
Get science-backed answers as you write with Paperpal's Research feature

How to Write a Conclusion for Research Papers (with Examples)
The conclusion of a research paper is a crucial section that plays a significant role in the overall impact and effectiveness of your research paper. However, this is also the section that typically receives less attention compared to the introduction and the body of the paper. The conclusion serves to provide a concise summary of the key findings, their significance, their implications, and a sense of closure to the study. Discussing how can the findings be applied in real-world scenarios or inform policy, practice, or decision-making is especially valuable to practitioners and policymakers. The research paper conclusion also provides researchers with clear insights and valuable information for their own work, which they can then build on and contribute to the advancement of knowledge in the field.
The research paper conclusion should explain the significance of your findings within the broader context of your field. It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered questions or areas requiring further investigation, your awareness of the broader research landscape can be demonstrated.
Remember to tailor the research paper conclusion to the specific needs and interests of your intended audience, which may include researchers, practitioners, policymakers, or a combination of these.
Table of Contents
What is a conclusion in a research paper, summarizing conclusion, editorial conclusion, externalizing conclusion, importance of a good research paper conclusion, how to write a conclusion for your research paper, research paper conclusion examples.
- How to write a research paper conclusion with Paperpal?
Frequently Asked Questions
A conclusion in a research paper is the final section where you summarize and wrap up your research, presenting the key findings and insights derived from your study. The research paper conclusion is not the place to introduce new information or data that was not discussed in the main body of the paper. When working on how to conclude a research paper, remember to stick to summarizing and interpreting existing content. The research paper conclusion serves the following purposes: 1
- Warn readers of the possible consequences of not attending to the problem.
- Recommend specific course(s) of action.
- Restate key ideas to drive home the ultimate point of your research paper.
- Provide a “take-home” message that you want the readers to remember about your study.

Types of conclusions for research papers
In research papers, the conclusion provides closure to the reader. The type of research paper conclusion you choose depends on the nature of your study, your goals, and your target audience. I provide you with three common types of conclusions:
A summarizing conclusion is the most common type of conclusion in research papers. It involves summarizing the main points, reiterating the research question, and restating the significance of the findings. This common type of research paper conclusion is used across different disciplines.
An editorial conclusion is less common but can be used in research papers that are focused on proposing or advocating for a particular viewpoint or policy. It involves presenting a strong editorial or opinion based on the research findings and offering recommendations or calls to action.
An externalizing conclusion is a type of conclusion that extends the research beyond the scope of the paper by suggesting potential future research directions or discussing the broader implications of the findings. This type of conclusion is often used in more theoretical or exploratory research papers.
Align your conclusion’s tone with the rest of your research paper. Start Writing with Paperpal Now!
The conclusion in a research paper serves several important purposes:
- Offers Implications and Recommendations : Your research paper conclusion is an excellent place to discuss the broader implications of your research and suggest potential areas for further study. It’s also an opportunity to offer practical recommendations based on your findings.
- Provides Closure : A good research paper conclusion provides a sense of closure to your paper. It should leave the reader with a feeling that they have reached the end of a well-structured and thought-provoking research project.
- Leaves a Lasting Impression : Writing a well-crafted research paper conclusion leaves a lasting impression on your readers. It’s your final opportunity to leave them with a new idea, a call to action, or a memorable quote.

Writing a strong conclusion for your research paper is essential to leave a lasting impression on your readers. Here’s a step-by-step process to help you create and know what to put in the conclusion of a research paper: 2
- Research Statement : Begin your research paper conclusion by restating your research statement. This reminds the reader of the main point you’ve been trying to prove throughout your paper. Keep it concise and clear.
- Key Points : Summarize the main arguments and key points you’ve made in your paper. Avoid introducing new information in the research paper conclusion. Instead, provide a concise overview of what you’ve discussed in the body of your paper.
- Address the Research Questions : If your research paper is based on specific research questions or hypotheses, briefly address whether you’ve answered them or achieved your research goals. Discuss the significance of your findings in this context.
- Significance : Highlight the importance of your research and its relevance in the broader context. Explain why your findings matter and how they contribute to the existing knowledge in your field.
- Implications : Explore the practical or theoretical implications of your research. How might your findings impact future research, policy, or real-world applications? Consider the “so what?” question.
- Future Research : Offer suggestions for future research in your area. What questions or aspects remain unanswered or warrant further investigation? This shows that your work opens the door for future exploration.
- Closing Thought : Conclude your research paper conclusion with a thought-provoking or memorable statement. This can leave a lasting impression on your readers and wrap up your paper effectively. Avoid introducing new information or arguments here.
- Proofread and Revise : Carefully proofread your conclusion for grammar, spelling, and clarity. Ensure that your ideas flow smoothly and that your conclusion is coherent and well-structured.
Write your research paper conclusion 2x faster with Paperpal. Try it now!
Remember that a well-crafted research paper conclusion is a reflection of the strength of your research and your ability to communicate its significance effectively. It should leave a lasting impression on your readers and tie together all the threads of your paper. Now you know how to start the conclusion of a research paper and what elements to include to make it impactful, let’s look at a research paper conclusion sample.
| Summarizing Conclusion | Impact of social media on adolescents’ mental health | In conclusion, our study has shown that increased usage of social media is significantly associated with higher levels of anxiety and depression among adolescents. These findings highlight the importance of understanding the complex relationship between social media and mental health to develop effective interventions and support systems for this vulnerable population. |
| Editorial Conclusion | Environmental impact of plastic waste | In light of our research findings, it is clear that we are facing a plastic pollution crisis. To mitigate this issue, we strongly recommend a comprehensive ban on single-use plastics, increased recycling initiatives, and public awareness campaigns to change consumer behavior. The responsibility falls on governments, businesses, and individuals to take immediate actions to protect our planet and future generations. |
| Externalizing Conclusion | Exploring applications of AI in healthcare | While our study has provided insights into the current applications of AI in healthcare, the field is rapidly evolving. Future research should delve deeper into the ethical, legal, and social implications of AI in healthcare, as well as the long-term outcomes of AI-driven diagnostics and treatments. Furthermore, interdisciplinary collaboration between computer scientists, medical professionals, and policymakers is essential to harness the full potential of AI while addressing its challenges. |

How to write a research paper conclusion with Paperpal?
A research paper conclusion is not just a summary of your study, but a synthesis of the key findings that ties the research together and places it in a broader context. A research paper conclusion should be concise, typically around one paragraph in length. However, some complex topics may require a longer conclusion to ensure the reader is left with a clear understanding of the study’s significance. Paperpal, an AI writing assistant trusted by over 800,000 academics globally, can help you write a well-structured conclusion for your research paper.
- Sign Up or Log In: Create a new Paperpal account or login with your details.
- Navigate to Features : Once logged in, head over to the features’ side navigation pane. Click on Templates and you’ll find a suite of generative AI features to help you write better, faster.
- Generate an outline: Under Templates, select ‘Outlines’. Choose ‘Research article’ as your document type.
- Select your section: Since you’re focusing on the conclusion, select this section when prompted.
- Choose your field of study: Identifying your field of study allows Paperpal to provide more targeted suggestions, ensuring the relevance of your conclusion to your specific area of research.
- Provide a brief description of your study: Enter details about your research topic and findings. This information helps Paperpal generate a tailored outline that aligns with your paper’s content.
- Generate the conclusion outline: After entering all necessary details, click on ‘generate’. Paperpal will then create a structured outline for your conclusion, to help you start writing and build upon the outline.
- Write your conclusion: Use the generated outline to build your conclusion. The outline serves as a guide, ensuring you cover all critical aspects of a strong conclusion, from summarizing key findings to highlighting the research’s implications.
- Refine and enhance: Paperpal’s ‘Make Academic’ feature can be particularly useful in the final stages. Select any paragraph of your conclusion and use this feature to elevate the academic tone, ensuring your writing is aligned to the academic journal standards.
By following these steps, Paperpal not only simplifies the process of writing a research paper conclusion but also ensures it is impactful, concise, and aligned with academic standards. Sign up with Paperpal today and write your research paper conclusion 2x faster .
The research paper conclusion is a crucial part of your paper as it provides the final opportunity to leave a strong impression on your readers. In the research paper conclusion, summarize the main points of your research paper by restating your research statement, highlighting the most important findings, addressing the research questions or objectives, explaining the broader context of the study, discussing the significance of your findings, providing recommendations if applicable, and emphasizing the takeaway message. The main purpose of the conclusion is to remind the reader of the main point or argument of your paper and to provide a clear and concise summary of the key findings and their implications. All these elements should feature on your list of what to put in the conclusion of a research paper to create a strong final statement for your work.
A strong conclusion is a critical component of a research paper, as it provides an opportunity to wrap up your arguments, reiterate your main points, and leave a lasting impression on your readers. Here are the key elements of a strong research paper conclusion: 1. Conciseness : A research paper conclusion should be concise and to the point. It should not introduce new information or ideas that were not discussed in the body of the paper. 2. Summarization : The research paper conclusion should be comprehensive enough to give the reader a clear understanding of the research’s main contributions. 3 . Relevance : Ensure that the information included in the research paper conclusion is directly relevant to the research paper’s main topic and objectives; avoid unnecessary details. 4 . Connection to the Introduction : A well-structured research paper conclusion often revisits the key points made in the introduction and shows how the research has addressed the initial questions or objectives. 5. Emphasis : Highlight the significance and implications of your research. Why is your study important? What are the broader implications or applications of your findings? 6 . Call to Action : Include a call to action or a recommendation for future research or action based on your findings.
The length of a research paper conclusion can vary depending on several factors, including the overall length of the paper, the complexity of the research, and the specific journal requirements. While there is no strict rule for the length of a conclusion, but it’s generally advisable to keep it relatively short. A typical research paper conclusion might be around 5-10% of the paper’s total length. For example, if your paper is 10 pages long, the conclusion might be roughly half a page to one page in length.
In general, you do not need to include citations in the research paper conclusion. Citations are typically reserved for the body of the paper to support your arguments and provide evidence for your claims. However, there may be some exceptions to this rule: 1. If you are drawing a direct quote or paraphrasing a specific source in your research paper conclusion, you should include a citation to give proper credit to the original author. 2. If your conclusion refers to or discusses specific research, data, or sources that are crucial to the overall argument, citations can be included to reinforce your conclusion’s validity.
The conclusion of a research paper serves several important purposes: 1. Summarize the Key Points 2. Reinforce the Main Argument 3. Provide Closure 4. Offer Insights or Implications 5. Engage the Reader. 6. Reflect on Limitations
Remember that the primary purpose of the research paper conclusion is to leave a lasting impression on the reader, reinforcing the key points and providing closure to your research. It’s often the last part of the paper that the reader will see, so it should be strong and well-crafted.
- Makar, G., Foltz, C., Lendner, M., & Vaccaro, A. R. (2018). How to write effective discussion and conclusion sections. Clinical spine surgery, 31(8), 345-346.
- Bunton, D. (2005). The structure of PhD conclusion chapters. Journal of English for academic purposes , 4 (3), 207-224.
Paperpal is a comprehensive AI writing toolkit that helps students and researchers achieve 2x the writing in half the time. It leverages 21+ years of STM experience and insights from millions of research articles to provide in-depth academic writing, language editing, and submission readiness support to help you write better, faster.
Get accurate academic translations, rewriting support, grammar checks, vocabulary suggestions, and generative AI assistance that delivers human precision at machine speed. Try for free or upgrade to Paperpal Prime starting at US$19 a month to access premium features, including consistency, plagiarism, and 30+ submission readiness checks to help you succeed.
Experience the future of academic writing – Sign up to Paperpal and start writing for free!
Related Reads:
- 5 Reasons for Rejection After Peer Review
- Ethical Research Practices For Research with Human Subjects
7 Ways to Improve Your Academic Writing Process
- Paraphrasing in Academic Writing: Answering Top Author Queries
Preflight For Editorial Desk: The Perfect Hybrid (AI + Human) Assistance Against Compromised Manuscripts
You may also like, how to write the first draft of a..., mla works cited page: format, template & examples, how to write a high-quality conference paper, academic editing: how to self-edit academic text with..., measuring academic success: definition & strategies for excellence, phd qualifying exam: tips for success , ai in education: it’s time to change the..., is it ethical to use ai-generated abstracts without..., what are journal guidelines on using generative ai..., quillbot review: features, pricing, and free alternatives.
Research Skills
Results, discussion, and conclusion, results/findings.
The Results (or Findings) section follows the Methods and precedes the Discussion section. This is where the authors provide the data collected during their study. That data can sometimes be difficult to understand because it is often quite technical. Do not let this intimidate you; you will discover the significance of the results next.
The Discussion section follows the Results and precedes the Conclusions and Recommendations section. It is here that the authors indicate the significance of their results. They answer the question, “Why did we get the results we did?” This section provides logical explanations for the results from the study. Those explanations are often reached by comparing and contrasting the results to prior studies’ findings, so citations to the studies discussed in the Literature Review generally reappear here. This section also usually discusses the limitations of the study and speculates on what the results say about the problem(s) identified in the research question(s). This section is very important because it is finally moving towards an argument. Since the researchers interpret their results according to theoretical underpinnings in this section, there is more room for difference of opinion. The way the authors interpret their results may be quite different from the way you would interpret them or the way another researcher would interpret them.
Note: Some articles collapse the Discussion and Conclusion sections together under a single heading (usually “Conclusion”). If you don’t see a separate Discussion section, don’t worry. Instead, look in the nearby sections for the types of information described in the paragraph above.
When you first skim an article, it may be useful to go straight to the Conclusion and see if you can figure out what the thesis is since it is usually in this final section. The research gap identified in the introduction indicates what the researchers wanted to look at; what did they claim, ultimately, when they completed their research? What did it show them—and what are they showing us—about the topic? Did they get the results they expected? Why or why not? The thesis is not a sweeping proclamation; rather, it is likely a very reasonable and conditional claim.
Nearly every research article ends by inviting other scholars to continue the work by saying that more research needs to be done on the matter. However, do not mistake this directive for the thesis; it’s a convention. Often, the authors provide specific details about future possible studies that could or should be conducted in order to make more sense of their own study’s conclusions.
- Parts of An Article. Authored by : Kerry Bowers. Provided by : University of Mississippi. Project : WRIT 250 Committee OER Project. License : CC BY-SA: Attribution-ShareAlike

Privacy Policy
When you choose to publish with PLOS, your research makes an impact. Make your work accessible to all, without restrictions, and accelerate scientific discovery with options like preprints and published peer review that make your work more Open.
- PLOS Biology
- PLOS Climate
- PLOS Complex Systems
- PLOS Computational Biology
- PLOS Digital Health
- PLOS Genetics
- PLOS Global Public Health
- PLOS Medicine
- PLOS Mental Health
- PLOS Neglected Tropical Diseases
- PLOS Pathogens
- PLOS Sustainability and Transformation
- PLOS Collections
- How to Write Discussions and Conclusions

The discussion section contains the results and outcomes of a study. An effective discussion informs readers what can be learned from your experiment and provides context for the results.
What makes an effective discussion?
When you’re ready to write your discussion, you’ve already introduced the purpose of your study and provided an in-depth description of the methodology. The discussion informs readers about the larger implications of your study based on the results. Highlighting these implications while not overstating the findings can be challenging, especially when you’re submitting to a journal that selects articles based on novelty or potential impact. Regardless of what journal you are submitting to, the discussion section always serves the same purpose: concluding what your study results actually mean.
A successful discussion section puts your findings in context. It should include:
- the results of your research,
- a discussion of related research, and
- a comparison between your results and initial hypothesis.
Tip: Not all journals share the same naming conventions.
You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript.
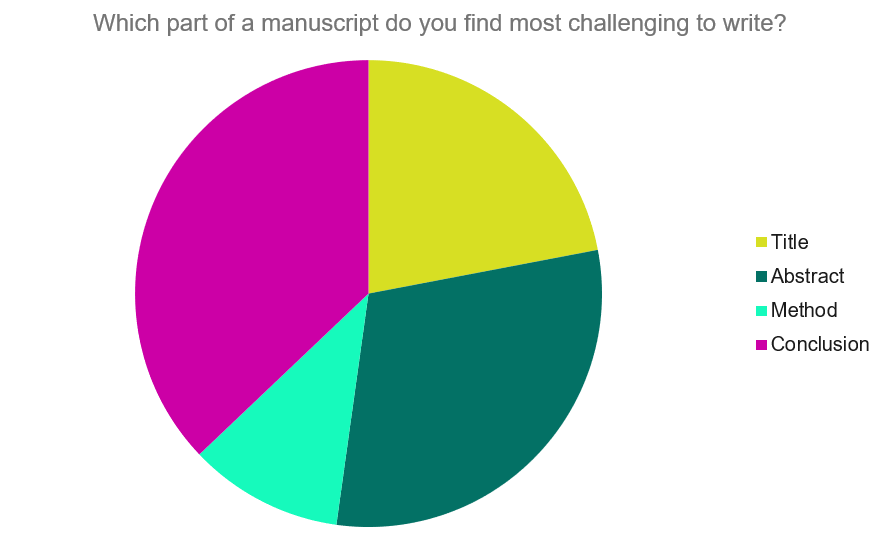
Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide provides questions to ask yourself, a basic structure to model your discussion off of and examples from published manuscripts.
Questions to ask yourself:
- Was my hypothesis correct?
- If my hypothesis is partially correct or entirely different, what can be learned from the results?
- How do the conclusions reshape or add onto the existing knowledge in the field? What does previous research say about the topic?
- Why are the results important or relevant to your audience? Do they add further evidence to a scientific consensus or disprove prior studies?
- How can future research build on these observations? What are the key experiments that must be done?
- What is the “take-home” message you want your reader to leave with?
How to structure a discussion
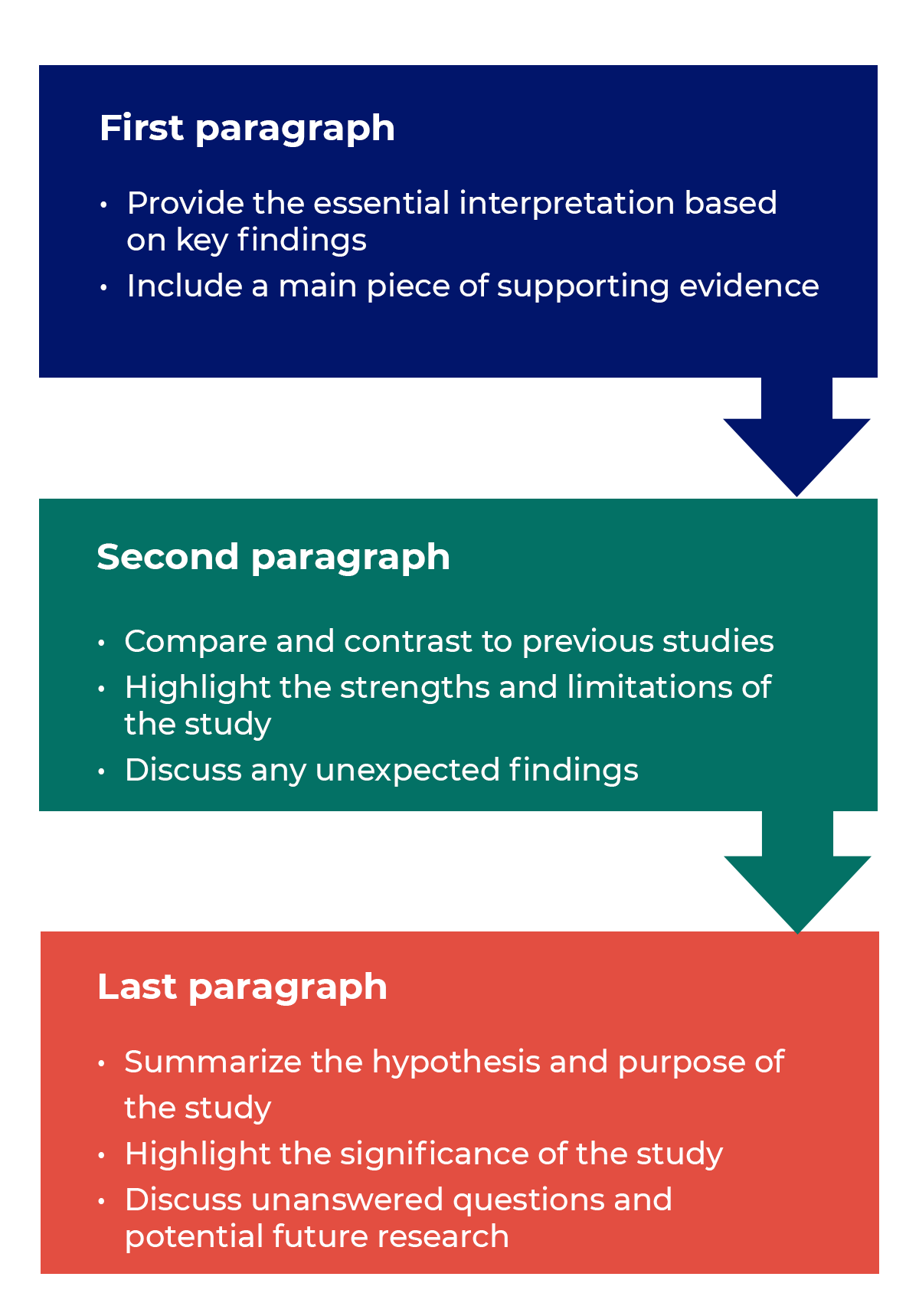
Trying to fit a complete discussion into a single paragraph can add unnecessary stress to the writing process. If possible, you’ll want to give yourself two or three paragraphs to give the reader a comprehensive understanding of your study as a whole. Here’s one way to structure an effective discussion:
Writing Tips
While the above sections can help you brainstorm and structure your discussion, there are many common mistakes that writers revert to when having difficulties with their paper. Writing a discussion can be a delicate balance between summarizing your results, providing proper context for your research and avoiding introducing new information. Remember that your paper should be both confident and honest about the results!

- Read the journal’s guidelines on the discussion and conclusion sections. If possible, learn about the guidelines before writing the discussion to ensure you’re writing to meet their expectations.
- Begin with a clear statement of the principal findings. This will reinforce the main take-away for the reader and set up the rest of the discussion.
- Explain why the outcomes of your study are important to the reader. Discuss the implications of your findings realistically based on previous literature, highlighting both the strengths and limitations of the research.
- State whether the results prove or disprove your hypothesis. If your hypothesis was disproved, what might be the reasons?
- Introduce new or expanded ways to think about the research question. Indicate what next steps can be taken to further pursue any unresolved questions.
- If dealing with a contemporary or ongoing problem, such as climate change, discuss possible consequences if the problem is avoided.
- Be concise. Adding unnecessary detail can distract from the main findings.

Don’t
- Rewrite your abstract. Statements with “we investigated” or “we studied” generally do not belong in the discussion.
- Include new arguments or evidence not previously discussed. Necessary information and evidence should be introduced in the main body of the paper.
- Apologize. Even if your research contains significant limitations, don’t undermine your authority by including statements that doubt your methodology or execution.
- Shy away from speaking on limitations or negative results. Including limitations and negative results will give readers a complete understanding of the presented research. Potential limitations include sources of potential bias, threats to internal or external validity, barriers to implementing an intervention and other issues inherent to the study design.
- Overstate the importance of your findings. Making grand statements about how a study will fully resolve large questions can lead readers to doubt the success of the research.
Snippets of Effective Discussions:
Consumer-based actions to reduce plastic pollution in rivers: A multi-criteria decision analysis approach
Identifying reliable indicators of fitness in polar bears
- How to Write a Great Title
- How to Write an Abstract
- How to Write Your Methods
- How to Report Statistics
- How to Edit Your Work
The contents of the Peer Review Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
The contents of the Writing Center are also available as a live, interactive training session, complete with slides, talking points, and activities. …
There’s a lot to consider when deciding where to submit your work. Learn how to choose a journal that will help your study reach its audience, while reflecting your values as a researcher…
Guide to Writing the Results and Discussion Sections of a Scientific Article
A quality research paper has both the qualities of in-depth research and good writing ( Bordage, 2001 ). In addition, a research paper must be clear, concise, and effective when presenting the information in an organized structure with a logical manner ( Sandercock, 2013 ).
In this article, we will take a closer look at the results and discussion section. Composing each of these carefully with sufficient data and well-constructed arguments can help improve your paper overall.
The results section of your research paper contains a description about the main findings of your research, whereas the discussion section interprets the results for readers and provides the significance of the findings. The discussion should not repeat the results.
Let’s dive in a little deeper about how to properly, and clearly organize each part.
How to Organize the Results Section
Since your results follow your methods, you’ll want to provide information about what you discovered from the methods you used, such as your research data. In other words, what were the outcomes of the methods you used?
You may also include information about the measurement of your data, variables, treatments, and statistical analyses.
To start, organize your research data based on how important those are in relation to your research questions. This section should focus on showing major results that support or reject your research hypothesis. Include your least important data as supplemental materials when submitting to the journal.
The next step is to prioritize your research data based on importance – focusing heavily on the information that directly relates to your research questions using the subheadings.
The organization of the subheadings for the results section usually mirrors the methods section. It should follow a logical and chronological order.
Subheading organization
Subheadings within your results section are primarily going to detail major findings within each important experiment. And the first paragraph of your results section should be dedicated to your main findings (findings that answer your overall research question and lead to your conclusion) (Hofmann, 2013).
In the book “Writing in the Biological Sciences,” author Angelika Hofmann recommends you structure your results subsection paragraphs as follows:
- Experimental purpose
- Interpretation
Each subheading may contain a combination of ( Bahadoran, 2019 ; Hofmann, 2013, pg. 62-63):
- Text: to explain about the research data
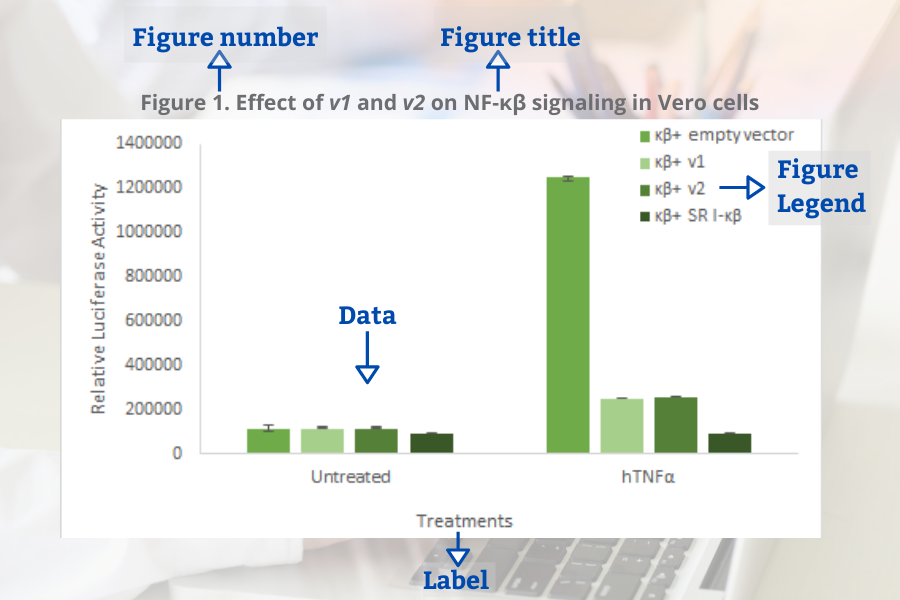
- Figures: to display the research data and to show trends or relationships, for examples using graphs or gel pictures.
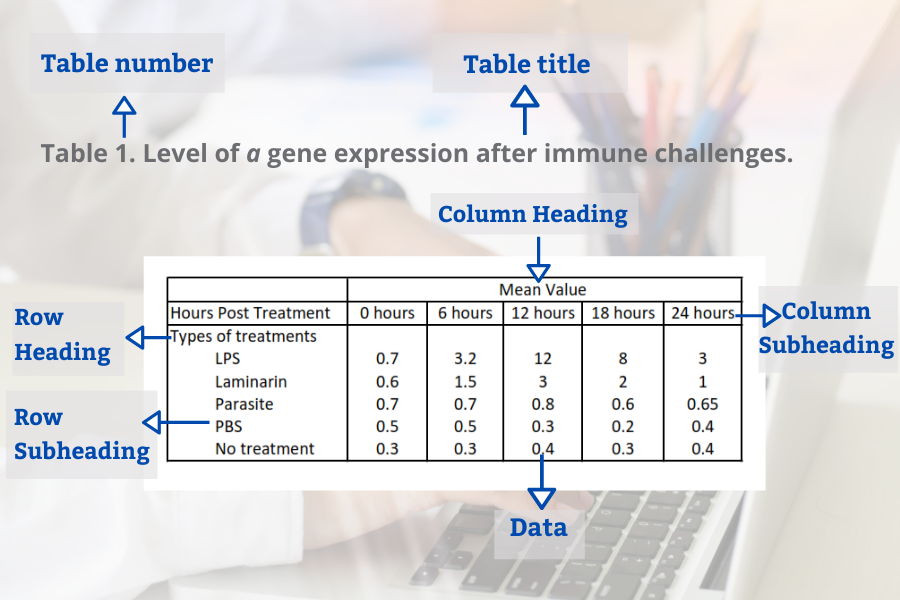
- Tables: to represent a large data and exact value
Decide on the best way to present your data — in the form of text, figures or tables (Hofmann, 2013).
Data or Results?
Sometimes we get confused about how to differentiate between data and results . Data are information (facts or numbers) that you collected from your research ( Bahadoran, 2019 ).

Whereas, results are the texts presenting the meaning of your research data ( Bahadoran, 2019 ).
One mistake that some authors often make is to use text to direct the reader to find a specific table or figure without further explanation. This can confuse readers when they interpret data completely different from what the authors had in mind. So, you should briefly explain your data to make your information clear for the readers.
Common Elements in Figures and Tables
Figures and tables present information about your research data visually. The use of these visual elements is necessary so readers can summarize, compare, and interpret large data at a glance. You can use graphs or figures to compare groups or patterns. Whereas, tables are ideal to present large quantities of data and exact values.
Several components are needed to create your figures and tables. These elements are important to sort your data based on groups (or treatments). It will be easier for the readers to see the similarities and differences among the groups.
When presenting your research data in the form of figures and tables, organize your data based on the steps of the research leading you into a conclusion.
Common elements of the figures (Bahadoran, 2019):
- Figure number
- Figure title
- Figure legend (for example a brief title, experimental/statistical information, or definition of symbols).
Tables in the result section may contain several elements (Bahadoran, 2019):
- Table number
- Table title
- Row headings (for example groups)
- Column headings
- Row subheadings (for example categories or groups)
- Column subheadings (for example categories or variables)
- Footnotes (for example statistical analyses)
Tips to Write the Results Section
- Direct the reader to the research data and explain the meaning of the data.
- Avoid using a repetitive sentence structure to explain a new set of data.
- Write and highlight important findings in your results.
- Use the same order as the subheadings of the methods section.
- Match the results with the research questions from the introduction. Your results should answer your research questions.
- Be sure to mention the figures and tables in the body of your text.
- Make sure there is no mismatch between the table number or the figure number in text and in figure/tables.
- Only present data that support the significance of your study. You can provide additional data in tables and figures as supplementary material.
How to Organize the Discussion Section
It’s not enough to use figures and tables in your results section to convince your readers about the importance of your findings. You need to support your results section by providing more explanation in the discussion section about what you found.
In the discussion section, based on your findings, you defend the answers to your research questions and create arguments to support your conclusions.
Below is a list of questions to guide you when organizing the structure of your discussion section ( Viera et al ., 2018 ):
- What experiments did you conduct and what were the results?
- What do the results mean?
- What were the important results from your study?
- How did the results answer your research questions?
- Did your results support your hypothesis or reject your hypothesis?
- What are the variables or factors that might affect your results?
- What were the strengths and limitations of your study?
- What other published works support your findings?
- What other published works contradict your findings?
- What possible factors might cause your findings different from other findings?
- What is the significance of your research?
- What are new research questions to explore based on your findings?
Organizing the Discussion Section
The structure of the discussion section may be different from one paper to another, but it commonly has a beginning, middle-, and end- to the section.
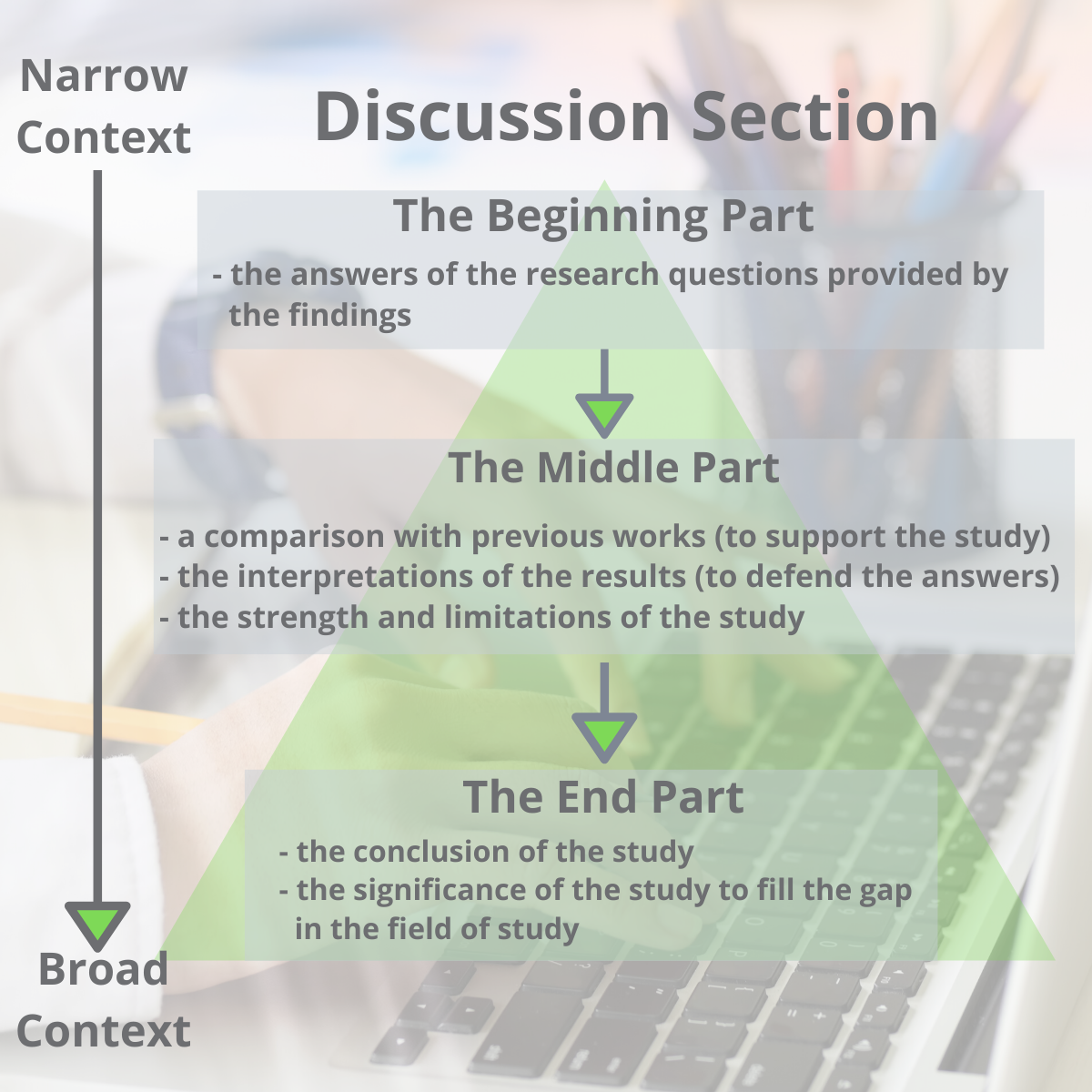
One way to organize the structure of the discussion section is by dividing it into three parts (Ghasemi, 2019):
- The beginning: The first sentence of the first paragraph should state the importance and the new findings of your research. The first paragraph may also include answers to your research questions mentioned in your introduction section.
- The middle: The middle should contain the interpretations of the results to defend your answers, the strength of the study, the limitations of the study, and an update literature review that validates your findings.
- The end: The end concludes the study and the significance of your research.
Another possible way to organize the discussion section was proposed by Michael Docherty in British Medical Journal: is by using this structure ( Docherty, 1999 ):
- Discussion of important findings
- Comparison of your results with other published works
- Include the strengths and limitations of the study
- Conclusion and possible implications of your study, including the significance of your study – address why and how is it meaningful
- Future research questions based on your findings
Finally, a last option is structuring your discussion this way (Hofmann, 2013, pg. 104):
- First Paragraph: Provide an interpretation based on your key findings. Then support your interpretation with evidence.
- Secondary results
- Limitations
- Unexpected findings
- Comparisons to previous publications
- Last Paragraph: The last paragraph should provide a summarization (conclusion) along with detailing the significance, implications and potential next steps.
Remember, at the heart of the discussion section is presenting an interpretation of your major findings.
Tips to Write the Discussion Section
- Highlight the significance of your findings
- Mention how the study will fill a gap in knowledge.
- Indicate the implication of your research.
- Avoid generalizing, misinterpreting your results, drawing a conclusion with no supportive findings from your results.
Aggarwal, R., & Sahni, P. (2018). The Results Section. In Reporting and Publishing Research in the Biomedical Sciences (pp. 21-38): Springer.
Bahadoran, Z., Mirmiran, P., Zadeh-Vakili, A., Hosseinpanah, F., & Ghasemi, A. (2019). The principles of biomedical scientific writing: Results. International journal of endocrinology and metabolism, 17(2).
Bordage, G. (2001). Reasons reviewers reject and accept manuscripts: the strengths and weaknesses in medical education reports. Academic medicine, 76(9), 889-896.
Cals, J. W., & Kotz, D. (2013). Effective writing and publishing scientific papers, part VI: discussion. Journal of clinical epidemiology, 66(10), 1064.
Docherty, M., & Smith, R. (1999). The case for structuring the discussion of scientific papers: Much the same as that for structuring abstracts. In: British Medical Journal Publishing Group.
Faber, J. (2017). Writing scientific manuscripts: most common mistakes. Dental press journal of orthodontics, 22(5), 113-117.
Fletcher, R. H., & Fletcher, S. W. (2018). The discussion section. In Reporting and Publishing Research in the Biomedical Sciences (pp. 39-48): Springer.
Ghasemi, A., Bahadoran, Z., Mirmiran, P., Hosseinpanah, F., Shiva, N., & Zadeh-Vakili, A. (2019). The Principles of Biomedical Scientific Writing: Discussion. International journal of endocrinology and metabolism, 17(3).
Hofmann, A. H. (2013). Writing in the biological sciences: a comprehensive resource for scientific communication . New York: Oxford University Press.
Kotz, D., & Cals, J. W. (2013). Effective writing and publishing scientific papers, part V: results. Journal of clinical epidemiology, 66(9), 945.
Mack, C. (2014). How to Write a Good Scientific Paper: Structure and Organization. Journal of Micro/ Nanolithography, MEMS, and MOEMS, 13. doi:10.1117/1.JMM.13.4.040101
Moore, A. (2016). What's in a Discussion section? Exploiting 2‐dimensionality in the online world…. Bioessays, 38(12), 1185-1185.
Peat, J., Elliott, E., Baur, L., & Keena, V. (2013). Scientific writing: easy when you know how: John Wiley & Sons.
Sandercock, P. M. L. (2012). How to write and publish a scientific article. Canadian Society of Forensic Science Journal, 45(1), 1-5.
Teo, E. K. (2016). Effective Medical Writing: The Write Way to Get Published. Singapore Medical Journal, 57(9), 523-523. doi:10.11622/smedj.2016156
Van Way III, C. W. (2007). Writing a scientific paper. Nutrition in Clinical Practice, 22(6), 636-640.
Vieira, R. F., Lima, R. C. d., & Mizubuti, E. S. G. (2019). How to write the discussion section of a scientific article. Acta Scientiarum. Agronomy, 41.
Related Articles

A quality research paper has both the qualities of in-depth research and good writing (Bordage, 200...
How to Survive and Complete a Thesis or a Dissertation
Writing a thesis or a dissertation can be a challenging process for many graduate students. There ar...

