- Find a hospital Results See all results Balashikha 1 hospitals Barnaul 2 hospitals Goryachinsk 1 hospitals Irkutsk 1 hospitals Ivanovo 2 hospitals Kaliningrad 2 hospitals Kazan 2 hospitals Kislovodsk 1 hospitals Korolev 1 hospitals Kovrov 1 hospitals Krasnodar 3 hospitals Krasnogorsk 1 hospitals Moscow 42 hospitals Nizhny Novgorod 3 hospitals Novokuibyshevsk 1 hospitals Novokuznetsk 1 hospitals Novosibirsk 5 hospitals Obninsk 1 hospitals Orenburg 1 hospitals Penza 1 hospitals Saint Petersburg 9 hospitals Samara 3 hospitals Surgut 1 hospitals Tomsk 1 hospitals Tula 1 hospitals Tyumen 1 hospitals Ulan-Ude 1 hospitals Ulyanovsk 2 hospitals Vladivostok 1 hospitals Volgograd 8 hospitals Vologda 1 hospitals Voronezh 1 hospitals Yalta 1 hospitals Yekaterinburg 2 hospitals All hospitals
- Find a sanatorium Results See all results Altai region 4 sanatoriums Buryatia 1 sanatoriums Crimea 4 sanatoriums Ingushetia 1 sanatoriums Karelia 1 sanatoriums Kislovodsk 1 sanatoriums Krasnodar region 2 sanatoriums Moscow region 5 sanatoriums Nizhny Novgorod Region 1 sanatoriums Saint Petersburg region 1 sanatoriums All sanatoriums
- Check the prices Allergology 29 hospitals Andrology 36 hospitals Bariatric surgery 18 hospitals Cardiology 47 hospitals Cosmetology 22 hospitals Dentistry 29 hospitals Dermatology 40 hospitals Dietetics 17 hospitals Endocrinology 46 hospitals Gastroenterology 43 hospitals Genetics 4 hospitals Gynecology 59 hospitals Hematology 21 hospitals IVF (In Vitro Fertilization) 15 hospitals Mammalogy 37 hospitals Maxillofacial Surgery 9 hospitals Narcology 3 hospitals Neurology 57 hospitals Neurosurgery 22 hospitals Obstetrics 15 hospitals Oncology 44 hospitals Ophthalmology 40 hospitals Orthopedics and traumatology 38 hospitals Otolaryngology (ENT) 42 hospitals Pediatrics 30 hospitals Phlebology 36 hospitals Plastic surgery 25 hospitals Proctology 33 hospitals Psychiatry 14 hospitals Pulmonology 28 hospitals Rehabilitation 21 hospitals Rheumatology 29 hospitals Speech therapy 6 hospitals Surgery 41 hospitals Urology 52 hospitals Venereology 24 hospitals
- List of diseases Aesthetic problems 27 hospitals Allergic diseases 31 hospitals Blood diseases 21 hospitals Cardiovascular diseases 49 hospitals Childhood diseases 28 hospitals Colon diseases 33 hospitals Diseases of the digestive system 48 hospitals Diseases of the mammary glands 38 hospitals Diseases of the musculoskeletal system and injuries 45 hospitals Diseases of veins and lymph nodes 39 hospitals Endocrine diseases 50 hospitals ENT (eye, nose, throat) diseases 43 hospitals Eye diseases 43 hospitals Female diseases 61 hospitals Genetic diseases 6 hospitals Infectious diseases 26 hospitals Male diseases 41 hospitals Mental disorders and phenomena 14 hospitals Narcological problems 6 hospitals Nervous diseases 60 hospitals Oncological diseases 46 hospitals Respiratory diseases 30 hospitals Rheumatic diseases 31 hospitals Skin diseases 41 hospitals Speech disorders 7 hospitals Teeth Diseases 30 hospitals Urological diseases 55 hospitals Venereal diseases 27 hospitals
- Our contacts

Dmitry Rogachev National Research Center of Pediatric Hematology, Oncology and Immunology

About hospital
Dmitry Rogachev National Research Center of Pediatric Hematology, Oncology and Immunology was created by order of the Government of Russian Federation.
Center is one of the largest hospitals in Europe. It contains the best achievements of modern medical science, designed to serve the health of children. The center is equipped with the latest medical equipment from the world’s leading manufacturers, and at its sites the most advanced and original technologies in the treatment of hematological and oncological diseases are successfully tested.
Aim of the Center
The aim of the center is to develop and introduce new methods of treatment and medical and social rehabilitation of children with diseases of the blood of the immune system, hemoblastosis, tumors of the nervous system and a number of other diseases associated with the activities of the clinic. The center conducts scientific research at the world level. On the basis of the constant work of a group of scientists from the two countries of Russia and Germany, the Moscow-Berlin protocol for the study of acute lymphoblastic leukemia in children was created.
Dmitry Rogachev National Research Center provides specialized high-tech medical care for children from Russia and foreign countries in a 24-hour and day hospital, as well as in an outpatient clinic. Patients aged from infants to 18-21 years old are being treated for various forms of oncological diseases. One of the priority areas is the treatment of leukemia in children, where the survival rate is 95%. There is no analogue of such treatment in other countries yet.
Hospital performs unique operations on bone marrow cell transplantation from related and unrelated donors living all over the world. More than 200 such operations are carried out annually.
Main directions of scientific and practical activities
- complex therapy of hemoblastosis, brain tumors and solid neoplasms in children, adolescents and young adults;
- high-tech surgery and radiation therapy for all types of cancer;
- transplantation of hematopoietic stem cells in cases of bone marrow insufficiency syndromes, immunodeficiencies, hematopoietic malignancies, oncological and hereditary diseases;
- diagnosis and treatment of immunodeficiency and autoimmune diseases in children;
- diagnosis and treatment of hemorrhagic diseases, thrombophilia, anemia, hereditary blood diseases and other pathological conditions;
- development of molecular biological methods for the diagnosis and treatment of hematological, oncological and immunodeficiency diseases in children;
- development of new methods of treatment for children with congenital and acquired aplasias of hematopoiesis;
- optimization of blood transfusion tactics and study of the peculiarities of procurement, storage and transplantation of hematopoietic stem cells;
- optimization of treatment regimens and improvement of the results of radiation diagnostics and therapy in children;
- molecular biological basis for the regulation of hematopoiesis, pathogenesis of erythron diseases and disorders of iron metabolism in children;
- development of complex methods of therapy for hemostasis disorders; epidemiology of hematological and oncological diseases in children and adolescents.
Specialization
What diseases are treated, additional services and facilities, booking of online-consultation.
After submitting this form our manager will get in touch with you to inform cost of consultation of selected specialist and agree with you date-time slot for online-talk with doctor.
Submitting Request to Dmitry Rogachev National Research Center of Pediatric Hematology, Oncology and Immunology
For reviewing your case by doctors you need to fill form below.
Coronavirus (COVID-19): Latest Updates | Visitation Policies Visitation Policies Visitation Policies Visitation Policies Visitation Policies | COVID-19 Testing | Vaccine Information Vaccine Information Vaccine Information
Department of Pediatrics
Center for children's health research.
- Research at the University of Rochester
The University of Rochester houses some of the world's premier basic and clinical biomedical and socioeconomic researchers in interdisciplinary centers and cutting-edge laboratories and clinical research facilities. This arrangement—with everything in close geographic proximity, with programmatic juxtaposition across departmental lines—makes intellectual interaction and translation of advances from the bench to the bedside and from the illness treatment setting to the prevention and wellness arena an everyday occurrence here.
- Biomedical Sciences Research at the University of Rochester
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Front Pediatr
Single Center Experience With Pediatric Patients With GATA2 Deficiency
Galina ovsyannikova.
1 Department of Pediatric Hematology and Oncology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia
Anna Pavlova
2 Laboratory of Molecular Biology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia
Ekaterina Deordieva
3 Department of Pediatric Immunology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia
Elena Raykina
Alexey pshonkin, alexey maschan, michael maschan.
