An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Eat Disord
- PMC10228434


Eating disorder outcomes: findings from a rapid review of over a decade of research
Jane miskovic-wheatley.
1 Faculty of Medicine and Health, InsideOut Institute for Eating Disorders, University of Sydney, Level 2, Charles Perkins Centre (D17), Sydney, NSW 2006 Australia
2 Sydney Local Health District, Sydney, Australia
Emma Bryant
Shu hwa ong, sabina vatter.
3 Healthcare Management Advisors, Melbourne, Australia
Stephen Touyz
Sarah maguire, associated data.
Not applicable—all citations provided.
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions that may reduce the detrimental impact of illness and to optimise recovery. This paper aims to synthesise the literature on outcomes for people with ED, including rates of remission, recovery and relapse, diagnostic crossover, and mortality.
This paper forms part of a Rapid Review series scoping the evidence for the field of ED, conducted to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031, funded and released by the Australian Government. ScienceDirect, PubMed and Ovid/MEDLINE were searched for studies published between 2009 and 2022 in English. High-level evidence such as meta-analyses, large population studies and Randomised Controlled Trials were prioritised through purposive sampling. Data from selected studies relating to outcomes for people with ED were synthesised and are disseminated in the current review.
Of the over 1320 studies included in the Rapid Review, the proportion of articles focused on outcomes in ED was relatively small, under 9%. Most evidence was focused on the diagnostic categories of AN, Bulimia Nervosa and Binge Eating Disorder, with limited outcome studies in other ED diagnostic groups. Factors such as age at presentation, gender, quality of life, the presence of co-occurring psychiatric and/or medical conditions, engagement in treatment and access to relapse prevention programs were associated with outcomes across diagnoses, including mortality rates.
Results are difficult to interpret due to inconsistent study definitions of remission, recovery and relapse, lack of longer-term follow-up and the potential for diagnostic crossover. Overall, there is evidence of low rates of remission and high risk of mortality, despite evidence-based treatments, especially for AN. It is strongly recommended that research in long-term outcomes, and the factors that influence better outcomes, using more consistent variables and methodologies, is prioritised for people with ED.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40337-023-00801-3.
Plain language summary
Eating disorders are complex psychiatric conditions that can seriously impact a person’s physical health. Whilst they are consistently associated with high mortality rates and significant psychosocial difficulties, lack of agreement on definitions of recovery, remission and relapse, as well as variations in methodology used to assess for standardised mortality and disability burden, means clear outcomes can be difficult to report. The current review is part of a larger Rapid Review series conducted to inform the development of Australia’s National Eating Disorders Research and Translation Strategy 2021–2031. A Rapid Review is designed to comprehensively summarise a body of literature in a short timeframe to guide policymaking and address urgent health concerns. This Rapid Review synthesises the current evidence-base for outcomes for people with eating disorders and identifies gaps in research and treatment to guide decision making and future clinical research. A critical overview of the scientific literature relating to outcomes in Western healthcare systems that may inform health policy and research in an Australian context is provided in this paper. This includes remission, recovery and relapse rates, diagnostic cross-over, the impact of relapse prevention programs, factors associated with outcomes, and findings related to mortality.
Introduction
Eating disorders (ED), especially Anorexia Nervosa (AN), have amongst the highest mortality and suicide rates in mental health. While there has been significant research into causal and maintaining factors, early identification efforts and evidence-based treatment approaches, global incidence rates have increased from 3.4% calculated between 2000 and 2006 to 7.8% between 2013 and 2018 [ 1 ]. While historically seen as a female illness, poorer outcomes are increasingly seen in other genders, including males [ 2 ].
Over 3.3 million healthy life years are lost worldwide due to ED each year, and many more lost to disability due to medical and psychiatric complications [ 3 ]. Suicide accounts for approximately 20% of non-natural deaths among people with ED [ 4 ]. As this loss of healthy life is preventable, there is a grave responsibility to better understand outcomes for people with ED, including factors which may minimise the detrimental impact they have on individuals, carers, and communities, as well as to optimise recovery.
There has been considerable debate within the clinical, scientific and lived experience (i.e., patient, consumer, carer) communities about the definition and measurement of key outcomes in ED, including ‘remission’ from illness (a period of relief from symptoms), ‘relapse’ (a resumption of symptoms) and ‘recovery’ (cessation of illness) [ 5 , 6 ], which can compromise outcome comparisons. Disparities include outcome variables relating to eating behaviours as well as medical, psychological, social and quality of life factors. There is increasing awareness in the literature of the elevated likelihood of diagnostic crossover [ 7 ]; research examining specific diagnostic profiles potentially misses outcomes where symptom experience transforms rather than alleviates. Methodological approaches in outcomes research are varied, the most significant being length of time to follow up, compromising direct study comparisons.
The aim of this Rapid Review (RR) is to synthesise the literature on outcomes for people with ED, including rates of remission, recovery and relapse, diagnostic crossover, and mortality. Factors influencing outcomes were summarised including demographic, illness, treatment, co-morbidities, co-occurring health conditions, societal factors, and impact of relapse prevention programs. This RR forms one of a series of reviews scoping the field of ED commissioned to inform the Australian National Eating Disorders Research and Translation Strategy 2021–2031 [ 8 ]. The objective is to evaluate the current literature in ED outcomes to identify areas of consensus, knowledge gaps and suggestions for future research.
The Australian Government Commonwealth Department of Health funded the InsideOut Institute for Eating Disorders (IOI) to develop the Australian Eating Disorders Research and Translation Strategy 2021–2031 [ 8 ] under the Psych Services for Hard to Reach Groups initiative (ID 4-8MSSLE). The strategy was developed in partnership with state and national stakeholders including clinicians, service providers, researchers, and experts by lived experience (including consumers and families/carers). Developed through a 2 year national consultation and collaboration process, the strategy provides the roadmap to establishing ED as a national research priority and is the first disorder-specific strategy to be developed in consultation with the National Mental Health Commission. To inform the strategy, IOI commissioned Healthcare Management Advisors (HMA) to conduct a series of RRs to broadly assess all available peer-reviewed literature on the six DSM-V [ 9 ] listed ED. RR’s were conducted in the following domains: (1) population, prevalence, disease burden, Quality of Life in Western developed countries; (2) risk factors; (3) co-occurring conditions and medical complications; (4) screening and diagnosis; (5) prevention and early intervention; (6) psychotherapies and relapse prevention; (7) models of care; (8) pharmacotherapies, alternative and adjunctive therapies; and (9) outcomes (including mortality) (current RR), with every identified paper allocated to only one of the above domains from abstract analysis by two investigators. Each RR was submitted for independent peer review to the Journal of Eating Disorders special edition, “Improving the future by understanding the present: evidence reviews for the field of eating disorders”.
A RR Protocol [ 10 ] was utilised to swiftly synthesise evidence to guide public policy and decision-making [ 11 ]. This approach has been adopted by several leading health organisations, including the World Health Organization [ 12 ] and the Canadian Agency for Drugs and Technologies in Health Rapid Response Service [ 13 ], to build a strong evidence base in a timely and accelerated manner, without compromising quality. RR was chosen as the most suitable design as it is conducted with broader search terms and inclusion criteria allowing to gain a better understanding of a specific field, returning a larger number of search results and providing a snapshot of key findings detailing the current state of a field at study [ 10 ]. A RR is not designed to be as comprehensive as a systematic review—it is purposive rather than exhaustive and provides actionable evidence to guide health policy [ 14 ].
The RR is a narrative synthesis adhering to the PRISMA guidelines [ 15 ]. It is divided by topic area and presented as a series of papers. Three research databases were searched: ScienceDirect, PubMed and Ovid/MEDLINE. To establish a broad understanding of the progress made in the field of eating disorders, and to capture the largest evidence base on the past 13 years (originally 2009–2019, but expanded to include the preceding two years), the eligibility criteria for included studies into the RR were kept broad. Therefore, included studies were published between 2009 and 2022, in English, and conducted within Western healthcare systems or health systems comparable to Australia in terms of structure and resourcing. The initial search and review process was conducted by three reviewers between 5 December 2019 and 16 January 2020. The re-run for the years 2020–2021 was conducted by two reviewers at the end of May 2021 and a final run for 2022 conducted in January 2023 to ensure the most up to date publications were included prior to publication.
The RR had a translational research focus with the objective of identifying evidence relevant to developing optimal care pathways. Searches, therefore, used a Population, Intervention, Comparison, Outcome (PICO) approach to identify literature relating to population impact, prevention and early intervention, treatment, and long-term outcomes. Purposive sampling focused on high-level evidence studies such as: meta-analyses; systematic reviews; moderately sized randomised controlled trials (RCTs) ( n > 50); moderately sized controlled-cohort studies ( n > 50), or population studies ( n > 500). However, the diagnoses Avoidant Restrictive Food Intake Disorder (ARFID), Eating Disorder Not Otherwise Specified (EDNOS), Other Specified Feeding or Eating Disorder (OSFED) and Unspecified Feeding or Eating Disorder (UFED) necessitated a less stringent eligibility criterion due to a paucity of published articles. As these diagnoses are newly captured in the DSM-V [ 9 ] (released in 2013, within the allocated search timeframe), the evidence base is emerging, and fewer studies have been conducted. Thus, smaller studies ( n ≤ 20) and narrative reviews were also considered and included. Grey literature, such as clinical or practice guidelines, protocol papers (without results) and Masters’ theses or dissertations, was excluded.
Full methodological details including eligibility criteria, search strategy and terms and data analysis are published in a separate protocol paper [ 10 ]. The full RR included a total of over 1320 studies (see Additional file 1 : Fig. S1). Data from included studies relating to outcomes for eating disorders were synthesised and are presented in the current review.
Of the 1320 articles included in the RR, the proportion of articles focused on outcomes in ED was relatively small, just less than 9% ( n = 116) (see Additional file 2 : Table S1). Studies typically examined outcomes in AN, Bulimia Nervosa (BN) and Binge Eating Disorder (BED), with limited research in other diagnostic groups. Whereas most outcome studies reported recovery, remission and relapse rates, others explored factors impacting outcomes, such as quality of life, co-occurring conditions, and outcomes from relapse prevention programs.
ED, particularly AN, have long been associated with an increased risk of mortality. The current review summarises best available evidence exploring this association. Several factors complicate these findings including a lack of consensus on definitions of remission, recovery and relapse, widely varying treatment protocols and research methodologies, and limited transdiagnostic outcome studies or syntheses such as meta-analyses. Table Table1 1 provides a summary of outcomes reported by studies identified in this review. There is considerable heterogeneity in the reported measures.
Summary of patient outcomes including predictors and mediators by eating disorder diagnosis
NB—Figures reported in the table for BN and BED are results from systematic review, which differentiated between treatment completer and intent to treat analysis [ 22 ]
*Any ED covers Feeding and/or Eating Disorders Not Otherwise Specified, OSFED
Overall outcomes
A good outcome for a person experiencing ED symptomatology is commonly defined as either remission or no longer meeting diagnostic criteria, as well as improved levels of psychosocial functioning and quality of life [ 28 , 29 ]. However, such a comprehensive approach is rarely considered, and there is no consensus on a definition for recovery, remission, or relapse for any of the ED diagnoses [ 30 , 31 ]. To contextualise this variation, definitions and determinants for these terms are presented in Table Table2 2 .
Sample of definitions of relapse, remission, and recovery in eating disorder research
NB—Ordered by diagnostic group then follow-up period. Where authors referred to definitions from a previous study, references included
a EDE Eating disorder examination
b %EBW Percent expected body weight for age, gender, and height
c EAT Eating Attitudes Test (EAT-26)
d EDE-Q Eating Disorder Examination—Questionnaire
e PSR Psychiatric Status Rating
The terms ‘remission’ and ‘recovery’ appear to be used interchangeably in the literature. Whilst ‘remission’ is usually defined by an absence of diagnostic symptomatology, and ‘recovery’ an improvement in overall functioning, the period in which an individual must be symptom-free to be considered ‘remitted’ or ‘recovered’ varies greatly between studies, follow-up (FU) time periods are inconsistent, and very few studies examine return to psychosocial function and quality of life (QoL) after alleviation of symptoms. The current review uses the terms adopted by the original studies. ‘Relapse’ is typically defined by a return of symptoms after a period of symptom relief. The reviewed studies report a variety of symptom determinants including scores on standardised psychological and behavioural interviews or questionnaires, weight criteria [including Body Mass Index (BMI) or %Expected Body Weight (%EBW)], clinical assessment by a multidisciplinary team, self-reported ED behaviours, meeting diagnostic criteria, or a combination of the above.
Remission, recovery, and relapse
In a global overview of all studies reviewed, remission or recovery rates were reported for around half of the cohort, regardless of diagnostic group. For example, a 30 month FU study of a transdiagnostic cohort of patients found 42% obtained full and 72% partial remission, with no difference between diagnostic groups for younger people; however, bulimic symptoms emerged frequently during FU, regardless of initial diagnosis [ 44 ]. A 6 year study following the course of a large clinical sample ( n = 793) reported overall recovery rates of 52% for AN, 50–52% for BN, 57% for EDNOS-Anorectic type (EDNOS-A), 60–64% for BED and 64–80% for EDNOS-Bulimic type (EDNOS-B) [ 7 ]. Of those who recorded full remission at end of treatment (EOT), relapse was highest for AN (26%), followed by BN (18%), and EDNOS-B (16%). Relapse was less common for individuals with BED (11–12%), and EDNOS-A (4%). Change in diagnosis (e.g., from AN to BN) was also seen within the relapse group [ 7 ].
