Home — Essay Samples — Social Issues — Euthanasia — Why Euthanasia Should Be Legal: Analysis of Arguments and Counterarguments

Why Euthanasia Should Be Legal: Analysis of Arguments and Counterarguments
- Categories: Assisted Suicide Euthanasia Right to Die
About this sample

Words: 1865 |
10 min read
Published: Aug 14, 2023
Words: 1865 | Pages: 4 | 10 min read
Table of contents
Introduction, why euthanasia should be legal, works cited, counterarguments.
- Corder, Mike. “Dutch Euthanasia Center Sees 22% Rise in Requests in 2019.” WAVY.com, 7 Feb. 2020, www.wavy.com/news/health/dutch-euthanasia-center-sees-22-rise-in-requests-in-2019/. Accessed 10 March 2020.
- Davis, Jacky. “Kevin Davis Deserved Choice.” Dignity in Dying, www.dignityindying.org.uk/story/kevin-davis/. Accessed 13 March 2020.
- De La Torre, Esther B. The Right to Assisted Suicide , www.lonestar.edu/rightto-assist-suicide.htm. Accessed 19 March 2020.
- “Euthanasia Laws - Information on the Law about Euthanasia.” Information on the Law about Euthanasia - Suicide, Life, Act, and Mercy - JRank Articles, law.jrank.org/pages/11858/Euthanasia.html. Accessed 10 March 2020.

Cite this Essay
Let us write you an essay from scratch
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Get high-quality help

Verified writer
- Expert in: Social Issues

+ 120 experts online
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
Related Essays
3 pages / 1552 words
1 pages / 670 words
5 pages / 2356 words
2 pages / 1011 words
Remember! This is just a sample.
You can get your custom paper by one of our expert writers.
121 writers online
Still can’t find what you need?
Browse our vast selection of original essay samples, each expertly formatted and styled
Related Essays on Euthanasia
The debate surrounding euthanasia is complex and multifaceted, involving considerations of ethics, religion, personal autonomy, and the value of human life. While advocates argue that euthanasia provides relief to those [...]
Euthanasia, also known as assisted suicide or mercy killing, has been a controversial topic for decades. The ethical, moral, and societal implications of euthanasia have sparked heated debates worldwide. While some argue that it [...]
End-of-life decisions have long been a topic of controversy and debate, with euthanasia being one of the most contentious subjects. Euthanasia or "merciful death" is defined as the act of intentionally ending a life to relieve [...]
Euthanasia, also known as mercy killing, is the act of intentionally ending a person's life to relieve their suffering. This controversial topic has been the subject of much debate and ethical consideration in the medical and [...]
Imagine facing a terminal illness with no hope for recovery, only prolonged suffering and pain. In such situations, the concept of euthanasia, or assisted suicide, becomes a controversial but increasingly relevant topic. [...]
Battin, M. P., Rhodes, R., & Silvers, A. (2015). The Patient as Victim and Vector: Can Ethics Abandon the Ideal of the Autonomous Patient? The American Journal of Bioethics, 15(3), 3-14.Pereira, J. M. (2011). Legalizing [...]
Related Topics
By clicking “Send”, you agree to our Terms of service and Privacy statement . We will occasionally send you account related emails.
Where do you want us to send this sample?
By clicking “Continue”, you agree to our terms of service and privacy policy.
Be careful. This essay is not unique
This essay was donated by a student and is likely to have been used and submitted before
Download this Sample
Free samples may contain mistakes and not unique parts
Sorry, we could not paraphrase this essay. Our professional writers can rewrite it and get you a unique paper.
Please check your inbox.
We can write you a custom essay that will follow your exact instructions and meet the deadlines. Let's fix your grades together!
Get Your Personalized Essay in 3 Hours or Less!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free
- Meeting report
- Open access
- Published: 15 January 2014
Should assisted dying be legalised?
- Thomas D G Frost 1 ,
- Devan Sinha 2 &
- Barnabas J Gilbert 3
Philosophy, Ethics, and Humanities in Medicine volume 9 , Article number: 3 ( 2014 ) Cite this article
69k Accesses
8 Citations
7 Altmetric
Metrics details
When an individual facing intractable pain is given an estimate of a few months to live, does hastening death become a viable and legitimate alternative for willing patients? Has the time come for physicians to do away with the traditional notion of healthcare as maintaining or improving physical and mental health, and instead accept their own limitations by facilitating death when requested? The Universities of Oxford and Cambridge held the 2013 Varsity Medical Debate on the motion “This House Would Legalise Assisted Dying”. This article summarises the key arguments developed over the course of the debate. We will explore how assisted dying can affect both the patient and doctor; the nature of consent and limits of autonomy; the effects on society; the viability of a proposed model; and, perhaps most importantly, the potential need for the practice within our current medico-legal framework.
Introduction
Over the past two centuries, the United Kingdom has experienced rapid population growth associated with a substantial decline in mortality from acute infectious diseases and poor nutrition [ 1 ]. As the average life expectancy has increased, so too have the rates of debilitating chronic illness – particularly coronary artery disease and cancers [ 2 ]. These diseases require years of treatment instead of the mere days to weeks that medicine once operated within [ 2 ]. Although healthcare systems have sought to adapt to such changes, aiming to prevent and treat such disease wherever possible, debate has arisen regarding those patients in the latter stages of chronic, incurable, terminal conditions [ 3 , 4 ]. Moreover, there is increasing recognition that the patient must be at the centre of health care decision-making, such that outcomes must be tailored to their individual needs and views. By extension, assisted dying might seem a logical step to help achieve these goals within the realm of end-of-life decision making [ 5 ]. Several jurisdictions, notably Oregon (1997) and the Netherlands (2001) have already legalised assisted dying in some form. These factors have contributed to ongoing legislative discussions within Parliaments for almost a decade, with current opinion polling suggesting a majority of medical practitioners and the public in favour of physician-assisted suicide [ 6 ].
Viability of assisted dying in practice
In the UK, a model for assisted dying has been developed from the legal structure found within the Assisted Dying Bill introduced by Lord Falconer in the House of Lords in 2013 [ 7 ]. Assisted dying could only be considered under circumstances in which a patient of legal age is diagnosed with a progressive disease that is irreversible by treatment and is “reasonably expected to die within six months” [ 7 ]. Registered medical practitioners would make such decisions for patients with terminal illnesses. Addressing the technicalities of ‘assisted dying’ requires distinction between ‘physician-assisted suicide’ (offering patients medical actions or cessation of actions by which they can end their own life) and ‘euthanasia’ (whereby the medical practitioner actively induces death). In light of the strong hostility of the medical profession towards active euthanasia, this proposed model, as with previous attempts to legalise assisted dying, permitted only the former [ 8 – 10 ].
However, there is concern that such distinction may be unrealistic in practice because medical practitioners could find themselves with a patient who had failed to successfully end their own life and was subsequently left in a state of greater suffering. Were such a patient no longer able to give consent, a heavy burden would then be placed on the physician regarding how to proceed. Moreover, the practice of physician-assisted suicide might be deemed discriminatory, for example by giving only patients with good mobility control over their own method of death.
The Assisted Dying Bill 2013 included the provision that any terminal prognosis must be confirmed and attested by a second registered practitioner. The strictness of such criteria has parallels to a similar double-physician requirement when procuring a legal abortion under the 1967 Abortion Act. The stated aims of the provision in both cases are as follows: first, to check the accuracy of the prognosis upon which the decision was being made; second, to ensure that the situation meets the required criteria; and third, to check that such a decision was taken by the patient after full consideration of all available options [ 11 , 12 ]. By having a second independent doctor, the legislation ensures that all three checks are met without prejudice or mistake.
Problematic for any protocol for assisted dying is the fact that estimates of life expectancy in terminal prognoses are erroneous in 80.3% of cases [ 13 ]. Furthermore, the accuracy of such prognoses deteriorates with increased length of clinical predicted survival. Forecasts of survival times are based largely on past clinical experience, and the inherent variability between patients makes this more of an art than a science. This brings to concern both the accuracy of any prognosis meeting the six-month threshold and the validity of requests for assisted dying based partly or wholly on predicted survival times. Whilst the majority of errors in life expectancy forecasts are a matter of over-optimism and hence would not affect either of those two concerns, many cases remain unaccounted for. Overly pessimistic forecasts occur in 17.3% of prognoses; hence we must decide whether the one in six patients making a decision based on an inaccurate prognosis is too high a cost to justify the use of this system. Patients requesting an assisted death often cite future expectations of dependency, loss of dignity, or pain [ 14 ]. If the hypothetical point at which the progression of their illness means they would consider life to be not worth living is not, as informed, mere weeks away but in fact many more months, then this information would have resulted in a different decision outcome and potentiated unnecessary loss of life.
Whilst the presence of a second doctor would be expected to mitigate such forecasting errors, the anchoring bias of the initial prediction may be enough to similarly reduce the accuracy of the second estimate. It is prudent to question the true independence of a second medical practitioner, and whether this second consultation could become more of a formality, as has now become the case with abortion [ 15 ].
Another challenge for an assisted dying system would be to recognise whether patients requesting death were legally competent to make that decision. Consider that any request for suicide from a patient with clinical depression is generally categorised as a manifestation of that mental disorder, thereby lacking capacity. It is arguably impossible to separate out the natural reactions to terminal illness and clinical depression. Indeed, there is evidence that major depressive disorders afflict between 25% and 77% of patients with terminal illness [ 16 , 17 ]. Any protocol for assisted dying must first determine what qualifies as a ‘fit mental state’ for a terminal patient.
The need for assisted dying
It could be argued that a doctor’s fundamental duty is to alleviate forms of suffering in the best interests of the patient. The avoidance of physical pain, as an obvious manifestation of suffering, might explain why assisted dying would be both necessary and within the duties of a doctor to provide. The evolving principle in common law known as the ‘Doctrine of Double Effect’ offers a solution to this problem [ 18 ]. This legal judgement stated that “[a doctor] is entitled to do all that is proper and necessary to relieve pain even if the measures he takes may incidentally shorten life”. This entails that a protocol already exists for patients searching for an escape from chronic pain. Furthermore, numerous retrospective studies have revealed very little correlation between opioid dose and mean survival times: one study of over 700 opioid-treated patients found that the variation in survival time from high-dose opioid treatment is less than 10% [ 19 – 21 ]. It can therefore be said that pain alone, if appropriately managed, should never be cause for considering assisted dying as an alternative.
By contrast, the ‘Doctrine of Double Effect’ might be seen as a subjective interpretation that has been applied unequally due to a lack of specialist training or knowledge [ 22 ]. Despite this, the principle can be easily understood and poor awareness can be remedied by improvements in medical education and standardisation of protocols. Moreover, should we choose to accept arguments for assisted dying that are based upon inadequate administration of pain medication, we set a precedent for conceding shortcomings in palliative care and other end-of-life treatments. Offering hastened death could become an alternative to actively seeking to improve such failings.
Whilst much has been made of the ‘pain argument’ here, the call for assisted dying is rarely this simple. Many patients also suffer a loss of dignity, often due to their lack of mobility – the inability to relieve oneself without help is a potent example. Beyond this are additional fears of further debilitation and the emotional costs of dealing with chronic illness, both for the patient and for their relatives and friends. A study of terminal patients in Oregon showed that these were the most significant reasons behind requests for assisted suicide, the next commonest reason being the perception of themselves as a ‘burden’ [ 14 ]. Clearly, we could seek to provide balanced, compassionate medical care for these patients, and still fail to address these points.
Developments in healthcare and technology may reduce this emotional burden, but remain an imperfect solution.
Rights of patients and limitations of their autonomy
J.S. Mill’s pithy dictum describes autonomy as follows: “over himself, over his own body and mind, the individual is sovereign” [ 23 ]. Not only has the sanctity of bodily autonomy profoundly influenced the development of liberal democracies, it has also provoked a holistic shift in making our healthcare systems more patient-centred – “care that meets and responds to patients’ wants, needs and preferences and where patients are autonomous and able to decide for themselves” [ 5 ]. The ethical principle of controlling the fate of one’s own body is inherently relevant to the debate on assisted dying. It is difficult to reconcile that citizens may have the right to do almost anything to and with their own bodies– from participating in extreme sports to having elective plastic surgery – yet a terminal patient cannot choose to avoid experiencing additional months of discomfort or loss of dignity in their final months of life.
Expectation of individual liberty has been codified in law. The right to bodily autonomy has been interpreted to be included under Article 8 - the right to privacy - of the European Convention on Human Rights (ECHR) and subsequently the Human Rights Act (HRA) [ 24 , 25 ]. Moreover, the ECHR underpins the right of individuals to ‘inherent dignity’ [ 26 ]. Hence, if an individual feels that dignity is unattainable due to the progression of a terminal illness, then taking recourse though assisted dying ought to be a legitimate option.
Conversely, there are two notable oversights in this interpretation of a right to assisted dying as an extension of the principles of bodily autonomy:
First, it would be wrong to view individual liberty as absolute. The HRA allows for exceptions to Article 8 on grounds of ‘health or morals’ [ 25 ]. The principle of autonomy is not inviolable. Governments have limited such privileges for the protection of individuals and society, for example by criminalizing the use of recreational drugs or the selling of one’s own organs. The preservation of life by denying assisted dying could fall within this category.
Second, the right of autonomy is not necessarily intrinsic to human beings but, as Kant argued, is dependent on our ‘rational nature’ [ 27 ]. This concept sees autonomy as an exercise of ‘evaluative choice’ [ 27 ], requiring rationality on the part of individuals to appreciate the nature of options and their consequences. To achieve true autonomy, there must be sufficient information to make those rational decisions; this is the basis of informed consent and why it is a fundamental duty of a doctor to offer a patient an informed series of treatment options [ 28 ]. The logistical issue is that doctors are unable to advise patients regarding the point at which their situation becomes less preferable to being dead. No doctor (or individual) has any knowledge or experience of what ‘death’ may be like. Hence, in this case, the idea of exercising true autonomy through informed consent might be considered meaningless.
Legalising assisted dying by attempting to establish an absolute right to bodily autonomy may undermine other individual and group rights. Vulnerable patients may feel pressured into assisted dying because of social, emotional, or financial strains placed on family and/or friends. This is exemplified by the trend showing that the proportion of patients stating ‘relief of burden’ on others as the reason for requesting assisted dying has risen from 17% to 25% in Oregon since legalisation [ 29 ]. One could even consider the risk of assisted dying becoming an expected choice rather than a free one. Thus, assisted dying may erode the elemental right to life of terminal patients as the value of their life becomes tied to relative costs to society and to those around them.
Moreover, by creating one class of individuals for whom life is expendable, that particular view may be extended by society to all groups possessing such attributes (e.g. the permanently disabled). There would be a definite risk to the rights of these vulnerable groups in the form of society being less willing to provide for their health and social care.
It is often raised that the limited legalisation of assisted dying would inevitably become extended in scope, but this is not necessarily a flaw. Even if the right to determine the manner of death were later extended to a wider group of people, posterity may reflect positively on such a change, just as extending the franchise to women ultimately led to legislation demanding equal pay.
Effect on health professionals and their role
‘To act in the best interest of the patient’ is often cited as a central duty of the doctor [ 28 ]. This concept of ‘best interest’ guiding the doctor’s action has seen the development of two important ethical principles: beneficence and non-maleficence. Beneficence mandates that the actions of the doctor must be aimed to bring about benefit (clinical improvement) for the patient, usually measured in terms of reduced morbidity or mortality; non-maleficence requires that the doctor not carry out treatment that is likely to cause overall harm the patient [ 30 ]. These traditional ethical imperatives on a doctor both conflict with intentionally hastening the death of a patient, and a resolution of this tension would require redefining what constitutes ‘acting in the best interest’.
A further dimension is the potential reluctance of health professionals to engage in a practice that contravenes their own ethical beliefs, particularly as this would affect doctors who never entered training in the knowledge that assisting patients to die would be an expected duty. This is certainly no argument against the introduction of assisted dying; indeed, a recent survey of a cohort of NHS doctors found that 46% would seriously consider requests from patients to undertake steps to hasten death [ 31 ]. It merely expresses the point that any early model would have to account for the fact that an initial 54% of the doctors in the NHS would be required to advise qualifying patients of assisted dying as a legitimate option, despite disagreeing with it in principle.
Furthermore, doctors who agree ethically with this practice may find themselves facing conflicts of interest. It is expensive to treat chronically ill patients, particularly in the final months of life [ 32 ]. Moreover, it would be difficult for commissioners to ignore the fact that the sustained treatment of one individual could deprive many others from access to surgery or access to novel drugs. Such an argument does not suggest that doctors or any other hospital staff would treat this practice without appropriate respect or care; rather it acknowledges the need for appropriate rationing of care and questions the intentions of service providers. The perception of an ulterior motive could negatively impact patient trust. One survey showed that a reasonable minority of patients (27%) – and particularly particularly the elderly – believe that legalising assisted dying would lessen their trust in their personal physician [ 33 ]. The costs of weakened trust in the doctor-patient relationship could far outweigh the benefits of assisted dying, particularly given the importance of trust when treating a chronic patient for an extended period of time.
There is no doubt that assisted dying would empower some patients to maximise control over the timing and manner of their own death. Such expression of autonomy would surely solidify moves towards a patient-centred approach to healthcare. However, the capacity for such consensual requests remains in doubt. Clinically, the patient’s state of mind and the reliability of diagnostic predictions are of issue; philosophically, the idea of informed consent for death is contradictory. The implications for patients, physicians and society have been weighed extensively within this article. The central tenet throughout has been the balancing of an individual’s right to escape a circumstance that they find intolerable, alongside the consequential changes to their other rights, and the rights and responsibilities of third parties. Ultimately, the challenge is for us as a society to decide where this balance lies.
About the debate
The Varsity Medical Debate was started in 2008 with the aim of allowing students, professors and members of the polis, to engage in discussion about ethics and policy within healthcare. Utilising the age-old rivalry between the two Universities, the debate encourages medical students from both Oxford and Cambridge to consider and articulate the arguments behind topics that will feature heavily in their future careers.
The debate was judged on the logic, coherence, and evidence in arguments, as well as flair in presentation. Although the debaters may not have necessarily agreed with their allocated side, the debate format required them to acknowledge a particular school of thought and present the key arguments behind it. Oxford, who opposed the motion, was awarded the victory in the debate; however, this does not mean that the judges believe that position ought to become public policy.
Colgrove J: The McKeown thesis: a historical controversy and its enduring influence. Am J Public Health. 2002, 92: 725-729. 10.2105/AJPH.92.5.725
Article Google Scholar
Yach D, Hawkes C, Linn Gould C, Hofman K: The global burden of chronic diseases: overcoming impediments to prevention and control. J Am Med Assoc. 2004, 291 (21): 2616-2622. 10.1001/jama.291.21.2616. doi:10.1001/jama.291.21.2616
Lankhorst EK, Spreeuwenberg C: Managing Chronic Conditions. Experience in Eight Countries. European Observatory on Health Systems and Policies. Edited by: Nolte E, Cécile K, Martin MK. 2008, The Netherlands: WHO Regional Office Europe
Google Scholar
Hudson PL, Kristjanson LJ, Ashby M: Desire for hastened death in patients with advanced disease and the evidence base of clinical guidelines: a systematic review. Palliat Med. 2006, 20: 693-701. 10.1177/0269216306071799
Hogg C: Patient-Centred Care - Tomorrow’s Doctors. 2004, GMC
Harris D, Richard B, Khanna P: Assisted dying: the ongoing debate. Postgrad Med J. 2006, 82 (970): 479-482. doi:10.1136/pgmj.2006.047530
House of Lords assisted Dying Bill: House of Lords. 2013, http://www.publications.parliament.uk/pa/bills/lbill/2013-2014/0024/2014024.pdf (accessed 23 October 2013)
House of Lords Assisted Dying for the Terminally Ill Bill: House of Lords. 2005, http://www.publications.parliament.uk/pa/ld200506/ldbills/036/2006036.pdf (accessed 15 Feb 2006)
Sanders K, Chaloner C: Voluntary euthanasia: ethical concepts and definitions. Nurs Stand. 2007, 21 (35): 41-44. 10.7748/ns2007.05.21.35.41.c4554. 10.7748/ns2007.05.21.35.41.c4554
Lee W, Price A, Rayner L, Hotopf M: Survey of doctors’ opinions of the legalisation of physician assisted suicide. BMC Med Ethics. 2009, 10: 2- 10.1186/1472-6939-10-2
House of Commons: Science and Technology Committee, Scientific Developments Relating to the Abortion Act 1967. 2007, London: tso, Volume 1
Royal College of Obstetricians and Gynecologists, Campaigns and Opinions. http://www.rcog.org.uk/what-we-do/campaigning-and-opinions/briefings-and-qas-/human-fertilisation-and-embryology-bill/brie-1
Christakis NA, Lamont EB: Extent and determinants of error in physicians’ prognoses in terminally ill patients. BMJ. 2000, 320: 469-473. 10.1136/bmj.320.7233.469
Ganzini L, Goy E, Dobscha S: Oregonians’ reasons for requesting physician aid in dying. J Am Med Assoc Int Med. 2009, 169 (5): 489-492. doi:10.1001/archinternmed.2008.579
Care Quality Commision. Findings of Termination of Pregnancy Inspections Published. 2012, http://www.cqc.org.uk/media/findings-termination-pregnancy-inspections-published , July
Watson M, Lucas C, Hoy A: Oxford Handbook of Palliative Care. 2005, Oxford: Oxford University Medical Press
Fine R: Depression, anxiety, and delirium in the terminally ill patient. Proc (Bayl Univ Med Cent). 2001, 14 (2): 130-133.
R v Adams [1957] Crim LR 773.
Morita T, Tsunoda J, Inoue S, Chihara S: Effects of high dose opioids and sedatives on survival in terminally ill cancer patients. J Pain Symptom Manage. 2001, 21 (4): 282-289. doi:10.1016/S0885-3924(01)00258-5
Bengoechea I, Gutiérrez S, Vrotsou K, Onaindia M, Lopez J: Opioid use at the end of life and survival in a hospital at home unit. J Palliat Med. 2010, 100828074323069: doi:10.1089/jpm.2010.0031
Thorns A, Sykes N: Opioid use in last week of life and implications for end-of-life decision-making. Lancet. 2000, 356 (9227): 398-399. doi:10.1016/S0140-6736(00)02534-4
Preston T, Patterson J: The rule of double effect. N Engl J Med. 1998, 338: 1389-1391.
Mill JS: “On Liberty” in On Liberty and Other Essays. 14-15.
Human Rights Act. 1998, HMSO
Judgment on the Merits Delivered by a Chamber. Y.F. v. TURKEY, no. 24209, /94, ECHR 2003-IV
McCrudden C: Human dignity and judicial interpretation of human rights. Eur J Int Law. 2008, 19 (4): 655-724. 10.1093/ejil/chn043. doi:10.1093/ejil/chn043
Savulescu J: Autonomy, the Good Life and Controversial Choices. 2006
General Medical Council: Good Medical Practice. 2013, GMC
Oregon Department of Human Services. Fifth Annual Report on Oregon’s Death with Dignity act. http://egov.oregon.gov/DHS/ph/pas/docs/year5.pdf
Campbell : Medical Ethics. 1997, Oxford: Oxford University Press
Ward B, Tate P: Attitudes among NHS doctors to requests for euthanasia. BMJ. 1994, 308: 1332- 10.1136/bmj.308.6940.1332
National Audit Office. End of Life Care : Report by the Comptroller and Auditor General. HC 1043 Session 2007-2008. 2008, NAO
Hall M, Trachtenberg M, Duggan E: The impact on patient trust of legalising physician aid in dying. J Med Ethics. 2005, 31 (12): 693-697. doi:10.1136/jme.2004.011452
Download references
Acknowledgements
For Cambridge University: Hilmi Bayri (Trinity), Alistair Bolger (Jesus), Casey Swerner (St Johns).
For Oxford University: Devan Sinha (Brasenose), Thomas Frost (Lincoln), Collis Tahzib (Lincoln).
Martin Farrell (Cambridge).
Baroness Finlay: Professor of Palliative Care Medicine and former President of the Royal Society of Medicine.
Dr. Roger Armour: Vascular Surgeon and Inventor of the Lens Free Ophthalmoscope.
Mr. Robert Preston: Director of Living and Dying Well.
Author information
Authors and affiliations.
Lincoln College, Turl Street, Oxford, OX1 3DR, UK
Thomas D G Frost
Brasenose College, Oxford, OX1 4AJ, UK
Devan Sinha
Green Templeton College, Woodstock Road, Oxford, OX2 6HG, UK
Barnabas J Gilbert
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Barnabas J Gilbert .
Additional information
Competing interests.
The authors declare that they have no competing interests.
Authors’ contributions
All authors planned and elucidated the layout. TDGF and DS drafted the manuscript which was critically edited and added to by BJG. All authors have read and approved the final draft.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver ( https://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Frost, T.D.G., Sinha, D. & Gilbert, B.J. Should assisted dying be legalised?. Philos Ethics Humanit Med 9 , 3 (2014). https://doi.org/10.1186/1747-5341-9-3
Download citation
Received : 12 November 2013
Accepted : 11 January 2014
Published : 15 January 2014
DOI : https://doi.org/10.1186/1747-5341-9-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Assisted dying
- Legalisation
- Physician-assisted suicide
Philosophy, Ethics, and Humanities in Medicine
ISSN: 1747-5341
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Skip to main content
- Keyboard shortcuts for audio player
Intelligence Squared U.S.
Debate: should physician-assisted suicide be legal.