12 Ways to Dramatically Improve your Research Manuscript Title and Abstract
The first thing a person doing literary research will see is a research publication title. After tha...

15 Laboratory Notebook Tips to Help with your Research Manuscript
Your lab notebook is a foundation to your research manuscript. It serves almost as a rudimentary dra...
Join our list to receive promos and articles.
- Competent Cells
- Lab Startup
- Z')" data-type="collection" title="Products A->Z" target="_self" href="/collection/products-a-to-z">Products A->Z
- GoldBio Resources
- GoldBio Sales Team
- GoldBio Distributors
- Duchefa Direct
- Sign up for Promos
- Terms & Conditions
- ISO Certification
- Agarose Resins
- Antibiotics & Selection
- Biochemical Reagents
- Bioluminescence
- Buffers & Reagents
- Cell Culture
- Cloning & Induction
- Competent Cells and Transformation
- Detergents & Membrane Agents
- DNA Amplification
- Enzymes, Inhibitors & Substrates
- Growth Factors and Cytokines
- Lab Tools & Accessories
- Plant Research and Reagents
- Protein Research & Analysis
- Protein Expression & Purification
- Reducing Agents
- Privacy Policy

Home » Research Paper Conclusion – Writing Guide and Examples
Research Paper Conclusion – Writing Guide and Examples
Table of Contents

Research Paper Conclusion
Definition:
A research paper conclusion is the final section of a research paper that summarizes the key findings, significance, and implications of the research. It is the writer’s opportunity to synthesize the information presented in the paper, draw conclusions, and make recommendations for future research or actions.
The conclusion should provide a clear and concise summary of the research paper, reiterating the research question or problem, the main results, and the significance of the findings. It should also discuss the limitations of the study and suggest areas for further research.
Parts of Research Paper Conclusion
The parts of a research paper conclusion typically include:
Restatement of the Thesis
The conclusion should begin by restating the thesis statement from the introduction in a different way. This helps to remind the reader of the main argument or purpose of the research.
Summary of Key Findings
The conclusion should summarize the main findings of the research, highlighting the most important results and conclusions. This section should be brief and to the point.
Implications and Significance
In this section, the researcher should explain the implications and significance of the research findings. This may include discussing the potential impact on the field or industry, highlighting new insights or knowledge gained, or pointing out areas for future research.
Limitations and Recommendations
It is important to acknowledge any limitations or weaknesses of the research and to make recommendations for how these could be addressed in future studies. This shows that the researcher is aware of the potential limitations of their work and is committed to improving the quality of research in their field.
Concluding Statement
The conclusion should end with a strong concluding statement that leaves a lasting impression on the reader. This could be a call to action, a recommendation for further research, or a final thought on the topic.
How to Write Research Paper Conclusion
Here are some steps you can follow to write an effective research paper conclusion:
- Restate the research problem or question: Begin by restating the research problem or question that you aimed to answer in your research. This will remind the reader of the purpose of your study.
- Summarize the main points: Summarize the key findings and results of your research. This can be done by highlighting the most important aspects of your research and the evidence that supports them.
- Discuss the implications: Discuss the implications of your findings for the research area and any potential applications of your research. You should also mention any limitations of your research that may affect the interpretation of your findings.
- Provide a conclusion : Provide a concise conclusion that summarizes the main points of your paper and emphasizes the significance of your research. This should be a strong and clear statement that leaves a lasting impression on the reader.
- Offer suggestions for future research: Lastly, offer suggestions for future research that could build on your findings and contribute to further advancements in the field.
Remember that the conclusion should be brief and to the point, while still effectively summarizing the key findings and implications of your research.
Example of Research Paper Conclusion
Here’s an example of a research paper conclusion:
Conclusion :
In conclusion, our study aimed to investigate the relationship between social media use and mental health among college students. Our findings suggest that there is a significant association between social media use and increased levels of anxiety and depression among college students. This highlights the need for increased awareness and education about the potential negative effects of social media use on mental health, particularly among college students.
Despite the limitations of our study, such as the small sample size and self-reported data, our findings have important implications for future research and practice. Future studies should aim to replicate our findings in larger, more diverse samples, and investigate the potential mechanisms underlying the association between social media use and mental health. In addition, interventions should be developed to promote healthy social media use among college students, such as mindfulness-based approaches and social media detox programs.
Overall, our study contributes to the growing body of research on the impact of social media on mental health, and highlights the importance of addressing this issue in the context of higher education. By raising awareness and promoting healthy social media use among college students, we can help to reduce the negative impact of social media on mental health and improve the well-being of young adults.
Purpose of Research Paper Conclusion
The purpose of a research paper conclusion is to provide a summary and synthesis of the key findings, significance, and implications of the research presented in the paper. The conclusion serves as the final opportunity for the writer to convey their message and leave a lasting impression on the reader.
The conclusion should restate the research problem or question, summarize the main results of the research, and explain their significance. It should also acknowledge the limitations of the study and suggest areas for future research or action.
Overall, the purpose of the conclusion is to provide a sense of closure to the research paper and to emphasize the importance of the research and its potential impact. It should leave the reader with a clear understanding of the main findings and why they matter. The conclusion serves as the writer’s opportunity to showcase their contribution to the field and to inspire further research and action.
When to Write Research Paper Conclusion
The conclusion of a research paper should be written after the body of the paper has been completed. It should not be written until the writer has thoroughly analyzed and interpreted their findings and has written a complete and cohesive discussion of the research.
Before writing the conclusion, the writer should review their research paper and consider the key points that they want to convey to the reader. They should also review the research question, hypotheses, and methodology to ensure that they have addressed all of the necessary components of the research.
Once the writer has a clear understanding of the main findings and their significance, they can begin writing the conclusion. The conclusion should be written in a clear and concise manner, and should reiterate the main points of the research while also providing insights and recommendations for future research or action.
Characteristics of Research Paper Conclusion
The characteristics of a research paper conclusion include:
- Clear and concise: The conclusion should be written in a clear and concise manner, summarizing the key findings and their significance.
- Comprehensive: The conclusion should address all of the main points of the research paper, including the research question or problem, the methodology, the main results, and their implications.
- Future-oriented : The conclusion should provide insights and recommendations for future research or action, based on the findings of the research.
- Impressive : The conclusion should leave a lasting impression on the reader, emphasizing the importance of the research and its potential impact.
- Objective : The conclusion should be based on the evidence presented in the research paper, and should avoid personal biases or opinions.
- Unique : The conclusion should be unique to the research paper and should not simply repeat information from the introduction or body of the paper.
Advantages of Research Paper Conclusion
The advantages of a research paper conclusion include:
- Summarizing the key findings : The conclusion provides a summary of the main findings of the research, making it easier for the reader to understand the key points of the study.
- Emphasizing the significance of the research: The conclusion emphasizes the importance of the research and its potential impact, making it more likely that readers will take the research seriously and consider its implications.
- Providing recommendations for future research or action : The conclusion suggests practical recommendations for future research or action, based on the findings of the study.
- Providing closure to the research paper : The conclusion provides a sense of closure to the research paper, tying together the different sections of the paper and leaving a lasting impression on the reader.
- Demonstrating the writer’s contribution to the field : The conclusion provides the writer with an opportunity to showcase their contribution to the field and to inspire further research and action.
Limitations of Research Paper Conclusion
While the conclusion of a research paper has many advantages, it also has some limitations that should be considered, including:
- I nability to address all aspects of the research: Due to the limited space available in the conclusion, it may not be possible to address all aspects of the research in detail.
- Subjectivity : While the conclusion should be objective, it may be influenced by the writer’s personal biases or opinions.
- Lack of new information: The conclusion should not introduce new information that has not been discussed in the body of the research paper.
- Lack of generalizability: The conclusions drawn from the research may not be applicable to other contexts or populations, limiting the generalizability of the study.
- Misinterpretation by the reader: The reader may misinterpret the conclusions drawn from the research, leading to a misunderstanding of the findings.
About the author
Muhammad Hassan
Researcher, Academic Writer, Web developer
You may also like

APA Table of Contents – Format and Example

Problem Statement – Writing Guide, Examples and...

Research Paper Title – Writing Guide and Example

Research Design – Types, Methods and Examples

Figures in Research Paper – Examples and Guide

Conceptual Framework – Types, Methodology and...
- SpringerLink shop
Discussion and Conclusions
Your Discussion and Conclusions sections should answer the question: What do your results mean?
In other words, the majority of the Discussion and Conclusions sections should be an interpretation of your results. You should:
- Discuss your conclusions in order of most to least important.
- Compare your results with those from other studies: Are they consistent? If not, discuss possible reasons for the difference.
- Mention any inconclusive results and explain them as best you can. You may suggest additional experiments needed to clarify your results.
- Briefly describe the limitations of your study to show reviewers and readers that you have considered your experiment’s weaknesses. Many researchers are hesitant to do this as they feel it highlights the weaknesses in their research to the editor and reviewer. However doing this actually makes a positive impression of your paper as it makes it clear that you have an in depth understanding of your topic and can think objectively of your research.
- Discuss what your results may mean for researchers in the same field as you, researchers in other fields, and the general public. How could your findings be applied?
- State how your results extend the findings of previous studies.
- If your findings are preliminary, suggest future studies that need to be carried out.
- At the end of your Discussion and Conclusions sections, state your main conclusions once again .
Back │ Next
- Communicating in STEM Disciplines
- Features of Academic STEM Writing
- STEM Writing Tips
- Academic Integrity in STEM
- Strategies for Writing
- Science Writing Videos – YouTube Channel
- Educator Resources
- Lesson Plans, Activities and Assignments
- Strategies for Teaching Writing
- Grading Techniques
IMRAD (Introduction, Methods, Results and Discussion)
Academic research papers in STEM disciplines typically follow a well-defined I-M-R-A-D structure: Introduction, Methods, Results And Discussion (Wu, 2011). Although not included in the IMRAD name, these papers often include a Conclusion.
Introduction
The Introduction typically provides everything your reader needs to know in order to understand the scope and purpose of your research. This section should provide:
- Context for your research (for example, the nature and scope of your topic)
- A summary of how relevant scholars have approached your research topic to date, and a description of how your research makes a contribution to the scholarly conversation
- An argument or hypothesis that relates to the scholarly conversation
- A brief explanation of your methodological approach and a justification for this approach (in other words, a brief discussion of how you gather your data and why this is an appropriate choice for your contribution)
- The main conclusions of your paper (or the “so what”)
- A roadmap, or a brief description of how the rest of your paper proceeds
The Methods section describes exactly what you did to gather the data that you use in your paper. This should expand on the brief methodology discussion in the introduction and provide readers with enough detail to, if necessary, reproduce your experiment, design, or method for obtaining data; it should also help readers to anticipate your results. The more specific, the better! These details might include:
- An overview of the methodology at the beginning of the section
- A chronological description of what you did in the order you did it
- Descriptions of the materials used, the time taken, and the precise step-by-step process you followed
- An explanation of software used for statistical calculations (if necessary)
- Justifications for any choices or decisions made when designing your methods
Because the methods section describes what was done to gather data, there are two things to consider when writing. First, this section is usually written in the past tense (for example, we poured 250ml of distilled water into the 1000ml glass beaker). Second, this section should not be written as a set of instructions or commands but as descriptions of actions taken. This usually involves writing in the active voice (for example, we poured 250ml of distilled water into the 1000ml glass beaker), but some readers prefer the passive voice (for example, 250ml of distilled water was poured into the 1000ml beaker). It’s important to consider the audience when making this choice, so be sure to ask your instructor which they prefer.
The Results section outlines the data gathered through the methods described above and explains what the data show. This usually involves a combination of tables and/or figures and prose. In other words, the results section gives your reader context for interpreting the data. The results section usually includes:
- A presentation of the data obtained through the means described in the methods section in the form of tables and/or figures
- Statements that summarize or explain what the data show
- Highlights of the most important results
Tables should be as succinct as possible, including only vital information (often summarized) and figures should be easy to interpret and be visually engaging. When adding your written explanation to accompany these visual aids, try to refer your readers to these in such a way that they provide an additional descriptive element, rather than simply telling people to look at them. This can be especially helpful for readers who find it hard to see patterns in data.
The Discussion section explains why the results described in the previous section are meaningful in relation to previous scholarly work and the specific research question your paper explores. This section usually includes:
- Engagement with sources that are relevant to your work (you should compare and contrast your results to those of similar researchers)
- An explanation of the results that you found, and why these results are important and/or interesting
Some papers have separate Results and Discussion sections, while others combine them into one section, Results and Discussion. There are benefits to both. By presenting these as separate sections, you’re able to discuss all of your results before moving onto the implications. By presenting these as one section, you’re able to discuss specific results and move onto their significance before introducing another set of results.
The Conclusion section of a paper should include a brief summary of the main ideas or key takeaways of the paper and their implications for future research. This section usually includes:
- A brief overview of the main claims and/or key ideas put forth in the paper
- A brief discussion of potential limitations of the study (if relevant)
- Some suggestions for future research (these should be clearly related to the content of your paper)
Sample Research Article
Resource Download
Wu, Jianguo. “Improving the writing of research papers: IMRAD and beyond.” Landscape Ecology 26, no. 10 (November 2011): 1345–1349. http://dx.doi.org/10.1007/s10980-011-9674-3.
Further reading:
- Organization of a Research Paper: The IMRAD Format by P. K. Ramachandran Nair and Vimala D. Nair
- George Mason University Writing Centre’s guide on Writing a Scientific Research Report (IMRAD)
- University of Wisconsin Writing Centre’s guide on Formatting Science Reports

- USC Libraries
- Research Guides
Organizing Your Social Sciences Research Paper
- 7. The Results
- Purpose of Guide
- Design Flaws to Avoid
- Independent and Dependent Variables
- Glossary of Research Terms
- Reading Research Effectively
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Applying Critical Thinking
- Choosing a Title
- Making an Outline
- Paragraph Development
- Research Process Video Series
- Executive Summary
- The C.A.R.S. Model
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tiertiary Sources
- Scholarly vs. Popular Publications
- Qualitative Methods
- Quantitative Methods
- Insiderness
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Writing Concisely
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Generative AI and Writing
- USC Libraries Tutorials and Other Guides
- Bibliography
The results section is where you report the findings of your study based upon the methodology [or methodologies] you applied to gather information. The results section should state the findings of the research arranged in a logical sequence without bias or interpretation. A section describing results should be particularly detailed if your paper includes data generated from your own research.
Annesley, Thomas M. "Show Your Cards: The Results Section and the Poker Game." Clinical Chemistry 56 (July 2010): 1066-1070.
Importance of a Good Results Section
When formulating the results section, it's important to remember that the results of a study do not prove anything . Findings can only confirm or reject the hypothesis underpinning your study. However, the act of articulating the results helps you to understand the problem from within, to break it into pieces, and to view the research problem from various perspectives.
The page length of this section is set by the amount and types of data to be reported . Be concise. Use non-textual elements appropriately, such as figures and tables, to present findings more effectively. In deciding what data to describe in your results section, you must clearly distinguish information that would normally be included in a research paper from any raw data or other content that could be included as an appendix. In general, raw data that has not been summarized should not be included in the main text of your paper unless requested to do so by your professor.
Avoid providing data that is not critical to answering the research question . The background information you described in the introduction section should provide the reader with any additional context or explanation needed to understand the results. A good strategy is to always re-read the background section of your paper after you have written up your results to ensure that the reader has enough context to understand the results [and, later, how you interpreted the results in the discussion section of your paper that follows].
Bavdekar, Sandeep B. and Sneha Chandak. "Results: Unraveling the Findings." Journal of the Association of Physicians of India 63 (September 2015): 44-46; Brett, Paul. "A Genre Analysis of the Results Section of Sociology Articles." English for Specific Speakers 13 (1994): 47-59; Go to English for Specific Purposes on ScienceDirect;Burton, Neil et al. Doing Your Education Research Project . Los Angeles, CA: SAGE, 2008; Results. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Kretchmer, Paul. Twelve Steps to Writing an Effective Results Section. San Francisco Edit; "Reporting Findings." In Making Sense of Social Research Malcolm Williams, editor. (London;: SAGE Publications, 2003) pp. 188-207.
Structure and Writing Style
I. Organization and Approach
For most research papers in the social and behavioral sciences, there are two possible ways of organizing the results . Both approaches are appropriate in how you report your findings, but use only one approach.
- Present a synopsis of the results followed by an explanation of key findings . This approach can be used to highlight important findings. For example, you may have noticed an unusual correlation between two variables during the analysis of your findings. It is appropriate to highlight this finding in the results section. However, speculating as to why this correlation exists and offering a hypothesis about what may be happening belongs in the discussion section of your paper.
- Present a result and then explain it, before presenting the next result then explaining it, and so on, then end with an overall synopsis . This is the preferred approach if you have multiple results of equal significance. It is more common in longer papers because it helps the reader to better understand each finding. In this model, it is helpful to provide a brief conclusion that ties each of the findings together and provides a narrative bridge to the discussion section of the your paper.
NOTE: Just as the literature review should be arranged under conceptual categories rather than systematically describing each source, you should also organize your findings under key themes related to addressing the research problem. This can be done under either format noted above [i.e., a thorough explanation of the key results or a sequential, thematic description and explanation of each finding].
II. Content
In general, the content of your results section should include the following:
- Introductory context for understanding the results by restating the research problem underpinning your study . This is useful in re-orientating the reader's focus back to the research problem after having read a review of the literature and your explanation of the methods used for gathering and analyzing information.
- Inclusion of non-textual elements, such as, figures, charts, photos, maps, tables, etc. to further illustrate key findings, if appropriate . Rather than relying entirely on descriptive text, consider how your findings can be presented visually. This is a helpful way of condensing a lot of data into one place that can then be referred to in the text. Consider referring to appendices if there is a lot of non-textual elements.
- A systematic description of your results, highlighting for the reader observations that are most relevant to the topic under investigation . Not all results that emerge from the methodology used to gather information may be related to answering the " So What? " question. Do not confuse observations with interpretations; observations in this context refers to highlighting important findings you discovered through a process of reviewing prior literature and gathering data.
- The page length of your results section is guided by the amount and types of data to be reported . However, focus on findings that are important and related to addressing the research problem. It is not uncommon to have unanticipated results that are not relevant to answering the research question. This is not to say that you don't acknowledge tangential findings and, in fact, can be referred to as areas for further research in the conclusion of your paper. However, spending time in the results section describing tangential findings clutters your overall results section and distracts the reader.
- A short paragraph that concludes the results section by synthesizing the key findings of the study . Highlight the most important findings you want readers to remember as they transition into the discussion section. This is particularly important if, for example, there are many results to report, the findings are complicated or unanticipated, or they are impactful or actionable in some way [i.e., able to be pursued in a feasible way applied to practice].
NOTE: Always use the past tense when referring to your study's findings. Reference to findings should always be described as having already happened because the method used to gather the information has been completed.
III. Problems to Avoid
When writing the results section, avoid doing the following :
- Discussing or interpreting your results . Save this for the discussion section of your paper, although where appropriate, you should compare or contrast specific results to those found in other studies [e.g., "Similar to the work of Smith [1990], one of the findings of this study is the strong correlation between motivation and academic achievement...."].
- Reporting background information or attempting to explain your findings. This should have been done in your introduction section, but don't panic! Often the results of a study point to the need for additional background information or to explain the topic further, so don't think you did something wrong. Writing up research is rarely a linear process. Always revise your introduction as needed.
- Ignoring negative results . A negative result generally refers to a finding that does not support the underlying assumptions of your study. Do not ignore them. Document these findings and then state in your discussion section why you believe a negative result emerged from your study. Note that negative results, and how you handle them, can give you an opportunity to write a more engaging discussion section, therefore, don't be hesitant to highlight them.
- Including raw data or intermediate calculations . Ask your professor if you need to include any raw data generated by your study, such as transcripts from interviews or data files. If raw data is to be included, place it in an appendix or set of appendices that are referred to in the text.
- Be as factual and concise as possible in reporting your findings . Do not use phrases that are vague or non-specific, such as, "appeared to be greater than other variables..." or "demonstrates promising trends that...." Subjective modifiers should be explained in the discussion section of the paper [i.e., why did one variable appear greater? Or, how does the finding demonstrate a promising trend?].
- Presenting the same data or repeating the same information more than once . If you want to highlight a particular finding, it is appropriate to do so in the results section. However, you should emphasize its significance in relation to addressing the research problem in the discussion section. Do not repeat it in your results section because you can do that in the conclusion of your paper.
- Confusing figures with tables . Be sure to properly label any non-textual elements in your paper. Don't call a chart an illustration or a figure a table. If you are not sure, go here .
Annesley, Thomas M. "Show Your Cards: The Results Section and the Poker Game." Clinical Chemistry 56 (July 2010): 1066-1070; Bavdekar, Sandeep B. and Sneha Chandak. "Results: Unraveling the Findings." Journal of the Association of Physicians of India 63 (September 2015): 44-46; Burton, Neil et al. Doing Your Education Research Project . Los Angeles, CA: SAGE, 2008; Caprette, David R. Writing Research Papers. Experimental Biosciences Resources. Rice University; Hancock, Dawson R. and Bob Algozzine. Doing Case Study Research: A Practical Guide for Beginning Researchers . 2nd ed. New York: Teachers College Press, 2011; Introduction to Nursing Research: Reporting Research Findings. Nursing Research: Open Access Nursing Research and Review Articles. (January 4, 2012); Kretchmer, Paul. Twelve Steps to Writing an Effective Results Section. San Francisco Edit ; Ng, K. H. and W. C. Peh. "Writing the Results." Singapore Medical Journal 49 (2008): 967-968; Reporting Research Findings. Wilder Research, in partnership with the Minnesota Department of Human Services. (February 2009); Results. The Structure, Format, Content, and Style of a Journal-Style Scientific Paper. Department of Biology. Bates College; Schafer, Mickey S. Writing the Results. Thesis Writing in the Sciences. Course Syllabus. University of Florida.
Writing Tip
Why Don't I Just Combine the Results Section with the Discussion Section?
It's not unusual to find articles in scholarly social science journals where the author(s) have combined a description of the findings with a discussion about their significance and implications. You could do this. However, if you are inexperienced writing research papers, consider creating two distinct sections for each section in your paper as a way to better organize your thoughts and, by extension, your paper. Think of the results section as the place where you report what your study found; think of the discussion section as the place where you interpret the information and answer the "So What?" question. As you become more skilled writing research papers, you can consider melding the results of your study with a discussion of its implications.
Driscoll, Dana Lynn and Aleksandra Kasztalska. Writing the Experimental Report: Methods, Results, and Discussion. The Writing Lab and The OWL. Purdue University.
- << Previous: Insiderness
- Next: Using Non-Textual Elements >>
- Last Updated: Jun 12, 2024 8:53 AM
- URL: https://libguides.usc.edu/writingguide
- How to Cite
- Language & Lit
- Rhyme & Rhythm
- The Rewrite
- Search Glass
What Is the Difference Between Results and Conclusions in a Scientific Experiment?
Five steps make up most scientific experiments, beginning with the research question. The next step is the formulation of a hypothesis, which is a statement of what you expect your project will show. The procedure is your step-by-step plan for the experiment. The final two steps are the results, or what happens, and, finally, the conclusion, or what the results showed.
The Results
When you record the results of a scientific experiment, you record what happens as you follow your procedure. Results should be raw data that is measurable rather than general observations, and it should relate directly to your research question and hypothesis. For example, if your experiment involves growing plants, the results will be data about one aspect of the plants’ growth, such as how much each plant grows over a particular period of time or which seed sprouts first. The results should also include notations of any variations in the conditions of the experiment, which in this case might be an unexpected overnight freeze or which seed received the most water.
Data Organization
At the end of your experiment’s procedure, you have data that tells what happened, but at this point it is just a collection of facts or numbers. The data needs to be organized before you can understand it, but how you organize the data depends on the factor tested in your experiment. If you entered the data into a chart as you collected it, you may already see a pattern. Another way to organize the data is with a line graph to show change over time, especially temperature changes. In the example of plant growth, a bar graph can illustrate how much each plant grew between measurements.
The Conclusion
After all the data is organized in a form that relates it to your hypothesis, you can interpret it and reach a conclusion about the experiment. The conclusion is simply a report about what you learned based on whether the results agree or disagree with your hypothesis. It usually contains a summary of the actual procedure and makes note of anything unexpected that happened during the experiment. Your conclusion should consider all possible explanations of the data, including any errors you might have made, such as forgetting to water the plants one day. It can also give you a point from which to create further hypotheses relating to the experiment.
No Right or Wrong
The conclusion, which is also sometimes called a discussion or interpretation, is a statement about the experiment’s results. As a report of your data, it can’t be considered wrong even if the results don’t support your hypothesis. You have learned that your hypothesis does not answer your original research question.
- Agriculture Is a Science: Parts of a Science Project
- Vermont EPSCoR Streams Project: Data Analysis Tutorial
Cynthia Gast began writing professionally over 25 years ago in the automotive magazine niche and has also taught preschoolers and elementary grades. She has been a full-time freelance writer since 2008. Gast holds a Bachelor of Arts in history from the University of Illinois.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Korean Med Sci
- v.37(16); 2022 Apr 25

