How to Write About Coronavirus in a College Essay
Students can share how they navigated life during the coronavirus pandemic in a full-length essay or an optional supplement.
Writing About COVID-19 in College Essays

Getty Images
Experts say students should be honest and not limit themselves to merely their experiences with the pandemic.
The global impact of COVID-19, the disease caused by the novel coronavirus, means colleges and prospective students alike are in for an admissions cycle like no other. Both face unprecedented challenges and questions as they grapple with their respective futures amid the ongoing fallout of the pandemic.
Colleges must examine applicants without the aid of standardized test scores for many – a factor that prompted many schools to go test-optional for now . Even grades, a significant component of a college application, may be hard to interpret with some high schools adopting pass-fail classes last spring due to the pandemic. Major college admissions factors are suddenly skewed.
"I can't help but think other (admissions) factors are going to matter more," says Ethan Sawyer, founder of the College Essay Guy, a website that offers free and paid essay-writing resources.
College essays and letters of recommendation , Sawyer says, are likely to carry more weight than ever in this admissions cycle. And many essays will likely focus on how the pandemic shaped students' lives throughout an often tumultuous 2020.
But before writing a college essay focused on the coronavirus, students should explore whether it's the best topic for them.

Writing About COVID-19 for a College Application
Much of daily life has been colored by the coronavirus. Virtual learning is the norm at many colleges and high schools, many extracurriculars have vanished and social lives have stalled for students complying with measures to stop the spread of COVID-19.
"For some young people, the pandemic took away what they envisioned as their senior year," says Robert Alexander, dean of admissions, financial aid and enrollment management at the University of Rochester in New York. "Maybe that's a spot on a varsity athletic team or the lead role in the fall play. And it's OK for them to mourn what should have been and what they feel like they lost, but more important is how are they making the most of the opportunities they do have?"
That question, Alexander says, is what colleges want answered if students choose to address COVID-19 in their college essay.
But the question of whether a student should write about the coronavirus is tricky. The answer depends largely on the student.
"In general, I don't think students should write about COVID-19 in their main personal statement for their application," Robin Miller, master college admissions counselor at IvyWise, a college counseling company, wrote in an email.
"Certainly, there may be exceptions to this based on a student's individual experience, but since the personal essay is the main place in the application where the student can really allow their voice to be heard and share insight into who they are as an individual, there are likely many other topics they can choose to write about that are more distinctive and unique than COVID-19," Miller says.
Opinions among admissions experts vary on whether to write about the likely popular topic of the pandemic.
"If your essay communicates something positive, unique, and compelling about you in an interesting and eloquent way, go for it," Carolyn Pippen, principal college admissions counselor at IvyWise, wrote in an email. She adds that students shouldn't be dissuaded from writing about a topic merely because it's common, noting that "topics are bound to repeat, no matter how hard we try to avoid it."
Above all, she urges honesty.
"If your experience within the context of the pandemic has been truly unique, then write about that experience, and the standing out will take care of itself," Pippen says. "If your experience has been generally the same as most other students in your context, then trying to find a unique angle can easily cross the line into exploiting a tragedy, or at least appearing as though you have."
But focusing entirely on the pandemic can limit a student to a single story and narrow who they are in an application, Sawyer says. "There are so many wonderful possibilities for what you can say about yourself outside of your experience within the pandemic."
He notes that passions, strengths, career interests and personal identity are among the multitude of essay topic options available to applicants and encourages them to probe their values to help determine the topic that matters most to them – and write about it.
That doesn't mean the pandemic experience has to be ignored if applicants feel the need to write about it.
Writing About Coronavirus in Main and Supplemental Essays
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form.
To help students explain how the pandemic affected them, The Common App has added an optional section to address this topic. Applicants have 250 words to describe their pandemic experience and the personal and academic impact of COVID-19.
"That's not a trick question, and there's no right or wrong answer," Alexander says. Colleges want to know, he adds, how students navigated the pandemic, how they prioritized their time, what responsibilities they took on and what they learned along the way.
If students can distill all of the above information into 250 words, there's likely no need to write about it in a full-length college essay, experts say. And applicants whose lives were not heavily altered by the pandemic may even choose to skip the optional COVID-19 question.
"This space is best used to discuss hardship and/or significant challenges that the student and/or the student's family experienced as a result of COVID-19 and how they have responded to those difficulties," Miller notes. Using the section to acknowledge a lack of impact, she adds, "could be perceived as trite and lacking insight, despite the good intentions of the applicant."
To guard against this lack of awareness, Sawyer encourages students to tap someone they trust to review their writing , whether it's the 250-word Common App response or the full-length essay.
Experts tend to agree that the short-form approach to this as an essay topic works better, but there are exceptions. And if a student does have a coronavirus story that he or she feels must be told, Alexander encourages the writer to be authentic in the essay.
"My advice for an essay about COVID-19 is the same as my advice about an essay for any topic – and that is, don't write what you think we want to read or hear," Alexander says. "Write what really changed you and that story that now is yours and yours alone to tell."
Sawyer urges students to ask themselves, "What's the sentence that only I can write?" He also encourages students to remember that the pandemic is only a chapter of their lives and not the whole book.
Miller, who cautions against writing a full-length essay on the coronavirus, says that if students choose to do so they should have a conversation with their high school counselor about whether that's the right move. And if students choose to proceed with COVID-19 as a topic, she says they need to be clear, detailed and insightful about what they learned and how they adapted along the way.
"Approaching the essay in this manner will provide important balance while demonstrating personal growth and vulnerability," Miller says.
Pippen encourages students to remember that they are in an unprecedented time for college admissions.
"It is important to keep in mind with all of these (admission) factors that no colleges have ever had to consider them this way in the selection process, if at all," Pippen says. "They have had very little time to calibrate their evaluations of different application components within their offices, let alone across institutions. This means that colleges will all be handling the admissions process a little bit differently, and their approaches may even evolve over the course of the admissions cycle."
Searching for a college? Get our complete rankings of Best Colleges.
10 Ways to Discover College Essay Ideas

Tags: students , colleges , college admissions , college applications , college search , Coronavirus
2024 Best Colleges

Search for your perfect fit with the U.S. News rankings of colleges and universities.
College Admissions: Get a Step Ahead!
Sign up to receive the latest updates from U.S. News & World Report and our trusted partners and sponsors. By clicking submit, you are agreeing to our Terms and Conditions & Privacy Policy .
Ask an Alum: Making the Most Out of College
You May Also Like
Takeaways from the ncaa’s settlement.
Laura Mannweiler May 24, 2024