Bioethicist Peter Singer argues that, under certain circumstances, people should have the right to die at a time of their choosing. Samuel La Hoz/Intelligence Squared U.S. hide caption
Bioethicist Peter Singer argues that, under certain circumstances, people should have the right to die at a time of their choosing.
Since Oregon legalized physician-assisted suicide for the terminally ill in 1997, more than 700 people have taken their lives with prescribed medication — including Brittany Maynard, a 29-year-old with an incurable brain tumor, who ended her life earlier this month.
Advocates of assisted-suicide laws believe that mentally competent people who are suffering and have no chance of long-term survival, should have the right to die if and when they choose. If people are have the right to refuse life-saving treatments, they argue, they should also have the freedom to choose to end their own lives.
Opponents say that such laws devalue human life. Medical prognoses are often inaccurate, they note — meaning people who have been told they will soon die sometimes live for many months or even years longer. They also argue that seriously ill people often suffer from undiagnosed depression or other mental illnesses that can impair their ability to make an informed decision.
At the latest event from Intelligence Squared U.S. , two teams addressed these questions while debating the motion, "Legalize Assisted Suicide."
Before the debate, the audience at the Kaufman Music Center in New York was 65 percent in favor of the motion and 10 percent against, with 25 percent undecided. After the debate, 67 percent favored the motion, with 22 percent against, making the team arguing against the motion the winner of this debate.
Those debating:
Web Resources
FOR THE MOTION
Peter Singer is a philosopher and author, best known for his work in ethics. He is the Ira W. DeCamp Professor of Bioethics in the University Center for Human Values at Princeton University, a position that he now combines with the part-time position of Laureate Professor at the University of Melbourne. Some of his more recent books include The Point of View of the Universe and The Life You Can Save: Acting Now to End World Poverty . In 2014 the Gottlieb Duttweiler Institute ranked him third on its list of Global Thought Leaders, and Time has ranked him among the world's 100 most influential people. An Australian, in 2012 he was made a Companion to the Order of Australia, his country's highest civilian honor.
Andrew Solomon is a writer, lecturer and a professor of clinical psychology at Columbia University. Solomon's newest book, Far From the Tree: Parents, Children, and the Search for Identity , won the National Book Critics Circle award for nonfiction and was chosen as one of the New York Times "Ten Best Books" of 2012. Solomon's previous book, The Noonday Demon: An Atlas of Depression won the National Book Award for nonfiction and was a finalist for the Pulitzer Prize. He is a director of the University of Michigan Depression Center and Columbia Psychiatry; a member of the board of visitors of Columbia University Medical Center; serves on the national advisory board of the Depression Center at the University of Michigan, and on the advisory board of the Depression and Bipolar Support Alliance. In 2011, he was appointed special advisor on Lesbian, Gay, Bisexual, and Transgender Mental Health at the Yale School of Psychiatry.

Dr. Daniel Sulmasy, with debate partner Ilora Finlay, argues that policies legalizing physician-assisted suicide are unethical. Samuel LaHoz/Intelligence Squared U.S. hide caption
Dr. Daniel Sulmasy, with debate partner Ilora Finlay, argues that policies legalizing physician-assisted suicide are unethical.
AGAINST THE MOTION
Baroness Ilora Finlay , a leading palliative care physician, is president of the British Medical Association, president of the Chartered Society of Physiotherapy, and is a past president of the Royal Society of Medicine. She has led the Palliative Care Strategy Implementation Board in Wales since 2008, and chaired the Welsh Medical and Dental Academic Advisory Board since 2012. Finlay was a general practitioner in inner-city Glasgow before returning to Cardiff to work full-time in care of the terminally ill. She works at the Velindre Cancer Centre, covering South East Wales when clinically on call. Finlay started the Marie Curie Hospice in Wales and since 2008 has responsibility on behalf of Welsh Government for strategic oversight of all hospice and palliative care services in Wales. Since 2001, Finlay has been an Independent Crossbench Peer in the House of Lords.
Dr. Daniel Sulmasy is the Kilbride-Clinton Professor of Medicine and Ethics in the Department of Medicine and Divinity School at the University of Chicago, where he serves as associate director of the MacLean Center for Clinical Medical Ethics and as director of the Program on Medicine and Religion. Sulmasy was appointed to the Presidential Commission for the Study of Bioethical Issues by President Obama in 2010. His research interests encompass both theoretical and empirical investigations of the ethics of end-of-life decision-making, ethics education and spirituality in medicine. He is the author or editor of six books, including Safe Passage: A Global Spiritual Sourcebook for Care at the End of Life . He also serves as editor-in-chief of the journal, Theoretical Medicine and Bioethics .
- physician-assisted suicide
- Harvard Division of Continuing Education
- DCE Theses and Dissertations
- Communities & Collections
- By Issue Date
- FAS Department
- Quick submit
- Waiver Generator
- DASH Stories
- Accessibility
- COVID-related Research
Terms of Use
- Privacy Policy
- By Collections
- By Departments
Euthanasia and the Law: The Rise of Euthanasia and Relationship With Palliative Healthcare
Citable link to this page
Collections.
- DCE Theses and Dissertations [1331]
Contact administrator regarding this item (to report mistakes or request changes)

