- Open access
- Published: 11 October 2023

A network system for the prevention and treatment of mushroom poisoning in Chuxiong Autonomous Prefecture, Yunnan Province, China: implementation and assessment
- Qunmei Yao 1 na1 ,
- Zhijun Wu 2 na1 ,
- Jiaju Zhong 1 ,
- Chengmin Yu 1 ,
- Haijiao Li 2 ,
- Qiuling Hu 3 ,
- Jianrong He 4 ,
- Jianping Du 5 &
- Chengye Sun 2
BMC Public Health volume 23 , Article number: 1979 ( 2023 ) Cite this article
943 Accesses
3 Citations
Metrics details
Mushroom poisoning is a major public health issue in China. The integration of medical resources from different institutes of different levels is crucial in reducing the harm of mushroom poisoning. However, few studies have provided comprehensive implementation procedures and postimplementation effectiveness evaluations. To reduce the harm caused by mushroom poisoning, a network system for the prevention and treatment of mushroom poisoning (NSPTMP) was established in Chuxiong, Yunnan Province, a high-risk area for mushroom poisoning.
The NSPTMP consists of three types of institutions, namely, centers for disease prevention, hospitals, and health administration departments, with each kind of institution comprising prefecture, county/city, town, and village levels. After three years of implementation, the network was evaluated by comparing the indices before and after network implementation using data from the “Foodborne Disease Outbreak Surveillance System” and 17 hospitals in Chuxiong. The indices included the fatalities caused by mushroom poisoning, the composition ratios of different types of mushrooms for both outpatients and inpatients and the hospitalization rates.
Compared to the average fatality rate of mushroom poisoning from 2015 to 2017, the average fatality rate from 2018 to 2020 significantly decreased from 0.57 to 0.06% ( P < 0.001). Regarding the poisonous genus containing lethal mushrooms, the outpatient and inpatient composition ratios significantly decreased for Amanita (9.36–2.91% and 57.23–17.68%, respectively) and Russula (15.27–8.41%) ( P < 0.05). Regarding poisonous mushrooms that caused mild symptoms, the outpatient and inpatient composition ratios significantly increased for Scleroderma (5.13–13.90% and 2.89–18.90%, respectively) and Boletaceae (19.08–31.71%) ( P < 0.05), and the hospitalization rates significantly increased for Scleroderma (6.33–18.02%) and Boletaceae (5.65–12.71%) ( P < 0.05).
Conclusions
These findings suggest that the NSPTMP effectively reduced the harm caused by mushroom poisoning. In addition to the integration of medical resources, the development of poisonous mushroom identification, hierarchical treatment systems in hospitals, public education, and professional training also played important roles in improving the system’s effectiveness. The establishment and evaluation of the NSPTMP in Chuxiong Prefecture can provide valuable insights and serve as a model for other regions facing similar challenges in managing mushroom poisoning.
Peer Review reports
Introduction
Mushroom poisoning occurs worldwide [ 1 , 2 , 3 ]. In Europe [ 4 , 5 , 6 , 7 ], the United States [ 8 , 9 , 10 ] and China [ 11 , 12 , 13 , 14 , 15 , 16 ], the consumption of wild mushrooms is a common practice and often leads to a high number of cases of toxic mushroom exposure. From 1999 to 2016, US poison centers reported 133,700 cases of mushroom poisoning, with 47,220 healthcare facility treatments and 52 deaths [ 10 ]. In Germany, from 2010 to 2018, 4441 patients were treated for mushroom poisoning in hospitals, and 32 deaths were recorded from diagnostic data [ 6 ]. However, a higher number of mushroom poisoning deaths and fatalities have been observed in China than in Europe and the US. Specifically, from 2004 to 2014, 3710 cases of mushroom poisoning were reported in “The Public Health Emergency Management Information System” in China, with 786 deaths [ 12 ]. Recent data from the “Foodborne Disease Outbreak Surveillance System” in China have shown that the proportion of foodborne disease-associated deaths caused by poisonous mushrooms is the highest [ 17 , 18 ], accounting for 37.78% (51/135), 57.6% (72/125), and 67.86% (76/112) of deaths in 2018, 2019 and 2021, respectively [ 19 , 20 , 21 ]. Thus, mushroom poisoning is a major public health problem in China.
Concern about mushroom poisoning in China has been a long-standing issue. Prior to 2000, China had neither a surveillance system that reflected national poisonous mushroom exposure nor a standardized mushroom poisoning prevention and treatment system. In 2000, a mushroom poisoning accident in Guangzhou (9 people were poisoned, and 8 died within a week) [ 22 ] sparked concern. Subsequent investigation of this incident revealed that some unique Chinese poisonous mushroom species were misidentified as common species found in Europe or the United States for many years. For example, the mushroom involved in the Guangzhou incident was not the common European species, Amanita verna , but a new species that had not yet been identified and was later named by fungal taxonomists Amanita exitialis [ 23 ]. In 2003, the severe acute respiratory syndrome (SARS) outbreak in China promoted the development of China’s public health system, including the establishment of the “Public Health Emergency Management Information System” by the Chinese Center for Disease Prevention (CCDC) in 2004. This system allows major mushroom poisoning cases to be reported as public health emergency events. At the same time, the surveillance system for foodborne diseases was established in 2001 and updated in 2013. Therefore, with the experience gained from field investigations, phone consultations from poisoning hotlines, and surveillance data analysis, the exposure properties of mushroom poisoning in China gradually became better understood. It became apparent that mushroom identification was crucial in the diagnosis and treatment of mushroom poisoning cases, which is also a consensus revealed in the relevant literature [ 6 , 7 , 9 , 23 ]. As a result, mycologists became involved in investigating mushroom poisoning incidents. In 2006, the “Toxic Biological Sample Bank” project was established by the CCDC to obtain the ecological characteristics of poisonous mushrooms and promote the taxonomy of mushrooms in China. Then, books and research papers on poisonous mushroom identification, prevention, and control were published [ 11 , 23 , 24 , 25 , 26 , 27 ]. These efforts have shifted the prevention and treatment of mushroom poisoning in China from an empirical mode to an evidence-based mode.
Over the years, experience in preventing, controlling, and treating mushroom poisoning in China has led to the recognition of two key characteristics. First, mushroom poisoning management involves multiple aspects, such as mushroom identification, standardization of clinical diagnosis and treatment, management of local health resources, and public education. Effective management of these aspects requires coordination across various institutions, including hospitals, CDCs, health administration departments (HADs), and research institutes. Second, it has been observed that over 80% of patients with mushroom poisoning experience mild symptoms [ 7 , 10 ], which suggests that a hierarchal treatment system should be established to ensure that patients with mild symptoms are treated in most healthcare institutions and that patients with severe symptoms are referred to hospitals with life-saving equipment as early as possible. Therefore, the integration of medical resources from different institutes of different levels is crucial in reducing the harm of mushroom poisoning [ 28 , 29 ]. To address these issues, in 2018, a network system for the prevention and treatment of mushroom poisoning (NSPTMP) was established in the most representative region, Chuxiong Autonomous Prefecture, Yunnan Province [ 28 , 30 ]. The NSPTMP was designed to reduce the harm of mushroom poisoning in Chuxiong Prefecture with two innovative principles, called “combination and connection”. This means (1) combining the job of prevention at the CDC, the treatment of patients in hospitals, and the authorities of the HAD; and (2) connecting the various levels, from the prefecture, through cities and counties, and down to the townships and villages. After three years of implementation, the effectiveness of the network was evaluated. Although many mushroom poisoning-related studies have proposed strategies to reduce mushroom poisoning risks by strengthening cooperation among various parties and enhancing public education, few have addressed the implementation of such strategies or evaluated their postimplementation effects.
The aim of our study was to reduce the harm caused by mushroom poisoning by establishing the NSPTMP in Chuxiong, Yunnan Province, a high-risk area for mushroom poisoning. This study comprises the following two main components. First, a comprehensive overview of the roles of each kind of institution and their interrelationship at each level within the NSPTMP is presented. Second, the effectiveness of the NSPTMP was evaluated using data from the Foodborne Disease Outbreak Surveillance System and diagnostic data from 17 key hospitals in Chuxiong Prefecture. The findings of this study offer valuable insights for the prevention, control, and management of mushroom poisoning.
Data collection
To assess the impact of the NSPTMP, two distinct data resources were used. First, the Foodborne Disease Outbreak Surveillance System in Chuxiong Prefecture provided insights into mushroom poisoning incidents reported by hospitals across 8 counties and 2 cities in Chuxiong Prefecture (including rural health centers) between 2015 and 2020. Second, data were collected from 17 hospitals within Chuxiong Prefecture, focusing on mushroom species information for patients in both outpatient and inpatient settings.
The surveillance data included the number of individuals who were poisoned and deaths resulting from mushroom poisoning. However, the data offered a general and coarse estimation of the situation, with regional distribution characteristics, but lacked detailed mushroom classification or identification. The hospital data provided a more detailed and specific assessment of mushroom poisoning incidents, helping to paint a more nuanced picture of the impact of the NSPTMP.
Statistical analysis
The data were analyzed using SPSS version 20.0. The count data are presented as the number of cases or as a percentage and were analyzed using the χ2 test. To assess the impact of the network, comparisons of the indices before and after network implementation were performed. The observed difference was deemed statistically significant at a p value of less than 0.05.
Establishment of the NSPTMP in Chuxiong Prefecture, Yunnan Province
The NSPTMP in Chuxiong Prefecture consists of three types of institutions arranged horizontally, namely, CDCs, hospitals, and HADs. This horizontal arrangement serves as the foundation of the “combination” principle (Fig. 1 A). Each of these institutions is vertically arranged into four levels, comprising the prefecture, counties/cities, towns, and villages, forming the basis of the “connection” principle, particularly for hospitals (Fig. 1 B).
HADs at the prefecture, city/county, and town levels
At the prefecture, city/county, and town levels, HADs play a vital role in the NSPTMP. First, HADs can facilitate the development of the NSPTMP and implementation of associated policies based on their organizational structure. Second, HAD authorities are responsible for allocating and coordinating hospitals, CDCs, and other health resources to address mushroom poisoning incidents.
