Case Report: Not Just Another Kidney Stone
- Reset your password
A 36-year-old woman with a history of nephrolithiasis presented to the ED for evaluation of increasing left flank pain and lightheadedness.
A 36-year-old woman with a 2-week history of left flank pain presented to the ED via emergency medical services. The patient, who had a history of nephrolithiasis, assumed her pain was due to another kidney stone. She stated that while waiting for the presumed stone to pass, the pain in her left flank worsened and she felt lightheaded and weak.
The patient’s vital signs at presentation were: heart rate, 96 beats/minute; blood pressure, 133/76 mm Hg; respiratory rate, 20 breaths/minute; and temperature, 98.9˚F. Oxygen saturation was 98% on room air. On physical examination, the patient had left lower quadrant pain and left costovertebral angle tenderness. Laboratory studies were remarkable for a negative urine pregnancy test, a hemoglobin level of 6.8 g/dL, and a hematocrit of 21.1%. Based on the patient’s history and symptoms, axial and coronal computed tomography (CT) scans were ordered, revealing a ruptured left renal calyx with hemorrhage from ureterolithiasis ( Figures 1a and 1b ).

Rupture of renal calyx and extravasation of blood or urine is a potential complication of nephrolithiasis. Stone size, degree of obstruction, and length of symptomatic presentation presumably contribute to complications from nephrolithiasis. Stones that are symptomatic for more than 4 weeks are estimated to have an increased complication rate of up to 20%. 1
Calyx or fornix rupture results from increased intraluminal pressure. Rupture of these structures is thought to be a type of “safety-valve” function to relieve obstructive uropathy. 2
Obstructions from small leaks to large urinomas can cause extravasation of urine. In most cases, urinary extravasation is confined to the subcapsular space or perirenal space within the Gerota’s fascia; 3 however, as seen in this patient, mixed hematoma/urinomas can form.
In cases of nontraumatic calyx rupture, the cause of the obstruction is most often a distal obstructing ureteral stone. 4 Other causes of rupture include extrinsic compression from malignant and benign masses, ureteric junction obstructions, or iatrogenic causes. 4 Interestingly, in one small study, the median size of the obstructing stone was only 4 mm. The same study also noted that proximal ureteral obstruction occurred when larger stones where present. 4
Conservative Versus Nonconservative Management
Potential complications of urinomas include abscess formation, sepsis, hydronephrosis, and paralytic ileus. 3 Despite possible adverse sequelae, uncomplicated urinomas may be managed conservatively with supportive care. According to a study by Chapman et al, 5 about 40% of patients managed conservatively recover without complications. In addition, in a retrospective study by Doehn et al 6 involving 160 cases of fornix rupture treated with endoscopic therapy or nephrostomy tube supplemented with antibiotics, no instances of perinephric abscess or other complications requiring a second procedure were noted.
Management of suspected ureterolithiasis in the ED is focused on analgesia and supportive care. Acute analgesia is often provided parenterally with opioids alone or with an opioid/nonsteroidal anti-inflammatory drug (NSAID) combination. 7 Frequent reassessment of the patient is required to ensure adequate pain control and to prevent sedation. Other symptoms, such as nausea, vomiting, and dehydration, may be treated with intravenous (IV) fluids and antiemetic medications. Further radiographic evaluation is needed once analgesia is achieved. 7,8
Imaging Studies
Radiological evaluation of patients with suspected ureterolithiasis may involve several imaging modalities. Noncontrast helical CT scan is the standard for rapid and efficient identification of ureteral stones while allowing visualization of other potential pathology (eg, urinoma). 7-9 Other modalities, such as ultrasonography; radiography of the kidneys, ureters, and bladder; and an IV pyelogram with contrasted CT, may be ordered if noncontrast helical CT scan is not available on-site or if there are comorbidities. In addition to imaging studies, basic laboratory studies (eg, serum creatinine and blood urea nitrogen testing) are indicated to assess overall renal function and direct the choice of radiological study. 7
Disposition
Clinical decision-making is key when recommending inpatient versus outpatient treatment in patients with ureterolithiasis. Patients with uncontrolled pain or vomiting may require inpatient admission for supportive care, while those demonstrating acute renal failure, pyuria with bacteriuria, complete bilateral ureteral obstruction, urinoma, or signs of sepsis demand emergent urology consultation. Specifically, patients with urinoma require ureteroscopy versus nephrostomy 6,10 to allow drainage while carefully monitoring for development of subsequent bleeding and infection.
When discharging patients from the ED, expulsive therapy using tamsulosin 9 and analgesia with combination of oral opioids and NSAIDs are most commonly effective. 11 Outpatient urology referrals are recommended for ureteral stones greater than 5 mm in size or if the stones have been present in the ureter for greater than 4 weeks. 1 Proper evaluation and management of ureterolithiasis in the ED is crucial for positive outcomes and to reduce long-term complications.
Case Conclusion
Computed tomography revealed a ruptured renal calyx on the left side with free fluid in the abdomen. Urology services were consulted and the patient was taken to the operating room for cystoscopy, ureteral stent placement, and laser lithotripsy. Following surgery, she subsequently developed urosepsis for which she was successfully treated with IV antibiotics and discharged on hospital day 15.
Mr Eisenstat is a fourth-year medical student at the University of South Carolina School of Medicine, Greenville. Dr Fabiano is an emergency physician, department of emergency medicine, Greenville Health Systems, Greenville, South Carolina. Dr Collins is family medicine physician, department of emergency medicine, Greenville Health Systems, Greenville, South Carolina.
- Hübner WA, Irby P, Stoller M. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993;24(2):172-176.
- Lin DY, Fang YC, Huang DY, Lin SP. Spontaneous rupture of the ureter secondary to urolithiasis and extravasation of calyceal fornix due to acute urinary bladder distension: four case reports. Chin J Radiology. 2004;29:269-275.
- Behzad-Noori M, Blandon JA, Negrin Exposito JE, Sarmiento JL, Dias AL, Hernandez GT. Urinoma: a rare complication from being between a rock and soft organ. El Paso Physician. 2010;33(6):5-6.
- Gershman B, Kulkarni N, Sahani DV, Eisner BH. Causes of renal forniceal rupture. BJU Int. 2011;108(11):1909-1911.
- Chapman JP, Gonzalez J, Diokno AC. Significance of urinary extravasation during renal colic. Urology. 1987;30(6):541-545.
- Doehn C, Fiola L, Peter M, Jocham D. Outcome analysis of fornix ruptures in 162 consecutive patients. J Endourol. 2010;24(11):1869-1873
- Portis AJ, Sundaram CP. Diagnosis and initial management of kidney stones. Am Fam Physician. 2001;63(7):1329-1338
- Smith RC, Verga M, Dalrymple N, McCarthy S, Rosenfield AT. Acute ureteral obstruction: value of secondary signs of helical unenhanced CT. AJR Am J Roentgenol. 1996;167(5):1109-1113.Burke TA, Wisniewski T, Ernst FR. Resource utilization and costs associated with chemotherapy-induced nausea and vomiting (CINV) following highly or moderately emetogenic chemotherapy administered in the US outpatient hospital setting. Support Care Cancer. 2011;19(1):131-140.
- Ha M, MacDonald RD. Impact of CT scan in patients with first episode of suspected nephrolithiasis. J Emerg Med. 2004;27(3):225-231.
- Tawfiek ER, Bagley DH. Management of upper urinary tract calculi with ureteroscopic techniques. Urology. 1999;53(1):25-31.
- Larkin GL, Peacock WF 4th, Pearl SM, Blair GA, D'Amico F. Efficacy of ketorolac tromethamine versus meperidine in the ED treatment of acute renal colic. Am J Emerg Med. 1999;17(1):6-10.