New Best Engineering Rankings June 18
Robert Morse and Eric Brooks May 24, 2024

Premedical Programs: What to Know
Sarah Wood May 21, 2024

How Geography Affects College Admissions
Cole Claybourn May 21, 2024

Q&A: College Alumni Engagement
LaMont Jones, Jr. May 20, 2024

10 Destination West Coast College Towns
Cole Claybourn May 16, 2024

Scholarships for Lesser-Known Sports
Sarah Wood May 15, 2024

Should Students Submit Test Scores?
Sarah Wood May 13, 2024

Poll: Antisemitism a Problem on Campus
Lauren Camera May 13, 2024

Federal vs. Private Parent Student Loans
Erika Giovanetti May 9, 2024

The complexity of managing COVID-19: How important is good governance?
- Download the essay
Subscribe to Global Connection
Alaka m. basu , amb alaka m. basu professor, department of global development - cornell university, senior fellow - united nations foundation kaushik basu , and kaushik basu nonresident senior fellow - global economy and development @kaushikcbasu jose maria u. tapia jmut jose maria u. tapia student - cornell university.
November 17, 2020
- 13 min read
This essay is part of “ Reimagining the global economy: Building back better in a post-COVID-19 world ,” a collection of 12 essays presenting new ideas to guide policies and shape debates in a post-COVID-19 world.
The COVID-19 pandemic has exposed the inadequacy of public health systems worldwide, casting a shadow that we could not have imagined even a year ago. As the fog of confusion lifts and we begin to understand the rudiments of how the virus behaves, the end of the pandemic is nowhere in sight. The number of cases and the deaths continue to rise. The latter breached the 1 million mark a few weeks ago and it looks likely now that, in terms of severity, this pandemic will surpass the Asian Flu of 1957-58 and the Hong Kong Flu of 1968-69.
Moreover, a parallel problem may well exceed the direct death toll from the virus. We are referring to the growing economic crises globally, and the prospect that these may hit emerging economies especially hard.
The economic fall-out is not entirely the direct outcome of the COVID-19 pandemic but a result of how we have responded to it—what measures governments took and how ordinary people, workers, and firms reacted to the crisis. The government activism to contain the virus that we saw this time exceeds that in previous such crises, which may have dampened the spread of the COVID-19 but has extracted a toll from the economy.
This essay takes stock of the policies adopted by governments in emerging economies, and what effect these governance strategies may have had, and then speculates about what the future is likely to look like and what we may do here on.
Nations that build walls to keep out goods, people and talent will get out-competed by other nations in the product market.
It is becoming clear that the scramble among several emerging economies to imitate and outdo European and North American countries was a mistake. We get a glimpse of this by considering two nations continents apart, the economies of which have been among the hardest hit in the world, namely, Peru and India. During the second quarter of 2020, Peru saw an annual growth of -30.2 percent and India -23.9 percent. From the global Q2 data that have emerged thus far, Peru and India are among the four slowest growing economies in the world. Along with U.K and Tunisia these are the only nations that lost more than 20 percent of their GDP. 1
COVID-19-related mortality statistics, and, in particular, the Crude Mortality Rate (CMR), however imperfect, are the most telling indicator of the comparative scale of the pandemic in different countries. At first glance, from the end of October 2020, Peru, with 1039 COVID-19 deaths per million population looks bad by any standard and much worse than India with 88. Peru’s CMR is currently among the highest reported globally.
However, both Peru and India need to be placed in regional perspective. For reasons that are likely to do with the history of past diseases, there are striking regional differences in the lethality of the virus (Figure 11.1). South America is worse hit than any other world region, and Asia and Africa seem to have got it relatively lightly, in contrast to Europe and America. The stark regional difference cries out for more epidemiological analysis. But even as we await that, these are differences that cannot be ignored.
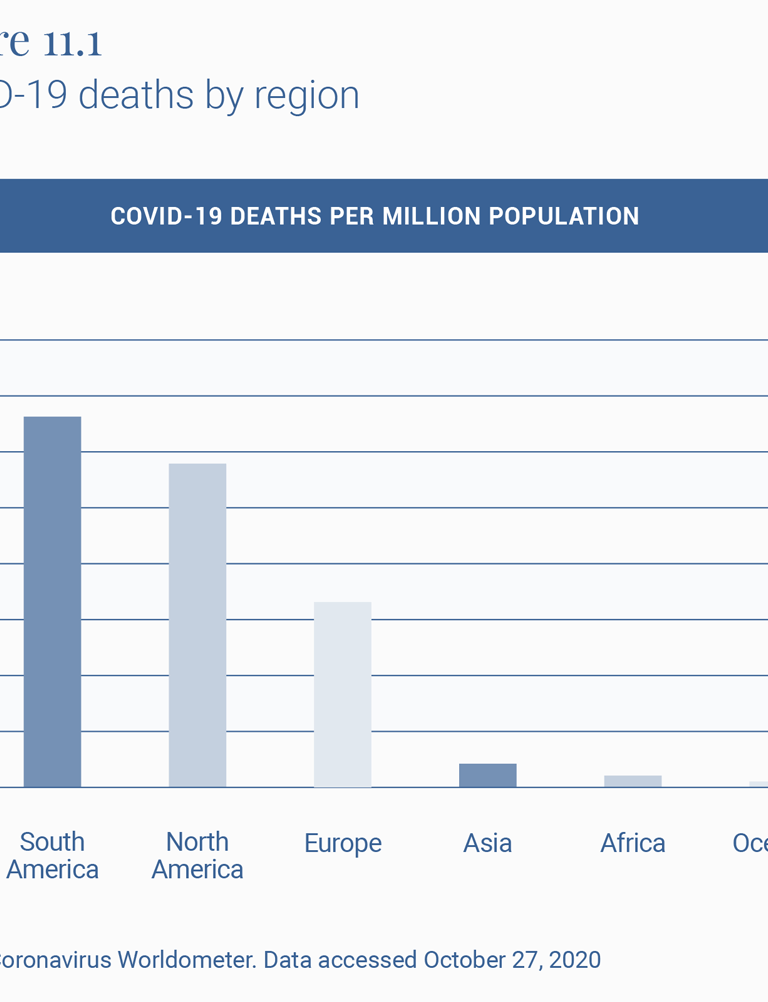
To understand the effect of policy interventions, it is therefore important to look at how these countries fare within their own regions, which have had similar histories of illnesses and viruses (Figure 11.2). Both Peru and India do much worse than the neighbors with whom they largely share their social, economic, ecological and demographic features. Peru’s COVID-19 mortality rate per million population, or CMR, of 1039 is ahead of the second highest, Brazil at 749, and almost twice that of Argentina at 679.
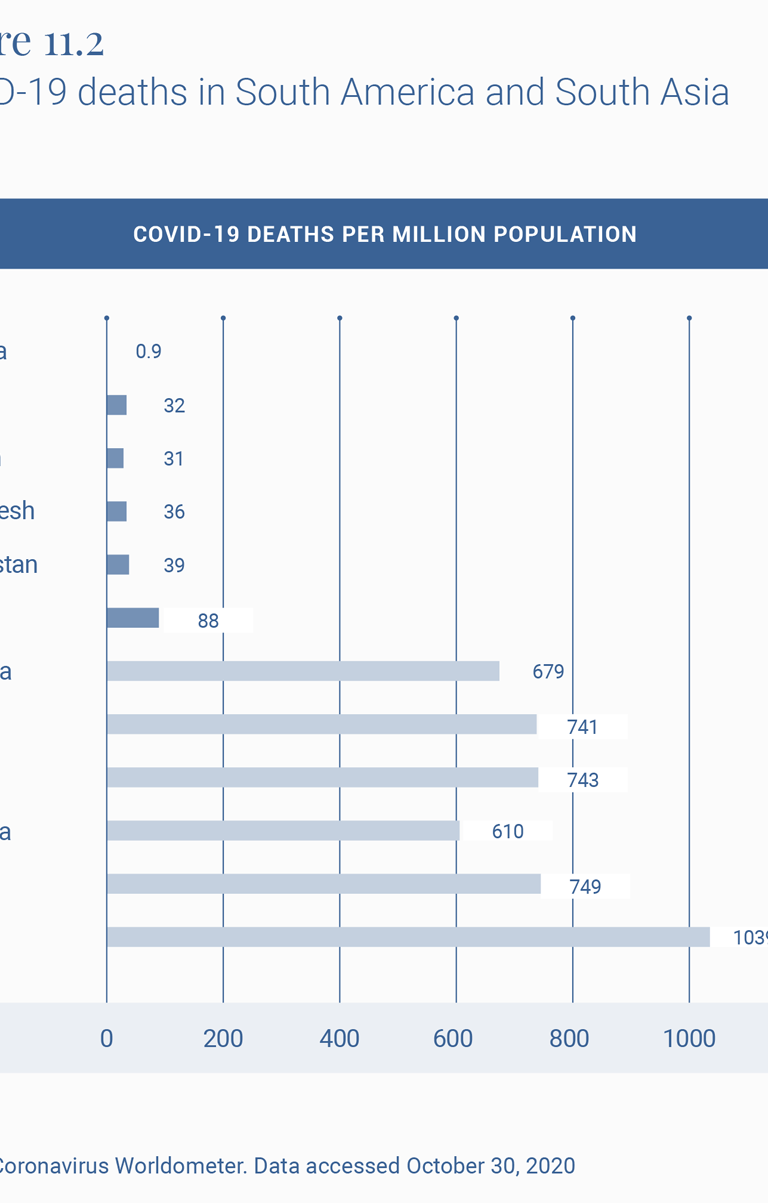
Similarly, India at 88 compares well with Europe and the U.S., as does virtually all of Asia and Africa, but is doing much worse than its neighbors, with the second worst country in the region, Afghanistan, experiencing less than half the death rate of India.
The official Indian statement that up to 78,000 deaths 2 were averted by the lockdown has been criticized 3 for its assumptions. A more reasonable exercise is to estimate the excess deaths experienced by a country that breaks away from the pattern of its regional neighbors. So, for example, if India had experienced Afghanistan’s COVID-19 mortality rate, it would by now have had 54,112 deaths. And if it had the rate reported by Bangladesh, it would have had 49,950 deaths from COVID-19 today. In other words, more than half its current toll of some 122,099 COVID-19 deaths would have been avoided if it had experienced the same virus hit as its neighbors.
What might explain this outlier experience of COVID-19 CMRs and economic downslide in India and Peru? If the regional background conditions are broadly similar, one is left to ask if it is in fact the policy response that differed markedly and might account for these relatively poor outcomes.
Peru and India have performed poorly in terms of GDP growth rate in Q2 2020 among the countries displayed in Table 2, and given that both these countries are often treated as case studies of strong governance, this draws attention to the fact that there may be a dissonance between strong governance and good governance.
The turnaround for India has been especially surprising, given that until a few years ago it was among the three fastest growing economies in the world. The slowdown began in 2016, though the sharp downturn, sharper than virtually all other countries, occurred after the lockdown.
On the COVID-19 policy front, both India and Peru have become known for what the Oxford University’s COVID Policy Tracker 4 calls the “stringency” of the government’s response to the epidemic. At 8 pm on March 24, 2020, the Indian government announced, with four hours’ notice, a complete nationwide shutdown. Virtually all movement outside the perimeter of one’s home was officially sought to be brought to a standstill. Naturally, as described in several papers, such as that of Ray and Subramanian, 5 this meant that most economic life also came to a sudden standstill, which in turn meant that hundreds of millions of workers in the informal, as well as more marginally formal sectors, lost their livelihoods.
In addition, tens of millions of these workers, being migrant workers in places far-flung from their original homes, also lost their temporary homes and their savings with these lost livelihoods, so that the only safe space that beckoned them was their place of origin in small towns and villages often hundreds of miles away from their places of work.
After a few weeks of precarious living in their migrant destinations, they set off, on foot since trains and buses had been stopped, for these towns and villages, creating a “lockdown and scatter” that spread the virus from the city to the town and the town to the village. Indeed, “lockdown” is a bit of a misnomer for what happened in India, since over 20 million people did exactly the opposite of what one does in a lockdown. Thus India had a strange combination of lockdown some and scatter the rest, like in no other country. They spilled out and scattered in ways they would otherwise not do. It is not surprising that the infection, which was marginally present in rural areas (23 percent in April), now makes up some 54 percent of all cases in India. 6
In Peru too, the lockdown was sudden, nationwide, long drawn out and stringent. 7 Jobs were lost, financial aid was difficult to disburse, migrant workers were forced to return home, and the virus has now spread to all parts of the country with death rates from it surpassing almost every other part of the world.
As an aside, to think about ways of implementing lockdowns that are less stringent and geographically as well as functionally less total, an example from yet another continent is instructive. Ethiopia, with a COVID-19 death rate of 13 per million population seems to have bettered the already relatively low African rate of 31 in Table 1. 8
We hope that human beings will emerge from this crisis more aware of the problems of sustainability.
The way forward
We next move from the immediate crisis to the medium term. Where is the world headed and how should we deal with the new world? Arguably, that two sectors that will emerge larger and stronger in the post-pandemic world are: digital technology and outsourcing, and healthcare and pharmaceuticals.
The last 9 months of the pandemic have been a huge training ground for people in the use of digital technology—Zoom, WebEx, digital finance, and many others. This learning-by-doing exercise is likely to give a big boost to outsourcing, which has the potential to help countries like India, the Philippines, and South Africa.
Globalization may see a short-run retreat but, we believe, it will come back with a vengeance. Nations that build walls to keep out goods, people and talent will get out-competed by other nations in the product market. This realization will make most countries reverse their knee-jerk anti-globalization; and the ones that do not will cease to be important global players. Either way, globalization will be back on track and with a much greater amount of outsourcing.
To return, more critically this time, to our earlier aside on Ethiopia, its historical and contemporary record on tampering with internet connectivity 9 in an attempt to muzzle inter-ethnic tensions and political dissent will not serve it well in such a post-pandemic scenario. This is a useful reminder for all emerging market economies.
We hope that human beings will emerge from this crisis more aware of the problems of sustainability. This could divert some demand from luxury goods to better health, and what is best described as “creative consumption”: art, music, and culture. 10 The former will mean much larger healthcare and pharmaceutical sectors.
But to take advantage of these new opportunities, nations will need to navigate the current predicament so that they have a viable economy once the pandemic passes. Thus it is important to be able to control the pandemic while keeping the economy open. There is some emerging literature 11 on this, but much more is needed. This is a governance challenge of a kind rarely faced, because the pandemic has disrupted normal markets and there is need, at least in the short run, for governments to step in to fill the caveat.
Emerging economies will have to devise novel governance strategies for doing this double duty of tamping down on new infections without strident controls on economic behavior and without blindly imitating Europe and America.
Here is an example. One interesting opportunity amidst this chaos is to tap into the “resource” of those who have already had COVID-19 and are immune, even if only in the short-term—we still have no definitive evidence on the length of acquired immunity. These people can be offered a high salary to work in sectors that require physical interaction with others. This will help keep supply chains unbroken. Normally, the market would have on its own caused such a salary increase but in this case, the main benefit of marshaling this labor force is on the aggregate economy and GDP and therefore is a classic case of positive externality, which the free market does not adequately reward. It is more a challenge of governance. As with most economic policy, this will need careful research and design before being implemented. We have to be aware that a policy like this will come with its risk of bribery and corruption. There is also the moral hazard challenge of poor people choosing to get COVID-19 in order to qualify for these special jobs. Safeguards will be needed against these risks. But we believe that any government that succeeds in implementing an intelligently-designed intervention to draw on this huge, under-utilized resource can have a big, positive impact on the economy 12 .
This is just one idea. We must innovate in different ways to survive the crisis and then have the ability to navigate the new world that will emerge, hopefully in the not too distant future.
Related Content
Emiliana Vegas, Rebecca Winthrop
Homi Kharas, John W. McArthur
Anthony F. Pipa, Max Bouchet
Note: We are grateful for financial support from Cornell University’s Hatfield Fund for the research associated with this paper. We also wish to express our gratitude to Homi Kharas for many suggestions and David Batcheck for generous editorial help.
- “GDP Annual Growth Rate – Forecast 2020-2022,” Trading Economics, https://tradingeconomics.com/forecast/gdp-annual-growth-rate.
- “Government Cites Various Statistical Models, Says Averted Between 1.4 Million-2.9 Million Cases Due To Lockdown,” Business World, May 23, 2020, www.businessworld.in/article/Government-Cites-Various-Statistical-Models-Says-Averted-Between-1-4-million-2-9-million-Cases-Due-To-Lockdown/23-05-2020-193002/.
- Suvrat Raju, “Did the Indian lockdown avert deaths?” medRxiv , July 5, 2020, https://europepmc.org/article/ppr/ppr183813#A1.
- “COVID Policy Tracker,” Oxford University, https://github.com/OxCGRT/covid-policy-tracker t.
- Debraj Ray and S. Subramanian, “India’s Lockdown: An Interim Report,” NBER Working Paper, May 2020, https://www.nber.org/papers/w27282.
- Gopika Gopakumar and Shayan Ghosh, “Rural recovery could slow down as cases rise, says Ghosh,” Mint, August 19, 2020, https://www.livemint.com/news/india/rural-recovery-could-slow-down-as-cases-rise-says-ghosh-11597801644015.html.
- Pierina Pighi Bel and Jake Horton, “Coronavirus: What’s happening in Peru?,” BBC, July 9, 2020, https://www.bbc.com/news/world-latin-america-53150808.
- “No lockdown, few ventilators, but Ethiopia is beating Covid-19,” Financial Times, May 27, 2020, https://www.ft.com/content/7c6327ca-a00b-11ea-b65d-489c67b0d85d.
- Cara Anna, “Ethiopia enters 3rd week of internet shutdown after unrest,” Washington Post, July 14, 2020, https://www.washingtonpost.com/world/africa/ethiopia-enters-3rd-week-of-internet-shutdown-after-unrest/2020/07/14/4699c400-c5d6-11ea-a825-8722004e4150_story.html.
- Patrick Kabanda, The Creative Wealth of Nations: Can the Arts Advance Development? (Cambridge: Cambridge University Press, 2018).
- Guanlin Li et al, “Disease-dependent interaction policies to support health and economic outcomes during the COVID-19 epidemic,” medRxiv, August 2020, https://www.medrxiv.org/content/10.1101/2020.08.24.20180752v3.
- For helpful discussion concerning this idea, we are grateful to Turab Hussain, Daksh Walia and Mehr-un-Nisa, during a seminar of South Asian Economics Students’ Meet (SAESM).
Global Economy and Development
The Brookings Institution, Washington DC
3:00 pm - 4:00 pm EDT
Robin Brooks
May 23, 2024
Gayle E. Smith
May 21, 2024
- Open access
- Published: 04 February 2022
Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies
- Yibeltal Assefa ORCID: orcid.org/0000-0003-2393-1492 1 ,
- Charles F. Gilks 1 ,
- Simon Reid 1 ,
- Remco van de Pas 2 ,
- Dereje Gedle Gete 1 &
- Wim Van Damme 2
Globalization and Health volume 18 , Article number: 10 ( 2022 ) Cite this article
36 Citations
10 Altmetric
Metrics details
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of Public Health Emergencies of International Concern. As of 12 January 2022, there were over 314 million cases and over 5.5 million deaths notified since the start of the pandemic. The COVID-19 pandemic takes variable shapes and forms, in terms of cases and deaths, in different regions and countries of the world. The objective of this study is to analyse the variable expression of COVID-19 pandemic so that lessons can be learned towards an effective public health emergency response.
We conducted a mixed-methods study to understand the heterogeneity of cases and deaths due to the COVID-19 pandemic. Correlation analysis and scatter plot were employed for the quantitative data. We used Spearman’s correlation analysis to determine relationship strength between cases and deaths and socio-economic and health systems. We organized qualitative information from the literature and conducted a thematic analysis to recognize patterns of cases and deaths and explain the findings from the quantitative data.
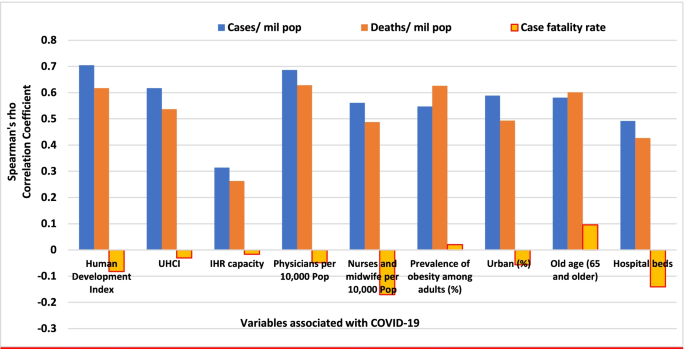
We have found that regions and countries with high human development index have higher cases and deaths per million population due to COVID-19. This is due to international connectedness and mobility of their population related to trade and tourism, and their vulnerability related to older populations and higher rates of non-communicable diseases. We have also identified that the burden of the pandemic is also variable among high- and middle-income countries due to differences in the governance of the pandemic, fragmentation of health systems, and socio-economic inequities.
The COVID-19 pandemic demonstrates that every country remains vulnerable to public health emergencies. The aspiration towards a healthier and safer society requires that countries develop and implement a coherent and context-specific national strategy, improve governance of public health emergencies, build the capacity of their (public) health systems, minimize fragmentation, and tackle upstream structural issues, including socio-economic inequities. This is possible through a primary health care approach, which ensures provision of universal and equitable promotive, preventive and curative services, through whole-of-government and whole-of-society approaches.
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of emerging infectious diseases that become Public Health Emergency of International Concern (PHEIC) [ 1 ]. The COVID-19 pandemic takes variable shapes and forms in how it affects communities in different regions and countries [ 2 , 3 ]. As of 12 January, 2022, there were over 314 million cases and over 5.5 million deaths notified around the globe since the start of the pandemic. The number of cases per million population ranged from 7410 in Africa to 131,730 in Europe while the number of deaths per million population ranged from 110 in Oceania to 2740 in South America. Case-fatality rates (CFRs) ranged from 0.3% in Oceania to 2.9% in South America [ 4 , 5 ]. Regions and countries with high human development index (HDI), which is a composite index of life expectancy, education, and per capita income indicators [ 6 ], are affected by COVID-19 more than regions with low HDI. North America and Europe together account for 55 and 51% of cases and deaths, respectively. Regions with high HDI are affected by COVID-19 despite their high universal health coverage index (UHCI) and Global Health Security index (GHSI) [ 7 ].
This seems to be a paradox (against the established knowledge that countries with weak (public) health systems capacity will have worse health outcomes) in that the countries with higher UHCI and GHSI have experienced higher burdens of COVID-19 [ 7 ]. The paradox can partially be explained by variations in testing algorithms, capacity for testing, and reporting across different countries. Countries with high HDI have health systems with a high testing capacity; the average testing rate per million population is less than 32, 000 in Africa and 160,000 in Asia while it is more than 800, 000 in HICs (Europe and North America). This enables HICs to identify more confirmed cases that will ostensibly increase the number of reported cases [ 3 ]. Nevertheless, these are insufficient to explain the stark differences between countries with high HDI and those with low HDI. Many countries with high HDI have a high testing rate and a higher proportion of symptomatic and severe cases, which are also associated with higher deaths and CFRs [ 7 ]. On the other hand, there are countries with high HDI that sustain a lower level of the epidemic than others with a similar high HDI. It is, therefore, vital to analyse the heterogeneity of the COVID-19 pandemic and explain why some countries with high HDI, UHCI and GHSI have the highest burden of COVID-19 while others are able to suppress their epidemics and mitigate its impacts.
The objective of this study was to analyse the COVID-19 pandemic and understand its variable expression with the intention to learn lessons for an effective and sustainable response to public health emergencies. We hypothesised that high levels of HDI, UHCI and GHSI are essential but not sufficient to prevent and control COVID-19.
We conducted an explanatory mixed-methods study to understand and explain the heterogeneity of the pandemic around the world. The study integrated quantitative and qualitative secondary data. The following steps were included in the research process: (i) collecting and analysing quantitative epidemiological data, (ii) conducting literature review of qualitative secondary data and (iii) evaluating countries’ pandemic responses to explain the variability in the COVID-19 epidemiological outcomes. The study then illuminated specific factors that were vital towards an effective and sustainable epidemic response.
We used the publicly available secondary data sources from Johns Hopkins University ( https://coronavirus.jhu.edu/data/new-cases ) for COVID-19 and UNDP 2020 HDI report ( http://hdr.undp.org/en/2019-report ) for HDI, demographic and epidemiologic variables. These are open data sources which are regularly updated and utilized by researchers, policy makers and funders. We performed a correlation analysis of the COVID-19 pandemic. We determined the association between COVID-19 cases, severity, deaths and CFRs at the 0.01 and 0.05 levels (2-tailed). We used Spearman’s correlation analysis, as there is no normal distribution of the variables [ 8 ].
The UHCI is calculated as the geometric mean of the coverage of essential services based on 17 tracer indicators from: (1) reproductive, maternal, newborn and child health; (2) infectious diseases; (3) non-communicable diseases; and, (4) service capacity and access and health security [ 9 ]. The GHSI is a composite measure to assess a country’s capability to prevent, detect, and respond to epidemics and pandemics [ 10 ].
We then conducted a document review to explain the epidemic patterns in different countries. Secondary data was obtained from peer-reviewed journals, reputable online news outlets, government reports and publications by public health-related associations, such as the WHO. To explain the variability of COVID-19 across countries, a list of 14 indicators was established to systematically assess country’s preparedness, actual pandemic response, and overall socioeconomic and demographic profile in the context of COVID-19. The indicators used in this study include: 1) Universal Health Coverage Index, 2) public health capacity, 3) Global Health Security Index, 4) International Health Regulation, 5) leadership, governance and coordination of response, 6) community mobilization and engagement, 7) communication, 8) testing, quarantines and social distancing, 9) medical services at primary health care facilities and hospitals, 10) multisectoral actions, 11) social protection services, 12) absolute and relative poverty status, 13) demography, and 14) burden of communicable and non-communicable diseases. These indicators are based on our previous studies and recommendation from the World Health Organization [ 3 , 4 ]. We conducted thematic analysis and synthesis to identify the factors that may explain the heterogeneity of the pandemic.
Heterogeneity of COVID-19 cases and deaths around the world: what can explain it?
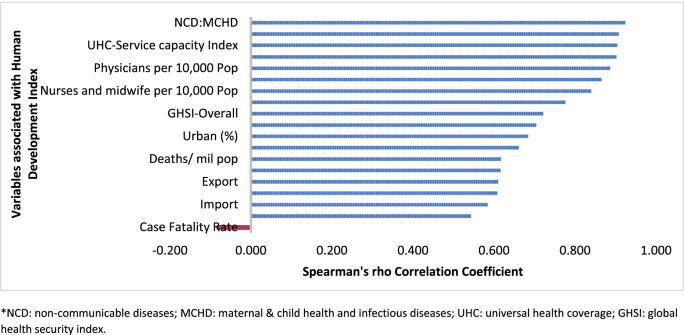
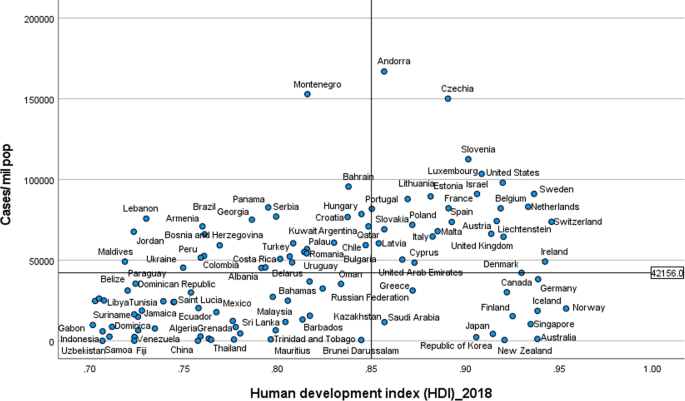
Table 1 indicates that the pandemic of COVID-19 is heterogeneous around regions of the world. Figure 1 also shows that there is a strong and significant correlation between HDI and globalisation (with an increase in trade and tourism as proxy indicators) and a corresponding strong and significant correlation with COVID-19 burden.
Human development index and its correlates associated with COVID-19 in 189 countries*
Globalisation and pandemics interact in various ways, including through international trade and mobility, which can lead to multiple waves of infections [ 11 ]. In at least the first waves of the pandemic, countries with high import and export of consumer goods, food products and tourism have high number of cases, severe cases, deaths and CFRs. Countries with high HDI are at a higher risk of importing (and exporting) COVID-19 due to high mobility linked to trade and tourism, which are drivers of the economy. These may have led to multiple introductions of COVID-19 into these countries before border closures.
The COVID-19 pandemic was first identified in China, which is central to the global network of trade, from where it spread to all parts of the world, especially those countries with strong links with China [ 12 ]. The epidemic then spread to Europe. There is very strong regional dimension to manufacturing and trading, which could be facilitate the spread of the virus. China is the heart of ‘Factory Asia’; Italy is in the heart of ‘Factory Europe’; the United States is the heart of ‘Factory North America’; and Brazil is the heart of ‘Factory Latin America’ [ 13 ]. These are the countries most affected by COVID-19 during the first wave of the pandemic [ 2 , 3 , 14 ].
It is also important to note that two-third of the countries currently reporting more than a million cases are middle-income countries (MICs), which are not only major emerging market economies but also regional political powers, including the BRICS countries (Brazil, Russia, India and South Africa) [ 3 , 15 ]. These countries participate in the global economy, with business travellers and tourists. They also have good domestic transportation networks that facilitate the internal spread of the virus. The strategies that helped these countries to become emerging markets also put them at greater risk for importing and spreading COVID-19 due to their connectivity to the rest of the world.
In addition, countries with high HDI may be more significantly impacted by COVID-19 due to the higher proportion of the elderly and higher rates of non-communicable diseases. Figure 1 shows that there is a strong and significant correlation between HDI and demographic transition (high proportion of old-age population) and epidemiologic transition (high proportion of the population with non-communicable diseases). Countries with a higher proportion of people older than 65 years and NCDs (compared to communicable diseases) have higher burden of COVID-19 [ 16 , 17 , 18 , 19 , 20 ]. Evidence has consistently shown a higher risk of severe COVID-19 in older individuals and those with underlying health conditions [ 21 , 22 , 23 , 24 , 25 ]. CFR is age-dependent; it is highest in persons aged ≥85 years (10 to 27%), followed by those among persons aged 65–84 years (3 to 11%), and those among persons aged 55-64 years (1 to 3%) [ 26 ].
On the other hand, regions and countries with low HDI have, to date, experienced less severe epidemics. For instance, as of January 12, 2022, the African region has recorded about 10.3 million cases and 233,000 deaths– far lower than other regions of the world (Table 1 ) [ 27 ]. These might be due to lower testing rates in Africa, where only 6.5% of the population has been tested for the virus [ 14 , 28 ], and a greater proportion of infections may remain asymptomatic [ 29 ]. Indeed, the results from sero-surveys in Africa show that more than 80% of people infected with the virus were asymptomatic compared to an estimated 40-50% asymptomatic infections in HICs [ 30 , 31 ]. Moreover, there is a weak vital registration system in the region indicating that reports might be underestimating and underreporting the disease burden [ 32 ]. However, does this fully explain the differences observed between Africa and Europe or the Americas?
Other possible factors that may explain the lower rates of cases and deaths in Africa include: (1) Africa is less internationally connected than other regions; (2) the imposition of early strict lockdowns in many African countries, at a time when case numbers were relatively small, limited the number of imported cases further [ 2 , 33 , 34 ]; (3) relatively poor road network has also limited the transmission of the virus to and in rural areas [ 35 ]; (4) a significant proportion of the population resides in rural areas while those in urban areas spend a lot of their time mostly outdoors; (5) only about 3% of Africans are over the age of 65 (so only a small proportion are at risk of severe COVID-19) [ 36 ]; (6) lower prevalence of NCDs, as disease burden in Africa comes from infectious causes, including coronaviruses, which may also have cross-immunity that may reduce the risk of developing symptomatic cases [ 37 ]; and (7) relative high temperature (a major source of vitamin D which influences COVID-19 infection and mortality) in the region may limit the spread of the virus [ 38 , 39 ]. We argue that a combination of all these factors might explain the lower COVID-19 burden in Africa.
The early and timely efforts by African leaders should not be underestimated. The African Union, African CDC, and WHO convened an emergency meeting of all African ministers of health to establish an African taskforce to develop and implement a coordinated continent-wide strategy focusing on: laboratory; surveillance; infection prevention and control; clinical treatment of people with severe COVID-19; risk communication; and supply chain management [ 40 ]. In April 2021, African Union and Africa CDC launched the Partnerships for African Vaccine Manufacturing (PAVM), framework to expanding Africa’s vaccine manufacturing capacity for health security [ 41 ].
Heterogeneity of the pandemic among countries with high HDI: what can explain it?
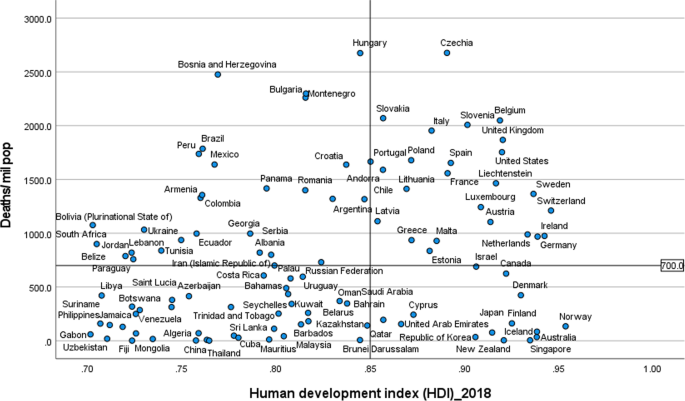
Figures 2 and 3 illustrate the variability of cases and deaths due to the COVID-19 pandemic across high-income countries (HICs). Contrary to the overall positive correlation between high HDI and cases, deaths and fatality rates due to COVID-19, there are outlier HICs, which have been able to control the epidemic. Several HICs, such as New Zealand, Australia, South Korea, Japan, Denmark, Iceland, and Norway, managed to contain their epidemics (Figs. 2 and 3 ) [ 15 , 42 , 43 ]. It is important to note that most of these countries (especially the island states) have far less cross-border mobility than other HICs.
Scatter plot of COVID-19 cases per million population in countries with high human development index (> 0.70)
Scatter plot of COVID-19 deaths per million population in countries with high human development index (> 0.70)
HICs that have been successful at controlling their epidemics have similar characteristics, which are related to governance of the response [ 44 ], synergy between UHC and GHS, and existing relative socio-economic equity in the country. Governance and leadership is a crucial factor to explain the heterogeneity of the epidemic among countries with high HDI [ 45 ]. There has been substantial variation in the nature and timing of the public health responses implemented [ 46 ]. Adaptable and agile governments seem better able to respond to their epidemics [ 47 , 48 ]. Countries that have fared the best are the ones with good governance and public support [ 49 ]. Countries with an absence of coherent leadership and social trust have worse outcomes than countries with collective action, whether in a democracy or autocracy, and rapid mobilisation of resources [ 50 ]. The erosion of trust in the United States government has hurt the country’s ability to respond to the COVID-19 crisis [ 51 , 52 ]. The editors of the New England Journal of Medicine argued that the COVID-19 crisis has produced a test of leadership; but, the leaders in the United States had failed that test [ 47 ].
COVID-19 has exposed the fragility of health systems, not only in the public health and primary care, but also in acute and long-term care systems [ 49 ]. Fragmentation of health systems, defined here to mean inadequate synergy and/ or integration between GHS and UHC, is typical of countries most affected by the COVID-19 pandemic. Even though GHS and UHC agendas are convergent and interdependent, they tend to have different policies and practices [ 53 ]. The United States has the highest index for GHS preparedness; however, it has reported the world’s highest number of COVID-19 cases and deaths due to its greatly fragmented health system [ 54 , 55 ]. Countries with health systems and policies that are able to integrate International Health Regulations (IHR) core capacities with primary health care (PHC) services have been effective at mitigating the effects of COVID-19 [ 50 , 53 ]. Australia has been able to control its COVID-19 epidemic through a comprehensive primary care response, including protection of vulnerable people, provision of treatment and support services to affected people, continuity of regular healthcare services, protection and support of PHC workers and primary care services, and provision of mental health services to the community and the primary healthcare workforce [ 56 ]. Strict implementation of public health and social intervention together with UHC systems have ensured swift control of the epidemics in Singapore, South Korea, and Thailand [ 57 ].
The heterogeneity of cases and deaths, due to COVID-19, is also explained by differences in levels of socio-economic inequalities, which increase susceptibility to acquiring the infection and disease progression as well as worsening of health outcomes [ 58 ]. COVID-19 has been a stress test for public services and social protection systems. There is a higher burden of COVID-19 in Black, Asian and Minority Ethnic individuals due to socio-economic inequities in HICs [ 59 , 60 ]. Poor people are more likely to live in overcrowded accommodation, are more likely to have unstable work conditions and incomes, have comorbidities associated with poverty and precarious living conditions, and reduced access to health care [ 59 ].
The epidemiology of COVID-19 is also variable across MICs, with HDI between 0.70 and 0.85, around the world. Overall, the epidemic in MICs is exacerbated by the rapid demographic and epidemiologic transitions as well as high prevalence of obesity. While India and Brazil witnessed rapidly increasing rates of cases and deaths, China, Thailand, Vietnam have experienced a relatively lower disease burden [ 15 ]. This heterogeneity may be attributed to a number of factors, including governance, communication and service delivery. Thailand, China and Vietnam have implemented a national harmonized strategic response with decentralized implementation through provincial and district authorities [ 61 ]. Thailand increased its testing capacity from two to over 200 certified facilities that could process between 10,000 to 100,000 tests per day; moreover, over a million village health volunteers in Thailand supported primary health services [ 62 , 63 ]. China’s swift and decisive actions enabled the country to contain its epidemic though there was an initial delay in detecting the disease. China has been able to contain its epidemic through community-based measures, very high public cooperation and social mobilization, strategic lockdown and isolation, multi-sector action [ 64 ]. Overall, multi-level governance (effective and decisive leadership and accountability) of the response, together with coordination of public health and socio-economic services, and high levels of citizen adherence to personal protection, have enabled these countries to successfully contain their epidemics [ 61 , 65 , 66 ].
On the other hand, the Brazilian leadership was denounced for its failure to establish a national surveillance network early in the pandemic. In March 2020, the health minister was reported to have stated that mass testing was a waste of public funding, and to have advised against it [ 67 ]. This was considered as a sign of a collapse of public health leadership, characterized by ignorance, neoliberal authoritarianism [ 68 ]. There were also gaps in the public health capacity in different municipalities, which varied greatly, with a considerable number of Brazilian regions receiving less funding from the federal government due to political tension [ 69 ]. The epidemic has a disproportionate adverse burden on states and municipalities with high socio-economic vulnerability, exacerbated by the deep social and economic inequalities in Brazil [ 70 ].
India is another middle-income country with a high burden of COVID-19. It was one of the countries to institute strict measures in the early phase of the pandemic [ 71 , 72 ]. However, the government eased restrictions after the claim that India had beaten the pandemic, which lead to a rapid increase in disease incidence. Indeed, on 12 January 2022, India reported 36 million cumulative cases and almost 485,000 total deaths [ 15 ]. The second wave of the epidemic in India exposed weaknesses in governance and inadequacies in the country’s health and other social systems [ 73 ]. The nature of the Indian federation, which is highly centripetal, has prevented state and local governments from tailoring a policy response to suit local needs. A centralized one-size-fits-all strategy has been imposed despite high variations in resources, health systems capacity, and COVID-19 epidemics across states [ 74 ]. There were also loose social distancing and mask wearing, mass political rallies and religious events [ 75 ]. Rapid community transmission driven by high population density and multigenerational households has been a feature of the current wave in India [ 76 ]. In addition, several new variants of the virus, including the UK (B.1.1.7), the South Africa (20H/501Y or B.1.351), and Brazil (P.1), alongside a newly identified Indian variant (B.1.617), are circulating in India and have been implicated as factors in the second wave of the pandemic [ 75 , 76 ].
Heterogeneity of case-fatality rates around the world: what can explain it?
The pandemic is characterized by variable CFRs across regions and countries that are negatively associated with HDI (Fig. 1 ). The results presented in Fig. 4 show that the proportion of elderly population and rate of obesity are important factors which are positively associated with CFR. On the other hand, UHC, IHR capacity and other indicators of health systems capacity (health workforce density and hospital beds) are negatively associated with the CFR (Figs. 1 and 4 ).
Correlates of COVID-19 cases, deaths and case-fatality rates in 189 countries
The evidence from several research indicates that heterogeneity can be explained by several factors, including differences in age-pyramid, socio-economic status, access to health services, or rates of undiagnosed infections. Differences in age-pyramid may explain some of the observed variation in epidemic severity and CFR between countries [ 77 ]. CFRs across countries look similar when taking age into account [ 78 ]. The elderly and other vulnerable populations in Africa and Asia are at a similar risk as populations in Europe and Americas [ 79 ]. Data from European countries suggest that as high as 57% of all deaths have happened in care homes and many deaths in the US have also occurred in nursing homes. On the other hand, in countries such as Mexico and India, individuals < 65 years contributed the majority of deaths [ 80 ].
Nevertheless, CFR also depends on the quality of hospital care, which can be used to judge the health system capacity, including the availability of healthcare workers, resources, and facilities, which affects outcomes [ 81 ]. The CFR can increase if there is a surge of infected patients, which adds to the strain on the health system [ 82 ]. COVID-19 fatality rates are affected by numerous health systems factors, including bed capacity, existence and capacity of intensive care unit (ICU), and critical care resources (such as oxygen and dexamethasone) in a hospital. Regions and countries with high HDI have a greater number of acute care facilities, ICU, and hospital bed capacities compared to lower HDI regions and countries [ 83 ]. Differences in health systems capacity could explain why North America and Europe, which have experienced much greater number of cases and deaths per million population, reported lower CFRs than the Southern American and the African regions, partly also due to limited testing capacity in these regions (Table 1 ) [ 84 , 85 , 86 ]. The higher CFR in Southern America can be explained by the relatively lower health systems surge capacity that could not adequately respond to the huge demand for health services [ 69 , 86 ]. The COVID-19 pandemic has highlighted existing health systems’ weaknesses, which are not able to effectively prepare for and respond to PHEs [ 87 ]. The high CFRs in the region are also exacerbated by the high social inequalities [ 69 ].
On the other hand, countries in Asia recorded lower CFRs (~ 1.4%) despite sharing many common risk factors (including overcrowding and poverty, weak health system capacity etc) with Africa. The Asian region shares many similar protective factors to the African region. They have been able to minimize their CFR by suppressing the transmission of the virus and flattening the epidemic curve of COVID-19 cases and deaths. Nevertheless, the epidemic in India is likely to be different because it has exceeded the health system capacity to respond and provide basic medical care and medical supplies such as oxygen [ 88 ]. Overall, many Asian countries were able to withstand the transmission of the virus and its effect due to swift action by governments in the early days of the pandemic despite the frequency of travel between China and neighbouring countries such as Hong Kong, Taiwan and Singapore [ 89 ]. This has helped them to contain the pandemic to ensure case numbers remain within their health systems capacity. These countries have benefited from their experience in the past in the prevention and control of epidemics [ 90 ].
There are a number of issues with the use of the CFR to compare the management of the pandemic between countries and regions [ 91 ], as it does not depict the true picture of the mortality burden of the pandemic. A major challenge with accurate calculation of the CFR is the denominator on number of identified cases, as asymptomatic infections and patients with mild symptoms are frequently left untested, and therefore omitted from CFR calculations. Testing might not be widely available, and proactive contact tracing and containment might not be employed, resulting in a smaller denominator, and skewing to a higher CFR [ 82 ]. It is, therefore, far more relevant to estimate infection fatality rate (IFR), the proportion of all infected individuals who have died due to the infection [ 91 ], which is central to understanding the public health impact of the pandemic and the required policies for its prevention and control [ 92 ].
Estimates of prevalence based on sero-surveys, which includes asymptomatic and mildly symptomatic infections, can be used to estimate IFR [ 93 ]. In a systematic review of 17 studies, seroprevalence rates ranged from 0.22% in Brazil to 53% in Argentina [ 94 ]. The review also identified that the seroprevalence estimate was higher than the cumulative reported case incidence, by a factor between 1.5 times in Germany to 717 times in Iran, in all but two studies (0.56 times in Brazil and 0.88 times in Denmark) [ 94 , 95 ]. The difference between seroprevalence and cumulative reported cases might be due to asymptomatic cases, atypical or pauci-symptomatic cases, or the lack of access to and uptake of testing [ 94 ]. There is only a modest gap between the estimated number of infections from seroprevalence surveys and the cumulative reported cases in regions with relatively thorough symptom-based testing. Much of the gap between reported cases and seroprevalence is likely to be due to undiagnosed symptomatic or asymptomatic infections [ 94 ].
Collateral effects of the COVID-19 pandemic
It is important to note that the pandemic has significant collateral effects on the provision of essential health services, in addition to the direct health effects [ 96 ]. Disruptions in the provision of essential health services, due to COVID-19, were reported by nearly all countries, though it is more so in lower-income than higher-income countries [ 97 , 98 ]. The biggest impact reported is on provision of day-to-day primary care to prevent and manage some of the most common health problems [ 99 ].
The causes of disruptions in service delivery were a mix of demand and supply factors [ 100 ]. Countries reported that just over one-third of services were disrupted due to health workforce-related reasons (the most common causes of service disruptions), supply chains, community mistrust and fears of becoming infected, and financial challenge s[ 101 ]. Cognizant of the disruptive effects of the pandemic, countries have reorganized their health system.
Countries with better response to COVID-19 have mobilized, trained and reallocated their health workforce in addition to hiring new staff, using volunteers and medical trainees and mobilizing retirees [ 102 ]. Several strategies have also been implemented to mitigate disruptions in service delivery and utilization, including: triaging to identify the most urgent patient needs, and postponing elective medical procedures; switching to alternative models of care, such as providing more home-based care and telemedicine [ 101 ].
This study identifies that the COVID-19 pandemic, in terms f cases and deaths, is heterogeneous around the world. This variability is explained by differences in vulnerability, preparedness, and response. It confirms that a high level of HDI, UHCI and GHSI are essential but not sufficient to control epidemics [ 103 ]. An effective response to public health emergencies requires a joint and reinforcing implementation of UHC, health emergency and disease control priorities [ 104 , 105 ], as well as good governance and social protection systems [ 106 ]. Important lessons have been learned to cope better with the COVID-19 pandemic and future emerging or re-emerging pandemics. Countries should strengthen health systems, minimize fragmentation of public health, primary care and secondary care, and improve coordination with other sectors. The pandemic has exposed the health effects of longstanding social inequities, which should be addressed through policies and actions to tackle vulnerability in living and working conditions [ 106 ].
The shift in the pandemic epicentre from high-income to MICs was observed in the second global wave of the pandemic. This is due to in part to the large-scale provision of vaccines in HICs [ 15 ] as well as the limitations in the response in LMICs, including inadequate testing, quarantine and isolation, contact tracing, and social distancing. The second wave of the pandemic in low- and middle-income countries spread more rapidly than the first wave and affected younger and healthier populations due to factors, including poor government decision making, citizen behaviour, and the emergence of highly transmissible SARS-CoV-2 variants [ 107 ]. It has become catastrophic in some MICs to prematurely relax key public health measures, such as mask wearing, physical distancing, and hand hygiene [ 108 ].
There is consensus that global vaccination is essential to ending the pandemic. Universal and equitable vaccine delivery, implemented with high volume, speed and quality, is vital for an effective and sustainable response to the current pandemic and future public health emergencies. There is, however, ongoing concern regarding access to COVID-19 vaccines in low-income countries [ 109 ]. Moreover, there is shortage of essential supplies, including oxygen, which has had a major impact on the prevention and control of the pandemic. It is, therefore, vital to transform (through good governance and financing mechanisms) the ACT-A platform to deliver vaccines, therapeutics, diagnostics, and other essential supplies [ 109 , 110 ]. The global health community has the responsibility to address these inequalities so that we can collectively end the pandemic [ 107 ].
The Omicron variant has a huge role in the current wave around the world despite high vaccine coverage [ 111 ]. Omicron appears to spread rapidly around the world ever since it was identified in November 2021 [ 112 ]. It becomes obvious that vaccination alone is inadequate for controlling the infection. This has changed our understanding of the COVID-19 pandemic endgame. The emergence of new variants of concern and their spread around the world has highlighted the importance of combination prevention, including high vaccination coverage in combination with other public health prevention measures [ 112 ].
Overall, the COVID-19 pandemic and the response to it emphasise valuable lessons towards an effective and sustainable response to public health emergencies. We argue that the PHC approach captures the different preparedness and response strategies required towards ensuring health security and UHC [ 113 ]. The PHC approach enables countries to progressively realize universal access to good-quality health services (including essential public health functions) and equity, empower people and communities, strengthen multi-sectoral policy and action for health, and enhance good governance [ 114 ]. These are essential in the prevention and control of public health emergencies, to suppress transmission, and reduce morbidity and mortality [ 115 ]. Access to high-quality primary care is at the foundation of any strong health system [ 116 ], which will, in turn, have effect on containing the epidemic, and reducing mortality and CFR [ 117 ]. Australia is a good example in this regard because it has implemented a comprehensive PHC approach in combination with border restrictions to ensure health system capacity is not exceeded [ 56 ]. The PHC approach will enable countries to develop and implement a context-specific health strategy, enhance governance, strengthen their (public) health systems, minimize segmentation and fragmentation, and tackle upstream structural issues, including discrimination and socio-economic inequities [ 118 ]. This is the type of public health approach (comprehensive, equity-focused and participatory) that will be effective and sustainable to tackle public health emergencies in the twenty-first century [ 119 , 120 ]. In addition, it is vital to transform the global and regional health systems, with a strong IHR and an empowered WHO at the apex [ 121 ]. We contend that this is the way towards a healthier and safer country, region and world.
The COVID-19 pandemic demonstrates that the world remains vulnerable to public health emergencies with significant health and other socio-economic impacts. The pandemic takes variable shapes and forms across regions and countries around the world. The pandemic has impacted countries with inadequate governance of the epidemic, fragmentation of their health systems and higher socio-economic inequities more than others. We argue that adequate response to public health emergencies requires that countries develop and implement a context-specific national strategy, enhance governance of public health emergency, build the capacity of their health systems, minimize fragmentation, and tackle socio-economic inequities. This is possible through a PHC approach that provides universal access to good-quality health services through empowered communities and multi-sectoral policy and action for health development. The pandemic has affected every corner of the world; it has demonstrated that “no country is safe unless other countries are safe”. This should be a call for a strong global health system based on the values of justice and capabilities for health.
Availability of data and materials
Data are available in a public, open access repository: Johns Hopkins University: https://coronavirus.jhu.edu/data/new-cases , and UNDP: http://hdr.undp.org/en/2019-report ; WHO: https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-22-december-2020
Abbreviations
Coronavirus Disease 2019
Case-fatality rates
Human development index
Universal health coverage index
Global Health Security index
High-income countries
Middle-income countries
El Zowalaty ME, Järhult JD. From SARS to COVID-19: A previously unknown SARS-CoV-2 virus of pandemic potential infecting humans–Call for a One Health approach. One Health. 2020;9:100124. https://doi.org/10.1016/j.onehlt.2020.100124 .
Van Damme W, Dahake R, Delamou A, Ingelbeen B, Wouters E, Vanham G, et al. The COVID-19 pandemic: diverse contexts; different epidemics—how and why? BMJ Glob Health. 2020;5(7):e003098.
Article PubMed Google Scholar
World Health Organization (WHO): Coronavirus disease ( COVID-19): situation report, 150. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200618-covid-19-sitrep-150.pdf .
Weekly epidemiological update - 22 December 2020 [ https://www.who.int/publications/m/item/weekly-epidemiological-update%2D%2D-22-december-2020 ].
Worldometer: COVID-19 coronavirus pandemic. 2020. https://www.worldometers.info/coronavirus/ .
Anand S, Sen A. Human Development Index: Methodology and Measurement. 1994. http://hdr.undp.org/en/content/human-development-index-methodology-and-measurement .
De Larochelambert Q, Marc A, Antero J, Le Bourg E, Toussaint J-F. Covid-19 mortality: a matter of vulnerability among nations facing limited margins of adaptation. Public Health. 2020;8. https://doi.org/10.3389/fpubh.2020.604339 .
de Winter JC, Gosling SD, Potter J. Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: a tutorial using simulations and empirical data. Psychol Methods. 2016;21(3):273.
World Health Organization. Universal health coverage [ http://www.who.int/universal_health_coverage/en/ ].
Johns Hopkins Center for Health Security. Global Health Security Index [ https://www.ghsindex.org/ ].
Pol Antràs SJR. Esteban Rossi-Hansberg: how do globalisation and pandemics interact? Surprising insights from a new model. In: #LSEThinks | CEP | global development vol. 2020. London: London School of Economics; 2020.
Google Scholar
Cai P. Understanding China’s belt and road initiative; 2017.
Baldwin R, Tomiura E. Thinking ahead about the trade impact of COVID-19. Economics in the Time of COVID-19. 2020;59. https://repository.graduateinstitute.ch/record/298220?ln=en .
Organization WH: Coronavirus disease ( COVID-19): situation report, 182. 2020.
Johns Hopkins University: COVID-19 Map - Johns Hopkins Coronavirus Resource Center. In. Edited by Security JHUCfH; 2021. https://coronavirus.jhu.edu/map.html .
Wang T, Du Z, Zhu F, Cao Z, An Y, Gao Y, et al. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet. 2020;395(10228):e52.
Article CAS PubMed PubMed Central Google Scholar
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. Jama. 2020;323(11):1061–9.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–13.
Hussain A, Bhowmik B, Do Vale Moreira NC. COVID-19 and diabetes: knowledge in progress. Diabetes Res Clin Pract. 2020;162:108142. https://doi.org/10.1016/j.diabres.2020.108142 . Epub 2020 Apr 9.
Covid C, COVID C, COVID C, Chow N, Fleming-Dutra K, Gierke R, Hall A, et al. Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019—United States, February 12–march 28, 2020. Morb Mortal Wkly Rep. 2020;69(13):382.
Group C-S. Characteristics of COVID-19 patients dying in Italy: report based on available data on March 20th, 2020. Rome: Instituto Superiore Di Sanita; 2020. https://www.epicentro.iss.it/coronavirus/bollettino/Report-COVID-2019_20_marzo_eng.pdf .
Guan W-j, Ni Z-y, Hu Y, Liang W-H, Ou C-Q, He J-X, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Article CAS PubMed Google Scholar
Arentz M, Yim E, Klaff L, Lokhandwala S, Riedo FX, Chong M, et al. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. Jama. 2020;323(16):1612–4.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the new York City area. JAMA. 2020;323(20):2052–9. https://doi.org/10.1001/jama.2020.6775 .
Covid C, Team R. Severe outcomes among patients with coronavirus disease 2019 (COVID-19)—United States, February 12–march 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–6.
Article Google Scholar
Mbow M, Lell B, Jochems SP, Cisse B, Mboup S, Dewals BG, et al. COVID-19 in Africa: dampening the storm? Science. 2020;369(6504):624–6.
Kavanagh MM, Erondu NA, Tomori O, Dzau VJ, Okiro EA, Maleche A, et al. Access to lifesaving medical resources for African countries: COVID-19 testing and response, ethics, and politics. Lancet. 2020;395(10238):1735–8.
Nordling L. Africa's pandemic puzzle: why so few cases and deaths? In: American Association for the Advancement of Science; 2020.
Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–7. https://doi.org/10.7326/M20-3012 . Epub 2020 Jun 3.
Nikolai LA, Meyer CG, Kremsner PG, Velavan TP. Asymptomatic SARS coronavirus 2 infection: invisible yet invincible. Int J Infect Dis. 2020;100:112–6. https://doi.org/10.1016/j.ijid.2020.08.076 . Epub 2020 Sep 3.
Rao C, Bradshaw D, Mathers CD. Improving death registration and statistics in developing countries: lessons from sub-Saharan Africa. Southern Afr J Demography. 2004:81–99.
Mehtar S, Preiser W, Lakhe NA, Bousso A, TamFum J-JM, Kallay O, et al. Limiting the spread of COVID-19 in Africa: one size mitigation strategies do not fit all countries. Lancet Glob Health. 2020;8(7):e881–3. Published online 2020 Apr 28. https://doi.org/10.1016/S2214-109X(20)30212-6 .
Nachega J, Seydi M, Zumla A. The late arrival of coronavirus disease 2019 (COVID-19) in Africa: mitigating pan-continental spread. Clin Infect Dis. 2020;71(15):875–8.
Gwilliam K, Foster V, Archondo-Callao R, Briceno-Garmendia C, Nogales A, Sethi K. Africa infrastructure country diagnostic: roads in sub-Saharan Africa: The World Bank; 2008.
Guengant J-P. Africa’s population: history, current status, and projections. In: Africa's Population: In Search of a Demographic Dividend: Springer; 2017. p. 11–31.
Collaborators GOD, Bernabe E, Marcenes W, Hernandez C, Bailey J, Abreu L, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: a systematic analysis for the global burden of disease 2017 study. J Dent Res. 2020;99(4):362–73.
Cambaza EM, Viegas GC, Cambaza C. Manuel a: potential impact of temperature and atmospheric pressure on the number of cases of COVID-19 in Mozambique, southern Africa. J Public Health Epidemiol. 2020;12(3):246–60.
Lawal Y. Africa’s low COVID-19 mortality rate: a paradox? Int J Infect Dis. 2021;102:118–22.
Nkengasong JN, Mankoula W. Looming threat of COVID-19 infection in Africa: act collectively, and fast. Lancet. 2020;395(10227):841–2.
African Union and Africa CDC. African union and Africa CDC launches partnerships for African vaccine manufacturing (PAVM), framework to achieve it and signs 2 MoUs: African Union and Africa CDC; 2021.
Forbes. What Do Countries With The Best Coronavirus Responses Have In Common? Women Leaders [ https://www.forbes.com/sites/avivahwittenbergcox/2020/04/13/what-do-countries-with-the-best-coronavirus-reponses-have-in-common-women-leaders/#603bd9433dec ].
University of Notre Dame. What can we learn from Austria’s response to COVID-19? [ https://keough.nd.edu/what-can-we-learn-from-austrias-response-to-covid-19/ ].
Stoller JK. Reflections on leadership in the time of COVID-19. BMJ Leader. 2020. https://doi.org/10.1136/leader-2020-000244 .
Houston Public Media. What 6 Of The 7 Countries With The Most COVID-19 Cases Have In Common [ https://www.npr.org/sections/goatsandsoda/2020/07/31/896879448/the-nations-with-the-most-to-lose-from-covid-19 ].
Hale T, Petherick A, Phillips T, Webster S. Variation in government responses to COVID-19. Blavatnik school of government working paper. 2020;31. https://en.unesco.org/inclusivepolicylab/sites/default/files/learning/document/2020/4/BSG-WP-2020-031-v3.0.pdf .
The Editors. Dying in a leadership vacuum. N Engl J Med. 2020;383(15):1479–80.
The Cable News Network. US and UK are bottom of the pile in rankings of governments' handling of coronavirus pandemic [ https://edition.cnn.com/2020/08/27/world/global-coronavirus-attitudes-pew-intl/index.html ].
Huston P, Campbell J, Russell G, Goodyear-Smith F, Phillips RL, van Weel C, et al. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4):bjgpopen20X101128. https://doi.org/10.3399/bjgpopen20X101128 .
Goodyear-Smith F, Kinder K, Eden AR, Strydom S, Bazemore A, Phillips R, et al. Primary care perspectives on pandemic politics. Glob Public Health. 2021;16(8-9):1304–19. https://doi.org/10.1080/17441692.2021.1876751 . Epub 2021 Jan 24.
Rutledge PE. Trump, COVID-19, and the war on expertise. Am Rev Public Adm. 2020;50(6-7):505–11.
Ugarte DA, Cumberland WG, Flores L, Young SD. Public attitudes about COVID-19 in response to president trump's social media posts. JAMA Netw Open. 2021;4(2):e210101.
Article PubMed PubMed Central Google Scholar
Lal A, Erondu NA, Heymann DL, Gitahi G, Yates R. Fragmented health systems in COVID-19: rectifying the misalignment between global health security and universal health coverage. Lancet. 2021;397(10268):61–7. https://doi.org/10.1016/S0140-6736(20)32228-5 . Epub 2020 Dec 1.
Tromberg BJ, Schwetz TA, Pérez-Stable EJ, Hodes RJ, Woychik RP, Bright RA, et al. Rapid scaling up of Covid-19 diagnostic testing in the United States—the NIH RADx initiative. N Engl J Med. 2020;383(11):1071–7.
Marwaha J, Halamka J, Brat G. Lifesaving ventilators will sit unused without a national data-sharing effort; 2020.
Kidd MR. Five principles for pandemic preparedness: lessons from the Australian COVID-19 primary care response. Br J Gen Pract. 2020;70(696):316–7. https://doi.org/10.3399/bjgp20X710765 . Print 2020 Jul.
Hsu LY, Tan M-H. What Singapore can teach the US about responding to COVID-19. STAT News. 2020. https://www.statnews.com/2020/03/23/singapore-teach-united-states-about-covid-19-response/ .
Horton R. Offline: COVID-19 is not a pandemic. Lancet (London, England). 2020;396(10255):874.
Article CAS Google Scholar
Raisi-Estabragh Z, McCracken C, Bethell MS, Cooper J, Cooper C, Caulfield MJ, et al. Greater risk of severe COVID-19 in black, Asian and minority ethnic populations is not explained by cardiometabolic, socioeconomic or behavioural factors, or by 25 (OH)-vitamin D status: study of 1326 cases from the UK biobank. J Public Health. 2020;42(3):451–60.
Hamidianjahromi A. Why African Americans are a potential target for COVID-19 infection in the United States. J Med Internet Res. 2020;22(6):e19934.
Tangcharoensathien V, Bassett MT, Meng Q, Mills A. Are overwhelmed health systems an inevitable consequence of covid-19? Experiences from China, Thailand, and New York State. BMJ. 2021;372. https://doi.org/10.1136/bmj.n83 .
Organization WH: COVID-19 health system response monitor, Thailand. 2020.
Narkvichien M. Thailand’s 1 million village health volunteers-“unsung heroes”-are helping guard communities nationwide from COVID-19. Nonthaburi: World Health Organization; 2020.
Kupferschmidt K, Cohen J. Can China's COVID-19 strategy work elsewhere? In: American Association for the Advancement of Science; 2020.
Al Saidi AMO, Nur FA, Al-Mandhari AS, El Rabbat M, Hafeez A, Abubakar A. Decisive leadership is a necessity in the COVID-19 response. Lancet. 2020;396(10247):295–8.
Forman R, Atun R, McKee M, Mossialos E. 12 lessons learned from the management of the coronavirus pandemic. Health Policy. 2020;124(6):577–80. https://doi.org/10.1016/j.healthpol.2020.05.008 .
Barberia LG, Gómez EJ. Political and institutional perils of Brazil's COVID-19 crisis. Lancet. 2020;396(10248):367–8.
Ortega F, Orsini M. Governing COVID-19 without government in Brazil: ignorance, neoliberal authoritarianism, and the collapse of public health leadership. Global Public Health. 2020;15(9):1257–77.
Ezequiel GE, Jafet A, Hugo A, Pedro D, Ana Maria M, Carola OV, et al. The COVID-19 pandemic: a call to action for health systems in Latin America to strengthen quality of care. Int J Qual Health Care. 2021;33(1):mzaa062.
Rocha R, Atun R, Massuda A, Rache B, Spinola P, Nunes L, et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. Lancet Glob Health. 2021;9(6):e782–92. https://doi.org/10.1016/S2214-109X(21)00081-4 . Epub 2021 Apr 12.
Lancet T. India under COVID-19 lockdown. Lancet (London, England). 2020;395(10233):1315.
Siddiqui AF, Wiederkehr M, Rozanova L, Flahault A. Situation of India in the COVID-19 pandemic: India’s initial pandemic experience. Int J Environ Res Public Health. 2020;17(23):8994.
Article CAS PubMed Central Google Scholar
Taneja P, Bali AS. India’s domestic and foreign policy responses to COVID-19. Round Table. 2021;110(1):46–61.
Choutagunta A, Manish G, Rajagopalan S. Battling COVID-19 with dysfunctional federalism: lessons from India. South Econ J. 2021;87(4):1267–99.
Mallapaty S. India's massive COVID surge puzzles scientists. Nature. 2021;592(7856):667–8.
Thiagarajan K. Why is India having a covid-19 surge? In: British Medical Journal Publishing Group; 2021.
Fisman DN, Greer AL, Tuite AR. Age is just a number: a critically important number for COVID-19 case fatality. Ann Intern Med. 2020;173(9):762–3.
Sudharsanan N, Didzun O, Bärnighausen T, Geldsetzer P. The contribution of the age distribution of cases to COVID-19 case fatality across countries: a 9-country demographic study. Ann Intern Med. 2020;173(9):714–20. https://doi.org/10.7326/M20-2973 . Epub 2020 Jul 22.
Think Global Health. The Myth of South Asian Exceptionalism. In: He Myth of South Asian Exceptionalism: South Asia's young population conceals the effects that COVID-19 has on its older and more vulnerable people. vol. 2020; 2020.
Ioannidis JP, Axfors C, Contopoulos-Ioannidis DG. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ Res. 2020;188:109890.
Kim D-H, Choe YJ, Jeong J-Y. Understanding and interpretation of case fatality rate of coronavirus disease 2019. J Korean Med Sci. 2020;35(12):e137. https://doi.org/10.3346/jkms.2020.35.e137 .
Rajgor DD, Lee MH, Archuleta S, Bagdasarian N, Quek SC. The many estimates of the COVID-19 case fatality rate. Lancet Infect Dis. 2020;20(7):776–7.
Sorci G, Faivre B, Morand S. Explaining among-country variation in COVID-19 case fatality rate. Sci Rep. 2020;10(1):1–11.
Sen-Crowe B, Sutherland M, McKenney M, Elkbuli A. A closer look into global hospital beds capacity and resource shortages during the COVID-19 pandemic. J Surg Res. 2021;260:56–63.
Li M, Zhang Z, Cao W, Liu Y, Du B, Chen C, et al. Identifying novel factors associated with COVID-19 transmission and fatality using the machine learning approach. Sci Total Environ. 2021;764:142810.
Undurraga EA, Chowell G, Mizumoto K. COVID-19 case fatality risk by age and gender in a high testing setting in Latin America: Chile, march–august 2020. Infect Dis Poverty. 2021;10(1):1–11.
Taylor L. How Latin America is fighting covid-19, for better and worse. BMJ. 2020;370:m3319. https://doi.org/10.1136/bmj.m3319 .
Bhuyan A. Covid-19: India looks to import oxygen as cases surge, overwhelming hospitals. In: British Medical Journal Publishing Group; 2021.
An BY, Tang S-Y. Lessons from COVID-19 responses in East Asia: institutional infrastructure and enduring policy instruments. Am Rev Public Adm. 2020;50(6-7):790–800.
Chen H, Shi L, Zhang Y, Wang X, Sun G. A cross-country core strategy comparison in China, Japan, Singapore and South Korea during the early COVID-19 pandemic. Glob Health. 2021;17(1):1–10.
Kahathuduwa CN, Dhanasekara CS, Chin S-H. Case fatality rate in COVID-19: a systematic review and meta-analysis. J Prev Med Hyg. 2021;62(2):E311–20. https://doi.org/10.15167/2421-4248/jpmh2021.62.2.1627 . eCollection 2021 Jun.
Meyerowitz-Katz G, Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection-fatality rates. Int J Infect Dis. 2020.
Seoane B. A scaling approach to estimate the COVID-19 infection fatality ratio from incomplete data. PLoS One. 2021;16(2):e0246831. https://doi.org/10.1371/journal.pone.0246831 . eCollection 2021.
Byambasuren O, Dobler CC, Bell K, Rojas DP, Clark J, McLaws M-L, et al. Comparison of seroprevalence of SARS-CoV-2 infections with cumulative and imputed COVID-19 cases: systematic review. PLoS One. 2021;16(4):e0248946.
Shakiba M, Nazemipour M, Salari A, Mehrabian F, Nazari SSH, Rezvani SM, et al. Seroprevalence of SARS-CoV-2 in Guilan Province, Iran, April 2020. Emerg Infect Dis. 2021;27(2):636.
Blanchet K, Alwan A, Antoine C, Cros MJ, Feroz F, Guracha TA, et al. Protecting essential health services in low-income and middle-income countries and humanitarian settings while responding to the COVID-19 pandemic. BMJ Glob Health. 2020;5(10):e003675.
Thome J, Coogan AN, Fischer M, Tucha O, Faltraco F. Challenges for mental health services during the 2020 COVID-19 outbreak in Germany. Psychiatry Clin Neurosci. 2020;74(7):407. https://doi.org/10.1111/pcn.13019 . Epub 2020 May 26.
Riley T, Sully E, Ahmed Z, Biddlecom A. Estimates of the potential impact of the COVID-19 pandemic on sexual and reproductive health in low-and middle-income countries. Int Perspect Sex Reprod Health. 2020;46:73–6.
World Health Organization (WHO): Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. In.: World Health Organization; 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 .
World Health Organization (WHO): Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. In.: World Health Organization; 2020. https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-EHS_continuity-survey-2020.1 .
World Health Organization (WHO): Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 22 April 2021. In.: World Health Organization; 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1 .
Organization WH. COVID-19: operational guidance for maintaining essential health services during an outbreak: interim guidance, 25 march 2020: World Health Organization; 2020.
Chen Y-Y, Assefa Y. The heterogeneity of the COVID-19 pandemic and national responses: an explanatory mixed-methods study. BMC Public Health. 2021;21(1):1–15.
World Health Organization (WHO). Thirteenth general programme of work 2019–2023. The seventy-first world health assembly. Geneva (Switzerland): World Health Organization; 2018.
Mahjour J, Mirza Z, Rashidian A, Atta H, Hajjeh R, Thieren M, et al. " promote health, keep the world safe, serve the vulnerable" in the eastern Mediterranean region. East Mediterr Health J. 2018;24(4):323–4.
Rollston R, Galea S. COVID-19 and the social determinants of health. Am J Health Promot. 2020;34(6):687–9. https://doi.org/10.1177/0890117120930536b .
Nachega JB, Sam-Agudu NA, Masekela R, van der Zalm MM, Nsanzimana S, Condo J, et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob Health. 2021;9(6):e746–8. https://doi.org/10.1016/S2214-109X(21)00097-8 . Epub 2021 Mar 10.
Skegg D, Gluckman P, Boulton G, Hackmann H, Karim SSA, Piot P, et al. Future scenarios for the COVID-19 pandemic. Lancet. 2021;397(10276):777–8.
Nhamo G, Chikodzi D, Kunene HP, Mashula N. COVID-19 vaccines and treatments nationalism: challenges for low-income countries and the attainment of the SDGs. Global Public Health. 2021;16(3):319–39.
Figueroa JP, Bottazzi ME, Hotez P, Batista C, Ergonul O, Gilbert S, et al. Urgent needs of low-income and middle-income countries for COVID-19 vaccines and therapeutics. Lancet. 2021;397(10274):562–4.
He X, Hong W, Pan X, Lu G, Wei X. SARS-CoV-2 omicron variant: characteristics and prevention. Med Comm (2020). 2021;2(4):838–45. https://doi.org/10.1002/mco2.110 .
Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398(10317):2126–8.
Sanders D, Nandi S, Labonté R, Vance C, Van Damme W. From primary health care to universal health coverage—one step forward and two steps back. Lancet. 2019;394(10199):619–21.
Hone T, Macinko J, Millett C. Revisiting Alma-Ata: what is the role of primary health care in achieving the sustainable development goals? Lancet. 2018;392(10156):1461–72.
Redwood-Campbell L, Abrahams J. Primary health care and disasters—the current state of the literature: what we know, gaps and next steps. Prehospital Disaster Med. 2011;26(3):184–91.
Bitton A, Ratcliffe HL, Veillard JH, Kress DH, Barkley S, Kimball M, et al. Primary health care as a foundation for strengthening health systems in low-and middle-income countries. J Gen Intern Med. 2017;32(5):566–71.
Dunlop C, Howe A, Li D, Allen LN. The coronavirus outbreak: the central role of primary care in emergency preparedness and response. BJGP Open. 2020;4(1):bjgpopen20X101041. https://doi.org/10.3399/bjgpopen20X101041 .
Assefa Y, Gilks CF, van de Pas R, Reid S, Gete DG, Van Damme W. Reimagining global health systems for the 21st century: lessons from the COVID-19 pandemic. BMJ Glob Health. 2021;6(4):e004882.
Loewenson R, Accoe K, Bajpai N, Buse K, Abi Deivanayagam T, London L, et al. Reclaiming comprehensive public health. BMJ Glob Health. 2020;5(9):e003886.
Rawaf S, Allen LN, Stigler FL, Kringos D, Quezada Yamamoto H, van Weel C, et al. Lessons on the COVID-19 pandemic, for and by primary care professionals worldwide. Eur J Gen Pract. 2020;26(1):129–33.
Gostin LO, Friedman EA. A retrospective and prospective analysis of the west African Ebola virus disease epidemic: robust national health systems at the foundation and an empowered WHO at the apex. Lancet. 2015;385(9980):1902–9.
Download references
Acknowledgements
Not applicable.
No funding was obtained for this study.
Author information
Authors and affiliations.
School of Public Health, the University of Queensland, Brisbane, Australia
Yibeltal Assefa, Charles F. Gilks, Simon Reid & Dereje Gedle Gete
Institute of Tropical Medicine, Antwerp, Belgium
Remco van de Pas & Wim Van Damme
You can also search for this author in PubMed Google Scholar
Contributions
YA conceived the idea of the research, collected and analysed the data, and prepared the first and subsequent drafts. DG participated in data collection and analysis. CFG, SR, RVDP, DG and WVD provided comments during subsequent drafts. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Yibeltal Assefa .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Assefa, Y., Gilks, C.F., Reid, S. et al. Analysis of the COVID-19 pandemic: lessons towards a more effective response to public health emergencies. Global Health 18 , 10 (2022). https://doi.org/10.1186/s12992-022-00805-9
Download citation
Received : 04 August 2021
Accepted : 14 January 2022
Published : 04 February 2022
DOI : https://doi.org/10.1186/s12992-022-00805-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Heterogeneity
Globalization and Health
ISSN: 1744-8603
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Numbers, Facts and Trends Shaping Your World
Read our research on:
Full Topic List
Regions & Countries
- Publications
- Our Methods
- Short Reads
- Tools & Resources
Read Our Research On:
Americans Reflect on Nation’s COVID-19 Response
Fewer than half say the country has given the right amount of priority to the needs of k-12 students, public health, quality of life, table of contents.
- Ratings of Biden’s, public officials’ response to the coronavirus outbreak
- What measures have worked to limit the spread of COVID-19?
- Vaccination rates, personal experiences with COVID-19 and testing
- Acknowledgments
- Methodology
- Appendix: Detailed charts and tables