CDCs at the prefecture, city/county, and town levels
CDCs operating at the prefecture, city/county, and town levels play a critical role in the NSPTMP. First, CDCs are tasked with conducting field epidemiological investigations, mushroom sampling, preservation, and, in certain cases, mushroom toxin detection (if feasible). Second, in some regions, the establishment of a poisonous mushroom sample library and an online platform for mushroom identification has been initiated to aid in the identification and classification of poisonous mushrooms.
Poisonous mushroom sample library
The National Institute of Occupational Health and Poison Control (NIOHP) at the Chinese Center for Disease Control and Prevention (China CDC) initiated a project in 2016 to establish a poisonous mushroom sample library in regions with a high prevalence of mushroom poisoning, such as Guizhou and Yunnan provinces. The goal of this project was to facilitate the standardized collection of mushroom samples by CDCs at all levels in a timely manner. With the successful implementation of this initiative, a searchable poisonous mushroom sample library was established.
Online poisonous mushroom identification
During the establishment of the national poisonous mushroom sample library, an effective online working system was developed among doctors, CDC staff, and mycologists, aided by the emergence of new communication tools, particularly the WeChat app. To identify poisonous mushrooms, doctors initially collect clinical symptoms from mushroom poisoning patients. Subsequently, CDC staff collect mushroom samples and upload pictures of these samples to the WeChat group as soon as possible. Third, mycologists conduct a preliminary online identification of the mushroom samples based on the pictures provided, providing feedback to the CDC staff or doctors, which is important information for further diagnosis and treatment. The NIOHP provides final confirmation of the mushroom species by molecular biological identification of mushroom samples sent by local CDCs.
Hospitals at the prefecture, city/county, and town levels
Hospitals at various levels, including village, town, county/city, and prefecture levels, exhibit different levels of expertise in recognizing, diagnosing, and treating patients affected by mushroom poisoning.
Village-level clinics
: These clinics should have the ability to make preliminary diagnoses of mushroom poisoning and provide simple treatment to patients, with the objective of conducting initial patient grading.
Town-level hospitals
: These hospitals should possess the capability to accurately categorize patients into high-, medium-, and low-risk groups and provide treatment for low-risk groups, with the aim of accepting patients with mild symptoms.
County-level hospitals
: These hospitals should have the capacity to recognize patients at high, medium, and low risk and provide appropriate treatment to patients in medium- and low-risk groups. Additionally, they should be equipped with life support technologies such as respiration and circulation systems, and when feasible, blood perfusion, to enable treatment of patients with mild to moderate symptoms that are not life threatening.
Emergency department of the prefecture-level hospital
: This department should have the capability to manage patients in all risk categories and provide guidance to lower-level hospitals on implementing standardized treatment protocols for mushroom poisoning. Additionally, the department should possess the expertise to identify poisonous mushroom species and detect mushroom toxins. The emergency intensive care unit (EICU) of this hospital should be equipped with advanced life support technologies, including respiration and circulation systems, artificial liver support, and bedside blood purification, to enable effective treatment of patients with complex and serious symptoms, as well as to offer guidance to lower-level hospitals in managing such cases.
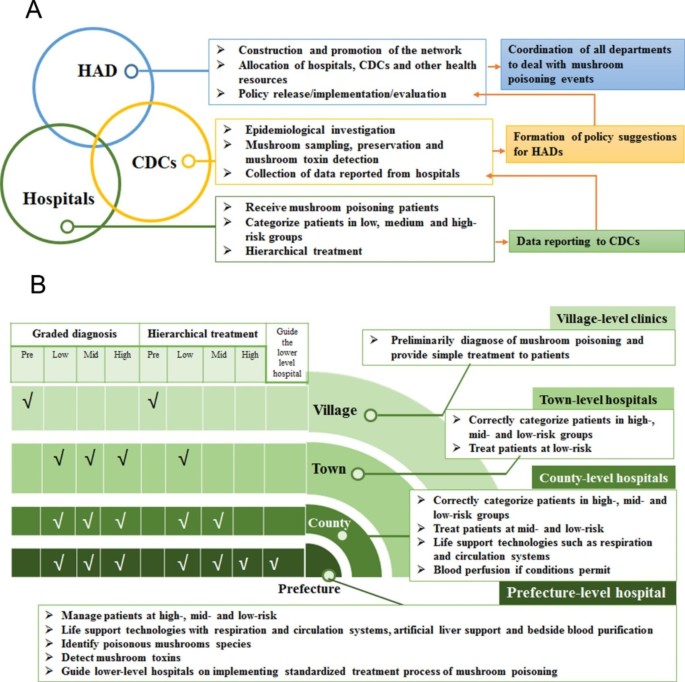
The structure of the NSPTMP. (A) Association among three kinds of institutions in the NSPTMP; (B) Association of four levels of hospitals in the NSPTMP
Implementation, practice, and promotion of the NSPTMP
Below, we present a description of the procedures and practical methods of the NSPTMP to enhance residents’ prevention awareness, develop doctors’ diagnostic and treatment standardization skills, and reinforce communication and consensus among relevant professionals.
Increasing residents’ awareness of prevention
Given that wild mushrooms are a traditional food in Chuxiong Prefecture, it is challenging for residents to abandon their habit of consuming them. To reduce the likelihood of severe mushroom poisoning, residents are advised against ingesting highly toxic mushrooms, such as Amanita and Russula subnigricans . If poisoning symptoms arise after consuming wild mushrooms, patients are recommended to seek medical attention immediately. Upon hospital admission, patients are urged to provide a detailed history of mushroom ingestion, along with photographs and mushroom samples whenever feasible to facilitate diagnosis and treatment. To increase public awareness, an advertising video on the clinical prevention and treatment of mushroom poisoning, a sitcom on the classification of diagnosis and treatment of mushroom poisoning, and a popular science exhibition on common poisonous mushrooms in Yunnan Province were produced. During the high-incidence season of mushroom poisoning, these materials are displayed in public gathering areas.
Outpatient doctors in hospitals: diagnosis
Physicians diagnose patients with suspected mushroom poisoning based on the criteria for mushroom poisoning patients (as follows):
Patients who provide mushroom pictures or samples, which are identified by experts as poisonous mushrooms;
Patients whose blood or urine test results show the presence of mushroom toxins detected by high-performance liquid chromatography or enzyme-linked immunosorbent assay;
Patients with a clear history of poisonous mushroom consumption and corresponding typical poisoning symptoms;
If the patients or their families are unable to provide pictures or samples of the mushrooms, they can identify the poisonous mushrooms using standard pictures of poisonous mushrooms.
Hospital admission/hospitalization/referral: risk classification
In China, mushroom poisoning symptoms include 7 clinical subtypes: acute liver failure, rhabdomyolysis, hemolysis, acute renal failure, gastroenteritis, psycho-neurological disorder, and photosensitive dermatitis, as well as other undetermined clinical types. To achieve the objective of a graded diagnosis, hierarchical treatment, and timely referral for patients, mushroom poisoning is classified into low, medium and high risk levels based on the clinical manifestations and mushroom species. Accordingly, patients can be treated appropriately or transferred to hospitals with better treatment equipment.
Low-risk group: The patients’ vital signs are stable, and the incubation period is generally less than 6 h. Highly toxic mushroom ingestion has been ruled out. In such cases, possible toxic mushrooms may include Boletaceae (with digestive tract symptoms), Chlorophyllum , Lactarius , Russula (excluding Russula subnigricans ), Scleroderma , Cordierites frondosus , and other species.
Medium-risk group: The patients’ symptoms include transient impaired consciousness, digestive tract symptoms leading to an internal environment disorder, organ function damage, and abnormal liver and kidney function indicators in laboratory examinations. Possible toxic mushrooms may include Boletaceae (which mainly cause neuropsychiatric symptoms), Amanita (which may cause neuropsychiatric symptoms or renal damage), and Cortinariaceae.
High-risk group: The patients’ symptoms are marked by unstable vital signs, impaired consciousness, organ dysfunction or failure, and severe internal environment disorder. Of mushroom poisoning fatalities, 70–90% are caused by acute liver failure induced by mushrooms containing amatoxins, which are primarily found in three genera: Amanita , Galerina , and Lepiota. Russula subnigricans and other mushrooms may also cause fatal poisoning.
Highly toxic mushrooms: consensus on diagnosis and treatment
The mushrooms that cause the highest fatality rates among all poisonous mushrooms are those containing amatoxins. In China, the Consensus on the clinical diagnosis and treatment of poisoning of mushrooms containing amanitin [ 31 ] was coedited by relevant professional committees, the NIOHP in the China CDC, and the People’s Hospital of Chuxiong Prefecture.
Hospitals, CDCs, and HAD authorities: communication and training
Communication and training among hospitals, CDCs, and HADs are conducted regularly and include:
Preparation and practice of the emergency plan for mushroom poisoning.
Development of a training course on the treatment of mushroom poisoning in hospitals.
Annually, the People’s Hospital of Chuxiong Prefecture provides further education for 5–10 medical and nursing personnel and offers training on rescue techniques for patients in medium- and high-risk groups for mushroom poisoning. Moreover, the hospital trains county-, town-, and village-level hospitals on the identification and treatment of poisonous mushrooms for mushroom poisoning patients through consultations, counterpart assistance, and medical union systems.
From 2017 to 2021, the People’s Hospital of Chuxiong Prefecture successfully hosted the Mushroom Poisoning Clinical Prevention and Control Conference annually. The conference attracted scholars from various fields related to mushroom poisoning and provided online and offline training to over 20,000 individuals.
Evaluation of the NSPTMP by data from the Foodborne Disease Outbreak Surveillance System
Table 1 presents the number of exposures and deaths caused by mushroom poisoning in Chuxiong Prefecture, which includes eight counties and two cities. Overall, between 2015 and 2020, there were 484 reported cases of mushroom poisoning in Chuxiong Prefecture, involving 6,306 individuals, of whom 20 died. After implementing the NSPTMP, although there was no significant change in the total number of mushroom poisoning incidents (3,174 vs. 3,132), the number of fatalities caused by mushroom poisoning substantially decreased (from 18 to 2). Consequently, the fatality rate decreased significantly from 0.57% (before implementation) to 0.06% (after implementation) ( P < 0.001). Table S1 and Figure S1 in the supplementary materials show the specific number of mushroom poisoning cases in Chuxiong Prefecture with regional information and annual trends.
