- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Author Guidelines
- Submission Site
- Open Access
- About Health Education Research
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Journals on Oxford Academic
- Books on Oxford Academic


Article Contents
Introduction, research design and method, opening of the encounter: developing a reciprocal relationship, active listening: power sharing, vision of the future: emphasizing the positive, conclusions.
- < Previous
Empowering counseling—a case study: nurse–patient encounter in a hospital
- Article contents
- Figures & tables
- Supplementary Data
Tarja Kettunen, Marita Poskiparta, Leena Liimatainen, Empowering counseling—a case study: nurse–patient encounter in a hospital , Health Education Research , Volume 16, Issue 2, April 2001, Pages 227–238, https://doi.org/10.1093/her/16.2.227
- Permissions Icon Permissions
This study illustrates practices that a nurse uses in order to empower patients. The emphasis is on speech formulae that encourage patients to discuss their concerns and to solicit information about impending surgery. The study is a part of a larger research project and a single case was selected for presentation in this article because it differed from the rest of the data by manifesting empowering practice. A videotaped nurse–patient health counseling session was conducted in a hospital and transcribed verbatim. The investigator interviewed the nurse and the patient after the conversation, and these interviews were transcribed as well. The encounter that is presented here as a case study is a concrete example of a counseling session during which the patient is free to discuss with the nurse. The empowering practices that the nurse employed were as follows: encouraging the patient to speak out, tactfully sounding out the patient's concerns and knowledge of impending surgery, listening to feedback, and building a positive vision of the future for the patient. We suggest that nurses should pay attention to verbal expression and forms of language. This enables them to gain self-awareness and discover new tools to work with.
In recent literature, empowerment has become an important concept of health education ( Feste and Anderson, 1995 ; van Ryn and Heaney, 1997 ), health promotion ( Labonte, 1994 ; Tones, 1994 , 1995 ; Williams, 1995 ; McWilliam et al. , 1997 ) and health counseling ( Poskiparta et al. , 2000 ). The process of empowerment has been related more to community and organizational levels than to micro levels of practice ( van Ryn and Heaney, 1997 ) where it is constantly crucial ( Tones, 1994 ). In addition, operationalization of the concept of empowerment has been relatively vague. According to Tones ( Tones, 1994 ), empowerment is a major goal of health promotion. This article focuses on health counseling as a means of interpersonal health education practice and uses health promotion as an umbrella term.
Empowerment is as much a process as an outcome of developing the skills and perceptions of clients. It is not only something that happens but a process that is facilitated. In interpersonal health counseling, the primary goal is not to change clients' behavior and seek their compliance with the presented message but rather to raise critical awareness through learning and support, to give clients tools for making changes on their own. The aim is personal empowerment, control and choice, which means that patients become aware of changes in their knowledge and understanding, decision-making skills, enhanced self-esteem/sense of personal control, and development of various social, health and life skills ( Labonte, 1994 ; Tones 1994 ; Anderson et al. , 1995 ; Feste and Anderson, 1995 ; van Ryn and Heaney, 1997 ; Kar et al. , 1999 ).
The basic point of departure for empowerment is taking into consideration the interactive nature of the individual and the environment: people are not completely controlled by their environment nor can they fully control their physical, social or economic circumstances ( Tones, 1994 ). Empowering health counseling is based on recognizing clients' competence, resources, explanations of action styles of coping and support networks. Client initiative, clients' realizations and clients' expressions of their opinions and interpretations are the basis on which clients can approach health issues in collaboration with professionals. They are of crucial importance for their decisions on future action ( Anderson, 1996 ). All this supports the notion that empowering health counseling is significant.
Because learning about personal health is complex, the key issue of empowering health counseling is partnership and reciprocal conversation in a confidential relationship. This means that clients not only analyze their situation but also have an opportunity to plan what to do next, and how to go on and to construct their own solutions to health issues. In this type of hospital health counseling, either patients raise the issues (i.e. determine the topics) or the nurses do so in a sensitive and non-threatening manner ( Poskiparta et al. , 2000 ). Nurses recognize and respect patients' experiences, knowledge and skills, and make their own professional knowledge and expertise available to them ( Williams, 1995 ; McWilliam, et al. , 1997 ), which are important aspects of nurse–patient relationships that are also reported by patients ( Häggman-Laitila and Åstedt-Kurki, 1994 ; Lindsey and Hartrick, 1996 ; Wiles 1997 ). The emphasis is placed on patient-driven [see ( Lindsey and Hartrick, 1996 )] health counseling, where patients' life situations are respected, patient-initiated actions are supported, and shared knowledge and deep understanding are nurtured.
The nurse's institutional task is not only to facilitate patient participation but also to promote patients' awareness of their routines and preconceptions as they are revealed to both interlocutors. This should lead to the aim of interaction, which is to activate self-reflection and re-evaluation and reorganization of patients' activities. The assumption is that new knowledge is gained in this process as a result of empirical realization and deliberation ( Feste and Anderson, 1995 ), which means that both patients and nurses have linked new knowledge to existing knowledge. Thus, patients learn to interpret and outline even familiar health problems in new ways that conform to their worldview [ cf . ( Mattus, 1994 )]. As for nurses, empowerment calls for not only sensitivity but also an ability to accurately perceive patients' messages.
From this point on, the focus is on the content of the interactive process. Tones ( Tones, 1994 ) discusses empowerment theoretically, Labonte ( Labonte, 1994 ) expresses ideas for practice in general, while Feste and Anderson ( Feste and Anderson, 1995 ) provide three empowerment tools for facilitating patients' empowering process: using questions, behavioral language and storytelling. According to them, questions maintain the process of pursuing wisdom, i.e. exploring the meaning of health problems in the context of everyday life. This kind of questioning involves broad questions that relate to one's personal philosophy and lifelong dreams. In addition, it includes practical, day-to-day issues of successfully integrating into one's personal, family, social and professional life. Behavioral language means using words such as `list', `describe', `identify', `decide', etc., in order to encourage patients to act and make choices instead of being satisfied with receiving information. Stories help to facilitate the process of self-discovery because diseases affect all areas of life and each individual's health status is unique.
Van Ryn and Heaney ( Van Ryn and Heaney, 1997 ) pay attention to interpersonal relations by suggesting concrete strategies and examples for empowering practice. In their article, they demonstrate two principles of interaction: (1) provide clients with unconditional positive regard and acceptance, and (2) facilitate client participation. Both principles include several practical strategies (Table I ).
However, the authors pay less attention to empirical findings ( Northouse, 1997 ). The present article describes some linguistic realizations of empowering practice. This article describes a nurse's empowering speech formulae during her efforts to give a patient information about an impending surgical operation and to strengthen her feelings of security by providing her with an opportunity to discuss her concerns. This study adopts a holistic approach to interaction and does not focus on isolated sentences or dialogue structure. The relationship of language and context in comprehension, as well as non-verbal communication, are also discussed.
This article describes a single case derived from qualitative data collected from a total of 38 counseling sessions in a Finnish hospital. Nurse–patient encounters were videotaped and transcribed verbatim. Interviews with the nurses and the patients after the sessions were transcribed as well. All participants volunteered to take part in the research, signed a research license and granted permission for the transcribed data to be used in publications. Nineteen nurses participated in this study. Each nurse conducted two videotaped counseling sessions with different patients. There was only one male nurse while the patient group consisted of 24 female and 14 male patients. The research material took shape as nurses volunteered in the hospital and it was found to be adequate for qualitative analysis. The length of the nurses' careers varied from 1 to 25 years. The ages of the nurses were between 24 and 50 years (mean age 36.9 years) while the patients' ages ranged from 18 to 70 years (mean age 47.9 years). The researcher did not attend the counseling sessions, which lasted from 5 to 45 min. The participating patients were experiencing diverse health problems. Various surgical problems, e.g. knee surgery, hernia operation, breast surgery, hip operation, back operation, post status of brain bleeding and post care of bypass surgery, were among the most representative. In addition to the health problems that had led to hospitalization, many patients also suffered from chronic diseases, such as hypertension, asthma, rheumatic illnesses or diabetes. Many patients also found themselves in an insecure situation when a chronic disease had suddenly been manifested or they were undergoing examinations. There were also some mothers in the group who had delivered recently and had no health problems.
The health counseling sessions were genuine counseling situations that were related to the patients' treatment. A single video camera was used, which meant that the observation of non-verbal communication was limited to examining the session as a whole, including only eye contact, smiles, laughter, tone of voice, gestures and, to some extent, facial expressions. Consequently, the emphasis of this study was examining verbal communication. Separate interviews with the nurses and the patients where both parties were encouraged to express their evaluations of the health counseling were used for partial support of the interpretations, e.g. when describing the patients' opinions about health counseling. We also checked if there were any nurses or patients who were nervous about the videotaping.
This article concentrates on videotaped data. When we examined all of the data we found many encounters that involved some empowering features from time to time, but there were none that were consistently empowering. In this article, we present a single case from the data. This particular encounter was selected because it differed from the rest of the data ( Stake, 1994 ) by manifesting empowering practice most widely. In order to study the interactive nature of communication, the coding and analysis of the videotaped data was based on principles of Conversation Analysis ( Drew and Heritage, 1998 ). The videotapes were transcribed word by word, including stammering, etc. At the same time, additional data were added to the transcriptions, such as pauses during and between turns, onset and termination of overlapping talk, intonation information, and some non-verbal communication. The following transcription symbols were used to indicate this information:
ha+ hands support speech
vo+ rising voice
vo– falling voice
[ ] at the beginning and end of overlapping speech, words enclosed
(( )) transcriber's comments, e.g. smile, laughter, body movements
(.) small but detectable pause
underlining emphasis
… omission of text
=no interval between the end of prior and start of next speech unit
°speech° speech in low volume, words enclosed
`speech'pitch change, words enclosed
The analysis was carried out on a turn-by-turn basis. The principle behind this analysis was to examine how turns were taken with regard to other participants' speech and what sequential implications each turn had for the next. After reading the transcript and watching the recording several times, we discovered a number of empowering expressions in the nurse's speech and concluded that this case was the one which best manifested empowering action in the data.
The particular case describes at the individual level information about the patient's situation, the nurse's interview after the encounter, an in-depth description of the nurse–patient conversation and the observational data derived from it. Pearson ( Pearson, 1991 ) and Patton ( Patton, 1990 ) indicate that a case study can be used, for example, for examining how different concepts emerge or change in particular contexts. However, an even more important question is what can be learned from a single case. Stake ( Stake, 1994 ) suggests that one should select a case that seems to offer an opportunity to learn and contributes to our understanding of specific phenomena. Here, a detailed single case analysis illustrates how empowerment may be practiced during health counseling and demonstrates how new working tools for empowerment can be developed on the basis of a single encounter ( Laitakari, 1998 ). The present study describes the speech of a nurse when she helped a patient to deal with anxiety and to receive information about surgery in an empowering way.
The nurse anesthetist has come to see a patient who is scheduled to have surgery the next day. The encounter involves, besides interviewing, producing a lot of information about the operation, counseling on the preparations for the surgery and advising how to manage after the surgery. The encounter takes place at a table, with the nurse and the patient facing each other. Both are women; the nurse is 50 and the patient 41 years old. The patient had had problems with her back for 10 years and was suddenly admitted to the hospital because of these problems. The patient has recently been examined and a decision has been made to operate on her the next morning. The interviewing session lasted 14 min.
At the beginning of a conversation the participants evaluate each others aims and concerns, and the communication situation as a whole, and this evaluation directs the entire discussion because the participants base their actions on it (Goffman, 1982). In a hospital, it is typical that nurses initiate a discussion ( Leino-Kilpi, 1991 ) and that is what happened in this case ( Extract 1 ). Professional dominance common in medical encounters ( Fairclough, 1992 ) is not so obvious in this conversation. After greeting the patient, the nurse refers to the goal of the discussion and individualizes it by using familiar `you' (line 1) instead of the formal, plural form of `you'. This form of address can be viewed as an act of communicating an appropriate degree of informality. It implies intimacy and mutual respect when a relationship is established ( van Ryn and Heaney, 1997 ).
1 N: Hello, Rose (.) you are going to have surgery 2 tomorrow…but now I would like to ask you 3 you well about the operation tomorrow if 4 there is (.) something that would influence 5 the preparations for your operation (.) and 6 then you ((ha+)) can bring things up ask well 7 er if something is unclear to you ((nod+)) If 8 you want to know anything about what's 9 going to happen to you tomorrow ((vo–))
((at first the nurse looks at papers on the table, while she speaks she turns her eyes to the patient and nods))
This opening was not typical of the other interviews in the data set, because in the data these encounters were usually initiated with the nurses' brief statements about the impending operation. They explained that they interviewed patients in advance in order to get information and that they could provide information to the patients as well. Nurses usually used formal, plural forms of address when speaking. When referring to the preoperative encounter, they used the plural, institutionalized form `we' [see ( Drew and Heritage, 1998 )], instead of first person singular `I', and plural `you', instead of the singular, when addressing the patient. Other nurses did not individualize their speech. On the contrary, they maintained a distance from the patients. In this particular case, a familiar mode of address reduces social distance, which is very important in health education practice [ cf . ( van Ryn and Heaney, 1997 )]. We explain our interpretations in more detail below.
The nurse uses the verb `ask' (line 2), but her remark further on (line 6–9) `then you can bring up ask well er if you were unclear about something if you want to know something about what's going to happen to you tomorrow' introduces a context for the discussion. Even though the nurse goes on to ask a question about previous operations, the interview becomes an interactive dialogue, with the patient actively participating. On her own initiative the patient discloses symptoms that she has experienced during the last few months, what happened when she needed to come to the hospital and the doctor's decision to perform surgery.
Thus, the nurse introduces the context of the discussion with her opening words [ cf . ( Peräkylä, 1995 )]. She expresses her acceptance by offering collaboration [ cf . ( van Ryn and Heaney, 1997 )] when asking questions. The verb form `would like to' (line 2) gives the discussion an air of voluntariness. The conditional form softens the notion of the necessity of the questions, and the verbal mode implies respect for the patient. At the beginning of the session (lines 1–9), the nurse combines two topics into a single long sentence, which also encourages (lines 6–9) the patient to clarify matters that are unclear to her. The nurse's words leave room for the patient's own thoughts and invites her to look for a personally meaningful way to connect the nurse's questions about the preparations (line 5) for the operation to her lack of information (lines 7–9). Encouraging statements can stimulate the patient to think in a way that is personally meaningful to her and to participate in the conversation ( van Ryn and Heaney, 1997 ; Tomm, 1988). Here, encouragement takes a form that is different from what Feste and Anderson ( Feste and Anderson, 1995 ) suggested; it is given in a more sophisticated manner. The opening words ( Extract 1 ) correspond with the goal that the nurse states later during the interview: `that the patient would receive the information she needs, what she wants to know and that she would feel safe to come, that at least those worst fears would be like forgotten. That she would feel safe'.
An encounter can threaten a patient's need for autonomy and freedom because it gives the nurse the legitimate power to request information about the patient's private life ( van Ryn and Heaney, 1997 ). Here, the nurse is mitigating her power by avoiding threatening terms and using tentative formulations (`would like to, well er, you you'), the emphasis being on the patient's needs. The opening of the interview by the nurse plays an important role in the development of the atmosphere. The act has been planned in advance but is not thoroughly thought out. In addition to conveying information, the main consideration in setting the goal for the discussion is to help the patient deal with her concerns. These are issues that have also been stressed in earlier studies ( Häggman-Laitila and Åstedt-Kurki, 1994 ; Breemhaar et al. , 1996 ; Leinonen et al. , 1996 ; Lindsey and Hartrick, 1996 ; Otte, 1996 ).
Tactful exploration: activation of reflection
Later during the interview, the patient mentions having thought about the impending surgery, which the nurse interprets as an indication of fear for the operation ( Extract 2 ). She indirectly gives the patient an opportunity to deal with her fears. The patient's words (lines 1, 3, 5 and 7) are related to the previous topic and her status during the operation and conclude the discussion. The nurse changes the subject (line 9) by praising the doctor's skill. The nurse and the patient look at each other.
1 P:mmm[think about during the day]= 2 N:[of] course ((nod+)) 3 P:=what's going to happen and (.) 4 N:right ((nod+)) 5 P:°like[that]° (.) 6 N:[mmm] 7 P:°it's[okay]° ((nod+, vo–)) 8 N: [that's] right (.) ((glance at papers: doctor's 9 name)) is is an excellent surgeon so in that 10 respect you can definitely (.) ((vo–)) feel 11 safe ((nod+)) that 12 P:yes of course I am 13 N:mmm 14 P: and and absolutely 110% (.) I trust that (.) 15 the thing is that (.) this is small case for 16 him but this is a horribly big thing for me…
The nurse's comment about the operating surgeon contains an allusion to fear of surgery. Instead of soothing the patient by telling her not to be afraid or asking if the patient is scared, the nurse indirectly comments on the doctor's professional skill (line 9) and emphasizes the expertise as a guarantee of success (line 10 and 11). Thus, the nurse allows the patient to save face when she leaves her to interpret her words. Her indirectness implies politeness and gives the patient options: if she does not want to deal with her fear, she may choose not to take the hint [see ( Brown and Levinson, 1987 )]. Here, politeness can also be linked to and interpreted through empowering practice, where the nurse holds the patient in high regard [ cf . ( van Ryn and Heaney, 1997 )].
The extract might have been interpreted as an example of the nurse cutting the patient off if one had not seen the videotape. Our interpretation is supported by a number of factors. First of all, the entire conversation until this extract has been tranquil and calm, the nurse has spoken and asked questions at a gentle pace, with pauses, and she has explored the patient's experiences. In this extract, the situation is similar, and she looks at the patient and nods. She speaks quite slowly, and her voice is low, friendly, and convincing ( van Ryn and Heaney, 1997 ). We can also see that the patient completes her speech by pausing (lines 3 and 5) and lowering her voice (lines 5 and 7). Therefore, after the nurse's words (lines 8–11), the patient presents her fear for discussion (lines 15 and 16) and also returns to the matter later during the interview. The extract shows how the issue has been constructed together by the nurse and the patient. The nurse raises the theme in a sensitive and non-threatening manner, and the patient continues the same topic. It also shows that the relationship is confidential enough for the patient to disclose her concerns and become aware of her own understanding, and thus contributes to empowerment. Salmon ( Salmon, 1993 ) has stressed that the main goal in the discussions between nurses and patients before surgery is not to reduce the patients' fears but to help them to deal with them.
Indirectness is a polite feature of discourse. There is `strategic indefiniteness' in indirectness that offers patients an opportunity to continue a discussion according to their own wishes ( Brown and Levinson, 1987 ). In general, nurses' empowering acts are mostly manifested in the form of questions ( Poskiparta et al. , 2000 ). In some cases, an indirect comment by a nurse, instead of a question, may encourage patients to talk about topics that they fear. Here it generates reflection in the patient. After disclosing her concerns, the patient analyzes the situation and recounts the conversation that she had with the doctor who explained the reason for her back surgery ( Extract 3 ).
Extract 3 .
1 P:this morning ((doctor's name)) said that 2 N:`this morning' ((surprised)) 3 P:this morning 4 N:that's recent for sure 4 P:yes 5 N:well it happened so 6 P: so it happened suddenly because yesterday 7 it became evident that (.) there was in the 8 X-ray ((doctor's name)) said that there was 9 a cause when I asked if there was anything 10 that caused the pain or if I was just imagining 11 it (.) so he said that yes there was a 12 genuine cause…
The amount of information given always depends on the situation and the nurse needs to continually evaluate the patient's needs: what it is that the patient knows, wants to know and how much she does want to know. This is also important because there are several persons that the patient sees before surgery ( Breemhaar et al. , 1996 ). Furthermore, nurses and doctors may deal with the same issues in their counseling. In Finland, the doctors, the surgeon and the consultant anaesthetist inform patients about the medical facts, risks, and benefits of operations. The patient also has an interview with a nurse on the surgical ward and, in addition to these encounters, there will occasionally be an encounter with a nurse anesthetist.
