An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Obstet Gynaecol India
- v.67(5); 2017 Oct


Influence of Research on Health Policy and Clinical Practice
Hafizur rahman.
Sikkim Manipal Institute of Medical Sciences, 5th Mile, Tadong, Gangtok, Sikkim India
Clinical research is a type of biomedical research conducted to aid and support the development of knowledge wherein there is involvement of patient. One of the key duties of healthcare professionals is to involve in research and change existing practice, when there is robust evidence in favour of new strategies that can have better patient care. Knowledge derived from research and experience may be of little value unless it is put into practice. Evidence-based medicine (EBM) is the diligent, clear, and wise use of current best research evidence in making decisions about clinical care of patients. The practice of EBM is incorporating clinician’s expertise with the best available clinical evidence from research. It leads to improved patient outcomes and promote critical thinking and reflective practice. Effective research utilization can enhance policy decisions, resource allocation for programmes, and decisions about how to deliver those services.
Introduction
Biomedical research is the basic research, applied research, or translational researches conducted to support evolution of new knowledge in the field of medicine. An important type of medical research is clinical research, which is distinguished by the involvement of patients. The increased lifespan of humans over the past century can be significantly attributed to advances resulting from medical research [ 1 ].
Clinical research or trials in obstetrics and gynaecology have significantly increased in number, size, and quality in the past few years. A well-planned and executed trial particularly multicentre trail or randomized trials can generate robust evidence that change health policy and clinical practice [ 2 ].
Why Participation in Research is Important in Obstetrics and Gynaecology?
Positive effects on the care of women.
Participation in research can improve women’s health services and outcomes. It is well recognized that research findings improve the future care of women. The improved outcomes observed in the women involved in a clinical trial may be due to positive change in the behaviour of the clinician, improved provision of care such as prompt action on the investigation findings, or better nursing care by virtue of being in a trial. Improved outcome may also because of strict compliance with the research protocol with standard guidelines, management with a new method that may be beneficial and positive attitude, knowledge, and clinical expertise of the clinicians involved in research, thereby improving the care of women [ 3 ].
Delivering the Duties of a Healthcare Professional
One of the key duties of healthcare professionals is to change existing interventions, when there is robust evidence in favour of new strategies that can improve the health of women. This objective cannot be achieved without participation in research. Clinicians are expected maintain high-standard safety measures in the care of women by working collaboratively with the women themselves and with professional colleagues, helping to resolve controversies and uncertainties in management [ 4 ].
Audit or Research?
Clinical audit and research have many similarities. Clinical audit is a quality enhancement process with objectives to improve patient care and outcomes through systematic review of provided care against standard criteria and the implementation of necessary changes. Systematic evaluation of the structure, procedures, and outcomes of care is compared against standard criteria. Where necessary, changes are implemented at an appropriate level and further evaluation is done to confirm improvement in healthcare standard. Review of evidence by National institute of Clinical Excellence (NICE) concluded that audit is an effective method for improving the standard of quality of clinical care [ 5 ].
Both research and audit start with a question, both aim to change or influence clinical practice, both require proper clinical data collection, and both depend on a rigorous methodology and design to achieve sound conclusions. The standards of audit in terms of design, data collection, and analysis should be as high as for research, as audit potentially leads to change more often than research does and often does much greater change. Both audit and research differ from normal clinical practice because normal clinical practice rarely involves in such high standard of data collection or analysis [ 6 ].
The major administrative difference between audit and research is that research aims to achieve new knowledge and finding out which treatments is the most effective, whereas clinical audit is about quality of care and to find out whether the best practice is being practised. Research gives information what we should be doing and clinical audit find out whether we are doing right thing what we should do [ 7 ].
Evidence-Based Medicine
Evidence-based medicine (EBM) is the diligent, clear, and wise use of current best research evidence in making decisions about clinical care of patients. The practice of EBM is integrating clinician’s expertise with the best available clinical evidence from systematic reviews or meta-analysis [ 7 , 8 ]. Individual clinical expertise is the proficiency and sound clinical judgment obtained through years of clinical experience and clinical practice. Increased expertise is observable in effective and logical diagnosis and in the more thoughtful identification and empathetic use of individual patients’ clinical situation, rights, and prerogative in making clinical decisions about their individual care. External clinical evidence both disproves previously accepted diagnostic tests and treatments and replaces them with new ones that are more robust, valid, effective, and guarded [ 8 ].
Good clinician uses both individual clinical expertise and the best available evidence, and so both are indispensable. Without clinical expertise, clinical practice is risky, for even excellent external evidence may be inapplicable to or inappropriate for an individual patient. Without up-to-date evidence, clinical practice runs out of date and may be harmful to patients. EBM is not restricted to meta-analyses and randomized controlled trials. It involves tracing out the best available evidence with which to answer clinical questions in a particular clinical situation [ 8 ].
Practice of True Evidence-Based Medicine
True EBM takes care of individual patients as its greatest importance, determining prime care method for particular clinical situation. To practise such clinical care, evidence must be individualized for the patient [ 9 ]. For research or evidence to be most user friendly, they must be expressed like the number needed to treat, number needed to harm, and number needed to screen and so that clinicians, together with their clients, can make a free voluntary decision on appropriate care method [ 10 ].
Practice of true EBM is based on sound clinical judgement not restricted by rules. A new clinician may work on a long history, clinical examination, and a number of diagnostic tests. On the other hand, an expert clinician makes a rapid initial differential diagnosis from a brief history and examinations, and then uses only a few selected tests to arrive at a diagnosis and to rule out other possibilities [ 11 ].
Practice of true EBM builds a strong bond between patient and clinician. It ensures uninterrupted care and empathetic listening of the patient, especially in grave clinical situations. Along with practice of EBM, clinicians are also expected to provide detailed information to patients and make ethical and clinical judgments, and socially accepted role to care, console, and ease to sufferings [ 11 ].
To deliver true evidence-based medicine, all the stakeholders must be proactive and diligent. Patients must demand better evidence, better presented, better explained, and applied in a more personalized way. Clinician’s training and knowledge should go beyond searching and critical appraisal of evidence to expertise in judgment and joint decision-making skills with patient. Producers of evidence and clinical guidelines need to clearly highlight who will use them, the scope, purposes, and situations. The publishers must raise their standard and publish studies fulfils usability standards with sound methodological ones [ 2 ]. To support true evidence-based practice, researchers, clinicians, and policy makers must avoid the instrumental generation and use of evidence by vested interests [ 12 ].
Real Evidence Influencing the Policy Makers
Use of research evidence in the management of health system and policy making is a big challenge. Knowledge translation and exchange among relevant stakeholders is essential to make use of the benefits of research advances in strengthening health systems and improving people’s health [ 13 ]. Much research evidence is not presented or communicated at appropriate manner, and most health managers and policy makers do not always have the appropriate skills and capacity to find and use research evidence [ 14 ].
Several factors can influence research evidence to put into decision and policymaking, e.g. the local context, poor communication among researchers, policy makers, and stakeholders, research evidence is not timely, relevant, or inappropriate [ 13 ]. The researchers and policy makers have to play an important role in dealing with these factors and make evidence into practice.
Caplan [ 15 ] described “two-community theory” to explain the poor associations between researchers and policy makers. The researchers and policy makers may have difference in awareness, attitude, and objectives to the problem that can cause miscommunication and sometimes rivalry among them [ 13 ]. Such miscommunication may put a lengthy and laborious study conducted over years may not find the attention of policy makers [ 16 ]. Frequently, a good research finds the right policy maker at the right time, but there are other factors (political forces, bureaucracies etc.) to play role in implementing agendas to be taken into account [ 16 ]. Sometime good evidence may not see appropriate light as the researcher does not communicate his research to a policy maker for fear of losing the autonomy of the research, or poorly trained or inexperienced policy makers using evidence in the first place [ 17 ]. A policy maker may not also incorporate research into decision-making because of a lack of contact with the researchers and research that is not timely, high quality, or relevant. One systematic review identified that factors such as interactions between researchers and healthcare policy makers and timing/timeliness appear to increase the prospects for research use among policy makers. It concluded that researchers could help to ensure that the future flow of evidence will better inform healthcare management and policymaking by involving healthcare managers and policy makers in their production and better highlighting information that is relevant for decisions [ 18 ].
Incorporating Evidence into Policy Making and Practice
Knowledge obtained from research and expertise is of little value unless it is put into practice. Knowledge translation and exchange become apparent to take up this challenge and to narrow the “know–do” gap [ 18 , 19 ]. To reduce this knowledge–practice gap and maximum utilization of research evidence, numerous frameworks have been designed. A very comprehensive framework taking a holistic view of the health system, different barriers, and influential factors on decision-making has been developed by world health organization [ 19 ]. This framework describes seven main domains that can be helpful in transferring knowledge to action—a) preparing a climate and context for research use, i.e. organization or institution undertakes activities to establish a climate and context where research evidence is used in decision-making, b) linkage and exchange efforts examine the relationships needed to enable the use of evidence, c) knowledge creation looks at the opportunities and existing capacity to conduct relevant research in the local context, d) push efforts, usually undertaken by researchers or intermediaries whether the information is pushed to different user groups to disseminate research evidence to potential users in appropriate formats, e) pull efforts are the efforts of policy makers to seek and use research on appropriate context, f) facilitating pull efforts relates to appropriate systems and infrastructure (technical infrastructure, “one-stop websites”, and unrestricted access to online resources and journals) in place that enable access to relevant research, g) evaluation efforts to monitor the implementation and to evaluate the impact of evidence on practice. It has to be noted that although this type of framework has been proposed to implement research into policy making, evidence is lacking on such frame work or ideas [ 20 ]. Further research is needed in this area.
Irrespective of the framework employed to narrow knowledge–action gap, ultimately research utilization enhances policy decisions, resource allocation for programmes, and decisions to deliver those services [ 21 ]. It leads to improved patient outcomes and promote critical thinking and reflective practice among health professionals. It also ensures safe and effective clinical practice based on relevant, scientifically sound knowledge. Effective research utilization validates researcher efforts, motivates researchers to continue to work for new knowledge, and reinforces professional responsibility [ 22 ].
Research utilization in policymaking may be instrumental, conceptual, or symbolic. Instrumental use is direct use of research finding in policy formulation; conceptual use is gradual incorporation of insight, theories, concepts, and perspectives, whereas symbolic use denotes use of research to support continuation of an already running protocol [ 23 ].
Evidence-Based Policy Making Role of Government and Professional Organizations
When health professionals are expected by public and politicians to practise best evidence-based care, it is reasonable that this should be applicable to Government health policy also [ 24 ]. If health professionals are expected to base their decisions on the findings of recent research politicians, policy makers and their policy should also follow the rule. Individual patients may be at less risk from non-evidence-based policymaking but the dangers for the community as a whole may be higher. The impact of policies that are poorly designed and untested may be disastrous. So all health policies are subject to rigorous research prior to and after implementation what is known as health systems research (HSR). HSR has proved to be a useful tool for health decision makers at all levels over the past twenty years in industrialized countries, providing them with the necessary data for informed decision-making [ 23 ].
The problem in many health policies is that politicians holding office and policy makers may avoid research on particular policy for fear that the results will be politically unfavourable. For this reason, there needs to be independent organizations, continuing source of ideas and funding to support research and analysis relevant to policy. Many non-government organizations are associated with community that influences health policy.
Although some organizations have professional or sectional interests, many organizations may have a position of independence from which they must both analyse government policies and propose policies of their own or fund others to carry out research on such policies or practices. Of particular notable organization in this aspect is Federation of Obstetrics & Gynaecological Societies of India and other professional organizations of clinicians. For example, there should be the initiative in establishing a research programme to evaluate the government’s current cervical cancer control programme, the success of which is disappointingly low in India. An organized screening programme reduced the incidence and mortality by 80% in developed countries [ 25 ]. Despite being effective, most of the women in developing and under-developed countries do not have access or people are not participating in screening programme [ 25 ]. There should be health system research on the policy for maximal access of screening procedure including involvement of nursing staffs and other paramedical health professionals, financial incentives, and free coupon distributions to improve participation. Such continuing research on health policy may provide new dimensions of care for disadvantageous sections in developing countries.
Participation in research improves patient care, and it is also duty of a healthcare professional to keep them updated and to change existing interventions, when there is robust evidence in favour of new interventions. Good clinician uses both individual clinical expertise and the best available evidence, so both are indispensable. Practice of true evidence-based medicine has the care of individual patients as its top priority, deciding best course of action for particular clinical situation. Practice of true evidence-based medicine is based on sound judgement. Health systems research has proved to be a useful tool for health decision makers at all levels providing them with the necessary data for informed decision and policy making. Researchers must ensure the future flow of evidence for better healthcare management and policymaking by involving healthcare managers and policy makers in their production and better highlighting information that is relevant for decisions and policy making. Such continuing research will provide new dimensions in health care for disadvantageous sections in developing countries.
Dr Hafizur Rahman
is a Professor of Obstetrics and Gynaecology at Sikkim Manipal Institute of Medical Sciences at Gangtok, India. He has over 50 scientific research publications in international indexed journals, peer reviewer of more than a dozen international journals and editorial board member of several international and national journals. Dr Rahman was awarded with prestigious Shan S. Ratnam Young Gynaecologist Award (SSR-YGA) and Community Fellowship (CFP) by Asia and Oceania Federation of Obstetrics and Gynaecology (AOFOG) at XXIV Asia and Oceania Congress of Obstetrics and Gynecology (AOCOG) held in Borneo Convention Centre at Kuching, Malaysia in 2015. He was awarded with FOGSI Dr Pravin Mehta Fellowship in Laparoscopy in 2015 by Federation of Obstetrics and Gynaecological Societies of India and was FOGSI Dr Kamini Rao Yuva Orator from east zone in the year 2015–16. Sikkim Manipal University awarded him A++ (A double plus), University’s highest performance achievement award consistently for last eight years. He has been regularly invited as faculty at RCOG, AOCOG and IFFS World congress and All India Congress of Obstetrics and Gynaecology (AICOG) and won several awards for his presentations. He has also featured as an external examiner at various Indian university examinations. Dr Rahman is the founder Secretary of the Gangtok Obstetrics and Gynaecological Society and organized many CMEs, practical and research methodology workshops including 26th NEOGSCON in 2015 at Gangtok.

Compliance with Ethical Standards
Conflicts of interest.
Dr Hafizur Rahman is a Professor of Obstetrics and Gynaecology, Sikkim Manipal Institute of Medical Sciences, Gangtok, India.
“ ‘The important thing is not to stop questioning.” -Albert Einstein.
- Search Menu
- Sign in through your institution
- Advance Articles
- Editor's Choice
- Supplements
- Open Access Articles
- Research Collections
- Review Collections
- Author Guidelines
- Submission Site
- Open Access Options
- Self-Archiving Policy
- About Health Policy and Planning
- About the London School of Hygiene and Tropical Medicine
- HPP at a glance
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Introduction, supplementary data, data availability, author contributions, reflexivity statement, ethical approval, conflict of interest statement.
- < Previous
Using health policy and systems research to influence national health policies: lessons from Mexico, Cambodia and Ghana
- Article contents
- Figures & tables
- Supplementary Data
Daniel Llywelyn Strachan, Kirsty Teague, Anteneh Asefa, Peter Leslie Annear, Abdul Ghaffar, Zubin Cyrus Shroff, Barbara McPake, Using health policy and systems research to influence national health policies: lessons from Mexico, Cambodia and Ghana, Health Policy and Planning , Volume 38, Issue 1, January 2023, Pages 3–14, https://doi.org/10.1093/heapol/czac083
- Permissions Icon Permissions
Health system reforms across Africa, Asia and Latin America in recent decades demonstrate the value of health policy and systems research (HPSR) in moving towards the goals of universal health coverage in different circumstances and by various means. The role of evidence in policy making is widely accepted; less well understood is the influence of the concrete conditions under which HPSR is carried out within the national context and which often determine policy outcomes. We investigated the varied experiences of HPSR in Mexico, Cambodia and Ghana (each selected purposively as a strong example reflecting important lessons under varying conditions) to illustrate the ways in which HPSR is used to influence health policy. We reviewed the academic and grey literature and policy documents, constructed three country case studies and interviewed two leading experts from each of Mexico and Cambodia and three from Ghana (using semi-structured interviews, anonymized to ensure objectivity). For the design of the study, design of the semi-structured topic guide and the analysis of results, we used a modified version of the context-based analytical framework developed by Dobrow et al . (Evidence-based health policy: context and utilisation. Social Science & Medicine 2004; 58 :207–17). The results demonstrate that HPSR plays a varied but essential role in effective health policy making and that the use, implementation and outcomes of research and research-based evidence occurs inevitably within a national context that is characterized by political circumstances, the infrastructure and capacity for research and the longer-term experience with HPSR processes. This analysis of national experiences demonstrates that embedding HPSR in the policy process is both possible and productive under varying economic and political circumstances. Supporting research structures with social development legislation, establishing relationships based on trust between researchers and policy makers and building a strong domestic capacity for health systems research all demonstrate means by which the value of HPSR can be materialized in strengthening health systems.
Health policy and systems research (HPSR) has emerged as a field that aims to generate and document contextually specific evidence regarding what policies (and policy content) are most appropriate and most effective in achieving health and health systems’ goals in a given setting.
HPSR, and specifically the use of evidence in policy formation, is influenced by contemporary yet historically determined factors that are both external (e.g. how the health system functions within a given economic and political context) and internal (e.g. the purpose of HPSR in a given setting as well as the process itself and the participants) to the policy development process.
Building HPSR capacity can improve a nation’s ability to: (1)
develop sustained, integrated and context-based, national health-system responses to local health challenges, and cumulatively monitor and evaluate them; (2)
support the implementation of interventions based on evidence obtained from abroad and locally, together with critical appraisal and appropriate adaptation to ensure their local suitability, feasibility and utility.
HPSR is crucial to policy development while recognizing that researchers and research institutes are one part of a larger process characterized by multiple stakeholders, all with particular interests. The role of HPSR in the policy process is most effective, and most efficient, where the research component is embedded within the wider health system.
In recent decades, Health Policy and Systems Research (HPSR) has emerged as a field that generates effective policies and policy content for achieving health and health system goals (see Shroff et al. , 2017 ). Health systems are influenced by local and international political, social and economic factors, and health policy must be based on evidence specific to the national context ( Bennett et al. , 2011 ; Norris et al. , 2019 ). Local ownership and embedding of HPSR in health system processes are a catalyst for research uptake ( Koon et al. , 2013 ; Vanyoro et al. , 2019 ). HPSR investigates both contextual variables and stakeholder interests (see Sheikh et al. , 2014 ; Ghaffar et al. , 2017 ), generates the data needed for effective interventions (see Dobrow et al. , 2004 ; Sheikh et al. , 2014 ; George et al. , 2019 ; Schleiff et al. , 2020 ) and encompasses a broad view of health and of the determinants of health, as recognized in the Sustainable Development Goals ( Peters, 2018 ; Vanyoro et al. , 2019 ).
Dobrow and colleagues suggest that context is a critical factor in evidence-based health policy and that it is more critical to understand how evidence is utilized than how it is defined ( Dobrow et al. , 2004 ). The purpose of the study was therefore to generate insights into the issues that affect the practice of HPSR through the analysis of three different, indicative country settings: Mexico, Cambodia and Ghana. The three countries were purposively selected (see Case selection below) as they illustrate conditions across three different continents, each operating under different economic and political conditions, each adopting HPSR in different ways and each with different levels of achievement.
Mexico is a democratic federal republic comprising 31 states and the Federal District. The health system was established with the provision of healthcare to workers at the time of industrialization, and public health initiatives emerged in the 1920s to address infectious diseases after the national revolution ( Birn, 2006 ; González-Block et al. , 2020a ). Services are provided at national and state level through social health insurance for the formally employed, government-funded care for the uninsured and a growing private sector ( Laurell, 2015a ; Urquieta-Salomón and Villarreal, 2016 ; Parker et al. , 2018 ; Reich, 2020 ; González-Block et al. , 2020a ). Mexico invested comparatively early in HPSR structures, fostered close relationships between researchers and government, and appointed researchers to senior policy positions. The governing 1983 General Health Law and subsequent legislation provided the foundation for the role of HPSR in health-policy making, within the context of frequently changing political circumstances and priorities.
Cambodia is a small, post-conflict, lower-middle-income country in Southeast Asia experiencing relative stability and strong economic growth since the 1990s. Cambodia faced the challenge of rebuilding its social and economic structures in the aftermath of its prolonged conflict ( Mam and Key, 1995 ; Annear, 1998 ). Following the peace agreements of 1989, almost all funding for infrastructure and health-system initiatives came from donor-funded programmes, while the Ministry of Health (MoH) carried the responsibility for planning, staffing and service delivery ( World Bank, 1994 ). Over time, the financial and human-resources capacity of the MoH has increased and the role of international partners has receded, although it remains strong. For 20 years from the mid-1990s, donors and government combined to pilot and evaluate ad hoc , experimental health system activities ( Chhun et al. , 2015 ), and the MoH looked for evidence to identify the most effective innovations (ERC1, expert respondent 1 from Cambodia) ( Ministry of Health, 2008 ; Walls et al. , 2017 ). Currently, Cambodia has a three-tiered (national, provincial, district), decentralized, government health service and a large but disparate private sector; the government funds ∼40% of total health expenditure ( Annear et al. , 2015 ). Cambodia’s health system and HPSR capacity grew organically in the post-conflict period from the early 1990s, based on a strong partnership between individuals in government, international donors and researchers.
Ghana is a lower-middle-income country in West Africa with a unitary constitutional democracy. In the 1970s and 1980s, Ghana experienced frequent military unrest and government changes affecting the economy and public services ( Aikins, 2016 ; Aikins and Koram, 2017 ). With increasing stability, reforms began within the MoH in 1995 ( Adua et al. , 2017 ). Significant health and health-system gains were made from 2000 under the government’s Poverty Reduction Strategy, including the establishment of the National Health Insurance Service (NHIS) in 2003 ( Aikins and Koram, 2017 ; Micah et al. , 2019 ; World Health Organization, 2019 ). Ghana faces new health challenges due to rising costs of healthcare, a multiple disease burden including increased incidence of non-communicable diseases, poverty and economic constraints ( Aikins, 2016 ; Adua et al. , 2017 ). Ghana embedded HPSR in routine government operations from the 1980s, enabling an accumulation of evidence that served to inform national and sub-national decision making; domestically generated research provides a strong local dimension alongside the activities of international development partners.
We drew on data from a review of the literature and semi-structured interviews in two rounds with strategically placed experts to construct three country case studies (see Scholz and Tietje, 2002 ). We made a cross-case comparison to identify similarities and differences and lessons learned. Central to our approach was iteration between the data generated from the literature and from the experts interviewed before synthesizing our findings. Where expert opinion appears in the text, we have cited this as ER (expert respondent) with M, C and G representing the three countries and a number according to respondent.
Analytical framework
We adopt the concept of ‘evidence-informed policy’ with an understanding that health-systems are complex adaptive systems operating within a context that is marked by national needs and priorities. While the concept of ‘evidence-based policy’ may be appropriate for clear-cut clinical concerns, HPSR faces a more complex environment, one affected by constantly changing external and internal factors (see below), and requires a more holistic approach. The conceptual framework developed by Dobrow and colleagues was modified and used to guide our approach, data collection and analysis ( Dobrow et al. , 2004 ). As illustrated in Figure 1 , this framework identifies four critical junctures in the use (or non-use) of evidence for decision making. It starts with sources used (A), before examining the process through which these sources of evidence are introduced (B), interpreted (C) and applied (D). Critically, it recognizes both external and internal contextual influences on the evidence cycle: ‘external contextual factors’ lie outside the influence of those directly involved in evidence-informed decision-making processes (e.g. national economic, structural and political processes); ‘internal contextual factors’ operate as a function of the parties directly involved (e.g. the individuals and institutions themselves, their purpose and approach).