A Practical Guide to Writing Quantitative and Qualitative Research Questions and Hypotheses in Scholarly Articles
Edward barroga.
1 Department of General Education, Graduate School of Nursing Science, St. Luke’s International University, Tokyo, Japan.
Glafera Janet Matanguihan
2 Department of Biological Sciences, Messiah University, Mechanicsburg, PA, USA.
The development of research questions and the subsequent hypotheses are prerequisites to defining the main research purpose and specific objectives of a study. Consequently, these objectives determine the study design and research outcome. The development of research questions is a process based on knowledge of current trends, cutting-edge studies, and technological advances in the research field. Excellent research questions are focused and require a comprehensive literature search and in-depth understanding of the problem being investigated. Initially, research questions may be written as descriptive questions which could be developed into inferential questions. These questions must be specific and concise to provide a clear foundation for developing hypotheses. Hypotheses are more formal predictions about the research outcomes. These specify the possible results that may or may not be expected regarding the relationship between groups. Thus, research questions and hypotheses clarify the main purpose and specific objectives of the study, which in turn dictate the design of the study, its direction, and outcome. Studies developed from good research questions and hypotheses will have trustworthy outcomes with wide-ranging social and health implications.
INTRODUCTION
Scientific research is usually initiated by posing evidenced-based research questions which are then explicitly restated as hypotheses. 1 , 2 The hypotheses provide directions to guide the study, solutions, explanations, and expected results. 3 , 4 Both research questions and hypotheses are essentially formulated based on conventional theories and real-world processes, which allow the inception of novel studies and the ethical testing of ideas. 5 , 6
It is crucial to have knowledge of both quantitative and qualitative research 2 as both types of research involve writing research questions and hypotheses. 7 However, these crucial elements of research are sometimes overlooked; if not overlooked, then framed without the forethought and meticulous attention it needs. Planning and careful consideration are needed when developing quantitative or qualitative research, particularly when conceptualizing research questions and hypotheses. 4
There is a continuing need to support researchers in the creation of innovative research questions and hypotheses, as well as for journal articles that carefully review these elements. 1 When research questions and hypotheses are not carefully thought of, unethical studies and poor outcomes usually ensue. Carefully formulated research questions and hypotheses define well-founded objectives, which in turn determine the appropriate design, course, and outcome of the study. This article then aims to discuss in detail the various aspects of crafting research questions and hypotheses, with the goal of guiding researchers as they develop their own. Examples from the authors and peer-reviewed scientific articles in the healthcare field are provided to illustrate key points.
DEFINITIONS AND RELATIONSHIP OF RESEARCH QUESTIONS AND HYPOTHESES
A research question is what a study aims to answer after data analysis and interpretation. The answer is written in length in the discussion section of the paper. Thus, the research question gives a preview of the different parts and variables of the study meant to address the problem posed in the research question. 1 An excellent research question clarifies the research writing while facilitating understanding of the research topic, objective, scope, and limitations of the study. 5
On the other hand, a research hypothesis is an educated statement of an expected outcome. This statement is based on background research and current knowledge. 8 , 9 The research hypothesis makes a specific prediction about a new phenomenon 10 or a formal statement on the expected relationship between an independent variable and a dependent variable. 3 , 11 It provides a tentative answer to the research question to be tested or explored. 4
Hypotheses employ reasoning to predict a theory-based outcome. 10 These can also be developed from theories by focusing on components of theories that have not yet been observed. 10 The validity of hypotheses is often based on the testability of the prediction made in a reproducible experiment. 8
Conversely, hypotheses can also be rephrased as research questions. Several hypotheses based on existing theories and knowledge may be needed to answer a research question. Developing ethical research questions and hypotheses creates a research design that has logical relationships among variables. These relationships serve as a solid foundation for the conduct of the study. 4 , 11 Haphazardly constructed research questions can result in poorly formulated hypotheses and improper study designs, leading to unreliable results. Thus, the formulations of relevant research questions and verifiable hypotheses are crucial when beginning research. 12
CHARACTERISTICS OF GOOD RESEARCH QUESTIONS AND HYPOTHESES
Excellent research questions are specific and focused. These integrate collective data and observations to confirm or refute the subsequent hypotheses. Well-constructed hypotheses are based on previous reports and verify the research context. These are realistic, in-depth, sufficiently complex, and reproducible. More importantly, these hypotheses can be addressed and tested. 13
There are several characteristics of well-developed hypotheses. Good hypotheses are 1) empirically testable 7 , 10 , 11 , 13 ; 2) backed by preliminary evidence 9 ; 3) testable by ethical research 7 , 9 ; 4) based on original ideas 9 ; 5) have evidenced-based logical reasoning 10 ; and 6) can be predicted. 11 Good hypotheses can infer ethical and positive implications, indicating the presence of a relationship or effect relevant to the research theme. 7 , 11 These are initially developed from a general theory and branch into specific hypotheses by deductive reasoning. In the absence of a theory to base the hypotheses, inductive reasoning based on specific observations or findings form more general hypotheses. 10
TYPES OF RESEARCH QUESTIONS AND HYPOTHESES
Research questions and hypotheses are developed according to the type of research, which can be broadly classified into quantitative and qualitative research. We provide a summary of the types of research questions and hypotheses under quantitative and qualitative research categories in Table 1 .
| Quantitative research questions | Quantitative research hypotheses |
|---|---|
| Descriptive research questions | Simple hypothesis |
| Comparative research questions | Complex hypothesis |
| Relationship research questions | Directional hypothesis |
| Non-directional hypothesis | |
| Associative hypothesis | |
| Causal hypothesis | |
| Null hypothesis | |
| Alternative hypothesis | |
| Working hypothesis | |
| Statistical hypothesis | |
| Logical hypothesis | |
| Hypothesis-testing | |
| Qualitative research questions | Qualitative research hypotheses |
| Contextual research questions | Hypothesis-generating |
| Descriptive research questions | |
| Evaluation research questions | |
| Explanatory research questions | |
| Exploratory research questions | |
| Generative research questions | |
| Ideological research questions | |
| Ethnographic research questions | |
| Phenomenological research questions | |
| Grounded theory questions | |
| Qualitative case study questions |
Research questions in quantitative research
In quantitative research, research questions inquire about the relationships among variables being investigated and are usually framed at the start of the study. These are precise and typically linked to the subject population, dependent and independent variables, and research design. 1 Research questions may also attempt to describe the behavior of a population in relation to one or more variables, or describe the characteristics of variables to be measured ( descriptive research questions ). 1 , 5 , 14 These questions may also aim to discover differences between groups within the context of an outcome variable ( comparative research questions ), 1 , 5 , 14 or elucidate trends and interactions among variables ( relationship research questions ). 1 , 5 We provide examples of descriptive, comparative, and relationship research questions in quantitative research in Table 2 .
| Quantitative research questions | |
|---|---|
| Descriptive research question | |
| - Measures responses of subjects to variables | |
| - Presents variables to measure, analyze, or assess | |
| What is the proportion of resident doctors in the hospital who have mastered ultrasonography (response of subjects to a variable) as a diagnostic technique in their clinical training? | |
| Comparative research question | |
| - Clarifies difference between one group with outcome variable and another group without outcome variable | |
| Is there a difference in the reduction of lung metastasis in osteosarcoma patients who received the vitamin D adjunctive therapy (group with outcome variable) compared with osteosarcoma patients who did not receive the vitamin D adjunctive therapy (group without outcome variable)? | |
| - Compares the effects of variables | |
| How does the vitamin D analogue 22-Oxacalcitriol (variable 1) mimic the antiproliferative activity of 1,25-Dihydroxyvitamin D (variable 2) in osteosarcoma cells? | |
| Relationship research question | |
| - Defines trends, association, relationships, or interactions between dependent variable and independent variable | |
| Is there a relationship between the number of medical student suicide (dependent variable) and the level of medical student stress (independent variable) in Japan during the first wave of the COVID-19 pandemic? | |
Hypotheses in quantitative research
In quantitative research, hypotheses predict the expected relationships among variables. 15 Relationships among variables that can be predicted include 1) between a single dependent variable and a single independent variable ( simple hypothesis ) or 2) between two or more independent and dependent variables ( complex hypothesis ). 4 , 11 Hypotheses may also specify the expected direction to be followed and imply an intellectual commitment to a particular outcome ( directional hypothesis ) 4 . On the other hand, hypotheses may not predict the exact direction and are used in the absence of a theory, or when findings contradict previous studies ( non-directional hypothesis ). 4 In addition, hypotheses can 1) define interdependency between variables ( associative hypothesis ), 4 2) propose an effect on the dependent variable from manipulation of the independent variable ( causal hypothesis ), 4 3) state a negative relationship between two variables ( null hypothesis ), 4 , 11 , 15 4) replace the working hypothesis if rejected ( alternative hypothesis ), 15 explain the relationship of phenomena to possibly generate a theory ( working hypothesis ), 11 5) involve quantifiable variables that can be tested statistically ( statistical hypothesis ), 11 6) or express a relationship whose interlinks can be verified logically ( logical hypothesis ). 11 We provide examples of simple, complex, directional, non-directional, associative, causal, null, alternative, working, statistical, and logical hypotheses in quantitative research, as well as the definition of quantitative hypothesis-testing research in Table 3 .
| Quantitative research hypotheses | |
|---|---|
| Simple hypothesis | |
| - Predicts relationship between single dependent variable and single independent variable | |
| If the dose of the new medication (single independent variable) is high, blood pressure (single dependent variable) is lowered. | |
| Complex hypothesis | |
| - Foretells relationship between two or more independent and dependent variables | |
| The higher the use of anticancer drugs, radiation therapy, and adjunctive agents (3 independent variables), the higher would be the survival rate (1 dependent variable). | |
| Directional hypothesis | |
| - Identifies study direction based on theory towards particular outcome to clarify relationship between variables | |
| Privately funded research projects will have a larger international scope (study direction) than publicly funded research projects. | |
| Non-directional hypothesis | |
| - Nature of relationship between two variables or exact study direction is not identified | |
| - Does not involve a theory | |
| Women and men are different in terms of helpfulness. (Exact study direction is not identified) | |
| Associative hypothesis | |
| - Describes variable interdependency | |
| - Change in one variable causes change in another variable | |
| A larger number of people vaccinated against COVID-19 in the region (change in independent variable) will reduce the region’s incidence of COVID-19 infection (change in dependent variable). | |
| Causal hypothesis | |
| - An effect on dependent variable is predicted from manipulation of independent variable | |
| A change into a high-fiber diet (independent variable) will reduce the blood sugar level (dependent variable) of the patient. | |
| Null hypothesis | |
| - A negative statement indicating no relationship or difference between 2 variables | |
| There is no significant difference in the severity of pulmonary metastases between the new drug (variable 1) and the current drug (variable 2). | |
| Alternative hypothesis | |
| - Following a null hypothesis, an alternative hypothesis predicts a relationship between 2 study variables | |
| The new drug (variable 1) is better on average in reducing the level of pain from pulmonary metastasis than the current drug (variable 2). | |
| Working hypothesis | |
| - A hypothesis that is initially accepted for further research to produce a feasible theory | |
| Dairy cows fed with concentrates of different formulations will produce different amounts of milk. | |
| Statistical hypothesis | |
| - Assumption about the value of population parameter or relationship among several population characteristics | |
| - Validity tested by a statistical experiment or analysis | |
| The mean recovery rate from COVID-19 infection (value of population parameter) is not significantly different between population 1 and population 2. | |
| There is a positive correlation between the level of stress at the workplace and the number of suicides (population characteristics) among working people in Japan. | |
| Logical hypothesis | |
| - Offers or proposes an explanation with limited or no extensive evidence | |
| If healthcare workers provide more educational programs about contraception methods, the number of adolescent pregnancies will be less. | |
| Hypothesis-testing (Quantitative hypothesis-testing research) | |
| - Quantitative research uses deductive reasoning. | |
| - This involves the formation of a hypothesis, collection of data in the investigation of the problem, analysis and use of the data from the investigation, and drawing of conclusions to validate or nullify the hypotheses. | |
Research questions in qualitative research
Unlike research questions in quantitative research, research questions in qualitative research are usually continuously reviewed and reformulated. The central question and associated subquestions are stated more than the hypotheses. 15 The central question broadly explores a complex set of factors surrounding the central phenomenon, aiming to present the varied perspectives of participants. 15
There are varied goals for which qualitative research questions are developed. These questions can function in several ways, such as to 1) identify and describe existing conditions ( contextual research question s); 2) describe a phenomenon ( descriptive research questions ); 3) assess the effectiveness of existing methods, protocols, theories, or procedures ( evaluation research questions ); 4) examine a phenomenon or analyze the reasons or relationships between subjects or phenomena ( explanatory research questions ); or 5) focus on unknown aspects of a particular topic ( exploratory research questions ). 5 In addition, some qualitative research questions provide new ideas for the development of theories and actions ( generative research questions ) or advance specific ideologies of a position ( ideological research questions ). 1 Other qualitative research questions may build on a body of existing literature and become working guidelines ( ethnographic research questions ). Research questions may also be broadly stated without specific reference to the existing literature or a typology of questions ( phenomenological research questions ), may be directed towards generating a theory of some process ( grounded theory questions ), or may address a description of the case and the emerging themes ( qualitative case study questions ). 15 We provide examples of contextual, descriptive, evaluation, explanatory, exploratory, generative, ideological, ethnographic, phenomenological, grounded theory, and qualitative case study research questions in qualitative research in Table 4 , and the definition of qualitative hypothesis-generating research in Table 5 .
| Qualitative research questions | |
|---|---|
| Contextual research question | |
| - Ask the nature of what already exists | |
| - Individuals or groups function to further clarify and understand the natural context of real-world problems | |
| What are the experiences of nurses working night shifts in healthcare during the COVID-19 pandemic? (natural context of real-world problems) | |
| Descriptive research question | |
| - Aims to describe a phenomenon | |
| What are the different forms of disrespect and abuse (phenomenon) experienced by Tanzanian women when giving birth in healthcare facilities? | |
| Evaluation research question | |
| - Examines the effectiveness of existing practice or accepted frameworks | |
| How effective are decision aids (effectiveness of existing practice) in helping decide whether to give birth at home or in a healthcare facility? | |
| Explanatory research question | |
| - Clarifies a previously studied phenomenon and explains why it occurs | |
| Why is there an increase in teenage pregnancy (phenomenon) in Tanzania? | |
| Exploratory research question | |
| - Explores areas that have not been fully investigated to have a deeper understanding of the research problem | |
| What factors affect the mental health of medical students (areas that have not yet been fully investigated) during the COVID-19 pandemic? | |
| Generative research question | |
| - Develops an in-depth understanding of people’s behavior by asking ‘how would’ or ‘what if’ to identify problems and find solutions | |
| How would the extensive research experience of the behavior of new staff impact the success of the novel drug initiative? | |
| Ideological research question | |
| - Aims to advance specific ideas or ideologies of a position | |
| Are Japanese nurses who volunteer in remote African hospitals able to promote humanized care of patients (specific ideas or ideologies) in the areas of safe patient environment, respect of patient privacy, and provision of accurate information related to health and care? | |
| Ethnographic research question | |
| - Clarifies peoples’ nature, activities, their interactions, and the outcomes of their actions in specific settings | |
| What are the demographic characteristics, rehabilitative treatments, community interactions, and disease outcomes (nature, activities, their interactions, and the outcomes) of people in China who are suffering from pneumoconiosis? | |
| Phenomenological research question | |
| - Knows more about the phenomena that have impacted an individual | |
| What are the lived experiences of parents who have been living with and caring for children with a diagnosis of autism? (phenomena that have impacted an individual) | |
| Grounded theory question | |
| - Focuses on social processes asking about what happens and how people interact, or uncovering social relationships and behaviors of groups | |
| What are the problems that pregnant adolescents face in terms of social and cultural norms (social processes), and how can these be addressed? | |
| Qualitative case study question | |
| - Assesses a phenomenon using different sources of data to answer “why” and “how” questions | |
| - Considers how the phenomenon is influenced by its contextual situation. | |
| How does quitting work and assuming the role of a full-time mother (phenomenon assessed) change the lives of women in Japan? | |
| Qualitative research hypotheses | |
|---|---|
| Hypothesis-generating (Qualitative hypothesis-generating research) | |
| - Qualitative research uses inductive reasoning. | |
| - This involves data collection from study participants or the literature regarding a phenomenon of interest, using the collected data to develop a formal hypothesis, and using the formal hypothesis as a framework for testing the hypothesis. | |
| - Qualitative exploratory studies explore areas deeper, clarifying subjective experience and allowing formulation of a formal hypothesis potentially testable in a future quantitative approach. | |
Qualitative studies usually pose at least one central research question and several subquestions starting with How or What . These research questions use exploratory verbs such as explore or describe . These also focus on one central phenomenon of interest, and may mention the participants and research site. 15
Hypotheses in qualitative research
Hypotheses in qualitative research are stated in the form of a clear statement concerning the problem to be investigated. Unlike in quantitative research where hypotheses are usually developed to be tested, qualitative research can lead to both hypothesis-testing and hypothesis-generating outcomes. 2 When studies require both quantitative and qualitative research questions, this suggests an integrative process between both research methods wherein a single mixed-methods research question can be developed. 1
FRAMEWORKS FOR DEVELOPING RESEARCH QUESTIONS AND HYPOTHESES
Research questions followed by hypotheses should be developed before the start of the study. 1 , 12 , 14 It is crucial to develop feasible research questions on a topic that is interesting to both the researcher and the scientific community. This can be achieved by a meticulous review of previous and current studies to establish a novel topic. Specific areas are subsequently focused on to generate ethical research questions. The relevance of the research questions is evaluated in terms of clarity of the resulting data, specificity of the methodology, objectivity of the outcome, depth of the research, and impact of the study. 1 , 5 These aspects constitute the FINER criteria (i.e., Feasible, Interesting, Novel, Ethical, and Relevant). 1 Clarity and effectiveness are achieved if research questions meet the FINER criteria. In addition to the FINER criteria, Ratan et al. described focus, complexity, novelty, feasibility, and measurability for evaluating the effectiveness of research questions. 14
The PICOT and PEO frameworks are also used when developing research questions. 1 The following elements are addressed in these frameworks, PICOT: P-population/patients/problem, I-intervention or indicator being studied, C-comparison group, O-outcome of interest, and T-timeframe of the study; PEO: P-population being studied, E-exposure to preexisting conditions, and O-outcome of interest. 1 Research questions are also considered good if these meet the “FINERMAPS” framework: Feasible, Interesting, Novel, Ethical, Relevant, Manageable, Appropriate, Potential value/publishable, and Systematic. 14
As we indicated earlier, research questions and hypotheses that are not carefully formulated result in unethical studies or poor outcomes. To illustrate this, we provide some examples of ambiguous research question and hypotheses that result in unclear and weak research objectives in quantitative research ( Table 6 ) 16 and qualitative research ( Table 7 ) 17 , and how to transform these ambiguous research question(s) and hypothesis(es) into clear and good statements.
| Variables | Unclear and weak statement (Statement 1) | Clear and good statement (Statement 2) | Points to avoid |
|---|---|---|---|
| Research question | Which is more effective between smoke moxibustion and smokeless moxibustion? | “Moreover, regarding smoke moxibustion versus smokeless moxibustion, it remains unclear which is more effective, safe, and acceptable to pregnant women, and whether there is any difference in the amount of heat generated.” | 1) Vague and unfocused questions |
| 2) Closed questions simply answerable by yes or no | |||
| 3) Questions requiring a simple choice | |||
| Hypothesis | The smoke moxibustion group will have higher cephalic presentation. | “Hypothesis 1. The smoke moxibustion stick group (SM group) and smokeless moxibustion stick group (-SLM group) will have higher rates of cephalic presentation after treatment than the control group. | 1) Unverifiable hypotheses |
| Hypothesis 2. The SM group and SLM group will have higher rates of cephalic presentation at birth than the control group. | 2) Incompletely stated groups of comparison | ||
| Hypothesis 3. There will be no significant differences in the well-being of the mother and child among the three groups in terms of the following outcomes: premature birth, premature rupture of membranes (PROM) at < 37 weeks, Apgar score < 7 at 5 min, umbilical cord blood pH < 7.1, admission to neonatal intensive care unit (NICU), and intrauterine fetal death.” | 3) Insufficiently described variables or outcomes | ||
| Research objective | To determine which is more effective between smoke moxibustion and smokeless moxibustion. | “The specific aims of this pilot study were (a) to compare the effects of smoke moxibustion and smokeless moxibustion treatments with the control group as a possible supplement to ECV for converting breech presentation to cephalic presentation and increasing adherence to the newly obtained cephalic position, and (b) to assess the effects of these treatments on the well-being of the mother and child.” | 1) Poor understanding of the research question and hypotheses |
| 2) Insufficient description of population, variables, or study outcomes |
a These statements were composed for comparison and illustrative purposes only.
b These statements are direct quotes from Higashihara and Horiuchi. 16
| Variables | Unclear and weak statement (Statement 1) | Clear and good statement (Statement 2) | Points to avoid |
|---|---|---|---|
| Research question | Does disrespect and abuse (D&A) occur in childbirth in Tanzania? | How does disrespect and abuse (D&A) occur and what are the types of physical and psychological abuses observed in midwives’ actual care during facility-based childbirth in urban Tanzania? | 1) Ambiguous or oversimplistic questions |
| 2) Questions unverifiable by data collection and analysis | |||
| Hypothesis | Disrespect and abuse (D&A) occur in childbirth in Tanzania. | Hypothesis 1: Several types of physical and psychological abuse by midwives in actual care occur during facility-based childbirth in urban Tanzania. | 1) Statements simply expressing facts |
| Hypothesis 2: Weak nursing and midwifery management contribute to the D&A of women during facility-based childbirth in urban Tanzania. | 2) Insufficiently described concepts or variables | ||
| Research objective | To describe disrespect and abuse (D&A) in childbirth in Tanzania. | “This study aimed to describe from actual observations the respectful and disrespectful care received by women from midwives during their labor period in two hospitals in urban Tanzania.” | 1) Statements unrelated to the research question and hypotheses |
| 2) Unattainable or unexplorable objectives |
a This statement is a direct quote from Shimoda et al. 17
The other statements were composed for comparison and illustrative purposes only.
CONSTRUCTING RESEARCH QUESTIONS AND HYPOTHESES
To construct effective research questions and hypotheses, it is very important to 1) clarify the background and 2) identify the research problem at the outset of the research, within a specific timeframe. 9 Then, 3) review or conduct preliminary research to collect all available knowledge about the possible research questions by studying theories and previous studies. 18 Afterwards, 4) construct research questions to investigate the research problem. Identify variables to be accessed from the research questions 4 and make operational definitions of constructs from the research problem and questions. Thereafter, 5) construct specific deductive or inductive predictions in the form of hypotheses. 4 Finally, 6) state the study aims . This general flow for constructing effective research questions and hypotheses prior to conducting research is shown in Fig. 1 .

Research questions are used more frequently in qualitative research than objectives or hypotheses. 3 These questions seek to discover, understand, explore or describe experiences by asking “What” or “How.” The questions are open-ended to elicit a description rather than to relate variables or compare groups. The questions are continually reviewed, reformulated, and changed during the qualitative study. 3 Research questions are also used more frequently in survey projects than hypotheses in experiments in quantitative research to compare variables and their relationships.
Hypotheses are constructed based on the variables identified and as an if-then statement, following the template, ‘If a specific action is taken, then a certain outcome is expected.’ At this stage, some ideas regarding expectations from the research to be conducted must be drawn. 18 Then, the variables to be manipulated (independent) and influenced (dependent) are defined. 4 Thereafter, the hypothesis is stated and refined, and reproducible data tailored to the hypothesis are identified, collected, and analyzed. 4 The hypotheses must be testable and specific, 18 and should describe the variables and their relationships, the specific group being studied, and the predicted research outcome. 18 Hypotheses construction involves a testable proposition to be deduced from theory, and independent and dependent variables to be separated and measured separately. 3 Therefore, good hypotheses must be based on good research questions constructed at the start of a study or trial. 12
In summary, research questions are constructed after establishing the background of the study. Hypotheses are then developed based on the research questions. Thus, it is crucial to have excellent research questions to generate superior hypotheses. In turn, these would determine the research objectives and the design of the study, and ultimately, the outcome of the research. 12 Algorithms for building research questions and hypotheses are shown in Fig. 2 for quantitative research and in Fig. 3 for qualitative research.

EXAMPLES OF RESEARCH QUESTIONS FROM PUBLISHED ARTICLES
- EXAMPLE 1. Descriptive research question (quantitative research)
- - Presents research variables to be assessed (distinct phenotypes and subphenotypes)
- “BACKGROUND: Since COVID-19 was identified, its clinical and biological heterogeneity has been recognized. Identifying COVID-19 phenotypes might help guide basic, clinical, and translational research efforts.
- RESEARCH QUESTION: Does the clinical spectrum of patients with COVID-19 contain distinct phenotypes and subphenotypes? ” 19
- EXAMPLE 2. Relationship research question (quantitative research)
- - Shows interactions between dependent variable (static postural control) and independent variable (peripheral visual field loss)
- “Background: Integration of visual, vestibular, and proprioceptive sensations contributes to postural control. People with peripheral visual field loss have serious postural instability. However, the directional specificity of postural stability and sensory reweighting caused by gradual peripheral visual field loss remain unclear.
- Research question: What are the effects of peripheral visual field loss on static postural control ?” 20
- EXAMPLE 3. Comparative research question (quantitative research)
- - Clarifies the difference among groups with an outcome variable (patients enrolled in COMPERA with moderate PH or severe PH in COPD) and another group without the outcome variable (patients with idiopathic pulmonary arterial hypertension (IPAH))
- “BACKGROUND: Pulmonary hypertension (PH) in COPD is a poorly investigated clinical condition.
- RESEARCH QUESTION: Which factors determine the outcome of PH in COPD?
- STUDY DESIGN AND METHODS: We analyzed the characteristics and outcome of patients enrolled in the Comparative, Prospective Registry of Newly Initiated Therapies for Pulmonary Hypertension (COMPERA) with moderate or severe PH in COPD as defined during the 6th PH World Symposium who received medical therapy for PH and compared them with patients with idiopathic pulmonary arterial hypertension (IPAH) .” 21
- EXAMPLE 4. Exploratory research question (qualitative research)
- - Explores areas that have not been fully investigated (perspectives of families and children who receive care in clinic-based child obesity treatment) to have a deeper understanding of the research problem
- “Problem: Interventions for children with obesity lead to only modest improvements in BMI and long-term outcomes, and data are limited on the perspectives of families of children with obesity in clinic-based treatment. This scoping review seeks to answer the question: What is known about the perspectives of families and children who receive care in clinic-based child obesity treatment? This review aims to explore the scope of perspectives reported by families of children with obesity who have received individualized outpatient clinic-based obesity treatment.” 22
- EXAMPLE 5. Relationship research question (quantitative research)
- - Defines interactions between dependent variable (use of ankle strategies) and independent variable (changes in muscle tone)
- “Background: To maintain an upright standing posture against external disturbances, the human body mainly employs two types of postural control strategies: “ankle strategy” and “hip strategy.” While it has been reported that the magnitude of the disturbance alters the use of postural control strategies, it has not been elucidated how the level of muscle tone, one of the crucial parameters of bodily function, determines the use of each strategy. We have previously confirmed using forward dynamics simulations of human musculoskeletal models that an increased muscle tone promotes the use of ankle strategies. The objective of the present study was to experimentally evaluate a hypothesis: an increased muscle tone promotes the use of ankle strategies. Research question: Do changes in the muscle tone affect the use of ankle strategies ?” 23
EXAMPLES OF HYPOTHESES IN PUBLISHED ARTICLES
- EXAMPLE 1. Working hypothesis (quantitative research)
- - A hypothesis that is initially accepted for further research to produce a feasible theory
- “As fever may have benefit in shortening the duration of viral illness, it is plausible to hypothesize that the antipyretic efficacy of ibuprofen may be hindering the benefits of a fever response when taken during the early stages of COVID-19 illness .” 24
- “In conclusion, it is plausible to hypothesize that the antipyretic efficacy of ibuprofen may be hindering the benefits of a fever response . The difference in perceived safety of these agents in COVID-19 illness could be related to the more potent efficacy to reduce fever with ibuprofen compared to acetaminophen. Compelling data on the benefit of fever warrant further research and review to determine when to treat or withhold ibuprofen for early stage fever for COVID-19 and other related viral illnesses .” 24
- EXAMPLE 2. Exploratory hypothesis (qualitative research)
- - Explores particular areas deeper to clarify subjective experience and develop a formal hypothesis potentially testable in a future quantitative approach
- “We hypothesized that when thinking about a past experience of help-seeking, a self distancing prompt would cause increased help-seeking intentions and more favorable help-seeking outcome expectations .” 25
- “Conclusion
- Although a priori hypotheses were not supported, further research is warranted as results indicate the potential for using self-distancing approaches to increasing help-seeking among some people with depressive symptomatology.” 25
- EXAMPLE 3. Hypothesis-generating research to establish a framework for hypothesis testing (qualitative research)
- “We hypothesize that compassionate care is beneficial for patients (better outcomes), healthcare systems and payers (lower costs), and healthcare providers (lower burnout). ” 26
- Compassionomics is the branch of knowledge and scientific study of the effects of compassionate healthcare. Our main hypotheses are that compassionate healthcare is beneficial for (1) patients, by improving clinical outcomes, (2) healthcare systems and payers, by supporting financial sustainability, and (3) HCPs, by lowering burnout and promoting resilience and well-being. The purpose of this paper is to establish a scientific framework for testing the hypotheses above . If these hypotheses are confirmed through rigorous research, compassionomics will belong in the science of evidence-based medicine, with major implications for all healthcare domains.” 26
- EXAMPLE 4. Statistical hypothesis (quantitative research)
- - An assumption is made about the relationship among several population characteristics ( gender differences in sociodemographic and clinical characteristics of adults with ADHD ). Validity is tested by statistical experiment or analysis ( chi-square test, Students t-test, and logistic regression analysis)
- “Our research investigated gender differences in sociodemographic and clinical characteristics of adults with ADHD in a Japanese clinical sample. Due to unique Japanese cultural ideals and expectations of women's behavior that are in opposition to ADHD symptoms, we hypothesized that women with ADHD experience more difficulties and present more dysfunctions than men . We tested the following hypotheses: first, women with ADHD have more comorbidities than men with ADHD; second, women with ADHD experience more social hardships than men, such as having less full-time employment and being more likely to be divorced.” 27
- “Statistical Analysis
- ( text omitted ) Between-gender comparisons were made using the chi-squared test for categorical variables and Students t-test for continuous variables…( text omitted ). A logistic regression analysis was performed for employment status, marital status, and comorbidity to evaluate the independent effects of gender on these dependent variables.” 27
EXAMPLES OF HYPOTHESIS AS WRITTEN IN PUBLISHED ARTICLES IN RELATION TO OTHER PARTS
- EXAMPLE 1. Background, hypotheses, and aims are provided
- “Pregnant women need skilled care during pregnancy and childbirth, but that skilled care is often delayed in some countries …( text omitted ). The focused antenatal care (FANC) model of WHO recommends that nurses provide information or counseling to all pregnant women …( text omitted ). Job aids are visual support materials that provide the right kind of information using graphics and words in a simple and yet effective manner. When nurses are not highly trained or have many work details to attend to, these job aids can serve as a content reminder for the nurses and can be used for educating their patients (Jennings, Yebadokpo, Affo, & Agbogbe, 2010) ( text omitted ). Importantly, additional evidence is needed to confirm how job aids can further improve the quality of ANC counseling by health workers in maternal care …( text omitted )” 28
- “ This has led us to hypothesize that the quality of ANC counseling would be better if supported by job aids. Consequently, a better quality of ANC counseling is expected to produce higher levels of awareness concerning the danger signs of pregnancy and a more favorable impression of the caring behavior of nurses .” 28
- “This study aimed to examine the differences in the responses of pregnant women to a job aid-supported intervention during ANC visit in terms of 1) their understanding of the danger signs of pregnancy and 2) their impression of the caring behaviors of nurses to pregnant women in rural Tanzania.” 28
- EXAMPLE 2. Background, hypotheses, and aims are provided
- “We conducted a two-arm randomized controlled trial (RCT) to evaluate and compare changes in salivary cortisol and oxytocin levels of first-time pregnant women between experimental and control groups. The women in the experimental group touched and held an infant for 30 min (experimental intervention protocol), whereas those in the control group watched a DVD movie of an infant (control intervention protocol). The primary outcome was salivary cortisol level and the secondary outcome was salivary oxytocin level.” 29
- “ We hypothesize that at 30 min after touching and holding an infant, the salivary cortisol level will significantly decrease and the salivary oxytocin level will increase in the experimental group compared with the control group .” 29
- EXAMPLE 3. Background, aim, and hypothesis are provided
- “In countries where the maternal mortality ratio remains high, antenatal education to increase Birth Preparedness and Complication Readiness (BPCR) is considered one of the top priorities [1]. BPCR includes birth plans during the antenatal period, such as the birthplace, birth attendant, transportation, health facility for complications, expenses, and birth materials, as well as family coordination to achieve such birth plans. In Tanzania, although increasing, only about half of all pregnant women attend an antenatal clinic more than four times [4]. Moreover, the information provided during antenatal care (ANC) is insufficient. In the resource-poor settings, antenatal group education is a potential approach because of the limited time for individual counseling at antenatal clinics.” 30
- “This study aimed to evaluate an antenatal group education program among pregnant women and their families with respect to birth-preparedness and maternal and infant outcomes in rural villages of Tanzania.” 30
- “ The study hypothesis was if Tanzanian pregnant women and their families received a family-oriented antenatal group education, they would (1) have a higher level of BPCR, (2) attend antenatal clinic four or more times, (3) give birth in a health facility, (4) have less complications of women at birth, and (5) have less complications and deaths of infants than those who did not receive the education .” 30
Research questions and hypotheses are crucial components to any type of research, whether quantitative or qualitative. These questions should be developed at the very beginning of the study. Excellent research questions lead to superior hypotheses, which, like a compass, set the direction of research, and can often determine the successful conduct of the study. Many research studies have floundered because the development of research questions and subsequent hypotheses was not given the thought and meticulous attention needed. The development of research questions and hypotheses is an iterative process based on extensive knowledge of the literature and insightful grasp of the knowledge gap. Focused, concise, and specific research questions provide a strong foundation for constructing hypotheses which serve as formal predictions about the research outcomes. Research questions and hypotheses are crucial elements of research that should not be overlooked. They should be carefully thought of and constructed when planning research. This avoids unethical studies and poor outcomes by defining well-founded objectives that determine the design, course, and outcome of the study.
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions:
- Conceptualization: Barroga E, Matanguihan GJ.
- Methodology: Barroga E, Matanguihan GJ.
- Writing - original draft: Barroga E, Matanguihan GJ.
- Writing - review & editing: Barroga E, Matanguihan GJ.

Organizing Academic Research Papers: 9. The Conclusion
- Purpose of Guide
- Design Flaws to Avoid
- Glossary of Research Terms
- Narrowing a Topic Idea
- Broadening a Topic Idea
- Extending the Timeliness of a Topic Idea
- Academic Writing Style
- Choosing a Title
- Making an Outline
- Paragraph Development
- Executive Summary
- Background Information
- The Research Problem/Question
- Theoretical Framework
- Citation Tracking
- Content Alert Services
- Evaluating Sources
- Primary Sources
- Secondary Sources
- Tertiary Sources
- What Is Scholarly vs. Popular?
- Qualitative Methods
- Quantitative Methods
- Using Non-Textual Elements
- Limitations of the Study
- Common Grammar Mistakes
- Avoiding Plagiarism
- Footnotes or Endnotes?
- Further Readings
- Annotated Bibliography
- Dealing with Nervousness
- Using Visual Aids
- Grading Someone Else's Paper
- How to Manage Group Projects
- Multiple Book Review Essay
- Reviewing Collected Essays
- About Informed Consent
- Writing Field Notes
- Writing a Policy Memo
- Writing a Research Proposal
- Acknowledgements
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of your points or a re-statement of your research problem but a synthesis of key points. For most essays, one well-developed paragraph is sufficient for a conclusion, although in some cases, a two-or-three paragraph conclusion may be required.
Importance of a Good Conclusion
A well-written conclusion provides you with several important opportunities to demonstrate your overall understanding of the research problem to the reader. These include:
- Presenting the last word on the issues you raised in your paper . Just as the introduction gives a first impression to your reader, the conclusion offers a chance to leave a lasting impression. Do this, for example, by highlighting key points in your analysis or findings.
- Summarizing your thoughts and conveying the larger implications of your study . The conclusion is an opportunity to succinctly answer the "so what?" question by placing the study within the context of past research about the topic you've investigated.
- Demonstrating the importance of your ideas . Don't be shy. The conclusion offers you a chance to elaborate on the significance of your findings.
- Introducing possible new or expanded ways of thinking about the research problem . This does not refer to introducing new information [which should be avoided], but to offer new insight and creative approaches for framing/contextualizing the research problem based on the results of your study.
Conclusions . The Writing Center. University of North Carolina; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion . San Francisco Edit, 2003-2008.
Structure and Writing Style
https://writing.wisc.edu/wp-content/uploads/sites/535/2018/07/conclusions_uwmadison_writingcenter_aug2012.pdf I. General Rules
When writing the conclusion to your paper, follow these general rules:
- State your conclusions in clear, simple language.
- Do not simply reiterate your results or the discussion.
- Indicate opportunities for future research, as long as you haven't already done so in the discussion section of your paper.
The function of your paper's conclusion is to restate the main argument . It reminds the reader of the strengths of your main argument(s) and reiterates the most important evidence supporting those argument(s). Make sure, however, that your conclusion is not simply a repetitive summary of the findings because this reduces the impact of the argument(s) you have developed in your essay.
Consider the following points to help ensure your conclusion is appropriate:
- If the argument or point of your paper is complex, you may need to summarize the argument for your reader.
- If, prior to your conclusion, you have not yet explained the significance of your findings or if you are proceeding inductively, use the end of your paper to describe your main points and explain their significance.
- Move from a detailed to a general level of consideration that returns the topic to the context provided by the introduction or within a new context that emerges from the data.
The conclusion also provides a place for you to persuasively and succinctly restate your research problem, given that the reader has now been presented with all the information about the topic . Depending on the discipline you are writing in, the concluding paragraph may contain your reflections on the evidence presented, or on the essay's central research problem. However, the nature of being introspective about the research you have done will depend on the topic and whether your professor wants you to express your observations in this way.
NOTE : Don't delve into idle speculation. Being introspective means looking within yourself as an author to try and understand an issue more deeply not to guess at possible outcomes.
II. Developing a Compelling Conclusion
Strategies to help you move beyond merely summarizing the key points of your research paper may include any of the following.
- If your essay deals with a contemporary problem, warn readers of the possible consequences of not attending to the problem.
- Recommend a specific course or courses of action.
- Cite a relevant quotation or expert opinion to lend authority to the conclusion you have reached [a good place to look is research from your literature review].
- Restate a key statistic, fact, or visual image to drive home the ultimate point of your paper.
- If your discipline encourages personal reflection, illustrate your concluding point with a relevant narrative drawn from your own life experiences.
- Return to an anecdote, an example, or a quotation that you introduced in your introduction, but add further insight that is derived from the findings of your study; use your interpretation of results to reframe it in new ways.
- Provide a "take-home" message in the form of a strong, succient statement that you want the reader to remember about your study.
III. Problems to Avoid Failure to be concise The conclusion section should be concise and to the point. Conclusions that are too long often have unnecessary detail. The conclusion section is not the place for details about your methodology or results. Although you should give a summary of what was learned from your research, this summary should be relatively brief, since the emphasis in the conclusion is on the implications, evaluations, insights, etc. that you make. Failure to comment on larger, more significant issues In the introduction, your task was to move from general [the field of study] to specific [your research problem]. However, in the conclusion, your task is to move from specific [your research problem] back to general [your field, i.e., how your research contributes new understanding or fills an important gap in the literature]. In other words, the conclusion is where you place your research within a larger context. Failure to reveal problems and negative results Negative aspects of the research process should never be ignored. Problems, drawbacks, and challenges encountered during your study should be included as a way of qualifying your overall conclusions. If you encountered negative results [findings that are validated outside the research context in which they were generated], you must report them in the results section of your paper. In the conclusion, use the negative results as an opportunity to explain how they provide information on which future research can be based. Failure to provide a clear summary of what was learned In order to be able to discuss how your research fits back into your field of study [and possibly the world at large], you need to summarize it briefly and directly. Often this element of your conclusion is only a few sentences long. Failure to match the objectives of your research Often research objectives change while the research is being carried out. This is not a problem unless you forget to go back and refine your original objectives in your introduction, as these changes emerge they must be documented so that they accurately reflect what you were trying to accomplish in your research [not what you thought you might accomplish when you began].
Resist the urge to apologize If you've immersed yourself in studying the research problem, you now know a good deal about it, perhaps even more than your professor! Nevertheless, by the time you have finished writing, you may be having some doubts about what you have produced. Repress those doubts! Don't undermine your authority by saying something like, "This is just one approach to examining this problem; there may be other, much better approaches...."
Concluding Paragraphs. College Writing Center at Meramec. St. Louis Community College; Conclusions . The Writing Center. University of North Carolina; Conclusions . The Writing Lab and The OWL. Purdue University; Freedman, Leora and Jerry Plotnick. Introductions and Conclusions . The Lab Report. University College Writing Centre. University of Toronto; Leibensperger, Summer. Draft Your Conclusion. Academic Center, the University of Houston-Victoria, 2003; Make Your Last Words Count . The Writer’s Handbook. Writing Center. University of Wisconsin, Madison; Tips for Writing a Good Conclusion . Writing@CSU. Colorado State University; Kretchmer, Paul. Twelve Steps to Writing an Effective Conclusion . San Francisco Edit, 2003-2008; Writing Conclusions . Writing Tutorial Services, Center for Innovative Teaching and Learning. Indiana University; Writing: Considering Structure and Organization . Institute for Writing Rhetoric. Dartmouth College.
Writing Tip
Don't Belabor the Obvious!
Avoid phrases like "in conclusion...," "in summary...," or "in closing...." These phrases can be useful, even welcome, in oral presentations. But readers can see by the tell-tale section heading and number of pages remaining to read, when an essay is about to end. You'll irritate your readers if you belabor the obvious.
Another Writing Tip
New Insight, Not New Information!
Don't surprise the reader with new information in your Conclusion that was never referenced anywhere else in the paper. If you have new information to present, add it to the Discussion or other appropriate section of the paper. Note that, although no actual new information is introduced, the conclusion is where you offer your most "original" contributions in the paper; it's where you describe the value of your research, demonstrate your understanding of the material that you’ve presented, and locate your findings within the larger context of scholarship on the topic.
- << Previous: Limitations of the Study
- Next: Appendices >>
- Last Updated: Jul 18, 2023 11:58 AM
- URL: https://library.sacredheart.edu/c.php?g=29803
- QuickSearch
- Library Catalog
- Databases A-Z
- Publication Finder
- Course Reserves
- Citation Linker
- Digital Commons
- Our Website
Research Support
- Ask a Librarian
- Appointments
- Interlibrary Loan (ILL)
- Research Guides
- Databases by Subject
- Citation Help
Using the Library
- Reserve a Group Study Room
- Renew Books
- Honors Study Rooms
- Off-Campus Access
- Library Policies
- Library Technology
User Information
- Grad Students
- Online Students
- COVID-19 Updates
- Staff Directory
- News & Announcements
- Library Newsletter
My Accounts
- Interlibrary Loan
- Staff Site Login
FIND US ON
Research Hypothesis In Psychology: Types, & Examples
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
A research hypothesis, in its plural form “hypotheses,” is a specific, testable prediction about the anticipated results of a study, established at its outset. It is a key component of the scientific method .
Hypotheses connect theory to data and guide the research process towards expanding scientific understanding
Some key points about hypotheses:
- A hypothesis expresses an expected pattern or relationship. It connects the variables under investigation.
- It is stated in clear, precise terms before any data collection or analysis occurs. This makes the hypothesis testable.
- A hypothesis must be falsifiable. It should be possible, even if unlikely in practice, to collect data that disconfirms rather than supports the hypothesis.
- Hypotheses guide research. Scientists design studies to explicitly evaluate hypotheses about how nature works.
- For a hypothesis to be valid, it must be testable against empirical evidence. The evidence can then confirm or disprove the testable predictions.
- Hypotheses are informed by background knowledge and observation, but go beyond what is already known to propose an explanation of how or why something occurs.
Predictions typically arise from a thorough knowledge of the research literature, curiosity about real-world problems or implications, and integrating this to advance theory. They build on existing literature while providing new insight.
Types of Research Hypotheses
Alternative hypothesis.
The research hypothesis is often called the alternative or experimental hypothesis in experimental research.
It typically suggests a potential relationship between two key variables: the independent variable, which the researcher manipulates, and the dependent variable, which is measured based on those changes.
The alternative hypothesis states a relationship exists between the two variables being studied (one variable affects the other).
A hypothesis is a testable statement or prediction about the relationship between two or more variables. It is a key component of the scientific method. Some key points about hypotheses:
- Important hypotheses lead to predictions that can be tested empirically. The evidence can then confirm or disprove the testable predictions.
In summary, a hypothesis is a precise, testable statement of what researchers expect to happen in a study and why. Hypotheses connect theory to data and guide the research process towards expanding scientific understanding.
An experimental hypothesis predicts what change(s) will occur in the dependent variable when the independent variable is manipulated.
It states that the results are not due to chance and are significant in supporting the theory being investigated.
The alternative hypothesis can be directional, indicating a specific direction of the effect, or non-directional, suggesting a difference without specifying its nature. It’s what researchers aim to support or demonstrate through their study.