Evaluation of the NSPTMP by data from 17 key hospitals in Chuxiong Prefecture
Between 2015 and 2020, a total of 4,841 patients with mushroom poisoning were admitted to the 17 hospitals we investigated in Chuxiong Prefecture. Among them, 57.34% (2,776/4,841) had information recorded regarding the identification of the mushroom species involved. This section only presents data on patients with documented species identification of poisonous mushrooms ingested.
Comparing the total number of outpatient and inpatient cases of mushroom poisoning before (2015–2017) and after the implementation of the NSPTMP (2018–2020), there was a relatively stable number of outpatients (1,539 vs. 1,237) and inpatients (172 vs. 164). However, the composition ratios of recorded mushroom species exhibited a significant change in both outpatient and inpatient cases.
Table 2 shows the changes in the composition ratios of recorded mushroom species among outpatient and inpatient cases of mushroom poisoning before and after the implementation of the NSPTMP. The data indicate that after the implementation of the NSPTMP, there was a significant decrease in the outpatient composition ratio regarding highly toxic Amanita mushroom poisoning from 9.36 to 2.91% ( P < 0.001), as well as a decrease in the outpatient composition ratio for Russula mushrooms (probably with highly toxic species) from 15.27 to 8.41% ( P < 0.001). Similarly, there was a decrease in the inpatient composition ratio for Amanita mushroom poisoning from 57.23 to 17.68% ( P < 0.001).
However, there were also changes in the composition ratios of nonlethal mushroom poisonings. The proportion of Scleroderma mushroom poisoning in outpatients increased from 5.13 to 13.90% ( P < 0.001), and the composition ratio of Boletaceae mushroom poisoning in inpatients increased from 19.08 to 31.71% ( P = 0.008). The composition ratio of Scleroderma mushroom poisoning inpatients also increased from 2.89 to 18.90% ( P < 0.001).
After the implementation of the NSPTMP, there was no significant change in the hospitalization rate for highly toxic mushroom poisoning ( Amanita and Russula ), while the hospitalization rate for nonlethal mushroom poisoning (Boletaceae and Scleroderma ) significantly increased. Table 3 shows that the hospitalization rate for Boletaceae mushroom poisoning increased significantly from 5.65% (33/584, before implementation) to 12.71% (52/409, after implementation, P < 0.001), and the hospitalization rate for Scleroderma mushroom poisoning increased significantly from 6.33% (5/79, before implementation) to 18.02% (31/172, after implementation, P = 0.014).
Various types of data resources reflect exposure to poisonous mushrooms, including health surveillance systems [ 6 , 7 , 10 ], hospital visit records [ 7 , 32 ], field surveys [ 11 ], telephone or online consultations [ 9 , 13 , 14 , 15 , 33 ], and literature reviews. Data from surveillance systems in China show that mushroom poisoning is one of the leading causes of death by foodborne poisoning. Over the past 20 years, as research and the understanding of mushroom poisoning in China have improved, it gradually became apparent that integrating the efforts of the CDC, hospitals, and HADs at various levels is a necessary step in reducing the harm of mushroom poisoning. In 2018, the NSPTMP was established in Chuxiong Prefecture, Yunnan Province, a representative high-risk area for mushroom poisoning in China, based on the principles of “combination and connection”. In this paper, we provided a comprehensive introduction to the NSPTMP and evaluated its effectiveness before and after its implementation. The evaluation showed that the implementation of the NSPTMP was effective in reducing the harm caused by mushroom poisoning, as evidenced by the following: (1) The total number of mushroom poisoning cases was almost stable before and after its implementation (3174 vs. 3132), but the number of mushroom poisoning deaths decreased from 18 to 2, with a significant decrease in the fatality rate (0.57% vs. 0.06%, P < 0.001). (2) After the implementation of the NSPTMP, the composition ratio for lethal mushrooms decreased significantly for outpatients ( Amanita and Russula ) and inpatients ( Amanita ), suggesting that residents reduced the consumption of mushrooms that can cause serious illness. (3) After the implementation of the NSPTMP, the composition ratios of mushrooms that caused minor symptoms significantly increased for both outpatients ( Scleroderma ) and inpatients (Boletaceae and Scleroderma ), indicating that with the decrease in highly toxic mushroom poisoning, mushrooms that caused mild symptoms received more attention.
The effectiveness of the NSPTMP is based on the development and standardization of the following three aspects: identification of poisonous mushrooms, hierarchical treatment in hospitals, and public education and professional training.
Identifying mushroom species is crucial for clinical diagnosis and hierarchical management. In China, research on the identification of poisonous mushrooms began relatively late compared to Europe and the United States. However, over the past two decades, Chinese scholars have conducted systematic research on poisonous mushrooms, and more than 520 species of poisonous mushrooms have been reported. The toxins of highly toxic poisonous mushrooms in China differ substantially from those of mushrooms in other countries. For example, the amatoxin levels in Amanita exitialis , unique to China, are 2–5 times higher than those in Amanita verna , a species common in Europe [ 34 , 35 ]. The poisonous mushroom identification rate in China has gradually increased, with 57% (2776/4841) of the mushroom poisoning cases received by 17 hospitals in Chuxiong Prefecture undergoing mushroom species determination from 2015 to 2020, compared to only 0.93% of mushroom poisoning events with mushroom specimen collection and identification from 2010 to 2014, as reported in the surveillance system [ 12 ]. However, the literature shows that the correct identification rate of mushroom species in mushroom poisoning events is quite low, ranging from 5 to 27% [ 2 , 7 , 36 , 37 , 38 , 39 ]. To improve identification accuracy, the basis for mushroom species determination has evolved from identification by pictures to standardized collection and preservation of mushroom samples and morphological and molecular biological identification. Additionally, research on mushroom taxonomy has promoted the detection of mushroom toxins and toxicity research of whole mushrooms or their toxins, which are of great value for toxin determination in clinical biological samples, poisoning mechanism research, and therapeutic drug development.
Hierarchical treatment in hospitals is an essential component of the NSPTMP. Although mushroom poisoning is a major public health issue, most cases are mild, and only a small proportion are severe and require hospitalization [ 10 , 32 ]. In Chuxiong Prefecture, between 2015 and 2020, of the 2776 outpatient cases of mushroom poisoning in 17 hospitals, the majority were poisoned by nonlethal mushrooms, such as Boletaceae, Scleroderma , and Lactarius , with Boletaceae being the most common (993 cases/2776 cases, 35.77%). Therefore, correct identification of mushrooms is crucial for appropriate hospital surveillance and management [ 7 , 36 , 37 , 38 ]. To address this, the NSPTMP adjusts medical resources based on diagnosis by grade and hierarchical treatment, resulting in more high-risk group patients being admitted by the People’s Hospital of Chuxiong Prefecture (Table S1 ). In 2021, the Yunnan Provincial Health Commission Office adopted the strategy of diagnosis by grade and hierarchical treatment” for the diagnosis and treatment of mushroom poisoning patients.
The NSPTMP also emphasizes public education and professional training. Regarding public education, some studies have shown that residents’ misrecognition of edible mushroom species is the most common cause of poisoning, which can be prevented through science popularization and public education [ 10 ]. As the consumption of delicious wild mushrooms is a way of life in Yunnan, it is impossible to persuade residents not to eat wild mushrooms at all. The NSPTMP focuses on the popular science work regarding highly toxic mushrooms by warning against the consumption of Amanita and Russula , which might be associated with the decrease in lethal mushroom consumption reflected by hospital outpatient records. Second, for professional training, the NSPTMP organizes regular training for medical staff, including the identification of mushroom species, clinical diagnosis, and treatment of mushroom poisoning. In addition, the program also provides training for village doctors, who are usually the first responders to mushroom poisoning cases in rural areas. Through training and education, medical staff and village doctors can improve their knowledge and skills in the diagnosis and treatment of mushroom poisoning, which can ultimately improve the quality of care for patients and reduce the fatality rate of mushroom poisoning cases. The NSPTMP also collaborates with local communities and stakeholders to raise awareness of the risks associated with wild mushroom consumption, promoting safe and responsible mushroom foraging practices to prevent mushroom poisoning.
However, there were still some limitations in our study. First, there was still a certain proportion of mushrooms listed as “unknown” mushroom species in the analysis of the mushroom species composition for outpatients (800/2776, 28.82%) and inpatients (44/336, 13.10%). It is necessary to analyze the causes of these “unknown” mushroom classifications in the future and identify more new species if possible. Second, we used only three years before and after the implementation of the NSPTMP to evaluate the NSPTMP, and more data need to be accumulated in the future to support the effectiveness of the NSPTMP.
Importantly, although mushroom poisoning may have regional characteristics, it is still a global public health issue. Some countries may lack reliable mushroom poisoning reporting systems and related death registries, and the risk of mushroom poisoning may be considerably underestimated. Studies have shown that in addition to China, other countries, such as Russia, Ukraine, Belarus, Poland, Turkey, Iran, Nepal, and Mexico, have high fatality rates from mushroom poisoning [ 1 ]. The establishment and evaluation of the NSPTMP in Chuxiong Prefecture can provide valuable insights and serve as a model for other regions facing similar challenges in managing mushroom poisoning.
In this paper, a network system for the prevention and treatment of mushroom poisoning was established in a high-risk area for mushroom poisoning, Chuxiong. The evaluation of the NSPTMP suggested that the network can effectively reduce the harm caused by mushroom poisoning. Overall, the successful implementation of the NSPTMP in Chuxiong Prefecture highlights the importance of a comprehensive and coordinated approach to public health issues. By adopting the principles of “combination and connection” and the three core foundations of the NSPTMP (identification of poisonous mushrooms, hierarchical treatment in hospitals, and public education and professional training), other regions can develop effective strategies for the prevention and control of mushroom poisoning. However, it is crucial to adapt these strategies to the local context, accounting for differences in the types of poisonous mushrooms, the availability of medical resources, and the cultural practices related to mushroom consumption.
Data Availability
The data will not be shared publicly; however, the data are available upon reasonable request. If someone wishes to request the data from this study, author Qunmei Yao ([email protected]) can be contacted.
Abbreviations
Network system for the prevention and treatment of mushroom poisoning
Center for Disease Control
Health administration department
National Institute of Occupational Health and Poison Control
Emergency intensive care unit
He MQ, Wang MQ, Chen ZH, et al. Potential benefits and harms: a review of poisonous mushrooms in the world. Fungal Biol Rev. 2022;42:56–68. https://doi.org/10.1016/j.fbr.2022.06.002 .
