Breastfeeding
Explore the latest in breastfeeding, including advances in understanding ways to encourage it and its long-term effects on child health.

Publication
Article type.
This systematic review and meta-analysis investigates the association between provision of a relaxation intervention and lactation outcomes.
This randomized clinical trial examines whether breast milk enemas can shorten the time to complete meconium evacuation and achievement of full enteral feeding for infants born preterm in China.
This cross-sectional study examines the prevalence of zero-food children (children who do not consume any food other than breast milk) aged 6 to 23 months across 92 low- and middle-income countries.
- Delivering on the Promise of Human Milk for Extremely Preterm Infants in the NICU JAMA Opinion January 30, 2024 Child Development Neonatology Nutrition Pediatrics Critical Care Medicine Full Text | pdf link PDF
This randomized clinical trial compares the effect of donor human milk on neurodevelopmental outcomes at 22 to 26 months’ corrected age compared with preterm infant formula among extremely preterm infants who received minimal maternal milk.
This study investigates whether ACA policies to increase access to breast pumps and lactation care were associated with innovation in the market for breast pumps.
This cross-sectional study analyzes lactation support policies at the top 50 US schools of medicine.
- Enhancing Lactation Accommodations for Physicians—An Opportunity for Tangible Investments in Our Workforce JAMA Network Open Opinion August 8, 2023 Equity, Diversity, and Inclusion Pregnancy Obstetrics Women's Health Obstetrics and Gynecology Full Text | pdf link PDF open access
This cohort study examines the association between improved lactation accommodation support and physician satisfaction at a large, urban academic health system.
This randomized clinical trial examines the development of egg allergy and sensitization in breastfed infants whose mothers ate eggs in the first 5 days after delivery.
This Viewpoint discusses 2 new programs of the Eunice Kennedy Shriver National Institute of Child Health and Human Development’s Pediatric Growth and Nutrition Branch that apply an ecological approach to understanding nutrition and public health.
This Patient Page describes the challenges of returning to work while breastfeeding, tips on how to transition back to work, and the advantages of breast milk.
- Maternal Opioid Treatment After Delivery Poses Low Risk to Infants JAMA News March 29, 2023 Neonatology Substance Use and Addiction Medicine Opioids Pediatrics Full Text | pdf link PDF free
This Viewpoint examines the current state of telelactation and its role in digital equity.
- Majority of Infant Formula Health Claims Are Poorly Supported JAMA News March 1, 2023 Child Development Neonatology Nutrition Pediatrics Full Text | pdf link PDF
This randomized clinical trial examines whether an exclusive human milk diet has an effect on gut bacterial richness, diversity, and proportions of specific taxa in preterm infants from enrollment to 34 weeks’ postmenstrual age.
This JAMA Insights Clinical Update reviews the risk factors for and symptoms of lactational mastitis and provides a potential treatment algorithm.
This cohort study investigates the presence of COVID-19 vaccine mRNA in the expressed breast milk of lactating individuals who received the vaccination within 6 months after delivery.
This review highlights recent literature regarding lactation in otolaryngology patients, including medication, radiologic imaging, perioperative considerations, and subspecialty-specific considerations for lactating patients.
This study aims to compare the antibody response in human milk after vaccination with mRNA-based and vector-based vaccines.
Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Disclaimer » Advertising
- HealthyChildren.org

- Previous Article
- Next Article
Milk Production and Transfer
Neonatal weight and output assessment, glucose stabilization, hyperbilirubinemia, immune development and the microbiome, supplementation, health system interventions: the baby-friendly hospital initiative, limitations and implications for future research, conclusions, acknowledgment, evidence-based updates on the first week of exclusive breastfeeding among infants ≥35 weeks.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
- Split-Screen
- Article contents
- Figures & tables
- Supplementary Data
- Peer Review
- CME Quiz Close Quiz
- Open the PDF for in another window
- Get Permissions
- Cite Icon Cite
- Search Site
Lori Feldman-Winter , Ann Kellams , Sigal Peter-Wohl , Julie Scott Taylor , Kimberly G. Lee , Mary J. Terrell , Lawrence Noble , Angela R. Maynor , Joan Younger Meek , Alison M. Stuebe; Evidence-Based Updates on the First Week of Exclusive Breastfeeding Among Infants ≥35 Weeks. Pediatrics April 2020; 145 (4): e20183696. 10.1542/peds.2018-3696
Download citation file:
- Ris (Zotero)
- Reference Manager
The nutritional and immunologic properties of human milk, along with clear evidence of dose-dependent optimal health outcomes for both mothers and infants, provide a compelling rationale to support exclusive breastfeeding. US women increasingly intend to breastfeed exclusively for 6 months. Because establishing lactation can be challenging, exclusivity is often compromised in hopes of preventing feeding-related neonatal complications, potentially affecting the continuation and duration of breastfeeding. Risk factors for impaired lactogenesis are identifiable and common. Clinicians must be able to recognize normative patterns of exclusive breastfeeding in the first week while proactively identifying potential challenges. In this review, we provide new evidence from the past 10 years on the following topics relevant to exclusive breastfeeding: milk production and transfer, neonatal weight and output assessment, management of glucose and bilirubin, immune development and the microbiome, supplementation, and health system factors. We focus on the early days of exclusive breastfeeding in healthy newborns ≥35 weeks’ gestation managed in the routine postpartum unit. With this evidence-based clinical review, we provide detailed guidance in identifying medical indications for early supplementation and can inform best practices for both birthing facilities and providers.
Exclusive breastfeeding significantly improves maternal and child health. Although US pediatricians’ recommendations are increasingly aligned with American Academy of Pediatrics (AAP) policies, their optimism about the potential for breastfeeding success has declined. 1 To maintain familiarity with the benefits of breastfeeding and the skills necessary to promote this positive health intervention, providers caring for neonates and/or new mothers need updated evidence-based information and tools to assess and manage breastfeeding.
In this review, we provide new evidence from the past 10 years on the following topics relevant to exclusive breastfeeding: milk production and transfer, neonatal weight and output assessment, glucose stabilization, hyperbilirubinemia, immune development and the microbiome, supplementation, and health system interventions. We focus on the early days of exclusive breastfeeding in healthy newborns ≥35 weeks’ gestation managed in the routine postpartum unit. 2 – 6 Tables 1 through 3 and Fig 1 provide summaries based on evidence and authors’ recommendations to provide concise and clear bullets on optimal management. The search strategy and tables of evidence for milk production and transfer, neonatal weight and output assessment, management of glucose, and hyperbilirubinemia are summarized in the Supplemental Information .
Breastfeeding Assessment During the First Postnatal Week
—, not applicable.
Mother, Infant, and Systems-Level Risk Factors for Breastfeeding Difficulties
Adapted from Evans A, Marinelli KA, Taylor JS; Academy of Breastfeeding Medicine. ABM clinical protocol #2: guidelines for hospital discharge of the breastfeeding term newborn and mother: “The going home protocol,” revised 2014. Breastfeed Med . 2014;9(1):4.
Risk Factors for Hypoglycemia
Adapted from Thornton PS, Stanley CA, De Leon DD, et al; Pediatric Endocrine Society. Recommendations from the Pediatric Endocrine Society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. J Pediatr . 2015;167(2):241 and Adamkin DH; Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics . 2011;127(3):576.

Supplementation decision algorithm.
Three stages of milk production, lactogenesis I to III, are defined on the basis of volume and composition of milk. For volume, Fig 2 shows estimated daily milk production. 16 In relation to composition, human milk changes dramatically over the first week of lactation. Colostrum, which is produced during the initial stage of lactation (lactogenesis I) in the first days after birth, contains more protein than mature milk. This highly dense early milk has a high concentration of immunoglobulins, activated macrophages, lymphocytes, neutrophils, and growth factors with essential roles in development of gut-associated lymphoid tissue. 17 As milk volume increases (lactogenesis II), sodium concentration and the sodium/potassium ratio decline rapidly with increased secretory activity of the lactocytes and closure of tight cellular junctions. 18 Production of fat-rich, higher-calorie mature milk typically occurs by ∼10 days post partum (lactogenesis III).

Milk volume estimated by breast milk transfer over the first 6 days in vaginal and cesarean births. *Adjusted difference P < .05. Adapted from Evans KC, Evans RG, Royal R, Esterman AJ, James SL. Effect of caesarean section on breast milk transfer to the normal term newborn over the first week of life. Arch Dis Child Fetal Neonatal Ed . 2003;88(5):F382.
Most, but not all, women experience lactogenesis II, referred to as “milk coming in,” by 72 hours post partum. In the Infant Feeding Practices Survey II, 19% of multiparous women and 35% of primiparous women reported milk coming in on day 4 or later. 19 Reasons for delayed lactogenesis II include primiparity, cesarean delivery, and BMI > 27. 20 – 22 Conditions associated with obesity, such as advanced maternal age (possibly related to reduced fertility associated with obesity-variant polycystic ovarian syndrome) and excessive gestational weight gain, may also lead to a delay. 23 , 24 Delayed lactogenesis II is associated with neonatal weight loss >10%. 20
Occasionally, a woman does not experience lactogenesis II and only produces small volumes of milk (prevalence 5%–8%). 19 , 25 The differential diagnosis includes breast pathology, previous breast surgery (with damage to ducts or augmentation for hypoglandular breasts), developmental anomalies of the breast tissue, hormonal disruptions (such as retained placental fragments and pituitary insufficiency, including Sheehan’s syndrome, hypothyroidism, polycystic ovarian syndrome, or theca-lutein ovarian cysts), and toxins (such as excessive tobacco exposure). 26 Occasionally, strategies described here to improve milk production and transfer are not effective, and long-term supplementation with either donor milk or infant formula is medically necessary.
Milk expression is safely and effectively achieved by both manual and mechanical methods and can be used to maintain milk supply in the event of separation from the infant. 27 Hand expression also facilitates milk transfer for the infant learning to breastfeed; both latch and an effective suckling pattern are key. Among mothers of term infants who were feeding poorly, those randomly assigned to hand expression versus electric pumps were more likely to still be breastfeeding at 2 months (96.1% vs 72.7%; P = .02). 28 Infrequent or inadequate signaling due to ineffective or infrequent breastfeeding or milk expression may trigger the autocrine-paracrine mechanisms of halting milk production and dismantling the mammary gland architecture. 29 Milk removal, either via direct breastfeeding or expression, is essential for continuation of milk production.
Some women experience engorgement with lactogenesis II. There is limited evidence regarding the optimal management of engorgement. However, because severe engorgement can impede infant removal of milk, breastfeeding mothers should learn hand expression and reverse pressure softening, which is positive pressure to the central subareolar region, 30 before discharge from maternity care. 31 , 32 If a mother is unable to hand express or her infant is unable to latch, she may require a breast massage 33 and/or use of an electric breast pump.
The components of a comprehensive breastfeeding assessment are described in Table 1 . 12 , 34 It is important to note that a mother’s pumped milk volume may be an inaccurate estimate of milk transfer because transfer also depends on the infant’s capabilities. Associated risk factors for suboptimal milk transfer are listed in Table 2 .
Painful latching deserves special attention as a contributor to low supply, impaired milk transfer, and early cessation of breastfeeding. 35 In an ultrasound study in which breastfeeding mothers with nipple pain were compared with those without, nipple pain was associated with abnormal infant tongue movement, restricted nipple expansion, and lower rates of milk transfer. 36 In a retrospective audit of an Australian breastfeeding center, 36% of visits were for nipple pain. 37 A US study revealed that nipple pain and trauma were among the most frequently cited reasons for early weaning. In a study of >1600 women with singleton births, ∼10% had nipple pain that persisted at postpartum day 7; 72% was attributed to inappropriate positioning and latching, 23% to tongue-tie in the infant, and 4% to oversupply. Women who received treatment recovered within 1 to 2 weeks, and 6-week exclusive breastfeeding rates were no different from those of mothers without nipple pain. 38 Although high-quality randomized controlled trials (RCTs) are needed, frenotomy has been shown to reduce maternal nipple pain in infants with congenital ankyloglossia. 39 There is no evidence that any one topical treatment is superior 40 ; the mainstay of management for nipple pain and fissuring is assistance with positioning and latching. 41
Healthy newborns experience physiologic weight loss after birth, 42 , 43 which, in the exclusively breastfed infant, typically plateaus as the mother’s milk transitions from lactogenesis I to lactogenesis II. The addition of infant formula, either as a supplement or in the form of exclusive formula feeding, is associated with rapid weight gain. This nonphysiologic weight trajectory is associated with childhood obesity. 44 Exclusive direct breastfeeding is inversely associated with the velocity of weight gain throughout the first year of life. 45 In one prospective cohort study of >300 newborns, weight gain >100 g during the first week after birth was independently associated with overweight status at age 2 (adjusted odds ratio [aOR] 2.3; 95% confidence interval [CI] 1.1 to 4.8). 44
Early infant weight loss should be evaluated in the context of the clinical status of the infant and the mother. Nomograms for newborn weight have been developed by using data from >100 000 healthy, exclusively breastfed infants in California. 46 Individual infant weights can be plotted against these nomograms by using the Newborn Early Weight Tool (NEWT) ( https://www.newbornweight.org ). Weight loss trajectory over time, combined with clinical information, provides a robust context for evidence-based decision-making. 47 Weight loss in the >75th percentile on NEWT nomograms for mode of delivery and infant age should prompt a thorough evaluation.
A term newborn’s weight is 75% water, compared with 60% for an adult. Urine output is usually low in the first 1 to 2 days after birth, after which a physiologic diuresis and loss of up to 7% to 10% of birth weight occurs. 48 , 49 Insufficient milk production and/or transfer in the exclusively breastfed newborn can contribute to excessive weight loss in the first few days of life. Low milk supply, often exacerbated by poor feeding or difficulty in suckling, correlates with elevated milk sodium levels. 50 Exclusively breastfed infants, especially those born via cesarean delivery, are at increased risk for greater weight loss, dehydration, and hypernatremia. 51 , 52 In a systematic review of hypernatremia among breastfed infants, significant risk factors included weight loss >10%, cesarean delivery, primiparity, breast anomalies, reported breastfeeding problems, excessive prepregnancy maternal weight, delayed first breastfeeding, lack of previous breastfeeding experience, and low maternal education. 53 Prevention strategies included daily weights coupled with lactation support during the first 4 to 5 days after birth.
Early weight loss nomograms for exclusively breastfed newborns can help identify those infants at risk for hypernatremic dehydration (HD), 54 , 55 a rare condition characterized by lethargy, restlessness, hyperreflexia, spasticity, hyperthermia, and seizures, with an estimated incidence of 20 to 70 per 100 000 births and up to 223 per 100 000 births among primiparous mothers. 56 Use of charts for weight loss with SD scores specifically to detect HD, combined with a policy of weight checks on days 2, 4, and 7 of life, had high sensitivity (97%) and specificity (98.5%) to detect HD. 47 However, given the low incidence of HD, the positive predictive value (PPV) of repeated weight checks alone was only 4.4%. 56
Importantly, elimination patterns during the first 2 days of life are neither sensitive nor specific as measures of infant intake. 49 Infants may be voiding and stooling despite insufficient intake or, more commonly, have decreased voiding and stooling compared with exclusively formula-fed infants despite adequate intake. In a cohort study of 313 infants, the frequency of urination and stooling was significantly decreased among exclusively breastfed infants compared with exclusively formula-fed infants during the first 3 days of life then rose and significantly surpassed that of exclusively formula-fed infants by day 6 of life. 49 Another prospective cohort study of 280 mother-infant pairs examined elimination patterns in relation to excessive weight loss (>10%) between 72 and 96 hours after birth. 48 The strongest association with weight loss >10% was with <4 stools after 72 hours or maternal perception of delayed lactogenesis II. Although term and late-preterm infants generally pass meconium within 48 hours (76%–83% in a study of 198 infants), delayed passage of meconium can be a marker for insufficient milk intake. 57 Correlations between infants’ intake and elimination are more reliable after the first 3 days (lactogenesis II).
To prepare for transitional energy needs, the third-trimester fetus stores glycogen, manufactures catecholamines, and deposits brown fat. Healthy newborns use these stores to maintain thermoregulation and meet their energy needs through metabolism of brown fat and the release of counterregulatory hormones such as glucagon, epinephrine, cortisol, and growth hormone. Combined with declining insulin secretion, these hormones mobilize glucose and alternative fuels, such as lactate and ketone bodies, to support organ functions. 58 , 59
Because oral intake is not the main energy source for healthy term neonates in the first days after birth, physiologic volumes of colostrum (16 kcal/oz) are sufficient to meet metabolic demands. As glycogen stores are depleted, coinciding with the transition from colostrum to mature milk, newborns transition from a catabolic state to reliance on enteral feeds, with approximately half of the caloric content derived from fat. 60
After placental detachment, neonatal glucose levels reach a physiologic nadir in the first hours after birth and then typically rise to adult levels a few days later. The threshold for neonatal glucose that is associated with neurotoxicity is unclear; a 2008 National Institutes of Health workshop concluded that “there is no evidence-based study to identify any specific plasma glucose concentration (or range of glucose values) to define pathologic hypoglycemia.” 61 In one cohort study, treatment of asymptomatic newborn hypoglycemia to maintain blood glucose levels >47 mg/dL had no effect on cognitive performance at 2 years; however, at 4.5 years, there were dose-dependent concerns regarding visual motor and executive function, with the highest risk in children exposed to severe (<36 mg/dL),and recurrent (≥3 episodes) hypoglycemia. 62 , 63
In the first hours after birth, healthy term neonates compensate for relatively low glucose levels by decreasing insulin production and increasing glycolysis, gluconeogenesis, and ketone production. Among at-risk newborns, early skin-to-skin care plus early feeding and blood glucose assessment at 90 minutes supports glucose homeostasis and is associated with decreased risk of hypoglycemia and NICU admission. 64 In a Cochrane review, early skin-to-skin contact increased glucose levels by 10.49 (95% CI 8.39 to 12.59) mg/dL or 0.6 (0.5 to 0.7) mmol/L. 65 Conversely, practices that separate the mother and infant and delay the first feeding increase hypoglycemia risk.
Glucose monitoring is recommended for infants with risk factors ( Table 3 ) and for any infant who exhibits symptoms of hypoglycemia. 66 Because operational thresholds for treating hypoglycemia and target glucose levels are not defined, clinical recommendations vary. Infants who require early or more frequent feedings should be supported to breastfeed and/or receive expressed milk. Authors of multiple studies confirm the benefits of using glucose gel rather than formula as an initial treatment of low glucose levels, and this practice has become increasingly commonplace. 67 – 73 Some institutions use pasteurized donor human milk (PDHM) as a treatment of hypoglycemia; however, there are, as yet, no published studies describing outcomes of this practice. The option of antenatal milk expression for lower-risk women with preexisting or gestational diabetes may also be considered because this technique may preserve exclusive breastfeeding without adversely affecting perinatal outcomes. 74 Infants requiring intravenous glucose should breastfeed, when able, during the therapy.
Persistent or late-onset hypoglycemia (>48 hours after birth) can occur in the setting of congenital endocrine disorders or, more commonly, perinatal stress due to birth asphyxia, intrauterine growth restriction, maternal preeclampsia, 75 or persistent problems establishing breastfeeding. 76 Infants with these risk factors may be more vulnerable to insufficient feeding, so skilled assessment is essential.
Management of hyperbilirubinemia in the exclusively breastfed newborn depends on whether the excess in bilirubin is pathologic or physiologic. Neonatal bilirubin levels rise after birth because of physiologic immaturity of glucuronyl transferase, which is exaggerated with each decreasing week of gestational age. Exclusively breastfed infants have higher serum bilirubin levels than formula-fed infants, possibly because of differences in fluid intake and bilirubin excretion and increased enterohepatic resorption of bilirubin. 77 Some individuals may also have a genetic predisposition to higher bilirubin levels. 78 , 79 Bilirubin is an antioxidant, and it has been hypothesized that moderate increases in bilirubin levels may be protective for the transition to extrauterine life. 77 , 80
In contrast, pathologic hyperbilirubinemia resulting from insufficient breastfeeding, sometimes referred to as breastfeeding jaundice, is better defined as suboptimal intake jaundice. 77 In the United States and Canada, it is recommended that all neonates undergo bilirubin risk screening at least once before hospital discharge. 81 The Academy of Breastfeeding Medicine and the AAP advise the use of Bhutani curves to assess risk and need for treatment of hyperbilirubinemia; clinical tools are available on mobile device applications. 77 , 81 , 82 This approach has led to a decrease in severe pathologic hyperbilirubinemia 83 ; however, concerns for overtreatment and the potential harm of phototherapy have arisen recently. 84 Using subthreshold bilirubin levels to initiate phototherapy as a mechanism to prevent readmission is not recommended because this approach increases length of stay and results in many infants receiving unnecessary treatment to reduce each case of readmission. 85
Breastfed infants with hyperbilirubinemia require assessment of milk production and transfer, feeding frequency, and neonatal weight loss. 86 – 91 If there is pathologic hyperbilirubinemia, and infant intake at the breast is sufficient, exclusive breastfeeding should be continued while the infant receives phototherapy. Although supplementation with infant formula may decrease the bilirubin level and risk of readmission for phototherapy, 85 it will also interfere with the establishment and continuation of breastfeeding. 92 If intake at the breast is insufficient and supplementation is medically necessary, expressed maternal milk is preferred. Despite the current lack of data on its benefits in reducing hyperbilirubinemia in term infants, the use of PDHM to preserve exclusive human-milk feeding is increasing. 93
Phototherapy for neonatal jaundice and concerns about insufficient milk can be anxiety provoking for parents, even in a supportive environment, and can be disruptive to successful breastfeeding. 94 Practices to minimize mother-infant separation, including providing phototherapy in the same room and maintaining safe skin-to-skin care with the infant’s mother, also promote exclusive breastfeeding. 95
Early colostrum and exclusive breastfeeding establish an optimal and intact immune system. Unlike infant formula, human milk has a dynamic composition of both macro- and micronutrients that varies within a feed, diurnally, and over the course of lactation. Protective proteins abound in human milk, including lactoferrin, secretory immunoglobulin A, transforming growth factor-β, and α-lactalbumin. These factors promote development of the infant’s immune system. 96 Additionally, lactoferrin has unique antibacterial properties important in the prevention of sepsis. Unique nonnutritive oligosaccharides that are specific to the mother-infant pair’s shared environment and exposures prevent binding of pathogenic bacteria and promote a healthy microbiome in the gut. 97 Differences in immune cell distributions based on neonatal diet can be detected through 6 months of age, with natural killer cells most significantly affected. 98
During vaginal birth, the newborn’s intestine and mucosal surfaces are colonized with maternal microbes that act synergistically with bioactive factors in mother’s milk to establish a robust lymphoid follicle replete with a healthy balance of T helper cells. 99 , 100 Surgical delivery is associated with aberrant colonization, which may lead to differences in the mother’s milk microbiome 101 only partially restored by vaginal secretions. 102 Formula supplementation may effect the most change in the newborn’s microbiome 103 , 104 and immune development. These basic science findings are supported by clinical studies.
Given the multiple mechanisms through which exclusive human milk impacts gut development, formula supplementation should always be avoided when the mother’s own milk is available. Although an exploratory study of early limited supplementation with extensively hydrolyzed formula followed by a return to exclusive breastfeeding did not reveal differences in the developing microbiome ( N = 15), 105 a longitudinal study among infants exclusively breastfeeding at 3 months ( N = 579) revealed alterations in the microbiome among infants exposed to formula as neonates ( n = 179). 106 Just as antimicrobial stewardship requires appropriate use of antibiotics, 107 supplementation stewardship requires judicious use of formula when medically indicated.
A systematic review of healthy, term, breastfed newborns revealed no benefit from routine supplementation with foods or fluids in the early postpartum period. 108 These findings are consistent with consensus recommendations for exclusive breastfeeding for the first 6 months, followed by continued breastfeeding with the addition of complementary foods until at least 12 months of age. 2 , 109 – 111 Early introduction of supplemental formula is associated with a greater than twofold increase in risk of early cessation of breastfeeding even when controlling for confounding variables. 112 – 114 Among almost 1500 women in the Infant Feeding Practices Study II, only early exclusive breastfeeding remained significant for achieving intended breastfeeding duration (aOR 2.3; 95% CI 1.8 to 3.1) after adjustment for relevant hospital practices. 113 This finding may be due in part to the supply and demand nature of milk production and the role of suckling, oxytocin release, and milk removal in establishing lactation.
If supplemental feeds are medically indicated, they should be accompanied by manual or mechanical milk expression, recognizing that direct breastfeeding usually provides more complete milk removal. 115 In a pilot RCT ( N = 40), early limited formula supplementation for infants with ≥5% weight loss increased exclusive breastfeeding at 3 months post partum. 116 In a subsequent larger study ( N = 164), early limited supplementation did not affect overall breastfeeding at 1 or 6 months but slightly increased rates of formula use at 1 month (36.7% vs 22.4%; P = .08), 105 decreased breastfeeding at 12 months (30% vs 48%; risk difference −18% [CI −34% to −3%]), and shortened the time to breastfeeding cessation (hazard ratio 0.65; 95% CI 0.43 to 0.97). 117
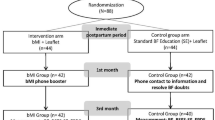
Because evidence continues to accrue that supplementation in the first days after birth has major health risks, 103 , 106 judicious use of supplementation is a critical goal, with a return to exclusivity whenever possible. If supplementation is indicated ( Fig 1 ), options in order of preference are (1) expressed milk from the infant’s own mother, 4 (2) PDHM, and (3) commercial infant formulas. The potential risks and benefits of these options should be considered in the context of the infant’s age, the volume required, and the impact on the establishment of breastfeeding. 4
Methods of supplemental feeding include spoon or cup feeds, supplemental nursing systems, syringe feeds, and paced bottle feeds. Methods should be tailored to staff training and family preferences. 7 Among late-preterm newborns, there is evidence that some may be more susceptible to feeding problems when supplemented via a bottle; in an RCT in which the 2 methods were compared, cup feeding was associated with a longer duration of exclusive breastfeeding compared with bottle-feeding. 118 Among term newborns, the manner in which supplementation is delivered, whether a bottle or alternative devices, has no apparent impact on continuation of breastfeeding. 119 If the supplement is the mother’s own expressed milk, avoidance of bottles and nipples may preserve a longer duration of breastfeeding, especially among late-preterm newborns. 120
To ensure milk removal, which is key to establishing a milk supply, a mother should be assisted to express milk each time her infant is supplemented, even if the infant is also “practicing” at the breast. 4 “Hands on” pumping, combining breast massage with pumping, has been shown to increase milk production in mothers of preterm infants who are hospitalized. 121
Physiologic early infant feeding is facilitated by keeping mothers close to their infants, beginning with skin-to-skin care immediately after birth and continuing with 24-hour rooming-in and feeding on cue. These are core practices of the recently updated World Health Organization’s Ten Steps to Successful Breastfeeding of the Baby-Friendly Hospital Initiative (BFHI). 7 Feeding on cue or “responsive feeding” is associated with more frequent breastfeeding throughout the day, more exclusive breastfeeding up to 6 months and beyond, 122 – 124 and decreased likelihood of abnormal rapid weight gain in infancy. 125
Several major health organizations, including the US Preventive Services Task Force and the Agency for Healthcare Research and Quality, have generated systematic reviews and quality improvement (QI) reports that demonstrate the positive impact of the BFHI on breastfeeding outcomes. 10 , 13 , 14 Implementation of maternity care practices aligned with any component of the BFHI is associated with improved in-hospital and postdischarge breastfeeding rates. 11 , 13 , 126 Best Fed Beginnings increased exclusive breastfeeding initiation from 39% to 61% ( t = 9.72; P < .001) at 89 hospitals over 2 years. 127 The Community and Hospitals Advancing Maternity Care Practices initiative reported that the BFHI helped to reduce racial disparities in breastfeeding in southern US states. 128
Since the initial implementation of the BFHI, safety concerns have emerged, including case reports of inadvertent bed-sharing, suffocation, falls, and increased risk of neonatal jaundice. 3 , 129 In this context, the World Health Organization conducted an extensive evidence-based review. 7 , 130 Key differences in the revised Ten Steps include highlighting the Code of Marketing of Breastmilk Substitutes, the need to collect ongoing data, a focus on safety and surveillance (especially as it relates to skin-to-skin care and rooming-in), and acknowledgment that there is insufficient evidence to limit pacifiers and other artificial nipples.
Step 10 of the BFHI requires a direct connection between the delivery hospital and the community for ongoing support. Referral for outpatient support as well as provision of contact information for those who can manage breastfeeding problems is paramount.
Given the importance of exclusive breastfeeding for maternal and child health, both intent and initiation are increasing. However, maternal conditions linked with delayed lactogenesis, such as advanced maternal age, obesity, and fertility treatment, are increasingly common. Priority research areas to help families meet their breastfeeding goals include accurate identification of women with risk factors for delay or absence of lactogenesis, more sensitive methods of identifying at-risk newborns, and exploration of the implications of early limited formula supplementation on infant outcomes such as ontogeny of the immune system and the microbiome, maternal self-efficacy, and continued breastfeeding.
Health care professionals’ support is critical for families to meet their infant feeding goals and achieve optimal health outcomes. All physicians who care for new mothers and infants need skills to evaluate early breastfeeding, perform maternal and infant risk stratification, understand the range of potential interventions in the context of the risk/benefit ratio of supplementation, and ensure appropriate follow-up.
Most mothers can produce adequate colostrum and mature milk, and most newborns are able to breastfeed exclusively. Nevertheless, conditions that require medical supplementation are common and important to recognize. The decision to supplement with infant formula requires thoughtful analysis of the risks and benefits, with consideration of the family’s informed choice. Early-term and late-preterm newborns are at a higher risk of complications. Therefore, more careful monitoring, detailed assessments, and case-based interventions are warranted. Further research is needed to identify the best methods to support exclusive breastfeeding in high-risk populations.
We thank Delali Lougou for organizing the articles used in this article to provide the original framework for the authors’ review.
Drs Feldman-Winter, Kellams, and Stuebe conceptualized and designed the review of the literature, conducted the literature review and analysis, drafted the initial manuscript, and reviewed and revised the manuscript; Dr Peter-Wohl made substantial contributions to the acquisition of data and to the analysis and interpretation of data, drafted the article, and revised it critically for important intellectual content; Dr Taylor made substantial contributions to conception and design and made critical revisions; Drs Lee and Terrell made substantial contributions to the design and to the acquisition of data and made critical revisions for important intellectual content; Drs Meek and Noble and Ms Maynor made substantial contributions to the conception, design, and analysis and interpretation of data and revised the article critically for important intellectual content; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: No external funding.
American Academy of Pediatrics
adjusted odds ratio
Baby-Friendly Hospital Initiative
confidence interval
hypernatremic dehydration
Newborn Early Weight Tool
pasteurized donor human milk
positive predictive value
quality improvement
randomized controlled trial
Competing Interests
Supplementary data.
Advertising Disclaimer »
Citing articles via
Email alerts.

