An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Clin Biochem Nutr
- v.73(2); 2023 Sep
- PMC10493209

Quality analysis of the clinical laboratory literature and its effectiveness on clinical quality improvement: a systematic review
Ahmed shabbir chaudhry.
1 Department of Medical Quality and Safety Science, Osaka City University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan
2 Department of Intensive Care Medicine, Osaka Women’s and Children’s Hospital, 840 Murodo-cho, Izumi, Osaka 594-1101, Japan
Etsuko Nakagami-Yamaguchi
3 Department of Medical Quality and Safety Science, Osaka Metropolitan University Graduate School of Medicine, 1-4-3 Asahi-machi, Abeno-ku, Osaka 545-8585, Japan
Associated Data
Quality improvement in clinical laboratories is crucial to ensure accurate and reliable test results. With increasing awareness of the potential adverse effects of errors in laboratory practice on patient outcomes, the need for continual improvement of laboratory services cannot be overemphasized. A literature search was conducted on PubMed and a web of science core collection between October and February 2021 to evaluate the scientific literature quality of clinical laboratory quality improvement; only peer-reviewed articles written in English that met quality improvement criteria were included. A structured template was used to extract data, and the papers were rated on a scale of 0–16 using the Quality Improvement Minimum Quality Criteria Set (QI-MQCS). Out of 776 studies, 726 were evaluated for clinical laboratory literature quality analysis. Studies were analyzed according to the quality improvement and control methods and interventions, such as training, education, task force, and observation. Results showed that the average score of QI-MQCS for quality improvement papers from 1981–2000 was 2.5, while from 2001–2020, it was 6.8, indicating continuous high-quality improvement in the clinical laboratory sector. However, there is still room to establish a proper system to judge the quality of clinical laboratory literature and improve accreditation programs within the sector.
Introduction
The robustness of the healthcare system relies upon the clinical laboratory because all the clinical decisions taken on patients by physicians mainly depend upon the clinical lab reports. ( 1 , 2 ) About 70–75% of medical diagnoses are obtained via clinical laboratory reports, making laboratory service quality directly impact healthcare quality. ( 3 , 4 ) Laboratory findings should be precise as possible, also at the same instance; all laboratory operations must be reliable with timely reporting resulting in a beneficial clinical setting. ( 5 ) Negligence during laboratory operations, including processing, assessing, and reporting, can cause severe consequences, including complications, lack of adequate treatment, and delay in correct and timely diagnosis, leading to unnecessary treatment and diagnostic testing. ( 6 – 8 ) A clinical laboratory is a complex set of cultures that include several activity steps, and many people make it unique and saucerful. The comprehensive set of these complex operations occurring during a testing process is called the path of the workflow. ( 9 ) The workflow path in a clinical laboratory initializes with the patient and finishes with reporting and comprehending the results. In any clinical lab setting, it is presumed that mistakes will be made in this process due to the high volume of samples, the limited number of staff, and the different steps implicated in the testing process. ( 10 , 11 ) Errors at any stage of the total testing process (TTP) can result in inaccurate laboratory outcomes. To guarantee the quality of the results, a reliable method for determining errors within the TTP is required. ( 12 )
Significance of quality in the medical laboratory
The term “quality” in the healthcare context has been properly defined by the Institute of Medicine (IOM). ( 13 ) It defines “quality of care as the extent to which health services for individuals and populations increase the probability of desired health outcomes and conform with current professional knowledge.” More recently, quality has been characterized as “doing the right things for the right people, at the right time and doing them right the first time.” In recent years, quality may entail different domains; there appears to be a consensus emerging that quality involves safety, effectiveness, appropriateness, responsiveness or patient-centered care, equity or access, and efficiency.
Importance of standardization
In the context of laboratory medicine, high-quality diagnostic testing (such as for patient safety) is often achieved through the application of standardized processes. Standardization helps to guarantee the accuracy and reproducibility of test outcomes and their appropriate application to the correct patient and also helps to ensure that the results are accurate. The accreditation agencies guarantee crucial points for standardization in laboratory medicine. There are several authorized CLIA accreditation agencies like the College of American Pathologists (CAP), Joint Commission (JCIA), Accreditation Commission for Health Care, Inc (ACHC), and American Association for Laboratory Accreditation, accreditation, which significantly influences quality improvement (QI) in medical laboratory. However, the international organization of standardization ISO is a non-governmental organization that offers a general framework for all procedural sections up to reporting results. Over the years, the establishment and maturity of each agency have brought significant improvement in the medical laboratory sector. The most crucial accreditation is ISO 15189 among all others because ISO 15189 fixates more on laboratory management systems and processes, e.g., The ISO 15189 standard includes requirements linked to the entire testing process, including pre-examination (i.e., pre-analytics), examination (i.e., analytics), and post-examination (i.e., post-analytics). These requirements include developing and implementing standard operating procedures, validation processes, staff training, internal and external quality control (EQC) measures, laboratory setup, and other aspects. In contrast, the other CLIA-approved laboratory accreditation program concentrates more on technical procedures implicated in testing, e.g., policy statement, certification standards, archive standards, and adequate laboratory testing.
The originality of this study
Several systematic analyses have been published on the quality and management of clinical laboratories, but none focus particularly on the overall QI of medical laboratories ( Supplemental Table 1 * ). This leaves a dent in our understanding of QI in clinical laboratory settings. ( 14 , 15 ) Regardless of the number of QIs in a medical laboratory context, the high-quality collective QI systematic review is insufficient, which limits our understating of this field and requires further advancement of QI reporting in the clinical laboratory.
Purpose of the study
This study sought to comprehensively review and evaluate published literature on QI in clinical laboratories. The goal was to provide researchers and professionals with a thorough overview of the present knowledge on quality control (QC) and improvement in medical laboratories. Furthermore, the study sought to determine areas for potential future research and developments in the field of QI in this setting.
Materials and Methods
Study design.
A systematic review is a technique for objectively summarizing prior research through a systematic and replicable process. ( 16 ) This review followed a three-stage design suggested by Tranfield et al. 2003. ( 16 , 17 ) During the planning stage, the choice of databases and keywords and the inclusion and exclusion criteria for selecting contextual articles were identified. The preferred reporting items for systematic reviews and Meta-analyses flow chart (Preferred Reporting Items for Systematic Reviews and Meta-Analyzes) was employed to illustrate selecting articles for inclusion in the final sample.
Data source
To guarantee comprehensive coverage of the literature, multiple databases were applied in the bibliometric analysis. ( 18 , 19 ) In this research, the Web of Science (WOS) core collection and PubMed were chosen for their significance to management and medical research. Three keywords were used to determine relevant articles: “quality control” in any of its forms, terms linked to quality processes such as “quality systems,” “quality improvement,” or “quality management,” and “clinical laboratory” to narrow the focus to the healthcare sector using different databases and these keywords helped to guarantee a comprehensive search of the literature on QC and improvement in clinical laboratories. ( 20 )
Study selection
The present analysis specializes in clinical laboratory QC and improvement research published between 1981 and 2021. To be added, the publication must be a research article and be written in English, with at least a title and summary available. Conference proceedings, letters, notes, reviews, editorials, summaries, and other types of publications were removed from the analysis.
Data processing
Before undertaking the study, we standardized the data to enhance the conformity of the results. We standardized the spelling of the author’s names and the formatting of journal affiliations and other data. We also revised to ensure that citations for each article were not counted multiple times when using both databases. Two authors worked independently to mitigate the risk of errors. Only articles that both reviewers agreed upon were included in the review, as displayed in Fig. 1 .

PRISMA (preferred reporting items for systematic reviews and meta-analyses)
Quality assessment of literature extracted
The QI Minimum Quality Criteria Set (QI-MQCS) (16) was used to assess this study. The QI-MQCS is employed in the evaluation of QI interventions in healthcare. The QI-MQCS comprises 16 operational and psychometrically dimensions being assessed to present a reliable and accurate assessment of different QI intervention evaluations. Two of the three reviewers in our study individually reviewed the publications. We allocated a score of 1 to each domain with the minimal criterion and a score of 0 to each area that was not satisfied; hence, each article was allocated a score between 0 and 16. The full review committee handled any score disagreements until a consensus was agreed upon. Although the QI-MQCS does not have a set threshold at which the quality of the articles is determined acceptable, “high quality” was defined in this study as a score between 14 and 16. ( 21 )
A total of 776 results were collected from PubMed and WOS bibliographic databases. Of these, 50 were duplicates, and 726 were screened based on their titles and abstracts. After an additional assessment, 224 of the remaining articles were deemed eligible for the QI study, and 53 met the inclusion criteria, as depicted in Fig. 1 . The selected papers were classified into QI ( n = 19) and QC ( n = 33), as presented in Table 1 . Most QI studies were performed in university hospital laboratories ( n = 34), while some of the QC studies were conducted in general community hospital laboratories ( n = 9). There was a great difference in the types of errors detected in these two categories of examinations. Preanalytical errors ( n = 12) were the most prevalent in the QI studies. In contrast, analytical errors ( n = 28) were the most prevalent error in QC studies.
Table 1.
Characteristics of selected papers
QI in the clinical laboratory focuses on preserving quality standards. The 19 extracted papers on QI were classified based on their themes, goals, methods, and interventions. The major theme among these papers was the improvement of clinical quality standards lab practice and training in the laboratory ( n = 8), followed by the improvement of problems in the reception area ( n = 5), the improvement of TTP ( n = 4), the management of preanalytical errors ( n = 4), and the evaluation and evolution of quality indicators ( n = 2). Accreditation ( n = 6) was the most prevalent method employed in these QI approaches. In contrast, training and education ( n = 17) were the most common interventions employed to achieve these goals, as highlighted in Table 2 .
Table 2.
Characteristics of quality improvement papers
PDSA, plan, do, study, act; DMAIC, define, measure, analyze, improve, control; TQM, total quality management.
The retrieved papers were classified based on their objectives, goals, and methods to examine the QC characteristics in the clinical laboratory. The core QC analytical processes in these papers included performance evaluation ( n = 10), QC assessment ( n = 7), improvement of laboratory practices ( n = 3), improvement of quality through the use of the sigma metric ( n = 8), and the QC criteria for susceptibility testing ( n = 7). These processes highlighted the objectives of QC standards in the clinical laboratory. They were implemented using various methods, including accreditation ( n = 22), six sigma ( n = 12), QC practices ( n = 4), statistical approaches ( n = 4), external quality assessment (EQA) ( n = 2), and EQC ( n = 1), as expressed in Table 3 .
Table 3.
Characteristics of quality control papers
EQA, external quality assessment; EQC, external quality control; POC, point of care; EBV, Epstein-Barr virus; IQC, internal quality control.
In this systematic review, we evaluated the present state of QI interventions, the frequency of errors in clinical laboratories, and the prevalence of issues in QI reporting by systematically examining QI articles in clinical laboratory contexts. As the number of QI publications in healthcare has elevated, so is the number of QI publications in clinical laboratories. ( 22 ) Laboratory errors can occur at any stage of the TTP and can promote increased healthcare costs, decreased patient satisfaction, delayed diagnosis, misdiagnosis, and adverse risks to patient health. ( 23 ) Despite the increasing automation of laboratory diagnostics, our research discovered that laboratories remain a source of errors that can influence patient care decisions.
Distribution of errors among QI and QC papers
Overall, errors in the preanalytical and postanalytical phases are more prevalent, accounting for most errors. ( 24 ) Errors within the analytical stage are generally fewer. ( 25 , 26 ) Our findings indicate that the frequency of errors within the analytical phase has declined in recent years. We categorized the papers into QI and QC to identify the prevalence of errors in each setting. Our findings revealed that preanalytical errors were most predominant in QI papers, comprising 12 out of 19 papers.
In contrast, analytical errors were mostly observed in QC papers, comprising 28 out of 33 papers, as presented in Table 1 . This disparity may be due to the focus of the papers in each category. QI papers often address training, education on safety teams, and other interventions that involve direct human interaction, such as phlebotomy, which may elucidate the higher prevalence of preanalytical errors in these papers. However, QC papers often assess methods or processes for improvement, such as six sigma, accreditation, QC practices, statistical approaches, and other related methods, which involve more analysis in the context.
GCLP is a potential source for QI
To prevent errors, the clinical laboratory must be accurate and precise in its testing. A quality assurance system based on GCLP guidelines can help with this, but it necessitates the commitment of both management and technical staff. A study executed by Horace Gumba et al. ( 27 ) has revealed that improving the workflow, increasing patient satisfaction, evaluating performance, and improving the test-treatment process can all contribute to QI in the clinical laboratory. Implementing GCLP guidelines also requires effective management, a solid foundation of best practices and a focus on quality culture, and training and education. Another study by Horace Gumba et al. 2018 ( 28 ) indicated that on-site training and education have been found to enhance the implementation of quality management systems considerably. Our previously reported data linked to QI supplement these ideas and propose that writing standard operating procedures, improving documentation practices, implementing GCLP guidelines, conducting improvement projects, and providing training on quality indicators can all be efficient interventions for improving the quality in the clinical laboratory, as expressed in Table 2 .
Performance evaluation
Performance evaluation in clinical laboratories is crucial for guaranteeing test results’ accuracy, precision, and reproducibility. This is typically accomplished through QC materials. These materials, which have prominent values, are used to validate the performance of the laboratory’s test systems. QC materials can be classified into internal and external types. Internal quality control (IQC) materials are used for consistent monitoring of the laboratory’s test systems, while EQC materials are used for comparison to those of other laboratories. A study was carried out by Loh et al. , ( 29 ) analyzed several methods used to assess clinical laboratories’ performance, including QC materials and inter-laboratory comparisons. The study highlighted the importance of constant improvement in the QC of clinical laboratories. Our QC paper intentionally highlights this concept in Table 3 .
Importance of accreditation in clinical laboratory
Accreditation of clinical laboratories is essential for promoting the quality of clinical laboratory practices. Our findings in Table 3 highlight the significance of accreditation in clinical laboratories, which conforms with the findings of research by Alkhenizan et al. ( 30 ) One of the main restrictions to implementing accreditation programs is the skepticism of healthcare professionals, particularly physicians, concerning the impact of accreditation on the quality of healthcare services. ( 31 , 32 ) In healthcare, QI activities are often promoted as part of a total quality management (TQM) strategy, including Kaizen/QI activities in nursing care, medical quality, logistics, administrative work, and patient services. In clinical laboratories, however, the influencing force behind the QI is often linked to accreditation, as it presents formal recognition and certification from a regulatory body that the laboratory is competent and operates effectively. ( 33 )
Influence of accreditation in QI and QC studies
To assess the trend of QI in clinical laboratories, we analyzed papers from 1981 to 2021 and made some intriguing findings. There was relatively minimal research on QI or control from the 1980s to 2000s, possibly due to insufficient quality infrastructure, barriers to globalization, and limited access to modern knowledge. Data categorization revealed that QI and QC trends increased considerably after 2000, suggesting a significant improvement in the laboratory sector. Several possible explanations abound for this trend, including increased awareness of the importance of quality healthcare and developing quality management systems. The most substantial factor is the establishment of accreditation agencies such as ISO 15189 and CAP. CAP and ISO 15189 have greatly impacted the clinical laboratory sector through several initiatives and guidelines. ( 34 ) CAP has had multiple changes from 1994 to 2020, including implementing training and unannounced inspection programs for pathology laboratories, establishing a multiyear initiative to promote the pathology specialty, and introducing CAP 15189 as a voluntary program. ISO 15189 was first published in 2003, offering information on the medical laboratory sector and outlining guidelines for sample procedures, results interpretation, reasonable turnaround times, patient sample collection, and the role of the laboratory in training and educating healthcare staff. It was revised in 2007 to conform with ISO/IEC 17205. A third edition was published in 2012, as depicted in Table 4 , which revised the prior layout and added a section on laboratory information management. ( 35 ) The effects of these changes on QI in clinical laboratories can be seen in our results in Fig. 2 from 2000 onwards, indicating a clear QI trend in medical laboratories.

Number of QI and QC papers per 5 years from 1981–2020. QC papers were the most published from 2001, indicating the gradual change of quality in clinical laboratory settings.
Table 4.
Introduction of accreditation agencies for the improvement of clinical laboratory
QI-MQCS as a psychometrically tool for quality publication
To determine the QI of clinical laboratory literature, we used the 16 domains of QI-MQCS. ( 21 ) Each paper was evaluated on these domains and scored on a scale of 0 to 16, with a score of 1 given if at least one reason was outlined. The QI papers generally followed the most domains. These papers were then classified by year of publication, and the average QI-MQCS score was determined. A substantial difference in QI-MQCS scores was detected in articles published between 2000 and 2020, as depicted in Fig. 3 . This disparity may be due to the implementation of laboratory QI standards and the accreditation of clinical laboratory facilities, which have been previously outlined.

This figure illustrates the scoring pattern of QI-MQCS concerning years of publication. The average score of QI-MQCS from 1981–2000 is 2.5, whereas, from 2001–2020, it is 6.8, which reveals the high quality of continuous enhancement in the clinical laboratory sector.
Limitations and strengths
One of the strengths of this analysis is its thorough analysis of all QI-related clinical laboratory papers. The clinical laboratory field is extensive and includes various subfields, but to our knowledge, only 12 reviews have previously addressed QI in the clinical laboratory. This research is the first to thoroughly evaluate all QI-related clinical laboratory papers in one review. There are some limitations to this research. Firstly, the lack of reporting or evaluation of clinical laboratory studies using QI-MQCS limits our comprehension of the QI process. Second, we assessed and scored all papers based on the 16 domains of QI-MQCS, even though some domains may not have been significant to medical laboratories ( Supplemental Table 2 * ). For example, spread (7%), sustainability (3%), penetration (3%), adherence/fidelity (7%), organizational readiness (11%), and intervention description (11%). This is because clinical laboratories do not typically entail delivering interventions or implementing evidence-based interventions in practice and do not usually require the analysis of performance measurements or process systems or developing connections between people.
The major function of the clinical laboratory is to offer diagnostic support to physicians, which can aid in the treatment process and contribute to further progress. However, the QI-MQCS was developed to help stakeholders determine high-quality studies in their field. QI techniques are diverse and distinct from clinical interventions, and the QI-MQCS is a psychometrically tested tool for evaluating the QI-specific characteristics of QI publications. This analysis has possible bias as it did not include other significant databases like Embase and EBSCOhost and only included articles in English.
This study investigated the trend and scope of QI and QC papers in clinical laboratory practice. Our findings revealed that the trend of QI and QC increased markedly after 2000, possibly due to the implementation of laboratory QI standards and the accreditation of clinical laboratory facilities. Our study emphasizes the importance of compliance with good clinical laboratory practice standards and the potential for collaboration between accredited and non-accredited organizations to enhance the quality management system and influence consistent improvement in the clinical laboratory sector.
Author Contributions
This research paper is the culmination of a joint effort between the author, the co-author YI, and the supervisor EN-Y. The study was conceptualized and designed through collaborative discussions between the author and the supervisor. The data collection process was a collaborative effort with significant contributions from YI, who provided valuable data visualization and analysis guidance. The supervisor was crucial in developing and refining the research framework, offering valuable insights that improved study conceptualization. The co-authors reviewed and revised the manuscript and provided critical feedback on presenting findings, including figures and tables.
Acknowledgments
We extend our heartfelt gratitude to the following colleagues for their invaluable contributions and support: Dr. Kaoru Nakatani, Mr. Nozomi Kamamemoto, Ms. Tomoko Honjo, and Mr. Atsushi Tokuwame. Additionally, we would like to acknowledge all those who have been a source of inspiration and motivation throughout the research process.
Abbreviations
Conflict of interest.
No potential conflicts of interest were disclosed.
Supplementary Material
Appointments at Mayo Clinic
Laboratory medicine and pathology.
Mayo Clinic staff members are actively engaged in research on several areas within Laboratory Medicine and Pathology. Mayo Clinic researchers continually study new and more efficient medical testing techniques and reflect their advances in tests offered internally at Mayo Clinic as well as externally though Mayo Clinic Laboratories .
Publications
See a list of publications by Mayo Clinic physicians on PubMed, a service of the National Library of Medicine.
Research profiles
Anatomic pathology.
- Keeney, Gary L. M.D. , Chair Minnesota
- Aubry, Marie Christine M.D. Minnesota
- Bell, Debra A. M.D. Minnesota
- Boland Froemming, Jennifer M. M.D. Minnesota
- Chen, Beiyun M.D., Ph.D. Minnesota
- Cheville, John C. M.D. Minnesota
- Cornell, Lynn D. M.D. Minnesota
- Erickson, Lori A. M.D. Minnesota
- Flotte, Thomas J. M.D. Minnesota
- Garcia, Joaquin J. M.D. Minnesota
- Giannini, Caterina M.D., Ph.D. Minnesota
- Grande, Joseph P. M.D., Ph.D. Minnesota
- Kipp, Benjamin R. Ph.D. Minnesota
- Maleszewski, Joseph J. M.D. Minnesota
- Mounajjed, Taofic M.D. Minnesota
- Roden, Anja C. M.D. Minnesota
- Salomao, Diva R. M.D. Minnesota
- Smyrk, Thomas C. M.D. Minnesota
- Visscher, Daniel W. M.D. Minnesota
- Yi, Joanne (Eunhee) E. M.D. Minnesota
- Zhang, Lizhi M.D. Minnesota
Clinical Biochemistry & Immunology
- Algeciras-Schimnich, Alicia Ph.D. , Chair Minnesota
- Baudhuin, Linnea M. Ph.D. Minnesota
- Black, John Logan M.D. Minnesota
- Grebe, Stefan K. M.D., Ph.D. Minnesota
- Klein, Christopher J. M.D. Minnesota
- Lachance, Daniel Honore M.D. Minnesota
- Lennon, Vanda A., M.D., Ph.D. Minnesota
- McKeon, Andrew M.B., B.Ch., M.D. Minnesota
- Pittock, Sean J. M.D. Minnesota
- Singh, Ravinder J. Ph.D. Minnesota
Clinical Core Laboratory Services
- Jaffe, Allan S. M.D. , Chair Minnesota
- Larson, Timothy S. M.D. Minnesota
Clinical Microbiology
- Patel, Robin M.D. , Chair Minnesota
- Pritt, Bobbi S. M.D. Minnesota
- Theel, Elitza S. Ph.D. Minnesota
- Wengenack, Nancy L. Ph.D. Minnesota
- Yao, Joseph D. M.D. Minnesota
Experimental Pathology and Laboratory Medicine
- Couch, Fergus J. Ph.D. , Chair Minnesota
- Cicek, Mine M. Ph.D. Minnesota
- Cunningham, Julie M. Ph.D. Minnesota
- Jen, Jin M.D., Ph.D. Minnesota
- Jenkins, Robert B. M.D., Ph.D. Minnesota
- Klee, George G. M.D., Ph.D. Minnesota
- Shridhar, Vijayalakshmi Ph.D. Minnesota
- Smith, David I. Ph.D. Minnesota
Hematopathology
- Chen, Dong M.D., Ph.D. Minnesota
- Feldman, Andrew L. M.D. Minnesota
- Hanson, Curtis A. M.D. Minnesota
- Heit, John A. M.D. Minnesota
- Kurtin, Paul J. M.D. Minnesota
- Macon, William R. M.D. Minnesota
- McPhail, Ellen D. M.D. Minnesota
- Pruthi, Rajiv K. M.B.B.S. Minnesota
- Rajkumar, S. Vincent M.D. Minnesota
Laboratory Genetics
- Matern, Dietrich M.D., Ph.D. , Chair Minnesota
Biochemical Genetics Laboratory
- Gavrilov, Dimitar K. M.D., Ph.D. Minnesota
- Matern, Dietrich M.D., Ph.D. Minnesota
- Oglesbee, Devin Ph.D. Minnesota
- Rinaldo, Piero M.D., Ph.D. Minnesota
- Tortorelli, Silvia M.D., Ph.D. Minnesota
Cytogenetics Laboratory
- Greipp, Patricia T. D.O. Minnesota
- Ketterling, Rhett P. M.D. Minnesota
- Thorland, Erik C. Ph.D. Minnesota
- Van Dyke, Daniel L. Ph.D. Minnesota
Molecular Genetics Laboratory
- Ferber, Matthew J. Ph.D. Minnesota
- Halling, Kevin C. M.D., Ph.D. Minnesota
- Rumilla, Kandelaria M. M.D. Minnesota
Transfusion Medicine
- Dietz, Allan B. Ph.D. Minnesota
- Gandhi, Manish J. M.D. Minnesota
- Santrach, Paula J. M.D. Minnesota
- Winters, Jeffrey L. M.D. Minnesota
- Medical Departments & Centers
- Laboratory Medicine & Pathology
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
- Search Menu
- Advance articles
- COVID-19 articles
- Editor's Choice
- CME/SAM Articles
- Author Guidelines
- Open Access
- Submission Site
- Why publish?
- Advertising and Corporate Services
- Advertising
- Reprints and ePrints
- Sponsored Supplements
- Branded Books
- About American Journal of Clinical Pathology
- About the American Society for Clinical Pathology
- Editorial Board
- Self-Archiving Policy
- Journals on Oxford Academic
- Books on Oxford Academic

