- Open access
- Published: 12 March 2019

Factors influencing unmet need for family planning among Ghanaian married/union women: a multinomial mixed effects logistic regression modelling approach
- Chris Guure 1 ,
- Ernest Tei Maya 2 ,
- Samuel Dery 1 ,
- Baaba da-Costa Vrom 1 ,
- Refah M. Alotaibi 3 ,
- Hoda Ragab Rezk 3 , 4 &
- Alfred Yawson 1
Archives of Public Health volume 77 , Article number: 11 ( 2019 ) Cite this article
17k Accesses
25 Citations
8 Altmetric
Metrics details
Unmet need for family planning is high (30%) in Ghana. Reducing unmet need for family planning will reduce the high levels of unintended pregnancies, unsafe abortions, maternal and neonatal morbidity and mortality. The purpose of this study was to examine factors that are associated with unmet need for family planning to help scale up the uptake of family planning services in Ghana.
This cross sectional descriptive and inferential study involved secondary data analysis of women in the reproductive age (15–49 years) from the Ghana Demographic and Health Survey 2014 data. The outcome variable was unmet need for family planning which was categorized into three as no unmet need, unmet need for limiting and unmet need for spacing. Chi-squared test statistic and bivariate multilevel multinomial mixed effects logistic regression model were used to determine significant variables which were included for the multivariable multilevel multinomial mixed effects logistic regression model. All significant variables ( p < 0.05) based on the bivariate analysis were included in the multinomial mixed effects logistic regression model via model building approach.
Women who fear contraceptive side effects were about 2.94 (95% CI, 2.28, 3.80) and 2.58 (95% CI, 2.05, 3.24) times more likely to have an unmet need for limiting and spacing respectively compared to those who do not fear side effects. Respondents’ age was a very significant predictor of unmet need for family planning. There was very high predictive probability among 45–49 year group (0.86) compared to the 15–19 year group (0.02) for limiting. The marginal predictive probability for spacing changed significantly from 0.74 to 0.04 as age changed from 15 to 19 to 45–49 years. Infrequent sexual intercourse, opposition from partners, socio-economic (wealth index, respondents educational level, respondents and partner’s occupation) and cultural (religion and ethnicity) were all significant determinants of both unmet need for limiting and spacing.
Conclusions
This study reveals that fear of side effect, infrequent sex, age, ethnicity, partner’s education and region were the most highly significant predictors of both limiting and spacing. These factors must be considered in trying to meet the unmet need for family planning.
Peer Review reports
Beyond the health benefits that accrue to women, children and men from family planning, it is a catalyst for environmental sustainability, [ 1 ] and economic growth of countries [ 2 ]. Thus, Ghana’s strive to improve its economic fortunes and health of the populace will be difficult if efforts are not made to reduce its high unmet need for family planning.
Unmet need for family planning is essentially the percentage of married/union women of reproductive age who are not using any method of family planning but who would like to postpone the next pregnancy (unmet need for spacing) or do not want to have any more children (unmet need for limiting) [ 3 ]. The concept of unmet need defines the gap between women’s reproductive intentions and their contraceptive behaviour. Unintended pregnancies have serious consequences for the health and well-being of women and their families, particularly in developing countries where maternal mortality is high and induced abortions are often unsafe. More than 358,000 women die of pregnancy-related causes every year, according to a report from the World Health Organization [ 4 ]. Couples who use contraception have the ability to control the number and spacing of their children thus preventing unintended pregnancies, abortions and deaths related to pregnancy and childbirth.
The recent Ghana Demographic and Health Survey 2014, estimated that 30 % of currently married women have an unmet need for family planning services, with 17% having an unmet need for spacing and 13% having an unmet need for limiting. Knowledge of contraceptives is universal in the developed world and almost universal in the developing world [ 5 ]. Globally, there is a high saturation of knowledge on contraceptive methods, with knowledge of at least one contraceptive method in sub-Saharan Africa being approximately 85%, [ 6 ].
The 2014 Ghana Demographic and Health Survey found that 99% of women and men knew of at least one contraceptive method [ 7 ]. The survey also showed that modern contraceptive methods were more known than traditional ones among women, with the male condom (96%), injectable (92%), and pills (91%) being the most commonly known methods. However, there is considerable variability in this knowledge across different population demographics such as, age, occupation, religion and ethnicity [ 8 ]. Knowledge however does not directly translate to use.
The United Nations [ 9 ] report on world contraceptive patterns shows that 63% of women of reproductive age who are married or in a union use a contraceptive method. Globally, female sterilization is the most common method of contraception, used by 19% of married/union women of reproductive age (15–49 years) group. The IUD, used by 14% of women of reproductive age who are married or in a union, is the second most widely used contraceptive method in the world, followed by the pill.
Ghana is a signatory to the Family Planning 2020 (FP2020) and has committed to increasing modern contraceptive use among married/in union women from 22% in 2012 to 30% in 2020, (Government of Ghana (GOG), 2016). In Ghana, the prevalence of modern contraceptive use among married/in union women is 22%; that of unmet need among married/in union women is 30% and the demand for modern contraceptive satisfied is 39% [ 7 ]. With just 2 years to 2020, there is the need to increase efforts to satisfy women’s need for contraception. It is therefore imperative to look at the magnitude of the individual determinants and their effects on unmet need for contraception after accounting for unobserved household and/or cluster variations. Unlike contraceptive prevalence which does not consider women’s ability to become pregnant and their wishes for children unmet need for family planning, takes these factors into consideration. We therefore concentrated on unmet need for family planning which gives the vital information about women’s need for family planning.
Study design and data source
This study used a secondary data from the 2014 Ghana Demographic and Health Survey for the analysis. The 2014 Ghana Demographic and Health Survey (GDHS) is a nationally representative household survey that collects very wide range of population, health and other important indicators covering all the ten regions of Ghana. Participants in the survey were asked retrospective questions spanning 5 years prior to the survey.
Sampling approach and study population
The 2014 GDHS followed a two-stage sample design and was intended to allow estimates of key indicators at the national level as well as for urban and rural areas and each of Ghana’s 10 administrative regions. The first stage involved selecting sample points (clusters) consisting of enumeration areas (EAs) delineated for the 2010 Ghana population and housing census (PHC). A total of 427 clusters were selected; 216 in urban areas and 211 in rural areas.
The second stage involved the systematic sampling of households. A household listing was undertaken in all the selected EAs in January–March 2014. The households included in the survey were randomly selected from the list. About 30 households were selected from each cluster to constitute the total sample size of 12,831 households. Because of the approximately equal sample sizes in each region, the sample is not self-weighting at the national level, and weighting factors have been added to the data file so that the results will be proportional at the national level [ 5 ]. In this current study, a total of 6503 (married/union) out of the 10,357 reproductive age women data were analysed in the 2014 GDHS.
Outcome variable, inclusion and exclusion criteria
The outcome variable of interest is unmet need for family planning. Unmet need for family planning was categorized into three; unmet need for spacing, unmet need for limiting and no unmet need. The categorization also conformed to the recently revised version of unmet need for family planning applied in DHS [ 10 ]. The number of participants who had their classification regarding unmet need for spacing, limiting and no unmet need after data manipulation and with only complete case analysis (respondents with no missing information) were 1708(26.26%), 2918(44.87%) and 1877(28.67%) respectively.
The inclusion criteria involved women in their reproductive ages, that is, 15–49 years and were either currently married or in a union. We included only married/ in union women with the reasonable assumption that they are exposed to regular sexual intercourse.
The exclusion criteria were married/in union women who had incomplete information (missing data).
Statistical analysis
The current analysis used both descriptive and inferential methods. Descriptive statistics used included frequencies and percentages. Both bivariate and multivariable techniques were used to assess statistical associations between the outcome variable and the predictors. The bivariate technique was applied to obtain predictors that had a statistically significant relationship with the outcome of interest (unmet need for family planning). In this approach, factors that were statistically significantly associated with the outcome were obtained via a simple multinomial mixed effects logistic regression model as well as chi-squared test of independence with the help of their confidence intervals (CI) and p -values. P -value less than or equal to 0.10 was used to retain and include variables in the multivariable analysis to obtain the risk ratios as a measure of association.
Further analysis were carried out with four selected variables (religion, region, education and age) to obtain predictive probabilities which enabled us observe the association between these predictor variables and the outcome. These were randomly picked for the purpose exploration. Although the simple multinomial mixed effects logistic regression model is complex, we used it because of the need to adjust and obtain parameter estimates through a fixed effects (multivariable) model, outcome variable categorized into three levels (referred to as multinomial), nesting nature of the GDHS data (multilevel) and the need to account for the cluster effects (via a random effects approach) which is not included in the data set.
The Ghana DHS 2014, is structured in such a way that women were nested within households and households were further nested within clusters. Due to the hierarchical nature of this survey, it is very important that a multilevel regression model be used in order to obtain a more accurate and reliable estimates of the model parameters. This modelling approach ensures that between household and cluster variations are properly accounted for in order to avoid parameter over-estimation. In accounting for these variations, enumeration areas referred to as clusters were considered as a level-2 variable while that of respondents or individual-level variables were assigned level-1. This statistical approach was implemented in STATA via a Generalized Structural Equation Modelling (with the logit link function and robust variance estimator for the standard error) approach in the STATA (Stata Statistical Software: Release 14. College Station, TX: StataCorp LP) software. We used Stata default number of iterations with convergence tolerances log likelihood of 1e^ (− 7). Four different models via nesting were specified and the final interpretation of coefficients were based on the best model among them. The best model was arrived at through the use of the log-likelihood ratio test and the Akaike information criteria. The predictive probabilities that were calculated and presented graphically were obtained using the robust approach to estimate the standard errors with vce (unconditional) option for the margins.
Model building with potential risk factors
The specifications of the models were based on variables that showed significant associations at the bivariate analysis with the Pearson’s chi-squared test statistic. Groupings of these variables were done according to socio-demographic, socio-economic, socio-cultural and psychosocial and other factors. Model-1 constituted our first model containing socio-demographic variables (region, age category and place of residence). Model-2 was formulated using Model-1 in addition to socio-economic factors (respondent’s educational level, wealth index of respondent’s household, respondent’s occupation and partner’s occupation). Model-3 involved Model-2 and socio-cultural factors (respondent’s religious beliefs and ethnicity). Model-3 was nested in Model-4 in addition to psychosocial and other factors (infrequent sex, partner’s opposition to contraceptive use, and fear of side effect). All these models were implemented via the multilevel modelling approach.
A total of 6503 married/union women met the inclusion criteria for this study. The mean (standard deviation (SD) age in years of the women was 35.27(7.1). Out of the 6503, 1877(28.9%) had no unmet need for family planning, 2918(44.9%) had unmet need for limiting while 1708(26.3%) had unmet need for spacing. The mean (SD) age in years of the respondents with no unmet need was 33.13(6.7) while that for those with unmet need for limiting and spacing were 39.19(5.7) and 30.94(6.1) respectively. Figures 1 , 2 , 3 , 4 , depict percentages of the four main variables (religion, region, age category and educational level) that were of primary interest in this study and grouped according to the outcome variable (unmet need for family planning) and further grouped according to place of residence (urban and rural). Majority (40.1%) of the respondents who had no unmet need were of the Islamic religion for urban setting. Those with unmet need for limiting and spacing were of the Charismatic religious belief for both the urban and rural residence. Respondents without any religious background had the least type of unmet need across both residential types.
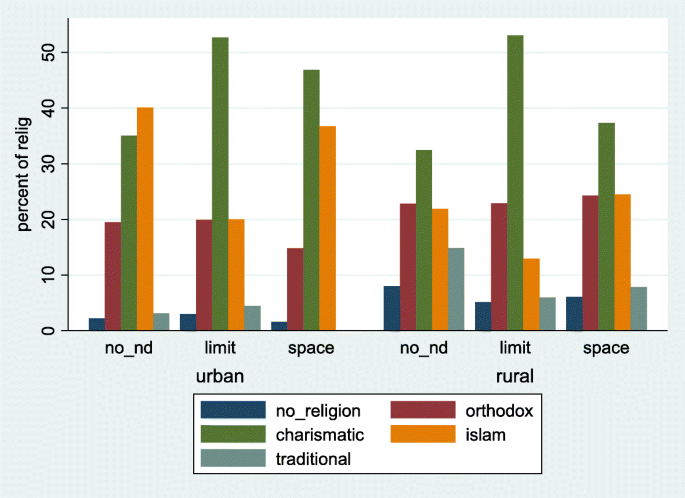
Distribution of unmet need for family planning among women (married or union) by religion and stratified by place of residence. Ghana Demographic and Health Survey, 2014. Legend: no_nd: no unmet need; limit: unmet need for limiting; space: unmet need for spacing
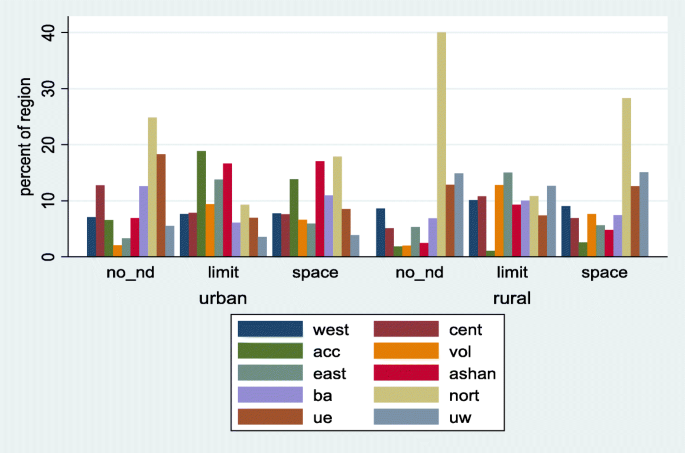
Distribution of unmet need for family planning among women (married or union) by region and stratified by place of residence. Ghana Demographic and Health Survey, 2014. Legend: no_nd: no unmet need; limit: unmet need for limiting; space: unmet need for spacing
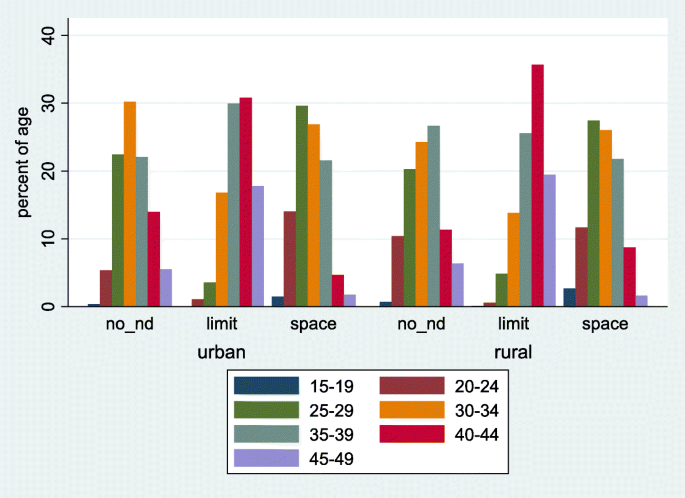
Distribution of unmet need for family planning among women (married or union) by age and stratified by place of residence. Ghana Demographic and Health Survey, 2014. Legend: no_nd: no unmet need; limit: unmet need for limiting; space: unmet need for spacing
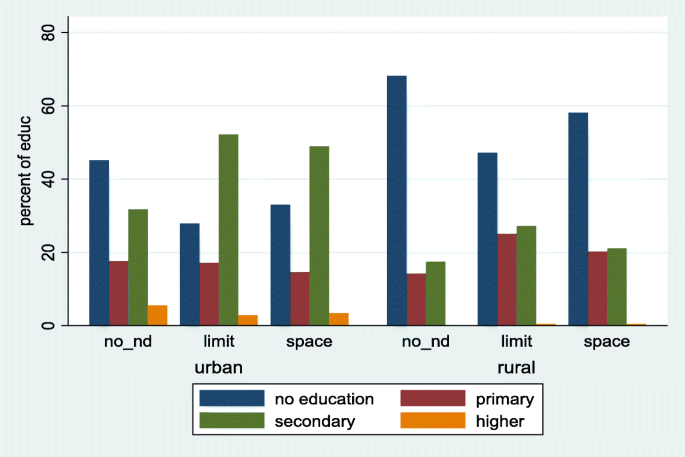
Distribution of unmet need for family planning among women (married or union) by education and stratified by place of residence. Ghana Demographic and Health Survey, 2014. Legend: no_nd: no unmet need; limit: unmet need for limiting; space: unmet need for spacing
With respect to regional distribution, majority of those with no unmet need for family planning were from the Northern region of Ghana for both urban (24.9%) and rural (40.1%) areas. Similarly, women in the Northern region had the highest unmet need for spacing for both urban (17.9%) and rural (28.3%) areas. Concerning unmet need for limiting, the Greater Accra region reported the highest (18.8%) for the rural areas while the Eastern region had the highest (15.0%) for the urban areas.
There was a high cluster effect at the multivariable analyses level. There were 8.88 and 3.95 for limiting and spacing respectively, Table 1 . The adjusted relative risk ratio results presented in Table 1 , constitute one out of the four Models specified in the model building subsection, though it contains all the variables in the other sub-models. The final Model was arrived at after calculating the goodness of fit of all the Models using the likelihood ratio test statistic and the Akaike information criteria, as presented in Table S1 (Additional file 1 ). The best model was selected on the basis that it had the lowest value of the Akaike information criteria (AIC). As stipulated in (Additional file 1 : Table S1, the more the significant variables were added to a Model, the better its fit. The Akaike information criteria was 8783.67 for Model-4 with its closest value being 8936.00 for Model-3, indicating that Model-4 is a better fit compared to Model-3, The difference between the two Models was 129.33. The likelihood ratio test for Model 4 compared to Model-3 was 164.33 with a p -value < 0.001, reinforcing the point that Model-4 is a better fit Model. Model-4 was therefore used for the final analysis. The calculated unobserved effect for the best fit Model (Model 4) was 8.88 implying a standard deviation of 2.98 for limiting. That for spacing was 3.95 implying a standard deviation of 1.99. The covariance between limiting and spacing was 2.73, an indication of a weak correlation (0.46) between them. Thus a 1-standard deviation of the random effects amounts to an exp. (2.98) = 19.69 and exp.(1.99) = 7.32 significant change in the relative risk ratio for limiting and spacing. Due to the type of model specified for these analyses, results are reported as relative risk ratios instead of odds ratios as expected if binary logistic regression is used for the analysis.
Demographic determinants of unmet need for family planning
Table 1 , shows both the bivariate and multivariable multinomial mixed effects logistic regression analyses results. Under the socio-demographic grouping approach with the adjusted relative risk ratio, there was a reduced risk of unmet need for limiting against no unmet need. A reduced risk of 99.9% (RR of 0.01 (95% CI, 0.00, 0.03, p -value < 0.001) was observed for people from the Upper West region compared to that of the Volta region. Also, a reduced risk of 88.8% (RR of 0.12 (95% CI, 0.22, 0.60, p -value = 0.01) for respondents from the Eastern region was observed against respondents from the Volta region. Similar observations for unmet need for spacing were made except that the highest relative risk among the ten regions was the Ashanti and Eastern regions for limiting as compared to no unmet need. Though the relative risk for the Upper West region was 0.20(95% CI, 0.05, 0.84, p -value = 0.028) and that of the Eastern region and Ashanti regions were 0.25 (95% CI, 0.07, 0.94, p -value = 0.040) and 0.80 (95% CI, 0.21, 3.12, p -value = 0.750) respectively, only Upper West was significant. This implies that the risk for unmet need for women from the Volta region in relation to those from the Upper West and Eastern regions for limiting were 205 and 9 times higher. That of spacing were 5 and 4 times higher. In terms of the age category, those within 15–19 were used as the reference group. The observations made were that a change in age from lower to higher corresponds to an increase risk of an unmet need for limiting compared to no unmet need. For instance, the risk of women aged 20–24 years had a risk ratio of 1.73 (95% CI, 0.22, 13.34, p -value = 0.600). The risk ratio for age group 35–39 years was 133 (95% CI, 18.12, 977.18, p -value < 0.001). The opposite was the case for all the year groups compared to the 15–19 years respondents for spacing. The risk of respondents aged 20–24 compared to 15–19 when evaluated under unmet need for spacing gave an RR of 0.29 (95% CI, 0.12, 0.71, p -value < 0.007) and that of 35–39 had an RR of 0.17 (95% CI, 0.07, 0.40, p -value < 0.001) times the risk for no unmet need. This shows that respondents within 15–19 years group were 3 and 6 times more likely to develop the need for spacing as against the 20–24 and 35–39 age groups. All the other age groupings were similarly related.
Figure 5 , contains the adjusted predictive probabilities of the types of unmet need for family planning according to regions and age categories of respondents. The marginal predictive probabilities for the unmet need for limiting is highest among respondents from the Volta region (0.80) followed by the Eastern region (0.66) with the smallest being the three regions of the Northern part of the country. For the age category, the marginal probabilities for limiting increased upwardly with a higher age. The predictive probability for wanting to limit was 0.86 for the 45–49 year group and as low as 0.02 among the 15–19 year group.
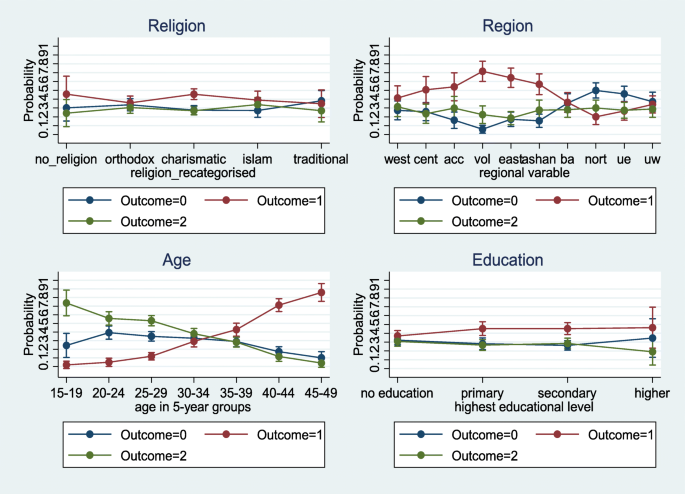
Adjusted probability of unmet need for family planning (no unmet need: outcome = 0); unmet need for limiting (outcome = 1); unmet need for spacing (outcome = 2)) among women (married or union). Results from a multinomial mixed effect logistic regression model. Ghana Demographic and Health Survey, 2014
Socio-economic determinants of unmet need for family planning
Four socio-economic factors were identified to be statistically significantly associated with unmet need for family planning. These were respondent’s educational level, wealth index of household, respondent’s occupation and partner’s occupation. With respect to wealth index, only the richest and poorer respondents showed a significant difference. The middle and the richer were insignificant statistically when compared to the poorest with regards to unmet need for limiting. Respondents who were poorest have 2 times (95% CI, 1.36, 2.97, p -value < 0.001) the risk of having an unmet need for limiting compared to the poorer respondents. Under spacing, the richest had approximately 32% more risk. The poorer had 89%more risk than the poorest respondents. Educational level did not demonstrate any statistical significant difference for spacing. For limiting, respondents with primary and secondary education had about 2 times the risk with a p -value < 0.001. With regards to respondent’s occupation, those in the services and professionals had an RR of 16.92 times (95% CI, 4.78, 59.97, p -value < 0.001) and 6.06 times (95% CI, 2.05, 17.92, p -value = 0.001) risk of having unmet need for limiting compared with those without any work. The marginal probabilities for educational levels, presented in Fig. 5 , shows that, the predictive probability for respondents classified under primary was the highest (0.47), followed by secondary (0.44) for limiting.
Socio-cultural determinants of unmet need for family planning
Respondents, religion and ethnicity were the only socio-cultural variables statistically significantly associated with unmet need for family planning. Religion was re-categorized into no religion, Orthodox, Charismatic, Islamic and Traditional for further analysis. The results showed that respondents without any religious affiliation had more than twice (with a p -value = 0.002) and 22% (with a p -value = 0.430) the risk of experiencing unmet need for limiting and spacing respectively compared to those with in traditional religion. Unmet need for family planning for the Charismatic group was approximately 3 with a p -value < 0.001 and 1.65 with a p -value < 0.011 times the risk for limiting and spacing than it was for traditional religion. From Fig. 2 , a higher predictive probability (0.46) was observed for respondents without any religious affiliation and those with the Charismatic faith (0.46) for limiting.
Psychosocial and other determinants of unmet need for family planning
All the variables identified under this category were insignificant except those who reported infrequent sex, partner’s opposition to use of contraceptives and respondents fear of side effects. Respondents who fear contraceptive side effects were 3 times (95% CI, 2.28, 3.80 p -value < 0.001) at risk of having unmet need for limiting and 2.58 times (95% CI, 2.05, 3.24, p -value < 0.001) more likely to experience an unmet need for spacing when compared to respondents who do not fear contraceptive side effects. Respondents who had infrequent sex were 4.6 times more likely to want to limit and 2.4 times more likely to space their children than those who had frequent sex.
Making use of the data for women in the reproductive age in the 2014 GDHS, this study used the most appropriate statistical model that has the power to control for unobserved effect estimates in the data set to determine the significant factors associated with unmet need for family planning in Ghana. This knowledge is important for policy makers and service providers to enable them put pragmatic measures in place to satisfy the unmet need for family planning.
Our study showed that a number of socio-demographic (age, religion and administrative region of residence), socio-economic (wealth index, respondents educational level, respondent’s and partner’s occupation), cultural (religion and ethnicity) as well as fear of contraceptive side effects, infrequent sex and opposition from partners were are all significant determinants of both unmet need for limiting and spacing.
Our analysis showed an upward trend of limiting for higher age groups. As women’s age changed from 15 to 19 group to 20–24 group, the likelihood of having an unmet need for FP only doubled but when 15–19 group was compared to 45–49 group, unmet need increased more than a thousand fold. For spacing, the likelihood of an unmet need decreased with an increasing age group. A similar conclusion was arrived at in a study by Wafula et al., in Kenya [ 11 ]. These findings are likely to be due to the fact that young women had not attained their desired family size and therefore their need is to space their children. On the other hand, older women might have attained their desired family size and would therefore not like to have any more children.
Religion was also observed to be a factor leading to having a higher unmet need for family planning as was found in other studies in India and Ethiopia [ 12 , 13 , 14 ]. Compared to those who professed traditional religion, women with no religious affiliation and those with the charismatic faith were twice more likely to have an unmet need for limiting. Women practicing Islamic religion were less likely to space birth compared with those practicing traditional religion. The different religious beliefs have varied perceptions and self-beliefs that could impact either negatively or positively in contraceptive use [ 11 ]. Members of Islamic religion and some Orthodox religions such as Catholics exhibit a strong opposition to contraceptive use. Overall, women who belonged to other religious beliefs other than traditional religion appeared to have a higher unmet need for limiting and spacing as compared to respondents who belonged to the traditional religion [ 11 ].