Article CAS Google Scholar
Govorushko S, Rezaee R, Dumanov J, et al. Poisoning associated with the use of mushrooms: a review of the global pattern and main characteristics. Food Chem Toxicol. 2019;128:267–79. https://doi.org/10.1016/j.fct.2019.04.016 .
Article CAS PubMed Google Scholar
Diaz JH. Evolving global epidemiology, syndromic classification, general management, and prevention of unknown mushroom poisonings. Crit Care Med. 2005;33(2):419–26. https://doi.org/10.1097/01.ccm.0000153530.32162.b7 .
Article PubMed Google Scholar
Jaeger A, Jehl F, Flesch F, Sauder P, Kopferschmitt J. Kinetics of amatoxins in human poisoning: therapeutic implications. J Toxicol Clin Toxicol. 1993;31(1):63–80. https://doi.org/10.3109/15563659309000374 .
Garcia J, Costa VM, Carvalho A. Amanita phalloides poisoning: mechanisms of toxicity and treatment. Food Chem Toxicol. 2015;86:41–55. https://doi.org/10.1016/j.fct.2015.09.008 .
Wennig R, Eyer F, Schaper A, et al. Mushroom poisoning. Dtsch Arztebl Int. 2020;117(42):701–8. https://doi.org/10.3238/arztebl.2020.0701 .
Article PubMed PubMed Central Google Scholar
Cervellin G, Comelli I, Rastelli G, et al. Epidemiology and clinics of mushroom poisoning in Northern Italy: a 21-year retrospective analysis. Hum Exp Toxicol. 2018;37(7):697–703. https://doi.org/10.1177/0960327117730882 .
Yamada EG, Mohle-Boetani J, Olson KR, Werner SB. Mushroom poisoning due to amatoxin. Northern California, Winter 1996–1997. West J Med. 1998;169(6):380–4.
CAS PubMed PubMed Central Google Scholar
Beug MW, Shaw M, Cochran KW. (2006) Thirty-Plus Years of Mushroom Poisoning: Summary of the Approximately 2,000 Reports in the NAMA Case Registry, https://namyco.org/docs/Poisonings30year.pdf .
Brandenburg WE, Ward KJ. Mushroom poisoning epidemiology in the United States. Mycologia. 2018;110(4):637–41. https://doi.org/10.1080/00275514.2018.1479561 .
Chen ZH, Zhang P, Zhang ZG. Investigation and analysis of 102 mushroom poisoning cases in southern China from 1994–2012. Fungal Divers. 2014;61(1):123–31. https://doi.org/10.1007/s13225-013-0260-7 .
Article Google Scholar
Zhou J, Yuan Y, Lang N, Yin Y, Sun CY. Analysis of hazard in mushroom poisoning incidents in China mainland. Chin J Emerg Med. 2016;25(6):724–8. https://doi.org/10.3760/cma.j.issn.1671-0282.2016.06.008 . (in Chinese).
Li HJ, Zhang HS, Zhang YZ, et al. Mushroom poisoning Outbreaks-China, 2019. China CDC weekly. 2020;2(2):19–24. https://doi.org/10.46234/ccdcw2020.005 .
Li HJ, Zhang HS, Zhang YZ, et al. Mushroom poisoning Outbreaks-China, 2020. China CDC Weekly. 2021;3(3):41–5. https://doi.org/10.46234/ccdcw2021.014 .
Article CAS PubMed PubMed Central Google Scholar
Li HJ, Zhang HS, Zhang YZ, et al. Mushroom poisoning Outbreaks-China, 2021. China CDC Weekly. 2022;4(3):35–40. https://doi.org/10.46234/ccdcw2022.010 .
Liu ZT, Zhao J, Li JJ. (2021) Epidemiologic features of the wild mushroom poisoning in Yunnan province during 2015–2020 and its trend prediction, Journal of Food Safety and Quality, 2021, 12(17): 7074–7079 (in Chinese)
Li WW, Liu ZT, Ma XC, et al. Surveillance of foodborne disease outbreaks in China, 2003–2017. Food Control. 2020;118:107359. https://doi.org/10.1016/j.foodcont.2020.107359 .
Li WW, Sara MP, Liu ZT, et al. Mushroom poisoning Outbreaks-China, 2010–2020. China CDC Weekly. 2021b;3(24):518–22. https://doi.org/10.46234/ccdcw2021.134 .
Han HH, Kou BY, Ma J, et al. Analysis of foodborne disease outbreaks in chinese mainland in 2018. Chin J Food Hyg. 2022;34(4):822–9. https://doi.org/10.13590/j.cjfh.2022.04.030 . (in Chinese).
Li HQ, Guo YC, Song ZZ, et al. Analysis of foodborne disease outbreaks in China in 2019. Chin J Food Hyg. 2021;33(6):650–6. https://doi.org/10.13590/j.cjfh.2021.06.003 .
Li HQ, Jia HY, Zhao S, et al. Analysis of foodborne disease outbreaks in chinese mainland in 2021. Chin J Food Hyg. 2022;34(4):816–21. https://doi.org/10.13590/j.cjfh.2022.04.029 . (in Chinese).
He JY, Ma L. Investigation and treatment of four cases of mushroom poisoning in Guangzhou. Chin J Food Hyg. 2001;13:29–31. (in Chinese).
CAS Google Scholar
Chen ZH, Yang ZL, Bau T et al. (2016) Poisonous mushrooms: recognition and poisoning treatment. Beijing Sci Press. 1–308 (in Chinese).
Mao XL. Poisonous mushrooms and their toxins in China. Mycosystema. 2006;25(3):345–63. (in Chinese).
Bau T, Bao HY, Li Y. (2014) A revised checklist of poisonous mushrooms in China, Mycosystema,33 (3): 517–48 (in Chinese). https://doi.org/10.13346/j.mycosystema.130256 .
Chen ZH. New advances in researches on poisonous mushrooms since 2000. Mycosystema. 2014;33(3):493–516. https://doi.org/10.13346/j.mycosystema.140041 . (in Chinese).
Dai YC, Yang ZL, Cui BK et al. (2021) Diversity and systematics of the important macrofungi in chinese forests, Mycosystema, 40: 770–805 (in Chinese). https://doi.org/10.13346/j.mycosystema.210036 .
YAO QM, Yu CM, Li CH, et al. Analysis of epidemiological characteristics and treatment of mushroom poisoning in Chuxiong of Yunnan province. J Clin Med. 2017;4(3):574–9. https://doi.org/10.16281/j.cnki.jocml.2017.03.132 . (in Chinese).
Li HJ, Zhang YZ, Liu ZT, et al. Species diversity of poisonous mushrooms causing poisoning incidents in Yunnan Province, Southwest China. Mycosystema. 2022;41(9):1416–29. https://doi.org/10.13346/j.mycosystema.210488 . (in Chinese).
Zhao J, Tang QL, Min XD, et al. Analysis on poisonous mushroom poisoning from 2010 to 2018 in Yunnan province. Capital J Public Health. 2019;13(6):280–2. https://doi.org/10.16760/j.cnki.sdggws.2019.06.001 .
Toxicology group of emergency medicine branch of Chinese Medical Association, emergency medical doctor branch of Chinese Medical Doctor Association, poisoning and treatment Committee of Chinese Society of Toxicology. Consensus on clinical diagnosis and treatment of poisoning of mushroom contained amanitin in China. Chin J Emerg. 2020;29(2):171–9. (in Chinese).
Google Scholar
Keller SA, Klukowska-Rötzler J, Schenk-Jaeger KM, et al. Mushroom Poisoning-A 17 year retrospective study at a Level I University Emergency Department in Switzerland. Int J Environ Res Public Health. 2018;14(12):2855–74. https://doi.org/10.3390/ijerph15122855 .
Beug MW. Summary of the Poisoning Reports in the NAMA Case Registry for 2006 through 2017. NAMA Toxicology Reports and Poison Case Registry; 2018. https://namyco.org/toxicology_reports.php .
Chen ZH, Hu JS, Zhang ZG, et al. Determination and analysis of the main amatoxins and phallotoxins in 28 species of Amanita from China. Mycosystema. 2003;22:565–73. (in Chinese).
Sun J, Niu YM, Zhang YT, et al. Toxicity and toxicokinetics of Amanita exitialis in beagle dogs. Toxicon. 2018;143:59–67. https://doi.org/10.1016/j.toxicon.2018.01.008 .
Trestrail JH 3rd. Mushroom poisoning in the United States: an analysis of 1989 United States poison center data. J Toxicol Clin Toxicol. 1991;29(4):459–65. https://doi.org/10.3109/15563659109025741 .
Pajoumand A, Shadnia S, Efricheh H, et al. A retrospective study of mushroom poisoning in Iran. Hum Exp Toxicol. 2005;24(12):609–13. https://doi.org/10.1191/0960327105ht572oa .
Schmutz M, Carron PN, Yersin B, et al. Mushroom poisoning: a retrospective study concerning 11-years of admissions in a swiss Emergency Department. Intern Emerg Med. 2018;13(1):59–67. https://doi.org/10.1007/s11739-016-1585-5 .
Mowry JB, Spyker DA, Cantilena LR et al. (2013) 2012 Annual report of the American association of poison control centers’ National Poison Data System (NPDS): 30th annual report. Clin. Toxicol. (Phila). 51(10): 949–1229. https://doi.org/10.3109/15563650.2013.863906 .
Download references
Acknowledgements
This work was supported by the Major Research Plan Foundation of Yunnan Province (2018ZF009), the Special Basic Cooperative Research Programs of Yunnan Provincial Undergraduate Universities (202001BA070001-046), and the National Natural Science Foundation of China (No. 82103886).
This work was supported by the Major Research Plan Foundation of Yunnan Province (2018ZF009); the Special Basic Cooperative Research Programs of Yunnan Provincial Undergraduate Universities (202001BA070001-046); and the National Natural Science Foundation of China (No. 82103886).
Author information
Qunmei Yao and Zhijun Wu contributed equally to the work and are co-first authors of the article.
