Loading metrics
Open Access
Peer-reviewed
Research Article

Assessing the impact of healthcare research: A systematic review of methodological frameworks
Roles Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Validation, Writing – original draft, Writing – review & editing
Affiliation Centre for Patient Reported Outcomes Research, Institute of Applied Health Research, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
Roles Conceptualization, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing
* E-mail: [email protected]
Roles Data curation, Formal analysis, Methodology, Validation, Writing – review & editing
Roles Formal analysis, Methodology, Supervision, Validation, Writing – review & editing
- Samantha Cruz Rivera,
- Derek G. Kyte,
- Olalekan Lee Aiyegbusi,
- Thomas J. Keeley,
- Melanie J. Calvert

- Published: August 9, 2017
- https://doi.org/10.1371/journal.pmed.1002370
- Reader Comments
Increasingly, researchers need to demonstrate the impact of their research to their sponsors, funders, and fellow academics. However, the most appropriate way of measuring the impact of healthcare research is subject to debate. We aimed to identify the existing methodological frameworks used to measure healthcare research impact and to summarise the common themes and metrics in an impact matrix.
Methods and findings
Two independent investigators systematically searched the Medical Literature Analysis and Retrieval System Online (MEDLINE), the Excerpta Medica Database (EMBASE), the Cumulative Index to Nursing and Allied Health Literature (CINAHL+), the Health Management Information Consortium, and the Journal of Research Evaluation from inception until May 2017 for publications that presented a methodological framework for research impact. We then summarised the common concepts and themes across methodological frameworks and identified the metrics used to evaluate differing forms of impact. Twenty-four unique methodological frameworks were identified, addressing 5 broad categories of impact: (1) ‘primary research-related impact’, (2) ‘influence on policy making’, (3) ‘health and health systems impact’, (4) ‘health-related and societal impact’, and (5) ‘broader economic impact’. These categories were subdivided into 16 common impact subgroups. Authors of the included publications proposed 80 different metrics aimed at measuring impact in these areas. The main limitation of the study was the potential exclusion of relevant articles, as a consequence of the poor indexing of the databases searched.
Conclusions
The measurement of research impact is an essential exercise to help direct the allocation of limited research resources, to maximise research benefit, and to help minimise research waste. This review provides a collective summary of existing methodological frameworks for research impact, which funders may use to inform the measurement of research impact and researchers may use to inform study design decisions aimed at maximising the short-, medium-, and long-term impact of their research.
Author summary
Why was this study done.
- There is a growing interest in demonstrating the impact of research in order to minimise research waste, allocate resources efficiently, and maximise the benefit of research. However, there is no consensus on which is the most appropriate tool to measure the impact of research.
- To our knowledge, this review is the first to synthesise existing methodological frameworks for healthcare research impact, and the associated impact metrics by which various authors have proposed impact should be measured, into a unified matrix.
What did the researchers do and find?
- We conducted a systematic review identifying 24 existing methodological research impact frameworks.
- We scrutinised the sample, identifying and summarising 5 proposed impact categories, 16 impact subcategories, and over 80 metrics into an impact matrix and methodological framework.
What do these findings mean?
- This simplified consolidated methodological framework will help researchers to understand how a research study may give rise to differing forms of impact, as well as in what ways and at which time points these potential impacts might be measured.
- Incorporating these insights into the design of a study could enhance impact, optimizing the use of research resources.
Citation: Cruz Rivera S, Kyte DG, Aiyegbusi OL, Keeley TJ, Calvert MJ (2017) Assessing the impact of healthcare research: A systematic review of methodological frameworks. PLoS Med 14(8): e1002370. https://doi.org/10.1371/journal.pmed.1002370
Academic Editor: Mike Clarke, Queens University Belfast, UNITED KINGDOM
Received: February 28, 2017; Accepted: July 7, 2017; Published: August 9, 2017
Copyright: © 2017 Cruz Rivera et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and supporting files.
Funding: Funding was received from Consejo Nacional de Ciencia y Tecnología (CONACYT). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript ( http://www.conacyt.mx/ ).
Competing interests: I have read the journal's policy and the authors of this manuscript have the following competing interests: MJC has received consultancy fees from Astellas and Ferring pharma and travel fees from the European Society of Cardiology outside the submitted work. TJK is in full-time paid employment for PAREXEL International.
Abbreviations: AIHS, Alberta Innovates—Health Solutions; CAHS, Canadian Academy of Health Sciences; CIHR, Canadian Institutes of Health Research; CINAHL+, Cumulative Index to Nursing and Allied Health Literature; EMBASE, Excerpta Medica Database; ERA, Excellence in Research for Australia; HEFCE, Higher Education Funding Council for England; HMIC, Health Management Information Consortium; HTA, Health Technology Assessment; IOM, Impact Oriented Monitoring; MDG, Millennium Development Goal; NHS, National Health Service; MEDLINE, Medical Literature Analysis and Retrieval System Online; PHC RIS, Primary Health Care Research & Information Service; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; PROM, patient-reported outcome measures; QALY, quality-adjusted life year; R&D, research and development; RAE, Research Assessment Exercise; REF, Research Excellence Framework; RIF, Research Impact Framework; RQF, Research Quality Framework; SDG, Sustainable Development Goal; SIAMPI, Social Impact Assessment Methods for research and funding instruments through the study of Productive Interactions between science and society
Introduction
In 2010, approximately US$240 billion was invested in healthcare research worldwide [ 1 ]. Such research is utilised by policy makers, healthcare providers, and clinicians to make important evidence-based decisions aimed at maximising patient benefit, whilst ensuring that limited healthcare resources are used as efficiently as possible to facilitate effective and sustainable service delivery. It is therefore essential that this research is of high quality and that it is impactful—i.e., it delivers demonstrable benefits to society and the wider economy whilst minimising research waste [ 1 , 2 ]. Research impact can be defined as ‘any identifiable ‘benefit to, or positive influence on the economy, society, public policy or services, health, the environment, quality of life or academia’ (p. 26) [ 3 ].
There are many purported benefits associated with the measurement of research impact, including the ability to (1) assess the quality of the research and its subsequent benefits to society; (2) inform and influence optimal policy and funding allocation; (3) demonstrate accountability, the value of research in terms of efficiency and effectiveness to the government, stakeholders, and society; and (4) maximise impact through better understanding the concept and pathways to impact [ 4 – 7 ].
Measuring and monitoring the impact of healthcare research has become increasingly common in the United Kingdom [ 5 ], Australia [ 5 ], and Canada [ 8 ], as governments, organisations, and higher education institutions seek a framework to allocate funds to projects that are more likely to bring the most benefit to society and the economy [ 5 ]. For example, in the UK, the 2014 Research Excellence Framework (REF) has recently been used to assess the quality and impact of research in higher education institutions, through the assessment of impact cases studies and selected qualitative impact metrics [ 9 ]. This is the first initiative to allocate research funding based on the economic, societal, and cultural impact of research, although it should be noted that research impact only drives a proportion of this allocation (approximately 20%) [ 9 ].
In the UK REF, the measurement of research impact is seen as increasingly important. However, the impact element of the REF has been criticised in some quarters [ 10 , 11 ]. Critics deride the fact that REF impact is determined in a relatively simplistic way, utilising researcher-generated case studies, which commonly attempt to link a particular research outcome to an associated policy or health improvement despite the fact that the wider literature highlights great diversity in the way research impact may be demonstrated [ 12 , 13 ]. This led to the current debate about the optimal method of measuring impact in the future REF [ 10 , 14 ]. The Stern review suggested that research impact should not only focus on socioeconomic impact but should also include impact on government policy, public engagement, academic impacts outside the field, and teaching to showcase interdisciplinary collaborative impact [ 10 , 11 ]. The Higher Education Funding Council for England (HEFCE) has recently set out the proposals for the REF 2021 exercise, confirming that the measurement of such impact will continue to form an important part of the process [ 15 ].
With increasing pressure for healthcare research to lead to demonstrable health, economic, and societal impact, there is a need for researchers to understand existing methodological impact frameworks and the means by which impact may be quantified (i.e., impact metrics; see Box 1 , 'Definitions’) to better inform research activities and funding decisions. From a researcher’s perspective, understanding the optimal pathways to impact can help inform study design aimed at maximising the impact of the project. At the same time, funders need to understand which aspects of impact they should focus on when allocating awards so they can make the most of their investment and bring the greatest benefit to patients and society [ 2 , 4 , 5 , 16 , 17 ].
Box 1. Definitions
- Research impact: ‘any identifiable benefit to, or positive influence on, the economy, society, public policy or services, health, the environment, quality of life, or academia’ (p. 26) [ 3 ].
- Methodological framework: ‘a body of methods, rules and postulates employed by a particular procedure or set of procedures (i.e., framework characteristics and development)’ [ 18 ].
- Pathway: ‘a way of achieving a specified result; a course of action’ [ 19 ].
- Quantitative metrics: ‘a system or standard of [quantitative] measurement’ [ 20 ].
- Narrative metrics: ‘a spoken or written account of connected events; a story’ [ 21 ].
Whilst previous researchers have summarised existing methodological frameworks and impact case studies [ 4 , 22 – 27 ], they have not summarised the metrics for use by researchers, funders, and policy makers. The aim of this review was therefore to (1) identify the methodological frameworks used to measure healthcare research impact using systematic methods, (2) summarise common impact themes and metrics in an impact matrix, and (3) provide a simplified consolidated resource for use by funders, researchers, and policy makers.
Search strategy and selection criteria
Initially, a search strategy was developed to identify the available literature regarding the different methods to measure research impact. The following keywords: ‘Impact’, ‘Framework’, and ‘Research’, and their synonyms, were used during the search of the Medical Literature Analysis and Retrieval System Online (MEDLINE; Ovid) database, the Excerpta Medica Database (EMBASE), the Health Management Information Consortium (HMIC) database, and the Cumulative Index to Nursing and Allied Health Literature (CINAHL+) database (inception to May 2017; see S1 Appendix for the full search strategy). Additionally, the nonindexed Journal of Research Evaluation was hand searched during the same timeframe using the keyword ‘Impact’. Other relevant articles were identified through 3 Internet search engines (Google, Google Scholar, and Google Images) using the keywords ‘Impact’, ‘Framework’, and ‘Research’, with the first 50 results screened. Google Images was searched because different methodological frameworks are summarised in a single image and can easily be identified through this search engine. Finally, additional publications were sought through communication with experts.
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (see S1 PRISMA Checklist ), 2 independent investigators systematically screened for publications describing, evaluating, or utilising a methodological research impact framework within the context of healthcare research [ 28 ]. Papers were eligible if they included full or partial methodological frameworks or pathways to research impact; both primary research and systematic reviews fitting these criteria were included. We included any methodological framework identified (original or modified versions) at the point of first occurrence. In addition, methodological frameworks were included if they were applicable to the healthcare discipline with no need of modification within their structure. We defined ‘methodological framework’ as ‘a body of methods, rules and postulates employed by a particular procedure or set of procedures (i.e., framework characteristics and development)’ [ 18 ], whereas we defined ‘pathway’ as ‘a way of achieving a specified result; a course of action’ [ 19 ]. Studies were excluded if they presented an existing (unmodified) methodological framework previously available elsewhere, did not explicitly describe a methodological framework but rather focused on a single metric (e.g., bibliometric analysis), focused on the impact or effectiveness of interventions rather than that of the research, or presented case study data only. There were no language restrictions.
Data screening
Records were downloaded into Endnote (version X7.3.1), and duplicates were removed. Two independent investigators (SCR and OLA) conducted all screening following a pilot aimed at refining the process. The records were screened by title and abstract before full-text articles of potentially eligible publications were retrieved for evaluation. A full-text screening identified the publications included for data extraction. Discrepancies were resolved through discussion, with the involvement of a third reviewer (MJC, DGK, and TJK) when necessary.
Data extraction and analysis
Data extraction occurred after the final selection of included articles. SCR and OLA independently extracted details of impact methodological frameworks, the country of origin, and the year of publication, as well as the source, the framework description, and the methodology used to develop the framework. Information regarding the methodology used to develop each methodological framework was also extracted from framework webpages where available. Investigators also extracted details regarding each framework’s impact categories and subgroups, along with their proposed time to impact (‘short-term’, ‘mid-term’, or ‘long-term’) and the details of any metrics that had been proposed to measure impact, which are depicted in an impact matrix. The structure of the matrix was informed by the work of M. Buxton and S. Hanney [ 2 ], P. Buykx et al. [ 5 ], S. Kuruvila et al. [ 29 ], and A. Weiss [ 30 ], with the intention of mapping metrics presented in previous methodological frameworks in a concise way. A consensus meeting with MJC, DGK, and TJK was held to solve disagreements and finalise the data extraction process.
Included studies
Our original search strategy identified 359 citations from MEDLINE (Ovid), EMBASE, CINAHL+, HMIC, and the Journal of Research Evaluation, and 101 citations were returned using other sources (Google, Google Images, Google Scholar, and expert communication) (see Fig 1 ) [ 28 ]. In total, we retrieved 54 full-text articles for review. At this stage, 39 articles were excluded, as they did not propose new or modified methodological frameworks. An additional 15 articles were included following the backward and forward citation method. A total of 31 relevant articles were included in the final analysis, of which 24 were articles presenting unique frameworks and the remaining 7 were systematic reviews [ 4 , 22 – 27 ]. The search strategy was rerun on 15 May 2017. A further 19 publications were screened, and 2 were taken forward to full-text screening but were ineligible for inclusion.
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pmed.1002370.g001
Methodological framework characteristics
The characteristics of the 24 included methodological frameworks are summarised in Table 1 , 'Methodological framework characteristics’. Fourteen publications proposed academic-orientated frameworks, which focused on measuring academic, societal, economic, and cultural impact using narrative and quantitative metrics [ 2 , 3 , 5 , 8 , 29 , 31 – 39 ]. Five publications focused on assessing the impact of research by focusing on the interaction process between stakeholders and researchers (‘productive interactions’), which is a requirement to achieve research impact. This approach tries to address the issue of attributing research impact to metrics [ 7 , 40 – 43 ]. Two frameworks focused on the importance of partnerships between researchers and policy makers, as a core element to accomplish research impact [ 44 , 45 ]. An additional 2 frameworks focused on evaluating the pathways to impact, i.e., linking processes between research and impact [ 30 , 46 ]. One framework assessed the ability of health technology to influence efficiency of healthcare systems [ 47 ]. Eight frameworks were developed in the UK [ 2 , 3 , 29 , 37 , 39 , 42 , 43 , 45 ], 6 in Canada [ 8 , 33 , 34 , 44 , 46 , 47 ], 4 in Australia [ 5 , 31 , 35 , 38 ], 3 in the Netherlands [ 7 , 40 , 41 ], and 2 in the United States [ 30 , 36 ], with 1 model developed with input from various countries [ 32 ].
https://doi.org/10.1371/journal.pmed.1002370.t001
Methodological framework development
The included methodological frameworks varied in their development process, but there were some common approaches employed. Most included a literature review [ 2 , 5 , 7 , 8 , 31 , 33 , 36 , 37 , 40 – 46 ], although none of them used a recognised systematic method. Most also consulted with various stakeholders [ 3 , 8 , 29 , 31 , 33 , 35 – 38 , 43 , 44 , 46 , 47 ] but used differing methods to incorporate their views, including quantitative surveys [ 32 , 35 , 43 , 46 ], face-to-face interviews [ 7 , 29 , 33 , 35 , 37 , 42 , 43 ], telephone interviews [ 31 , 46 ], consultation [ 3 , 7 , 36 ], and focus groups [ 39 , 43 ]. A range of stakeholder groups were approached across the sample, including principal investigators [ 7 , 29 , 43 ], research end users [ 7 , 42 , 43 ], academics [ 3 , 8 , 39 , 40 , 43 , 46 ], award holders [ 43 ], experts [ 33 , 38 , 39 ], sponsors [ 33 , 39 ], project coordinators [ 32 , 42 ], and chief investigators [ 31 , 35 ]. However, some authors failed to identify the stakeholders involved in the development of their frameworks [ 2 , 5 , 34 , 41 , 45 ], making it difficult to assess their appropriateness. In addition, only 4 of the included papers reported using formal analytic methods to interpret stakeholder responses. These included the Canadian Academy of Health Sciences framework, which used conceptual cluster analysis [ 33 ]. The Research Contribution [ 42 ], Research Impact [ 29 ], and Primary Health Care & Information Service [ 31 ] used a thematic analysis approach. Finally, some authors went on to pilot their framework, which shaped refinements on the methodological frameworks until approval. Methods used to pilot the frameworks included a case study approach [ 2 , 3 , 30 , 32 , 33 , 36 , 40 , 42 , 44 , 45 ], contrasting results against available literature [ 29 ], the use of stakeholders’ feedback [ 7 ], and assessment tools [ 35 , 46 ].
Major impact categories
1. primary research-related impact..
A number of methodological frameworks advocated the evaluation of ‘research-related impact’. This encompassed content related to the generation of new knowledge, knowledge dissemination, capacity building, training, leadership, and the development of research networks. These outcomes were considered the direct or primary impacts of a research project, as these are often the first evidenced returns [ 30 , 62 ].
A number of subgroups were identified within this category, with frameworks supporting the collection of impact data across the following constructs: ‘research and innovation outcomes’; ‘dissemination and knowledge transfer’; ‘capacity building, training, and leadership’; and ‘academic collaborations, research networks, and data sharing’.
1 . 1 . Research and innovation outcomes . Twenty of the 24 frameworks advocated the evaluation of ‘research and innovation outcomes’ [ 2 , 3 , 5 , 7 , 8 , 29 – 39 , 41 , 43 , 44 , 46 ]. This subgroup included the following metrics: number of publications; number of peer-reviewed articles (including journal impact factor); citation rates; requests for reprints, number of reviews, and meta-analysis; and new or changes in existing products (interventions or technology), patents, and research. Additionally, some frameworks also sought to gather information regarding ‘methods/methodological contributions’. These advocated the collection of systematic reviews and appraisals in order to identify gaps in knowledge and determine whether the knowledge generated had been assessed before being put into practice [ 29 ].
1 . 2 . Dissemination and knowledge transfer . Nineteen of the 24 frameworks advocated the assessment of ‘dissemination and knowledge transfer’ [ 2 , 3 , 5 , 7 , 29 – 32 , 34 – 43 , 46 ]. This comprised collection of the following information: number of conferences, seminars, workshops, and presentations; teaching output (i.e., number of lectures given to disseminate the research findings); number of reads for published articles; article download rate and number of journal webpage visits; and citations rates in nonjournal media such as newspapers and mass and social media (i.e., Twitter and blogs). Furthermore, this impact subgroup considered the measurement of research uptake and translatability and the adoption of research findings in technological and clinical applications and by different fields. These can be measured through patents, clinical trials, and partnerships between industry and business, government and nongovernmental organisations, and university research units and researchers [ 29 ].
1 . 3 . Capacity building , training , and leadership . Fourteen of 24 frameworks suggested the evaluation of ‘capacity building, training, and leadership’ [ 2 , 3 , 5 , 8 , 29 , 31 – 35 , 39 – 41 , 43 ]. This involved collecting information regarding the number of doctoral and postdoctoral studentships (including those generated as a result of the research findings and those appointed to conduct the research), as well as the number of researchers and research-related staff involved in the research projects. In addition, authors advocated the collection of ‘leadership’ metrics, including the number of research projects managed and coordinated and the membership of boards and funding bodies, journal editorial boards, and advisory committees [ 29 ]. Additional metrics in this category included public recognition (number of fellowships and awards for significant research achievements), academic career advancement, and subsequent grants received. Lastly, the impact metric ‘research system management’ comprised the collection of information that can lead to preserving the health of the population, such as modifying research priorities, resource allocation strategies, and linking health research to other disciplines to maximise benefits [ 29 ].
1 . 4 . Academic collaborations , research networks , and data sharing . Lastly, 10 of the 24 frameworks advocated the collection of impact data regarding ‘academic collaborations (internal and external collaborations to complete a research project), research networks, and data sharing’ [ 2 , 3 , 5 , 7 , 29 , 34 , 37 , 39 , 41 , 43 ].
2. Influence on policy making.
Methodological frameworks addressing this major impact category focused on measurable improvements within a given knowledge base and on interactions between academics and policy makers, which may influence policy-making development and implementation. The returns generated in this impact category are generally considered as intermediate or midterm (1 to 3 years). These represent an important interim stage in the process towards the final expected impacts, such as quantifiable health improvements and economic benefits, without which policy change may not occur [ 30 , 62 ]. The following impact subgroups were identified within this category: ‘type and nature of policy impact’, ‘level of policy making’, and ‘policy networks’.
2 . 1 . Type and nature of policy impact . The most common impact subgroup, mentioned in 18 of the 24 frameworks, was ‘type and nature of policy impact’ [ 2 , 7 , 29 – 38 , 41 – 43 , 45 – 47 ]. Methodological frameworks addressing this subgroup stressed the importance of collecting information regarding the influence of research on policy (i.e., changes in practice or terminology). For instance, a project looking at trafficked adolescents and women (2003) influenced the WHO guidelines (2003) on ethics regarding this particular group [ 17 , 21 , 63 ].
2 . 2 . Level of policy impact . Thirteen of 24 frameworks addressed aspects surrounding the need to record the ‘level of policy impact’ (international, national, or local) and the organisations within a level that were influenced (local policy makers, clinical commissioning groups, and health and wellbeing trusts) [ 2 , 5 , 8 , 29 , 31 , 34 , 38 , 41 , 43 – 47 ]. Authors considered it important to measure the ‘level of policy impact’ to provide evidence of collaboration, coordination, and efficiency within health organisations and between researchers and health organisations [ 29 , 31 ].
2 . 3 . Policy networks . Five methodological frameworks highlighted the need to collect information regarding collaborative research with industry and staff movement between academia and industry [ 5 , 7 , 29 , 41 , 43 ]. A policy network emphasises the relationship between policy communities, researchers, and policy makers. This relationship can influence and lead to incremental changes in policy processes [ 62 ].
3. Health and health systems impact.
A number of methodological frameworks advocated the measurement of impacts on health and healthcare systems across the following impact subgroups: ‘quality of care and service delivering’, ‘evidence-based practice’, ‘improved information and health information management’, ‘cost containment and effectiveness’, ‘resource allocation’, and ‘health workforce’.
3 . 1 . Quality of care and service delivery . Twelve of the 24 frameworks highlighted the importance of evaluating ‘quality of care and service delivery’ [ 2 , 5 , 8 , 29 – 31 , 33 – 36 , 41 , 47 ]. There were a number of suggested metrics that could be potentially used for this purpose, including health outcomes such as quality-adjusted life years (QALYs), patient-reported outcome measures (PROMs), patient satisfaction and experience surveys, and qualitative data on waiting times and service accessibility.
3 . 2 . Evidence-based practice . ‘Evidence-based practice’, mentioned in 5 of the 24 frameworks, refers to making changes in clinical diagnosis, clinical practice, treatment decisions, or decision making based on research evidence [ 5 , 8 , 29 , 31 , 33 ]. The suggested metrics to demonstrate evidence-based practice were adoption of health technologies and research outcomes to improve the healthcare systems and inform policies and guidelines [ 29 ].
3 . 3 . Improved information and health information management . This impact subcategory, mentioned in 5 of the 24 frameworks, refers to the influence of research on the provision of health services and management of the health system to prevent additional costs [ 5 , 29 , 33 , 34 , 38 ]. Methodological frameworks advocated the collection of health system financial, nonfinancial (i.e., transport and sociopolitical implications), and insurance information in order to determine constraints within a health system.
3 . 4 . Cost containment and cost-effectiveness . Six of the 24 frameworks advocated the subcategory ‘cost containment and cost-effectiveness’ [ 2 , 5 , 8 , 17 , 33 , 36 ]. ‘Cost containment’ comprised the collection of information regarding how research has influenced the provision and management of health services and its implication in healthcare resource allocation and use [ 29 ]. ‘Cost-effectiveness’ refers to information concerning economic evaluations to assess improvements in effectiveness and health outcomes—for instance, the cost-effectiveness (cost and health outcome benefits) assessment of introducing a new health technology to replace an older one [ 29 , 31 , 64 ].
3 . 5 . Resource allocation . ‘Resource allocation’, mentioned in 6frameworks, can be measured through 2 impact metrics: new funding attributed to the intervention in question and equity while allocating resources, such as improved allocation of resources at an area level; better targeting, accessibility, and utilisation; and coverage of health services [ 2 , 5 , 29 , 31 , 45 , 47 ]. The allocation of resources and targeting can be measured through health services research reports, with the utilisation of health services measured by the probability of providing an intervention when needed, the probability of requiring it again in the future, and the probability of receiving an intervention based on previous experience [ 29 , 31 ].
3 . 6 . Health workforce . Lastly, ‘health workforce’, present in 3 methodological frameworks, refers to the reduction in the days of work lost because of a particular illness [ 2 , 5 , 31 ].
4. Health-related and societal impact.
Three subgroups were included in this category: ‘health literacy’; ‘health knowledge, attitudes, and behaviours’; and ‘improved social equity, inclusion, or cohesion’.
4 . 1 . Health knowledge , attitudes , and behaviours . Eight of the 24 frameworks suggested the assessment of ‘health knowledge, attitudes, behaviours, and outcomes’, which could be measured through the evaluation of levels of public engagement with science and research (e.g., National Health Service (NHS) Choices end-user visit rate) or by using focus groups to analyse changes in knowledge, attitudes, and behaviour among society [ 2 , 5 , 29 , 33 – 35 , 38 , 43 ].