Analytical framework for context-based, evidence-based decision making ( Dobrow et al. , 2004 )
Case selection
Mexico, Cambodia and Ghana were purposively selected as case studies because they have each been, in various ways, early adopters of HPSR and provide diverse examples of HPSR development and implementation. The three countries have unique and interesting characteristics that make them the primary subjects of the study. The policy process and HPSR in Mexico have been essentially top down, national in scale, supported by legislation and inevitably influenced by political decision making; the Seguro Popular reform of social health protection measures (now superseded) was supported by increased total health expenditure equal to 1% of gross domestic product (GDP). While published research on the Mexican reform process is extensive (see González-Block et al. , 2020a , for a recent summary), much less is available on the influence of political decision making affecting the replacement of the Seguro Popular reform and the contested use of HPSR by different actors.
In Cambodia, the HPSR process has been essentially bottom-up and organic, relying mainly on the participation of international donors and researchers working in close collaboration with the MoH and its agencies. Significant HPSR activities were translated into policy through the strategic planning process, based on the close (informal) working relationships between researchers and policy makers ( Ir et al. , 2010 ; RDI Network, 2017 ). In tight economic and fiscal circumstances, targeted national funding for ongoing HPSR has not been available. More recently, less attention has been given in the published literature to understanding the development of Cambodia’s HPSR system.
In Ghana, HPSR was embedded into routine government operations as early as the 1980s, enabling managers of the health system to use an accumulating evidence base to direct and refine innovations in health-financing, maternal-health and human-resources policy. The Kintampo, Dodowa and Navrongo Health Research Centres have, with public funding and longstanding collaborations with foreign research institutes, produced evidence commonly discussed and utilized in Ghanaian health policy fora. Evidence generated in part from studies of community-based health insurance conducted by the Ghana Health Service (GHS)’s Dodowa Health Research Centre provided the foundation for establishment of Ghana’s NHIS (which emerged following political campaign promises) ( Aikins and Koram, 2017 ). The domestic origins of this policy, combined with commentary regarding the enduring influence on health policy of foreign development partners over time, make Ghana a nuanced setting for the appraisal of HPSR ( Aikins and Koram, 2017 ).
Please refer to the supplementary file for the approach taken to data collection and analysis.
Limitations
In implementing our study, we faced two main limitations. First, the topic of enquiry is large, contested and affected by context. Our expert respondents were used not to survey the field of practice in each country but rather to provide specialist insight on the findings from our literature reviews. While the number of expert respondents was limited, we targeted those best-placed to provide their intimate knowledge of the issues under consideration; this generated important points of agreement at country level and when analysing across settings. It also oriented our literature review towards their perspectives and experience, albeit through the authors’ interpretive lens rather than through a systematic approach. Secondly, under conditions created by a global pandemic, our research could not include extensive field work or consultation with a wide range of local officials and experts. In studies of this nature, local expertise is invaluable, and we made efforts to draw on those with longstanding experiential insights into the national context (including among the authors).
Ethical approval was obtained from the Human Ethics Sub-Committee at the Melbourne School of Population and Global Health, Human Ethics Advisory Group at the University of Melbourne, Australia (Ethics ID: 2057979.1). This article is based on a more extensive research report delivered to the Alliance for Health Policy and Systems Research, World Health Organization; the report may be shared on reasonable request to the corresponding author.
HPSR development in Mexico
Mexico has a long history of public health research, and since the 1980s has institutionalized HPSR training and capacity, following a largely Mexican-led research agenda. The School of Public Health of Mexico (ESPM), established in 1922, and the National Autonomous University of Mexico (UNAM) are the seminal teaching and research institutions, together with the Autonomous Metropolitan University (UAM), which has a social medicine postgraduate programme (ERM1). The National Institute of Public Health (INSP) was established in 1987 as a confederation of various research institutes and today houses the majority of HPSR researchers; ESPM merged with INSP in 1995 as part of a strategy to integrate quality academic training and research generation ( González-Block, 2009 ).
Among the wider HPSR community, The Mexican Social Security Institute (IMSS), the main social health insurer and significant health care provider, produces considerable health service delivery research, although not research on health system development or universal health coverage (ERM1). The public universities and some private universities and smaller foundations also produce HPSR (ERM1). A study examining HPSR publication trends from Latin America, including Mexico, indicated an average annual growth of 27.5% in HPSR papers between 2000–2018, where the global increase over the same period was 11.4% ( González-Block et al. , 2020b ).
At the centre of this upsurge in HPSR publications was the assessment and promotion of the nationwide Seguro Popular national health insurance programme introduced in 2003, funded by an increase in the health budget equal to 1% of GDP. An extensive debate followed, much of it recorded in the pages of The Lancet (for example, see LANCET, 2006 ). On one side were the designers and promoters ( Frenk, 2006 ), who documented the need for and the effectiveness of the scheme; on the other side were the critics ( Laurell, 2007 ; 2015a ), who emphasized the shortcomings of the programme, which did not achieve universal coverage. This rich discussion of policy options for improved health coverage paved the way first for the introduction of Seguro Popular and later for its replacement. A similar experience was evident in the introduction of the 2014 sugar-sweetened beverage tax. The literature underlying these policy discussions is further discussed below.
Significant events in the development of HPSR capacity
The appointment of Guillermo Soberón as Minister of Health during 1982–1988, a doctor and highly regarded academic from UNAM, saw health reform placed on the agenda and HPSR supported by decision makers. Research capacity then grew steadily, producing a close relationship between HPSR researchers and the Federal MoH (ERM1, ERM2) ( González-Block, 2009 ). The inter-disciplinary range and balance of HPSR during this period expanded beyond the boundaries of public health, particularly incorporating health economics, psychology, sociology and anthropology (ERM1, ERM2).
As health minister, Soberón secured the social right to health care through constitutional amendment, passed the General Health Law, instigated development of HPSR institutions and championed evidence-informed health reforms In 1984, the Centre for Public Health Research (CISP) was established within the MoH with Julio Frenk (who was later to become Minster for Health during 2000–2006) as founding director, with funding largely from foundations and international organizations ( Frenk et al. , 1986 ; Bobadilla et al. , 1989 ; ESPM, 2009 ). CISP was then incorporated into INSP in 1987. In 1985, the Mexican Health Foundation (FUNSALUD) was established as a private, not-for-profit, evidence-based policy think-tank funded largely by transnational corporations. FUNSALUD established a strong relationship with INSP and mobilizes the private sector ( González-Block et al. , 2020a ).
In 1996, the Centre for Health Systems Research (CISS) was established within INSP, and by the early 2000s the national infrastructure to produce, fund and regulate HPSR, with close institutional relationships, was in place ( González-Block, 2009 ; Oxman et al. , 2010 ; Martínez-Martínez et al. , 2012 ). Under the 2002 Law for Science and Technology, a number of public health insurance institutes were established along with the National Council for Science and Technology (CONACYT), an organization that regulates trust funds in specific areas including health research ( Martínez-Martínez et al. , 2012 ). Public entities, primarily federal and state ministries of health, contribute to these pooled funds ( González-Block et al. , 2020a ). The evaluation of social development policies (including health) was mandated by the 2004 General Social Development Law, which established the autonomous National Council for the Evaluation of Social Development Policy (CONEVAL) ( Oxman et al. , 2010 ; Valle, 2016 ).
Political will and contextual influences on HPSR
The political environment has had a major (although inconsistent) impact on health and health-research policies in Mexico, characterized by an often close relationship between research and decision makers (ERM1, ERM2). During Frenk’s tenure as Minister, the institutional structures supporting HPSR played a major role in developing and monitoring a programme of health system reforms headlined by the 2003 creation of the Seguro Popular, designed to provide coverage to those previously excluded from health insurance ( Frenk, 2006 ). Demonstrating international recognition of these achievements, the reforms were promoted in a Lancet series, with key contributions authored by the leading individuals in this network of institutions ( LANCET, 2006 ).
Domestically, however, the close network of relationships between stakeholders in government, the research community and private industry that produced this research evidence have been the subject of scrutiny and criticism. The independence of the research agenda, the evidence generated and its interpretation have all been questioned ( Lakin, 2010 ) and at times critiqued as one part of a neo-liberal enterprise spanning three decades ( Laurell, 2007 ; 2015a ; 2015b ; Homedes and Ugalde, 2009 ). Critics have, for instance, noted the influence of industry in blocking a larger-scale and more progressive reform than the Seguro Popular that had aimed to create a universal health insurance system (ERM1).
In following years, under a new government, relationships between different parts of the health research community were strained, particularly as tensions rose between industry-based research interests and the HPSR and public-health institutions. For example, close relations between INSP and FUNSALUD were strained when FUNSALUD was seen to have supported contradictory evidence related to non-communicable diseases and the obesity epidemic (ERM1) ( Barquera et al. , 2013 ; Turnbull et al. , 2019 ; Barquera and Rivera, 2020 ). Tensions reached a peak over enactment of the 2014 sugar-sweetened beverage tax after a long period of contestation pitting the beverage industry against the public-health and HSPR communities ( Fuster et al. , 2020 ). In the debate over policy, both industry and health researchers engaged in evidence production and interpretation ( Gómez, 2019 ; Carriedo et al. , 2020 ; James et al. , 2020 ; Ojeda et al. , 2020 ).
The current centre-left government has restructured and reduced the volume of research funding, and some of the trust funds have been disbanded. In 2020, it replaced Seguro Popular (calling it a foreign, neo-liberal initiative) with a return to a centralized health system with public financing and service delivery and reduced private participation, justified as a move towards universal health care ( Argen, 2020 ). Reich (2020) interprets this as a pro-statist and anti-market bias, in contradiction to current global health system trends. Widespread recognition of the persistent inequities in health care and health financing under Seguro Popular were also evident. According to one view, evidence is often used in support of political decisions based on values rather than science, just as true for the introduction of Seguro Popular (under Frenk) as for its recent disbanding; this was not seen simply as an ideological issue, as all policy making is inherently political (ERM2).
Organic development of HPSR
The development of HPSR capacity has largely been informal and organic, in step with the experimentation occurring within the public health system. Two major interventions that received considerable attention were health equity funds for the poor and the contracting of government health services (see Annear, 2010 ; Khim et al. , 2017 ; Annear et al. , 2019 ). In general, much of this activity was carried out by international and local researchers (non-government organizations, donor partners, research institutes) working in close partnership with the MoH and its newly-founded National Institute of Public Health (NIPH). Externally initiated research is welcomed by government when it focuses on established health priorities (ERC1).
This work was accompanied by a growing body of published literature on health systems, health care and the evidence-to-policy process (see Ir et al. , 2010 ; Goyet et al. , 2015 ; RDI Network, 2017 ; Liverani et al. , 2018 ; Witter et al. , 2019 ). Research carried out by and with local institutions, supported by international agencies, played a major role in informing MoH and government decision making, including the adoption of the health equity fund model, abandonment of official community-based health insurance and modifications to the contracting model (see e.g. Ir et al. , 2010 ; RDI Network, 2017 ). This process has also contributed significantly to the formation of a new generation of qualified Cambodian researchers, although in limited numbers. Research capacity has grown through the NIPH, the University of Health Sciences and some non-government research organizations (such as the Cambodian Development Resource Institute, the Reproductive Health Association of Cambodia; see e.g. NIPH, 2015 ). Nonetheless, following the period of experimentation, the number of HPSR activities has fallen, and the challenge of institutionalizing HPSR remains; often, policy development moves ahead more quickly than does the capacity to generate evidence (ERC1).
Officials in the MoH and the NIPH are conscious of the need to build permanent in-house research capacity, although funding and human resources are especially constrained (ERC1). An informal health system researchers’ forum was convened in 2015 ( NIPH, 2015 ), and in 2018 the NIPH and MoH initiated thinking (in collaboration with international research partners) about a national agenda for heath-systems research at an inaugural workshop ( NIPH, 2018 ) (ERC1). Research personnel with the expertise, time and resources are needed, although Treasury has yet to commit the targeted funding required (ERC1). The challenge of putting HPSR at the centre of the national health agenda and budget remains ( Goyet et al. , 2015 ; Liverani et al. , 2018 ).
Significant events in the development of Cambodian HPSR capacity
In an environment rich with donor activities and health system experimentation, HPSR emerged largely as a partnership activity between the MoH, local researchers and international agencies, in which the results of evaluation and research provided input to the national health planning process, characterized by the MoH’s successive national health strategic plans. The policy outcomes often followed vigorous debate among partners on the meaning and significance of research outcomes. The most conspicuous reforms to travel this path were the health equity funds (HEF) and contracting of government health service delivery. HEFs emerged from 2000 as district-level donor-non-governmental organisation (NGO) projects to fund user-fees for the poor, accompanied by a growing body of research (for a summary, see Annear, 2010 ; Annear et al. , 2019 ). The evidence was influential (ERC1); the HEF was scaled-up to national population coverage of the poor and became a central part of the Government’s National Social Protection Policy Framework 2016–2025 (see Chhun et al. , 2015 ).
Contracting of government district-health service delivery to NGOs was first piloted by the Asian Development Bank (ADB) in five selected districts in 1997, and internal ADB research suggested it improved elements of service delivery (despite limitations in the research design) (see Bloom et al. , 2006 ; Lagarde and Palmer, 2009 ). At the same time, traditional methods of NGO support for MoH district health services achieved (in some cases) equally good results. Because the MoH took responsibility for service delivery, it was reluctant to hand over domestic and donor funding to NGOs. The contracting model evolved over three phases ( Khim et al. , 2017 ): (1) 1997–2002, the ADB pilot study; (2) 2003–2009, a ‘hybrid’ model; and (3) from 2009, an ‘internal’ contracting model in which higher levels of the MoH structure ‘contracted’ service delivery to lower levels as one part of a government-wide administrative reform known as Special Operating Agencies. In this case, national imperatives related to the affordability of contracting, and MoH concern that donor funding it expected to receive for service delivery may be allocated instead to NGOs, prevailed. The internal contracting model is being gradually scaled up.
Institutional and structural developments conducive to HPSR include an improved health information system, increased availability of surveys and research products, the existence of participatory mechanisms in which evidence can be presented to local and international stakeholders and improved channels for the circulation of evidence across the MoH ( Liverani et al. , 2018 ). Regular Technical Working Group for Health meetings have brought together MoH and donor officials, although, at times, policy discussions have been constrained ( Wilkinson, 2012 ). Established in 1997, the NIPH has, alongside its principal laboratory functions, developed public-health and health-systems research and teaching functions funded through the health budget together with donor support. Periodic demographic and health surveys have been carried out since 2000, providing data on population health, health status and health-seeking behaviours, referred to in some cases as the most important evidence for health policy ( Liverani et al. , 2018 ).
HPSR activities have progressed mainly through the building of relationships between the main actors in the MoH and government services and those from international agencies and research institutes. With the focus shifting more recently to scaling up of proven interventions, research activities have somewhat receded and domestic HPSR capacity and career opportunities remain modest (ERC1).
Political will and contextual influences on HPSR in Cambodia
Consistent economic growth, an expanding health budget and an ongoing process of government administrative reform all create the context in which various arms of government (Cabinet, Health, Finance) have both willingly moved to adopt policies confirmed by evidence (such as HEF) and made political decisions to modify the implementation of certain interventions in line with perceived national needs (as in the case of contracting). The imperative to reduce national poverty played a large role in generating political support for HEF expansion; a sentiment in favour of reinforcing government service delivery contributed to the move to internal contracting. The interpretation and application of research evidence has, in various ways, reflected prevailing conditions related to the role of donors, the perceived needs of the Cambodian government and the relationships developed between local and foreign stakeholders. More recently, the policy-making process has increasingly been characterized by the broader process of government administrative reform, the role of the Council of Ministers (national cabinet) in health policy-making and the increasing experience and capacity of the MoH. However, as health officials point out (ERC1), guidelines about the way in which evidence should be appraised and used in the policy process are lacking and the use of evidence varies depending on political will and the skills of individual managers.
HPSR development in Ghana
The development of HPSR capacity in Ghana has run in parallel with structural reforms The 1990s were marked by key health reforms, including the 1997 launch of the rolling Five Year Program of Work that guides strategy and policy with regard to health service delivery and inauguration of the government’s development programme, Ghana: Vision 2020, which aspired to move the country to middle-income country status (attained in 2010) ( Dovlo, 1998 ; Aikins, 2016 ; Aikins and Koram, 2017 ). These reforms created a platform for sustained progress in the generation and use of evidence for policymaking, including HPSR ( Aikins and Koram, 2017 ).
Significant events in the development of Ghanaian HPSR capacity
Central to the development of HPSR capacity has been the establishment of training and evidence-generating institutions and their close relationship with stakeholders, including the MoH. Building on earlier initiatives in which district medical officers were sent overseas to gain a degree in public health (beginning in 1994, particularly to the UK), the School of Public Health at the University of Ghana has produced Masters of Public Health (MPH) graduates and continues to conduct collaborative research and academic teaching of HPSR for cadres in the MoH and its agencies, including the National Health Insurance Authority ( Agyepong et al. , 2015 ). An MPH from the School of Public Health was seen as critical for career progression within the MoH (ERG3). Other academic institutions—such as the Kwame Nkrumah University of Science and Technology (founded 1959), the Ghana Institute of Management and Public Administration (founded 1961; university status 2004) and the University of Health and Allied Sciences (founded 2011)—have all contributed to HPSR capacity through practical training in evidence gathering and interpretation (ERG2, ERG3).
A strong foundation for domestic HPSR was built by the 1996 formation of the GHS in collaboration with the World Health Organization. The GHS was established as an autonomous agency under the MoH to deliver government health services while the MoH focused on policy-related endeavours. The GHS produces the bulk of domestic evidence related to health system development and has established three health research centres in different parts of the country at Dodowa, Kintampo and Navrongo ( Aikins, 2016 ). These centres, which carry out operational research and track health system performance (ERG2), have had an enduring influence.
Significant research findings from many of these institutions in the 1990s paved the way for the foundation of Ghana’s NHIS, including analyses of national health financing, cost-recovery initiatives, user fees and health seeking behaviours ( Asenso-Okyere, 1995 : Asenso-Okyere et al ., 1998 ; Nyonator and Kutzin, 1999 ). The 2001 NHIS bill was based largely on evidence of community-based health insurance (CBHI) implementation in one district produced by the Dodowa Research Centre ( Agyepong and Adjei, 2008 ). HPSR has been embedded in the NHIS to track its progress and support corrective actions ( National Health Insurance Authority, 2013 ). The NHIS has an expert technical committee, led by a health economist, that collects and synthesizes evidence from various sources. For example, the delayed reimbursement of expenditures to health facilities necessitated out-of-pocket payments from clients and, reportedly, poorer quality of care, leading the committee to examine health sector expenditure review data and suggest a monthly payment schedule to facilities ( National Health Insurance Authority, 2013 ; Dalinjong et al. , 2017 ).
Strengthening the NHIS in terms of coverage, uptake and quality has been attributed, at least in part, to the perspectives, insights and contributions of a diverse range of researchers and research groups ( Seddoh and Akor, 2012 ; Aryeetey et al. , 2016 ; Alhassan et al. , 2016a ; 2016b ; Aikins and Koram, 2017 ; Okoroh et al. , 2018 ; Agbanyo, 2020 ). Academics, think tanks, professional associations, academic institutions and civil society organizations were reportedly engaged in the 2012 revision of the NHIS act, which drew on evidence related to improving NHIS financing mechanisms ( Seddoh and Akor, 2012 ).
Another example is the 1999 Community-based Health Planning and Services (CHPS) initiative, based on a Navrongo health research centre pilot study of community-level health service provision (ERG3) ( Binka et al. , 2007 ; Bawah et al ., 2019 ; Kweku et al. , 2020 ). The CHPS was ostensibly a national programme for universal access based on a ‘best practice model’ of community engagement and empowerment with task shifting to community health workers (CHWs). Even so, in common with other CHW strategies in Sub-Saharan Africa and elsewhere, scale-up has been difficult ( Perry et al. , 2014 ; GHS, 2017 ). Health-systems challenges—including supply bottlenecks and issues of CHW support and performance specific to the operational setting—are central to the difficulties, causing a drift away from the intended community-based primary health care model (ERG3) ( Bawah et al ., 2019 , Kweku et al. , 2020 ). Consequently, the 2010 Ghana Essential Health Intervention Program (GEHIP) was launched to generate evidence (using an implementation science approach) for designing strategies to address the scale-up and sustainability of the CHPS ( Awoonor‐Williams et al. , 2016 , Bawah et al ., 2019 ; Kanmiki et al. , 2019 ). The reported result was 100% CHPS population coverage achieved in target districts compared to ∼50% in non-GEHIP comparison districts ( Awoonor‐Williams et al. , 2016 ).
The revised Ghana National Health Policy, launched in 2020, emphasizes the need for strengthening research capacity, aiming, for example, to identify the key barriers to enrolment in the NHIS and to support evidence-oriented policy decision-making ( Ministry of Health, 2020 ).
Political will and contextual influences on HPSR development and utility in Ghana
The GHS and the MoH both play an active role in promoting HPSR through the policy-making process in collaboration with major stakeholders. Personal contact between specialists at the GHS health research centres, MoH officials and the public health research institutions—such as the School of Public Health at the University of Ghana, the Kwame Nkrumah University of Science and Technology, the Ghana Institute of Management and Public Administration, the University of Health and Allied Sciences—remains the main means for processing research activities (ERG1, ERG2). Formally, evidence is channelled to the Policy, Planning, Monitoring and Evaluation division of the GHS and to the Policy, Planning, Budgeting, Monitoring and Evaluation unit at the MoH. The GHS policy division operates as a conduit for the use of this evidence in the MoH’s decision making process. The MoH policy division gathers relevant evidence from routine health-services data, ad hoc evaluation reports and policy reviews.
The MoH leads the technical synthesis of existing evidence in collaboration with its local and international partners. As one part of this process, the MoH hosts annual 3-day summits with a topical theme where researchers convene with the MoH, NGOs, international development partners and other stakeholders to review the year past and plan for the year to come ( Ministry of Health, 2021 ). The MoH also convenes technical working groups with invited specialists and health stakeholders that focus on speciality areas, such as health financing. The technical working groups introduce evidence to decision makers through formal and informal communication platforms, including the annual MoH summit.
As they provide significant financial and technical support for the delivery of various health services, international donor organizations continue to have a powerful influence on the strategic direction of the health system and the policy process, playing a key role in the annual health summit and the technical working groups. While local officials often see this simply as a funding-based reality (ERG1, ERG2, ERG3), there is also a feeling that priorities may sometimes be at odds with national needs. One example may be the perceived disproportionate investment in communicable disease control despite rising incidence of chronic and non-communicable diseases (ERG3).
The various experiences of Mexico, Cambodia and Ghana demonstrate the value and the complexity of developing HPSR capacity and the use of evidence in policy-making. HPSR provides the foundation for sustained, integrated and context-based national health-system responses to local health challenges. Nonetheless, because health is a social and governmental issue, decision making about health policy generally takes place within an environment characterized by national needs, national objectives and political imperatives. The process of introducing, interpreting and applying evidence takes place within this context, characterized also by the activities of stakeholders and participants ( Dobrow et al. , 2004 ).
The conceptual framework developed by Dobrow and colleagues proved to be a useful tool for the analysis of the complex, contextually dependent story of HPSR in each of the case-study countries. The framework provided our starting point; in the process of synthesizing the lessons from each country, we used this foundation to move beyond the confines of the framework to identify the main themes arising from the data collected, including the critical influence of development partners and other international players in Ghana and Cambodia, and the level of maturity of the Mexican health research system. The framework itself is built on the understanding that there cannot be a linear progression across the domains, and these sorts of issues overlay the four domains (the source, introduction, interpretation and application of HPSR). Maintaining HPSR is a function not only of the initial investment in capacity but also of ongoing experience associated with policy-making influence. Our work demonstrates that the HPSR system is one element of broader policy networks, not a set of actors or activities external to them.
Introducing and using evidence in the policy development process
The case study results confirm that the pathways of evidence into policy making are influenced by both the production and the consumption functions of research evidence ( Peterson, 2018 ). In general, the use of HPSR in policy development appears to be more likely where a trust-based relationship exists between policy makers and researchers. At the same time, health policy, which is itself a political issue, is often the product of national imperatives or changes in political leadership, as in Cambodia or Mexico.
In Mexico, the appointment of Guillermo Soberón and subsequently further academics as Minister of Health, established a clear role for the consumption of HPSR in policy making. This was reinforced through legislative pathways and investment in HPSR research capacity, based in decentralized institutions. Even so, political decision making resulting from changes in government has at times taken precedence over the evidence-to-policy transition.
In Cambodia, the process evolved informally. The early activities of donor partners and international NGOs experimenting with various health-system interventions during reconstruction initiated a process of piloting, research and evaluation. Much of this activity was carried out with MoH approval and participation and was supported by the then nascent NIPH. More widely, both international agencies and government leaders demanded evidence of effectiveness before adopting pilot programmes into national strategy. This organic process both fostered and relied on close and respectful working relationships between researchers and policy makers at the local and the international level.
In Ghana, the MoH’s annual summit of health officials, donors and researchers is an important conduit for interpreting and moving evidence into policy. A steady stream of MPH graduates from the University of Ghana have become increasingly influential in evidence-to-policy processes. In Cambodia, the MoH’s periodic national health strategic plan is the most common vehicle through which proven initiatives enter national policy, and intermittent national health policy forums act to assemble and reflect on evidence to support policy development (ERC1). Both Ghana and Cambodia have technical working groups for health led by the MoH and comprising government and development partners to interpret evidence and consider policy. Both countries have MoH policy and planning departments that draw, wherever possible, on research-based evidence. These examples have in common a relationship-based progression through the introduction, interpretation and application of evidence.
The Dobrow et al . (2004) approach focuses attention on the influence of external (health, economic, political) and internal (purpose, process, participants) factors that influence the introduction, interpretation and application of evidence.
External factors and politics
Health is a national issue, and health systems function within a given economic, structural and political context ( Dobrow et al. , 2004 ). Commercial interests, the political climate, prevailing legislation and many other external factors have influenced the development and implementation of the health system policies explored in these case studies. In Ghana and Cambodia, HPSR has evolved alongside the earlier stages of health-system structural development. In Mexico, HPSR had initially to find a role within a more established national structure, where economic and political interest groups were well entrenched.
It is evident that, within a context of changing external conditions, maintaining an independent HPSR structure to produce evidence in a timely fashion opens the path to necessary policy reform when political conditions allow. In Mexico, where the integrity and weight of evidence used in policy development have been shaped by intermittent power shifts between social-reform and conservative political parties, the decision-making pathway nonetheless remained open to ongoing research inputs. The design and introduction of the Seguro Popular—which was based on extra-jurisdictional evidence of universal coverage processes globally and extensive national research—was cited to be determined politically by the neo-liberal approach of the newly elected centre-right National Action Party. On the other hand, as the circumstances surrounding the introduction of the sugar-sweetened-beverage tax demonstrate, the use of evidence can provide the leverage needed to achieve a public good while steering away from undue commercial interests. In Cambodia and Ghana, research-based evidence of the impact of certain interventions (such as revisions made to the contracting model in Cambodia) has at times been weighed and assessed against broader national considerations that the government (or MoH) deems necessary to meet its own objectives.
Internal factors and the HPSR community
The purpose of HPSR, the process of research and the actors who participate in the evidence-to-policy continuum comprise the internal factors that influence policy outcomes. Within complex adaptive systems, like healthcare, policy outcomes are the product of the contest between the independent activities of each stakeholder, from researcher to policymaker, to healthcare provider or representative of an interest group. As Sheikh et al . (2014) say, understanding policy making from the perspectives of the people working within the system is a HPSR task. Our case studies demonstrate the crucial role of HPSR in policy formulation and evaluation, especially in creating locally generated evidence, even where policy choices are contested. Building an evidence-informed policy culture and embedding it within the health system is recognized as the means to maintain HPSR under changing objective conditions ( Koon et al. , 2013 ; Barasa et al. , 2017 ).
The process is often strengthened, as in Ghana, where the evidence-informed policy culture includes regional as well as national agencies. In the more long-standing Mexican HPSR environment, the value of institutionalizing HPSR through legislation (and building permanent HPSR institutions) provided the foundation and the resources for health system researchers to continue producing objective evidence despite swings in the political leadership. In Cambodia and Ghana, the challenge has often been to manage the influence of international development partners.
Whatever the circumstances, the use of HPSR to initiate, monitor and evaluate the implementation of policies in a cumulative way provides timely data for appropriate reforms when the opportunity arises. With economic growth and rising fiscal strength, Cambodia has been able to direct increasing health resources into proven programmes to expand service coverage and financial protection, especially for poorer communities. In Ghana, domestically generated evidence has been used to influence debates around reform of the NHIS. In Mexico, where the politics of health policy formation can dominate the narrative, an embedded HPSR community continues to monitor and track health system performance and policy development.
Mexico, Cambodia and Ghana have each been early adopters of HPSR, with differing starting points. Their contrasting pathways demonstrate the pre-requisites for the growth and influence of HPSR within the national context. Each country must determine its own path while making best use of international experience and lessons learned. The experiences of these three diverse countries illustrate how HPSR is of most value when it is embedded as a routine part of the health system, and not a parallel or ad hoc activity, as the emergence of social-protection mechanisms in Cambodia, or evaluation of national insurance structures in Ghana, demonstrate. Mexico—as an example of a more mature, long-standing HPSR structure—may be seen as demonstrating the natural tension between a predominantly technical approach to HPSR and health reform and an approach that is influenced by wider political and values-based commitments.
Both historical and contemporary contexts influence health-system development and the HPSR agenda. These factors also influence the formation and sustainability of policy networks, including the agency and symbolic capital of their main players, the generation of evidence and its influences on policy. The resilience of evidence-informed policy making in the face of changing economic and political circumstances is made stronger with the development of independent HPSR structures embedded within the wider health system and with the capacity to shepherd the consistent use of evidence through the policy process, as the case of Mexico demonstrates most clearly.
Recommendations for countries developing evidence-informed health-systems policy processes include the following.
Build HPSR capacity and practice as an integral part of the health system, not parallel to it; support the HPSR function with social development legislation; HPSR requires a variety and number of individual researchers and institutions (both national and international); building long-term relationships between the main players is essential.
Implement HPSR with a commitment to reflecting and accounting for the national context within which health policy is determined; an understanding of the sources, introduction, interpretation and application of evidence is the foundation for the wider analysis of policy directions.
Maintain the independence of HPSR institutions to guarantee the objectivity of evidence created; ensure sustainable career paths for HPSR researchers equal to other career options; recognize and manage the influence of external and internal forces on the research process.
The role of HPSR in shaping health systems, health, and, ultimately, development outcomes—which is one part of the Sustainable Development Goals—is analogous to the concept of ‘emergence’ as coined by complexity theorists ( Barasa et al. , 2017 ; Kitson et al. , 2018 ). Emergence describes the interaction of constituent parts of a system producing organized or patterned outcomes that are not conscious or planned by the constituent parts. While investment in HPSR is a conscious and planned activity, researchers and research institutes operate as only one part of the larger whole characterized by multiple stakeholders, all with particular interests. As our case studies demonstrate, the role of HPSR in the policy process is most effective, and most efficient, where the research component is embedded within the wider health system.
Supplementary data is available at Health Policy and Planning Journal online.
The data underlying this article cannot be shared publicly due to the need to maintain the privacy of individuals that participated in the study in accordance with the conditions for ethical approval. The data will be shared on reasonable request to the corresponding author.
This work was supported by the Alliance for Health Policy and Systems Research, World Health Organization. The Alliance is supported through both core funding as well as project-specific designated funds. The full list of Alliance donors is available at: https://ahpsr.who.int/about-us/funders .
B.McP., A.G. and Z.C.S. conceived and B.McP., D.L.S. and P.A. designed the study. D.L.S., K.T., A.A.B. and P.L.A. collected and analysed the data and, with B.McP., interpreted it. D.L.S., K.T. and P.L.A. drafted the article and critically revised it with contributions from A.A.B. and B.McP. and critical feedback from A.G. and Z.C.S. All authors approved the final version of the paper.
The authors include two females and five males and span multiple levels of seniority. All authors have engaged for several years in research activities with a health policy and systems focus with three authors having done so for more than 30 years. Collectively, the authors have applied research experience in Mexico, Cambodia and Ghana. The authors’ academic training is diverse with two being health economists, two with first degrees in medicine, one a social psychologist, one originally trained in occupational therapy and one in nursing. All authors have several years’ experience conducting qualitative research and literature reviews.
The team of authors conducted the study of experiences in three disparate countries as an objective, outside view supported by anonymous contribution from in-country experts. While the focus of the article is the experience of health policy and systems research in Mexico, Cambodia and Ghana, and expert respondents with significant experience at national level were recruited as key informants to the study, these individuals are not named as authors. This decision was taken for two reasons. First, to enable separation of expert national respondent testimony from the analysis and interpretation of it. Second, in accordance with the ethical approval granted for the study based on the preservation of anonymity of expert national respondents.
Ethical approval was received from the Human Ethics Sub-Committee at the Melbourne School of Population and Global Health, Human Ethics Advisory Group at the University of Melbourne, Australia (Ethics ID: 2057979.1).
None declared.
Adua E , Frimpong K , Li X , wang W . 2017 . Emerging issues in public health: a perspective on Ghana’s healthcare expenditure, policies and outcomes . EPMA Journal 8 : 197 – 206 .
Google Scholar
Agbanyo R . 2020 . Ghana’s national health insurance, free maternal healthcare and facility-based delivery services . African Development Review 32 : 27 – 41 .
Agyepong IA , Adjei S . 2008 . Public social policy development and implementation: a case study of the Ghana National Health Insurance scheme . Health Policy & Planning 23 : 150 – 60 .
Agyepong IA , Anniah K , Aikins M et al. 2015 . Health policy, health systems research and analysis capacity assessment of the School of Public Health, University of Ghana . Ghana Medical Journal 49 : 200 – 13 .
Aikins ADEG . 2016 . Health policy and systems research in Ghana: a preliminary review of the evidence. In: Aryeety, E. B-D , Sackey B , Arfranie S (eds). Contemporary Social Policy Issues in Ghana . Chap. 9. Accra, Ghana : Sub Saharan Publishers .
Google Preview
Aikins ADEG Koram K . 2017 . Health and Healthcare in Ghana, 1957–2017. In: Aryeetey E , Kanbur R (eds). The Economy of Ghana Sixty Years after Independence . Chap. 22. UK : Oxford University Press , 365–84.
Alhassan RK , Nketiah-amponsah E , Arhinful DK , Coles JA . 2016a . A review of the national health insurance scheme in ghana: what are the sustainability threats and prospects? PLoS One 11 : e0165151.
Alhassan RK , Nketiah-Amponsah E , Spieker N , Arhinful DK , Rinke de Wit TF . 2016b . Perspectives of frontline health workers on Ghana’s National Health Insurance Scheme before and after community engagement interventions . BMC Health Services Research 16 : 192.
Annear P . 1998 . Health and development in Cambodia . Asian Studies Review 22 : 193 – 221 .
Annear P . 2010 . Health Equity Funds in Cambodia: a comprehensive review of the literature and annotated bibliography . Health Policy and Health Financing Knowledge Hub Working Paper. Number 9, November 2010 . Melbourne : Nossal Institute for Global Health .
Annear PL , Grundy J , Ir P et al. 2015 . The Kingdom of Cambodia health system review. In: Annear PL (ed). Health Systems in Transition , Vol. 5 . Manila : World Health Organization, Regional Office for the Western Pacific .
Annear PL , Lee JT , Khim KV et al. 2019 . Protecting the poor? Impact of the national health equity fund on utilization of government health services in Cambodia, 2006-2013 . BMJ Global Health 4 : e001679.
Argen D . 2020 . Farewell seguro popular . The Lancet 395 : 549 – 50 .
Aryeetey GC , Nonvignon J , Amissah C , Buckle G , Aikins M . 2016 . The effect of the National Health Insurance Scheme (NHIS) on health service delivery in mission facilities in Ghana: a retrospective study . Globalization and Health 12 : 1 – 9 .
Asenso-Okyere WK . 1995 . Financing health care in Ghana . World health forum 16 : 86 – 91 .
Asenso-Okyere WK , Anum A , Osei-Akoto I , Adukonu A . 1998 . Cost recovery in Ghana: are there any changes in health care seeking behaviour? . Health Policy and Planning 13 : 181 – 8 .
Awoonor‐Williams JK , Phillips JF , Bawah AA . 2016 . Catalyzing the scale‐up of community‐based primary healthcare in a rural impoverished region of northern Ghana . International Journal of Health Planning and Management 31 : e273 – 89 .
Barasa EW , Cloete K , Gilson LJ . 2017 . From bouncing back, to nurturing emergence: reframing the concept of resilience in health systems strengthening . Health Policy & Planning 32 : iii91 – 4 .
Barquera S , Campos I , Rivera JA . 2013 . Mexico attempts to tackle obesity: the process, results, push backs and future challenges . Obesity Reviews 14 : 69 – 78 .
Barquera S , Rivera JA . 2020 . Obesity in Mexico: rapid epidemiological transition and food industry interference in health policies . The Lancet Diabetes & Endocrinology 8 : 746 – 7 .
Bawah AA , Awoonor-Williams JK , Asuming PO et al. 2019 . The child survival impact of the Ghana Essential Health Interventions Program: a health systems strengthening initiative in a rural region of Northern Ghana . PLoS One 14 : e0218025.
Bennett S , Agyepong IA , Sheikh K et al. 2011 . Building the field of health policy and systems research: an agenda for action . PLoS Medicine 8 : e1001081.
Binka FN , Bawah AA , Phillips JF et al. 2007 . Rapid achievement of the child survival millennium development goal: evidence from the Navrongo experiment in Northern Ghana . Tropical Medicine & International Health 12 : 578 – 93 .
Birn A-E . 2006 . Marriage of Convenience: Rockefeller Internationl Health and Revolutionary Mexico . Rochester, New York: University of Rochester Press (Boydell & Brewer) .
Bloom E , Bhushan I , Clingingsmith D et al. 2006 . Contracting for Health: Evidence from Cambodia . Asian Development Bank, World Bank . https://www.brookings.edu/wp-content/uploads/2016/06/20060720cambodia.pdf , accessed 12 July 2022 .
Bobadilla JL , Infante C , Langer A , Lozano R , Frenk Mora J . 1989 . Advances in public health investigation. 5 years’ work of the Center for Research in Public Health, 1984-1989 . Salud Publica Mexico 31 : 550 – 68 .
Carriedo A , Lock K , Hawkins B . 2020 . Policy process and Non-State Actors’ Influence on the 2014 Mexican Soda Tax . Health Policy & Planning 35 : 941 – 52 .
Chhun C , Kimsun T , Yu G , Ensor T , Mcpake B . 2015 . Impact of health financing policies on household spending: evidence from Cambodia Socio-Economic Surveys 2004 and 2009 . ReBUILD Consortium. CDRI Working Paper Series No.106 . Cambodia Development Resource Institute, Phnom Penh .
Dalinjong PA , Wang AY , Homer CSE . 2017 . The operations of the free maternal care policy and out of pocket payments during childbirth in rural Northern Ghana . Health Economics Review 7 : 41.
Dobrow MJ , Goel V , Upshur RE . 2004 . Evidence-based health policy: context and utilisation . Social Science & Medicine 58 : 207 – 17 .
Dovlo D . 1998 . Health sector reform and deployment, training and motivation of human resources towards equity in health care: issues and concerns in Ghana . Division of Human Resources . Acra : Ministry of Health .
ESPM . 2009 . Centro de Investigación en Salud Poblacional . Primera edición/septiembre 2009© Instituto Nacional de Salud PúblicaAv. Universidad 655, colonia Santa María Ahuacatitlán 62100 Cuernavaca, Morelos, México . https://www.insp.mx/centros/salud-poblacional.html , accessed 12 July 2022 .
Frenk J . 2006 . Bridging the divide: global lessons from evidence-based health policy in Mexico . The Lancet 368 : 954 – 61 .
Frenk J , Bobadilla JL , Sepúlveda J et al. 1986 . An innovative approach to public health research: the case of a new center in Mexico . Journal of Health Administration Education 4 : 467 – 81 .
Fuster M , Burrowes S , Cuadrado C et al. 2020 . Understanding policy change for obesity prevention: learning from sugar-sweetened beverages taxes in Mexico and Chile . Health Promotion International 36 : 155 – 64 .
George A , Olivier J , Glandon D , Kapilashrami A , Gilson L . 2019 . Health systems for all in the SDG era: key reflections based on the Liverpool statement for the fifth global symposium on health systems research . Health Policy & Planning 34 : ii135 – 8 .
Ghaffar A , Tran N , Langlois E , Shroff Z , Javadi D . 2017 . Alliance for health policy and systems research: aims, achievements and ambitions . Public Health Research & Practice 27 : 2711703.
GHS . 2017 . Policy, Planning, Monitoring and Evaluation Division . Accra : Ghana Health Service . https://www.ghanahealthservice.org/ghs-division.php?ghs&ghsdid=9 , accessed 15 November 2020.
Gómez EJ . 2019 . Coca-Cola’s political and policy influence in Mexico: understanding the role of institutions, interests and divided society . Health Policy & Planning 34 : 520 – 8 .
González-Block MÁ . 2009 . Leadership, institution building and pay-back of health systems research in Mexico . Health Research Policy & Systems 7 : 22.
González-Block MÁ , Arroyo Laguna J , Cetrángolo O et al. 2020b . Health policy and systems research publications in Latin America warrant the launching of a new specialised regional journal . Health Research Policy & Systems 18 : 59.
González-Block MÁ , Reyes Morales H , Cahuana Hurtado L et al. 2020a . Mexico: Health System Review . Health Systems in Transition , Vol. 22 No. 2. World Health Organization. Regional Office for Europe . https://apps.who.int/iris/handle/10665/334334 , accessed 12 July 2022 .
Goyet S , Touch S , Ir P et al. 2015 . Gaps between research and public health priorities in low income countries: evidence from a systematic literature review focused on Cambodia . Implementation Science 10 : 32.
Homedes N , Ugalde A . 2009 . Twenty-five years of convoluted health reforms in Mexico . PLoS Medicine 6 : e1000124.
Ir P , Bigdeli M , Meessen B , Van Damme W . 2010 . Translating knowledge into policy and action to promote health equity: a case study of health equity funds to improve access to health services for the poor in Cambodia . Health Policy 96 : 200 – 9 .
James E , Lajous M , Reich MR . 2020 . The politics of taxes for health: an analysis of the passage of the sugar-sweetened beverage tax in Mexico . Health Systems & Reform 6 : e1669122.
Kanmiki EW , Akazili J , Bawah AA et al. 2019 . Cost of implementing a community-based primary health care strengthening program: the case of the ghana essential health interventions program in northern Ghana . PLoS One 14 : e0211956.
Khim KV , Ir P , Annear PL . 2017 . Factors driving changes in the design, implementation and scaling-up of the contracting of health services in rural Cambodia, 1997–2015 . Health Systems & Reform 3 : 105 – 16 .
Kitson A , Brook A , Harvey G et al. 2018 . Using complexity and network concepts to inform healthcare knowledge translation . International Journal of Health Policy and Management 7 : 231 – 43 .
Koon AD , Rao KD , Tran NT , Ghaffar A . 2013 . Embedding health policy and systems research into decision-making processes in low- and middle-income countries . Health Research Policy and Systems 11 : 30.
Kweku M , Amu H , Awolu A et al. 2020 . Community-based health planning and services plus programme in Ghana: a qualitative study with stakeholders in two Systems Learning Districts on improving the implementation of primary health care . PLoS One 15 : e0226808.
Lagarde M , Palmer N . 2009 . The impact of contracting out on health outcomes and use of health services in low and middle-income countries . Cochrane Database of Systematic Reviews CD008133.
Lakin J . 2010 . The end of insurance? Mexico’s Seguro Popular, 2001-2007 . Journal of Health Politics, Policy and Law 35 : 313 – 52 .
LANCET . 2006 . Mexico: Health System Reform [Series form the Lancet journals ] . www.thelancet.com/series/health-system-reform-in-mexico , accessed 12 July 2022 .
Laurell AC . 2007 . Health system reform in Mexico: a critical review . International Journal of Health Services 37 : 515 – 35 .
Laurell AC . 2015a . The Mexican popular health insurance: myths and realities . International Journal of Health Services 45 : 105 – 25 .
Laurell AC . 2015b . Three decades of neoliberalism in Mexico: the destruction of society . International Journal of Health Services 45 : 246 – 64 .
Liverani M , Chheng K , Parkhurst J . 2018 . The making of evidence-informed health policy in Cambodia: knowledge, institutions and processes . BMJ Global Health 3 : e000652.
Mam BH , Key PJ . 1995 . Cambodian health in transition . British Medical Journal (International Edition) 311 : 435.
Martínez-Martínez E , Zaragoza ML , Solano E et al. 2012 . Health research funding in Mexico: the need for a long-term agenda . PLoS One 7 : e51195.
Micah AE , Chen CS , Zlavog BS et al. 2019 . Trends and drivers of government health spending in sub-Saharan Africa, 1995-2015 . BMJ Global Health 4 : e001159.
Ministry of Health . 2008 . Health Strategic Plan 2008-2015: Accountability, Efficiency, Quality, Equity . Phnom Penh, Cambodia . https://www.yumpu.com/en/document/view/36645842/health-strategic-plan-2008-2015-ministry-of-health , accessed 12 July 2022 .
Ministry of Health . 2020 . National Health Policy: ensuring healthy lives for all . Accra, Ghana .
Ministry of Health . 2021 . Strengthening the Resilience of Ghana’s Health System to Better Respond to Emergencies . Acra, Ghana . https://2021.healthsummitgh.org , accessed 12 July 2022 .
National Health Insurance Authority . 2013 . 2013 annual report . Accra, Ghana : National Health Insurance Authority .
NIPH . 2015 . Mapping and Planning Health Systems Research in Cambodia: Building the Evidence base for Policy and Practice . Report of the Cambodia Health Researchers’ Forum . https://www.gov.uk/research-for-development-outputs/mapping-and-planning-health-systems-research-in-cambodia-building-the-evidence-base-for-policy-and-practice-report-of-the-cambodia-health-researchers-forum , accessed 12 July 2022 .
NIPH . 2018 . First consultative workshop on developing a National Agenda for health systems research . 17 August . Phnom Penh, Cambodia (available from the authors).
Norris SL , Rehfuess EA , Smith H et al. 2019 . Complex health interventions in complex systems: improving the process and methods for evidence-informed health decisions . BMJ Global Health 4 : e000963.
Nyonator F , Kutzin J . 1999 . Health for some? The effects of user fees in the Volta Region of Ghana . Health Policy and Planning 14 : 329 – 41 .
Ojeda E , Torres C , Carriedo Á et al. 2020 . The influence of the sugar-sweetened beverage industry on public policies in Mexico . International Journal of Public Health 65 : 1037 – 44 .
Okoroh J , Essoun S , Seddoh A et al. 2018 . Evaluating the impact of the national health insurance scheme of Ghana on out of pocket expenditures: a systematic review . BMC Health Services Research 18 : 426.
Oxman AD , Bjørndal A , Becerra-Posada F et al. 2010 . A framework for mandatory impact evaluation to ensure well informed public policy decisions . The Lancet 375 : 427 – 31 .
Parker SW , Saenz J , Wong R . 2018 . Health insurance and the aging: evidence from the seguro popular program in Mexico . Demography 55 : 361 – 86 .
Perry H , Crigler L , Hodgins SL (eds.) 2014 . Developing and Strengthening Community Health Worker Programs at Scale: A Reference Guide for Program Managers and Policy Makers . USAID . https://pdf.usaid.gov/pdf_docs/pa00jxwd.pdf , accessed 12 July 2022 .
Peters DH . 2018 . Health policy and systems research: the future of the field . Health Research Policy and Systems 16 : 1 – 4 .
Peterson MA . 2018 . In the shadow of politics: the pathways of research evidence to health policy-making . Journal of Health Politics, Policy & Law 43 : 341 – 76 .
RDI Network . 2017 . From Evidence to Impact: Development contribution of Australian Aid funded research–A study based on research undertaken through the Australian Development Research Awards Scheme 2007–2016 . Authored by Debbie Muirhead with Juliet Willetts, Joanne Crawford, Jane Hutchison and Philippa Smales . https://rdinetwork.org.au/wp-content/uploads/2020/02/From-Evidence-to-Impact-Full-Report.pdf , accessed 12 July 2022 .
Reich MR . 2020 . Restructuring health reform, mexican style . Health Systems & Reform 6 : 1 – 11 .
Schleiff MJ , Kuan A , Ghaffar A . 2020 . Comparative analysis of country-level enablers, barriers and recommendations to strengthen institutional capacity for evidence uptake in decision-making . Journal of Health Research Policy and Systems 18 : 78.
Scholz RW , Tietje O . 2002 . Embedded Case Study Methods: Integrating Quantitative and Qualitative Knowledge . USA : Sage Publications .
Seddoh A , Akor SA . 2012 . Policy initiation and political levers in health policy: lessons from Ghana’s health insurance . BMC Public Health 12 : S10.
Sheikh K , George A , Gilson L . 2014 . People-centred science: strengthening the practice of health policy and systems research . Journal of Health Research Policy and Systems 12 : 1 – 8 .
Shroff ZC , Javadi D , Gilson L , Kang R , Ghaffar A . 2017 . Institutional capacity to generate and use evidence in LMICs: current state and opportunities for HPSR . Journal of Health Research Policy and Systems 15 : 94.
Turnbull B , Gordon SF , Martínez-Andrade GO , González-Unzaga M . 2019 . Childhood obesity in Mexico: a critical analysis of the environmental factors, behaviours and discourses contributing to the epidemic . Health Psychology Open 6 : 2055102919849406.
Urquieta-Salomón JE , Villarreal HJ . 2016 . Evolution of health coverage in Mexico: evidence of progress and challenges in the Mexican health system . Health Policy & Planning 31 : 28 – 36 .
Valle AM . 2016 . The Mexican experience in monitoring and evaluation of public policies addressing social determinants of health . Global Health Action 9 : 29030.
Vanyoro KP , Hawkins K , Greenall M et al. 2019 . Local ownership of health policy and systems research in low-income and middle-income countries: a missing element in the uptake debate . BMJ Global Health 4 : e001523.
Walls H , Liverani M , Chheng K , Parkhurst J . 2017 . The many meanings of evidence: a comparative analysis of the forms and roles of evidence within three health policy processes in Cambodia . Journal of Health Research Policy and Systems 15 : 95.
Wilkinson D . 2012 . Review of the functioning of the Technical Working Group for Health . Report prepared for the TWGH Secretariat . Phnom Penh. (Available from the authors.)
Witter S , Anderson I , Annear P et al. 2019 . What, why and how do health systems learn from one another? Insights from eight low-and-middle-income country case studies . BMC Health Research Policy and Systems 17 : 9.
World Bank . 1994 . Cambodia: From Rehabilitation to Reconstruction . East Asia and Pacific Region, Country Department 1, Phnom Penh . https://documents.worldbank.org/en/publication/documents-reports/documentdetail/408971468743782412/cambodia-from-rehabilitation-to-reconstruction-an-economic-report , accessed 12 July 2022 .
World Health Organization . 2019 . Trends in Maternal Mortality: 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division . Geneva, Switzerland : World Health Organization . https://apps.who.int/iris/handle/10665/327596 , accessed 12 July 2022 .
- health policy
- health care systems
Email alerts
Citing articles via.
- Recommend to Your Librarian
Affiliations
- Online ISSN 1460-2237
- Copyright © 2024 The London School of Hygiene and Tropical Medicine and Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 28 May 2019
Transforming evidence for policy and practice: creating space for new conversations
- Kathryn Oliver ORCID: orcid.org/0000-0002-4326-5258 1 &
- Annette Boaz 2
Palgrave Communications volume 5 , Article number: 60 ( 2019 ) Cite this article
18k Accesses
54 Citations
157 Altmetric
Metrics details
- Science, technology and society
A Correction to this article was published on 29 August 2019
This article has been updated
For decades, the question of how evidence influences policy and practice has captured our attention, cutting across disciplines and policy/practice domains. All academics, funders, and publics have a stake in this conversation. There are pockets of great expertise about evidence production and use, which all too often remains siloed. Practical and empirical lessons are not shared across disciplinary boundaries and theoretical and conceptual leaps remain contained. This means that we are not making the most of vast and increasing investment in knowledge production. Because existing lessons about how to do and use research well are not shared, funders and researchers are poorly equipped to realise the potential utility of research, and waste resources on—for example—ineffective strategies to create research impact. It also means that the scarce resources available to study evidence production and use are misspent on overly-narrow or already-answered questions. Patchy and intermittent funding has failed to build broadly relevant empirical or theoretical knowledge about how to make better use of evidence, or to build the communities required to act on this knowledge. To transform how we as a community think about what evidence is, how to generate it, and how to use it well, we must better capture lessons being learned in our different research and practice communities. We must find ways to share this knowledge, to embed it in the design of our research systems and practices, and work jointly to establish genuine knowledge gaps about evidence production and use. This comment sets out one vision of how that might be accomplished, and what might result.
Are we investing wisely in research for society?
For decades, conversations between research funders, users, and producers have focused on different aspects of what evidence is, the roles it plays in policy and practice, and the different ways in which roles can be enhanced and supported. Most researchers feel unequivocally that ‘more research’ is always better—and funders and governments seem to agree (Sarewitz, 2018 ). Governments are increasingly using investments explicitly to help create the evidence base for better decision-making. For example, funding has been explicitly focused on the United Nation’s Sustainable Development Goals (UKRI-UNDP, 2018 ). The UK government has made several targeted investments, including the £1.5 billion Global Challenges Research Fund to address substantive social problems, (Gov. UK, 2016 ; UKRI, 2017 ), and in health, the thirteen (up from nine) Collaborations for Leadership in Applied Health Research and Care, which received £232 million 2008–2019 (NIHR, 2009 ). This investment looks set to continue with a further £150 million allocated to the Applied Research Collaborations (NIHR, 2018 ). In the US, the Trump administration recently signed into law $176.8 billion for research and development, of which $543 million is specifically for translational health research (Science, 2018 ). These funds are made available to researchers with an effective proviso that the research is targeted towards questions of direct interest to policymakers and practitioners.