4 Department of Hematopoietic Stem Cell Transplantation, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia
Associated Data
The NGS datasets presented in this study are available upon request from the author (Galina Ovsyannikova) by email: [email protected] .
GATA2 deficiency is one of the most common predisposing conditions for MDS in young individuals. It is characterized by autosomal dominant inheritance and a high rate of de novo mutations. Here we describe the clinical phenotype and hematological presentation of 10 pediatric patients with GATA2 deficiency presented to the Dmitry Rogachev Center between 2013 and 2020. All patients had been referred for neutropenia or suspected aplastic anemia. While some patients presented with an immunological phenotype, others displayed monosomy 7 and MDS. The clinical presentation with MDS in infancy and the constitutional phenotypes in our patients underline the great variability in clinical manifestation. Careful description of cohorts with GATA2 deficiency from different countries and genetic backgrounds will help to unravel the enormous heterogeneity of this recently discovered genetic disorder.
Introduction
Establishing the correct diagnosis in children with cytopenia has recently become more challenging. Clinical and laboratory features of a number of genetic disorders, specifically germline disease predisposing to myeloid neoplasia, the classical inherited bone marrow failure syndromes (BMFS) and primary immunodeficiencies, can overlap. In addition, these inherited conditions need to be differentiated from acquired disorders such as aplastic anemia.
GATA2 deficiency is one of the most common predisposing conditions for MDS in young individuals. It is characterized by autosomal dominant inheritance with a high rate of de novo mutations. GATA2 syndrome exhibits incomplete penetrance and heterogeneity in clinical presentation with manifestation of myeloid neoplasia at any age ( 1 ). GATA2 encodes a zinc finger transcription factor critical to early hematopoiesis, mononuclear development, and alveolar macrophage activity ( 2 , 3 ). Heterozygous germline mutations in GATA2 lead to complex and heterogeneous clinical phenotypes including MonoMAC syndrome (monocytopenia and mycobacterial infections)/DCML deficiency (dendritic cell, monocyte, B and natural killer (NK) lymphoid deficiency) ( 2 – 7 ), lymphedema (Emberger syndrome) ( 8 , 9 ) and familial MDS/AML ( 10 ). In addition, other recurrent phenotypes have been described such as primary pediatric MDS ( 11 ), chronic neutropenia ( 12 ), aplastic anemia ( 13 ), pulmonary alveolar proteinosis ( 14 ), dermatological ( 15 ), autoimmune or vascular features ( 16 ).
A continuous review of clinical and genetic data on patients with GATA2 deficiency in different parts of the world will help to understand the heterogeneity of presenting features. Careful description of patient series with this rare disorder will facilitate the development of standards of care for patients and healthy gene carriers. This manuscript describes the clinical and hematological phenotype of 10 children with GATA2 deficiency diagnosed at the Dmitry Rogachev National Research Center in Moscow.
Materials and Methods
Peripheral blood samples from patients or family members had been obtained with informed consent. The study was approved by the local ethics committee. Metaphase karyotyping, chromosome banding analyses of diagnostic bone marrow specimens were performed according to standard procedures. Genetic testing was done by Sanger sequencing for single gene analysis or target next-generation sequencing on the MiSeq/NextSeq (Illumina, USA) using BMFS custom gene panel. The BMFS custom gene panel consists of 197 genes ( Supplementary Table 1 ). Population frequency evaluation of the identified variants was performed using the data from the gnomAD Exomes and gnomAD Genomes projects. Computational pathogenicity assessment of missense variants was performed using the following prediction tools: SIFT, Provean, PolyPhen-2, and UMD Predictor. Computational effect prediction of the splice site and splice site region alterations was performed with Human Splicing Finder 3.0 and NNSplice. Evaluation of variant clinical relevance was performed using Online Mendelian Inheritance in Man and the Human Gene Mutation Database. The clinical significance of the identified variants has been assigned based on the American College of Medical Genetics and Genomics recommendations ( 17 ).
Characteristics of hematopoietic stem cell transplantation are presented in the Supplementary Table 2 .
GATA2 deficiency was diagnosed in 10 patients referred for a diagnosis of cytopenia between 2013 and 2020 ( Table 1 ). In all 10 patients GATA2 mutations located in zinc finger 2; mutations were missense in 4 cases, and truncating in 6 with 4 nonsense and 2 frameshift changes. Genetic analysis in non-hematological tissue demonstrated germline origin in all six cases analyzed.
Clinical and hematological characteristics of patients with GATA2 deficiency.
N, normal; ND, no data; BM, bone marrow; M, Male; F, Female; CBC, complete blood count; WBC, white blood cells; ANC, absolute neutrophil count; Plt, Platelets. E, erythropoiesis; G, granulopoiesis; M, megakaryopoiesis ;
% ,GATA2 mutational study not performed .
Eight of the 10 patients had physical abnormalities ( Table 2 ); 5 of them showed an Emberger-like phenotype with deafness and/or lymphedema/hydrocele, 3 had abnormalities of the genitourinary tract, 2 constitutional heart disease and one patient gallbladder anomaly. Genetic evaluation of family members established the de novo origin of the identified mutation in 6 cases ( Table 1 ). The father of one patient was known to have lymphedema, but mutational analysis was not feasible due to absent material.
Constitutional phenotype and infections.
M, Male; F, Female ;
Median age at onset of cytopenia was 10.5 years (range 2.8–17.6), and the median duration between first cytopenia and consultation in our referral center was 2.8 years (range 0.1–10.2). Leukopenia (9/10 patients), neutropenia (10/10) and profound monocytopenia (10/10) were the most prevalent hematological manifestations; median values for the absolute neutrophil and monocyte count were 0.59 G/L (range 0.32–1.10) and 0.06 G/L (range 0.01–0.18), respectively ( Table 1 ). In contrast, none of the patients had a platelet count below 100 G/L (range 106–469, median 217). Median hemoglobin level was 10.8 g/dl (range 7.2–14.6), one patient required red cell transfusions prior to diagnosis. Red cells were macrocytic for age in 8/10 patients. In all patients, the bone marrow blast percentage was <5%, and in 8 out of the 10 cases the marrow was hypocellular. Chromosomal analysis showed monosomy 7 in 4/10 patients, one patient had trisomy 8 ( Table 1 ).
Recurrent or severe infections at diagnosis or during the clinical course were observed in all patients. One patient (Pt 2) succumbed to varicella zoster encephalitis 4.9 years after diagnosis; she had a normal karyotype, normal IgG levels, but a profound decrease in B-cells as well as neutropenia and monocoytopenia. In 6 patients immunoglobulin G serum levels were available and within the normal range. The analysis of lymphocyte subpopulations showed a reduction in number of B-cells (CD19+; median 0.02 G/L, range 0.01–0.03) and NK-cells (CD16+/CD56+; median 0.052 G/L, range 0.013–0.124) in the five patients studied; 3 of these patients also demonstrated T-cell deficiency (CD3+, median 1.14 G/L, range 0.44–1.71).
Allogeneic hematopoietic stem cell transplantation (HSCT) was not readily available for all patients. Four of the 10 patients were transplanted a median time of 4.0 years (range 0.5–6.7) from onset of cytopenia ( Supplemental Table 2 ). Two of these 4 patients had presented with monosomy 7, one with trisomy 8, and none of them had an increased blast percentage. One patient was grafted from a matched unrelated donor (MUD), while the other 3 patients received a haploidentical graft. In 2 of the 3 patients with a haploidentical parental transplant, a second grafting procedure was necessary because of primary graft failure.
Six patients were followed in the absence of HSCT. Median time from onset of cytopenia to last follow-up was 3.9 years (range 1.0–10.2). One of these patients (Pt 8) experienced disease progression with increase in blast percentage 1.2 years from onset of cytopenia. He was found to have monosomy 7, progressed rapidly to AML and succumbed to candida sepsis shortly thereafter. In one patient (Pt 9), monosomy 7 with trisomy 8 was diagnosed 5.7 years after hematological presentation.
