- Open access
- Published: 21 September 2021

Local government responses for COVID-19 management in the Philippines
- Dylan Antonio S. Talabis 1 , 2 ,
- Ariel L. Babierra 1 , 2 ,
- Christian Alvin H. Buhat 1 , 2 ,
- Destiny S. Lutero 1 , 2 ,
- Kemuel M. Quindala III 1 , 2 &
- Jomar F. Rabajante 1 , 2 , 3
BMC Public Health volume 21 , Article number: 1711 ( 2021 ) Cite this article
555k Accesses
25 Citations
6 Altmetric
Metrics details
Responses of subnational government units are crucial in the containment of the spread of pathogens in a country. To mitigate the impact of the COVID-19 pandemic, the Philippine national government through its Inter-Agency Task Force on Emerging Infectious Diseases outlined different quarantine measures wherein each level has a corresponding degree of rigidity from keeping only the essential businesses open to allowing all establishments to operate at a certain capacity. Other measures also involve prohibiting individuals at a certain age bracket from going outside of their homes. The local government units (LGUs)–municipalities and provinces–can adopt any of these measures depending on the extent of the pandemic in their locality. The purpose is to keep the number of infections and mortality at bay while minimizing the economic impact of the pandemic. Some LGUs have demonstrated a remarkable response to the COVID-19 pandemic. The purpose of this study is to identify notable non-pharmaceutical interventions of these outlying LGUs in the country using quantitative methods.
Data were taken from public databases such as Philippine Department of Health, Philippine Statistics Authority Census, and Google Community Mobility Reports. These are normalized using Z-transform. For each locality, infection and mortality data (dataset Y ) were compared to the economic, health, and demographic data (dataset X ) using Euclidean metric d =( x − y ) 2 , where x ∈ X and y ∈ Y . If a data pair ( x , y ) exceeds, by two standard deviations, the mean of the Euclidean metric values between the sets X and Y , the pair is assumed to be a ‘good’ outlier.
Our results showed that cluster of cities and provinces in Central Luzon (Region III), CALABARZON (Region IV-A), the National Capital Region (NCR), and Central Visayas (Region VII) are the ‘good’ outliers with respect to factors such as working population, population density, ICU beds, doctors on quarantine, number of frontliners and gross regional domestic product. Among metropolitan cities, Davao was a ‘good’ outlier with respect to demographic factors.
Conclusions
Strict border control, early implementation of lockdowns, establishment of quarantine facilities, effective communication to the public, and monitoring efforts were the defining factors that helped these LGUs curtail the harm that was brought by the pandemic. If these policies are to be standardized, it would help any country’s preparedness for future health emergencies.
Peer Review reports
Introduction
Since the emergence of the COVID-19 pandemic, the number of cases have already reached 82 million worldwide at the end of 2020. In the Philippines, the number of cases exceeded 473,000. As countries around the world face the continuing threat of the COVID-19 pandemic, national governments and health ministries formulate, implement and revise health policies and standards based on recommendations by world health organization (WHO), experiences of other countries, and on-the-ground experiences. Early health measures were primarily aimed at preventing and reducing transmission in populations at risk. These measures differ in scale and speed among countries, as some countries have more resources and are more prepared in terms of healthcare capacity and availability of stringent policies [ 1 , 2 ].
During the first months of the pandemic, several countries struggled to find tolerable, if not the most effective, measures to ‘flatten’ the COVID-19 epidemic curve so that health facilities will not be overwhelmed [ 3 , 4 ]. In responding to the threat of the pandemic, public health policies included epidemiological and socio-economic factors. The success or failure of these policies exposed the strengths or weaknesses of governments as well as the range of inequalities in the society [ 5 , 6 ].
As national governments implemented large-scale ‘blanket’ policies to control the pandemic, local government units (LGUs) have to consider granular policies as well as real-time interventions to address differences in the local COVID-19 transmission dynamics due to heterogeneity and diversity in communities. Some policies in place, such as voluntary physical distancing, wearing of face masks and face shields, mass testing, and school closures, could be effective in one locality but not in another [ 7 – 9 ]. Subnational governments like LGUs are confronted with a health crisis that have economic, social and fiscal impact. While urban areas have been hot spots of the COVID-19 pandemic, there are health facilities that are already well in placed as compared to less developed and deprived rural communities [ 10 ]. The importance of local narratives in addressing subnational concerns are apparent from published experiences in the United States [ 11 ], China [ 12 , 13 ], and India [ 14 ].
In the Philippines, the Inter-Agency Task Force on Emerging Infectious Diseases (IATF) was convened by the national government in January 2020 to monitor a viral outbreak in Wuhan, China. The first case of local transmission of COVID-19 was confirmed on March 7, 2020. Following this, on March 8, the entire country was placed under a State of Public Health Emergency. By March 25, the IATF released a National Action Plan to control the spread of COVID-19. A community quarantine was initially put in place for the national capital region (NCR) starting March 13, 2020 and it was expanded to the whole island of Luzon by March 17. The initial quarantine was extended up to April 30 [ 5 , 15 ]. Several quarantine protocols were then implemented based on evaluation of IATF:
Community Quarantine (CQ) refers to restrictions in mobility between quarantined areas.
In Enhanced Community Quarantine (ECQ), strict home quarantine is implemented and movement of residents is limited to access essential goods and services. Public transportation is suspended. Only economic activities related to essential and utility services are allowed. There is heightened presence of uniformed personnel to enforce community quarantine protocols.
Modified Enhanced Community Quarantine (MECQ) is implemented as a transition phase between ECQ and GCQ. Strict home quarantine and suspension of public transportation are still in place. Mobility restrictions are relaxed for work-related activities. Government offices operates under a skeleton workforce. Manufacturing facilities are allowed to operate with up to 50% of the workforce. Transportation services are only allowed for essential goods and services.
In General Community Quarantine (GCQ), individuals from less susceptible age groups and without health risks are allowed to move within quarantined zones. Public transportation can operate at reduced vehicle capacity observing physical distancing. Government offices may be at full work capacity or under alternative work arrangements. Up to 50% of the workforce in industries (except for leisure and amusement) are allowed to work.
Modified General Community Quarantine (MGCQ) refers to the transition phase between GCQ and the New Normal. All persons are allowed outside their residences. Socio-economic activities are allowed with minimum public health standard.
LGUs are tasked to adopt, coordinate, and implement guidelines concerning COVID-19 in accordance with provincial and local quarantine protocols released by the national government [ 16 ].
In this study, we identified economic and demographic factors that are correlated with epidemiological metrics related to COVID-19, specifically to the number of infected cases and number of deaths [ 17 , 18 ]. At the regional, provincial, and city levels, we investigated the localities that differ with the other localities, and determined the possible reasons why they are outliers compared to the average practices of the others.
We categorized the data into economic, health, and demographic components (See Table 1 ). In the economic setting, we considered the number of people employed and the number of work hours. The number of health facilities provides an insight into the health system of a locality. Population and population density, as well as age distribution and mobility, were used as the demographic indicators. The data (as of November 10, 2020) from these seven factors were analyzed and compared to the number of deaths and cumulative cases in cities, provinces or regions in the Philippines to determine the outlier.
The Philippine government’s administrative structure and the availability of the data affected its range for each factor. Regional data were obtained for the economic component. For the health and demographic components, data from cities and provinces were retrieved from the sources. Due to the NCR exhibiting the highest figures in all key components, an investigation was conducted to identify an outlier among its cities. The z -transform
where x is the actual data, μ is the mean and σ is the standard deviation were applied to normalize the dataset. Two sets of normalized data X and Y were compared by assigning to each pair ( x , y ), where x ∈ X and y ∈ Y , its Euclidean metric d given by d =( x − y ) 2 . Here, the Y ’s are the number of COVID-19 cases and deaths, and X ’s are the other demographic indicators. Since 95% of the data fall within two standard deviations from the mean, this will be the threshold in determining an outlier. This means that if a data pair ( x , y ) exceeds, by two standard deviations, the mean of the Euclidean metric values between the sets X and Y , the pair is assumed to be an outlier.
To identify a good outlier, a bias computation was performed. In this procedure, Y represents the normalized data set for the number of deaths or the number of cases while X represents the normalized data set for every factor that were considered in this study. The bias is computed using the metric
for all x in X and y in Y . To categorize a city, province, or region as a good outlier, the bias corresponding to this locality must exceed two standard deviations from the mean of all the bias computations between the sets X and Y .
Results and discussion
The data used were the reported COVID-19 cases and deaths in the Philippines as of November 10, 2020 which is 240 days since community lockdowns were implemented in the country. Figure 1 shows the different lockdowns implemented per province since March 15. It can be seen that ECQ was implemented in Luzon and major cities in the country in the first few weeks since March 15, and slowly eased into either GCQ or MGCQ as time progressed. By August, the most stringent lockdown was MECQ in the National Capital Region (NCR) and some nearby provinces. Places under MECQ on September were Iloilo City, Bacolod City, and Lanao del Sur, with the last province as the lone community to be placed under MECQ the month after. By November 1, 2020, communities were either placed under GCQ or MGCQ.
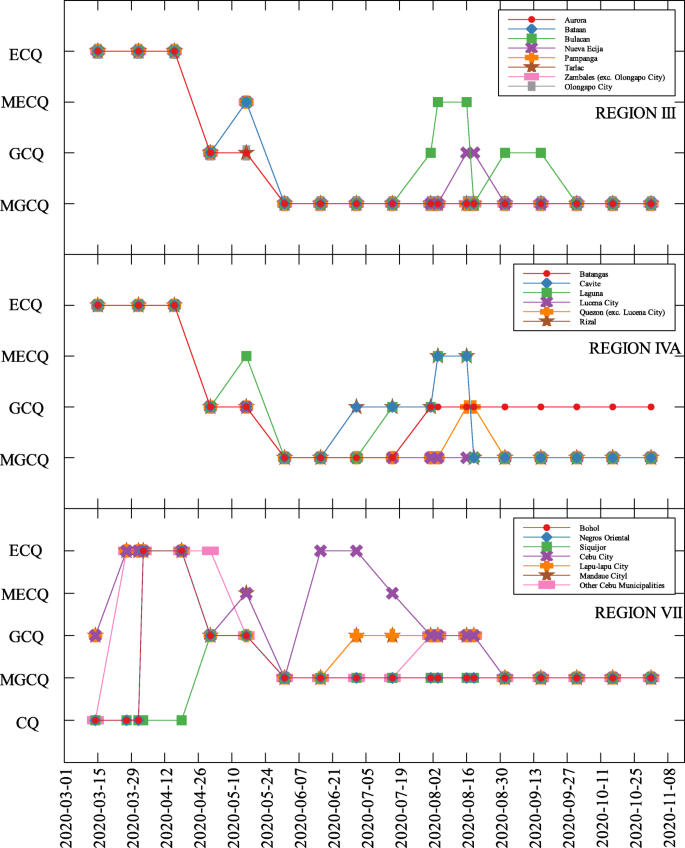
COVID-19 community quarantines in Regions III, IVA and VII
Comparison of economic, health, and demographic components and COVID-19 parameters
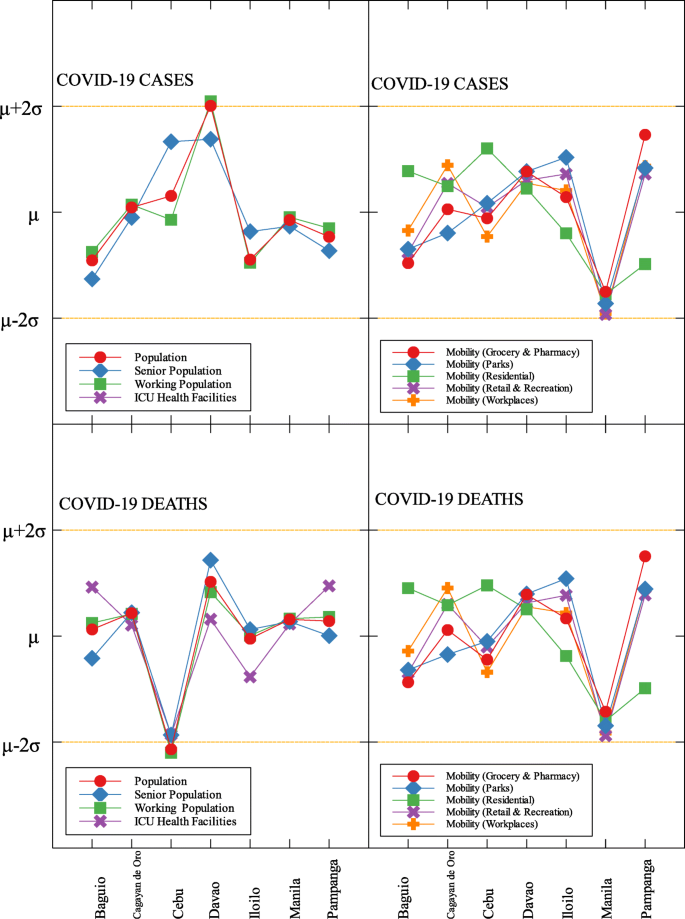
The economic, health and demographic components were compared to COVID-19 cases and deaths. These comparisons were done for different community levels (regional, provincial, city/metropolitan) (See Tables 2 , 3 , and 4 ). Figure 2 summarizes the correlation of components to COVID-19 cases and deaths at the regional level. In all components, correlations with other parameters to both COVID-19 cases and deaths are close. Every component except Residential Mobility and GRDP have slightly higher correlation coefficient for COVID-19 cases as compared to COVID-19 deaths.
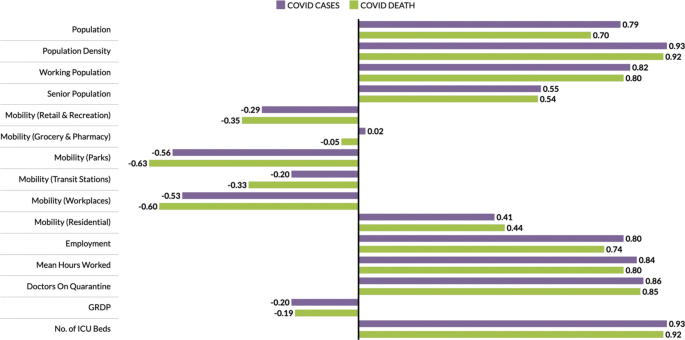
Correlation of components to COVID-19 cases and deaths at the regional level
Among the components, the number of ICU beds component has the highest correlation with COVID-19 parameters. This makes sense as this is one of the first-degree measures of COVID-19 transmission. Population density comes in second, followed by mean hours worked and working population, which are all related to how developed the region is economy-wise. Regions having larger population density also have a huge working population and longer working hours [ 24 ]. Thus, having a huge population density implies high chance of having contact with each other [ 25 , 26 ]. Another component with high correlation to the cases and deaths is the number of doctors on quarantine, which can be looked at two ways; (i) huge infection rate in the region which is the reason the doctors got exposed or are on quarantine, and (ii) lots of doctors on quarantine which resulted to less frontliners taking care of the infected individuals. All definitions of mobility and the GDP are not strongly correlated to any of the COVID-19 measures.
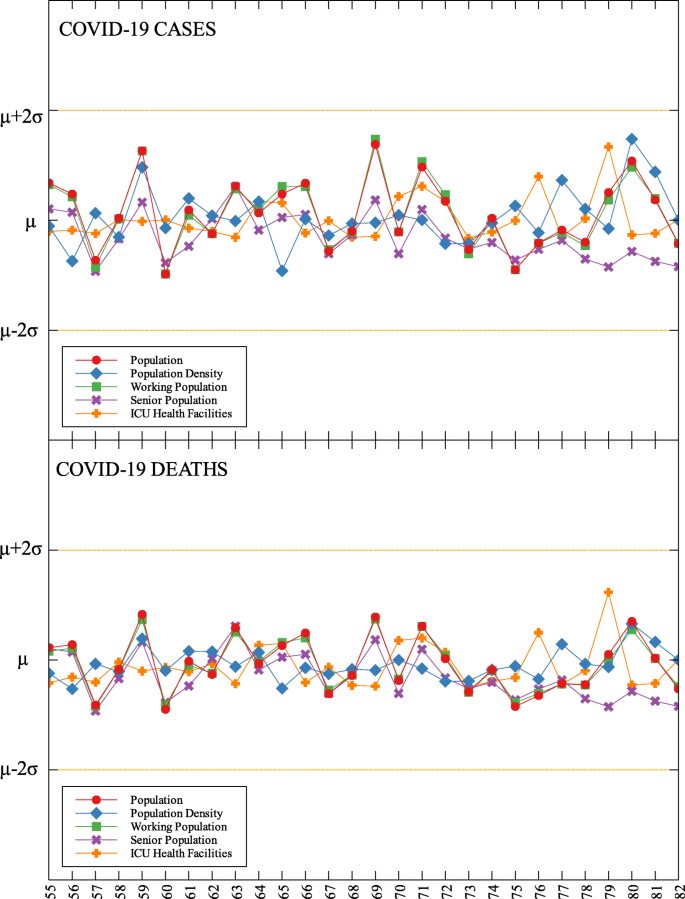
In each data set, outliers were identified depending on their distance from the mean. For simplicity, we denote components that are compared with COVID-19 cases by (C) and with COVID-19 deaths by (D). The summary of outliers among regions in the Philippines is shown in Figs. 3 and 4 . Data is classified according to groups of component. In each outlier region, non-pharmaceutical interventions (NPI) implemented and their timing are identified.
