- PRO Courses Guides New Tech Help Pro Expert Videos About wikiHow Pro Upgrade Sign In
- EDIT Edit this Article
- EXPLORE Tech Help Pro About Us Random Article Quizzes Request a New Article Community Dashboard This Or That Game Popular Categories Arts and Entertainment Artwork Books Movies Computers and Electronics Computers Phone Skills Technology Hacks Health Men's Health Mental Health Women's Health Relationships Dating Love Relationship Issues Hobbies and Crafts Crafts Drawing Games Education & Communication Communication Skills Personal Development Studying Personal Care and Style Fashion Hair Care Personal Hygiene Youth Personal Care School Stuff Dating All Categories Arts and Entertainment Finance and Business Home and Garden Relationship Quizzes Cars & Other Vehicles Food and Entertaining Personal Care and Style Sports and Fitness Computers and Electronics Health Pets and Animals Travel Education & Communication Hobbies and Crafts Philosophy and Religion Work World Family Life Holidays and Traditions Relationships Youth
- Browse Articles
- Learn Something New
- Quizzes Hot
- This Or That Game
- Train Your Brain
- Explore More
- Support wikiHow
- About wikiHow
- Log in / Sign up
- Education and Communications
- College University and Postgraduate
- Academic Writing
- Research Papers

How to Write a Medical Research Paper
Last Updated: February 5, 2024 Approved
This article was co-authored by Chris M. Matsko, MD . Dr. Chris M. Matsko is a retired physician based in Pittsburgh, Pennsylvania. With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award for Excellence. He holds a BS in Nutritional Science from Cornell University and an MD from the Temple University School of Medicine in 2007. Dr. Matsko earned a Research Writing Certification from the American Medical Writers Association (AMWA) in 2016 and a Medical Writing & Editing Certification from the University of Chicago in 2017. wikiHow marks an article as reader-approved once it receives enough positive feedback. In this case, 89% of readers who voted found the article helpful, earning it our reader-approved status. This article has been viewed 202,819 times.
Writing a medical research paper is similar to writing other research papers in that you want to use reliable sources, write in a clear and organized style, and offer a strong argument for all conclusions you present. In some cases the research you discuss will be data you have actually collected to answer your research questions. Understanding proper formatting, citations, and style will help you write and informative and respected paper.
Researching Your Paper

- Pick something that really interests you to make the research more fun.
- Choose a topic that has unanswered questions and propose solutions.

- Quantitative studies consist of original research performed by the writer. These research papers will need to include sections like Hypothesis (or Research Question), Previous Findings, Method, Limitations, Results, Discussion, and Application.
- Synthesis papers review the research already published and analyze it. They find weaknesses and strengths in the research, apply it to a specific situation, and then indicate a direction for future research.

- Keep track of your sources. Write down all publication information necessary for citation: author, title of article, title of book or journal, publisher, edition, date published, volume number, issue number, page number, and anything else pertaining to your source. A program like Endnote can help you keep track of your sources.
- Take detailed notes as you read. Paraphrase information in your own words or if you copy directly from the article or book, indicate that these are direct quotes by using quotation marks to prevent plagiarism.
- Be sure to keep all of your notes with the correct source.
- Your professor and librarians can also help you find good resources.

- Keep all of your notes in a physical folder or in a digitized form on the computer.
- Start to form the basic outline of your paper using the notes you have collected.
Writing Your Paper

- Start with bullet points and then add in notes you've taken from references that support your ideas. [1] X Trustworthy Source PubMed Central Journal archive from the U.S. National Institutes of Health Go to source
- A common way to format research papers is to follow the IMRAD format. This dictates the structure of your paper in the following order: I ntroduction, M ethods, R esults, a nd D iscussion. [2] X Research source
- The outline is just the basic structure of your paper. Don't worry if you have to rearrange a few times to get it right.
- Ask others to look over your outline and get feedback on the organization.
- Know the audience you are writing for and adjust your style accordingly. [3] X Research source

- Use a standard font type and size, such as Times New Roman 12 point font.
- Double-space your paper.
- If necessary, create a cover page. Most schools require a cover page of some sort. Include your main title, running title (often a shortened version of your main title), author's name, course name, and semester.

- Break up information into sections and subsections and address one main point per section.
- Include any figures or data tables that support your main ideas.
- For a quantitative study, state the methods used to obtain results.

- Clearly state and summarize the main points of your research paper.
- Discuss how this research contributes to the field and why it is important. [4] X Research source
- Highlight potential applications of the theory if appropriate.
- Propose future directions that build upon the research you have presented. [5] X Research source
- Keep the introduction and discussion short, and spend more time explaining the methods and results.

- State why the problem is important to address.
- Discuss what is currently known and what is lacking in the field.
- State the objective of your paper.
- Keep the introduction short.

- Highlight the purpose of the paper and the main conclusions.
- State why your conclusions are important.
- Be concise in your summary of the paper.
- Show that you have a solid study design and a high-quality data set.
- Abstracts are usually one paragraph and between 250 – 500 words.

- Unless otherwise directed, use the American Medical Association (AMA) style guide to properly format citations.
- Add citations at end of a sentence to indicate that you are using someone else's idea. Use these throughout your research paper as needed. They include the author's last name, year of publication, and page number.
- Compile your reference list and add it to the end of your paper.
- Use a citation program if you have access to one to simplify the process.

- Continually revise your paper to make sure it is structured in a logical way.
- Proofread your paper for spelling and grammatical errors.
- Make sure you are following the proper formatting guidelines provided for the paper.
- Have others read your paper to proofread and check for clarity. Revise as needed.
Expert Q&A

- Ask your professor for help if you are stuck or confused about any part of your research paper. They are familiar with the style and structure of papers and can provide you with more resources. Thanks Helpful 0 Not Helpful 0
- Refer to your professor's specific guidelines. Some instructors modify parts of a research paper to better fit their assignment. Others may request supplementary details, such as a synopsis for your research project . Thanks Helpful 0 Not Helpful 0
- Set aside blocks of time specifically for writing each day. Thanks Helpful 0 Not Helpful 0

- Do not plagiarize. Plagiarism is using someone else's work, words, or ideas and presenting them as your own. It is important to cite all sources in your research paper, both through internal citations and on your reference page. Thanks Helpful 4 Not Helpful 2
You Might Also Like

- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3178846/
- ↑ http://owl.excelsior.edu/research-and-citations/outlining/outlining-imrad/
- ↑ http://china.elsevier.com/ElsevierDNN/Portals/7/How%20to%20write%20a%20world-class%20paper.pdf
- ↑ http://intqhc.oxfordjournals.org/content/16/3/191
- ↑ http://www.ruf.rice.edu/~bioslabs/tools/report/reportform.html#form
About This Article

To write a medical research paper, research your topic thoroughly and compile your data. Next, organize your notes and create a strong outline that breaks up the information into sections and subsections, addressing one main point per section. Write the results and discussion sections first to go over your findings, then write the introduction to state your objective and provide background information. Finally, write the abstract, which concisely summarizes the article by highlighting the main points. For tips on formatting and using citations, read on! Did this summary help you? Yes No
- Send fan mail to authors
Reader Success Stories
Joshua Benibo
Jun 5, 2018
Did this article help you?
Dominic Cipriano
Aug 16, 2016
Obiajulu Echedom
Apr 2, 2017
Noura Ammar Alhossiny
Feb 14, 2017
Dawn Daniel
Apr 20, 2017

