Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
Enter the email address you signed up with and we'll email you a reset link.
- We're Hiring!
- Help Center


Chapter 4: Research Ethics

2014, Doing Research in the Real World, 3rd edn
Related Papers
Journal of Emergency Nursing
Anne Manton
Bangladesh Journal of Physiology and Pharmacology
Mohammad Uzire Azam Khan
Ethics in research involving humans were first codified in 1946 as Nuremberg code. Subsequently other ethical declarations and guide lines were developed to protect the research participants as well as the researchers. The basic research bioethics includes three principles-respects for person, beneficence, and justice. To make a research with human subjects ethically sound the research protocol should have social and scientific values, fair subject selection, favorable risk benefit ratio, independent review, and informed consent of and respect for the participants. Above all the researcher should be honest and responsible enough to safeguard the rights and welfare of the research subjects. DOI: 10.3329/bjpp.v24i1.5734Bangladesh J Physiol Pharmacol 2008; 24(1&2) : 24-26
Reaz Mazumdar
Research involving human subjects are important to develop new therapeutics for the betterment of the human race. To take part in such research as volunteers is moral duty of any human. But such experiments should be justifiable and minimal risky for the participants. History of unethical research involving humans led to the development of many guidelines to make such research ethical as well as to gain maximum possible output. Several guidelines have been formulated to ensure research with human participants ethical. All the guidelines emphasize on one thing in particular- informed consent of the human subjects. Other considerations include rational benefit-harm ration, beneficence, justice, adequate research design and approval from proper authorities. All these guidelines aim to prevent any unethical research involving humans against their will.
Journal of Oral Health and Community Dentistry
sripriya nagarajan
Ghada Al Tajir
The twentieth century witnessed a succession of heinous experiments on human subjects in the name of science. The deplorable nature of these experiments led to the development of several guidelines that laid down the principles of research ethics. Respect, bene cence, and justice are the principles that form the foundation of research ethics today. These principles should be implemented through the channels of the informed consent process, privacy and con dentiality, risk bene t analysis, and fair recruitment. Proper implementation of research ethics ensures the protection of the rights and well-being of the participants. Some individuals are considered to be “vulnerable” in the research context because their autonomy is either diminished or lacking. Examples include children, some elderly persons, those with temporary or permanent cognitive impairment, prisoners, and refugees. Vulnerable groups require additional protection measures if they are involved in research. Public health research differs from general health research that necessitates additional ethical considerations. Research involving public health interventions or research conducted during public emergencies, such as natural disasters and disease outbreaks, has unique ethical challenges. Furthermore, in public health research, an understanding or familiarity with the community in which the research will be done is essential to ethical conduct of research. research ethics committees [otherwise known as institutional review boards (IRB)] play a central role in research involving human participants. The proposed research must be reviewed and approved prior to initiation and monitored thereafter with ongoing reviews of safety reports, progress reports, and emerging information or circumstances that may impact the study. A substantial number of conditions need to be met to ensure research starts and then remains ethical. Researchers should be quali ed by education, training, and experience to take on the role of investigators. The scienti c aspects of the research should be robust and valid and the research itself should be purposeful. It is important that ethical considerations be a constant, integrated into the research undertaking, from inception right through to the dissemination and or sharing of the results.
Amanda Hunn
Bodija Journal
Titilola H . Olojede
Ethical abuse of human subjects is still prevalent in researches. Biomedical research as the use of modern day medical technology to test hypothesis so as to deduce conclusions that are generalisable as theories and principles involve human subjects. If such research is not morally guided, it runs the danger of abusing the sacredness of human life and dehumanising the human person. Therefore, ethics as the philosophical science, which establishes the moral order of human acts would necessarily be required to check and balance the procedural systems of such research. It is within this context that this paper interrogates the role of ethics in biomedical research. This paper carefully and critically analyses how and why researchers abuse the human subject. Appealing to the Kantian moral imperatives, it opines that human subjects should never be treated as means to an end but as end in themselves. It succinctly points out the relevance of ethics in researches involving human subjects, particularly, biomedical research.
udo schuklenk
ABSTRACT This module will introduce you to the ethical concepts underlying applied ethical decision-making in the area of research involving human participants. We will also learn what the issues are that people involved in research on research ethics are concerned with. Ethics without an understanding of historical and legal context makes arguably little sense. It is for this reason that this module will begin with a brief history of research ethics and ends with a brief overview of the relevant national and international guidelines pertaining to ethical issues in research involving human participants.