Affiliations
- Editorial Board
- Editorial Policies
- Journal Blogs
- Pediatrics On Call
- Online ISSN 1098-4275
- Print ISSN 0031-4005
- Pediatrics Open Science
- Hospital Pediatrics
- Pediatrics in Review
- AAP Grand Rounds
- Latest News
- Pediatric Care Online
- Red Book Online
- Pediatric Patient Education
- AAP Toolkits
- AAP Pediatric Coding Newsletter
First 1,000 Days Knowledge Center
Institutions/librarians, group practices, licensing/permissions, integrations, advertising.
- Privacy Statement | Accessibility Statement | Terms of Use | Support Center | Contact Us
- © Copyright American Academy of Pediatrics
This Feature Is Available To Subscribers Only
Sign In or Create an Account
The Benefits of Breast Feeding
Affiliation.
- 1 Institute for Pediatric Gastroenterology, Nutrition and Liver Diseases, Schneider Children's Medical Center, Petach Tivka, and Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel.
- PMID: 27336781
- DOI: 10.1159/000442724
Human milk is considered as the gold standard for infant feeding. Breastfeeding advantages extend beyond the properties of human milk itself. A complex of nutritional, environmental, socioeconomic, psychological as well as genetic interactions establish a massive list of benefits of breastfeeding to the health outcomes of the breastfed infant and to the breastfeeding mother. For this reason, exclusive breastfeeding is recommended for about 6 months and should be continued as long as mutually desired by mother and child. The evidence in the literature on the effect of breastfeeding on health outcomes is based on observational studies due to the fact that it is unethical and practically impossible to randomize children to be breastfed or not. As such, multiple confounders cloud the evidence and one must base conclusions on the accumulating evidence when not contradictory and on the only intervention study, PROBIT (Promotion of Breastfeeding Intervention Trial). This review highlights some of the health outcomes related to breastfeeding such as the prevention of infections, the effect of breastfeeding on neurodevelopmental outcome, obesity, allergy and celiac disease. Available evidence as well as some of the contradictory results is discussed.
© 2016 Nestec Ltd., Vevey/S. Karger AG, Basel.
Publication types
- Breast Feeding*
- Celiac Disease / prevention & control
- Communicable Diseases / diet therapy
- Health Promotion
- Hypersensitivity / prevention & control
- Infant Nutritional Physiological Phenomena
- Meta-Analysis as Topic
- Milk, Human / chemistry*
- Neurodevelopmental Disorders / prevention & control
- Obesity / prevention & control
- Observational Studies as Topic
- Randomized Controlled Trials as Topic
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 19 May 2024
The role of breastfeeding and formula feeding regarding depressive symptoms and an impaired mother child bonding
- Clara Carvalho Hilje 1 , 2 ,
- Nicola H. Bauer 3 ,
- Daniela Reis 1 , 2 ,
- Claudia Kapp 4 ,
- Thomas Ostermann 4 ,
- Franziska Vöhler 5 &
- Alfred Längler 1 , 2
Scientific Reports volume 14 , Article number: 11417 ( 2024 ) Cite this article
407 Accesses
1 Altmetric
Metrics details
- Paediatrics
Associations between depressive symptoms and breastfeeding are well documented. However, evidence is lacking for subdivisions of feeding styles, namely exclusive breastfeeding, exclusive formula feeding and a mixed feeding style (breastfeeding and formula feeding). In addition, studies examining associations between mother-child-bonding and breastfeeding have yielded mixed results. The aim of this study is to provide a more profound understanding of the different feeding styles and their associations with maternal mental health and mother-child-bonding. Data from 307 women were collected longitudinally in person (prenatally) and by telephone (3 months postnatally) using validated self-report measures, and analyzed using correlational analyses, unpaired group comparisons and regression analyses. Our results from a multinomial regression analysis revealed that impaired mother-child-bonding was positively associated with mixed feeding style ( p = .003) and depressive symptoms prenatal were positively associated with exclusive formula feeding ( p = .013). Further studies could investigate whether information about the underlying reasons we found for mixed feeding, such as insufficient weight gain of the child or the feeling that the child is unsatiated, could help prevent impaired mother-child-bonding. Overall, the results of this study have promising new implications for research and practice, regarding at-risk populations and implications for preventive measures regarding postpartum depression and an impaired mother-child-bonding.
Similar content being viewed by others

Exclusive breastfeeding promotion policies: whose oxygen mask are we prioritizing?