At the time of writing seven patients are alive, one patient died due to varicella zoster encephalitis (Pt 2), one patient died after the second HSCT due to infectious complications (Pt 9), and another one due to infectious complications during intensive chemotherapy (Pt 8) ( Table 1 ).
All patients with GATA2 deficiency presented in this retrospective cohort had neutropenia. More strikingly, the absolute neutrophil count in all patients was severely decreased with a range between 0.32–1.10 G/L at time of first evaluation. In contrast to what has been reported in the largest series of GATA2 deficiency in pediatric MDS ( 1 – 11 ), all patients presented here had monocytopenia with an absolute monocyte count ranging between 0.01 and 0.18 G/L. Also, thrombocytopenia and anemia were less common, likely indicating that some patients presented here had an immunodeficiency - type of manifestation rather than an MDS-type presentation.
Median age at diagnosis in the largest series of GATA2 deficiency in pediatric MDS was 12 years, in fact, all patients were above the age of 3 years at presentation ( 11 ). In this consecutive study of EWOG-MDS patients, 70% of GATA2 deficient cases had monosomy 7. Infants with MDS and monosomy 7 are more likely to have an underlying SAMD9/SAMD9 syndrome than GATA2 deficiency ( 18 ). The youngest patient included in the series presented here, was 2.8 years and had monosomy 7 at diagnosis. This observation emphasizes that despite the different age distribution in presentation between GATA2 deficiency and SAMD9/SAMD9L syndrome, all patients need complete diagnostic work-up for all genetic disorders irrespective of age.
Physical examination with constitutional abnormalities in 8 of the 10 patients had already raised the suspicion of a genetic disorder prior to molecular testing. Interestingly, 3 of the 8 patients had abnormalities of the genitourinary tract, possibly indicating that this organ system is more commonly affected than previously appreciated ( 8 – 16 ). In addition, we describe biliary tract and cardiac anomalies as potential novel constitutional features of GATA2 deficiency. The exact description of the spectrum of constitutional abnormalities related to GATA2 deficiency will require large carefully selected patient cohorts. For instance, although café au lait spots were noted in one of our patients and had previously been described in GATA2 deficiency ( 19 ), they are also not very common in the general population. Furthermore, syndactyly of the foot in one of our patients is likely not related to GATA2 deficiency since his father with GATA2 wild type had syndactyly of his fingers.
Taking into account that more than 80% of patients with GATA2 deficiency present with a hematologic malignancy around the age of 40 years ( 16 ), HSCT is generally considered early in the clinical course. Indeed, most patients with MDS and monosomy 7 are transplanted as soon as a suitable donor is available. Progression to MDS and AML may be very rapid as observed in one of our patients who died from infectious complications while receiving intensive chemotherapy for AML. Also, profound neutropenia or other signs of immunodeficiency should result in timely HSCT to avoid severe infectious complication. One of our patients died from severe varicella infection. If a MUD is not available, a haploidentical HSCT can be performed. Stem cell source and type of donor does not significantly influence HSCT outcome in GATA2 deficiency, while abnormal karyotype and blast percentage are the main risk factors for poor outcome ( 20 ). HSCT must be carefully considered in all individuals with GATA2 deficiency, and timely grafting when indicated will most likely improve outcome for this group of patients.
Conclusions
In this retrospective study, we expand the clinical and genetic phenotype of GATA deficiency by outlining previously undescribed constitutional abnormalities and novel mutations. Thus, our work underlines the broad heterogeneity of the predisposition syndrome.
Data Availability Statement
Ethics statement.
The studies involving human participants were reviewed and approved by the Local Ethics Committee of Dmitry Rogachev National Research Center of pediatric oncology, hematology and immunology. Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin.
Author Contributions
GO collected and analyzed data and wrote the manuscript. AP and ER performed genetic data analysis. ED and AP participated in data collection. AM and MM reviewed the manuscript and supervised the project. All authors contributed to the study design.
This study is supported by a grant from the Charitable Foundation Science for Children in the Russian Federation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors cordially thank Prof. Dr. Charlotte M. Niemeyer (Children‘s Hospital University Medical Center Freiburg, Germany) for helpful comments, helping to prepare the manuscript, and for preparing tables.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2022.801810/full#supplementary-material
- UTHealth Houston
- Pediatric Research Center
- Keynote Speakers
- Research Team
- Selected Publications
- Lab Members
- Selected Publications and Recent Preprints
- Contact Information
- Publications
- Recent Lab News
- Resident Collaborators
- Former Lab Members
- Lab News via Twitter
- Publication
- Bone Disease Program Seminar Series
- Data Exchange Seminar Series
- PRC/CCR Seminar Series
Komatsu Lab
Understanding Craniofacial Development and Disease
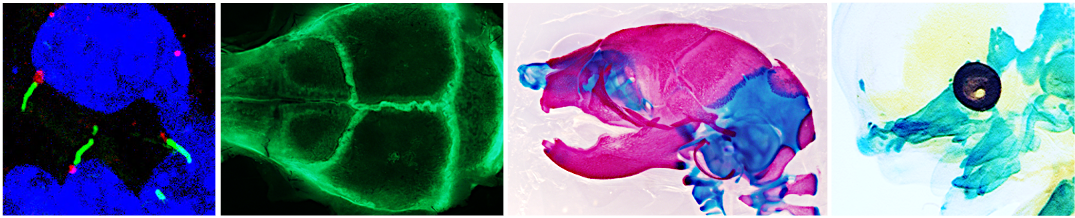
Welcome to the Komatsu lab. Our research has focused on understanding the molecular mechanisms responsible for human congenital diseases, with an emphasis on craniofacial abnormalities. Our ultimate long-term goal is to acquire the molecular knowledge for understanding craniofacial skeletal defects and to develop strategies for craniofacial skeletal tissue regeneration.
- McGovern Medical School Facebook Page
- McGovern Medical School X Page
- McGovern Medical School Instagram Page
- McGovern Medical School YouTube Page
- McGovern Medical School LinkedIn Page
- Medical School IT (MSIT)
- Campus Carry
- Emergency Info
- How to report sexual misconduct
- University Website Policies
- Open access
- Published: 30 May 2024
Hospitalization information and burden of pediatric inpatients in transport accidents
- Jing Yu 1 na1 ,
- Lin Mei 2 na1 ,
- Yanni Wang 1 ,
- Guoshuang Feng 3 ,
- Yueping Zeng 4 ,
- Xinyu Wang 3 &
- Jing Liu 1
BMC Public Health volume 24 , Article number: 1446 ( 2024 ) Cite this article
Metrics details
Transport accidents are one of the leading causes of child morbidity and mortality worldwide and represent a significant public health burden. This study aimed to investigate the hospitalization information and burden of pediatric inpatients in transport accidents in China.
In this study, we collected the cover page of the medical records of pediatric inpatients in transport accidents using the Futang Research Center of Pediatric Development (FRCPD) database from January 1, 2016 to December 31, 2021. Then, we extracted the epidemiological characteristics, including demographic characteristics, cases distribution, disease information, and hospitalization burden.
Among 36,455 included inpatients, males, aged 1–3 years, East China, July were dominant in different subgroups. In transport accidents, pedestrians were the most frequently type of injury (65.69%). Of all known lesions, craniocerebral/nerve injury was the more common results in pediatric inpatients in transport accidents (33.93%). In addition to pedal cyclists more susceptible to sport system injury, other types of injured person with transport accidents were mainly craniocerebral/nerve injury. In terms of the type of discharge, occupant of heavy transport vehicle or bus and people with craniocerebral/nerve injury had the highest mortality rate after hospitalization in all type and lesion of injured person groups, respectively. The largest hospitalization burden in the type of injured person was occupant of heavy transport vehicle or bus.
Conclusions
This study revealed that epidemiological characteristics and the main factor influencing the hospitalization information and burden of children with traffic accidents in China.