Longer-term FU studies may more accurately reflect the high rates of relapse and diagnostic crossover associated with ED. A 17 year outcome study of ED in adult patients found only 29% remained fully recovered, with 21% partially recovered and half (50%) remaining ill [ 52 ], noting the protracted nature of illness for adults with longstanding ED. Relapse is observed at high rates (over 30%) among people with AN and BN at 22 year FU [ 61 ]. In a large clinical study using predictive statistical modelling, full remission was more likely for people with BED (47.4%) and AN (43.9%) compared to BN (25.2%) and OSFED (23.2%) [ 41 ]. This result is distinct from other studies citing AN to have the worst clinical outcomes within the diagnostic profiles [ 52 ]. The cut‐off points for the duration of illness associated with decreased likelihood of remission were 6–8 years for OSFED, 12–14 years for AN/BN and 20–21 years for BED [ 41 ]. As with recovery rates, reported rates of relapse are highly variable due to differing definitions and study methodologies used by researchers in FU studies [ 35 , 61 ].
Evidence from a meta-analysis of 16 studies found four factor clusters that significantly contributed to relapse; however, also noted a substantial variability in procedures and measures compromising study comparison [ 62 ]. Factors contributing to heightened risk of relapse included severity of ED symptoms at pre- and post-treatment, presence and persistence of co-occurring conditions, higher age at onset and presentation to assessment, and longer duration of illness. Process treatment variables contributing to higher risk included longer duration of treatment, previous engagement in psychiatric and medical treatment (including specialist ED treatment) and having received inpatient treatment. These variables may indicate more significant illness factors necessitating a higher intensity of treatment.
Importantly, full recovery is possible, with research showing fully recovered people may be indistinguishable from healthy controls (HCs) on all physical, behavioural, and psychological domains (as evaluated by a battery of standardised assessment measures), except for anxiety (those who have fully recovered may have higher general anxiety levels than HCs) [ 29 ].
Diagnostic crossover
Most studies reported outcomes associated with specific ED diagnoses; however, given a significant proportion of individuals will move between ED diagnoses over time, it can be challenging to determine diagnosis-specific outcomes. Results from a 6 year FU study indicated that overall individuals with ED crossed over to other ED diagnoses during the FU observational period, most commonly AN to BN (23–27%), then BN to BED (8–11%), BN to AN (8–9%) and BED to BN (7–8%) [ 7 ]. Even higher crossover trends were observed in the subgroup reporting relapse during the FU period, with 61.5% of individuals originally diagnosed with AN developing BN, 27.2% and 18.1% of individuals originally diagnosed with BN developing AN and BED respectively, and 18.7% of people with a previous diagnosis of BED developing BN [ 7 ].
A review of 79 studies also showed a significant number of individuals with BN (22.5%) crossed over to other diagnostic groups (mostly OSFED) at FU [ 63 ]. A large prospective study of female adolescents and young adults in the United States ( n = 9031) indicated that 12.9% of patients with BN later developed purging disorder and between 20 and 40% of individuals with subthreshold disorders progressed to full threshold disorders [ 64 ]. Progression from subthreshold to threshold eating disorders was higher for BN and BED (32% and 28%) than for AN (0%), with researchers suggesting higher risk for binge eating [ 66 ]. Progression from subthreshold to full threshold BN and BED was also common in adolescent females over the course of an 8 year observational study [ 33 ]. Some researchers contend that such diagnostic ‘instability’ demonstrates a need for ‘dimensional’ approaches to research and treatment which have greater focus on the severity rather than type of symptoms [ 7 ]. Diagnostic crossover is common and should be considered in the long-term management and monitoring of people with an ED.
Anorexia nervosa (AN)
People with restrictive-type ED have the poorest prognosis compared to the other diagnostic groups, particularly individuals displaying severe AN symptomatology (including lower weights and higher body image concerns) [ 44 ]. There is a paucity of effective pharmacological and/or psychological treatments for AN [ 65 ]. Reported rates of recovery vary and include 18% [ 56 ] to 52% at 6 year FU [ 7 ] to 60.3% at 13 year FU [ 20 ] and 62.8% at 22 year-FU [ 61 ]. Reported relapse rates in AN also vary, for example, 41.0% at 1 year post inpatient/day program treatment [ 35 ] to 30% at 22 year FU [ 61 ]. Average length of illness across the reviewed studies also varies from 6.5 years [ 56 ] to 14 years [ 41 ].
A variety of reported outcomes from treatment studies is likely due to the breadth of treatments under investigation, diverse study protocols and cohorts. For example, in a mixed cohort of female adult patients with AN and Atypical AN (A-AN), 33% were found to have made a full recovery at 3 year FU after treatment with cognitive behavioural therapy (CBT) [ 57 ], while 6.4% had a bad outcome and 6.4% a severe outcome. However, in a 5–10 year FU study of paediatric inpatients (mean age 12.5 years) approximately 41% had a good outcome, while 35% had intermediate and 24% poor outcome [ 66 ]. Multimodal treatment approaches including psychiatric, nutritional, and psychological rehabilitation have been found to be most efficacious for moderate to severe and enduring AN but noting a discrete rate of improvement [ 67 ].
Very few factors were able to predict outcomes in AN. Higher baseline BMI was consistently found to be the strongest predictor of recovery, and better outcomes were associated with shorter duration of illness [ 7 , 55 , 61 , 66 ]. Earlier age of illness onset [ 59 , 68 , 69 ] and older age at presentation to treatment [ 30 ] were related to chronicity of illness and associated with poorer outcome.
There was a consensus across a variety of studies that engagement in binge/purge behaviours (Anorexia Nervosa Binge/Purge subtype; AN-BP) was associated with a poorer prognosis [ 20 , 56 , 70 ]. Similarly, individuals with severe and enduring AN restrictive sub-type (AN-R) are likely to have a better outcome than individuals with AN-BP. AN-BP was associated with a two-fold greater risk of relapse compared to AN-R [ 30 , 35 ]. Some studies, however, were unable to find an association between AN subtype and outcome [ 55 ]. Other factors leading to poorer outcome and higher probability of relapse were combined ED presentations, such as combined AN/BN [ 35 ], higher shape concern [ 57 ], lower desired weight/BMI [ 44 ], more ED psychopathology at EOT, low or decreasing motivation to recover, and comorbid depression [ 35 , 61 ].
Preliminary genetic work has found associations between a single nucleotide polymorphism (SNP) in a ghrelin production gene (TT genotype at 3056 T-C) and recovery from AN-R [ 71 ], and the S-allele of the 5-HTTLPR genotype increasing the risk susceptibility for both depressive comorbidity and diagnostic crossover at FU of AN patients [ 72 ]. These studies, however, need to be interpreted with caution as they were conducted over a decade ago and have not since been replicated. Research in eating disorder genetics is a rapidly emerging area with potential clinical implications for assessment and treatment.
Bulimia nervosa (BN)
Overall, studies pertaining to a diagnostic profile of BN report remission recovery rates of around 40–60%, depending on criteria and FU period, as detailed below. Less than 40% of people achieved full symptom abstinence [ 73 ] and relapse occurred in around 30% of individuals [ 61 ]. A meta-analysis of 79 case series studies reported rates of recovery for BN at 45.0% for full recovery and 27.0% for partial remission, with 23.0% experiencing a chronic course and high rates of treatment dropout [ 63 ]. At 11 year FU, 38.0% reported remission in BN patients, increasing to 42.0% at 21 year [ 45 ]. At 22 year FU, 68.2% with BN were reported to have recovered [ 41 ]. Higher frequency of both objective binge episodes and self-induced vomiting factors influencing poorer outcomes [ 44 ].
Considering impact of treatment, analysis of engagement in self-induced vomiting as a predictor for outcome indicated there were no differences between groups in treatment dropout or response to CBT among a sample of 152 patients with various types of EDs (AN-BP, BN, EDNOS) at EOT [ 74 ]. Meta-analysis of results from 45 RCTs on psychotherapies for BN found 35.4% of treatment completers achieved symptom abstinence [ 73 ] with other studies indicating similar rates of recovery (around 52–59% depending on DSM criteria) [ 7 ].
Studies delivering CBT or other behavioural therapies reported the best outcomes for BN [ 73 ]. Specifically, early treatment progression, elimination of dietary restraint and normalisation of eating behaviour resulted in more positive outcomes [ 22 ]. These findings are supported by results from a study comparing outcomes of CBT and integrative cognitive-affective therapy (ICAT) [ 75 ]. Additional moderating effects were shown at FU (but not EOT), with greater improvements for those with less baseline depression, higher stimulus seeking (the need for excitement and stimulation) and affective lability (the experience of overly intense and unstable emotions) in the ICAT-BN group and lower stimulus seeking in the Enhanced Cognitive Behavioural Therapy (CBT-E) group. Lower affective lability showed improvements in both treatment groups [ 75 ]. Such findings indicate personality factors may deem one treatment approach more suitable to an individual than another.
A review of 4 RCTs of psychotherapy treatments for BN in adolescents (including FBT and CBT) reported overall psychological symptom improvement by EOT predicting better outcomes at 12 months, which underscored the need for not only behavioural but psychological improvement during 6 month treatment [ 31 ]. Other factors leading to poorer outcomes included less engagement in treatment, higher drive for thinness, less global functioning, and older age at presentation [ 45 ]. More research is needed into consistent predictors, mediators and moderators focused on treatment engagement and outcomes [ 22 ].
While many studies combine findings for BN and BED, one study specifically considered different emotions associated with binge eating within the two diagnostic profiles [ 60 ]. At baseline, binge eating was associated with anger/frustration for BN and depression for BED. At FU, objective binge eating (OBE) reduction in frequency (a measure of recovery) was associated with lower impulsivity and shape concern for BN but lower emotional eating and depressive symptoms for BED. These differences may provide approaches for effective intervention targets for differing presentations; however, how these may play out within a transdiagnostic approach requires further enquiry.
Binge eating disorder (BED)
BED is estimated to affect 1.5% of women and 0.3% of men worldwide, with higher prevalence (but more transient) in adolescents. Most adults report longstanding symptoms, 94% lifetime mental health conditions and 23% had attempted suicide, yet only half were in recognised healthcare or treatment [ 76 ].
Compared with AN and BN, long-term outcomes, and treatment success for individuals with BED were more favourable. Meta-analysis of BED abstinence rates suggests available psychotherapy and behavioural interventions are more effective for this population [ 77 ]. Additionally, stimulant medication (i.e., Vyvanse) has been found to be particularly effective to reduce binge eating [see [ 78 ] for full review]. Results from a study of people who received 12 months of CBT for BED indicated high rates of treatment response and favourable outcomes, maintained to 4 year FU. Significant improvements were observed with binge abstinence increasing from 30.0% at post-treatment to 67.0% at FU [ 79 ]. A meta-analysis reviewing psychological or behavioural treatments found Interpersonal Therapy (IPT) to be the treatment producing the greatest abstinence rates [ 73 ]. In a comparative study of IPT and CBT, people receiving CBT experienced increased ED symptoms between treatment and 4 year FU, while those who received IPT improved during the same period. Rates of remission at 4 year FU were also higher for IPT (76.7%) versus CBT (52.0%) [ 80 ].
One study specifically explored clinical differences between ED subtypes with and without lifetime obesity over 10 years. Prevalence of lifetime obesity in ED was 28.8% (ranging from 5% in AN to 87% in BED), with a threefold increase in lifetime obesity observed over the previous decade. Observed with temporal changes, people with ED and obesity had higher levels of childhood and family obesity, older-age onset, longer ED duration, higher levels of ED (particularly BED and BN) and poorer general psychopathology than those who were not in the obese weight range [ 81 ], suggesting greater clinical severity and poorer outcomes for people of higher weight.
Comparison of 6 year treatment outcomes between CBT and Behavioural Weight Loss Treatment (BWLT) found CBT more effective at post-treatment but fading effectiveness over time, with remission rates for both interventions lower than other reported studies (37%) [ 82 ]. A meta-analytic evaluation of 114 published and unpublished psychological and medical treatments found psychological treatments, structured self-help, and a combination of the two were all effective at EOT and 12 month FU but noted a wide variation in study design and quality, and the need for longer term FU. Efficacy and FU data for pharmacological and surgical weight loss treatments were lacking [ 77 ].
Whilst high weight and associated interventions (such as bariatric surgery) can be associated with any ED, they are frequently studied in relation to BED. A significant proportion of individuals seeking bariatric surgery (up to 42%) displayed binge eating symptomatology [ 83 ], yet little is known about the effect of these interventions on ED psychopathology and whether this differs by type of intervention. A systematic review of 23 studies of changes in ED behaviour following three different bariatric procedures found no specific procedure led to long term changes in ED profiles or behaviours [ 84 ]; however, another study investigating the placement of an intragastric balloon in obese patients found post-surgical reductions in grazing behaviours, emotional eating and EDNOS scores [ 85 ]. Bariatric surgery in general is associated with a reduction in ED, binge eating and depressive symptoms [ 86 ].