Legalizing Euthanasia
- Markkula Center for Applied Ethics
- Focus Areas
- Bioethics Resources
Medical Perspectives on Death and Dying
Several states have begun to consider legislation that would legalize active voluntary euthanasia.
Several states have begun to consider legislation that would legalize active voluntary euthanasia. To address some of the ethical issues raised by such legislation, the Center for Applied Ethics sponsored a symposium entitled Legalizing Euthanasia: Ethical Perspectives on Medicine and Dying . Principal speakers were Derek Humphry, founder and president of the Hemlock Society, and author of the current best-seller, Final Exit , a suicide manual for the terminally ill; and Richard Gula, S.S., Ph.D., a professor of moral theology at St. Patrick's Seminary in Menlo Park, California. The symposium was funded in part by the California Council for the Humanities, a state program of the National Endowment for the Humanities. The following excerpts highlight the remarks of Mr. Humphry and Father Gula.
Derek Humphry Let me explain how I became involved with the subject of euthanasia. In 1974 my first wife, Jean, was dying of bone cancer. Thrombosis had set in, her bones were cracking and she was losing control of her bowels. One day, after a very close brush with death, she sat up in her hospital bed and said to me, "Will you help me die?" That is when I first encountered the issue of euthanasia; from across my late wife's hospital bed.
After she made her request, I asked myself, "What if I were sitting in that hospital bed? What if I had had two years of pain and agony? What if I faced an imminent death? What if I was losing control of my bowels and my bones were cracking and so-forth?" I realized then that I would be asking her to help me to die. That, ladies and gentlemen, is my simple reason for what I did. It was an act of love.
Jean had been a good wife to me for 22 years. She stood by me in good times and bad. And when she was experiencing a bad time, I felt it was my duty to support her in her decision. I am not a Christian. I am an atheist. So, for me there was no question of consulting any god. It was a matter of situational ethics.
In 1980, five years after Jean's death, I helped to establish the Hemlock Society. This organization seeks to change certain laws regarding suicide. We want the government to decriminalize the actions taken by physicians in the assisted suicides of terminally ill patients.
We believe that a mentally competent adult who is dying should be able to submit a written request to their doctor that would state, "I've had all I can take. The pain and suffering are too much. I wish to die. Help me."
The physician, according to the Hemlock movement's prepared law, would have to obtain the opinion of a second doctor. They would both have to agree that the person is dying. The first doctor could then end the life of the patient with an oral or intravenous drug overdose, without the threat of prosecution or lawsuit. Our laws also state that the doctor could elect not to assist the patient with such an action.
There are those who agree with what the Hemlock movement is saying at the present time, but are fearful that such an ideology would result in a system of euthanasia similar to that used by Nazi forces. It is true that the Nazis introduced a program which they called euthanasia. They murdered about 100,000 people who were physically or mentally handicapped. No senior citizens or terminally ill people were allowed to voluntarily end their own lives.
But how can you say to a person who is dying of throat cancer today that they cannot have voluntary euthanasia because of what the Germans did in 1940 and 1942? I think that the person would respond, "It's not relevant. It's me. It's my body. It's my liberty. It's my life. And it's my death. Let me have control."
I would claim that this is the ultimate civil liberty. If we cannot go to our deaths in the manner of our own choosing, what liberty do we have?
Richard Gula Most of the focus on euthanasia so far has been dominated by what I'm going to call the paradigm of individual case analysis. My position is that euthanasia is not primarily an individual issue; it's a societal one. So discussion about euthanasia should not be governed primarily by individual case ethics, but by societal ethics.
The sanctity of life principle is probably the common ground principle. There are two extreme positions that can give sanctity of life as a principle a bad name. One extreme is what I call vitalism, and that is the extreme that tries to absolutize physical life making an idol out of biological existence. This principle says no cost is too great to keep this biological life going. The other extreme interpretation leads to what I'm calling a utilitarian perspective, which values life for its usefulness. This is the interpretation that says only the strongest and the fittest ought to survive. The danger here is the abuse of undertreatment.
I want to think about the sanctity of life from the middle position. This is the interpretation of the principle that recognizes we have limited dominion over life. It's the interpretation that says we are stewards of life, that we ought to care for life and promote it and enhance it in order to allow our lives to flourish and to achieve our potential. This is the interpretation that wants to respect life in all its forms and in all its stages. Interpreting sanctity of life in this way entails two obligations: a positive one--to nurture and support life„and a negative obligation not to harm life. Therefore, to appeal to sanctity of life in a discussion of euthanasia is to create a presumption in favor of life.
The second principle is the principle against the prohibition of killing. I want to look at three ways of interpreting this principle. The first says there is no moral difference between killing and allowing to die -- that once you decide that life no longer needs to be sustained, because the use of treatment would be futile, then it makes no difference whether you actively intervene or simply withhold or withdraw treatment.
The second interpretation is that there is a qualified moral difference. That qualified moral difference is that the distinction holds but gives way at a certain point. Some will say when the person has gone beyond the reach of human care, when there is no longer the capacity to receive love, or to receive comfort, then the distinction dissolves. Others will say when the person is in intractable pain and there's nothing more that can be done to relieve the pain, then the distinction between killing and allowing to die dissolves. Others would say when the patient is overtaken by the dying process -- that is to say, once you have decided that nothing more needs to be done, that life has reached its limits, then it makes no difference whether you withhold treatment or intervene, because in that condition, you are not usurping the dominion that is not yours. Then there's the third position that says the distinction holds all the way through.
The next principle is the principle of autonomy, which is probably going to be at the core of this discussion of whether euthanasia ought to be legalized. In our culture, we interpret autonomy as the right to self determination. The prevailing interpretation of autonomy in our culture is that autonomy is there to maximize self-interest. That means that we are able to pursue our own goals and life plans without external constraints. When we interpret autonomy this way, we answer the question "whose life is it anyway?" in favor of the one whose life is in question. This is solid ground for supporting euthanasia.
Can the principle of autonomy be used to challenge euthanasia? Some argue that the very interpretation of autonomy that says that you have the freedom to have another person intervene to take your life is a contradiction of what autonomy means -- that actually what you're doing is giving away your freedom. The other way of looking at it is to say that euthanasia is not primarily a private affair. It's a public or societal action that involves others, and therefore it is something that ought to be treated as a form of public action.
The third principle is the principle of the common good. To show that euthanasia ought to be sanctioned as a public practice, we need to be able to show that we can justify it in more than the individual case. This is the principle that says that when we establish a policy, we are sanctioning actions as a common practice. When we apply that principle to euthanasia, we need to ask, "how does the goal of my own private killing contribute towards making society the context in which human life can flourish?"
Now let's turn to the perspective of virtue. Virtue asks whether or not a policy on euthanasia creates the right kind of relationship between the physician and the patient, and would a policy on euthanasia create the right kind of community in which health care is delivered. The perspective of virtue asks that the physician deliver compassionate care within the limits of the physician's role. The trust that we extend to the medical profession to heal and protect life is something that we would want to sustain and the perspective of virtue asks whether that kind of trusting relationship would be enhanced or hindered if euthanasia became part of the options that are available to the physician. The perspective of virtue looks on ourselves as a community of interdependents in which we are partners to one another. It sustains the community of trust and care by promising not to abandon anyone, and it tries to be realistic about accepting the limits about what it means to be human. We recognize that life will not be free of suffering, that life will be burdensome, and there will be tragedy. The perspective of virtue tries to be realistic about accepting that. It encourages us to construct structures of support which will enable us to raise those who suffer into the network of the supportive, caring community.
Ultimately we cannot convert individual cases into public policy without having something remaining. The common good resists the temptation. How do the burdens to one individual compare to the burdens and the benefit on society as a whole? I think all of this ultimately is going to turn not on the basis of principles we argue with, but on the kind of people we are. Are we a virtuous people that creates a community of caring or are we going to compromise that in the way we allow euthanasia to become a practice in our healing society?
Videotapes of the symposium are available for $16.50 by writing to the Center for Applied Ethics, Santa Clara University, Santa Clara, CA 95053.
This article was originally published in Issues in Ethics - V. 5, N. 2 Fall 1991
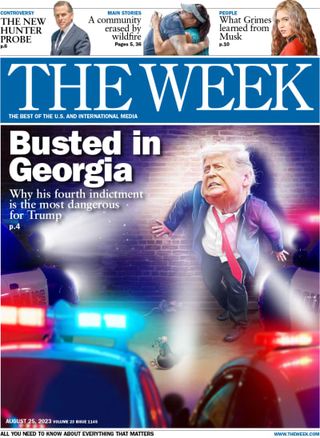
The pros and cons of legalising euthanasia
Help to end suffering for terminal patients could put disabled, elderly and unwell people at risk, opponents warn
- Newsletter sign up Newsletter

Pro: an end to suffering
Con: losing legal protection, pro: ending 'mercy killings', con: 'slippery slope', pro: shifting opinion, con: religious concerns.
Demonstrations calling for the decriminalisation of assisted dying are to take place in central London today to coincide with a debate among MPs in Westminster.
The Commons debate – which will not be followed by a vote – was triggered after a petition backed by campaigner Esther Rantzen gained more than 200,000 signatures.
Rantzen, who has stage four lung cancer, revealed last year that she had joined the assisted dying clinic Dignitas, in Switzerland, but that under current UK law her family could be at risk of prosecution if they helped her travel there to end her life.
Subscribe to The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.
Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
"The Great British Bake Off" judge Prue Leith, actor Susan Hampshire and rights campaigner Peter Tatchell are all expected to attend the protests calling for a change in the law. A previous bill in favour of assisted dying was defeated in the Commons by 330 votes to 118 in 2015.
Also known as euthanasia , assisted dying is a controversial issue for legislatures worldwide, with widely cited arguments both for and against a practice that is legal in some countries while totally taboo in others.
It is currently banned in England, Wales, and Northern Ireland – although not a specific criminal offence in Scotland – and carries a maximum prison sentence of 14 years.
Allowing patients to end their suffering is not only morally justified but also essential to upholding the right to personal and bodily autonomy, advocates argue.
A major parliamentary inquiry set up last year to explore whether assisted dying should be legalised in the UK received tens of thousands of submissions from people facing "uncontrollable" pain and "unbearable suffering", which palliative care alone cannot fix, The Guardian reported.
Paul Lamb, a paralysed former builder from Leeds who died in June 2021, had lost his legal case to challenge UK laws on assisted dying seven months earlier.
"I cannot understand, in a civilised society like ours, why I should be forced to suffer when millions of people around the world already have the choice I asked for," he said in November 2020.
It is currently a criminal offence under the 1961 Suicide Act to help someone take their own life, punishable by up to 14 years in prison.
Some people believe that legalising euthanasia would put too much power in the hands of doctors, who could abuse their position, or relatives.
Rita Marker, executive director of the International Task Force on Euthanasia and Assisted Suicide in the US, has argued: "Euthanasia and assisted suicide are not about the right to die. They are about the right to kill."
The UK's anti-euthanasia Care Not Killing alliance said that the law is also in place to protect the vulnerable "from being pressured into ending their lives".
Making her case against any law change, Ilora Finlay, a crossbench peer and palliative care physician, told the parliamentary inquiry that legalising euthanasia in Britain could result in between 5,800 and 58,000 assisted deaths a year, based on extrapolated data from countries where it is already legal. "Such demand would divert an already stretched workforce of NHS clinicians," she said.
According to Dignity in Dying , 44% of people would break the law and help a loved one to die, risking 14 years in prison.
In 2022 the Crown Prosecution Service (CPS) said it was considering revising its stance on so-called mercy killings so that defendants are less likely to face criminal charges.
"We are not decriminalising any offence," Max Hill, director of public prosecutions and head of the CPS, told the i news site, but in offences "born solely out of compassion", justice can sometimes "be achieved by not prosecuting".
Campaigners claim that UK police are also increasingly turning a blind eye to people travelling to other countries to assist loved ones to end their life.
Opponents argue that normalising euthanasia would be a move towards legalised murder.
This "slippery slope is real", said James Mildred of Care (Christian Action Research and Education), which campaigns against assisted suicide. In a 2018 article in The Economist , Mildred cited "a steady increase year on year in the number of people being killed or helped to commit suicide by their doctors" in countries that have legalised assisted suicide, as the rules are loosened over time.
"Critics say this is happening in Canada," said New Scientist , "with the criteria for assisted dying having expanded once already and a further change planned for next year." Canada, which introduced Medical Assistance in Dying, or MAID, in 2016, has seen the number of people choosing to end their life rise steadily ever since, with MAID deaths comprising 4.1% of all deaths in 2022.
There has been a significant shift in recent years among both the public and professional medical opinion regarding assisted dying for people with a terminal illness.
Polling for The Guardian last August found 65% of people in the UK believe it should become legal for a doctor to assist an adult of sound mind with less than six months to live to voluntarily end their own life, subject to High Court confirmation.
Dignity in Dying claims this number is even higher, and also that 54% of GPs are supportive or neutral to a law change on assisted dying.
Many religious people, especially Catholics, believe that life is the ultimate gift and that taking that away is usurping power that belongs to God only.
In 2020, the Vatican reiterated the Roman Catholic Church's opposition to assisted suicide and euthanasia, describing them as "intrinsically evil" acts "in every situation or circumstance", The New York Times reported.
Sign up for Today's Best Articles in your inbox
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com

In The Spotlight Republicans expected to make hay from Biden Junior's latest legal entanglement
By Chas Newkey-Burden, The Week UK Published 3 June 24

The Explainer Officials 'openly threatening' to build nuclear bomb, as watchdog finds large increase in enriched uranium stockpile
By Harriet Marsden, The Week UK Published 3 June 24

Today's Big Question Turbulent coalition talks 'could decide between two very different directions' for the country
By Elliott Goat, The Week UK Published 3 June 24
- Contact Future's experts
- Terms and Conditions
- Privacy Policy
- Cookie Policy
- Advertise With Us
The Week is part of Future plc, an international media group and leading digital publisher. Visit our corporate site . © Future US, Inc. Full 7th Floor, 130 West 42nd Street, New York, NY 10036.
You are using an outdated browser. Upgrade your browser today or install Google Chrome Frame to better experience this site.
Mercy killing debate: should euthanasia be legalized?