Pew Research Center conducted this study to understand how Americans are continuing to respond to the coronavirus outbreak. For this analysis, we surveyed 10,282 U.S. adults from May 2 to 8, 2022.
Everyone who took part in the survey is a member of the Center’s American Trends Panel (ATP), an online survey panel that is recruited through national, random sampling of residential addresses. This way, nearly all U.S. adults have a chance of selection. The survey is weighted to be representative of the U.S. adult population by gender, race, ethnicity, partisan affiliation, education and other categories. Read more about the ATP’s methodology .
Here are the questions used for this report , along with responses, and its methodology .
As levels of public concern over the coronavirus outbreak recede, Americans offer a lackluster evaluation of how the country has balanced priorities during the outbreak. A majority of U.S. adults say the country has given too little priority to meeting the educational needs of K-12 students since the outbreak first took hold in February 2020. Assessments of the nation’s response across other domains are little better: Fewer than half of Americans say the country has done about the right amount to support quality of life and economic activity or to protect public health.
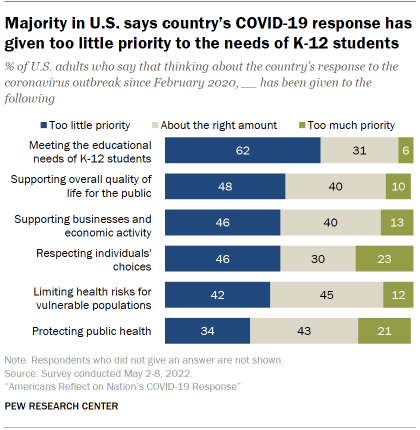
When asked to take stock of what measures have worked to limit the spread of the coronavirus, the public is conflicted. Vaccines and masks rank at the top of the list of effective steps; but even for these public health tools, sizable shares of Americans describe them as no more than somewhat effective at limiting the spread of the coronavirus.
A Pew Research Center survey of 10,282 U.S. adults conducted from May 2 to 8, 2022, finds 62% of Americans say the country has given too little priority to meeting the educational needs of K-12 students during its response to the coronavirus outbreak; far fewer (31%) say this has received about the right amount of priority since the outbreak first began in February of 2020 (just 6% say it’s received too much priority).
On balance, larger shares of Americans also say too little priority – rather than the right amount – has been given to supporting the public’s overall quality of life, supporting businesses and economic activity, and respecting individuals’ choices.
When it comes to the central goal of protecting public health, Americans have decidedly mixed views: 43% say the country has given about the right amount of priority to protecting public health, while 34% say this has received too little priority and 21% say it has received too much.
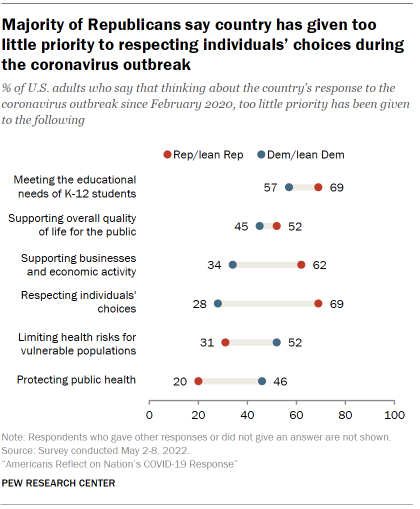
The overall findings reflect two competing critiques of the nation’s response. One, widely expressed among Republicans, is that the country has not focused enough on business concerns and respecting individual choices. The other, more widely held by Democrats, centers concern around efforts to protect public health and limit health risks for vulnerable populations.
In short, neither Republicans nor Democrats think the country has hit the mark in its response to the outbreak – one that has spanned the presidential administrations of both Donald Trump and Joe Biden.
Among Democrats and Democratic-leaning independents, larger shares say protecting public health has received too little priority than say it has received too much (46% vs. 7%), while 46% say it has gotten about the right amount of priority. Republicans and Republican leaners offer a very different assessment: More say public health has received too much priority (40%) than say it’s been given too little (20%), while 38% say it’s gotten about the right amount of priority.
Majorities of Republicans say the country has done too little during the outbreak when it comes to respecting individuals’ choices (69%) and supporting businesses and economic activity (62%). Relatively small shares of Democrats express these views. In fact, half of Democrats say there has been about the right amount of attention given to supporting businesses and economic activity. And Democrats are roughly as likely to say too much priority has been given to respecting individuals’ choices as to say too little (33% and 28%, respectively). See the Appendix for more details on this question .
Amid these contrasting views of the nation’s response to the coronavirus outbreak stands a notable point of general partisan agreement: Majorities of both Republicans (69%) and Democrats (57%) say the country has given too little priority to meeting the educational needs of K-12 students. A January survey by the Center found a majority of parents of K-12 students expressed concern about academic progress when it came to decisions about whether to keep schools open for in-person instruction.
Over the past two years, public health and elected officials have invested extensively in communicating ways to limit the spread of the coronavirus. For Americans, vaccines rank at the top of the list of what they believe has worked, followed by mask-wearing and limiting interactions with other people. Still, not all Americans see these measures as particularly effective.
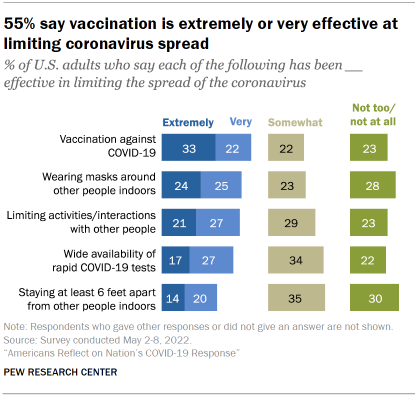
For instance, a narrow majority (55%) says vaccination against COVID-19 has been extremely or very effective at limiting the spread of the coronavirus; 22% say this has been somewhat effective and 23% say it has been not too or not at all effective.
About half say wearing masks around people indoors (48%) and limiting activities and interactions with other people (47%) have been extremely or very effective at limiting the spread of the coronavirus. The remainder of Americans describe these two steps as no more than somewhat effective.
The partisan gaps over the effectiveness of these interventions are about as wide as any seen in the survey. For instance, 75% of Democrats say COVID-19 vaccines have been extremely or very effective at limiting the spread of the coronavirus; 16% say they have been somewhat effective and just 9% describe them as not too or not at all effective.
Republicans offer a much more skeptical view: A slightly larger share of Republicans say vaccines have been not too or not at all effective at limiting the spread of the coronavirus than say they have been extremely or very effective (39% vs. 32%); 29% fall between these two views and say vaccines have been somewhat effective.
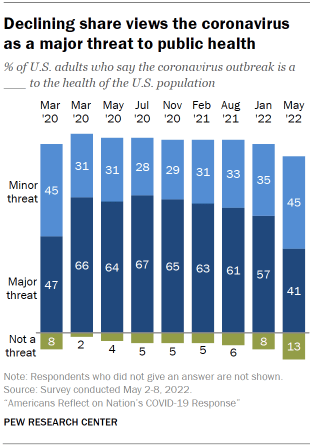
Asked to assess where the country stands at this stage of the outbreak, about three-quarters of Americans (76%) say the worst of the country’s problems from the coronavirus are behind us. And declining shares express deep personal concern about getting the coronavirus themselves.
But while the intensity of public concern about the coronavirus outbreak has waned, cases in the U.S. remain stubbornly high and 86% of Americans say the outbreak remains at least a minor threat to the health of the U.S. population.
To date, over a million Americans have died from COVID-19 . Firsthand connections to people who have experienced serious cases of COVID-19 are common among the public: 81% of U.S. adults – including 88% of Black and 86% of Hispanic adults – say they know someone personally who has been hospitalized or died from the coronavirus. See the Appendix for more details .
Four months ahead of the November midterm elections, President Joe Biden’s standing on the issue of the coronavirus outbreak has diminished. A majority of adults (56%) say he is doing an only fair or poor job responding to the outbreak, compared with 43% who say he is doing an excellent or good job.
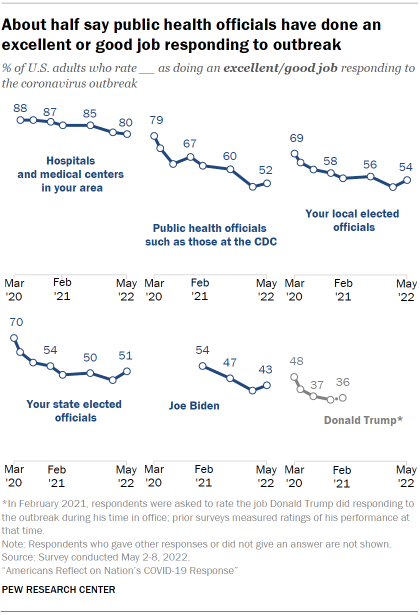
In October of 2020, Biden held a clear advantage over Donald Trump as the candidate voters saw as better able to handle the public health impact of the outbreak – among the issues voters identified as most important to the election. And at the start of Biden’s term, 65% of Americans said they were confident in his ability to deal with the outbreak.
Biden is not the only official, or set of officials, to see their ratings fall over the course of the outbreak. Ratings for state and local elected officials as well as for public health officials – such as those at the Centers for Disease Control and Prevention – are all lower today than at early stages of the outbreak, though they are about the same as they were in January of this year.
Ratings for the performance of local hospitals and medical centers stand well above those of other groups. Eight-in-ten Americans say hospitals and medical centers in their area are doing an excellent or good job responding to the coronavirus outbreak – far higher than ratings of all other groups and individuals included in the survey. The gap between ratings for local hospitals and medical centers and those for other groups, including public health and state and local officials, is much wider today than at early stages of the outbreak.
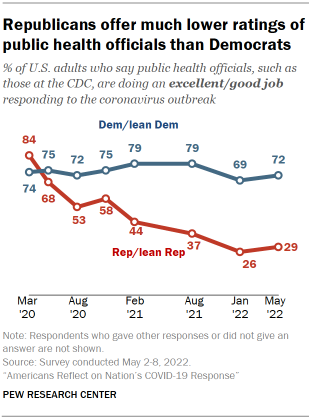
Ratings of public health officials are an example of intensifying partisan differences that have formed over the course of the outbreak. Democrats and those who lean to the Democratic Party are far more likely than Republicans and GOP leaners (72% vs. 29%) to say public health officials, such as those at the CDC, have done an excellent or good job responding to the coronavirus outbreak. In the early stages of the outbreak, majorities of both Republicans and Democrats gave public health officials positive ratings.
While the overall decline in ratings for public health officials has been driven by sharply lower assessments among Republicans, the declines in ratings for state and local elected officials have occurred among both Republicans and Democrats.
National preparedness for a future global health emergency
Asked to consider preparedness for a future global health emergency, 59% of Americans say they have either a great deal (15%) or some confidence (44%) in the U.S. health care system to handle a future global health emergency. Four-in-ten say they have not too much or no confidence at all in the U.S. health care system to handle a future global health emergency.
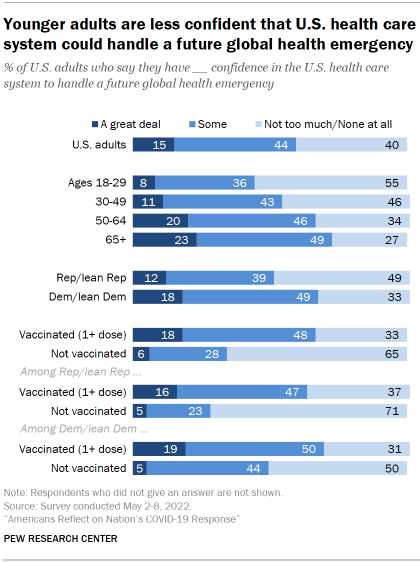
Overall views are similar to those measured in February of 2021 , when 55% of Americans said they had at least some confidence in the health care system to handle a future global health emergency.
However, views among partisans have changed considerably over the last year. Democrats are now significantly more likely than Republicans to say they have a great deal of or some confidence in the health care system to handle a future emergency (67% vs. 51%). In February 2021, during the final days of the Trump administration, Republicans (57%) were about as likely as Democrats (54%) to express this level of confidence in the preparedness of the U.S. health care system.
Attitudes also differ on this question by vaccination status. A majority of adults (67%) who have received at least one dose of a COVID-19 vaccine say they have a great deal of or some confidence in the health care system to handle a future emergency, compared with just 34% of those who have not received a vaccine. Republicans and Democrats who have received a vaccine are each more likely to express confidence in the health care system than unvaccinated members of their respective parties.
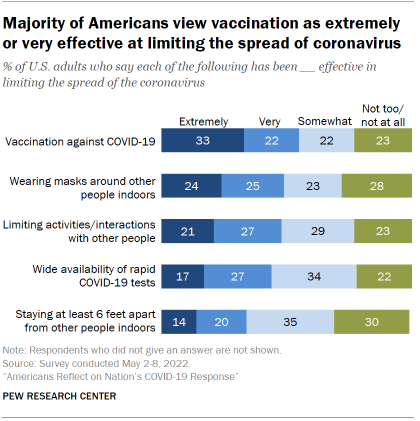
Overall, 55% of Americans say vaccination against COVID-19 has been extremely (33%) or very (22%) effective at limiting the spread of the coronavirus; 22% say vaccines have been somewhat effective and 23% say they have been not too or not at all effective.
About half of Americans (48%) say wearing masks around other people indoors has been extremely or very effective at limiting the spread of the coronavirus. A similar share (47%) say limiting activities and interactions with other people has been extremely or very effective. Still, for both measures, roughly as many Americans describe these actions as no more than somewhat effective at limiting the spread of the coronavirus.
The wide availability of rapid COVID-19 tests is seen as very or extremely effective at limiting the spread of the coronavirus by 43% of the public. Relatively fewer (35%) say staying six feet apart from other people indoors has been extremely or very effective at limiting the spread of the coronavirus.
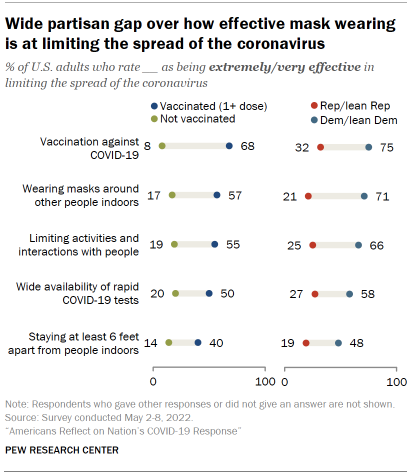
Democrats are much more likely than Republicans to view all five measures as extremely or very effective at limiting the spread of the coronavirus. For instance, 71% of Democrats say wearing masks around other people indoors is extremely or very effective at limiting the spread of the coronavirus; a considerably smaller share of Republicans (21%) say the same.
Across the five public health tools asked about in the survey, wide differences in views are also seen between adults that have received at least one dose of a COVID-19 vaccine and those that have not been vaccinated. Among respondents that have received at least one dose of a vaccine, a majority views several of these measures – vaccines, wearing masks and limiting social interactions – as extremely or very effective at limiting the spread of the coronavirus. Among the much smaller share of Americans who have not been vaccinated, no more than two-in-ten say any of these five measures are extremely or very effective.
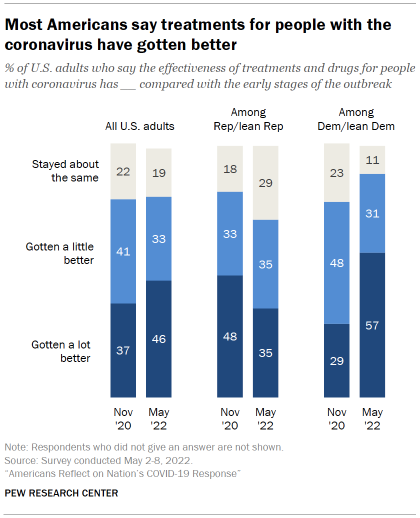
A majority of Americans think treatments and drugs for those with the coronavirus have gotten a lot (46%) or a little (33%) better since the early stages of the outbreak. The share who say they have gotten a lot better is up 9 points from 37% in November of 2020, when this question was last asked.
Democrats and Democratic leaners are now more likely than Republicans and Republican leaners to say the effectiveness of treatments for the coronavirus has gotten a lot better (57% vs. 35%) since the early stages of the outbreak.
Democrats’ views about the improvement of medical treatments for COVID-19 have become more positive since November 2020, during the last months of the Trump administration. By contrast, Republicans are less likely today to say medical treatments have improved over the course of the outbreak than they were in November 2020.
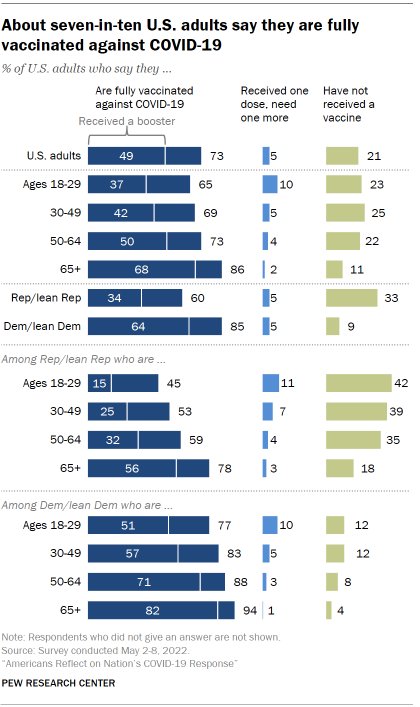
Overall, 73% of U.S. adults say they are fully vaccinated for coronavirus as of May 2022. This share is the same as it was in a January 2022 Pew Research Center survey. According to the Centers for Disease Control and Prevention (CDC), “fully vaccinated” means having received two doses of Pfizer or Moderna vaccines or one dose of the Johnson & Johnson.
A relatively small share of U.S. adults say they have received one dose of a vaccine but need one more (5%); 21% say they have not received a vaccine for COVID-19. Both shares are virtually unchanged from January 2022.
Republicans and Republican-leaning independents (60%) continue to be less likely than Democrats and Democratic leaners (85%) to say they are fully vaccinated.
Older adults also continue to be more likely than younger adults to say they are fully vaccinated, a pattern that holds true within each party.
As in the past, those who live in urban or suburban communities (76% each) are more likely than those living in rural areas (64%) to say they are fully vaccinated.
When it comes to booster shots, about half (49%) of the public say they are fully vaccinated and have received a booster shot within the past six months. The share is about the same as it was in January 2022.
Differences by partisanship persist in both the shares who say they are fully vaccinated and in the shares who say they’ve received a booster shot among fully vaccinated adults. A narrow majority of fully vaccinated Republicans (56%) have received a booster shot. This group makes up 34% of all Republicans. Meanwhile, a larger majority (75%) of fully vaccinated Democrats – or 64% of all Democrats – say they have received a booster shot.
Among both partisan groups, younger adults who are fully vaccinated remain less likely than older adults who are fully vaccinated to say they have received a COVID-19 booster shot.
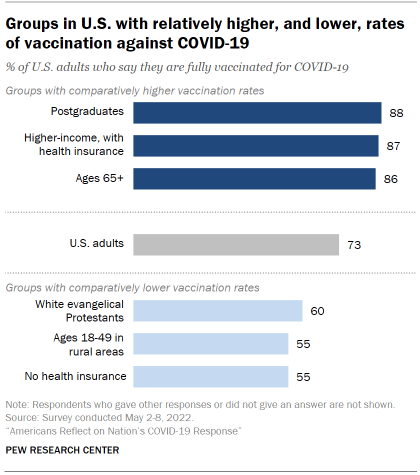
With vaccination rates among U.S. adults leveling off in recent months, differences across groups in the country have crystalized.
Looking across a wide range of characteristics associated with the decision to get a vaccine, some of those most likely to be fully vaccinated in the U.S. include those with a postgraduate degree, those in higher-income households with health insurance, and Americans ages 65 and older.
At the other end of the spectrum, those relatively less likely to be fully vaccinated include White evangelical Protestants, adults younger than 50 living in rural areas, and those without health insurance. See the Appendix for more details about vaccination rates across groups .
When it comes to personal experiences with the coronavirus, 46% of U.S. adults say they have tested positive for COVID-19 or been pretty sure they have had it.
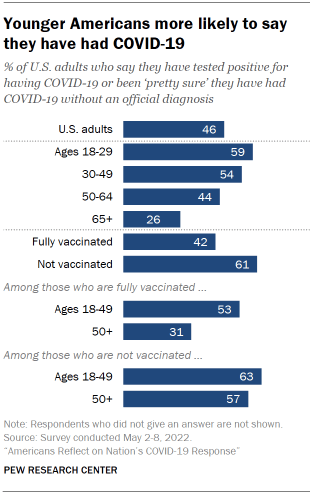
The share of Americans who say they have had COVID-19 has risen since August 2021, when three-in-ten (30%) said this.
Across age groups, younger adults are more likely than older adults to say they have tested positive for COVID-19 or been pretty sure they had it. A majority (59%) of adults ages 18 to 29 say this, compared with 26% of adults 65 and older.
Those who are fully vaccinated (42%) are less likely to say they have had COVID-19 than those who are not vaccinated (61%). (The survey did not ask respondents whether they got COVID-19 before or after being vaccinated.)
Among those who are fully vaccinated, younger adults are more likely than older adults to say they have had COVID-19.
When vaccination status and exposure to COVID-19 are taken together, 90% of Americans report some level of immune response to COVID-19 (78% have received at least one dose of a vaccine and an additional 12% are not vaccinated but say they’ve had the coronavirus). Public health experts are continuing to evaluate how long immunity from vaccination or previous infection last as coronavirus variants evolve.
Use of at-home testing is highest among young adults
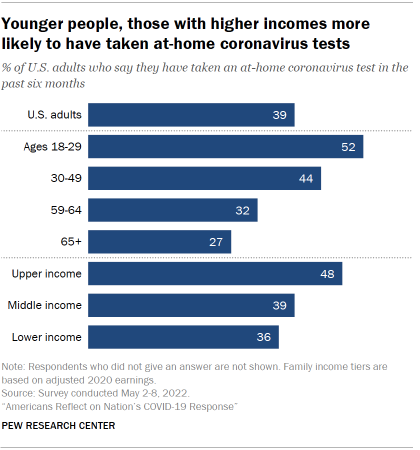
The CDC recommends the use of at-home coronavirus tests as one way for Americans to help reduce the spread of COVID-19.
About four-in-ten U.S. adults (39%) say they have taken an at-home COVID-19 test in the past six months.
Across age groups, younger adults are more likely to say that they have taken an at-home coronavirus test in the past six months. Around half (52%) of adults ages 18 to 29 say this, compared with 27% of those 65 and older.
Upper-income adults (48%) are more likely than middle-income (39%) or lower-income (36%) adults to say that they have taken an at-home COVID-19 test in the past six months.
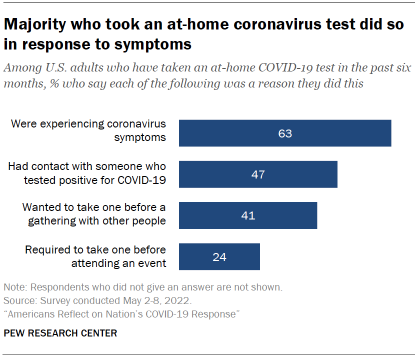
When the 39% of Americans who have taken an at-home COVID-19 test in the past six months were asked about their reasons for doing so, a majority of this group (63%) say that a reason was that they were experiencing coronavirus symptoms.
Around four-in-ten or more say that a reason they had taken an at-home COVID-19 test was that they had contact with someone who tested positive (47%) or wanted to take one before attending a gathering with other people (41%).
About a quarter (24%) say that a reason they have taken an at-home COVID-19 test was that they were required to do so before an event.
For each of the possible reasons listed for taking a COVID-19 test, younger adults are generally more likely than older adults to say that each had been a factor. For example, 57% of adults ages 18 to 29 say that having contact with someone who tested positive for COVID-19 was a reason they had done an at-home test, compared with 37% of adults 65 and older.
Personal concern over virus lower than earlier in the outbreak
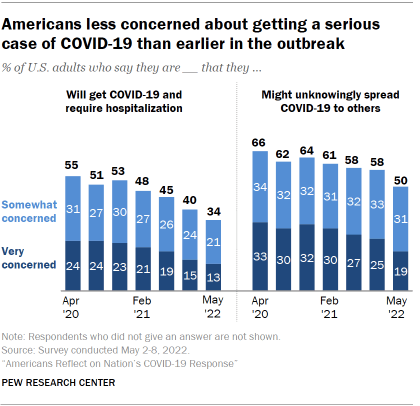
About a third of Americans (34%) say they are at least somewhat concerned that they will get COVID-19 and require hospitalization, a much smaller share than said this at earlier stages of the outbreak.
Half of Americans say they are at least somewhat concerned that they might unknowingly spread COVID-19 to others. This share has declined steadily since November 2020, when about two-thirds (64%) of U.S. adults said this.
Consistent with these declines, Americans are also less likely to see the coronavirus outbreak as a major threat to their personal health than at earlier stages of the outbreak. About a quarter (23%) now say this, down from 30% in January 2022. See the Appendix for more details .
Sign up for our weekly newsletter
Fresh data delivery Saturday mornings
Sign up for The Briefing
Weekly updates on the world of news & information
- Coronavirus (COVID-19)
- COVID-19 & Politics
- COVID-19 & Science
- Trust in Science
How Americans View the Coronavirus, COVID-19 Vaccines Amid Declining Levels of Concern
Online religious services appeal to many americans, but going in person remains more popular, about a third of u.s. workers who can work from home now do so all the time, how the pandemic has affected attendance at u.s. religious services, mental health and the pandemic: what u.s. surveys have found, most popular, report materials.
1615 L St. NW, Suite 800 Washington, DC 20036 USA (+1) 202-419-4300 | Main (+1) 202-857-8562 | Fax (+1) 202-419-4372 | Media Inquiries
Research Topics
- Email Newsletters
ABOUT PEW RESEARCH CENTER Pew Research Center is a nonpartisan fact tank that informs the public about the issues, attitudes and trends shaping the world. It conducts public opinion polling, demographic research, media content analysis and other empirical social science research. Pew Research Center does not take policy positions. It is a subsidiary of The Pew Charitable Trusts .
Copyright 2024 Pew Research Center
- Search Menu
- Sign in through your institution
- Advance articles
- Editor's Choice
- Supplements
- Author Guidelines
- Submission Site
- Open Access
- About Journal of Public Health
- About the Faculty of Public Health of the Royal Colleges of Physicians of the United Kingdom
- Editorial Board
- Self-Archiving Policy
- Dispatch Dates
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
- < Previous
Adapting to the culture of ‘new normal’: an emerging response to COVID-19
- Article contents
- Figures & tables
- Supplementary Data
Jeff Clyde G Corpuz, Adapting to the culture of ‘new normal’: an emerging response to COVID-19, Journal of Public Health , Volume 43, Issue 2, June 2021, Pages e344–e345, https://doi.org/10.1093/pubmed/fdab057
- Permissions Icon Permissions
A year after COVID-19 pandemic has emerged, we have suddenly been forced to adapt to the ‘new normal’: work-from-home setting, parents home-schooling their children in a new blended learning setting, lockdown and quarantine, and the mandatory wearing of face mask and face shields in public. For many, 2020 has already been earmarked as ‘the worst’ year in the 21st century. Ripples from the current situation have spread into the personal, social, economic and spiritual spheres. Is this new normal really new or is it a reiteration of the old? A recent correspondence published in this journal rightly pointed out the involvement of a ‘supportive’ government, ‘creative’ church and an ‘adaptive’ public in the so-called culture. However, I argue that adapting to the ‘new normal’ can greatly affect the future. I would carefully suggest that we examine the context and the location of culture in which adaptations are needed.
To live in the world is to adapt constantly. A year after COVID-19 pandemic has emerged, we have suddenly been forced to adapt to the ‘new normal’: work-from-home setting, parents home-schooling their children in a new blended learning setting, lockdown and quarantine, and the mandatory wearing of face mask and face shields in public. For many, 2020 has already been earmarked as ‘the worst’ year in the 21st century. 1 Ripples from the current situation have spread into the personal, social, economic and spiritual spheres. Is this new normal really new or is it a reiteration of the old? A recent correspondence published in this journal rightly pointed out the involvement of a ‘supportive’ government, ‘creative’ church and an ‘adaptive’ public in the so-called culture. 2 However, I argue that adapting to the ‘new normal’ can greatly affect the future. I would carefully suggest that we examine the context and the location of culture in which adaptations are needed.
The term ‘new normal’ first appeared during the 2008 financial crisis to refer to the dramatic economic, cultural and social transformations that caused precariousness and social unrest, impacting collective perceptions and individual lifestyles. 3 This term has been used again during the COVID-19 pandemic to point out how it has transformed essential aspects of human life. Cultural theorists argue that there is an interplay between culture and both personal feelings (powerlessness) and information consumption (conspiracy theories) during times of crisis. 4 Nonetheless, it is up to us to adapt to the challenges of current pandemic and similar crises, and whether we respond positively or negatively can greatly affect our personal and social lives. Indeed, there are many lessons we can learn from this crisis that can be used in building a better society. How we open to change will depend our capacity to adapt, to manage resilience in the face of adversity, flexibility and creativity without forcing us to make changes. As long as the world has not found a safe and effective vaccine, we may have to adjust to a new normal as people get back to work, school and a more normal life. As such, ‘we have reached the end of the beginning. New conventions, rituals, images and narratives will no doubt emerge, so there will be more work for cultural sociology before we get to the beginning of the end’. 5
Now, a year after COVID-19, we are starting to see a way to restore health, economies and societies together despite the new coronavirus strain. In the face of global crisis, we need to improvise, adapt and overcome. The new normal is still emerging, so I think that our immediate focus should be to tackle the complex problems that have emerged from the pandemic by highlighting resilience, recovery and restructuring (the new three Rs). The World Health Organization states that ‘recognizing that the virus will be with us for a long time, governments should also use this opportunity to invest in health systems, which can benefit all populations beyond COVID-19, as well as prepare for future public health emergencies’. 6 There may be little to gain from the COVID-19 pandemic, but it is important that the public should keep in mind that no one is being left behind. When the COVID-19 pandemic is over, the best of our new normal will survive to enrich our lives and our work in the future.
No funding was received for this paper.
UNESCO . A year after coronavirus: an inclusive ‘new normal’. https://en.unesco.org/news/year-after-coronavirus-inclusive-new-normal . (12 February 2021, date last accessed) .
Cordero DA . To stop or not to stop ‘culture’: determining the essential behavior of the government, church and public in fighting against COVID-19 . J Public Health (Oxf) 2021 . doi: 10.1093/pubmed/fdab026 .
Google Scholar
El-Erian MA . Navigating the New Normal in Industrial Countries . Washington, D.C. : International Monetary Fund , 2010 .
Google Preview
Alexander JC , Smith P . COVID-19 and symbolic action: global pandemic as code, narrative, and cultural performance . Am J Cult Sociol 2020 ; 8 : 263 – 9 .
Biddlestone M , Green R , Douglas KM . Cultural orientation, power, belief in conspiracy theories, and intentions to reduce the spread of COVID-19 . Br J Soc Psychol 2020 ; 59 ( 3 ): 663 – 73 .
World Health Organization . From the “new normal” to a “new future”: A sustainable response to COVID-19. 13 October 2020 . https: // www.who.int/westernpacific/news/commentaries/detail-hq/from-the-new-normal-to-a-new-future-a-sustainable-response-to-covid-19 . (12 February 2021, date last accessed) .
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1741-3850
- Print ISSN 1741-3842
- Copyright © 2024 Faculty of Public Health
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Understanding the US...
Understanding the US failure on coronavirus—an essay by Drew Altman
Read our latest coverage of the coronavirus outbreak.
- Related content
- Peer review
- Drew Altman , president and CEO
- Henry J Kaiser Family Foundation, San Francisco, CA
- drewA{at}kff.org
The world has been staggered by the US’s disjointed response to covid-19, resulting in by far the highest case and death count globally. The die was cast by two fundamental policy decisions taken by the Trump administration, writes Drew Altman
On 9 August, the US passed the five million mark in cases of covid-19, representing slightly more than a quarter of all global cases. That day, more than half the states in the US qualified as coronavirus hot spots. 1
The same day in South Dakota, the small town of Sturgis with a population of less than 7000 prepared to welcome 250 000 bikers to its annual biker rally. With no social distancing or face masks required by that mostly conservative rural state, it would be the largest known public gathering in the world in the middle of the covid-19 pandemic.
At the same time, 40 million Californians were living with that state’s mandatory mask order imposed by the governor when the state’s decision to open up its economy led to a resurgence in covid-19 infections.
In Georgia, the Republican governor and the Democratic mayor of Atlanta continued to spar over the mayor’s desire to take more stringent measures to protect public health than the governor, a Trump loyalist, wanted to allow. Similar tensions between Democratic mayors and pro-Trump Republican governors were playing out in Texas and Florida, two large states where cases of the virus were increasing.
In New York, where the state had come through the worst epidemic in the US after deploying strict public health measures, the infection rate was low enough that the governor, whose daily press conferences had become national television events, announced he was ready to open schools.
And so goes the American response to covid-19: a patchwork of responses by state and local governments, divided sharply along partisan lines.
Our lamentable performance is not the product of a famously fragmented, market driven healthcare system. The US medical system has in many ways performed well and even valiantly, increasing capacity when needed, and saving lives when possible. Uninsured people and working people are faced with much higher out-of-pocket costs and surprise costs than they are in other countries, but our deaths per case of covid-19 compare favourably with other developed nations that have significant numbers of cases. 2 We celebrate our heroic frontline workers with cheers and applause just as other countries do.
No, the disappointing US response to covid-19 has been because of a failure of policy and leadership, not healthcare, and largely owing to two fateful policy decisions.
The federal government as back-up
After first casting himself as a wartime president, in April President Trump made a fundamental policy shift that has shaped the US response to the pandemic ever since. He announced that states would have primary responsibility for containing the virus, with the federal government in a “back-up” role. 3
A state role in public health is traditional in the US, and any national plan would allow for customisation to reflect regional and state circumstances. Delegating primary responsibility to states in a crisis is unprecedented. It was, as far as I know, the first time a sitting US president has sought to decentralise authority and responsibility during a national crisis.
The motivation for the policy shift was never clearly articulated. While consistent with conservative principles to let state and local governments customise solutions to local circumstances, it may also have been an effort, however futile in retrospect, to offload political accountability for a growing pandemic with the presidential election looming.
As a former state commissioner of human services experienced in the vagaries of state government, I felt at the time that the consequences were predictable. On 5 April, I tweeted 4 :
“This is the result when you leave it to states to decide what to do on their own with the federal government as “back-up.” Pacesetters, a muddled middle, and laggards, often in the South. The consequences this time may be tragic.”
In practice the ramifications were even more complex, with states, counties, and cities all filling the vacuum created by the lack of an overall national response.
The US has 3141 counties. Some are rural with no health departments; others are as large as states and have health directors with strong independent authority to implement public health measures, such as stay-at-home orders. Three hundred cities in the US have populations of 100 000 or more. In some jurisdictions, county and city authorities overlap. A city may deliver health services and a county may control public health. A school system may operate independently of both. Virtually every combination exists across the country.
In the absence of a centralised federal response, this fragmentation resulted in extreme variation in our national response to covid-19 by and within states. For example, at the time of writing, 33 states had instituted mandatory mask orders, while other states imposed softer orders or none at all. 5
This variation had significant public health consequences. Some states opened up their economies earlier than others—and, in general, the states that opened up their economies earlier suffered larger outbreaks. 6
This led directly to the second fateful policy decision shaping the US response: the Trump administration’s decision to push for an opening up of the economy before the virus was contained—and the fracturing of the country along partisan lines in response.
A starkly partisan pandemic response
Initially, the White House sought to impose so called “gating criteria” to be met by states before they opened up. 7 These guidelines could have imposed greater discipline on the fragmented response of state and local government. But the criteria were abandoned with the president pushing initially for opening up as early as Easter, then moving that timetable back in the face of pandemic reality.
The response has been the defining and most troubling characteristic of the American response to the pandemic: the states and the American people split strikingly along partisan lines in their response to covid-19, as if the country has both red and blue pandemics. When that happened, the public’s willingness to prevent the spread of the virus substantially collapsed across red America.
The partisan divide can be seen on almost every dimension of the epidemic. Democrats are about twice as likely as Republicans to say the worst is still yet to come on the pandemic in the US ( fig 1 ), 8 and a wide gulf has opened between Democrats and Republicans in the debate around opening schools. 9