Peer Review reports
Introduction
Transport accidents are one of the leading causes of child morbidity and mortality worldwide and represent a significant public health burden. According to the World Health Organization (WHO)’s 2018 Global Status Report on Road Safety, more than 10 million children are injured in transport accidents every year, and up to 186,300 children lose their lives [ 1 ]. In China, transport accidents are the second leading cause of injury and death among children. A previous report showed that in 2019, 19.619 children under the age of 15 were injured and 2,593 were killed in transport accidents [ 2 ]. Faced with severe transport accidents problems, children are the vulnerable groups that need special attention in road traffic safety. However, as a country with a huge number of children, China does not have adequate epidemiological information about the pediatric inpatients in transport accidents.
The Futang Research Center of Pediatric Development (FRCPD) is a large medical consortium that promotes the development of children’s medical research [ 3 ]. It covers 47 tertiary children’s hospitals, 28 of which have agreed and uploaded the annual summary reports of discharged patients since 2016 in China. Herein, we retrospectively analyzed the epidemiological characteristics of pediatric inpatients in transport accidents using the FRCPD database, aiming to investigate the current situation of transport accidents among children in China and carry out targeted intervention activities.

Methodology
Data source and categories.
The FRCPD was established as a multi-tiered pediatric diagnosis and treatment network. The data uploading docking and format standards are referred to the requirements made by the Hospital Quality Monitoring System (HQMS) for the collection of first-page information of inpatient medical records in the performance appraisal and medical quality management of national tertiary public hospitals (2019). In this study, the data came from the cover page of the medical records of discharged children using FRCPD database from January 1, 2016 to December 31, 2021. Detailed information regarding the FRCPD is learned at http://www.futang.org/about/fu-tang-jie-shao.htm . The inclusion criteria & exclusion criteria were shown in Table 1 .
Next, we extracted the epidemiological characteristics of pediatric inpatients in transport accidents, including demographic characteristics (gender, age), cases distribution (region, month of hospitalization), disease information (type/lesion of injured person, type of discharge), hospitalization burden (length of hospital stay/LOS and hospitalization expenses). Then, we divided age of hospitalization into five categories: < 1 years old, 1–3 years old, 4–6 years old, 7–12 years old, and 13–18 years old. Then, the lesion of injured person was summarized into five groups including craniocerebral/nerve injury, sports system injury, visceral-related injury, skin injury, and others. Next, the type of discharge was divided into discharge with doctor’s advice, discharge without doctor’s advice, death, transfer with doctor’s advice, transfer to community health service agencies/township health center with doctor’s advice, others. Furthermore, this 28 provincial and municipal hospitals were respectively belong to Northeast, North, East, Northwest, Southwest, South, and Central China regions (Sup Table 1 ).
Categorical variables, including gender, age, region, month of hospitalization, type/lesion of injured person, type of discharge were expressed as numbers (N), and were compared among different groups using the Pearson chi-square tests. Continuous variables including LOS and hospitalization expenses, were both non-normally distributed based on the Shapiro-Wilk tests. Therefore, they were expressed as median and interquartile ranges, and compared using Kruskal-Wallis tests. Post-hoc tests were conducted using the Steel-Dwass method. P < 0.05 was assessed as statistically significant. Statistical analyses were conducted with the JMP Pro 15 software.
Demographic characteristics and cases distribution of pediatric inpatients in transport accidents
Firstly, over 7 million cover pages of the medical records were screened from the FRCPD database, and 36,455 pediatric inpatients in transport accidents were included in this study. As shown in Table 2 , the included males accounted for 62.78% ( n = 22,886), and females 37.22% ( n = 13,569), with a male-female ratio of 1.68:1. The results showed that 1–3 years old inpatients were dominant ( n = 12,258, 33.63%), followed by 4–6 years old ( n = 11,388, 31.24%), 7–12 years old ( n = 9970, 27.35%), 13–18 years old ( n = 1698, 4.66%), and < 1 years old ( n = 1141, 3.13%) (Table 2 ).
Since this 28 hospitals of FRCPD database belonged to seven different regions in China, Fig. 1 ; Table 2 revealed that the top 3 regions with the highest numbers of patients with transport accidents were East China ( n = 15,080, 41.37%), North China ( n = 10,258, 28.14%), and Northwest China ( n = 3504, 9.61%). Basing the month of hospitalization, the proportion of patients with transport accidents in July was largest (Fig. 2 and Sup Table 2 ).
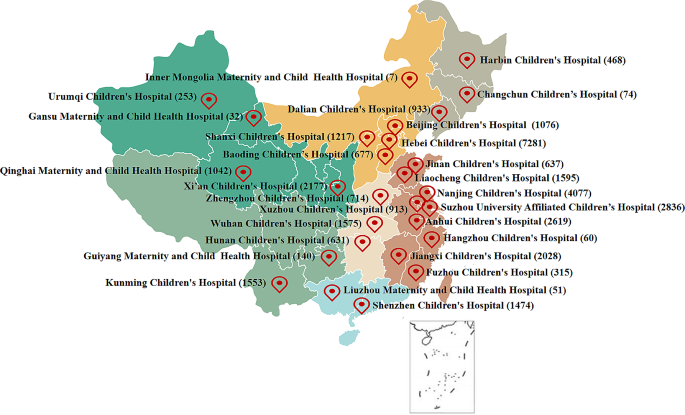
The region and hospital distribution of pediatric inpatients in traffic accidents
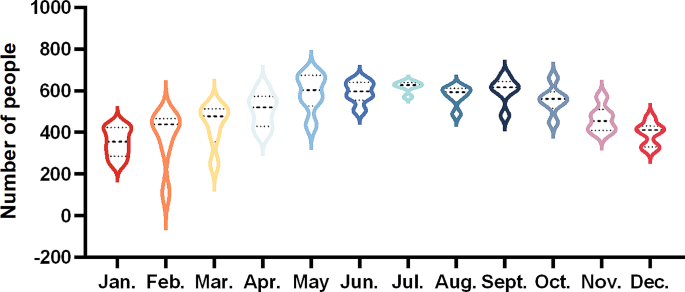
Total number of pediatric inpatients in traffic accidents per month, 2016 to 2021
Disease information of pediatric inpatients in transport accidents
Our findings confirmed that among 36,455 hospitalization cases, pedestrians were the most common type of injured person ( n = 23,949, 65.69%, Table 2 ). Males with transport accidents were markedly more than females in all type of injured person groups (Fig. 3 A and Sup Table 3 ). Except for the types of injured persons < 1 year old were mainly motorcycle rider or occupant of three-wheeled motor vehicle ( n = 238), the other four age groups were mainly pedestrians (1–3 years old/ n = 3707, 4–6 years old/ n = 4222, 7–12 years old/ n = 3544, 13–18 years old/ n = 789, Fig. 4 A and Sup Table 3 ). In the type of injured person group, pedal cyclists more susceptible to sport system injury (38.88%). On the other hand, pedestrian (30.21%), motorcycle rider or occupant of three-wheeled motor vehicle (51.26%), occupant of car, pick-up truck or van (50.78%), occupant of heavy transport vehicle or bus (39.33%) were mainly lead to craniocerebral/nerve injury (Table 3 ). Moreover, the type of injured person were significantly different with the gender (χ 2 = 88.38, p < 0.001), age (χ 2 = 2677.02, p < 0.001), lesion of injured person (χ 2 = 1702.32, p < 0.001) in pediatric inpatients.