Null Hypothesis
The null hypothesis states no relationship exists between the two variables being studied (one variable does not affect the other). There will be no changes in the dependent variable due to manipulating the independent variable.
It states results are due to chance and are not significant in supporting the idea being investigated.
The null hypothesis, positing no effect or relationship, is a foundational contrast to the research hypothesis in scientific inquiry. It establishes a baseline for statistical testing, promoting objectivity by initiating research from a neutral stance.
Many statistical methods are tailored to test the null hypothesis, determining the likelihood of observed results if no true effect exists.
This dual-hypothesis approach provides clarity, ensuring that research intentions are explicit, and fosters consistency across scientific studies, enhancing the standardization and interpretability of research outcomes.
Nondirectional Hypothesis
A non-directional hypothesis, also known as a two-tailed hypothesis, predicts that there is a difference or relationship between two variables but does not specify the direction of this relationship.
It merely indicates that a change or effect will occur without predicting which group will have higher or lower values.
For example, “There is a difference in performance between Group A and Group B” is a non-directional hypothesis.
Directional Hypothesis
A directional (one-tailed) hypothesis predicts the nature of the effect of the independent variable on the dependent variable. It predicts in which direction the change will take place. (i.e., greater, smaller, less, more)
It specifies whether one variable is greater, lesser, or different from another, rather than just indicating that there’s a difference without specifying its nature.
For example, “Exercise increases weight loss” is a directional hypothesis.
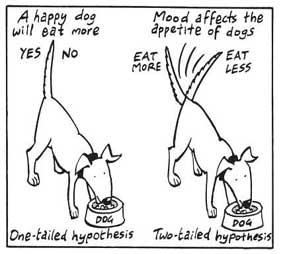
Falsifiability
The Falsification Principle, proposed by Karl Popper , is a way of demarcating science from non-science. It suggests that for a theory or hypothesis to be considered scientific, it must be testable and irrefutable.
Falsifiability emphasizes that scientific claims shouldn’t just be confirmable but should also have the potential to be proven wrong.
It means that there should exist some potential evidence or experiment that could prove the proposition false.
However many confirming instances exist for a theory, it only takes one counter observation to falsify it. For example, the hypothesis that “all swans are white,” can be falsified by observing a black swan.
For Popper, science should attempt to disprove a theory rather than attempt to continually provide evidence to support a research hypothesis.
Can a Hypothesis be Proven?
Hypotheses make probabilistic predictions. They state the expected outcome if a particular relationship exists. However, a study result supporting a hypothesis does not definitively prove it is true.
All studies have limitations. There may be unknown confounding factors or issues that limit the certainty of conclusions. Additional studies may yield different results.
In science, hypotheses can realistically only be supported with some degree of confidence, not proven. The process of science is to incrementally accumulate evidence for and against hypothesized relationships in an ongoing pursuit of better models and explanations that best fit the empirical data. But hypotheses remain open to revision and rejection if that is where the evidence leads.
- Disproving a hypothesis is definitive. Solid disconfirmatory evidence will falsify a hypothesis and require altering or discarding it based on the evidence.
- However, confirming evidence is always open to revision. Other explanations may account for the same results, and additional or contradictory evidence may emerge over time.
We can never 100% prove the alternative hypothesis. Instead, we see if we can disprove, or reject the null hypothesis.
If we reject the null hypothesis, this doesn’t mean that our alternative hypothesis is correct but does support the alternative/experimental hypothesis.
Upon analysis of the results, an alternative hypothesis can be rejected or supported, but it can never be proven to be correct. We must avoid any reference to results proving a theory as this implies 100% certainty, and there is always a chance that evidence may exist which could refute a theory.
How to Write a Hypothesis
- Identify variables . The researcher manipulates the independent variable and the dependent variable is the measured outcome.
- Operationalized the variables being investigated . Operationalization of a hypothesis refers to the process of making the variables physically measurable or testable, e.g. if you are about to study aggression, you might count the number of punches given by participants.
- Decide on a direction for your prediction . If there is evidence in the literature to support a specific effect of the independent variable on the dependent variable, write a directional (one-tailed) hypothesis. If there are limited or ambiguous findings in the literature regarding the effect of the independent variable on the dependent variable, write a non-directional (two-tailed) hypothesis.
- Make it Testable : Ensure your hypothesis can be tested through experimentation or observation. It should be possible to prove it false (principle of falsifiability).
- Clear & concise language . A strong hypothesis is concise (typically one to two sentences long), and formulated using clear and straightforward language, ensuring it’s easily understood and testable.
Consider a hypothesis many teachers might subscribe to: students work better on Monday morning than on Friday afternoon (IV=Day, DV= Standard of work).
Now, if we decide to study this by giving the same group of students a lesson on a Monday morning and a Friday afternoon and then measuring their immediate recall of the material covered in each session, we would end up with the following:
- The alternative hypothesis states that students will recall significantly more information on a Monday morning than on a Friday afternoon.
- The null hypothesis states that there will be no significant difference in the amount recalled on a Monday morning compared to a Friday afternoon. Any difference will be due to chance or confounding factors.
More Examples
- Memory : Participants exposed to classical music during study sessions will recall more items from a list than those who studied in silence.
- Social Psychology : Individuals who frequently engage in social media use will report higher levels of perceived social isolation compared to those who use it infrequently.
- Developmental Psychology : Children who engage in regular imaginative play have better problem-solving skills than those who don’t.
- Clinical Psychology : Cognitive-behavioral therapy will be more effective in reducing symptoms of anxiety over a 6-month period compared to traditional talk therapy.
- Cognitive Psychology : Individuals who multitask between various electronic devices will have shorter attention spans on focused tasks than those who single-task.
- Health Psychology : Patients who practice mindfulness meditation will experience lower levels of chronic pain compared to those who don’t meditate.
- Organizational Psychology : Employees in open-plan offices will report higher levels of stress than those in private offices.
- Behavioral Psychology : Rats rewarded with food after pressing a lever will press it more frequently than rats who receive no reward.
Related Articles
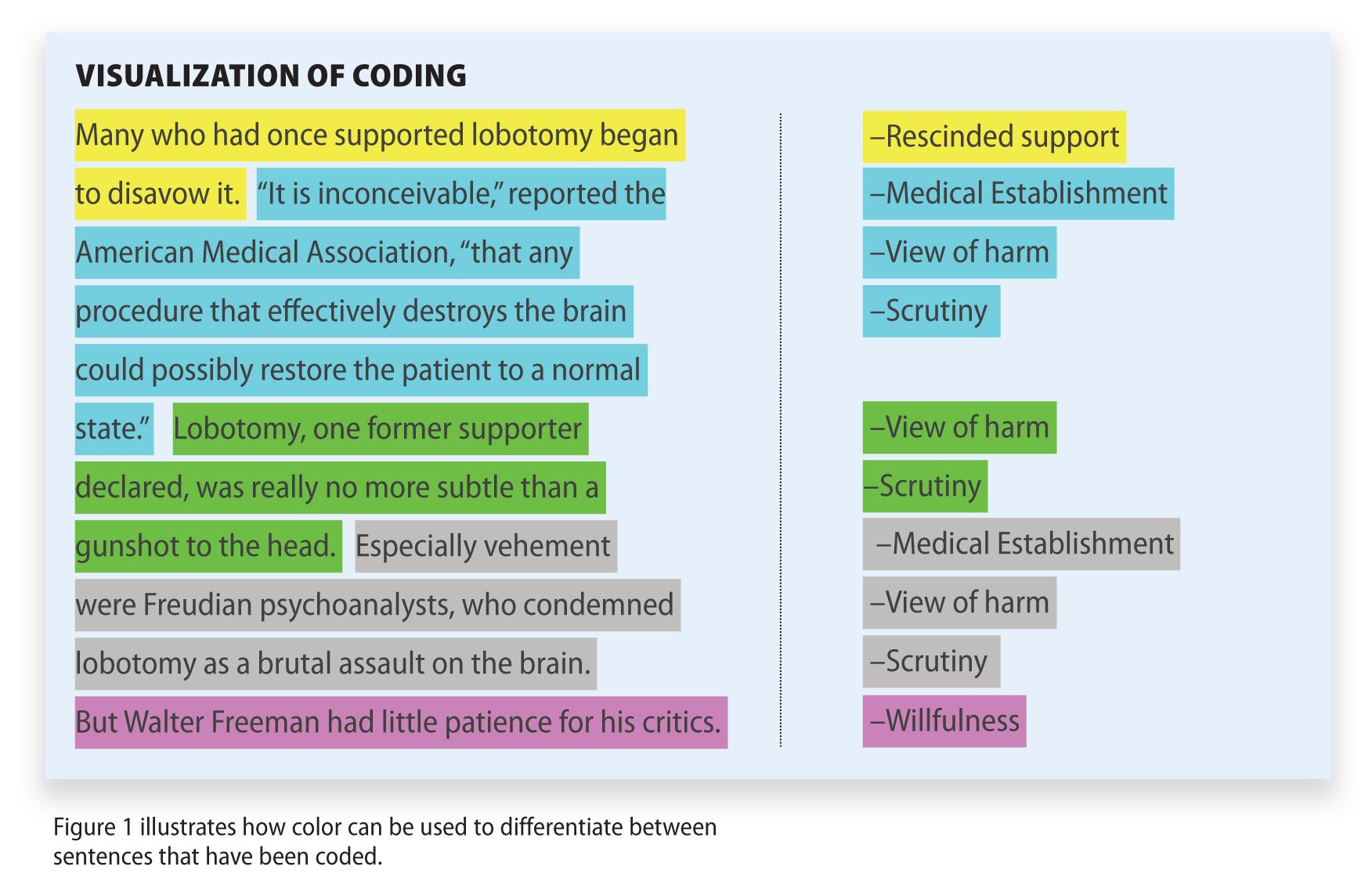
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
- Open access
- Published: 01 July 2022
Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden
- Lena Petersson 1 ,
- Ingrid Larsson 1 ,
- Jens M. Nygren 1 ,
- Per Nilsen 1 , 2 ,
- Margit Neher 1 , 3 ,
- Julie E. Reed 1 ,
- Daniel Tyskbo 1 &
- Petra Svedberg 1
BMC Health Services Research volume 22 , Article number: 850 ( 2022 ) Cite this article
28k Accesses
62 Citations
30 Altmetric
Metrics details
Artificial intelligence (AI) for healthcare presents potential solutions to some of the challenges faced by health systems around the world. However, it is well established in implementation and innovation research that novel technologies are often resisted by healthcare leaders, which contributes to their slow and variable uptake. Although research on various stakeholders’ perspectives on AI implementation has been undertaken, very few studies have investigated leaders’ perspectives on the issue of AI implementation in healthcare. It is essential to understand the perspectives of healthcare leaders, because they have a key role in the implementation process of new technologies in healthcare. The aim of this study was to explore challenges perceived by leaders in a regional Swedish healthcare setting concerning the implementation of AI in healthcare.
The study takes an explorative qualitative approach. Individual, semi-structured interviews were conducted from October 2020 to May 2021 with 26 healthcare leaders. The analysis was performed using qualitative content analysis, with an inductive approach.
The analysis yielded three categories, representing three types of challenge perceived to be linked with the implementation of AI in healthcare: 1) Conditions external to the healthcare system; 2) Capacity for strategic change management; 3) Transformation of healthcare professions and healthcare practice.
Conclusions
In conclusion, healthcare leaders highlighted several implementation challenges in relation to AI within and beyond the healthcare system in general and their organisations in particular. The challenges comprised conditions external to the healthcare system, internal capacity for strategic change management, along with transformation of healthcare professions and healthcare practice. The results point to the need to develop implementation strategies across healthcare organisations to address challenges to AI-specific capacity building. Laws and policies are needed to regulate the design and execution of effective AI implementation strategies. There is a need to invest time and resources in implementation processes, with collaboration across healthcare, county councils, and industry partnerships.
Peer Review reports
The use of artificial intelligence (AI) in healthcare can potentially enable solutions to some of the challenges faced by healthcare systems around the world [ 1 , 2 , 3 ]. AI generally refers to a computerized system (hardware or software) that is equipped with the capacity to perform tasks or reasoning processes that we usually associate with the intelligence level of a human being [ 4 ]. AI is thus not one single type of technology but rather many different types within various application areas, e.g., diagnosis and treatment, patient engagement and adherence, and administrative activities [ 5 , 6 ]. However, when implementing AI technology in practice, certain problems and challenges may require an optimization of the method in combination with the specific setting. We may therefore define AI as complex sociotechnical interventions as their success in a clinical healthcare setting depends on more than the technical performance [ 7 ]. Research suggests that AI technology may be able to improve the treatment of many health conditions, provide information to support decision-making, minimize medical errors and optimize care processes, make healthcare more accessible, provide better patient experiences and care outcomes as well as reduce the per capita costs of healthcare [ 8 , 9 , 10 ]. Even if the expectations for AI in healthcare are great [ 2 ], the potential of its use in healthcare is far from having been realized [ 5 , 11 , 12 ].
Most of the research on AI in healthcare focuses heavily on the development, validation, and evaluation of advanced analytical techniques, and the most significant clinical specialties for this are oncology, neurology, and cardiology [ 2 , 3 , 11 , 13 , 14 ]. There is, however, a current research gap between the development of robust algorithms and the implementation of AI systems in healthcare practice. The conclusion in newly published reviews addressing regulation, privacy and legal aspects [ 15 , 16 ], ethics [ 16 , 17 , 18 ], clinical and patient outcomes [ 19 , 20 , 21 ] and economic impact [ 22 ], is that further research is needed in a real-world clinical setting although the clinical implementation of AI technology is still at an early stage. There are no studies describing implementation frameworks or models that could inform us concerning the role of barriers and facilitators in the implementation process and relevant implementation strategies of AI technology [ 23 ]. This illustrates a significant knowledge gap on how to implement AI in healthcare practice and how to understand the variation of acceptance of this technology among healthcare leaders, healthcare professionals, and patients [ 14 ]. It is well established in implementation and innovation research that novel technologies, such as AI, are often resisted by healthcare leaders, which contributes to their slow and variable uptake [ 13 , 24 , 25 , 26 ]. New technologies often fail to be implemented and embedded in practice because healthcare leaders do not consider how they fit with or impact existing healthcare work practices and processes [ 27 ]. Although, understanding how AI technologies should be implemented in healthcare practice is unexplored.
Based on literature from other scientific fields, we know that the leaders’interest and commitment is widely recognized as an important factor for successful implementation of new innovations and interventions [ 28 , 29 ]. The implementation of AI in healthcare is thus supposed to require leaders who understand the state of various AI systems. The leaders have to drive and support the introduction of AI systems, the integration into existing or altered work routines and processes, and how AI systems can be deployed to improve efficiency, safety, and access to healthcare services [ 30 , 31 ]. There is convincing evidence from outside the healthcare field of the importance of leadership for organizational culture and performance [ 32 ], the implementation of planned organizational change [ 33 ], and the implementation and stimulation of organizational innovation [ 34 ]. The relevance of leadership to implementing new practices in healthcare is reflected in many of the theories, frameworks, and models used in implementation research that analyses barriers to and facilitators of its implementation [ 35 ]. For example, Promoting Action on Research Implementation in Health Services [ 36 ], Consolidated Framework for Implementation Research (CFIR) [ 37 ], Active Implementation Frameworks [ 38 ], and Tailored Implementation for Chronic Diseases [ 39 ] all refer to leadership as a determinant of successful implementation. Although these implementation models are available and frequently used in healthcare research, they are highly abstract and not tailored to the implementation of AI systems in healthcare practices. We thus do not know if these models are applicable to AI as a socio-technical system or if other determinants are important for the implementation process. Likewise, based on a new literature study, we found no AI-specific implementation theories, frameworks, or models that could provide guidance for how leaders could facilitate the implementation and realize the potential of AI in healthcare [ 23 ]. We thus need to understand what the unique challenges are when implementing AI in healthcare practices.
Research on various types of stakeholder perspectives on AI implementation in healthcare has been undertaken, including studies involving professionals [ 40 , 41 , 42 , 43 ], patients [ 44 ], and industry partners [ 42 ]. However, very few studies have investigated the perspectives of healthcare leaders. This is a major shortcoming, given that healthcare leaders are expected to have a key role in the implementation and use of AI for the development of healthcare. Petitgand et al.’s study [ 45 ] serves as a notable exception. They interviewed healthcare managers, providers, and organizational developers to identify barriers to integrating an AI decision-support system to enhance diagnostic procedures in emergency care. However, the study did not focus on the leaders’ perspectives, and the study was limited to one particular type of AI solution in one specific care department. Our present study extends beyond any specific technology and encompasses the whole socio-technical system around AI technology. The present study thus aimed to explore challenges perceived by leaders in a regional Swedish healthcare setting regarding implementation of AI systems in healthcare.
This study took an explorative qualitative approach to understanding healthcare leaders’ perceptions in contexts in which AI will be developed and implemented. The knowledge generated from this study will inform the development of strategies to support an AI implementation and help avoid potential barriers. The analysis was based on qualitative content analysis, with an inductive approach [ 46 ]. Qualitative content analysis is widely used in healthcare research [ 46 ] to find similarities and differences in the data, in order to understand human experiences [ 47 ]. To ensure trustworthiness, the study is reported in accordance with the Consolidated Criteria for Reporting Qualitative Research 32‐item checklist [ 48 ].
The study was conducted in a county council (also known as “region”) in the south of Sweden. The Swedish healthcare system is publicly financed based on local taxation; residents are insured by the state and there is a vision that healthcare should be equally accessible across the population. Healthcare responsibility is decentralized to 21 county councils, whose responsibilities include healthcare provision and promotion of good health for citizens.
The county council under investigation has since 2016 invested financial, personnel and service resources to enable agile analysis (based on machine learning models) of clinical and administrative data of patients in healthcare [ 49 , 50 ]. The ambition is to gain more value from the data, utilizing insights drawn from machine learning on healthcare data to make facts-based decisions on how healthcare is managed, organized, and structured in routines and processes. The focus is thus on overall issues around management, staffing, planning and standardization for optimization of resource use, workflows, patient trajectories and quality improvement at system level. This includes several layers within the socio-technical ecosystem around the technology, dealing with: a) generating, cleaning, and labeling data, b) developing models, verifying, assuring, and auditing AI tools and algorithms, c) incorporating AI outputs into clinical decisions and resource allocation, and d) the shaping of new organizational structures, roles, and practices. Given that AI thus extends beyond any specific technology and encompasses the whole socio-technical system around the technology, in the context of this article, it is hereafter referred to generically as ‘AI systems’. We deliberately sought to understand the broad perspectives on healthcare leaders in a region that has a high level of support for AI developments and our study thus focuses on the potential of a wide range of AI systems that could emerge from the regional investments, rather than a specific AI application or AI algorithms.
Participants
Given the focus on understanding healthcare leaders’ perceptions, we purposively recruited leaders who were in a position to potentially influence the implementation and use of AI systems in relation to the setting described above. To achieve potential variability, these leaders belonged to three groups: politicians at the highest county council level, managers at various levels, such as the hospital director, manager for primary care, manager for knowledge and evidence, head of research and development center, and quality developers and strategists with responsibilities for strategy-based work at county council level or development work in various divisions in the county council healthcare organization.
The ambition was to include leaders who had a range of experiences, interests and with different mandates and responsibilities in relation to funding, running, and sustaining the implementation of AI systems in practice. A sample of 28 healthcare leaders was invited through snowball recruitment; two declined and 26 agreed to participate (Table 1 ). This sample comprised five individuals originally identified on the basis of their knowledge and insights. They were interviewed and they then identified and suggested other leaders to interview.
Data collection
Individual semi-structured interviews were conducted between October 2020 and May 2021 via phone or video communication by one of the authors (LP or DT). We start from a broad perspective on AI focusing on healthcare leaders’ perceptions bottom-up and not on the views of AI experts or healthcare professionals who work with specific AI algortihms in clinical practice. The interviews were based on an interview guide, structured around: 1) the roles and previous experiences of the informants regarding the application of AI systems in practice, 2) the opportunities and problems that need to be considered to support implementation of AI systems, 3) beliefs and attitudes towards the possibilities of using AI systems to support healthcare improvements, and 4) the obstacles, opportunities and facilitating factors that need to be considered to enable AI systems to fit into existing processes, methods and systems. The interview guide was thus based on important factors previously identified in terms of implementing technology in healthcare [ 51 , 52 ]. Interviews lasted between 30 and 120 min, with a total length of 23 h and 49 min and were audio-recorded.
Data analysis
An inductive qualitative content analysis [ 46 ] was used to analyze the data. First, the interviews were transcribed verbatim and read several times by the first (LP) and second (IL) authors, to gain familiarity. Then, the first (LP) and second (IL) authors conducted the initial analyses of the interviews, by identifying and extracting meaning units and/or phrases with information relevant to the object of the study. The meaning units were then abstracted into codes, subcategories, and categories. The analytical process was discussed continuously between authors (LP, IL, JMN, PN, MN, PS). Finally, all authors, who are from different disciplines, reviewed and discussed the analysis to increase the trustworthiness and rigour of the analysis. To further strengthen the trustworthiness, the leaders’ quotations used in this paper were translated from Swedish to English by a native English-speaking professional proofreader and were edited only slightly to improve readability.
Three categories consisting of nine sub-categories emerged from the analysis of the interviews with the healthcare leaders (Fig. 1 ). Conditions external to the healthcare system concern various exogenous conditions and circumstances beyond the direct control of the healthcare system that the leaders believed could affect AI implementation. Capacity for strategic change management reflects endogenous influences and internal requirements related to the healthcare system that the leaders suggested could pose challenges to AI implementation. Transformation of healthcare professions and healthcare practice concerns challenges to AI implementation observed by the leaders, in terms of how AI might change professional roles and relations and its impact on existing work practices and routines.
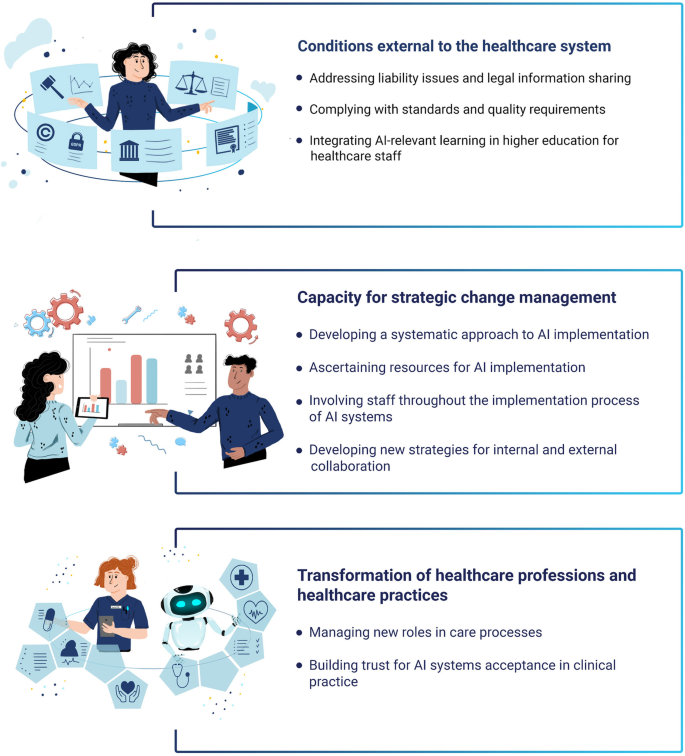
Categories and subcategories
Conditions external to the healthcare system
Addressing liability issues and legal information sharing.
The healthcare leaders described the management of existing laws and policies for the implementation of AI systems in healthcare as a challenge and an issue that was essential to address. According to them, the existing laws and policies have not kept pace with technological developments and the organization of healthcare in today’s society and need to be revised to ensure liability.
The accountability held among individuals, organizations, and AI systems regarding decisions based on support from an AI algorithm was perceived as a risk and an element that needs to be addressed. However, accountability is not addressed in existing laws, which were perceived by the leaders to present problematic uncertainties in terms of responsibilities. They raised concerns about where responsibilities lie in relation to decisions made by AI algorithms, such as when an AI algorithm run in one part of the system identifies actions that should be taken in another part of the system. For example, if a patient is given AI-based advice from a county council-operated patient portal for triaging suggesting self-care, and the advice instead should have been to visit the emergency department, who has the responsibility, is it the AI system itself, the developers of the system or the county council. Additionally, concerns were raised about accountability, if it turns out that the advice was not accurate.
The issue of accountability is a very difficult one. If I agree with what doctor John (AI systems) recommended, where does the burden of proof lie? I may have looked at this advice and thought that it worked quite well. I chose to follow this advice, but can I blame Doctor John? The legislation is a risk that we have to deal with. Leader 7.
Concerns were raised as to how errors would be handled when AI systems contributed to decision making, highlighting the need for clear laws and policies. The leaders emphasized that, if healthcare professionals made erroneous decisions based on AI systems, they could be reported to the Patients Advisory Committee or have their medical license revoked. This impending threat could lead to a stressful situation for healthcare professionals. The leaders expressed major concerns about whether AI systems would be support systems for healthcare professionals’ decisions or systems that could take automated and independent decisions. They believed based on the latter interpretation that there would be a need for changes in the laws before they could be implemented in practice. Nevertheless, some leaders anticipated a development where some aspects of care could be provided without any human involvement.
If the legislation is changed so that the management information can be automated, that is to say that they start acting themselves, but they’re not allowed to do that yet. It could, however, be so that you open an app in a few years’ time, then you furnish the app with the information that it needs about your health status. Then the app can write a prescription for medication for you, because it has all the information that is needed. That is not allowed at present, because the judicial authority still need an individual to blame when something goes wrong. But even that aspect will be gradually developed. Leader 2.
According to the leaders, legislation and policies also constituted obstacles to the foundation in the implementation of AI systems in healthcare: collecting, using, merging, and analyzing patient information. The limited opportunities to legally access and share information about patients within and between organizations were described as a crucial obstacle in implementing and using AI systems. Another issue was the legal problems when a care provider wanted to merge information about patients from different providers, such as the county council and a municipality. For this to take place, it was perceived that a considerable change of the laws regulating the possibilities of sharing information across different care providers would be required. Additionally, there are challenges in the definition of personal data in laws regulating personal integrity and in the risk of individuals being identified when the data is used for computerized advanced analytics. The law states that it is not legal to share personal data, but the boundaries of what is constituted by personal data in today’s society are changing, due to the increasing amounts of data and opportunities for complex and intelligent analysis.
You are not allowed to share any personal information. No, we understand that but what is personal information and when is personal information no longer personal information? Because legally speaking it is definitely not just the case of removing the personal identity number and the name, as a computer can still identify who you are at an individual level. When can it not do that? Leader 2.
Thus, according to the healthcare leaders, laws and regulations presented challenges for an organization that want to implement AI systems in healthcare practice, as laws and regulations have different purposes and oppose each other, e.g., the Health and Medical Services Act, the Patient Act and the Secrecy Act. Leaders described how outdated laws and regulations are handled in healthcare practice, by stretching current regulations and attempts to contribute to changing laws . They aimed to not give up on visions and ideas, but to try to find gaps in existing laws and to use rather than break the laws. When possible, another way to approach this was to try to influence decision-makers on the national political level to change the laws. The leaders reported that civil servants and politicians in the county council do this lobbying work in different contexts, such as the parliament or the Swedish Association of Local Authorities and Regions (SALAR).
We discuss this regularly with our members of parliament with the aim of influencing the legislative work towards an enabling of the flow of information over boundaries. It’s all a bit old-fashioned. Leader 16.
Complying with standards and quality requirements
The healthcare leaders believed it could be challenging to follow standardized care processes when AI systems are implemented in healthcare. Standardized care processes are an essential feature that has contributed to development and improved quality in Swedish healthcare. However, some leaders expressed that the implementation of AI systems could be problematic because of uncertainties regarding when an AI algorithm is valid enough to be a part of a standardized care process. They were uncertain about which guarantees would be required for a product or service before it would be considered “good enough” and safe to use in routine care. An important legal aspect for AI implementation is the updated EU regulation for medical devices (MDR) that came into force in May 2021. According to one of the leaders, this regulation could be problematic for small innovative companies, as they are not used to these demands and will not always have the resources needed to live up to the requirements. Therefore, the leaders perceived that the county council should support AI companies to navigate these demands, if they are to succeed in bringing their products or services to implementation in standardized care processes.
We have to probably help the narrow, supersmart and valuable ideas to be realized, so that there won’t be a cemetery of ideas with things that could have been good for our patients, if only the companies had been given the conditions and support to live up to the demands that the healthcare services have and must have in terms of quality and security. Leader 2.
Integrating AI-relevant learning in higher education for healthcare staff
The healthcare leaders described that changes needed to be made in professional training, so that new healthcare professionals would be prepared to use digital technology in their practical work. Some leaders were worried that basic level education for healthcare professionals, such as physicians, nurses, and assistant nurses has too little focus on digital technology in general, and AI systems in particular. They stated that it is crucial that these educational programs are restructured and adapted to prepare students for the ongoing digitalization of the healthcare sector. Otherwise, recently graduated healthcare professionals will not be ready to take part in utilizing and implementing new AI systems in practice.
I am fundamentally quite concerned that our education, mainly when it comes to the healthcare services. Both for doctors and nurses and also assistant nurses for that matter. That it isn’t sufficiently proactive and prepare those who educate themselves for what will come in the future. // I can feel a certain concern for the fact that our educations do not actually sufficiently prepare our future co-workers for what everybody is talking now about that will take place in the healthcare services. Leader 15.
Capacity for strategic change management
Developing a systematic approach to ai implementation.
The healthcare leaders described that there is a need for a systematic approach and shared plans and strategies at the county council level, in order to meet the challenge of implementing AI systems in practice. They recognized that it will not be successful if the change is built on individual interests, instead of organizational perspectives. According to the leaders, the county council has focused on building the technical infrastructure that enables the use of AI algorithms. The county council have tried to establish a way of working with multi-professional teams around each application area for AI-based analysis. However, the leaders expressed that it is necessary to look beyond the technology development and plan for the implementation at a much earlier stage in the development process. They believed that their organization generally underestimated the challenges of implementation in practice. Therefore, the leaders believed that it was essential that the politicians and the highest leadership in the county council both support and prioritize the change process. This requires an infrastructure for strategic change management together with clear leadership that has the mandate and the power to prioritize and support both development of AI systems and implementation in practice. This is critical for strategic change to be successful.
If the County Council management does not believe in this, then nothing will come of it either, the County Council management have to indicate in some way that this is a prioritized issue. It is this we are going to work with, then it’s not sufficient for a single executive director who pursues this and who thinks it’s interesting. It has to start at the top and then filter right through, but then the politicians have to also believe in this and think that it’s important. Leader 4.
Additionally, the healthcare leaders experienced that there was increasing interest among unit managers within the organization in using data for AI-based analysis and that there might be a need to make more prioritizations of requests for data analysis in the future. The leaders expressed that it would not be enough to simply have a shared core facility supporting this. Instead, management at all levels should also be involved and active in prioritization, based on their needs. They also perceived that the implementation of AI systems will demand skilled and structured change management that can prioritize and that is open to new types of leadership and decision-making processes. Support for innovative work will be needed, but also caution so that change does not proceed too quickly and is sufficiently anchored among the staff. The implementation of AI systems in healthcare was anticipated to challenge old routines and replace them with new ones, and that, as a result, would meet resistance from the staff. Therefore, a prepared plan at the county council level was perceived to be required for the purpose of “anchoring” with managers at the unit level, so that the overall strategy would be aligned with the needs and views of those who would have to implement it and supported by the knowledge needed to lead the implementation work.
It’s in the process of establishing legitimacy that we have often erred, where we’ve made mistakes and mistakes and mistakes all the time, I’ve said. That we’re not at the right level to make the decisions and that we don’t follow up and see that they understand what it’s about and take it in. It’s from the lowest manager to the middle manager to executive directors to politicians, the decisions have to have been gained legitimacy otherwise we’ll not get the impetus. Leader 21.
The leaders believed that it was essential to consider how to evaluate different parts of the implementation process. They expressed that method development is required within the county council, because, at the moment, there is a lack of knowledge and guidelines on how to evidence-base the use of AI systems in practice. There will be a need for a support organization spanning different levels within the county council, to guide and supervise units in the systematic evaluation of AI implementations. There will also be a need for quantitative evaluation of the clinical and organizational effects and qualitative assessment that focuses on how healthcare professionals and patients experience the implementation. Additionally, validation and evaluation of AI algorithms will be needed, both before they can be used in routine care, and afterwards, to provide evidence of quality improvements and optimizations of resources.
I believe that one needs to get an approval in some way, perhaps not from the Swedish Medical Products Agency, but the AI Agency or something similar. I don’t know. The Swedish National Board of Health and Welfare or some agency needs to go in and check that it is a sufficiently good foundation that they have based this algorithm on. So that it can be approved for clinical use. Leader 10.
Furthermore, the leaders described a challenge around how the implementation of AI systems in practice could be sustainable and last over time. They expressed that the county council should develop strategies in the organization so that they are readied for sustainability and long-term implementation. At the same time, this is an area with fast development and high uncertainty about the future, and thus what AI systems and services will look like in five or ten years, and how healthcare professionals and patients will use them. This is a challenge and requires that both leaders and staff are prepared to adjust and change their ways of working during the implementation process, including continuous improvements and uptake, updating and evolution of technologies and work practices.
The rate of change where digitalization, technology, new technology and AI is concerned is so high and the rate of implementation is low, so this will entail that as soon as we are about to implement something then there is something else in the market that is better. So I think it’s important to dare to implement something that is a little further on in the future. Leader 13.
Ascertaining resources for AI implementation
The leaders emphasized the importance of training for implementation of AI systems in healthcare. The county council should provide customized training at the workplace and extra knowledge support for certain professions. This could result in difficult decisions regarding what and whom to prioritize. The leaders discussed whether there was a need to provide all staff with basic training on AI systems or if it would be enough to train some of them, such as quality developers, and provide targeted training for some healthcare professionals who are close to the implementation of the AI system at a care unit. Furthermore, the leaders described that the training had to be connected to implementing the AI system at a specific care unit, which could present a challenge for the planning and realization. They emphasized that it could be a waste of resources to educate the staff beforehand. They need to be educated in close connection to the implementation of a specific AI system in their workplace, which thus demands organizational resources and planning.
I think that we often make the mistake of educating first, and then you have to use it. But you have been educated, so now you should know this? Yes, but it is not until we use something that the questions arise. Leader 13.
There could also be a need for patient education and patient guidance, if they are to use AI systems for self-care or remote monitoring. Thus, it is vital to give all citizens the same opportunities to access and utilize new technical solutions in healthcare.
We treat all our patients equally now, everyone will receive the same invitation, and everyone will need to ring about their appointment, although 99% could really book and do this themselves. Then we should focus on that, and thus return the impetus and the power to the patient and the population for them to take care of this themselves to a greater extent. But then of course information is needed and that in turn needs intuitive systems. That is not something we are known for. Leader 14.
Many of the healthcare leaders found financial resources and time, especially the prioritization of time, to be critical to the implementation process of AI system. There is already time pressure in many care units, and it can be challenging to set aside time and other resources for the implementation.
Involving staff throughout the implementation process of AI systems
The healthcare leaders stated that anchoring and involving staff and citizens is crucial to the successfully implementation of AI systems. The management has to be responsible for the implementation process but also ensure that the staff are aware of and interested in the implementation, based on their needs. Involvement of the staff together with representatives from patient groups was considered key to successful implementation and to limit risks of perceiving the AI system as unnecessary and erroneously used. At the same time, the leaders described that it would be important for unit managers to “stand up” for the change that is required, if their staff questioned the implementation.
I think for example that if you’re going to make a successful implementation then you have to perhaps involve the co-workers. You can’t involve all of them, but a representative sample of co-workers and patients and the population who are part of it. // We mess it up time after time, and something comes that we have to implement with short notice. So we try to force it on the organization, so we forget that we need to get the support of the co-workers. Leader 4.
The propensity for change differs both among individuals and within the organization. According to the leaders, that could pose a challenge, since the support and needs differ between individuals. The motivational aspect could also vary between different actors, and some leaders claim that it is crucial to arouse curiosity among healthcare professionals. If the leaders are not motivated and do not believe that the change benefits them, implementation will not be successful. To increase healthcare professionals’ motivation and engagement, the value that will be created for the clinicians has to be made obvious, along with whether the AI system will support them in their daily work.
It has to be beneficial for the clinics otherwise it’s meaningless so to speak. A big risk with AI is that you work and work with data and then algorithms emerge that are sort of obvious. Everyone can do this. It’s why it’s important to have clinical staff in the small agile teams, that there really is a clinical benefit, this actually improves it. Leader 10.
Developing new strategies for internal and external collaboration
The healthcare leaders believed that there was a need for new forms of collaboration and communication within the county council, at both organizational and professional levels. Professionals need to interact with professions other than their own, thus enabling new teamwork and new knowledge. The challenge is for different groups to talk to each other, since they do not always have the same professional language. However, it was perceived that, when these kinds of team collaborations are successful, there will be benefits, such as automation of care processes that are currently handled by humans.
To be successful in getting a person with expert knowledge in computer science to talk to a person with expert knowledge in integrity legislation, to a one who has expert knowledge in the clinical care of a patient. Even if all of them go to work with exactly the same objective, that one person or a few people can live a bit longer or feel a bit better, then it’s difficult to talk with each other because they use essentially different languages. They don’t know much about what knowledge the other has, so just getting that altogether. Leader 2.
Leaders’ views the implementation of AI systems would require the involvement and collaboration of several departments in the county council across organizational boundaries, and with external actors. A perceived challenge was that half of the primary care units are owned by private care providers, where the county council has limited jurisdiction, which challenges the dissemination of common ways of working. Additionally, the organization in the county council and its boundaries might have to be reviewed to enable different professions to work together and interact on an everyday basis.
The complexity in terms of for example apps is very, very, very much greater, we see that now. Besides there being this app, so perhaps the procurement department must be involved, the systems administration must definitely be involved, the knowledge department must be involved and the digitalization department, there are so many and the finance department of course and the communication department, the system is thus so complex. Leader 9.
There was also consensus among the healthcare leaders that the county council should collaborate with companies in AI systems implementation and should not handle such processes on their own. An eco-system of actors working in AI systems implementation is required, who have shared goals for the joint work. The leaders expressed that companies must be supported and invited to collaborate within the county council’s organization at an early stage. In that way, pitfalls regarding legal or technical aspects can be discovered early in product development. Similar relations and dialogues are also needed with patients to succeed with implementation that is not primarily based on technical possibilities, but patients’ needs. Transparency is essential to patients’ awareness of AI systems’ functions and for the reliability in outcomes.
This is born out of a management philosophy, which is based on the principle of not being able to command everything oneself, one has to be humble, perceptive about not being able to do it. One needs to invite others to be there and help with the solution. Leader 16.
Transformation of healthcare professions and healthcare practices
Managing new roles in care processes.
The healthcare leaders described a need for new professions and professional roles in healthcare for AI systems implementation. All professional groups in today’s healthcare sector were expected to be affected by these changes, particularly the work unit managers responsible for daily work processes and the physicians accountable for the medical decisions. The leaders argued that the changes could challenge traditions, hierarchies, conventional professional roles and division of labour. There might be changes regarding the responsibilities for specific work tasks, changes in professional roles, a need for new professions that do not exist in today’s labour market and the AI systems might replace some work tasks and even professions. A change towards more combined positions at both the county council and a company or a university might also be a result of the development and implementation of AI systems. However, the leaders perceived that, for some healthcare professionals, these ideas are unthinkable, and it may take several years before these changes in roles and care processes become a reality in the healthcare sector.
I think I will be seeing other professions in the healthcare services who have perhaps not received a healthcare education. It will be a culture shock, I think. It also concerns that you may perhaps not need to be medically trained, for sitting there and checking those yellow flags or whatever they are, or it could perhaps be another type of professional group. I think that it would actually be good. We have to start economizing with the competencies we now have and it’s difficult enough to manage. Leader 15.
The acceptance of the AI systems may vary within and between professional groups, ages, and areas of specialized care. The leaders feared that the implementation of AI systems would change physicians’ knowledge base and that there would be a loss of knowledge that could be problematic in the long run. The leaders argued that younger, more recently graduated physicians would never be able to accumulate the experience-based knowledge to the extent that their older colleagues have done, as they will rely more on AI systems to support their decisions. Thus, on one hand, professional roles and self-images might be threatened when output from the AI systems is argued to be more valid than the recommendation by an experienced physician. However, on the other hand, physicians who do not “work with their hands” can utilize such output as decision support to complement their experience-based knowledge. Thus, it is important that healthcare professionals have trust in recommendations from the AI systems in clinical practice. If some healthcare professionals do not trust the AI systems and their output, there is a risk that they will not use them in clinical practice and continue to work in the way they are used to, resulting in two parallel systems. This might be problematic, both for the work environment and the healthcare professionals’ wellbeing. The leaders emphasized that this would represent a challenge for the implementation of AI systems in healthcare.
We can’t add anything more today without taking something else away, I’d say it was impossible. // The level of burden is so high today so it’s difficult to see, it’s not sufficient to say that this will be of use to us in two years’ time. Leader 20.
Implementing AI systems can change existing care processes and change the role of the patient. The leaders described that, in primary care, AI systems have the best potential to change existing work processes and make care more efficient, for example through an automatic AI-based triage for patients. The AI system could take the anamnesis, instead of the healthcare professionals, and do this when patients still are at home, so the healthcare professionals will not meet the patient unless the AI system has decided that it is necessary. The AI system can also autonomously discover something in a patient’s health status and suggest that the patient contact healthcare staff for follow-up. This use of AI systems could open up opportunities for more proactive and personalized care.
The leaders also described that the implementation of AI systems in practice could facilitate an altered patient role. The development that is taking place in the healthcare sector with, for instance, patient-reported data, enables and, in some cases, requires an active and committed patient that takes part in his or her care process. The leaders mentioned that there might be a need for patient support. Otherwise, there might be a risk that only patients with high digital literacy would be able to participate with valid data. The leaders described that AI systems could facilitate this development, by recommending self-care advice to patients or empowering them to make decisions. Still, there were concerns that not all patients would benefit from AI systems, due to variations in patients’ capabilities and literacy.
We also deal with people who are ill, we must also have respect for that. Everyone will not be able to use these tools. Leader 7.
Building trust for AI systems acceptance in clinical practice
A challenge and prerequisite for implementing AI systems in healthcare is that the technology meets expectations on quality to support the healthcare professionals in their practical work, such as having a solid evidence base, being thoroughly validated and meeting requirements for equality. It is important to have confidence in the validity of the data, the algorithms and their output. A key challenge pointed out was the need to have a sufficiently large population base, the “right” type of data and the right populations to build valid AI systems. For common conditions, where rich data exists to base AI algorithms, leaders believed the reliability would be high. For unusual conditions, there were concerns that there would be lower accuracy. Questions were also raised about how AI systems take aspects around equity and equality into account, such as gender and ethnicity. The leaders expressed concern that, due to these obstacles, in relation to certain unusual or complex conditions AI systems might not be suitable.
Then there is a challenge with the new technology, whether it’s Ok to apply it. Because it’s people who are affected, people’s health and lives that are affected by the new technology. How can we guarantee that it delivers what it says it will deliver? It must be safe and reviewed, validated and evidence-based in order for us to be able to use it. If a bug is built in then the consequences can be enormous. Leader 2.
Lack of confidence in the reliability of AI systems was also described and will place higher demands and requirements on their accuracy than on similar assessments made by humans. Thus, acceptance depends on confidence in AI systems as highly sensitive and that they can diagnose conditions at earlier stages than skilled healthcare professionals. The leaders perceived that the “black box” needs to be understood in order to be reliable, i.e. what the AI algorithms calculations are based on. Thus, reliance on the outputs from AI algorithms depends on reliance on the algorithm itself and the data used for its calculation.
There are a number of inherent problems with AI. It’s a little black box. AI looks at all the data. AI is not often easy to explain, “oh, you’ve got a risk, that it passed the cut-off value for that person or patient”, no because it weighs up perhaps a hundred different dimensions in a mathematical model. AI models are often called a black box and there have been many attempts at opening that box. The clinics are a bit skeptical then when they are not able to, they just get a risk score, I would say. Leader 10.
Big data sets are important for quality, but the leaders stated that too much information about a patient also could be problematic. There is a risk that information about a patient is available to healthcare professionals who should not have that information. The leaders believed that this could already be a problem today, but that it would be an increased risk in the future. This challenge needs to be handled as the amount of patient information increases, and as more healthcare professionals get access to such information when it’s being used in AI systems, regardless of the reason for the patient’s contact with the healthcare unit. Another challenge and prerequisite for implementing AI systems in healthcare is that the technology is user-friendly and create value for both healthcare professionals and patients. The leaders expected AI systems to be user-friendly, self-instructing, and easy to use, without requiring too much prior knowledge or training. In addition to being easy to use, the AI systems must also be time-saving and never time-consuming or dependent on the addition of yet more digital operative systems to work with. Using AI systems should, in some cases, be equated with having a second opinion from a colleague, when it comes to simplicity and time consumption.
An easy way to receive this support is needed. One needs to ask a number of questions in order to receive the correct information. But it mustn’t be too complicated, and it mustn’t take time, then nothing will come of it. Leader 4.
The leaders expected that AI systems would place the patients in focus and thereby contribute to more person-centred care. These expectations are based on a large amount of data on which AI algorithms are built, which leaders perceive will make it possible to individualize assessments and treatment options. AI systems would enable more person-centred and value-creating care for patients. AI systems could potentially contribute to making healthcare efficient without compromising quality. It was seen as an opportunity to meet future increasing needs for care among the citizens, combined with a reduced number of healthcare professionals. Smart and efficient AI systems used in investigations, assessments, and treatments can streamline care and allow more patients to receive care. Making healthcare efficient was also about the idea that AI systems should contribute to improved communication within and between caregivers for both public and private care. Using AI systems to follow up the given care and to evaluate the quality of care with other caregivers was highlighted, along with the risk that the increased efficiency provided by AI systems could result in a loss of essential values for healthcare and in impaired care.
I think that automatization via AI would be a safe way and it would be perfect for the primary care services. It would have entailed that we have more hands, that we can meet the patients who need to be met and that we can meet more often and for longer periods and perhaps do more house calls and just be there where we are needed a little more and help these a bit more easily. Leader 13.
The perspectives of the challenges described by leaders in the present study are an important contribution to improving knowledge regarding the determinants influencing the implementation of AI systems in healthcare. Our results showed that healthcare leaders perceived challenges to AI implementation concerning the handling of conditions external to the healthcare system, the building of internal capacity for strategic change management and the transformation of professional roles and practices. While implementation science has advanced the knowledge concerning determinants for successful implementation of digital technology in healthcare [ 53 ], our study is one of the few that have investigated leaders’ perceptions of the implementation of AI systems in healthcare. Our findings demonstrate that the leaders concerns do not lie so much with the specific technological nuances of AI, but with the more general factors relating to how such AI systems can be channeled into routine service organization, regulation and practice delivery. These findings demonstrate the breadth of concerns that leaders perceive are important for the successful application of AI systems and therefore suggest areas for further advancements in research and practice. However, the findings also demonstrate a potential risk that, even in a county council where there is a high level of investment and strategic support for AI systems, there is a lack of technical expertise and awareness of AI specific challenges that might be encountered. This could cause challenges to the collaboration between the developers of AI systems and healthcare leaders if there is a cognitive dissonance about the nature and scope of the problem they are seeking to address, and the practical and technical details of both AI systems and healthcare operational issues [ 7 ]. This suggests the need for people who are conversant in languages of both stakeholder groups maybe necessary to facilitate communication and collaboration across professional boundaries [ 54 ]. Importantly, these findings demonstrate that addressing the technological challenges of AI alone is unlikely to be sufficient to support their adoption into healthcare services, and AI developers are likely to need to collaborate with those with expertise in healthcare implementation and improvement scientists in order to address the wider systems issues that this study has identified.
The healthcare leaders perceived challenges resulting from external conditions and circumstances, such as ambiguities in existing laws and sharing data between organizations. The external conditions highlighted in our study resonate with the outer setting in the implementation framework CFIR [ 37 ], which is described in terms of governmental and other bodies that exercise control, with the help of policies and incentives that influence readiness to implement innovations in practice. These challenges described in our study resulted in uncertainties concerning responsibilities in relation to the development and implementation of AI systems and what one was allowed to do, giving rise to legal and ethical considerations. The external conditions and circumstances were recognized by the leaders as having considerable impact on the possibility of implementing AI systems in practice although they recognized that these were beyond their direct influence. This suggests that, when it comes to the implementation of AI systems, the influence of individual leaders is largely restricted and bounded. Healthcare leaders in our study perceived that policy and regulation cannot keep up with the national interest in implementing AI systems in healthcare. Here, concerted and unified national authority initiatives are required according to the leaders. Despite the fact that the introduction of AI systems in healthcare appears to be inevitable, the consideration of existing regulatory and ethical mechanisms appears to be slow [ 16 , 18 ]. Additionally, another challenge attributable to the setting was the lack of to increase the competence and expertise among professionals in AI systems, which could be a potential barrier to the implementation of AI in practice. The leaders reflected on the need for future higher education programs to provide healthcare professionals with better knowledge of AI systems and its use in practice. Although digital literacy is described as important for healthcare professionals [ 55 , 56 ], higher education faces many challenges in meeting emerging requirements and demands of society and healthcare.
The healthcare leaders addressed the fact that the healthcare system’s internal capacity for strategic change management is a hugh challenge, but at the same time of great importance for successful and sustainable implementation of AI systems in the county council. The leaders highlighted the need to create an infrastructure and joint venture, with common structures and processes for the promotion of the capability to work with implementation strategies of AI systems at a regional level. This was needed to obtain a lasting improvement throughout the organization and to meet organizational goals, objectives, and missions. Thus, this highlights that the implementation of change within an organization is a complex process that does not solely depend on individual healthcare professionals’ change responses [ 57 ]. We need to focus on factors such as organisational capacity, climate, culture and leadership, which are common factors within the “inner context” in CFIR [ 37 ]. The capacity to put the innovations into practice consists of activities related to maintaining a functioning organization and delivery system [ 58 ]. Implementation research has most often focused on implementation of various individual, evidence-based practices, typically (digitally) health interventions [ 59 ]. However, AI implementation represents a more substantial and more disruptive form of change than typically involved in implementing new practices in healthcare [ 60 ]. Although there are likely many similarities between AI systems and other new digital technologies implemented in healthcare, there may also be important differences. For example, our results and other AI research has acknowledged that the lack of transparency (i.e. the “black box” problem) might yield resistance to some AI systems [ 61 ]. This problem is probably less apparent when implementing various evidence-based practices based on empirical research conducted according to well-established principles to be trustworthy [ 62 ]. Ethical and trust issues were also highlighted in our study as playing a more prominent role in AI implementation, perhaps more prominently than in “traditional” implementation of evidence-based practices. There might thus be AI-specific characteristics that are not really part of existing frameworks and models currently used in implementation science.
Transformation of healthcare professions and healthcare practice
The healthcare leaders perceived that the use of AI in practice could transform professional roles and practices and this could be an implementation challenge. They reflected on how the implementation of AI systems would potentially impact provider-patient relationships and how the shifts in professional roles and responsibilities in the service system could potentially lead to changes in clinical processes of care. The leaders’ concerns related to the compatibility of new ways of working with existing practice, which is an important innovation characteristic highlighted in the Diffusion of Innovation theory [ 63 ]. According to the theory, compatibility with existing values and past experiences facilitates implementation. The leaders in our study also argued that it was important to see the value of AI systems for both professionals and service-users. Unless the benefits of using AI systems are observable healthcare professionals will be reluctant to drive the implementation forward. The importance of observability for adoption of innovations is also addressed in the Diffusion of Innovation theory [ 63 ], being the degree to which the results of an innovation are visible to the users. The leaders in our study conveyed the importance for healthcare professionals of having trust and confidence in the use of AI systems. They discussed uncertainties regarding accountability and liability in situations where AI systems impacts directly or indirectly on human healthcare, and how ambiguity and uncertainty about AI systems could lead to healthcare workers having a lack of trust in the technology. Trust in relation to AI systems is well reflected on as a challenge in research in healthcare [ 30 , 41 , 64 , 65 , 66 ]. The leaders also perceived that the expectations of patient-centeredness and usability (efficacy and usefulness) for service users could be a potential challenge in connection with AI implementation. Their concerns are echoed in a review by Buchanan et al. [ 67 ], in which it was observed that the use of AI systems could serve to weaken the person-centred relationships between healthcare professionals and patients.
In summary, the expectations for AI in healthcare are high in society and the technological impetus is strong. A lack of “translation” of the technology is in some ways part of the initial difficulties of implementing AI, because implementation strategies still need to be developed that might facilitate testing and clinical use of AI to demonstrate its value in regular healthcare practice. Our results relate well to the implementation science literature, identifying implementation challenges attributable to both external and internal conditions and circumstances [ 37 , 68 , 69 ] and the characteristics of the innovation [ 37 , 63 ]. However, the leaders in our study also pointed out the importance of establishing an infrastructure and common strategies for change management on the system level in healthcare. Thus, introducing AI systems and the required changes in healthcare practice should not only be dependent on early adopters at the particular units. This resonates with the Theory of Organizational Readiness for Change [ 70 ], which emphasizes the importance of an organization being both willing and able to implement an innovation [ 71 ]. The theory posits that, although organizational willingness is one of the factors that may facilitate the introduction of an innovation into practice, both the organization’s general capacities and its innovation-specific capacities for adoption and sustained use of an innovation are key to all phases in the implementation process [ 71 ].
Methodological considerations
In qualitative research, the concepts credibility, dependability, and transferability are used to describe different aspects of trustworthiness [ 72 ]. Credibility was strengthened by the purposeful sample of participants with various experiences and a crucial role in any implementation process. It is considered of great relevance to investigate the challenges that leaders in the county council expressed concerning the implementation of various AI systems in healthcare, albeit the preparation for implementing AI systems is a current issue in many Swedish county councils. Furthermore, the research team members’ familiarity with the methodology, together with their complementary knowledge and backgrounds enabled a more nuanced and profound, in-depth analysis of the empirical material and was another strength of the study.
Dependability was strengthened by using an interview guide to ensure that the same opening questions were put to all participants and that they were encouraged to talk openly. Because this study took place during the COVID-19 pandemic, the interviews were performed either at a distance, using the Microsoft Teams application, or face-to-face, the variation might be a limitation. However, according to Archibald et al. [ 73 ], distance interviewing with videoconferencing services, such as Microsoft Teams, could be beneficial and even preferred. Based on the knowledge gap regarding implementation of AI systems in healthcare, the authors chose to use an inductive qualitative approach to the exploration of healthcare leaders’ perceptions of implementation challenges. It might be that the implementation of AI systems largely aligns with the implementation of other digital technologies or techniques in healthcare. A strength of our study is that it focuses on perceptions on AI systems in general regardless of the type of AI algorithm or the context or area of application. However, one potential limitation of this approach is the possibility that more specific AI systems and or areas of applications may become associated with somewhat different challenges. Further studies specifying such boundaries will provide more specific answers but will probably also require the investigation be conducted in connection with the actual implementation of a specific AI systems and based on participants' experiences of having participated in the implementation process. With this in mind, we encourage future research to take this into account when deciding upon study designs.
Transferability was strengthened by a rich presentation of the results along with appropriate quotations. However, a limitation could be that all healthcare leaders work in the same county council, so transferability to other county councils must be considered with caution. In addition, an important contextual factor that might have an impact on whether, and how, the findings observed in this study will occur in other settings as well, concerns the nature of, and approach to, AI implementation. AI could be considered a rather broad concept, and while we adopted a broad and general approach to AI systems in order to understand healthcare leader’s perceptions, we would, perhaps, expect that more specific AI systems and or areas of applications become associated with different challenges. Taken together, these are aspects that may affect the possibilities for our results to be portable or transferred to other contexts. We thus suggest that the perceptions of healthcare leaders in other empirical contexts and the involvement of both more specific and broader AI systems are utilized in the study designs of future research.
In conclusion, the healthcare leaders highlighted several implementation challenges in relation to AI within the healthcare system and beyond the healthcare organization. The challenges comprised conditions external to the healthcare system, internal capacity for strategic change management, and transformation of healthcare professions and healthcare practice. Based on our findings, there is a need to see the implementation of AI system in healthcare as a changing learning process at all organizational levels, necessitating a healthcare system that applies more nuanced systems thinking. It is crucial to involve and collaborate with stakeholders and users inside the regional healthcare system itself and other actors outside the organization in order to succeed in developing and applying system thinking on implementation of AI. Given that the preparation for implementing AI systems is a current and shared issue in many (Swedish) county councils and other countries, and that our study is limited to one specific county council context, we encourage future studies in other contexts, in order to corroborate the findings.
Availability of data and materials
Empirical material generated and/or analyzed during the current study are not publicly available, but are available from the corresponding author on reasonable request.
Buch VH, Ahmed I, Maruthappu M. Artificial intelligence in medicine: current trends and future possibilities. Br J Gen Pract. 2018;68(668):143–4.
Article PubMed PubMed Central Google Scholar
Mehta N, Pandit A, Shukla S. Transforming healthcare with big data analytics and artificial intelligence: A systematic mapping study. J Biomed Inform. 2019;100: 103311.
Article PubMed Google Scholar
Horgan D, Romao M, Morré SA, Kalra D. Artificial Intelligence: Power for Civilisation - and for Better Healthcare. Public Health Genomics. 2019;22(5–6):145–61.
Union E. A definition of AI: Main capabilities and scientific disciplines. https://ec.europa.eu/futurium/en/system/files/ged/ai_hleg_definition_of_ai_18_december_1.pdf ; 2018.
Davenport T, Kalakota R. The potential for artificial intelligence in healthcare. Future Healthc J. 2019;6(2):94–8.
Shaw J, Rudzicz F, Jamieson T, Goldfarb A. Artificial Intelligence and the Implementation Challenge. J Med Internet Res. 2019;21(7):e13659.
Elish MC. The Stakes of Uncertainty: Developing and Integrating Machine Learning in Clinical Care. Ethnographic Praxis in Industry Conference Proceedings. 2018;2018(1):364–80.
Article Google Scholar
Lee JC. The perils of artificial intelligence in healthcare: Disease diagnosis and treatment. J Comput Biol Bioinformatics Res. 2019;9(1):1–6.
Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56.
Article CAS PubMed Google Scholar
Technology EIoIa. Transforming healthcare with AI. https://eithealth.eu/wp-content/uploads/2020/03/EIT-Health-and-McKinsey_Transforming-Healthcare-with-AI.pdf ; 2020.
Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol. 2017;2(4):230–43.
De Nigris S, Craglia M, Nepelski D, Hradec J, Gomez-Gonzales E, Gomez Gutierrez E, et al. AI Watch : AI Uptake in Health and Healthcare. 2020.
He J, Baxter SL, Xu J, Xu J, Zhou X, Zhang K. The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25(1):30–6.
Article CAS PubMed PubMed Central Google Scholar
Alhashmi S, Alshurideh M, Al Kurdi B, Salloum S. A Systematic Review of the Factors Affecting the Artificial Intelligence Implementation in the Health Care Sector. 2020. p. 37–49.
Google Scholar
Asan O, Bayrak AE, Choudhury A. Artificial Intelligence and Human Trust in Healthcare: Focus on Clinicians. J Med Internet Res. 2020;22(6):e15154.
Gooding P, Kariotis T. Ethics and Law in Research on Algorithmic and Data-Driven Technology in Mental Health Care: Scoping Review. JMIR Ment Health. 2021;8(6):e24668.
Beil M, Proft I, van Heerden D, Sviri S, van Heerden PV. Ethical considerations about artificial intelligence for prognostication in intensive care. Intensive Care Med Exp. 2019;7(1):70.
Murphy K, Di Ruggiero E, Upshur R, Willison DJ, Malhotra N, Cai JC, et al. Artificial intelligence for good health: a scoping review of the ethics literature. BMC Med Ethics. 2021;22(1):14.
Choudhury A, Asan O. Role of Artificial Intelligence in Patient Safety Outcomes: Systematic Literature Review. JMIR Med Inform. 2020;8(7):e18599.
Fernandes M, Vieira SM, Leite F, Palos C, Finkelstein S, Sousa JMC. Clinical Decision Support Systems for Triage in the Emergency Department using Intelligent Systems: a Review. Artif Intell Med. 2020;102:101762.
Yin J, Ngiam KY, Teo HH. Role of Artificial Intelligence Applications in Real-Life Clinical Practice: Systematic Review. J Med Internet Res. 2021;23(4):e25759.
Wolff J, Pauling J, Keck A, Baumbach J. The Economic Impact of Artificial Intelligence in Health Care: Systematic Review. J Med Internet Res. 2020;22(2):e16866.
Gama F, Tyskbo D, Nygren J, Barlow J, Reed J, Svedberg P. Implementation Frameworks for Artificial Intelligence Translation Into Health Care Practice: Scoping Review. J Med Internet Res. 2022;24(1):e32215.
Safi S, Thiessen T, Schmailzl KJ. Acceptance and Resistance of New Digital Technologies in Medicine: Qualitative Study. JMIR Res Protoc. 2018;7(12):e11072.
Whitelaw S, Mamas MA, Topol E, Van Spall HGC. Applications of digital technology in COVID-19 pandemic planning and response. Lancet Digit Health. 2020;2(8):e435–40.
Alami H, Lehoux P, Denis J-L, Motulsky A, Petitgand C, Savoldelli M, et al. Organizational readiness for artificial intelligence in health care: insights for decision-making and practice. J Health Organ Manag. 2021;35(1):106–14.
Reed JE, Howe C, Doyle C, Bell D. Simple rules for evidence translation in complex systems: A qualitative study. BMC Med. 2018;16(1):92.
Reichenpfader U, Carlfjord S, Nilsen P. Leadership in evidence-based practice: a systematic review. Leadersh Health Serv (Bradf Engl). 2015;28(4):298–316.
Nilsen P, Bernhardsson S. Context matters in implementation science: a scoping review of determinant frameworks that describe contextual determinants for implementation outcomes. BMC Health Serv Res. 2019;19(1):189.
Chen M, Decary M. Artificial intelligence in healthcare: An essential guide for health leaders. Healthc Manage Forum. 2020;33(1):10–8.
Loh E. Medicine and the rise of the robots: a qualitative review of recent advances of artificial intelligence in health. BMJ Leader. 2018;2(2):59.
Ogbonna E, Harris LC. Leadership style, organizational culture and performance: empirical evidence from UK companies. Int J Human Res Manage. 2000;11(4):766–88.
Battilana J, Gilmartin M, Sengul M, Pache A-C, Alexander JA. Leadership competencies for implementing planned organizational change. Leadersh Q. 2010;21(3):422–38.
Denti L, Hemlin S. Leadership and innovation in organizations: a systematic review of factors that mediate or moderate the relationship. Int J Innov Manag. 2012;16(03):1240007.
Nilsen P. Overview of theories, models and frameworks in implementation science. In: Nilsen P, Birken, S. A., editor. Handbook on Implementation Science. Cheltenham: Edward Elgar Publishing Limited; 2020. p. 8–31. https://www.elgaronline.com/view/edcoll/9781788975988/9781788975988.xml .
Kitson A, Harvey G, McCormack B. Enabling the implementation of evidence based practice: a conceptual framework. Qual Health Care. 1998;7(3):149–58.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JCJIS. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. 2009;4.
Blase KA, Van Dyke M, Fixsen DL, Bailey FW. Key concepts, themes, and evidence for practitioners in educational psychology. In: Handbook of implementation science for psychology in education. New York, NY, US: Cambridge University Press; 2012. p. 13–34.
Chapter Google Scholar
Flottorp SA, Oxman AD, Krause J, Musila NR, Wensing M, Godycki-Cwirko M, et al. A checklist for identifying determinants of practice: A systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci. 2013;8(1):35.
Wangmo T, Lipps M, Kressig RW, Ienca M. Ethical concerns with the use of intelligent assistive technology: findings from a qualitative study with professional stakeholders. BMC Med Ethics. 2019;20(1):98.
Shinners L, Aggar C, Grace S, Smith S. Exploring healthcare professionals’ understanding and experiences of artificial intelligence technology use in the delivery of healthcare: An integrative review. Health Informatics J. 2020;26(2):1225–36.
Laï MC, Brian M, Mamzer MF. Perceptions of artificial intelligence in healthcare: findings from a qualitative survey study among actors in France. J Transl Med. 2020;18(1):14.
Diprose WK, Buist N, Hua N, Thurier Q, Shand G, Robinson R. Physician understanding, explainability, and trust in a hypothetical machine learning risk calculator. J Am Med Inform Assoc. 2020;27(4):592–600.
Nelson CA, Pérez-Chada LM, Creadore A, Li SJ, Lo K, Manjaly P, et al. Patient Perspectives on the Use of Artificial Intelligence for Skin Cancer Screening: A Qualitative Study. JAMA Dermatol. 2020;156(5):501–12.
Petitgand C, Motulsky A, Denis JL, Régis C. Investigating the Barriers to Physician Adoption of an Artificial Intelligence- Based Decision Support System in Emergency Care: An Interpretative Qualitative Study. Stud Health Technol Inform. 2020;270:1001–5.
PubMed Google Scholar
Graneheim UH, Lindgren BM, Lundman B. Methodological challenges in qualitative content analysis: A discussion paper. Nurse Educ Today. 2017;56:29–34.
Krippendorff K. Content analysis : an introduction to its methodology. Thousand Oaks, Calif: SAGE; 2013.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–57.
Ashfaq A, Lingman M, Sant’Anna A, Nowaczyk S. Readmission prediction using deep learning on electronic health records. J Biomed Inform. 2019;97:103256.
Ashfaq A, Lönn S, Nilsson H, Eriksson JA, Kwatra J, Yasin ZM, et al. Data Resource Profile: Regional healthcare information platform in Halland. Sweden Int J Epidemiol. 2020;49(3):738–9.
Wärnestål P, Nygren J. Building an experience framework for a digital peer support service for children surviving from cancer. New York, New York, USA: Proceedings of the 12th International Conference on Interaction Design and Children Association for Computing Machinery; 2013. p. 269–72.
Reed MS, Curzon R. Stakeholder mapping for the governance of biosecurity: a literature review. J Integr Environ Sci. 2015;12(1):15–38.
Vis C, Bührmann L, Riper H, Ossebaard HC. Health technology assessment frameworks for eHealth: A systematic review. Int J Technol Assess Health Care. 2020;36(3):204–16.
Rosen MA, DiazGranados D, Dietz AS, Benishek LE, Thompson D, Pronovost PJ, et al. Teamwork in healthcare: Key discoveries enabling safer, high-quality care. Am Psychol. 2018;73(4):433–50.
Booth RG, Strudwick G, McBride S, O’Connor S, Solano López AL. How the nursing profession should adapt for a digital future. BMJ. 2021;373:n1190.
Article PubMed Central Google Scholar
Foadi N, Varghese J. Digital competence - A Key Competence for Todays and Future Physicians. J Eur CME. 2022;11(1):2015200.
Nilsen P, Schildmeijer K, Ericsson C, Seing I, Birken S. Implementation of change in health care in Sweden: a qualitative study of professionals’ change responses. Implement Sci. 2019;14(1):51.
Wandersman A, Duffy J, Flaspohler P, Noonan R, Lubell K, Stillman L, et al. Bridging the gap between prevention research and practice: the interactive systems framework for dissemination and implementation. Am J Community Psychol. 2008;41(3–4):171–81.
Nilsen P, Birken S. Prologue. In: Nilsen P, Birken, S. A., editor. Handbook on Implementation Science. Cheltenham: Edward Elgar Publishing Limited; 2020. p. 1–6. https://www.elgaronline.com/view/edcoll/9781788975988/9781788975988.xml .
Scott WR. Institutional change and healthcare organizations : from professional dominance to managed care. Chicago: University of Chicago Press; 2000.
von Eschenbach WJ. Transparency and the Black Box Problem: Why We Do Not Trust AI. Philosophy & Technology. 2021;34:1607+.
Li S-A, Jeffs L, Barwick M, Stevens B. Organizational contextual features that influence the implementation of evidence-based practices across healthcare settings: a systematic integrative review. Syst Rev. 2018;7(1):72.
Rogers EM. Diffusion of innovations. New York: Free Press; 1995.
Matheny ME, Whicher D, Thadaney IS. Artificial Intelligence in Health Care: A Report From the National Academy of Medicine. JAMA. 2020;323(6):509–10.
Moorman LP. Principles for Real-World Implementation of Bedside Predictive Analytics Monitoring. Appl Clin Inform. 2021;12(4):888–96.
Lee D, Yoon SN. Application of Artificial Intelligence-Based Technologies in the Healthcare Industry: Opportunities and Challenges. Int J Environ Res Public Health. 2021;18(1):271.
Buchanan C, Howitt ML, Wilson R, Booth RG, Risling T, Bamford M. Predicted Influences of Artificial Intelligence on the Domains of Nursing: Scoping Review. JMIR Nursing. 2020;3(1):e23939.
Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Med Care Res Rev. 2012;69(2):123–57.
Powell BJ, Fernandez ME, Williams NJ, Aarons GA, Beidas RS, Lewis CC, et al. Enhancing the Impact of Implementation Strategies in Healthcare: A Research Agenda. Front Public Health. 2019;7:3.
Weiner BJ. A theory of organizational readiness for change. Implement Sci. 2009;4(1):67.
Scaccia JP, Cook BS, Lamont A, Wandersman A, Castellow J, Katz J, et al. A practical implementation science heuristic for organizational readiness: R = MC(2). J Community Psychol. 2015;43(4):484–501.
Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12.
Archibald MM, Ambagtsheer RC, Casey MG, Lawless M. Using Zoom Videoconferencing for Qualitative Data Collection: Perceptions and Experiences of Researchers and Participants. Int J Qual Methods. 2019;18:1609406919874596.
World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–4.
Article CAS Google Scholar
Council SR. Good Research Practice: Swedish Research Council; 2017 [Available from: https://www.vr.se/download/18.5639980c162791bbfe697882/1555334908942/Good-Research-Practice_VR_2017.pdf .
Download references
Acknowledgements
The authors would like to thank the participants who contributed to this study with their experiences.
All authors belong to the Healthcare Improvement Research Group at Halmstad University, https://hh.se/english/research/our-research/research-at-the-school-of-health-and-welfare/healthcare-improvement.html
Open access funding provided by Halmstad University. The funders for this study are the Swedish Government Innovation Agency Vinnova (grant 2019–04526) and the Knowledge Foundation (grant 20200208 01H). The funders were not involved in any aspect of study design, collection, analysis, interpretation of data, or in the writing or publication process.
Author information
Authors and affiliations.
School of Health and Welfare, Halmstad University, Box 823, 301 18, Halmstad, Sweden
Lena Petersson, Ingrid Larsson, Jens M. Nygren, Per Nilsen, Margit Neher, Julie E. Reed, Daniel Tyskbo & Petra Svedberg
Department of Health, Medicine and Caring Sciences, Division of Public Health, Faculty of Health Sciences, Linköping University, Linköping, Sweden
Department of Rehabilitation, School of Health Sciences, Jönköping University, Jönköping, Sweden
Margit Neher
You can also search for this author in PubMed Google Scholar
Contributions
LP, JMN, JR, DT and PS together identified the research question and designed the study. Applications for funding and coproduction agreements were put in place by PS and JMN. Data collection (the interviews) was carried out by LP and DT. Data analysis was performed by LP, IL, JMN, PN, MN and PS and then discussed with all authors. The manuscript was drafted by LP, IL, JMN, PN, MN and PS. JR and DT provided critical revision of the paper in terms of important intellectual content. All authors have read and approved the final submitted version.
Corresponding author
Correspondence to Lena Petersson .
Ethics declarations
Ethics approval and consent to participate.
The study conforms to the principles outlined in the Declaration of Helsinki (74) and was approved by the Swedish Ethical Review Authority (no. 2020–06246). The study fulfilled the requirements of Swedish research: information, consent, confidentiality, and safety of the participants and is guided by the ethical principles of: autonomy, beneficence, non-maleficence, and justice (75). The participants were first informed about the study by e-post and, at the same time, were asked if they wanted to participate in the study. If they agreed to participate, they were verbally informed at the beginning of the interview about the purpose and the structure of the study and that they could withdraw their consent to participate at any time. Participation was voluntary and the respondents were informed about the ethical considerations of confidentiality. Informed consent was obtained from all participants prior to the interview.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Petersson, L., Larsson, I., Nygren, J.M. et al. Challenges to implementing artificial intelligence in healthcare: a qualitative interview study with healthcare leaders in Sweden. BMC Health Serv Res 22 , 850 (2022). https://doi.org/10.1186/s12913-022-08215-8
Download citation
Received : 04 April 2022
Accepted : 20 June 2022
Published : 01 July 2022
DOI : https://doi.org/10.1186/s12913-022-08215-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Artificial intelligence
- Digital transformation
- Implementation
- Healthcare leaders
- Organizational change
- Qualitative methods
- Stakeholders
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
What is decision making?