Journal of the American Dietetic Association
Maureen Moran
Australasian Journal of Dermatology
David Wendler
RELATED PAPERS
ZPE 214, 257–260
Werner Eck , Andreas Pangerl
RAIRO - Theoretical Informatics and Applications
Journal for ImmunoTherapy of Cancer
Ashenafi Tilahun
cenatav.co.cu
Eduardo Llanos
Acta Pharmaceutica
Veeresh Veerapur
Journal of Cellular Physiology
Francesca Truzzi
Genetics in Medicine
Jozef Hertecant
Scientific reports
Girish Mishra
Aquatic Toxicology
Marie Therese soleil
Pan Arab Journal of Rhinology
Tharwat Omara
Nayan Barua
nayan barua
AL-ISHLAH: Jurnal Pendidikan
Dwi Suryani Alfa
The Journal of Urology
Matthew Rutman
New Economics Foundation
Frank van Lerven
Revista do Serviço Público
Revista do Serviço Público - RSP
Cuadernos del Centro de Estudios en Diseño y Comunicación
Valeria Stefanini
InTechOpen, London
Heimo Mikkola
Semina: Ciências Agrárias
Ana Claudia Nascimento Campos
Cornell University - arXiv
Daniel Ríos cruz
IEEE Access
Somayeh Raiesdana
Revista de la Sociedad Argentina de Diabetes
Raúl A. David
Revista Contabilidade & Finanças
RELATED TOPICS
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024

- My presentations
Auth with social network:
Download presentation
We think you have liked this presentation. If you wish to download it, please recommend it to your friends in any social system. Share buttons are a little bit lower. Thank you!
Presentation is loading. Please wait.
Ethics in Medical Research
Published by Herman Lesmono Modified over 5 years ago
Similar presentations
Presentation on theme: "Ethics in Medical Research"— Presentation transcript:
Basic Principles of Research Ethics
Allyn & Bacon 2003 Social Work Research Methods: Qualitative and Quantitative Approaches Topic 5: Ethics and Politics in Social Work Research.
Ethics Relating to Children in Research in FP7
Chapter 10 Ethical Issues in Nursing Research. Perspectives for Assessing Ethical Acceptability Utilitarian Perspective - the good of a project is defined.
Introduction to basic principles
Ethical Considerations when Developing Human Research Protocols A discipline “born in scandal and reared in protectionism” Carol Levine, 1988.
Research Ethics The American Psychological Association Guidelines
Obtaining Informed Consent: 1. Elements Of Informed Consent 2. Essential Information For Prospective Participants 3. Obligation for investigators.
THE ETHICS OF HUMAN PARTICIPANT RESEARCH Office for Research Protections The Pennsylvania State University.
Use of Children as Research Subjects What information should be provided for an FP7 ethical review?
PPA 691 – Seminar in Public Policy Analysis Lecture 1d – The Belmont Report.
Detectives in the Classroom - Investigation 2-3: What's Wrong with This Picture? What's Wrong with This Picture?
Ethics in research involving human subjects
Chapter 3 Ethics in research.
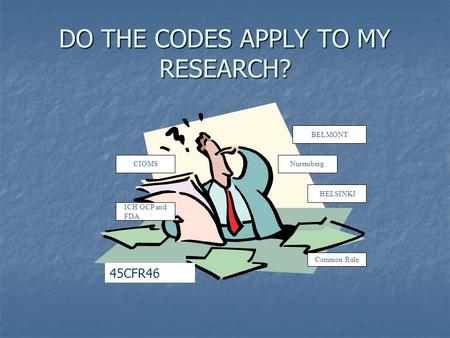
DO THE CODES APPLY TO MY RESEARCH?
Good Clinical Practice GCP

Idara C.E.. Three ethical principles guides research with human participants. principle of Autonomy 1. The principle of Autonomy requires investigators.

Research Raymond Martin Methodologies.

Human Research Ethics and Obtaining Ethics Approval
Regulatory Authority Governing Clinical Trials Anthony J. Minisi, MD Director, Cardiology Fellowship Program.
About project
© 2024 SlidePlayer.com Inc. All rights reserved.
Artificial intelligence is being used in healthcare for everything from answering patient questions to assisting with surgeries and developing new pharmaceuticals.
According to Statista , the artificial intelligence (AI) healthcare market, which is valued at $11 billion in 2021, is projected to be worth $187 billion in 2030. That massive increase means we will likely continue to see considerable changes in how medical providers, hospitals, pharmaceutical and biotechnology companies, and others in the healthcare industry operate.
Better machine learning (ML) algorithms, more access to data, cheaper hardware, and the availability of 5G have contributed to the increasing application of AI in the healthcare industry, accelerating the pace of change. AI and ML technologies can sift through enormous volumes of health data—from health records and clinical studies to genetic information—and analyze it much faster than humans.
Healthcare organizations are using AI to improve the efficiency of all kinds of processes, from back-office tasks to patient care. The following are some examples of how AI might be used to benefit staff and patients:
- Administrative workflow: Healthcare workers spend a lot of time doing paperwork and other administrative tasks. AI and automation can help perform many of those mundane tasks, freeing up employee time for other activities and giving them more face-to-face time with patients. For example, generative AI can help clinicians with note-taking and content summarization that can help keep medical records as thoroughly as possible. AI might also help with accurate coding and sharing of information between departments and billing.
- Virtual nursing assistants: One study found that 64% of patients are comfortable with the use of AI for around-the-clock access to answers that support nurses provide. AI virtual nurse assistants—which are AI-powered chatbots, apps, or other interfaces—can be used to help answer questions about medications, forward reports to doctors or surgeons and help patients schedule a visit with a physician. These sorts of routine tasks can help take work off the hands of clinical staff, who can then spend more time directly on patient care, where human judgment and interaction matter most.
- Dosage error reduction: AI can be used to help identify errors in how a patient self-administers medication. One example comes from a study in Nature Medicine , which found that up to 70% of patients don’t take insulin as prescribed. An AI-powered tool that sits in the patient’s background (much like a wifi router) might be used to flag errors in how the patient administers an insulin pen or inhaler.