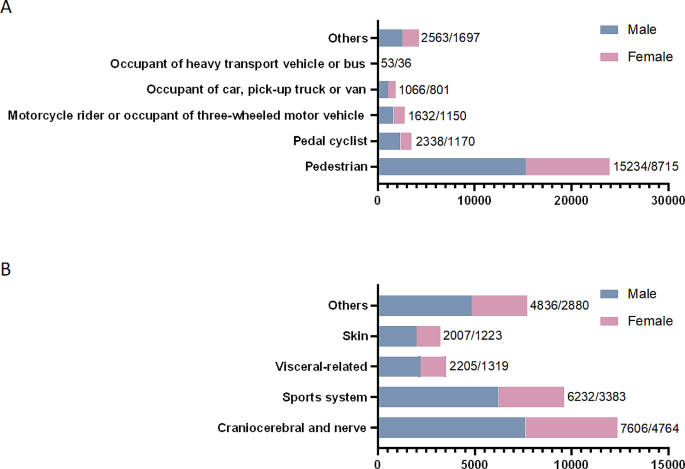
Gender distribution of pediatric inpatients in different type (A) and lesion (B) of injured person groups
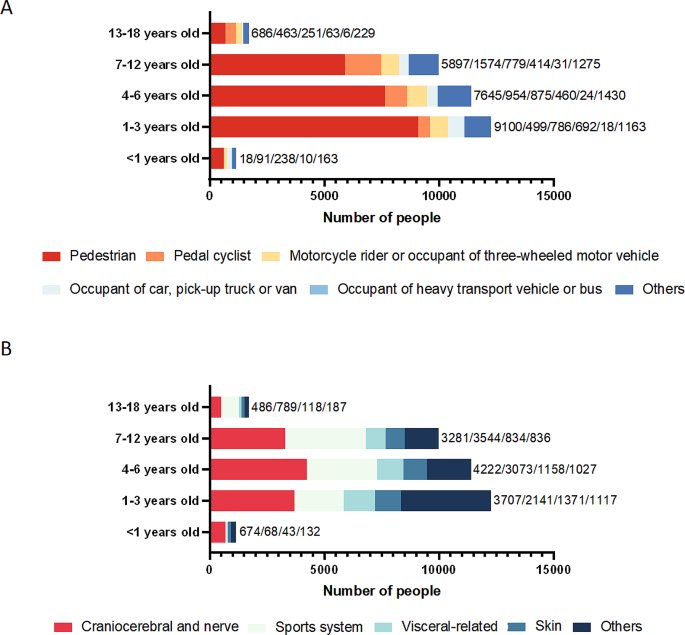
Age distribution of pediatric inpatients in different type (A) and lesion (B) of injured person groups
Of all known lesions, craniocerebral/nerve injury was the more common results in pediatric inpatients in transport accidents ( n = 12,370, 33.93%, Table 2 ), and the number of male patients is higher in all kinds of injuries (Fig. 3 B and Sup Table 4 ). Specifically, children younger than 1 year old ( n = 674), 1–3 years old ( n = 3707), and 4–6 years old ( n = 4222) were the most likely to cause craniocerebral/nerve injury, and children 7–12 years old ( n = 3544) and 13–18 years old ( n = 789) are the most likely to cause sports injury (Fig. 4 B and Sup Table 4 ). Furthermore, the lesion of injured person was significantly different with the gender (χ 2 = 26.57, p < 0.001) and age (χ 2 = 2623.64, p < 0.001) of patients.
In addition, Table 2 showed the number of children who were discharged in different ways, among which the vast majority of pediatric inpatients were discharged with doctor’s advice ( n = 32,907, 90.27%). Furthermore, the type of discharge were significantly different with the type of injured person (χ 2 = 316.27, p < 0.001) and lesion of injured person (χ 2 = 713.24, p < 0.001) in pediatric inpatients (Sup Table 5 ). Specially, occupant of heavy transport vehicle or bus (2.25%) and people with craniocerebral/nerve injury (0.97%) respectively had the highest mortality rate after hospitalization in all type and lesion of injured person groups (Sup Table 5 ).
Hospitalization burden of pediatric inpatients in transport accidents
With the benefit of this multi-center database, we were able to better understand the average hospitalization burden of children after traffic accidents. As shown in Table 4 , the largest hospitalization burden (included LOS and hospitalization expenses) in the type of injured person was occupant of heavy transport vehicle or bus. Interestingly, among the different lesions of injured person, the hospitalization expense was highest in sports system group, while the LOS was the longest in the visceral-related group. In the end, our results found important differences in the hospitalization burden of patients stratified by the type and lesion of injured person groups.
With the continuous development of the automobile industry and the increasing diversification of transportation modes, traffic accidents have long been a global health challenge. As the leading cause of death for children over the age of five, traffic accidents place a huge physical, psychological and financial burden on children and families [ 4 , 5 , 6 ]. In China, the risk of children being injured in traffic accidents is also increasing rapidly, and it has become the second leading cause of death for children aged 1–10 and the first leading cause of death for children aged 15–18 [ 7 ]. However, to date, only a few studies have reported on the epidemiological characteristics and hospitalization burden of children suffer from traffic accidents.
Based on a large-scale and multi-center FRCPD database, we reported a national cross-sectional study on the hospitalization information and financial burden of pediatric inpatients in transport accidents, aiming to increase people’s attention to children’s traffic accidents and provide clinical basis for the diagnosis and treatment of children’s traffic accidents. Our results showed that the incidence of road traffic injuries among children in North and East China was higher than in other regions of China. The rate of injury was higher among boys than girls, and among children who had not yet attended kindergarten compared to those in other grades. The skull, brain and nervous system was the most vulnerable body part for younger children. When road traffic injuries occurred, walking was the primary activity for children. Additionally, our results found important differences in the hospitalization burden of patients stratified by the type and lesion of injured person groups.
First, our study also found that boys accounted for the majority of pediatric inpatients in traffic accidents (1.68:1). Similarly, a previous report indicated that boys are more likely to be injured in traffic accidents than girls (1.76: 1) [ 8 ]. The possible reason may be that boys are more active, faster, and less caution than girls. Second, given the age of the patients, our results found that children aged 1–3 years were more easily to suffer traffic accidents. Children under 3 years of age do not receive adequate road safety education, due to they are not enrolled in the kindergarten. Therefore, the incidence of traffic accidents will increase when children with poor mobility and judgment ability are walking, playing, and crossing the road [ 9 ]. In addition, the number of children aged < 1 or 13–18 in traffic accidents obviously decreased compared to other age groups in our study. Children < 1 year old can’t walk very well, and are generally looked by caregivers for a long time. Children aged 13–18 have better safety awareness, and children > 14 years old are often admitted to adult hospitals in China [ 8 , 10 ]. In addition, the number of children hospitalized due to traffic accidents peaked in July. Similarly, a study reported that the hospitalization peak of pediatric traumatic brain injury was the third quarter of the year, which may be related to children’ easier outdoor activities during the summer vacation [ 15 ].
Then, the number of hospitalization children in traffic accidents were significantly higher in North and East China than in other regions in the current study. On the one hand, many scholars believe that the high degree of urbanization, large population density and large vehicle flow are the risk factors that lead to frequent traffic accidents [ 11 ]. Due to the economic conditions, terrain characteristics and other factors in different regions of a country, the incidence and death rate of traffic accidents are also different [ 2 ]. Thus, as the economically developed regions, North and East China have higher incident of traffic accidents [ 11 , 13 , 14 ]. On the other hand, a previous study found that as the number of health facilities increased, the number of deaths from traffic accidents decreased, so the investment of health facilities located in the area needed to be improved [ 12 ]. Thus, a large number of patients will also be treated and transferred to North and East China, due to the backward medical resources in other regions. Unfortunately, this FRCPD database does not cover and extract the hospitalization information of children’s hospitals such as Guangzhou and Shanghai, so the regions analysis remain limitations.
Next, our study found that pedestrian was the most common type of injured person in the FRCPD database. Possible explanations for this results were that active children are unable to judge the distance and speed of cars approaching them in a timely and accurate manner, and the parents often ignore the dangers of their children as pedestrians [ 11 ]. Furthermore, the patients with craniocerebral/nerve injury were mainly 4–6 years old, the patients with sport injury were 7–12 years old and 13–18 years old, and the patients with visceral-related or skin injury were 1–3 years old. In addition to pedal cyclists more susceptible to sport system injury, other types of injured person with transport accidents were mainly craniocerebral/nerve injury in our results. Past studies have reported that children on the road are usually impacted by the front end of the vehicle, and the head and lower extremity are the most vulnerable areas to suffer moderate and severe injuries [ 13 , 14 ]. In motor vehicle collisions, head injuries are most common in children, which is independent of the age of the child, whether the child was restrained by a seat belt, or crash direction [ 15 , 16 , 17 ]. Body proportions of children change dramatically throughout the growing period. The head accounts for about a quarter of the body length at birth, and only about 1/7 of the body length in adulthood [ 18 ]. A study has found that children under the age of 6 are more likely to suffer craniocerebral/nerve injury [ 17 ]. This may be related to the higher head weight of children in this age group, and the head is more likely to hit the ground first in traffic accidents, resulting in craniocerebral/nerve injury. With the increase of children’s age, the proportion of craniocerebral/nerve injury gradually decreased, but sport system injuries increased correspondingly. Adolescents have an increased subconscious self-protection reflex in dangerous, and they often use their limbs for emergency protection, which leads to an increased possibility of damage to the sport system. A cohort study has confirmed that the extremities (47.7%) are the most likely to be injured in bicycle-related trauma [ 19 ].