Kidney stones: pathophysiology, diagnosis and management
Affiliations.
- 1 PhD student and undergraduate nursing teaching assistant, Queen's University Belfast, Northern Ireland.
- 2 Lecturer Health Services Research, Queen's University Belfast, Northern Ireland.
- 3 Senior Lecturer (Education), Queen's University Belfast, Northern Ireland.
- 4 Clinical Teaching Fellow, Queen's University Belfast, Northern Ireland.
- PMID: 27834524
- DOI: 10.12968/bjon.2016.25.20.1112
The prevalence of kidney stones is increasing, and approximately 12 000 hospital admissions every year are due to this condition. This article will use a case study to focus on a patient diagnosed with a calcium oxalate kidney stone. It will discuss the affected structures in relation to kidney stones and describe the pathology of the condition. Investigations for kidney stones, differential diagnosis and diagnosis, possible complications and prognosis, will be discussed. Finally, a detailed account of management strategies for the patient with kidney stones will be given, looking at pain management, medical procedures and dietary interventions.
Keywords: Calcium oxalate; Kidney stones; Medical expulsion therapy; Nephrolithiasis; Renal colic; Renal obstruction.
Publication types
- Case Reports
- Anti-Inflammatory Agents, Non-Steroidal / therapeutic use*
- Diet Therapy*
- Disease Management
- Fluid Therapy / methods*
- Kidney Calculi / chemistry
- Lithotripsy / methods*
- Nephrolithiasis / diagnosis
- Nephrolithiasis / nursing*
- Nephrolithiasis / physiopathology
- Nephrolithiasis / therapy
- Nurse's Role
- Pain Management
- Anti-Inflammatory Agents, Non-Steroidal
Supplementary concepts
- Nephrolithiasis, Calcium Oxalate
7 Urolithiasis (Renal Calculi) Nursing Care Plans
Deliver effective care to patients with urolithiasis with this nursing care plan and management guide. Gain insights into nursing assessment , interventions, goals, and diagnosis customized for their specific needs. Enhance your ability to provide specialized care for patients with renal calculi.
Table of Contents
What is urolithiasis, nursing problem priorities, nursing assessment, nursing diagnosis, nursing goals, 1. managing pain, 2. promoting effective urinary elimination, 3. promoting optimal fluid balance, 4. providing patient education and teachings for lifestyle changes, 5. administering medications and pharmacologic support, 6. assessing and monitoring for potential complications, 7. monitoring laboratory and diagnostic procedures, recommended resources.
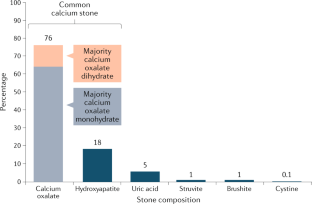
Urolithiasis is the process of forming stones in the kidney , bladder , and/or urethra (urinary tract). Kidney stones (calculi) are formed of mineral deposits, most commonly calcium oxalate and calcium phosphate; however, uric acid, struvite, and cystine are also calculus formers. Although renal calculi can form anywhere in the urinary tract, they are most commonly found in the renal pelvis and calyces. Renal calculi can remain asymptomatic until passed into a ureter and/or urine flow is obstructed when the potential for renal damage is acute.
There are four main types of kidney stones — calcium stones, uric acid stones, struvite stones, and cystine stones.
Nursing Care Plans and Management
Nursing goals for patients with urolithiasis aim to provide comprehensive care to manage pain , prevent complications, and facilitate the passage of kidney stones.
The following are the nursing priorities for patients with urolithiasis:
- Acute pain management. Managing acute pain is a top priority to provide immediate relief and improve the patient’s comfort .
- Infection control . Prompt identification and treatment of any infection is crucial to prevent further complications and ensure the patient’s well-being.
- Stone removal. The primary goal of treatment is to eliminate kidney stones.
- Prevention of stone recurrence. Implementing preventive measures, such as lifestyle modifications, dietary changes, and appropriate medical therapies, is important to reduce the risk of future stone formation.
- Renal function preservation. Protecting renal function through early intervention and appropriate management strategies is essential to maintain the overall health of the patient’s urinary system .
- Education and patient awareness. Informing patients about the causes, prevention strategies, signs of complications, and the importance of regular follow-ups to monitor their condition is important.
- Lifestyle modifications. Encouraging lifestyle changes, such as increased fluid intake, dietary adjustments (e.g., reduced sodium and oxalate intake), and regular physical activity , can help prevent stone recurrence and promote overall urinary health.
Assess for the following subjective and objective data :
- Urgency and frequency; oliguria (retention)
- Questions; request for information; statement of misconception
- Inaccurate follow-through of instructions, development of preventable complications
Assess for factors related to the cause of urolithiasis:
- Increased frequency/force of ureteral contractions
- Tissue trauma , edema formation; cellular ischemia
- Possibly evidenced by
- Reports of colicky pain
- Guarding/distraction behaviors, restlessness, moaning, self-focusing, facial mask of pain, muscle tension
- Autonomic responses
- Stimulation of the bladder by calculi, renal or ureteral irritation
- Mechanical obstruction, inflammation
- Nausea / vomiting (generalized abdominal and pelvic nerve irritation from renal or ureteral colic )
- Post obstructive diuresis
- Lack of exposure/recall; information misinterpretation
- Unfamiliarity with information resources
Following a thorough assessment , a nursing diagnosis is formulated to specifically address the challenges associated with urolithiasis based on the nurse ’s clinical judgment and understanding of the patient’s unique health condition. While nursing diagnoses serve as a framework for organizing care, their usefulness may vary in different clinical situations. In real-life clinical settings, it is important to note that the use of specific nursing diagnostic labels may not be as prominent or commonly utilized as other components of the care plan. It is ultimately the nurse’s clinical expertise and judgment that shape the care plan to meet the unique needs of each patient, prioritizing their health concerns and priorities.
Goals and expected outcomes may include:
- The patient will report relief of pain with spasms controlled.
- The patient will appear relaxed and will be able to sleep /rest appropriately.
- The patient will void in normal amounts and usual pattern.
- The patient will experience no signs of obstruction.
- The patient will maintain adequate fluid balance as evidenced by vital signs and weight within patient’s normal range, palpable
- The patient will demonstrate peripheral pulses, moist mucous membranes, and good skin turgor .
- The patient will verbalize understanding of disease process and potential complications.
- The patient will be able to correlate symptoms with causative factors.
- The patient will verbalize understanding of therapeutic needs.
- The patient will initiate necessary lifestyle changes and participate in treatment regimen.
Nursing Interventions and Actions
Therapeutic interventions and nursing actions for patients with urolithiasis may include:
Acute pain is common in patients with urolithiasis because the passage of kidney stones through the urinary tract can cause irritation, inflammation, and obstruction, leading to intense pain. The severity of the pain can vary depending on the size and location of the stone. Effective pain management in patients with urolithiasis serves several important purposes. First and foremost, it aims to provide relief and alleviate suffering. The excruciating pain associated with kidney stones can significantly impact the patient’s physical and emotional well-being, impairing their daily activities and overall quality of life. By effectively managing pain, healthcare professionals can alleviate distress and improve the patient’s comfort .
1. Determine and note location, duration, intensity (0–10 scale), and radiation . Document nonverbal signs such as elevated BP and pulse, restlessness, moaning, thrashing about. Aids to evaluate site of obstruction and progress of calculi movement . Flank pain suggests that stones are in the kidney area, upper ureter. Flank pain radiates to back, abdomen, groin, genitalia because of proximity of nerve plexus and blood vessels supplying other areas. Sudden, severe pain may precipitate apprehension, restlessness, and severe anxiety .
2. Justify and clarify cause of pain and the need of notifying caregivers of changes in pain occurrence and characteristics. Provides opportunity for timely administration of analgesia (helpful in enhancing patient’s coping ability and may reduce anxiety ) and alerts caregivers to possibility of passing of stone and developing complications. Sudden cessation of pain usually indicates stone passage.
3. Implement comfort measures (back rub, restful environment). Promotes relaxation, reduces muscle tension and enhances coping.
4. Encourage use of focused breathing, guided imagery, and diversional activities. Redirects attention and helps in muscle relaxation.
5. Assist with frequent ambulation as indicated and increased fluid intake of at least 3–4 L a day within cardiac tolerance. Renal colic can be worse in the supine position. Vigorous hydration promotes passing of stones, prevents urinary stasis, and aids in prevention of further stone formation.
6. Document reports of increased and persistent abdominal pain. Complete obstruction of ureter can cause perforation and extravasation of urine into perirenal space. This represents an acute surgical emergency.
7. Apply warm compresses to the back. Relieves muscle tension and may reduce reflex spasms.
8. Check and sustain patency of catheters when used. Prevents urinary stasis or retention, and reduces risk of increased renal pressure and infection.
Because the presence of kidney stones in the urinary tract can cause blockages or partial obstructions, impaired urinary elimination is a common problem in patients with urolithiasis. This can result in urinary retention , urinary tract infections, and other complications. Effective urinary elimination aims to ensure the proper passage of urine, aid in the elimination of kidney stones, and maintain the overall health of the urinary system. The goals of promoting effective urinary elimination in patients with urolithiasis are multifaceted. First and foremost, it aims to relieve urinary obstruction and restore the normal flow of urine. By facilitating the passage of urine, healthcare professionals can help alleviate pain, reduce urinary stasis, and prevent further complications, such as urinary tract infections or renal damage.
1. Record I&O and characteristics of urine. Provides information about kidney function and presence of complications (infection and hemorrhage ). Bleeding may indicate increased obstruction or irritation of ureter. Note: Hemorrhage due to ureteral ulceration is rare.
2. Determine patient’s normal voiding pattern and note variations. Calculi may cause nerve excitability, which causes sensations of urgent need to void. Usually frequency and urgency increase as calculus nears ureterovesical junction.
3. Encourage the patient to walk if possible. To facilitate spontaneous passage.
4. Promote sufficient intake of fluids. Increased hydration flushes bacteria, blood, and debris and may facilitate stone passage.
5. Offer fruit juices, particularly cranberry juice. To help acidify urine.
6. Strain all urine. Document any stones expelled and send to laboratory for analysis. Retrieval of calculi allows identification of type of stone and influences choice of therapy.
7. Investigate reports of bladder fullness; palpate for suprapubic distension. Note decreased urine output, and presence of periorbital and dependent edema . Urinary retention may develop, causing tissue distension (bladder, kidney), and potentiates risk of infection, and renal failure .
8. Observe for changes in mental status, behavior, or level of consciousness. Accumulation of uremic wastes and electrolyte imbalances can be toxic to the CNS.
9. Maintain patency of indwelling catheters (urethral, urethral, or nephrostomy) when used. May be required to facilitate urine flow and prevent retention and corresponding complications. Note: Tubes may be occluded by stone fragments.
10. Irrigate with acid or alkaline solutions as indicated. Changing urine pH may help dissolve stones and prevent further stone formation.
11. Check laboratory studies ( electrolytes , BUN, Cr). Elevated BUN, Cr, and certain electrolytes indicate presence and degree of kidney dysfunction.
12. Obtain urine for culture and sensitivities. Determines presence of UTI, which may be causing or complicating symptoms
Patients with urolithiasis are at risk for inadequate fluid volume due to factors such as dehydration , reduced oral intake, and increased urinary output resulting from the formation and passage of kidney stones. Additionally, after the obstruction caused by a kidney stone is relieved, some patients may experience post-obstructive diuresis, which can further increase urinary output and exacerbate fluid and electrolyte imbalances . Achieving and maintaining appropriate fluid balance is essential in preventing stone recurrence, promoting stone passage, and preserving urinary system health. Effective management of fluid balance aims to ensure adequate hydration, promote urinary flow, and prevent the recurrence of kidney stones.
1. Monitor and document I&O and daily weight. Comparing actual and anticipated output may aid in evaluating presence and degree of renal stasis or impairment. Note: Impaired kidney functioning and decreased urinary output can result in higher circulating volumes with signs and symptoms of HF.
2. Note incidence and document characteristics and frequency of vomiting and diarrhea , as well as accompanying or precipitating events. Nausea and vomiting and diarrhea are commonly associated with renal colic because celiac ganglion serves both kidneys and stomach . Documentation may help rule out other abdominal occurrences as a cause for pain or pinpoint calculi.
3. Promote fluid intake to 3–4 L a day within cardiac tolerance. Maintains fluid balance for homeostasis and “washing” action that may flush the stone(s) out. Dehydration and electrolyte imbalance may occur secondary to excessive fluid loss ( vomiting and diarrhea ).
4. Monitor vital signs. Evaluate pulses, capillary refill, skin turgor, and mucous membranes. Indicators of hydration and circulating volume and need for intervention. Note: Decreased GFR stimulates production of renin, which acts to raise BP in an effort to increase renal blood flow.
5. Weigh daily. Rapid weight gain may be related to water retention.
6. Check Hb and Hct, electrolytes. Assesses hydration and effectiveness or need for interventions.
7. If patient can’t drink required amount of fluids, supplemental IV fluids may be given. Maintains circulating volume (if oral intake is insufficient), promoting renal function.