Featured Articles

Trending Articles

Watch Articles

- Terms of Use
- Privacy Policy
- Do Not Sell or Share My Info
- Not Selling Info
wikiHow Tech Help Pro:
Develop the tech skills you need for work and life
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Why all doctors should...
Why all doctors should be involved in research
- Related content
- Peer review
- Hannah Jacob , academic clinical fellow
- 1 UCL Institute of Child Health, London WC1N 1EH
- hcjacob{at}gmail.com
Neena Modi tells Hannah Jacob about her career in research and why this is a fundamental part of every doctor’s job
Neena Modi is president of the Royal College of Paediatrics and Child Health and professor of neonatal medicine at Imperial College, London. She is a practising clinician and academic lead of a neonatal research programme focusing on nutritional and other perinatal determinants of lifelong metabolic health. After a period as vice president for science and research at the college, she was elected president in April 2015.
How did you become interested in research?
I realised that what I was being taught during my training was wrong, and my very enlightened consultant challenged me to design a trial to back my contention. There were no training posts in neonatal medicine when I started my paediatric training, but there were lots of opportunities to learn and undertake research because the rate of change was so great. That was really exciting.
Which research projects are you most proud of? Which do you think has had the biggest impact?
We did a series of studies to develop methods for measuring body water compartments in extremely preterm babies and to describe the postnatal alterations in fluid balance. We also tested the hypothesis that immediate sodium supplementation in babies with respiratory distress syndrome was harmful. That was a big achievement.
Most recently we have identified possible biological mechanisms that underpin the epidemiological associations between early onset of features of the metabolic syndrome and being born extremely preterm. That is of real interest as we learn more about the long term effects of extremely preterm birth.
How have you coped with the inevitable setbacks of a career in clinical research?
Real life is about being refused things and carrying on anyway, so I have developed resilience. There was no academic training route when I started out, so I have had to forge my own way. People will always tell you that it cannot be done. You have to pursue the things you are passionate about.
Do you have any advice for junior doctors interested in doing research?
Work out what interests you, and then find the person who is going to help you do it. Being approached by an enthusiastic junior doctor is always well received, and once you have found the right senior person they can support you in achieving your goals. Do not lose heart if you don’t get an academic training post as they are not the only way into research. Some of the best research students I have worked with have not come through the standard path.
What would you say to doctors who have no interest in doing research?
I would argue that they may not be thinking broadly enough about what research actually is. Every clinician is responsible for evaluating their own practice, and to do that in a robust and meaningful way you need to use the tools of research. We all need to be able to critically review research done by others. For example, the guidelines used in everyday clinical practice are based on meta-analyses and systematic reviews. So I think all doctors need to be involved in research in some way, and that may be different for different people.
How can undertaking research help doctors in their careers?
It’s not just a help, it’s essential. There are few absolutes in science, and without inquiring minds medicine will stand still. Participation in research enables doctors to evaluate their practice objectively and to be involved in advancing their discipline. You can learn so many skills that make you a better clinician around appraising the evidence and thinking critically about a situation.
What are the benefits and downsides of doing research—both on a personal and professional level?
The benefits come from knowing you are contributing to the science of medicine as well as the art, and are able to question, evaluate, and test different approaches objectively. Everyone has a role in supporting research—many will contribute, and some will be research leaders.
As for downsides, life has ups and downs, and research is no different. You have to not be too disheartened when a grant application gets rejected. When you want to achieve something, you have to keep speaking to the powers that be until you find someone who can be an advocate.
How do you juggle the research, clinical, and leadership aspects of your working life?
It is a balance that is evolving all the time and that provides me with a huge stimulus. Every time I have been presented with an opportunity I have had to evaluate its potential effect on the other components of my work. I always say yes to the things that interest me and follow my muse. We are very privileged as doctors to have such a range of tremendous opportunities available to us.
Do you have a particular philosophy that has guided you in your career?
When life offers you an opportunity, do not turn it down. I believe you must do what grabs your interest, and if you are still doing it years later you know you made the right decision. When you lose the excitement, it is time for a change. The future lies with junior doctors, and you can be a part of shaping it in the way you think is right.
Is there anything you would do differently if you had your career again?
I would have much greater confidence to fight for something I believed in.
Competing interests: I have read and understood BMJ policy on declaration of interests and declare that I am the academic officer for the Paediatric Educators Special Interest Group of the Royal College of Paediatrics and Child Health.
- Open access
- Published: 04 March 2022
“ Not yet a doctor”: medical student learning experiences and development of professional identity
- Gyu Mi Park 1 &
- Ah Jeong Hong 1
BMC Medical Education volume 22 , Article number: 146 ( 2022 ) Cite this article
8238 Accesses
9 Citations
2 Altmetric
Metrics details
To become a good doctor, developing a professional identity is as important as having the right knowledge and skills. Great attention has been given to professional identity in medical school because it plays an important role in the transition from student to doctor. Nonetheless, the necessity of acquiring a tremendous amount of knowledge and skill during medical school training does not create sufficient opportunities for students to develop their professional identities. Thus, this paper pays careful attention to how students’ learning experiences in medical school affect this development. The research questions are as follows. 1) How do medical students’ perceptions of doctors change or strengthen after entering medical school in the process of professional identity development? 2) What kinds of knowledge have medical students accumulated while attending medical school? How do their learning experiences affect professional identity development? 3) What is a doctor’s role and the career’s meaning to medical students, and what understanding does this awareness bring to their learning experiences and lives as future doctors?
In-depth semi-structured interviews were conducted with 20 Korean students in their fourth year of medical school; all had more than one year of experience in clinical settings. The students’ learning experiences and professional identity development were used to analyze the data using inductive thematic analysis.
When students first entered medical school, they perceived their identities as “given to” them by society. However, various learning experiences during the medical school years affected them, causing them to think about becoming a doctor according to their own perceptions and the meaning of becoming a doctor in the profession. Although an isolated medical community and a competitive student culture hindered them from searching for their professional identities, informal learning experiences, including active interaction with patients, senior doctors, and others outside the medical community, enabled them to develop their professional identities. The medical students experienced a conflict between individual and professional values as they considered what kind of doctor they would be in the future.
Conclusions
The findings noted in this study extend the understanding of professional identity and informal learning experiences in medical school.
Peer Review reports
A layperson becomes a professional doctor through completion of medical school. In medical education, developing a "professional identity" is essential to becoming a future doctor [ 1 , 2 , 3 ] in addition to medical knowledge and skills. Professional identity is “a representation of self, achieved in stages over time during which the medical profession's characteristics, values, and norms are internalized, resulting in an individual thinking, acting, and feeling like a physician” [ 4 ]. This identity enables students to gain confidence in what they are doing as doctors and affects their relationships with co-workers, professional groups, and patients [ 5 ].
However, medical students have not yet fully developed their professional identity as preliminary doctors. Most students enter medical school without an understanding of a doctor’s value [ 6 ]. Moreover, they have few opportunities to reflect on their professional identity after attending medical school [ 7 ]. As a result, many students have struggled to interact with patients and adopt the doctor role [ 8 ]. The lack of professional identity has returned to medical students as a negative impact on them [ 7 , 8 , 9 ].
One of the reasons that medical students cannot develop their professional identity can be found in medical education. Medical education has become a source of biased learning that excludes the humanistic aspects of medicine [ 10 ]. The way doctors' attitudes are reflected and reproduced in clinical practice has been ignored [ 11 ]. This is also related to the “dehumanization in medicine” problem caused by medical education, which mainly focuses on medical knowledge and technical skills [ 12 , 13 , 14 ]. Therefore, it is necessary to attract academic attention to medical education and professional identity development to make educational suggestions for creating better future doctors.
Earlier research has stated that medical students learn not only through the formal curriculum but through the informal learning of clinical practice to develop their professional identity [ 15 ]. Informal learning is “any activity involving the pursuit of understanding, knowledge or skill which occurs without the presence of externally imposed curricular criteria” [ 16 ]. Informal learning also occurs in a space surrounded by events and activities with a formal educational purpose [ 17 ]. For example, patient interaction in clinical practice [ 18 , 19 , 20 , 21 , 22 , 23 ], positive and negative role models [ 24 , 25 , 26 , 27 ], authentic experiences [ 28 ], and the medical community [ 29 , 30 ] are aspects of informal learning that can affect professional identity. However, little attention has been paid to how students respond to informal learning in developing professional identity.
Adult learning is an individualized process that moves away from institutionalized learning and focuses on the meaning of individual learning and identity [ 31 ]. After entering school, adult learners reconstruct their identities in various learning experiences [ 32 ]. Thus, it is crucial to examine what unique learning experiences are accumulated in medical school and their meaning to medical students.
The research started with careful attention to how medical students develop their professional identity through learning experiences. Using the perspectives of informal learning and identity theory, this exploratory research focused on medical students' learning experiences within the social-cultural context of the Korean medical school’s learning environment and the meaning it provides to their professional identity development as future doctors. The research questions are as follows.
In the professional identity development process, how do medical students’ perceptions of doctors change or strengthen after entering medical school?
What kinds of knowledge have medical students accumulated while attending medical school? How do their learning experiences affect professional identity development?
What is a doctor’s role and the career’s meaning to medical students, and what understanding has this awareness brought to their learning experiences and lives as future doctors?
To this end, qualitative research was conducted with 20 Korean medical students in their fourth year. The study allows understanding of the medical students’ identity development and learning experiences, and it provides research implications, including suggestions for a better learning environment to educate medical professionals.
Qualitative research is helpful to understand the in-depth meaning of individual experience [ 33 ]. This study was conducted to grasp the context of medical students’ learning experiences and deeply examine how these are involved in their professional identity development. To this end, the qualitative research method was adopted.
Participants and setting
The participants consisted of 20 students in their fourth year at two Korean medical schools. A purposive sampling method was used to select suitable participants for the research purpose. Details on the setting and the criteria for selecting participants are as follows.
The Korean medical school program is six years long; the first two years are pre-medical courses that are followed by four years of clinical studies. The final one and a half years are usually based on clinical practice education. Korean medical students can become doctors if they pass the Korean Medical Licensing Examination (KMLE) national exam. After graduation, they can apply for an internship in a hospital. Their school records and KMLE scores determine the hospital where they can be an intern.
According to the Medical Act, Korean medical students can practice medical treatment such as history taking, physical examination, and clinical skills without a license. They must perform all medical activities under the guidance and supervision of their advisor, and they are responsible for performing medical treatment based on patient safety. Clinical practice is one of the essential educational strategies in medical school to develop medical students into primary clinicians with expertise and a sense of responsibility.
Considering the system of Korean medical education, it was most appropriate to select fourth-year undergraduate students with more than one year of experience in clinical settings as participants in this research. The researchers judged that they had had relatively enough time to think about the meaning of their learning experiences in medical school and had formed their professional identity through their career decisions.
The researchers contacted professors and doctors working in a university hospital to recruit the participants. Medical students who voluntarily agreed to participate in an interview and had been recommended by their professors and doctors were recruited. Finally, 20 fourth year students from two medical schools were selected; 14 were males, and 6 were females. Their ages ranged from the mid-20 s to the mid-30 s. They had completed most of their medical education course and were studying for the KMLE. The participants attended medical schools located in Seoul and Daegu city in Korea. Their schools’ names and other personal information were omitted to guarantee their anonymity.
Data collection
To grasp the medical school curriculum in advance, the researcher referred to the medical school web page, which includes general information such as course types, teaching methods, credits, academic programs, and educational goals.
The data were collected through individual interviews. The participants were informed about the research purpose, content, and research ethics. The researcher and each participant had a conversation for about an hour in a classroom. All interviews were recorded with the consent of the participants. The recorded files were transcribed verbatim in Korean and translated into English later.
The interviews were conducted using semi-structured questions. A conceptual framework for the research questions was developed based on a literature review. The interview questions were based on the research questions. The key questions are as follows: “What motivated you to attend medical school?”, “What are the (dis)advantages of clinical practice in becoming a doctor?”, “What kind of (positive or negative) role models have you formed in your clinical practice?”, “What is the unique culture of the medical school?”, “What are the special perceptions of people toward doctors?”, “What would a “good doctor” look like?”, “When you compare yourself right after entering medical school with now, how has the image of the doctor you would like to become changed?” As the interviews progressed, the questions were elaborated on and enhanced to address the research questions better.
Data analysis
In a qualitative study, data collection ends when it reaches data saturation in which new information cannot be obtained, and data collection cannot trigger new theoretical insights [ 34 ]. It has been recommended that between 16 and 24 interviews be conducted to reach a saturation of in-depth meaning in the responses to the research question [ 35 ]. A total of 20 interviews were conducted in this study when saturation was reached.
Data analysis was focused on medical students' learning experiences closely related to professional identity. This study used inductive thematic analysis [ 36 ] as a qualitative data coding and analysis method. Inductive thematic analysis is a flexible method for organizing and analyzing patterns in collected data. The analysis followed six steps: familiarizing with data, generating initial codes, searching for themes, reviewing themes, naming themes, and producing a report [ 36 ].
The researchers read the transcripts repeatedly to familiarize themself with the data and developed initial coding schemes extracting key ideas related to the research questions that emerged from the participants' interviews. Initial coding is the process of organizing the collected data, discovering meanings, and conceptualizing the results [ 34 ]. After that, the researchers categorized the data related to the themes: changes in the perception of doctors after entering medical school, common social perceptions of doctors and medical students, unique characteristics of the medical school community, informal learning (interaction, role models, authentic and a contextualized learning field) in clinical practice, and identity conflict as a prospective doctor were categorized. These were grouped into three overriding categories: job search and preparation, medical school learning experiences, and the meaning of a doctor’s profession. Each theme was named to clarify the analysis. Finally, vivid extracted examples were selected and produced to the research question.
In qualitative research, the trustworthiness of data must be considered [ 37 ]. The study used strategies to ensure trustworthiness. After explaining the study purpose to the participants, the interview was conducted, with the interviewer keeping a distance from categorizing the data. Two researchers reviewed the transcripts independently. They met weekly to cross-examine the categorization and interpretation of the data.
Becoming a doctor: job search and preparation
The research participants who entered medical school with the dream of becoming a doctor began to explore the job by coming to understand a doctor’s life and the social perception of doctors in medical school over several years. This experience catalyzed the developing psychological readiness of ordinary students to become professional doctors while changing or strengthening their perceptions of doctors.
After entering medical school: from looking at to understanding a doctor’s life
The participants entered medical school for different reasons, such as their parent’s recommendation that they should become a doctor, the expectation of high job security, and people’s recognition that excellent students should attend medical school. The common theme in why they chose medical school is that they simply had followed others’ perceptions of a doctor.
It goes without saying that the best students go to medical school. (Student 1, male)
When I was a high school student, I heard that doctors make a lot of money. I think I’ve been motivated by that. (Student 16, male)
However, the participants changed their thinking after entering medical school and observing doctors' real lives. Before entering medical school, Student 11 thought the same as other people, "A doctor has a wonderful job respected by many people and earns a lot of money." But after clinical practice, she realized that a real doctor’s life was different from her earlier thought. A doctor’s role is never a job to earn lots of money and live comfortably. Student 6 also believed that a doctor could earn money easily. However, now she realized that being a doctor was not an easy job and that it takes much effort and time to become one.
Doctors have to study continuously. They also must work in extreme situations with sick people. If you think being a doctor is a job to earn a lot of money and live comfortably, it's not such a job at all. (Student 11, female)
I didn’t know that it’s so hard. (…) I just knew that doctors earn lots of money and have a stable job, and they would be respected by other people. (…) But actually, it takes a lot of effort and time to become a doctor. It's a tough job. (Student 6, female)
Social perception regarded medical students as “predetermined” doctors: a given identity
The participants were aware that the public gives special attention to medical students.
When talking to my friends or relatives, I can feel that they envy me. Once, they said to me, “Our future doctor’s here.” (Student 11, female)
There is a perception that doctors can make or break lives. This external perspective on doctors is being passed on to medical students.
People usually think that doctors can make or break patients’ lives. So, it’s like; it makes me believe that human lives are in my hand. (Student 7, female)
Student 6 said doctors and medical students have a sense of privilege because doctors are licensed and hold socially promising jobs. Those students who belong to the medical school community were identified as predetermined doctors.
I think not only doctors but even medical students seem to have a sense of privilege. A doctor has a license, and it’s a socially promising job that has a bright future. (Student 6, female)
Learning experiences in medical school
From the perspective of informal learning, several characteristics of medical school learning experiences are closely related to professional identity development. The fiercely competitive, closed, and strongly authoritarian culture of the medical school community encourages passive learners who lack professional attitudes. On the other hand, the authentic learning environment of clinical practice gradually refines them into future doctors with professional competence, values, and attitudes.
Keen competition culture in medical school: a passive learning attitude
The participants describe that medical school looks quite similar to high school. The competition among students in Korean high schools with high “education fever” derived from the belief that entering a good university would guarantee one’s quality of life. A similar belief justified competition in medical school, assuming that choosing a popular specialty would guarantee a happy life. Korean medical students had to get better grades than others to choose such a specialty. In this competitive structure, the problem is that the issue of professional identity has been hidden by the student focus on picking a popular specialty because of their good grades. Instead of sufficient consideration of what kind of doctor they would be, they were chasing a popular specialty to occupy a better position than others and survive the competition.