The nurse's empowering approach is manifested in how she raises issues or questions from time to time as if with hesitation. A pause precedes questions [`I don't have any (.) questions to ask you any more but do you—you have anything to ask from me like such things about tomorrow that worry you') ((looks at the patient))]. She asks the questions more quietly than normal and looks at the patient. According to Beck and Ragan's ( Beck and Ragan, 1992 ) study, nurses' softening words and their hesitant and tentative manner of speaking indicate discretion and tact and are aimed at not embarrassing patients. In our data, slow and hesitant speech also encourages the patients to comment more than nurses' more usual and brief question does: `Do you have any questions?'.
The nurse's tentative manner of asking questions makes it easier for the patient to start dealing with her concerns. She repeatedly pauses briefly and, in addition to the closed questions in the medical history questionnaire, she asks open-ended questions that explore the patient's experiences: `What kind of memories do you have of previous operations?' `Is there anything else you remember (.) is there something?'. Open-ended questions encourage the patient to speak and participate, e.g. in the naming and solving of a problem [ cf . ( Feste and Anderson, 1995 ; van Ryn and Heaney, 1997 )]. In this particular case, indirectness and hesitation are polite speech formulae that help the patient to save face ( Fairclough, 1992 ). They can also serve as empowering strategies that provide unconditional positive regard and acceptance for patients.
Despite these quite extensive empowering acts, the nurse subsequently evaluated her information skills only. She indicated how difficult it was for her to decide what kind of information to give to the patient:
I wondered if I should have maintained a more professional role, I mean more facts, if the patient got all that she wanted. Because this is not really medical science, you know, that's up to the doctor. It has to happen on the patient's terms, what she wants to know. I tried to check the patient's needs several times.
The content of the session satisfied the patient as well:
I got enough information about the operation, things that occupied my mind, so I didn't, she even told me before I asked. There's nothing to find out any more. As I said to her, I'm terribly afraid but I'll go ahead with confidence.
The nurse's way of posing questions builds up interaction. With her questions she steers the discussion thematically. This is how she controls the conversation. On the other hand, it is the patient who determines the content of the discussion. Her answers are reflective and bring up new issues. When the patient speaks, the nurse supports her with various feedback (e.g. Extracts 2 and 3) `mmm, right, of course, yes, exactly' and sometimes by paraphrasing. She nods a lot, bends toward the patient and looks at her. The feedback also occasionally includes completing the patient's sentences. According to van Ryn and Heaney ( van Ryn and Heaney, 1997 ), such non-verbal cues signal acceptance and, according to Caris-Verhallen et al. ( Caris-Verhallen et al. , 1999 ), they are patient-centered. With her feedback the nurse shows that she is there to listen to the patient, that she does not want to interrupt. Her feedback encourages the patient to speak in a similar way as in the doctor–patient conversation of an alternative medical interview described by Fairclough ( Fairclough, 1992 ). The patient interprets the feedback as encouragement, goes on to discuss the matter, and indicates her intention to continue by using the expressions `What I have been wondering…', `I did that when…' and `on the other hand, it's…'. This is how the nurse supports the patient's right to speak, which is not necessarily typical of a medical conversation ( Fairclough, 1992 ). The nurse's multi-facetted listening feedback is empowering, and this can be seen here and there in the data [see also ( Poskiparta et al. , 2000 )]. In this encounter, the feedback is exceptional because it disregards the participant's status. Generally, this type of feedback is directed to the dominant person ( Hakulinen, 1989 ). In a medically oriented environment, the hospital staff are viewed as superior to patients in knowledge ( van Ryn and Heaney, 1997 ; Tones, 1994 ). In this particular case, the nurse's listening feedback manifests power sharing.
When the patient discusses the reason for her admission to the hospital, the nurse builds up a positive, healthier vision of the future through other patients' experiences ( Extract 4 ). She makes her professional knowledge and expertise available to the patient ( Williams, 1995 ; McWilliam et al. , 1997 ). This lends a touch of reality and possibly builds on the patient's strengths ( van Ryn and Heaney, 1997 ) in this situation. The nurse attempts to dispel the patient's concerns about the risks of the operation. Her tone is convincing, and her non-verbal messages also inspire confidence: she looks at the patient, reinforces her message by nodding her head and gestures with her hands. Encouraged by the nurse, the patient can have a vision of her postoperative future.
Extract 4 .
1 N:these these ((ha+)) back operations are 2 like such that patients in them are usually 3 really grateful ((nod+)) after the operation 4 because if the operation like succeeds and 5 something is found (.) then the pain will be 6left in the operating room (.) ((ha+)) and 7 in that in that this is like like different from 8 other operations (.) and then because the 9 woundpainisinthebacksomehowit's 10 different than in here if the wound was here 11 inthestomach(ha+))andit'snotthatthat 12bad when it is if[you]= 13 P:[yeah] 14 N:=afterthosestomachoperationsyouoften 15 often hear that these patients who have had 16their back operated are such fortunate 17((nod+)) cases in the sense [that]= 18 P:[yeah] ((nod+)) 19 N:= because the pain will be left in the 20 operating room and and that's it then 21 ((nod+/ha+))
The nurse encourages the patient to examine her life at some hypothetical future point of time when the operation will have succeeded. Hypothetical questions encourage patients to discuss issues that they fear [ cf . ( Peräkylä, 1995 ; Tomm, 1987 )], while a hypothetical positive situation encourages patients indirectly. In this case, discussing the past would not calm the patient but rather lead her thoughts to the incident that caused her hospitalization. The vision of the future that the nurse provides to the patient with may help relieve her. A positive example is an empowering message and displays the nurse's understanding of the patient's anxiety. This vision can tap new resources in the patient for facing the future that is suddenly uncertain [ cf . ( van Ryn and Heaney, 1997 )]. Some manifestations of this can be seen in the patient's words: `…I'm very happy that if it's going to be over (.) yes I'm ready though I feel nervous' or `…I'm going ahead with confidence…'. A skilful use of future focus by the nurse helps the patient to find new solutions to her problems [ cf . ( Tomm, 1987 )]. As Atwood ( Atwood, 1995 ) suggests, confining the clients' thoughts to their problems is not sufficient in therapy work (focus on the past). In addition, we need to assist clients to expand their outlook by re-visioning their lives (future focus).
The encounter that is presented here as a case study demonstrates empowering nursing practice in hospital. It is a concrete example of a discussion during which the official and formal nature that characterizes the role of an institutional nurse is not emphasized. It actually emphasizes partnership and reciprocal conversation [ cf . ( van Ryn and Heaney, 1997 ; Poskiparta et al. , 2000 )], with the nurse's social interaction skills at the heart of the encounter [ cf . ( Wiles, 1997 )]. The patient is free to discuss her thoughts, concerns, experiences and even fears with the nurse, and the nurse adopts an empowerment strategy in order to facilitate the patient's participation. This encounter included the following empowering practices: (1) opening the session in an encouraging and constructive manner, which improves the atmosphere, (2) tactful exploration when examining the patient's need for information and concerns for surgery, (3) active, power sharing listening, and (4) building up a positive vision of the future.
The descriptions of empowerment strategies reported by van Ryn and Heaney ( van Ryn and Heaney, 1997 ) support our findings. However, we agree with Northouse's ( Northouse, 1997 ) criticism that the reported strategies are not completely separated. In our study, empowerment was manifested through intimacy and mutual respect. The nurse's encouragement of the patient's participation and her attempt to share power signaled acceptance, and perhaps gave the patient new insights for controlling her feelings about the impending surgery. Furthermore, the perceptions of active listening feedback and questioning are consistent with our previous studies ( Poskiparta et al. , 1998 , 2000 ; Kettunen et al. , 2000 ), where we found them to be a means of activating patients' self-evaluation and self-determination. In this study, we did not find evidence for empowering stories or questions that relate to patients' personal philosophy, as mentioned by Feste and Anderson ( Feste and Anderson, 1995 ). In addition, the nurse's encouragement was more sophisticated than what Feste and Anderson suggest with their empowering tools.
Our research data consisted of only one videotaped session per patient. Thus we have no evidence about how patients' decision-making skills develop or their self-esteem improves. During the interviews we did not ask the patients' opinion on the effects of counseling and that is why the patients evaluated conversations at a quite general level. In this particular case, the patient said that an encounter was ` illuminating ' for her. She mentioned that she received enough information and again spoke about her fears but used the same words as the nurse did when she emphasized a positive vision of future (see Extract 4 , lines 5, 6, 19 and 20): `if it's a fact that the pain will be left in the operating room, if it really is possible…that there's going to be an operation and they'll do it tomorrow, then that's how it's going to be'. This could, perhaps, signify some kind of relief or new resources to face an uncertain future. During the interview it also became evident that the patient's fears had not been diminished, but she talked about them and stressed a strong reliance on the professionals and on the operation as a whole: `I believe what I'm told'. This is in line with the perspective of Salmon ( Salmon, 1993 ), who emphasized that patients' anxiety about surgery should not be seen as a problem but rather as a normal phenomenon, a sign of patients' emotional balance, of an ability to feel fear. Thus, the nurse's task is not to diminish the patient's fears but to facilitate the patient's disclosure and offer help for dealing with fear.
With caution, we can speculate on the factors behind this kind of empowering practice, which became evident during the subsequent interviews. There was no evidence that nurses' or patients' age, education or work experience influenced the format of the counseling. What makes this case different from traditional rigid counseling sessions is that the nurse had a goal that she had planned in advance and pursued flexibly. This indicates that she had reflected on the significance of this situation from the patient's perspective. In most cases, nurses approached counseling without any goal or the hospital provided a detailed agenda based on professional knowledge of diseases, their care and prevention. Then, different kinds of institutionalized health counseling packages seemed to restrict nurses' communication, and health counseling often followed the standard institutional order of phases mentioned by Drew and Heritage ( Drew and Heritage 1998 ).
This study highlights empowering opportunities that arise in actual situations and that nurses can consciously use in their work. The results of this study can be applied to other health counseling practices and we would argue that every nurse should consider how (s)he initiates discussion. The analysis of the encounter shows that a tentative discussion style gives the patient a chance to deal with her concerns and to absorb the information that she needs. Thus, the patient has an opportunity to participate more actively in the discussion from the beginning than she could in the case of filling out a questionnaire in a strict predetermined order.
Clearly there are limitations to the generalizability of these findings. For example, both interlocutors were women, and this could in part explain the nature of the conversation since the highest levels of empathic and positive behavior occur between females [see ( Coates, 1986 ; Roter and Hall, 1993 ), p. 63]. There is also some concern whether the nurse may have been subject to a performance bias because she was aware of being videotaped and possibly behaved differently. However, we think that this was limited because only two nurses discussed this type of bias in the interviews afterwards and other nurses did not even notice the camera or did so only briefly at the beginning of counseling [see also ( Caris-Verhallen et al. , 1998 )]. Techniques to enhance the credibility of the findings included data and methodological triangulation of research data ( Patton, 1990 ; Stake, 1994 ; Begley, 1996 ), and acquiring data that included both verbal and non-verbal communication from the videotaped health counseling sessions and the subsequent interviews. In addition, team analysis sessions (investigator triangulation) ensured the accuracy of data interpretation (Polit and Hunger 1995). Different expertise helped us to get more complete picture from this case and empowerment philosophy when we discussed interpretations together.
However, in the last analysis, the effect of an empowering encounter could be checked after the operation by checking the patient's perspective, e.g. her satisfaction, recovery rate, etc. Evidence from nursing and medical staff might also be offered as additional evidence. Further research from larger numbers of patients is needed and more evidence from different settings will be required for a more extensive description of empowering practice. We will continue our research, and, for example, present qualitative analysis of interaction by describing how power features and patients' taciturnity are manifested in nurse–patient counseling. In addition, we will investigate how student nurses make progress in empowering counseling.
We suggest that nurses should pay attention to verbal expression and forms of language, in addition to non-verbal messages, because then they can empower patients by opening new and important perspectives for them. Nurses' every question, remark or piece of advice leads to individualized understanding and interpretation by the patient. It is important to remember that each communication situation is a unique, dynamic and transforming process. Nurses should observe what figures of speech they use and thus gain self-awareness and discover new tools to work with. We suggest a training program where the development of health care professionals' empowering skills can occur in practical, dynamic communication situations, be videotaped and transcribed for later theoretical, conscious and instructive evaluation. Analyzing the transcripts of video or tape-recorded counseling sessions opens up the possibility of an exact evaluation of empowering skills.
In health counseling, it is important that patients are able to maintain and strengthen a positive image of themselves as communicators. Positive experiences build up patients' self-esteem and increase their confidence in their ability to influence their care. The mere opportunity to discuss one's opinions and interpretations or different health concerns with a nurse may have the effect of unlocking patients' mental resources. This article demonstrates particularly how unconditional acceptance and facilitation of participation can be used in interpersonal counseling [see ( van Ryn and Heaney, 1997 )]. The empowering practices that are presented in this article should not be regarded as rigid and formalistic, rather they should be adapted to one's personal style.
Empowering principles of interpersonal practice ( van Ryn and Heaney, 1997 )
This study was supported by the Ministry of Health and Social Affairs of Finland and by the Finnish Cultural Foundation. We are sincerely grateful to all that participated in this study.
Anderson, J. M. ( 1996 ) Empowering patients: issues and strategies. Social Science and Medicine , 43 , 697 –705.
Anderson, R. M., Funnell, M. M., Butler, P. M., Arnold, M. S., Fitzgerald, J. T. and Feste, C. C. ( 1995 ) Patient empowerment. Results of randomized controlled trial. Diabetes Care , 18 , 943 –949.
Atwood, J. D. ( 1995 ) A social constructionist approach to counseling the single parent family. Journal of Family Psychotherapy , 6 , 1 –32.
Beck, C. S. and Ragan, S. L. ( 1992 ) Negotiating interpersonal and medical talk: frame shifts in the gynaecologic exam. Journal of Language and Social Psychology , 11 , 47 –61.
Begley, C. M. ( 1996 ) Using triangulation in nursing research. Journal of Advanced Nursing , 24 , 122 –128.
Breemhaar, B., van den Born, H. W. and Mullen, P. D. ( 1996 ) Inadequacies of surgical patient education. Patient Education and Counseling , 28 , 31 –44.
Brown, P. and Levinson, S. C. (1987) Politeness. Some Universals in Language Usage. Cambridge University Press, Cambridge.
Caris-Verhallen, W. M. C. M., Kerkstra, A., van der Heijden, P. G. M. and Bensing, J. M. ( 1998 ) Nurse–elderly patient communication in home care and institutional care: an explorative study. International Journal of Nursing Studies , 35 , 95 –108.
Caris-Verhallen, W. M. C. M., Kerkstra, A. and Bensing, J. M. ( 1999 ) Non-verbal behaviour in nurse–elderly patient communication. Journal of Advanced Nursing , 29 , 808 –818.
Coates, J. (1986) Women , Men and Language. A Sociolinguistic Account of Sex Differences in Language. Longman, New York.
Drew, P. and Heritage, J. (1998) Analyzing talk at work: an introduction. In Drew, P. and Heritage, J. (eds), Talk at Work. Interaction in Institutional Settings. Cambridge University Press, Cambridge, pp. 3–65.
Fairclough, N. (1992) Discourse and Social Change. Polity Press, Cambridge, pp. 134–168.
Feste, C. and Anderson, R. M. ( 1995 ) Empowerment: from philosophy to practice. Patient Education and Counseling , 26 , 139 –144.
Goffman, E. (1967/1982) Interaction Ritual. Doubleday, New York, pp. 5–45.
Hakulinen, A. (1989) Keskustelun luonnehtimisesta konteksti- ja funktionaalisten tekijöiden nojalla. [Characterizing the conversation according to contextual and functional factors]. In Hakulinen, A. (eds), Kieli 4 Suomalaisen Keskustelun Keinoja I. Helsingin Yliopiston Suomen Kielen Laitos, Helsinki, pp. 41–72.
Häggman-Laitila, A. and Åstedt-Kurki, P. ( 1994 ) What is expected of nurse–client interaction and how these expectations are realized in Finnish health care. International Journal of Nursing Studies , 31 , 253 –261.
Kar, S. B., Pascual, C. A. and Chickering, K. L. ( 1999 ) Empowerment of women for health promotion: a meta-analysis. Social Science and Medicine , 49 , 1431 –1460.
Kettunen, T., Poskiparta M. and Liimatainen, L. (2000) Communicator styles of hospital patients during nurse–patient counseling. Patient Education and Counseling , in press.
Labonte, R. ( 1994 ) Health promotion and empowerment: reflections on professional practice. Health education quarterly , 21 , 253 –268.
Laitakari, J. ( 1998 ) How to develop one's counseling—demonstration of the use of single-case studies as a practical tool for evaluating the outcomes of counseling. Patient Education and Counseling , 33 , S39 –S46.
Leino-Kilpi, H. ( 1991 ) Good nursing care—the relationship between client and nurse. Hoitotiede , 3 , 200 –206.
Leinonen, T., Leino-Kilpi, H. and Katajisto, J. ( 1996 ) The quality of intraoperative nursing care: the patient's perspective. Journal of Advanced Nursing , 24 , 843 –852.
Lindsey, E. and Hartrick, G. ( 1996 ) Health-promoting nursing practice: the demise of the nursing process? Journal of Advanced Nursing , 23 , 106 –112.
Mattus, M.-R. (1994) Interview as intervention: strategies to empower families of children with disabilities. In Leskinen, M. (ed.), Family in Focus. New Perspectives on Early Childhood Special Education. Jyväskylä Studies in Education, Psychology and Social Research 108. Jyväskylä University Printing House, Jyväskylä, pp. 87–107.
McWilliam, C. L., Stewart, M., Brown, J. B., McNair, S., Desai K., Patterson, M. L., Del Maestro, N. and Pittman, B. J. ( 1997 ) Creating empowering meaning: an interactive process of promoting health with chronically ill older Canadians. Health Promotion International , 12 , 111 –123.
Northouse P. G. 1997 . Effective helping relationships: the role of power and control. Health Education and Behavior , 24 , 703 –706.
Otte, D. I. ( 1996 ) Patients' perspectives and experiences of day case surgery. Journal of Advanced Nursing , 23 1226 –1237.
Patton, M. G. (1990) Qualitative Evaluation and Research Methods. Sage, Newbury Park, CA, pp. 388–390.
Pearson, P. ( 1991 ) Clients' perceptions: the use of case studies in developing theory. Journal of Advanced Nursing , 16 , 521 –528.
Peräkylä, A. (1995) AIDS Counselling. Institutional Interaction and Clinical Practice . Cambridge University Press, Cambridge.
Polit, D. F. and Hungler, B. P. (1995) Nursing Research. Principles and Methods. Lippincott, Philadelphia, PA.
Poskiparta, M., Kettunen, T. and Liimatainen, L. ( 1998 ) Reflective questions in health counseling. Qualitative Health Research , 8 , 682 –693.
Poskiparta, M., Kettunen, T. and Liimatainen, L. ( 2000 ) Questioning and advising in health counseling. Results from a study of Finnish nurse counselors. Health Education Journal , 95 , 47 –67.