8. Encourage appropriate diet, clear liquids, and bland foods as tolerated. Easily digested foods decrease GI activity and irritation and help maintain fluid and nutritional balance.
9. Administer medications as indicated Reduces nausea and vomiting .
Providing patient education and teachings for lifestyle changes is a crucial component of care for patients with urolithiasis, a condition characterized by the formation of kidney stones in the urinary tract. Urolithiasis is influenced by various lifestyle factors, including diet, fluid intake, and physical activity . Educating patients about these factors and empowering them to make necessary lifestyle modifications is essential in preventing stone recurrence, promoting overall urinary health, and improving long-term outcomes.
1. Recall and analyze disease process and future expectations. Provides knowledge base from which patient can make informed choices.
2. Review dietary regimen, as individually appropriate:
- 2.1. Low-purine diet Decreases oral intake of uric acid precursors.
- 2.2. Low-calcium diet Reduces risk of calcium stone formation. Note: Research suggests that restricting dietary calcium is not helpful in reducing calcium-stone formation, and researchers, although not advocating high-calcium diets, are urging that calcium limitation be reexamined.
- 2.3. Low-oxalate diet Reduces calcium oxalate stone formation.
- 2.4. Short regimen: low-calcium or phosphorus diet with aluminum carbonate gel 30–40 mL, 30 min pc or hs. Prevents phosphatic calculi by forming an insoluble precipitate in the GI tract, reducing the load to the kidney nephron . Also effective against other forms of calcium calculi. Note: May cause constipation .
3. Emphasize importance of increased fluid intake of 3–4L a day or as much as 6–8 L a day. Flushes renal system, decreasing opportunity for urinary stasis and stone formation.
4. Encourage patient to notice dry mouth and excessive diuresis and diaphoresis and to increase fluid intake whether or not feeling thirsty. Increased fluid losses or dehydration require additional intake beyond usual daily needs.
5. Discuss medication regimen; avoidance of OTC drugs, and read all product or food ingredient labels. Drugs will be given to acidify or alkalize urine, depending on underlying cause of stone formation. Ingestion of products containing individually contraindicated ingredients (calcium, phosphorus) potentiates recurrence of stones.
6. Promote regular activity and exercise program. Inactivity contributes to stone formation through calcium shifts and urinary stasis.
7. Active-listen concerns about therapeutic regimen and lifestyle changes. Helps patient work through feelings and gain a sense of control over what is happening.
8. Identify signs and symptoms requiring medical evaluation (recurrent pain, hematuria, oliguria). With increased probability of recurrence of stones, prompt interventions may prevent serious complications.
9. Demonstrate proper care of incisions and catheters if present. Promotes competent self-care and independence.
Medications play a vital role in the management of urolithiasis by addressing various aspects of the condition, including pain control, prevention of stone formation, and treatment of associated complications. The administration of medications and pharmacologic support in patients with urolithiasis requires close collaboration between healthcare professionals and patients. Healthcare providers play a crucial role in assessing the patient’s condition, determining the appropriate medications, and monitoring their effectiveness and potential side effects. Patient education is also important, ensuring that patients understand the purpose, dosage , and potential adverse effects of their prescribed medications.
1. Analgesics These medications are used to relieve pain associated with kidney stones. They help alleviate the intense pain caused by stone movement and obstruction in the urinary tract. Commonly used analgesics include nonsteroidal anti-inflammatory drugs ( NSAIDs ) like ibuprofen and naproxen , as well as opioids such as morphine or oxycodone .
2. Alpha-blockers Alpha-blockers are prescribed to relax the smooth muscles of the ureter, facilitating the passage of kidney stones. They help reduce ureteral spasms, allowing the stones to move more easily through the urinary tract. Tamsulosin is a commonly used alpha-blocker for this purpose.
3. Diuretics Diuretics are medications that increase urine production and promote the flushing out of kidney stones. They may be prescribed to help increase urinary flow and facilitate the passage of stones. Thiazide diuretics, such as hydrochlorothiazide , are sometimes used to reduce calcium excretion and prevent the formation of certain types of stones.
4. Alkalinizing agents These medications are used to increase the pH of urine, making it more alkaline. Alkalinizing agents are helpful in preventing the formation of uric acid stones, as they make the urine less acidic and reduce the solubility of uric acid. Potassium citrate is a commonly prescribed alkalinizing agent for patients with uric acid stones.
5. Uricosuric agents Uricosuric agents are prescribed to reduce the concentration of uric acid in the urine by increasing its excretion. By promoting the elimination of uric acid, these medications help prevent the formation of uric acid stones. Probenecid is an example of a uricosuric agent.
6. Antibiotics In cases where urinary tract infections (UTIs) occur concurrently with urolithiasis, antibiotics are prescribed to treat the infection and prevent its recurrence. The choice of antibiotic depends on the specific bacteria causing the infection and its susceptibility to different antibiotics.
Urolithiasis can give rise to various complications that require vigilant assessment and ongoing monitoring to ensure timely intervention and optimal patient outcomes . Urolithiasis, the presence of kidney stones in the urinary tract, can lead to a range of complications that can significantly impact patient health and well-being. These complications may include urinary tract infections (UTIs), obstructive uropathy, hydronephrosis, sepsis , renal impairment, and stone recurrence. Proactive assessment and ongoing monitoring of patients with urolithiasis are essential to identify potential complications, initiate timely interventions, and prevent further adverse outcomes.
1. Perform a comprehensive assessment of the patient’s medical history , including previous episodes of urolithiasis, associated symptoms, and risk factors such as family history, diet, and fluid intake. A thorough assessment helps identify the patient’s specific risk factors, contributing factors, and potential complications associated with urolithiasis.
2. Monitor vital signs regularly, including temperature, heart rate , blood pressure , and respiratory rate, to detect any signs of infection or systemic complications. Vital signs provide important information about the patient’s overall condition, including the presence of fever , which may indicate infection or other systemic complications.
3. Evaluate the intensity, location, and duration of the patient’s pain using a standardized pain assessment tool. Assess the effectiveness of pain relief measures and administer analgesics as prescribed. Pain assessment is crucial for determining the severity of the patient’s symptoms and evaluating the effectiveness of pain management interventions, ensuring optimal comfort and promoting recovery.
4. Monitor the patient’s fluid intake and output to ensure an adequate urine output and prevent dehydration . Encourage the patient to maintain a high fluid intake unless contraindicated. Adequate hydration helps promote urine flow and prevents the concentration of substances that can contribute to stone formation. Monitoring fluid balance helps prevent dehydration , which can worsen symptoms and increase the risk of complications.
5. Monitor the characteristics of the patient’s urine, including color, clarity, and presence of blood or sediment. Document any changes in urine output and report abnormal findings promptly. Changes in urine characteristics can indicate the presence of infection, obstruction, or renal impairment. Monitoring urine output helps identify any decrease in urinary flow, which may be a sign of complications.
6. Monitor renal function by assessing laboratory values such as blood urea nitrogen (BUN), creatinine , and electrolyte levels. Notify the healthcare provider of any significant changes that may indicate renal impairment or obstruction. Monitoring renal function through laboratory values helps identify any impairment or changes in kidney function, which may be caused by complications of urolithiasis, such as obstruction or infection.
7. Assess for signs and symptoms of urinary tract infection (UTI), such as fever, chills, dysuria , and increased frequency or urgency of urination . Collect urine samples for culture and sensitivity testing as indicated. Patients with urolithiasis are at an increased risk of developing UTIs. Prompt identification and treatment of UTIs help prevent further complications and promote recovery.
8. Educate the patient about common symptoms associated with urolithiasis, such as flank pain, hematuria, and urinary urgency. Provide appropriate interventions to alleviate discomfort and promote patient comfort. Patient education on urolithiasis symptoms helps patients recognize potential complications and seek timely medical intervention. Providing comfort measures helps alleviate discomfort and improve the patient’s overall well-being.
9. Administer prescribed medications accurately, including analgesics, antibiotics for infection, and medications to facilitate stone passage (if applicable). Monitor the patient for any adverse drug reactions and provide patient education regarding medication use and potential side effects. Medications are often used to manage pain, treat infections, and facilitate the passage of urinary stones. Proper administration and monitoring of medications help ensure their effectiveness and prevent adverse reactions.
10. Collaborate with the healthcare team, including physicians, urologists, and radiologists, to ensure timely diagnostic tests, such as ultrasound or CT scan , and interventions, such as lithotripsy or surgical intervention , are implemented as necessary. Collaborating with urologists allows for specialized knowledge and skills in managing the condition, providing optimal care for the patient. Collaboration allows for comprehensive evaluation and discussion of treatment options. Each patient’s case may vary, and having input from multiple specialists ensures that treatment plans are tailored to the individual patient’s needs and circumstances. Collaboration ensures that all team members work together towards a common goal, optimizing patient outcomes and providing comprehensive care.
Laboratory and diagnostic tests provide valuable information about the patient’s kidney function, stone composition, and overall health status, aiding in accurate diagnosis, treatment planning , and monitoring of potential complications. Monitoring laboratory and diagnostic procedures allows healthcare professionals to identify complications, determine stone characteristics, and guide appropriate treatment strategies. By closely monitoring these parameters, healthcare professionals can promptly identify any changes, tailor interventions, and ensure effective management of urolithiasis, ultimately improving the patient’s quality of life.
1. Urinalysis Urinalysis helps assess the presence of blood, crystals, infection, and other abnormalities in the urine. It aids in diagnosing urinary tract infections (UTIs), identifying urinary stones, and evaluating the overall health of the urinary system.
2. Complete Blood Count (CBC) CBC measures various components of blood, including red and white blood cells , hemoglobin , and platelets . It helps identify signs of infection, anemia , and other systemic abnormalities associated with urolithiasis or its complications.
3. Serum Creatinine and Blood Urea Nitrogen (BUN) levels These tests measure the levels of waste products (creatinine and urea nitrogen) in the blood to assess kidney function. Monitoring creatinine and BUN levels helps detect renal impairment or kidney damage caused by urolithiasis or related complications.
4. Serum Electrolyte Levels ( Sodium , Potassium , Calcium) This test measures the levels of various electrolytes in the blood. It helps assess electrolyte imbalances that may result from kidney dysfunction or abnormal urinary stone formation.
5. Stone Analysis Stone analysis involves the chemical and physical examination of retrieved urinary stones. It helps determine the composition of the stone, such as calcium oxalate, uric acid, or struvite. This information guides treatment and preventive measures.
6. Imaging Studies
- X-ray X-rays help identify the presence, location, and size of urinary stones.
- Ultrasound Ultrasound uses sound waves to visualize the urinary tract, detect stones, and assess complications such as hydronephrosis or obstruction.
- Computed Tomography (CT) Scan CT scan provides detailed imaging of the urinary tract, allowing precise identification of stones, their size, and locations.
- Intravenous Pyelogram (IVP) IVP involves injecting a contrast dye into a vein and taking X-ray images to visualize the kidneys, ureters , and bladder, helping identify stones and obstructions.
7. Stone Density Analysis This analysis measures the density of urinary stones, usually using Hounsfield units (HU). Stone density analysis helps determine the potential effectiveness of certain treatment options, such as shock wave lithotripsy (SWL), based on stone composition and density.
8. 24-Hour Urine Collection This test involves collecting all urine passed in a 24-hour period for analysis. It provides information on urine volume, pH, and levels of substances (e.g., calcium, oxalate, citrate) to identify risk factors for stone formation and guide preventive measures.
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ! Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch.
- Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
Other care plans and nursing diagnoses related to reproductive and urinary system disorders:
- Acute Glomerulonephritis | 4 Care Plans
- Acute Renal Failure | 6 Care Plans
- Benign Prostatic Hyperplasia (BPH) | 5 Care Plans
- Chronic Renal Failure | 10 Care Plans
- Hemodialysis | 3 Care Plans
- Hysterectomy (TAHBSO) | 6 Care Plans
- Mastectomy | 15 Care Plans
- Menopause | 6 Care Plans
- Nephrotic Syndrome | 5 Care Plans
- Peritoneal Dialysis | 6 Care Plans
- Prostatectomy | 6 Care Plans
- Urolithiasis (Renal Calculi) | 4 Care Plans
- Urinary Tract Infection | 4 Care Plans
- Vesicoureteral Reflux (VUR) | 5 Care Plans
Leave a Comment Cancel reply
- Practice Test
- Fundamentals of Nursing
- Anatomy and Physiology
- Medical and Surgical Nursing
- Perioperative Nursing
- Psychiatric Mental Health Nursing
- Maternal & Child Nursing
- Community Health Nursing
- Pathophysiology
- Nursing Research
- Study Guide and Strategies
- Nursing Videos
- Work for Us!
- Privacy Policy