4 . 2 . Improved equity , inclusion , or cohesion and human rights . Other methodological frameworks, 4 of the 24, suggested capturing improvements in equity, inclusion, or cohesion and human rights. Authors suggested these could be using a resource like the United Nations Millennium Development Goals (MDGs) (superseded by Sustainable Development Goals [SDGs] in 2015) and human rights [ 29 , 33 , 34 , 38 ]. For instance, a cluster-randomised controlled trial in Nepal, which had female participants, has demonstrated the reduction of neonatal mortality through the introduction of maternity health care, distribution of delivery kits, and home visits. This illustrates how research can target vulnerable and disadvantaged groups. Additionally, this research has been introduced by the World Health Organisation to achieve the MDG ‘improve maternal health’ [ 16 , 29 , 65 ].
4 . 3 . Health literacy . Some methodological frameworks, 3 of the 24, focused on tracking changes in the ability of patients to make informed healthcare decisions, reduce health risks, and improve quality of life, which were demonstrably linked to a particular programme of research [ 5 , 29 , 43 ]. For example, a systematic review showed that when HIV health literacy/knowledge is spread among people living with the condition, antiretroviral adherence and quality of life improve [ 66 ].
5. Broader economic impacts.
Some methodological frameworks, 9 of 24, included aspects related to the broader economic impacts of health research—for example, the economic benefits emerging from the commercialisation of research outputs [ 2 , 5 , 29 , 31 , 33 , 35 , 36 , 38 , 67 ]. Suggested metrics included the amount of funding for research and development (R&D) that was competitively awarded by the NHS, medical charities, and overseas companies. Additional metrics were income from intellectual property, spillover effects (any secondary benefit gained as a repercussion of investing directly in a primary activity, i.e., the social and economic returns of investing on R&D) [ 33 ], patents granted, licences awarded and brought to the market, the development and sales of spinout companies, research contracts, and income from industry.
The benefits contained within the categories ‘health and health systems impact’, ‘health-related and societal impact’, and ‘broader economic impacts’ are considered the expected and final returns of the resources allocated in healthcare research [ 30 , 62 ]. These benefits commonly arise in the long term, beyond 5 years according to some authors, but there was a recognition that this could differ depending on the project and its associated research area [ 4 ].
Data synthesis
Five major impact categories were identified across the 24 included methodological frameworks: (1) ‘primary research-related impact’, (2) ‘influence on policy making’, (3) ‘health and health systems impact’, (4) ‘health-related and societal impact’, and (5) ‘broader economic impact’. These major impact categories were further subdivided into 16 impact subgroups. The included publications proposed 80 different metrics to measure research impact. This impact typology synthesis is depicted in ‘the impact matrix’ ( Fig 2 and Fig 3 ).
CIHR, Canadian Institutes of Health Research; HTA, Health Technology Assessment; PHC RIS, Primary Health Care Research & Information Service; RAE, Research Assessment Exercise; RQF, Research Quality Framework.
https://doi.org/10.1371/journal.pmed.1002370.g002
AIHS, Alberta Innovates—Health Solutions; CAHS, Canadian Institutes of Health Research; IOM, Impact Oriented Monitoring; REF, Research Excellence Framework; SIAMPI, Social Impact Assessment Methods for research and funding instruments through the study of Productive Interactions between science and society.
https://doi.org/10.1371/journal.pmed.1002370.g003
Commonality and differences across frameworks
The ‘Research Impact Framework’ and the ‘Health Services Research Impact Framework’ were the models that encompassed the largest number of the metrics extracted. The most dominant methodological framework was the Payback Framework; 7 other methodological framework models used the Payback Framework as a starting point for development [ 8 , 29 , 31 – 35 ]. Additional methodological frameworks that were commonly incorporated into other tools included the CIHR framework, the CAHS model, the AIHS framework, and the Exchange model [ 8 , 33 , 34 , 44 ]. The capture of ‘research-related impact’ was the most widely advocated concept across methodological frameworks, illustrating the importance with which primary short-term impact outcomes were viewed by the included papers. Thus, measurement of impact via number of publications, citations, and peer-reviewed articles was the most common. ‘Influence on policy making’ was the predominant midterm impact category, specifically the subgroup ‘type and nature of policy impact’, in which frameworks advocated the measurement of (i) changes to legislation, regulations, and government policy; (ii) influence and involvement in decision-making processes; and (iii) changes to clinical or healthcare training, practice, or guidelines. Within more long-term impact measurement, the evaluations of changes in the ‘quality of care and service delivery’ were commonly advocated.
In light of the commonalities and differences among the methodological frameworks, the ‘pathways to research impact’ diagram ( Fig 4 ) was developed to provide researchers, funders, and policy makers a more comprehensive and exhaustive way to measure healthcare research impact. The diagram has the advantage of assorting all the impact metrics proposed by previous frameworks and grouping them into different impact subgroups and categories. Prospectively, this global picture will help researchers, funders, and policy makers plan strategies to achieve multiple pathways to impact before carrying the research out. The analysis of the data extraction and construction of the impact matrix led to the development of the ‘pathways to research impact’ diagram ( Fig 4 ). The diagram aims to provide an exhaustive and comprehensive way of tracing research impact by combining all the impact metrics presented by the different 24 frameworks, grouping those metrics into different impact subgroups, and grouping these into broader impact categories.
NHS, National Health Service; PROM, patient-reported outcome measure; QALY, quality-adjusted life year; R&D, research and development.
https://doi.org/10.1371/journal.pmed.1002370.g004
This review has summarised existing methodological impact frameworks together for the first time using systematic methods ( Fig 4 ). It allows researchers and funders to consider pathways to impact at the design stage of a study and to understand the elements and metrics that need to be considered to facilitate prospective assessment of impact. Users do not necessarily need to cover all the aspects of the methodological framework, as every research project can impact on different categories and subgroups. This review provides information that can assist researchers to better demonstrate impact, potentially increasing the likelihood of conducting impactful research and reducing research waste. Existing reviews have not presented a methodological framework that includes different pathways to impact, health impact categories, subgroups, and metrics in a single methodological framework.
Academic-orientated frameworks included in this review advocated the measurement of impact predominantly using so-called ‘quantitative’ metrics—for example, the number of peer-reviewed articles, journal impact factor, and citation rates. This may be because they are well-established measures, relatively easy to capture and objective, and are supported by research funding systems. However, these metrics primarily measure the dissemination of research finding rather than its impact [ 30 , 68 ]. Whilst it is true that wider dissemination, especially when delivered via world-leading international journals, may well lead eventually to changes in healthcare, this is by no means certain. For instance, case studies evaluated by Flinders University of Australia demonstrated that some research projects with non-peer-reviewed publications led to significant changes in health policy, whilst the studies with peer-reviewed publications did not result in any type of impact [ 68 ]. As a result, contemporary literature has tended to advocate the collection of information regarding a variety of different potential forms of impact alongside publication/citations metrics [ 2 , 3 , 5 , 7 , 8 , 29 – 47 ], as outlined in this review.
The 2014 REF exercise adjusted UK university research funding allocation based on evidence of the wider impact of research (through case narrative studies and quantitative metrics), rather than simply according to the quality of research [ 12 ]. The intention was to ensure funds were directed to high-quality research that could demonstrate actual realised benefit. The inclusion of a mixed-method approach to the measurement of impact in the REF (narrative and quantitative metrics) reflects a widespread belief—expressed by the majority of authors of the included methodological frameworks in the review—that individual quantitative impact metrics (e.g., number of citations and publications) do not necessary capture the complexity of the relationships involved in a research project and may exclude measurement of specific aspects of the research pathway [ 10 , 12 ].
Many of the frameworks included in this review advocated the collection of a range of academic, societal, economic, and cultural impact metrics; this is consistent with recent recommendations from the Stern review [ 10 ]. However, a number of these metrics encounter research ‘lag’: i.e., the time between the point at which the research is conducted and when the actual benefits arise [ 69 ]. For instance, some cardiovascular research has taken up to 25 years to generate impact [ 70 ]. Likewise, the impact may not arise exclusively from a single piece of research. Different processes (such as networking interactions and knowledge and research translation) and multiple individuals and organisations are often involved [ 4 , 71 ]. Therefore, attributing the contribution made by each of the different actors involved in the process can be a challenge [ 4 ]. An additional problem associated to attribution is the lack of evidence to link research and impact. The outcomes of research may emerge slowly and be absorbed gradually. Consequently, it is difficult to determine the influence of research in the development of a new policy, practice, or guidelines [ 4 , 23 ].
A further problem is that impact evaluation is conducted ‘ex post’, after the research has concluded. Collecting information retrospectively can be an issue, as the data required might not be available. ‘ex ante’ assessment is vital for funding allocation, as it is necessary to determine the potential forthcoming impact before research is carried out [ 69 ]. Additionally, ex ante evaluation of potential benefit can overcome the issues regarding identifying and capturing evidence, which can be used in the future [ 4 ]. In order to conduct ex ante evaluation of potential benefit, some authors suggest the early involvement of policy makers in a research project coupled with a well-designed strategy of dissemination [ 40 , 69 ].
Providing an alternate view, the authors of methodological frameworks such as the SIAMPI, Contribution Mapping, Research Contribution, and the Exchange model suggest that the problems of attribution are a consequence of assigning the impact of research to a particular impact metric [ 7 , 40 , 42 , 44 ]. To address these issues, these authors propose focusing on the contribution of research through assessing the processes and interactions between stakeholders and researchers, which arguably take into consideration all the processes and actors involved in a research project [ 7 , 40 , 42 , 43 ]. Additionally, contributions highlight the importance of the interactions between stakeholders and researchers from an early stage in the research process, leading to a successful ex ante and ex post evaluation by setting expected impacts and determining how the research outcomes have been utilised, respectively [ 7 , 40 , 42 , 43 ]. However, contribution metrics are generally harder to measure in comparison to academic-orientated indicators [ 72 ].
Currently, there is a debate surrounding the optimal methodological impact framework, and no tool has proven superior to another. The most appropriate methodological framework for a given study will likely depend on stakeholder needs, as each employs different methodologies to assess research impact [ 4 , 37 , 41 ]. This review allows researchers to select individual existing methodological framework components to create a bespoke tool with which to facilitate optimal study design and maximise the potential for impact depending on the characteristic of their study ( Fig 2 and Fig 3 ). For instance, if researchers are interested in assessing how influential their research is on policy making, perhaps considering a suite of the appropriate metrics drawn from multiple methodological frameworks may provide a more comprehensive method than adopting a single methodological framework. In addition, research teams may wish to use a multidimensional approach to methodological framework development, adopting existing narratives and quantitative metrics, as well as elements from contribution frameworks. This approach would arguably present a more comprehensive method of impact assessment; however, further research is warranted to determine its effectiveness [ 4 , 69 , 72 , 73 ].
Finally, it became clear during this review that the included methodological frameworks had been constructed using varied methodological processes. At present, there are no guidelines or consensus around the optimal pathway that should be followed to develop a robust methodological framework. The authors believe this is an area that should be addressed by the research community, to ensure future frameworks are developed using best-practice methodology.
For instance, the Payback Framework drew upon a literature review and was refined through a case study approach. Arguably, this approach could be considered inferior to other methods that involved extensive stakeholder involvement, such as the CIHR framework [ 8 ]. Nonetheless, 7 methodological frameworks were developed based upon the Payback Framework [ 8 , 29 , 31 – 35 ].
Limitations
The present review is the first to summarise systematically existing impact methodological frameworks and metrics. The main limitation is that 50% of the included publications were found through methods other than bibliographic databases searching, indicating poor indexing. Therefore, some relevant articles may not have been included in this review if they failed to indicate the inclusion of a methodological impact framework in their title/abstract. We did, however, make every effort to try to find these potentially hard-to-reach publications, e.g., through forwards/backwards citation searching, hand searching reference lists, and expert communication. Additionally, this review only extracted information regarding the methodology followed to develop each framework from the main publication source or framework webpage. Therefore, further evaluations may not have been included, as they are beyond the scope of the current paper. A further limitation was that although our search strategy did not include language restrictions, we did not specifically search non-English language databases. Thus, we may have failed to identify potentially relevant methodological frameworks that were developed in a non-English language setting.
In conclusion, the measurement of research impact is an essential exercise to help direct the allocation of limited research resources, to maximise benefit, and to help minimise research waste. This review provides a collective summary of existing methodological impact frameworks and metrics, which funders may use to inform the measurement of research impact and researchers may use to inform study design decisions aimed at maximising the short-, medium-, and long-term impact of their research.
Supporting information
S1 appendix. search strategy..
https://doi.org/10.1371/journal.pmed.1002370.s001
S1 PRISMA Checklist. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist.
https://doi.org/10.1371/journal.pmed.1002370.s002
Acknowledgments
We would also like to thank Mrs Susan Bayliss, Information Specialist, University of Birmingham, and Mrs Karen Biddle, Research Secretary, University of Birmingham.
- View Article
- PubMed/NCBI
- Google Scholar
- 3. HEFCE. REF 2014: Assessment framework and guidance on submissions 2011 [cited 2016 15 Feb]. Available from: http://www.ref.ac.uk/media/ref/content/pub/assessmentframeworkandguidanceonsubmissions/GOS%20including%20addendum.pdf .
- 8. Canadian Institutes of Health Research. Developing a CIHR framework to measure the impact of health research 2005 [cited 2016 26 Feb]. Available from: http://publications.gc.ca/collections/Collection/MR21-65-2005E.pdf .
- 9. HEFCE. HEFCE allocates £3.97 billion to universities and colleges in England for 2015–1 2015. Available from: http://www.hefce.ac.uk/news/newsarchive/2015/Name,103785,en.html .
- 10. Stern N. Building on Success and Learning from Experience—An Independent Review of the Research Excellence Framework 2016 [cited 2016 05 Aug]. Available from: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/541338/ind-16-9-ref-stern-review.pdf .
- 11. Matthews D. REF sceptic to lead review into research assessment: Times Higher Education; 2015 [cited 2016 21 Apr]. Available from: https://www.timeshighereducation.com/news/ref-sceptic-lead-review-research-assessment .
- 12. HEFCE. The Metric Tide—Report of the Independent Review of the Role of Metrics in Research Assessment and Management 2015 [cited 2016 11 Aug]. Available from: http://www.hefce.ac.uk/media/HEFCE,2014/Content/Pubs/Independentresearch/2015/The,Metric,Tide/2015_metric_tide.pdf .
- 14. LSE Public Policy Group. Maximizing the impacts of your research: A handbook for social scientists. http://www.lse.ac.uk/government/research/resgroups/LSEPublicPolicy/Docs/LSE_Impact_Handbook_April_2011.pdf . London: LSE; 2011.
- 15. HEFCE. Consultation on the second Research Excellence Framework. 2016.
- 18. Merriam-Webster Dictionary 2017. Available from: https://www.merriam-webster.com/dictionary/methodology .
- 19. Oxford Dictionaries—pathway 2016 [cited 2016 19 June]. Available from: http://www.oxforddictionaries.com/definition/english/pathway .
- 20. Oxford Dictionaries—metric 2016 [cited 2016 15 Sep]. Available from: https://en.oxforddictionaries.com/definition/metric .
- 21. WHO. WHO Ethical and Safety Guidelines for Interviewing Trafficked Women 2003 [cited 2016 29 July]. Available from: http://www.who.int/mip/2003/other_documents/en/Ethical_Safety-GWH.pdf .
- 31. Kalucy L, et al. Primary Health Care Research Impact Project: Final Report Stage 1 Adelaide: Primary Health Care Research & Information Service; 2007 [cited 2016 26 Feb]. Available from: http://www.phcris.org.au/phplib/filedownload.php?file=/elib/lib/downloaded_files/publications/pdfs/phcris_pub_3338.pdf .
- 33. Canadian Academy of Health Sciences. Making an impact—A preferred framework and indicators to measure returns on investment in health research 2009 [cited 2016 26 Feb]. Available from: http://www.cahs-acss.ca/wp-content/uploads/2011/09/ROI_FullReport.pdf .
- 39. HEFCE. RAE 2008—Guidance in submissions 2005 [cited 2016 15 Feb]. Available from: http://www.rae.ac.uk/pubs/2005/03/rae0305.pdf .
- 41. Royal Netherlands Academy of Arts and Sciences. The societal impact of applied health research—Towards a quality assessment system 2002 [cited 2016 29 Feb]. Available from: https://www.knaw.nl/en/news/publications/the-societal-impact-of-applied-health-research/@@download/pdf_file/20021098.pdf .
- 48. Weiss CH. Using social research in public policy making: Lexington Books; 1977.
- 50. Kogan M, Henkel M. Government and research: the Rothschild experiment in a government department: Heinemann Educational Books; 1983.
- 51. Thomas P. The Aims and Outcomes of Social Policy Research. Croom Helm; 1985.
- 52. Bulmer M. Social Science Research and Government: Comparative Essays on Britain and the United States: Cambridge University Press; 2010.
- 53. Booth T. Developing Policy Research. Aldershot, Gower1988.
- 55. Kalucy L, et al Exploring the impact of primary health care research Stage 2 Primary Health Care Research Impact Project Adelaide: Primary Health Care Research & Information Service (PHCRIS); 2009 [cited 2016 26 Feb]. Available from: http://www.phcris.org.au/phplib/filedownload.php?file=/elib/lib/downloaded_files/publications/pdfs/phcris_pub_8108.pdf .
- 56. CHSRF. Canadian Health Services Research Foundation 2000. Health Services Research and Evidence-based Decision Making [cited 2016 February]. Available from: http://www.cfhi-fcass.ca/migrated/pdf/mythbusters/EBDM_e.pdf .
- 58. W.K. Kellogg Foundation. Logic Model Development Guide 2004 [cited 2016 19 July]. Available from: http://www.smartgivers.org/uploads/logicmodelguidepdf.pdf .
- 59. United Way of America. Measuring Program Outcomes: A Practical Approach 1996 [cited 2016 19 July]. Available from: https://www.bttop.org/sites/default/files/public/W.K.%20Kellogg%20LogicModel.pdf .
- 60. Nutley S, Percy-Smith J and Solesbury W. Models of research impact: a cross sector review of literature and practice. London: Learning and Skills Research Centre 2003.
- 61. Spaapen J, van Drooge L. SIAMPI final report [cited 2017 Jan]. Available from: http://www.siampi.eu/Content/SIAMPI_Final%20report.pdf .
- 63. LSHTM. The Health Risks and Consequences of Trafficking in Women and Adolescents—Findings from a European Study 2003 [cited 2016 29 July]. Available from: http://www.oas.org/atip/global%20reports/zimmerman%20tip%20health.pdf .
- 70. Russell G. Response to second HEFCE consultation on the Research Excellence Framework 2009 [cited 2016 04 Apr]. Available from: http://russellgroup.ac.uk/media/5262/ref-consultation-response-final-dec09.pdf .
- Open access
- Published: 26 May 2022
Structural changes in the Russian health care system: do they match European trends?
- Sergey Shishkin ORCID: orcid.org/0000-0002-0807-3277 1 ,
- Igor Sheiman ORCID: orcid.org/0000-0002-5238-4187 2 ,
- Vasily Vlassov ORCID: orcid.org/0000-0001-5203-549X 2 ,
- Elena Potapchik ORCID: orcid.org/0000-0001-7004-3100 1 &
- Svetlana Sazhina ORCID: orcid.org/0000-0002-2023-3384 1
Health Economics Review volume 12 , Article number: 29 ( 2022 ) Cite this article
7408 Accesses
3 Citations
2 Altmetric
Metrics details
In the last two decades, health care systems (HCS) in the European countries have faced global challenges and have undergone structural changes with the focus on early disease prevention, strengthening primary care, changing the role of hospitals, etc. Russia has inherited the Semashko model from the USSR with dominance of inpatient care, and has been looking for the ways to improve the structure of service delivery. This paper compares the complex of structural changes in the Russian and the European HCS.
We address major developments in four main areas of medical care delivery: preventive activities, primary care, inpatient care, long-term care. Our focus is on the changes in the organizational structure and activities of health care providers, and in their interaction to improve service delivery. To describe the ongoing changes, we use both qualitative characteristics and quantitative indicators. We extracted the relevant data from the national and international databases and reports and calculated secondary estimates. We also used data from our survey of physicians and interviews with top managers in medical care system.
The main trends of structural changes in Russia HCS are similar to the changes in most EU countries. The prevention and the early detection of diseases have developed intensively. The reduction in hospital bed capacity and inpatient care utilization has been accompanied by a decrease in the average length of hospital stay. Russia has followed the European trend of service delivery concentration in hospital-physician complexes, while the increase in the average size of hospitals is even more substantial. However, distinctions in health care delivery organization in Russia are still significant. Changes in primary care are much less pronounced, the system remains hospital centered. Russia lags behind the European leaders in terms of horizontal ties between providers. The reasons for inadequate structural changes are rooted in the governance of service delivery.
The structural transformations must be intensified with the focus on strengthening primary care, further integration of care, and development of new organizational structures that mitigate the dependence on inpatient care.
In the last two decades, health care systems in the European Union countries have faced global challenges, including aging populations, a substantial rise in chronic and multiple diseases, the emergence of new medical and information technologies, and a growing citizen awareness of the role of a healthy lifestyle in disease prevention [ 1 ]. The responses of health systems to these challenges included structural changes in their organization with a focus on the promotion of healthy lifestyles and disease prevention, the growing scale of screening for early disease detection, strengthening primary care, changing the role of the hospitals, the development of chronic disease management programs, etc. [ 2 , 3 ]
Studies of these trends address mostly Western countries. Much less attention has been paid to the post-Soviet countries. In this paper, we study structural changes in the health care in Russia. Russian health care has inherited the Semashko model of health care organization. Its main distinction is state-centered financing, regulation, and provision of health care. The model has specific forms of provider organization, for example, outpatient clinics (polyclinics) with a large number of various specialists, the separation of care for adults and children, and large highly-specialized hospitals [ 4 ].
The Soviet and post-Soviet health systems have been underfunded. Public health funding in the 1990s dropped almost by one third in real terms [ 5 ]. The organization of medical care in the 1990s has not changed significantly relative to Soviet times, and the system has adapted through the reduction in the volume of services and increased payments by patients, frequently informal [ 6 ]. The surge in oil prices after 2000 allowed health funding to increase and while encouraged noticeable changes in service delivery.
The changes in the Russian health system have been discussed in the literature mostly focusing on specific sectors and health finance reforms [ 5 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 ]. But these changes in different sectors were not analyzed together, from a single methodological position, as changes in the structural characteristics of the Russian health care system, i.e. the changes in the ratio of different types of medical care, in the structure of medical service providers, in functionalities and modes of their interaction.
The objective of this paper is to explore the entire complex of structural changes over the past two decades in comparison with European trends. What were the structural changes in European health care systems, what were they like in Russia, and how can their differences be explained?
Study design
We followed a six-step methodological framework. The first stage involved designation of the types of medical care and the types of structural changes for identification and comparison. We considered four main areas of medical care delivery: preventive activities, primary care, inpatient care, long-term care. We focused on three different dimensions of structural changes: i) changes in the organizational structure of medical service providers; ii) changes in the structure of their activities (in its types and in their coverage of the population / patients); iii) changes in the organization of interaction between different service providers.
The second stage consisted of identifying for each type of medical care the changes in these three dimensions in the last twenty years before the COVID-19 pandemic. We described the changes that met two criteria: 1) these changes are assessed in the OECD, WHO, and World Bank reviews, and other review publications on this topic as the most noteworthy characteristics of the development of European health care systems, and 2) they have spread in a large number of European countries.
The changes identified according to the formulated criteria cover not all dimensions of structural changes for each type of medical care. For preventive activities, there are changes in the types of activities and in their coverage of the population. In primary and inpatient care, there are changes in the organizational structure of service providers, in the structure of their activities, and in the organization of interaction with other providers. In long-term care, there are changes in the structure of developed activities and their coverage of the population.
To describe the ongoing changes, we use both qualitative characteristics and, if possible, quantitative indicators that highlight them to the greatest extent.
The third stage involved detection of structural changes in four main areas of medical care delivery in Russia. We used the results of our previous studies and conducted an additional search for data characterizing structural changes in health care, using new statistical data, evidence derived from our survey of physicians and interviews with top managers in medical care system.
On the fourth stage we compared the identified structural changes in European health care systems (HCS) with the changes taking place in Russian health care. We identified the presence or absence of similar types of structural changes and the differences between them. The fifth stage was the consideration of the driving forces of structural changes in the Russian health care system. The sixth stage included discussion of the reasons for the distinctions with European developments.
Data sources
To identify the main structural changes in medical care delivery during last twenty years we searched the literature addressing both European HCS and Russia in the all aspects of changes of health care system indicators, better classified by MeSH term “health care reform”. We searched MEDLINE using the query: (russia OR europ* OR “european union” OR semashko) AND health care reform [mh] AND 2000:2021[dp]). All 788 findings were checked manually and 86 were relevant. We also used sources snowballed from these reports and the grey literature related to Russian health care, including those in limited circulation, unpublished documents, memorandums, and presentations from our personal collections covering more than twenty years.
We also used data from an online survey of 999 primary care physicians (further – survey) conducted by the authors in April–May 2019. The respondents representing 82 out of 85 regions of the Russian Federation were asked about implementation of the national prophylactic medical examination program. We also interviewed four leading specialists of the national Ministry of Health on the criteria for the inclusion of the components into the program.
To identify the driving forces of structural changes in the Russian health care system, we used materials from 10 interviews on the issues of implementing state health care programs that we conducted in 2019 with current and former top-managers in the federal government and in five regional governments. We also used the grey literature as well as published reports.
We used statistical data from the international databases of OECD [ 18 ], WHO [ 19 ], World Bank [ 20 ], as well as the Russian sources — the Federal State Statistics Service [ 21 ] and the Russian Research Instuitute of Health [ 22 ]. The data was analyzed for the period from 2000 to the latest date with available data for both EU member states and Russia. To ensure the comparability of the composition of countries in different years, the analysis of the dynamics of some indicators was limited to EU 19 members, i.e. excluding Cyprus, Greece, Croatia, Bulgaria, Luxemburg, Malta, Netherland, Poland, and Romania. The averages for EU 19 estimates are based on population size-weighted averages. If the studied publications and databases did not contain the necessary indicators, we made our own estimates.