There has also been an increase in the infrastructure governments provide, such as scientific advisory posts and professionals (Doubleday and Wilsdon, 2012 ; Gluckman, 2014 ), and a range of secondments and fellowship opportunities designed to ‘solve’ the problem of limited academic-policy engagement (Cairney and Oliver, 2018 ). The UK Government recently asked departments to produce research priority areas (Areas of Research Interest (ARIs)), to guide future academic-policy collaboration (Nurse, 2015 ). Yet, there has been almost no evaluation of these activities. There is limited evidence about how to build the infrastructure to use evidence in impactful ways and limited evidence about the impact of this investment (Kislov et al., 2018 ). We simply do not know whether the growth of funding, infrastructure, or initiatives has actually improved research quality, or led to improvements for populations, practice or policy.
Thus, despite our ever-growing knowledge about our world, physical and social, it is not easy to find answers to the challenges facing us and our governments. Spending ever-increasing amounts on producing research evidence is not likely to help, if we do not understand how to make the most of these investments. Discussions about wastage within the research system often focus on valid concerns about reproducibility and quality (Bishop, 2019 ), but until we also understand the broader political and societal pressure shaping what evidence is produced and how, we will not be able to reduce this waste (Sarewitz, 2018 ). In short, our research systems are not guided by current theory about what types of knowledge are most valuable to help address societal problems, or how to produce useful evidence, or how to use this knowledge in policy and practice setting.
Who knows about how to improve evidence production and use?
Fortunately, even if under-used, there is a significant body of academic and practical knowledge about how evidence is produced and used. Several disciplines take the question of evidence production and use as a core concern, and this inherently transdisciplinary space has become populated by research evidence from different academic and professional traditions, jurisdictions and contexts.
Much of the funded research into knowledge production and use has been conducted in health and health care, and other applied disciplines. Although there are perennial inquiries about the ‘best’ research methods which should inform policy and practice (Haynes et al., 2016 ), this field has offered some very practical insights, from identifying factors which influence evidence use (Innvaer et al., 2002 ; Oliver et al., 2014 ; Orton et al., 2011 ), to identifying types of evidence used in different contexts (Dobrow et al., 2004 ; Oliver and de Vocht, 2015 ; Whitehead et al., 2004 ). Researchers have explored strategies to increase evidence use (Dobbins et al., 2009 ; Haynes et al., 2012 ; Lavis et al., 2003 ), and developed structures to support knowledge production and use—in the UK, see, for example, the What Works Centres, Policy Research Units, Health Research Networks and so forth (Ferlie, 2019 ; Gough et al., 2018 ). Similar examples can be found in the US (Tseng et al., 2018 ; Nutley and Tseng, 2014 ) and the Netherlands (Wehrens et al., 2010 ). Alongside these practical tools, critical research has helped us to understand the importance of diverse evidence bases (e.g., Brett et al., 2014 ; Goodyear-Smith et al., 2015 ), of including patients and stakeholders in decision-making (Boaz et al., 2016 ; Liabo and Stewart, 2012 ), and to contextualise the drive for increased impact outcomes (Boaz et al., 2019 ; Locock and Boaz, 2004 ; Nutley et al., 2000 ).
The social sciences have provided research methods to investigate the various interfaces between different disciplines and their potential audiences. Acknowledging insights from philosophy, critical theory and many other field (see, e.g., Douglas, 2009 ), we highlight two particular perspectives. Firstly, policy studies has helped us to understand the processes of decision-making and the (political) role of evidence within it (Dye, 1975 ; Lindblom, 1990 ; Weiss, 1979 ). A subfield of ‘the politics of evidence-based policymaking’ has grown up, using an explicitly political-science lens to examine questions of evidence production and use (Cairney, 2016b ; Hawkins and Ettelt, 2018 ; Parkhurst, 2017 ). Political scientists have commented on the ways in which political debate has been leveraged by scientific knowledge, with particular focuses on social justice, and the uses of evidence to support racist and sexist oppression (Chrisler, 2015 ; Emejulu, 2018 ; Lopez and Gadsden, 2018 ; Malbon et al., 2018 ; Scott, 2011 ).
Secondly, the field of Science and Technology studies (STS) treats the practice and purpose science itself as an object of study. Drawing on philosophies of science and sociologies of knowledge and practice, early theorists described science as an esoteric activity creating knowledge through waves of experimentation (Kuhn, 1970 ; Popper, 1963 ). This was heavily critiqued by social constructivists, who argue that all knowledge was inherently bound to cultural context and practices (Berger and Luckmann, 1966 ; Collins and Evans, 2002 ; Funtowicz and Ravetz, 1993 ). Although some took this to mean that science was just another way of interpreting reality of equal status with other belief systems, most see these insights as demonstrating the importance of understanding the social context within which scientific practices and objects were conducted and described (Latour and Woolgar, 2013 ; Shapin, 1995 ). Similarly, Wynne showed how social and cultural factors determine what we consider ‘good’ evidence or expertise (Wynne, 1992 ). More recently, scholars have focused on how science and expertise is politicised through funding and assessment environments (Hartley et al., 2017 ; Jasanoff, 2005 ; Jasanoff and Polsby, 1991 ; Prainsack, 2018 ), the cultures and practices of research (Fransman, 2018 ; Hartley, 2016 ), through the modes of communication with audiences, and on the role for scientific advice around emerging technologies and challenges (Lee et al., 2005 ; Owen et al., 2012 ; Pearce et al., 2018 ; Smallman, 2018 ; Stilgoe et al., 2013 ).
Are we acting on these lessons?
However, funders and researchers rarely draw on the learning from these different fields; nor is learning shared between disciplines and professions (Oliver and Boaz, 2018 ). Thus, we have sociologists of knowledge producing helpful theory about the complex and messy nature of decision-making and the political nature of knowledge (e.g., Lancaster, 2014 ); but this is not drawn on by designers of research partnerships or evaluators of research impact (Chapman et al., 2015 ; Reed and Evely, 2016 ; Ward, 2017 ). This leaves individual researchers with the imperative to do high quality research and to demonstrate impact, but with little useful advice about how as individuals or institutions they might achieve or measure impact (Oliver and Cairney, 2019 ), leading to enormous frustration, duplicated and wasted effort. Even more damagingly, researchers produce poor policy recommendations, or naively engage in political debates with no thought about the possible costs and consequences for themselves, the wider sector, or publics.
We recognise that engaging meaningfully with literatures from multiple disciplines is too challenging a labour for many. The personal and institutional investment required to engage with the practical and scholarly knowledge about evidence production and use is—on top of other duties—beyond most of us. Generating consensus about the main lessons is itself challenging, although initial attempts have been made (Oliver and Pearce, 2017 ). Across the diverse literature on evidence use, terms are defined and mobilised differently. Working out what the terms are implying and what is at stake in the alternative mobilisation of these terms is a huge task. Many researchers are only briefly able to enter this broader debate, through tacked-on projects attached to larger grants. There is no obvious career pathway for those who want to remain at this higher level. There are simply too many threads pulling researchers and practitioners back into their ‘home’ disciplines and domains, which prevents people undertaking the labour of learning the key lessons from multiple fields.
Yet the history of research in this area, scattered and patchy though it is, shows us how necessary this labour is if useful, meaningful research is to be done and used (DuMont, 2019 ). Too much time and energy has been spent investigating questions which have been long-since answered—such as whether RCTs should be used to investigate policy issues, whether we need a pluralistic approach to research design; whether to invest in relationships as well as data production. But governments and universities have also failed to create environments where knowledge producers are welcome and useful in decision-making environments; where their own staff feel able to freely discuss and experiment with ideas; and universities consistently fail to reward or support those who want to create social change or work at the interfaces between knowledge production and use.
This failure to draw together key lessons also means that the scarce resources allocated to the study of evidence production and use have been misspent. There has been no sustained interdisciplinary funding for empirical research studies into evidence production and use in the UK, and in the US only over the last 15 years (DuMont, 2019 ). This has led to a dearth of shared empirical and theoretical evidence, but also a lack of community, which has had a detrimental effect on the scholarship in this space. All too often, research funding goes towards already-answered questions (such as whether bibliometrics are a good way to capture impact). We must ensure that new research on evidence production and use addresses genuine gaps. That can only be done by making existing knowledge more widely available and working together to generate collaborative research agendas.
An unfortunate side-effect of this lack of community is that many who enter it do so with the sense that it is a new, ‘emerging’ field, which will generate silver-bullet solutions for researchers and funders. Because it is new to them, researchers feel it must be new to all—not realising that their own journey has been undertaken by many others before them. For instance, there are many initiatives which claim to be ‘newly addressing’ the problem of ‘evidence use’, ‘research on research’, the ‘science of science’, ‘meta-science’, or some other variant. Whether they explore the allocation and impact of research funding and evaluation, the infrastructure of policy research units or the practice of collaborative research, they all make vital contributions. But to claim as many do that it is an ‘emerging field’ illustrates how easy it is, even with the best of intentions, to ignore existing expertise on the production and use of evidence. We must better articulate the difference between these pieces of the puzzle, and the difference those differences make. Too many are claiming that their piece provides the whole picture. In turn, funders feel they have done their part by funding this small piece of research, but remain ignorant of the existing knowledge, and indeed of the real gaps.
Research on evidence production and use is often therefore not as useful as it should be. Failing to draw on existing literature, the solutions proposed by most commentators on the evidence-policy/practice ‘gap’ often do not take into account the realities of complex and messy decision-making, or the contested and political nature of knowledge construction—leading to a situation where an author synthesising lessons from across the field can end up sharing a set of normative statements that might imply that there has been no conceptual leap in 20 years (see e.g., French, 2018 ; Gamoran, 2018 ).
Evidence and policy/practice studies: our tasks
There are therefore two key tasks for those primarily engaged in researching and teaching evidence production and use for policy and practice, which are to (1) identify and share key lessons more effectively and (2) to build a community enabling transdisciplinary evidence to be produced and used, which addresses real gaps in the evidence base and helps decision-makers transform society for the better. We close with some suggestions about possible steps we can take towards these goals.
Firstly, we must better communicate our key lessons. We would like to help people articulate the hard-won, often disciplinary-specific lessons from their own work for others—and to work with partners to embed them into the design, practice and evaluation of research. For instance, critical perspectives on power can describe the lines of authority and the institutional governance surrounding decision-making (Bachrach and Baratz, 1962 ; Crenson, 1971 ; Debnam, 1975 ); the interpersonal dynamics which determine everything from the credibility of evidence to the placement of topics on policy agendas (Oliver and Faul, 2018 ; Tchilingirian, 2018 ; White, 2008 ); to the practice of research itself, and the ways in which assumed and enacted power leads to the favouring of certain methodologies and narratives (Hall and Tandon, 2017 ; Pearce and Raman, 2014 ). How might this translate into infrastructure and funding to support equitable research partnerships (Fransman et al., 2018 )? What other shared theory and practical insights might help us transform how we do and use research?
Secondly, we must generate research agendas collaboratively. In our view, the only way to avoid squandering resources on ineffective research on research is to work together to share emerging ideas, and to produce genuinely transdisciplinary questions. We made a start on this task at recent meetings. A 2018 Nuffield Foundation-funded symposium brought together leading scholars, practitioners and policymakers, and funders, to share learning about evidence use and to identify key gaps. We followed this meeting with a broader discussion at the William T. Grant Use of Research Evidence meeting in March 2019 which has also contributed to our thinking.
We initiated the conversation with a Delphi exercise to identify key research questions prior to the meeting. We refined the list, and during the meeting we asked participants to prioritise these. This was a surprisingly challenging process, which revealed that even to reach common understanding about the meaning of a research question, let alone the importance, discussants had to wade through decades-worth of assumptions, biases, preferences, language nuances and habits.
Based on this analysis, we identify three main areas of work which are required to transform how we think about to create and use evidence (Table 1 ):
Transforming knowledge production
Transforming translation and mobilisation
Transforming decision-making
The topics below were selected to indicate the broad range of empirical and normative questions which need broader discussion, and are by no means definitive. Of course, much research on some topics has already been done, but we have included them—because even if research already exists, it is not widely enough known to routinely inform research users, funders or practitioners about how to better produce or use evidence. We observe that much of the very limited funding to investigate evidence production and use has gone to either developing metrics (responsible or otherwise, Row 2 column 4) or tools to increase uptake (Row 2, column 4), to the relative neglect of everything else. There are significant gaps which can only be addressed jointly across disciplines and sectors, and we welcome debates, additions, and critiques about how to do this better.
A shared research agenda
As we note above, these topics are drawn from proposed questions and discussions by an interdisciplinary group of scholars, practitioners, funders and other stakeholders. It became clear during this process that many were unaware of relevant research which had already been undertaken under these headings. These topics reflect our own networks and knowledge of the field, so cannot be regarded as definitive. We need and welcome partnership with others working in this space to attempt to broaden the conversation as much as possible. We have selected a proportion of the selected topics to illustrate a number of points.
First, that no one discipline or researcher could possibly have the skills or knowledge to answer all of these questions. Interdisciplinary teams can be difficult to assemble, but clearly required. We need leadership in this space to help spot opportunities to foster interdisciplinary research and learning.
Second that all of these topics could be framed and addressed in multiple ways, and many have been. Many are discussed, but there is little consensus; or there is consensus within disciplines but not between them. Some topics have been funded and others have not. We feel there is an urgent need to identify where research investment is required, where conversations need to be supported, and where and how to draw out the value of existing knowledge. Again, we need leadership to help us generate collaborative research agendas.
Third, that while we all have our own interests, the overall picture is far more diverse, and that there is a need for all working in this area to clearly define what their contributions are in relation to the existing evidence and communities. A shared space to convene and learn from one another would help us all understand the huge and exciting space within which we are working.
Finally, this is an illustrative set of topics, and not an exhaustive one. We would not claim to be setting the definitive research agenda in this paper. Rather, we are setting out the need to learn from one another and to work together in the future. Below, we describe some examples of the type of initial discussions which might help us to move forward, using our three themes of knowledge production, knowledge mobilisation, and decision-making. We have cited relevant studies which set out research questions or provide insights. By doing so, we hope to demonstrate the breadth of disciplines and approaches which are being used to explore these questions; and the potential value of bringing these insights together.
Firstly, we must understand who is involved in shaping and producing the evidence base. Much has been written about the need to produce more robust, meaningful research which minimises research waste through improving quality and reporting (Chalmers et al., 2014 ; Glasziou and Chalmers, 2018 ; Ioannidis, 2005 ), and the infrastructure, funding and training which surround knowledge production and evaluation have attracted critical perspectives (Bayley and Phipps, 2017 ; Gonzalez Hernando and Williams, 2018 ; Katherine Smith and Stewart, 2017 ). Current discourses around ‘improving’ research focus on making evidence more rigorous, certain, and relevant; but how are these terms interpreted locally in different policy and practice contexts? How are different forms of knowledge and evidence assessed, and how do these criteria shape the activities of researchers?
Enabling researchers to reflect on their own role in the ‘knowledge economy’—that is, the production and services attached to knowledge-intensive activities (usually but not exclusively referring to technological innovation (Powell and Snellman, 2004 ))—requires engagement with this history.
This might mean asking questions about who is able to participate in the practice and evaluation of research. Who is able to ask and answer questions? What questions are asked and why? Who gets to influence research agendas? We know that there are barriers to participation in research for minority groups, and for many research users (Chrisler, 2015 ; Duncan and Oliver, 2017 ; Scott et al., 2009 ). At a global level, how are research priorities set by, for example, international funders and philanthropists? How can we ensure that local and indigenous interests and priorities are not ignored by predominantly Western research practices? How are knowledge ‘gaps’ or areas of ‘non-knowledge’ constructed, and what are the power relationships underpinning that process (Nielsen and Sørensen, 2017 )? There are important questions about what it means to do ethical research in the global society, with honesty about normative stances and values (Callard and Fitzgerald 2015 ), which apply to the practices we engage in as much as the substantive topics we focus on (Prainsack et al., 2010 ; Shefner et al., 2014 ).
It might also mean asking about how we do research. Many argue that research (particularly funded through responsive-mode arrangements) progresses in an incremental way, with questions often driven by ease, rather than public need (Parkhurst, 2017 ). Is this the most efficient way to generate new knowledge? How does this compare with, for example, random research funding (Shepherd et al., 2018 )? Stakeholder engagement is said to be required for impact, yet we know it is costly and time-consuming (Oliver et al., 2019 , 2019a ). How can universities and funders support researchers and users to work together long-term, with career progression and performance management untethered from simplistic (or perhaps any) metrics of impact? Is coproduced research truly more holistic, useful, and relevant? Or does inviting in different interests to deliberate on research findings, even processes, distort agendas and politicise research (Parkhurst and Abeysinghe, 2016 )? What are the costs and benefits to these different systems and practices? We know little about whether (and if so how well) each of these modes of evidence production leads to novel, useful, meaningful knowledge; nor how these modes influence the practice or outputs of research.
Transforming evidence translation and mobilisation
Significant resources are put into increasing ‘use’ of evidence, through interventions (Boaz et al., 2011 ) or research partnerships (Farrell et al., 2019 ; Tseng et al., 2018 ). Yet ‘use’ is not a straightforward concept. Using research well implies the existence of a diverse and robust evidence base; a range of pathways for evidence to reach decision-makers; both users and producers of knowledge having the capacity and willingness to engage in relationship-building and deliberation about policy and practice issues; research systems supporting individuals and teams to develop and share expertise.
More attention should be paid to how evidence is discussed, made sense of, negotiated and communicated—and the consequences of different approaches. This includes examining the roles of people involved in the funding of research, through to the ways in which decision-makers access and discuss evidence of different kinds. How can funders and universities create infrastructure and incentives to support researchers to do impactful research, and to inhabit boundary spaces between knowledge production and use? We know that potential users of research may sit within or outside government, with different levels and types of agency, making different types of decisions in different contexts (Cairney, 2018 ; Sanderson, 2000 ). Yet beyond ‘tailoring your messages’, existing advice to academics does not help them navigate this complex system (Cairney and Oliver, 2018 ). To take this lesson seriously, we might want to think about the emergence of boundary spanning- organisations and individuals which help to interface between research producers (primarily universities, but also civil society) and users (Bednarek et al., 2016 ; Cvitanovic et al., 2016 ; Stevenson, 2019 ). What types of interfacing are effective, and how—and how do interactions between evidence producers and users shape both evidence and policy? How might policies on data sharing and open science influence innovation and knowledge mobilisation practices?
Should individual academics engage in advocacy for policy issues (Cairney, 2016a ; Smith et al., 2015 ), using emotive stories or messaging to best communicate (Jones and Crow, 2017 ; Yanovitzky and Weber, 2018 ), or rather be ‘honest brokers’ representing without favour a body of work (Pielke, 2007 )? Or should this type of dissemination work be undertaken by boundary organisations or individuals who develop specific skills and networks? There is little empirical evidence about how best to make these choices (Oliver and Cairney, 2019 ), or how these consequences affect the impact or credibility of evidence (Smith and Stewart, 2017 ); nor is there good quality evidence about the most effective strategies and interventions to increase engagement or research uptake by decision-makers or between researchers and their audiences (Boaz et al., 2011 ). It seems likely that some researchers may get involved and others stay in the hinterlands (Locock and Boaz, 2004 ), depending on skills and preference. However, it is not clear how existing studies can help individuals navigate these complex and normative choices.
Communities (of practice, within policy, amongst diverse networks) develop their own languages and rationalities. This will affect how evidence is perceived and discussed (Smallman, 2018 ). Russell and Greenhalgh have shown how competing rationalities affect the reasoning and argumentation deployed in decision-making contexts (Greenhalgh and Russell, 2006 ; Russell and Greenhalgh, 2014 ); how can we interpret local meanings and sense-making in order to better communicate about evidence? Much has been written about the different formats and tailored outputs which can be used to ‘increase uptake’ by decision-makers (Lavis et al., 2003 ; Makkar et al., 2016 ; Traynor et al., 2014 )—although not with conclusive findings—yet we know so little about how these messages are received. Researchers may be communicating particularly messages, but how can we be sure that decision-makers are comprehending and interpreting those messages in the same way? Theories of communication (e.g., Levinson, 2000 ; Neale, 1992 ) must be applied to this problem.
Similarly, drawing on psychological theories of behaviour change, commentators have argued for greater use of emotion, narrative and story-telling by researchers in an attempt to influence decision-making (Cairney, 2016b ; Davidson, 2017 ; Jones and Crow, 2017 ). Are these effective at persuading people and if so how do they work? What are the ethical questions surrounding such activities and how does this affect researcher identity? Should researchers be aiming to communicate simple messages about which there is broad consensus?
Discussions of consensus often ask whether agreement is a laudable aim for researchers, or how far consensus is achievable (De Kerckhove et al., 2015 ; Lidskog and Sundqvist, 2004 ; Rescher, 1993 ). We are also interested in the tension between scientific and politician consensus, and how differences in interpretations of knowledge can be leveraged to influence political consensus (Beem, 2012 ; Montana, 2017 ; Pearce et al., 2017 ). What tools can be used to generate credibility? Is evidence persuasive of itself; can it survive the translation process; and is it reasonable to expect individual researchers to broadcast simple messages about which there is broad consensus, if that is in tension with their own ethical practices and knowledge (even if the most effective way to influence policy? Is consensus required for the credibility of science and scientists, or can am emphasis on similarity in fact reduce the value of research and the esteem of the sector? Is it the task of scientists to surface conflicts and disagreements, and how far does this duty extend into the political sphere (Smith and Stewart, 2017 )?
Transforming decision-making, and the role of evidence within it
Finally, we need to understand how research and researchers can support decision-making given what we know about the decision-making context or culture, and how this influences evidence use (Lin, 2008 ). This means better understanding the roles of professional and local cultures of evidence use, governance arrangements, and roles of public dialogues so that we can we start to investigate empirically-informed strategies to increase impact (Locock and Boaz, 2004 ; Oliver et al., 2014 ). This would include empirical examination of individual strategies to influence decision-making, as well as more institutional infrastructures and roles; case studies of different types of policymaking and the evidence diets consumed in these contexts; and how different people embody different imperatives of the evidence/policy nexus. We need to bring together examples of the policy and practice lifecycles, and examine the roles of different types of evidence throughout those processes (Boaz et al., 2011 , 2016 ).
We want to know what shapes the credibility afforded to different experts and forms of expertise, and how to cultivate credibility to enable better decision-making (Grundmann, 2017 ; Jacobson and Goering, 2006 ; Mullen, 2016 ; Williams, 2018 ). What does credibility enable (greater attention or influence; greater participation by researchers in policy processes; a more diverse debate)? What is the purpose of increasing credibility? What is the ultimate aim of attempting to become credible actors in policy spaces? How far should universities and researchers go—should we be always aiming for more influence? Or should we recognise and explore the diversity of roles research and researchers can play in decision-making spaces?
Ultimately, methods must be found to evaluate the impact of evidence on policy and practice change, and on populations—including unintended or unwanted consequences (Lorenc and Oliver, 2013 ; Oliver et al., 2019 , 2019a ). Some have argued that the primary role for researchers is to demonstrate the consequences of decisions and to enable debate. This requires the development and application of methods to evaluate changes, understand mechanisms, and develop theory and substantive and normative debates, as well as engage in the translation and mobilisation of evidence. It also requires increased transparency to enable researchers to understand evidence use (Nesta, 2012 ), while also allowing others like Sense about Science to check the validity of evidence claims on behalf of the public (Sense about Science, 2016 ).
Next steps and concrete outputs
These illustrative examples demonstrate the vast range of discussions which are happening, and need to happen to help us transform how we produce and use evidence. We are not the first to identify the problems of research wastage (Glasziou and Chalmers, 2018 ) or to emphasise the need to maximise the value of research for society (Duncan and Oliver, 2017 ). Nor are we the first to note that all the parts of the research system play a role achieving this, from funding (Geuna and Martin, 2003 ), to research practices (Bishop, 2019 ; Fransman, 2018 ), to translational activities (Boaz et al. 2019 ; Nutley and Tseng, 2014 ), professional science advice (Doubleday and Wilsdon, 2012 ) and public and professional engagement (Holliman and Warren, 2017 ). There have been sustained attempts to build communities and networks to attempt ways to improve parts of this system Footnote 1 . However, most of these initiatives are rooted in particular disciplines or professional activities. We see a need for a network which bridges these initiatives, helping each other articulate their key lessons for one another, and progressing our conversations about how to do better research about evidence production and use.
Researchers, funders, decision-makers and publics will approach and inhabit this space from different, sometimes very different directions. We do not claim to be writing the definitive account. But we would like to open the door to more critical accounts of evidence production and use which are specifically aimed at multi-disciplinary and sectoral audiences. Our aim is to welcome and support debate, to introduce parts of our diverse community to each other, and to enable our individual perspectives and knowledge to be more widely valued.
We anticipate disagreement and discussion, and support a multitude of ways of approaching the issues we identify above. Some may feel that our energies should be directed to democratising knowledge for all and ensuring that this is mobilised to maximise equality and fairness (Stewart et al., 2018 ). Others may feel that our task is to observe, problematise and critique these processes, rather than engage in them directly (Fuller, 1997 ). Our view is that both normative and critical approaches are vital; as are empirical and theoretical contributions to our understanding of high-level research systems, down to micro-interactions in evidence production and use. Our contention is that we must keep this space vibrant and busy, producing new knowledge together, and learning from each other. This requires investment in research on evidence production and use, in virtual and literal spaces to hold conversations, as well as in capacity and capability. There are significant and important gaps in what we know about evidence production and use, but identifying the particular and specific research agendas for each of these gaps must be a collaborative process.
We also see a need to support those who are new to this space. Many come to the problem of evidence use without any training in the history of research in this space. We see a need to provide an accessible route into these debates, and welcome opportunities to collaborate on textbooks or learning resources to support new students, non-academics and those new to the field.
The Nuffield Foundation meeting which led to this paper demonstrated how valuable these opportunities are to enable learning and relationship-building through face-to-face interactions. We will continue to create opportunities for greater transdisciplinary and academic-partner conversations, to share learning across spheres of activity and to build capacity, and to use these new perspectives to generate fresh avenues of enquiry, through the new Transforming Evidence Footnote 2 collaboration.
Finally, we argue for increased investment to maximise the learning we already have, and to support more effective knowledge production and use. Too much money and expertise has been wasted, and too many opportunities to build on existing expertise have been squandered. We must find better ways to make this learning accessible, and to identify true knowledge gaps. Indeed, we believe that collaboration across disciplinary and sectoral boundaries is the only way in which this space will both progress and demonstrate its true value. We must prevent the waste of limited resources to understand how to transform evidence production and use for the benefit of society. Putting what we already know into practice would be an excellent place to start.
Change history
29 august 2019.
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
See, for example https://www.alliance4usefulevidence.org/ , https://www.ingsa.org/ , https://4sonline.org/ , https://www.metascience2019.org/ , http://www.alltrials.net/
See Transforming Evidence site, https://transformure.wordpress.com/
Bachrach P, Baratz MS (1962) Two faces of power. Am Polit Sci Rev. https://doi.org/10.2307/1952796
Article Google Scholar
Bayley JE, Phipps D (2017) Building the concept of research impact literacy. Evid Policy . https://doi.org/10.1332/174426417x15034894876108
Bednarek AT, Shouse B, Hudson CG et al. (2016) Science-policy intermediaries from a practitioner’s perspective: The Lenfest Ocean Program experience. Sci Pub Policy. https://doi.org/10.1093/scipol/scv008
Beem B (2012) Learning the wrong lessons? Science and fisheries management in the Chesapeake Bay blue crab fishery Public Underst Sci 21(4):401–417. https://doi.org/10.1177/0963662510374177
Article PubMed Google Scholar
Berger PL, Luckmann T (1966) The social construction of reality: A treatise in the sociology of knowledge. Doubleday, Garden City, NY
Bishop D (2019) Rein in the four horsemen of irreproducibility. Nature 568(7753):435–435. https://doi.org/10.1038/d41586-019-01307-2
Article ADS CAS PubMed Google Scholar
Boaz A, Baeza J, Fraser A (2011) Effective implementation of research into practice: An overview of systematic reviews of the health literature. BMC Res Notes. https://doi.org/10.1186/1756-0500-4-212
Boaz A, Robert G, Locock L et al. (2016) What patients do and their impact on implementation. J Health Organiz Manag. https://doi.org/10.1108/JHOM-02-2015-0027
Boaz A, Davies H, Fraser A et al. (2019) What works now? Evidence-based policy and practice revisited. Policy press. Available at: https://policy.bristoluniversitypress.co.uk/what-works-now . (Accessed 17 July 2018)
Brett J, Staniszewska S, Mockford C et al. (2014) A systematic review of the impact of patient and public involvement on service users, researchers and communities. Patient 7(4):387–395. https://doi.org/10.1007/s40271-014-0065-0
Cairney P (ed) (2016a) Health and advocacy: What are the barriers to the use of evidence in policy? In: The politics of evidence-based policy making. Palgrave Macmillan, London, UK, pp 51–84. https://doi.org/10.1057/978-1-137-51781-4_3
Google Scholar
Cairney P (2016b) The politics of evidence-based policy making. Springer, London, pp 1–137. https://doi.org/10.1057/978-1-137-51781-4
Cairney P (2018) Three habits of successful policy entrepreneurs. Policy Polit 46(2):199–215. https://doi.org/10.1332/030557318X15230056771696
Cairney P, Oliver K (2018) How should academics engage in policymaking to achieve impact? Polit Stud Rev . https://doi.org/10.1177/1478929918807714
Callard F, Des Fitzgerald (2015) Rethinking interdisciplinarity across the social sciences and neurosciences. https://doi.org/10.1057/9781137407962
Book Google Scholar
Chalmers I, Bracken MB, Djulbegovic B et al. (2014) How to increase value and reduce waste when research priorities are set. Lancet 383(9912):156–165. https://doi.org/10.1016/S0140-6736(13)62229-1
Chapman JM, Algera D, Dick M et al. (2015) Being relevant: Practical guidance for early career researchers interested in solving conservation problems. Glob Ecol Conserv 4:334–348. https://doi.org/10.1016/j.gecco.2015.07.013
Chrisler AJ (2015) Humanizing research: Decolonizing qualitative inquiry with youth and communities. J Fam Theory Rev 7(3):333–339. https://doi.org/10.1111/jftr.12090
Collins HM, Evans R (2002) The third wave of science studies. Soc Stud Sci 32(2):235–296. https://doi.org/10.1177/0306312702032002003
Crenson MA (1971) The un-politics of air pollution; a study of non-decisionmaking in the cities. Johns Hopkins Press, Baltimore and London
Cvitanovic C, McDonald J, Hobday AJ (2016) From science to action: Principles for undertaking environmental research that enables knowledge exchange and evidence-based decision-making. J Environ Manage. https://doi.org/10.1016/j.jenvman.2016.09.038
Article CAS PubMed Google Scholar
Davidson B (2017) Storytelling and evidence-based policy: Lessons from the grey literature. Palgrave Commun. https://doi.org/10.1057/palcomms.2017.93
De Kerckhove DT, Rennie MD, Cormier R (2015) Censoring government scientists and the role of consensus in science advice: A structured process for scientific advice in governments and peer-review in academia should shape science communication strategies. EMBO Rep 16(3):263–266. https://doi.org/10.15252/embr.201439680
Article CAS PubMed PubMed Central Google Scholar
Debnam G (1975) Nondecisions and Power: The Two Faces of Bachrach and Baratz. Am Political Sci Rev 69(03):889–899. https://doi.org/10.2307/1958397
Dobbins M, Robeson P, Ciliska D et al. (2009) A description of a knowledge broker role implemented as part of a randomized controlled trial evaluating three knowledge translation strategies. Implement Sci 4(1). https://doi.org/10.1186/1748-5908-4-23
Dobrow MJ, Goel V, Upshur REG (2004) Evidence-based health policy: context and utilisation. Soc Sci Med. https://doi.org/10.1016/S0277-9536(03)00166-7
Doubleday R, Wilsdon J (2012) Science policy: Beyond the great and good. Nature. https://doi.org/10.1038/485301a .
Douglas H (2009) Science, Policy, and the Value-Free Ideal. University of Pittsburgh Press, Pittsburgh
DuMont K (2019) Reframing evidence-based policy to align with the evidence|William T. Grant foundation. Available at: http://wtgrantfoundation.org/digest/reframing-evidence-based-policy-to-align-with-the-evidence . (Accessed 28 Jan 2019)
Duncan S, Oliver S (2017) Editorial. Res All 1(1):1–5. https://doi.org/10.18546/RFA.01.1.01
Article MathSciNet Google Scholar
Dye TR (1975) Understanding public policy. Prentice-Hall. Available at: http://agris.fao.org/agris-search/search.do?recordID=US201300519645 . (Accessed 18 Jan 2019)
Emejulu A (2018) On the problems and possibilities of feminist solidarity: The Women’s March one year on. IPPR Progress Rev 24(4):267–273. https://doi.org/10.1111/newe.12064
Farrell CC, Harrison C, Coburn CE (2019) What the hell is this, and who the hell are you? role and identity negotiation in research-practice partnerships. AERA Open 5(2):233285841984959. https://doi.org/10.1177/2332858419849595
Ferlie E (2019) The politics of management knowledge in times of austerity. Available at: https://books.google.co.uk/books?hl=en&lr=&id=Ok5yDwAAQBAJ&oi=fnd&pg=PP1&dq=info:XZBJCDoqIowJ:scholar.google.com&ots=Vg1eZHL9e_&sig=fS2Bf8w7VtyDKfZ3InQWq-npbuk&redir_esc=y#v=onepage&q&f=false . (Accessed 14 Feb 2019)
Fransman J (2018) Charting a course to an emerging field of ‘research engagement studies’: A conceptual meta-synthesis Res All 2(2):1–49. http://www.ingentaconnect.com/contentone/ioep/rfa/2018/00000002/00000002/art00002#
Fransman J, Hall B, Hayman R et al. (2018) Promoting fair and equitable research partnerships to respond to global challenges. Rethinking research collaborative. Available at: http://oro.open.ac.uk/57134/ . (Accessed 25 Apr 2019)
French RD (2018) Lessons from the evidence on evidence-based policy. Can Public Adm 61(3):425–442. https://doi.org/10.1111/capa.12295
Fuller S (1997) Constructing the high church-low church distinction in STS textbooks. Bull Sci, Technol Soc 17(4):181–183. https://doi.org/10.1177/027046769701700408
Funtowicz SO, Ravetz JR (1993) Science for the post-normal age. Futures. https://doi.org/10.1016/0016-3287(93)90022-L
Gamoran A (2018) Evidence-based policy in the real world: A cautionary view Ann Am Acad Political Soc Sci 678(1):180–191. https://doi.org/10.1177/0002716218770138
Geuna A, Martin BR (2003) University research evaluation and funding: An international comparison. Kluwer Academic Publishers, Minerva. https://doi.org/10.1023/B:MINE.0000005155.70870.bd
Glasziou P, Chalmers I (2018) Research waste is still a scandal—an essay by Paul Glasziou and Iain Chalmers. BMJ 363:k4645. https://doi.org/10.1136/BMJ.K4645
Gluckman P (2014) Policy: The art of science advice to government. Nature 507(7491):163–165. https://doi.org/10.1038/507163a
Gonzalez Hernando M, Williams K (2018) Examining the link between funding and intellectual interventions across universities and think tanks: a theoretical framework. Int J Polit, Cult Soc 31(2):193–206. https://doi.org/10.1007/s10767-018-9281-2
Goodyear-Smith F, Jackson C, Greenhalgh T (2015) Co-design and implementation research: challenges and solutions for ethics committees. BMC Med Eth. https://doi.org/10.1186/s12910-015-0072-2
Gough D, Maidment C, Sharples J (2018) UK What Works Centres: Aims, methods and contexts. London. Available at: https://eppi.ioe.ac.uk/cms/Default.aspx?tabid=3731 . (Accessed 27 Feb 2019)
Gov.UK (2016) Science and research funding allocation: 2016 to 2020-GOV.UK. Available at: https://www.gov.uk/government/publications/science-and-research-funding-allocation-2016-to-2020 . (Accessed 14 Feb 2019)
Greenhalgh T, Russell J (2006) Reframing evidence synthesis as rhetorical action in the policy making drama. Healthcare Policy|Politiques de Santé. https://doi.org/10.12927/hcpol.2006.17873
Article PubMed PubMed Central Google Scholar
Grundmann R (2017) The problem of expertise in knowledge societies. Minerva 55(1):25–48. https://doi.org/10.1007/s11024-016-9308-7
Hall BL, Tandon R (2017) Decolonization of knowledge, epistemicide, participatory research and higher education. Res All 1(1):6–19. https://doi.org/10.18546/RFA.01.1.02
Hartley S (2016) Policy masquerading as science: an examination of non-state actor involvement in European risk assessment policy for genetically modified animals. J Eur Public Policy. https://doi.org/10.1080/13501763.2015.1049196 .
Hartley S, Pearce W, Taylor A (2017) Against the tide of depoliticisation: the politics of research governance. Policy Polit 45(3):361–377. https://doi.org/10.1332/030557316X14681503832036
Hawkins B, Ettelt S (2018) The strategic uses of evidence in UK e-cigarettes policy debates. Evid Policy. https://doi.org/10.1332/174426418X15212872451438
Haynes A, Brennan S, Redman S et al. (2016) Figuring out fidelity: A worked example of the methods used to identify, critique and revise the essential elements of a contextualised intervention in health policy agencies. Implement Sci 11(1). https://doi.org/10.1186/s13012-016-0378-6
Haynes AS, Derrick GE, Redman S et al. (2012) Identifying trustworthy experts: How do policymakers find and assess public health researchers worth consulting or collaborating with?. PLoS ONE 7(3):e32665. https://doi.org/10.1371/journal.pone.0032665 .
Article ADS CAS PubMed PubMed Central Google Scholar
Holliman R, Warren CJ (2017) Supporting future scholars of engaged research. Res All. https://doi.org/10.18546/rfa.01.1.14
Innvaer S, Vist G, Trommald M et al. (2002) Health policy-makers’ perceptions of their use of evidence: a systematic review. J health Serv Res policy 7(4):239–44. https://doi.org/10.1258/135581902320432778
Ioannidis JPA (2005) Why most published research findings are false. PLoS Med 2(8):e124. https://doi.org/10.1371/journal.pmed.0020124
Jacobson N, Goering P (2006) Credibility and credibility work in knowledge transfer. Evid Policy. https://doi.org/10.1332/174426406777068894
Jasanoff S (2005) Judgment under siege: The three-body problem of expert legitimacy. In: Maasen S, Weingart P (eds) Democratization of expertise? Springer-Verlag, Berlin/Heidelberg, pp 209–224. https://doi.org/10.1007/1-4020-3754-6_12
Jasanoff S, Polsby NW (1991) The fifth branch: Science advisers as policymakers. Contemp Sociol 20(5):727. https://doi.org/10.2307/2072218
Jones M, Crow D (2017) How can we use the ‘science of stories’ to produce persuasive scientific stories. Palgrave Commun 3(1):53. https://doi.org/10.1057/s41599-017-0047-7
Kislov R, Wilson PM, Knowles S et al. (2018) Learning from the emergence of NIHR Collaborations for Leadership in Applied Health Research and Care (CLAHRCs): a systematic review of evaluations. Implement Sci 13(1):111. https://doi.org/10.1186/s13012-018-0805-y
Kuhn TS (1970) The structure of scientific revolutions. The physics teacher. https://doi.org/10.1017/CBO9781107415324.004
Lancaster K (2014) Social construction and the evidence-based drug policy endeavour. Int J Drug Policy 25(5):948–951. https://doi.org/10.1016/j.drugpo.2014.01.002
Latour B, Woolgar S (2013) Laboratory life: The construction of scientific facts. 1986. https://doi.org/10.1017/CBO9781107415324.004
Lavis JN, Robertson D, Woodside JM et al. (2003) How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q 81(2):221–248. https://doi.org/10.1111/1468-0009.t01-1-00052
Lee CJ, Scheufele DA, Lewenstein BV (2005) Public attitudes toward emerging technologies: Examining the interactive effects of cognitions and affect on public attitudes toward nanotechnology. Sci Commun 27(2):240–267. https://doi.org/10.1177/1075547005281474
Levinson SC (2000) Presumptive meanings: The theory of generalized conversational implicature. language, speech, and communication series. https://doi.org/10.1162/coli.2000.27.3.462
Liabo K, Stewart R (2012) Involvement in research without compromising research quality. J Health Serv Res Policy. https://doi.org/10.1258/jhsrp.2012.011086
Lidskog R, Sundqvist G (2004) From consensus to credibility: New challenges for policy-relevant science. Innovation 17(3):205–226. https://doi.org/10.1080/1351161042000241144
Lin V (2008) Evidence-Based public health policy. In: Quah, Stella R (eds) International encyclopedia of public health. Elsevier, Oxford. https://doi.org/10.1016/B978-012373960-5.00234-3
Chapter Google Scholar
Lindblom CE (1990) Inquiry and change: The troubled attempt to understand and shape society. Yale University Press, JSTOR. http://www.jstor.org/stable/j.ctt1dszwww
Locock L, Boaz A (2004) Research, policy and practice–worlds apart? Soc Pol Soc. https://doi.org/10.1017/S1474746404002003
Lopez N, Gadsden VL (2018) Health inequities, social determinants, and intersectionality. NAM Perspect. 6(12). https://doi.org/10.31478/201612a
Lorenc T, Oliver K (2013) Adverse effects of public health interventions: a conceptual framework. J Epidemiol Community Health 68(3):288–290. https://doi.org/10.1136/jech-2013-203118
Makkar SR, Howe M, Williamson A et al. (2016) Impact of tailored blogs and content on usage of Web CIPHER–an online platform to help policymakers better engage with evidence from research. Health Res Policy Syst 14(1):85. https://doi.org/10.1186/s12961-016-0157-5
Malbon E, Carson L, Yates S (2018) What can policymakers learn from feminist strategies to combine contextualised evidence with advocacy? Palgrave Commun. https://doi.org/10.1057/s41599-018-0160-2
Montana J (2017) Accommodating consensus and diversity in environmental knowledge production: Achieving closure through typologies in IPBES. Environ Sci Policy 68:20–27. https://doi.org/10.1016/J.ENVSCI.2016.11.011
Mullen EJ (2016) Reconsidering the ‘idea’ of evidence in evidence-based policy and practice. European journal of social work 19(3–4):310–335
Neale S (1992) Paul Grice and the philosophy of language. Linguist Philos. https://doi.org/10.1007/BF00630629
Nesta (2012) The red book for evidence. Available at: https://www.nesta.org.uk/blog/red-book-evidence/ . (Accessed 14 Feb 2019)
Nielsen KH, Sørensen MP (2017) How to take non-knowledge seriously, or “the unexpected virtue of ignorance”. Public Underst Sci 26(3):385–392. https://doi.org/10.1177/0963662515600967
NIHR (2009) NIHR collaborations for leadership in applied health research and care (CLAHRCs): implementation plan 5.8. Available at: https://www.nihr.ac.uk/about-us/how-we-are-managed/our-structure/infrastructure/collaborations-for-leadership-in-applied-health-research-and-care.htm . (Accessed 14 Feb 2019)
NIHR (2018) NIHR announces £150m investment in applied health research. Available at: https://www.nihr.ac.uk/news/nihr-announces-150m-investment-in-applied-health-research/8800 . (Accessed 25 Apr 2019)
Nurse P (2015) Ensuring a successful UK research endeavour: A review of the UK Research councils. BIS/15/625, Department for Business, Innovation and Skills, London
Nutley SM, Smith PC, Davies HTO (eds) (2000) What works?: Evidence-based policy and practice in public services. Policy Press, Bristol
Oliver K, Boaz A (2018) What makes research useful? We still don’t know. Available at: https://www.researchresearch.com/news/article/?articleId=1377811 . (Accessed 18 Jan 2019)
Oliver K, Cairney P (2019) The do's and don’ts of influencing policy: a systematic review of advice to academics. Palgrave Commun 5(1):21
Oliver K, Faul MV (2018) Networks and network analysis in evidence, policy and practice. Evid Policy 14(3):369–379. https://doi.org/10.1332/174426418X15314037224597
Oliver K, Pearce W (2017) Three lessons from evidence-based medicine and policy: increase transparency, balance inputs and understand power. Palgrave Commun 3(1):43. https://doi.org/10.1057/s41599-017-0045-9
Oliver K, Innvar S, Lorenc T et al. (2014) A systematic review of barriers to and facilitators of the use of evidence by policymakers. BMC Health Serv Res 14(1):2. https://doi.org/10.1186/1472-6963-14-2
Oliver K, Lorenc T, Innvær S (2014) New directions in evidence-based policy research: A critical analysis of the literature. Health Res Policy Syst 12(1):34. https://doi.org/10.1186/1478-4505-12-34
Oliver K, Tinker J, Lorenc T et al. (2019a) Evaluating unintended consequences: new insights into solving practical, ethical, and political challenges of evaluation. Evaluation (in press)
Oliver K, Kothari A, Mays N (2019) The dark side of coproduction: do the costs outweigh the benefits for health research? Health Res Policy Syst 17(1):33
Oliver A, de Vocht F (2015) Defining ‘evidence’ in public health: a survey of policymakers’ uses and preferences. Eur J Public Health: ckv082. https://doi.org/10.1093/eurpub/ckv082
Orton L, Lloyd-Williams F, Taylor-Robinson D et al. (2011) The use of research evidence in public health decision making processes: Systematic review. PLoS ONE. https://doi.org/10.1371/journal.pone.0021704
Owen R, Macnaghten P, Stilgoe J (2012) Responsible research and innovation: From science in society to science for society, with society. Sci Public Policy. https://doi.org/10.1093/scipol/scs093
Parkhurst J (2017) The politics of evidence: From evidence-based policy to the good governance of evidence. Routledge Studies in Governance and Public Policy. Routledge, London. https://doi.org/10.4324/9781315675008
Parkhurst JO, Abeysinghe S (2016) What constitutes “Good” evidence for public health and social policy-making? From hierarchies to appropriateness. Soc Epistemol 30(5–6):665–679. https://doi.org/10.1080/02691728.2016.1172365
Pearce W, Raman S (2014) The new randomised controlled trials (RCT) movement in public policy: challenges of epistemic governance. Policy Sci 47(4):387–402. https://doi.org/10.1007/s11077-014-9208-3
Pearce W, Grundmann R, Hulme M et al. (2017) Beyond counting climate consensus. Environ Commun 11(6):723–730. https://doi.org/10.1080/17524032.2017.1333965
Pearce W, Mahony M, Raman S (2018) Science advice for global challenges: Learning from trade-offs in the IPCC. Environ Sci Policy 80:125–131. https://doi.org/10.1016/j.envsci.2017.11.017
Pielke RA (2007) The honest broker: Making sense of science in policy and politics. Cambridge University Press, Cambridge. https://doi.org/10.1017/CBO9780511818110
Popper K (1963) Science as Falsification. Conjectures and refutations, readings in the philosophy of science. Routledge, London. https://doi.org/10.2307/3517358
Powell WW, Snellman K (2004) The knowledge economy. Annu Rev Sociol 30(1):199–220. https://doi.org/10.1146/annurev.soc.29.010202.100037
Prainsack B (2018) The “We” in the “Me”: Solidarity and health care in the era of personalized medicine. Sci Technol Hum Values 43(1):21–44. https://doi.org/10.1177/0162243917736139
Prainsack B, Svendsen MN, Koch L et al. (2010) How do we collaborate? Social science researchers’ experience of multidisciplinarity in biomedical settings. BioSocieties 5(2):278–286. https://doi.org/10.1057/biosoc.2010.7
Reed M, Evely A (2016) How can your research have more impact? Five key principles and practical tips for effective knowledge exchange. LSE Impact blog: 1–5. Available at: http://blogs.lse.ac.uk/impactofsocialsciences/2015/07/07/how-can-your-research-have-more-impact-5-key-principles-tips/ . (Accessed 10 July 2018)
Rescher N (1993) Pluralism: against the demand for consensus. Clarendon Press, Oxford University Press, Oxford
Russell J, Greenhalgh T (2014) Being ‘rational’ and being ‘human’: How National Health Service rationing decisions are constructed as rational by resource allocation panels. Health (United Kingdom). https://doi.org/10.1177/1363459313507586
Sanderson I (2000) Evaluation in complex policy systems. Evaluation 6(4):433–454. https://doi.org/10.1177/13563890022209415 .
Sarewitz D (2018) Of cold mice and isotopes or should we do less science? In: Science and politics: Exploring relations between academic research, higher education, and science policy summer school in higher education research and science studies, Bonn, 2018. Available at: https://sfis.asu.edu/sites/default/files/should_we_do_less_science-revised_distrib.pdf
Science (2018) Congress approve largest U.S. research spending increase in a decade. https://doi.org/10.1126/science.aat6620
Scott J, Lubienski C, Debray-Pelot E (2009) The politics of advocacy in education. Educ Policy. https://doi.org/10.1177/0895904808328530
Scott JT (2011) Market-driven education reform and the racial politics of advocacy. Peabody J Educ. https://doi.org/10.1080/0161956X.2011.616445
Sense about Science (2016) Missing evidence. Available at: https://senseaboutscience.org/activities/missing-evidence/ . (Accessed 14 Feb 2019)
Shapin S (1995) Here and everywhere: sociology of scientific knowledge. Ann Rev Sociol. https://doi.org/10.1146/annurev.soc.21.1.289
Shefner J Dahms HF Jones RE (eds) (2014) Social justice and the university. Palgrave Macmillan UK, London. https://doi.org/10.1057/9781137289384
Shepherd J, Frampton GK, Pickett K et al. (2018) Peer review of health research funding proposals: A systematic map and systematic review of innovations for effectiveness and efficiency. PLoS ONE 13(5):e0196914. https://doi.org/10.1371/journal.pone.0196914
Smallman M (2018) Science to the rescue or contingent progress? Comparing 10 years of public, expert and policy discourses on new and emerging science and technology in the United Kingdom. Public Underst Sci. https://doi.org/10.1177/0963662517706452
Article MathSciNet PubMed Google Scholar
Smith K, Stewart E (2017) We need to talk about impact: Why social policy academics need to engage with the UK’s research impact agenda. J Soc Policy 109–127. https://doi.org/10.1017/S0047279416000283
Smith K, Stewart E, Donnelly P et al. (2015) Influencing policy with research-public health advocacy and health inequalities. Health Inequalities. https://doi.org/10.1093/acprof:oso/9780
Smith KE, Stewart EA (2017) Academic advocacy in public health: Disciplinary ‘duty’ or political ‘propaganda’? Soc Sci Med 189:35–43. https://doi.org/10.1016/j.socscimed.2017.07.014
Stevenson O (2019) Making space for new models of academic-policy engagement. Available at: http://www.upen.ac.uk/blogs/?action=story&id=41 . (Accessed 12 Apr 2019)
Stewart R, Langer L, Erasmus Y (2018) An integrated model for increasing the use of evidence by decision-makers for improved development. Dev Southern Africa. 1–16. https://doi.org/10.1080/0376835X.2018.1543579
Stilgoe J, Owen R, Macnaghten P (2013) Developing a framework for responsible innovation. Res Policy. https://doi.org/10.1016/j.respol.2013.05.008
Tchilingirian JS (2018) Producing knowledge, producing credibility: British think-tank researchers and the construction of policy reports. Int J Polit Cult Soc 31(2):161–178. https://doi.org/10.1007/s10767-018-9280-3
Traynor R, DeCorby K, Dobbins M (2014) Knowledge brokering in public health: A tale of two studies. Public Health 128(6):533–544. https://doi.org/10.1016/j.puhe.2014.01.015
Nutley SM, Tseng V (2014) Building the infrastructure to improve the use and usefulness of research in education. In: Finnigan KS, Daly AJ (eds) Using research evidence in education: From the schoolhouse door to Capitol Hill. Policy implications of research in education, vol. 2. Springer, pp 163–175. https://doi.org/10.1007/978-3-319-04690-7_11
Tseng V, Easton JQ, Supplee LH (2018) Research-practice partnerships: Building two-way streets of engagement. Soc Policy Report. https://doi.org/10.1002/j.2379-3988.2017.tb00089.x
UKRI-UNDP (2018) UKRI-UNDP joint report: ‘How science, research and innovation can best contribute to meeting the sustainable development goals for developing countries’ full application guidance -applications by invitation only. Available at: https://www.ukri.org/research/global-challenges-research-fund/ukri-undp-joint-report-how-science-research-and-innovation-can-best-contribute-to-meeting-the-sustainable-development-goals-for-developing-countries/ . (Accessed 14 Feb 2019)
UKRI (2017) UK strategy for the global challenges research fund (GCRF). Available at: https://www.ukri.org/files/legacy/research/gcrf-strategy-june-2017/%0A%0A
Ward V (2017) Why, whose, what and how? A framework for knowledge mobilisers. Evid Policy. https://doi.org/10.1332/174426416X14634763278725
Wehrens R, Bekker M, Bal R (2010) The construction of evidence-based local health policy through partnerships: Research infrastructure, process, and context in the Rotterdam ‘Healthy in the City’ programme. J Public Health Policy. https://doi.org/10.1057/jphp.2010.33
Weiss CH (1979) The many meanings of research utilization. Public Adm Rev 39(5):426. https://doi.org/10.2307/3109916
White HC (2008) Identity and control: How social formations emerge. Princeton University Press, Princeton. https://doi.org/10.1007/s13398-014-0173-7.2
Whitehead M, Petticrew M, Graham H et al. (2004) Evidence for public health policy on inequalities: 2: Assembling the evidence jigsaw. J Epidemiol Community Health 2004:817–821. https://doi.org/10.1136/jech.2003.015297
Williams K (2018) Three strategies for attaining legitimacy in policy knowledge: Coherence in identity, process and outcome. Public Admin. https://doi.org/10.1111/padm.12385
Wynne B (1992) Misunderstood misunderstanding: Social identities and public uptake of science. Public Understand Sci. 1281–304. https://doi.org/10.1088/0963-6625/1/3/004
Yanovitzky I, Weber M (2018) Analysing use of evidence in public policymaking processes: a theory-grounded content analysis methodology. Evid Policy. https://doi.org/10.1332/174426418x15378680726175
Download references
Acknowledgements
We thank the Nuffield Foundation, the Wellcome Trust and the William T Grant Foundation for financial support for a meeting on Transforming the use of Research Evidence, held in London in 2018. We are grateful to both the participants at this meeting and those attending the William T Grant Foundation Use of Research Evidence meeting in Washington 2019. In particular, we very much appreciate the contribution of Kim DuMont, Paul Cairney and Warren Pearce who commented on drafts of this paper before submission. Our thanks to you all.
Author information
Authors and affiliations.
London School of Hygiene and Tropical Medicine, London, UK
Kathryn Oliver
Kingston University, London, UK
Annette Boaz
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Kathryn Oliver .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Oliver, K., Boaz, A. Transforming evidence for policy and practice: creating space for new conversations. Palgrave Commun 5 , 60 (2019). https://doi.org/10.1057/s41599-019-0266-1
Download citation
Received : 19 February 2019
Accepted : 14 May 2019
Published : 28 May 2019
DOI : https://doi.org/10.1057/s41599-019-0266-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Public engagement for inclusive and sustainable governance of climate interventions.
- Livia Fritz
- Chad M. Baum
- Benjamin K. Sovacool
Nature Communications (2024)
Combining public health evidence, policy experience and communications expertise to inform preventive health: reflections on a novel method of knowledge synthesis
- Maddie Heenan
- Alexandra Chung
- Lucie Rychetnik
Health Research Policy and Systems (2023)
Developing, implementing, and monitoring tailored strategies for integrated knowledge translation in five sub-Saharan African countries
- Kerstin Sell
- Nasreen S. Jessani
- Lisa M. Pfadenhauer
Barriers to evidence use for sustainability: Insights from pesticide policy and practice
- Benjamin Hofmann
- Karin Ingold
- Sabine Hoffmann
Ambio (2023)
Building evidence into youth health policy: a case study of the Access 3 knowledge translation forum
- Daniel Waller
- Fiona Robards
- Melissa Kang
Health Research Policy and Systems (2022)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Influence of Research on Health Policy and Clinical Practice
Affiliation.
- 1 Sikkim Manipal Institute of Medical Sciences, 5th Mile, Tadong, Gangtok, Sikkim India.
- PMID: 28867881
- PMCID: PMC5561754
- DOI: 10.1007/s13224-017-1013-4
Clinical research is a type of biomedical research conducted to aid and support the development of knowledge wherein there is involvement of patient. One of the key duties of healthcare professionals is to involve in research and change existing practice, when there is robust evidence in favour of new strategies that can have better patient care. Knowledge derived from research and experience may be of little value unless it is put into practice. Evidence-based medicine (EBM) is the diligent, clear, and wise use of current best research evidence in making decisions about clinical care of patients. The practice of EBM is incorporating clinician's expertise with the best available clinical evidence from research. It leads to improved patient outcomes and promote critical thinking and reflective practice. Effective research utilization can enhance policy decisions, resource allocation for programmes, and decisions about how to deliver those services.
Keywords: Audit; Evidence; Health policy; Health practice; Research.
Advertisement
Influence of Research on Health Policy and Clinical Practice
- Invited Mini Review
- Published: 07 June 2017
- Volume 67 , pages 319–323, ( 2017 )
Cite this article