Association between maternal postpartum depressive symptoms, socioeconomic factors, and birth outcomes with infant growth in South Africa
A randomised controlled trial evaluating the effect of a brief motivational intervention to promote breastfeeding in postpartum depression
Introduction.
Pregnancy and the birth of a child is an extraordinary and overwhelming event for many women. It is accompanied by intense positive emotions 1 , 2 . However, the birth of a child is associated with several changes and can cause intense stress 2 , 3 . Peri- and postpartum depression is defined as an episode of major depression that is associated with childbirth 4 . With a prevalence ranging from 10 to 15%—or even higher in lower- and middle-income countries—postpartum depression (PPD) is a widespread illness 5 , 6 , 7 , 8 . Its effects on maternal and the infant’s health, is a well-recognized issue 9 . Several studies have examined developmental disturbances in children of (severely) depressed mothers 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , such as behavioral problems, lower math scores, or a sevenfold risk of depression during adolescence 16 . PPD is furthermore associated with an impaired mother-child-bonding 14 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , which poses an increased risk of impaired emotional, social and cognitive development in the child 25 , 26 . Mother-child-bonding is described as a general tendency in the first weeks and months after birth to engage in social interaction with each other 27 . It is conceived as the maternal bond towards the child and the child's attachment towards the mother 28 . Disruption of this process has a long history in research 29 and has been described as a disorder of mother-child - bonding 19 , 30 . The mother’s emotional response to the child is considered an essential symptom of bonding disorder and may reach the level of hatred and rage 29 . Mother-child-bonding disorders include a lack of maternal emotion to the extent that it can cause distress, irritability, hostile and aggressive impulses, pathological ideas, and outright rejection of the child 19 . Numerous further studies provide evidence for an association between PPD and mother–child bonding disorders 14 , 18 , 19 , 20 , 24 , 31 .
A possibility to prevent adverse outcomes such as PPD and an impaired mother-child-bonding might be breastfeeding . Previous studies found supportive evidence that (exclusive) breastfeeding prevents PPD and a poor mother-child-bonding 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 and vice versa, as PPD is associated with early cessation of breastfeeding 42 , 43 , 44 . Numerous other studies provide evidence of an association between weaning and maternal depression 45 , 46 , 47 , 48 , 49 , 50 . In addition, 60% to 90% of women indicate breastfeeding difficulties, which may be an additional source of stress 51 , 52 . This can lead to a vicious cycle, as breastfeeding difficulties are an additional stressor for the mother and may promote depression 53 , 54 , 55 .
Studies examining associations between mother-child-bonding and breastfeeding, as well as attachment—which focuses more on how the infant builds up a relationship with its primary caregiver 56 —and breastfeeding, have found mixed results 37 , 38 , 57 , 58 , 59 , 60 , 61 . Keller et al. (2016) found that the Postpartum Bonding Questionnaire (PBQ) factor “anxiety about care” negatively predicted breastfeeding duration beyond six months 62 . Besides the educational level of the mothers, this was found to be the most important influential factor on the duration of breastfeeding in a regression analysis. Systematic reviews of the associations between breastfeeding and mother-child-bonding found that maternal sensitivity and secure attachment were the aspects of mother-child-bonding most often associated with breastfeeding 63 , 64 . Regarding the associations between breastfeeding difficulties and mother-child-bonding, emotional availability was found to be negatively correlated with objective (e.g. cracked nipples) as well as subjective breastfeeding difficulties (e.g. perceived insufficiency of milk supply 65 ). In another study, secure attachment also appears to play an important role in breastfeeding continuation when breastfeeding difficulties occur 66 . In addition, breastfeeding confidence was found to be positively associated with higher levels of maternal attachment 67 . A study by Smith and Ellwood (2011) reported a descending pattern from exclusive to mixed to no breastfeeding and receipt of emotional care from the mother. The authors suggest that the time invested in breastfeeding and the associated close contact between mother and child strengthens the bond between the two. More time may also improve breastfeeding itself 68 . However, to our knowledge, no study so far differentiated exclusive, mixed and no breastfeeding patterns with regard to mother-child-bonding in particular.
Further research on the association of breastfeeding on PPD and mother-child-bonding may contribute in a meaningful way to the prevention of subsequent disorders and the reduction of long-term consequences for mother and child. The aforementioned influence of mother-child-bonding on breastfeeding behavior led us to include bonding as an independent variable in the study. The study design explained below led us to examine the influence of depressive symptoms in pregnant women and the influence of depressive symptoms in postpartum mothers, also as independent variables, in relation to the different feeding practices. The aim of this study is to examine whether PPD and poor mother-child-bonding are associated with different feeding practices (exclusive, mixed and no breastfeeding) in order to gain a better understanding of the associations between feeding practices and adverse psychological outcomes, such as PPD. In addition, to better understand such associations, we investigated the reasons for non-breastfeeding or adding formula in our study. We hypothesized that mothers who breastfed (exclusively) at the time point of three months postpartum would show significantly less symptoms of PPD and would report a better bonding towards their child, than mothers who did not breastfeed at that time.
Study design and procedure
The present work was embedded in a larger research project “Baby-Friendly and Breastfeeding” (in the following BaSti-study ) and is a longitudinal observational cohort design. We recruited women between December 2017 and November 2019 vis-a-a-vis prenatal (participants were at least in their 16th week of pregnancy) as well as postpartum (three months after birth) via phone after the participants gave their informed consent. Recruitment took place before and after midwife consultations and gynecological examinations, delivery room information evenings and, for only postpartum surveys, through the hospital staff at the neonatal wards. Four pilot surveys were conducted prior to actual implementation. The participating hospitals were two university teaching hospitals in Germany. Inclusion criteria were delivery in one of the participating hospitals, a minimum age of 18 years and sufficient German language skills. Stillbirths or early postnatal death led to an exclusion of the study. The final study sample comprised N = 307. Of the total sample, 90 women (29.3%) were surveyed during pregnancy. To ensure that the conditions of the surveys were as comparable as possible, the procedure was always as follows: participants received (1) an information sheet, (2) the consent form, (3) a questionnaire on sociodemographic data and the test battery. Prior to the introduction of the EPDS, the following standardized introduction was presented to the participants by the person conducting the survey: " I would like to move on to topics that may be uncomfortable for you. If you do not wish to answer a question, you are of course free to do so. It is important for me to emphasize at this point that negative thoughts and feelings about yourself and the child can be common during and after pregnancy and are, to a certain extent, quite normal. However, it is possible for these feelings to persist for several days or weeks, leading to what is known as PPD. It is important to us that this topic receives more attention and recognition in the future and is not made taboo, as this leaves those affected alone with it". We filled in the answers given in the postpartum telephone survey in the questionnaire and sent it to the participants upon request.
All research was performed in accordance with relevant guidelines. The participants proved written informed consent to participate in the study. This study was conducted in accordance with the Declaration of Helsinki. The Ethics Committee of the University Witten/Herdecke approved all components of the project 86/2017.
Instruments
Edinburgh postnatal depression scale (epds).
To assess the occurrence of depressive symptoms we used the German version 69 of the 10-item self-report scale EPDS 70 as a screening tool. The EPDS was originally developed as a screening instrument for the postnatal period 71 , but because it has been validated in numerous studies as an applicable tool for both pre- and postpartum assessment 72 , we included it in both settings. Each item is scored on a 4-point scale ranging from 0 to 3—with a higher sum score indicating more depressive symptoms 20 , 69 . Responses are based on the mental state over the past seven days 69 . The data revealed a Cronbach’s α of 0.82 (prepartum) and 0.79 (postpartum) in our sample.
Postpartum Bonding Questionnaire (PBQ)
To investigate mother–infant bonding, we used the German version of the self-report PBQ 19 , 23 , which assesses a mother’s feelings or behaviors toward her infant 73 . In contrast to the original version, which consists of 25 items and proposes a four factor solution, the German version of the screening instrument consists of 16 Items and proposes a solution with only one general factor “impaired bonding” 23 . The Likert scaling of the PBQ ranges from 0 (always) to 5 (never), with a higher sum score indicating impaired bonding 20 . In our sample, the internal consistency was α = 0.80.
Questionnaire “Feeling Comfortable During Pregnancy” (original: Schwanger Wohlfühlen)
To assess possible covariates such as subjective mental and physical well-being, coping during pregnancy and partner relationship/social support, we administered the questionnaire “Feeling Comfortable During Pregnancy” 74 during pregnancy. The questionnaire was originally developed in German and consists of 38 items. They reflect the dimensions “ affective well-being ”, “ physical well-being ” and “ coping during pregnancy ”. Responses are given on a Likert scale ranging from 1 (does not apply at all) to 7 (fully applicable). In our sample, the overall internal consistency reached Cronbach’s α = 0.82 and for the three underlying dimensions affective well-being α = 0.82, physical well-being α = 0.42 and coping during pregnancy α = 0.66.
Statistical analysis
All analyses were performed using IBM SPSS Statistics 27.0 (IBM Corp 2020). Decisions regarding the use of parametric or non-parametric tests are, besides the scale levels of the variables, based on the examination of outliers and the following assumptions: additivity and linearity, homoscedasticity, independence of residual terms and multicollinearity 75 . We tested normality with regard to sample sizes ˂ 30 75 , 76 . To use either parametric or non-parametric tests was decided for each test individually.
Hypothesis testing was conducted in two steps. First, unpaired group comparisons and correlational analyses were performed. All significant interactions with more than two groups were analyzed with post hoc tests. Due to different sample sizes, we chose to use Hochberg’s GT2 as a post hoc test 75 . Second, logistic regression analyses containing the significant results out of step one were performed. Because the regression analyses were hierarchical 75 , we focused primarily on the Akaike information criterion (AIC) to decide on a model. The final model of the regression analyses was bootstrapped ( N = 1000 samples, 95% confidence interval), to ensure its explanatory value.
Potential covariates
Given previous research on the EPDS postpartum, the PBQ and the success of breastfeeding 20 , 23 , 77 , 78 , 79 , 80 , 81 , we included the following covariates (see Table 1 ) to minimize potential confounding.
Descriptive statistics
Women were aged between 19 and 57 years ( M = 32.93, SD = 4.50) and 87.6% of the women were born in Germany. 10.1% of the women have previously had a psychological illness. 12.7% of the children had to be transferred to the pediatric clinic after birth. See Table 2 for additional demographic characteristics.
Feeding styles and its associations with PPD and mother–child-bonding
A t -test did not reveal significant differences between the breastfeeding (n = 263) and the non-breastfeeding group (n = 43) concerning the postpartum EPDS, t (304) = 1.695, p = 0.09. Due to an outlier we found, we additionally performed a Mann–Whitney U -Test, which confirmed our results, U (43,263) = 4647.00, Z = −1.881, p = 0.060. However, a tendency was evident here. No significant difference could be shown with respect to PBQ scores either, t (304) = −1.320, p = 0.188.
Examining exclusive breastfeeding vs. mixed feeding vs. non-breastfeeding, an ANOVA revealed significant differences in EPDS scores postpartum, F (2, 304) = 3.323, p = 0.037, r = 0.145, with a small effect size 82 , as well as in PBQ scores, F (2, 304) = 4.689, p = 0.010, r = 0.173. For EPDS scores, post hoc tests did not reveal significant differences between the groups. For PBQ scores, post hoc tests showed significant differences between the breastfeeding group and the mixed feeding group, M Diff = −2.801, 95% CI [− 5.24, − 0.37], p = 0.018, with d = 0.551, indicating a medium effect size 82 , as well as between the non-breastfeeding group and the mixed feeding group, M Diff = − 3.610, 95% CI [− 6.57, − 0.65], p = 0.011, with d = 0.677, also indicating a medium effect size 82 .
Based on these findings, we conducted multinomial regression analyses. Table 3 shows all correlations of potential variables relevant to exclusive breastfeeding. Significant correlations were included in the regression analyses. In order to obtain a feasibly parsimonious model, we decided to use a hierarchical method 75 .
Our final regression model (Table 4 ) included the PBQ score and EPDS score prenatal as significant variables relevant to the different breastfeeding states (AIC = 148.514). The Likelihood Ratio test was significant, χ 2 (4, N = 86) = 17.647, p ˂ 0.001, and Nagelkerke’s R 2 = 0.221 (Cox and Snell’s R 2 = 0.184) can be considered as acceptable 83 . Both, Pearson test ( p = 0.554) and deviance ( p = 0.954), indicated that the model was a good fit to the data 75 . Bootstrapped regression weights (Table 5 ) confirm our results.
We furthermore investigated partner relationship/social support for breastfeeding and reasons for non-breastfeeding or adding formula as well as associations with breastfeeding difficulties . Regarding partner relationship/social support, no significant difference was found between the groups, χ 2 (2, N = 200) = 3.293, p = 0.193. Table 6 shows the reasons given by the groups. Mothers who added formula reported more often than mothers who did not breastfeed, that they were unsure whether the infant was satiated/were sure that they were not satiated, and that the infant did not gain enough weight. In terms of any breastfeeding difficulties, correlations with the EPDS postpartum, η = 0.033, p = 0.568, and the PBQ, η = 0.077, p = 0.181, were both not significant. Regarding the quantity of breastfeeding difficulties no significant correlation was found with the EPDS postpartum, r (307) = 0.058, p = 0.311, 95% CI [− 0.054, 0.169], nor with the PBQ, r (307) = 0.080, p = 0.160, 95% CI [− 0.032, 0.191], either.
The aim of this study was to investigate associations between depressive symptoms, mother–child-bonding and different feeding practices (exclusive, mixed, and no breastfeeding). We found that higher EPDS scores prepartum were associated with non-breastfeeding rather than with exclusive breastfeeding three months after birth. The association with the postpartum EPDS score was less clear. Nevertheless, an association between depressive symptoms occurring around pregnancy and birth and non-breastfeeding at three months after delivery was, as hypothesized, definitely reflected in our results and supports previous studies which found similar relations 36 , 40 , 46 , 47 , 48 . Another study that focused on the factor of a "breastfeeding method" found that exclusive or non-exclusive breastfeeding did not significantly affect depression, anxiety, or mother–child-bonding in the early postpartum period nor vice versa 84 . However the authors attributed these results to the short observation period of one month after birth, among other factors.
Considerations that PPD could be triggered by breastfeeding difficulties 54 , 55 as a common source of stress 51 , 52 , are not supported by our results. According to Roth et al. (2021) breastfeeding difficulties are associated with lower bonding while postpartum depression has a negative impact on bonding quality regardless of breastfeeding difficulties: “The effect of breastfeeding difficulties on bonding persists over and above the effect of postnatal depressive symptoms” 85 . The authors concluded that postpartum depression and breastfeeding difficulties provide unique pathways for understanding bonding. A better understanding of bonding is relevant because studies have confirmed its importance, especially the importance of maternal sensitivity, for child development 86 . Furthermore, we found that with a higher PBQ score, mothers were signficantly more likely to report adding formula at the time point of three months than to exclusively breastfeed. To our knowledge, no study so far differentiated exclusive, mixed and formula feeding patterns with regard to mother-child-bonding in particular. Higher oxytocin levels may be of explanatory value for differences between exclusive and mixed breastfeeding. The quality of mother–child interrelations and maternal oxytocin levels appear to be positively correlated 87 , 88 , 89 , 90 . Oxytocin has also been found to be lower in patients with major depression 91 and with higher depression symptoms postpartum 47 , 92 .
However, following the argument of oxytocin levels and breastfeeding, it remains unclear why mothers who had not breastfed also reported a better bonding quality than mothers who practiced mixed feeding, which is different from our hypothesis. Mothers who added formula reported reasons such as insufficient weight gain and non-satiation of the infant for doing so significantly more often than mothers who did not breastfed. Clayton et al. (2013) already found that infant hunger was a predominant reason for mixed feeding, rather than bottle-feeding alone 93 . In addition, no mother who added formula cited self-referred reasons, such as convenience, less dependency, stress or simply “not feeling like it” for their decision, whereas mothers who did not breastfeed did report such reasons. These results indicate that the underlying impulses and prior experiences that lead to the decision whether to add formula or to wean differ. First, women who decide to wean seem to be more likely to make decisions in their own favor, as the postpartum period has negative effects on their quality of life 94 . Second, these women may have more self-confidence to face potential stigmas associated with the role of the mother and (discontinued) breastfeeding. Hence, they may be able to see their bond with their child as unaffected by less successful breastfeeding. The relationship between self-confidence, self-care and bonding has been well investigated 95 , 96 , 97 and may be of important explanatory value for our findings. Third, thinking that the child is not gaining enough weight or might be hungry could lead to feelings of guilt and cause stress. Postpartum stress decreases maternal self-confidence and affects the relationship between mother and child 98 . The decision to wean might be a relief for some women and reduce one source of postpartum stress. Symon et al. (2013) furthermore found the antenatal breastfeeding intention to be an important factor regarding satisfaction 99 . Maternal satisfaction scores were highest, when breastfeeding goals were reached, regardless of whether the goal was to breastfeed or intentionally not to do so 99 . Subsequently, regarding the given reasons to add formula, a possible explanation for higher PBQ scores of mixed feeding mothers in our sample could be, that they did not reach their breastfeeding goal, which subsequently resulted in a poorer rating of the bonding to their infant. However, more research is needed to prove our findings and conclusions, as the breastfeeding patterns, as distributed by us, and their association to mother–child-bonding, are to our knowledge still unexplored.
Our findings can be highly beneficial in terms of designing and disassembling preventive programs. They support for example indications to provide universal screening of previous depressive symptoms during pregnancy. It should be noted that screening in itself does not mean that depression can be definitively identified in an individual. Screening aims to identify as accurately as possible subpopulations with a high prevalence. A full diagnostic evaluation can only be made based on gold-standard clinical criteria 100 . Furthermore, peripartum maternal mental health is complex, as it comprises a variety of possible mental health problems 1 .
Screening should also be conducted postpartum, comprehensively, and with a special focus on at-risk populations. Especially reasons and impacts concerning a mixed feeding-style should be addressed in future research, to enable drawing more profound conclusions. Breastfeeding mothers with infants that do not gain enough weight or are not being sufficiently satiated, should especially be supported postpartum, as they tend to characterize their bonding as poorer, respectively. Education over these problems and possible solutions for them should get more attention during hospitalization and antepartum. According to our findings, mother–child-bonding seems to be an important variable in the issue of different feeding practices (exclusive, mixed, and non-breastfeeding). Depressive symptoms prepartum also seem to be an important variable in this context. We have not investigated to what extent the two are related. Although breastfeeding has many benefits for both the mother and the infant, the relationship between maternal mental health and breastfeeding is complex. It should be taken into consideration that breastfeeding may not be the most effective or viable option for all mothers 101 .
Limitations
Several points limiting our findings should be considered. Although we included several possible covariates in our analyses, confounding factors might remain. We also did not impute the missing values (this refers especially to the prepartum data). When recruiting participants for the study, we were aware that this was a sensitive issue and that we did not want to commit to the sample size initially. We did not perform a power analysis prior to recruitment. Besides that, we did not evaluate our data with respect to dropouts. Hence, we cannot completely rule out an attrition bias. Future studies should collect data concerning information over their dropouts, as previous studies already reported for example higher depression rates in groups with missing data 16 . However, inclusion in our study was not very restrictive and data collection took place in different in-hospital environments. This led to a large sample that is representative of the facilities in which they were collected. The reliability of the subscales physical well-being and coping during pregnancy of the Questionnaire "Feeling Comfortable During Pregnancy" was lower than expected and not significant in the correlations (Table 3 ) and thus excluded from the regression analyses, which needs to be addressed here. Even though all screening tools used in our study were established and validated, it should be noted that we exclusively used self-report measures. These can cause biases, for example through answering in a socially desirable manner 102 , 103 , 104 , which could be crucial for our findings regarding associations between poor bonding and high education 23 , 81 . Reck et al. (2006) reported similar findings and hypothesized that higher educated mothers would have a greater tendency to answer in a less socially desirable manner, rather than actually suffering from poorer bonding to their infants 23 . Mixed-measure designs could prevent such biases. Future studies should for example consider including structured diagnostic interviews, video observations of maternal behavior or biochemical analyses. Depressed women furthermore tend to rate themselves as worse parents than they are, due to a low self-esteem and negative thoughts 105 , 106 , which could have affected some of the associations we found.
Our findings provide important implications for future directions. These concern information regarding populations that may be at higher risk of developing PPD or a poor mother-child-bonding, such as antenatal depressive symptoms, or, representing to our knowledge a new finding, a mixed feeding style. However, more research is needed to get a more profound understanding of associations between mother–child-bonding and a mixed feeding style. Especially information about underlying reasons we found for performing mixed feeding, such as insufficient weight gain of the child or the feeling that the child was unsatiated, could contribute in a meaningful way to prevent impaired mother–child-bonding. We suggest implementing more measures supporting aspects such as self-efficacy and postpartum well-being of the mother in preventive programs.
Data availability
Due to the strict European General Data Protection Regulation the dataset generated in this study can not be deposited in a public repository. A request for access to the pseudonymized data for researchers who meet the criteria for access to confidential data must be submitted to the author: Clara Carvalho Hilje, email: [email protected].
Jomeen, J. in Mayes’ Midwifery , edited by S. Macdonald & G. Johnson (Elsevier, 2017), Vol. 15 186–199.
Razurel, C., Bruchon-Schweitzer, M., Dupanloup, A., Irion, O. & Epiney, M. Stressful events, social support and coping strategies of primiparous women during the postpartum period: a qualitative study. Midwifery 27 , 237–242 (2011).
Article CAS PubMed Google Scholar
Razurel, C., Kaiser, B., Sellenet, C. & Epiney, M. Relation between perceived stress, social support, and coping strategies and maternal well-being: A review of the literature. Women Health 53 , 74–99 (2013).
Article PubMed Google Scholar
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-5 , 5th ed (American Psychiatric Publishing, 2013).
Dorn, A. & Mautner, C. Postpartale depression. Interdisziplinäre Behandlung. Die Gynäkologie 51 , 94–101 (2018).
Article Google Scholar
Gaynes B. N. et al. in AHRQ Evidence Report Summaries , edited by B. N. Gaynes, et al. (Agency for Healthcare Research and Quality (US), 2005).
Howard, L. M. et al. Non-psychotic mental disorders in the perinatal period. Lancet 384 , 1775–1788 (2014).
Munk-Olsen, T., Laursen, T. M., Pedersen, C. B., Mors, O. & Mortensen, P. B. New parents and mental disorders: A population-based register study. JAMA 296 , 2582–2589 (2006).
Grigoriadis, S. et al. The impact of maternal depression during pregnancy on perinatal outcomes: A systematic review and meta-analysis. J. Clin. Psychiatry 74 , e321–e341 (2013).
DiPietro, J. A., Novak, M. F. S. X., Costigan, K. A., Atella, L. D. & Reusing, S. P. Maternal psychological distress during pregnancy in relation to child development at age two. Child Dev. 77 , 573–587 (2006).
Field, T. Prenatal depression risk factors, developmental effects and interventions: A review. J. Pregnancy Child Health 4 , 66 (2017).
Google Scholar
Gelaye, B., Rondon, M. B., Araya, R. & Williams, M. A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 3 , 973–982 (2016).
Article PubMed PubMed Central Google Scholar
Kim-Cohen, J., Caspi, A., Rutter, M., Tomás, M. P. & Moffitt, T. E. The caregiving environments provided to children by depressed mothers with or without an antisocial history. Am. J. Psychiatry 163 , 1009–1018 (2006).
Moehler, E., Brunner, R., Wiebel, A., Reck, C. & Resch, F. Maternal depressive symptoms in the postnatal period are associated with long-term impairment of mother–child bonding. Arch. Womens Ment. Health 9 , 273–278 (2006).
Murray, L., Halligan, S. L., Goodyer, I. & Herbert, J. Disturbances in early parenting of depressed mothers and cortisol secretion in offspring: A preliminary study. J. Aff. Disord. 122 , 218–223 (2010).
Article CAS Google Scholar
Netsi, E. et al. Association of persistent and severe postnatal depression with child outcomes. JAMA Psychiatry 75 , 247–253 (2018).
Öztop, D. & Uslu, R. Behavioral, interactional and developmental symptomatology in toddlers of depressed mothers: A preliminary clinical study within the DC:0–3 framework. Turk. J. Pediatr. 49 , 171–178 (2007).
PubMed Google Scholar
Behrendt, H. F. et al. Postnatal mother-to-infant attachment in subclinically depressed mothers: Dyads at risk?. Psychopathology 49 , 269–276 (2016).
Brockington, I. F. et al. A screening questionnaire for mother–infant bonding disorders. Arch. Womens Ment. Health 3 , 133–140 (2001).
Dubber, S., Reck, C., Müller, M. & Gawlik, S. Postpartum bonding: The role of perinatal depression, anxiety and maternal-fetal bonding during pregnancy. Arch. Womens Ment. Health 18 , 187–195 (2015).
Friedman, S. H. & Resnick, P. J. Postpartum depression: An update. Women’s Health 5 , 287–295 (2009).
Nonnenmacher, N., Noe, D., Ehrenthal, J. C. & Reck, C. Postpartum bonding: The impact of maternal depression and adult attachment style. Arch. Womens Ment. Health 19 , 927–935 (2016).
Reck, C. et al. The German version of the postpartum bonding instrument: Psychometric properties and association with postpartum depression. Arch. Womens Ment. Health 9 , 265–271 (2006).
Song, M. et al. Maternal depression and mother-to-infant bonding: The association of delivery mode, general health and stress markers. OJOG 07 , 155–166 (2017).
Fitzsimons, E. & Vera-Hernández, M. Breastfeeding and child development. Am. Econ. J. Appl. Econ. 14 , 329–366 (2022).
Smith-Nielsen, J., Tharner, A., Krogh, M. T. & Vaever, M. S. Effects of maternal postpartum depression in a well-resourced sample: Early concurrent and long-term effects on infant cognitive, language, and motor development. Scand. J. Psychol. 57 , 571–583 (2016).
Bowlby, J. Attachment and Loss (Basic Books, 1980).
Jansen, J., de Weerth, C. & Riksen-Walraven, J. M. Breastfeeding and the mother–infant relationship—A review. Dev. Rev. 28 , 503–521 (2008).
Brockington, I. F., Aucamp, H. M. & Fraser, C. Severe disorders of the mother–infant relationship: Definitions and frequency. Arch. Womens Ment Health 9 , 243–251 (2006).
Kumar, R. C. “Anybody’s child”: Severe disorders of mother-to-infant bonding. Br. J. Psychiatry 171 , 175–181 (1997).
Field, T., Healy, B. T., Goldstein, S. & Guthertz, M. Behavior-state matching and synchrony in mother–infant interactions of nondepressed versus depressed dyads. Dev. Psychol. 26 , 7–14 (1990).
Alimi, R., Azmoude, E., Moradi, M. & Zamani, M. The association of breastfeeding with a reduced risk of postpartum depression: A systematic review and meta-analysis. Breastfeed Med. 17 , 290–296 (2022).
Figueiredo, B., Canário, C. & Field, T. Breastfeeding is negatively affected by prenatal depression and reduces postpartum depression. Psychol. Med. 44 , 927–936 (2014).
Govoni, L. et al. Breastfeeding pathologies: Analysis of prevalence, risk and protective factors. Acta Biomed. 90 , 56–62 (2019).
Ip, S. et al. Breastfeeding and maternal and infant health outcomes in developed countries. Evid. Rep. Technol. Assess 66 , 1–186 (2007).
McCoy, S. J. B., Beal, M. J., Shipman, S. B. M., Payton, M. E. & Watson, G. H. Risk factors for postpartum depression: A retrospective investigation at 4-weeks postnatal and a review of the literature. Int. J. Osteopath. Med. 106 , 193–198 (2006).
Mezzacappa, E. S. & Katlin, E. S. Breast-feeding is associated with reduced perceived stress and negative mood in mothers. Health Psychol. 21 , 187–193 (2002).
Strathearn, L., Mamun, A. A., Najman, J. M. & O’Callaghan, M. J. Does breastfeeding protect against substantiated child abuse and neglect? A 15-year cohort study. Pediatrics 123 , 483–493 (2009).
Weaver, J. M., Schofield, T. J. & Papp, L. M. Breastfeeding duration predicts greater maternal sensitivity over the next decade. Dev. Psychol. 54 , 220–227 (2018).
Webber, E. & Benedict, J. Postpartum depression: A multi-disciplinary approach to screening, management and breastfeeding support. Arch. Psychiatr. Nurs. 33 , 284–289 (2019).
Xia, M., Luo, J., Wang, J. & Liang, Y. Association between breastfeeding and postpartum depression: A meta-analysis. J. Aff. Disord. 308 , 512–519 (2022).
Dias, C. C. & Figueiredo, B. Breastfeeding and depression: A systematic review of the literature. J. Aff. Disord. 171 , 142–154 (2015).
Seimyr, L., Edhborg, M., Lundh, W. & Sjögren, B. In the shadow of maternal depressed mood: Experiences of parenthood during the first year after childbirth. J. Psychosom. Obstet. Gynaecol. 25 , 23–34 (2004).
Silva, C. S. et al. Association between postpartum depression and the practice of exclusive breastfeeding in the first three months of life. Jornal de Pediatria 93 , 356–364 (2017).
Dennis, C.-L. & McQueen, K. The relationship between infant-feeding outcomes and postpartum depression: a qualitative systematic review. Pediatrics 123 , e736–e751 (2009).
Kendall-Tackett, K., Cong, Z. & Hale, T. W. The effect of feeding method on sleep duration, maternal well-being, and postpartum depression. Clin. Lactation 2 , 22–26 (2011).
Lara-Cinisomo, S., McKenney, K., Di Florio, A. & Meltzer-Brody, S. Associations between postpartum depression, breastfeeding, and oxytocin levels in latina mothers. Breastfeed Med. 12 , 436–442 (2017).
Nishioka, E. et al. A prospective study of the relationship between breastfeeding and postpartum depressive symptoms appearing at 1–5 months after delivery. J. Aff. Disord. 133 , 553–559 (2011).
Taveras, E. M. et al. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics 112 , 108–115 (2003).
Watkins, S., Meltzer-Brody, S., Zolnoun, D. & Stuebe, A. Early breastfeeding experiences and postpartum depression. Obstet. Gynecol. 118 , 214–221 (2011).
Brown, A., Rance, J. & Bennett, P. Understanding the relationship between breastfeeding and postnatal depression: The role of pain and physical difficulties. J. Adv. Nurs. 72 , 273–282 (2016).
Chaput, K. H., Nettel-Aguirre, A., Musto, R., Adair, C. E. & Tough, S. C. Breastfeeding difficulties and supports and risk of postpartum depression in a cohort of women who have given birth in Calgary: A prospective cohort study. CMAJ Open 4 , E103–E109 (2016).
Borra, C., Iacovou, M. & Sevilla, A. New evidence on breastfeeding and postpartum depression: The importance of understanding women’s intentions. Matern. Child Health J. 19 , 897–907 (2015).
Henshaw, E. J., Fried, R., Siskind, E., Newhouse, L. & Cooper, M. Breastfeeding self-efficacy, mood, and breastfeeding outcomes among primiparous women. J. Hum. Lact. 31 , 511–518 (2015).
Lion, C. Ph.D. (Walden University, 2011).
Ettenberger, M., Bieleninik, Ł, Epstein, S. & Elefant, C. Defining attachment and bonding: Overlaps, Differences and implications for music therapy clinical practice and research in the neonatal intensive care unit (NICU). Int. J. Environ. Res. Public Health 18 , 66 (2021).
Davis, A. M. B. & Sclafani, V. Birth experiences, breastfeeding, and the mother–child relationship: Evidence from a large sample of mothers. Can. J. Nurs. Res. 54 , 518–529 (2022).
Else-Quest, N. M., Hyde, J. S. & Clark, R. Breastfeeding, bonding, and the mother–infant relationship. Merrill Palmer Q 49 , 495–517 (2003).
Hairston, I. S., Handelzalts, J. E., Lehman-Inbar, T. & Kovo, M. Mother–infant bonding is not associated with feeding type: a community study sample. BMC Pregnancy Childb. 19 , 125 (2019).
Minamida, T. et al. Do postpartum anxiety and breastfeeding self-efficacy and bonding at early postpartum predict postpartum depression and the breastfeeding method?. Infant Ment. Health J. 41 , 662–676 (2020).
Papp, L. M. Longitudinal associations between breastfeeding and observed mother–child interaction qualities in early childhood. Child Care Health Dev. 40 , 740–746 (2014).
Keller, N., Medved, V. & Armano, G. The influence of maternal personality and risk factors for impaired mother–infant bonding on breastfeeding duration. Breastfeed Med. 11 , 532–537 (2016).
Linde, K., Lehnig, F., Nagl, M. & Kersting, A. The association between breastfeeding and attachment: A systematic review. Midwifery 81 , 102592 (2020).
Peñacoba, C. & Catala, P. Associations between breastfeeding and mother–infant relationships: A systematic review. Breastfeed Med. 14 , 616–629 (2019).
Whittingham, K. & Mitchell, A. E. Birth, breastfeeding, psychological flexibility and self-compassion as predictors of mother–infant emotional availability in a cross-sectional study. Infant Ment. Health J. 42 , 718–730 (2021).
Scharfe, E. Maternal attachment representations and initiation and duration of breastfeeding. J. Hum. Lact. 28 , 218–225 (2012).
Kim, S.-H. Factors associated with maternal attachment of breastfeeding mothers. Child Health Nurs. Res. 25 , 65–73 (2019).
Smith, J. P. & Ellwood, M. Feeding patterns and emotional care in breastfed infants. Soc. Indic. Res. 101 , 227–231 (2011).
Bergant, A. M., Nguyen, T., Heim, K., Ulmer, H. & Dapunt, O. Deutschsprachige Fassung und Validierung der “Edinburgh postnatal depression scale”. Dtsch Med Wochenschr 123 , 35–40 (1998).
Cox, J. L., Holden, J. M. & Sagovsky, R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 150 , 782–786 (1987).
Cox, J. L., Chapman, G., Murray, D. & Jones, P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J. Aff. Disord. 39 , 185–189 (1996).
Matthey, S., Henshaw, C., Elliott, S. & Barnett, B. Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale: Implications for clinical and research practice. Arch. Womens Ment. Health 9 , 309–315 (2006).
Wittkowski, A., Wieck, A. & Mann, S. An evaluation of two bonding questionnaires: A comparison of the Mother-to-Infant Bonding Scale with the Postpartum Bonding Questionnaire in a sample of primiparous mothers. Arch. Womens Ment. Health 10 , 171–175 (2007).
Ayerle, G. & Gross, M. Psychometric assessment of subjective well-being and coping in pregnancy. Z. Med. Psychol. 19 , 12–20 (2010).
Field, A. Discovering Statistics Using IBM SPSS Statistics. And Sex and Drugs and Rock 'n' Roll 4th ed. (Sage, 2013).
Lumley, T., Diehr, P., Emerson, S. & Chen, L. The importance of the normality assumption in large public health data sets. Annu. Rev. Public Health 23 , 151–169 (2002).
Declercq, E., Labbok, M. H., Sakala, C. & O’Hara, M. Hospital practices and women’s likelihood of fulfilling their intention to exclusively breastfeed. Am. J. Public Health 99 , 929–935 (2009).
Goecke, T. W. et al. The association of prenatal attachment and perinatal factors with pre- and postpartum depression in first-time mothers. Arch. Gynecol. Obstet. 286 , 309–316 (2012).
Handelzalts, J. E. et al. Associations of rooming-in with maternal postpartum bonding: The impact of mothers’ pre-delivery intentions. Midwifery 95 , 102942 (2021).
Hawkins, S. S., Stern, A. D., Baum, C. F. & Gillman, M. W. Compliance with the baby-friendly hospital initiative and impact on breastfeeding rates. Arch. Dis. Child Fetal. Neonatal Ed. 99 , F138–F143 (2014).
van Bussel, J. C. H., Spitz, B. & Demyttenaere, K. Three self-report questionnaires of the early mother-to-infant bond: Reliability and validity of the Dutch version of the MPAS, PBQ and MIBS. Arch. Womens Ment. Health 13 , 373–384 (2010).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences 2nd ed. (Erlbaum, 1988).
Backhaus, K., Erichson, B., Plinke, W. & Weiber, Rs. Multivariate Analysemethoden. Eine anwendungsorientierte Einführung , 13th ed. (Springer, 2011).
Fukui, N. et al. Exclusive breastfeeding is not associated with maternal–infant bonding in early postpartum, considering depression, anxiety, and parity. Nutrients 13 , 66 (2021).
Roth, M. C., Humphreys, K. L., King, L. S., Gotlib, I. H. & Robakis, T. K. Breastfeeding difficulties predict mothers’ bonding with their infants from birth to age six months. Matern. Child Health J. 25 , 777–785 (2021).
Soares, H., Barbieri-Figueiredo, M., Pereira, S., Silva, M. & Fuertes, M. Parents attending to nurse visits and birth age contribute to infant development: A study about the determinants of infant development. Early Hum. Dev. 122 , 15–21 (2018).
Galbally, M., Lewis, A. J., van Ijzendoorn, M. & Permezel, M. The role of oxytocin in mother–infant relations: A systematic review of human studies. Harv. Rev. Psychiatry 19 , 1–14 (2011).
Levine, A., Zagoory-Sharon, O., Feldman, R. & Weller, A. Oxytocin during pregnancy and early postpartum: Individual patterns and maternal-fetal attachment. Peptides 28 , 1162–1169 (2007).
McErlean, R. & Eape, V. in Perinatal Depression , edited by M. Graciela Rojas Castillo 39–54 (IntechOpen, 2012).
Meyer-Lindenberg, A., Domes, G., Kirsch, P. & Heinrichs, M. Oxytocin and vasopressin in the human brain: Social neuropeptides for translational medicine. Nat. Rev. Neurosci. 12 , 524–538 (2011).
Scantamburlo, G. et al. Plasma oxytocin levels and anxiety in patients with major depression. Psychoneuroendocrinology 32 , 407–410 (2007).
Stuebe, A. M., Grewen, K. & Meltzer-Brody, S. Association between maternal mood and oxytocin response to breastfeeding. J. Womens Health 22 , 352–361 (2013).
Clayton, H. B., Li, R., Perrine, C. G. & Scanlon, K. S. Prevalence and reasons for introducing infants early to solid foods: Variations by milk feeding type. Pediatrics 131 , e1108–e1114 (2013).
Özdemir, F., Öztürk, A., Karabulutlu, Ö. & Tezel, A. Determination of the life quality and self-care ability of the mothers in post-partum period. J. Pak. Med. Assoc. 68 , 210–215 (2018).
Barbosa, E. M. G. et al. Educational technologies to encourage (self) care in postpartum women. Rev. Bras Enferm 69 , 582–590 (2016).
Kadiroğlu, T. & Güdücü Tüfekci, F. Effect of infant care training on maternal bonding, motherhood self-efficacy, and self-confidence in mothers of preterm newborns. Matern. Child Health J. 26 , 131–138 (2022).
Zietlow, A.-L., Schlüter, M. K., Nonnenmacher, N., Müller, M. & Reck, C. Maternal self-confidence postpartum and at pre-school age: The role of depression, anxiety disorders, maternal attachment insecurity. Matern. Child Health J. 18 , 1873–1880 (2014).
Moghaddam Tabrizi, F. & Nournezhad, H. The effect of family support based counselling on postnatal perceived stress and mother–child bonding in nulliparous women to health centers in Urmia in 2016–2017. Nurs. Midwif. J. 16 , 109–121 (2018).
Symon, A. G., Whitford, H. & Dalzell, J. Infant feeding in Eastern Scotland: A longitudinal mixed methods evaluation of antenatal intentions and postnatal satisfaction—The Feeding Your Baby study. Midwifery 29 , e49-56 (2013).
Fisher, J., Rahman, A., Cabral de Mello, M., Chandra, P. S. & Herrman, H. in Parenthood and Mental Health , edited by S. Tyano, M. Keren, H. Herrman & J. Cox 429–442 (Wiley, 2010).
Vanderkruik, R., Lemon, E. & Dimidjian, S. Breastfeeding support and messaging: A call to integrate public health and psychological perspectives. Matern. Child Health J. 19 , 2545–2547 (2015).
Cuixia, L., Jian, X. & Zhongfang, Y. A compromise between self-enhancement and honesty: Chinese self-evaluations on social desirability scales. Psychol. Rep. 92 , 291–298 (2003).
Tourangeau, R., Rips, L. J. & Rasinski, K. The Psychology of Survey Response (Cambridge University Press, 2000).
Wlömert, N., Pellenwessel, D., Fox, J.-P. & Clement, M. Multidimensional assessment of social desirability bias: An application of multiscale item randomized response theory to measure academic misconduct. J. Surv. Stat. Methodol. 7 , 365–397 (2019).
Frankel, K. A. & Harmon, R. J. Depressed mothers: They don’t always look as bad as they feel. J. Am. Acad. Child Adolesc. Psychiatry 35 , 289–298 (1996).
Hornstein, C., Schenk, S., Wortmann-Fleischer, S., Downing, G. & Schwarz, M. Videotherapie bei postpartalen Störungen. Psychotherapeut 51 , 363–368 (2006).
Download references
Acknowledgements
We would like to thank the women who were willing to participate in this study. Furthermore, we would like to thank the Gerhard-Kienle-Foundation for supporting the study.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and affiliations.
Department of Pediatrics, Gemeinschaftskrankenhaus Herdecke, Herdecke, Germany
Clara Carvalho Hilje, Daniela Reis & Alfred Längler
Professorship for Integrative Pediatrics, Institute for Integrative Medicine, Witten/Herdecke University, Witten, Germany
Institute of Midwifery Science, Faculty of Medicine, University of Cologne, Cologne, Germany
Nicola H. Bauer
Department of Psychology and Psychotherapy, Faculty of Health, Witten/Herdecke University, Witten, Germany
Claudia Kapp & Thomas Ostermann
Department of Obstetrics, Gemeinschaftskrankenhaus Herdecke, Herdecke, Germany
Franziska Vöhler
You can also search for this author in PubMed Google Scholar
Contributions
C.C.H., F.V., N.B., C.K. and A.L. conceived and designed the idea for the study and the manuscript, while C.K. was mainly supporting the data collection. C.C.H. wrote the manuscript of the paper and created together with D.R. the tables. C.C.H., N.B., D.R., C.K., T.O., F.V. and A.L. reviewed and edited the draft of the paper independently until consensus was reached on the final version. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Daniela Reis .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Carvalho Hilje, C., Bauer, N.H., Reis, D. et al. The role of breastfeeding and formula feeding regarding depressive symptoms and an impaired mother child bonding. Sci Rep 14 , 11417 (2024). https://doi.org/10.1038/s41598-024-62168-y
Download citation
Received : 06 February 2024
Accepted : 14 May 2024
Published : 19 May 2024
DOI : https://doi.org/10.1038/s41598-024-62168-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
May 22, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
Health and economic benefits of breastfeeding quantified
by Public Library of Science
Breastmilk can promote equitable child health and save health care costs by reducing childhood illnesses and health care utilization in the early years, according to a new study published in the open-access journal PLOS ONE by Tomi Ajetunmobi of the Glasgow Center for Population Health, Scotland, and colleagues.
Breastfeeding has previously been found to promote development and prevent disease among infants. In Scotland—as well as other developed countries—low rates of breastfeeding in more economically deprived areas are thought to contribute to inequalities in early childhood health. However, government policies to promote child health have made little progress and more evidence on the effectiveness of interventions may be needed.
In the new study, researchers used administrative datasets on 502,948 babies born in Scotland between 1997 and 2009. Data were available on whether or not infants were breastfed during the first 6–8 weeks, the occurrence of ten common childhood conditions from birth to 27 months, and the details of hospital admissions, primary care consultations and prescriptions.
Among all infants included in the study, 27% were exclusively breastfed, 9% mixed fed and 64% formula fed during the first 6-8 weeks of life. The rates of exclusively breastfed infants ranged from 45% in the least deprived areas to 13% in the most deprived areas.
The researchers found that, within each quintile of deprivation, exclusively breastfed infants used fewer health care services and incurred lower costs compared to infants fed any formula milk.
On average, breastfed infants had lower average costs of hospital care per admission (£42) compared to formula-fed infants (£79) in the first six months of life and fewer GP consultations (1.72, 95% CI: 1.66–1.79) than formula-fed infants (1.92 95% CI: 1.88–1.94). At least £10 million of health care costs could have been avoided if all formula-fed infants had instead been exclusively breastfed for the first 6–8 weeks of life, the researchers calculated.
The authors conclude that breastfeeding has a significant health and economic benefit and that increasing breastfeeding rates in the most deprived areas could contribute to the narrowing of inequalities in the early years.
Explore further
Feedback to editors