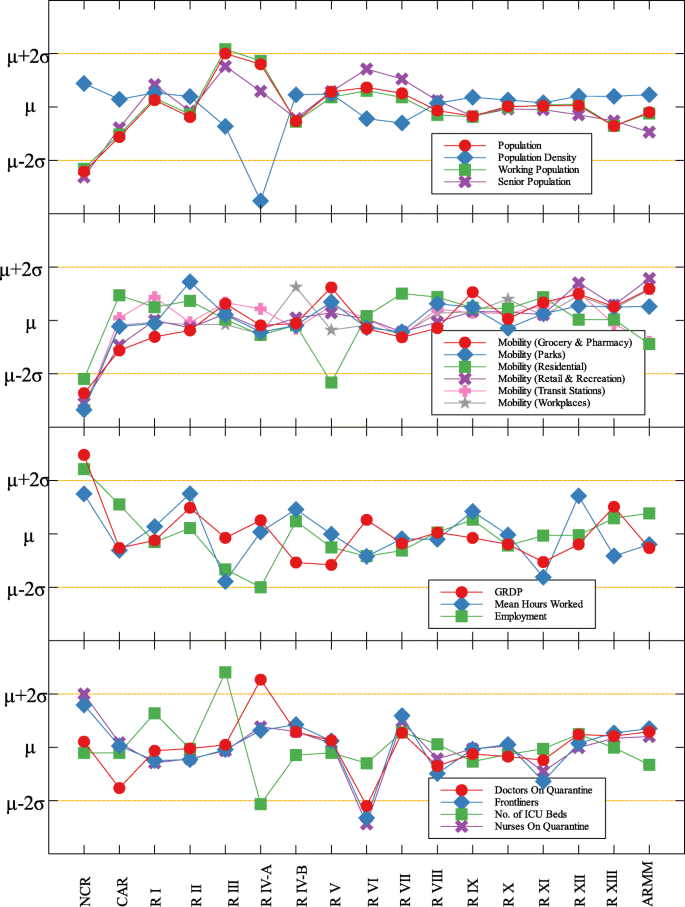
Outliers among regions in the Philippines with respect to COVID-19 cases
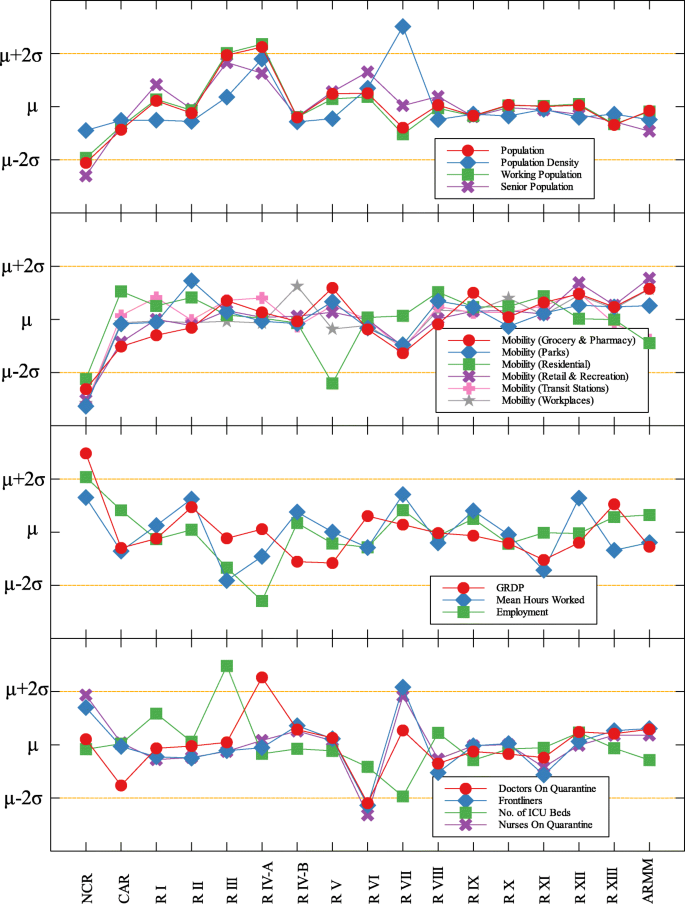
Outliers among regions in the Philippines with respect to COVID-19 deaths
Region III is an outlier in terms of working population (C) and the number of ICU beds (C) (see Fig. 5 and Table 5 ). This means that considering the working population of the region, the number of COVID-19 infections are better than that of other regions. Same goes with the number of ICU beds in relation to COVID-19 deaths. Region III is comprised of Aurora, Bataan, Nueva Ecija, Pampanga, Tarlac, Zambales, and Bulacan. This good performance might be attributed to their performance especially on their programs against COVID-19. As early as March 2020, the region had been under a community lockdown together with other regions in Luzon. Being the closest to NCR, Bulacan has been the most likely to have high number of COVID-19 cases in the region. But the province responded by opening infection control centers which offer free healthcare, meals, and rooms for moderate-severe COVID-19 patients [ 27 ]. They have also implemented strict monitoring of entry-exit borders, organization of provincial task force and incident command center, establishment of provincial quarantine facilities for returning overseas Filipino workers, mandated municipal quarantine facilities for asymptomatic cases, and mass testing, among others [ 27 ]. Most of which have been proven effective in reducing the number of COVID-19 cases and deaths [ 28 ].
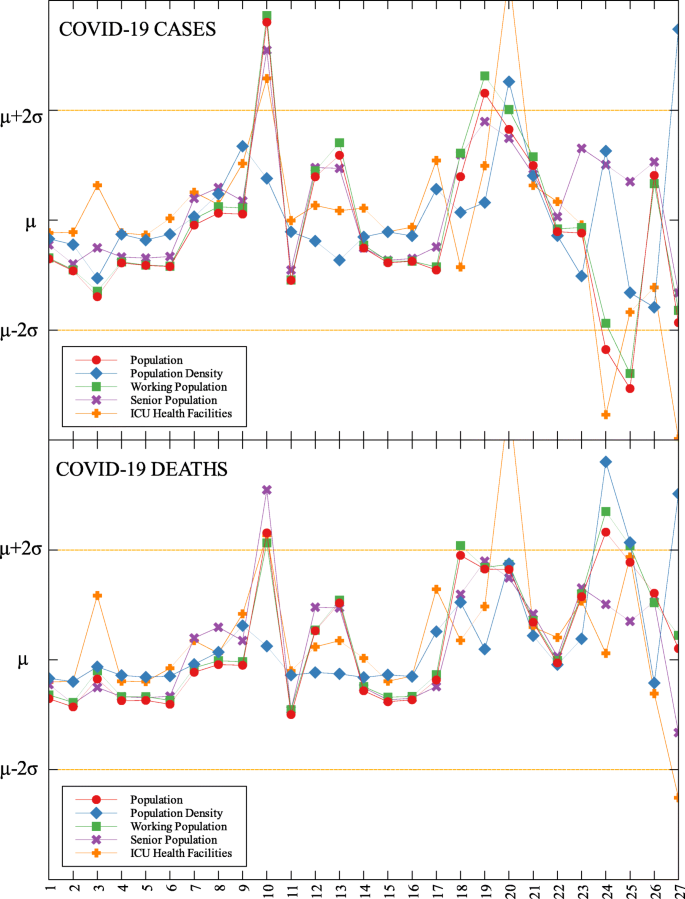
Outliers among the provinces in Luzon with respect to COVID-19 cases and deaths
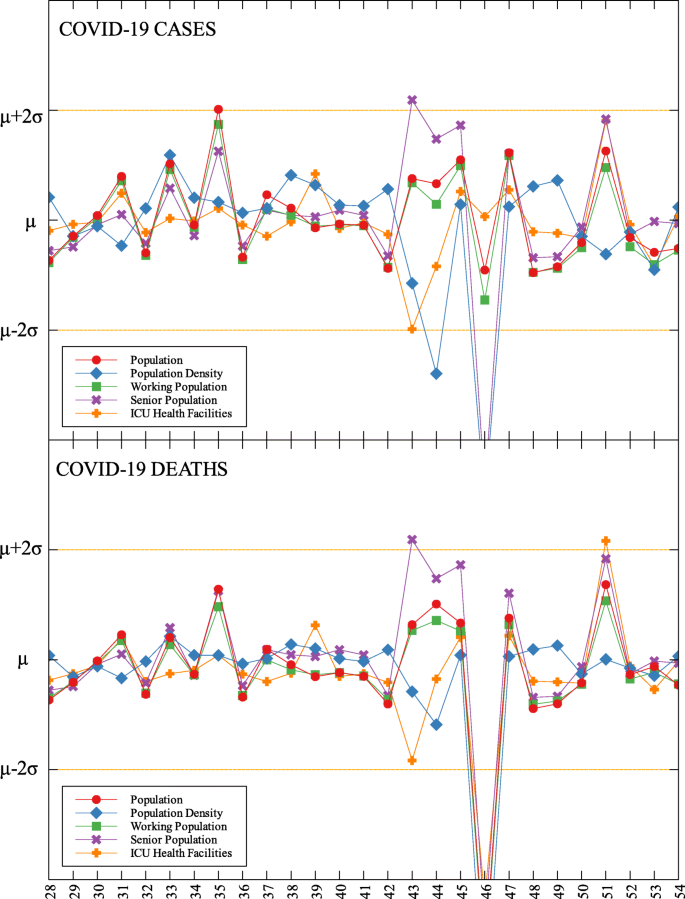
Outliers among the provinces in Visayas with respect to COVID-19 cases and deaths
Outliers among the provinces in Mindanao with respect to COVID-19 cases and deaths
Region IV-A is an outlier in terms of population and working population (D) and doctors on quarantine (D) (see Fig. 5 and Table 5 ). Considering their population and working population, the COVID-19 death statistics show better results compared to other regions. Same goes with the number of doctors in the region which are in quarantine in relation to the reported COVID-19 deaths. This shows that the region is doing well in terms of decreasing the COVID-19 fatalities compared to other regions in terms of populations and doctors on quarantine. Region IV-A is comprised of Batangas, Cavite, Laguna, Quezon, and Rizal. Same with Region III, they have been under the community lockdown since March of last year. Provinces of the region such as Rizal have been proactive in responding to the epidemic as they have already suspended classes and distributed face masks even before the nationwide lockdown [ 29 ]. Despite being hit by natural calamities, the region still continue ramping up the response to the pandemic through cash assistance, first aid kits, and spreading awareness [ 30 ].
An interesting result is that NCR, the center of the country and the most densely populated, is a good outlier in terms of GRDP (C) and GRDP (D). Cities in the region launched various programs in order to combat the disease. They have launched mass testings with Quezon City, Taguig City, and Caloocan City starting as early as April 2020. Pasig City started an on-the-go market called Jeepalengke. Navotas, Malabon, and Caloocan recorded the lowest attack rate of the virus. Caloocan city had good strategies for zoning, isolation and even in finding ways to be more effective and efficient. Other programs also include color-coded quarantine pass, and quarantine bands. It is also possible that NCR may just have a very high GRDP compared to other regions. A breakdown of the outliers within NCR can be seen in Fig. 8 .
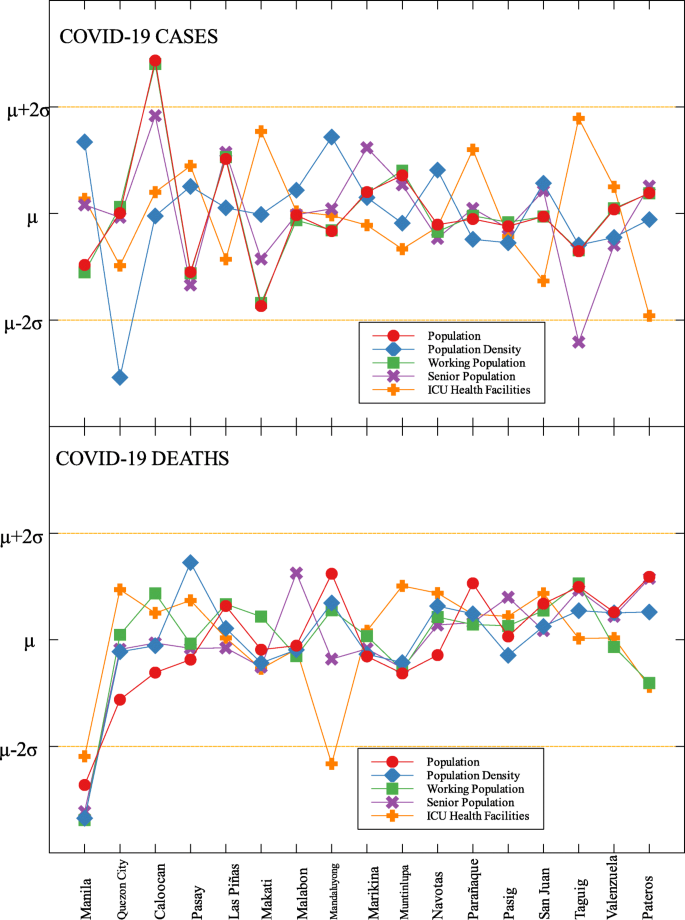
Outliers in the national capital region with respect to COVID-19 cases and deaths
Region VII is also an outlier in terms of population density (D) and frontliners (D) (see Fig. 6 and Table 5 ). This means that given the population density and the number of frontliners in the region, their COVID-related deaths in the region is better than the rest of the country. This region consists of four provinces (Cebu, Bohol, Negros Oriental, and Siquijor) and three highly urbanized cities (Cebu City, Lapu-Lapu City, and Mandaue City), referred to as metropolitan Cebu. This significant decline may be explained by how the local government responded after they were placed in stricter community quarantine measures despite the rest of the country easing in to more lenient measures. Due to the longer and stricter quarantine in Cebu, the lockdown had a greater impact here than in other areas where restrictions were eased earlier [ 31 ]. Dumaguete was one of the destinations of the first COVID case in the Philippines [ 32 ], their local government was able to keep infections at bay early on. Siquijor was also COVID-19-free for 6 months [ 33 ]. The compounded efforts of the different provinces in the region can account for the region being identified as an outlier.
Among the metropolitan cities, Davao came out as a good outlier in terms of population (C) and working population (C) (see Figs. 7 , 9 , and Table 5 ). This result may be attributed to their early campaign on consistent communication of COVID-19-related concerns to the public [ 34 ]. They were also able to set up transportation for essential workers early on [ 35 ].
Outliers among metropolitan areas in the Philippines with respect to COVID-19 cases and deaths
This study identified outliers in each data group and determined the NPIs implemented in the locality. Economic, health and demographic components were used to identify these outliers. For the regional data, three regions in Luzon and one in Visayas were identified as outliers. Apart from the minimum IATF recommended NPIs, various NPIs were implemented by different regions in containing the spread of COVID-19 in their areas. Some of these NPIs were also implemented in other localities yet these other localities did not come out as outliers. This means that one practice cannot be the sole explanation in determining an outlier. The compounding effects of practices and their timing of implementation are seen to have influenced the results. A deeper analysis of daily data for different trends in the epidemic curve is considered for future research.
Correlation tables, outliers and community quarantine timeline
Availability of data and materials.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Phil D, Cowling BJ, Yang B, Leung GM, Feng Z. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med. 2020; 382(13):1199–207.
Article CAS Google Scholar
Hsiang S, Allen D, Annan-Phan S, Bell K, Bolliger I, Chong T, Druckenmiller H, Huang LY, Hultgren A, Krasovich E, Lau P, Lee J, Rolf E, Tseng J, Wu T. The effect of large-scale anti-contagion policies on the covid-19 pandemic. Nature. 2020; 584:262–67.
Anderson R, Heesterbeek JAP, Klinkenberg D, Hollingsworth T. Comment how will country-based mitigation measures influence the course of the covid-19 epidemic?Lancet. 2020; 395. https://doi.org/10.1016/S0140-6736(20)30567-5 .
Buhat CA, Torres M, Olave Y, Gavina MK, Felix E, Gamilla G, Verano KV, Babierra A, Rabajante J. A mathematical model of covid-19 transmission between frontliners and the general public. Netw Model Anal Health Inform Bioinforma. 2021; 10. https://doi.org/10.1007/s13721-021-00295-6 .
Ocampo L, Yamagishic K. Modeling the lockdown relaxation protocols of the philippine government in response to the covid-19 pandemic: an intuitionistic fuzzy dematel analysis. Socioecon Plann Sci. 2020; 72. https://doi.org/10.1016/j.seps.2020.100911 .
Weible C, Nohrstedt D, Cairney P, Carter D, Crow D, Durnová A, Heikkila T, Ingold K, McConnell A, Stone D. Covid-19 and the policy sciences: initial reactions and perspectives. Policy Sci. 2020; 53:225–41. https://doi.org/10.1007/s11077-020-09381-4 .
Article Google Scholar
Wibbens PD, Koo WW-Y, McGahan AM. Which covid policies are most effective? a bayesian analysis of covid-19 by jurisdiction. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0244177 .
Mintrom M, O’Connor R. The importance of policy narrative: effective government responses to covid-19. Policy Des Pract. 2020; 3(3):205–27. https://doi.org/10.1080/25741292.2020.1813358 .
Google Scholar
Chin T, Kahn R, Li R, Chen JT, Krieger N, Buckee CO, Balsari S, Kiang MV. Us-county level variation in intersecting individual, household and community characteristics relevant to covid-19 and planning an equitable response: a cross-sectional analysis. BMJ Open. 2020; 10(9). https://doi.org/10.1136/bmjopen-2020-039886 .
OECD. The territorial impact of COVID-19: managing the crisis across levels of government. 2020. https://www.oecd.org/coronavirus/policy-responses/the-territorial-impact-of-covid-19-managing-the-crisis-across-levels-of-government-d3e314e1/#biblio-d1e5202 . Accessed 20 Feb 2007.
White ER, Hébert-Dufresne L. State-level variation of initial covid-19 dynamics in the united states. PLoS ONE. 2020; 15. https://doi.org/10.1371/journal.pone.0240648 .
Lin S, Huang J, He Z, Zhan D. Which measures are effective in containing covid-19? — empirical research based on prevention and control cases in China. medRxiv. 2020. https://doi.org/10.1101/2020.03.28.20046110 . https://www.medrxiv.org/content/early/2020/03/30/2020.03.28.20046110.full.pdf .
Mei C. Policy style, consistency and the effectiveness of the policy mix in China’s fight against covid-19. Policy Soc. 2020; 39(3):309–25. https://doi.org/10.1080/14494035.2020.1787627. http://arxiv.org/abs/https: //doi.org/10.1080/14494035.2020.1787627.
Dutta A, Fischer HW. The local governance of covid-19: disease prevention and social security in rural india. World Dev. 2021; 138:105234. https://doi.org/10.1016/j.worlddev.2020.105234 .
Vallejo BM, Ong RAC. Policy responses and government science advice for the covid 19 pandemic in the philippines: january to april 2020. Prog Disaster Sci. 2020; 7:100115. https://doi.org/10.1016/j.pdisas.2020.100115 .
Inter-Agency Task Force for the Management of Emerging Infectious Diseases. Omnibus guidelines on the implementation of community quarantine in the Philippines. 2020. https://doh.gov.ph/node/27640 . Accessed 20 Feb 2020.
Roy S, Ghosh P. Factors affecting covid-19 infected and death rates inform lockdown-related policymaking. PloS ONE. 2020; 15(10):0241165. https://doi.org/10.1371/journal.pone.0241165 .
Pullano G, Valdano E, Scarpa N, Rubrichi S, Colizza V. Evaluating the effect of demographic factors, socioeconomic factors, and risk aversion on mobility during the covid-19 epidemic in france under lockdown: a population-based study. Lancet Digit Health. 2020; 2(12):638–49.