Democrats twice as likely as Republicans to say worst of coronavirus is yet to come. Source: KFF health tracking poll (conducted July 14-19 2020)
- Download figure
- Open in new tab
- Download powerpoint
Strikingly, in a late August poll CBS and YouGov found that 90% of Democrats said the number of coronavirus deaths in the US was unacceptable. But a majority (57%) of Republicans said it was acceptable, in part because they believe the death count has been exaggerated. 10 It is an open question whether attitudes and behaviour will change as the virus spreads through red and rural America.
Not too late
Other reasons account for the poor performance in the US. The historic neglect and underfunding of our state and local public health system have also contributed to the weak US response. 11 And our country’s public health system also operates independently of our healthcare system, which does not help.
Overall, however, the US response to the pandemic has much more to do with fundamental policy decisions made—and not made—in the White House than the nature of our much debated health system.
The distribution of a vaccine in the US may well be built on a similar state by state architecture, allowing for customisation but also substantial variation in performance, depending on the degree of oversight exercised by federal public health agencies.
The decentralised structure of the US response could have worked more effectively had the role of the federal government as “back-up” been buttressed by a national plan overlaying state responses and more fulsome federal support for testing, contact tracing, personal protective equipment, school reopening, and other elements of the response that require a national policy and resources targeted to state and local conditions.
The US coronavirus failure was not inevitable and does not have to be permanent. But it is historically aberrant for our federal government to follow and not lead in a national crisis, and equally unusual for our country to divide rather than unify in a time of crisis. This too is the product of the policy decisions that have been made and can be altered or unmade by the current or a future administration.
Drew Altman is president and CEO of the Henry J Kaiser Family Foundation (KFF). He is an innovator in the world of foundations and non-profit organisations and a leading expert on national health policy who publishes and speaks widely on health issues.
He founded the present day KFF in the early 1990s. He is also founding publisher of KFF’s Kaiser Health News , the largest health newsroom in the US, distributing coverage of health issues through major news outlets across the country.
He was commissioner of the Department of Human Services for the state of New Jersey, director of health and human services at the Pew Charitable Trusts, vice president of the Robert Wood Johnson Foundation, and served in the Carter administration. He is a member of the National Academy of Medicine and the Council on Foreign Relations and serves on numerous advisory committees.
Drew Altman earned his PhD in political science at Massachusetts Institute of Technology and completed his post-doctoral work at Harvard University before moving on to public service. He holds an honorary doctorate from the Morehouse School of Medicine.
Commissioned; not externally peer reviewed.
Competing interests The BMJ has judged that there are no disqualifying financial ties to commercial companies. The author declares the following other interests: none.
This article is made freely available for use in accordance with BMJ's website terms and conditions for the duration of the covid-19 pandemic or until otherwise determined by BMJ. You may use, download and print the article for any lawful, non-commercial purpose (including text and data mining) provided that all copyright notices and trade marks are retained.
- ↵ Kates J, Tolbert J, Orgera K, Michaud J, Levitt L. Where are the COVID-19 Hotspots? Tracking State Outbreaks. KFF. 2020. https://www.kff.org/coronavirus-covid-19/issue-brief/where-are-the-covid-19-hotspots-tracking-state-outbreaks/
- ↵ Craig J. Charts: how the US ranks on covid-19 deaths per capita—and by case count. Goats and Soda . 2020. https://www.npr.org/sections/goatsandsoda/2020/08/05/899365887/charts-how-the-u-s-ranks-on-covid-19-deaths-per-capita-and-by-case-count?t=1599118732041
- ↵ Yen H, Woodward C. AP fact check: Trump, ‘wartime’ pandemic leader or ‘backup’? AP 2020. https://apnews.com/a64cf7fd5095d4d3b002dc4830e32119
- ↵ Altman D. Twitter. 2020. https://twitter.com/DrewAltman/status/1246817341846896645
- ↵ KFF. State actions to mitigate the spread of covid-19. 2020. https://www.kff.org/other/state-indicator/state-actions-to-mitigate-the-spread-of-covid-19/
- ↵ Leonhardt D. The unique US failure to control the virus. New York Times 2020. https://www.nytimes.com/2020/08/06/us/coronavirus-us.html
- ↵ White House. Guidelines: opening up America again. 2020. https://www.whitehouse.gov/openingamerica/
- ↵ Hamel L, Kearney A, Kirzinger A, Lopes L, Muñana C, Brodie M. KFF health tracking poll–July 2020. 2020. https://www.kff.org/coronavirus-covid-19/report/kff-health-tracking-poll-july-2020/
- ↵ Menasce Horowitz J. Republicans, Democrats differ over factors K-12 schools should consider in deciding whether to reopen. Pew Research Center. 2020. https://www.pewresearch.org/fact-tank/2020/08/05/republicans-democrats-differ-over-factors-k-12-schools-should-consider-in-deciding-whether-to-reopen/
- ↵ Salvanto A, de Pinto J, Backus F, Khanna K, Cox E. Republicans see US as better off now than four years ago ahead of convention—Battleground Tracker poll. CBS News 2020. https://www.cbsnews.com/news/republicans-economy-coronavirus-opinion-poll-cbs-news-battleground-tracker/
- ↵ Weber L, Ungar L, Smith MR, Recht H, Barry-Jester AM. Hollowed-out public health system faces more cuts amid virus. Kaiser Health News 2020. https://khn.org/news/us-public-health-system-underfunded-under-threat-faces-more-cuts-amid-covid-pandemic/
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic
a School of Information Systems and Modelling, Faculty of Engineering and Information Technology, University of Technology Sydney, NSW 2007, Australia
I.M. Rizwanul Fattah
Md asraful alam.
b School of Chemical Engineering, Zhengzhou University, Zhengzhou 450001, China
A.B.M. Saiful Islam
c Department of Civil and Construction Engineering, College of Engineering, Imam Abdulrahman Bin Faisal University, Dammam 31451, Saudi Arabia
Hwai Chyuan Ong
S.m. ashrafur rahman.
d Biofuel Engine Research Facility, Queensland University of Technology (QUT), Brisbane, QLD 4000, Australia
e Tarbiat Modares University, P.O.Box: 14115-111, Tehran, Iran
f Science and Math Program, Asian University for Women, Chattogram 4000, Bangladesh
Md. Alhaz Uddin
g Department of Civil Engineering, College of Engineering, Jouf University, Sakaka, Saudi Arabia
T.M.I. Mahlia
COVID-19 has heightened human suffering, undermined the economy, turned the lives of billions of people around the globe upside down, and significantly affected the health, economic, environmental and social domains. This study aims to provide a comprehensive analysis of the impact of the COVID-19 outbreak on the ecological domain, the energy sector, society and the economy and investigate the global preventive measures taken to reduce the transmission of COVID-19. This analysis unpacks the key responses to COVID-19, the efficacy of current initiatives, and summarises the lessons learnt as an update on the information available to authorities, business and industry. This review found that a 72-hour delay in the collection and disposal of waste from infected households and quarantine facilities is crucial to controlling the spread of the virus. Broad sector by sector plans for socio-economic growth as well as a robust entrepreneurship-friendly economy is needed for the business to be sustainable at the peak of the pandemic. The socio-economic crisis has reshaped investment in energy and affected the energy sector significantly with most investment activity facing disruption due to mobility restrictions. Delays in energy projects are expected to create uncertainty in the years ahead. This report will benefit governments, leaders, energy firms and customers in addressing a pandemic-like situation in the future.
1. Introduction
The newly identified infectious coronavirus (SARS-CoV-2) was discovered in Wuhan and has spread rapidly since December 2019 within China and to other countries around the globe ( Zhou et al., 2020 ; Kabir et al., 2020 ). The source of SARS-CoV-2 is still unclear ( Gorbalenya et al., 2020 ). Fig. 1 demonstrates the initial timeline of the development of SARS-CoV-2 ( Yan et al., 2020 ). The COVID-19 pandemic has posed significant challenges to global safety in public health ( Wang et al., 2020 ). On 31 st January 2020, the World Health Organization (WHO), due to growing fears about the rapid spread of coronavirus, announced a global epidemic and on 11 th March, the disease was recognised as a pandemic ( Chowdhury et al., 2021 ). COVID-19 clinical trials indicate that almost all patients admitted to hospital have trouble breathing and pneumonia-like symptoms ( Holshue et al., 2020 ). Clinical diagnosis has identified that COVID-19 (disease caused by SARS-CoV-2) patients have similar indications to other coronavirus affected patients, e.g. Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS) ( Wang and Su, 2020 ). The initial indication of a COVID-19 infection is coughing, fever, and short breath, and in the later stages, it can damage the kidney, cause pneumonia, and unexpected death ( Mofijur et al., 2020 ). The vulnerability of the elderly (>80 years of age) is high, with a fatality rate of ~22% of cases infected by COVID-19 ( Abdullah et al., 2020 ). The total number of confirmed COVID-19 cases has reached over 33 million as of 29 th September 2020, with more than 213 countries and regions affected by the pandemic ( Worldometer, 2020 ). Over 1,003,569 people have already passed away ( Worldometer, 2020 ) due to COVID-19. Most countries are currently trying to combat the virus spread by screening for COVID-19 in large numbers and maintaining social distancing policies with an emphasis on the health of human beings.

The initial stage development timeline for COVID-19 ( Yan et al., 2020 ).
Fig. 2 shows infections and replication cycle of the coronavirus. In extreme cases, the lungs are the most severely damaged organ of a SARS-CoV-2 infected person (host). The alveoli are porous cup-formed small cavities located in the structure of the lungs where the gas exchange of the breathing process take place. The most common cells on the alveoli are the type II cells.

Infections and replication cycle of the coronavirus ( Acter et al., 2020 ).
It has been reported that travel restrictions play a significant role in controlling the initial spread of COVID-19 ( Chinazzi et al., 2020 ; Aldila et al., 2020 ; Beck and Hensher, 2020 ; Bruinen de Bruin et al., 2020 ; de Haas et al., 2020 ). It has been reported that staying at home is most useful in controlling both the initial and last phase of infectious diseases ( de Haas et al., 2020 ; Cohen, 2020 , Pirouz et al., 2020 ). However, since the start of the COVID-19 pandemic, quarantines, entry bans, as well as other limitations have been implemented for citizens in or recent travellers to several countries in the most affected areas ( Sohrabi et al., 2020 ). Also, most of the industries were shutdown to lower mobility. A potential benefit of these measures is the reduction of pollution by the industrial and transportation sector, improving urban sustainability ( Jiang et al., 2021 ). Fig. 3 shows the global responses to lower the impact of the COVID-19 outbreak. There have been negative economic and social implications due to restrictions and decreased travel readiness worldwide ( Leal Filho et al., 2020 ). A fall in the volume of business activity and international events and an increase in online measures could have a long-term impact. The status of global transport and air activity as a result of the COVID-19 pandemic is shown in Fig. 4 ( International Energy Agency (IEA), 2020 ). By March 2020, the average global road haulage activity in regions with lockdowns had declined to almost 50% of the 2019 standard. Air travel has almost completely stopped in certain regions with aviation activity decreasing by over 90% in some European countries. Air activity in China recovered slightly from a low in late February, with lockdown measures somewhat eased. Nevertheless, as lockdowns spread, by the end of Q1 2020, global aviation activity decreased by a staggering 60%.

Initial preventive measures to lower the COVID-19 outbreak ( Bruinen de Bruin et al., 2020 ).