- Hafizur Rahman 1
248 Accesses
2 Citations
Explore all metrics
“ ‘The important thing is not to stop questioning.” -Albert Einstein.
Clinical research is a type of biomedical research conducted to aid and support the development of knowledge wherein there is involvement of patient. One of the key duties of healthcare professionals is to involve in research and change existing practice, when there is robust evidence in favour of new strategies that can have better patient care. Knowledge derived from research and experience may be of little value unless it is put into practice. Evidence-based medicine (EBM) is the diligent, clear, and wise use of current best research evidence in making decisions about clinical care of patients. The practice of EBM is incorporating clinician’s expertise with the best available clinical evidence from research. It leads to improved patient outcomes and promote critical thinking and reflective practice. Effective research utilization can enhance policy decisions, resource allocation for programmes, and decisions about how to deliver those services.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others

Research for Improving Patient Care

Evidence-Based Medicine in Theory and Practice: Epistemological and Normative Issues

“Basic Science”. Association of American Medical Colleges. www.aamc.org . Accessed 20 March 2017.
Contopoulos-Ioannidis DJ, Gilbody SM, Trikalinos TA, et al. Comparison of large versus smaller randomized trials for mental health-related interventions. Am J Psychiatry. 2005;162:578–84.
Article PubMed Google Scholar
Shakila T, Khan SK. Participation in research as a means of improving quality of care: the role of a principal investigator in multicentre clinical trials. Obstet Gynaecol. 2015;17:55–61.
Google Scholar
National Health Service. The NHS Plan. Cmd. 4818. London: Stationery Office, 2000. [ http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_4002960 ] Accessed 20 March 2017.
NHS, National Institute for Clinical Excellence, Commission for Health Improvement, Royal College of Nursing, University of Leicester. Principles for Best Practice in Clinical Audit. Oxford: Radcliffe Medical Press; 2002. [ http://www.uhbristol.nhs.uk/files/nhs-ubht/best_practice_clinical_audit.pdf ] Accessed 21 March 2017.
Warlow C. Clinical research under the cosh again. This time it is ethics committees. BMJ. 2004;329:241–2.
Article PubMed PubMed Central Google Scholar
Smith R. Audit and research. BMJ. 1992;305:905–6.
Article CAS PubMed PubMed Central Google Scholar
Sackett DL, Rosenberg WMC, Gray JAM, et al. Evidence based medicine: what it is and what it isn’t. BMJ. 1996;312:71–2.
Montgomery K. How doctors think: clinical judgement and the practice of medicine. Oxford: Oxford University Press; 2006.
Gigerenzer G, Gaissmaier W, Kurz-Milcke E, et al. Helping doctors and patients make sense of health statistics. Psychol Sci Public Interest. 2007;8:53–96.
Greenhalgh T, Howick J, Maskrey. Evidence based medicine: a movement in crisis? BMJ. 2014;348:1–7.
Article Google Scholar
Lenzer J. Why we can’t trust clinical guidelines. BMJ. 2013;346:f3830.
Pablos-Mendez A, Shademani R. Knowledge translation in global health. J Contin Educ Health Prof. 2006;26:81–6.
Lavis JN, Catallo C, Permanand G, et al. BRIDGE study team: BRIDGE summary 1—communicating clearly: enhancing information-packaging mechanisms to support knowledge brokering in European health systems. Brussels: European Observatory on Health Systems and Policies; 2011.
Caplan N. The two communities theory and knowledge utilization. Am Behav Sci. 1979;22:459–70.
Hyder AA, Corluka A, Winch PJ, et al. National policy-makers speak out: are researchers giving them what they need? Health Policy Plan. 2011;26:73–82.
Ross SE, Lavis JN, Rodriguez C, et al. Partnership experiences: involving decision-makers in the research process. J Health Serv Res Policy. 2003;8:26–34.
Lavis JN, Davies H, Oxman AD, et al. Towards systematic reviews that inform health care management and policymaking. J Health Serv Res Policy. 2005;10:35–48.
Ellen ME. Knowledge translation on ageing and health: a framework for policy development. Geneva: World Health Organization; 2012.
Dobbins M, Ciliska D, Cockerill R, et al. A framework for the dissemination and utilization of research for health-care policy and practice. Online J Knowl Synth Nurs. 2002;9:7.
PubMed Google Scholar
Hennink M, Stephenson R. Using research to inform health policy: barriers and strategies in developing countries. J Health Commun. 2005;10(2):163–80.
Gillis A, Jackson W. Research for nurses: methods and interpretation. Philadelphia: F.A. Davis Company; 2002.
Hanney SR, Gonzalez-Block MA, Buxton MJ, et al. The utilisation of health research in policy-making: concepts, examples and methods of assessment. Health Res Policy Syst. 2003;1(1):2.
Morrison I, Smith R. The future of medicine. BMJ. 1994;309:1099–100.
Rahman H, Kar S. Knowledge, attitudes and practice toward cervical cancer screening among Sikkimese nursing staff in India. Indian J Med Paediatr Oncol. 2015;36:105–10.
Download references
Author information
Authors and affiliations.
Sikkim Manipal Institute of Medical Sciences, 5th Mile, Tadong, Gangtok, Sikkim, India
Hafizur Rahman
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hafizur Rahman .
Ethics declarations
Conflicts of interest, additional information.
Dr Hafizur Rahman is a Professor of Obstetrics and Gynaecology, Sikkim Manipal Institute of Medical Sciences, Gangtok, India.
Rights and permissions
Reprints and permissions
About this article
Rahman, H. Influence of Research on Health Policy and Clinical Practice. J Obstet Gynecol India 67 , 319–323 (2017). https://doi.org/10.1007/s13224-017-1013-4
Download citation
Received : 19 April 2017
Accepted : 16 May 2017
Published : 07 June 2017
Issue Date : October 2017
DOI : https://doi.org/10.1007/s13224-017-1013-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health policy
- Health practice
- Find a journal
- Publish with us
- Track your research

How can research findings influence policy on health?
26 September 2019
- Newsletter feature
- Improvement research
- Share on Twitter
- Share on LinkedIn
- Share on Facebook
- Share on WhatsApp
- Share by email
- Link Copy link
Stephen Aldridge is Director for Analysis and Data at the Ministry of Housing, Communities and Local Government. A government economist by background, he was previously Chief Economist and then Director of the Strategy Unit in the Cabinet Office. He is a member of the advisory group for our Social and Economic Value of Health research programme . We spoke to Stephen about the programme, and how research findings can influence policy.
Why is it so important to build and spread knowledge about the value of health to society and the economy?
Understanding that health has value over and above its impact on our personal wellbeing – for example, because it helps to improve work productivity or wider prosperity – is clearly really important when making policy decisions.
It’s not just about how much we should spend on health care, but it helps to inform what specific interventions we should be making to improve health, on the basis that more effective interventions will improve human capital (the skills, knowledge, capacity and capability of the population) and the outcomes for society and the economy that we’re interested in.
You are part of the advisory group for the first round of grants issued through the Health Foundation's Social and Economic Value of Health research programme. Why is this programme important?
You only have to read the titles of the projects in the research programme to appreciate their potential significance. One project is looking at the relationship between childhood obesity and its impacts on human capital development; another is on health and labour market outcomes; and there’s a project looking at parental and childhood health and educational attainment. Having an understanding of, for example, the relationship between health and the labour market would enable us better to design policies to ensure both better health and better labour market outcomes.
The researchers are using very large datasets and bringing data analytics to bear in new ways in order to really try and pin down the nature of these relationships. It’s very important to understand whether we are saying that better health leads to better labour market outcomes, or that better labour market outcomes lead to improved health. That changes what you might do in the light of the research findings.
Whether in health or other spheres, research findings will have an impact and help to inform and improve many important decisions. However, it may take time and it may be a challenge, because sometimes evidence can be complicated or counterintuitive.
How can policymakers find out about new research like this?
Within government departments, there are analysts like me who act as intermediaries between policymakers and academia. Personally, I try to build strong links with relevant experts in the areas on which my team is providing analytical advice, so we can help policymakers access that research. Within my department, we run seminars and host roundtables with external experts. The importance of bringing people together and sharing knowledge shouldn’t be underestimated.
There are other important intermediaries – indeed, the Health Foundation is one, with its role not just in funding research, but in making it available in ways that are accessible to policymakers. There are also the research councils, which run various activities to make sure that research findings are shared with policymakers.
I’ve been involved in the establishment of a number of What Works centres and one of their roles is to synthesise evidence on what we know works in achieving different policy goals. There’s the Centre for Ageing Better, the Early Intervention Foundation, the Centre for Local Economic Growth, the recently established Centre for Homelessness Impact and a number of others. They’re an example of the intermediaries that exist to help channel evidence to policymakers in a clear and timely way.
What can researchers do to make the evidence they build more accessible to policymakers?
The key thing is that researchers need to think about how they present their findings clearly – and in plain English! Some of the What Works centres have developed dashboards to summarise evidence on what works in achieving different policy outcomes and which interventions are most cost-effective.
It’s also very important for researchers to build relationships with policymakers and vice versa. I’m closely involved with the Centre for Science and Policy at the University of Cambridge. They arrange really excellent policy fellowships, which mean that civil servants and people from other sectors can meet academic researchers to discuss issues of mutual interest and to improve the sharing of knowledge. We’re all busy, but we need to redouble our efforts to make use of these types of opportunities.
How can the research community ensure the topics they study are relevant for policymakers?
My department and others have developed short documents detailing our areas of research interest and I think this type of communication is really important.
It’s also important for policymakers and researchers to engage directly. Researchers can reach out to analysts like me in government departments, and use us as intermediaries to the policy community. The What Works centres and similar bodies – including the Health Foundation – can also facilitate connections and conversations about the topics on which it would be most useful to have more research.
I run a series of economic and social research seminars, inviting people from academia, think tanks and elsewhere to come and talk to people in the department. Many government departments have programmes of engagement with the research community and I’d really encourage researchers to take up those opportunities.
For more information contact Stephen ( [email protected] or via twitter @saldridg ).
This content originally featured in our email newsletter, which explores perspectives and expert opinion on a different health or health care topic each month.
Also in this newsletter
Share this page:
You might also like...
Health Foundation @HealthFdn
- Work with us
We look for talented and passionate individuals as everyone at the Health Foundation has an important role to play.
The Q community
Q is an initiative connecting people with improvement expertise across the UK.
Quick links
- News and media
- Events and webinars
Hear from us
Receive the latest news and updates from the Health Foundation
- 020 7257 8000
- [email protected]
- The Health Foundation Twitter account
- The Health Foundation LinkedIn account
- The Health Foundation Facebook account
Copyright The Health Foundation 2024. Registered charity number 286967.
- Accessibility
- Anti-slavery statement
- Terms and conditions
- Privacy policy

- Systematic review
- Open access
- Published: 18 April 2017
Using media to impact health policy-making: an integrative systematic review
- Lama Bou-Karroum 1 , 2 ,
- Fadi El-Jardali 1 , 2 , 3 ,
- Nour Hemadi 2 ,
- Yasmine Faraj 2 ,
- Utkarsh Ojha 4 ,
- Maher Shahrour 5 ,
- Andrea Darzi 1 , 6 ,
- Maha Ali 7 , 8 ,
- Carine Doumit 9 ,
- Etienne V. Langlois 10 ,
- Jad Melki 11 ,
- Gladys Honein AbouHaidar 12 &
- Elie A. Akl 1 , 3 , 13
Implementation Science volume 12 , Article number: 52 ( 2017 ) Cite this article
32k Accesses
60 Citations
32 Altmetric
Metrics details
Introduction
Media interventions can potentially play a major role in influencing health policies. This integrative systematic review aimed to assess the effects of planned media interventions—including social media—on the health policy-making process.
Eligible study designs included randomized and non-randomized designs, economic studies, process evaluation studies, stakeholder analyses, qualitative methods, and case studies. We electronically searched Medline, EMBASE, Communication and Mass Media Complete, Cochrane Central Register of Controlled Trials, and the WHO Global Health Library. We followed standard systematic review methodology for study selection, data abstraction, and risk of bias assessment.
Twenty-one studies met our eligibility criteria: 10 evaluation studies using either quantitative ( n = 7) or qualitative ( n = 3) designs and 11 case studies. None of the evaluation studies were on social media. The findings of the evaluation studies suggest that media interventions may have a positive impact when used as accountability tools leading to prioritizing and initiating policy discussions, as tools to increase policymakers’ awareness, as tools to influence policy formulation, as awareness tools leading to policy adoption, and as awareness tools to improve compliance with laws and regulations. In one study, media-generated attention had a negative effect on policy advocacy as it mobilized opponents who defeated the passage of the bills that the media intervention advocated for. We judged the confidence in the available evidence as limited due to the risk of bias in the included studies and the indirectness of the evidence.
There is currently a lack of reliable evidence to guide decisions on the use of media interventions to influence health policy-making. Additional and better-designed, conducted, and reported primary research is needed to better understand the effects of media interventions, particularly social media, on health policy-making processes, and the circumstances under which media interventions are successful.
Trial registration
PROSPERO 2015: CRD42015020243
Peer Review reports
Media interventions are defined as organized and purposive activities that utilize a variety of media channels to inform, persuade, or motivate populations [ 1 ]. In health care, media interventions can convey health-related information including research evidence to the public, policymakers, and health professionals [ 2 – 6 ]. They can also influence individual health behaviors [ 7 ]. For instance, media campaigns were shown to be effective in decreasing tobacco uptake, reducing alcohol-impaired driving and alcohol-related crashes and influencing health services utilization [ 8 – 10 ].
In the area of policy-making, media can contribute to setting the agenda for the press, the public, and policymakers through highlighting what issues are newsworthy at a particular time [ 11 ]. Media can also influence how the public and policymakers view or think about certain issues through selecting some aspects of a perceived reality and making them more salient in a communicating text [ 12 ]. Another way media can influence policymakers is through shaping public opinion, which in turn, exerts pressure on policymakers to respond [ 13 ]. For instance, media advocacy is known as a popular strategy in public health that can assist in increasing public awareness and mobilizing decision-makers for policy change [ 14 , 15 ].
When examining the various functions that media interventions can play in the health field, it is important to consider new interactive information and communication platforms, particularly social media including blogs, social networking sites, and interactive websites. While traditional media, mainly television, still account for a large audience, the influence of social media is constantly increasing and cannot be ignored [ 16 , 17 ]. Social media increase user interaction, provide peer support, and extend access to health interventions [ 16 , 17 ]. Social media also bring a new dimension to health care as they provide the public, patients, and health professionals with a platform to exchange on different health matters potentially affecting population health outcomes [ 18 ].
A number of systematic reviews on the impact of media interventions on health behavior and their use in increasing awareness and education exist [ 16 , 19 , 20 ]. However, to our knowledge, there is no systematic review assessing the role of media interventions in the different stages of health policy-making. Our objective is to better inform those considering the use of media interventions to influence health policy-making. Therefore, we conducted this integrative review to assess the effects of planned media interventions on the health policy-making process.
Protocol and registration
A protocol for this review is registered in PROSPERO International prospective register of systematic reviews under registration number PROSPERO 2015:CRD42015020243 [ 21 ]. While we had planned in the protocol to start the search with the year 2000, following our discussion with a media expert, we changed the date to the year 2005—the year of the rise of “web 2.0”. Web 2.0 allowed users of the web to interact and generate content especially through social media [ 22 ]. Around that time, traditional mainstream media also started to more seriously integrate social media within their operations.
Methodology
We used the integrative review methodology that aims to include a range of studies from different methodological approaches (both experimental and non-experimental). We followed the five stages of an integrative review by Whittmore et al.: problem formulation, literature search, data evaluation, data analysis, and data presentation [ 23 ]. This methodology is meant to protect against bias, enhance rigor, and improve accuracy of conclusions [ 23 ].
Problem formulation
Herein the definitions of terms used in the research question:
- Media interventions
Media interventions are described as organized and purposive activities that utilize a variety of media channels to inform, persuade, or motivate populations [ 1 ]. Given that the goal of this review was to inform those interested in using media interventions to affect health policy-making, we restricted our eligibility to studies where the primary purpose of using media was to affect policy-making (i.e., media as planned intervention). For example, we excluded studies where unplanned media coverage influenced health policy-making or where media coverage followed a health policy change. To make this distinction, we adopted the terminology used by a published Cochrane review on a related topic—effects of mass media on the utilization of health services—to distinguish between the two approaches: planned campaigns/interventions and unplanned media coverage [ 10 ].
Public policy
Public policy referred to government policy such as any statement or position taken by the government or government departments [ 13 ]. We only considered public policies pertaining to health. We adopted the stages heuristic framework that divides the public policy process into five stages: agenda-setting, policy formulation, adoption, implementation, and evaluation. Agenda-setting is the stage during which issues or subjects reach the policy agenda and get the attention of policymakers. In the formulation and adoption stages, legislatures and other decision-makers design policies and adopt policy solutions in the form of legislation or rules. In the implementation stage, governments carry out an adopted policy and resources are mobilized. Finally, the evaluation stage aims at assessing whether policies have achieved their intended objectives [ 24 , 25 ].
Outcomes of interest
Our outcomes of interest were the impact of the intervention on the different stages of the policy process, as defined above: agenda-setting, policy formulation, adoption, implementation, and evaluation. We only included studies that assessed the effects of media on policy outcome. For this purpose, we used a framework that provides indicators to assess the influence of media advocacy on policy outcomes. Some of the indicators include speeches and statements, mentions in official documents, new policy or legislation, and increased enforcement of a policy. We did not consider surrogate outcomes such as the impact on media coverage, community, or public opinion [ 26 ].
Literature search
Eligibility criteria.
We considered as eligible for this integrative review the following:
Study designs: randomized studies, non-randomized studies, economic studies, process evaluation studies, stakeholder analyses, qualitative studies, and case studies. We excluded editorials, commentaries, news articles, letters, conference papers, proposals, reviews, and studies published only in abstract format;
Planned media interventions (e.g., advocacy activities, media campaigns) implemented as stand-alone or as part of multicomponent interventions, including social media (Facebook, Twitter, blogs), broadcast media (radio, television), print media (newspapers, newsletters, magazines, leaflets, posters, and pamphlets), and electronic media (websites). The media interventions should have targeted a specific population such as specific communities, policymakers, groups, or associations;
Setting: any country, state, or community;
Studies that assessed the impact of media interventions on one of the policy stages as defined in the stages heuristic framework: agenda-setting (setting the policy agenda and establishing priorities), policy formulation, adoption, implementation, and evaluation [ 24 ]. We excluded studies that did not formally assess the association between media exposure and policy-making (e.g., assessed surrogate outcomes such as increasing exposure, engagement, and preferences of the public for certain policies).
Search strategy
We searched Medline, EMBASE, Communication and Mass Media Complete, Cochrane Central Register of Controlled Trials (CENTRAL), and the WHO Global Health Library. We developed the search strategies used in the different databases in consultation with an expert librarian. We used both free text search terms and MeSH terms (see details for the different electronic databases in Additional file 1 ). We ran the search from January 2005 until June 2015. We did not restrict the search to specific languages. We also screened the reference lists of included studies to retrieve additional studies, and we contacted experts in the field (including authors of included studies) to get additional material.
Selection process
We imported the search results into Endnote X7 and removed duplicates. Before starting the selection process, and in order to ensure its reliability, all the reviewers participated in a calibration exercise using a randomly chosen sample of 100 citations.
The selection process consisted of two stages:
Title and abstract screening: Teams of two reviewers (LBK, MS, AD, MA, CD) used the eligibility criteria to screen titles and abstracts of identified citations in duplicate and independently for potential eligibility. Then, they retrieved the full-texts for citations judged as potentially eligible by at least one of the two reviewers.
Full-text screening: Teams of two reviewers (LBK, NH, YF, UO, MS) used the same eligibility criteria to screen the full-texts in duplicate and independently for eligibility. At this stage, the two reviewers compared results and resolved disagreement by discussion. The reviewers aimed not to force consensus, and when consensus could not be reached, a third reviewer (FJ or EAA) made the final decision. We used standardized and pilot-tested screening forms. We documented the reason for study exclusion.
We used Fleiss’ Kappa coefficient to calculate agreement between reviewers for full-text screening. We used the following values to judge the degree of agreement: 0.21–0.40 for fair agreement, 0.41–0.60 for moderate agreement, 0.61–0.80 for substantial agreement, and 0.81–1.00 for almost perfect agreement [ 27 ].
Data evaluation
Throughout the process of data abstraction, two reviewers abstracted data from eligible studies in duplicate and independently. We used standardized and piloted data abstraction forms. We conducted a calibration exercise on a randomly chosen sample to ensure adequate agreement. The reviewers resolved their disagreements by discussion or with the help of a third reviewer when consensus could not be reached.
We collected the following information from each included evaluation study: objectives, type of study design, details of the methodology, study setting (health topic and jurisdiction), population, characteristics of the media intervention, type of media used, outcome assessed, study theme, results, and limitations of the study. We abstracted from each included case study the study’s name and country, health topic, type of media used, characteristics of the media intervention, and policy outcome.
As part of data evaluation, we appraised the methodological quality of included studies using tools appropriate to the study design. Two reviewers (LBK, NH) assessed the quality of included studies independently and resolved disagreements through discussion or with the help of a third reviewer when needed. We considered the following tools for assessing the risk of bias (quantitative) and quality of reporting (qualitative) of the included studies:
The Cochrane Risk of Bias tool for randomized trials;
A modified version of the Cochrane Risk of Bias tool for non-randomized studies (A Cochrane Risk Of Bias Assessment Tool: for Non-Randomized Studies of Interventions (ACROBAT-NRSI);
The Cochrane Effective Practice and Organization of Care (EPOC) risk of bias criteria for controlled before and after studies and interrupted time series;
The Critical Appraisal Skills Program (CASP) tool for qualitative studies;
A tool adapted from Lotfi et al. [ 28 ] to assess the methodological features of quantitative studies using surveys including the following criteria: sample size calculation, reporting of a sampling frame, the sampling method, the response rate, and the validity of the survey.
Data analysis and presentation
We stratified the studies based on the stages of the policy-making process. We conducted thematic analysis of all papers reflecting the role of media as reported in each study and presented the results in a narrative summary by stage. Two reviewers (LBK, NH) identified the themes. A third reviewer (GH) settled any discrepancy. We did not identify a mix of quantitative and qualitative data for any of the stages we examined; therefore, we could not conclude whether the included studies confirmed, refuted, or complemented each other [ 29 ].
As for case studies, we summarized them in a table (see Additional file 2 ) listing the study’s name and country, health topic, type of media used, and characteristics of the media intervention and policy outcome.
Study selection
Figure 1 shows the PRISMA flow chart summarizing the study selection process. Out of 13,674 citations, we identified 21 eligible studies: 10 evaluation studies and 11 case studies. We excluded 530 articles at the full-text screening phase for the following reasons: not an intervention of interest ( n = 148), not about public health policy ( n = 155), not an outcome of interest ( n = 164), and not the design of interest ( n = 63). Additional file 2 provides detailed descriptions of the 11 case studies [ 30 – 40 ]. We provide below the characteristics and results of the 10 evaluation studies [ 41 – 50 ].
PRIMSA flowchart for study selection process
Characteristics of the included evaluation studies
Table 1 describes the characteristics of the 10 eligible evaluation studies [ 41 – 50 ], including study design, setting, population, media intervention (type and nature), and outcome assessed.
Study design
The designs of the 10 evaluation studies were
Quantitative ( n = 7): before and after design ( n = 2) [ 47 , 48 ], event history analysis ( n = 1) [ 45 ], media and document analysis ( n = 1) [ 44 ], and cross-sectional survey ( n = 3) [ 42 , 43 , 46 ]. Two of those studies included qualitative components that were not relevant to our question [ 42 , 43 ].
Qualitative ( n = 3): interviews ( n = 1) [ 41 ], media analysis ( n = 1) [ 50 ], and content analysis ( n = 1) [ 49 ].
Setting and population
Except for one study that was conducted in Pakistan [ 41 ], the included studies were conducted in high-income countries: USA ( n = 4), New Zealand ( n = 1), Australia ( n = 1), Canada ( n = 2), and Sweden ( n = 1). One study targeted policymakers only [ 41 ], three targeted the public only [ 46 – 48 ], and six targeted both [ 42 – 45 , 49 , 50 ].
The health topics were water fluoridation ( n = 2), alcohol control ( n = 2), tobacco control ( n = 1), road safety ( n = 1), maternal and newborn health ( n = 1), nursing education ( n = 1), access to health care ( n = 1), and food insecurity ( n = 1).
Type of media assessed
All campaigns relied on the use of traditional media (including broadcast and print media); none included social media. Media activities included a combination of paid media and earned media, where the topic received recognition and gained publicity for free. Examples of encountered media activities were advertisements ( n = 1) [ 48 ], news coverage of events and campaigns ( n = 3) [ 44 , 48 , 50 ], media interviews ( n = 3) [ 42 , 44 , 50 ], TV talk shows ( n = 1) [ 41 ], creating videos ( n = 2) [ 42 , 49 ], launching of websites ( n = 1) [ 42 ], framing and releasing of news and press releases ( n = 3) [ 43 , 45 , 50 ], letters to the editor ( n = 3) [ 42 , 43 , 46 ], provision of information kits to media ( n = 2) [ 43 , 46 ], press conferences ( n = 2) [ 47 , 49 ], and media events ( n = 1) [ 45 ].
Nature of the intervention
In four studies, the media intervention was part of a multi-component intervention, where authors assessed the effect of the whole intervention on policy outcome. Other components included enforcement campaign [ 48 ], parent meetings, merchant meetings, visits to shops, postcards to parents, letters to merchants, training of staff [ 47 ], policy advocacy and community action projects [ 43 ], and a public forum [ 46 ].
In three studies, the media activities were part of a broad intervention program but authors assessed the effect of the media component on policy outcome [ 42 , 44 , 45 ].
In three studies, the media intervention was implemented alone and the effect of the media on policy outcome was explored [ 41 , 49 , 50 ].
Outcomes assessed
Impact on agenda-setting assessed as change in policy priorities/approach of policymakers and as stimulating inquiries and discussions from policymakers [ 41 , 49 ].
Impact on policy formulation assessed as change in content of government policy [ 50 ].
Impact on policy adoption assessed as passage of bills and ordinances [ 44 , 45 ], as change in policies or increased funding to clinics [ 42 ], and as adoption of a new policy [ 43 , 46 ].
Impact on policy implementation assessed as increased enforcement of law, in particular change in seat belt usage rates [ 48 ] and change in availability of beer to the under-aged [ 47 ].
Methodological appraisal
Additional file 3 summarizes the detailed assessment of the methodological appraisal of the 10 evaluation studies. Using the CASP tool, we judged the qualitative study to be of high quality as it reported on 8 of 10 criteria of the tool [ 41 ]. Using the tool adapted from Lotfi et al. [ 28 ], we judged the three quantitative survey studies to be at high risk of bias since they suffered from a number of methodological limitations [ 42 , 43 , 46 ]. The same applied to the controlled before and after study [ 47 ], using the EPOC risk of bias criteria. We were not able to find tools to assess the methodological quality of the other five studies. So we assessed their limitations narratively (see Additional file 3 ). Overall, they all suffered from at least one major limitation (mainly related to confounding), so we judged them to be at high risk of bias.
Effects of media interventions on policy outcomes
Additional file 4 provides themes and results of individual studies. We present below the findings organized according to the stages heuristic framework of the public policy process and present the overarching effect of media on each stage highlighted in italic font [ 24 ].
Agenda-setting
Two qualitative studies have assessed media interventions as stand-alone interventions and found positive perceptions regarding the impact of media on agenda-setting.
Haq et al. [ 41 ] used a qualitative study design to examine the use of media as accountability tools leading to prioritizing and initiating policy discussions . The study evaluated a television talk show in Pakistan aiming to get on-camera commitments from key officials and policymakers belonging to district health policy. The interviews with the officials and policymakers 6 months following the TV talk show suggested that this media accountability tool was an “effective” strategy in setting maternal and newborn health as a priority health issue in the targeted districts, as perceived by the interviewees. The effectiveness of television talk show was based on the perceptions of the interviewees [ 41 ].
Rock et al. [ 49 ] used a content analysis design to qualitatively examine media as tools to increase policymakers’ awareness in Canada in 2008. The media intervention intended to convey the message that income-related food insecurity is a serious population health problem. The authors of this study reported that the media intervention generated interest within the Government of Canada and the Government of Alberta, in particular, stimulated discussion in the Alberta Legislature and sparked inquiries from the Senate Committee on Social Affairs Subcommittee on Cities and from a political staff member [ 49 ].
Policy formulation
Leurer [ 50 ] used a qualitative media analysis to examine the role of media as advocacy tools to influence policy formulation . The authors of the study reported that media advocacy efforts of nursing stakeholders in Saskatchewan, Canada, increased public pressure that in return led the government to revise its policy that originally intended to impose a 3-year diploma entry requirement despite opposition from the licensing body. They also noted that what happened in Saskatchewan “stands in contrast to the neighboring province of Manitoba where the government’s announcement of a reintroduction of the diploma entry requirement in 2000, within weeks of the Saskatchewan announcement, was implemented” [ 50 ].
Policy adoption
All the five studies that examined the effect of media on policy adoption were quantitative [ 42 – 46 ]. All five focused on media as awareness tools leading to policy adoption . The differences were in the targets of the planned media. All but one study, Harwood et al. [ 44 ], suggested that media interventions were successful in achieving the intended goals.
Harwood et al. [ 44 ] assessed the association between media attention to alcohol issues and the legislative success of related bills. A detailed analysis of media covers four alcohol policies: bans on minors in bars, increases in alcohol taxes, beer keg registration, and zero tolerance for teen driving under the influence of alcohol. The analysis showed that out of the five bills that successfully passed, four received little or no media attention while all the bills that were defeated received intense media coverage. The authors speculated that press attention may have hindered the passage of bills through mobilizing opponents but they provided no details on those “opponents” or whether they run any counter campaigns. The authors also concluded that press inattention may give stakeholders the opportunity to compromise during negotiations on bill content and wording [ 44 ].
Niederdeppe et al. [ 45 ] suggested that media awareness efforts implemented as part of the Florida Tobacco Control Program (FTCP) in FL, USA, were effective in generating news coverage and promoting policy change—the passage of the tobacco product placement ordinances (TPPO). TPPO are designed to reduce youth smoking by removing the visual and physical availability of cigarettes, requiring retailers to place cigarettes and other tobacco products behind the counter. The study found that a one-unit increase in news coverage on Students Working Against Tobacco, a part of the FTCP, was associated with a 94% increase in the odds of counties enacting a TPPO ( p value <0.05). The effect persisted when the analysis controlled for community mobilization and pro-tobacco marketing influences [ 45 ].
Two studies (Sivaneswaran et al. and Gowda et al.) assessed the role of media as awareness tools to gain public support leading to policy adoption [ 43 , 46 ]. Sivaneswaran et al. [ 46 ] explored the role of a multicomponent education campaign including the use of media to educate and increase awareness about the importance of water fluoridation. The purpose of the campaign was to gain public support before the adoption and implementation of the water fluoridation policy in two rural towns in New South Wales, Australia, in 2005. Thus, the Mid-Western Regional Council commissioned an independent rural research organization to survey households in those two communities to assess their support of the fluoridation. The survey found that newspapers followed by radio and television ( n = 80) were the most common sources of information (86%). Among those who were informed, 59% indicated that they were supportive of the policy compared with 47% among those not informed. Although the authors do not explicitly provide evidence for the link between public opinion and policy adoption, they make a clear statement supporting that link: “the pro-fluoridation decision was influenced by the majority of community support for the measure” [ 46 ].
Gowda et al. [ 43 ] evaluated a fluoridation advocacy program implemented in Northland, New Zealand. Media were employed as part of the advocacy program to raise awareness and to promote water fluoridation among the community and decision-makers. The authors reported on a community consultation survey that showed that the public was in favor of fluoridation in two districts of Northland (53 and 56%). Although Gowda et al. did not explicitly provide evidence for the link between public opinion and policy adoption, they clearly stated that obtaining “a simple majority in favor of fluoridation led directly to the District Council’s resolution to fluoridate” . The authors of the study judged that positive publicity and messages, the timing, and the reopening of the fluoridation issue were important in gaining support for fluoridation from other health providers, health organizations, and the community [ 43 ].
Gardner et al. [ 42 ] explored the role of media advocacy as tools for increasing awareness of policymakers on community clinics’ issues and leading to policy adoption. A survey of policymakers, community leaders, and stakeholders in 2003 and 2004 reported that 60% of the 2003 and 42% of the 2004 respondents perceived Clinic Consortia media activities to be “very effective” at increasing their awareness of community clinics’ issues. Nearly all (95%) clinic organizations and associations surveyed rated media as “effective” in increasing policymaker awareness. However, only 20% of the clinic organizations and associations reported that the media were successful in achieving a policy change or increasing funding to the clinics [ 42 ]. The effectiveness of media advocacy in this paper was based on the perceptions of the respondents.
Policy implementation
Two before and after studies examined media as awareness tools to improve compliance with laws and regulations. While the two studies found positive effects on compliance with laws and regulations, media interventions were part of multi-component interventions [ 47 , 48 ].
Rehnman et al. [ 47 ] explored the effects of “the beer campaign” conducted in 1999 and 2000 in Stockholm, Sweden. The campaign aimed to reduce the sale of beer to under-aged youths. The media advocacy campaign was not clearly described and was only one of many components of the intervention that also involved parent meetings, merchant meetings, visits to shops (with feedback and commitment for the 2000 intervention), postcards to parents, letters to merchants, and training of staff. The authors of this study reported on a comparison area but did not specify whether any intervention was implemented there. The study found that in the intervention area, the percentage of successful beer purchase attempts varied from 66% at baseline to 73% at the end of the first year and to 44% at the end of the second year. The values in the comparison area were respectively 60, 86, and 44%. This study provides insufficient evidence on the role of media advocacy in the observed results [ 47 ].
Vasudevan et al. [ 48 ] assessed the effects of media and a “seat belt” law enforcement campaign in the state of NV, USA, on increasing the seat belt usage rates. The campaign, Click it or Ticket, was conducted during the month of May over 3 years (2003–2005). The authors collected seat belt usage rates among both drivers and passengers pre-campaign (March and April) and post campaign (June and August). They found that the overall seat belt usage rate significantly increased from 73.9 to 78.9% in 2003 ( p value <0.001), from 81.8 to 86.6% in 2004 ( p value <0.001), and from 88.4 to 94.8% in 2005 ( p value <0.001). The authors of this study concluded that “effectively coupling media and enforcement campaigns” led to a “significant increase in seat belt usage” [ 48 ].
Policy evaluation
No studies were found to examine the role of media in policy evaluation.
Summary of findings
This integrative systematic review identified 10 eligible studies that evaluated the effects of planned media interventions on the different stages of the health policy-making process, except for the policy evaluation stage. None of the evaluation studies assessed social media interventions. We judged all 10 studies to be at high risk of bias. The findings of the evaluation studies suggest that media interventions may have a positive impact when used as accountability tools leading to prioritizing and initiating policy discussions, as tools to increase policymakers’ awareness, as tools to influence policy formulation, as awareness tools leading to policy adoption (and to gain public support leading to policy adoption), and as awareness tools to improve compliance with laws and regulations. In one study, media-created attention had a negative effect on policy advocacy as it mobilized opponents who defeated the passage of the bills that the media intervention advocated for [ 44 ]. One could speculate that the reason for such defeat may be due to more effective counter-media interventions funded and supported by powerful special interests and stakeholders.
In addition, the available evidence suggested a number of factors as possible predictors of the success of the interventions. These include the timing of media publicity, building relationships with the media, the mobilization of opponents, and the concomitant use of other strategies such as enforcement campaigns and community mobilization and engagement [ 42 – 44 , 46 , 49 ]. This suggests that media interventions do not occur in isolation and a number of factors should be taken in consideration while designing a media campaign for policy change.
Research gaps in the field
A methodological review of published evidence maps found that the most popular domains used to classify evidence gaps were study design, interventions, setting, population, and outcomes [ 51 ]. We present in Table 2 the research gaps relevant to the “use of media to impact health policy-making” according to those domains. Similarly, we used a framework developed by Robinson et al. to discuss the reasons behind the research gaps [ 52 ]. Using that framework, we identified three reasons related to the topic under review: (1) the bias in conducting research, (2) the indirectness of the evidence, and (3) the insufficiency of information. First, the included studies suffered from at least one major methodological limitation, mainly confounding, that makes their findings potentially biased. Second, in the majority of the studies, the media intervention was part of a multi-component intervention or part of larger programs, making the evidence indirect. Consequently, it was not possible to isolate the effects of media as stand-alone interventions. This approach to intervention design may be due to the fact that using media as stand-alone interventions might not be sufficient when aiming to impact policy [ 42 ], given the multiple and complex factors that affect the policy-making process [ 13 ]. One additional limitation is that in the survey and interview studies, the outcomes were assessed based on perceptions of respondents on effectiveness of media interventions and not actual evaluation of effectiveness.
The aforementioned challenges and limitations of the included studies made it difficult to make any inferences on effectiveness as the authors of these papers do not explicitly provide an evidence for the link between the intervention and the outcome. Thus, we reported the results cautiously and relied on what the authors of the included papers reported. Third, our review showed limited quantity of research on the effects of planned media interventions and social media in particular on health policy-making.
Another major challenge in the reporting of most of the included studies is the very limited description of the media interventions, knowing that these qualify as complex interventions. This makes it difficult to understand the specific media intervention that was tested, and what component of that complex intervention might have been effective. Indeed, two other systematic reviews examining the effectiveness of mass media on health services utilization [ 10 ] and on reducing alcohol-impaired driving and alcohol-related crashes [ 53 ] identified similar limitations in terms of the description of the intervention.
There is also a dearth of studies reporting on the effectiveness of media interventions on health policies in low middle-income countries (LMIC). This may be linked to the fact that the production of Health Policy and Systems Research (HPSR) is still in its infancy in these countries [ 54 – 56 ].
We are aware of a number of systematic reviews assessing the use of media/social media in clinical medicine and public health. For instance, media interventions were assessed for their impact on smoking cessation [ 8 ], reducing the risk of alcohol-related injuries or crashes [ 53 ], increasing child survival in LMICs [ 57 ], and changing health behavior in fields such as HIV prevention [ 20 , 58 ] and physical activity [ 19 , 59 ]. Two reviews identified evidence that mass media campaigns can in fact have positive impact [ 8 , 57 ]. Patel et al. showed that using social media, especially Facebook and blogs, likely improves care for patients with chronic disease [ 60 ]. Stellefson et al. reported that Web 2.0 can benefit older adults in managing their diseases [ 61 ]. Social media were also shown to be used for a variety of conditions and purposes in child health [ 62 ].
Implications for research and policy
This systematic review can inform researchers and funders interested in understanding the interaction between the media and the policy worlds. Researchers are encouraged to conduct more and better-designed primary research studies on social media interventions given the rise of their use in the recent decade and potential impact on policy-making. Researchers should develop and follow guidelines for designing and evaluating complex media interventions. Moreover, there is a need for better reporting of studies in this field, taking into consideration guidelines for the reporting of complex interventions when describing the media intervention used [ 63 – 65 ].
This systematic review highlighted the challenges of evaluating the impact of media advocacy on health policy given the difficulties in applying experimental methods, the complex nature of these interventions, and the multiple factors influencing the policy-making process [ 13 , 26 ]. Future primary studies and systematic reviews should include process evaluation and qualitative components to explore factors behind successes and failures, the impact of the context, and elements of best practices in health policy-making media campaigns [ 66 ]. Furthermore, future research should focus on the influence of media on health policy-making in diverse settings. Examining the role of media in these LMICs is important to design context-specific strategies and understand how the impact of media campaigns and interventions can differ across various health systems and socioeconomic realities. Funding agencies are also called to support future studies particularly in LMICs, where research production is still at its early stages, and support capacity building for research in the field of HPSR.
Our findings can also inform, to some extent, civil society organizations, advocacy groups, and researchers working to influence policy-making when considering media as tools for policy change. One particular important finding that emerged is the unintended effects of media campaigns to energize opponents. This implies that any media intervention has to be carefully designed and thought through to take into account such situations.
Strengths and limitations
This review has two main strengths. First, and to our knowledge, this is the first systematic review examining the effects of planned media interventions, including social media, on health policy-making. Second, we have conducted the review using standard, explicit, and rigorous methods [ 67 ] and we followed standard methods for reporting systematic reviews [ 68 ]. This includes a very comprehensive search, including of the Communication and Mass Media Complete database, the main database for media-related articles. One limitation of this review is the use of stages heuristic framework while some academics consider it to assume linearity of the public policy process that does not exist in real world. However, it did help us synthesize the identified evidence by providing a simplified and useful way in viewing the entire public policy process [ 24 ].
Sixsmith J, Fox K-A, Doyle P, Barry MM. A literature review on health communication campaign evaluation with regard to the prevention and control of communicable diseases in Europe. 2014.
Google Scholar
Wilson K, et al. The reporting of theoretical health risks by the media: Canadian newspaper reporting of potential blood transmission of Creutzfeldt-Jakob disease. BMC Public Health. 2004;4(1):1–9.
Article PubMed PubMed Central Google Scholar
Lavis JN, et al. Bridging the gaps between research, policy and practice in low- and middle-income countries: a survey of researchers. CMAJ. 2010;182(9):E350–61.
Cheung A, et al. Climate for evidence-informed health systems: a print media analysis in 44 low- and middle-income countries that host knowledge-translation platforms. Health Res Policy Sys. 2011;9(1):1–7.
Article Google Scholar
El-Jardali F, et al. Use of health systems evidence by policymakers in eastern Mediterranean countries: views, practices, and contextual influences. BMC Health Serv Res. 2012;12(1):1–20.
Phillips DP, et al. Importance of the lay press in the transmission of medical knowledge to the scientific community. N Engl J Med. 1991;325:1180–3.
Article CAS PubMed Google Scholar
Wakefield MA, Loken B and Hornik RC. Use of mass media campaigns to change health behaviour. The Lancet. 2010;376(9748):1261–71.
Bala MM, et al. Mass media interventions for smoking cessation in adults. Cochrane Database Syst Rev. 2013(6): p. Cd004704.
Elder RW, et al. Effectiveness of mass media campaigns for reducing drinking and driving and alcohol-involved crashes: a systematic review. Am J Prev Med. 2004;27(1):57–65.
Article PubMed Google Scholar
Grilli R, Ramsay C and Minozzi S. Mass media interventions: effects on health services utilisation. Cochrane Database Syst Rev. 2002(1): p. Cd000389.
Lancaster K, et al. Illicit drugs and the media: models of media effects for use in drug policy research. Drug Alcohol Rev. 2011;30(4):397–402.
Entman RM. Framing: toward clarification of a fractured paradigm. J Commun. 1993;43(4):51–8.
Buse K, Nicholas M, Walt G. Making health policy. secondth ed. Maidenhead: Open University Press; 2012.
Chapman S. Advocacy for public health: a primer. J Epidemiol Community Health. 2004;58(5):361–5.
Article CAS PubMed PubMed Central Google Scholar
Wallack L, Dorfman L. Media advocacy: a strategy for advancing policy and promoting health. Health Educ Q. 1996;23(3):293–317.
Williams G, et al. Social media interventions for diet and exercise behaviours: a systematic review and meta-analysis of randomised controlled trials. BMJ Open. 2014;4(2):e003926.
Oxman AD, et al. SUPPORT Tools for evidence-informed health Policymaking (STP) 15: engaging the public in evidence-informed policymaking. Health Res PolicySys. 2009;7(1):1–9.
Moorhead SA, et al. A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res. 2013;15(4):e85.
Brown DR, et al. Stand-alone mass media campaigns to increase physical activity: a community guide updated review. Am J Prev Med. 2012;43(5):551–61.
LaCroix JM, et al. Effectiveness of mass media interventions for HIV prevention, 1986–2013: a meta-analysis. J Acquir Immune Defic Syndr. 2014;66 Suppl 3:S329–40.
Akl E, E.-J.F., Bou-Karroum L, Ali M, El-Eid J, Darzi A, Melki, Langlois E, Farha A. Impact of media on health policy making: a systematic review protocol. 2015; Available from: http://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42015020243 . last Accessed August 2016.
Kaplan AM, Haenlein M. Users of the world, unite! The challenges and opportunities of Social Media. Bus Horiz. 2010;53(1):59–68.
Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546–53.
Sabatier PA (ed.). Theories of the policy process. First edition ed. 1999. United States: Westview Press.
Walt G, et al. ‘Doing’ health policy analysis: methodological and conceptual reflections and challenges. Health Policy Plan. 2008;23(5):308–17.
Stead M, Hastings G, Eadie D. The challenge of evaluating complex interventions: a framework for evaluating media advocacy. Health Educ Res. 2002;17(3):351–64.
Fleiss JL, Levin B and Paik MC. The measurement of interrater agreement, in statistical methods for rates and proportions. United States: John Wiley & Sons, Inc.2014; p. 598–626.
Lotfi T, et al. Knowledge, beliefs and attitudes of physicians in low and middle-income countries regarding interacting with pharmaceutical companies: a systematic review. BMC Health Serv Res. 2016;16(1):1–11.
Sandelowski M, Voils CI, Barroso J. Defining and designing mixed research synthesis studies. Res Sch. 2006;13(1):29.
PubMed PubMed Central Google Scholar
Arnott D, et al. Comprehensive smoke-free legislation in England: how advocacy won the day. Tob Control. 2007;16(6):423–8.
Bhojani U, Venkataraman V, Manganawar B. Challenging ties between state and tobacco industry: advocacy lessons from India. Health Promot Perspect. 2013;3(1):102–12.
Gomm M, et al. Planning and implementing a community-based public health advocacy campaign: a transport case study from Australia. Health Promot Int. 2006;21(4):284–92.
Jernigan DH. Framing a public health debate over alcohol advertising: The Center on Alcohol Marketing and Youth 2002–2008. J Public Health Policy. 2011;32(2):165–79.
Kreger M, et al. Creating an environmental justice framework for policy change in childhood asthma: a grassroots to treetops approach. Am J Public Health. 2011;101 Suppl 1:S208–16.
Lane C u H, Carter MI. The role of evidence-based media advocacy in the promotion of tobacco control policies El papel de la abogacía en medios de comunicación para la promoción de políticas del control del tabaco. Salud Publica Mex. 2012;54(3):281–8.
PubMed Google Scholar
Madhab A, Prasad VM, Kapur A. Gestational diabetes mellitus: advocating for policy change in India. Int J Gynecol Obstet. 2011;115 SUPPL 1:S41–4.
Okonofua F, et al. Advocacy for free maternal and child health care in Nigeria—results and outcomes. Health Policy. 2011;99(2):131–8.
Tataru V. Media advocacy in anti-tobacco campaign in the Republic of Moldova. Pneumologia (Bucharest, Romania). 2009;58(3):163–5.
Vaughan K. Campaigning for children’s oral health: a case study. New Dir Youth Dev. 2009;124:97–102.
Weiler R, Neyndorff C. BJSM social media contributes to health policy rethink: a physical activity success story in Hertfordshire. Br J Sports Med. 2013;47(9):593–4.
Haq ZU, et al. Using TV talk show for public health media advocacy: a case study. J Pak Med Assoc. 2010;60(6):460–4.
Gardner A, et al. Clinic consortia media advocacy capacity: partnering with the media and increasing policymaker awareness. J Health Commun. 2010;15(3):293–306.
Gowda S, Thomas DR. The Northland fluoridation advocacy programme: an evaluation. N Z Dent J. 2008;104(4):134–8.
Harwood EM, et al. Media advocacy and underage drinking policies: a study of Louisiana news media from 1994 through 2003. Health Promot Pract. 2005;6(3):246–57.
Niederdeppe J, Farrelly MC, Wenter D. Media advocacy, tobacco control policy change and teen smoking in Florida. Tob Control. 2007;16(1):47–52.
Sivaneswaran S, Chong GT. Investing in professional advocacy: a case study of a successful fluoridation campaign in rural New South Wales, Australia. Community Dent Health. 2011;28(3):243–7.
CAS PubMed Google Scholar
Rehnman C, Larsson J, Andréasson S. The beer campaign in Stockholm—attempting to restrict the availability of alcohol to young people. Alcohol. 2005;37(2):65–71.
Vasudevan V, et al. Effectiveness of media and enforcement campaigns in increasing seat belt usage rates in a state with a secondary seat belt law. Traffic Inj Prev. 2009;10(4):330–9.
Rock MJ, et al. A media advocacy intervention linking health disparities and food insecurity. Health Education Research. 2011.
Leurer MD. Lessons in media advocacy: a look back at Saskatchewan’s nursing education debate. Policy Polit Nurs Pract. 2013;14(2):86–96.
Miake-Lye IM, et al. What is an evidence map? A systematic review of published evidence maps and their definitions, methods, and products. Syst Rev. 2016;5(1):28.
Robinson KA, S.I., Mckoy NA., Frameworks for determining research gaps during systematic reviews. Methods Future Research Needs Report No. 2. June 2011.
Yadav R-P, Kobayashi M. A systematic review: effectiveness of mass media campaigns for reducing alcohol-impaired driving and alcohol-related crashes. BMC Public Health. 2015;15(1):1–17.
Article CAS Google Scholar
Law T, et al. Climate for evidence-informed health systems: a profile of systematic review production in 41 low- and middle-income countries, 1996–2008. J Health Serv Res Policy. 2012;17(1):4–10.
El-Jardali F, et al. Health policy and systems research in twelve eastern Mediterranean countries: a stocktaking of production and gaps (2000–2008). Health Res Policy Sys. 2011;9(1):1–12.
Wilson MG, Moat KA, Lavis JN. The global stock of research evidence relevant to health systems policymaking. Health Res Policy Sys. 2013;11(1):1–13.
Naugle DA, Hornik RC. Systematic review of the effectiveness of mass media interventions for child survival in low- and middle-income countries. J Health Commun. 2014;19(sup1):190–215.
Taggart T, et al. Social media and HIV: a systematic review of uses of social media in HIV communication. J Med Internet Res. 2015;17(11):e248.
Leavy JE, et al. Physical activity mass media campaigns and their evaluation: a systematic review of the literature 2003–2010. Health Educ Res. 2011;26(6):1060–85.
Patel R, et al. Social media use in chronic disease: a systematic review and novel taxonomy. Am J Med. 2015;128(12):1335–50.
Stellefson M, et al. Web 2.0 chronic disease self-management for older adults: a systematic review. J Med Internet Res. 2013;15(2):e35.
Hamm MP, et al. A systematic review of the use and effectiveness of social media in child health. BMC Pediatr. 2014;14(1):1–15.
Craig P, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655.
Lamb SE, et al. Reporting of complex interventions in clinical trials: development of a taxonomy to classify and describe fall-prevention interventions. Trials. 2011;12:125.
Möhler R, Köpke S, Meyer G. Criteria for Reporting the Development and Evaluation of Complex Interventions in healthcare: revised guideline (CReDECI 2). Trials. 2015;16(1):1–9.
Moore GF, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258.
Higgins JPT, G.S., Cochrane handbook for systematic reviews of interventions. Version 5.1.0 ed: The Cochrane Collaboration; 2011.
Moher D. et al. The PRISMA group: preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Download references
Acknowledgements
We would like to thank Ms. Aida Farha for her help in designing the search strategy. We would also like to thank Drs. Sunitha Gowda, Jeff Niederdeppe, Marie Leurer, Annette Gardner, Friday Okonufua, and Richard Weiler for responding to our request to check the validity of our data abstraction of their papers and Drs. Marie Leurer, Jeff Niederdeppe, and Dr. Monika Gehner for their expert input.
This systematic review was funded by the Alliance for Health Policy and Systems Research, WHO, Geneva, with support from the Norwegian Government Agency for Development Cooperation (Norad), the Swedish International Development Cooperation Agency (Sida), and the UK Department for International Development (DFID). The funding body had no role in the design of the study, collection, analysis, and interpretation of data, and in writing the manuscript.
Availability of data and materials
All relevant data are within the paper and its additional files.
Authors’ contributions
EA, FJ, and LBK conceived the study. EA, FJ, LBK, GH, EL, and JM contributed to the study design. LBK designed and run the search strategy. LBK, NH, YF, MS, UO, AD, CD, and MA screened the articles for eligibility. LBK, NH, YF, MS, and UO abstracted the data from papers. LBK, EA, and GH contributed to the analysis, interpretation of results, and write up of the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Center for Systematic Review for Health Policy and Systems Research, American University of Beirut, Beirut, Lebanon
Lama Bou-Karroum, Fadi El-Jardali, Andrea Darzi & Elie A. Akl
Department of Health Management and Policy, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon
Lama Bou-Karroum, Fadi El-Jardali, Nour Hemadi & Yasmine Faraj
Department of Health Research Methods, Evidence, and Impact (HE&I), McMaster University, Hamilton, Canada
Fadi El-Jardali & Elie A. Akl
Imperial College London, London, UK
Utkarsh Ojha
Al-Makassed Hospital, Jerusalem, Palestine
Maher Shahrour
AUB GRADE Center, Clinical Research Institute, American University of Beirut, Beirut, Lebanon
Andrea Darzi
Department of Nutrition and Food Sciences, Faculty of Agricultural and Food Sciences, American University of Beirut, Beirut, Lebanon
Leeds Institute of Health Sciences, Faculty of Medicine and Health, University of Leeds, Leeds, UK
Department of Health Promotion and Community Health, Faculty of Health Sciences, American University of Beirut, Beirut, Lebanon
Carine Doumit
Alliance for Health Policy and Systems Research, World Health Organization, Geneva, Switzerland
Etienne V. Langlois
Department of Communication Arts, Lebanese American University, Beirut, Lebanon
Hariri School of Nursing, American University of Beirut, Beirut, Lebanon
Gladys Honein AbouHaidar
Department of Internal Medicine, American University of Beirut, P.O. Box 11–0236, Riad-El-Solh Beirut, 1107 2020, Beirut, Lebanon
Elie A. Akl
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Elie A. Akl .
Additional files
Additional file 1:.
Search strategies for electronic databases. (DOCX 24 kb)
Additional file 2:
Included case studies. (DOCX 35 kb)
Additional file 3:
Methodological appraisal. (DOCX 23 kb)
Additional file 4:
Results table. (DOCX 22 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Bou-Karroum, L., El-Jardali, F., Hemadi, N. et al. Using media to impact health policy-making: an integrative systematic review. Implementation Sci 12 , 52 (2017). https://doi.org/10.1186/s13012-017-0581-0
Download citation
Received : 06 September 2016
Accepted : 06 April 2017
Published : 18 April 2017
DOI : https://doi.org/10.1186/s13012-017-0581-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Media campaigns
- Health communication
- Health policy-making
Implementation Science
ISSN: 1748-5908
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Internet Explorer is no longer supported by Microsoft. To browse the NIHR site please use a modern, secure browser like Google Chrome, Mozilla Firefox, or Microsoft Edge.