Authors and Affiliations
Department of Emergency Medicine, The People’s Hospital of Chuxiong Yi Autonomous Prefecture, Chuxiong, 675000, Yunnan, China
Qunmei Yao, Jiaju Zhong & Chengmin Yu
National Institute for Occupational Health and Poison Control, Chinese Center for Disease Control and Prevention, Beijing, 100050, China
Zhijun Wu, Haijiao Li & Chengye Sun
Chuxiong Yi Minority Autonomous Prefecture Center for Disease Control and Prevention, Chuxiong, 675000, Yunnan, China
Chuxiong Health Commission, Chuxiong, 675000, Yunnan, China
Jianrong He
Dayao People’s Hospital, Dayao, 675400, Yunnan, China
Jianping Du
You can also search for this author in PubMed Google Scholar
Contributions
QMY led the data collection and analysis. ZJW wrote the main manuscript. JJZ, CMY, QLH, JRH, and JPD collected the data. HJL reviewed the data. CYS led the research project. All authors reviewed the manuscript.
Corresponding author
Correspondence to Chengye Sun .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Ethics Committee of the People’s Hospital of Chuxiong Yi Autonomous Prefecture (2022-41). In this study, data were obtained from patients’ records, and their data remained confidential. Therefore, the need for informed consent to participate was waived by the Ethics Committee of the People’s Hospital of Chuxiong Yi Autonomous Prefecture. All methods in this study were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yao, Q., Wu, Z., Zhong, J. et al. A network system for the prevention and treatment of mushroom poisoning in Chuxiong Autonomous Prefecture, Yunnan Province, China: implementation and assessment. BMC Public Health 23 , 1979 (2023). https://doi.org/10.1186/s12889-023-16042-7
Download citation
Received : 20 March 2023
Accepted : 02 June 2023
Published : 11 October 2023
DOI : https://doi.org/10.1186/s12889-023-16042-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mushroom poisoning
- Implementation
- Mushroom identification
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
Mushroom Poisoning: A Rare Etiology of Acute Liver Failure
Affiliations.
- 1 Respiratory Medicine, University Hospital of North Durham, Durham, GBR.
- 2 Internal Medicine, Grantham and District Hospital, Grantham, GBR.
- PMID: 38283455
- PMCID: PMC10811487
- DOI: 10.7759/cureus.51144
Acute liver failure is defined as a rapid deterioration in liver function, manifested by symptoms and signs of hepatic encephalopathy and disturbed synthetic function in a patient without Pre-existing cirrhosis and with an illness of less than 26 weeks duration. Mushroom poisoning as a cause of acute liver injury is rare but associated with deadly outcomes if not early recognized and treated. The mortality is very high in the case of amatoxin-containing mushrooms ingestion and liver transplantation is the only lifesaving option. Therefore, early recognition of a suspected patient who came with features of mushroom-related food poisoning, timely referral to a liver transplantation center, and adequate supportive management remain the main approaches of management in a patient with acute liver injury. We present a patient with gastroenteritis who ingested wild mushroom 14 hours prior to hospital admission with subsequent severe acute liver failure due to mushroom poisoning, successfully treated with urgent liver transplantation. This case study highlighted that careful evaluation of the symptoms and signs of acute liver failure in a patient with a history of mushroom ingestion can result in early referral to a liver transplant center, especially if the patient is systemically unwell.
Keywords: acute liver failure (alf); amanitn phalloides; amatoxin poisoning; mushroom poisoning; n-acetyl cysteine; orthotropic liver transplantation.
Copyright © 2023, Mohammed et al.
Publication types
- Case Reports
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Clinics (Sao Paulo)
- v.65(5); 2010 May
Mushroom poisoning: retrospective analysis of 294 cases
Sevki hakan eren.
I Department of Emergency Medicine, Cumhuriyet University Medical Faculty - Sivas, Turkey
Yeltekin Demirel
II Department of Family Medicine, Cumhuriyet University Medical Faculty - Sivas, Turkey
Serdal Ugurlu
III Division of Rheumatology, Department of Medicine, Cerrahpasa Medical Faculty, University of Istanbul - Istanbul, Turkey
Ilhan Korkmaz
IV Department of Emergency Medicine, Yeditepe University Medical Faculty – Istanbul, Turkey, Email: moc.liamtoh@nerenakahs
Fatma Mutlu Kukul Güven
The objective of this study was to present special clinical and laboratory features of 294 cases of mushroom poisoning.
MATERIALS AND METHODS
In this retrospective study, 294 patients admitted to the Pediatric and Adult Emergency, Internal Medicine and ICU Departments of Cumhuriyet University Hospital were investigated.
Of 294 patients between the ages of 3 and 72 (28.97 ± 19.32), 173 were female, 121 were male and 90 were under the age of 16 years. One hundred seventy-three patients (58.8%) had consumed the mushrooms in the early summer. The onset of mushroom toxicity symptoms was divided into early (within 6 h after ingestion) and delayed (6 h to 20 d). Two hundred eighty-eight patients (97.9%) and six (2.1%) patients had early and delayed toxicity symptoms, respectively. The onset of symptoms was within two hours for 101 patients (34.3%). The most common first-noticed symptoms were in the gastrointestinal system. The patients were discharged within one to ten days. Three patients suffering from poisoning caused by wild mushrooms died from fulminant hepatic failure.
Education of the public about the consumption of mushrooms and education of health personnel working in health centers regarding early treatment and transfer to hospitals with appropriate facilities are important for decreasing the mortality.
INTRODUCTION
Various types of wild mushrooms grow in forests and meadows, and it is common for the local population to consume them. 1 It is estimated that there are over 5000 species of mushrooms worldwide. Only 20–25% of mushrooms have been named, and 3% of these are poisonous. 2 Previous experience and observation make it possible to discriminate between poisonous and non-poisonous mushrooms. 1 Mushroom poisoning constitutes the main portion of plant toxicities in Turkey. In addition to occurring in rural areas, gathering of mushrooms is a habit in Istanbul among villagers who have moved to the city and settled in the vicinity of a forest. 3 During the four-year period from 1994 to 1998 in Sivas, Turkey, mushroom poisoning represented 10.9% of the different analyzed poisonings. 4 However, these cases were not analyzed toxicologically.
Depending on the type of mushroom, the adverse effects range from mild gastrointestinal (GI) symptoms to major cytotoxic effects resulting in organ failure and death. Toxicity may also vary depending on the amount and age of the mushroom, the season, the geographic location and the way in which the mushroom was prepared prior to ingestion. Consumption of poisonous mushrooms can cause various types of reactions, such as allergic gastroenteritis, psychological relaxation and fatal liver intoxication. 1 , 5 , 6 Mushroom poisoning occurs among four main groups of individuals: young children who ingest mushrooms inadvertently, wild-mushroom foragers, individuals attempting suicide or homicide and individuals looking for a hallucinatory high. Identification of the ingested mushroom can be difficult and time consuming. In all cases, treatment should be directed by the patient’s symptoms rather than by attempts at mushroom identification. 6
Today, emergency department physicians have increasing occasions to treat mushroom poisoning. Interest in eating mushrooms has risen dramatically in recent years as part of the back-to-nature and organic food movement. In addition, some people are eating certain mushrooms for their hallucinogenic components, leading to an increase in mushroom poisonings. 7
This study’s aim was to determine the demographic and clinical features of adult and pediatric patients who were admitted to the hospital (ED) due to mushroom poisoning, and to emphasize the significance of mushroom poisoning. We contribute one of the largest series to be applied to the same hospital concerning mushroom poisoning, which has been seen frequently in developing countries and will increase in developed countries due to the rise of natural nutrition. Furthermore, to establish this study as the largest serial study concerning mushroom poisoning in Turkey, we will present extensive information about mushroom poisonings in our country.
A retrospective descriptive/epidemiologic study was designed, and all patients with mushroom poisoning admitted to the Pediatric and Adult Emergency, Internal Medicine and ICU departments in the Cumhuriyet University Hospital in Sivas between 2000 and 2007 were studied. Two hundred ninety-four patients with mushroom poisoning were included in the study. We collected data on the season and location where the mushrooms were picked, method of cooking, symptoms, onset time for symptoms, laboratory findings, type of treatment administered and results of therapies. The laboratory evaluation included blood glucose, bilirubin, liver function, complete blood cell count, coagulation profile, electrolyte and renal function tests. Diagnosis was made according to the physical features of the mushrooms, time of appearance of symptoms, clinical conditions of the patients and laboratory parameters. The mushrooms toxins could not be analyzed. The onset times of mushroom toxicity symptoms were divided into early (within 6 h after ingestion) and delayed (6 h to 20 d). Patients with early symptoms were treated by stomach irrigation, the maintenance of the fluid-electrolyte balance, forced diuresis and the administration of activated charcoal, whereas patients with severe toxicity symptoms were treated by adding crystallized penicillin. In patients with fulminant hepatic failure, maintenance therapy was given, but liver transplantation could not be performed. Data are presented as the mean (SD) or percentage.
All data were analyzed with SPSS software, version 16.0. A detailed multiple-variable database was formed. Statistical comparisons were carried out using the Mann-Whitney U-test and Student’s t -test. The Pearson test was used to evaluate correlations among variables. P values of 0.05 or less were considered to be statistically significant.
Two hundred ninety-four patients aged between three and seventy-two years (28.97 ± 19.32) were studied. Of these, 204 (69.4) were adults, and 90 (30.6%) were in the pediatric age group. In the adult group, 121 patients were female, and 83 were male. In the pediatric group, 52 patients were female, and 38 were male. It was established that 173 (58.8%) patients had consumed the mushrooms in the early summer, 84 (28.6%) in the spring, 22 (7.5%) in the autumn and 15 (5.1%) in the winter. Two hundred seventy-six (93.8%) patients had foraged for the mushrooms in nature (hills, riverbanks, fields), and eighteen (6.2%) had bought cultivated mushrooms. The methods of cooking were as follows: the mushrooms were grilled by 112 (38.1%) patients, roasted by 78 (26.5 %), cooked into the meal by 45 (15.3%) and consumed uncooked by 59 (20.1%). In total, 112 (38.1%) patients were seen in the emergency care unit, 59 (20.1%) in the internal service, 33 (11.2%) in the intensive care unit and 90 (30.6%) in the pediatric service.
Laboratory abnormalities were found in 112 (38.1%) patients and included hematological abnormalities (leukocytosis, thrombocytopenia, prolonged prothrombin time), elevated liver enzymes, hematuria, glucosuria, impaired renal functions, hyponatremia, hypernatremia and hypoglycemia ( Table 1 ).
Laboratory data.
