134 Childhood Obesity Essay Topics & Examples
If you’re writing an academic paper or speech on kids’ nutrition or weight loss, you will benefit greatly from our childhood obesity essay examples. Besides, our experts have prepared a list of original topics for your work.

Childhood Obesity - Free Essay Samples And Topic Ideas
Childhood Obesity is a serious medical condition where excess body fat negatively affects a child’s health or well-being. Essays might discuss the causes, consequences, prevention and management of childhood obesity, as well as the role of parents, schools, and healthcare providers in addressing this issue. A vast selection of complimentary essay illustrations pertaining to Childhood Obesity you can find in Papersowl database. You can use our samples for inspiration to write your own essay, research paper, or just to explore a new topic for yourself.
Problem: Childhood Obesity in America
As you've probably heard, more children are becoming overweight today in America than ever before. Experts are calling this an "obesity epidemic." To first understand childhood obesity we must ask ourselves what is obesity? Obesity is a diet-related chronic disease involving excessive body fat that increases the risk of health problems. Many doctors have expressed obesity has an increasing problem in today's youth as obesity can lead to many health issues such as type 2 diabetes, high blood pressure, heart […]
Childhood Obesity Parents are the Blame
In current years, children becoming more obese in their entire childhood development has become common. Obesity in children could be due to various reasons such as family structure, busy family life experienced in the modern days, and insufficient knowledge of foods containing high calories. Parents ought to be accountable for what they do or fail to do that amounts to a negative influence on their children's weight and cause them to be overweight or obese during their childhood period. When […]
Childhood and Adolescents Obesity Prevention
Obesity in children and adolescents is a serious and growing problem in America. Overweight children are becoming overweight adults and that is causing life-threatening, chronic diseases such as diabetes and heart disease. There are multiple reasons for childhood obesity. The most common reasons are genetic factors, lack of physical activity, unhealthy eating patterns, or a combination of all three factors (“Obesity in Children,” 2018). Today, there are many children that spend a lot of time being inactive and eating junk […]
We will write an essay sample crafted to your needs.
Childhood Obesity – Causes and Potential Long-Term Effects
Abstract There is growing concern about the state of children’s health. Every year there is an increase in the number of overweight and obese children. What causes this and what does it mean for them long-term? There are many contributing factors to children’s weight issues. Some of these factors are limited access to healthy food, more time spent in front of a screen, and less physical activity. Long-term health affects include a rising risk of Type 2 diabetes, coronary heart […]
How are Fast Food Advertising and Childhood Obesity Related
By 1950s, fast food industry boom was in full swing. It was secured in 1951. In the 1950s, McDonald has become a staple of the American diet. Fast food restaurants have been grown more and more and by now, there are over one hundred and sixty thousands fast food restaurants in the United States, becoming a one hundred and ten billion dollar industry. One can’t deny that fast food has become really important in American life nowadays. Whether Americans are […]
Obesity in Childhood
There are numerous issues that society faces on a daily basis. One of the issues that society faces is obesity. It is one of the leading risks of death and has been ongoing since the 1960s and 1970s. Obesity is an issue that continues to grow not only in the United States but also in developing countries as well. Not only does obesity affect adults but it has become a serious issue for children. According to an article, "approximately 12.7 […]
Childhood Obesity a Serious Problem in the USA
Childhood obesity is a serious problem in the United States. Obesity is condition in which a child is significantly overweight for his or her age and height. It is a very common condition and is estimated to have around 3 million cases in the United States each year. Every day more children are getting diagnosed with obesity, and some as young as 4 years old. When a child gets diagnosed with obesity at a young age, it can be very […]
Childhood Obesity is an Epidemic in the USA
Introduction Childhood obesity has become an epidemic in the United States and other western industrialized societies. "Childhood obesity affects more than 18 percent of children in the United States, making it the most common chronic disease of childhood" (Obesity Action Coalition). According to the OAC, the percentage of children suffering from childhood obesity has tripled since 1980. A child is considered obese if their body mass index for their age is greater than 95 percent. Childhood obesity is both an […]
Obese Kids and Low Self-esteem
Those who are in poverty are predominately people of color and as you can see from the chart above there is a high percentage of children of color who were diagnosed with childhood obesity. According to Centers of Disease Control, "Overall, non-Hispanic black and Hispanic adults and youth had a higher prevalence of obesity compared with other race and Hispanic-origin groups. Obesity prevalence was lower among non-Hispanic Asian men and women compared with other race and Hispanic-origin groups. Among men, […]
Childhood Obesity Today
In America, childhood obesity is on a rise today. Children can gain obsessive weight because of environmental factors. Vending machines, low cost on snacks, and a increase in the fast food chain are contributing factors towards obesity. Genetics can also play a part in childhood obesity. Many children come from a generation of overweight families. Most parents don't see the harm in letting their children gain tons of weight. Obesity can cause many health problems. Childhood obesity affects the health […]
Childhood Obesity in the American Nation
Childhood obesity is still rising in this nation. One out of three Americans is obese. The outlook for children is not much better, as adolescent obesity has quadrupled over the last thirty years. "As of 2012, almost 18 percent of children aged 6-11 years were obese" (Newman, 1). Despite the considerable public awareness of the negative impacts of obesity, this challenge persists. The situation for youngsters is hardly brighter; over the last few decades, the rate of youth obesity has […]
Child and Adolescent Obesity in the United States
Child and adolescent obesity in the United States has nearly tripled sincethe 70s. About 1 out of every 5 children suffer from childhood obesity. It is the duty ofmothers and fathers to prevent and find solutions to child and adolescent obesity. Thispaper will seek to explain the many causes and current results which parents can execute.Child and adolescent obesity comprises of several likely causes such as poor diet and lowphysical activity including numerous adverse effects. Therefore, changes in familyhousehold structures […]
The Causes and Preventions of Childhood Obesity
When trying to find out if a child is considered for obesity, they need to have a body mass index that is between the ranges of the 85th percentile and the 95th percentile. When speaking about childhood obesity it is for children between the ages of infancy and early adulthood which is eighteen years of age. Obesity is one of the most preventable diseases especially if caught early enough. There are many different reasons for the cause of childhood obesity, […]
The Effects of the Epidemic Childhood Obesity
Childhood obesity has become a growing epidemic in more than just the U.S. However, over the past three decades, childhood obesity rates have tripled in the U.S. and today, the country has some of the highest obesity rates in the world: One out of six children is obese, and one out of three children is overweight. Chubby children were once thought of as cute, it was there baby fat and they would soon emerge into healthy adults, however this isn't […]
Tackling Childhood Obesity in Rural Mississippi
Childhood obesity is a growing health issue in the United States. Children with higher Body Mass Indexes than the recommended by the National Institutes of Health are more prone to adverse health effects later in life. Obesity in early age can translate into adulthood and increases the risk of developing cardiovascular diseases and diabetes (Franks 2010). The highest rates of childhood obesity can be observed in the southeastern corner of the United States, Mississippi, in particular, with the highest prevalence […]
Childhood Obesity, a Crisis that could be Cure
Obesity is a crisis that is affecting many countries, their most vulnerable citizens being children. Bad eating habits, high calorie intake, genetics, and lack of activity or exercise are some of the elements that, either combined or individually, are the cause for childhood obesity in America, Latin America, and many other nations. In the United States, rural areas have higher rates of childhood obesity, as do Hispanics and Blacks (Davis 2011). Keywords: Obesity, Childhood. Childhood Obesity, a Crisis that could […]
Childhood Obesity: Global Epidemic and Ethical Concerns
Abstract Numbers continue to climb for those who have childhood obesity. This serious issue has been brought to the attention of the public who have been taking preventative measures and action in hopes to reduce the number of cases. In a number of countries, public policies have been implemented to prevent obesity. However, in the U.S. efforts made are not enough or have not been effective to stop the obesity rate from increasing. Proposals for solutions to this health problem […]
Childhood Obesity and Unhealthy Diets
Over the years childhood obesity has become an epidemic. Working as a medical assistant in family practice for the past ten years, I have witnessed a lot of children struggling with being overweight and obese. Many children now in days lack whole foods that contain proper macronutrients for their bodies to use as energy adequately. Processed foods and sugary beverages can cause more complications over time when overconsumed. Along with lack of proper nutrition, a lot of children seem to […]
The Social Environment and Childhood Obesity
I, Marisol Nuñez, reside in South Gate the reason for this letter is that I am very concerned about the prevention of childhood obesity. Residents in our city lack the resources of acquiring healthy nutritious foods for their families, the resources in our city are very limited. The city has a farmer’s market once a week, and the likelihood of working families purchasing healthier foods is very limited. We need more resources for our families can eat highly nutritious foods. […]
Childhood Obesity and Physical Activity
Most children and teens have access to a tablet, smartphone, television, laptop or a video console. They are sitting around on-screen time more and more as the days go by. Research from the CDC states obesity has nearly doubled since the 1970s in the United States. It is estimated now that 20 percent of children and adolescents are affected by obesity. Too much screen time, the accessibility to the internet and not enough physical activity are the biggest reasons the […]
Childhood Obesity and Adolesence
Childhood obesity can be prevented in many ways. Parents are the main ones with a say so on obesity. They allow their children to digest all kinds of bad foods. Parents should introduce on a daily basis different kinds of healthy foods. They should also promote is by showing children how healthy food are good for the body. You have some children that won’t eat healthy things because of the color and the way it looks. Obesity is one of […]
Several Factors in Childhood Obesity
Childhood obesity is widely described as excess in body fat in children and teenagers. There is, however, no agreement about exactly how much body fat is excessive in relation to the group. The Center for Disease Control and Prevention on its part defined overweight as at or above the 95th percentile of body mass index (BMI) for age and "at risk for overweight" as between 85th to 95th percentile of BMI for age (Krushnapriya Sahoo). In general clinic environments, the […]
Factors that Influence Childhood Obesity
The cause of pediatric obesity is multifactorial (1). There is not a single cause, nor solution, found that leads to all cases of pediatric obesity. Parental discipline in regard to the child is not proven to lead to less adiposity or obesity in children. Parental feeding strategy may actually be a cause of obesity with restrictive approach to food by the parent shown to increase the proclivity for the restricted foods (2). Likewise, when parents allowed their children to have […]
Childhood Obesity, Disease Control and Prevention
According to the Centers for Disease Control and Prevention, identifying effective intervention strategies that can target both improvements in physical activity and providing a nutritious diet to reduce childhood obesity are important" (Karnik, 21). There has been a rising concern on whether or not the government needs to be involved in this childhood obesity epidemic. Sameera, Karnik, and Amar Kanekar give an amazing detailed article on how important it is to get involved with children through the government and through […]
The Impact of Childhood Obesity on Health
Childhood Obesity has become an ongoing problem across the United States. Obesity kills about 34 children every hour in the world, making it a serious issue. Many leaders and people have come together to attempt to prevent the issue, but some strategies have failed. Most people disregard the fact that what they feed their children can affect them in many ways, specifically become obese. Childhood obesity can lead to becoming obese in the future, being susceptible to different diseases and […]
What is Childhood Obesity?
Introduction Childhood obesity has become a widespread epidemic, especially in the United States. Twenty five percent of children in the United States are overweight and eleven percent are obese (Dehghan, et al, 2005). On top of that, about seventy percent of those children will grow up to be obese adults (Dehgan, et al, 2005). There are many different causes that can be attributed to the childhood obesity. Environmental factors, lifestyle preferences, and cultural environment play pivotal roles in the rising […]
Problem of Childhood Obesity in the United States
Among the many issues that the United States is facing, there is no doubt that Childhood Obesity is a timely and relevant debatable topic that has brought many consequences and health issues among our nation’s children. Many debates in regard to childhood obesity have formed. Because the prevalence of childhood obesity is on the rise, there have been varying opinions about what leading factors contribute to this issue. Although some health professionals and parents believe that childhood obesity stems from […]
A Big Problem – Bad Healthcare is Aiding Childhood Obesity
A study done in 2002 found that, almost 14 million children are obese, that is 24 percent of the U.S. population from ages 2 to 17. This number just keeps rising as the years go by. Some people would argue that the increasing numbers are due to sugary dinks and foods sold in vending machines at schools, or not enough healthy food options. Other parties can argue that this number keeps increasing because of bad healthcare and not enough opportunities […]
Childhood Obesity Rate Can be Decreased
Child obesity has become a major concern as it continues to increase every year in the US. Many parents are uneducated about the risks of childhood obesity. Parental awareness and increasing physical activity are steps towards making a change in the rates of childhood obesity. There are many side effects of childhood obesity that can obstruct a child’s future. However, positive changes to children’s health can be achieved through the influence of adults. Child obesity has become a more critical […]
Additional Example Essays
- The Mental Health Stigma
- Psychiatric Nurse Practitioner
- Substance Abuse and Mental Illnesses
- Homeschooling vs Public School
- Socioautobiography Choices and Experiences Growing up
- A Research Paper on Alzheimer's Disease
- The Effect of Alcohol on College Students
- Is Sexual Orientation Determined At Birth?
- Nursing Shortage: solutions of the problem
- End Of Life Ethical Issues
- Beauty Pageants for Children Should Be Banned: Protecting Child Well-being
- Live Free and Starve, by Chitra Divakaruni
How To Write an Essay About Childhood Obesity
Understanding childhood obesity.
Writing an essay about childhood obesity requires a comprehensive understanding of the topic. Childhood obesity is a serious public health issue that has grown significantly in recent years. It's characterized by children having a body mass index (BMI) at or above the 95th percentile for children of the same age and sex. Start by exploring the causes of childhood obesity, which can include genetic factors, poor dietary habits, lack of physical activity, and environmental influences. Also, consider the short and long-term health implications, such as an increased risk of chronic diseases like diabetes and heart disease. This foundational knowledge sets the stage for a deeper analysis in your essay.
Developing a Focused Thesis Statement
Your essay should be guided by a clear, focused thesis statement. This statement should present a specific angle or argument about childhood obesity. For instance, you might argue the importance of early intervention programs, the role of schools in promoting healthy lifestyles, or the impact of advertising and media on children’s eating habits. Your thesis will determine the direction of your essay, guiding your analysis and ensuring a structured approach to the topic.
Gathering and Analyzing Data
An effective essay on childhood obesity should be supported by relevant data and research. This includes statistics on the prevalence of obesity, studies on its causes and effects, and evaluations of intervention programs. Use this information to support your thesis, incorporating both national and global perspectives. Analyze the data critically, acknowledging any limitations and considering different viewpoints. This approach adds depth to your essay and strengthens your arguments.