How researchers can influence policy and practice

Published: 09 July 2019
Version: 1.0 - July 2019
Researchers are good at producing and exchanging scientific knowledge but need help in transforming that into practical knowledge.
- We say: How can we get research into policymaking?
- What we mean is: How can researchers influence policymakers?
- What we need to know is: How are policymakers influenced?
What is evidence-based commissioning?
The ‘art of commissioning’ entails juggling competing agendas, priorities, power relationships, demands and personal inclinations to build a persuasive, compelling case. Commissioning involves :
- National and regional performance managers
- Evidence purveyors
- Healthcare providers
- Internal colleagues
- Service users
Researchers define evidence as research, while commissioners have a much broader definition of ‘evidence’. Commissioners influence and collaborate with external and internal interested parties to build a cohesive, compelling case for taking a particular course of action.
Where do commissioners get information from?
Commissioners are highly pragmatic – if information is not helpful, they will not use it.
Commissioners get empirical evidence from :
- National Service Framework Guidelines
- NICE guidance
- Government publications (e.g. guidance on the commissioning of cancer services for improving colorectal cancer)
- Clinical guidelines (e.g. choice of ACE inhibitors in the primary care management of adults with symptomatic heart failure)
- Guidance from professional associations e.g. the Royal College of Surgeons
- Secondary sources (e.g. NHS evidence)
- Published cost-effectiveness analyses
- Work commissioned to academic researchers
- General published literature (e.g. journal articles)
Commissioners get practical evidence from:
- Local public health intelligence (e.g. population data, needs analysis, health outcomes, activity and capacity modelling etc.)
- Expert advice either from colleagues or external experts (e.g. from the local authority, Department of Health and Social Care etc.)
- Examples of best practice from other organisations
- Their own personal experience
- Local policies and plans (e.g. the strategic plan, the operating plan, clinical policies, risk registers)
- Benchmarking data with other organisations (e.g. investment levels, outcomes, National Clinical and Health Outcomes Knowledge Base data)
Commissioners tend to seek information from trusted colleagues via conversations. Interpersonal relationships were the most crucial in influencing commissioning decisions. This has been confirmed by systematic reviews :
The most frequently reported facilitators [of the use of research] were collaboration between researchers and policymakers, and improved relationships and skills.
NB Review includes 13 other systematic reviews and studies from outside healthcare field e.g. criminal justice.
Information is modified by organisational pressures and tensions.
What about academic research?
Commissioners are predisposed to using research, but find it difficult to access, understand and apply.
Commissioners rely on public health departments to supply and interpret research. Evidence reviews are difficult to incorporate into decision-making.
Local evaluations more helpful than academic research, because local evaluations include useful contextual information.
NICE guidelines are “crucial” to decision-making, but commissioners only follow the most “doable” as otherwise they would go “bust”.
Academics try to reach policymakers by publishing written material in scientific journals that policymakers do not (or cannot) access from outside policymaking organisations. But policymakers are influenced by regular conversations with trusted colleagues whom they know, usually from within their own organisation.
How can researchers influence policymakers and practitioners?
Researchers can influence policymakers and practitioners through knowledge mobilisation.
Knowledge mobilisation is the process(es) that can lead to the outcome of impact by catalysing change through:
- Engagement & networking
- Educational events
- Co-production
- Embedding procedures & practices
- Commercialisation
- Science communication
- Social media
- Targeted dissemination
Engaging research users is crucial.
NB Knowledge mobilisation is NOT implementation. Knowledge mobilisation needs to happen for implementation to occur.
Two approaches
Researchers might want to take an outside track or an inside track to knowledge mobilisation .
Outside track
- Targets large number of individuals
- Uses public messaging and campaigning
- Uses social and traditional media (social, press)
Inside track
- Collaborative
- Involves direct interaction with policymakers through formal negotiations & meetings
- Uses informal face-to-face meetings
National School for Primary Care Research study of gambling
- Key finding = 25% men b/t 18-24 presenting at GP surgeries have gambling problems
- Comms officer + PI working together
- Scientific paper + press release + blog + infographic + Twitter
- Coverage in The Times, Guardian, BBC World Service, Pulse, the Conversation
- Top 10 read for 6 months in British Journal of General Practice
Influencing through ‘expertise into practice’
- CCG transformation programme of diabetes services
- Researcher in residence + management fellow carried out before & after evaluation of 2 GP practices’ implementation of new intervention
- Presented findings to several CCG committees who continued or changed their plans
- Management fellow learnt evaluation skills later applied in several other projects

Health Policy
Goal: use health policy to prevent disease and improve health..