Article Contents
Materials and methods, conclusions.
- < Previous
The Value of Artificial Intelligence in Laboratory Medicine: Current Opinions and Barriers to Implementation
- Article contents
- Figures & tables
- Supplementary Data
Ketan Paranjape, Michiel Schinkel, Richard D Hammer, Bo Schouten, R S Nannan Panday, Paul W G Elbers, Mark H H Kramer, Prabath Nanayakkara, The Value of Artificial Intelligence in Laboratory Medicine: Current Opinions and Barriers to Implementation, American Journal of Clinical Pathology , Volume 155, Issue 6, June 2021, Pages 823–831, https://doi.org/10.1093/ajcp/aqaa170
- Permissions Icon Permissions
As laboratory medicine continues to undergo digitalization and automation, clinical laboratorians will likely be confronted with the challenges associated with artificial intelligence (AI). Understanding what AI is good for, how to evaluate it, what are its limitations, and how it can be implemented are not well understood. With a survey, we aimed to evaluate the thoughts of stakeholders in laboratory medicine on the value of AI in the diagnostics space and identify anticipated challenges and solutions to introducing AI.
We conducted a web-based survey on the use of AI with participants from Roche’s Strategic Advisory Network that included key stakeholders in laboratory medicine.
In total, 128 of 302 stakeholders responded to the survey. Most of the participants were medical practitioners (26%) or laboratory managers (22%). AI is currently used in the organizations of 15.6%, while 66.4% felt they might use it in the future. Most had an unsure attitude on what they would need to adopt AI in the diagnostics space. High investment costs, lack of proven clinical benefits, number of decision makers, and privacy concerns were identified as barriers to adoption. Education in the value of AI, streamlined implementation and integration into existing workflows, and research to prove clinical utility were identified as solutions needed to mainstream AI in laboratory medicine.
This survey demonstrates that specific knowledge of AI in the medical community is poor and that AI education is much needed. One strategy could be to implement new AI tools alongside existing tools.
Artificial intelligence (AI) is used in 15.6% of the organizations while 66.4% felt they might use AI in the future. Key uses of AI include diagnostics, review risk profile of patients, laboratory results, and financial analytics.
To implement AI, the laboratory community will need education on the technology and usage, as well as research into generating clinical evidence and addressing implementation challenges.
We believe AI in laboratory medicine can help with reducing health care costs, improve access to generate better insights, and enhance the quality of care delivered to the patient.
Advances in our understanding of biology, disease, and molecular medicine have created a central role for laboratory medicine in the diagnostic workup of many, if not most, diseases. It is estimated that 70% of decisions regarding a patient’s diagnosis, treatment, and discharge are in part based on results of laboratory tests. 1 Unfortunately, the main cause of medical errors in the United States is inaccurate diagnosis. 2-5 The ever-increasing workload, high health care costs, and need for improved precision call for continuous optimization of the laboratory processes. 6 With both health care and laboratory medicine 7 transitioning into an era of big data and artificial intelligence (AI), the ability to provide accurate, readily available, and contextualized data is crucial. AI in health care is the use of complex algorithms and software to emulate human cognition in the analysis of complicated medical data generated from diagnostics, medical records, claims, clinical trials, and so on. AI algorithms can only properly function with reliable and accurate laboratory data. 8 Automation and AI can fundamentally change the way medicine is practiced, as demonstrated by the recent applications in ophthalmology 9 and dermatology. 10 Some possible applications of AI specific to laboratory medicine are presented in Table 1 . With the increasing role of laboratory medicine in many diseases, AI has the potential to improve diagnostics through more accurate detection of pathology, better laboratory workflows, improved decision support, and reduced costs, leading to higher efficiencies. 8 , 11 , 12
Baseline Characteristics of Survey Respondents (n = 128)
AI, artificial intelligence.
As laboratory medicine continues to undergo digitalization and automation, clinical laboratorians will likely be confronted with the challenges associated with evaluating, implementing, and validating AI algorithms, both inside and outside their laboratories. Understanding what AI is good for and where it can be applied, along with the state-of-the-art and limitations, will be useful to practicing laboratory professionals and clinicians. On the other hand, the introduction of new technologies requires willingness to change the current structure and mindset toward these technologies, which are not always well understood. Historically, there has been resistance to the adoption of new technologies in the medical community. 13
With a web-based survey among stakeholders in laboratory medicine in the United States, we aimed to evaluate their current perspectives on the value of AI in the diagnostics space and identify anticipated challenges with the introduction of AI in this field, as well as resistance to introduction of this new technology in today’s practice.
Today, AI is occasionally used in laboratory medicine for enabling the effective use of resources, avoiding unnecessary tests, improving patient safety, and alerting for abnormal results. 14-18 AI is also being used in limited clinical usage for molecular/genomic testing 19-21 by accurately identifying variants and matching it to possible treatments.
Survey Development
A web-based survey on the use of AI in laboratory medicine was designed in several independent steps. First, 98 stakeholders participated in a 2-week online discussion board on AI in diagnostics in August 2019. These participants were part of Roche’s Strategic Advisory Network (SAN), a group consisting of laboratory medicine decision makers, practicing physicians and surgeons, point-of-care coordinators, anatomic pathologists, laboratory management, information technology (IT) management, and senior leadership. Roche does not know the identity of the community members to protect their privacy. The online discussion board was moderated by C-space and developed questions to gain insights on potentially important topics to discuss in the survey. Open-ended as well as multiple-choice questions were formulated based on content of the discussion board.
Next, two 1-hour online group chats were organized on October 2 and 3, 2019, to discuss these questions and fine-tune their phrasing and to refine the answer possibilities to the multiple-choice questions. In these group chats, a total of 11 practitioners in laboratory medicine were asked to answer the initial survey questions one at the time, after which they could comment on each other’s answers and discuss their opinions on and interpretations of the questions.
This thoroughly discussed survey was fielded to a group of 302 laboratory medicine practitioners who are part of SAN via email. These individuals were both available for completing surveys and in a position to decide on embracing or refraining from using technologies such as AI in their respective organizations. The survey was available from October 21 until November 1, 2019. The data were collected using a software platform called Confirmit, and all participants gave informed consent for their input to be used for research purposes.
Finally, as there are multiple different definitions of AI, for the sake of the survey we defined AI as follows: “ Artificial intelligence (AI) in health care is the use of complex algorithms and software to emulate human cognition in the analysis of complicated medical data generated from diagnostics, medical records, claims, clinical trials, and so on. AI is truly the ability for computer algorithms to approximate conclusions without direct human input.”
In the survey, we posed 21 questions that ranged from collecting demographic information to answering questions about if the respondents used AI in their organizations, what kind of improvements they would like to see in the current use of AI, how valuable they think AI will be in their practice, and what challenges they feel exist. A full list of all the questions can be found in the Supplement (all supplemental material can be found at American Journal of Clinical Pathology online).
Data Analysis
Quantitative data.
Categorical data were analyzed using a Pearson χ 2 test, considering a P value less than .05 to be statistically significant. The perceived value of AI was compared for different age groups and different experience levels with AI. The analyses were performed in Microsoft Excel. Data from the multiple-choice questions were presented as percentages per category.
The number of participants who could be reached was highly dependent on the number of available advisers in the SAN network. With 302 available advisers and an acceptable response rate of above 40%, we got responses from 128 participants. The study was powered to detect a 20% difference across subgroups in how they valued AI.
Qualitative Data
An inductive approach 22 of direct content analysis was used to analyze the open-ended questions. First, two researchers, B.S. (psychologist) and M.S. (internal medicine doctor), independently screened the answers and drafted a rough framework of themes. After consensus on the overarching themes, answers were independently coded with this framework by both researchers. Then conflicts were resolved by consensus to account for different interpretations of the answers. Coding was performed and bar charts were created in Excel.
Demographics
The survey was fielded to 302 stakeholders in laboratory medicine, of whom 128 (42%) responded. The modal age group was aged between 41 and 50 years (32.0%), while 23 (18.0%) of the respondents were younger than 41 years. The top three participants were physicians, laboratory managers, and pathologists. See Table 1 for further details on demographic information.
Qualitative Analysis
Based on the data, six main themes were derived (attitude, quality of care, organizational value, data analysis, prerequisites, and education). The “attitude” theme was further categorized into three subthemes (positive, unsure, and negative). To prevent losing valuable information, multiple themes could be assigned to an answer. The specific content of these themes is presented in Table 2 , as well as in subsequent paragraphs, along with quotes from the survey participants. It should be noted that the attitude theme could be interpreted as being a separate sentiment analysis. However, this is not the case. Attitude was merely a theme in which many answers could be categorized according to both researchers.
List of Six Themes Derived From the Survey
AI, artificial intelligence; IT, information technology.
In 173 (73%) of the 237 coded cases, there was an initial agreement on the codes to be assigned. In 64 (27%) cases, when there was a discrepancy between codes assigned by the two different coders, an extensive consensus procedure was followed. This resulted in a 100% agreement between coders after this consensus procedure.
Current Uses of AI in Laboratory Medicine
AI is currently used in the organizations of 20 (15.6%; 95% confidence interval [CI], 9.8%-23.1%) of the participants, while 85 (66.4%; 95% CI, 57.5%-74.5%) felt they might use it in the future and 8 (6.3%; 95% CI, 2.7%-11.9%) felt that they would never use AI. Respondents who have AI in their practice use it for diagnosing diseases from images (30%), reviewing patients’ risk profiles for certain conditions (40%), preempting rapid response solutions (30%), and automatically releasing laboratory results and financial analytics (10%). Examples of specific use cases include AI to perform digital cell analysis for peripheral blood, analyze medical record laboratory data to determine which patients are at risk of infection, improve patients’ outcomes and length of stays and readmissions, or preempt rapid response situations in hospitals and automated sepsis alerts to identify patients early.
When asked how respondents felt that these current applications could be improved, most of them answered that certain prerequisites (eg, user interface, IT support, and better software) were needed. All 20 participants who currently use AI answered this question; see Figure 1 for counts against themes. For example, respondent 119 answered, “reduce the number of pop-ups in the EMR [electronic medical record],” and respondent 70 said, “We use AI for chatbots about common questions for diagnostics. The AI chatbots are not very intelligent. Need to make AI smarter.”

Answers to the survey question “How can current AI applications in your organization be improved?”—categorized as counts per theme. AI, artificial intelligence.
Value of AI in Practice
Regarding the potential use of AI in the diagnostics space, of the 90 (81%; 95% CI, 72.6%-87.9%) participants who felt AI will be valuable in their organization within the next 5 years, 20 (18%; 95% CI, 11.4%-26.5%) labeled it as expected to be extremely valuable. Twenty-one (19%; 95% CI, 12.1%-27.5%) of the respondents felt like AI will not be valuable in their organization within the next 5 years. There were missing data on this question for 17 participants. To further examine whether the results were different in subgroups of respondents, we dichotomized the answers to finding AI valuable (including extremely valuable, very valuable, and somewhat valuable; n = 90) or not valuable at all (n = 21). A χ 2 test showed no significant difference in how participants in the different age groups valued AI in the diagnostics space (χ 2 = 5.0947 [4 degrees of freedom]; P = .28). Also, there was no significant difference in how AI was valued between respondents who currently use AI in their practice (n = 17) compared with respondents who have not used it yet (χ 2 = 0.6698 [1 degree of freedom]; P = .41). Table 3 shows the number of respondents to find AI valuable or not valuable in the different subgroups.
Categorized Subgroup Results for Finding AI Valuable or Not Valuable in the Diagnostics Space a
a Percentage calculated row-wise.
Respondents were also given the opportunity to elaborate on why they thought AI would or would not be valuable in their organizations. A plethora of reasons were given, and all were coded by theme, as shown in Figure 2 . Most answers indicated that AI could be valuable because of the “organizational value” (eg, quicker results, reduced redundancy, and resource management). As an example, respondent 87 answered, “it could make the lab more efficient by streamlining work flow.” Another frequently reported theme was “quality of care” (eg, accessibility of care, accuracy, and early recognition). This was illustrated by respondent 100, who said, “might help in keeping patients informed of test results/appointments/follow up more efficiently,” and respondent 47 believed “could have some useful clinical algorithms to identify problems before they are known by humans, but the technology is still in early development.” Another substantial part of respondents, who thought AI would be valuable, were not sure about the reasons for this (“attitude—unsure”), as suggested by respondent 68: “I’m not entirely sure, I just know something is there!”

Answers to the survey question “Why will AI be valuable in your organization?”—categorized as counts per theme. AI, artificial intelligence.
Not Valuable
The 19% (95% CI, 12.1%-27.5%) of respondents who did not consider AI to be valuable in their organizations in the next 5 years had more uniform responses. The answers were largely split between the themes’ “prerequisites” (eg, budget and strategic plan) and an unsure attitude. See Figure 3 for more details. The missing prerequisites, for example, were presented by respondent 47: “very expensive and we have very limited capital dollars that we need to use to refresh old technology,” and respondent 106 said, “it’s not in our strategic plan to implement AI at this time.” The unsure attitude toward AI was summed up by respondent 75: “I’m not sure about the use of AI.”

Answers to the survey question “Why will AI not be valuable in your organization?”—categorized as counts per theme. AI, artificial intelligence.
Requirements for Implementing AI
Participants were asked what they would need to feel comfortable with using AI in the diagnostics space. Most respondents had an “unsure attitude” toward what they needed most to adopt AI in their practice. For example, respondent 69 said, “this seems like too forward thinking of a question that we aren’t yet prepared to answer.” Others felt like they need education (eg, specific to tools and on AI in general). Respondent 40 answered “specific training to device” and respondent 46 said “AI short course training.” Most of the remaining group felt like they needed various prerequisites (eg, support systems, certifications, and evidence of benefits) to feel comfortable to adopt AI in their practice. There were missing data for 23 of the participants; see Figure 4 for the counts per theme.