Each section of the paper contains a brief description of the main trends in the European countries, and then provides a comparative analysis of the corresponding changes in Russian health care. The comparison is followed by a discussion of the driving forces and the limitations of structural changes in Russia compared to the main European trends. We limited our analysis to the pre – COVID-19 pandemic years.
The development of preventive activities
European hcs.
Most of them have implemented health check-ups, and population and opportunistic screenings for the early detection of diseases. These activities are viewed as a way to improve outcomes by ensuring that health services can focus on diagnosing and treating disease earlier [ 23 ]. The population covered by screenings is high and growing. In Germany 81% of population between 50 and 74 years in 2014 had been tested for colorectal cancer at least once, in Austria 78%, France 60%, Great Britain 48% [ 24 ].
The impact of these activities on health outcomes depends on the selection of preventive services, as well as on their implementation in specific national contexts. The selection of preventive services is increasingly based on research into their potential impact on mortality and other health indicators, as well as their cost effectiveness, with some services being declined because of their inadequate input into health gains [ 25 ]. It is particularly important that screenings are focused on socially disadvantaged groups with the highest probability of disease identification and the expected benefits of their management. Therefore, screening programs are based on the evaluation of local needs. Physicians have discretion in the choice of patients for screenings, depending on their importance for specific groups of the population, and individual risks and preferences.
It is increasingly common for a screening program to include follow-up management of any detected illnesses, with the implication that policy makers design such programs as a set of interrelated preventive and curative activities [ 26 ].
The original Semashko model and the current legislation prioritize preventive activities, while their implementation has been limited by the chronic underfunding of the health system. In the 2000s, the priority of prevention campaigns was revitalized in the form of a national prophylactic medical examination program (Prophylactic Program, called Dispanserization) that is a set of health check-ups and screenings. The major expectation from this Prophylactic Program is the same as in European HCS [ 27 ].
To supplement the analysis of the Prophylactic Program, we analyzed the evidence base for the components of the program and interviewed leading specialists of the federal Ministry of Health on the criteria for the inclusion of the components into the program. We found that some screenings were not evidence based and effect on the population health and/or health of participants is small [ 28 ]. The screening package of the dispanserization was expanded and reduced couple of times, but still number of ineffective screenings are included in the package (electrocardiography (ECG) screening of healthy subjects, prostate specific antigen (PSA) screening of middle age and adult men, urinalysis and routine blood tests, mammography from age 40 etc.).
Primary care physicians play a major role in conducting screenings and check-ups as well as subsequent interventions. There are also public health units responsible exclusively for these preventive activities in big polyclinics. Polled in 2019, primary care physicians responded that in 11% of polyclinics check-ups are carried out in these departments only, and in 24% of primary care organizations the check-ups are conducted by district physicians as well as by staff of these preventive units.
Under the current Prophylactic Program, people over 40 are supposed to have a set of check-ups annually; those 18–39 every three years. Most children go through physicals only. The official estimates of the coverage of the eligible population in the Prophylactic Program are around 100% [ 29 ], while service providers are less optimistic. According to the survey, more than half of the respondents reported that this share was less than 60%, while 17.4% reported less than 20% [ 27 ].
An important shortcoming of the Prophylactic Program design and implementation is the gap between its major objective and the capacity of primary care. The shortage of primary care physicians does not allow the target groups to be provided with all preventive services. Physicians have to distort the service to their registered population and to underprovide the follow-up care of detected cases. The lack of a systematic approach, less focus on local conditions, and the lack of a professional autonomy of providers are the major distinctions between Russian prevention campaigns and similar activities in Europe.
The Prophylactic Program is built on the presumption that preventive activities should include the follow-up management of any detected conditions. There is some evidence, however, that this is not taking place: according to our survey, a half of primary care physicians are unaware of the results of check-ups and screenings. The reported coverage and quality of the follow-up management of identified cases are low: a half of the respondents indicate that less than 60% of patients with identified diseases become objects of the follow-up disease management. Only 7.7% of respondents indicate that a set of disease management services corresponds to a pattern of dispensary surveillance issued by the federal Ministry of Health. The majority reports that these requirements are met only for some patients or are not met at all.
Disease management of newly identified chronic and multiple cases is focused on process rather than outcome indicators. The information on the latter is very fragmented. According to our survey, a decrease in the number of disability days of chronic patients is reported by only 14% of physicians. More than a half of respondents are unaware of the number of emergency care visits and hospital admissions of their chronic patients.
Strengthening primary care
There is a trend of multi-disciplinary primary care practices or networks development and promotion of teamwork and providers coordination in response to the growing complexity of patients. In Spain, France, and the UK it is increasingly common for large general practices to serve more than 20,000 people and provide a wider spectrum of services than in traditional solo and group practices. These emerging extended practices include pharmacists, mental care professionals, dieticians, and sometimes 2–3 specialists [ 30 , 31 ]. The role of nurses is also expanding. Most advanced nurses independently see patients, provide immunizations, health promotion, routine checks for chronically ill patients in all EU member states [ 32 ]. Related to these extended practices is the growing concentration of primary care providers via mergers and reconfigurations that increase the size of the units. The major benefits are economies of scale and scope through staff sharing and better integrated care.
There is also a general trend to strengthen the links with the local community, social care and hospitals [ 32 ]. Primary care providers are increasingly involved in chronic disease management programs together with other professionals in and out of general practices. Links with hospitals are developing beyond simple referral systems [ 33 ].
The trend of multidisciplinary practices development has greatly affected Russian health care. However, this trend in Russia differs significantly from the European HCS. It began in the 1980s, when large numbers of specialists were employed by polyclinics, which are the major providers of both primary care and outpatient specialty care. Today, large urban polyclinics employ 15–20 categories of specialists, and polyclinics in small towns 3–5 categories. The generalist who serves for the catchment area (district doctors) is limited in the scope of services they provide. Multidisciplinary practices are built through employing new specialists, while in European countries mainly through nurses and other categories of staff. Specialists in Russian polyclinics do not supplement, but essentially replace district doctors: they accounted for 66% of visits in 2019. Footnote 1
The scope of district doctors’ services is limited: at least 30–40% of initial visits end with referrals to a specialist or to a hospital, while in Europe only 5–15% [ 35 , 36 ]. Gatekeeping is promoted, but district doctors are overloaded and not interested in expanding the scope of their services. Specialists in polyclinics have insufficient training and poorly equipped, e.g. urologists do not do ureteroscopy and ophthalmologists do not practice surgery.
Since the 1990s, some regions started replacing district doctors and pediatricians with general practitioners. But this initiative has not been supported by the federal Ministry of Health, therefore the institution of a general practitioner is not accepted throughout the country. Currently, the share of general practitioners in the total number of generalists serving a catchment area is only 15% (Fig. 1 ). The model of general practice is used only in some regions. The main part of the primary care in the country is provided by district doctors and pediatricians, whose task profile remains narrower than that of general practitioners. The division of primary care for children and adults is preserved. The family is not a whole object of medical care. This division is actively defended by Russian pediatricians with references to specific methods of managing child diseases.
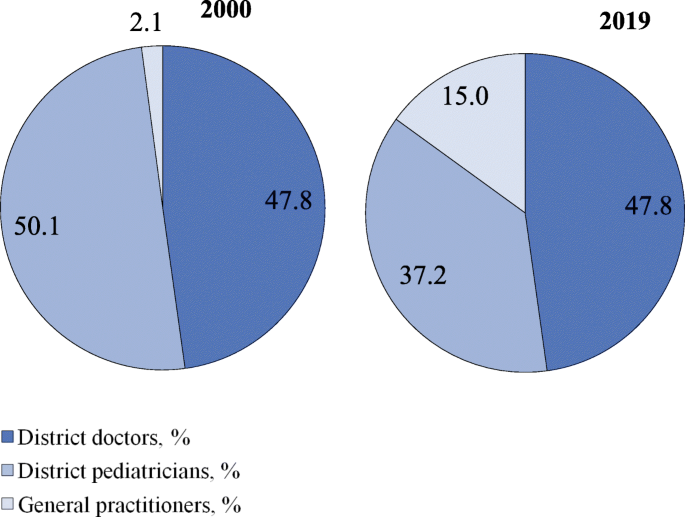
Distribution of generalists in Russia by categories in 2000, 2019. Source: Calculated from RRIH [ 22 , 37 ]
The prevailing trend in all European HCS is to increase the role of nurses. In Russia, the participation of nurses in medical care is limited to fulfilling doctors’ prescriptions and performing ancillary functions.
The transformation of inpatient care
Due to increased costs, technological advances in diagnosis and treatment, there were changes in patterns of diseases and patients treated in hospitals. A substantial amount of inpatient care has been moved to outpatient settings with a respective decrease in bed capacity. This is an almost universal trend in European HCS [ 19 ].
Hospitals continue to be centers of high-tech care, which concentrate most difficult cases and intensify inpatient care with a corresponding decrease in the average length of stay. These changes have been promoted by the move to diagnostic related groups based payment systems and a growing integration with other sectors of service delivery.
In many European countries, most hospitals no longer act as discrete entities and have become units of hospital-physician systems which are multi-level complex adaptive structures [ 3 ]. A new function of hospital specialists is their involvement in chronic disease management in close collaboration with general practitioners, outpatient specialists, and rehabilitative and community care providers [ 38 ].
Over the past two decades the treatment of relatively simple cases and preoperative testing have gradually moved to day care wards and polyclinics. In annual health funding, the federal government sets decreasing targets of inpatient care which are obligatory and which regions use to plan their inpatient care. However, inpatient care discharges per 100 people have been almost stable (21.9 in 2000 and 22.4 in 2018) in contrast to the EU 19 members Footnote 2 (18.4 in 2000 and 16.9 in 2018) [ 18 ]. The pressure of decreasing targets resulted in a drop in the average length of hospital stays (Fig. 2 ) and the total bed-days per person (Fig. 3 ). These indicators, along with bed supply (Fig. 4 ), decreased even faster than in the EU.
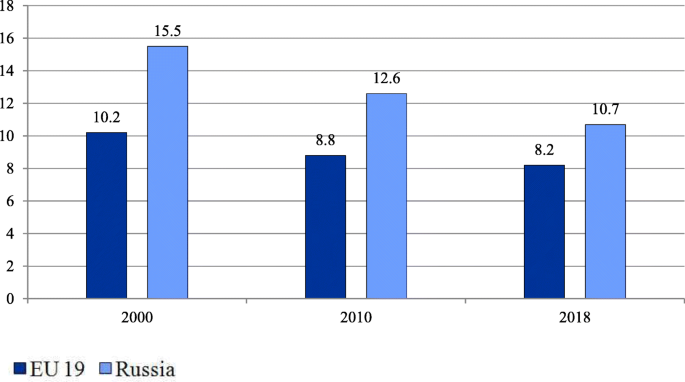
Average length of stay in hospital in EU members and Russia (days). Note: Calculated for EU 19 member states (see Methods). The EU 19 average length of hospital stay estimates are calculated as the sum of the products of inpatient care discharges by the average length of stay for each country, weighted average by the total inpatient care discharges. Source: OECD Health Statistics [ 18 ]
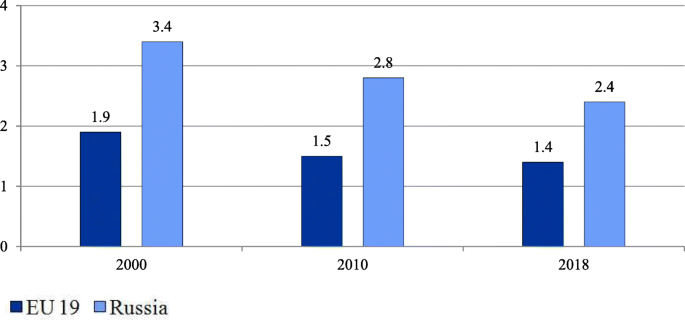
Number of bed-days per person in the EU and Russia. Note: Calculated for EU 19 member states (see Methods). EU 19 estimates are calculated as the sum of the products of inpatient care discharges by the average length of stay for each country weighted by the total population. Source: OECD Health Statistics [ 18 ]

Hospital beds per 1000 people in the EU and Russia. Note: Calculated as the average for all EU 28 members weighted by the total population. Source: World Bank [ 20 ]
At the same time, the intensity of medical care processes in hospitals in Russia remains significantly lower than in European countries. An indicator of this is the gap in the number of hospital employees per 1000 discharged (Table 1 ).
Over the past 20 years, significant efforts have been made to deploy day wards, both in hospitals and polyclinics, to reduce the burden on hospitals. As a result, the proportion of patients treated in day wards in the total number of patients treated in hospitals increased from 7.6% in 2000 to 20.8% in 2016 [ 21 ]. However, there is fragmentary evidence that this figure is still noticeably lower than in Europe. The share of cataract surgery carried out as ambulatory cases varies in most European countries between 80 to 99% [ 24 ] but is negligible in Russia.
Despite these positive trends, the health system remains hospital centered. The number of bed-days per person remains nearly twice as high as the EU average (Fig. 3 ).
An important trend is the increasing concentration of hospitals. The number of hospitals halved between 2000 and 2018, mostly due to mergers, but also due to the closures of inadequately equipped hospitals. This process has led to an increase in the average size of hospitals from 156 beds in 2000 to 223 beds in 2018 [ 21 ]. This figure is higher today than in Western countries with large territories. The average hospital size in France was 130 beds in 2018 and in Germany 215 beds in 2017 [ 18 ]. In Russia, with its very low population density, the reduction in the number of small rural hospitals resulted in some accessibility problems.
At the same time, the incorporation of previously independent polyclinics into hospitals is under way. The proportion of independent polyclinics in the total number of polyclinics has decreased from 35% in 2000 to 19% in 2014 [ 36 ].
The development of long-term care
Over the last 20 years, most European countries have increasingly developed the public provision of long-term care. The number of nursing and elderly home beds per 100,000 people in the EU increased from 581.7 in 2000 to 748.3 in 2014 [ 19 ], although the pace of changes, the coverage of citizens in need of long-term care, and its organization and funding differ substantially across countries [ 39 ]. Many countries control costs by keeping people in their homes longer and shifting the responsibility for non-institutional forms of care to communities [ 40 ]. An expected outcome of investment in long-term care is the reduction of informal care utilization.
Compared to European HCS, long-term care is underdeveloped in Russia. The number of nursing care beds declined from 14.7 per 100,000 people in 2011 to 10.6 in 2019 [ 22 ]. The share of citizens over working age and people with disabilities receiving outpatient and inpatient care within the long-term care system in the total number of citizens over working age and people with disabilities in need of long-term care, was only 2.9% in 2019 [ 41 ].
In contrast to the European HCS, Russia has not built a strong long-term care sector with the capacity to reduce the workload of acute inpatient care settings. Hospitals have to keep some patients longer resulting in a relatively higher length of stay. Palliative care as another sector of the long-term care which started to develop only a few years ago.
Driving forces and tools of structural changes in the Russian health care system
These changes have been driven by the federal and regional governments. They use two main tools to manage structural changes: 1) setting health care targets for the entire country and for regions, and 2) implementing vertical health care programs.
Since 1998, the federal government has annually approved a program of benefit packages for health (the Program). It sets targets for the utilization of medical care for each sector of service delivery, as well as unit cost targets. The Program is designed to balance the volumes of care with the amount of public funding. The annual versions of the Program gradually reduced the targets for inpatient care to encourage a shift to outpatient care. The federal targets are used in regional health planning. In the first decade of using the Program, the changes in the actual volume of medical care were small, but in the second decade, pressure from the federal center on the regions increased, and the gap between the federal targets and the actual utilization of care has noticeably narrowed (Table 2 ).
The development of the legislation on the delimitation of responsibility between levels of government, carried out in the last two decades, has consistently strengthened the regional governments role in restructuring medical care delivery. In 2012, almost all resources of health care governance were transferred from the municipal to the regional level (including the governance of primary health care. During the period 2000–2019 the number of public hospitals has decreased by 2.2 times, the number of hospital beds by 1.5 times, polyclinics 1.3 times, feldsher-obstetric posts 1.3 times. Footnote 3
When oil prices increased, the federal government poured additional resources into vertical programs. They are administered by the federal Ministry of Health and regional governments. The major programs: the ‘Priority national health project’ (2004–2012), the Prophylactic Program (2008 – ongoing), and regional programs for the modernization of health care (2011–2013). All additional and some basic resources are earmarked in an attempt to develop the highest priority activities: preventive care, obstetric care, cardiovascular surgery, oncology, etc.
The role of the centralized administration of these priority programs is controversial. The federal government initiated them, provided regions with additional funding, and made the program’s targets a priority of health policy. According to interviews with federal and regional officials, the implementation of programs is heavily controlled by the federal government: practically all decisions on specific activities, target indicators and resource allocation are approved on the federal level. The Russian regions have low flexibility to respond to local needs such as variation in disease incidence, the capacity of health care, or vulnerable population groups.
Structural changes in the provision of inpatient care were prompted by the introduction of a diagnostic related groups based payment system in the early 2010s. This was initiated by the federal government and implemented with the participation of the World Bank experts. It makes more profitable for hospitals to reduce the duration of hospitalizations and to complicate the structure of inpatient treatment [ 44 ].
We found that despite significant differences in health care organization, some structural changes in Russia have followed the general European trends. A similar rise in the coverage of the population with screenings is underway in Russia. There is a clear tendency to replace some inpatient care with day care. The volume of inpatient care is reducing —mostly due to a significant decrease in the length of stays, while the rate of hospital admission remains relatively stable. As in the most European HCS, the concentration of medical organizations and the formation of large outpatient and inpatient complexes is developing.
However, there are some substantial differences: the development of prevention programs is relatively less focused on the most vulnerable target groups and on local needs; primary care specialization is much stronger than in European HCS; the role of first contact generalists is waning; the worldwide tendency of increasing the role of nurses is almost invisible in Russia; long-term care is starting to develop but is still at a very low level and palliative care is in its infancy; integration in the health system are much less pronounced—both at the level of individual medical organizations and between health sectors.
The reasons for these differences are rooted in the specific features of health governance in Russia.
The Semashko model, by virtue of its genesis, reproduces the state administration patterns of a planned economy. The main driving force of changes is the bureaucracy. Its managerial activities are guided by the mechanism described by J. Kornai: ‘postponement, putting out the fire, postponement’ [ 45 ]. The governance focuses on mobilizing and distributing available resources to solve or mitigate the most pressing problems - ‘fire fighting’. This is what determines the fragmentation of structural changes in Russian health care compared to structural changes in European countries.
Materials of interviews with heads of federal and regional health authorities suggest that in the existing governance system each of its levels must demonstrate the success of its activity exclusively to the higher levels of management. It is easier to achieve success when solving problems of optimizing the volume of medical care and the organizational structure of medical institutions, and much more difficult when solving problems of improving the efficiency of all elements of medical care system, which requires changes in their functionality and ways of interaction. It requires more financial resources and better management at all levels of health governance.
A number of deeply rooted limitations for carrying out structural transformations in Russian health care can be highlighted.
Firstly, the low capacity of primary care providers and to some extent the unwillingness of patients to replace inpatient care with outpatient treatment prevents a shift of patients from hospitals to polyclinics.
Secondly, a feature of the Russian health care system is the weak development of horizontal links between medical organizations related to different levels of medical care, and between medical workers within medical organizations working in different departments [ 36 , 46 , 47 ]. The interaction of different providers is carried out mostly through vertical channels. This is a serious obstacle to the development of horizontal integration [ 36 ].
Thirdly, democratic institutions for the development of health care are historically underdeveloped in Russia and this influences the choice of health policy priorities. According to interviews with heads of regional health authorities, the role of local communities is negligible, and the role of the medical community is marginal. Professional organizations are rarely involved in decision-making on health issues. The input of public councils to government bodies is largely imitative. Information about the activities of the system as a whole and of individual medical organizations is restricted for public use. This enables health authorities to focus on achievements in their reports, while hiding shortcomings. Feedback from patients, and society as a whole, is poorly expressed.
Conclusions
Russian health care, whose genetic basis was the Soviet Semashko model, after a difficult ‘survival’ period in the 1990s, underwent significant structural changes over the next two decades. To a large extent, the directions of these changes have coincided with European trends. The prevention and the early detection of diseases have developed intensively. The reduction in hospital bed capacity and inpatient care was accompanied by an intensification of inpatient treatment and a decrease in the average length of stay. Russia has followed the European trend of service delivery concentration in hospital-physician complexes, while the increase in the average size of hospitals is even more substantial. Structural changes in primary care are much less pronounced. The resources and competences of providers and the governance of primary care are still not enough to abolish the hospital-centered model of service delivery. Russia has intensively implemented vertical health care programs to develop the priority activities, but still significantly lags in the level of development of horizontal ties among services providers.
Specific structural changes in Russia are rooted in the organization and governance of service delivery. The interests of federal and regional bureaucracies, which act as the main drivers of changes, are pushing them to prioritize the changes in volumes of medical care and organizational structure of health care providers and not spend a lot of effort on improving their functionality and modes of interaction between providers of medical care. An important role is also played by the low capacity of primary care units to provide quality care.
To respond effectively to modern global challenges, reduce mortality, and improve the health of the population, structural transformations in Russian health care must be intensified with the focus on strengthening primary care, the further integration of care, and an accelerated development of new structures that mitigate the dependence on inpatient care.
Availability of data and materials
The data used and analysed during the current study are publicly available.
Calculated using data from [ 34 ].
See Methods.
Calculated using data from [ 21 ].
Abbreviations
European Union
Health Care System
Organization for Economic Co-operation and Development
World Health Organization
World Health Organization. Better Health for Europe: more equitable and sustainable. Copenhagen: WHO; 2019. https://apps.who.int/iris/bitstream/handle/10665/327427/9789289054225-eng.pdf . Accessed 9 Mar 2021.
Kringos D, Boerma W, Bourgueil Y, et al. The strength of primary care in Europe: an international comparative study. Br J Gen Pract. 2013;63(616):e742–50. https://doi.org/10.3399/bjgp13X674422 .
Article PubMed PubMed Central Google Scholar
McKee M, Merkur S, Edwards N, Nolte E, eds. The changing role of the Hospital in European Health Systems. European Observatory on Health Systems and Policies. Cambrige University Press; 2020. https://www.euro.who.int/__data/assets/pdf_file/0010/448048/Changing-role-of-hospitals-eng.pdf . Accessed 11 Feb 2021.
Davis C. Priority and the shortage model: the medical system in the socialist economy. In: Davis C, Charemza W, editors. Models of disequilibrium and shortage in centrally planned economies. London: Chapman and Hall; 1989. p. 427–59.
Chapter Google Scholar
Shishkin S. Russia’s health care system: difficult path of reform. In: Alexeev M, Weber S, editors. The Oxford handbook of the Russian economy. Oxford: Oxford University Press; 2013. p. 748–74.
Google Scholar
Shishkin SV, Vlassov VV. Russia's healthcare system: in need of modernisation. BMJ. 2009;338:b2132. https://doi.org/10.1136/bmj.b2132 .
Rese A, Balabanova D, Danishevski K, McKee M, Sheaff R. Implementing general practice in Russia: getting beyond the first steps. BMJ. 2005;331(7510):204–7. https://doi.org/10.1136/bmj.331.7510.204 .
Human Rights in Patient Care. Stockholm Region Office in St.Petersburg. Russian Healthcare System Overview. St. Petersburg, 2010. 2010. https://health-rights.org/index.php/cop/item/russian-healthcare-system-overview . Accessed 29 Nov 2020.
Gordeev VS, Pavlova M, Groot W. Two decades of reforms. Appraisal of the financial reforms in the Russian public healthcare sector. Health Policy. 2011;102(2-3):270–7. https://doi.org/10.1016/j.healthpol.2010.08.009 .
Popovich L, Potapchik E, Shishkin S, Richardson E, Vacroux A, Mathivet B. Russian Federation: health system review. Health Syst Transit. 2011;13(7):1-190, xiii-xiv.
PubMed Google Scholar
Bochkareva VK. Health-care reform and ensuring equal access to free medical services. Probl Econ Transit. 2013;55(12);12-31. https://doi.org/10.2753/PET1061-1991551203 .
Sheiman I, Shevski V. Evaluation of health care delivery integration: the case of the Russian Federation. Health Policy. 2014. https://doi.org/10.1016/j.healthpol.2013.12.011 .
Kontsevaya A, Sabgaida T, Ivanova A, Leon DA, McKee M. How has the management of acute coronary syndrome changed in the Russian Federation during the last 10 years? Health Policy. 2017;121(12):1274-9. https://doi.org/10.1016/j.healthpol.2017.09.018 .
Tagaeva TO, Kazantseva LK. Public health and health Care in Russia. Probl Econ Transit. 2017;59(11-12):973-90. https://doi.org/10.1080/10611991.2017.1431488 .
Belova N. Health Care in Rural Areas. Sociol Res. 2018;57(2):123-35. https://doi.org/10.1080/10610154.2018.1577621 .
Sheiman I, Shishkin S, Shevsky V. The evolving Semashko model of primary health care: the case of the Russian Federation. Risk Manag Healthc Policy. 2018;11:209-20. https://doi.org/10.2147/RMHP.S168399 .
Somanathan A, Sheiman I, Salakhutdinova S, Buisman L. Universal health coverage in Russia: extending coverage for the poor in the post-soviet era. Universal health coverage study series. Washington, DC: Universal Health Coverage Study Series The World Bank Group; 2018. p. 37. https://openknowledge.worldbank.org/handle/10986/30026 . Accessed 10 Mar 2021.
OECD. Health Statistics. OECD; 2020. https://stats.oecd.org/Index.aspx?ThemeTreeId=9 . Accessed 01 Dec 2020.
World Health Organization (WHO). European Health for All database (HFA-DB). WHO; 2020. https://gateway.euro.who.int/ru/datasets/european-health-for-all-database/ . Accessed 29 Nov 2020.