Health policy can have a major impact on health and well-being. Healthy People 2030 focuses on keeping people safe and healthy through laws and policies at the local, state, territorial, and federal level.
Evidence-based health policies can help prevent disease and promote health. For example, smoke-free policies can help prevent smoking initiation and increase quit attempts. Similarly, policies requiring community water systems to provide fluoridated water can improve oral health.
Establishing informed policies is key to improving health nationwide.
Objective Status
Learn more about objective types
Related Objectives
The following is a sample of objectives related to this topic. Some objectives may include population data.
Health Policy — General
- Environmental Health
- Tobacco Use
Other topics you may be interested in
- Oral Conditions
The Office of Disease Prevention and Health Promotion (ODPHP) cannot attest to the accuracy of a non-federal website.
Linking to a non-federal website does not constitute an endorsement by ODPHP or any of its employees of the sponsors or the information and products presented on the website.
You will be subject to the destination website's privacy policy when you follow the link.
- Open access
- Published: 29 May 2024
The implementation of person-centred plans in the community-care sector: a qualitative study of organizations in Ontario, Canada
- Samina Idrees 1 ,
- Gillian Young 1 ,
- Brian Dunne 2 ,
- Donnie Antony 2 ,
- Leslie Meredith 1 &
- Maria Mathews 1
BMC Health Services Research volume 24 , Article number: 680 ( 2024 ) Cite this article
Metrics details
Person-centred planning refers to a model of care in which programs and services are developed in collaboration with persons receiving care (i.e., persons-supported) and tailored to their unique needs and goals. In recent decades, governments around the world have enacted policies requiring community-care agencies to adopt an individualized or person-centred approach to service delivery. Although regional mandates provide a framework for directing care, it is unclear how this guidance is implemented in practice given the diversity and range of organizations within the sector. This study aims to address a gap in the literature by describing how person-centred care plans are implemented in community-care organizations.
We conducted semi-structured interviews with administrators from community-care organizations in Ontario, Canada. We asked participants about their organization’s approach to developing and updating person-centred care plans, including relevant supports and barriers. We analyzed the data thematically using a pragmatic, qualitative, descriptive approach.
We interviewed administrators from 12 community-care organizations. We identified three overarching categories or processes related to organizational characteristics and person-centred planning: (1) organizational context, (2) organizational culture, and (3) the design and delivery of person-centred care plans. The context of care and the types of services offered by the organization were directly informed by the needs and characteristics of the population served. The culture of the organization (e.g., their values, attitudes and beliefs surrounding persons-supported) was a key influence in the development and implementation of person-centred care plans. Participants described the person-centred planning process as being iterative and collaborative, involving initial and continued consultations with persons-supported and their close family and friends, while also citing implementation challenges in cases where persons had difficulty communicating, and in cases where they preferred not to have a formal plan in place.
Conclusions
The person-centred planning process is largely informed by organizational context and culture. There are ongoing challenges in the implementation of person-centred care plans, highlighting a gap between policy and practice and suggesting a need for comprehensive guidance and enhanced adaptability in current regulations. Policymakers, administrators, and service providers can leverage these insights to refine policies, advocating for inclusive, flexible approaches that better align with diverse community needs.
Peer Review reports
The community-care sector facilitates the coordination and administration of in-home and community-based health and social services. Community-care services include supports for independent living, residential services, complex medical care, and community-participation services to support personal and professional goals (e.g., education, employment, and recreation-based supports) [ 1 ]. There is substantial heterogeneity in the clinical and demographic characteristics of the community-care population, including individuals with physical and developmental disabilities, and complex medical needs [ 2 ]. We refer to the individuals served by these organizations as ‘persons-supported’ in line with person-first language conventions [ 3 , 4 ].
In recent decades, governments across the world have enacted policies requiring community-care agencies to adopt an individualized or person-centred approach to service delivery [ 5 , 6 , 7 , 8 ]. Person-centred care encompasses a broad framework designed to direct care delivery, as opposed to a singular standardized process. In the context of community-care, person-centred planning refers to a model of care provision in which programs and services are developed in collaboration with persons-supported and tailored to their unique needs and desired outcomes [ 9 , 10 ].
In Ontario, Canada, community-care services are funded by the Ministry of Health (MOH) and the Ministry of Children, Community and Social Services (MCCSS). Service agreements between these ministries and individual agencies can be complex and contingent on different factors including compliance with a number of regulatory items and policies [ 7 , 11 ]. MOH provides funding for health-based services including in-home physiotherapy, respiratory therapy, and personal support services, among several others. MOH funds Home and Community Care Support Services (HCCSS), a network of organizations responsible for coordinating the delivery of in-home and community-based care in the province. MCCSS funds social service agencies including those providing community participation and residential support for people with intellectual and developmental disabilities (IDDs).
Several tools and resources have been developed to aid organizations in providing person-centred care and organizations may differ in their use of these tools and their specific approach. Although regional mandates provide a framework for directing care delivery, it is unclear how this guidance is implemented in practice given the diversity and range of organizations within the sector. In addition, as noted by a recent scoping review, there is limited literature on the implementation process and impact of person-centred planning on individual outcomes [ 12 ]. Using a pragmatic, qualitative, descriptive approach [ 13 ], we outline how community-care organizations enact a person-centred approach to care and the factors that shape their enactment. By describing existing practices in the context of the community-care sector, we aim to provide insight on how to optimize care delivery to improve outcomes and inform current policy. This study is part of a larger, multi-methods project examining the implementation of person-centred care plans in the community-care sector. This project encompasses qualitative interviews with representatives from different community-care organizations, as well as staff and persons-supported at a partner community-care organization. This paper focuses on analyzing data from interviews with representatives from different community-care organizations.
We conducted semi-structured interviews with administrators from community-care organizations in Southwestern Ontario (roughly the Ontario Health West Region) between October 2022 and January 2023. We included community-care organizations funded by MOH or MCCSS. We excluded organizations that did not provide services in Southwestern Ontario. We identified eligible organizations and participants by searching online databases, including community resource lists, as well as through consultation with members of the research team.
We used maximum variation sampling [ 14 ], to recruit participants from organizations with a wide range of characteristics including location (i.e., urban, rural), organization type (i.e., for-profit, not-for-profit), and types of services provided (e.g., residential, recreation, transportation, etc.) We contacted eligible organizations via email, providing them with study information and inviting them to participate. We recruited until the data reached saturation, defined as the point at which there was sufficient data to enable rigorous analysis [ 14 , 15 ].
In each interview, we asked participants about their organization’s approach to developing and updating individual service agreements or person-centred care plans, and the supports and barriers (e.g., organizational, funding, staffing, etc.) that facilitate or hinder the implementation of these plans (Supplementary Material 1 : Interview Guide). We also collected information on relevant participant and organizational characteristics, including participant gender, position, years of experience, organization location, type (i.e., for-profit, not-for-profit), services offered, years in operation, and client load. The interviews were approximately one hour in length and conducted virtually via Zoom (Zoom Video Communications Inc.) or by telephone. The interviews were audio-recorded and transcribed verbatim. Interviewer field notes were also used in data analysis.
We analyzed the data thematically [ 16 ]. The coding process followed a collaborative and multi-step approach. Initially, three members of the research team independently reviewed and coded a selection of transcripts to identify key ideas and patterns in the data, and form a preliminary coding template. We then met to consolidate individual coding efforts. We compared coding of each transcript, resolving conflicts through discussion and consensus. In coding subsequent transcripts and through a series of meetings, we worked together to finalize the codebook to reflect more analytic codes. We used the finalized template to code all interview transcripts in NVivo (QSR International), a software designed to facilitate qualitative data analysis. We refined the codebook on an as-needed basis by incorporating novel insights gleaned from the coding of additional transcripts, reflecting the iterative nature of the analysis.
We increased the robustness of our methodology by pre-testing interview questions, documenting interview and transcription protocols, using experienced interviewers, and confirming meaning with participants in interviews [ 14 , 15 , 16 ]. We kept detailed records of interviews, field notes, and drafts of the coding template. We made efforts to identify negative cases and provided rich descriptions and illustrative quotes [ 17 ]. We included individuals directly involved in the administration of community-care services on our research team. These individuals provided important context and feedback at each stage of the research process.
This study was approved by the research ethics board at Western University. We obtained informed consent from participants prior to the onset of interviews. We maintained confidentiality through secure storage of interview data (e.g., audio recordings), password-protection of sensitive documents, and the de-identification of transcripts.
Positionality
The authors represent a multidisciplinary team of researchers, clinicians, and community-care leaders. The community-care leaders and clinicians on our team provided key practical expertise to inform the development of interview questions and the analysis of study findings.
We interviewed administrators across 12 community-care organizations in Southwestern Ontario. The sample included representatives from seven organizations that received funding from MCCSS, three organizations that received funding from MOH, and two organizations that received funding from both MCCSS and MOH (Table 1 ). Eleven organizations were not-for-profit, one was a for-profit agency. The organizations provided care in rural ( n = 3), urban ( n = 4), or both rural and urban populations ( n = 5). Seven of the 12 participants were women, nine had been working with their organization for more than 11 years, and all had been working in the community-care sector for more than 12 years (Table 2 ).
We identified three key categories or processes relating to organizational characteristics and their impact on the design and delivery of person-centred care plans: (1) organizational context, (2) organizational culture, and (3) the development and implementation of person-centred care plans.
Organizational context
Organizational context refers to the characteristics of persons-supported, and the nature of services provided. Organizational context accounts for the considerable heterogeneity across organizations in the community-care sector and their approach to person-centred care plans.
Populations served
The majority of organizations included in the study supported individuals with IDDs: “all of the people have been identified as having a developmental disability. That’s part of the eligibility criteria for any funded developmental service in Ontario.” [P10]. Participants described how eligibility was ascertained through the referral process: “ the DSO [Developmental Services Ontario] figures all of that out and then refers them to us .” [P08]. These descriptions highlighted a common access point for publicly-funded adult developmental services in the province. Accordingly, these organizations were primarily funded by MCCSS. Other organizations focused on medically complex individuals including those with acquired brain injuries or those unable to access out-patient services due to physical disabilities: “the typical reason for referral is going to be around a physical impairment… But, with this medically complex population, you’re often seeing comorbidities where there may be some cognitive impairment, early dementia.” [P04]. In these organizations, eligibility and referral were usually coordinated by HCCSS. These insights highlighted the diverse characteristics of community-care populations, emphasizing the need to consider both physical and cognitive health challenges in care provision approaches.
Services offered
The characteristics of persons-supported informed the context of care and the type of services offered by the organization. The different dimensions of services offered within this sector include social and medical care, short and long-term care provision, in-home and community-care, and full and part-time care.
Nature of care: social vs. medical
Many organizations serving individuals with IDDs employed a holistic, psychosocial model of care, designed to support all areas of an individual’s life including supports for independent-living, and community-based education, employment, and recreation services to support personal and professional goals: “we support people in their homes, so residential supports. We also support people in the community, to be a part of the community, participate in the community and also to work in the community.” [P06]. These descriptions reflect a comprehensive approach to care, aiming to address needs within and beyond residential settings to promote active participation within the broader community. In contrast, some organizations followed a biomedical model of care, designed to support specific health needs: “We provide all five therapies… physiotherapy, occupational therapy, speech, social work, and nutrition. In some locations we provide visiting nursing, at some locations shift nursing. We have some clinic-nursing… and we provide personal support and home-making services in a number of locations as well.” [P04]. These organizations adopted a more clinically-focused approach to care. In either instance, the care model and the nature of services offered were largely determined by an organization’s mandate including which gaps they aimed to fill within the community. Many organizations described providing a mixture of social and medical care for individuals with complex needs. However, the implementation of care plans could be impacted by the lack of integration between social and medical care sectors, as some participants spoke to the importance of “[integrating] all of the different healthcare sector services… [including] acute care and public health and home and community care and primary care, and mental health and addictions.” [P04].
Duration of care: short-term vs. long-term
The duration of care also varied based on the needs of persons-supported. Organizations serving individuals with IDDs usually offered support across the lifespan: “We support adults with developmental disabilities and we support them from 18 [years] up until the end of their life.” [P06]. Some organizations provided temporary supports aimed at addressing specific health needs: “For therapies – these are all short-term interventions and typically they’re very specific and focused on certain goals. And so, you may get a referral for physiotherapy that is authorized for three visits or five visits” [P04], or crisis situations (e.g., homelessness): “Our services are then brought in to help provide some level of support, guidance, stabilization resource, and once essentially sustainability and positive outcomes are achieved—then our services are immediately withdrawn.” [P12]. One organization employed a model of care with two service streams, an initial rehabilitation stream that was intended to be short-term and an ongoing service stream for individuals requiring continuing support.
In-home vs. community-based care
Many organizations provided in-home care and community-based supports, where residential supports were designed to help individuals lead independent lives, and community-based supports encouraged participation in community activities to further inclusion and address personal and professional goals. One participant spoke about the range of services offered in the home and community:
“There’s probably two big categories of [services we offer]: community support services—so that includes things like adult day programs, assisted living, meals on wheels, transportation, friendly visiting … and things like blood pressure clinics, exercise programs… and then on the other side we do home care services. In the home care basket, we provide personal support, and we also provide social work support.” [P05].
Likewise, another participant spoke in further detail on the types of services that allow individuals to live independently within their homes, or in community-based residential settings (e.g., long-term care facilities):
“We provide accommodation supports to about 100 people living in our community—which means that we will provide support to them in their own homes. So, anywhere from an hour a week to 24 hours a day. And that service can include things from personal care to home management to money management, cooking, cleaning, and being out and about in communities—so community participation. We also provide supports for about 50 people living in long-term care facilities and that is all community participation support. So, minus the last 2 and a half years because of the pandemic, what that means is that a person living in a long-term care facility with a developmental disability can have our support to get out and about for 2 or 3 hours a week, on average.” [P10].
Full-time vs. part-time support
The person-supported’s needs also determined whether they would receive care within their homes and if they would be supported on a full-time (i.e., 24 h a day, 7 days a week) or part-time basis:
“ It really does range from that intensive 24- hour/7 day a week support, which we actually do provide that level of intense support in the family home, if that’s needed. And then, all the way through to just occasional advocacy support and phone check-in.” [P01].
Organizational Culture
Organizational culture was described as a key influence in the development and implementation of person-centred care plans. The culture of the organization includes their perceptions, attitudes and beliefs surrounding persons-supported; their model of care provision; as well as their willingness to evolve and adapt service provision to optimize care delivery.
Perceptions, attitudes, and beliefs regarding persons-supported
Participants described their organization’s view of persons-supported, with many organizations adopting an inclusionary framework where persons-supported were afforded the same rights and dignities as others in the community. This organizational philosophy was described as being deeply intertwined with an organization’s approach to personalizing programs and services:
“…an organization needs to be able to listen to the people who are receiving the service… and support them, to learn more, figure out, articulate, whatever it is, the service or the supports that they need in order to get and move forward with their life.” [P10].
The focus on the person-supported, their needs, likes, and dislikes, was echoed across organizations, with an emphasis on the impact of “culture and trying to embed for each person who delivers service the importance of understanding the individual.” [P05]. Participants also described their organization’s approach to allowing persons-supported to take risks, make mistakes, and live life on their own terms:
“You have to go and venture out and take some [risks]… We try to exercise that philosophy - people with disabilities should have the same rights and responsibilities as other people in the community. Whether that’s birthing or education, getting a job, having a house they can be proud of, accessing community supports, whether that be [a] library or community centre, or service club, whatever that is.” [P03].
Model of care provision
The model of care provision was heavily influenced by the organization’s values and philosophy. Several organizations employed a flexible model of care where supports were developed around the needs, preferences, and desired outcomes of the person-supported:
“…if we don’t offer [the program they want], we certainly build it. Honestly, most of our programs were either created or built by someone coming to us [and] saying ‘I want to do this with my life,’ or …‘my son would like to do art.’” [P02].
Although there were similarities in models across the different organizations, one participant noted that flexibility can be limited in the congregate care setting as staff must tend to the needs of a group as opposed to an individual:
“Our typical plan of operation outside of the congregate setting is we design services around the needs of the person. We don’t ask them to fit into what we need, we build services for what they need. Within the congregate care setting, we have a specific set of rules and regulations for safety and well-being of the other people that are here.” [P11].
Evolving service orientation
In organizations serving individuals with IDDs, many described shifting from program-based services to more individualized and community-based supports: “The goal was always to get people involved in their community and build in some of those natural supports … [we] are looking to support people in their own communities based on their individual plans.” [P07]. One participant described this model as a person-directed approach as opposed to person-centred, citing the limitations of program-based services in meeting individual needs:
“[Persons-supported] couldn’t [do] what they wanted because they were part of a bigger group. We would listen to the bigger group, but if one person didn’t want to go bowling … we couldn’t support them because everybody had to go bowling.” [P06].
The focus on individualized support could potentially lead to increased inclusion for persons-supported in their communities:
“… people go to Tim Horton’s, and if they go every day at 9 they probably, eventually will meet other people that go at 9 o’clock and maybe strike up a conversation and get to know somebody and join a table … and meet people in the community.” [P02].
By creating routines centred on individual preferences, the person-supported becomes a part of a community with shared interests and values.
Person-centred care plans
Community-care organizations enacted a person-centred approach by creating person-centred care plans for each person-supported. Although all participants said their organization provided person-centred services, there was considerable variation in the specific processes for developing, implementing, and updating care plans.
Developing a person-centred care plan
The development of a care plan includes assessment, consultation, and prioritization. The initial development of the care plan usually involved an assessment of an individual’s needs and goals. Participants described agency-specific assessment processes that often incorporated information from service referrals: “ In addition to the material we get from the DSO [Disability Services Ontario] we facilitate the delivery of an intake package specifically for our services. And that intake package helps to further understand the nature and needs of an individual.” [P12]. Agency-specific assessment processes differed by the nature of services provided and the characteristics of the population. However, most organizations included assessments of “not only physical functioning capabilities, but also cognitive.” [P01]. Assessment also included an appraisal of the suitability of the organization’s services. In instances where persons-supported were seeking residential placements or independent-living support, organizations assessed their ability to carry out the activities of daily living:
“[Our internal assessment] is an overview of all areas of their life. From, ‘do they need assistance with baking, cooking, groceries, cleaning, laundry? Is there going to be day program opportunities included in that residential request for placement? What the medical needs are?’” [P02].
In contrast, the person-supported’s community-based activities were primarily informed by their interests and desired outcomes: “We talk about what kinds of goals they want to work on. What kind of outcomes we’re looking for…” [P06].
The development of the care plan also included a consultation phase, involving conversations with the person-supported, their family members, and potentially external care providers: “We would use the application information, we’d use the supports intensity scale, but we’d also spend time with the person and their connections, their family and friends, in their home to figure out what are the kinds of things that this person needs assistance with.” [P10]. Participants described the person-supported’s view as taking precedence in these meetings: “We definitely include the family or [alternate] decision-maker in that plan, but the person-supported ultimately has the final stamp of approval.” [P08]. Many participants also acknowledged the difficulty of identifying and incorporating the person-supported’s view in cases where opinions clash and the person-supported has difficulty communicating and/or is non-verbal: “Some of the people we support are very good at expressing what they want. Some people are not. Some of our staff are really strong in expressing what they support. …And some of the family members are very strong. So you have to be very careful that the [person-supported] is not being lost in the middle of it.” [P06].
Participants also noted that some persons-supported preferred not to have a care plan:
“Some of the people say ‘I hate [the plans] I don’t want to do them’…. we look at it in a different way then. We’ll use graphic art, we’ll use video, we’ll think outside the box to get them to somehow—because at the end of the day when we’re audited by MCCSS every [person-supported] either has to have [a plan]… or there has to be [an approval of] why it wasn’t completed.” [P02].
Plan development may also include a prioritization process, particularly in cases where resources are limited. A person-supported’s goals could be prioritized using different schemas. One participant noted that “the support coordinator takes the cue from the person-supported - … what they’ve identified as ‘have to have’ and ‘nice to have’. … because the ‘have to haves’ are prioritized.” [P09]. Likewise, the person-supported’s preference could also be identified through “[an] exercise, called ‘what’s important for and what’s important to .’” [P06]. This model, based on a Helen Sanderson approach [ 18 ], was described as being helpful in highlighting what is important to the person-supported, as opposed to what others (i.e., friends, family, staff, etc.) feel is important for them.
Several organizations updated care plans throughout the year, to document progress towards goals, adapt to changing needs and plan for future goals: “We revisit the plan periodically through the year. And if they say the goal is done, we may set another goal.” [P06]. Organizations may also change plans to adapt to the person-supported’s changing health status or personal capacity.
Implementing a person-centred care plan
The implementation of care plans differed based on the nature of services provided by the organization. The delivery of health-based or personal support services often involved matching the length and intensity of care with the individual’s needs and capacity:
“Sometimes that is a long time, sometimes it’s a short time, sometimes it’s an intervention that’s needed for a bit, and then the person is able to function.” [P05].
In contrast, the delivery of community-based services involved matching activities and staff by interests: “[if] a person-supported wants to go out and be involved in the music community, then we pull the staff pool in and match them up according to interest.” [P06].
Broad personal goals were broken down into smaller, specific activities. For example, one participant described their organization’s plan in helping a person-supported achieve his professional goal of securing employment:
“[The person-supported] said ‘Okay, I want a job.’ So for three weeks he was matched up with a facilitator. They came up with an action plan in terms of how to get a job, what kind of job he’s looking for, where he wants to go, where he wants to apply, how to conduct an interview. And after three weeks he got a job.” [P09].
Organizations that provided residential services focused on developing independent-living skills. One participant described their organization’s plan to empowering persons-supported by allowing them to make their own financial decisions:
“If one month they’re looking after their own finances, and they’ve overspent. Well, maybe we help them out with a grocery card or something and say ‘okay, next month how are you going to do this?’ [The person-supported may say], ‘well, maybe I’ll put so much money aside each week rather than doing a big grocery shop the first week and not having enough money left at the end of the month.’” [P03].
The participant noted that “a tremendous amount of learning [happens] when a person is allowed to [take] risks and make their own decisions.” [P03].
Likewise, participants representing organizations that provided residential services described tailoring care to the persons-supported’s sleeping schedule and daily routine:
“We develop a plan and tweak it as we go. With [the person-supported] coming to the home, what worked well was, we found that he wanted to sleep in, so we adjusted the [staff] time. We took a look at his [medication] times in the morning… and [changed] his [medication] times. We found that he wanted to sleep [until] later in the day, so he would get up at 10 o’clock, so then instead of having breakfast, lunch, and supper he would just have a bigger brunch. Just really tailoring the plan around the person-supported, and it’s worked out well.” [P08].
These examples highlight how organizational context and culture influence how organizations operationalize person-centred care plans; the same individual may experience different approaches to care and engage in different activities depending on the organization they receive services from.
In this paper, we described key elements of the person-centred planning process across different community-care organizations in Southwestern Ontario. We also identified that the context and culture of an organization play a central role in informing the process by which services are personalized to an individual’s needs. These findings shed light on the diversity of factors that influence the implementation of person-centred care plans and the degree to which organizations are able to address medical and social needs in an integrated fashion. They also inform future evaluations of person and system-related outcomes of person-centred planning.
There are regulations around individualizing services delivered by community-care organizations, whereby care providers must allow persons-supported to participate in the development and evaluation of their care plans. HCCSS or MOH-funded services are largely focused on in-home rehabilitation or medical care. In contrast, MCCSS-funded organizations often focus on developing independent living skills or promoting community participation, thus highlighting the role of the funding agency in determining organizational context as well as the nature of services and personalization of care plans.
We also identified organizational culture as a key influence in the person-centred planning process. In previous reports, organizational culture, and specifically the way in which staff perceive and view persons-supported and their decision-making capabilities can impact the effective delivery of person-centred care [ 19 ]. Staff support, including their commitment to persons-supported and the person-centred process, has been regarded as one of the most powerful predictors of positive outcomes and goal attainment in the developmental services sector [ 20 , 21 ]. Moreover, in order to be successful, commitment to this process should extend across all levels of the organization, be fully integrated into organizational service delivery, and be reflected in organizational philosophy, values and views of persons-supported [ 22 , 23 , 24 ].
MCCSS mandates that agencies serving individuals with IDDs develop an individual service plan (ISP) for each person-supported, one “that address[es] the person’s goals, preferences and needs.” [ 7 ]. We reference ISPs as person-centred care plans, as is in line with the view of participants in interviews. There are a series of checklists designed to measure compliance with these policies, and the process is iterative, with mandated annual reviews of care plans and active participation by the person-supported [ 25 ]. In our study, the agencies funded by MCCSS adhered to the general framework outlined by these regulations and informed service delivery accordingly. However, participants also described areas for improvement with respect to the implementation of these policies in practice. These policies, while well-intentioned, may imply a one-size-fits-all approach and appear more as an administrative exercise as opposed to a meaningful endeavor designed to optimize care. Participants spoke about individuals who preferred not to have an ISP, and how that in and of itself is a person-centred approach, respecting the person’s wishes. Additionally, we heard about how the goal-setting process may not be realistic as it can be perceived as unnatural to have goals at each point in one’s life. Moreover, participants noted challenges in implementing person-centred care in shared residential settings (e.g., group homes) or in cases where persons-supported had difficulty communicating.
Prior research indicates that individuals living in semi-independent settings fare better across several quality-of-life measures relative to individuals living in group homes, including decreased social dissatisfaction, increased community participation, increased participation in activities of daily living, and increased empowerment [ 26 ]. Furthermore, a recent study by İsvan et al. (2023) found that individuals living in the community (e.g., own home, family home, or foster home) exhibit greater autonomy in making everyday and life decisions, and greater satisfaction with their inclusion in the community [ 27 ]. These findings may be indicative of a reduced focus on person-centred care plan development and implementation in congregate care settings, where limited staff capacity can make it difficult to tend to the needs of everyone in the home. However, poor outcomes may also be explained by potentially more complex health challenges or more severe disability in persons-supported living in congregate care settings. The challenges described in our study are consistent with calls to improve the quality of care provided in residential group home settings [ 28 , 29 ].
In line with our findings, previous literature also describes challenges in implementing person-centred planning for individuals who have difficulty communicating or are non-verbal [ 19 , 30 , 31 , 32 ]. Communication has also been identified as a barrier to patient-centred care for adults with IDDs in healthcare settings [ 33 , 34 ]. Other reports have identified a need for increased training and awareness of diverse communication styles (including careful observation of non-verbal cues) to aid staff in including persons-supported in the development of care plans [ 35 , 36 , 37 ]. Importantly, these methods take substantial time which is often limited, and compounded by staffing shortages that are widespread across the sector [ 38 ]. Similar barriers were identified in interviews with staff and persons-supported at a partner community-care agency within our larger project [ 39 ]; other papers from the project examine strategies used by the organization to overcome these barriers.
Limitations
The findings from this study should be interpreted in the context of the following limitations. There is a risk for social desirability bias, whereby participants may feel pressure to present their care plan process in a more positive light due to societal norms and expectations [ 40 ]. Additionally, the experiences and views of community-care organizations may vary by region and organization type (i.e., for-profit vs. not-for-profit). In this study, we limited participation to agencies providing services in Southwestern Ontario and we were only able to interview one for-profit agency, despite concerted recruitment efforts. Consequently, we may not have fully captured how financial pressures, or different contextual and cultural components of an organization impact their implementation of care plans.
The person-centred planning process in community-care organizations is largely informed by the characteristics of the population served and the nature of services offered (i.e., organizational context). This process usually involves initial and continued consultations with persons-supported to tailor plans to their specific needs and desired outcomes. There are ongoing challenges in the implementation of person-centred planning, including a need for increased adaptability and clarity in current regulations. In some areas, there may be benefit to incorporating nuance in the application of policies (e.g., in cases where a person-supported does not want to have a formal plan in place). In other areas, it may be helpful to have increased guidance on how to optimize care delivery to improve outcomes (e.g., in cases where a person-supported has difficulty communicating, or is residing in a group home). Policymakers, administrators, and service providers can leverage these insights to refine policies, advocating for inclusive, flexible approaches that better align with diverse community needs.
Data availability
The datasets generated and analyzed in the current study are not publicly available to maintain participant confidentiality, however access may be granted by the corresponding author upon reasonable request.
Abbreviations
Acquired Brain Injury
Disability Services Ontario
Home and Community Care Support Services
Intellectual and Developmental Disabilities
Individual Service Plan
Ministry of Children, Community and Social Services
Ministry of Health
Purbhoo D, Wojtak A. Patient and family-centred home and community care: realizing the opportunity. Nurs Leadersh Tor Ont. 2018;31(2):40–51.
Article PubMed Google Scholar
Lin E, Balogh RS, Durbin A, Holder L, Gupta N, Volpe T et al. Addressing gaps in the health care services used by adults with developmental disabilities in Ontario. ICES. 2019 [cited 2023 Aug 30]. https://www.ices.on.ca/publications/research-reports/addressing-gaps-in-the-health-care-services-used-by-adults-with-developmental-disabilities-in-ontario/
American Psychological Association. APA Guidelines for Assessment and Intervention with Persons with Disabilities: (502822022-001). 2022 [cited 2023 Aug 30]; http://doi.apa.org/get-pe-doi.cfm?doi=10.1037/e502822022-001
Dunn DS, Andrews EE. Person-first and identity-first language: developing psychologists’ cultural competence using disability language. Am Psychol. 2015;70(3):255–64.
Burke C. Building a stronger system for people with developmental disabilities: a six-month progress report from Commissioner Courtney Burke. New York Office for People with Developmental Disabilities; 2011. https://opwdd.ny.gov/system/files/documents/2019/12/6_month_progress_report_0.pdf
Government of Manitoba. Agency service coordination manual: 5.1 person-centred planning. 2021. https://www.gov.mb.ca/fs/clds/asc-manual/pubs/5.1-person-centred-planning.pdf
Government of Ontario. Services and supports to promote the social inclusion of Persons with Developmental Disabilities Act, 2008. 2008 [cited 2023 Aug 30]. https://www.ontario.ca/laws/regulation/100299#:~:text=O.-,Reg.,and other relevant clinical assessments
State of Michigan. Person Centered Planning.pdf. 2018.
O’Brien CL, O’Brien J. The origins of person-centered planning: a community of practice perspective.
Sanderson H. Person Centred Planning. York, Joseph Rowntree Foundation; 2000.
Government of Ontario. Ontario.ca. 2019 [cited 2023 Sep 4]. Connecting Care Act, 2019: Home and Community Care Services. https://www.ontario.ca/laws/regulation/220187#BK17
Dong M. Examining individualized participatory approaches to care for individuals with intellectual and developmental disabilities. University of Western Ontario; 2023. https://ir.lib.uwo.ca/etd/9517
Doyle L, McCabe C, Keogh B, Brady A, McCann M. An overview of the qualitative descriptive design within nursing research. J Res Nurs. 2020;25(5):443–55.
Creswell JW. Research design: qualitative, quantitative, and mixed methods approaches. SAGE; 2014. p. 305.
Berg BL. Qualitative research methods for the social sciences: 2nd ed. Bostan, MA: Allyn and Bacon; 1995. p. 421.
Google Scholar
Guest G, MacQueen KM, Namey EE. Applied Thematic Analysis. SAGE; 2012. p. 321.
Yin RK. Case study research design and methods. 5th ed. Thousand Oaks, CA: SAGE; 2014. p. 282.
Helen Sanderson Associates. Helen Sanderson Associates. [cited 2023 Oct 31]. Sorting important to/for. http://helensandersonassociates.co.uk/person-centred-practice/person-centred-thinking-tools/sorting-important-tofor/
Hughes CA. The benefits and barriers to person centered planning for adults with developmental disabilities. [Saint Paul, Minnesota, USA]: St. Catherine University; 2013. https://sophia.stkate.edu/msw_papers/191
Heller T, Miller AB, Hsieh K, Sterns H. Later-life planning: promoting knowledge of options and choice-making. Ment Retard. 2000;38(5):395–406.
Article CAS PubMed Google Scholar
Ratti V, Hassiotis A, Crabtree J, Deb S, Gallagher P, Unwin G. The effectiveness of person-centred planning for people with intellectual disabilities: a systematic review. Res Dev Disabil. 2016;57:63–84.
Kaehne A, Beyer S. Person-centred reviews as a mechanism for planning the post-school transition of young people with intellectual disability. J Intellect Disabil Res. 2014;58(7):603–13.
Parley FF. Person-centred outcomes: are outcomes improved where a person-centred care model is used? J Learn Disabil. 2001;5(4):299–308.
Article Google Scholar
Sanderson H, Thompson J, Kilbane J. The emergence of person-centred planning as evidence‐based practice. J Integr Care. 2006;14(2):18–25.
Government of Ontario. Ministry of Children, Community and Social Services. Developmental service (DS) compliance inspection: indicator list. 2021 [cited 2023 Sep 4]. https://www.mcss.gov.on.ca/documents/en/mcss/developmental/EN_DS_Indicator_List.pdf
Stancliffe RJ, Keane S. Outcomes and costs of community living: a matched comparison of group homes and semi-independent living. J Intellect Dev Disabil. 2000;25(4):281–305.
İsvan N, Bonardi A, Hiersteiner D. Effects of person-centred planning and practices on the health and well-being of adults with intellectual and developmental disabilities: a multilevel analysis of linked administrative and survey data. J Intellect Disabil Res. 2023 [cited 2023 Sep 4]; https://onlinelibrary.wiley.com/doi/abs/ https://doi.org/10.1111/jir.13015
Office of the Auditor General of Ontario. 3.10: residential services for people with developmental disabilities. 2014. https://www.auditor.on.ca/en/content/annualreports/arreports/en14/310en14.pdf
Office of the Auditor General of Ontario. 1.10 residential services for people with developmental disabilities. 2016. https://www.auditor.on.ca/en/content/annualreports/arreports/en16/v2_110en16.pdf
Robertson J, Emerson E, Hatton C, Elliott J, McIntosh B, Swift P, et al. Person-centred planning: factors associated with successful outcomes for people with intellectual disabilities. J Intellect Disabil Res JIDR. 2007;51(Pt 3):232–43.
Everson JM, Zhang D, Person-Centered Planning. Characteristics, inhibitors, and supports. Educ Train Ment Retard Dev Disabil. 2000;35(1):36–43.
Claes C, Van Hove G, Vandevelde S, van Loon J, Schalock RL. Person-centered planning: analysis of research and effectiveness. Intellect Dev Disabil. 2010;48(6):432–53.
Stringer K, Terry AL, Ryan BL, Pike A. Patient-centred primary care of adults with severe and profound intellectual and developmental disabilities. Can Fam Physician. 2018;64(Suppl 2):S63–9.
PubMed PubMed Central Google Scholar
Badcock E, Sakellariou D. Treating him… like a piece of meat: poor communication as a barrier to care for people with learning disabilities. Disabil Stud Q. 2022 [cited 2023 Sep 4];42(1). https://dsq-sds.org/index.php/dsq/article/view/7408
Mansell J, Beadle-Brown J. Person-centred planning or person-centred action? Policy and Practice in Intellectual Disability Services. J Appl Res Intellect Disabil. 2004;17(1):1–9.
Bigby C, Frawley P. Social work practice and intellectual disability: working to support change. Bloomsbury Publishing; 2018. p. 253.
Taylor JE, Taylor JA. Person-centered planning: evidence-based practice, challenges, and potential for the 21st century. J Soc Work Disabil Rehabil. 2013;12(3):213–35.
Zijlstra R, Vlaskamp C, Buntinx W. Direct-care staff turnover: an indicator of the quality of life of individuals with profound multiple disabilities. Eur J Mental Disabil. 2001;(22):39–55.
Canadian Institutes of Health Research (CIHR), CIHR-Institute of Health Services and Policy Research (CIHR-IHSPR) and partners. Evidence brief booklet: quadruple aim & equity catalyst grants. 2024 [cited 2024 Apr 2]. https://face2face.events/wp-content/uploads/2024/01/Evidence-Brief-Booklet-Quadruple-Aim-and-Equity-EN.pdf
Bergen N, Labonté R. Everything is perfect, and we have no problems: detecting and limiting social desirability bias in qualitative research. Qual Health Res. 2020;30(5):783–92.
Download references
Acknowledgements
The authors thank Ruth Armstrong, from PHSS - Medical & Complex Care in Community, for her valuable feedback and support throughout the research process.
This research was funded by the Canadian Institutes of Health Research. The funding agency had no role in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and affiliations.
Department of Family Medicine, Schulich School of Medicine & Dentistry, Western University, 1151 Richmond St, London, ON, N6A 5C1, Canada
Samina Idrees, Gillian Young, Leslie Meredith & Maria Mathews
PHSS - Medical & Complex Care in Community, 620 Colborne St, London, ON, N6B 3R9, Canada
Brian Dunne & Donnie Antony
You can also search for this author in PubMed Google Scholar
Contributions
S.I. conducted the interviews, developed the coding template, coded the data, thematically analyzed the data, and prepared the manuscript. G.Y. helped develop the coding template, and reviewed and approved the final manuscript. B.D. and D.A. helped conceptualize the study, aided in the interpretation and analysis of study findings, and reviewed and approved the final manuscript. L.M. coordinated research activities, aided in the interpretation and analysis of study findings, and reviewed and approved the final manuscript. M.M. conceptualized the study, supervised its implementation, and was a major contributor in reviewing and editing the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Correspondence to Maria Mathews .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the research ethics board at Western University. We obtained informed consent from participants prior to the onset of interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Idrees, S., Young, G., Dunne, B. et al. The implementation of person-centred plans in the community-care sector: a qualitative study of organizations in Ontario, Canada. BMC Health Serv Res 24 , 680 (2024). https://doi.org/10.1186/s12913-024-11089-7
Download citation
Received : 14 February 2024
Accepted : 08 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1186/s12913-024-11089-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Person-centred planning
- Community-based care
- Integrated care
- Social services
- Health services
- Organizational culture
- Qualitative study
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
- What We’re Learning About the Patient…
What We’re Learning About the Patient Navigator Role in Supporting Behavioral Health Access and Utilization: Discussing Insights with Dr. Jennifer Mautone
Date posted:.

In a 2023 blog post , we explored how pediatric researchers and clinicians are using patient navigation to support children and families in accessing behavioral health care. This approach builds on patient navigation research for children with special health care needs , which finds improved health and well-being for families and children when navigation services are available. Related to behavioral health, emerging research and pilot studies find families are more likely to complete mental health assessments, connect to care and to stay engaged in care once connected when they work with patient navigators.
Today, I am following up with my PolicyLab colleague Dr. Jennifer Mautone who works with patient navigators to connect families to health care providers and resources, provide brief interventions, support family engagement in care, advocate for the patient and family, or help the caregiver problem-solve. I sat down with her to learn more about what they are observing in their research and patient care.
In your research, how are you considering the navigators’ impact on patient care? What are you learning so far?
With our study about the effectiveness of an enhanced behavior therapy program for families of children with ADHD, Partnering to Achieve School Success (PASS) , we call our patient navigator a Community Health Partner (CHP). The CHP is part of the team and promotes family engagement in treatment and cultural effectiveness of care. In this role, the patient navigator is working to establish trust, listen attentively and use motivational interviewing strategies. We are seeing that the more contacts families have with the patient navigator, the more likely they are to attend therapy sessions. Behavioral health clinicians and families have also indicated that the patient navigator is an extremely helpful extension of the care team.
And what are you learning about the patient navigator role?
In PASS , we are finding that the patient navigator spends most of their time working with patients’ families on scheduling, reminding them about appointments and assisting in overcoming barriers to care. Occasionally, the navigator supports parents with implementation of strategies they learn in therapy sessions, such as how to consistently provide positive attention to their children and limit their use of punishment. The patient navigator has also become involved in supporting family-school collaborations.
What do you see as priorities for future research related to patient navigators supporting families in engaging in behavioral health care?
Our study is unique in that we are connecting children with ADHD to care and also providing the intervention, so our patient navigators are critical in supporting families’ initial attendance and ongoing engagement in care. We believe that higher levels of engagement will result in better child and family outcomes. As such, one question that we hope to answer is how the patient navigator role influences outcomes for children with ADHD.
Additionally, we are thinking about how this position could be sustained in the care team. We are exploring if these activities could be billable as part of collaborative care or case management, and we are collaborating with health systems leaders to consider other options for sustainability.
Putting this conversation into context
In reflecting on my conversation with Dr. Mautone about PASS and the context about other interventions that engage patient navigators, I noticed a few themes:
Patient navigators’ time is primarily focused on helping patients get to appointments and connect to resources responsive to families’ needs and what is available in the community. These roles might be able to be expanded to more fully support patient and family engagement in care and adherence to care plans.
Care teams are observing improved attendance at appointments. This metric is valuable and perhaps a major indicator of success as attributing the impact of patient navigation on the child’s health is complex. There is going to be variability in individual family needs and the subsequent referrals made. And, unless a standard intervention is offered—as is the case with PASS—the care received following the referral will be individualized, making it difficult to get a full understanding of the link between navigation and health outcomes.
Sustaining these service models will be reliant on a flexible reimbursement mechanism that can accommodate different applications and patient populations.
We also know that continued research related to patient navigator roles and their contributions to improved patient outcomes is needed to justify the cost of these professionals and sustain their involvement in clinical services. We look forward to continuing to explore how to best support families through this unique role.
Latest Blog Posts
Understanding infant and caregiver mental health: what is the impact of the covid-19 pandemic and systemic racism.
Mental Health Awareness Month offers an opportunity to reflect on the importance of our health and well-being—including for the littlest amongst us…