Discussing Solutions and Interventions
A significant portion of your essay should be dedicated to discussing potential solutions and interventions for childhood obesity. This can include public health policies, educational programs, changes in food industry practices, or community-based initiatives. Evaluate the effectiveness of these solutions, drawing on case studies or research findings. Discussing both the successes and challenges in tackling childhood obesity will provide a balanced view and demonstrate a comprehensive understanding of the topic.
Concluding the Essay
Conclude your essay by summarizing the main points of your discussion and restating your thesis in light of the evidence presented. Your conclusion should tie together your analysis and emphasize the significance of addressing childhood obesity. This is also an opportunity to reflect on potential future developments in the field or to suggest areas for further research.
Reviewing and Refining the Essay
After completing your essay, it's important to review and refine it. Check for coherence in your arguments and clarity in your writing. Ensure that your essay is well-organized and free from grammatical errors. Consider seeking feedback from peers, teachers, or health professionals to further improve your work. A well-crafted essay on childhood obesity should not only inform but also engage readers in considering the complexities of this public health issue and the collective efforts required to address it.
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 30 May 2024
Epidemiology and Population Health
Childhood adversity trajectories and weight status in young adult men: a register-based study including 359,783 Danish men
- Cathrine L. Wimmelmann ORCID: orcid.org/0000-0002-8718-1654 1 , 2 ,
- Christoffer Sejling ORCID: orcid.org/0000-0002-4128-9299 3 ,
- Rebecca B. Clarke ORCID: orcid.org/0000-0002-2328-2480 1 ,
- Leonie K. Elsenburg ORCID: orcid.org/0000-0002-9824-9837 4 ,
- Thorkild I. A. Sørensen ORCID: orcid.org/0000-0003-4821-430X 2 , 4 , 5 &
- Naja H. Rod 4
International Journal of Obesity ( 2024 ) Cite this article
Metrics details
- Epidemiology
- Risk factors
Childhood adversity has previously been associated with overweight and obesity in adult life, but there is a need for larger population-based studies using prospectively obtained adversity trajectories across childhood to confirm these associations. Moreover, childhood adversity may also be associated with underweight, which is less often studied. The aim of the current study is to investigate the association between childhood adversity trajectories from 0–15 years with weight categories in young adult men.
The Danish Life Course Cohort (DANLIFE) was linked with the Danish Conscription Registry resulting in a study sample of 359,783 men, who have been assigned to one of five previously identified adversity trajectories from 0–15 years: “low adversity”, “early material deprivation”, “persistent material deprivation”, “loss or threat of loss”, and “high adversity”. Height and weight in young adulthood was assessed at a draft board examination at age 18–26 years. Associations of adversity trajectories and weight categories were investigated in multinomial regression models.
Compared with the “low adversity” group, the four other adversity groups had higher risks of underweight, overweight, and obesity. The “high adversity” group showed the strongest associations with both underweight (1.44 (1.32, 1.58)) and obesity (1.50 (1.39, 1.61)) when adjusted for parental origin, birth year, age at draft board examination, and maternal age.
Childhood adversity, experienced between 0 and 15 years of life, was associated with a higher risk of underweight, overweight, and obesity in young adulthood among men.
Introduction
A rapid and continued rise in overweight and obesity in most parts of the world is of major public health concern. Overweight and obesity have serious short and long-term consequences for physical, mental, and socioeconomic aspects of life [ 1 ]. Research has indicated that especially weight status in young adulthood (around ages 20–30) is of importance for later health outcomes [ 2 , 3 ]. The path to young adult obesity may be established during childhood [ 4 ], making it central to study childhood predictors of body mass index (BMI) in young adulthood. Along these lines, adverse childhood experiences have received increasing attention in recent years as a potential risk factor for unhealthy weight development [ 5 ]. Childhood adversity can be defined as intense stressors or traumatic events that disrupt a child’s sense of safety and stability, potentially leading to mental and physiological consequences that can extend into adulthood [ 6 ]. Studies have shown that such childhood adversities are common, even in developed countries where reports indicate that around half of all adults have experienced at least one type of adversity [ 7 , 8 , 9 ].
Childhood adversities, such as parental divorce, poverty, parental or sibling death, and family drug abuse, have been found to have strong and enduring effects on health in adulthood [ 5 , 6 , 9 , 10 ] and systematic reviews have consistently reported that individuals who have experienced adversities in childhood have higher risk of developing overweight and obesity in adulthood [ 11 , 12 ]. Several potential mechanisms for the association between childhood adversity and later obesity have been proposed including both biological and stress-related pathways [ 13 , 14 ], and behavioral pathways [ 15 , 16 , 17 ]. Furthermore, according to both the Food Insecurity Hypothesis [ 18 , 19 ] and the more recent Adiposity Force Theory [ 20 ], the perception of poor social resources, which is a consequence of many types of adversities [ 21 ], triggers a mechanism encoding the body to store fat [ 20 ]. Thus, both theories propose the existence of an evolutionary developed biological reaction to difficult early life conditions, which increases the risk of developing overweight and obesity.
Though the association between childhood adversity and obesity in adulthood is relatively well-established [ 5 ], several questions remain unresolved. Previous studies are mainly based on selected and small samples, and there is a need for studies replicating the findings in large population-based samples. Also, the majority of the previous studies have used retrospectively obtained measures of single adversities [ 9 , 22 , 23 , 24 , 25 ], but adversities tend to cluster and focusing on single events may have resulted in an underestimation of the effect of adversities on weight status. Studies investigating the accumulation of adverse events in childhood with weight status have generally found a dose-response relation between number of adversities and obesity [ 9 , 26 ]. Finally, most studies used self-reported measures of BMI [ 22 , 24 , 25 ] and investigated associations between adverse experiences in childhood and obesity defined as BMI ≥ 30 kg/m 2 rather than the full range of weight categories. However, it has been indicated that adversities in childhood may also be associated with underweight in adulthood, yet results are inconsistent [ 22 ].
The aim of the present study is to investigate associations of adversity trajectories (prospectively obtained from 0–15 years) on the whole range of weight categories in adulthood (underweight, normal weight, overweight, and obesity) in a large population-based sample of Danish men. Based on theoretical and empirical considerations, it was hypothesized that men who experienced adversities in childhood would show greater risk of both underweight, overweight, and obesity compared with those who have experienced no or few adversities during childhood.
Study sample
The Danish Life Course Cohort (DANLIFE) [ 27 ] was linked with the Danish Conscription Registry (DCR) [ 28 ] to investigate the aim of the current study. DANLIFE contains information on childhood adversity for all children born in Denmark between January 1st 1980 and December 31st 2015. In this study, a sample was used consisting of children born 1980–2001, who could be followed their entire childhood until 15 years of age ( n = 1,283,955). The DCR includes information on mental and physical health, such as height and weight, for all Danish men appearing at a draft board examination during the period from January 1st 2006 to October 19th 2022 ( n = 658,943). All men who reside in Denmark are required by law to appear at the examination during the calendar year they turn 18. The examination can be postponed until age 26 upon request, but most men appear before they turn 19. We only had access to height and weight data from DCR starting from year 2006, and information on height and weight was therefore missing for a substantial part of participants born before 1988. To prevent selection bias, all DCR records of men born before 1988 ( n = 34,054) were excluded. The current study sample consists of a total of 359,783 men born in 1988 or later, who are both in the DANLIFE cohort and have information on height and weight assessed at a draft board examination.
Childhood adversity
Childhood adversity trajectories were derived from an earlier study using DANLIFE data [ 6 ]. In that study, group-based multi-trajectory modeling (using package TRAJ for Stata) was applied to the yearly count of adversities from 0–15 years across the following three dimensions: material deprivation (i.e., poverty and parental long-term unemployment), loss or threat of loss (i.e., parental or sibling somatic illness or death), family dynamics (i.e., foster care placement, maternal separation, parental alcohol or drug abuse, parental or sibling psychiatric illness). Zero-inflated Poisson regressions with a cubic trajectory function were used to model childhood adversities, resulting in the identification of five groups of adversity trajectories: (1) Low adversity is characterized by yearly adversity counts close to zero within all three assessed dimensions. (2) Early life material deprivation is characterized by a high rate of material deprivation during the first years of life followed by a decreasing rate of yearly counts on this dimension. The yearly count of adversities across the other two dimensions was close to zero for this group. (3) Persistent material deprivation is characterized by a high rate of material deprivation throughout childhood combined with yearly counts close to zero on the other two dimensions. (4) Loss or threat of loss is characterized by a moderate to high and increasing rate of loss or threat of loss across childhood, including death or somatic illness in the family, combined with relatively low rates in the two other dimensions. (5) High adversity is characterized by a high and increasing annual rate of adversities in all three dimensions. For a graphical visualization of the trajectories, please see Rod et al. [ 6 ]. The strong association of these five trajectory groups with later mortality and morbidity attests to their adequacy and validity [ 6 , 10 , 29 , 30 ]. All individuals in the current study were allocated to the adversity trajectory they were most likely to belong to. The childhood adversity groups were thus included as exhaustive and exclusive categorical variable in all analyses.
Body mass index in young adulthood
BMI is calculated using height and weight measured at the draft board examination. The examinations are carried out by medical staff using standardized methods for measurement of height and weight. BMI was used as a categorical variable applying the weight categories defined by the World Health Organization (WHO): Underweight BMI < 18.5; Normal weight BMI 18.5–24.9; Overweight BMI 25.0–29.9; Obesity BMI ≥ 30.0.
Several potential confounders of the association between childhood adversity and weight status in young adulthood were considered based on previous research. Information on birth year, age at draft board examination, parental country of origin, maternal age at birth, parental cardiometabolic disease, preterm birth, size for gestational age, and parental education was extracted from Danish nationwide registries. Birth year refers to the calendar year the child was born. Age at draft board examination is a continuous variable and refers to the age the individual had when appearing at the draft board examination. Parental country of origin is a binary variable classifying parents as either Western (if one or both parents had a European, North American, Australian, or New Zealand nationality) or non-Western (if both parents had another nationality). Maternal age was applied as a categorical variable classifying mother’s age at birth as younger (<20 years), average (20–30 years), or older (>30 years). Parental cardiometabolic disease in the 3 years before child birth was identified in either the Danish National Patient register or the Danish Register of Causes of Death as the presence of any of the following diagnoses: ischemic heart disease (ICD8: 410–414/ICD10: I20.0, I20.1, I21–159, I25), cerebrovascular disease (ICD8: 430–438/ICD10: I60–I69), congestive heart failure (ICD8: 427.09–427.11, 427.19, 160 428.99, 782.49/ICD10: I50, I11.0, I13.0, I13.2), peripheral vascular disease (ICD8: 440–445/ICD10: I70–I74, I77), type 1 diabetes (ICD8: 249/ICD10: E10), or type 2 diabetes (ICD8: 250/ICD10: E11). Preterm birth was a binary variable classifying the children as “preterm” if they were born prior to gestational week 37 and as “not preterm” if they were born in gestational week 37 or later. Size for gestational age was used as a categorical variable depicting small (<10th), average (≥10th–≤90th), and large (>90th) gestational size at birth according to percentiles of age- and sex-specific intrauterine growth reference curves. Parental education refers to the household’s highest educational level at the time of birth and was used as a categorical variable classifying parental education as either low ( < 10 years) corresponding to elementary school, medium (10–12 years) corresponding to high-school, or high (>12 years) corresponding to a higher degree.
Statistical analyses
We used descriptive statistics to examine participant characteristics. Associations of the childhood adversity trajectories with the categorical weight status variable were analyzed using multinomial logistic regression models, with low adversity as the reference group [ 31 ]. Model 1 (the main model) included age at draft board examination, birth year, parental origin, and maternal age where the relationships between the link function and the covariates birth year and age at draft board examination were modeled with flexible splines. Parental cardiometabolic disease, size for gestational age, and preterm birth may have been influenced by family adversity before birth of the child, whereas parental education is closely related to childhood adversity, especially the dimension of material deprivation. Thus, these variables were not included in the main analysis, but were instead presented in three supplementary models: Supplementary Model 1 included parental cardiometabolic disease in addition to variables in Model 1. Supplementary Model 2 additionally included size for gestational age and preterm birth. Finally, Supplementary Model 3 included parental education in addition to the covariates in Supplementary Model 1 .
The majority (58.2%) of men belonged to the low adversity group, 20.1% were in the early material deprivation group, 9.7% in the persistent material deprivation group, 9.4% in the loss or threat of loss group, and 2.6% of the men belonged to the high adversity group.
Table 1 presents participant characteristics according to childhood adversity trajectory. The largest differences between the adversity groups were observed for maternal age and parental education. The low adversity group had a lower percentage of mothers in the younger category and a higher percentage of parents with a higher education than the other adversity groups. Table 2 presents the frequency of underweight, normal weight, overweight, and obesity across the five adversity groups. Group differences were observed across all weight groups with the lowest percentage of underweight and obesity observed in the low adversity group, whereas the highest percentage of underweight and obesity was observed in the high adversity group.
Results of the multinomial regression models investigating associations of adversity trajectory groups and weight status category are presented in Fig. 1 and Supplementary Fig. S1a–c . The plots present risk ratios (RR) for having underweight, overweight, and obesity compared with normal weight. RR estimates for all analyses are presented in Supplementary Table 1 . Overall, results show that men in the adversity groups have higher risks of underweight, overweight, or obesity, compared with the low adversity group. In the main model, adjusted for birth year, age at draft board examination, parental origin, and maternal age (Fig. 1 ), the strongest associations with underweight (RR 1.44; 95% CI: 1.32, 1.58) and obesity (1.50; 1.39, 1.61) were found for the high vs. low adversity group. The highest RR for overweight (1.14 (1.11, 1.17)) was found for the persistent material deprivation group compared with the low adversity group . These results remained similar when additionally adjusting for cardiometabolic disease (Fig. S1a ), and for cardiometabolic disease, size for gestational age and preterm birth (Fig. S1b ). When adjusting for parental education (Fig. S1c ), the RR estimates were attenuated for all adversity groups, and particularly for the high adversity group. After adjustment for parental education, high adversity was associated with a slightly lower risk of overweight (0.90 (0.85, 0.95)) when compared to the low adversity group.

The figure presents risk ratios (RR) with 95% confidence intervals (CI) for underweight, overweight, and obesity for each adversity group compared with the low adversity group. The RRs are adjusted according to Model 1: birth year, age at draft board examination, parental origin, and maternal age.
Results from this large prospective population-based study showed that young men with a history of childhood adversity during the first 15 years of life had a higher risk of underweight, overweight, and obesity compared with men who experienced low childhood adversity. For instance, men in the high adversity group had a 44% and 50% higher risk of underweight and obesity respectively, than men in the low adversity group. These results were not explained by confounding from risk factors such as parental origin, maternal age, parental cardiometabolic disease, size for gestational age, or preterm birth. However, results were attenuated when adjusting for parental education.