World Bank. World Bank Open Data. The World Bank Group, 2020. https://data.worldbank.org/ .
Federal State Statistics Service website (Rosstat). Health care in Russia. Moscow: 2020. https://rosstat.gov.ru/folder/210/document/13218 . Accessed 02 Dec 2020.
Russian Research Institute for Health (RRIH). Health statistics. Moscow: 2020. https://mednet.ru/napravleniya/mediczinskaya-statistika . Accessed 29 Nov 2020.
International Agency for Research on Cancer. Cancer Screening in the European Union. Report on the implementation of the Council Recommendation on cancer screening. Lyon: European Commission; 2017. https://ec.europa.eu/health/sites/default/files/major_chronic_diseases/docs/2017_cancerscreening_2ndreportimplementation_en.pdf . Accessed 19 Dec 2020.
OECD. Health at a Glance 2019: OECD Indicators. Paris: OECD Publishing; 2019.
Book Google Scholar
McKee M, Rechel B. Screening. In: Rechel B and McKee M eds. Facets of public health in Europe. WHO Observatory for health systems and health reforms. Berkshire: Open University Press; 2014. https://www.euro.who.int/__data/assets/pdf_file/0003/271074/Facets-of-Public-Health-in-Europe.pdf . Accessed 21 Mar 2021.
Sagan A, McDaid D, Rajan S, Farrington J, McKee M. Screening: When is it appropriate and how can we get it right? European Observatory on health systems and health reforms. European Observatory Policy Brief. 35. Copenhagen, 2020. https://apps.who.int/iris/bitstream/handle/10665/330810/Policy-brief-35-1997-8073-eng.pdf . Accessed 20 Apr 2021.
Sheiman IM, Shishkin SV, Shevsky VI, Sazhina SV, Ponkratova OF. Regular medical check-ups in Russia: expectations and reality. Mir Rossii. 2021;30(4):6-29. https://doi.org/10.17323/1811-038X-2021-30-4-6-29 .
Rebrova OI, Fedyaeva VK, Omel'ianovskiĭ VV, Ilyin MA. Stage 1 screenings of periodical health check: a systematic review of long-term efficiency. Profilakticheskaya Meditsina. 2017;20(3):55-59. https://doi.org/10.17116/profmed201720355-59 .
Federal Fund of Mandatory Health Insurance. Report about the mandatory health insurance system activity in the Russian Federation in 2019. Mandatory Med Insur Russian Federat. 2020;4:22.
Dedeu T, Marti T. Multiprofile primary health care teams in Catalonia, Spain: a population-based effective model of service delivery. WHO; 2018. https://www.euro.who.int/__data/assets/pdf_file/0009/366498/HSS-NCDs-Policy-brief-cat.pdf . Accessed 15 Feb 2020.
Kumpunen S, Curry N, Farnworth M, Rosen R. Collaboration in general practice: surveys of GP practice and clinical commissioning groups. Nuffield trust, Royal College of General Practitioners; 2017. https://www.nuffieldtrust.org.uk/files/2017-10/collaboration-in-general-practice-2017-final.pdf . Accessed 20 Dec. 2020.
OECD. Realizing the full potential of primary care. Policy Brief. OECD; 2019. https://www.oecd.org/health/health-systems/OECD-Policy-Brief-Primary-Health-Care-May-2019.pdf . Accessed 11 Dec 2020.
Damiani G, Pascucci D, Sindoni A, et al. The bigger, the better? A systematic review on the impact of mergers on primary care organizations. Eur J Pub Health. 2021;31(2):244-52. https://doi.org/10.1093/eurpub/ckaa248 .
The Ministry of Health of the Russian Federation. The accounting form No. 30 of the Federal Statistical Surveillance for 2019 (raw data) (not in the public domain).
Kringos DE, WGW B, Hutchinson A, Saltman R. Building primary Care in a Changing Europe. Eur Observ Health Syst Health. Observatory Studies Series. 2015;38;172.
Sheiman I, Shevsky V. Concentration of health care providers: does it contribute to integration of service delivery? Risk Manag Healthc Policy. 2019;12:153-66. https://doi.org/10.2147/RMHP.S205905 .
Rugol LV, Son IM, Starodubov VI, Pogonin AV. Some results of healthcare reforming. Soc Aspects Popul. Health. 2021;67(1):4. https://doi.org/10.21045/2071-5021-2018-64-6-1 .
Article Google Scholar
Urbanski D, Reichert A, Amelung V. Discharge and Transition Management in Integrated Care. In: Amelung V, Stein V, Goodwin N, Balicer R, Nolte E, Suter E, editors. Handbook Integrated Care; 2017. p. 97–111.
Hernández-Quevedo C, Maresso A, Merkur S, Quentin W, Richardson E, Ginneken E. 20 years of health system reforms in Europe: what’s new? Eurohealth. 2018;24(2):23–8.
Spasova S, Baeten R, Vanhercke B. Challenges in long-term care in Europe. Eurohealth. 2018;24(4):7–12.
The presidium of the presidential Council for the Strategic Development and Priority Projects. The Federal Project ‘the senior generation’. Protocol No 16 dated December 24, 2018. The Ministry of Labour and Social Protection; 2018. https://mintrud.gov.ru/ministry/programms/demography/3 . Accessed 15 Nov 2020.
Government of the Russian Federation. Resolutions of the government of the Russian Federation ‘on the program of the state guarantees of free provision of medical care to Citizens’ 1998–2018. The Federal Compulsory Medical Insurance Fund. 2018. https://www.ffoms.gov.ru/system-oms/about-fund/questions-oms/programm-gos-guarantee/ . Accessed 11 Sept 2021.
The Ministry of Health of the Russian Federation. Reports on the implementation of the program of the state guarantees of free provision of medical care to Citizens, 1999–2019. Moscow: The Ministry of Health of the Russian Federation, 2000-2019.
Avxentyeva MV, Omelyanovskiy VV, Petrovskiy AV, et al. New approaches to the development of diagnostic related groups for Cancer pharmacotherapy in Russian Federation. Med Technol Assess Choice. 2018;2(32):8–22.
Kornai J. Economics of shortage. Amsterdam: Elsevier Science. 1980.
Kuhlmann E, Shishkin S, Richardson E, et al. Understanding the role of physicians within the managerial structure of Russian hospitals. Health Policy. 2019;123(8):773-81. https://doi.org/10.1016/j.healthpol.2019.05.020 .
Sazhina SV, Shevsky VI, Sheiman IM, Shishkin SV. Interaction of health care providers: physicians' survey outcomes. Soc Aspects Popul Health. 2021;67(1):4 http://vestnik.mdnet.ru/content/view/1230/30/lang,ru/ .
Download references
Acknowledgements
Authors’ information (optional).
Sergey Shishkin – DSc in Economics, Director, Centre for Health Policy, HSE University.
Igor Sheiman – PhD in Economics, Professor, Health Economics and Management Department, HSE University.
Vasily Vlassov – DSc in Internal Diseases, Professor, Health Economics and Management Department, HSE University.
Elena Potapchik – PhD in Economics, Leading Research Fellow, Centre for Health Policy, HSE University.
Svetlana Sazhina – MPA, Leading Analyst, Centre for Health Policy, HSE University.
The study was funded by the grant provided by the Ministry of Science and Higher Education of the Russian Federation (Grant Agreement No. 075–15–2020-928).
Author information
Authors and affiliations.
Centre for Health Policy, National Research University Higher School of Economics, 4 Slavyanskaya Ploshchad, Building 2, Moscow, Russia, 109074
Sergey Shishkin, Elena Potapchik & Svetlana Sazhina
Department of Health Care Administration and Economics, School of Politics and Governance, Faculty of Social Sciences, National Research University Higher School of Economics, 20 Myasnitskaya Ulitsa, Moscow, Russia, 101000
Igor Sheiman & Vasily Vlassov
You can also search for this author in PubMed Google Scholar
Contributions
Sergey Shishkin conceptualized, designed the study and supervised the work. All authors collected, analyzed and interpreted the data. Elena Potapchik, Svetlana Sazhina made statistical analysis. Sergey Shishkin, Igor Sheiman and Vasily Vlassov wrote a first draft of the manuscript. All authors critically reviewed the draft. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Sergey Shishkin .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Shishkin, S., Sheiman, I., Vlassov, V. et al. Structural changes in the Russian health care system: do they match European trends?. Health Econ Rev 12 , 29 (2022). https://doi.org/10.1186/s13561-022-00373-z
Download citation
Received : 19 January 2022
Accepted : 05 May 2022
Published : 26 May 2022
DOI : https://doi.org/10.1186/s13561-022-00373-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health care system
- Health service provision
- Primary care
- Inpatient care
- Structural changes
- Semashko model
Health Economics Review
ISSN: 2191-1991
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Open access
- Published: 28 May 2024
Epidemic preparedness and innovations in digital healthcare: enhancing post-pandemic speech-language pathology services for child and adolescent mental health in Qatar
- Abdullah Amro 1 ,
- Hanan Abdallah Kotkot 1 ,
- Yahia Albobali 1 ,
- Prem Chandra 2 &
- Yasser Saeed Khan 1 , 3
BMC Health Services Research volume 24 , Article number: 673 ( 2024 ) Cite this article
1 Altmetric
Metrics details
This paper discusses the critical importance of epidemic preparedness and innovations in digital health care by examining the transformative impact on speech-language pathology (SLP) services in a specialist outpatient child and adolescent service (CAMHS).
This retrospective review analyzes referral data from three periods: pre-pandemic (15 March 2019–14 March 2020), pandemic (15 March 2020–14 March 2021), and post-pandemic (15 March 2021–14 March 2022). Statistical analyses assess trends in referrals and diagnoses during these periods. Feedback was also obtained from Parents of children who received virtual consultations during the pandemic.
The results reveal an increase in the demand for SLP services during and after the pandemic, with a surge in referrals (increased from 9.7 to 12.9% when compared pre-pandemic to post-pandemic periods; Chi-Square value 3.33, P = 0.068) for children with social communication challenges and autism spectrum disorder. Phone and video consultations were effectively adopted. Feedback from families shows a positive response (69%–98% of participants responded as strongly agreed and agreed on various items listed in feedback form specifically designed in line with the service objectives) to telehealth interventions, with many parents finding virtual consultations effective and helpful.
Conclusions
The study emphasizes the importance of telehealth SLP services in meeting the increasing demand for mental health interventions among children and adolescents. It suggests integrating telehealth into clinical practice beyond the pandemic and highlights the need for long-term evaluation and addressing potential barriers to access.
Peer Review reports
Introduction
Epidemic preparedness regarding children’s development and mental health has gained unprecedented importance, particularly in the wake of the COVID-19 pandemic. The pandemic rendered children and adolescents with neurodevelopmental and mental disorders vulnerable in the sense that they faced unique challenges, disrupting their routines, isolating them from peers, and affecting their access to essential healthcare services. With nearly half of all mental disorders beginning by the age of 14 years [ 1 ], and up to 20% of children and adolescents who have a disabling mental disorder each year globally [ 2 ] the vulnerability of this specific patient population to epidemic disruptions is undeniable. Mental health services for children and adolescents around the world have been under strain for several years, more so since the onset of the COVID-19 pandemic [ 3 ]. There has been an escalation in the treatment demand for mental health problems in childhood and adolescence [ 4 , 5 , 6 ]. A study in Ireland reported a significant increase in the number of referrals to a child and adolescent mental health service one year after the COVID-19 pandemic [ 7 ].
The COVID-19 pandemic and the associated social restrictions rendered children and adolescents with neurodevelopmental disorders particularly vulnerable [ 8 , 9 ]. There have been reports of an increase in externalizing behaviors in children with neurodevelopmental disorders due to reduced therapy [ 10 ]. Given the higher prevalence of communication challenges in this group of individuals, the need and delivery of speech-language pathology (SLP) services gained paramount importance. It is understood that precautionary measures taken during the pandemic (wearing masks, canceling in-person activities, social isolation) may have impacted children’s communication and language skills during their critical development years [ 11 ].
In this paper, we report the impact of the COVID-19 pandemic on the SLP referral trends in a specialist outpatient child and adolescent service (CAMHS) in Hamad Medical Corporation (HMC), Qatar. HMC is the largest public healthcare provider in Qatar, and its multidisciplinary CAMHS service receives referrals from multiple sources including primary care, schools, and general hospitals [ 12 ]. We also describe how the SLP service in HMC CAMHS remained functional during the COVID-19 pandemic through the utilisation of virtual modalities of care. It outlines how the demand for speech-language interventions for children and adolescents with neurodevelopmental and mental disorders surged during the pandemic, underscoring the critical need for innovative approaches such as telehealth to bridge the service gap.
By examining the impact of the pandemic on SLP referral trends and evaluating the efficacy of telehealth interventions, this study contributes to the ongoing discourse on advancing epidemic preparedness for health systems, especially concerning the vulnerable population of children and adolescents. As the world navigates post-pandemic challenges, it is imperative to prioritize the developmental and mental well-being of young individuals through proactive and adaptable approaches within healthcare systems. The feedback provided by families who received care during the pandemic and future directions are also discussed.
Ethical considerations
This service evaluation initiative involved a retrospective analysis of existing data. No new patients were recruited. The data used was fully anonymized and not linked to any patient-identifiable information to ensure data protection and confidentiality. The study did not meet the requirements for ethical approval by the institutional review board and necessary departmental approval was obtained from the leadership of mental health services, in line with the advice provided by the medical research centre.
Referral data
The referral pathway to SLP services in HMC CAMHS is such that most referrals to the two speech-language pathologists are made internally by other members of the multidisciplinary team. A typical example could be a child or young person receiving a diagnosis of autism spectrum disorder (ASD) by the ASD assessment team and then being referred to SLP services for follow-on work focusing on communication. Occasionally, referrals may be received from external providers for children and young people who may have been discharged from other services e.g., Developmental Paediatrics due to age limit, but may require continued SLP intervention. In this case, the referral is discussed by the CAMHS Triage team with the speech-language pathologists in the team to ensure it is appropriate for the service.
We compared three different time periods to ascertain if any trends existed in the number and nature of referrals to SLP services. COVID-19 restrictions were implemented in the state of Qatar during the second week of March 2020. The first period reviewed was 15 March 2019–14 March 2020 (pre-pandemic period), followed by 15th March 2020–14th March 2021 (pandemic period) and 15th March 2021- 14th March 2022 (post-pandemic period).
Statistical analyses
Anonymous data were collected using a specific standard data collection tool and entered into a database designed in view of the study design and objectives. Descriptive statistics were used to summarize and determine the participants’ characteristics and distribution of various considered parameters related to demographics and diagnosis of the participants across three periods (Pre-pandemic period, Pandemic period, and Post-pandemic period). Quantitative data were presented using mean and standard deviation (SD). Categorical data were summarized using frequencies and percentages. The Mantel-Haenszel Chi-Square test was employed to examine and statistically evaluate the linear trend in the percentage (%) of referrals to SLP. Associations between two or more qualitative variables across three periods were examined and assessed using Pearson Chi-square or Yates corrected Chi-Square tests as appropriate. Quantitative data (mean age) measured across three periods were compared using one-way analysis of variance (ANOVA) followed by the Bonferroni multiple-comparison test. The most crucial findings were graphically represented using appropriate statistical graphs. All P values presented were two-tailed, and P values < 0.05 was considered statistically significant. All Statistical analyses were done using statistical packages SPSS version 27.0 (Armonk, NY: IBM Corp) and Epi Info 2000 (Centers for Disease Control and Prevention, Atlanta, GA).
Feedback questionnaires
We collected responses from parents on feedback questionnaires designed to obtain their views about the quality of the service received. The original questionnaire was developed in English Language which was forward-translated into Arabic and further back-translated into English by experienced Psychiatrists in the local Child and Adolescent mental health services with excellent proficiency in both English and Arabic languages. It was ensured that the original and the translated versions achieved conceptual and linguistic equivalence. The translated questionnaires were piloted on the first five respondents. Their understanding of each item on the questionnaire and its response was explored to ensure the translated items retained the same meaning as the original items. The questionnaires comprised six questions and were offered in English or Arabic language.
Referral and diagnosis trends
Two hundred forty-eight children and young people were referred to the SLP service in HMC CAMHS over the 3 years. Of these 248, 175 were boys and 73 were girls. The age range was 3–18 years. Figure 1 displays a box plot illustrating the distribution of ages across the three periods. Children and young people referred to SLP services were categorized into three groups based on age range: young children (Group 1: aged 3 years to < 9 years), older children (Group 2: aged 9 years to < 13 years), and adolescents (Group 3: aged 13 years to < 18 years).
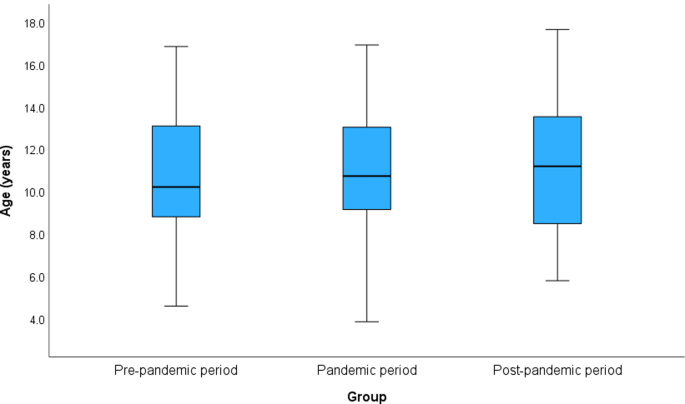
Box plot depicts Age distribution across the c periods
Expatriates formed 70.6% and natives 29.4% of the total patients, and the percentage of patients was observed to be significantly ( P = 0.008) lower in the pandemic period (58%) compared to the pre-pandemic period (82%) and post-pandemic period (73%) (Table 1 ).
Mantel-Haenszel Chi-Square test indicated an increased linear trend in the percentage of referrals to SLP (pre-pandemic 9.7%, pandemic 12.1% and post-pandemic, 13%); however, this difference was statistically insignificant (Chi-Square for linear trend 3.33, P = 0.068) as shown in Table 2 ; Fig. 2 . Moreover, a consistent increase was noted over the 3 periods in the absolute percentage of patients referred to the SLP service. It increased by 26.2% between the pre-pandemic and pandemic periods and a further increase of 42.8% was noted between the pandemic and the post-pandemic periods. Furthermore, the number escalated by 80.3% when the post and pre-pandemic periods were compared (Table 1 ).
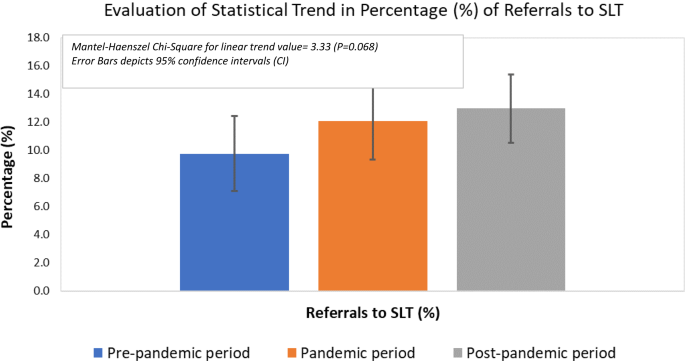
Evaluation of statistical trend in percentage (%) of referrals to SLT
A breakdown of diagnoses for the 248 children and young people was also included in Table 1 . In the case of coexisting conditions, the primary diagnosis with the most impairing impact on the functioning of the child/young person was prioritised. Social (Pragmatic) communication disorder is mentioned separately given its relevance with CAMHS. Stuttering, Language Disorder, and Speech Sound Disorder were included in the “others” category. The majority of children and young people referred over the 3 years had a primary diagnosis of autism spectrum disorder followed by Attention deficit and hyperactivity disorder (ADHD), social (pragmatic) communication disorder, others, and intellectual/learning disability in decreasing order. The largest and most consistent increase over the three years was noted in the referrals received for patients with social (pragmatic) communication disorders. Various specific primary diagnoses outlined showed no significant association across three periods ( P = 0.088).
Clinical activity and contact modalities during the pandemic
The modality of routine healthcare provision in the state of Qatar had to be switched from in-person to virtual (phone/video) consultations during the peak of the pandemic to contain the dissemination of the deadly virus [ 13 ]. The mental health service at HMC responded quickly to the developing situation. The community mental health services including the outpatient CAMHS service were provided video equipment and software to ensure continuity of care to the patient population.
The online SLP interventions were conducted in real-time audio and/or video connection through high-speed internet to create an experience close to that achieved in an in-person encounter. The parent/caregiver was expected to attend the session to facilitate the intervention. Parents were trained to support the learning of their children during sessions through prior completion of training tasks. The tasks were emailed to parents/caregivers in between sessions to facilitate their preparedness for the session. The SLP activities included direct tasks involving auditory or auditory-visual stimulation. Several resources were used e.g. flashcards, social squad videos, games focusing on the enhancement of several communication skills, and conversational activities, etc. The use of social squad videos combined with checking the child’s understanding of facial expressions, gestures, intonations, etc. proved particularly helpful in engaging children with ADHD, ASD (high functioning), and social communication disorder.
The challenges associated with this sudden transition to virtual modalities of treatment were twofold. Firstly, the impact on patients, particularly those who were at a higher risk of deterioration in their mental state and behaviour due to this sudden change. Secondly, the challenge of speech-language pathologists having to adapt to a new way of delivering therapy since many were using this delivery method for the first time globally [ 14 ].
The CAMHS outpatient service at HMC has two speech-language pathologists as part of its MDT (one male and one female). In terms of the clinical activity in the two clinics, a total of 709 appointments (new and follow-up) were offered during the pre-pandemic period, 1601 during the pandemic, and 1668 during the post-pandemic year. The relatively lower number in the pre-pandemic period could be explained by the absence of a dedicated speech-language pathologist between March 2019 and August 2019 due to the previous therapist leaving the service. This gap was bridged to some extent by a visiting therapist who could offer limited input only. To make a more reliable comparison, we also reviewed the average number of sessions per month and the number of time units consumed (each unit comprising 15 min) per month during the three periods. It was noted that the average number of sessions offered increased across the three periods and by 65.3% between the pre-pandemic and post-pandemic periods. The increase in the number of time units (90-minute new-patient and 45-minute follow-up appointments) was even more pronounced.
We also reviewed the utilisation of different contact modalities (Telephone, video, in-person) during the pandemic and post-pandemic periods. We were able to obtain the contact modality record for 1428 appointments out of 1601 for the pandemic period and 1387 out of 1668 for the post-pandemic period. We noted that 58.3% of all appointments during the pandemic were conducted via telephone, followed by video (22.2%) and in-person contact (19.5%). The high number of telephone appointments during this year can be explained by the fact that between March 15 and Jul 1, 2020, in-person contact had to be almost discontinued due to the severity of the pandemic (first wave peaking in May 2020) and until suitable video equipment and privileges were put in place.
Telephone consultations during the first three months mainly involved providing counseling to existing patients during follow-up appointments. Telephone interventions were complemented with the completion of worksheets (emailed soft copies) to make the virtual learning experience more productive. The post-pandemic period, however, saw a major decrease in the proportion of telephone appointments (22%) whereas video and in-person appointments increased to 39.7% and 38.3% respectively. A total of 868 appointments were held via video over the two years which formed 30.8% of all appointments offered during the two years.
Feedback from families
Previously, high patient satisfaction has been reported with telehealth across ages and conditions for paediatric patients [ 15 ]. We were interested to know whether the provision of virtual SLP services by HMC CAMHS to children and young people during the pandemic had impacted the quality of care and service standards. Parents were asked to rate their responses on a typical Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). Levels 2, 3, and 4 corresponded to “disagree”, “neutral”, and “agree” respectively.
A total of 32 families provided their feedback. 84.4% agreed or strongly agreed when asked whether their expectations from the sessions were met and whether they believed progress was made toward the goals. Interestingly, more than two-thirds of parents found the virtual intervention as effective as an in-person session for their children. Three-quarters of the parents found a virtual consultation more helpful than canceling the appointment altogether, in situations where an in-person consultation could not be carried out (Table 3 ).
In the context of advancing epidemic preparedness for health systems, the impact of the COVID-19 pandemic on healthcare services, particularly for children and adolescents, has come to the forefront. This study sheds light on the dynamic response of speech-language pathology (SLP) services within a specialized outpatient child and adolescent mental health service (CAMHS) to the challenges posed by the pandemic. The surge in demand for SLP services, particularly for social communication challenges and autism spectrum disorder, highlights the significance of early intervention in maintaining the developmental trajectory of this population. It was anticipated at the beginning of the pandemic that disruption to SLP services for children could contribute to the persistence of speech and language problems among them. To meet this challenge, the need for SLP clinicians to actively provide telehealth interventions during the pandemic was therefore recommended [ 16 ].
A considerable amount of literature in recent times has highlighted the potential impact of the pandemic on the social and communication development of children, particularly those with vulnerabilities [ 17 , 18 ]. The social restrictions during the COVID-19 pandemic adversely impacted the learning disability population significantly [ 19 ] as it caused disruption to their access to healthcare services, including SLP interventions. A study in the United Kingdom concluded that many parents observed a worsening of social-communication skills among their children with autism spectrum disorder during COVID-19 [ 20 ]. This conclusion is consistent with the notable finding of our study of the number of referrals for children and adolescents with social communication challenges increasing consistently over the 3 years. Furthermore, the number of these specific referrals increased more than 3-fold when the pre and post-pandemic periods were compared. The number of referrals for children with autism spectrum disorder, a condition characterized by social communication deficits and often associated with speech delay, also increased by 60%. The findings of this study highlight the significant impact of the COVID-19 pandemic on Speech-language pathology (SLP) services in a specialized outpatient child and adolescent mental health service (CAMHS). The surge in demand for SLP services for children and adolescents suggests the profound effect of the pandemic on the mental health, speech, and social communication of this special population.