- Less invasive surgeries: AI-enabled robots might be used to work around sensitive organs and tissues to help reduce blood loss, infection risk and post-surgery pain.
- Fraud prevention: Fraud in the healthcare industry is enormous, at $380 billion/year, and raises the cost of consumers’ medical premiums and out-of-pocket expenses. Implementing AI can help recognize unusual or suspicious patterns in insurance claims, such as billing for costly services or procedures that are not performed, unbundling (which is billing for the individual steps of a procedure as though they were separate procedures), and performing unnecessary tests to take advantage of insurance payments.
A recent study found that 83% of patients report poor communication as the worst part of their experience, demonstrating a strong need for clearer communication between patients and providers. AI technologies like natural language processing (NLP), predictive analytics, and speech recognition might help healthcare providers have more effective communication with patients. AI might, for instance, deliver more specific information about a patient’s treatment options, allowing the healthcare provider to have more meaningful conversations with the patient for shared decision-making.
According to Harvard’s School of Public Health , although it’s early days for this use, using AI to make diagnoses may reduce treatment costs by up to 50% and improve health outcomes by 40%.
One use case example is out of the University of Hawaii , where a research team found that deploying deep learning AI technology can improve breast cancer risk prediction. More research is needed, but the lead researcher pointed out that an AI algorithm can be trained on a much larger set of images than a radiologist—as many as a million or more radiology images. Also, that algorithm can be replicated at no cost except for hardware.
An MIT group developed an ML algorithm to determine when a human expert is needed. In some instances, such as identifying cardiomegaly in chest X-rays, they found that a hybrid human-AI model produced the best results.
Another published study found that AI recognized skin cancer better than experienced doctors. US, German and French researchers used deep learning on more than 100,000 images to identify skin cancer. Comparing the results of AI to those of 58 international dermatologists, they found AI did better.
As health and fitness monitors become more popular and more people use apps that track and analyze details about their health. They can share these real-time data sets with their doctors to monitor health issues and provide alerts in case of problems.
AI solutions—such as big data applications, machine learning algorithms and deep learning algorithms—might also be used to help humans analyze large data sets to help clinical and other decision-making. AI might also be used to help detect and track infectious diseases, such as COVID-19, tuberculosis, and malaria.
One benefit the use of AI brings to health systems is making gathering and sharing information easier. AI can help providers keep track of patient data more efficiently.
One example is diabetes. According to the Centers for Disease Control and Prevention , 10% of the US population has diabetes. Patients can now use wearable and other monitoring devices that provide feedback about their glucose levels to themselves and their medical team. AI can help providers gather that information, store, and analyze it, and provide data-driven insights from vast numbers of people. Using this information can help healthcare professionals determine how to better treat and manage diseases.
Organizations are also starting to use AI to help improve drug safety. The company SELTA SQUARE, for example, is innovating the pharmacovigilance (PV) process , a legally mandated discipline for detecting and reporting adverse effects from drugs, then assessing, understanding, and preventing those effects. PV demands significant effort and diligence from pharma producers because it’s performed from the clinical trials phase all the way through the drug’s lifetime availability. Selta Square uses a combination of AI and automation to make the PV process faster and more accurate, which helps make medicines safer for people worldwide.
Sometimes, AI might reduce the need to test potential drug compounds physically, which is an enormous cost-savings. High-fidelity molecular simulations can run on computers without incurring the high costs of traditional discovery methods.
AI also has the potential to help humans predict toxicity, bioactivity, and other characteristics of molecules or create previously unknown drug molecules from scratch.
As AI becomes more important in healthcare delivery and more AI medical applications are developed, ethical, and regulatory governance must be established. Issues that raise concern include the possibility of bias, lack of transparency, privacy concerns regarding data used for training AI models, and safety and liability issues.
“AI governance is necessary, especially for clinical applications of the technology,” said Laura Craft, VP Analyst at Gartner . “However, because new AI techniques are largely new territory for most [health delivery organizations], there is a lack of common rules, processes, and guidelines for eager entrepreneurs to follow as they design their pilots.”
The World Health Organization (WHO) spent 18 months deliberating with leading experts in ethics, digital technology, law, and human rights and various Ministries of Health members to produce a report that is called Ethics & Governance of Artificial Intelligence for Health . This report identifies ethical challenges to using AI in healthcare, identifies risks, and outlines six consensus principles to ensure AI works for the public’s benefit:
- Protecting autonomy
- Promoting human safety and well-being
- Ensuring transparency
- Fostering accountability
- Ensuring equity
- Promoting tools that are responsive and sustainable
The WHO report also provides recommendations that ensure governing AI for healthcare both maximizes the technology’s promise and holds healthcare workers accountable and responsive to the communities and people they work with.
AI provides opportunities to help reduce human error, assist medical professionals and staff, and provide patient services 24/7. As AI tools continue to develop, there is potential to use AI even more in reading medical images, X-rays and scans, diagnosing medical problems and creating treatment plans.
AI applications continue to help streamline various tasks, from answering phones to analyzing population health trends (and likely, applications yet to be considered). For instance, future AI tools may automate or augment more of the work of clinicians and staff members. That will free up humans to spend more time on more effective and compassionate face-to-face professional care.