Decisions, decisions. When was the last time you struggled with a choice? Maybe it was this morning, when you decided to hit the snooze button—again. Perhaps it was at a restaurant, with a miles-long menu and the server standing over you. Or maybe it was when you left your closet in a shambles after trying on seven different outfits before a big presentation. Often, making a decision—even a seemingly simple one—can be difficult. And people will go to great lengths—and pay serious sums of money—to avoid having to make a choice. The expensive tasting menu at the restaurant, for example. Or limiting your closet choices to black turtlenecks, à la Steve Jobs.
Get to know and directly engage with senior McKinsey experts on decision making
Aaron De Smet is a senior partner in McKinsey’s New Jersey office, Eileen Kelly Rinaudo is McKinsey’s global director of advancing women executives and is based in the New York office, Frithjof Lund is a senior partner in the Oslo office, and Leigh Weiss is a senior adviser in the Boston office.
If you’ve ever wrestled with a decision at work, you’re definitely not alone. According to McKinsey research, executives spend a significant portion of their time— nearly 40 percent , on average—making decisions. Worse, they believe most of that time is poorly used. People struggle with decisions so much so that we actually get exhausted from having to decide too much, a phenomenon called decision fatigue.
But decision fatigue isn’t the only cost of ineffective decision making. According to a McKinsey survey of more than 1,200 global business leaders, inefficient decision making costs a typical Fortune 500 company 530,000 days of managers’ time each year, equivalent to about $250 million in annual wages. That’s a lot of turtlenecks.
How can business leaders ease the burden of decision making and put this time and money to better use? Read on to learn the ins and outs of smart decision making—and how to put it to work.
Learn more about our People & Organizational Performance Practice .
How can organizations untangle ineffective decision-making processes?
McKinsey research has shown that agile is the ultimate solution for many organizations looking to streamline their decision making . Agile organizations are more likely to put decision making in the right hands, are faster at reacting to (or anticipating) shifts in the business environment, and often attract top talent who prefer working at companies with greater empowerment and fewer layers of management.
For organizations looking to become more agile, it’s possible to quickly boost decision-making efficiency by categorizing the type of decision to be made and adjusting the approach accordingly. In the next section, we review three types of decision making and how to optimize the process for each.
What are three keys to faster, better decisions?
Business leaders today have access to more sophisticated data than ever before. But it hasn’t necessarily made decision making any easier. For one thing, organizational dynamics—such as unclear roles, overreliance on consensus, and death by committee—can get in the way of straightforward decision making. And more data often means more decisions to be taken, which can become too much for one person, team, or department. This can make it more difficult for leaders to cleanly delegate, which in turn can lead to a decline in productivity.
Leaders are growing increasingly frustrated with broken decision-making processes, slow deliberations, and uneven decision-making outcomes. Fewer than half of the 1,200 respondents of a McKinsey survey report that decisions are timely, and 61 percent say that at least half the time they spend making decisions is ineffective.
What’s the solution? According to McKinsey research, effective solutions center around categorizing decision types and organizing different processes to support each type. Further, each decision category should be assigned its own practice—stimulating debate, for example, or empowering employees—to yield improvements in effectiveness.
Here are the three decision categories that matter most to senior leaders, and the standout practice that makes the biggest difference for each type of decision.
- Big-bet decisions are infrequent but high risk, such as acquisitions. These decisions carry the potential to shape the future of the company, and as a result are generally made by top leaders and the board. Spurring productive debate by assigning someone to argue the case for and against a potential decision can improve big-bet decision making.
- Cross-cutting decisions, such as pricing, can be frequent and high risk. These are usually made by business unit heads, in cross-functional forums as part of a collaborative process. These types of decisions can be improved by doubling down on process refinement. The ideal process should be one that helps clarify objectives, measures, and targets.
- Delegated decisions are frequent but low risk and are handled by an individual or working team with some input from others. Delegated decision making can be improved by ensuring that the responsibility for the decision is firmly in the hands of those closest to the work. This approach also enhances engagement and accountability.
In addition, business leaders can take the following four actions to help sustain rapid decision making :
- Focus on the game-changing decisions, ones that will help an organization create value and serve its purpose.
- Convene only necessary meetings, and eliminate lengthy reports. Turn unnecessary meetings into emails, and watch productivity bloom. For necessary meetings, provide short, well-prepared prereads to aid in decision making.
- Clarify the roles of decision makers and other voices. Who has a vote, and who has a voice?
- Push decision-making authority to the front line—and tolerate mistakes.