New study shows heat waves increase risk of preterm, early-term birth

New therapy proven effective against rejection in kidney transplantation
2 hours ago

Cell-targeting technology can isolate neuronal subpopulations and link them to behavioral states

First seizure clinics reduce the need for future health care, researchers find

International study reveals surprising twist in how diabetes drugs help the heart
3 hours ago

Sanfilippo syndrome: Research team resolves structure of crucial enzyme for the first time

Physical frailty may put people at greater risk of depression, study finds

Study demonstrates how gut microbes process steroids—using flatulence

Eating more fruits and vegetables may lead to optimal sleep duration

Study finds feeding infants peanut products protects against allergy into adolescence
Related stories.

Study compares stools of breastfed and formula-fed infants
Nov 7, 2018

Weaning occurs earlier for infants with in-hospital formula feeding
Jun 10, 2020

Breastfed babies less likely to be given treats, sweetened drinks before 12 months: Study
Feb 21, 2024

Low-dose iron supplementation has no benefit for breastfed infants, shows study
May 20, 2024

Infant gut microbes have their own circadian rhythm: Study finds diet has little impact on how the microbiome assembles
Apr 2, 2024

Exclusive breastfeeding in hospital associated with longer breastfeeding duration
Mar 12, 2018
Recommended for you

Integration of pharmacies with physician practices has little impact on cancer drug expenditures, study finds
May 24, 2024

Poor access to essential surgery is costing lives, says study
May 23, 2024

Exposure to endocrine-disrupting chemicals in utero associated with higher odds of metabolic syndrome in children

Mental disorders may spread in young people's social networks
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy

Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Health and economic benefits of breastfeeding quantified
Among half a million scottish infants, those exclusively breastfed were less likely to use healthcare services and incurred lower costs to the healthcare system.
Breastmilk can promote equitable child health and save healthcare costs by reducing childhood illnesses and healthcare utilization in the early years, according to a new study published this week in the open-access journal PLOS ONE by Tomi Ajetunmobi of the Glasgow Centre for Population Health, Scotland, and colleagues.
Breastfeeding has previously been found to promote development and prevent disease among infants. In Scotland -- as well as other developed countries -- low rates of breastfeeding in more economically deprived areas are thought to contribute to inequalities in early childhood health. However, government policies to promote child health have made little progress and more evidence on the effectiveness of interventions may be needed.
In the new study, researchers used administrative datasets on 502,948 babies born in Scotland between 1997 and 2009. Data were available on whether or not infants were breastfed during the first 6-8 weeks, the occurrence of ten common childhood conditions from birth to 27 months, and the details of hospital admissions, primary care consultations and prescriptions.
Among all infants included in the study, 27% were exclusively breastfed, 9% mixed fed and 64% formula fed during the first 6-8 weeks of life. The rates of exclusively breastfed infants ranged from 45% in the least deprived areas to 13% in the most deprived areas.
The researchers found that, within each quintile of deprivation, exclusively breastfed infants used fewer healthcare services and incurred lower costs compared to infants fed any formula milk. On average, breastfed infants had lower average costs of hospital care per admission (£42) compared to formula-fed infants (£79) in the first six months of life and fewer GP consultations (1.72, 95% CI: 1.66 -- 1.79) than formula-fed infants (1.92 95% CI: 1.88 -- 1.94). At least £10 million of healthcare costs could have been avoided if all formula-fed infants had instead been exclusively breastfed for the first 6-8 weeks of life, the researchers calculated.
The authors conclude that breastfeeding has a significant health and economic benefit and that increasing breastfeeding rates in the most deprived areas could contribute to the narrowing of inequalities in the early years.
- Breastfeeding
- Infant's Health
- Today's Healthcare
- Health Policy
- Public Health
- Disaster Plan
- Poverty and Learning
- Education and Employment
- Early childhood education
- Upper respiratory tract infection
- Social inclusion
- Health science
- Evidence-based medicine
Story Source:
Materials provided by PLOS . Note: Content may be edited for style and length.
Journal Reference :
- Omotomilola Ajetunmobi, Emma McIntosh, Diane Stockton, David Tappin, Bruce Whyte. Levelling up health in the early years: A cost-analysis of infant feeding and healthcare . PLOS ONE , 2024; 19 (5): e0300267 DOI: 10.1371/journal.pone.0300267
Cite This Page :
Explore More
- Future Climate Impacts Put Whale Diet at Risk
- Charge Your Laptop in a Minute?
- Caterpillars Detect Predators by Electricity
- 'Electronic Spider Silk' Printed On Human Skin
- Engineered Surfaces Made to Shed Heat
- Innovative Material for Sustainable Building
- Human Brain: New Gene Transcripts
- Epstein-Barr Virus and Resulting Diseases
- Origins of the Proton's Spin
- Symbiotic Bacteria Communicate With Plants
Trending Topics
Strange & offbeat.
- Open access
- Published: 26 May 2024
State paid family leave policies and breastfeeding duration: cross-sectional analysis of 2021 national immunization survey-child
- Julia Rosenberg 1 ,
- Deanna Nardella 1 , 2 &
- Veronika Shabanova 1 , 3
International Breastfeeding Journal volume 19 , Article number: 37 ( 2024 ) Cite this article
Metrics details
Paid parental leave policies may promote breastfeeding, which can have short- and long-term health benefits for both members of the birthing person-infant dyad. In the United States, where 56% of the workforce qualifies for unpaid federal medical leave, certain states have recently enacted paid parental and family leave policies. We aimed to assess the extent to which living in states with versus without paid family leave was associated with feeding regimens that included breastfeeding.
In this cross-sectional analysis of the 2021 National Immunization Survey-Child, we assessed feeding outcomes: (1) exclusively breastfed (only fed breastmilk—never infant formula—both before and after six months of age), (2) late mixed breastfeeding (formula after six months), (3) early mixed breastfeeding (breastfed, formula before six months), and (4) never breastfed. We conducted Pearson χ 2 to compare social-demographic characteristics and multivariable nominal regression to assess extent to paid family leave was associated with breastfeeding regimens, compared with never breastfeeding.
Of the 35,995 respondents, 5,806 (25% of weighted respondents) were from states with paid family leave policies. Compared with never breastfeeding, all feeding that incorporated breastfeeding—exclusive breastfeeding, late mixed feeding (breastfed, formula introduced after six months), and early mixed feeding (breastfed, formula introduced before six months)—were more prevalent in states with paid family leave policies. The adjusted prevalence ratio (aPR) and differences in adjusted prevalence compared with never breastfeeding in states with versus without paid family leave policies were: aPR 1.41 (95% CI 1.15, 1.73), 5.36% difference for exclusive breastfeeding; aPR 1.25 (95% CI 1.01, 1.53), 3.19% difference for late mixed feeding, aPR 1.32 (95% CI 1.32, 1.97), 5.42% difference for early mixed feeding.
States with paid family leave policies have higher rates of any breastfeeding and of exclusive breastfeeding than states without such policies. Because all feeding types that incorporate breastfeeding were higher in states with paid family leave policies, expansion of paid family leave may improve breastfeeding rates.
The short- and long-term benefits of breastfeeding for both members of the birthing person-infant dyad have been well-established. The American Academy of Pediatrics, the American College of Obstetrics and Gynecology, and the World Health Organization promote exclusive breastfeeding for six months followed by continued breastfeeding until one to two years of age [ 1 , 2 , 3 ]. For newborns, sustained breastfeeding is associated with decreased adverse health consequences including lower rates of infant mortality and lower incidence of sudden infant death syndrome; respiratory, ear, and gastrointestinal infections; asthma; eczema; autoimmune conditions; and diabetes [ 2 ]. While exclusive breastfeeding without infant formula introduction is recommended to maximize benefits, data suggest protective effects of any breastfeeding against gastrointestinal illnesses, ear infections, asthma, and obesity [ 4 , 5 , 6 ]. For birthing people, breastfeeding is associated with decreased rates of hypertension, diabetes, and certain types of cancer [ 1 , 2 ]. In addition to the individual benefits, breastfeeding promotes dyadic health with opportunities for bonding and benefits for mental and physical health [ 7 ]. According to the Centers for Disease Control and Prevention (CDC) breastfeeding report card, in 2019, only 25% of infants born in the United States (US) exclusively breastfed until six months of age and about 36% were breastfeeding at one year [ 8 ], falling short of the US Healthy People 2030 targets of 42.4% and 54.1%, respectively [ 9 ].
A major barrier to sustained breastfeeding can be caregivers returning to work. Globally, longer maternity leave is associated with higher rates of breastfeeding [ 10 ]. In the US, exclusive breastfeeding decreases by approximately 25% within the first week of life, nearly 50% by three months, and 70% by six months, correlating with return to work for many parents [ 8 ].
With nearly two-thirds of females participating in the US workforce having a child under three years of age [ 11 ], the need to establish and evaluate policies that protect breastfeeding for working lactating persons has been underscored in formal recommendations, including through the Surgeon General’s Calls to Action to Support Breastfeeding and to Improve Maternal Health and the 2022 White House National Strategy on Hunger, Nutrition and Health [ 12 , 13 , 14 ]. Despite these recommendations, the US is the only country in the Organization for Economic Cooperation and Development (OECD) to not offer a paid federal family leave policy [ 15 , 16 ].
Federal US Legislation supporting unpaid leave and lactation includes the 1993 Family Medical Leave Act (FMLA), the 2010 Patient Protection and Affordable Care Act, and the 2021 Providing Urgent Maternal Protections for Nursing Mothers (PUMP) Act [ 17 ]. Federal FMLA stipulates 12 weeks of unpaid, job-protective leave for care of a child [ 18 ]. A growing number of states and regions have enacted paid family leave policies. As of 2024, 17 US states and Washington, DC have active paid family leave policies, with five states’ legislation to be enacted in future years (Fig. 1 ) [ 19 ].
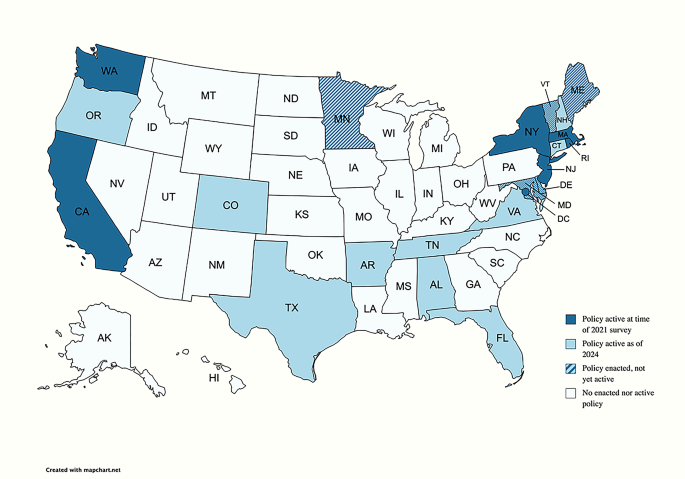
Primary exposure of interest: paid family leave policy status by US state
In this cross-sectional study, we aimed to assess the relationship of paid family leave with a spectrum of breastfeeding outcomes, including metrics of breastfeeding duration and exclusivity, at the population level. We hypothesized that residence in US states with paid family leave policies is associated with higher rates of both exclusive and any breastfeeding.
Data source
This cross-sectional, secondary dataset analysis was conducted using data from the 2021 National Immunization Survey-Child (NIS-C), which included the fifty US states and Washington, DC. The National Immunization Surveys (NIS), which includes NIS-C, are telephone surveys administered via random digit dialing to a stratified representative US sample, conducted by the CDC’s National Center for Immunization and Respiratory Disease. The NIS-C incorporates data from parent/guardian interviews and from questionnaires sent to medical providers to evaluate multiple domains of health, including immunization, breastfeeding, and usage of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) program. The 2021 NIS-C target population included US families of children who were 19–35 months old during calendar year 2021. The survey was translated into English and Spanish, and other languages were queried using telephonic interpretation [ 20 , 21 ].
The NIS-C is a publicly available, de-identified dataset. Its use is not considered Human Subjects Research, and we did not obtain a determination of this status from the Institutional Review Board. We followed the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines for cross-sectional observational data (Additional File 1 ) [ 22 ].
Study variable terminology
When analyzing and presenting data, we used terminology as reported in the NIS-C dataset, which includes terms such as breastfeeding and mother, rather than gender-inclusive terms such as chest feeding and birthing person [ 23 , 24 ].
States with and without paid family leave policies
The locations with paid family leave policies at the time of the 2021 NIS-C included California, Massachusetts, New Jersey, New York, Rhode Island, Washington, and Washington, DC (Fig. 1 ). All other states without active paid family leave policies were grouped together, and Puerto Rico was excluded. Three locations—Washington DC, Massachusetts, and Washington—had aspects of their policies enacted in 2020, so some of the surveyed families may have given birth before full enactment. Thus, post-hoc sensitivity analyses were also conducted with these locations removed from analyses.
Primary outcome
The primary outcome was a composite variable reflecting breastmilk and infant formula feeding. To construct this variable, we accounted for three NIS-C variables that assessed if the child ever was fed breastmilk, duration of breastfeeding, and the date of first formula introduction. The finalized infant feeding primary outcome is summarized in Fig. 2 and includes four categories: (1) exclusively breastfed for the duration captured by data (without formula introduction), (2) late mixed breastfeeding (breastfed exclusively until six months, introduced formula after 6 months), and (3) early mixed breastfeeding (breastfed, introduced formula either before six months of age or at unknown time), and (4) never breastfed. “Exclusively breastfed” refers to receiving breastmilk and never infant formula as source of nutrition but may include supplementary, non-infant formula foods. Because the primary outcome centered around breastfeeding, the 141 respondents with unknown breastfeeding data were excluded from the analysis (see Additional File 2 for characteristics of excluded respondents, who could be considered as non-respondents generally due to high rates of missingness for other variables).
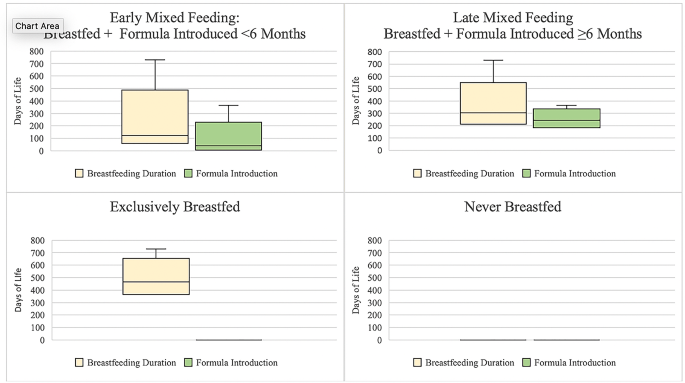
Total days of breastfeeding duration and first day of formula by primary outcome of infant feeding category. Legend: “Exclusively breastfed” refers to receiving breastmilk and never infant formula as source of nutrition but may include supplementary, non-infant formula foods. Figure includes maximum (upper whisker) but not minimum values, as some respondents who reported exclusive breastfeeding had very few days of breastfeeding reported, which we assumed to be errors in reporting. Box indicates upper and lower quartiles. Line indicates median. Adjusted n’s: Exclusively Breastfed n = 6,579.82, Late Mixed Feeding n = 5,899.27, Early Mixed Feeding n = 16,312.40, Never Breastfed n = 5,9343.9
Covariate selection
Based on prior studies of breastfeeding outcomes and available data in the NIS-C, selected covariates included: maternal age, infant age, infant sex, infant race and ethnicity (as reported by the NIS-C dataset), household size, children in the home, maternal education, marital status, language of interviews, poverty level, and WIC enrollment [ 2 ]. In order to control for policies that may affect breastfeeding outcomes at the state level, we also developed a covariate to account for workplace lactation protection policies; thirty states and the District of Columbia have such protections in place [ 25 ].
Statistical analyses
Since the data were collected using stratified random sampling, survey responses have been weighted by the weights provided by the NIS-C, to reflect strata and non-response. Simple descriptive statistics (count, percent) and Pearson χ 2 tests were used to describe and compare the social and demographic characteristics of children and mothers from states that did and did not have active paid family leave policies in 2021 (Table 1 ).
We used multivariable nominal regression to examine the extent to which the primary exposure variable of residence in states with and without paid family leave policies in 2021 was associated with the primary outcome of any infant feeding regimen that included breastfeeding, compared with never breastfeeding. In this multivariable regression, we controlled for a priori chosen covariates, all of which were retained in the adjusted model and are displayed in Tables 1 and 2 . Results are reported as adjusted estimates of prevalence of each feeding regimen (as percentages within each outcome level); differences between adjusted prevalence of breastfeeding outcomes (exclusive, late mixed, early mixed) and adjusted prevalence of never breastfeed; and unadjusted and adjusted prevalence ratios (PR, aPR) with 95% confidence intervals (CI), which were obtained postestimation via linear combinations of relevant parameters and use of marginal mean statement [ 26 ]. As noted in the description of the independent variable (states with and without family leave policies), we also conducted post-hoc sensitivity analyses without states where implementation of policies occurred during the study period. Because we were interested in the effect of paid family leave on a spectrum of breastfeeding outcomes that corresponded to independent hypotheses, we did not adjust for multiple comparisons [ 27 , 28 ].
Given the predetermined sample size by the NIS-C, our conclusions are based on the magnitude of the PR and surrounding 95% CI, rather than the p-values [ 29 , 30 ]. We further defined a meaningful magnitude of difference in the prevalence of breastfeeding at the 1% point, which reflects the change noted in the prior three years of exclusive breastfeeding in the United States, per Healthy People 2030 [ 9 ].
We completed analyses in Stata Version 15 (StataCorp College Station, Texas).
Sociodemographic characteristics by state paid family leave policy
As shown in Table 1 , of the 34,722 NIS-C unweighted survey respondents from 2021, 5,806 were from states with paid family leave policies, and they accounted for 25% of weighted survey respondents. We did not observe a meaningful difference between states with and without paid family leave policies in terms of infant sex, infant age, or household size. Differences were noted when assessing breastfeeding workplace policies, maternal age, number of children in the home, parental education, marital status, language of the interview, poverty level, and WIC enrollment (Table 1 ). Families in states with paid parental leave policies were more likely to reside in states that had workplace breastfeeding protections, report that the mother was over 29 years old, the infant was of Hispanic/Latino ethnicity, there were fewer children in the home, the mother graduated college, the mother was married, and that the income was above poverty and above $75,000. They were less likely to report being enrolled in WIC (Table 1 ).
Infant feeding patterns by state paid family leave policy
Exclusive breastfeeding was more prevalent in states with paid family leave policies than in states without such policies: 20.36% (95% CI 18.46%, 22.26%) in states with policies vs. 18.48% (95% CI 17.74%, 19.22%) in states without policies. Late mixed breastfeeding was similar in states with vs. without paid family leave: 16.78% (95% CI 14.97%, 18.60%) vs. 17.09% (95% CI 16.30%, 17.88%). Early mixed breastfeeding was more prevalent in states with vs. without paid family leave: 48.48% (95% CI 46.00%, 50.97%) vs. 46.55% (95% CI 45.47%, 47.64%). Fewer reported never breastfeeding in states with paid family leave: 14.38% (95% CI 12.52%, 16.23%) vs. 17.87% (95% CI 16.98%, 18.76%) (Fig. 3 ).
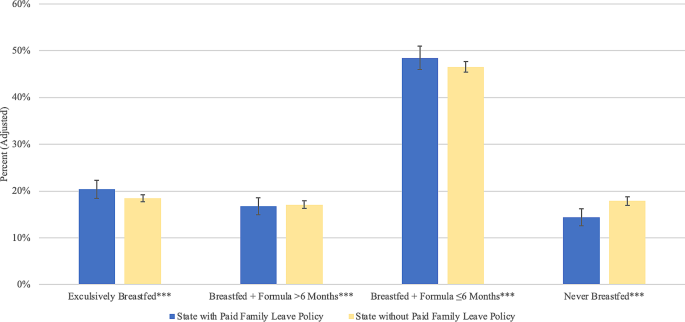
Adjusted prevalence of breastfeeding outcomes by US state paid family leave policies, National Immunization Survey-Child, 2021. Legend: Reported values are estimated prevalence of each feeding type. Error bars correspond to 95% confidence intervals
As shown in Table 2 ; Fig. 4 , compared with never breastfeeding, the adjusted prevalence of exclusive breastfeeding was higher by 5.36% (aPR = 1.41) in states with paid family leave vs. in states without paid family leave. Similarly, the adjusted prevalence of late mixed breastfeeding was higher by 3.19% (aPR = 1.25), and early mixed breastfeeding was higher by 5.42% (aPR = 1.32).
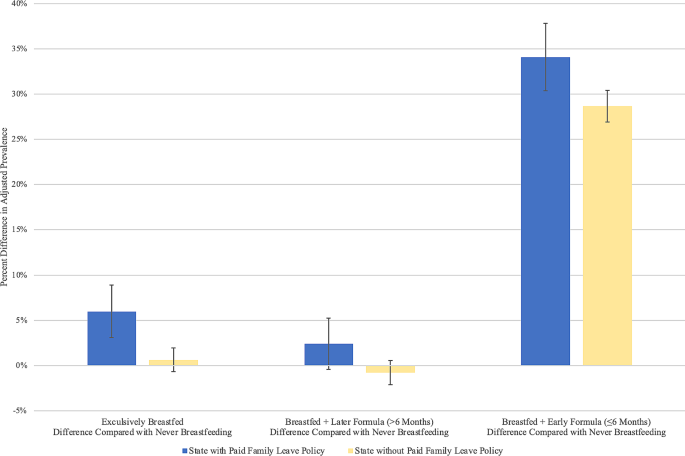
Difference in adjusted prevalence of breastfeeding outcomes and prevalence of never breastfeeding by US state paid family leave policies, National Immunization Survey-Child, 2021. Legend: Reported values are estimated differences in adjusted prevalence of each feeding type. Error bars correspond to 95% confidence intervals
A sensitivity analysis which excluded states that enacted family leave policies during the study period (Washington DC, Washington, and Massachusetts) found similar results across all feeding types (Additional File 3 ).
Covariates associated with breastfeeding
As shown in Table 2 , several covariates remained associated with breastfeeding outcomes in the adjusted model.
Workplace breastfeeding policies were positively associated with all types of breastfeeding.
Women with income below poverty had lower aPR of late mixed breastfeeding. Women who were married had greater aPR of all breastfeeding outcomes. Respondents who reported the race/ethnicity of their child as non-Hispanic/Latino Black had lower aPR of exclusively breastfeeding compared with non-Hispanic/Latino White children. Respondents who identified their children as Hispanic/Latino had higher aPR of late mixed feeding compared with non-Hispanic/Latino White children. Compared with English-speaking respondents, Spanish-speaking respondents had higher aPR of all breastfeeding types. Respondents with lower education levels had lower aPR of all breastfeeding outcomes. WIC enrollees also had lower aPR of all types of breastfeeding.
In this secondary dataset analysis using a US representative sample, we found that, after adjusting for covariates, all feeding types that incorporate breastfeeding (exclusive breastfeeding, late mixed feeding, and/or early mixed feeding) were higher in states with paid family leave compared with states without paid family leave policies. These findings offer novel insight into various feeding approaches indicative of real-world infant feeding practices among breastfeeding persons in the labor force. Even after controlling for state-level workplace breastfeeding policies, paid family leave policies are associated with exclusive breastfeeding and with a spectrum of feeding types that incorporate breastfeeding. These results demonstrate that the paid family leave policies are positively associated with breastfeeding, and thus may reflect health benefits for the parent/baby dyad that accompany any degree of breastfeeding [ 2 , 4 , 5 , 6 ].
Paid family leave policies have previously been associated with improvements in breastfeeding duration and with health and economic benefits [ 31 , 32 , 33 , 34 , 35 , 36 ]. After California was the first US state to provide eight weeks of partial paid family leave in 2004, Huang et al. utilized the CDC Infant Feeding Practices Study and found contemporaneous increases in the rates of breastfeeding in California compared with other US states, with difference-in-differences of 15.8%, 17.4%, and 18.4% in the rates of any breastfeeding at three, six, and nine months, respectively [ 37 , 38 ]. Globally, parental leave after childbirth has been associated with reduced maternal and infant morbidity and mortality [ 15 , 39 , 40 , 41 , 42 ]. In high-income countries, paid parental leave has been associated with increases in exclusive breastfeeding, downstream earning potential, workforce retention, and infant vaccination rates and with reductions in maternal medical and mental health morbidity [ 16 , 43 ]. Data suggest higher degrees of benefit with increasingly generous leave, including longer breastfeeding duration and higher maternal pay [ 44 ].