Source: This image was created for netivist.org. If you want to use it you simply need to attribute it by linking to this page or to https://netivist.org . Thanks
Many new cases of physician-assisted suicide or mercy killing are emerging in Western countries. Some of them have regulated it. Do you think euthanasia should be legalized? Under what circumstances? Do we have the right to die as we choose?
Mercy Killing Debate
Euthanasia or physician- assisted suicide , also know as mercy killing , is becoming a prominent public debate . The implications of legalizing assisted suicide are wide-ranging from a medical , legal, political and ethical point of view.
The term euthanasia means "good death" in Greek. With the progress of medicine in multiple domains (e.g. anesthesiology, pain medicine) came the problem of the decision of death. Some countries, like for instance Belgium, The Netherlands, and some states in the USA, including New Mexico, Montana, Oregon and Vermont, have passed laws allowing voluntary euthanasia. But the legality of choosing the moment of death is an extremely controversial subject because it appeals to personal views on ethics and morality and is highly emotional and linked to religious beliefs. Most countries still consider euthanasia a crime . Some people consider allowing euthanasia to risk opening a slippery slope where killing may become more common, and risk the killing of people misinformed or against their will. These people also worry about the risk of killing any person with some sort of suffering (e.g. mental disability, physical handicap). Supporters of euthanasia claim it is an individual right to decide when to die, to keep control of their fate when it is still possible.
Types of euthanasia
There are different types of euthanasia according to whether the will of the patient has been expressed.
- Voluntary euthanasia : to intentionally end the life of someone who asked for it to relieve physical pain and psychological suffering. It can be considered as assisted suicide. Patient gives informed consent. An official signed document in which one declares one wants to be euthanized.
- Non-voluntary euthanasia : consent of the patient is unavailable. Usually family members are asked about the possible will of the patient as well as their own wish.
- Involuntary euthanasia is against the patient’s will and is illegal, considered as murder, in most countries.
Euthanasia can also be divided into:
- Passive euthanasia: when the family or medical staff withhold life support (e.g. medication, respiratory machine, feeding or liquids) from the patient.
- Active euthanasia: when the patient is administered (e.g. injected) a lethal dose of any chemical substance to end her/life.
And you? Do you support mercy killing ? Should euthanasia be legalized? Before voting and commenting you may want to consider the pros and cons of legalizing physician-assisted suicide (see below).
Watch this video on the mercy killing debate
Euthanasia pros and cons
- Dying with dignity: some people are deeply sick, postrated and unable to do even the most basic human actions, such as eating, changing clothes, washing themselves or using the toilets. They often find their state degrading and humilliating and may prefer to die with dignity and stop being a burden to those around them.
- End to human suffering: people with terminal illness and no chance of recovery often suffer great physical pain and emotional distress. Ending their lives, if they wish so, can spare them from an unnecessary suffering.
- Legal certainty: according to research conducted in the Netherlands, regulating euthanasia has improved legal certainty and has contributed to the carefulness of assisted suicide.
- Healthcare spending: keeping alive terminal patients who are suffering and not able to recover is also very expensive and detracts medical resources from other patients who could heal or need treatments. Families of the patients who want to end their lives may also face bills which can very negatively affect their finances.
- Autonomy and self-determination: opposing to someone's will of ending her/his life goes against that person freedom and right of deciding on their future.
- Moral and ethical problems: physician assisted death clashes with religious beliefs. Many religions state that human life end should not be decided by people but by God.
- Misunderstandings and errors: there are cases in which doctors have wrongfully diagnosed a terminal disease or have thought that a patient is without hope of recovery. However, medicine evolves and cures may be found. Some new treatments may become effective were others failed. So terminating someone's life even with her/his consent may be a mistake.
- Legalizing murder: regulating euthanasia for some extreme cases may mean crossing a line. It has been argued that this could be a slippery slope which could end up with the legalization of an increasing number of cases for ending a life for utilitarian reasons.
- Abuse: if euthanasia is legal, there may be an incentive to exaggerate the negative condition of patients so that the family decides to "disconnect" them so that the hospital or insurance company saves money.
- Complexity: even if countries decide to legalize euthanasia, there may be great difficulties in agreeing with the cases and situations in which these mercy killings are acceptable and with the legal procedures that should be respected.
Taking all these pros and cons into consideration and the experience in the territories where it has been legalized, what would you recommend doing?
You may also want to participate in our debates on the legalization of cannabis , prostitution , and same sex marriage .
Vote to see result and collect 1 XP. Your vote is anonymous. If you change your mind, you can change your vote simply by clicking on another option.
Voting results
New to netivist?
Join with confidence, netivist is completely advertisement free. You will not receive any promotional materials from third parties.
Or sign in with your favourite Social Network:
Join the debate
In order to join the debate you must be logged in.
Already have an account on netivist? Just login . New to netivist? Create your account for free .

Report Abuse and Offensive language
Was there any kind of offensive or inappropriate language used in this comment.
If you feel this user's conduct is unappropriate, please report this comment and our moderaters will review its content and deal with this matter as soon as possible.
NOTE: Your account might be penalized should we not find any wrongdoing by this user. Only use this feature if you are certain this user has infringed netivist's Terms of Service .
Our moderators will now review this comment and act accordingly. If it contains abusive or inappropriate language its author will be penalized.
Posting Comment
Your comment is being posted. This might take a few seconds, please wait.
Error Posting Comment
error.
We are having trouble saving your comment. Please try again .
Most Voted Debates
Start a Debate
Would you like to create a debate and share it with the netivist community? We will help you do it!
Found a technical issue?

Are you experiencing any technical problem with netivist? Please let us know!
Help netivist
Help netivist continue running free!
Please consider making a small donation today. This will allow us to keep netivist alive and available to a wide audience and to keep on introducing new debates and features to improve your experience.

- What is netivist?
- Entertainment
- Top Debates
- Top Campaigns
- Provide Feedback

Follow us on social media:

Share by Email
There was an error...
Email successfully sent to:

Join with confidence, netivist is completely advertisement free You will not recive any promotional materials from third parties
Join netivist
Already have a netivist account?
If you already created your netivist account, please log in using the button below.
If you are new to netivist, please create your account for free and start collecting your netivist points!
You just leveled up!
Congrats you just reached a new level on Netivist. Keep up the good work.

Together we can make a difference
Follow us and don't miss out on the latest debates!
Euthanasia – For Legalizing
There are many arguments for and against legalizing euthanasia. It has ethical benefits as well as downsides. Should euthanasia be legalized? Essay samples like this one will help you understand the issue.
Introduction
There is no respect for autonomy, justice is denied, sympathy for the suffering of others, individual liberty vs. state interest, the voice of the u.s. public.
The legality issue of Euthanasia has been a subject of heated debate since long. On the global scene, the Netherlands was the first country to legalize Euthanasia in April 2002, followed a month later by Belgium.
Switzerland legalized the practice in December 2005 (Reuters U.K). In the U.K where public support for legalization of Euthanasia rose from 69% in 1976 to 82% in 2004, it is widely expected that Parliament will soon legalize the practice (News-medical.net).
In the U.S, many states have been debating the legality issue of Euthanasia but only Oregon has legalized it since 1997 (Reuters U.K). It is my contention that Euthanasia should be legalized all over the country.
The word ‘Euthanasia’ comes from the Greek word ‘Euthanatos’ meaning ‘good health.’ Euthanasia is defined as the deliberate ending of a person’s life by anther person at the specific request of the former. Euthanasia is not the same as other practices such as Physician-Assisted Suicide, Terminal Sedation or Withholding/Withdrawing Life-Sustaining Treatments.
Physician-Assisted Suicide takes place when a physician, responding to specific request from patients, gives information {for example, a prescription for a fatal dose of sleeping pills}, and/or the means {such as a supply of carbon monoxide gas} of committing suicide to patients so that they can easily hasten their death (Religious tolerance.org).
Terminal Sedation occurs in cases where the physician administers sufficient sedatives to cause a terminally ill, competent patient to become unconscious, then permitting the patient to die of starvation, dehydration and the disease which has been contracted (Braddock et al.).
Withholding/Withdrawing Life-Sustaining Treatments takes place where a competent patient refuses to continue taking on-going life-sustaining treatment (Braddock et al.) such as the use of ventilators, dialysis, intravenous fluids and feeding tubes.
There are 3 kinds of Euthanasia. Active Euthanasia takes place when a person is put to death as a direct consequence of a request from him or her.
A famous example is the 1998 case involving Jack Kevorkian who caused the death {by lethal injection} of a patient suffering from ALS {Lou Gehrig’s Disease} who begged for a swift and painless death. Passive Euthanasia occurs when the death of a person is speeded up by changing some type of life-support being administered to him or her, thereby paving the way for nature to take its own course.
Examples of Passive Euthanasia include unplugging a respirator, ceasing administration of medications or not performing CPR {cardio-pulmonary resuscitation} on a person whose heart has ceased functioning. Involuntary Euthanasia involves putting to death persons who have not specifically asked for assistance in dying.
This usually occurs in case of those who have slipped into a Persistent Vegetative State and will in all likelihood never regain consciousness (Religioustolerance.org).
Taking decisions about the time and method of one’s death is considered very personal and confidential. Persons who are terminally ill patients with deadly diseases like ALS, AIDS, Alzheimer’s or Multiple Sclerosis know they will soon die and simply want to exercise control over the process. They cannot tolerate the loss of personal dignity as they are no longer self-sufficient, but have to constantly depend on others for care (Religioustolerance.org).
Secondly, such terminally ill persons do not wish to reduce their financial assets by having to constantly pay massive hospital bills as their death draws nearer; they would prefer to die quickly so that their inheritors of their assets will benefit to a greater degree by way of savings of such heavy hospital expenses.
Heavily underlying these reasons is the inescapable fact that they are living in excessive, chronic pain fully knowing that there is no cure for their ailment and that death is inevitable (Religioustolerance.org).
The Constitution of the country dictates that all persons have the freedom of choice. The freedom of choice in this case refers to the right of all persons – whether in good health, slightly ill or terminally ill – to choose if they want to go on living or if they are restrained so heavily by circumstances such as terminal illness to take the decision that they do not want to continue living and that they would be better off dead.
By not legalizing Euthanasia, terminally ill patients are denied the right to court speedier death by taking matters into their own hands. For some of them, death does not come as speedily as they wish, with the result that they have only one option left – death (Braddock et al.). By denying them the right to escape a life of pain that will anyway end in nothing by death, the State is denying terminally ill persons their Constitutional right
Some illnesses, besides causing intense physical suffering, also cause unbearable psychological burdens to patients (Braddock et al.). A classic example is AIDS. Sufferers of this disease endure horrific suffering as the disease progresses. Their bodily resistance steadily deteriorates, weakness sets in and they literally wither away to death.
Their physical anguish is accompanied by extreme mental suffering as they know that even with the best treatment, their burden of physical and metal suffering will at the most be slight, and that too temporarily, relieved but the onset of death is inevitable.
If these patients may request Euthanasia hasten death, do their loved ones not have the moral duty to end their physical and metal suffering? The key word in this scenario is ‘inevitability.’
The persons who have been entrusted by the patient to administer Euthanasia knows that death is inevitable, therefore, if such death is allowed to come in earlier than scheduled, it is a matter of showing sympathy for the suffering of the patient. In this context, Euthanasia is seen as a compassionate reaction to intense suffering.
There is no doubt that the State has a strong interest in preserving the life of its citizens. It is understandable and widely expected as a sign of a well-run State because such interest stems from the responsibility entrusted to the State.
Therefore when the State takes precautionary measures to safeguard its citizens such as apprehending thieves and muggers, or interning drug dealers and human smugglers, or punishing rapists and wife batterers, or sentencing serial killers to life imprisonment or capital punishment, these actions are viewed as signs of a government correctly doing the job that it was elected to do.
However, when it turns into a matter of private {as opposed to the above various forms of public safeguards}, the intensity of such State interest does not match the interest of terminally ill individuals who opt for death to end life. This lopsided {against the State} level of interest, if strengthened by prohibition by the State, is seen as an infringement on the personal liberty of the individual (Braddock et al.).
Perhaps the greatest U.S President of all time, Abraham Lincoln, described democracy as a rule “by the people, of the people and for the people.” It therefore follows that in this great democracy called the United States of America, it is the voice of the people that is paramount.
It also therefore follows that the voice of the people in case of legalizing Euthanasia should be treated with the greatest of importance. The voice of the people states that Euthanasia should be legalized.
While almost all the U.S states may have been intimated by the 1997 U.S Supreme Court landmark ruling against Euthanasia, the U.S public certainly has not been similarly affected. A 2005 Harris Poll involving 1,010 adults in the U.S discovered that as many as 64% of them disagreed with the 1997 Supreme Court ruling.
It was therefore not surprising that the same poll also found that 70% of them were in favor of legalizing Euthanasia. The greatest support was reserved for Involuntary Euthanasia with an overwhelming 72% of respondents declaring that they would go to the extent of expressly authorizing the administration of Euthanasia against themselves in their last wills and testaments (Taylor).
In addition to the above cited arguments, hard facts show that the most potent argument against legalizing Euthanasia {that it will increase the number of deaths of terminally ill persons} has been soundly refuted. Data from areas that have legalized Euthanasia do not show any marked changes as a result of this action. A good example is the U.S state of Oregon.
Ever since the passing of the Death with Dignity Act, the number of Euthanasia cases has hardly registered any noticeable change as compared to data of previous years. But what did change however, in Oregon as well as all those nations that have legalized Euthanasia, is the great relief that was made available to terminally ill patients – much needed relief that was cruelly denied to them before such legalization.
Their relief has been well articulated by Professor Torbjorn Tannsjo: “They [terminally ill patients] would know that, if, when their turn comes, and things turn out to be terrible, they have a way out” (News-medical.net).
Braddock C.H. & Tonelli M.R. “Physician-Assisted Suicide.” University of Washington. 2008.
“ British Medical Journal Publishes Euthanasia Opinions .” News-medical.net. 2005.
“ Euthanasia & Physician-Assisted Suicide .” Religioustolerance.org. 2002.
“ FACTBOX – Legal Status of Euthanasia around the World .” Reuters U.K. 2007.
Taylor, H. “Poll: U.S Adults Favor Euthanasia & Physician Assisted Suicide.” Death with Dignity National Center. 2005.
Cite this paper
- Chicago (N-B)
- Chicago (A-D)
StudyCorgi. (2020, January 10). Euthanasia – For Legalizing. https://studycorgi.com/euthanasia-for-legalizing/
"Euthanasia – For Legalizing." StudyCorgi , 10 Jan. 2020, studycorgi.com/euthanasia-for-legalizing/.
StudyCorgi . (2020) 'Euthanasia – For Legalizing'. 10 January.
1. StudyCorgi . "Euthanasia – For Legalizing." January 10, 2020. https://studycorgi.com/euthanasia-for-legalizing/.
Bibliography
StudyCorgi . "Euthanasia – For Legalizing." January 10, 2020. https://studycorgi.com/euthanasia-for-legalizing/.
StudyCorgi . 2020. "Euthanasia – For Legalizing." January 10, 2020. https://studycorgi.com/euthanasia-for-legalizing/.
This paper, “Euthanasia – For Legalizing”, was written and voluntary submitted to our free essay database by a straight-A student. Please ensure you properly reference the paper if you're using it to write your assignment.
Before publication, the StudyCorgi editorial team proofread and checked the paper to make sure it meets the highest standards in terms of grammar, punctuation, style, fact accuracy, copyright issues, and inclusive language. Last updated: June 10, 2022 .
If you are the author of this paper and no longer wish to have it published on StudyCorgi, request the removal . Please use the “ Donate your paper ” form to submit an essay.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Why active euthanasia...
Why euthanasia should not be legalised
Rapid response to:
Why active euthanasia and physician assisted suicide should be legalised
- Related content
- Article metrics
- Rapid responses
Rapid Response:
In response to the editorial regarding the legalisation of active euthanasia and physician-assisted suicide,1 I present the following arguments against the legalisation of active euthanasia.
Active euthanasia is unnecessary because alternative treatments exist
It is widely believed that there are only two options for patients with terminal illness: either they die suffering or receive euthanasia. Recent research in palliative medicine has shown that virtually all unpleasant symptoms experienced in terminal illness can be relieved or alleviated by existing techniques.
Requests for active euthanasia are rarely free and active.
A person with terminal illness is vulnerable, lacking the skills and knowledge to alleviate their symptoms. It is very difficult for him to be entirely objective about his own situation. Their capacity for decision-making may equally be affected by confusion, dementia or symptoms, which could be relieved with appropriate treatment. Patients who on admission say "let me die" usually after effective treatment are grateful that their request was not acceded to.
Active euthanasia gives too much power to doctors
Ironically, active euthanasia legislation makes doctors less accountable and gives them more power. Patients generally decide in favour of euthanasia on the basis of information given to them by doctors. If a doctor confidently suggests a certain course of action, it can be difficult for a patient to resist. However, diagnoses may be mistaken and prognoses may be widely misjudged. Active euthanasia gives the medical practitioner power, which in turn can be abused.
Active euthanasia leads inevitably to involuntary euthanasia
When active euthanasia has been previously accepted and legalised, it has led inevitably to inactive euthanasia.
Holland is moving rapidly down the slippery slope with the public conscience changing quickly to accept such action as acceptable. The Royal Dutch Medical Association has recommended that the termination of the lives of patients suffering from dementia is acceptable under certain conditions. Case reports include a woman killed at her own request for reasons of "mental suffering".[2]
Such a progression requires only four accelerating factors: favourable public opinion, willing doctors, economic pressure and a law allowing it. In most Western countries the first three ingredients are present already. When legislation comes into effect and political and economic interests are brought to bear, the generated momentum inevitably follows.
Dr Liz Croton SHO A&E City Hospital NHS Trust, Dudley Rd,Birmingham B18 7QH [email protected]
1. Doyle L, Doyle L. Why active euthanasia and physician assisted suicide should be legalised. BMJ 2001:323;1079-80.
Competing interests: No competing interests
Why Euthanasia Should not be Legalized
A Reflection on the Dutch Experiment
Cite this chapter