Answers to the survey question “What requirements are necessary in order for you to feel more comfortable with adopting AI?”—categorized as counts per theme. AI, artificial intelligence.
In the next question, participants were asked to specify how they would like to be trained to use AI. Twenty-three (22%) of 105 (95% CI, 14.4%-31.0%) participants felt that they were not able to speak to how they should be educated on these new technologies.
Finally, we asked participants to select persons within their organizations who they felt should be involved in the selection of AI equipment. Up to 10 individuals across an organization were identified who could be involved in evaluating a potential AI diagnostic solution. Respondent 56 said, “Medical staff committees and physicians and mid-level providers that use AI, utilization review staff that monitor provider performance, IT department and leadership that maintain AI software.”
With this survey, we aimed to evaluate the thoughts of stakeholders in laboratory medicine on the value of AI in the diagnostics space and identify anticipated challenges with the introduction of AI in this field. About four in five respondents believed AI will be valuable in their organization within the next 5 years, mostly because of organizational and patient-oriented benefits. One in five respondents do not see any value in AI, which is often because of the lack of prerequisites such as budget for the implementation and not being adopted as part of an overall strategic initiative. Maybe this is because of the bias management might have toward AI.
The Value of AI
The quantitative results in this survey are similar to those found in surveys on this subject among other health care professionals. Similar to our findings, surveys on AI for pathologists, 23 medical students, 24 physicians, 25 and radiologists 26 all found that about 80% of participants believe AI will be influential or valuable in their practice in the upcoming years. Interestingly enough, a 2019 survey shows that 84% of the general population in the United States thinks that AI will be at the center of the next technological revolution. 27
All surveys on this subject in the medical community seem to show similar results regarding the perceived value of AI, independent of age or experience with AI in clinical practice. The fact that these results also overlap with the value of AI as perceived by the general population raises concerns that specific knowledge on this subject has not yet penetrated the medical community at large and that the surveys on this subject just reflect the ongoing AI hype. Our survey adds to this concern by showing that many respondents are unsure about why AI would or would not be valuable, what is needed to comfortably adopt AI, or how to be educated on AI.
There certainly seems to be a disconnect between the more positive views of information experts on AI and views of the medical community. 28 To get all the benefits AI presents, while keeping its drawbacks to a minimum, drastic changes are needed in the medical community. There is a need for general AI training to the various health care stakeholders as identified in a recent publication on the need to introduce AI training in medical education. 29 In the meantime, training on new AI tools should also be the responsibility of the companies who provide the algorithms through extensive web-based training, along with on-site hands-on training.
Health Care Costs
Another highlight from this survey was the potential of AI to target high health care expenditure, since it can reduce and replace repetitive manual labor. Recent study has shown that AI can help reduce the waste in the US health care system in the range from $760 billion to $935 billion in 2019. 30 Respondents believe AI can make the diagnostics process more efficient and decrease costs. 1 For example, safely reducing the number of laboratory tests ordered or the frequency of ordering repeat tests is illustrated with a quote from respondent 94: “Alert me to the fact that a lab test I ordered was already completed at another hospital system in the past week.”
Impact on Jobs
Finally, we learned from the discussion board conducted prior to developing the survey that advisers also mentioned that they know AI is rapidly increasing in importance and value and want it to evolve their roles rather than replace them. 31 “AI will become an integral concept for health care. Whether diagnosis or process improvement in medicine, AI will impact the industry. For personalized medicine and improving diagnostic accuracy AI will drive decision making in the hands of providers,” said respondent 12, an executive at a large integrated health network. Laboratory managers similarly think that AI could create efficiencies that expedite their workflows but want to ensure that they are still in control. Respondent 31 believes, “AI needs to be used in the right spaces and not to eliminate med techs but to supplement them.”
Implementation Strategies
In this survey, 19% of respondents did not see the added value of implementing AI in laboratory medicine, partially because of the high initial investment costs. This will be a limiting factor as long as the return on investment and clinical benefits of these tools are not well understood. A recent narrative review on the clinical applications of AI for sepsis validates this idea by identifying that a large gap still remains between the development of AI algorithms and their clinical implementation. 32 The question remains whether this gap between development and clinical implementation might be caused by the resistance to implementing new technologies. Unfortunately, this can hold back research on this subject and thereby delay the gathering of evidence on whether AI tools can be beneficial and cost-effective in clinical practice on a large scale.
Although it was not mentioned in the survey itself, an interesting strategy to implement AI in laboratory medicine was discussed in one of the group chats that was used to shape the final survey. One of the participants disclosed that in their hospital, a new AI tool was introduced alongside an existing tool that was used in routine clinical practice. The old tool was still used but as a backup for when the AI tool failed. Practitioners were encouraged to try the AI tool but could choose either of the available options. They gradually got familiar with the AI tool and could see the added value firsthand. They ended up switching to the AI tool completely. This illustrates a viable way to integrate AI tools in health care. Although more expensive, this provides an opportunity to compare these tools in practice and allow the practitioners to feel comfortable with the tool before having to rely on it completely. See Table 4 for our key recommendations.
Key Recommendations for Implementing AI in Laboratory Medicine
Patient Viewpoint
The overarching goal of implementing AI in clinical practice is to benefit the patient. Therefore, the patient’s perspective should also be discussed. One of the respondents posed an interesting question in the online group chat: “Should the patients be informed that some of the decisions are being recommended by AI?” Another question is whether we should inform patients when an AI recommendation is not followed. Unfortunately, this burdens the patient as they now have to choose between the physician and the computer. Many algorithms are already being used in medicine, like the YEARS criteria 33 for pulmonary embolisms. Their role in the diagnostic process is rarely explained to or discussed with the patient, as only trained physicians can interpret the results of these algorithms. We therefore believe that a similar approach might be best when using more advanced algorithms, in which explainability and interpretation are an even larger problem. These tools and algorithms are an aid to complement the health care practitioners who are eventually responsible for the diagnostic process and decision making. Finally, from a provider’s viewpoint, they will need to know details of the algorithms they use to make decisions.
Strengths of the Survey
We addressed a target population of participants who are currently in a position to influence organizational policies to either embrace new technologies or refrain from using them in their laboratories. Any specific intervention to encourage the introduction of AI in the diagnostics space should be tailored to such a population of decision makers. Another strength is that the results were independently analyzed by two researchers with different backgrounds, thereby minimalizing the chance of interpretation bias. Finally, the questions were extensively scrutinized in the initial discussion board and group chats prior to fielding the final survey.
Limitations of the Survey
The participants did not represent the entire population of practitioners who will be using AI in a diagnostic setting. We cannot generalize these findings to all laboratory medicine practitioners across multiple types of settings. Finally, the study population (n = 128) was relatively small for quantitative analyses, perhaps causing the nonsignificance of the χ 2 tests. Only a large difference in how AI was valued between groups would have shown significant results in the quantitative analysis.
This survey shows that many stakeholders in laboratory medicine think that AI will be valuable to them in the near future, mostly given the “organizational value” and expected improvements in “quality of care,” although vital prerequisites such as support systems, strategic plans, and budgets need to be provided. The overall response to this and other similar surveys raises the concern that specific knowledge on AI in the medical community at large is still poor. AI education in the medical community is much needed. As suggested by one respondent, one strategy to the implement new AI tools could be to implement it alongside existing tools, so that practitioners can feel comfortable with the new tools and experience their added value in practice firsthand while awaiting further research studies on the clinical evidence, implementation, and benefits of AI.
Roche funded the C-space consultancy.
Ketan Paranjape wrote this article as part of his PhD studies. He is a vice president at Roche. There is no conflict of interest with his employment at Roche.
Badrick T . Evidence-based laboratory medicine . Clin Biochem Rev. 2013 ; 34 : 43 - 46 .
Google Scholar
Makary MA , Daniel M . Medical error—the third leading cause of death in the US . BMJ. 2016 ; 353:i2139 .
Institute of Medicine Committee on Quality of Health Care in America. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System . Washington, DC : National Academies Press ; 2000 .
Google Preview
Brennan TA , Leape LL , Laird NM , et al. Incidence of adverse events and negligence in hospitalized patients . N Engl J Med. 1991 ; 324 : 370 - 376 .
Leape LL , Brennan TA , Laird N , et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II . N Engl J Med. 1991 ; 324 : 377 - 384 .
Naugler C , Church DL . Automation and artificial intelligence in the clinical laboratory . Crit Rev Clin Lab Sci. 2019 ; 56 : 98 - 110 .
Tizhoosh HR , Pantanowitz L . Artificial intelligence and digital pathology: challenges and opportunities . J Pathol Inform. 2018 ; 9 : 38 .
Cabitza F , Banfi G . Machine learning in laboratory medicine: waiting for the flood? Clin Chem Lab Med. 2018 ; 56 : 516 - 524 .
Gulshan V , Peng L , Coram M , et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs . JAMA. 2016 ; 316 : 2402 - 2410 .
Esteva A , Kuprel B , Novoa RA , et al. Dermatologist-level classification of skin cancer with deep neural networks . Nature. 2017 ; 542 : 115 - 118 .
Zhang Z . The role of big-data in clinical studies in laboratory medicine . J Lab Precis Med. 2017 ; 2 : 34 - 34 .
Durant T . Machine learning and laboratory medicine: now and the road ahead. 2019 . https://www.aacc.org/publications/cln/articles/2019/march/machine-learning-and-laboratory-medicine-now-and-the-road-ahead . Accessed April 17, 2020.
Safi S , Thiessen T , Schmailzl KJ . Acceptance and resistance of new digital technologies in medicine: qualitative study . JMIR Res Protoc. 2018 ; 7 : e11072 .
Cismondi F , Celi LA , Fialho AS , et al. Reducing unnecessary lab testing in the ICU with artificial intelligence . Int J Med Inform. 2013 ; 82 : 345 - 358 .
Gunčar G , Kukar M , Notar M , et al. An application of machine learning to haematological diagnosis . Sci Rep. 2018 ; 8 : 411 .
Gruson D , Helleputte T , Rousseau P , et al. Data science, artificial intelligence, and machine learning: opportunities for laboratory medicine and the value of positive regulation . Clin Biochem. 2019 ; 69 : 1 - 7 .
Li L , Georgiou A , Vecellio E , et al. The effect of laboratory testing on emergency department length of stay: a multihospital longitudinal study applying a cross-classified random-effect modeling approach . Acad Emerg Med. 2015 ; 22 : 38 - 46 .
Garcia E , Kundu I , Ali A , et al. The American Society for Clinical Pathology’s 2016-2017 vacancy survey of medical laboratories in the United States . Am J Clin Pathol. 2018 ; 149 : 387 - 400 .
Xu J , Yang P , Xue S , et al. Translating cancer genomics into precision medicine with artificial intelligence: applications, challenges and future perspectives . Hum Genet. 2019 ; 138 : 109 - 124 .
Serag A , Ion-Margineanu A , Qureshi H , et al. Translational AI and deep learning in diagnostic pathology . Front Med (Lausanne). 2019 ; 6 : 185 .
Dias R , Torkamani A . Artificial intelligence in clinical and genomic diagnostics . Genome Med. 2019 ; 11 : 70 .
Thomas DR . A general inductive approach for analyzing qualitative evaluation data . Am J Eval. 2006 ; 27 : 237 - 246 .
Sarwar S , Dent A , Faust K , et al. Physician perspectives on integration of artificial intelligence into diagnostic pathology . NPJ Digit Med. 2019 ; 2 : 28 .
Pinto Dos Santos D , Giese D , Brodehl S , et al. Medical students’ attitude towards artificial intelligence: a multicentre survey . Eur Radiol. 2019 ; 29 : 1640 - 1646 .
Oh S , Kim JH , Choi SW , et al. Physician confidence in artificial intelligence: an online mobile survey . J Med Internet Res. 2019 ; 21 : e12422 .
Collado-Mesa F , Alvarez E , Arheart K . The role of artificial intelligence in diagnostic radiology: a survey at a single radiology residency training program . J Am Coll Radiol. 2018 ; 15 : 1753 - 1757 .
Edelman. 2019 Artificial Intelligence Survey. https://www.edelman.com/research/2019-artificial-intelligence-survey . Accessed December 22, 2019 .
Blease C , Bernstein MH , Gaab J , et al. Computerization and the future of primary care: a survey of general practitioners in the UK . PLoS One. 2018 ; 13 : e0207418 .
Paranjape K , Schinkel M , Nannan Panday R , et al. Introducing artificial intelligence training in medical education . JMIR Med Educ. 2019 ; 5 : e16048 .
Shrank WH , Rogstad TL , Parekh N . Waste in the US health care system . JAMA. 2019 ; 322 : 1501 .
Obermeyer Z , Emanuel EJ . Predicting the future—big data, machine learning, and clinical medicine . N Engl J Med. 2016 ; 375 : 1216 - 1219 .
Schinkel M , Paranjape K , Panday RSN , et al. . Clinical applications of artificial intelligence in sepsis: a narrative review . Comput Biol Med. 2019 ;115: 103488 .
van der Hulle T , Cheung WY , Kooij S , et al. ; YEARS Study Group . Simplified diagnostic management of suspected pulmonary embolism (the YEARS study): a prospective, multicentre, cohort study . Lancet. 2017 ; 390 : 289 - 297 .
Yuan C , Ming C , Chengjin H . UrineCART, a machine learning method for establishment of review rules based on UF-1000i flow cytometry and dipstick or reflectance photometer . Clin Chem Lab Med. 2012 ; 50 : 2155 - 2161 .
Putin E , Mamoshina P , Aliper A , et al. Deep biomarkers of human aging: application of deep neural networks to biomarker development . Aging (Albany NY). 2017 ; 8 : 1021 - 1033 .
Razavian N , Blecker S , Schmidt AM , et al. Population-level prediction of type 2 diabetes from claims data and analysis of risk factors . Big Data. 2015 ; 3 : 277 - 287 .
Nelson DW , Rudehill A , MacCallum RM , et al. Multivariate outcome prediction in traumatic brain injury with focus on laboratory values . J Neurotrauma. 2012 ; 29 : 2613 - 2624 .
Lin C , Karlson EW , Canhao H , et al. Automatic prediction of rheumatoid arthritis disease activity from the electronic medical records . PLoS One. 2013 ; 8 : e69932 .
Liu KE , Lo CL , Hu YH . Improvement of adequate use of warfarin for the elderly using decision tree-based approaches . Methods Inf Med. 2014 ; 53 : 47 - 53 .
Supplementary data
Email alerts, citing articles via.
- Recommend to your Library
Affiliations
- Online ISSN 1943-7722
- Print ISSN 0002-9173
- Copyright © 2024 American Society for Clinical Pathology
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Accessibility
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
Masks Strongly Recommended but Not Required in Maryland, Starting Immediately
Due to the downward trend in respiratory viruses in Maryland, masking is no longer required but remains strongly recommended in Johns Hopkins Medicine clinical locations in Maryland. Read more .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
Find a Research Lab
Featured research topics.
- Clinical Trials
- Neurological Disorders
- Brain Science Institute
- Institute for Basic Biomedical Sciences (IBBS)
- Institute for Cell Engineering (ICE)
- Institute for Clinical and Translational Research (ICTR)
- Institute for Computational Medicine (ICM)
- Institute for Genetic Medicine (IGM)
Participate in a Clinical Trial at Johns Hopkins
- Search all Clinical Trials
- Search Cancer Clinical Trials
Resources for: Medical Laboratory Science

- MEDLINE (Ovid) Searches MEDLINE, which is the primary source of journal articles for the health sciences (fields of medicine, nursing, dentistry, veterinary medicine, public health, health care systems, and basic sciences). Ovid MEDLINE is optimized for advanced literature searches. Coverage is from the 1940s to the present.
- PubMed Searches MEDLINE, which is the primary source of journal articles for the health sciences (fields of medicine, nursing, dentistry, veterinary medicine, public health, health care systems, and basic sciences). Coverage is from the 1940s to the present. View this tutorial to learn how to go from a general idea to a very precise set of results of journal articles and scholarly materials.
- CINAHL Ultimate (Nursing & Allied Health) Covers nursing and allied health journal articles, book chapters, and dissertations, as well as providing summarized evidence-based resources such as care sheets and quick lessons.
- Current Protocols Current Protocols is a collection of updatable, step-by-step, reproducible laboratory methods.
- Google Scholar (Setup connection to get to PDFs) Use Google Scholar to find articles from academic publishers, professional societies, research institutes, and scholarly repositories from colleges and universities. If you are using from off-campus access, change the "Library Settings" to University of Minnesota Twin Cities. Look for the "FindIt@U of M Twin Cities" links in your Google Scholar search results to access full text and PDFs. View this tutorial to learn how to go from a general idea to a very precise set of results of journal articles and scholarly materials.
- Merck Index: An Encyclopedia of Chemicals, Drugs, and Biologicals Classic reference source for chemists with over 10,000 entries on drugs and pharmaceuticals, common organic chemicals and laboratory reagents. The entries include data such as chemical names, molecular formula, chemical structure, physical data, and literature references.
- SciFinder-n SciFinder-n is the updated version of SciFinder and is the best database for topics related to chemistry and adjacent fields. It includes journal articles, book chapters, dissertations, and patents. Find substance and reaction information as well as suppliers and chemical regulatory data. more... less... Registration is required, and you must download the Virtual Private Network (VPN) from UMN Office of Information Technology, set up new account if you don't have one and then log in to it for off-campus access.
E-Books in Medical Laboratory Science
E-books available at the University of Minnesota Libraries. Requires authentication/log-in with current University internet ID and password.
Journals in Medical Laboratory Science
Selected list of Journals in Medical Laboratory Science and related disciplines. Requires a current University of Minnesota internet ID and password to access. See library catalog for more titles.
Clinical laboratory science (Online). (1988). The Society.
Annals of clinical and laboratory science (Online). (1971). Association of Clinical Scientists.
Laboratory medicine (Online). (1970). [American Society of Clinical Pathologists, etc.].
Archives of pathology & laboratory medicine (Online). (1976). College of American Pathologists.
Clinical chemistry. (1955). P.B. Hoeber.
Alternatives to laboratory animals : ATLA . (1981). FRAME.
Microscopy research and technique (Online). (1992). Wiley-Liss.
Journal of clinical laboratory analysis (Online). (1987). [Alan R. Liss].
Journal of clinical microbiology . (1975). American Society for Microbiology.
Journal of clinical pathology (Online). (1947). British Medical Association.
Selected Internet Resources
Freely available selected internet resources on laboratory tests and clinical laboratory medicine
- PubChem : PubChem is an open chemistry database at the National Institutes of Health (NIH) . PubChem is the world's largest collection of freely accessible chemical information. Search chemicals by name, molecular formula, structure, and other identifiers. Find chemical and physical properties, biological activities, safety and toxicity information, patents, literature citations and more.
- Medical Tests: List of common medical tests, including iwhat the tests are used for, why a doctor may order a test, how a test will feel, and what the results may mean.
- Laboratory Tests : Set of resources aimed at the consumer
- Testing.com (formerly LabTestsOnline.org): Testing.com is a health information digital resource designed to help people understand the many lab tests that are a vital part of health care. The site contains a library of over 400 expert-reviewed guides on specific lab tests and laboratory topics.
- Clinical Laboratory Improvement Amendments (CLIA) : The Clinical Laboratory Improvement Amendments of 1988 (CLIA) regulations include federal standards applicable to all U.S. facilities or sites that test human specimens for health assessment or to diagnose, prevent, or treat disease.
Normal Laboratory Values (Merck Manual, Professional)
Normal Laboratory Values: Blood, Plasma, and Serum
Normal Laboratory Values: Urine
Normal Laboratory Values: CSF
Normal Laboratory Values: Stool
Normal Laboratory Values: Other
Commonly Used Panels
Bayot ML, Lopes JE, Naidoo P. Clinical Laboratory. [Updated 2022 Dec 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-.
Minnesota State Resources
- Environmental Laboratory
Clinical Guide to Services - List of Tests
- Newborn Screening Laboratory
- Laboratory Emergency Preparedness
- UNC Chapel Hill
What is Clinical Laboratory Science?
Clinical Laboratory Science, also called Medical Laboratory Science or Medical Technology, is the health profession that provides laboratory information and services needed for the diagnosis and treatment of disease. Clinical Laboratory Scientists perform a variety of laboratory tests, ensure the quality of the test results, explain the significance of laboratory tests, evaluate new methods and study the effectiveness of laboratory tests. Examples of laboratory tests performed by Clinical Laboratory Scientists include:

- the detection of the abnormal cells that cause leukemia
- the analysis of cardiac enzyme activity released during a heart attack
- the identification of the type of bacteria causing an infection
- the detection of DNA markers for genetic diseases
Molecular Diagnostic Science is a specialized area of Clinical Laboratory Science that uses sensitive and specific techniques to detect and identify biomarkers at the most basic level: that of nucleic acids (DNA and RNA). Common applications of molecular methods include medical diagnosis, establishing prognosis, monitoring the course of disease, and selecting optimal therapies. Molecular methods are also used in both forensic and non-forensic identification. A variety of biological materials can be used for molecular testing including fetal cells from amniotic fluid, dried blood spots from newborn screening programs, blood samples, buccal (mouth) swabs, bone, and hair follicles.
Molecular diagnostic tests are increasingly used in many major areas of medicine including genetic disorders, infectious diseases, cancer, pharmacogenetics and identity testing. Examples include:
- Genetic disorders: Molecular methods are used to detect common inherited diseases such as cystic fibrosis, hemochromatosis, and fragile X syndrome.
- Infectious diseases: Many diseases – including hepatitis, tuberculosis, human immunodeficiency virus (HIV), human papilloma virus (HPV), Chlamydia, Neisseria gonorrhoeae, and methicillin-resistant Staphylococcus aureus (MRSA) – can be identified faster and more accurately using molecular techniques as compared to traditional culture or antibody assays.
- Cancer: Some leukemias and solid tumor cancers can be detected and identified by molecular probes which target the abnormal gene rearrangements occurring in these disorders.
- Pharmacogenetics. Molecular testing can be used to individualize a specific dosing schedule for patients on a common blood thinner, warfarin, and thereby reduce the likelihood of overmedication and potential bleeding problems.
- Identity testing: Molecular diagnostic tests are used in determining the identity of combat casualties, in analyzing crime scene evidence, in determining paternity, and identifying foreign DNA in transplantation medicine.
These examples are only a small sample of the many clinical and other applications of molecular testing methods.
Vignettes of the Profession of Clinical Laboratory Science [ pdf file ] by Barbara Thornton, CLS(NCA), MT(ASCP), M.Ed.
- Laboratories
Narrow your search
- Areas of Research
- active Find a research lab with a name beginning with the letter A A
- Find a research lab with a name beginning with the letter B B
- Find a research lab with a name beginning with the letter C C
- Find a research lab with a name beginning with the letter D D
- Find a research lab with a name beginning with the letter E E
- Find a research lab with a name beginning with the letter F F
- Find a research lab with a name beginning with the letter G G
- Find a research lab with a name beginning with the letter H H
- Find a research lab with a name beginning with the letter I I
- No research labs names begin with the letter J J
- Find a research lab with a name beginning with the letter K K
- Find a research lab with a name beginning with the letter L L
- Find a research lab with a name beginning with the letter M M
- Find a research lab with a name beginning with the letter N N
- Find a research lab with a name beginning with the letter O O
- Find a research lab with a name beginning with the letter P P
- No research labs names begin with the letter Q Q
- Find a research lab with a name beginning with the letter R R
- Find a research lab with a name beginning with the letter S S
- Find a research lab with a name beginning with the letter T T
- No research labs names begin with the letter U U
- Find a research lab with a name beginning with the letter V V
- No research labs names begin with the letter W W
- No research labs names begin with the letter X X
- No research labs names begin with the letter Y Y
- Find a research lab with a name beginning with the letter Z Z
- Advanced Endoscopy Innovation Translation and Clinical Trials Group: Barham Abu Dayyeh
- Advanced Medical Imaging Technology: Richard L. Ehman
- Aerospace Medicine and Vestibular Research: Michael J. Cevette, Jan Stepanek
- Aging and Dementia Imaging Research (ADIR): Clifford R. Jack Jr.; Kejal Kantarci; Prashanthi Vemuri
- Aging and Immune Restoration: Jessica N. Lancaster
- Allergic Diseases: Hirohito Kita
- Anesthesia Outcomes: Juraj Sprung
- Anesthesiology Systematic Review: W. Michael Hooten
- Anticancer Drug Action: Scott H. Kaufmann
- Artificial Liver and Liver Transplantation: Scott L. Nyberg
- Artificial Pancreas: Yogish C. Kudva
- Assistive and Restorative Technology: Kristin D. Zhao
- Atherosclerosis and Lipid Genomics: Iftikhar J. Kullo
More about research at Mayo Clinic
- Research Faculty
- Core Facilities
- Centers & Programs
- Departments & Divisions
- Clinical Trials
- Institutional Review Board
- Postdoctoral Fellowships
- Training Grant Programs
- Publications
Mayo Clinic Footer
- Request Appointment
- About Mayo Clinic
- About This Site
Legal Conditions and Terms
- Terms and Conditions
- Privacy Policy
- Notice of Privacy Practices
- Notice of Nondiscrimination
- Manage Cookies
Advertising
Mayo Clinic is a nonprofit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
- Advertising and sponsorship policy
- Advertising and sponsorship opportunities
Reprint Permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Volume 15 Supplement 2
Accomplishing Career Transitions 2019: Professional Development for Postdocs and Tenure-track Junior Faculty in the Biomedical Sciences
- Open access
- Published: 22 June 2021
A guide to setting up and managing a lab at a research-intensive institution
- Bob Goldstein 1 &
- Prachee Avasthi 2 , 3 , 4
BMC Proceedings volume 15 , Article number: 8 ( 2021 ) Cite this article
20k Accesses
8 Citations
67 Altmetric
Metrics details
Postdocs who land faculty jobs at research-intensive institutions need to juggle several new large-scale tasks: identifying space and equipment needs for their lab, negotiating the hiring package, outfitting the lab with supplies, building a team, and learning to manage time in ways that can promote productivity and happiness. Here we share tips to help new hires think clearly about each of these tasks.
Introduction
You’re on the job market, and you’ve just been offered a job. Congratulations! Now brace yourself, because the next steps will involve some quick decision making. You’ll be asked for a start-up list detailing the costs of equipment and supplies that you’ll need to set up your lab, and you’ll be negotiating important job details — all while thinking about how you’ll build a team, a career, and a life as an independent scientist.
This short guide covers some advice that we’ve shared with postdocs who had just been offered faculty positions at research-intensive institutions, or to postdocs who were thinking ahead to a time when this may happen. Here, we cover how to set up and manage a lab. (A separate article in this series covers steps that follow toward tenure [ 1 ]). We have prepared this written guide to contribute to leveling the playing field for newly hired faculty, by demystifying some key steps to success that we learned little-by-little from various sources.
This guide is not exhaustive. Rather, it seeks to raise some points that can be useful to consider at this stage. We recommend using this guide, together with other sources [ 2 , 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 ] and those referenced throughout this guide, as starting places for discussions with peers to brainstorm ideas for setting up your own lab. Discussions with peers facing similar challenges can be invaluable for your own success and to help you face the challenges with some optimism that you can succeed. For this reason, we recommend forming networks of peers who face similar issues. The possible avenues for forming such networks may come naturally to some. You may want to ask peers locally to gather on occasion for informal meetings; use conferences in your field to get together with groups of people who are not well represented at your own institution; and use communities like Future PI Slack [ 19 ] and New PI Slack [ 20 ] to communicate about problems you’re facing, to seek solutions, and to create new channels within those platforms for building needed spaces. However, it is not unusual for many new PIs to feel like outsiders because of issues they face that some of their peers do not. Videoconferencing tools and messaging platforms like Slack make it easier than before to initiate groups who share related challenges. A little work on cultivating the community you need if it doesn’t already exist can go a long way, and if a gap exists in the support landscape for you, it likely does for others as well. This shared need is what binds a nascent group together. People are in general happy to meet informally to learn from each other.
An important point to keep in mind: As a newly hired PI, you can make mistakes, and you can be sure that you will. We all do. It is common for early-stage principal investigators (PIs) to regret some of the decisions they make regarding hires or equipment purchases. Many early-stage PIs repeatedly and subtly change their approaches on exactly how to interact productively with their lab members. There are many paths to success. Some trial and error to finding your own path is inevitable. Rather than expecting perfection, it can be healthy to view some trial and error as valuable in your learning process.