When patients need help, they don’t want to (or can’t) wait on hold. Healthcare facilities’ resources are finite, so help isn’t always available instantaneously or 24/7—and even slight delays can create frustration and feelings of isolation or cause certain conditions to worsen.
IBM® watsonx Assistant™ AI healthcare chatbots can help providers do two things: keep their time focused where it needs to be and empower patients who call in to get quick answers to simple questions.
IBM watsonx Assistant is built on deep learning, machine learning and natural language processing (NLP) models to understand questions, search for the best answers and complete transactions by using conversational AI.
Get email updates about AI advancements, strategies, how-tos, expert perspective and more.
See IBM watsonx Assistant in action and request a demo
Get our newsletters and topic updates that deliver the latest thought leadership and insights on emerging trends.
History of Medical Ethics
Jul 18, 2014
300 likes | 776 Views
History of Medical Ethics. PH 350 Norwich University Spring 2010. Learning Objectives. To understand early medicinal thought, especially the concept of paternalism To highlight some of the major events in history that developed patient autonomy To review the goals of medicine
Share Presentation
- sexual relations
- advance directives
- tuskegee syphilis study
- average life expectancy
- final decision

Presentation Transcript
History of Medical Ethics PH 350 Norwich University Spring 2010
Learning Objectives • To understand early medicinal thought, especially the concept of paternalism • To highlight some of the major events in history that developed patient autonomy • To review the goals of medicine • To understand the major principles of modern-day medical ethics
Early Medicinal Thought • Paternalism -Medical treatment as a father/child relationship -Guiding principle: physician decides what is best for the patient and tries to follow that course of action -Focus: patient care and outcomes, not the patient’s needs or rights -Argument: maximum patient benefit can only be achieved when the doctor makes the final decision
Paternalism…Continued • Types of Paternalism -Positive vs. Negative Positive = promotes the patient’s good Negative = seeks to prevent an existing harm -Soft vs. Hard Soft = appeals to the patient’s values Hard = applies another’s values over the patient -Direct vs. Indirect Direct = benefits the patient who has been restricted Indirect = benefits a person other than the one restricted
The Father of Medicine • Hippocrates -Rejected medical views of his time -Based his medical practice on observations and study of the human body -Believed that illness has a rational explanation -Treated body as a whole unit, not just parts -Founded a medical school on the island of Cos, Greece to teach his beliefs
Hippocratic Oath • Original vs. Contemporary -language and content has been updated to fit modern beliefs about medicine -spells out physician responsibilities to both the patient and the medical profession
Evolution to Autonomy • Making the shift from paternalism -Patient given opportunity to determine benefit vs. harm - The Patient’s Bill of Rights -Questions being raised regarding the patient’s wishes as to what is ethical -How much do you tell the patient? -Do they even want to know?
Notable Cases in History • Nuremberg Code: 1946 -Limits on medical research following Nazi testing of hypothermia & antimicrobial agents -Subjects were put in ice tanks for 3 hours, wounds were inflicted & purposely infected with bacteria -Concepts of informed consent, avoiding all unnecessary physical & mental suffering, proper preparation & facilities, ability for subjects to opt out, basing human experiments on results of animal testing
Notable Cases…Continued • Tuskegee Syphilis Study: 1929 -Use of placebos in studies -Participants were illiterate, black sharecroppers thought to have “bad blood” -Deaths, chronic illness, and transmission to wives & children resulted
Notable Cases…Continued • Nancy Cruzan: 1983 -Was maintained in a persistent vegetative state for several years -Parents requested that artificial hydration and nutrition be withdrawn -Courts rule in their favor, but healthcare team appeals the decision -Incompetent patients need to be protected by law -Encouraged the development of advance directives and appointment of a health care proxy to carry out patient’s wishes
Goals of Medicine • Relieve suffering - Example: The use of Chloroform and Ether Chloroform was used more often because it was faster acting, less was needed to put someone under, and it was non-flammable. However, it was more dangerous than using Ether. The risk of drug overdose was greater with Chloroform.
Goals…Continued • Promote health - Flintstones Vitamins - Acne Treatment - Weight loss
Goals…Continued • To cure disease and preserve life 1900 – Average life expectancy was 49 2003 – Average Life expectancy is 78 • Vaccinations Definition: “A preparation of a weakened or killed pathogen, such as a bacterium or virus, or of a portion of the pathogen's structure that upon administration stimulates antibody production or cellular immunity against the pathogen but is incapable of causing severe infection.” -Swine Flu • Cures - Breast Cancer
Principles of Medical Ethics • Confidentiality -HIPAA (Health Insurance Portability & Accountability Act) • Honesty -Telling patients what they need to know • Justice -Treating all patients without discrimination • Gatekeeping -Patients access to medicine through doctors • Report impaired colleagues
Principles…Continued • Avoid sexual relations with patients • Conflicts of interest • Scope of practice -Range of responsibility, abilities • Gaming the system -Using patients to make more money
Thank you to all of our viewers! The End Produced by: J. Bielski, H. Black, V. Bruce, & J. Davis
- More by User
Medical Ethics
Medical Ethics. Introduction. What is Ethics?. What is medical science?. How are medical science and ethics related?. Why Ethics Become Important?.