Department of Health. COVID-19 tracker. 2020. https://doh.gov.ph/covid19tracker . Accessed 25 Nov 2020.
Authority PS. Philippine population density (based on the 2015 census of population). 2020. https://psa.gov.ph/content/philippine-population-density-based-2015-census-population . Accessed 11 Apr 2020.
Google. COVID-19 community mobility report. 2020; https://www.google.com/covid19/mobility?hl=en. Accessed 25 Nov 2020.
Authority PS. Labor force survey. 2020. https://psa.gov.ph/statistics/survey/labor-and-employment/labor-force-survey?fbclid=IwAR0a5GS7XtRgRmBwAcGl9wGwNhptqnSBm-SNVr69cm8sCVd9wVmcoKHRCdU . Accessed 11 Apr 2020.
Authority PS. https://psa.gov.ph/grdp/tables?fbclid=IwAR3dKvo3B5eauY7KcWQG4VXbuiCrzFHO4b-f1k5Od76ccAlYxUimUIaqs94 . Accessed 11 Apr 2020. 2020.
Peterson E. The role of population in economic growth. SAGE Open. 2017; 7:215824401773609. https://doi.org/10.1177/2158244017736094 .
Buhat CA, Duero JC, Felix E, Rabajante J, Mamplata J. Optimal allocation of covid-19 test kits among accredited testing centers in the philippines. J Healthc Inform Res. 2021; 5. https://doi.org/10.1007/s41666-020-00081-5 .
Hamidi S, Sabouri S, Ewing R. Does density aggravate the covid-19 pandemic?: early findings and lessons for planners. J Am Plan Assoc. 2020; 86:1–15. https://doi.org/10.1080/01944363.2020.1777891 .
Philippine News Agency. Bulacan shares anti-COVID-19 best practices. 2020. https://mb.com.ph/2020/08/16/bulacan-shares-anti-covid-19-best-practices/ . Accessed Mar 2020.
Buhat CA, Villanueva SK. Determining the effectiveness of practicing non-pharmaceutical interventions in improving virus control in a pandemic using agent-based modelling. Math Appl Sci Eng. 2020; 1:423–38. https://doi.org/10.5206/mase/10876 .
Hallare K. Cainta, Rizal suspends classes, distributes face masks over coronavirus threat. 2020. https://newsinfo.inquirer.net/1238217/cainta-rizal-suspends-classes-distributes-face-masks-over-coronavirus-threat . Accessed Mar 2020.
Relief International. Responding to COVID-19 in the Aftermath of Volcanic Eruption. 2020. https://www.ri.org/projects/responding-to-covid-19-in-the-aftermath-of-volcanic-eruption/. Accessed Mar 2020.
Macasero R. Averting disaster: how Cebu City flattened its curve. 2020. https://www.rappler.com/newsbreak/explainers/how-cebu-city-flattened-covid-19-curve/ . Accessed Mar 2020.
Edrada EM, Lopez EB, Villarama JB, Salva-Villarama EP, Dagoc BF, Smith C, Sayo AR, Verona JA, Trifalgar-Arches J, Lazaro J, Balinas EGM, Telan EFO, Roy L, Galon M, Florida CHN, Ukawa T, Villaneuva AMG, Saito N, Nepomuceno JR, Ariyoshi K, Carlos C, Nicolasor AD, Solante RM. First covid-19 infections in the philippines: a case report. Trop Med Health. 2020; 48(30). https://doi.org/10.1186/s41182-020-00218-7 .
Macasero R. Coronavirus-free for 6 months, Siquijor reports first 2 cases. 2020. https://www.rappler.com/nation/siquijor-coronavirus-cases-august-2-2020 . Accessed Mar 2020.
Davao City. Mayor Sara, disaster radio journeying with dabawenyos. 2020. https://www.davaocity.gov.ph/disaster-risk-reduction-mitigation/mayor-sara-disaster-radio-journeying-with-dabawenyos . Accessed Mar 2020.
Davao City. Davao city free rides to serve GCQ-allowed workers. 2020. https://www.davaocity.gov.ph/transportation-planning-traffic-management/davao-city-free-rides-to-serve-gcq-allowed-workers/ . Accessed Mar 2020.
Download references
Acknowledgements
JFR is supported by the Abdus Salam International Centre for Theoretical Physics Associateship Scheme.
This research is funded by the UP System through the UP Resilience Institute.
Author information
Authors and affiliations.
Institute of Mathematical Sciences and Physics, University of the Philippines Los Baños, Laguna, Philippines
Dylan Antonio S. Talabis, Ariel L. Babierra, Christian Alvin H. Buhat, Destiny S. Lutero, Kemuel M. Quindala III & Jomar F. Rabajante
University of the Philippines Resilience Institute, University of the Philippines, Quezon City, Philippines
Faculty of Education, University of the Philippines Open University, Laguna, Philippines
Jomar F. Rabajante
You can also search for this author in PubMed Google Scholar
Contributions
All authors are involved in drafting the manuscript and in revising it. The author(s) read and approved the final manuscript.
Corresponding author
Correspondence to Dylan Antonio S. Talabis .
Ethics declarations
Ethics approval and consent to participate.
Not applicable. We used secondary data. These are from the public database of the Philippine Department of Health ( https://www.doh.gov.ph/covid19tracker ) and Philippine Statistics Authority Census ( https://psa.gov.ph )
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
S. Talabis, D.A., Babierra, A.L., H. Buhat, C.A. et al. Local government responses for COVID-19 management in the Philippines. BMC Public Health 21 , 1711 (2021). https://doi.org/10.1186/s12889-021-11746-0
Download citation
Received : 19 April 2021
Accepted : 30 August 2021
Published : 21 September 2021
DOI : https://doi.org/10.1186/s12889-021-11746-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Local government
- Quantitative methods
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 10, Issue 11
- The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA study): a protocol study
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0001-5621-1833 Adrian I Espiritu 1 , 2 ,
- http://orcid.org/0000-0003-1135-6400 Marie Charmaine C Sy 1 ,
- http://orcid.org/0000-0002-1241-8805 Veeda Michelle M Anlacan 1 ,
- http://orcid.org/0000-0001-5317-7369 Roland Dominic G Jamora 1
- 1 Department of Neurosciences , College of Medicine and Philippine General Hospital, University of the Philippines Manila , Manila , Philippines
- 2 Department of Clinical Epidemiology, College of Medicine , University of the Philippines Manila , Manila , Philippines
- Correspondence to Dr Adrian I Espiritu; aiespiritu{at}up.edu.ph
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes.
Objectives The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA) study investigators will conduct a nationwide, multicentre study involving 37 institutions that aims to determine the neurological manifestations and factors associated with clinical outcomes in COVID-19 infection.
Methodology and analysis This is a retrospective cohort study (comparative between patients with and without neurological manifestations) via medical chart review involving adult patients with COVID-19 infection. Sample size was determined at 1342 patients. Demographic, clinical and neurological profiles will be obtained and summarised using descriptive statistics. Student’s t-test for two independent samples and χ 2 test will be used to determine differences between distributions. HRs and 95% CI will be used as an outcome measure. Kaplan-Meier curves will be constructed to plot the time to onset of mortality (survival), respiratory failure, intensive care unit (ICU) admission, duration of ventilator dependence, length of ICU stay and length of hospital stay. The log-rank test will be employed to compare the Kaplan-Meier curves. Stratified analysis will be performed to identify confounders and effects modifiers. To compute for adjusted HR with 95% CI, crude HR of outcomes will be adjusted according to the prespecified possible confounders. Cox proportional regression models will be used to determine significant factors of outcomes. Testing for goodness of fit will also be done using Hosmer-Lemeshow test. Subgroup analysis will be performed for proven prespecified effect modifiers. The effects of missing data and outliers will also be evaluated in this study.
Ethics and dissemination This protocol was approved by the Single Joint Research Ethics Board of the Philippine Department of Health (SJREB-2020–24) and the institutional review board of the different study sites. The dissemination of results will be conducted through scientific/medical conferences and through journal publication. The lay versions of the results may be provided on request.
Trial registration number NCT04386083 .
- adult neurology
- epidemiology
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-040944
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms Study is a nationwide, multicentre, retrospective, cohort study with 37 Philippine sites.
Full spectrum of neurological manifestations of COVID-19 will be collected.
Retrospective gathering of data offers virtually no risk of COVID-19 infection to data collectors.
Data from COVID-19 patients who did not go to the hospital are unobtainable.
Recoding bias is inherent due to the retrospective nature of the study.
Introduction
The COVID-19 has been identified as the cause of an outbreak of respiratory illness in Wuhan, Hubei Province, China, in December 2019. 1 The COVID-19 pandemic has reached the Philippines with most of its cases found in the National Capital Region (NCR). 2 The major clinical features of COVID-19 include fever, cough, shortness of breath, myalgia, headache and diarrhoea. 3 The outcomes of this disease lead to prolonged hospital stay, intensive care unit (ICU) admission, dependence on invasive mechanical ventilation, respiratory failure and mortality. 4 The specific pathogen that causes this clinical syndrome has been named SARS-CoV-2, which is phylogenetically similar to SARS-CoV. 4 Like the SARS-CoV strain, SARS-CoV-2 may possess a similar neuroinvasive potential. 5
A study on cases with COVID-19 found that about 36.4% of patients displayed neurological manifestations of the central nervous system (CNS) and peripheral nervous system (PNS). 6 The associated spectrum of symptoms and signs were substantially broad such as altered mental status, headache, cognitive impairment, agitation, dysexecutive syndrome, seizures, corticospinal tract signs, dysgeusia, extraocular movement abnormalities and myalgia. 7–12 Several reports were published on neurological disorders associated with patients with COVID-19, including cerebrovascular disorders, encephalopathy, hypoxic brain injury, frequent convulsive seizures and inflammatory CNS syndromes like encephalitis, meningitis, acute disseminated encephalomyelitis and Guillain-Barre syndrome. 7–16 However, the estimates of the occurrences of these manifestations were based on studies with a relatively small sample size. Furthermore, the current description of COVID-19 neurological features are hampered to some extent by exceedingly variable reporting; thus, defining causality between this infection and certain neurological manifestations is crucial since this may lead to considerable complications. 17 An Italian observational study protocol on neurological manifestations has also been published to further document and corroborate these findings. 18
Epidemiological data on the proportions and spectrum of non-respiratory symptoms and complications may be essential to increase the recognition of clinicians of the possibility of COVID-19 infection in the presence of other symptoms, particularly neurological manifestations. With this information, the probabilities of diagnosing COVID-19 disease may be strengthened depending on the presence of certain neurological manifestations. Furthermore, knowledge of other unrecognised symptoms and complications may allow early diagnosis that may permit early institution of personal protective equipment and proper contact precautions. Lastly, the presence of neurological manifestations may be used for estimating the risk of certain important clinical outcomes for better and well-informed clinical decisions in patients with COVID-19 disease.
To address this lack of important information in the overall management of patients with COVID-19, we organised a research study entitled ‘The Philippine COVID-19 Outcomes: a Retrospective study Of Neurological manifestations and Associated symptoms (The Philippine CORONA Study)’.
This quantitative, retrospective cohort, multicentre study aims: (1) to determine the demographic, clinical and neurological profile of patients with COVID-19 disease in the Philippines; (2) to determine the frequency of neurological symptoms and new-onset neurological disorders/complications in patients with COVID-19 disease; (3) to determine the neurological manifestations that are significant factors of mortality, respiratory failure, duration of ventilator dependence, ICU admission, length of ICU stay and length of hospital stay among patients with COVID-19 disease; (4) to determine if there is significant difference between COVID-19 patients with neurological manifestations compared with those COVID-19 patients without neurological manifestations in terms of mortality, respiratory failure, duration of ventilator dependence, ICU admission, length of ICU stay and length of hospital stay; and (5) to determine the likelihood of mortality, respiratory failure and ICU admission, including the likelihood of longer duration of ventilator dependence and length of ICU and hospital stay in COVID-19 patients with neurological manifestations compared with those without neurological manifestations.
Scope, limitations and delimitations
The study will include confirmed cases of COVID-19 from the 37 participating institutions in the Philippines. Every country has its own healthcare system, whose level of development and strategies ultimately affect patient outcomes. Thus, the results of this study cannot be accurately generalised to other settings. In addition, patients with ages ≤18 years will be excluded in from this study. These younger patients may have different characteristics and outcomes; therefore, yielded estimates for adults in this study may not be applicable to this population subgroup. Moreover, this study will collect data from the patient records of patients with COVID-19; thus, data from patients with mild symptoms who did not go to the hospital and those who had spontaneous resolution of symptoms despite true infection with COVID-19 are unobtainable.
Methodology
To improve the quality of reporting of this study, the guidelines issued by the Strengthening the Reporting of Observational Studies in Epidemiology Initiative will be followed. 19
Study design
The study will be conducted using a retrospective cohort (comparative) design (see figure 1 ).
- Download figure
- Open in new tab
- Download powerpoint
Schematic diagram of the study flow.
Study sites and duration
We will conduct a nationwide, multicentre study involving 37 institutions in the Philippines (see figure 2 ). Most of these study sites can be found in the NCR, which remains to be the epicentre of the COVID-19 pandemic. 2 We will collect data for 6 months after institutional review board approval for every site.
Location of 37 study sites of the Philippine CORONA study.
Patient selection and cohort description
The cases will be identified using the designated COVID-19 censuses of all the participating centres. A total enumeration of patients with confirmed COVID-19 disease will be done in this study.
The cases identified should satisfy the following inclusion criteria: (A) adult patients at least 19 years of age; (B) cases confirmed by testing approved patient samples (ie, nasal swab, sputum and bronchoalveolar lavage fluid) employing real-time reverse transcription PCR (rRT-PCR) 20 from COVID-19 testing centres accredited by the Department of Health (DOH) of the Philippines, with clinical symptoms and signs attributable to COVID-19 disease (ie, respiratory as well as non-respiratory clinical signs and symptoms) 21 ; and (C) cases with disposition (ie, discharged stable/recovered, home/discharged against medical advice, transferred to other hospital or died) at the end of the study period. Cases with conditions or diseases caused by other organisms (ie, bacteria, other viruses, fungi and so on) or caused by other pathologies unrelated to COVID-19 disease (ie, trauma) will be excluded.
The first cohort will involve patients with confirmed COVID-19 infection who presented with any neurological manifestation/s (ie, symptoms or complications/disorder). The comparator cohort will compose of patients with confirmed COVID-19 infection without neurological manifestation/s.
Sample size calculation
We looked into the mortality outcome measure for the purposes of sample size computation. Following the cohort study of Khaledifar et al , 22 the sample size was calculated using the following parameters: two-sided 95% significance level (1 – α); 80% power (1 – β); unexposed/exposed ratio of 1; 5% of unexposed with outcome (case fatality rate from COVID19-Philippines Dashboard Tracker (PH) 23 as of 8 April 2020); and assumed risk ratio 2 (to see a two-fold increase in risk of mortality when neurological symptoms are present).
When these values were plugged in to the formula for cohort studies, 24 a minimum sample size of 1118 is required. To account for possible incomplete data, the sample was adjusted for 20% more. This means that the total sample size required is 1342 patients, which will be gathered from the participating centres.
Data collection
We formulated an electronic data collection form using Epi Info Software (V.7.2.2.16). The forms will be pilot-tested, and a formal data collection workshop will be conducted to ensure collection accuracy. The data will be obtained from the review of the medical records.
The following pertinent data will be obtained: (A) demographic data; (B) other clinical profile data/comorbidities; (C) neurological history; (D) date of illness onset; (E) respiratory and constitutional symptoms associated with COVID-19; (F) COVID-19 disease severity 25 at nadir; (G) data if neurological manifestation/s were present at onset prior to respiratory symptoms and the specific neurological manifestation/s present at onset; (H) neurological symptoms; (i) date of neurological symptom onset; (J) new-onset neurological disorders or complications; (K) date of new neurological disorder or complication onset; (L) imaging done; (M) cerebrospinal fluid analysis; (N) electrophysiological studies; (O) treatment given; (P) antibiotics given; (Q) neurological interventions given; (R) date of mortality and cause/s of mortality; (S) date of respiratory failure onset, date of mechanical ventilator cessation and cause/s of respiratory failure; (T) date of first day of ICU admission, date of discharge from ICU and indication/s for ICU admission; (U) other neurological outcomes at discharge; (V) date of hospital discharge; and (W) final disposition. See table 1 for the summary of the data to be collected for this study.
- View inline
Data to be collected in this study
Main outcomes considered
The following patient outcomes will be considered for this study:
Mortality (binary outcome): defined as the patients with confirmed COVID-19 who died.
Respiratory failure (binary outcome): defined as the patients with confirmed COVID-19 who experienced clinical symptoms and signs of respiratory insufficiency. Clinically, this condition may manifest as tachypnoea/sign of increased work of breathing (ie, respiratory rate of ≥22), abnormal blood gases (ie, hypoxaemia as evidenced by partial pressure of oxygen (PaO 2 ) <60 or hypercapnia by partial pressure of carbon dioxide of >45), or requiring oxygen supplementation (ie, PaO 2 <60 or ratio of PaO 2 /fraction of inspired oxygen (P/F ratio)) <300).
Duration of ventilator dependence (continuous outcome): defined as the number of days from initiation of assisted ventilation to cessation of mechanical ventilator use.
ICU admission (binary outcome): defined as the patients with confirmed COVID-19 admitted to an ICU or ICU-comparable setting.
Length of ICU stay (continuous outcome): defined as the number of days admitted in the ICU or ICU-comparable setting.
Length of hospital stay (continuous outcome): defined as the number of days from admission to discharge.
Data analysis plan
Statistical analysis will be performed using Stata V.7.2.2.16.
Demographic, clinical and neurological profiles will be summarised using descriptive statistics, in which categorical variables will be expressed as frequencies with corresponding percentages, and continuous variables will be pooled using means (SD).
Student’s t-test for two independent samples and χ 2 test will be used to determine differences between distributions.
HRs and 95% CI will be used as an outcome measure. Kaplan-Meier curves will be constructed to plot the time to onset of mortality (survival), respiratory failure, ICU admission, duration of ventilator dependence (recategorised binary form), length of ICU stay (recategorised binary form) and length of hospital stay (recategorised binary form). Log-rank test will be employed to compare the Kaplan-Meier curves. Stratified analysis will be performed to identify confounders and effects modifiers. To compute for adjusted HR with 95% CI, crude HR of outcomes at discrete time points will be adjusted for prespecified possible confounders such as age, history of cardiovascular or cerebrovascular disease, hypertension, diabetes mellitus, and respiratory disease, COVID-19 disease severity at nadir, and other significant confounding factors.