- Henk Jochemsen 8
Part of the book series: International Library of Ethics, Law, and the New Medicine ((LIME,volume 12))
248 Accesses
1 Citations
The experience of the Netherlands continues to be cited as illustrative of the euthanasia debate that is going on in many countries. The parliamentary debates on the legalization of euthanasia (November 2000 in the Second Chamber and April 2001 First Chamber) have drawn a lot of international attention. But, before this legalization in the Penal Code this country had adopted a legal regulation of euthanasia and, before and after that, extensive surveys into the practice of euthanasia had been carried out. The fact that the Dutch example is cited both by those who favor the legislation of euthanasia and those who reject it demonstrates that empirical data in themselves do not settle an ethical or juridical issue.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Baar, F.P.M. 1999. Palliatieve zorg voor terminale patienten in verpleeghuizen [palliative care for terminal patients in nursing homes]. Pro Vita Humana 6 (6): 169–75.
Google Scholar
Beauchamp, T.L., and J.F. Childress. 1994. Principles of biomedical ethics , 4th ed. Oxford: Oxford University Press.
Callahan, D. 1989. Can we return death to disease? Hasting Center Report 19 (1): 4–6.
Article Google Scholar
Callahan, D. 1990. What kind of life? The limits of medical progress . New York: Simon 0000 Schuster.
Callahan, D. 1992. When self-determination runs amok. Hastings Center Report 22 (2): 52–5.
Article PubMed CAS Google Scholar
Cameron, N.M.S. 1996. Autonomy and the “right to die.” In Dignity and dying: A Christian appraisal , J.F. Kilner, A.B. Miller, and E.D. Pellegrino, 23–33. Grand Rapids (MI): Eerdmans. Cassell, E.J. 1993. The sorcerer’s broom. Hastings Center Report 23(6): 32–9.
Danhof, E. 1999. Palliatieve zorg is gebaat bij een bundeling van krachten tot een loket. [Palliative care would benefit from concentrating efforts in one desk]. Pallium 1(5) : 12–14.
Dillmann RJM. 1998. Euthanasie: de morde legitimatie van de arts [Euthanasia: the moral legitimation of the physician]. In Levensbeëindigend handelen door een arts: tussen norm en praktijk [Life terminating acting by a physician: between norm and practice] , eds. J. Legemaate, and R.J.M Dillmann, 11–25. Houten: Bohn Stafleu Van Loghum.
Doyal, L. 1993. Making sense of debates about euthanasia. [Editorial comment] Current medical literature. Anaesthesiology 7 (2): 35–9.
Drion, H. 1992. Het zelfgewilde einde van oude mensen [The selfchosen end of elderly people]. Amsterdam: Balans.
Editorial. 1970. A new ethic for medicine and society California Medicine 113(3): 67–8. Fenigsen, R. 1989. A case against Dutch euthanasia. Hastings Center report 19 (1): S22 - S30
Fenigsen, R 1995. Physician-assisted death: Impact on long-term care. Issues in law 0000 medicine 11 (3): 283–97.
CAS Google Scholar
Francke, A.L., A. Persoon, D. Temmink, and A. Kerkstra. 1997. Palliatieve zorg in Nederland . Utrecht: Nivel.
Gadamer, H.G. 1996. The enigma of health-the art of healing in a scientific age . Stanford: Stanford University Press
Jaspers, K. 1989. The physician in the technological age. Theoretical Medicine 10(2): 251–67. 262. Jochemsen, H. 1994. Euthanasia in Holland: an ethical critique of the new law. Journal of Medical Ethics 20 (1994), 212–7.
Jochemsen, H. 1998a. Dutch court decisions on non voluntary euthanasia critically reviewed. Issues in Law 0000 Medicine 13 (4): 447–458.
Jochemsen, H 1998b. The range of objections to euthanasia, In Asking to die. Inside the Dutch debate about euthanasia , eds. D.C. Thomasma, T. Kimbrough-Kushner, G.K. Kimsma, and C. Ciesielski-Carlucci, 227–40. Dordrecht: Kluwer Academic Publishers.
Chapter Google Scholar
Jochemsen, H 2001. Update: The legalization of euthanasia in the Netherlands. Ethics 0000 Medicine 17 (1): 7–12.
Jochemsen, H., and J. Keown. 1999. Voluntary euthanasia under control? Further empirical evidence from the Netherlands. Journal of Medical Ethics 25: 16–21.
Kastelein, W.R. 1995. Standpunt hoofdbestuur KNMG inzake euthanasie , [Position General Committee KNMG on Euthanasia]. Utrecht, August.
Keown, J. 1995. Euthanasia in the Netherlands: Sliding down the slippery slope? In Euthanasia examined , ed. J. Keown, 261–96. Cambridge: Cambridge University Press.
Keown, J. 1999. Double effect and palliative care: A legal and ethical outline. Ethics 0000 Medicine 15 (2): 53–4.
Kimsma, G.K., and E. Van Leeuwen. 1998. Euthanasia and assisted suicide in the Netherlands and the USA: Comparing practices, justifications and key concept in bioethics and laws. In Asking to die. Inside the Dutch debate about euthanasia , eds. D.C. Thomasma, T. Kimbrough-Kushner, G.K. Kimsma, and C. Ciesielski-Carlucci, 35–71. Dordrecht: Kluwer Academic Publishers.
Leenen, H.J.J. 1989. Dying with dignity: Developments in the field of euthanasia in the Netherlands. Medicine and Law 8: 517–526.
PubMed CAS Google Scholar
Mayo, D.J., and M. Gunderson. 1993. Physician assisted death and hard choices. Journal of Medicine and Philosophy 18: 329–41.
Muskin, P.R. 1998. The request to die. Role for a psychodynamic perspective on physician-assisted suicide. Journal of the American Medical Association 279 (4): 323–8.
Pijnenborg, L. 1995. End-of-life decisions in Dutch medical practice . PhD. Diss. Erasumus University. Rotterdam.
Pool, R. 1996. Vragen om te sterven. Euthanasie in een Nederlands ziekenhuis. [Asking to die. Euthanasia in a Dutch hospital] . Rotterdam: WYT Uitgeefgroep.
Reich, W., ed. 1978. Acting and refraining. In Encyclopedia of Bioethics , 33–5. New York: Free Press. Reichel, W., and A.J. Dyck. 1989. Euthanasia: A contemporary moral quandary. The Lancet ii: 1321–3. Reitman, J.S. 1995. The debate on assisted suicide-redefining morally appropriate care for people with intractable suffering. Issues in law 0000 medicine 11(3) : 317–8.
Schipperges, H. 1978. Motivation und Legitimation des Arztliche Handelns. In Krankheit , Heilkunst , Heilung , eds. H. Schipperges, E. Seidler, and P.U. Unschuld, 447–489. München: Alber.
Schulte, B.P.M. 1988. Over euthanasia en in het bijzonder over de relatie tussen hersenfunctie en vrijwilligheid bij euthanasie [On euthanasia and in particular on the relation between brain functioning and voluntariness of euthanasia]. Vita Humana XV (1): 9–12.
Select Committee of the House of Lords (UK). 1994. Report of the Select Committee on Medical Ethics . House of Lords, Session 1993–94. London: HSMO.
Singer, P.A., and M. Siegler. 1990. Euthanasia–a critique. New England Journal of Medicing 32 (26): 1881–3.
Sorgdrager, W., and E. Borst-Eilers. 1995. Euthanasie. De stand van zaken. Medisch Contact 50 (12): 381–4.
The Appleton International Conference: developing guidelines for decisions to forgo life-prolonging medical treatment. 1992. Journal of Medical Ethics 18(suppl.) : 3–5.
Twycross, R. 1995. Where there is hope, there is life: a view from the hospice. In: Euthanasia examined. Ethical , clinical and legal perspectives , ed. J. Keown, 141–68. Cambridge: Cambridge University Press.
Van der Maas, P.J., 1991. Medische beslissingen rond het levenseinde . Den Haag: SDU Uitgeverij. [Published in translation as Euthanasia and Other Medical Decisions Concerning the End of Life . Amsterdam: Elsevier 1992.]
Van der Maas, P.J., G. Van der Wal, I. Haverkate, C.L.M. de Graaff, J.G.C. Kester, B.D. OnwuteakaPhilipsen, A. van der Heide, J.M. Bosma, and D.L. Willems, Dick L. 1996. Euthanasia, physician-assisted suicide, and other medical practices involving the end of life in the Netherlands 1990–1995. New England Journal of Medicine 335: 1699–1705.
Van der Wal, G., and P.J. Van der Maas. 1996. Euthanasie en andere medische beslissingen rond het levenseinde. De praktijk en de meldingsprocedure . [Euthanasia and other medical decisions concerning the end of life. Practice and reporting procedure.] Den Haag: SDU uitgevers.
Van der Wal, G., P.J. Van der Maas, J.M. Bosma, B.D. Onwuteaka-Philipsen, D.L. Willems, I. Haverkate, and P.J. Kostense. 1996. Evaluation of the notification procedure for physician-assisted death in the Netherlands. New England Journal of Medicine 335: 1706–11.
Article PubMed Google Scholar
Velaers, J. 1996. Het leven, de dood en de grondrechten — juridische beschouwing over zelfdoding en euthanasie [Life, death and fundamental rights — juridical discours on suicide and euthanasia. In Over
zichzelf beschikken? Juridische en ethische bijdragen over het leven , het lichaam en de dood [Self determination? Juridical and ethical essays on life , the body and death] ,469–574. Reeks: Het recht in de samenleving, van het Centrum Grondslagen van het Recht, Universiteit Antwerpen. Antwerpen: Maklu uitgevers.
Verhagen, S. 2000. Behandeling depressiviteit: altijd zinvol, vaak effectief [treatment of depression: always useful, often effective]. Pallium 2 (2): 13–7.
Willems, J.H.P.H. 1987. Euthanasie en noodtoestand. Nederlands Juristenblad 22: 694–8.
Zylicz Z. 1998. Palliative care: Dutch hospice and euthanasia. In Asking to die. Inside the Dutch debate about euthanasia , eds. D.C. Thomasma, T. Kimbrough-Kushner, G.K. Kimsma, and C. CiesielskiCarlucci, 187–203. Dordrecht: Kluwer Academic Publishers.
Download references
Author information
Authors and affiliations.
Free University of Amsterdam, Ede, The Netherlands
Henk Jochemsen ( Lindeboom Chair of Medical Ethics, Director, Prof. dr. G.A. Lindeboom Institute )
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Faculté de Médicine, Université de Montréal, Canada
David N. Weisstub ( Philippe Pinel Professor of Legal Psychiatry and Biomedical Ethics ) ( Philippe Pinel Professor of Legal Psychiatry and Biomedical Ethics )
Neiswanger Institute for Bioethics and Health Policy, Loyola University of Chicago Medical Center, USA
David C. Thomasma ( Professor and Fr. English Chair of Medical Ethics ) ( Professor and Fr. English Chair of Medical Ethics )
Centre for Studies on Aging, Faculty of Medicine, McGill University, Canada
Serge Gauthier ( Professor of Neurology, Neurosurgery and Psychiatry ) ( Professor of Neurology, Neurosurgery and Psychiatry )
Faculty of Law, University of Sydney, Australia
George F. Tomossy ( Ross Waite Parsons Scholar ) ( Ross Waite Parsons Scholar )
Rights and permissions
Reprints and permissions
Copyright information
© 2001 Springer Science+Business Media Dordrecht
About this chapter
Jochemsen, H. (2001). Why Euthanasia Should not be Legalized. In: Weisstub, D.N., Thomasma, D.C., Gauthier, S., Tomossy, G.F. (eds) Aging: Decisions at the End of Life. International Library of Ethics, Law, and the New Medicine, vol 12. Springer, Dordrecht. https://doi.org/10.1007/978-94-015-9682-4_5
Download citation
DOI : https://doi.org/10.1007/978-94-015-9682-4_5
Publisher Name : Springer, Dordrecht
Print ISBN : 978-90-481-5898-0
Online ISBN : 978-94-015-9682-4
eBook Packages : Springer Book Archive
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Indian J Med Res
- v.136(6); 2012 Dec
Euthanasia: Right to life vs right to die
Suresh bada math.
Department of Psychiatry National Institute of Mental Health & Neuro Sciences (Deemed University) Bangalore 560 029, India
Santosh K. Chaturvedi
The word euthanasia, originated in Greece means a good death 1 . Euthanasia encompasses various dimensions, from active (introducing something to cause death) to passive (withholding treatment or supportive measures); voluntary (consent) to involuntary (consent from guardian) and physician assisted (where physician's prescribe the medicine and patient or the third party administers the medication to cause death) 2 , 3 . Request for premature ending of life has contributed to the debate about the role of such practices in contemporary health care. This debate cuts across complex and dynamic aspects such as, legal, ethical, human rights, health, religious, economic, spiritual, social and cultural aspects of the civilised society. Here we argue this complex issue from both the supporters and opponents’ perspectives, and also attempts to present the plight of the sufferers and their caregivers. The objective is to discuss the subject of euthanasia from the medical and human rights perspective given the background of the recent Supreme Court judgement 3 in this context.
In India abetment of suicide and attempt to suicide are both criminal offences. In 1994, constitutional validity of Indian Penal Code Section (IPC Sec) 309 was challenged in the Supreme Court 4 . The Supreme Court declared that IPC Sec 309 is unconstitutional, under Article 21 (Right to Life) of the constitution in a landmark judgement 4 . In 1996, an interesting case of abetment of commission of suicide (IPC Sec 306) came to Supreme Court 5 . The accused were convicted in the trial court and later the conviction was upheld by the High Court. They appealed to the Supreme Court and contended that ‘right to die’ be included in Article 21 of the Constitution and any person abetting the commission of suicide by anyone is merely assisting in the enforcement of the fundamental right under Article 21; hence their punishment is violation of Article 21. This made the Supreme Court to rethink and to reconsider the decision of right to die. Immediately the matter was referred to a Constitution Bench of the Indian Supreme Court. The Court held that the right to life under Article 21 of the Constitution does not include the right to die 5 .
Regarding suicide, the Supreme Court reconsidered its decision on suicide. Abetment of suicide (IPC Sec 306) and attempt to suicide (IPC Sec 309) are two distinct offences, hence Section 306 can survive independent of Section 309. It has also clearly stated that a person attempts suicide in a depression, and hence he needs help, rather than punishment. Therefore, the Supreme Court has recommended to Parliament to consider the feasibility of deleting Section 309 from the Indian Penal Code 3 .