With regards to education, this study revealed a higher unmet need for both limiting and spacing among respondents who had completed either primary or secondary education compared to those without any formal education; similar conclusions were drawn from other studies [ 15 , 16 ]. A non-significant effect between higher and no educated respondents were observed and this is contrary to findings from Kenya [ 11 ]. They observed a higher unmet need for women with low educational background. The high unmet need for family planning in educated Ghanaian women may explain why induced abortion tends to be higher in them as compared to women with no education [ 17 , 18 ]. It has been suggested that induced abortion may be an integral factor in the control of fertility among educated Ghanaian women [ 17 ]. It is also possible that highly educated women may have knowledge about potential contraceptives side effects which may translate into low use among this demographic group. It was further observed that place of residence was a statistically insignificant contributor to unmet need for family planning, though rural residents were less likely to have an unmet need. This finding is again contrary to findings of Genet et al., in Ethiopia [ 19 ], which stipulated that rural respondents were twice more likely to have unmet need. There are a number of possibilities that could have influenced our findings. Family planning services have also been an integral part of health services provided in rural areas in Ghana and this high level of awareness created in these areas may have had positive impact on FP.
Our study has also shown that, the fear of side effects, infrequent sexual intercourse and opposition from partners are all significant factors contributing to the high unmet need for family planning in Ghana. Similarly, demographic and health surveys from 52 countries spanning the period from 2005 to 2014 have shown that about 7 out of 10 married women with unmet need for family planning cite either fear of side effects or health risks, infrequent or no sex and opposition to contraception (either by they themselves or from significant others) as their reason for not using modern contraception [ 20 ]. This is an indication that satisfying the needs of women with unmet need for family planning will get a big boost if these factors are tackled with the seriousness they deserve.
In many countries contraceptive prevalence have stalled and this has been attributed partly to the poor quality of counselling and hence the call for new approaches to counselling [ 21 ]. Good counselling should pay attention to dealing with misconceptions, how to prepare new clients to handle common side effects and also how continuing clients can cope with side effects [ 22 ].
A recent study from five urban family planning centres in Ghana revealed that even though over two thirds of women adopting a family planning methods were counselled to expect side effects, over a third of these same women were not counselled on common side effects of their chosen methods [ 23 ]. In the same study, about 7 out of 10 family planning acceptors chose methods whose side effects they had stated earlier will cause them to stop the said method. This shows that much importance was not attached to side effects of clients before they were given their chosen methods. In addition, women wary of side effects could also be educated on natural FP methods which they may not be familiar with. Studies have shown that mobile application for contraception based on a woman’s natural cycle is effective in preventing pregnancies [ 24 ]. Such tools on fertility-awareness may be the solution for women for whom side effects are positive predictors of unmet needs on limiting and spacing [ 23 , 24 ]. Quality of family planning services which includes, good counselling is associated with clients selecting family planning methods that best suits their individual needs. This will enable them navigate through side effects effectively and to continue to use their choice of methods [ 25 ].
Respondents who had infrequent sexual intercourse were about four and two times more likely to have an unmet need for limiting and spacing respectively. It is possible that women who had infrequent sexual intercourse may not want to be to be using a method continuously when they do not know when they next will have sexual intercourse. They are however at risk of unintended pregnancies and need to be abreast with emergency contraception and barrier methods in order to avoid unintended pregnancies.
For those whose partners oppose their contraceptive use, there will be the need to get them involved in order for them to appreciate the benefits of family planning. Some men have the wrong impression that their spouses may become promiscuous once they are using contraceptives [ 26 ].
While acknowledging that factors such as level of education, wealth index and religion will require multi-sectoral approach to handle, dealing with side effects, getting women with infrequent sex to use emergency contraception or barrier methods, and educating partners on the benefits of family planning lies mostly in the domain of service providers. There is the need to start dealing with the high unmet need for family planning by tackling these three factors first.
Strengths and limitations of the study
This study derives its strengths from the fact that, the use of a nationally representative sample allows for the generalizability of study findings to the whole country. In addition, demographic and health surveys are well planned and executed surveys and therefore the data is usually of high quality. Furthermore, the number of observations with complete dataset that met the inclusion criteria was large. The use of the multilevel mixed effects logistic model addresses the issues of cluster variations by appropriately accounting for those unobserved effects that are not usually measured by the dataset. The coefficient estimates obtained in this study are more accurate and generalizable due to our modelling approach.
This study also had some limitations. To begin with, the data was obtained through a cross-sectional study and so causations could not be established. Secondly, there were delays in model convergence due to the complex nature of the model proposed and applied to the dataset but that did not have an effect on the parameters estimates. The survey obtained retrospective information which was self-reported from participants spanning a 5-year period prior to the survey and so the likelihood of recall bias was high. Recall bias has some consequences on coefficient estimates and overall significant testing and so interpretations/use of the results should be done cautiously.
This study reveals that socio-demographic factors such as respondents region, age and not place of residence contribute to predicting unmet need for family planning. Also, socio-economic (partner’s occupation) and cultural (religion and ethnicity) as well as side effects are all significant determinants of both unmet need for limiting and spacing. Variables such as, educational level, wealth index and respondents occupation overall were significant in predicting only unmet need for limiting but insignificant for predicting unmet need for spacing. The fear of side effect on the use of contraceptives as well as infrequent sex among respondents are both high predictors of unmet need for family planning. Overall, fear of side effect, infrequent sex, age, ethnicity, partner’s education and region were the most highly significant predictors of both limiting and spacing. The Ministry of Health need to work more closely with the Ghana Health Service to train its service providers to ensure that prospective family planning acceptors are counselled adequately on common side effects of their methods of choice and to also address misconceptions. All stakeholders in family planning must do their best to extol the virtues of family planning to men and help involve them in family planning.
Abbreviations
Confidence Interval
Exponential
Family Planning
Ghana Demographic Health Survey
Intrauterine Device
Campbell M, Cleland J, Ezeh A, Prata N. Return of the population growth factor. Science. 2007;315(5818):1501.
CAS PubMed Google Scholar
Sinding SW. Population, poverty and economic development. Philos Trans R Soc Lond Ser B Biol Sci. 2009;364(1532):3023–30.
Google Scholar
Westoff CF. The potential demand for family planning: a new measure of unmet need and estimates for five Latin American countries. Int Fam Plan Perspect. 1988;14(2):45–53.
Der E, Moyer C, Gyasi R, Akosa A, Tettey Y, Akakpo P, Blankson A, Anim J. Pregnancy related causes of deaths in Ghana: a 5-year retrospective study. Ghana Med J. 2013;47(4):158.
CAS PubMed PubMed Central Google Scholar
Longwe A, Huisman J, Smits J. Effects of knowledge, acceptance and use of contraceptives on household wealth in 26 African countries, Nijmegen Center for Economics working paper; 2013. p. 12–109.
Sedgh G, Hussain R, Bankole A, Singh S. Women with an unmet need for contraception in developing countries and their reasons for not using a method, Occasional report, vol. 37; 2007. p. 5–40.
Ghana Statistical Service (GSS), Ghana Health Service (GHS), and ICF Macro. Accra: Ghana Demographic and Health Survey 2008, 2009.
Apanga PA, Adam MA. Factors influencing the uptake of family planning services in the Talensi District, Ghana. Pan Afr Med J. 2015;20:10. https://doi.org/10.11604/pamj.2015.20.10.5301 .
Bongaarts J. United nations department of economic and social affairs, population division world mortality report 2005. Popul Dev Rev. 2006;32(3):594–6.
Bradley SE, Croft TN, Fishel JD, Westoff CF. Revising unmet need for family planning; 2012.
Wafula SW. Regional differences in unmet need for contraception in Kenya: insights from survey data. BMC Womens Health. 2015;15(1):86.
PubMed PubMed Central Google Scholar
Barman S. Socio-economic and demographic determinants of unmet need for family planning in India and its consequences. J Res Humanit Soc Sci. 2013;3(3):62–75.
Gebre G, Birhan N, Gebreslasie K. Prevalence and factors associated with unmet need for family planning among the currently married reproductive age women in Shire-Enda-Slassie, northern west of Tigray, Ethiopia 2015: a community based cross-sectional study. Pan Afr Med J. 2016;23:195. https://doi.org/10.11604/pamj.2016.23.195.8386 .
Westoff CF, Bankole A. Unmet need: 1990–1994; 1995.
Kumar A, Bhardwaj P, Srivastava J, Gupta P. A study on family planning practices and methods among women of urban slums of Lucknow city. Indian J Community Health. 2011;23(2):75–7.
Mekonnen W, Worku A. Determinants of low family planning use and high unmet need in Butajira District, South Central Ethiopia. Reprod Health. 2011;8(1):37.
Geelhoed DW, Nayembil D, Asare K, Van Leeuwen J, Van Roosmalen J. Contraception and induced abortion in rural Ghana. Tropical Med Int Health. 2002;7(8):708–16.
CAS Google Scholar
Ahiadeke C. Incidence of induced abortion in southern Ghana. Int Fam Plan Perspect. 2001:27(2):96–101 & 108.
Genet E, Abeje G, Ejigu T. Determinants of unmet need for family planning among currently married women in Dangila town administration, Awi zone, Amhara regional state; a cross sectional study. Reprod Health. 2015;12(1):42.
Sedgh G, Ashoford LS, Hussain R. Unmet need for contraception in developing countries: examining women’s reasons for not using a method, New york: Guttmacher Institute; 2016. http://www.guttmacher.org/report/unmet-need-for-contraception-in-developing-countries .
Berglund Scherwitzl E, Lindén Hirschberg A, Scherwitzl R. Identification and prediction of the fertile window using NaturalCycles. Eur J Contracept Reprod Health Care. 2015;20(5):403–8.
PubMed Google Scholar
Alam M-E, Bradley J, Shabnam F. IUD use and discontinuation in Bangladesh. E&R study# 8. New York: Engender Health/The ACQUIRE Project; 2007.
Rominski SD, Morhe ES, Maya E, Manu A, Dalton VK. Comparing Women's contraceptive preferences with their choices in 5 urban family planning clinics in Ghana. Glob Health Sci Pract. 2017;5(1):65–74.
Berglund Scherwitzl E, Gemzell Danielsson K, Sellberg JA, Scherwitzl R. Fertility awareness-based mobile application for contraception. Eur J Contracept Reprod Health Care. 2016;21(3):234–41.
Heerey M, Merritt AP, Kols AJ. Improving the quality of care. Quality improvement projects from the Johns Hopkins University Bloomberg School of Public Health Center for Communication Programs; 2003.
Kabagenyi A, Jennings L, Reid A, Nalwadda G, Ntozi J, Atuyambe L. Barriers to male involvement in contraceptive uptake and reproductive health services: a qualitative study of men and women’s perceptions in two rural districts in Uganda. Reprod Health. 2014;11(1):21.
Download references
Acknowledgements
Not applicable.
The authors did not obtain any funding for this research.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the Ghana demographic and health repository, http://dhsprogram.com/data/available-datasets.cfm .
Author information
Authors and affiliations.
Department of Biostatistics, School of Public Health, University of Ghana, Legon, Accra, Ghana
Chris Guure, Samuel Dery, Baaba da-Costa Vrom & Alfred Yawson
Department of Population, Family and Reproductive Health, School of Public Health, University of Ghana, Legon, Accra, Ghana
Ernest Tei Maya
Department of Mathematical Sciences, Faculty of Science, Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Refah M. Alotaibi & Hoda Ragab Rezk
Princess Nourah bint Abdulrahman University, Riyadh, Saudi Arabia
Hoda Ragab Rezk
You can also search for this author in PubMed Google Scholar
Contributions
CG and SD conceptualized the present study. CG led the data extraction and analysis and wrote the first draft of the manuscript. ETM contributed in the write-up of the different sections of the manuscript. CG, ETM, SD, BDV, RMA, HRR and AY reviewed the draft manuscript and contributed to the final version of the manuscript. All authors read and approved the final manuscript before submission.
Corresponding author
Correspondence to Ernest Tei Maya .
Ethics declarations
Ethics approval and consent to participate.
The Ghana Health Service Institutional Review Board (IRB) approved the study protocol, survey instruments and materials prior to the commencement of the surveys. Individual consent was also obtained during the data collection process. An application requesting for the use of the 2014 Ghana Demographic and Health Survey data was sent to the Ghana Statistical Service (GSS) representative. Data was then used after approval was obtained.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Table S1. Model building strategy: unmet need for family planning among women (married or union), Ghana Demographic and Health Survey, 2014. (DOCX 27 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Guure, C., Maya, E.T., Dery, S. et al. Factors influencing unmet need for family planning among Ghanaian married/union women: a multinomial mixed effects logistic regression modelling approach. Arch Public Health 77 , 11 (2019). https://doi.org/10.1186/s13690-019-0340-6
Download citation
Received : 28 June 2018
Accepted : 20 February 2019
Published : 12 March 2019
DOI : https://doi.org/10.1186/s13690-019-0340-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family planning
- Estimating unobserved effects
- Multilevel modelling
Archives of Public Health
ISSN: 2049-3258
- General enquiries: [email protected]
Factors influencing the uptake of family planning services in the Talensi District, Ghana
Affiliation.
- 1 Ghana Health Service, Talensi district, Upper East Region, Ghana.
- PMID: 25995807
- PMCID: PMC4430143
- DOI: 10.11604/pamj.2015.20.10.5301
Introduction: Usage of family planning services in developing countries have been found to avert unintended pregnancies, reduce maternal and child mortality, however, it's usage still remains low. Hence, the objective of this study was to investigate the factors that influence the decision of women in fertility age to go for family planning services.
Methods: This was a descriptive cross-sectional study conducted in Talensi district in the Upper East Region of Ghana. Systematic random sampling was used to recruit 280 residents aged 15-49 years and data was analysed using SPSS version 21.0.
Results: The study revealed that 89% (249/280), of respondents were aware of family planning services, 18% (50/280) of respondents had used family planning services in the past. Parity and educational level of respondents were positively associated with usage of family planning services (P<0.05). Major motivating factors to the usage of family planning service were to space children, 94% (47/50) and to prevent pregnancy and sexual transmitted infections 84% (42/50). Major reasons for not accessing family planning services were opposition from husbands, 90% (207/230) and misconceptions about family planning, 83% (191/230).
Conclusion: Although most women were aware of family planning services in the Talensi district, the uptake of the service was low. Thus, there is the need for the office of the district health directorate to intensify health education on the benefits of family planning with male involvement. The government should also scale up family planning services in the district to make it more accessible.
Keywords: Family planning; Ghana; Talensi district; contraceptives; uptake.
- Contraception Behavior / statistics & numerical data
- Cross-Sectional Studies
- Family Planning Services / statistics & numerical data*
- Ghana / epidemiology
- Health Knowledge, Attitudes, Practice
- Middle Aged
- Socioeconomic Factors
- Surveys and Questionnaires
- Young Adult
- Open access
- Published: 23 January 2021
Towards achieving the family planning targets in the African region: a rapid review of task sharing policies
- Leopold Ouedraogo ORCID: orcid.org/0000-0001-5842-1842 1 ,
- Desire Habonimana ORCID: orcid.org/0000-0003-0832-5558 2 ,
- Triphonie Nkurunziza 1 ,
- Asmani Chilanga 3 ,
- Elamin Hayfa 4 ,
- Tall Fatim 3 ,
- Nancy Kidula 4 ,
- Ghislaine Conombo 5 ,
- Assumpta Muriithi 1 &
- Pamela Onyiah 1
Reproductive Health volume 18 , Article number: 22 ( 2021 ) Cite this article
6925 Accesses
14 Citations
Metrics details
Expanding access and use of effective contraception is important in achieving universal access to reproductive healthcare services, especially in low- and middle-income countries (LMICs), such as those in sub-Saharan Africa (SSA). Shortage of trained healthcare providers is an important contributor to increased unmet need for contraception in SSA. The World Health Organization (WHO) recommends task sharing as an important strategy to improve access to sexual and reproductive healthcare services by addressing shortage of healthcare providers. This study explores the status, successes, challenges and impacts of the implementation of task sharing for family planning in five SSA countries. This evidence is aimed at promoting the implementation and scale-up of task sharing programmes in SSA countries by WHO.
Methodology and findings
We employed a rapid programme review (RPR) methodology to generate evidence on task sharing for family planning programmes from five SSA countries namely, Burkina Faso, Cote d’Ivoire, Ethiopia, Ghana, and Nigeria. This involved a desk review of country task sharing policy documents, implementation plans and guidelines, annual sexual and reproductive health programme reports, WHO regional meeting reports on task sharing for family planning; and information from key informants on country background, intervention packages, impact, enablers, challenges and ways forward on task sharing for family planning. The findings indicate mainly the involvement of community health workers, midwives and nurses in the task sharing programmes with training in provision of contraceptive pills and long-acting reversible contraceptives (LARC). Results indicate an increase in family planning indicators during the task shifting implementation period. For instance, injectable contraceptive use increased more than threefold within six months in Burkina Faso; contraceptive prevalence rate doubled with declines in total fertility and unmet need for contraception in Ethiopia; and uptake of LARC increased in Ghana and Nigeria. Some barriers to successful implementation include poor retention of lower cadre providers, inadequate documentation, and poor data systems.
Conclusions
Task sharing plays a role in increasing contraceptive uptake and holds promise in promoting universal access to family planning in the SSA region. Evidence from this RPR is helpful in elaborating country policies and scale-up of task sharing for family planning programmes.
Introduction
L'élargissement de l'accès et de l'utilisation d’une contraception efficace est important pour parvenir à l'accès universel aux services de santé reproductive, en particulier dans les pays à revenu faible et intermédiaire, comme ceux de l'Afrique subsaharienne. L’insuffisance de prestataires de soins de santé qualifiés est un facteur important de l'augmentation des besoins non satisfaits en matière de contraception en Afrique subsaharienne. L'Organisation mondiale de la Santé (OMS) recommande le partage des tâches comme stratégie importante pour améliorer l'accès aux services de santé sexuelle et reproductive en s’attaquant à la pénurie des prestataires de soins de santé. Cette étude explore l'état des lieux, les réussites, les défis et les impacts de la mise en œuvre du partage des tâches pour la planification familiale dans cinq pays d'Afrique subsaharienne. Ces données factuelles visent à promouvoir la mise en œuvre et l'extension des programmes de partage des tâches dans les pays d'Afrique sub-saharienne par l'OMS.
Méthodologie et résultats
Nous avons utilisé la méthodologie de la revue rapide des programmes (RPR) pour générer des données sur le partage des tâches pour les programmes de planification familiale de cinq pays d'Afrique subsaharienne, à savoir le Burkina Faso, la Côte d'Ivoire, l'Éthiopie, le Ghana et le Nigéria. Cela impliquait la revue documentaire des documents de politique nationale de partage des tâches, des plans de mise en œuvre et des directives, des rapports annuels sur les programmes de santé sexuelle et reproductive, des rapports des réunions régionales de l'OMS sur le partage des tâches pour la planification familiale; et des informations provenant des informateurs clés sur le contexte du pays, les programmes d'intervention, l'impact, les catalyseurs, les défis et les voies à suivre pour le partage des tâches pour la planification familiale. Les résultats indiquent principalement l'implication des agents de santé communautaires, des sages-femmes et des infirmières dans les programmes de partage des tâches avec une formation liée à l’approvisionnement de pilules contraceptives et de contraceptifs réversibles à longue durée d’action (LARC). Les résultats indiquent une augmentation des indicateurs de planification familiale pendant la période de mise en œuvre du partage des tâches. Par exemple, l'utilisation des contraceptifs injectables a plus que triplé en six mois au Burkina Faso; le taux de prévalence de la contraception a doublé avec une baisse de la fécondité totale et des besoins non satisfaits en matière de contraception en Éthiopie; et l'adoption du LARC a augmenté au Ghana et au Nigéria. Certains obstacles à la réussite de la mise en œuvre comprennent une faible rétention des prestataires de niveau inférieur, une documentation inadéquate et des systèmes peu performants de gestion des données.
Le partage des tâches joue un rôle important dans l'augmentation de l'utilisation de la contraception et dans la promotion de l'accès universel à la planification familiale dans la région Afrique subsaharienne. Les données de ce RPR sont utiles pour l'élaboration des politiques nationales et l'intensification du partage des tâches pour les programmes de planification familiale.
Plain English summary
Correct and consistent use of contraceptives has been shown to reduce pregnancy and childbirth related maternal deaths and generally improve reproductive health. However, statistics show that many women of reproductive age in SSA who ought to be using contraceptives are not using them. As a result, high rates of maternal deaths from pregnancy or childbirth-related complications have been recorded in the region. One of the key barriers to accessing family planning in SSA is the shortage of healthcare providers. To address this problem, WHO recommends task sharing as an intervention to improve access and use of sexual and reproductive health services including family planning. While task sharing guidelines have been developed and disseminated in many SSA countries, limited evidence exists on their adoption, implementation and outcomes to promote scale-up. This study undertook a rapid programme review of evidence from policy documents, implementation plans and guidelines, annual sexual and reproductive health programme reports, regional meeting reports and key stakeholder reports on task sharing to explore the status, successes, challenges and impacts of the implementation of task sharing for family planning in five SSA countries: Burkina Faso, Cote d’Ivoire, Ethiopia, Ghana, and Nigeria. We found that task sharing programmes mainly involved community health workers, midwives and nurses. The intervention led to increased modern contraception access and use and general improvement in family planning indicators during the implementation periods. Some barriers to successful implementation of task sharing include poor retention of lower cadre providers, inadequate documentation, and poor data systems.
Peer Review reports
The World Bank projects a ten-fold increase in the population of sub-Saharan Africa (SSA) between 1960 and 2050, reaching 9.7 billion people in 2050 [ 1 ]. This escalation indicates Africa’s growing fertility rate [ 2 ]. Notably, while the global fertility rate between 1990 and 2019 fell from 3.2 to 2.5 births per woman, this indicator only dropped from 6.3 to 4.6 births per woman for SSA [ 2 ]. Evidently, other regions have recorded much higher declines compared to SSA (from 4.5 to 3.4 in Oceania, from 4.4 to 2.9 in Northern Africa and Western Asia, from 3.3 to 2.0 in Latin America and the Caribbean, and from 2.5 to 1.8 in Eastern and South-Eastern Asia) [ 2 ]. This decline in fertility rate continues to occur at a much slower pace in SSA as compared to the rest of the world. In other words, while it took 19 years for fertility rates in Northern Africa and Western Asia to drop from 6 to 4 births per woman (1974 to 1993), a similar decline is expected to materialise after 34 years (1995 to 2029) in SSA [ 2 ]. With weak health systems present in fragile economies, the higher fertility rates present greater risks of unpropitious pregnancy outcomes in SSA countries [ 3 , 4 , 5 ].
In the light of the evidence above, a wealth of literature has established a correlation between higher fertility rates, poverty and pregnancy-related deaths/complications. For instance, of some 830 women who die daily from pregnancy or childbirth-related complications around the world, 99% of such deaths occur in low-income and middle-income countries (LMICs) [ 6 ]. It is also estimated that of the 2.6 million stillbirths that occurred globally in 2015, 98% were in LMICs [ 7 ]. Furthermore, the risk of a woman in a LMIC dying from a maternal-related cause during her lifetime is about 33 times higher compared to her counterpart in a high-income country [ 8 ]. Fortunately, interventions such as modern contraception which space and limit pregnancies significantly improve the overall health of women of reproductive age [ 9 ]. Although this remains true, SSA continues to register higher proportions of unmet contraception expectations to date [ 10 , 11 ].
In SSA, 16% of women of reproductive age who desire to either terminate or postpone childbearing do not currently use a contraceptive method [ 12 ]. Most importantly, in this region, the rate of unmet needs for family planning is about 21% among married women or those living in union [ 12 ]. Such trends represent barriers to the achievement of universal access to sexual and reproductive healthcare services including for family planning by 2030 in SSA, as stipulated in the third and fifth Sustainable Development Goals (SDGs) targets: 3.1, 3.7, 3.8, and 5.6 [ 13 , 14 ]. One of the key barriers to the availability and accessibility of family planning services in sub-Saharan Africa is the critical dearth of qualified health care providers. On the one hand, while reaffirming that human resources is at the core of each health care system around the world, the health workforce remains inequitably distributed in most sub-Saharan African countries, with rural areas suffering chronic and severe shortages of competent health care providers [ 15 , 16 ]. On the other hand, lack of motivation and absenteeism of health care providers in impoverished countries widens the gap in quality family planning services [ 17 ]. In the bid to assuage human resource shortages, many countries have started to train less experienced health workers perform tasks that should otherwise be performed by qualified doctors or other highly-trained healthcare workers [ 18 ].
The World Health Organization (WHO), like many other stakeholders, recognise task sharing as a promising strategy to address the serious lack of health care workers to provide reproductive, maternal and new-born care in less wealthy countries [ 19 , 20 , 21 ]. By definition, task sharing involves the safe expansion of tasks and procedures that are usually performed by higher-level staff (i.e. physicians) to lay- and mid-level healthcare professionals (i.e. midwives, nurses, and auxiliaries) [ 22 ]. In the same perspective, WHO recommends that midwives be empowered to provide all family planning services except tubal ligation and vasectomy (Box 1 ). Also, initiation and maintenance of injectable contraceptives (standard syringe) can be performed by auxiliary nurses. Following WHO recommendations on “Optimizing the roles of health personnel through the delegation of tasks to improve access to maternal and new-born health interventions” (2012), regions including the Regional Office for Africa have started to mobilise local efforts with an aim to initiate and expand task sharing policies for family planning across respective member countries.
For the above reason, WHO Regional Office for Africa, in partnership with member countries and other key players such as the Ouagadougou Partnership for Family Planning Coordination Unit (UCPO), the West Africa Health Organisation (WAHO), and the United Nations Population Fund (UNFPA), organized a regional consultation meeting on task sharing in September 2016 with the aim of aiding nine pilot countries in developing action plans for the implementation of task sharing recommendations. Moreover, WHO Regional Office for Africa conducted an intensive advocacy which yielded a special resolution relating to task sharing for family planning endorsed by governments of the Economic Community of West African States (ECOWAS) region. In December 2019, a second regional advocacy meeting was held to expand the task sharing policies to an additional 11 English-speaking countries.
Four years after the first advocacy meeting, this paper explores the lessons learnt in relation to task sharing for family planning in five countries in the WHO African region. Specifically, the paper documents the status of task sharing for family planning policy implementation, its effect in coverage and use of family planning services, gauges key achievements, enablers and challenges to form a basis for the implementation monitoring and planning of task sharing initiatives for family planning in the region.
Box 1 Table of guideline recommendations for task sharing of contraception

The study applied the Rapid Programme Review (RPR) methodology to generate evidence on what WHO Regional Office for Africa and member countries can do to build on successes and tackle challenges with an aim to scale-up task sharing programmes for family planning region-wide. A rapid review is a knowledge synthesis method in which components of the systematic review process are simplified or omitted to produce information in a short period of time [ 23 ]. A RPR focuses on synthesizing information regarding a programme (task sharing programme for family planning in this case) through desk-review of programme documents, reports and key stakeholder information. The RPR methodology generates strong evidence and saves both time and costs, rather than conducting full programme reviews which are time-consuming and effort-intensive [ 24 ]. The method allows a rapid and progressive learning with conscious exploration and flexible use of methods without following a blueprint programme [ 25 ]. The review triangulated data from secondary sources with information from key informants in four countries which have already piloted the task sharing programmes for family planning. A trend analysis was done alongside an overview of system-level implementation enablers and barriers to successful implementation of task sharing programmes in the African context.
Data collection
Data was collected in two steps. In the first instance, data for the RPR were obtained through a desk review of country task sharing for family planning policy documents, relevant implementation plans and guidelines, and annual sexual and reproductive health programme reports. In addition, data presented during the second Africa regional meeting on task sharing for family planning organised by WHO Regional Office for Africa was exploited to supplement document reviews. During this meeting, five countries which are piloting or implementing programmes on task sharing for family planning (Burkina Faso, Cote d’Ivoire, Ethiopia, Ghana, and Nigeria) presented success stories as well as challenges, lessons learnt and ways forward. A full list of countries that participated in the meeting is provided in Box 2 .