Roter, D. L. and Hall, J. A. (1993) Doctors Talking with Patients/Patients Talking with Doctors . Greenwood, Westport, CT.
van Ryn, M. and Heaney, C. A. ( 1997 ) Developing effective helping relationships in health education practice. Health Education and Behavior , 24 , 683 –702.
Salmon, P. ( 1993 ) The reduction of anxiety in surgical patients: an important nursing task or the medicalization of preparatory worry? International Journal of Nursing Studies , 30 , 323 –330.
Stake, R. E. (1994) Case studies. In Denzin, N. K. and Lincoln, Y. S. (eds), Handbook of Qualitative Research. Sage, Newbury Park, CA, pp. 236–247.
Tomm, K. ( 1987 ) Interventive interviewing: part II. Reflexive questioning as a means to enable self-healing. Family Process , 26 , 197 –183.
Tones, K. (1994) Health promotion, empowerment and action competence. In Jensen B. B and Schnack, K. (eds), Action and Action Competence as Key Concepts in Critical Pedagogy. Studies in Educational Theory and Curriculum . Royal Danish School of Educational Studies, vol. 12, pp. 163–183.
Tones, K. ( 1995 ) Editorial. Health Education Research , 10 , i –v.
Wiles, R. ( 1997 ) Empowering practice nurses in the follow-up of patients with established heart disease: lessons from patients' experiences. Journal of Advanced Nursing , 26 , 729 –735.
Williams, J. ( 1995 ) Education for empowerment: implications for professional development and training in health promotion. Health Education Journal , 54 , 37 –47.
Email alerts
Citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1465-3648
- Print ISSN 0268-1153
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
- Section One: Introduction
- Section Two: Learning and Teaching Resources to Support Integration of Mental Health and Addiction in Curricula
- Section Three: Faculty Teaching Modalities and Reflective Practice
- Section Four: Student Reflective Practice and Self-Care in Mental Health and Addiction Nursing Education
- Section Five: Foundational Concepts and Mental Health Skills in Mental Health and Addiction Nursing
- Section Six: Legislation, Ethics and Advocacy in Mental Health and Addiction Nursing Practice
- Section Seven: Clinical Placements and Simulations in Mental Health and Addiction Nursing Education
- Section Eight: Reference and Bibliography
- Section Nine: Appendices and Case Studies
Section Nine
Case studies, also in this section.
- Alignment between CASN/ CFMHN Entry-to-Practice Mental Health and Addiction Competencies and Sections in the Nurse Educator Mental Health and Addiction Resource
- Process Recording
- Criteria for Validation: Process Recording
- Criteria for Phase of Relationship: Process Recording
- Journaling Activity
- Safety and Comfort Plan Template
- Advocacy Groups for Mental Health in Canada
- Tips for Engaging Lived Experience
- Glossary of Terms
- Case Study 1
- Case Study 2
- Case Study 3
- Case Study 4
- Case Study 5
- Case Study 6
- Case Study 7
- Case Study 8
- Case Study 9
The case study is an effective teaching strategy that is used to facilitate learning, improve critical thinking, and enhance decision-making Sprang, (2010). Below are nine case studies that educators may employ when working with students on mental illness and addiction. The case studies provided cover major concepts contained in the RNAO Nurse Educator Mental Health and Addiction Resource.
While not exhaustive, the case studies were developed and informed by the expert panel. It is recommended that educators use the case studies and tweak or add questions as necessary to impart essential information to students. Also, educators are encouraged to modify them to suit the learning objective and mirror the region in which the studies are taking place. Potential modifications include:
- demographics (age, gender, ethnicity);
- illness and addiction, dual diagnosis or additional co-morbidities such as cardiovascular disease; and
- setting (clinical, community).
Suggested “Student questions” explore areas of learning, while “Educator elaborations” recommend ways to modify the case study. Discussion topics are a limited list of suggested themes.
When using these case studies, it is essential that this resource is referenced.
See Engaging Clients Who Use Substances BPG appendices for examples
- Printer-friendly version
- Skip to content

State Resources
National Resources
Nursing Organizations
- MNWC Initiatives
Maryland Nursing Workforce Center
- NextGen NCLEX
Faculty Case Studies
The purpose of this project was to develop a repository of NextGen NCLEX case studies that can be accessed by all faculty members in Maryland.
Detailed information about how faculty members can use these case students is in this PowerPoint document .
The case studies are in a Word document and can be modified by faculty members as they determine.
NOTE: The answers to the questions found in the NextGen NCLEX Test Bank are only available in these faculty case studies. When students take the Test Bank questions, they will not get feedback on correct answers. Students and faculty should review test results and correct answers together.
The case studies are contained in 4 categories: Family (13 case studies), Fundamentals and Mental Health (14 case studies) and Medical Surgical (20 case studies). In addition the folder labeled minireviews contains PowerPoint sessions with combinations of case studies and standalone items.
Family ▾
- Attention Deficit Hyperactivity Disorder - Pediatric
- Ectopic Pregnancy
- Febrile Seizures
- Gestational Diabetes
- Intimate Partner Violence
- Neonatal Jaundice
- Neonatal Respiratory Distress Syndrome
- Pediatric Hypoglycemia
- Pediatric Anaphylaxis
- Pediatric Diarrhea and Dehydration
- Pediatric Intussusception
- Pediatric Sickle Cell
- Postpartum Hemmorhage
- Poststreptococcal Glomerulonephritis Pediatric
- Preeclampsia
Fundamentals and Mental Health ▾
- Abdominal Surgery Postoperative Care
- Anorexia with Dehydration
- Catheter Related Urinary Tract Infection
- Deep Vein Thrombosis
- Dehydration Alzheimers
- Electroconvulsive Therapy
- Home Safety I
- Home Safety II
- Neuroleptic Maligant Syndrome
- Opioid Overdose
- Post Operative Atelectasis
- Post-traumatic Stress
- Pressure Injury
- Substance Use Withdrawal and Pain Control
- Suicide Prevention
- Tardive Dyskinesia
- Transfusion Reaction
- Urinary Tract infection
Medical Surgical ▾
- Acute Asthma
- Acute Respiratory Distress
- Breast Cancer
- Chest Pain (MI)
- Compartment Syndrome
- Deep Vein Thrombosis II
- End Stage Renal Disease and Dialysis
- Gastroesphageal Reflux
- Heart Failure
- HIV with Opportunistic Infection
- Ketoacidosis
- Liver Failure
- Prostate Cancer
- Spine Surgery
- Tension Pneumothorax
- Thyroid Storm
- Tuberculosis
Community Based ▾
Mini Review ▾
- Comprehensive Review
- Fundamentals
- Maternal Newborn Review
- Medical Surgical Nursing
- Mental Health Review
- Mini Review Faculty Summaries
- Mini Review Training for Website
- Mini Reviews Student Worksheets
- Pediatric Review
- Research article
- Open access
- Published: 16 April 2019
Recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings: a cross national comparative mixed methods study
- Michael Coffey ORCID: orcid.org/0000-0002-0380-4704 1 ,
- Ben Hannigan 2 ,
- Sally Barlow 3 ,
- Martin Cartwright 4 ,
- Rachel Cohen 5 ,
- Alison Faulkner 6 ,
- Aled Jones 2 &
- Alan Simpson 3 , 7
BMC Psychiatry volume 19 , Article number: 115 ( 2019 ) Cite this article
55k Accesses
47 Citations
52 Altmetric
Metrics details
Involving mental health service users in planning and reviewing their care can help personalised care focused on recovery, with the aim of developing goals specific to the individual and designed to maximise achievements and social integration. We aimed to ascertain the views of service users, carers and staff in acute inpatient wards on factors that facilitated or acted as barriers to collaborative, recovery-focused care.
A cross-national comparative mixed-methods study involving 19 mental health wards in six service provider sites in England and Wales. This included a survey using established standardised measures of service users ( n = 301) and staff ( n = 290) and embedded case studies involving interviews with staff, service users and carers ( n = 76). Quantitative and qualitative data were analysed within and across sites using descriptive and inferential statistics, and framework method.
For service users, when recovery-oriented focus was high, the quality of care was rated highly, as was the quality of therapeutic relationships. For staff, there was a moderate correlation between recovery orientation and quality of therapeutic relationships, with considerable variability. Staff members rated the quality of therapeutic relationships higher than service users did. Staff accounts of routine collaboration contrasted with a more mixed picture in service user accounts. Definitions and understandings of recovery varied, as did views of hospital care in promoting recovery. Managing risk was a central issue for staff, and service users were aware of measures taken to keep them safe, although their involvement in discussions was less apparent.
Conclusions
There is positive practice within acute inpatient wards, with evidence of commitment to safe, respectful, compassionate care. Recovery ideas were evident but there remained ambivalence on their relevance to inpatient care. Service users were aware of efforts taken to keep them safe, but despite measures described by staff, they did not feel routinely involved in care planning or risk management decisions. Research on increasing therapeutic contact time, shared decision making in risk assessment and using recovery focused tools could further promote personalised and recovery-focused care planning.
This paper arises from a larger study published by National Institute for Health Research (Simpson A, et al, Health Serv Deliv Res 5(26), 2017).
Peer Review reports
Improving the treatment and care of people with mental illness is amongst key priorities for health and social care in both England and Wales [ 1 ]. However, despite the shift to community-based models of care, considerable resources are still spent on acute inpatient beds: as much as £585million in 2009–10 [ 2 ].
In England in 2016–17, 101,589 people in contact with mental health and learning disability services spent time in hospital, with an estimated 45,864 people detained under the Mental Health Act (MHA) 1983 [ 3 ]. In Wales, 8723 admissions to hospital for mental illness took place in 2016–17, with 1776 of these taking place using sections of the MHA 1983 [ 4 ]. This volume of admissions requires considerable planning and coordination to ensure effective care is delivered consistently.
Health care is a devolved responsibility in the UK meaning that the context and delivery of mental health care is diverging between countries, providing a rich geographical comparison for research. In England the care programme approach (CPA), and in Wales care and treatment plans (CTPs), oblige providers to: comprehensively assess health/social care needs and risks; develop a written care plan; allocate a care co-ordinator; and regularly review care. CPA/CTP processes are now also expected to reflect a philosophy of recovery and to promote personalised care [ 5 , 6 ]. These similarities between CPA and CTP mask an important difference too however. CPA in England is central guidance while CTP in Wales is legislative and places legal obligations on health boards and local authorities. CTP in Wales uniquely has an associated code of practice, stipulating for example that only specifically qualified workers (e.g. registered mental health nurses, occupational therapists and clinical psychologists) can act as care co-ordinators [ 7 ].
The concept of recovery in mental health was initially developed by service users and refers to “a way of living a satisfying, hopeful, and contributing life even with limitations caused by illness,” while developing new purpose or meaning [ 8 ]. (p527) The importance of addressing personal recovery, alongside more conventional ideas of clinical recovery [ 9 ] is now supported in guidance for all key professions [ 10 , 11 , 12 , 13 ]. To this has been added the idea of personalisation. This aims to see people and their families taking more control over their support and treatment options, alongside new levels of partnership and collaboration between service users (or citizens) and professionals [ 14 ]. (p3) Recovery and personalisation in combination mean tailoring support to fit the specific needs of the individual and enabling social integration through greater involvement of local communities [ 15 ].
The CPA/CTP are central to modern mental health care [ 16 ] yet there are few studies that explicitly explore the practices of care planning and coordination in community services and even fewer focusing on inpatient care planning [ 17 ]. A relatively rare example of the former is the recently completed COCAPP study [ 18 , 19 ]. In the UK national quality statements include the requirement that service users can jointly develop a care plan with mental health professionals, are given a copy with an agreed date to review it, and are routinely involved in shared decision-making [ 20 ]. National policies [ 1 , 6 ] outline expectations of recovery and involvement in decisions about treatment. This holds true for both informal and detained inpatients, with a requirement that reasonable adjustments are made where necessary to ensure that people are supported to live as full and socially participative lives as possible [ 21 ]. However, national quality reviews reveal limited evidence of service users’ views being listened to, with concerns being raised that control and containment are prioritised over treatment and support [ 21 ].
Earlier national reviews across both nations found that service users remained largely mystified by the care planning and review process itself, with significant proportions not understanding their care plans, not receiving written copies of their plan and often not feeling involved in the writing of care plans and setting of goals [ 22 , 23 ]. Clearly, there are significant problems with inpatient care planning with the Care Quality Commission (CQC) noting “significant gap between the realities observed in practice and the ambitions of the national mental health policy” [ 21 ]. (p5) The House of Commons Health Committee [ 24 ] subsequently reported widespread concerns about delays in care planning and an imbalance between a focus on risk rather than recovery.
Previously, the Healthcare Commission [ 25 ] measured performance on 554 wards across 69 NHS Trusts providing mental health acute inpatient services. They found that almost two-fifths of trusts (39%) scored weak on involving service users and carers; 50% of care plans sampled did not record the service user’s views; and nearly a third of care records (30%) did not record whether or not the service user had a carer. A third of all care records sampled (33%) showed that community care coordinators provided input into the service users’ care review meetings only “some or none of the time”.
The aim of this study was to identify factors that facilitate or hinder recovery-focused personalised care planning and coordination in acute inpatient mental health settings. As an exploratory study guided by the Medical Research Council (MRC) [ 26 ] Complex Interventions Framework we aimed to generate empirical data, new theoretical knowledge and greater understanding of the complex relationships between collaborative care planning, recovery and personalisation.
We conducted a cross-national comparative study of recovery-focused care planning and coordination in inpatient mental healthcare settings, employing a concurrent transformative mixed methods approach with embedded case studies [ 27 ]. A full account of our methods is provided elsewhere [ 28 ].
In summary, our study was informed by systems ideas emphasising connections between macro, meso and micro levels of organisation [ 29 ]. Cross-national comparative research involves “comparisons of political and economic systems …and social structures” [ 30 ] (p93) where “one or more units in two or more societies, cultures or countries are compared in respect of the same concepts and concerning the systematic analysis of phenomena, usually with the intention of explaining them and generalising from them” [ 31 ]. (p1–2) In this study, devolved government and the emergence of similar but distinct health policy, legislation and service development in England and Wales provided the macro-level national context.
A case study method [ 32 ] allows the exploration of a particular phenomenon within dynamic contexts where multiple influencing variables are difficult to isolate [ 33 ]. It allows consideration of historical and social contexts [ 34 ] and is especially useful in explaining real-life links that are potentially too complex for survey or experimental approaches [ 35 ]. The definitions of the case studies were predetermined [ 36 ], focusing on selected NHS Trust/Health Boards. Data collection at this meso-level included identifying local policy and service developments alongside empirical investigations of care planning and inpatient care, recovery, personalisation, therapeutic relationships and empowerment, employing mixed quantitative and qualitative methods. This design is represented in Fig. 1 .
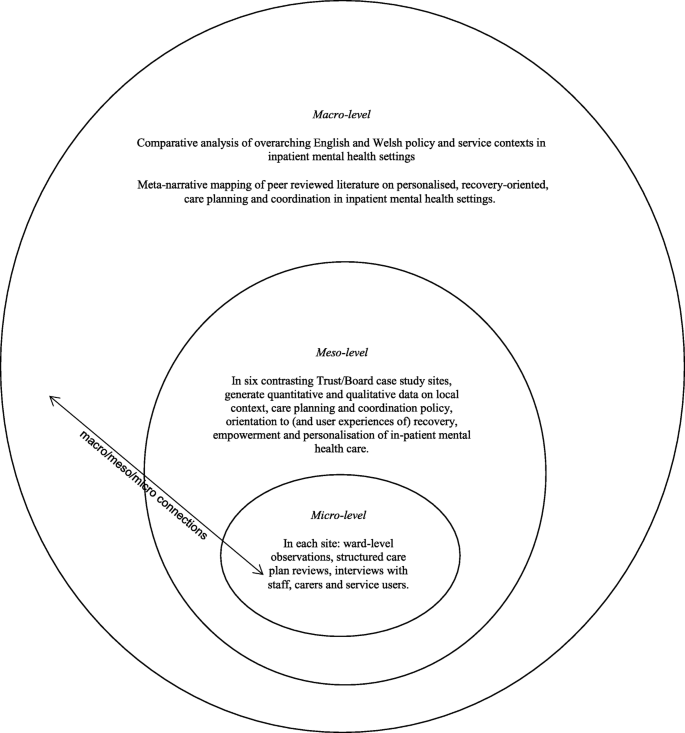
Diagram illustrating embedded case study design and integration of care planning and coordination in acute inpatient mental health settings
We selected six case study sites to match our earlier community study [ 18 ] so that comparisons and connections between community and inpatient services could be drawn [ 32 ]. These consisted of four NHS Trusts in England and two Local Health Boards in Wales that are commissioned to provide inpatient mental health services. In total 19 acute wards were selected for data collection. These sites reflected a mix of rural, urban and inner city settings in which routine inpatient care is provided to people with complex and enduring mental health problems. In each site, a single acute inpatient ward was chosen for further in-depth investigation and up to six service users, six multidisciplinary staff and four informal carers were sampled as embedded micro-level case studies [ 27 ]. Inclusion criteria for wards included that these were providing acute mental health care admissions facilities to the local adult population and had an established ward manager/team leader in post. Inclusion criteria for service user participants included that they were currently admitted to the in-patient facility, had been on the ward for a minimum of 7 days, 18 years or older, with a history of severe mental illness and able to provide informed consent. Staff inclusion criteria were staff working on inpatient wards involved in care planning or review. Full inclusion and exclusion criteria are provided elsewhere [ 28 ].
Sample size calculations
For the survey, an a priori sample size calculation was conducted using the G*Power software (version 3.1) [ 37 ]. The estimated sample size for service users was calculated for the global effect of a one-way multivariate analysis of variance (MANOVA) with six groups (sites), 17 outcomes (Recovery Self-Assessment Scale total (+ 5 sub-scales), Scale To Assess the Therapeutic Relationship total (+ 3 sub-scales), Empowerment Scale total (+ 5 sub-scales) and the Views of Inpatient Care Scale total), an α level of 0.05, power of 0.8 and a small effect size (f 2 = 0.029). This calculation suggested that a total of 276 service user participants was required.
We anticipated that with non-response and incomplete measures we would need to oversample, we therefore decided to recruit 300 service users ( n = 50 per Trust/Health Board) and 300 inpatient staff ( n = 50 per site). We anticipated that we would not achieve this sample size for informal carers and therefore aimed to recruit 150 informal carers ( n = 25 per Trust/Health Board). This was because not every service user would have a carer, therefore analysis for the informal carers would be underpowered (estimated power was 0.44). The data for the informal carers was therefore anticipated to be exploratory.
Sample size calculations for qualitative interviews were based on previous research with similar populations by the co-investigators and others. Calculations were based on understanding of the practicalities and time commitments of recruiting and interviewing participants and analysing in-depth qualitative data; and the numbers required to feel confident that the findings would be transferable to other similar settings.
Instrumentation
The data collection measures reported in this paper are;
The Recovery Self-Assessment Scale (RSA) [ 38 ]: a 36-item scale measuring the extent of recovery-oriented practices. The scale addresses the domains of life goals, involvement, treatment options, choice and individually tailored services. Acceptable internal consistency of the RSA with Cronbach’s alpha has previously been demonstrated [ 18 ]. It was completed by service users, carers and ward staff. In the current study Cronbach’s alpha for the Total RSA scale for service users was 0.98 ( N = 103) and for staff was 0.95 ( N = 186); Life Goals subscale, for service users was 0.93 ( N = 179) and for staff was 0.86 ( N = 246); Involvement subscale, for service users 0.91 ( N = 163) and for staff was 0.85 ( N = 225); Diversity of Treatment options subscale, for service users was 0.81 ( N = 172) and for staff was 0.77 (N = 225); Choice subscale, for service users was 0.81 ( N = 217) and for staff was 0.68 ( N = 254) and Individually Tailored Services subscale for service users was 0.85 ( N = 159) and for staff was 0.71 ( N = 253).