Recognizing Cross-sector Collaborations That Can Improve Financial Wellness and Educational Opportunities in 200 Words
Education pays. That truth underlies the role education plays in addressing poverty, and is part of why education has been acknowledged as a …
Utilizing Behavioral Health Research to Inform Policy: A Conversation with Dr. Rhonda Boyd
As the youth behavioral health crisis has grown in the past several years, members of PolicyLab’s Behavioral Health portfolio have continued to think…
Check out our new Publications View Publications
Adolescent Health & Well-Being
Behavioral health, population health sciences, health equity, family & community health.
- Open access
- Published: 06 March 2021
How to bring research evidence into policy? Synthesizing strategies of five research projects in low-and middle-income countries
- Séverine Erismann 1 , 2 ,
- Maria Amalia Pesantes 3 ,
- David Beran 4 ,
- Andrea Leuenberger 1 , 2 ,
- Andrea Farnham 1 , 2 ,
- Monica Berger Gonzalez de White 1 , 2 , 5 ,
- Niklaus Daniel Labhardt 1 , 2 , 6 ,
- Fabrizio Tediosi 1 , 2 ,
- Patricia Akweongo 7 ,
- August Kuwawenaruwa 1 , 2 , 8 ,
- Jakob Zinsstag 1 , 2 ,
- Fritz Brugger 9 ,
- Claire Somerville 10 ,
- Kaspar Wyss 1 , 2 &
- Helen Prytherch 1 , 2
Health Research Policy and Systems volume 19 , Article number: 29 ( 2021 ) Cite this article
25k Accesses
19 Citations
11 Altmetric
Metrics details
Addressing the uptake of research findings into policy-making is increasingly important for researchers who ultimately seek to contribute to improved health outcomes. The aims of the Swiss Programme for Research on Global Issues for Development (r4d Programme) initiated by the Swiss National Science Foundation and the Swiss Agency for Development and Cooperation are to create and disseminate knowledge that supports policy changes in the context of the 2030 Agenda for Sustainable Development. This paper reports on five r4d research projects and shows how researchers engage with various stakeholders, including policy-makers, in order to assure uptake of the research results.
Eleven in-depth interviews were conducted with principal investigators and their research partners from five r4d projects, using a semi-structured interview guide. The interviews explored the process of how stakeholders and policy-makers were engaged in the research project.
Three key strategies were identified as fostering research uptake into policies and practices: (S1) stakeholders directly engaged with and sought evidence from researchers; (S2) stakeholders were involved in the design and throughout the implementation of the research project; and (S3) stakeholders engaged in participatory and transdisciplinary research approaches to coproduce knowledge and inform policy. In the first strategy, research evidence was directly taken up by international stakeholders as they were actively seeking new evidence on a very specific topic to up-date international guidelines. In the second strategy, examples from two r4d projects show that collaboration with stakeholders from early on in the projects increased the likelihood of translating research into policy, but that the latter was more effective in a supportive and stable policy environment. The third strategy adopted by two other r4d projects demonstrates the benefits of promoting colearning as a way to address potential power dynamics and working effectively across the local policy landscape through robust research partnerships.
Conclusions
This paper provides insights into the different strategies that facilitate collaboration and communication between stakeholders, including policy-makers, and researchers. However, it remains necessary to increase our understanding of the interests and motivations of the different actors involved in the process of influencing policy, identify clear policy-influencing objectives and provide more institutional support to engage in this complex and time-intensive process.
Peer Review reports
Increasingly, research funders are asking their grantees to address the uptake of research findings into decision-making processes and policy-making [ 1 , 2 ]. This growing trend is a response to a need for real-world and context-sensitive evidence to respond to and address complex health systems and health service delivery bottlenecks faced by policy-makers, health practitioners, communities and other actors that require more than single interventions to induce large-scale change [ 3 ]. Moreover, there is growing pressure for applied and implementation research to be relevant, demonstrate value for money and result in high-impact publications. The relevance of ensuring the translation of research into practice is also reflected in growing support for research projects with concrete requirements regarding the evaluation of their impact of science on society [ 4 ].
One example of the above is the Swiss Programme for Research on Global Issues for Development (r4d Programme) initiated by the Swiss National Science Foundation (SNSF) and the Swiss Agency for Development and Cooperation (SDC) covering the period 2012–2022. The r4d Programme is aimed at researchers in Switzerland and low-and middle-income countries (LMICs) conducting projects that specifically focus on poverty reduction and the protection of public goods in developing countries. Its specific objectives are to create and disseminate knowledge that supports policy-making in the area of global development and foster research on global issues in the context of the 2030 Agenda for Sustainable Development [ 5 , 6 ].
While the linkage of research to policy is strongly encouraged by research funding agencies, the uptake of research evidence by policy-makers to establish new laws and regulations or to improve policies to solve a problem or enhance implementation effectiveness, especially in LMICs, remains weak [ 2 , 7 ]. This is often referred to as the gap between research and policy [ 8 ]. One of the factors that was identified with the dearth of research uptake in previous studies is a lack of evidence that is context sensitive, timely and relevant for policy-makers; other factors include difficulties in accessing existing evidence, challenges with correctly interpreting and using existing evidence [ 7 , 9 ] and also a lack of interest from policy-makers in the use and uptake of evidence [ 10 ]. Using the SNSF r4d funding scheme, our aim is to show how researchers have engaged with stakeholders, including policy-makers, from the onset of a research project, in order to identify strategies for evidence uptake and use.
As part of the r4d Programme, several synthesis initiatives have been launched to disseminate the research evidence from the r4d projects and increase its impact ( http://www.r4d.ch/r4d programme/synthesis ). The aim of one of these synthesis initiatives is to support knowledge translation and exchange, as well as knowledge diffusion and dissemination among 15 r4d projects focusing on public health. More specifically, the aim is to facilitate the uptake of findings for the benefit of societies in LMICs, especially with regards to social inclusion and gender equity in the drive towards universal health coverage (UHC) and the 2030 Agenda for Sustainable Development [ 6 ]. The present study and resulting article are part of this synthesis initiative.
In this article, we present—through five case studies—strategies to translate and bridge evidence emerging from research into policy-making and decision-making. We rely on the experiences of five public health projects within the r4d research initiative. This paper describes these experiences, reports on the lessons learnt and outlines important features and challenges of engaging in this process using the researchers’ perspectives. This paper contributes to the body of literature on research translation by highlighting concrete examples and successful strategies for the uptake of research evidence in policy formulation.
Invitations were sent out to researchers working on projects within the r4d Programme to share their experiences with the project. Based on the interest shown by researchers, five projects were selected by the authors to demonstrate the different approaches and strategies used in the r4d projects with the aim to influence policy. Researchers were asked to share descriptions of the different approaches used in seeking to influence the uptake of research results by policy-makers. Each project represents a case study with emphasis on the main features of their translational approaches and the challenges, enablers and successes encountered.
The different research–policy engagement strategies were identified through data analysis of the interviews conducted within the framework of the five r4d case studies and were inspired by the work conducted by Uzochukwu and colleagues in Nigeria [ 2 ], who described four detailed strategies to support evidence-informed policy-making: (1) policy-makers and stakeholders seeking evidence from researchers; (2) involving stakeholders in designing objectives of a research project and throughout the research period; (3) facilitating policy-maker–researcher engagement in optimizing ways of using research findings to influence policy and practice; (4) active dissemination of own research findings to relevant stakeholders and policy-makers (see Table 1 ).
In using the term stakeholder, we apply the following definition by Brinkerhoff and Crosby [ 11 ]: “A stakeholder is an individual or group that makes a difference or that can affect or be affected by the achievement of the organization’s objectives”. Hence, individual stakeholders can include politicians (heads of state and legislators), government bureaucrats and technocrats from various sectors (e.g. health), but also representatives of civil society organizations and support groups [ 12 ].
Data collection
Eleven in-depth interviews with principal investigators and their research partners from five r4d projects were conducted by the first author, using a semi-structured interview guide. The interview guide covered the following themes: (1) How were stakeholders involved in the research project? (2) Was there uptake of research evidence in national/international policies? (3) How were research results disseminated? (4) What were the challenges or obstacles encountered in disseminating and translating evidence from research to policy? The interview duration was between 30 and 45 min. Seven interviews were conducted with researchers based in Switzerland and four with researchers in LMICs. At least two interviews were conducted for each r4d case study.
Data management and analysis
Of the 11 interviews, nine were audio recorded and notes taken. Audio files were transcribed verbatim by the same researcher. Two interviews were not recorded, but detailed notes were taken during the interview.
A qualitative content analysis method was used in order to organize and structure both the manifest and latent content [ 13 ]. Aligned to overall study questions, essential content was identified by the first author, which involved a process of generating a provisional list of themes of interest that were based on the study objectives, including stakeholder involvement in the generation of research questions, research process, generation of results and dissemination of research findings, as well as challenges to research dissemination and policy uptake. In a next step, the transcripts were sorted and grouped by the first author according to the coding scheme for analysis. This involved using the content summary analysis method, which consists of reducing the textual content and preserving only the essential content in order to produce a short text [ 14 ]. As several co-authors were interviewed, they validated that their perspective was not misinterpreted or misrepresented.
Three key strategies were identified for research uptake into policy and practice throughout the data collection of this synthesis initiative: (S1) stakeholders directly engaged with and sought evidence from researchers; (S2) stakeholders were involved in the design and throughout the implementation of the research project; and (S3) stakeholders engaged in participatory and transdisciplinary research approaches to co-produce knowledge and inform policy. The first two strategies (S1, S2) are in line with Uzochukwu and colleagues’ work [ 2 ], and the third strategy (S3) is an additional category based on the experiences of researchers in r4d projects [ 2 ]. Each r4d project is described in more detail as a case study in one of these three strategies (Table 2 ).
S1: stakeholders directly engaged with and sought evidence from researchers
In this strategy, international stakeholders requested evidence from the research team. This is a unique (and rare) strategy, as stated by Uzochukwu et al. [ 2 ], and often involves a policy window of opportunity in which stakeholders, including policy-makers, are looking to solve a particular problem, which coincides with the publishing of a scientific report or paper and the interests of these same groups [ 15 , 16 ].
Improving the HIV care cascade in Lesotho: towards 90-90-90—a research collaboration with the Ministry of Health of Lesotho
In this r4d project, the research team was approached by the International Aids Society (IAS) and the World Health Organization (WHO) in Geneva, based on the publication of their study protocol [ 17 ], introducing their innovative research approach of same-day antiretroviral therapy (ART) initiation in rural communities in Lesotho:
“They [international stakeholders] were all keen of getting the results out and requested evidence of the randomized controlled trials. We shared the results confidentially with WHO as soon as we had the data and thereafter published the results in a journal with a wide reach. WHO as well as other international guidelines and policy committees took up the recommendation of same-day ART initiation and informed global guidelines” (Researcher 1).
As a result, many HIV programmes in sub-Saharan Africa as well as in the global north have adopted the practice of offering rapid-start ART to persons who test HIV positive even outside a health facility. In this example, the policy window and direct stakeholder engagement was crucial for the effective translation and uptake of research evidence.
Furthermore, by closely collaborating with national policy-makers, the research team advocated for the setting up of a research database and of knowledge management units within the Ministry of Health (MoH) of Lesotho, which have been successfully established. The members of the research project consortia have also initiated a national research symposium on a bi-annual basis, which is chaired by the MoH with the aim of facilitating the dissemination and uptake of research findings.
S2: Stakeholders were involved in the design and throughout the implementation of the research project
In this strategy, policy uptake is facilitated through stakeholder engagement from the beginning as well as during the conduct of research activities, through participating at workshops or functioning in the governance of the projects. Two r4d projects illustrate this strategy.
Health system governance for an inclusive and sustainable social health protection in Ghana and Tanzania
This project established a Country Advisory Group (CAG) at the start that included representatives of the main stakeholders of the social health protection systems. The CAGs were involved in all phases of the project, from the definition of the research plans to the dissemination of the results. The specific research questions addressed by the project emerged from the interactions with these main stakeholders, i.e. national policy-makers, healthcare providers and members of the social health protection schemes (the NHIS and the Livelihood Empowerment Against Poverty schemes in Ghana; and the National Health Insurance Fund, the Community Health Funds and the Tanzania Social Action Fund in Tanzania). Specifically in Ghana, the following stakeholders played a major role in shaping the research plan: the Ministry of Gender Children and Social Protection (MGCSP), the Ghana Health Service (Policy Planning and Monitoring and Evaluation Division; Research and Development Division), the National Health Insurance Authority (NHIA) and the Associations of Private Health Care Providers. In Tanzania, a major role was played by the Ministry of Health, Community, Development, Gender, Elderly and Children, the President’s Office—Regional Administration and Local Government, by representatives of civil society organizations, such as Sikika, by the SDC (Swiss Agency for Development and Cooperation) Health Promotion and System Strengthening project and by the SDC-supported development programme.
These stakeholders were subsequently involved in steering the research, as captured by a researcher:
“In Ghana, it was a balanced relationship. They were involved since the very beginning of the project in articulating what the information gap at policy level is, formulating the research questions and understanding the methods/what is feasible. In Tanzania, where the policy landscape is more fragmented, it was very important to listen to the voices of several different stakeholders” (Researcher 2).
The stakeholder consultations in Ghana and Tanzania initially involved discussions on the relevance of the research plans to address the existing gaps in strengthening the social health protection scheme, the synergies with other research initiatives and the feasibility of implementing the proposed research. Later on in the project, the consultation process involved reviewing and discussing the focus of the research and the appropriateness of the research aims in light of decisions and reforms that were under discussion by the government but not in the public domain. This led to revision of the research questions as they would have become redundant when such reforms were made public, especially in Ghana. These consultation processes were more formal in Ghana and more informal in Tanzania, but they were very informative and had a tangible impact on the research plans, which were revised according to the feedback received. However, the research teams were always independent in deciding on the research methodology and in interpreting the results. The in-country dissemination of the results at the end of the first phase of the project informed the decisions to be made on the research plan for the second phase and provided the opportunity to discuss policy implications based on the results of the first phase. Because of this close collaboration and engagement with stakeholders, the results of the studies were widely disseminated in Ghana. Two of the main findings of the project were particularly considered by these stakeholders. According to the researcher:
“First, the study results showed that even though people registered with the NHIS they continued to pay out of pocket for health services. The reasons for this were delays in reimbursement by NHIS, escalating prices of drugs and medical products, low tariffs, lack of trust between providers and NHIA and inefficiencies. Secondly, the results showed that the current system of targeting the poor is not working properly, with more than half of people registered in the NHIS as indigents being in the non-poor socio-economic groups. These results contributed to inform decisions regarding the revision of the NHIA reimbursement tariffs, and to improve the identification of the poor to be exempted from paying the NHIS premium, in collaboration with the MGCSP” (Researcher 3).
In Tanzania, research was conducted to assess the effects of the public private partnership, referred as the Jazia Prime Vendor System (Jazia PVS), on improving access to medicines in the Dodoma and Morogoro regions in Tanzania. This is one of the reforms in the area of supply chain management taking place in the country. Results showed that a number of accountability mechanisms (inventory and financial auditing, close monitoring of standard operating procedures) implemented in conjunction with Jazia PVS contributed positively to the performance of Jazia PVS. Participants’ acceptability of Jazia PVS was influenced by the increased availability of essential medicines at the facilities, higher-order fulfilment rates and timely delivery of the consignment [ 18 , 19 , 20 ].
The findings from this study were disseminated during the national meeting attended by various stakeholders, including CAG members, government officials and policy-makers. In addition, the findings were used to inform the national scale-up of the Jazia PVS intervention as the government of Tanzania decided to scale up the Jazia PVS to all the 23 regions in 2018. Moreover, the results/manuscripts were published or submitted to peer-reviewed journals [ 18 , 19 , 20 ], enabling other countries intending to adopt such innovate public–private partnerships for improvement of the in-country pharmaceutical supply chain to learn from Jazia PVS in Tanzania.
Health impact assessment for engaging natural resource extraction projects in sustainable development in producer regions (HIA4SD)
In this r4d project, stakeholders were involved from the outset through their participation in the project launch meeting and in regular consortium meetings. The project is a collaboration between the Swiss Tropical and Public Health Institute (Swiss TPH), the Center for Development and Cooperation (NADEL) at the Swiss Federal Institute of Technology in Zurich/Switzerland and national research institutes, namely the Institut de Recherches en Sciences de la Santé in Burkina Faso, the University of Health and Allied Sciences in Ghana, the Centro de Investigação em Saúde de Manhiça in Mozambique and the Ifakara Health Institute in Tanzania [ 21 ]. The involvement of key stakeholders from the government, civil society, private sector and research community in an engaged dialogue from the beginning iss of central importance in this project, as in most cases mining is a highly politicized topic. To promote the immediate integration of research findings into policy, the project is organized into two streams, namely an “impact research stream” and a “governance stream”, that work in parallel. While the impact research stream is focused on evidence generation to support the uptake of health impact assessment (HIA) in Africa, the governance stream is focused on understanding the policy terrain and consequently the pathways that need to be utilized to support translation of the evidence into policy and practice. The second phase of the study is devoted to the dissemination of research findings into policy at the national and local levels, including capacity-building activities for national stakeholders. As the HIA4SD project examines operational questions of relevance for guiding both policy-making and decision-making, team members sought to regularly engage with and inform the national stakeholders. According to the researcher:
“Strategies employed to influence policy vary according to the country, but included regular stakeholder workshops, participation in a new national platform launched to discuss issues around mining in Mozambique, development of policy briefs, strengthened collaborations with national ministries of health, discussion of results and advocacy with policy makers, and conference presentation of findings” (Researcher 4).
In these two case examples, continuous stakeholder engagement was considered essential to translate and disseminate research evidence. Thus, beyond the stage of setting the objectives, contact with stakeholders was active and maintained on a regular basis through regular exchanges with stakeholder groups during workshops or meetings, which facilitated the dissemination and uptake of the research results. While the time and level of meaningful interaction varied across the countries and workshops, all meetings were well attended by participants from varied levels of government, MoHs, nongovernmental organizations and private industry, prompting spirited discussion and insight from these groups. All stakeholders were willing to attend these workshops as part of the scope of their professional duties.
S3: stakeholders engaged in participatory and transdisciplinary research approaches to co-produce knowledge and inform policy
In the two examples presented in this section, the research questions and approaches arose through community and stakeholder participation in the research and intervention design itself. The methodology adopted allowed them to engage, design research, act, share and sustain partnerships between the communities, the involved stakeholders and researchers [ 22 ]. These participatory research approaches facilitated grassroot-level policy and practice changes which were not researcher nor policy maker led, and that show promising approaches for developing culturally aligned solutions [ 23 ]. Policy makers at both the regional and national levels were invited to be part of the participatory research approach: they were interviewed during the initial stage, then the research results were presented and discussed with them; thereafter, we had several meetings to co-create potential interventions to address the identified problems, with the aim to directly engage in the research and intervention design itself in partnerships with the community stakeholders, including local leaders, and the researchers.
Surveillance and response to zoonotic diseases in Maya communities of Guatemala: a case for OneHealth
The research was embedded in a collaboration between the Universidad del Valle in Guatemala, the MoH, the Ministry of Animal Production and Health, the Maya Qéqchi’ Council of Elders, TIGO Telecommunications Foundation and the community development councils. The objective of this r4d programme was to set up integrated animal–human disease surveillance (OneHealth) in Maya communities in Guatemala. The research approach arose from a context of medical pluralism, where communities have access to and use two different medical systems: (1) the modern Western medical system and (2) traditional Maya medicine [ 24 ].
Researchers and community members collaborated at all stages of the research process, including the planning stage. Even before the grant proposal was finalized, researchers met with the communities that, should the funding come through, would be invited to participate in the research. According to the researchers:
“The project was set up through a transdisciplinary process, with academic and non-academic actors—including national, local and traditional authorities—involved in the problem through a collaborative design, analysis, dissemination and research translation. It was a co-producing transformative process—transferring knowledge between academic and non-academic stakeholders in plenary sessions and through group work. These meetings were held every year to continuously follow up the progress of the process” (Researcher 7).
The active engagement and collaboration by the community and stakeholders facilitated the acceptability of the study results and hence its dissemination, captured by the researchers as follows:
“The main result was that they allowed a frank discussion between Maya medical exponents in human–animal health and Western medicine, which allowed the patients and the animal holders to avoid the cognitive dissonance and so that the patients or the animal holders can choose freely what they want. Cognitive dissonance exists if one system dominates the other—or refutes the other” (Researcher 7).
“After all stakeholders discussed the research evidence produced jointly, an unprecedented process of collaboration between Government authorities and communities followed to develop three joint responses: a) education campaigns led by local teachers in tandem with the Ministry of Education, b) communication strategies at regional levels led by the Human and Animal Health authorities along with traditional Maya Ajilonel (medicine specialists), and c) a policy framework for producing a OneHealth approach led by Central Government authorities” (Researcher 8).
The process of mutual learning throughout the project produced a new level of awareness, facilitating culturally pertinent and socially robust responses that overcame a historical tendency of unilateral policy making based solely on Western values and preferences. As the project implemented a new approach to monitoring animal and human populations, the involvement of regional teams from the different ministries (Health, Livestock and Agriculture) throughout all the phases of methodological design, data collection, posterior data analysis and design of specific interventions for the local population (transformation of scientific results into actions for public health improvement) was essential to ensuring that the approach used secured the regional authorities’ commitment to defining new policies for immediate application in their territory. Accordingly, this also contributed towards the development of a OneHealth national strategy for Guatemala in which ministries start to cooperate to take up priority issues.
Addressing the double burden of disease: improving health systems for non-communicable and neglected tropical diseases (Community Health System Innovation [COHESION])
Together with three Swiss academic partners, this r4d project examined the challenges of a double burden of non-communicable and neglected tropical diseases at the primary healthcare level in vulnerable populations in Mozambique, Nepal and Peru. Community participation and co-creation were key elements of the project’s approach. The work conducted in Peru illustrates this approach:
“At the beginning, the people who were involved were respondents, but then they became active participants. So it was this active engagement and the changing of roles, giving feedback not just from the research responses but also from being involved in the process, which helped to design and create interventions together with the research team” (Researcher 5).
This participatory approach to co-creation actively sought a diverse range of stakeholders, including community members, primary healthcare workers, and regional and national health authorities. The co-creation approach to participatory research enables context-specific variation in methodological design, a critical element when studying three very different countries and health systems. Central to all aspects was a feedback loop whereby early findings were shared with research participants for further elaboration and iteration.
As active co-creators of the research process, local communities developed high levels of trust in the methodology and data, with the result that researchers achieved deeper “buy-in” which in turn is known to enhance the uptake of findings by decision-makers [ 25 ] as communities in which research is being undertaken play a central role in the decision-making process [ 26 ].
Challenges to research uptake in health policy identified by r4d researchers
During the interviews, r4d researchers identified several challenges to research utilization and uptake into policy. These challenges are summarized and highlighted in Table 3 .
Three key strategies identified for research uptake in policy and practice are described in this paper, namely: (S1) stakeholders directly engaged with and sought evidence from researchers; (S2) stakeholders were involved in the design and throughout the implementation of the research project; and (S3) stakeholders engaged in participatory and transdisciplinary research approaches to co-produce knowledge and inform policy. These strategies are in line with the overall objectives of the r4d projects, which are to generate scientific knowledge and research-based solutions to reduce poverty and global risks in LMICs, and also to offer national and international stakeholders integrated approaches to solving problems [ 5 ]. In the course of our synthesis work, we found that several lessons could be learned from the three strategies identified for research uptake in policy and practice.
S1: raising awareness of planned research to attract stakeholder involvement
The actual uptake of research findings in policy was most direct in the case of the first strategy (S1), in which IAS and WHO stakeholders were wanting new knowledge on HIV and same-day ART initiation, and were actively seeking new evidence on these specific topics. The findings published in peer-reviewed journals were then taken up by these stakeholders to update international policies and guidelines on rapid ART initiation [ 27 ]. This was also found in other studies, highlighting the importance of the timeliness and relevance of findings and the production of credible and trustworthy reports, among others, as key factors in promoting the use of research evidence in policy [ 2 , 28 ].
S2: sustainable collaborations in a supportive policy environment with stakeholder engagement from early on and throughout the research process
With regards to the second strategy (S2), we found that constant collaboration with an advisory and steering group composed of diverse stakeholders, including policy-makers, from early on promotes the uptake and use of research evidence. In line with findings from other studies [ 2 ], the experiences encountered in the r4d public health projects show that early involvement of stakeholders in the processes to identify the research problem and set the priorities facilitated the continuous exchange of information that might ultimately influence policy. The r4d project on social governance mechanisms in Ghana highlight that the evidence produced influenced policy documents (identification of the poor and tariff adjustments), but that frequent changes government officials made it difficult to maintain a close relationship between the researchers and the governmental agencies/policy stakeholders. From this, we draw the conclusion that research approaches need to be more adaptive and flexible to be successful in an unsupportive or unstable policy environment to ensure continuity in promoting the dissemination and uptake of research evidence in policy-making. One possible manner to secure this transformation is for researchers to apply for additional funding after the grant is finished. Other studies have also come to this conclusion, thereby demonstrating the key role of a supportive and effective policy environment that includes some degree of independence in governance and financing, strong links to stakeholders that facilitate trust and influence and also the capacity within the government workforce to process and apply policy advice developed by the research findings [ 29 ]. By involving stakeholders in the process of identifying research objectives and designing the project, as seen particularly in the r4d case studies on social health protection in Ghana and Tanzania and the HI4SD, but also in the HIV care cascade in Lesotho, the research approach responded to the need of locally led and demand-driven research in these countries, strengthening local research capacities and institutions, but also investing in research that is aligned with the national research priorities. As highlighted by other authors, advantages of this “demand-driven” approach is that it tailors research questions to local needs, helps to strengthen local individual and organizational capacities and provides a realized stringent framework on which a research project should deliver outcomes [ 30 , 31 ].
S3: co-creation and equal partnerships
The third strategy with a strong participatory approach, such as that adopted by two r4d projects, OneHealth in Guatemala and COHESION, demonstrates benefits to promoting co-learning as a way to minimize the impact of unequal power dynamics and to work effectively across the local policy landscape through equal partnerships. It also facilitates identifying solutions that are culturally pertinent, socially more robust and implementable.
The approaches of co-creation, equal participation and stakeholder involvement used in the research projects raise questions of ‘governance’, that is the way rules, norms and actions are structured, sustained and regulated by public and para-public actors to condition the engagement and impact of public involvement activities [ 32 , 33 ]. Through stakeholder involvement in setting the agenda and designing the research projects, as shown in the case studies on social protection in Ghana and Tanzania and the HI4SD project, but particularly in the two projects using a co-creation approach, the engagement of a range of stakeholders serves to make the health research systems a participaant in the endeavor that then has the capacity to promote changes in the healthcare system it aims to serve. By establishing a shared vision with a public involvement agenda and through the collaborative efforts of various stakeholders, as we found particularly in the co-creation approach, supportive health research systems are established. This leads to greater public advancement through collaborative actions, thereby tackling the stated problems of the health systems [ 34 ].
There were four key challenges mentioned by the respondents during the interviews to research uptake in policy making. The first was the necessary time investment by researchers to translate the result and develop policy advocacy products for the different audiences. This challenge is all the more difficult because research evidence and tangible products only become available towards the end of a research project, leaving only a short window of opportunity for exchange and engagement. There seems to be a need for wider discussion on the role of researchers in influencing policy. The concerns raised included whether influencing policy is actually a role for researchers and whether researchers have the right skills to be effective in persuasion or network formation [ 35 ]. Conversely, researchers may be in a good position to engage in the policy process if they enjoy finding solutions to complex problems while working with diverse and collaborative groups in partnerships [ 36 , 37 ]. The rationale for engaging in such a process needs to be clarified in advance: is the aim to frame an existing problem, or is it to simply measure the issues at stake and provide sound evidence according to an existing frame? Regarding the the former, how far should researchers go to be useful and influential in the policy process or to present challenges faced by vulnerable populations [ 37 ]? While fully engaging in the policy process may be the best approach for researchers to achieve credibility and impact, there may also be significant consequences, such as the risk of political interests undermining the methodological rigour of academic research (being considered as academic ‘lightweight’ among one’s peer group) [ 38 , 39 , 40 , 41 ]. For researchers there is also considerable opportunity costs because engaging in the policy-influencing process is a time-consuming activity [ 35 ], with no clear guarantee of the impact of success [ 37 ]. It is therefore crucial to consider the investment and overall time researchers may have to spend to engage [ 35 ], and how this time and investment can be distributed between actual research and the production of outreach products, such as policy briefs, presentation of research findings as policy narratives [ 35 ] and the setting-up of alliances, building of networks and exploitation of windows of opportunity for policy change [ 37 ].
The second challenge included the issue of scale and objectivity, as most of the projects are not scaled or national-level studies and thus are highly context specific. The difficulty to measure the contributions of a single research project or study in terms of policy outcomes was also highlighted, particularly in view of the different understandings among researchers and funders on the possible policy impacts of the research, which can range from guiding policy-makers to understand a situation or problem (awareness raising) to influencing a particular course of action by establishing new or revising existing policies. This has also been emphasized in the Evidence Peter Principle [ 42 ], showing that single studies are often inappropriately used to make global policy statements for which they are not suitable. To make global policy statements, an assessment of the global evidence in systematic reviews is needed [ 42 , 43 ].
The third challenge mentioned was the frequent changes in staff at the governmental level, which demanded continuous interactions between r4d researchers and stakeholders, highlighting the need for more adaptive and flexible research approaches. These should include a thorough analytical process prior to implementation in historical, sociopolitical and economic aspects, power differentials and context; backward planning exercises to check assumptions; and conflict transformation and negotiation skills in order to be able to constantly adapt to changing contexts. In line with our research findings, when researchers make the time investment needed to engage in the policy-influencing process, an opportunity is provided to getting know the involved stakeholders better and improve their understanding of the policy world in practice, but also to build diverse and longer-term networks [ 37 , 44 ] and to identify policy problems and the appropriate stakeholders to work with [ 45 , 46 ]. Engaging a diverse range of stakeholders through co-designing the research is widely held to be practically the best way to guarantee the uptake and use of evidence in policy through a more dynamic research approach [ 47 ]. However, the development of networks and contacts for collaboration, as well as the skills to do so, takes time and effort and is an ongoing process [ 48 ], factors which need to be acknowledged more widely.
Lastly, the fourth challenge related to research uptake was the diverging interests between researchers, research funding bodies and stakeholders. Time was identified as a limiting factor from the perspective of the design of the research project. Most research projects, including the r4d projects, are funded for 3–4 years [ 5 ]. It takes a considerable amount of time to generate new research results, and often these are more likely to be produced for further use at the end of a project. If researchers should engage more fully in the policy process to secure meaningful impact, it is critical to discuss the extent to which they have the skills, resources and institutional support to do so [ 37 ], as well as how projects could be set up differently. This could be done either by the funders in providing the necessary support that allows researchers to have the means to impact policy, or by the researchers in the design of their project to take on board the different strategies to influence evidence use and uptake. In moving forward, defining shared goals from the outset between funders and the researchers might translate to more achievable milestones in terms of which policy issue, theme or process a research project aims to change in order to effectively influence policy [ 49 ]. This would help to identify the resources and budget needed by the funders in order for the researchers to engage with more resources over a longer time span in this process.
Limitations
Interviews were limited to researchers of the r4d projects and did not include local stakeholders. Therefore, the synthesis work, including the analysis and results, reflects solely the perspective of researchers. We are aware that had we included a range of stakeholders, including policy-makers, in the sample, we would have potentially been able to identify additional factors relating to social, cultural and political barriers to the use and uptake of research findings in politics and practice. However, constraints such as access to local stakeholders, language barriers and time zones drove our decision to focus on researchers. A future synthesis effort would need to include the other voices.
There is ever growing awareness of how critical it is to close the gap between policy-makers, practitioners and researchers. Using the researchers’ perspectives, in this article we give insight into three different strategies that can facilitate this process, with the first strategy requiring proactive searching for the latest findings on the part of well-informed policy-makers, the second requiring researchers to take steps to ensure an active exchange of ideas and information with diverse stakeholders when designing the research project and ensuring the latter’s involvement throughout; and the third using a transdisciplinary and/or co-creation approach to establish equal partnerships and trust among all involved stakeholders.
The five case studies reported here also show some of the difficulties that prevail for research to be taken up into policy and practice, despite everyone’s best intentions and efforts. Researchers may not always be best placed for communication, dissemination and advocacy work, all activities which are very time intensive or become important only towards the end of a research project when clear and high-quality evidence is produced. Moreover, it takes a strong body of evidence, advocacy and coalition building with appropriate stakeholders to influence policy, and then a further major effort of resources to see policy followed through into practice. It is through experiences such as this synthesis initiative that precious insights and learning can be gained for the common good of all involved moving forward, and it is crucial that funders continue to support and/or adapt their funding schemes to ensure some of these strategies are implemented.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Antiretroviral therapy
Country Advisory Group
Community Health System Innovation
Health impact assessment
Health impact assessment for engaging natural resource extraction projects in sustainable development in producer regions
Human immunodeficiency virus
International Aids Society
Jazia Prime Vendor System
Low- and middle-income countries
Ministry of Health
Ministry of Gender Children and Social Protection
Center for Development and Cooperation at the Swiss Federal Institute of Technology
National Health Insurance Authority
National Health Insurance Scheme
Swiss Programme for Research on Global Issues for Development
Swiss Agency for Development and Cooperation
Swiss National Science Foundation
Swiss Tropical and Public Health Institute
Universal health coverage
World Health Organization
Court J, Young J. Bridging research and policy in international development: an analytical and practical framework. J Dev Pract. 2006;16(1):85–90.
Article Google Scholar
Uzochukwu B, Onwujekwe O, Mbachu C, Okwuosa C, Etiaba E, Nyström ME, Gilson L. The challenge of bridging the gap between researchers and policy makers: experiences of a Health Policy Research Group in engaging policy makers to support evidence informed policy making in Nigeria. Glob Health. 2016;12(1):67.
Di Ruggiero E, Edwards N. The interplay between participatory health research and implementation research: Canadian research funding perspectives. Biomed Res Int. 2018;2018:1519402.
Rau H, Goggins G, Fahy F. From invisibility to impact: recognising the scientific and societal relevance of interdisciplinary sustainability research. Res Policy. 2018;47(1):266–76.
Swiss National Science Foundation: Swiss Programme for Research on Global Issues for Development (r4d programme). http://www.r4d.ch/r4d programme/portrait . Accessed 20 Jan 2020.
United Nations: Sustainable Development Goals. https://sustainabledevelopment.un.org/ . Accessed 17 Dec 2019.
Shroff ZC, Javadi D, Gilson L, Kang R, Ghaffar A. Institutional capacity to generate and use evidence in LMICs: current state and opportunities for HPSR. Health Res Policy Syst. 2017;15(1):94.
McKee M. Bridging the gap between research and policy and practice Comment on “CIHR health system impact fellows: reflections on ‘driving change’ within the health system.” Int J Health Policy Manag. 2019;8(9):557–9.
World Health Organization. Sound choices: enhancing capacity for evidence-informed health policy. In: Bennett S, Green A, editors. Geneva: WHO; 2007.
Stoker G, Evans M. Evidence-based policy making in the social sciences: methods that matter. Bristol: Policy Press; 2016.
Book Google Scholar
Brinkerhoff DW, Crosby B. Managing policy reform: concepts and tools for decision-makers in developing and transitioning countries. Sterling: Kumarian Press; 2002.
Google Scholar
Hardee KFI, Boezwinkle J, Clark B. A framework for analyzing the components of family planning, reproductive health, maternal health, and HIV/AIDS policies. Wilmette: The Policy Circle; 2004.
Mayring P. Qualitative Inhaltsanalyse. In: Mey G, Mruck K, editors. Handbuch qualitative Forschung in der Psychologie. Wiesbaden: Springer; 2010. pp. 601–613.
Mayring P, Fenzl T. Qualitative Inhaltsanalyse. In: Baur N, Blasius J, editors. Handbuch Methoden der empirischen Sozialforschung. Wiesbaden: Springer; 2014. pp. 543–556.
Rose DC, Amano T, González-Varo JP, Mukherjee N, Robertson RJ, Simmons BI, Wauchope HS, Sutherland WJ. Calling for a new agenda for conservation science to create evidence-informed policy. Biol Conserv. 2019;238:108222.
Shiffman J, Smith S. Generation of political priority for global health initiatives: a framework and case study of maternal mortality. Lancet. 2007;370(9595):1370–9.
Labhardt ND, Ringera I, Lejone TI, Klimkait T, Muhairwe J, Amstutz A, Glass TR. Effect of offering same-day ART vs usual health facility referral during home-based HIV testing on linkage to care and viral suppression among adults with HIV in Lesotho: the CASCADE randomized clinical trial. JAMA. 2018;319(11):1103–12.
Kuwawenaruwa A, Wyss K, Wiedenmayer K, Metta E, Tediosi F. The effects of medicines availability and stock-outs on household’s utilization of healthcare services in Dodoma region, Tanzania. Health Policy Plan. 2020;35(3):323–33.
Kuwawenaruwa A TF, Metta E, Obrist B, Wiedenmayer K, Msamba V, Wyss K. Acceptability of a prime vendor system in public healthcare facilities in Tanzania. Int J Health Policy Manag. 2020. (in press).
Kuwawenaruwa ATF, Obrist B, Metta E, Chiluda F, Wiedenmayer K, Wyss K. The role of accountability in the performance of Jazia prime vendor system in Tanzania. J Pharm Policy Pract. 2020;2020(13):25.
Farnham A, Cossa H, Dietler D, Engebretsen R, Leuenberger A, Lyatuu I, Nimako B, Zabre HR, Brugger F, Winkler MS. Investigating health impacts of natural resource extraction projects in Burkina Faso, Ghana, Mozambique, and Tanzania: protocol for a mixed methods study. JMIR Res Protoc. 2020;9(4):e17138.
Beran D, Lazo-Porras M, Cardenas MK, Chappuis F, Damasceno A, Jha N, Madede T, Lachat S, Perez Leon S, Aya Pastrana N, Pesantes MA, Singh SB, Sharma S, Somerville C, Suggs LS, Miranda JJ. Moving from formative research to co-creation of interventions: insights from a community health system project in Mozambique, Nepal and Peru. BMJ Gob Health. 2018;3(6):e001183.
Mertens DM. Advancing social change in South Africa through transformative research. S Afr Rev Sociol. 2016;47(1):5–17.
Berger-González M, Stauffacher M, Zinsstag J, Edwards P, Krütli P. Transdisciplinary research on cancer-healing systems between biomedicine and the Maya of Guatemala: a tool for reciprocal reflexivity in a multi-epistemological setting. Qual Health Res. 2016;26(1):77–91.
Theron LC. Using research to influence policy and practice: the case of the pathways-to-resilience study (South Africa). In: Abubakar A, van de Vijver FJR, editors. Handbook of applied developmental science in sub-Saharan Africa. New York: Springer; 2017. pp. 373–87.
Baum F, MacDougall C, Smith D. Participatory action research. J Epidemiol Community Health. 2006;60(10):854–7.
WHO. Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy. Geneva: World Health Organization; 2017.
Lavis JN, Oxman AD, Lewin S, Fretheim A. SUPPORT Tools for evidence-informed health policymaking (STP) 3: setting priorities for supporting evidence-informed policymaking. Health Res Policy Syst. 2009;7(S1):I3.
Bennett S, Corluka A, Doherty J, Tangcharoensathien V, Patcharanarumol W, Jesani A, Kyabaggu J, Namaganda G, Hussain AMZ, de-Graft Aikins A. Influencing policy change: the experience of health think tanks in low- and middle-income countries. Health Policy Plan. 2011;27(3):194–203.
Kok MO, Gyapong JO, Wolffers I, Ofori-Adjei D, Ruitenberg EJ. Towards fair and effective North–South collaboration: realising a programme for demand-driven and locally led research. Health Res Policy Syst. 2017;15(1):96.
Wolffers I, Adjei S. Research-agenda setting in developing countries. Lancet. 1999;353(9171):2248–9.
Article CAS Google Scholar
Dodgson R, Lee K, Drager N. Global health governance: a conceptual review. London: Centre on Global Change and Health, London School of Hygiene & Tropical Medicine/World Health Organization; 2018.
Saltman RB, Ferroussier-Davis O. The concept of stewardship in health policy. Bull World Health Organ. 2000;78(6):732–9.
CAS PubMed PubMed Central Google Scholar
Miller FA, Patton SJ, Dobrow M, Marshall DA, Berta W. Public involvement and health research system governance: a qualitative study. Health Res Policy Syst. 2018;16(1):87.
Lloyd J. Should academics be expected to change policy? Six reasons why it is unrealistic for research to drive policy change. https://blogs.lse.ac.uk/impactofsocialsciences/2016/05/25/should-academics-be-expected-to-change-policy-six-reasons-why-it-is-unrealistic/ . Accessed 28 May 2020.
Petes LE, Meyer MD. An ecologist’s guide to careers in science policy advising. Front Ecol Environ. 2018;16(1):53–4.
Oliver KCP. The dos and don’ts of influencing policy: a systematic review of advice to academics. Palgrave Commun. 2019;5(1):21.
Hutchings JA, Stenseth NC. Communication of science advice to government. Trends Ecol Evol. 2016;31(1):7–11.
Maynard A. Is public engagement really career limiting?. https://www.timeshighereducation.com/blog/public-engagement-really-career-limiting . Accessed 27 May 2020.
Haynes AS, Derrick GE, Chapman S, Redman S, Hall WD, Gillespie J, Sturk H. From “our world” to the “real world”: exploring the views and behaviour of policy-influential Australian public health researchers. Soc Sci Med. 2011;72(7):1047–55.
Crouzat E, Arpin I, Brunet L, Colloff MJ, Turkelboom F, Lavorel S. Researchers must be aware of their roles at the interface of ecosystem services science and policy. Ambio. 2018;47(1):97–105.
White H. The Evidence Peter Principle: the misuse and abuse of evidence Reflections on the evidence architecture. https://www.campbellcollaboration.org/blog/the-evidence-peter-principle-the-misuse-and-abuse-of-evidence.html?utm_source=Campbell+Collaboration+newsletters&utm_campaign=4dfa01ec7d-Newsletter+September+2019&utm_medium=email&utm_term=0_ab55bacb0c-4dfa01ec7d-199138457 . Accessed 29 Jan 2020.
Caird J, Sutcliffe K, Kwan I, Dickson K, Thomas J. Mediating policy-relevant evidence at speed: are systematic reviews of systematic reviews a useful approach? Evid Policy J Res Debate Pract. 2015;11(1):81–97.
Evans MC, Cvitanovic C. An introduction to achieving policy impact for early career researchers. Palgrave Commun. 2018;4(1):88.
Echt L. Context matters:” a framework to help connect knowledge with policy in government institutions. LSE Impact Blog. https://blogs.lse.ac.uk/impactofsocialsciences/2017/12/19/context-matters-a-framework-to-help-connect-knowledge-with-policy-in-government-institutions/ . Accessed 13 July 2020.
Lucey JM, Palmer G, Yeong KL, Edwards DP, Senior MJM, Scriven SA, Reynolds G, Hill JK. Reframing the evidence base for policy-relevance to increase impact: a case study on forest fragmentation in the oil palm sector. J Appl Ecol. 2017;54(3):731–6.
Green D: How academics and NGOs can work together to influence policy: insights from the InterAction report. LSE Impact blog https://blogs.lse.ac.uk/impactofsocialsciences/2016/09/23/how-academics-and-ngos-can-work-together-to-influence-policy-insights-from-the-interaction-report/ . Accessed 13 July 2020.
Boaz A, Hanney S, Borst R, O’Shea A, Kok M. How to engage stakeholders in research: design principles to support improvement. Health Res Policy Syst. 2018;16(1):60.
Tilley HSL, Rea J, Ball L, Young J. 10 things to know about how to influence policy with research. London: Overseas Development Institute; 2017.
Download references
Acknowledgements
The authors would like to acknowledge the contribution of Dr Claudia Rutte from the r4d programme/SNSF for her inputs to the history and background of the r4d programme.
The r4d synthesis initiative is implemented by the Swiss Tropical and Public Health Institute, which funded the costs of publishing this paper.
Author information
Authors and affiliations.
Swiss Tropical and Public Health Institute, Basel, Switzerland
Séverine Erismann, Andrea Leuenberger, Andrea Farnham, Monica Berger Gonzalez de White, Niklaus Daniel Labhardt, Fabrizio Tediosi, August Kuwawenaruwa, Jakob Zinsstag, Kaspar Wyss & Helen Prytherch
University of Basel, Basel, Switzerland
CRONICAS Centre of Excellence in Chronic Diseases, Universidad Peruana Cayetano Heredia, Lima, Peru
Maria Amalia Pesantes
Division of Tropical and Humanitarian Medicine, University of Geneva and Geneva University Hospitals, Geneva, Switzerland
David Beran
Centro de Estudios en Salud, Universidad del Valle de Guatemala, Guatemala, Guatemala
Monica Berger Gonzalez de White
Department of Infectious Diseases and Hospital Epidemiology, University Hospital Basel, Basel, Switzerland
Niklaus Daniel Labhardt
School of Public Health, College of Health Sciences, University of Ghana, Accra, Ghana
Patricia Akweongo
Ifakara Health Institute, Plot 463, Kiko Avenue Mikocheni, Dar es Salaam, Tanzania
August Kuwawenaruwa
Swiss Federal Institute of Technology Zurich, Zurich, Switzerland
Fritz Brugger
Gender Centre, Graduate Institute of International and Development Studies, Geneva, Switzerland
Claire Somerville
You can also search for this author in PubMed Google Scholar
Contributions
All authors contributed to the writing of this manuscript. Each author contributed with synthesizing their project experiences and with the discussion and recommendations. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Séverine Erismann or Helen Prytherch .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Erismann, S., Pesantes, M.A., Beran, D. et al. How to bring research evidence into policy? Synthesizing strategies of five research projects in low-and middle-income countries. Health Res Policy Sys 19 , 29 (2021). https://doi.org/10.1186/s12961-020-00646-1
Download citation
Received : 15 July 2020
Accepted : 15 October 2020
Published : 06 March 2021
DOI : https://doi.org/10.1186/s12961-020-00646-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Evidence-based policy-making
- Research for development
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Open access
- Published: 28 May 2024
Knowledge level and constructs of the theory of planned behaviour (TPB) to the practice of unsafe abortion among postnatal mothers attending Mkonze health center, Dodoma Region, Tanzania
- Immaculata Alphonce Samila 1 &
- Joanes Faustine Mboineki 1
BMC Public Health volume 24 , Article number: 1427 ( 2024 ) Cite this article
Metrics details
Unsafe abortion is now a global agenda because 45% of all global abortions are unsafe, and 97% are occurring in developing countries. In Tanzania, one million reproductive-aged women face unplanned pregnancies per year, and 39% end up with abortion. About 16% of maternal deaths are reported per year in Tanzania, and unsafe abortion takes the second position. There are several efforts to prevent and intervene unsafe abortions, such as equipping healthcare facilities across all levels of healthcare, approval of Misoprostol use, establishment of comprehensive post-abortion care (PAC), revising policy guidelines and standards, provision of emergency contraceptives, and capacity building of healthcare providers. There is little documentation about how the constructs of the theory of planned behaviour, knowledge, and sociodemographics influence the practice of abortion.
To assess the association of knowledge level, sociodemographic characteristics, and constructs of the theory of planned behaviour (TPB) to the practice of unsafe abortion among postnatal mothers at Mkonze Health Center in the Dodoma region.
Methodology
It is an analytical cross-sectional study design conducted in Dodoma-Tanzania and involved 206 postnatal women. A validated questionnaire was used and analysis was performed in the Statistical Package for the Social Sciences (SPSS), through descriptive and inferential statistics.
The practice of unsafe abortion in the current study is 28/206 (13.6%), influenced bytheir lower educational level and being single women. It was found that the majority had adequate knowledge of unsafe abortion 129 (62.6%), positive attitude 130 (63.1%), good subjective norms 113 (54.9%), and positive perceived behavioral control111 (53.9%). Knowledge, attitude, subjective norms, and perceived behavioral control were not significantly associated with the practice of unsafe abortion.
The majority of the respondents had high knowledge, attitudes, subjective norms, and perceived behavior control on unsafe abortion. This is an indicator that the implemented initiatives are effective. Maintaining the ongoing effort and improving strategies are promising to mitigate the burden of unsafe abortion. Future research needs to find out hidden factors associated with attitude and how health beliefs might influence someone’s attitude towards unsafe abortion.
Peer Review reports
Introduction
Abortion is a global issue that has been taking the attention of different cultures, religions, and social, psychological, and country laws [ 1 ]. Abortion has become a major issue across the country’s boundaries whereby some countries’ policies accept it in special scenarios such as life-threatening conditions and emergencies while others such as United States and Canada allow women to abort depending on their reasons such as medical, psychology, rape, financial hardship, incest, and fetal abnormalities [ 2 ]. Out of 210 million pregnancies per year, 46 million pregnancies end in abortion [ 3 ].
Unsafe abortion is now a global agenda because 45% of all global abortions are unsafe, with 97% occurring in developing countries and 3% in developed countries [ 4 ]. Out of 55.7 million abortions that occurred globally between 2010 and 2014, 25.1 million of these were unsafe every year [ 5 ]. It is approximated that there are 20 million unsafe abortions annually and one out of 250 end to death and maternal disabilities [ 6 ]. This is supported by another study reporting that 13% of unsafe abortions end in maternal death each year [ 7 ]. While a huge burden of unsafe abortion is in Sub-Saharan countries, East Africa accounts for 75% of unsafe abortions [ 8 ].
Different reasons contribute to the decision of unsafe abortion among many women and adolescent girls, including unpreparedness for pregnancy, poor access to contraceptives, education level, and sexual education, economic issue, rape, marital status, victim of incest, support from partner and parents, society norms, religion, stigma, health care system and laws of the countries [ 9 ]. All these have contributed to unsafe abortion among women in countries where there is no accessibility of safe abortion due to restrictive laws of abortion [ 10 ]. The rate of unsafe abortion is increasing proportionally especially in restrictive countries due to the influence of demographics, low community awareness, socioeconomic and cultural factors such as financial issues, and peer groups, to continue their education, secure their future aspiration, relationship status, stigma, risk measuring, and availability and accessibility of methods of abortion such as misoprostol [ 11 ]. According to research done in Zambia, 77 women out of 362 had unsafe abortions whereby most of them fall into the group of unmarried, living in high density, having a history of unplanned pregnancy and a history of miscarriage [ 12 ]. Generally, the higher proportions of unsafe abortion are confined to countries with highly restrictive abortion laws [ 13 , 14 ], and countries with difficulty accessing health facilities [ 15 ]. Abortion is the termination or expulsion of the fetus before 20 weeks of gestation [ 16 ]. Abortion can be spontaneous or induced, whereby it is induced abortion when there is termination of unwanted pregnancy by use of external methods (medically or by dilation and curettage) [ 17 ]. On the other side, spontaneous abortion refers to a miscarriage or purely accidental abortion [ 18 ]. When the abortion is carried out using a method recommended by WHO, appropriate to the pregnancy duration, and by someone with the necessary skills, it is considered a safe abortion [ 19 ]. Meanwhile, unsafe abortion refers to a procedure of pregnancy termination either by persons lacking the necessary skills or in an environment that does not conform to minimal medical standards or both [ 7 ].
In Tanzania, one million reproductive-aged women face unplanned pregnancies per year, and 39% end up with abortion [ 20 ]. About 16% of maternal deaths are reported per year in Tanzania, and unsafe abortion takes the second position [ 21 ]. Several efforts are observed in Tanzania to combat unsafe abortion by improving post-abortion care and provision of emergency contraceptives and safe abortion services to women underwent incest and rape [ 8 ]. In addition, the efforts of tackling unsafe abortion in the country have been through identification and prioritizing unsafe abortion services to zones with the highest rates of abortion, promotion of men’s involvement in family planning, equipping healthcare facilities across all levels of the healthcare system to provide basic post-abortion care, implementation of national Road Map Strategic Plan, approval of Misoprostol, and building on a comprehensive post-abortion care (PAC) training program [ 22 ]. Moreover, there have been new and revised policy guidelines and standards to guide the extension of post-abortion care, capacity building of healthcare providers, developing networks, and platforms to promote understanding of abortion issues [ 23 ]. It is reported that one-third of hospital admissions due to pregnancy complications are due to unsafe abortion while one-quarter lead to maternal death [ 20 ]. Unsafe abortion in Tanzania is due to unintended pregnancy and inaccessibility of contraceptives [ 24 ]. Most studies in Tanzania regarding abortion have focused on incidence, abortion-seeking practices, and service delivery [ 21 ]. There is little documentation about how the constructs of the theory of planned behavior and knowledge influence abortion practice. Therefore, the study aimed to assess the association of knowledge level, sociodemographic characteristics, and constructs of the theory of planned behaviour (TPB) to the practice of unsafe abortion among postnatal mothers at the Mkonze health center in Dodoma region.
The theory of planned behavior (TPB) which is a cognitive theory by Azjen (1985), states that an individual’s decision to engage in a specific behavior can be predicated by their intention to engage in that behaviour [ 25 ]. The theory has four constructs; attitude, subjective norms, perceived behavior control, and intention [ 26 ]. The specific objectives of this study are; ① To determine the knowledge about unsafe abortion among postnatal mothers at Mkonze health center in Dodoma regional ② To assess the attitude towards unsafe abortion among postnatal mothers at Mkonze health center in Dodoma regional ③ To predict subjective norms leading to unsafe abortion among postnatal mothers at Mkonze health center in Dodoma regional ④ To determine perceived behavior control about unsafe abortion among postnatal mother at Mkonze health center in Dodoma regional and ⑤ To evaluate the intention practice towards unsafe abortion among postnatal mother at Mkonze health center in Dodoma regional.
Study design
An analytical cross-sectional study design was employed to use the construsts of the theory of planned behavior and knowledge to assess the intentional practice of unsafe abortion among postnatal mothers at the Mkonze health center in Dodoma region.
The study was carried out in Dodoma City at Mkonze Health Center. Dodoma city was chosen as the study area because it has the highest magnitude of teenage pregnancies (29–39%) compared to other regions of Tanzania [ 27 , 28 ]. Moreover, it is a marked region with relatively low utilization of contraceptives [ 29 ].
Study population
The study population included all postnatal women attending or admitted to Mkonze Health Centre. Participants were excluded if had sickness to impair their responses, could not comprehend the instructions, and were not willing to participate because of self-reported tiredness and busy.
Sample size calculation and sampling technique
Sample size calculation.
The sample size was calculated using the sample size formula:
n = (Z² * P * (1 - P)) / E².
n = Sample size,
Z = Standard normal deviation (for a 95% confidence interval, Z = 1.96),
P = Proportion of target population. The prevalence of 16% for unsafe abortion in Tanzania [ 22 ].
E = Marginal error on the quantity to be estimated (5%).
Therefore, the calculated sample size was 206.
Sampling technique
Probability sampling especially systematic random sampling was used in the study. The postnatal ward at the health center had a daily recorded number of admitted postnatal women in the register. The required number of participants per day was 6 postnatal women, therefore, the nth number was calculated by dividing the number of required postnatal women over the total admitted number of postnatal women of a particular day. The participants were then selected at the interval of the nth number in the register.
Data collection procedure and data collection tools
Data were collected from Mkonze Health Centre from 25th May to 30th June 2023 by a principal investigator with an assistant. The questionnaire which was used in the data collection was developed and validated by a principal investigator. The development started with a literature review to identify items for each variable, followed by content validity where the experts were invited to rate how well was the tool. The tool was pre-tested to 20% of the actual sample size, and internal consistent reliability was determined. Through principal component analysis (PCA), the weak items were modified, making the final tool to have consisted six parts, (1) socio-demographic information, (2) attitude (3) practice (4) knowledge (5) perceived behavior control, and (6) subjective norms among postnatal mothers. Different parts contained varying numbers of items related to the study’s context. For instance, the practice toward unsafe abortion among postnatal mothers was assessed using 8 questions, with response 1 for Yes and 2 for No, the knowledge toward unsafe abortion among postnatal mothers was assessed using 13 questions having responses of 1-Yes and 2-No.Attitude toward unsafe abortion among postnatal mothers was assessed using five items on a 5-Likert scale (1-strongly disagree,2-disagree, 3-neutral, 4-agree, 5-strongly agree). The higher the score (strongly agree) the more positive attitude of the participants. Subjective norms toward unsafe abortion among postnatal mothers were assessed using five items having a response of 1 for Yes and 2 for No. Participants who responded as “Yes” in each item, were considered to get the correct answer. Perceived behavior control toward unsafe abortion among postnatal mothers was assessed using three items 5-Likert scale (1-strongly disagree, 2-disagree, 3-neutral, 4-agree, and 5-strongly agree). The increased number indicates a correct answer, with the maximum (strongly agree).
The questionnaire was translated from English to Swahili’s native language for the convenience of participants.
Data analysis
Regarding measures and data processing, knowledge, subjective norms, and practices of unsafe abortion were measured through binary responses of Yes/No, but attitude and perceived behavioral control were measured through a 5-Likert scale. In each variable, the average of items were computed and the scores were categorized. The cut-off point for each variable was 50%, the above 50%, the higher score, and vice versa.Data were entered and analyzed in the Statistical Package for the Social Sciences. Descriptive statistics summarize the data in the form of frequency, percentage, and mean. A cross-tabulation was carried out to look association between sociodemographic data and factors. A P -value of less than 0.05 was considered statistically significant.
Social demographic characteristics of the respondents
The study recruited 206 postnatal women in the study. The majority of the respondents 56 (27.2%) were aged 25–29 followed by 52 (25.2%) aged 30–34. It was found that 159 (77.2%) of participants lived in urban areas. The participants were married 133 (64.6%), single 33 (16.0%), divorced 28 (13.6%), and windowed 12 (5.8%). Regarding the occupation, participants were entrepreneurs 82 (39.8%), peasant 67 (32.5%), employed 32 (15.5%), and housewife 25 (12.1%). Regarding the education status of the respondents, they had a primary level of education of 92 (44.7%), secondary level education of 54 (26.2%) college or university 23 (11.2%), and never attended school 37 (18%). Refer to Table 1 .
The practice of unsafe abortion among the participants
The majority of the participants about two-thirds seemed not to have had an abortion in the course of their lives 161 (78.2%) and those who had abortions were about one-third 45 (21.8%) of the total participants. Of those who had abortions, 17 (38%) had safe abortions and 28 (62.2%) had an unsafe abortion. Therefore, the practice of unsafe abortion in the current study is 28/206 (13.6%). The highly useful method for unsafe was medication 89 (43.2%) and home remedies 84 (40.8%). Three-quarters did not practice unsafe abortion in the past two years 177 (85.9%) and those who practiced it were 29 (14.1%). Reasons for unsafe abortion are highly due to the advice from friends and parents 129 (62.6%), rape 97 (47.1%) pregnancies rejected by their partners 89 (43.1%), and those in need to continue with studies 88 (42.7%). From those who practiced unsafe abortion, the high frequency of having an unsafe abortion was once in a life lifetime 26 (12.6%). Refer to Table 2 . A total score was computed whereas a score above 4 was regarded as good practice toward unsafe abortion and a score below 4 was regarded as poor practice toward unsafe abortion. By summing up the scores of practices, it was found that the majority of participants had practiced unsafe abortion 147 (71.4%) and 59 (28.6%) had practiced safe abortion.
Knowledge of unsafe abortion among participants
Most of the participants had heard of safe 150 (72.8%), and unsafe abortion 150 (72.8%). Participants agreed that unsafe abortion is a problem in our current society 116 (56.3%). Regarding the source of information on unsafe abortion, most of the participants got information through friends 132 (64.1%), social media 116 (56.3%), health professionals 112 (54.4%), and relatives/family 114 (55.3%). It was found that 158 (76.6%) of participants had never experienced unwanted pregnancy in their lives and further responded that in case they become pregnant unwillingly they would continue and give birth 176 (85.4%). Most women knew the gestation age when abortion is unsafe to be 3 months of pregnancy 126 (61.2%). On the signs and symptoms of unsafe abortion, participants agree that the following are signs and symptoms of unsafe abortion; abdominal pain 148 (71.8%), vaginal infection 152 (73.8%), vaginal bleeding 165 (80.1%), shock 149 (72.3%), and heavy bleeding 151 (73.3%). Participants mentioned that unsafe abortion has complications 157 (66.5%) like infertility 142 (68.9%) and future pregnancy problem 133 (64.6%). The majority knew that abortion is illegal in Tanzania 151 (73.3%) and agreed with the presence of home remedies used in abortion 133 (64.6%) but reported that the use of home remedies for abortion is not safe 154 (74.8%). Refer to Table 3 . A total score was computed whereas a score above 7 was regarded as adequate knowledge toward unsafe abortion and a score below 7 was regarded as inadequate knowledge toward unsafe abortion. The summation of the total score was performed to categorize variables into adequate and inadequate knowledge. Finally, the majority of the participants had adequate knowledge of unsafe abortion 129 (62.6%) and the rest had inadequate knowledge 77 (37.4%). Refer to Fig. 1 .
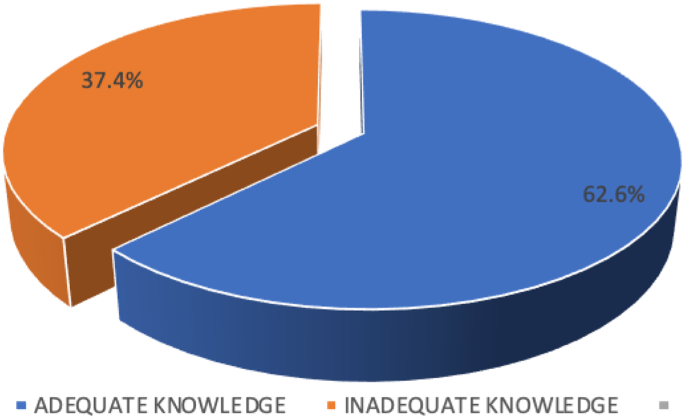
Knowledge level of unsafe abortion among study participants
The association between sociodemographic and knowledge level of participants
Only age was significantly associated with the knowledge of participants, such that respondents of 30–34 had adequate knowledge of safe abortion compared to other age groups (χ 2 = 12.897; P = 0.024). Other sociodemographic characteristics were not significantly associated with knowledge level; place of residence (χ 2 = 2.313; P = 0.128), marital status (χ 2 = 2.248; P = 0.522), occupation (χ 2 = 3.704; P = 0.295), and education level (χ 2 = 0.130; P = 0.988). Refer to Table 4 .
The association knowledge level and practice of unsafe abortion
Among postnatal women who had adequate knowledge, 94 (72.9%) had unsafe abortion. While, those who had inadequate knowledge, 53 (68.8%) had unsafe abortions. Generally, the result has shown that there was no significant association between knowledge level and practice of unsafe abortion (χ 2 = 0.385; P = 0.535).
Attitudes toward unsafe abortion among participants
Participants strongly agreed on the following items; unsafe abortion is an unhealthy procedure for a woman 101 (49%), and unsafe abortion can cause complications to a woman 91 (44.2%). The remaining three items indicate that the majority of participants agreed; that unsafe abortion can cause death to a woman 66 (32%), unsafe abortion can lead to sepsis to a woman 68 (33%), and unsafe abortion is a bad thing 75 (36.4%). Refer to Table 5 . A total score was computed whereas a score above 10 was a positive attitude toward unsafe abortion while a score below 10 was regarded as a negative attitude toward unsafe abortion. The majority of participants, 130 (63.1%) had positive attitudes toward unsafe abortion compared to those with negative attitudes 76 (36.9%). Refer to Fig. 2 .
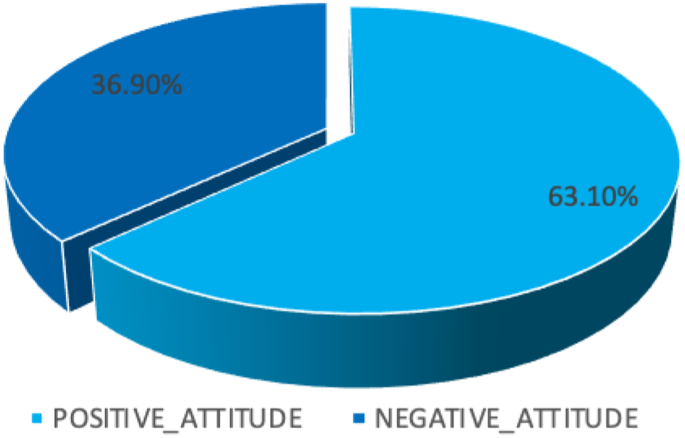
Attitude towards unsafe abortion among study participants
The association between sociodemographics and the attitude of participants
None of the sociodemographic characteristics was significantly associated with attitude towards unsafe abortion among participants; age group (χ 2 = 10.216; P = 0.069), place of residence (χ 2 = 2.571; P = 0.109), marital status (χ 2 = 4.801; P = 0.187), Occupation (χ 2 = 2.453; P = 0.484), and education level (χ 2 = 2.853; P = 0.415). Refer to Table 6 .
The association attitude and practice of unsafe abortion
The results show that the attitude towards unsafe abortion was not significantly associated with the practice χ 2 = 1.066 ; P = 0.302.
Subjective norms towards unsafe abortion
Participants answered correctly on the following items: in your family and society is unsafe abortion viewed as a sin 123 (59.7%), When someone is known she had an abortion she is viewed as a killer 129 (62.6%), and when someone is known she had an abortion she is viewed as bad person 120 (58.3%). However, in two items, participants were incorrectly; when someone is known she had an abortion should be stigmatized 118 (57.3%) and do social norms a source of information about unsafe abortion 113 (54.9%). Refer to Table 7 . A total score was computed whereas a score above 2 was regarded as good subjective norms toward unsafe abortion while a score below 2 was regarded as poor subjective norms. Through summation of scores, 113 (54.9%) had good subjective norms compared to 93 (45%) who had poor subjective norms. Refer to Fig. 3 .
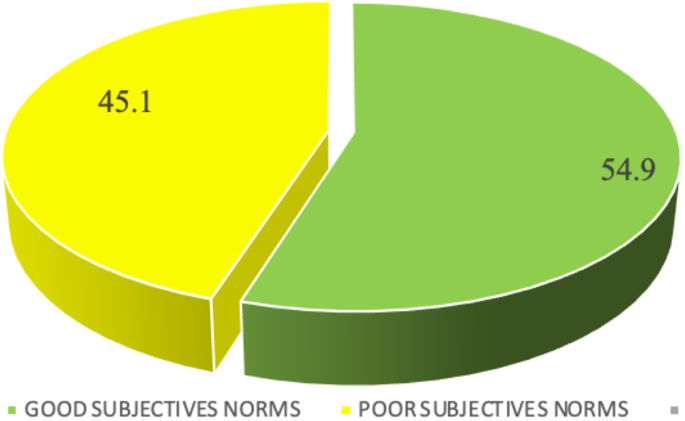
Subjective norms towards unsafe abortion among study participants
The association between sociodemographic and subjective norms of participants
There were no sociodemographic characteristics significantly associated with subjective norms towards unsafe abortion; age group (χ 2 = 3.732; P = 0.589), place of residence (χ 2 = 3.031; P = 0.082), marital status (χ 2 = 3.175; P = 0.365), occupation (χ 2 = 7.749; P = 0.051), and education level (χ 2 = 6.190; P = 0.103). Refer to Table 8 .
The association of subjective norms and the practice of unsafe abortion
Among participants with good subjective norms, 65 (69.9%) had unsafe abortion. Those who had poor subjective norms, 82 (72.6%) had unsafe abortions. Generally, the results indicate that subjective norms towards unsafe abortion were not significantly associated with the practice (χ 2 = 0.178 ; P = 0.673).
- Perceived behavioral control
Participants agreed on items stating that I cannot practice unsafe abortion because it is illegal in Tanzania 70 (34%) while many participants 58 (28.2%) disagreed on the item “I’m confident that I cannot practice unsafe abortion”. Participants were neutral 54 (26.2%) and others agreed 54 (26.2%) when responding to the item “Regardless I get unwanted pregnancy I cannot practice unsafe abortion”. Refer to Table 9 . A total score was computed whereas a score above 6 was regarded as positive perceived behavior control toward unsafe abortion and a score below 6 was regarded as negative perceived behavior control toward unsafe abortion. After the summation of all scores, most of the participants 111 (53.9%) had positive perceived behavioral control while 95 (46.1%) had negative perceived behavioral control.
The association between sociodemographic and perceived behavioral control of participants
It was found that none of the sociodemographic characteristics of participants was significantly associated with perceived behavioral control; age group (χ 2 = 5.849; P = 0.321), place of residence (χ 2 = 2.075; P = 0.15), marital status (χ 2 = 2.595; P = 0.458), occupation (χ 2 = 5.384; P = 0.146), and education level (χ 2 = 3.905; P = 0.272). Refer to Table 10 .
The association of perceived behavioral control and practice of unsafe abortion
The results show that perceived behavioral control towards unsafe abortion was not significantly associated with the practice χ 2 = 0.466; P = 0.495).
The association of sociodemographic characteristics and practice of abortion
The result indicates that only two sociodemographic characteristics (Marital status and educational level) were significantly associated with the safe abortion. In such a way respondents who were divorced had high good practice 16 (57.1%) compared to other participants who belonged to other marital statuses (χ 2 = 13.515; P = 0.004) and participants who had secondary educational level had safe abortion 73 (79.3%) than other participants with different educational levels (χ 2 = 10.146; P = 0.017). Other sociodemographic characteristics were significantly association with safe abortion; age (χ 2 = 8.751 P = 0.119), place of residence (χ 2 = 0.029; P = 0.866), and occupation (χ 2 = 4.663; P = 0.198). Refer to Table 11 .
Interaction of knowledge, attitude, and perceived behavioral control
Knowledge level of unsafe abortion was not significantly associated with attitude (χ2 = 3.657; P = 0.056). Refer to Supplementary Table ( 1 ) In the same way, there was no significant association between knowledge level and perceived behavioral control (χ2 = 3.537; P = 0.06). Refer to Supplementary Table ( 2 ) Meanwhile, there was a significant association between attitude and perceived behavioral control in such a way that 61 (55%) participants who had a positive attitude towards unsafe abortion had positive perceived behavioral control (χ2 = 3.657; P = 0.056). Refer to supplement Table 3.
Knowledge of unsafe abortion among the participants
The current study found that most of the participants 129 (62.6%) had adequate knowledge of unsafe abortion. This indicates the effectiveness of the ongoing national approaches for promoting public understanding of unsafe abortion. Further, it is because the majority were aged 30–34 and probably had been exposed to previous health education from antenatal care visits. The adequate knowledge of unsafe abortion (91%) is also reported in the previous study [ 30 ].
Attitude on unsafe abortion among participants
In this study, two-thirds of the participants 130 (63.1%) had positive attitudes. health beliefs (perceived susceptibility, perceived severity, perceived benefits) might be a reason for a positive attitude. For instance, when a woman feels susceptible to sepsis after an unsafe abortion might help her to avoid practicing unsafe abortion. Same way, the woman will avoid unsafe abortion if believes that she may end up with complications and unfertile. The previous study supports that health beliefs influence attitude [ 31 ]. Moreover, another study pinpoints that health beliefs and attitudes have a significant association with lifestyle change and risks in primary care [ 32 ].
Subjective norms on unsafe abortion among participants
From the results of our study, most participants had good subjective norms toward unsafe abortion 113 (54.9%) because the participants encounter pressure from a society that considers unsafe abortion sin, the doer of unsafe abortion as a killer, and anyone involved in unsafe abortion needs to be stigmatized. The finding is aligned with previous findings by Connell [ 33 ].
Perceived behavior control among participants
From the results of our study, the majority 111 (53.9%) had positive perceived behavior control, which has been influenced by the positive attitude participants possessed. It is surprising to find out that the current study finding is contrary to the theory of planned behaviour since the theory is silent on whether attitude influences perceived behavioral control.
The practice of unsafe abortion among participants
Most participants 147 (71.4%) were found to practice unsafe abortion due to marital status and educational level. Since most of the participants in this study were single women and abortion in Tanzania is illegal, if a single woman becomes pregnant while still having a plan to develop a career, unsafe abortion is the alternative. Meanwhile, if a single woman becomes pregnant but the pregnancy is rejected by a partner, this triggers the woman to perform an unsafe abortion. Regarding education level, participants with lower educational levels or those who have never attended the school practice unsafe abortion. The school is the place with health clubs, teaching, and guiding students in all health-related matters with unsafe abortion inclusively. The more a woman advances her education level, the more she is exposed to teachings on unsafe abortion. Out of health clubs, the curriculum may contain courses with the content of unsafe abortion. The finding is consistent with the previous study reported that unsafe abortion is higher among less educated women [ 34 ].
Study limitation
The study was carried out in a single region of Tanzania and at a single healthcare facility which may limit the generalization of the current findings. It seems that most of the important factors for unsafe abortion were left out as none of the independent variables in the current study were significantly associated with the practice of unsafe abortion.
Most of the respondents had high knowledge, attitudes, subjective norms, and perceived behavior control on unsafe abortion. This is an indicator that the implemented initiatives are effective. Maintaining the ongoing effort and improving strategies are promising to mitigate the burden of unsafe abortion. Future research needs to find out hidden factors associated with attitude and how health beliefs might influence someone’s attitude towards unsafe abortion. Even though the theory does not support the attitude to influence perceived behavioral control, extensive studies need to be conducted to confirm the association between these two variables.
Data availability
The data set and other supplementary documents are available upon request. Point of contact, Dr. Joanes Faustine Mboineki, Email: [email protected], Mobile number: +255756310634.
Saeed S, Jain S, Emma N, Afzali H, Razaqi N, Yousufi M, et al. Knowledge and attitude towards abortion among women in Afghanistan. Razi Int Med J. 2022;2:52–62.
Article Google Scholar
Sitaula S, Basnet T, Agrawal A, Manandhar T, Das D, Shrestha P. Prevalence and risk factors for maternal mortality at a tertiary care centre in Eastern Nepal – retrospective cross sectional study. BMC Pregnancy Childbirth. 2021;:1–8.
Mukanga B, Daka V, Mulenga D, Knowledge, attitude and practice towards unsafe abortions among tertiary education female students in KITWE., ZAMBIA. 2020; January.
World Health Organization. Abortion: Key facts. World Health Organization. 2021. https://www.who.int/news-room/fact-sheets/detail/abortion . Accessed 26 Aug 2023.
Ganatra B, Gerdts C, Rossier C, Ronald B Jr, Tunçalp J et al. Ö,. Global, regional, and subregional classification of abortions by safety, 2010–14 : estimates from a Bayesian hierarchical model. 2017;390.
Ermeko T, Knowledge. Attitude and practice on unsafe abortion among female students in Batu Terara Preparatory School Goba Town. Southeast Ethiopia. 2018;9:1–6.
Google Scholar
Gebremedhin M, Semahegn A, Usmael T, Tesfaye G. Unsafe abortion and associated factors among reproductive aged women in Sub-saharan Africa: a protocol for a systematic review and meta-analysis. BMC Syst Reviews. 2018. https://doi.org/10.1186/s13643-018-0775-9 .
Namagembe I, Nakimuli A, Byamugisha J, Moffett A, Bchir MB, Aiken A, et al. Preventing death following unsafe abortion: a case series from urban Uganda. AJOG Global Rep. 2022;2:100039.
Cresswell JA, Schroeder R, Dennis M, Owolabi O, Vwalika B, Musheke M et al. Women ’ s knowledge and attitudes surrounding abortion in Zambia: a cross-sectional survey across three provinces. 2016;:1–10.
Loi UR, Lindgren M, Faxelid E, Oguttu M, Klingberg-allvin M. Decision-making preceding induced abortion: a qualitative study of women ’ s experiences in Kisumu. Kenya. 2018;:1–12.
Lokubal P, Corcuera I, Balil M, Frischer R, Kayemba N. Articles Abortion decision-making process trajectories and determinants in low- and middle-income countries: a mixed-methods systematic review and meta-analysis. eClinicalMedicine. 2022;54:101694.
Article PubMed PubMed Central Google Scholar
Chavkin W, Baffoe P, Awoonor-williams K, Bank U. Implementing safe abortion in Ghana: we must tell our story and tell it well. Table 1. 2018;143:25–30.
Faundes A, Comendant R, Dilbaz B, Jaldesa G, Leke R, Mukherjee B et al. Preventing unsafe abortion: Achievements and challenges of a global FIGO initiative. Best Practice and Research: Clinical Obstetrics and Gynaecology. 2020;62 xxxx:101–12.
Singh S. Hospital admissions resulting from unsafe abortion: estimates from 13 developing countries. Lancet. 2006;368:1887–92.
Article PubMed Google Scholar
Cioffi A, Cioffi F, Rinaldi R. Reflections about abortion limitation. Ciencia E Saude Coletiva. 2021;26:3787–90.
MIchelle Mouri H, Hall, Timothy J. Rupp. Threatened abortion: Continuing Education Activity. StatPearls [Internet]; 2022.
Romano C, Bekele A. Assessment of Knowledge, attitude and practice towards the Use of Medication Abortion among female regular undergraduate students in Faculty of Health Science,. 2020;4:127–42.
Zheng D, Li C, Wu T, Tang K. Factors associated with spontaneous abortion: a cross-sectional study of Chinese populations. Reproductive Health. 2017;14:1–9.
Article CAS Google Scholar
World Health Orangization. Abortion: Key facts. World Health Orangization. 2021. https://www.who.int/news-room/fact-sheets/detail/abortion . Accessed 13 Feb 2024.
Center for Reproductive Rights. Open Secret: The Toll of Unsafe Abortion in Tanzania. 2020;:1–4.
Sambaiga R, Haukanes H, Moland KM, Blystad A. Health, life and rights : a discourse analysis of a hybrid abortion regime in Tanzania. Int J Equity Health. 2019;18.
Keogh SC, Kimaro G, Muganyizi P, Philbin J, Kahwa A, Ngadaya E, et al. Incidence of Induced Abortion and Post-abortion Care in Tanzania. PLoS ONE. 2015;10:e0133933.
Mutashobya G, Shingale M, Garfinkel D, Agarwal A. Transforming Postabortion and Comprehensive Abortion Care in Zanzibar: Lessons Learned from EngenderHealth’s Expanding Access to Postabortion Care Project in Tanzania. Washington, DC; 2022.
Guttmacher. Unsafe Abortion Is Common In Tanzania and Is A Major Cause of Maternal Death. Guttmacher. 2016. https://www.guttmacher.org/news-release/2016/unsafe-abortion-common-tanzania-and-major-cause-maternal-death . Accessed 26 Aug 2023.
Elisabeth Brookes. The theory of Planned Behavior: behavioral intention. Simply Psychol. 2023;:438–59.
Bosnjak M, Ajzen I, Schmidt P. The theory of planned behavior: selected recent advances and applications. Europe’s J Psychol. 2020;16:352–6.
Moshi FV, Tilisho O. The magnitude of teenage pregnancy and its associated factors among teenagers in Dodoma Tanzania: a community – based analytical cross – sectional study. Reproductive Health. 2023;20:1–13.
Munuo U, Moshi FV. Assessing motivators for utilizing family planning services among youth students in higher learning institutions in Dodoma, Tanzania: protocol for analytical cross sectional study. PLoS ONE. 2023;18(3 March):1–10.
Kara WSK, Benedicto M, Mao J. Knowledge, attitude, and practice of Contraception methods among female undergraduates in Dodoma, Tanzania. Cureus. 2019;11.
Bahadur R, Id K, Poudel S, Raj P, Id G. Factors associated with unsafe abortion practices in Nepal: pooled analysis of the 2011 and 2016 Nepal demographic and health surveys. PLoS ONE. 2019;14:e0223385.
Kim HY, Shin SH, Lee EH. Effects of Health Belief, Knowledge, and attitude toward COVID-19 on Prevention Behavior in Health College Students. Int J Environ Res Public Health. 2022;19.
Mäntyselkä P, Kautiainen H, Miettola J. Beliefs and attitudes towards lifestyle change and risks in primary care - A community-based study. BMC Public Health. 2019;19:1–9.
Connell KAO, Kebede AT, Menna BM, Woldetensay MT, Fischer SE, Samandari G, et al. Signs of a turning tide in social norms and attitudes toward abortion in Ethiopia: findings from a qualitative study in four regions. Reproductive Health. 2022;19:1–13.
Arambepola C, Rajapaksa LC, Attygalle D, Moonasinghe L. Relationship of family formation characteristics with unsafe abortion: is it confounded by women’s socio-economic status? - a case-control study from Sri Lanka. Reproductive Health. 2016;13:1–9.
Download references
Acknowledgements
We acknowledge individual and organizational support received during the research process. We thank Dr Fabiola Moshi, for guidance, expertise, and continuous encouragement. We appreciate Maria Luambano and Irene Maina for their valuable assistance in enriching the depth of this research. The opinions and suggestions from Dr Stephen Kibusi were constructive and enabled the accomplishment of the study.
Authors received no research fund.
Author information
Authors and affiliations.
Department of Nursing Management and Education, School of Nursing and Public Health, The University of Dodoma, P. O. Box 259, Dodoma, Tanzania
Immaculata Alphonce Samila & Joanes Faustine Mboineki
You can also search for this author in PubMed Google Scholar
Contributions
IAS developed a protocol draft, collected data, performed the data analysis, and prepared the research report. JFM supervised the development of a protocol, determined the significance of the study, prepared the data collection tools, supervised the data analysis, and revised the prepared manuscript.
Corresponding author
Correspondence to Joanes Faustine Mboineki .
Ethics declarations
Ethics approval and consent to participate.
Ethical clearance was obtained from the University of Dodoma research review committee. A written informed consent was obtained from each participant before their involvement. The informed consent of participants under 16 years of age was completed by their guardians on behalf of the participants. Moreover, legal guardians completed the informed consent for individuals with no formal education, who were considered incapable of providing informed consent for their participation. Clear instructions were given to participants, emphasizing voluntary participation and the option to withdraw at any time. Confidentiality was maintained, and the data obtained were stored securely by the researcher. The research was conducted based on the standard.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Samila, I.A., Mboineki, J.F. Knowledge level and constructs of the theory of planned behaviour (TPB) to the practice of unsafe abortion among postnatal mothers attending Mkonze health center, Dodoma Region, Tanzania. BMC Public Health 24 , 1427 (2024). https://doi.org/10.1186/s12889-024-18921-z
Download citation
Received : 05 September 2023
Accepted : 22 May 2024
Published : 28 May 2024
DOI : https://doi.org/10.1186/s12889-024-18921-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Unsafe abortion
- Subjective norms
- Sociodemographic characteristics
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Correctional Health
- Reentry for Formerly Incarcerated
- CDC Recommendations
Public Health Considerations for Correctional Health
- To provide people who are justice system-involved, correctional facility staff, public health professionals, community organizations, and anyone else with an interest in correctional health with resources.
- Review CDC resources, guidelines, and data on correctional health and justice-involved populations