Identifying space and equipment needs
One note before we get to space and equipment needs: Back when you were initially interviewing for jobs, each interview was really a two-way interview – they were considering you for the job, and you were considering them as colleagues and their institution as a place to settle into. But in general, initial interviews are biased heavily in one of those directions: in most searches, they are generally interviewing their top five or so candidates from hundreds of applicants for just one job. As a result, it’s generally wise to try to enjoy the interviews by focusing on your shared interests in science, not money, and to avoid saying anything that could be perceived as a demand at this stage. It’s a good idea to ask relevant questions, for example about availability of graduate students and support for graduate students during rotations, but it’s generally not a good time for expressing expectations about start-up or salary totals (which we discuss more below). If your needs are typical, then saying so is a useful answer to any questions you’re asked at this stage about your start-up needs – to settle a chair’s worry that you’ll have atypical needs that can’t possibly be met, for example. Then pivot right back to your shared scientific interests.
Once you have a verbal job offer in hand, things change. You’ll plan a second visit to see the lab space and to think concretely about your equipment needs. You’ll build your start-up list, which will commonly be the basis for negotiations with a department chair (or sometimes a dean) before you accept the job offer. If you and your partner are both seeking jobs, this is when you’ll raise that. Remember that you are negotiating with a future colleague, so always negotiate in good faith. With any communication about your start-up needs, you might like to also re-express enthusiasm about the job and gratitude to the chair for helping to work out the details. It’s important to find a good balance where you are clear about any needs to accomplish what they’re hiring you for, while also starting off on friendly and professional terms with your future colleague. In general, the department chair is on your team: the chair will want new hires to be set up well to succeed. Be clear that you’re enthusiastic and that you just want to make sure you will be set up for a strong start there. Work to arm the chair with relevant information, including any other offers you have, to help them justify start-up costs to a dean, provost, or other institution sources.
You can envision your space needs as one bench and one desk per person, plus common space for equipment, shared resources, and other needs, and some room for growth including temporary summer students and rotation students. Looking at the benches and common spaces in your postdoctoral lab will be a useful guide, but be sure to consider all of the spaces, for example the spaces used for incubators, freezers, microscopes, tissue culture, and any equipment that’s outside of the lab in shared equipment rooms. If you want to really make sure the space will be adequate, consider the footprints of any atypical equipment or setup you’ll use. For example, this could include space for maintenance of your research organisms, microscopes, or custom-built rigs for specialty applications. Space discussions after accepting the job can be contentious, so this is a good time to ensure that you’ll be comfortable with your lab’s space.
Interviews can be an opportunity to ask to see the space, if a specific space is designated. Just as with meeting potential future colleagues, seeing a space can give you a gut feeling about a place that can contribute to your decision about whether to accept an offer. Some PIs like their office connected to the lab, where they can interact with lab members and catch any misconceptions in conversations. Others prefer a space that is separated from the lab for quiet writing and thinking or for more frequent interactions with other PIs. Nearby labs can affect a lab’s atmosphere significantly too. Consider the value of having colleagues nearby with whom you anticipate camaraderie, as well as potential collaborators and PIs who might serve as natural mentors to you. Physical proximity can contribute to productive collaboration [ 21 ]. Even a reasonably short distance can be the difference between interacting with colleagues and not. Note that in some institutions, and particularly in some medical schools, space is linked to funding using a specific space formula in which square feet of lab space is determined for each lab by how much grant funding they are bringing in. After you have a job offer, it is a good idea to ask the chair if a space formula is used, and how frequently it is calculated (i.e., will you lose lab space if you have a brief gap in funding, and conversely how quickly can your space grow if your grant funding grows).
Building and negotiating the start-up package
Once you’ve landed a job offer and you’ve replied that you’re interested in the offer, you’ll likely be asked for your start-up list. It’s a good idea to at least get a start on putting one together in advance. The start-up list is where you will be clear about your itemized needs to set up your lab. If you are being recruited in part for a specific skill, and they don’t have the infrastructure you need, it is important to say so. You should be clear about things that are absolutely required to bring the strengths they want. You sold them on your strengths in your job talk(s), so your start-up needs should not be a surprise to anyone. Indeed, sometimes recruitment is the department’s chance to justify investing in expensive equipment that they’ve been wanting.
Your start-up list is often the best opportunity you will have to secure equipment that is necessary for your research but that is too expensive to be paid for from most grants. In rare cases of an especially expensive piece of equipment, you might propose that it be shared to help make the case for utility to the department, but in general you will want full access to your own lab’s equipment instead. For such large pieces of equipment, consider whether your usage will be enough to justify covering maintenance costs from your grants and/or efforts by you and your lab for maintenance, or whether some equipment might be better to propose as a shared departmental resource in an existing core facility. These different models each come with their own strengths and drawbacks. For instance, in core facilities, usually you will need to pay by the hour for use of equipment, and your lab’s access may be limited, but the equipment will be maintained by someone else in a core space.
Rather than reinventing the wheel by building a start-up list from scratch, most people collect multiple start-up lists from peers and/or communities like Future PI Slack [ 19 ] and use those as examples as they build their own list. Just as with envisioning your space needs, it can be useful to take stock of what you’re using in your postdoc that you’ll need in your own lab, along with things you’d like to upgrade, as technology advances quickly. If you ask, companies will bring expensive equipment like microscopes to you to try out (such a demonstration of equipment is referred to as a “demo”), which can allow you to compare equipment and support from different companies. As you build your start-up list, look back at your application materials. What did you say your research goals would be? Are you requesting what you’ll need to pursue those goals?
The amount of money that is reasonable to expect for start-up varies tremendously by type of job and institution. It can be helpful to talk to colleagues at peer institutions or to use communities like Future PI Slack [ 19 ] to get an idea for what the market is offering. After initial startup costs, personnel are often the biggest cost. Most people will request 1–3 years of personnel costs to cover the cost of initial personnel until the first grant is awarded, for example for a technician and your first 1–2 graduate students. At some institutions, you will also be covering part of your own salary from start-up (and later from grants). For all personnel, remember to include fringe benefit costs as well as salary, or tuition for students if you are expected to cover this. You can contact your future department’s accountants to ask for useful information on the standard fringe costs for grad students, postdocs, and technicians. Certain potential costs in your lab may be covered by other sources in the long term, for example when graduate students land 1–2 year spots on training grants, but be sure to gauge the likelihood that this will happen on average, for example by asking for the success rates of graduate students applying for training grant spots. If you are choosing between multiple verbal offers, be wary of comparing start-up totals when deciding which offer to accept. What is included in start-up totals can vary between institutions, and being somewhere you can succeed in your goals and enjoy your colleagues will be far more important in the long run.
Once you and the chair iron out details, you should receive an official offer letter. At this stage, it is wise to find some new and experienced PIs whom you trust (for example, PIs at your postdoc institution) to check over your offer letter. They can help spot important gaps, and they can help build your comfort with negotiating as needed. Getting such input at this stage can be invaluable, because the offer letter is generally treated like a contract by institutions, and yet initial offer letters are often missing some critical details. As a result, it is not unusual to tactfully ask the chair for a revised offer letter that details all important points and expectations, including the precise teaching load, any restrictions on when and how your start-up total is spent, what space the lab will occupy and well-defined arrangements for any shared space, and specific plans laid out in case the space is not fully ready when you start, with everything (including gas lines and air lines) working. Spaces that require significant renovations come with a potential drawback: it is not unusual for schedules to stretch out for longer than planned because of unforeseen issues either with the space or with other jobs affecting engineering and facilities’ workers schedules. It is helpful to also have a specific statement that any needed infrastructure repairs or renovations will be completed before the lab opens, with contingency plans if that cannot happen, and that lab furniture (lab benches and chairs) will not be charged to your start-up allocation. Most institutions will give faculty two pre-tenure semesters of relief from teaching, to help with getting a research program off the ground. You will want to be strategic about when you use these (it can be helpful for starting the lab to have one semester away from teaching as you begin, and you might delay the other semester if possible until closer to tenure, although different PIs have different preferences). You also might consider in your teaching assignment whether you can teach courses that first year graduate students take, to give you exposure to potential rotation students. Be sure that your start date is specified and understand what the process would be if there were a need to adjust it, and by how much. Be sure that your chair has explained to you how your start date will play into your promotions and tenure timeline, your teaching roles, and your recruitment of graduate students.
If you are enthusiastic about the written job offer but you have any remaining major unmet needs that seem reasonable, then consider picking one major need and requesting that. For example, if more than one lab space is available, and one option is near colleagues that you dream of being near, it would be fine to tell the chair this. If some important details are still omitted from an initial or revised offer letter and yet you’re keen to accept the offer, it can help to email a conditional acceptance stating your own understanding of some specific unwritten details, so that a chair can correct any misconceptions at this stage, and so that you will have some record of verbal understandings to refer to in case the department chair changes.
With all of your negotiations, remember again that your chair will want you to succeed; they’re expending significant effort and significant resources for your benefit; and you’re beginning a long-term professional relationship. With these things in mind, while you need to be clear during any needed negotiations, you’ll also want to be tactful, and maintain a friendly, professional tone.
Once you’ve formally accepted the job, celebrate!
Opening the lab, onboarding new lab members, and building a team
After celebrating, you’ll have a chance to get wheels in motion for selected things that will benefit from some early action. Two things are useful to consider tackling first: (1) So that incoming graduate students and undergraduate students will see your new lab as a possibility, get yourself added to your new department’s and/or graduate program’s website; build your own lab’s website; and use social media to announce your lab. (2) Request demos of large pieces of equipment, like microscopes, from companies. Companies can generally offer to demo equipment on site at your postdoc lab. If you make decisions on big pieces of equipment early, this accommodates lead time often necessary to get the equipment delivered to your new lab so that your first rotation students can start in the lab without too much delay. Large pieces of equipment can sometimes have specific parts on backorder, and any resulting delays can create problems. For example, the microscope you need will feel like a useless doorstop until the most critical lens arrives. Some institutions will allow you to spend some start-up funds before you arrive, so that you can begin to place orders early. If support from equipment company representatives is important after purchase, as it can be for microscopes (a rep that can loan parts that need repair can save a lot of headaches), then be sure to ask your future colleagues about the effectiveness of reps for different companies before making major purchasing decisions.
Sometimes another lab is closing down or moving and leaving glassware, pipettors, and equipment behind. Once you’ve accepted a job offer, it’s a good idea to ask the chair if this is anticipated, and plan to scavenge useful items with permission when they become available.
Before you arrive in your new position, you might consider hiring a short-term personnel to start when you do, or even earlier, to help with purchasing and unpacking. In general, hiring people is governed by more defined rules than is buying materials, because hiring is regulated by employment laws. These laws can require openly posting positions, which can help you get a larger and more diverse set of applicants than you might otherwise. You can further grow and diversify the applicant pool by encouraging people to apply, soliciting recommendations for such people from other new PIs through New PI Slack [ 20 ], Twitter, and from colleagues, especially junior faculty at your new institution. You may also consider recent graduates or gap year students. You can also hire work-study students at your new institution to help with setting up the lab. Your new department’s human resources specialists can advise you on navigating hiring requirements.
Equipment and supply purchases are sometimes governed by contracts negotiated between vendors and the university. Your department’s accountants can explain any equipment and supply purchase rules and whether you are required to complete any training to make purchases. Product representatives from multiple suppliers may reach out to you as new PIs often make many purchases at once. New investigators can sometimes negotiate discounts. While not all of the lab startup deals from suppliers are in fact a deal, some significant discounts are possible when buying in bulk. Ask other labs what they pay for frequently-used services like DNA sequencing and for ordering primers so that you can be aware of discounts to request from your sales reps. Some institutions allow purchases from Amazon, or eBay for used equipment. As you begin purchasing equipment and supplies for the lab, you will spend some time trying to cut costs on big purchases and frequent purchases. It will take some practice to minimize the time you spend researching economical purchases. At some point, you may delegate the supplies purchasing role to a technician or assistant that you hire, or have each person in the lab make their own supplies purchases as needed, but it will be useful for you to learn the ropes at first so that you can be aware of any unanticipated issues.
Some newly hired PIs will get a start on writing their first grant proposal, or even submit one, before arriving. Grant writing strategies are covered in a separate article [ 1 ]; here, we review just selected matters that may help with envisioning the process in advance. Once you have a suitable funding source (like NIH) identified, it can be helpful to email a program officer there that handles grants in your subfield to ask for a short phone or video meeting. Program officers can evaluate whether the aims you plan to propose are suitable for a specific funding mechanism or review panel, and sometimes they will share other advice. You can also start to collect a list of awards specific to junior faculty such as Pew and Searle Scholars programs and ask your new chair about being nominated for ones that only accept limited numbers of proposals from each institution; some applicants will ask about being nominated for these before accepting a job offer. Some institutions keep especially useful resources of funding opportunities that anyone can access online, including funding opportunities reserved for early-career faculty and underrepresented minority researchers [ 22 , 23 ]. Other junior faculty may share lists of grants they have applied for, and they may share successful proposals to use as models as you prepare your own. For all grant proposals that you plan to write, be sure to contact your new institution’s office that handles grant submission (commonly called a Sponsored Projects office or a Sponsored Research office) as well as the administrative people handling grant proposals in your department to find out what they will need. Within-institution deadlines are commonly a few days to a week before a funding agency’s deadline, because they will need to check proposal paperwork for problems and sign off on proposals. Administrative people within your own department can sometimes help with preparing budgets and other paperwork parts of proposals; it’s a good idea to ask faculty in your new department about the help that department administrators can typically provide.
Upon arriving in your new position, you’ll start to build a team. For many new PIs, building a strong team can become one of their most satisfying new roles in science. Building a strong team can also be challenging, and it can be critical to your success as a PI. You will want to consider the extent to which you will micromanage lab members’ work and/or encourage and support independence, and for people to work independently vs. in teams, to promote both your scientific goals and your lab members’ career development. Even in labs where each lab member has a completely independent project, the group of people has the potential to interact in healthy ways that can help everyone. People may have skills and interests that complement each other (like the old Super Friends cartoons — Wonder Woman stops the bullets, the Wonder Twins transform into useful forms, and Aquaman takes care of underwater tasks, or teaches others how to do so). It can be helpful to seek lab members with these criteria in mind. Diversity in multiple senses can help contribute to a strong team [ 24 , 25 ]. For this reason, it is important to fight the urge to look for clones of yourself in prospective hires. And it can be helpful to consider your own goals, as you framed them in your job talk(s) or in grant proposals that you are envisioning. Sometimes lab members with specific interests can help relieve demands on your time; for example, a lab member interested in microscopy might be happy to serve as a second point person for interacting with microscope companies.
As you’re considering taking on new lab members, keep in mind whether potential lab members have emotional maturity too. A strong experimentalist who cannot interact well with a diverse team and respect others (often described as a “dominant negative” lab member) can harm team dynamics and/or slow other people’s research progress. Interviews and rotations can be an opportunity to look for healthy interactions between people. There may be a temptation to avoid conflict or hang on too long to a poor fit, but all lab members contribute to the collective environment, and a PI’s inaction often can be damaging. And a group with healthy interactions will contribute strongly to their own team building atmosphere. It can be helpful to watch for natural team-building initiative among lab members and to encourage it.
You’ll want to make your lab a welcoming place for potential lab members both in terms of the atmosphere among lab members and in terms of how the lab space is organized. As your salary will generally jump up in the transition from postdoc to PI, it may be helpful to consider the last $1000 or so of your annual PI salary as for the lab — for a lab coffee machine, bluetooth speakers, a food fridge, and in the longer term, for lab dinners and other social events. You’ll thank yourself later! Also remember that such perks are not a substitute for the culture you’ll seek to build: it’s even more important for lab members to feel nurtured and supported. If you’re naturally shy, develop regular habits to be in the lab interacting with people. In general, people in the lab will appreciate when their opinions are solicited and considered, for example when you are considering adding new lab members or making major purchases. You may not always agree with the feedback you get. You may even overrule the feedback for important reasons, but listening and understanding the perspectives of those who will be interacting most frequently with new people and equipment is invaluable [ 26 , 27 ].
It’s wise to give yourself plenty of chances to interact with potential rotation students: interview as many prospective grad students visiting your department or graduate program each spring as possible, seek opportunities to meet the new grad students who arrive each fall. In your first couple of years, consider volunteering for the admissions committee that reviews graduate school applications for your program. Become aware, though, of the time you would be committing first. It’s a good idea to try to limit your committee work before you have your first grant supporting the lab’s research (and chairs and colleagues will generally respect this need, assigning you to a light load of select committees at first), but the admissions committee can be a valuable one to join when you’re seeking graduate students if the time required is not too burdensome at your institution. For campuses with large numbers of partially overlapping departments and programs, you might also explore whether you can be affiliated with multiple graduate programs on your campus, to recruit from multiple pools of incoming graduate students each year. Having access to multiple pools of graduate students may aid in your goal to find graduate students who are good fits for your lab.
The graduate students who start in your first year or two will have incentives well aligned with your own goals toward tenure: making discoveries and reporting them in publications in your pre-tenure years (hence the advice above about setting yourself up to take rotation students into a fully functioning lab as early as possible). In general, when your own incentives and the incentives of the people in your lab are well aligned, this can help many things in your lab go smoothly. For this reason, and because you’ll be working toward healthy relationships with the people in your new lab, it’s a good idea to get to know what motivates the people in your lab both as you’re considering taking people on and as their goals evolve over time [ 28 ]. Do they have enough freedom to encourage their own creative thinking and for them to grow as independent scientists? Having an atmosphere where people feel comfortable taking some risks and also talking about their motivations can help. It is especially important to consider the challenges and circumstances of those who may come from a different background than you. You can encourage lab members to complete any of several types of individual developmental plans, for example MyIDP [ 29 ], at least annually, as an opportunity to review their long-term career goals and to review whether they’re working toward those goals. Graduate students and postdocs have diverse career interests and skills they’re seeking to develop [ 30 , 31 , 32 , 33 ]. They will need to spend some of their time exploring options for their continued careers, for example by attending workshops, gaining teaching experience and experience in scientific outreach. Your support toward their own goals will be appreciated. Often, time spent cultivating one’s soft skills, career path, and network will energize, refocus, and motivate their science as well [ 34 ].
Recruiting postdocs when you’re a junior faculty member can be difficult because you will be less well known than many of your senior colleagues. Some new PIs work on developing an online presence, for example on Twitter, to help students and colleagues become aware of their work. Twitter can be a great place to share what you do, solicit feedback, and work on community building. Opportunities to interact with graduate students at other institutions — for example giving invited seminars, contributing a little to courses that students travel to, or meeting graduate students at conferences — can also contribute to recruitment of postdocs to your lab. These opportunities also serve the reason that most of us do science in the first place, i.e. to make discoveries and to share the discoveries with each other. Sometimes these opportunities can seem hard to come by as a new faculty member, but consider adding your name to lists of seminar speakers at New PI Slack or other initiatives that serve to increase speaking opportunities for early career or underrepresented groups. Once you have postdoc applicants, it’s a good idea to talk to their PhD advisor directly, because conversations often produce more candid evaluations of strengths and weaknesses than a letter will.
Undergraduate students can also contribute to a lab environment. Training undergraduates has the potential to contribute to both your graduate students’ and postdocs’ career development. From large undergraduate student populations, there is a great potential to recruit ethnically and racially diverse undergraduates, who can contribute to strengthening your lab and the scientific field more generally by bringing diverse perspectives. Use your colleagues’ input on how to recruit undergraduate researchers at your institution and how to structure the undergraduate research experience to support benefits to both the student and the lab’s research goals.
These days, PIs often generate an onboarding document that outlines lab policies and expectations — what you expect from lab members, and what they can expect from you [ 35 , 36 ]. These documents can save time and reduce miscommunication. It is helpful to spend considerable reflective time envisioning the type of lab dynamics and culture that you want to build. Create a prioritized list of the character traits, work ethics, diversity, and professional behaviors that you envision in your group, considering expert advice [ 9 , 24 , 25 ], and use these to build a mission statement for the document. Once you have members in the lab, it can be useful to rebuild this document on occasion with everyone’s input, to help make the document more useful and to increase everyone’s genuine support for a useful set of expectations. As you gain lab members, you will likely want to improve your ability as a mentor; online resources can help [ 37 , 38 , 39 ], and some institutions offer local training workshops.
Maintain a professional relationship with your lab members. Being a new PI can be lonely at times, and it can be tempting to put yourself on equal footing as one of the group. But keep in mind that there is an inevitable power dynamic: they will generally be aware that you have a great deal of control over their ability to succeed [ 40 , 41 ]. Ignoring the existing power dynamics can lead to issues down the road. To promote a healthy environment, it can be useful to encourage lab members to cultivate broad networks of peers and additional PIs to give them input, to acknowledge that you and members of the lab may have interpersonal conflicts at times, and to start off relationships stating that you are committed to working through any conflicts that do arise.
In a position now where you have some responsibility for others (mentoring, teaching, serving on admissions committees, etc.), you should consider with some care not just what you’re doing but also what you’re not doing. In positions of responsibility, people are reasonably held responsible for both, which can be an equally daunting and exciting challenge to aim to meet. Take some time to read and/or discuss with colleagues issues that are important to the practice of science — for example, diversity issues and inclusive environments, unconscious bias, mental health issues, and ethical conduct.
There are many ways to be a successful independent scientist. For example, some PIs choose to work at the bench their entire career with a small number of PhD students. Some prefer challenging themselves to run effectively as big a lab as possible. Some prefer a lab of mostly postdocs, or mostly PhD students, or undergraduate students. Some choose to focus on developing new techniques for a field. Some keep research topics continuous from each lab member to the next, and others prefer to try new lines of research frequently. Keep in mind that you don’t need to be all of these things. Your colleagues in your institution and your field provide you a variety of useful models to consider as you shape your own ideas of the kind of scientist you’d like to be.
Managing your time for productivity and happiness
You’ve made it to a highly sought-after position, so you’ll thank yourself later for some thinking at this stage about how you’ll develop your career in a form that will contribute to your long-term well being.
Every new PI establishes relationships with many people beyond their own lab members. Among these people, other junior faculty can serve as an important peer support group, because you’ll be going through some experiences in common. It can be helpful to schedule informal gatherings with this group, as well as gatherings focusing on topics like teaching or specific scientific topics. Many new PIs are surprised to learn that some thorny issues they face have already been faced by other new PIs. The solutions that your peers have found for their own productivity and happiness can be useful to consider. It can also be valuable to cultivate relationships with people who can serve as informal mentors, i.e. more senior faculty who share your vision for how to run a lab, and who can provide input on your grants and manuscripts (and when you do share grants and manuscripts, it’s courteous to let people know a few weeks in advance the specific date when you’ll share something, and to ask if they can return comments within a week, so that they can schedule in advance some time for reading and commenting). If your department does not have a formal process for existing PIs to mentor new PIs, you can ask your chair to recommend some informal mentors. Also consider mentors from outside of your own institution who might agree to an occasional meeting by video or at conferences. As you collect wisdom from peers and mentors, consider practices they use in common as well as input from the outliers whom you admire. Remember that there are many paths to success and almost as many ways to do the job as there are people doing it [ 42 ]. For this reason, it’s important to decide what you value, and keep an eye toward liking the person you’ll become to get tenure and the job that you’ll have at that stage. It is important to stay true to your values rather than solely ensuring that you meet expectations required to keep and advance your career.
You will also establish new relationships with administrative staff members of your department — accountants, human resources specialists, facilities maintenance people, and others. Be sure to treat administrative staff members respectfully, and be friendly. Some PIs make the mistake of finding themselves in a position of some authority for the first time and, in the interest of time efficiency, losing a little of their naturally friendly and human demeanor when interacting with staff members. You will likely know these people for a long time. Administrative staff can be tremendously effective at navigating quirks of institutional rules, so remember that you stand to learn a lot from them.
Your own time management is important. Your research effort and time allocation will be completely unlike what it was as a postdoc. At first, you are, in a sense, your own best postdoc, so it can be wise to continue bench work yourself at least until lab members are well trained. In the long run, your time management will likely involve some trial and error in figuring out what works best for you, as well as trying out new habits now and then throughout your career. The pace of work may feel ramped up at first, given your role in multiple projects in the lab at the same time. This change typically involves an attitude and skills adjustment to manage more projects. You’ll need to be strategic about your research goals, not spreading yourself too thin across too many distantly related projects, and you’ll need to find your own best balance for effort toward research, teaching, and other roles. Teaching a course for the first time generally involves a bigger time commitment than new faculty anticipate, both for preparing the material to be taught and for learning how to manage a course effectively and efficiently. You’ll want to do a job you’re proud of in research, teaching, and your other roles, but remember that in the end you will need to find a balance that you can be comfortable with. If it takes you longer than you expect for setting up your lab and beginning to teach, give yourself a break by reminding yourself that this is a common experience for new PIs. You’ll likely improve at juggling multiple roles over time. Help is available for faculty looking to improve their abilities to do so [ 14 ].
One key issue of time management is how to respond to others’ expectations of your contributions in your department or in the field. It will be important to be a good citizen by doing your share of work in your department and in your field of science, but you’ll also need to learn to say “no” in order to avoid overextending yourself. For example, for reviewing papers and grants, a good rule of thumb for being a good citizen is to only review those that are within your own field and to review roughly as many grants and manuscripts as one’s own lab’s work incurs (for example, plan to review roughly 2–3 manuscripts per manuscript that you submit for peer review). It’s always okay to respond to requests with a polite, “I’m overbooked with other commitments and wouldn’t be able to take this on” whenever this is the case. A good option when turning down a request is to recommend a colleague or trainee that could use the opportunity. This makes it easier to say no, solves a problem for the requester, and helps others.
When deciding if you are indeed overbooked with other commitments, be sure to reserve time both for things that are urgent and things that are important but not urgent. Important but not urgent tasks are often key to long-term success, but are also the easiest to postpone. These tasks will be challenging to complete unless you specifically set aside time in your schedule. For example, grant proposals become increasingly urgent as a deadline approaches, and beginning early to set out a plan and stick with it may require you to mark out planned milestones month-to-month on your calendar. Commonly used grant application guides can help with planning out a useful schedule for yourself [ 43 ] . For important tasks, it is also common to fill up all available time with a specific task. This may result in spending a week to prepare a lecture or complete a first draft of a piece of writing that could have been done in a focused day. A useful method of dealing with this phenomenon is to allocate dedicated time, and no more, in one’s schedule for a specific activity (sometimes called “timeboxing”). The increased focus can reduce anxiety when sufficient time is protected for an activity. This practice can also reduce the amount of overall time spent, thereby increasing productivity. There is no shortage of management hacks taken from the business world that can benefit a new PI balancing many productivity, hiring, leadership, and organizational challenges for the first time. We are often not trained for many of the new roles that a PI takes on, but existing resources can help [ 6 , 8 , 9 , 44 , 45 ].
Another trick for making good use of your time is to double up on use of commitments when possible. Consider whether certain of your commitments can double as useful topics for lab meetings, or training opportunities for grad students and postdocs. For example, some journals will permit reviewing a manuscript together with a member of your lab. Doing so can satisfy multiple of your goals — contributing to your good citizenship in the field, keeping you and a lab member discussing ongoing research in your field, and serving as a valuable training experience for the lab member.
Keep in mind that some opportunities may not have a clear proximal benefit but may increase your exposure in the community and with your colleagues, and/or allow you to get to know colleagues you admire. Your reputation as a scientist is one criterion for tenure, as reflected by letters that your tenure committee will solicit from colleagues of your choosing and of their choosing. This reputation will be based in large part on what you discover and publish. For this reason, it can feel especially satisfying to say yes to opportunities that increase your exposure in the field specifically when you have discoveries that you’re especially proud to share; in this way, you can bring something of value to others, for example in invited talks you give, and you can gain input on your work in the process. There is a firehose of research out there, and it is not necessarily anyone’s job to pay particular attention to your or your lab members’ discoveries. It is important to appropriately credit your lab members for their discoveries in talks and on social media, and colleagues in your field will appreciate learning about these discoveries.
Lastly, don’t forget to do what you need beyond your job – time with family and friends, and doing other things you enjoy! You can expect to experience some failure and resulting stress at work, along with some successes, and overworking can be emotionally draining. If you’re the kind of person who feels guilty taking time away from work, you can comfort yourself by remembering that you’ll likely be a more creative scientist and a better mentor if you are taking time to do what you enjoy and what’s important to you outside of work.
Availability of data and materials
Not applicable.
Abbreviations
Principal investigator
Boyce M, Aguilera R. Preparing for tenure at a tesearch-intensive university. BMC Proc. 2021;15(2).
Making the Right Moves: A Practical Guide to Scientific Management for Postdocs and New Faculty. https://www.hhmi.org/science-education/programs/making-right-moves . Accessed 7 Jul 2020.
Barker K. At the helm: leading your laboratory: Cold Spring Harbor Laboratory Press; 2010.
Google Scholar
Noor MAF. You’re hired! Now what?: a guide for New science faculty: Sinauer Associates; 2012.
Jahren H. Lab girl. New York: Alfred A. Knopf; 2016.
Newport C. Deep work : rules for focused success in a distracted world. New York: Grand Central Publishing; 2016.
Cohen CM. Cohen SL. Lab Dynamics: Management Skills for Scientists. Cold Spring Harbor Laboratory Press; 2005.
Bungay SM. The coaching habit: Toronto Box of Crayons Press; 2016.
Coyle D. The culture code: the secrets of highly successful groups: Random House Publishing Group; 2018.
Somerville LH, Cunningham WA, Gruber J, Van Bavel JJ, Lewis NA. Three keys to launching your own lab: Science | AAAS; 2019. https://www.sciencemag.org/careers/2019/08/three-keys-launching-your-own-lab . Accessed 7 Jul 2020
Book Google Scholar
Petry S. Learning the art of leading a lab. ASCB. 2017; https://www.ascb.org/careers/learning-art-leading-lab/ . Accessed 7 Jul 2020.
EMBO Lab Leadership Courses. https://lab-management.embo.org/ . Accessed 7 Jul 2020.
National Institute of General Medical Sciences. Starting Your Own Lab with Dr. Olivia S. Rissland and Dr. Prachee Avasthi. 2020. https://www.youtube.com/watch?v=dHIbiBN8Pgw . Accessed 7 Jul 2020.
Faculty Diversity: On-demand access to the mentoring, tools, and support you need to be successful in the Academy. https://www.facultydiversity.org/ . Accessed 15 Jul 2020.
Career development courses, workshops, and programs from ASCB. https://www.ascb.org/career-development/ . Accessed 15 Jul 2020.
Careers in Biology. iBiology. https://www.ibiology.org/careers-in-biology/ . Accessed 21 Jul 2020.
SACNAS Webinars. https://www.sacnas.org/what-we-do/webinars/ . Accessed 18 Sep 2020.
SACNAS Professional Programs. https://www.sacnas.org/what-we-do/professional-programs/ . Accessed 18 Sep 2020.
Future PI Slack. https://futurepislack.wordpress.com/ . Accessed 7 Jul 2020.
New PI Slack. https://newpislack.wordpress.com/ . Accessed 7 Jul 2020.
Claudel M, Massaro E, Santi P, Murray F, Ratti C. An exploration of collaborative scientific production at MIT through spatial organization and institutional affiliation. PLoS One. 2017;12(6):e0179334. https://doi.org/10.1371/journal.pone.0179334 .
Article CAS PubMed PubMed Central Google Scholar
Funding Opportunities. Vice provost for research at Johns Hopkins University. 2016. https://research.jhu.edu/rdt/funding-opportunities/ . Accessed 21 Jul 2020.
Funding Opportunities for Women and Minorities, UC Berkeley Sponsored Projects Office. https://spo.berkeley.edu/fund/womenminority.html . Accessed 21 Jul 2020.
Rock D, Grant H. Why Diverse Teams Are Smarter: Harvard Business Review; 2016. https://hbr.org/2016/11/why-diverse-teams-are-smarter . Accessed 21 Jul 2020
Taylor TA. Diversity, Inclusion and Culture. In: How to Build Great Teams: The New York Times; 2018. https://open.nytimes.com/diversity-inclusion-and-culture-steps-for-building-great-teams-ca157bd98c07 . Accessed 21 Jul 2020.
Scott K. Radical candor: fully revised & updated edition: be a kick-ass boss without losing your humanity: St. Martin’s Publishing Group; 2019.
Stone D, Heen S. Thanks for the feedback: the science and art of receiving feedback well (even when it is off base, unfair, poorly delivered, and frankly, You’re not in the mood): Penguin; 2014.
Teater B. 7 qualities to look for in a scientific mentor. The Jackson Laboratory https://www.jax.org/news-and-insights/2015/october/seven-qualities-to-look-for-in-a-scientific-mentor . Accessed 7 Jul 2020.
myIDP. http://myidp.sciencecareers.org/ . Accessed 8 Jul 2020.
National Postdoctoral Association. NPA core competencies. 2009. https://www.nationalpostdoc.org/page/CoreCompetencies .
Tracking Career Outcomes at Institutions. Future of Research. 2018. https://www.futureofresearch.org/tracking-career-outcomes-at-institutions/ . Accessed 7 Jul 2020.
Postdocs’ Guide to Gaining Independence. https://www.niaid.nih.gov/grants-contracts/postdoc-guide . Accessed 7 Jul 2020.
iBiology Courses. https://courses.ibiology.org/courses . Accessed 7 Jul 2020.
Avasthi P. Synergy of science and career development | ASCB: ASCB; 2019. https://www.ascb.org/publications-columns/career-navigator/synergy-of-science-and-career-development/ . Accessed 8 Jul 2020
Mehr S. Lab handbooks tweet thread: Twitter. https://twitter.com/samuelmehr/status/1139733291899080705 . Accessed 8 Jul 2020
Masters KS, Kreeger PK. Ten simple rules for developing a mentor-mentee expectations document. PLoS Comput Biol. 2017;13(9):e1005709. https://doi.org/10.1371/journal.pcbi.1005709 .
Office of Intramural Training & Education at the National Institutes of Health. https://www.training.nih.gov/ . Accessed 12 Jul 2020.
NIH OITE videos. https://www.youtube.com/channel/UCQQHo_QnuBxdfcsRy4INGGw . Accessed 12 Jul 2020.
The Science of Effective Mentoring in STEMM. https://www.nationalacademies.org/our-work/the-science-of-effective-mentoring-in-stemm . Accessed 12 Jul 2020.
Tintori SC. Turning the microscope on power dynamics in the lab. Mol Biol Cell. 2018;29(26):3064–6. https://doi.org/10.1091/mbc.E18-10-0684 .
Article CAS PubMed Central Google Scholar
National Academies of Sciences, Engineering, and Medicine, Policy and Global Affairs, Board on Higher Education and Workforce, Committee on Revitalizing Graduate STEM Education for the 21st Century. Graduate STEM Education for the 21st Century: National Academies Press; 2018.
Heppert J, Heikes K, Bowie E, Siripurapu V. How cell biologists work column: ASCB. https://www.ascb.org/tag/how-cell-biologists-work/ . Accessed 7 Jul 2020
Workbooks - Grant Writers’ Seminars & Workshops. http://www.grantcentral.com/workbooks/ . Accessed 7 Jul 2020.
Smart G, Street R. Who: solve your #1 problem. In: Ballantine Books; 2008.
The National Center for Faculty Development & Diversity’s Faculty Success Program. https://www.facultydiversity.org/fsp-bootcamp . Accessed 15 Jul 2020.
Download references
Acknowledgments
The contents of this article grew out of panels in ASCB’s Accomplishing Career Transitions program, a program for underrepresented minority postdocs and new faculty or postdocs and new faculty at primarily minority-serving institutions. We are grateful to Veronica Segarra, Ashanti Edwards, Jim Vigoreaux, Maria Elena Zavala, and Erika Shugart for developing this program, to the National Institutes of Health IPERT for support of the ACT program, to program fellows at the panels and to panel members for highlighting some key issues facing new hires, and to Veronica Segarra for guidance on writing the article. For helpful input on the manuscript we thank Katherine Aird, Amanda Amodeo, Kerry Bloom, Emily Bowie, Kathleen Caron, Courtney Clark-Hachtel, Brad Dickerson, Daniel Dickinson, Rob Dowen, David Drubin, Kacy Gordon, Jonathan Hibshman, Toshi Hige, Dan Kiehart, George Langford, Zack Nimchuk, Ariel Pani, Olivia Rissland, Pam Rosato, Celia Shiau, and two anonymous reviewers.
About this supplement
This article has been published as part of BMC Proceedings, Volume 15, Supplement 2, 2021: Accomplishing Career Transitions 2019: Professional Development for Postdocs and Tenure-track Junior Faculty in the Biomedical Sciences. The full contents of the supplement are available at https://bmcproceedings.biomedcentral.com/articles/supplements/volume-15-supplement-2 .
The ACT program and the Article Processing Charge (APC) for this article is supported by an Innovative Programs to Enhance Research Training (IPERT) grant from the National Institute of General Medical Sciences (NIGMS) awarded to the American Society for Cell Biology (award number 2R25GM116707). BG is supported by NIH R35GM134838 and NSF IOS 2028860. PA is supported by NIH R35GM128702.
Author information
Authors and affiliations.
Biology Department and Lineberger Comprehensive Cancer Center, The University of North Carolina at Chapel Hill, Chapel Hill, NC, 27599, USA
Bob Goldstein
Department of Anatomy and Cell Biology, University of Kansas Medical Center, Kansas City, KS, 66103, USA
Prachee Avasthi
Department of Ophthalmology, University of Kansas Medical Center, Kansas City, KS, 66103, USA
Department of Biochemistry and Cell Biology, The Geisel School of Medicine at Dartmouth, Hanover, NH, 03755, USA
You can also search for this author in PubMed Google Scholar
Contributions
BG and PA wrote and edited the manuscript. Both authors have read and approved the final version of the manuscript.
Corresponding authors
Correspondence to Bob Goldstein or Prachee Avasthi .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Goldstein, B., Avasthi, P. A guide to setting up and managing a lab at a research-intensive institution. BMC Proc 15 (Suppl 2), 8 (2021). https://doi.org/10.1186/s12919-021-00214-7
Download citation
Published : 22 June 2021
DOI : https://doi.org/10.1186/s12919-021-00214-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Career development
BMC Proceedings
ISSN: 1753-6561
- Submission enquiries: [email protected]
- General enquiries: [email protected]
The National Laboratories
Pushing the boundaries of science
The transformative science and technology solutions being discovered across the 17 National Laboratories are changing the way the world sees innovation.
Learn More →
Looking for the best & brightest
Internships, fellowships, and opportunities to further your research await you at the National Laboratories.
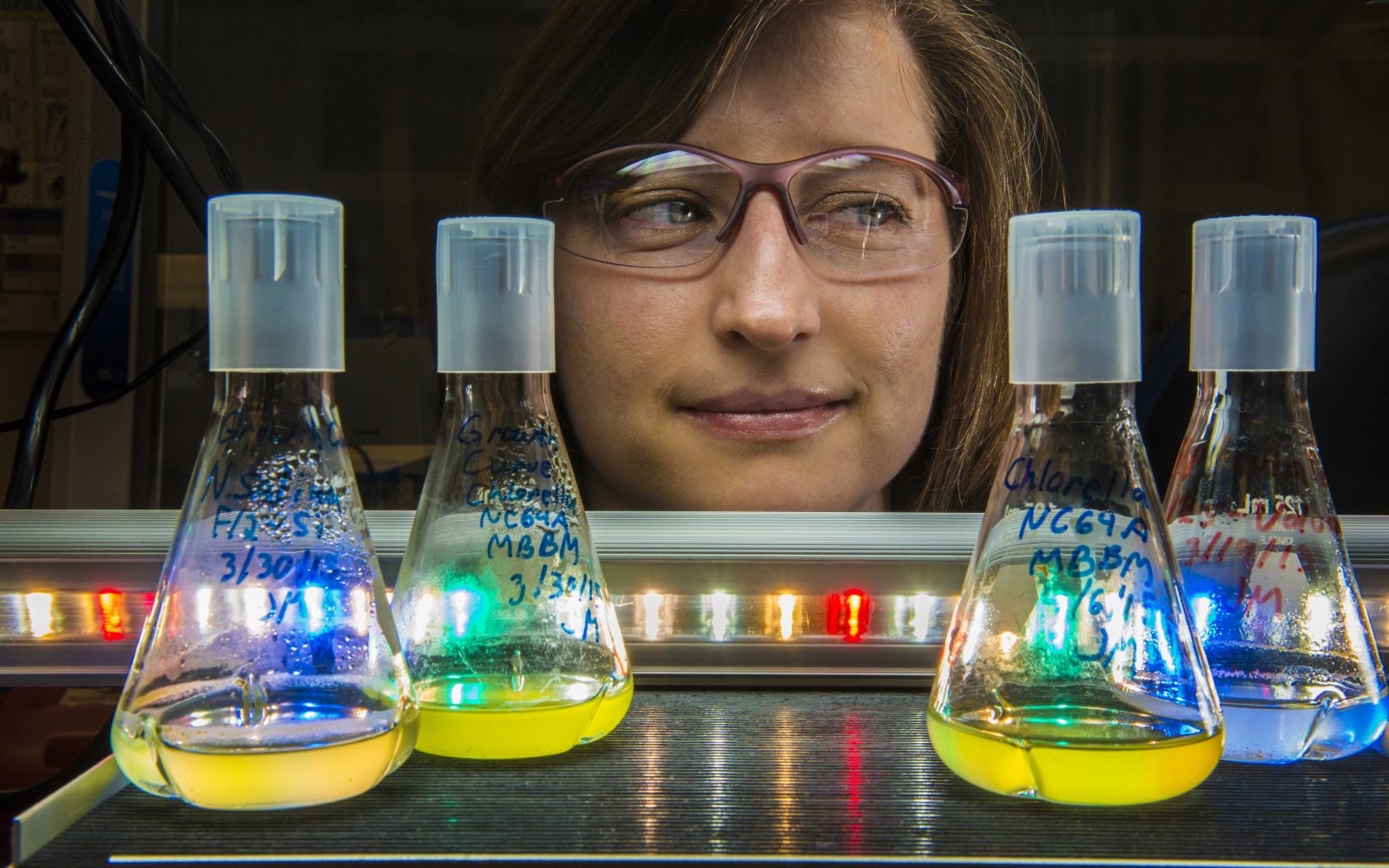
Innovation drives us
By recruiting and retaining a diverse workforce, the National Laboratories can better fulfill their mission to deliver scientific breakthroughs.
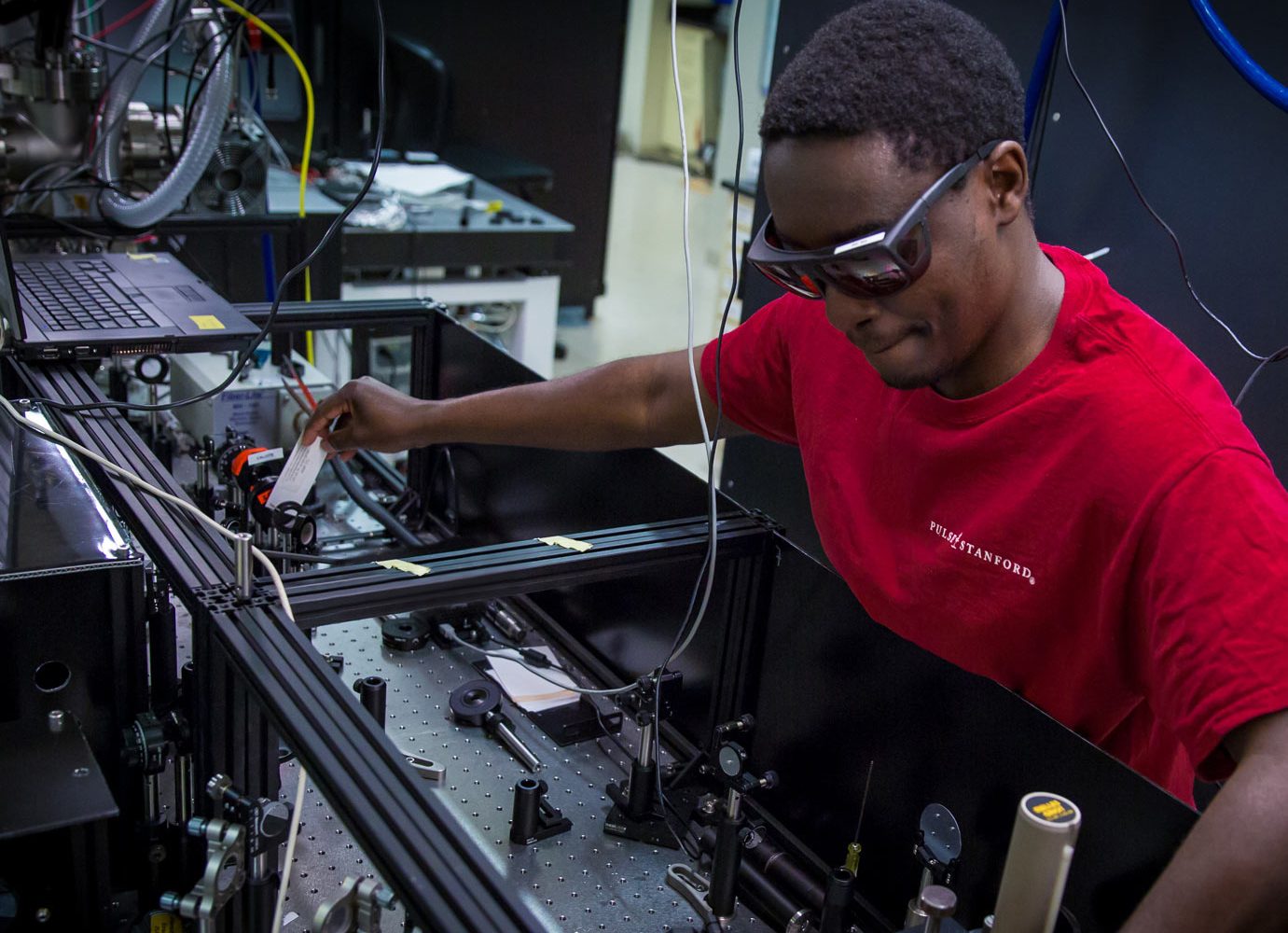
Get to know our workforce
The National Labs’ success depends on the unique insights and perspectives enabled by a diverse workforce.
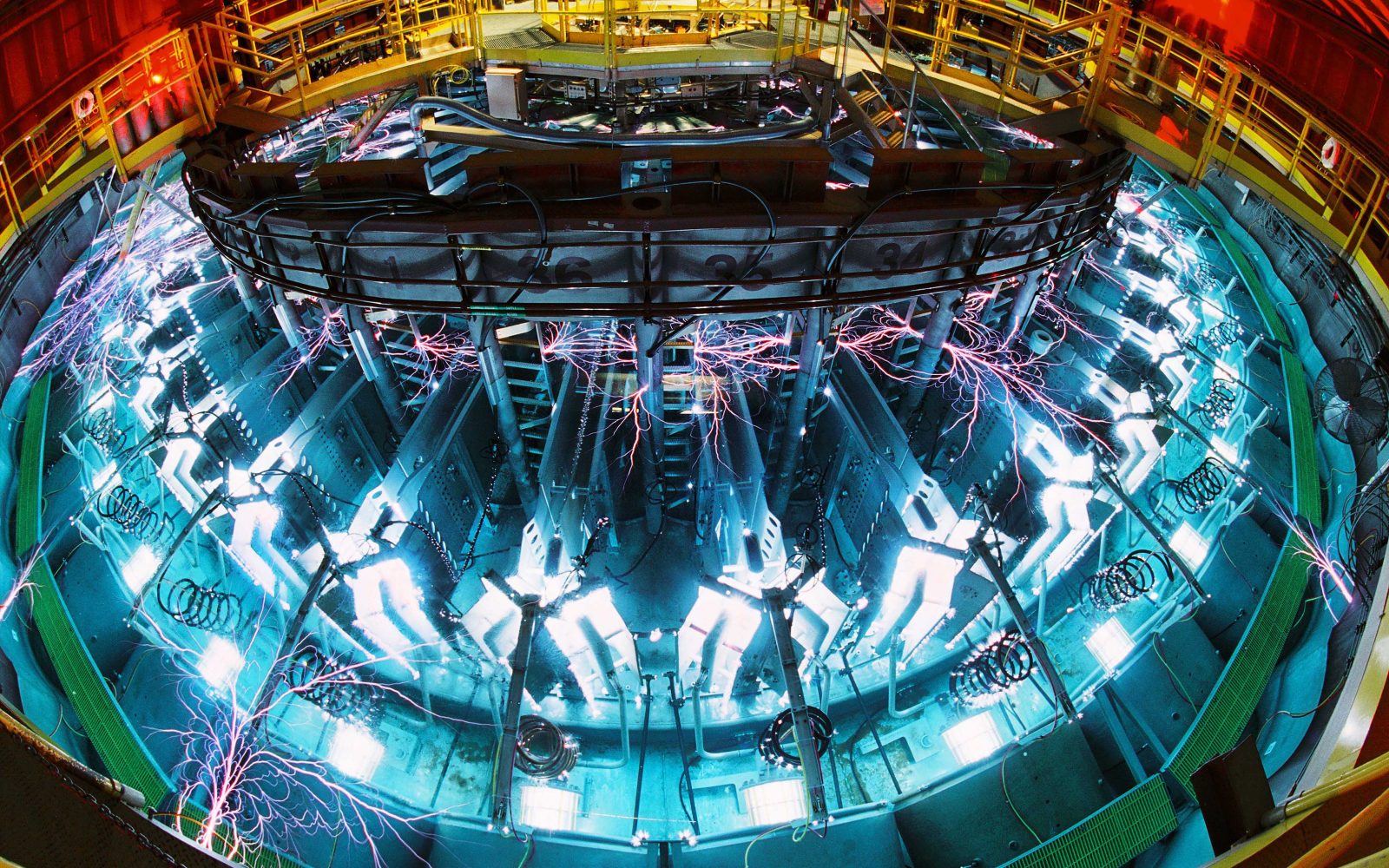
Improving lives
Innovation is at the heart of everything done inside the National Laboratories. Our scientists strive to make our world a safer, better place for all.
The Department of Energy’s 17 National Laboratories are powerhouses of science and technology whose researchers tackle some of the world’s toughest challenges. The Laboratories support scientists and engineers from academia, government, and industry with access to specialized equipment, world-class research facilities, and skilled technical staff. Together, they are working to solve some of the world’s greatest scientific challenges.