Eventually, a man who graduated from a famous university would have a good career and meet a pretty girlfriend. That’s the way things go. Now, I will have to graduate medical school with good grades to select the best specialty and then finish my internship here in the university hospital. After that, finally, I’ll become a doctor. The way of success in one’s life is quite similar. (Student 1, male)
The participants were studying hard to get good grades. This means that there is no need to learn more than given tasks. In Student 3’s case, he would be willing to study hard only if it is necessary to graduate from medical school. The participants pointed to the “passive” learning attitudes of medical students.
They are very passive, really. (Interviewer: Then, if it would be asked in the exam, would you?) Of course, I will study hard. If 20 credits for social participation are requirements for graduation, I will definitely do so. But if not, why do I need to do that? (Student 3, male)
Medical students trapped in the cage of medical school
Doctors and students coexist in a medical school community. Doctors teach students, while students learn medicine from doctors. The relationship continues for a long time, even after students start working as qualified doctors. The study notes the characteristics of the medical school community and relationships with the community members to find how they influence students' identity development. One of the prominent characteristics of the Korean medical school community is that it is a “closed group.”
It seems to be the problem of the medical group itself. It’s too closed. I think it may be worse than the army. (Student 3, male)
The exclusiveness of the medical school community appeared as two types. The first was characterized by a lack of interaction among the community members. Some medical students with similar backgrounds formed an exclusive small group. Student 4 described that the tendency of such an exclusive small group was the expansion of a closed medical community, interrupting communication with patients and other doctors.
There is a kind of culture that medical students usually hang out only with a group of friends who have similar backgrounds, making an invisible exclusive boundary around them. Many doctors and professors in medical school are exclusive, too. I think everything starts from those groups. Medical students become doctors who are not good at communicating with others outside of their group. (Student 4, male)
The interaction between doctors and students in medical school is also restricted. According to participants who experienced a clear hierarchy in the community through clinical practice, there is a strong authoritarian culture.
I thought if I do well, like providing good care for patients, everyone would like it. But what I’ve experienced in clinical practice was very different from my expectation. There’s a clear hierarchy among doctors and lots of constraints more than I thought. A hospital was another organizational society. (Student 1, male)
The second type of closed medical school community is related to a lack of interaction with other academic groups. Medical school started with physical and psychological separation from non-medical groups due to the geographical location of medical school and the different school curricula. It caused indifference to people and society, restricting learning from interaction with various people.
They should look for the outside world. Medical students have very narrowed and limited relationships. They don’t know anything other than medicine. (Student 8, female)
A doctor’s job is a stable one with a great social safety net. They don’t have to make efforts so as not to fall behind. Medical students are becoming complacent doctors, including me. I used to read many books and newspapers, finding out what happened these days in our society. But after four years have passed, now I don’t have any interest in that. (Student 3, male)
Authentic learning
Clinical practice complements the limitations of lecture classes. The participants could understand the medical knowledge they had memorized in the class, observing diseases and symptoms. Some students regained interest in medicine and conducted self-directed learning through hands-on training.
It’s no use just taking a class or looking at the picture of jaundice. Once you just look at the real patient, you will realize, “Oh, that's it.” No matter how hard I try to memorize the disease or accept it as an image, it can’t be better than observing real patients. (Student 3, male)
Another advantage of clinical practice is that it can integrate medical knowledge learned only in a fragmentary way through a book. Beyond simply memorizing each disease along with its symptoms and treatment, students can identify the actual process by which medical knowledge applies to clinical practice. Student 5 said that while textbooks cover only one disease and treatment, priorities and treatment methods can be learned simultaneously when a patient has multiple diseases. These are not covered in textbooks.
I’ve learned in a textbook about the treatment of a single disease, not the case of several diseases at the same time. In fact, the priority of treatment is not considered at all in the book. But in the case of clinical practice, it is helpful to understand the real treatment on how to care for patients who are suffering from many diseases at once. (Student 5, male)
The experience of clinical practice was also helpful in specialty choice. Medical students were helped in their selection through contact with real patients and learning the workplace environment. Student 17 explained that students could choose their specialty based on their practice experiences considering their interest and aptitude.
I think it’s the most important meaning of practice. Just as students are going to be different before and after entering medical school, practice also can change their minds about specialty choice. So, students may exclude some specialties that they didn’t really fit in with during practice, “I should not choose it. It does not fit me.” (Student 17, male)
Finding a “good doctor” role model: A "friendly" doctor to patients
The key role models for medical students were the doctors they met in practice. Interestingly, the common characteristic of good role models was “kindness.” The participants chose doctors as good role models who stood out for their human side, not losing their kindness toward patients because of their busy schedules. Student 3 expressed his opinion that the doctor’s personality will emerge as an essential virtue in the future as much as the doctor’s competence.
In the past, the doctor who knows every disease and treatment was judged as a competent doctor. But now, if you don’t know about something very well, then you can just look it up on the computer, smartphone, or something. All the information is showing up on the screen. So, I think it’s not really far away until the day of admitting the doctor who has a good personality rather than skills. If the doctor’s skill is 9 and the personality is 1, then it’s gonna be 7 to 3, or it’ll be possibly 6 to 4 in the future. (Student 3, male)
The participants had not only positive but negative role models. Patient-friendly doctors were good role models. On the contrary, doctors who neglect patients and prescribe without making eye contact were negative role models.
I’ve seen a professor who didn’t make eye contact with patients at all. The professor who lectured about how to treat patients in the hospital did it that way. Well, that is the gap between reality and ideals. (Student 4, male)
Patients make good doctors
Clinical practice has become an essential learning space for medical students to develop identities through interaction with various people. The relationship with patients is critical to developing a medical student’s identity. The participants interacted directly with patients and formed values and attitudes as preliminary doctors. Student 13 notes that the perception of a specialty could change due to the relationship with patients.
I was not interested in the specialty. But after the practice, I could feel lots of things by talking and communicating with patients so we could get to know each other. I changed my perspective on the specialty by myself. (Student 13, male)
Meeting with patients greatly influenced identity formation. The participants interacted directly with patients and formed values and attitudes as preliminary doctors. Student 15 observed a patient with an incurable disease who could not accept it and missed a treatment period. Student 15 realized that a doctor could not cure every disease. Also, he learned that the competence to explain well to patients and help them accept their condition is necessary.
I realized that doctors could not cure all illnesses. (…) I think if a doctor had explained better to the patient the disease the first time, the patient would have been able to accept rather than deny it for a long time. (…) At that moment, I felt that it’s important for doctors to cure patients, and it’s also important to help patients accept themselves by explanation. (Student 15, male)
Medical students participating in practice have identities both as a “student” and a “doctor.” From the patient’s viewpoint, they are a doctor, while they are a student to doctors. These two identities conflict in the hospital. Patients were cooperating in treatment believing that medical students were real doctors. As medical students also knew about the belief, they were concealing who they were.
If I don’t tell them (patients) I’m a student; they describe their symptoms very specifically. The people really trust me who believe that I’m a doctor. Then, it’s going to be very easy for me. But once I tell them the truth, they rarely come to talk to me and just say “yes” to all of my questions. (Student 14, female)
On the other hand, medical students were viewed as students still training to become doctors by professors and senior doctors. They do not belong to the hospital, nor are they qualified as doctors. They think of themselves as students evaluated by doctors, referring to "their weakest position" in the hospital.
We’re students in the weakest position who are always conscious of doctors and professors. I thought, “If I do something wrong, I can’t get good grades.” So, I couldn’t be active in practice. I was going to be uncomfortable with doctors and professors only because of their one word. (Student 13, male)
The participants regarded themselves as students rather than preliminary doctors, avoiding their responsibilities to the patients in clinical practice. Student 8 added, as she was reflecting on herself, that she was indifferent to patients because they were not her patients.
I tend not to examine patients’ conditions in detail. When I get feedback from my professor, I thought, “Did I miss it because they are not my patients?” (Student 8, female)
The participants gave various responses to the question of “when will you admit you are a doctor?” The responses were, “after graduating from medical school, have opportunities to participate in treatment directly,” “when becoming one’s doctor and get some experience,” or “take on a doctor’s role and responsibility.” The common element in the responses is that the students think abundant clinical experience is necessary to admit they are a real doctor.
Interns are doctors. They have a name card. If I’m an intern, I will meet patients confidently. Interns can draw blood for testing and get consent from patients or something. But students can’t do those things. Actually, nothing could be done by students. (Student 14, female)
I’ll do better when I become someone’s doctor. Interns just do a job with chores. They don’t have their own patients. So, I think it would be different after I have my own patients later. (Student 8, male)
I think the doctor’s role is different depending on the position. For example, as an intern, if you can draw blood and release patients with discomfort at night, I guess it’s enough to say I am in an intern’s position. So, what I want to say is that I should admit I am a doctor, like, "Oh, I think I am a doctor now.” (Student 20, male)
The meaning of being a doctor
While attending medical school, the participants developed their own awareness of the doctor’s role and the career’s meaning. The awareness clarified why they had to learn in a certain way in medical school and what values they must pursue as future doctors.
Becoming a doctor
Most of the participants expressed that they had difficulty studying. They had to memorize large amounts of medical knowledge and confirm it through tests. This type of learning environment is far from one that encourages them to be interested in medical study.
Doctors always looked cool to me. But now, I know it’s not easy to live as a doctor. I have too much work to do. Rote learning seems to make me lose any interest in studying. (Student 8, female)
Even though the participants had trouble adapting to medical classes focusing on memorizing a large amount of content, they regarded it as an inevitable strategic choice associated with becoming a doctor. Student 15 thought that medical knowledge is essential for doctors, so rote learning was the most effective way to absorb such knowledge in a short time. Therefore, the medical classes were neither interesting nor unsatisfying to him.
To get a lot of knowledge in a limited time, efficiency is the most important thing. I also think the most important thing for a doctor is knowledge, not creativity. I believe that I need to know what I need to know. So, I don’t have any fun along the way, but I don’t complain, either. (Student 15, male)
Realizing that there was not much time until they received a doctor's license, the participants worried about what they had learned in medical school and how much they knew about it. A doctor's duty to treat patients with accurate medical knowledge without any mistakes has come to mean fear and responsibility. The resolution to be faithful to the doctor’s duties became a driving force to study hard.
I have some worries about myself. For example, I didn’t know that before, but now that it’s about time to get a doctor’s license, I feel like I have a tremendous responsibility for my judgments. That makes me extremely nervous. (Student 7, female)
It’s most important to know medical knowledge accurately. (…) We are the ones who can do harm to others if we don’t know exactly. So, all of us think that it’s really important to know precisely and correctly. That’s why we have to study hard. (Student 6, female)
As for the specific atmosphere of the hospital and medical school, the participants pointed out some problems but deemed to some degree their necessity as well. As mentioned above, medical schools and hospitals are characterized by a strong hierarchy and authoritarian culture. The participants regarded that this culture was formed in an effort to keep health services safe.
The hospital itself is a place where we are treating human life, and it’s where we should be alert. (Student 13, male)
There is a distinct culture in medical school. Having attended another school, Student 6 talked about the special culture only seen in medical school. At the school from which she had graduated, idiosyncratic personalities were naturally accepted. In contrast, the medical school had a “standardized framework.” In medical school, exhibiting behaviors that stood out was regarded as “strange.” Student 15 thought that hiding their unique personality was related to the characteristics of doctors’ work. The act of emphasizing one’s personality, such as through creativity and challenging behavior, could threaten a patient’s life. It is a top priority for doctors to treat patients safely by precisely applying earlier treatment rather than engaging in challenges or creativity.
Doctors are not supposed to be challenging. I think it’s not right to reveal individual creativity in medical treatment. It can put patients at risk. (…) So I think the individual character should not be emphasized. So, the culture and atmosphere are quite understandable. (Student 15, male)
Conflict between individual value and professional value
There were two conditions for choosing a popular specialty among medical students. First, a field’s associated income level should be good. Second, its work intensity should not be high.
Popular specialties usually meet two conditions. The income should be good, and then the working hours should be short, which means that the work intensity is weak. (Student 15, male)
The participants' conflicts between personal and professional values increased their concerns about career choices. They were conflicted between a specialty in which it is easy to manage both work and household and the specialty in which they truly want to work. Student 7 was deep in thought about whether she should choose the specialty she wanted or another, which is considered to be good for quality of life. Her decision became more complicated after she heard a professor’s story. The professor chose to do minor surgery instead of major surgery to manage both work and childrearing.
The older I get, the more I want quality of life. One day the professor told me her story. She wanted to become a great surgeon in the past. But after she married and then gave birth to a child, she decided to do small surgeries. She said priorities are changed in a lifetime. (…) I hope to be a ○ ○ doctor if I could, but should I have to live so hard? (Student 7, female)
Student 20 considered high income a top priority in specialty choice, but his values changed as he participated in clinical practice. He could understand the meaning of chronic illness in a patient's life that the books never revealed. Now he considers a specialty that requires interaction with patients who may give meaning to his life as a doctor. He said, "I’m not old enough yet,” as the purpose of becoming a doctor is stepping away from money and trying to pursue something more than material value.
Money couldn’t be ignored. (…) Material is, of course, it’s good. But I guess there is something more than material. Maybe I’m not old enough yet. (Student 20, male)
When an ordinary student forms a professional identity as a preliminary doctor from entrance to graduation from medical school, it is a dynamic process. At first, the students who entered medical school followed the perceptions of others about doctors, and they simply admired doctors as people commonly do. In addition, they identified themselves as predetermined doctors, showing a sense of privilege, pride, and self-confidence. In Korea, education is regarded as the path of success to occupy a higher socio-economic status, demonstrating the effects of a Confucian cultural heritage [ 38 ]. The social perception of doctors revealed in the study also reflected the common belief from Confucian culture that top students will certainly enter medical school and be educated to become doctors who can live successful lives with high social status. They thus were absorbing an identity derived from the social perception of medical students as doctors, which means that success is a foregone conclusion.
Medical students’ professional identity shows their “possible selves,” which means the self-presentation of what they would like to become and what they are afraid of becoming [ 39 , 40 ]. The doctor's identity reveals a possible self for medical students in clinical practice. This identity has a weaker social binding power than the current self. Meanwhile, the current self, the student identity, remains stable due to social feedback such as that associated with assimilation into the medical organizational culture. Multiple selves are activated in accordance with the social environment [ 39 ].
The situation changes as they continue their school life. They withdraw from the image of a doctor derived from social perception and start to think for themselves about what it is like to be a doctor. The given identity reflects the social expectation that a medical student can be a promising doctor who can treat every disease. The participants were confident and had adopted the given identity, but they were afraid of its expectations simultaneously. They clearly recognized the limitation that a doctor never cures all illnesses. The fact that they have to take care of patients has come with heavy responsibility.
The study shows that identity is formed dynamically by the intricate entanglement of individuals and society rather than in a linear or fixed way [ 1 , 41 ] through the professional identity development of medical students. The identity of a medical student is not merely that of a doctor but that of a person who would be reborn as a doctor with congruent professional behaviors, attitudes, and values. The participants hoped to be a warm-hearted doctor like their role models who treat patients well. The way to become the doctor they hope to be depends on developing professional identity through their rich clinical experiences, passion, and effort. The medical students must become “agents” [ 42 ] who can lead their own professional identity formation.
The first step toward becoming an agent of identity is to embrace a doctor’s life as it is. The participants found out why they should keep learning by rote and why they should assimilate into the culture of the medical community. Rote learning was the best choice for them to acquire more knowledge of medicine in a short period to become a decent doctor. The medical community's authoritarian and strongly hierarchical culture was a necessary evil that protects patients.
The meaning of professional identity to medical students could be interpreted as taking on a “social identity” [ 43 ] which concentrates on social group attributes. The social identity is individual self-conception, derived from membership in a social group, and accompanied by the values and emotions fixed in membership [ 44 ]. Having a social identity means performing actions similar to other group members, employing the group’s perspective, and reinforcing the group's consistent values, perceptions, and behaviors [ 45 ]. The participants tend to frame their behaviors to mimic other medical students rather than emphasize their individuality. This shows "deindividuation," which refers to a contextual change of identity from an individual to a group member [ 46 ]. One unique individual, a medical student, acquires social identity in being labeled a professional group member.
In becoming a doctor, medical students are confronted with a new conflict. The conflict is the question of what value should they bring to the job, an individual value or a professional one? The struggle with the choice between work and family [ 47 ] represents a person who has undertaken various social roles with multiple identities in society [ 48 ]. The internal confusion of medical students in this conflict is related to psychology’s identity theory that links individual roles to identity [ 43 ]. Individuals with multiple identities negotiate their roles with identity role partners, manipulate the environment to control the resources responsible for the roles, and meet role expectations [ 45 ]. The study participants looked for their roles in two different social spaces, the hospital, and the household. In the hospital, they negotiated their roles with the role partners of patients and doctors. In their personal lives, they were concerned about their roles as heads of present or future families. The career choice accounting for their reality represents an attempt to manipulate the surrounding environment to fulfill the responsibilities accompanying both their work and individual lives.