- Nursing Care Plan
Kidney Stone (Urolithiasis) Nursing Care Plan
Kidney stones or Renal calculi are hard masses formed in the different sites of the urinary tract. The process of stone formation is called urolithiasis , renal lithiasis, or nephrolithiasis . The most common mineral deposits are calcium oxalate and calcium phosphate, and it is commonly found in the renal pelvis and calyces.
Stones are more common to people with underlying diseases like hypertension and short bowel syndrome and those persons with a diet high in protein or those who do not consume enough water. Sometimes the formation of stones can be caused by urinary tract infection , which can be evidenced by struvite stones or also known as infection stones.
A renal calculus is asymptomatic until it passes through the ureter. Obstruction of urine flow becomes the triggering indicator for renal damage, which is then considered acute. Excruciating pain is the primary basis for the diagnosis of renal calculi . It is accompanied by tenderness over the back and groin, and a urinalysis may show the presence of blood or pus in the urine.
Kidney Stone Nursing Care Plan
Nursing diagnosis: acute pain.
Possible Etiologies: (Related to)
- Increased frequency or force or ureteral contractions
- Tissue trauma
- Edema formation
- Cellular ischemia
Defining Characteristics: (Evidenced by)
Subjective Data:
“This pain is bothering me a lot.”
Cries or moans frequently.
Rates pain as 7/10 when asked to rate pain on a scale of 1 to 10, with 10 as the highest.
Objective Data:
- Guarding behavior/ protective
- Restlessness
- Creasing eyebrows
- Tensed muscles
- Frequent grimacing
- Autonomic responses:
-Blood pressure, pulse, and respiratory rates changes
Blood pressure ranging from 140/90 – 130/ 100
Pulse rate ranging from 95 – 105 beats per minute
Respiratory rate ranging from 18 – 22 breaths per minute
Objectives:
Short term goal:
Client will be able to report and demonstrate behaviors signaling a relief or control of pain.
Long term goal:
Client will be able to know and perform activities that do not only provide relief from pain but are helpful in dealing with the disease condition.
Outcome Criteria:
Client will be able to report that the pain is relieved or controlled and demonstrates behaviors like decrease in the frequency of guarding behavior, restlessness, and grimacing; also present vital signs of being stable with BP of 110/70mmHg – 120/80mmHg, pulse rate of 60 – 75 beats per minute and respiratory rate of 16 – 20 breaths per minute within 3 days of nursing intervention.
Client will be able to learn and perform relaxation skills like deep breathing exercises and diversional activities like guided imagery etc., for pain relief, as well as other activities like proper diet planning, BP monitoring, and compliance to medications and treatment regimens.
Nursing Interventions:
RELATED ARTICLES MORE FROM AUTHOR
Urinary tract infection nursing care plan, anemia nursing care plan, hiatal hernia nursing care plan, diarrhea nursing care plan, pulmonary embolism nursing care plan, pleural effusion nursing care plan, leave a reply cancel reply.
Save my name, email, and website in this browser for the next time I comment.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 04 August 2020
Determining the true burden of kidney stone disease
- Charat Thongprayoon ORCID: orcid.org/0000-0002-8313-3604 1 ,
- Amy E. Krambeck ORCID: orcid.org/0000-0001-8255-598X 2 &
- Andrew D. Rule 1 , 3
Nature Reviews Nephrology volume 16 , pages 736–746 ( 2020 ) Cite this article
4243 Accesses
133 Citations
112 Altmetric
Metrics details
- Renal calculi
- Risk factors
The incidence and prevalence of kidney stones have increased over the past four decades. However, the diagnosis of ‘kidney stone’ can range from an incidental asymptomatic finding of limited clinical significance to multiple painful episodes of ureteral obstruction with eventual kidney failure. Some general strategies may be useful to prevent the recurrence of kidney stones. In particular, greater attention to kidney stone classification, approaches to assessing the risk of recurrence and individualized prevention strategies may improve the clinical care of stone formers. Although there have been some advances in approaches to predicting the recurrence of kidney stones, notable challenges remain. Studies of kidney stone prevalence, incidence and recurrence have reported inconsistent findings, in part because of the lack of a standardized stone classification system. A kidney stone classification system based on practical and clinically useful measures of stone disease may help to improve both the study and clinical care of stone formers. Any future kidney stone classification system should be aimed at distinguishing asymptomatic from symptomatic stones, clinically diagnosed symptomatic stone episodes from self-reported symptomatic stone episodes, symptomatic stone episodes that are confirmed from those that are suspected, symptomatic recurrence from radiographic recurrence (that is, with radiographic evidence of a new stone, stone growth or stone disappearance from presumed passage) and determine stone composition based on mutually exclusive categories.
Kidney stones can range from an asymptomatic incidental finding with limited clinical significance to a painful recurrent disorder with substantial morbidity.
The prevalence and incidence of kidney stones has increased worldwide, but some of this increase is due to improvements in medical imaging with increased utilization of CT.
Classifying stone formers according to their clinical presentation and stone composition can help to predict the risk of future symptomatic stone episodes and aid personalization of stone prevention strategies.
The wide range of recurrence rates reported between different studies might largely be due to the use of different definitions that include various degrees of symptomatic evidence of recurrence and/or radiographic manifestations of recurrence.
Risk factors for symptomatic kidney stone recurrence include younger age, male gender, family history of stones, obesity, pregnancy, rarer stone compositions, higher radiographic kidney stone burden, number of past symptomatic kidney stone episodes and fewer years since last kidney stone episode.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
24,99 € / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
195,33 € per year
only 16,28 € per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others