Cox proportional regression models will be used to determine significant factors of outcomes. Testing for goodness of fit will be done using Hosmer-Lemeshow test. Likelihood ratio tests and other information criteria (Akaike Information Criterion or Bayesian Information Criterion) will be used to refine the final model. Statistical significance will be considered if the 95% CI of HR or adjusted HR did not include the number one. A p value <0.05 (two tailed) is set for other analyses.
Subgroup analyses will be performed for proven prespecified effect modifiers. The following variables will be considered for subgroup analyses: age (19–64 years vs ≥65 years), sex, body mass index (<18.5 vs 18.5–22.9 vs ≥23 kg/m 2 ), with history of cardiovascular or cerebrovascular disease (presence or absence), hypertension (presence or absence), diabetes mellitus (presence or absence), respiratory disease (presence or absence), smoking status (smoker or non-smoker) and COVID-19 disease severity (mild, severe or critical disease).
The effects of missing data will be explored. All efforts will be exerted to minimise missing and spurious data. Validity of the submitted electronic data collection will be monitored and reviewed weekly to prevent missing or inaccurate input of data. Multiple imputations will be performed for missing data when possible. To check for robustness of results, analysis done for patients with complete data will be compared with the analysis with the imputed data.
The effects of outliers will also be assessed. Outliers will be assessed by z-score or boxplot. A cut-off of 3 SD from the mean can also be used. To check for robustness of results, analysis done with outliers will be compared with the analysis without the outliers.
Study organisational structure
A steering committee (AIE, MCCS, VMMA and RDGJ) was formed to direct and provide appropriate scientific, technical and methodological assistance to study site investigators and collaborators (see figure 3 ). Central administrative coordination, data management, administrative support, documentation of progress reports, data analyses and interpretation and journal publication are the main responsibilities of the steering committee. Study site investigators and collaborators are responsible for the proper collection and recording of data including the duty to maintain the confidentiality of information and the privacy of all identified patients for all the phases of the research processes.
Organisational structure of oversight of the Philippine CORONA Study.
This section is highlighted as part of the required formatting amendments by the Journal.
Ethics and dissemination
This research will adhere to the Philippine National Ethical Guidelines for Health and Health-related Research 2017. 26 This study is an observational, cohort study and will not allocate any type of intervention. The medical records of the identified patients will be reviewed retrospectively. To protect the privacy of the participant, the data collection forms will not contain any information (ie, names and institutional patient number) that could determine the identity of the patients. A sequential code will be recorded for each patient in the following format: AAA-BBB where AAA will pertain to the three-digit code randomly assigned to each study site; BBB will pertain to the sequential case number assigned by each study site. Each participating centre will designate a password-protected laptop for data collection; the password is known only to the study site.
This protocol was approved by the following institutional review boards: Single Joint Research Ethics Board of the DOH, Philippines (SJREB-2020-24); Asian Hospital and Medical Center, Muntinlupa City (2020- 010-A); Baguio General Hospital and Medical Center (BGHMC), Baguio City (BGHMC-ERC-2020-13); Cagayan Valley Medical Center (CVMC), Tuguegarao City; Capitol Medical Center, Quezon City; Cardinal Santos Medical Center (CSMC), San Juan City (CSMC REC 2020-020); Chong Hua Hospital, Cebu City (IRB 2420–04); De La Salle Medical and Health Sciences Institute (DLSMHSI), Cavite (2020-23-02-A); East Avenue Medical Center (EAMC), Quezon City (EAMC IERB 2020-38); Jose R. Reyes Memorial Medical Center, Manila; Jose B. Lingad Memorial Regional Hospital, San Fernando, Pampanga; Dr. Jose N. Rodriguez Memorial Hospital, Caloocan City; Lung Center of the Philippines (LCP), Quezon City (LCP-CT-010–2020); Manila Doctors Hospital, Manila (MDH IRB 2020-006); Makati Medical Center, Makati City (MMC IRB 2020–054); Manila Medical Center, Manila (MMERC 2020-09); Northern Mindanao Medical Center, Cagayan de Oro City (025-2020); Quirino Memorial Medical Center (QMMC), Quezon City (QMMC REB GCS 2020-28); Ospital ng Makati, Makati City; University of the Philippines – Philippine General Hospital (UP-PGH), Manila (2020-314-01 SJREB); Philippine Heart Center, Quezon City; Research Institute for Tropical Medicine, Muntinlupa City (RITM IRB 2020-16); San Lazaro Hospital, Manila; San Juan De Dios Educational Foundation Inc – Hospital, Pasay City (SJRIB 2020-0006); Southern Isabela Medical Center, Santiago City (2020-03); Southern Philippines Medical Center (SPMC), Davao City (P20062001); St. Luke’s Medical Center, Quezon City (SL-20116); St. Luke’s Medical Center, Bonifacio Global City, Taguig City (SL-20116); Southern Philippines Medical Center, Davao City; The Medical City, Pasig City; University of Santo Tomas Hospital, Manila (UST-REC-2020-04-071-MD); University of the East Ramon Magsaysay Memorial Medical Center, Inc, Quezon City (0835/E/2020/063); Veterans Memorial Medical Center (VMMC), Quezon City (VMMC-2020-025) and Vicente Sotto Memorial Medical Center, Cebu City (VSMMC-REC-O-2020–048).
The dissemination of results will be conducted through scientific/medical conferences and through journal publication. Only the aggregate results of the study shall be disseminated. The lay versions of the results may be provided on request.
Protocol registration and technical review approval
This protocol was registered in the ClinicalTrials.gov website. It has received technical review board approvals from the Department of Neurosciences, Philippine General Hospital and College of Medicine, University of the Philippines Manila, from the Cardinal Santos Medical Center (San Juan City) and from the Research Center for Clinical Epidemiology and Biostatistics, De La Salle Medical and Health Sciences Institute (Dasmariñas, Cavite).
Acknowledgments
We would like to thank Almira Abigail Doreen O Apor, MD, of the Department of Neurosciences, Philippine General Hospital, Philippines, for illustrating figure 2 for this publication.
- Adhikari SP ,
- Wu Y-J , et al
- Department of Health
- Philippine Society for Microbiology and Infectious Diseases
- Hu Y , et al
- Li Yan‐Chao ,
- Bai Wan‐Zhu ,
- Hashikawa T ,
- Wang M , et al
- Paterson RW ,
- Benjamin L , et al
- Hall JP , et al
- Varatharaj A ,
- Ellul MA , et al
- Mahammedi A ,
- Vagal A , et al
- Collantes MEV ,
- Espiritu AI ,
- Sy MCC , et al
- Merdji H , et al
- Sharifi Razavi A ,
- Poyiadji N ,
- Noujaim D , et al
- Zhou H , et al
- Moriguchi T ,
- Goto J , et al
- Nicholson TR , et al
- Ferrarese C ,
- Priori A , et al
- von Elm E ,
- Altman DG ,
- Egger M , et al
- Li J , et al
- Centers for Disease Control and Prevention
- Khaledifar A ,
- Hashemzadeh M ,
- Solati K , et al
- McGoogan JM
- Philippine Research Ethics Board
VMMA and RDGJ are joint senior authors.
AIE and MCCS are joint first authors.
Twitter @neuroaidz, @JamoraRoland
Collaborators The Philippine CORONA Study Group Collaborators: Maritoni C Abbariao, Joshua Emmanuel E Abejero, Ryndell G Alava, Robert A Barja, Dante P Bornales, Maria Teresa A Cañete, Ma. Alma E Carandang-Concepcion, Joseree-Ann S Catindig, Maria Epifania V Collantes, Evram V Corral, Ma. Lourdes P Corrales-Joson, Romulus Emmanuel H Cruz, Marita B Dantes, Ma. Caridad V Desquitado, Cid Czarina E Diesta, Carissa Paz C Dioquino, Maritzie R Eribal, Romulo U Esagunde, Rosalina B Espiritu-Picar, Valmarie S Estrada, Manolo Kristoffer C Flores, Dan Neftalie A Juangco, Muktader A Kalbi, Annabelle Y Lao-Reyes, Lina C Laxamana, Corina Maria Socorro A Macalintal, Maria Victoria G Manuel, Jennifer Justice F Manzano, Ma. Socorro C Martinez, Generaldo D Maylem, Marc Conrad C Molina, Marietta C Olaivar, Marissa T Ong, Arnold Angelo M Pineda, Joanne B Robles, Artemio A Roxas Jr, Jo Ann R Soliven, Arturo F Surdilla, Noreen Jhoanna C Tangcuangco-Trinidad, Rosalia A Teleg, Jarungchai Anton S Vatanagul and Maricar P Yumul.
Contributors All authors conceived the idea and wrote the initial drafts and revisions of the protocol. All authors made substantial contributions in this protocol for intellectual content.
Funding Philippine Neurological Association (Grant/Award Number: N/A). Expanded Hospital Research Office, Philippine General Hospital (Grant/Award Number: N/A).
Disclaimer Our funding sources had no role in the design of the protocol, and will not be involved during the methodological execution, data analyses and interpretation and decision to submit or to publish the study results.
Map disclaimer The depiction of boundaries on the map(s) in this article does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. The map(s) are provided without any warranty of any kind, either express or implied.
Competing interests None declared.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication Not required.
Provenance and peer review Not commissioned; externally peer reviewed.
Read the full text or download the PDF:
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Study Protocol
Assessing the effect of the COVID-19 pandemic, shift to online learning, and social media use on the mental health of college students in the Philippines: A mixed-method study protocol
Roles Funding acquisition, Writing – original draft
Affiliation College of Medicine, University of the Philippines, Manila, Philippines
Roles Methodology, Supervision, Visualization, Writing – original draft, Writing – review & editing
Affiliations Department of Clinical Epidemiology, College of Medicine, University of the Philippines, Manila, Philippines, Institute of Clinical Epidemiology, National Institutes of Health, University of the Philippines, Manila, Philippines
Roles Methodology
Affiliation Department of Psychiatry, College of Medicine, University of the Philippines, Manila, Philippines
Roles Conceptualization, Funding acquisition, Project administration, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
- Leonard Thomas S. Lim,
- Zypher Jude G. Regencia,
- J. Rem C. Dela Cruz,
- Frances Dominique V. Ho,
- Marcela S. Rodolfo,
- Josefina Ly-Uson,
- Emmanuel S. Baja

- Published: May 3, 2022
- https://doi.org/10.1371/journal.pone.0267555
- Peer Review
- Reader Comments
Introduction
The COVID-19 pandemic declared by the WHO has affected many countries rendering everyday lives halted. In the Philippines, the lockdown quarantine protocols have shifted the traditional college classes to online. The abrupt transition to online classes may bring psychological effects to college students due to continuous isolation and lack of interaction with fellow students and teachers. Our study aims to assess Filipino college students’ mental health status and to estimate the effect of the COVID-19 pandemic, the shift to online learning, and social media use on mental health. In addition, facilitators or stressors that modified the mental health status of the college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning will be investigated.
Methods and analysis
Mixed-method study design will be used, which will involve: (1) an online survey to 2,100 college students across the Philippines; and (2) randomly selected 20–40 key informant interviews (KIIs). Online self-administered questionnaire (SAQ) including Depression, Anxiety, and Stress Scale (DASS-21) and Brief-COPE will be used. Moreover, socio-demographic factors, social media usage, shift to online learning factors, family history of mental health and COVID-19, and other factors that could affect mental health will also be included in the SAQ. KIIs will explore factors affecting the student’s mental health, behaviors, coping mechanism, current stressors, and other emotional reactions to these stressors. Associations between mental health outcomes and possible risk factors will be estimated using generalized linear models, while a thematic approach will be made for the findings from the KIIs. Results of the study will then be triangulated and summarized.
Ethics and dissemination
Our study has been approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2021-099-01). The results will be actively disseminated through conference presentations, peer-reviewed journals, social media, print and broadcast media, and various stakeholder activities.
Citation: Lim LTS, Regencia ZJG, Dela Cruz JRC, Ho FDV, Rodolfo MS, Ly-Uson J, et al. (2022) Assessing the effect of the COVID-19 pandemic, shift to online learning, and social media use on the mental health of college students in the Philippines: A mixed-method study protocol. PLoS ONE 17(5): e0267555. https://doi.org/10.1371/journal.pone.0267555
Editor: Elisa Panada, UNITED KINGDOM
Received: June 9, 2021; Accepted: April 11, 2022; Published: May 3, 2022
Copyright: © 2022 Lim et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This project is being supported by the American Red Cross through the Philippine Red Cross and Red Cross Youth. The funder will not have a role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: The authors have declared that no competing interests exist.
The World Health Organization (WHO) declared the Coronavirus 2019 (COVID-19) outbreak as a global pandemic, and the Philippines is one of the 213 countries affected by the disease [ 1 ]. To reduce the virus’s transmission, the President imposed an enhanced community quarantine in Luzon, the country’s northern and most populous island, on March 16, 2020. This lockdown manifested as curfews, checkpoints, travel restrictions, and suspension of business and school activities [ 2 ]. However, as the virus is yet to be curbed, varying quarantine restrictions are implemented across the country. In addition, schools have shifted to online learning, despite financial and psychological concerns [ 3 ].
Previous outbreaks such as the swine flu crisis adversely influenced the well-being of affected populations, causing them to develop emotional problems and raising the importance of integrating mental health into medical preparedness for similar disasters [ 4 ]. In one study conducted on university students during the swine flu pandemic in 2009, 45% were worried about personally or a family member contracting swine flu, while 10.7% were panicking, feeling depressed, or emotionally disturbed. This study suggests that preventive measures to alleviate distress through health education and promotion are warranted [ 5 ].
During the COVID-19 pandemic, researchers worldwide have been churning out studies on its psychological effects on different populations [ 6 – 9 ]. The indirect effects of COVID-19, such as quarantine measures, the infection of family and friends, and the death of loved ones, could worsen the overall mental wellbeing of individuals [ 6 ]. Studies from 2020 to 2021 link the pandemic to emotional disturbances among those in quarantine, even going as far as giving vulnerable populations the inclination to commit suicide [ 7 , 8 ], persistent effect on mood and wellness [ 9 ], and depression and anxiety [ 10 ].
In the Philippines, a survey of 1,879 respondents measuring the psychological effects of COVID-19 during its early phase in 2020 was released. Results showed that one-fourth of respondents reported moderate-to-severe anxiety, while one-sixth reported moderate-to-severe depression [ 11 ]. In addition, other local studies in 2020 examined the mental health of frontline workers such as nurses and physicians—placing emphasis on the importance of psychological support in minimizing anxiety [ 12 , 13 ].
Since the first wave of the pandemic in 2020, risk factors that could affect specific populations’ psychological well-being have been studied [ 14 , 15 ]. A cohort study on 1,773 COVID-19 hospitalized patients in 2021 found that survivors were mainly troubled with fatigue, muscle weakness, sleep difficulties, and depression or anxiety [ 16 ]. Their results usually associate the crisis with fear, anxiety, depression, reduced sleep quality, and distress among the general population.
Moreover, the pandemic also exacerbated the condition of people with pre-existing psychiatric disorders, especially patients that live in high COVID-19 prevalence areas [ 17 ]. People suffering from mood and substance use disorders that have been infected with COVID-19 showed higher suicide risks [ 7 , 18 ]. Furthermore, a study in 2020 cited the following factors contributing to increased suicide risk: social isolation, fear of contagion, anxiety, uncertainty, chronic stress, and economic difficulties [ 19 ].
Globally, multiple studies have shown that mental health disorders among university student populations are prevalent [ 13 , 20 – 22 ]. In a 2007 survey of 2,843 undergraduate and graduate students at a large midwestern public university in the United States, the estimated prevalence of any depressive or anxiety disorder was 15.6% and 13.0% for undergraduate and graduate students, respectively [ 20 ]. Meanwhile, in a 2013 study of 506 students from 4 public universities in Malaysia, 27.5% and 9.7% had moderate and severe or extremely severe depression, respectively; 34% and 29% had moderate and severe or extremely severe anxiety, respectively [ 21 ]. In China, a 2016 meta-analysis aiming to establish the national prevalence of depression among university students analyzed 39 studies from 1995 to 2015; the meta-analysis found that the overall prevalence of depression was 23.8% across all studies that included 32,694 Chinese university students [ 23 ].
A college student’s mental status may be significantly affected by the successful fulfillment of a student’s role. A 2013 study found that acceptable teaching methods can enhance students’ satisfaction and academic performance, both linked to their mental health [ 24 ]. However, online learning poses multiple challenges to these methods [ 3 ]. Furthermore, a 2020 study found that students’ mental status is affected by their social support systems, which, in turn, may be jeopardized by the COVID-19 pandemic and the physical limitations it has imposed. Support accessible to a student through social ties to other individuals, groups, and the greater community is a form of social support; university students may draw social support from family, friends, classmates, teachers, and a significant other [ 25 , 26 ]. Among individuals undergoing social isolation and distancing during the COVID-19 pandemic in 2020, social support has been found to be inversely related to depression, anxiety, irritability, sleep quality, and loneliness, with higher levels of social support reducing the risk of depression and improving sleep quality [ 27 ]. Lastly, it has been shown in a 2020 study that social support builds resilience, a protective factor against depression, anxiety, and stress [ 28 ]. Therefore, given the protective effects of social support on psychological health, a supportive environment should be maintained in the classroom. Online learning must be perceived as an inclusive community and a safe space for peer-to-peer interactions [ 29 ]. This is echoed in another study in 2019 on depressed students who narrated their need to see themselves reflected on others [ 30 ]. Whether or not online learning currently implemented has successfully transitioned remains to be seen.
The effect of social media on students’ mental health has been a topic of interest even before the pandemic [ 31 , 32 ]. A systematic review published in 2020 found that social media use is responsible for aggravating mental health problems and that prominent risk factors for depression and anxiety include time spent, activity, and addiction to social media [ 31 ]. Another systematic review published in 2016 argues that the nature of online social networking use may be more important in influencing the symptoms of depression than the duration or frequency of the engagement—suggesting that social rumination and comparison are likely to be candidate mediators in the relationship between depression and social media [ 33 ]. However, their findings also suggest that the relationship between depression and online social networking is complex and necessitates further research to determine the impact of moderators and mediators that underly the positive and negative impact of online social networking on wellbeing [ 33 ].
Despite existing studies already painting a picture of the psychological effects of COVID-19 in the Philippines, to our knowledge, there are still no local studies contextualized to college students living in different regions of the country. Therefore, it is crucial to elicit the reasons and risk factors for depression, stress, and anxiety and determine the potential impact that online learning and social media use may have on the mental health of the said population. In turn, the findings would allow the creation of more context-specific and regionalized interventions that can promote mental wellness during the COVID-19 pandemic.