Global transport and aviation activity in the first quarter of the year 2020 ( International Energy Agency (IEA), 2020 ).
The spread of COVID-19 continues to threaten the public health situation severely ( Chinazzi et al., 2020 ) and greatly affect the global economy. Labour displacement, business closures and stock crashes are just some of the impacts of this global lockdown during the pandemic. According to the International Monetary Fund (IMF), the effect of COVID-19 will result in a worldwide economic decline in 2020 and a decline in the economic growth to 3% ( International Monetary Fund (IMF) ). COVID-19 has a detrimental impact on economic growth due to two primary factors. In the beginning, the exponential growth of the global epidemic directly contributed to considerable confusion about instability in the financial and capital markets. Secondly, countries have strictly regulated human movement and transport to monitor the growth of the epidemic and significantly reduced economic activity, putting pressure on both consumer and productive economic activity.
Since the 1970s, the link between economic growth and pollution has been an important global concern. The assessment of energy and financial efficiency is usually connected to environmental pollution research. Green practices at a national level, the inclusion of renewable energy, regulatory pressure and the sustainable use of natural resources are associated with environmental sustainability ( Khan et al., 2020 ). One study has shown that environmental pollution increases with economic growth and vice versa ( Cai et al., 2020 ). The strict control over movement and business activity due to COVID-19 has led to an economic downturn, which is in turn, expected to reduce environmental pollution. This paper systematically assesses how the novel coronavirus has had a global effect on society, the energy sector and the environment. This study presents data compiled from the literature, news sources and reports (from February 2020 to July 2020) on the management steps implemented across the globe to control and reduce the impact of COVID-19. The study will offer guidelines for nations to assess the overall impact of COVID-19 in their countries.
2. Impact of COVID-19 on the environmental domain
2.1. waste generation.
The generation of different types of waste indirectly creates a number of environmental concerns ( Schanes et al., 2018 ). The home isolation and pop-up confinement services in countries that have experienced major impacts of COVID-19 are standard practise, as hospitals are given priority to the most serious cases. In some countries, hotels are being used to isolate travellers for at least two weeks on entry. In several countries, such quarantine measures have resulted in consumers increasing their domestic online shopping activity that has increased domestic waste. In addition, food bought online is packaged, so inorganic waste has also increased. Medical waste has also increased. For instance, Wuhan hospitals produced an average of 240 metric tonnes of medical waste during the outbreak compared to their previous average of fewer than 50 tonnes ( Zambrano-Monserrate et al., 2020 ). This unusual situation poses new and major obstacles in the implementation of waste collection services, thus creating a new challenge for waste collection and recycling groups. With the global adaptation to exponential behavioural and social shifts in the face of COVID-19 challenges, municipal services such as waste collection and management need to alter their operations to play an important role in reducing the spread of infectious diseases.
2.1.1. Lifespan of COVID-19 on different waste media
SARS-CoV-2′s transmission activity has major repercussions for waste services. SARS-CoV-2 attacks host cells with ACE2 proteins directly. ACE2 is a cell membrane-associated enzyme in the lungs, heart and kidneys. When all the resources in the host cell are infected and depleted, the viruses leave the cell in the so-called shedding cycle ( Nghiem et al., 2020 ). Clinical and virological evidence suggests that the elimination of the SARS-CoV-2 virus is most relevant early on, right before and within a couple of days of the onset of the illness ( AEMO, 2020 ). Fomites are known as major vectors for the replication of other infectious viruses during the outbreak ( Park et al., 2015 ). Evidence from SARS-CoV-2 and other coronaviruses show that they remain effective for up to a few days in the atmosphere and on a variety of surfaces ( Fig. 5 ). The survival time of SARS-CoV-2 on hard and plastic surfaces is up to three days indicating that waste materials from COVID-19 patients may contain coronavirus and be a source of infection spread ( Chin et al., 2020 ). During the early stages of this epidemic, updated waste disposal methods to tackle COVID-19 were not implemented on the broader community. The concept of clinical waste essentially also applies to waste from contaminated homes and quarantine facilities. Throughout this pandemic, huge volumes of domestic and hospital waste, particularly plastic waste, has been generated. This has already impeded current efforts to reduce plastic waste and decrease its disposal in the environment. More effort should be made to find alternatives to heavily used plastics.

The lifespan of SARS-CoV-2 on different media ( Chin et al., 2020 ; van Doremalen et al.; 2020 ; Ye et al., 2016 )
2.1.2. Waste recycling service
COVID-19 has already had significant effects on waste recycling. Initially, as the outbreak spread and lockdowns were implemented in several countries, both public authorities and municipal waste management officials had to adjust to the situation quickly. Waste disposal has also been a major environmental problem for all technologically advanced nations, as no clear information was available about the retention time of SARS-CoV-2 ( Liu et al., 2020 ). Recycling is a growing and efficient means of pollution control, saving energy and conserving natural resources ( Ma et al., 2019 ). Recycling projects in various cities have been put on hold due to the pandemic, with officials worried about the possibility of COVID-19 spreading to recycling centres. Waste management has been limited in affected European countries. For example, Italy prohibited the sorting of waste by infected citizens. Extensive waste management during the pandemic is incredibly difficult because of the scattered nature of the cases and the individuals affected. The value of implementing best management practises for waste handling and hygiene to minimise employee exposure to potentially hazardous waste, should be highlighted at this time. Considering the possible role of the environment in the spread of SARS-CoV-2 ( Qu et al., 2020 ), the processing of both household and quarantine facility waste is a crucial point of control. Association of Cities and Regions for sustainable Resource management (ACR+) has reported on the provision of separate collection services to COVID-19 contaminated households and quarantine facilities to protect frontline waste workers in Europe, as shown in Fig. 6 . ACR+ also suggests a 72-hour delay in waste disposal (the possible lifespan of COVID-19 in the environment) ( Nghiem et al., 2020 ). Moreover, the collected waste should be immediately transported to waste incinerators or sites without segregation.

Recommended waste management during COVID-19 ( ACR+ 2020 ).
2.2. NO 2 emissions
Without the global pandemic, we had naively anticipated that in 2020 global emissions would rise by around 1% on a five-year basis. Instead, the sharp decline in economic activity in response to the current crisis will most probably lead to a modest drop in global greenhouse emissions. The European Space Agency (ESA), with its head office in Paris, France, is an intergovernmental body made up of 22 European countries committed to exploring the international space. To monitor air pollution in the atmosphere, the ESA uses the Copernicus Sentinel-5P Satellite. In addition to the compound contents measurement, the Copernicus Sentinel-5P troposphere monitor (TROPOMI) and other specified precision equipment measure ozone content, sulphur dioxide, carbon monoxide, and methane. Table 1 shows NO 2 emissions data acquisition by ESA using Sentinel-5P across different regions of Europe ( Financial Times, 2020 ).
NO 2 emissions data acquisition by ESA using Sentinel-5P across different regions of Europe ( Financial Times, 2020 ).
Burning fossil fuels, such as coal, oil, gas and other fuels, is the source of atmospheric nitrogen dioxide ( Munawer, 2018 ). The bulk of the NO 2 in cities, however, comes from emissions from motor vehicles (approximately 80%). Other NO 2 sources include petroleum and metal refining, coal-fired electricity, other manufacturing and food processing industries. Some NO 2 is naturally produced by lightning in the atmosphere and from the soil, water, and plants, which, taken together, constitutes not even 1% of the total NO 2 found in the air of our localities. Due to pollution variations as well as changes in weather conditions, the levels of the NO 2 in our atmosphere differ widely every day. Anthropogenic pollution is estimated to contain around 53 million tonnes of NO 2 annually. Nitrogen dioxide, together with nitrogen oxide (NO), are considered the major components of oxides of nitrogen (NOx) ( M Palash et al., 2013 ; Fattah et al., 2013 ). NO, and NO 2 are susceptible to other chemicals and form acid rain that is toxic to the environment ( Mofijur et al., 2013 ; Ashraful et al., 2014 ), WHO lists NO 2 as one of the six typical air contaminants in the atmosphere. For this reason, the amount of NO 2 in the atmosphere is used as a precise measure for determining whether the COVID-19 outbreak affects environmental pollution.
NO 2 is an irritating reddish-brown gas with an unpleasant smell, and when cooled or compressed, it becomes a yellowish-brown liquid ( Wang and Su, 2020 ). NO 2 inflames the lung linings and can decrease lung infection immunity. High levels of NO 2 in the air we breathe can corrode our body's lung tissues . Nitrogen dioxide is a problematic air pollutant because it leads to brown photochemical smog formation, which can have significant impacts on human health ( Huang et al., 2020 ). Brief exposure to high concentrations of NO 2 can lead to respiratory symptoms such as coughing, wheezing, bronchitis, flu, etc., and aggravate respiratory illnesses such as asthma. Increased NO 2 levels can have major effects on individuals with asthma, sometimes leading to frequent and intense attacks ( Munawer, 2018 ). Asthmatic children and older individuals with cardiac illness are most vulnerable in this regard. However, its main drawback is that it produces two of the most harmful air pollutants, ozone and airborne particles. Ozone gas affects our lungs and the crops we eat.

2.2.1. NO₂ emissions across different countries
According to the ESA ( European Space Agency (ESA), 2020 ), average levels of NO 2 declined by 40% between 13 th March 2020 to 13 th April 2020. The reduction was 55% compared to the same period in 2019. Fig. 7 compares the 2019-2020 NO 2 concentration ( European Space Agency (ESA), 2020 ). The displayed satellite image was captured with the TROPOMI by ESA satellite Sentinel-5P. The percentage reductions in average NO 2 emissions in European countries during the COVID-19 outbreak from 1 st April to 30 th April 2020 can be seen in Fig. 8 ( Myllyvirta, 2020 ). Portugal, Spain, Norway, Croatia, France, Italy, and Finland are the countries that experienced the largest decrease in NO 2 levels, with 58%, 48%, 47%, 43% and 41%, respectively.

Comparison of the NO 2 concentration between 2019 and 2020 in Europe ( European Space Agency (ESA), 2020 ).

Changes in average NO 2 emission in different countries ( Myllyvirta, 2020 ).
The average 10-day animation of NO 2 emissions throughout Europe (from 1 st January to 11 th March 2020), demonstrated the environmental impact of Italy's economic downturn, see Fig. 9 ( European Space Agency (ESA), 2020 ). In the recent four weeks (Last week of February 2020 to the third week of March 2020) the average concentration of NO 2 in Milan, Italy, has been at least 24% less than the previous four weeks. In the week of 16 – 22 March, the average concentration was 21% lower than in 2019 for the same week. Over the last four weeks of January 2020, NO 2 emissions in Bergamo city has been gradually declining. During the week of 16–22 March, the average concentration was 47% less than in 2019. In Rome, NO 2 rates were 26–35% lower than average in the last four weeks (third week of January 2020 to the third week of February 2020) than they were during the same week of 2019 ( Atmosphere Monitoring Service, 2020 ).

Changes of NO 2 emission (a) over entire Italy (b) capital city (c) other cities ( European Space Agency (ESA), 2020 ; Atmosphere Monitoring Service, 2020 ).
Fig. 10 shows a comparison of NO 2 volumes in Spain in March 2019 and 2020. As per ( European Space Agency (ESA), 2020 ), Spain's NO 2 pollutants decreased by up to 20–30% due to lockdown, particularly across big cities like Madrid, Barcelona, and Seville. ESA Sentinel-5P captured the satellite image using TROPOMI. Satellite images of the 10 days between 14 th and 25 th March 2020 show that NO 2 tropospheric concentration in the areas of Madrid, Barcelona, Valencia, and Murcia ranges from 0–90 mg/m 3 . The NO 2 tropospheric concentration for Seville is almost 0 mg/m 3 for the same time. For March 2019, the average NO 2 tropospheric concentration for the Madrid area was between 90 and 160 mg/m 3 . At the same time, the range of NO 2 tropospheric concentration for Barcelona, Valencia, and Seville area was between 90–140 mg/m 3 , 90-130 mg/m 3 , and 30–50 mg/m 3 , respectively.

Comparison between before and after lockdown NO 2 emissions in Spain ( European Space Agency (ESA), 2020 ).
Fig. 11 shows the reduction in the amount of NO 2 emissions in France in March 2019 and 2020 ( European Space Agency (ESA), 2020 ). In France, levels of NO 2 have been reduced by 20% to 30%. The ESA Sentinel-5P satellite image was captured with the TROPOMI. In Paris and other major cities, the emission levels of NO 2 considerably lowered due to lockdown. The three major areas of France where NO 2 tropospheric concentration was significant are Paris, Lyon, Marseille and their surroundings. Satellite images of the ten days between 14 th and 25 th March 2020 show that NO 2 tropospheric concentration of the Paris, Lyon, Marseille areas ranges 30–90 mg/m 3 , 20–40 mg/m 3 and 40–80 mg/m 3 , respectively. For March 2019, the average NO 2 tropospheric concentration for the same areas was reported as 100–160 mg/m 3 , 30–60 mg/m 3, and 90–140 mg/m 3 , respectively.

Comparison of NO 2 emissions in France before and after lockdown ( European Space Agency (ESA), 2020 ).
Various industries across the UK have been affected by COVID-19, which has influenced air contamination. As shown in Fig. 12 , there were notable drops in the country's NO 2 emissions on the first day of quarantine ( Khoo, 2020 ). Edinburgh showed the most significant reduction. The average NO 2 emissions on 26 th March 2020, were 28 μg/m 3 while on the same day of 2019, this was 74 μg/m 3 ( Khoo, 2020 ). The second biggest reduction was observed in London Westminster where emissions reduced from 58 µg/m 3 to 30 µg/m 3 . Not all cities have seen such a significant decrease, with daily air pollution reducing by 7 μg/m 3 compared to the previous year in Manchester Piccadilly, for example ( Statista, 2020 ).

(a) Changes in NO 2 emissions in the UK during lockdown ( European Space Agency (ESA), 2020 ); (b) comparison of NO 2 emissions in 2019 and 2020 ( Khoo, 2020 ).
2.3. PM emission
The term particulate matter, referred to as PM, is used to identify tiny airborne particles. PM forms in the atmosphere when pollutants chemically react with each other. Particles include pollution, dirt, soot, smoke, and droplets. Pollutants emitted from vehicles, factories, building sites, tilled areas, unpaved roads and the burning of fossil fuels also contribute to PM in the air ( Baensch-Baltruschat et al., 2020 ). Grilling food (by burning leaves or gas grills), smoking cigarettes, and burning wood on a fireplace or stove also contribute to PM. The aerodynamic diameter is considered a simple way to describe PM's particle size as these particles occur in various shapes and densities. Particulates are usually divided into two categories, namely, PM 10 that are inhalable particles with a diameter of 10 μm or less and PM 2.5 which are fine inhalable particle with a diameter of 2.5 μm or less. PM 2.5 exposure causes relatively severe health problems such as non-fatal heart attacks, heartbeat irregularity, increased asthma, reduced lung function, heightened respiratory symptoms, and premature death ( Weitekamp et al., 2020 ).
PM 2.5 also poses a threat to the environment, including lower visibility (haze) in many parts of the globe. Particulates can be transported long distances then settle on the ground or in water sources. In these contexts and as a function of the chemical composition, PM 2.5 may cause acidity in lakes and stream water, alter the nutrient balance in coastal waters and basins, deplete soil nutrients and damage crops on farms, affect the biodiversity in the ecosystem, and contribute to acid rain. This settling of PM, together with acid rain, can also stain and destroy stones and other materials such as statues and monuments, which include valuable cultural artefacts ( Awad et al., 2020 ).
2.3.1. PM emission in different countries
Due to the COVID-19 outbreak, PM emission in most countries has been reduced ( Chatterjee et al., 2020 ; Ghahremanloo et al., 2021 ; Gualtieri et al., 2020 ; Sharifi and Khavarian-Garmsir, 2020 ; Srivastava, 2020 ). Fig. 13 shows the impact of COVID19 on PM emission in a number of some countries around the world ( Myllyvirta, 2020 ). The largest reductions in PM pollution took place in Portugal, with 55%, followed by Norway, Sweden, and Poland with reductions of 32%, 30%, and 28%, respectively. Spain, Poland, and Finland recorded PM emission reductions of 19%, 17% and 16%, respectively. Both Romania and Croatia recorded no changes in PM level, with Switzerland and Hungary recording about a 3% increase in PM emission.

Reduction of PM emission in different countries ( Myllyvirta, 2020 ).
PM emissions have been significantly reduced during the epidemic in most regions of Italy. Fig. 14 illustrates the changes in COVID-19 containment emissions before and after a lockdown in major cities in Italy. According to a recent study by Sicard et al. ( Sicard et al., 2020 ), lockdown interventions have had a greater effect on PM emission. They found that confinement measures reduce PM 10 emissions in all major cities by “around 30% to 53%” and “around 35% to 56%”.

Comparison of PM emission in Italy (a) PM 2.5 emission (b) Changes of PM 2.5 emission (c) PM 10 emission (d) Changes of PM 10 emission ( Sicard et al., 2020 ).
2.4. Noise emission
Noise is characterised as an undesirable sound that may be produced from different activities, e.g. transit by engine vehicles and high volume music. Noise can cause health problems and alter the natural condition of ecosystems. It is among the most significant sources of disruption in people and the environment ( Zambrano-Monserrate and Ruano, 2019 ). The European Environment Agency (EEA) states that traffic noise is a serious environmental problem that negatively affects the health and security of millions of citizens in Europe. The consequences of long-term exposure to noise include sleep disorders, adverse effects on the heart and metabolic systems, and cognitive impairment in children. The EEA estimates that noise pollution contributes to 48,000 new cases of heart disease and 12,000 early deaths per year. They also reported chronic high irritation for 22 million people and a chronic high level of sleep disorder for 6.5 million people ( Lillywhite, 2020 ).
Most governments have imposed quarantine measures that require people to spend much more time at home. This has considerably reduced the use of private and public transport. Commercial activities have almost completely stopped. In most cities in the world, these changes have caused a significant decline in noise levels. This was followed by a significant decline in pollution from contaminants and greenhouse gas emissions. Noise pollution from sources like road, rail or air transport has been linked to economic activity. Consequently, we anticipate that the levels of transport noise will decrease significantly due to the decreased demand for mobility in the short term ( Ro, 2020 ).
For example, it was obvious that environmental noise in Italy was reduced after 8 th March 2020 (the lockdown start date) due to a halt in commercial and recreational activities. A seismograph facility in Lombardy city in Italy that was severely affected by the COVID-19 pandemic indicated how the quarantine measures reduce both traffic and noise emissions. The comparison of the 24-hour seismic noise data before and after the lockdown period indicates a considerable drop in environmental noise in Italy ( Bressan, 2020 ).
3. Impact of COVID-19 on the socio-economic domain
COVID-19 has created a global health crisis where countless people are dying, human suffering is spreading, and people's lives are being upended ( Nicola et al., 2020 ). It is not only just a health crisis but also a social and economic crisis, both of which are fundamental to sustainable development ( Pirouz et al., 2020 ). On 11 th March 2020, when WHO declared a global pandemic, 118,000 reported cases spanning 114 countries with over 4,000 fatalities had been reported. It took 67 days from the first reported case to reach 100,000 cases, 11 days for the second 100,000, and just four days for the third ( United Nations Development Programme (UNDP), 2020 ). This has overwhelmed the health systems of even the richest countries with doctors being forced to make the painful decision of who lives and who dies. The COVID-19 pandemic has pushed the world into uncertainty and countries do not have a clear exit strategy in the absence of a vaccine. This pandemic has affected all segments of society. However, it is particularly damaging to vulnerable social groups, including people living in poverty, older persons, persons with disabilities, youths, indigenous people and ethnic minorities. People with no home or shelter such as refugees, migrants, or displaced persons will suffer disproportionately, both during the pandemic and in its aftermath. This might occur in multiple ways, such as experiencing limited movement, fewer employment opportunities, increased xenophobia, etc. The social crisis created by the COVID-19 pandemic may also increase inequality, discrimination and medium and long-term unemployment if not properly addressed by appropriate policies.
The protection measures taken to save lives are severely affecting economies all over the world. As discussed previously, the key protection measure adopted universally is the lockdown, which has forced people to work from home wherever possible. Workplace closures have disrupted supply chains and lowered productivity. In many instances, governments have closed borders to contain the spread. Other measures such as travel bans and the prohibition of sporting events and other mass gatherings are also in place. In addition, measures such as discouraging the use of public transport and public spaces, for example, restaurants, shopping centres and public attractions are also in place in many parts of the world. The situation is particularly dire in hospitality-related sectors and the global travel industry, including airlines, cruise companies, casinos and hotels which are facing a reduction in business activity of more than 90% ( Fernandes, 2020 ). The businesses that rely on social interactions like entertainment and tourism are suffering severely, and millions of people have lost their jobs. Layoffs, declines in personal income, and heightened uncertainty have made people spend less, triggering further business closures and job losses ( Ghosh, 2020 ).
A key performance indicator of economic health is Gross Domestic Product (GDP), typically calculated on a quarterly or annual basis. IMF provides a GDP growth estimate per quarter based on global economic developments during the near and medium-term. According to its estimate, the global economy is projected to contract sharply by 3% in 2020, which is much worse than the 2008 global financial crisis ( International Monetary Fund (IMF), 2020 ). The growth forecast was marked down by 6% in the April 2020 World Economic Outlook (WEO) compared to that of the October 2019 WEO and January 2020 WEO. Most economies in the advanced economy group are expected to contract in 2020, including the US, Japan, the UK, Germany, France, Italy and Spain by 5.9%, 5.4%, 6.5%, 7.0%, 7.2%, 9.1%, and 8.0% respectively. Fig. 15 a shows the effect of COVID-19 on the GDP of different countries around the globe. On the other hand, economies of emerging market and developing economies, excluding China, are projected to contract by only 1.0% in 2020. The economic recovery in 2021 will depend on the gradual rolling back of containment efforts in the latter part of 2020 that will restore consumer and investor confidence. According to the April 2020 WEO, the level of GDP at the end of 2021 in both advanced and emerging market and developing economies is expected to remain below the pre-virus baseline (January 2020 WEO Update), as shown in Fig. 15 b.