Outcomes among patients receiving bariatric surgery with and without BED were assessed where weight loss was comparable between the groups at 1 year FU. However, compared with participants receiving a BWLT-based lifestyle modification intervention instead of surgery, bariatric surgery patients lost significantly less weight at a 10.3% difference between groups. There was no significant difference between lifestyle modification and surgery groups in BED remission rates [ 87 ]. These results indicate that BLWT-type interventions are more effective than surgery at promoting weight loss in individuals with BED over a 1 year FU period, and people with BED and higher BMI were able to maintain weight loss in response to psychotherapy (CBT) at up to 5 year FU [ 88 ]. In analysis of health-related quality of life (HRQoL) in people with BED who received various levels of CBT (therapist-led, therapist-assisted and self-help), evaluation indicated that all modalities resulted in improvements to HRQoL. Poorer outcomes were associated with obesity and ED symptom severity at presentation, stressing the importance of early detection and intervention measures [ 89 ]. Research into the role of CBT in strengthening the effect of bariatric surgery for obesity is ongoing but promising [ 90 ].
EDNOS, OSFED and UFED
Similarly to BED, a diagnosis of DSM-IV EDNOS (now OSFED) was associated with a more favourable outcome than AN or BN, including shorter time to remission. One study reported remission rates for both EDNOS and BED at 4 year FU of approximately 80% [ 21 ]. The researchers suggested that an ‘otherwise specified’ diagnostic group might be comprised of individuals transitioning into or out of an ED rather than between diagnostic categories; however, more work is needed in this area to fully understand this diagnostic profile. The reported recovery rate from EDNOS-A has been found to be much lower at 57% than for EDNOS-B at 80% (DSM-V). One factor suggested leading to poorer outcomes for EDNOS-A was a higher association with a co-occurring condition of major depression and/or dysthymia not found in other EDNOS subtypes [ 7 ]. Another study found purging occurred in 6.7% from total (cross-diagnostic) ED referrals, but this subtype did not have different post-treatment remission rates or completion rates compared to non-purging profiles [ 91 ], so results are mixed.
Acknowledging the scarcity of research within these diagnostic groups, remission rates for adolescents including those with a diagnosis of Other Specified Feeding or Eating Disorder (OSFED) and Unspecified Feeding or Eating Disorder (UFED) was reported to be 23% at 12 month FU in the one study reviewed, but no detail was provided on recovery rates by diagnosis [ 26 ]. No available evidence was identified specifically for the DSM-V disorders OSFED or UFED for adults.
Avoidant/Restrictive Food Intake Disorder (ARFID)
Research into outcomes for people with ARFID is lacking, with only three studies meeting criteria for the review [ 23 – 25 ]. While, like AN, recovery for people with ARFID is usually measured by weight gain targets, one of the three studies [ 63 ] identified by this review instead reported on outcomes in terms of meeting a psychiatric diagnosis, making comparison between the studies difficult.
In a cross-diagnostic inpatient study, individuals presenting with ARFID were younger, had fewer reported ED behaviours and co-occurring conditions, less weight loss and were less likely to be bradycardic than individuals presenting with AN [ 25 ]. Although both groups received similar caloric intakes, ARFID patients relied on more enteral nutrition and required longer hospitalisations but had higher rates of remission and fewer readmissions than AN patients at 12 months. This study highlights the need for further investigation into inpatient treatment optimisation for different diagnostic profiles.
People with ARFID who had achieved remission post-treatment were able to maintain remission until 2.5 year FU, with most continuing to use outpatient treatment services [ 23 ]. In a 1 year FU study assessing ARFID, 62.0% of patients had achieved remission as defined by weight recovery and no longer meeting DSM-V criteria [ 25 ]. In a study following children treated for ARFID to a mean FU of 16 years post-treatment (age at FU 16.5–29.9 years), 26.3% continued to meet diagnostic criteria for ARFID with no diagnostic crossover, suggesting symptom stability [ 24 ]. Rates of recovery for ARFID patients in this study were not significantly different to the comparison group who had childhood onset AN, indicating similar prognoses for these disorders. No predictors of outcome for patients with ARFID were identified by the articles reviewed [ 63 ].
Community outcomes
While most outcome studies derive from health care settings, two studies were identified exploring outcomes of ED within the community. The first reported the 8 year prevalence, incidence, impairment, duration, and trajectory of ED via annual diagnostic interview of 496 adolescent females. Controlling for age, lifetime prevalence was 7.0% for BN/subthreshold BN, 6.6% for BED/subthreshold BED, 3.4% for purging disorder, 3.6% for AN/atypical AN, and 11.5% for feeding and eating disorders not otherwise classified. Peak onset age across the ED diagnostic profiles was 16–20 years with an average episode duration ranging from 3 months for BN to a year for AN; researchers noted that these episodes were shorter than the average duration estimates reported in similar research and may be representative of the transient nature of illness rather than longer term prognosis. ED were associated with greater functional impairment, distress, suicidality, and increased use of mental health treatment [ 27 ].
A second study followed 70 young people (mean age of 14 years at study commencement) meeting DSM-IV criteria for a binge eating or purging ED and found 44% no longer met criteria at ages 17 or 20, while 25% still met criteria at age 20 (the latter individuals were more likely to have externalising behaviour problems and purging behaviour at age 17). Those who experienced a persistent ED were less likely to complete secondary education and report higher depressive and anxiety symptoms at age 20, indicating the ongoing impacts of ED on education and quality of life [ 92 ]. These studies provide information about the course and outcome of early onset ED at the population level with indicators of predictive and maintaining factors.
Factors relating to outcomes
Several factors relating to outcomes have been studied across ED presentations and in specific diagnostic profiles. These include predictors of outcome, moderators or mediators of outcome, and illness reinforcers, considering age of presentation and duration of illness, ED symptomatology, presence of co-occurring medical and psychiatric conditions, and treatment characteristics.
Age of presentation
Age of presentation to treatment has been shown to have a significant impact on outcome in all diagnoses. One study considering ED in general (including AN, BN and EDNOS) showed presentation at mid-life drastically decreased chances of achieving a good outcome in response to treatment (“good” outcome defined as BMI ≥ 18.5, 3 month remission of symptoms and Eating Disorder Examination Questionnaire (EDE-Q) scores within or better than normal range). Six percent of mid-life (≥ 40 years) presentations achieved a good outcome post-treatment compared to 14% of young adults (18–39 years) and 28% of younger people (< 18 years) [ 28 ]. This finding has also been seen in research comparing 22 year outcomes of AN and BN [ 61 ].
People presenting in mid-life often have more complex medical and psychiatric profiles as well as life circumstances. They are also far more likely to have a sustained length of illness by the time of initial presentation: 27.8 years compared with 1.2 years for youths [ 28 ]. Longer duration of illness is associated with greater increase in self-reported clinical impairment [ 93 ]; however, illness duration does not necessarily influence treatment outcome, though wide variation in study protocol and quality limit the interpretability of these findings [ 37 , 94 ]. The disparity in rates of favourable outcome between age groups highlights the importance of prevention, screening, awareness of ED in primary care settings and early intervention programs, as well as targeted programs for those presenting with more complex psychosocial and life challenges.
Clinical features and co-occurring conditions
A systematic review assessed the average duration of untreated illness duration in help-seeking populations at first contact to treatment services at 29.9 months for AN, 53.0 months for BN and 67.4 months for BED [ 69 ]. ED clinical factors significantly influence outcomes, with poorer prognosis in those with time of untreated illness, primary diagnosis of AN [ 95 ], lower BMI at presentation [ 93 ], and presence of binge/purge symptomatology [ 20 , 56 ]. Certain ED behaviours and cognitions at intake predict better outcome such as lower rates of purging behaviour, higher rates of body image flexibility [ 96 ], and lower EDE-Q scores at baseline [ 97 ].
There is strong evidence for the presence of co-occurring medical and psychiatric conditions as a predictor of outcome in ED. At 22 year FU, the presence of co-occurring psychiatric conditions including Major Depressive Disorder (MDD) and Substance Use Disorder (SUD) were negatively correlated with recovery, with those who had recovered from an ED being 2.17 times less likely to have MDD and 5.33 times less likely to have SUD [ 98 ]. Co-occurring mood disorders consistently lead to poorer outcomes [ 47 , 51 , 55 , 99 ] and greater chance of moving between ED diagnoses [ 7 ]. In one study, presence of a mood disorder was the strongest predictor of classification of AN-R (but not AN-BP) [ 61 ]. Comorbid personality disorder was found in several studies to be the most common predictor of poorer outcome in ED [ 20 , 41 , 44 , 67 ].
In an adolescent sample, 39% of individuals with AN met criteria for at least one other psychiatric disorder and poorer prognosis was associated with co-occurring diagnoses of Obsessive Compulsive Disorder (OCD) and autistic traits [ 59 ]. In a large community childhood health longitudinal study, presence of any ED profile was predictive of later anxiety and mood disorders. AN was prospectively associated with long term low weight, while BN and BED with obesity, drug use and deliberate self-harm compared to age-matched children who did not have an ED profile [ 100 ].
Personality traits have also been found to be associated with poorer outcomes such as low persistence and harm avoidance in AN, lower self-directedness (BN) and reward dependence (BED) [ 41 ]. Higher perfectionism at intake predicted a lower likelihood of remission at 12 months in an adolescent sample [ 26 ], a finding consistent with previous research in adult cohorts [ 41 ].
Medical comorbidities such as malnutrition [ 72 ], concurrent type 1 diabetes [ 39 , 42 ], bodily pain [ 55 ] and viral infections [ 72 ] have been identified as risk factors for poorer outcomes and increased rates of relapse. Other co-occurring factors associated with poorer outcomes for people with ED include anxiety [ 47 , 56 , 93 ], dissociative experiences [ 101 ], impulsivity [ 56 ], adjustment disorder [ 95 ], use of psychotropic medications [ 30 ], and autistic traits have been associated with greater use of ED treatment [ 102 ].
Psychosocial, environmental and health factors
A large United States community study found positive correlation between higher rates of smoking behaviour and ED in women [ 99 ]. The same study also reported birth-related outcomes in women with ED including having a later first birth, pregnancy health concerns, experience of miscarriage or abortion [ 99 ], and women with ED may have increased experience of adverse pregnancy and neonatal outcomes, and lower numbers of children [ 3 ]. For women with a history of ED, ED symptoms tend to alleviate during pregnancy; however, they commonly resurface during the postnatal period, and up to a third of women with ED report postnatal depression [ 103 , 104 ].
Demographic factors leading to poorer prognosis include being male [ 72 ], of the LGBTQIA + community [ 105 ], being from a non-white ethnic background, low family education levels [ 99 ], lower socioeconomic status, living in a remote or rural area [ 72 ], poor employment and social adjustment [ 30 ], functional impairment [ 47 ], and having a family member with an ED [ 99 ]. Complicating prognosis are additional factors such as financial stress (individuals with ED face yearly health care costs 48% higher than the general population, while the presence of co-occurring psychiatric conditions is associated with 48% lower yearly earnings [ 3 ]. These financial challenges limit ability to access evidence-based treatments (especially in countries lacking in publicly funded health care) which may prolong illness.
There is strong evidence to suggest QoL is reduced in people with an ED [ 3 , 106 ]. It is important to consider associations between QoL, ED symptomatology and treatment outcome. Evidence-based treatments have demonstrated positive effects on QoL in addition to reduction in ED symptomatology, for example, improvements in QoL and psychological functioning and well-being were seen in response to CBT in a cross-diagnostic sample [ 43 ]. However, a meta-analysis of ED outcome studies found that the QoL of recovered ED patients remained lower than in healthy populations, highlighting the importance of prevention efforts [ 107 ] and restoration of QoL in relapse prevention. These studies highlight the high public health and clinical burden of eating disorders and the need to consider co-occurring medical and psychiatric conditions during comprehensive assessment history-taking, treatment planning and provision.
Treatment factors
Early progression in treatment can provide indication of treatment outcomes. In an RCT comparing Family Based Treatment (FBT) and Adolescent Focused Therapy (AFT) for adolescents with AN, most people who achieved remission at 1 year FU maintained recovery to 4 years FU regardless of treatment arm with remission rates tended to remain stable after 1 year [ 108 ]. The First Episode Rapid Early Intervention for Eating Disorders (FREED) service model for young adults with AN reported significant and rapid clinical improvements in over 53.2% of people compared to 17.9% TAU and also reported more cost-effective treatment [ 109 ]. In a transdiagnostic study comparing inpatient vs outpatient settings, rapid response to treatment (defined here as a clinically meaningful reduction in disorder-specific symptoms within the first ten sessions) was the only outcome predictor accounting for 45.6% of variance in ED symptoms, suggesting future work should evaluate mediators and moderators of rapid response [ 37 ]. A systematic review of outcome predictors and mediators in response to CBT indicated that early behavioural and cognitive change was associated with positive outcomes across ED diagnoses [ 22 ]. Similarly, a recent systematic review and meta-analysis of 20 years of accumulated evidence concluded early response to treatment the most robust predictor of better treatment outcomes, however, only half of people investigated across numerous studies showed early change, and more research was needed to determine outcome predictors [ 110 ]. Ongoing assessment to identify individuals who do not show early response to treatment (defined by healthy weight and absence of ED behaviours at 12 month FU), as well as provision of targeted engagement approaches, may improve outcomes [ 47 ].