From innovations in energy technologies and sustainable building design to medical discoveries and improved national security, National Laboratory scientists and engineers are inventing solutions that make America and the world safer, healthier, and more sustainable.
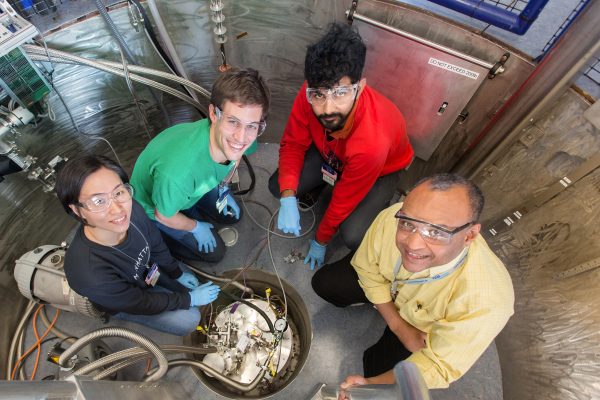
The U.S. Department of Energy’s 17 National Laboratories lead the nation in advancing the frontiers of scientific knowledge, keeping our nation secure, and fueling our clean energy economy. The innovation at the heart of the Laboratories’ past and future success benefits from the fusion of diverse talents and inclusive perspectives.
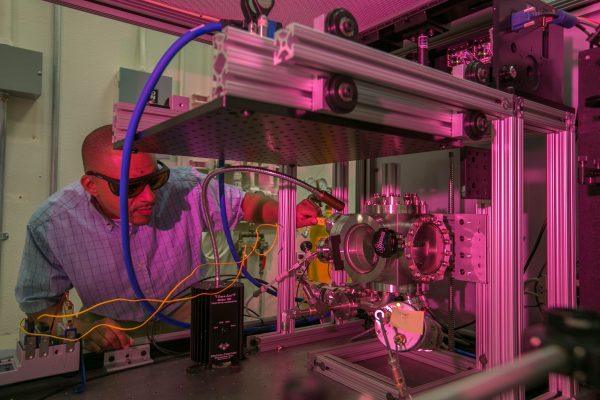
The Department of Energy’s 17 National Laboratories are powerhouses of science and technology.