In the second instance, WHO country offices were contacted to identify and obtain key informants on task sharing for family planning programmes in the five aforementioned countries. Through written communication (electronic mails), National Focal Points (NFPs) on sexual and reproductive health provided information on the country background, intervention packages, intervention impact, system-level enablers and challenges, and information on ways forward.
The country background helped to understand the baseline picture. Specifically, we collected information on the date when the first task sharing programme was piloted, the rollout process and, most importantly, the significant baseline family planning indicators. A list of full family planning indicators for Burkina Faso before (2010) and after (2019) implementation of the task sharing for family planning programme is shown in Table 1 . Secondly, data on the type of task sharing intervention packages were collected. In addition, geographical reach and the type of tasks and healthcare professionals involved were documented. If available and applicable, an illustrative picture was also shared to demonstrate lay- and auxiliary-level cadres performing family planning tasks previously performed by higher healthcare professionals. Thirdly, we used Table 1 and collected data on key family planning indicators during the period of implementation of task sharing for family planning. Given the availability of enough data-points, baseline and midterm data were used to trace an indicator trend line. We also documented system-level levers and challenges that played an important role in the successful/unsuccessful implementation of task sharing programmes. This information is necessary for policymakers amid the aim by WHO Regional Office for Africa and member states of rolling-out and expanding task sharing for family planning programmes region-wide. Lastly, each country provided information on the next steps with concrete actions to be undertaken in the near future with regards to task sharing for family planning.
Box 2. List of countries that participated to the WHO regional meeting on task sharing for family planning, 16–19 December 2019
Burkina Faso*
Cote d’Ivoire*
South Africa
* Countries piloting or implementing programmes on task sharing for family planning
Data analysis
Data was analysed in two steps. Step one consisted of compiling information from the country background, the task sharing intervention packages, the system-level enablers and challenges, and the ways forward. All data sources were verified to ensure reliability of reported information. In the event of missing data, a request was resent to the respective NFP who was asked to provide feedback within two weeks. Beyond a period of two weeks, the data was confirmed as “missing information”. For example, Cote d’Ivoire was excluded from analysis due to substantial missing data. Step Two consisted of a trend analysis of key family planning indicators. Owing to the limited number of data-points (often only two data-points), a trend line was only possible for Ghana and Nigeria. For Burkina Faso and Ethiopia, we compared proportions before and during task sharing interventions.
Results are mainly presented as text boxes of country overviews. In each box, we summarised findings on the country background, described existing task sharing intervention packages, quantified midterm programme impact, analysed system-level enablers and barriers, and suggested ways forward.
Box 3. Burkina Faso
Burkina Faso is a West African country struggling with severe health workforce shortages [ 26 ]. On average there is less than one physician per 10,000 people and 2.39 midwives per 10,000 people [ 27 ]. This is way lesser than the WHO doctor-population ratio of 1:1000. Burkina Faso piloted the first task sharing programme between 2015 and 2016 across 17,688 villages in the Hauts Bassin region, Boucle de Mouhoun region, Central West region, and Central region. Each participating village received two community health workers (CHWs) trained to provide injectable contraception (Sayana press) in addition to contraceptive pills. Task sharing was also piloted at health facility level where midwives were trained to perform long acting reversible contraception (LARC) procedures—the intrauterine contraceptive device (IUCD) and implants. Evaluation of the pilot programme yielded promising results, leading to the validation and nationwide rollout of the task sharing programme in November 2017.
Task sharing intervention packages
CHWs and midwives received comprehensive specific training needed for performing new family planning tasks. The training was provided by the Ministry of Health. There were also adequate post-training follow-up and monitoring of the health workers. Furthermore, in addition to an effective supply chain of services, mechanisms for quality control were put in place. Additionally, advocacy meetings and community mass mobilisation campaigns were regularly conducted. Joint-field monitoring and evaluation missions were conducted to enable an early detection of potential enabling factors and challenges that affect the successful programme implementation. Results were disseminated through regional and sub-regional meetings in Burkina Faso, Ghana, Kenya, and Cote d’Ivoire.
Partial results showed an increase in new users. For instance, within a period of six months (February to September 2017) during the implementation of task sharing for family planning by trained CHWs and midwives, a total 1225 implants—of which 857 were new users—were administered. A total of 384 IUCDs, of which 238 were new users, were provided by newly trained midwives. In the same period, CHWs provided 3541 injectable contraceptives (Medroxyprogesterone acetate)—of which 1013 were new users— and 1257 contraceptive pills, of which 241 were new users. Other family planning indicators are presented in Table 1 .
It stood out that the strong commitment and stewardship of health authorities from the top to the bottom levels, the expansion of contraceptive options, the community involvement, and the improved financial and geographic accessibility of family planning services played an important facilitating role.
Notable challenges included data reporting, as routine paper-based reporting system was solely used, and financial constraints. Also, the programme was fraught with insufficient funding causing great irregularities in the payment of CHWs incentives. Evidence has confirmed that such a financial challenge has potential for reducing provider motivation [ 28 , 29 ].
Ways forward
A commitment maker since 2012 and a member of both the Ouagadougou Partnership and SWEDD (Sahel Women’s Empowerment and Demographic Dividend project), Burkina Faso has taken its FP2020 commitment seriously through its 2017–2020 RH/FP strategy, which incorporates task sharing for family planning [ 30 ]. Burkina Faso vowed to build on successes to strengthen task sharing programmes through the recruitment and training of lay- and auxiliary-level healthcare providers by the Ministry of Health. Furthermore, there is a robust financial pledge and advocacy from political and administrative authorities, technical and financial partners and non-governmental associations working in the field of family planning.
On the one hand, time comparison shows an increase in the number of women of reproductive age and that of expected and real pregnancies. On the other hand, there has been a decrease in fertility rate and maternal mortality ratio. Overall, Burkina Faso showed promising results for family planning services. Key improvement features of family planning include an increase in contraceptive prevalence which more than doubled (105% increase), the increase in numbers of couples using a contraceptive method which nearly tripled (183% increase), and an increase in family planning expenditures. Moreover, in 2019, family planning averted 11.56% of expected pregnancies (comparison of expected and real pregnancies in 2019).
Box 4. Ethiopia
Ethiopia has a total population of 100 million people of whom 83.6% live in rural areas [ 31 ]. Majority of Ethiopia’s population is made up of young people, with 45% representing those under 15 years old and 71% under 30 years old [ 32 ]. Women of reproductive age account for 24% of Ethiopia’s population [ 31 ]. Each year, Ethiopia expects a total number of 3 million pregnancies. The country’s population growth rate is 2.6% per year and the total fertility rate is 2.3 births per woman in urban settings and 5.2 births in rural areas [ 31 ].
In Ethiopia, the task sharing programme was piloted in three different phases. Phase one involved the Implanon programme which was first piloted in 8 districts in 2009. Provision of Implanon was shifted from healthcare facility level to community level. Phase Two, which started in 2011, was the IUCD task sharing programme which was piloted in one region where the device was inserted and removed by midwives and nurses rather than physicians. Phase Three was where the IUCD provision was further lowered to auxiliary nurses in 2016 across 66 selected health posts.
Within a period of 12 months (from July 2018 to June 2019), 1.43 million clients received a LARC method (1,362,149 women received Implanon and 64,073 women received IUCD). Moreover, contraceptive prevalence rate has doubled every five years from 2000 (CPR = 6.1%) to 2019 (CPR = 41%). Another supporting point is the decline in total fertility rate which fell from 6.0 to 4.6 in the same period. Similarly, unmet contraceptive needs were higher in 2011 (25.3% of unmet contraceptive needs) as compared to 2019 (22% of unmet contraceptive needs). Equally important, IUCD utilization rate increased from less than 2% in 2011 to more than 11% in 2019.
The successful implementation of Ethiopia’s task sharing pilot programme was a result of political commitment. There has been a visible political will and support by the Government of Ethiopia. Specifically, the Government signed international family planning policies, elaborated national policies and strategies in support of the implementation of family planning standards, promoted and stimulated demand for family planning services, and continuously increased the overall health budget over the past decade.
Key challenges included lack of awareness and misconceptions regarding some contraception methods such as long-acting family planning (LAFP) methods among the target population, shortages of medical equipment and logistics, poor infrastructure (electricity, water, and roads), and poor mentorship and supporting supervision.
Looking ahead, Ethiopia aims to accelerate strategies to increase the demand for family planning services until the very remote communities, to enhance service availability and accessibility, to improve provider competency and performance, and to strengthen mentorship and supportive supervision. Ethiopia has committed to the FP2020 call to action that urges global health and development partners to adopt task sharing as a key solution for increasing access to contraception [ 33 ].
Box 5. Ghana
Despite Ghana having halved the maternal mortality ratio in the past 20 years (760 maternal deaths per 100,000 live births in 1990s versus 310 maternal deaths per 100,000 live births in 2019), the country still has one of the lowest contraceptive prevalence rates in the region (22.2% in 2014) [ 34 ]. In this country, task sharing programmes for family planning started in 2008 when 33 Community Health Nurses (CHNs) from 6 regions received training in Jadelle insertion and removal. After the Jadelle programme, nurses and midwives from across Ghana started receiving tailored training on Implant provision nationally in 2013.
From 2013, Implants were inserted and removed by CHNs, nurses, and midwives.
Implant users increased from 11 users per provider in 2013 to 18 users per provider as of 2018 (DHIMS2). Contraception prevalence rate among married women increased from 18.6% in 2008 to 19.8% in 2014 among rural residents and from 15.1% in 2008 to 24.6% in 2014 among urban women. The trend in Implants (Jadelle and Implanon) utilisation is depicted in Fig. 1 below. As can be seen, the number of Implant users tripled from the onset of countrywide task sharing programme (2013) to 2018.
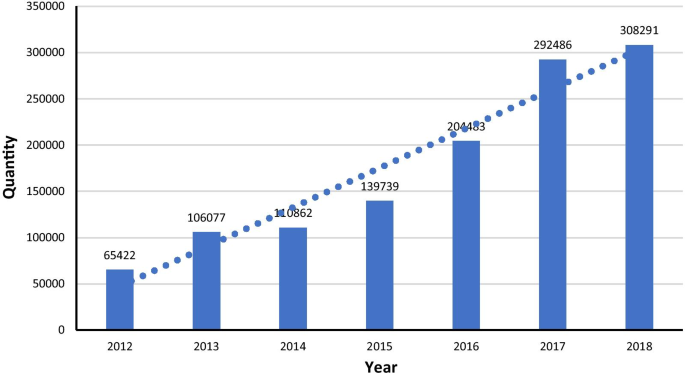
(Source: Ghana Maternal Health Survey 2017. 2018)
Trend in implant utilisation in Ghana
Like for other countries, levers of success included the political will and commitment of Ghanaian Leaders, concerted advocacy programmes, stakeholder involvement, quality monitoring and supervision, and support by regional resource teams.
A couple of notable challenges concerned funding gaps and the uneven distribution of CHNs in task sharing.
Ghana’s main next step in task sharing for family planning is to initiate a Midwifery Assistant programme. This programme will enable the training of CHNs as “Midwifery Assistants” who will be sent across the country. Following the training, Ghana projects to further select and train 72 Midwifery Assistants on IUCD in a one-year pilot programme followed by an evaluation and countrywide rollout. Furthermore, as part of its commitment to the FP2020 targets to increase the number of women and girls using modern contraception from 1.5 million to 1.9 million by improved access to and availability of quality family planning services, Ghana aims to support capacity building of Community Health Nurses through task sharing of LARC provision to strengthen the provision of FP services nationally [ 35 ].
Box 6. Nigeria
Nigeria has an estimated population of 200 million with 45 million women of reproductive age [ 36 ]. The total fertility rate is 5.3 with current contraceptive prevalence rate of 12%. While unmet need for contraception was 19% in 2018, the country aims to attain 27% of contraceptive coverage by 2020 [ 36 ]. The Federal Government of Nigeria passed the task sharing policy in 2014 through which Community Health Extension Workers (CHEWs) received training on LARC and a subsequent authorisation to provide and remove Implants and IUCD.
From 2014, nurses, midwives, and CHEWs became responsible for the provision of the entire family planning arsenal except tubal ligation and vasectomy (Box 1 ). They provided family planning counselling and education, promoted dual protection for HIV positive women, inserted and removed Implants and IUCD, and provided injectable contraception.
Implementation of the task sharing policy for family planning increased the uptake of LARC. Figure 2 illustrates the uptake in implants increased by 80% within a period of four years (2015 to 2019).

(Source: Nigeria Demographic and Health Survey 2018)
Trend in implants uptake in Nigeria
In Nigeria, there was collaboration with professional bodies which enhanced acceptance and ownership of task sharing programmes. Another lever was the ability of majority of CHEWs to fast-learn and absorb training materials.
Adverse circumstances were limited to a small number of poor-performing family planning providers. Also, the programme required intense follow-ups and mentoring which meant that it became costly despite benefits outweighing the costs.
Preliminary results were a powerful tool to advocate for the scaling up of task sharing for family planning programmes. Therefore, from 2019, Nigeria embarked on rolling out the pilot project at country level. As part of their FP2020 commitments, Nigeria plans to train at least 3700 community health workers (CHWs) for the delivery of LARC and support task shifting so CHWs in rural areas can provide multiple methods [ 37 ].
This rapid review set out to identify lessons learnt from the task sharing for family planning pilot programmes in four African countries with an aim to assist WHO Regional Office for Africa in identifying areas and strategies to strengthen advocacy for policy expansion region-wide. Data was collected, analysed, and presented according to five subdomains: country background, task sharing intervention packages, impact, enablers and challenges, and ways forward.
The findings of this review confirm that African countries share a similar background characterised by higher fertility and population growth rates, younger and mostly rural populations, lower contraceptive coverage rates, higher rates of unmet needs for contraception, severe human resource shortages with existing health workforce being unevenly and inequitably distributed; among others. This population trend, which hinders the attainment of development and health goals in Africa, has existed for more than two decades and will continue to rise unless substantial changes are made [ 38 , 39 , 40 ].
Common task sharing interventions involved CHWs, midwives, and nurses. There may have been different naming based on country-specific contexts, but they all referred to the above three categories of healthcare providers. For all countries studied, CHWs, midwives, and nurses were trained on the provision of contraceptive pills and LARC namely, Implants and IUCD. Based on WHO recommendations in Box 1 , however, it is not recommended for lay-level health workers to insert and remove IUCD. Likewise, Auxiliary nurses are not allowed to insert and remove IUCD unless in the context of rigorous research (Box 1 ). Unfortunately, we did not obtain data on adverse effects that could have resulted from CHWs and midwives inserting and removing IUCD. Although this may be true, previous studies from the African context did not report side effects or incidents from CHWs providing LARC namely IUCD. Instead, CHWs increased uptake of IUCD utilisation in Rwanda [ 41 ] and in Ethiopia [ 42 ]. This evidence corroborates our findings.
Our findings indicated an increase in family planning indicators resulting from the task sharing programmes. In Burkina Faso, LARC uptake increased by greater than three times within a period of six months with 232.9% new implant users and 163.0% new IUCD users. There was a slower uptake for Depo-Provera and contraceptive pills with 40.1% and 23.7% of new users, respectively. Most importantly, the new contraception programme averted 11.7% of expected pregnancies in 2019. In Ethiopia, results from this study showed a doubling contraceptive prevalence rate with declining rates of total fertility and unmet needs for contraception. In Ghana and Nigeria, there has been an increase in the number of new users with a significant uptake of Implants and IUCDs. Similar results have been found in many other African contexts. For instance, the Democratic Republic of Congo (DRC) is one of the countries that have suffered the most from human resource shortages in the whole world. A new task sharing programme that sought to promote LARC in remote areas was able to achieve 38,662 new users within a period of 5 years [ 43 ].
To summarise, despite countries being at different stages in terms of promotion and implementation of task sharing policies, they have some achievements in common. These include the presence of policies, regulations, or laws on task sharing; the presence of community health strategies and programmes, ongoing dialogues and discussions on task sharing, in-country communication strategies and governmental support. Countries also share some common challenges mainly the difficulties in retention of lower cadres due to financial constraints (incentives), inadequate documentation of successful processes to support internal learning and external lessons sharing, and difficulties capturing data on service provision. Moreover, they share common priorities: advocacy, capacity building, and financial pledge for impact sustainability.
Task sharing is important to ensuring that everyone has access to family planning services they need to space or limit childbearing. Task sharing for family planning should be contextualised to align with country situations. Furthermore, training and monitoring of lay- and auxiliary-level cadres remains a dire necessity. Country plans for task sharing for family planning should be positioned within the broader national objectives of Universal Health Coverage (UHC) and Primary Health Care (PHC) in order to achieve the SDGs agenda. Plans should be specific on and include documented best practices and promote mentoring (i.e. through South-South learning) as a viable solution to support the advancement of best practices. Evidence from the present review point to possible association between task sharing for family planning and increased contraceptive uptake, which makes task sharing a potential viable intervention. It is against this evidence that we recommend WHO Regional Office for Africa and member states to build on the evidence from Burkina Faso, Ethiopia, Ghana, and Nigeria in elaborating country policies for task sharing in family planning.
Limitations
The small sample size of key informants who provided information to the RPR could be considered a limitation to the study. Furthermore, the collection of electronic information rather than verbal could have limited the depth of information provided. However, current and available documents on task sharing for family planning ably supplemented the information provided. It is important to mention that attribution of the family planning outcomes to the task shifting intervention should be handled with caution as the RPR cannot be used in place of causal studies. Therefore, we recommend additional studies that can statistically attribute outcomes to the task sharing intervention.
Availability of data and materials
Data and materials used for this review are available either online (policies and country reports) or from the corresponding author (meeting presentations, information from key informant interviews).
Abbreviations
World Health Organization
Sub-Saharan Africa
Rapid programme Review
Long-acting reversible contraceptives
Low- and middle-income countries
Ouagadougou Partnership for Family Planning Coordination Unit
United Nations Population Fund
Economic Community of West African States
National Focal Points
Community health workers
Intra-utérine device
Intra-utérine contraceptive device
Human Immunodeficiency virus
Long-acting family planning
Sustainable Development Goals
Community Health Extension Workers
Community Health Nurse
World Bank Data Catalog. Population Estimates And Projections. 2020. https://datawrapper.dwcdn.net/V12Gh/3/ . Accessed 22 Aug 2020 at 22:36 (GMT+2).
United Nations. Department of Economics and Social Affairs. World Fertility and Family Planning 2020. 2020. https://www.un.org/en/development/desa/population/publications/pdf/family/Ten_key_messages%20for%20WFFP2020_highlights.pdf . Accessed 22 Aug 2020 at 23:05 (GMT+2).
Adeniyi OV, et al. High rate of unplanned pregnancy in the context of integrated family planning and HIV care services in South Africa. BMC Health Serv Res. 2018;18(1):1–8.
Article Google Scholar
Londero AP, et al. Maternal age and the risk of adverse pregnancy outcomes: a retrospective cohort study. BMC Pregnancy Childbirth. 2019;19(1):261.
Kietpeerakool C, et al. Pregnancy outcomes of women with previous caesarean sections: secondary analysis of World Health Organization Multicountry Survey on Maternal and Newborn Health. Sci Rep. 2019;9(1):1–9.
Article CAS Google Scholar
Alkema L, et al. Global, Regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030. Obstetric Anesthesia Digest. 2016;36(4):191.
WHO, World Health Organization (WHO). WHO Recommendations on antenatal care for a positive pregnancy experience: summary. Geneva, Switzerland: WHO; 2018. Licence: CC BY-NC-SA 3.0 IGO. 2018.
WHO et al. UNFPA, World Bank Group and the United Nations Population Division. Trends in maternal mortality: 1990 to 2015. Estimates by WHO, UNICEF. 2015, UNFPA, World Bank group and the united nations population division.
Ganatra B, Faundes A. Role of birth spacing, family planning services, safe abortion services and post-abortion care in reducing maternal mortality. Best Pract Res Clin Obstet Gynaecol. 2016;36:145–55.
Ahinkorah BO. Predictors of unmet need for contraception among adolescent girls and young women in selected high fertility countries in sub-Saharan Africa: a multilevel mixed effects analysis. PLoS ONE. 2020;15(8):e0236352.
Darroch JE, et al. Costs and benefits of meeting the contraceptive needs of adolescents. New York: Guttmacher Institute; 2016.
Google Scholar
The United Nations Population Fund. World Population Dashboard. 2020. https://www.unfpa.org/data/world-population-dashboard . Accessed 23 Aug 2020 at 00:37 (GMT+2).
Division of Sustainable Development Goals. Transforming our world: the 2030 Agenda for Sustainable Development. New York: Division for Sustainable Development Goals; 2015.
Kumar S, Kumar N, Vivekadhish S. Millennium development goals (MDGS) to sustainable development goals (SDGS): Addressing unfinished agenda and strengthening sustainable development and partnership. Indian J Commun Med. 2016;41(1):1.
Afriyie DO, Nyoni J, Ahmat A. The state of strategic plans for the health workforce in Africa. BMJ Glob Health. 2019;4(Suppl 9):e001115.
Miseda MH, et al. The implication of the shortage of health workforce specialist on universal health coverage in Kenya. Hum Resour Health. 2017;15(1):80.
Tweheyo R, et al. ‘Nobody is after you; it is your initiative to start work’: a qualitative study of health workforce absenteeism in rural Uganda. BMJ Glob Health. 2017;2(4).
Sharma N, et al. Community health workers involvement in preventative care in primary healthcare: a systematic scoping review. BMJ Open. 2019;9(12):e031666.
Janowitz B, Stanback J, Boyer B. Task sharing in family planning. Stud Fam Plann. 2012;43(1):57–62.
Okyere E, Mwanri L, Ward P. Is task-shifting a solution to the health workers’ shortage in Northern Ghana? PLoS ONE. 2017;12(3):e0174631.
Millogo T, et al. Task sharing for family planning services, Burkina Faso. Bull World Health Organ. 2019;97(11):783.
Kim C, Sorhaindo A, Ganatra B. WHO guidelines and the role of the physician in task sharing in safe abortion care. Best Pract Res Clin Obstet Gynaecol. 2020;63:56–66.
Khangura S, et al. Evidence summaries: the evolution of a rapid review approach. Syst Rev. 2012;1(1):10.
Barua A, et al. Adolescent health programming in India: a rapid review. Reproductive Health. 2020;17:1–10.
Chambers R. Rapid but relaxed and participatory rural appraisal: towards applications in health and nutrition. International Nutrition Foundation for Developing Countries. 1992.
Global Health Workforce Alliance, -.W. Country responses - Burkina Faso. 2020. https://www.who.int/workforcealliance/countries/bfa/en/ .
National Statistics Council Burkina Faso, Burkina Faso Health Statistical Yearbook 2010. 2010: Burkina Faso.
Ormel H, et al. Salaried and voluntary community health workers: exploring how incentives and expectation gaps influence motivation. Hum Resour Health. 2019;17(1):59.
Singh D, et al. The effect of payment and incentives on motivation and focus of community health workers: five case studies from low-and middle-income countries. Hum Resour Health. 2015;13(1):1–12.
Ministère de la Santé, Plan National d’Accélération de Planification Familiale du Burkina Faso 2017–2020. 2017.
Central Statistical Agency (CSA). Ethiopia Demographic and Health Survey,. Addis Ababa, Ethiopia, and Rockville: Central Statistical Agency (CSA); 2017.
Agency, C.S., Ethiopia Mini Demographic and Health Survey 2014 2014: Addis Ababa, Ethiopia.
Health, M.o., COSTED IMPLEMENTATION PLAN FOR FAMILY PLANNING IN ETHIOPIA 2015/16–2020. 2016: Addis Ababa, Ethiopia.
Ghana Statistical Service (GSS), Ghana Maternal Health Survey. 2018: Accra. Ghana: GSS, GHS, and ICF; 2017.
Family Planning 2020, Ghana FP2020 Actions for Acceleration (2018–2019)—Fact Sheet. 2019.
National Population Commission (NPC). Nigeria Demographic and Health Survey 2018. Abuja, Nigeria, and Rockville, Maryland, USA: NPC and ICF; 2019.
2020, F.P. Nigeria FP2020 Commitment. 2012. https://www.familyplanning2020.org/news/nigeria-fp2020-commitment .
Groth H, and May JF. Africa's population: In search of a demographic dividend. 2017; Springer.
Kamarudin MKA, et al. Population growth and economic development in developing and developed countries. Int J Eng Technol. 2018;7(4.34):123–7.
De la Croix D, Gobbi PE. Population density, fertility, and demographic convergence in developing countries. J Dev Econ. 2017;127:13–24.
Mazzei A, et al. Community health worker promotions increase uptake of long-acting reversible contraception in Rwanda. Reprod Health. 2019;16(1):75.
Teklu AM. et al. Competency of Level-4 Health Extension Workers to provide Long acting reversible contraceptives: a task shifting initiative in Ethiopia. 2020.
Castle S, et al. Successful programmatic approaches to facilitating IUD uptake: CARE’s experience in DRC. BMC Women’s Health. 2019;19(1):104.
Download references
Acknowledgements
Not applicable.
This study was funded by the WHO Regional Office for Africa.
Author information
Authors and affiliations.
Reproductive, Maternal Health and Ageing Team, World Health Organization, Regional Office for Africa, Brazzaville, Republic of the Congo
Leopold Ouedraogo, Triphonie Nkurunziza, Assumpta Muriithi & Pamela Onyiah
Department of Community Medicine, Research and Innovation Unit, Faculty of Medicine, University of Burundi, Bujumbura, Burundi
Desire Habonimana
Reproductive, Maternal Health and Ageing Team, Intercountry Support Team for West Africa, World Health Organization, Ouagadougou, Burkina Faso
Asmani Chilanga & Tall Fatim
Reproductive, Maternal Health and Ageing Team, Intercountry Support Team for East and Southern Africa, World Health Organization, Harare, Zimbabwe
Elamin Hayfa & Nancy Kidula
Reproductive, Maternal Health and Ageing Team, Intercountry Support Team for Central Africa, World Health Organization, Libreville, Gabon
Ghislaine Conombo
You can also search for this author in PubMed Google Scholar
Contributions
LO conceptualized the study, developed the research methodology, analysed the data, and prepared the initial draft manuscript. DH facilitated data collection and proofread the initial draft manuscript. TN validated the content and edited the manuscript before submission. AC validated the content and edited the manuscript before submission. EH validated the content and edited the manuscript before submission. TF validated the content and edited the manuscript before submission. NK validated the content and edited the manuscript before submission. GC validated the content and edited the manuscript before submission. AM validated the content and edited the manuscript before submission. PO validated the content and edited the manuscript before submission. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Leopold Ouedraogo .
Ethics declarations
Ethics approval and consent to participate.