Due to the frequent need for medical stabilisation in the early and acute stages of AN, the role of hospitalisation needs to be considered in the evaluation of treatment outcomes. In a large patient cohort study ( n = 7505) with 5 year FU, a clear trend was observed with the per-patient 5 year cumulated number of inpatient days decreasing by 6% per annum after adjustment for age at diagnosis, parental mental health, and household income. The number of hospital admissions decreased by 2% per year, although there was no change in outpatient visits [ 111 ]. Factors contributing to better outcomes were not identified in this study, but in other research, early change in %EBW and ED psychopathology in adolescent inpatients predicted later change in the same ED variables [ 18 ]. Another study showed longer first admission predicted increased use of the health system in young adults [ 112 ].
In a multicentre RCT there was no difference between higher or lower calorie refeeding on clinical remission or medical hospitalisation to 12 month FU [ 113 ]. A systematic scoping review of 49 studies found adolescent day programs (intensive treatment programmes that do not involve an overnight stay at the treatment facility) can be an effective alternative to inpatient hospitalisation or step up/down in treatment intensity and are generally associated with weight gain and improvements in ED and comorbid psychopathology [ 114 ]. Outcomes in the review were sustained from 3 months to 2 years from EOT; however, due to large variability in the content, structure and theoretical underpinnings of reviewed programs, findings should be interpreted with caution.
Difficulties with emotion regulation are also associated with poor outcome across diagnostic profiles. There is evidence to suggest emotion-focused treatment is beneficial both to emotional functioning and mood as well as ED severity for people with elevated emotion regulation issues at baseline with positive effects lasting up to 5 years FU [ 115 ].
Self-esteem, self-compassion, and motivation
There is little conclusive evidence regarding predictors of poor response to evidence-based treatments [ 22 , 58 ]; however, low self-esteem has been implicated across all ED diagnoses [ 98 , 101 ], particularly AN [ 55 ]. A meta-analysis exploring the role of self-esteem on treatment outcomes indicated that while self-esteem did not predict remission or long-term weight related outcomes, it did mediate progression during inpatient treatment (greater increase in self-esteem during inpatient treatment was associated with higher remission and lower relapse rates at FU) [ 116 ]. Relatedly, high fear of self-compassion was associated with greater severity of ED symptoms in individuals with an active ED, suggesting that a fearful unwillingness to become more self-compassionate, rather than the absence of self-compassion, may lead to more detrimental outcomes [ 117 ].
Greater pre-treatment motivation has also been associated with ED symptom improvement and management of co-occurring anxiety and depression, in a systematic review and meta-analysis of 42 longitudinal studies [ 118 ]. Therapeutic interventions that include enhancement of motivation, self-esteem and self-compassion have been shown across studies to improve treatment outcomes across diagnostic profiles [ 117 ].
Relapse prevention programs
Whilst the role of treatment is crucial in the alleviation of symptoms and restoration of wellbeing, active provision of evidence-based post-treatment recovery care may be an important determining factor in relapse prevention. Research suggests the period in which individuals are at greatest risk of relapse is between four and nine-months following discharge [ 35 ], with between 31 and 41% relapsing at one to two years post-discharge [ 62 ].
To reduce readmission among a group of females receiving inpatient treatment for AN at an Australian specialist child and adolescent ED service, a 10 week transition ‘day’ program was developed and evaluated. The delivered program allowed for a ‘step down’ option and was found to have significant benefit for participants, who achieved an average weight gain of over 1 BMI point and decreased ED symptomatology at six-month FU [ 65 ]. Promising findings were also seen in a 6-session post-(inpatient and/or outpatient) treatment relapse prevention program designed by clinicians, parents, and patients in the Netherlands, which included a take-home workbook and appointments up to 18 months (frequency dependent on patient progress). Evaluated with young people with AN-R and AN-BP, 70% maintained post-discharge recovery to the end of the study period [ 36 ]. Such programs were evaluated in the context of a comprehensive specialist service with no control group comparison to measure the impact of the specific intervention, and there was no FU assessment following conclusion of the intervention to assess maintenance. Although more work is needed, these studies indicate the value of targeted relapse prevention programs.
Online relapse prevention programs
There is emerging evidence to support the safety and efficacy of internet-based relapse prevention programs aimed at preventing readmission to intensive ED treatment following discharge. These programs have the potential to be widely disseminated to individuals who may otherwise disengage from ongoing support due to access issues (e.g., living in an underserviced area, financial burden) or personal reasons such as stigma or shame [ 119 , 120 ].
A 9-session (1/month) CBT-based online relapse prevention program for women with AN discharged from inpatient treatment (baseline BMI x ̄ = 17.7) found participants who completed the program had significant gains in BMI at end of program ( x ̄ = 19.1) while the treatment as usual (TAU) control group did not ( x ̄ = 17.7). Of note, participants who were 1–2 sessions short of completing the program maintained a higher BMI ( x ̄ = 18.0) than the TAU group, whereas participants with less than 50% completion had a significantly lower BMI than any group including TAU ( x ̄ = 17.0) [ 121 ]. A similar CBT-based online program targeted toward women discharged from inpatient treatment for BN found that the intervention group reported 46.0% fewer vomiting episodes compared to TAU, with some improvement in symptom abstinence (intervention group: 21.4%, TAU control = 18.9%), although this finding was not statistically significant [ 122 ].
In Hungary, an internet-based aftercare support program for individuals who had received inpatient or outpatient treatment for BN or related EDNOS in the 12 months prior to the study included information and support offered via 30 min chat sessions with peers and clinicians. Results showed 40.6% of the intervention group reported improvement compared to TAU waitlist controls (24.4%), although this difference was not statistically significant. The study noted that, although on the waitlist for the internet-based aftercare support program, the TAU group could still access additional treatment if so required. Evaluation findings report the program was feasible and well accepted [ 123 ].
Text messaging-based interventions have also been trialled to maintain engagement post-treatment, whereby participants send regular symptom reports to the clinical team with feedback provided. A 12 week ‘mobile therapy’ study with a group of women exiting CBT treatment for BN resulted in significant improvement in binge/purge frequency, ED and depressive symptoms from baseline to FU, with high rates of protocol adherence (87.0%), although there was no control group comparison [ 124 ]. Further evidence was provided in a 16 week weekly symptom report study of women with BN following inpatient discharge, with a significantly larger proportion of the intervention group achieving remission (51%) compared with TAU (36%) at 8 months FU. There was no significant difference between groups in terms of outpatient service use [ 125 ]. Results from these studies conflict with evidence from a systematic review of 15 studies, which was unable to support the effectiveness of text messaging-based programs for people with ED as either a sole or adjunctive component of the intervention [ 126 ]; however, this review noted the lack of a common evaluation framework making comparison difficult.
Despite advances in awareness and treatment, ED, particularly AN, continue to be associated with increased risk of mortality [ 4 ]. Studies identified that focus on the assessment of ED mortality, as well as data from the Global Burden of Disease Study 2016 are discussed in this section. Importantly, there are several different metrics used to report mortality. These include the Standardised Mortality Ratio (SMR), or the number of observed deaths in a cohort versus the number of expected deaths in a reference population (where a rate greater than one is interpreted as excess mortality); Weighted Mortality Ratio (WMR), or the weighted average of age-specific mortality rates per 100,000 persons; Crude Mortality Rate (CMR) , or the number of deaths in a given period divided by the population exposed to risk of death in that period; and Years of Life Lost (YLL), a summary measure of premature mortality calculated by subtracting the age at death from the standard life expectancy in a reference population.
Standardised, weighted, and crude mortality
AN is consistently described as having the highest mortality rate of the ED, but actual rate difference varies between studies. A summary of Standardised Mortality Ratios across studies is presented in Table Table3. 3 . SMRs from a meta-analysis suggest that measured mortality of AN is approximately three times as high as for other ED diagnoses, and in a UK study of ED patients ( n = 1892) accessing services between 1992 and 2004, the SMR for AN was almost five times higher than other ED [ 127 ]. This is consistent with other research (a meta-analysis summarising 41 studies) reporting people with AN were 5.2 [3.7–7.5] times more likely to die prematurely from any cause [ 128 ]. A longitudinal study ( n = 246) found SMR of AN to be only twice as high compared to BN, but still 6.5 times the rate expected in the general population [ 49 ].
Standardised mortality rate by eating disorder diagnosis across included studies
*Mortality rate is reported by per 1000 person-year
Some studies did not report higher SMR for AN compared to other ED, however, methodological differences need to be considered. For example, some studies reported comparable SMR for AN to other ED, but subthreshold AN cases were included (previously catagorised as EDNOS) which may have reduced the calculated AN SMR [ 104 , 108 ]. In a British study using English National Hospital Episodes Statistics (2001–2009) comparing AN and BN, little difference in SMRs was reported [ 132 ]. The diagnosis of BN was less likely than other diagnosis to be recorded as the primary diagnosis and may not have been representative.
In a 22 year trial FU of a large sample of inpatients treated for BN, 2.4% had died [ 45 ]; the CMR for BN was 0.32% [ 63 ] and in severely malnourished patients, the crude mortality rate rose to 11.5% with SMR 15.9 [CI 95% (11.6–21.4)], just over 5 years post-treatment [ 137 ]. WMR has been found to be 5.1 for AN, 1.7 for BN, and 3.3 for EDNOS. SMRs were 5.86 for AN, 1.93 for BN, 1.92 for EDNOS [ 4 ] and 1.5–1.8 for BED [ 76 ].
Mortality rates in AN were highest during the first year after admission to treatment, while in BN it is in the first two years [ 134 ], with a higher risk in adolescence [ 140 ]. In AN, peak age of risk of death has been reported to be 15 years of age, BN 22 years and EDNOS 18–22 years [ 141 ]. Substance use disorders (including alcohol and/or cannabis) increased mortality in people with eating disorders across the diagnostic profiles [ 142 ].
In ED, peak age of risk for males may be earlier than females [ 141 ]. SMRs are higher for males (SMR = 7.24; 95% CI 6.58–7.96) relative to females (SMR = 4.59; 95% CI 4.34–4.85) overall, and in all age groups [ 131 ]. This may be due to the lower likelihood of males to self-identify or be identified with ED resulting in treatment delays and higher severity of illness when finally seeking help [ 131 ]. In mortality research conducted with a male-only sample, similarly high SMRs for males with BN and particularly AN as in majority female samples [ 2 ] were reported; however, mortality rates of EDNOS in males were considerably higher than those reported in female-dominant or female-only samples. Moreover, a case-controlled study found there was a sex difference across all diagnostic categories in CMR, with male to female being 15–5% in AN, 8–3% in BN, and 4–3% in EDNOS, but there were no significant sex differences in SMR for any diagnostic group, with males showing a shorter survival time after onset [ 2 ]. Researchers have suggested that increased mortality in males could be due to several factors, including reluctance to seek treatment and current treatment approaches being less effective in males [ 138 ]. Further research in males with ED is required to better understand the impact and response in male patients. Regardless of the mortality metric used, these studies indicate the vital importance of considering elevated mortality risk across the range of ED diagnoses.
Years of life lost/years lived with disability
The Global Burden of Disease Study 2016 reported that YLL due to premature death attributable to AN was 0.4 per 100,000. No YLL were attributed to BN; however, cause-specific mortality (CSM)—where each death is attributed to a single underlying cause—was, per thousand, 0.5 for AN (with a 2.9% increase from 1980 to 2016) and 0.1 for BN (21.8% increase from 1980 to 2016) [ 143 ]. The 2019 extension advocated for the inclusion of BED and OSFED in the Global Burden of Disease Study, previously excluded, as both diagnostic groups accounted for the majority of global ED cases and accounted for an unrepresented 41.9 million people living with ED [ 144 ].
Estimates are that over 3.3 million healthy life years are lost per year worldwide due to eating disorders. Years lived with a disability (YLDs) have increased from 2007 to 2017 for both AN (6.2% increase) and BN (10.3%), a higher rate than other mental disorders (− 0.1%). ED outcomes include reduced self-reported quality of life and estimated health care costs at 48% higher than for the general population [ 3 ].
Risk factors
Little is known about specific risk factors for mortality, although some variables have been reported in the literature. People who receive inpatient treatment for AN have more than five to seven times mortality risk when matched to age and gender and compared to other ED diagnoses [ 3 , 131 , 133 ]. For individuals receiving AN or BN treatment in outpatient settings, the risk is still twice that of controls [ 3 ]. Older age of presentation is a significant risk; adult presentations are associated with much higher mortality rates than adolescent presentations likely due to longer duration of illness at presentation, higher rates of medical and psychiatric complications and less engagement in treatment [ 4 , 28 , 68 , 137 , 139 ]. Higher mortality rates (especially in AN) are associated with lower BMI, longer duration of illness at service presentation [ 4 , 49 , 68 , 137 , 139 ], diuretic use [ 68 ], and occurrence of an in-hospital suicide attempt [ 68 , 137 ]. Certain treatment factors may be associated with higher risk of mortality, including transfer to medical intensive care unit, discharge against medical advice, and shorter hospital stays [ 137 ]. Other factors associated with increased risk of mortality include poor psychosocial functioning, substance use [ 28 , 49 ] and absence of family ED history [ 28 ].