Correctional health is community health

Correctional health encompasses all aspects of health and well-being for adults and juveniles who are justice system*-involved. This starts at the point of arrest, continues at detention or incarceration, and carries through after they return to their community (called "reentry"). Correctional health also includes the health of families and communities of persons who are justice system-involved, as well as the health administrators and staff who work in facilities.
Justice System-Involved
Persons who are justice system-involved are more likely to experience risk factors for HIV, viral hepatitis, sexually transmitted infections (STIs), tuberculosis (TB), latent TB infection (LTBI), and traumatic brain injuries (TBI) and concussions . The prevalence of these infections, diseases, and injuries is higher than in the general population. Additionally, a high proportion of people with justice system involvement have a history of unstable housing and mental health and substance use disorders, which increases vulnerability and risk for HIV, viral hepatitis, STIs, tuberculosis/latent tuberculosis infection, and injuries like TBI. This puts many in need of linkage to substance use and mental health treatment, employment, and permanent housing upon release. Justice-involvement also leads to family and community instability and adverse childhood events , with 1 in 28 children having a caregiver who is incarcerated.
Taken together, these multiple health conditions and social determinates of health contribute to the health disparities found in this population and their communities.
CDC has worked to provide people who are justice system-involved, correctional facility staff, public health professionals, community organizations, and anyone else with an interest in correctional health with data, testing and treatment guidelines, educational materials, and other correctional health resources.
How CDC supports correctional health
Community support.
- Funds partners working with health departments to improve health in the communites of justice-involved persons, particularly related to priority pathogens such as HIV, hepatitis, STIs, and TB.
- Develops programs and guidance that address community health disparities and social determinants of health (SDOH).
Intake / entry
- Develops intake screening and treatment guidance for use by clinicians/administrators of correctional health services and health departments.
During incarceration
- Works with state, tribal, local, and territorial health departments to investigate disease outbreaks.
- Develops and provides useful health education materials for staff and justice-involved persons.
- Supports projects that improve the continuity of care for people returning to their communities.
- Offers policy and planning guidance that support efforts to improve the continuity of care within communities.
Surveillance
- Identifies/monitors cases and potential exposures to HIV, viral hepatitis, STIs, TB, and other pathogens among persons who are justice-involved or work in correctional facilities.

According to the U.S. Bureau of Justice Statistics , over 5 million people are estimated to be under the supervision of U.S. adult correctional systems (in prison or jail, or on probation or parole). Many persons who are justice-involved experience multiple risk factors for HIV, viral hepatitis, sexually transmitted infections (STIs), tuberculosis (TB) and latent TB infection (LTBI), and traumatic brain injuries (TBI) and concussions . The prevalence of these infections, diseases, and injuries among people who are incarcerated is higher than in the general population.
- In 2021, about 1.1% of persons incarcerated in state and federal prisons were known to be persons with HIV; this rate was three times higher than the prevalence in the general U.S. population.
- In 2021, 16 U.S. states conducted mandatory HIV testing of all persons under state law enforcement custody, and 23 states and the U.S. Federal Bureau of Prisons offered opt-out HIV testing, accounting for 84% of all persons admitted and sentenced to more than 1 year in the custody of state and federal correctional authorities.
- In a 2013 survey of women across 20 metropolitan areas with high HIV prevalence, women who were recently incarcerated were significantly more likely to have factors that increase their risk for HIV infection than those who were never incarcerated, including receiving money or drugs in exchange for sex with a partner, multiple casual partners, multiple casual condomless partners, and sexually transmitted infection (STI) diagnosis.
More information on HIV Surveillance in the United States .
Viral hepatitis
- In 2009, a systematic review of 23 studies from incarcerated populations in the U.S. reported a wide chronic hepatitis B virus (HBV) prevalence range of 0.9%–11.4%.
- HBV prevalence has been estimated to be 3 to 38 times higher in correctional settings than in the general population in 2009.
- From 2013–2016, people who were incarcerated were estimated to have a rate of current hepatitis C virus (HCV) infection 10 times higher (10.7% vs 1%) than persons in the general population.
- Approximately 30% of all persons infected with HCV in the United States spend at least part of the year in correctional facilities.
More information on viral hepatitis surveillance in the United States.
- Males and females 35 years of age and younger in juvenile and adult detention facilities have been reported to have higher rates of chlamydia and gonorrhea than nonincarcerated persons in the community.
- Jail-based chlamydia screen-and-treat programs can potentially decrease chlamydia prevalence in communities with higher incarceration rates —as much as 13% in large communities and 54% in small communities.
More information on STIs among persons detained or incarcerated .
Tuberculosis (TB)
- In 2021, 2.4% of persons 15 years of age or older diagnosed with tuberculosis were current residents of correctional facilities at the time of diagnosis.
- From 2003–2013, annual median tuberculosis incidence was about 6 times higher for persons in jails and federal prisons compared with the general population.
- An analysis during 2011–2019 demonstrated that large tuberculosis outbreaks still occur in state prisons and account for a large proportion of total tuberculosis cases in some states.
For more information on Tuberculosis cases by residence in and type of correctional facility .
Traumatic brain injury (TBI)
- Research in the United States and from other countries suggests almost half (46%) of people in correctional or detention facilities such as prisons and jails have a history of TBI, but the exact number is not known.
- Studies show an association between people in correctional or detention facilities with a history of TBI and mental health problems, such as severe depression and anxiety, substance use disorders, difficulty controlling anger, and suicidal thoughts and/or attempts.
- People in correctional or detention facilities with TBI-related problems may not be screened for a TBI or may face challenges with getting TBI-related care. These challenges may continue after a person is released from the facility.
Find more information about TBI and other brain injuries .
CDC guidance and resources

HIV, viral hepatitis, STIs, and tuberculosis
- At-A-Glance: CDC Recommendations for Correctional and Detention Settings for Testing, Vaccination, and Treatment for HIV, Viral Hepatitis, TB, and STIs – Summary of current CDC guidelines and recommendations for testing, vaccination, and treatment of HIV, viral hepatitis, TB, and STIs for persons who are detained or incarcerated. Links to full guidance documents are included.
- Guidance on Management of COVID-19 in Homeless Service Sites and in Correctional and Detention Facilities – Guidance that can be used to inform COVID-19 prevention actions in homeless service sites and correctional and detention facilities.
Worker safety
- Safe and Proper Use of Disinfectants to Reduce Viral Surface Contamination in Correctional Facilities – Steps to reduce viral surface contamination through safe and proper use of disinfectants for persons who work in correctional facilities, including a companion printable poster to be displayed throughout the facility. The poster is available in English and Spanish.
- Reducing Work-Related Needlestick and Other Sharps Injuries Among Law Enforcement Officers (PDF) – Provides recommendations for reducing needlesticks and other sharps injuries to law enforcement officers, which specifically includes guidance for correctional employees.
Overdose prevention
- Partnerships Between Public Health and Public Safety – Overview of CDC partnerships built through multiple public health and public safety collaborations to strengthen and improve efforts to reduce drug overdoses.
- Public Health and Public Safety Resources – Resources for jails and prisons that support public health and public safety related to overdose prevention and medication-assisted treatment (MAT) for opioid use disorder.
- What Health Departments Need to Know When Responding to Mumps Outbreaks in Correctional and Detention Facilities – Job-aid with guidance for health departments and facilities during mumps outbreaks.
- LM Maruschak. HIV in Prisons, 2021—Statistical Tables. U.S. Department of Justice, Bureau of Justice Statistics, Washington, DC (Published May 2022). https://bjs.ojp.gov/document/hivp21st.pdf , Accessed 16 Mar 2023
- Wise A, Finlayson T, Nerlander L, Sionean C, Paz-Bailey G; NHBS Study Group. Incarceration, Sexual Risk-related Behaviors, and HIV Infection Among Women at Increased Risk of HIV Infection, 20 United States cities. J Acquir Immune Defic Syndr. 2017 Jul 1;75 Suppl 3:S261-S267. Incarceration, Sexual Risk-Related Behaviors, and HIV Infection Among Women at Increased Risk of HIV Infection, 20 United States Cities – PubMed (nih.gov)
- Harzke AJ, Goodman KJ, Mullen PD, Baillargeon J. Heterogeneity in Hepatitis B Virus (HBV) Seroprevalence Estimates from U.S. Adult Incarcerated Populations. Ann Epidemiol. 2009;19(9):647-650. doi:10.1016/j.annepidem.2009.04.001. Heterogeneity in Hepatitis B Virus (HBV) Seroprevalence Estimates from U.S. Adult Incarcerated Populations | Elsevier Enhanced Reader
- Roberts H, Kruszon-Moran D, Ly KN, Hughes E, Iqbal K, Jiles RB, Holmberg SD. Prevalence of Chronic Hepatitis B Virus (HBV) Infection in U.S. Households: National Health and Nutrition Examination Survey (NHANES), 1988-2012. Hepatology. 2016 Feb;63(2):388-97. doi: 10.1002/hep.28109. Epub 2015 Oct 27. PMID: 26251317. Prevalence of chronic hepatitis B virus (HBV) infection in U... : Hepatology (lww.com)
- Hofmeister MG, Rosenthal EM, Barker LK, et al. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016. Hepatology. 2019;69(3):1020-1031. doi:10.1002/hep.30297. Estimating Prevalence of Hepatitis C Virus Infection in the United States, 2013-2016 – PubMed (nih.gov)
- CDC 2021 Sexually Transmitted Infections (STI) Treatment Guidelines: Persons in Correctional Facilities
- Bernstein KT, Chow JM, Pathela P, Gift TL. Bacterial Sexually Transmitted Disease Screening Outside the Clinic–Implications for the Modern Sexually Transmitted Disease Program. Sex Transm Dis. 2016;43(2 Suppl 1):S42-S52. Bacterial Sexually Transmitted Disease Screening Outside the Clinic–Implications for the Modern Sexually Transmitted Disease Program – PubMed (nih.gov)
- Owusu-Edusei K Jr, Gift TL, Chesson HW, Kent CK. Investigating the potential public health benefit of jail-based screening and treatment programs for chlamydia. Am J Epidemiol. 2013 Mar 1;177(5):463-73. doi: 10.1093/aje/kws240. Epub 2013 Feb 12. PMID: 23403986. Investigating the potential public health benefit of jail-based screening and treatment programs for chlamydia – PubMed (nih.gov)
- CDC Tuberculosis Data & Statistics: Reported Tuberculosis in the United States, 2021 in Residents of Correctional Facilities https://www.cdc.gov/tb/statistics/reports/2020/risk_factors.htm Lambert LA, Armstrong LR, Lobato MN, Ho C, France AM, Haddad MB. Tuberculosis in Jails and Prisons: United States, 2002-2013. Am J Public Health. 2016 Dec;106(12):2231-2237. doi: 10.2105/AJPH.2016.303423. Epub 2016 Sep 15. PMID: 27631758; PMCID: PMC5104991. Tuberculosis in Jails and Prisons: United States, 2002-2013 – PubMed (nih.gov)
- Stewart RJ, Raz KM, Burns SP, Kammerer JS, Haddad MB, Silk BJ, Wortham JM. Tuberculosis Outbreaks in State Prisons, United States, 2011 – 2019. Am J Public Health. 2022, 112(8), 1170-1179. PMID: 35830666; PMCID: PMC934802. Doi: 10.2105/AJPH.2022.306864
- Hunter S, Kois L, Peck A, Elbogen E, LaDuke C. (2023). The prevalence of traumatic brain injury (TBI) among people impacted by the criminal legal system: An updated meta-analysis and subgroup analyses. Law and Human Behavior , 47(5), 539–565.
- Moore E, Indig D, Haysom L. Traumatic brain injury, mental health, substance use, and offending among incarcerated young people. Journal of Head Trauma Rehabilitation. 2014;29(3):239-247.
- Ray B, Sapp D, Kincaid A. Traumatic brain injury among Indiana state prisoners. Journal of Forensic Sciences. 2014;59(5):1248-1253.
- Walker R, Hiller M, Staton M, Leukefeld C. Head injury among drug abusers: An indicator of co-occurring problems. Journal of Psychoactive Drugs. 2003;35(3):343-353.
- Slaughter B, Fann J, Ehde D. Traumatic brain injury in a county jail population: Prevalence, neuropsychological functioning and psychiatric disorders. Brain Injury. 2003;17(9):731-741.
- Blaauw E, Arensman E, Kraaij V, Winkel F, Bout R. Traumatic life events and suicide risk among jail inmates: The influence of types of events, time period and significant others. Journal of Traumatic Stress. 2002;15(1):9-16.
- Allely C. Prevalence and assessment of traumatic brain injury in prison inmates: A systematic PRISMA review. Brain Injury. 2016;30(10):1161-1180.
- Williams W, Mewse A, Tonks J, Mills S, Burgess C, Cordan G. Traumatic brain injury in a prison population: Prevalence and risk for re-offending. Brain Injury. 2010;24(10):1184-1188.
- “Criminal legal system” may also be used as an alternative to “justice system” to reflect historic and current challenges to achieving justice in the U.S. criminal legal system.
CDC provides health resources to protect the health of people in correctional settings who are at higher risk for HIV, Viral Hepatitis, STIs, and Tuberculosis.

IMAGES
VIDEO
COMMENTS
Real Evidence Influencing the Policy Makers. Use of research evidence in the management of health system and policy making is a big challenge. Knowledge translation and exchange among relevant stakeholders is essential to make use of the benefits of research advances in strengthening health systems and improving people's health .
In the last century, public health research, policy and practice have contributed to a 30-year life expectancy increase. ... Policies influence the public health system and impact our lives due to their long-term effects (Johnson, 2009). Gradually now, health programmes are being implemented with a focus on policy change of priority.
Introduction. In recent decades, Health Policy and Systems Research (HPSR) has emerged as a field that generates effective policies and policy content for achieving health and health system goals (see Shroff et al., 2017).Health systems are influenced by local and international political, social and economic factors, and health policy must be based on evidence specific to the national context ...
For decades, the question of how evidence influences policy and practice has captured our attention, cutting across disciplines and policy/practice domains. ... Health Research Policy and Systems ...
Health policy and systems research (HPSR) has changed considerably over the last 20 years, but its main purpose remains to inform and influence health policies and systems. Whereas goals that underpin health systems have endured - such as a focus on health equity - contexts and priorities change, research methods progress, and health organisations continue to learn and adapt, in part by ...
Nurses acting together with other disciplines can combine our efforts around these issues and influence important policy changes to 1) expand the number of diseases for which Medicare will pay for oral health care, 2) expand the variety of professions that use the title "Dr." in California and if applicable in other states, and 3) prevent ...
draws on policy framing research and provides evidence that the way global health issues are framed—as threats, ethical imperatives, and wise investments—can shape the amount of attention and resources these issues receive from global health organisations and national governments. ... because political processes and decisions influence and ...
Clinical research is a type of biomedical research conducted to aid and support the development of knowledge wherein there is involvement of patient. One of the key duties of healthcare professionals is to involve in research and change existing practice, when there is robust evidence in favour of new strategies that can have better patient ...
Clinical research is a type of biomedical research conducted to aid and support the development of knowledge wherein there is involvement of patient. One of the key duties of healthcare professionals is to involve in research and change existing practice, when there is robust evidence in favour of new strategies that can have better patient care. Knowledge derived from research and experience ...
A government economist by background, he was previously Chief Economist and then Director of the Strategy Unit in the Cabinet Office. He is a member of the advisory group for our Social and Economic Value of Health research programme. We spoke to Stephen about the programme, and how research findings can influence policy.
The use of health policy and systems research (HPSR) to inform health policy-making is an international challenge. Incorporating HPSR into decision-making primarily involves two groups, namely researchers (knowledge producers) and policy-makers (knowledge users). The purpose of this study was to compare the perceptions of Israeli health systems and policy researchers and health services policy ...
Furthermore, future research should focus on the influence of media on health policy-making in diverse settings. Examining the role of media in these LMICs is important to design context-specific strategies and understand how the impact of media campaigns and interventions can differ across various health systems and socioeconomic realities.
Researchers can influence policymakers and practitioners through knowledge mobilisation. Knowledge mobilisation is the process (es) that can lead to the outcome of impact by catalysing change through: Engagement & networking. Educational events. Co-production. Embedding procedures & practices. Commercialisation. Science communication.
Goal: Use health policy to prevent disease and improve health. Health policy can have a major impact on health and well-being. Healthy People 2030 focuses on keeping people safe and healthy through laws and policies at the local, state, territorial, and federal level. Evidence-based health policies can help prevent disease and promote health.
Background In order to understand and measure the policy impact of research we need a definition of research impact that is suited to the task. This article systematically reviewed both peer-reviewed and grey literature for definitions of research impact to develop a definition of research impact that can be used to investigate how public health research influences policy. Method Keyword ...
Background Person-centred planning refers to a model of care in which programs and services are developed in collaboration with persons receiving care (i.e., persons-supported) and tailored to their unique needs and goals. In recent decades, governments around the world have enacted policies requiring community-care agencies to adopt an individualized or person-centred approach to service ...
The establishment of policy is key to the implementation of actions for health. We review the nature of policy and the definition and directions of health policy. In doing so, we explicitly cast a health political science gaze on setting parameters for researching policy change for health. A brief overview of core theories of the policy process for health promotion is presented, and ...
In a 2023 blog post, we explored how pediatric researchers and clinicians are using patient navigation to support children and families in accessing behavioral health care.This approach builds on patient navigation research for children with special health care needs, which finds improved health and well-being for families and children when navigation services are available.
Increasingly, research funders are asking their grantees to address the uptake of research findings into decision-making processes and policy-making [1, 2].This growing trend is a response to a need for real-world and context-sensitive evidence to respond to and address complex health systems and health service delivery bottlenecks faced by policy-makers, health practitioners, communities and ...
Future research needs to find out hidden factors associated with attitude and how health beliefs might influence someone's attitude towards unsafe abortion. ... levels of healthcare, approval of Misoprostol use, establishment of comprehensive post-abortion care (PAC), revising policy guidelines and standards, provision of emergency ...
Develops and provides useful health education materials for staff and justice-involved persons. Reentry. Supports projects that improve the continuity of care for people returning to their communities. Offers policy and planning guidance that support efforts to improve the continuity of care within communities. Surveillance