Just over half (56%) of the US workforce qualifies for federal FMLA, which is unpaid [ 45 ]. There are also limited opportunities for paid leave in the United States, which results in suboptimal breastfeeding initiation and duration [ 41 ]. Cross-sectional US studies have found that 59% of women did not receive paid leave, and, even when it was received, paid leave averaged about three weeks, with reduced salary [ 46 ]. Current FMLA policies and qualifications tend to support families who can afford unpaid time off work and have stable employment from large employers [ 18 ]. Women facing social and structural barriers to breastfeeding, such as low income, lower educational attainment, and membership in minority racial and ethnic groups, disproportionately do not benefit from federal FMLA policies. In this multivariable analysis, we found disparities in breastfeeding was associated with multiple factors that are also related to disparities in medical leave policies.
When evaluating income, we found that, in the adjusted model, women below the poverty level were less likely to exclusively breastfeed for the first six months before introducing infant formula. Families with lower incomes have previously been shown to have less paid and unpaid leave. One 2014 cross-sectional study found that only 20% of families making under $35,000 per year received paid leave, averaging 1.5 weeks in duration, compared with a respective 55% and 4.5 weeks for families making over $75,000 per year [ 46 ]. The 2018 US Department of Labor FMLA surveys demonstrated that low-wage workers making $15 per hour or less were least likely to take needed medical leave, citing the inability to afford unpaid time off from work and fear of job loss [ 45 ].
Similar to other studies, we found that marital status was positively associated with breastfeeding [ 47 ]. The US Department of Labor reports that approximately 95% of fathers with children under three years of age are working, highlighting the potential importance of parental leave for all caregivers in the workforce [ 11 ].
Our findings also reflected known racial and ethnic disparities in breastfeeding stemming from complex policies and histories related to structural and ongoing racism [ 8 , 48 , 49 ]. After adjusting for covariates, we found that, compared with respondents who identified their children as non-Hispanic White, non-Hispanic Black respondents were less likely to exclusively breastfeed. Racial and ethnic disparities extend to FMLA eligibility; studies have found that more Black and Hispanic/Latino workforce members (60.2% and 66.9%, respectively) reported being ineligible for or unable to afford unpaid leave than White workers (55.3%) [ 39 ]. Because Black women experience higher rates of pregnancy complications and preterm delivery compared to other races, current federal FMLA policies, which count time from pregnancy complications as part of leave, may further exacerbate racial inequities [ 50 , 51 , 52 ]. We also found that Hispanic/Latino respondents had higher rates of late mixed feeding but lower rates of exclusive breastfeeding compared with non-Hispanic White women. A 2021 study examining feeding goals found that despite Hispanic/Latina women having higher intentions to breastfeeding compared with non-Hispanic/Latina White women, they had lower odds of meeting their goals [ 53 ]. Inequitable access to FMLA policies may be contributing to this gap, as Hispanic/Latina women are less likely to qualify for both paid and unpaid leave, which may be related to part-time work status or working for small employers [ 39 , 54 , 55 ].
Employment and education have also previously been associated with breastfeeding outcomes and may be related to access to FMLA [ 47 ]. While NIS-C does not include employment data, in the unadjusted and adjusted analyses, we found that women with lower education levels, which are associated with employment opportunities, were less likely to breastfeed. Return to work is among the top reasons for interrupted breastfeeding [ 33 , 56 ], and women who take six months or more of leave from work have a 30% higher likelihood of any breastfeeding at six months [ 57 ].
We also found that women enrolled in WIC were less likely to report breastfeeding across all adjusted and unadjusted analyses. For breastfeeding individuals, WIC distributes breast pumps, offers nutritional support, and supports breastfeeding peer counselor programs [ 58 ]. WIC also subsidizes formula purchases, which can result in sales benefits for formula manufactures [ 59 ]. Multi-level strategies have been found to enhance breastfeeding for WIC participants, including supporting early WIC enrollment, assessing breastfeeding intentions, and funding peer counseling [ 60 ]. However, formula provision may be an incentive for WIC enrollment for some income-eligible individuals, and prior studies have found that some enrollees perceive WIC as a formula provider and appreciate the financial support for formula supplementation [ 61 ]. These findings underscore the need to further enrich the lactation-supporting capacity of WIC while considering financial implications and regulations for formula provision.
Limitations of this cross-sectional, secondary dataset analysis included baseline differences between the states with and without paid family leave policies. Respondents in states with paid family leave policies were more likely to report older age, Hispanic/Latina ethnicity, smaller household size, college degree, married status, higher income levels, and lower WIC enrollment. While we adjusted for these characteristics and for workplace breastfeeding policies, there were potentially other unmeasured confounding factors that may have differed between states with and without paid family leave policies, including maternal employment status. Although more generous leave has been found to be associated with greater benefits for breastfeeding-related outcomes, this study did not account for state-by-state variation in leave policies [ 44 ]. Several states had policies that went into effect during the survey lookback period, but sensitivity analyses showed similar outcomes regardless of inclusion or exclusion of these states in analyses. Additionally, there were limited data for families who prefer languages other than English or Spanish, and birthing people with varying gender identities may have been excluded.
Despite the limitations of the cross-sectional analysis, it is important to assess differences in breastfeeding outcomes, including mixed breast and formula feeding, as more states enact paid family leave policies. Future prospective studies can evaluate changes in breastfeeding after policy enactment and can assess breastfeeding prevalence in the workforce.
Conclusions
In the United States, all feeding types that incorporate breastfeeding were higher in states with paid family leave compared with states without paid family leave policies. Although multilevel interventions are needed to support breastfeeding, expansion of policies that grant working families and caregivers paid time to raise children can positively affect breastfeeding, which in turn could improve preventative health and economic benefits for individuals and society.
Data availability
The datasets analyzed during the current study are available in the repository which is available from the Centers for Disease Control and Prevention at: https://www.cdc.gov/vaccines/imz-managers/nis/datasets.html.
Abbreviations
Adjusted prevalence ratio
Centers for Disease Control and Prevention
Confidence Interval
- Family Medical Leave Act
National Immunization Surveys
National Immunization Survey-Child
Organization for Economic Cooperation and Development
Prevalence Ratio
Providing Urgent Maternal Protections for Nursing Mothers Act
STrengthening the Reporting of OBservational studies in Epidemiology
United States
Special Supplemental Nutrition Program for Women, Infants, and Children
Practice advisory to update the duration of breastfeeding. https://www.acog.org/en/clinical/clinical-guidance/practice-advisory/articles/2023/02/duration-of-breastfeeding-update . Accessed 18 March 2024.
Meek JY, Noble L. Technical report: breastfeeding and the use of human milk. Pediatrics. 2022;150:e2022057989. https://doi.org/10.1542/peds.2022-057988 .
Article PubMed Google Scholar
World Health Organization. Breastfeeding. https://www.who.int/westernpacific/health-topics/breastfeeding . Accessed 18 March 2024.
Frank NM, Lynch KF, Uusitalo U, Yang J, Lönnrot M, Virtanen SM, et al. The relationship between breastfeeding and reported respiratory and gastrointestinal infection rates in young children. BMC Pediatr. 2019;19:339. https://doi.org/10.1186/s12887-019-1693-2 .
Article CAS PubMed PubMed Central Google Scholar
Güngör D, Nadaud P, Dreibelbis C, LaPergola C, Terry N, Wong YP et al. Shorter versus longer durations of exclusive human milk feeding prior to the introduction of infant formula and food allergies, allergic rhinitis, atopic dermatitis, and asthma: a systematic review. Alexandria (VA): USDA Nutrition Evidence Systematic Review; 2019. http://www.ncbi.nlm.nih.gov/books/NBK580356/ . Accessed 10 April 2023.
Dewey K, Bazzano L, Davis T, Donovan S, Taveras E, Kleinman R et al. The duration, frequency, and volume of exclusive human milk and/or infant formula consumption and overweight and obesity: a systematic review. Alexandria (VA): USDA Nutrition Evidence Systematic Review; 2020. http://www.ncbi.nlm.nih.gov/books/NBK578873/ . Accessed 10 April 2023.
Glazer KB, Zeitlin J, Howell EA. Intertwined disparities: applying the maternal-infant dyad lens to advance perinatal health equity. Semin Perinatol. 2021;45(4):151410. https://doi.org/10.1016/j.semperi.2021.151410 .
Article PubMed PubMed Central Google Scholar
CDC. 2022 Breastfeeding report card. Center for Disease Control and Prevention. 2022. https://www.cdc.gov/breastfeeding/data/reportcard.htm . Accessed 23 Feb 2023.
Increase the proportion of infants who. are breastfed exclusively through age 6 months — MICH–15 - Healthy People 2030 | health.gov. https://health.gov/healthypeople/objectives-and-data/browse-objectives/infants/increase-proportion-infants-who-are-breastfed-exclusively-through-age-6-months-mich-15 . Accessed 23 Feb 2023.
Steurer LM. Maternity leave length and workplace policies’ impact on the sustainment of breastfeeding: global perspectives. Public Health Nurs. 2017;34:286–94. https://doi.org/10.1111/phn.12321 .
Labor force participation rates | U.S. Department of Labor. https://www.dol.gov/agencies/wb/data/latest-annual-data/labor-force-participation-rates#Labor-Force-Participation-Rate-of-Mothers-and-Fathers-by-Age-of-Youngest-Child . Accessed 1 May 2023.
CDC. The Surgeon General’s call to action to support breastfeeding. Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/breastfeeding/resources/calltoaction.htm . Accessed 30 March 2023.
The Surgeon General’. s call to action to improve maternal health - Healthy People 2030 | health.gov. https://health.gov/healthypeople/tools-action/browse-evidence-based-resources/surgeon-generals-call-action-improve-maternal-health . Accessed 10 April 2023.
The White House. Biden-Harris administration national strategy on hunger, nutrition, and health. 2022. https://www.whitehouse.gov/briefing-room/statements-releases/2022/09/27/executive-summary-biden-harris-administration-national-strategy-on-hunger-nutrition-and-health/ . Accessed 10 April 2023.
Nandi A, Jahagirdar D, Dimitris MC, Labrecque JA, Strumpf EC, Kaufman JS, et al. The impact of parental and medical leave policies on socioeconomic and health outcomes in OECD countries: a systematic review of the empirical literature. Milbank Q. 2018;96:434–71.
Heymann J, Sprague AR, Nandi A, Earle A, Batra P, Schickedanz A, et al. Paid parental leave and family wellbeing in the sustainable development era. Public Health Rev. 2017;38:21. https://doi.org/10.1111/1468-0009.12340 .
Rep, Maloney. CB [D-N-12. H.R.3110–117th Congress (2021–2022): PUMP for Nursing Mothers Act. 2021. http://www.congress.gov/ . Accessed 10 April 2023.
Department of Labor. Family and Medical Leave (FMLA). http://www.dol.gov/general/topic/benefits-leave/fmla . Accessed 1 May 2023.
Bipartisan Policy Center. State paid family leave laws across the U.S https://bipartisanpolicy.org/explainer/state-paid-family-leave-laws-across-the-u-s/ . Accessed 10 December 2023.
U.S. Department of Health and Human Services (DHHS) National Center for Immunization and Respiratory Diseases. The 2021 National Immunization Survey - Child. Atlanta, GA: Centers for Disease Control and Prevention. 2022. https://www.cdc.gov/vaccines/imz-managers/nis/downloads/NIS-PUF21-DUG.pdf . Accessed 18 March 2024.
Centers for Disease Control and Prevention. NIS-Child data tables for 2015 to present. 2023. https://www.cdc.gov/vaccines/imz-managers/nis/datasets.html . Accessed 23 February 2023.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008 .
Article Google Scholar
Dinour LM. Speaking out on breastfeeding terminology: recommendations for gender-inclusive language in research and reporting. Breastfeed Med. 2019;14:523–32. https://doi.org/10.1089/bfm.2019.0110 .
National Institutes of Health (NIH). Inclusive and gender-neutral language. https://www.nih.gov/nih-style-guide/inclusive-gender-neutral-language . Accessed 1 May 2023.
National Conference of State Legislatures. Breastfeeding state laws. 2021. https://www.ncsl.org/health/breastfeeding-state-laws . Accessed 6 December 2023.
Stata. mlogit — multinomial (polytomous) logistic regression. https://www.stata.com/manuals/rmlogit.pdf . Accessed 27 May 2023.
Rubin M. When to adjust alpha during multiple testing: a consideration of disjunction, conjunction, and individual testing. Synthese. 2021;199:10969–1000. https://doi.org/10.1007/s11229-021-03276-4 .
Rubin M. There’s no need to lower the significance threshold when conducting single tests of multiple individual hypotheses. Acadademia Lett. 2021. https://doi.org/10.20935/AL610 .
Poole C. Low p-values or narrow confidence intervals: which are more durable? Epidemiology. 2001;12:291–4. https://doi.org/10.1097/00001648-200105000-00005 .
Article CAS PubMed Google Scholar
Sullivan GM, Feinn R. Using effect size—or why the p value is not enough. J Grad Med Educ. 2012;4:279–82. https://doi.org/10.4300/JGME-D-12-00156.1 .
Navarro-Rosenblatt D, Garmendia M-L. Maternity leave and its impact on breastfeeding: a review of the literature. Breastfeed Med. 2018;13:589–97. https://doi.org/10.1089/bfm.2018.0132 .
Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices? Lancet. 2016;387:491–504. https://doi.org/10.1016/S0140-6736(15)01044-2 .
Baker M, Milligan K. Maternal employment, breastfeeding, and health: evidence from maternity leave mandates. J Health Econ. 2008;27:871–87. https://doi.org/10.1016/j.jhealeco.2008.02.006 .
Andres E, Baird S, Bingenheimer JB, Markus AR. Maternity leave access and health: a systematic narrative review and conceptual framework development. Matern Child Health J. 2016;20:1178–92. https://doi.org/10.1007/s10995-015-1905-9 .
Hamad R, Modrek S, White JS. Paid family leave effects on breastfeeding: a quasi-experimental study of US policies. Am J Public Health. 2019;109:164–6. https://doi.org/10.2105/AJPH.2018.304693 .
Kortsmit K, Li R, Cox S, Shapiro-Mendoza CK, Perrine CG, D’Angelo DV, et al. Workplace leave and breastfeeding duration among postpartum women, 2016–2018. Am J Public Health. 2021;111:2036–45. https://doi.org/10.2105/AJPH.2021.306484 .
Huang R, Yang M. Paid maternity leave and breastfeeding practice before and after California’s implementation of the nation’s first paid family leave program. Econ Hum Biol. 2015;16:45–59. https://doi.org/10.1016/j.ehb.2013.12.009 .
Centers for Disease Control and Prevention. Why it matters. 2023. https://www.cdc.gov/breastfeeding/about-breastfeeding/why-it-matters.html . Accessed 10 April 2023.
Sprague A, Earle A, Moreno G, Raub A, Waisath W, Heymann J. National policies on parental leave and breastfeeding breaks: racial, ethnic, gender, and age disparities in access and implications for infant and child health. Public Health Rep. 2023;333549231151661. https://doi.org/10.1177/00333549231151661 .
Webster JL, Paul D, Purtle J, Locke R, Goldstein ND. State-level social and economic policies and their association with perinatal and infant outcomes. Milbank Q. 2022;100:218–60. https://doi.org/10.1111/1468-0009.12571 .
Ruhm CJ. Parental leave and child health. J Health Econ. 2000;19:931–60. https://doi.org/10.1016/s0167-6296(00)00047-3 .
Burtle A, Bezruchka S. Population health and paid parental leave: what the United States can learn from two decades of research. Healthcare. 2016;4:30. https://doi.org/10.3390/healthcare4020030 .
Raub A, Nandi A, Earle A, de Guzman Chorny N, Wong E, Chung P et al. Paid parental leave: a detailed look at approaches across OECD countries. UCLA WORLD Policy Analysis Center; 2018. https://www.worldpolicycenter.org/sites/default/files/WORLD%20Report%20-%20Parental%20Leave%20OECD%20Country%20Approaches_0.pdf . Accessed 18 March 2024.
Heshmati A, Honkaniemi H, Juárez SP. The effect of parental leave on parents’ mental health: a systematic review. Lancet Public Health. 2023;8:e57–75. https://doi.org/10.1016/S2468-2667(22)00311-5 .
Abt Associates. Assessing FMLA: results from 2018 surveys. https://www.abtassociates.com/insights/publications/report/assessing-fmla-results-from-2018-surveys . Accessed 11 May 2023.
Shepherd-Banigan M, Bell JF. Paid leave benefits among a national sample of working mothers with infants in the United States. Matern Child Health J. 2014;18:286–95. https://doi.org/10.1007/s10995-013-1264-3 .
Mandal B, Roe BE, Fein SB. The differential effects of full-time and part-time work status on breastfeeding. Health Policy. 2010;97:79–86. https://doi.org/10.1016/j.healthpol.2010.03.006 .
Griswold MK, Crawford SL, Perry DJ, Person SD, Rosenberg L, Cozier YC, et al. Experiences of racism and breastfeeding initiation and duration among first-time mothers of the black women’s health study. J Racial Ethn Health Disparities. 2018;5:1180–91. https://doi.org/10.1007/s40615-018-0465-2 .
Manuck TA. Racial and ethnic differences in preterm birth: a complex, multifactorial problem. Semin Perinatol. 2017;41:511–8. https://doi.org/10.1053/j.semperi.2017.08.010 .
Bornstein E, Eliner Y, Chervenak FA, Grünebaum A. Racial disparity in pregnancy risks and complications in the US: temporal changes during 2007–2018. J Clin Med. 2020;9:1414. https://doi.org/10.3390/jcm9051414 .
Martin JA, Hamilton BE, Osterman MJK. Births in the United States, 2019. NCHS Data Brief. 2020;1–8.
KFF. Preterm Births as a Percent of All Births by Race/Ethnicity. 2023. https://www.kff.org/other/state-indicator/preterm-births-by-raceethnicity/ . Accessed 11 May 2023.
Hamner HC, Beauregard JL, Li R, Nelson JM, Perrine CG. Meeting breastfeeding intentions differ by race/ethnicity, infant and toddler feeding practices Study-2. Matern Child Nutr. 2020;17:e13093. https://doi.org/10.1111/mcn.13093 .
Ann Bartell, Soohyun K, Nam J, Rossin-Slater M, Ruhm C, Waldfogel J. June. Racial and ethnic disparities in access to and use of paid family and medical leave: evidence from four nationally representative datasets: monthly labor review: U.S. Bureau of Labor Statistics. https://www.bls.gov/opub/mlr/2019/article/racial-and-ethnic-disparities-in-access-to-and-use-of-paid-family-and-medical-leave.htm . Accessed 2 2023.
Goodman JM, Richardson DM, Dow WH. Racial and ethnic inequities in paid family and medical leave: United States, 2011 and 2017–2018. Am J Public Health. 2022;112:1050–8. https://doi.org/10.2105/AJPH.2022.306825 .
Schwartz K, D’Arcy HJS, Gillespie B, Bobo J, Longeway M, Foxman B. Factors associated with weaning in the first 3 months postpartum. J Fam Pract. 2002;51:439–44.
PubMed Google Scholar
UNICEF USA. The ost of not breastfeeding. https://www.unicefusa.org/stories/cost-not-breastfeeding . Accessed 11 May 2023.
Food and Nutrition Service. Breastfeeding promotion in WIC: current federal requirements https://www.fns.usda.gov/wic/breastfeeding-promotion-wic-current-federal-requirements . Accessed 12 May 2023.
Choi YY, Ludwig A, Andreyeva T, Harris JL. Effects of United States WIC infant formula contracts on brand sales of infant formula and toddler milks. J Public Health Policy. 2020;41:303–20. https://doi.org/10.1057/s41271-020-00228-z .
Houghtaling B, Shanks CB, Jenkins M. Likelihood of breastfeeding within the USDA’s Food and Nutrition Service Special Supplemental Nutrition Program for women, infants, and children population: a systematic review of the literature. J Hum Lact off J Int Lact Consult Assoc. 2017;33:83–97. https://doi.org/10.1177/0890334416679619 .
Almeida R, Alvarez Gutierrez S, Whaley SE, Ventura AK. A qualitative study of breastfeeding and formula-feeding mothers’ perceptions of and experiences in WIC. J Nutr Educ Behav. 2020;52:615–25. https://doi.org/10.1016/j.jneb.2019.12.006 .
Download references
Acknowledgements
Not applicable.
Support for Dr. Rosenberg was made possible by CTSA Grant Number KL2 TR001862 from the National Center for Advancing Translational Science (NCATS), components of the National Institutes of Health (NIH), and NIH roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Support for Dr. Nardella was made possible by the Yale National Clinician Scholars Program and by CTSA Grant Number TL1 TR001864 from the National Center for Advancing Translational Science (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Author information
Authors and affiliations.
Department of Pediatrics, Yale School of Medicine, 333 Cedar St, New Haven, CT, USA
Julia Rosenberg, Deanna Nardella & Veronika Shabanova
National Clinician Scholars Program, Yale University, 333 Cedar St, New Haven, CT, USA
Deanna Nardella
Department of Biostatistics, Yale School of Public Health, 333 Cedar St, New Haven, CT, USA
Veronika Shabanova
You can also search for this author in PubMed Google Scholar
Contributions
JR: conceptualization, methodology, validation, formal analysis, investigation, resources, data curation, writing – original draft, review, editing, visualization, project administration, funding acquisition. DN: validation, investigation, resources, writing – original draft, review, and editing. VS: conceptualization, methodology, validation, formal analysis, writing – review and editing, supervision. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Julia Rosenberg .
Ethics declarations
Ethics approval and consent to participate.
Not applicable. The National Immunization Survey is a publicly available, de-identified dataset. Its use is not considered Human Subjects Research, and we did not obtain a determination of this status from the Institutional Review Board.
Consent for publication
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Rosenberg, J., Nardella, D. & Shabanova, V. State paid family leave policies and breastfeeding duration: cross-sectional analysis of 2021 national immunization survey-child. Int Breastfeed J 19 , 37 (2024). https://doi.org/10.1186/s13006-024-00646-9
Download citation
Received : 16 December 2023
Accepted : 18 May 2024
Published : 26 May 2024
DOI : https://doi.org/10.1186/s13006-024-00646-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Breastfeeding
- National Immunization Survey
International Breastfeeding Journal
ISSN: 1746-4358
- General enquiries: [email protected]
- Member Login