This rapid programme review was approved by the World Health Organization Regional Office for Africa. All key informants provided informed consent before participation in the study.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ouedraogo, L., Habonimana, D., Nkurunziza, T. et al. Towards achieving the family planning targets in the African region: a rapid review of task sharing policies. Reprod Health 18 , 22 (2021). https://doi.org/10.1186/s12978-020-01038-y
Download citation
Received : 27 August 2020
Accepted : 05 November 2020
Published : 23 January 2021
DOI : https://doi.org/10.1186/s12978-020-01038-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Family planning
- Task sharing
- World health organisation
- African region
- planification familiale
- partage des tâches
- Organisation mondiale de la Santé
- Région africaine
Reproductive Health
ISSN: 1742-4755
- General enquiries: [email protected]
- Open access
- Published: 24 August 2021
Equity and access to maternal and child health services in Ghana a cross-sectional study
- Samuel George Anarwat 1 ,
- Mubarik Salifu 2 &
- Margaret Atosina Akuriba 2
BMC Health Services Research volume 21 , Article number: 864 ( 2021 ) Cite this article
5705 Accesses
4 Citations
4 Altmetric
Metrics details
Inequities in the distribution of and access to maternal and child health care services is pervasive in Ghana. Understanding the drivers of inequity in maternal and child health (MCH) is important to achieving the universal health coverage component of the Sustainable Development Goals (SDGs) and poverty reduction in developing countries. However, there is increasing disparities in MCH services, especially in rural -urban, and income quintiles. The study aimed to examine the disparities in maternal and child health care services in Ghana for policy intervention.
Data for this study was extracted from the nationally representative Ghana Statistical Service (GSS) Multiple Indicator Cluster Survey (MICS) round 4, 2011. Respondents of this survey were women of reproductive age 15–49 years with a sample size of 10,627 households. The models were estimated using multivariate regression analysis together with concentration index (CI) and risk ratio (RR) to assess the distribution of MCH indicator groups across the household wealth index.
The results show that women with secondary school level and above were more likely to receive family planning, prenatal care, and delivery by a skilled health professional than those without formal education. Mothers with low level of educational attainment were 87% more likely to have their first pregnancy before the age of 20 years, and 78% were more likely to have children with under-five mortality, and 45% more likely to have children who had diarrhoea. teenage pregnancy (CI = − 0.133, RR =0.679), prenatal care by skilled health worker (CI = − 0.124, RR =0.713) under five mortality, child underweight, reported diarrhoea, and suspected pneumonia, though not statistically significant, were more concentrated in the poorer than in the richer households, The RR between the top and bottom quintiles ranged from 0.77 for child underweight to 0.82 for child wasting.
Geographic location, income status and formal education are key drivers of maternal and child health inequities in Ghana. Government can partner the private sector to implement health policies to address inequalities in MCH services through primary health care, and resource allocation skewed towards rural areas and the lower wealth quintile to bridge the inequality gaps and improve MCH outcomes. The government and the private sectors should prioritize female education, as that can improve maternal and child health.
Peer Review reports
Improved maternal and child health is imperative for the survival of every nation and global population. However, inequities in the distribution of and access to maternal and child health care services is pervasive in Ghana. Understanding the drivers of inequity in maternal and child health (MCH) is important to achieving the universal health coverage component of the Sustainable Development Goals (SDGs) and poverty reduction in Low – and Middle-Income Countries. The study aimed to examine inequities in maternal and child health care services among population groups especially, the upper and lower wealth quintiles on one hand and geographical (Rural-Urban) disparities in access to MCH on the other hand. The study contributes to filling in the gaps in literature and inadequacy of equity in MCH data in Low -and Middle-Income Countries (LMICs) for evidence-based MCH policy and programme implementation. Knowing the gaps and the determinant factors of inequities in MCH can aid in effective resource allocation and MCH programs implementation to improve health outcomes.
Ghana has embarked on several interventions and efforts aimed at preventing and reducing maternal and infant mortality. These interventions span enhancing utilisation of health care through the National Health Insurance Scheme (NHIS), Free Maternal Care programme, launched in 2007 for pregnant women to enhance their utilisation of delivery care services, Healthcare Network (CHN)-On-The-Go, Kangaroo Baby Care, Mobile Technology for Community Health (MOTECH), and Millennium Development Goal Acceleration Framework (MAF), and Expanded Program on Immunization, among others. It is expected that the NHIS will improve provision of basic health care services to persons resident in the country.
Inequities in the distribution of health care services is gaining global attention in public health [ 1 ]. Inequities in maternal and child health services are among the prominent reasons for high maternal and child morbidities and mortalities in Sub-Saharan Africa and the world at large [ 2 ]. Like other Sub-Saharan countries, Ghana experiences unequal distribution in maternal and child health care services [ 3 ]. Quality and equitably access to MCH is critical for the improvement of health outcomes and health status of women and children. However, inequitable spread of MCH services increases mortality in resource poor regions. Infant, child, and maternal mortality are highest in Northern Ghana, where poverty is rife and access to MCH services are woefully in short supply. The poor MCH services in Northern Ghana is worse than the economically endowed Southern Ghana (Greater Accra and Ashanti) regions. It is estimated that 1 in 27 infants in Ghana die before their first birthday, and 1 in 19 children die before age five [ 4 ].
In 2017, the Maternal Mortality Ratio was estimated at 310 per 100,000 deaths, with a lifetime risk of maternal death estimated at 1% of all women dying from maternal causes. A stunning 517 pregnant women die of maternal causes, annually in Ghana, for lack of quality maternal health care services, and inequitable distribution of MCH services [ 4 ]. Surprisingly, most of the maternal and infant mortalities are preventable [ 5 ]. Ghana’s key health status indicators on MCH, such as maternal mortality rate (MMR), infant mortality rate (IMR), family planning, and neonatal mortality rate (NMR) improved steadily over the MDG period. This achievement was praised by the international community as a remarkable success. Nonetheless, there were large inequalities in health coverage and strong overall performance marks significant disparities between income groups and regions [ 6 ]. Much is still left to be accomplished in the areas of equity in maternal and child health status among the lower wealth quintile of the population. The 2017/2018 Ghana Multiple Indicator Cluster Survey (MICS), round six report showed a reduction in infant mortality rate (IMR) from 49 per every 1000 to 41 children per 1000 live births, according to the Ghana Statistical Services data in 2018. This statistic is far from achieving the SDG Goal 3-Target 3.2 of “ending preventable deaths of new-borns and children under 5 years with all countries aiming to reduce neonatal mortality.
Low or no education of mothers also hampers their maternal and child health status and well-being. In Ghana low education of mothers is still a problem, considering that as many as 79 maternal deaths were associated with mothers with no education while 53 deaths for mothers with at least secondary education [ 7 ]. Inequality creates serious obstacles to achieving the Sustainable Development Goals (SDGs), especially, overcoming poverty, achieving universal health coverage and reduced inequalities by the year 2030 (SDG1, 3 and 10). The widening and persistent inequality in the distribution of social services including maternal and child health care is harmful to countries as well as individuals as agreed by policy makers [ 8 ]. Between 2016 and 2017, 82% of the wealth generated went to the richest 1% of the global population, while the poorest half saw no increase [ 6 ]. Over 800 women die globally every day from complications in pregnancy and childbirth due to the disparities in maternal and child health services utilization [ 7 ]. For every woman who dies, approximately 20 others suffer serious injuries, infections or disabilities and almost all maternal deaths (99%) occur in developing country regions [ 7 ]. According to the Population Reference Bureau [ 9 ] the maternal mortality rates (MMR) for Africa and West Africa are 490 per 100,000 live births and 674 per 100,000 live births, respectively. These statistics are worrying since no woman should die giving birth. The survival of mothers has become very important since saving them implies saving the lives of the more than one million children who are left motherless.
Research shows that educated women are more likely to start antenatal care (ANC) visits earlier than less educated women [ 10 ], and utilisation of delivery care depends largely on the women’s educational level [ 11 ]. Most maternal health studies in Ghana [ 12 , 13 ], have focused mostly on the general population, and in some instances on some regions. Arthur (2012), for instance, identified wealth, age, education, number of children, transportation, and health insurance among women between 15 and 49 years to influence antenatal use in Ghana as contributory factors of maternal health care service utilisation. Other variables such as long travel distance and long waiting times affect the use of ANC within communities [ 14 ]. We present in the next few paragraphs, previous literature on maternal health, family planning, and child health in Ghana.
Maternal health
Ghana has made good progress in recent years in many social development indicators including health. Maternal and child health status are determined by several variables such as the conditions of the place of residence, school environment, and work environment, which determines their health risks and outcomes. Environmental and social variables such as, health care and early health care seeking and treatment; educational attainment of households especially mothers, employment, social support and economic opportunities, family incomes, health insurance coverage, significantly influence maternal health care behaviors and health status [ 13 ]. These variables that influence maternal health equally affect pregnancy outcomes and child health status [ 15 ].
Evidence suggests high unmet need for family planning among unmarried adolescents while modern use of family planning methods is higher among married than unmarried adolescents [ 3 ]. Adolescent girls in rural areas and those among the poorest and less educated are at a higher risk of early childbearing in Ghana [ 3 ]. Ample evidence indicates that 14% of adolescent women aged 15–19 are mothers or pregnant with their first child [ 3 ].
Family planning
Family planning has been an integral component of government of Ghana’s maternal health programs for decades. Family Planning is an important factor in the population management and national development outlined in many national development plans [ 16 ].
Family planning aims to assist couples and individuals of reproductive age to achieve their reproductive aspirations. Despite the high premium placed on family planning programs in Ghana, funding remains a daunting challenge. Family planning intake is highest (69%) among women between 15 and 19 years and lowest (33%) among women within 45–49 years. The demand for family planning is also highest (59%) among women in rural areas. Those women with at least primary or high school education use more family planning services and women in the middle three quintiles (60–61%) [ 17 ].
Although there is a huge progress in family planning services intake, there is still about 50% unmet need for family planning services in Ghana, especially among young women within the 15–19 years (51%) and lowest among women aged 45–59 (14%). Also women in rural dwelling have slightly higher (31%) unmet needs of family planning than their counterparts in urban areas (29%) [ 17 ].
Delivery by skilled health personnel is another key indicator of maternal health. There has been progress in this indicator, about 68% of all births in the last 2 years preceding the MICS survey round 6 were delivered by skilled personnel. Education plays an important role in deliveries by skilled health personnel. Educated woman were more likely to have assisted delivered by a skilled health personnel. Assisted delivery by skilled health personnel for mothers with no formal education constituted only 44% of all deliveries compared to 95% for women with secondary or higher education. Also, poor women were less likely to deliver using skilled personnel (39%), compared to rich women (98%). Despite the progress made in delivery by skill personnel deliveries at home is still highly significant as 1 in 3 births take place at home without a skilled health personnel [ 18 ]. This needs to be addressed to reduce preventable maternal mortality which might emanate from complications or blood loss.
Promoting and ensuring deliveries in health facilities can reduce the health risks to both the mother and the baby. Proper medical attention and hygienic conditions during delivery can also reduce the risks of complications and infection that can cause morbidity and mortality to either the mother or the baby [ 18 ].
Child health
The health of children is a global concern. Over the years, many countries and institutions have worked towards improving the health of children to reduce infant mortality. Despite the significant investments and improvement in child health in the past few decades, many children still lose their lives to diseases before their 5th birthday globally, and inequity in health is still a huge challenge [ 19 ]. Technical and medical solutions such as disease control and medical care of illnesses that cause the most deaths in children are critical in making fundamental improvements in health equity.
Diarrhoea and pneumonia have been the most frequent childhood illnesses and causes of attendance at health facilities in low-income and middle-income countries [ 20 ]. These diseases have been regarded as the “biggest child killers” in the last century [ 21 ]. In 2011 for instance, diarrhoea and pneumonia caused about 700,000 and 1, 300,000 global deaths respectively in children under 5 years [ 20 ]. The plan was necessitated by some alarming statistics that pneumonia and diarrhoea together accounted for 30% of all childhood deaths [ 22 ]. The prevalence rate of diarrhoea in children under 5 years in Ghana is reported to be 13% in the 2011MICS, with Oral Rehydration Treatment (ORT) being higher in urban areas (64%) than in rural areas (56%) [ 18 ]. Childhood diarrhoea in Ghana is also said to show inequities that are to the disadvantage of the poorest [ 23 ]. Thus, cases recorded in urban areas or in relatively rich homes are properly managed compared to those in rural and/or poor homes. In 2011, the incidence of suspected pneumonia in children under 5 years in Ghana was 3% [ 18 ]. The main intervention in treating pneumonia is antibiotics. Of the 3% suspected pneumonia cases reported in Ghana, 41% of them were taken to an appropriate health provider and 56% received antibiotics. Children in rural areas and/or poor homes are disadvantaged in terms of care seeking behaviour [ 18 ].
WHO estimates that at least 10 million deaths were prevented between 2010 and 2015 globally due to vaccinations; and many lives were protected from suffering and disability associated with diseases such as pneumonia, diarrhoea, whooping cough, measles, and polio [ 21 ]. However, in Ghana many children still suffer from nutrition deficiency illnesses and other preventable childhood diseases. For instance, children under 5 years suffered from stunting (18.8%) underweight (11.0%) and wasting (4.7%) [ 18 ]. There are also significant variations in stunting, underweight, and wasting across wealth quintiles and geographic regions [ 24 ]. An estimated 19% of Ghanaian children are chronically malnourished, with stunting less than two standard deviations (SD) below the national average, and 5% are stunted (below − 3 SD). This represents a 17% decrease (improvement) since the MICS in 2011 and a 47% decrease (improvement) since the DHS in 2008 [ 22 ].
Stunting becomes more common as children get older, peaking at 28% among children aged 24–35 months. Stunting affects a significantly higher percentage of males (20%) than females (17%), and stunting is more prevalent in rural areas (22%) than in urban areas (15%). Stunting rates vary by area, ranging from 10% in Greater Accra to 33% in the Northern region. Education and income are inversely linked to stunting. For example, 25% of children in the lowest two wealth quintiles are stunted, while only 9% of children in the highest quintile are stunted [ 22 ].
Data sources
Data for this study was extracted from the 2011 Ghana Multiple Indicator Cluster Survey, round four (MICS4 (19). The Ghana Multiple Cluster Indicator survey (MICS) is a nationally representative survey which contains valuable data on the condition of children, women, and men in Ghana. Unlike the previous MICS, the Ghana MICS4 2011 included three “malaria biomarkers,” such as anaemia testing, malaria testing using rapid diagnostic tests (RDTs), and thick blood smear samples prepared on microscope slides.
Study settings
The data were collected in all regions of Ghana namely, Greater Accra, Central, Western, Volta, Eastern, Volta, Ashanti, Brong Ahafo, Northern, Eastern, Upper East and Upper West regions. The estimated population of Ghana, as of July 2021 was estimated at 31,754,995 people based on Worldometer elaboration of the latest United Nations data. The population density is estimated at 137 per Km 2 (354 people per mi 2 ), and the Urban Population was 56.7% (17,625,567 people in 2020). The total land area is 227,540 Km2 (87,854 sq. miles). https://www.worldometers.info/world-population/ghana-population
Sample design
The MICS 2011 used a cross-sectional sample design to collect data on multiple indicators about children, women, and men, nationwide, stratified into urban and rural areas and the 10 geographical regions of Ghana.
Questionnaires/instruments
The Ghana MICS4, 2011, used four different sets of questionnaires in the survey:1) Household questionnaire which collected information on usual residents, the household, and the dwelling, 2) Women’s questionnaire data on women aged 15–49 years, 3) Under-5 questionnaire administered to mothers or caretakers for all children under 5 living in the household, 4) Men’s questionnaire administered in each third household to all men aged 15–59 years.
The household questionnaire contained Household listing form, Education, Water and Sanitation, Household Characteristics, Insecticide Treated Nets, Indoor Residual Spraying, Child Labor, Child Discipline, Handwashing, and Salt Iodization.
The Women questionnaire included Women’s Background, Access to Mass Media and Use of Information/Communication Technology, Child Mortality, Desire for Last Birth, Maternal and Newborn Health, Post-natal Health Checks, Illness Symptoms, Contraception, Unmet Need, Female Genital Mutilation/Cutting, Behaviour Change Communication on Malaria, Attitudes Towards Domestic Violence, Marriage/Union, Sexual Behaviour, HIV/AIDS, and National Health Insurance.
The Children Under-Five Questionnaire (administered to mothers or caretakers of children under- 5 years of age) included, Age, Birth Registration, Early Childhood, Development, Breastfeeding, Diet Diversity, Care of Illness, Malaria, Immunization, National Health Insurance, Anthropometry, Anaemia, and Malaria Testing.
The Men Questionnaire (administered to men aged 15–59 years living in each third Household) contained Men’s Background, Access to Mass media and use of Information/Communication Technology, Marriage/Union, Attitude Towards Contraception, Behaviour Change Communication on Malaria, Attitudes Towards Domestic Violence, Sexual Behaviour, HIV/AIDS National, Health Insurance.
The questionnaires were pre-tested in two districts: Ga West district in Greater Accra region and Akwapim South district in Eastern region and finalized. For the study, we used the composite household questionnaire.
Sampling method
The sampling frame used for the sampling was the 2000 Ghana Population and Housing Census data. The urban and rural areas of each region served as the key sampling strata. Two stage sampling method was used. In each stratum, the established population census enumeration areas were then systematically selected using probability proportional to size. There is no self-weighting because some of the regions namely Central, Northern, Upper East and Upper West regions were over-sampled. However, sample weights are used in reporting national level results.
The sample consists of women within the ages of 15–49 years with a live birth in the last 5 years preceding the survey. Of the 12,150 households sampled, 10,963 women aged 15–49 years were interviewed, with a response rate of 97%. Children under the age of 5 years constituted 7626. Responses were obtained from their mothers or caregivers with a response rate of 99%. The male survey involved 3511 men aged 15–59 years with a response rate of 95%. The questionnaire had questions on demographic indicators, health status, illness and visits to a doctor, health behaviour such as smoking, drinking alcohol, physical activity, and eating habits. We obtained our variables from the composite household survey, cleaned for missing values, and analyzed.
Inclusion and exclusion criteria
Only the composite household questionnaires with questions on MCH were included for the analysis based on our variables. All the other questionnaires were not included in the analysis which did not have data on the key variables of interest were not included.
Data analysis
Measurement of inequities.
We measured inequities in maternal and child health outcomes and access to health care interventions by three steps: i) Identification of the health outcome or intervention whose distribution is to be measured; ii) classification of the population into different strata by a selected equity stratifier; and iii) measuring the degree of inequality [ 23 ]. Finally, we tried to understand the drivers of these inequities in MCH utilization. The variables of interest, maternal and child health outcomes and interventions are listed in Table 1 . In the Multiple Indicator Cluster Survey, the socio-economic stratifier used is household wealth, which is derived from the household ownership of assets such as television, car etc. and dwelling characteristics such as flooring material and source of drinking water. In this study, we have used wealth quintiles that are provided in the MICS 4 report [ 18 ]. Each asset was assigned a weight (factor score) generated through principal components analysis, and the resulting asset scores were standardised in relation to a normal distribution with a mean of zero and standard deviation of one. Each household was then assigned a score for each asset, and the scores were summed for each household; individuals were ranked according to the total score of the household in which they resided. The sample was then divided into quintiles from one (lowest) to five (highest). A single asset index was developed for the whole sample; separate indices were not prepared for the urban and rural populations [ 24 ].
To date, various measures have been used in the measurement of inequities in health and health care. However, of the available measures only the slope index of inequality (SII), the relative index of inequality (RII) and the concentration index (CI) have been commonly used giving their desirable characteristics: (i) they reflect the socio-economic dimension of health inequalities; (ii) they reflect the experience of the entire population rather than only two groups such as wealth quintiles one and five and (iii) they are sensitive to changes in the distribution of the population across socio-economic groups [ 25 ].
The concentration index
In this study, inequities in maternal and child health are measured using the concentration index. The concentration index is defined with reference to the concentration curve, which is used to identify whether socioeconomic inequality in some health sector variable exists and whether it is more pronounced at one point in time than another or in one country than another. But a concentration curve does not give a measure of the magnitude of inequality that can be compared conveniently across many time periods, countries, regions, or whatever may be chosen for comparison. However, the concentration index quantifies the degree of socioeconomic related inequality in a health variable [ 26 , 27 ]. The CI has been used, for example, to measure and to compare the degree of socioeconomic-related inequality in child mortality [ 28 ], child malnutrition [ 29 ], health subsidies [ 30 ], and health care utilization [ 31 ].
Formally, the concentration index is defined as:
The index is bounded between − 1 and 1. For a discrete living standards variable, it can be written as:
where h i is the health sector variable, μ is its mean, and r i = i , N is the fractional rank of individual i in the living standards distribution, with i = 1 for the poorest and i = N for the richest. For computation, a more convenient formula for the concentration index defines it in terms of the covariance between the health variable and the fractional rank in the living standards distribution [ 26 , 32 , 33 ].
The sign of the concentration index indicates the direction of any relationship between the health variable and position in the living standards distribution, and its magnitude reflects both the strength of the relationship and the degree of variability in the health variable.
Equity stratifies and measures
Health equity is the absence of unjust, avoidable differences in health care access, quality, or outcomes. Measuring health inequalities allows us to identify differences that can be acted on and can be used to measure progress toward achieving health equity. Disaggregating health indicators using equity stratifiers can identify inequalities between subpopulations. An equity stratifier refers to a characteristic such as a demographic, social, economic, racial, or geographic descriptor that can identify population subgroups for the purpose of measuring differences in health and health care that may be considered unfair or unjust [ 34 ].
To assess wealth, the study used selected assets and durables in a sample household, because asset ownership tends to fluctuate less than individual income or expenditure. The assets considered in houses were permanent floors, roofs, or walls; flush or pour-flush toilets; transportation - including bicycles, motorcycles, cars or trucks; and electrical equipment, including radios, televisions, line or mobile telephones, refrigerators and computers. Households with these assets were considered richer than those without. The study also used principal component analysis of all household samples to generate a wealth index for each household and use this as an equity stratifier. This was done by measuring final use of goods and services, and money payments to obtain them and measures asset ownership, housing and/or access to services. This was then used to construct asset indices using methods such as principal component analysis. Using the concentration standard method, the study summarized the distribution of each MCH indicator over a gradient of the wealth index by a concentration index (CI) and a concentration curve (CC). The CI, which ranges from − 1.0 to + 1.0, captures the extent to which health outcomes and service use were concentrated among different population groups: the richest and the poorest. A CI of zero means an equal distribution of a particular indicator throughout the economic gradients. A negative CI indicates a concentration among those who are poorer (i.e., the CC lies above the equality line of 45 degrees), and a positive CI reflects a concentration among those who are richer (i.e. the CC lies below the equality line).
The study also compared the prevalence of health outcomes and the coverage of the MCH interventions between the richest and the poorest subgroups using a risk ratio (RR). All households were ranked according to their wealth indices, which was divided equally into quintile [ 5 ] and decile [ 9 ] subgroups. Only the top (richest) and bottom (poorest) quintiles and deciles were selected for the RR calculation, to demonstrate any disparity between rich and poor urban and rural domiciles and educated and uneducated.
Multiple regression models were then used to assess the drivers of inequity in the MCH outcomes using CI and RR as dependent variables. Data was analysed using STATA 13 statistical software.
Disparities among the poor and the rich in MCH
Tables 1 , 2 , 3 and 4 , summarizes equity measures for all MCH indicators in terms of CI and RR between the richest and poorest quintiles and deciles.
Economic disparities in health outcomes
We discovered substantial differences between income classes and geographic areas, suggesting that household wealth has a significant impact on child survival and that the poor have a higher risk of child mortality. Teenage pregnancy (CI = − 0.133, RR =0.679), Prenatal care by skilled health worker (CI = − 0.124, RR =0.713) (See Table 1 ); low birth weight (CI = − 0.021) (though not statistically significant), under five mortality (CI = − 0.247, RR = 0.426); all child malnourishment indicators: underweight, stunting and wasting (CI =, − 0.055, − 0,029, − 0.003, RR =0.772, 0.738, 0.822) respectively, and child disease all showed economic inequalities in MCH (See Table 2 ). The poorer subgroups were more likely to have negative health effects (as shown by the negative CIs in Tables 1 and 2 ). The poor had the highest concentration, which was statistically important for child underweight. The CI for stunting and wasting in children was negative. In terms of magnitude of concentration, teenage pregnancy was ranked third among the poor. Children under the age of 5 years old with suspected pneumonia and diarrhoea were also more prevalent among the poor, though not statistically significant (Table 2 ). The RRs were compatible with the computed CI when comparing MCH outcomes between the top and bottom income quintiles. Teenage pregnancy, under-five mortality, underweight children, and confirmed diarrhoea and suspected pneumonia were all more common in poorer households than in wealthier ones. The RR between the upper and bottom quintiles ranged from 0.77 for underweight children to 0.82 for wasting children (Table 2 ). Low birth weight was less clearly associated with economic disparities. The negative CI represented the fact that it was concentrated in relatively poor families, but it had no statistical significance.
Economic disparities in service coverage
The results indicate that the primary MCH interventions were spread more evenly across economic strata than the health outcomes (Table 2 ). Prenatal service by a professional health worker was statistically significant and concentrated among the poor, while delivery care in a health facility was also statistically significant and concentrated among the wealthy. The magnitude of the CI, on the other hand, was high, and the RR between the wealthiest and poorest groups was not close to one, suggesting a large disparity between the wealthy and the poor. The poorest quintile had the highest coverage of oral rehydration salts/oral rehydration therapy for diarrhoea. The wealthiest quintile and decile, on the other hand, had the highest coverage of adequate health-care services for suspected pneumonia. Table 2 shows that the CIs of the four vaccine types for childhood immunization coverage ranged from 0.054 to 0.069, and the CI for family planning (at 0.076) is all statistically different from zero. As a result, since all the indicators were clustered around the richest quintiles and deciles, there were inequalities in service coverage for these indicators. The RR for these indicators had mixed results (Tables 1 and 2 ); both had more than one for comparisons between the first and fifth quintiles, as well as between the first and tenth deciles.
Geographic inequity of MCH
Health outcome prevalence’s were as follows: teenage pregnancy among all mothers, 7.93%; low birth weight, 16.73%; and child stunting, 16.56% (Table 4 ). Service coverage was less equitable; for example, on average, less than 26% of respondents had prenatal care delivered either by skilled health workers or in health facilities, and less than 15% of children had received all vaccinations.
Tables 3 and 4 also summarizes the urban–rural and educational disparities in MCH, as reflected by the RR. The four vaccines (BCG, MMR, DPT and yellow fever) and the coverage indicator appropriate provider for pneumonia were all concentrated in the urban areas than rural areas (thus, by 47, 52, 53 and 56% respectively) while low birth, under five mortality, underweight, stunting, wasting, child illness (diarrhoea and suspected pneumonia) and coverage indicator ORS/ORT for diarrhoea were more concentrated in rural than in urban areas. The most profound health gap was under-five mortality, which was 33% more prevalent in rural than in urban areas.
The urban–rural gap for MCH service coverage was quite large. For instance, women living in rural areas were 30% less likely than those in urban areas to receive prenatal and delivery care from a skilled health worker. Although family planning was concentrated in the urban areas than rural, this was not statistically significant. Again, teenagers in urban areas were 73% less risky in getting expose to teenage issues compared to their counterparts in the rural areas. Also, there was a sharp gap between urban and rural women usage of print/electronic media and technology, thus women in urban areas were 4.9–78% more likely to use newspapers, radio, television, computer, and internet than their counterparts in the rural areas.
Educational inequity and MCH disparity
Mothers’ or caregivers’ formal schooling is a significant determinant of MCH inequity. Our findings show that more educated mothers or caregivers did better on all outcome indicators. The disparity was most noticeable when it came to teenage pregnancy. Women with less than a secondary school education were 87% more likely than those with a secondary school education to have their first pregnancy before the age of 20. Mothers or caregivers with no formal education were more likely (78% and 45%, respectively) to have under-five mortality and children with diarrhoea than those with a secondary education (Table 3 ).