Materials and methods
The study’s general objective is to assess the mental health status of college students and determine the different factors that influenced them during the COVID-19 pandemic. Specifically, it aims:
- To describe the study population’s characteristics, categorized by their mental health status, which includes depression, anxiety, and stress.
- To determine the prevalence and risk factors of depression, anxiety, and stress among college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning.
- To estimate the effect of social media use on depression, anxiety, stress, and coping strategies towards stress among college students and examine whether participant characteristics modified these associations.
- To estimate the effect of online learning shift on depression, anxiety, stress, and coping strategies towards stress among college students and examine whether participant characteristics modified these associations.
- To determine the facilitators or stressors among college students that modified their mental health status during the COVID-19 pandemic, quarantine, and subsequent shift to online learning.
Study design
A mixed-method study design will be used to address the study’s objectives, which will include Key Informant Interviews (KIIs) and an online survey. During the quarantine period of the COVID-19 pandemic in the Philippines from April to November 2021, the study shall occur with the population amid community quarantine and an abrupt transition to online classes. Since this is the Philippines’ first study that will look at the prevalence of depression, anxiety, and stress among college students during the COVID-19 pandemic, quarantine, and subsequent shift to online learning, the online survey will be utilized for the quantitative part of the study design. For the qualitative component of the study design, KIIs will determine facilitators or stressors among college students that modified their mental health status during the quarantine period.
Study population
The Red Cross Youth (RCY), one of the Philippine Red Cross’s significant services, is a network of youth volunteers that spans the entire country, having active members in Luzon, Visayas, and Mindanao. The group is clustered into different age ranges, with the College Red Cross Youth (18–25 years old) being the study’s population of interest. The RCY has over 26,060 students spread across 20 chapters located all over the country’s three major island groups. The RCY is heterogeneously composed, with some members classified as college students and some as out-of-school youth. Given their nationwide scope, disseminating information from the national to the local level is already in place; this is done primarily through email, social media platforms, and text blasts. The research team will leverage these platforms to distribute the online survey questionnaire.
In addition, the online survey will also be open to non-members of the RCY. It will be disseminated through social media and engagements with different university administrators in the country. Stratified random sampling will be done for the KIIs. The KII participants will be equally coming from the country’s four (4) primary areas: 5–10 each from the national capital region (NCR), Luzon, Visayas, and Mindanao, including members and non-members of the RCY.
Inclusion and exclusion criteria
The inclusion criteria for the online survey will include those who are 18–25 years old, currently enrolled in a university, can provide consent for the study, and are proficient in English or Filipino. The exclusion criteria will consist of those enrolled in graduate-level programs (e.g., MD, JD, Master’s, Doctorate), out-of-school youth, and those whose current curricula involve going on duty (e.g., MDs, nursing students, allied medical professions, etc.). The inclusion criteria for the KIIs will include online survey participants who are 18–25 years old, can provide consent for the study, are proficient in English or Filipino, and have access to the internet.
Sample size
A continuity correction method developed by Fleiss et al. (2013) was used to calculate the sample size needed [ 34 ]. For a two-sided confidence level of 95%, with 80% power and the least extreme odds ratio to be detected at 1.4, the computed sample size was 1890. With an adjustment for an estimated response rate of 90%, the total sample size needed for the study was 2,100. To achieve saturation for the qualitative part of the study, 20 to 40 participants will be randomly sampled for the KIIs using the respondents who participated in the online survey [ 35 ].
Study procedure
Self-administered questionnaire..
The study will involve creating, testing, and distributing a self-administered questionnaire (SAQ). All eligible study participants will answer the SAQ on socio-demographic factors such as age, sex, gender, sexual orientation, residence, household income, socioeconomic status, smoking status, family history of mental health, and COVID-19 sickness of immediate family members or friends. The two validated survey tools, Depression, Anxiety, and Stress Scale (DASS-21) and Brief-COPE, will be used for the mental health outcome assessment [ 36 – 39 ]. The DASS-21 will measure the negative emotional states of depression, anxiety, and stress [ 40 ], while the Brief-COPE will measure the students’ coping strategies [ 41 ].
For the exposure assessment of the students to social media and shift to online learning, the total time spent on social media (TSSM) per day will be ascertained by querying the participants to provide an estimated time spent daily on social media during and after their online classes. In addition, students will be asked to report their use of the eight commonly used social media sites identified at the start of the study. These sites include Facebook, Twitter, Instagram, LinkedIn, Pinterest, TikTok, YouTube, and social messaging sites Viber/WhatsApp and Facebook Messenger with response choices coded as "(1) never," "(2) less often," "(3) every few weeks," "(4) a few times a week," and “(5) daily” [ 42 – 44 ]. Furthermore, a global frequency score will be calculated by adding the response scores from the eight social media sites. The global frequency score will be used as an additional exposure marker of students to social media [ 45 ]. The shift to online learning will be assessed using questions that will determine the participants’ satisfaction with online learning. This assessment is comprised of 8 items in which participants will be asked to respond on a 5-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree.’
The online survey will be virtually distributed in English using the Qualtrics XM™ platform. Informed consent detailing the purpose, risks, benefits, methods, psychological referrals, and other ethical considerations will be included before the participants are allowed to answer the survey. Before administering the online survey, the SAQ shall undergo pilot testing among twenty (20) college students not involved with the study. It aims to measure total test-taking time, respondent satisfaction, and understandability of questions. The survey shall be edited according to the pilot test participant’s responses. Moreover, according to the Philippines’ Data Privacy Act, all the answers will be accessible and used only for research purposes.
Key informant interviews.
The research team shall develop the KII concept note, focusing on the extraneous factors affecting the student’s mental health, behaviors, and coping mechanism. Some salient topics will include current stressors (e.g., personal, academic, social), emotional reactions to these stressors, and how they wish to receive support in response to these stressors. The KII will be facilitated by a certified psychologist/psychiatrist/social scientist and research assistants using various online video conferencing software such as Google Meet, Skype, or Zoom. All the KIIs will be recorded and transcribed for analysis. Furthermore, there will be a debriefing session post-KII to address the psychological needs of the participants. Fig 1 presents the diagrammatic flowchart of the study.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0267555.g001
Data analyses
Quantitative data..
Descriptive statistics will be calculated, including the prevalence of mental health outcomes such as depression, anxiety, stress, and coping strategies. In addition, correlation coefficients will be estimated to assess the relations among the different mental health outcomes, covariates, and possible risk factors.
Several study characteristics as effect modifiers will also be assessed, including sex, gender, sexual orientation, family income, smoking status, family history of mental health, and Covid-19. We will include interaction terms between the dichotomized modifier variable and markers of social media use (total TSSM and global frequency score) and shift to online learning in the models. The significance of the interaction terms will be evaluated using the likelihood ratio test. All the regression analyses will be done in R ( http://www.r-project.org ). P values ≤ 0.05 will be considered statistically significant.
Qualitative data.
After transcribing the interviews, the data transcripts will be analyzed using NVivo 1.4.1 software [ 50 ] by three research team members independently using the inductive logic approach in thematic analysis: familiarizing with the data, generating initial codes, searching for themes, reviewing the themes, defining and naming the themes, and producing the report [ 51 ]. Data familiarization will consist of reading and re-reading the data while noting initial ideas. Additionally, coding interesting features of the data will follow systematically across the entire dataset while collating data relevant to each code. Moreover, the open coding of the data will be performed to describe the data into concepts and themes, which will be further categorized to identify distinct concepts and themes [ 52 ].
The three researchers will discuss the results of their thematic analyses. They will compare and contrast the three analyses in order to come up with a thematic map. The final thematic map of the analysis will be generated after checking if the identified themes work in relation to the extracts and the entire dataset. In addition, the selection of clear, persuasive extract examples that will connect the analysis to the research question and literature will be reviewed before producing a scholarly report of the analysis. Additionally, the themes and sub-themes generated will be assessed and discussed in relevance to the study’s objectives. Furthermore, the gathering and analyzing of the data will continue until saturation is reached. Finally, pseudonyms will be used to present quotes from qualitative data.
Data triangulation.
Data triangulation using the two different data sources will be conducted to examine the various aspects of the research and will be compared for convergence. This part of the analysis will require listing all the relevant topics or findings from each component of the study and considering where each method’s results converge, offer complementary information on the same issue, or appear to contradict each other. It is crucial to explicitly look for disagreements between findings from different data collection methods because exploration of any apparent inter-method discrepancy may lead to a better understanding of the research question [ 53 , 54 ].
Data management plan.
The Project Leader will be responsible for overall quality assurance, with research associates and assistants undertaking specific activities to ensure quality control. Quality will be assured through routine monitoring by the Project Leader and periodic cross-checks against the protocols by the research assistants. Transcribed KIIs and the online survey questionnaire will be used for recording data for each participant in the study. The project leader will be responsible for ensuring the accuracy, completeness, legibility, and timeliness of the data captured in all the forms. Data captured from the online survey or KIIs should be consistent, clarified, and corrected. Each participant will have complete source documentation of records. Study staff will prepare appropriate source documents and make them available to the Project Leader upon request for review. In addition, study staff will extract all data collected in the KII notes or survey forms. These data will be secured and kept in a place accessible to the Project Leader. Data entry and cleaning will be conducted, and final data cleaning, data freezing, and data analysis will be performed. Key informant interviews will always involve two researchers. Where appropriate, quality control for the qualitative data collection will be assured through refresher KII training during research design workshops. The Project Leader will check through each transcript for consistency with agreed standards. Where translations are undertaken, the quality will be assured by one other researcher fluent in that language checking against the original recording or notes.
Ethics approval.
The study shall abide by the Principles of the Declaration of Helsinki (2013). It will be conducted along with the Guidelines of the International Conference on Harmonization-Good Clinical Practice (ICH-GCP), E6 (R2), and other ICH-GCP 6 (as amended); National Ethical Guidelines for Health and Health-Related Research (NEGHHRR) of 2017. This protocol has been approved by the University of the Philippines Manila Research Ethics Board (UPMREB 2021-099-01 dated March 25, 2021).
The main concerns for ethics were consent, data privacy, and subject confidentiality. The risks, benefits, and conflicts of interest are discussed in this section from an ethical standpoint.
Recruitment.
The participants will be recruited to answer the online SAQ voluntarily. The recruitment of participants for the KIIs will be chosen through stratified random sampling using a list of those who answered the online SAQ; this will minimize the risk of sampling bias. In addition, none of the participants in the study will have prior contact or association with the researchers. Moreover, power dynamics will not be contacted to recruit respondents. The research objectives, methods, risks, benefits, voluntary participation, withdrawal, and respondents’ rights will be discussed with the respondents in the consent form before KII.
Informed consent will be signified by the potential respondent ticking a box in the online informed consent form and the voluntary participation of the potential respondent to the study after a thorough discussion of the research details. The participant’s consent is voluntary and may be recanted by the participant any time s/he chooses.
Data privacy.
All digital data will be stored in a cloud drive accessible only to the researchers. Subject confidentiality will be upheld through the assignment of control numbers and not requiring participants to divulge the name, address, and other identifying factors not necessary for analysis.
Compensation.
No monetary compensation will be given to the participants, but several tokens will be raffled to all the participants who answered the online survey and did the KIIs.
This research will pose risks to data privacy, as discussed and addressed above. In addition, there will be a risk of social exclusion should data leaks arise due to the stigma against mental health. This risk will be mitigated by properly executing the data collection and analysis plan, excluding personal details and tight data privacy measures. Moreover, there is a risk of psychological distress among the participants due to the sensitive information. This risk will be addressed by subjecting the SAQ and the KII guidelines to the project team’s psychiatrist’s approval, ensuring proper communication with the participants. The KII will also be facilitated by registered clinical psychologists/psychiatrists/social scientists to ensure the participants’ appropriate handling; there will be a briefing and debriefing of the participants before and after the KII proper.
Participation in this study will entail health education and a voluntary referral to a study-affiliated psychiatrist, discussed in previous sections. Moreover, this would contribute to modifications in targeted mental-health campaigns for the 18–25 age group. Summarized findings and recommendations will be channeled to stakeholders for their perusal.
Dissemination.
The results will be actively disseminated through conference presentations, peer-reviewed journals, social media, print and broadcast media, and various stakeholder activities.
This study protocol rationalizes the examination of the mental health of the college students in the Philippines during the COVID-19 pandemic as the traditional face-to-face classes transitioned to online and modular classes. The pandemic that started in March 2020 is now stretching for more than a year in which prolonged lockdown brings people to experience social isolation and disruption of everyday lifestyle. There is an urgent need to study the psychosocial aspects, particularly those populations that are vulnerable to mental health instability. In the Philippines, where community quarantine is still being imposed across the country, college students face several challenges amidst this pandemic. The pandemic continues to escalate, which may lead to fear and a spectrum of psychological consequences. Universities and colleges play an essential role in supporting college students in their academic, safety, and social needs. The courses of activities implemented by the different universities and colleges may significantly affect their mental well-being status. Our study is particularly interested in the effect of online classes on college students nationwide during the pandemic. The study will estimate this effect on their mental wellbeing since this abrupt transition can lead to depression, stress, or anxiety for some students due to insufficient time to adjust to the new learning environment. The role of social media is also an important exposure to some college students [ 55 , 56 ]. Social media exposure to COVID-19 may be considered a contributing factor to college students’ mental well-being, particularly their stress, depression, and anxiety [ 57 , 58 ]. Despite these known facts, little is known about the effect of transitioning to online learning and social media exposure on the mental health of college students during the COVID-19 pandemic in the Philippines. To our knowledge, this is the first study in the Philippines that will use a mixed-method study design to examine the mental health of college students in the entire country. The online survey is a powerful platform to employ our methods.
Additionally, our study will also utilize a qualitative assessment of the college students, which may give significant insights or findings of the experiences of the college students during these trying times that cannot be captured on our online survey. The thematic findings or narratives from the qualitative part of our study will be triangulated with the quantitative analysis for a more robust synthesis. The results will be used to draw conclusions about the mental health status among college students during the pandemic in the country, which will eventually be used to implement key interventions if deemed necessary. A cross-sectional study design for the online survey is one of our study’s limitations in which contrasts will be mainly between participants at a given point of time. In addition, bias arising from residual or unmeasured confounding factors cannot be ruled out.
The COVID-19 pandemic and its accompanying effects will persistently affect the mental wellbeing of college students. Mental health services must be delivered to combat mental instability. In addition, universities and colleges should create an environment that will foster mental health awareness among Filipino college students. The results of our study will tailor the possible coping strategies to meet the specific needs of college students nationwide, thereby promoting psychological resilience.
OCTA as an independent science advice provider for COVID-19 in the Philippines
- Benjamin M. Vallejo Jr 1 &
- Rodrigo Angelo C. Ong 1
Humanities and Social Sciences Communications volume 9 , Article number: 104 ( 2022 ) Cite this article
6161 Accesses
4 Citations
7 Altmetric
Metrics details
- Health humanities
- Science, technology and society
- Social science
We comment on science advice in the political context of the Philippines during the COVID 19 pandemic. We focus on the independent science advisor OCTA Research, whose publicly available epidemiological forecasts have attracted media and government attention. The Philippines government adopted a COVID-19 suppression or “flattening of the curve” policy. As such, it required epidemiological forecasts from science advisors as more scientific information on SARS CoV 2 and COVID 19 became available from April to December 2020. The independent think-tank, OCTA Research has emerged the leading independent science information advisor for the public and government. The factors that made OCTA Research as the dominant science advice source are examined, the diversity of scientific evidence, processes of evidence synthesis and, of evidence brokerage for political decision makers We then describe the dynamics between the government, academic science research and science advisory actors and the problem of science advice role conflation. We then propose approaches for a largely independent government science advisory system for the Philippines given these political dynamics.
Similar content being viewed by others

The Dutch see Red: (in)formal science advisory bodies during the COVID-19 pandemic

An evaluation of North Carolina science advice on COVID-19 pandemic response
Mobilization of science advice by the Canadian federal government to support the COVID-19 pandemic response
Introduction.
Pandemic science before COVID 19 presumed “predictable challenges” (Lipsitch et al., 2009 ) that informs government response especially in planning for containment interventions such as lockdowns. The success of government response is in the public perception of a positive outcome and this is reducing the number of infections. The COVID 19 pandemic is a crisis in which the orderly functioning of social and political institutions are placed into disorder and uncertainty (Boin et al., 2016 ). In political institutions this may be a threat to accepted political power arrangements and requires a response which because of their urgency, are occasions for political leaders to demonstrate leadership. However, to do so they will have to rely on actors who provide science, economic and social information and advice. In many cases these actors are within the government bureaucracy itself, as specialized agencies. Academic research institutions also provide advice. Civil society organizations with science and technology advocacies may provide advice. Science advice provided by civil society organizations, citizen science advocacy organizations and non-government think tanks are independent science advice providers. These organizations are a feature of the technical and science advice ecosystems of liberal democracies.
How governments use science advice and decide in a crisis strengthens political legitimacy. In the United Kingdom with its formal structures of government science advice such as the Science Advisory Group for Emergencies (SAGE) a key outcome is lowering SARS CoV 2 transmission (R) rate and the way this can be achieved is to institute a lockdown. SAGE was placed in a high degree of public, media and political scrutiny in its recommendations. While formal science advice structures may work well in countries with a large and well-established science community, in countries with small science communities, independent science advice actors may be more effective than formal science advice actors.
Previous studies on the use of science advice by governments have revealed a dichotomy. Knowledge producers (e.g., academic science community) perceive high uncertainty in scientific results and consequentially become guarded in their science advice or even dispense with it in recognition of their political costs. In contrast knowledge users (e.g. politicians and science advisors in government) perceive less uncertainty in science advice and require assurances in outcomes (MacKenzie, 1993 ). This present challenges for science advice practitioners since differentiating the roles of science knowledge generation and science knowledge users, both of which can be played by academic scientists, can be conflated, and may result in political risks and opportunities.
To remedy this conflation, science advice mechanisms emphasizing independent knowledge brokerage (Gluckman, 2016a ) define a particular role for scientists in listing down science informed options for politicians and policy makers. These roles have their theoretical basis from post-normal science approaches (Funtowicz and Ravetz, 1993 , 1994 ; Ravetz, 1999 ) which place a premium on managing uncertainty in crises through consensus building and identifying of science informed policy options. The science advice “knowledge broker” will not be functioning as part of the knowledge generation constituency but in a purely advisory capacity identifying policy options. This is the model promoted by the International Network for Government Science Advice (INGSA). This also insulates the science advisor from undue political interference.
