Health Rep (New Rochelle). 2020;1(1):529–42.
Heitmann K, Svendsen HC, Sporsheim IH, Holst L. Nausea in pregnancy: attitudes among pregnant women and general practitioners on treatment and pregnancy care. Scand J Prim Health Care. 2016;34(1):13–20.
Roper JC, Amber N, Wan OYK, Sultan AH, Thakar R. Review of available national guidelines for obstetric anal sphincter injury. Int Urogynecol J. 2020;31(11):2247–59.
The Australian Commission on Safety and Quality in Health Care. Third and Fourth Degree Perineal Tears Clinical Care Standard. Sydney: The Australian Commission on Safety and Quality in Health Care; 2021. Cited 2024 Feb 20. Available from: https://www.safetyandquality.gov.au/standards/clinical-care-standards/third-and-fourth-degree-perineal-tears-clinical-care-standard .
Foucault M, Sheridan A. The birth of the clinic: an archaeology of medical perception. 3rd ed. London: Routledge; 2003.
Scarf VL, Rossiter C, Vedam S, Dahlen HG, Ellwood D, Forster D, et al. Maternal and perinatal outcomes by planned place of birth among women with low-risk pregnancies in high-income countries: a systematic review and meta-analysis. Midwifery. 2018;62:240–55.
Offerhaus P, Jans S, Hukkelhoven C, de Vries R, Nieuwenhuijze M. Women’s characteristics and care outcomes of caseload midwifery care in the Netherlands: a retrospective cohort study. BMC Pregnancy Childbirth. 2020;20(1):517.
Forster DA, McLachlan HL, Davey MA, Biro MA, Farrell T, Gold L, et al. Continuity of care by a primary midwife (caseload midwifery) increases women’s satisfaction with antenatal, intrapartum and postpartum care: results from the COSMOS randomised controlled trial. BMC Pregnancy Childbirth. 2016;16:28.
Brady S, Lee N, Gibbons K, Bogossian F. Woman-centred care: an integrative review of the empirical literature. Int J Nurs Stud. 2019;94:107–19.
Findlay D. The medical gaze: medical models, power, and women’s health. Atlantis. 1992;18(1&2):104–24.
Samulowitz A, Gremyr I, Eriksson E, Hensing G. “Brave Men” and “Emotional Women”: a theory-guided literature review on gender bias in health care and gendered norms towards patients with chronic pain. Pain Res Manag. 2018;2018:6358624.
Fielding-Singh P, Dmowska A. Obstetric gaslighting and the denial of mothers’ realities. Soc Sci Med (1982). 2022;301:114938.
Sebring JCH. Towards a sociological understanding of medical gaslighting in western health care. Sociol Health Ill. 2021;43(9):1951–64.
Jones CE. Wandering wombs and “female troubles”: the hysterical origins, symptoms, and treatments of endometriosis. Women Stud. 2015;44(8):1083–113.
Tasca C, Rapetti M, Carta MG, Fadda B. Women and hysteria in the history of mental health. Clin Pract Epidemiol Ment Health. 2012;8:110–9.
Young K, Fisher J, Kirkman M. “Do mad people get endo or does endo make you mad?”: Clinicians’ discursive constructions of Medicine and women with endometriosis. Fem Psychol. 2019;29(3):337–56.
The Swedish Ministry of Health and Social Affairs. Överenskommelse om en förbättrad förlossningsvård och insatser för kvinnors hälsa [Agreement on improving maternity care and women's health] [Internet]. Stockholm: The Swedish Government; 2015. S2015/07777/FS. [cited 2024 Maj 8]. Available from: https://www.regeringen.se/overenskommelser-och-avtal/2015/12/overenskommelse-om-en-forbattrad-forlossningsvard-och-insatser-for-kvinnors-halsa/ .
Boddy CR. Sample size for qualitative research. Qual Mark Res. 2016;19(4):426–32.
Malterud K, Siersma VD, Guassora AD. Sample size in qualitative interview studies: guided by information power. Qual Health Res. 2016;26(13):1753–60.
Download references
Acknowledgements
We want to thank the participating women for generously sharing their experiences.
Open access funding provided by Umea University. This work was supported by the Research Lift (SWE: Forskningslyftet) and Strategic Research Area Health Care Science (SFO-V), Umeå University. The funders had no specific role in the conceptualisation, design, data collection, analysis, publication decision, or manuscript preparation.
Author information
Authors and affiliations.
Department of Nursing, Umeå University, 901 87, Umeå, Sweden
Katharina Tjernström, Inger Lindberg & Margareta Persson
Department of Community Medicine and Rehabilitation, Section of Physiotherapy, Umeå University, 901 87, Umeå, Sweden
Maria Wiklund
You can also search for this author in PubMed Google Scholar
Contributions
KT: conceptualisation; data curation; formal analysis; investigation; methodology; validation; visualisation; writing - original draft; writing - review & editing. IL: conceptualisation; methodology; supervision; visualisation; writing - review & editing. MW: conceptualisation; methodology; supervision; visualisation; writing - review & editing. MP: conceptualisation; data curation; funding acquisition; methodology; project administration; supervision; visualisation; writing - review & editing. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Katharina Tjernström .
Ethics declarations
Ethics approval and consent to participate.
The Swedish Ethical Review Authority approved the study. An amendment to the original ethical approval of the research project to further explore the experiences of encounters with healthcare services was obtained (Dnr: 2020-035410908 and Dnr: 2022-02784-02). The study was undertaken in compliance with research ethics guidelines. All participation was voluntary, and participants received oral and written information about the study and provided written informed consent before the interviews. No interview questions were mandatory, and the women decided if and how detailed they wanted to share their experiences.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12913_2024_11037_moesm1_esm.pdf.
Additional file 1. Semi-structured interview guide for individual interviews; contains interview questions aimed at highlighting the experience of everyday life and working life after suffering 3 rd or 4 th degree perineal laceration at childbirth (i.e., severe perineal trauma [SPT]).
Additional file 2. Consolidated criteria for reporting qualitative studies (COREQ): 32-item checklist.
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Tjernström, K., Lindberg, I., Wiklund, M. et al. Overlooked by the obstetric gaze – how women with persistent health problems due to severe perineal trauma experience encounters with healthcare services: a qualitative study. BMC Health Serv Res 24 , 610 (2024). https://doi.org/10.1186/s12913-024-11037-5
Download citation
Received : 11 September 2023
Accepted : 23 April 2024
Published : 09 May 2024
DOI : https://doi.org/10.1186/s12913-024-11037-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Persistent health problems
- Qualitative content analysis
- Healthcare encounters
- Postpartum healthcare
- Normalisation
- Access to care
- Empowerment
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- Open access
- Published: 13 May 2024
Sexual and reproductive health implementation research in humanitarian contexts: a scoping review
- Alexandra Norton 1 &
- Hannah Tappis 2
Reproductive Health volume 21 , Article number: 64 ( 2024 ) Cite this article
202 Accesses
6 Altmetric
Metrics details
Meeting the health needs of crisis-affected populations is a growing challenge, with 339 million people globally in need of humanitarian assistance in 2023. Given one in four people living in humanitarian contexts are women and girls of reproductive age, sexual and reproductive health care is considered as essential health service and minimum standard for humanitarian response. Despite growing calls for increased investment in implementation research in humanitarian settings, guidance on appropriate methods and analytical frameworks is limited.
A scoping review was conducted to examine the extent to which implementation research frameworks have been used to evaluate sexual and reproductive health interventions in humanitarian settings. Peer-reviewed papers published from 2013 to 2022 were identified through relevant systematic reviews and a literature search of Pubmed, Embase, PsycInfo, CINAHL and Global Health databases. Papers that presented primary quantitative or qualitative data pertaining to a sexual and reproductive health intervention in a humanitarian setting were included.