Women with education beyond secondary school were 30–46% more likely than those without any formal education to receive family planning, maternal care, and delivery by a professional health worker or in a health facility. Higher educational attainment was also associated with a consistent improvement in maternal care coverage, with a large difference (RR: 1.304–1.457; P < 0.01). Surprisingly, children born to mothers or cared for by someone with a post-secondary education were 57–66% more likely than those who were not in this subgroup to receive all forms of vaccination before the age of 1 year.
The study analysed data from the Ghana Statistical Service’s (GSS) Multiple Indicator Cluster Survey (MICS 4, 2011) to unearth inequities in maternal and child health services delivery and access in Ghana. The results can inform policy planning to improve maternal and child health services, especially in the disadvantage areas and populations subgroups .
In 2016, Ghana’s MMR was 319 per 100,000 live births [ 32 ]. This demonstrates that MDG 5 [ 5 ], which aimed to reduce maternal mortality by three-quarters (190 deaths per 100,000 live births) by 2015, was not met. This means that if Ghana is to meet the Sustainable Development Goal (SDG) three [ 3 ], it will need to make more thoughtful and pragmatic efforts. Addressing and closing the disparities between rich and poor, educated, and uneducated, and social gradients in general are important first steps toward improving the well-being of mothers, infants, and children. Mothers’ and children’s health and socioeconomic well-being will have an impact on future generations’ health and make predicting future public health challenges for families, societies, and the health-care system easier. Much has been accomplished in terms of necessary child immunization, but ANC still has much room for improvement [ 22 ]. The sharp drop in ANC threatens to undo the country’s advances in maternal health care. With regional, location, mothers’ education, and wealth quintile inequalities, ANC coverage has dropped from 93.08% in 2012 to 81.3% in 2017 [ 33 ].
Major differences in MCH care measures were discovered in the literature across many geographical areas, maternal, economic, and socio-demographic factors in many developing countries. What is unknown are the factors that contribute to inequities in MCH service access and distribution.
Government health expenditure has a less progressive effect on inequality in Ghana than in many other nations, accounting for just one-third of the reduction in Gini Co-efficient [ 4 ]. Again, the government’s annual allocation to the health sector has fluctuated and remains below the Abuja Declaration target of 15% (ISSER, 2018), implying that less money is going into Maternal and Child Health services, further widening the country’s health disparities.
Assessing inequalities’ drivers is critical for making evidence-based decisions and allocating scarce public resources to those who are most in need. The existence of health-care inequities that disadvantage the poor, rural dwellers, and women with low education makes achieving the relevant health-related SDG targets difficult. This study sends a strong policy message: universal access to health care is critical to achieving the objective of health equity or reducing inequalities between sub-groups such as the poor and the wealthy, rural and urban dwellers, and those who have completed secondary school and those who have not completed secondary school.
In Ghana, child immunization was given to all mothers or caregivers regardless of their economic status. Surprisingly, immunization coverage was marginally higher in urban areas and among children whose mothers or caregivers had completed secondary school than in rural areas and among those who had not completed secondary school. These results indicate that urban areas have higher service coverage than rural areas.
Government’s low commitment to investment in health infrastructure and expansion of health insurance coverage over the past decades can explain Ghana’s relatively unequal distribution of MCH service coverage – between the wealthy and the poor, urban and rural populations [ 7 ]. Over the last few decades, the regional reach of district hospitals and sub-district health centers has tended to increase in favor of the urban and wealthy. District health systems, which include hospitals and health centers, are leading the way in offering a wide variety of curative, preventative, and health-promotion programs, including MCH.
In Ghana, there is still some difference in child health results between the rich and the poor, as well as between urban and rural areas. The country’s CIs for diarrhoea, malnutrition, underweight, and stunting, for example, are equivalent to the MICS for developing countries.
One of the most significant social determinants of health inequity is education. The education disparities for measures of teenage pregnancy and child malnutrition were far greater than the urban–rural differential, according to this report. As the mother’s or caregiver’s formal education level increased, the prevalence of adolescent pregnancy and infant malnutrition decreased. Teenage pregnancy was found to be much less common among those who had completed high school. This and other studies [ 12 ] show that maternal education is an important component of MCH policies.
In Ghana, access to MCH services is inequitable in the form of universal health coverage. Inequity in health outcomes is a problem, and social determinants (such as poverty, maternal education, and other structural social inequities) are significant, even though they are often beyond the health sector’s mandate. In this study, 16.13% of children were underweight, 16.56% were stunted, and 16.76% of children were wasting. Wasting in children suggests acute malnutrition, whereas stunting indicates chronic malnutrition, which is usually caused by long-term poverty in the home. Policies should tackle inequity from birth; for example, they should address problems including low birth weight, teen pregnancy, and infant malnutrition, for which the World Health Organization recommends multi-sectoral interventions. Inequity at birth has long-term consequences; undernutrition, for example, is linked to a loss of human capital (i.e., the skills and knowledge that enable people to work and thus produce economic value).
Limitation of the study
The data for the study is somehow old and could have potential policy gaps. Many factors might have changed within the period 2011 to 2021. However, current literature on MCH has been incorporated into the paper to account for the limitations. Though the MICS4 data is somewhat old, the analysis is relevant for comparing the results with future studies that uses current MICS data. Also, the study would have benefited from in-depth qualitative understanding of the inequalities in MCH which was not conducted. Further qualitative research is needed to complement and enhance the understanding of the drivers of inequalities in MCH in Ghana.
Major challenges remain in inequity in health outcomes, particularly in the areas of child mortality, teenage pregnancy, child malnourishment. The gaps between rich and poor and between urban and rural areas reveal a similar pattern. Mothers’ education is the main determinant of health inequity. Key policy leverage and multi-sectoral actions are needed to close these gaps. Inequities in most of the maternal and child health interventions in Ghana are widespread among sub-groups (rich-poor, urban-rural and high educated-less educated) to the detriment of poor, rural dwellers, and less-educated. Thus, tackling inequalities in resource allocation through primary health care services is key to fighting the extreme geographical and wealth inequality in Ghana. For instance, upping maternal and child health education and promotion, and improving the quality of primary health care clinics in the most disadvantage rural districts resource allocation using equity formulas can improve quality and equity of maternal and child health care in Ghana. Further research, especially qualitative research is needed to unravel the social dimensions of the inequalities and the congruent factors responsible for the MCH inequalities.
Availability of data and materials
The data that support the findings of this study are available from Ghana Statistical Service, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from Mubarik Salifu, (our author who managed the data) upon reasonable request and with permission of Ghana Statistical Service.
Yaya S, Bishwajit G, Shah V. Wealth, Education and Urban–rural Inequality and maternal healthcare service usage in Malawi. BMJ Global Health. 2016;1:e000085. https://doi.org/10.1136/bmjgh-2016-000085 .
Article PubMed PubMed Central Google Scholar
Birmeta K, Dibaba Y, Wo D. Determinants of maternal health care utilization in Holeta town, Central Ethiopia. BMC Health Serv Res. 2013;13(1):256. https://doi.org/10.1186/1472-6963-13-256 .
Ghana Statistical Service, Multiple Indicator Cluster Survey (MICS 2017/18), Survey Findings Report. Accra, Ghana, GSS; 2018.
Ghana Statistical Service (GSS), Ghana Health Service (GHS), ICF. Ghana Maternal Health Survey 2017, Key indicators report, Accra, Ghana: GSS, GHS, ICF; 2018.
Pfaller B, Sathananthan G, Grewal J, Mason J, D'Souza R, Spears D, et al. Preventing complications in pregnant women with cardiac disease. J Am Coll Cardiol. 2020;75(12):1443–52. https://doi.org/10.1016/j.jacc.2020.01.039 .
Article PubMed Google Scholar
OXFAM International. Building a more equal Ghana. A five-point action plan to close the gap between the rich and the rest. Oxford: OXFAM International, ISBN 978–1– 78748-298-2; 2018.
UNICEF. Maternal and newborn health; 2015. available from https://www.uncef.org/healt/index_maternalhealth.html . retrieved January 12, 2019.
Gould ED, Hijzen A. Inequality We Trust. Finance and Development; 2017.
Google Scholar
Population Reference Bureau. World Population Data Sheet 2016. Available from: https://www.prb.org/2016-world-population-data-sheet/2016 . Retrieved May, 2020.
Miles-Doan R, Brewster KL. The impact of type of employment on women’s use of prenatal care services and family planning in urban Cebu, the Philipines. Stud Fam Plann. 1998:69–78, 29, 1, https://doi.org/10.2307/172182 .
Raguparthy S. Education and the use of maternal health care in Thailand. Soc Sci Med. 1996;43(4):459–71. https://doi.org/10.1016/0277-9536(95)00411-4 .
Article Google Scholar
Arthur E. Wealth and antenatal care use: implications for maternal health care utilisation in Ghana. Health Econ Rev. 2012;e2:14. https://doi.org/10.1186/2191-1991-2-14 .
Ganle JK, Parker M, Fitzpatrick R, Otupri E. A qualitative study of health system barriers to accessibility and utilization of maternal and newborn healthcare services in Ghana after user-fee abolition. BMC Pregnancy Childbirth. 2014;14:425. https://doi.org/10.1186/s12884-014-0425-8 .
Owoo NS, Lambon-Quayefio MP. National health insurance, social influence and antenatal care use in Ghana. Health Econ Review. 2013;3:19. https://doi.org/10.1186/2191-1991-3-19 .
Braveman PA, Egerter SA, Mockenhaupt RE. Broadening the focus: the need to address the social determinants of health. Am J Prev Med. 2011;40(Suppl 1):S4–18. https://doi.org/10.1016/j.amepre.2010.10.002 .
Government of Ghana, National Development Planning Commission (NDPC). Medium-term national development policy framework: Ghana Shared Growth and Development Agenda (GSGDA) II, 2014–2017, Volume I: Policy framework. Accra: Government of Ghana, NDPC; 2014.
Ghana Statistical Service -GSS, Ghana Health Service -GHS, and ICF International. Ghana Demographic and Health Survey 2014. Rockville, Maryland, USA: GSS, GHS, and ICF International; 2015.
Ghana Statistical Service. Ghana Multiple Indicator Cluster Survey, with an Enhanced Malaria Module and Biomarker 2011, Final Report, Accra, Ghana, Ghana Statistical Service, 2012.
GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect Dis. 2018;18(1):1211–28.
Walker CLF, Rudan I, Liu L, Nair H, Theodoratou E. Childhood Pneumonia and Diarrhoea: Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405–16. https://doi.org/10.1016/S0140-6736(13)60222-6 .
World Health Organization. Maternal, newborn, child, and adolescent health. [Internet]. 2017. Available from: WHO, (2017). Maternal, newborn, http://www.who.int/maternal_child_adolescent/topics/maternal/skilled_birth/en/ . Retrieved, June 2019.
Liu I, Johnson HI, Cousens S, Perian J. Global , regional , and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379(9832):2151–61. https://doi.org/10.1016/S0140-6736(12)60560-1 .
Zere E, Tumusiime P, Walker O, Kirigia J, Mwikisa C, Mbeeli T. Inequities in utilization of maternal health interventions in Namibia: implications for progress towards MDG 5 targets. Int J Equity Health. 2010. https://doi.org/10.1186/475-9276-9-16 .
Ghana Statistical Service (GSS). Ghana Living Standard Survey 6: Poverty Profile. Accra: GSS; 2014.
Wagstaff A, van Doorslaer E, Watanabe N. On decomposing the causes of health sector inequalities, with an application to malnutrition inequalities in Vietnam. J Econ. 2003;112(1):219–27.
Kakwani N. Income inequality and poverty: methods of estimation and policy applications. Oxford: Oxford University Press; 1980.
Wagstaff A, van Doorslaer E, Paci P. Equity in the finance and delivery of health care: some tentative cross-country comparisons. Oxf Rev Econ Policy. 1989;5(1):89–112. https://doi.org/10.1093/oxrep/5.1.89 .
Wagstaff A. Socioeconomic inequalities in child mortality: comparisons across nine developing countries. Bull World Health Organ. 2000;78(1):19–29.
CAS PubMed PubMed Central Google Scholar
Wagstaff A, Watanabe N. What difference does the choice of SES make in health inequality measurement? Health Econ. 2003;12(10):885–90. https://doi.org/10.1002/hec.805 .
O’Donnell O, van Doorslaer E, Rannan-Eliya RP, Somanathanl A, Adhikari SR, Harbianto D, et al. The incidence of public spending on healthcare: comparative evidence from Asia. World Bank Econ Rev. 2007;2007(21):93–123. https://doi.org/10.1093/wber/lhl009 .
van Doorslaer E, Masseria C, Kool X. Inequalities in access to medical care by income in developed countries. Can Med Assoc J. 2006;174(2):7–83. https://doi.org/10.1503/cmaj.050584 .
Jenkins SP. Calculating income distribution indices from micro-data. Natl Tax J. 1988;41(1):139–42. https://doi.org/10.1086/NTJ41788716 .
Lerman R. I, Yitzhaki S. improving the accuracy of estimates of Gini coefficients. iJournal of econometrics. Elsevier. 1989;42(1):3–7.
Canadian Institute for Health Information. In pursuit of health equity: defining Stratifiers for measuring health inequality. A focus on age, sex, gender, income, education, and geographic location. Ottawa: CIHI; 2018.
Download references
Acknowledgments
We dully acknowledge the contribution of Dr. Mahamudu Akudugu, the coordinator of the Ghana Inclusive Development Research Network, of the University for Development Studies, Tamale for his technical advice and coordination of the research. We are very grateful to UNICEF for their funding support, and the Ghana Statistical Service for providing the datasets for this research. Finally, we extend our gratitude to our mentor, Professor Seidu Al-hassan for his coaching in carrying out this research.
Funding for this study was made possible by grants from UNICEF through the Ghana Inclusive Development Research Network (GIDRN)-University for Development Studies, Tamale.
Author information
Authors and affiliations.
School of Public Health, Department of Health Services, Policy, Planning, Management and Economics (HSPPME), University for Development Studies, Tamale, Ghana
Samuel George Anarwat
School of Applied Economics and Management Sciences, Department of Economics, University for Development Studies, Tamale, Ghana
Mubarik Salifu & Margaret Atosina Akuriba
You can also search for this author in PubMed Google Scholar
Contributions
SGA, MS, and MA contributed to the conception of the study and design. MS managed data analysis, while all authors contributed to the methodological design, interpretation of results, discussions and findings, conclusion, and the intellectual content including, writing, editing and proof reading for accuracy. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Samuel George Anarwat .

Ethics declarations
Ethics approval and consent to participate.
Since, this study was an empirical analysis of an existing data, it did not require ethical clearance.
Consent for publication
Not applicable.
Competing interests
We the authors for this research declare that we have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Anarwat, S.G., Salifu, M. & Akuriba, M.A. Equity and access to maternal and child health services in Ghana a cross-sectional study. BMC Health Serv Res 21 , 864 (2021). https://doi.org/10.1186/s12913-021-06872-9
Download citation
Received : 12 April 2021
Accepted : 09 August 2021
Published : 24 August 2021
DOI : https://doi.org/10.1186/s12913-021-06872-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Maternal and child health
- Health service access and delivery
- Concentration index
- Risk ratios
- Universal health coverage
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 07 November 2022
Exposure to family planning messages and contraceptive use among women of reproductive age in sub-Saharan Africa: a cross-sectional program impact evaluation study
- Duah Dwomoh 1 ,
- Susan Ama Amuasi 2 ,
- Emefa Modey Amoah 3 ,
- Winfred Gborgbortsi 4 &
- John Tetteh 5
Scientific Reports volume 12 , Article number: 18941 ( 2022 ) Cite this article
1682 Accesses
4 Citations
7 Altmetric
Metrics details
- Health care
- Medical research
Many women of reproductive age in sub Saharan Africa are not utilizing any contraceptive method which is contributing to the high burden of maternal mortality. This study determined the prevalence, trends, and the impact of exposure to family planning messages (FPM) on contraceptive use (CU) among women of reproductive age in sub-Saharan Africa (SSA). We utilized the most recent data from demographic and health surveys across 26 SSA countries between 2013 and 2019. We assessed the prevalence and trends and quantified the impact of exposure to FPM on contraceptive use using augmented inverse probability weighting with regression adjustment. Sensitivity analysis of the impact estimate was conducted using endogenous treatment effect models, inverse probability weighting, and propensity score with nearest-neighbor matching techniques. The study involved 328,386 women of reproductive age. The overall prevalence of CU and the percentage of women of reproductive age in SSA exposed to FPM were 31.1% (95% CI 30.6–31.5) and 38.9% (95% CI 38.8–39.4) respectively. Exposure to FPM increased CU by 7.1 percentage points (pp) (95% CI 6.7, 7.4; p < 0.001) among women of reproductive age in SSA. The impact of FPM on CU was highest in Central Africa (6.7 pp; 95% CI 5.7–7.7; p < 0.001) and lowest in Southern Africa (2.2 pp; 95% CI [1.3–3.0; p < 0.001). There was a marginal decline in the impact estimate among adolescents (estimate = 6.0 pp; 95% CI 5.0, 8.0; p < 0.001). Exposure to FPM has contributed to an increase in CU among women of reproductive age. Programs that are geared towards intensifying exposure to FPM through traditional media in addition to exploring avenues for promoting the appropriate use of family planning method using electronic media remain critical.
Similar content being viewed by others
Exploring rise of pregnancy in Bangladesh resulting from contraceptive failure
Factors influencing the uptake of short-term contraceptives among women in Afghanistan

Risk factors and knowledge associated with high unintended pregnancy rates and low family planning use among pregnant women in Papua New Guinea
Introduction.
Currently, the global estimates of maternal mortality (MM), although indicative of improvements, remain unacceptably high 1 , 2 . In 1987, the Safe Motherhood Initiative (SMI) was launched as an initiative to enhance the quality of maternal health. The focus of the initiative was channeled to people living in low-and-middle-income countries (LMICs). The SMI envisages that in making an impact to minimize MM, all women must have access to essential health services including family planning 3 . However, many women of reproductive age are not utilizing any contraceptive method which is contributing to the high burden of MM. It has been established that a considerable number of MM would be avoided if the contraceptive prevalence rate (CPR) increased, and the unmet need for FP decreased 4 . Contraceptive use reduces the risk of unplanned pregnancy 5 , 6 , and provides substantial social and economic benefits including improved educational and employment opportunities 7 . Additionally, contraceptive use reduces unwanted fertility which is a major public health problem in developing countries 4 .
Globally, 172 million women are currently not using any method of contraception even though they desire to avoid pregnancy 8 . In 2013, Darroch and colleagues found that the unmet need for modern contraceptives in sub-Saharan Africa (SSA) was 60% of the 89 million population 9 . The non-use of contraceptives varies across the continent. However, unmet needs, health concerns, infrequent sex, opposition from others, lack of knowledge, and other less reported factors are the key barriers hindering contraceptive use (CU) 10 , 11 .
In low and middle-income countries, it is estimated that a quarter of women of reproductive age wish to avoid pregnancy but are not utilizing effective contraceptive methods 7 . Among women aged 15–49 years in 47 developing countries, this was observed to be higher at an average of 40.9% who needed contraception but are not using any technique 12 .
All sexually active women should be informed about their risk of becoming pregnant as well as the many techniques available to prevent unplanned or unintended pregnancies. Countries in SSA are currently facing the challenges of high birth rates that may be attributable to inadequate access and use of contraceptive methods. In response to this, the governments of these countries are focusing on the need for mass communication campaigns to encourage the use of contraceptives. The empirical evidence documented in some studies although limited in scope, geographical boundaries, and in some cases statistical analysis rigor has shown that exposure to family planning (FP) information remains critical if we intend to increase contraceptive use among women of reproductive age 13 , 14 , 15 . In addition, the investment made in FP education over the years has been enormous. For instance, the direct and indirect annual cost (program support, information and education on family planning, construction and maintenance of facilities, and supply chain management) of providing modern contraceptive services to 671 million users in developing regions was estimated to be US$6.3 billion 14 . Despite this huge investment in FP campaign messages, there is a paucity of evidence regarding the effectiveness of FP messages on contraceptive use in sub-Saharan Africa. In Africa, some studies have estimated the pooled prevalence of contraceptive use and determined associated factors among reproductive women using nationally stratified surveys 16 , 17 , however, none of them have assess the effectiveness of FP messages on contraceptive use. Using the most recent demographic and health survey data, we determine the prevalence trends and quantify the impact of exposure to FPM on CU among women of reproductive age in SSA.
This study followed the standard guidelines for reporting observational studies using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
Data source
This study utilized secondary data from the most recent and available Demographic and Health Survey (DHS) conducted in 26 SSA countries between 2013 and 2019 (Supplementary Table 1 ). The DHS is a nationally representative household survey with similar data collection instruments and study designs conducted in LMICs with the primary goal of generating estimates for indicators that are comparable across the sub-region. The DHS provides data for a wide range of monitoring and impact evaluation indicators in the areas of population, health, and nutrition. Specifically, the DHS collects data on family planning (knowledge and use of contraceptives), maternal health (antenatal, delivery, and postnatal care), household wealth, parity, education, place of residence, and demographics, amongst other variables with sample sizes (usually between 5000 and 30,000 households) and typically are conducted in every 5 years, to allow comparisons over time. The survey employs a multi-stage stratified cluster sampling design where the index country is stratified into distinct geographical regions or provinces during the first phase of the design. The first phase of sampling involves the random sampling of clusters or enumeration areas (EA) using probability proportional to the size of the EA and the subsequent sampling of a fixed number of households within each of the sampled enumeration areas using a systematic random sampling approach. A complete household listing was carried out to update the sampling frame before the random sampling of households. Trained field data collectors were assigned to these sampled enumeration areas for the household survey. Details on the study design and procedures for data collection have been published elsewhere 18 .
The DHS data is publicly available upon reasonable written request at the DHS website ( https://dhsprogram.com/data/available-datasets.cfm ).
All standard DHS surveys have been reviewed and approved by ICF Institutional Review Board (IRB). Additionally, country-specific DHS survey protocols are reviewed by the ICF IRB and typically by an IRB in the host country ( https://dhsprogram.com/Methodology/Protecting-the-Privacy-of-DHS-Survey-Respondents.cfm ). This study did not require country-specific ethical approval since we only analyze secondary data from the DHS program that has obtained ethical approval for all countries for the different survey years and all study participants have been de-identified.
DHS is one of the few nationally representative household surveys with very high response rate (> 95%). Because of this high response rate, we assumed that missing data will be missing completely at random. This implies that there would be no systematic differences in the observed characteristics between participants with missing data and those with complete data.
Outcome variable
The primary outcome measure in this study was contraceptive use. Contraceptive use as defined by DHS was among women of reproductive age who currently use any standard method of contraceptive (traditional or modern). Contraceptive use was classified as a binary variable that takes the value of 1 if the woman is currently using a traditional or modern contraception method and a value of 0 if otherwise. The modern methods include women who use female sterilization (tubal ligation, laparotomy, voluntary surgical contraception), male sterilization (vasectomy, voluntary surgical contraception), the contraceptive pill (oral contraceptives), intrauterine contraceptive device (IUD), injectables (Depo-Provera), implant (Norplant), female condom, the male condom (prophylactic, rubber), diaphragm, contraceptive foam and contraceptive jelly, lactational amenorrhea method (LAM), standard days method (SDM) and country-specific modern methods. Respondents mentioned other modern contraceptive methods (including cervical cap, contraceptive sponge, and others), but do not include abortions and menstrual regulation 19 .
Primary exposure
Exposure to FPM was defined as individual women of reproductive age who heard or saw FPM on the radio, on television, in a newspaper or magazine, or on a mobile phone in the past few months 19 .
Confounders
Variables considered as possible confounders were selected based on an extensive literature review of factors that could potentially influence access to FPM and contraceptive use among women of reproductive age . The following variables were accounted for in all the multivariable models: the age of the household head (categorized as ≤ 29, 30–39, 40–49, 50–59, and 60+), sex of the household head (male or female), household wealth Index (poorest, poorer, middle, richer, richest), place of residence (rural or urban), religion (Islam, Christian or Others), respondent age (15–19, 20–29, 30–39, 40–49), marital status (widowed, never married, married or divorced), educational level (no formal education, primary, secondary, higher), currently working (no, yes), children ever born (no child, 1 child, 2 children, 3 + children) 20 , 21 . These variables have been found to either increase contraceptive use, exposure to family planning messages or both.
Statistical analysis
Assessing trend and factors associated with contraceptive use.
We explored the trend of FPM and CU between 2013 and 2019 using tools from time series line graphs and estimated the weighted prevalence of FPM and CU over the period by adjusting for sampling weight for all point and interval estimates including regression models. Factors contributing to CU and FPM were assessed using the Poisson regression model with a cluster-robust standard error that generates prevalence ratios and their respective confidence intervals. Sensitivity analysis of the point estimates and corresponding confidence interval (CI) was conducted using the multivariable binary logistic regression model that reports odds ratio and CI. The Poisson model was preferred to the logistic regression model as the odds ratio may overestimate the prevalence ratio, the measure of choice in cross-sectional studies 22 .
Assessing impact of family planning messages on contraceptive use
Augmented inverse-probability weighting (AIPW) was used to estimate the average treatment effect of FPM from cross-sectional data. The AIPW estimator is classified among the estimators with the doubly-robust property as it combines aspects of regression adjustment and inverse-probability-weighted methods to reduce bias associated with the impact estimate. The model accounted for sampling weight and used cluster-robust standard errors to address the methodological challenges (stratification, clustering, weighting) associated with complex survey design. Since different impact estimation procedures may lead to slightly different impact estimates especially when the data originates from crossectional studies instead of the more rigorous experimental design, sensitivity analysis of the impact estimate was conducted using endogenous treatment effect models, inverse probability weighting, propensity scores, and nearest-neighbor matching techniques. Estimating the impact of an intervention, program or policy becomes difficult due to endogeneity. For instance, genetic predisposition, personal values, conservative lifestyle, religious beliefs, and other unmeasured confounders may simultaneously affect exposure to family planning messages and utilization of contraception 13 . The standard regression models (e.g., Poisson, Negative Binomial, binary logistic, probit, and ordinary least square assume that these unmeasured covariates do not correlate with both the outcome measure (contraceptive use) and exposure to FPM. This assumption is largely violated in the context of observational data where both the outcome and exposure are usually measured at the same time and may correlate with unobserved confounders. We anticipated these problems, and as part of the sensitivity analyses that were conducted, we used endogenous treatment regression models to address endogeneity. Having radio or television was used as the instrumental variable since it met the exclusion restriction criteria recommended for instrumental variable regression analysis (that is, having a radio or television sets influence the ability to listen to FPM directly, it does not influence the use of contraceptives directly, but only through the family planning message and we assume that it is not influenced by other factors).
All statistical analyses were conducted using Stata version 17 (StataCorp, College Station, Texas, USA) and a p-value of less than 0.05 was considered statistically significant.
Ethics approval and consent to participants
This is a secondary data analysis of publicly available data with de-identified participants' information.
Characteristics of the study participants
The study involved 328,386 women of reproductive age (15–49 years) in SSA with an average of 30.5 years (standard deviation 8.9 years). Approximately 61% of the women lived in rural areas and 73% were married. About 30% of the women had no formal education. The sociodemographic characteristics of the women can be found in supplementary Table 2 .