Introducing McKinsey Explainers : Direct answers to complex questions
How can business leaders effectively delegate decision making.
Business is more complex and dynamic than ever, meaning business leaders are faced with needing to make more decisions in less time. Decision making takes up an inordinate amount of management’s time—up to 70 percent for some executives—which leads to inefficiencies and opportunity costs.
As discussed above, organizations should treat different types of decisions differently . Decisions should be classified according to their frequency, risk, and importance. Delegated decisions are the most mysterious for many organizations: they are the most frequent, and yet the least understood. Only about a quarter of survey respondents report that their organizations make high-quality and speedy delegated decisions. And yet delegated decisions, because they happen so often, can have a big impact on organizational culture.
The key to better delegated decisions is to empower employees by giving them the authority and confidence to act. That means not simply telling employees which decisions they can or can’t make; it means giving employees the tools they need to make high-quality decisions and the right level of guidance as they do so.
Here’s how to support delegation and employee empowerment:
- Ensure that your organization has a well-defined, universally understood strategy. When the strategic intent of an organization is clear, empowerment is much easier because it allows teams to pull in the same direction.
- Clearly define roles and responsibilities. At the foundation of all empowerment efforts is a clear understanding of who is responsible for what, including who has input and who doesn’t.
- Invest in capability building (and coaching) up front. To help managers spend meaningful coaching time, organizations should also invest in managers’ leadership skills.
- Build an empowerment-oriented culture. Leaders should role model mindsets that promote empowerment, and managers should build the coaching skills they want to see. Managers and employees, in particular, will need to get comfortable with failure as a necessary step to success.
- Decide when to get involved. Managers should spend effort up front to decide what is worth their focused attention. They should know when it’s appropriate to provide close guidance and when not to.
How can you guard against bias in decision making?
Cognitive bias is real. We all fall prey, no matter how we try to guard ourselves against it. And cognitive and organizational bias undermines good decision making, whether you’re choosing what to have for lunch or whether to put in a bid to acquire another company.
Here are some of the most common cognitive biases and strategies for how to avoid them:
- Confirmation bias. Often, when we already believe something, our minds seek out information to support that belief—whether or not it is actually true. Confirmation bias involves overweighting evidence that supports our belief, underweighting evidence against our belief, or even failing to search impartially for evidence in the first place. Confirmation bias is one of the most common traps organizational decision makers fall into. One famous—and painful—example of confirmation bias is when Blockbuster passed up the opportunity to buy a fledgling Netflix for $50 million in 2000. (Actually, that’s putting it politely. Netflix executives remember being “laughed out” of Blockbuster’s offices.) Fresh off the dot-com bubble burst of 2000, Blockbuster executives likely concluded that Netflix had approached them out of desperation—not that Netflix actually had a baby unicorn on its hands.
- Herd mentality. First observed by Charles Mackay in his 1841 study of crowd psychology, herd mentality happens when information that’s available to the group is determined to be more useful than privately held knowledge. Individuals buy into this bias because there’s safety in the herd. But ignoring competing viewpoints might ultimately be costly. To counter this, try a teardown exercise , wherein two teams use scenarios, advanced analytics, and role-playing to identify how a herd might react to a decision, and to ensure they can refute public perceptions.
- Sunk-cost fallacy. Executives frequently hold onto underperforming business units or projects because of emotional or legacy attachment . Equally, business leaders hate shutting projects down . This, researchers say, is due to the ingrained belief that if everyone works hard enough, anything can be turned into gold. McKinsey research indicates two techniques for understanding when to hold on and when to let go. First, change the burden of proof from why an asset should be cut to why it should be retained. Next, categorize business investments according to whether they should be grown, maintained, or disposed of—and follow clearly differentiated investment rules for each group.
- Ignoring unpleasant information. Researchers call this the “ostrich effect”—when people figuratively bury their heads in the sand , ignoring information that will make their lives more difficult. One study, for example, found that investors were more likely to check the value of their portfolios when the markets overall were rising, and less likely to do so when the markets were flat or falling. One way to help get around this is to engage in a readout process, where individuals or teams summarize discussions as they happen. This increases the likelihood that everyone leaves a meeting with the same understanding of what was said.
- Halo effect. Important personal and professional choices are frequently affected by people’s tendency to make specific judgments based on general impressions . Humans are tempted to use simple mental frames to understand complicated ideas, which means we frequently draw conclusions faster than we should. The halo effect is particularly common in hiring decisions. To avoid this bias, structured interviews can help mitigate the essentializing tendency. When candidates are measured against indicators, intuition is less likely to play a role.
For more common biases and how to beat them, check out McKinsey’s Bias Busters Collection .
Learn more about Strategy & Corporate Finance consulting at McKinsey—and check out job opportunities related to decision making if you’re interested in working at McKinsey.
Articles referenced include:
- “ Bias busters: When the crowd isn’t necessarily wise ,” McKinsey Quarterly , May 23, 2022, Eileen Kelly Rinaudo , Tim Koller , and Derek Schatz
- “ Boards and decision making ,” April 8, 2021, Aaron De Smet , Frithjof Lund , Suzanne Nimocks, and Leigh Weiss
- “ To unlock better decision making, plan better meetings ,” November 9, 2020, Aaron De Smet , Simon London, and Leigh Weiss
- “ Reimagine decision making to improve speed and quality ,” September 14, 2020, Julie Hughes , J. R. Maxwell , and Leigh Weiss
- “ For smarter decisions, empower your employees ,” September 9, 2020, Aaron De Smet , Caitlin Hewes, and Leigh Weiss
- “ Bias busters: Lifting your head from the sand ,” McKinsey Quarterly , August 18, 2020, Eileen Kelly Rinaudo
- “ Decision making in uncertain times ,” March 24, 2020, Andrea Alexander, Aaron De Smet , and Leigh Weiss
- “ Bias busters: Avoiding snap judgments ,” McKinsey Quarterly , November 6, 2019, Tim Koller , Dan Lovallo, and Phil Rosenzweig
- “ Three keys to faster, better decisions ,” McKinsey Quarterly , May 1, 2019, Aaron De Smet , Gregor Jost , and Leigh Weiss
- “ Decision making in the age of urgency ,” April 30, 2019, Iskandar Aminov, Aaron De Smet , Gregor Jost , and David Mendelsohn
- “ Bias busters: Pruning projects proactively ,” McKinsey Quarterly , February 6, 2019, Tim Koller , Dan Lovallo, and Zane Williams
- “ Decision making in your organization: Cutting through the clutter ,” McKinsey Quarterly , January 16, 2018, Aaron De Smet , Simon London, and Leigh Weiss
- “ Untangling your organization’s decision making ,” McKinsey Quarterly , June 21, 2017, Aaron De Smet , Gerald Lackey, and Leigh Weiss
- “ Are you ready to decide? ,” McKinsey Quarterly , April 1, 2015, Philip Meissner, Olivier Sibony, and Torsten Wulf.

Want to know more about decision making?
Related articles.
What is productivity?

What is the future of work?

What is leadership?
Frequently asked questions
What’s the difference between results and discussion.
The results chapter or section simply and objectively reports what you found, without speculating on why you found these results. The discussion interprets the meaning of the results, puts them in context, and explains why they matter.
In qualitative research , results and discussion are sometimes combined. But in quantitative research , it’s considered important to separate the objective results from your interpretation of them.
Frequently asked questions: Dissertation
Dissertation word counts vary widely across different fields, institutions, and levels of education:
- An undergraduate dissertation is typically 8,000–15,000 words
- A master’s dissertation is typically 12,000–50,000 words
- A PhD thesis is typically book-length: 70,000–100,000 words
However, none of these are strict guidelines – your word count may be lower or higher than the numbers stated here. Always check the guidelines provided by your university to determine how long your own dissertation should be.
A dissertation prospectus or proposal describes what or who you plan to research for your dissertation. It delves into why, when, where, and how you will do your research, as well as helps you choose a type of research to pursue. You should also determine whether you plan to pursue qualitative or quantitative methods and what your research design will look like.
It should outline all of the decisions you have taken about your project, from your dissertation topic to your hypotheses and research objectives , ready to be approved by your supervisor or committee.
Note that some departments require a defense component, where you present your prospectus to your committee orally.
A thesis is typically written by students finishing up a bachelor’s or Master’s degree. Some educational institutions, particularly in the liberal arts, have mandatory theses, but they are often not mandatory to graduate from bachelor’s degrees. It is more common for a thesis to be a graduation requirement from a Master’s degree.
Even if not mandatory, you may want to consider writing a thesis if you:
- Plan to attend graduate school soon
- Have a particular topic you’d like to study more in-depth
- Are considering a career in research
- Would like a capstone experience to tie up your academic experience
The conclusion of your thesis or dissertation should include the following:
- A restatement of your research question
- A summary of your key arguments and/or results
- A short discussion of the implications of your research
The conclusion of your thesis or dissertation shouldn’t take up more than 5–7% of your overall word count.
For a stronger dissertation conclusion , avoid including:
- Important evidence or analysis that wasn’t mentioned in the discussion section and results section
- Generic concluding phrases (e.g. “In conclusion …”)
- Weak statements that undermine your argument (e.g., “There are good points on both sides of this issue.”)
Your conclusion should leave the reader with a strong, decisive impression of your work.
While it may be tempting to present new arguments or evidence in your thesis or disseration conclusion , especially if you have a particularly striking argument you’d like to finish your analysis with, you shouldn’t. Theses and dissertations follow a more formal structure than this.
All your findings and arguments should be presented in the body of the text (more specifically in the discussion section and results section .) The conclusion is meant to summarize and reflect on the evidence and arguments you have already presented, not introduce new ones.
A theoretical framework can sometimes be integrated into a literature review chapter , but it can also be included as its own chapter or section in your dissertation . As a rule of thumb, if your research involves dealing with a lot of complex theories, it’s a good idea to include a separate theoretical framework chapter.
A literature review and a theoretical framework are not the same thing and cannot be used interchangeably. While a theoretical framework describes the theoretical underpinnings of your work, a literature review critically evaluates existing research relating to your topic. You’ll likely need both in your dissertation .
While a theoretical framework describes the theoretical underpinnings of your work based on existing research, a conceptual framework allows you to draw your own conclusions, mapping out the variables you may use in your study and the interplay between them.
A thesis or dissertation outline is one of the most critical first steps in your writing process. It helps you to lay out and organize your ideas and can provide you with a roadmap for deciding what kind of research you’d like to undertake.
Generally, an outline contains information on the different sections included in your thesis or dissertation , such as:
- Your anticipated title
- Your abstract
- Your chapters (sometimes subdivided into further topics like literature review , research methods , avenues for future research, etc.)
When you mention different chapters within your text, it’s considered best to use Roman numerals for most citation styles. However, the most important thing here is to remain consistent whenever using numbers in your dissertation .
In most styles, the title page is used purely to provide information and doesn’t include any images. Ask your supervisor if you are allowed to include an image on the title page before doing so. If you do decide to include one, make sure to check whether you need permission from the creator of the image.
Include a note directly beneath the image acknowledging where it comes from, beginning with the word “ Note .” (italicized and followed by a period). Include a citation and copyright attribution . Don’t title, number, or label the image as a figure , since it doesn’t appear in your main text.
Definitional terms often fall into the category of common knowledge , meaning that they don’t necessarily have to be cited. This guidance can apply to your thesis or dissertation glossary as well.
However, if you’d prefer to cite your sources , you can follow guidance for citing dictionary entries in MLA or APA style for your glossary.
A glossary is a collection of words pertaining to a specific topic. In your thesis or dissertation, it’s a list of all terms you used that may not immediately be obvious to your reader. In contrast, an index is a list of the contents of your work organized by page number.
The title page of your thesis or dissertation goes first, before all other content or lists that you may choose to include.
The title page of your thesis or dissertation should include your name, department, institution, degree program, and submission date.
Glossaries are not mandatory, but if you use a lot of technical or field-specific terms, it may improve readability to add one to your thesis or dissertation. Your educational institution may also require them, so be sure to check their specific guidelines.
A glossary or “glossary of terms” is a collection of words pertaining to a specific topic. In your thesis or dissertation, it’s a list of all terms you used that may not immediately be obvious to your reader. Your glossary only needs to include terms that your reader may not be familiar with, and is intended to enhance their understanding of your work.
A glossary is a collection of words pertaining to a specific topic. In your thesis or dissertation, it’s a list of all terms you used that may not immediately be obvious to your reader. In contrast, dictionaries are more general collections of words.
An abbreviation is a shortened version of an existing word, such as Dr. for Doctor. In contrast, an acronym uses the first letter of each word to create a wholly new word, such as UNESCO (an acronym for the United Nations Educational, Scientific and Cultural Organization).
As a rule of thumb, write the explanation in full the first time you use an acronym or abbreviation. You can then proceed with the shortened version. However, if the abbreviation is very common (like PC, USA, or DNA), then you can use the abbreviated version from the get-go.
Be sure to add each abbreviation in your list of abbreviations !
If you only used a few abbreviations in your thesis or dissertation , you don’t necessarily need to include a list of abbreviations .
If your abbreviations are numerous, or if you think they won’t be known to your audience, it’s never a bad idea to add one. They can also improve readability, minimizing confusion about abbreviations unfamiliar to your reader.
A list of abbreviations is a list of all the abbreviations that you used in your thesis or dissertation. It should appear at the beginning of your document, with items in alphabetical order, just after your table of contents .
Your list of tables and figures should go directly after your table of contents in your thesis or dissertation.
Lists of figures and tables are often not required, and aren’t particularly common. They specifically aren’t required for APA-Style, though you should be careful to follow their other guidelines for figures and tables .
If you have many figures and tables in your thesis or dissertation, include one may help you stay organized. Your educational institution may require them, so be sure to check their guidelines.
A list of figures and tables compiles all of the figures and tables that you used in your thesis or dissertation and displays them with the page number where they can be found.
The table of contents in a thesis or dissertation always goes between your abstract and your introduction .
You may acknowledge God in your dissertation acknowledgements , but be sure to follow academic convention by also thanking the members of academia, as well as family, colleagues, and friends who helped you.
A literature review is a survey of credible sources on a topic, often used in dissertations , theses, and research papers . Literature reviews give an overview of knowledge on a subject, helping you identify relevant theories and methods, as well as gaps in existing research. Literature reviews are set up similarly to other academic texts , with an introduction , a main body, and a conclusion .
An annotated bibliography is a list of source references that has a short description (called an annotation ) for each of the sources. It is often assigned as part of the research process for a paper .
In a thesis or dissertation, the discussion is an in-depth exploration of the results, going into detail about the meaning of your findings and citing relevant sources to put them in context.
The conclusion is more shorter and more general: it concisely answers your main research question and makes recommendations based on your overall findings.
In the discussion , you explore the meaning and relevance of your research results , explaining how they fit with existing research and theory. Discuss:
- Your interpretations : what do the results tell us?
- The implications : why do the results matter?
- The limitation s : what can’t the results tell us?
Results are usually written in the past tense , because they are describing the outcome of completed actions.
The results chapter of a thesis or dissertation presents your research results concisely and objectively.
In quantitative research , for each question or hypothesis , state:
- The type of analysis used
- Relevant results in the form of descriptive and inferential statistics
- Whether or not the alternative hypothesis was supported
In qualitative research , for each question or theme, describe:
- Recurring patterns
- Significant or representative individual responses
- Relevant quotations from the data
Don’t interpret or speculate in the results chapter.
To automatically insert a table of contents in Microsoft Word, follow these steps:
- Apply heading styles throughout the document.
- In the references section in the ribbon, locate the Table of Contents group.
- Click the arrow next to the Table of Contents icon and select Custom Table of Contents.
- Select which levels of headings you would like to include in the table of contents.
Make sure to update your table of contents if you move text or change headings. To update, simply right click and select Update Field.
All level 1 and 2 headings should be included in your table of contents . That means the titles of your chapters and the main sections within them.
The contents should also include all appendices and the lists of tables and figures, if applicable, as well as your reference list .
Do not include the acknowledgements or abstract in the table of contents.
The abstract appears on its own page in the thesis or dissertation , after the title page and acknowledgements but before the table of contents .
An abstract for a thesis or dissertation is usually around 200–300 words. There’s often a strict word limit, so make sure to check your university’s requirements.
In a thesis or dissertation, the acknowledgements should usually be no longer than one page. There is no minimum length.
The acknowledgements are generally included at the very beginning of your thesis , directly after the title page and before the abstract .
Yes, it’s important to thank your supervisor(s) in the acknowledgements section of your thesis or dissertation .
Even if you feel your supervisor did not contribute greatly to the final product, you must acknowledge them, if only for a very brief thank you. If you do not include your supervisor, it may be seen as a snub.
In the acknowledgements of your thesis or dissertation, you should first thank those who helped you academically or professionally, such as your supervisor, funders, and other academics.
Then you can include personal thanks to friends, family members, or anyone else who supported you during the process.
Ask our team
Want to contact us directly? No problem. We are always here for you.
- Email [email protected]
- Start live chat
- Call +1 (510) 822-8066
- WhatsApp +31 20 261 6040