A growing body of research has investigated associations of adverse childhood experiences and adult obesity, and the findings are generally in line with those of the present study. A systematic review of the literature ( n = 253,719) combining cross-sectional, case-control, and cohort studies found an odds ratio for adult overweight or obesity of 1.39 (CI = 1.13, 1.71) among individuals who had been exposed to childhood adversity when compared with individuals who had not [ 5 ]. A more recent review of ten population-based cross-sectional studies ( n = 118,691) found a 46% higher odds of obesity (OR(CI)1.46 (1.28, 1.64)) in adulthood following exposure to multiple adverse childhood experiences [ 11 ]. Few studies have investigated longitudinal associations between childhood adversities and adult obesity specifically. A cross-sectional study of 26,615 mid to late life individuals who were asked to recall exposure on childhood adversities identified a dose-repose relationship between number of adversities and risk of obesity [ 9 ]. Adults who reported four to eight adversities had 54% higher risk of obesity (1.54 (1.28, 1.75)) than adults who did not report adversities in childhood. A meta-analysis of associations between accumulation of adversity or trauma in childhood and overweight during childhood and adolescence [ 32 ] found a pooled OR of 1.12 (1.01, 1.25), which is substantially lower than the OR reported in studies of adult obesity. This may indicate that it takes several years for childhood adversities to manifest their effects on obesity in adulthood [ 33 ]. Our study contributes to these previous findings by using prospectively collected information on childhood adversity from a large population-based sample with measured BMI in young adulthood, which is a critical window for later weight developments.
It is highly plausible that exposure to childhood adversity combined with genetic predisposition contributes to obesity development both within and across generations [ 34 ]. A systematic review of population-based studies found that social disruption, health behavior, and chronic stress responses were the most likely explanations for the association between childhood adversity and adult obesity [ 11 ]. Several other mechanisms may contribute to explaining the observed association. A recent theory suggests that childhood adversity triggers an evolutionary developed mechanism, which originally had the function of storing fat when the prospect of having social support and therefore food was uncertain [ 20 ]. This may indicate that social factors such as childhood adversities have a direct effect on weight status through biological pathways. This notion is supported by findings linking early stressful life conditions and social factors, such as poverty, to increased HPA axis reactivity that may lead to increased fat deposits [ 11 , 35 ]. Another possible explanation is that childhood adversity has indirect effects on weight status in adulthood by inducing other factors with presumed direct influence on obesity development. Individuals who have been exposed to childhood adversity are more likely to engage in unhealthy behaviors such as eating a poor quality diet [ 17 ] and limited physical activity [ 36 ]. Also, early adverse experiences have consistently been linked to negative psychological outcomes such as depression [ 37 , 38 ], which in turn are known to influence an individuals’ eating patterns and weight status [ 39 ].
In the current study, childhood adversity was also associated with underweight. Specifically, men in the high adversity group had a higher risk of underweight than men in the low adversity group. While previous results are overall inconsistent [ 22 , 33 ], the association between childhood adversities and underweight has been found in previous studies [ 40 , 41 , 42 ]. Childhood adversities may lead to the development of underweight through psychological and behavioral factors, such as poor mental health [ 43 , 44 ] maladaptive coping and self-harm behaviors including drug abuse and restricted or disordered eating [ 45 , 46 ]. Also, a low BMI in young adulthood may be indicative of chronic physical disease, which has also been associated with childhood adversities.
There is a conceptual overlap between parental education and childhood adversity, particularly concerning the material deprivation dimension within trajectories, which include indicators such as poverty and prolonged parental unemployment. It is therefore interesting to see that associations of childhood adversities with underweight persisted even when adjusting for parental education, while they as expected attenuated for obesity (Supplementary Model 3 ). This indicates that the underlying mechanisms linking childhood adversities with body weight may differ across weight categories. The association of childhood adversity with overweight (BMI ≥ 25) was modest indicating that childhood adversity may be an important predictor of the more extreme weight categories (i.e., underweight and obesity) rather than the weight categories within the broader normal range.
A major strength of the present study is the prospective population-based design minimizing recall bias and selective inclusion. Additional strengths include the large sample, the nationwide register-based information on yearly incidence of different childhood adversities and their accumulation across childhood with proven associations with later morbidity and mortality [ 6 , 10 ]. Finally, the study included extensive information on potential early life confounding factors.
Some limitations of this study are that we did not have direct measurements of childhood adversities, such as family violence, sexual abuse, or neglect, nor measures on social dynamics in schools such as bullying, which have been related to various health outcomes [ 47 ]. Neither do we have information on manifested effects of the adversities on the individual children, which was the key exposure in a previous study, showing a much stronger relation of parental neglect in childhood with later obesity in young adulthood [ 48 ]. Likewise, we did not have information on parental BMI, which is a well-established genetic and shared familial environmental predictor of the child’s BMI, and it may also affect the conditions under which the child grow up [ 49 , 50 ]. This is especially relevant for the loss and threat of loss group, which is often associated with parental somatic disease. We did, however, adjust for parental cardiometabolic disease as a crude indicator of parental BMI, which only had very minor impact on the results. Furthermore, we did not have information on other weight status indicators than BMI. This is a limitation as the accuracy of BMI on the individual level may be questioned.
Finally, the study sample included only men, and some previous studies have indicated sex differences in the association between childhood adversities and obesity with a stronger association among women than men [ 51 , 52 ]. Thus, this suggests that the associations in our study might be stronger had we had the possibility to study them in young women. Overall, the current study provides solid evidence of an association between adversity trajectories in childhood and young adult weight status. Future research should focus on investigating the underlying mechanisms of this association, for instance, whether the risk of underweight and obesity is driven by different types of adversities. Also, there is a need for large population-based studies investigating the effect of adversity trajectories in childhood on weight status throughout adulthood.
Findings from this large population-based study showed that men who had encountered childhood adversity within the first 15 years of their life faced a higher risk of underweight, overweight, and obesity in young adulthood when compared with those with low adversity. These findings emphasize the importance of early life experiences in shaping healthy weight trajectories across the lifespan. Young adulthood represents a critical phase in weight development, carrying potential implications for later-life health and overall well-being. Addressing childhood adversity within social and familial contexts could serve as central intervention opportunities for public health initiatives.
Data availability
The data material contains personally identifiable and sensitive information. According to the Act on Processing of Personal Data, such data cannot be made publicly available. Inquiries about secure access to data under conditions stipulated by the Danish Data Protection Agency should be directed to the principal investigator of DANLIFE, NHR ([email protected]).
Williams EP, Mesidor M, Winters K, Dubbert PM, Wyatt SB. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr Obes Rep. 2015;4:363–70.
Article PubMed Google Scholar
Hirko KA, Kantor ED, Cohen SS, Blot WJ, Stampfer MJ, Signorello LB. Body mass index in young adulthood, obesity trajectory, and premature mortality. Am J Epidemiol. 2015;182:441–50.
Article PubMed PubMed Central Google Scholar
Cheng HL, Medlow S, Steinbeck K. The health consequences of obesity in young adulthood. Curr Obes Rep. 2016;5:30–7.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17:95–107. https://doi.org/10.1111/obr.12334 .
Article CAS PubMed Google Scholar
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. Lancet Public Health. 2017;2:e356–66.
Rod NH, Bengtsson J, Budtz-Jørgensen E, Clipet-Jensen C, Taylor-Robinson D, Andersen AMN, et al. Trajectories of childhood adversity and mortality in early adulthood: a population-based cohort study. Lancet. 2020;396:489–97.
Bellis MA, Hughes K, Leckenby N, Hardcastle KA, Perkins C, Lowey H. Measuring mortality and the burden of adult disease associated with adverse childhood experiences in England: a national survey. J Public Health. 2015;37:445–54.
Article CAS Google Scholar
Chu WWE, Chu NF. Adverse childhood experiences and development of obesity and diabetes in adulthood—a mini review. Obes Res Clin Pr. 2021;15:101–5.
Article Google Scholar
De Rubeis V, Gonzalez A, Tarride JÉ, Griffith LE, Anderson LN. A longitudinal study evaluating adverse childhood experiences and obesity in adulthood using the Canadian Longitudinal Study on Aging (CLSA). Int J Epidemiol. 2023;52:1100–11.
Rod NH, Bengtsson J, Elsenburg LK, Taylor-Robinson D, Rieckmann A. Hospitalisation patterns among children exposed to childhood adversity: a population-based cohort study of half a million children. Lancet Public Health. 2021;6:e826–35.
Wiss DA, Brewerton TD. Adverse childhood experiences and adult obesity: a systematic review of plausible mechanisms and meta-analysis of cross-sectional studies. Physiol Behav. 2020;223:112964.
Vámosi M, Heitmann BL, Kyvik KO. The relation between an adverse psychological and social environment in childhood and the development of adult obesity: a systematic literature review. Obes Rev. 2010;11:177–84.
Tomiyama AJ. Stress and obesity. Annu Rev Psychol. 2019;70:703–18.
Taheri S. The link between short sleep duration and obesity: we should recommend more sleep to prevent obesity. Arch Dis Child. 2006;91:881–4.
Article CAS PubMed PubMed Central Google Scholar
Rønningen R, Wammer ACP, Grabner NH, Valderhaug TG. Associations between lifetime adversity and obesity treatment in patients with morbid obesity. Obes Facts. 2019;12:1–13.
Mahmood S, Li Y, Hynes M. Adverse childhood experiences and obesity: a one-to-one correlation? Clin Child Psychol Psychiatry. 2023;28:785–94.
Aquilina SR, Shrubsole MJ, Butt J, Sanderson M, Schlundt DG, Cook MC, et al. Adverse childhood experiences and adult diet quality. J Nutr Sci. 2021;10:e95.
Nettle D, Andrews C, Bateson M. Food insecurity as a driver of obesity in humans: the insurance hypothesis. Behav Brain Sci. 2017;40:e105.
Bateson M, Pepper GV. Food insecurity as a cause of adiposity: evolutionary and mechanistic hypotheses. Philos Trans R Soc Lond B Biol Sci. 2023;378:20220228.
Sørensen TIA. An adiposity force induces obesity in humans independently of a normal energy balance system—a thought experiment. Philos Trans R Soc B Biol Sci. 2023;378:20220203.
Ejlskov L, Bøggild H, Kuh D, Stafford M. Social relationship adversities throughout the lifecourse and risk of loneliness in later life. Ageing Soc. 2020;40:1718–34.
Davis L, Barnes AJ, Gross AC, Ryder JR, Shlafer RJ. Adverse childhood experiences and weight status among adolescents. J Pediatr. 2019;204:71–6.e1.
Doom JR, Young ES, Farrell AK, Roisman GI, Simpson JA. Behavioral, cognitive, and socioemotional pathways from early childhood adversity to BMI: evidence from two prospective, longitudinal studies. Dev Psychopathol. 2023;35:749–65.
Hazzard VM, Yoon C, Emery RL, Mason SM, Crosby RD, Wonderlich SA, et al. Adverse childhood experiences in relation to mood-, weight-, and eating-related outcomes in emerging adulthood: does self-compassion play a buffering role? Child Abus Negl. 2021;122:105307.
Gunstad J, Paul RH, Spitznagel MB, Cohen RA, Williams LM, Kohn M, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res. 2006;142:31–7.
Friedman EM, Montez JK, Sheehan CM, Guenewald TL, Seeman TE. Childhood adversities and adult cardiometabolic health: does the quantity, timing, and type of adversity matter? J Aging Health. 2015;27:1311–38.
Bengtsson J, Dich N, Rieckmann A, Hulvej Rod N. Cohort profile: the DANish LIFE course (DANLIFE) cohort, a prospective register-based cohort of all children born in Denmark since 1980. BMJ Open. 2019;9:e027217.
Christensen GT, Skogstad S, Nissen LR, Osler M. Data resource profile: Danish Conscription Registry Data (DCRD). Int J Epidemiol. 2018;47:1023–4e.
Bengtsson J, Elsenburg LK, Andersen GS, Larsen ML, Rieckmann A, Rod NH. Childhood adversity and cardiovascular disease in early adulthood: a Danish cohort study. Eur Heart J. 2023;44:586–93.
Elsenburg LK, Bengtsson J, Rieckmann A, Rod NH. Childhood adversity and risk of type 2 diabetes in early adulthood: results from a population-wide cohort study of 1.2 million individuals. Diabetologia. 2023;66:1218–22.
Ripley B, Venables W. Package nnet: feed-forward neural networks and multinomial log-linear models. 2023. https://cran.r-project.org/web/packages/nnet/index.html .
Elsenburg LK, van Wijk KJE, Liefbroer AC, Smidt N. Accumulation of adverse childhood events and overweight in children: a systematic review and meta-analysis. Obesity. 2017;25:820–32.
Elsenburg LK, Rieckmann A, Bengtsson J, Lange T, Baker JL, Sørensen TIA, et al. Early childhood adversity and body mass index in childhood and adolescence: linking registry data on adversities with school health records of 53,401 children from Copenhagen. Int J Obes. 2023. https://doi.org/10.1038/s41366-023-01355-9 .
Hemmingsson E, Nowicka P, Ulijaszek S, Sørensen TIA. The social origins of obesity within and across generations. Obes Rev J Int Assoc Study Obes. 2023;24:e13514.
van der Valk ES, Savas M, van Rossum EFC. Stress and obesity: are there more susceptible individuals? Curr Obes Rep. 2018;7:193–203.
Kestilä L, Mäki-Opas T, Kunst AE, Borodulin K, Rahkonen O, Prättälä R. Childhood adversities and socioeconomic position as predictors of leisure-time physical inactivity in early adulthood. J Phys Act Health. 2015;12:193–9.
Liu RT. Childhood adversities and depression in adulthood: current findings and future directions. Clin Psychol Sci Pr. 2017;24:140–53.
Ho TC, King LS. Mechanisms of neuroplasticity linking early adversity to depression: developmental considerations. Transl Psychiatry. 2021;11:1–13.
Lang UE, Beglinger C, Schweinfurth N, Walter M, Borgwardt S. Nutritional aspects of depression. Cell Physiol Biochem. 2015;37:1029–43.
Hanć T, Bryl E, Szcześniewska P, Dutkiewicz A, Borkowska AR, Paszyńska E, et al. Association of adverse childhood experiences (ACEs) with obesity and underweight in children. Eat Weight Disord. 2022;27:1751–63.
Lown EA, Lui CK, Karriker-Jaffe K, Mulia N, Williams E, Ye Y, et al. Adverse childhood events and risk of diabetes onset in the 1979 National longitudinal survey of youth cohort. BMC Public Health. 2019;19:1007.