It is suggested that medical education should facilitate professional identity formation so that students can discern robust and compelling values as future doctors. As society has become more complex, the difficulties of harmonizing multiple identities have increased [ 49 ]. A robust professional identity will help promote mature career decision-making by assisting the integration of self and occupation [ 50 ]. Therefore, if educational support for the development of professional identity within the medical school learning environment is achieved, students’ identity confusion and value conflict would be reduced. As agents of identity, they would find what their job means in life.
This research reveals that medical students’ professional identity is affected by various types of learning experiences in medical school. The most striking feature of the Korean medical school community is its closed structure, marked by competition and an authoritarian culture that hinders interaction among people. In this environment, the participants had great difficulty communicating with others. It was promoting doctors who are indifferent to patients and society, preferring to pursue their own interests. The purpose of becoming a “good student,” not a “good doctor,” has overtaken the opportunity to grow as a social being.
Based on the results, it is necessary to have a learning environment that enables medical students to interact with people to develop a professional demeanor. This can be discussed within the category of informal learning. Informal learning is contextualized [ 51 ]. The greatest advantage of clinical practice is that students encounter patients and doctors in a context-based clinical environment. Some participants started to think about the meaning of diseases in patients’ lives and behaviors as a doctor through clinical immersion. Interaction with other doctors also provided meaningful learning. Medical students took as role models doctors good at interacting with patients; they then behaved in ways that reflected the role models’ behaviors. While living in a hospital with doctors, medical students learned a way of doing and a way of thinking. The rich learning space enabled them to use existing knowledge to deeper understand and develop personal and professional values. The study shows that improved doctor-patient interaction is needed to foster good doctors [ 52 ]. Therefore, efforts to provide an interactive learning environment should be attempted to understand patients and care for them according to the humanistic aspects of medicine.
The study has some limitations. A small sample from two Korean medical schools was used in the research. Since the government controls the nationwide medical school curriculum in Korea, it is expected that there would be little regional variation in exploring students’ learning experiences.
It is worth examining or comparing professional identity development according to students’ unique informal learning experiences as adult learners using larger samples from Korea and other countries. For example, a study conducted in Brazil confirmed the impact of the hidden curriculum of the professional identity, a “speeding up” culture that requires quick work and pressure to learn as much as possible without sufficient reflection on clinical experience, which ends with a lack of awareness of students’ professional identity in the context of a chaotic health care system [ 53 ]. Another study, conducted in an Australian university, found that students from diverse cultural backgrounds had two main senses of their professional identity [ 54 ]. One is professional inclusivity which is formed when they are treated as future doctors. The other is social exclusivity which is developed by socially separating themselves from non-medical students [ 54 ]. Future research can be expected in international studies conducted in similar or different socio-cultural contexts from that of Korea.
This study investigates medical students’ professional identity development through informal learning experiences in a distinctive Korean educational environment. The study indicates that medical students, in their earlier years, accept a “given identity” provided by social perception. The limited interaction in the medical school community and competition culture obstructs professional identity formation. On the other hand, informal learning in clinical practice, full of interaction, contexts, and authenticity, facilitates students’ thinking about what kind of doctor they would be as the agent of their identity. They experience a conflict between individual and professional values, in considering what kind of doctor they will be in the future. In the process, difficulties in medical school were accepted as preparation for becoming a doctor by medical students. The findings noted in this study extend the understanding of professional identity and learning experiences in medical school.
Availability of data and materials
The raw data supporting the conclusions of this article will be made available by the authors without undue reservation.
Abbreviations
Korean Medical Licensing Examination
Niemi PM. Medical students’ professional identity: self-reflection during the preclinical years. Med Educ. 1997;31(6):408–15.
Article Google Scholar
Vagan A. Medical students’ perceptions of identity in communication skills training: a qualitative study. Med Educ. 2009;43(3):254–9.
White MT, Borges NJ, Geiger S. Perceptions of factors contributing to professional identity development and specialty choice: a survey of third- and fourth-year medical students. Ann Behav Sci Med Educ. 2011;17(1):18–23.
Brennan N, Corrigan O, Allard J, Archer J, Barnes R, Bleakley A, Collett T, De Bere SR. The transition from medical student to junior doctor: today’s experiences of tomorrow’s doctors. Med Educ. 2010;44(5):449–58.
Monrouxe LV. Identity, identification and medical education: why should we care? Med Educ. 2010;44(1):40–9.
Cooke M, Irby DM, O’Brien BC. Educating physicians: a call for reform of medical school and residency. San Francisco: Jossey-Bass; 2010.
Google Scholar
Ban DJ. Physician’s professionalism and Hippocratic oath. Philos Med. 2011;12:73–93.
Roper L, Foster K, Garlan K, Jorm C. The challenge of authenticity for medical students. Clin Teach. 2015;13(2):130–3.
Wilson I, Cowin LS, Johnson M, Young H. Professional identity in medical students: pedagogical challenges to medical education. Teach Learn Med. 2013;25(4):369–73.
An JH, Kwon I, Lee SN, Han JJ, Jeong JE. Study on medical humanities and social sciences curriculum in Korean medical school: current teaching status and learning subjects. Korean Med Educ. 2008;20(2):133–44.
Lingard L, Garwood K, Schryer CF, Spafford MM. A certain art of uncertainty: case presentation and the development of professional identity. Soc Sci Med. 2003;56(3):603–16.
Meng KH. Teaching medical humanities in Korean medical schools: tasks and prospect. Korean Med Educ. 2007;19(1):5–11.
Serodio A, Kopelman BI, Bataglia PU. The promotion of medical students’ moral development: a comparison between a traditional course on bioethics and a course complemented with the Konstanz method of dilemma discussion. Int J Eth Educ. 2016;1(1):81–9.
Amin S, Chin J, Terrell MA, Lomiguen CM. Addressing challenges in humanistic communication during COVID-19 through medical education. Front Commun. 2021;6:1–6.
Goldie J. The formation of professional identity in medical students: considerations for educators. Med Teach. 2012;34(9):641–8.
Livingstone DW. Adults’ informal learning: definitions, findings, gaps, and future research. In: In NALL working paper No. 21. Toronto: Ontario Inst; 2001.
Eraut M. Informal learning in the workplace. Stud Contin Educ. 2004;26(2):247–73.
Pitkala KH, Mantyranta T. Professional socialization revised: medical students’ own conceptions related to adoption of the future physician’s role-a qualitative study. Med Teach. 2003;25(2):155–60.
Harrell PL, Kearl GW, Reed EL, Grigsby DG, Caudill TS. Medical students’ confidence and the characteristics of their clinical experiences in a primary care clerkship. Acad Med. 1993;68(7):577–9.
Newton BW, Barber L, Clardy J, Cleveland E, OʼSullivan P. Is there hardening of the heart during medical school? Acad Med. 2008;83(3):244–9.
Woodhead S, Lindsley I, Micallef C, Agius M. The doctor patient relationship: what if communication skills are not used? a maltese story. Psychiatr Danubina. 2015;27(1):34–40.
Litzelman DK, Cottingham AH. The new formal competency-based curriculum and informal curriculum at Indiana university school of medicine: overview and five-year analysis. Acad Med. 2007;82(4):410–21.
Bleakley A, Bligh J. Students learning from patients: let’s get real in medical education. Adv Health Sci Educ. 2008;13(1):89–107.
Wong A, Trollope-Kumar K. Reflections: an inquiry into medical students’ professional identity formation. Med Educ. 2014;48(5):489–501.
Karnieli-Miller O, Vu TR, Holtman MC, Clyman SG, Inui TS. Medical students’ professionalism narratives: a window on the informal and hidden curriculum. Acad Med. 2010;85(1):124–33.
Foster K, Roberts C. The heroic and the villainous: a qualitative study characterizing the role models that shaped senior doctors’ professional identity. BMC Med Educ. 2016;16(1):206.
Maudsley RF. Role models and the learning environment. Acad Med. 2001;76(5):432–4.
Manninen K. Experiencing authenticity–the core of student learning in clinical practice. Perspect Med Educ. 2016;5(5):308–11.
Egan T, Jaye C. Communities of clinical practice: the social organization of clinical learning. Health. 2009;13(1):107–25.
Lovell B. ‘We are a tight community’: social groups and social identity in medical undergraduates. Med Educ. 2015;49(10):1016–27.
Merriam SB, Caffarella RS, Baumgartner LM. Learning in adulthood: a comprehensive guide. San Francisco: Jossey-Bass; 2007.
Hong AJ. Reconstructing self through learning: adults’ learning experience in higher education. Andragogy Today. 2009;12(4):185–218.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. Thousand Oaks: Sage; 2009.
Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London, UK: SAGE publications; 2006.
Hennink MM, Kaiser BN, Marconi VC. Code saturation versus meaning saturation: how many interviews are enough? Qual Health Res. 2017;27(4):591–608.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
Lincoln YS, Guba EG. Naturalistic inquiry. California: Sage; 1985.
Book Google Scholar
Choi SJ. Schooling, learning disposition, and life course transitions: a life history study on Korean elite adult learners. Adult Educ Quart. 2017;67(3):167–85.
Markus H, Nurius P. Possible selves. Am Psychol. 1986;41(9):954–69.
Oyserman D, Markus HR. Possible selves and delinquency. J Pers Soc Psychol. 1990;59(1):112–25.
Volkmann MJ, Anderson MA. Creating professional identity: dilemmas and metaphors of a first-year chemistry teacher. Sci Educ. 1998;82(3):293–310.
Coldron J, Smith R. Active location in teachers’ construction of their professional identities. J Curr Stud. 1999;31(6):711–26.
Thoits P, Virshup L. Me’s and we’s. In: Ashmore RD, Jussim L, editors. Self and identity: fundamental issues. New York: Oxford University Press; 1997. p. 106–33.
Tajfel H. Human groups and social categories: studies in social psychology. Cambridge: Cambridge University Press; 1981.
Stets JE, Burke PJ. Identity theory and social identity theory. Soc Psychol Q. 2000;63(3):224–37.
Hogg MA, Terry DJ, White KM. A tale of two theories: a critical comparison of identity theory with social identity theory. Soc Psychol Q. 1995;58(4):255–69.
Greenhaus JH, Parasuraman S, Collins KM. Career involvement and family involvement as moderators of relationships between work–family conflict and withdrawal from a profession. J Occup Health Psychol. 2001;6(2):91–100.
Lobel SA. Allocation of investment in work and family roles: alternative theories and implications for research. Acad Manage Rev. 1991;16(3):507–21.
Stryker S, Burke PJ. The past, present, and future of an identity theory. Soc Psychol Q. 2000;63(4):284–97.
Saunders DE, Peterson GW, Sampson JP, Reardon RC. Relation of depression and dysfunctional career thinking to career indecision. J Vocational Behav. 2000;56(2):288–98.
Gunderman RB. Achieving excellence in medical education. London, UK: Springer; 2006.
Sadati AK, Iman MT, Lankarani KB, Ebrahimzadeh N. From good to great physician: a critical ethnography based on patients’ views. J Med Ethic Hist Med. 2016;9:18.
Silveira GL, Campos LK, Schweller M, Turato ER, Helmich E, de Carvalho-Filho MA. “Speed up”! the influences of the hidden curriculum on the professional identity development of medical students. Health Prof Educ. 2019;5(3):198–209.
Weaver R, Peters K, Koch J, Wilson I. ‘Part of the team’: professional identity and social exclusivity in medical students. Med Educ. 2011;45(12):1220–9.
Download references
Acknowledgements
The authors thank the students who shared their experiences for this study.
The study participants were named under numbers to protect their anonymity.
This work was supported by the Ministry of Education of the Republic of Korea and the National Research Foundation of Korea (NRF-2020S1A3A2A02091529).
Author information
Authors and affiliations.
Department of Education, Chung-Ang University, Seoul, 06974, Republic of Korea
Gyu Mi Park & Ah Jeong Hong
You can also search for this author in PubMed Google Scholar
Contributions
GMP: Led all aspects of the research project and manuscript writing. AJH: Advisor of GMP for her PhD program. Provided theoretical framework and insight into the qualitative methodology used and revised manuscript drafts. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Ah Jeong Hong .
Ethics declarations
Ethics approval and consent to participate.
This study was performed in accordance with the relevant guidelines and ethical principles contained in the Declaration of Helsinki and was approved by the Ethics Committee of Chung-Ang University (Ref. C2012063(758)/ 1041078–201708-HRSB-158–01). The study participants provided their written informed consent to participate in this study.
Consent for publication
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication. The study participants have consented to publish their own quotes.
Competing interests
There are no competing interests to report.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Park, G.M., Hong, A.J. “ Not yet a doctor”: medical student learning experiences and development of professional identity. BMC Med Educ 22 , 146 (2022). https://doi.org/10.1186/s12909-022-03209-w
Download citation
Received : 31 July 2021
Accepted : 24 February 2022
Published : 04 March 2022
DOI : https://doi.org/10.1186/s12909-022-03209-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Professional identity
- Learning experiences
- Medical students
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Introduction
- Article Information
Results are from logistic regression models controlling for age, Hispanic or Latina/x ethnicity, marital status, parity, tobacco use, prenatal visit utilization, stillbirth, and placental abruption. Other race includes Alaska Native, American Indian, Chinese, Filipino, Guam/Chamorro Hawaiian, Indian, Japanese, Korean, Other Asian/Pacific Islander, Samoan, and Vietnamese. In the sample, 4100 patients had a history of substance use, and 33 760 had no history of substance use; 4636 had a urine toxicology test, and 2199 had any positive test result at labor and delivery. Error bars indicate 95% CIs.
Data Sharing Statement
See More About
Select your interests.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Others Also Liked
- Download PDF
- X Facebook More LinkedIn
Jarlenski M , Shroff J , Terplan M , Roberts SCM , Brown-Podgorski B , Krans EE. Association of Race With Urine Toxicology Testing Among Pregnant Patients During Labor and Delivery. JAMA Health Forum. 2023;4(4):e230441. doi:10.1001/jamahealthforum.2023.0441
Manage citations:
© 2024
- Permissions
Association of Race With Urine Toxicology Testing Among Pregnant Patients During Labor and Delivery
- 1 Department of Health Policy and Management, University of Pittsburgh School of Public Health, Pittsburgh, Pennsylvania
- 2 Friends Research Institute, Baltimore, Maryland
- 3 Department of Obstetrics, Gynecology, and Reproductive Sciences, University of California, San Francisco
- 4 Department of Obstetrics, Gynecology & Reproductive Sciences, University of Pittsburgh School of Medicine, Pittsburgh, Pennsylvania
- 5 Magee-Womens Research Institute, Pittsburgh, Pennsylvania
An estimated 16% of pregnant persons in the US use alcohol (10%) or an illicit substance (6%, including cannabis). 1 Urine toxicology testing (UTT) is often performed at the time of labor and delivery for pregnant patients to evaluate substance use. 2 , 3 We sought to elucidate associations between race and receipt of UTT and a positive test result among pregnant patients admitted to the hospital for delivery.
This cohort study followed the STROBE reporting guideline. Data were extracted from electronic medical records (EMRs) of patients with a live or stillbirth delivery between March 2018 and June 2021 in a large health care system in Pennsylvania. The study was approved by the University of Pittsburgh institutional review board. Informed consent was waived because the research constituted minimal risk. All patients presenting for delivery were verbally screened for substance use using questions adapted from the National Institute on Drug Abuse Quick Screen. 4 Policy specified UTT would be performed for those with a positive screen result, history of substance use in the year prior to delivery, few prenatal visits, or abruption or stillbirth without a clear medical explanation.
We studied 2 binary outcomes: the receipt of UTT (point of care presumptive testing) and a positive test result at delivery. The primary variable of interest, patient race, was conceptualized as a social construct that could manifest in biased or discriminatory delivery of health care. Self-reported race was categorized as Black, White, and other (Alaska Native, American Indian, Chinese, Filipino, Guam/Chamorro Hawaiian, Indian, Japanese, Korean, Other Asian/Pacific Islander, Samoan, and Vietnamese). Substance use history was defined as having a diagnosis of an alcohol, cannabis, opioid, or stimulant use or disorder during pregnancy in the EMR within 1 year prior through delivery. A positive UTT result was defined as at least 1 positive result of a test component, including amphetamines, barbiturates, benzodiazepines, buprenorphine, cocaine, cannabis, methadone, opiates, or phencyclidine. We used multivariable logistic regression models including race and substance use history, adjusting for age, Hispanic or Latina/x ethnicity, marital status, parity, tobacco use, prenatal visit utilization, stillbirth, and placental abruption. We derived mean predicted probabilities of outcomes by race and substance use history. 5 Analyses were conducted using Stata, version 17.
Among 37 860 patients (100% female; mean [SD] age, 29.8 [5.5] years), 16% Black, 76% were White, and 8% were other race ( Table ). Overall, 11% had a history of substance use; opioid use was more common among White patients (40% of all substance use), whereas cannabis use was most common among Black patients (86% of all substance use). The mean predicted probability of having a UTT at delivery was highest among Black patients compared with White patients and other racial groups regardless of history of substance use ( Figure ). For Black patients without a history of substance use, the mean predicted probability of receiving a UTT at delivery was 6.9% (95% CI, 6.4%-7.4%) vs 4.7% (95% CI, 4.4%-4.9%) among White patients. Among Black patients with a history of substance use, the mean predicted probability of receiving a UTT at delivery was 76.4% (95% CI, 74.8%-78.0%) vs 68.7% (95% CI, 67.3%-70.1%) among White patients. In contrast, among those with a history of substance use, the mean predicted probability of having a positive test result was 66.7% (95% CI, 64.8%-68.7%) among White patients and 58.3% (95% CI, 55.5%-61.1%) among Black patients.
In this cohort study, Black patients, regardless of history of substance use, had a greater probability of receiving a UTT at delivery compared with White patients and other racial groups. However, Black patients did not have a higher probability of a positive test result than other racial groups. Limitations of the study include a lack of a sufficient sample size to investigate other racial and ethnic minoritized groups, such as Alaska Native and American Indian patients, and that data were from a single geographical area and may not generalize nationally. To address racial biases, health care systems should examine drug testing practices and adhere to evidence-based practices.
Accepted for Publication: February 4, 2023.
Published: April 14, 2023. doi:10.1001/jamahealthforum.2023.0441
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2023 Jarlenski M et al. JAMA Health Forum .
Corresponding Author: Marian Jarlenski, PhD, MPH, University of Pittsburgh School of Public Health, 130 DeSoto St, A619, Pittsburgh, PA 15261 ( [email protected] ).
Author Contributions: Dr Jarlenski and Mr Shroff had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Jarlenski, Terplan, Krans.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Jarlenski, Krans.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Shroff, Terplan, Brown-Podgorski, Krans.
Obtained funding: Jarlenski, Krans.
Administrative, technical, or material support: Krans.
Supervision: Jarlenski, Krans.
Conflict of Interest Disclosures: Dr Roberts reported receiving grants from the Foundation for Opioid Response Efforts and the University of California, San Francisco CSF Bixby Center for Global Reproductive Health and National Center of Excellence in Women's Health outside the submitted work. Dr Krans reported receiving grants from the National Institutes of Health, Merck, and Gilead outside the submitted work. No other disclosures were reported.
Funding/Support: This work was supported by grant R01DA049759 from the National Institute on Drug Abuse (Dr Jarlenski and Krans).
Role of the Funder/Sponsor: The National Institute on Drug Abuse had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 04 March 2022
An online cursive handwritten medical words recognition system for busy doctors in developing countries for ensuring efficient healthcare service delivery
- Shaira Tabassum 1 ,
- Nuren Abedin 1 ,
- Md Mahmudur Rahman 2 ,
- Md Moshiur Rahman 3 ,
- Mostafa Taufiq Ahmed 4 ,
- Rafiqul Islam 2 , 5 &
- Ashir Ahmed 1 , 2
Scientific Reports volume 12 , Article number: 3601 ( 2022 ) Cite this article
24k Accesses
8 Citations
12 Altmetric
Metrics details
- Health services
- Information technology
- Scientific data
Doctors in developing countries are too busy to write digital prescriptions. Ninety-seven percent of Bangladeshi doctors write handwritten prescriptions, the majority of which lack legibility. Prescriptions are harder to read as they contain multiple languages. This paper proposes a machine learning approach to recognize doctors’ handwriting to create digital prescriptions. A ‘Handwritten Medical Term Corpus’ dataset is developed containing 17,431 samples of 480 medical terms. In order to improve the recognition efficiency, this paper introduces a data augmentation technique to widen the variety and increase the sample size. A sequence of line data is extracted from the augmented images of 1,591,100 samples and fed to a Bidirectional Long Short-Term Memory (LSTM) network. Data augmentation includes pattern Rotating, Shifting, and Stretching (RSS). Eight different combinations are applied to evaluate the strength of the proposed method. The result shows 93.0% average accuracy (max: 94.5%, min: 92.1%) using Bidirectional LSTM and RSS data augmentation. This accuracy is 19.6% higher than the recognition result with no data expansion. The proposed handwritten recognition technology can be installed in a smartpen for busy doctors which will recognize the writings and digitize them in real-time. It is expected that the smartpen will contribute to reduce medical errors, save medical costs and ensure healthy living in developing countries.
Similar content being viewed by others