ALT: Alanine aminotransferase, AST:Aspartate aminotransferase
PT:Protrombintime
PTT:Activated Parsiyel tromboplastin time BUN:Blood Urea Nitrogen
Two hundred eighty-eight (97.9%) patients had early and six (2.1%) had delayed toxicity symptoms. The onset of symptoms was within two hours for 101 (34.3%) patients. The signs and symptoms included cardiovascular, gastrointestinal and central nervous system symptoms ( Table 2 ). In both adult and pediatric groups, the most common first symptom was nausea and vomiting (84.8% and 78.8%, respectively) ( Table 3 ).
Signs and symptoms of poisoning.
First symptoms of poisoning.
One hundred seventy-seven (60.2%) patients were treated by stomach irrigation and the administration of activated charcoal. One hundred eleven (37.7%) patients who had severe clinical manifestations were treated with stomach irrigation as well as administration of activated charcoal and penicillin G. Six patients (2.1%) rejected therapy.
Four patients were pregnant. Neither the mothers nor the fetuses showed any problems. All of the patients were discharged within one to ten days. However, three patients (child=1, adult=2) who consumed raw mushrooms and were treated in the ICU died due to acute hepatic failure ( Table 4 ). The mortality rate was 1.02%. There was a significant (p<0.001) relationship between mortality, hepatic failure and consuming raw mushrooms.
Laboratory parameters of deceased patients.
ALT: Alanine aminotransferase, AST:Aspartate aminotransferase PT:Protrombintime
Mushroom poisoning presents a major health risk in rural areas. It is estimated that there are over 5000 species of mushroom worldwide. 2 Foraging for wild mushrooms is popular in Europe, the United States and the Far East. 8 – 12 The exact identification of mushroom species can be difficult. Substantial morphologic variations can occur in the same mushroom species depending on the season, geographic location and maturity of the fungus. Most ingested mushrooms are either nontoxic or only gastrointestinal irritants, resulting in mild to moderate toxic effects. 13
The pathogenicity of mushrooms depends on cyclopeptide toxins. The type of mushroom is unknown in >90% of cases of digestion. 5 , 14 Amatoxins, which account for 90% of fatal mushroom poisonings, have their most significant impact on the liver. 15
Mushroom poisonings occur every year between June and December. 16 A study performed in Japan reported that mushroom poisoning happened most frequently in September and October. 17 A similar study performed in Iran reported that mushroom poisoning usually happened in autumn and spring. 18 Unluoglu et al. reported that mushroom poisoning cases were seen in the spring or early summer. 19 Ergüven et al. reported that mushroom poisoning cases were seen in the autumn. 20 Another study performed in Turkey reported that mushroom poisoning usually happened in October and November. 21
In our study, 58.8% of the patients consumed the mushrooms in the early summertime. While the winter is very long and the rains start in May and June, mushroom collecting is increased during these months, and mushroom poisonings were seen at this time in Sivas. A seasonal variation was also seen in the present study that is consistent with the characteristics of the seasons, i.e., it rains during the spring, when mushrooms are prevalent.
Mushroom poisoning is caused not only by toxic mushrooms (true intoxications) but also, under certain conditions, by edible mushrooms (false intoxications and pseudo-intoxications). 22 In our study, most of the mushroom poisonings were due to the consumption of foraged mushrooms, but 6.2% arose from commercially cultivated mushrooms. In another study, 5.6% of the patients were poisoned with cultivated mushrooms. 19 A two-year survey conducted by the Food and Drug Administration showed that 21% of cultivated mushrooms were contaminated with toxic look–alike species. 23
Cultivated mushroom poisoning did not result in adverse outcomes in our study. This shows that sanitation and hygienic conditions are inadequate during mushroom production.
Many preparation methods were used for the mushrooms before ingestion. In our study, grilling (38.1%) and roasting (26.5%) of the mushrooms were the most common. The toxicity may vary based on the amount ingested and the way in which the mushroom was prepared prior to ingestion. The cooking of wild mushrooms was relatively safe. Raw mushroom ingestion was very dangerous. In our study, the three patients who died from mushroom poisoning had ingested the mushrooms raw. Children are especially susceptible to this risky endeavor. They can easily find mushrooms in nature and eat them without cooking. Families must be careful to prevent accidental mushroom ingestion among children.
Clinically, mushroom toxicity is divided into early (within 6 h after ingestion) and delayed (6 h to 20 d). 5 In our study, most of the patients (97.9%) had early toxicity symptoms. Only 2.1% of the patients had delayed toxicity symptoms. The most common first-noticed symptoms were gastrointestinal. A total of 37.7% of the patients had laboratory abnormalities. Alterations in hematological parameters and elevated transaminase levels were the most common laboratory findings. A considerable portion of amatoxin is taken up by hepatocytes, excreted into the bile and reabsorbed by the enterohepatic cycle. 24 , 25 The amatoxins bind to RNA polymerase II and thus inhibit the hepatic formation of mRNA. 26 As a result of this, Amanita species cause increases of AST(Aspartate aminotransferase) and ALT(Alanine aminotransferase) levels in the serum. 27
Pajoumand et al. showed increases in ALT and AST levels in 17 of 25 patients. 18 In another study examining 6317 cases, an increase in transaminase levels was reported for 0.5% of the patients. 28 In the present study, 8.1% of the cases were found to have increased levels of AST and ALT. The patients who died had very high AST and ALT levels, with AST values between 2075–3464 U/L and ALT values between 2345–4048 U/L. As the AST and ALT values rose, hepatic coma followed. There was a significant relationship between mortality and liver enzyme levels (AST, ALT). This indicates that liver enzyme levels (AST, ALT) are a good prognostic marker of mushroom poisoning or an indication for liver transplantation.
Because the goal of the total prevention of mushroom poisoning is likely never to be reached, it is important for clinicians to focus on diagnosis and treatment. The diagnosis of mushroom poisoning must at least be considered in patients with appropriate symptoms. The most common toxic symptoms recorded in this study’s subjects, including nausea, vomiting, fatigue, abdominal pain, dizziness, diarrhea, headache and loss of consciousness, have also been reported in the literature. 29 , 30
Most patients present with gastrointestinal symptoms. It is important to establish the latency period of symptoms after ingestion. Late toxicities (symptom onset >6 hrs after ingestion) are life-threatening due to liver and renal failure. Patients who have jaundice after an acute gastrointestinal episode are suspected to be poisoned with amatoxins. Symptoms of mushroom poisonings with amatoxins begin at six to twenty-four hours after the initial ingestion of the mushroom. 31 , 32 In our study, most of the mushroom-poisoned patients had early toxicity symptoms.
In total, 10.2% of our patients were discharged after 24 hours of admission, while 49.7% required hospitalization for 72 hours. According to the patients’ symptoms and doctors’ decisions, the patients were observed in the hospital for 24 hours to 72 hours. The patients who had no clinical manifestations or laboratory abnormalities were discharged from the hospital after the 24 hours of observation. Only 11.2% of the patients required intensive care unit admission. The patients who had delayed toxicity symptoms were required to undergo observation in the intensive care unit. The patients who had moderate clinical and laboratory findings were observed in the emergency observation unit. If a patient had no clinical and laboratory findings in 24 hours, they could be safely discharged from the hospital.
The patients who had histories of wild mushroom consumption were treated. The patients who had mild clinical symptoms were treated by stomach irrigation and the administration of activated charcoal, while those who had severe clinical manifestations were treated with stomach irrigation and the administration of activated charcoal in addition to penicillin G. The patients who had clinical symptoms from the cultivated mushrooms were treated symptomatically.
In this study, 294 patients with mushrooms poisoning, 3 of whom died (one child, two adults), were admitted to the Cumhuriyet University Hospital of the Faculty of Medicine in Sivas between 2000 and 2007. The mortality rate in this study was 1.02%. Unluoglu et al. reported a mortality rate of 2.8%. 19 In another study in Turkey the mortality rate was 17.9%. 20 In a study in Istanbul the mortality rate was 21.4%. 20 The mortality rate of mushroom poisoning in Iran, one of our neighboring countries, was 12%. 18 The low mortality rate in our study was due to early presentation to the hospital, early treatment by hemoperfusion and intoxication by species other than Amanita. An additional reason could be that the wild mushrooms in our region were less poisonous.
Mushroom poisoning is a public health problem. People and health care providers must be educated about this poison. The species of mushrooms are numerous, and there are various clinical presentations depending on the ingested species. There are no guidelines about the treatment of mushroom toxicity in the emergency department, so diagnosis and treatment must be based on the history of ingestion and associated clinical presentations. Patients showing delayed toxicity symptoms should be observed in intensive care units. Despite treatment, the prognosis can be mortal. These types of patients must be transferred immediately to hospitals where liver transplantations can be performed. Children are a high-risk group for wild and uncooked mushroom poisonings.

Health Benefits of Mushrooms
Mushrooms are defined as the fruiting bodies of filamentous fungi that grow above the ground. Within culinary use, they are categorized as white vegetables.
There are about 1,600 mushroom species, but only 100 have been recognized as edible and 33 species are cultivated for consumption throughout the world. Many cultures have consumed mushrooms for centuries. The Romans considered mushrooms to be "food of God" and the Chinese designated them as an elixir of life.
Mushrooms are low in calories and provide a range of nutrients, including antioxidants, fiber, B vitamins, and minerals. Mushrooms exposed to UV light can also be an abundant source of vitamin D.
The consumption of edible mushrooms has been linked to numerous health benefits, including improved gut and brain health, and protection against obesity, type 2 diabetes, certain cancers, high blood pressure, and more. They have been referred to as the main underutilized nutritious food.
Has Anti-Inflammatory Properties
Mushrooms are ranked as one of the top anti-inflammatory foods. Chronic inflammation in the body is linked to autoimmune conditions and chronic diseases, including heart disease, cancers, and neurodegenerative diseases, like Alzheimer’s.
Several bioactive compounds found in mushrooms have been shown to exhibit anti-inflammatory effects, which may protect against a number of illnesses. These include beta-glucans, which regulate pro-inflammatory compounds called cytokines linked to systemic long-term inflammation.
May Help Diabetes Prevention and Treatment
Mushrooms are low in calories and have a low glycemic index, a measure of how quickly blood sugar rises after consuming a food. And while research is limited, studies have shown natural compounds in mushrooms help reduce blood sugar levels by inhibiting the absorption of glucose (sugar) from the digestive tract into the bloodstream. They may also improve both pancreatic function and insulin release.