Our team helps students graduate by offering:
- A world-class citation generator
- Plagiarism Checker software powered by Turnitin
- Innovative Citation Checker software
- Professional proofreading services
- Over 300 helpful articles about academic writing, citing sources, plagiarism, and more
Scribbr specializes in editing study-related documents . We proofread:
- PhD dissertations
- Research proposals
- Personal statements
- Admission essays
- Motivation letters
- Reflection papers
- Journal articles
- Capstone projects
Scribbr’s Plagiarism Checker is powered by elements of Turnitin’s Similarity Checker , namely the plagiarism detection software and the Internet Archive and Premium Scholarly Publications content databases .
The add-on AI detector is powered by Scribbr’s proprietary software.
The Scribbr Citation Generator is developed using the open-source Citation Style Language (CSL) project and Frank Bennett’s citeproc-js . It’s the same technology used by dozens of other popular citation tools, including Mendeley and Zotero.
You can find all the citation styles and locales used in the Scribbr Citation Generator in our publicly accessible repository on Github .
- Open access
- Published: 07 June 2024
Effects of intensive lifestyle changes on the progression of mild cognitive impairment or early dementia due to Alzheimer’s disease: a randomized, controlled clinical trial
- Dean Ornish 1 , 2 ,
- Catherine Madison 1 , 3 ,
- Miia Kivipelto 4 , 5 , 6 , 7 ,
- Colleen Kemp 8 ,
- Charles E. McCulloch 9 ,
- Douglas Galasko 10 ,
- Jon Artz 11 , 12 ,
- Dorene Rentz 13 , 14 , 15 ,
- Jue Lin 16 ,
- Kim Norman 17 ,
- Anne Ornish 1 ,
- Sarah Tranter 8 ,
- Nancy DeLamarter 1 ,
- Noel Wingers 1 ,
- Carra Richling 1 ,
- Rima Kaddurah-Daouk 18 ,
- Rob Knight 19 ,
- Daniel McDonald 20 ,
- Lucas Patel 21 ,
- Eric Verdin 22 , 23 ,
- Rudolph E. Tanzi 13 , 24 , 25 , 26 &
- Steven E. Arnold 13 , 27
Alzheimer's Research & Therapy volume 16 , Article number: 122 ( 2024 ) Cite this article
14k Accesses
726 Altmetric
Metrics details
Evidence links lifestyle factors with Alzheimer’s disease (AD). We report the first randomized, controlled clinical trial to determine if intensive lifestyle changes may beneficially affect the progression of mild cognitive impairment (MCI) or early dementia due to AD.
A 1:1 multicenter randomized controlled phase 2 trial, ages 45-90 with MCI or early dementia due to AD and a Montreal Cognitive Assessment (MoCA) score of 18 or higher. The primary outcome measures were changes in cognition and function tests: Clinical Global Impression of Change (CGIC), Alzheimer’s Disease Assessment Scale (ADAS-Cog), Clinical Dementia Rating–Sum of Boxes (CDR-SB), and Clinical Dementia Rating Global (CDR-G) after 20 weeks of an intensive multidomain lifestyle intervention compared to a wait-list usual care control group. ADAS-Cog, CDR-SB, and CDR-Global scales were compared using a Mann-Whitney-Wilcoxon rank-sum test, and CGIC was compared using Fisher’s exact test. Secondary outcomes included plasma Aβ42/40 ratio, other biomarkers, and correlating lifestyle with the degree of change in these measures.
Fifty-one AD patients enrolled, mean age 73.5. No significant differences in any measures at baseline. Only two patients withdrew. All patients had plasma Aβ42/40 ratios <0.0672 at baseline, strongly supporting AD diagnosis. After 20 weeks, significant between-group differences in the CGIC ( p = 0.001), CDR-SB ( p = 0.032), and CDR Global ( p = 0.037) tests and borderline significance in the ADAS-Cog test ( p = 0.053). CGIC, CDR Global, and ADAS-Cog showed improvement in cognition and function and CDR-SB showed significantly less progression, compared to the control group which worsened in all four measures. Aβ42/40 ratio increased in the intervention group and decreased in the control group ( p = 0.003). There was a significant correlation between lifestyle and both cognitive function and the plasma Aβ42/40 ratio. The microbiome improved only in the intervention group ( p <0.0001).
Conclusions
Comprehensive lifestyle changes may significantly improve cognition and function after 20 weeks in many patients with MCI or early dementia due to AD.
Trial registration
Approved by Western Institutional Review Board on 12/31/2017 (#20172897) and by Institutional Review Boards of all sites. This study was registered retrospectively with clinicaltrials.gov on October 8, 2020 (NCT04606420, ID: 20172897).
Increasing evidence links lifestyle factors with the onset and progression of dementia, including AD. These include unhealthful diets, being sedentary, emotional stress, and social isolation.
For example, a Lancet commission on dementia prevention, intervention, and care listed 12 potentially modifiable risk factors that together account for an estimated 40% of the global burden of dementia [ 1 ]. Many of these factors (e.g., hypertension, smoking, depression, type 2 diabetes, obesity, physical inactivity, and social isolation) are also risk factors for coronary heart disease and other chronic illnesses because they share many of the same underlying biological mechanisms. These include chronic inflammation, oxidative stress, insulin resistance, telomere shortening, sympathetic nervous system hyperactivity, and others [ 2 ]. A recent study reported that the association of lifestyle with cognition is mostly independent of brain pathology, though a part, estimated to be only 12%, was through β-amyloid [ 3 ].
In one large prospective study of adults 65 or older in Chicago, the risk of developing AD was 38% lower in those eating high vs low amounts of vegetables and 60% lower in those consuming omega-3 fatty acids at least once/week, [ 4 ] whereas consuming saturated fat and trans fats more than doubled the risk of developing AD [ 5 ].A systematic review and meta-analysis of 243 observational prospective studies and 153 randomized controlled trials found a similar relationship between these and similar risk factors and the onset of AD [ 6 ].
The multifactorial etiology and heterogeneity of AD suggest that multidomain lifestyle interventions may be more effective than single-domain ones for reducing the risk of dementia, and that more intensive multimodal lifestyle interventions may be more efficacious than moderate ones at preventing dementia [ 7 ].
For example, in the Finnish Geriatric Intervention Study (FINGER) study, a RCT of men and women 60-77 in age with Cardiovascular Risk Factors, Aging, and Incidence of Dementia (CAIDE) dementia risk scores of at least 6 points and cognition at mean or slightly lower, a multimodal intervention of diet, exercise, cognitive training, vascular risk monitoring maintained cognitive function after 2 years in older adults at increased risk of dementia [ 8 ]. After 24 months, global cognition in the FINGER intervention group was 25% higher than in the control group which declined. Moreover, the FINGER intervention was equally beneficial regardless of several demographic and socioeconomic risk factors [ 9 ] and apolipoprotein E (APOE) ε4 status [ 10 ].
The FINGER lifestyle intervention also resulted in a 13-20% reduction in rates of cardiovascular disease events (stroke, transient ischemic attack, or coronary), providing more evidence that “what’s good for the heart is good for the brain”(and vice versa) [ 11 ]. Other large-scale multidomain intervention studies to determine if this intervention can help prevent dementia are being conducted or planned in over 60 countries worldwide, as part of the World-Wide FINGERS network, including the POINTER study in the U.S. [ 12 , 13 ].
More recently, a similar dementia prevention-oriented RCT showed that a 2-year personalized multidomain intervention led to modest improvements in cognition and dementia risk factors in those at risk for (but not diagnosed with) dementia and AD [ 14 ].
All these studies showed that lifestyle changes may help prevent dementia. The study we are reporting here is the first randomized, controlled clinical trial to test whether intensive lifestyle changes may beneficially affect those already diagnosed with mild cognitive impairment (MCI) or early dementia due to AD.
In two earlier RCTs, we found that the same multimodal lifestyle intervention described in this article resulted in regression of coronary atherosclerosis as measured by quantitative coronary arteriography [ 15 ] and ventricular function, [ 16 ] improvements in myocardial perfusion as measured by cardiac PET scans, and 2.5 times fewer cardiac events after five years, all of which were statistically significant [ 17 ]. Until then, it was believed that coronary heart disease progression could only be slowed, not stopped or reversed, similar to how MCI or early dementia due to AD are viewed today.
Since AD and coronary heart disease share many of the same risk factors and biological mechanisms, and since moderate multimodal lifestyle changes may help prevent AD, [ 18 ] we hypothesized that a more intensive multimodal intervention proven to often reverse the progression of coronary heart disease and some other chronic diseases may also beneficially affect the progression of MCI or early dementia due to AD.
We report here results of a randomized controlled trial to determine if the progression of MCI or early dementia due to AD may be slowed, stopped, or perhaps even reversed by a comprehensive, multimodal, intensive lifestyle intervention after 20 weeks when compared to a usual-care randomized control group. This lifestyle intervention includes (1) a whole foods, minimally processed plant-based diet low in harmful fats and low in refined carbohydrates and sweeteners with selected supplements; (2) moderate exercise; (3) stress management techniques; and (4) support groups.
This intensive multimodal lifestyle modification RCT sought to address the following questions:
Can the specified multimodal intensive lifestyle changes beneficially affect the progression of MCI or early dementia due to AD as measured by the AD Assessment Scale–Cognitive Subscale (ADAS-Cog), CGIC (Clinical Global Impression of Change), CDR-SB (Clinical Dementia Rating Sum of Boxes), and CDR-G (Clinical Dementia Rating Global) testing?
Is there a significant correlation between the degree of lifestyle change and the degree of change in these measures of cognition and function?
Is there a significant correlation between the degree of lifestyle change and the degree of change in selected biomarkers (e.g., the plasma Aβ42/40 ratio)?
Participants and methods
This study was a 1:1 multi-center RCT during the first 20 weeks of the study, and these findings are reported here. Patients who met the clinical trial inclusion criteria were enrolled between September 2018 and June 2022.
Participants were enrolled who met the following inclusion criteria:
Male or female, ages 45 to 90
Current diagnosis of MCI or early dementia due to AD process, with a MoCA score of 18 or higher (National Institute on Aging–Alzheimer’s Association McKhann and Albert 2011 criteria) [ 19 , 20 ]
Physician shared this diagnosis with the patient and approved their participation in this clinical trial
Willingness and ability to participate in all aspects of the intervention
Availability of spouse or caregiver to provide collateral information and assist with study adherence
Patients were excluded if they had any of the following:
Moderate or severe dementia
Physical disability that precludes regular exercise
Evidence for other primary causes of neurodegeneration or dementia, e.g., significant cerebrovascular disease (whose primary cause of dementia was vascular in origin), Lewy Body disease, Parkinson's disease, FTD
Significant ongoing psychiatric or substance abuse problems
Fifty-one participants with MCI or early-stage dementia due to AD who met these inclusion criteria were enrolled between September 2018 and June 2022 and underwent baseline testing. 26 of the enrolled participants were randomly assigned to an intervention group that received the multimodal lifestyle intervention for 20 weeks and 25 participants were randomly assigned to a usual habits and care control group that was asked not to make any lifestyle changes for 20 weeks, after which they would be offered the intervention. Patients in both groups received standard of care treatment managed by their own neurologist.
The intervention group received the lifestyle program for 20 weeks (initially in person, then via synchronous Zoom after March 2020 due to COVID-19). Two participants who did not want to continue these lifestyle changes withdrew during this time, both in the intervention group (one male, one female). Participants in both groups completed a follow-up visit at 20 weeks, where clinical and cognitive assessments were completed. Data were analyzed comparing the baseline and 20 week assessments between the groups.
In a drug trial, access to an investigational new drug can be restricted from participants in a randomized control group. However, we learned in our prior clinical trials of this lifestyle intervention with other diseases that it is often difficult to persuade participants who are randomly assigned to a usual-care control group to refrain from making these lifestyle changes for more than 20 weeks, which is why this time duration was chosen. If participants in both groups made similar lifestyle changes, then it would not be possible to show differences between the groups. Therefore, to encourage participants randomly assigned to the control group not to make lifestyle changes during the first 20 weeks, we offered to provide them the same lifestyle program at no cost to them for 20 weeks after being in the usual-care control group and tested after 20 weeks.
We initially planned to enroll 100 patients into this study based on power calculations of possible differences between groups in cognition and function after 20 weeks. However, due to challenges in recruiting patients, especially with the COVID-19 emergency and that many pharma trials began recruiting patients with similar criteria, it took longer to enroll patients than initially planned [ 21 ]. Because of this, we terminated recruitment after 51 patients were enrolled. This decision was based only on recruitment issues and limited funding, without reviewing the data at that time.
Patients were recruited from advertisements, presentations at neurology meetings, referrals from diverse groups of neurologists and other physicians, and a search of an online database of patients at UCSF. We put a special emphasis on recruiting diverse patients, although we were less successful in doing so than we hoped (Table 1 ).
This clinical trial was approved by the Western Institutional Review Board on 12/31/2017 (approval number: 20172897) and all participants and their study partners provided written informed consent. The trial protocol was also approved by the appropriate Institutional Review Board of all participating sites, and all subjects provided informed consent. Due to the COVID-19 emergency, planned MRI and amyloid PET scans were no longer feasible, and the number of cognition and function tests was decreased. An initial inclusion criterion of “current diagnosis of mild to moderate dementia due to AD (McKhann et al., 2011)” was further clarified to include a MoCA score of 18 or higher. This study was registered with clinicaltrials.gov on October 8, 2020 (NCT04606420, Unique Protocol ID: 20172897) retrospectively due to an administrative error. None of the sponsors who provided funding for this study participated in its design, conduct, management, or reporting of the results. Those providing the lifestyle intervention were separate from those performing testing and from those collecting and analyzing the data, who were blinded to group assignment. All authors contributed to manuscript draft revisions, provided critical comment, and approved submission for publication.
Any modifications in the protocol were approved in advance and in writing by the senior biostatistician (Charles McCulloch PhD) or the senior expert neuropsychologist (Dorene Rentz PsyD), and subsequently approved by the WIRB.
Patients were initially recruited only from the San Francisco Bay area beginning October 2018 and met in person until February 2020 when the COVID-19 pandemic began. Subsequently, this multimodal lifestyle intervention was offered to patients at home in real time via Zoom.
Offering this intervention virtually provided an opportunity to recruit patients from multiple sites, including the Massachusetts General Hospital/Harvard Medical School, Boston, MA; the University of California, San Diego; and Renown Regional Medical Center, Reno, NV, as well as with neurologists in the San Francisco Bay Area. These participants were recruited and tested locally at each site and the intervention was provided via Zoom and foods were sent directly to their home.
Patient recruitment
This is described in the Supplemental Materials section.
Intensive multimodal lifestyle intervention
Each patient received a copy of a book which describes this lifestyle medicine intervention for other chronic diseases. [ 2 ]
A whole foods minimally-processed plant-based (vegan) diet, high in complex carbohydrates (predominantly fruits, vegetables, whole grains, legumes, soy products, seeds and nuts) and especially low in harmful fats, sweeteners and refined carbohydrates. It was approximately 14-18% of calories as total fat, 16-18% protein, and 63-68% mostly complex carbohydrates. Calories were unrestricted. Those with higher caloric needs were given extra portions.
To assure the high adherence and standardization required to adequately test the hypothesis, 21 meals/week and snacks plus the daily supplements listed below were provided throughout the 40 weeks of this intervention to each study participant and his or her spouse or study partner at no cost to them. Twice/week, we overnight shipped to each patient as well as to their spouse or study partner three meals plus two snacks per day that met the nutritional guidelines as well as the prescribed nutritional supplements.
We asked participants to consume only the food and nutritional supplements we sent to them and no other foods. We reasoned that if adherence to the diet and lifestyle intervention was high, whatever outcomes we measured would be of interest. That is, if patients in the intervention group were adherent but showed no significant benefits, that would be a disappointing but an important finding. If they showed improvement, that would also be an important finding. But if they did not follow the lifestyle intervention sufficiently, then we would not have been able to adequately test the hypotheses.
Aerobic (e.g., walking) at least 30 minutes/day and mild strength training exercises at least three times per week from an exercise physiologist in person or with virtual sessions. Patients were given a personalized exercise prescription based on age and fitness level. All sessions were overseen by a registered nurse.
- Stress management
Meditation, gentle yoga-based poses, stretching, progressive relaxation, breathing exercises, and imagery for a total of one hour per day, supervised by a certified stress management specialist. The purpose of each technique was to increase the patient’s sense of relaxation, concentration, and awareness. They were also given access to online meditations. Patients had the option of using flashing-light glasses at a theta frequency of 7.83 Hz plus soothing music as an aid to meditation and insomnia [ 22 ]. They were also encouraged to get adequate sleep.
Group support
Participants and their spouses/study partners participated in a support group one hour/session, three days/week, supervised by a licensed mental health professional in a supportive, safe environment to increase emotional support and community as well as communication skills and strategies for maintaining adherence to the program. They also received a book with memory exercises used periodically during group sessions [ 23 ].
To reinforce this lifestyle intervention, each patient and their spouse or study partner met three times/week, four hours/session via Zoom: 2
one hour of supervised exercise (aerobic + strength training)
one hour of stress management practices (stretching, breathing, meditation, imagery)
one hour of a support group
one hour lecture on lifestyle
Additional optional exercise and stress management classes were provided.
Supplements
Omega-3 fatty acids with Curcumin (1680 mg omega-3 & 800 mg Curcumin, Nordic Naturals ProOmega CRP, 4 capsules/day). Omega-3 fatty acids: In those age 65 or older, those consuming omega-3 fatty acids once/week or more had a 60% lower risk of developing AD, and total intake of n-3 polyunsaturated fatty acids was associated with reduced risk of Alzheimer disease [ 24 ]. Curcumin targets inflammatory and antioxidant pathways as well as (directly) amyloid aggregation, [ 25 ] although there may be problems with bioavailability and crossing the blood-brain barrier [ 26 ].
Multivitamin and Minerals (Solgar VM-75 without iron, 1 tablet/day). Combinatorial formulations demonstrate improvement in cognitive performance and the behavioral difficulties that accompany AD [ 27 ].
Coenzyme Q10 (200 mg, Nordic Naturals, 2 soft gels/day). CoQ10. May reduce mitochondrial impairment in AD [ 28 ].
Vitamin C (1 gram, Solgar, 1 tablet/day): Maintaining healthy vitamin C levels may have a protective function against age-related cognitive decline and AD [ 29 ].
Vitamin B12 (500 mcg, Solgar, 1 tablet/day): B12 hypovitaminosis is linked to the development of AD pathology [ 30 ].
Magnesium L-Threonate (Mg) (144 mg, Magtein, 2 tablets/day). A meta-analysis found that Mg deficiency may be a risk factor of AD and Mg supplementation may be an adjunctive treatment for AD [ 31 ].
Hericium erinaceus (Lion’s Mane, Stamets Host Defense, 2 grams/day): Lion’s mane may produce significant improvements in cognition and function in healthy people over 50 [ 32 ] and in MCI patients compared to placebo [ 33 ].
Super Bifido Plus Probiotic (Flora, 1 tablet/day). A meta-analysis suggests that probiotics may benefit AD patients [ 34 ].
Primary outcome measures: cognition and function testing
Four tests were used to assess changes in cognition and function in these patients. These are standard measures of cognition and function included in many FDA drug trials: ADAS-Cog; Clinical Global Impression of Change (CGIC); Clinical Dementia Rating Sum of Boxes (CDR-SB); Clinical Dementia Rating Global (CDR Global). All cognition and function raters were trained psychometrists with experience in administering these tests in clinical trials. Efforts were made to have the same person perform cognitive testing at each visit to reduce inter-observer variability. Those doing ADAS-Cog assessments were certified raters and tested patients in person. The CGIC and CDR tests were administered for all patients via Zoom by different raters than the ADAS-cog. Also, raters were blind to treatment arm to the degree possible.
Secondary outcome measures: biomarkers and microbiome
These are described in the Supplemental Materials section. These include blood-based biomarkers (such as the plasma Aβ42/40 ratio) and microbiome taxa (organisms).
Statistical methods
These are described in the Supplemental Materials section.
The recruitment effort for this trial lasted from 01/23/2018 to 6/16/2022. The most effective recruitment method was referral from the subjects’ physician or healthcare provider. Additional recruitment efforts included advertising in print and digital media; speaking to community groups; mentioning the study during podcast and radio interviews; collaborating with research institutions that provide dementia diagnosis and treatment; and contracting a clinical trials recruitment service (Linea). A total of 1585 people contacted us; of these, 1300 did not meet the inclusion criteria, 102 declined participation, and 132 were screening incomplete when enrollment closed, resulting in the enrollment of 51 participants (Fig. 1 ).
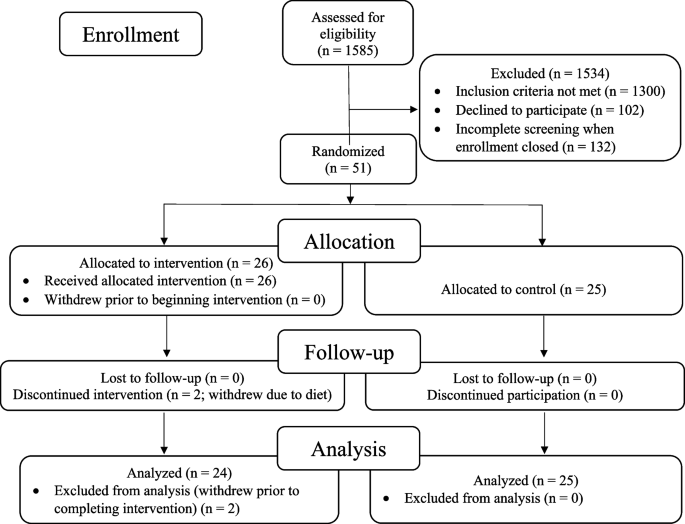
CONSORT flowchart: patients, demographics, and enrollment
The remaining 51 patients were randomized to an intervention group (26 patients) that received the lifestyle intervention for 20 weeks or to a usual-care control group (25 patients) that was asked not to make any lifestyle changes. Two patients in the intervention group withdrew during the intervention because they did not want to continue the diet and lifestyle changes. No patients in the control group withdrew prior to 20-week testing. Analyses were performed on the remaining 49 patients. No patients were lost to follow-up.
All of these 49 patients had plasma Aβ42/40 ratios <0.089 (all were <0.0672), strongly supporting the diagnosis of Alzheimer’s disease [ 35 ].
At baseline, there were no statistically significant differences between the intervention group and the randomized control group in any measures, including demographic characteristics, cognitive function measures, or biomarkers (Table 1 and Table 2 ).
Cognition and function testing: primary analysis
Results after 20 weeks of a multimodal intensive lifestyle intervention in all patients showed overall statistically significant differences between the intervention group and the randomized control group in cognition and function in the CGIC ( p = 0.001), CDR-SB ( p = 0.032), and CDR Global ( p = 0.037) tests and of borderline significance in the ADAS-Cog test ( p = 0.053, Table 3 ). Three of these measures (CGIC, CDR Global, ADAS-Cog) showed improvement in cognition and function in the intervention group and worsening in the control group, and one test (CDR-SB) showed significantly less progression when compared to the randomized control group, which worsened in all four of these measures.
PRIMARY ANALYSIS (with outlier included), Table 3 :
CGIC (Clinical Global Impression of Change)
These scores improved in the intervention group and worsened in the control group.
(Fisher’s exact p -value = 0.001). 10 people in the intervention group showed improvement compared to none in the control group. 7 people in the intervention group and 8 people in the control group were unchanged. 7 people in the intervention group showed minimal worsening compared to 14 in the control group. None in the intervention group showed moderate worsening compared to 3 in the control group.
CDR-Global (Clinical Dementia Rating-Global)
These scores improved in the intervention group (from 0.69 to 0.65) and worsened in the randomized control group (from 0.66 to 0.74), mean difference = 0.12, p = 0.037 (Table 3 and Fig. 2 ).
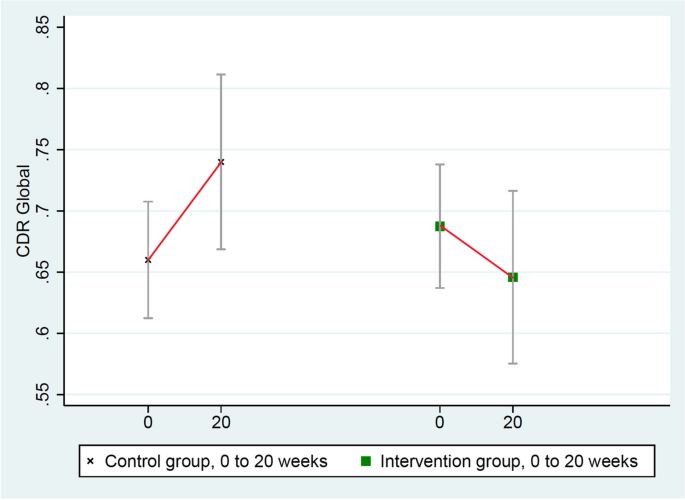
Changes in CDR-Global (lower = improved)
ADAS-Cog (Alzheimer’s Disease Assessment Scale)
These scores improved in the intervention group (from 21.551 to 20.536) and worsened in the randomized control group (from 21.252 to 22.160), mean group difference of change = 1.923 points, p = 0.053 (Table 3 and Fig. 3 ). (ADAS-Cog testing in one intervention group patient was not administered properly so it was excluded.)
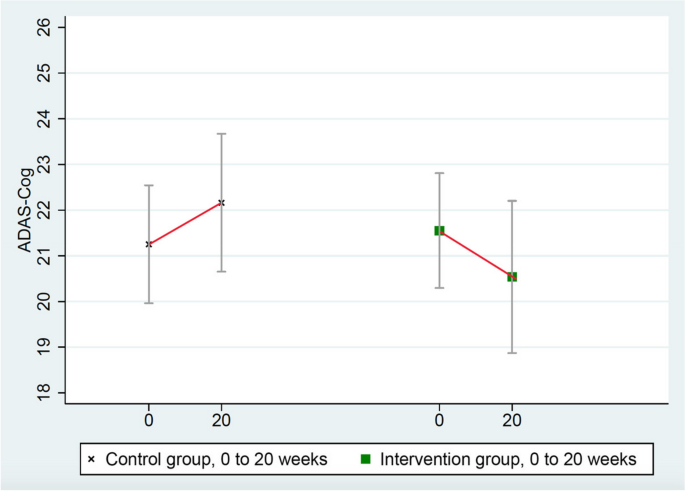
Changes in ADAS-Cog (lower = improved)
CDR-SB (Clinical Dementia Rating Sum of Boxes)
These scores worsened significantly more in the control group (from 3.34 to 3.86) than in the intervention group (from 3.27 to 3.35), mean group difference = 0.44, p = 0.032 (Table 3 and Fig. 4 ).
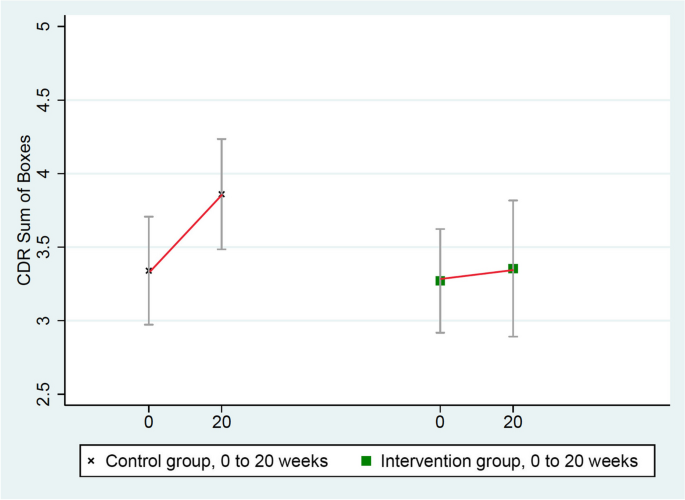
Changes in CDR-SB (lower = improved)
There were no significant differences in depression scores as measured by PHQ-9 between the intervention and control groups.
Secondary sensitivity analyses
One patient in the intervention group was a clear statistical outlier in his cognitive function testing based on standard mathematical definitions (none was an outlier in the control group) [ 36 ]. Therefore, this patient’s data were excluded in a secondary sensitivity analysis. These results showed statistically significant differences in all four of these measures of cognition and function (Table 4 ). Three measures (ADAS-Cog, CGIC, and CDR Global) showed significant improvement in cognition and function and one (CDR-SB) showed significantly less worsening when compared to the randomized control group, which worsened in all four of these measures.
Sensitivity analysis (with outlier excluded)
There were no significant differences in depression scores as measured by PHQ-9 between the intervention and control groups in either analysis.
A reason why this patient might have been a statistical outlier is that he reported intense situational stress before his testing. As a second sensitivity analysis, this same outlier patient was retested when he was calmer, and all four measures (ADAS-Cog, CGIC, CDR Global, and CDR-SB) showed significant improvement in cognition and function, whereas the randomized control group worsened in all four of these measures.
Biomarker results
We selected biomarkers that have a known role in the pathophysiology of AD (Table 5 ). Of note is that the plasma Aβ42/40 ratio increased in the intervention group but decreased in the randomized control group ( p = 0.003, two-tailed).
Correlation of lifestyle index and cognitive function
In the current clinical trial, despite the inherent limitations of self-reported data, we found statistically significant correlations between the degree of lifestyle change (from baseline to 20 weeks) and the degree of change in three of four measures of cognition and function as well as correlations between the adherence to desired lifestyle changes at just the 20-week timepoint and the degree of change in two of the four measures of cognition and function and borderline significance in the fourth measure.
Correlation with lifestyle at 20 weeks: p = 0.052; correlation: 0.241
Correlation with degree of change in lifestyle: p = 0.015; correlation: 0.317
Correlation with lifestyle at 20 weeks: p = 0.043; correlation: 0.251
Correlation with degree of change in lifestyle: p = 0.081; correlation: 0.205
Correlation with lifestyle at 20 weeks: p = 0.065; correlation: 0.221
Correlation with degree of change in lifestyle: p = 0.024; correlation: 0.286
Correlation with lifestyle at 20 weeks: p = 0.002
Correlation with degree of change in lifestyle: p = 0.0005
(CGIC tests are non-parametric analyses, so standard effect size calculations are not included for this measure.)
Also, we also found a significant correlation between dietary total fat intake and changes in the CGIC measure ( p = 0.001), but this was not significant for the other three measures.
Correlation of lifestyle index and biomarker data
In the current clinical trial, despite the inherent limitations of self-reported data, we found statistically significant correlations between the degree of lifestyle change (from baseline to 20 weeks) and the degree of change in many of the key biomarkers, as well as correlations between the degree of lifestyle change at 20 weeks and the degree of change in these biomarkers:
Plasma Aβ42/40 ratio
Correlation with lifestyle at 20 weeks: p = 0.035; correlation: 0.306
Correlation with degree of change in lifestyle: p = 0.068; correlation: 0.266
Correlation with lifestyle at 20 weeks: p = 0.011; correlation: 0.363
Correlation with degree of change in lifestyle: p = 0.007; correlation: 0.383
LDL-cholesterol
Correlation with lifestyle at 20 weeks: p < 0.0001; correlation: 0.678
Correlation with degree of change in lifestyle: p < 0.0001; correlation: 0.628
Beta-Hydroxybutyrate (ketones)
Correlation with lifestyle at 20 weeks: p = 0.013; correlation: 0.372
Correlation with degree of change in lifestyle: p = 0.034; correlation: 0.320
Correlation with lifestyle at 20 weeks: p = 0.228; correlation: 0.177
Correlation with degree of change in lifestyle: p = 0.135; correlation: 0.219
GFAP/glial fibrillary acidic protein
Correlation with lifestyle at 20 weeks: p = 0.096; correlation: 0.243
Correlation with degree of change in lifestyle: p =0.351; correlation: 0.138
What degree of lifestyle change is correlated with improvement in cognitive function tests?
What degree of lifestyle is needed to stop or improve the worsening of MCI or early dementia due to AD? In other words, what % of adherence to the lifestyle intervention was correlated with no change in MCI or dementia across both groups? Higher adherence than this degree of lifestyle change was associated with improvement in MCI or dementia.
Correlation with lifestyle at 20 weeks: 71.4% adherence
Correlation with lifestyle at 20 weeks: 120.6% adherence
CDR-Global:
Correlation with lifestyle at 20 weeks: 95.6%
Microbiome results
There was a significant and beneficial change in the microbiome configuration in the intervention group but not in the control group.
Several taxa (groups of microorganisms) that increased only in the intervention group were consistent with those involved in reduced AD risk in other studies. For example, Blautia, which increased during the intervention in the intervention group, has previously been associated with a lower risk of AD, potentially due to its involvement in increasing γ-aminobutyric acid (GABA) production [ 37 ]. Eubacterium also increased during the intervention in the intervention group, and prior studies have identified Eubacterium genera (namely Eubacterium fissicatena) as a protective factor in AD [ 38 ].
Also, there was a decrease in relative abundance of taxa involved in increased AD risk in the intervention group, e.g., Prevotella and Turicibacter , the latter of which has been associated with relevant biological processes such as 5-HT production. Prevotella and Turicibacter have previously been shown to increase with disease progression, [ 39 ] and these taxa decreased over the course of the intervention.
These results support the hypothesis that the lifestyle intervention may beneficially modify specific microbial groups in the microbiome: increasing those that lower the risk of AD and decreasing those that increase the risk of AD. (Please see Supplement for more detailed information.)
We report the first randomized, controlled trial showing that an intensive multimodal lifestyle intervention may significantly improve cognition and function and may allay biological features in many patients with MCI or early dementia due to AD after 20 weeks.
After 20 weeks of a multimodal intensive lifestyle intervention, results of the primary analysis when all patients were included showed overall statistically significant differences between the intervention group and the randomized control group in cognition and function as measured by the CGIC ( p = 0.001), CDR-SB ( p = 0.032), and CDR Global ( p = 0.037) tests and of borderline significance in the ADAS-Cog test ( p = 0.053).
Three of these measures (CGIC, CDR Global, ADAS-Cog) showed improvement in cognition and function in the intervention group and worsening in the randomized control group, and one test (CDR-SB) showed less progression in the intervention group when compared to the control group which worsened in all four of these measures.
These differences were even clearer in a secondary sensitivity analysis when a mathematical outlier was excluded. These results showed statistically significant differences between groups in all four of these measures of cognition and function. Three of these measures showed improvement in cognition and function and one (CDR-SB) showed less deterioration when compared to the randomized control group, which worsened in all four of these measures.
The validity of these changes in cognition and function and possible biological mechanisms of improvement is supported by the observed changes in several clinically relevant biomarkers that showed statistically significant differences in a beneficial direction after 20 weeks when compared to the randomized control group.
One of the most clinically relevant biomarkers is the plasma Aβ42/40 ratio, which increased by 6.4% in the intervention group and decreased by 8.3% in the randomized control group after 20 weeks, and these differences were statistically significant ( p = 0.003, two-tailed).
In the lecanemab trial, plasma levels of the Aβ42/40 biomarker increased in the intervention group over 18 months with the presumption that this reflected amyloid moving from the brain to the plasma [ 40 ]. We found similar results in the direction of change in the plasma Aβ42/40 ratio from this lifestyle intervention but in only 20 weeks. Conversely, this biomarker decreased in the control group (as in the lecanemab trial), which may indicate increased cerebral uptake of amyloid.
Other clinically relevant biomarkers also showed statistically significant differences (two-tailed) in a beneficial direction after 20 weeks when compared to the randomized control group. These include hemoglobin A1c, insulin, glycoprotein acetyls (GlycA), LDL-cholesterol, and β-Hydroxybutyrate (ketone bodies).
Improvement in these biomarkers provides more biological plausibility for the observed improvements in cognition and function as well as more insight into the possible mechanisms of improvement. This information may also help in predicting which patients are more likely to show improvements in cognition and function by making these intensive lifestyle changes.
Other relevant biomarkers were in a beneficial direction of change in the intervention group compared with the randomized control group after 20 weeks. These include pTau181, GFAP, CRP, SAA, and C-peptide. Telomere length increased in the intervention group and was essentially unchanged in the control group. These differences were not statistically significant even when there was an order of magnitude difference between groups (as with GFAP and pTau181) or an almost four-fold difference (as with CRP), but these changes were in a beneficial direction. At least in part, these findings may be due to a relatively small sample size and/or a short duration of only 20 weeks.
We found a statistically significant dose-response correlation between the degree of lifestyle changes in both groups (“lifestyle index”) and the degree of change in many of these biomarkers. This correlation was found in both the degree of change in lifestyle from baseline to 20 weeks as well as the lifestyle measured at 20 weeks. These correlations also add to the biological plausibility of these findings.
We also found a statistically significant dose-response correlation between the degree of lifestyle changes in both groups (“lifestyle index”) and changes in most measures of cognition and function testing. In short, the more these AD patients changed their lifestyle in the prescribed ways, the greater was the beneficial impact on their cognition and function. These correlations also add to the biological plausibility of these findings. This variation in adherence helps to explain in part why some patients in the intervention group improved and others did not, but there are likely other mechanisms that we do not fully understand that may play a role. These statistically significant correlations are especially meaningful given the greater variability of self-reported data, the relatively small sample size, and the short duration of the intervention.
These findings are consistent with earlier clinical trials in which we used this same lifestyle intervention and the same measure of lifestyle index and found significant dose-response correlations between this lifestyle index (i.e., the degree of lifestyle changes) and changes in the degree of coronary atherosclerosis (percent diameter stenosis) in coronary heart disease; [ 41 , 45 ] changes in PSA levels and LNCaP cell growth in men with prostate cancer; [ 42 ] and changes in telomere length [ 43 ].
We also found significant differences between the intervention and control groups in several taxa (groups of micro-organisms) in the microbiome which may be beneficial.
There were no significant differences in depression scores as measured by PHQ-9 between the intervention and control groups. Therefore, reduction in depression is unlikely to account for the overall improvements in cognition and function seen in the intervention group patients.
We also found that substantial lifestyle changes were required to stop the progression of MCI in these patients. In the primary analysis, this ranged from 71.4% adherence for ADAS-Cog to 95.6% adherence for CDR-Global to 120.6% adherence for CDR-SB. In other words, extensive lifestyle changes were required to stop or improve cognition and function in these patients. This helps to explain why other studies of less-intensive lifestyle interventions may not have been sufficient to stop deterioration or improve cognition and function.
For example, comparing these results to those of the MIND-AD clinical trial provides more biological plausibility for both studies [ 44 ]. That is, more moderate multimodal lifestyle changes may slow the rate of worsening of cognition and function in MCI or early dementia due to early-stage AD, whereas more intensive multimodal lifestyle changes may result in overall average improvements in many measures of cognition and function when compared to a randomized usual-care control group in both clinical trials.
Lifestyle changes may provide additional benefits to patients on drug therapy. Anti-amyloid antibodies have shown modest effects on slowing progression, but they are expensive, have potential for adverse events, are not yet widely available, and do not result in overall cognitive improvement [ 40 ]. Perhaps there may be synergy from doing both.
Limitations
This study has several limitations. Only 51 patients were enrolled and randomized in our study, and two of these patients (both in the intervention group) withdrew during the trial. Showing statistically significant differences across different tests of cognition and function and other measures despite the relatively small sample size suggests that the lifestyle intervention may be especially effective and has strong internal validity.
However, the smaller sample size limits generalizability, especially since there was much less racial and ethnic diversity in this sample than we strived to achieve. Also, we measured these differences despite the relative insensitivity of these measures, which might have increased the likelihood of a type II error.
Raters were blinded to the group assignment of the participants. However, unlike a double-blind placebo-controlled drug trial, it is not possible to blind subjects in a lifestyle intervention about whether or not they are receiving the intervention. This might have affected outcome measures, although to reduce positive expectations and because it was true, patients were told during the study that we did not know whether or not this lifestyle intervention would be beneficial, and we said that whatever we showed would be useful.
Also, 20 weeks is a relatively short time for any intervention with MCI or early dementia due to AD. We did not include direct measures of brain structure in this trial, so we cannot determine whether there were direct impacts on markers of brain pathology relevant to AD. However, surrogate markers such as the plasma Aβ42/40 ratio are becoming more widely accepted.
Not all patients in the intervention group improved. Of the 24 patients in the intervention group, 10 showed improvement as measured by the CGIC test, 7 were unchanged, and 7 worsened. In the control group, none improved, 8 were unchanged, and 17 worsened. In part, this may be explained by variations in adherence to the lifestyle intervention, as there was a significant relationship between the degree of lifestyle change and the degree of change in cognition and function across both groups. We hope that further research may further clarify other factors and mechanisms to help explain why cognition and function improved in some patients but not in others.
The findings on the degree of lifestyle change required to stop the worsening or improve cognition and function need to be interpreted with caution. Since data from both groups were combined, it was no longer a randomized trial for this specific analysis, so there could be unknown confounding influences. Also, it is possible that those with improved changes in cognition were better able to adhere to the intervention and thus have higher lifestyle indices.
In summary, in persons with mild cognitive impairment or early dementia due to Alzheimer’s disease, comprehensive lifestyle changes may improve cognition and function in several standard measures after 20 weeks. In contrast, patients in the randomized control group showed overall worsening in all four measures of cognition and function during this time.
The validity of these findings was supported by the observed changes in plasma biomarkers and microbiome; the dose-response correlation of the degree of lifestyle change with the degree of improvement in all four measures of cognition and function; and the correlation between the degree of lifestyle change and the degree of changes in the Aβ42/40 ratio and the changes in some other relevant biomarkers in a beneficial direction.
Our findings also have implications for helping to prevent AD. Newer technologies, some aided by artificial intelligence, enable the probable diagnosis of AD years before it becomes clinically apparent. However, many people do not want to know if they are likely to get AD if they do not believe they can do anything about it. If intensive lifestyle changes may cause improvement in cognition and function in MCI or early dementia due to AD, then it is reasonable to think that these lifestyle changes may also help to prevent MCI or early dementia due to AD. Also, it may take less-extensive lifestyle changes to help prevent AD than to treat it. Other studies cited earlier on the effects of these lifestyle changes on diseases such as coronary heart disease support this conclusion. Clearly, intensive lifestyle changes rather than moderate ones seem to be required to improve cognition and function in those suffering from early-stage AD.
These findings support longer follow-up and larger clinical trials to determine the longer-term outcomes of this intensive lifestyle medicine intervention in larger groups of more diverse AD populations; why some patients beneficially respond to a lifestyle intervention better than others besides differences in adherence; as well as the potential synergy of these lifestyle changes and some drug therapies.
Availability of data and materials
The datasets used and/or analyzed during the current study may be available from the corresponding author on reasonable request. Requesters will be asked to submit a study protocol, including the research question, planned analysis, and data required. The authors will evaluate this plan (i.e., relevance of the research question, suitability of the data, quality of the proposed analysis, planned or ongoing analysis, and other matters) on a case-by-case basis.
Livingston G, Huntley J, Sommerlad A, Ames D, Ballard C, Banerjee S, Brayne C, Burns A, Cohen-Mansfield J, Cooper C, Costafreda SG, Dias A, Fox N, Gitlin LN, Howard R, Kales HC, Kivimäki M, Larson EB, Ogunniyi A, Orgeta V, Ritchie K, Rockwood K, Sampson EL, Samus Q, Schneider LS, Selbæk G, Teri L, Mukadam N. Dementia prevention, intervention, and care: 2020 report of the Lancet Commission. Lancet. 2020;396(10248):413–46. https://doi.org/10.1016/S0140-6736(20)30367-6 . (Epub 2020 Jul 30. Erratum in: Lancet. 2023 Sep 30;402(10408):1132. PMID: 327389 PMCID: PMC7392084).
Article PubMed PubMed Central Google Scholar
Ornish D, Ornish A. UnDo It. New York: Ballantine Books; 2019.
Google Scholar
Dhana K, Agarwal P, James BD, Leurgans SE, Rajan KB, Aggarwal NT, Barnes LL, Bennett DA, Schneider JA. Healthy Lifestyle and Cognition in Older Adults With Common Neuropathologies of Dementia. JAMA Neurol. 2024. https://doi.org/10.1001/jamaneurol.2023.5491 . Epub ahead of print. PMID: 38315471.
Morris MC, Evans DA, Tangney CC, Bienias JL, Wilson RS. Associations of vegetable and fruit consumption with age-related cognitive change. Neurology. 2006;67(8):1370–6. https://doi.org/10.1212/01.wnl.0000240224.38978.d8 . (PMID:17060562;PMCID:PMC3393520).
Article CAS PubMed Google Scholar
Morris MC, Evans DA, Bienias JL, Tangney CC, Bennett DA, Aggarwal N, Schneider J, Wilson RS. Dietary fats and the risk of incident Alzheimer disease. Arch Neurol. 2003;60(2):194–200. https://doi.org/10.1001/archneur.60.2.194 . (Erratum.In:ArchNeurol.2003Aug;60(8):1072 PMID: 12580703).
Article PubMed Google Scholar
Yu JT, Xu W, Tan CC, Andrieu S, Suckling J, Evangelou E, Pan A, Zhang C, Jia J, Feng L, Kua EH, Wang YJ, Wang HF, Tan MS, Li JQ, Hou XH, Wan Y, Tan L, Mok V, Tan L, Dong Q, Touchon J, Gauthier S, Aisen PS, Vellas B. Evidence-based prevention of Alzheimer’s disease: systematic review and meta-analysis of 243 observational prospective studies and 153 randomised controlled trials. J Neurol Neurosurg Psychiatry. 2020;91(11):1201–9. https://doi.org/10.1136/jnnp-2019-321913 . (Epub 2020 Jul 20. PMID: 32690803; PMCID: PMC7569385).
Blumenthal JA, Smith PJ, Mabe S, Hinderliter A, Lin PH, Liao L, et al. Lifestyle and neurocognition in older adults with cognitive impairments: A randomized trial. Neurology. 2019;92(3):e212–23. https://doi.org/10.1212/WNL.0000000000006784 . (Epub 2018/12/21. PubMed PMID: 30568005; PubMed Central PMCID: PMCPMC6340382).
Ngandu T, Lehtisalo J, Solomon A, Levälahti E, Ahtiluoto S, Antikainen R, Bäckman L, Hänninen T, Jula A, Laatikainen T, Lindström J, Mangialasche F, Paajanen T, Pajala S, Peltonen M, Rauramaa R, Stigsdotter-Neely A, Strandberg T, Tuomilehto J, Soininen H, Kivipelto M. A 2 year multidomain intervention of diet, exercise, cognitive training, and vascular risk monitoring versus control to prevent cognitive decline in at-risk elderly people (FINGER): a randomised controlled trial. Lancet. 2015;385(9984):2255–63. https://doi.org/10.1016/S0140-6736(15)60461-5 . (Epub 2015 Mar 12 PMID: 25771249).
Rosenberg A, Ngandu T, Rusanen M, Antikainen R, Backman L, Havulinna S, et al. Multidomain lifestyle intervention benefits a large elderly population at risk for cognitive decline and dementia regardless of baseline characteristics: The FINGER trial. Alzheimers Dement. 2018;14(3):263–70. https://doi.org/10.1016/j.jalz.2017.09.006 . (Epub 2017/10/23. PubMed PMID: 29055814).
Solomon A, Turunen H, Ngandu T, Peltonen M, Levalahti E, Helisalmi S, et al. Effect of the apolipoprotein e genotype on cognitive change during a multidomain lifestyle intervention: a subgroup analysis of a randomized clinical trial. JAMA Neurol. 2018;75(4):462–70. https://doi.org/10.1001/jamaneurol.2017.4365 . (Epub 2018/01/23. PubMed PMID: 29356827; PubMed Central PMCID: PMCPMC5885273).
Lehtisalo J, Rusanen M, Solomon A, Antikainen R, Laatikainen T, Peltonen M, et al. Effect of a multi-domain lifestyle intervention on cardiovascular risk in older people: the FINGER trial. Eur Heart J. 2022. https://doi.org/10.1093/eurheartj/ehab922 . Epub 2022/01/21. PubMed PMID: 35051281.
Kivipelto M, Mangialasche F, Snyder HM, Allegri R, Andrieu S, Arai H, et al. World-Wide FINGERS Network: a global approach to risk reduction and prevention of dementia. Alzheimers Dement. 2020;16(7):1078–94. https://doi.org/10.1002/alz.12123 . (Epub 2020/07/07. PubMed PMID: 32627328).
Kivipelto M, Mangialasche F, Snyder H M, Allegri R, Andrieu S, Arai H, Baker L, Belleville S, Brodaty H, Brucki SM, Calandri I, Caramelli P, Chen C, Chertkow H, Chew E, Choi S H, Chowdhary N, Crivelli L, De La Torre R, Du Y, Dua T, Espeland M, Feldman H H, Hartmanis M, Hartmann T, Heffernan M, Henry C J, Hong C H, Håkansson K, Iwatsubo T, Jeong J H, Jimenez‐Maggiora G, Koo E H, Launer L J, Lehtisalo J, Lopera F, Martínez‐Lage P, Martins R, Middleton L, Molinuevo J L, Montero‐Odasso M, Moon S Y, Morales‐Pérez K, Nitrini R, Nygaard H B, Park Y K, Peltonen M, Qiu C, Quiroz Y T, Raman R, Rao N, Ravindranath V, Rosenberg A, Sakurai T, Salinas R M, Scheltens P, Sevlever G, Soininen H, Sosa A L, Suemoto C K, Tainta‐Cuezva M, Velilla L, Wang Y, Whitmer R, Xu X, Bain L J, Solomon A, Ngandu T, Carillo, M C. World‐Wide FINGERS Network: A global approach to risk reduction and prevention of dementia. Alzheimer's Dement. 2020, https://doi.org/10.1002/alz.12123 .
Yaffe K, Vittinghoff E, Dublin S, Peltz CB, Fleckenstein LE, Rosenberg DE, Barnes DE, Balderson BH, Larson EB. Effect of personalized risk-reduction strategies on cognition and dementia risk profile among older adults: the SMARRT randomized clinical trial. JAMA Intern Med. 2023:e236279. https://doi.org/10.1001/jamainternmed.2023.6279 . Epub ahead of print. PMID: 38010725; PMCID: PMC10682943
Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001–7. https://doi.org/10.1001/jama.280.23.2001 . (Erratum.In:JAMA1999Apr21;281(15):1380 PMID: 9863851).
Ornish D, Scherwitz LW, Doody RS, Kesten D, McLanahan SM, Brown SE, DePuey E, Sonnemaker R, Haynes C, Lester J, McAllister GK, Hall RJ, Burdine JA, Gotto AM Jr. Effects of stress management training and dietary changes in treating ischemic heart disease. JAMA. 1983;249(1):54–9 (PMID: 6336794).
Gould KL, Ornish D, Scherwitz L, Brown S, Edens RP, Hess MJ, Mullani N, Bolomey L, Dobbs F, Armstrong WT, et al. Changes in myocardial perfusion abnormalities by positron emission tomography after long-term, intense risk factor modification. JAMA. 1995;274(11):894–901. https://doi.org/10.1001/jama.1995.03530110056036 . (PMID: 7674504).
Dhana K, Evans DA, Rajan KB, Bennett DA, Morris MC. Healthy lifestyle and the risk of Alzheimer dementia: Findings from 2 longitudinal studies. Neurology. 2020;95(4):e374–83. https://doi.org/10.1212/WNL.0000000000009816 . (Epub 2020 Jun 17. PMID: 32554763; PMCID: PMC7455318).
Article CAS PubMed PubMed Central Google Scholar
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR Jr, Kawas CH, Klunk WE, Koroshetz WJ, Manly JJ, Mayeux R, Mohs RC, Morris JC, Rossor MN, Scheltens P, Carrillo MC, Thies B, Weintraub S, Phelps CH. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7(3):263–9. https://doi.org/10.1016/j.jalz.2011.03.005 . (Epub 2011 Apr 21. PMID: 21514250; PMCID: PMC3312024).
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9.
McDonald K, Seltzer E, Lu M, Gaisenband SD, Fletcher C, McLeroth P, Saini KS. Quantifying the impact of the COVID-19 pandemic on clinical trial screening rates over time in 37 countries. Trials. 2023;24(1):254. https://doi.org/10.1186/s13063-023-07277-1 . (PMID:37013558;PMCID:PMC10071259).
Tang HY, Vitiello MV, Perlis M, Mao JJ, Riegel B. A pilot study of audio-visual stimulation as a self-care treatment for insomnia in adults with insomnia and chronic pain. Appl Psychophysiol Biofeedback. 2014;39(3–4):219–25. https://doi.org/10.1007/s10484-014-9263-8 . (PMID:25257144;PMCID:PMC4221414).
Horsley K. Unlimited Memory. Granger Indiana: TCK Publishing; 2016.
Morris MC, Evans DA, Bienias JL, Tangney CC, Bennett DA, Wilson RS, et al. Consumption of fish and n-3 fatty acids and risk of incident Alzheimer disease. Arch Neurol. 2003;60(7):940–6. https://doi.org/10.1001/archneur.60.7.940 . (Epub 2003/07/23. PubMed PMID: 12873849).
Voulgaropoulou SD, van Amelsvoort T, Prickaerts J, Vingerhoets C. The effect of curcumin on cognition in Alzheimer’s disease and healthy aging: A systematic review of pre-clinical and clinical studies. Brain Res. 2019;1725:146476. https://doi.org/10.1016/j.brainres.2019.146476 . Epub 2019/09/29. PubMedPMID:31560864.
Ringman JM, Frautschy SA, Teng E, Begum AN, Bardens J, Beigi M, Gylys KH, Badmaev V, Heath DD, Apostolova LG, Porter V, Vanek Z, Marshall GA, Hellemann G, Sugar C, Masterman DL, Montine TJ, Cummings JL, Cole GM. Oral curcumin for Alzheimer’s disease: tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimers Res Ther. 2012;4(5):43. https://doi.org/10.1186/alzrt146 . (PMID:23107780;PMCID:PMC3580400).
Shea TB, Remington R. Nutritional supplementation for Alzheimer’s disease? Curr Opin Psychiatry. 2015;28(2):141–7. https://doi.org/10.1097/YCO.0000000000000138 . (Epub 2015/01/21. PubMed PMID: 25602242).
Pradhan N, Singh C, Singh A. Coenzyme Q10 a mitochondrial restorer for various brain disorders. Naunyn Schmiedebergs Arch Pharmacol. 2021;394(11):2197–222. https://doi.org/10.1007/s00210-021-02161-8 . (Epub 2021/10/02 PubMed PMID: 34596729).
Harrison FE. A critical review of vitamin C for the prevention of age-related cognitive decline and Alzheimer’s disease. J Alzheimers Dis. 2012;29(4):711–26. https://doi.org/10.3233/JAD-2012-111853 . (Epub 2012/03/01. PubMed PMID: 22366772; PubMed Central PMCID: PMCPMC3727637).
Lauer AA, Grimm HS, Apel B, Golobrodska N, Kruse L, Ratanski E, et al. Mechanistic Link between Vitamin B12 and Alzheimer's Disease. Biomolecules. 2022;12(1). https://doi.org/10.3390/biom12010129 . Epub 2022/01/22. PubMed PMID: 35053277; PubMed Central PMCID: PMCPMC8774227.
Du K, Zheng X, Ma ZT, Lv JY, Jiang WJ, Liu MY. Association of Circulating Magnesium Levels in Patients With Alzheimer’s Disease From 1991 to 2021: A Systematic Review and Meta-Analysis. Front Aging Neurosci. 2021;13:799824. https://doi.org/10.3389/fnagi.2021.799824 . (Epub 2022/01/28. PubMed PMID: 35082658; PubMed Central PMCID: PMCPMC8784804).
Saitsu Y, Nishide A, Kikushima K, Shimizu K, Ohnuki K. Improvement of cognitive functions by oral intake of Hericium erinaceus. Biomed Res. 2019;40(4):125–31. https://doi.org/10.2220/biomedres.40.125 . (Epub 2019/08/16. PubMed PMID: 31413233).
Mori K, Inatomi S, Ouchi K, Azumi Y, Tuchida T. Improving effects of the mushroom Yamabushitake (Hericium erinaceus) on mild cognitive impairment: a double-blind placebo-controlled clinical trial. Phytother Res. 2009;23(3):367–72. https://doi.org/10.1002/ptr.2634 . (Epub 2008/10/11. PubMed PMID: 18844328).
Xiang S, Ji JL, Li S, Cao XP, Xu W, Tan L, et al. Efficacy and Safety of probiotics for the treatment of alzheimer’s disease, mild cognitive impairment, and Parkinson’s Disease: a systematic review and meta-analysis. Front Aging Neurosci. 2022;14:730036. https://doi.org/10.3389/fnagi.2022.730036 . (Epub 2022/02/22. PubMed PMID: 35185522; PubMed Central PMCID: PMCPMC8851038).
Fogelman I, West T, Braunstein JB, Verghese PB, Kirmess KM, Meyer MR, Contois JH, Shobin E, Ferber KL, Gagnon J, Rubel CE, Graham D, Bateman RJ, Holtzman DM, Huang S, Yu J, Yang S, Yarasheski KE. Independent study demonstrates amyloid probability score accurately indicates amyloid pathology. Ann Clin Transl Neurol. 2023;10(5):765–78. https://doi.org/10.1002/acn3.51763 . (Epub 2023 Mar 28. PMID: 36975407; PMCID: PMC10187729).
Exploratory data analysis. John W. Tukey, 1977. Addison-Wesley, Reading MA. https://doi.org/10.1002/bimj.4710230408 .
Zhuang Z, Yang R, Wang W, Qi L, Huang T. Associations between gut microbiota and Alzheimer’s disease, major depressive disorder, and schizophrenia. J Neuroinflammation. 2020;17(1):288. https://doi.org/10.1186/s12974-020-01961-8 . (PMID:33008395;PMCID:PMC7532639).
Cammann D, Lu Y, Cummings MJ, Zhang ML, Cue JM, Do J, Ebersole J, Chen X, Oh EC, Cummings JL, Chen J. Genetic correlations between Alzheimer’s disease and gut microbiome genera. Sci Rep. 2023;13(1):5258. https://doi.org/10.1038/s41598-023-31730-5 . (PMID:37002253;PMCID:PMC10066300).
Borsom EM, Conn K, Keefe CR, Herman C, Orsini GM, Hirsch AH, Palma Avila M, Testo G, Jaramillo SA, Bolyen E, Lee K, Caporaso JG, Cope EK. Predicting Neurodegenerative Disease Using Prepathology Gut Microbiota Composition: a Longitudinal Study in Mice Modeling Alzheimer’s Disease Pathologies. Microbiol Spectr. 2023;11(2):e0345822. https://doi.org/10.1128/spectrum.03458-22 . (Epub ahead of print. PMID: 36877047; PMCID: PMC10101110).
van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, Kanekiyo M, Li D, Reyderman L, Cohen S, Froelich L, Katayama S, Sabbagh M, Vellas B, Watson D, Dhadda S, Irizarry M, Kramer LD, Iwatsubo T. Lecanemab in Early Alzheimer’s Disease. N Engl J Med. 2023;388(1):9–21. https://doi.org/10.1056/NEJMoa2212948 . (Epub 2022 Nov 29 PMID: 36449413).
Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280(23):2001–7. https://doi.org/10.1001/jama.280.23.2001 .
Ornish D, Weidner G, Fair WR, Marlin R, Pettengill EB, Raisin CJ, Dunn-Emke S, Crutchfield L, Jacobs FN, Barnard RJ, Aronson WJ, McCormac P, McKnight DJ, Fein JD, Dnistrian AM, Weinstein J, Ngo TH, Mendell NR, Carroll PR. Intensive lifestyle changes may affect the progression of prostate cancer. J Urol. 2005;174(3):1065–9. https://doi.org/10.1097/01.ju.0000169487.49018.73 . (discussion 1069-70. PMID: 16094059).
Ornish D, Lin J, Chan JM, Epel E, Kemp C, Weidner G, Marlin R, Frenda SJ, Magbanua MJM, Daubenmier J, Estay I, Hills NK, Chainani-Wu N, Carroll PR, Blackburn EH. Effect of comprehensive lifestyle changes on telomerase activity and telomere length in men with biopsy-proven low-risk prostate cancer: 5-year follow-up of a descriptive pilot study. Lancet Oncol. 2013;14(11):1112–20. https://doi.org/10.1016/S1470-2045(13)70366-8 . (Epub 2013 Sep 17 PMID: 24051140).
Kivipelto M et al. Multimodal preventive trial for Alzheimer’s disease. Alzheimer’s Dement. 2021;17(Suppl.10):e056105. https://alz-journals.onlinelibrary.wiley.com/doi/abs/10.1002/alz.056105 .
Ornish D, Brown SE, Scherwitz LW, Billings JH, Armstrong WT, Ports TA, McLanahan SM, Kirkeeide RL, Brand RJ, Gould KL. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet. 1990;336(8708):129–33. https://doi.org/10.1016/0140-6736(90)91656-u . (PMID: 1973470).
Download references
Acknowledgements
We are grateful to each of the following people who made this study possible. Paramount among these are all of the study participants and their spouse or support person. Their commitment was inspiring, and without them this study would not have been possible. Each of the staff who provided and supported this program is exceptionally caring and competent, and includes: Heather Amador, who coordinated and administered all grants and infrastructure; Tandis Alizadeh, who is chief of staff; as well as Lynn Sievers, Nikki Liversedge, Pamela Kimmel, Stacie Dooreck, Antonella Dewell, Stacey Dunn-Emke, Marie Goodell, Emily Dougherty, Kamala Berrio, Kristin Gottesman, Katie Mayers, Dennis Malone, Sarah & Mary Barber, Steven Singleton, Kevin Lane, Laurie Case, Amber O’Neill, Annie DiRocco, Alison Eastwood, Sara Henley, Sousha Naghshineh, Sarah Reinhard, Laura Kandell, Alison Haag, Sinead Lafferty, Haley Perkins, Chase Delaney, Danielle Marquez, Ava Hoffman, Sienna Lopez, and Sophia Gnuse. Dr. Caitlin Moore conducted much of the cognition and function testing along with Dr. Catherine Madison, Trevor Ragas, Andrea Espinosa, Lorraine Martinez, Davor Zink, Jeff Webb, Griffin Duffy, Lauren Sather, and others. Dr. Cecily Jenkins trained the ADAS-Cog rater. Dr. Jan Krumsiek and Dr. Richa Batra performed important analyses in Dr. Rima Kaddurah-Daouk’s lab. Dr. Pia Kivisåkk oversaw biomarker assays in Dr. Steven Arnold's lab. We are grateful to all of the referring neurologists. Board members of the nonprofit Preventive Medicine Research Institute provided invaluable oversight and support, including Henry Groppe, Jenard & Gail Gross, Ken Hubbard, Brock Leach, and Lee Stein, as well as Joel Goldman.
Author’s information
DO is the corresponding author. RT contributed as the senior author.
We are very grateful to Leonard A. Lauder & Judith Glickman Lauder; Gary & Laura Lauder; Howard Fillit and Mark Roithmayr of The Alzheimer’s Drug Discovery Foundation; Mary & Patrick Scanlan of the Mary Bucksbaum Scanlan Family Foundation; Laurene Powell Jobs/Silicon Valley Community Foundation; Pierre & Pamela Omidyar Fund/Silicon Valley Community Foundation (Pat Christen and Jeff Alvord); George Vradenburg Foundation/Us Against Alzheimer’s; American Endowment Foundation (Anna & James McKelvey); Arthur M. Blank Family Foundation/Around the Table Foundation (Elizabeth Brown, Natalie Gilbert, Christian Amica); John Paul & Eloise DeJoria Peace Love & Happiness Foundation (Constance Dykhuizen); Maria Shriver/Women’s Alzheimer’s Movement (Sandy Gleysteen, Laurel Ann Gonsecki, Erin Stein); Mark Pincus Family Fund/Silicon Valley Community Foundation; Christy Walton/Walton Family Foundation; Milken Family Foundation; The Cleveland Clinic Lou Ruvo Center for Brain Health (Larry Ruvo); Jim Greenbaum Foundation; R. Martin Chavez; Wonderful Company Foundation (Stewart & Lynda Resnick); Daniel Socolow; Anthony J. Robbins/Tony Robbins Foundation; John Mackey; John & Lisa Pritzker and the Lisa Stone Pritzker Family Foundation; Ken Hubbard; Greater Houston Community Foundation (Jenard & Gail Gross); Henry Groppe; Brock & Julie Leach Family Charitable Foundation; Bucksbaum/Baum Foundation (Glenn Bucksbaum & April Minnich); YPO Gold Los Angeles; Lisa Holland/Betty Robertson; the Each Foundation (Lionel Shaw); Moby Charitable Fund; California Relief Program; Gary & Lisa Schildhorn; McNabb Foundation (Ricky Rafner); Renaissance Charitable Foumdation (Stephen & Karen Slinkard); Network for Good; Ken & Kim Raisler Foundation; Miner Foundation; Craiglist Charitable Fund (Jim Buckmaster and Annika Joy Quist); Gaurav Kapadia; Healing Works Foundation/Wayne Jonas; and the Center for Innovative Medicine (CIMED) at the Karolinska Institutet, Hjärnfonden, Stockholms Sjukhem, Research Council for Health Working Life and Welfare (FORTE). In-kind donations were received from Alan & Rob Gore of Body Craft Recreation Supply (exercise equipment), Dr. Andrew Abraham of Orgain, Paul Stamets of Fungi Perfecta ( Host Defense Lion’s Mane), Nordic Naturals, and Flora. Dr. Rima Kaddurah-Daouk at Duke is PI of the Alzheimer Gut Microbiome Project (funded by NIA U19AG063744). She also received additional funding from NIA that has enabled her research (U01AG061359 & R01AG081322).
The funders had no role in the conceptualization; study design; data collection; analysis; and interpretation; writing of the report; or the decision to submit for publication.
Author information
Authors and affiliations.
Preventive Medicine Research Institute, 900 Bridgeway, Sausalito, CA, USA
Dean Ornish, Catherine Madison, Anne Ornish, Nancy DeLamarter, Noel Wingers & Carra Richling
University of California, San Francisco and University of California, San Diego, USA
Dean Ornish
Ray Dolby Brain Health Center, California Pacific Medical Center, San Francisco, CA, USA
Catherine Madison
Division of Clinical Geriatrics, Department of Neurobiology, Care Sciences and Society, Karolinska Institute, Karolinska vägen 37 A, SE-171 64, Solna, Sweden
Miia Kivipelto
Theme Inflammation and Aging, Karolinska University Hospital, Karolinska vägen 37 A, SE-171 64, Stockholm, Solna, Sweden
The Ageing Epidemiology (AGE) Research Unit, School of Public Health, Imperial College London, St Mary’s Hospital, Norfolk Place, London, W2 1PG, United Kingdom
Institute of Public Health and Clinical Nutrition, University of Eastern Finland, Yliopistonranta 8, 70210, Kuopio, Finland
Clinical Services, Preventive Medicine Research Institute, Bridgeway, Sausalito, CA, 900, USA
Colleen Kemp & Sarah Tranter
Division of Biostatistics, Department of Epidemiology & Biostatistics, UCSF, San Francisco, CA, USA
Charles E. McCulloch
Neurosciences, University of California, San Diego, CA, USA
Douglas Galasko
Clinical Neurology, School of Medicine, University of Nevada, Reno, USA
Renown Health Institute of Neurosciences, Reno, NV, USA
Harvard Medical School, Boston, MA, USA
Dorene Rentz, Rudolph E. Tanzi & Steven E. Arnold
Center for Alzheimer Research and Treatment, Boston, MA, USA
Dorene Rentz
Mass General Brigham Alzheimer Disease Research Center, Boston, MA, USA
Elizabeth Blackburn Lab, UCSF, San Francisco, CA, USA
UCSF, San Francisco, CA, USA
Departments of Medicine and Psychiatry, Duke University Medical Center and Member, Duke Institute of Brain Sciences, Durham, NC, USA
Rima Kaddurah-Daouk
Department of Pediatrics; Department of Computer Science & Engineering; Department of Bioengineering; Center for Microbiome Innovation, Halıcıoğlu Data Science Institute, University of California, San Diego, La Jolla, CA, USA
Department of Pediatrics and Scientific Director, American Gut Project and The Microsetta Initiative, University of California San Diego, La Jolla, CA, USA
Daniel McDonald
Bioinformatics and Systems Biology Program; Rob Knight Lab; Medical Scientist Training Program, University of California, San Diego, La Jolla, CA, USA
Lucas Patel
Buck Institute for Research on Aging, San Francisco, CA, USA
Eric Verdin
University of California, San Francisco, CA, USA
Genetics and Aging Research Unit, Boston, MA, USA
Rudolph E. Tanzi
McCance Center for Brain Health, Boston, MA, USA
Massachusetts General Hospital, Boston, MA, USA
Interdisciplinary Brain Center, Massachusetts General Hospital, Boston, MA, USA
Steven E. Arnold
You can also search for this author in PubMed Google Scholar
Contributions
DO, CM, MK, CK, DG, JA, DR, CEM, JL, KN, AO, ST, ND, NW, CR, RKD, RK, EV, RT, and SEA were involved in the study design and conduct. DO conceptualized the study hypotheses (building on the work of MK), obtained funding, prepared the first draft of the manuscript, and is the principal investigator. CEM oversaw the statistical analyses and interpretation, and DR oversaw the cognition and function testing and interpretation. CK and ST oversaw all clinical operations and patient recruitment, including the IRB. JL conducted the telomere analyses. CM oversaw patient selection. AO developed the learning management system and community platform for patients and providers. KN managed an IRB. ND co-led most of the support groups, and CR oversaw all aspects involving nutrition. All authors participated in writing the manuscript. NW and ST oversaw data collection and prepared the databases other than the microbiome databases which were overseen by RK and prepared by DM and LP who helped design this part of the study. CM, CK, JL, RKD, RK, DM, and LP were involved in the acquisition of data. SA, RT, and RKD did biomarker analyses. All authors contributed to critical review of the manuscript and approved the final manuscript.
Corresponding author
Correspondence to Dean Ornish .
Ethics declarations
Competing interests.
MK is one of the Editors-in-Chief of this journal and has no relevant competing interests and recused herself from the review process. RKD is an inventor on key patents in the field of metabolomics and holds equity in Metabolon, a biotech company in North Carolina. In addition, she holds patents licensed to Chymia LLC and PsyProtix with royalties and ownership. DO and AO have consulted for Sharecare and have received book royalties and lecture honoraria and, with CK, have received equity in Ornish Lifestyle Medicine. RK is a scientific advisory board member and consultant for BiomeSense, Inc., has equity and receives income. He is a scientific advisory board member and has equity in GenCirq. He is a consultant and scientific advisory board member for DayTwo, and receives income. He has equity in and acts as a consultant for Cybele. He is a co-founder of Biota, Inc., and has equity. He is a cofounder of Micronoma, and has equity and is a scientific advisory board member. The terms of these arrangements have been reviewed and approved by the University of California, San Diego in accordance with its conflict of interest policies. DM is a consultant for BiomeSense. RT is a co-founder and equity holder in Hyperion Rx, which produces the flashing-light glasses at a theta frequency of 7.83 Hz used as an optional aid to meditation. The rest of the authors declare that they have no competing interests.
Ethics approval and consent to participate
This clinical trial was approved by the Western Institutional Review Board on 12/31/2017 (approval number: 20172897) and all participants and their study partners provided written informed consent. The trial protocol was also approved by the appropriate Institutional Review Board of all participating sites; and all subjects provided informed consent.
Consent for publication
Informed consent was received from all patients. All data from research participants described in this paper is de-identified.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1. , rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ornish, D., Madison, C., Kivipelto, M. et al. Effects of intensive lifestyle changes on the progression of mild cognitive impairment or early dementia due to Alzheimer’s disease: a randomized, controlled clinical trial. Alz Res Therapy 16 , 122 (2024). https://doi.org/10.1186/s13195-024-01482-z
Download citation
Received : 21 February 2024
Accepted : 15 May 2024
Published : 07 June 2024
DOI : https://doi.org/10.1186/s13195-024-01482-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Alzheimer’s
- Lifestyle medicine
- Social support
Alzheimer's Research & Therapy
ISSN: 1758-9193
- General enquiries: [email protected]