(a) Quarterly World GDP. 2019:Q1 =100, dashed line indicates estimates from January 2020 WEO; (b) GDP fall due to lockdown in selected countries.
A particular example of a country hardest hit by COVID-19 is Italy. During the early days of March, the Italian government imposed quarantine orders in major cities that locked down more than seventeen million people ( Andrews, 2020 ). The mobility index data by Google for Italy shows there has been a significant reduction in mobility (and therefore economic activity) across various facets of life. The reported decline of mobility in retail and recreation, grocery and pharmacy, transit stations and workplaces were 35%, 11%, 45% and 34% respectively ( Rubino, 2020 ). The Italian economy suffered great financial damage from the pandemic. The tourism, and hospitality sectors were among those most severely affected by foreign countries prohibiting travel to and from Italy, and by the government's national lockdowns in early March ( Brunton, 2020 ). A March 2020 study in Italy showed that about 99% of the companies in the housing and utility sector said the epidemic had affected their industry. In addition, transport and storage was the second most affected sector. Around 83% of companies operating in this sector said that their activities had been affected by the coronavirus ( Statista, 2020 ) pandemic. In April 2020, Italian Minister Roberto Gualtieri estimated a 6% reduction in the GDP for the year 2020 ( Bertacche et al., 2020 ). The government of Italy stopped all unnecessary companies, industries and economic activities on 21 st March 2020. Therefore The Economist estimates a 7% fall in GDP in 2020 ( Horowitz, 2020 ). The Economist predicted that the Italian debt-to-GDP ratio would grow from 130% to 180% by the end of 2020 ( Brunton, 2020 ) and it is also assumed that Italy will have difficulty repaying its debt ( Bertacche et al., 2020 ).
4. Impact of COVID-19 on the energy domain
COVID-19 has not only impacted health, society and the economy but it has also had a strong impact on the energy sector ( Chakraborty and Maity, 2020 ; Abu-Rayash and Dincer, 2020 ). World energy demand fell by 3.8% in the first quarter (Q1) of 2020 compared with Q1 2019. In Q1 of 2020, the global coal market was heavily impacted by both weather conditions and the downturn in economic activity resulting in an almost 8% fall compared to Q1 2019. The fall was primarily in the electricity sector as a result of substantial declines in demand (-2.5%) and competitive advantages from predominantly low-cost natural gas. The market for global oil has plummeted by almost 5%. Travel bans, border closures, and changes in work routines significantly decreased the demand for the use of personal vehicles and air transport. Thus rising global economic activity slowed down the use of fuel for transportation ( Madurai Elavarasan et al., 2020 ). In Q1 2020, the output from nuclear energy plants decreased worldwide, especially in Europe and the US, as they adjusted for lower levels of demand. Demand for natural gas dropped significantly, by approximately 2% in Q1 2020, with the biggest declines in China, Europe, and the United States. In the Q1 2020, the need for renewable energy grew by around 1.5%, driven in recent years by the increasing output of new wind and solar plants. Renewable energy sources substantially increased in the electricity generation mix, with record hourly renewable energy shares in Belgium, Italy, Germany, Hungary, and East America. The share of renewable energy sources in the electricity generation mix has increased. Table 2 shows the effect of COVID-19 outbreak on the energy demand around the world.
Impact of COVID-19 on global energy sector ( AEMO, 2020 ; CIS Editorial, 2020 ; Eurelectric, 2020 ; Livemint, 2020 ; Renewable Energy World, 2020 ; S&P Global, 2020 ; Madurai Elavarasan et al., 2020 ).
Different areas have implemented lockdown of various duration. Therefore, regional energy demand depends on when lockdowns were introduced and how lockdowns influence demand in each country. In Korea and Japan, the average impact on demand is reduced to less than 10%, with lower restrictions. In China, where the first COVID-19 confinement measures were introduced, not all regions faced equally stringent constraints. Nevertheless, virus control initiatives have resulted in a decline of up to 15% in weekly energy demand across China. In Europe, moderate to complete lockdowns were more radical. On average, a 17% reduction in weekly demand was experienced during temporary confinement periods. India's complete lockdown has cut energy requirements by approximately 30%, which indicates yearly energy needs are lowered by 0.6% for each incremental lockdown week ( International Energy Agency (IEA) 2020 ).
The International Energy Agency (IEA) has predicted an annual average decline in oil production of 9% in 2020, reflecting a return to 2012 levels. Broadly, as electricity demand has decreased by about 5% throughout the year, coal production may fall by 8%, and the output of coal-fired electricity generation could fall by more than 10%. During the entire year, gas demand may fall far beyond Q1 2020 due to a downward trend in power and industrial applications. Nuclear energy demand will also decrease in response to reduced electricity demand. The demand for renewable energies should grow due to low production costs and the choice of access to many power systems. Khan et al. (2020) reported that international trade is significantly and positively dependent on renewable energy. In addition, sustainable growth can be facilitated through the consumption of renewable energy which improves the environment, enhances national image globally and opens up international trade opportunities with environmentally friendly countries ( Khan et al., 2021 ). As such, policies that promote renewables can result in economic prosperity, create a better environment as well as meet critical goals for sustainable development ( Khan et al., 2020 ).
5. Preventive measures to control COVID-19 outbreak
COVID-19 is a major crisis needing an international response. Governments will ensure reliable information is provided to assist the public in combating this pandemic. Community health and infection control measures are urgently needed to reduce the damage done by COVID-19 and minimise the overall spread of the virus. Self-defence techniques include robust overall personal hygiene, face washing, refraining from touching the eyes, nose or mouth, maintaining physical distance and avoiding travel. In addition, different countries have already taken preventive measures, including the implementation of social distancing, medicine, forestation and a worldwide ban on wildlife trade. A significant aim of the community health system is to avoid SARS-CoV-2 transmission by limiting large gatherings. COVID-19 is transmitted by direct communication from individual to individual. Therefore, the key preventive technique is to limit mass gatherings. Table 3 shows the impact of lockdown measures on the recovery rate of COVID-19 infections. The baseline data for this table is the median value, for the corresponding day of the week, during the 5-week period 3 rd January to 6 th February 2020.
Mobility index report of different countries ( Ghosh, 2020 ; Johns Hopkins University (JHU), 2020 ; Worldometer, 2020 ).
As of today, no COVID-19 vaccine is available. Worldwide scientists are racing against time to develop the COVID-19 vaccine, and WHO is now monitoring more than 140 vaccine candidates. As of 29 th September 2020, about 122 candidates have been pre-clinically checked, i.e. determining whether an immune response is caused when administering the vaccine to animals ( Biorender, 2020 ). About 45 candidates are in stage I where tests on a small number of people are conducted to decide whether it is effective ( Biorender, 2020 ). About 29 candidates are in Phase II where hundreds of people are tested to assess additional health issues and doses ( Biorender, 2020 ). Only 14 candidates are currently in Phase III, where thousands of participants are taking a vaccine to assess any final safety concerns, especially with regard to side effects ( Biorender, 2020 ). 3 candidates are in Phase IV, where long-term effects of the vaccines on a larger population is observed ( Biorender, 2020 ). The first generation of COVID-19 vaccines is expected to gain approval by the end of 2020 or in early 2021 ( Peiris and Leung, 2020 ). It is anticipated that these vaccines will provide immunity to the population. These vaccines can also reduce the transmission of SARS-CoV-2 and lead to a resumption of a pre-COVID-19 normal. Table 4 shows the list of vaccines that have been passed in the pre-clinical stage. In addition, according to the COVID-19 vaccine and therapeutics tracker, there are 398 therapeutic drugs in development. Of these, 83 are in the pre-clinical phase, 100 in Phase I, 224 in Phase II, 119 in Phase III and 46 in Phase IV ( Biorender, 2020 ).
List of vaccines that have passed the pre-clinical stage ( Biorender, 2020 ).
In addition to the above, forestation and a worldwide ban on wildlife trade can also play a significant role in reducing the spread of different viruses. More than 30% of the ground area is covered with forests. The imminent increase in population contributes to deforestation in agriculture or grazing for food, industries and property. The rise in ambient temperature, sea levels and extreme weather events affects not only the land and environment but also public health ( Ruscio et al., 2015 ; Arora and Mishra, 2020 ). Huge investment has been made into treatments, rehabilitation and medications to avoid the impact of this epidemic. However, it is important to focus on basic measures, e.g. forestation and wildlife protection. The COVID-19 infection was initially spread from the Seafood Market, Wuhan, China. Therefore, China temporarily banned wildlife markets in which animals are kept alive in small cages. It has been reported that 60% of transmittable diseases are animal-borne, 70% of which are estimated to have been borne by wild animals ( Chakraborty and Maity, 2020 ). Deforestation is also related to various kinds of diseases caused by birds, bats, etc. ( Afelt et al., 2018 ). For example, COVID-19 is a bat-borne disease that is transmitted to humans. Therefore, several scientists have advised various countries to ban wildlife trade indefinitely so that humans can be protected from new viruses and global pandemics like COVID-19.
6. Conclusion
In this article, comprehensive analyses of energy, environmental pollution, and socio-economic impacts in the context of health emergency events and the global responses to mitigate the effects of these events have been provided. COVID-19 is a worldwide pandemic that puts a stop to economic activity and poses a severe risk to overall wellbeing. The global socio-economic impact of COVID-19 includes higher unemployment and poverty rates, lower oil prices, altered education sectors, changes in the nature of work, lower GDPs and heightened risks to health care workers. Thus, social preparedness, as a collaboration between leaders, health care workers and researchers to foster meaningful partnerships and devise strategies to achieve socio-economic prosperity, is required to tackle future pandemic-like situations. The impact on the energy sector includes increased residential energy demand due to a reduction in mobility and a change in the nature of work. Lockdowns across the globe have restricted movement and have placed people primarily at home, which has, in turn, decreased industrial and commercial energy demand as well as waste generation. This reduction in demand has resulted in substantial decreases in NO 2, PM, and environmental noise emissions and as a consequence, a significant reduction in environmental pollution. Sustainable urban management that takes into account the positive benefits of ecological balance is vital to the decrease of viral infections and other diseases. Policies that promote sustainable development, ensuring cities can enforce recommended measures like social distancing and self-isolation will bring an overall benefit very quickly. The first generation of COVID-19 vaccines is expected to gain approval by the end of 2020 or in early 2021, which will provide immunity to the population. It is necessary to establish preventive epidemiological models to detect the occurrence of viruses like COVID-19 in advance. In addition, governments, policymakers, and stakeholders around the world need to take necessary steps, such as ensuring healthcare services for all citizens, supporting those who are working in frontline services and suffering significant financial impacts, ensuring social distancing, and focussing on building a sustainable future. It is also recommended that more investment is required in research and development to overcome this pandemic and prevent any similar crisis in the future.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Dr. Syed Abdul Rehman Khan
- Abdullah S., et al. Air quality status during 2020 Malaysia movement control order (MCO) due to 2019 novel coronavirus (2019-nCoV) pandemic. Sci. Total Environ. 2020; 729 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Abu-Rayash A., Dincer I. Analysis of the electricity demand trends amidst the COVID-19 coronavirus pandemic. Energy Res. Soc. Sci. 2020; 68 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- ACR+, Municipal waste management and COVID-19. URL: https://www.acrplus.org/en/municipal-waste-management-covid-19 . Date accessed: 22nd September, 2020. 2020.
- Acter T., et al. Evolution of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) as coronavirus disease 2019 (COVID-19) pandemic: a global health emergency. Sci. Total Environ. 2020; 730 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- AEMO, COVID-19 demand impact in Australia. https://aemo.com.au/en/news/demand-impact-australia-covid19 . Date accessed: 21st September, 2020. 2020.
- Afelt A., Frutos R., Devaux C. Bats, coronaviruses, and deforestation: toward the emergence of novel infectious diseases? Front. Microbiol. 2018; 9 702-702. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Aldila D., et al. A mathematical study on the spread of COVID-19 considering social distancing and rapid assessment: the case of Jakarta, Indonesia. Chaos Solitons Fractals. 2020; 139 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Andrews, F., Before and after: Italy's tourist attractions left deserted amid coronavirus lockdown. https://www.thenational.ae/lifestyle/travel/before-and-after-italy-s-tourist-attractions-left-deserted-amid-coronavirus-lockdown-1.991274 . Date accessed: 21st September, 2020, in The National. 2020: Abu Dhabi.
- Arora N.K., Mishra J. COVID-19 and importance of environmental sustainability. Environ. Sustain. 2020; 3 (2):117–119. [ Google Scholar ]
- Ashraful A.M., et al. Production and comparison of fuel properties, engine performance, and emission characteristics of biodiesel from various non-edible vegetable oils: a review. Energy Convers. Manage. 2014; 80 :202–228. [ Google Scholar ]
- Atmosphere Monitoring Service. Air quality information confirms reduced activity levels due to lockdown in Italy. https://atmosphere.copernicus.eu/air-quality-information-confirms-reduced-activity-levels-due-lockdown-italy . Date accessed: 21st September, 2020. 2020.
- Awad O.I., et al. Particulate emissions from gasoline direct injection engines: a review of how current emission regulations are being met by automobile manufacturers. Sci. Total Environ. 2020; 718 [ PubMed ] [ Google Scholar ]
- Baensch-Baltruschat B., et al. Tyre and road wear particles (TRWP) - a review of generation, properties, emissions, human health risk, ecotoxicity, and fate in the environment. Sci. Total Environ. 2020; 733 [ PubMed ] [ Google Scholar ]
- Beck M.J., Hensher D.A. Insights into the impact of COVID-19 on household travel and activities in Australia – the early days under restrictions. Transp. Policy. 2020; 96 :76–93. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bertacche, M., Orihuela, R., and Colten, J., Italy struck by deadliest day as virus prompts industry shutdown. https://www.bloomberg.com/news/articles/2020-03-21/germany-plans-extra-spending-of-eu150-billion-scholz-says . Date accessed: 21st September, 2020, in Bloomberg. 2020.
- Biorender, COVID-19 vaccine & therapeutics tracker. URL: https://biorender.com/covid-vaccine-tracker . Date accessed: 28th September, 2020. 2020.
- Bressan, D., Coronavirus lockdowns cause worldwide decrease in man-made seismic noise. https://www.forbes.com/sites/davidbressan/2020/04/04/coronavirus-lockdowns-cause-worldwide-decrease-in-man-made-seismic-noise/#1643453464da . Date accessed: 21st September, 2020, in Forbes. 2020.
- Bruinen de Bruin Y., et al. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf. Sci. 2020; 128 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Brunton, J., Nothing less than a catastrophe': Venice left high and dry by coronavirus. https://www.theguardian.com/travel/2020/mar/17/nothing-less-than-a-catastrophe-venice-left-high-and-dry-by-coronavirus . date accessed: 21st September, 2020, in The Guardian. 2020.
- Cai C., et al. Temperature-responsive deep eutectic solvents as green and recyclable media for the efficient extraction of polysaccharides from Ganoderma lucidum. J. Cleaner Prod. 2020; 274 [ Google Scholar ]
- Chakraborty I., Maity P. COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci. Total Environ. 2020; 728 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chatterjee A., et al. High rise in carbonaceous aerosols under very low anthropogenic emissions over eastern Himalaya, India: impact of lockdown for COVID-19 outbreak. Atmos. Environ. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chin A.W.H., et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet Microbe. 2020; 1 (1):e10. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chinazzi M., et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020; 368 (6489):395–400. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- CIS Editorial, Coronavirus impact on energy markets. URL: https://www.icis.com/explore/resources/news/2020/04/08/10482507/topic-page-coronavirus-impact-on-energy-markets . Date accessed: 2nd September, 2020. 2020.
- Cohen M.J. Does the COVID-19 outbreak mark the onset of a sustainable consumption transition? Sustainability. 2020; 16 (1):1–3. [ Google Scholar ]
- Chowdhury, M. A., M. B. A. Shuvho, M. A. Shahid, A. K. M. M. Haque, M. A. Kashem, S. S. Lam, H. C. Ong, M. A. Uddin and M. Mofijur (2021). "Prospect of biobased antiviral face mask to limit the coronavirus outbreak." Environmental Research 192: 110294. [ PMC free article ] [ PubMed ]
- de Haas M., Faber R., Hamersma M. How COVID-19 and the Dutch ‘intelligent lockdown’ change activities, work and travel behaviour: evidence from longitudinal data in the Netherlands. Transp. Res. Interdiscip. Perspect. 2020; 6 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Eurelectric, Impact of COVID 19 on customers and society. URL: https://cdn.eurelectric.org/media/4313/impact_of_covid_19_on_customers_and_society-2020-030-0216-01-e-h-584D2757.pdf . Date accessed: 28th Spetember, 2020. 2020.
- European Space Agency (ESA). Sentinel-5P. https://www.esa.int/Applications/Observing_the_Earth/Copernicus/Sentinel-5P . Date accessed: 21st September, 2020. 2020.
- Fattah I.M.R., et al. Impact of various biodiesel fuels obtained from edible and non-edible oils on engine exhaust gas and noise emissions. Renew. Sustain. Energy Rev. 2013; 18 :552–567. [ Google Scholar ]
- Fernandes, N., Economic effects of coronavirus outbreak (COVID-19) on the world economy. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3557504 . Date accessed: 21st September, 2020. 2020.
- Financial Times, Coronavirus: is Europe losing Italy? https://www.ft.com/content/f21cf708-759e-11ea-ad98-044200cb277f . Date accessed: 21st September, 2020, in Financial Times. 2020.
- Ghahremanloo M., et al. Impact of the COVID-19 outbreak on air pollution levels in East Asia. Sci. Total Environ. 2021; 754 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ghosh, I. The road to recovery: which economies are reopening? URL: https://www.visualcapitalist.com/the-road-to-recovery-which-economies-are-reopening-covid-19/ . Date accessed: 22nd September, 2020. 2020 [cited 2020 25th July, 2020]; Available from: https://www.visualcapitalist.com/the-road-to-recovery-which-economies-are-reopening-covid-19/.
- Gorbalenya A.E., et al. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat. Microbiol. 2020; 5 (4):536–544. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gualtieri G., et al. Quantifying road traffic impact on air quality in urban areas: a Covid19-induced lockdown analysis in Italy. Environ. Pollut. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Holshue M.L., et al. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020; 382 (10):929–936. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Horowitz, J., Italy locks down much of the country's north over the coronavirus. URL: https://www.nytimes.com/2020/03/07/world/europe/coronavirus-italy.html . Date accessed: 21st September, 2020, in The New York Times. 2020.
- Huang, Y., W.-c. Mok, Y.-s. Yam, J. L. Zhou, N. C. Surawski, B. Organ, E. F. C. Chan, M. Mofijur, T. M. I. Mahlia and H. C. Ong (2020). Evaluating in-use vehicle emissions using air quality monitoring stations and on-road remote sensing systems. Science of The Total Environment 740: 139868. [ PubMed ]
- International Energy Agency (IEA) IEA; Paris: 2020. Global Energy Review. https://www.iea.org/reports/global-energy-review-2020 Date accessed: 21st September, 2020. 2020. [ Google Scholar ]
- International Monetary Fund (IMF), World Economic Outlook, April 2020: The Great Lockdown. https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020 . Date accessed: 22nd September, 2020. 2020.
- International Monetary Fund (IMF), World economic outlook, April 2020: The Great Lockdown. URL: https://www.imf.org/en/Publications/WEO/Issues/2020/04/14/weo-april-2020 . Date accessed: 21st September, 2020. 2020.
- Jiang P., et al. Spatial-temporal potential exposure risk analytics and urban sustainability impacts related to COVID-19 mitigation: a perspective from car mobility behaviour. J. Cleaner Prod. 2021; 279 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Johns Hopkins University (JHU). COVID-19 dashboard by the center for systems science and engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html . Date accessed: 25th July, 2020. 2020.
- Kabir M.T., et al. nCOVID-19 pandemic: from molecular pathogenesis to potential investigational therapeutics. Front. Cell Dev. Biol. 2020; 8 616-616. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Khan S.A.R., et al. Measuring the impact of renewable energy, public health expenditure, logistics, and environmental performance on sustainable economic growth. Sustain. Dev. 2020; 28 (4):833–843. [ Google Scholar ]
- Khan S.A.R., et al. Investigating the effects of renewable energy on international trade and environmental quality. J. Environ. Manage. 2020; 272 [ PubMed ] [ Google Scholar ]
- Khan S.A.R., et al. Determinants of economic growth and environmental sustainability in South Asian association for regional cooperation: evidence from panel ARDL. Environ. Sci. Pollut. Res. 2020 [ PubMed ] [ Google Scholar ]
- Khan S.A.R., et al. A state-of-the-art review and meta-analysis on sustainable supply chain management: future research directions. J. Cleaner Prod. 2021; 278 [ Google Scholar ]
- Khoo, A., Coronavirus lockdown sees air pollution plummet across UK. https://www.bbc.com/news/uk-england-52202974 . Date accessed: 21st September, 2020, in BBC News. 2020.
- Leal Filho W., et al. COVID-19 and the UN sustainable development goals: threat to solidarity or an opportunity? Sustainability. 2020; 12 (13):5343. [ Google Scholar ]
- Lillywhite, R., Air quality and wellbeing during COVID-19 lockdown. https://www.newswise.com/coronavirus/air-quality-and-wellbeing-during-covid-19-lockdown/?article_id=730455 . Date accessed: 21st September, 2020, in Newswise. 2020: USA.
- Liu M., et al. Waste paper recycling decision system based on material flow analysis and life cycle assessment: a case study of waste paper recycling from China. J. Environ. Manage. 2020; 255 [ PubMed ] [ Google Scholar ]
- Livemint. India's energy demand falls by 30% due to COVID-19 lockdown. URL: https://www.livemint.com/news/world/lockdown-cuts-india-s-energy-demand-by-30-says-iea-11588235067694.html . Date accessed: 28th September, 2020. 2020.
- M Palash S., et al. Impacts of biodiesel combustion on NOx emissions and their reduction approaches. Renewable Sustainable Energy Rev. 2013; 23 (0):473–490. [ Google Scholar ]
- Ma B., et al. Recycle more, waste more? When recycling efforts increase resource consumption. J. Cleaner Prod. 2019; 206 :870–877. [ Google Scholar ]
- Madurai Elavarasan R., et al. COVID-19: impact analysis and recommendations for power sector operation. Appl. Energy. 2020; 279 115739-115739. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Madurai Elavarasan R., et al. COVID-19: impact analysis and recommendations for power sector operation. Appl. Energy. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mofijur M., et al. A study on the effects of promising edible and non-edible biodiesel feedstocks on engine performance and emissions production: a comparative evaluation. Renew. Sustain. Energy Rev. 2013; 23 (0):391–404. [ Google Scholar ]
- Munawer M.E. Human health and environmental impacts of coal combustion and post-combustion wastes. J. Sustain. Min. 2018; 17 (2):87–96. [ Google Scholar ]
- Myllyvirta, L., 11,000 air pollution-related deaths avoided in Europe as coal, oil consumption plummet. https://energyandcleanair.org/air-pollution-deaths-avoided-in-europe-as-coal-oil-plummet/ . Date accessed: 21st September, 2020. 2020.
- Mofijur, M., I. M. Rizwanul Fattah, A. B. M. Saiful Islam, M. N. Uddin, S. M. Ashrafur Rahman, M. A. Chowdhury, M. A. Alam and M. A. Uddin (2020). "Relationship between Weather Variables and New Daily COVID-19 Cases in Dhaka, Bangladesh." Sustainability 12(20): 8319.
- Nghiem L.D., et al. The COVID-19 pandemic: considerations for the waste and wastewater services sector. Case Stud. Chem. Environ. Eng. 2020; 1 [ Google Scholar ]
- Nicola M., et al. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020; 78 :185–193. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Park G.W., et al. Evaluation of a new environmental sampling protocol for detection of human norovirus on inanimate surfaces. Appl. Environ. Microbiol. 2015; 81 (17):5987–5992. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peiris M., Leung G.M. What can we expect from first-generation COVID-19 vaccines? Lancet North Am. Ed. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pirouz B., et al. Investigating a serious challenge in the sustainable development process: analysis of confirmed cases of COVID-19 (new type of coronavirus) through a binary classification using artificial intelligence and regression analysis. Sustainability. 2020; 12 (6):2427. [ Google Scholar ]
- Qu G., et al. An imperative need for research on the role of environmental factors in transmission of novel coronavirus (COVID-19) Environ. Sci. Technol. 2020; 54 (7):3730–3732. [ PubMed ] [ Google Scholar ]
- Renewable Energy World, Renewables achieve clean energy record as COVID-19 hits demand. URL: https://www.renewableenergyworld.com/2020/04/06/renewables-achieve-clean-energy-record-as-covid-19-hits-demand/ . Date accessed: 28th September, 2020. 2020.
- Ro, C., Is coronavirus reducing noise pollution? https://www.forbes.com/sites/christinero/2020/04/19/is-coronavirus-reducing-noise-pollution/#2fe787d5766f . Date accessed: 21st September, 2020, in Forbes. 2020.
- Rubino, d.M., Coronavirus, il decreto del governo: tutte le misure per la zona arancione e quelle per il resto d'Italia. URL: https://www.repubblica.it/cronaca/2020/03/08/news/coronavirus_i_decreti_del_governo-250617415/ . Date accessed: 21st September, 2020, in la Repubblica. 2020.
- Ruscio B.A., et al. One health - a strategy for resilience in a changing arctic. Int. J. Circumpolar Health. 2015; 74 :27913. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- S&P Global, Japan, Singapore lockdowns to stifle Asian gas, power demand further. https://www.spglobal.com/platts/en/market-insights/latest-news/natural-gas/040720-japan-singapore-lockdowns-to-stifle-asian-gas-power-demand-further . Date accessed: 21st September, 2020. 2020.
- Schanes K., Dobernig K., Gözet B. Food waste matters - a systematic review of household food waste practices and their policy implications. J. Cleaner Prod. 2018; 182 :978–991. [ Google Scholar ]
- Sharifi A., Khavarian-Garmsir A.R. The COVID-19 pandemic: impacts on cities and major lessons for urban planning, design, and management. Sci. Total Environ. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sicard P., et al. Amplified ozone pollution in cities during the COVID-19 lockdown. Sci. Total Environ. 2020; 735 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sohrabi C., et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020; 76 :71–76. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Srivastava A. COVID-19 and air pollution and meteorology-an intricate relationship: a review. Chemosphere. 2020 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Statista, Perceived impact of coronavirus (COVID-19) among Italian companies in March 2020, by macro sector. https://www.statista.com/statistics/1103017/perceived-impact-of-coronavirus-covid-19-among-italian-companies-by-sector/ . Date accessed: 21st September, 2020. 2020.
- Statista, COVID-19 lockdown affect on nitrogen dioxide (NO2) emissions in UK cities in March 2020 compared with March 2019. https://www.statista.com/statistics/1111519/no2-emissions-decrease-due-to-lockdown-united-kingdom/ . Date accessed: 21st September, 2020. 2020.
- United Nations Development Programme (UNDP), The social and economic impact of COVID-19 in the Asia-Pacific region. https://www.undp.org/content/undp/en/home/librarypage/crisis-prevention-and-recovery/the-social-and-economic-impact-of-covid-19-in-asia-pacific.html . Date accessed: 21st September, 2020. 2020.
- van Doremalen N., et al. Aerosol and Surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N. Engl. J. Med. 2020; 382 (16):1564–1567. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang D., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020; 323 (11):1061–1069. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang Q., Su M. A preliminary assessment of the impact of COVID-19 on environment – a case study of China. Sci. Total Environ. 2020; 728 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Weitekamp C.A., et al. Health effects from freshly emitted versus oxidatively or photochemically aged air pollutants. Sci. Total Environ. 2020; 704 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Worldometer, Reported cases and deaths by country, territory, or conveyance. https://www.worldometers.info/coronavirus/ . Date accessed: 25th July, 2020. 2020.
- Worldometer, Reported cases and deaths by country, territory, or conveyance. https://www.worldometers.info/coronavirus/ . Date accessed: 22nd September, 2020. 2020.
- Yan Y., et al. The first 75 days of novel coronavirus (SARS-CoV-2) outbreak: recent advances, prevention, and treatment. Int. J. Environ. Res. Public Health. 2020; 17 (7):2323. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ye Y., et al. Survivability, partitioning, and recovery of enveloped viruses in untreated municipal wastewater. Environ. Sci. Technol. 2016; 50 (10):5077–5085. [ PubMed ] [ Google Scholar ]
- Zambrano-Monserrate M.A., Ruano M.A. Does environmental noise affect housing rental prices in developing countries? Evidence from Ecuador. Land Use Policy. 2019; 87 [ Google Scholar ]
- Zambrano-Monserrate M.A., Ruano M.A., Sanchez-Alcalde L. Indirect effects of COVID-19 on the environment. Sci. Total Environ. 2020; 728 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhou P., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020; 579 (7798):270–273. [ PMC free article ] [ PubMed ] [ Google Scholar ]
March 11, 2021
12 min read
How the U.S. Pandemic Response Went Wrong—and What Went Right—during a Year of COVID
On the anniversary of this global disaster, we take a look back at some of the biggest mistakes, surprising successes and lingering questions
By Tanya Lewis

Faced with the unimaginable, health care workers continued to show up for patients.
Go Nakamura Getty Images
When the World Health Organization first called COVID-19 a pandemic on March 11, 2020, few people had any idea what the world was in for. The progression was swift: borders clamped shut, authorities issued stay-at-home orders, and public life ground to a near halt. Most of the world had no experience dealing with an infectious disease outbreak of this scale. The previously unknown virus, now called SARS-CoV-2, could spread through the air, often before (or, in some cases, possibly without ever) causing any symptoms. COVID—though mild for many people—struck down elderly and more vulnerable individuals (and occasionally very healthy ones) with a vengeance, launching a wave of fear, suffering and death unlike any in recent memory.
“In the beginning, when this started a year ago, we knew that it was spreading. And we knew that it also was lethal in some percentage of people,” says Stanley Perlman, a virologist at the University of Iowa, who is an expert on coronaviruses, a group that includes SARS-CoV-2. “But I don't think we had a full appreciation about how bad it was.”
Among the biggest shocks was that the U.S. fared worse than most other countries, with more than 29 million cases and nearly 530,000 deaths as of this writing. “We absolutely can’t say that we had the most robust response to the pandemic, up till this point, because we have had a higher death rate per capita than so many other places,” says Monica Gandhi, a professor of medicine at the University of California, San Francisco.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing . By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
As the country raced to react to this new and terrifying scourge, mistakes were made that together cost hundreds of thousands of lives. Yet the tireless efforts of health care workers, along with an unprecedented vaccine push, have saved countless others. Scientific American interviewed scientists and public health experts about the biggest mistakes in the U.S.’s response, some of the key successes and the lingering questions that still need to be answered.
A lot of effort has been spent on cleaning surfaces even though the virus is thought to be spread mainly by air.
Credit: Victor J. Blue and New York Times REDUX
What Went Wrong
Downplaying the danger and sidelining experts. During the pandemic’s crucial early days and weeks, then president Donald Trump and other authority figures actively minimized the virus’s threat. Trump dismissed it as no worse than the flu and said the pandemic would be over by Easter.
“One thing that shouldn’t have been done is people downplaying the infection,” Perlman says. “That was a real big problem, because if you let the pandemic get out of control and don’t take it seriously, it gets worse.” The U.S. Centers for Disease Control and Prevention initially told the media that the threat to the American public was low. When a CDC spokesperson acknowledged in late February that disruptions to daily life could be “severe,” the agency was quickly sidelined—and Trump himself became the government’s main conduit for COVID updates through his daily briefings. “The Trump administration really tightly controlled what [the CDC] could put out,” says Angela Rasmussen, a virologist at the Georgetown University Center for Global Health Science and Security. This muzzling of the CDC and top government health experts made it hard for them to communicate accurate and lifesaving scientific information to the public. Under President Joe Biden’s administration, government science agencies and health officials have been given renewed respect and independence. But rebuilding public trust in these authorities will still take time.
Slow and flawed testing. The CDC developed its own test for the virus rather than employing a German-developed one used by the World Health Organization . But the CDC test was flawed , causing a deadly delay while scientists worked out the problem. The agency was not designed to produce tests at the scale needed to spot the infections as they silently spread through the population. Meanwhile the Food and Drug Administration was slow to approve tests made by private companies, says Caitlin Rivers, an epidemiologist at the Johns Hopkins Center for Health Security. She also says the earliest criteria for getting a test were too stringent—one often had to have been hospitalized with severe symptoms and have recently traveled to a “high-risk” area. As a result of these hurdles, the virus spread undetected for weeks. By the time testing became somewhat more available, community spread was already rampant in many places, making it difficult or impossible to do contact tracing and isolate people before they infected others. “In this pandemic, things moved so quickly that when you screwed up for two or three weeks, it made a difference,” Perlman says.
Testing availability has improved but remains uneven. Some experts have argued for the use of widespread rapid antigen testing, a type that is cheap, does not require sophisticated laboratory processing and could be done at homes, schools or offices. But some scientists still have concerns about the accuracy of these tests, and the FDA has been slow to approve them .
Inadequate tracing, isolating and quarantines. The timeworn methods of combatting an infectious disease—testing people who may be sick, tracing their contacts, and isolating or quarantining those who are positive or exposed—worked for COVID as well. The WHO repeatedly stressed the importance of these measures, and countries that followed this advice closely (such as Vietnam, Thailand, New Zealand and South Korea) succeeded in controlling their outbreaks. In addition to its test problems, the U.S. did not do an adequate job of isolating those who were known or suspected to be infected (or had recently traveled to a high-risk area), tracing their contacts or requiring quarantines for those who were exposed. China imposed extremely strict, city-wide quarantines. Other countries required those who may have been exposed to stay at a government-approved hotel or other facility for a quarantine ranging from a few days to a couple of weeks. Such policies would likely have been harder to implement in the U.S., a nation that prides itself on personal freedoms. But not doing so came at the expense of keeping the virus in check.
Confusing mask guidance. Although face masks are now widely considered a crucial part of stopping transmission, U.S. and global health authorities were slow to recommend them for public use. Many countries in East and Southeast Asia, including China and Japan, had normalized mask wearing well before the pandemic—in part because of the SARS outbreak in 2002–2003. Unlike the SARS virus, however, scientists now know that SARS-CoV-2 often spreads before a carrier develops symptoms (and possibly even if they never do). In the early weeks and months of the COVID outbreak, the CDC and WHO stated that face masks were not necessary for the general public unless a person was experiencing symptoms or caring for someone who was. The agencies also initially urged people not to buy high-filtration N95 and surgical masks because they were needed for health care workers and were in short supply because of inadequate government stockpiles. Though perhaps well-meaning, the WHO’s and CDC’s guidances sent a mixed message about masks’ effectiveness—and about who deserves protection. The CDC changed course and recommended cloth face coverings in April . The WHO did not do so until June , citing inadequate evidence of their efficacy before then. The CDC did not respond to a request for comment, and the WHO referred Scientific American to press briefings that addressed these issues. In these briefings , experts pointed to a lack of high-quality evidence for mask use. The WHO’s director general also stated that, in the absence of other public health measures, “masks alone will not protect you from COVID-19.”
Even after health experts reached a consensus that masks were effective, Trump refused to set an example by wearing one in public. Instead he mocked people who wore them, and many of his supporters rejected masks as well. “I don’t think it should ever become a political issue,” Rivers says. “It’s a straightforward public health intervention.” A study in Nature Medicine published online in October estimated that universal mask wearing could have saved nearly 130,000 lives during the fall and winter of 2020–2021. Most states did ultimately institute mask requirements, and Biden has made them mandatory in government buildings and on interstate transit. Yet several states, such as Texas and Mississippi , have just removed mask mandates and other restrictions entirely. “We’ve seen this happen over and over again: Where the virus picks back up, they implement more restrictions in various states and localities. It goes down a little bit, and then they just open back up again rather than saying, ‘Hey, you know, maybe this became a huge problem in the first place because we opened back up,’” Rasmussen says. “We haven’t seemed to learn from our mistakes.”
Airborne spread and “hygiene theater.” Early in the pandemic, U.S. health authorities believed the virus spread primarily by direct contact or relatively large droplets from a nearby cough or sneeze—not by far smaller droplets, called aerosols, that linger in the air. As a result, officials placed a huge emphasis on washing one’s hands and cleaning surfaces. Scientists now believe transmission from surfaces is not the main way the virus spreads and that aerosols play a much larger role. Ensuring proper ventilation and wearing well-fitted, high-quality masks are much more effective ways to reduce transmission than deep cleaning surfaces. Yet the latter—which critics have dubbed “hygiene theater” —continues to be a focus of many offices and businesses.
Structural racism fueled health inequities. The pandemic exposed and exacerbated deep-rooted racial and economic inequities in health and health care. Black and Hispanic individuals and other people of color were sickened with, and died of, COVID at disproportionately high rates. Many people in Black and brown communities had already long suffered from high rates of underlying conditions such as obesity and diabetes as a result of inadequate health care, lack of access to nutritious foods and outdoor space, and higher exposure to pollution. They also comprise a large percentage of essential workers in frontline industries with an inherently high risk of COVID exposure, such as nursing homes, meatpacking plants and restaurant kitchens. The uneven death toll is a wake-up call that far too many people of color lack access to preventative health care, as well as protections such as paid sick leave or hazard pay. “I do think the pandemic has laid bare some of those inequalities,” Rivers says. Public health experts have been tackling this problem for a long time, she notes, adding, “we need to draw on these lessons about underlying vulnerabilities from other disciplines that have such a deep understanding of how communities are affected and how to engage effectively with hard-to-reach communities.”
Decentralized response. The U.S. government’s structure meant that much of the pandemic response was left up to state and local leaders. In the absence of a strong national strategy, states implemented a patchwork of largely uncoordinated policies that did not effectively suppress the spread of the virus. This caused sudden, massive spikes of infections in many local outbreaks, placing enormous strain on health care systems and leaving no region untouched by the disease. “Every district, every county, every state could make decisions and keep them to themselves,” Gandhi says. “And we just have uneven applications of public health recommendations in a way that I can’t imagine any other country does. The Trump administration has been widely criticized for how the pandemic played out here. But Gandhi adds that the U.S. government’s decentralized nature would likely have been an obstacle under any president.
What Went Well
Despite the many mistakes and bad policy choices in the U.S. response, there were some incredible success stories, too.
Vaccines. Perhaps the clearest success amid this crisis has been the development of several vaccines in record time. Less than a year after the virus was genetically sequenced, two vaccines—one made by Pfizer and BioNTech and another developed by Moderna—were found to have roughly 95 percent efficacy in preventing symptomatic COVID and were authorized for emergency use in the U.S. The Johnson & Johnson vaccine, with efficacies of 66 percent in preventing moderate to severe disease and 85 percent in preventing severe illness alone, was recently authorized as well. (The Johnson & Johnson vaccine’s efficacy cannot be directly compared with that of the Pfizer or Moderna vaccines because the former was tested in a different population at a time when more dangerous variants of the virus were circulating.) All three vaccines prevent severe disease, hospitalization and death. “We are in an incredible place, with this pandemic, to have developed vaccines this quickly and that are that effective,” Gandhi says. Public-private partnerships were a big part of that success, she adds. Several other vaccines have been authorized or approved in other countries, and more are in development.
Vaccine development was one of the biggest success stories of the pandemic.
Credit: APU Gomes Getty Images
But the remarkable success in creating vaccines is tempered by the fact that most of the world still lacks access to them. And early rollout efforts in the U.S. had a slow and stumbling start, largely because the federal government did not provide states with the resources for distributing the vaccines. Further, Black and Hispanic people are being vaccinated at far lower rates than white people. And more work is needed to overcome vaccine hesitancy in some populations, including Republican voters. Yet the pace of vaccinations is picking up, and Biden has said the country is on track to have enough vaccine doses for every U.S. adult by the end of May , fueling promise of a return to some normality in the coming months.
Heroic efforts of health care workers. Faced with unprecedented levels of sickness and death, health care workers stepped up and risked their lives to care for COVID patients. Nurses, aides and orderlies cared for the elderly and most vulnerable individuals as the virus ravaged nursing homes . Paramedics responded to calls at all hours of the night. Doctors, nurses and other hospital staff comforted dying patients as they struggled to breathe—and held their hand when they said goodbye over video calls to family members who were not allowed in the room with them. Over time, medical professionals learned better techniques for treating the disease: these ranged from pharmaceuticals such as steroids and monoclonal antibodies to low-tech interventions, including “proning,” or simply turning some patients onto their stomach so they can breathe more easily. Even as nursing homes and hospitals became overwhelmed with COVID patients, hardworking staff kept showing up, shift after shift, facing down terror, exhaustion and despair.
The public (mostly) did its part. Despite COVID becoming a part of the country’s bitter and escalating political divide, many Americans followed public health guidance regarding mask wearing, social distancing and avoiding unnecessary risks. Surveys show the majority of people wear masks when they go out, Johns Hopkins’s Rivers says. “I am really heartened by the sense of purpose—the willingness for the whole country to come together and change their lives and protect themselves and their communities,” she says.
Combatting misinformation. In a media environment where misinformation and disinformation can reach millions through a single tweet, sorting out the signal from the noise has been an enormous challenge. But for the most part, science journalists confronted the informational chaos with clear, evidence-based reporting. When Trump made unsupported claims about safety levels or mask wearing or dubious COVID “treatments,” journalists and high-profile scientists such as Anthony Fauci quickly set the record straight. But as conspiracy theorists continue to circulate misinformation about the disease and vaccines, it is more important than ever that media outlets remain on guard.
Lingering Questions
As the world passes this one-year milestone in the pandemic, many unknowns remain.
What will happen with the new variants? Several novel strains of SARS-CoV-2 have emerged that could threaten progress against the disease. A variant called B.1.1.7, first identified in the U.K., is deadlier and more transmissible than the original—and it is on track to become the dominant variant in the U.S. this spring. Another variant that was initially spotted in South Africa, called B.1.351, has mutations that appear to help it to at least partially evade some of the vaccines. A third variant that was first seen in Brazil, called P.1, has overrun parts of that country and also contains worrisome mutations. Currently these variants are in a race with the vaccines, and scientists hope enough people can be vaccinated quickly enough to outmaneuver the new strains. Some vaccine makers are already working on booster shots , should they be necessary.
How long will immunity last? The duration of immunity to COVID—whether from natural infection or vaccination—remains unknown. A large study demonstrated that people who had recovered from infection still had antibodies, as well as so-called memory B cells and memory T cells, six to eight months later . A number of reinfections have occurred with some of the new variants, however. The CDC recently released guidelines stating that, with a few exceptions, fully vaccinated people who are exposed to the virus do not need to quarantine if they do not show symptoms. Time will tell whether vaccination provides immunity that lasts months or years and if booster shots will be needed.
Why do some people become COVID “long haulers”? A certain percentage of people who get COVID develop lingering symptoms that persist for months after their initial infection. Symptoms range from extreme fatigue to brain fog to problems sleeping. Scientists do not yet fully understand why some individuals experience these disturbing effects, although other viral infections have been known to produce similar syndromes. The National Institutes of Health has announced plans to invest $1 billion to study “long COVID.” But the illness’s true impact on people’s lives may not be known for decades.
What is the future of SARS-CoV-2? Exactly what will happen to the virus over time remains a mystery. Most scientists think it will never go away completely but could become less common and milder as more people are vaccinated against it—or as they build up some immunity through natural infection. It may ultimately become something like the flu, a virus that circulates every year and causes some severe infections and deaths—but does not shut down society. Eventually it could evolve into a less virulent form like some strains of the common cold. But that could take many years.
Read more about the coronavirus outbreak from Scientific American here . And read coverage from our international network of magazines here .
Mission: Recovering Education in 2021