10.37k views • 49 slides
Medical Ethics. Introduction. The Origins of the Field and Its Current Status. The Beginnings: a) The Nuremburg Code, 1948 b) Life Magazine article on dialysis selection committees, November 1962 . Earlier Points of Origin: Babylonian Codes Hippocratic Code/Oath Islamic Codes
520 views • 18 slides

Principles of Medical Ethics
Principles of Medical Ethics. Autonomy Nonmaleficence Beneficence Justice/Equity. Ethical Issues in Research. Informed consent Explanation of the research: risks/benefits Protection of the subject’s well being Confidentiality of data Control group issues Ethical review/decision process
1.01k views • 9 slides
MEDICAL ETHICS
MEDICAL ETHICS. A Brief Introductory Lecture Ms Shirley Chan / EL Dept / JJC. 2010. What is ethics?. Ethics is a system of moral principles They affect how people make decisions and lead their lives Ethics is concerned with what is good for individuals and society
1.27k views • 57 slides

Medical Ethics. http://www.youtube.com/watch?v=VU_rTX23V7Q. Psalm 139. Psalm 139: 13-16 You formed my inmost being; You knit me in my mother’s womb. I praise you, so wonderfully you made me; Wonderful are your works! My very self you knew; My bones were not hidden from you,
541 views • 13 slides
Medical Ethics. Nigel Calvert. Plan. Short presentation on basic medical ethics concepts Group Work – written material Discussion Group Work – My Sister’s Keeper Discussion Conclusions. Concepts in Medical Ethics. Non-maleficence Beneficence Autonomy Truth-telling Confidentiality
420 views • 10 slides
Medical Ethics. Learning Objectives:- To understand the nature of medical ethics in terms of both beginning life and maintaining life. To consider the meaning and effectiveness of IVF AID/H and surrogacy in fertility treatments.
765 views • 7 slides
Ethics of Medical Research
Ethics of Medical Research. Professor Ahmed A. Adeel. Objectives . Identify the main principles of medical research ethics. Discuss the balance of research and clinical care. Describe requirements of ethics review committees , including definition of informed consent.
1.4k views • 63 slides
Medical Ethics. Rev. Donna Field, M. Div . BSN PCCN Medical Ethics Fellow 2013-2014 North Shore LIJ Division of Medical Ethics, Department of Medicine. BIOETHICS. Arises from dilemmas or conflicts encountered in moral choices about clinical issues in the care of patients.
702 views • 22 slides
HISTORY OF MEDICAL ETHICS JEOPARDY
HISTORY OF MEDICAL ETHICS JEOPARDY . NOTABLE CASES. PATERNALISM. HIPPOCRATES. PRINCIPLES. MISC. 100. 100. 100. 100. 100. 200. 200. 200. 200. 200. 300. 300. 300. 300. 300. 400. 400. 400. 400. 400. 500. 500. 500. 500. 500. PATERNALISM FOR 100.
658 views • 52 slides
Medical Ethics. Fall 2011 Philosophy 2440 Prof. Robert N. Johnson Friday, August 8, 2014. MIDTERM NEXT THURSDAY (11/13) IN YOUR DISCUSSION LAB DESCRIPTION AND ESSAY QUESTIONS: http:// web.missouri.edu /~ johnsonrn /midtermFS11.htm. Advanced Directives. HELGA WANGLIE.
579 views • 10 slides
Medical Ethics. Antony Vaughan General Practitioner. Medical ethics principles. Beneficence Non-maleficence Autonomy Justice Dignity Truthfulness. Medical Business Environmental Legal Political. Feminism Animal rights Bioethics Gay rights.
1.33k views • 34 slides
Medical ethics
Medical ethics. Dr D Grace MD. FFARCSI. Dip.ICM. Dept of Anaesthesia & Critical Care Medicine Altnagelvin Area Hospital. 1. Aims. Consider medical ethics & clinical practice Outline and define ethical principles Outline practicalities & challenging issues arising in medical practice. 2.
507 views • 24 slides
Medical Ethics. Advancement in medicine creates new problems. Medical Ethics. How will the recipient of an organ be chosen? Who will be allowed to receive experimental drugs? How will the creation of in vitro embryos be ethically managed?
484 views • 10 slides
Medical Ethics. Fall 2011 Philosophy 2440 Prof. Robert N. Johnson Wednesday, November 12, 2014. Do animals have rights?. Carl Cohen: No Rights are claims among a community of moral agents. Animals are not moral agents. Therefore, animals have no rights. Do animals have rights?.
510 views • 30 slides
Medical Ethics. Fall 2011 Philosophy 2440 Prof. Robert N. Johnson Thursday, November 13, 2014. Utilitarianism and Voluntary Euthanasia. Hentoff: Physicians are bad at palliative care. The only meaningful difference between terminal sedation and euthanasia is that the former takes longer.
582 views • 15 slides
Medical Ethics. Fall 2011 Philosophy 2440 Prof. Robert N. Johnson Thursday, November 20, 2014. The Cruzan Case and Advanced Directives. Missouri Supreme Court, 1988. 1) Treatment vs. Care Special Status of Nutrition and Hydration: Treatment is treatment Nutrition and hydration is care
231 views • 9 slides
MEDICAL ETHICS. Dr. Riyaz Mather. ETHICS. Described as the ‘science’ of morality. And defines systems of moral values. Medical ethics The standards of conduct and competence expected of medical professionals, some of which are captured in legislation.