The patient and clinician versions of the Scale To Assess the Therapeutic Relationship (STAR-P and STAR-C) [ 39 ]: a 12-item scale assessing therapeutic relationships. A total STAR score is obtained by summing individual items. The subscales measure positive collaborations (possible scores 0–24), positive clinician input (possible score 0–12) and non-supportive clinician input in the patient version and emotional difficulties in the staff version (possible score 0–12). It was completed by service users and ward staff. Cronbach’s alpha for the total STAR-P scale for service users was 0.89 ( N = 264) and for staff was 0.81 ( N = 263); Positive Collaboration subscale, for service users was 0.92 ( N = 279) and for staff was 0.81 ( N = 269); Positive clinician input subscale, for service users was 0.72 ( N = 282) and for staff was 0.56 ( N = 268); and Non-Supportive clinician input subscale, for service users was 0.67 ( N = 284) and for staff was 0.63 ( N = 273).
The Empowerment Scale (ES) [ 40 ]: a 28-item questionnaire with five subscales: self-esteem, power, community activism, optimism and righteous anger. A total empowerment score is obtained by summing individual items and dividing them by the number of items. Subscale values can also be provided for ‘self-esteem-self-efficacy’, ‘power-powerlessness’, community activism and autonomy’, ‘optimism and control over the future’ and ‘righteous anger’. This scale was completed by service users. Cronbach’s alpha for the total Empowerment scale for service users was 0.82 ( N = 255); Self-esteem-self-efficacy subscale, 0.91 ( N = 272); Power-Powerlessness subscale 0.56 ( N = 271); Community activism and autonomy subscale, 0.58 ( N = 276); Optimism and control, 0.70 ( N = 275) and Righteous anger, 0.40 ( N = 281).
The Views of Inpatient Care Scale (VOICE) [ 41 ]: a 19-item patient-reported outcome measure of perceptions of acute mental health care that includes questions on involvement in care planning and ward round discussions. VOICE total score was obtained by summing individual item scores, possible total scores range from 19 to 114. The higher the total score for the VOICE the more negative the perception of the quality of care on the ward. It was completed by service users.
We further investigated internal consistency using alternative approaches, mean item-total correlations and Spearman-Brown prediction values (see Additional file 1 ). These additional analyses suggested that all subscales had acceptable internal consistency, although two subscales of the Empowerment Scale would merit further psychometric development.
We additionally conducted semi-structured interviews with ward staff, service users and carers. Interview schedules were based on our previous study and refined in consultation with our Scientific Steering Committee and Lived Experience Advisory Group (LEAG) and drawing on relevant literature. The aim of all interviews was to explore participants’ views and experiences of care planning and co-ordination, safety and risk, recovery and personalisation, and the context within which these operated. Care plan reviews and observations of ward rounds were also conducted but are not reported in this paper. In some cases participants on the case study sites completed surveys and research interviews but this was not a requirement of the study and the majority chose to participate in one part of the study only.
Research ethics
The study received NHS Research Ethics approval from the NRES Committee NRES Committee London – Fulham (Ref: 13/LO/2062) on 29th December 2014.
Considerable attention was given to ensuring the welfare of service user, carer and other participants and of the researchers. This included providing opportunities to pause or withdraw from interviews, assurances of anonymity and confidentiality and responding to concerns for people’s welfare.
Public and patient involvement (PPI) and study oversight
The study was developed and designed with full involvement of co-investigator and independent service user researcher (AF) and in consultation with SUGAR (Service User and Carer Group Advising on Research [ 42 ]). In addition, a Lived Experience Advisory Group (LEAG) met every 4/6 months during the study, consisting of seven service users and one carer with direct experience of inpatient mental health care.
The 12-member independently chaired Scientific Steering Committee (SSC) consisted of representatives with a clinical or research background from each of the participating NHS Trusts/Health Boards, as well as independent academics. One service user and one carer member also represented the LEAG.
Three Service User Researcher Assistants (SURAs)/Service User Project Assistants (SUPAs) were employed to recruit participants and conduct research interviews. All received training and ongoing support throughout the study.
Suitable local wards meeting inclusion criteria were identified with the assistance of local NHS Trust/Health Board principal investigators. Ward managers were approached by a researcher who explained the study, responded to any queries and invited them to participate. No service declined to take part. We sought approval to participate from two or three wards in each area and one of the three wards was then selected for in-depth case study of care planning including interviews. Each site was given a pseudonym to help maintain anonymity of participants. French names were chosen to avoid any accidental connection with English or Welsh sites or regions. The site names are:
All managers and ward staff involved in care planning or care plan review received written and verbal information about the study and were invited to participate in the survey (target n = 50 per Trust/Health Board).
Staff from participating wards were asked to identify service users who had been on that ward for a minimum of seven days, and who in their view potentially had the capacity to participate in the study. The service user was provided with written and verbal information by a researcher, who then ensured the person was able to provide informed consent to participate. Each participant was then given a survey pack to complete, with assistance if required. A thank you gift of £10 was given to service user participants on completion of the survey pack.
Ward staff were asked to give carer survey packs to carers (family members and friends) visiting service users on the ward (target n = 25 per Trust/Health Board). The packs included an information sheet and a Freepost return envelope. Researchers working on the ward also approached carers to invite them to participate by completing measures.
Semi-structured interviews
Key personnel (registered nurses, ward managers, occupational therapists, psychologists and psychiatrists) were identified using purposive sampling to reflect meso and micro level functions. They were invited to participate in research interviews for the in-depth case study (target n = 6 per case study ward; total n = 36). Micro-level refers to the level at which face-to-face care is organised, provided and received. For our purposes meso-level refers to management functions that enable or structure micro-level work. Staff were given written materials describing the purpose of the study including the option to decline or withdraw at any time. Informed consent procedures were followed.
Service users approaching discharge were invited to participate in an interview about their experiences of care planning and jointly review their care plan (target n = 6 per case study ward; total n = 36). Informed consent procedures were followed. A thank you gift of £10 was given to service user participants on completion of the research interview.
Service users were asked to identify a carer (if applicable) to take part in an interview (target n = 4 per case study ward; total n = 24). Carers were contacted by telephone or when visiting, in the presence of the service user if possible. Informed consent procedures were followed.
Data management and analysis
Qualitative and quantitative data in each of the sites were considered on a within-group basis prior to a cross-case analysis aimed at identifying common themes and divergences. The between-group analysis of the quantitative data compared service users and staff across sites on key markers of the service user experience (recovery-oriented care, therapeutic relationship and empowerment). The quantitative analyses were conducted alongside the qualitative analyses in a convergent parallel design that facilitates the integration of mixed methods data [ 27 ]. Large scale survey data provides a broad picture while the interview data offers more micro detail. This is a pragmatic approach to mixed method research that can generate a more complete understanding of complex phenomena or processes. Quantitative and qualitative data analyses were conducted independently and subsequently synthesised to generate understanding of the links across micro, meso and macro levels than either approach could achieve alone.
Quantitative data
Data from the questionnaires were entered into SPSS version 21 [ 43 ] and distribution of the data assessed for normality using descriptive quantitative measures of skewness and kurtosis. There were few deviations from normality (2 of 27 scale outcomes exceeded the conservative criteria of +/− 1), one was small in the extent of deviation (within +/− 2) however one scale displayed larger deviation of skewness (Emotional differences subscale, Staff outcome on the STAR-C).
A missing value analysis was completed for the 27 scale outcomes. Moderate to high levels of missing data, not missing at random, were identified on a small number of items (mean level of missing data across the 27 scales/subscales was 20%, range from 6 to 55%). The service user version of the RSA questionnaire in particular had a moderate amount of missing data. Mean replacement was used to avoid unnecessary loss of cases from the analysis. The mean of the available items for the scale and participant were used for replacement of the missing values on the scale. A series of sensitivity analyses were conducted to determine what effect mean replacement would have in the primary analyses at different levels of replacement ranging from 20 to 50% replacement. Utilising a 50% mean replacement had no substantive changes in the key statistical parameters ( p -values and associated effect sizes) and the inferences drawn, therefore it was deemed appropriate to maximise the number of cases included in the analyses.
Descriptive statistics were calculated for the four measures (VOICE, RSA, STAR and ES). Where appropriate these scores were compared against reference values (VOICE, STAR and ES) or to the participant groups (RSA). Several unadjusted one-way Analysis of Variance (ANOVA) were conducted to compare differences between the six sites on the RSA, STAR, ES and VOICE measures. Subsequent Tukey post hoc tests were conducted to ascertain which measures differed between which locations. A series of one-way analysis of covariance (ANCOVA) were completed to adjust the analyses for potential confounders. The demographic variables that were chosen for service users were: age; gender; ethnicity and living status. Three care-related variables were chosen for service users: previous admissions; time in mental health services and time on the ward. The demographic variables that were chosen for staff were: age, gender, ethnicity, personal experience of mental illness and family experience of mental illness. Two clinical variables were also chosen: time working in mental health services and time working on the ward. The criteria for adjusted analysis between the ANOVA and ANCOVA were the p -value from the omnibus test, the adjusted means and the p-value from the post-hoc test. If the p-value from the omnibus test for the ANCOVAs were not substantively different from the ANOVAs then no further post –hoc analyses were completed. A series of independent t-tests were completed to determine if there were differences between service users and staff on the outcome measures.
Correlations of the service user data were completed to identify if there was a relationship between the scores on the outcome measures used. Six Pearson’s correlations were conducted to identify if there were relationships between the mean total scores for the measures RSA and VOICE; RSA and STAR-P; RSA and ES; STAR-P and ES; STAR-P and VOICE and VOICE and ES for all service user participants and by individual site. Cohen’s [ 44 ] effect sizes were used to describe the data (Small, r = 0.10, medium r = 0.30 and large r = 0.50). A Pearson correlation was also completed for staff on the mean total scores for the RSA and STAR-C.
For all the ANOVA and ANCOVA analysis the statistical significance level was set at a level of 0.05. To account for multiple comparisons for the t-tests the significance threshold was raised to 0.005 to accommodate for the number of tests applied ( n = 10).
Qualitative data
All digital interview recordings were professionally transcribed and checked against original recordings for accuracy and identifying information redacted, before being imported into QSR International’s NVivo10 qualitative data analysis software [ 45 ] for analysis using Framework method [ 46 , 47 ]. The Framework matrix used was developed a priori from the interview schedules, with sections focusing on organisational background and developments, care planning, recovery, personalisation, safety and risk, and recommendations for improvement. Each matrix section also had an ‘other’ column for the inclusion of data-led emergent categories. Once all charting was completed, second-level summarising was undertaken to further précis data and to identify commonalities and differences.
Data collection across the six sites is summarised in Table 1 and consisted of n = 301 service users (target was 300), n = 290 members of staff (target was 300), n = 28 carers (target 150) completing survey measures.
We completed 31 research interviews with staff (target was 36), 36 with service users (target was 36); and nine with carers (target was 24).
Cross-site analyses will be presented for the four service user questionnaires (VOICE, RSA, STAR-P and ES) followed by a cross-site analysis of the two staff questionnaires (RSA and STAR-C).
Service users
To explore cross-site differences one-way ANOVAs of all total score and subscales were conducted and revealed that there were no global differences across the sites for any of the four measures. Table 2 shows the mean item scores, alongside the parameters of significance for service user participants.
For staff, one-way ANOVAs were conducted for the mean RSA and STAR-C total scores and the subscales (Table 3 ). There was a significant difference between the research sites in the mean RSA total score (F 5, 279) = 6.35, p < 0.001, η 2 = 0.32) and the mean total score for the STAR-C (F 5, 273) = 3.02, p = 0.011, η 2 = 0.23). There were also significant differences found in all of the mean item subscale scores of the RSA and the positive collaboration subscale for the STAR-C. Table 3 shows summary scores for staff.
When using Artois and Champagne as reference sites (the sites with the lowest scores) Provence and Dauphine sites scored significantly higher for the mean RSA total score indicating more recovery focused care (see Fig. 2 ). This scale measures some important perceptions that may have a significant effect on patient outcomes and concordance to care and collaboration with service users. Subsequent Tukey post-hoc tests revealed that staff in Artois (3.36, s.d. = 0.59) score significantly lower than Provence (3.76, s.d. = 0.56, p = 0.009, CI.95–0.73, − 0.07, Cohen’s d = 0.69) and Dauphine (3.74, s.d. = 0.53, p = 0.009, CI.95–0.70, − 0.06, Cohen’s d = 0.68). Staff in Champagne (3.21, s.d. = 0.46) score significantly lower than Provence ( p < 0.001, CI.95–0.92, − 0.19, Cohen’s d = 1.07) and Dauphine ( p < 0.001, CI.95–0.88, − 0.19, Cohen’s d = 1.07).
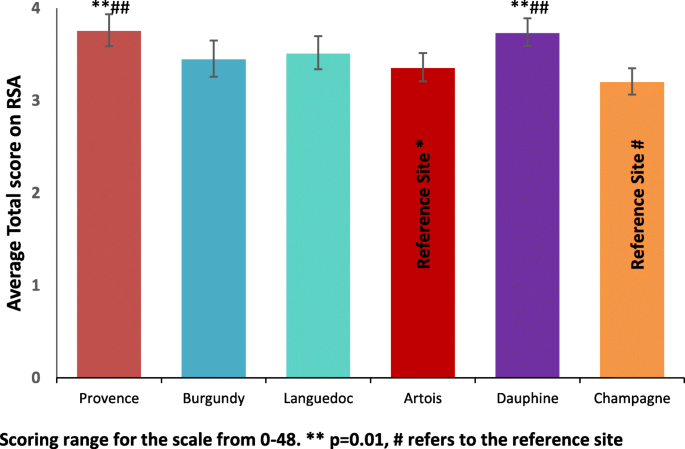
Mean Total RSA score for staff +_95% CI
STAR-C questionnaire
There were no significant differences in the staff responses across sites for the Positive Clinician Input subscale (F (5,272) = 1.53, p = 0.182, η 2 = 0.16) and the Emotional Difficulties subscale (F (5,270) = 1.91, p = 0.092, η 2 = 0.16) There were however significant differences found between sites for the Positive Collaboration subscale (F (5, 274) = 2.42, p = 0.036, η 2 = 0.20) and the STAR-C Total score (F (5, 273) = 3.02, p = 0.011, η 2 = 0.23).
STAR-C positive collaboration
Burgundy performs significantly better for the mean Positive collaboration subscale score than Artois (see Fig. 3 ). This scale measures some important perceptions around rapport and shared understanding of goals focused on mutual openness and trust. Subsequent Tukey post-hoc tests revealed that staff in Artois (17.17, s.d. = 2.65) score significantly lower on the subscale than Burgundy (18.86, s.d. = 2.57, p = 0.019, CI.95–3.20, − 0.18, Cohen’s d = 0.65). There were no significant differences between all of the other sites on this subscale.
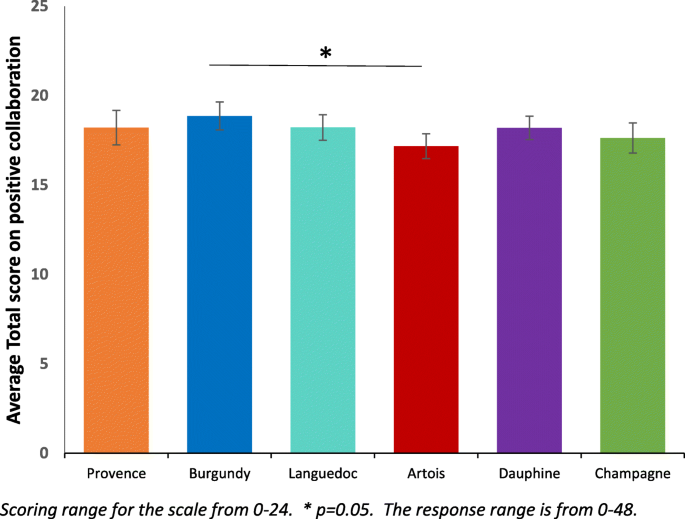
Mean Positive Collaboration subscale score for staff ±95% CI
STAR-C Total
Burgundy performs significantly better for the mean positive collaboration subscale score than Artois (see Fig. 4 ). This scale measures some important perceptions that may have a significant effect on patient outcomes and concordance to care and collaboration with service users. Subsequent Tukey post-hoc tests revealed that staff in Artois (36.08, s.d. = 4.18) score significantly lower on the subscale than Burgundy (39.33, s.d. = 4.31, p = 0.011, CI.95–5.76, − 0.75, Cohen’s d = 0.77). There were no significant differences between all of the other sites on total score.
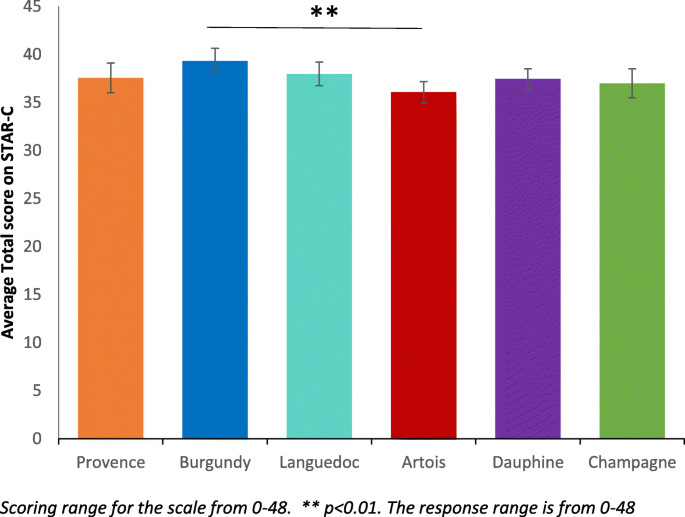
Mean STAR-C Total score for staff ±95% CI
Correlations between outcome measures
Pearson’s correlations were used for the service user survey scores to determine if there were associations between responses on the four scales. Table 4 shows that there is a strong negative correlation between the RSA and VOICE ( r = −.70, n = 285, p < 0.001). This shows that there is an inverse association between the recovery-oriented focus and the negative perception of quality of care amongst service users meaning when recovery-oriented focus was high the quality of care was viewed highly. There is also a positive correlation between the RSA and the STAR-P ( r = .61, n = 282, p < 0.001), indicating an association between the recovery-oriented focus and ratings of the quality of therapeutic relationships amongst service users. There is also a strong negative correlation between the STAR-P and VOICE scale ( r = −.64, n = 294, p < 0.001). There is also an inverse association between the quality of therapeutic relationships and the negative perception of quality of care meaning that when therapeutic relationships are scored highly the perception of quality of care is also scored highly. There are negligible relationships between the RSA and ES; STAR-P and ES and the VOICE and ES.
A Pearson’s correlation was completed at the global level with all participants to determine if there were associations for staff scores between the responses on the two questionnaire scales. This correlation were completed using pairwise deletion. There is a small to moderate correlation between the RSA and STAR-C ( r = −.28, n = 279 p < 0.001).