Arguments against euthanasia
Eliminating the invalid : Euthanasia opposers argue that if we embrace ‘the right to death with dignity’, people with incurable and debilitating illnesses will be disposed from our civilised society. The practice of palliative care counters this view, as palliative care would provide relief from distressing symptoms and pain, and support to the patient as well as the care giver. Palliative care is an active, compassionate and creative care for the dying 6 .
Constitution of India : ‘Right to life’ is a natural right embodied in Article 21 but suicide is an unnatural termination or extinction of life and, therefore, incompatible and inconsistent with the concept of ‘right to life’. It is the duty of the State to protect life and the physician's duty to provide care and not to harm patients. If euthanasia is legalised, then there is a grave apprehension that the State may refuse to invest in health (working towards Right to life). Legalised euthanasia has led to a severe decline in the quality of care for terminally-ill patients in Holland 7 . Hence, in a welfare state there should not be any role of euthanasia in any form.
Symptom of mental illness : Attempts to suicide or completed suicide are commonly seen in patients suffering from depression 8 , schizophrenia 9 and substance users 10 . It is also documented in patients suffering from obsessive compulsive disorder 11 . Hence, it is essential to assess the mental status of the individual seeking for euthanasia. In classical teaching, attempt to suicide is a psychiatric emergency and it is considered as a desperate call for help or assistance. Several guidelines have been formulated for management of suicidal patients in psychiatry 12 . Hence, attempted suicide is considered as a sign of mental illness 13 .
Malafide intention : In the era of declining morality and justice, there is a possibility of misusing euthanasia by family members or relatives for inheriting the property of the patient. The Supreme Court has also raised this issue in the recent judgement 3 . ‘Mercy killing’ should not lead to ‘killing mercy’ in the hands of the noble medical professionals. Hence, to keep control over the medical professionals, the Indian Medical Council (Professional Conduct, Etiquette and Ethics) Regulations, 2002 discusses euthanasia briefly in Chapter 6, Section 6.7 and it is in accordance with the provisions of the Transplantation of Human Organ Act, 1994 14 . There is an urgent need to protect patients and also medical practitioners caring the terminally ill patients from unnecessary lawsuit. Law commission had submitted a report (no-196) to the government on this issue 15 .
Emphasis on care : Earlier majority of them died before they reached the hospital but now it is converse. Now sciences had advanced to the extent, life can be prolonged but not to that extent of bringing back the dead one. This phenomenon has raised a complex situation. Earlier diseases outcome was discussed in terms of ‘CURE’ but in the contemporary world of diseases such as cancer, Aids, diabetes, hypertension and mental illness are debated in terms best ‘CARE’, since cure is distant. The principle is to add life to years rather than years to life with a good quality palliative care. The intention is to provide care when cure is not possible by low cost methods. The expectation of society is, ‘cure’ from the health professionals, but the role of medical professionals is to provide ‘care’. Hence, euthanasia for no cure illness does not have a logical argument. Whenever, there is no cure, the society and medical professionals become frustrated and the fellow citizen take extreme measures such as suicide, euthanasia or substance use. In such situations, palliative and rehabilitative care comes to the rescue of the patient and the family. At times, doctors do suggest to the family members to have the patient discharged from the hospital wait for death to come, if the family or patient so desires. Various reasons are quoted for such decisions, such as poverty, non-availability of bed, futile intervention, resources can be utilised for other patients where cure is possible and unfortunately majority of our patient's family do accordingly. Many of the terminally ill patients prefer to die at home, with or without any proper terminal health care. The societal perception needs to be altered and also the medical professionals need to focus on care rather in addition to just cure. The motive for many euthanasia requests is unawareness of alternatives. Patients hear from their doctors that ‘nothing can be done anymore’. However, when patients hear that a lot can be done through palliative care, that the symptoms can be controlled, now and in the future, many do not want euthanasia anymore 16 .
Commercialisation of health care : Passive euthanasia occurs in majority of the hospitals across the county, where poor patients and their family members refuse or withdraw treatment because of the huge cost involved in keeping them alive. If euthanasia is legalised, then commercial health sector will serve death sentence to many disabled and elderly citizens of India for meagre amount of money. This has been highlighted in the Supreme Court Judgement 3 , 17 .
Research has revealed that many terminally ill patients requesting euthanasia, have major depression, and that the desire for death in terminal patients is correlated with the depression 18 . In Indian setting also, strong desire for death was reported by 3 of the 191 advanced cancer patients, and these had severe depression 19 . They need palliative and rehabilitative care. They want to be looked after by enthusiastic, compassionate and humanistic team of health professionals and the complete expenses need to be borne by the State so that ‘Right to life’ becomes a reality and succeeds before ‘Right to death with dignity’. Palliative care actually provides death with dignity and a death considered good by the patient and the care givers.
Counterargument of euthanasia supporters
Caregivers burden : ‘Right-to-die’ supporters argue that people who have an incurable, degenerative, disabling or debilitating condition should be allowed to die in dignity. This argument is further defended for those, who have chronic debilitating illness even though it is not terminal such as severe mental illness. Majority of such petitions are filed by the sufferers or family members or their caretakers. The caregiver's burden is huge and cuts across various domains such as financial, emotional, time, physical, mental and social. Hence, it is uncommon to hear requests from the family members of the person with psychiatric illness to give some poison either to patient or else to them. Coupled with the States inefficiency, apathy and no investment on health is mockery of the ‘Right to life’.
Refusing care : Right to refuse medical treatment is well recognised in law, including medical treatment that sustains or prolongs life. For example, a patient suffering from blood cancer can refuse treatment or deny feeds through nasogastric tube. Recognition of right to refuse treatment gives a way for passive euthanasia. Many do argue that allowing medical termination of pregnancy before 16 wk is also a form of active involuntary euthanasia. This issue of mercy killing of deformed babies has already been in discussion in Holland 20 .
Right to die : Many patients in a persistent vegetative state or else in chronic illness, do not want to be a burden on their family members. Euthanasia can be considered as a way to upheld the ‘Right to life’ by honouring ‘Right to die’ with dignity.
Encouraging the organ transplantation : Euthanasia in terminally ill patients provides an opportunity to advocate for organ donation. This in turn will help many patients with organ failure waiting for transplantation. Not only euthanasia gives ‘Right to die’ for the terminally ill, but also ‘Right to life’ for the organ needy patients.
Constitution of India reads ‘right to life’ is in positive direction of protecting life. Hence, there is an urgent need to fulfil this obligation of ‘Right to life’ by providing ‘food, safe drinking water and health care’. On the contrary, the state does not own the responsibility of promoting, protecting and fulfilling the socio-economic rights such as right to food, right to water, right to education and right to health care, which are basic essential ingredients of right to life. Till date, most of the States has not done anything to support the terminally ill people by providing for hospice care.
If the State takes the responsibility of providing reasonable degree of health care, then majority of the euthanasia supporters will definitely reconsider their argument. We do endorse the Supreme Court Judgement that our contemporary society and public health system is not matured enough to handle this sensitive issue, hence it needs to be withheld. However, this issue needs to be re-examined again after few years depending upon the evolution of the society with regard to providing health care to the disabled and public health sector with regard to providing health care to poor people.
The Supreme Court judgement to withhold decision on this sensitive issue is a first step towards a new era of health care in terminally ill patients. The Judgment laid down is to preserve harmony within a society, when faced with a complex medical, social and legal dilemma. There is a need to enact a legislation to protect terminally ill patients and also medical practitioners caring for them as per the recommendation of Law Commission Report-196 15 . There is also an urgent need to invest in our health care system, so that poor people suffering from ill health can access free health care. Investment in health care is not a charity; ‘Right to Health’ is bestowed under ‘Right to Life’ of our constitution.
- The Courts Today By LatestLaws.com| 04.06.2024 |
- Delhi High Court Protects Indian Law Firm's Trademark in Landmark Ruling
- Vloggers shooting Videos from inside of Driver's Cabin of moving Vehicle to be booked under MV Act: High Court [Read Order]
- 6th International Conference on Leveraging the Digital Transformation for Environmental Sustainability-Envisioning A Developed India 2040 [June 21-22]: Register by June 15
- CfP: 4th International Conference on Human Rights and Constitutional Law by Centre for Legal Research and Studies [Online, June 9]: Submit Abstract by June 6
- CfP: Conference on Development and Energy Needs of Global South- Addressing inequity in Climate Policy Framework at IIT Bombay [Offline; Dec 6-8]: Submit by June 30
- CfP: 21st Virtual Seminar on Cyber Crime- Issues, Challenges, and Prevention by the Kerala Law Academy Law College, Trivandrum: Submit Abstract by June 10
- बहराइच में मासूम से रेप और हत्या के आरोपी को फांसी की सजा, कोर्ट ने जुर्माना भी लगाया
- मनीष सिसोदिया को आबकारी नीति मामले में बड़ा झटका, अदालत ने कहा- जमानत याचिका पर अभी सुनवाई नहीं
- High Court dismisses plea against appointment of NSIDC Chairman
- Lok Sabha Elections 2024: Surat seat's uncontested result challenged in Gujarat High Court
- साइफर सहित दो मामले में Ex.PM इमरान खान और शाह महमूद कुरैशी बरी
- Delhi HC asks MCD to respond to plea for seizure of Horse drawn carts illegally plying in Delhi
- हमारा मजाक उड़ाया जा रहा है? सुप्रीम कोर्ट ने हाईकोर्ट के फैसले पर क्यों की ये टिप्पणी
- Internship Opportunity at Abhidhvaj Law Journal (12th Aug to 12thSept): Apply by August 12
- Central Acts
- Latest News
- Corporate Law News
- Human Rights News
- Intellectual Property News
- Did you Know?
- International News
- हिंदी न्यूज़
- Law Firm News
- Marriage and Divorce News
- Tourism News
- World of Petroleum & Natural Gas
- Case Analysis Supreme Court High Courts Tribunal Courts
- Cheque Bounce News
- Legal Services News
- Petroleum News
Supreme Court Judgments
- Supreme Court
High Court Judgments
- Delhi High Court
- Allahabad High Court
- Bombay High Court
- Calcutta High Court
- Madras High Court
- Punjab & Haryana High Court
- Andhra High Court
- Chattisgarh High Court
- Gauhati High Court
- Gujarat High Court
- Himachal Pradesh High Court
- Jammu & Kashmir High Court
- Jharkhand High Court
- Karnataka High Court
- Kerala High Court
- Madhya Pradesh High Court
- Meghalaya High Court
- Manipur High Court
- Orissa High Court
- Patna High Court
- Rajasthan High Court
- Sikkim High Court
- Tripura High Court
- Telangana High Court
- Uttarakhand High Court
- Arbitration
- Conciliation
Campus Buzz
- Call for Papers
- Conferences & Seminars
- Courses & Workshops
- Debate Competitions
- Essay Competitions
- Fellowships
- Fests, MUNs and Other Competitions
- International Opportunities
- Internships
- Moot Court Competitions
- Scholarships
- Legal Documents
- Legal Forms for Advocates
- Legal Dictionary
- SC Collegium Resolutions
- Law Commission of India Reports
- NCRB Reports
- Justice Verma Committee Report, 2013
- Justice BN Srikrishna Report on Institutionalisation of Arbitration
- Legal Maxims
- Web Links Directory
Legal Education
- Law School Entrance Exams
- Law Schools and Colleges in India
- Overseas Law Schools
- Careers in Law
Circulars & Notices
- RBI Circulars
- RBI Notices
- SEBI Circulars
- SEBI Notices
- MCA Circulars
- MCA Notices
- Supreme Court Calendar 2023
- Supreme Court Bar Association
- Supreme Court Advocate-On-Record
- All High Courts Calendar
- High Courts Portals
- Judicial Exam Notice Board
- Judicial Services Exam Question Papers
- Bar Councils
- Bar Associations