THE CONTEXT
The COVID-19 pandemic has caused abrupt and profound changes around the world. This is the worst shock to education systems in decades, with the longest school closures combined with looming recession. It will set back progress made on global development goals, particularly those focused on education. The economic crises within countries and globally will likely lead to fiscal austerity, increases in poverty, and fewer resources available for investments in public services from both domestic expenditure and development aid. All of this will lead to a crisis in human development that continues long after disease transmission has ended.
Disruptions to education systems over the past year have already driven substantial losses and inequalities in learning. All the efforts to provide remote instruction are laudable, but this has been a very poor substitute for in-person learning. Even more concerning, many children, particularly girls, may not return to school even when schools reopen. School closures and the resulting disruptions to school participation and learning are projected to amount to losses valued at $10 trillion in terms of affected children’s future earnings. Schools also play a critical role around the world in ensuring the delivery of essential health services and nutritious meals, protection, and psycho-social support. Thus, school closures have also imperilled children’s overall wellbeing and development, not just their learning.
It’s not enough for schools to simply reopen their doors after COVID-19. Students will need tailored and sustained support to help them readjust and catch-up after the pandemic. We must help schools prepare to provide that support and meet the enormous challenges of the months ahead. The time to act is now; the future of an entire generation is at stake.
THE MISSION
Mission objective: To enable all children to return to school and to a supportive learning environment, which also addresses their health and psychosocial well-being and other needs.
Timeframe : By end 2021.
Scope : All countries should reopen schools for complete or partial in-person instruction and keep them open. The Partners - UNESCO , UNICEF , and the World Bank - will join forces to support countries to take all actions possible to plan, prioritize, and ensure that all learners are back in school; that schools take all measures to reopen safely; that students receive effective remedial learning and comprehensive services to help recover learning losses and improve overall welfare; and their teachers are prepared and supported to meet their learning needs.
Three priorities:
1. All children and youth are back in school and receive the tailored services needed to meet their learning, health, psychosocial wellbeing, and other needs.
Challenges : School closures have put children’s learning, nutrition, mental health, and overall development at risk. Closed schools also make screening and delivery for child protection services more difficult. Some students, particularly girls, are at risk of never returning to school.
Areas of action : The Partners will support the design and implementation of school reopening strategies that include comprehensive services to support children’s education, health, psycho-social wellbeing, and other needs.
Targets and indicators
2. All children receive support to catch up on lost learning.
Challenges : Most children have lost substantial instructional time and may not be ready for curricula that were age- and grade- appropriate prior to the pandemic. They will require remedial instruction to get back on track. The pandemic also revealed a stark digital divide that schools can play a role in addressing by ensuring children have digital skills and access.
Areas of action : The Partners will (i) support the design and implementation of large-scale remedial learning at different levels of education, (ii) launch an open-access, adaptable learning assessment tool that measures learning losses and identifies learners’ needs, and (iii) support the design and implementation of digital transformation plans that include components on both infrastructure and ways to use digital technology to accelerate the development of foundational literacy and numeracy skills. Incorporating digital technologies to teach foundational skills could complement teachers’ efforts in the classroom and better prepare children for future digital instruction.
While incorporating remedial education, social-emotional learning, and digital technology into curricula by the end of 2021 will be a challenge for most countries, the Partners agree that these are aspirational targets that they should be supporting countries to achieve this year and beyond as education systems start to recover from the current crisis.
3. All teachers are prepared and supported to address learning losses among their students and to incorporate digital technology into their teaching.
Challenges : Teachers are in an unprecedented situation in which they must make up for substantial loss of instructional time from the previous school year and teach the current year’s curriculum. They must also protect their own health in school. Teachers will need training, coaching, and other means of support to get this done. They will also need to be prioritized for the COVID-19 vaccination, after frontline personnel and high-risk populations. School closures also demonstrated that in addition to digital skills, teachers may also need support to adapt their pedagogy to deliver instruction remotely.
Areas of action : The Partners will advocate for teachers to be prioritized in COVID-19 vaccination campaigns, after frontline personnel and high-risk populations, and provide capacity-development on pedagogies for remedial learning and digital and blended teaching approaches.
Country level actions and global support
UNESCO, UNICEF, and World Bank are joining forces to support countries to achieve the Mission, leveraging their expertise and actions on the ground to support national efforts and domestic funding.
Country Level Action
1. Mobilize team to support countries in achieving the three priorities
The Partners will collaborate and act at the country level to support governments in accelerating actions to advance the three priorities.
2. Advocacy to mobilize domestic resources for the three priorities
The Partners will engage with governments and decision-makers to prioritize education financing and mobilize additional domestic resources.
Global level action
1. Leverage data to inform decision-making
The Partners will join forces to conduct surveys; collect data; and set-up a global, regional, and national real-time data-warehouse. The Partners will collect timely data and analytics that provide access to information on school re-openings, learning losses, drop-outs, and transition from school to work, and will make data available to support decision-making and peer-learning.
2. Promote knowledge sharing and peer-learning in strengthening education recovery
The Partners will join forces in sharing the breadth of international experience and scaling innovations through structured policy dialogue, knowledge sharing, and peer learning actions.
The time to act on these priorities is now. UNESCO, UNICEF, and the World Bank are partnering to help drive that action.
Last Updated: Mar 30, 2021
- (BROCHURE, in English) Mission: Recovering Education 2021
- (BROCHURE, in French) Mission: Recovering Education 2021
- (BROCHURE, in Spanish) Mission: Recovering Education 2021
- (BLOG) Mission: Recovering Education 2021
- (VIDEO, Arabic) Mission: Recovering Education 2021
- (VIDEO, French) Mission: Recovering Education 2021
- (VIDEO, Spanish) Mission: Recovering Education 2021
- World Bank Education and COVID-19
- World Bank Blogs on Education
This site uses cookies to optimize functionality and give you the best possible experience. If you continue to navigate this website beyond this page, cookies will be placed on your browser. To learn more about cookies, click here .
- Contributors
- Mission and Values
- Submissions
- The Regulatory Review In Depth

Lessons Learned From COVID-19
Lee a. fleisher and matthew a. fleisher.

The COVID-19 response illustrates steps officials should take to ensure the effectiveness of vaccine mandates.
The COVID-19 pandemic was the worst public health emergency of the last century. Despite aggressive attempts to contain the virus by social isolation, masking, and medical management, over 1.1 million Americans died between January 31, 2020, when the U.S. Department of Health and Human Services (HHS) declared COVID-19 a public health emergency, and March 11, 2023, when HHS declared the public health emergency over. Of those that perished, there was a particularly tremendous loss among the elderly, immunocompromised, and those in nursing homes.
In December 2020, the U.S. Food and Drug Administration issued emergency use authorizations for the Pfizer-BioNTech and Moderna COVID-19 vaccines . Despite the widespread availability of the vaccines at no cost, their adoption varied considerably. For this reason, physicians and public health officials soon called for a COVID-19 vaccine mandate.
In August 2021, President Joseph R. Biden directed the Centers for Medicare and Medicaid Services (CMS) to require nursing homes to ensure their workers were fully vaccinated against COVID-19 as a condition of participating in the Medicare and Medicaid programs. The Social Security Act provides that facilities participating in Medicare must meet certain requirements and that the HHS Secretary may impose additional requirements deemed necessary to protect the health and safety of patients in hospitals, nursing homes, and other CMS-certified facilities.
HHS’s emergency declarations authorized its component agencies, such as CMS, to issue new health and safety regulations. In addition, outside of public health emergencies, CMS has the authority to oversee healthcare delivery systems. CMS issued its vaccine mandate based on substantial evidence demonstrating that the prevalence of nursing home COVID-19 cases was related to low levels of vaccination among care staff. Furthermore, evidence that many nursing homes were not implementing standard infection control practices accelerated vaccine mandate drafting and execution.
The Administrative Procedure Act requires that agencies that wish to forgo notice-and-comment rulemaking during a public health emergency must demonstrate that undergoing notice-and-comment would be “impracticable, unnecessary, or contrary to the public interest.” The Biden Administration concluded on this basis that it could create an emergency regulation to require vaccines in nursing homes. Nevertheless, as CMS was developing its emergency regulation, nursing homes expressed concern that the mandate could trigger widespread staff shortages because workers would refuse to receive the vaccine. The industry feared that a staffing shortage could lead to worse health outcomes for residents.
While developing the vaccine mandate, the CMS Center for Clinical Standards and Quality convened several listening sessions from all corners of the healthcare industry. During this feedback period, several states issued their own vaccine mandates in both nursing homes and hospitals, and individual nursing home chains and hospital systems also proposed vaccine mandates. This patchwork approach further complicated efforts to limit the spread of COVID-19.
Hospitals and nursing homes were concerned that the variation between states’ rules could lead staff to move to different states to avoid a vaccine mandate. Several providers pushed for a national mandate. A marked increase in the proportion of nurses who sought employment through traveling services during the public health emergency validated this concern. Several national leaders suggested that a national mandate would be useful to manage interstate variability.
Because of these concerns, CMS and HHS began to explore the medical benefits of a national mandate for all healthcare facilities that receive Medicare funding. Data from the National Healthcare Safety Network demonstrated that COVID-19 rates among long-term care facilities were higher in facilities with lower vaccination coverage among staff. The agencies also explored the legal basis for a mandate. Critically, they determined that systems for documenting medical and religious exemptions to the vaccine mandate would be needed.
Ultimately, CMS issued its regulation in November 2021. Shortly thereafter, 14 states challenged the regulation and argued that CMS had exceeded its statutory authority under the Social Security Act. In January 2022, the U.S. Supreme Court, in a 5–4 decision, upheld the mandate, explaining that:
The Secretary of Health and Human Services determined that a COVID-19 vaccine mandate will substantially reduce the likelihood that healthcare workers will contract the virus and transmit it to their patients. He accordingly concluded that a vaccine mandate is “necessary to promote and protect patient health and safety” in the face of the ongoing pandemic. The rule thus fits neatly within the language of the statute.
Importantly, the Court found that the HHS Secretary had examined sufficient evidence justifying the decision to “(1) impose the vaccine mandate instead of a testing mandate; (2) require vaccination of employees with ‘natural immunity’ from prior COVID-19 illness; and (3) depart from the agency’s prior approach of merely encouraging vaccination.”
After the Biden Administration declared the public health emergency over in March 2023, CMS ended its vaccine mandate in August. In the end, the mandate did not substantially disrupt the healthcare ecosystem, and staff resignations due to the mandate did not produce national adverse health outcomes.
It is difficult to analyze the precise effects of the vaccine mandate because there were many states and local facilities that had already mandated the vaccine. Nonetheless, there are at least three important lessons public health officials can learn for the future from CMS’s experience in imposing a COVID-19 vaccine mandate.
First, it will be important to address the non-uniform manner in which states and local healthcare facilities adopt a mandatory vaccination policy during any future pandemic. There should be a national vaccine for healthcare facilities as soon as a safe and effective vaccine is approved. Early adoption can ensure national uniformity, which can in turn help prevent localized staffing shortages. The federal government should also monitor and evaluate the impact of any such mandate and adjust the manner of implementation as needed.
Second, public health officials should proactively collect evidence to demonstrate the health and safety implications of unvaccinated staff in Medicare-certified facilities to justify the need to forgo notice and comment rulemaking. This evidence can also help justify a national vaccine mandate if challenged in the courts.
Finally, public health officials should develop and implement rigorous standards for determining who is exempt from the vaccine mandate by balancing civil rights with healthcare concerns. Rigorous standards will help ensure vaccines succeed in cutting community transmission.
The political debate around vaccination continues to this day but these three lessons can help public health officials prepare for future public health emergencies.

Lee A. Fleisher is an emeritus professor of anesthesiology and critical care at the University of Pennsylvania Perelman School of Medicine .

Matthew A. Fleisher is the chief operating officer and managing director of Rubrum Advising .
Related Essays

Regulating the Great Indoors
Scholar argues that environmental law and policy should expand its scope to inside areas.

Cutting Corners on COVID-19 Treatments?
Scholars analyze FDA’s emergency use authorizations during the COVID-19 pandemic.

How Fixing the Past May Create Future Regulatory Problems
Scholar argues that generational amnesia may lead to ineffective regulatory solutions in the future.

- May 26, 2024 | This Week @NASA: Imaging Faraway Planets, X-59 Aircraft Milestone, Dream Chaser Launch Preparation
- May 26, 2024 | New Study Predicts Major Leap in Global Life Expectancy by 2050
- May 26, 2024 | From Black Gold to Green Energy: Mining Rare Earths Alongside Coal
- May 26, 2024 | Dartmouth Researchers Have Mapped How the Brain Regulates Emotions
- May 26, 2024 | Innovative NASA Solutions for Cleaning Up Space Debris Efficiently
Evolving With the Virus: Repeat COVID-19 Shots Neutralizing Beyond the Expected
By Washington University School of Medicine May 22, 2024

New research indicates that unlike flu vaccines, previous COVID-19 immunizations may enhance the efficacy of subsequent vaccines by fostering broad-spectrum neutralizing antibodies, suggesting annual updates could help combat emerging variants and related viruses.
The response to an updated vaccine is influenced by previous vaccinations but also produces broadly neutralizing antibodies.
The COVID-19 pandemic has ended, yet the virus responsible continues to circulate, hospitalizing thousands weekly and frequently producing new variants. Due to the virus’s remarkable capacity for mutation and immune evasion, the World Health Organization (WHO) advises yearly updates to COVID-19 vaccines.
However, some scientists worry that the remarkable success of the first COVID-19 vaccines may work against updated versions, undermining the utility of an annual vaccination program. A similar problem plagues the annual flu vaccine campaign; immunity elicited by one year’s flu shots can interfere with immune responses in subsequent years, reducing the vaccines’ effectiveness.
A new study by researchers at Washington University School of Medicine in St. Louis helps to address this question. Unlike immunity to influenza virus, prior immunity to SARS-CoV-2 , the virus that causes COVID-19, doesn’t inhibit later vaccine responses. Rather, it promotes the development of broadly inhibitory antibodies, the researchers report.
Benefits of Repeated Vaccination
The study, available online in Nature , shows that people who were repeatedly vaccinated for COVID-19 — initially receiving shots aimed at the original variant, followed by boosters and updated vaccines targeting variants — generated antibodies capable of neutralizing a wide range of SARS-CoV-2 variants and even some distantly related coronaviruses. The findings suggest that periodic re-vaccination for COVID-19, far from hindering the body’s ability to recognize and respond to new variants, may instead cause people to gradually build up a stock of broadly neutralizing antibodies that protect them from emerging SARS-CoV-2 variants and some other coronavirus species as well, even ones that have not yet emerged to infect humans.
“The first vaccine an individual receives induces a strong primary immune response that shapes responses to subsequent infection and vaccination, an effect known as imprinting,” said senior author Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine. “In principle, imprinting can be positive, negative, or neutral. In this case, we see strong imprinting that is positive, because it’s coupled to the development of cross-reactive neutralizing antibodies with remarkable breadth of activity.”

Healthcare workers received the first doses of the COVID-19 vaccine in December 2020. A study by researchers at Washington University School of Medicine in St. Louis has found that repeat vaccination with updated versions of the COVID-19 vaccine promotes the development of antibodies that neutralize a wide range of variants of the virus that causes COVID-19, as well as related coronaviruses. Credit: Matt Miller/Washington University
Imprinting is the natural result of how immunological memory works. A first vaccination triggers the development of memory immune cells. When people receive a second vaccination quite similar to the first, it reactivates memory cells elicited by the first vaccine. These memory cells dominate and shape the immune response to the subsequent vaccine.
In the case of the flu vaccine, imprinting has negative effects. Antibody-producing memory cells crowd out new antibody-producing cells, and people develop relatively few neutralizing antibodies against the strains in the newer vaccine. But in other cases, imprinting can be positive, by promoting the development of cross-reactive antibodies that neutralize strains in both the initial and subsequent vaccines.
Study on Imprinting and Its Effects
To understand how imprinting influences the immune response to repeat COVID-19 vaccination, Diamond and colleagues including first author Chieh-Yu Liang, a graduate student, studied the antibodies from mice or people who had received a sequence of COVID-19 vaccines and boosters targeting first the original and then omicron variants. Some of the human participants also had been naturally infected with the virus that causes COVID-19.
The first question was the strength of the imprinting effect. The researchers measured how many of the participants’ neutralizing antibodies were specific for the original variant, the omicron variant, or both. They found that very few people had developed any antibodies unique to omicron, a pattern indicative of strong imprinting by the initial vaccination. But they also found few antibodies unique to the original variant. The vast majority of neutralizing antibodies cross-reacted with both.
The next question was how far the cross-reactive effect extended. Cross-reactive antibodies, by definition, recognize a feature shared by two or more variants. Some features are shared only by similar variants, others by all SARS-CoV-2 variants or even all coronaviruses. To assess the breadth of the neutralizing antibodies, the researchers tested them against a panel of coronaviruses, including SARS-CoV-2 viruses from two omicron lineages; a coronavirus from pangolins; the SARS-1 virus that caused the 2002-03 SARS epidemic; and the Middle Eastern Respiratory Syndrome (MERS) virus. The antibodies neutralized all the viruses except MERS virus, which comes from a different branch of the coronavirus family tree than the others.
Further experiments revealed that this remarkable breadth was due to the combination of original and variant vaccines. People who received only the vaccines targeting the original SARS-CoV-2 variant developed some cross-reactive antibodies that neutralized the pangolin coronavirus and SARS-1 virus, but the levels were low. After boosting with an omicron vaccine, though, the cross-reactive neutralizing antibodies against the two coronavirus species increased.
Taken together, the findings suggest that regular re-vaccination with updated COVID-19 vaccines against variants might give people the tools to fight off not only the SARS-CoV-2 variants represented in the vaccines, but also other SARS-CoV-2 variants and related coronaviruses, possibly including ones that have not yet emerged.
“At the start of the COVID-19 pandemic, the world population was immunologically naïve, which is part of the reason the virus was able to spread so fast and do so much damage,” said Diamond, also a professor of molecular microbiology and of pathology & immunology. “We do not know for certain whether getting an updated COVID-19 vaccine every year would protect people against emerging coronaviruses, but it’s plausible. These data suggest that if these cross-reactive antibodies do not rapidly wane — we would need to follow their levels over time to know for certain — they may confer some or even substantial protection against a pandemic caused by a related coronavirus.”
Reference: “Imprinting of serum neutralizing antibodies by Wuhan-1 mRNA vaccines” by Chieh-Yu Liang, Saravanan Raju, Zhuoming Liu, Yuhao Li, Guha Asthagiri Arunkumar, James Brett Case, Suzanne M. Scheaffer, Seth J. Zost, Cory M. Acreman, Matthew Gagne, Shayne F. Andrew, Deborah Carolina Carvalho dos Anjos, Kathryn E. Foulds, Jason S. McLellan, James E. Crowe Jr., Daniel C. Douek, Sean P. J. Whelan, Sayda M. Elbashir, Darin K. Edwards and Michael S. Diamond, 15 May 2024, Nature . DOI: 10.1038/s41586-024-07539-1
The study was funded by the National Institutes of Health , the Vaccine Research Center, and Moderna.
More on SciTechDaily
NASA PREFIRE Postponed: Arctic Heat Mission Launch Delayed Due to Severe Storms

Angry Bees Produce Better Venom – Effective Treatment for Degenerative and Infectious Diseases
The ultimate fate of a star shredded by a black hole: spaghettified at 22 million miles per hour.

Ancient Underwater Landslide Discovery Could Help Middle Eastern Nations Realize Tsunami Hazards

Inflammation in the Elderly: Could Vitamin D Be the Answer?
Discovery Alert: Water Vapor Detected on “Super Neptune” Exoplanet

New Nasal Spray COVID Vaccine Uses Gene Transfer Technology

Rapidly Adjusting Moderna and Pfizer mRNA COVID Vaccines: How Scientists Can Update Coronavirus Vaccines for Omicron
Be the first to comment on "evolving with the virus: repeat covid-19 shots neutralizing beyond the expected", leave a comment cancel reply.
Email address is optional. If provided, your email will not be published or shared.
Save my name, email, and website in this browser for the next time I comment.
This paper is in the following e-collection/theme issue:
Published on 3.2.2021 in Vol 23 , No 2 (2021) : February
Using Twitter to Understand the COVID-19 Experiences of People With Dementia: Infodemiology Study
Authors of this article:

Original Paper
- Juanita-Dawne Bacsu 1 , PhD ;
- Megan E O'Connell 1 , PhD ;
- Allison Cammer 2 , PhD ;
- Mahsa Azizi 3 , MSc ;
- Karl Grewal 1 , BSc ;
- Lisa Poole 4 , BA ;
- Shoshana Green 1 , MEd ;
- Saskia Sivananthan 5 , PhD ;
- Raymond J Spiteri 3 , PhD
1 Department of Psychology, University of Saskatchewan, Saskatoon, SK, Canada
2 College of Pharmacy and Nutrition, University of Saskatchewan, Saskatoon, SK, Canada
3 Department of Computer Science, University of Saskatchewan, Saskatoon, SK, Canada
4 Dementia Advocacy Canada, Calgary, AB, Canada
5 Alzheimer Society of Canada, Toronto, ON, Canada
Corresponding Author:
Megan E O'Connell, PhD
Department of Psychology
University of Saskatchewan
9 Campus Drive
Saskatoon, SK, S7N 5A5
Phone: 1 306 966 2496
Email: [email protected]
Background: The COVID-19 pandemic is affecting people with dementia in numerous ways. Nevertheless, there is a paucity of research on the COVID-19 impact on people with dementia and their care partners.
Objective: Using Twitter, the purpose of this study is to understand the experiences of COVID-19 for people with dementia and their care partners.
Methods: We collected tweets on COVID-19 and dementia using the GetOldTweets application in Python from February 15 to September 7, 2020. Thematic analysis was used to analyze the tweets.
Results: From the 5063 tweets analyzed with line-by-line coding, we identified 4 main themes including (1) separation and loss; (2) COVID-19 confusion, despair, and abandonment; (3) stress and exhaustion exacerbation; and (4) unpaid sacrifices by formal care providers.
Conclusions: There is an imminent need for governments to rethink using a one-size-fits-all response to COVID-19 policy and use a collaborative approach to support people with dementia. Collaboration and more evidence-informed research are essential to reducing COVID-19 mortality and improving the quality of life for people with dementia and their care partners.
Introduction
The COVID-19 pandemic is having an impact on people with dementia. In Canada, almost two-thirds of all COVID-19–related deaths have been people with dementia [ 1 ]. In the United Kingdom, 50% of COVID-19–related deaths in care homes have been people with dementia [ 2 ].
In comparison to other groups, people with dementia are among the most vulnerable to the COVID-19 pandemic [ 3 ]. Although people with dementia are not necessarily more susceptible to COVID-19, advancing age, frailty, and coexisting health conditions often associated with dementia (eg, cardiovascular disease, hypertension, or diabetes) increase the risk of complications [ 4 , 5 ]. Moreover, social isolation measures (eg, stay-at-home orders, visitation bans, and lockdowns in care facilities) from COVID-19 may increase the risk of hospitalization and mortality for people with dementia [ 6 ].
People with dementia also face a heightened risk of COVID-19 exposure due to cognitive impairment and memory loss [ 3 ]. For example, people with dementia may have challenges remembering or understanding self-protection protocols such as wearing a mask, using proper hand hygiene, and maintaining physical distance from others [ 7 , 8 ]. Despite these challenges, there is a paucity of knowledge on the COVID-19 pandemic’s impact on people with dementia.
There is an urgent need to understand the experiences of people with dementia and their care partners in the COVID-19 pandemic [ 8 - 10 ]. Mitigation strategies that include physical distancing make it difficult to conduct timely and collaborative research, with many universities suspending recruitment and in-person studies during the pandemic [ 11 ]. Given these difficulties, examining the impact of COVID-19 requires ingenuity and innovation.
With over 330 million monthly users [ 12 ], the microblogging and social networking website Twitter [ 13 ] presents an innovative opportunity to examine the COVID-19 impact on people with dementia. For example, Twitter users are publicly sharing lived experiences of COVID-19 and dementia. The purpose of this study is to use Twitter to understand the COVID-19 experiences of people with dementia and their care partners.
Recruitment
We scraped tweets posted in the English language containing synonyms for dementia (eg, “Alzheimer’s disease” and “Lewy Body disease”) and synonyms for COVID-19 (including nontechnical phrases such as “Corona”) during the period from February 15 to September 7, 2020, from Twitter using the GetOldTweets application programming interface in Python [ 14 ]. The Tweets were not geo-tagged.
Twitter is a social media and microblogging website where users share their posts with the public. Following on existing studies, there is a general consensus that tweets posted publicly on Twitter can be used for research [ 15 , 16 ]. Tweets on the Twitter website are located within the public domain; informed consent was not obtained.
Data Exclusion
From the approximately 20,800 tweets that were gathered using these criteria, we applied filters referring to candidates for the US presidential election (eg, synonyms for “Donald Trump” and “Joe Biden”). In addition, the filter “Tom Seaver“ was used to delete tweets of public reactions to the major league baseball player who was reported to have died on August 31, 2020, of complications due to COVID-19 and dementia with Lewy bodies. Retweets and nonoriginal tweets were also excluded. Finally, to increase the likelihood of scraping tweets that described personal experiences with dementia during the era of COVID-19, we excluded tweets that did not include synonyms for familial relationships (eg, “father,” “mother,” and “grandparent”) or friends and acquaintances (eg, “buddy,” “pal,” and “neighbour”). This filtering procedure resulted in a total of 5063 tweets that were extracted into an Excel (Microsoft Corporation) spreadsheet for qualitative line-by-line coding as the basis for thematic analysis.
Data Analysis: Coding and Intercoder Consistency
To develop a robust codebook, authors JDB and MEO read and reread 300 tweets. The researchers independently assigned codes to each of the 300 tweets. After coding the tweets, the two researchers met to discuss their code lists and developed an initial codebook. The initial codebook consisted of 18 codes with code definitions, keywords, and specific examples (eg, tweets).
To test intercoder consistency, a team of six researchers pilot-tested 100 tweets by independently coding the tweets according to the codebook. Once the team finished their coding, the codes were compared with a coding example sheet that JDB and MEO developed. Following this pilot test, a group coding workshop was held to collectively pilot-code 50 tweets and discuss any inconsistencies in the interpretation of the codes. During this workshop, group discussion resolved coding uncertainties and disputes, leading to the refinement of the codebook (eg, overlapping codes or unused codes). The final version of the codebook consisted of 9 codes including (1) death, (2) fear for person with dementia’s health and well-being, (3) challenges and unmet needs, (4) separation or restricted visiting, (5) formal care provider challenges, (6) supports described, (7) informal caregiver’s health and well-being, (8) stories of survival, and (9) user identifies as a person with dementia (used as a second tag vs a primary code).
The tweets (n=5063) were then divided among the seven authors (approximately 723 tweets each) for descriptive analysis, with JDB managing intercoder consistency throughout the coding process. For 7 consecutive days, each coder completed approximately 100 codes per day and sent them to JDB. Coders flagged any tweets of which they were unsure or uncertain for JDB to review. In addition to reviewing the flagged tweets, the JDB randomly reviewed 10% of each coder’s work and provided feedback (eg, flagged tweets or any inconsistencies) for each day of coding. Throughout the coding process, JDB worked in direct collaboration with the MEO to discuss any discrepancies or uncertainties within the data. Once the coding was completed, two team meetings were held to identify and discuss the key themes arising from the data.
From the 5063 tweets analyzed, we identified 4 main themes including (1) separation and loss; (2) COVID-19 confusion, despair, and abandonment; (3) stress and exhaustion; and (4) risks of exposure and personal sacrifices faced by formal care providers. Illustrative tweets are provided and are unedited for grammar.
Separation and Loss
This theme captures the psychological sense of loss due to physical barriers that create separation. Many personal descriptions included discussion of the physical separation, which includes separation due to death, separation during the process of dying during the COVID-19 pandemic, and separation due to visitation bans because of COVID-19. Underlying these descriptors of physical separation is a clear psychological disconnection accompanied by feelings of loss. Separation creates a psychological sense of loss. A notable subtheme in separation and loss is the expression of the sense of loss expressed by care partners at the acceleration of decline perceived in persons with dementia during COVID-19, which was frequently blamed on the visitation bans and imposed lockdowns in care homes and health facilities. The intersection of the multiple dimensions of loss and separation are highlighted in the following illustrative quotes:
Yesterday I lost my mom. Due to covid [sic] I was unable to see her for the last few months. I did get to FaceTime twice and we did chat on the phone until her dementia made it difficult for her to do so. There will be no memorial until it is cleared to do so. My heart is broken.
...My husband passed away a few days ago, victim of Covid [sic] protocol! He had dementia, didn’t understand why I couldn’t visit him. He lost hope, 36 lbs in 23 days; could not be saved. This is so cruel to do to our seniors/he was a veteran!!! WRONG!!!
...Dad had dementia and was otherwise healthy. He had daily visitors even though he had little memory of who they were. Covid [sic] closed the nursing home to visitors and he stopped eating. He lost 40lbs and died in June. It’s another aspect of the Covid [sic]. Dying Alone.
Let me tell you what this covid [sic] lockdown did, it killed my daddy. He had dementia and he was still doing good, then the lockdown, we weren't there to hold him and to help feed him. When we went to see him, he was a shell, there was nothing left of him. I am so angry.
COVID-19 Confusion, Despair, and Abandonment
Another predominant theme was feelings of despair and abandonment among people with dementia from COVID-19 confinement and visitation bans. Many tweets described difficulties understanding COVID-19 displayed or experienced by persons with dementia and negative psychological consequences due to this confusion about COVID-19. Many reported that people with dementia could not understand the changes necessitated by the pandemic response; they required constant teaching, reminders, and reassurance. For some, this lack of understanding of COVID-19 led to challenges (described or implied) of living with the new policies for social distancing, mask wearing, and other sanitary precautions, which engendered feelings of hopelessness and despair. For many others, the lack of understanding the physical distancing restrictions due to COVID-19 led to feelings of abandonment and subsequent despair. For example, many described that their loved one could not understand why visits were no longer being made and why they could not have physical contact. The following tweets illustrate these issues:
Or live alone with dementia and all the trouble I have. I can't even drive myself to a doctor. I don't remember all the rules myself. I'm terrible at wearing a mask. Someone pointed out I had it inside out at the covid [sic] testing place. Im gonna [sic] die, I hope. Im [sic] tired of life.
You are told your Covid [sic] positive Mum is being discharged to you Covid [sic] negative dad. She has dementia. He is told to keep 2m away in their 3 bed bungalow. Is this NHS policy?
I’ve lost count of how many times I’ve been on the phone with my grandmother telling her that it’s not safe for her to leave the house because of COVID-19. Life with a loved one who has dementia right now is frustrating. Constantly re-teaching and remaining patient.
Hardest thing to hear is my mom trying to explain to my grandmother, who has Alzheimer and dementia, that we can’t see her because of the corona [sic]. My grandmother repeating that she is in jail. Asking where we are.
Stress and Exhaustion Exacerbation
Care partners described stress and exhaustion (eg, mental, emotional, and physical) related to providing care for people with dementia in the context of the COVID-19 pandemic. Increased workload, disruption to routine, financial strain, mental health issues, social isolation, and loneliness were common features described.
COVID-19 confinement and lockdown measures substantially increased the workload of informal care partners by limiting or terminating access to support services such as day care programs, home care, respite, meal programs, medical specialists, and adequate care home options. As such, many described the difficulty of dealing with household chores, social isolation, and the increasing workload, which often led to feelings of mental, emotional, and physical exhaustion. Moreover, care partners described difficulties managing behavioral changes and worsening neuropsychiatric symptoms (eg, anxiety, agitation, anger, and depression) of their loved ones with dementia.
Care partners also discussed stress related to the fear of COVID-19 exposure and concern for the person with dementia’s health and well-being. This fear was especially apparent among care partners with loved ones staying in care homes or hospitals. Others noted that COVID-19 precautions were confusing to people with dementia and made appointments and outings more difficult not only for the person with dementia but also for the care partner. Some reported balancing decisions on whether to pursue health services based on how distressing the experience would be for their loved one (eg, due to being alone without care partner support). Many reported strain due to financial pressures related to losing work coupled with unease for the future of their loved one. Difficulty obtaining care services or relocation to long-term care due to the pandemic were noted. Further, some care partners described feeling a need to bring people with dementia home from long-term care to ensure their well-being. The following tweets highlight the challenges faced by informal care partners:
I've lost some income but the hardest part is being stuck 24/7 in the house with my Mom who has severe dementia. It is hell! She had a daycare but it closed. I can't get respite bc [sic] I'm terrified of exposing her to covid [sic]. I fight loneliness, depression and boredom everyday [sic]!
The services for people with dementia have had to fall into line with COVID rules and there are of course personal restrictions. A devastating combination for people who need safety, routine and gentle stimulation.
Another horrifying day. We are in isolation with my beloved 93 yo [sic] Mom. She has descended into terrifying hallucinations and extreme anger because of dementia. We can't get her into nursing care because of a Covid [sic] outbreak. Just getting thru [sic] each hour.
Unpaid Sacrifices by Formal Care Providers
Formal care providers identified numerous sacrifices beyond their paid jobs. Formal care providers commonly expressed emotional connection to people with dementia and a sense of duty related to care, noting that this was more than simply a job. Formal care providers also described making personal sacrifices to work and provide care during the COVID-19 pandemic. For example, care providers discussed sacrificing their participation in family gatherings, parenting responsibilities, and social activities to help protect their patients and family members from potential exposure to the virus. Consequently, many expressed concern for the health of their families due to exposures at work and made trade-offs to help ensure the safety of their patients or residents, such as limiting their outside contacts. They also noted that caring for people with dementia involved a sacrifice of their own safety because of the lack of personal protective equipment (eg, gowns, gloves, masks, eye protection, and face shields), leading to stress of exposure. Finally, they reported their frustration with the reduced ability to support quality of life for people with dementia in the face of an increased workload due to COVID-19.
The workforce challenges experienced by formal care providers are captured in the following tweets:
People were discharged from hospital with covid [sic] and placed directly into my work. Trying to isolate a dementia patient with covid [sic] is impossible in a care home, they've already wandered down the corridor before we could even get our gloves on
I'm a mental health nurse working in a dementia specialist nursing home. My fight is to keep corona [sic] out of the building. There are many of us who will be in hiding to protect our residents…
I’m a nurse with COVID, probably from reusing dirty N95s and working with dementia patients who simply could not grasp the need to wear a mask and social distance. I worked so hard to try not to get COVID.
Principal Results
Using Twitter, the aim of this study is to understand the COVID-19 experiences of people with dementia and their care partners. People with dementia are among the most vulnerable to the pandemic in terms of exposure risk, social isolation, hospitalization, and mortality [ 4 ]. Understanding the impact of COVID-19 is urgently needed to reduce mortality and improve the quality of life for people with dementia and their care partners during the pandemic. Given the current COVID-19 context, Twitter provided a valuable means to support timely and innovative research during the pandemic.
In analyzing the 5063 tweets, this study found that people with dementia are experiencing substantial burden from the COVID-19 pandemic. For example, separation and institutional visiting bans were described as having a detrimental impact on people with dementia. Numerous tweets identified the effects of visitation bans on people with dementia, such as despair, loss, abandonment, social isolation, not eating, losing the will to live, and dying alone. Tweets also identified challenges faced by informal care partners, such as financial struggles, mental health issues, lack of formal supports, inadequate care home options, fear of COVID-19 exposure, and difficulties explaining COVID-19 (eg, quarantine, self-isolation, social distancing, and protective equipment) to people with dementia. In addition, tweets addressed workforce issues experienced by formal care providers, ranging from insufficient access to personal protective equipment to understaffing and having to sacrifice family responsibilities to provide formal care.
This study has significant implications for COVID-19 policy and practice. For example, findings from this study suggest that prohibitive visitation policies (eg, visitation bans and institutional lockdowns) in care homes and health facilities may not be advantageous or acceptable for people with dementia. Numerous tweets emphasized the issue of separation on mortality for people with dementia. Emerging data from the United Kingdom showed that, in care homes, more people have died from dementia than from COVID-19 [ 2 ]. Similarly, data from Canada [ 17 , 18 ] and the United States [ 1 ] mirror this trend, documenting thousands of excess dementia deaths in care homes throughout the pandemic. These findings suggest that secondary effects of the COVID-19 pandemic (eg, social isolation) may be causing rapid deterioration and mortality of people with dementia. Consequently, COVID-19 policies (eg, visitation bans and institutional lockdowns) that were initially intended to protect people from the virus may be causing significant harm to people with dementia. Accordingly, there is an imminent need for governments to rethink using a one-size-fits-all response to COVID-19 policy and use instead a collaborative approach to support people with dementia and their care partners. In moving forward, collaboration and partnerships with people with dementia are essential to developing targeted policies to protect people with dementia and their care partners.
Formal care providers desperately need additional resources (eg, allocated funding, personal protective equipment, adequate staffing, and mental health supports) to support people with dementia during the pandemic. Findings from this study identify a range of workforce challenges such as understaffing and lack of adequate personal protective equipment. Formal care providers in care homes and health facilities cannot provide optimal care and prevent COVID-19 exposure without having access to required resources and supports. Consequently, additional resources are needed to provide safeguards to protect both formal care providers and people with dementia during the pandemic.
Research is needed on the COVID-19 impact from the perspective of people with dementia and their care partners. Although several editorials, letters to the editor, and commentaries have discussed anticipated challenges of COVID-19 for people with dementia [ 8 - 10 , 19 - 21 ], few studies have involved people with dementia. Research is needed to examine the lived experiences of COVID-19 among people with dementia. Accordingly, more evidence-informed research is required to reduce mortality and understand the impact of COVID-19 on people with dementia and their care partners.
Limitations
Twitter has a 280-character limit for each tweet. Given this limit, the user’s story and experience is confined to these restrictions. For example, important information and relevant details (eg, context, background, and confounding factors) may not be captured in the tweet. Consequently, qualitative interviews may provide a more comprehensive and in-depth perspective of the COVID-19 impact on people with dementia. In addition, given that Twitter is in the public domain, people may not feel comfortable sharing their full perspectives and lived experiences. Future research requires collaboration and partnerships with people with dementia to develop more in-depth knowledge on the impact of COVID-19 on people with dementia and their care partners.
In addition, there are some limitations related to the generalizability of our findings from Twitter. For example, no demographic information was collected in this study, and findings from Twitter may not be fully generalizable or representative of the general public living with dementia and their care partners (eg, age, gender, ethnicity, education, income, or employment background). However, existing data show that Twitter users are 56% male and 44% female, with the largest age groups of users being in the categories of 18-29 years (38%), 30-49 years (27%), and 50-64 years (17%) [ 22 ]. Since no demographic information was collected, another study limitation relates to sex and gender. Without any demographic information, it is impossible to make any inferences or draw specific conclusions regarding the impact of COVID-19 in relation to sex or gender. As such, more research is needed to examine the impact of COVID-19 in relation to the sex and gender of people with dementia and their care partners.
A final limitation of these data is the cross-sectional nature of our analysis and geographically blind nature of the data. It is possible that experiences of people with dementia and their care partners will vary over time, particularly over waves of the pandemic. We believe these current data captured what might be described as wave one of the pandemic. It is likely, however, that any temporal variability in experiences with COVID-19 and dementia will be related to geography. It is clear that there are geographic differences in the experiences of the pandemic. Future research to compare temporal variability in experiences of COVID-19 and dementia with publicly available databases detailing country-level COVID-19 disease burden and mitigation strategies is needed.
Conclusions
The purpose of this study was to use Twitter to understand the COVID-19 experiences of people with dementia and their care partners. Through an analysis of 5063 tweets, this study found that people are experiencing substantial burden from the COVID-19 pandemic. Specifically, four main issues were identified, including separation and loss, despair and abandonment, informal care partner challenges, and workforce issues experienced by formal care providers.
There is an imminent need for governments to rethink using a one-size-fits-all response to COVID-19 policy and use a collaborative approach to support people with dementia. More specifically, collaboration and partnerships are essential to developing effective COVID-19 policies to support people with dementia and their care partners. Moreover, there is a critical need for additional resources (eg, personal protective equipment, adequate staffing, safeguards, and mental health supports) to address workforce challenges and support formal care providers of people with dementia during the pandemic. Research is needed on the impact of COVID-19 from the perspective of people with dementia. Collaboration and more evidence-informed research are essential to reducing COVID-19–related mortality and improving the quality of lives for people with dementia and their care partners.
Acknowledgments
JDB is a postdoctoral fellow, KG is a doctoral student, and MA and SG were research assistants whose salaries were partially funded by Team 15 in the Canadian Consortium on Neurodegeneration in Aging (CCNA). CCNA is supported by a grant from the Canadian Institutes of Health Research with funding from several partners including the Saskatchewan Health Research Foundation, the Centre for Aging and Brain Health, and the Alzheimer Society of Canada (ASC). The ASC COVID Task Force (of which MEO, LP, and SS are members) was a particular catalyst for this study.
Authors' Contributions
MEO conceived the idea with LP. MEO, MA, and RJS devised the Twitter scraping approach, and MA scraped Twitter. MEO and JDB devised the codebook. MEO, AC, MA, KG, LP, SG, and RJS coded tweets, JDB double-coded a random sample of these for quality control, and MEO was the final arbiter. All authors contributed example tweets. MEO and AC performed the thematic analysis. JDB wrote the first draft of the manuscript, and all authors revised the manuscript.
Conflicts of Interest
None declared.
- Suárez-González A, Livingston G, Low LF, Cahill S, Hennelly N, Dawson WD, et al. Impact and mortality of COVID-19 on people living with dementia: cross-country report. International Long-Term Care Policy Network. 2020. URL: https://ltccovid.org/wp-content/uploads/2020/08/International-report-on-the-impact-of-COVID-19-on-people-living-with-dementia-19-August-2020.pdf [accessed 2020-10-19]
- ONS report shows 52% increase in excess deaths of people dying of dementia – Alzheimer’s Society comments. Alzheimer's Society. 2020. URL: https://www.alzheimers.org.uk/news/2020-06-05/ons-report-shows-52-increase-excess-deaths-people-dying-dementia-alzheimers-society [accessed 2020-10-23]
- COVID-19 deaths disproportionately affecting people with dementia. Alzheimer's Disease International. 2020. URL: https://www.alzint.org/news/covid-19-deaths-disproportionately-affecting-people-with-dementia/ [accessed 2020-10-23]
- Azarpazhooh MR, Amiri A, Morovatdar N, Steinwender S, Rezaei Ardani A, Yassi N, et al. Correlations between COVID-19 and burden of dementia: an ecological study and review of literature. J Neurol Sci 2020 Sep 15;416:117013 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Older adults. Centers for Disease Control and Prevention. 2020. URL: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html [accessed 2020-10-21]
- National Academies of Sciences, Engineering, and Medicine, Division of Behavioral and Social Sciences and Education, Health and Medicine Division, Board on Behavioral, Cognitive, and Sensory Sciences, Board on Health Sciences Policy, Committee on the Health and Medical Dimensions of Social Isolation and Loneliness in Older Adults. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Washington, DC: National Academies Press; 2020.
- Vaitheswaran S, Lakshminarayanan M, Ramanujam V, Sargunan S, Venkatesan S. Experiences and needs of caregivers of persons with dementia in India during the COVID-19 pandemic-a qualitative study. Am J Geriatr Psychiatry 2020 Nov;28(11):1185-1194 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wang H, Li T, Barbarino P, Gauthier S, Brodaty H, Molinuevo JL, et al. Dementia care during COVID-19. Lancet 2020 Apr 11;395(10231):1190-1191 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Canevelli M, Bruno G, Cesari M. Providing simultaneous COVID-19-sensitive and dementia-sensitive care as we transition from crisis care to ongoing care. J Am Med Dir Assoc 2020 Jul;21(7):968-969 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Migliaccio R, Bouzigues A. Dementia and COVID-19 lockdown: more than a double blow for patients and caregivers. J Alzheimers Dis Rep 2020 Jul 06;4(1):231-235 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Clay RA. Conducting research during the COVID-19 pandemic. American Psychological Association. 2020. URL: https://www.apa.org/news/apa/2020/03/conducting-research-covid-19 [accessed 2020-10-23]
- Clement J. Number of monthly active Twitter users worldwide from 1st quarter 2010 to 1st quarter 2019. Statista. 2019. URL: https://www.statista.com/statistics/282087/number-of-monthly-active-twitter-users/ [accessed 2020-10-19]
- Twitter. URL: https://twitter.com/ [accessed 2020-10-19]
- Henrique J. A project written in Python to get old tweets which could bypass some limitations of Twitter official API. GitHub. URL: https://github.com/Jefferson [accessed 2020-10-21]
- Moreno MA, Goniu N, Moreno PS, Diekema D. Ethics of social media research: common concerns and practical considerations. Cyberpsychol Behav Soc Netw 2013 Sep;16(9):708-713 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Talbot CV, O'Dwyer ST, Clare L, Heaton J, Anderson J. How people with dementia use twitter: a qualitative analysis. Comput Hum Behav 2020 Jan;102:112-119. [ CrossRef ]
- Hsu AT, Lane N, Sinha SK, Dunning J, Dhuper M, Kahiel Z, et al. Impact of COVID-19 on residents of Canada’s long-term care homes – ongoing challenges and policy responses. International Long-Term Care Policy Network. 2020. URL: https://ltccovid.org/wp-content/uploads/2020/05/LTCcovid-country-reports_Canada_Hsu-et-al_May-10-2020-2.pdf [accessed 2020-10-23]
- McMichael TM, Currie DW, Clark S, Pogosjans S, Kay M, Schwartz NG, Public Health–Seattle and King County, EvergreenHealth, and CDC COVID-19 Investigation Team. Epidemiology of Covid-19 in a long-term care facility in King County, Washington. N Engl J Med 2020 May 21;382(21):2005-2011 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Brown EE, Kumar S, Rajji TK, Pollock BG, Mulsant BH. Anticipating and mitigating the impact of the COVID-19 pandemic on Alzheimer's disease and related dementias. Am J Geriatr Psychiatry 2020 Jul;28(7):712-721 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Korczyn AD. Dementia in the COVID-19 period. J Alzheimers Dis 2020;75(4):1071-1072 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Velayudhan L, Aarsland D, Ballard C. Mental health of people living with dementia in care homes during COVID-19 pandemic. Int Psychogeriatr 2020 Oct;32(10):1253-1254 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Clement J. Percentage of U.S. adults who use Twitter as of February 2019, by age group. Statista. URL: https://www.statista.com/statistics/265647/share-of-us-internet-users-who-use-twitter-by-age-group/ [accessed 2020-10-19]
Abbreviations
Edited by G Eysenbach; submitted 03.12.20; peer-reviewed by B Chakalov, C Basch; comments to author 24.12.20; accepted 19.01.21; published 03.02.21
©Juanita-Dawne Bacsu, Megan E O'Connell, Allison Cammer, Mahsa Azizi, Karl Grewal, Lisa Poole, Shoshana Green, Saskia Sivananthan, Raymond J Spiteri. Originally published in the Journal of Medical Internet Research (http://www.jmir.org), 03.02.2021.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on http://www.jmir.org/, as well as this copyright and license information must be included.
Advertisement
Supported by
Countries Fail to Agree on Treaty to Prepare the World for the Next Pandemic
Negotiators plan to ask for more time. Among the sticking points are equitable access to vaccines and financing to set up surveillance systems.
- Share full article

By Apoorva Mandavilli
Countries around the globe have failed to reach consensus on the terms of a treaty that would unify the world in a strategy against the inevitable next pandemic, trumping the nationalist ethos that emerged during Covid-19.
The deliberations, which were scheduled to be a central item at the weeklong meeting of the World Health Assembly beginning Monday in Geneva, aimed to correct the inequities in access to vaccines and treatments between wealthier nations and poorer ones that became glaringly apparent during the Covid pandemic.
Although much of the urgency around Covid has faded since the treaty negotiations began two years ago, public health experts are still acutely aware of the pandemic potential of emerging pathogens, familiar threats like bird flu and mpox, and once-vanquished diseases like smallpox.
“Those of us in public health recognize that another pandemic really could be around the corner,” said Loyce Pace, an assistant secretary at the Department of Health and Human Services, who oversees the negotiations in her role as the United States liaison to the World Health Organization.
Negotiators had hoped to adopt the treaty next week. But canceled meetings and fractious debates — sometimes over a single word — stalled agreement on key sections, including equitable access to vaccines.
The negotiating body plans to ask for more time to continue the discussions.
“I’m still optimistic,” said Dr. Jean Kaseya, director general of Africa Centers for Disease Control and Prevention. “I think the continent wants this agreement. I think the world wants this agreement.”
Once adopted, the treaty would set legally binding policies for member countries of the W.H.O., including the United States, on surveillance of pathogens, rapid sharing of outbreak data, and local manufacturing and supply chains for vaccines and treatments, among others.
Contrary to rhetoric from some politicians in the United States and Britain , it would not enable the W.H.O. to dictate national policies on masking, or use armed troops to enforce lockdowns and vaccine mandates.
Next week’s deadline was self-imposed, and some public health experts have said it was far too ambitious — most treaties take many years — for such a complex endeavor. But negotiators were scrambling to ratify the treaty before elections in the United States and multiple European countries.
“Donald Trump is in the room,” said Lawrence Gostin, director of the W.H.O. Center on Global Health Law, who has helped to draft and negotiate the treaty.
“If Trump is elected, he will likely torpedo the negotiations and even withdraw from W.H.O.,” Mr. Gostin said.
During his tenure as president, Mr. Trump severed ties with the W.H.O. , and he has recently signaled that, if re-elected, he might shutter the White House pandemic preparedness office.
Among the biggest bones of contention in the draft treaty is a section called Pathogen Access and Benefits Sharing, under which countries would be required to swiftly share genetic sequences and samples of emerging pathogens. This information is crucial for rapid development of diagnostic tests, vaccines and treatments.
Low-income nations, including those in Africa, want to be compensated for the information with quick and equitable access to the developed tests, vaccines and treatments. They have also asked that pharmaceutical manufacturers share information that would allow local companies to manufacture the products at low cost.
“We don’t want to see Western countries coming to collect pathogens, going with pathogens, making medicines, making vaccines, without sending back to us these benefits,” Dr. Kaseya said.
Member countries have only ever agreed to one other health treaty, the 2003 Framework Convention on Tobacco Control , which strengthened control of the tobacco industry and decreased smoking rates in participating countries. But they were jolted by the devastation of the Covid pandemic and the inequities it reinforced to embark on a second.
The countries are also working on bolstering the W.H.O.’s International Health Regulations, which were last revised in 2005 and set detailed rules for countries to follow in the event of an outbreak that may breach borders.
In May 2021, an independent review of the global reaction to Covid-19 “found weak links at every point in the chain of preparedness and response.”
The pandemic also deepened mistrust between wealthier nations and poorer ones. By the end of 2021, more than 90 percent of people in some high-income countries had received two doses of Covid vaccines, compared with less than 2 percent in low-income nations. The lack of access to vaccines is thought to have caused more than a million deaths in low-income nations.
The treaty would be an acknowledgment of sorts that an outbreak anywhere threatens the entire globe, and that providing vaccines and other resources is beneficial to everyone. Variants of the coronavirus that emerged in countries with large unvaccinated populations swiftly swept across the world.
“Nearly half of U.S. deaths came from variants, so it’s in everybody’s interest to have a strong accord,” said Peter Maybarduk, who directs Public Citizen’s Access to Medicines program.
In December 2021, the W.H.O. established a group of negotiators to develop a legally binding treaty that would enable every country to prevent, detect and control epidemics, and allow for equitable allocation of vaccines and drugs.
More than two years into the negotiations, negotiators have agreed, at least in principle, on some sections of the draft.
But much of the good will generated during Covid has evaporated, and national interests have returned to the fore. Countries like Switzerland and the United States have been reluctant to accept terms that may affect the pharmaceutical industry; others like Argentina have fought against strict regulations on meat exports.
“It’s evident that people have very short memories,” said Dr. Sharon Lewin, director of the Cumming Global Center for Pandemic Therapeutics in Melbourne.
“But it can happen again, and it can happen with a pathogen that is far trickier to deal with than Covid was,” she warned.
One proposal for the Pathogen Access and Benefits Sharing section would require manufacturers to set aside 10 percent of vaccines to be donated, and another 10 percent to be provided at cost to the W.H.O. for distribution to low-income nations.
But that idea proved to be too complicated, said Roland Driece, who is one of the leaders of the negotiations. “We found along the way that that was too ambitious in the time frame.”
Instead, a working group established by the World Health Assembly will be tasked with hammering out the details of that section by May 2026, Mr. Driece said.
The terms of the proposed agreement have generated some confusion. In Britain, Nigel Farage, the conservative broadcaster and populist politician, and some other conservative politicians have claimed that the W.H.O. would force richer countries to give away 20 percent of their vaccines.
But that is an incorrect reading of the proposed agreement, Mr. Driece said. “It’s not the countries that have to come up with those vaccines, it’s the companies,” he said. Pharmaceutical companies would commit to the system in exchange for guaranteed access to data and samples needed to make their products.
Britain will not sign the treaty unless “it is firmly in the U.K. national interest and respects national sovereignty,” a spokesperson for the country’s health department told Reuters earlier this month.
In the United States, Republican senators have demanded that the Biden administration reject the treaty because it would “potentially weaken U.S. sovereignty.”
Dr. Tedros Adhanom Ghebreyesus, W.H.O.’s director general, has roundly criticized what he called the “the litany of lies and conspiracy theories,” noting that the organization does not have the authority to dictate national public health policies, nor does it seek such power.
The secrecy surrounding the negotiations has made it difficult to counter misinformation, said James Love, director of Knowledge Ecology International, one of the few nonprofits with a window into the negotiations.
Having more people allowed into the discussion rooms or to see the drafts as they evolve would help clarify complicated aspects of the treaty, Mr. Love said.
“Also, the public could relax a bit if they’re actually reading the actual agreement on a regular basis,” he said.
Some proposals in the draft treaty would require massive investments, another sticking point in the negotiations.
To monitor emerging pathogens, wealthier nations endorse a so-called One Health strategy, which recognizes the interconnections between people, animals, plants and their shared environment. They want low-income countries to regulate live animal markets and limit trade in animal products — a big economic blow for some nations.
Last month, the Biden administration released its own strategy for global health security , with a focus on bilateral partnerships aimed at helping 50 countries bolster their pandemic response systems. The administration hopes to expand the list to 100 countries by the end of the year.
American support would help the countries, most of which are in Asia and Africa, strengthen their One Health systems and better manage outbreaks.
The U.S. strategy is meant to be complementary to the global treaty, and cannot serve as an alternative, public health experts said.
“In my view, this is the most important moment in global health since W.H.O. was founded in 1948,” Mr. Gostin said. “It would just be an unforgivable tragedy if we let this slip away after all the suffering of Covid.”
Apoorva Mandavilli is a reporter focused on science and global health. She was a part of the team that won the 2021 Pulitzer Prize for Public Service for coverage of the pandemic. More about Apoorva Mandavilli
- MyServiceNSW
- Manage account
- Logout of MyServiceNSW
Protecting yourself from COVID-19
How to help protect yourself and your community from COVID-19 infection.

COVID-19 update – 23 May 2024
COVID-19 remains at moderate levels.
Read the latest data from NSW Health .
Continue to protect other people. Please stay home if you have any cold or flu symptoms. Wear a mask if you need to leave home.
Steps to keep yourself safe
Stay home if you have cold or flu symptoms. Wear a mask if you need to leave home.
You may be required to wear a mask in high risk settings.
Stay up to date with your recommended COVID-19 vaccinations .
Don't visit people who are at higher risk if you have COVID-19 or symptoms.
Talk with your doctor now if you're at higher risk . You may need a PCR test and be eligible for antivirals.
Gather outdoors or in well-ventilated indoor spaces.
Guidance on protecting other people
Advice for parents of children in childcare and schools.
Find out what COVID-safe measures are in place at NSW early childhood education centres and schools.
Visiting people in high-risk settings
If you're visiting someone in aged care or disability care, find out what you can do to keep them safe.
Advice for workers
Guidance for workers affected by COVID-19.
Advice for people at higher risk of severe illness
Find the full list of people who are considered at higher risk .
People over 70
People with disability, pregnant women and new parents, aboriginal communities, easy read and translated resources, easy read information on covid-19, in-language and translated covid-19 support, contact us and find translation help.
- Service NSW – information and advice for NSW residents and businesses. Phone 13 77 88
- Healthdirect – government-funded 24-hour health advice. Phone 1800 022 222
- Disability Gateway – information for people with disability. Phone 1800 643 787
- Mental health support, services and programs
- Service NSW Savings Finder – find rebates and vouchers relevant to you
- Business Concierge – tailored advice from Business Connect advisors. Phone 13 77 88
- Translating and Interpreting Service (TIS National) – free service provided by the Australian Government. Phone 13 14 50

IMAGES
VIDEO
COMMENTS
This essay is an opportunity to share your pandemic experience and the lessons learned. The college admissions process has experienced significant changes as a result of COVID-19, creating new challenges for high school students. Since the onset of the pandemic, admissions officers have strongly emphasized a more holistic review process.
Students can choose to write a full-length college essay on the coronavirus or summarize their experience in a shorter form. To help students explain how the pandemic affected them, The Common App ...
The Covid-19 pandemic is a case in point. We need to save lives now while also improving the way we respond to outbreaks in general. The first point is more pressing, but the second has crucial ...
Here are some essay topic ideas related to Covid-19: 1. The impact of Covid-19 on mental health: Discuss how the pandemic has affected individuals' mental well-being and explore potential solutions for addressing mental health challenges during this time. 2.
This essay examines key aspects of social relationships that were disrupted by the COVID-19 pandemic. It focuses explicitly on relational mechanisms of health and brings together theory and emerging evidence on the effects of the COVID-19 pandemic to make recommendations for future public health policy and recovery. We first provide an overview of the pandemic in the UK context, outlining the ...
Even in the lead up to the COVID-19 pandemic, U.S. resource allocation for combating infectious diseases and developing biodefense was woefully inadequate. In 2014, the U.S. allocated $6 billion ...
In both its war on drugs and its COVID-19 response, the government has relied on brute force to eliminate its perceived enemy, and it has peddled a narrative of a bifurcated nation. ... securitization of illegal drugs and the return of national boss rule. In: Curato N. (ed.), A Duterte Reader: Critical Essays on Rodrigo Duterte's Early ...
This essay is part of "Reimagining the global economy: Building back better in a post-COVID-19 world," a collection of 12 essays presenting new ideas to guide policies and shape debates in a ...
The social cost of COVID-19 was only just beginning to emerge, but the mental health impact was already considerable,2 3 and the inequality of the health burden stark.4 Knowledge of the epidemiology of COVID-19 accrued rapidly, but evidence of the most effective policy responses remained uncertain. The initial response to COVID-19 in the UK was
vCal. iCal. AACOMAS, AADSAS, and OPTCOMCAS have all added a new prompt that asks you how your path to medical, dental, or optometry school has been impacted by COVID-19. This seminar is specifically designed to assist applicants in writing a strong response to this essay that is authentic, compelling, and reflective.
In response to a request from The New York Times, more than 900 seniors submitted the personal essays they wrote for their college applications. Reading them is like a trip through two of the ...
1. Introduction. The coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented changes in people's daily lives, with implications for mental health and well-being [1-4], both at the level of a given country's population, and when considering specific vulnerable groups [5-7].In order to mitigate the untoward impact of the pandemic (including lockdown) and support mental health ...
Abstract. Low- and middle-income countries (LMICs) with weak health systems are especially vulnerable during the COVID-19 pandemic. In this paper, we describe the challenges and early response of the Philippine Government, focusing on travel restrictions, community interventions, risk communication and testing, from 30 January 2020 when the ...
The pandemic of Coronavirus Disease 2019 (COVID-19) is a timely reminder of the nature and impact of Public Health Emergencies of International Concern. As of 12 January 2022, there were over 314 million cases and over 5.5 million deaths notified since the start of the pandemic. The COVID-19 pandemic takes variable shapes and forms, in terms of cases and deaths, in different regions and ...
Reading time: 3 min (864 words) The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work. The economic and social disruption caused by the pandemic is devastating: tens of millions of people are at risk of falling into extreme poverty ...
In the 20 months since the World Health Organization declared covid-19 to be a pandemic, more than 250 million cases have been confirmed. More than 5 million deathshave occurred disproportionately by country, with 10% of countries reporting 80% of cases. 1 In a new pandemic, with no vaccines prepared, non-pharmaceutical interventions are the only response.
A Pew Research Center survey of 10,282 U.S. adults conducted from May 2 to 8, 2022, finds 62% of Americans say the country has given too little priority to meeting the educational needs of K-12 students during its response to the coronavirus outbreak; far fewer (31%) say this has received about the right amount of priority since the outbreak ...
To live in the world is to adapt constantly. A year after COVID-19 pandemic has emerged, we have suddenly been forced to adapt to the 'new normal': work-from-home setting, parents home-schooling their children in a new blended learning setting, lockdown and quarantine, and the mandatory wearing of face mask and face shields in public.
The world has been staggered by the US's disjointed response to covid-19, resulting in by far the highest case and death count globally. The die was cast by two fundamental policy decisions taken by the Trump administration, writes Drew Altman On 9 August, the US passed the five million mark in cases of covid-19, representing slightly more than a quarter of all global cases. That day, more ...
This essay is a commentary on the U.S. Federal government response to the 2020 COVID-19 outbreak. The focus is on the response of the Trump Administration during the first 3 months of the outbreak, specifically the period between January 20, 2020, and May 15, 2020.
COVID-19 is a major crisis needing an international response. Governments will ensure reliable information is provided to assist the public in combating this pandemic. Community health and infection control measures are urgently needed to reduce the damage done by COVID-19 and minimise the overall spread of the virus.
When the World Health Organization first called COVID-19 a pandemic on March 11, 2020, few people had any idea what the world was in for. The progression was swift: borders clamped shut ...
The COVID-19 pandemic has caused abrupt and profound changes around the world. This is the worst shock to education systems in decades, with the longest school closures combined with looming recession. It will set back progress made on global development goals, particularly those focused on education. The economic crises within countries and ...
This essay explores the origins, impact, and response to the COVID-19 pandemic, highlighting the lessons learned and the path forward towards recovery and resilience. COVID-19 is believed to have originated in Wuhan, China, where the first cases were reported in December 2019.
Then, determine which essay circumstances group you fall into. 1. None of your target programs include a supplemental essay question equivalent to the Life Experiences essay. If none of the PA programs you'll be applying to include secondary essays similar to the life experience topic, then you definitely don't want to skip the optional CASPA ...
The COVID-19 pandemic was the worst public health emergency of the last century. Despite aggressive attempts to contain the virus by social isolation, masking, and medical management, over 1.1 million Americans died between January 31, 2020, when the U.S. Department of Health and Human Services (HHS) declared COVID-19 a public health emergency, and March 11, 2023, when HHS declared the public ...
The response to an updated vaccine is influenced by previous vaccinations but also produces broadly neutralizing antibodies. The COVID-19 pandemic has ended, yet the virus responsible continues to circulate, hospitalizing thousands weekly and frequently producing new variants. Due to the virus's remarkable capacity for mutation and immune evasion, the World Health Organization (WHO) advises ...
Conclusions: There is an imminent need for governments to rethink using a one-size-fits-all response to COVID-19 policy and use a collaborative approach to support people with dementia. Collaboration and more evidence-informed research are essential to reducing COVID-19 mortality and improving the quality of life for people with dementia and ...
In May 2021, an independent review of the global reaction to Covid-19 "found weak links at every point in the chain of preparedness and response." The pandemic also deepened mistrust between ...
Wear a mask if you need to leave home. You may be required to wear a mask in high risk settings. Stay up to date with your recommended COVID-19 vaccinations. Don't visit people who are at higher risk if you have COVID-19 or symptoms. Talk with your doctor now if you're at higher risk. You may need a PCR test and be eligible for antivirals.