Isohookana R, Marttunen M, Hakko H, Riipinen P, Riala K. The impact of adverse childhood experiences on obesity and unhealthy weight control behaviors among adolescents. Compr Psychiatry. 2016;71:17–24.
Merrick MT, Ports KA, Ford DC, Afifi TO, Gershoff ET, Grogan-Kaylor A. Unpacking the impact of adverse childhood experiences on adult mental health. Child Abus Negl. 2017;69:10–9.
Sheffler JL, Stanley I, Sachs-Ericsson N. Chapter 4—ACEs and mental health outcomes. In: Asmundson GJG, Afifi TO, editors. Adverse childhood experiences. Academic Press, Elsevier Inc, London, United Kingdom; 2020. pp. 47–69. https://www.sciencedirect.com/science/article/pii/B9780128160657000045 .
Jaite C, Schneider N, Hilbert A, Pfeiffer E, Lehmkuhl U, Salbach-Andrae H. Etiological role of childhood emotional trauma and neglect in adolescent anorexia nervosa: a cross-sectional questionnaire analysis. Psychopathology. 2012;45:61–6.
Jacobi C, Hayward C, de Zwaan M, Kraemer HC, Agras WS. Coming to terms with risk factors for eating disorders: application of risk terminology and suggestions for a general taxonomy. Psychol Bull. 2004;130:19–65.
Rivara F, Adhia A, Lyons V, Massey A, Mills B, Morgan E, et al. The effects of violence on health. Health Aff. 2019;38:1622–9.
Lissau I, Sørensen TI. Parental neglect during childhood and increased risk of obesity in young adulthood. Lancet. 1994;343:324–7.
Sørensen TI, Holst C, Stunkard AJ. Childhood body mass index-genetic and familial environmental influences assessed in a longitudinal adoption study. Int J Obes Relat Metab Disord. 1992;16:705–14.
PubMed Google Scholar
Whitaker KL, Jarvis MJ, Beeken RJ, Boniface D, Wardle J. Comparing maternal and paternal intergenerational transmission of obesity risk in a large population-based sample. Am J Clin Nutr. 2010;91:1560–7.
Fuller-Thomson E, Sinclair DA, Brennenstuhl S. Carrying the pain of abuse: gender-specific findings on the relationship between childhood physical abuse and obesity in adulthood. Obes Facts. 2013;6:325–36.
Bentley T, Widom CS. A 30-year follow-up of the effects of child abuse and neglect on obesity in adulthood. Obesity. 2009;17:1900–5.
Download references
The study was made possible by a grant from Helsefonden (project number: 21B_0093). Open access funding provided by Copenhagen University.
Author information
Authors and affiliations.
Section of Environmental Health, Department of Public Health, University of Copenhagen, Øster Farimagsgade 5A, Copenhagen, Denmark
Cathrine L. Wimmelmann & Rebecca B. Clarke
Centre for Childhood Health, Islands Brygge 41, 2300 Copenhagen S, Copenhagen, Denmark
Cathrine L. Wimmelmann & Thorkild I. A. Sørensen
Section of Biostatistics, Department of Public Health, University of Copenhagen, Øster Farimagsgade 5A, Copenhagen, Denmark
Christoffer Sejling
Section of Epidemiology, Department of Public Health, University of Copenhagen, Øster Farimagsgade 5A, Copenhagen, Denmark
Leonie K. Elsenburg, Thorkild I. A. Sørensen & Naja H. Rod
Section on Genomic Physiology and Translation, Novo Nordisk Foundation Center for Basic Metabolic Research, University of Copenhagen, Blegdamsvej 3B, 2200 Copenhagen N, Copenhagen, Denmark
Thorkild I. A. Sørensen
You can also search for this author in PubMed Google Scholar
Contributions
CLW, TIAS and NHR conceived the idea and designed the study. All authors discussed the statistical analyses. CS conducted the analyses. CLW wrote the first draft of the manuscript. All authors discussed the results and contributed significantly to the final manuscript. All authors approved the final manuscript.
Corresponding author
Correspondence to Cathrine L. Wimmelmann .

Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
DANLIFE has been approved by the Danish Data Protection Agency (record number 514-0641/21-3000), who ensures that the project is in accordance with national and EU legislation. In Denmark, ethical approval is not required for this type of project, and it was therefore not requested. Also, as all data in the current study are retrieved from registries, it was not required to obtain written consent from participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary figures, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Wimmelmann, C.L., Sejling, C., Clarke, R.B. et al. Childhood adversity trajectories and weight status in young adult men: a register-based study including 359,783 Danish men. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01540-4
Download citation
Received : 24 November 2023
Revised : 06 May 2024
Accepted : 09 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1038/s41366-024-01540-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 27 May 2024
Predicting higher child BMI z-score and obesity incidence in Malaysia: a longitudinal analysis of a dynamic cohort study
- Ruth Salway 1 , 2 ,
- Miranda Armstrong 1 ,
- Jeevitha Mariapun 3 ,
- Daniel D Reidpath 4 ,
- Sophia Brady 1 ,
- Mohamed Shajahan Yasin 3 ,
- Tin Tin Su 5 na1 &
- Laura Johnson 2 na1
BMC Public Health volume 24 , Article number: 1408 ( 2024 ) Cite this article
82 Accesses
Metrics details
To target public health obesity prevention, we need to predict who might become obese i.e. predictors of increasing Body Mass Index (BMI) or obesity incidence. Predictors of incidence may be distinct from more well-studied predictors of prevalence, therefore we explored parent, child and sociodemographic predictors of child/adolescent BMI z-score and obesity incidence over 5 years in Malaysia.
The South East Asia Community Observatory in Segamat, Malaysia, provided longitudinal data on children and their parents ( n = 1767). Children were aged 6–14 years at baseline (2013-14) and followed up 5 years later. Linear multilevel models estimated associations with child BMI z-score at follow-up, adjusting for baseline BMI z-score and potential confounders. Predictors included parent cardiometabolic health (overweight/obesity, central obesity, hypertension, hyperglycaemia), and socio-demographics (ethnicity, employment, education). Logistic multilevel models explored predictors of obesity incidence.
Higher baseline BMI z-score predicted higher follow-up BMI z-score both in childhood to late adolescence (0.60; 95% CI: 0.55, 0.65) and early to late adolescence (0.76; 95% CI: 0.70, 0.82). There was inconsistent evidence of association between child BMI z-score at follow-up with parent cardiometabolic risk factors independent of baseline child BMI z-score. For example, maternal obesity, but not overweight, predicted a higher BMI z-score in childhood to early adolescence (overweight: 0.16; 95% CI: -0.03, 0.36, obesity: 0.41; 95% CI: 0.20, 0.61), and paternal overweight, but not obesity, predicted a higher BMI z-score in early to late adolescence (overweight: 0.22; 95% CI: 0.01, 0.43, obesity: 0.16; 95% CI: -0.10, 0.41). Parental obesity consistently predicted five-year obesity incidence in early to late adolescence, but not childhood to early adolescence. An adolescent without obesity at baseline with parents with obesity, had 3–4 times greater odds of developing obesity during follow-up (incidence OR = 3.38 (95% CI: 1.14–9.98, mother) and OR = 4.37 (95% CI 1.34–14.27, father) respectively).
Conclusions
Having a higher BMI z-score at baseline was a stronger predictor of a higher BMI z-score at follow-up than any parental or sociodemographic factor. Targeting prevention efforts based on parent or sociodemographic factors is unwarranted but early childhood remains a key period for universal obesity prevention.
Peer Review reports
Obesity is a major public health concern, which increases the risk of developing non-communicable diseases (NCDs) such as diabetes, stroke and cardiovascular disease [ 1 ]. Children and adolescents with obesity are five times more likely to become adults with obesity, with approximately 80% of adolescents with obesity remaining so in adulthood [ 2 ]. Obesity in childhood and adolescence is independently associated with the development of NCDs later in life [ 3 ]. To date, no childhood obesity treatments show long-term success [ 4 , 5 ], so preventing new incidence of obesity in childhood and adolescence is vital for long-term NCD prevention. Prevention is particularly important in low-and-middle-income countries (LMICs) where the prevalence of NCDs is lower but increasing rapidly [ 6 ]. In Malaysia, NCDs are the most common cause of death [ 7 ], and obesity prevalence in children and adolescents has more than doubled between 2011 and 2019 (6% and 15% respectively) [ 8 , 9 ], pointing to a need to understand new incidence of obesity. Obesity rates differ by ethnicity, with higher rates among Malay and Indian and lower among Chinese ethnicities [ 9 , 10 ]. Increasing obesity prevalence in Asian LMICs is generally attributed to changes in dietary and physical activity patterns caused by economic factors and urbanisation [ 11 ]. These include shifts towards more calorie-dense westernized foods and an increase in sedentary, indoor behaviours driven by a lack of open spaces or neighbourhood safety [ 12 , 13 ]. Universal prevention efforts to improve eating and activity behaviours are generally ineffective, often because long-term behaviour change requires intensive and sustained interventions. In resource poor settings, targeting prevention strategies at populations subgroups most likely to develop obesity could be more cost-effective. Thus understanding predictors of obesity incidence as well as prevalence is essential to identifying such subgroups before they develop obesity.
Parent obesity is consistently associated with child obesity prevalence, but less is known about associations with incidence. Two meta-analyses estimated the odds of childhood obesity for a child with parents with overweight/obesity to be double that of a child with parents of healthy weight [ 14 , 15 ]. Cross-sectional associations are also seen between parent and child body mass index (BMI), with stronger associations for those children with higher BMIs, suggesting an intergenerational transmission of risk for a high BMI [ 16 , 17 ]. Maternal pre-pregnancy BMI is prospectively associated with offspring BMI in both childhood and adulthood [ 18 ], but it is not clear whether associations are gender-specific, with some studies showing a stronger maternal association [ 17 , 19 ] while others show no differences between mothers and fathers [ 14 , 20 , 21 ]. Most studies of obesity prevalence are in high income countries, and systematic reviews suggest weaker associations in LMICs [ 14 , 15 ]. In Malaysia, a previous cross-sectional analysis found a two-fold higher obesity prevalence among children with one or more parents with obesity or central obesity [ 22 ], and the prevalence of overweight mother-child pairs increased from 15 to 22% between 2006 and 2015 [ 23 ]. While prevalence studies identify groups in need of treatment, understanding predictors of greater BMI gain over time and obesity incidence could identify targets for prevention. Annual obesity incidence estimates decrease with age, from 3.2% in 5–13 year-olds to 1.8% in 13–18 year-olds in the US [ 24 ] with similar patterns in other high-income countries [ 25 , 26 ]. However, obesity incidence is often lower in LMICs [ 27 ], and less is known about how incidence is related to parental risk factors in these countries. Identifying those children who may be at risk of developing obesity in future, based on current parental risk factors may allow intervention before obesity develops and thus reduce new incidence and future prevalence.
Few studies have explored the relationship between broader parental cardiometabolic risk factors, such as hypertension and hyperglycaemia, with child obesity although associations have been reported with parent cardiovascular health [ 28 ]and diabetes in parents [ 29 , 30 ]. Intergenerational transmission of risk of NCDs could be via genetic or lifestyle mechanisms, and parents with hypertension or hyperglycaemia may have poorer diets and lower physical activity that may be shared with their children [ 31 , 32 ]. To our knowledge, no studies have described differences in BMI or obesity incidence among children in Malaysia and little is known about the factors associated with higher gains in BMI and the development of obesity in this population. Therefore, we aimed to explore how parental weight status and cardiometabolic risk factors are longitudinally associated with child BMI z-score (follow-up adjusted for baseline) and obesity incidence.
Analysis is reported following STROBE guidelines (Supplement). Data are from two health surveys from the South East Asia Community Observatory (SEACO) health and demographic surveillance system cohort in Malaysia [ 33 ], which undertakes annual enumeration of households within five of 11 sub-districts of the Segamat district. Population-wide individual level health surveys of participants aged 5 years and above were undertaken in 2013–14 and 2018-19, and collected questionnaire and biophysical measurement data on around 25,000 participants in each round (55–56% response rate of the total SEACO population), with around 10,000 participating at both timepoints.
We analysed individual data on children aged 6–14 years at baseline (11–19 years at follow-up) and their parents from the SEACO health surveys, using household structure information taken from the enumeration in 2013-14 and 2018-19 to match parents and children [ 33 ]. Participants and households were linked across surveys using a unique SEACO participant ID. The analysis sample consisted of all children who had data at both timepoints and were matched to at least one parent with data. Fig. 1 shows the flow of participants from baseline to main analysis. We treated data for 59 mothers who were pregnant as missing and excluded one pregnant adolescent. Of the 4,388 children available at baseline, 1,855 (42%) had data at follow-up, with 1,768 (95%; 40% of the baseline cohort) matched to at least one parent, and 1,341 (72%; 31% of the baseline) having two parents identified. The final analysis sample size after multiple imputation (see below) was 1,768 (40% of baseline cohort).
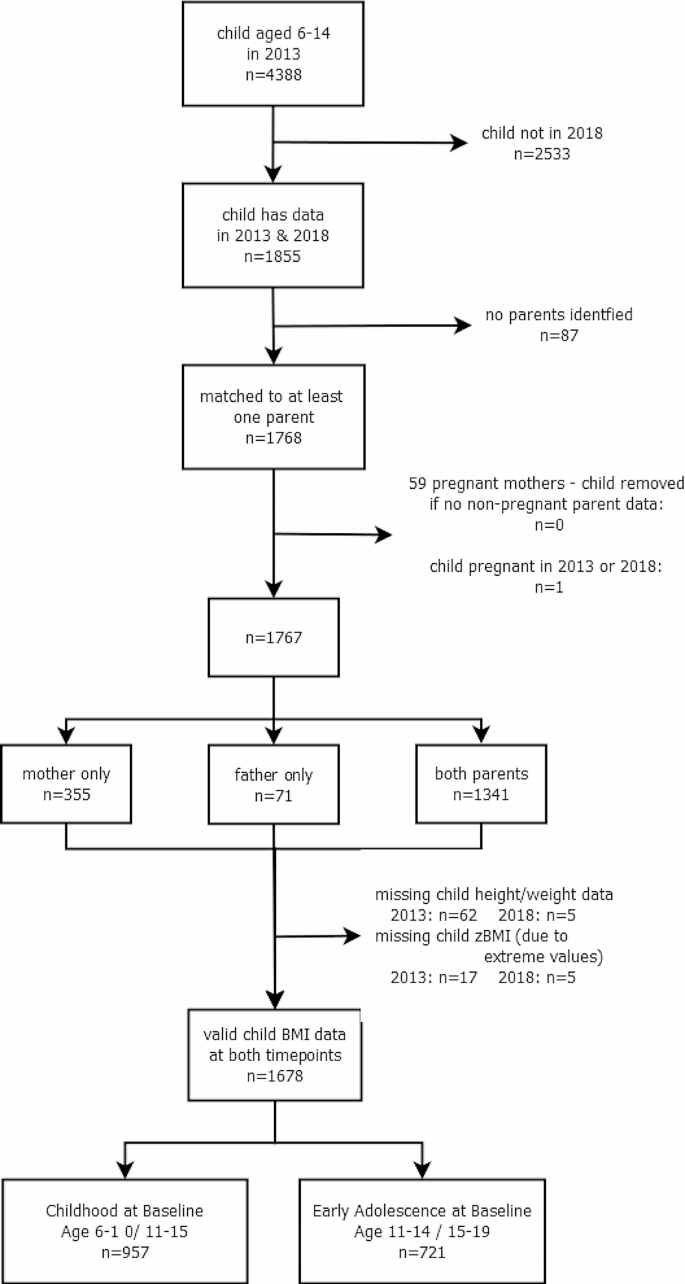
Flow diagram of participants
Ethical considerations
Ethics approval for both surveys were obtained through the Monash University Human Research Ethics Committee: MUHREC (3837) for the Health Round Survey 2013 and MUHREC (13,242) for the Health Round Survey 2018. All participants gave informed consent which allows for secondary analysis without additional consent, and data was provided in anonymised form. As part of the SEACO Health Round surveys, adult participants received free health screenings (blood pressure, blood glucose, BMI and waist circumference), with referral letters provided to high-risk respondents for future health check-ups at local clinics.