However, in countries where the science community is small and politically underrepresented, performing these well-defined functions will be difficult due to a lack of experts and the range of scientific expertise they can provide. In small science communities, the problems of role conflation become more apparent and may place the science advisor prone to political pressure. Vallejo and Ong ( 2020 ) reviewed the Philippines government response and science advice for COVID 19 from when the World Health Organization (WHO) advised UN member states of a pandemic health emergency on January 6 to April 30, 2020 when the Philippines government began relaxing quarantine regulations. They noted the roles of various science advice knowledge generation actors such as individual scientists, academe, national science academies and organizations and how these were eventually considered by the Inter Agency Task Force on Emerging Infectious Diseases (IATF-EID) which is the government’s policy recommending body for COVID 19 suppression. Of these advisory actors, the private and independent OCTA Research Group hereafter referred to as OCTA, which consists of a multi-disciplinary team of academics from the medical, social, economic, environmental, and mathematical sciences mostly from the University of the Philippines, became the most prominent source of government science advice with its proactive but unsolicited provision of government science advice.
Because of this engagement, like SAGE in the UK, OCTA became a focus of intense media, public, and political interest and could represent an effective modality for independent science advice especially in newly industrialized countries where the science community is small but gaining a larger base of expertise. While science advice in this context may involve a conflation of science advice roles, we look into this conflation and their political dynamics in pandemic uncertainty and how consensus was formed in COVID 19 policy advice. This paper explores on how independent science advice has proved to be the chief source science advice in a polarized political environment in a Southeast Asian nation from the start of the pandemic in January 2020–October 2021.
The Philippine science advice ecosystem
Science advice in the Philippines takes on formal (with government mandate), informal (without government mandate) solicited and unsolicited modalities. Formal science advice to the President of the Philippines is provided by the National Academy of Science and Technology (NAST) by virtue of Presidential Executive Order Number 812. The government solicits science advice from the NAST which provides advice as position or white papers to cabinet for consideration. The NAST is not a wholly independent body from government. It is attached to the Department of Science and Technology (DOST) for administrative and fiscal purposes.
Other sources of science advice are from the universities such as the University of the Philippines (UP). The UP is designated by charter (Republic Act Number 8500) as the national, research and graduate university. This mandates it to provide science advice to the government. Academics in their individual capacities, as members of think-tanks or civil society organizations provide unsolicited and informal science advice to government through the publication of scientific and position papers as well as technical reports. Academics who are part of non-government science academies such as the Philippine American Academy of Science and Engineering (PAASE) provide similar advice. The science advice system in the Philippines is diverse with each actor having its own political and development advocacy. The system is largely ad hoc and informal, and science advice are largely unsolicited. This dynamic determines its role with the government. Also, when these science advice actors are consulted by the government, they are all primuses inter pares in dealing with political actors in government. Members of the science advisory bodies are mostly active academics. They are all knowledge producers and users at the same time.
There are few studies that directly examine the politics of science advice and uncertainty in the Philippines, and these are in disaster risk reduction management (DRRM). This can serve as a template for analysis for the COVID 19 pandemic in the Philippines which has been construed by government and the public as a global disaster. The strengths and weaknesses of the present science advisory system may be seen in DRRM advice.
DRRM as a framework for government science advice in the Philippines
Disasters which have affected the Philippines in the first decade of the 21st century such as Typhoon Ketsana (Philippine name “Ondoy”) in 2009 which flooded much of the National Capital Region, have resulted in several studies investigating the resilience of urban communities and how science advice is used in crafting urban resilience policies and governance. This disaster was also the major impetus for disaster legislation with enactment of the DRRM law (Republic Act Number 10121). This law institutionalizes and mainstream the development of capacities in disaster management at every level of governance, disaster risk reduction in physical and land-use planning, budget, infrastructure, education, health, environment, housing, and other sectors. The law also institutes the establishment of DRRM councils at each level of government. The councils are composed of members from government departments, the armed forces and police, civil society, humanitarian agencies but most notably, does not include academic research scientists. Science advice is given by CSOs but that is in accordance with their particular advocacies and their political objectives.
A study commissioned by the independent think tank Odi.org and by researchers of De La Salle University in Manila (Pellini et al., 2013 ) concluded that there is a “low uptake of research and analysis” to inform local decision in DRRM. It also identified a reactionary response to disasters rather than a response to disaster risks. Formal and informal science advice is most effective in local government if local executives prioritize risk reduction with consensus building at the local level. In general, formal, and informal science advice is less effective at the national level. The Philippine science advisory ecosystem is focused on formal science advice at the national level and thus the effectiveness of science advice is placed into question. The disaster-prone province of Albay is held as an example where science advice is more effective at a devolved level from the national (Bankoff and Hilhorst, 2009 ; Pellini et al., 2013 ).
At the lower levels of governance, informal science advice is predominant and is provided by science advice actors such as non-government organizations (NGO) or by civil society organizations (CSO). While NGOs, CSOs and, the government communicate using a consensus vocabulary (Funtowicz and Ravetz, 1994 ) in DRRM, differing risk perceptions have resulted in different domains of political engagement (Bankoff and Hilhorst, 2009 ) tied to different interpretations of the risk vocabulary in terms of political costs. And so the dominant paradigm remains disaster reactive with a general trend in “dampening uncertainties” (Pearce, 2020 ) in order to come up with positive political outcomes for the science advisors and the government.
While the present DRRM law institutionalizes consultation and collaboration, the law does not mandate a science or technical advisor to sit on DRRM councils at each level of governance. This is one possible reason for the “low uptake of research and analysis” at higher levels of governance while at lower levels of governance, science advice is provided by CSO and other advocacy organizations in an independent and ad hoc manner as they are more effective in establishing collaborative relationships with local government executives and councils.
IATF-EID and OCTA Research as an independent science advisor
Vallejo and Ong ( 2020 ) review the timeline for the Philippines government COVID 19 response, the formation of the Inter-agency Task Force on Emerging Infectious Diseases (IATF-EID), the science advisory ecosystem, and how the science community began to dispense informal science advice for consideration by IATF-EID. IATF-EID is the government’s policy recommending body for COVID 19 suppression and is composed of members from the cabinet and health agencies of the government. Informal science advice initially came from individual or groups of academics modeling the initial epidemiological trajectory of COVID 19. The IATF-EID is not a science evidence synthesizing or peer review body. It must rely on many science advisory actors as consultants. The University of the Philippines COVID 19 Pandemic Response Team is a major actor as its scientists are well known in the medical and disaster sciences. But it was OCTA which is composed mainly of academics from the University of the Philippines and the University of Santo Tomas. OCTA that has emerged as the leading government science advice actor for COVID 19.
OCTA bills itself as a “polling, research and consultancy firm”(Fig. 1 ). That OCTA has been identified in media reports as the “University of the Philippines OCTA Research group” is to be expected as academic credibility is a premium in the Philippines as like in other countries (Doubleday and Wilsdon, 2012 ). This however can constrain its political relationship with government science advice actors and so OCTA had to publish disclaimers that while it is composed of mostly University of the Philippines academics, it claims to be an independent entity. OCTA’s polling function is separate from its science advice advocacy which is performed by volunteer scientists as testified by OCTA President Ranjit S Rye to the Philippine Congress Committee on Public Accountability on 3 October 2021. The polling function is supported by paid subscribers while the science advice advocacy is supported by unpaid volunteers. Volunteer OCTA epidemiological modelers and policy analysts have provided robust estimates on the COVID 19 reproductive number R0, positivity rates, hospital capacity and attack rates at the national, provincial, and local government levels every fortnight beginning April 27, 2020. It has since issued 76 advisories and updates (Fig. 2 ). Local and provincial governments have used their forecasts in deciding quarantine and lockdown policies in their jurisdictions. OCTA publicly released these forecasts in academic websites, institutional media and social media. This allowed for public vetting and extended peer review with other independent scientists validating its forecast estimates. Some independent scientists contest methodologies and OCTA has appropriately responded to these.
OCTA is a primarily polling organization but has taken on COVID-19 monitoring, forecasting and advice services.
An OCTA COVID-19 forecast update (7 March 2021).
OCTA like other science advice actors, based its epidemiological analyses on the Philippines Department of Health (DOH) Data Drop whose data quality was publicly perceived as poor even though steps have been taken to improve data quality. The DOH in the interest of transparency began Data Drop on April 15, 2020. Data Drop has information on the number of active cases, recovered cases, and hospital admissions. With Data Drop, OCTA was able to issue its first epidemiological forecast.
OCTA does not belong to the formal structures of science advice in the Philippines but is part of the informal science advice community. Its volunteer experts are publicly known. OCTA has emerged as the leading information and science advice provider for the public. How did it become the leading source of science advice and often cited by social and mainstream media and acknowledged by government?
Uncertainty perception in COVID-19 suppression and the political context of role conflation
OCTA became the leading source of science advice when by publishing weekly forecasts on COVID-19 epidemiological trends, it reduced public perception of uncertainty of the pandemic. The bulletins estimated national and regional R0, attack rates, hospital capacity and ICU bed capacity. While most countries worldwide have adopted suppression as the main strategy (Allen et al., 2020 ) a few countries most notably New Zealand, adopting a COVID 19 elimination strategy. The Philippines decided on a suppression policy or a strategy of “flattening the curve” which necessitated lockdowns with the outcome of reducing R0 and COVID-19 hospital admissions.
The most socially and economically disruptive intervention is lockdown with is tied with the uncertainty of lifting quarantine (Caulkins et al., 2020 ). The Philippines instituted a national lockdown beginning 14 March 2020 and instituted a graded system of “community quarantine” which allowed for almost cessation of economic activity and mobility in enhanced community quarantine (ECQ), a modified enhanced community quarantine (MECQ) which allows for the opening of critical services and a limited operation of public transport, to a near open economy and unimpeded local mobility in modified general community quarantine (MGCQ) and a low risk general community quarantine (GCQ) which allows for most economic activities subject to health protocols (Vallejo and Ong, 2020 ) which regulated mobility between quarantine zones.
It is in lockdown policies that uncertainty perception takes on a large political dimension (Gluckman, 2016b ; Pearce, 2020 ). Science advisors have to provide forecasts on the trajectory of R0 for politicians to make a decision on tightening or relaxing of quarantine. In this manner OCTA has provided not only the quarantine grade option but the best option while recognizing that the constraint to lessening the perception of uncertainty lies on data quality itself (Johns, 2020 ). OCTA has raised this concern questions on the accuracy and timeliness of DOH’s Data Drop. In doing so, it has done multiple scenario models to assess the accuracy of data. If the government takes on lockdown as the main strategy for COVID 19 suppression, then it must ensure that science advisory actors are able to deal with the multiple uncertainties that data quality will generate. Science advisory actors can be both knowledge generators and users and this conflation has several consequences such as a tension between knowledge production and use which is called as the “uncertainty monster” (Van der Sluijs, 2005 ).
OCTA it its business model has role conflation. While its polling services are paid for by subscribers, the science advice advocacy function in COVID-19 is volunteer based. This conflation was questioned by members of Congress. Thus, the political context for OCTA is within the problem of role conflation in science in a particular political and academic context which may be the norm in developing countries. The politics of conflation in science advice in the UK was demonstrated when two esteemed epidemiologists belonging to two research groups, Professor Neil Ferguson of the Imperial College London (ICL) and Professor John Edmunds of the London School of Hygiene and Tropical Medicine (LSHTM) released R0 estimates to the public. ICL and LSHTM provided advisories to media and the UK government SAGE, with two different estimates for R0. The ICL estimate (2.0–2.6) were earlier made known to media while the LSHTM estimate (2.7–3.99) underwent peer review and was published in Lancet Public Health (Davies et al., 2020 ). The two estimates became the focus of controversy as the UK Chief Science Advisor Professor Patrick Vallance echoed Edmund’s claim of a case doubling time of 5–6 days. The SAGE consensus was 3–4 days, thus necessitating a sooner rather than later lockdown. The question on when to impose a lockdown is also a political matter. This placed SAGE and its established protocols of keeping experts anonymous under public criticism and scrutiny.
Pearce ( 2020 ) reviews the problem of role conflation of knowledge providers (the modelers) and the knowledge users (government) if they occupy both positions at the same time. Edmunds is a SAGE member (knowledge user) as well as a producer of science information as an academic. This conflation of roles resulted in the “dampening of uncertainties” for political reasons. The government is not acutely aware that this ultimately stems from poor data quality and the resulting scientific uncertainty has great political costs (UP COVID-19 Pandemic Response Team, 2020 ).
Similarly, OCTA has faced questions in its R0 estimates which differs from estimates by other scientists. OCTA’s estimates are higher (2.3) than what government initially used (2.1) in characterizing the surge in cases beginning Feb 2021. With R0 and positivity rates increasing, OCTA recommended an ECQ for the 2021 Easter break which was extended to a MECQ until 30 April 2021 (CNN Philippines, 2021 ). Like in the UK, this will affect policy decision making based on doubling time and the allocation of health resources. But unlike in the UK where there is a formal process of science peer review, in the ad hoc nature of science advice review in the Philippines, much of this “open peer review” by academics was on social media thus giving a polarizing political environment in policy decision.
OCTA has long been aware of the problem of role conflation which is a problem in a country with a small national science community. The national science community is small with only 189 scientists per million people. It thus has sought the expertise of overseas Filipino scientists to expand its advisory bench and to reduce possible role conflation. The overseas scientists are not associated with government health research agencies and so could act more independently. This was a strategy to deal with the possibility of “dampening of evidence”. The Presidential Spokesperson Mr. Harry Roque said that OCTA should cease reporting results to the public and rather send these “privately” to government (Manila Bulletin, 2020 ; Philippine Star, 2020 ). Roque is misconstruing the role of OCTA as a formal government science advisory body when it is not. The statements of the government spokesman may reflect debates in cabinet about the necessity and role of government science advice in and outside of government and their political costs. IATF-EID has its own experts as internal government science advisors. However, their advice must still be subject to peer review and so a mechanism must be found for these experts to compare forecasts with independent advisors such as OCTA. This will minimize public perception that the government silencing OCTA to dampen uncertainties for political outcomes. Public trust in government science advice has always been low if there is no transparency (Dommett and Pearce, 2019 ).
OCTA forecasts have been criticized by government economic planners especially in tourism (Philippine Daily Inquirer, 2020 ) as the forecasts directly affect plans to reopen important economic sectors. Some criticism is apparently political (Manila Times, 2020 ) and implies alienation of OCTA from its academic institutional linkage base. OCTA forecasts have been more and more adopted by the IATF-EID (ABS-CBN, 2021 ) This is a political dynamic for science advice actors sitting in government. Internal science advice actors will have to deal with populist interests in government and their advice may be “written off” (Boin et al., 2016 ). Independent science advice actors do not want their government science advice to be written off and so are likely to take the public route in presenting their synthesis of evidence and options.
Pandemic policy response is all about the management of multiple epidemiological uncertainties. This is when inability of government to manage it became apparent when doctors through the Healthcare Professionals Alliance Against COVID-19 (HPAAC), an organization which is comprised of the component and affiliate societies of the Philippine Medical Association admonished the government to increase quarantine restrictions from General Community Quarantine to Modified Enhanced Community Quarantine for a period of 2 weeks in August to allow the health workers to recover from exhaustion (One News, 2020 ). This is due to the surge in new cases and the overburdening of the healthcare capacity which OCTA earlier forecasted (David et al., 2020 ). The threat of a “doctors strike” would have been politically damaging to the government and the President decided to heed the doctors’ request.
The Philippines response is not very different from response of the majority of 22 countries examined by INGSA’s COVID 19 policy tracker (Allen et al., 2020 ), where these countries embarked on a monitoring and surveillance policy from January to March 2020. The INGSA study also shows that few countries have utilized internal and external formal science advisory bodies in the first 3 months of the pandemic. The Philippines is not one of the countries which INGSA tracked but similarly it started to seek the advice of individual experts by March 2020. Many of these experts posted their unsolicited science advice on social media.
Like most of the 22 INGSA tracked countries, after the 3rd month of the pandemic, the Philippines enacted legislation to deal with the social and economic impact of lockdowns. But this has not yet resulted in legislation passed in the Philippines Congress to deal with developing and improving systems for pandemic response through research and development initiatives although the late Senator Miriam Defensor Santiago filed Senate Bill 1573 “Pandemic and All Hazards Act” in September 2013 (Senate of the Philippines 16th Congress, 2013 ) in response to MERS and Senator Manny Villar in April 2008 filed Senate Bill 2198 “The Pandemic Preparedness Act” (Senate of the Philippines 14th Congress, 2008 ). Both bills institute a Pandemic Emergency Fund and mandates a Pandemic Emergency Council or Task Force, roughly along the lines of the DRRM Law. Defensor-Santiago’s bill was refiled by Senator Grace Poe as Senate Bill 1450 “An Act Strengthening National Preparedness and Response to Public Health Emergencies by Creating a Center for Disease Control” during the first session of the 18th Congress on 27 April 2020 (Senate of the Philippines 18th Congress, 2020 ). Poe’s bill updates Defensor-Santiago’s bill by proposing the creation of Center for Disease Control
These bills have not been enacted into law. The Philippines also did not enact legislation or executive on creating or strengthening science advisory capacity which 12 of the 22 countries INGSA tracked did. However, a senator has recently approached OCTA for policy input in developing formal crisis science advice legislation.
Prospects for independent government science advice in the Philippines
The Philippines government’s COVID 19 suppression policy is based on science informed advice. However, this has been provided informally by individual experts consulted by IATF-EID and this advice is not subjected to formal peer review. This has exposed experts to political criticism and attack as their identities and roles have been spun by media and government media spokespersons as integral to IATF-EID. At least one expert has resigned from providing science advice due to possible conflicts of interests. In this science advice gap, entered OCTA Research in the second quarter of 2020 and continued to 2021 and 2022.
The informal science advice actors more often give their forecasts directly to the media while the formal actors give it to the government agency that commissioned it. The government uses the evidence in determining what quarantine status to implement nationally and regionally through the recommendation of the IATF-EID.
The government’s policy decisions on COVID 19 suppression are chiefly based on a single statistical estimate, R0 but more recently has included positivity rate and hospital capacity. Science advisory bodies must defend R0 and the other estimates to the government and in the public sphere. The estimates will have incorporated all statistical uncertainties in this number. OCTA has done this by publicly reporting low, moderate and high R0 scenarios and the consequent projections for new cases, hospital utilization and attack rates at the national, regional and local government level. The government has used these estimates in its monthly policy responses.