The significant increase in the adoption of virtual modes of contact for speech and language intervention during the pandemic served the purpose of a “window of opportunity” for both healthcare services and families to consider remotely delivered interventions in the longer term. This was demonstrated by the two-fold increase in the utilisation of video contact in HMC CAMHS even after the end of the worst period of the pandemic. The successful adoption of telehealth technology for delivering SLP services emerged as a significant outcome of this study. Telehealth SLP interventions proved to be an effective alternative to in-person sessions during the pandemic. Many families reported satisfaction with the service, as it offered convenience and accessibility and yet remained reasonably effective. Telehealth SLP services may therefore have the potential to be integrated into clinical practice even beyond the pandemic as demonstrated in this study. Incorporating telehealth SLP services into CAMHS can improve mental health provision and address the surge in demand for SLP services. The barriers that may still exist (no access to suitable equipment or broadband and lack of training) globally preventing judicious and effective utilisation of tele/video consultations in SLP services [ 14 , 21 ] will need addressing as a matter of priority to embrace this much-needed intervention effectively.

Lessons gained and future directions
The lessons gained from this paper provide valuable insights into the opportunities and challenges presented by the COVID-19 pandemic in the context of speech-language pathology (SLP) services for children and adolescents with neurodevelopmental and mental disorders. This paper highlights the significant impact of the pandemic on the demand for SLP services, particularly among individuals with social communication challenges and autism spectrum disorder. The adoption of telehealth modalities, including phone and video consultations, proved to be an effective and accessible alternative during the pandemic. Feedback from families indicated a positive response to telehealth interventions, with many parents finding them effective and helpful. Importantly, the study underscores the potential of integrating telehealth SLP services into clinical practice beyond the pandemic to meet the increasing demand for mental health interventions among children and adolescents. The findings emphasize the need for long-term evaluation of telehealth services and for addressing potential barriers to access, such as availability of suitable equipment and broadband. The paper’s insights have implications for the future of healthcare delivery, suggesting the importance of sustaining telehealth options, training healthcare professionals in virtual care delivery, and engaging policymakers to ensure equitable access to these services. By highlighting these lessons, the paper contributes to advancing epidemic preparedness for health systems by showcasing innovative practices that can enhance the resilience of healthcare services in the face of challenges like pandemics.
This study provides a timely contribution to the discourse on advancing epidemic preparedness for health systems. The findings of this study suggest several future directions that can be considered to optimize care for children and adolescents receiving SLP interventions. There is a need for long-term evaluation in the form of conducting longitudinal studies to explore the lasting impact of telehealth SLP services on treatment outcomes and service satisfaction. Studies allowing comparison of the effectiveness of telehealth interventions with conventional in-person therapy may identify new horizons for children and adolescents with different neurodevelopmental and behavioral disorders.
There is a need for investigating potential barriers in accessing telehealth SLP services, particularly among low-income families and those living in remote areas with no access to Internet. The training of SLP clinicians in delivering telehealth interventions is crucial and needs to be expanded across services. Furthermore, the engagement of policymakers to ensure sustainable funding for training and securing telehealth equipment will help support the long-term integration of telehealth SLP services into mainstream healthcare systems. The aforementioned suggestions can help CAMHS in responding effectively to the increased global demand of SLP service and continue to provide high-quality care to its patient population as we emerge from the pandemic.
The pandemic has impacted considerably on the social communication of children who have underlying neurodevelopmental or mental disorders. Telehealth services can be helpful in supporting children with speech and language and social communication challenges in outpatient CAMHS settings. The demand for CAMHS services including the need for SLP interventions has escalated even further since the onset of the pandemic. The successful implementation of telehealth interventions underscores the potential for innovation in service delivery, identifying digital healthcare as a key tool for future epidemic preparedness.
Data availability
No further data is available other than what is being published.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602.
Article PubMed Google Scholar
Costello EJ, Mustillo S, Keeler G, Angold A. Prevalence of Psychiatric disorders in Childhood and Adolescence. In: Levin BL, Petrila J, Hennessy KD, editors. Mental health services: a public health perspective. Oxford University Press; 2004. pp. 111–28.
Huang HC, Ougrin D. Impact of the COVID-19 pandemic on child and adolescent mental health services. BJPsych Open. 2021;7(5):e145.
Werling AM, Walitza S, Eliez S, Drechsler R. The impact of the COVID-19 pandemic on mental health care of children and adolescents in Switzerland: results of a survey among mental health care professionals after one year of COVID-19. Int J Environ Res Public Health. 2022;19(6):3252.
Article CAS PubMed PubMed Central Google Scholar
Rafferty G, Legris Z, Parker S, Doody B. Referrals and admissions from pediatric and medical hospitals to a child and adolescent inpatient mental health service: a longitudinal analysis over the period of the COVID-19 pandemic.
Ayraler Taner H, Akın Sarı B, Kaba D. How did the COVID-19 pandemic affect child and adolescent psychiatry outpatient clinic admissions? A single-center, retrospective study. Clin Child Psychol Psychiatry. 2022;(3):824–35.
McNicholas F, Kelleher I, Hedderman E, Lynch F, Healy E, Thornton T, Barry E, Kelly L, McDonald J, Holmes K, Kavanagh G. Referral patterns for specialist child and adolescent mental health services in the Republic of Ireland during the COVID-19 pandemic compared with 2019 and 2018. BJPsych Open. 2021;7(3):e91.
Kawaoka N, Ohashi K, Fukuhara S, Miyachi T, Asai T, Imaeda M, Saitoh S. Impact of school closures due to COVID-19 on children with neurodevelopmental disorders in Japan. J Autism Dev Disord. 2022;52(5):2149–55.
Guller B, Yaylaci F, Eyuboglu D. Those in the shadow of the pandemic: impacts of the COVID-19 outbreak on the mental health of children with neurodevelopmental disorders and their parents. Int J Dev Disabil. 2022;68(6):943–55.
Bentenuto A, Mazzoni N, Giannotti M, Venuti P, de Falco S. Psychological impact of Covid-19 pandemic in Italian families of children with neurodevelopmental disorders. Res Dev Disabil. 2021;109:103840.
Charney SA, Camarata SM, Chern A. Potential impact of the COVID-19 pandemic on communication and language skills in children. Otolaryngol Head Neck Surg. 2021;165(1):1–2.
Khan YS, Al-Shamlawi M, Phiri L, Alabdulla M. Triage of referrals in a child and adolescent mental health service in Qatar: reducing waiting times and promoting needs-based prioritization. BJPsych Int. 2021;18(3):67–70.
Article PubMed PubMed Central Google Scholar
Law J, Dornstauder M, Charlton J, Gréaux M. Tele-practice for children and young people with communication disabilities: employing the COM‐B model to review the intervention literature and inform guidance for practitioners. Int J Lang Commun Disord. 2021;56(2):415–34.
Fong R, Tsai CF, Yiu OY. The implementation of telepractice in speech language pathology in Hong Kong during the COVID-19 pandemic. Telemed e-Health. 2021;27(1):30–8.
Article Google Scholar
Tenforde AS, Borgstrom H, Polich G, Steere H, Davis IS, Cotton K, O’Donnell M, Silver JK. Outpatient physical, occupational, and speech therapy synchronous telemedicine: a survey study of patient satisfaction with virtual visits during the COVID-19 pandemic. Am J Phys Med Rehabil. 2020.
Tohidast SA, Mansuri B, Bagheri R, Azimi H. Provision of speech-language pathology services for the treatment of speech and language disorders in children during the COVID-19 pandemic: problems, concerns, and solutions. Int J Pediatr Otorhinolaryngol. 2020;138:110262.
Rocha PM. The Covid-19 pandemic and its possible consequences to language/speech development and delay in children: an urgent issue. Audiology-Commun Res. 2021;26.
Patel K. Mental health implications of COVID-19 on children with disabilities. Asian J Psychiatry. 2020;54:102273.
Hughes N, Anderson G. The experience of the COVID-19 pandemic in a UK learning disability service: lost in a sea of ever changing variables–a perspective. Int J Dev Disabil. 2022;68(3):374–7.
Morris PO, Hope E, Foulsham T, Mills JP. Parent-reported social-communication changes in children diagnosed with autism spectrum disorder during the COVID-19 pandemic in the UK. Int J Dev Disabil. 2023;69(2):211–25.
Monaghesh E, Hajizadeh A. The role of telehealth during COVID-19 outbreak: a systematic review based on current evidence. BMC Public Health. 2020;20:1–9.
Download references
Acknowledgements
We would like to thank Dr. Majid Alabdulla (Chairman, MHS), Mr. Iain Tulley (Chief Executive Officer, MHS), Dr. Raed Amro (Assistant Executive Director, MHS), and Dr. May Jasim Almeraisi (Clinical Director, CAMHS) for their support with the arrangement of necessary equipment and training during the pandemic. Their role was instrumental in the continuity of speech and language pathology services during the pandemic. We would also like to acknowledge the ongoing support of Ms. Eman Al-Mulla (Chief of Speech-language pathology department at HMC) and Mr. Ibrahim Alayaseh (Speech-language pathologists supervisor, HMC) to the CAMHS speech-language pathology service in CAMHS. Open access for this article was funded by Qatar National Library.
Not applicable.
Author information
Authors and affiliations.
Child and Adolescent Mental Health Service, Hamad Medical Corporation, Doha, Qatar
Abdullah Amro, Hanan Abdallah Kotkot, Yahia Albobali & Yasser Saeed Khan
Medical Research Centre, Hamad Medical Corporation, Doha, Qatar
Prem Chandra
College of Medicine, Qatar University, Doha, Qatar
Yasser Saeed Khan
You can also search for this author in PubMed Google Scholar
Contributions
YSK wrote the initial manuscript. AA, HAK, and YA reviewed the data, prepared the tables, and suggested useful edits to the initial draft. PC supported with statistical analysis and prepared the figures. All authors reviewed and approved the final draft of the manuscript.
Corresponding author
Correspondence to Yasser Saeed Khan .
Ethics declarations
Ethics approval and consent to participate.
This service evaluation initiative involved a retrospective analysis of existing data and did not involve any experiments on humans. No new patients were recruited and therefore consent to participate was not required. The data used was fully anonymized and not linked to any patient-identifiable information to ensure data protection and confidentiality. The need for informed consent and ethical approval by the institutional review board (medical research centre) was deemed unnecessary and waived by Abhath, the online submission support service for researchers at Hamad Medical Corporation, and mental health service departmental approval was advised. The necessary ethical approval and informed consent waiver were obtained from the leadership of the mental health services department. The study was performed in accordance with the relevant guidelines and regulations as outlined in the Declaration of Helsinki.
Consent for publication
Competing interests.
No potential conflict of interest was reported by the authors
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Amro, A., Kotkot, H.A., Albobali, Y. et al. Epidemic preparedness and innovations in digital healthcare: enhancing post-pandemic speech-language pathology services for child and adolescent mental health in Qatar. BMC Health Serv Res 24 , 673 (2024). https://doi.org/10.1186/s12913-024-10989-y
Download citation
Received : 08 September 2023
Accepted : 14 April 2024
Published : 28 May 2024
DOI : https://doi.org/10.1186/s12913-024-10989-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
- Speech-Language pathology
- Digital health
- Adolescents
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
Academia.edu no longer supports Internet Explorer.
To browse Academia.edu and the wider internet faster and more securely, please take a few seconds to upgrade your browser .
- We're Hiring!
- Help Center
Health Care System
- Most Cited Papers
- Most Downloaded Papers
- Newest Papers
- Save to Library
- Last »
- Quality of services Follow Following
- International Management Follow Following
- International HRM Follow Following
- Business Follow Following
- Health Care Follow Following
- Public health systems and services research Follow Following
- Mathematical Sciences Follow Following
- Optometry and Ophthalmology Follow Following
- History of Public Health Follow Following
- Caesarean Section Follow Following
Enter the email address you signed up with and we'll email you a reset link.
- Academia.edu Publishing
- We're Hiring!
- Help Center
- Find new research papers in:
- Health Sciences
- Earth Sciences
- Cognitive Science
- Mathematics
- Computer Science
- Academia ©2024
- Open access
- Published: 27 May 2024
Decentralization of the health system – experiences from Pakistan, Portugal and Brazil
- Shafaq Mahmood ORCID: orcid.org/0000-0002-8139-7040 1 ,
- Rita Sequeira 2 ,
- Muhammad Muneeb Ullah Siddiqui 1 ,
- Marcos Batista Araujo Herkenhoff 3 ,
- Patrícia Pita Ferreira 2 , 4 ,
- Adalberto Campos Fernandes 2 &
- Paulo Sousa 2
Health Research Policy and Systems volume 22 , Article number: 61 ( 2024 ) Cite this article
81 Accesses
2 Altmetric
Metrics details
Decentralization of a health system is a complex and multidimensional phenomenon that demands thorough investigation of its process logistics, predisposing factors and implementation mechanisms, within the broader socio-political environment of each nation. Despite its wide adoption across both high-income countries (HICs) and low-and-middle-income countries (LMICs), empirical evidence of whether decentralization actually translates into improved health system performance remains inconclusive and controversial. This paper aims to provide a comprehensive description of the decentralization processes in three countries at different stages of their decentralization strategies – Pakistan, Brazil and Portugal.
This study employed a systematic analysis of peer-reviewed academic journals, official government reports, policy documents and publications from international organizations related to health system decentralization. A comprehensive search was conducted using reputable databases such as PubMed, Google Scholar, the WHO repository and other relevant databases, covering the period up to the knowledge cutoff date in June 2023. Information was systematically extracted and organized into the determinants, process mechanics and challenges encountered during the planning, implementation and post-decentralization phases. Although decentralization reforms have achieved some success, challenges persist in their implementation. Comparing all three countries, it was evident that all three have prioritized health in their decentralization reforms and aimed to enhance local decision-making power. Brazil has made significant progress in implementing decentralization reforms, while Portugal and Pakistan are still in the process. Pakistan has faced significant implementation challenges, including capacity-building, resource allocation, resistance to change and inequity in access to care. Brazil and Portugal have also faced challenges, but to a lesser extent. The extent, progress and challenges in the decentralization processes vary among the three countries, each requiring ongoing evaluation and improvement to achieve the desired outcomes.
Notable differences exist in the extent of decentralization, the challenges faced during implementation and inequality in access to care between the three countries. It is important for Portugal, Brazil and Pakistan to address these through reinforcing implementation strategies, tackling inequalities in access to care and enhancing monitoring and evaluation mechanism. Additionally, fostering knowledge sharing among these different countries will be instrumental in facilitating mutual learning.
Peer Review reports
Accelerating economic growth and social advancement in a country through the promotion of good governance is widely recognized as a crucial pillar of sustainable development [ 1 ]. To achieve the Sustainable Development Goals (SDGs), nations worldwide, regardless of their development status, have undertaken numerous reforms in their health systems [ 2 ]. One such reform is decentralization, which has been widely implemented across both high-income countries (HICs) and low-and-middle-income countries (LMICs) in an attempt to improve the health system performance [ 3 ]. This decentralization movement began in the latter half of the 20th century, and received strong support from the international development and donor agencies, leading to its adoption in more than 80% of countries worldwide, albeit in various degrees and forms [ 3 , 4 ]. However, despite its wide adoption, empirical evidence of whether decentralization actually translates into improved health system performance remains inconclusive and controversial [ 5 ].
The term “decentralization” often means transfer of responsibilities, planning, management, decision-making authority and resources from the national to sub-national government entities (for example, regional, state and district/municipal levels) with the aim of tailoring the health system to meet local needs more effectively and responsively [ 6 ]. It is usually argued that a decentralized governance of health services bridges the gap between communities and decision-makers; improves equity, accessibility and accountability of local service providers; and fosters innovation and technical efficiency in healthcare provision [ 7 , 8 ]. However, preliminary data from various countries worldwide has yielded mixed results. A recent systematic review studying the effects of decentralization in LMICs reported that decentralization of governance, financing and service delivery had positive effects on the performance of health system. Nevertheless, in the absence of adequate training and accountability mechanisms, decentralized resource management posed significant challenges and adversely affected health system performance indicators [ 9 ]. Similarly, evidence from Uganda and Indonesia suggested that, in the absence of transparent accountability mechanisms, transferring discretionary powers for resource allocation to local governments produced harmful effects on health sector [ 10 , 11 ].
In contrast, some countries, including Argentina, China, India, Spain and Canada, have reported beneficial impacts of fiscal decentralization on population health, such as improved mortality rates, reduced regional disparities and higher life expectancy [ 12 , 13 , 14 , 15 , 16 ]. Some differences in the effects of decentralization also seem to be influenced by the income group of the country. For instance, a study examining the relationship between political decentralization and immunization coverage in 140 LMICs found that, for the low-income group, decentralized nations had higher coverage rates than centralized ones, whereas the opposite was true for the middle-income group [ 17 ]. As a result, significant disagreements and gaps persist in the assessments of decentralization conducted across different regions of the world.
It is crucial to underscore that decentralization is a complex and multidimensional phenomenon that demands thorough investigation and a deep understanding of the specific conditions within each country. These mixed findings across the literature suggest that the design and implementation of decentralization processes vary significantly and are contingent upon various contextual and socio-political factors [ 18 ]. For example, the decentralization process in Colombia unfolded gradually in phases over nearly 3 decades, whereas in other countries, such as Indonesia and Pakistan, the change happened overnight as a result of a sudden policy revolution [ 19 , 20 , 21 ]. Therefore, to make cross-country comparisons of decentralization’s impact on health system outcomes, it is first essential to describe and understand the process logistics, predisposing factors and implementation mechanisms in detail within the broader socio-political environment of each nation.
This research selects Brazil, Pakistan and Portugal as case studies for analysing decentralization processes within health systems. These countries have been chosen due to their varying levels of maturity and the diverse, insightful experiences each offers. Brazil’s extensive implementation of the unified health system Sistema Único de Saúde (SUS) since 1988 provides valuable insights into the long-term effects and challenges of decentralizing healthcare services, making it a pertinent case for comparative analysis. Pakistan’s inclusion is motivated by its notable decentralization efforts aimed at enhancing healthcare access, particularly in rural and underserved areas, which offers valuable lessons on decentralization dynamics in resource-constrained settings. Additionally, Portugal’s experience with decentralization reforms, including the establishment of regional health administrations, offers a contrasting perspective within the context of European healthcare systems, enabling nuanced comparisons and insights into the adaptability of decentralization strategies across diverse political and institutional frameworks. Through examining the decentralization experiences of these countries, each with distinct socio-economic backgrounds, this study aims to gain comprehensive insights into the determinants, process mechanics and challenges encountered during the planning, implementation and post-decentralization phases of this critical health sector reform. To the best of our knowledge, this would be the first narrative to compare and contrast the decentralization process and performance between LMICs and HICs. As a result, this study is expected to make a significant and valuable contribution to the expanding body of literature in this field.
Methodology
Research design.
This study employs a literature and document review approach to comprehensively investigate the decentralization processes within the health sectors of Pakistan, Brazil and Portugal. The choice of this study design was deliberate, aiming to systematically analyse a wide range of academic/scientific papers, national and international reports, policy documents and relevant literature pertaining to decentralization within the chosen countries. By synthesizing existing knowledge and insights from various sources, this approach allows for a thorough examination of the determinants, mechanics and challenges associated with decentralization in the health sector. Through this comprehensive analysis, we aim to contribute valuable insights to the existing literature on health system governance and policy-making.
Data collection
The primary data sources for this study included peer-reviewed academic journals, official government reports, policy documents and publications from international organizations related to health system decentralization. A comprehensive search was conducted using reputable databases such as PubMed, Google Scholar, the WHO repository and other relevant databases, covering the period up to the knowledge cutoff date in June 2023.
The initial search was carried out using relevant keywords and Medical Subject Headings (MeSH) terms in combination with Boolean operators. The MeSH terms were utilized to enhance the precision and specificity of the search.
The primary keywords and MeSH terms used for the search included “decentralization”, “health sector reform”, “health system”, “governance”, “policy implementation”, “Pakistan”, “Brazil” and “Portugal”. Synonyms and related terms were also considered to capture a wider range of relevant literature.
Inclusion and exclusion criteria
The inclusion criteria for selecting relevant literature was based on papers and documents that specifically focused on the decentralization process in the health sector within Pakistan, Brazil and Portugal. The documents covered the planning, implementation and post-decentralization phases of the reform. Additionally, papers providing insights into the socio-political context and challenges encountered during decentralization were also considered.
In our review, a subset of strategic or explanatory documents were presented in their original language, necessitating their inclusion in the analysis. While the majority of documents were in English, a limited number were in Portuguese. To ensure comprehensive understanding, these Portuguese documents were diligently translated by native speakers proficient in both languages.
The exclusion criteria was mainly the literature not directly related to the health sector decentralization in the specified countries, and those published after the knowledge cutoff date were also excluded from the review.
Data extraction
Information from the selected literature was systematically extracted and organized, including details on the decentralization timeline, implementation strategies, mechanism for resource allocation, accountability mechanisms, challenges and any reported health system performance indicators. Key findings and insights related to the decentralization experience of each country were documented.
Data analysis
A thematic analysis approach was employed to categorize and synthesize the extracted data. Key themes and patterns related to the determinants, mechanics and challenges of decentralization were identified. Additionally, the performance outcomes reported in the literature were compared and contrasted between the developed and developing countries to draw relevant conclusions (Table 1 ).
Pakistan – country profile
Pakistan, situated in the South Asian region and bordered by India, China, Afghanistan, Iran and the Arabian Sea, stands as the fifth most populous country globally, with a current population of 232 million, projected to increase to 281 million by 2030 [ 22 ]. Encompassing an area of 881 913 km 2 , Pakistan ranks as the 33rd-largest country and maintains a population density of 302.08 people/km 2 . The country is divided into four provinces: Punjab, Sindh, Khyber Pakhtunkhwa (KPK) and Baluchistan. In addition, there are three federating units: Azad Jammu and Kashmir (AJK), Gilgit Baltistan (GB) and Islamabad Capital Territory (ICT) [ 23 ]. Currently, Pakistan has a gross domestic product (GDP) of 376.53 billion US$, gross national income (GNI) per capita of 1580 US$, and a GDP growth rate (annual %) of 6.2. As per the World Bank’s country classification, Pakistan is classified as a lower-middle-income economy [ 24 ]. The government current expenditure on health accounts for 1.2% of the total GDP.
Pre-decentralization scenario
Pakistan’s health system is characterized by a mixed structure, comprising various vertical and horizontal institutions, including the public sector, private sector, parastatal organizations, philanthropists and donor agencies. Health services are organized into a three-tiered delivery system, encompassing primary, secondary and tertiary levels of care. Prior to the decentralization, the constitution contained two legislative lists: the federal legislative list (FLL) and the concurrent legislative list (CLL), which determined the division of legislative authorities between the federal and provincial governments. Under this setup, the central government had exclusive power to formulate laws with respect to any matter listed in the FLL while both the central and provincial governments had the authority to make laws related to matters in the CLL. Matters not specified in either list fell under the jurisdiction of the provincial assemblies. Consequently, a majority of health functions fell within the jurisdiction of the federal ministry of health (MoH). The MoH assumed several stewardship responsibilities such as planning and policy formulation, service delivery programming, health financing, coordination with international agencies, human resource management and drug regulation and implementation of the 11 vertical health programs, as well as monitoring and evaluation of health services. Although the provincial governments played a co-financing role in most of these important health functions, their involvement was primarily administrative and passive in nature [ 25 ].
The decentralization reform
Decentralization is often classified into three forms:
Deconcentration (equivalent to opening a branch office in another region);
Delegation (transferring certain responsibilities to a sub-national government);
Devolution (a complete take-over of functions and authority from the central government by a lower tier) [ 26 ].
In Pakistan, the decentralization reform was preceded by a change in resource allocation formula for the federal and provincial authorities in 2009. This led to the adaptation of an equity-based distribution of resources, with a larger share (56–58%) going to the provinces based on their developmental requirements and local challenges [ 27 , 28 ]. Subsequently, the unanimous passing of the 18th constitutional amendment by all political parties in 2010–2011 marked a radical, politically driven decentralization process, implemented in its strongest form – devolution [ 29 , 30 ]. As a result, 17 federal ministries, including health to the provinces, were dissolved, transferring functional, jurisdictional and fiscal responsibilities to the four sub-national governments [ 31 ]. The amendment also led to the abolition of the CLL, granting provinces greater autonomy in exercising full administrative and financial control over their health systems [ 30 , 32 ].
However, the devolution process was abrupt and inadequately planned. Provinces lacked prior experience in independently assuming stewardship functions (such as budgeting and policy formulation), leading to a chaotic situation [ 21 ]. Moreover, with the abolition of the CLL, many of the functions previously being managed by the MoH were dispersed across various federal institutions, including the Economic Affairs Division, Ministry of Inter Provincial Coordination, Federal Bureau of Statistics and Capital Administration and Development [ 21 ]. Due to the demolition of a central governing body, several difficulties were raised in managing national and international coordination for global health commitments, licensing of medical and paramedical practitioners and health regulation, particularly drug regulation and licensing. As a result, a recentralization process was initiated within 2 years to consolidate the dispersed central functions under a single federal entity. In 2013, the new federal ministry named Ministry of National Health Services Regulation and Coordination (MoNHSR&C) was quickly reconstituted the basis of recommendations of a multi-donor WHO mission [ 30 ]. The federal government assumed responsibilities for managing international trade and agreements, drug pricing and licensing, human resource regulation, surveillance of ports and borders and co-financing important vertical health programs [ 33 ].
Post-decentralization – progress and challenges
After the devolution, the provinces in Pakistan took several planning and governance initiatives to fulfil their new stewardship role in the health sector. For the first time, each province formulated its own context-specific health policy and action plan, outlining a strategic direction for the sector for the next 10 years. This also opened doors for the international donor agencies to engage directly with the provinces in alignment with their provincial priorities. Moreover, two provinces, Sindh and KPK, undertook district-level planning to implement essential service delivery reforms [ 21 ].