STEM Resources
The National Laboratories are committed to advancing Science, Technology, Engineering, and Mathematics (STEM) in our nation’s schools.
The National Laboratories are a diverse and inclusive career destination for the next generation of scientists and engineers aspiring to make an impact through their research.
- MTS Health Sciences Clinical Lab Science vs. Clinical Research
- Anesthesia Technician
- Audiologist & SLP
- Cardiovascular Technologist
- Dental Assistant
- Dental Hygienist
- Diagnostic Medical Sonographer
- Dialysis Technician
- EKG Technician
- EMT & Paramedic
- Kinesiologist
- Mammography Technologist
- Medical Assistant
- MRI Technologist
- Neurodiagnostic Technologist
- Nuclear Medicine Technologist
- Ophthalmic Technician
- Pharmacy Technician
- Phlebotomist
- Physical Therapist Assistant & Aide
- Psychiatric & Mental Health Technician
- Radiation Therapist
- Radiologic Technologist
- Respiratory Therapist
- Surgical Technologist
- Cytologist (Cytotechnologist)
- Dental Lab Technician
- Histotechnologist
- Medical Lab Assistant
- Medical Lab Technician
- Biological Sciences
- Biomedical Science
- Biotechnology
- Health Sciences
- Medical Laboratory Scientist
- Nutritionist & Dietitian
- Pathologists' Assistant (PathA)
- Pre-Vet (Veterinarian)
- Biomedical Equipment Technician
- Biomedical Informatics
- Health Informatics
- Health Information Management
- Health Information Technology
- Healthcare Administration
- Medical Billing & Coding
- Nursing Informatics
- Sterile Processing Technician
- Patient-Facing Technology Programs
- Laboratory Technology programs
- Natural & Clinical Lab Science
- Medical IT & Administrative
Certification Guides
Career guides, interviews & features, clinical lab science vs. clinical research, search for schools.
When you click on a sponsoring school or program advertised on our site, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
While they may operate in similar settings, clinical laboratory science, and clinical research are two vastly different fields of medicine.
Clinical laboratory scientists, sometimes called medical laboratory scientists, specialize in laboratory information and services that inform the diagnosis, treatment, and monitoring of medical conditions. They may perform tests, interpret results, or develop entirely new laboratory tests and processes.
On the other hand, clinical researchers use scientific investigation methods to study human health and illness and answer specific questions about medicine and behavior. They may design or administer studies investigating a particular disease or evaluate a new drug’s effectiveness and impact.
Clinical researchers often attain graduate-level education through doctoral degrees in medicine or philosophy (MD or PhD). According to the United States Bureau of Labor Statistics (BLS), many pursue both due to increased job opportunities and higher starting salaries. Further certification through a professional society such as the Association for Clinical Research Professionals (ACRP) can distinguish a clinical researcher further in a field that is expected to grow almost twice as fast as the average for all occupations, according to the BLS.
Clinical laboratory science and clinical research take a scientific and investigative approach to answering medical questions. Still, each involves different methodological approaches, institutional certifications, work responsibilities, and educational requirements. When choosing between the two fields of study, it is essential to dig into the details to determine precisely what separates them.
For those considering a career in either field, here is a side-by-side chart comparing and contrasting the disciplines of clinical lab science and clinical research, including career requirements and educational programs.

Matt Zbrog is a writer and researcher from Southern California. Since 2018, he’s written extensively about emerging topics in medical technology, particularly the modernization of the medical laboratory and the network effects of both health data management and health IT. In consultation with professors, practitioners, and professional associations, his writing and research are focused on learning from those who know the subject best. For MedicalTechnologySchools.com, he’s interviewed leaders and subject matter experts at the American Health Information Management Association (AHIMA), the American Society of Clinical Pathology (ASCP), and the Department of Health and Human Services (HHS).
Related Articles
- Upskilling in the Allied Health Professions
- Single-use Plastics in Medicine Raise Concerns About Sustainability
- Clinical Research Certification - CCRA, CCRC, CPI
- How to Become a Clinical Research Associate
- Online Master’s in Clinical and Translational Research Programs
Related Programs

Clinical Research vs Lab Research: An In-depth Analysis

Clinical research , a cornerstone in advancing patient care, involves human subjects to test the safety and effectiveness of new treatments , ranging from drugs to diagnostic tools. Unlike clinical research , laboratory research focuses on the foundational science behind medicine without direct human involvement , contributing significantly to medical lab science.
The contrast between clinical research vs lab research highlights the diverse approaches in the scientific pursuit of better healthcare, where every medical advancement once relied on volunteer participation in clinical studies 1 . Bridging these two fields promises to accelerate the translation of lab discoveries into practical medical applications, underscoring the importance of collaboration in future developments in medical lab science 1 2 .
The Evolution of Clinical Research
The evolution of clinical research traces its origins back to ancient times, with the world's first recorded clinical tria l found in the "Book of Daniel" where a dietary intervention was observed to improve health after 10 days. This historical milestone was followed by significant advancements including Avicenna's rules for drug testing in his ‘ Canon of Medicine’ and Ambroise Pare's accidental trial in 1537 , which introduced a novel therapy for wounded soldiers. The modern era of clinical trials was marked by James Lind's controlled trial on scurvy in 1747 , laying the foundational principles for contemporary clinical research methodologies. The progression from these early experiments to the structured, ethical, and scientifically rigorous trials of today highlights the dynamic nature of clinical research. This evolution was further shaped by the introduction of the placebo in the early 1800s and the establishment of ethical frameworks , starting with the Hippocratic Oath and later formalized by the Nuremberg Code in 1947 . The development of clinical research has been instrumental in advancing medical science, with each phase of clinical trials meticulously designed to ensure the safety and efficacy of new treatments for the benefit of patient care.
Key Components of Laboratory Research
Clinical Research Facility Sciences, pivotal in the realm of medical lab science, leverage laboratory data and services extensively for disease diagnosis, monitoring, and treatment 2 4 . These sciences are underpinned by professionals who, after obtaining a Bachelor's degree in fields such as clinical research facility science or biomedical sciences from NAACLS-accredited programs, perform crucial laboratory tests, analyze specimens, and furnish healthcare providers with critical insights into the results' significance and validity 2 . Notably, these activities are conducted in laboratory settings without involving human subjects, emphasizing the distinction between clinical and laboratory research 2 .
The infrastructure of laboratories is meticulously designed to support the complex and sensitive nature of laboratory tests and analyses. This includes sturdy tables and ample counter space for heavy equipment, overhead and adjustable shelving for efficient space utilization, and cabinets and drawers for organized storage. Additionally, the deployment of fume hoods, customized for specific research needs, is essential for the safe handling of chemicals. Compliance with safety regulations and proper storage of flammable items underscore the operational standards necessary for high-quality testing and analysis in medical breakthroughs 6 .
The scientific process in laboratory research unfolds through several key steps: hypothesis formulation, experiment design, data collection, data analysis, and report writing. This structured approach begins with formulating a tentative explanation for a phenomenon, followed by planning and conducting experiments using appropriate methods and tools. The subsequent collection and analysis of data facilitate testing the hypothesis, culminating in the documentation of the entire process and findings in a formal report or paper 7 . This systematic methodology underscores the rigorous and methodical nature of laboratory research, contributing significantly to advancements in medical lab science.
Bridging the Gap: Collaboration between Clinical and Laboratory Research
Bridging the gap between clinical and laboratory research involves fostering collaborative environments that leverage the strengths of both fields to advance medical science. Medical scientific studies bifurcate into clinical laboratory scientists, who interpret critical data for healthcare professionals, and clinical researchers, who lay the groundwork for medical education and understanding 4 . This collaboration is pivotal for both building the future of medicine and administering its current benefits 4 . Enhanced operational efficiency is achieved through cross-departmental synergy, reducing redundancies in resource and personnel utilization, and fostering faster adoption of best practices and innovations across the lab 8 . These collaborations are exemplified by real-world success stories from renowned institutions like Mayo Clinic and Stanford Health Care, which have demonstrated the profound impact of integrated efforts on medical advancements 8 .
Key strategies for effective collaboration include regular meetings to address challenges, the integration of digital communication platforms with lab databases for swift sharing of results, and the establishment of clear guidelines for consistency in sample collection and result dissemination 8 . Unified objectives ensure that despite methodological differences, the end goals of improving patient care and advancing medical knowledge remain aligned 8 . Furthermore, the adoption of cloud-based data systems and AI technologies not only facilitates seamless data sharing but also automates routine tasks, thereby enhancing productivity and enabling the discovery of new insights 9 .
Challenges such as competition, ethics reviews, insufficient research funds, and the recruitment of project managers underscore the complexities of collaborative efforts 9 . However, the benefits, including improved reputation, publication quality, knowledge transfer, and acceleration of the research process, often outweigh the costs and risks associated with collaboration 9 . Collaborative relationships in Translational Medical Research (TMR) among clinicians highlight a strong willingness to collaborate, with preferences varying across different stages of research and between preferring independent and interdependent relationships 9 . This willingness to collaborate is crucial for bridging the gap between clinical and laboratory research, ultimately leading to groundbreaking advancements in medical science.
Future Trends in Clinical and Laboratory Research
The future of clinical and laboratory research is poised for transformative changes, driven by technological advancements and evolving healthcare needs. Notably:
Greater Efficiency through Automation : The integration of automation in research processes promises to streamline workflows, reducing manual labor and enhancing precision 13 .
Collaboration and Capacity Sharing : Partnerships between research institutions will facilitate shared resources and expertise, optimizing research outputs 13 .
Remote Sample Support and Diagnostic Data Interoperability : These advancements will enable more inclusive research and improved patient care by allowing data to flow seamlessly between different healthcare systems 13 .
Artificial Intelligence and Machine Learning : AI and machine learning are set to revolutionize both clinical and laboratory research by providing advanced data analysis, predictive modeling, and personalized medicine approaches 13 14 .
Staffing Solutions and Digital Workflows : Addressing staffing shortages through innovative solutions, alongside the adoption of digital workflows, will be crucial for maintaining research momentum 14 .
New Diagnostic Technologies : The development of novel diagnostic methods and technologies, including next-generation sequencing and biomarker-based screenings, will enhance disease diagnosis and treatment 14 .
Regulatory Changes and Patient-Centric Approaches : Increased FDA oversight of laboratory-developed tests and a shift towards patient-centric research models will ensure safer and more effective healthcare solutions 14 16 .
Precision Medicine and Big Data Analytics : The focus on precision medicine, supported by real-world evidence and big data analytics, will tailor treatments to individual patient needs, improving outcomes 15 .
Decentralized Clinical Trials and Digital Health Technologies : The rise of decentralized trials and digital health tools, including remote monitoring, will make research more accessible and patient-friendly 15 .
Innovation in Testing and Consumer Health : Laboratories will explore new frontiers in diagnostics, such as multi-drug-of-abuse testing and T-cell testing, while also responding to consumer health trends with at-home testing services 14 18 .
These trends underscore a dynamic shift towards more efficient, patient-centered, and technologically advanced clinical and laboratory research, setting the stage for groundbreaking discoveries and innovations in healthcare 13 14 15 16 18 .
Through this detailed exploration, we have seen the distinct yet intertwined roles that clinical and laboratory research play in the advancement of medical science and patient care. By comparing their methodologies, evolution, and collaborative potential, it becomes clear that both domains are crucial for fostering innovations that can bridge the gap between theoretical knowledge and practical healthcare solutions. The synergy between clinical and laboratory research, as highlighted by various examples and future trend predictions, establishes an essential framework for the continual improvement of medical practices and patient outcomes.
As we look toward the future, the significance of embracing technological advancements, enhancing collaboration, and adopting patient-centric approaches cannot be overstressed. These elements are pivotal in navigating the challenges and leveraging the opportunities within clinical and laboratory research landscapes. The potential impacts of such advancements on the field of medicine and on societal health as a whole are immense, underscoring the imperative for ongoing research, dialogue, and innovation in bridging the gap between the laboratory bench and the patient's bedside.
What distinguishes clinical research from laboratory research? Clinical research involves studies that include human participants, aiming to understand health and illness and answer medical questions. Laboratory research, on the other hand, takes place in environments such as chemistry or biology labs, typically at colleges or medical schools, and does not involve human subjects. Instead, it focuses on experiments conducted on non-human samples or models.
How does a clinical laboratory differ from a research laboratory? Clinical laboratories are specialized facilities where laboratory information and services are utilized to diagnose, monitor, and treat diseases. Research laboratories, in contrast, are settings where scientific investigation is conducted to study illness and health in humans to answer medical and behavioral questions.
In what ways do clinical research and scientific research differ? Clinical research is a branch of medical research that directly applies knowledge to improve patient care, often through the study of human subjects. Scientific research, including basic science research, aims to understand the mechanisms of diseases and biological processes, which may not have immediate applications in patient care.
Can you outline the various types of medical research analysis? Medical research can be categorized into three primary types based on the study's nature: basic (experimental) research, clinical research, and epidemiological research. Clinical and epidemiological research can be further divided into interventional studies, which actively involve treating or intervening in the study subjects, and noninterventional studies, which observe outcomes without intervention.