Seven thousand thirty-six unique records were screened for inclusion, and 69 papers met inclusion criteria. Of these, six papers explicitly described the use of an implementation research framework, three citing use of the Consolidated Framework for Implementation Research. Three additional papers referenced other types of frameworks used in their evaluation. Factors cited across all included studies as helping the intervention in their presence or hindering in their absence were synthesized into the following Consolidated Framework for Implementation Research domains: Characteristics of Systems, Outer Setting, Inner Setting, Characteristics of Individuals, Intervention Characteristics, and Process.
This review found a wide range of methodologies and only six of 69 studies using an implementation research framework, highlighting an opportunity for standardization to better inform the evidence for and delivery of sexual and reproductive health interventions in humanitarian settings. Increased use of implementation research frameworks such as a modified Consolidated Framework for Implementation Research could work toward both expanding the evidence base and increasing standardization.
Plain English summary
Three hundred thirty-nine million people globally were in need of humanitarian assistance in 2023, and meeting the health needs of crisis-affected populations is a growing challenge. One in four people living in humanitarian contexts are women and girls of reproductive age, and provision of sexual and reproductive health care is considered to be essential within a humanitarian response. Implementation research can help to better understand how real-world contexts affect health improvement efforts. Despite growing calls for increased investment in implementation research in humanitarian settings, guidance on how best to do so is limited. This scoping review was conducted to examine the extent to which implementation research frameworks have been used to evaluate sexual and reproductive health interventions in humanitarian settings. Of 69 papers that met inclusion criteria for the review, six of them explicitly described the use of an implementation research framework. Three used the Consolidated Framework for Implementation Research, a theory-based framework that can guide implementation research. Three additional papers referenced other types of frameworks used in their evaluation. This review summarizes how factors relevant to different aspects of implementation within the included papers could have been organized using the Consolidated Framework for Implementation Research. The findings from this review highlight an opportunity for standardization to better inform the evidence for and delivery of sexual and reproductive health interventions in humanitarian settings. Increased use of implementation research frameworks such as a modified Consolidated Framework for Implementation Research could work toward both expanding the evidence base and increasing standardization.
Peer Review reports
Over the past few decades, the field of public health implementation research (IR) has grown as a means by which the real-world conditions affecting health improvement efforts can be better understood. Peters et al. put forward the following broad definition of IR for health: “IR is the scientific inquiry into questions concerning implementation – the act of carrying an intention into effect, which in health research can be policies, programmes, or individual practices (collectively called interventions)” [ 1 ].
As IR emphasizes real-world circumstances, the context within which a health intervention is delivered is a core consideration. However, much IR implemented to date has focused on higher-resource settings, with many proposed frameworks developed with particular utility for a higher-income setting [ 2 ]. In recognition of IR’s potential to increase evidence across a range of settings, there have been numerous reviews of the use of IR in lower-resource settings as well as calls for broader use [ 3 , 4 ]. There have also been more focused efforts to modify various approaches and frameworks to strengthen the relevance of IR to low- and middle-income country settings (LMICs), such as the work by Means et al. to adapt a specific IR framework for increased utility in LMICs [ 2 ].
Within LMIC settings, the centrality of context to a health intervention’s impact is of particular relevance in humanitarian settings, which present a set of distinct implementation challenges [ 5 ]. Humanitarian responses to crisis situations operate with limited resources, under potential security concerns, and often under pressure to relieve acute suffering and need [ 6 ]. Given these factors, successful implementation of a particular health intervention may require different qualities than those that optimize intervention impact under more stable circumstances [ 7 ]. Despite increasing recognition of the need for expanded evidence of health interventions in humanitarian settings, the evidence base remains limited [ 8 ]. Furthermore, despite its potential utility, there is not standardized guidance on IR in humanitarian settings, nor are there widely endorsed recommendations for the frameworks best suited to analyze implementation in these settings.
Sexual and reproductive health (SRH) is a core aspect of the health sector response in humanitarian settings [ 9 ]. Yet, progress in addressing SRH needs has lagged far behind other services because of challenges related to culture and ideology, financing constraints, lack of data and competing priorities [ 10 ]. The Minimum Initial Service Package (MISP) for SRH in Crisis Situations is the international standard for the minimum set of SRH services that should be implemented in all crisis situations [ 11 ]. However, as in other areas of health, there is need for expanded evidence for planning and implementation of SRH interventions in humanitarian settings. Recent systematic reviews of SRH in humanitarian settings have focused on the effectiveness of interventions and service delivery strategies, as well as factors affecting utilization, but have not detailed whether IR frameworks were used [ 12 , 13 , 14 , 15 ]. There have also been recent reviews examining IR frameworks used in various settings and research areas, but none have explicitly focused on humanitarian settings [ 2 , 16 ].
Given the need for an expanded evidence base for SRH interventions in humanitarian settings and the potential for IR to be used to expand the available evidence, a scoping review was undertaken. This scoping review sought to identify IR approaches that have been used in the last ten years to evaluate SRH interventions in humanitarian settings.
This review also sought to shed light on whether there is a need for a common framework to guide research design, analysis, and reporting for SRH interventions in humanitarian settings and if so, if there are any established frameworks already in use that would be fit-for-purpose or could be tailored to meet this need.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews was utilized to guide the elements of this review [ 17 ]. The review protocol was retrospectively registered with the Open Science Framework ( https://osf.io/b5qtz ).
Search strategy
A two-fold search strategy was undertaken for this review, which covered the last 10 years (2013–2022). First, recent systematic reviews pertaining to research or evaluation of SRH interventions in humanitarian settings were identified through keyword searches on PubMed and Google Scholar. Four relevant systematic reviews were identified [ 12 , 13 , 14 , 15 ] Table 1 .
Second, a literature search mirroring these reviews was conducted to identify relevant papers published since the completion of searches for the most recent review (April 2017). Additional file 1 includes the search terms that were used in the literature search [see Additional file 1 ].
The literature search was conducted for papers published from April 2017 to December 2022 in the databases that were searched in one or more of the systematic reviews: PubMed, Embase, PsycInfo, CINAHL and Global Health. Searches were completed in January 2023 Table 2 .
Two reviewers screened each identified study for alignment with inclusion criteria. Studies in the four systematic reviews identified were considered potentially eligible if published during the last 10 years. These papers then underwent full-text review to confirm satisfaction of all inclusion criteria, as inclusion criteria were similar but not fully aligned across the four reviews.
Literature search results were exported into a citation manager (Covidence), duplicates were removed, and a step-wise screening process for inclusion was applied. First, all papers underwent title and abstract screening. The remaining papers after abstract screening then underwent full-text review to confirm satisfaction of all inclusion criteria. Title and abstract screening as well as full-text review was conducted independently by both authors; disagreements after full-text review were resolved by consensus.
Data extraction and synthesis
The following content areas were summarized in Microsoft Excel for each paper that met inclusion criteria: publication details including author, year, country, setting [rural, urban, camp, settlement], population [refugees, internally displaced persons, general crisis-affected], crisis type [armed conflict, natural disaster], crisis stage [acute, chronic], study design, research methods, SRH intervention, and intervention target population [specific beneficiaries of the intervention within the broader population]; the use of an IR framework; details regarding the IR framework, how it was used, and any rationale given for the framework used; factors cited as impacting SRH interventions, either positively or negatively; and other key findings deemed relevant to this review.
As the focus of this review was on the approach taken for SRH intervention research and evaluation, the quality of the studies themselves was not assessed.
Twenty papers underwent full-text review due to their inclusion in one or more of the four systematic reviews and meeting publication date inclusion criteria. The literature search identified 7,016 unique papers. After full-text screening, 69 met all inclusion criteria and were included in the review. Figure 1 illustrates the search strategy and screening process.