When comparing the correlation between the RSA and STAR-C (see Table 5 ) there is a considerable amount of variability across sites. There is a large correlation in Burgundy ( r = 0.50, n = 43, p = 0.001). There are moderate or small to moderate correlations in Artois ( r = 0.28, n = 56, p = 0.034), Languedoc ( r = 0.35, n = 47, p = 0.015) and Provence ( r = 0.28, n = 56, p = 0.034). Only small correlations were found in Champagne ( r = 0.16, n = 41, p = 0.331) and Dauphine ( r = 0.35, n = 50, p = 0.015).
Across all of the six research sites staff score significantly higher than service users on the scale to assess therapeutic relationships. In Burgundy and Dauphine the same pattern is present across all of the subscales. Positive clinician input was scored higher by staff than service users across the six sites (see Table 2 ).
Qualitative findings
Table 1 summarises the characteristics of each of the six meso-level case study sites and the types and quantity of data generated in each. Illustrative quotations used below are labelled with the initial of the site pseudonym; then ST, SU, or CA for staff, service user or carer; and their unique number, e.g. B-ST-001 (Burgundy-Staff-001).
Care planning and coordination
Staff across sites talked of the importance of collaborative care planning. Many also spoke of the value of plans being kept up-to-date with service users actively involved, and of plans being used as a way of collecting multidisciplinary contributions and of helping manage transitions between hospital and community. For example,
“[B]ringing a person’s care all together really, so it’s like a standard to work around, that it’s all centred around the patient’s care, so everything works for them in the best way, I think.” (L-ST-103)
However, staff, service user and carer interviews all revealed gaps between shared aspirations and realities, even where service users drew attention to receiving good quality care. Staff accounts of routine collaboration with service users in care planning contrasted with service user accounts which pointed to lack of involvement. In all sites some service users report that they were not involved in the planning of their care, were unaware of the content of their care plans or had not received copies, or did not feel a sense of care plan ownership. For example,
“There isn’t a treatment plan. There’s no treatment, there’s just containment. Walking to the shop to get a newspaper isn’t treatment. There’s no therapy here.” (C-SU-103)
Staff sometimes spoke of service users’ unwillingness or inability to collaborate in care planning, or of the barriers to collaborating brought about by the introduction of electronic records. Lack of a shared language was cited as a barrier in one inner city site (Dauphine). Staff in Burgundy said how the all-Wales CTP template was not well-suited to the short-term nature of acute hospital care with some domains (e.g., housing) emerging as higher priority than others.
“I think I struggle with the principles [of CTP] and how that fits perhaps into the ward – the confusion that still exists is very much present in terms of the fundamentals of it.” (B-ST-102)
Coherence and continuity in care across hospital and community interfaces were identified as important by many of those taking part, and examples of detailed and collaborative discharge planning involving staff and service users were given. Innovations were also described, such as ‘interim discharge summaries’. However, rapidly arranged discharges caused some concern with little time then available for considered planning, one service user recalled being ‘pulled in out of the blue’ to be told ‘right, you can go’ (P-SU-102).
Two types of care plan review were described: formal, typically weekly, multidisciplinary meetings chaired invariably by consultant psychiatrists and daily handovers where care on a more immediate basis was reviewed by staff. Formal ward rounds were described as key events by staff and as places where progress and plans could be reviewed in a multidisciplinary context. Service user views and experiences of these differed, within and across sites. For some they were helpful, serving as opportunities for catching up with psychiatrists and the whole multidisciplinary team.
“Sometimes you’ve got a load of people in there and you sort of feel a bit like you’re on stage, you know like the spotlight’s on you, sort of thing. But yeah. I’ve had problems with ward rounds but more recently things have been OK, I’ve been able to sort of express myself more.” (P-SU-104)
Some service users also described the opportunity to plan and prepare for formal ward round participation. Others spoke of limited time to fully consider their needs, of excessive jargon being used and of inflexibility over ward round scheduling.
Safety and risk
Assessing and managing risk were customarily seen by staff as central parts of the work of planning and providing care so that risk assessments were described as proliferating so much they were “ coming out of your eyeballs” (P-ST-101). Formal ward round-based review meetings were named as a place for risks to be discussed although not necessarily in the presence of service users. Some staff also talked of the particular issues surrounding risk and decision-making in the care of service users who were detained. Risks mentioned by staff included those to self and others, with some also noting the dangers of over-estimating risks and the importance of attending to strengths and of positive risk-taking.
“ if you let the risk rule over the actual care plan then you’re never going to get anywhere .” (L-ST-102)
Most service users talked of their safety being considered and attended to, sometimes giving specific examples of this in action (e.g., through removal of objects and the use of observations), even though risk assessments and management plans were often not actively discussed with them. Others did, however, talk of feeling unsafe in hospital and of asking for more staff.
Definitions and understandings of recovery varied amongst staff, service users and carers, as did views of the role of hospitals in promoting this. Participants, in many cases, were also aware of the disparate meanings of ‘recovery’. Some staff (e.g., in Artois) viewed recovery as problematic in the inpatient context, saying that this raised expectations or was too poorly understood to help effective care planning.
“ I think it’s about being realistic as well. … certainly it’s about fostering hope, looking for things as well, and working towards those things, but in an acute ward where people can’t … leave [the ward] ” (A-ST-106)
In Languedoc, antipathy to the idea of recovery was reported by some staff who challenged both its meaning and utility. Most service users said that hospital had helped (e.g., to stabilise medication), though some complained of having been largely left to their own devices or subjected to containment. The use of tools to aid recovery (e.g., Recovery Star) were occasionally mentioned (e.g., in Burgundy), but in most cases these were either not deployed or were described as being more suitable beyond the acute hospital care context. Service users and carers revealed a range of views around recovery, from the cure of symptoms, to the prospects of life without medication, to the idea of coming to terms with difficulties.
“getting rid of the voices and what I see. That’s my recovery” (P-SU-101).
- Personalisation
The term ‘personalisation’ was not a familiar one, with few revealing knowledge of personal budgets, “ It doesn’t mean anything, it just sounds like a made-up word .” (L-SU-102).
In all settings there was recognition of the idea that care and services should be oriented to the individual. Whilst some staff talked of inpatient care as being person-centred there was also widespread recognition of the challenges to this (e.g., tensions between different approaches to providing care, the fact that staff only get to know people as patients, and the relative (un)availability of resources). Within and across sites there were differences in service user views and experiences of individually tailored care. Some were clear that hospital had been pivotal in their care, “ without this place it would be the end of me ” (C-SU-105). Others were equally clear that their care had not been personalised, or talked of their care at home being more personalised. Carers gave positive accounts of care provided although most remained uncertain about the term personalisation,
“ I guess personalisation means the way her treatment was personalised for her and I guess it was, because everyone is different and everyone needs different help, but I don’t really know what you mean.” (P-CA-101)
The aim of this study was to identify factors that facilitate or hinder recovery-focused personalised care planning and coordination in acute inpatient mental health settings. The intention was to generate new theoretical knowledge and greater understanding of the complex relationships between collaborative care planning, recovery and personalisation.
Comparison and consideration of our survey results and interview data across sites provides some reason for optimism concerning the overall quality of mental health inpatient care but also indicators of areas where greater attention may be required.
We found no global differences across the six sites on the service user measures. The VOICE measure [ 41 ] examined service users’ perceptions of inpatient care and found marginally lower scores than the reference value [42]. However, the mean scores in all six research sites in this study were lower (so more positive) than those reported in a recently published study which examined different inpatient service models over a period from 2008 to 2010 [ 48 ]. We found that service users leaned towards a positive perception of the wards but there was wide variation within sites, suggesting a mix of views. These results converge with our research interview data showing service users being largely positive about their care, acknowledging being treated with dignity, respect and compassion. This was irrespective of legal status. Those carers interviewed also spoke positively about care provided and attitudes of staff.
Staff spoke of the challenges of collaborating on care planning with service users in severe mental distress or lacking insight and this is likely to include those formally detained. However, despite specific questions related to the legal status of services users, this was not explicitly identified as an issue perhaps reflecting the now high proportion of inpatients legally detained.
On ratings of the quality of therapeutic relationships, across all six sites staff consistently rated these relationships significantly more positively than did service users. The STAR-P measure used was initially designed for rating the one-to-one relationships that service users have with care coordinators in community teams [ 15 ] so it may be that, despite having a ‘named nurse’, the more dispersed nature of relationships with a number of ward staff over days and weeks, across shifts and 24-h care weaken any rating. Inpatient care also includes the greater likelihood of restrictions, limitations, rules and regulations necessary to provide a safe environment [ 49 ]. First- or second-hand experience of coercion and containment are also likely to be more prevalent in an inpatient setting [ 50 ]. Nevertheless, the need for further investigation to identify how positive relationships can be mutually achieved is indicated.
There was a strong perception across sites that staff were aware of policy drives to provide a greater focus on recovery, to provide respectful, compassionate and dignified care. Most staff articulated clear values and understandings reflecting core components of the focus on recovery as well as other initiatives that have been promoted in an attempt to improve inpatient services, such as the Royal College of Psychiatrists’ Accreditation for Inpatient Mental Health Services (AIMS) [ 51 ], Bright charity’s Star Wards [ 52 ] and most recently, the mental health nurse-led evidence-based intervention, SafeWards [ 53 ].
Staff participants suggested that severity of illness and/or lack of insight sometimes means that collaborative care planning is difficult to achieve, that there was often insufficient time to devote to this task, or that some service users were unwilling or unable to collaborate on care planning. Staff found it difficult to discuss care with service users especially where there was a mismatch in goals and expectations and limited advice on what a good care plan looks like or on how to identify achievable goals. Some of these barriers such as staff views on severity of illness have been found in other studies and highlighted in systematic reviews of barriers to involvement [ 54 ] and the consistency of this finding across our study sites can be read in a number of ways. First, it is undoubtedly the case that some people admitted to inpatient services are in severe distress and the process of discussing and negotiating a care plan in those first few days is unlikely to be a priority for them.
A second reading is that mental health professionals despite their claimed interest and support of involvement actually struggle to put this idea into practice and may need some guidance to achieve the aspiration of true collaboration. A possible contributor here was highlighted by both service users and staff and this relates to inflexible documentation and information technology on inpatient wards. In tandem these two elements prevent service users and staff writing care plans together as staff have to leave to type up a care plan once discussed, service users feel removed from the process and unable to alter the document which can often be presented to them without adequate explanation.
Services are also pressured to meet organisational demands and staff may simply not prioritise collaboration with service users. Service users report that time with staff is highly valued but for the most part was a limited resource. Time is an important and taken for granted feature of social life; it is used by individuals to impose order, understand and handle discontinuities [ 55 , 56 ]. A universal expectation reported by staff and service users in this current study was that individual one to one time would provide the means for problem resolution, help establish rapport and trust and ultimately engender a sense of collaboration towards preferred goals. However, time was a scarce resource and organisational schedules were reported to quickly over-ride those of the service user and their primary nurse.
Interprofessional ward rounds were of critical importance to service users and staff alike as the site for discussion, planning and review. Service users and staff may experience the timetabling of ward rounds differently, for example there may be diverse perceptions of scheduling delays or contradictory understandings of what happened [ 57 ]. For service users in our study ward rounds involved anxious hours waiting to be called, followed by sometimes short but overwhelming or intimidating experiences in the meeting itself [ 58 ]. It was noted that few service users were adequately prepared on what to expect. Some told us they had expected to meet only the doctor but found themselves shown into a room full of unfamiliar faces, others felt that their contributions were not valued or that they had been poorly treated. For people who are already distressed and anxious about their treatment or future outcomes it seems ward rounds handled poorly can worsen their sense of efficacy and discourage attempts to achieve involvement.
Both staff and service users said that reviewing care plans in ward rounds would help mark progress towards agreed goals. This finding from our research interviews aligns with our quantitative survey showing that participants rated highly the recovery language used by staff and the regular monitoring of progress towards recovery goals. Additionally, the information needs of service users could be better met by helping them prepare for ward rounds, including determining expectations and the agenda. In addition it was suggested to us that service users be given summaries of ward round outcomes.
Recovery, therapeutic relationships and care planning
The focus of recovery for many service users was around medication and symptom suppression (perhaps reflecting the primary focus of inpatient care) indicating a more ‘clinical’ as opposed to a ‘personal’ concept of recovery [ 9 ]. In some sites, there was greater ambivalence around the suitability or relevance of ‘recovery’ in inpatient care, particularly where people are very unwell. There may be tensions with working in recovery-focused ways when people are formally detained. It is possible however that this is the very time where a recovery-focused approach would be most powerful.
Our data on recovery shows convergence between results from standardised measures and findings from qualitative research interviews. Across five of the six sites service user participants rated highly the use of recovery language from workers and services alongside their perspective that workers believe that people can recover and participate in their own life choices. Service users also rated highly that there is regular monitoring of progress towards their recovery goals. Workers rated these items highly too suggesting that notions of recovery and therapeutic optimism were supported. Qualitative data indicate staff recognised the complex and individual nature of recovery. For example some staff saw a more recent orientation towards recovery focused care as representing the shift from previous authoritarian and prescriptive asylum based care to more collaborative models that encourage patient and family involvement.
There was a strong association amongst service users between their perceptions of recovery-oriented care and their perception of the quality of care on the ward. Likewise there were close correlations between the therapeutic relationships and the perception of quality of care. These findings were robust and consistent across all research sites. Whilst it is not possible to determine which factor might be influencing which, it does suggest an important interrelationship between service users’ subjective valuing of their relationships with staff, the quality of inpatient care and the recovery-focus of the service.
Across all sites staff consistently scored practices as more recovery-oriented than did service users. Our interviews, however, revealed ambivalence and a range of staff perspectives on recovery in line with previous research [ 59 ]. The concern that recovery creates ‘unrealistic’ expectations can perhaps be read as anxiety about what services have to offer to achieve this desired outcome. It may be that participants are simply acknowledging that recovery opportunities are hindered in settings where insufficient space is afforded to wider structural and social issues that give rise to and maintain mental distress. All participants appear to recognise the non-linear complex nature of recovery but place the emphasis differently.
One site that scored recovery highly, Dauphine, had made local attempts to introduce innovations such as service user-focused ‘This is Me’ care plans and short summary ‘management plans’, but these are in addition to standard documents and care plans, adding to workload. Interestingly, in Wales service user participants recognized that their goals were being monitored on a regular basis. This was appreciated to a lesser extent in England with just one site scoring this highly which may be a positive indication of the use of the structured care and treatment plan (CTP) approach in Wales.
Risk and safety remain key concerns for mental health workers [ 60 ] and issues around safety and risk are reported to be central to inpatient work for staff. In the mental health system more widely risk is constructed as an unwanted outcome arising from the actions or behaviours of individuals with mental health problems. In this sense risk is seen to emanate from the person who is seen as the chief agent of unwanted harmful behaviours. Harm does occur of course and mental health services appear to be chiefly concerned with harms from the person to themselves or others. For example, there are approximately 5500 suicides each year in the UK, 30% of which are known to mental health services [ 61 , 62 , 63 ]. Risk of suicide in the transition from inpatient care is now firmly established [ 64 ] and there is some suggestion that this risk has been transferred from inpatient to crisis resolution and home treatment services [ 65 , 66 ]. Harm to others is a much rarer event but nevertheless is likely to have significant negative consequences for the victim, the individual with mental health problems and their family, and the wider system including individual workers such that risk averse practice is common [ 67 ]. The pressure to ensure safety and avoid blame appears to be omnipresent in mental health services.
Coherence and continuity in care across hospital and community interfaces is known to be important in delivering safe, supportive mental health care [ 68 ] and were identified as important by many of those taking part in this study, with examples of detailed and collaborative discharge planning involving staff and service users given. Innovations were also described, such as ‘interim discharge summaries’. However, participants also reported rapidly arranged discharges with little time for discussion or planning. Decisions on movement through phases of inpatient treatment will in part depend on the presenting symptomatology of the person, an assessment of their risk status, their needs for treatment and an assessment of their post discharge needs such as accommodation [ 69 ].
Staff acknowledged tensions around sensitive discussions and especially with people detained. Workers openly acknowledged that this was to avoid difficult conversations but others seemed less aware that in denying service users access to knowledge about their risk that they are effectively excluding people from participation in decisions about their care [ 70 ]. Previously we have noted that workers position risk assessment as legitimate work despite limitations in the predictive power of these judgements as one way of gaining normative certainty [ 71 ].
Here, unlike in the community study [ 18 , 71 ], service users seemed to be more aware of their safety being considered and managed in that they understood why certain items were removed or restrictions were imposed. Some service users spoke of not feeling safe on wards as reported in previous studies [ 72 , 73 ] and this needs to be considered in ongoing discussions and policy developments on safe staffing [ 74 ]. It remained a curious finding that while workers saw risk assessment as central to their efforts that they appear to largely exclude the service user from meaningful discussions about these.
Drawing on the evidence presented here, personalisation is not widely recognized as a concept and not actively used in inpatient services by staff or service users, although there was wide discussion amongst staff of aiming to provide personal care or a personalised approach to care.
Staff spoke about some of the constraints and challenges in trying to work in a personalised way and these included a lack of resources, short ward stays, service users being formally detained, disagreements, risk behaviours, limited capacity, and a primary focus on medical treatment. It was recognised that to enable personalised care, it was necessary to have the time to get to know people as individuals and to provide some element of continuous care. Too often this was difficult to achieve in inpatient settings. Staff in the Welsh sites thought that the format of the CTP process and care plan was supportive of working in a personalised way and helped service users and staff get to know each other better.
Some service users were clear that their care was very personalized and that staff had considered their unique needs with several good examples provided. Others felt that inpatient care was more routine and standard for all and that individually tailored care was less possible in hospital, especially when people are detained. However, it was notable that some wards and staff were able to provide care in a more personalised way and support should continue to be given to achieve this everywhere. Personalisation is an integral component of a recovery-focused approach to mental health care and needs to be promoted and supported as such [ 75 ].
Strengths and limitations
Achieving our target numbers for each grouping on the survey was challenging. Service user numbers were achieved but fell just short for staff. To achieve our target recruitment figures we approached all eligible participants meaning that our sample was not randomly selected. Despite considerable efforts we were unable to recruit sufficient numbers of carers. Researchers in the field reported how few carers visit wards, often preferring to meet service users elsewhere. The difficulties of involving carers in studies of inpatient mental health services has been reported elsewhere [ 76 ] and poses a particular challenge for researchers keen to include the views of family members and friends.
Due to the nature of the survey it is not possible to make comparisons between responders and non-responders as we had no access to data for non-participants. There was a moderate level of missing data for the RSA scale completed by service users, possibly due to some of the difficult language used and the community focus of the measure. As a consequence, more detailed analysis of covariations within the data was restricted by lack of power.
The interview data is rich and the framework method provided a time-consuming but structured and visible method of organising, analysing and comparing that data within and across sites. We believe the framework method and detailed presentation of results supports the transferability of these findings to other similar services. The involvement of service users and carers throughout the study as researchers and advisors has also provided added value to the study through additional viewpoints and interpretations.
The findings of this cross-national, multi-site mixed methods study suggests positive practice is taking place within acute inpatient wards with evidence of a widespread commitment amongst staff to provide safe, respectful, compassionate care with strong values underpinning practice. Whilst ideas of recovery were evident amongst staff there was some uncertainty and discrepancy about the relevance of recovery ideals to inpatient care or the ability of people experiencing high levels of distress to engage in recovery-focused approaches. However, service users saw inpatient admissions as a necessary stage in stabilising their mental state, with medication an important component, and often appreciated the efforts that were made to keep them safe and to help them take the next tentative steps on their recovery. They also rate highly staff using recovery-focused language and values. Many spoke of care being personalised with examples given of staff being very responsive and considerate to particular needs or concerns. Carers often similarly described positive views of patient care. However, whilst service users valued the relationships they have with staff on the wards, they do not rate these as highly as staff. As discussed earlier, this is perhaps not surprising given all the tensions and anxieties associated with an inpatient stay, but this perhaps can best be summarised as ‘doing well, but could do better’.