Height and weight were measured without footwear or head gear (except a light scarf or veil) using a Transtek digital weighing scale with height gauge, (model GBS-721) by trained data collectors, with one measurement taken following the SEACO Standard Operating Protocol (SOP). Child BMI was calculated from weight and height and converted to age-adjusted standardised z-scores (BMI z-score) using the sex-specific World Health Organization (WHO) 2007 BMI reference for children aged 5–19. Children were classified with thinness, overweight or obesity according to WHO definitions [ 34 ] if the standardised BMI z-score was <-2 standard deviations (SD), >1SD and > 2SD, respectively, with all remaining children classified as healthy weight.
Parent risk factors
Anthropometric measurements of all participating parents (mothers and fathers) were taken by trained data collectors in the participant’s home, with parent height and weight measured in the same way as for children, following the SEACO SOP. Waist circumference was measured using an AccuFitness Myotape, with the measurement taken at the midpoint between the lower margin of the tip of the rib and the upper point of the iliac crest (hip bone), following the WHO STEPS protocol [ 35 ]. Blood pressure was recorded after participants had been sitting for at least 15 min. Three blood pressure measurements were taken using an Omron automated blood pressure monitor (HEM-7203) with 30–60 s between subsequent measurements, and the mean of the final two readings used, according to the SEACO SOP. Participants were asked how long since they had taken food or drink (other than water), and random non-fasting blood glucose was measured using a finger-prick Omron blood glucose monitoring system, (HGM-111). BMI (kg/m 2 ) was calculated from height and weight and classified with thinness (< 18 kg/m 2 ), overweight (> 25 kg/m 2 and < 30 kg/m 2 ), obesity (≥ 30 kg/m 2 ), and of healthy weight otherwise [ 36 ], in line with previous analyses of the SEACO data [ 22 ]. Central obesity was defined using International Diabetes Federation (IDF) recommendations for Asian populations [ 37 ], as waist circumference ≥ 90 cm in men and ≥ 80 cm in women. Hypertension was defined as either systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg [ 38 ]. Hyperglycaemia was defined as random non-fasting blood glucose ≥ 11.1 mmol/l [ 39 ].
Confounders
Parent and child age, gender and ethnicity were self-reported in the main SEACO census. Inconsistencies between the two timepoints were checked using date of birth and date of data collection with precedence given to age at baseline in 2013. We grouped children into two age groups, corresponding to Malaysian primary and secondary school ages: childhood at baseline (aged 6–10 years at baseline, aged 11–15 at follow-up) and adolescence at baseline (aged 11–14 years at baseline, aged 15–19 at follow-up)). Ethnicity was recoded into four groups: Malay, Chinese, Indian and Other (comprising indigenous (Orang Asli) and Other, grouped due to low numbers). Missing child ethnicity was derived from parent ethnicity, with preference given to 2013 data. Parental working status was classified as Working (part-time, full-time, casual) or Not Working (unemployed, housewife, student, retired). Highest parental education (up to primary, secondary, tertiary) was recorded for each parent.
Statistical analysis
Baseline sample characteristics (child: age, gender, ethnicity, BMI z-score and weight category, and parent: age, gender, highest education, employment status, weight category, central obesity, hypertension and hyperglycaemia) were described using means and SDs, or percentages, as appropriate, by child gender and age group (results provided in main document). Child and Head of Household characteristics were compared for baseline and analysis samples, and for children with zero, one and two identified parents (see Appendix). Five-year incidence rate of obesity was calculated as the percentage without obesity at baseline with obesity at follow-up. Similarly, five-year remission rates were calculated as the percentage of those with obesity who were without obesity at follow-up, and five-year persistence rate as the percentage who remained with obesity (main document).
To investigate associations between parental risk factors (overweight/obesity, central obesity, hypertension and hyperglycaemia) and change in child BMI z-score, we modelled child BMI z-score in 2018 adjusted for baseline [ 40 ]. While concerns have been raised around the use of BMI z-scores for assessing change in child BMI for children with extreme BMIs, in particular those with severe obesity [ 41 ], this study focuses on estimating associations for the general population where BMI z-score has been found to be suitable for assessing change [ 42 , 43 ] and so distortion in the extremes will have less of an impact, although associations will be underestimated for children with very high BMI. We fitted a linear multilevel model for children nested within parents, with child BMI z-score at follow-up as the outcome, adjusted for time to follow-up and baseline child BMI z-score; this assumes a linear change between baseline and follow-up. We first fitted models for each parental risk factor separately. We then fitted adjusted models, controlling for child characteristics (gender, age, ethnicity) and parent sociodemographic characteristics (age, working status and education Associations with parent hypertension and hyperglycaemia models were additionally adjusted for parent BMI category. The adjusted estimates are illustrated in Fig. 3 in the main document; estimates for unadjusted and adjusted models are given in the Appendix. We also fit models for the association between follow-up BMI z-score adjusted for baseline BMI z-score, and sociodemographic variables, specifically ethnicity, parental age, education and employment status. In a post-hoc analysis, we investigated associations between parental risk factors and obesity incidence, which focuses on children with higher BMI moving to a weight status of higher risk, and does not suffer from the same issues as using BMI z-score. We used logistic multilevel models, with a binary outcome for child with obesity at follow-up, restricted to those who were without obesity at baseline, and adjusted for time to follow-up, child characteristics, parent sociodemographic characteristics, and other parental risk factors as described above (main document). All analyses were stratified by age group, with separate models for mothers and fathers. A test for gender interactions did not support the need for stratification by gender, therefore results are reported for the whole sample combined. Adjusted models excluded child ethnicity ’Other’ due to small numbers. Descriptive summaries were performed in Stata v17 [ 44 ] and multilevel models were run in MLwiN v3.05 via the Stata command runmlwin, using restrictive iterative generalised least squares. Sensitivity analyses compared adjusted model estimates using imputed data with complete case analyses, and we repeated the analysis, first using Asian population BMI cut-offs for parental overweight (> 23 kg/m 2 and < 25 kg/m 2 ) and obesity (> 25 kg/m 2 ) and second excluding children with thinness, as for these children an increase in BMI might be considered beneficial thus potentially violating the linearity assumption (Appendix).
Missing data
We restricted analysis to children with BMI data at both timepoints who could be matched to at least one parent ( n = 1678; 38% of baseline). Missing data on gender, age and ethnicity for children and parents was taken from the other timepoint where available. Multiple imputation was used for parent risk factors to maximise the information used in the study and increase the precision of estimates [ 45 ]. We imputed missing parent data if they were included for at least one timepoint; note we did not impute child data at missing timepoints or BMI z-score.
Missing data was imputed using the jomo package in R (v4.0.2) via a simulation-based approach with a multivariate normal model to account for the multilevel structure. All analysis variables were included, and variables associated with missingness: total size of household, number of children and household structure (children/ parents, children/grandparents, and multi-generational/complex households). Continuous parental risk factors were imputed on a log scale, and parent BMI, central obesity, hypertension and hyperglycaemia were calculated from these. Twenty imputation datasets were created for each age group separately, using a burn-in of 500 iterations and 500 iterations between imputation datasets, selected by visual inspection. Model estimates were combined across the imputation datasets using Rubin’s rules [ 46 ].
There were 1,678 children included at both timepoints, with valid child BMI data, were not pregnant and were matched to at least one parent (Fig. 1 ). At baseline, 957 were aged 6–10 years (childhood at baseline) and 721 aged 11–14 (adolescence at baseline). Of these, 68% were Malay, 16% Chinese, 13% Indian and 2% Other, and 56% were female (Table 1 ). At baseline, 16% had obesity, 16% overweight and 16% thinness, with similar prevalences at follow-up. Compared to those excluded owing to missing child BMI data at a single timepoint, the children in the longitudinal analysis sample were a year younger, had lower baseline BMI z-score, were less likely to be male or Chinese, and came from households where the Head of Household had higher education and was less likely to be Indian (Table S1 ). Children with matched parents had higher BMI z-scores, were more likely to be male and were less likely to be Chinese (Table S2 ). Missing data varied between 8 and 27% for maternal and 20–36% for paternal variables (Table S3 ), primarily due to missing hypertension and hyperglycaemia. We imputed data on 9% of mothers and 24% of fathers; baseline characteristics were broadly similar between collected data and imputed data (Table S3 ). The average age of mothers was 41 years, with father slightly older at 45 years. Most parents (70%) were educated to secondary level, with most fathers in employment (91%) while mothers less likely to be employed (31%).
BMI z-score was higher at follow-up compared to baseline for girls, the childhood age-group at baseline. Whereas BMI z-score was lower at follow-up compared to baseline for the adolescent age-group at baseline (Table 1 ). Obesity prevalence was 16–18%, with movement between weight categories over time (Fig. 2 ). Five-year obesity incidence was higher in childhood (at baseline) than adolescence (at baseline) (10.8% and 6.1% respectively; Table 2 ). Five-year obesity remission rates of 42% were observed (Table 2 ). Of those participants with a healthy weight at baseline, 19% developed overweight or obesity at follow-up, compared to 7% developing thinness.
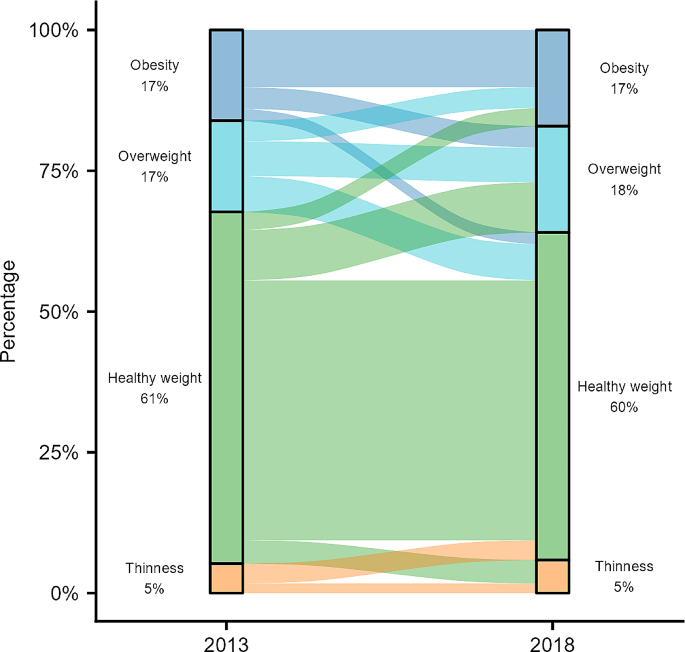
Change in child BMI category between 2013 and 2018
Fig. 3 (and Table S4 & S5 ) shows modelled associations between parent cardiometabolic health and child BMI z-score at follow-up. For all models, higher child BMI z-score at baseline was the strongest predictor of a higher child BMI z-score at follow-up. Each unit of baseline BMI z-score was associated with a 0.60 (95% CI: 0.55, 0.65) higher follow-up BMI z-score for childhood to early adolescence and 0.76 (95% CI: 0.70, 0.82) higher for early to late adolescence. Associations with parental cardiometabolic risk factors were much smaller with weak or no evidence of association. In childhood to early adolescence, compared to healthy maternal weight, obesity (B = 0.41 (95% CI: 0.20, 0.61)), but not overweight (B = 0.16 (95% CI: -0.03, 0.36)) was associated with an increase in child BMI z-score of at follow-up (Table S4 ). While not associated with higher BMI z-score among younger participants (childhood to early adolescence), compared to a healthy paternal weight, overweight (B = 0.22 (95% CI: 0.01, 0.43)) but not obesity (B = 0.16 (95% CI: -0.10, 0.41)) showed small associations with a higher BMI z-score in older participants (early to late adolescence) (Table S4 ). Parental BMI and waist circumference were strongly correlated (0.73–0.75) and so associations with central obesity followed the same patterns as parental overweight/obesity. Associations between child BMI z-score at follow-up and baseline parent hypertension and hyperglycaemia (Table S4 ), ethnicity, parent employment status or educational attainment (Table S5 ) were small with weak or no evidence of association.
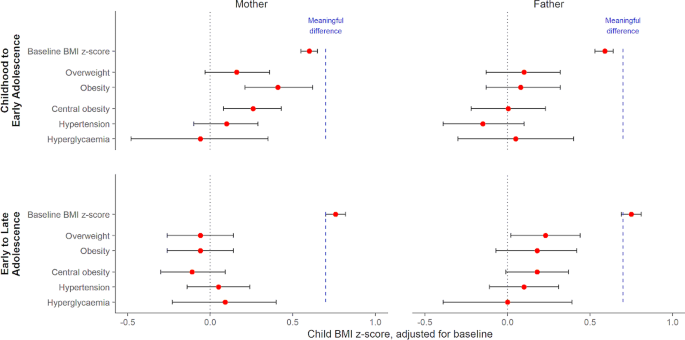
Association between parental risk factors and baseline-adjusted child BMI z-score at follow-up
Model estimates and 95% confidence intervals by age strata and parent (see also Table S4 ). Models adjusted for baseline BMI z-score, time interval, child (gender, age, ethnicity) and relevant parent characteristics (age, education, other cardiometabolic risk factors). The dashed blue line represents the minimum change in BMI z-score for a meaningful clinical impact on child and adolescent lipids and blood pressure, based on a recent meta-analysis (El-Medany et al., 2020).