Cause of death
Results from a large prospective 20 year (1985–2005) longitudinal study of individuals admitted to inpatient services in Germany ( n = 5839) showed people with AN were likely to die from health issues caused by their disorder, most commonly circulatory failure, cachexia, and multiple organ failure [ 133 ]. Other studies have identified somatic risk factors including anaemia, dysnatremia, infection, cardiac complications and haematological comorbidities [ 137 ]. A 2021 study reported rates of medical complications for severe AN, which included anaemia (79%), neutropenia (53.9%), hypertransaminasemia (53.7%), osteoporosis (46.3%), hypokalemia (39.5%), hypophosphatemia (26%), hypoglycaemia (13.8%), infectious complications (24.3%), cardiac dysfunction (7.1%), and proven gelatinous bone marrow transformation (6.5%). Five (1.4%) of the patients in this study died of the following causes: septic shock of pulmonary origin ( n = 1), septic shock of urinary origin ( n = 1) and suicide ( n = 3) [ 145 ].
Suicide is the most common non-natural cause of death in people with AN, BN, BED and EDNOS [ 133 ]. High rates of suicidality were reported in a meta-analysis of 36 studies published between 1966 and 2010 with data showing one in five individuals who died from an ED did so by suicide [ 4 ]. Risk of suicide may be particularly elevated in AN [Hazard Ratio (HR) 5.07; 95% CI 1.37–18.84] and BN (HR 6.07; 95% CI 2.47–14.89) even when specialised treatments are available [ 134 ]: people with AN are 18.1 [11.5–28.7] times more likely to die by suicide than 15–34 year old females in the general population [ 128 ]. This is supported by results from a meta-review exploring risk of all-cause and suicide across major mental disorders. 1.7 million patients and over a quarter of a million deaths were examined, finding all mental health disorders had an increased mortality rate to the general population; however, substance use and AN were the highest, translating into 10–20 year reductions in life expectancy, with borderline personality disorder, AN, depression and bipolar disorder having the highest suicide risk [ 146 ].
This rapid review, which synthesised the available literature on ED remission, relapse and recovery rates including associated moderating and mediating variables such as psychosocial and treatment characteristics, highlighted significant challenges of synthesising outcome literature. This includes a wide variety of ways in which key outcomes ‘remission’, ‘relapse’ and ‘recovery’ are not only defined but also how they are measured and analysed. There is no consensus among clinical or research communities on these definitions for any of the ED diagnoses [ 30 , 31 , 94 ]; thus, comparison between studies is challenging.
As EDs have amongst the highest rates of mortality of the mental health disorders, including one in five deaths caused by suicide, research into preventable causes of death, mitigatable risk, prevention and treatment efficacy is of paramount importance. It is noteworthy that current reported YLL and YLD for ED are likely an underestimate due to lack of robust epidemiological data, methodological limitations of burden of disease studies, absence of the illness group from national surveys and underreporting of mortality [ 147 ].
‘Relapse’ is typically defined by a return of symptoms after a period of reduced symptomatology; however, reviewed studies report a variety of methods to measure this, including multidisciplinary healthcare team assessment, scores on standardised psychological and behavioural interviews or questionnaires, weight criteria (including BMI or %EBW), reported eating disorder behaviours, meeting DSM (IV or V) diagnostic criteria, or a combination of the above. More difficult is determining if there is a difference between ‘remission’ and ‘recovery’, with remission usually determined by an absence of diagnostic symptomatology (again, characterised by a variety of methods), and recovery an improvement in overall functioning. Many studies report remission and recovery interchangeably, and very few incorporate returns to psychosocial functioning and QoL post alleviation of symptoms [ 29 ]. More standardised definitions may progress research [ 148 ] by allowing direct comparison between outcome studies, improving the ability of future investigations to predict and report relapse versus recovery rates and to comprehensively evaluate intervention and relapse prevention approaches.
An additional challenge across studies is a highly variable period between initial assessment or baseline and the time at which ‘outcome’ is assessed—ranging from as little as one week up to 25 years. As rates of relapse increase with illness progression, relatively short FU periods may compromise the understanding of true long-term outcomes. Longer-term FU studies are crucial to understand optimised models of care for sustained recovery and wellbeing.
Along with illness progression over time in individuals, the shift of diagnostic profiles among the individual may differ the definition of relapse or remission and thus impacts on outcome measures. Most research protocols adopt a firm inclusion/exclusion criterion, focusing on specific diagnostic profiles; however, findings from this review suggest considering a transdiagnostic approach in outcomes research which may better reflect the potentially transient nature of ED symptomatology [ 44 ]. This may have implications for diagnoses such as OSFED, potentially a transient category [ 21 ], rather than categorisation in or out of full ED diagnostic syndromes. Identification and consideration of transdiagnostic profiles, combined ED presentations and co-occurring mental health conditions should be considered in the long-term management and monitoring of individuals.
Studies within this review reported on cohorts of individuals with a formal diagnosis and research conducted within treatment settings. However, previous research has suggested that incidence rates within the community are considerable, and yet help-seeking of any type for a problem related to ED symptoms is uncommon, ranging between 22 and 40% [ 106 ] and there can be a significant time delay from first symptom experience [ 69 ]. A recent large community survey of the impact of COVID-19 on people with ED reported up to 70% of people who experienced ED symptoms were not in treatment [ 149 ] suggesting a significant proportion of people with an ED are not captured within this outcome review. Outcomes for this population are largely unknown [ 150 ] but preliminary research suggests they may be less favourable [ 151 , 152 ].
Improved QoL has been shown to be a significant predictor of positive outcome and is an opportunity for broader scope interventions for people with ED [ 107 ], and yet consistent and more wholistic markers of life quality are rarely integrated into research or clinical decision making [ 153 , 154 ]. It is also noted that outcome determinants in the reviewed studies are predominantly biometric (e.g., weight) and ED symptom related, whereas qualitative lived experience evidence suggests a broader range of person-centred metrics should be used to measure outcome. These include supportive relationships (e.g., receiving support, advice and encouragement from others, including family, friends, and/or professional carers), sense of hope, identity, meaning and purpose, feelings of empowerment and self-compassion [ 155 ]. Involvement of those to whom the work pertains (i.e., individuals with lived experience) is essential in future outcomes research to add richness and utility to theoretical frameworks, methodological approaches and conclusions [ 156 ].
Key findings
ED frequently take a chronic course, with less than half of individuals achieving recovery at long-term FU [ 41 , 44 , 52 ]. Between 30 and 41% of people will relapse within two years of receiving treatment [ 35 , 61 ], and between 20 and 61% will experience more than one type of eating disorder [ 7 , 63 , 64 ]. As with much of the extant ED literature, most outcome research has been conducted in AN. Restrictive ED are consistently associated with the poorest prognosis. This review identified recovery rates in the range of 18–60% for AN and an average length of illness of between 6.5 and 14 years [ 41 , 56 ]. Binge/purge symptomatology within AN is associated with worse outcome [ 20 , 56 ]. Recovery rates for BN are slightly more optimistic at 35–59% [ 7 , 45 , 63 , 157 ], and similarly for BED at 37–77% [ 79 , 80 , 82 ]. There is limited data available on outcomes in ARFID, OSFED, and UFED.
Factors associated with a more positive long-term outcome include lower age of presentation [ 28 , 61 ], shorter duration of illness at first presentation [ 69 , 93 , 94 ], higher pre-treatment motivation to recover [ 116 ], and demonstrated early response to treatment [ 18 , 75 , 110 , 112 ]. Factors associated with poorer outcome are lower BMI at presentation [ 93 ], presence of binge/purge symptomatology [ 20 , 30 , 44 , 56 ], and presence of comorbid psychiatric condition/s such as depression, anxiety, or personality disorder [ 44 , 47 , 51 , 55 , 67 , 98 , 99 ]. Males, LGBTQIA + community [ 104 , 105 ], neurodiversity [ 102 ], individuals from non-white/ethnic backgrounds, and those from lower socioeconomic brackets or rural/remote communities are also more likely to experience a poor outcome [ 18 , 72 , 76 , 77 ].
Relapse following ED treatment is common [ 11 , 35 , 36 , 62 , 148 ] and is most likely to occur 4–9 months post discharge [ 35 ]. Up to 41% of individuals will relapse by the second-year post-discharge [ 62 ]. Aftercare relapse prevention programs, including online and face-to-face initiatives such as text-message based interventions, daily feedback to clinicians and intensive day programs have been shown to increase chance of maintaining recovery [ 121 , 123 – 125 ]. The implementation of such programs may be key to improving long-term recovery rates particularly for those individuals who may otherwise disengage from treatment for access reasons (such as living in an underserviced area) or because of the stigma of engaging with mental health care [ 119 , 120 ]. There is emerging evidence in the effectiveness of online intervention for preventing relapse and promoting treatment gains when individuals are motivated to change; however, evidence is not conclusive potentially due to the high variability of the interventions and evaluations of such programs.
ED are associated with unacceptably high mortality rates, and particularly high risk of suicide [ 128 , 133 ]. Of the ED, AN carries the highest mortality risk [ 49 , 127 , 128 ]. Standardised mortality ratios (SMRs) identified by this review ranged between 1.2 and 15.9 for AN; 1.4 and 4.8 for BN; 1.01 and 3.3 for BED; and 1.3 to 4.7 for EDNOS/OSFED [ 2 , 4 , 20 , 121 , 127 , 128 , 132 , 134 , 135 , 137 , 139 ]. Factors associated with increased risk of mortality include having received inpatient treatment [ 3 , 131 , 133 ], longer duration of untreated illness [ 4 , 28 , 68 , 68 , 137 , 139 ] and lower BMI at presentation [ 4 , 49 , 68 , 137 , 139 ]. Males are at higher risk of death than females [ 2 ].
Strengths and limitations
This rapid review has several strengths inherent to the methodological approach of the series, conducted to inform the Australian Eating Disorders Research and Translation Strategy 2021–2031 [ 1 ]. The RR process broadly assessed all available high-level evidence peer-reviewed literature swiftly [ 24 ], included all diagnostic categories covering transdiagnostic continuums, considered the full demographic range available and reported a variety of methodological designs including clinical trials (across a variety of settings), systematic reviews, meta-analyses, and population-level research. It aimed to provide the most comprehensive and current review possible with coordination of complex findings into a more cohesive structure. It was noted where applicable the limitations of conclusions drawn from this review, such as the widely disparate definitions and measurements for key outcome data (i.e., remission, relapse, and recovery rates), crossover from DSM-IV to DSM-V criteria (due to timeframe of search), vastly different periods of follow up impacting findings, and conflicting evidence. As with the series of rapid reviews, the inclusion criteria of evidence may have potentially excluded relevant evidence, and it is noted that evidence is always emerging.
This RR of outcomes in ED identified several gaps in current knowledge and provides direction for future strategic research directives, specifically, defining the key outcomes of remission, recovery, and relapse, with consensus of determinants and inclusion of broader QoL measures and lived experience. Identifying and refining risk factors, mediating and moderating factors that may influence outcomes is ongoing, with longer-term FU research needed to track remission versus relapse, diagnostic crossover and optimisation of treatment engagement and recovery. Regarding mortality literature, this review noted considerable gaps [ 146 ], with variety reporting methods, a paucity of research between population level reporting and small hospital outcome studies, and minimal investigation into life circumstances relating to death, especially as many of these deaths may be preventable. With low rates of remission despite evidence-based care and high risk of mortality, especially for AN, it is strongly recommended that focused, long-term follow-up research is prioritised for people with ED.