Staff were clearly able to articulate the care planning processes and documentation required of them and described some of their frustrations with lengthy, unwieldy forms and at times distancing computerised systems that required more time in front of monitors than in conversation with service users. Most staff also spoke of their understanding and efforts to involve service users, and carers and families where possible, in the care planning process. However, most service users did not really appreciate the written care plan as an integral or important part of their experience and many did not have copies or could not find them. The majority of service users did not feel they had been genuinely involved in the process. Unfortunately, in relation to service users receiving sufficient time with nursing staff and being involved in planning their care, very little progress appears to have made since the report of the Healthcare Commission of nearly a decade ago [ 25 ].
Issues of risk and safety are ever-present in mental health services and it was clear that this was central to the work of staff, whilst they displayed an awareness of the sensitivities and challenges involved. Service users, and carers, were often aware of efforts being made by staff to keep them safe. However, involvement of service users in discussions about personal risk factors and safety is challenging and requires greater training and support to encourage staff to develop the skills and confidence to undertake such sensitive and important work with confidence.
Abbreviations
Analysis of Covariance
Analysis of Variance
Care Programme Approach
Care Quality Commission
Care and Treatment Planning
Empowerment Scale
Lived Experience Advisory Group
Multivariate Analysis
Multidisciplinary Team
Medical Research Council
National Health Service
National Research Ethics Service
Recovery Self-Assessment
Scientific Steering Committee
Scale to Assess the Therapeutic Relationship – Clinician version
Scale to Assess the Therapeutic Relationship – Patient version
Service User and Carer Group Advising on Research
Service User Project Assistants
Service User Researcher Assistants
United Kingdom
Views of Inpatient Care Scale
HM Government. No health without mental health: a cross-government mental health outcomes strategy for people of all ages. London: HM Government; 2011.
Google Scholar
Naylor C, Bell A. Mental health and the productivity challenge. Improving quality and value for money. London: Kings Fund; 2010.
Health and Social Care Information Centre: Mental Health Bulletin, 2016–17 Annual Report. Leeds: Health and Social Care Information Centre; 2017.
Statistics for Wales. Admission of patients to mental health facilities in Wales, 2016–17. Cardiff: Welsh Government; 2018.
Department of Health. Refocusing the care Programme approach: policy and positive practice guidance. London: Department of Health; 2008.
Welsh Government. Together for mental health: a strategy for mental health and wellbeing in Wales. Cardiff: Welsh Government; 2012.
Welsh Government. Code of practice to parts 2 and 3 of the mental health (Wales) measure 2010. In. Cardiff: Welsh Government; 2012.
Anthony WA. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial Rehabilitation Journal. 1993;16(4):11–23.
Article Google Scholar
Slade M. Personal recovery from mental illness: a guide for mental health professionals. Cambridge: Cambridge University Press; 2009.
Book Google Scholar
British Psychological Society: Understanding Mental Illness: Recent advances in understanding mental illness and psychotic experiences. In . Leicester: British Psychological Society; 2000.
COT. Recovering Ordinary Lives. London: College of Occupational Therapists; 2006.
CNO/DH. From values to action: The Chief Nursing Officer's review of mental health nursing. London: Department of Health; 2007.
RCPsych. Fair Deal for Mental Health. London: Royal College of Psychiatrists; 2008.
Duffy S. Personalisation in mental health. Sheffield: Centre for Welfare Reform; 2010.
Shepherd G, Boardman J, Rinaldi M, Roberts G. Supporting recovery in mental health services: quality and outcomes. London: Implementing Recovery Through Organisational Change; 2014.
Coffey M, Hannigan B, Simpson A. Care planning and coordination: Imperfect solutions in a complex world. J. Psychiatr. Ment. Health Nurs. 2017;24(6):333–4.
Article PubMed Google Scholar
Jones A, Hannigan B, Coffey M, Simpson A. Traditions of research into community mental health care planning and care coordination: a meta narrative review. PloSOne. 2018;13(6):e0198427.
Article CAS Google Scholar
Simpson A, Hannigan B, Coffey M, Barlow S, Cohen R, Jones A, Všetečková J, Faulkner A, Thornton A, Cartwright M. Recovery-focused care planning and coordination in England and Wales: a cross-national mixed methods comparative case study. BMC Psychiatry. 2016;16(1):1–18.
Simpson A, Hannigan B, Coffey M, Jones A, Barlow S, Cohen R, Všetečková J, Faulkner A: Cross-national comparative mixed-methods case study of recovery-focused mental health care planning and co-ordination: Collaborative Care Planning Project (COCAPP). Health Serv Deliv Res 2016, 4(5).
NICE: NICE Guidance on improving the experience of care for people using adult NHS mental health services. NICE; 2011.
CQC: Monitoring the Mental Health Act in 2011/12. Newcastle-Upon-Tyne: Care Quality Commission; 2013.
CQC: Community mental health services survey 2011. Newcastle-Upon-Tyne: Care Quality Commission; 2011.
WAO. Adult mental health services: follow up report. Cardiff: Wales Audit Office; 2011.
House of Commons Health Committee: Post-legislative scrutiny of the Mental Health Act 2007: HC584, First Report of Session 2013–14, vol. HC584. London: The Stationery Office Limited; 2013.
Healthcare Commission. The pathway to recovery. A review of NHS acute inpatient mental health services. London: Healthcare Commission; 2008.
MRC. Developing and evaluating complex interventions. London: Medical Research Council; 2008.
Creswell J. Research design: qualitative, quantitative and mixed methods approaches. London: Sage; 2009.
Simpson A, Coffey M, Hannigan B, Barlow S, Cohen R, Jones A, Faulkner A, Thornton A, Všetečková J, et al. Cross-national mixed-methods comparative case study of recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings (COCAPP-A). Health Serv Deliv Rese. 2017;5(26).
Byrne DS. Complexity theory and the social sciences: an introduction. London: Routledge; 1998.
Kohn M. Cross-National Research in Sociology. Newbury Park: Sage; 1993.
Hantrais L, Mangen S. cross-National Research Methods in the social sciences. London: Pinter; 1996.
Stake RE. The art of case study research. London: Sage; 1995.
Fitzgerald L. Case studies as a research tool. Quality in health care: QHC. 1999;8(2):75.
Article CAS PubMed PubMed Central Google Scholar
Platt J. Case study in American methodological thought. Curr Sociol. 1992;40(1):17–48.
Yin RK. Case study: design and methods. Newbury Park: Sage Publications; 1994.
Robson C. Real world research: a resource for social scientists and practitioners-researchers. Oxford: Blackwell; 1993.
Faul F, Erdfelder E, Lang AG, Buchner A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–91.
O'Connell M, Tondora J, Croog G, Evans A, Davidson L. From rhetoric to routine: assessing perceptions of recovery-oriented practices in a state mental health and addiction system. Psychiatric Rehabilitation Journal. 2005;28(4):378.
Mcguire-Snieckus R, McCabe R, Catty J, Hansson L, Priebe S. A new scale to assess the therapeutic relationship in community mental health care: STAR. Psychol Med. 2007;37(1):85–95.
Rogers ES, Chamberlin J, Ellison ML, Crean T. A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatr Serv. 1997;48(8):1042–7.
Article CAS PubMed Google Scholar
Evans J, Rose D, Flach C, Csipke E, Glossop H, McCrone P, Craig T, Wykes T. VOICE: developing a new measure of service users' perceptions of inpatient care, using a participatory methodology. J Ment Health. 2012;21(1):57–71.
Article PubMed PubMed Central Google Scholar
Simpson A, Barlow S, Cox L, Jones J. SUGAR : adding SUGAR: collaborating with service users and carers in mental health nursing research. J Psychosoc Nurs Health Serv. 2014;52(1):22–30.
IBM Corp: IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp; Released 2012.
Cohen J. A power primer. Psychol Bull. 1992;112(1):155–9.
QSR International Pty Ltd. NVivo qualitative data analysis software; version 10. Doncaster: QSR International Pty Ltd; 2012.
Ritchie J, Lewis J, Nicholls CM, Ormston R. Qualitative research practice: a guide for social science students and researchers. London: Sage; 2013.
Ritchie J, Spencer L. The analysis of qualitative data: an approach to analysis for applied social policy research. In: Bryman A, RG B, editors. Analyzing qualitative data. London: Routledge; 1993.
Csipke E, Williams P, Rose D, Koeser L, McCrone P, Wykes T, Craig T. Following the Francis report: investigating patient experience of mental health in-patient care. Br J Psychiatry. 2016;209(1):35-39.
Bowers L, Simpson A, Alexander J, Hackney D, Nijman H, Grange A, Warren J. The nature and purpose of acute psychiatric wards: the Tompkins acute Ward study. J Ment Health. 2005;14(6):625–35.
Whittington R, Bowers L, Nolan P, Simpson A, Neil L. Approval ratings of inpatient coercive interventions in a national sample of mental health service users and staff in England. Psychiatr Serv. 2009;60(6):792–8.
Cresswell J, Beavon M. Accreditation for inpatient mental health services (AIMS): standards for inpatient wards-working-age adults. London: Royal College of Psychiatrists; 2010.
Star Wards’ 75 Ideas. http://www.starwards.org.uk/ . Accessed 5 Apr 2019.
Bowers L, James K, Quirk A, Simpson A, SUGAR, Stewart D, Hodsoll J. Reducing conflict and containment rates on acute psychiatric wards: the Safewards cluster randomised controlled trial. Int J Nurs Stud. 2015;52:1412–22.
Storm M, Davidson L. Inpatients’ and providers’ experiences with user involvement in inpatient care. Psychiatry Q. 2010;81:111–25.
Roth JA. Timetables: structuring the passage of time in hospital treatment and other careers. Bobbs-Merrill: Indianapolis; 1963.
Coffey M. Time and its uses in accounts of conditional discharge in forensic psychiatry. Sociology of Health and Illness. 2013;35(8):1181–95.
Klitzman R. "patient-time", "doctor-time", and "institution-time": perceptions and definitions of time among doctors who become patients. Patient Educ Couns. 2007;66(2):147–55.
White R, Karim B. Patients’ views of the ward round: a survey. Psychiatrist. 2005;29(6):207–9.
Aston V, Coffey M. Recovery: what mental health nurses and service users say about the concept of recovery. J Psychiatr Ment Health Nurs. 2012;19(3):257–63.
Dixon J. Balancing risk and recovery in mental health: an analysis of the way in which policy objectives around risk and recovery affect professional practice in England. In: Chamberlain M, editor. Medicine, Power, and Discourse. London: Taylor & Francis; 2015.
Cavanagh B, Ibrahim S, Roscoe A, Bickley H, While D, Windfuhr K, Appleby L, Kapur N. The timing of general population and patient suicide in England, 1997–2012. J Affect Disord. 2016;197:175–81.
Coope C, Gunnell D, Hollingworth W, Hawton K, Kapur N, Fearn V, Wells C, Metcalfe C. Suicide and the 2008 economic recession: who is most at risk? Trends in suicide rates in England and Wales 2001–2011. Soc Sci Med. 2014;117:76–85.
National Confidential Inquiry into homicide and suicide by people with mental illness: annual report: England, Northern Ireland, Scotland and Wales July 2015 . . Manchester: University of Manchester; 2015.
Meehan J, Kapur N, Hunt IM, Turnbull P, Robinson J, Bickley H, Parsons R, Flynn S, Burns J, Amos T. Suicide in mental health in-patients and within 3 months of discharge. Br J Psychiatry. 2006;188(2):129–34.
Johnson S. Crisis resolution and home treatment teams: an evolving model. Adv Psychiatr Treat. 2013;19(2):115–23.
Hunt IM, Rahman MS, While D, Windfuhr K, Shaw J, Appleby L, Kapur N. Safety of patients under the care of crisis resolution home treatment services in England: a retrospective analysis of suicide trends from 2003 to 2011. Lancet Psychiatry. 2014;1(2):135–41.
Coffey M. A risk worth taking? Value differences and alternative risk constructions in accounts given by patients and their community workers following conditional discharge from forensic mental health services. Health Risk and Society. 2012;14(5):465–82.
Weaver N, Coffey M, Hewitt J. Concepts, models and measurement of continuity of care in mental health services: a systematic appraisal of the literature. J Psychiatr Ment Health Nurs. 2017;24(6):431–50.
Bowers L, Chaplin R, Quirk A, Lelliott P. A conceptual model of the aims and functions of acute inpatient psychiatry. J Ment Health. 2009;18(4):316–25.
Fricker M. Epistemic injustice: power and the ethics of knowing. Oxford: Oxford University Press; 2007.
Coffey M, Cohen R, Faulkner A, Hannigan B, Simpson A, Barlow S. Ordinary risks and accepted fictions: how contrasting and competing priorities work in risk assessment and mental health care planning. Health Expect. 2017;20(3):471–83.
Jones J, Nolan P, Bowers L, Simpson A, Whittington R, Hackney D, Bhui K. Psychiatric wards: places of safety? J Psychiatr Ment Health Nurs. 2010;17(2):124–30.
Quirk A, Lelliott P, Seale C. Service users’ strategies for managing risk in the volatile environment of an acute psychiatric ward. Soc Sci Med. 2004;59(12):2573–83.
NHS Improvement accused of 'dismantling' NICE safe staffing work. https://www.hsj.co.uk/workforce/exclusive-nhs-improvement-accused-of-dismantling-nice-safe-staffing-work/7005462.article . Accessed 5 Apr 2019.
Alakeson V, Perkins R. Recovery, personalisation and personal budgets. London: Centre for Mental Health; 2012.
Nolan F: An evaluation of protected engagement time on staff and patient outcomes in acute mental health inpatient wards: implications for mental health nursing and research . In: Network for Psychiatric Nursing Research . University of Warwick; 2013.
Download references
Acknowledgements
All members of the Lived Experience Advisory Group, the Study Steering Group, the service user researchers and research staff who ensured the success of the study.
The project reported in this article was commissioned and funded by the National Institute for Health Research (NIHR) Health Services and Delivery Research Programme (HS&DR 13/10/75). The NIHR had no role in the design of the study and collection, analysis, and interpretation of data or in writing of the manuscript. The views and opinions expressed here are those of the authors and do not necessarily reflect those of the HS&DR programme, NIHR, the National Health Service (NHS) or the Department of Health and Social Care.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and affiliations.
Department of Public Health, Policy and Social Sciences, Swansea University, Singleton Park, Swansea, SA2 8PP, UK
Michael Coffey
School of Healthcare Sciences, Cardiff University, Cardiff, CF24 0AB, UK
Ben Hannigan & Aled Jones
Centre for Mental Health Research, School of Health Sciences, City, University of London, Northampton, Square, EC1V 0HB, UK
Sally Barlow & Alan Simpson
Centre for Health Services Research, School of Health Sciences, City, University of London, Square, EC1V 0HB, Northampton, UK
Martin Cartwright
Centre for Academic Mental Health, Bristol Medical School, University of Bristol, Oakfield House, Oakfield Grove, Clifton, Bristol, BS8 2BN, UK
Rachel Cohen
Independent Service User Researcher Consultant, London, UK
Alison Faulkner
East London NHS Foundation Trust, 9 Alie St, London, E1 8DE, UK
Alan Simpson
You can also search for this author in PubMed Google Scholar
Contributions
MCo contributed to the design of the study, data collection, analysis, interpretation, write-up and final edit of the paper. BH contributed to the design of the study, data collection, analysis, interpretation, and write-up of the paper. SB contributed to data collection, led on quantitative analysis, contributed to qualitative analysis, interpretation, and write-up of the paper. MCa advised and contributed to statistical analysis and write-up of the paper. RC contributed to data collection, qualitative analysis, interpretation, and write-up of the paper. AF contributed to the design of the study, data collection, analysis, interpretation, and write-up of the paper. AJ led on the literature review and contributed to interpretation and write-up of the paper. AS contributed to the design of the study, analysis, interpretation and write-up of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Michael Coffey .
Ethics declarations
Ethics approval and consent to participate.
The study received NHS Research Ethics approval from the NRES Committee NRES Committee London – Fulham (Ref: 13/LO/2062) on 29th December 2014. All participants provided written informed consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:.
Reliability Assessment.docx showing additional reliability checks for the internal consistency of the scales and subscales. (DOCX 23 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions

About this article
Cite this article.
Coffey, M., Hannigan, B., Barlow, S. et al. Recovery-focused mental health care planning and co-ordination in acute inpatient mental health settings: a cross national comparative mixed methods study. BMC Psychiatry 19 , 115 (2019). https://doi.org/10.1186/s12888-019-2094-7
Download citation
Received : 12 June 2018
Accepted : 27 March 2019
Published : 16 April 2019
DOI : https://doi.org/10.1186/s12888-019-2094-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Care planning
- Inpatient care
- Therapeutic relationships
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Mental Health and Psychiatric Nursing
The field of mental health often seems a little unfamiliar or mysterious, making it hard to imagine what the experience will be like or what nurses do in this area. This is an overview of the history of mental illness, advances in treatment, current issues in mental health, and the role of the psychiatric nurse .
Table of Contents
Mental health, mental illness, diagnostic and statistical manual of mental disorders, ancient times, period of enlightenment and creation of mental institutions, sigmund freud and treatment of mental disorders, development of psychopharmacology, mental illness in the 21st century, psychiatric nursing practice, mental health and mental illness.
Mental health and mental illness are difficult to define precisely. The culture of any society strongly influences its beliefs and values, and this in turn affects how that society defines health and illness.
No single universal definition of mental health exists. Generally, a person’s behavior can provide clues to his or her mental health.
- In most cases, mental health is a state of emotional, psychological, and social wellness evidenced by satisfying interpersonal relationships , effective behavior and coping, positive self-concept, and emotional stability.
- Factors influencing a person’s mental health can be categorized as individual, interpersonal, and social/cultural.
- Individual , or personal, factors include a person’s biologic make up, autonomy and independence, self-esteem , capacity for growth, vitality, ability to find meaning in life, emotional resilience or hardiness, sense of belonging, reality orientation, and coping or stress management abilities.
- Interpersonal , or relationship, factors include effective communication , ability to help others, intimacy, and a balance of separateness and connectedness.
- Social/cultural , or environmental, factors include a sense of community, access to adequate resources, intolerance of violence, support of diversity among people, mastery of the environment, and a positive, yet realistic, view of one’s world.
The American Psychiatric Association (APA, 2000) defines a mental disorder as “a clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and is associated with present distress or with a significantly increased risk of suffering death , pain , disability, or an important loss of freedom.
- General criteria to diagnose mental disorders include dissatisfaction with one’s characteristics, abilities, and accomplishments; ineffective or unsatisfying relationships; dissatisfaction with one’s place in the world; ineffective coping with life events; and lack of personal growth.
- Factors contributing to mental illness also can be viewed within individual, interpersonal, and social/cultural categories.
- Individual factors include biologic make up, intolerable or unrealistic worries or fears, inability to distinguish reality from fantasy, intolerance of life’s uncertainties, a sense of disharmony in life, and a loss of meaning in one’s life.
- Interpersonal factors include ineffective communication , excessive dependency on or withdrawal from relationships, no sense of belonging, inadequate social support, and loss of emotional control.