Recent News
Euthanasia: should it be legalized in india.

The Author, Urvashi Trivedi, is a 2nd-year, BA.LLB student at University of Petroleum and Energy Studies, Dehradun. She is currently interning with LatestLaws.com.
Introduction
The term “euthanasia” comes from the liaison of the two Greek words: “eu” and “thantos”, meaning good and death, respectively. It is therefore considered the practice of ending an individual’s life of suffering and misery caused due to a condition that is beyond repair or a terminal illness, through suspension of medical facilities or injection, in order to rid the person off of the intolerable pain. It is often termed as an act of intentional taking of a person’s life in a painless manner, which is not worth living or, ‘mercy killing’ where the individual is set free off the irremediable life condition of suffering and pain.
To understand the complexity of the concept of euthanasia, one must know the classification of euthanasia and the terms related to it.
Physician Assisted Suicide (PAS), wherein the doctor knowingly provides medical assistance to an individual to end their life, who is likely to be experiencing persistent and intolerable suffering and pain. The physician provides for a complete analysis of the medical condition and determines the most painless and effective method of dying.
Voluntary Euthanasia, when the individual wishes through a conscious decision of ending their help with the help of another. It requires full consent and awareness of the concept and process.
Non-Voluntary Euthanasia, whereas the decision of ending an individual’s life is taken by another, like a family member or your partner. This takes place when the individual is in a state of permanent unconsciousness and incapacitated beyond treatment.
Active Euthanasia means where the doctor can directly end an individual’s life. The other names given to this process are, ‘Positive Euthanasia’ or ‘Aggressive Euthanasia’. The doctor may directly intervene and prescribe a painless method to end an individual’s life. The main element under this remains consent of the individual whose sufferings are irremediable and endless. This is a quicker method of dying through a lethal and high dose of drug or by injecting a lethal drug.
Passive Euthanasia or ‘Negative Euthanasia’ or ‘Non-Aggressive Euthanasia’ is the practice of intentionally causing the death of an individual by withdrawing the necessary and essential care, food or water. It is an intentional discontinuation which also implies the removal of artificial life support facilities. It is considered as a slow killer and is more comfortable than the active method. It is only aided when the individual no longer remains mentally and physically alert. There are medical tests and scales like Glasgow Coma Scales (GCS) to ensure the mental vegetative state of the individual. In many countries and states, this is a legal right provided to individuals usually on medical life support.
In the ancient, or often considered traditional times, euthanasia was labelled as a practice against the culture, religion and even the ethical human values. The transition from it being considered a malpractice to a legal right, was due to the term and extension of the practice of “Palliative Care”. The medical practice of providing care to those patients who suffer from any terminal illness. Under this, the patient’s needs and wants are taken care of and the process of decay and prolonged death is made comfortable in any way possible.
Every individual is born with a basic shield of human rights and amongst all such rights, Right to Life is the most essential right. It is the basic and fundamental right which states that every human being has the right to live and cannot be killed by another being. This right is the umbrella right under which other rights get their light and backing.
Chronology of the Legal Advancements
Article 21 of the Constitution of India provides this right to every person. Soon enough the people of the state began to question, “whether the right to life also entails the right to die?”. This started a massive debate and deliberations on the concept and its relevance in the Indian context. The two cases, M.S. Dubal v. State of Maharashtra (1986) and Chenna Jagadeeswar v. State of AP (1987), dealt with the positive and negative aspect of the rights given to the people and the violative nature of certain articles, respectively. Both the cases contradict one another on the “Right of Life includes Right to Die” topic.
In the case of M.S. Dubal v State of Maharashtra (1986), the conflict took place on the negative and positive aspects of the rights that were provided to the people. The court ruled that Right to Life under article 21 also contains the Right not to live.
The Court observed that “ those who make the suicide attempt on account of the mental disorders require psychiatric treatment and not confinement in the prison cells where their condition is bound to worsen leading to further mental derangement. Those on the other hand who make the suicide attempt on account of acute physical ailments, incurable diseases, torture or decrepit physical state induced by old age or disablement need nursing homes and not prisons to prevent them from making the attempts again .”
The submission made in the court regarding the right to live with dignity was as follows,
“By the term 'life' as here used something more is meant than mere animal existence. The inhibition against its deprivation extends to all these limits and faculties by which life is enjoyed. The provision equally prohibits the mutilation of the body or amputation of an arm or leg or the putting out of an eye or the destruction of any other organ of the body through which the soul communicates with the outer world...by the term liberty, as used in the provision something more is meant than mere freedom from physical restraint or the bonds of a prison.”
While in the latter case, the High Court of Andhra Pradesh contradicted the former and established the constitutional validity of the Section 309 of the Indian Penal Code which criminalized the offence of suicide, meaning taking one’s own life.
This debate was furthered in the case of P. Rathinam v. Union of India (1994), which gave the verdict in favor of the motion and legalized assisted suicide. It was later contradicted and overruled in Gian Kaur v. State of Punjab (1996), where it was held that Article 21 cannot include right to die or be killed.
In the case of Gian Kaur v. State of Punjab, the five-judge bench, headed by Justice J.S. Verma, brought the Section 309 of the Indian Penal Code, 1860 back and the judgement that was passed stated that, under the ambit of Article 21 of the Indian Constitution, the part of Right To Live only includes the aspect of life and thereof and nowhere includes the aspect of right to die. It was because of this particular case that passive Euthanasia and Assisted Suicide were made unlawful.
The debate over this topic continued amongst the people on various platforms and soon in the path breaking judgment in the case of Aruna Shaunbaug v. Union of India (2011), the Supreme Court with its 5 judge bench remarked the relevance of the concept of euthanasia and the right to life can be interpreted as the right to a life of dignity and worth. This much awaited judgment which in itself was a hard battle, helped push the awareness quotient on this topic and the debate for the legalization of passive euthanasia thus entered into our society, but with the exception of it being practiced only on terminally ill patients and through the removal of medical life support. The recent case of Aruna Shaunbaug generated a plethora of opinions and also made us look towards the status of the law in other countries and states which have legalized the practice.
In furtherance to such landmark cases, the Law Commission gave various recommendations in its reports time to time.
In the 42 nd Report in 1971, it was stated that after reviewing Manu’s code and the law commentaries on it, it held that the commission of suicide was considered valid when the people was diseased and was living under miserable life conditions. It referred to the Vedic texts which upheld the values and importance of the persons who got rid of his own self as someone who would find salvation as they left the earthly pleasures. It considered the legal provisions of suicide as harsh and unjustifiable.
Later in the year 1997, the 156 th Law Commission’s report held the validity of the criminalization of the offence of suicide and gave the credit to medical science and law. It supported the judgement given in the Gian Kaur case and the validity of the Penal section and supported the argument further with the prevalent societal evils like drug and trafficking and the existence of terrorism and those who attempted suicide under these events.
In 2008, the Law Commission in its 210 th Report recommended the decriminalization of the section which punishes though who commit the offence of attempt to suicide, which is section 309 of the IPC. It also proposed amendments to the IPC.
In 2017, the nation welcomed its Mental Healthcare Act , repealing the previous act and de-criminalizing the “attempt to suicide” section. Section 115 of the act states:
“Notwithstanding anything contained in Section 309 of the IPC, any person who attempts to commit suicide shall be presumed to have severe stress and shall not be tried and punished under this Code; and
The government is duty bound to provide care, treatment and rehabilitation to such a person in order to reduce the risk of recurrence of attempt to commit suicide.”
As every individual has the right to live, they also have the right to form guided and well-aided opinions on matters that concern the most crucial decision of their lives. As citizens of a growing and developing nation, we must be aware and well guided through the examples set by other nations as well as their mistakes. When we look at the rate and usage of the medical facility of practicing euthanasia, we must understand that in this day and age, the misuse of such a practice is more likely than its benefits. To be able to equip the medical institutions with the facilities of euthanasia is a great risk as a collective effort. For a nation like India, it is a slippery slope to tread on as this practice may be done by those who are corrupted or by the weaker minds. It may become a tool in hands of the corrupt to demand and misguide a person’s will and consent in the name of “living will” or “PAS” or even “non-voluntary euthanasia”. As the practice not only encompasses the physical state of an individual but also the emotional and psychological aspects, there needs to be a greater sense of understanding before allowing active euthanasia or ‘ living will’.
It is also considered medically unethical and it goes against the notions of nursing, healing and care giving oaths that medical officials undertake. To understand the dilemma of the family and the doctors while prescribing passive euthanasia is a painful and necessary task to the rid the person off of the futile resources and time without any assurance to the normalcy of life in the future. It is the level of mental consciousness that determines whether the individual receives the consent for passive killing. Therefore, such a decision is far more risk bearing and complex when the person is mentally alert.
To better the medical facilities in India with regard to Palliative Care of the terminally ill people can be an alternative approach. In other countries where such practices are legal have their rules and exceptions. In Netherlands and Belgium, it is permitted only in the case of terminally ill children and in Switzerland it is allowed only in the case of advanced malignancy or intractable pain and suffering.
Similarly, euthanasia means the practice of ending the life of a person who is suffering from terminal illness which is irremediable or has persistent pain or suffering and is not a life worth living. Therefore, the question to be understood and addressed are many. The debate remains ongoing on the subject and the factors that one must consider while deciding whether their life is not worth living any longer. The limelight remains on the allowance of active euthanasia and its implications. Whether the approval to this would bring justice to the people suffering or become the cause of the sufferings in the long run. It remains a conflict between the social norms and values, medical needs of the patient and his will and consent. It questions the standards and scales which define and measure the quality of a persons’ life and whether such life can be ended on the individual’s consent.
It is proven that euthanasia provides a way to relieve the individual from the mammoth of sufferings as though they are alive on a burning pyre of intolerable pain. It gives the right to the beings to evaluate their essence of life and live and end it in a dignified manner without any force. The underlying principle of this is the consent and choice of the person. The battle of euthanasia as a legal remedy is tough and complex. It needs careful examination of the status quo of India, the mindset of the people, the acceptance and the presence of required equipment. If at all, it were to be legalized in India, there would be a requirement of stringent and well-structured laws that would guarantee the consent and will of the individual, monitoring the failure of all medical resources and methods to revive the person, intentions of the caregivers and medical officials, proper ways to ensure that no abuse of the law takes place and the review of circumstances under which the euthanasia is to be allowed.
References-
- http://www.legalservicesindia.com/article/787/Euthanasia-in-India.html - Euthanasia in India
- https://www.britannica.com/topic/euthanasia - Euthanasia
- https://www.thehindu.com/opinion/op-ed/should-euthanasia-be-allowed/article22524514.ece - Should euthanasia be allowed?
- https://www.latestlaws.com/articles/euthanasia-india-team-latest-laws/ - 'All about Euthanasia in India’
- https://www.researchgate.net/publication/320054647_Should_Euthanasia_be_Legalised_in_India- Should we legalize Euthanasia?
- M.S Dubal v. State of Maharastra, CrLJ 549 AIR 1987
- Chenna Jagadeeswar v. State of A.P, CrLJ 549 AIR 1988
- P.Rathinam v. Union of India, 3 scc 394, AIR 1994
- Gian Kaur v. State of Punjab, 2 scc 648, AIR 1996
- Aruna Ramachandra Shanbaug v. Union of India, (2011) 4 SCC 454 s 140
Picture Source :

You May Also Like :
Trending news :.

LatestLaws.com presents: Lexidem Offline Internship Program, 2024

LatestLaws.com presents 'Lexidem Online Internship, 2024', Apply Now!

LatestLaws Guest Court Correspondent

Publish Your Article

Campus Ambassador

Media Partner

The Essential Role of the 7th Amendment in American Democracy
This essay is about the significance of the 7th Amendment in the United States Constitution, which guarantees the right to a jury trial in certain civil cases. It explains how the amendment ensures that disputes can be resolved by a jury of peers rather than solely by judges, reflecting the Founding Fathers’ intent to protect against governmental overreach and maintain impartiality. The essay highlights the amendment’s role in involving ordinary citizens in the judicial process, promoting fairness and democratic principles. It also addresses the challenges posed by modern, complex cases and suggests that the collective wisdom of juries remains crucial for balanced and just outcomes. Ultimately, the essay underscores the 7th Amendment’s enduring importance in upholding justice and accountability in the American legal system.
How it works
The 7th Amendment to the United States Constitution stands as a pivotal element in ensuring justice within the American legal framework. Adopted in 1791 as part of the Bill of Rights, it guarantees the right to a jury trial in certain civil cases, underscoring the importance of citizen participation in the judicial process. Although its wording is straightforward, its implications are profound and continue to shape the legal landscape.
At its core, the 7th Amendment ensures that individuals involved in civil disputes can have their case decided by a jury of their peers rather than solely by a judge.
This provision applies to federal civil cases where the value in controversy exceeds twenty dollars—a threshold set in the 18th century that reflects a different economic reality but emphasizes the principle rather than the specific amount. The amendment aims to preserve the traditional role of the jury as a fundamental component of the justice system, ensuring that ordinary citizens can play a direct role in legal proceedings.
The inclusion of the 7th Amendment was driven by the Founding Fathers’ deep mistrust of potential governmental overreach. They believed that judges, appointed by the government, might be influenced by political pressures or corruption. By contrast, juries composed of ordinary citizens were seen as less likely to be swayed by such factors and more likely to deliver fair and impartial verdicts based on the evidence presented. This belief in the impartiality and common sense of the average citizen was a cornerstone of early American democratic ideals.
Over the years, the 7th Amendment has significantly impacted the development of the American legal system. It has ensured that many disputes involving contracts, property, and personal injuries, among other matters, are subject to jury trials. This has reinforced the idea that legal decisions should not be the exclusive domain of legal professionals but should include input from the broader community. Juries bring diverse perspectives and collective judgment, which can often lead to more balanced and equitable outcomes.
However, the application of the 7th Amendment is not without challenges. The legal system has evolved, and so have the complexities of civil cases. Some critics argue that juries in modern, highly technical cases may struggle to understand intricate legal and factual issues. Despite this, supporters of the amendment contend that the collective wisdom of a jury can often cut through complexities and focus on the essential facts and fairness of a case. Moreover, judges can still play a crucial role by guiding juries on legal standards and ensuring that trials are conducted fairly.
The 7th Amendment also highlights the enduring tension between direct democratic participation and professional expertise in the legal system. While some aspects of modern law may benefit from specialized knowledge, the amendment insists on the value of lay participation in judicial decisions. This reflects a broader democratic principle that government and its functions, including the judiciary, should remain accessible and accountable to the people.
In contemporary legal practice, the right to a jury trial in civil cases remains a fundamental protection. It acts as a check on judicial power and serves as a reminder of the foundational democratic values that underpin the American legal system. While the specifics of civil litigation have evolved, the principle that ordinary citizens should have a voice in resolving disputes remains as relevant as ever.
The 7th Amendment’s impact extends beyond the courtroom. It is a testament to the democratic ethos that pervades American society. By involving ordinary citizens in the judicial process, it fosters a sense of community and shared responsibility for justice. Jurors, drawn from diverse backgrounds, bring their unique experiences and perspectives to the deliberation process, enriching the decision-making framework. This collective approach often leads to more nuanced and empathetic outcomes, reflecting the community’s moral and ethical standards.
Moreover, the 7th Amendment serves as a crucial educational tool. Participation in jury duty exposes citizens to the legal system’s workings, enhancing their understanding of civic duties and rights. It demystifies legal proceedings, making the law more transparent and accessible. This educational aspect of jury duty contributes to a more informed and engaged citizenry, capable of critically evaluating legal and political issues.
Despite its enduring significance, the 7th Amendment faces contemporary challenges. The increasing complexity of civil cases, driven by advancements in technology and specialized industries, poses a challenge for lay jurors. In response, some legal scholars advocate for a hybrid approach, where juries are supplemented by expert advisors who can clarify technical details. This compromise aims to preserve the jury’s democratic essence while ensuring informed and accurate verdicts.
Additionally, the 7th Amendment’s role in promoting fairness and impartiality is more critical than ever in an era of heightened polarization. By entrusting ordinary citizens with the power to decide civil disputes, the amendment reinforces the principle that justice should transcend political and ideological divides. It underscores the idea that justice is a communal endeavor, requiring the collective wisdom and judgment of the populace.
In conclusion, the 7th Amendment’s guarantee of a jury trial in certain civil cases is a cornerstone of the American justice system. It enshrines the principle of citizen participation, providing a vital check on judicial power and ensuring that legal decisions reflect the community’s values and standards. Despite the evolving complexities of modern law, the amendment’s core principles remain steadfast, upholding the democratic ideals of fairness, accountability, and citizen involvement. The 7th Amendment’s enduring legacy is a testament to the foresight of the Founding Fathers and their commitment to a just and equitable society.
Cite this page
The Essential Role of the 7th Amendment in American Democracy. (2024, Jun 01). Retrieved from https://papersowl.com/examples/the-essential-role-of-the-7th-amendment-in-american-democracy/
"The Essential Role of the 7th Amendment in American Democracy." PapersOwl.com , 1 Jun 2024, https://papersowl.com/examples/the-essential-role-of-the-7th-amendment-in-american-democracy/
PapersOwl.com. (2024). The Essential Role of the 7th Amendment in American Democracy . [Online]. Available at: https://papersowl.com/examples/the-essential-role-of-the-7th-amendment-in-american-democracy/ [Accessed: 4 Jun. 2024]
"The Essential Role of the 7th Amendment in American Democracy." PapersOwl.com, Jun 01, 2024. Accessed June 4, 2024. https://papersowl.com/examples/the-essential-role-of-the-7th-amendment-in-american-democracy/
"The Essential Role of the 7th Amendment in American Democracy," PapersOwl.com , 01-Jun-2024. [Online]. Available: https://papersowl.com/examples/the-essential-role-of-the-7th-amendment-in-american-democracy/. [Accessed: 4-Jun-2024]
PapersOwl.com. (2024). The Essential Role of the 7th Amendment in American Democracy . [Online]. Available at: https://papersowl.com/examples/the-essential-role-of-the-7th-amendment-in-american-democracy/ [Accessed: 4-Jun-2024]
Don't let plagiarism ruin your grade
Hire a writer to get a unique paper crafted to your needs.