Acknowledgements
The InsideOut Institute is a collaboration between the University of Sydney and Sydney Local Health District. We thank all the staff from the Institution for their support of this significant project. The authors would like to thank and acknowledge the hard work of Healthcare Management Advisors (HMA) who were commissioned to undertake the Rapid Review. Additionally, the authors would like to thank all members of the consortium and consultation committees for their advice, input, and considerations during the development process. Further, a special thank you to the carers, consumers and lived experience consultants that provided input to the development of the Rapid Review and wider national Eating Disorders Research & Translation Strategy. Finally, thank you to the Australian Government—Department of Health for their support of the current project. National Eating Disorder Research Consortium Members (alphabetical order of surname): *indicates named authors. Phillip Aouad InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Sarah Barakat InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Robert Boakes School of Psychology, Faculty of Science, University of Sydney, NSW Australia. Leah Brennan School of Psychology and Public Health, La Trobe University, Victoria, Australia. Emma Bryant* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Susan Byrne School of Psychology, Western Australia, Perth, Australia. Belinda Caldwell Eating Disorders Victoria, Victoria, Australia. Shannon Calvert Perth, Western Australia, Australia. Bronny Carroll InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. David Castle Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia. Ian Caterson School of Life and Environmental Sciences, University of Sydney, Sydney, New South Wales, Australia. Belinda Chelius Eating Disorders Queensland, Brisbane, Queensland, Australia. Lyn Chiem Sydney Local Health District, New South Wales Health, Sydney, Australia. Simon Clarke Westmead Hospital, Sydney, New South Wales, Australia. Janet Conti Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Lexi Crouch Brisbane, Queensland, Australia. Genevieve Dammery InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Natasha Dzajkovski InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Jasmine Fardouly School of Psychology, University of New South Wales, Sydney, New South Wales, Australia. John Feneley New South Wales Health, New South Wales, Australia. Amber-Marie Firriolo University of Sydney, NSW Australia. Nasim Foroughi Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Mathew Fuller-Tyszkiewicz School of Psychology, Faculty of Health, Deakin University, Victoria, Australia. Anthea Fursland School of Population Health, Faculty of Health Sciences, Curtain University, Perth, Australia. Veronica Gonzalez-Arce InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Bethanie Gouldthorp Hollywood Clinic, Ramsay Health Care, Perth, Australia. Kelly Griffin InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Scott Griffiths Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia. Ashlea Hambleton InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Amy Hannigan Queensland Eating Disorder Service, Brisbane, Queensland, Australia. Mel Hart Hunter New England Local Health District, New South Wales, Australia. Susan Hart St Vincent’s Hospital Network Local Health District, Sydney, New South Wales, Australia. Phillipa Hay Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Ian Hickie Brain and Mind Centre, University of Sydney, Sydney, Australia. Francis Kay-Lambkin School of Medicine and Public Health, University of Newcastle, New South Wales, Australia. Ross King School of Psychology, Faculty of Health, Deakin University, Victoria, Australia. Michael Kohn Paediatrics & Child Health, Children's Hospital, Westmead, Sydney, Australia. Eyza Koreshe InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Isabel Krug Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia. Jake Linardon School of Psychology, Faculty of Health, Deakin University, Victoria, Australia. Randall Long College of Medicine and Public Health, Flinders University, South Australia, Australia. Amanda Long Exchange Consultancy, Redlynch, New South Wales, Australia. Sloane Madden Eating Disorders Service, Children’s Hospital at Westmead, Sydney, New South Wales, Australia. Sarah Maguire* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Danielle Maloney InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Peta Marks InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Sian McLean The Bouverie Centre, School of Psychology and Public Health, La Trobe University, Victoria, Australia. Thy Meddick Clinical Excellence Queensland, Mental Health Alcohol and Other Drugs Branch, Brisbane, Queensland, Australia. Jane Miskovic-Wheatley* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Deborah Mitchison Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Richard O’Kearney College of Health & Medicine, Australian National University, Australian Capital Territory, Australia. Shu Hwa Ong* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Roger Paterson ADHD and BED Integrated Clinic, Melbourne, Victoria, Australia. Susan Paxton La Trobe University, Department of Psychology and Counselling, Victoria, Australia. Melissa Pehlivan InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Genevieve Pepin School of Health & Social Development, Faculty of Health, Deakin University, Geelong, Victoria, Australia. Andrea Phillipou Swinburne Anorexia Nervosa (SWAN) Research Group, Centre for Mental Health, School of Health Sciences, Swinburne University, Victoria, Australia. Judith Piccone Children's Health Queensland Hospital and Health Service, Brisbane, Queensland, Australia. Rebecca Pinkus School of Psychology, Faculty of Science, University of Sydney, NSW Australia. Bronwyn Raykos Centre for Clinical Interventions, Western Australia Health, Perth, Western Australia, Australia. Paul Rhodes School of Psychology, Faculty of Science, University of Sydney, NSW Australia. Elizabeth Rieger College of Health & Medicine, Australian National University, Australian Capital Territory, Australia. Karen Rockett New South Wales Health, New South Wales, Australia. Sarah-Catherine Rodan InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Janice Russell Central Clinical School Brain & Mind Research Institute, University of Sydney, New South Wales, Sydney. Haley Russell InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Fiona Salter Ramsay Health Care, Perth, Australia. Susan Sawyer Department of Paediatrics, The University of Melbourne, Australia. Beth Shelton National Eating Disorders Collaboration, Victoria, Australia. Urvashnee Singh The Hollywood Clinic Hollywood Private Hospital, Ramsey Health, Perth, Australia. Sophie Smith Sydney, New South Wales, Australia. Evelyn Smith Translational Health Research Institute, Western Sydney University, Sydney NSW Australia. Karen Spielman InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Sarah Squire The Butterfly Foundation, Sydney, Australia. Juliette Thomson The Butterfly Foundation, Sydney, Australia. Stephen Touyz* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Ranjani Utpala The Butterfly Foundation, Sydney, Australia. Lenny Vartanian School of Psychology, University of New South Wales, Sydney, New South Wales, Australia. Sabina Vatter* InsideOut Institute, Central Clinical School, Faculty of Medicine and Health, University of Sydney, NSW Australia. Andrew Wallis Eating Disorder Service, The Sydney Children’s Hospital Network, Westmead Campus, Sydney, Australia. Warren Ward Department of Psychiatry, University of Queensland, Brisbane, Australia. Sarah Wells University of Tasmania, Tasmania, Australia. Eleanor Wertheim School of Psychology and Public Health, La Trobe University, Victoria, Australia. Simon Wilksch College of Education, Psychology and Social Work, Flinders University, South Australia, Australia. Michelle Williams Royal Hobart, Tasmanian Health Service, Tasmania, Australia.
Abbreviations
Author contributions.
AL carried out and wrote the initial review from the first search; JMW conducted subsequent reviews, analysed results, wrote the first manuscript and the final edit; EB, SHO and SV contributed to specific sections, detailed tables and figures, responded to review comments and contributed to ongoing drafts to manuscript completion; the National Eating Disorder Research Consortium reviewed and provided expert feedback; ST and SM provided project direction, methodological design, comprehensively reviewed the manuscript and provided overall supervision and leadership. All authors read and approved the final manuscript.
The RR was in-part funded by the Australian Government Department of Health in partnership with other national and jurisdictional stakeholders. As the organisation responsible for overseeing the National Eating Disorder Research & Translation Strategy, InsideOut Institute commissioned Healthcare Management Advisors to undertake the RR as part of a larger, ongoing, project. Role of Funder: The funder was not directly involved in informing the development of the current review.
Availability of data and materials
Declarations.
Not applicable.
ST receives royalties from Hogrefe and Huber, McGraw Hill and Taylor and Francis for published books/book chapters. He has received honoraria from the Takeda Group of Companies for consultative work, public speaking engagements and commissioned reports. He has chaired their Clinical Advisory Committee for Binge Eating Disorder. He is the Editor in Chief of the Journal of Eating Disorders. He is a committee member of the National Eating Disorders Collaboration as well as the Technical Advisory Group for Eating Disorders. AL undertook work on this RR while employed by HMA. JMW and SM are guest editors of the special issue “Improving the future by understanding the present: evidence reviews for the field of eating disorders.”
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Phillip aouad, sarah barakat, robert boakes.
4 School of Psychology, Faculty of Science, University of Sydney, Sydney, NSW Australia
Leah Brennan
5 School of Psychology and Public Health, La Trobe University, Victoria, Australia
Susan Byrne
6 School of Psychology, Perth, Western Australia Australia
Belinda Caldwell
7 Eating Disorders Victoria, Victoria, Australia
Shannon Calvert
8 Perth, Australia
Bronny Carroll
David castle.
9 Medicine, Dentistry and Health Sciences, University of Melbourne, Victoria, Australia
Ian Caterson
10 School of Life and Environmental Sciences, University of Sydney, Sydney, NSW Australia
Belinda Chelius
11 Eating Disorders Queensland, Brisbane, QLD Australia
12 Sydney Local Health District, New South Wales Health, Sydney, Australia
Simon Clarke
13 Westmead Hospital, Sydney, NSW Australia
Janet Conti
14 Translational Health Research Institute, Western Sydney University, Sydney, NSW Australia
Lexi Crouch
15 Brisbane, Australia
Genevieve Dammery
Natasha dzajkovski, jasmine fardouly.
16 School of Psychology, University of New South Wales, Sydney, NSW Australia
Carmen Felicia
17 University of Sydney, Sydney, NSW Australia
John Feneley
18 New South Wales Health, Sydney, NSW Australia
Amber-Marie Firriolo
Nasim foroughi, mathew fuller-tyszkiewicz.
19 School of Psychology, Faculty of Health, Deakin University, Victoria, Australia
Anthea Fursland
20 School of Population Health, Faculty of Health Sciences, Curtain University, Perth, Australia
Veronica Gonzalez-Arce
Bethanie gouldthorp.
21 Hollywood Clinic, Ramsay Health Care, Perth, Australia
Kelly Griffin
Scott griffiths.
22 Melbourne School of Psychological Sciences, University of Melbourne, Victoria, Australia
Ashlea Hambleton
Amy hannigan.
23 Queensland Eating Disorder Service, Brisbane, QLD Australia
24 Hunter New England Local Health District, New Lambton, NSW Australia
25 St Vincent’s Hospital Network Local Health District, Sydney, NSW Australia
Phillipa Hay
26 Brain and Mind Centre, University of Sydney, Sydney, Australia
Francis Kay-Lambkin
27 School of Medicine and Public Health, University of Newcastle, Newcastle, NSW Australia
Michael Kohn
28 Westmead Hospital, Sydney, Australia
Eyza Koreshe
Isabel krug, jake linardon, randall long.
29 College of Medicine and Public Health, Flinders University, Adelaide, SA Australia
Amanda Long
30 Exchange Consultancy, Redlynch, NSW Australia
Sloane Madden
31 Eating Disorders Service, Children’s Hospital at Westmead, Sydney, NSW Australia
Danielle Maloney
Sian mclean.
32 The Bouverie Centre, School of Psychology and Public Health, La Trobe University, Victoria, Australia
Thy Meddick
33 Clinical Excellence Queensland, Mental Health Alcohol and Other Drugs Branch, Brisbane, QLD Australia
Deborah Mitchison
Richard o’kearney.
34 College of Health and Medicine, Australian National University, Canberra, ACT Australia
Roger Paterson
35 ADHD and BED Integrated Clinic, Melbourne, VIC Australia
Susan Paxton
36 Department of Psychology and Counselling, La Trobe University, Victoria, Australia
Melissa Pehlivan
Genevieve pepin.
37 School of Health and Social Development, Faculty of Health, Deakin University, Geelong, VIC Australia
Andrea Phillipou
38 Swinburne Anorexia Nervosa (SWAN) Research Group, Centre for Mental Health, School of Health Sciences, Swinburne University, Victoria, Australia
Judith Piccone
39 Children’s Health Queensland Hospital and Health Service, Brisbane, QLD Australia
Rebecca Pinkus
Bronwyn raykos.
40 Centre for Clinical Interventions, Western Australia Health, Perth, WA Australia
Paul Rhodes
Elizabeth rieger, sarah-catherine rodan, karen rockett, janice russell.
41 Central Clinical School Brain & Mind Research Institute, University of Sydney, Sydney, NSW Australia
Haley Russell
Fiona salter.
42 Ramsay Health Care, Perth, Australia
Susan Sawyer
43 Department of Paediatrics, The University of Melbourne, Parkville, Australia
Beth Shelton
44 National Eating Disorders Collaboration, Victoria, Australia
Urvashnee Singh
45 The Hollywood Clinic Hollywood Private Hospital, Ramsey Health, Perth, Australia
Sophie Smith
46 Sydney, Australia
Evelyn Smith
Karen spielman, sarah squire.
47 The Butterfly Foundation, Sydney, Australia
Juliette Thomson
Ranjani utpala, lenny vartanian, andrew wallis.
48 Eating Disorder Service, The Sydney Children’s Hospital Network, Westmead Campus, Sydney, Australia
Warren Ward
49 Department of Psychiatry, University of Queensland, Brisbane, Australia
Sarah Wells
50 University of Tasmania, Hobart, TAS Australia
Eleanor Wertheim
Simon wilksch.
51 College of Education, Psychology and Social Work, Flinders University, Adelaide, SA Australia
Michelle Williams
52 Royal Hobart, Tasmanian Health Service, Hobart, TAS Australia
Introduction to Eating Disorders
Eating disorders involve a persistent disturbance of eating or of behavior related to eating that
Alters consumption or absorption of food
Significantly impairs physical health and/or psychosocial functioning
Specific eating disorders include
Anorexia nervosa
Avoidant/restrictive food intake disorder
Binge eating disorder
Bulimia nervosa
Rumination disorder
Anorexia nervosa is characterized by a relentless pursuit of thinness, a morbid fear of obesity, a distorted body image, and restriction of intake relative to requirements, leading to a significantly low body weight to the point where health is harmed. This disorder may or may not include purging (eg, self-induced vomiting).
Avoidant/restrictive food intake disorder is characterized by avoidance of food or restriction of food intake that results in significant weight loss, nutritional deficiency, dependence on nutritional support, and/or marked disturbance of psychosocial functioning. But unlike anorexia nervosa and bulimia nervosa, this disorder does not include concern about body shape or weight.
Binge eating disorder is characterized by recurrent episodes in which people consume large amounts of food and feel as if they have lost control. Episodes are not followed by inappropriate compensatory behavior (eg, self-induced vomiting).
Bulimia nervosa is characterized by recurrent episodes of binge eating followed by some form of inappropriate compensatory behavior such as purging (self-induced vomiting, laxative or diuretic abuse), fasting, or driven exercise.