- Social/cultural factors include lack of resources, violence, homelessness, poverty, an unwarranted negative view of the world, and discrimination.
The Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM-IV-TR) is a taxonomy published by the APA.
- The DSM-IV-TR describes all mental disorders, outlining specific diagnostic criteria for each based on clinical experience and research.
- The DSM-IV-TR has three purposes:
- To provide a standardized nomenclature and language for all mental health professionals.
- To present defining characteristics or symptoms that differentiate specific diagnoses.
- To assist in identifying the underlying causes of disorders.
- The multiaxial classification system that involves assessment on several axes, or domains of information, allows the practitioner to identify all the factors that relate to a person’s condition.
- Axis I is for identifying all major psychiatric disorders except mental retardation and personality disorders .
- Axis II is for reporting mental retardation and personality disorders as well as prominent maladaptive personality features and defense mechanisms .
- Axis III is for reporting current medical conditions that are potentially relevant to understanding or managing the person’s mental disorder as well as medical conditions that might contribute to understanding the person.
- Axis IV for reporting psychosocial and environmental problems that may affect the diagnosis, treatment, and prognosis of mental disorders.
- Axis V presents a Global Assessment of Functioning, which rates the person’s overall psychological functioning on a scale of 0 to 100; this represents the clinician’s assessment of the person’s current level of functioning.
Historical Perspectives of the Treatment of Mental Illness
- People of ancient times believed that any sickness indicated displeasure of the gods and in fact was punishment for sins and wrongdoing.
- Those with mental disorders were viewed as either divine or demonic, depending on their behavior.
- Later, Aristotle attempted to relate mental disorders to physical disorders and developed his theory that the amounts of blood , water, and yellow and black bile in the body controlled the emotions.
- These four substances, or humors, corresponded with happiness, calmness, anger, and sadness; imbalances of the four humors were believed to cause mental disorders, so treatment was aimed at restoring balance through bloodletting, starving, and purging.
- In early Christian times, all diseases were again blamed on demons, and the mentally ill were viewed as possessed; priests perform exorcism to to rid evil spirits.
- During the Renaissance, people with mental illness were distinguished from criminals in England; those considered harmless were allowed to wander the countryside and or live in rural communities, but the more “dangerous lunatics” were thrown in prison, chained, and starved.
- In 1547, the Hospital of St. Mary of Bethlehem was officially declared a hospital for the insane, the first of its kind; by 1775, visitors at the institution were charged a fee for the privilege of viewing and ridiculing the intimates, who were seen as animals, less than human.
- In the 1790s, a period of enlightenment concerning persons with mental illness began.
- Phillipe Pinel in France and William Tukes in England formulated the concept of asylum as a safe refuge or haven offering protection at institutions where people had been whipped, beaten, or starved just because they were mentally ill (Gollaher, 1995).
- In the United States, Dorothea Dix (1802-1887) began a crusade to reform the treatment of mental illness after a visit to Tukes’ institution in England; she was instrumental in opening 32 state hospitals that offered asylum to the suffering.
- The period of scientific study and treatment of mental disorders began with Sigmund Freud (1856-1939) and others, such as Emil Kraeplin (1856-1926) and Eugene Bleuler (1857-1939).
- With these men, the study of psychiatry and the diagnosis and treatment of mental illness started in earnest.
- Freud challenged society to view human beings objectively; he studied the mind, its disorders, and their treatment as no one had before.
- Kraeplin began classifying mental disorders according to their symptoms, and Bleuler coined the term schizophrenia .
- A great leap in the treatment of mental illness began in about 1950 with the development of psychotropic drugs, or drugs used to treat mental illness.
- Chlorpromazine ( Thorazine ) an antipsychotic drug, and lithium, an antimanic agent, were the first drugs to be developed.
- Over the following 10 years, monoamine oxidase inhibitor antidepressants , haloperidol ( Haldol ), an antipsychotic; tricyclic antidepressants ; and antianxiety agents, called benzodiazepines , were introduced.
The National Institute of Mental Health (NIMH) estimates that more than 26% of Americans aged 18 years and older have a diagnosable mental disorder- approximately 57.7 million persons each year (2006).
- Furthermore, mental illness or serious emotional disturbances impair daily activities for an estimated 10 million adults and 4 million children and adolescents.
- Mental disorders are the leading cause of disability in the United States and Canada for persons 15 to 44 years of age.
- Homelessness is a major problem in the United States today; the National Resource and Training Center on Homelessness and Mental Illness (2006) estimates that one-third of adult homeless persons have a serious mental illness and that more than one half also have substance abuse problems.
- In 1993, the federal government created and funded Access to Community Care and Effective Services and Support (ACCESS) to begin to address the needs of people with mental illness who were homeless either all or part of the time.
- In 1873, Linda Richards graduated from the New England Hospital for Women and Children in Boston; she went on to improve nursing care in psychiatric hospitals and organized educational programs in state mental hospitals in Illinois.
- Richards is called the first American psychiatric nurse; she believed that “the mentally sick should be at least as well cared for as the physically sick” (Doona, 1984).
- The first training of nurses to work with persons with mental illness was in 1882 at McLean Hospital in Belmont, Massachusetts.
- The care was primarily custodial and focused on nutrition , hygiene , and activity.
- The role of psychiatric nurses expanded as somatic therapies for the treatment of mental disorders were developed.
- Treatments such as insulin shock therapy (1935), psychosurgery (1936), and electroconvulsive therapy (1937) required nurses to use their medical- surgical skills more extensively.
- The first psychiatric nursing textbook, Nursing Mental Diseases by Harriet Bailey was published in 1920; in 1913, John Hopkins was the first school of nursing to include a course in psychiatric nursing in its curriculum.
- In 1973, the division of psychiatric and mental health practice of the American Nurses Association (ANA) developed standards of care, which it revised in 1982, 1994, and 2000.
- Standards of care are authoritative statements by professional organizations that describe the responsibilities for which nurses are accountable.
- The goal of self-awareness is to know oneself so that ones’ values, attitudes, and beliefs are not projected to the client, interfering with nursing care; self-awareness does not mean having to change one’s values and beliefs unless one desires to do so.
1 thought on “Mental Health and Psychiatric Nursing”
Such a useful information in brief, really appreciate the efforts of writer Marianne
Leave a Comment Cancel reply
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Mental health case studies
Driving up quality in mental health care.
Mental health care across the NHS in England is changing to improve the experiences of the people who use them. In many areas, a transformation is already under way, offering people better and earlier access as well as more personalised care, whilst building partnerships which reach beyond the NHS to create integrated and innovative approaches to mental health care and support.
Find out more through our case studies and films about how mental health care across the NHS is changing and developing to better meet people’s needs.
- Children and young people (CYP)
- Community mental health
- Crisis mental health
- Early intervention in psychosis (EIP)
- Improving access to psychological therapies (IAPT)
- Perinatal mental health
- Severe mental illness (SMI)
- Staff mental health and wellbeing
- Other mental health case studies
- Archived mental health case studies
- NICE Guidance
- Conditions and diseases
- Mental health, behavioural and neurodevelopmental conditions
Common mental health problems: identification and pathways to care
Clinical guideline [CG123] Published: 25 May 2011
This guideline has been stood down. All of the recommendations are now covered in other NICE guidelines, or are out of date and no longer relevant to clinical practice.
For guidance on common mental health problems, see our guidelines on:
- Depression in adults
- Depression in adults with a chronic physical health problem
- Depression in children and young people
- Generalised anxiety disorder and panic disorder in adults
- Obsessive-compulsive disorder and body dysmorphic disorder
- Social anxiety disorder
Mental Health Nursing
At a glance, grahame smith.
- Your Feedback
- Become a reviewer
- More student books
- Student Apps
- Join an e-mail list

Buy now/find out more
Case Studies
Case 3: john.
John, a 26-year-old man, presented at the local A & E department and has now been referred to the mental health liaison team after drinking a large amount of alcohol and taking 100 paracetamol tablets. He woke up the next morning surprised that he was alive but also concerned about his actions. On this basis he asked his next-door neighbour to take him to hospital.
Over the last year John has been experiencing symptoms of anxiety; John describes himself as a constant worrier but recently he has felt "more panicky", to the point that he finds it more and more difficult to engage in everyday activities such as talking to other people. The impact of these distressing symptoms is that John has now been off sick from work for the last three months.
John indicates that he now has significant difficulty in controlling his "worrying", he constantly feels restless and irritable, is physically tense, has difficulty concentrating on everyday tasks, and has difficulty sleeping. John also mentions that to help him sleep he has been drinking four to five cans of strong lager every night.
(a) How would the mental health nurse build a therapeutic relationship with John?
Show Answer
- selecting the right words to use;
- knowing when to talk and when to be silent;
- using the right verbal and non-verbal responses;
- adapting non-verbal communication to suit the situation.
- an active listener;
- genuinely interested;
- accepting the person;
- caring and compassionate.
(b) How should the nurse mange the risk element when building a therapeutic relationship with John?
- considering John's perspective;
- balancing the "rules" against this perspective;
- preserving the person-centred element of this perspective;
- fully representing this perspective in the decision-making process.
(c) How would the nurse formally describe John's drinking?
Correct answer: Alcohol use is usually described in terms of safe limits: 21 units of alcohol per week for men and 14 units for women (a unit of alcohol is approximately a small glass of wine or half a pint of beer). In John's case his alcohol use can be described as harmful drinking, which in men is consuming over 50 units weekly.
(d) What negative impact could John's alcohol intake have upon his health?
- disturbances of consciousness and perception;
- damage to John's health and social functioning;
- physical and psychological withdrawal;
- hallucinations and delusions;
- memory and cognitive impairments.
(e) What other symptoms of anxiety might John be experiencing?
- increased vigilance;
- hyperactivity;
- palpitations;
- abdominal discomfort and nausea;
- hot flushes;
- outbursts of anger;
- ruminating thoughts and compulsions.
(f) What types of psychological interventions would the nurse consider delivering, bearing in mind John's alcohol consumption?
- build a collaborative and therapeutic relationship;
- motivational and brief intervention work;
- guided self-help ;
- breathing and relaxation exercises;
- identifying, challenging and replacing negative thoughts;
- harm reduction;
- coping strategy work;
- health promotion;
- contingency approaches – using incentives to change behaviour.
John is progressing well; he feels that he has recovered and has now returned to work; subsequently John has been discharged from the community mental health nurse's case load.
(a) What potential conflict could there possibly be between John's and the nurse's understanding of recovery, and what would be the best way forward?
- promoting wellbeing;
- maximising opportunity;
- empowering individuals to take control;
- facilitating and supporting the individual in finding meaning and purpose.
(b) John returning to work can be viewed as a factor that positively influences the recovery process. What other factors are there?
- positive and sustainable relationships;
- meaningful activity;
- resilience;
- personal growth;
- a healthy living environment;
- a supportive social network.
(c) How should the nurse use their experiences of working with John in their journey towards being a clinical expert?
Correct answer: Key to being an expert is the use of reflection; this process enables the nurse to develop their self-awareness to a level where they are able to clearly identify their strengths and also the areas that they need to develop further. It is important to recognise that knowledge accrued through the reflective process is useful knowledge especially as it is experience-based knowledge. Like scientific knowledge this form of knowledge should not be used in isolation; rather it should be used to complement scientific knowledge in a way that anchors both forms of knowledge to the nurse's ongoing practice experiences.
Consider Chapters 27 and 38.
Print Answers | « Previous Case | Next Case »
- Children's mental health case studies
- Food, health and nutrition
- Mental wellbeing
- Mental health
Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and feedback for the user. Use these cases on your own or in classes and training events
Each case study:
- Explores the experiences of a child and family over time.
- Introduces theories, research and practice ideas about children's mental health.
- Shows the needs of a child at specific stages of development.
- Invites users to “try on the hat” of different specific professionals.
By completing a case study participants will:
- Examine the needs of children from an interdisciplinary perspective.
- Recognize the importance of prevention/early intervention in children’s mental health.
- Apply ecological and developmental perspectives to children’s mental health.
- Predict probable outcomes for children based on services they receive.
Case studies prompt users to practice making decisions that are:
- Research-based.
- Practice-based.
- Best to meet a child and family's needs in that moment.
Children’s mental health service delivery systems often face significant challenges.
- Services can be disconnected and hard to access.
- Stigma can prevent people from seeking help.
- Parents, teachers and other direct providers can become overwhelmed with piecing together a system of care that meets the needs of an individual child.
- Professionals can be unaware of the theories and perspectives under which others serving the same family work
- Professionals may face challenges doing interdisciplinary work.
- Limited funding promotes competition between organizations trying to serve families.
These case studies help explore life-like mental health situations and decision-making. Case studies introduce characters with history, relationships and real-life problems. They offer users the opportunity to:
- Examine all these details, as well as pertinent research.
- Make informed decisions about intervention based on the available information.
The case study also allows users to see how preventive decisions can change outcomes later on. At every step, the case content and learning format encourages users to review the research to inform their decisions.
Each case study emphasizes the need to consider a growing child within ecological, developmental, and interdisciplinary frameworks.
- Ecological approaches consider all the levels of influence on a child.
- Developmental approaches recognize that children are constantly growing and developing. They may learn some things before other things.
- Interdisciplinary perspectives recognize that the needs of children will not be met within the perspectives and theories of a single discipline.
There are currently two different case students available. Each case study reflects a set of themes that the child and family experience.
The About Steven case study addresses:
- Adolescent depression.
- School mental health.
- Rural mental health services.
- Social/emotional development.
The Brianna and Tanya case study reflects themes of:
- Infant and early childhood mental health.
- Educational disparities.
- Trauma and toxic stress.
- Financial insecurity.
- Intergenerational issues.
The case studies are designed with many audiences in mind:
Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others.
Professionals in training, including those attending graduate or undergraduate classes.
The broader community.
Each case is based on the research, theories, practices and perspectives of people in all these areas. The case studies emphasize the importance of considering an interdisciplinary framework. Children’s needs cannot be met within the perspective of a single discipline.
The complex problems children face need solutions that integrate many and diverse ways of knowing. The case studies also help everyone better understand the mental health needs of children. We all have a role to play.
These case has been piloted within:
Graduate and undergraduate courses.
Discipline-specific and interdisciplinary settings.
Professional organizations.
Currently, the case studies are being offered to instructors and their staff and students in graduate and undergraduate level courses. They are designed to supplement existing course curricula.
Instructors have used the case study effectively by:
- Assigning the entire case at one time as homework. This is followed by in-class discussion or a reflective writing assignment relevant to a course.
- Assigning sections of the case throughout the course. Instructors then require students to prepare for in-class discussion pertinent to that section.
- Creating writing, research or presentation assignments based on specific sections of course content.
- Focusing on a specific theme present in the case that is pertinent to the course. Instructors use this as a launching point for deeper study.
- Constructing other in-class creative experiences with the case.
- Collaborating with other instructors to hold interdisciplinary discussions about the case.
To get started with a particular case, visit the related web page and follow the instructions to register. Once you register as an instructor, you will receive information for your co-instructors, teaching assistants and students. Get more information on the following web pages.
- Brianna and Tanya: A case study about infant and early childhood mental health
- About Steven: A children’s mental health case study about depression
Cari Michaels, Extension educator
Reviewed in 2023
© 2024 Regents of the University of Minnesota. All rights reserved. The University of Minnesota is an equal opportunity educator and employer.
- Report Web Disability-Related Issue |
- Privacy Statement |
- Staff intranet
Mental health associated with the cluster of childhood trauma and resilience among nursing students: A cross-sectional study
Affiliation.
- 1 School of Nursing, Wenzhou Medical University.
- PMID: 37227834
- DOI: 10.1037/tra0001527
Objective: This study aimed to propose clusters of the association between childhood trauma and resilience in nursing students and to examine their mental health according to these clusters.
Method: A cross-sectional study was carried out between September 2018 and May 2019. A total of 1,245 undergraduate nursing students (104 male, 1,141 female) were enrolled in a medical university in East China to complete the Childhood Trauma Questionnaire, Connor-Davidson Resilience Scale, Self-Rating Anxiety Scale, and Self-Rating Depression Scale.
Results: The cluster analysis identified three clusters as follows: the self-healing group (40.7%), the mildly traumatized with low resiliency group (22.2%), and the healthy group (37.1%). The logistic regression analysis revealed that the levels of anxiety and depression significantly differed between the three clusters, with the mildly traumatized with low resiliency group having the highest odds to have anxiety and depression.
Conclusion: This study identified three clusters of the association between childhood trauma and resilience in undergraduate nursing students and indicated that each cluster was associated with a different level of anxiety and depression. The unique characteristics of the three clusters may help identify and develop appropriate interventions to promote the mental health of undergraduate nursing students. (PsycInfo Database Record (c) 2024 APA, all rights reserved).
- Adverse Childhood Experiences*
- Cross-Sectional Studies
- Education, Nursing, Baccalaureate*
- Mental Health
- Psychological Tests*
- Resilience, Psychological*
- Self Report*
- Students, Nursing* / psychology
Supplementary concepts
- Connor-Davidson Resilience Scale
- Childhood Trauma Questionnaire
Grants and funding
- Ministry of Education
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Med (Lausanne)
- PMC10390251
Burnout syndrome and work engagement in nursing staff: a systematic review and meta-analysis
Miguel Ángel vargas-benítez.
1 San Cecilio Clinical University Hospital, Granada, Spain
Francisco José Izquierdo-Espín
2 Critical Care Unit, General University Hospital of Jaén, Jaén, Spain
Nuria Castro-Martínez
3 Internal Medicine Service, General University Hospital of Jaen, Jaén, Spain
José L. Gómez-Urquiza
4 School of Health Sciences, University of Granada, Cortadura del Valle s/n, Ceuta, Spain
Luis Albendín-García
5 Casería de Montijo Health Centre, Granada-Metropolitan Health District, Granada, Spain
6 Instituto de Investigación Biosanitaria (ibs.GRANADA), Granada, Spain
Almudena Velando-Soriano
Guillermo a. cañadas-de la fuente.
7 School of Health Sciences, University of Granada, Granada, Spain
8 Brain, Mind and Behaviour Research Centre (CIMCYC), University of Granada, Granada, Spain
Associated Data
The original contributions presented in the study are included in the article/ Supplementary material , further inquiries can be directed to the corresponding author.
A difficult and demanding work environment, such as that often experienced in healthcare, can provoke fatigue, anxiety, distress, and discomfort. This study considers factors that may influence levels of burnout and work engagement among nurses and seeks to determine the relationship between these conditions.
A systematic scoping review was performed, in accordance with the PRISMA Extension for Scoping Reviews, based on data obtained from a search of the PubMed/MEDLINE and Scopus databases carried out in 2022 using the search equation: “work engagement AND nurs * AND burnout.” This search identified nine quantitative primary studies suitable for inclusion in our analysis.
Work overload, type of shift worked, and/or area of hospital service, among other elements, are all relevant to the development of burnout. This syndrome can be countered by social support and appropriate personal resources and values, which are all positively associated with work engagement. Our analysis revealed a significant correlation between work engagement and the different domains of burnout. The correlation effect size between burnout and work engagement was −0.46 (95% CI −0.58, −0.31), with p < 0.001.
Well-targeted interventions in the healthcare work environment can reduce burnout levels, strengthen work engagement, and enhance the quality of healthcare.