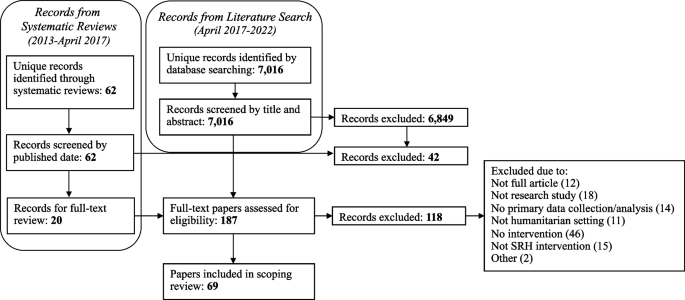
Flow chart of paper identification
Papers published in each of the 10 years of the review timeframe (2013–2022) were included. 29% of the papers originated from the first five years of the time frame considered for this review, with the remaining 71% papers coming from the second half. Characteristics of included publications, including geographic location, type of humanitarian crisis, and type of SRH intervention, are presented in Table 3 .
A wide range of study designs and methods were used across the papers, with both qualitative and quantitative studies well represented. Twenty-six papers were quantitative evaluations [ 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 ], 17 were qualitative [ 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 ], and 26 used mixed methods [ 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 ]. Within the quantitative evaluations, 15 were observational, while five were quasi-experimental, five were randomized controlled trials, and one was an economic evaluation. Study designs as classified by the authors of this review are summarized in Table 4 .
Six papers (9%) explicitly cited use of an IR framework. Three of these papers utilized the Consolidated Framework for Implementation Research (CFIR) [ 51 , 65 , 70 ]. The CFIR is a commonly used determinant framework that—in its originally proposed form in 2009—is comprised of five domains, each of which has constructs to further categorize factors that impact implementation. The CFIR domains were identified as core content areas influencing the effectiveness of implementation, and the constructs within each domain are intended to provide a range of options for researchers to select from to “guide diagnostic assessments of implementation context, evaluate implementation progress, and help explain findings.” [ 87 ] To allow for consistent terminology throughout this review, the original 2009 CFIR domains and constructs are used.
Guan et al. conducted a mixed methods study to assess the feasibility and effectiveness of a neonatal hepatitis B immunization program in a conflict-affected rural region of Myanmar. Guan et al. report mapping data onto the CFIR as a secondary analysis step. They describe that “CFIR was used as a comprehensive meta-theoretical framework to examine the implementation of the Hepatitis B Virus vaccination program,” and implementation themes from multiple study data sources (interviews, observations, examination of monitoring materials) were mapped onto CFIR constructs. They report their results in two phases – Pre-implementation training and community education, and Implementation – with both anchored in themes that they had mapped onto CFIR domains and constructs. All but six constructs were included in their analysis, with a majority summarized in a table and key themes explored further in the narrative text. They specify that most concerns were identified within the Outer Setting and Process domains, while elements identified within the Inner Setting domain provided strength to the intervention and helped mitigate against barriers [ 70 ].
Sarker et al. conducted a qualitative study to assess provision of maternal, newborn and child health services to Rohingya refugees residing in camps in Cox’s Bazar, Bangladesh. They cite using CFIR as a guide for thematic analysis, applying it after a process of inductive and deductive coding to index these codes into the CFIR domains. They utilized three of the five CFIR domains (Outer Setting, Inner Setting, and Process), stating that the remaining two domains (Intervention Characteristics and Characteristics of Individuals) were not relevant to their analysis. They then proposed two additional CFIR domains, Context and Security, for use in humanitarian contexts. In contrast to Guan et al., CFIR constructs are not used nor mentioned by Sarker et al., with content under each domain instead synthesized as challenges and potential solutions. Regarding the CFIR, Sarker et al. write, “The CFIR guided us for interpretative coding and creating the challenges and possible solutions into groups for further clarification of the issues related to program delivery in a humanitarian crisis setting.” [ 51 ]
Sami et al. conducted a mixed methods case study to assess the implementation of a package of neonatal interventions at health facilities within refugee and internally displaced persons camps in South Sudan. They reference use of the CFIR earlier in the study than Sarker et al., basing their guides for semi-structured focus group discussions on the CFIR framework. They similarly reference a general use of the CFIR framework as they conducted thematic analysis. Constructs are referenced once, but they do not specify whether their application of the CFIR framework included use of domains, constructs, or both. This may be in part because they then applied an additional framework, the World Health Organization (WHO) Health System Framework, to present their findings. They describe a nested approach to their use of these frameworks: “Exploring these [CFIR] constructs within the WHO Health Systems Framework can identify specific entry points to improve the implementation of newborn interventions at critical health system building blocks.” [ 65 ]
Three papers cite use of different IR frameworks. Bolan et al. utilized the Theoretical Domains Framework in their mixed methods feasibility study and pilot cluster randomized trial evaluating pilot use of the Safe Delivery App by maternal and newborn health workers providing basic emergency obstetric and newborn care in facilities in the conflict-affected Maniema province of the Democratic Republic of the Congo (DRC). They used the Theroetical Domains Framework in designing interview questions, and further used it as the coding framework for their analysis. Similar to the CFIR, the Theoretical Domains Framework is a determinant framework that consists of domains, each of which then includes constructs. Bolan et al. utilized the Theoretical Domains Framework at the construct level in interview question development and at the domain level in their analysis, mapping interview responses to eight of the 14 domains [ 83 ]. Berg et al. report using an “exploratory design guided by the principles of an evaluation framework” developed by the Medical Research Council to analyze the implementation process, mechanisms of impact, and outcomes of a three-pillar training intervention to improve maternal and neonatal healthcare in the conflict-affected South Kivu province of the DRC [ 67 , 88 ]. Select components of this evaluation framework were used to guide deductive analysis of focus group discussions and in-depth interviews [ 67 ]. In their study of health workers’ knowledge and attitudes toward newborn health interventions in South Sudan, before and after training and supply provision, Sami et al. report use of the Conceptual Framework of the Role of Attitudes in Evidence-Based Practice Implementation in their analysis process. The framework was used to group codes following initial inductive coding analysis of in-depth interviews [ 72 ].
Three other papers cite use of specific frameworks in their intervention evaluation [ 19 , 44 , 76 ]. As a characteristic of IR is the use of an explicit framework to guide the research, the use of the frameworks in these three papers meets the intention of IR and serves the purpose that an IR framework would have in strengthening the analytical rigor. Castle et al. cite use of their program’s theory of change as a framework for a mixed methods evaluation of the provision of family planning services and more specifically uptake of long-acting reversible contraception use in the DRC. They describe use of the theory of change to “enhance effectiveness of [long-acting reversible contraception] access and uptake.” [ 76 ] Thommesen et al. cite use of the AAAQ (Availability, Accessibility, Acceptability and Quality) framework in their qualitative study assessing midwifery services provided to pregnant women in Afghanistan. This framework is focused on the “underlying elements needed for attainment of optimum standard of health care,” but the authors used it in this paper to evaluate facilitators and barriers to women accessing midwifery services [ 44 ]. Jarrett et al. cite use of the Centers for Disease Control and Prevention’s (CDC) Guidelines for Evaluating Public Health Surveillance Systems to explore the characteristics of a population mobility, mortality and birth surveillance system in South Kivu, DRC. Use of these CDC guidelines is cited as one of four study objectives, and commentary is included in the Results section pertaining to each criteria within these guidelines, although more detail regarding use of these guidelines or the authors’ experience with their use in the study is not provided [ 19 ].
Overall, 22 of the 69 papers either explicitly or implicitly identified IR as relevant to their work. Nineteen papers include a focus on feasibility (seven of which did not otherwise identify the importance of exploring questions concerning implementation), touching on a common outcome of interest in implementation research [ 89 ].
While a majority of papers did not explicitly or implicitly use an IR framework to evaluate their SRH intervention of focus, most identified factors that facilitated implementation when they were present or served as a barrier when absent. Sixty cite factors that served as facilitators and 49 cite factors that served as barriers, with just three not citing either. Fifty-nine distinct factors were identified across the papers.