However, despite these efforts, the implementation of the newly formed health sector strategies remained limited and ineffective due to weak institutional capacities and insufficient budgets [ 21 ]. A comprehensive review by Zaidi et al. in 2018 revealed a significant increase in healthcare budgetary spending across all provinces, with a greater portion of the increased health spending being allocated to salaries and administrative costs [ 21 ]. Delayed release of budgetary transfers from the federal government also hindered the effective functioning of vertical health programs at the provincial level [ 21 , 34 ]. Nonetheless, provinces managed these challenges by generating their own resources or seeking additional support from external donor agencies.
Provinces also made substantial progress in improving the governance and delivery of the primary healthcare through multiple reforms and innovations. Initiatives included implementing public–private partnership (PPP) models at the district level, contracting out of primary healthcare services to private providers and integrating overlapping vertical health programs [ 21 , 35 , 36 ]. Despite these positive steps, the influence of local bureaucracies and the political influence of provincial elites posed some serious challenges in maintaining merit and transparency across all levels of provincial health management.
Despite the shortcomings in planning and execution, the devolution in Pakistan did result in increased ownership of healthcare by provincial stakeholders and bureaucrats. Moreover, the devolution fostered a sense of healthy competition among all four provincial governments, driving them to deliver better healthcare and to gain increased political support from their communities. Hence, this transition to a decentralized health system, though abrupt, laid the groundwork for several legislative and innovative reforms at the provincial health level.
While no formal evaluation to measure the impact of the decentralization reform in Pakistan has been conducted thus far, the country’s health indicators have shown considerable improvement over time, potentially attributable to the health sectors reforms and initiatives undertaken by local governments following devolution. For instance, the infant mortality rate in Pakistan decreased from 74 per 1000 live births in 2012 to 62 per 1000 live births in 2018. Likewise, the under-5-year-old mortality rate also exhibited a reduction from 89 per 1000 live births in 2012 to 74 per 1000 live births in 2018 [ 37 ]. However, it is strongly recommended that a systematic evaluation of the health system indicators be conducted in future to ascertain the actual impact of decentralization on the health sector performance and efficiency in Pakistan. Such an evaluation would provide valuable insights into the successes and challenges of the decentralization process and help inform further improvements in the country’s healthcare system.
Portugal – country profile
Portugal is a coastal country located in the Southern European region. The mainland, located in the southwest of the Iberian Peninsula, shares its borders with Spain to the north and east, while being bordered by the Atlantic Ocean to the west and south. In addition to the mainland, Portugal includes two autonomous regions located in the Atlantic Ocean: the archipelagos of Azores and Madeira. In terms of territory, Portugal covers a total area of 92 212 km 2 and has a population of approximately 10 million habitants resulting in a population density of 112.6 habitants/km 2 . The country is administratively divided into seven regions: North, Centre, Lisbon Metropolitan Area, Alentejo, Algarve, Azores and Madeira [ 38 , 39 ].
In 2021, Portugal’s GDP stood at 249.89 billion US$, with an annual growth rate of 4.9%. The gross national income (GNI) per capita based on purchasing power parity was of 35 470$, experiencing an annual growth rate of 4.5% [ 40 ]. Regarding healthcare, the government’s current expenditure on health in 2022 amounted to 10.6% of the total GDP [ 41 ].
Since 1976, Portugal has been undergoing an ongoing decentralization process as an integral part of the constitution of the Portuguese Republic. The Portuguese health system was established in 1979, evolving from the integration and complementarity of various response levels, including primary, hospital, continuing and palliative care. This health system is characterized by the coexistence of three distinct systems: the national health system (NHS), public and private insurance schemes for certain professions (health subsystems) and private voluntary health insurance. The healthcare delivery system in Portugal comprises a network of public, social and private healthcare providers. The Ministry of Health holds the responsibility for developing health policies, with its principal function centred on the planning, regulation and management of the NHS [ 42 , 43 ]. Through this decentralized approach, Portugal has established a healthcare system that integrates multiple sectors and strives to provide comprehensive care to its population.
The principles for the organization and functioning of the health system in Portugal were introduced by the 1990 Basic Law on Health. According to this law, the NHS would be supervised by the Minister of Health and administered at the region health level by the respective regional health administrations (RHAs). A significant milestone in the Portuguese health system occurred in 1993 when administrative regionalization was established, leading to the creation of five RHAs: North, Centre, Lisbon and Tagus Valley, Alentejo and Algarve [ 44 ].
The RHAs played crucial roles in the healthcare system, including:
Developing activity and budget plans for the NHS in their respective regions;
Representing the NHS at the regional level;
Guiding, coordinating and monitoring the regional areas of the NHS;
Regulating demand among healthcare establishments and services in the region and overseeing their operations;
Contracting with private healthcare providers to offer healthcare services to NHS beneficiaries;
Coordinating patient/beneficiaries’ transport to ensure accessibility to healthcare services.
Through the establishment of RHAs, Portugal aimed to enhance regional coordination and management of healthcare services, bringing healthcare decision-making closer to the local level and promoting more efficient and effective healthcare delivery across different regions.
In 1999, a new law was introduced in Portugal that assigned new health functions to municipalities. These functions included the management, construction and maintenance of primary healthcare centres. The aim was to decentralize certain responsibilities to the local level and empower municipalities to play a more active role in the provision of primary healthcare services. However, despite the enactment of this legislation, it was not fully implemented in the subsequent years. As a result, the intended decentralization and involvement of municipalities in managing primary healthcare centres did not materialize to its full extent, and the status quo in health service management may have remained largely unchanged at the time.
The implementation of various laws and reforms in Portugal led to significant changes in the decentralization process of the health system. As a result, each regional health administration (RHA) gained local influence and assumed a central role at the regional level. The management of hospitals, primary healthcare centres and other health institutions came under the authority of the RHAs, enabling them to make agreements with the private sector and develop health plans on the basis of the specific needs of the population in their regions [ 43 ].
While hospitals remained public property, a different management model was introduced through PPP contracts. These contracts ensured the construction and maintenance of hospital infrastructures, as well as the provision of healthcare services. This approach aimed to improve the efficiency and quality of healthcare delivery by involving private sector expertise while still upholding the public ownership of healthcare facilities [ 42 ]. Furthermore, with the decentralization process, managers of health institutions were locally recruited, giving considerable power and autonomy to the new regional boards. This local management approach allowed for a more tailored and responsive decision-making process, as managers were well-acquainted with the specific health needs and challenges of their respective regions [ 43 ].
In 2019, a significant development occurred in Portugal’s health system with the approval of a new Basic Law on Health (Lei no. 95/2019 de 4 de setembro). This law marked a shift in the organization of the NHS towards regionalization and decentralized, participative management [ 45 ]. Furthermore, in 2019, the framework for the transfer of competencies to municipal bodies and intermunicipal organizations in the health domain was completed. This transfer of competencies aimed to further strengthen the role of local municipalities in the provision and management of healthcare services. By empowering municipal bodies and intermunicipal organizations, the health system aimed to foster more responsive and locally tailored healthcare solutions. Under this framework, municipal authorities in Portugal were granted several competencies that further reinforced their role in the health domain. Municipalities were empowered to take proactive measures to promote health and well-being within their communities, implementing programs and campaigns to raise awareness about healthy lifestyles and disease prevention. Additionally, they were tasked with fostering initiatives to support active ageing and improve the quality of life for elderly citizens. Another crucial aspect of the competencies granted to municipalities was the responsibility for maintaining healthcare buildings and facilities, ensuring that the infrastructure remained in optimal conditions to deliver quality healthcare services to the public. Furthermore, the law emphasized the importance of involving municipalities in shaping local health policies, allowing them to contribute valuable insights based on their unique understanding of the health needs and priorities of their respective populations. By entrusting municipalities with these competencies, the health system sought to foster a more community-centred approach to healthcare, promoting inclusivity and empowering local authorities to play an active role in the well-being of their citizens.
In addition to the Basic Law on Health, other legislative resolutions have been implemented in Portugal to further advance the health decentralization process. The 21st Government Program played a significant role in this regard by emphasizing the importance of democratic decentralization of public administration as an essential state reform, aligning with the principles enshrined in the Portuguese constitution (no. 1 of the 6th article).
In theory, decentralization has been incorporated into the constitutional and legal frameworks of the NHS in Portugal over the past decades. Proposals for devolution and delegation of authority from the central government to regional units have been put forward. However, in practice, the responsibility for planning and resource allocation in the Portuguese health system has remained highly centralized. The administrative devolution has not fully materialized, leading to a gradual decentralization process that primarily focuses on bringing healthcare services closer to citizens and addressing their specific needs. This process has been predominantly centred around primary healthcare.
While RHAs have been granted some autonomy, particularly in budget setting and spending, their jurisdiction has largely been limited to primary care. Most public hospitals still fall under the central administration, and their financial resources primarily come from the state budget. Decisions regarding staff allocation, technical guidance and organizational rules for these hospitals are also predominantly made at the central level [ 46 ].
As a result, the decentralization process in the Portuguese health system has been slow and constrained, with limited impact on the management and decision-making processes at higher levels of healthcare services. The focus has primarily been on strengthening primary healthcare services and improving accessibility and quality of care at the local level. However, achieving a more comprehensive and fully decentralized health system remains a challenge due to the prevailing centralization of resources and decision-making authority in the hospital sector.
It is anticipated that, by the end of 2023, the RHAs will be eliminated, marking a significant step towards complete devolution of authority from the central government to local health units (LHUs). These LHUs are envisioned to encompass a comprehensive range of health services, including primary care, hospital care, palliative and continuing care and public health initiatives. With the elimination of RHAs, LHUs are expected to assume greater autonomy in managing the majority of health competences. This shift will foster a close and collaborative partnership between LHUs and municipal bodies, allowing for more localized decision-making and tailored health policies that reflect the specific needs and priorities of different communities. This complete devolution of authority to LHUs is anticipated to lead to a more decentralized and citizen-centred health system in Portugal, with a focus on delivering responsive, efficient and equitable healthcare services across the nation.
The process of decentralization of health in Portugal is a dynamic and ongoing endeavour. As the country continues to implement changes in its health system organization and management, there is a pressing need for further research and evaluation. To assess various dimensions such as effectiveness, efficiency, access, patient-centredness safety and equity, this is crucial to understanding its impact on the health system’s overall performance.
Brazil – country profile
Brazil is a vast federative republic situated in South America, covering an area of 8.5 million km 2 , making it the fifth-largest country globally. With a population estimated at 203 million in 2022, and an annual growth rate of 0.52%, Brazil ranks as the seventh most populous nation in the world, with population density of 23.86 people/km 2 . The political structure of Brazil is organized into three levels of government: the federal government, 26 states/provinces and one federal district, and 5563 municipalities. Currently, Brazil’s GDP is about 1.92 trillion US$, GNI per capita is 8917.7 US$, and GDP growth rate is +2.9% annually [according to the Brazilian Institute of Geography and Statistics (IBGE)]. The country’s government consumption expenditure on health stands at around 3.8% of the GDP, while the total consumption expenditure on health amounts to 9.6% of the GDP, with a significant portion spent by households and non-profit institutions serving households. With respect to its economic status, Brazil is classified as an upper-middle-income economy by the World Bank.
The decentralization process of the health system in Brazil occurred during the establishment of the national public health system, called the Sistema Único de Saúde (SUS), in the early 1990s. Prior to the creation of SUS, the Brazilian health system comprised a mix of health services established at different periods, including public and private services, and philanthropic institutions. At that time, public health assistance in Brazil was the responsibility of the Social Security and Assistance Ministry (MPAS), primarily provided through the National Social Security Healthcare Institute (INAMPS), which was created in 1977 to centralize various public health services [ 47 ].
The Ministry of Health, in contrast, was primarily focused on epidemiological vigilance, sanitary control and collective health actions, and was relatively underfunded compared with the INAMPS. The assistance services provided by the INAMPS were accessible only to workers with formal employment and their dependents, who received care through public hospitals and ambulatory centres, as well as private services contracted by the state. Meanwhile rural workers, informal labourers and unemployed citizens relied on philanthropic institutions for their healthcare needs.
During the 1970s and the 1980s, Brazil witnessed significant progress in health coverage supported by funding from the federal government [ 48 ]. This funding was directed not only towards the private sector through contracting private services but also towards expanding public health initiatives and actions. Initiatives such as the Integrated Health Actions (AIS) and the Program of Interiorization of Health and Sanitation Actions (PIASS) were introduced, promoting regionalization and establishing a hierarchy between municipalities, states and the federal government [ 47 ]. The AIS and PIASS were integral to the maturation of the public health debate in Brazil, paving the way to the Sanitary Reform Movement. This movement played a crucial role in formulating both the theoretical and political basis for the establishment of the SUS in 1990. The creation of the SUS and the decentralization process in Brazil aimed to address the issue of centralized resources and power within the federal government. Furthermore, the new health system sought to transform the existing health model, which heavily emphasized hospitalization and disease treatment, into one that prioritized prevention and health promotion actions. Recognizing the importance of preventive measures in improving overall population health, the SUS aimed to shift the focus from solely providing curative care to actively promoting wellness and disease prevention. This change in approach was deemed essential for achieving better health outcomes and ensuring a more sustainable and efficient health system for the Brazilian population [ 49 ].
- Decentralization
The concept of decentralization, involving the sharing of management and decision-making power with the municipalities and states, was fundamental guiding principle stated inside the Health section of the Federal Constitution of 1988. This principle was further formalized and solidified with the approval of Law no. 8080/1990, which officially established the SUS in 1990. The process of decentralization and the establishment of the SUS occurred gradually during the early years of the 1990s, in line with the prevailing political and governmental priorities.
Indeed, Brazil’s decentralization process within the health sector can be considered a devolution process. In this context, subnational governments, including municipalities and states, not only assume responsibility for providing healthcare services but also gain control over the planning and decision-making aspects of health policies [ 50 ].
The SUS Organic Law (Law no. 8080) outlines a clear division of competencies among different levels of government in Brazil’s health system. According to this law, municipalities have the responsibility to manage and provide public health services to their local populations. In contrast, states and the federal government play a role in coordinating, evaluating and participating in the formulation of health policies. Their specific tasks include areas such as health vigilance, epidemiology, sanitation, health norms and financial cooperation [ 51 ].
An important feature of the decentralization process in Brazil’s health system was the establishment of tripartite and bipartite commissions. These commissions include representatives from the federal, state and municipal governments, and they serve as platforms for shared decision-making on health policies. This collaborative approach ensures that decisions are made collectively, taking into account the perspectives and needs of all levels of government. Additionally, health conferences and councils were introduced as mechanisms for social participation. These platforms allow citizens and civil society organizations to actively engage in the policy-making process, providing valuable input and feedback on health issues [ 52 ].
The process of decentralization in Brazil’s health system during the 1990s was characterized by different phases, influenced by changes in the norms that governed the transition to a decentralized management model. These norms, known as the Norms of Basic Operationalization (NOB), were introduced in 1991, 1993 and 1996, respectively. The NOBs established terms and guidelines for local governments to adhere to the management transition plan in various stages, based on their capacity and willingness to take on responsibilities, while adhering to the structural and organizational conditions specified by these norms [ 49 , 51 ].
A significant aspect of the NOBs was the requirement for every level of government to establish health councils, with representatives of users occupying at least half of the seats. This emphasis on social participation through health councils underscores the priority given to involving citizens and civil society in the formulation of health policies, as mandated by the regulatory laws of the SUS. By ensuring that health councils have a significant user representation, the goal was to foster greater transparency, inclusivity and responsiveness in decision-making processes related to health services. The effects of decentralization were felt as an important increase in the participation of municipalities during the 1980s and the 1990s in health actions. For example, the percentage of health facilities managed by the municipalities rose from 22% of the facilities in 1981 to 69% in 1992. In terms of employment, the municipalities, which were responsible for employing 16% of the public health workers in 1981, rose to 44% of the total amount of workers inside the public health system in 1992 [ 51 ].
Post-decentralization
Over its more than 30-year trajectory, the Brazilian SUS has undergone significant changes and adaptations, particularly in terms of funding and organization. The decentralization guidelines, established by regulatory norms such as the NOB and the Operational Norms of Health Assistance (NOAS) played a crucial role in inducing the transition to a decentralized model during the 1990s and early 2000s,
The NOBs and NOAS provided guidelines and incentives for municipalities to take on greater responsibilities in managing their health systems. As a result of these efforts, by the year 2000, an impressive 99% of Brazilian municipalities were fully (9.4%) or partially in charge of the management of their health systems. This marked a significant shift towards greater local autonomy and ownership in the delivery of healthcare services. The funding system of SUS has seen continuous improvement through the same norms, incorporating new sets of rules to define financing to municipalities and states [ 53 ].
In the 2000s, a significant step was taken to ensure adequate financing for the health system. A constitutional amendment was approved, mandating that states and municipalities allocate a minimum of 12% and 15% of their yearly revenue, respectively, to the health system. Meanwhile, the federal government’s minimum allocation was defined on the basis of the previous year’s health expenditure, adjusted for inflation and GDP growth. This amendment aimed to secure a stable and sufficient funding base for the SUS, promoting financial sustainability and stability.
The impact of these funding measures has been substantial. Between 1989 and 2014, real health expenditure per capita in Brazil increased by an impressive 149%. This growth was divided between the public sector, which contributed 46% of the increase, and the private sector, which contributed the remaining 54%. The increased investment in the health system has led to significant improvements in healthcare access, infrastructure and services, benefiting both the public and private sectors [ 52 ].
Regionalization emerged as a crucial aspect of the public health agenda in Brazil during the late 1990s and early 2000s. It was seen as a complementary approach to decentralization, aiming to address fragmentation and improve the delivery of healthcare services by optimizing available resources through regional networks with shared planning and programming. Official regulation of regionalization was introduced through NOAS in 2001 and was further reinforced by the Pact for Health in 2006.
The implementation of regionalization, however, has yielded heterogeneous results across different regions of the country. Some regions have made significant advances in successfully executing regionalization, leading to improved service integration, resource utilization and healthcare outcomes. However, certain regions have faced challenges in fully executing regionalization [ 54 ].
Overall, since the implementation of the decentralized and primary-care-based SUS, there have been notable improvements in the delivery of healthcare services, particularly through the Family Health Strategy (PSF) [ 55 ]. The SUS has contributed to better health outcomes for the population. In terms of access and utilization of health services, significant progress has been observed. From 1998 to 2013, the percentage of the population that had visited a doctor within the last 12 months increased from 54.7% to 74.2%. These figures demonstrate improved access to healthcare services and a greater utilization of medical care among the Brazilian population.
Moreover, health outcomes have seen remarkable advancements. The infant mortality rate has significantly decreased from 53.4 per 1000 live births in 1990 to 14 per 1000 live births in 2015. Similarly, the under-5-year-old mortality rate has also declined from 64.2 per 1000 live births in 2012 to 15.7 per 1000 live births in 2015 [ 52 ].
Although there is evidence that the decentralized SUS has contributed to these positive health outcomes, it is important to acknowledge that other factors have also played a role in the improvements. These factors include broader societal advancements and public health initiatives, such as improved access to water and sanitation, enhanced immunization coverage and other public health initiatives, making it challenging to isolate the specific effects of the decentralization process alone.
As such, the specific impact of decentralization on the health system in Brazil remains a subject of debate and requires further investigation. Future research should aim to disentangle the various factors that have contributed to the observed improvements in health outcomes, providing a more nuanced understanding of the role of decentralization in shaping Brazil’s healthcare landscape [ 56 ].
Decentralization involves transferring technical, managerial and financial responsibilities from the centre to the periphery, such as provinces or districts [ 57 ]. It is advocated at the top level as an essential element for achieving universal health coverage [ 58 ]. In theory, decentralization offers several benefits, including faster decision-making at the local level, consideration of local customs and perspectives and a more responsive health system. However, successful implementation relies on strong democratic values, accountability systems and professional standards within the local governments.
In this study, we examined the experiences of three countries from different continents with distinct socioeconomic profiles, each having unique experiences in implementing and advancing decentralization. Our aim was to assess the impact of this bold political move on the health of the population in these countries, evaluating both the positive and negative aspects. In Pakistan, the implementation of decentralization faced challenges common to other LMICs. Issues at the local level included inadequate technical skills, ineffective delegation of decision-making power and a lack of local interest. A rapid implementation led to coordination problems between central and local authorities, particularly during political conflicts. Nevertheless, positive effects on the health system were observed, such as improvements in financing, governance and service delivery. Studies from Pakistan have also reported an increase in community participation after decentralization, as it required more engagement from the community in healthcare planning [ 59 ]. Decentralization reforms in Pakistan prioritized health, leading to increased investment in the sector and granting local decision-making power, resulting in more responsive and effective healthcare services. Local managers are better adapted to local needs and demands, leading to better-quality care.
When comparing Portugal to other European countries it becomes evident that decentralization efforts have been undertaken in several countries across the continent. Countries such as Sweden, Norway, Finland and Denmark have embraced decentralization as a general principle in their health systems to achieve efficiency and improved healthcare outcomes [ 60 ]. Similarly, the United Kingdom has decentralized its health system, granting devolved powers to regions such as Wales, Northern Ireland and Scotland, enabling them to manage and deliver healthcare services according to their specific needs [ 61 ].
In Southern European countries such as Italy, Portugal and France, decentralization has also been implemented to a lesser extent, and the impact varies. It is essential to acknowledge that each country has its own unique context, political structure and healthcare system, influencing the success and outcomes of their decentralization efforts. Portugal’s decentralization process started a decade later than other European countries and has been relatively slow [ 46 ]. The intention was to enhance access to healthcare services, improve quality of care and optimize resource utilization [ 43 ]. However, potential drawbacks, including service fragmentation, unequal access to care, lack of standardization and increased bureaucracy, need to be addressed to ensure high-quality and accessible healthcare services [ 62 ]. As of now, the decentralization in Portugal does not cover all domains, with most public hospitals still belonging to the central administration [ 63 ].
Brazil, in contrast, has implemented successful decentralization reforms in its health system since the establishment of SUS in the 1990s [ 64 ]. These reforms aimed to transfer decision-making authority to sub-national levels, focusing on financing, management and inter-managerial agreements. This decentralization has facilitated the provision, financing, management and regulation of a wide range of health services, with substantial collaboration between all three levels of government. However, challenges remain, including disparities in services and quality across the country, unstable funding streams and expenditure allocation not fully based on the level of need [ 64 ]. Other South American countries have also adopted decentralization reforms to improve health outcomes and increase local decision-making power, albeit with variations in approaches depending on their unique contexts and healthcare systems [ 65 ].
Although decentralization reforms have achieved some success, challenges persist in their implementation. These challenges include capacity-building, resource limitations and resistance to change. Decentralization can also lead to inequality in access to care, with some regions having better access to healthcare services than others. This can lead to disparities in health outcomes, fragmented services and inefficiencies in care coordination across different levels of care [ 66 ].
Comparing all three countries, it is evident that all three have prioritized health in their decentralization reforms and aimed to enhance local decision-making power. Brazil has made significant progress in implementing decentralization reforms, while Portugal and Pakistan are still in the process of doing so. The decentralization context of these three countries holds significant relevance beyond their respective borders, offering valuable insights and lessons that can inform decentralization efforts elsewhere. Despite their diverse socioeconomic backgrounds and healthcare systems, these countries share common challenges and successes in their decentralization journeys. The experiences of Pakistan highlight the complexities and implementation challenges faced by many LMICs striving to devolve power and resources to local levels. Portugal’s slow but deliberate approach underscores the importance of addressing potential drawbacks, such as service fragmentation and unequal access, to ensure the success of decentralization initiatives. Brazil’s remarkable progress in decentralization, particularly in the health sector, serves as a beacon of success for countries seeking to improve service delivery and governance through greater local autonomy. The extent, progress and challenges in the decentralization processes vary among the three countries, each requiring ongoing evaluation and improvement to achieve the desired outcomes. By analysing and synthesizing the decentralization experiences of these countries, policy-makers and stakeholders worldwide can gain valuable insights into the contextual factors, implementation strategies and accountability mechanisms that contribute to successful decentralization reforms.
The study may be limited by the availability and scope of the literature on health sector decentralization in the selected countries. Additionally, the data used in this review will be up to the knowledge cutoff date, and any subsequent developments or changes in the decentralization strategies may not be captured.
In conclusion, all three countries have undertaken decentralization reforms in their health systems with the shared goal of improving health outcomes and empowering local decision-making. However, notable differences exist in the extent of decentralization, the challenges faced during implementation and inequality in access to care between the three countries. Thus, additional research is needed to obtain more rigorous evidence that can allow to learn from different experiences in LMIC and HICs countries.
Way forward
Moving forward, it is important for Portugal, Brazil and Pakistan to address the challenges encountered during their decentralization processes. This can be achieved through reinforcing implementation strategies, tackling inequalities in access to care, and enhancing monitoring and evaluation mechanism. Additionally, fostering knowledge sharing among these different countries will be instrumental in facilitating mutual learning.
By proactively addressing these aspects, Portugal, Brazil and Pakistan can continue refining and strengthening their decentralization efforts in the health sector. This, in turn, will help reduce disparities in healthcare, improve accessibility to services and ultimately lead to better health outcomes for their respective populations. Collaborative efforts and continuous improvement will be essential in achieving the overarching goal of equitable and high-quality healthcare for all.
Availability of data and materials
Not applicable.
Abbreviations
Integrated Health Actions
Azad Jammu and Kashmir
Concurrent legislative list
Federal legislative list
Gilgit Baltistan
Gross domestic product
Gross national income
The Brazilian Institute of Geography and Statistics
Islamabad Capital Territory
National Social Security Healthcare Institute
Khyber Pakhtunkhwa
Social Security and Assistance Ministry
National health system
Operational Norms of Health Assistance
Norms of Basic Operationalization
Program of Interiorization of Health and Sanitation Actions
Public–private partnerships
Family health strategy
Regional health administration
Sistema Único de Saúde
Siddiqi S, Masud TI, Nishtar S, Peters DH, Sabri B, Bile KM, et al. Framework for assessing governance of the health system in developing countries: gateway to good governance. Health Policy. 2009;90(1):13–25.