Childhood to early adolescence group were aged 6–10 at baseline (11–15 at follow-up) and early to late adolescence group aged 11–14 at baseline (16–19 at follow-up).
We saw similar patterns for obesity incidence, with stronger maternal associations in childhood to early adolescence, and paternal associations in early to late adolescence (Table 3 ). In childhood to early adolescence, the odds of obesity incidence were similar among those with a parent with overweight vs. a healthy weight parent (paternal OR = 0.67 (95% CI 0.33–1.37); maternal OR = 1.33 (95% CI: 0.71–2.48)). Obesity incidence odds were higher among the older age group, especially for those with a parent with obesity at 3–4 times higher (paternal OR = 4.37 (95% CI 1.34–14.27); maternal OR = 3.38 (95% CI: 1.14–9.98)). Associations with parental central obesity followed similar patterns, especially for maternal central obesity, where odds were higher than for BMI-based overweight/obesity (Table 3 ). There were no marked associations with parent hypertension or hyperglycaemia (ORs between 0.5 and 1.5 with wide confidence intervals).
Complete case analysis showed similar associations (Table S6 ), with slightly stronger associations for mothers with overweight. Sensitivity analyses were run for the association between child BMI z-score at follow-up and parental weight category using the overweight/obesity definition for Asian populations, which has lower BMI thresholds (Table S7 ). We saw similar patterns of associations to before, but with parental obesity rather than parental overweight; specifically associations with maternal obesity for those in childhood to early adolescence, and associations with paternal obesity for those in early to late adolescence. As the linearity assumption between baseline and follow-up BMI z-score did not hold for low values of baseline BMI z-score (Figure S1 )., we repeated the analysis excluding children with thinness (Table S8 ) but found no difference in the reported associations between child BMI z-score at follow-up and parental cardiometabolic risk factors.
We have reported how parental cardiometabolic factors (overweight, obesity, central obesity, hypertension and hyperglycaemia) are associated with child BMI z-score at five-year follow-up, and the development of obesity in Malaysian children. Five-year increases in BMI z-score depended on child age at baseline, with larger increases between childhood and early adolescence compared to early and late adolescence. Previous cross-sectional analyses highlight associations between parental weight status and sociodemographic factors and child BMI z-score at a single timepoint [ 21 , 22 ]. We found parental obesity was weakly associated with child BMI z-score differences, below values considered clinically meaningful, but associated with high odds of developing obesity, suggesting that targeted childhood obesity prevention strategies may need to focus on children of parents with obesity who may not be immediately at risk. For example, existing adult weight management programmes, such as ‘My body is fit and fabulous’ in Malaysia aimed at housewives [ 47 ], could also include advice and support aimed at the whole family to target children in childhood and early adolescence before they develop obesity.
In Segamat, obesity prevalence was estimated at 16% in 6–10 year olds, 18% in 10–14 year olds and 16% in those aged 15 or more, with overweight prevalence at 15%, 20% and 15% respectively. This is consistent with overweight and obesity prevalences of 15% across ages 5–18 reported for Malaysian children in the National Health and Morbidity Survey 2019 and elsewhere [ 9 , 21 , 23 ], but highlights variation with age, with higher rates during the early adolescent period. While obesity prevalence was relatively stable, this masked substantial change. Over five years, new obesity incidence was 8.8%, while 42% of those with obesity at baseline were without obesity at follow-up. Both the incidence and remission rates are slightly lower than those reported in high-income countries [ 24 , 25 ] and we did not observe higher remission rates among younger children as other studies have reported [ 48 , 49 , 50 ]. In general, the majority of children who shift between BMI categories tend to do so at the boundaries. While some of the remission may be attributable to measurement error or regression to the mean, it may also be due to individual behaviour change, timing of maturation [ 48 ], or lower odds of remission associated with low birthweight [ 50 ].
Malaysia has a double burden of both thinness and overweight/obesity but we found more children with healthy weight at baseline developing overweight/obesity than thinness at follow-up (19% and 7% respectively). Our findings may reflect differences in LMICs where obesity rates are still increasing, with higher incidence in childhood not balanced by higher remission rates, leading to an increasing obesity prevalence over time, although conclusions are limited by having only two time points.
In childhood to early adolescence, maternal overweight/obesity were associated with higher mean BMI z-score at follow-up compared to mothers of healthy weight, whilst in early to late adolescence the associations of higher offspring BMI z-score were strongest with paternal overweight and obesity. Note that we have used WHO international BMI thresholds for parental overweight/obesity, but we found similar maternal and paternal patterns by child age group when using lower risk thresholds suggested for Asian populations, with the key difference being associations with parental obesity but not overweight, reflecting the shift in the thresholds. We observed similar patterns for central obesity, which is in line with the strong correlation between BMI and waist circumference. A recent meta-analysis [ 51 ] indicates a minimum mean increase in BMI z-score for a clinical impact on lipid profiles and blood pressure in 4–19 year olds is 0.7 z-scores. The associations we observed are over five years, and estimates (and confidence interval bounds) are much smaller than 0.7 and thus do not suggest associations are substantial enough to alter metabolic health in a clinically-relevant way. While larger cross-sectional associations between parental overweight/obesity and children’s BMI z-score [ 14 , 15 , 22 ] may be due to genetic predisposition to obesity, common obesogenic lifestyles, including diet and physical activity, due to shared living environment and/or behavioural factors passed down from parent to child [ 14 ], our analysis suggests these factors have a far smaller impact on the five-year difference in BMI z-score. We note, however, that our results may underestimate the association for those children with very high BMIs, and so further research on associations for children with severe obesity may be warranted.
There were no marked associations with parental hypertension, hyperglycaemia, or socioeconomic status, thus our study suggests that childhood obesity prevention strategies may be best targeted at those who have parents with overweight or obesity. The strongest associations observed were with BMI z-score at baseline, as children with higher initial BMI experienced larger five-year increases than expected compared to WHO references.
While increasing BMI z-scores can indicate growth in excess of normal expectations for a given age and sex, higher-than-average BMI is not in itself a cause for concern if children remain on the same trajectories into adolescence, because they will stay within the healthy BMI range. Both BMI z-score and overweight/obesity definitions in children are based on comparison to a historic cross-sectional reference population (in this study, the WHO reference population) and thus differences we observe may be a result of different underlying characteristics of populations, such as the timing of pubertal growth spurts, rather than necessarily cause for concern. Figure S2 (see Appendix) shows that median BMI was higher than the WHO growth reference at all ages for boys and girls, with the rate of change in BMI temporally shifted, so the fastest rate of increase occurred 1–2 years younger. The strong associations with baseline BMI z-score suggest that excessive growth trajectories are initiated earlier in childhood and are perpetuated into adolescence [ 52 , 53 , 54 ]. Thus, the small associations between parental risk factors and offspring BMI z-score may be because those children predisposed to obesity, having already lived with overweight or obesity from a young age. However, these difficulties in assessing change in BMI in childhood make it challenging to interpret results.
Five-year obesity incidence was higher between childhood and early adolescence than between early and late adolescence (10.8% and 6.1% respectively), consistent with patterns elsewhere of higher incidence at younger ages [ 24 , 25 ], and in line with the theory that excessive growth tends to occur earlier in childhood. Associations between parental overweight/obesity and child obesity incidence were larger in early to late adolescence than in childhood to early adolescence with parental overweight associated with a doubling in odds of five-year obesity incidence and parental obesity associated with a 3–4 times higher odds. Note that BMI changes considerably during puberty with a growth spurt and the adiposity rebound, which will occur predominantly within the childhood to early adolescence group, and may account for the weaker associations within this group. In contrast, the stronger associations in the early to late adolescence group, once puberty is more established, highlights that a child with one or both parents with obesity may not develop obesity until late adolescence, and so may not have been identified as at risk when younger. This is of concern because associations with obesity in adulthood are stronger for those with obesity in adolescence than in childhood [ 2 ], and thus indicate that this group of children may require targeting at a younger age even if they do not yet have obesity. Associations between parental obesity and adolescent obesity incidence but not BMI z-score may indicate a differential importance of parent weight for child BMI across the distribution of child BMI [ 16 , 17 ]. For example, children with higher baseline BMI z-scores would need a smaller increase in BMI z-score (such as is associated with having a parent with obesity) to move into the overweight or obesity category. Thus, parental obesity may have a stronger association for children closer to the cut-off for obesity at baseline, especially in early adolescence.
We saw some evidence of different associations by parent gender, with maternal weight dominating in childhood to early adolescence and paternal weight in early to late adolescence. Maternal obesity before and during pregnancy (a key developmental period) is associated with offspring BMI in childhood, potentially driven by intrauterine, genetic or lifestyle factors such as smoking [ 53 , 55 ]. Some cross-sectional studies have found stronger maternal associations [ 17 , 19 ] and our results suggest that associations may continue into childhood, possibly reflecting the common role of the mother as primary caregiver in younger children, especially in more traditional communities, with more influence over lifestyle factors such as diet and physical activity. However, we found this was replaced by a weaker paternal association in early to late adolescence. Thus maternal associations in childhood may thus result in earlier puberty [ 56 ], and an earlier adolescent increase in BMI, while paternal weight is associated with higher BMI at the end of adolescence. However, all these associations were small and other evidence is inconclusive, especially for fathers. While much of the current evidence focuses on maternal associations, fathers are under-represented, and more research is needed to determine the paternal role throughout childhood and adolescence. Understanding further our findings of a stronger paternal association in early to late adolescence is of particular importance as this is a critical time for BMI trajectories into adulthood.
Strengths and limitations
This study uses prospective data with a robust sampling design in the SEACO cohort, resulting in high levels of parental data, especially for fathers who are typically under-represented, with most studies focusing on mothers [ 23 ]. Parental cardiometabolic risk factors were measured objectively rather than using self-report measures. However, because data were collected at household level, matching children to parents was difficult especially with multiple families in a household and we were unable to distinguish between biological and non-biological parents. We also excluded a substantial number of children due to missing data at follow-up, and did not have data on lifestyle factors such as diet or physical activity. While multiple imputation maximises the available information in the data, this is under a missing at random assumption. Exploring changes in BMI in this age group is challenging due to puberty and childhood growth patterns, and so care should be taken in interpreting results. Furthermore, Segamat is a semi-rural region so is not generalisable to the wider Malaysian population, although overweight/obesity estimates are similar [ 23 ]. Finally, our analysis focuses on the general population; estimates of associations may be underestimated for those children with severe obesity.
In this Malaysian cohort, child/adolescent obesity prevalence was stable at 16–18%, with a five-year incidence of obesity at 8.8%. Parental overweight/obesity was prospectively associated with slightly higher child BMI z-score after adjusting for baseline, but the largest follow-up BMI z-scores were among children with a higher baseline BMI z-score. These findings support the importance of childhood as a key period for obesity prevention, rather than later intervention based on parent cardiometabolic risk. However, those in early adolescence with higher BMI z-score and at least one parent with obesity may be at an increased risk of becoming obese during late adolescence.
Data availability
Data are from an ongoing prospective cohort study and are available from SEACO by completion of a data application form to: https://www.monash.edu.my/seaco/research-and-training/how-to-collaborate-with-seaco.
Abbreviations
Body mass index
International Diabetes Federation
Low-and-middle-income country
Non-communicable disease
South East Asia Community Observatory
World Health Organization
World Health Organization. Global Health Risks: Mortality and burden of disease attributable to selected major risks. In. Geneva: World Health Organization; 2009.
Simmonds M, Llewellyn A, Owen CG, Woolacott N. Predicting adult obesity from childhood obesity: a systematic review and meta-analysis. Obes Rev. 2016;17(2):95–107.
Article CAS PubMed Google Scholar
Lin X, Xu Y, Xu J, Pan X, Song X, Shan L, Zhao Y, Shan PF. Global burden of noncommunicable disease attributable to high body mass index in 195 countries and territories, 1990–2017. Endocrine. 2020;69(2):310–20.
Mead E, Brown T, Rees K, Azevedo LB, Whittaker V, Jones D, Olajide J, Mainardi GM, Corpeleijn E, O’Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese children from the age of 6 to 11 years. Cochrane Database Syst Rev. 2017;6:CD012651.
PubMed Google Scholar
Al-Khudairy L, Loveman E, Colquitt JL, Mead E, Johnson RE, Fraser H, Olajide J, Murphy M, Velho RM, O’Malley C, et al. Diet, physical activity and behavioural interventions for the treatment of overweight or obese adolescents aged 12 to 17 years. Cochrane Database Syst Rev. 2017;6:CD012691.
Miranda JJ, Barrientos-Gutierrez T, Corvalan C, Hyder AA, Lazo-Porras M, Oni T, Wells JCK. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat Med. 2019;25(11):1667–79.
Low WY, Lee YK, Samy AL. Non-communicable diseases in the Asia-Pacific region: prevalence, risk factors and community-based prevention. Int J Occup Med Environ Health. 2015;28(1):20–6.
Institute for Public Health (IPH). National Health and Morbidity Survey 2015 (NHMS 2015). Vol. II: Non-Communicable Diseases, Risk Factors & Other Health Problems. In. Malaysia; 2015.
Institute for Public Health: National Health and Morbidity Survey (NHMS). 2019: Vol. I: NCDs – Non-Communicable Diseases: Risk Factors and other Health Problems. In. Malaysia: Institute for Public Health, National Institutes of Health, Ministry of Health; 2020.
Rampal L, Rampal S, Khor GL, Zain AM, Ooyub SB, Rahmat RB, FGhani S, N, Krishnan J. A national study on the prevalence of obesity among 16,127 malaysians. Asia Pac J Clin Nutr. 2007;16(3):561–6.
Li M, Dibley M, Baur L, Twigg S, Magnusson R. Child and adolescent obesity in Asia. A modern epidemic: Expert perspectives on obesity and diabetes. Sydney, NSW: Sydney University; 2012.
Google Scholar
Gupta N, Goel K, Shah P, Misra A. Childhood obesity in developing countries: epidemiology, determinants, and prevention. Endocr Rev. 2012;33(1):48–70.
Misra A, Khurana L. Obesity and the metabolic syndrome in developing countries. J Clin Endocrinol Metab. 2008;93(11 Suppl 1):S9–30.
Wang Y, Min J, Khuri J, Li M. A systematic examination of the Association between parental and child obesity across Countries. Adv Nutr. 2017;8(3):436–48.
Article PubMed PubMed Central Google Scholar
Lee JS, Jin MH, Lee HJ. Global relationship between parent and child obesity: a systematic review and meta-analysis. Clin Exp Pediatr. 2022;65(1):35–46.