Three of the six studies that explicitly used an IR framework used the CFIR, and the CFIR is the only IR framework that was used by multiple studies. As previously mentioned, Means et al. put forth an adaptation of the CFIR to increase its relevance in LMIC settings, proposing a sixth domain (Characteristics of Systems) and 11 additional constructs [ 2 ]. Using the expanded domains and constructs as proposed by Means et al., the 59 factors cited by papers in this review were thematically grouped into the six domains: Characteristics of Systems, Outer Setting, Inner Setting, Characteristics of Individuals, Intervention Characteristics, and Process. Within each domain, alignment with CFIR constructs was assessed for, and alignment was found with 29 constructs: eight of Means et al.’s 11 constructs, and 21 of the 39 standard CFIR constructs. Three factors did not align with any construct (all fitting within the Outer Setting domain), and 14 aligned with a construct label but not the associated definition. Table 5 synthesizes the mapping of factors affecting SRH intervention implementation to CFIR domains and constructs, with the construct appearing in italics if it is considered to align with that factor by label but not by definition.
Table 6 lists the CFIR constructs that were not found to have alignment with any factor cited by the papers in this review.
This scoping review sought to assess how IR frameworks have been used to bolster the evidence base for SRH interventions in humanitarian settings, and it revealed that IR frameworks, or an explicit IR approach, are rarely used. All four of the systematic reviews identified with a focus on SRH in humanitarian settings articulate the need for more research examining the effectiveness of SRH interventions in humanitarian settings, with two specifically citing a need for implementation research/science [ 12 , 13 ]. The distribution of papers across the timeframe included in this review does suggest that more research on SRH interventions for crisis-affected populations is taking place, as a majority of relevant papers were published in the second half of the review period. The papers included a wide range of methodologies, which reflect the differing research questions and contexts being evaluated. However, it also invites the question of whether there should be more standardization of outcomes measured or frameworks used to guide analysis and to facilitate increased comparison, synthesis and application across settings.
Three of the six papers that used an IR framework utilized the CFIR. Guan et al. used the CFIR at both a domain and construct level, Sarker et al. used the CFIR at the domain level, and Sami et al. did not specify which CFIR elements were used in informing the focus group discussion guide [ 51 , 65 , 70 ]. It is challenging to draw strong conclusions about the applicability of CFIR in humanitarian settings based on the minimal use of CFIR and IR frameworks within the papers reviewed, although Guan et al. provides a helpful model for how analysis can be structured around CFIR domains and constructs. It is worth considering that the minimal use of IR frameworks, and more specifically CFIR constructs, could be in part because that level of prescriptive categorization does not allow for enough fluidity in humanitarian settings. It also raises questions about the appropriate degree of standardization to pursue for research done in these settings.
The mapping of factors affecting SRH intervention implementation provides an example of how a modified CFIR framework could be used for IR in humanitarian contexts. This mapping exercise found factors that mapped to all five of the original CFIR domains as well as the sixth domain proposed by Means et al. All factors fit well within the definition for the selected domain, indicating an appropriate degree of fit between these existing domains and the factors identified as impacting SRH interventions in humanitarian settings. On a construct level, however, the findings were more variable, with one-quarter of factors not fully aligning with any construct. Furthermore, over 40% of the CFIR constructs (including the additional constructs from Means et al.) were not found to align with any factors cited by the papers in this review, also demonstrating some disconnect between the parameters posed by the CFIR constructs and the factors cited as relevant in a humanitarian context.
It is worth noting that while the CFIR as proposed in 2009 was used in this assessment, as well as in the included papers which used the CFIR, an update was published in 2022. Following a review of CFIR use since its publication, the authors provide updates to construct names and definitions to “make the framework more applicable across a range of innovations and settings.” New constructs and subconstructs were also added, for a total of 48 constructs and 19 subconstructs across the five domains [ 90 ]. A CFIR Outcomes Addendum was also published in 2022, based on recommendations for the CFIR to add outcomes and intended to be used as a complement to the CFIR determinants framework [ 91 ]. These expansions to the CFIR framework may improve applicability of the CFIR in humanitarian settings. Several constructs added to the Outer Setting domain could be of particular utility – critical incidents, local attitudes, and local conditions, each of which could help account for unique challenges faced in contexts of crisis. Sub-constructs added within the Inner Setting domain that seek to clarify structural characteristics and available resources would also be of high utility based on mapping of the factors identified in this review to the original CFIR constructs. As outcomes were not formally included in the CFIR until the 2022 addendum, a separate assessment of implementation outcomes was not undertaken in this review. However, analysis of the factors cited by papers in this review as affecting implementation was derived from the full text of the papers and thus captures content relevant to implementation determinants that is contained within the outcomes.
Given the demonstrated need for additional flexibility within an IR framework for humanitarian contexts, while not a focus of this review, it is worth considering whether a different framework could provide a better fit than the CFIR. Other frameworks have differing points of emphasis that would create different opportunities for flexibility but that do not seem to resolve the challenges experienced in applying the CFIR to a humanitarian context. As one example, the EPIS (Exploration, Preparation, Implementation, Sustainment) Framework considers the impact of inner and outer context on each of four implementation phases; while the constructs within this framework are broader than the CFIR, an emphasis on the intervention characteristics is missing, a domain where stronger alignment within the CFIR is also needed [ 92 ]. Alternatively, the PRISM (Practical, Robust Implementation and Sustainability Model) framework is a determinant and evaluation framework that adds consideration of context factors to the RE-AIM (Reach, Effectiveness, Adoption, Implementation, Maintenance) outcomes framework. It has a stronger emphasis on intervention aspects, with sub-domains to account for both organization and patient perspectives within the intervention. While PRISM does include aspects of context, external environment considerations are less robust and intentionally less comprehensive in scope, which would not provide the degree of alignment possible between the Characteristics of Systems and Outer Setting CFIR domains for the considerations unique to humanitarian environments [ 93 ].
Reflecting on their experience with the CFIR, Sarker et al. indicate that it can be a “great asset” in both evaluating current work and developing future interventions. They also encourage future research of humanitarian health interventions to utilize the CFIR [ 51 ]. The other papers that used the CFIR do not specifically reflect on their experience utilizing it, referring more generally to having felt that it was a useful tool [ 65 , 70 ]. On their use of an evaluation framework, Berg et al. reflected that it lent useful structure and helped to identify aspects affecting implementation that otherwise would have gone un-noticed [ 67 ]. The remaining studies that utilized an IR framework did not specifically comment on their experience with its use [ 72 , 83 ]. While a formal IR framework was not engaged by other studies, a number cite a desire for IR to contribute further detail to their findings [ 21 , 37 ].
In their recommendations for strengthening the evidence base for humanitarian health interventions, Ager et al. speak to the need for “methodologic innovation” to develop methodologies with particular applicability in humanitarian settings [ 7 ]. As IR is not yet routinized for SRH interventions, this could be opportune timing for the use of a standardized IR framework to gauge its utility. Using an IR framework to assess factors influencing implementation of the MISP in initial stages of a humanitarian response, and interventions to support more comprehensive SRH service delivery in protracted crises, could lend further rigor and standardization to SRH evaluations, as well as inform strategies to improve MISP implementation over time. Based on categorizing factors identified by these papers as relevant for intervention evaluation, there does seem to be utility to a modified CFIR approach. Given the paucity of formal IR framework use within SRH literature, it would be worth conducting similar scoping exercises to assess for explicit use of IR frameworks within the evidence base for other health service delivery areas in humanitarian settings. In the interim, the recommended approach from this review for future IR on humanitarian health interventions would be a modified CFIR approach with domain-level standardization and flexibility for constructs that may standardize over time with more use. This would enable use of a common analytical framework and vocabulary at the domain level for stakeholders to describe interventions and the factors influencing the effectiveness of implementation, with constructs available to use and customize as most appropriate for specific contexts and interventions.