IMAGES
VIDEO
COMMENTS
The conclusion in a research paper is the final section, where you need to summarize your research, presenting the key findings and insights derived from your study. ... It restates how your results contribute to the existing body of knowledge and whether they confirm or challenge existing theories or hypotheses. Also, by identifying unanswered ...
The conclusion of a research paper restates the research problem, summarizes your arguments or findings, and discusses the implications. FAQ About us . Our editors ... (you will have presented your in-depth results and discussion already), but do clearly express the answers to the research questions you investigated.
Research Results. Research results refer to the findings and conclusions derived from a systematic investigation or study conducted to answer a specific question or hypothesis. These results are typically presented in a written report or paper and can include various forms of data such as numerical data, qualitative data, statistics, charts, graphs, and visual aids.
The way the authors interpret their results may be quite different from the way you would interpret them or the way another researcher would interpret them. Note: Some articles collapse the Discussion and Conclusion sections together under a single heading (usually "Conclusion"). If you don't see a separate Discussion section, don't worry.
the results of your research, a discussion of related research, and; ... You can apply the advice in this article to the conclusion, results or discussion sections of your manuscript. Our Early Career Researcher community tells us that the conclusion is often considered the most difficult aspect of a manuscript to write. To help, this guide ...
Tips to Write the Results Section. Direct the reader to the research data and explain the meaning of the data. Avoid using a repetitive sentence structure to explain a new set of data. Write and highlight important findings in your results. Use the same order as the subheadings of the methods section.
Here are a few best practices: Your results should always be written in the past tense. While the length of this section depends on how much data you collected and analyzed, it should be written as concisely as possible. Only include results that are directly relevant to answering your research questions.
Research Paper Conclusion. Definition: A research paper conclusion is the final section of a research paper that summarizes the key findings, significance, and implications of the research. It is the writer's opportunity to synthesize the information presented in the paper, draw conclusions, and make recommendations for future research or ...
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of the main topics covered or a re-statement of your research problem, but a synthesis of key points derived from the findings of your study and, if applicable, where you recommend new areas for future research.
Step 2: Summarize and reflect on your research. Step 3: Make future recommendations. Step 4: Emphasize your contributions to your field. Step 5: Wrap up your thesis or dissertation. Full conclusion example. Conclusion checklist. Other interesting articles. Frequently asked questions about conclusion sections.
The conclusion is where you describe the consequences of your arguments by justifying to your readers why your arguments matter (Hamilton College, 2014). Derntl (2014) also describes conclusion as the counterpart of the introduction. Using the Hourglass Model (Swales, 1993) as a visual reference, Derntl describes conclusion as the part of the ...
Discuss your conclusions in order of most to least important. Compare your results with those from other studies: Are they consistent? If not, discuss possible reasons for the difference. Mention any inconclusive results and explain them as best you can. You may suggest additional experiments needed to clarify your results.
Conclusion. The Conclusion section of a paper should include a brief summary of the main ideas or key takeaways of the paper and their implications for future research. This section usually includes: A brief overview of the main claims and/or key ideas put forth in the paper; A brief discussion of potential limitations of the study (if relevant)
For most research papers in the social and behavioral sciences, there are two possible ways of organizing the results. Both approaches are appropriate in how you report your findings, but use only one approach. Present a synopsis of the results followed by an explanation of key findings. This approach can be used to highlight important findings.
The Conclusion. After all the data is organized in a form that relates it to your hypothesis, you can interpret it and reach a conclusion about the experiment. The conclusion is simply a report about what you learned based on whether the results agree or disagree with your hypothesis. It usually contains a summary of the actual procedure and ...
The results section of a research paper tells the reader what you found, while the discussion section tells the reader what your findings mean. The results section should present the facts in an academic and unbiased manner, avoiding any attempt at analyzing or interpreting the data. Think of the results section as setting the stage for the ...
Option 3: Results, discussion, and conclusion in separate sections. ... While writing a discussion section, writers compare the results of their study with previous research as well as speculate on the explanations for such findings. Common Moves in Results Sections. Below are some moves, sub-moves, and language commonly used in results and ...
Results are findings of the study or research, discussion is the relationship between results and literature review while conclusion is the relationship between the study aims/objectives and and ...
INTRODUCTION. Scientific research is usually initiated by posing evidenced-based research questions which are then explicitly restated as hypotheses.1,2 The hypotheses provide directions to guide the study, solutions, explanations, and expected results.3,4 Both research questions and hypotheses are essentially formulated based on conventional theories and real-world processes, which allow the ...
The conclusion is intended to help the reader understand why your research should matter to them after they have finished reading the paper. A conclusion is not merely a summary of your points or a re-statement of your research problem but a synthesis of key points. For most essays, one well-developed paragraph is sufficient for a conclusion ...
Qualitative research aims to produce rich and detailed descriptions of the phenomenon being studied, and to uncover new insights and meanings. Quantitative data is information about quantities, and therefore numbers, and qualitative data is descriptive, and regards phenomenon which can be observed but not measured, such as language.
A research hypothesis, in its plural form "hypotheses," is a specific, testable prediction about the anticipated results of a study, established at its outset. It is a key component of the scientific method. Hypotheses connect theory to data and guide the research process towards expanding scientific understanding.
What Is Data Analysis? (With Examples) Data analysis is the practice of working with data to glean useful information, which can then be used to make informed decisions. "It is a capital mistake to theorize before one has data. Insensibly one begins to twist facts to suit theories, instead of theories to suit facts," Sherlock Holme's proclaims ...
An abstract is a 150- to 250-word paragraph that provides readers with a quick overview of your essay or report and its organization. It should express your thesis (or central idea) and your key points; it should also suggest any implications or applications of the research you discuss in the paper. According to Carole Slade, an abstract is ...
In conclusion, healthcare leaders highlighted several implementation challenges in relation to AI within and beyond the healthcare system in general and their organisations in particular. ... For example, our results and other AI research has acknowledged that the lack of transparency (i.e. the "black box" problem) might yield resistance to ...
According to McKinsey research, executives spend a significant portion of their time— nearly 40 percent, on average—making decisions. Worse, they believe most of that time is poorly used. People struggle with decisions so much so that we actually get exhausted from having to decide too much, a phenomenon called decision fatigue.
Research to date has found that the Z chromosome in birds typically carries an excess of non-synonymous polymorphisms relative to the autosomes, implicating genetic drift as the mechanism driving fast-Z in birds [6,10,11,13] (although see for more mixed results across three species of sparrow).
The results chapter or section simply and objectively reports what you found, without speculating on why you found these results. The discussion interprets the meaning of the results, puts them in context, and explains why they matter. In qualitative research, results and discussion are sometimes combined. But in quantitative research, it's ...
Requesters will be asked to submit a study protocol, including the research question, planned analysis, and data required. The authors will evaluate this plan (i.e., relevance of the research question, suitability of the data, quality of the proposed analysis, planned or ongoing analysis, and other matters) on a case-by-case basis.
Generating power. Generating electricity and heat by burning fossil fuels causes a large chunk of global emissions. Most electricity is still generated by burning coal, oil, or gas, which produces ...