Pica is persistent eating of nonnutritive, nonfood material that is not developmentally appropriate (ie, pica is not diagnosed in children < 2 years) and not part of a cultural tradition.
Rumination disorder is repeated regurgitation of food after eating.
Eating disorders are more common among women, especially younger women, than among men.
See also the American Psychiatric Association’s Practice Guidelines: Treatment of Patients With Eating Disorders, 3rd Edition and guidelines from the National Institute for Clinical Excellence [NICE] , December, 2020.

- Cookie Preferences

Copyright © 2024 Merck & Co., Inc., Rahway, NJ, USA and its affiliates. All rights reserved.
Home — Essay Samples — Nursing & Health — Public Health Issues — Eating Disorders
Essay Examples on Eating Disorders
What makes a good eating disorders essay topic.
When it comes to selecting a topic for your eating disorders essay, it's crucial to consider a multitude of factors that can elevate your writing to new heights. Below are some innovative suggestions on how to brainstorm and choose an essay topic that will captivate your readers:
- Brainstorm: Begin by unleashing a storm of ideas related to eating disorders. Delve into the various facets, such as causes, effects, treatment options, societal influences, and personal narratives. Ponder upon what intrigues you and what will engage your audience.
- Research: Embark on a comprehensive research journey to accumulate information and gain a profound understanding of the subject matter. This exploration will enable you to identify distinctive angles and perspectives to explore in your essay. Seek out scholarly sources such as academic journals, books, and reputable websites.
- Cater to your audience: Reflect upon your readers and their interests to tailor your topic accordingly. Adapting your subject matter to captivate your audience will undoubtedly make your essay more engaging. Consider the age, background, and knowledge level of your readers.
- Unveil controversies: Unearth the controversies and debates within the realm of eating disorders. Opting for a topic that ignites discussion will infuse your essay with thought-provoking and impactful qualities. Delve into various viewpoints and critically analyze arguments for and against different ideas.
- Personal connection: If you possess a personal connection or experience with eating disorders, contemplate sharing your story or delving into it within your essay. This will add a unique and personal touch to your writing. However, ensure that your personal anecdotes remain relevant to the topic and effectively support your main points.
Overall, a remarkable eating disorders essay topic should be meticulously researched, thought-provoking, and relevant to your audience's interests and needs.
Best Eating Disorders Essay Topics
Below, you will find a compilation of the finest eating disorders essay topics to consider:
1. The captivating influence of social media on promoting unhealthy body image. 2. Breaking free from stereotypes: Exploring eating disorders among male athletes. 3. The profound impact of diet culture on body image and self-esteem. 4. Unraveling the intricate link between eating disorders and the pursuit of perfection. 5. The portrayal of eating disorders in popular media: Dissecting the battle between glamorization and reality.
Best Eating Disorders Essay Questions
Below, you will find an array of stellar eating disorders essay questions to explore:
1. How does social media contribute to the development and perpetuation of eating disorders? 2. What challenges do males with eating disorders face, and how can these challenges be addressed? 3. To what extent does the family environment contribute to the development of eating disorders? 4. What role does diet culture play in fostering unhealthy relationships with food? 5. How can different treatment approaches be tailored to address the unique needs of individuals grappling with eating disorders?
Eating Disorders Essay Prompts
Below, you will find a collection of eating disorders essay prompts that will kindle your creative fire:
1. Craft a personal essay that intricately details your voyage towards recovery from an eating disorder, elucidating the lessons you learned along the way. 2. Picture yourself as a parent of a teenager burdened with an eating disorder. Pen a heartfelt letter to other parents, sharing your experiences and providing valuable advice. 3. Fabricate a fictional character entangled in the clutches of binge-eating disorder. Concoct a short story that explores their odyssey towards self-acceptance and recovery. 4. Construct a persuasive essay that fervently argues for the integration of comprehensive education on eating disorders into school curricula. 5. Immerse yourself in the role of a therapist specializing in eating disorders. Compose a reflective essay that delves into the challenges and rewards of working with individuals grappling with eating disorders.
Writing Eating Disorders Essays: Frequently Asked Questions
Below, you will find answers to some frequently asked questions about writing eating disorders essays:
Q: How can I effectively commence my eating disorders essay? A: Commence your essay with a captivating introduction that ensnares the reader's attention and provides an overview of the topic. Consider starting with an intriguing statistic, a powerful quote, or a personal anecdote.
Q: Can I incorporate personal experiences into my eating disorders essay? A: Absolutely! Infusing your essay with personal experiences adds depth and authenticity. However, ensure that your personal anecdotes remain relevant to the topic and effectively support your main points.
Q: How can I make my eating disorders essay engaging? A: Utilize a variety of rhetorical devices such as metaphors, similes, and vivid descriptions to transform your essay into an engaging masterpiece. Additionally, consider incorporating real-life examples, case studies, or interviews to provide concrete evidence and make your essay relatable.
Q: Should my essay focus solely on one specific type of eating disorder? A: While focusing on a specific type of eating disorder can provide a narrower scope for your essay, exploring the broader theme of eating disorders as a whole can also be valuable. Strive to strike a balance between depth and breadth in your writing.
Q: How can I conclude my eating disorders essay effectively? A: In your conclusion, summarize the main points of your essay and restate your thesis statement. Additionally, consider leaving the reader with a thought-provoking question or a call to action, encouraging further reflection or research on the topic.
Argumentative Essay on Eating Disorders
Eating disorders and methods of its treatment, made-to-order essay as fast as you need it.
Each essay is customized to cater to your unique preferences
+ experts online
The Correlation Between Social Media and The Development of Eating Disorders
The damages of eating disorders, stereotypes around eating disorders, anorexia – a growing issue in teenage girls, let us write you an essay from scratch.
- 450+ experts on 30 subjects ready to help
- Custom essay delivered in as few as 3 hours
Examining Eating Disorders and Social Learning Theory to Draw Useful Conclusions
Photoshopping images and how it impacts eating disorders, nutrition intervention for eating disorders, how beauty pageants can cause health difficulties, get a personalized essay in under 3 hours.
Expert-written essays crafted with your exact needs in mind
A Look into The Life of People with Anorexia Nervosa
Bulimia nervosa: causes, symptoms and treatment, the prevention and treatment of anorexia nervosa, food addiction: does it really exist, depiction of anorexia nervosa in the movie to the bone, a study of eating disorders in judaism and the impact of patriarchal values and pressures, the differences between anorexia and bulimia, social media as the reason of body dissatisfaction and eating disorders, the role of society in the development of anorexia in teen girls, exploring solutions for fighting the obesity epidemic, jane martin’s beauty, eating disorders in adolescents.
Eating disorders refer to a complex set of mental health conditions characterized by disturbances in one's eating behaviors and attitudes towards food, leading to severe consequences on an individual's physical and psychological well-being.
Anorexia Nervosa: Anorexia nervosa is a psychological disorder characterized by an intense fear of gaining weight and a distorted perception of one's body image. People with this disorder exhibit extreme food restriction, leading to significant weight loss and the possibility of reaching dangerously low levels of body weight. Anorexia nervosa is often accompanied by obsessive thoughts about food, excessive exercise routines, and a constant preoccupation with body shape and size. Bulimia Nervosa: Bulimia nervosa involves a cyclic pattern of binge eating followed by compensatory behaviors aimed at preventing weight gain. During binge episodes, individuals consume large quantities of food in a short period and experience a loss of control over their eating. To counteract the caloric intake, these individuals may resort to self-induced vomiting, excessive exercising, or the misuse of laxatives. It is important to note that unlike anorexia nervosa, individuals with bulimia nervosa typically maintain a body weight within the normal range or slightly above. Binge Eating Disorder: Binge eating disorder is characterized by recurrent episodes of consuming a significant amount of food in a short period, accompanied by a feeling of loss of control. Unlike other eating disorders, individuals with binge eating disorder do not engage in compensatory behaviors such as purging or excessive exercise.
Distorted Body Image: Individuals with eating disorders often have a distorted perception of their body, seeing themselves as overweight or unattractive, even when they are underweight or at a healthy weight. Obsession with Food and Weight: People with eating disorders may constantly think about food, calories, and their weight. They may develop strict rules and rituals around eating, such as avoiding certain food groups, restricting their intake, or engaging in excessive exercise. Emotional and Psychological Factors: Eating disorders are often associated with underlying emotional and psychological issues, such as low self-esteem, perfectionism, anxiety, depression, or a need for control. Physical Health: Eating disorders can have severe physical health consequences, including malnutrition, electrolyte imbalances, hormonal disruptions, gastrointestinal problems, and organ damage. These complications can be life-threatening and require medical intervention. Social Isolation and Withdrawal: Individuals struggling with eating disorders may experience a withdrawal from social activities, distancing themselves from others due to feelings of shame, guilt, and embarrassment related to their eating behaviors or body image. This social isolation can intensify the challenges they face and contribute to a sense of loneliness and emotional distress. Co-occurring Disorders: Eating disorders frequently co-occur with other mental health conditions, creating complex challenges for those affected. It is common for individuals with eating disorders to also experience anxiety disorders, depression, substance abuse issues, or engage in self-harming behaviors. The coexistence of these disorders can exacerbate the severity of symptoms and necessitate comprehensive and integrated treatment approaches.
Genetic and Biological Factors: Research suggests that there is a genetic predisposition to eating disorders. Individuals with a family history of eating disorders or other mental health conditions may be at a higher risk. Biological factors, such as imbalances in brain chemicals or hormones, can also contribute to the development of eating disorders. Psychological Factors: Psychological factors play a significant role in the development of eating disorders. Factors such as diminished self-worth, a relentless pursuit of perfection, dissatisfaction with one's body, and distorted perceptions of body image can play a significant role in the onset and perpetuation of disordered eating patterns. Sociocultural Influences: Societal pressures and cultural norms surrounding body image and beauty standards can contribute to the development of eating disorders. Media portrayal of unrealistic body ideals, peer influence, and societal emphasis on thinness can impact individuals' self-perception and increase the risk of developing an eating disorder. Traumatic Experiences: The impact of traumatic events, be it physical, emotional, or sexual abuse, can heighten the vulnerability to developing eating disorders. Such distressing experiences have the potential to instigate feelings of diminished self-worth, profound body shame, and a compelling desire to exert control over one's body and eating behaviors. Dieting and Weight-related Practices: Restrictive dieting, excessive exercise, and weight-focused behaviors can serve as triggers for the development of eating disorders. These behaviors may start innocently as an attempt to improve one's health or appearance but can spiral into disordered eating patterns.
Psychotherapy: Various forms of psychotherapy, such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and family-based therapy (FBT), are employed to address the underlying psychological factors contributing to eating disorders. These therapies aim to challenge distorted thoughts and beliefs about body image, develop healthier coping mechanisms, and improve self-esteem. Nutritional Counseling: Working with registered dietitians, individuals receive personalized guidance on developing a balanced and healthy relationship with food. Nutritional counseling focuses on establishing regular eating patterns, promoting mindful eating practices, and debunking harmful dietary myths. Medical Monitoring: This involves regular check-ups to assess physical health, monitor vital signs, and address any medical complications arising from the disorder. Medication: In some cases, medication may be prescribed to manage associated symptoms like depression, anxiety, or obsessive-compulsive disorder. Medications can complement therapy and help stabilize mood, regulate eating patterns, or address co-occurring mental health conditions. Support Groups and Peer Support: Joining support groups or engaging in peer support programs can provide individuals with a sense of community and understanding. Interacting with others who have faced similar challenges can offer valuable insights, encouragement, and empathy.
Films: Movies like "To the Bone" (2017) and "Feed" (2017) shed light on the struggles individuals with eating disorders face. These films delve into the psychological and emotional aspects of the disorders, emphasizing the importance of seeking help and promoting recovery. Books: Novels such as "Wintergirls" by Laurie Halse Anderson and "Paperweight" by Meg Haston offer intimate perspectives on the experiences of characters grappling with eating disorders. These books provide insights into the complexities of these conditions, including the internal battles, societal pressures, and the journey towards healing. Documentaries: Documentaries like "Thin" (2006) and "Eating Disorders: Surviving the Silence" (2019) offer real-life accounts of individuals living with eating disorders. These documentaries provide a raw and authentic portrayal of the challenges faced by those affected, raising awareness and encouraging empathy.
1. As per the data provided by the National Eating Disorders Association (NEDA), it is estimated that around 30 million individuals residing in the United States will experience an eating disorder during their lifetime. 2. Research suggests that eating disorders have the highest mortality rate of any mental illness. Anorexia nervosa, in particular, has a mortality rate of around 10%, emphasizing the seriousness and potential life-threatening nature of these disorders. 3. Eating disorders can affect individuals of all genders and ages, contrary to the common misconception that they only affect young women. While young women are more commonly affected, studies indicate that eating disorders are increasingly prevalent among men and can also occur in older adults and children.