This review had a number of limitations. As this was a scoping review and a two-part search strategy was used, the papers summarized here may not be comprehensive of those written pertaining to SRH interventions over the past 10 years. Papers from 2013 to 2017 that would have met this scoping review’s inclusion criteria may have been omitted due to being excluded from the systematic reviews. The review was limited to papers available in English. Furthermore, this review did not assess the quality of the papers included or seek to assess the methodology used beyond examination of the use of an IR framework. It does, however, serve as a first step in assessing the extent to which calls for implementation research have been addressed, and identify entry points for strengthening the science and practice of SRH research in humanitarian settings.
With one in 23 people worldwide in need of humanitarian assistance, and financing required for response plans at an all-time high, the need for evidence to guide resource allocation and programming for SRH in humanitarian settings is as important as ever [ 94 ]. Recent research agenda setting initiatives and strategies to advance health in humanitarian settings call for increased investment in implementation research—with priorities ranging from research on effective strategies for expanding access to a full range of contraceptive options to integrating mental health and psychosocial support into SRH programming to capturing accurate and actionable data on maternal and perinatal mortality in a wide range of acute and protracted emergency contexts [ 95 , 96 ]. To truly advance guidance in these areas, implementation research will need to be conducted across diverse humanitarian settings, with clear and consistent documentation of both intervention characteristics and outcomes, as well as contextual and programmatic factors affecting implementation.
Conclusions
Implementation research has potential to increase impact of health interventions particularly in crisis-affected settings where flexibility, adaptability and context-responsive approaches are highlighted as cornerstones of effective programming. There remains significant opportunity for standardization of research in the humanitarian space, with one such opportunity occurring through increased utilization of IR frameworks such as a modified CFIR approach. Investing in more robust sexual and reproductive health research in humanitarian contexts can enrich insights available to guide programming and increase transferability of learning across settings.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Availability, Accessibility, Acceptability and Quality
Centers for Disease Control and Prevention
Consolidated Framework for Implementation Research
Democratic Republic of the Congo
Exploration, Preparation, Implementation, Sustainment
- Implementation research
Low and middle income country
Minimum Initial Service Package
Practical, Robust Implementation and Sustainability Model
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Reach, Effectiveness, Adoption, Implementation, Maintenance
- Sexual and reproductive health
World Health Organization
Peters DH, et al. Implementation research: what it is and how to do it. RESEARCH METHODS. 2013;347:7.
Means AR, et al. Evaluating and optimizing the consolidated framework for implementation research (CFIR) for use in low- and middle-income countries: a systematic review. Implement Sci. 2020;15(1):17.
Article PubMed PubMed Central Google Scholar
Alonge O, et al. How is implementation research applied to advance health in low-income and middle-income countries? BMJ Glob Health. 2019;4(2):e001257.
Ridde V, Pérez D, Robert E. Using implementation science theories and frameworks in global health. BMJ Glob Health. 2020;5(4):e002269.
Gaffey MF, et al. Delivering health and nutrition interventions for women and children in different conflict contexts: a framework for decision making on what, when, and how. Lancet (London, England). 2021;397(10273):543–54.
Article PubMed Google Scholar
Singh NS, et al. Delivering health interventions to women, children, and adolescents in conflict settings: what have we learned from ten country case studies? The Lancet. 2021;397(10273):533–42.
Article Google Scholar
Ager A, et al. Strengthening the evidence base for health programming in humanitarian crises. Science. 2014;345(6202):1290–2.
Article CAS PubMed Google Scholar
Blanchet K, et al. Evidence on public health interventions in humanitarian crises. The Lancet. 2017;390(10109):2287–96.
Sphere A. The Sphere Handbook | Standards for quality humanitarian response. 2018.
Google Scholar
Barot S. In a State of Crisis: Meeting the Sexual and Reproductive Health Needs of Women in Humanitarian Situations. Guttmacher Policy Rev. 2017;20:7.
Crisis, I.-A.W.G.f.R.H.i., Minimum Initial Service Package. 2020: https://www.unfpa.org/resources/minimum-initial-service-package-misp-srh-crisis-situations .
Casey SE. Evaluations of reproductive health programs in humanitarian settings: a systematic review. Confl Heal. 2015;9(1):S1.
Singh NS, et al. A long way to go: a systematic review to assess the utilisation of sexual and reproductive health services during humanitarian crises. BMJ Glob Health. 2018;3(2):e000682.
Singh NS, et al. Evaluating the effectiveness of sexual and reproductive health services during humanitarian crises: A systematic review. PLoS ONE. 2018;13(7):e0199300.
Warren E, et al. Systematic review of the evidence on the effectiveness of sexual and reproductive health interventions in humanitarian crises. BMJ Open. 2015;5(12):e008226.
Dadich A, Piper A, Coates D. Implementation science in maternity care: a scoping review. Implement Sci. 2021;16(1):16.
Tricco AC, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73.
Devine A, et al. Strategies for the prevention of perinatal hepatitis B transmission in a marginalized population on the Thailand-Myanmar border: a cost-effectiveness analysis. BMC Infect Dis. 2017;17(1):552.
Jarrett P, et al. Evaluation of a population mobility, mortality, and birth surveillance system in South Kivu. Democratic Republic of the Congo Disasters. 2020;44(2):390–407.
PubMed Google Scholar
Logie CH, et al. A Psycho-Educational HIV/STI Prevention Intervention for Internally Displaced Women in Leogane, Haiti: Results from a Non-Randomized Cohort Pilot Study. PLoS ONE. 2014;9(2):e89836.
O’Laughlin KN, et al. A cohort study to assess a communication intervention to improve linkage to HIV care in Nakivale Refugee Settlement. Uganda Glob Public Health. 2021;16(12):1848–55.
Adam I. The influence of maternal health education on the place of delivery in conflict settings of Darfur. Sudan Conflict and Health. 2015;9:31.
Adam IF, et al. Relationship between implementing interpersonal communication and mass education campaigns in emergency settings and use of reproductive healthcare services: evidence from Darfur, Sudan. BMJ Open. 2015;5(9):e008285.
Edmond K, et al. Mobile outreach health services for mothers and children in conflict-affected and remote areas: a population-based study from Afghanistan. Arch Dis Child. 2020;105(1):18–25.
Nasir S, et al. Dissemination and implementation of the e-MCHHandbook, UNRWA’s newly released maternal and child health mobile application: a cross-sectional study. BMJ Open. 2020;10(3):e034885.
O’Laughlin KN, et al. Feasibility and acceptability of home-based HIV testing among refugees: a pilot study in Nakivale refugee settlement in southwestern Uganda. BMC Infect Dis. 2018;18(1):332.
Adam I. Evidence from cluster surveys on the association between home-based counseling and use of family planning in conflict-affected Darfur. Int J Gynecol Obstet. 2016;133(2):221–5.
Casey S, et al. Availability of long-acting and permanent family-planning methods leads to increase in use in conflict-affected northern Uganda: Evidence from cross-sectional baseline and endline cluster surveys. Glob Public Health. 2013;8(3):284–97.
Corna F, et al. Supporting maternal mental health of Rohingya refugee women during the perinatal period to promote child health and wellbeing: a field study in Cox’s Bazar. Intervention, the Journal of Mental Health & Psychosocial Support in Conflict Affected Areas. 2019;17(2):160–8.
Glass N, et al. Effectiveness of the Communities Care programme on change in social norms associated with gender-based violence (GBV) with residents in intervention compared with control districts in Mogadishu, Somalia. BMJ Open. 2019;9(3):e023819.
James LE, et al. Development and Testing of a Community-Based Intervention to Address Intimate Partner Violence among Rohingya and Syrian Refugees: A Social Norms-Based Mental Health-Integrated Approach. Int J Environ Res Public Health. 2021;18(21):11674.