Considering that both use the same DOH Data Drop dataset, dissonance between OCTA and government scientists’ recommendations have been reported in print, broadcast, and social media. This involves largely the differences in interpreting the framework of quarantine status and risks, with government experts tending to question OCTA’s projections with a very conservative precautionary interpretation of evidence. One doctor with the IATF-EID has accuses OCTA of using “erroneous” and “incomplete” data (Kho, 2021 ). This dissonance has led politicians to label OCTA as “alarmist” (David, 2021 ).
OCTA is a knowledge producer in science advice since it constructs DOH epidemiological data into models informed by epidemiological theory. Even if OCTA has decided to remain completely independent as a science advisory body, it is not completely insulated from political attack. Political attack is a result of perceived role conflation in the science advice ecosystem and process which is exacerbated by the nature of uncertainty in science advice leading to accusations of OCTA being “alarmist. OCTA was misconstrued by the government as its own knowledge producer and its critics demanded that it be completely alienated from its academic institutional linkages. OCTA’s weakness and the weakness of the Philippines crisis science advisory system overall, is the lack of external and extended peer review. This is a consequence of a small science community where there are few actors who can perform this role with citizen scientists. In a postnormal science advisory environment, the role of extended peer review is important in validating policy options and creating public consensus.
OCTA has recently partnered with Go Negosyo, a small and medium business entrepreneurship (SME) advocacy, headed by Presidential advisor for entrepreneurship, Joey Concepcion. Mr. Concepcion has a minister’s portfolio. OCTA in this arrangement will provide data analytics services and science advice for SMEs for a business friendly COVID exit policy with a safe reopening of the economy based on vaccination prioritization strategies (Cordero, 2021 ). This move also evidences OCTA’s influence in setting new policy directions in government’s adoption of a new quarantine classification system of Alert Levels, an idea first proposed by OCTA Fellow and medical molecular biologist Rev Dr. Nicanor Austriaco OP and mathematical modeler Dr. Fredegusto Guido David. This is a political move on OCTA’s part to deflect critics in Congress as the business sector has a large political clout in government.
While a pandemic crisis like COVID 19 gives political leaders an advantageous occasion to demonstrate personal leadership, their constituencies will tend to expect a more personalistic crisis management. In this independent science advice plays a crucial political dynamic by building public trust, ensuring reliable statistical estimates reviewed by the academic science community, and managing political advantages and risks. These are all in the context of epidemiological uncertainties. In the Philippines, public criticism of the pandemic response is fierce due to the primarily law and order policing approach which raised concerns on human rights violations (Hapal, 2021 ) as well as those cases began to rise in the first quarter of 2021 (Robles and Robles, 2021 ). The failure to deal with uncertainties in science without effective science advice may entail large political costs. Managing public perception and the use of government scientific and technical advice is a delicate balancing act in liberal democracies. The press and media will report and scrutinize science informed decisions while shaping public opinion of crisis decisions. Academic science and civil society organizations not part of the advisory system provide another level of scrutiny and critique. Social media has extremely broadened the venue for public scrutiny and, open or extended peer review of crisis decisions.
These realities were not faced by political leaders as recently as 30 years ago. However unfair or unrealistic the critique by constituencies and the press, public expectation is real in political terms. And while politicians can “write off” certain social and political sectors in deciding which crisis response is best, this is no longer tenable in democracies in the 21st century.
In these realities emerge new actors of engaged independent academic science advisors such as OCTA. It has certainly played the role of a knowledge generator and to some extent a knowledge broker. And like any science advice actor, OCTA was not immune to political attack, and this would suggest that SAGE with its embeddedness in the administrative and ministerial structures in the UK, largely missing in the Philippines (Berse, 2020 ), will be subject to great political interference which may limit its effectiveness. Political interference may masquerade as technical in nature (Smallman, 2020 ).
The Philippines government response to COVID 19 has been described as “deficient in strategic agility” (Aguilar Jr, 2020 ) partly due to its inability to mobilize scientific expertise and synthesize science informed advice options in governance. Thus, a plausible proposal to strengthen science advice is in reframing the DRRM policy and advisory structures and applying these to crisis in order to strengthen science advice capacity at all levels of governance. As Berse ( 2020 ) suggests “tweaking the National Disaster Risk Reduction and Management Council structure, which has a seat for an academic representative, might do the trick. This national set-up is replicated by law at the provincial, city and municipal levels”.
Berse also suggests that an academic should be appointed to sit at each of these councils. The major constraint is that there are very few academics willing to sit as this will expose them to political criticism and interference. If academics are appointed, then their expertise should not be unduly constrained by political interference. They should be backed by several researchers and citizen scientists coming from multiple disciplines in reviewing science informed policies. More and more citizen scientists have come up with science advice which for consistency of policy should be reviewed in extended consensus by scientists and stakeholders (Funtowicz and Ravetz, 1993 ; Marshall and Picou, 2008 ).
The closed and elitist system of science advice in the Philippines with its handful of actors, mainly appointed by government, are inordinately prone to political pressure. This necessitates the role of independent science advisors. Independent science advisors can act as a “challenge function” to government experts whose recommendation if ignored contributes to further erosion of public trust in government (Dommett and Pearce, 2019 ). Independent science advice when framed in the context of parliamentary democracy can be likened to “shadow cabinets” in this way they provide a check, balance and review of science evidence and is called “shadow science advice” (Pielke, 2020 )
As pandemics and other environmentally related public health emergencies are expected to be more frequent in the 21st century, the public will be less tolerant of social and political instability and demand a clear science informed response from their politicians. However, most politicians do not have enough scientific and technical competency to do so and so will have to rely on science informed advice which has degrees of outcome uncertainty (Gluckman, 2016b ). If science informed options are ignored for political gains, this is not a result of broken science advice and knowledge generation systems but a dysfunctional political and governance system. The huge cost in life and economic opportunity left by the pandemic demands functional government informed by science advice.
Furthermore, any government to cement its legacy must find a COVID 19 crisis exit strategy after the operational aspects such as a mass vaccination strategy have been met and the social, health (Dickens et al., 2020 ), economic and political situation has been stabilized (Gilbert et al., 2020 ). In COVID 19, this is a gradual relaxation of lockdown and quarantine (Leung and Wu, 2020 ) with the roll out of vaccines.
Vaccination is the main COVID-19 exit strategy of the government (Congress of the Philippines, 2021 ) and given the large existing vaccine hesitancy of 46% as OCTA estimated in February 2021 (Tomacruz, 2021 ), there is a need to increase public confidence on vaccines (Vergara et al., 2021 ). Public distrust of vaccines became a major public health concern due to the Dengvaxia vaccine rollout controversy in November 2017 when Sanofi publicly released a warning that vaccination posed a risk if given to people who never had a dengue infection (Larson et al., 2019 ). The political impact was damaging to the Benigno Aquino III presidential administration, which rolled out the vaccine in 2016 before Aquino III’s term ended. The drop in vaccine confidence was significant, from 93% in 2015 to 32% in 2018. The new presidential administration of Rodrigo Duterte placed the blame on Aquino III, and this resulted in social and political polarization, loss of trust in the public health system which have continued in the COVID-19 pandemic. The “blame game” is political risk in any liberal democracy. This can be a long drawn out affair where government will have to establish accountability and the “blame game” is expected with various independent boards and blue ribbon committees setting the narrative (Boin et al., 2016 ). In the Philippines, several hearings in the House and Senate in which Sanofi and previous Department of Health leadership were called to give testimonies, further worsened political and social polarization to vaccination. These independent boards, blue ribbon committees and fact-finding investigations, however, are prone to agency capture by ruling party politics. This is evident in the Philippines. The government exit strategy for COVID-19 is clouded by these polarizations. OCTA will be expected by the public to provide government science advice on vaccination policies, and this will have great political costs for independent science advice. As vaccination in the Philippines has become a political issue more than as a public health issue, other think tanks and academic research institutions which have investigated Dengvaxia, and vaccine compliance have been more guarded as not to attract undue negative political comment. OCTA to its credit, has successfully navigated political risks in its COVID-19 forecasts and in a political move, has allied with a SME advocacy headed by a close Presidential advisor on economic affairs. OCTA can continue to maintain its credibility by periodically issuing forecasts and policy option recommendations and reducing social and political polarizations through consensus building with the public, government, and science community. Here is where the independent science advice actors will have a place, and that is to set the objective bases for science informed policy decisions while recognizing the political dynamic. How independent science advice will result in lasting policy impacts in the Philippines remains to be seen. The government and the public have relied on OCTA forecasts because of OCTA’s increasing presence in broadcast, print, and social media. This is evidence of the effective science communication strategy of the organization. But with the Government increasingly using OCTA’s forecasts and policy recommendations, this is evidence that government science advice has political dividends and risks which may affect politicians’ political standing with the electorate in the 2022 election.
Data availability
COVID-19 open data cited in this paper can be accessed through the Philippines Department of Health Data Drop https://doh.gov.ph/covid19tracker and through OCTA Research https://www.octaresearch.com/ .
ABS-CBN (2021) Metro Manila COVID-19 surge begins ahead of Christmas: OCTA Research. https://news.abs-cbn.com/news/12/22/20/metro-manila-covid-19-surge-begins-ahead-of-christmas-octa-research . Accessed 3 Jan 2021
Aguilar Jr FV (2020) Preparedness, agility, and the Philippine response to the Covid-19 pandemic the early phase in comparative Southeast Asian perspective. Philipp Stud Hist Ethnogr Viewp 68(3):373–421
Article Google Scholar
Allen K, Buklijas T, Chen A, Simon-Kumar N, Cowen L, Wilsdon J, Gluckman P (2020) Tracking global knowledge-to-policy pathways in the coronavirus crisis: a preliminary report from ongoing research. INGSA. https://www.ingsa.org/wp-content/uploads/2020/09/INGSA-Evidence-to-Policy-Tracker_Report-1_FINAL_17Sept.pdf
Bankoff G, Hilhorst D (2009) The politics of risk in the Philippines: comparing state and NGO perceptions of disaster management. Disasters. 33(4):686–704
Berse K (2020) In science we trust? Science advice and the COVID-19 response in the Philippines https://www.ingsa.org/covidtag/covid-19-commentary/berse-philippines/ . Accessed 3 Jan 2021.
Boin A, Stern E, Sundelius B (2016) The politics of crisis management: Public leadership under pressure. Cambridge University Press, Cambridge
Book Google Scholar
Caulkins J, Grass D, Feichtinger G, Hartl R, Kort PM, Prskawetz A, Seidl A, Wrzaczek S (2020) How long should the COVID-19 lockdown continue? PLoS ONE 15(12):e0243413
Article CAS Google Scholar
CNN Philippines (2021) OCTA Research: four-week MECQ to “knock out” COVID-19 case surge. https://cnnphilippines.com/news/2021/3/24/OCTA-Research-4-week-MECQ-knock-out-surge.html . Accessed 16 Apr 2021
Congress of the Philippines (2021) An act establishing the coronavirus disease 2019 (COVID-19) vaccination program expediting the vaccine procurement and administration. Providing Funds Therefor, and for Other Purposes, Manila. https://www.officialgazette.gov.ph/downloads/2021/02feb/20210226-RA-11525-RRD.pdf . Accessed 16 Apr 2021
Cordero T (2021) Go Negosyo, OCTA Research ink partnership on data-sharing, proposals to reopen economy. GMA News Online. https://www.gmanetwork.com/news/money/companies/807569/go-negosyo-octa-research-ink-partnership-on-data-sharing-proposals-to-reopen-economy/story/ . Accessed 25 Oct 2021.
David G, Rye R, Agbulos M, Alampay E, Brillantes E, Lallanam R, Ong R, Vallejo B, Tee M (2020) COVID-19 forecasts in the Philippines: NCR, Cebu and COVID-19 hotspots as of June 25, 2020. OCTA Research, Quezon City, Philippines
Google Scholar
David R (2021) Probing OCTA. Philippine Daily Inquirer https://opinion.inquirer.net/142869/probing-octa . Accessed 25 Oct 2021.
Davies NG, Kucharski AJ, Eggo RM, Gimma A, Edmunds WJ, Jombart T, O’Reilly K, Endo A, Hellewell J, Nightingale ES et al. (2020) Effects of non-pharmaceutical interventions on COVID-19 cases, deaths, and demand for hospital services in the UK: a modelling study. Lancet Public Health 5(7):e375–e385. https://doi.org/10.1016/S2468-2667(20)30133-X
Article PubMed PubMed Central Google Scholar
Dickens BL, Koo JR, Lim JT, Park M, Quaye S, Sun H, Sun Y, Pung R, Wilder-Smith A, Chai LYA et al. (2020) Modelling lockdown and exit strategies for COVID-19 in Singapore. Lancet Reg Health-West Pac 1:100004. https://doi.org/10.1016/j.lanwpc.2020.100004
Dommett K, Pearce W (2019) What do we know about public attitudes towards experts? Reviewing survey data in the United Kingdom and European Union. Public Underst Sci 28(6):669–678
Doubleday R, Wilsdon J (2012) Beyond the great and good. Nature 485(7398):301–302. https://doi.org/10.1038/485301a
Article ADS CAS PubMed Google Scholar
Funtowicz SO, Ravetz JR (1993) Science for the post-normal age. Futures 25:739–755. https://doi.org/10.1016/0016-3287(93)90022-L
Funtowicz SO, Ravetz JR (1994) Uncertainty, complexity, and post‐normal science. Environ Toxicol Chem Int J 13(12):1881–1885
Gilbert M, Dewatripont M, Muraille E, Platteau J-P, Goldman M (2020) Preparing for a responsible lockdown exit strategy. Nat Med 26(5):643–644. https://doi.org/10.1038/s41591-020-0871-y
Article CAS PubMed PubMed Central Google Scholar
Gluckman P (2016a) The science–policy interface. Science 353(6303):969. https://doi.org/10.1126/science.aai8837
Gluckman P (2016b) Making decisions in the face of uncertainty: understanding risk Auckland. Office of the Prime Minister’s Chief Science Advisor, Auckland, New Zealand
Hapal K (2021). The Philippines’ COVID-19 response: securitising the pandemic and disciplining the pasaway. J Curr Southeast Asian Aff. https://doi.org/10.1177/1868103421994261
Kho R (2021) House inquiry sought on OCTA Research group. Businessworld https://www.bworldonline.com/house-inquiry-sought-on-octa-research-group/ . Accessed 25 Oct 2021.
Larson HJ, Hartigan-Go K, de Figueiredo A (2019) Vaccine confidence plummets in the Philippines following dengue vaccine scare: why it matters to pandemic preparedness. Hum Vaccines Immunother 15(3):625–627. https://doi.org/10.1080/21645515.2018.1522468
Leung K, Wu JT (2020) The gradual release exit strategy after lockdown against COVID-19. Lancet Reg Health–West Pac 1. https://doi.org/10.1016/j.lanwpc.2020.100008 . Accessed 4 Jan 2021
Lipsitch M, Riley S, Cauchemez S, Ghani AC, Ferguson NM (2009) Managing and reducing uncertainty in an emerging influenza pandemic. N Engl J Med 361(2):112–115. https://doi.org/10.1056/NEJMp0904380
MacKenzie DA (1993) Inventing accuracy: a historical sociology of nuclear missile guidance. MIT press, Cambridge, MA
Manila Bulletin (2020) OCTA Research reporting continues. https://mb.com.ph/2020/10/15/octa-research-reporting-continues/ . Accessed 3 Jan 2021.
Manila Times (2020) Time for UP OCTA research team to account for its Covid forecasting. https://www.manilatimes.net/2020/07/20/opinion/editorial/time-for-up-octa-research-team-to-account-for-its-covid-forecasting/743476/ . Accessed 3 Jan 2021.
Marshall BK, Picou JS (2008) Postnormal science, precautionary principle, and worst cases: the challenge of twenty‐first century catastrophes. Sociol Inq 78(2):230–247
UP COVID-19 Pandemic Response Team (2020) Prevailing data issues in the time of COVID-19 and the need for open data. University of Philippines. https://www.up.edu.ph/prevailing-data-issues-in-the-time-of-covid-19-and-the-need-for-open-data/ . Accessed 4 Jan 2021
Johns S (2020) Neil Ferguson talks modelling, lockdown and scientific advice with MPs. Imperial News. Imperial College London https://www.imperial.ac.uk/news/198155/neil-ferguson-talks-modelling-lockdown-scientific/ . Accessed 2 Jan 2021.
One News.ph (2020) NO REVOLUTION: medical frontliners tell Duterte they had to go public as distress calls went unanswered. https://www.onenews.ph/no-revolution-medical-frontliners-tell-duterte-they-had-to-go-public-as-distress-calls-went-unanswered . Accessed 4 Jan 2021.
Pearce W (2020) Trouble in the trough: how uncertainties were downplayed in the UK’s science advice on Covid-19. Humanit Soc Sci Commun 7(1):1–6. https://doi.org/10.1057/s41599-020-00612-w
Article MathSciNet Google Scholar
Pellini A, Jabar M, Era M, Erasga D (2013) Towards policy-relevant science and scientifically informed policy: political economy of the use of knowledge and research evidence. ODI, Manila
Philippine Daily Inquirer (2020). Baguio tourism industry objects to OCTA ‘high risk’ tag. INQUIRER.net https://newsinfo.inquirer.net/1364601/baguio-tourism-industry-objects-to-octa-high-risk-tag . Accessed 3 Jan 2021.
Philippine Star (2020) Palace tells UP, UST experts to stop publicizing quarantine status recommendations. Oct 10th, 2013. https://www.philstar.com/headlines/2020/10/13/2049279/palace-tells-experts-stop-publicizing-quarantine-status-recommendations . Accessed 3 Jan 2021.
Pielke RJ (2020) On shadow science advice https://youtu.be/PktWL5xNanc . Accessed 24 March 2021
Ravetz IR (1999) What is post-normal science. Futur-J Forecast Plan Policy 31(7):647–654
Robles A, Robles R. 2021. Where did the Philippines’ pandemic response go wrong? South China Morning Post. https://www.scmp.com/week-asia/health-environment/article/3122257/late-and-slow-motion-where-philippines-pandemic . Accessed Apr 16 2021.
Senate of the Philippines 14th Congress (2008) An act establishing a pandemic preparedness plan and for other purposes therefor. 14th Congress first regular session https://legacy.senate.gov.ph/lis/bill_res.aspx?congress=14&q=SBN-2198 . Accessed 15 Jan 2021
Senate of the Philippines 16th Congress (2013) An act strengthening national preparedness and response to public health emergencies. 16th Congress first regular session https://legacy.senate.gov.ph/lis/bill_res.aspx?congress=16&q=SBN-1573 . Accessed 15 Jan 2021
Senate of the Philippines 18th Congress (2020) An Act Strengthening National Preparedness and Response to Public Health Emergencies by Creating a Center for Disease Control 18th Congress. First regular session http://legacy.senate.gov.ph/lisdata/3260429469!.pdf . Accessed 15 Jan 2021
Smallman M (2020) ‘Independent Sage’ group is an oxymoron. Res Prof News. https://www.researchprofessionalnews.com/rr-news-political-science-blog-2020-5-independent-sage-group-is-an-oxymoron/ . Accessed 4 Jan 2021.