263 views • 12 slides
Medical ethics. Introduction to basic principles. Ethics are not …. Ethics is not the same as feelings Ethics is not religion Ethics is not following the law Ethics is not following culturally accepted norms Ethics is not science. Ethics are …. Moral Principles What is good and bad
415 views • 20 slides
Medical Ethics. Basic Concepts of Medical ethics. Confidentiality. Confidentiality. The doctor patient relation ship is an extremely confidential one All information that the doctor has acquired professionally should be kept strictly confidential (Professional secrecy). Confidentiality….
613 views • 39 slides
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
- Public Health
Perspective
When pto stands for 'pretend time off': doctors struggle to take real breaks.
Mara Gordon

A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off. Wolfgang Kaehler/LightRocket via Getty Images hide caption
A survey shows that doctors have trouble taking full vacations from their high-stress jobs. Even when they do, they often still do work on their time off.
A few weeks ago, I took a vacation with my family. We went hiking in the national parks of southern Utah, and I was blissfully disconnected from work.
I'm a family physician, so taking a break from my job meant not seeing patients. It also meant not responding to patients' messages or checking my work email. For a full week, I was free.
Taking a real break — with no sneaky computer time to bang out a few prescription refill requests — left me feeling reenergized and ready to take care of my patients when I returned.
But apparently, being a doctor who doesn't work on vacation puts me squarely in the minority of U.S. physicians.
Research published in JAMA Network Open this year set out to quantify exactly how doctors use their vacation time — and what the implications might be for a health care workforce plagued by burnout, dissatisfaction and doctors who are thinking about leaving medicine.
"There is a strong business case for supporting taking real vacation," says Dr. Christine Sinsky , the lead author of the paper. "Burnout is incredibly expensive for organizations."

Shots - Health News
Health workers know what good care is. pandemic burnout is getting in the way.
Researchers surveyed 3,024 doctors, part of an American Medical Association cohort designed to represent the American physician workforce. They found that 59.6% of American physicians took 15 days of vacation or less per year. That's a little more than the average American: Most workers who have been at a job for a year or more get between 10 and 14 days of paid vacation time , according to the U.S. Bureau of Labor Statistics.
However, most doctors don't take real vacation. Over 70% of doctors surveyed said they worked on a typical vacation day.
"I have heard physicians refer to PTO as 'pretend time off,'" Sinsky says, referring to the acronym for "paid time off."
Sinsky and co-authors found that physicians who took more than three weeks of vacation a year had lower rates of burnout than those who took less, since vacation time is linked to well-being and job satisfaction .
And all those doctors toiling away on vacation, sitting poolside with their laptops? Sinsky argues it has serious consequences for health care.
Physician burnout is linked to high job turnover and excess health care costs , among other problems.
Still, it can be hard to change the culture of workaholism in medicine. Even the study authors confessed that they, too, worked on vacation.
"I remember when one of our first well-being papers was published," says Dr. Colin West , a co-author of the new study and a health care workforce researcher at the Mayo Clinic. "I responded to the revisions up at the family cabin in northern Minnesota on vacation."
Sinsky agreed. "I do not take all my vacation, which I recognize as a delicious irony of the whole thing," she says.
She's the American Medical Association's vice president of professional satisfaction. If she can't take a real vacation, is there any hope for the rest of us?
I interviewed a half dozen fellow physicians and chatted off the record with many friends and colleagues to get a sense of why it feels so hard to give ourselves a break. Here, I offer a few theories about why doctors are so terrible at taking time off.
We don't want to make more work for our colleagues
The authors of the study in JAMA Network Open didn't explore exactly what type of work doctors did on vacation, but the physicians I spoke to had some ideas.
"If I am not doing anything, I will triage my email a little bit," says Jocelyn Fitzgerald , a urogynecologist at the University of Pittsburgh who was not involved in the study. "I also find that certain high-priority virtual meetings sometimes find their way into my vacations."
Even if doctors aren't scheduled to see patients, there's almost always plenty of work to be done: dealing with emergencies, medication refills, paperwork. For many of us, the electronic medical record (EMR) is an unrelenting taskmaster , delivering a near-constant flow of bureaucratic to-dos.
When I go on vacation, my fellow primary care doctors handle that work for me, and I do the same for them.
But it can sometimes feel like a lot to ask, especially when colleagues are doing that work on top of their normal workload.
"You end up putting people in kind of a sticky situation, asking for favors, and they [feel they] need to pay it back," says Jay-Sheree Allen , a family physician and fellow in preventive medicine at the Mayo Clinic.
She says her practice has a "doctor of the day" who covers all urgent calls and messages, which helps reduce some of the guilt she feels about taking time off.
Still, non-urgent tasks are left for her to complete when she gets back. She says she usually logs in to the EMR when she's on vacation so the tasks don't pile up upon her return. If she doesn't, Allen estimates there will be about eight hours of paperwork awaiting her after a week or so of vacation.
"My strategy, I absolutely do not recommend," Allen says. But "I would prefer that than coming back to the total storm."