Prevalence of contraceptive use and exposure to family planning messages
The overall prevalence of contraceptive use among women of reproductive age and adolescents in SSA between 2013 and 2019 was estimated as 31.1% (95%CI 30.6, 31.5) and 22.6% (95% CI 21.9–23.2) respectively (Table 1 ). The prevalence of contraceptive use was highest in Southern Africa [52.3% (95% CI 41.6–52.9)] and lowest in West Africa [0.4% (95% CI 19.9–20.9)]. By country, the Chad Republic recorded the lowest prevalence of contraceptive use [6.2% (95% CI 5.3–7.2)] with Zimbabwe recording the highest prevalence of contraceptive use [59.6% (95% CI 58.0–61.1)]. Approximately 39% (95% CI 38.8–39.4) and 32% (95% CI 31.36–32.94) of the women and adolescents were exposed to FPM in SSA between 2013 and 2019 respectively (Table 2 ). Eastern African countries were highly exposed to family planning messages [49.5%; 95% CI (48.3–50.6)] and the Central African countries were the least exposed to FPM [26.5%; 95% CI (25.4–27.7)]. By Country, Uganda recorded the highest exposure to FPM [70.1 (68.7–71.5)] and Chad recorded the least exposure to FPM [11.3 (9.9–12.9)]. The geospatial distribution of contraceptive use and exposure to FP messages can be found in Fig. 1 .
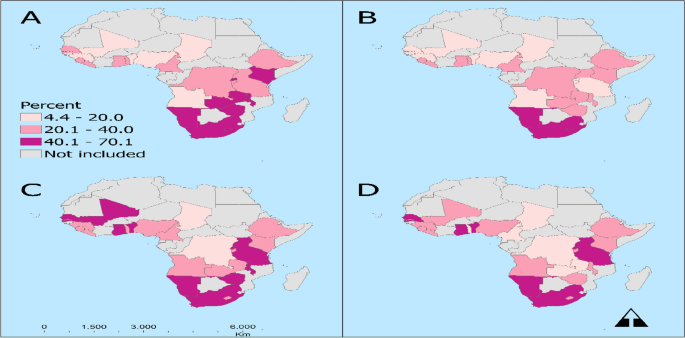
The geospatial distribution of contraceptive use and exposure to FP messages. Prevalence of contraceptive use by ( A ) general population, ( B ) adolescents and the exposure to family planning messages by ( C ) general population, and ( D ) adolescents among women of reproductive age in Sub-Saharan Africa, evidence from DHS surveys.
Trend analysis of contraceptive use and exposure to family planning messages
The trend analysis showed that the prevalence of contraceptive use among women of reproductive age and adolescence fluctuated between 2013 and 2019 but increased marginally between 2015 and 2017. Contraceptive use among women of reproductive age increased between 2013 and 2015 and declined between 2015 to 2017. Among adolescents, CU increased between 2013 and 2015 and remained fairly constant between 2015 and 2017 but declined between 2017 and 2018 before increasing marginally in 2019 (Fig. 2 ). There was a positive correlation between exposure to FPM and CU as a higher prevalence of CU was associated with higher exposure to FPM and vice versa (Fig. 2 ).
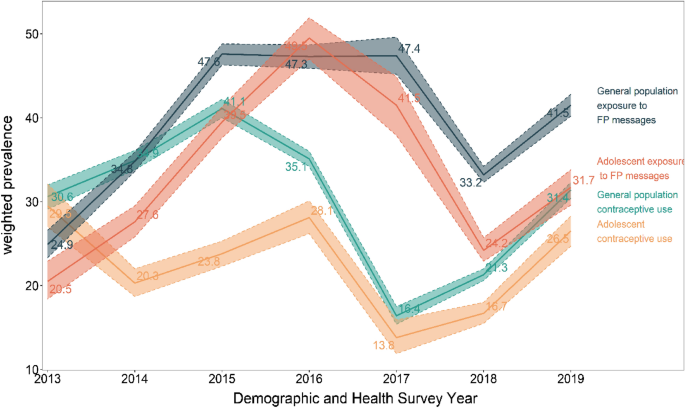
Trend of contraceptive use and exposure to family planning among women in their reproductive year in sub-Saharan countries, evidence from DHS study. FP family planning.
Factors associated with access to family planning message
The following factors were found to be associated with access to family planning messages: age of the respondent, female household heads, higher socio-economic status measured via household wealth, living in urban areas, religion, marital status, higher education level, parity and women who were currently working at the time of the survey were found to be associated with a higher prevalence of access to FPM (Supplementary Table 3 ).
Factors associated with contraceptive use
The results from the multivariable Poisson regression model showed that the age of the household head, sex of household head, higher socio-economic status measured via household wealth, living in urban areas, religion, marital status, higher education level, parity, and exposure to FPM were found to be associated with contraceptive use (Supplementary Table 4 ).
Impact of exposure to family planning information messages on contraceptive use among women of reproductive age: evidence from DHS study
Table 2 shows the results from the augmented inverse probability weighting with regression adjustment and sensitivity analysis of the impact estimate among women of reproductive age. Exposure to FPM increased contraceptive use by 7.1 percentage points (pp) (95% CI 6.7, 7.4) among women of reproductive age in SSA. The impact of FPM on contraceptive use was highest in Central Africa [6.7 pp; 95% CI: (5.7–7.7) and lowest in Southern Africa (2.2 pp; 95% CI: (1.3–3.0)]. Cameroon recorded the highest impact of FPM on contraceptive use (6.7 pp; 95% CI: (4.4–9.0)] but exposure to FPM did not have a statistically significant effect on contraceptive use in Rwanda, Namibia, and Liberia.
Impact of exposure to family planning information messages on contraceptive use among adolescents: evidence from DHS study
Table 3 shows the results from the augmented inverse probability weighting with regression adjustment and sensitivity analysis of the impact estimate of FPM among adolescents. Exposure to FPM increased CU by 6.0 percentage points (pp) (95% CI 5.0, 8.0) among adolescents in SSA. The impact of FPM on CU was highest in Southern Africa [7.0 pp; 95% CI: (4.0–9.0)] and lowest in Eastern Africa [2.0 pp; 95% CI: (−0.00, −3.0)]. Cameroon recorded the highest impact of FPM on contraceptive use among adolescents [impact estimate 17.0 pp; 95% CI: (9.0–25.0)].
This study assessed the prevalence, trends, and impact of exposure to FPM on contraceptive use among women of reproductive age in SSA and further conducted a sub-group analysis among the adolescent class of women using augmented inverse probability to treatment weighting with regression adjustment. Different sensitivity analyses were performed as a robustness check to confirm the results of augmented inverse probability to treatment weighting with regression adjustment. The empirical evidence presented in this manuscript allows us to draw four important conclusions. First, the prevalence of contraceptive use among women of reproductive age (general population aged from 15 to 49 years) and the adolescent sub-class largely varies among countries and geographic groupings in SSA and changes significantly over time. The high fluctuations in the prevalence of contraceptive use based on the trend analysis could be attributed to the variations in the level of intensity of family planning campaigns over the period, access and affordability of contraceptives in the sub-region.
The marginal increase in CU among the general population coupled with the declining CU among adolescents despite their increased exposure to FPM would indicate that regardless of exposure to messages, barriers to use persists.
Second, our final multivariable regression analyses showed that exposure to FPM does increase the likelihood of using contraceptive methods among women of reproductive age and adolescents sub-class in SSA although the effect size estimate varies by country and regional block. The regional and national diversity of SSA may play a key role in the diffusion of fertility regulating ideas and practices adopted by women 17 . Evidence of this is seen as contraceptive use among women of reproductive age and adolescents is higher in Southern Africa compared to Central, Eastern, and Western African countries. Eastern African countries are the most exposed to FPM this has been documented to be attributable to the government’s investments in improving access to SRH services through health insurance schemes, involvement of religious leaders in FP counseling and education, and introduction of health extension workers 23 . It is plausible that the structural and developmental changes such as that accompany urbanization such as the establishment of telecommunications networks and increased proliferation of cellular and smartphones could also be used to accelerate the spread of information on sexual and reproductive health. Policymakers and other stakeholders should intensify exposure to FPM using diverse media outlets such as television, radio, and print, and explore avenues for the appropriate use of electronic media.
Our third observation is that among the 26 SSA countries studied, there was a wide range of geographical differences in the prevalence of modern CU and exposure to FPM. Especially among the general population of women aged 15–49 years, the pattern of CU showed a decreasing array. Within the sub-regions, the lowest use of conceptive was among reproductive was observed among women residents in the WA region with approximately one-fifth prevalence rate. The need to address misinformation and fears of side effects as barriers to method use remains a critical area to be addressed in WA 24 . The prevalence of contraceptive use is a major public health concern in WA since the sub-region lagging in the use of contraceptives has been consistently so for more than two decades now 25 . Interestingly, the low utilization of contraceptives in WA is evident in the high total fertility rate compared with the general SSA region (5.1 versus 2.4) 26 .
Among the general population of women and adolescents, the high prevalence of CU and exposure to FPM in SSA occurred among women in Southern Africa and specifically Zimbabwe. Zimbabwean women have benefited from the strong post-independence encouragement of contraceptive use by their government 27 . For CU, approximately less than and a little more than one-twentieth of adolescents utilize contraceptives among adolescents and the general population respectively. The lowest prevalence of CU in Chad has also been confirmed by Ahinkorah et al., 2021 28 . Chad is at a disadvantage in both the use of contraceptives and exposure to FPM which needs urgent attention for improvement This calls for the adoption of new strategies to include adolescents in exposure to FPM programs since non-exposure to FPM directly translates into a high unmet need for FP among adolescents 29 . Communication is a vital mechanism connecting social factors and health outcomes.
Finally, we infer that exposure to FPM was found to be associated with CU among participants. Exposure to FPM was defined as hearing or seeing an FPM on the radio, television, in a newspaper or magazine, or on a mobile phone in the past few months. By using a counterfactual control group in this current study, the impact of exposure to FPM significantly increased the utilization of contraceptives in the SSA region. Findings envisage that the average conceptive use among women of reproductive age who are exposed to FPM significantly increased as compared with those who are not exposed. This finding corroborates the findings that exposure to FPM enhances the use of CU among reproductive-age women 30 .
Our study has provided empirical evidence to support the incessant calls for policymakers, external donor funding agencies, Civil Society and NGOs to prioritize and increase the resources for implementing family planning communication interventions in low-and middle-income countries. We proposed diverse country-specific policies, programs, and interventions that incorporate the different dynamics of socio-political, cultural, and other contextual factors that hinder access to family planning messages and the use of contraceptives in SSA.
Assessing the impact of health interventions poses a great challenge in situations where the data used for the analysis were from observational studies due to the problem of endogeneity (unobserved factors correlate with the treatment variable and the outcome measure of interest). Although a more rigorous statistical technique and sensitivity analysis of the impact estimates were conducted to generate an unbiased estimate of the program impact that addresses the problems of endogeneity, we believe that other unmeasured covariates (unobserved factors) such as health-related conditions, genetic predisposition, socio-cultural factors and area-specific inherent traditions in some part of SSA and many other factors may contribute to the observed change in the contraceptive use.
Notwithstanding these limitations, this impact evaluation study represents one of the few efforts to examine the effects of FPM on contraceptive use in SSA using data that originate from observation studies compared to the more preferred experimental study designs. It is the first study to assess the effect of family planning messages in SSA. In addition, the main outcomes were self-reported, which are subject to participants’ recall bias or socially desirable responses because the DHS asked the participant to recall over the past 30 days.
Prevalence of CU and exposure to FPM varies significantly across countries in SSA and the exposure to family planning messages increased the use of contraceptive among women of reproductive age. Despite disparities observed, exposure to FPM has contributed to an increase in CU among women of reproductive age and the adolescent sub-class. We emphasized the need to implement policies that incorporate social-cultural and political support to encourage women to adopt contraceptive methods following exposure to messages. Funding for family planning education via print and electronic media should continue unabated.
Data availability
The datasets that were used in the study are publicly available on the DHS website ( https://dhsprogram.com/data/available-datasets.cfm ).
Abbreviations
Augmented inverse probability weighting
Contraceptive use
Demographic and health survey
Endogenous treatment effect
Family planning messages
Inverse probability weighting
Maternal mortality
Propensity score matching
Safe motherhood initiative
Sub-Saharan Africa
Hogan, M. C. et al. Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet 375 , 1609–1623 (2010).
Article PubMed Google Scholar
WHO. Maternal Mortality . https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (2019).
Mahler, H. The safe motherhood initiative: A call to action. Lancet 1 , 668–670 (1987).
Article CAS PubMed Google Scholar
Utomo, B. et al. The impact of family planning on maternal mortality in Indonesia: What future contribution can be expected?. Popul. Health Metrics 19 , 2 (2021).
Article Google Scholar
Adeniyi, O. V. et al. High rate of unplanned pregnancy in the context of integrated family planning and HIV care services in South Africa. BMC Health Serv. Res. 18 , 140 (2018).
Article PubMed PubMed Central Google Scholar
Bukenya, J. N. et al. Contraceptive use, prevalence and predictors of pregnancy planning among female sex workers in Uganda: A cross sectional study. BMC Pregnancy Childb. 19 , 121 (2019).
Singh, S., Darroch, J. E. & Ashford, L. S. Adding It Up: The Costs and Benefits of Investing in Sexual and Reproductive Health 2014 . https://www.guttmacher.org/report/adding-it-costs-and-benefits-investing-sexual-and-reproductive-health-2014 (2014).
United Nations Department of Economic and Social Affairs, Population Division. World Family Planning 2020 Highlights: Accelerating Action to Ensure Universal Access to Family Planning (ST/ESA/SER.A/450). https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Sep/unpd_2020_worldfamilyplanning_highlights.pdf (2020).
Darroch, J. E. & Singh, S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: An analysis of national surveys. Lancet 381 , 1756–1762 (2013).
Camara, B. S., Sidibe, S. & Dioubaté, N. Non-Use of Contraceptive Methods Among Married: Analysis of the 2018 Guinea Demographic and Health Survey . (2020).
Sedgh, G., Ashford, L. S. & Hussain, R. Unmet Need for Contraception in Developing Countries: Examining Women’s Reasons for Not Using a Method . (2016).
Moreira, L. R., Ewerling, F., Barros, A. J. D. & Silveira, M. F. Reasons for nonuse of contraceptive methods by women with demand for contraception not satisfied: An assessment of low and middle-income countries using demographic and health surveys. Reprod. Health 16 , 148 (2019).
Babalola, S., Folda, L. & Babayaro, H. The effects of a communication program on contraceptive ideation and use among young women in northern Nigeria. Stud. Fam. Plann. 39 , 211–220 (2008).
Guttmacher Institute. Adding It Up: Investing in Contraception and Maternal and Newborn Health, 2017—Estimation Methodology . https://www.guttmacher.org/report/adding-it-up-investing-in-contraception-maternal-newborn-health-2017-methodology (2018).
Hutchinson, P. & Wheeler, J. Advanced methods for evaluating the impact of family planning communication programs: Evidence from Tanzania and Nepal. Stud. Fam. Plann. 37 , 169–186 (2006).
Ba, D. M., Ssentongo, P., Agbese, E. & Kjerulff, K. H. Prevalence and predictors of contraceptive use among women of reproductive age in 17 sub-Saharan African countries: A large population-based study. Sex. Reprod. Healthc. 21 , 26–32 (2019).
Tsui, A. O., Brown, W. & Li, Q. Contraceptive practice in sub-Saharan Africa. Popul. Dev. Rev. 43 , 166–191 (2017).
ICF International. Demographic and Health Survey Sampling and Household Listing Manual . (2012).
Croft, T. N., Aileen, M. J. M. & Courtney, K. A. Guide to DHS Statistics . (2018).
Abdulai, M. et al. Demographic and socio-cultural factors influencing contraceptive uptake among women of reproductive age in Tamale Metropolis, Northern Region, Ghana. Ghana Med. J. 54 , 64–72 (2020).
Idris, I. M. & Idris, I. M. Factors influencing contraception usage: A cross-sectional study among mothers receiving abortion services in Orotta Maternity Hospital, Eritrea. Int. J. Sex. Reprod. Health Care 3 , 070–074 (2020).
Martinez, B. A. F. et al. Odds ratio or prevalence ratio? An overview of reported statistical methods and appropriateness of interpretations in cross-sectional studies with dichotomous outcomes in veterinary medicine. Front. Vet. Sci. 4 , 193 (2017).
Tilahun, T., Dibaba, Y., Bangha, M., Gatura, C., Doughman, D., & Izugbara, C. Contraceptive Use in East Africa: What Do the Numbers Tell Us? (Africa Population and Health Reserach Centre, 2018).
Hindin, M. J., McGough, L. J. & Adanu, R. M. Misperceptions, misinformation and myths about modern contraceptive use in Ghana. J. Fam. Plann. Reprod. Health Care 40 , 30–35 (2014).
Population Reference Bureau. Family Planning in West Africa. PRB https://www.prb.org/resources/family-planning-in-west-africa/ (2008).
Population Reference Bureau. Total Fertility Rate: International Data . PRB https://www.prb.org/international/ (2021).
Akim, M. & Kembo, J. Falling fertility and increase in use of contraception in Zimbabwe. Afr. J. Reprod. Health 15 , 31–44 (2011).
Google Scholar
Ahinkorah, B. O. et al. Factors associated with modern contraceptive use among women with no fertility intention in sub-Saharan Africa: Evidence from cross-sectional surveys of 29 countries. Contracept. Reprod. Med. 6 , 22 (2021).
UNFPA. Facing the Facts: Adolescent Girls and Contraception . https://www.unfpa.org/sites/default/files/resource-pdf/UNFPA_Adolescent_brochure.pdf (2015).
Das, P. et al. Association between media exposure and family planning in Myanmar and Philippines: Evidence from nationally representative survey data. Contracept. Reprod. Med. 6 , 11 (2021).
Download references
Author information
Authors and affiliations.
Department of Biostatistics, School of Public Health, University of Ghana, Accra, Ghana
Duah Dwomoh
Department of Physician Assistantship, School of Medicine and Health Sciences, Central University College, Accra, Greater Accra, Ghana
Susan Ama Amuasi
Department of Population, Family and Reproductive Health, School of Public Health, University of Ghana, Accra, Ghana
Emefa Modey Amoah
School of Geography and Environmental Science, University of Southampton, Highfield, SO17BJ, UK
Winfred Gborgbortsi
Department of Community Health, University of Ghana Medical School, University of Ghana, Accra, Ghana
John Tetteh
You can also search for this author in PubMed Google Scholar
Contributions
D.D. conceived and design the study. D.D. and J.T. performed all the statistical analyses. E.M.A., S.A.M., W.G. reviewed the initial draft, contributed to the write-up of the results section and wrote the discussion sections of the manuscript.
Corresponding author
Correspondence to Duah Dwomoh .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Dwomoh, D., Amuasi, S.A., Amoah, E.M. et al. Exposure to family planning messages and contraceptive use among women of reproductive age in sub-Saharan Africa: a cross-sectional program impact evaluation study. Sci Rep 12 , 18941 (2022). https://doi.org/10.1038/s41598-022-22525-1
Download citation
Received : 10 July 2022
Accepted : 17 October 2022
Published : 07 November 2022
DOI : https://doi.org/10.1038/s41598-022-22525-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Individual and community level factors for modern contraceptives utilization among reproductive aged women in amhara region, mixed effect multi-level modeling, data from mini-edhs, 2019.
- Fassikaw Kebede Bizuneh
- Tsehay Kebede Bizuneh
- Berihun Mulu Yayeh
Contraception and Reproductive Medicine (2023)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Research article
- Open access
- Published: 23 April 2020
Patterns of access to reproductive health services in Ghana and Nigeria: results of a cluster analysis
- Oluwasegun Jko Ogundele 1 ,
- Milena Pavlova 1 &
- Wim Groot 1 , 2
BMC Public Health volume 20 , Article number: 549 ( 2020 ) Cite this article
2530 Accesses
3 Citations
6 Altmetric
Metrics details
Inequalities in access to health care result in systematic health differences between social groups. Interventions to improve health do not always consider these inequalities. To examine access to reproductive health care services in Ghana and Nigeria, the patterns of use of family planning and maternal care by women in these countries are explored.
We used population-level data from the Ghana and Nigeria Demographic Health Surveys of 2014 and 2013 respectively. We applied a two-step cluster analysis followed by multinomial logistic regression analysis.
The initial two-step cluster analyses related to family planning identified three clusters of women in Ghana and Nigeria: women with high, medium and poor access to family planning services. The subsequent two-step cluster analyses related to maternal care identified five distinct clusters: higher, high, medium, low and poor access to maternal health services in Ghana and Nigeria. Multinomial logistic regression showed that compared to women with secondary/higher education, women without education have higher odds of poor access to family planning services in Nigeria (OR = 2.54, 95% CI: 1.90–3.39) and in Ghana (OR = 1.257, 95% CI: 0.77–2.03). Compared to white-collar workers, women who are not working have increased odds of poor access to maternal health services in Nigeria (OR = 1.579, 95% CI: 1.081–2.307, p ≤ 0.01). This association is not observed for Ghana. Household wealth is strongly associated with access to family planning services and maternal health care services in Nigeria. Not having insurance in Ghana is associated with low access to family planning services, while this is not the case in Nigeria. In both countries, the absence of insurance is associated with poor access to maternal health services.
Conclusions
These differences confirm the importance of a focused context-specific approach towards reproductive health services, particularly to reduce inequality in access resulting from socio-economic status. Interventions should be focused on the categorization of services and population groups into priority classes based on needs assessment. In this way, they can help expand coverage of quality services bottom up to improve access among these vulnerable groups.
Peer Review reports
Inequalities in access to health care can result in health differences between social groups. Interventions to create universal access to health care and to improve health outcomes, do not always consider these inequalities. Women are exposed to unequal access to health care services globally [ 1 ]. This is particularly the case for reproductive health care services [ 2 ], which include contraceptives, maternal health services, and services related to sexual health [ 3 , 4 , 5 ]. Targets have been set to improve these services. For example, the Sustainable Development Goal 3 aims to ensure universal access to reproductive health care services [ 6 ].
Factors that determine access to reproductive health services are related to both demand and supply and can be divided into social and economic factors [ 7 ]. Education, occupation, wealth and possession of insurance, among others, are significant predictors of inequality in access to reproductive health services in Sub-Saharan Africa [ 8 , 9 , 10 , 11 , 12 , 13 ]. However, previous studies have mostly focused on the determinants of service use in a country or region [ 11 , 14 , 15 ]. There is a need for cross-country comparisons to shed light on similarities and/or dissimilarities between groups of users of reproductive health services in Sub-Saharan African countries.
This study examines access to reproductive health care services among women of reproductive age in Ghana and Nigeria. We use data from the Demographic Health Surveys (DHS) of Ghana carried out in 2014 and that of Nigeria carried out in 2013. The two countries are selected for this study based on the similarities in trends, health outcomes as well as data availability. At the same time, their health care systems are different. For example, Ghana has an established national health insurance system, while there is no such well-established system in Nigeria [ 16 ]. Ghana and Nigeria introduced a minimal user fee in the early 1970s, which was later abandoned in both countries due to cash crunches [ 17 ]. Ghana offers free-of-charge maternal care. The health insurance scheme in the country is reported to cover 65% of the population, which reduces the out-of-pocket health expenditure (66% of total health spending) [ 18 ]. One study using a cluster analysis method has shown that there are differences in the adequacy of maternal care available in Ghana and that there are disparities in the socio-demographic characteristics that determine access [ 8 ]. Insurance in Nigeria covers 3.5% of the population with out-of-pocket health expenditure amounting to over 90% of total health spending [ 17 , 18 ]. These differences are expected to result in differences in access to reproductive health services, which we investigate in this paper.
The DHS are nationally representative cross-sectional surveys carried out in low- and middle-income countries periodically [ 19 , 20 ]. The DHS adopts a multi-stage sampling design. Samples selected for enumeration, are ensured to be representative and comparative across countries. The DHS of Ghana and Nigeria included in this study, involved a two-stage sampling procedure: first selecting the location and then, selecting households per location at random [ 19 , 20 ]. Within a household, respondents were selected by gender for the different questionnaire types. A respondent was included if he/she was a usual member of the household or had spent the night preceding the survey, in the household.
We only used data for women of reproductive age (15–49 years) in Ghana and Nigeria who had given birth during the last 5 years before the survey and were able to provide information on the use of reproductive health services. Our study included 4142 women from the DHS of Ghana and 7725 women from the DHS of Nigeria. The indicators of reproductive care that we used in the cluster analysis are categorized as family planning services and maternal health services and are shown in Appendix A of the supplementary file .
We first performed two-step cluster analyses, which provided insight into the patterns of reproductive health services use among women of reproductive age in both countries. Cluster analysis is a method to classify similarities or dissimilarities based on respondents’ data [ 21 ]. Four cluster analyses were carried out, namely one for family planning services and another one for maternal health services for each of the two countries. The clusters generated by the cluster analysis procedure are shown in Appendix A in the supplementary file . In particular, the two-step clustering procedure uses the Schwarz’s Bayesian Information Criterion (BIC) method to determine the number of clusters. Different clustering solutions are compared and the clustering solution with the lowest BIC is selected by the procedure. We inspected this clustering and accept it as adequate. The stability and reliability of the cluster analyses were confirmed by repeating the clustering procedure produced no less than 10 times. The repeated analyses resulted in the same cluster quality. The two-step cluster analysis procedure specifies the clustering quality based on the Silhouette Index (SI). The SI indicates how well each subject/object lies within its cluster, and thus, it validates the clustering outcomes. The SI ranges from − 1 to 1. SI greater or equal to 0.5 indicates good clustering quality.
We titled the clusters based on the quality and adequacy of medical care used by women in each cluster compared to what is usually provided in government-licensed medical facilities. Thus, in the poor access cluster, on average, women reported using less and lower quality care than the care usually provided at government-licensed facilities, and in the high access cluster, women reported using more and better care. Details about the cluster composition variables, patterns, and quality are presented in Appendix A in the supplementary file .
Multinomial logistic regression was used to identify factors associated with the cluster membership determined during the cluster analyses. A total of four regression analyses were conducted. The cluster membership generated in each cluster analysis was the dependent variable in the multinomial logistic regression analyses. The explanatory variables consisted of women’s background characteristics that were found to be associated with the use of family planning services and maternal health services in previous studies and were available in our dataset. Sample weights were applied for the multinomial logistic regression. Software package SPSS version 23 was used for all data analyses.
Descriptive statistics on the socio-economic characteristics of the two samples and primary results of the two-steps cluster analyses can be found in the appendices ( supplementary files ). Below, we present the key findings of the cluster analyses as well as the results of the regression analyses.
Cluster analysis
The two-step cluster analysis of family planning service use in Ghana automatically produced 3 distinct clusters. In the two-step cluster analysis of family planning service use in Nigeria, the number of clusters (3 clusters) was fixed in advance to be able to produce meaningful clusters. The clusters are presented in Table 1 . The clusters were inspected and labeled as high, medium, and poor access to family planning services based on the services used by women in each cluster (see Methods section). The cluster with high access to family planning services captures 19.1 and 21.4% of women in Nigeria’s and Ghana’s sample respectively. The other extreme is the third cluster that consists of women whose access can be described as poor; 71.5% of women in Nigeria’s sample belong to this cluster and 64.2% of women in Ghana’s sample.