Long-term kidney outcomes of semaglutide in obesity and cardiovascular disease in the SELECT trial

Noninvasive assessment of organ-specific and shared pathways in multi-organ fibrosis using T1 mapping

Chronic kidney disease and the global public health agenda: an international consensus
Scales, C. D. Jr., Smith, A. C., Hanley, J. M. & Saigal, C. S. Urologic Diseases in America Project. Prevalence of kidney stones in the United States. Eur. Urol. 62 , 160–165 (2012).
Article PubMed PubMed Central Google Scholar
Stamatelou, K. K., Francis, M. E., Jones, C. A., Nyberg, L. M. & Curhan, G. C. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 63 , 1817–1823 (2003).
Article PubMed Google Scholar
Trinchieri, A. et al. Increase in the prevalence of symptomatic upper urinary tract stones during the last ten years. Eur. Urol. 37 , 23–25 (2000).
Article CAS PubMed Google Scholar
Hesse, A., Brandle, E., Wilbert, D., Kohrmann, K. U. & Alken, P. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur. Urol. 44 , 709–713 (2003).
Penniston, K. L., McLaren, I. D., Greenlee, R. T. & Nakada, S. Y. Urolithiasis in a rural Wisconsin population from 1992 to 2008: narrowing of the male-to-female ratio. J. Urol. 185 , 1731–1736 (2011).
Liu, Y. et al. Epidemiology of urolithiasis in Asia. Asian J. Urol. 5 , 205–214 (2018).
Sorokin, I. et al. Epidemiology of stone disease across the world. World J. Urol. 35 , 1301–1320 (2017).
Pearle, M. S., Calhoun, E. A. & Curhan, G. C. Urologic Diseases of America Project. Urologic diseases in America project: urolithiasis. J. Urol. 173 , 848–857 (2005).
Kittanamongkolchai, W. et al. The changing incidence and presentation of urinary stones over 3 decades. Mayo Clin. Proc. 93 , 291–299 (2018).
Dwyer, M. E. et al. Temporal trends in incidence of kidney stones among children: a 25-year population based study. J. Urol. 188 , 247–252 (2012).
Tasian, G. E. et al. Annual incidence of nephrolithiasis among children and adults in South Carolina from 1997 to 2012. Clin. J. Am. Soc. Nephrol. 11 , 488–496 (2016).
Article CAS PubMed PubMed Central Google Scholar
Edvardsson, V. O., Indridason, O. S., Haraldsson, G., Kjartansson, O. & Palsson, R. Temporal trends in the incidence of kidney stone disease. Kidney Int. 83 , 146–152 (2013).
Edvardsson, V. O., Ingvarsdottir, S. E., Palsson, R. & Indridason, O. S. Incidence of kidney stone disease in Icelandic children and adolescents from 1985 to 2013: results of a nationwide study. Pediatr. Nephrol. 33 , 1375–1384 (2018).
Yasui, T., Iguchi, M., Suzuki, S. & Kohri, K. Prevalence and epidemiological characteristics of urolithiasis in Japan: national trends between 1965 and 2005. Urology 71 , 209–213 (2008).
Krambeck, A. E. et al. Effect of age on the clinical presentation of incident symptomatic urolithiasis in the general population. J. Urol. 189 , 158–164 (2013).
Brisbane, W., Bailey, M. R. & Sorensen, M. D. An overview of kidney stone imaging techniques. Nat. Rev. Urol. 13 , 654–662 (2016).
Semins, M. J. & Matlaga, B. R. Kidney stones during pregnancy. Nat. Rev. Urol. 11 , 163–168 (2014).
Smith-Bindman, R. et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N. Engl. J. Med. 371 , 1100–1110 (2014).
Sternberg, K. M. et al. Is hydronephrosis on ultrasound predictive of ureterolithiasis in patients with renal colic? J. Urol. 196 , 1149–1152 (2016).
Chi, T., Miller, J. & Stoller, M. L. Randall plaque versus renal stone? Transl. Androl. Urol. 1 , 66–70 (2012).
PubMed PubMed Central Google Scholar
Dhondup, T. et al. Risk of ESRD and mortality in kidney and bladder stone formers. Am. J. Kidney Dis. 72 , 790–797 (2018).
Emamian, S. A., Nielsen, M. B., Pedersen, J. F. & Ytte, L. Sonographic evaluation of renal appearance in 665 adult volunteers. Correlation age obesity. Acta Radiol. 34 , 482–485 (1993).
Oshibuchi, M., Nishi, F., Sato, M., Ohtake, H. & Okuda, K. Frequency of abnormalities detected by abdominal ultrasound among Japanese adults. J. Gastroenterol. Hepatol. 6 , 165–168 (1991).
Buchholz, N. P. et al. The prevalence of silent kidney stones — an ultrasonographic screening study. J. Pak. Med. Assoc. 53 , 24–25 (2003).
CAS PubMed Google Scholar
Passerotti, C. et al. Ultrasound versus computerized tomography for evaluating urolithiasis. J. Urol. 182 , 1829–1834 (2009).
Brenner, D. J. & Hall, E. J. Computed tomography — an increasing source of radiation exposure. N. Engl. J. Med. 357 , 2277–2284 (2007).
Lorenz, E. C. et al. Clinical characteristics of potential kidney donors with asymptomatic kidney stones. Nephrol. Dial. Transpl. 26 , 2695–2700 (2011).
Article Google Scholar
Durbin, J. M. et al. Genitourinary abnormalities in an asymptomatic screening population: findings on virtual colonoscopy. Clin. Nephrol. 77 , 204–210 (2012).
D’Costa, M. R. et al. Symptomatic and radiographic manifestations of kidney stone recurrence and their prediction by risk factors: a prospective cohort study. J. Am. Soc. Nephrol. 30 , 1251–1260 (2019).
Li, X. et al. Outcomes of long-term follow-up of asymptomatic renal stones and prediction of stone-related events. BJU Int. 123 , 485–492 (2019).
Goldsmith, Z. G. & Lipkin, M. E. When (and how) to surgically treat asymptomatic renal stones. Nat. Rev. Urol. 9 , 315–320 (2012).
Selby, M. G. et al. Quantification of asymptomatic kidney stone burden by computed tomography for predicting future symptomatic stone events. Urology 85 , 45–50 (2015).
Dropkin, B. M., Moses, R. A., Sharma, D. & Pais, V. M. Jr. The natural history of nonobstructing asymptomatic renal stones managed with active surveillance. J. Urol. 193 , 1265–1269 (2015).
Kang, H. W. et al. Natural history of asymptomatic renal stones and prediction of stone related events. J. Urol. 189 , 1740–1746 (2013).
Burgher, A., Beman, M., Holtzman, J. L. & Monga, M. Progression of nephrolithiasis: long-term outcomes with observation of asymptomatic calculi. J. Endourol. 18 , 534–539 (2004).
Assimos, D. et al. Surgical management of stones: American Urological Association/Endourological Society guideline, part I. J. Urol. 196 , 1153–1160 (2016).
Assimos, D. et al. Surgical management of stones: American Urological Association/Endourological Society guideline, part II. J. Urol. 196 , 1161–1169 (2016).
Curhan, G. C., Willett, W. C., Speizer, F. E. & Stampfer, M. J. Twenty-four-hour urine chemistries and the risk of kidney stones among women and men. Kidney Int. 59 , 2290–2298 (2001).
Chooi, Y. C., Ding, C. & Magkos, F. The epidemiology of obesity. Metabolism 92 , 6–10 (2019).
Taylor, E. N., Stampfer, M. J. & Curhan, G. C. Obesity, weight gain, and the risk of kidney stones. JAMA 293 , 455–462 (2005).
Geiss, L. S. et al. Prevalence and incidence trends for diagnosed diabetes among adults aged 20 to 79 years, United States, 1980–2012. JAMA 312 , 1218–1226 (2014).
Taylor, E. N., Stampfer, M. J. & Curhan, G. C. Diabetes mellitus and the risk of nephrolithiasis. Kidney Int. 68 , 1230–1235 (2005).
Meyer, K. A. et al. Twenty-two-year population trends in sodium and potassium consumption: the Minnesota Heart Survey. J. Am. Heart Assoc. 2 , e000478 (2013).
Article PubMed PubMed Central CAS Google Scholar
Sorensen, M. D. et al. Impact of nutritional factors on incident kidney stone formation: a report from the WHI OS. J. Urol. 187 , 1645–1649 (2012).
Muldowney, F. P., Freaney, R. & Moloney, M. F. Importance of dietary sodium in the hypercalciuria syndrome. Kidney Int. 22 , 292–296 (1982).
Curhan, G. C., Willett, W. C., Speizer, F. E., Spiegelman, D. & Stampfer, M. J. Comparison of dietary calcium with supplemental calcium and other nutrients as factors affecting the risk for kidney stones in women. Ann. Intern. Med. 126 , 497–504 (1997).
Daniel, C. R., Cross, A. J., Koebnick, C. & Sinha, R. Trends in meat consumption in the USA. Public. Health Nutr. 14 , 575–583 (2011).
Taylor, E. N., Stampfer, M. J. & Curhan, G. C. Dietary factors and the risk of incident kidney stones in men: new insights after 14 years of follow-up. J. Am. Soc. Nephrol. 15 , 3225–3232 (2004).
Breslau, N. A., Brinkley, L., Hill, K. D. & Pak, C. Y. Relationship of animal protein-rich diet to kidney stone formation and calcium metabolism. J. Clin. Endocrinol. Metab. 66 , 140–146 (1988).
Gross, L. S., Li, L., Ford, E. S. & Liu, S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am. J. Clin. Nutr. 79 , 774–779 (2004).
Curhan, G. C., Willett, W. C., Knight, E. L. & Stampfer, M. J. Dietary factors and the risk of incident kidney stones in younger women: Nurses’ Health Study II. Arch. Intern. Med. 164 , 885–891 (2004).
Lemann, J. Jr., Piering, W. F. & Lennon, E. J. Possible role of carbohydrate-induced calciuria in calcium oxalate kidney-stone formation. N. Engl. J. Med. 280 , 232–237 (1969).
Bleich, S. N., Wang, Y. C., Wang, Y. & Gortmaker, S. L. Increasing consumption of sugar-sweetened beverages among US adults: 1988–1994 to 1999–2004. Am. J. Clin. Nutr. 89 , 372–381 (2009).
Ferraro, P. M., Taylor, E. N., Gambaro, G. & Curhan, G. C. Soda and other beverages and the risk of kidney stones. Clin. J. Am. Soc. Nephrol. 8 , 1389–1395 (2013).
Fakheri, R. J. & Goldfarb, D. S. Ambient temperature as a contributor to kidney stone formation: implications of global warming. Kidney Int. 79 , 1178–1185 (2011).
Soucie, J. M., Coates, R. J., McClellan, W., Austin, H. & Thun, M. Relation between geographic variability in kidney stones prevalence and risk factors for stones. Am. J. Epidemiol. 143 , 487–495 (1996).
Soucie, J. M., Thun, M. J., Coates, R. J., McClellan, W. & Austin, H. Demographic and geographic variability of kidney stones in the United States. Kidney Int. 46 , 893–899 (1994).
Boscolo-Berto, R. et al. Do weather conditions influence the onset of renal colic? A novel approach to analysis. Urol. Int. 80 , 19–25 (2008).
Chen, Y. K., Lin, H. C., Chen, C. S. & Yeh, S. D. Seasonal variations in urinary calculi attacks and their association with climate: a population based study. J. Urol. 179 , 564–569 (2008).
Chauhan, V., Eskin, B., Allegra, J. R. & Cochrane, D. G. Effect of season, age, and gender on renal colic incidence. Am. J. Emerg. Med. 22 , 560–563 (2004).
Brikowski, T. H., Lotan, Y. & Pearle, M. S. Climate-related increase in the prevalence of urolithiasis in the United States. Proc. Natl Acad. Sci. USA 105 , 9841–9846 (2008).
Rule, A. D. et al. The ROKS nomogram for predicting a second symptomatic stone episode. J. Am. Soc. Nephrol. 25 , 2878–2886 (2014).
Vaughan, L. E. et al. Predictors of symptomatic kidney stone recurrence after the first and subsequent episodes. Mayo Clin. Proc. 94 , 202–210 (2019).
Singh, P. et al. Stone composition among first-time symptomatic kidney stone formers in the community. Mayo Clin. Proc. 90 , 1356–1365 (2015).
Lieske, J. C. et al. Stone composition as a function of age and sex. Clin. J. Am. Soc. Nephrol. 9 , 2141–2146 (2014).
Knoll, T. et al. Urolithiasis through the ages: data on more than 200,000 urinary stone analyses. J. Urol. 185 , 1304–1311 (2011).
Daudon, M. et al. Sex- and age-related composition of 10 617 calculi analyzed by infrared spectroscopy. Urol. Res. 23 , 319–326 (1995).
Ye, Z. et al. The status and characteristics of urinary stone composition in China. BJU Int. 125 , 801–809 (2019).
Article CAS Google Scholar
Worcester, E. M., Bergsland, K. J., Gillen, D. L. & Coe, F. L. Mechanism for higher urine pH in normal women compared with men. Am. J. Physiol. Renal Physiol 314 , F623–F629 (2018).
Kohri, K. et al. Relationship between metabolic acidosis and calcium phosphate urinary stone formation in women. Int. Urol. Nephrol. 23 , 307–316 (1991).
Maalouf, N. M. Metabolic syndrome and the genesis of uric acid stones. J. Ren. Nutr. 21 , 128–131 (2011).
Sakhaee, K. & Maalouf, N. M. Metabolic syndrome and uric acid nephrolithiasis. Semin. Nephrol. 28 , 174–180 (2008).
Morgan, M. S. & Pearle, M. S. Medical management of renal stones. BMJ 352 , i52 (2016).
Pearle, M. S. et al. Medical management of kidney stones: AUA guideline. J. Urol. 192 , 316–324 (2014).
Qaseem, A. et al. Dietary and pharmacologic management to prevent recurrent nephrolithiasis in adults: a clinical practice guideline from the American College of Physicians. Ann. Intern. Med. 161 , 659–667 (2014).
Skolarikos, A. et al. Metabolic evaluation and recurrence prevention for urinary stone patients: EAU guidelines. Eur. Urol. 67 , 750–763 (2015).
D’Costa, M. R., Pais, V. M. & Rule, A. D. Leave no stone unturned: defining recurrence in kidney stone formers. Curr. Opin. Nephrol. Hypertens. 28 , 148–153 (2019).
Sternberg, K. M. et al. Ultrasonography significantly overestimates stone size when compared to low-dose, noncontrast computed tomography. Urology 95 , 67–71 (2016).
Williams, R. E. Long-term survey of 538 patients with upper urinary tract stone. Br. J. Urol. 35 , 416–437 (1963).
Marshall, V., White, R. H., De Saintonge, M. C., Tresidder, G. C. & Blandy, J. P. The natural history of renal and ureteric calculi. Br. J. Urol. 47 , 117–124 (1975).
Sutherland, J. W., Parks, J. H. & Coe, F. L. Recurrence after a single renal stone in a community practice. Min. Electrolyte Metab. 11 , 267–269 (1985).
CAS Google Scholar
Steyerberg, E. W. et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21 , 128–138 (2010).
Iremashvili, V. et al. External validation of the recurrence of kidney stone nomogram in a surgical cohort. J. Endourol. 33 , 475–479 (2019).
Emmott, A. S., Brotherhood, H. L., Paterson, R. F., Lange, D. & Chew, B. H. Complications, re-intervention rates, and natural history of residual stone fragments after percutaneous nephrolithotomy. J. Endourol. 32 , 28–32 (2018).
Chew, B. H. et al. Natural history, complications and re-intervention rates of asymptomatic residual stone fragments after ureteroscopy: a report from the EDGE research consortium. J. Urol. 195 , 982–986 (2016).
Alexander, C. E., Gowland, S., Cadwallader, J., Reynard, J. M. & Turney, B. W. Shock wave lithotripsy (SWL): outcomes from a national SWL database in New Zealand. BJU Int. 117 (Suppl. 4), 76–81 (2016).
Javanmard, B., Kashi, A. H., Mazloomfard, M. M., Ansari Jafari, A. & Arefanian, S. Retrograde intrarenal surgery versus shock wave lithotripsy for renal stones smaller than 2 cm: a randomized clinical trial. Urol. J. 13 , 2823–2828 (2016).
PubMed Google Scholar
Albala, D. M. et al. Lower pole I: a prospective randomized trial of extracorporeal shock wave lithotripsy and percutaneous nephrostolithotomy for lower pole nephrolithiasis-initial results. J. Urol. 166 , 2072–2080 (2001).
Bozzini, G. et al. A prospective randomized comparison among SWL, PCNL and RIRS for lower calyceal stones less than 2 cm: a multicenter experience: a better understanding on the treatment options for lower pole stones. World J. Urol. 35 , 1967–1975 (2017).
Ferraro, P. M., Curhan, G. C., D’Addessi, A. & Gambaro, G. Risk of recurrence of idiopathic calcium kidney stones: analysis of data from the literature. J. Nephrol. 30 , 227–233 (2017).
Fink, H. A. et al. Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians clinical guideline. Ann. Intern. Med. 158 , 535–543 (2013).
Download references
Author information
Authors and affiliations.
Division of Nephrology and Hypertension, Mayo Clinic, Rochester, MN, USA
Charat Thongprayoon & Andrew D. Rule
Department of Urology, Indiana University, Indianapolis, IN, USA
Amy E. Krambeck
Division of Epidemiology, Mayo Clinic, Rochester, MN, USA
Andrew D. Rule
You can also search for this author in PubMed Google Scholar
Contributions
C.T. and A.D.R. researched data for the article. All authors contributed to discussion of the article’s content, writing and review/editing of the manuscript before submission.
Corresponding author
Correspondence to Andrew D. Rule .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Peer review information.
Nature Reviews Nephrology thanks D. Goldfarb and R. Pálsson for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Recurrence of Kidney Stone (ROKS) tool: https://qxmd.com/calculate/calculator_438/roks-recurrence-of-kidney-stone-2018
A procedure for treating stones in the kidney or ureter using a high-energy shock wave from outside the body to break stones into fragments that are small enough to spontaneously pass in urine.
A procedure in which a small scope is inserted into the ureter via the urethra and bladder to diagnose and treat a variety of problems in the urinary tract. In the case of urinary stones, it allows the urologist to actually look into the ureter or kidney, find the stone and remove or fragment the stone.
A procedure used to remove kidney stones from the body when they cannot pass spontaneously.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Thongprayoon, C., Krambeck, A.E. & Rule, A.D. Determining the true burden of kidney stone disease. Nat Rev Nephrol 16 , 736–746 (2020). https://doi.org/10.1038/s41581-020-0320-7
Download citation
Accepted : 23 June 2020
Published : 04 August 2020
Issue Date : December 2020
DOI : https://doi.org/10.1038/s41581-020-0320-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The sox4/ezh2/slc7a11 signaling axis mediates ferroptosis in calcium oxalate crystal deposition-induced kidney injury.
- Xinzhou Yan
Journal of Translational Medicine (2024)
Exploring the impact of digital health literacy on quality of life in patients undergoing retrograde intrarenal surgery for kidney stone treatment: a prospective, single-center study
- Ahmet Keles
- Ozgur Arikan
- Asif Yildirim
Urolithiasis (2024)
Cymbopogon proximus and Petroselinum crispum seed ethanolic extract/Gum Arabic nanogel emulsion: Preventing ethylene glycol and ammonium chloride-induced urolithiasis in rats
- Hend A. Essa
- Alaa M. Ali
- Mona A. Saied
Surgical procedure and recurrence of upper urinary tract stone: a national-wide study based on hospitalized patients
- Ming-Hui Zhao
World Journal of Urology (2024)
Gaps in kidney stone disease management: From clinical theory to patient reality
- Agnieszka Pozdzik
- Viridiana Grillo
- Khashayar Sakhaee
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