A new dataset for mongolian online handwritten recognition

EMD-based data augmentation method applied to handwriting data for the diagnosis of Essential Tremor using LSTM networks

BEHRT: Transformer for Electronic Health Records
Introduction.
A global study reports that Bangladeshi physicians spend less than a minute on each primary consultation whereas physicians of Sweden spend 22.5 min 1 . This happens due to the massive population and limited number of physicians available for them in developing countries. The ideal doctor to population ratio recommended by World Health Organization (WHO) is 1:1000, while on the contrary, the ratio in Bangladesh is only 0.304:1000 2 . The consultation time of doctors includes listening to patients’ problems, inspecting test reports, writing a prescription, explaining the patients’ condition and giving advises. As they serve a large number of patients in a very short time, they are left with less time for writing a prescription. Thus, the handwriting on the prescription becomes cursive and indecipherable for the patients and pharmacists. As a result, the pharmacists misread the prescriptions due to the similar appearances or sounds of thousands of medication names 3 and end up providing the patients with wrong medicines.
This research conducted an online survey to understand the current state of handwritten prescription usage in the medical practice of Bangladesh. The survey reports that 97.1% of Bangladeshi doctors still generate handwritten prescriptions. According to Bhuiyan et al. 4 , incompetency of understanding doctors’ handwritten prescriptions is an obstacle for getting quality health services. The difficulty of reading these prescriptions often causes adverse medical consequences such as selecting wrong medicine, improper number of dosage, and even death. National Academies of Science Institute reports that 7000 deaths occur in the US due to the sloppy handwriting of doctors’ 5 . Doctors can be trained to write legible prescriptions, but they get a very short period of time to serve each patient.
This paper proposes a machine learning approach to assist the doctors by recognizing cursive handwriting of doctors and converting them into readable digital prescriptions. The handwriting recognition system consists of several steps: handwritten data collection, data prepossessing for simplification, increasing data samples using data augmentation, and building a machine learning model for predicting doctors’ handwriting.
Bangladeshi prescriptions are a mixture of Bangla and English words with Latin abbreviations of medical terms 4 . Due to the unavailability of enough Bangladeshi prescriptions online, this research started its journey by creating a ‘Handwritten Medical Term Corpus’. Initially, a medical words corpus is created using the 8,324 Bangladeshi prescriptions of the Portable Health Clinic (PHC). PHC is a remote healthcare system which provides affordable and sustainable health services to the base of the pyramid population of developing countries 6 7 to ensure universal healthcare coverage targeting rurality, poverty, and disability 8 . The PHC data has been used for predicting health status of the existing patients 9 10 in terms of healthcare cost reduction 11 , understanding consumer behavior 12 . However, none of these works considered the doctors’ role in the PHC system.
The ultimate performance of a remote healthcare system depends on the decision made by the doctor. As mentioned earlier, 97% of Bangladeshi doctors still write handwriting prescriptions. The trend is changing to digital prescriptions. The analog prescriptions are not archived in digital forms and are difficult to search for previous medical history. In order to create real-time digital prescriptions, a real-time handwriting recognition system is necessary. At the first step, a ‘Medical Term Corpus’ is needed. We have created a corpus considering the most used words that appeared in the PHC prescriptions. The corpus contains 480 medical-related words (English: 320 and Bangla:120). Afterward, the handwriting of 39 healthcare professionals of these 480 words are collected for the recognition purpose. Thus, the ‘Handwritten Medical Term Corpus’ has 17,431 handwritten instances.
Recognizing different types of handwriting requires a large dataset collected from various sources which is both costly and time-consuming. One way to deal with this problem is data augmentation 13 . This paper proposes a new data augmentation technique - Rotate, Shift, and Stretch (RSS) to generate multitudes of handwriting variations. RSS method takes each stroke of a handwritten word and creates new data by updating the coordinates. After applying RSS, the extended dataset has 1,591,100 samples. For predicting the handwritten words, Bidirectional LSTM model is used due to the recent popularity of Recurrent Neural Network (RNN) in the area of handwriting recognition. According to Zhang et al. 14 , sequence data can contain rich details of handwriting than static image-like representations.
The proposed handwritten technology can be used in a smartpen, specifically designed for doctors. The smartpen will digitize the handwriting of doctors into readable texts. The database will store each doctors’ writings individually to learn the unique pattern of writing of that particular doctor. This will lead the tool to recognize the handwriting of each doctor more efficiently. The smartpen will benefit the doctors by saving time and reducing typographical errors of digital prescriptions.
The rest of the article starts with a review on related researches in “ Related work ”, introduces a handwritten dataset of Bangladeshi doctors in “ Handwritten medical term corpus ”, demonstrates the steps of recognition methodology in “ Methodology of handwriting recognition ”, “ Results and discussion ” reports the results and findings including the idea of a smartpen, and finally, the conclusion is given in “ Conclusion ”.
Related work
Over the last few decades, multitudes of deep learning approaches have been proposed for efficient handwriting recognition using several handwritten datasets of different languages. This section discusses similar research works in the following four sectors:
Doctors’ handwriting dataset
Few online datasets are available to design a doctors’ handwriting recognition system. Dibyajyoti et al. 15 introduced HP_DocPres dataset with 11,340 samples of handwritten and printed words collected from various medical prescriptions. This dataset is prepared to differentiate between handwritten and printed texts. However, the words are not labeled so they can’t be used to recognize the written words by doctors. Another doctors’ handwriting dataset is introduced by Farjado et al. 16 . This dataset contains 1800 images of 12 medicine names collected from 50 doctors from clinics and hospitals of Metro Manila, Quezon City, and Taytay, Rizal in the Philippines. However, this dataset is not suitable for recognizing doctors’ handwriting in Bangladeshi prescriptions due to the limited number of medical terms it contains and the region of data collected being different from our study region.
Although doctors’ handwriting dataset is scarce, there are multitudes of available handwriting datasets both for English and Bangla languages. IAM Dataset by the University of Bern 17 is one of the most popular datasets with the largest handwriting collection in English. This dataset contains 13,353 images of handwritten lines of text created by 657 writers. A similar dataset in Bangla is the Bangla handwriting recognition dataset by Bappaditya et al. 18 that has obtained 79,000 handwritten Bangla word samples written by 77 different writers. BanglaLekha-Isolated 19 and ISI 20 dataset comes with a vast number of handwriting samples of individual Bangla characters with numerals. Another popular dataset is CMATERdb1 21 that has 100 handwritten Bangla pages and 50 handwritten English and Bangla combined pages with ground-truth annotations. However, these datasets do not contain doctors’ handwriting or any medical terms, hence might perform poorly in recognizing doctors’ handwriting.
Offline handwritten character recognition: using image data as input
Automatic conversion of handwritten texts into images for recognition using Convolutional Neural Network (CNN) is called Offline Character Recognition 22 . Shahariar et al. 23 proposed a lightweight CNN model for Bangla handwriting recognition. The model has 13 convolutional layers with 2 sub-layers. The sub-layers are joined together to pass through a max-pooling layer with one 0.25 weighted dropout layer. This model has attained 98%, 96.8% and 96.4% accuracy in BanglaLekha, CMATERdb, and ISI datasets. A modified LeNet-5 CNN model by Yuan et al. 24 obtained an accuracy of 93.7% for uppercase and 90.2% for lowercase for the recognition for English Language characters. Yang et al. 25 presented a path-signature feature method using deep CNN for identifying Chinese character writers. The method was 99.52% accurate with DropStroke data augmentation.
Online handwritten character recognition: using time-series data as input
Online character recognition considers a sequence of times which is captured by the movements of a specialized pen. The recognition rate of the online system is more efficient and higher than the offline system 22 . RNN has recently been widely used in the area of handwriting recognition for showing better recognition performance. The RNNs work with sequence data of coordinates which contain vast information than static images 14 . Bappaditya et al. 18 used bidirectional LSTM using 65,620 handwritten Bangla words dataset and has obtained 79% accuracy. Zhang et al. 14 proposed a conditional RNN-based generative model combining LSTM and Gated Recurrent Units (GRU). The model is built for recognizing Chinese handwritten characters and has achieved 98.15% recognition accuracy. Farjado et al. 16 used Convolutional RNN (CRNN) for recognizing doctors’ cursive handwriting which contained 13 convolutional layers followed by 3 bidirectional LSTM layers and has attained 72% accuracy. However, Achkar et al. 26 reported obtaining 95% accuracy using the similar CRNN model with a different dataset for recognizing medical handwritten prescriptions.
Handwriting recognition with data augmentation
In our previous work, SRP (Stroke Rotation and Parallel-shift) data augmentation technique was applied for expanding the doctors’ cursive handwritten dataset. However, the minimum accuracy of that system was only 68.0% 27 . For recognizing Bangla handwriting characters, Shahariar et al. 23 applied three data augmentation methods on 10% of the dataset: shifted height and width, rotated images by 10 degrees, and zoomed in the images. Another data augmentation method named ‘DropStroke’ was used for Chinese character recognition. Chinese characters are very complex as they have many strokes. Thus, the DropStroke method randomly excludes several strokes and generates new handwritten characters using the combination of the remaining strokes 14 25 . Hayashi et al. 13 used a data augmentation technique using probability distribution for handwriting recognition. This method calculates probability distribution from the features related to the structure of the character. Then, it generates strokes based on the distribution and forms multitudes of new characters.
Ethics approval
All the authors mentioned in the manuscript have agreed for authorship, read and approved the manuscript, and given consent for submission and subsequent publication of the manuscript.
Consent to participate
The written informed consent was obtained from all subjects prior to collecting their handwritten samples in these studies.
Consent for publication
Handwritten medical term corpus.
In developing countries, Doctors’ handwriting becomes illegible as they have to serve a lot of patients in a short span of time. The writings get more difficult to read as Bangladeshi prescriptions are a mixture of different languages. A sample of Bangladeshi prescription is given in Fig. 1 . Due to the shortage of available Bangladeshi prescriptions online, this research has introduced a handwriting prescription dataset collected from Bangladeshi doctors. This section describes the data collection and preparation process for creating a handwritten medical term corpus.
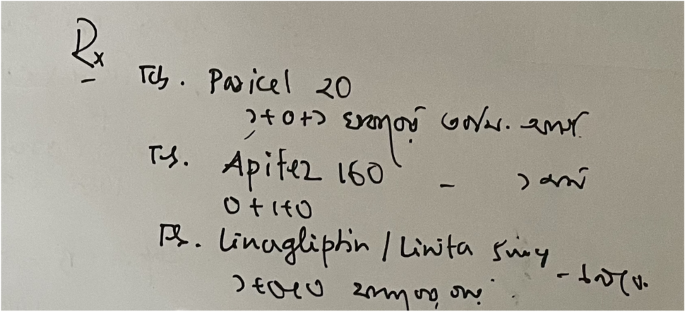
A sample image of Bangladeshi handwritten prescription.
Creating medical corpus from digital prescriptions
Medical terms were collected from the remote healthcare prescription database of PHC. PHC system maintains an electronic journal of patients’ health records. There are major five categories of data in the journal: (1) registration data, (2) survey data, (3) clinical data, iv) conversation data, and v) prescription data. The foremost section of ‘Handwritten Medical Term Corpus’ is collected from the digital prescriptions of PHC. Figure 2 shows a sample of PHC prescription data.
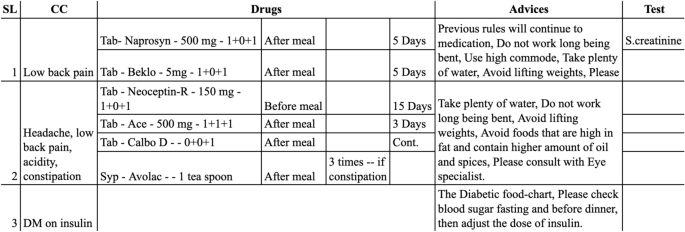
Sample of digital prescription of PHC.
A total of 8324 digital prescriptions were found in the PHC database. Each prescription contained several columns such as symptoms, medicine names, advises. Initially, a corpus of medical terms is created using the most frequently appeared words in these columns. The corpus has selected 360 English and 120 Bangla words. These words are sorted according to the frequency of their appearance in the prescriptions, as shown in Fig. 3 .
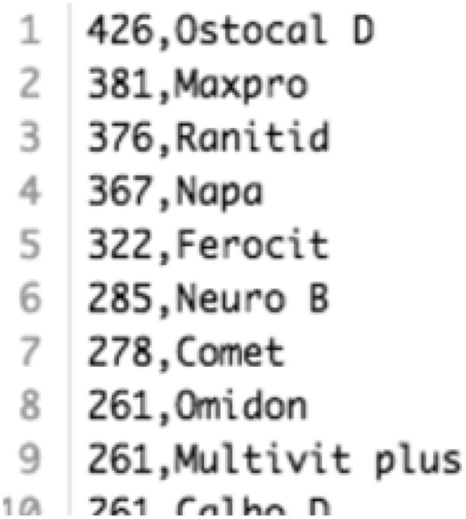
A segment from the Medical Term Corpus.
Obtaining handwritten data via android application
A simple android app has been developed to obtain real handwriting data from doctors and medical professionals. The app displays medical words on the device screen one by one from the ‘Medical Term Corpus’. Then, the data providers write the corresponding words shown on the screen. Samsung Galaxy Tab S3 was used to capture data as it contains a stylus pen. The data providers write down on the screen using the stylus pen and the application stores the handwritten words in the database. Besides the writings, the application also receives detailed information such as pen movements (xy coordinates) and the status of the pen. Status indicates the state of the pen whether it is up or down. Collected information is stored in the database along with the writings as sequential data. The ‘Handwritten Medical Term Corpus’ also contains the original corpus data to use as truth value while training the machine learning model. The complete data collection process is shown in Fig. 4 a.
Dataset profile
There are 480 medical words (360 English and 120 Bangla) in the ‘Handwritten Medical Term Corpus’. These words are chosen based on the number of appearances in 8324 Bangladeshi prescriptions. The handwritings are collected from 39 medical professionals and doctors of Bangladesh. Due to receiving incomplete data from 12 data providers, 1,289 samples are missing in the dataset. Hence, the dataset has 17,431 handwritten instances of 480 medical-related words. All the data were collected by maintaining authenticity, security, and privacy of the data providers, and the experiments were performed in accordance with relevant guidelines and regulations.