Our writers will help you fix any mistakes and get an A+!
Please check your inbox.
You can order an original essay written according to your instructions.
Trusted by over 1 million students worldwide
1. Tell Us Your Requirements
2. Pick your perfect writer
3. Get Your Paper and Pay
Hi! I'm Amy, your personal assistant!
Don't know where to start? Give me your paper requirements and I connect you to an academic expert.
short deadlines
100% Plagiarism-Free
Certified writers
Advertisement
After Trump’s Conviction, a Wary World Waits for the Fallout
Already braced for uncertainty about the U.S. election, countries in Europe and Asia are now even more unclear about the future of American diplomacy.
- Share full article

By Hannah Beech and Paul Sonne
- May 31, 2024
The world does not vote in American presidential elections. Nor do its jurors play a part in the American judicial system. Nevertheless, the conviction of Donald J. Trump on all 34 felony counts in a hush-money trial in a New York court on Thursday has again made clear how consequential what happens in the United States is for the rest of the planet.
Many America-watchers are grappling with the same questions posed by people in the United States: Can Mr. Trump still run for president? (Yes.) And if so, will the guilty verdicts cut into the support from his political base? (Unclear.)
Foreign observers also began wondering if Mr. Trump, already a volatile force, would become even less likely to stay within the guardrails of normal politics and diplomacy if he won the presidency again in November.
Mr. Trump’s supporters in anti-immigrant, right-wing nationalist circles abroad quickly jumped to his defense. Viktor Orban, Hungary’s Kremlin-friendly prime minister, called Mr. Trump “a man of honor” in a post on X and said the American people should deliver their own verdict in November.
Matteo Salvini, Italy’s deputy prime minister and the leader of the hard-right League party, expressed “solidarity and full support,” and called Mr. Trump a “victim of judicial harassment.”
“This verdict is a disgrace,” Nigel Farage, the pro-Brexit campaigner and Trump supporter, who is honorary president of Reform UK, a small right-wing party in Britain, wrote on social media. “Trump will now win big.”
President Vladimir V. Putin of Russia did not immediately respond to the verdict but has seized on the situation more broadly to undermine American influence. Mr. Putin last year called the various proceedings against Mr. Trump political “ persecution ” and said they had revealed the “rottenness of the American political system, which cannot pretend to teach others about democracy.”
His spokesman, Dmitri S. Peskov, reiterated the point on Friday in response to the verdict, saying it was clear to the entire world that the U.S. authorities were trying to eliminate political rivals “by all possible legal and illegal means.”
The convictions by a Manhattan jury come as the question of American engagement has become central in several global crises.
In Ukraine, the war effort against Russia has been stymied after Republicans in Congress delayed American military aid for months.
In Europe, leaders reliant on the United States for their defense are jittery about a return to a more acrimonious relationship with Washington and a possible withdrawal of American support for hardening defenses against Russia.
In Asia, where the Biden administration perceives a growing Chinese threat and worries about a possible invasion of Taiwan, American allies are concerned about the sanctity of defense treaties that have long girded the regional security order.
On the campaign trail, Mr. Trump has said he would encourage Russia to attack any NATO member that doesn’t pay sufficiently for its defense and has questioned whether the United States should defend South Korea, a treaty ally that hosts a large American military presence. He is considering the Ohio senator J.D. Vance, one of Washington’s most vociferous opponents of military aid for Ukraine, as a possible running mate.
Foreign analysts worry that Mr. Trump’s favored currency, unpredictability, could again shake up the global order.
Concern about his possible return to the White House is particularly palpable in Germany, the object of Mr. Trump’s ire for much of his first term and the host of more than 35,000 U.S. troops.
Andrea Römmele, vice president of the Hertie School, a public policy-focused graduate school in Berlin, said many Germans watching the Trump verdict were relieved to see that even a former president was not above the law in the United States. But she said Germans remained very anxious about a Trump victory.
“I think everyone is much more prepared to think the unthinkable,” she said.
Prime Minister Donald Tusk of Poland, whose right-wing domestic opponents accuse him of using the judiciary to settle political scores, hailed the conviction of Mr. Trump in New York as “an American lesson” for Polish politicians.
“The law determines guilt and punishment, regardless of whether the perpetrator is a president or a minister,” Mr. Tusk said in a message posted on X. A veteran centrist, Mr. Tusk took office after an October election that ousted a nationalist government that cultivated close ties with Mr. Trump during and after his time in the White House.
Still, on Friday, most foreign governments, forced to surf every shift in the American political mood, reacted cautiously.
“I would like to refrain from commenting on matters related to judicial procedures in other countries,” Yoshimasa Hayashi, Japan’s chief cabinet secretary, said at a news conference in Tokyo on Friday.
In Britain, where a national election campaign is underway, Prime Minister Rishi Sunak refused to discuss the Trump case. His Labour Party opponent, Keir Starmer, a former top prosecutor, said he respected the court’s decision and called the situation unprecedented.
“Ultimately whether he is elected president will be a matter for the American people and obviously, if we’re privileged to come in to serve, we would work with whoever they choose as their president,” Mr. Starmer told BBC Radio Scotland.
Mao Ning, a spokeswoman for China’s foreign ministry, declined to comment on the verdict. She said she hoped whoever was elected president would “be committed to developing healthy and stable China-U. S. relations.”
The possibility of Mr. Trump’s return to the White House is a source of anxiety for U.S. allies in Asia that rely on Washington for their defense.
When Prime Minister Fumio Kishida of Japan made a state visit to Washington in April, President Biden called relations between the countries the most important bilateral alliance in the world. With American concern rising over China’s expanding military footprint, Mr. Biden has strengthened American defense partnerships with Japan, South Korea, the Philippines and others in Asia.
By contrast, while president, Mr. Trump called for Japan, which hosts more than 50,000 American troops on its soil, to pay $8 billion for the upkeep of American bases there. (It never happened.)
Still, the fundamental tension in regional geopolitics — the contest between the United States and China — will continue no matter who wins the American presidential election.
“Beijing has no illusion about Trump or Biden, given their anti-China solid stance,” said Lau Siu-kai, an adviser to the Chinese government on Hong Kong policy. “Beijing is all set for a more intense confrontation with the U.S. over technology, trade and Taiwan.”
Officials in China’s embassy in the United States and its consulates around the country are most likely scrambling to assess how the verdict could affect the election, said Willy Lam, an analyst of Chinese politics at the Jamestown Foundation in Washington.
“The majority of Xi Jinping’s advisers now think a Trump presidency might be worse for U.S.-China relations,” Mr. Lam said of China’s top leader. “If Trump were to win, given the now peculiar circumstances of his victory, he might gravitate towards unpredictable actions to assert his authority.”
There is a sense in Asia that the region is perennially overlooked and underappreciated by U.S. presidents, particularly as crises in Europe and the Middle East have monopolized Mr. Biden’s attention. That sentiment was also felt acutely during Mr. Trump’s presidency, and for American partners in Asia it was made worse by his affinity for regional strongmen.
In addition to occasional expressions of admiration for Mr. Putin and Kim Jong-un of North Korea, Mr. Trump invited to the White House a former army chief who led a coup in Thailand and installed himself as prime minister. Mr. Trump drew accolades from Rodrigo Duterte, formerly the president of the Philippines and now under investigation by the International Criminal Court over his deadly war on drugs.
The Philippines is now led by the son of the longtime dictator Ferdinand E. Marcos, who died in exile in Hawaii. He has reoriented the country away from China back toward the United States.
In at least one regard — the prosecution of former leaders — the rest of the world is far ahead of the United States. South Korea, where four former presidents have been convicted of corruption and abuse of power, has made something of a national sport of imprisoning disgraced leaders. The former French presidents Nicolas Sarkozy and Jacques Chirac were convicted of corruption.
Jacob Zuma, the former president of South Africa, has been charged with money laundering, among other crimes. And Luiz Inácio Lula da Silva was sentenced to years in prison for corruption after leading Brazil. His convictions were eventually annulled. He is again president of the country.
Reporting was contributed by Stephen Castle, Elisabetta Povoledo, Roger Cohen, Zixu Wang, Andrew Higgins, Camille Elemia , Choe Sang-Hun , Motoko Rich , Alexandra Stevenson , Sui-Lee Wee and Sameer Yasir .
An earlier version of this article misstated the length of Rodrigo Duterte’s term in office. It was six years, not eight years.
How we handle corrections
Hannah Beech is a Times reporter based in Bangkok who has been covering Asia for more than 25 years. She focuses on in-depth and investigative stories. More about Hannah Beech
Paul Sonne is an international correspondent, focusing on Russia and the varied impacts of President Vladimir V. Putin’s domestic and foreign policies, with a focus on the war against Ukraine. More about Paul Sonne
Our Coverage of the Trump Hush-Money Trial
Guilty Verdict : Donald Trump was convicted on all 34 counts of falsifying records to cover up a sex scandal that threatened his bid for the White House in 2016, making him the first American president to be declared a felon .
What Happens Next: Trump’s sentencing hearing on July 11 will trigger a long and winding appeals process , though he has few ways to overturn the decision .
Reactions: Trump’s conviction reverberated quickly across the country and around the world . Here’s what voters , New Yorkers , Republicans , Trump supporters and President Biden had to say.
The Presidential Race : The political fallout of Trump’s conviction is far from certain , but the verdict will test America’s traditions, legal institutions and ability to hold an election under historic partisan tension .
Making the Case: Over six weeks and the testimony of 20 witnesses, the Manhattan district attorney’s office wove a sprawling story of election interference and falsified business records.
Legal Luck Runs Out: The four criminal cases that threatened Trump’s freedom had been stumbling along, pleasing his advisers. Then his good fortune expired .

IMAGES
VIDEO
COMMENTS
Palliative Care. Physician Obligation. Financial Motivations. 1. Legalization. "The right to die should be a matter of personal choice. We are able to choose all kinds of things in life from who we marry to what kind of work we do and I think when one comes to the end of one's life, whether you have a terminal illness or whether you're ...
This highlights the importance of considering why euthanasia should be legal in this essay. Granting patients the autonomy to make this decision would honor their right to choose how they wish to approach their final moments and put an end to their unbearable suffering. Moreover, legalizing euthanasia could ease the burden on families by ...
Conversely, there are two notable oversights in this interpretation of a right to assisted dying as an extension of the principles of bodily autonomy: First, it would be wrong to view individual liberty as absolute. The HRA allows for exceptions to Article 8 on grounds of 'health or morals' [ 25 ].
Definition and current legal framework. Assisted dying is a general term that incorporates both physician-assisted dying and voluntary active euthanasia.Voluntary active euthanasia includes a physician (or third person) intentionally ending a person's life normally through the administration of drugs, at that person's voluntary and competent request. 2, 3 Facilitating a person's death ...
Why active euthanasia and physician assisted suicide should be legalised - PMC. Journal List. BMJ. v.323 (7321); 2001 Nov 10. PMC1121585. As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of Health.
Assisted dying is a general term that incorporates both physician-assisted dying and voluntary active euthanasia.Voluntary active euthanasia includes a physician (or third person) intentionally ending a person's life normally through the administration of drugs, at that person's voluntary and competent request. 2,3 Facilitating a person's death without their prior consent incorporates ...
Euthanasia, also called mercy killing, refers to the administration of a lethal medication to an incurably suffering patient. It may be voluntary (the patient requests it) or involuntary. Euthanasia is illegal in the United States, but voluntary euthanasia is legal in Belgium, Colombia, Luxembourg, and Canada.
Existential Suffering as a Legitimization of Euthanasia - Volume 32 Issue 1. Introduction. The controversial nature of the issue of whether it should be legal to perform euthanasia or assist in another's suicide has waned, and several countries have legalized these options, but it would not be realistic to expect a universally accepted perspective to be forthcoming.
Bioethicist Peter Singer argues that, under certain circumstances, people should have the right to die at a time of their choosing. Since Oregon legalized physician-assisted suicide for the ...
because life and death are God's business with which we shouldn't interfere. because most people don't want to die. because it violates our autonomy in a drastic way. The first two reasons form ...
Euthanasia is one of the issues that has been the subject of intense debate over time. It has been a pertinent issue in human rights discourse as it also affects ethical and legal issues ...
Active euthanasia is criminal while passive euthanasia is non criminal. The big debate surrounding euthanasia is whether to consider it as voluntary thus becoming a suicide or involuntary murder. Further, there have been numerous arguments as to whether a certain death could be considered easy, happy, painless or wrongful.
Abstract. Acting as the conductor on the train of impending death, a divisive turn to the left will hasten human pain and end life; while a swerve to the right will prolong human life, but also, extend unbearable human pain and suffering. One could make sound arguments that both of these grim decisions are equally acts of compassion or malice.
Several states have begun to consider legislation that would legalize active voluntary euthanasia. To address some of the ethical issues raised by such legislation, the Center for Applied Ethics sponsored a symposium entitled Legalizing Euthanasia: Ethical Perspectives on Medicine and Dying.Principal speakers were Derek Humphry, founder and president of the Hemlock Society, and author of the ...
pros and cons. The pros and cons of legalising euthanasia. Help to end suffering for terminal patients could put disabled, elderly and unwell people at risk, opponents warn. Assisted dying is a ...
Mercy Killing Debate. Euthanasia or physician- assisted suicide, also know as mercy killing, is becoming a prominent public debate. The implications of legalizing assisted suicide are wide-ranging from a medical, legal, political and ethical point of view. The term euthanasia means "good death" in Greek.
The word 'Euthanasia' comes from the Greek word 'Euthanatos' meaning 'good health.'. Euthanasia is defined as the deliberate ending of a person's life by anther person at the specific request of the former. Euthanasia is not the same as other practices such as Physician-Assisted Suicide, Terminal Sedation or Withholding ...
Introduction. Euthanasia is defined as "the act of deliberately ending a person's life to relieve suffering". People seek euthanasia as it provides a solution to problems that many views as insurmountable; more specifically to deal with "unbearable" suffering that may arise in life, and or death.
Active euthanasia gives the medical. practitioner power, which in turn can be abused. Active euthanasia leads inevitably to involuntary euthanasia. When active euthanasia has been previously accepted and. legalised, it has led inevitably to inactive euthanasia. Holland is moving rapidly down the slippery slope with the.
But, before this legalization in the Penal Code this country had adopted a legal regulation of euthanasia and, before and after that, extensive surveys into the practice of euthanasia had been carried out. ... Juridical and ethical essays on life, the body and death],469-574. Reeks: Het recht in de samenleving, van het Centrum Grondslagen van ...
All twenty subjects were for euthanasia, and said that it should be legalised in the UK, but the questionnaire (See appendix 1) brought out differing views regarding, under what circumstances it should be made legal, for example only for terminal illness. The research findings showed that there were a higher number of participants that believed ...
If euthanasia is legalised, then there is a grave apprehension that the State may refuse to invest in health (working towards Right to life). Legalised euthanasia has led to a severe decline in the quality of care for terminally-ill patients in Holland 7. Hence, in a welfare state there should not be any role of euthanasia in any form.
Essay Map. Euthanasia should be legalized because it relieves the terminally ill patient from undergoing adverse pain and suffering and also saves the family and friends from having to see their loved one going through such immense pain and suffering knowing that there is nothing that could be done to improve their situation. Other than that, euthanasia is not just a necessity for terminally ...
Voluntary Euthanasia, when the individual wishes through a conscious decision of ending their help with the help of another. It requires full consent and awareness of the concept and process. Non-Voluntary Euthanasia, whereas the decision of ending an individual's life is taken by another, like a family member or your partner. This takes place when the individual is in a state of permanent ...
The 7th Amendment to the United States Constitution stands as a pivotal element in ensuring justice within the American legal framework. Adopted in 1791 as part of the Bill of Rights, it guarantees the right to a jury trial in certain civil cases, underscoring the importance of citizen participation in the judicial process.
By New York Times Opinion. June 2, 2024. Now that Donald Trump has been convicted on 34 felony counts, his sentencing hearing looms on July 11. Below are two legal experts weighing in on the ...
Mr. Grasso is a retired New York City administrative judge. I spent almost 13 years as a judge in Brooklyn, Queens and the Bronx. I supervised judges presiding over a wide spectrum of cases ...
The Supreme Court Could Make the President a King. The high court's decision in the Trump immunity case appears to set the stage for future abuses of the pardon power. Supreme Court Police ...
Donald J. Trump in New York after his conviction on Thursday. Hiroko Masuike/The New York Times. The world does not vote in American presidential elections. Nor do its jurors play a part in the ...