Mushrooms can also be a significant source of vitamin D. Research has shown a link between low vitamin D intakes and insulin resistance. Insulin resistance occurs when cells don’t respond well to insulin, which prevents sugar from being cleared from the blood properly. This can lead to type 2 diabetes.
Offers Obesity Support
Mushrooms may help combat obesity. A review of research found this may be partly due to mushrooms’ anti-inflammatory effects.
Mushrooms have several features that positively impact weight management. They’re low in calories, take more time to chew, and their fluid and fiber contents are filling. They also slow stomach emptying and boost feelings of satiety.
Additionally, mushrooms have been shown to shift the makeup of gut microbes and increase levels of anti-obesogenic (obesity-causing) gut bacteria.
Mushrooms also support weight regulation when they are used as a meat alternative. In one clinical trial in 73 obese adults, mushrooms were substituted for red meat in the participants regular diets. At the end of one year, the mushroom eaters consumed fewer calories and had reduced body weights and smaller waist measurements.
Another 10-day study found replacing meat with mushrooms resulted in reduced calorie intakes and weight loss.
May Improve Blood Pressure Regulation
High blood pressure or hypertension is a risk factor for heart disease and stroke. A recent research review states mushrooms contain bioactive compounds known to help reduce blood pressure. Some of these compounds relax blood vessels, which opens up circulation.
Mushrooms may also contribute to blood pressure control due to their vitamin D content, as low blood vitamin D levels are tied to increased hypertension risk.
May Reduce Depression Risk
Major depression is one of the most common mental health illnesses in the United States. Approximately 21 million U.S. adults (8.3% of the population) have had at least one major depressive episode.
Research has found mushrooms contain numerous bioactive compounds that may be associated with anxiety reduction, including vitamin B12 , antioxidants, and anti-inflammatory agents.
The research is based on data from the 2005–2016 National Health and Nutrition Examination Survey, which is representative of all U.S. adults.
Among the almost 25,000 participants, people with a moderate mushroom consumption had decreased odds of depression compared to participants with the lowest mushroom intakes.
Mushrooms are also the highest dietary source of an amino acid called ergothioneine. Ergothioneine acts as an antioxidant and other studies have linked it to mental health benefits, including depression prevention.
Supports Brain Health
Mushrooms may help fend off cognitive impairment, the stage between normal age-related cognitive decline and the more serious condition of dementia .
A study from Singapore assessed 663 participants aged 60 and above. Compared with participants who consumed mushrooms less than once per week, adults who ate more than two portions per week had reduced odds of developing cognitive impairment.
The association was independent of several factors, including age, gender, education, cigarette smoking, alcohol consumption, high blood pressure, diabetes, heart disease, stroke, physical activities, and social activities. Researchers concluded the data supported the potential role of mushrooms and their bioactive compounds for delaying neurodegeneration.
Offers Immune Support
The gut microbiome, often referred to as the body’s “forgotten organ,” plays a significant role in human health and disease, including immune function. The gut microbiome is the community of microorganisms—such as fungi, bacteria, and viruses—that live in the human gut. Gut microbiota are the specific microbes in the gut, which change in response to factors like diet and exercise.
A research review found mushrooms have a significant effect on the gut microbiome due to their prebiotics, which essentially serve as food for beneficial probiotic microbes. This impact supports healthy immune function, generates anti-inflammatory compounds in the gut, and strengthens the gut barrier. Strengthening the gut barrier helps to prevent harmful substances from being absorbed from the gut into the bloodstream.
Mushrooms also support immune health through their natural antibacterial, antifungal, and antiviral activities, including the ability to combat Escherichia coli (E. coli), Staphylococcus aureus (staph), and flu viruses.
May Help Protect Against Cancer
Mushrooms have been studied for their ability to prevent cancer and reduce its progression. A recent research review states edible mushrooms may prevent cancer from developing, growing, and spreading, and provide immune support during cancer recovery.
Previous studies have shown mushroom consumption may be inversely associated with the risk of breast cancer, although the research is mixed. One study found each one-gram-per-day increase in dietary mushroom intake appeared to decrease breast cancer risk by 3%.
Another study found the relative risk for breast cancer was 35% lower in mushroom eaters compared to those who did not consume them. However, studies conducted in different countries yielded different results.
Other research has shown mushrooms may also be protective against cancers of the liver, uterus, pancreas, and stomach, as well as acute leukemia. However, more research is needed to understand if and how much mushrooms may reduce cancer risk.
Nutrition of Mushrooms
Mushrooms provide several key nutrients, but the levels vary by type. One cup of sliced raw brown or crimini mushrooms provides:
- Calories: 15.8
- Fat: 0 grams (g)
- Sodium: 4.32 milligrams (mg)
- Carbohydrates: 3.1 g
- Fiber: 0.432 g
- Protein: 1.8 g
- Selenium: 18.7 micrograms (mcg) (34% of the Daily Value)
Selenium is a mineral that helps your body make special proteins, called antioxidant enzymes, which play a role in preventing cell damage, which may be linked to cancer prevention.
One study found the addition of an 84 gram serving (just over one cup) of commonly consumed raw mushrooms (white, crimini, and portabella) to USDA Food Patterns—the national recommended amounts of each food group—resulted in a minimal or no impact on saturated fat or cholesterol. The addition of mushrooms also resulted in a:
- 1% increase in calories
- 2–3% increase in fiber
- 8–12% increase in potassium
- 12–18% increase in riboflavin
- 11–26% increase in niacin
- 11–23% increase in selenium
- 16–26% increase in copper
Mushrooms exposed to ultraviolet (UV) light to increase their vitamin D levels to 200 IU per serving also increased vitamin D consumption by 67–90%.
A scientific paper reported UV vitamin D-enhanced mushrooms contain high concentrations of vitamin D2, a form that is readily available to the body and relatively stable during storage and cooking. Scientists concluded the consumption of vitamin D-enhanced mushrooms could substantially help alleviate vitamin D deficiency, which is a global public health issue.
Risks of Mushrooms
Humans have consumed mushrooms since prehistory. Today most mushrooms are farmed commercially, ensuring safer consumption. Foraging for wild mushrooms may result in accidental harm if a poisonous species is misidentified as edible.
The effects of mushroom poisoning can range from generalized gastrointestinal upset to liver or kidney failure, seizures, and even death. To avoid these risks, make sure to only purchase mushrooms from reputable suppliers.
Tips for Consuming Mushrooms
Mushrooms can be consumed raw or cooked. Microwaving and grilling have been shown to be the best cooking methods to maintain mushrooms’ nutritional profile compared to boiling and deep frying. Microwaving and grilling were also shown to increase mushrooms’ antioxidant activity.
There are many ways to enjoy mushrooms. For example, you can:
- Blend mushrooms into smoothies.
- Add mushrooms to egg or chickpea-based breakfast scrambles.
- Slice mushrooms as a topping for avocado toast.
- Slice or chop mushrooms and add them to garden salads, soups, stews, chili, or stir fries.
- Stuff mushroom caps with a bean and vegetable mixture and bake as an appetizer.
- Skewer mushrooms, alternating with other vegetables, and grill as kabobs.
- Mince mushrooms and combine them with cooked lentils as a ground beef alternative for tacos or pasta sauce.
- Incorporate mushrooms into meatless burgers and meatballs.
- Sauté mushrooms with onions and herbs in vegetable broth and blend into gravy.
- Sauté mushrooms in extra virgin olive oil as side dish or topping for hummus or baked potatoes.
A Quick Review
Edible mushrooms are low in calories, nutritious, anti-inflammatory, and help support immune health. Their consumption has been linked to protection against a number of conditions, including cognitive decline, diabetes, and high blood pressure. Mushrooms can be enjoyed in a number of dishes, but to avoid poisonous varieties be sure to purchase them from reliable sources.
For more Health.com news, make sure to sign up for our newsletter!
Read the original article on Health.com .

Mercury poisoning near Grassy Narrows First Nation worsened by ongoing industrial pollution, study suggests
New research shows sulfate, organic matter are exacerbating methylmercury levels.

Social Sharing
A new study from the University of Western Ontario suggests mercury contamination in northwestern Ontario's English-Wabigoon River has been made worse by ongoing industrial pollution.
Contamination of the river system dates back to the 1960s and 70s , when the pulp and paper mill dumped an estimated nine tonnes of mercury into the water.
The mercury has impacted generations of people living in Grassy Narrows First Nation, also known as Asubpeeschoseewagong Netum Anishinabek, a community about 150 kilometres from Dryden near the Ontario-Manitoba border, and Wabaseemoong Independent Nation.
However, the new study, published Thursday, has found that discharge of wastewater from the Dryden Paper Mill, combined with existing mercury, has created high levels of methylmercury – an even more toxic compound.
"Other forms of mercury don't accumulate as strongly as methylmercury, but because it accumulates, it builds up to high levels in organisms, presenting that greater risk," said Brian Branfireun, a biology professor at the University of Western Ontario. "It's actually more serious than I even imagined."

The experiment was conducted by masters student Eric Grimm under Branfireun's supervision.
Dianne Loewen, communications and engagement co-ordinator for Dryden Fibre Canada, the owner of the Dryden Paper Mill, said in an email to CBC News on Wednesday that she could not comment on the study.
"Dryden Fibre Canada only recently acquired the mill from Domtar. We are not in a position to comment as we have not seen, nor have we been briefed on, Dr. Branfireun's report."
Dryden Fibre Canada took over the mill from Domtar in August 2023.
Poison through the food chain
While the wastewater coming from the mill today does not contain mercury, it does contain high levels of sulfate and organic matter, which "feed the bacteria that produce methylmercury from inorganic mercury in the environment," the study says.
These toxins build up in the river's fish, which are then passed on to the people that consume them.
"The accumulation of methylmercury in the human body causes neuromuscular problems and can also lead to death," Branfireun said.

Grassy Narrows Chief Rudy Turtle reacts to new mercury research
Just under 1,000 people live in Grassy Narrows First Nation, and fish are a staple part of the community's diet.
"Most of the families continue to fish, they continue to eat the fish. It's something they've done for hundreds of years – you can't really stop them," said Grassy Narrows Chief Rudy Turtle in an interview with CBC News.