NurseStudy.Net
Nursing Education Site

Renal Calculi Nursing Diagnosis and Nursing Care Plan
Last updated on August 19th, 2022 at 07:09 am
Renal Calculi Nursing Care Plans Diagnosis and Interventions
Renal Calculi NCLEX Review and Nursing Care Plans
Renal calculi are made of minerals and acid salts that form in the kidney. This health condition is known as nephrolithiasis. These kidney stones can travel to the rest of the urinary tract such as the ureters, bladder, and urethra, and can result to urolithiasis.
Renal calculi begin to form when there is a high concentration of these crystal-forming substances than the fluid in the urine the kidneys can dilute.
Collections of these stones can cause obstruction and infection in severe cases. Although renal stones are commonly mild and can be treated symptomatically it accounts for 1 million emergency visits annually in the U.S.
Signs and Symptoms of Renal Calculi
The signs and symptoms of renal calculi may vary depending on the location of the kidney stone ranging from asymptomatic to severe infection or hemodynamic instability. These may include:
- Sudden or gradual onset of unilateral, abdominal/flank colicky pain
- Radiating pain in the back , lower abdomen, or groin with fluctuating intensity
- Pain or burning sensation upon urination
- Frequent urgency to urinate with small amounts of urine
- Nausea or vomiting
- Fever and chills
- Dark-color urine or blood in the urine (usually seen microscopically)
- Soft, non-distended abdomen
- Pediatric patients may be seen as restless, irritable, and crying
- In severe cases, the patient may present with mild confusion due to metabolic abnormalities.
Causes of Renal Calculi
There are different types of waste particles or crystal-forming substances that can cause the formation of kidney stones such as:
- Calcium Stones. These are composed of calcium oxalate, phosphate, or maleate. While it is true that calcium is the most abundant mineral in our body, consuming a diet high in calcium does not contribute to the formation of these stones but certain foods with high oxalates do such as spinach, beet, nuts, and chocolates. Certain medications like fish oil, vitamin C and high-dose vitamin D can cause calcium stone formation. Metabolic conditions such as type 2 diabetes mellitus, obesity, and hyperlipidemia are associated with calcium oxalate and uric acid stones. It is also the most common type of kidney stone that accounts for 80% of the cases.
- Struvite Stones. This is also called the infection stone as it is commonly formed secondary to a urinary tract infection. It is composed of magnesium ammonia phosphate from an elevated urine pH caused by Proteus or Klebsiella infections. This accounts for 10% of kidney stone cases.
- Uric Acid Stones. Certain metabolic disorders like diabetes, obesity, chronic diarrhea, or malabsorption can cause the formation of these stones. Diets high in animal protein can increase the uric acid level. 9% of kidney stone cases are uric acid stones.
- Cystine Stones. This is a rare type of kidney stone caused by a congenital disorder called cystinuria caused by a defective cystine metabolism and transport leading to stones. This rare type of kidney stone accounts for 1% of the cases.
Risk Factors to Renal Calculi
The risk of having renal calculi increases because of any condition that causes an obstruction or reduction in urinary flow. Certain risk factors increase the incidence of a stone formation such as:
- Gender. Men have a higher incidence in most cases, but women are more likely to have struvite stones because they tend to have urinary tract infections frequently.
- Race. White and non-Hispanic have high incidence than black people.
- Age. It is common among the ages 20 to 50 or the working-age population with rising incidence due to lifestyle and diet influences in the working environment.
- Family history. It is most likely to acquire kidney stones if it runs in the family or had it previously.
- Obesity. Associated with calcium oxalate and uric acid stone formation.
- Dehydration. Reduced body fluid affects the dilution of the urine by decreasing urine output and increasing urine pH leading to the formation of stones.
- Diet. High sodium, oxalate, fat, sugar, and animal protein diet contribute to different substances the kidney must filter leading to renal stone formation. High sodium intake also increases the amount of calcium in the urine.
- Medications. Diuretics , antacids , antiseizure, vitamin C, and a high dose of vitamin D increase the risk of kidney stone formation.
- Metabolic disorder. Diabetes , inflammatory bowel disease, or chronic diarrhea causes changes in the absorption of water increasing crystal-forming substances in the urine.
- Surgery and other medical conditions. Gastric bypass surgery, cystinuria, or repeated urinary tract infection increase the risk of kidney stones.
Complications of Renal Calculi
The presence of renal calculi can be asymptomatic until serious complications arise which commonly cause excruciating pain and serious medical emergency. This includes:
- Sepsis. Severe infections such as septicemia are one of the most common and most life-threatening complications of renal stones as they may block the urine flow causing urinary retention and septicemia. Sepsis or blood poisoning is the body’s deadly response to infection.
- Renal scarring. It is the kidney’s response to injury which reduce its ability to filter waste products leading to progressive renal failure. Frequent urinary tract infections and renal calculi can cause this injury. This condition doesn’t have a cure and is considered irreversible.
- Obstruction. This is the latest and most painful manifestation of renal calculi. The obstruction may lead to the dilation of the ureter and hydronephrosis which eventually lead to renal failure. Unilateral obstruction can be asymptomatic but bilateral obstruction usually present with renal failure and requires prompt treatment.
- Anuria. This is also called anuresis, defined as non-passage of at least 100mL of urine per day where the kidney cannot produce urine. This is usually caused by a large kidney stone stuck in the urethra leading to complete bladder blockage and urinary retention.
- Urinary Tract Infection. Recurrent infection related to kidney stones can cause damage over time through inflammation and scarring of kidney tissues.
- Renal failure. Severe blockage and untreated renal obstruction will eventually cause kidney atrophy and loss of function. Although this rarely happens this can lead to a serious medical condition and lifetime treatment.
Diagnosis of Renal Calculi
Early detection can help prevent the development of complications of renal calculi. The diagnostic tests usually include:
- Urinalysis. This is the primary test used to detect the presence of blood in the urine ( hematuria ), leukocytes, bacteria, crystals, increased WBC, and pH level of the urine.
- Blood tests. Complete blood count detects elevated white blood cell count that signifies an infection. Basic Metabolic Panel (BMP) can also be used to measure the level of glucose and electrolytes such as calcium, sodium, and potassium which are indicators of kidney dysfunction.
- Physical assessment. A thorough physical assessment along with the signs and symptoms can help in determining the location of the stones.
- Patient history. Complete medical history should include family history, previous surgery, diet, and medical conditions.
- CT Scan. An abdominal or pelvic CT scan is the ideal diagnostic test to use as it can detect renal calculi as small as 3mm in size.
- KUB Ultrasound. This is a non-invasive procedure ideal for pediatric and pregnant patients that can quickly measure and detect renal stone location.
- MRI. This can be used adjunctively with ultrasound as it provides 3-dimension imaging without radiation and is reliable in determining hydronephrosis.
- X-ray. This is commonly used in monitoring stone growth for radiopaque stones such as calcium oxalate and phosphate.
- Kidney stone analysis. This test is used to determine the composition of the stone to determine the cause and appropriate treatment.
Treatment for Renal Calculi
Treatment of patients with renal calculi may vary depending on the present condition and complications associated which includes conservative and surgical interventions such as:
- Analgesics. NSAIDs are the first choice of treatment for pain. Opioids are used for severe refractory pain.
- Antiemetics. Used to relieve nausea and vomiting.
- Antibiotics. Management of urinary tract infections that can cause struvite stones.
- Diuretics. Help prevent calcium stones from forming.
- Alpha-blocker. Muscle relaxant that facilitates passage of stones by relaxing the muscles in the ureter.
- IV Fluids. Help the patient stay hydrated and act as natural diuretics that may help in flushing out kidney stones.
- Extracorporeal shockwave lithotripsy (ESWL). This procedure uses shockwave to break the stones into smaller pieces that can be passed into the urine. A follow-up ureteral stent placement may be done to facilitate the passage of the stones.
- Flexible ureteroscopy (URS). This method uses an endoscopic approach to remove blocked stones in the lower urinary tract or ureter.
- Indwelling urinary catheter. This is used as an urgent management for patients with acute renal obstruction to decompress the bladder.
- Percutaneous nephrolithotomy (PCNL). This is used for stones greater than 20mm in size located in the upper urinary tract such as kidneys and proximal ureter. A ureteroscope is also used over a small incision at the back to remove the stones.
- Nephrostomy tube. This is an emergent, minimally invasive procedure that is used to bypass the obstruction and drain urine from the body to prevent permanent renal damage.
Nursing Diagnosis for Renal Calculi
Nursing care plan for renal calculi 1.
Nursing Diagnosis: Acute Pain related to tissue trauma secondary to the excretion of renal calculi as evidenced by hematuria and burning pain with urination.
Desired Outcomes:
- The patient will be able to urinate normally without any pain and discomfort.
- The patient will be able to perform activities that provide relief and control of pain.
Nursing Care Plan for Renal Calculi 2
Impaired Urinary Elimination
Nursing Diagnosis: Impaired Urinary Elimination related to mechanical obstruction secondary to renal calculi formation s evidenced by oliguria and distended bladder.
- The patient will be able to achieve a normal elimination amount and pattern.
- The patient will verbalize techniques to prevent urinary retention.
Nursing Care Plan for Renal Calculi 3
Risk for Deficient Fluid Volume
Nursing Diagnosis: Risk for Deficient Fluid Volume related to vomiting secondary to the presence of renal calculi.
- The patient will be able to tolerate fluids without vomiting within 24 hours.
- The patient will have an adequate and equal amount of intake and output within 24 hours.
Nursing Care Plan for Renal Calculi 4
Deficient Knowledge
Nursing Diagnosis: Deficient Knowledge related to unfamiliarity with information resources about renal calculi as evidenced by frequent questions and clarification
- The patient will verbalize understanding of the disease process and potential complications of having renal calculi.
- The patient will participate and comply with the treatment plan.
Nursing Care Plan for Renal Calculi 5
Hyperthermia
Nursing Diagnosis: Hyperthermia related to urinary tract infection secondary to renal calculi as evidenced by high body temperature and flushed skin.
Desired Outcome: The patient will be able to maintain a normal body temperature after 4 hours of intervention and treatment.
Nursing References
Ackley, B. J., Ladwig, G. B., Makic, M. B., Martinez-Kratz, M. R., & Zanotti, M. (2020). Nursing diagnoses handbook: An evidence-based guide to planning care . St. Louis, MO: Elsevier. Buy on Amazon
Gulanick, M., & Myers, J. L. (2022). Nursing care plans: Diagnoses, interventions, & outcomes . St. Louis, MO: Elsevier. Buy on Amazon
Ignatavicius, D. D., Workman, M. L., Rebar, C. R., & Heimgartner, N. M. (2020). Medical-surgical nursing: Concepts for interprofessional collaborative care . St. Louis, MO: Elsevier. Buy on Amazon
Silvestri, L. A. (2020). Saunders comprehensive review for the NCLEX-RN examination . St. Louis, MO: Elsevier. Buy on Amazon
Disclaimer:
Please follow your facilities guidelines, policies, and procedures.
The medical information on this site is provided as an information resource only and is not to be used or relied on for any diagnostic or treatment purposes.
This information is intended to be nursing education and should not be used as a substitute for professional diagnosis and treatment.
Anna Curran. RN, BSN, PHN
Leave a Comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Int J Mol Med
Recent advances on the mechanisms of kidney stone formation (Review)
1 Department of Urology, People's Hospital of Longhua, Southern Medical University, Shenzhen, Guangdong 518109, P.R. China
2 Central Laboratory, People's Hospital of Longhua, Southern Medical University, Shenzhen, Guangdong 518109, P.R. China
Jianwen Zhang
Associated data.
Not applicable.
Kidney stone disease is one of the oldest diseases known to medicine; however, the mechanisms of stone formation and development remain largely unclear. Over the past decades, a variety of theories and strategies have been developed and utilized in the surgical management of kidney stones, as a result of recent technological advances. Observations from the authors and other research groups suggest that there are five entirely different main mechanisms for kidney stone formation. Urinary supersaturation and crystallization are the driving force for intrarenal crystal precipitation. Randall's plaques are recognized as the origin of calcium oxalate stone formation. Sex hormones may be key players in the development of nephrolithiasis and may thus be potential targets for new drugs to suppress kidney stone formation. The microbiome, including urease-producing bacteria, nanobacteria and intestinal microbiota, is likely to have a profound effect on urological health, both positive and negative, owing to its metabolic output and other contributions. Lastly, the immune response, and particularly macrophage differentiation, play crucial roles in renal calcium oxalate crystal formation. In the present study, the current knowledge for each of these five aspects of kidney stone formation is reviewed. This knowledge may be used to explore novel research opportunities and improve the understanding of the initiation and development of kidney stones for urologists, nephrologists and primary care.
1. Introduction
Kidney stone disease, also known as nephrolithiasis or urolithiasis, is one of the oldest diseases known to medicine. It is estimated that 1-15% individuals suffer from kidney stone formation at some point during their lifetime, and the prevalence and incidence of kidney stone is reported to be increasing worldwide ( 1 , 2 ). A recent study concluded that the prevalence of kidney stones was 5.8% among Chinese adults (6.5% in men and 5.1% in women), with about 1 in 17 adults currently affected ( 3 ). Without proper treatment, kidney stones can cause the blockage of the ureter, blood in the urine, frequent urinary tract infections, vomiting or painful urination, culminating in the permanent functional damage of the kidneys ( 4 ). The worldwide prevalence of urolithiasis has increased over the past decades. Urolithiasis is often a recurrent and lifelong disease with a recurrence rate of 50% within 5-10 years and 75% within 20 years ( 5 ). Some studies have indicated that an increase in kidney stone occurrence is expected, due to multiple environmental factors, including changes in lifestyle and dietary habits, as well as global warming ( 1 , 4 , 6 ). However, precise factors responsible for the upward prevalence and recurrence of urolithiasis have not been identified yet. Due to its high prevalence in adults of working age, kidney stone disease has a substantial impact on the individual and society, and has become a public health issue, particularly in populations residing in regions with a hot and dry climate ( 7 , 8 ).
There are mainly five types of kidney stones according to the mineralogical composition, including calcium oxalate (CaOx; 65.9%), carbapatite (15.6%), urate (12.4%), struvite [(magnesium ammonium phosphate), 2.7%], brushite (1.7%) ( 9 , 10 ). Kidney stones can be broadly categorized into calcareous (calcium containing) stones and non-calcareous stones. The most common types of human kidney stones are CaOx and calcium phosphate (CaP), either alone or combined, which are calcareous and radio-opaque stones ( 9 , 11 ). Kidney stones form at a foundation of CaP termed Randall's plaques (RPs), which begins at the basement membranes of thin limbs of the loop of Henle on the renal papillary surface ( 12 ). CaOx and urate stones exhibit a higher occurrence in males, whereas higher percentages of carbapatite and struvite stones are observed in females than in males ( 10 , 13 ). However, the role of sex differences in the pathophysiological mechanisms of urinary stone disease are not yet fully understood.
Regardless of the type, kidney stone formation is a complex and multistep process that includes urinary supersaturation, crystal nucleation, growth and aggregation ( 11 , 14 ). Kidney stone formation is associated with systemic disorders, including diabetes ( 15 ), obesity, cardiovascular diseases, hypertension and metabolic syndrome ( 16 , 17 ). Conversely, nephrolithiasis patients [also known as kidney stone formers (KSF)] are at a risk of developing hypertension ( 18 ), chronic kidney disease (CKD) ( 19 ) and progression to end-stage renal disease (ESRD) ( 20 , 21 ). Multiple promoting factors and inhibitors have been reported to play critical roles in kidney stone formation. For example, hyperoxaluria, hyperuricosuria and phosphaturia are common promoting factors linked to kidney stone formation ( 22 , 23 ); inter-α-inhibitor (IαI), a member of the protease inhibitor family, has been shown to inhibit CaOx crystallization in vitro ( 24 ).
Although details of human stone formation have accumulated, kidney stone formation and growth mechanisms are far from being clarified. The present review provides an update on the mechanisms of kidney stone formation, in order to improve the understanding of kidney stones for urologists, nephrologists and primary care givers.
2. Physicochemical mechanism of kidney stone formation
Urinary supersaturation and crystallization are the driving force for intrarenal crystal precipitation and is mainly caused by inherited or acquired diseases associated with renal function impairment. Additionally, urinary supersaturation and crystallization are influenced by urine pH and specific concentrations of substance excess, including CaOx, CaP, uric acids and urates, struvite, amino acids (cysteine), purines (2,8-dihydroxyadenine and xanthine) and drugs (e.g., atazanavir, sulfamethoxazole, amoxicillin, ceftriaxone) ( 25 , 26 ). Additionally, crystal formation and development are influenced by multiple modulator molecules, which are known as receptors, promoters and inhibitors.
Promoters of stone formation
A number of receptors or receptor-like features have been reported to play critical roles in crystal-cell interaction, which is recognized as the most important process for crystal retention in kidney ( 8 , 27 ). Recently, protein alterations in a CaOx monohydrate (COM) crystal-cell interaction model were screened by the authors, and 1,141 differentially expressed proteins (DEPs) were identified in COM treated HK-2 cells ( 28 ). Proteins and glycosaminoglycan like CD44, nucleolin, hyaluronan (HA), heat shock protein 90 (HSP90) ( 29 ), Annexin II ( 30 ) and osteopontin (OPN) ( 28 , 31 ), have been reported to act as stone formation modulators, which has been thoroughly reviewed previously ( 32 ). Several structures and molecular components also play the role of receptor in crystal attachments, including the phosphatidylserine component of the lipid bilayer and the acidic side chains of proteins ( 33 ). Calcium, oxalate, urate and phosphate ions are the main promoters of crystal formation, which can promote crystallization of stone constituents or their aggregation through the activation of several mechanisms. Ketha et al ( 34 ) demonstrated that the first time nephrolithiasis patients had increased serum calcium and 1,25(OH)2D levels than the corresponding healthy individual serum calcium levels, suggesting that stone formation is a manifestation of altered calcium and vitamin D regulation. Higher serum calcium concentration acts as a promoter in lithogenesis, which directly regulated by the calcium-sensing receptor (CaSR) through different pathways ( 35 ). Similarly, urate and phosphate ions have also been reported to promote heterogeneous nucleation and enhance the attachment of crystals to epitheliums ( 36 , 37 ). Another important promoter of stone formation is urine pH ( 38 ). Low pH urine may lead to CaOx crystallization and crystal precipitation ( 39 ). High-alkaline urine may also promote precipitation and nucleation of CaOx crystals ( 40 , 41 ). Lysozyme and lactoferrin are two most recently identified proteins that promote COM growth through the acceleration of layer advancement rate on crystal surfaces ( 42 ).
Inhibitors of stone formation
Normal urine contains numerous inhibitors that act both in competition and cooperation, consequently decrease crystallization and inhibit crystals aggregation and/or adhesion to the tubular epithelial cells ( 43 , 44 ). These inhibitors can be divided into three groups: Anions, metallic cations and macromolecules. Anions such as citrate, can inhibit crystal growth very efficiently, at concentrations above 0.1 mM ( 45 , 46 ). A majority of nephrolithiasis patients exhibited a decrease in citrate excretion. Alkali supplements are widely used for hypocitraturic recurrent nephrolithiasis patients to restore citrate excretion ( 47 , 48 ). Hydroxycitrate is a structural analog of citrate, which has been reported to show equivalent capacity in forming complexes with calcium, in order to inhibit crystallization ( 49 , 50 ). Metallic cations such as magnesium, have been reported to inhibit crystal growth and aggregation, which is synergistic with citrate in acidic environments ( 51 - 53 ). Macromolecules are the most effective inhibitors of crystal growth. More specifically, OPN, Tamm-Horsfall protein (THP), urinary prothrombin fragment 1 (UPTF-1), nephrocalcin (NC) and some subunits of the serum IαI are able to inhibit crystal growth, aggregation and/or adhesion to the tubular cells ( 11 , 38 , 45 ).
However, there is a competition between supersaturation and inhibitors of crystallization as mentioned above, which ultimately determines the pattern of crystalluria in nephrolithiasis patients and healthy individuals ( 54 ). As a consequence of the increased promoters and reduced inhibitors, crystal formation and kidney stone occurrence have been observed ( Fig. 1 ).