May 27, 2024
National Osteoporosis Awareness and Prevention Month
Lam and neuroendocrine effects on fertility and bone: a review.
By: Magdalene Lederer
Director’s Note: Since May is also National Osteoporosis Awareness and Prevention Month, this week we feature a 2022 review by Calik-Ksepka et al [1] published in the International Journal of Molecular Sciences titled, “Lactational Amenorrhea: Neuroendocrine Pathways Controlling Fertility and Bone Turnover.” The review article, summarized by former FACTS elective participant Magdalene Lederer, addresses the link between breastfeeding and bone turnover. Not only is breastfeeding relevant for the family planning applications of the lactational amenorrhea method , but this article also explores the influence of lactation on neuroendocrine pathways with widespread effects in the body.
Breastfeeding Physiology
The article by Calik-Ksepka et al [1] reviewed the available research on the physiology of both the lactational amenorrhea method (LAM) and the bone turnover that occurs during breastfeeding. Before understanding how lactation can induce amenorrhea, it is important to explain the physiology behind lactation. To prepare for lactation, breasts require a change and development within the glandular tissue. This process relies on estrogen, progesterone, and prolactin, and their changes in prevalence during pregnancy and postpartum.
“To prepare for lactation, breasts require a change and development within the glandular tissue. This process relies on estrogen, progesterone, and prolactin.”
Estrogen plays two roles: it promotes physical changes in the breast, including ductal development, and stimulates prolactin secretion. During pregnancy, however, estrogen is unable to promote significant prolactin secretion because the high progesterone levels inhibit this effect until after delivery of the placenta. This is one reason for the different types of milk seen at the end of pregnancy through day one, typically referred to as colostrum, transitional milk from days 2-5, and mature milk produced from day 5. When suckling occurs, mechanoreceptors at the breast trigger oxytocin release, which stimulates the let-down reflex that mediates breastfeeding. Oxytocin increases contraction within the breast to allow milk to flow toward the nipple and also stimulates prolactin release, which leads to a positive feedback loop: continued breastfeeding empties the breast, further increasing prolactin release as well as the milk supply.
Lactational Amenorrhea
The neurochemical control of lactational amenorrhea has not been fully researched. It is clear that the female hypothalamus-pituitary-ovarian (HPO) axis is affected by both pregnancy and breastfeeding. During pregnancy, placental hormones inhibit the HPO axis. After pregnancy, breastfeeding can maintain amenorrhea. Studies reveal that follicle stimulating hormone (FSH) returns to levels similar to that of the follicular phase by 4 weeks postpartum. Luteinizing hormone (LH) has also been demonstrated to return to low normal levels by 4 weeks postpartum. With both hormones needed for menstruation present, it seems another mechanism is at play.
In a menstruating woman, LH is released in pulses. Breastfeeding and suckling in particular disrupt this pulsatile nature of LH secretion, which results in anovulation. The LH release corresponds with gonadotropin-releasing hormone (GnRH) release. Kisspeptin is a stimulator of GnRH. Although research has only been conducted in rats, suppression of kisspeptin may be the main suppressor of GnRH, which in turn would suppress LH pulsatile release. The exact mechanism of this phenomenon needs more research to identify differences in moms who exclusively breastfeed, moms who breastfeed and pump, and moms who exclusively pump.
“Breastfeeding and suckling in particular disrupt this pulsatile nature of LH secretion, which results in anovulation.”

Lactational Amenorrhea Method
Studies demonstrate LAM can be 98% effective when used alone under these conditions:
- up to 6 months from delivery,
- exclusive or nearly exclusive breastfeeding, and
- no return of menses.
If any one of these conditions is no longer met, another method should be used for family planning. Exclusive or nearly exclusive breastfeeding is an important aspect of the success of this method. Any food or liquids given could delay the frequency and/or duration of infant suckling and thus affect HPO axis suppression, which could lead to ovulation. Initial return of menses is most likely anovulatory, but once it has returned, the possibility of ovulation increases significantly.
Lactation and Bone Turnover
Lactation does more than affect the menstrual cycle; it can also lead to bone turnover. Estrogen is lower during lactation, leading to bone remodeling. Yet, estrogen rises upon discontinuation of breastfeeding, and bone formation occurs. In patients with pre-existing risk factors for osteoporosis, pregnancy-and-lactation-induced osteoporosis can occur and can lead to fractures. While the extent of bone loss varies among breastfeeding women, there is a consistent change when compared to mothers who choose formula rather than breastfeed. The greatest bone losses tend to be in the lumbar spine. Once lactation ends, however, these changes typically reverse and mineral content within the skeleton is restored to baseline.
“Estrogen is lower during lactation, leading to bone remodeling. Yet, estrogen rises upon discontinuation of breastfeeding, and bone formation occurs.”
In conclusion, breastfeeding has many effects on the lactating mother. Amenorrhea is a significant physiological change that deserves more attention in research. Bone turnover for the calcium in breastmilk is significant during the breastfeeding period but resolves quickly once lactation ends. This article demonstrated the significant gaps in research connecting lactation and the menstrual cycle. Potential differences between breastfeeding and pumping at the neurochemical level also need to be explored. Such differences would impact the usefulness of LAM for women who are unable to breastfeed without pumping, particularly in the U.S. where there is no guaranteed maternity leave and many women return to work well before their newborn is 6 months old.
Despite conflicting data regarding bone turnover and its mechanism, consistent evidence shows bone turnover during breastfeeding is temporary, and women return to baseline after lactation ends. On the other hand, women with preexisting risk factors for osteoporosis may need more calcium support to prevent fractures.
This article [1] provides insight into information and data to investigate further about female physiology. It also reinforces the value of exclusive breastfeeding for the first 6 months postpartum, which needs to be recognized at both the individual and societal level to maximize its benefits.
[1] Calik-Ksepka A, Stradczuk M, Czarnecka K, Grymowicz M, Smolarczyk R. Lactational Amenorrhea: Neuroendocrine Pathways Controlling Fertility and Bone Turnover. Int J Mol Sci. 2022 Jan 31;23(3):1633. doi: 10.3390/ijms23031633. PMID: 35163554; PMCID: PMC8835773.
ABOUT THE AUTHOR
Magdalene lederer.
Magdalene Lederer is a fourth-year medical student at Rowan-Virtua School of Osteopathic Medicine in Stratford, NJ. She completed her undergraduate education at Liberty University in Lynchburg, VA and will begin residency in obstetrics and gynecology this summer at Saint Peter’s University in New Brunswick, NJ. She is excited to provide informed consent to her patients about family planning options, from contraception to infertility.

- Breastfeeding & Pregnancy
- Charting and the Science of the Cycle
- FABM Effectiveness for Pregnancy Prevention
- FABM Training Programs and Education
- FABMs for Infertility And Achieving Pregnancy
- FABMs Personal Stories
- Fertility Apps and FEMM Tech
- In The News
- Miscellaneous
- Psychosocial Aspects of NFP/FABMs
- Women's Health & FABMs
Pin It on Pinterest
Username or Email Address
Remember Me
Pregnancy Checklist
Be prepared for the big day with this pregnancy to-do list by trimester and month.
This article is based on reporting that features expert sources.
With all the logistics that arise with planning for conception and pregnancy, it’s no surprise that the 40-week-long endeavor brings out many challenges.
Whether you’re hoping for a positive pregnancy test in the near future or already have a baby on the way, here’s a list of useful tips to help with how to prepare for pregnancy.
First Trimester Pregnancy Checklist