Le Roux E, et al. Engaging with faith groups to prevent VAWG in conflict-affected communities: results from two community surveys in the DRC. BMC Int Health Hum Rights. 2020;20(1):27.
Morris CN, et al. When political solutions for acute conflict in Yemen seem distant, demand for reproductive health services is immediate: a programme model for resilient family planning and post-abortion care services. Sex Reprod Health Matters. 2019;27(2):1610279.
Anibueze AU, et al. Impact of counseling visual multimedia on use of family planning methods among displaced Nigerian families. Health Promot Int. 2022;37(3):daac060.
Doocy S, et al. Cash-based assistance and the nutrition status of pregnant and lactating women in the Somalia food crisis: A comparison of two transfer modalities. PLoS ONE. 2020;15(4):e0230989.
Article CAS PubMed PubMed Central Google Scholar
Draiko CV, et al. The effect of umbilical cord cleansing with chlorhexidine gel on neonatal mortality among the community births in South Sudan: a quasi-experimental study. Pan Afr Med J. 2021;38:78.
Edmond KM, et al. Can community health worker home visiting improve care-seeking and maternal and newborn care practices in fragile states such as Afghanistan? A population-based intervention study. BMC Med. 2018;16(1):106.
Edmond KM, et al. Conditional cash transfers to improve use of health facilities by mothers and newborns in conflict affected countries, a prospective population based intervention study from Afghanistan. BMC Pregnancy Childbirth. 2019;19(1):193.
Bakesiima R, et al. Effect of peer counselling on acceptance of modern contraceptives among female refugee adolescents in northern Uganda: A randomised controlled trial. PLoS ONE. 2021;16(9):e0256479.
Greene MC, et al. Evaluation of an integrated intervention to reduce psychological distress and intimate partner violence in refugees: Results from the Nguvu cluster randomized feasibility trial. PLoS ONE. 2021;16(6):e0252982.
Gupta J, et al. Gender norms and economic empowerment intervention to reduce intimate partner violence against women in rural Côte d’Ivoire: a randomized controlled pilot study. BMC Int Health Hum Rights. 2013;13(1):46.
Hossain M, et al. Working with men to prevent intimate partner violence in a conflict-affected setting: a pilot cluster randomized controlled trial in rural Côte d’Ivoire. BMC Public Health. 2014;14(1):339.
Vaillant J, et al. Engaging men to transform inequitable gender attitudes and prevent intimate partner violence: a cluster randomised controlled trial in North and South Kivu, Democratic Republic of Congo. BMJ Glob Health. 2020;5(5):e002223.
Thommesen T, et al. “The midwife helped me … otherwise I could have died”: women’s experience of professional midwifery services in rural Afghanistan - a qualitative study in the provinces Kunar and Laghman. BMC Pregnancy Childbirth. 2020;20(1):140.
Awasom-Fru A, et al. Doctors’ experiences providing sexual and reproductive health care at Catholic Hospitals in the conflict-affected North-West region of Cameroon: a qualitative study. Reprod Health. 2022;19(1):126.
Kabakian-Khasholian T, Makhoul J, Ghusayni A. “A person who does not have money does not enter”: a qualitative study on refugee women’s experiences of respectful maternity care. BMC Pregnancy and Childbirth. 2022;22(1):748.
Lilleston P, et al. Evaluation of a mobile approach to gender-based violence service delivery among Syrian refugees in Lebanon. Health Policy Plan. 2018;33(7):767–76.
Mugo NS, et al. Barriers Faced by the Health Workers to Deliver Maternal Care Services and Their Perceptions of the Factors Preventing Their Clients from Receiving the Services: A Qualitative Study in South Sudan. Matern Child Health J. 2018;22(11):1598–606.
Persson M, et al. A qualitative study on health care providers’ experiences of providing comprehensive abortion care in Cox’s Bazar, Bangladesh. Conflict and Health. 2021;15(1):6.
Phanwichatkul T, et al. The perceptions and practices of Thai health professionals providing maternity care for migrant Burmese women: An ethnographic study. Women Birth. 2022;35(4):e356–68.
Sarker M, et al. Effective maternal, newborn and child health programming among Rohingya refugees in Cox’s Bazar, Bangladesh: Implementation challenges and potential solutions. PLoS ONE. 2020;15(3):e0230732.
Tousaw E, et al. “Without this program, women can lose their lives”: migrant women’s experiences with the Safe Abortion Referral Programme in Chiang Mai. Thailand Reprod Health Matters. 2017;25(51):58–68.
Tousaw E, et al. “It is just like having a period with back pain”: exploring women’s experiences with community-based distribution of misoprostol for early abortion on the Thailand-Burma border. Contraception. 2018;97(2):122–9.
West L, et al. Factors in use of family planning services by Syrian women in a refugee camp in Jordan. Journal of Family Planning and Reproductive Health Care. 2017;43(2):96–102.
O’Connell KA, et al. Meeting the Sexual and Reproductive Health Needs of Internally Displaced Persons in Ethiopia’s Somali Region: A Qualitative Process Evaluation. Glob Health Sci Pract. 2022;10(5):e2100818.
Orya E, et al. Strengthening close to community provision of maternal health services in fragile settings: an exploration of the changing roles of TBAs in Sierra Leone and Somaliland. BMC Health Serv Res. 2017;17(1):460.
Perera SM, et al. Barriers to seeking post-abortion care in Paktika Province, Afghanistan: a qualitative study of clients and community members. BMC Womens Health. 2021;21(1):390.
Tanabe M, et al. Piloting community-based medical care for survivors of sexual assault in conflict-affected Karen State of eastern Burma. Confl Heal. 2013;7(1):12.
Tran NT, et al. Clinical outreach refresher trainings in crisis settings (S-CORT): clinical management of sexual violence survivors and manual vacuum aspiration in Burkina Faso, Nepal, and South Sudan. Reprod Health Matters. 2017;25(51):103–13.
Yankah E, et al. Feasibility and acceptability of mobile phone platforms to deliver interventions to address gender-based violence among Syrian adolescent girls and young women in Izmir. Turkey Vulnerable Children and Youth Studies. 2020;15(2):133–43.
Muuo S, et al. Barriers and facilitators to care-seeking among survivors of gender-based violence in the Dadaab refugee complex. Sex Reprod Health Matters. 2020;28(1):1722404.
Amsalu R, et al. Essential newborn care practice at four primary health facilities in conflict affected areas of Bossaso, Somalia: a cross-sectional study. Conflict and Health. 2019;13(13):27.
Myers A, et al. Facilitators and barriers in implementing the Minimum Initial Services Package (MISP) for reproductive health in Nepal post-earthquake. Conflict and Health. 2018;12:35.
Santo L.C.d, et al. Feasibility and acceptability of a video library tool to support community health worker counseling in rural Afghan districts: a cross-sectional assessment. Conflict and Health. 2020;14:56.
Sami S, et al. Understanding health systems to improve community and facility level newborn care among displaced populations in South Sudan: a mixed methods case study. BMC Pregnancy Childbirth. 2018;18(1):325.
Amsalu R, et al. Effectiveness of clinical training on improving essential newborn care practices in Bossaso, Somalia: a pre and postintervention study. BMC Pediatr. 2020;20(1):215.
Berg M, Mwambali SN, Bogren M. Implementation of a three-pillar training intervention to improve maternal and neonatal healthcare in the Democratic Republic Of Congo: a process evaluation study in an urban health zone. Glob Health Action. 2022;15(1):2019391.
Castillo M, et al. Turning Disaster into an Opportunity for Quality Improvement in Essential Intrapartum and Newborn Care Services in the Philippines: Pre- to Posttraining Assessments. Biomed Res Int. 2016;2016:1–9.