1. Introduction
In nursing, highly complex tasks must be performed and decisions are taken in situations that are often difficult and stressful. Moreover, appropriate attention must be provided not only to patients but also to visiting family members. The working environment can include long days, rotating shifts, a severe emotional burden, and sometimes aggression expressed by patients, their families, or even colleagues ( 1 ). If this circumstance persists for an extended period of time, it can provoke fatigue, anxiety, distress, and discomfort, any or all of which may reduce the quality of care provided and heighten the probability of error. In such a case, there may be an evident imbalance between the human resources available and the demands placed on them ( 2 ).
The tasks performed by nurses are determined, on the one hand, by the day-to-day healthcare demands encountered, and on the other hand, by the resources available—personal, situational, and organizational. This balance is reflected in the job demands–resources model (JD-R) ( 3 ). Occupational demands may be physiological and/or psychological, and each type imposes a cost on the individual. In many situations, workers are subjected to stress and heavy workloads, although these may be counteracted by the application of situational resources ( 4 ), such as companionship, autonomy, opportunities to learn, institutional recognition, and the possibility of promotion, as well as personal resources such as resilience, self-efficacy, and optimism ( 5 ). Both types of resources help the professional adapt to the work environment, fostering the ability to cope ( 6 ), generating motivation and work engagement (WE), and thus reducing the probability of burnout ( 7 , 8 ).
Burnout is a consequence of long-term harmful stress in the workplace. If the individual lacks resources to deal with this situation, the response made may be maladaptive and prolonged ( 9 ). Maslach and Leiter defined three domains of burnout syndrome: emotional exhaustion, depersonalization, and low personal accomplishment ( 10 ). It may be counteracted, however, by high levels of WE, that is, a state of satisfaction, commitment, and motivation. This, too, consists of three domains: vigor (effort, self-generated energy, and resolve), dedication (exaltation, empowerment, and active assistance), and absorption (immersion and high levels of concentration in the activity being performed) ( 11 ).
Traditionally, the concepts of burnout and WE have been considered opposing and independent. Paradoxically, however, some studies have observed the simultaneous presence of burnout ( 12 ) and WE ( 13 – 15 ), which suggests that these concepts, while independent, have a certain negative correlation ( 3 , 16 ). Nevertheless, demanding occupational conditions are associated with burnout, while the availability of appropriate resources contributes to WE ( 16 ), although the beneficial impact of these resources varies according to the population considered and the environment in question.
As members of the multidisciplinary team in critical and emergency care services, nurses play a vital role in improving the quality of care and in reducing morbidity, mortality, and their associated health costs ( 17 ). Moreover, incorporating nurses into the multidisciplinary oncology team benefits the team's overall performance and can shorten the duration of treatment ( 18 ). Therefore, a good understanding of the working conditions experienced by nurses and other health workers will facilitate an organizational approach to help prevent burnout and foster WE, thus enhancing the care provided ( 19 ).
In summary, the aim of this study is to identify and analyse the factors that affect WE and burnout in nurses and then to determine the relationship between these reactions to the occupational environment.
2.1. Search strategy
A systematic scoping review was performed, in accordance with the PRISMA Extension for Scoping Reviews ( 20 ), based on data obtained from a search of the PubMed/MEDLINE and Scopus databases carried out in September 2022 using the Medical Subject Headings (MeSH search equation: “work engagement AND nurs * AND burnout”).
2.2. Inclusion and exclusion criteria
The following inclusion criteria were applied:
- - Primary full-text sources in English or Spanish.
- - Quantitative articles with sample populations of nurses.
- - Articles that measure the correlation between WE and burnout, or establish their predictive characteristics.
- - Studies published between 2016 and 2022.
The exclusion criteria were as follows:
- - Doctoral thesis.
- - Articles with mixed samples without independent data on the nursing staff.
- - Articles whose main objective is not correlated with the subject of study.
The selection of articles for analysis was carried out in three steps: First, the titles and abstracts were read, followed by a full-text reading of those remaining for analysis. Finally, a critical reading was conducted of each text finally selected, in order to assess the method applied and to detect any publication bias.
2.3. Level of evidence
The quality of the studies included in this review was assessed in accordance with the levels of evidence and degrees of recommendation stipulated by the Oxford Centre for Evidence-Based Medicine (OCEBM) ( 21 ).
2.4. Variables, data collection, and data analysis
The following data, obtained from each study/article, are summarized in Table 1 : (1) author, year of publication, country of the study; (2) design; (3) sample; (4) results; (5) level of evidence (OCEBM); and (6) grade of recommendation ( Table 1 ). A correlation effect size meta-analysis was calculated using StatsDirect software. Random effects were used for the calculation, and heterogeneity was assessed by i 2 . The Egger test was used to test for publication bias, and a sensitivity analysis was performed to check that none of the studies significantly affected the effect size.
General information on the studies considered.
DASS21, Depression Anxiety Stress Scale-21; GR, Grade of Recommendation; JDRQ, Job demands–resources Questionnaire; LE, level of evidence; MBI, Maslach Burnout Inventory; MBI-HSS, Maslach Burnout Inventory—Human Services Survey; PINS, Professional Identity in Nursing Survey; QEEW, Questionnaire on the Experience and Evaluation of Work; QNWLS, Quality of Nursing Work Life Scale; SIMPH, Short Inventory to Monitor Psychosocial Hazards; UWES, Utrecht Work Engagement Scale; WE, Work engagement.
The literature search obtained 404 articles. After excluding duplicates and applying the inclusion and exclusion criteria, 65 remained for full-text reading. This led to a further 58 being excluded, leaving seven for the final analysis review. In addition, a reverse search performed on these articles led to another two being included. Thus, nine studies were finally reviewed ( Figure 1 ).

PRISMA flowchart of the study selection process. Adapted from Page et al. ( 31 ), licensed CC-BY-4.0.
3.1. Burnout risk factors
Among the burnout risk factors for nurses, a positive correlation was observed between emotional exhaustion (a dimension of burnout) and workload. This dimension was also aggravated by emotional demands on the nurses. The longer the nurses had been employed in the service, and the more prolonged or unstable their working hours (for example, in the form of rotating shifts), the more likely they were to suffer burnout ( 25 ). Nurses who work in critical care units are more liable to suffer burnout than those working in other departments. Other factors that are positively associated with the presence of burnout syndrome include lengthy work schedules, anxiety, depression, stress, and problems with interpersonal relationships ( 26 ). Finally, a strong correlation between burnout and workload has been reported, with the latter being a significant predictor of the syndrome ( 26 , 32 ).
3.2. Protective factors of work engagement
According to the studies analyzed, good organizational values and practices, together with support from co-workers and leaders, are positively correlated with the WE of healthcare professionals. Vigor and dedication, which both contribute to WE, are positively associated with the presence of clearly stated corporate objectives, rules, and procedures ( 28 ). Other factors that favor WE include control over one's work, decision-making powers and abilities, the development of professional skills, the perception of social support, and the existence of learning opportunities—in short, satisfactory job quality ( 25 – 27 , 32 ).
Nurses working in surgical areas tend to present greater WE than those in emergency or medical care units. Moreover, hospital nurses often have lower levels of WE than those who work in health clinics ( 28 ). The specific characteristics of the job and the work environment, and even the age of the individual may also influence the development or otherwise of WE ( 30 ).
3.3. Correlation between work engagement and the dimensions of burnout
The dimensions of burnout considered were emotional exhaustion, depersonalization, and low personal accomplishment, while those of WE were vigor, dedication, and absorption.
Low levels of vigor are associated with a high risk of developing burnout due to emotional exhaustion (a perfect linear correlation has been reported in this respect). Burnout may also arise from low personal fulfillment, even if high levels of vigor are reported. Among the professionals who present low or very low dedication, there is a very high probability (90–100%) of burnout due to emotional exhaustion ( 23 ).
In addition, vigor is a significant negative predictor of emotional exhaustion, while absorption is a significant positive predictor of this condition. On the other hand, it is not significantly predicted by dedication. With respect to depersonalization, another dimension of burnout, none of the WE domains were significant mediators or direct predictors. Finally, dedication is a positive direct predictor of personal fulfillment, but neither vigor nor absorption is a significant predictor in any sense ( 22 , 23 ).
According to several studies, WE is most frequently (around 50% of cases) classified as moderate, in terms of the three domains considered (vigor, dedication, and absorption). The correlation between WE and burnout is reported to be negative and highly significant ( 22 , 23 , 27 , 29 ).
3.4. Meta-analysis of the correlation between burnout and work engagement
Five studies were included in the meta-analysis, with a total sample size of 1,506 nurses. The correlation effect size between burnout and WE was −0.46 (95%CI −0.58, −0.31) with p < 0.001 and the heterogeneity (i 2 ) was 89%. The Egger test did not reveal any publication bias, and the sensitivity analysis did not suggest any publication that had to be excluded ( Figure 2 ).

Forestplot of the correlation between burnout and work engagement.
4. Discussion
This study aims to enhance our understanding of how personal characteristics and workplace-related factors may influence WE and trigger the presence of burnout among nurses. Given this information, appropriate measures can be adopted to reduce the risk of burnout and to foster greater participation and commitment by these workers.
Our analysis shows that nurses' WE is favored by environments in which they have autonomy of decision-making, where they are given sufficient resources to carry out their work, and where there is greater altruism among workers ( 33 ). In other words, WE benefits from a strengthening of the nursing identity, which generates pride in job performance and enhances the working experience ( 34 ). In turn, higher levels of support among nurses will decrease the burnout experienced ( 33 , 35 ). The hospital area in which a nurse work is also relevant to WE and job satisfaction, which are both affected by the emotional impact or workload experienced in different areas of health care ( 36 ). According to previous research, when WE is high, nurses are less likely to request a transfer to a different work unit or service. Moreover, favorable occupational health conditions are expected to improve relationships and collaboration among workers, which enhances the care provided, and thus generates a positive gains spiral ( 24 ).
Among the factors found to increase the risk of burnout is the hospital area in which the nurses work. Those employed in an Accident and Emergency (A&E) department are more likely to generate a psychologically distant relationship with patients, as a consequence of the high level of burnout experienced ( 16 ). This, in turn, can cause patients to have negative perceptions of the quality, effectiveness, and efficiency of the healthcare received ( 37 , 38 ). Another relevant factor is the type of work shift performed; thus, nurses who work night shifts have been shown to present higher levels of burnout. In short, professionals who undergo high levels of stress and fatigue are more liable to present detachment and dysfunctional attitudes ( 39 ). Burnout can also be caused by lengthy employment in the same medical unit/service. In response, and seeking to alleviate this condition, long-standing workers might request to be transferred elsewhere ( 40 ). In addition to the above, many other elements can influence the appearance of burnout syndrome among nurses, such as the female stereotype of the profession, the lack of recognition of the ‘invisible' tasks performed, and an excessive level of bureaucracy, as pointed out by Manzano Garcia et al. in their qualitative e-Delphi study ( 41 ). These questions have received little previous research attention.
Finally, consideration should be given to the COVID-19 pandemic, which has had a negative impact on the mental health of critical care nurses and their families, as public safety considerations have been prioritized over those of patient care. This situation has generated great unhappiness among the nurses affected, despite the support received from friends and colleagues ( 42 , 43 ).
After considering the factors relevant to burnout and WE, we then determined the relationship between them, taking into account the three dimensions of each. Our analysis confirms previous findings that there is indeed a close relationship between the two concepts, and specifically that greater WE (as concerns each of its constituent elements) reduces the risk of burnout ( 40 , 44 ).
A lack of vigor is associated with higher levels of emotional exhaustion. This is in line with the Utrecht Work Engagement Scale, according to which there is a strong interaction between these two dimensions ( 45 ). Therefore, the goal of recognizing WE among nurses and establishing strategies to promote it may be limited by the presence of emotional exhaustion ( 46 ). Conversely, dedication is inversely related to the presence and impact of burnout. Some of the studies in our analysis concluded that professionals who were unable to perform the work expected of them, or who were unable to meet the needs raised, whether by the patient or by the organization, due to decreased levels of dedication and perceptions of insufficiency, were at a high risk of developing burnout ( 47 ). In this respect, too, some authors indicate that a feeling of low personal fulfillment may arise from the view that the tasks performed are not considered important or productive. This impression would tend to reduce dedication and hence WE ( 48 ). Finally, high levels of absorption might provoke burnout, if this absorption prevents the worker from achieving an objective emotional balance ( 37 , 40 ).
Our study is subject to certain limitations, which should be acknowledged. First, by restricting the articles considered to those published in English or Spanish, we may have omitted potentially significant research findings from studies published in other languages which otherwise met the inclusion requirements. Furthermore, the studies included did not all use the same measurement instruments, so the results presented may not be homogeneous. Finally, the relationship between burnout and WE has only recently been the object of academic study, and so relatively few articles are available for consideration.
5. Conclusion
The correlation between low WE and burnout in nurses not only impacts these professionals but also has damaging consequences for patients and the health system in general.
The studies considered in our review describe varying degrees of burnout and WE. The relevant factors identified include employment conditions (such as work overload and type of shift or service area), personal characteristics (such as perceived support and the individual's own values), and organizational resources. All of these factors influence WE and hence the possibility of burnout.
The results obtained from our analysis highlight the need to design and implement effective interventions in the workplace in order to address the problematic areas identified and thus reduce the risk or degree of burnout among nursing personnel. This, in turn, would enhance levels of WE. Failure to do so might be damaging not just for the workers concerned but also for the quality and safety of public healthcare.
As a final observation, further studies in this area are needed in order to better understand the phenomenon of burnout among nursing staff.
Data availability statement
Author contributions.
MAV-B, FJI-E, and GAC-F: conceptualization. FJI-E, AV-S, and LA-G: data curation. NC-M, JLG-U, and AV-S: formal analysis. MAV-B, JLG-U, and AV-S: investigation. AV-S, JLG-U, and GAC-F: methodology. MAV-B and AV-S: resources. JLG-U: software. LA-G and GAC-F: supervision. JLG-U, NC-M, and GAC-F: visualization and validation. MAV-B, NC-M, and FJI-E: writing—original draft, review, and editing. GAC-F: funding acquisition and project administration. All authors contributed to the article and approved the submitted version.
Acknowledgments
This study forms part of the Doctoral Thesis of the FJI-E, working within the Clinical Medicine and Public Health Doctoral Programme of the University of Granada (Spain).
Funding Statement
This article has been funded by the FEDER/Consejería de Universidad, Investigación e Innovación de la Junta de Andalucía, Project P20-00627.
Abbreviations
WE, Work engagement; A&E, Accident and Emergency department.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2023.1125133/full#supplementary-material

IMAGES
VIDEO
COMMENTS
This case study aims to describe the implementation of the decision-making process in mental health nursing given the care needs identified in a person with Alzheimer's disease at home. The cognitive assessment, supported by the cognitive decision algorithm, revealed that the patient presented moderate dementia, with visuospatial disorganization, memory changes, orientation, evocation, and ...
A stigma around mental health issues within healthcare and nursing itself has created a culture of perfectionism in the workplace, and nurses struggle to live up to the expectations while pushing aside their feelings, thoughts, and needs. Inspired by one author's personal experiences, this article explores mental health issues many nurses confront today.
Therapeutic alliance is a core part of the nursing role and key to the attainment of positive outcomes for people utilising mental health care services. However, these relationships are sometimes difficult to develop and sustain, and nursing staff would arguably benefit from evidence-based support to foster more positive relationships.
To evaluate the effectiveness of a mental health screening form for early identification and care escalation of mental health issues in general settings. A secondary aim was to explore general nurses' use of the form and their confidence to discuss mental health issues with patients.
Mental health nursing is acknowledged internationally as being a demanding profession; however, little is known about the range of experience and complexity of workplace challenges or their impacts on mental health nurses (MHN). This qualitative descriptive study aimed to examine and describe the range of challenging workplace situations experienced by MHN and is reported according to the ...
The investigator interviewed the nurse and the patient after the conversation, and these interviews were transcribed as well. The encounter that is presented here as a case study is a concrete example of a counseling session during which the patient is free to discuss with the nurse.
These findings provided an enhanced understanding of mental health complexities among nurses, and shed light on policy enactment to alleviate the negative impact of mental health problems on nurses. Addressing mental health among nurses should be a top priority.
This study has provided knowledge of the importance and role of the nurses' attitude in the context of the nurse-patient therapeutic relationship based on the reflections of nurses in mental health units regarding their own practice.
The Journal of Psychiatric and Mental Health Nursing is a bi-monthly international mental health journal that publishes research and scholarly papers relevant to psychiatric nursing or mental health nursing and people with lived experiences of mental health problems.
The case study is an effective teaching strategy that is used to facilitate learning, improve critical thinking, and enhance decision-making Sprang, (2010). Below are nine case studies that educators may employ when working with students on mental illness and addiction. The case studies provided cover major concepts contained in the RNAO Nurse Educator Mental Health and Addiction Resource.
This study provides information based on mental health nurses' experiences. It explains the home environment, the therapeutic relationship and the process of mental health nursing care during a crisis.
Examples of recommended interventions in the treatment of depression across the lifespan, including interpersonal psychotherapy for adults, behavioral therapy and cognitive therapy.
The case studies are contained in 4 categories: Family (13 case studies), Fundamentals and Mental Health (14 case studies) and Medical Surgical (20 case studies). In addition the folder labeled minireviews contains PowerPoint sessions with combinations of case studies and standalone items.
Chapter 1: Psychiatric-mental Health Nursing and Evidence-based Practice, Case Studies
A cross-national comparative mixed-methods study involving 19 mental health wards in six service provider sites in England and Wales. This included a survey using established standardised measures of service users ( n = 301) and staff ( n = 290) and embedded case studies involving interviews with staff, service users and carers ( n = 76). Quantitative and qualitative data were analysed within ...
The purpose of this descriptive-exploratory study was to identify profiles of mental health among undergraduate nursing students to understand the relationship between student's mental health profiles and relevant risk and protective factors at the onset of COVID-19. Latent Class Analysis (LCA) was employed to cull these students' mental health profiles (yielding 3 profiles) using data ...
In most cases, mental health is a state of emotional, psychological, and social wellness evidenced by satisfying interpersonal relationships, effective behavior and coping, positive self-concept, and emotional stability. Factors influencing a person's mental health can be categorized as individual, interpersonal, and social/cultural.
Case 5: Denise. Denise, a 19-year-old woman, has been admitted informally to an acute mental health ward; this is Denise's first admission. Denise was being treated for depression by her GP; prior to her admission Denise attempted to kill herself by cutting her wrists. Subsequently a short admission was arranged with the aim of devising a ...
This descriptive and exploratory study with a qualitative design aimed to describe and analyze discussions in online chats about mental disorders in a psychiatric nursing course as part of an ...
Find out more through our case studies and films about how mental health care across the NHS is changing and developing to better meet people's needs.
For guidance on common mental health problems, see our guidelines on: Depression in adults. Depression in adults with a chronic physical health problem. Depression in children and young people. Generalised anxiety disorder and panic disorder in adults. Obsessive-compulsive disorder and body dysmorphic disorder. Social anxiety disorder.
Case 3: John. John, a 26-year-old man, presented at the local A & E department and has now been referred to the mental health liaison team after drinking a large amount of alcohol and taking 100 paracetamol tablets. He woke up the next morning surprised that he was alive but also concerned about his actions.
Mental health. Children's mental health case studies. Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and ...
This study identified three clusters of the association between childhood trauma and resilience in undergraduate nursing students and indicated that each cluster was associated with a different level of anxiety and depression.
A difficult and demanding work environment, such as that often experienced in healthcare, can provoke fatigue, anxiety, distress, and discomfort. This study considers factors that may influence levels of burnout and work engagement among nurses and seeks ...
Search for DHS Pages and Documents Department of Human Services