Methodology of handwriting recognition
After the data collection phase (Fig. 4 a), the research is administered in three steps, as shown in Fig. 4 b–d. First, the collected dataset is analyzed and preprocessed. Then, the proposed RSS (Rotation, Shift, and Stretch) data augmentation technique is applied to the preprocessed dataset to expand the number of instances. In this step, sequence line data is generated from the extended dataset. Finally, a bidirectional LSTM model uses the sequence data as input and predicts handwritten medical terms.
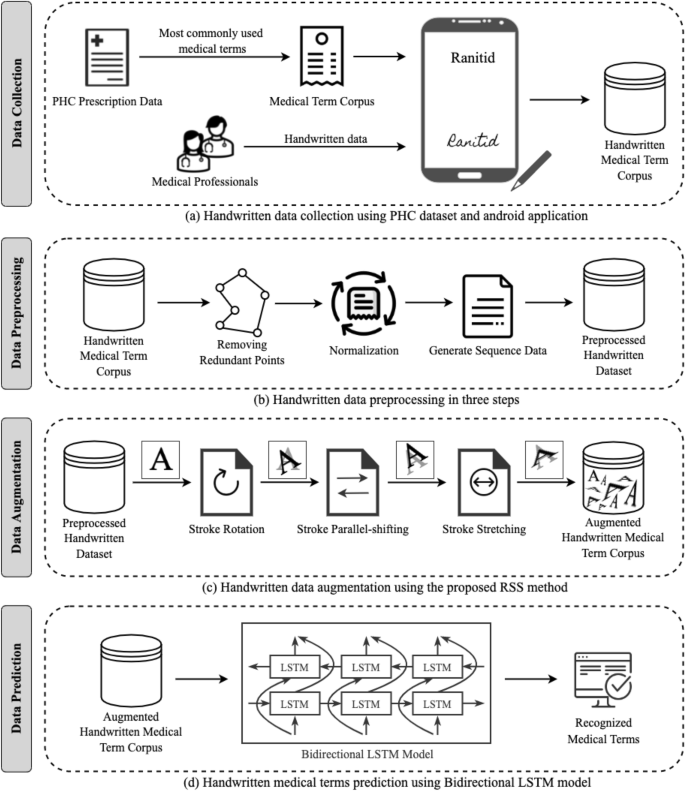
Overview of the handwritten medical terms recognition system.
Data preprocessing
Image-like representations provide very general information about the data. Whereas raw data is rich with information such as spatial and temporal details. These spatio-temporal information can be constituted in a sequence of variable length 14 , given in equation ( 1 ). Here, \(x_i\) and \(y_i\) denotes the xy-coordinates of pen movements and \(s_i\) states the stroke number of any point i .
As shown in Fig. 4 b, the preprocessing is done in three steps. The images are simplified through removing nearby repetitive points and normalization. Then, a six-dimensional vector is extracted sequentially for each stroke to generate machine learning model input data. The three segments are described below:
Remove redundant points
Different styles of handwriting can be found even in a group of people with the same language. Different people follow different ways of writing such as small, regular, flat, cursive. Each writer creates distinct sampling points even if they are writing the same character. Thus, a general format for each character can be created by removing nearby redundant points for efficiently estimating the handwritten words. To remove all the redundant points from any handwritten word or character, consider a particular point \((x_i, y_i, s_i)\) where point i lies in the same stroke with its nearby points, as such \(s_{i-1} = s_i = s_{i+1}\) . There are two conditions to determine if point i should be removed:
Distance between points: If the distance between two points i and \(i-1\) is very small, then point i is removed. In the given Eq. ( 2 ), the threshold \(T_{dist}\) = \(0.005 * max(H,W)\) , where H indicates the vertical and W indicates the horizontal widths of the handwriting text input place. Besides, two connecting points lying on a straight line is also be removed.
Cosine similarity: Cosine similarity determines the similarity of an inner product space between two non-zero vectors. Point i is removed if similarity between two points i and \(i-1\) is greater than the threshold cosine angle value. In the given Eq. ( 3 ), the threshold \(T_{cos}\) is set to 0.99.
Point i is considered as a redundant point if one of the given conditions is satisfied. After removing the redundant points, the shape of the handwritten character is well-preserved and each point of the recreated form contains more information 14 . An example of removing redundant points on a sample handwritten medical term is shown in Fig. 5 .
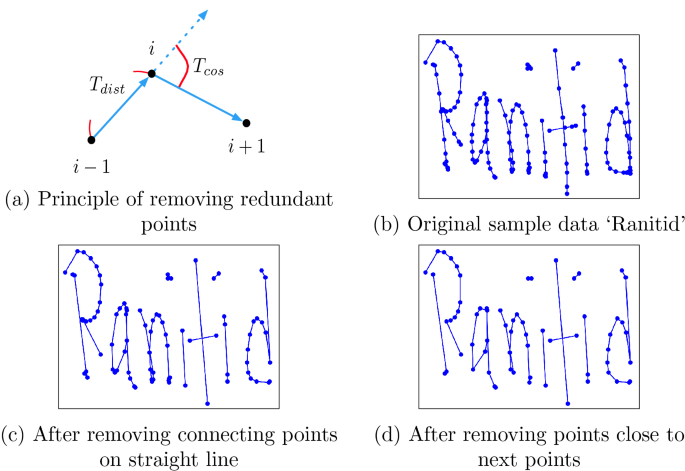
Remove redundant points from handwritten data.
Normalization
After removing the redundant points, the data is normalized for simplification. For x and y coordinates, the maximum \(x_{max}\) , \(y_{max}\) and the minimum \(x_{min}\) , \(y_{min}\) is calculated from each data point. Then, x as X and y as Y coordinates is normalized to \(X_{nor}\) and \(Y_{nor}\) using Eq. ( 4 ). Thus, the ( x , y ) coordinates data is scaled between the value of 0 and 1.
Generate sequence data
After the data preprocessing steps, this research has connected the normalized points to form straight lines. Then, a six-dimensional vector is generated from the straight line as \(L_i\) with two connecting points i and \(i+1\) , as shown in Eq. ( 5 ).
In the given equation, \(x_i\) and \(y_i\) are the xy-coordinates which states the starting position of a line. The direction of pen movements in x and y axis is denoted by \(\Delta {x_i}\) and \(\Delta {y_i}\) . The last two expressions determine the status of the pen ([0, 1] indicates pen-up, [1, 0] indicates pen-down). The term \(I(s_i=s_{i+1}) = 1\) indicates that the starting and ending points of the straight line lies on the same stroke. The last expression \(I(s_i \ne s_{i+1}) = 1\) states that the line has moved to the next stroke. Thus, a new sequence of vectors \([L_1, L_2, \ldots , L_{n-1}]\) is formed from the ( x , y , s ) coordinates. This newly generated sequence is denoted as \([x_1,x_2,\ldots ,x_k]\) for simplification, where each \(x_i\) represents one six-dimensional vector 14 .
Data augmentation
This research has used data augmentation on the preprocessed data in order to increase the number of instances of ‘Handwritten Medical Term Corpus’. A new data augmentation approach named RSS (Rotation, Shift, and Stretch) is proposed in this article. RSS method expands data by rotation, shifting, and stretching the shape of character, as shown in Fig. 4 c. This method is specifically designed to expand the variety of handwriting styles.
Rotate (stroke rotation)
In stroke rotation, the middle point of a stroke ( a , b ) is determined using the starting point \((x_f, y_f)\) and ending point \((x_l, y_l)\) coordinates, as in Eq. ( 6 ). Then, all the points lying on the middle point of that stroke are rotated. The principle of the rotation process is shown in Fig. 6 a.
Stroke rotation process uses Eq. ( 7 ) to rotate a point ( x , y ) in \(\theta \) angle around the middle point of the stroke ( a , b ). The rotated point is ( X , Y ).
This equation is applied to all of the points on the stroke to rotate the entire stroke around the midpoint of the stroke. Figure 6 b is a sample example where the blue color is the original instance and the red color is the instance after rotation. This method is applied to the strokes with random values of angles in order to create new augmented data in different forms.
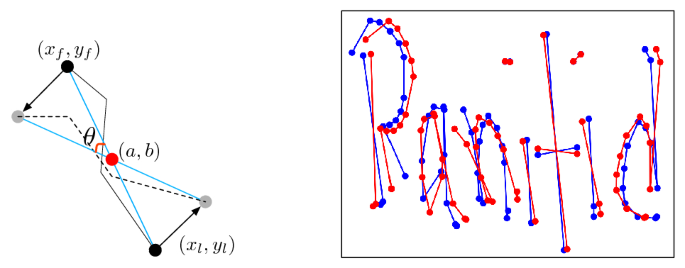
( a ) Principle of rotation, ( b ) sample data after preprocessing (blue) and after rotation (red).
Shift (stroke parallel-shift)
In this second method, all of the points on the stroke are added to a constant number ( x , y ) in order to shift the strokes in parallel. The principle of parallel-shifting is given in Fig. 7 a. One certain point ( x , y ) is shifted to a new point ( X , Y ) following Eq. ( 8 ).
The entire stroke is shifted by ( dx , dy ) after applying this equation to every point on the stroke. Figure 7 b is a sample example where the blue color is the original instance and the red color is the instance after shifting. This method is applied to the strokes with random values of dx and dy in order to create new augmented data in different forms.
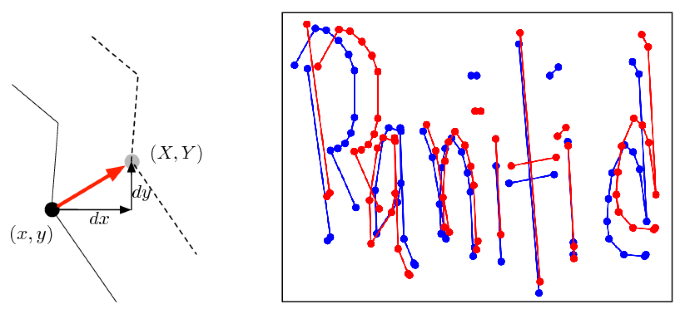
( a ) Principle of shifting, b sample data after preprocessing (blue) and after Shifting (red).
Stretch (stroke stretching)
When a writer writes very quickly and roughly, the letters may be stretched vertically or horizontally. Hence, the stroke stretching method is proposed which takes all the strokes of a word and stretches the strokes to change the ratio of the handwritten word. The principle of this method is shown in Fig. 8 a. First, the average value of the y-coordinates is calculated for all the points of a stroke as the reference value Y . If a certain point \((x_i, y_i)\) has larger y-coordinate that Y , then the value of \(y_i\) is multiplied by \((1 + r)\) , otherwise it’s multiplied by \((1 - r)\) , shown in Eq. ( 9 ). Here, r is the changing ratio rate and is set to 0.02.
However, when the writing is stretched, the points do not overlap and do not break the shape of the character. Figure 8 b is a sample example where the blue color is the original instance and the red color is the instance after stretching. According to the findings of this research, this is an effective method for identifying rough handwriting.
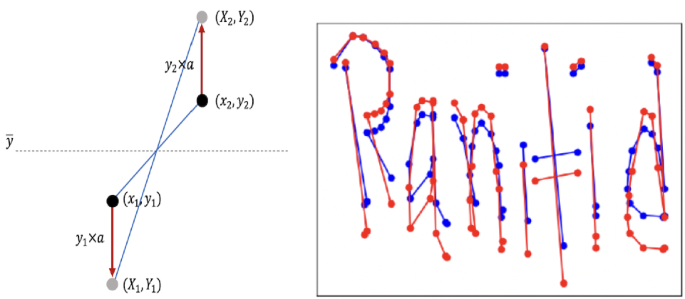
( a ) Principle of stretching, ( b ) sample data after preprocessing (blue) and after stretching (red).
Regenerating sequence data
The original dataset contains six-dimensional vectors for all the instances. After data augmentation, the vectors need to be regenerated for the new augmented images by updating the parameters. For the rotated images, the values are updated by adding \(\theta \) with \(\Delta {x_i}\) and \(\Delta {y_i}\) , Eq. ( 10 ). To update the vector for parallel-shifting, dx and dy is added to \(x_i\) and \(y_i\) , Eq. ( 11 ). Finally, the values of \(x_i\) and \(y_i\) are multiplied with r for the stretched images, Eq. ( 12 ). However, the values of \(I(s_i=s_{i+1})\) and \(I(s_i \ne s_{i+1})\) remain unchanged.
The RSS data augmentation is designed specifically targeting handwriting data as the operations are done by updating the strokes. It can also be used for other datasets if the data are obtained as time series—a sequence of coordinates. If the time series data is converted into images, it can also be used for the expansion of offline characters. The augmented data is stored in the ‘Augmented Handwritten Medical Term Corpus’ dataset, as shown in Fig. 4 c.
Machine learning model: bidirectional LSTM
Handwriting contains multiple strokes with several points. Writing style, speed, order, shape of the character varies from person to person which information is difficult to achieve from static images. Hence, this research has dealt with raw sequential data rather than generating image-like representations in order to get rich information about doctors’ handwriting.
This research has used Bidirectional LSTM to develop a complete end-to-end recognition system by operating the sequence data extracted from the line data of the augmented handwritten dataset, as shown in Fig. 4 d. Bidirectional LSTM uses both past and future inputs for prediction, as shown in Fig. 9 , whereas the original LSTM considers only past inputs 28 . In this research, the machine learning model has used both past and future line data to calculate parameters and predict handwritten medical words.
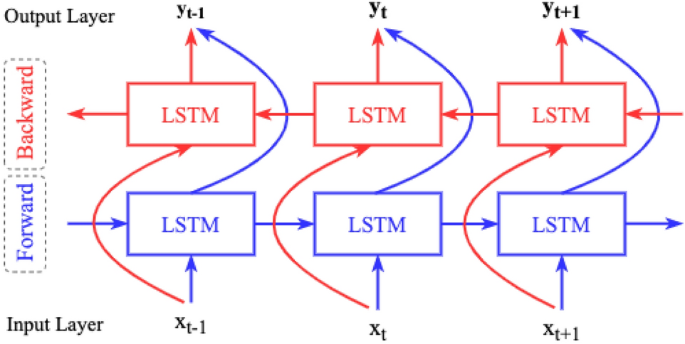
Concept of bidirectional LSTM.
The model architecture for this research is developed using Keras - a neural network library of python. The maximum length of each data is set to 260 by padding zeroes by the end of the instances. There are 300 hidden LSTM layers with corresponding pooling layers. In order to avoid over-fitting, Dropout is used between pooling layer and dense layer 29 . As the model learns the same data many times due to using data augmentation, the Early Stopping method is also used to circumvent overfitting 30 . The Bidirectional LSTM model has the following parameters:
Activation function: Softmax 31
Batch size: 512 32
Learning rate: 0.001 32
Number of epochs: 5 32
Loss function: Categorical cross-entropy 33
Optimization function: Adam 34
Dropout: 0.3 29
Results and discussion
The ‘Handwritten Medical Term Corpus’ contains 17,431 handwritten samples of 480 medical words. The writings are obtained from 39 medical professionals. Among the 39 sets, there are 27 complete sets of instances due to receiving incomplete data from 12 writers. Three sets of 480 words are randomly selected from the complete sets as test data. Thus, the train data has 15,911 and the test data has 1440 handwritten samples. The data augmentation methods are applied only to the train data. Thus, the Bidirectional LSTM model is trained using the extended sequence data and is evaluated based on its performance on the test set.
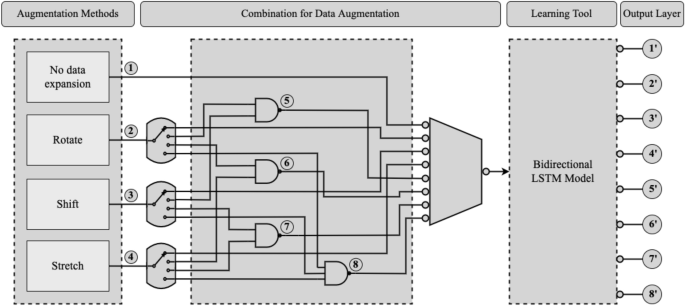
Training bidirectional LSTM model by different combination of data augmentation methods.
This research has performed eight sets of experiments by training the model with eight different mixtures of handwritten data. Figure 10 demonstrates the applied eight datasets expanded using different combination of data augmentation methods. The performance of the model is evaluated based on its accuracy on the same test set. The findings from the model evaluation are as follows, given in Table 1 :
No data expansion: First, the bidirectional LSTM model is trained on the original ‘Handwritten Medical Term Corpus’ with 15,911 instances without applying any data augmentation method. This case has attained the lowest accuracy.
Rotate: This case has trained by model by applying only Rotation data augmentation method. Rotation is applied 100 times on each instances and the data size becomes 1,591,100. This experiment has achieved high maximum accuracy, but the lowest and unacceptable minimum accuracy which is only 3.33%.
Shift: Shifting data augmentation is used 100 times on the train data. It has shown overall good performance in all the above three measurements.
Stretch: Stretching data augmentation is applied similarly on the train data and the expanded data size is 1,591,100. This experiment has achieved similar results to Shifting data augmentation.
Rotate + Shift: This experiment has combined the Rotate and Shift data augmentation methods. First, each instance is rotated ten (10) times and the data size becomes 159,110. Then, Shift method is performed for another ten (10) times on the expanded instances. Thus, the final data size gets 1,591,100 instances. The maximum accuracy is quite high but the minimum accuracy is comparatively low.
Rotate + Stretch: The combined Rotation and Stretching methods are applied in this experiment in the similar way. This case has attained the highest maximum accuracy. However, the average and minimum accuracy is low comparing to the other cases.
Shift + Stretch: Shifting and Stretching data augmentation methods are combined in this case. The data size is 1,591,100 by applying the methods ten (10) times each. This experiment has also accomplished overall considerable accuracy, but better results were observed when these two methods are applied individually on the training data (case 3 and 4 ).
Rotate + Shift + Stretch (RSS): Finally, this is the proposed data augmentation technique of this research. It applies all the three methods on the training data one by one. First, the instances are rotated five (5) times. Then, shifting is performed for another five (5) times on the expanded 79,555 instances. The data size becomes 397,775 where we have applied the stretch method for four (4) times. Thus, this research introduces the ‘Augmented Handwritten Medical Term Corpus’ which contains 1,591,100 handwritten medical term samples. The Bidirectional LSTM model with RSS data augmentation has achieved the highest average and minimum accuracy. It could not reach the highest maximum accuracy but the accuracy never plunged under 92.1%. Thus, this experiment can be considered as the best possible method for recognizing doctors’ cursive handwriting.
IoT smartpen for doctors: an application example
The handwriting recognition tool can be installed in a doctor’s smartpen, which is an ongoing work at our research institution. As shown in Fig. 11 , the smartpen has seven major modules. The same recognition tool can also be installed in tablet PCs. The Handwriting Stroke Detector contains a sensor in the nib of the pen to collect words written by a doctor. The Fingertip Sensor will recognize the authorized user of the pen so that unauthorized person can not use the pen. The Memory will store all the prescriptions so that the doctor can easily find previous health records. It can also store new patterns of words written by the doctor.
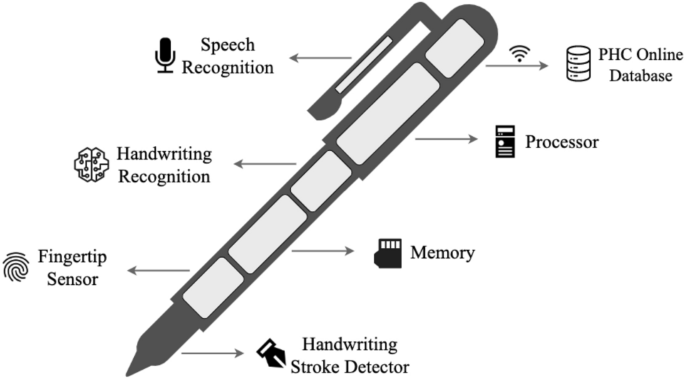
IoT smartpen design for doctors.
In this way, the data set will get larger day by day. The system will also able to capture the unique handwriting habit of that particular doctor. The Handwriting Recognition tool will recognize the words written by the doctor and convert them into text to store it to the memory. A copy of the prescription will also be stored in PHC Online Database that can be accessed by the patient, authorized pharmacy and family members. The Speech Recognition will be used as a sound recorder to generate prescriptions from doctors’ speech through voice recognition. However, that module will use a different technology which is not part of this particular research of handwriting recognition.
As mentioned above, the smartpen is still in the concept level where our handwriting recognition technique can be applied. This smartpen will handle sensitive information such as patients’ identification, medical history, doctors’ profiles including bio-metric information. The smartpen development process will follow relevant privacy security guidelines such as data privacy for m-health patients 35 , location based privacy 36 , privacy protection of health records from search engines 37 .
The objective of this research has been to recognize doctors’ handwriting and digitize the prescriptions in real time. Towards this goal, this paper contributes in three steps- (a) develop a medical term corpus (b) introduce a unique data augmentation technique and (c) use a machine learning approach for final recognition. It also compares the recognition accuracy in different augmentation stages.
The machine learning approach was designed for recognizing particularly doctors’ cursive handwriting and converting them into digital printed texts. A dataset named ‘Handwritten Medical Term Corpus’ was created from digital prescriptions of PHC that contains 17,431 handwritten texts of 480 Bangla and English medical-related words. A data augmentation method RSS was proposed for enriching the variety of doctors’ handwriting. RSS method expanded the data set to 1,591,100 instances which was also introduced in this paper named ‘Augmented Handwritten Medical Term Corpus’. Bidirectional LSTM model was used to create an online character recognition system for predicting doctors’ handwriting. This research performed eight experiments on the handwritten data set and achieved 93.0% average accuracy (max: 94.5%, min: 92.1%) using Bidirectional LSTM and RSS data augmentation. This accuracy was 19.6% higher than the recognition result with no data expansion.
The current accuracy needs to be improved. The proposed recognition methodology can be implemented in a smartpen for doctors. A brief system architecture of the proposed smartpen is introduced. Doctors will use the smartpen for writing and the tool will automatically convert the handwriting texts into digital prescriptions. Apart from the proposed method for data augmentation, other representative computational intelligence algorithms can be used to solve similar problems like Monarch Butterfly Optimization (MBO) 38 , Earthwarm Optimization Algorithm (EOA) 39 , Elephant Herding Optimization (EHO) 40 , Moth Search (MS) Algorithm 41 , and Harris Hawk Optimization (HHO) 42 . More samples will be collected and will be automatically stored in the corpus. Doctors personal handwriting habit will also be captured. More samples will improve the recognition accuracy.
Data availability
The data and materials are available in the Social Technology Lab page at http://socialtech.gramweb.net/media-archive/codes .
Code availability
All codes are available in the Social Technology Lab page at http://socialtech.gramweb.net/media-archive/codes .
Irving, G. et al. International variations in primary care physician consultation time: A systematic review of 67 countries. BMJ Open 7 (10), e017902 (2017).
Article Google Scholar
Kumar, R. & Pal, R. India achieves WHO recommended doctor population ratio: A call for paradigm shift in public health discourse!. J. Family Med. Primary Care 7 (5), 841 (2018).
Jeetu, G. & Girish, T. Prescription drug labeling medication errors: A big deal for pharmacists. J. Young Pharm. 2 (1), 107–111 (2010).
Article CAS Google Scholar
Bhuiyan, B. et al. Assessing whether medical language is a barrier to receiving healthcare services in Bangladesh: An exploratory study. BJGP Open 3 (2), 1–9 (2019).
Brits, H. et al. Illegible handwriting and other prescription errors on prescriptions at National District Hospital. Bloemfontein. Prof. Nurs. Today 21 (2), 53–56 (2017).
Google Scholar
Ahmed, A., Inoue, S., Kai, E., Nakashima, N., & Nohara, Y. Portable Health Clinic: A pervasive way to serve the unreached community for preventive healthcare. In International Conference on Distributed, Ambient, and Pervasive Interactions (pp. 265–274). Springer (2013).
Ahmed, A., Rebeiro-Hargrave, A., Nohara, Y., Maruf, R., Ghosh, P., Nakashima, N., & Yasuura, H. Portable health clinic: A telehealthcare system for unreached communities. In Smart Sensors and Systems (pp. 447–467). Springer, Cham (2015).
Podder, K., Tabassum, S., Khan, L., Salam, K., Maruf, R., & Ahmed, A. Design of a sign language transformer to enable the participation of persons with disabilities in remote healthcare systems for ensuring universal healthcare coverage. In 2021 IEEE Technology and Engineering Management Conference-Europe (TEMSCON-EUR) (pp. 1–6). IEEE (2021).
Tabassum, S., Sampa, M., Islam, R., Yokota, F., Nakashima, N., & Ahmed, A. A data enhancement approach to improve machine learning performance for predicting health status using remote healthcare data. In 2020 2nd International Conference on Advanced Information and Communication Technology (ICAICT) (pp. 308–312). IEEE (2020).
Sampa, M. et al. Blood uric acid prediction with machine learning: Model development and performance comparison. JMIR Med. Inform. 8 (10), e18331 (2020).
Tabassum, S., Sampa, M., Maruf, R., Yokota, F., Nakashima, N., & Ahmed, A. An analysis on remote healthcare data for future health risk prediction to reduce health management cost. In APAMI 2020: 11th Biennial Conference of the Asia-Pacific Association for Medical Informatics (pp. 115–119). (2020).
Hossain, M., Okajima, H., Kitaoka, H., Yokota, F., & Ahmed, A. eHealth Consumer Behavior. In Behavior Engineering and Applications (pp. 129–147). Springer, Cham (2018).
Hayashi, T., Gyohten, K., Ohki, H., & Takami, T. A study of data augmentation for handwritten character recognition using deep learning. In 2018 16th International Conference on Frontiers in Handwriting Recognition (ICFHR) (pp. 552–557). IEEE (2018).
Zhang, X. Y., Yin, F., Zhang, Y. M., Liu, C. L. & Bengio, Y. Drawing and recognizing Chinese characters with recurrent neural network. IEEE Trans. Pattern Anal. Mach. Intell. 40 (4), 849–862 (2017).
Dhar, D., Garain, A., Singh, P. & Sarkar, R. HP_DocPres: A method for classifying printed and handwritten texts in doctor’s prescription. Multimed. Tools Appl. 80 (7), 9779–9812 (2020).
Fajardo, L., Sorillo, N., Garlit, J., Tomines, C., Abisado, M., Imperial, J., Rodriguez, R., & Fabito, B. Doctor’s cursive handwriting recognition system using deep learning. In 2019 IEEE 11th International Conference on Humanoid, Nanotechnology, Information Technology, Communication and Control, Environment, and Management (HNICEM) (pp. 1–6). IEEE (2019).
Bunke, H. IAM handwriting database (INF, University of Bern, Research Group on Computer Vision and Artificial Intelligence, 2000).
Chakraborty, B., Mukherjee, P., & Bhattacharya, U. Bangla online handwriting recognition using recurrent neural network architecture. In Proceedings of the Tenth Indian Conference on Computer Vision, Graphics and Image Processing (pp. 1–8) (2016).
Biswas, Mithun et al. BanglaLekha-Isolated: A multi-purpose comprehensive dataset of Handwritten Bangla Isolated characters. Data Brief. 12 , 103–107 (2017).
Bhattacharya, U. & Chaudhuri, B. B. Handwritten numeral databases of Indian scripts and multistage recognition of mixed numerals. IEEE Trans. Pattern Anal. Mach. Intell. 31 (3), 444–457 (2009).
Sarkar, R. et al. CMATERdb1: A database of unconstrained handwritten Bangla and Bangla-English mixed script document image. Int. J. Doc. Anal. Recognit. (IJDAR) 15 (1), 71–83 (2012).
Priya, A., Mishra, S., Raj, S., Mandal, S., & Datta, S. Online and offline character recognition: A survey. In 2016 International Conference on Communication and Signal Processing (ICCSP) (pp. 0967–0970). IEEE (2016).
Rabby, A., Haque, S., Islam, S., Abujar, S. & Hossain, S. Bornonet: Bangla handwritten characters recognition using convolutional neural network. Proc. Comput. Sci. 143 , 528–535 (2018).
Yuan, A., Bai, G., Jiao, L., & Liu, Y. Offline handwritten English character recognition based on convolutional neural network. In 2012 10th IAPR International Workshop on Document Analysis Systems (pp. 125–129). IEEE. (2012).
Yang, W., Jin, L., & Liu, M. Character-level Chinese writer identification using path signature feature, dropstroke and deep CNN. arXiv preprint arXiv:1505.04922 . (2015).
Achkar, R., Ghayad, K., Haidar, R., Saleh, S., & Al Hajj, R. Medical Handwritten Prescription Recognition Using CRNN. In 2019 International Conference on Computer, Information and Telecommunication Systems (CITS) (pp. 1–5). IEEE (2019).
Tabassum, S., Takahashi, R., Rahman, M., Imamura, Y., Sixian, L., Rahman, M., & Ahmed, A. Recognition of doctors’ cursive handwritten medical words by using bidirectional LSTM and SRP data augmentation. In 2021 IEEE Technology & Engineering Management Conference-Europe (TEMSCON-EUR) (pp. 1–6). IEEE (2021).
Schuster, M. & Paliwal, K. Bidirectional recurrent neural networks. IEEE Trans. Signal Process. 45 (11), 2673–2681 (1997).
Article ADS Google Scholar
Srivastava, N., Hinton, G., Krizhevsky, A., Sutskever, I. & Salakhutdinov, R. Dropout: A simple way to prevent neural networks from overfitting. J. Mach. Learn. Res. 15 (1), 1929–1958 (2014).
MathSciNet MATH Google Scholar
Prechelt, L. Early Stopping—but when?. In Neural Networks: Tricks of the Trade: Second Edition (pp. 53–67). Springer, Berlin, Heidelberg (2012).
Nwankpa, C., Ijomah, W., Gachagan, A., & Marshall, S. Activation functions: Comparison of trends in practice and research for deep learning. arXiv preprint arXiv:1811.03378 (2018).
Nagaoka, T. Hyperparameter optimization for deep learning-based automatic melanoma diagnosis system. Adv. Biomed. Eng. 9 , 225–232 (2020).
Zhang, Z., & Sabuncu, M. R. Generalized cross entropy loss for training deep neural networks with noisy labels. In 32nd Conference on Neural Information Processing Systems (NeurIPS). (2018).
Kingma, D. P., & Ba, J. Adam: A method for stochastic optimization. arXiv preprint arXiv:1412.6980 . (2014).
Regulation, G. D. P. General data protection regulation (GDPR). Intersoft Consulting, Accessed in January 2022. (2018).
Wu, Z. et al. A location privacy-preserving system based on Query range cover-up or location-based services. IEEE Trans. Veh. Technol. 69 (5), 5244–5254 (2020).
Wu, Z., Shen, S., Lian, X., Su, X. & Chen, E. A dummy-based user privacy protection approach for text information retrieval. Knowl. Based Syst. 195 , 105679 (2020).
Wang, G. G., Deb, S. & Cui, Z. Monarch butterfly optimization. Neural Comput. Appl. 31 (7), 1995–2014 (2019).
Wang, G. G., Deb, S. & Coelho, L. D. S. Earthworm optimisation algorithm: a bio-inspired metaheuristic algorithm for global optimisation problems. Int. J. Bio-Inspired Comput. 12 (1), 1–22 (2018).
Wang, G. G., Deb, S., & Coelho, L. D. S. Elephant herding optimization. In 2015 3rd International Symposium on Computational and Business Intelligence (ISCBI) (pp. 1–5). IEEE (2015).
Wang, G. G. Moth search algorithm: A bio-inspired metaheuristic algorithm for global optimization problems. Memetic Comput. 10 (2), 151–164 (2018).
Heidari, A. A. et al. Harris hawks optimization: Algorithm and applications. Futur. Gener. Comput. Syst. 97 , 849–872 (2019).
Download references
Acknowledgements
The authors are grateful to the team in Global Communication Center (GCC) in Grameen Communications, Bangladesh for collecting data samples for creating the ‘Medical Term Corpus’. Kaze Shindo and Ryo Takahashi of our Social Tech Lab conducted the data augmentation experiments.
No funding has been received for the research work undertaken in this manuscript.
Author information
Authors and affiliations.
Faculty of Information Science and Electrical Engineering, Kyushu University, Fukuoka, Japan
Shaira Tabassum, Nuren Abedin & Ashir Ahmed
Global Communication Center, Grameen Communications, Dhaka, Bangladesh
Md Mahmudur Rahman, Rafiqul Islam & Ashir Ahmed
Graduate School of Biomedical and Health Sciences, Hiroshima University, Hiroshima, Japan
Md Moshiur Rahman
M A G Osmani Medical College, Sylhet, Bangladesh
Mostafa Taufiq Ahmed
Medical Information Center, Kyushu University Hospital, Fukuoka, Japan
Rafiqul Islam
You can also search for this author in PubMed Google Scholar
Contributions
S.T., N.A., and A.A. conducted the experiments, concluded results and findings, and wrote the whole manuscript. M.Ma.R. assisted in data collection. R.I. assisted in data collection and provided guidance in data privacy. M.Mo.R. and M.T.A provided knowledge on current medical prescription mechanisms in Bangladesh, introduced medical professionals for data collection and commented on the findings.
Corresponding author
Correspondence to Shaira Tabassum .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Tabassum, S., Abedin, N., Rahman, M.M. et al. An online cursive handwritten medical words recognition system for busy doctors in developing countries for ensuring efficient healthcare service delivery. Sci Rep 12 , 3601 (2022). https://doi.org/10.1038/s41598-022-07571-z
Download citation
Received : 19 October 2021
Accepted : 21 February 2022
Published : 04 March 2022
DOI : https://doi.org/10.1038/s41598-022-07571-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: AI and Robotics newsletter — what matters in AI and robotics research, free to your inbox weekly.