The hospitalization burden of traffic accidents (including LOS and hospitalization expenses) will have a huge impact on the families and society. Therefore, this paper analyzed the factors affecting the hospitalization burden of children of traffic accidents. Among the different lesions of injured person in our study, the hospitalization expense was highest in sports system group, while the LOS was the longest in the visceral-related group. In traffic accidents, children with visceral-related injury often have visceral rupture, so clinical treatment such as indwelling drainage tube is needed. Patients with these injuries generally need to stop eating and drinking for a long time, and the recovery process may be prolonged, ultimately resulting in a longer LOS. Additionally, hospitalization costs include treatment, drugs, materials, tests, care and other costs. For those with sports injuries, surgery often involves the use of expensive medical materials, such as fixation frames and Kirschner wires, which can significantly increase the expenses of hospitalization.
This study used a relatively large-scale, multi-center representative sample from China in recent years, presenting evidence-based epidemiological characteristics and hospitalization burden for pediatric inpatients in transport accidents. Therefore, the prevention of road traffic injuries among children in China remains urgent and requires a multi-pronged approach. Publicity and enforcement of traffic laws should be strengthened, especially in the eastern and northern regions. It is proposed to add helmets for cyclists to traffic regulations, strengthen traffic safety education starting from kindergartens, and strengthen penalties for pedestrians violating traffic safety laws.
Data availability
The original data presented in the study are included in the article material, further inquiries can be directed to the corresponding authors.
Abbreviations
The Futang Research Center of Pediatric Development
World Health Organization
Hospital Quality Monitoring System
Length of hospital stay
Heather E, Rosen I, Bari N, Paichadze M, Peden M, Khayesi. Jesús Monclús, Adnan A Hyder; global road safety 2010-18: an analysis of global Status reports. Injury. 2022. https://doi.org/10.1016/j.injury.2022.07.030 .
Article Google Scholar
Wang X, Yu H, Nie C, Zhou Y, Wang H. Road traffic injuries in China from 2007 to 2016: the epidemiological characteristics, trends and influencing factors. PeerJ. 2019;7:e7423. https://doi.org/10.7717/peerj.7423 .
Article PubMed PubMed Central Google Scholar
Xinyu Wang Y, Zeng J, Tian H, Xu F, Song Y, Guo X, Xu G, Feng. Xin Ni; a brief introduction to the FUTang updating medical REcords (FUTURE) database. Pediatr Invest. 2021;5(3):247–8. https://doi.org/10.1002/ped4.12297 .
Huarong Wang C, Morgan D, Li R, Huang, David C. Schwebel; Children’s fear in traffic and its association with pedestrian decisions. J Saf Res 2021 02;76:56–63 https://doi.org/10.1016/j.jsr.2020.11.010 .
Mikko Nurmi S, Järvelä, Ville M, Mattila TM, Luoto. Satu-Liisa Pauniaho; paediatric traffic accidents-current epidemiological trends at a Finnish university hospital. Injury. 2020;51(10):2179–85. https://doi.org/10.1016/j.injury.2020.07.030 .
Article PubMed Google Scholar
Chang F-R, Huang H-L, Schwebel DC, Alan HS, Chan, Guo-Qing H. Global road traffic injury statistics: challenges, mechanisms and solutions. Chin J Traumatol = Zhonghua Chuang shang za zhi. 2020;23(4):216–8. https://doi.org/10.1016/j.cjtee.2020.06.001 .
Ma S, Li Q, Zhou M, Duan L. David Bishai; Road traffic injury in China: a review of national data sources. Traffic Inj Prev. 2012;13(Suppl 1):57–63. https://doi.org/10.1080/15389588.2011.633945 .
Xiaomei Dong C, Peek-Asa J, Yang S, Wang X, Chen G, Chi M. The association of road safety knowledge and risk behaviour with paediatric road traffic injury in Guangzhou, China. Injury Prevention: J Int Soc Child Adolesc Injury Prev. 2011;17(1):15–20. https://doi.org/10.1136/ip.2010.027540 .
Yuxi Liu M, Wang L, Kang C, He L, Miao L, Chen S, Zhong J, Zhu J, Liang Q, Li Y, Wang. Hanmin Liu; Social and environmental risk factors for road traffic injuries among children under five in rural China. Medicine. 2020;99(17):e19825. https://doi.org/10.1097/MD.0000000000019825 .
Huarong Wang L, Shi, David C. Relations between adolescent sensation seeking and traffic injury: multiple-mediating effects of road safety attitudes, intentions and behaviors. Traffic Inj Prev. 2019;20(8):789–95. https://doi.org/10.1080/15389588.2019.1666982 .
Li-Min Hsu BS, Wiratama P-L, Chen W, Saleh H-A, Lin. Chih-Wei Pai; Pediatric Traffic Injuries on Halloween in the United Kingdom: Prevalence and Injury Severity. Int J Environ Res Public Health 2021 08 28;18(17) https://doi.org/10.3390/ijerph18179093 .
Miao Qi X, Hu X, Li X, Wang X. Analysis of road traffic injuries and casualties in China: a ten-year nationwide longitudinal study. PeerJ. 2022;10:e14046. https://doi.org/10.7717/peerj.14046 .
Huiting Yu C, Nie Y, Zhou X, Wang H, Wang. Xiuquan Shi; characteristic and introspection of Road Traffic injuries in China from 2012 to 2017. Iran J Public Health. 2021;50(7):1381–8. https://doi.org/10.18502/ijph.v50i7.6627 .
Smith AC, Jones SJ. David Hanna; Epidemiology and mapping of child road casualties. Archives Disease Child 2022 06;107(6):540–2 https://doi.org/10.1136/archdischild-2021-323331 .
Li Y, Chen F, Zhang J, Li G, Yang X, Lu Q, Xia X, Zhang X, Qiu J, Zhang J. Jihong Zhou, Yongqin Kuang, Jianwen Gu; epidemiological characteristics of Chinese paediatric traumatic brain injury inpatients. Brain Injury. 2017;31(8):1094–101. https://doi.org/10.1080/02699052.2017.1298004 .
Kristy B, Arbogast S, Wozniak CM, Locey MR, Maltese, Mark R. Head impact contact points for restrained child occupants. Traffic Inj Prev. 2012;13(2):172–81. https://doi.org/10.1080/15389588.2011.642834 .
Li G, Wang F, Otte D. Accid Anal Prev. 2019;129:362–6. https://doi.org/10.1016/j.aap.2019.05.007 . Ciaran Simms; Characteristics of pedestrian head injuries observed from real world collision data.
Yunzhu Meng, Costin D, Untaroiu, A Review of Pediatric Lower Extremity Data for Pedestrian Numerical Modeling. Injury Epidemiology, anatomy, Anthropometry, Structural, and Mechanical properties. Appl Bionics Biomech. 2018;2018:6271898. https://doi.org/10.1155/2018/6271898 .
Zaki Arshad M, Majeed A, Thahir F, Anwar J, Rawal P, Hull. Andrew Carrothers, Daud Tai Shan Chou; Cycling-related trauma admissions to the major trauma centre in the cycling capital of the United Kingdom. Injury. 2022;53(12):3970–7. https://doi.org/10.1016/j.injury.2022.09.016 .
Download references
Acknowledgements
We are grateful to investigators from members of the FRCPD.