We did not predefine the number of clusters for maternal health services. For both countries, the two-step cluster analyses of maternal health services use resulted in five clusters, which we inspected and labeled as higher, high, medium, low and poor access to maternal health services (see Table 1 ). The higher-access cluster captures 29.6% of women in Nigeria’s sample and 26.3% of the women in Ghana’s sample. Relative to the other four clusters, a larger proportion of members of this cluster report that they accessed government hospitals for antenatal care and used institutional maternal care more. The high-access cluster consists of 21.6% of women in Nigeria’s sample and 23.0% of women in Ghana’s sample. For both countries, this cluster has a lower proportion of women who accessed government health centers for antenatal care or got assistance from physicians during childbirth. Members of the medium-access cluster in both countries used private facilities for antenatal care as well as for childbirth. This cluster of women makes up 25.9% of Nigeria’s sample and 18.2% of the Ghana sample. Members of the low-access cluster in both countries mostly report that they accessed government health posts/dispensaries for antenatal care but did not have skilled assistance during childbirth. In Nigeria’s sample, 4.4% of women fall into this cluster and in the Ghana’s sample, this share is 7.1%. Lastly, 18.5 and 25.4% of women from the Nigeria’s and Ghana’s sample respectively are members of the poor-access cluster. Members of this cluster mostly did not receive institutionalized maternal care. For both countries, the poor-access cluster has a high proportion of members who had home childbirth and used traditional birth attendants during childbirth.
Regression analysis
The dependent variables in the four multinomial logistic regressions were the four cluster membership variables generated in the cluster analyses. Tables 2 and 3 present the odds ratios for the four regressions. Information about the independent variables used and the full results of the regression analyses can be found in Appendix B of the supplementary file .
For family planning services, the results in Table 2 show that in both countries, women with no education, compared to women with secondary or higher education, have higher odds to belong to the poor-access family planning cluster (in Nigeria OR = 2.544, 95% CI:1.907–3.395, p ≤ 0.01 and in Ghana OR = 1.527, 95% CI: 1.173–1.988, p ≤ 0.01). Increased odds of having poor-access to family planning services are found for women in Ghana who do not belong to white-collar workers but not among women who live in rural areas, and also not among women in any of the wealth quintiles. Higher odds of poor-access to family planning services are also found for women in Nigeria who belong to the service-occupational category (OR = 1.283, 95% CI: 1.002–1.642, p ≤ 0.05), compared with white-collar workers. The odds of poor-access are as much as three times higher among the poorest quintile (95% CI: 1.825–6.396, p ≤ 0.01) than the richest quintile; and among those who have no insurance (OR = 1.374, 95% CI: 1.011–1.867, p ≤ 0.05) compared to those with insurance.
Table 3 shows the regression results on access to maternal health services in Nigeria and Ghana. In Nigeria’s sample, women with primary or no education have higher odds to have poor-access (OR = 1.387, 95% CI: 1.140–1.687, p ≤ 0.01) or low-access (OR = 1.786, 95% CI: 1.247–2.557, p ≤ 0.01) to maternal health services. In Nigeria’s sample, women who are not working have higher odds to belong to the cluster of poor-access maternal health services only (OR = 1.579, 95% CI 1.081–2.307, p ≤ 0.01). Compared to women in the white-collar occupational group, women in other occupational categories in Nigeria also have higher odds to belong to the poor-access cluster. Women in other occupational categories in Nigeria also have higher odds to belong to the poor-access cluster. Women in all household wealth quintiles have higher odds to have high- or poor-access to maternal health services; women without insurance have higher odds to have high or poor-access to maternal health services. Results for Ghana show that women with primary (OR = 1.38, 95% CI: 1.036–1.838, p ≤ 0.05) or no education (OR = 1.542, 95% CI: 1.115–2.132, p ≤ 0.01) have higher odds of poor-access to maternal health services. Only women in the agriculture occupational group have higher odds of high-access to maternal health services compared to women in the white-collar sector. Women without health insurance have higher odds of access to maternal health care services.
As shown by our results, access to reproductive health services varies among women of reproductive age in Ghana and Nigeria. A large proportion of women in Ghana’s and Nigeria’s samples have poor access to family planning services. Most women do not have access to modern contraceptives. They use traditional birth control methods and do not have the means for needed services. These differences in access to maternal health services in both countries reflect a broader gap in health care use between women who access antenatal care at government hospitals for childbirth with a physician present and women who are not able to access such services. In particular, women in the low-access cluster are restricted to services at government health posts without skilled assistance during childbirth, or to services of antenatal care private vendors. This confirms that among women of reproductive age in Ghana and Nigeria, there is unequal access to reproductive health services.
This suggests a dysfunctional organization structure that creates constraints to use preventive and medical procedures provided by well-trained professionals [ 4 , 18 , 22 ].
Our results show that educational attainment is associated with access to family planning and maternal health services. Low educational attainment reduces the ability to overcome access barriers, particularly to maternal health services. This finding supports similar results in other studies on the importance of education in improving access to reproductive health services [ 10 , 11 , 12 , 23 ]. Our results indicate that some women with low education intend to use contraceptives later while others use traditional contraceptive methods of family planning. Notably, the cluster with poor access to family planning services for a large part consists of women who have no intention of future contraceptive use. Lower-educated women seem to be less able to act on their intentions due to difficulties in overcoming access barriers or limited knowledge about the benefits of family planning [ 24 ]. The connection between education and socio-economic status could also explain this observation because low education attainment usually implies less access to resources [ 10 , 25 , 26 ]. This result further confirms what is known about the educational level as an indirect predictor of access to health care services [ 9 ].
Our results suggest that wealth/finance related inequality in access to reproductive health services is prominent in both Nigeria and Ghana. Considering finance-related inequality between the two countries, we find that women without insurance coverage in Ghana are less likely to access family planning services. This is dissimilar when compared to women without insurance in Nigeria; women in Nigeria who have poor-access to family planning opt for services such as traditional methods of contraception. These findings are consistent with other studies on the use of family planning services in the two countries and other parts of Africa [ 10 ]. This can be partially attributed to the inaccessibility of family planning services due to a cost-reducing scheme, which inadvertently increases the preference for traditional contraceptives among some women [ 27 ]. Another study also found a situation similar to Ghana among women in Burkina Faso and concluded that affordability of insurance premium varies by household income [ 13 ]. The poor access to reproductive health services in any of the wealth quintiles in Nigeria is expected considering the lack of insurance. The low coverage of insurance schemes such as the NHIS, particularly among informal workers or uneducated women, magnifies the effect of household wealth [ 17 , 18 ].
There is an association between maternal occupation and access to maternal health services in both countries. Other studies have also reported associations between care use and occupation [ 14 , 22 , 23 ]. However, where associations between maternal occupation and access to reproductive health services are observable, disparity by type of livelihood is not unusual [ 22 ]. We observe such differences between Ghana and Nigeria as well. In particular, the group of white-collar workers seems to have better access to family planning services in Ghana but no such differences are found for maternal care. The results for Nigeria are just the opposite; occupation does not explain poor access to family planning services in Nigeria but white-collar workers seem to have access to maternal care. In Nigeria, the cost of maternal health services has to be endured by women themselves while in Ghana, these services are available to women through the free maternal care policy [ 28 , 29 ]. Out-of-pocket payments for health have been consistently high in Nigeria compared to those in Ghana while insurance coverage is better in Ghana, particularly in the informal sector [ 27 , 30 ].
This study has some limitations that need to be acknowledged. There was not much variation in some response variables and they had to be excluded from the analysis. The inclusion of country-specific variables helps to better reflect the women’s situation but this also creates some dissimilarities in the countries’ analytical models.
This study provided evidence on inequalities in access to reproductive health services in Ghana and Nigeria. A key observation is the varied composition of services available for use at different access levels. Several imperative factors contribute to inequality in access to these services. After controlling for the effects of maternal-related variables, findings showed significant inequalities by educational attainment, household wealth, insurance status and woman’s occupational type. Much of the inequality in access to family planning services that are seen in Nigeria and Ghana is related to education. The contribution of household wealth and insurance status in creating unequal access was also evidenced in the study. Health programs, which seek to stimulate the use of reproductive health services in Ghana and Nigeria, could take into account the variation in access reported in this study to assure the user-centeredness of these programs. It is important to identify and prioritize services for the needs of vulnerable groups.
Availability of data and materials
The data used for this study can be accessed through the following link: https://dhsprogram.com/data/dataset_admin/login_main.cfm?CFID=15554769&CFTOKEN=6d6c1572de0c435a-5BA70A19-BD9F-EDBD-DBC0BB52339CAF30
Cook RJ. International human rights and women's reproductive health. Stud Fam Plan. 1993;24(2):73–86.
Article CAS Google Scholar
Braveman P, Tarimo E. Social inequalities in health within countries: not only an issue for affluent nations. Soc Sci Med. 2002;54(11):1621–35.
Article Google Scholar
Canning D, Schultz TP. The economic consequences of reproductive health and family planning. Lancet. 2012;380(9837):165–71.
Koblinsky MA, Campbell O, Heichelheim J. Organizing delivery care: what works for safe motherhood? Bull World Health Organ. 1999;77(5):399–406.
CAS PubMed PubMed Central Google Scholar
Gavin L, Moskosky S, Carter M, Curtis K, Glass E, Godfrey E, Marcell A, Mautone-Smith N, Pazol K, Tepper N, et al. Providing quality family planning services: Recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recommendations Reports. 2014;63(RR-04):1–54.
PubMed Google Scholar
Sustainable Development Knowledge Platform [ https://sustainabledevelopment.un.org/sdg3 ]. Accessed 26 Apr 2016.
Gulliford M, Figueroa-Munoz J, Morgan M, Hughes D, Gibson B, Beech R, Hudson M. What does 'access to health care' mean? J Health Serv Res Policy. 2002;7(3):186–8.
Ayanore MA, Pavlova M, Groot W. Unmet reproductive health needs among women in some west African countries: a systematic review of outcome measures and determinants. Reprod Health. 2016;13:5.
Solar O, Irwin A: A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). In . ; 2010.
Darroch JE, Singh S. Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys. Lancet. 2013;381(9879):1756–62.
Overbosch GB, Nsowah-Nuamah NNN, van den Boom GJM, Damnyag L. Determinants of antenatal care use in Ghana. J Afr Econ. 2004;13(2):277–301.
Kabir M, Iliyasu Z, Abubakar IS, Asani A. Determinants of utilization of antenatal care services in Kumbotso Village, northern Nigeria. Trop Dr. 2005;35(2):110–1.
Dong H, Kouyate B, Cairns J, Sauerborn R. Inequality in willingness-to-pay for community-based health insurance. Health Policy. 2005;72(2):149–56.
Addai I. Determinants of use of maternal-child health services in rural Ghana. J Biosoc Sci. 2000;32(1):1–15.
Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria--looking beyond individual and household factors. BMC Pregnancy Childb. 2009;9(1):43.
Dixon J, Tenkorang EY, Luginaah I. Ghana's National Health Insurance Scheme: a national level investigation of members' perceptions of service provision. BMC Int Health Hum Rights. 2013;13(1):35.
Ibiwoye A, Adeleke IA. Does National Health Insurance Promote Access to quality health care? Evidence from Nigeria. Geneva Papers on Risk Insurance - Issues Practice. 2008;33(2):219–33.
Odeyemi IA, Nixon J. Assessing equity in health care through the national health insurance schemes of Nigeria and Ghana: a review-based comparative analysis. Int J Equity Health. 2013;12(1):9.
Ghana Statistical Service, Ghana Health Service, ICF International. Ghana Demographic and Health Survey. Ghana Demographic and Health Survey 2014. Rockville: GSS, GHS, and ICF International; 2014.
Google Scholar
NPC NPC, ICF II. Nigeria demographic and health survey 2013. Abuja, Nigeria and Rockville, Maryland: NPC and ICF International; 2014.
Romesburg C: Cluster analysis for researchers: Lulu. com; 2004.
Onah HE, Ikeako LC, Iloabachie GC. Factors associated with the use of maternity services in Enugu, southeastern Nigeria. Soc Sci Med. 2006;63(7):1870–8.
Mekonnen Y, Mekonnen A. Utilization of maternal health care services in Ethiopia. In: DHS Further Analysis Reports No 38. Calverton, Maryland: ORC Macro; 2002.
Ashford L. Unmet need for family planning: recent trends and their implications for programs: population reference bureau; 2003.
Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One. 2010;5(6):e11190.
Ochako R, Fotso JC, Ikamari L, Khasakhala A. Utilization of maternal health services among young women in Kenya: insights from the Kenya demographic and health survey, 2003. BMC Pregnancy Childb. 2011;11(1):1.
Singh K, Osei-Akoto I, Otchere F, Sodzi-Tettey S, Barrington C, Huang C, Fordham C, Speizer I. Ghana's National Health insurance scheme and maternal and child health: a mixed methods study. BMC Health Serv Res. 2015;15:108.
Aremu O, Lawoko S, Dalal K. Neighborhood socioeconomic disadvantage, individual wealth status and patterns of delivery care utilization in Nigeria: a multilevel discrete choice analysis. Int J Women's Health. 2011;3:167–74.
Asante F, Chikwama C, Daniels A, Armar-Klemesu M. Evaluating the economic outcomes of the policy of fee exemption for maternal delivery care in Ghana. Ghana Med J. 2007;41(3):110–7.
PubMed PubMed Central Google Scholar
Olakunde B. Public health care financing in Nigeria: which way forward? Ann Nigerian Med. 2012;6(1):4.
Download references
Acknowledgments
Not applicable.
Author information
Authors and affiliations.
Department of Health Services Research; CAPHRI, Maastricht University Medical Center; Faculty of Health, Medicine and Life Sciences; Maastricht University, PO Box 616, 6200MD, Maastricht, The Netherlands
Oluwasegun Jko Ogundele, Milena Pavlova & Wim Groot
United Nations University-Maastricht Economic and Social Research Institute on Innovation and Technology, Maastricht, The Netherlands
You can also search for this author in PubMed Google Scholar
Contributions
JO and MP designed the study. JO analyzed the data and drafted the manuscript. JO, MP, and WG subsequently revised the manuscript and approved the final draft for submission. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Oluwasegun Jko Ogundele .
Ethics declarations
Ethics approval and consent to participate.
Administrative permissions were required and obtained from the Demographic and Health Survey program to access the data used in this study. We made use of secondary DHS data from Ghana and Nigeria. Therefore, our study did not require a formal ethics approval and the study complied with Maastricht University code of ethics for research in the social and behavioral sciences involving human participants, and also with the national guidelines (nietWMOplichtig onderzoek or the Medical Research Involving Human Subjects Act (WMO) Link: https://www.maastrichtuniversity.nl/research/integrity-ethics/ethics-review and https://nwmostudies.nl/nwmo/
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ogundele, O.J., Pavlova, M. & Groot, W. Patterns of access to reproductive health services in Ghana and Nigeria: results of a cluster analysis. BMC Public Health 20 , 549 (2020). https://doi.org/10.1186/s12889-020-08724-3
Download citation
Received : 23 October 2019
Accepted : 16 April 2020
Published : 23 April 2020
DOI : https://doi.org/10.1186/s12889-020-08724-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Reproductive services
- Maternal care
- Family planning
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 06 May 2024
Prevalence and factors associated with antepartum depression among adolescent women in the assin north district of Ghana: a cross-sectional study
- Hannah Amoquandoh Asante ORCID: orcid.org/0000-0002-5964-2521 1 ,
- Shadrach Tetteh Boyetey ORCID: orcid.org/0009-0002-8496-2196 2 ,
- Ebenezer Essaw 1 ,
- Christopher Amoah Nyame ORCID: orcid.org/0000-0002-5497-1414 3 ,
- Bertha Mante ORCID: orcid.org/0000-0002-6306-9553 4 ,
- Louisa Dziwornu ORCID: orcid.org/0000-0001-6826-0392 5 &
- Paul Okyere ORCID: orcid.org/0000-0001-7756-2085 1
BMC Women's Health volume 24 , Article number: 276 ( 2024 ) Cite this article
112 Accesses
Metrics details
Globally, depression is a leading cause of disease-related disability among women. In low-and-middle-income countries (LMICs), the prevalence rate of antepartum depression is estimated to range between 15% and 57% and even higher in adolescent antepartum women. Although a number of studies have shown that depression is common in adolescent pregnancies and has a prevalence rate between 28% and 67% among adolescent mothers, there currently exists no literature on depression among adolescent pregnant women in Ghana. The study aimed to determine the prevalence of antepartum depression and identify the factors associated with it among pregnant adolescent women.
A quantitative cross-sectional study design was adopted by randomly recruiting 220 adolescent pregnant women visiting antenatal clinics in five selected health facilities in five communities in the Assin North District of Ghana. Data were collected using the Edinburgh Postnatal Depression Scale (EPDS). Data analysis was performed using Stata version 14. Both descriptive and inferential analyses were performed. A chi-square analysis was conducted to identify the association between independent and dependent variables. A multivariate logistic regression analysis was carried out to identify the independent variables that were significantly associated with the dependent variable. In all analyses, p-values ≤ 0.05 were deemed statistically significant at a 95% confidence interval.
The results indicated prevalence of depression was 38.6% using the EPDS cut-off ≥ 13. Respondents who were cohabiting were less likely to experiencing antepartum depression compared to those who were single (AOR = 0.36, 95% CI: 0.20–0.64, p = 0.001). Also, Respondents who had completed Junior High School had a lower likelihood of experiencing antepartum depression compared to those who had no formal education (AOR = 0.19, 95% CI: 0.05–0.76, p = 0.019). Respondents who perceived pregnancy-related items to be costly had higher odds of experiencing antepartum depression (AOR = 2.05, 95% CI: 1.02–4.12, p = 0.042). Lastly, adolescent pregnant women who reported that pregnancy-related items are costly were likely to experience antepartum depression compared to those who did not report such costs (AOR = 2.12, 95% CI: 1.20–3.75, p < 0.001).
The results of this study highlight the importance of a multi-pronged strategy for combating antepartum depression in adolescents and improving the overall health and well-being of pregnant adolescents. Considering that adolescence is a transitional period occasioned by several bio-psycho-social challenges, setting up systems to ensure that young girls are motivated and supported to stay in school will enhance their economic prospects and improve their standards of life while providing psycho-social support will benefit their health and general well-being.
Peer Review reports
Introduction
Depression is a leading cause of disease-related disability among women globally [ 1 ]. Characterized by the Massachusetts General Hospital Comprehensive Clinical Psychiatry as the presence of depressed mood or loss of interest, most of the day, more days than not, depression presents numerous symptoms including changes in appetite and sleep patterns, feelings of guilt, poor self-esteem, poor concentration, psychomotor agitation, fatigue, and even suicide. The prevalence of depression is deeply concerning with an estimated 280 million people living with the disease globally [ 1 ]. Among women with a history of pregnancy and/or childbirth, depression in the period before childbirth was common with a prevalence rate as high as 25% [ 2 ]. In low-and-middle-income countries (LMICs), the prevalence rate of antepartum depression is estimated to range between 15% and 57% [ 3 ] and it is slightly higher than postpartum depression ranging between 14% and 50% [ 4 ]. Evidence shows that when not treated, antepartum depression can continue to the postpartum period [ 5 ].
Traditionally, pregnancy was perceived to protect women from depression since it was thought to be a period of wellness and happiness but recent evidence suggests otherwise as the incidence of depression diagnoses during childbirth has been on the rise, with a sevenfold increase in 2015 compared to the year 2000 [ 6 ]. According to a recent Center for Disease Control(CDC) study, depression during pregnancy is not easily noticeable though its prevalence is high [ 2 ]. Evidence suggests it is difficult to diagnose depression during the first trimester because there is usually an overlap between symptoms of pregnancy and symptoms of depression [ 7 ]; nonetheless, a systematic review [ 8 ] documented a 7.4% prevalence of depression during the first trimester in their study. This figure rose to 12.8% during the second trimester and remained at 12% during the last trimester. Another longitudinal study in Sweden [ 9 ], found a 17% rate of antepartum depression. These patients were then followed into the postpartum period and depression rates were found to have decreased by 4–13% by the 8th week after delivery and maintained at 6 months postpartum. Two studies [ 10 , 11 ] have revealed the risk factors connected with depression during pregnancy; personal and family history of depression, childhood abuse, domestic or partner violence, smoking/substance abuse, single motherhood, inadequate social support, lower educational levels, lack of employment and adolescent pregnancies.
Adolescent pregnancy is widely seen as a public health problem due to its health and social implications. Studies show that 11% of all deliveries worldwide and about 14% of all maternal deaths globally are among adolescents aged between 15 and 19 years old with over 90% of such adolescent births occurring in LMICs [ 1 , 12 ]. Each year, about 21 million girls aged 15–19 years in low-income and middle-income countries (LMICs) experience pregnancy, with around 12 million of them delivering babies [ 13 ]. Ghana’s adolescent pregnancy situation is no different from other LMICs [ 14 ]. Ghana continues to record high cases of adolescent pregnancies. Research reveals that about one in ten females between 15 and 19 years of age had begun childbearing in cities whereas the situation in rural settings is twice as high as those in urban settings [ 15 ]. The 2014 Ghana Demography and Health Survey (GDHS) report revealed that 14% of adolescents aged 15–19 years had begun childbearing with 11% having had a live birth and 3% pregnant with their first child [ 16 ]. Adolescent pregnancies are associated with health, psychosocial and economic consequences that make it a disturbing public health concern [ 8 , 17 ]. Some studies suggest that adolescent pregnancies have a higher incidence of health-related complications such as serious maternal and neonatal outcomes [ 17 , 18 ]. These include preterm birth, low birth weight, anemia, Sexually Transmitted Infections (STIs), postpartum hemorrhage, and mental disorders such as depression.
Studies have documented several factors that may contribute to adolescent pregnancy. Some societies put pressure on girls to marry and bear children, especially because there is more value on motherhood and marriage [ 19 ]. Girls may also choose to become pregnant when there are limited educational and job opportunities [ 1 , 20 ]. These may be because of lack of access to contraceptives, knowledge gaps, financial constraints, sexual violence, and lack of autonomy among many other constraints [ 21 ].
Women living in developing countries such as Ghana are particularly vulnerable to multiple exposures to depression. Studies in Africa show that rates of depression during pregnancy are generally significantly higher and may have longer durations than those in developed countries [ 4 , 22 ]. Ghana has over 2.3 million people living with various mental health conditions, yet mental health care remains a challenge, with a 98% treatment gap [ 23 , 24 ]. Another study in Ghana, which looked at the prevalence and risk factors of postpartum depression among 153 mothers of sick and hospitalized infants in a tertiary hospital, found 32.4% mild, 27.4% moderate, and 9.8% severe depression [ 4 ]. A separate study [ 25 ], also investigated postpartum depression among HIV-positive women in Ghana and established that 10% of the respondents had symptoms of depression at the time of birth and a further 9% six [ 26 ] months after birth. Yet another study by [ 27 ] compared three screening instruments for postpartum depression. It was found that 11% of the 160 respondents had scores that represent clinically major depression [ 16 , 28 ] and these are all studies among adult women who are not adolescents. Although some studies have shown that depression is common in adolescent pregnancies and has between 28% and 67% among adolescent mothers [ 27 , 29 ], there currently exists no literature on depression among adolescent pregnant women in Ghana. Thus, this study aimed to contribute to the evidence base on antepartum depression among adolescent women in Ghana by placing it in a larger context of prevalence and factors associated with it.
Study design and sampling
This study employed a quantitative cross-sectional approach conducted within health facilities. Participants were recruited through a simple random sampling strategy from five health facilities in the Assin North district of the Central region of Ghana. Overall, 220 pregnant adolescent girls were recruited. The sample size was determined using the Cochran [ 17 ] formula for estimating sample size based on 5% level of precision/absolute error and a type 1 error of 5%. The expected proportion of the outcome variable in the population-based on previous studies was 17%.
Participant recruitment procedures
The research units were chosen using a multistage sampling process. First, five health facilities were selected from the 27 health facilities in the district which were stratified based on the levels of care provided. These five (5) health facilities included one (1) Community-Based Health Planning Services (CHPS), two (2) health centers, one (1) polyclinic and one (1) district hospital. They were selected from five out of the seven sub-districts. One CHPS which represents the largest in the district was chosen to represent the selected level of care in the subdistrict. Also to ensure fair geographical representation, two health centers were chosen in their respective sub-districts. Each health facility was representative of the five sub-districts chosen for the study. The sample size was allotted in tens to each selected health facility using the proportional allocation technique. The district hospital had 80 respondents, polyclinic had 40 respondents, the two health centers had 35 respondents each and the CHPS had 30 respondents. Finally, using the lottery approach, study respondents were randomly selected using the antenatal clinic register. Respondents were then contacted during their antenatal clinic visitations at the five selected health facilities. Follow-up home visitations and phone calls were used to contact respondents who were not present at the facilities. Respondents were included on the basis of being a female, aged (10–19) years, pregnant, living in or around the study area, enrolled in a maternal health program (antenatal care) in a health facility in the study area, willing to participate in the study, and written informed consent was obtained to be a part of the study. Respondents were excluded from the study if they were below 10 years and above 19 years of age, pregnant but had serious health issues that may prevent participation, did not live in or around the study area, and did not give informed consent to be a part of the study. All data collection was conducted face-to-face at the selected health facilities.
Data collection instrument
The Edinburg Postnatal Depression Scale (EPDS) was administered to serve as a data collection tool since it is one of the most acceptable and internationally recognized standard questionnaires used for studies on depression [ 30 , 31 ]. One study [ 32 ], concluded with preference for the EPDS for measuring depressive symptoms in the peripartum populations. The EPDS is made of ten standardized questions with answers and scores. It asks questions such as “in the past seven days, have you felt happy, been able to laugh and see the funny side of things, looked forward with enjoyment to things, etc? Respondents with a score > 10 were considered to be have probable depression (mild) with 30 being the highest score and showing severe depression. In this study, respondents with scores ≥ 13 were considered to have screened positive for depression as comparable to other studies in Ghana which used the EPDS with such a cutoff point. The data gathering instrument also included questions on respondents’ background characteristics and additional questions about social determinants of health. Data were collected from September to November, 2021. All COVID-19 safety protocols were followed during data collection. This involved the use of face masks by data collectors and maintenance of adequate social distance. There was no physical contact with participants however hand sanitizers were used after signing of consent forms.
Data Collection Method
The data collection method involved presenting the questionnaire in English and administering it electronically through a Google Form by trained data collectors. Respondents proficient in English were given the questionnaire to self-administer, while those requiring assistance had the questions read aloud by data collectors.
Additionally, some respondents expressed a preference for the local language (Twi). In such cases, translation and validation of questionnaire items were conducted by data collectors proficient in both English and Twi. These data collectors were responsible for ensuring the accuracy and equivalence of the translations during this process.
Prior to the main data collection, pretests were conducted to validate the translated questionnaire and responses. This validation approach aimed to maintain the integrity and reliability of the data collected in the preferred language of the respondents, ensuring accuracy, clarity, and cultural relevance.
Data analysis
Data analysis was performed using Stata version 14. Both the descriptive and inferential analyses were performed. A chi-square analysis was conducted to identify the association between independent and dependent variables. A multivariate logistic regression analysis was carried out to identify the independent variables that were significantly associated with the dependent variable. In all analyses, p-values ≤ 0.05 were deemed statistically significant at a 95% confidence interval.