Foster AM, Arnott G, Hobstetter M. Community-based distribution of misoprostol for early abortion: evaluation of a program along the Thailand-Burma border. Contraception. 2017;96(4):242–7.
Guan TH, et al. Implementation of a neonatal hepatitis B immunization program in rural Karenni State, Myanmar: A mixed-methods study. PLoS ONE. 2021;16(12):e0261470.
Logie, C.H., et al., Mixed-methods findings from the Ngutulu Kagwero (agents of change) participatory comic pilot study on post-rape clinical care and sexual violence prevention with refugee youth in a humanitarian setting in Uganda. Global Public Health, 2022((Logie C.H., [email protected]) Factor-Inwentash Faculty of Social Work, University of Toronto, Toronto, Canada(Logie C.H., [email protected]) Women’s College Research Institute, Women’s College Hospital, Toronto, Canada(Logie C.H., carmen.l).
Sami S, et al. “You have to take action”: changing knowledge and attitudes towards newborn care practices during crisis in South Sudan. Reprod Health Matters. 2017;25(51):124–39.
Smith JR, et al. Clinical care for sexual assault survivors multimedia training: a mixed-methods study of effect on healthcare providers’ attitudes, knowledge, confidence, and practice in humanitarian settings. Confl Heal. 2013;7(1):14.
Stevens A, et al. Folate supplementation to prevent birth abnormalities: evaluating a community-based participatory action plan for refugees and migrant workers on the Thailand-Myanmar border. Public Health. 2018;161:83–9.
Nguyen Toan T, et al. Strengthening healthcare providers’ capacity for safe abortion and postabortion care services in humanitarian settings: lessons learned from the clinical outreach refresher training model (S-CORT) in Uganda, Nigeria, and the Democratic Republic of Congo. Conflict and Health. 2021;15(1):20.
Castle S, et al. Successful programmatic approaches to facilitating IUD uptake: CARE’s experience in DRC. BMC Womens Health. 2019;19(1):104.
Deitch J, et al. “They Love Their Patients”: Client Perceptions of Quality of Postabortion Care in North and South Kivu, the Democratic Republic of the Congo. Global health, science and practice. 2019;7(Suppl 2):S285–98.
Ferreyra C, et al. Evaluation of a community-based HIV test and start program in a conflict affected rural area of Yambio County, South Sudan. PLoS ONE. 2021;16(7):e0254331.
Ho LS, Wheeler E. Using Program Data to Improve Access to Family Planning and Enhance the Method Mix in Conflict-Affected Areas of the Democratic Republic of the Congo. Glob Health Sci Pract. 2018;6(1):161–77.
Klabbers RE, et al. Health Worker Perspectives on Barriers and Facilitators of Assisted Partner Notification for HIV for Refugees and Ugandan Nationals: A Mixed Methods Study in West Nile Uganda. AIDS Behav. 2021;25(10):3206–22.
Turner C, et al. Neonatal Intensive Care in a Karen Refugee Camp: A 4 Year Descriptive Study. PLoS ONE. 2013;8(8):e72721.
Vries Id, et al. Key lessons from a mixed-method evaluation of a postnatal home visit programme in the humanitarian setting of Gaza. Eastern Mediterr Health J. 2021;27(6):546–52.
Bolan NE, et al. mLearning in the Democratic Republic of the Congo: A Mixed-Methods Feasibility and Pilot Cluster Randomized Trial Using the Safe Delivery App. Global health, science and practice. 2018;6(4):693–710.
Khan MN, et al. Evaluating feasibility and acceptability of a local psycho-educational intervention for pregnant women with common mental problems affected by armed conflict in Swat, Pakistan: A parallel randomized controlled feasibility trial. Int J Soc Psychiatry. 2017;63(8):724–35.
Hynes M, et al. Using a quality improvement approach to improve maternal and neonatal care in North Kivu, Democratic Republic of Congo. Reprod Health Matters. 2017;25(51):140–50.
Gibbs A, et al. The impacts of combined social and economic empowerment training on intimate partner violence, depression, gender norms and livelihoods among women: an individually randomised controlled trial and qualitative study in Afghanistan. BMJ Glob Health. 2020;5(3):e001946.
Damschroder L, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science: IS; 2009.
Moore GF, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258.
Proctor E, et al. Outcomes for Implementation Research: Conceptual Distinctions, Measurement Challenges, and Research Agenda. Adm Policy Ment Health. 2011;38(2):65–76.
Damschroder LJ, et al. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75.
Damschroder LJ, et al. Conceptualizing outcomes for use with the Consolidated Framework for Implementation Research (CFIR): the CFIR Outcomes Addendum. Implement Sci. 2022;17(1):7.
Aarons GA, Hurlburt M, Horwitz SM. Advancing a Conceptual Model of Evidence-Based Practice Implementation in Public Service Sectors. Administration and Policy in Mental Health and Mental Health Services Research. 2011;38(1):4–23.
Feldstein AC, Glasgow RE. A Practical, Robust Implementation and Sustainability Model (PRISM) for Integrating Research Findings into Practice. The Joint Commission Journal on Quality and Patient Safety. 2008;34(4):228–43.
OCHA. Global Humanitarian Overview 2023. 2022 [cited 2023 8/3/2023]; Available from: https://humanitarianaction.info/node/13073/article/glance-0 . Accessed 8 Mar 2023.
Kobeissi L, et al. Setting research priorities for sexual, reproductive, maternal, newborn, child and adolescent health in humanitarian settings. Confl Heal. 2021;15(1):16.
Save the, C., et al. Roadmap to Accelerate Progress for Every Newborn in Humanitarian Settings 2020 – 2024. 2020. p. 52.
Inter-Agency Working Group on Reproductive Health in, C. Inter-Agency Field Manual on Reproductive Health in Humanitarian Settings. 2018.
Download references
Acknowledgements
Not applicable.
The authors received no funding for this study.
Author information
Authors and affiliations.
Duke University School of Medicine, 40 Duke Medicine Circle, Durham, NC, 27710, USA
Alexandra Norton
Johns Hopkins Bloomberg School of Public Health, 615 N. Wolfe St, Baltimore, MD, 21205, USA
Hannah Tappis
You can also search for this author in PubMed Google Scholar
Contributions
AN and HT designed the scoping review. AN conducted the literature search. AN and HT screened records for inclusion. AN extracted data from included studies. Both authors contributed to synthesis of results. AN drafted the manuscript and both authors contributed to editorial changes.
Corresponding author
Correspondence to Alexandra Norton .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
. Literature search terms: Exact search terms used in literature search, with additional detail on the methodology to determine search terms and definitions used for each component of the search
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Norton, A., Tappis, H. Sexual and reproductive health implementation research in humanitarian contexts: a scoping review. Reprod Health 21 , 64 (2024). https://doi.org/10.1186/s12978-024-01793-2
Download citation
Received : 06 November 2023
Accepted : 12 April 2024
Published : 13 May 2024
DOI : https://doi.org/10.1186/s12978-024-01793-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Humanitarian settings
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]

COMMENTS
20th International Congress of Qualitative Inquiry. May 15-18, 2024 (in person) May 29-31 (virtual) We shall not cease from exploration/ And the end of all our exploring/ Will be to arrive where we started/ And know the place for the first time (T. S. Eliot, No. 4 of Four Quartets, 1942). The 20 th International Congress of Qualitative Inquiry ...
34 th Annual Conference on Ethnographic and Qualitative Conference (EQRC). March 21-22, 2022, held virtually. March 21-22, 2022, held virtually. Proposal Submission Portal will open January 4 th , 2022 and the deadline is February 22, 2022.