The study was supported by Beijing Natural Science Foundation (No. 7244337 and 7244334), and 2022 Scientific Research Project of Chronic Diseases Control and Health Education (No. BJMB0012022028010).
Author information
Jing Yu and Lin Mei contributed equally to this work.
Authors and Affiliations
Department of Burn and Plastic Surgery, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, 56 Nanlishi Rd, Xicheng, Beijing, 100045, China
Jing Yu, Yanni Wang & Jing Liu
Department of Otolaryngology, Head and Surgery, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, China
Big Data Center, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, 56 Nanlishi Rd, Xicheng, Beijing, 100045, China
Guoshuang Feng & Xinyu Wang
Medical Record Management Office, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, China
Yueping Zeng
Information Center, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, China
You can also search for this author in PubMed Google Scholar
Contributions
JL and XW contributed to the conception and design of the study. JY, LM, YW, GF, YZ, XX contributed to acquisition, analysis and interpretation of the data. JY, LM wrote the MS. JL and XW revised the MS. All authors read and approved the final manuscript.
Corresponding authors
Correspondence to Xinyu Wang or Jing Liu .
Ethics declarations
Ethics approval and consent to participate.
Ethical approval to hold and analyse the data set was obtained from the Ethics Committee of Beijing Children’s Hospital, Capital Medical University (Approval Number: 2020-k-10). The requirement for informed consent was waived by the Ethics Committee of Beijing Children’s Hospital, Capital Medical University because of the retrospective nature of the study.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Yu, J., Mei, L., Wang, Y. et al. Hospitalization information and burden of pediatric inpatients in transport accidents. BMC Public Health 24 , 1446 (2024). https://doi.org/10.1186/s12889-024-18891-2
Download citation
Received : 12 December 2023
Accepted : 20 May 2024
Published : 30 May 2024
DOI : https://doi.org/10.1186/s12889-024-18891-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Hospitalization information
- Hospitalization burden
- Traffic accidents
BMC Public Health
ISSN: 1471-2458
- General enquiries: [email protected]
COLUMBIA UNIVERSITY IN THE CITY OF NEW YORK

Technician B
- Columbia University Medical Center
- Opening on: May 25 2024
- Technical Grade 4
- Job Type: Support Staff - Union
- Bargaining Unit: SSA
- Regular/Temporary: Regular
- End Date if Temporary:
- Hours Per Week: 35
- Standard Work Schedule:
- Salary Range: $51,839.00 - $51,839.00
Position Summary
The Nurture Science Program at Columbia University, as it expands nationally and underscores the importance of human connectedness, is currently searching for a Technician B . The Technician B role within the COVID-19 Mother Baby Outcomes (Combo) Initiative/Nurture Science Program (NSP) Study research team is an integral part of our mission to advance scientific understanding in human connectedness including neurodevelopment, growth, maternal cognitive function, socioemotional function, and much more. Working under the supervision of senior researchers, the Technician B will play a hands-on role in conducting experiments, collecting data, and assisting with the coordination of research activities.
At CUIMC, we are leaders in teaching, research, and patient care and are proud of the service and support we provide to our community. We apply the same rigor in our commitment to fostering an inclusive, thriving community and caring for our employees and their loved ones. We offer immediate eligibility and invest in our employee's families through comprehensive Health and Welfare, Employee Assistance, Tuition Programs, and Retirement Benefits.
Responsibilities
- Data Collection and Analysis: Accurately record data and maintain detailed records of procedures and outcomes.
- Assist in the analysis of data under the guidance of senior researchers.
- Will be responsible for assuring compliance with study protocols, including IRB, and HIPPA.
- Assist with management of the lab including ordering, maintaining inventory of laboratory supplies.
- Screen, schedule, and assist with research participants.
- Interpreting and presenting data, and participating in manuscript preparation.
- REDCap management, project setup, and customize project settings and forms based on the requirements of individual research studies.
- Performs related duties & responsibilities as assigned/requested.
Minimum Qualifications
- Bachelor's degree in chemistry, biology or physics or a completed animal husbandry program or equivalent in education, training and experience.
Preferred Qualifications
- Knowledge of various related laboratory procedures and techniques preferred.
- One year of related experience preferred.
Equal Opportunity Employer / Disability / Veteran
Columbia University is committed to the hiring of qualified local residents.
Commitment to Diversity
Columbia university is dedicated to increasing diversity in its workforce, its student body, and its educational programs. achieving continued academic excellence and creating a vibrant university community require nothing less. in fulfilling its mission to advance diversity at the university, columbia seeks to hire, retain, and promote exceptionally talented individuals from diverse backgrounds. , share this job.
Thank you - we'll send an email shortly.
Other Recently Posted Jobs
Communication Manager
Manager, guest services, student admin worker, welcome center.
Refer someone to this job

- ©2022 Columbia University
- Accessibility
- Administrator Log in
Wait! Before you go, are you interested in a career at Columbia University? Sign up here!
Thank you, for sharing your information. A member of our team will reach out to you soon!
This website uses cookies as well as similar tools and technologies to understand visitors' experiences. By continuing to use this website, you consent to Columbia University's usage of cookies and similar technologies, in accordance with the Columbia University Website Cookie Notice .
Efficacy of combined immunosuppression with or without eltrombopag in children with newly diagnosed aplastic anemia
Affiliations.
- 1 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology, and Immunology, Moscow, Russia.
- 2 Pirogov Russian Clinical Children's Hospital, Moscow, Russia.
- 3 St. Petersburg Children's City Hospital No 1, St. Petersburg, Russia.
- 4 Almazov National Medical Research Center, St. Petersburg, Russia.
- 5 Krasnoyarsk Regional Clinical Hospital, Krasnoyarsk, Russia.
- 6 Shustov University Clinical Hospital No 3 of Razumovsky Saratov State Medical University, Saratov, Russia.
- 7 Samara Regional Clinical Children's Hospital, Samara, Russia.
- 8 Perm Regional Clinical Hospital, Perm, Russia.
- 9 Ekaterinburg Regional Clinical Children's Hospital, Ekaterinburg, Russia.
- 10 Voronezh Regional Clinical Children's Hospital No 1, Voronezh, Russia.
- 11 Regional Clinical Children's Hospital, Nizhniy Novgorod, Russia.
- 12 Piotrovich Regional Clinical Children's Hospital, Khabarovsk, Russia.
- PMID: 35446936
- PMCID: PMC10027512
- DOI: 10.1182/bloodadvances.2021006716
We compared the efficacy and safety of eltrombopag (ELTR) combined with immunosuppressive therapy (IST) and IST alone in treatment-naïve children with severe (SAA) and very severe (vSAA) aplastic anemia. Ninety-eight pediatric patients were randomized to receive horse antithymocyte globulin (hATG) and cyclosporin A (CsA) with (n = 49) or without (n = 49) ELTR. The primary endpoint was the overall response rate (ORR) at 4 months. After 4 months, nonresponders were crossed over to the alternative group. In all patients, the ORR in ELTR + IST and IST groups was similar (65% vs 53%; P = .218); however, the complete response (CR) rate was significantly higher in the ELTR + IST group (31% vs 12%; P = .027). In severity subgroups, the ORR was 89% vs 57% (P = .028) in favor of IST + ELTR in SAA, but it did not differ in patients with vSAA (52% vs 50%; P = .902). At 6 months after the crossover, 61% of initial ELTR(-) patients achieved a response compared with 17% of initial ELTR(+) patients (P = .016). No significant difference in ELTR + IST and IST groups was observed in the 3-year overall survival (OS) (89% vs 91%; P = .673) or the 3-year event-free survival (EFS) (53% vs 41%; P = .326). There was no unexpected toxicity related to ELTR. Adding ELTR to standard IST was well tolerated and increased the CR rate. The greatest benefit from ELTR combined with IST was observed in patients with SAA but not in those with vSAA. The second course of IST resulted in a high ORR in initial ELTR(-) patients who added ELTR and had limited efficacy among patients who received ELTR upfront. This trial was registered at Clinicaltrials.gov as #NCT03413306 .