Tomacruz S (2021) 46% of adult Filipinos still unwilling to get vaccinated vs. COVID-19. Rappler https://www.rappler.com/nation/octa-research-filipinos-covid-19-vaccine-willingness-february-2021 . Accessed 15 Apr 2021
Vallejo BM, Ong RAC (2020) Policy responses and government science advice for the COVID 19 pandemic in the Philippines: January to April 2020. Prog Disaster Sci 7:100115. https://doi.org/10.1016/j.pdisas.2020.100115
Van der Sluijs J (2005) Uncertainty as a monster in the science–policy interface: Four coping strategies. Water Sci Technol 52(6):87–92
Vergara RJD, Sarmiento PJD, Lagman JDN (2021) Building public trust: a response to COVID-19 vaccine hesitancy predicament. J Public Health Oxf Engl 43(2):e291–e292. https://doi.org/10.1093/pubmed/fdaa282
Download references
Acknowledgements
The authors thank the University of the Philippines Bayanihan Research Grants for COVID-19 for funding support. We also thank Assistant Professor Ranjit Singh and Dr. Fredegusto Guido David of OCTA Research for providing OCTA COVID-19 forecasts and epidemiological model and Mr. Fil Elefante for proofreading. Many thanks also to Prof. Roger Pielke at the University of Colorado at Boulder and EsCAPE ( www.escapecovid19.org ) for encouraging the publication of this paper.
Author information
Authors and affiliations.
University of the Philippines Diliman, Quezon City, Philippines
Benjamin M. Vallejo Jr & Rodrigo Angelo C. Ong
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Benjamin M. Vallejo Jr .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors. Ethics review is not required.
Informed consent
All statements attributed to specific individuals used in this study are in the public record and no informed consent from individuals is required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Vallejo, B.M., Ong, R.A.C. OCTA as an independent science advice provider for COVID-19 in the Philippines. Humanit Soc Sci Commun 9 , 104 (2022). https://doi.org/10.1057/s41599-022-01112-9
Download citation
Received : 17 June 2021
Accepted : 23 February 2022
Published : 30 March 2022
DOI : https://doi.org/10.1057/s41599-022-01112-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Psychological impact of COVID-19 pandemic in the Philippines
Affiliations.
- 1 Department of Physiology, College of Medicine, University of the Philippines Manila, Taft Avenue, Manila 1000, Philippines; Philippine One Health University Network. Electronic address: [email protected].
- 2 Department of Pediatrics, College of Medicine, University of the Philippines Manila, Taft Avenue, Manila 1000, Philippines. Electronic address: [email protected].
- 3 Department of Psychiatry and Behavioral Medicine, College of Medicine, University of the Philippines Manila, Taft Avenue, Manila 1000, Philippines.
- 4 School of Statistics, University of the Philippines Diliman, Philippines.
- 5 South East Asia One Health University Network. Electronic address: [email protected].
- 6 Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Kent Ridge 119228, Singapore. Electronic address: [email protected].
- PMID: 32861839
- PMCID: PMC7444468
- DOI: 10.1016/j.jad.2020.08.043
Background: The 2019 coronavirus disease (COVID-19) pandemic poses a threat to societies' mental health. This study examined the prevalence of psychiatric symptoms and identified the factors contributing to psychological impact in the Philippines.
Methods: A total of 1879 completed online surveys were gathered from March 28-April 12, 2020. Collected data included socio-demographics, health status, contact history, COVID-19 knowledge and concerns, precautionary measures, information needs, the Depression, Anxiety and Stress Scales (DASS-21) and the Impact of Events Scale-Revised (IES-R) ratings.
Results: The IES-R mean score was 19.57 (SD=13.12) while the DASS-21 mean score was 25.94 (SD=20.59). In total, 16.3% of respondents rated the psychological impact of the outbreak as moderate-to-severe; 16.9% reported moderate-to-severe depressive symptoms; 28.8% had moderate-to-severe anxiety levels; and 13.4% had moderate-to-severe stress levels. Female gender; youth age; single status; students; specific symptoms; recent imposed quarantine; prolonged home-stay; and reports of poor health status, unnecessary worry, concerns for family members, and discrimination were significantly associated with greater psychological impact of the pandemic and higher levels of stress, anxiety and depression (p<0.05). Adequate health information, having grown-up children, perception of good health status and confidence in doctors' abilities were significantly associated with lesser psychological impact of the pandemic and lower levels of stress, anxiety and depression (p<0.05).
Limitations: An English online survey was used.
Conclusion: During the early phase of the pandemic in the Philippines, one-fourth of respondents reported moderate-to-severe anxiety and one-sixth reported moderate-to-severe depression and psychological impact. The factors identified can be used to devise effective psychological support strategies.
Keywords: Anxiety; COVID-19; Depression; Philippines; Psychological impact; Stress.
Copyright © 2020 Elsevier Ltd. All rights reserved.
- Age Factors
- Anxiety / epidemiology*
- Anxiety / psychology
- Betacoronavirus
- Coronavirus Infections*
- Depression / epidemiology*
- Depression / psychology
- Health Personnel / psychology
- Health Personnel / statistics & numerical data
- Health Status
- Mental Health
- Middle Aged
- Philippines / epidemiology
- Pneumonia, Viral*
- Sex Factors
- Single Person
- Stress, Psychological / epidemiology*
- Stress, Psychological / psychology
- Students / psychology
- Students / statistics & numerical data
- Surveys and Questionnaires
- Young Adult
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Oxford University Press - PMC COVID-19 Collection

Telehealth during the COVID-19 pandemic in the Philippines
Dalmacito a cordero, jr.
Department of Theology and Religious Education (DTRE), De La Salle University, 1004 Taft Avenue, Manila, Philippines
To the Editor,
In a very timely Editorial published in this journal, Fisher and Magin rightfully concluded that during this COVID-19 pandemic, telehealth has the potential to bridge healthcare inequity and increase access for vulnerable and disadvantaged populations. At the same time, they also added that it has the potential to exacerbate existing inequity. 1 With these interesting perspectives, I would like to validate and flesh these claims by pointing out both their advantages and disadvantages, especially in the Philippine primary care context.
In the Philippine healthcare system, health outcomes are generally improving, but the stagnant maternal mortality ratio and neonatal mortality rate, and the sluggish rate of improvement in health outcomes compared to neighboring countries, are worrisome. Addressing health system inefficiencies and health inequities due to disorganized governance, fragmented health financing, and devolved and pluralistic service delivery remain critical challenges to the Philippine health system. 2 Primary care can play a significant role in the COVID-19 response by differentiating patients with respiratory symptoms from those with COVID-19, making an early diagnosis, helping vulnerable people cope with their anxiety about the virus, and reducing the demand for hospital services. 3 Telehealth or telemedicine is one way of improving the country’s healthcare system. Telemedicine is a method of seeking professional medical help with the use of technologies and devices such as smartphones to remotely gain information regarding their health status. 4 The technical support provided by this alternative method matters a lot. One example of this is H4D’s Consult Station. H4D is an international company specializing in clinical telemedicine that enjoined the international effort to fight the COVID-19 pandemic by offering healthcare facilities, local authorities, and senior residences a fast, efficient, and reliable solution to facilitate patient care. The Consult Station allows patients not only to take their own vital signs but also to carry out teleconsultations with a doctor through a videoconference. These teleconsultations are done with the assistance of all the instruments and sensors necessary to perform a clinical examination, a diagnosis, and a prescription if necessary. 5 Teleconsultations in the Philippines can now be done through COVID-19 hotlines, websites, and mobile apps launched by several agencies and businesses. These include the Department of Health (DOH), Medgate, KonsultaMD, Medifi, HealthNow, AIDE, DOCPH, Yo-Vivo Health, and Lifeline. 6 Some doctors also have their personal Facebook pages and Viber accounts utilizing the respective video app for online consultations. The Philippine Health department engaged with more than 100,000 patients a month in the first quarter of 2021 on Cisco Webex, a video conferencing platform developed by Cisco Philippines. The agency conducted 17,400 sessions over Webex in 2020, equivalent to more than 2.3 million minutes of meetings and teleconsultations. 7 In addition, Albay 2nd District Representative Joey Salceda has filed a bill that would enable the telemedicine and electronic health industry to expand in the country. This is House Bill No. 7422 or the Philippine E-Health and Telemedicine Development Act of 2020, which would be beneficial as the country continues to grapple with the COVID-19 pandemic, especially as more services could be provided to underserved communities. 8 This bill will basically promote the delivery of health and medical services through the use of information and communication technology. The practice has proven to be useful and worth considering in some situations. The proven benefits include reduction of the risk of spreading the virus by patients, chronic health management, comprehensive family engagement with the doctor, and many others.
On the other hand, telemedicine is not always applicable to all situations. A thorough analysis of the patient’s condition must be taken into consideration since there are also disadvantages that are pointed out by health experts. These considerations cannot be taken for granted as it involves an appropriate diagnosis by doctors, which is a must for all types of patients, immunocompromised or not. What then are the disadvantages of telemedicine? First, the basic procedure of a physical checkup done on a patient is traditionally the use of a stethoscope by a doctor. The stethoscope is an instrument used for listening to sounds produced by the body. It is used primarily to detect and study heart, lung, stomach, and other sounds in adult humans, human fetuses, and animals. Using it, the doctor can hear normal and abnormal respiratory, cardiac, pleural, arterial, venous, uterine, fetal, and intestinal sounds. 9 It is still one of the most efficient tools in helping doctors to find an accurate diagnosis, especially for cardiovascular disease. In a teleconsultation, the doctor makes an initial diagnosis by hearing the sound data that is obtained from an interactive stethoscope since the traditional type is not possible. However, when other electronic devices such as cell phones are present, digital stethoscopes sometimes tend to malfunction, interfering with the typical optimal performance they have become known for. 10 The accuracy of the initial diagnosis may be sacrificed at times. The patient cannot just simply describe this sound to the doctor by self-listening. In relation to this, doctors must rely heavily on patient self-reports during the online checkup and this may require doctors to ask more questions to ensure that they get a comprehensive health history. If a patient leaves out an important symptom that might have been noticeable during in-person care, this can compromise treatment. 11 Second, telemedicine may also cause security and privacy issues. There can be a lack of transparency between health care professionals and their patients and the difficulty in verifying their respective identities. It is hard to know if the doctor on one end and/or the patient on the other are really who they say they are. The doctor may also ask for more data for the medical record of a patient. When the records are shared with other health care professionals or organizations for referral or billing services or are supplied to third-party service providers, the confidentiality, integrity, and availability of the data may be compromised. 12 Hackers and other criminals may be able to access a patient’s medical data, especially if the patient accesses telemedicine on a public network or via an unencrypted channel. Lastly, when a patient needs emergency care, accessing telemedicine first may delay treatment, particularly since a doctor cannot provide life-saving care or laboratory tests digitally. 11
Telemedicine provides a range of benefits for both patients and healthcare providers. However, it has also limitations and may not be applicable at all times. It is important to understand its benefits and limitations to avoid any potentially dangerous situations or cause health inequity. I argue that this method must be availed only on a case-by-case basis, that is if the patient is limited by his/her physical capacity to go to the hospital for a checkup or any medical procedure. This can also include a situation where the hospital is too far from the patient’s location and traveling for a longer period of time will be too risky and requires much effort. In the same way, one has to consider the strength of internet connections and the clear quality of equipment to be used for audiovisual data. Telehealth is a helpful alternative to the traditional patient-doctor appointment especially during a pandemic, but it cannot guarantee the same high level of healthcare management like that of the in-person setup.
Conflict of interest
The author declares that he has no competing interests.

IMAGES
COMMENTS
COVID-19 dynamics in the Philippines are driven by age, contact structure, mobility, and MHS adherence. Continued compliance with low-cost MHS should help the Philippines control the epidemic until vaccines are widely distributed, but disease resurgence may be occurring due to a combination of low population immunity and detection rates and new variants of concern.
The Philippine population of 110 million comprises a relatively young population. On May 22, 2021, the number of confirmed COVID-19 cases reported in the country is 1,171,403 with 55,531 active ...
Overview of the Philippine COVID-19 surveillance system. The Philippines is an archipelago of three island groups and 17 regions subdivided into 81 provinces covering 146 cities and 1488 municipalities [].COVID-19 surveillance, like majority of health service delivery, is decentralised to local government units (LGUs), i.e. provinces, cities and municipalities.
The novel coronavirus disease 2019 (COVID-19, caused by SARS-CoV-2) has spread globally since its first report in Wuhan, China on December 31, 2019. On January 30, the Philippines reported its first two imported cases of COVID-19 in a couple from Wuhan. One of them died on February 1st, becoming the first COVID-19 death outside China.
Low- and middle-income countries (LMICs) with weak health systems are especially vulnerable during the COVID-19 pandemic. In this paper, we describe the challenges and early response of the Philippine Government, focusing on travel restrictions, community interventions, risk communication and testing, from 30 January 2020 when the first case was reported, to 21 March 2020.
Methods We calculated the crude (CMR) and age-standardised mortality rates (ASMR) of the Philippine provinces from the national COVID-19 surveillance data from January 18, 2020 to May 9, 2023.
Responses of subnational government units are crucial in the containment of the spread of pathogens in a country. To mitigate the impact of the COVID-19 pandemic, the Philippine national government through its Inter-Agency Task Force on Emerging Infectious Diseases outlined different quarantine measures wherein each level has a corresponding degree of rigidity from keeping only the essential ...
Introduction The SARS-CoV-2, virus that caused the COVID-19 global pandemic, possesses a neuroinvasive potential. Patients with COVID-19 infection present with neurological signs and symptoms aside from the usual respiratory affectation. Moreover, COVID-19 is associated with several neurological diseases and complications, which may eventually affect clinical outcomes. Objectives The ...
WHO Philippines situation reports by date. 20 December 2023. COVID-19 in the Philippines Situation Report 142. 27 November 2023. COVID-19 in the Philippines Situation Report 141. 12 November 2023. COVID-19 in the Philippines Situation Report 140. 29 October 2023.
With the emergence of the highly transmissible Omicron variant, large-scale vaccination coverage is crucial to the national and global pandemic response, especially in populous Southeast Asian countries such as the Philippines and Malaysia where new information is often received digitally. The main aims of this research were to determine levels of hesitancy and confidence in COVID-19 vaccines ...
The Philippines is contending with one of the worst COVID-19 outbreaks in southeast Asia. As of April 18, 2021, there were 926 052 cases of SARS-CoV-2 infection and 15 810 deaths recorded. WHO has warned that the country's health-care system risks being overwhelmed. From March 29, 2021, a new round of lockdown was implemented in Manila and four ...
The World Bank, in collaboration with the Department of Social Welfare and Development (DSWD), conducted two rounds of a high frequency social monitoring survey that aimed to assess the impact of COVID-19 pandemic on the poorest and most vulnerable rural communities. This survey aimed to also determine the level of understanding and source of ...
The Philippine government mounted a multi-sectoral response to the COVID-19, through the Interagency Task Force (IATF) on Emerging Infectious Diseases chaired by the Department of Health (DOH). Through the National Action Plan (NAP) on COVID-19, the government aims to contain the spread of COVID-19 and mitigate its socioeconomic impacts.
3.5. Knowledge and concerns about COVID-19 and association with psychological impact. The proportions of respondents who perceive that the routes of transmission of the virus for COVID-19 were via droplets, via contaminated objects and airborne were 98.6%, 96.7% and 35.3%, respectively (Table 4). About 76.8% were satisfied to very satisfied ...
Introduction The COVID-19 pandemic declared by the WHO has affected many countries rendering everyday lives halted. In the Philippines, the lockdown quarantine protocols have shifted the traditional college classes to online. The abrupt transition to online classes may bring psychological effects to college students due to continuous isolation and lack of interaction with fellow students and ...
We comment on science advice in the political context of the Philippines during the COVID 19 pandemic. We focus on the independent science advisor OCTA Research, whose publicly available ...
COVID-19 in the Philippines Abstract Lockdowns and policy actions to curtail the transmission of COVID-19 have widespread health system, economic, and societal impacts. Health systems of low-to-middle-income countries may have fewer buffering resources and capacity against shocks from a pandemic. This paper presents
Background: The 2019 coronavirus disease (COVID-19) pandemic poses a threat to societies' mental health. This study examined the prevalence of psychiatric symptoms and identified the factors contributing to psychological impact in the Philippines. Methods: A total of 1879 completed online surveys were gathered from March 28-April 12, 2020.
In contrast, Chinese respondents requested more health information about COVID-19. For the Philippines, student status, low confidence in doctors, dissatisfaction with health information, long daily duration spent on health information, worries about family members contracting COVID-19, ostracization, and unnecessary worries about COVID-19 were ...
The COVID-19 pandemic in the Philippines was a part of the worldwide pandemic of coronavirus disease 2019 caused by severe acute respiratory syndrome coronavirus 2 (). As of May 14, 2024, there have been 4,140,383 reported cases, and 66,864 reported deaths, the fifth highest in Southeast Asia, behind Vietnam, Indonesia, Malaysia, and Thailand.The first case in the Philippines was identified on ...
The first suspected case in the Philippines was investigated on January 22, 2020, and 633 suspected cases were reported as of March 1. We describe the clinical and epidemiological aspects of the first two confirmed COVID-19 cases in the Philippines, both admitted to the national infectious disease referral hospital in Manila.
Despite facing setbacks from the COVID-19 pandemic, the Philippines aspires to achieve upper-middle-income status by 2025 and envisions becoming one of the largest economies in the Asia Pacific by 2033. Economic planners maintain their optimism, citing a robust post-pandemic rebound and positive evaluations from credit rating agencies.
The study stresses the necessity for education stakeholders to blend technology with pedagogical strategies, a need further accentuated by the COVID-19 pandemic. The study's major contribution lies in its comprehensive synthesis of TELL's current landscape and for both future research and education endeavours in the field of English TELL.
This is House Bill No. 7422 or the Philippine E-Health and Telemedicine Development Act of 2020, which would be beneficial as the country continues to grapple with the COVID-19 pandemic, especially as more services could be provided to underserved communities. 8 This bill will basically promote the delivery of health and medical services ...