We have too little flexibility about when we take vacation
Lawren Wooten , a resident physician in pediatrics at the University of California San Francisco, says she takes 100% of her vacation time. But there are a lot of stipulations about exactly how she uses it.
She has to take it in two-week blocks — "that's a long time at once," she says — and it's hard to change the schedule once her chief residents assign her dates.
"Sometimes I wish I had vacation in the middle of two really emotionally challenging rotations like an ICU rotation and an oncology rotation," she says, referring to the intensive care unit. "We don't really get to control our schedules at this point in our careers."
Once Wooten finishes residency and becomes an attending physician, it's likely she'll have more autonomy over her vacation time — but not necessarily all that much more.
"We generally have to know when our vacations are far in advance because patients schedule with us far in advance," says Fitzgerald, the gynecologist.
Taking vacation means giving up potential pay
Many physicians are paid based on the number of patients they see or procedures they complete. If they take time off work, they make less money.
"Vacation is money off your table," says West, the physician well-being researcher. "People have a hard time stepping off of the treadmill."
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount regardless of patient volume. That means the more patients doctors cram into their schedules, the more money they make. Going on vacation could decrease their take-home pay.
But West says it's important to weigh the financial benefits of skipping vacation against the risk of burnout from working too much.
Physician burnout is linked not only to excess health care costs but also to higher rates of medical errors. In one large survey of American surgeons , for example, surgeons experiencing burnout were more likely to report being involved in a major medical error. (It's unclear to what extent the burnout caused the errors or the errors caused the burnout, however.)
Doctors think they're the only one who can do their jobs
When I go on vacation, my colleagues see my patients for me. I work in a small office, so I know the other doctors well and I trust that my patients are in good hands when I'm away.

Doctors have their own diagnosis: 'Moral distress' from an inhumane health system
But ceding that control to colleagues might be difficult for some doctors, especially when it comes to challenging patients or big research projects.
"I think we need to learn to be better at trusting our colleagues," says Adi Shah , an infectious disease doctor at the Mayo Clinic. "You don't have to micromanage every slide on the PowerPoint — it's OK."
West, the well-being researcher, says health care is moving toward a team-based model and away from a culture where an individual doctor is responsible for everything. Still, he adds, it can be hard for some doctors to accept help.
"You can be a neurosurgeon, you're supposed to go on vacation tomorrow and you operate on a patient. And there are complications or risk of complications, and you're the one who has the relationship with that family," West says. "It is really, really hard for us to say ... 'You're in great hands with the rest of my team.'"
What doctors need, says West, is "a little bit less of the God complex."
We don't have any interests other than medicine
Shah, the infectious disease doctor, frequently posts tongue-in-cheek memes on X (formerly known as Twitter) about the culture of medicine. Unplugging during vacation is one of his favorite topics, despite his struggles to follow his own advice.
His recommendation to doctors is to get a hobby, so we can find something better to do than work all the time.
"Stop taking yourself too seriously," he says. Shah argues that medical training is so busy that many physicians neglect to develop any interests other than medicine. When fully trained doctors are finally finished with their education, he says, they're at a loss for what to do with their newfound freedom.
Since completing his training a few years ago, Shah has committed himself to new hobbies, such as salsa dancing. He has plans to go to a kite festival next year.
Shah has also prioritized making the long trip from Minnesota to see his family in India at least twice a year — a journey that requires significant time off work. He has a trip there planned this month.
"This is the first time in 11 years I'm making it to India in summer so that I can have a mango in May," the peak season for the fruit, Shah says.
Wooten, the pediatrician, agrees. She works hard to develop a full life outside her career.
"Throughout our secondary and medical education, I believe we've really been indoctrinated into putting institutions above ourselves," Wooten adds. "It takes work to overcome that."
Mara Gordon is a family physician in Camden, N.J., and a contributor to NPR. She's on X as @MaraGordonMD .
- American Medical Association

IMAGES
VIDEO
COMMENTS
May 8, 2018 • Download as PPTX, PDF •. 27 likes • 6,632 views. A. Ashok Kulkarni. Ethics in Medical research. Health & Medicine. 1 of 23. Download now. 12. ethics in medical research - Download as a PDF or view online for free.
NSF. (1) Fabrication means making up data or results and recording or reporting them. (2) Falsification means manipulating research materials, equipment, or processes, or changing or omitting data or results such that the research is not accurately represented in the research record. (3) Plagiarism means the appropriation of another person's ...
introduction to medical ethics and bioethics. Apr 16, 2021 • Download as PPTX, PDF •. 4 likes • 2,032 views. AI-enhanced description. R. RamiAboali. This document discusses medical ethics and legal medicine. It begins by defining ethics, morality, values, and their relationship. It then discusses the principles of medical ethics including ...
Focus on relationships involving care, responsibility, and trust 6 E THICAL T HEORY …. TO A CTION Theory Principle Rule Action. An introduction to Bioethics A Modified presentation by Nicole M. Deming, J.D., M.A. Assistant Professor of Bioethics Case Western Reserve University School of Medicine. HTML view of the presentation.