© 2023 by The American Society of Hematology. Licensed under Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0), permitting only noncommercial, nonderivative use with attribution. All other rights reserved.
Publication types
- Randomized Controlled Trial
- Anemia, Aplastic* / diagnosis
- Anemia, Aplastic* / drug therapy
- Immunosuppression Therapy
- Immunosuppressive Agents* / adverse effects
- Treatment Outcome
- Immunosuppressive Agents
- eltrombopag
Associated data
- ClinicalTrials.gov/NCT03413306

IMAGES
VIDEO
COMMENTS
Our Center, Dmitry Rogachev National Research Center of Pediatric Hematology, Oncology and Immunology - is one of the largest institutions in the field of cancer, inborn and acquired blood disorders and immune deficiencies. Physicians of more than 38 subspecialties work in the Center and over 200 of them have the PhD degree.
Affiliations 1 Immunology, Dmitry Rogachev National Medical Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia.; 2 Nephrology, Dmitry Rogachev National Medical Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia.; 3 Nephrology, Y. Veltischev Research and Clinical Institute for Pediatrics at N. Pirogov Russian National Research Medical University, Moscow ...
1 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, 1, Samory Mashela Str., 117997, Moscow, Russia. [email protected]. 2 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, 1, Samory Mashela Str., 117997, Moscow, Russia.
Affiliations 1 Department of Immunology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia.; 2 Department of Pathology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia.; 3 Department of Radiology, Dmitry Rogachev National Medical Research Center of Pediatric ...
Dmitry Rogachev National Research Center provides specialized high-tech medical care for children from Russia and foreign countries in a 24-hour and day hospital, as well as in an outpatient clinic. Patients aged from infants to 18-21 years old are being treated for various forms of oncological diseases.
Pirogov Russian National Research Medical University: Moscow, RU . 2020-09-01 to present ... Kirill R. Butov Dmitry Rogachev National Research Center of Pediatric Hematology, Oncology and Immunology: Moscow, RU . 2017 to present | Researcher (Department of Hematology and Immunology) Employment
Research at the University of Rochester. The University of Rochester houses some of the world's premier basic and clinical biomedical and socioeconomic researchers in interdisciplinary centers and cutting-edge laboratories and clinical research facilities. This arrangement—with everything in close geographic proximity, with programmatic ...
Russian National Research Medical University. / 55.64722°N 37.49028°E / 55.64722; 37.49028. Pirogov Russian National Research Medical University (formerly known as Russian State Medical University or RSMU) is a medical higher education institution in Moscow, Russia founded in 1906. It is fully accredited and recognized by Russia's ...
1 11. Median age at diagnosis in the largest series of GATA2 deficiency in pediatric MDS was 12 years, in fact, all patients were above the age of 3 years at presentation ( 11 ). In this consecutive study of EWOG-MDS patients, 70% of GATA2 deficient cases had monosomy 7. Infants with MDS and monosomy 7 are more likely to have an underlying ...
Affiliations 1 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia.; 2 Hematopoietic Stem Cell Transplantation Department, Morozov Children Hospital, Moscow, Russia.; 3 Hematology and Chemotherapy Department №1, Russian Children's Clinical Hospital, Moscow, Russia.; 4 Pediatric Hematology and Oncology Department, Piotrovich ...
Our research has focused on understanding the molecular mechanisms responsible for human congenital diseases, with an emphasis on craniofacial abnormalities. Our ultimate long-term goal is to acquire the molecular knowledge for understanding craniofacial skeletal defects and to develop strategies for craniofacial skeletal tissue regeneration.
Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Ministry of Health of Russia, 1 Samory Mashela St., 117997 Moscow, Russia Irina Shubina Research Institute of Experimental Diagnostics and Therapy of Tumors of N.N. Blokhin National Medical Research Centre of Oncology, Ministry of Health of Russia ...
• Pediatric Research and Clinical Center for Infectious Diseases under the Federal Medical Biological Agency, St. Petersburg • Federal Research Centre of Nutrition, Biotechnology and Food Safety, Moscow • Dmitry Rogachev National Research Center of the Ministry of Health of the Russian Federation, Moscow
Affiliations 1 Research Department, Belarusian Research Center for Pediatric Oncology, Hematology and Immunology, Minsk Region, Belarus.; 2 Department of Immunology, Children's Memorial Health Institute, Warsaw, Poland.; 3 Department of Immunology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia.
Dmitriy AVERCHENKOV | Cited by 44 | of Pirogov Russian National Research Medical University, Moscow (RNRMU) | Read 4 publications | Contact Dmitriy AVERCHENKOV
The study was supported by the National Institute of Mental Health (R01MH127046, R01MH128814 and R01MH103284), the National Institute of Child Health and Development (P50 HD093079) and the MIND Institute Intellectual and Developmental Disabilities Research Center (P50 HD103526). Read the full paper
Anastasia KHOKHLOVA, Student of Pirogov Russian National Research Medical University, Moscow (RNRMU) | Read 4 publications | Contact Anastasia KHOKHLOVA
8 Department of Hematopoietic Stem Cell Transplantation, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia. PMID: 34697698 PMCID: PMC8821066 DOI: 10.1007/s10875-021-01155-8 Abstract Purpose: WHIM (warts, hypogammaglobulinemia, infections, and myelokathexis) syndrome is a rare ...
The Futang Research Center of Pediatric Development (FRCPD) is a large medical consortium that promotes the development of children's medical research . It covers 47 tertiary children's hospitals, 28 of which have agreed and uploaded the annual summary reports of discharged patients since 2016 in China.
4 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology Oncology and Immunology, Institute of Oncology, Radiology and Nuclear Medicine, Moscow, Russian Federation. PMID: 37058324 DOI: 10.1111/ijlh.14072 Abstract Introduction ...
Job Type: Support Staff - Union Bargaining Unit: SSA Regular/Temporary: Regular End Date if Temporary: Hours Per Week: 35 Standard Work Schedule: Building: Salary Range: $51,839.00 - $51,839.00 The salary of the finalist selected for this role will be set based on a variety of factors, including but not limited to departmental budgets, qualifications, experience, education, licenses, specialty ...
17 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia. 18 Department of Pediatric Hematology and Oncology, Félix Guyon University Hospital, St Denis, Réunion Island, France. PMID: 34174157 DOI: 10.1002/pbc.29112 Abstract ...
Affiliations 1 Department of Immunology, Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia; Translational and Clinical Research Institute, Newcastle University, Newcastle upon Tyne, United Kingdom. Electronic address: [email protected]. 2 Department of Immunology, Dmitry Rogachev National Medical Research Center of ...
13 Serbsky National Medical Research Center on Psychiatry and Addictions, Moscow, Russian Federation. 14 Veltischev Research and Clinical Institute for Pediatrics, the Pirogov Russian National Research Medical University, Moscow, Russian Federation. 15 Privolzhskiy Research Medical University, Nizhny Novgorod, Russian Federation.
5 Clinical Center, Dmitriy Rogachev National Medical Center of Pediatric Hematology, Oncology and Immunology, Moscow, Russia. ... Oncology and Radiation Therapy, Pirogov Russian National Research Medical University, Moscow, Russia. [email protected]. PMID: 33594278 DOI: 10.1038/s41409-021-01232-x Abstract Depletion of αβ T cells from the ...
35 Sean N. Parker Center for Allergy and Asthma Research at Stanford University, Stanford University, Stanford, Calif. 36 Department of Pediatrics, Russian National Research Medical University of MoH RF, Moscow, Russia. 37 Center of Allergic Diseases of Upper Respiratory Ways, National Academy of Medical Sciences of Ukraine, Kyiv, Ukraine.
1 Dmitry Rogachev National Medical Research Center of Pediatric Hematology, Oncology, and Immunology, Moscow, Russia. 2 Pirogov Russian Clinical Children's Hospital, Moscow, Russia. 3 St. Petersburg Children's City Hospital No 1, St. Petersburg, Russia. 4 Almazov National Medical Research Center, St. Petersburg, Russia.