Article PubMed Google Scholar
Sreeramareddy CT, Sathyanarayana T. Decentralised versus centralised governance of health services. Cochrane Database Syst Rev. 2019;2019(9):CD010830.
PubMed Central Google Scholar
Manor J. The political economy of democratic decentralization. Washington, DC: The World Bank; 1999.
Book Google Scholar
World Bank. World development report 1993: investing in health, vol. 1. Washington, DC: The World Bank; 1993.
Martinussen PE, Rydland HT. Is a decentralised health policy associated with better self-rated health and health services evaluation? A comparative study of European countries. Int J Health Policy Manag. 2021;10(2):55–66.
PubMed Google Scholar
OECD. Making decentralisation work: a handbook for policy-makers, OECD multi-level governance studies. Paris: OECD Publishing; 2019. https://doi.org/10.1787/g2g9faa7-en .
Peckham S, Exworthy M, Powell M, Greener I. Decentralisation, centralisation and devolution in publicly funded health services: decentralisation as an organisational model for health-care in England. 2005. https://researchonline.lshtm.ac.uk/id/eprint/3582134 .
Bossert TJ, Beauvais JC. Decentralization of health systems in Ghana, Zambia, Uganda and the Philippines: a comparative analysis of decision space. Health Policy Plan. 2002;17(1):14–31.
Cobos Muñoz D, Merino Amador P, Monzon Llamas L, Martinez Hernandez D, Santos Sancho JM. Decentralization of health systems in low and middle income countries: a systematic review. Int J Public Health. 2017;62(2):219–29.
Akin J, Hutchinson P, Strumpf K. Decentralisation and government provision of public goods: the public health sector in Uganda. J Dev Stud. 2005;41(8):1417–43.
Article Google Scholar
Kruse I, Pradhan M, Sparrow R. Marginal benefit incidence of public health spending: evidence from Indonesian sub-national data. J Health Econ. 2012;31(1):147–57.
Habibi N, Huang C, Miranda D, et al. Decentralization in Argentina. New Haven: Yale University, Economic Growth Center; 2001.
Google Scholar
Yee E. The effects of fiscal decentralization on health care in China. Univ Avenue Undergrad J Econ. 2001;5(1):5.
Asfaw A, Frohberg K, James K, Jütting J. Fiscal decentralization and infant mortality: empirical evidence from rural India. J Dev Areas. 2007;41:17–35.
Cantarero D, Pascual M. Analysing the impact of fiscal decentralization on health outcomes: empirical evidence from Spain. Appl Econ Lett. 2008;15(2):109–11.
Rubio DJ. The impact of decentralization of health services on health outcomes: evidence from Canada. Appl Econ. 2011;43(26):3907–17.
Khaleghian P. Decentralization and public services: the case of immunization. Soc Sci Med. 2004;59(1):163–83.
Dwicaksono A, Fox AM. Does decentralization improve health system performance and outcomes in low- and middle-income countries? A systematic review of evidence from quantitative studies. Milbank Q. 2018;96(2):323–68.
Article PubMed PubMed Central Google Scholar
Faguet J-P, Sánchez F. Decentralization and access to social services in Colombia. Public Choice. 2014;160(1):227–49.
Hodge A, Firth S, Jimenez-Soto E, Trisnantoro L. Linkages between decentralisation and inequalities in neonatal health: evidence from Indonesia. J Dev Stud. 2015;51(12):1634–52.
Zaidi SA, Bigdeli M, Langlois EV, Riaz A, Orr DW, Idrees N, et al. Health systems changes after decentralisation: progress, challenges and dynamics in Pakistan. BMJ Glob Health. 2019;4(1): e001013.
Pakistan Bureau of Statistics (PBS). 6th population and housing census-2017. How many we are? What do we need? Block wise provisional summary results of 6th Population & Housing Census – 2017; 2018. https://www.pbs.gov.pk/sites/default/files/2022-04/population_Census_2017_Results.pdf
Safi MM, Zaidi SRM, Yousaf J, Bashir U, Zulfiqar W, Javed M. Pakistan: 2021 monitoring report – universal health coverage. Health Planning, System Strengthening and Information Analysis Unit (HPSIU). Ministry of National Health Services, Regulations and Coordination, 2021 Dec 2021. https://phkh.nhsrc.pk/sites/default/files/202208/Universal%20Health%20Coverage%20Monitoring%20Report%20Pakistan%202021.pdf .
World Bank. Pakistan country profile – world development indicators database. https://databank.worldbank.org/ . Accessed 24 July 2023.
Pakistan TNAo. The Constitution of 1973 Pakistan; 1973.
Karmel E. Decentralising government what you need to know. Democr Rep Int Brief Paper. 2017;87:1–13.
Ur-Rehman S, Khan N, SA Gill. Fiscal decentralization in Pakistan. In: 7th NFC award as case study public policy and administration research, vol. 4. 2014. p. 81–7.
Mustafa U. Fiscal federalism in Pakistan: the 7th National Finance Commission award and its implications. PIDE-Working Papers. 2011;73. https://file.pide.org.pk/pdfpideresearch/wp-0073-fiscal-federalism-in-Pakistan-the-7th-national-finance-commission-awardand-its-implications.pdf .
National School of Public Policy. Strategic appraisal of 18th amendment: federal/provincial roles and impact on service delivery. Senior management wing. National Management College, Islamabad: NSPP; 2012. http://www.nspp.gov.pk/guideline/strategic-appraisal-of-18th-amendment.pdf .
Nishtar S. Health and the 18th Amendment. Retaining national functions in devolution: heart file. 2011. http://www.heartfile.org/pdf/HEALTH_18AM_FINAL.pdf .
Government of Pakistan. Overview of the constitution (eighteenth amendment) act, 2010; 2010. https://ipc.gov.pk/SiteImage/Misc/files/Year%20Books/Final%20Report%20of%20Implementation%20Commission.pdf .
Government of Pakistan. The 18th amendment to the constitution of the Islamic Republic of Pakistan. Cabinet Division, Islamabad; 2010. http://pakistanconstitutionlaw.org/18thamendment-2010 .
Shehla Zaidi AR, Idrees N. Primary healthcare systems (PRIMASYS): case study from Pakistan. Geneva: World Health Organization; 2016.
Kundi A. Factors making LHWs say enough is enough Dawn; 2012. https://www.dawn.com/news/712404/factors-making-lhws-say-enough-is-enough .
Shehla Zaidi RS, Bhutta ZA, Ansari S. Public private partnerships for improving maternal and neonatal health service delivery a review of the evidence. Islamabad: Research and Advocacy Fund, British Council; 2013.
Pukhtunkhwa GoK. PC1-integrated health programme Khyber Pakhtunkhwa. In: Health do; 2016. https://phkh.nhsrc.pk/sites/default/files/2019-06/Integrated%20PC-1%20Khyber%20Pakhtunkhwa%202012-15.pdf .
National Institute of Population Studies (NIPS) [Pakistan] and ICF. 2019. Pakistan demographic and health survey 2017–18. Islamabad, Pakistan, and Rockville, Maryland, USA: NIPS and ICF.
About Portugal. https://portaldiplomatico.mne.gov.pt/en/about-portugal . Accessed 24 July 2023.
Censos 2021 – população. https://censos.ine.pt/xportal/xmain?xpgid=censos21_populacao&xpid=CENSOS21 .
World Bank. Portugal country profile – world development indicators database. https://data.worldbank.org/country/portugal . Accessed 24 July 2023.
Current expenditure on health care in % of GDP. In: Pordata. https://www.pordata.pt/Portugal/Despesa+corrente+em+cuidados+de+sa%C3%BAde+em+percentagem+do+PIB-610 . Accessed 24 July 2023.
de Almeida SJ, Augusto GF, Fronteira I, Hernandez-Quevedo C. Portugal: health system review. Health Syst Transit. 2017;19(2):1–184.
Nunes AM, Ferreira DC. A critical analysis of decentralizing the Portuguese public healthcare provision services. Int J Environ Res Public Health. 2022;19(20):13390.
Ferreira DC, Nunes AM. Technical efficiency of Portuguese public hospitals: a comparative analysis across the five regions of Portugal. Int J Health Plan Manag. 2019;34(1):e411–22.
Law-Decree n. 23/2019 of 30 January. https://dre.pt/dre/detalhe/decreto-lei/23-2019-118748850 . Accessed 4 July 2022.
Correia de Campos A. Decentralization and privatization in Portuguese health reforms. Rev Port Saude Publica. 2004;4: 7–20.
Paiva C, Teixeira L. Reforma sanitária e a criação do Sistema Único de Saúde: notas sobre contextos e autores. Hist Cienc Saude-Manguinhos. 2014;21:15–35.
Paim J, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet. 2011;377(9779):1778–97.
Descentralização das ações e serviços de saúde: a ousadia de cumprir e fazer cumprir a lei./Brasil. Ministério da Saúde. Sistema Único de Saúde. [Brasília]; 1993.
Pasche DF, Righi LB, Thomé HI, Stolz ED. Paradoxos das políticas de descentralização de saúde no Brasil. Rev Panam Salud Publica. 2006;20(6):416–22.
Costa NDR, Barros PL, Ribeiro JM. A descentralização do sistema de saúde no Brasil. Rev Serv Público. 2014;50(3):32–55.
Castro MC, Massuda A, Almeida G, Menezes-Filho NA, Andrade MV, de Souza Noronha KVM, et al. Brazil’s unified health system: the first 30 years and prospects for the future. Lancet. 2019;394(10195):345–56.
Viana AL, Heimann LS, de Lima LD, de Oliveira RG, Rodrigues SH. Significant changes in the health system decentralization process in Brazil. Cad Saude Publica. 2002;18(Suppl):139–51.
Vargas I, Mogollón-Pérez AS, Unger JP, da-Silva MR, De Paepe P, Vázquez ML. Regional-based integrated healthcare network policy in Brazil: from formulation to practice. Health Policy Plan. 2015;30(6):705–17.
Hanley J. Does Brazil’s decentralized system improve primary care with the family health program? Clin Soc Work Health Interv. 2016;7(4):41–5.
Atkinson S, Haran D. Back to basics: does decentralization improve health system performance? Evidence from Ceara in north-east Brazil. Bull World Health Organ. 2004;82(11):822–7.
PubMed PubMed Central Google Scholar
Mills A, Vaughan JP, Smith DL, Tabibzadeh I, World Health Organization. Health system decentralization: concepts, issues and country experience. Geneva: World Health Organization; 1990.
O’Connell TS, Sharkey A. Reaching universal health coverage: using a modified Tanahashi model sub-nationally to attain equitable and effective coverage. New York: UNICEF; 2013.
Shaikh S, Naeem I, Nafees A, Zahidie A, Fatmi Z, Kazi A. Experience of devolution in district health system of Pakistan: perspectives regarding needed reforms. J Pak Med Assoc. 2012;62(1):28–32.
Sorens J. The partisan logic of decentralization in Europe. Reg Federal Stud. 2009;19:255–72.
Saltman RB, Bankauskaite V. Conceptualizing decentralization in European health systems: a functional perspective. Health Econ Policy Law. 2006;1(Pt 2):127–47.
Ferrinho P, Conceição C, Biscaia A, Fronteira I, Antunes A. Sixty years of reform in the Portuguese health system: what is the situation with regard to decentralisation? Viewpoint. Rev Fr Aff Soc. 2006;6:297–312.
Nunes AM, Ferreira DC. Reforms in the Portuguese health care sector: challenges and proposals. Int J Health Plan Manag. 2019;34(1):e21–33.
Collins C, Araujo J, Barbosa J. Decentralising the health sector: issues in Brazil. Health Policy. 2000;52(2):113–27.
Article CAS PubMed Google Scholar
Bossert T. Decentralization of health systems in Latin America: a comparative study of Chile, Colombia, and Bolivia. Publications of the Latin America and the Caribbean Regional Health Sector Reform Initiative, mimeo. 2000 Jun 22.
Bossert TJ, Mitchell AD. Health sector decentralization and local decision-making: decision space, institutional capacities and accountability in Pakistan. Soc Sci Med. 2011;72(1):39–348.
Download references
Acknowledgements
The present publication was funded by Fundaçao para a Ciência e Tecnologia, IP National support through Comprehensive Health Research Centre - CHRC (UIDP/04923/2020).
Author information
Authors and affiliations.
Community Health Sciences, The Aga Khan University, Karachi, Pakistan
Shafaq Mahmood & Muhammad Muneeb Ullah Siddiqui
NOVA National School of Public Health, Public Health Research Centre, Comprehensive Health Research Center (CHRC), NOVA University Lisbon, Lisbon, Portugal
Rita Sequeira, Patrícia Pita Ferreira, Adalberto Campos Fernandes & Paulo Sousa
Federal University of Espirito Santo, Vitoria, ES, Brazil
Marcos Batista Araujo Herkenhoff
Unidade de Saúde Pública Zé Povinho, ACES Oeste Norte, Caldas da Rainha, Portugal
Patrícia Pita Ferreira
You can also search for this author in PubMed Google Scholar
Contributions
SM and RS contributed substantially to concept/design of study, acquisition and interpretation of data and drafting/revising of manuscript. MS, MH, PF and AF contributed substantially to acquisition and interpretation of data and drafting/revising of manuscript. PS contributed substantially to concept/design of study, acquisition and interpretation of data and drafting/revising of manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Shafaq Mahmood .
Ethics declarations
Ethics approval and consent to participate.
As this study is based solely on the analysis of existing literature and document sources, ethical approval was not required. All sources used in this review are appropriately cited and referenced to acknowledge the authors’ contributions.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Mahmood, S., Sequeira, R., Siddiqui, M.M.U. et al. Decentralization of the health system – experiences from Pakistan, Portugal and Brazil. Health Res Policy Sys 22 , 61 (2024). https://doi.org/10.1186/s12961-024-01145-3
Download citation
Received : 28 July 2023
Accepted : 25 April 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12961-024-01145-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Health sector reform
- Performance of health systems
- Developed country
Health Research Policy and Systems
ISSN: 1478-4505
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Variance Analysis in the Health Care System Research Paper
Introduction, month variances, additional data.
In healthcare facilities, many factors can affect deviations from the original budget. To establish and track budget variances, it is essential to keep a record of finances through variance analysis. Each new budget is built based on the previous variance data and the standard method of calculating the required items. However, healthcare institutions cannot, in any case, accurately calculate the probable overrun of funds. This work aims to consider the deviations present in the submitted report for the last month and highlight additional data to describe them. In addition, a strategy has been developed to correct deviations to create a more accurate budget plan.
As seen from the table, several deviations have recently been noted in the institution. Discrepancies in the originally budgeted budget and the final amount can be traced in many points of the report. The most considerable difference is noted in such items as ambulatory surgery, supplies, and net assets released. Areas that go far beyond the planned budget require closer attention, as they can significantly impact the organization’s financial position (Drury, 2018). In addition, this indicates that the calculations need to be corrected, and these areas require significant investments.
Furthermore, some items slightly exceeded the given budget. If the organization considers this in the context of one month, then the discrepancy seems insignificant. However, this happens all the time, and looking at finances over a long period can play a significant role. Nevertheless, not only negative discrepancies are observed from the provided report, which increases the financial gap. Some items show the use of less funding than initially offered. For example, Inpatient Revenue and Other Patient Revenue show a decline of $960 and $326. In this case, it is essential to reconsider the budget distribution and strengthen those areas lacking funding (Kouvelis et al., 2018). This can lead to a more sustainable system with a well-defined budget.
However, additional data must be considered to explain the details thoroughly. First, it is essential to understand that the influx of patients calculated in the budget is nominal and may not reflect the actual reality. Accordingly, one of the main points in the additional data is the exact number of clients compared with the prediction made (Jones et al., 2018). Thus, the healthcare organization can hire other employees in case of a large flow of clients. This will require supplementary costs that were not originally foreseen. Further, with a large flow of customers, staff can stay at the workplace for more hours. Since the overtime rate is increased, the nurse manager must account for this factor in the budget. Nevertheless, as the report shows, salaries and wages were $345 less than previously estimated monthly. This may be because many patients did not visit the health facility, and some staff needed to be more involved.
In addition, more than the flow of patients can explain the lower number of salaries. There could be an outbreak of a viral disease among the staff, spreading to many workers. As a result, many of them could not attend the workplace, resulting in a shortage of staff and lower pay (Hansen et al., 2021). Furthermore, any catastrophes or natural disasters can become an additional factor. This may explain the high budget overruns in ambulatory surgery. These are quick one-day interventions that do not require the patient to stay in the hospital. This includes the treatment of wounds and burns, suturing, and other manipulations that do not keep the patient in the department. Supplies are an essential item in the process of protecting the health of patients. The report shows additional budget spending in this area, possibly due to a need for more materials. Thus, the nurse manager is forced to order more necessary items than were initially included in the finances. To a greater extent, this is due to the difference in the estimated and actual volume of procedures associated with these resources, including X-ray examinations and laboratory tests.
In case of discrepancies between the planned and actual budget, a strategy for correcting the variances should be developed. First, it is crucial to determine where the most remarkable difference in the budget can be traced and detail the reason. The next step is to analyze the discrepancies and highlight the most critical areas. It is necessary to establish whether the deviations are single or increase over time (Dai et al., 2021). This will help to understand how vulnerable this or that side of the system is. An equally significant step is the definition of the nature of the dispersion, that is, positive or negative. Those areas that consistently use less than the gold budget can be used for those with a constant shortage. Thus, such a strategy will help to correct the difference between the forecast and the actual budget.
In conclusion, variance analysis is a critical tool for the health care system. It highlights the organization’s effectiveness and allows one to trace the distribution of financial flows. In addition, it helps to predict the possible costs of payments, procedures, etc. If it is necessary to fix deviations, it is essential to highlight the main points and outline whether they are positive or negative. In this way, a successful budget adjustment can be made.
Dai, M., Jin, H., Kou, S., & Xu, Y. (2021). A dynamic mean-variance analysis for log returns . Management Science , 67 (2), 1093-1108. Web.
Drury, C. (2018). Cost and management accounting . Cengage Learning.
Hansen, D. R., Mowen, M. M., & Heitger, D. L. (2021). Cost management . Cengage Learning.
Jones, C., Finkler, S. A., Kovner, C. T., & Mose, J. (2018). Financial Management for Nurse Managers and Executives-E-Book . Elsevier Health Sciences.
Kouvelis, P., Pang, Z., & Ding, Q. (2018). Integrated commodity inventory management and financial hedging: A dynamic mean‐variance analysis . Production and Operations Management , 27 (6), 1052-1073. Web.
- Patient Safety in Ambulatory Healthcare
- Managed Care: Ambulatory Health Care Accreditation
- Discrepancies Between Aspirations and Reality in Healthcare
- Home Healthcare Providers: Sepsis Review
- Ecological Systems Theory and Social Determinants of Health Model
- Reducing Catheter-Associated Urinary Tract Infections by Atkins et al.
- The Pregnant Woman's Smoking Cessation
- Primary vs. Review Articles in Scientific Literature
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2024, May 25). Variance Analysis in the Health Care System. https://ivypanda.com/essays/variance-analysis-in-the-health-care-system/
"Variance Analysis in the Health Care System." IvyPanda , 25 May 2024, ivypanda.com/essays/variance-analysis-in-the-health-care-system/.
IvyPanda . (2024) 'Variance Analysis in the Health Care System'. 25 May.
IvyPanda . 2024. "Variance Analysis in the Health Care System." May 25, 2024. https://ivypanda.com/essays/variance-analysis-in-the-health-care-system/.
1. IvyPanda . "Variance Analysis in the Health Care System." May 25, 2024. https://ivypanda.com/essays/variance-analysis-in-the-health-care-system/.
Bibliography
IvyPanda . "Variance Analysis in the Health Care System." May 25, 2024. https://ivypanda.com/essays/variance-analysis-in-the-health-care-system/.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Guidelines and Guidance Library
- Core Practices
- Isolation Precautions Guideline
- Disinfection and Sterilization Guideline
- Environmental Infection Control Guidelines
- Hand Hygiene Guidelines
- Multidrug-resistant Organisms (MDRO) Management Guidelines
- Catheter-Associated Urinary Tract Infections (CAUTI) Prevention Guideline
- Tools and resources
- Evaluating Environmental Cleaning
What to know
This guideline provides recommendations for isolation precautions in healthcare settings.
Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007)
Print Version of Guidelines
Updates, infection control.
CDC provides information on infection control and clinical safety to help reduce the risk of infections among healthcare workers, patients, and visitors.
For Everyone
Health care providers, public health.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Springer Nature - PMC COVID-19 Collection

Modern Development Problems of Russian Healthcare (Part 1)
V. n. ivanov.
Institute of Economic Forecasting, Russian Academy of Sciences, Moscow, Russia
A. V. Suvorov
Abstract—.
The paper (part 1) analyzes the dynamics of indicators characterizing the state of health of the Russian population. A comparative analysis of the development of healthcare in Russia and other countries is carried out. The conclusion is confirmed that the main problem in the development of Russian healthcare is the insufficient volume of public funding. The drawbacks and limited potential of the adopted funding model are assessed. A possible way to increase public funding is proposed. It is shown that the availability of medical care is reduced as a result of the so-called optimization of healthcare. A possible way to improve the territorial organization of medical services is considered. The effectiveness of the Russian healthcare system in the fight against the coronavirus pandemic is assessed.
The current state of the national healthcare system raises justified concern. The high morbidity and mortality of the population of Russia persist. Sociological studies record a low level of satisfaction of the population with the quality and level of accessibility of medical care. Representatives of the medical community are increasingly criticizing the government’s policy in the field of healthcare, the adopted directions of reforming the industry. At the same time, many of the shortcomings of the implemented strategy for organizing healthcare have been clearly manifested during the epidemic of coronavirus infection COVID-19 and caused significant damage to the socio-economic development of the country.
The state of health of the population. According to official data, in 2018 the total number of registered diseases in the country’s residents amounted to 240 mln, i.e., on average, 1.6 diseases per person. 1 Every fourth person has a disease of the circulatory system; in a population sample of 100 people, 13 were diagnosed with diseases of the musculoskeletal system, 12 had diseases of the genitourinary system, 11 had digestion diseases, 10 had eye diseases, 8 had diseases of the endocrine system, and 5 had neoplasms.
The fastest growing morbidity in the Russian population was observed in the first half of the 1990s during the period of change in the social system, which was characterized by a sharp drop in the level and deterioration of living conditions of the population. An increase in morbidity was observed in relation to almost all classes of diseases, including curable diseases, which were considered almost completely eliminated in the Soviet period. So, for example, in comparison with 1991, the number of patients with a diagnosis of active tuberculosis established for the first time in their life increased by the mid-1990s by more than two times, and the number of patients with a diagnosis of syphilis grew 30 times.
In the 2000s, as compared to the previous decade, the rate of growth in the incidence of diseases of the circulatory system (the number of registered diseases in patients diagnosed for the first time in their lives) increased, while it decreased in many other classes of diseases ( Table 1 ). At the same time, the incidence rate in 2019 was lower than in 1991 only for infectious diseases. Meanwhile, over the past almost thirty years, the number of detected diseases of the endocrine system has increased three and a half times, the number of detected diseases of the circulatory system has grown more than three times, and the number of neoplasms has twice increased. The last two classes of diseases as well as external causes (accidents, traffic injuries, homicides and suicides) are currently the main causes of mortality in the population.
Table 1.
The incidence rate for main classes of diseases (registered diseases in patients with a diagnosis established for the first time in life), thousands
The dynamics of the mortality rate of the population include three time intervals: 1991–1995, 1995–2005, and 2005–2019. In the early 1990s, there was a maximum increase in the overall mortality of the population, which was due, first of all, to a significant deterioration in the socio-economic situation in the country: a deep economic recession, a sharp drop in the standard of living for the majority of the population and an accompanying increase in socio-psychological tension as a result of the inability adapt to new economic conditions [ 1 ]. Moreover, this inability was most characteristic of the younger age cohorts of the population. This is confirmed by the significantly higher growth in mortality at the working age ( Table 2 ).
Table 2.
Mortality from the main death causes (deaths from all causes per 100 000 people)
The increase in mortality in 1991–1995 was noted for all major classes of death causes, while the increase in mortality from external causes was the greatest, which was a direct consequence of the growth of socio-psychological tension. In this regard, it should be noted that social and psychological stress is recognized by WHO experts as main among socioeconomic factors that negatively affect the health of the population and lead to the development of cardiovascular diseases, an increase in mortality from accidents, homicides and suicides; at the same time, this influence is most pronounced in the countries that are carrying out accelerated economic transformations without an adequate social policy [ 2 ].
The degradation of the medical care system also contributed to the growth in mortality in the first half of the 1990s. As radical economic transformations began, funding for Russian healthcare collapsed. The reduction in funding and the deterioration of the material and technical support of the healthcare system resulted in the transition to simplified medical technologies, which in many cases did not provide the previously achieved quality of medical care. This could not but lead to a decrease in its effectiveness.
During the next time interval (1995–2005), the growth rate of total mortality decreased significantly. At the same time, mortality from external causes, primarily in the working age, had a clear tendency to decrease, while mortality from cardiovascular diseases (the main cause of mortality in the population) continued to grow and increased by almost one and a half times compared with 1991. It is due to mortality from diseases of the circulatory system that the increase in the total mortality of the population occurred in the period under review.
It became possible to reverse the growth trend in mortality only in the middle of the 2000s as a result of both an improvement in the socio-economic situation and living conditions of the population and improvement in the medical care system. The latter was facilitated primarily by implementing measures for strengthening the material and technical base of healthcare within the framework of the “Health” national project, which was launched in 2006: large-scale procurement of modern medical equipment, and introduction of modern medical technologies.