It is estimated that 90 per cent of Grassy Narrows' population has symptoms of mercury poisoning, which causes problems including tremors, insomnia, memory loss, neuromuscular effects, headaches and cognitive and motor dysfunction.
- Grassy Narrows chief calls out feds amid 'ridiculous' delays to mercury treatment centre construction
- As First Nations chiefs in northern Ontario call for health-care action, youth demand more involvement
For years, Turtle has called for the paper mill to be closed and for the river to be cleaned up. The community has also been anxiously awaiting the construction of a Mercury Care Home, for which the federal government signed a funding agreement in 2020.
"We continue to be poisoned," said Turtle, who himself has shared his experiences with mercury poisoning.
Mercury Care Home construction slated for summer
Anispiragas Piragasanathar, a spokesperson for Indigenous Services Canada (ISC), provided CBC News an emailed statement about the Mercury Care Home.
Piragasanathar said the federal government has committed:
- $77M to build the Mercury Care Home.
- $68.9M for operations, maintenance and specialized service delivery.
"ISC continues to support Grassy Narrows leadership as they take steps toward realizing their vision for health-care delivery in their community through the Mercury Care Home," Piragasanathar said.
- In Depth NWMO reaffirms safety of Canada's 1st nuclear waste repository but there's still heavy pushback
- Mining claims jump in northern Ontario's Ring of Fire as EV battery interest grows
"Together, we have developed key construction milestones to ensure that the Mercury Care Home is built in a timely manner."
Construction is planned to begin by July 1 and take about two to three years to complete.
Turtle said he is pleased with the additional funds the government has committed to the project this year, and that a ceremony will be held in the community once the shovels hit the ground.
No simple solutions
It is possible to remove the methylmercury from the water – but it won't be easy, Branfireun said.
"We are talking about potentially hundreds of kilometres of rivers and lakes and wetlands in a very complicated landscape that is not developed," he said.
While cleaning up the river will take substantial time and resources, removing the sulfate and organic matter is a more manageable solution for the short-term, Branfireun said.
"It wouldn't completely solve the mercury problem in fish in this river, but it would dramatically improve it while these other remediation strategies are being implemented over the next few decades."
Michael Rennie is an associate professor at Lakehead University's biology department, as well as a research fellow at the International Institute for Sustainable Development (IISD) Experimental Lakes Area.
While he was not involved in the methylmercury study, he said he is not surprised by the results.
We are talking about potentially hundreds of kilometres of rivers and lakes and wetlands in a very complicated landscape that is not developed. - Brian Branfireun, University of Western Ontario
"It shows a pretty clear role for the impact that the mill has on the system now just from the effluent that's going into it from the current operations," Rennie said in an interview with CBC News.
There are ways to reduce the impact of mill operations on the river, Rennie said, such as settling ponds or new environmental policies, but the level of contamination throughout the system means there are no simple solutions.
"I don't think this is saying, 'Oh my God, we have to close the mill.'
"What I think it's saying is there are likely industrial processes that can be put in to help reduce sulfate concentrations that are coming out of that effluent to help reduce organic matter, that will at least not make the problem continue to be worse," he said.
Branfireun is expected to share the study's findings on Thursday morning at the Earth Sciences Centre in Toronto.

Study shows ongoing pollution at Grassy Narrows First Nation
About the author.

Sarah Law is a CBC News reporter based in Thunder Bay, Ont., and has also worked for newspapers and online publications elsewhere in the province. Have a story tip? You can reach her at [email protected]
With files from Brett Forester and Philip Lee-Shanok
Related Stories

IMAGES
COMMENTS
Worldwide, special attention has been paid to wild mushrooms-induced poisoning. This review article provides a report on the global pattern and characteristics of mushroom poisoning and identifies the magnitude of mortality induced by mushroom poisoning. In this work, reasons underlying mushrooms-in …
Mushroom poisoning can be divided into two major categories depending on the interval (latency) from mushroom ingestion to the onset of the first symptoms of poisoning: ... Poliwoda A, et al. Research on acute toxicity and the behavioral effects of methanolic extract from psilocybin mushrooms and psilocin in mice. Toxins (Basel) 2015; 7:1018 ...
A significant portion of these global numbers is attributable to mushroom poisoning. There are numerous mushroom poisoning cases in different countries each year. In 1998, 1,675 mushroom poisoning cases were reported in France and approximately 8,000 to 10,000 cases are estimated to be on record. Mushrooms have long attracted a great deal of ...
In this paper, we provide a review focusing on poisonous mushrooms, their toxins, symptoms and utilizations. In addition, this paper establishes a poisonous mushroom list which includes 643 species from two phyla, 16 orders, 51 families and 148 genera. ... Thus, genomic studies are becoming another hot spot of poisonous mushroom research.
The gathering and consumption of wild mushrooms is a traditional social outing in Europe, Asia, and the United States. 1-5 Mushrooms were described also as popular remedies in ancient oriental documents, and some of them became ingredients in traditional medicine. 6 The consumption of wild mushrooms is very popular in Poland. An estimated figure of over 10 million Poles participate in ...
The problem of mushroom poisoning is quite serious in some Asian countries. The highest mortality rates are reported from China, with the highest number of deaths occurring in Yunnan and Guizhou provinces (Sun et al., 2018). In Nepal, the annual mortality due to ingestion of poisonous mushrooms is 15-20 people (Adhikari et al., 2005).
A two-and-a-half-month-old baby on breast milk is the youngest patient admitted with mushroom poisoning. Out of 53 patients with mushroom poisoning, 33 (62.26%) were reported in six clusters, and 20 (37.74%) were admitted as individual mushroom poisoning patients. The majority, 40 (75.47%), of the patients survived and got discharged.
Background: Poisonous mushrooms are eaten by mushroom hunters out of ignorance, after misidentification as edible mushrooms, or as a psychoactive drug. Mushroom poisoning commonly leads to consultation with a poison information center and to hospitalization. Methods: This review is based on pertinent publications about the syndromes, toxins, and diagnostic modalities that are presented here ...
In the past few decades, mushrooms have become popular in the human diet as a result of their exquisite taste and texture, protein content, and an expanding body of scientific research supporting their health benefits (Cheung, 2010).The increased public demand for wild edible mushrooms contributes to an increased interest in their picking and consumption (Pilz and Molina, 2002), which enhances ...
In 2006, the "Toxic Biological Sample Bank" project was established by the CCDC to obtain the ecological characteristics of poisonous mushrooms and promote the taxonomy of mushrooms in China. Then, books and research papers on poisonous mushroom identification, prevention, and control were published [11, 23,24,25,26,27]. These efforts have ...
The earliest publication related to mushroom poisoning dates back to 1837. To date, bibliometric analysis related to the field of mushroom poisoning has not been published. This study aimed to assess the most significant publications in this field as well as the associated trends and important drivers in the research related to mushroom poisoning.
Poisoning from ingestion of mushrooms, primarily from, but not restricted to, toxic varieties. | Explore the latest full-text research PDFs, articles, conference papers, preprints and more on ...
symptoms, treatment, autopsy findin gs and. histopathological examination along wi th their analysis. according to fore nsic casework samples of commonly. encountered poisonous mushrooms ...
Mushroom poisoning is difficult to diagnose and treat since the symptoms are similar to those of other disorders. In terms of chemistry, mushroom poisoning is associated with extraordinarily strong toxins, meaning that isolating and identifying toxins has substantial scientific relevance, especially in understanding the lethal components of ...
Of these 33 reviewed studies, the most countries that conducted research on mushroom poisoning were the United States with 7 studies, China with 6 studies, and Iran with 5 studies. The highest study duration was 30 years in France, 21 years in Italy, and 18 years in America. ... This paper is the first study in mortality rate of mushroom ...
In addition, this paper establishes a poisonous mushroom list which includes 643 species from two phyla, 16 orders, 51 families and 148 genera. ... Discover the world's research. 25+ million ...
Amatoxin-containing mushrooms are responsible for most fatal mushroom ingestions as a result of delayed-onset hepatocellular necrosis. 1 Amatoxin-containing mushroom poisonings are increasing worldwide as young adults mistake poisonous mushrooms for hallucinogenic ones, immigrants mistake poisonous mushrooms for edible ones from their home country, and trekkers inadvertently ingest poisonous ...
Toxicity studies of mushroom species have demonstrated that mushroom poisoning can cause adverse effects such as liver failure, bradycardia, chest pain, seizures, gastroenteritis, intestinal fibrosis, renal failure, erythromelalgia, and rhabdomyolysis. Correct categorization and better understanding are essential for the safe and healthy ...
Mushroom poisoning as a cause of acute liver injury is rare but associated with deadly outcomes if not early recognized and treated. The mortality is very high in the case of amatoxin-containing mushrooms ingestion and liver transplantation is the only lifesaving option. Therefore, early recognition of a suspected patient who came with features ...
Lethal mushrooms in the Amanita genus contain two major groups of cyclopeptides, the bicyclic octapeptide amatoxins and bicyclic heptapeptide phallotoxins. Some contain monocyclic virotoxin peptides as well. The thermostable amatoxins are 10-20 times more toxic than the others, but is the only toxin class of the three that is actually absorbed and therefore responsible for poisoning and ...
Of 294 patients between the ages of 3 and 72 (28.97 ± 19.32), 173 were female, 121 were male and 90 were under the age of 16 years. One hundred seventy-three patients (58.8%) had consumed the mushrooms in the early summer. The onset of mushroom toxicity symptoms was divided into early (within 6 h after ingestion) and delayed (6 h to 20 d).
Wild mushroom poisoning is a global public health concern, with mushrooms containing amatoxins being the main cause of fatalities. ... In this paper, we report a case of amatoxin-containing Mushrooms poisoning, which resulted in three individuals being poisoned and two fatalities. ... research has found that even in the later stages, toxins may ...
2-3% increase in fiber. 8-12% increase in potassium. 12-18% increase in riboflavin. 11-26% increase in niacin. 11-23% increase in selenium. 16-26% increase in copper. Mushrooms exposed ...
Numerous mushroom species have psychoactive toxins. They ar e poisonous and a. serious threat to health [9]. Some mushrooms are very toxic and are dangerous. even in very small quantities. Many ...
A new study suggests historic problems in northwestern Ontario from mercury contamination in the 1960s and 70s are being made worse by ongoing industrial pollution.