Socio-demographic characteristics of study respondents
Table 1 shows the socio-demographic characteristics of study respondents. The total number of respondents that completed the survey questionnaire was 220 adolescent pregnant women. The mean age of study respondents was 17.5 (± 1.6). More than half ( n = 119/ 54.1%) of the respondents were single. Nearly half ( n = 103/ 48%) of the respondents were in school with over 56.4% ( n = 124) of the respondents being in JHS.
Nearly half ( n = 108/ 49.1%) were living with their parents. Most ( n = 213/ 96.8%) of the respondents were in households with an estimated monthly income of less than or equal to GH₡500.00.
Prevalence of antepartum depression among adolescent pregnant women
Out of a total of 220 adolescent pregnant women, more than a third ( n = 85/ 38.6%) experienced antepartum depression (EPDS ≥ 13) while the remaining 135 (61.4%) did not experience it. The prevalence of depression in this study was found to be 38.6%.
Factors associated with antenatal depression among pregnant adolescent women
Socio-demographic/social determinants level factors.
Table 2 shows the socio-demographic/social determinants factors associated with antenatal depression among study respondents.Respondent’s relationship status ( p = 0.002), level of education ( p = 0.001), maternal level of education ( p = 0.041), paternal occupation ( p = 0.009), who you are living with ( p < 0.001), high cost of pregnancy related items ( p < 0.001), denial of pregnancy by partner ( p = 0.023), and denial of responsibility by man’s family ( p = 0.010).
Other factors which showed statistically significant association with antepartum depression among the study respondents were sexual abuse ( p = 0.001), gravidity ( p = 0.006), and planning life independent of partner ( p = 0.009) were significantly associated with antenatal depression as illustrated in Table 2 .
Table 3 shows the multivariate logistic regression analysis of the factors associated with antenatal depression. After adjusting for all the variables, respondents that had JHS education ( p = 0.019), had a mother with primary level education ( p = 0.04), and less costly pregnancy-related items ( p = 0.038) were the most significant factors associated with antenatal depression.
The results of this study indicated that 38.6% of the respondents screened positive for depression using the Edinburg Postnatal Depression Scale (EPDS) of cut-off ≥ 13. To the best of our knowledge, this is the first study in Ghana on antepartum depression focusing on adolescent pregnant women. The EPDS has shown a good clinical value and it is compatible with studies conducted in many countries all over the world including Ghana and other SSA countries as a screening tool for depression studies [ 4 , 10 ]. It is also the most commonly used depression screening tool used for the adolescent population [ 33 ].
The study revealed a high proportion (38.6%) of pregnant adolescents with depressive symptoms in the five health facilities in the Assin North District. This is comparable with previous studies [ 2 , 34 ]. For example, a study conducted in South Africa in a peri-urban area outside of Cape Town reported a prevalence of antepartum depression and Post- Partum Depression (PPD) of 39% and 34.7% respectively [ 28 ].
Other studies reported a much higher prevalence of antepartum depression. For example, in a study of rural pregnant women in KwaZulu-Natal, South Africa, 47% of the women showed positive signs of depression, and 45% of those who were depressed were HIV-positive [ 33 ]. Uthaipaisanwong et al. [ 26 ], recorded 46% whilst a 43.9% prevalence was found by a study conducted on prenatal depression among pregnant adolescents in the Maha Sarakham province [ 35 ]. In Ghana, one study found a point prevalence of 69.9.% among mothers with sick infants in Kumasi and currently the highest prevalence of depression in the country [ 4 ].
In contrast, there are studies that reported a lower prevalence of antepartum depression. Bindt et al. [ 8 ], reported antenatal depression of 26% prevalence, Lillie et al. [ 36 ], reported 19.7% whereas Woebong et al. [ 20 ], reported 9.9% in studies conducted in Ghana. A study by Birkeland et al. [ 29 ], in the United States of America (USA) on adolescent motherhood and depression found a prevalence of 29%. Another study on the association of social support and antepartum depression among pregnant Peruvian women reported a roughly 25%-point prevalence of antepartum depression [ 20 ]. Dibaba et al. [ 4 ], recorded a point prevalence of 19.9%. In a study conducted in Nepal, depression among women during their antepartum period visiting public health centers was recorded to be 18% [ 37 ], while one study in Nigeria reported 16.4% antepartum depression [ 38 ] with Gelaye et al. [ 5 ], reporting a 10.3% prevalence of antepartum depression in Peru.
The differences in prevalence rate for antepartum depression are influenced by many factors. These factors consist of the study design, the screening tool used and cut-offs, the respondents involved, and the study location. The original EPDS has a minimum cut-off of 10 which indicates signs of mild depression [ 4 ]. The revised EPDS guide [ 39 ], employs a minimum of 9-11to show mild depression. In this study, the EPDS with a cut of point of 13 and above was employed as the main depression tool. The study was also cross-sectional and conducted in a rural district of Ghana focusing on adolescents. Theses may have explained the relatively high prevalence of depression found in this study since, for example, adolescent mothers are reported to experience a high rate of antepartum depression due to the fact that they are joggling with their identities and responsibilities as adolescents and having to add motherhood to the many challenges they face [ 40 ]. Other studies which used the EPDS with cut off of 13 and above include ( P = 33.1%) [ 8 ], ( P = 32.9%) [ 34 ], ( P = 21.5%) [ 38 ]. Studies using the EPDS of 10 and above include Gold et al., ( p = 37%) [ 4 ], and Joshi et al., ( p = 18%) [ 36 ]. Another study used the EPDS of 11 and above and recorded a point prevalence of antepartum depression to be 46% [ 40 ]. These are suggestive that perhaps, the EPDS depression scale yields a relatively high depression prevalence.
Conversely, there were studies that utilized other screening tools like the Patient Health Questionnaire (PHQ-9) the Structural Clinical Interview for Depression (SCID) or a combination of SCID and EPDS or PHQ-9 and EPDS. For instance, in Friedman et al. [ 20 ] used the PHQ-9 with a cut-off of 15 and above was used to assess the association between social support and antepartum depression among pregnant Peruvian women, reporting a prevalence of nearly 25% [ 20 ]. In another study conducted in Ghana and Cote D’Ivoire, the PHQ-9 was used to screen for depressive symptoms yielding a prevalence of 26% and 32% respectively [ 16 ]. Rochat et al. [ 33 ] used a combination of the EPDS ≥ 13 and the SCID which resulted in a prevalence of 44.5% and 47% correspondingly.
Association between socio-demographic characteristics and antepartum depression among adolescent pregnant women
The present study found perceived low cost of pregnancy-related items, respondents and maternal levels of education to be significantly associated with adolescent antepartum depression. It revealed that those who perceived the cost of pregnancy-related items to be low were 59% less likely to develop antepartum depression as compared with those who perceived the cost of pregnancy-related items to be high. Though the study did not find poor socio-economic status as a precursor for adolescent antepartum depression, it is understandable that people with poor socio-economic status most likely will find pregnancy-related items costly especially in a rural setting like the Assin North District. Besides, other studies have found associations between poor socio-economic status and antepartum depression [ 34 , 38 , 41 ]. indicated in their findings that poor socioeconomic status and lower-income among pregnant women including adolescents were considerably linked to developing antepartum depression than those with higher income. Being financially dependent and unable to provide their basic needs/care without external support are reasons that can lead to extreme stress and depression among pregnant adolescents. This shows that perhaps, inadequate financial resources may contribute to the concern of not being able to support the financial needs of the upcoming child.
The study also revealed that respondents with JHS education and those whose mothers had primary education were 81% and 79% less likely to be depressed compared to those with primary and no education respectively. Possibly, this is an indication of the importance of formal education on the health and well-being of adolescent girls. Education increase job or economic prospect and those with little or no education are to be at risk of developing antepartum depression [ 42 ]. Also, perhaps if the adolescent’s mother is educated, she will understand and give better support to their girl children as love and support are protective factors against the development of adolescent antepartum depression [ 38 ]. These results indicate that more attention should be given to adolescents’ health and wellbeing by focusing on ways to improve their educational achievement as well as economic opportunities.
Conclusions
In conclusion, this study successfully determined that 38.6% of pregnant adolescent women in the Assin North District of Ghana screened positive for antepartum depression using the EPDS with a cut-off of ≥ 13. Factors such as perceived cost of pregnancy-related items, maternal education levels, and socioeconomic status were identified as significant contributors to antepartum depression among this population. These findings highlight the urgent need for targeted interventions aimed at improving access to mental health support, reducing financial barriers to maternal care, and enhancing educational opportunities for pregnant adolescents in Ghana.
Moving forward, tailored strategies focusing on addressing these specific factors are crucial in mitigating the prevalence of antepartum depression and promoting the overall well-being of pregnant adolescent women in the region.
Limitations
This study has a few limitations. First, the cross-sectional nature of the study precludes any suggestion of causality. Secondly, data were collected in only one district in the Central region of Ghana and the fairly small sample size may not allow for the generalization of the results to all adolescent pregnant women in Ghana. A longitudinal study on the prevalence and associated factors on antepartum depression among pregnant adolescents is thus encouraged.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Committee on Human Research, Publications, and Ethics
Edinburgh Postnatal Depression Scale
Ghana Demography and Health Survey
In low-and-middle-income countries
Patient Health Questionnaire
Post- Partum Depression
Sexually Transmitted Infections
Structural Clinical Interview for Depression
Organization WH. Depressive disorder (depression): Factsheet, World Health Organization. Accessed: Oct. 30, 2023. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/depression .
Bavle AD, Chandahalli AS, Phatak AS, Rangaiah N, Kuthandahalli SM, Nagendra PN. Antenatal Depression in a Tertiary Care Hospital. Indian J Psychol Med. 2016;38(1):31–5. https://doi.org/10.4103/0253-7176.175101 .
Article PubMed PubMed Central Google Scholar
Shidhaye P, Giri P. Maternal depression: a hidden burden in developing countries. Ann Med Health Sci Res. Jul. 2014;4(4):463–5. https://doi.org/10.4103/2141-9248.139268 .
Gold KJ, Spangenberg K, Wobil P, Schwenk TL. Depression and risk factors for depression among mothers of sick infants in Kumasi, Ghana., Int. J. Gynaecol. Obstet. Off. organ Int. Fed. Gynaecol. Obstet , vol. 120, no. 3, pp. 228–231, Mar. 2013, https://doi.org/10.1016/j.ijgo.2012.09.016 .
Gelaye B, et al. Poor sleep quality, antepartum depression and suicidal ideation among pregnant women. J Affect Disord. Feb. 2017;209:195–200. https://doi.org/10.1016/j.jad.2016.11.020 .
Haight SC, Byatt N, Moore Simas TA, Robbins CL, Ko JY. Recorded Diagnoses of Depression During Delivery Hospitalizations in the United States, 2000–2015., Obstet. Gynecol , vol. 133, no. 6, pp. 1216–1223, Jun. 2019, https://doi.org/10.1097/AOG.0000000000003291 .
Ryan D, Milis L, Misri N. Depression during pregnancy., Can. Fam. Physician , vol. 51, no. 8, pp. 1087–1093, Aug. 2005.
HA B, Einarson A, Taddio A, Koren G, TR E. Of T. Faculty of Pharmacy 19 Russell Street, Toronto, ON M5S 2S2, Canada, [email protected], prevalence of depression during pregnancy: systematic review. Obstet Gynecol. 2004;103(4):698–709. https://doi.org/10.1097/01.AOG.0000116689.75396.5f .
Article Google Scholar
Josefsson A, Berg G, Nordin C, Sydsjö G. Prevalence of depressive symptoms in late pregnancy and postpartum. Acta Obstet Gynecol Scand. Mar. 2001;80(3):251–5. https://doi.org/10.1034/j.1600-0412.2001.080003251.x .
Field T. Prenatal depression risk factors, Developmental effects and interventions: a review. J Pregnancy Child Heal. Feb. 2017;4(1). https://doi.org/10.4172/2376-127X.1000301 .
Marcus SM, Flynn HA, Blow FC, Barry KL. Depressive symptoms among pregnant women screened in obstetrics settings. J Womens Health (Larchmt). May 2003;12(4):373–80. https://doi.org/10.1089/154099903765448880 .
Patton GC, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet (London England). Sep. 2009;374(9693):881–92. https://doi.org/10.1016/S0140-6736(09)60741-8 .
Sully EA, Biddlecom A, Daroch J, Riley T, Ashford L, Lince-Deroche N et al. Adding It Up: Investing in Sexual and Reproductive Health 2019. Guttmacher Institute 2020,., 2019.
Ghana U. Adolescent Pregnancy in Ghanaian Communities – A worrying trend amid MTCT of HIV. Accessed: Apr. 10, 2024. [Online]. Available: https://ghana.unfpa.org/en/news/adolescent-pregnancy-ghanaian-communities-–-worrying-trend-amid-mtct-hiv-0 .
Service GS. Ghana Demographic and Housing Survey, 2009. [Online]. Available: https://www.dhsprogram.com/pubs/pdf/FR221/FR221%5B13Aug2012%5D.pdf .
Service GS. Ghana Demographic and Health Survey, 2014. [Online]. Available: https://www2.statsghana.gov.gh/docfiles/DHS_Report/Ghana_DHS_2014-KIR-21_May_2015.pdf .
Statistics NB. Demographic and Health Survey,2014. National Bureau of Statistics, Kenya, ICF international, Kenya, 2015. [Online]. Available: https://www.dhsprogram.com/pubs/pdf/sr227/sr227.pdf .
Control CforD. Vital signs: teen pregnancy–United States, 1991–2009., MMWR. Morb. Mortal. Wkly. Rep , vol. 60, no. 13, pp. 414–420, Apr. 2011.
Güner Ö, Öztürk R. The development of pressure scale toward marriage and fertility in social structure., Women Health , vol. 63, no. 8, pp. 587–598, Sep. 2023, https://doi.org/10.1080/03630242.2023.2249119 .
Friedman LE, Gelaye B, Sanchez SE, Williams MA. Association of social support and antepartum depression among pregnant women., J. Affect. Disord , vol. 264, pp. 201–205, Mar. 2020, https://doi.org/10.1016/j.jad.2019.12.017 .
Organization WH, Factsheet AP, World Health Organization. Accessed: Oct. 30, 2023. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy .
Organization WH. Global Burden of Disease 2004 Update, 2008. [Online]. Available: https://www.who.int/publications-detail-redirect/9789241563710 .
Organization WH, WHO/AFRICA/GHANA/NEWS. Sustaining the mental health agenda in Ghana,. Accessed: Oct. 05, 2023. [Online]. Available: https://www.afro.who.int/countries/ghana/news/sustaining-mental-health-agenda-ghana .
Organization Africa WH. Redefining mental healthcare in Ghana. Accessed: Oct. 31, 2023. [Online]. Available: https://www.afro.who.int/countries/ghana/news/redefining-mental-healthcare-ghana .
Okronipa HET, Marquis GS, Lartey A, Brakohiapa L, Perez-Escamilla R, Mazur RE. Postnatal depression symptoms are associated with increased diarrhea among infants of HIV-positive Ghanaian mothers., AIDS Behav , vol. 16, no. 8, pp. 2216–2225, Nov. 2012, https://doi.org/10.1007/s10461-012-0153-x .
D’Alfonso A, Iovenitti P, Casacchia M, Carta G. Disturbances of humour in postpartum: our experience. Clin Exp Obstet Gynecol. 2002;29(3):207–11.
PubMed Google Scholar
Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: systematic review. Obstet Gynecol. Apr. 2004;103(4):698–709. https://doi.org/10.1097/01.AOG.0000116689.75396.5f .
Hartley M, et al. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health. May 2011;8:9. https://doi.org/10.1186/1742-4755-8-9 .
Birkeland R, Thompson JK, Phares V. Adolescent motherhood and postpartum depression., J. Clin. child Adolesc. Psychol. Off. J. Soc. Clin. Child Adolesc. Psychol. Am. Psychol. Assoc. Div. 53 , vol. 34, no. 2, pp. 292–300, Jun. 2005, https://doi.org/10.1207/s15374424jccp3402_8 .
Zhong Q, et al. Comparative performance of Patient Health Questionnaire-9 and Edinburgh postnatal depression scale for screening antepartum depression. J Affect Disord. Jun. 2014;162:1–7. https://doi.org/10.1016/j.jad.2014.03.028 .
Liu W, et al. Comparison of the EPDS and PHQ-9 in the assessment of depression among pregnant women: similarities and differences. J Affect Disord. 2024;351:774–81. https://doi.org/10.1016/j.jad.2024.01.219 .
Article PubMed Google Scholar
Stefana A, et al. Comparing the factor structures and reliabilities of the EPDS and the PHQ-9 for screening antepartum and postpartum depression: a multigroup confirmatory factor analysis. Arch Womens Ment Health. 2023;26(5):659–68. https://doi.org/10.1007/s00737-023-01337-w .
Rochat TJ, Tomlinson M, Newell M-L, Stein A. Detection of antenatal depression in rural HIV-affected populations with short and ultrashort versions of the Edinburgh Postnatal Depression Scale (EPDS)., Archives of Women’s Mental Health , vol. 16, no. 5. Springer, Rochat, Tamsen J.: Africa Centre for Health and Population Studies, University of KwaZulu-Natal, Mtubatuba, South Africa, [email protected], pp. 401–410, 2013. https://doi.org/10.1007/s00737-013-0353-z .
Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. Apr. 2008;8. https://doi.org/10.1186/1471-244X-8-24 .
Jantasin B, Yoosook W, Thaewpia S. Predictive statistical model for the factors associated with prenatal depression among pregnant adolescents in Maha Sarakham province, Thailand [version 2; peer review: 1 approved, 1 not approved], F1000Research , vol. 8, no. 1921, 2020, https://doi.org/10.12688/f1000research.21007.2 .
Lillie M, et al. Prevalence and correlates of Depression among pregnant women enrolled in a maternal and Newborn Health Program in Rural Northern Ghana: a cross-sectional survey. Glob Soc Welf Res Policy Pract. 2020;7(2):131–40. https://doi.org/10.1007/s40609-020-00170-8 .
Joshi D, Shrestha S, Shrestha N. Understanding the antepartum depressive symptoms and its risk factors among the pregnant women visiting public health facilities of Nepal. PLoS ONE. 2019;14(4):e0214992. https://doi.org/10.1371/journal.pone.0214992 .
Article CAS PubMed PubMed Central Google Scholar
Leplatte D, Rosenblum KL, Stanton E, Miller N, Muzik M. Mental health in primary care for adolescent parents. Ment Health Fam Med. Jan. 2012;9(1):39–45.
Services P. Edinburgh Postnatal/Postpartum Depression Scale (EPDS) Scoring Guide. Accessed: Oct. 31, 2023. [Online]. Available: http://www.perinatalservicesbc.ca/Documents/Resources/HealthPromotion/EPDS/EPDSScoringGuide_March2015.pdf .
Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the mental health needs of pregnant and parenting adolescents., Pediatrics , vol. 133, no. 1, pp. 114–122, Jan. 2014, https://doi.org/10.1542/peds.2013-0927 .
Bawahab JA, Alahmadi JR, Ibrahim AM. Prevalence and determinants of antenatal depression among women attending primary health care centers in Western Saudi Arabia., Saudi Med. J , vol. 38, no. 12, pp. 1237–1242, Dec. 2017, https://doi.org/10.15537/smj.2017.12.21262 .
Rahman A, Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: prospective study from Rawalpindi, Pakistan., J. Affect. Disord , vol. 100, no. 1–3, pp. 115–121, Jun. 2007, https://doi.org/10.1016/j.jad.2006.10.004 .
Download references
Acknowledgements
The researchers would like to express their gratitude to the personnel of the Assin North District Directorate of Health and the staff of all the health facilities used in the conduct of this study for their invaluable assistance. We would also want to express our appreciation to all of our respondents for their contributions to this study.
There was no external funding for this research work.
Author information
Authors and affiliations.
Department of Health Promotion and Disability Studies, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Hannah Amoquandoh Asante, Ebenezer Essaw & Paul Okyere
Department of Health Policy, Management and Economics, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Shadrach Tetteh Boyetey
Department of Occupational and Environmental Health and Safety, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Christopher Amoah Nyame
Department of Real Estate and Land Management, University for Development Studies, Tamale, Ghana
Bertha Mante
Department of Sociology and Social Work, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana
Louisa Dziwornu
You can also search for this author in PubMed Google Scholar
Contributions
H.A.A is responsible for the design of this manuscript. She is involved in the write up, ethics approval, data collection, analysis and manuscript drafting. S.T.B is responsible for data analysis and reviewed the final draft. H.A.A, E.E, B.M, L.D and C.A.N are responsible for data collection. P.O reviewed and edited the final draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Hannah Amoquandoh Asante .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval for this study was obtained from the Committee on Human Research, Publications, and Ethics, an institutional review board of the School of Medicine and Dentistry, Kwame Nkrumah University of Science and Technology, Ghana with reference number CHRPE/AP/501/21 . Permission was also obtained from the Director of Health Services in the Assin North district and the heads of the various selected health facilities. Written and signed informed consent/assent were obtained from all consenting respondents. Each participant was assured of her confidentiality in the study. The selection of adolescent pregnant women was based on their willingness to participate, the completion of the consent and assent form, and availability to be utilized in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Asante, H.A., Boyetey, S.T., Essaw, E. et al. Prevalence and factors associated with antepartum depression among adolescent women in the assin north district of Ghana: a cross-sectional study. BMC Women's Health 24 , 276 (2024). https://doi.org/10.1186/s12905-024-03111-1
Download citation
Received : 10 November 2023
Accepted : 23 April 2024
Published : 06 May 2024
DOI : https://doi.org/10.1186/s12905-024-03111-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Antepartum depression
- Pregnant women
- Mental health
BMC Women's Health
ISSN: 1472-6874
- Submission enquiries: [email protected]
- General enquiries: [email protected]

COMMENTS
Background Unmet need for family planning is high (30%) in Ghana. Reducing unmet need for family planning will reduce the high levels of unintended pregnancies, unsafe abortions, maternal and neonatal morbidity and mortality. The purpose of this study was to examine factors that are associated with unmet need for family planning to help scale up the uptake of family planning services in Ghana ...
Ghana has long prioritized Family Planning (FP) as a key strategy for addressing the country's health, social and economic issues. Ghana's first organized efforts towards scaling up FP started in 1969 when an advisory team on population affairs led by Prof. Fred T. Sai helped to establish the Family Planning
Introduction. Ghana pioneered family planning program policy in West Africa (Machiyama & Cleland, 2014).Although fertility declines have occurred since the 1970s, from 6.4 births per woman to 3.9 births per woman (Ghana Statistical Service (GSS), Ghana Health Service (GHS) & ICF, 2018), the rate of decline has currently stalled (Bongaarts, 2005, 2017).
A systematic review of the literature of family planning and contraception services ... important barrier to reproductive health and adoption of family planning methods. Using the 2008 Ghana ...
The Ghana Demographic and Health Survey (GDHS) observed that a large number of women have an unmet need for family planning as the acceptor rate for family planning services remains low . It is on this note the Ghana Health Service argues that the lives of mothers and children will be improved and maternal mortality reduced if family planning ...
Literature Review on Family Planning in Ghana - Free download as PDF File (.pdf), Text File (.txt) or read online for free. literature review on family planning in ghana
Objective: to identify enablers and barriers to the quality of care of family planning services in Ghana and provide evidence of best practices and recommendations to inform decision making. Methods: A literature review of published studies on the quality of family planning services in Ghana using the Bruce quality of care framework.
CHAPTER TWO: LITERATURE REVIEW . Introduction 14 . Conceptual Issues 14 . ... 3 Conceptual Framework for Unmet Need for Family Planning 52 4 Map of Ghana Showing Regional Proportions of Young Women (15-24years) with Unmet Need for Family Planning 58 Digitized by Sam Jonah Library
In Ghana, despite a 38 percent decline in the total fertility rate from 1988 to 2008, unmet need for family planning among married women exposed to pregnancy risk declined only modestly in this period: from 50 percent to 42 percent.
To be included in this review the studies had to: 1) be published in English; 2) use quantitative analysis; 3) use an observational or experimental study design; 4) analyse data from lower- and middle-income countries; 5) examine at least one family planning outcome (current or ever use of family planning, unmet need, future intentions, participation in family planning decision-making, spousal ...
Parity and educational level of respondents were positively associated with usage of family planning services (P<0.05). Major motivating factors to the usage of family planning service were to space children, 94% (47/50) and to prevent pregnancy and sexual transmitted infections 84% (42/50). Major reasons for not accessing family planning ...
The World Bank projects a ten-fold increase in the population of sub-Saharan Africa (SSA) between 1960 and 2050, reaching 9.7 billion people in 2050 [].This escalation indicates Africa's growing fertility rate [].Notably, while the global fertility rate between 1990 and 2019 fell from 3.2 to 2.5 births per woman, this indicator only dropped from 6.3 to 4.6 births per woman for SSA [].
In 2015, Ghana mounted a family planning program which had as its objective to increase the contraceptive prevalence rate (CPR) of married women aged 15-49 from 22.2 to 29.7 percent, and that of unmarried women from 31.7 to 40 percent by 2020 (GFPCIP, 2015). The implementation of the program has been successful, the CPR is
As Ghana, like many parts of rural Africa, is a highly underdeveloped and pro-natalist area, this article concludes that family planning programs have the ability to influence reproductive attitudes and behavior, even under conditions of limited development.
Family planning aims to assist couples and individuals of reproductive age to achieve their reproductive aspirations. Despite the high premium placed on family planning programs in Ghana, funding remains a daunting challenge. Family planning intake is highest (69%) among women between 15 and 19 years and lowest (33%) among women within 45-49 ...
This review is aimed to investigate family planning knowledge, attitudes, and practices in east African countries. through published papers.A re view was conducted on knowledge, attitude and ...
This study determined the prevalence, trends, and the impact of exposure to family planning messages (FPM) on contraceptive use (CU) among women of reproductive age in sub-Saharan Africa (SSA).
Background Inequalities in access to health care result in systematic health differences between social groups. Interventions to improve health do not always consider these inequalities. To examine access to reproductive health care services in Ghana and Nigeria, the patterns of use of family planning and maternal care by women in these countries are explored. Methods We used population-level ...
The median number of new family planning clients receiving services in a facility each month has decreased from eight in 1993 to six in 1996, to five in 2002. The mean, while increasing in 1996 (from 15 to 18 new clients per month) remains essentially the same (19 new clients per month in 2002) (Table 3.12).
Literature review. Health information needs of women in rural communities ... They appear to require information on reproductive health, which includes family planning, delivery, and good menstruation practices. More crucially, women in Ghana required information on how to prevent and treat common urban ailments such as malaria, diarrhoea, and ...
We found the overall prevalence of use at 21%, similar to the 22% reported by the Ghana Demographics and Health Survey , but below the Ghana Health Service's national family planning target rate of 23.3% . A previous study conducted in Iran reported usage of modern contraceptive at 55% . This higher rate, compared to the 21% found in this ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on FAMILY PLANNING. Find methods information, sources, references or conduct a literature review on ...
Nearly half (n = 108/ 49.1%) were living with their parents.Most (n = 213/ 96.8%) of the respondents were in households with an estimated monthly income of less than or equal to GH₡500.00.Prevalence of antepartum depression among adolescent pregnant women. Out of a total of 220 adolescent pregnant women, more than a third (n = 85/ 38.6%) experienced antepartum depression (EPDS ≥ 13) while ...