Article PubMed Google Scholar
Dolton P, Xiao M. The intergenerational transmission of body mass index across countries. Econ Hum Biol. 2017;24:140–52.
Johnson PCD, Logue J, McConnachie A, Abu-Rmeileh NME, Hart C, Upton MN, Lean M, Sattar N, Watt G. Intergenerational change and familial aggregation of body mass index. Eur J Epidemiol. 2011;27(1):53–61.
Heslehurst N, Vieira R, Akhter Z, Bailey H, Slack E, Ngongalah L, Pemu A, Rankin J. The association between maternal body mass index and child obesity: a systematic review and meta-analysis. PLoS Med. 2019;16(6):e1002817.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in Young Adulthood from Childhood and parental obesity. New Eng J Med 1997(13):869–73.
Davey Smith G, Steer C, Leary S, Ness A. Is there an intrauterine influence on obesity? Evidence from parent child associations in the Avon Longitudinal Study of parents and children (ALSPAC). Arch Dis Child. 2007;92(10):876–80.
Ahmad A, Zulaily N, Shahril MR, Wafa SW, Mohd Amin R, Piernas C, Ahmed A. Obesity determinants among Malaysian 12-year old school adolescents: findings from the HAT study. BMC Pediatr. 2021;21(1):418.
Partap U, Young EH, Allotey P, Sandhu MS, Reidpath DD. Anthropometric and cardiometabolic risk factors in parents and child obesity in Segamat, Malaysia. Int J Epidemiol. 2017;46(5):1523–32.
Mohamed NN, Rohana AJ, Hamid NAA, Hu FB, Malik VS, Mohd Yusoff MF, Aris T, The Global N. Epidemiologic transition Initiative G: Intergenerational Transmission of Obesity from mothers to their offspring: Trends and Associated factors derived from the Malaysian National Health and Morbidity Survey (NHMS). Nutrients 2022, 14(11).
Cheung PC, Cunningham SA, Narayan KM, Kramer MR. Childhood Obesity Incidence in the United States: a systematic review. Child Obes. 2016;12(1):1–11.
Hughes AR, Sherriff A, Lawlor DA, Ness AR, Reilly JJ. Incidence of obesity during childhood and adolescence in a large contemporary cohort. Prev Med. 2011;52(5):300–4.
Ikeda N, Nishi N. First incidence and associated factors of overweight and obesity from preschool to primary school: longitudinal analysis of a national cohort in Japan. Int J Obes (Lond). 2019;43(4):751–60.
Do LM, Tran TK, Eriksson B, Petzold M, Ascher H. Prevalence and incidence of overweight and obesity among Vietnamese preschool children: a longitudinal cohort study. BMC Pediatr. 2017;17(1):150.
Muchira JM, Gona PN, Mogos MF, Stuart-Shor E, Leveille SG, Piano MR, Hayman LL. Temporal trends and Familial Clustering of Ideal Cardiovascular Health in parents and offspring over the Life Course: An Investigation using the Framingham Heart Study. J Am Heart Assoc. 2020;9(12):e016292.
Article CAS PubMed PubMed Central Google Scholar
Linares Segovia B, Gutierrez Tinoco M, Izquierdo Arrizon A, Guizar Mendoza JM, Amador Licona N. Long-term consequences for offspring of paternal diabetes and metabolic syndrome. Exp Diabetes Res. 2012;2012:684562.
Kawasaki M, Arata N, Miyazaki C, Mori R, Kikuchi T, Ogawa Y, Ota E. Obesity and abnormal glucose tolerance in offspring of diabetic mothers: a systematic review and meta-analysis. PLoS ONE. 2018;13(1):e0190676.
Niermann CYN, Spengler S, Gubbels JS. Physical activity, screen time, and dietary intake in families: a cluster-analysis with Mother-Father-Child triads. Front Public Health. 2018;6:276.
Bogl LH, Silventoinen K, Hebestreit A, Intemann T, Williams G, Michels N, Molnar D, Page AS, Pala V, Papoutsou S et al. Familial resemblance in Dietary intakes of children, adolescents, and parents: does Dietary Quality play a role? Nutrients 2017, 9(8).
Partap U, Young EH, Allotey P, Soyiri IN, Jahan N, Komahan K, Devarajan N, Sandhu MS, Reidpath DD. HDSS Profile: the South East Asia Community Observatory Health and Demographic Surveillance System (SEACO HDSS). Int J Epidemiol. 2017;46(5):1370–g1371.
WHO. Growth Reference 5–19 Years - Application Tools. In. Geneva: World Health Organization; 2014.
STEPwise approach to NCD risk factor surveillance (STEPS). https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps.
World Health Organization. Obesity and overweight. In. Geneva: World Health Organization; 2015.
IDF. The IDF Consensus on the Definition of the Metabolic Syndrome in Children and Adolescents. In. Brussels: International Diabetes Federation; 2007.
Whitworth J. World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertensb. 2003;21:1983–92.
Article Google Scholar
WHO, IDF. Definition and diagnosis of diabetes Mellitus and Intermediate Hyperglycemia. In. Geneva: World Health Organization; 2006.
Tennant PWG, Arnold KF, Ellison GTH, Gilthorpe MS. Analyses of ‘change scores’ do not estimate causal effects in observational data. Int J Epidemiol. 2022;51(5):1604–15.
Freedman DS, Berenson GS. Tracking of BMI z scores for severe obesity. Pediatrics. 2017;140(3):e20171072.
Kakinami L, Henderson M, Chiolero A, Cole TJ, Paradis G. Identifying the best body mass index metric to assess adiposity change in children. Arch Dis Child. 2014;99(11):1020–4.
Inokuchi M, Matsuo N, Takayama JI, Hasegawa T. BMI z-score is the optimal measure of annual adiposity change in elementary school children. Ann Hum Biol. 2011;38(6):747–51.
StataCorp.: Stata Statistical Software: Release 17. In. College Station, TX: StataCorp LLC; 2021.
Dong Y, Peng C-Y. Principled missing data methods for researchers. SpringerPlus. 2013;2:222.
Rubin D. Multiple imputation after 18 years. J Am Stat Assoc. 1996;91(434):473–89.
Ambak R, Mohamad Nor NS, Puteh N, Mohd Tamil A, Omar MA, Shahar S, Ahmad NA, Aris T. The effect of weight loss intervention programme on health-related quality of life among low income overweight and obese housewives in the MyBFF@home study. BMC Womens Health. 2018;18(Suppl 1):111.
Kim J, Must A, Fitzmaurice GM, Gillman MW, Chomitz V, Kramer E, McGowan R, Peterson KE. Incidence and remission rates of overweight among children aged 5 to 13 years in a district-wide school surveillance system. Am J Public Health. 2005;95(9):1588–94.
von Kries R, Beyerlein A, Muller MJ, Heinrich J, Landsberg B, Bolte G, Chmitorz A, Plachta-Danielzik S. Different age-specific incidence and remission rates in pre-school and primary school suggest need for targeted obesity prevention in childhood. Int J Obes (Lond). 2012;36(4):505–10.
Luan D, Mezuk B, Bauer KW. Remission of obesity among a nationally representative sample of US children. Pediatr Obes 2019, 14(1).
El-Medany A, Birch L, Hunt L, Matson R, Chong A, Beynon R, Hamilton-Shield J, Perry R. What change in body Mass Index is required to Improve Cardiovascular outcomes in Childhood and adolescent obesity through Lifestyle interventions: a Meta-regression. Child Obes. 2020;16(7):449–78.
Dos Santos CS, Picoito J, Nunes C, Loureiro I. Early individual and Family Predictors of Weight Trajectories from Early Childhood to adolescence: results from the Millennium Cohort Study. Front Pediatr. 2020;8:417.
Nedelec R, Miettunen J, Mannikko M, Jarvelin MR, Sebert S. Maternal and infant prediction of the child BMI trajectories; studies across two generations of Northern Finland birth cohorts. Int J Obes (Lond). 2021;45(2):404–14.
Magarey AM, Daniels LA, Boulton TJ, Cockington RA. Predicting obesity in early adulthood from childhood and parental obesity. Int J Obes. 2003;27(4):505–13.
Article CAS Google Scholar
Bond TA, Karhunen V, Wielscher M, Auvinen J, Mannikko M, Keinanen-Kiukaanniemi S, Gunter MJ, Felix JF, Prokopenko I, Yang J, et al. Exploring the role of genetic confounding in the association between maternal and offspring body mass index: evidence from three birth cohorts. Int J Epidemiol. 2020;49(1):233–43.
Chen YC, Fan HY, Yang C, Hsieh RH, Pan WH, Lee YL. Assessing causality between childhood adiposity and early puberty: a bidirectional mendelian randomization and longitudinal study. Metabolism. 2019;100:153961.
Download references
Acknowledgements
The authors would like to express their appreciation to the SEACO Field Teams and survey participants. The research described in this paper was supported by the South East Asia Community Observatory (SEACO, https://www.monash.edu.my/seaco ). The views, however, are those of the authors and there is no real or implied endorsement by SEACO.
This work was supported by funding from UK Medical Research Council and the Malaysian Ministry of Higher Education/UK-MY Joint Partnership on Non-Communicable Diseases 2019/MR/T018984/1. Monash University funds the SEACO health and demographic surveillance system. Co-authors of this study are also supported by the National Institute for Health and Care Research Bristol Biomedical Research Centre (MA). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Tin Tin Su and Laura Johnson share the joint senior authorship.
Authors and Affiliations
Centre for Exercise, Nutrition & Health Sciences, School for Policy Studies, University of Bristol, 8 Priory Road, Bristol, BS8 1TZ, UK
Ruth Salway, Miranda Armstrong & Sophia Brady
Population Health Sciences, Bristol Medical School, University of Bristol, Canynge Hall, Bristol, BS8 2PN, UK
Ruth Salway & Laura Johnson
Clinical School Johor Bahru, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Subang Jaya, Malaysia
Jeevitha Mariapun & Mohamed Shajahan Yasin
Institute for Global Health and Development, Queen Margaret University, Edinburgh, EH21 6UU, Scotland
Daniel D Reidpath
South East Asia Community Observatory (SEACO), and Global Public Health, Jeffrey Cheah School of Medicine and Health Sciences, Monash University Malaysia, Subang Jaya, Malaysia
You can also search for this author in PubMed Google Scholar
Contributions
The study was conceived by LJ and TTS, and funding was obtained by LJ, TTS, MA, DR and MY. The analyses were planned by LJ and RS, who wrote the analysis plan with input from TTS, JM, DR, MY and MA. LJ supervised the analysis and drafting and RS undertook the analysis and wrote the first draft of the article. All authors critically reviewed the article and approved the final manuscript.
Corresponding author
Correspondence to Ruth Salway .
Ethics declarations
Ethics approval and consent to participate.
Ethics approval for both surveys were obtained through the Monash University Human Research Ethics Committee: MUHREC (3837) for the Health Round Survey 2013 and MUHREC (13242) for the Health Round Survey 2018. All participants gave informed consent which allows for secondary analysis without additional consent, and data was provided in anonymised form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. For transparency: LJ has received, for research unrelated to the current paper, institutional funding from UKRI, World Cancer Research Fund, National Institute for Health Research UK, Joint Programs Initiative EU FP7, Alpro foundation, Danone Baby Nutrition, Kellogg Europe, and the Wellcome Trust. MA has received, for research unrelated to the current paper, institutional funding from the Centre for Aging Better, NIHR and Cancer Research UK.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Salway, R., Armstrong, M., Mariapun, J. et al. Predicting higher child BMI z-score and obesity incidence in Malaysia: a longitudinal analysis of a dynamic cohort study. BMC Public Health 24 , 1408 (2024). https://doi.org/10.1186/s12889-024-18917-9
Download citation
Received : 20 November 2023
Accepted : 21 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12889-024-18917-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents
- Intergenerational obesity
- Cardiometabolic risk factors
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Phenome-Wide Investigation of the Causal Associations Between Pre-Pregnancy Obesity Traits and Gestational Diabetes: A Two-Sample Mendelian Randomization Analyses
- Reproductive Endocrinology: Original Article
- Published: 24 May 2024
Cite this article

- Mengjin Hu ORCID: orcid.org/0000-0003-0473-6077 1 na1 ,
- Xiaosong Li 2 na1 ,
- Jiangong Wu 3 ,
- Boyu Li 1 ,
- Jinggang Xia 1 ,
- Yuejin Yang 2 &
- Chunlin Yin 1
60 Accesses
Explore all metrics
Pre-pregnancy obesity was associated with gestational diabetes in observational studies, but whether this relationship is causal remains to be determined. To evaluate whether pre-pregnancy obesity traits causally affect gestational diabetes risk, a two-sample Mendelian randomization (MR) analysis was performed utilizing summary-level statistics from published genome-wide association studies (GWAS). Obesity-related traits included body mass index (BMI), overweight, obesity, obesity class 1, obesity class 2, obesity class 3, childhood obesity, waist circumference (WC), hip circumference (HC), waist-to-hip ratio (WHR), percent liver fat, visceral adipose tissue volume, abdominal subcutaneous adipose tissue volume. Effect estimates were evaluated using the inverse-variance weighting method. Weighted median, MR-Egger, simple mode, and weighted mode were performed as sensitivity analyses. Genetically predicted pre-pregnancy BMI [odds ratio (OR) = 1.68; 95% confidence interval (CI): 1.45–1.95; P = 9.13 × 10 –12 ], overweight (OR = 1.49; 95% CI: 1.21–1.85; P = 2.06 × 10 –4 ), obesity (OR = 1.25; 95% CI: 1.18–1.33; P = 8.01 × 10 –13 ), obesity class 1 (OR = 1.31; 95% CI: 1.17–1.46; P = 1.49 × 10 –6 ), obesity class 2 (OR = 1.26; 95% CI: 1.16–1.37; P = 5.23 × 10 –8 ), childhood obesity (OR = 1.33; 95% CI: 1.23–1.44; P = 4.06 × 10 –12 ), and WHR (OR = 2.35; 95% CI: 1.44–3.83; P = 5.89 × 10 –4 ) were associated with increased risk of gestational diabetes. No significant association was observed with obesity class 3, WC, HC, percent liver fat, visceral adipose tissue volume, or abdominal subcutaneous adipose tissue volume. Similar results were observed in sensitivity analyses. Therefore, genetically predicted pre-pregnancy obesity traits may increase the risk of gestational diabetes. Weight control before pregnancy may be beneficial to prevent gestational diabetes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
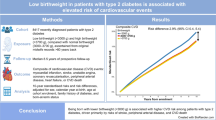
Low birthweight in patients with type 2 diabetes is associated with elevated risk of cardiovascular events and mortality
The epidemiology of obesity: a big picture.