Prevent CRA Fraud: 5 Strategies to Protect Your CRO Team
Everything you need to know about clinical research studies.
Advertisement
Supported by
U.S. Tightens Rules on Risky Virus Research
A long-awaited new policy broadens the type of regulated viruses, bacteria, fungi and toxins, including those that could threaten crops and livestock.
- Share full article

By Carl Zimmer and Benjamin Mueller
The White House has unveiled tighter rules for research on potentially dangerous microbes and toxins, in an effort to stave off laboratory accidents that could unleash a pandemic.
The new policy, published Monday evening, arrives after years of deliberations by an expert panel and a charged public debate over whether Covid arose from an animal market or a laboratory in China.
A number of researchers worried that the government had been too lax about lab safety in the past, with some even calling for the creation of an independent agency to make decisions about risky experiments that could allow viruses, bacteria or fungi to spread quickly between people or become more deadly. But others warned against creating restrictive rules that would stifle valuable research without making people safer.
The debate grew sharper during the pandemic, as politicians raised questions about the origin of Covid. Those who suggested it came from a lab raised concerns about studies that tweaked pathogens to make them more dangerous — sometimes known as “gain of function” research.
The new policy, which applies to research funded by the federal government, strengthens the government’s oversight by replacing a short list of dangerous pathogens with broad categories into which more pathogens might fall. The policy pays attention not only to human pathogens, but also those that could threaten crops and livestock. And it provides more details about the kinds of experiments that would draw the attention of government regulators.
The rules will take effect in a year, giving government agencies and departments time to update their guidance to meet the new requirements.
“It’s a big and important step forward,” said Dr. Tom Inglesby, the director of the Johns Hopkins Center for Health Security and a longtime proponent of stricter safety regulations. “I think this policy is what any reasonable member of the public would expect is in place in terms of oversight of the world’s most transmissible and lethal organisms.”
Still, the policy does not embrace the most aggressive proposals made by lab safety proponents, such as creating an independent regulatory agency. It also makes exemptions for certain types of research, including disease surveillance and vaccine development. And some parts of the policy are recommendations rather than government-enforced requirements.
“It’s a moderate shift in policy, with a number of more significant signals about how the White House expects the issue to be treated moving forward,” said Nicholas Evans, an ethicist at University of Massachusetts Lowell.
Experts have been waiting for the policy for more than a year. Still, some said they were surprised that it came out at such a politically fraught moment . “I wasn’t expecting anything, especially in an election year,” Dr. Evans said. “I’m pleasantly surprised.”
Under the new policy, scientists who want to carry out experiments will need to run their proposals past their universities or research institutions, which will to determine if the work poses a risk. Potentially dangerous proposals will then be reviewed by government agencies. The most scrutiny will go to experiments that could result in the most dangerous outcomes, such as those tweaking pathogens that could start a pandemic.
In a guidance document , the White House provided examples of research that would be expected to come under such scrutiny. In one case, they envisioned scientists trying to understand the evolutionary steps a pathogen needed to transmit more easily between humans. The researchers might try to produce a transmissible strain to study, for example, by repeatedly infecting human cells in petri dishes, allowing the pathogens to evolve more efficient ways to enter the cells.
Scientists who do not follow the new policy could become ineligible for federal funding for their work. Their entire institution may have its support for life science research cut off as well.
One of the weaknesses of existing policies is that they only apply to funding given out by the federal government. But for years , the National Institutes of Health and other government agencies have struggled with stagnant funding, leading some researchers to turn instead to private sources. In recent years, for example, crypto titans have poured money into pandemic prevention research.
The new policy does not give the government direct regulation of privately funded research. But it does say that research institutions that receive any federal money for life-science research should apply a similar oversight to scientists doing research with support from outside the government.
“This effectively limits them, as the N.I.H. does a lot of work everywhere in the world,” Dr. Evans said.
The new policy takes into account the advances in biotechnology that could lead to new risks. When pathogens become extinct, for example, they can be resurrected by recreating their genomes. Research on extinct pathogens will draw the highest levels of scrutiny.
Dr. Evans also noted that the new rules emphasize the risk that lab research can have on plants and animals. In the 20th century, the United States and Russia both carried out extensive research on crop-destroying pathogens such as wheat-killing fungi as part of their biological weapons programs. “It’s significant as a signal the White House is sending,” Dr. Evans said.
Marc Lipsitch, an epidemiologist at Harvard and a longtime critic of the government’s policy, gave the new one a grade of A minus. “I think it’s a lot clearer and more specific in many ways than the old guidance,” he said. But he was disappointed that the government will not provide detailed information to the public about the risky research it evaluates. “The transparency is far from transparent,” he said.
Scientists who have warned of the dangers of impeding useful virus research were also largely optimistic about the new rules.
Gigi Gronvall, a biosafety specialist at the Johns Hopkins Bloomberg School of Public Health, said the policy’s success would depend on how federal health officials interpreted it, but applauded the way it recognized the value of research needed during a crisis, such as the current bird flu outbreak .
“I was cautiously optimistic in reading through it,” she said of the policy. “It seems like the orientation is for it to be thoughtfully implemented so it doesn’t have a chilling effect on needed research.”
Anice Lowen, an influenza virologist at Emory University, said the expanded scope of the new policy was “reasonable.” She said, for instance, that the decision not to create an entirely new review body helped to alleviate concerns about how unwieldy the process might become.
Still, she said, ambiguities in the instructions for assessing risks in certain experiments made it difficult to know how different university and health officials would police them.
“I think there will be more reviews carried out, and more research will be slowed down because of it,” she said.
Carl Zimmer covers news about science for The Times and writes the Origins column . More about Carl Zimmer
Benjamin Mueller reports on health and medicine. He was previously a U.K. correspondent in London and a police reporter in New York. More about Benjamin Mueller
Research Laboratory Specialist Intermediate
How to apply.
A cover letter is required for consideration for this position and should be attached as the first page of your resume. The cover letter should address your specific interest in the position and outline skills and experience that directly relate to this position.
The Biomedical Research Core Facilities Advanced Genomics Core is looking for a skilled research technician to join us full time as a Research Laboratory Specialist. The incumbent will assist in developing, deploying and executing protocols on DNA/RNA for our research community. This role will support next generation sequencing by performing library preparations, quality control, and in operations of many of our sequencing instruments.
Mission Statement
Michigan Medicine improves the health of patients, populations and communities through excellence in education, patient care, community service, research and technology development, and through leadership activities in Michigan, nationally and internationally. Our mission is guided by our Strategic Principles and has three critical components; patient care, education and research that together enhance our contribution to society.
Why Join Michigan Medicine?
Michigan Medicine is one of the largest health care complexes in the world and has been the site of many groundbreaking medical and technological advancements since the opening of the U-M Medical School in 1850. Michigan Medicine is comprised of over 30,000 employees and our vision is to attract, inspire, and develop outstanding people in medicine, sciences, and healthcare to become one of the world?s most distinguished academic health systems. In some way, great or small, every person here helps to advance this world-class institution. Work at Michigan Medicine and become a victor for the greater good.
What Benefits can you Look Forward to?
- Excellent medical, dental and vision coverage effective on your very first day
- 2:1 Match on retirement savings
Responsibilities*
- Prepare libraries for both short and long read next-generation sequencing platforms, starting from RNA or DNA specimens. Ensure that the input RNA and DNA conform to the core's standards for library creation by performing a range of quality control tests, such as fluorescent, spectrophotometric, and electrophoretic assays. Assist with implementation of new protocols for DNA and RNA library preparation and sequencing, with a focus on high-throughput process development.
- Conduct quality control assessments for both in-house and client-prepared libraries. Evaluate the size of the library inserts and their quality parameters. Identify and record any samples or batches that do not pass the quality control checks. Adhere to the core's standard operating procedures to decide on subsequent actions. Keep accurate records indicating when samples are cleared to advance to the subsequent phase of the sequencing process. Prepare libraries for pooling and sequencing using multiple QC results qPCR results as a guide to balance the data output.
- Operation of sequencing instruments from Illumina, Singular Genomics, and Oxford Nanopore, encompassing library clustering and sequencing adhering to proven protocols. Responsibilities involve performing post-run and regular maintenance cleaning procedures, conducting diagnostic checks for troubleshooting purposes, and liaising with vendor technical support by providing relevant feedback. Monitoring the progress and quality metrics of sequencing runs is also a key duty. Additional instrumentation responsibilities include use of existing programs on automated liquid handlers.
- Assist in developing, deploying and executing protocols to improve operations in the Advanced Genomics Core. Tasks may include but are not limited to inventory management, quality control tracking, and efficiency enhancement.
Required Qualifications*
Candidates should possess a bachelor's degree in a related field such as biochemistry, cell biology, or molecular biology, though a master's degree is preferred. They should also have 4-5 years of practical experience with fundamental molecular biology techniques like DNA/RNA extraction, PCR, gel electrophoresis, and sequencing. A thorough understanding of core lab practices is critical, including adeptness in pipetting, making reagents, and ensuring aseptic conditions to prevent contamination. Experience with common molecular biology instruments, including centrifuges, thermocyclers, spectrophotometers, microscopes, and high-throughput sequencing devices, is important. Computer proficiency is mandatory for the role, specifically with standard office programs like Microsoft Word and Excel. An ideal applicant will be detailed-oriented in the laboratory and with documentation, capable of working autonomously and collaboratively within a diverse team, particularly when tasked with delivering prompt results under time constraints.
Desired Qualifications*
Preferred qualifications include proficiency in handling and programming a range of laboratory apparatuses, including instrumentation from Hamilton, Formulatrix, Tecan, Beckman Coulter, Eppendorf, or similar platforms. Practical knowledge of next-generation sequencing library preparation and the operation of instruments from PacBio, Illumina, Singular Genomics, Oxford Nanopore, or Element Biosciences is highly desirable. Additional experience with cellular techniques, immunohistochemistry, in situ hybridization, and the preparation of tissue samples including fixation, cryopreservation, and the sectioning of both paraffin-embedded and frozen specimens will be considered an asset.
Work Locations
Position is located at the North Campus Research Complex. Not eligible for remote work.
Additional Information
Michigan Medicine values a culture of diversity, equity, and inclusion. Here at the Biomedical Research Core Facilities (BRCF), our dedication to customer service is inseparable from our commitment to diversity, equity and inclusion. It is central to our mission as an institutional resource to ensure that each member of our community has full opportunity to thrive in our environment, for we believe that diversity is key to individual flourishing, educational excellence and the advancement of knowledge.
Background Screening
Michigan Medicine conducts background screening and pre-employment drug testing on job candidates upon acceptance of a contingent job offer and may use a third party administrator to conduct background screenings. Background screenings are performed in compliance with the Fair Credit Report Act. Pre-employment drug testing applies to all selected candidates, including new or additional faculty and staff appointments, as well as transfers from other U-M campuses.
Application Deadline
Job openings are posted for a minimum of seven calendar days. The review and selection process may begin as early as the eighth day after posting. This opening may be removed from posting boards and filled anytime after the minimum posting period has ended.
U-M EEO/AA Statement
The University of Michigan is an equal opportunity/affirmative action employer.
Suggested Searches
- Climate Change
- Expedition 64
- Mars perseverance
- SpaceX Crew-2
- International Space Station
- View All Topics A-Z
- Humans in Space
Earth & Climate
The solar system, the universe, aeronautics, learning resources, news & events.

Welcome Back to Planet Earth, Expedition 70 Crew!
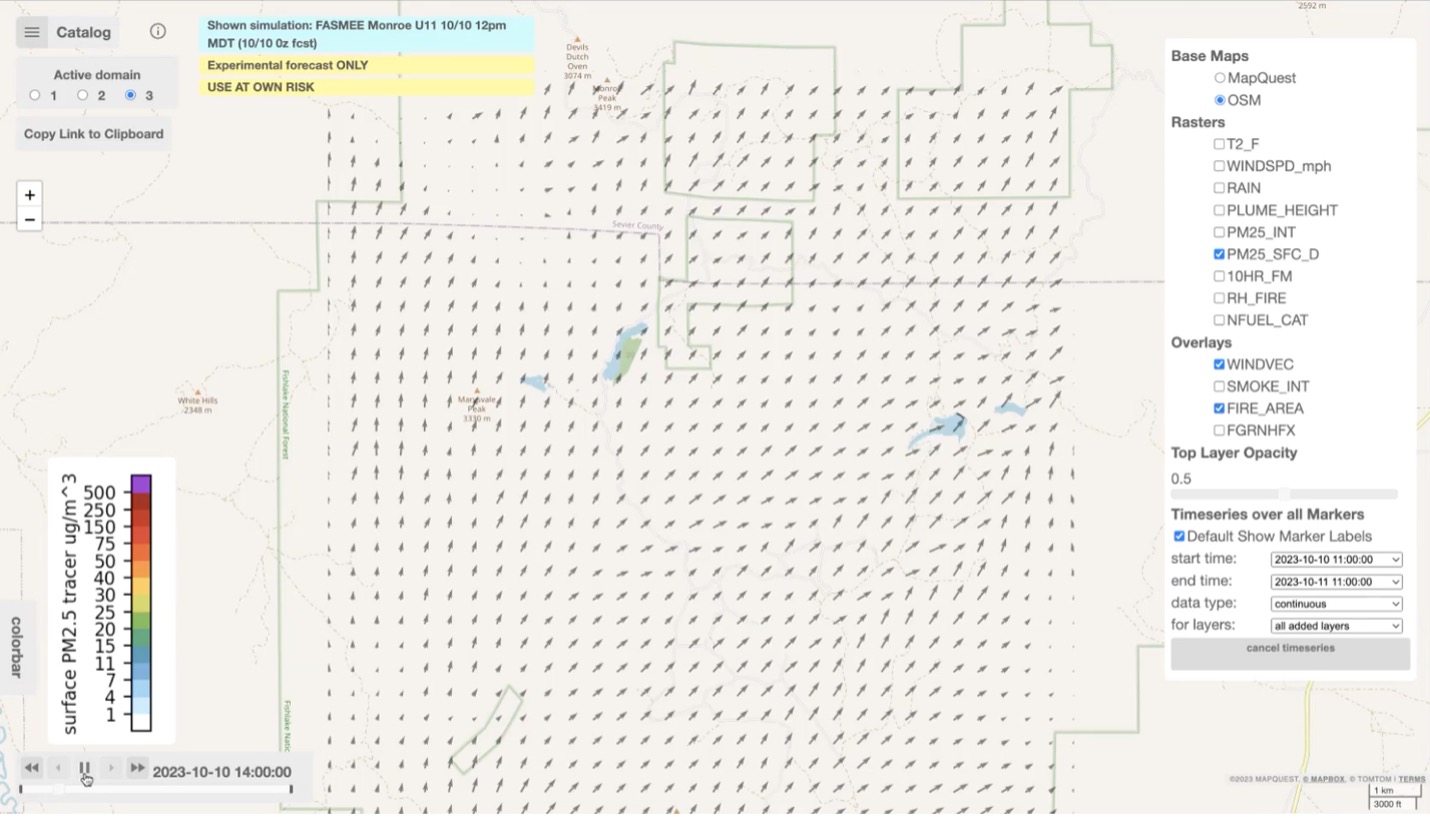
NASA “Wildfire Digital Twin” Pioneers New AI Models and Streaming Data Techniques for Forecasting Fire and Smoke
NASA Study Provides New Look at Orbital Debris, Potential Solutions
- Search All NASA Missions
- A to Z List of Missions
- Upcoming Launches and Landings
- Spaceships and Rockets
- Communicating with Missions
- James Webb Space Telescope
- Hubble Space Telescope
- Why Go to Space
- Astronauts Home
- Commercial Space
- Destinations
- Living in Space
- Explore Earth Science
- Earth, Our Planet
- Earth Science in Action
- Earth Multimedia
- Earth Science Researchers
- Pluto & Dwarf Planets
- Asteroids, Comets & Meteors
- The Kuiper Belt
- The Oort Cloud
- Skywatching
- The Search for Life in the Universe
- Black Holes
- The Big Bang
- Dark Energy & Dark Matter
- Earth Science
- Planetary Science
- Astrophysics & Space Science
- The Sun & Heliophysics
- Biological & Physical Sciences
- Lunar Science
- Citizen Science
- Astromaterials
- Aeronautics Research
- Human Space Travel Research
- Science in the Air
- NASA Aircraft
- Flight Innovation
- Supersonic Flight
- Air Traffic Solutions
- Green Aviation Tech
- Drones & You
- Technology Transfer & Spinoffs
- Space Travel Technology
- Technology Living in Space
- Manufacturing and Materials
- Science Instruments
- For Kids and Students
- For Educators
- For Colleges and Universities
- For Professionals
- Science for Everyone
- Requests for Exhibits, Artifacts, or Speakers
- STEM Engagement at NASA
- NASA's Impacts
- Centers and Facilities
- Directorates
- Organizations
- People of NASA
- Internships
- Our History
- Doing Business with NASA
- Get Involved
- Aeronáutica
- Ciencias Terrestres
- Sistema Solar
- All NASA News
- Video Series on NASA+
- Newsletters
- Social Media
- Media Resources
- Upcoming Launches & Landings
- Virtual Events
- Sounds and Ringtones
- Interactives
- STEM Multimedia
Discovery Alert: Mini-Neptune in Double Star System is a Planetary Puzzle

NASA Tool Gets Ready to Image Faraway Planets

Astronaut Exercise

Eleasa Kim: Pioneering CLDP Payload Operations and Cultural Integration

5 Things to Know About NASA’s Tiny Twin Polar Satellites

How ‘Glowing’ Plants Could Help Scientists Predict Flash Drought
NASA’s Juno Provides High-Definition Views of Europa’s Icy Shell

The Next Full Moon is the Flower, Corn, or Corn Planting Moon

Binoculars: A Great First Telescope
Webb Cracks Case of Inflated Exoplanet
NASA, Industry to Start Designing More Sustainable Jet Engine Core
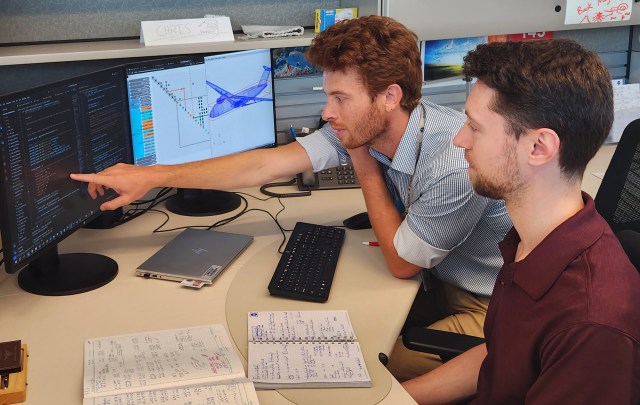
Aviary: A New NASA Software Platform for Aircraft Modelling

NASA’s X-59 Passes Milestone Toward Safe First Flight

Tech Today: From Spacesuits to Racing Suits
Tech Today: A NASA-Inspired Bike Helmet with Aerodynamics of a Jet

NASA Challenge Gives Artemis Generation Coders a Chance to Shine
Kan Yang: Translating Science Ideas into Engineering Concepts
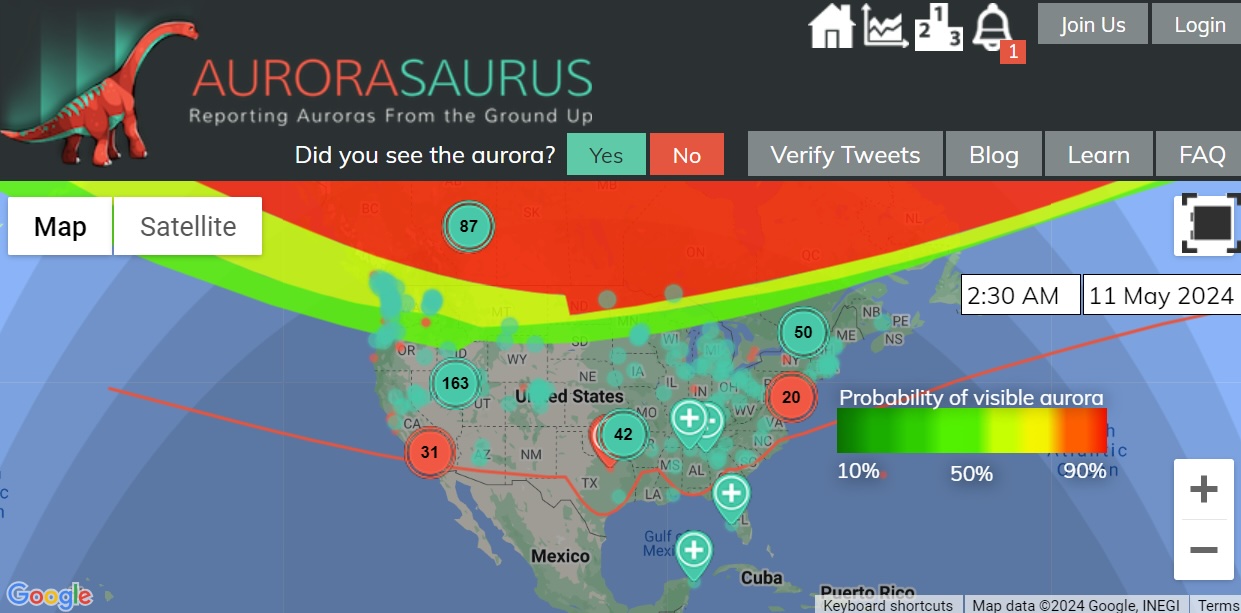
Aurorasaurus Roars During Historic Solar Storm

Johnson Celebrates AA and NHPI Heritage Month: Anima Patil-Sabale

Diez maneras en que los estudiantes pueden prepararse para ser astronautas

Astronauta de la NASA Marcos Berríos
Resultados científicos revolucionarios en la estación espacial de 2023
Station science 101 | research in microgravity: higher, faster, longer.