Physicochemical mechanisms of kidney stone formation. The reduced inhibitors (left panel) and increased promoters (right panel) are suggested to play critical roles in kidney stone formation.
3. Randall's plaque and calcium oxalate stone formation
RPs, first proposed by Alexander Randall in 1937 ( 55 ), are regions of subepithelial mineralized tissue at the papillary tip, surrounding the openings of the ducts of Bellini containing CaP ( 56 ). Scanning electron microscopy (SEM) examination has shown that RP are made of a mixing of tubules with calcified walls and of tubules obstructed by CaP plugs ( 57 ). RP consists of CaP crystals mixed with an organic matrix that is rich in various proteins and lipids, and includes membrane-bound vesicles or exosomes, collagen fibers, as well as other components of the extracellular matrix ( 58 ). An increasing number of studies have suggested that RPs are the origin of renal stones ( 57 - 60 ). Winfree et al ( 61 ) clarified that kidney stones develop as an overgrowth on RP, which contains unique organic composition (fibrillar collagen) that can be differentiated from the stone overgrowth by specific autofluorescence signatures. Of note, a previous study using a murine mode of RP revealed that vitamin D supplementation and calcium intake could notably accelerate RP formation ( 60 ). However, the precise mechanisms of RP formation remain unclear.
Recently, studies indicated that long non-coding RNAs (lcnRNAs) H19 and MALAT1 mediated osteogenic differentiation of human renal interstitial fibroblasts (hRIFs) and participated in RP formation ( 62 - 64 ). lcnRNA H19 has been shown to be significantly upregulated in RP, which can promote the osteogenic differentiation of hRIFs by activating Wnt/β-catenin signaling ( 63 ). lcnRNA H19 can also serve as a facilitator in the process of CaOx nephrocalcinosis-induced oxidative stress and renal tubular epithelial cell injury through the interaction with miR-216b and exerts its effect via the HMGB1/TLR4/NF-κB signaling pathway ( 64 ). lcnRNA MALAT1 can function as a competing endogenous RNA (ceRNA) that sponges miR-320a-5p, upregulates Runx2 expression and thus promotes the osteogenic phenotype of hRIFs ( 62 ).
These studies provide novel insight into the pathogenesis of RP-mediated kidney stone disease, while further studies are urgently anticipated to explore the mechanisms of RP formation, as well as additional roles of RP in the context of stone formation.
4. Role of sex hormones in calcium oxalate nephrolithiasis
Statistical analyses have revealed that males have a higher incidence of CaOx nephrolithiasis than females at a ratio of 2-3:1 ( 4 , 65 ); however, the exact mechanism remain unclear. Previous studies have indicated that androgens increase and estrogens decrease urinary oxalate excretion, plasma oxalate concentration and kidney CaOx crystal deposition. Additionally, enhanced androgen signaling may be responsible for the association between sex and kidney stone formation ( 65 - 68 ). Androgen receptor (AR) signaling can directly upregulate hepatic glycolate oxidase ( 69 ) and kidney epithelial nicotinamide adenine dinucleotide phosphate oxidase (NAPDH), subunit p22-PHOX at the transcriptional level, so as to increase oxalate biosynthesis, ultimately leading to kidney stone formation ( 70 ). Peng et al ( 71 ) reported that testosterone contributes to nephrolithiasis development through the induction of renal tubular epithelial cells apoptosis and necrosis through HIF-1α/BNIP3 pathway. Changtong et al ( 72 ) revealed that testosterone could promote kidney stone disease via the enhanced COM crystal-cell adhesion by the increased surface α-enolase. Zhu et al ( 73 ) demonstrated that AR can inhibit the recruitment of macrophages and suppress the COM crystals phagocytic ability of macrophages via the decrease of the colony-stimulating factor 1 (CSF-1) signals, through miR-185-5p upregulation. These findings suggest that androgen receptor signaling may be a key player in the development of nephrolithiasis ( Fig. 2 ).

Role of sex hormones in calcium oxalate nephrolithiasis. The AR signaling could induce TECs apoptosis and necrosis and kidney tubular injury, promote COM crystallization and oxalate biosynthesis; however, macrophage recruitment and crystal phagocytosis are inhibited. Conversely, ER signaling can reduce ROS-mediated kidney tubular injury and COM crystallization. COM, calcium oxalate monohydrate; AR, androgen receptor; ER, estrogen receptor; ROS, reactive oxygen species.
Theoretically, AR may be a new potential target and can be evaluated for novel therapeutics for the suppression of kidney stone formation. The 5α-reductase inhibitor, finasteride, has been reported to abolish the promoting effect of testosterone on COM crystallization ( 74 ). Another newly developed AR degradation enhancer, dimethylcurcumin (ASC-J9), has been reported to suppress oxalate crystal formation via the modulation of oxalate biosynthesis and reactive oxygen species (ROS)-induced kidney tubular epithelial cell injury in a rat model ( 73 ). Reversely, estrogen may serve as a protective factor against kidney stone formation. An in vitro study demonstrated that estrogen led to changes in the cellular proteome of [Madin darby canine kidney (MDCK)] renal tubular cells that led to the decreased CaOx crystal receptor surface expression (annexin A1 and α-enolase), reduced intracellular ATP, and enhanced cell proliferation and renal tubular cell tissue healing ( 75 ). There is evidence to suggest that estrogen receptor β (ERβ) can suppress oxalate-induced oxidative stress via transcriptional suppression of the NADPH oxidase subunit 2 (NOX2) through the direct binding to the estrogen response elements (EREs) on the NOX2 5′ promoter ( 76 ), which exerts protective effects on renal CaOx crystal deposition.
All these findings may partly explain why a higher incidence of nephrolithiasis is encounter in males than in females. Targeting AR may be developed as a potential therapy for CaOx crystal-related kidney stone disease. However, these studies were performed in vitro and in vivo , using only cell lines or animal models. Further validation and clinical studies are required. Finasteride and ASC-J9 have been demonstrated to suppress a number of AR-mediated diseases, including prostate cancer ( 77 , 78 ), liver cancer and spinal and bulbar muscular atrophy neuron disease ( 79 ). However, additional future studies are necessary before the clinical application of finasteride and ASC-J9 in kidney stone prevention, considering the side-effects, including sexual dysfunction ( 80 ).
5. Role of the microbiome in stone formation
Emerging evidence has indicated that microorganisms belonging to the human microbiome, including microorganisms of the kidney and urinary tract, are likely to have a profound effect on urological health, both positive and negative, due to their metabolic output and other contributions ( 81 ).
Urease-producing bacteria
Urease-producing bacteria, such as Proteus mirabilis, Klebsiella pneumonia, Staphylococcus aureus, Pseudomonas aeruginosa, Providentia stuartii, Serratia and Morganella morganii , are always associated with struvite stone formation and recurrence ( 82 , 83 ). The bacterial urease degrades urea and promotes ammonia and carbon dioxide formation, leading to urine alkalinization and phosphate salt formation ( Fig. 3 ).

Role of urease-producing bacteria in stone formation. The urease-producing bacteria split urea and promote the formation of ammonia and carbon dioxide, leading to kidney tubular injury and urine alkalinization and subsequent formation of phosphate salts.
Urinary acidification and urease inhibitors have been proposed and implemented for the prevention and/or dissolution of struvite stones and encrustations in patients with infection by urea-degrading bacteria; however, their long term use is limited due to their ineffectiveness and toxicity ( 84 ). Secondarily infected stones caused by non-urease-producing bacteria, including Escherichia coli and Enterococcus spp., have also been described ( 85 , 86 ). However, whether kidney stones form and become secondarily infected or result from a nidus of infection that propagates stone formation remains largely unclear.
Nanobacteria (NB)
NB have been isolated from kidney stones for >30 years ( 87 - 89 ); however, the nature and the mechanisms involved remain obscure. Ansari et al ( 90 ) demonstrated that the size of cultured NB varies between 60 and 160 nm, and that they could infect patients with apatite kidney stone. Kajander et al ( 91 ) indicated that NB can adapt to growing in plain DMEM or RPMI-1640, through self-proliferation. In the study by Ciftçioglu et al ( 92 ), it was demonstrated that 70 out of 72 (97.2%) kidney stones contained NB. The presence of NB was independent of the stone type, although apatite-based kidney stones presented the highest immunopositivity ( 91 ). NB are considered to play roles in calcium nucleation, as they can produce sufficient calcium apatite in their cell walls to initiate pathologic calcifications and stone formation ( 93 - 95 ). This evidence is strongly in favor of the suggestion that NB are living organisms.
However, an increasing number of studies have indicated that NB, also termed 'Calcifying nanoparticles (CNPs)', 'nanobacteria-like particles' or 'Nanobes', are merely mineral protein nanoparticles with biomimetic functions ( 88 , 89 ). Although the definition and nature of these nanoparticles remains controversial ( 96 ), their roles in kidney stone diseases has been widely reported. CNPs have been identified in RPs and have been proven to be cytotoxic to 3T6 fibroblasts and HK-2 cells in vitro ( 89 ), which contributes to the renal tubular epithelial cell injury linked to kidney stone formation. Hong et al ( 97 ) demonstrated that catalase (CAT) and malonaldehyde (MDA) levels were significantly higher in CNP-treated HK-2 cells than the HK-2 control group, suggesting that CNPs may induce lipid peroxidation and result in damaging HK-2 cells. Wu et al ( 89 ) demonstrated that the CNPs may: Induce ROS production through JNK activation; decrease mitochondrial membrane potential and promote cell apoptosis through the downregulation of Bcl-2 expression and the upregulation of Bax expression; lead to autophagy through the upregulation of microtubule-associated proteins 1A/1B light chain 3B (LC3-II) and Beclin-1 expression ( Fig. 4 ).

Role of nanobacteria in stone formation. The nanobacteria may induce ROS production through the JNK/p-JNK signaling induction, may decrease mitochondrial membrane potential and promote cell apoptosis through the downregulation of Bcl-2 expression and the upregulation of Bax expression. Additionally, nanobacteria may lead to autophagy through the upregulation of LC3-II and Beclin-1 expression. ROS, reactive oxygen species; LC3-II, microtubule-associated proteins 1A/1B light chain 3B.
According to currently available findings in the literature, NB are localized in high concentrations in kidneys, excreted in urine, are isolated from RPs and the majority of renal stones, and play the role of the initiator, by favoring nucleation and crystal formation. Continued investigations are required, in order to solve the controversy of whether NB are living or non-living, as well as the mechanisms through which NB induce calcification and stone formation.
Intestinal microbiota
The intestinal microbiome, which has been a recent area of wide interest, has been reported to play a role in both the pathogenesis and prevention of kidney stone disease ( 87 , 98 - 100 ). Oxalobacter formigenes is the most well-studied Gram-negative anaerobic bacterium that degrades oxalate in the intestinal tract and has potential probiotic characteristics for the prevention of CaOx kidney stone formation.
In a pilot study, Stern et al ( 101 ) investigated the distinct differences in the gut microbiome of nephrolithiasis patients, as compared with patients without kidney stone formation. Their results demonstrated that the genus Bacteroides were 3.4-fold more abundant in the kidney stone group, while the genus Prevotella were 2.8-fold more abundant in the non-stone control group. A 24 h urine analysis revealed that the genus Eubacterium was inversely associated with oxalate levels and the genus Escherichia trended to an inverse correlation with citrate level ( 101 ). However, the potential causative role of pre-existing dysbiosis of gut microbiome in kidney stone disease is still unclear, and the association of urinary oxalate excretion and oxalate-degrading bacteria abundances remain limited ( 87 , 98 , 102 , 103 ).
Both absorptive and secretory pathways for oxalate have been identified in the proximal and distal segments of the colon, regulated by neuro-hormones that direct net oxalate level. Thus, it has been suggested that intestinal tract participates significantly in oxalate balance and subsequent oxalate homeostasis ( 104 - 106 ). The intestinal tract is also where oxalate-degrading bacteria tend to reside, particularly Oxalobacter formigenes , which requires a strict anaerobic environment to survive. One hypothesis for the role of the microbiome in the prevention of kidney stone has been that specific functional bacteria, such as the oxalate-degrading bacteria (such as Oxalobacter formigenes , Bifidobacterium sp. Porphyromonas gingivalis and Bacillus sp.) in human gut and intestinal tract, which use oxalate as their carbon energy source and thrive in the presence of the oxalate anion, exhibit growth inhibition in the CaOx crystallization in the kidney ( 102 , 107 , 108 ) ( Fig. 5 ).