Getty Images
During the first trimester, you’ll experience hormonal changes as your body demonstrates the earliest signs of pregnancy.
You may not know you’re pregnant during the first month of pregnancy. The first probable signs of pregnancy may appear around 12 to 15 days after ovulation at the earliest. This is when levels of human chorionic gonadotropin (hCG), a hormone produced by the placenta, are high enough to become detectable on a pregnancy test .
At this time, you may experience other presumptive signs of pregnancy, such as:
- Sore breasts
- A missed period
- Nausea and vomiting
During the first month, check a few early pregnancy tasks off your list, including:
- Choose your pregnancy and birth provider, like an OB-GYN, midwife or family medicine OB provider
- Select which hospital you plan to give birth at, if your provider has delivery privileges at multiple locations
- Schedule your initial prenatal appointment
- Treat any comorbid conditions and review your current medications, as some may need to be changed during pregnancy
Dr. Kecia Gaither, a double board-certified OB-GYN and maternal-fetal medicine provider, suggests treating conditions like:
- Thyroid disease
- Hypertension
“Comorbid conditions, especially uncontrolled diabetes, can significantly increase the risk of congenital abnormalities,” explains Gaither, who also serves as director of perinatal services and maternal-fetal medicine at New York City Health + Hospitals, Lincoln in the Bronx.
Congratulations! Month two is when most women discover their pregnancies.
As soon as you learn you're pregnant, it’s important to stop smoking , drinking or using drugs. Talk with your medical provider about which prescription medications you may need to start, stop or change at this time.
You will also likely begin taking supplements under the direction of your medical provider. Gaither emphasizes the importance of optimizing your pregnancy meal plan and maintaining healthy iron and folate levels for optimal fetal development.
This is because key fetal development occurs during month two, such as:
- Development of the neural tube, which will later become organs in the nervous system, like the brain and spinal cord
- Digestive tract development
- Bone formation
Month three
Month three is often an exciting time in pregnancy, when most people have the first chance to hear the baby’s heart rate. The heart rate may be detectable as early as six weeks, but most initial prenatal appointments occur between eight and 12 weeks.
By this point, you may already be experiencing morning sickness, which is nausea or vomiting, most commonly during the first three months of pregnancy.
To combat these symptoms, try:
- Eating small, frequent meals
- Staying hydrated
- Eating a small snack, like a few crackers, before getting out of bed
While morning sickness is common, reach out to your provider if you experience the following:
- Nausea or vomiting that is preventing you from your daily activities
- Inability to stay hydrated
- Feeling faint, dizzy or confused due to your symptoms
- Vomiting multiple times a day, unrelieved by home care
You may need a hydration infusion to keep you hydrated, or your provider may prescribe medications to combat your symptoms.
Second Trimester Checklist
By the second trimester, the reality of preparing for a baby will start to set in. During this trimester, the early stages of nesting – a drive to prepare your home and lifestyle to accommodate your new addition – may begin.
Around week 10, you’ll have an opportunity to perform noninvasive prenatal genetic testing (NIPT), which uses the mother's blood to screen for chromosome balance and genetic conditions, such as Down syndrome.
By this time your pregnancy may also start to show. If you haven’t already, make sure to add some maternity and loose-fitting clothing to your wardrobe.
Dr. Andrea Braden, a board-certified OB-GYN and lactation consultant, suggests not to wait on purchasing new bras.
“Your breast size starts to increase during pregnancy and for preparation for nursing after," she explains. "Typically, you'll need to buy a new bra as it is, so I would say go ahead and buy bras that have the dual function of being a pregnancy bra in a nursing bra.”
Make sure that by month five, you have a stable exercise routine or movement plan to ensure a healthy pregnancy.
According to the American College of Obstetrics and Gynecology, exercise during pregnancy is essential to:
- Reduce aches and pains
- Relieve constipation
- Decrease the risk of pregnancy complications
Month five is also when you may feel some of the first signs of fetal movement.
Month six is a great opportunity to start the first stages of nesting.
Consider the following nesting activities:
- Planning baby purchases or creating a baby registry
- Planning for potential projects around the house or in the nursery
- If you are working, start to consider how you will handle medical leave and time off to recover after birth and bond with your baby
Third Trimester Checklist
You’re in the final stretch! The third trimester is a great time to finalize your plans and preferences for labor and delivery.
Month seven
Taking a hospital birth class? Best to take it in the third trimester so your memory is fresh, explains Kristin Revere, the owner and founder of Gold Coast Doulas in Grand Rapids, Michigan. If you’re opting for a birth without an epidural, she explains you may consider taking birth classes like hypnobirthing or Lamaze as early as six weeks into pregnancy if you want to get a head start. This will help you mentally prepare to cope with labor pain.
Since you're starting your third trimester, it's a good idea to start preparing for your baby to enter the world.
- Choose your baby's pediatrician .
- Purchase a car seat and have it inspected and properly installed.
- Build a crib or bassinet for the nursery.
Month eight
By month eight, you may be experiencing significant pregnancy-related aches and pains or having trouble sleeping. Ashley Mareko, surrogate program director at Surrogate First, says she used acupuncture and chiropractic services throughout her pregnancy but began going once a week in her third trimester.
Many pregnant women, like Mareko, share anecdotal evidence of acupuncture and chiropractic services helping with reducing pregnancy and labor pain or assisting with labor induction. Researchers acknowledge that the body of evidence supporting acupuncture is limited, but ACOG does not discourage acupuncture or acupressure use in pregnancy. The American Pregnancy Association shares that there are no major concerns with chiropractic care during pregnancy.
At the beginning of month nine, it’s helpful to start planning for birth and the postpartum period.
Here are a few tips:
- Cook some make-ahead freezer meals for nutritious, easy meals after birth.
- Start packing your hospital bag for delivery , just in case the baby comes a few weeks early.
- Finalize your birth plan, and ask the hospital about any pertinent birth or visitation policies.
Bottom Line
The course of your pregnancy will bring new challenges and learning experiences, and no two pregnancies are exactly the same. Consult with your pregnancy provider to get pregnancy advice tailored to your health and wellness.
Antidepressants During Pregnancy
Payton Sy June 1, 2023

The U.S. News Health team delivers accurate information about health, nutrition and fitness, as well as in-depth medical condition guides. All of our stories rely on multiple, independent sources and experts in the field, such as medical doctors and licensed nutritionists. To learn more about how we keep our content accurate and trustworthy, read our editorial guidelines .
Braden is a board-certified OB-GYN based in Atlanta and a breastfeeding medicine specialist at Lybbie, a lactation innovation company.
Gaither is a double board-certified OB-GYN and maternal fetal medicine provider. She is also the director of perinatal services and maternal-fetal medicine at New York City Health and Hospitals, Lincoln in the Bronx.
Mareko is the surrogate program director at SurrogateFirst, a surrogacy matching service. She is based in Los Angeles.
Revere is the founder of Gold Coast Doulas in Grand Rapids, Michigan.
Tags: pregnancy , patient advice
Most Popular

Patient Advice

Second Opinion

health disclaimer »
Disclaimer and a note about your health ».

Your Health
A guide to nutrition and wellness from the health team at U.S. News & World Report.
You May Also Like
20 questions to ask your oncologist.
Lisa Esposito , Elaine K. Howley and Payton Sy May 24, 2024

Colon Cancer Symptoms
Barbara Sadick May 23, 2024

Are More Young Adults Getting Cancer?
Payton Sy May 23, 2024
Who Needs a Medigap Plan?
Ruben Castaneda and Paul Wynn May 23, 2024
What to Know After a Knee Replacement
Christine Comizio and Heidi Godman May 23, 2024
Hospital Rankings to Expand Use of Data
Ben Harder and Min Hee Seo May 22, 2024
Having a Baby After Cancer
Christine Comizio May 21, 2024
10 Signs of Strep Throat
Elaine K. Howley May 20, 2024

Early Pregnancy Signs
Vanessa Caceres May 17, 2024

Prostate Cancer: Questions to Ask
Ruben Castaneda and Payton Sy May 16, 2024

An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Breastfeeding.
Saieda M. Kalarikkal ; Jennifer L. Pfleghaar .
Affiliations
Last Update: April 8, 2023 .
- Definition/Introduction
Breastfeeding is an important part of the neonatal and infant periods. Breastfeeding or lactation provides total nutritional support and promotes the emotional dependency of the baby on the breastfeeding parent. A strong emotional bond facilitates the successful prolongation of breastfeeding. [1] Breast milk is recommended as the optimal and exclusive source of early nutrition for all infants from birth to at least six months of age. Maternal milk is crucial for development. [2]
Milk production is regulated by the hypothalamic-pituitary tract and its associated hormones. Oxytocin and prolactin are the main hormones in milk production and the resulting let-down reflex. [3]
Milk production occurs in stages, the first of which usually begins before the birth of the infant. The first milk is colostrum and is available after labor. Occasionally, there is pre-colostrum before the postpartum stage. Colostrum is high in protein, sodium, and immunoglobulins and is low in lactose. [4] After 30 to 40 hours postpartum, the milk composition is characterized by an increase in lactose content; dilution of other constituents occurs due to increased milk volume.
Vitamin D supplementation should be started within the first few days of life. Initial dosing of 400 IU daily should be increased to 600 IU daily at one year of age.
Maintenance of lactation follows an autonomous pattern wherein infant suckling and emptying of the breast are the main factors regulating the milk flow. [5]
- Issues of Concern
Establishing smooth bonding between the breastfeeding parent and the neonate is essential for successful breastfeeding. [6]
Skin-to-skin contact in the first two hours after birth is important for initiating lactation. The breast crawl of the alert neonate that occurs soon after birth will initiate the bonding process. The breast crawl is when the neonate is placed on the birthing parent's abdomen after birth and finds its way to the breast to suckle. [6] [7]
Successful neonatal breastfeeding factors include proper latching and an alert neonate with intact rooting and suckling reflexes. Although lactation is a natural process, parental support and education for proper positioning and latching are often required. [8] The ability of the neonate to empty the breast will determine the subsequent milk volume. [9] [5]
Limiting factors like pain, anxiety, and emotional instability, among others, should be addressed before and after delivery. Lactation consultants or knowledgeable nurses can facilitate the successful initiation of breastfeeding. [10] Non-breastfeeding parents and other supportive individuals, including physicians, also have an important role in education and support. [11] [12]
Achieving a correct latch on the nipple is imperative. Incorrect latch resulting from poor neonate positioning or issues such as lip or tongue tie may result in cracked nipples or pain while breastfeeding. [13] An evaluation by a lactation consultant or other healthcare provider who is comfortable troubleshooting breastfeeding difficulties is often helpful.
Medication use needs to be monitored and addressed during breastfeeding. The need for a complete cessation of breastfeeding due to medication use is uncommon; adjusting the medication regimen to safe alternatives while breastfeeding may be necessary. Some studies show an increase in medication use while breastfeeding compared to pregnancy. [14]
- Clinical Significance
Colostrum contains a high amount of immunoglobulins. [15] It is often referred to as the first immunization. Colostrum provides mucosal immunity to the gastrointestinal (GI) tract by delivering secretory IgA (sIgA), IgM, and IgG. These vital immunoglobulins provide barrier protection to the gut and offer protection from some infectious processes.
Milk contains microbiota like Bifidobacterium and Lactobacillus, which confer anti-bacterial activity to the gut along with the delivered oligosaccharides. [16] [17] Furthermore, this facilitates the synthesis of essential nutrients such as vitamins B12, B6, K, and folate. Early introduction of breastfeeding will colonize the neonatal gut with these safe micro-organisms derived from the breastfeeding parent, crowding out organisms from the hospital room and other caretakers. Early rooming-in, where the neonate stays with the breastfeeding parent, is advised when possible.
Lactoferrin is also transmitted via breastmilk; it confers immunoprotection against bacterial, viral, fungal, and parasitic infections by prohibiting the sequestration and degradation of iron by microbes. [18]
Produced breast milk can be classified as foremilk and hindmilk. Foremilk contains higher levels of lactose, while hindmilk contains a higher proportion of proteins and fats. The nutritional needs of the neonate control the quantity of milk and its components. Understanding milk composition will help the breastfeeding parent regulate the feed from both breasts. [19]
Evidence shows that breastfeeding lowers the risk of upper respiratory tract infections and diarrhea in newborns. Other postulated benefits include a lower risk of developing asthma, type 1 diabetes, food allergies, and obesity. Breastfeeding may also delay the return of menstruation and offers cost benefits. In the United States, while approximately 75% of neonates are breastfed, numbers decline within a few months of life. Cigarette smoking and alcohol or caffeine use are not valid reasons to stop breastfeeding. Generally, breastfeeding can be stopped between 6 to 12 months of age, although some children are breastfed until they are 2 to 4 years old.
Lactation consultants are trained, certified healthcare professionals who can support the breastfeeding dyad with education and support. They are trained to promote positive attitudes towards breastfeeding by boosting the confidence of the breastfeeding parent through positive counseling. The entire healthcare team should take care to use positive and supportive language, avoiding terms like "problem," "difficulty," "inadequate," or "improper." The presence of postpartum disorders like depression and psychosis may be subtle in presentation and can rapidly deter breastfeeding. These conditions should be considered while managing the postpartum and breastfeeding periods. A lactation consultant should be provided during the hospital stay and after discharge. [10]
- Nursing, Allied Health, and Interprofessional Team Interventions
Breast milk jaundice is a commonly encountered condition in the neonatal period. Addition of 5 ml of artificial baby milk (ABM) in every feed (minimum six feeds) for three days before initiation of breast milk will lower the neonatal bilirubin to safe levels; bilirubin levels tend to remain in a safe zone once normalized. Breastfeeding parents who receive this regimen should be counseled not to continue with ABM supplementation once bilirubin is normalized. [20]
Another treatment regimen for breast milk jaundice includes a 10% solution of chicory distillate (50 ml every 12 hours) to promote bilirubin normalization; a random controlled clinical trial showed this to be helpful. [21] This regimen also promotes colonization of the neonatal gut with normal flora. [22]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Saieda Kalarikkal declares no relevant financial relationships with ineligible companies.
Disclosure: Jennifer Pfleghaar declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Kalarikkal SM, Pfleghaar JL. Breastfeeding. [Updated 2023 Apr 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Expansion of the baby-friendly hospital initiative ten steps to successful breastfeeding into neonatal intensive care: expert group recommendations. [J Hum Lact. 2013] Expansion of the baby-friendly hospital initiative ten steps to successful breastfeeding into neonatal intensive care: expert group recommendations. Nyqvist KH, Häggkvist AP, Hansen MN, Kylberg E, Frandsen AL, Maastrup R, Ezeonodo A, Hannula L, Haiek LN, Baby-Friendly Hospital Initiative Expert Group. J Hum Lact. 2013 Aug; 29(3):300-9. Epub 2013 May 31.
- Review Breastfeeding and its gamut of benefits. [Minerva Pediatr. 2016] Review Breastfeeding and its gamut of benefits. Gertosio C, Meazza C, Pagani S, Bozzola M. Minerva Pediatr. 2016 Jun; 68(3):201-12. Epub 2015 May 29.
- The relationship between perceived milk supply and exclusive breastfeeding during the first six months postpartum: a cross-sectional study. [Int Breastfeed J. 2020] The relationship between perceived milk supply and exclusive breastfeeding during the first six months postpartum: a cross-sectional study. Sandhi A, Lee GT, Chipojola R, Huda MH, Kuo SY. Int Breastfeed J. 2020 Jul 17; 15(1):65. Epub 2020 Jul 17.
- Improved general health status in an unselected infant population following an allergen reduced dietary intervention programme. The ZUFF-study-programme. Part I: Study design and 6-month nutritional behaviour. [Eur J Nutr. 2000] Improved general health status in an unselected infant population following an allergen reduced dietary intervention programme. The ZUFF-study-programme. Part I: Study design and 6-month nutritional behaviour. Exl BM, Deland U, Secretin MC, Preysch U, Wall M, Shmerling DH. Eur J Nutr. 2000 Jun; 39(3):89-102.
- Review Early additional food and fluids for healthy breastfed full-term infants. [Cochrane Database Syst Rev. 2016] Review Early additional food and fluids for healthy breastfed full-term infants. Smith HA, Becker GE. Cochrane Database Syst Rev. 2016 Aug 30; 2016(8):CD006462. Epub 2016 Aug 30.
Recent Activity
- Breastfeeding - StatPearls Breastfeeding - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

IMAGES
VIDEO
COMMENTS
The collection of data on 'infant feeding at hospital discharge' is used to monitor breastfeeding outcomes, health service benchmarking, and research. While some Australian states have clear definitions of thi...
Here, we provide a non-exhaustive review of the empirical evidence, showing that breastfeeding impacts children's brain, cognitive, and socio-emotional development. In mothers, research is presented indicating that breastfeeding influences mood, affect, stress, and maternal care. The current review aims to provide a broad overview of existing ...
Despite public health efforts to promote breastfeeding, global rates of breastfeeding continue to trail behind the goals identified by the World Health Organization. While the literature exploring breastfeeding beliefs and practices is growing, it offers various and sometimes conflicting explanations regarding women's attitudes towards and experiences of breastfeeding. This research explores ...
Optimal breastfeeding (BF) practices are essential for child survival and proper growth and development. The purpose of this overview is to evaluate the effectiveness of different interventions for promoting and optimizing breastfeeding.We included systematic ...
In this Series paper, we examine how mother and baby attributes at the individual level interact with breastfeeding determinants at other levels, how these interactions drive breastfeeding outcomes, and what policies and interventions are necessary to achieve optimal breastfeeding. About one in three neonates in low-income and middle-income countries receive prelacteal feeds, and only one in ...
Explore the latest in breastfeeding, including advances in understanding ways to encourage it and its long-term effects on child health.
Breastfeeding has proven health benefits for both mothers and babies in high-income and low-income settings alike. Yet, less than 50% of babies worldwide are breastfed according to WHO recommendations. For decades, the commercial milk formula industry has used underhand marketing strategies, designed to prey on parents' fears and concerns, to turn the feeding of infants and young children ...
Journal of Human Lactation. Journal of Human Lactation (JHL) is an international multi-disciplinary quarterly, peer-reviewed journal publishing original research, original theoretical and conceptual articles, discussions regarding clinical practice and policy issues, and special features … | View full journal description.
This article examines the effects of breastfeeding on physical and cognitive development in children, using data from a large-scale longitudinal study in Brazil.
Novel insights into the health impacts of exclusive breastfeeding provide compelling evidence to support its establishment while also identifying medical indications for supplementation.
The complexity and challenges involved in designing, delivering, and evaluating multicomponent breastfeeding support programmes that operate across the different levels of the socioecological model is important to acknowledge.4Although much more implementation science research is needed, the evidence makes clear the importance for breastfeeding ...
Human milk is considered as the gold standard for infant feeding. Breastfeeding advantages extend beyond the properties of human milk itself. A complex of nutritional, environmental, socioeconomic, psychological as well as genetic interactions establish a massive list of benefits of breastfeeding to …
By contrast, our systematic review was restricted to qualitative research on perceptions and experiences of breastfeeding in public spaces within OECD countries, to reduce heterogeneity across findings and shape the design of future interventions aimed at reducing barriers to breastfeeding outside of the home in high- and middle-income countries.
Further research on the association of breastfeeding on PPD and mother-child-bonding may contribute in a meaningful way to the prevention of subsequent disorders and the reduction of long-term ...
Breastfeeding is the normal way of providing young infants with the nutrients they need for healthy growth and development. Virtually, all mothers can breastfeed, provided they have accurate information and the support of their family, the health care system and society at large. Colostrum, the yellowish, sticky breast milk produced at the end ...
BackgroundBreast engorgement and breast pain are the most common reasons for the early cessation of exclusive breastfeeding by mothers.Research Aims (1) To examine the influence of breastfeeding edu...
Worldwide, breastfeeding saves the lives of infants and reduces their disease burden. Breastfeeding also reduces the disease burden for mothers. This article examines who chooses to breastfeed and for how long in the American context. It also reviews ...
The authors conclude that breastfeeding has a significant health and economic benefit and that increasing breastfeeding rates in the most deprived areas could contribute to the narrowing of ...
Breastmilk can promote equitable child health and save healthcare costs by reducing childhood illnesses and healthcare utilization in the early years, according to a new study.
Background Paid parental leave policies may promote breastfeeding, which can have short- and long-term health benefits for both members of the birthing person-infant dyad. In the United States, where 56% of the workforce qualifies for unpaid federal medical leave, certain states have recently enacted paid parental and family leave policies. We aimed to assess the extent to which living in ...
The article by Calik-Ksepka et al [1] reviewed the available research on the physiology of both the lactational amenorrhea method (LAM) and the bone turnover that occurs during breastfeeding. Before understanding how lactation can induce amenorrhea, it is important to explain the physiology behind lactation.
The research emphasises the need for realistic rather than idealistic antenatal preparation and the importance of timely and parent-centred breastfeeding support, particularly in the immediate postnatal weeks. The findings suggest that effective social support, combined with reassurance and guidance from skilled practitioners, can help women to overcome difficulties and find confidence in ...
The research could make a big difference in perceptions of pregnancy needs, said Dr. Eve Feinberg, associate professor of obstetrics and gynecology at Northwestern University's Feinberg School ...
Braden is a board-certified OB-GYN based in Atlanta and a breastfeeding medicine specialist at Lybbie, a lactation innovation company.
Breastfeeding is an important part of the neonatal and infant periods. Breastfeeding or lactation provides total nutritional support and promotes the emotional dependency of the baby on the breastfeeding parent. A strong emotional bond facilitates the successful prolongation of breastfeeding.[1] Breast milk is recommended as the optimal and exclusive source of early nutrition for all infants ...
Research is ongoing to learn more about whether or not phosphatidylserine is safe to take if you're pregnant or thinking about becoming pregnant or breastfeeding (chestfeeding). Many manufacturers don't recommend taking this medication if you're pregnant or planning on becoming pregnant or breastfeeding.