Over the past 15 years (2005–2019), the rate of mortality from diseases of the circulatory system and external causes has decreased most significantly. As the socio-economic situation in the country began to improve, mortality from external causes began to decline rapidly and decreased by a third by 2019 compared to 1991. The reduction in mortality from diseases of the circulatory system must be attributed—in contrast to the decrease in mortality from external causes—to achievements of healthcare as a result of the modernization of the system of medical care for patients with cardiovascular diseases: the organization of a network of vascular centers and vascular departments of hospitals, a multiple increase in the number of surgeries on the heart and blood vessels. At the same time, it should be noted that mortality from diseases of the circulatory system in Russia continued to remain at a significantly higher level compared to most economically developed countries [ 3 ]. There is also reason to believe that the rate of mortality from diseases of the circulatory system officially registered in recent years is artificially underestimated. Experts explain this by the fact that the achievement of the target rates of mortality from cardiovascular diseases defined by the 2012 presidential decrees in May is one of the criteria for assessing the performance of regional leaders. As a result, the regions often indicate another concomitant disease of the patient as the cause of death at the suggestion of their leaders [ 4 ]. This is probably the reason for the hard-to-explain increase in mortality from “other diseases” just in elderly patients who usually have several diseases (see Table 2 ).
A generalizing characteristic of the mortality rate and one of the main indicators for assessing the health of the population and the effectiveness of the functioning of the healthcare system is the indicator of average life expectancy (life expectancy at birth). The dynamics of the average life expectancy indicator also include three time intervals ( Table 3 ).
Table 3.
Average life expectancy (years)
In the early 1990s, there was a sharp decline in life expectancy, which was unprecedented in peacetime, primarily for men (see Table 2 ). From the mid-1990s to the mid-2000s, the values of this indicator remained almost unchanged. The observed insignificant increase in the average life expectancy with a simultaneous growth in the total mortality of the population during this period is mainly explained by the decrease in mortality from external causes during this period due to the significantly lower average age of death in comparison with other death causes.
During 2005–2019, the average life expectancy grew, while the difference in the average life expectancy between men and women also decreased due to the higher growth rates for men (see Table 3 ). A significant increase in average life expectancy during this period was primarily due to a decrease in mortality from cardiovascular diseases and mortality from external causes. At the same time, the decrease in mortality from external causes not only made a significant contribution to the growth of average life expectancy, but also largely determined the decrease in the difference in the average life expectancy between women and men due to the lower average age of death from this cause with a fourfold excess of its level in men compared to women. Along with the reduction in mortality from diseases of the circulatory system, a significant decrease in infant mortality must be attributed to the unconditional achievements of domestic healthcare, which contribute to an increase in average life expectancy. The infant mortality rate (the number of children who died under one year of age per 1000 live births) decreased almost three times: from 11.0 in 2005 to 4.1 in 2019.
Despite the observed upward trend in the average life expectancy of the population, Russia is still among the second hundred countries of the world in the WHO ranking for this indicator [ 5 ]. In most developed countries, the average life expectancy of the population is eight to ten years higher than in Russia, and the difference in the life expectancy between women and men is two times less ( Table 4 ). The reasons for Russia’s lag behind other developed countries have a more than half a century history and are explained, first of all, by insufficient financing of the Russian healthcare system.
Table 4.
Life expectancy (in 2019) in Russia and in a number of developed countries, years
Health financing. A global trend is a change in the so-called epidemiological revolutions. By the middle of the 20th century, developed countries almost completed the first epidemiological revolution, which was characterized by significant successes in the fight against diseases that are curable in nature. One of the main results was a significant decrease in mortality, primarily in infant mortality and mortality in working age. As a result, average life expectancy increased by 1960 to about 70 years in most developed countries.
The second epidemiological revolution meant a replacement of the strategy of “treatment up to recovery” with the strategy of prevention and “postponement of fatal complications” of chronic diseases (atherosclerosis, diseases associated with metabolism, etc.), i.e., “moving deaths from these causes to older ages, an increase in the average age of death from them, and, ultimately, a significant increase in life expectancy” [ 6 ].
The implementation of such a strategy requires the development and introduction of new medical technologies, diagnostic and therapeutic equipment, an increase in the number of people employed in healthcare, and the development of pharmaceutical production. All this leads to a significant rise in the cost of medical care and, accordingly, to a significant increase in healthcare costs.
As a result, the dynamics of spending on healthcare have become an indicator of the dynamics of the volume of medical services of the quality required to solve the problems of the second epidemiological revolution. At the same time, it is considered that one of the most adequate indicators of not only the quality, but also the availability of medical care for the population is the value of public expenditures on healthcare and, in particular, the indicator of the share of these expenditures in the gross domestic product (GDP), which allows for cross-country comparisons, including comparison of countries with different levels of economic development. This indicator to the greatest extent reflects the state of health of the population, mortality rate and average life expectancy.
As the analysis shows, there has been a rapid increase in healthcare expenditures since the 1960s in almost all foreign developed countries. At the same time, the growth rates of public healthcare financing significantly exceeded the rates of economic growth of the countries; as a result, the share of these expenditures in GDP increased by no less than 2–3 times by 1990 compared to 1960. Simultaneously, the average life expectancy increased by 5–7 years in most developed countries (see Table 4 ).
In our country, the problems of the first epidemiological revolution were solved quite successfully. As a result, life expectancy increased from 43 years in 1926–1927 (data for the European part of the Russian Soviet Federative Socialist Republic) up to 68.8 years in 1960. The country entered the top twenty countries of the world by this indicator, being only slightly inferior to the leading countries. However, in the next 30 years, the average life expectancy did not increase and in 1990 it was equal to only 69.2 years. At the same time, as calculations show, the amount of public health spending that was calculated as a share of GDP remained almost unchanged. This indicator ( Table 5 ) in 1990 remained at the level of spending in most developed countries in the 1960s.
Table 5.
Public health spending (% of GDP) and average life expectancy (years) in the Soviet Union and other countries in 1960–1990*
* The data for the Russian Soviet Federative Socialist Republic barely differed from the data for the Soviet Union. Data for foreign countries were calculated according to [ 7 , 8 ].
The development of domestic healthcare in the period under review followed the path of building up the network of medical institutions and increasing the training of medical personnel. As a result, the number of hospital beds and the number of doctors in the Russian Soviet Federative Socialist Republic increased more than twice. Given the size of the country’s territory and the nature of the population’s settlement, such an extensive direction of healthcare development seems to be a fully justified way of ensuring universal access to medical care. At the same time, insufficient funding did not make it possible to ensure an improvement in the quality of medical care by the technical and technological re-equipment of domestic healthcare, which was necessary to solve the problems of the second epidemiological revolution. Calculations show, in particular, that the cost of purchasing equipment in total healthcare spending in the period under review was only about 2% [ 9 ].
As a result of insufficient funding, the provision of medical organizations with modern diagnostic and treatment equipment, the use of advanced medical technologies remained at an extremely low level. The provision of modern medicines was also very low. In addition, insufficient funding led to low wages in healthcare. Despite the high educational and professional levels of people employed in this sector, the average salary in healthcare was a quarter lower than the average for the national economy. Our country also lagged significantly behind other developed countries in terms of the ratio of the average wages in healthcare to the this indicator in the economy as a whole.
In the early 1990s, there was a collapse in funding for Russian healthcare. The scale of the fall in public spending is evidenced, first of all, by a sharp decline in wages for people employed in healthcare, which is the main item of expenditure of medical organizations. Calculations show that this indicator decreased in constant prices three times in the first year of radical reforms, and in 1995 it amounted to 47% of the 1991 level. Due to the unreliability of statistics on the values of the deflator of GDP elements in 1992, it is difficult to give an accurate estimate of the magnitude of the fall in total public health spending from 1991 to 1995. According to our calculations with corrections of data for 1992, public health financing decreased about twice over this period.
Table 6 shows the dynamics of the indicator of public health spending for the period from 1995 to 2018 in constant prices, which was calculated on the basis of the deflator of final consumption as an element of the use of GDP.
Table 6.
Public health spending (at constant 1995 prices) and average life expectancy
* In 1995—bln Rubles.
As can be seen from the cited data, public health spending continued to decline in the second half of the 1990s, and the 2000s brought about an increase in financing for healthcare along with the growth of the economy. Given the two-fold drop in funding in the first half of the 1990s, this growth is a recovery growth. The level of funding in 1991 was achieved only in 2010. It is interesting to note that the indicator of average life expectancy in 2010 (68.9 years) became exactly the same as in 1991.
In the second half of the 2000s at a relatively high growth rate of public expenditures (average annual growth was 2.8%), the state of the material and technical base of healthcare improved. The coefficient of renewal of fixed assets increased several times—up to 6% in 2010. At the same time, the share of machinery and equipment in the structure of fixed assets grew (up to 39% in 2010). As noted above, large-scale purchases of modern diagnostic and treatment equipment were carried out during these years within the implementation of the “Health” national project, which made it possible to switch to the use of advanced medical technologies, at least at some medical organizations. First of all, this applies to federal specialized medical centers, the network of which significantly increased, including through the creation of such centers outside Moscow and St. Petersburg.
In general, all this led to an improvement in the quality of medical care and, accordingly, to an increase in its effectiveness. For the first time in Russian history, average life expectancy exceeded the 70‑year threshold in the 2010s and continued to grow until recently. At the same time, the success of the Russian healthcare system significantly lags behind the majority of developed foreign countries. Russia’s lag behind these countries in terms of life expectancy not only has not decreased, but has increased over the past three decades. A similar trend is also observed for the difference in public health expenditures calculated as a share of these expenditures in GDP. As for per capita public spending in comparable prices at purchasing power parity (PPP), the scale of Russia’s lag behind most developed countries is especially large. In terms of per capita financing, Russia lags almost three times behind the average financing for the countries of the Organization for Economic Cooperation and Development (OECD) and 3.5–5 times behind the countries such as Austria, Germany, Canada, Norway, France, and Japan ( Table 7 ).
Table 7.
Public health spending and average life expectancy in the Russian Federation and other countries in 2018*
* Data for the OECD countries are given according to [ 10 ]. ** Per capita spending is calculated using PPP of final consumption in GDP.
Against the background of low public funding in post-Soviet Russia, private spending on healthcare began to grow rapidly: household spending on the purchase of medicines and medical supplies, payments for medical services, and contributions to voluntary medical insurance increased. For the period 1995–2018 in comparable prices, spending for the purchase of medicines and medical goods increased almost 12 times, and spending for payments for medical services grew almost seven times. An advancing growth in private spending was accompanied by an increase in its share in total expenditures on healthcare.
As can be seen from Table 8 , the commercialization of Russian healthcare has become an obvious trend.
Table 8.
Structure of healthcare expenditures and their share in GDP in 1995 and 2018
At the same time, the vector of development was directly opposite to that observed in most developed foreign countries. Historically, the improvement of healthcare systems in these countries followed the path of strengthening the role of the state, the transition from private to public funding. As a result, the current share of private financing in total health spending in developed foreign countries (23% in Belgium and France, 22% in Germany, 21% in Great Britain, 16% in Japan, 15% in Norway [ 10 ]) is significantly lower than in Russia (39%).
As many years of world experience have shown, public funding not only ensures universal access to healthcare, but also allows more efficient use of health resources. In Russia, this experience was ignored, including the conclusions of experts that “private financing of healthcare threatens its values and is ineffective in comparison with public financing” [ 11 ]. In this regard, it should be noted that healthcare is the most costly in the United States, where private funding dominated until recently. Thus, total expenditures on healthcare in the United States in 2018 amounted to 16.9% of GDP, which is almost twice more than the average for OECD countries [ 10 ]. At the same time, the United States occupies one of the last places in terms of average life expectancy (78.6 years) among the countries with a high level of economic development.
The commercialization of Russian healthcare has resulted in the increased inequality in the availability of medical care for the population due to the lack of funds for paid medicine among the majority of the population, especially among its poorest strata. So, for example, according to the data from a sample survey of households cited by Federal State Statistics Service, in 2018 20% of the wealthiest citizens accounted for 70% of paid medical services and 20% of the poorest people accounted for less than 1.5%, or a share almost 50 times less. According to sample studies, every seventh resident of the country and every fifth pensioner could not purchase the medicines necessary for treatment due to a lack of funds.
At the beginning of the period under review, a reform of public health financing took place: in addition to state budget financing, a compulsory health insurance system (CHI) was introduced in 1993, which provides for employers paying insurance premiums for employees to the state federal and territorial CHI funds. It should be emphasized that financing through the CHI, i.e., financing by the introduction of compulsory payments for the working population was originally regarded precisely as an addition to financing from the state budget in the context of a sharp decline in the incomes of the latter. This made it possible to dampen the drop in budget financing to a certain extent.
However, later the CHI system began to be considered as the main model for financing healthcare. A transition was made to a one-channel system of financing, in which the budgets of the constituent entities of the Russian Federation transfer certain amounts (contributions) for the nonworking population to the territorial CHI funds. Territorial funds that also receive employers’ insurance contributions from the federal CHI fund transfer the accumulated funds to private insurance companies that finance the activities of medical organizations. Meanwhile, some types of medical care as well as capital expenditures, including the purchase of expensive equipment, are financed exclusively from the state budget.
The above-described complex and contradictory scheme of healthcare financing (public expenditures are carried out by private insurance companies) is only one of the characteristics of the adopted CHI model. Leaving aside for now the assessment of all the negative consequences of the application of this model, we note two important circumstances. First, as international comparative studies show, the CHI model is more costly compared to the system of financing from the state budget and, moreover, does not provide greater efficiency of medical care, in particular, reduction in the mortality rate of the population (for example, see [ 12 ]).
Second, despite the declared transition to universal compulsory health insurance, the main source of public funding for healthcare is still the state budget rather than personalized insurance premiums for each insured person, as in other countries applying the CHI model. As calculations show, employers’ insurance premiums for employees at a statutory rate amounted in 2018 to just over a third (36%) of public health spending despite the increase in this rate from 3.6% during the introduction of CHI to 5.1% in recent years, and budgetary appropriations accounted for the remaining almost two-thirds (calculations were made according to [ 13 ]).
Proceeding from these two facts, a natural question arises about the expediency of maintaining funding according to the adopted CHI model. Recently, proposals to return to the state budget financing system have been increasingly formulated by many experts (see, for example, [ 14 – 16 ]), including due to the ineffectiveness of the CHI model under the conditions of the coronavirus pandemic. In 2020, the state allocated additional budgetary funding for the development of a network of covid hospitals and additional payments to doctors working with coronavirus patients. At the same time, due to a sharp decrease in the number of patients in polyclinics and noncovid hospitals under the conditions of the pandemic, their financing through compulsory medical insurance decreased, which resulted in large accounts payable of medical organizations to insurance companies that pay for their services under compulsory medical insurance [ 17 ].
Summarizing the above, one cannot but agree with the experts’ conclusion that the fundamental limitation of the financial capabilities of the CHI system is becoming more and more obvious [ 16 ]. Moreover, to restore economic growth, it is necessary to increase consumer demand at the expense of the growth in household incomes. Therefore, it seems reasonable to reduce the insurance burden on the wages of employees. In such a situation, in our opinion, the abandonment of the CHI model and the transition to a system of budgetary financing must be considered fully justified.
Under these conditions, an urgent task is to increase significantly state budget spending on healthcare, which is necessary not only to compensate for falling insurance payments, but also to achieve an acceptable level of financing for healthcare in general. The way to solve this problem is also obvious—the state budget revenues must be increased. Until recently, the revenues of the RF consolidated budget amounted to only 35% of the GDP. This is significantly less than in most developed countries: this figure is 45% on average for the EU countries, and in Belgium, Denmark and Finland it exceeds 50% [ 18 ].
It is currently recognized that one of the main problems of economic development is an increase in the income gap with an increasing concentration of income among one percent of the population. The importance of solving this problem was acknowledged by the President of the Russian Federation in his speech at the last Davos Forum [ 19 ].
In developed foreign countries, a decrease in income concentration is stimulated by high tax rates on incomes of the richest citizens from work and property. As a result, one percent of taxpayers account for most of the collected income tax (in the United States, for example, more than 40% [ 20 ]), which is one of the main items of state budget revenues.
In our opinion, the introduction of a high income tax rate in Russia similarly to developed countries in relation to the incomes of the richest citizens must be considered the first step in solving the problem of increasing the incomes of the consolidated budget of the Russian Federation and, accordingly, increasing public spending on healthcare. The relevance of such a solution is defined as extremely high. According to available estimates, the concentration of income in Russia for one percent of the Russian population corresponds to that in the United States. In both countries, especially in Russia, the authorities are realizing the urgent need to reduce this concentration.
It should be emphasized that we are not talking about the introduction of progressive taxation with a multilevel scale of tax rates in Russia. Objections to the introduction of such a system are to a certain extent justified, given the low income of the vast majority of citizens and the complexity of the administration of such taxation. It is proposed not to go beyond the establishment of an increased tax rate on that part of the income of the richest taxpayers, which exceeds a certain threshold value with maintaining the existing tax rate on all incomes below the established threshold, i.e., incomes of the absolute majority of the population. The amount of the threshold income, above which an increased rate must be applied, as well as the amount of this rate can be determined taking into account the experience of taxation in developed foreign countries: the maximum tax rate they use for that part of an individual’s income that exceeds the established threshold. The corresponding calculations for a number of countries [ 21 – 23 ] are given in Table 9 .
Table 9.
The maximum personal income tax rate and the amount of the annual income above which the maximum rate is applied
* Based on the results of international comparisons for 2017.
1 Here and below, if a specific reservation is not made, the indicators are based on the data of the Federal State Statistics Service published in the “Russian Statistical Yearbook,” statistical collections “Healthcare in Russia,” “Demographic Yearbook of Russia,” “Social Position and Living Standard of the Population of Russia,” and “Regions of Russia.”
Translated by L. Solovyova

COMMENTS
The flaws of the U.S. health care system have been exposed and exacerbated by the coronavirus pandemic. This paper posits three underlying causes of our persistent poor performance: flawed assumptions; inadequate information; and fragmented delivery, payment, and insurance systems that make it easier to profit by shifting risk or costs to others than by improving value.
Health system research is a part of health research. It. closely links eld evidences and applies its results for the. improvement of the health system. Initially, it was known as. health service ...
The current paper discuses opportunities and challenges around global health care systems in next 25-30 years. The paper will analyze the future needs of healthcare in next 30 years and review key achievements and challenges faced globally both in developing and developed countries. ... The research from Advisory Board shows that increasing ...
Introduction. Healthcare systems around the world face significant challenges in achieving the 'quadruple aim' for healthcare: improve population health, improve the patient's experience of care, enhance caregiver experience and reduce the rising cost of care. 1-3 Ageing populations, growing burden of chronic diseases and rising costs of healthcare globally are challenging governments ...
Healthcare quality assessments evaluate health systems' effectiveness to provide patient care that is timely, affordable, and based on reliable evidence. This section of the report provides a broad portrait of U.S. healthcare in consideration of those fundamental measures as well as additional factors that influence disparities in care. This information is provided to support contextual ...
Since the 1980s, markets have turned increasingly to intangible goods - healthcare, education, the arts, and justice. Over 40 years, the authors investigated healthcare commoditisation to produce policy knowledge relevant to patients, physicians, health professionals, and taxpayers. This paper revisits their objectives, methods, and results to enlighten healthcare policy design and research.
Methods and findings. Two independent investigators systematically searched the Medical Literature Analysis and Retrieval System Online (MEDLINE), the Excerpta Medica Database (EMBASE), the Cumulative Index to Nursing and Allied Health Literature (CINAHL+), the Health Management Information Consortium, and the Journal of Research Evaluation from inception until May 2017 for publications that ...
Content last reviewed March 2023. Agency for Healthcare Research and Quality, Rockville, MD. Health systems research provides evidence that, when applied can make healthcare affordable, safe, effective, equitable, accessible, and patient-centered. AHRQ invests in research to generate new evidence to help health care systems and health care ...
Health-care systems comprise heterogeneous actors who perform distinct but related tasks (Djellal and Gallouj, 2005, ... The second exclusion criterion applied to the identification of relevant prior art concerned literature other than research papers, that is, papers that do not aim to increase scholarly knowledge about a particular question. ...
S. W. Gillani and M. I. Mohammad Abdul: Public health care system, a quasi-experi mental study: A cceptance and a itude to implicate clinica l services, Acta Pharm. 67 (2017) 71-83.
Вackground In the last two decades, health care systems (HCS) in the European countries have faced global challenges and have undergone structural changes with the focus on early disease prevention, strengthening primary care, changing the role of hospitals, etc. Russia has inherited the Semashko model from the USSR with dominance of inpatient care, and has been looking for the ways to ...
The paper describes an intellectual model of clinical risk management (CRM) for a general hospital based on Failure Mode and Effects Analysis (FMEA), Route Cause Analysis (RCA) and Systems Engineering Initiative in Patient Safety (SEIPS) model. Input and output parameters of the CRM model, management resources and corrective interventions were ...
Other papers assessed e-health on basis of accessibility, feasibility and medium of education in clinical practice. ... Maiti A. K., Chakraborty C. (2017). Web-enabled distributed health-care framework for automated malaria parasite classification: An E-Health approach. Journal of Medical System. 41 ... Healthcare Informatics Research, 22(4 ...
History of Health Services Research. The history of HSR is generally considered to have begun in the 1950s and 1960s with the first funding of grants for health services research focused on the impact of hospital organizations. 19, 20 On the contrary, HSR began with Florence Nightingale when she collected and analyzed data as the basis for improving the quality of patient care and outcomes. 21 ...
India Health System Review Health Systems in Transition Vol. 11 No. 1 2022 Written by: Sakthivel Selvaraj, Public Health Foundation of India, Delhi, India Anup K Karan, Indian Institute of Public Health, Delhi, India Swati Srivastava, Medical Faculty and University Hospital, Heidelberg University, Germany Nandita Bhan, Center on Gender Equity and Health, India
This paper provides empirical evidence using two studies to explain the primary factors facilitating electronic health record (EHR) systems adoption through the lens of the resource advantage theory. We aim to address the following research questions: What are the main organizational antecedents of EHR implementation? What is the role of monitoring in EHR system implementation?
This paper discusses the critical importance of epidemic preparedness and innovations in digital health care by examining the transformative impact on speech-language pathology (SLP) services in a specialist outpatient child and adolescent service (CAMHS). This retrospective review analyzes referral data from three periods: pre-pandemic (15 March 2019-14 March 2020), pandemic (15 March 2020 ...
A health care system evaluation and a series of school parasitaemia surveys and health facility-based surveys were carried out during the dry season in of 2003, applying standard Rapid Urban Malaria Appraisal (RUMA) methodology. ... This paper discusses the findings of research exploring the conduct of portfolio-based performance appraisal ...
Decentralization of a health system is a complex and multidimensional phenomenon that demands thorough investigation of its process logistics, predisposing factors and implementation mechanisms, within the broader socio-political environment of each nation. Despite its wide adoption across both high-income countries (HICs) and low-and-middle-income countries (LMICs), empirical evidence of ...
Motivation and Scope. There is a large body of recently published review/conceptual studies on healthcare and data mining. We outline the characteristics of these studies—e.g., scope/healthcare sub-area, timeframe, and number of papers reviewed—in Table 1.For example, one study reviewed awareness effect in type 2 diabetes published between 2001 and 2005, identifying 18 papers [].
In conclusion, variance analysis is a critical tool for the health care system. It highlights the organization's effectiveness and allows one to trace the distribution of financial flows. In addition, it helps to predict the possible costs of payments, procedures, etc. If it is necessary to fix deviations, it is essential to highlight the ...
In 2023, the median annual list price for a new drug was $300,000, an increase of 35% from the prior year. 2023 saw the most drug shortages in over a decade; there were an average of 301 drugs in shortage per quarter, an increase of 13% from the previous year. Hospitals' labor costs, which on average accounts for 60% of a hospital's budget ...
This publication is the first peer-reviewed quantum computing paper from the Cleveland ... Cleveland Clinic is a nonprofit multispecialty academic medical center that integrates clinical and hospital care with research and education. Located in Cleveland, Ohio, it was founded in 1921 by four renowned physicians with a vision of providing ...
Appendix A: Type and Duration of Precautions Recommended for Selected Infections and Conditions. Appendix A: Table 1. History of Guidelines for Isolation Precautions in Hospitals. Appendix A: Table 2. Clinical Syndromes or Conditions Warranting Empiric Transmission-Based Precautions in Addition to Standard Precautions. Appendix A. Table 3.
Introduction. The evolution in the digital era has led to the confluence of healthcare and technology resulting in the emergence of newer data-related applications [].Due to the voluminous amounts of clinical data generated from the health care sector like the Electronic Health Records (EHR) of patients, prescriptions, clinical reports, information about the purchase of medicines, medical ...
Robotics Education was aimed at equipping students with knowledge through robotics constructions. It dates back to the 1960s, when Logo programming language commenced being implemented widely through recruiting programmable devices based on project-based learning (Papert, 1980).Based on this research, it is obvious that children who were actively involved in robotics classes gained more ...
To Canadians, the notion that access to health care should be based on need, not ability to pay, is a defining national value. This value survives despite a shared border with the USA, which has the most expensive and inequitable health-care system in the developed world. 4 Canadian Medicare is more than a set of public insurance plans: more than 90% of Canadians view it as an important source ...
Overview. Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources. DHS Executive Leadership.
Objectives. Smart hospitals involve the application of recent information and communications technology (ICT) innovations to medical services; however, the concept of a smart hospital has not been rigorously defined. In this study, we aimed to derive the definition and service types of smart hospitals and investigate cases of each type.
The effectiveness of the Russian healthcare system in the fight against the coronavirus pandemic is assessed. ... Thomson, T. Foubister, and E. Mossialos, Financing Health Care in the European Union (WHO Regional Office ... Social Health Insurance vs. Tax-Financed Health Systems—Evidence From The OECD. Policy Research Working Paper No. WPS ...