Melissa L. Gaskill
Microgravity, a unique orbit, crewed laboratory, twenty years and counting, adding subjects adds time.
The International Space Station provides unique features that enable innovative research, including microgravity, exposure to space, a unique orbit, and hands-on operation by crew members.
The space station provides consistent, long-term access to microgravity. Eliminating the effects of Earth’s gravity on experiments is a game-changer across many disciplines, including research on living things and physical and chemical processes. For example, without gravity hot air does not rise, so flames become spherical and behave differently. Removing the forces of surface tension and capillary movement allows scientists to examine fluid behavior more closely.
The speed, pattern, and altitude of the space station’s orbit provide unique advantages. Traveling at 17,500 miles per hour, it circles the planet every 90 minutes, passing over a majority of Earth’s landmass and population centers in daylight and darkness. Its 250-mile-high altitude is low enough for detailed observation of features, atmospheric phenomena, and natural disasters from different angles and with varying lighting conditions. At the same time, the station is high enough to study how space radiation affects material durability and how organisms adapt and examine phenomena such as neutron stars and blackholes. The spacecraft also places observing instruments outside Earth’s atmosphere and magnetic field, which can interfere with observations from the ground.
Other satellites in orbit contain scientific experiments and conduct Earth observations, but the space station also has crew members aboard to manage and maintain scientific activities. Human operators can respond to and assess events in real time, swap out experiment samples, troubleshoot, and observe results first-hand. Crew members also pack experiment samples and send them back to the ground for detailed analysis.
Thanks to the space station’s longevity, experiments can continue for months or even years. Scientists can design follow-up studies based on previous results, and every expedition offers the chance to expand the number of subjects for human research.
One area of long-term human research is on changes in vision, first observed when astronauts began spending months at a time in space. Scientists wondered whether fluids shifting from the lower to the upper body in microgravity caused increased pressure inside the head that changed eye shape. The Fluid Shifts investigation began in 2015 and continued to measure the extent of fluid shifts in multiple astronauts through 2020. 1
Whether the original study is long or short, it can take years for research to go from the lab into practical applications. Many steps are involved, some of them lengthy. First, researchers must come up with a question and a possible answer, or hypothesis. For example, Fluid Shifts questioned what was causing vision changes and a possible answer was increased fluid pressure in the head. Scientists must then design an experiment to test the hypothesis, determining what data to collect and how to do so.

Getting research onto the space station in the first place takes time, too. NASA reviews proposals for scientific merit and relevance to the agency’s goals. Selected investigations are assigned to a mission, typically months in the future. NASA works with investigators to meet their science requirements, obtain approvals, schedule crew training, develop flight procedures, launch hardware and supplies, and collect any preflight data needed. Once the study launches, in-flight data collection begins. When scientists complete their data collection, they need time to analyze the data and determine what it means. This may take a year or more.
Scientists then write a paper about the results – which can take many months – and submit it to a scientific journal. Journals send the paper to other experts in the same field, a process known as peer review. According to one analysis, this review takes an average of 100 days. 2 The editors may request additional analysis and revisions based on this review before publishing.
Aspects of research on the space station can add more time to the process. Generally, the more test subjects, the better – from 100 to 1,000 subjects for statistically significant results for clinical research. But the space station typically only houses about six people at a time.
Lighting Effects shows how the need for more subjects adds time to a study. This investigation examined whether adjusting the intensity and color of lighting inside the station could help improve crew circadian rhythms, sleep, and cognitive performance. To collect data from enough crew members, the study ran from 2016 until 2020.
Other lengthy studies about how humans adapt to life in space include research on loss of heart muscle and a suite of long-term studies on nutrition, including producing fresh food in space.

For physical science studies, investigators can send batches of samples to the space station and collect data more quickly, but results can create a need for additional research. Burning and Suppression of Solids ( BASS ) examined the characteristics of a wide variety of fuel samples from 2011 to 2013, and BASS-II continued that work through 2017. The Saffire series of fire safety demonstrations began in 2016 and wrapped up in 2024. Researchers have answered many burning (pun intended) questions, but still have much to learn about preventing, detecting, and extinguishing fires in space.
The timeline for scientific results can run long, especially in microgravity. But those results can be well worth the wait.
Melissa Gaskill International Space Station Research Communications Team Johnson Space Center
Search this database of scientific experiments to learn more about those mentioned above.
1 Macias BR, Liu JHK, Grande-Gutierrez N, Hargens AR. Intraocular and intracranial pressures during head-down tilt with lower body negative pressure. Aerosp Med Hum Perform. 2015; 86(1):3–7. https://www.ingentaconnect.com/content/asma/amhp/2015/00000086/00000001/art00004;jsessionid=31bonpcj2e8tj.x-ic-live-01
2 Powell K. Does it take too long to publish research? Nature 530, pages148–151 (2016). https://www.nature.com/articles/530148a
Discover More Topics
Station Science 101

Latest News from Space Station Research
Space Station Research and Technology Resources

Station Benefits for Humanity
Related Terms
- ISS Research
- International Space Station (ISS)
- Johnson Space Center
Natural Resources Job Board
OUR SPONSORS AND PARTNERS

USDA-ARS Research Fellowship in Laboratory Quality Assurance
Oak Ridge Associated Universities (ORAU) (Private) | https://orise.orau.gov/index.html
Description
View location.
A member of Texas A&M AgriLife
Texas A&M AgriLife Extension Service | Texas A&M AgriLife Research | Texas A&M Forest Service | Texas A&M AgriLife Veterinary Medical Diagnostic Lab | College of Agriculture & Life Sciences

- Careers Home
- Working Here
- Living Here
- Graduate - Education & Internship Opportunities
- Scientific Leadership
- Biology and Environment
- Clean Energy
- Fusion and Fission
- National Security
- Neutron Science
- Postdoctoral
- Supercomputing
- Business and Administrative Support
- Craft and Skilled Labor
- University of Tennessee-Oak Ridge Innovation Institute
- Join Talent Community
- View All Jobs
Research Operations Support Professional
Date: May 21, 2024
Location: Oak Ridge, TN, US, 37830
Company: Oak Ridge National Laboratory
Requisition Id 13078
Overview:
We are hiring an entry-level Research Operations Support Professional to support operation tasks associated with work control of science and engineering activities. You will also provide support to researchers in maintaining compliance with applicable federal and state laws, DOE orders, and ORNL policies and procedures regarding work control. This position resides in the Integrated Research Operations Support group in the Safety & Operations Services Division, in the Environment, Safety, Health & Quality Directorate, at Oak Ridge National Laboratory (ORNL).
As a U.S. Department of Energy (DOE) Office of Science national laboratory, ORNL has an extraordinary 80-year history of solving the nation’s biggest problems. We have a dedicated and creative staff of over 6,000 people! Our vision for diversity, equity, inclusion, and accessibility (DEIA) is to cultivate an environment and practices that foster diversity in ideas and in the people across the organization, as well as to ensure ORNL is recognized as a workplace of choice. These elements are essential for enabling the execution of ORNL’s broader mission to accelerate scientific discoveries and their translation into energy, environment, and security solutions for the nation.
Major Duties/Responsibilities:
Serve as a Divisional point-of contact (POC) for work control as it relates to research safety summaries (RSS) and documentation for hazard identification and control.
Coordinate RSS reviews to ensure sufficient review between peers and SMEs and ensure all RSSs are approved and authorized within the allocated timeframe.
Help ensure that operational activities required for research objectives are completed safely and compliantly, either through the work control process or as requested by researchers.
Schedule and participate in laboratory compliance walkthroughs.
Abide by and promote the Battelle Safe Conduct of Research principles including being personally responsible for ensuring safe operations, raising safety concerns, using a questioning mentality, considering hazards for every task and where learning never stops.
Continually seek ways to increase operational efficiencies and improve safety culture in support of the research mission and champion initiatives to do so.
Deliver ORNL’s mission by aligning behaviors, priorities, and interactions with our core values of Impact, Integrity, Teamwork, Safety, and Service. Promote diversity, equity, inclusion, and accessibility by encouraging a respectful workplace – in how we treat one another, work together, and measure success.
Other responsibilities may include:
Support the integration of Integrated Safety Management (ISM) into work planning and execution, working alongside a diverse operations team.
Participate in the review and development of division or directorate level procedures and guidelines as needed.
Basic Qualifications:
A BS in science, operations, health and safety, industrial hygiene, environmental management, project management, engineering, operations, or a related field of study and zero (0) to two (2) years of technical experience is required.
Preferred Qualifications:
Experience collaborating as a team member in a dynamic, diverse organizational setting, involving interactions with management, researchers, facility users, and operations staff across different subject areas and tasks.
Experience with work control processes in a research and development environment and/or industrial environment.
Experience working in multi-disciplinary R&D environment or supporting industrial, radiological, nuclear, or secure facilities and operations.
Proven excellence in interpersonal, verbal, and written communication skills.
Ability to prioritize work and manage multiple projects simultaneously.
Strong organizational and time management skills and ability to meet inflexible delivery schedules on own initiative.
Experience in DOE and ORNL systems such as the Research Hazard Analysis and Control System and/or Integrated Safety Management.
Special Requirements:
Work involves various physical requirements and working conditions. As such, a pre-hire physical will be required after offer.
Visa sponsorship is not available for this position.
This position requires the ability to obtain and maintain a clearance from the Department of Energy. As such, this position is a Workplace Substance Abuse (WSAP) testing designated position. WSAP positions require passing a pre-placement drug test and participation in an ongoing random drug testing program.
Benefits at ORNL:
ORNL offers competitive pay and benefits programs to attract and retain dedicated people. The laboratory offers many employee benefits, including medical and retirement plans and flexible work hours, to help you and your family live happy and healthy. Employee amenities such as on-site fitness, banking, and cafeteria facilities are also provided for convenience.
Other benefits include the following: Prescription Drug Plan, Dental Plan, Vision Plan, 401(k) Retirement Plan, Contributory Pension Plan, Life Insurance, Disability Benefits, Generous Vacation and Holidays, Parental Leave, Legal Insurance with Identity Theft Protection, Employee Assistance Plan, Flexible Spending Accounts, Health Savings Accounts, Wellness Programs, Educational Assistance, Relocation Assistance, and Employee Discounts.
Having difficulty using the online application system or need an accommodation to apply due to a disability? Please email: [email protected] or call 1.866.963.9545.
This position will remain open for a minimum of 5 days after which it will close when a qualified candidate is identified and/or hired.
We accept Word (.doc, .docx), Adobe (unsecured .pdf), Rich Text Format (.rtf), and HTML (.htm, .html) up to 5MB in size. Resumes from third party vendors will not be accepted; these resumes will be deleted and the candidates submitted will not be considered for employment.
If you have trouble applying for a position, please email [email protected].
ORNL is an equal opportunity employer. All qualified applicants, including individuals with disabilities and protected veterans, are encouraged to apply. UT-Battelle is an E-Verify employer.
Nearest Major Market: Knoxville
- Privacy Policy
- UT-Battelle
- Department of Energy
- Search Jobs
All Comments © Copyright 2017 All Rights Reserved
- Stavropol Tourism
- Stavropol Hotels
- Stavropol Bed and Breakfast
- Flights to Stavropol
- Stavropol Restaurants
- Things to Do in Stavropol
- Stavropol Travel Forum
- Stavropol Photos
- Stavropol Map
- All Stavropol Hotels
- Stavropol Hotel Deals
- Things to Do
- Restaurants
- Vacation Rentals
- Travel Stories
- Rental Cars
- Add a Place
- Travel Forum
- Travelers' Choice
- Help Center
Safety in Stavropol' - Stavropol Forum
- Europe
- Russia
- North Caucasian District
- Stavropol Krai
- Stavropol
Safety in Stavropol'
- United States Forums
- Europe Forums
- Canada Forums
- Asia Forums
- Central America Forums
- Africa Forums
- Caribbean Forums
- Mexico Forums
- South Pacific Forums
- South America Forums
- Middle East Forums
- Honeymoons and Romance
- Business Travel
- Train Travel
- Traveling With Disabilities
- Tripadvisor Support
- Solo Travel
- Bargain Travel
- Timeshares / Vacation Rentals
- Stavropol Krai forums
- Stavropol forum

I am hoping to spend some time in Stavropol' (the city itself) to conduct research for my graduate degree. I am having a hard time figuring out very much about the city, however. Is it a safe place to stay for a young woman? Is it far enough away from some of the more dangerous areas of the Northern Caucasus to be safe for travel? Any advice about the city is much appreciated, thanks!
- Employment in Stavropol Area of Russia Dec 02, 2021
- Stavropol safety for American Jan 30, 2018
- How to get from Stavropol to Tbilisi? Aug 18, 2016
- Services for persons with disabilities Apr 06, 2016
- Safety in Stavropol' Jan 25, 2015
- Safety in Stavropol Oct 30, 2012
- Security Situation Jan 21, 2010
- Safety in Stavropol 2 replies
- Employment in Stavropol Area of Russia 10 replies

COMMENTS
Laboratory medicine has undergone a profound evolution in organizational, methodological, and cultural terms in recent decades [].From the organizational point of view, we are living in the era of consolidation, i.e., the formation of networks of consolidated laboratories with marked automation and integration of the various branches of laboratory medicine [].
The clinical laboratory field is extensive and includes various subfields, but to our knowledge, only 12 reviews have previously addressed QI in the clinical laboratory. This research is the first to thoroughly evaluate all QI-related clinical laboratory papers in one review. There are some limitations to this research.
Research. Mayo Clinic staff members are actively engaged in research on several areas within Laboratory Medicine and Pathology. Mayo Clinic researchers continually study new and more efficient medical testing techniques and reflect their advances in tests offered internally at Mayo Clinic as well as externally though Mayo Clinic Laboratories.
A medical laboratory or clinical laboratory is a laboratory where tests are conducted out on clinical specimens to obtain information about the health of a patient to aid in diagnosis, treatment, and prevention of disease. [1] Clinical medical laboratories are an example of applied science, as opposed to research laboratories that focus on ...
Explore the latest full-text research PDFs, articles, conference papers, preprints and more on MEDICAL LABORATORY TECHNOLOGY. Find methods information, sources, references or conduct a literature ...
Research: Research on AI in laboratory medicine should focus on generating clinical evidence of benefits and implementation: AI, artificial intelligence. Open in new tab Patient Viewpoint. The overarching goal of implementing AI in clinical practice is to benefit the patient. Therefore, the patient's perspective should also be discussed.
Nadine Lerret, PhD, MLS (ASCP) CM Director of Research (312) 942-2780. At Rush University, we believe that basic, clinical and translational research activities serve as the foundation for advances in patient care. Our graduate students are introduced to research related to medical laboratory science early on — in the first academic quarter ...
Clinical Research at Johns Hopkins Medicine. Offices and Policies. Hopkins Synergy. Events Calendar. Advancements in Research. Home Research. Find a Research Lab. Search for a research area, principal investigator, or keyword. Search. Browse an A-Z Listing. A B C ...
Resources for Clinical Laboratory Science, also called Medical Laboratory Science or Medical Technology, is the health profession that provides laboratory information and services needed for the diagnosis and treatment of disease. ... UPDATED content includes the latest research relating to accuracy of tests, diagnostic value of results, and ...
Clinical Laboratory Science, also called Medical Laboratory Science or Medical Technology, is the health profession that provides laboratory information and services needed for the diagnosis and treatment of disease. Clinical Laboratory Scientists perform a variety of laboratory tests, ensure the quality of the test results, explain the significance of laboratory tests, evaluate new methods ...
A. Advanced Endoscopy Innovation Translation and Clinical Trials Group: Barham Abu Dayyeh. Advanced Medical Imaging Technology: Richard L. Ehman. Aerospace Medicine and Vestibular Research: Michael J. Cevette, Jan Stepanek. Aging and Dementia Imaging Research (ADIR): Clifford R. Jack Jr.; Kejal Kantarci; Prashanthi Vemuri.
Postdocs who land faculty jobs at research-intensive institutions need to juggle several new large-scale tasks: identifying space and equipment needs for their lab, negotiating the hiring package, outfitting the lab with supplies, building a team, and learning to manage time in ways that can promote productivity and happiness. Here we share tips to help new hires think clearly about each of ...
Medical laboratory scientists have a wide variety of responsibilities and duties. They can: Cross-match blood for transfusion. Create quality assurance programs to monitor and ensure the accuracy ...
The Department of Energy's 17 National Laboratories are powerhouses of science and technology whose researchers tackle some of the world's toughest challenges. The Laboratories support scientists and engineers from academia, government, and industry with access to specialized equipment, world-class research facilities,…
Research advisor: Diana Huang, PhD. Laboratory Results for Clostridium difficile Infection: Correlation with Patient Symptoms and History By Marie Mohrbacher Research advisor: Kamaljit Singh, MD. Analysis of RBC Handling and Waste Reduction in a Large Academic Medical Center Operating Room By Kristi Mosher Research advisor: Yolanda Garcia, MS
Medical lab scientists work in a variety of settings like hospitals, clinics, forensic or public health laboratories, research institutions, and in many industries such as pharmaceutical and biotechnology. Work hours may vary based on the work setting; but typically labs are run 24 hours a day, seven days a week.
As September approaches, a new cohort of junior faculty members are taking up their first positions as research group leaders. I was there 3 years ago, making career-shaping decisions—sometimes without much mentoring or support. I learned a lot in my first years—how to write a grant, manage rejection, and supervise students, to name just a few—and it was all trial by fire. Though I made ...
Clinical laboratory science uses laboratory information and services to help diagnose, monitor, and treat disease. Clinical research uses scientific investigation to study the health and illness of people and answer questions about medicine and behavior. Requirements to Join Career. Clinical laboratory scientists typically complete a bachelor ...
Clinical research involves studies that include human participants, aiming to understand health and illness and answer medical questions. Laboratory research, on the other hand, takes place in environments such as chemistry or biology labs, typically at colleges or medical schools, and does not involve human subjects.
By Carl Zimmer and Benjamin Mueller. May 7, 2024. The White House has unveiled tighter rules for research on potentially dangerous microbes and toxins, in an effort to stave off laboratory ...
The Biomedical Research Core Facilities Advanced Genomics Core is looking for a skilled research technician to join us full time as a Research Laboratory Specialist. The incumbent will assist in developing, deploying and executing protocols on DNA/RNA for our research community. This role will support next generation sequencing by performing ...
The Rune-Lens Research Laboratory. As you enter the Rune-Lens Research Lab, before heading forward, head on the path to your left. This path has a red chest containing a useful Anti-Confuse Scarf ...
Estimated Market Value (USD) in 2023. $2.52 Billion. Forecasted Market Value (USD) by 2029. $3.08 Billion. Compound Annual Growth Rate. 3.4%. A selection of companies mentioned in this report ...
The space station provides consistent, long-term access to microgravity. Eliminating the effects of Earth's gravity on experiments is a game-changer across many disciplines, including research on living things and physical and chemical processes. For example, without gravity hot air does not rise, so flames become spherical and behave ...
The Agricultural Research Service (ARS) is the U.S. Department of Agriculture's chief scientific in-house research agency with a mission to find solutions to agricultural problems that affect Americans every day from field to table. ARS will deliver cutting-edge, scientific tools and innovative solutions for American farmers, producers ...
Research Operations Support Professional. Apply now ». Date: May 21, 2024. Location: Oak Ridge, TN, US, 37830. Company: Oak Ridge National Laboratory. Requisition Id 13078. Overview: We are hiring an entry-level Research Operations Support Professional to support operation tasks associated with work control of science and engineering activities.
Through research conducted over the course of two years in 2008 and 2009, supplemented by an analysis of research conduced by NGOs and independent researchers, I document post-Soviet ethnic ...
INL is the nation's center for nuclear energy research and development, celebrating 75 years of scientific innovations in 2024. The laboratory performs research in each of DOE's strategic goal areas: energy, national security, science and the environment. Follow us on social media: Facebook, Instagram, LinkedIn and X.
Categories: krai of Russia and locality. Location: Southern Russia, Russia, Eastern Europe, Europe. View on OpenStreetMap. Latitude. 44.8633° or 44° 51' 48" north. Longitude. 43.4407° or 43° 26' 27" east. Population.
Stavropol forums. 703historybuff89. Boulder, Colorado. 1 post. Safety in Stavropol'. 9 years ago. Save. I am hoping to spend some time in Stavropol' (the city itself) to conduct research for my graduate degree. I am having a hard time figuring out very much about the city, however.