“The Doctor as a Humanist”: The Viewpoint of the Students
Conference Report and Reflection by Poposki Ognen (University Pompeu Fabra); Castillo Gualda Paula (University of Balearic Islands); Barbero Pablos Enrique (University Autonoma de Madrid); Pogosyan Mariam (Sechenov University); Yusupova Diana (Sechenov University); and Ahire Akash (Sechenov University)

The practice of Medicine as a profession has become very technical; doctors rely on fancy investigations, treatment algorithms and standardized guidelines in treating patients. In a lot of universities, medical students and residents are trained without appreciating the importance of art and the humanities in delivering good care to patients and their families. Factual knowledge is imposed on us, as students, from scientific evidence delivered by highly specialized professionals: those who know more and more about niche subjects.
As a result, when someone decides to become a doctor , it seems that scientific training is the sole priority, with most attention being given to the disease-treatment model. As medical students, we are taught very specific subjects, leaving little or no space or time for any cultural enrichment programs. And yet, Personal growth as a doctor and a human being cannot be achieved unless one is exposed to the whole range of human experience. Learning from art and artists can be one such means of gaining these enriching experiences. We can learn from historians, and from eminent painters, sculptors, and writers, as well as from great scientists. How do we achieve these ends? The following essay summarizes and reviews one attempt at providing answers. The 2nd “Doctor as a Humanist” Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment.
To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference. Culture is a complex phenomenon that includes knowledge, beliefs, artistic production, morals, customs and skills acquired by being part of a society, which can be transmitted consciously or unconsciously, by individuals to others and through different generations.
The humanities are academic disciplines that study the cultural aspects and frailties of being human, and use methods that are primarily analytical, critical, or speculative, which distinguish them from the approaches of the natural sciences. Humanism is the practice of making the human story central. Consequently, the studies of humanities, so invested in human stories, is one aspect of practicing humanism.
Technological and practical progress in medicine has been impressive in the past fifty years. Nevertheless, patients still suffer from chronic conditions such as heart failure, chronic lung disease, depression, and many others. These are conditions where technology cannot significantly change the outcomes or reverse the underlying condition. One of the ways to alleviate suffering is through compassion and empathy where the doctor is a professional who listens to, understands and comforts the patient, as well as engaging the patient as a fellow human being. We need arts and humanities as doctors’ tools to comfort and, perhaps, even to heal. We also need them to remind us that we are ‘merely human’ ourselves, and that we share our humanity with our patients, as equals.
Unquestionably, there are fundamental requirements that every physician must internalize; the conference goal was to explain that one such requirement is the humanistic view. Opera, poetry, philosophy, history, the study of dialectics, biographical readings, and even volunteering abroad can be means of engaging the world for positive change. Sometimes called “soft” skills, these are in fact necessary and valuable qualities to empower ourselves as persons, as well as doctors. The 2nd The Doctor as a Humanist Symposium placed the corner stone in a global project that aims to understand medicine as a multidisciplinary subject, and to establish the concept of humanistic medicine both as a science and an art where the patient and the doctor are human beings working together.

STUDENT PARTICIPATION
The event united experts in Medicine and the Humanities from all over the world. The speakers (doctors, nurses and students) were from Russia, the USA, the UK, Spain, Italy, Germany, Mexico and more. Each day’s program was both intense and diverse, and included plenary lectures and panel sessions. Medical students were highly involved in all parts of the conference, offering us a great chance to introduce our projects, share our opinions on various topics, and discuss our questions connected with the role of the humanities in medicine.We participated in roundtable discussions, which were chaired by experts from different countries. Even though this made us nervous, at the same time it was very important for us, as students, to be a part of it. We discussed the future of medical humanities from various perspectives, and above all our thoughts and ideas were listened to and commented on, on an equal basis with the world’s experts. For once, we could see that our views were being taken into consideration, and we hope that in the future this will be the norm and NOT the exception. We are the future of medicine, and our voices should be heard, too.
At the end of the first day there was a students’ session, where we gave our opinions on the relative importance of the medical humanities from a multicultural viewpoint, and on this particular roundtable there were students from Russia, Spain, Iran, Mexico, Italy, as well as a Nursing resident. One of the students during the session shared her view that “I would like to see medicine through the lens of humanism and empathy, and also implement all its principles in my professional life on a daily basis”. All participants agreed, and although we were representing different countries and cultures there was no disagreement about this. Even though we have not yet faced many of the obstacles of the world of medicine, we can see the role of compassion in clinical practice better perhaps than our seniors. We shared our points of view about this question and its relevance in the different countries. It was an incredible moment, as experts and professors demonstrated a great interest in our ideas.
The program was extremely diverse; however, the main idea that most speakers expressed was how to find, sustain and not lose humanist goals. Brandy Schillace gave an impressive presentation entitled “Medical Humanities today: a publisher’s perspective”, which studied the importance of writing and publishing not only clinical trials, but also papers from historians, literary scholars, sociologists, and patients with personal experiences. The nurses Pilar d’Agosto and Maria Arias made a presentation on the topic of the Nursing Perspective that is one of the main pillars of medical practice. Professor Jacek Mostwin (Johns Hopkins University) shared his thoughts on patients’ memoirs. An Italian student, Benedetta Ronchi presented the results of an interview on medical humanities posed to the participants and speakers during the symposium. The plurality of perspectives made this conference an enriching event and showed us how diverse ideas can help us become better doctors. More importantly, it reminded us of our common humanity.
A significant part of the symposium was dedicated to Medicine and Art. Prof Josep Baños and Irene Canbra Badii spoke about the portrayal of physicians in TV medical dramas during the last fifty years. The book “The role of the humanities in the teaching of medical students” was presented by these authors and then given to participants as gifts. Dr Ourania Varsou showed how Poetry can influence human senses through her own experience in communicating with patients. She believed that many of the opinions and knowledge that we have internalized should be unlearned in order to have a better understanding of the human mind. The stimulus of poetry makes this possible. Poetry allows us to find new ways to express ourselves, and thus increase our emotional intelligence and understanding of other people’s feelings.
One of the most impressive lectures was by Dr Joan.B Soriano, who spoke about “Doctors and Patients in Opera” and showed how the leading roles of physicians in opera have changed over the centuries. People used to consider the doctor as the antihero, but with time this view has transformed into a positive one that plays a huge role in history.
It is important to be professional in your medical career, but also to be passionate about the life surrounding you; for instance, Dr Soriano is also a professional baritone singer. For students, this Symposium was full of obvious and hidden messages, which gave us much lot of food for thought. As Edmund Pellegrino, the founding editor of the Journal of Medicine and Philosophy , said: “Medicine is the most humane of sciences, the most empiric of arts, and the most scientific of humanities.”

CHOOSING ONE WORD
To conclude our summary of the students’ viewpoint each of us chose One word to encapsulate our thoughts about the symposium.
The Doctor as a Humanist is a multicultural event where everyone can learn and contribute to this global necessity to put the heart and soul back into medicine. Of course, we are aware and delighted that other organizations are championing the cause of the Humanities in Medicine, and in some cases, such as https://www.dur.ac.uk/imh/ , they have been doing so for many years.
As medical students, we appreciate how we have been placed at the centre of the symposium, which we believe has made this new initiative rather special. We hope that students of Medicine and from other disciplines come and participate in future symposia.
If you want to learn more, and see how you can participate, please contact the International student representatives, Mariam ( [email protected] ) and David ( [email protected] ).
Acknowledgements
Assistance provided by Jonathan McFarland (c) and Joan B. Soriano (University Autonoma de Madrid) was greatly appreciated during the planning and the development of the article.
Analysis and discussion of research | Updates on the latest issues | Open debate
All BMJ blog posts are published under a CC-BY-NC licence
BMJ Journals
share this!
May 16, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
First-generation medical students face unique challenges and need more targeted support, say researchers
by University of Chicago Medical Center

Medical research is increasingly informed by recognition of diversity's key role in addressing health equity. But when it comes to medical education, there's a group that has remained not just underrepresented but also under-researched: first-generation (first-gen) medical students—those whose parents have not earned bachelor's degrees.
These students are more likely to be older, identify as racial or ethnic minorities, be immigrants or children of immigrants, or come from low-income families . Along with anecdotal evidence, the minimal previous research indicates that these students face some unique struggles on top of the common challenges most medical students encounter.
"It became clear to me that schools—even the great ones that are intentional and diligent about building diverse classes—are not truly ready to receive first-gen students," said Catherine Havemann, MD, an emergency medicine chief resident at UChicago Medicine. "Admission isn't the same as full access to the institution. Sometimes support doesn't exist, and other times it's off-target."
To increase understanding of the first-gen experience and identify opportunities for educators and administrators to provide the most meaningful support, Havemann helped lead a team of researchers to perform an in-depth qualitative study . They analyzed data collected in interviews with a diverse group of medical students recruited from 27 medical schools across the U.S.
The results, published in JAMA , have the potential to inform efforts at increasing educational equity at both the institutional and individual level.
Struggles shared among a diverse first-generation population
Overall, the study confirmed that first-gen medical students feel that they face disproportionate adversity throughout their education and do not receive the support they need to compensate for that. Participants identified four main themes: feelings of isolation and exclusion; difficulties accessing basic resources such as food, rent, transportation and textbooks; a general lack of institutional support; and pressure to rely on personal "grit" and resilience for survival.
Some issues highlighted in the data were relatively unsurprising, such as financial difficulties.
"No matter which subset of first-gen students we talk to, money is a foundational part of the challenges they face—even if they're not technically low-income," said Havemann, the paper's first author. "Within the medical community, we need to talk more about the discomfort of disadvantaged students entering incredibly wealthy institutions with mostly wealthy peers. What does it mean to create some basic degree of equity?"
Other issues emerged as more persistent than the researchers had anticipated. For example, interviewees frequently mentioned transportation problems, such as situations where student loans don't cover the cost of having a car but medical school necessitates one. An especially striking theme was that many students reported being overtly discouraged by mentors or teachers during their education.
"People who meet the criteria for medical school admission are being told 'This is not for you,'" Havemann said. "It's disheartening to see, and it makes me think differently about my career as an aspiring educator. Saying 'yes'—even in a small way—to someone who has heard a lifetime of 'no' can make all the difference. To think there are people out there discouraging others is frankly appalling."
Responding to the findings
Havemann said the paper resonated strongly with student communities online following its publication.
"Responses ranged from 'This is obvious' and 'Water is wet' to 'Why doesn't my school understand this?' or 'We knew this already—where are the solutions?'" she said.
As a former first-gen student herself, she was struck by the consistency of experience revealed by the study's results. "It was validating as a researcher but also profoundly validating as a person."
But while the student response online served as important confirmation that the study's findings are representative, the real target audience is the educators who have the power to make a difference.
"I would love for them to read this paper and feel what a powerful position they're in to make a more equitable world," Havemann said. "Even the little things matter a lot."
Even as she and others conduct more research on this topic, Havemann said institutions can and should already be taking steps to provide better support for first-generation medical students .
"People like to talk about using holistic review in admissions to look at the whole student—we also have to look at holistic support once they enroll," she said.
Future studies will dive deeper into themes like professional identity formation, financial challenges, burnout and sense of belonging. Now that the qualitative groundwork has been laid, researchers can design more nuanced quantitative and mixed-method studies.
"For example, I'd like to quantify the percentage of first-gen students who are not only trying to support themselves but also keeping the lights on for their parents," Havemann said. "I think the answers would be gutting."
Journal information: Journal of the American Medical Association , JAMA Network Open
Provided by University of Chicago Medical Center
Explore further
Feedback to editors

Saturday Citations: The cheapness horizon of electric batteries; the battle-worthiness of ancient armor; scared animals
2 hours ago

Cosmic leap: NASA Swift satellite and AI unravel the distance of the farthest gamma-ray bursts
4 hours ago

Scientists discover CO₂ and CO ices in outskirts of solar system

Charge your laptop in a minute? Supercapacitors can help; new research offers clues
5 hours ago

New study discovers tiny target on RNA to short-circuit inflammation

Researchers develop organic photoredox catalysts with enhanced stability and recyclability
19 hours ago

Theory and experiment combine to shine a new light on proton spin
20 hours ago

On repeat: Biologists observe recurring evolutionary changes, over time, in stick insects

New findings on fertility: Sperm can adapt to sexually transmitted microbes
21 hours ago

Observing mammalian cells with superfast soft X-rays
Relevant physicsforums posts, physics education is 60 years out of date, is "college algebra" really just high school "algebra ii".
May 14, 2024
Plagiarism & ChatGPT: Is Cheating with AI the New Normal?
May 13, 2024
Physics Instructor Minimum Education to Teach Community College
May 11, 2024
Studying "Useful" vs. "Useless" Stuff in School
Apr 30, 2024
Why are Physicists so informal with mathematics?
Apr 29, 2024
More from STEM Educators and Teaching
Related Stories

Exploring challenges in learning for nursing students in Morocco
May 6, 2024

Taking a leave of absence can harm medical students' match prospects, finds study
Apr 16, 2024

First study on teacher effectiveness for students with and without disabilities
Mar 25, 2024

Minority students more likely to leave medical school: study
Jul 19, 2022

Study finds clear instruction, parental support predict students' sense of school belonging
Mar 27, 2024

Medical students with disabilities are at higher risk of burnout than peers
Jan 10, 2024
Recommended for you

Investigation reveals varied impact of preschool programs on long-term school success
May 2, 2024

Training of brain processes makes reading more efficient
Apr 18, 2024

Researchers find lower grades given to students with surnames that come later in alphabetical order
Apr 17, 2024

Earth, the sun and a bike wheel: Why your high-school textbook was wrong about the shape of Earth's orbit
Apr 8, 2024