Role of oxalate-degrading bacteria in stone formation. Oxalate-degrading bacteria use oxalate as a carbon energy source and thrive in the presence of the oxalate anion, reduce urinary oxalate level and exhibit growth inhibition in the calcium oxalate crystallization in the kidney.
The activity of oxalate-degrading bacteria mediates extra-renal elimination of oxalate in the intestines and has a significantly impact on the homeostatic levels of oxalate in plasma and urine ( 109 ). This activity exhibits a strong association with the occurrence of CaOx stone formation.
6. Immune response to urinary crystals
Macrophage accumulation and macrophage-related inflammation or anti-inflammation is the main immune response alteration observed in kidney stone disease, which has been widely reported to play a crucial role in renal CaOx crystal formation ( 110 ).
Firstly, the recruited macrophages could promote the development of COM crystals via the interaction of CD44 with OPN and fibronectin (FN) ( 111 ), which are upregulated in renal tubular cells induced by crystals. Secondly, macrophages have been evidenced to secrete various mediators via classical secretory pathways that cause renal interstitial inflammation ( 112 , 113 ), particularly macrophage inhibitory protein-1, monocyte chemoattractant protein-1 and interleukin-8 (IL-8) ( 112 ). These chemokines consequently enhance the recruitment of various immune cells, including monocytes, macrophages, neutrophils, dendritic cells and T-cells into the inflammatory locale ( 114 , 115 ). Several studies have demonstrated that macrophage-derived exosomes following COM exposure are involved in kidney stone pathogenesis ( 112 , 113 , 116 ). A set of proteins in COM-treated macrophage exosomes were previously identified as proteins involved mainly in immune processes, including T-cell activation and homeostasis, Fcγ receptor-mediated phagocytosis, interferon-γ (IFN-γ) regulation and cell migration ( 112 ). Additionally, infiltrated monocytes could differentiate into different macrophage subtypes with a wide range of clinical manifestations, presentations and histological phenotypes ( 110 , 117 ), display protective or pathogenic activities in kidney stone development ( 110 ).
Increasing evidence has revealed that M1/M2-macrophage differentiation plays an important role in renal CaOx crystal formation ( 111 , 115 , 118 - 120 ). However, whether M1 macrophage-mediated inflammation that contributes to stone formation will initiate stone promoters and reduce stone inhibitors remains controversial. Khan et al ( 58 ) demonstrated that M1 macrophages could cause acute tissue injury, which was associated with crystal deposition and RP formation. Conversely, Taguchi et al ( 121 ) concluded that there was no association between renal dysfunction and increased crystal deposition, based on their observation that no changes were observed in urinary variables in lipopolysaccharide (LPS)-induced M1 macrophage-mediated acute renal injury. M2 anti-inflammatory macrophages can phagocytize and degrade CaOx kidney stone fragments through a clathrin-dependent mechanism ( 110 , 113 , 115 , 120 , 121 ) ( Fig. 6 ).

Immune response to urinary crystals. Macrophage accumulation and macrophage-related inflammation or anti-inflammation is the main immune response alteration observed as a result of kidney stone formation. M1 macrophages are important effectors of CaOx stone formation, while M2 macrophages could prevent CaOx inflammatory damage through crystal phagocytosis. CaOx, calcium oxalate.
Given the critical role of immune-response in CaOx crystal formation and development, the immunotherapy approach has been proposed to prevent stone recurrences in certain individuals through the modulation of the immune response, in order to degrade CaOx crystals and thus prevent stones from developing ( 122 ). However, investigations into immunotherapeutic targets for kidney stone disease are urgently required.
7. Conclusion and future perspectives
In the present review article, emerging concepts of mechanisms contributing to stone formation were summarized, by reviewing novel insight into kidney stone disease related-metabolic risk factors, receptors, promoters and inhibitors, through the examination of the roles of immune-response, microbiome and sex hormones in stone formation and development. The pathophysiology of kidney stone disease cannot be completely explained by crystallization processes alone. However, due to current limitations in research, there are still some research areas in kidney stone formation that remain poorly understood, and were not been discussed herein. Future comprehensive studies are mandatory to further elucidate the mechanisms of the microbiome and immune response in kidney stone formation, in order to develop novel prophylactic and therapeutic approaches.
Acknowledgments
Funding statement.
The present study was supported by the National Natural Science Foundation of China (grant no. 81802566), and Shenzhen Science and Technology Program (Basic Research Project, grant no. JCYJ20180228163919346).
Availability of data and materials
Authors' contributions.
ZW and YZ prepared and drafted the manuscript. ZW obtained funding for the study, and drafted and revised the manuscript. QD, JZ and HL assisted in obtaining data for the review article, drafted the manuscript and provided critical revision of the manuscript for intellectual content. ZW and HL confirm the authenticity of all the raw data. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
Patient consent for publication, competing interests.
The authors declare that they have no competing interests.

IMAGES
VIDEO
COMMENTS
Case study. History. ... The majority of kidney stones contain calcium (approximately 90% in men and 70% in women) while the remainder consist of cystine (<1%), pure uric acid (10-15%) and struvite (10-15%). 7 Calcium based stones are most commonly composed of calcium oxalate, calcium phosphate or both. Several factors can affect stone ...
Although a 24-hour urine study provides valuable information regarding the contents of a patient's urine and their metabolic status, it does not substitute for stone analysis. Per the most recent AUA guideline for the medical management of kidney stones, when a stone is available, it should be sent for analysis. 16
This case study explores the presentation of Sally Jones, a 56-year-old lady that shows signs of kidney stones and AKI as she presents to the ED. The case discussion will include the pathophysiology of kidney stones and AKI that includes the clinical manifestations by Ms. Jones during the admissions.
Urinary tract stones are a general term for stone disease in various parts of the urinary system and are common diseases of the urinary system. According to the location of the stone, it is divided into kidney stones, ureteral stones, bladder stones, urethra stones. Total urinary calculi occur less frequently, usually accompanied by severe ...
Urolithiasis, commonly known as renal calculi or kidney stones, is a prevalent and painful condition that affects millions of individuals worldwide. These solid mineral and salt deposits form within the urinary tract and can cause excruciating pain and complications if left untreated. As nurses, it is imperative to have a comprehensive understanding of urolithiasis to provide effective care ...
Bradley G. Collins, MD. Case. A 36-year-old woman with a 2-week history of left flank pain presented to the ED via emergency medical services. The patient, who had a history of nephrolithiasis, assumed her pain was due to another kidney stone. She stated that while waiting for the presumed stone to pass, the pain in her left flank worsened and ...
Kidney stones: pathophysiology, diagnosis and management. A case study approach. Abstract The prevalence of kidney stones is increasing, and approximately 12,000 hospital admissions every year are due to this condition. This article will use a case study to focus on a patient diagnosed with a calcium oxalate kidney stone.
sound or abdominal (kidney-ureter-bladder, KUB) radiograph may be used. However, operator experience may affect ultrasound results; and some stones are radiolucent on a KUB radiograph. Additional studies such as serum uric acid, para-thyroid hormone, and 25-hydroxy vitamin D may be needed based on the results of these initial studies.
Case study Figure. DH, a 70-year-old White male, accompanied by his son, arrived at the ED with complaints of excruciating left flank pain. ... Renal calculi, also known as kidney stone disease or nephrolithiasis, ... Nursing interventions include performing a focused abdominal assessment, placing a 20 gauge or larger I.V. access, providing ...
A case study appr oach. Abstract. The prevalence of kidney stones is increasing, and approximately 12,000 hospital admissions. every year are due to this condition. This article will use a case ...
The prevalence of kidney stones is increasing, and approximately 12 000 hospital admissions every year are due to this condition. This article will use a case study to focus on a patient diagnosed with a calcium oxalate kidney stone. It will discuss the affected structures in relation to kidney stones and describe the pathology of the condition.
Two case studies in this article describe the diagnosis and management of cystinuria, the most common rare kidney stone disorder. Keywords: Genetic kidney disease, tiopronin, disorders of amino acids, kidney stones, nephrolithiasis, urolithiasis. Kidney stones, particularly those that present in childhood, may be due to rare inherited metabolic ...
There are four main types of kidney stones — calcium stones, uric acid stones, struvite stones, and cystine stones. Nursing Care Plans and Management. Nursing goals for patients with urolithiasis aim to provide comprehensive care to manage pain, prevent complications, and facilitate the passage of kidney stones. Nursing Problem Priorities
Kidney stones or renal calculi are hard deposits formed from minerals and salts in the kidneys that cause pain and complications as they move through the urinary tract. ... Educate on performing a 24-hour urine study. ... home health, case management, travel nursing, and telehealth, but her passion lies in educating through writing for other ...
Case 5 • 73 year old male • 1st stone at age 24 • Prior R open pyelotomy, L PCNL, SWL x 12 • Previous stone CaOx, now CaP • Told previous needed to increase fluid hydration • Labs: Creatinine 1.09, calcium 8.2 • CT imaging: L hydronephrosis with 10, 17, 7 mm renal and 6mm ureteral stone, R 6, 9, 1 mm
227. Renal Calculi: An Evidence Based Case Study. Dr. Abhijit Chakma *. Qualification : MD (Homoeopathy) Designation : Senior Research Fellow (Homoeopathy) Place of work : Clinical Researc h Unit ...
Kidney Stone (Urolithiasis) Nursing Care Plan. Kidney stones or Renal calculi are hard masses formed in the different sites of the urinary tract. The process of stone formation is called urolithiasis, renal lithiasis, or nephrolithiasis. The most common mineral deposits are calcium oxalate and calcium phosphate, and it is commonly found in the ...
A study of bone mineral density scores showed an inverse relation to urinary calcium excretion in individuals who form kidney stones but not in those without kidney stones. 40 In an analysis of NHS postmenopausal women without baseline osteoporosis, a history of kidney stones was associated with an 18% higher risk of wrist fracture, but there ...
Among first-time symptomatic kidney stone formers in the community, the recurrence rate for a confirmed symptomatic episode resulting in clinical care is 11% at 2 years, 20% at 5 years, 31% at 10 ...
Diets high in animal protein can increase the uric acid level. 9% of kidney stone cases are uric acid stones. Cystine Stones. This is a rare type of kidney stone caused by a congenital disorder called cystinuria caused by a defective cystine metabolism and transport leading to stones. This rare type of kidney stone accounts for 1% of the cases.
References ARUPConsult.com UpToDate.com Coe F, Parks J, Asplin J. The pathogenesis and treatment of kidney stones. New Eng J Med 1992;327:1141-1151 Daudon M, Marfisi C, Lacour B, Bader C. Investigation of urinary crystals by Fourier Transform Infrared Microscopy. Clin Chem 1991; 37:83.87. Jager P. Genetic versus environmental factors in renal stone disease.
Kidney stone disease is a crystal concretion formed usually within the kidneys. It is an increasing urological disorder of human health, affecting about 12% of the world population. It has been associated with an increased risk of end-stage renal failure. The etiology of kidney stone is multifactorial. The most common type of kidney stone is ...
Traditionally, the building stones used in the architectural heritage of Galicia (Spain) during the past were mainly extracted from quarries located in the surrounding areas of the historical buildings. Thus, a great variety of monuments were built with the same type of granite but with different degrees of weathering depending on local conditions, geological context (facies), and period of ...
1. Introduction. Kidney stone disease, also known as nephrolithiasis or urolithiasis, is one of the oldest diseases known to medicine. It is estimated that 1-15% individuals suffer from kidney stone formation at some point during their lifetime, and the prevalence and incidence of kidney stone is reported to be increasing worldwide (1,2).A recent study concluded that the prevalence of kidney ...