Panel Fri137 and Fri150: "Autoethnography: "All in!The Curiosity of Norman Denzin in the present tense," Dominique Hill snd Durell Callier; Claudio Moreira and Marcelo Diversi; David Carless & Kitrina Douglas; Bryant Keith Alexander; Carolyn Ellis; Art Bochner; Jonathan Wyatt & Ken Gale; Cynthia Lubin Langtiw; Dan Harris & Stacy Holman Jones; Tami Spry; Charles Vanover
The 9th World Conference on Qualitative Research (WCQR2025) will be held from 4 to 6 February 2025 at Jagiellonian University, in Kraków, Poland, and from 11 to 13 February 2025 Online. Each edition brings together researchers from 40+ countries, world-renowned authors, and research groups sharing their experiences in the field, making the WCQR one of the most relevant platforms for ...
Qualitative Health Research (QHR) is a peer-reviewed monthly journal that provides an international, interdisciplinary forum to enhance health care and further the development and understanding of qualitative research in health-care settings.QHR is an invaluable resource for researchers and academics, administrators and others in the health and social service professions, and graduates who ...
World Conference on Qualitative Research. Search within this conference. Search. 2023 WCQR 2023. 25-27 January; Algarve, Portugal; Computer Supported Qualitative Research. 23 Papers. 1 Volume. 2022 WCQR 2022. 26-28 January; Barcelona, Spain; Computer Supported Qualitative Research ... 2018 WCQR 2018. 17-19 October; Lisbon, Portugal; Computer ...
Qualitative Health Research Conference (QHR) Tell a Friend Since the first QHR conference in 1994, the world in which we live, work and research has undergone unprecedented change. On the 20th anniversary of the QHR conference, progress seems ever quicker and change deeper and more widespread. 10/21/2014 to 10/23/2014: When: ...
Registration extended deadline is Monday, MARCH 14, 2022. Virtual Conference. Due to the c ontinuing Covid-19 pandemic circumstances, EQRC will be held again as a "virtual conference," during March 21-22, 2022. Both pre-recorded lecture sessions as well as poster sessions will be posted on the conference website in an open-view format.
Find out more about our past conferences below: 2021 conference: Negotiating Trust: Exploring power, belief, truth and knowledge in health and care. 2019 conference: Crafting the Future of Qualitative Health Research in a Changing World. 2017 symposium: Engagement, co-production, and collaborative meaning-making: collaboration in qualitative ...
Towards a shared understanding of the learning health system in a large academic-based health system: A qualitative analysis. ... Acad Med 2022: 97: 1564-1572 ... Frantsve-Hawley J, Jolles MP, Embedded Research Conference Priorities and Methods Workgroup, et al. Methods to identify and prioritize research projects and perform embedded ...
Date TBD (Day One) - Qualitative Health Research: Meanings and Methods. The conference is postponed to a date TBD in 2021. 08:00-9:00 Participant Registration. 9:00-10:00 Official Greetings and Introduction to the Conference. Moderators: Ausilia Pulimeno, Stefano Casciato 10:00-10:30 Kyung Rim Shin (Korea) The art of nursing science driven from phenomenology
11-13 February 2025. See the Full Program. The World Conference on Qualitative Research (WCQR) is an annual event that aims to bring together researchers, academics and professionals, promoting the sharing and discussion of knowledge, new perspectives, experiences and innovations on the field of Qualitative Research.
Qualitative research methods explore and provide deep contextual understanding of real world issues, including people's beliefs, perspectives, and experiences. Whether through analysis of interviews, focus groups, structured observation, or multimedia data, qualitative methods offer unique insights in applied health services research that other approaches cannot deliver. However, many ...
WCQR 2025 9th World Conference on Qualitative Research The World Conference on Qualitative Research (WCQR) is an annual event that brings together researchers, world-renowned authors, and research groups from 40+ countries, sharing their experiences with qualitative methods, making the WCQR one of the most relevant platforms for discussing and disseminating the best scientific production in […]
The UCL Qualitative Health Research Network (UCL QHRN) is a cross-faculty and transdisciplinary initiative to support the use and development of qualitative research in health, illness and care. Aim Our aim is to encourage an intellectually dynamic yet supportive atmosphere for debate and discussion that examines the place of qualitative ...
At the 14th Annual TQR Conference in February 2023, we invite you to share papers in which you describe what you have learned from your qualitative inquiries on all aspects of life from all around the world. We would also love to learn how your work as a qualitative researcher and educator has changed and evolved to meet these challenging times ...
Spotlight on qualitative research. Welcome to this first issue of Nursing in Critical Care for 2022, and our new editorial style of introducing the journal's collection of papers. In October, this year, the British Association of Critical Care Nurses will mark their first joint conference; a collaborative event with the Irish Association of ...
Please choose one category to submit your abstract. Panel submissions are comprised of at least four (4) but not more than five (5) papers, each paper with full abstract and author information. Proposals with incomplete abstract/author information will not be considered. Panels are guaranteed an 75-minute slot (individual paper presentations ...
Thank You to our 2024 Annual Partners. QRCA is a global association of the world's most innovative, collaborative and passionate research professionals dedicated to maximizing the power of qualitative. For additional information, contact us at 651-290-7491 or 888-674-7722.
For younger quallies, our 2025 conference will have programming that meets their needs and enhances their skill set and knowledge. It's all happening February 11-14, 2025, in Philadelphia, PA. It's been a while since the annual gathering was in the Northeastern United States. The QRCA Conference for 2025 brings this classic back with a ...
On behalf of the International Society of Qualitative Research in Sport and Exercise, we are delighted to announce that our International Conference (QRSE) returns in 2024 - July 29th (pre-conference workshops), 30th, 31st & August 1st (main conference). The conference is hosted by the Centre for Qualitative Research and the Department of Health, University of Bath, UK.
Proceedings of the 2022 3rd International Conference on Mental Health, Education and Human Development (MHEHD 2022) ... So critical assessment of quantitative and qualitative research can help researchers better choose the appropriate research method in their studies. ... Xueting Xiong PY - 2022 DA - 2022/07/11 TI - Critical Review of ...
THE 5TH QUALITATIVE RESEARCH CONFERENCE 2022 (QRC 2022) 12 October 2022.
"Exploring progress: qualitative health research through crisis, disruption and emergence". Than you to everyone who presented, attended, sponsored, and organised the 2024 conference that took place on the 28 th and 29 th February 2024. This was a virtual conference with a pre-conference in-person workshop day held at University College London a few weeks before (16th of February).
The 40th Annual Qualitative Analysis Conference:"Origin Stories:" Tracing the Origin of Ideas, Selves, and CommunitiesJune 26-28, 2024. Our plenary speakers for 2024 are set! We look forward to welcoming Keynote Speaker Scott Grills (Brandon University), and Featured Speakers Dan Henhawk (University of Manitoba) and Jacqueline Low (Univeristy ...
The field of psychedelics is in an important era, with a significant focus on the potential role of psychedelic compounds in the treatment of mental health and substance use disorders. In 2022, a scientific research conference was held in Toronto to bring together stakeholders from a variety of disciplines and to promote dialogue and collaboration. This Special Issue includes 8 papers based on ...
This research aimed to explore the emotion impact factors and emotion management strategies for college students quarantined as close contacts during the COVID-19 outbreak by analyzing data collected in real time (Lee et al. in DARPA information survivability conference and exposition II, DISCEX'01, vol 1, pp 89-100, IEEE, 2001), and built an emotion impact factors—emotion management ...
Background During the first year postpartum, about 25 per cent of Swedish women with severe perineal trauma (SPT), i.e., a third- or fourth-degree perineal laceration at childbirth, are unsatisfied with their healthcare contacts. Further, there is a lack of research on the more long-term experiences of healthcare encounters among women with persistent SPT-related health problems. This study ...
Background Meeting the health needs of crisis-affected populations is a growing challenge, with 339 million people globally in need of humanitarian assistance in 2023. Given one in four people living in humanitarian contexts are women and girls of reproductive age, sexual and reproductive health care is considered as essential health service and minimum standard for humanitarian response ...