Non-linear Mendelian randomization: detection of biases using negative controls with a focus on BMI, Vitamin D and LDL cholesterol
Data availability.
Our data and materials will be shared upon reasonable request by contacting the corresponding author.
WHO. Obesity and overweight. Switzerland: WHO; 2016. http://www.who.int/mediacentre/factsheets/fs311/en/
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2014;384(9945):766–81.
Article PubMed PubMed Central Google Scholar
Chu SY, Callaghan WM, Kim SY, Schmid CH, Lau J, England LJ, et al. Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care. 2007;30(8):2070–6.
Article PubMed Google Scholar
Fattah C, Farah N, Barry SC, O’Connor N, Stuart B, Turner MJ. Maternal weight and body composition in the first trimester of pregnancy. Acta Obstet Gynecol Scand. 2010;89(7):952–5.
Abrams B, Selvin S. Maternal weight gain pattern and birth weight. Obstet Gynecol. 1995;86(2):163–9.
Article CAS PubMed Google Scholar
Stegenga H, Haines A, Jones K, Wilding J. Identification, assessment, and management of overweight and obesity: summary of updated NICE guidance. BMJ. 2014;349:g6608.
Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN, et al. Meta-analysis of genome-wide association studies for height and body mass index in ∼700000 individuals of European ancestry. Hum Mol Genet. 2018;27(20):3641–9.
Article CAS PubMed PubMed Central Google Scholar
Berndt SI, Gustafsson S, Mägi R, Ganna A, Wheeler E, Feitosa MF, et al. Genome-wide meta-analysis identifies 11 new loci for anthropometric traits and provides insights into genetic architecture. Nat Genet. 2013;45(5):501–12.
Bradfield JP, Taal HR, Timpson NJ, Scherag A, Lecoeur C, Warrington NM, et al. A genome-wide association meta-analysis identifies new childhood obesity loci. Nat Genet. 2012;44(5):526–31.
Shungin D, Winkler TW, Croteau-Chonka DC, Ferreira T, Locke AE, Mägi R, et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature. 2015;518(7538):187–96.
Liu Y, Basty N, Whitcher B, Bell JD, Sorokin EP, van Bruggen N, et al. Genetic architecture of 11 organ traits derived from abdominal MRI using deep learning. Elife. 2021;10:e65554.
Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity Analyses for Robust Causal Inference from Mendelian Randomization Analyses with Multiple Genetic Variants. Epidemiology. 2017;28(1):30–42.
Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–25.
Wei YM, Yang HX, Zhu WW, Liu XY, Meng WY, Wang YQ, et al. Risk of adverse pregnancy outcomes stratified for pre-pregnancy body mass index. J Matern Fetal Neonatal Med. 2016;29(13):2205–9.
Singh J, Huang CC, Driggers RW, Timofeev J, Amini D, Landy HJ, et al. The impact of pre-pregnancy body mass index on the risk of gestational diabetes. J Matern Fetal Neonatal Med. 2012;25(1):5–10.
Kivelä J, Sormunen-Harju H, Girchenko PV, Huvinen E, Stach-Lempinen B, Kajantie E, et al. Longitudinal metabolic profiling of maternal obesity, gestational diabetes, and hypertensive pregnancy disorders. J Clin Endocrinol Metab. 2021;106(11):e4372–88.
Tinius RA, Blankenship MM, Furgal KE, Cade WT, Pearson KJ, Rowland NS, et al. Metabolic flexibility is impaired in women who are pregnant and overweight/obese and related to insulin resistance and inflammation. Metabolism. 2020;104:154142.
Ritchie SC, Würtz P, Nath AP, Abraham G, Havulinna AS, Fearnley LG, et al. The biomarker glyca is associated with chronic inflammation and predicts long-term risk of severe infection. Cell Syst. 2015;1(4):293–301.
Houttu N, Mokkala K, Laitinen K. Overweight and obesity status in pregnant women are related to intestinal microbiota and serum metabolic and inflammatory profiles. Clin Nutr. 2018;37(6 Pt A):1955–66.
Goodpaster BH, Sparks LM. Metabolic flexibility in health and disease. Cell Metab. 2017;25(5):1027–36.
Ross R, Neeland IJ, Yamashita S, Shai I, Seidell J, Magni P, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR working group on visceral obesity. Nat Rev Endocrinol. 2020;16(3):177–89.
Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25(10):1862–8.
De Souza LR, Berger H, Retnakaran R, Maguire JL, Nathens AB, Connelly PW, et al. First-trimester maternal abdominal adiposity predicts dysglycemia and gestational diabetes mellitus in midpregnancy. Diabetes Care. 2016;39(1):61–4.
Heslehurst N, Ngongalah L, Bigirumurame T, Nguyen G, Odeniyi A, Flynn A, et al. Association between maternal adiposity measures and adverse maternal outcomes of pregnancy: Systematic review and meta-analysis. Obes Rev. 2022;23(7):e13449.
Censin JC, Nowak C, Cooper N, Bergsten P, Todd JA, Fall T. Childhood adiposity and risk of type 1 diabetes: A Mendelian randomization study. PLoS Med. 2017;14(8):e1002362.
Wang C, Wei Y, Zhang X, Zhang Y, Xu Q, Sun Y, et al. A randomized clinical trial of exercise during pregnancy to prevent gestational diabetes mellitus and improve pregnancy outcome in overweight and obese pregnant women. Am J Obstet Gynecol. 2017;216(4):340–51.
Ługowska K, Kolanowski W. The nutritional behaviour of pregnant women in Poland. Int J Environ Res Public Health. 2019;16(22):4357.
Lewandowska M, Więckowska B, Sajdak S. Pre-pregnancy obesity, excessive gestational weight gain, and the risk of pregnancy-induced hypertension and gestational diabetes mellitus. J Clin Med. 2020;9(6):1980.
Bell R, Hayes L, Pasecinic N, Heslehurst N. Implementation of national screening guidelines for gestational diabetes: A national survey of maternity units in England. Diabetes Res Clin Pract. 2018;146:58–66.
Chen Z, Du J, Shao L, Zheng L, Wu M, Ai M, et al. Prepregnancy body mass index, gestational weight gain, and pregnancy outcomes in China. Int J Gynaecol Obstet. 2010;109(1):41–4.
Download references
Acknowledgements
This work was supported by the National Key R&D Program of China (2023YFC3605000).
Author information
Mengjin Hu and Xiaosong Li contributed equally to this work.
Authors and Affiliations
Xuanwu Hospital, Capital Medical University, Beijing, 100053, China
Mengjin Hu, Boyu Li, Jinggang Xia & Chunlin Yin
State Key Laboratory of Cardiovascular Disease, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, 100037, China
Xiaosong Li & Yuejin Yang
Fenyang Center for Disease Control and Prevention, Fenyang, 032200, Shanxi Province, China
Jiangong Wu
You can also search for this author in PubMed Google Scholar
Corresponding authors
Correspondence to Yuejin Yang or Chunlin Yin .
Ethics declarations
Conflict of interest.
All authors declared no conflicts of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (TIF 33254 KB)
Supplementary file2 (tif 18083 kb), supplementary file3 (tif 17545 kb), supplementary file4 (tif 18889 kb), supplementary file5 (docx 96 kb), rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Hu, M., Li, X., Wu, J. et al. Phenome-Wide Investigation of the Causal Associations Between Pre-Pregnancy Obesity Traits and Gestational Diabetes: A Two-Sample Mendelian Randomization Analyses. Reprod. Sci. (2024). https://doi.org/10.1007/s43032-024-01577-w
Download citation
Received : 08 February 2024
Accepted : 19 April 2024
Published : 24 May 2024
DOI : https://doi.org/10.1007/s43032-024-01577-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Waist circumference
- Visceral adipose tissue volume
- Gestational diabetes
- Mendelian randomization
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
15. On how many of the past 7 days did you exercise or take part in physical activity that made your heart beat fast and made you breathe hard for at least 20 minutes. (For example: basketball, soccer, running, or jogging, fast dancing, swimming laps, tennis, fast bicycling, or similar aerobic activities). 16.
Thesis Advisor: Andrew Wise, PhD. ABSTRACT. This study evaluated the effectiveness of the Coordinated School Health Program model. in reducing childhood obesity rates using state-level data collected by the Centers for Disease. Control and Prevention (CDC) for the years 1994, 2000, and 2006.
According to Wang. and Lim (2012), the global prevalence of overweight and obesity in preschool-aged children increased from 4% to 7% within a 10-year span. An estimated 43 million. children worldwide are obese or overweight and 35 million of these children live in less-. developed countries (Wang & Lim, 2012).
By analyzing other children's eating behaviors, physical activities, and other determinants of obesity, the children will be able to increase their awareness on obesity. Childhood Obesity. The condition occurs when the weight of a child is over 120 percent of the median weight in relation to the height of the child.
impacted by childhood obesity. Therefore, the objective of this dissertation was to explore the contextual factors that influence rapid weight gain, non-responsive feeding practices, and diet quality in infants and young children at increased risk for developing obesity. We developed a conceptual model using self-determination theory and
This dissertation focused on childhood obesity among preschool aged children in the United States, using data from the Early Childhood Longitudinal Study Birth Cohort. ... Results: Unweighted baseline sample size included ~7200 children. Overall, 54.6% of children were white, 23.1% Hispanic, 15.7% African-American, 3.4% Asian, 2.8% American ...
The prevalence of childhood obesity continues to rise despite decades of clinical and public health efforts. Early identification of children at risk of developing obesity is essential using newer electronic health systems, which move beyond traditional growth charts to provide a wealth of information about body mass index and other relevant parameters such as social determinants of health and ...
Childhood obesity has become a national epidemic, affecting 17% of children in the United States (Ogden, Carroll, Kit, & Flegal, 2014). The Centers for Disease Control and Prevention (CDC) (2017) reported that one in five school-aged children suffers from childhood obesity. It is known to predispose the child to chronic illnesses as he or she
Abstract. Childhood obesity has become a global pandemic in developed countries, leading to a host of medical conditions that contribute to increased morbidity and premature death. The causes of obesity in childhood and adolescence are complex and multifaceted, presenting researchers and clinicians with myriad challenges in preventing and ...
A thesis submitted to The University of Birmingham for the degree of DOCTOR OF PHILOSOPHY Unit of Public Health, Epidemiology and Biostatistics ... Childhood obesity is a major global concern but there is little evidence for effective childhood obesity prevention strategies. People of South Asian origin are a specific target group for
As indicated in Table 3, the data suggests that 44.1% of children between the ages. of 10 and 14 were overweight or obese whereas 55.9% of the children were not. overweight or obese. The sample was composed of 19.6% Hispanic children, 26% Non-Hispanic blacks and 54.4% Non-Hispanic white children.
Introduction. Childhood obesity is a major public health challenge, with one in three US children between the ages of 2 and 5 meeting criteria for overweight or obesity. 1 The urgency to reverse the course of childhood obesity has led to significant growth in the scientific literature evaluating childhood obesity interventions. Extant reviews of this research have provided limited guidance ...
Childhood Obesity 2 Abstract Obesity is a chronic health condition that is increasing at alarming rates in the United States, particularly among low-income children. This literature review examines several of the factors that place low-income children at risk for developing obesity: environmental (i.e., lack of access
Introduction. Excess weight in children is prevalent worldwide. Although plateauing trends were observed in many high-income countries in Europe, in medium and low-income countries childhood obesity prevalence has increased in the last decade ().In Romania, almost one in four children has overweight or obesity, as shown in a pooled analysis of more than 25,000 school age Romanian children and ...
CHILDHOOD OBESITY AND FAMILY INFLUENCE ON CHILDREN'S NUTRITION INTAKE, PHYSICAL ACTIVITY PATTERNS, AND BMI Z-SCORES IN OMAN Basma Al Yazeedi A dissertation submitted to the faculty at the University of North Carolina at Chapel Hill in partial fulfillment of the requirements for the degree of Doctor of Philosophy in the School of Nursing.
The undersigned certify that they have read and hereby recommend for acceptance by the University of Dar es Salaam a dissertation entitled: Prevalence and Implications of Overweight and Obesity in Children's health and Learning Behaviour, in fulfillment of the requirements for the degree of Masters of Arts (Education) of the
The purpose of this study was to examine the relationship between weight status, nutrition intake, and physical activity patterns of Omani middle age children and explore the familial factors that influence them. The sample of the study consisted of 204 Omani mother-child dyads. The mean age of children was 7.74 years (SD ± 1.161).
29 essay samples found. Childhood Obesity is a serious medical condition where excess body fat negatively affects a child's health or well-being. Essays might discuss the causes, consequences, prevention and management of childhood obesity, as well as the role of parents, schools, and healthcare providers in addressing this issue.
research with larger, more representative samples to address these limitations are made. Overall, this dissertation makes a unique contribution to the psychological understanding of overweight and obesity, which has the potential to enhance treatment outcomes and suggests useful avenues for further research.
Abstract. Childhood obesity is a major concern in today's society. Research suggests the inclusion of the views and understandings of a target group facilitates strategies that have better efficacy. The objective of this study was to explore the concepts and themes that make up children's understandings of the causes and consequences of obesity.
This updated synthesis of obesity prevention interventions for children aged 6-18 years, found a small beneficial impact on child BMI for school-based obesity prevention interventions. A more comprehensive assessment of interventions is required to identify mechanisms of effective interventions to inform future obesity prevention public health policy, which may be particularly salient in for ...
Finally, the study sample included only men, and some previous studies have indicated sex differences in the association between childhood adversities and obesity with a stronger association among ...
Childhood Obesity: Thesis Statement. This essay sample was donated by a student to help the academic community. Papers provided by EduBirdie writers usually outdo students' samples. Childhood obesity, an ongoing disease burden in various parts of the world, is a serious medical condition where the body stores excessive body fat.
To target public health obesity prevention, we need to predict who might become obese i.e. predictors of increasing Body Mass Index (BMI) or obesity incidence. Predictors of incidence may be distinct from more well-studied predictors of prevalence, therefore we explored parent, child and sociodemographic predictors of child/adolescent BMI z-score and obesity incidence over 5 years in Malaysia.
The committee reviewed and considered a broad array of information in its work on issues potentially involved in the prevention of obesity and overweight in children and youth. Information sources included the primary research literature in public health, medicine, allied health, psychology, sociology, education, and transportation; reports, position statements, and other resources (e.g ...
Pre-pregnancy obesity was associated with gestational diabetes in observational studies, but whether this relationship is causal remains to be determined. To evaluate whether pre-pregnancy obesity traits causally affect gestational diabetes risk, a two-sample Mendelian randomization (MR) analysis was performed utilizing summary-level statistics from published genome-wide association studies ...