Touchibo, a robot that fosters inclusion in education through touch
Apr 5, 2024

More than money, family and community bonds prep teens for college success: Study
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Phys.org in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Australas Med J
- v.5(8); 2012
Doctors and Medical Science
Are practicing medical doctors up to date on the latest advances in their field? Is published research valid and reliable? Why are doctors seldom involved in research? The aim of this editorial is to explore some of these complex issues.
Prescribing habits and therapeutic advance
Patients may believe that their doctor is a source of impartial and up to date information in his or her field but how do doctors keep up to date? Gabbayay and Le May reported the following:
‘…clinicians rarely accessed, appraised, and used explicit evidence directly from research or other formal sources; rare exceptions were where they might consult such sources after dealing with a case that had particularly challenged them. Instead, they relied on what we have called “mindlines,” collectively reinforced, internalised tacit guidelines, which were informed by brief reading, but mainly by their interactions with each other…opinion leaders, patients…pharmaceutical representatives and by other sources of largely tacit knowledge that built on their early training and their own and their colleagues' experience’ . 1
Are doctors who prescribe the latest drugs more likely to be up to date? General practitioners for example have been found to be reactive and opportunistic recipients of new drug information, and rarely report undertaking an active information search. The decision to initiate a new drug is heavily influenced by advertising, endorsement by colleagues and hospital consultants. 2 Furthermore new medications offer little, if any, incremental value over existing therapies. The combination of inadequate information about the potential side effects of new drugs plus their limited value strongly argues against their early use except in exceptional circumstances. 3
It is telling that drug companies are spending billions every year promoting their products. 4 It is also notable that many new drugs are withdrawn within a very short time of their launch. 5 Worryingly, there is sometimes a relative lack of urgency when a drug is clearly shown to be harming patients. For example 19.8 million patients were prescribed five questionable drugs before action was taken to remove them from the market. This included painkillers, anti-histamines, drugs used to treat obesity and anti-hypertensive drugs. Not one of these were lifesaving nor, in many cases, were they the only drugs available for that indication.In another case physicians prescribed a new painkiller to 2.5 million patients with acute pain, even though many well-tested similar drugs were available and the drug was known to elevate liver enzymes. Similarly the rationale for not withdrawing an anti-histamine from the market as soon as researchers clearly identified it as causing deaths has not been explained. 6 It is surprising that the drug was not removed from the market when the adverse effects were identified, but only after the manufacturer had developed a new product to substitute for it.
For some relatively rare conditions practicing doctors may know little more than they knew when they first qualified. 7 Physicians who have been in practice for a long time may be at greatest risk of being out of date in their recommendations and practice. Therefore, this group of physicians may need support to be kept abreast of research. 8 Older physicians also seem less likely to adopt newly proven therapies and may be less receptive to new standards of care. 9 - 10 So what is the role of so-called peer reviewed publication?
Publication and medical science
It is estimated that there are 1.29 papers published in the peer reviewed medical literature every minute. 11 Even if a doctor were able to keep up with this volume of reading, it is said that much of what is published is flawed. Richard Smith, former editor of the British Medical Journal (BMJ), is quoted as saying that only 5% of published papers reached minimum standards of scientific soundness and clinical relevance, and in most journals the figure was less than 1%. 12
In the period from 2000–2010 a total of 788 papers have been retracted, i.e. expunged from the public record. 13 Approximately three-quarters of these papers had been withdrawn because of a serious error; the rest of the retractions were attributed to fraud (data fabrication or falsification). The fakes were more likely to appear in leading publications with a high “impact factor”. The impact factor is a proxy measure of how often research is cited in other peer reviewed journals. More than half (53%) of the faked research papers had been written by a first author who was a “repeat offender”. This was the case in only one in five (18%) of the erroneous papers. 13 At about the same time it was estimated that the number of articles published between 1950 and 2004 that ought to be retracted should have been as many as 100,000 and at least 10,000. 14 The authors further conclude that although high impact journals tend to have fewer undetected flawed articles than their lower-impact peers, even the most vigilant journals potentially host papers that should be retracted. 14
Retraction or not, one would like to think that doctors are able to spot flawed papers and, better still, are unlikely to have their clinical practice misled by poor science or glossy leaflets for new and untested treatments. Let us start with the first question: do doctors read research papers? Here is a quote from a doctor writing in the BMJ:
‘The volume of statistical argument [in research papers] also seems part of the same disingenuous process. How many doctors have a clue what it means? Of all the areas of mathematics, probability, and its inscrutable daughter statistics, are the most slippery to grasp. Yet authors routinely drop large chunks of this extremely difficult stuff into papers that are supposed to be there to illuminate practice for doctors. But most doctors, including myself, don’t understand it’. 15
What is the point of publishing research papers that cannot be absorbed by the target audience? One author suggested a possible answer:
‘Authors are eager to get their names in print not because they are bursting to tell us something but for more solemn reasons. Another paper means another line on a curriculum vitae, another step towards a job or a research grant.’ 16
Publishers and medical science
Journals rely on ‘peers’ to decide which papers merit publication and which should be jettisoned. The process of peer review is recognised to be flawed. 17 The quality of the reviews varies. There may be divergent views expressed in the review and it is sometimes difficult to determine why an editor rejects or indeed accepts a submission without concluding that the editor’s biases have played a significant role in that decision. In many cases, especially in niche areas a competitor who may or may not declare a conflict of interest may be invited to review the paper. If the identity of the reviewer is kept from the authors, the reviewer is free to recommend rejection or publication without fear of recrimination in what is known as “blind” peer review. In very specialised topics the identity of authors can be very hard to conceal from an expert in the field at the time of review. Secondly publishing is a powerful, prestigious and lucrative business. No journal yet has taken up a long-standing suggestion to remove the names of authors from published papers. This would ensure that papers are published only for the sake of disseminating information. However to do so would be to make the journal much less attractive to authors and therefore advertisers and other cash cows. 18
To fully appreciate the value of journal articles to their target audience, namely university researchers, and their host institutions one might consider the value of a paper in a highly-rated journal (impact factor >40) compared to one in a more modestly rated one (impact factor <2). A paper in the high impact journal may have an Eigenfactor score of 0.67. The Eigenfactor score calculation is based on the number of times articles from the journal published in the past five years have been cited in the year. 19 A paper published in a ‘lesser’ journal has a Eigenfactor score of 0.003. Naturally a university dean would be impressed with work cited frequently rather than seldom. But what is even more likely is that the academic with the paper in a so-called high impact journal will be more likely to be successful on grant applications and be invited to speak at national and international conferences. All of which may attract postgraduate students, competitive grants and lucrative collaborations. In Australia, for example, universities who employ academics who publish on a predetermined list of journals are more likely to be rewarded with a larger share of government grants and subsidies. 20
That is not to say that publication in the high impact journals means living happily ever after. The reputation of a top rated medical journal was damaged by a controversy involving its response to problems with research on a drug used to treat pain. 21 A study was published in the journal in 2000 which noted an increase in myocardial infarction amongst those using the drug. 21 Concerns about the robustness of that study were raised with the journal in August 2001. At the same time both the US Food and Drug Administration and another major journal also cast doubt on the interpretation of the data that had been published in the journal. However it was not until 2005 that the journal published concern about the original study. During that five-year period funded reprints of the original article were used to promote the offending drug.
Publishing and profit
Most journals are peer reviewed by an unpaid army of academics and editors. The journals may then be sold to libraries. An annual subscription to some journals may be over $20,000. Publishers make substantial profits. Here is a list of published subscription rates for various top-rated journals:
A major publisher of medical journals is a global company based in Amsterdam, employing more than 7,000 people in 24 countries. It claims a global community of 7,000 journal editors, 70,000 editorial board members, 300,000 reviewers and 600,000 authors. In July 2010 the company posted interim profit results with a revenue of almost 3 billion GBP and adjusted profits of 758 million GBP in the six months ending 30 June. 22 This is also the company that was reported to have been paid an undisclosed sum by a pharmaceutical company to produce several volumes of a publication that had the look of a peer-reviewed medical journal, but contained only reprinted or summarised articles, most of which presented data favourable to its products with no disclosure of company sponsorship. 23
Doctors and research
Despite the fact that doctors are key to delivering health care they are seldom involved in research and far less often cited as leaders on research teams. The relationship between the research organisations and doctors is the key to understanding their limited involvement in innovation. ‘Good’ research is a painstaking science in which clearly defined research questions are articulated, appropriate methods are applied, data is efficiently collected and appropriate analysis is conducted to craft conclusions that take into account the limitations and strengths of the study. Seldom, if ever, does a single study, no matter how large, offer robust conclusions that will lead to change in practice. The design and execution of high quality research requires expertise which takes many years of further training and experience. The acquisition of these skills may take doctors out of clinics and at a significant personal opportunity cost.
The subject of clinical research, i.e. patients, must give informed consent before they can be included in a study. This is more complicated than working with uncomplaining rats in a sanitised laboratory. In practice limited control over research subjects means that most clinical research cannot be generalised and is therefore less likely to be published in high impact journals. Most research is also conducted at universities, directly or indirectly. Universities and medical schools have to generate a surplus income to grow in size and influence. Very little research in primary care or public health has a commercial value, therefore to profit from clinical research universities rely on government funding. The government agenda may be driven by political imperative. Therefore a government minister unveiling shiny new machines makes for a far more voter friendly photo opportunity than one launching a more efficient way to rehabilitate people with mental illness or manage incontinence in general practice.
Therefore funding is heavily weighted towards biomedical sciences. Here the focus is on cure rather than prevention or more efficient service delivery. Genetic research, nano particles and the study of prions, is therefore more likely to get generously funded than research on system design that would allow people to die in comfort in their own homes.
In 2010 the Australian National Health and Medical Research Council divided its research funding so that 39% of the funds were awarded to preventive medicine and public health. At the same time the majority of government funding on health care in practice is on so-called primary care services. 24 For universities the return on investment does not favour clinical research, so that laboratory-based research on a cure for cancer makes a far more compelling case than research involving therapists in the community or models of disease self-management. And yet, in the scheme of things, research in how to deliver an equitable health service is going to make more of an impression on the community in the short term than research on a cure for cancer that may be 20 years away.
Academics understand that universities are financially rewarded for adopting this paradigm by a system that is driven by priorities related to a return on investment. Given the competitive nature of those who enrol in medical school this is a considerable disincentive and drives clinicians out of research. As if that was not sufficient disincentive, there are major challenges to recruiting participants in clinical practice. 25 Patients do not seek help from doctors only to spend most of their consultation negotiating an opportunity to participate in research that may or may not benefit them directly. When the patient is paying for the doctor’s time, as is the case in many countries, doctors have no incentive to introduce distractions to that consultation. In reality many of the patients in clinical practice are excluded from research designs which usually favour young, articulate, English speaking, literate, relatively healthy people and not those living with the conditions for whom the evidence has apparently been generated. 26
Doctors are not generally actively involved in research, they may not critically appraise research articles and their knowledge of recent advances in their field may be out of date. For example there are cases of doctors continuing to prescribe drugs that have been reported to cause harm. A vast number of research papers are published every year and most of these have significant limitations and some poor science may even be published in the most influential journals. Publishers and manufacturers of pharmaceuticals have sometimes colluded in ways that do not necessarily benefit patients. The need for specialist research skills as well as research funding structures mean that those most closely involved with patients neither lead research nor participate in research projects. Much of the most generously funded research is aimed at long-term commercial goals rather than to benefit patients.
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The author is the editor in chief of the AMJ
Please cite this paper as: Jiwa M. Doctors and Medical Science AMJ 2012, 5, 8, 462-467. http//dx. doi.org/10.4066/AMJ. 2012.1491

Research involvement of medical students in a medical school of India: exploring knowledge, attitude, practices, and perceived barriers
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Abhinav Jha
- ORCID record for Deepak Dhamnetiya
- For correspondence: [email protected]
- ORCID record for Ravi Prakash Jha
- Info/History
- Preview PDF
Introduction Research in the medical discipline significantly impacts society by improving the general well-being of the population, through improvements in diagnostic and treatment modalities. However, of 579 Indian medical colleges, 332 (57.3%) did not publish a single paper from the year 2005 to 2014," indicating a limited contribution from medical fraternity In order to probe in to the cause of this a study was conducted to assess the knowledge, attitude, practices (KAP) and perceived barriers to research among students of a medical school in Delhi, India.
Methods A cross-sectional study was conducted among medical students and the data on academic-cum-demographic information, assessment of knowledge, attitude, practices and barriers to research was collected using a pre-tested, semi-structured questionnaire. Chi-square test was used to check the association of various factors with the KAP of research. A p-value less than 0.05 was considered significant.
Results A total of 402 (N) subjects were enrolled in the study. Majority were male (79.6%) and from clinical professional years (57%). Majority (266, 66.2%) of the subjects had adequate knowledge. Of the study subjects (61,15%) having inadequate knowledge of research, sixty percent were from pre- and para-clinical years, while around 70 % of those having good knowledge were from clinical professional years. However, only 16.9% of the participants had participated in a research project, and only 4.72% had authored a publication. Sixty one percent of study subjects having a positive attitude towards research, were from pre- and para-clinical years. Among the study subjects having a positive attitude towards research, over 60% were from pre- and para-clinical years. The barriers for conducting research were mostly; lack of funds/laboratory equipment/infrastructure (85.1%), lack of exposure to opportunities for research in the medical (MBBS) curriculum (83.8%), and lack of time (83.3%). There was a statistically significant association between knowledge and attitude towards research with a professional year of study.
Conclusions The study revealed that while most of the students had a positive attitude towards research as well as an adequate knowledge of research, there was a poor level of participation in research. These challenges can be overcome by incorporating research as a part of the medical school curriculum from early years on, setting aside separate time for research, and establishing student research societies that can actively promote research.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This study did not receive any funding.
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
The ethics committee of Dr Baba Saheb Ambedkar Medical College and Hospital, New Delhi gave ethical approval for this work.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Email id: jhaabhinav677{at}gmail.com , manas.shah1999{at}gmail.com , Ritikgoyal152{at}gmail.com , drdeepakdhamnetiya{at}gmail.com , apoorv1729{at}gmail.com , raviprakashjha{at}gmail.com , dr.prachi.obg{at}bsamch.in
Data Availability
All data produced in the present study are available upon reasonable request to the authors.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Medical Education
- Addiction Medicine (324)
- Allergy and Immunology (632)
- Anesthesia (168)
- Cardiovascular Medicine (2399)
- Dentistry and Oral Medicine (289)
- Dermatology (207)
- Emergency Medicine (381)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (850)
- Epidemiology (11795)
- Forensic Medicine (10)
- Gastroenterology (705)
- Genetic and Genomic Medicine (3766)
- Geriatric Medicine (350)
- Health Economics (637)
- Health Informatics (2408)
- Health Policy (939)
- Health Systems and Quality Improvement (905)
- Hematology (342)
- HIV/AIDS (786)
- Infectious Diseases (except HIV/AIDS) (13346)
- Intensive Care and Critical Care Medicine (769)
- Medical Education (368)
- Medical Ethics (105)
- Nephrology (401)
- Neurology (3523)
- Nursing (199)
- Nutrition (528)
- Obstetrics and Gynecology (679)
- Occupational and Environmental Health (667)
- Oncology (1832)
- Ophthalmology (538)
- Orthopedics (221)
- Otolaryngology (287)
- Pain Medicine (234)
- Palliative Medicine (66)
- Pathology (447)
- Pediatrics (1037)
- Pharmacology and Therapeutics (426)
- Primary Care Research (424)
- Psychiatry and Clinical Psychology (3187)
- Public and Global Health (6178)
- Radiology and Imaging (1290)
- Rehabilitation Medicine and Physical Therapy (751)
- Respiratory Medicine (832)
- Rheumatology (380)
- Sexual and Reproductive Health (373)
- Sports Medicine (324)
- Surgery (403)
- Toxicology (50)
- Transplantation (172)
- Urology (147)

IMAGES
VIDEO
COMMENTS
The New England Journal of Medicine (NEJM) is a weekly general medical journal that publishes new medical research and review articles, and editorial opinion on a wide variety of topics of ...
JAMA - The Latest Medical Research, Reviews, and Guidelines. Home New Online Issues For Authors. Editor's Choice: New CDC Survey on H5N1 Preparedness. ATS International Conference: New Trials in Pulmonary and Critical CareMay 19, 2024Original Investigation Pamrevlumab for Idiopathic Pulmonary Fibrosis: The ZEPHYRUS-1 Randomized Clinical Trial ...
Methods. Thirteen semi-structured interviews of English-speaking medical doctors of any specialty were conducted. Recruitment was achieved through the authors' network; contacting authors of relevant research papers; and Bond University's General Practitioner recruitment program.
Explore this issue of The New England Journal of Medicine (Vol. 0 No. 0).
High impact medical journal. Champion of better research, clinical practice & healthcare policy since 1840. For GPs, hospital doctors, educators, policymakers.
The proportions of term or late preterm births after exposure to early antenatal corticosteroids, and outcomes. August 2, 2023. Can't find what you're looking for? Continue to all research articles. Original research studies that can improve decision making in clinical medicine, public health, health care policy, medical education, or ...
Writing a medical research paper is similar to writing other research papers in that you want to use reliable sources, write in a clear and organized style, and offer a strong argument for all conclusions you present. ... With over 25 years of medical research experience, Dr. Matsko was awarded the Pittsburgh Cornell University Leadership Award ...
Abstract. Effective doctor-patient communication is a central clinical function in building a therapeutic doctor-patient relationship, which is the heart and art of medicine. This is important in the delivery of high-quality health care. Much patient dissatisfaction and many complaints are due to breakdown in the doctor-patient relationship.
Overall, the associative algorithm performs on par with the average doctor, achieving a mean accuracy across all trails of 72.52 ± 2.97% vs 71.4 ± 3.01% for doctors. The algorithm scores higher ...
BMC Medical Ethics (2024) Artificial intelligence (AI) is poised to broadly reshape medicine, potentially improving the experiences of both clinicians and patients. We discuss key findings from a ...
Every clinician is responsible for evaluating their own practice, and to do that in a robust and meaningful way you need to use the tools of research. We all need to be able to critically review research done by others. For example, the guidelines used in everyday clinical practice are based on meta-analyses and systematic reviews.
A clinician should continuously strive to increase knowledge by reviewing and critiquing papers, thoughtfully considering how to integrate new data into practice. This is the essence of evidence-based medicine (EBM).[1] When new clinical queries arise, one should seek answers in the published literature. The ability to read a scientific or medical manuscript remains vitally important ...
Your success in getting published shouldn't start with a complete paper. It should start right when you conceptualize your research. Edward Livingston, MD, deputy editor of clinical content for the Journal of the American Medical Association (JAMA), said it all begins with asking the right questions."Re-examine what's in front of you," Dr. Livingston told physicians in training at a ...
A layperson becomes a professional doctor through completion of medical school. In medical education, developing a "professional identity" is essential to becoming a future doctor [1,2,3] in addition to medical knowledge and skills.Professional identity is "a representation of self, achieved in stages over time during which the medical profession's characteristics, values, and norms are ...
Dr. Cummings was a medical student conducting research in the Carolina Health Workforce Research Center at the time this work was conducted. Declaration of Conflicting Interests The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
The JAMA Network - Published continuously since 1883, JAMA is an international peer-reviewed general medical journal published 48 times per year in print/online issues, and new articles are published several times a week online. JAMA is the most widely circulated medical journal in the world. See submission guidelines.
Importantly, to recognize and navigate the complexities of clinical AI research, medical training and education should deliver interdisciplinary knowledge about AI and its implementation in ...
Dmitry SALIMOV, Medical Doctor | Cited by 12 | of Central Clinical Hospital, Moscow, Moscow | Read 6 publications | Contact Dmitry SALIMOV
Data were extracted from electronic medical records (EMRs) of patients with a live or stillbirth delivery between March 2018 and June 2021 in a large health care system in Pennsylvania. The study was approved by the University of Pittsburgh institutional review board. Informed consent was waived because the research constituted minimal risk.
Abstract. Between 2009 and 2012, I taught principles of evidence-based medicine and clinical research in Russia, Tatarstan, Moldova, and Kazakhstan. The Soviet Union left a medical legacy characterized by balkanization of top tier medicine in highly specialized centers, so there was little capability for multidiscipinary care.
Ilya BORISOV, Medical Doctor | Cited by 30 | of Moscow State University of Medicine and Dentistry, Moscow (MSMSU) | Read 33 publications | Contact Ilya BORISOV
This paper proposes a machine learning approach to recognize doctors' handwriting to create digital prescriptions. A 'Handwritten Medical Term Corpus' dataset is developed containing 17,431 ...
The 2nd "Doctor as a Humanist" Symposium took place at Sechenov University in Moscow from the 1 st to the 3 rd of April, 2019, to explore the holistic perspective of interpersonal treatment. To begin our essay, we would like to clarify some key concepts, such as culture, humanism and humanities, as they were employed at the conference.
Medical research is increasingly informed by recognition of diversity's key role in addressing health equity. But when it comes to medical education, there's a group that has remained not just ...
Publishers and medical science. Journals rely on 'peers' to decide which papers merit publication and which should be jettisoned. The process of peer review is recognised to be flawed. 17 The quality of the reviews varies. There may be divergent views expressed in the review and it is sometimes difficult to determine why an editor rejects or indeed accepts a submission without concluding ...
Introduction: Research in the medical discipline significantly impacts society by improving the general well-being of the population, through improvements in diagnostic and treatment modalities. However, of 579 Indian medical colleges, 332 (57.3%) did not publish a single paper from the year 2005 to 2014," indicating a limited contribution from medical fraternity In order to probe in to the ...