See Full PDFDownload PDF. Ethics in research involving humans were first codified in 1946 as Nuremberg code. Subsequently other ethical declarations and guide lines were developed to protect the research participants as well as the researchers. The basic research bioethics includes three principles-respects for person, beneficence, and justice.
Ethical Principles of Research Hippocrates was the first physician to define the ethical principles of research in humans. These principles are still valid today: Autonomy - to respect the autonomy of the participant or of their representative; Beneficence - to act always in the best interest of the participant; Non-maleficence - to do as little harm as possible to the participant ...
Ethics in Healthcare: Current Ethics, Ethical vs Unethical Research through 1970. If you have any questions about the program you have just watched, you may call us at: (800) 424-4888 or fax (806) 743-2233. Direct your inquiries to Customer Service. Be sure to include the program number, title and speaker.
Writing Strategies and Ethical Considerations. Pages Sage Publishers 2003. Download ppt "ETHICS IN BIOMEDICAL RESEARCH". LEARNING OBJECTIVES Define the term "ethics" in health research Recognize the need for adherence to ethical principles in health research Describe the general ethical principles in health research Justify the role of ...
1 INTRODUCTION TO MEDICAL ETHICS. Assist.Prof.Dr. Mehmet KARATAS Dept. of History of Medicine and Ethics. 2 CONCEPTS ETHICS MORALS DEONTOLOGY BIOETHICS BIOMEDICAL ETHİCS ACTION. VIRTUE. 3 ETHICS In Greek "Ethos" Good, well, temperament, character. The code of ethics are defined by the reactions of the society It has no legal obligation It ...
Ethics of Medical Research Professor Ahmed A. Adeel. Objectives • Identify the main principles of medical research ethics. • Discuss the balance of research and clinical care. • Describe requirements of ethics review committees, including definition of informed consent. • Identify the key international and national references for the ...
Module for Teaching Medical Ethics to Undergraduates iii Contributors Acknowledgement A team of academic staff members from Faculty of Medicine, University of ... • Principles of research ethics and research publication 1 e.g. medical tourism, conflict situations, female foeticide, female genital mutilation. ...
INTRODUCTION TO MEDICAL ETHICS Assist.Prof.Dr. Mehmet KARATAŞ Department of History of MedicineandEthics. CONCEPTS • ETHICS • MORALS • DEONTOLOGY • BIOETHICS • ACTION • VIRTUE. ETHICS • In Greek "Ethos" • Good, well • The code of ethics are defined by the reactions of the society • It has no legal obligation • It ...
Presentation Transcript. Ethics of Medical Research Professor Ahmed A. Adeel. Objectives By the end of this lecture the student should be able to • Identify the main principles of medical research ethics. • Discuss the balance of research and clinical care. • Describe requirements of ethics review committees, including definition of ...
Phase 1 and Phase 2. Ethics is the discipline that systematically analyzes and rationally justifies our moral choices (Pellegrino). Knowledge of ethics is critical to the professional development of the physician (Hafferty). Ethical decision making deals with concrete judgments in situations in which action must be taken despite uncertainty.
Ethics of medical research on human subjects must be clinically justified and scientifically sound. Informed consent is a mandatory component of any clinical research. Investigators are obligated to design research protocols that establish standards of scientific integrity, safeguard ethical and legislative issues of the human subjects, and ...
PK !!Zï C [Content_Types].xml ¢ ( Ę[o›0 †ï'õ? ßVÁI·uÝ RUÝvµC¥v?Àƒ/Ä >È6YóïgC'ÑŠ Œ¸A1öû¾ >±¼~dE´ ¥©à ZÄs OEFyž ŸgW(Ò†ðŒ ‚C‚v ÑõêìÕòa'AGVÍu‚6ÆÈ ët ŒèXHà¶g- #Æ6UŽ%I " ðÅ|~‰SÁ p33Î - aMÊÂDŸ íëšDò E·õ8 • ʜ޽NJ_ Ú%UG»FA¡Ÿiˆ" M‰±ýx˳gs™íç [e5Fo¨ÔçvÀ‰ ×s:`¯ûnÿE3ˆîˆ2ß ³ ...
Download ppt "Ethics in Medical Research" Similar presentations . Basic Principles of Research Ethics. Allyn & Bacon 2003 Social Work Research Methods: Qualitative and Quantitative Approaches Topic 5: Ethics and Politics in Social Work Research.
Research Methodology and Biostatistics syllabus: Medical Research: History, values in medical ethics, autonomy, beneficence, non-maleficence, double effect, conflicts between autonomy. Medical research has a long and varied history. It has evolved from rudimentary practices to sophisticated, evidence-based methodologies.
According to Statista, the artificial intelligence (AI) healthcare market, which is valued at $11 billion in 2021, is projected to be worth $187 billion in 2030.That massive increase means we will likely continue to see considerable changes in how medical providers, hospitals, pharmaceutical and biotechnology companies, and others in the healthcare industry operate.
History of Medical Ethics. PH 350 Norwich University Spring 2010. Learning Objectives. To understand early medicinal thought, especially the concept of paternalism To highlight some of the major events in history that developed patient autonomy To review the goals of medicine. Download Presentation. sexual relations. advance directives. indirect.
A 2022 research brief from the American Medical Association estimated that over 55% of U.S. physicians were paid at least in part based on "productivity," as opposed to earning a flat amount ...