The topic of eating disorders is of significant importance when it comes to raising awareness, promoting understanding, and addressing the challenges faced by individuals who experience these disorders. Writing an essay on this topic allows for a deeper exploration of the complexities surrounding eating disorders and their impact on individuals, families, and society. First and foremost, studying eating disorders is crucial for shedding light on the psychological, emotional, and physical aspects of these conditions. By delving into the underlying causes, risk factors, and symptoms, we can gain a better understanding of the complex interplay between biological, psychological, and sociocultural factors that contribute to the development and maintenance of eating disorders. Furthermore, discussing eating disorders helps to challenge societal misconceptions and stereotypes. It allows us to debunk harmful beliefs, such as the notion that eating disorders only affect a specific gender or age group, and instead emphasizes the reality that anyone can be susceptible to these disorders. Writing an essay on eating disorders also provides an opportunity to explore the impact of media, societal pressures, and body image ideals on the development of disordered eating behaviors. By analyzing these influences, we can advocate for more inclusive and body-positive narratives that promote self-acceptance and well-being. Moreover, addressing the topic of eating disorders is crucial for raising awareness about the available treatment options and support systems. It highlights the importance of early intervention, comprehensive treatment approaches, and access to mental health resources for those affected by these disorders.
1. American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing. 2. Arcelus, J., Mitchell, A. J., Wales, J., & Nielsen, S. (2011). Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry, 68(7), 724-731. 3. Brown, T. A., Keel, P. K., & Curren, A. M. (2020). Eating disorders. In D. H. Barlow (Ed.), Clinical handbook of psychological disorders: A step-by-step treatment manual (6th ed., pp. 305-357). Guilford Press. 4. Fairburn, C. G., & Harrison, P. J. (2003). Eating disorders. The Lancet, 361(9355), 407-416. 5. Herpertz-Dahlmann, B., & Zeeck, A. (2020). Eating disorders in childhood and adolescence: Epidemiology, course, comorbidity, and outcome. In M. Maj, W. Gaebel, J. J. López-Ibor, & N. Sartorius (Eds.), Eating Disorders (Vol. 11, pp. 68-82). Wiley-Blackwell. 6. Hudson, J. I., Hiripi, E., Pope, H. G., & Kessler, R. C. (2007). The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry, 61(3), 348-358. 7. Jacobi, C., Hayward, C., de Zwaan, M., Kraemer, H. C., & Agras, W. S. (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130(1), 19-65. 8. Keski-Rahkonen, A., & Mustelin, L. (2016). Epidemiology of eating disorders in Europe: Prevalence, incidence, comorbidity, course, consequences, and risk factors. Current Opinion in Psychiatry, 29(6), 340-345. 9. Smink, F. R. E., van Hoeken, D., & Hoek, H. W. (2012). Epidemiology of eating disorders: Incidence, prevalence and mortality rates. Current Psychiatry Reports, 14(4), 406-414. 10. Stice, E., Marti, C. N., & Rohde, P. (2013). Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal of Abnormal Psychology, 122(2), 445-457.
Relevant topics
- Drug Addiction
- Mental Health
By clicking “Check Writers’ Offers”, you agree to our terms of service and privacy policy . We’ll occasionally send you promo and account related email
No need to pay just yet!
We use cookies to personalyze your web-site experience. By continuing we’ll assume you board with our cookie policy .
- Instructions Followed To The Letter
- Deadlines Met At Every Stage
- Unique And Plagiarism Free

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Eating Disorders
What are eating disorders.
There is a commonly held misconception that eating disorders are a lifestyle choice. Eating disorders are actually serious and often fatal illnesses that are associated with severe disturbances in people’s eating behaviors and related thoughts and emotions. Preoccupation with food, body weight, and shape may also signal an eating disorder. Common eating disorders include anorexia nervosa, bulimia nervosa, and binge-eating disorder.
What are the signs and symptoms of eating disorders?
Anorexia nervosa.
Anorexia nervosa is a condition where people avoid food, severely restrict food, or eat very small quantities of only certain foods. They also may weigh themselves repeatedly. Even when dangerously underweight, they may see themselves as overweight.
There are two subtypes of anorexia nervosa: a "restrictive " subtype and a "binge-purge " subtype.
- In the restrictive subtype of anorexia nervosa, people severely limit the amount and type of food they consume.
- In the binge-purge subtype of anorexia nervosa, people also greatly restrict the amount and type of food they consume. In addition, they may have binge-eating and purging episodes—eating large amounts of food in a short time followed by vomiting or using laxatives or diuretics to get rid of what was consumed.
Anorexia nervosa can be fatal. It has an extremely high death (mortality) rate compared with other mental disorders. People with anorexia are at risk of dying from medical complications associated with starvation. Suicide is the second leading cause of death for people diagnosed with anorexia nervosa.
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
Symptoms include:
- Extremely restricted eating
- Extreme thinness (emaciation)
- A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight
- Intense fear of gaining weight
- Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape, or a denial of the seriousness of low body weight
Other symptoms may develop over time, including:
- Thinning of the bones (osteopenia or osteoporosis)
- Mild anemia and muscle wasting and weakness
- Brittle hair and nails
- Dry and yellowish skin
- Growth of fine hair all over the body (lanugo)
- Severe constipation
- Low blood pressure
- Slowed breathing and pulse
- Damage to the structure and function of the heart
- Brain damage
- Multiorgan failure
- Drop in internal body temperature, causing a person to feel cold all the time
- Lethargy, sluggishness, or feeling tired all the time
- Infertility
Bulimia nervosa
Bulimia nervosa is a condition where people have recurrent and frequent episodes of eating unusually large amounts of food and feeling a lack of control over these episodes. This binge-eating is followed by behavior that compensates for the overeating such as forced vomiting, excessive use of laxatives or diuretics, fasting, excessive exercise, or a combination of these behaviors. People with bulimia nervosa may be slightly underweight, normal weight, or over overweight.
- Chronically inflamed and sore throat
- Swollen salivary glands in the neck and jaw area
- Worn tooth enamel and increasingly sensitive and decaying teeth as a result of exposure to stomach acid
- Acid reflux disorder and other gastrointestinal problems
- Intestinal distress and irritation from laxative abuse
- Severe dehydration from purging of fluids
- Electrolyte imbalance (too low or too high levels of sodium, calcium, potassium, and other minerals) which can lead to stroke or heart attack
Binge-eating disorder
Binge-eating disorder is a condition where people lose control over their eating and have reoccurring episodes of eating unusually large amounts of food. Unlike bulimia nervosa, periods of binge-eating are not followed by purging, excessive exercise, or fasting. As a result, people with binge-eating disorder often are overweight or obese. Binge-eating disorder is the most common eating disorder in the U.S.
- Eating unusually large amounts of food in a specific amount of time, such as a 2-hour period
- Eating even when you're full or not hungry
- Eating fast during binge episodes
- Eating until you're uncomfortably full
- Eating alone or in secret to avoid embarrassment
- Feeling distressed, ashamed, or guilty about your eating
- Frequently dieting, possibly without weight loss
Avoidant restrictive food intake disorder
Avoidant restrictive food intake disorder (ARFID), previously known as selective eating disorder, is a condition where people limit the amount or type of food eaten. Unlike anorexia nervosa, people with ARFID do not have a distorted body image or extreme fear of gaining weight. ARFID is most common in middle childhood and usually has an earlier onset than other eating disorders. Many children go through phases of picky eating, but a child with ARFID does not eat enough calories to grow and develop properly, and an adult with ARFID does not eat enough calories to maintain basic body function.
- Dramatic restriction of types or amount of food eaten
- Lack of appetite or interest in food
- Dramatic weight loss
- Upset stomach, abdominal pain, or other gastrointestinal issues with no other known cause
- Limited range of preferred foods that becomes even more limited (“picky eating” that gets progressively worse)
What are the risk factors for eating disorders?
Eating disorders can affect people of all ages, racial/ethnic backgrounds, body weights, and genders. Eating disorders frequently appear during the teen years or young adulthood but may also develop during childhood or later in life.
Researchers are finding that eating disorders are caused by a complex interaction of genetic, biological, behavioral, psychological, and social factors. Researchers are using the latest technology and science to better understand eating disorders.
One approach involves the study of human genes. Eating disorders run in families. Researchers are working to identify DNA variations that are linked to the increased risk of developing eating disorders.
Brain imaging studies are also providing a better understanding of eating disorders. For example, researchers have found differences in patterns of brain activity in women with eating disorders in comparison with healthy women. This kind of research can help guide the development of new means of diagnosis and treatment of eating disorders.

How are eating disorders treated?
It is important to seek treatment early for eating disorders. People with eating disorders are at higher risk for suicide and medical complications. People with eating disorders can often have other mental disorders (such as depression or anxiety) or problems with substance use. Complete recovery is possible.
Treatment plans are tailored to individual needs and may include one or more of the following:
- Individual, group, and/or family psychotherapy
- Medical care and monitoring
- Nutritional counseling
- Medications
Psychotherapies
Family-based therapy, a type of psychotherapy where parents of adolescents with anorexia nervosa assume responsibility for feeding their child, appears to be very effective in helping people gain weight and improve eating habits and moods.
To reduce or eliminate binge-eating and purging behaviors, people may undergo cognitive behavioral therapy (CBT), which is another type of psychotherapy that helps a person learn how to identify distorted or unhelpful thinking patterns and recognize and change inaccurate beliefs.
Evidence also suggests that medications such as antidepressants, antipsychotics, or mood stabilizers may also be helpful for treating eating disorders and other co-occurring illnesses such as anxiety or depression. The Food and Drug Administration’s (FDA) website has the latest information on medication approvals, warnings, and patient information guides.
How can I find a clinical trial for an eating disorder?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials
- Clinicaltrials.gov: Current Studies on Eating Disorders : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Where can I learn more about eating disorders?
Free brochures and shareable resources.
- Eating Disorders: About More Than Food : A brochure about the common eating disorders anorexia nervosa, bulimia nervosa, and binge-eating disorder, and various approaches to treatment. Also available en español .
- Let’s Talk About Eating Disorders : An infographic with facts that can help shape conversations around eating disorders. Also available in en español .
- Shareable Resources on Eating Disorders : Help support eating disorders awareness and education in your community. Use these digital resources, including graphics and messages, to spread the word about eating disorders.
- Mental Health Minute: Eating Disorders : Take a mental health minute to watch this video on eating disorders.
- Let’s Talk About Eating Disorders with NIMH Grantee Dr. Cynthia Bulik : Learn about the signs, symptoms, treatments, and the latest research on eating disorders.
Research and statistics
- NIMH Eating Disorders Research Program : This program supports research on the etiology, core features, longitudinal course, and assessment of eating disorders.
- Journal Articles : References and abstracts from MEDLINE/PubMed (National Library of Medicine).
- Statistics: Eating Disorders
Last Reviewed: January 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.
- Patient Care & Health Information
- Diseases & Conditions
- Eating disorders
Eating disorders are serious health conditions that affect both your physical and mental health. These conditions include problems in how you think about food, eating, weight and shape, and in your eating behaviors. These symptoms can affect your health, your emotions and your ability to function in important areas of life.
If not treated effectively, eating disorders can become long-term problems and, in some cases, can cause death. The most common eating disorders are anorexia, bulimia and binge-eating disorder.
Most eating disorders involve focusing too much on weight, body shape and food. This can lead to dangerous eating behaviors. These behaviors can seriously affect the ability to get the nutrition your body needs. Eating disorders can harm the heart, digestive system, bones, teeth and mouth. They can lead to other diseases. They're also linked with depression, anxiety, self-harm, and suicidal thoughts and behaviors.
With proper treatment, you can return to healthier eating habits and learn healthier ways to think about food and your body. You also may be able to reverse or reduce serious problems caused by the eating disorder.
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Symptoms vary, depending on the type of eating disorder. Anorexia, bulimia and binge-eating disorder are the most common eating disorders. People with eating disorders can have all different body types and sizes.
Anorexia (an-o-REK-see-uh), also called anorexia nervosa, can be a life-threatening eating disorder. It includes an unhealthy low body weight, intense fear of gaining weight, and a view of weight and shape that is not realistic. Anorexia often involves using extreme efforts to control weight and shape, which often seriously interfere with health and daily life.
Anorexia may include severely limiting calories or cutting out certain kinds of foods or food groups. It may involve other methods to lose weight, such as exercising too much, using laxatives or diet aids, or vomiting after eating. Efforts to reduce weight can cause severe health problems, even for those who continue eating throughout the day or whose weight isn't extremely low.
Bulimia (buh-LEE-me-uh), also called bulimia nervosa, is a serious, sometimes life-threatening eating disorder. Bulimia includes episodes of bingeing, commonly followed by episodes of purging. Sometimes bulimia also includes severely limiting eating for periods of time. This often leads to stronger urges to binge eat and then purge.
Bingeing involves eating food — sometimes an extremely large amount — in a short period of time. During bingeing, people feel like they have no control over their eating and that they can't stop. After eating, due to guilt, shame or an intense fear of weight gain, purging is done to get rid of calories. Purging can include vomiting, exercising too much, not eating for a period of time, or using other methods, such as taking laxatives. Some people change medicine doses, such as changing insulin amounts, to try to lose weight.
Bulimia also involves being preoccupied with weight and body shape, with severe and harsh self-judgment of personal appearance.
Binge-eating disorder
Binge-eating disorder involves eating food in a short amount of time. When bingeing, it feels like there's no control over eating. But binge eating is not followed by purging. During a binge, people may eat food faster or eat more food than planned. Even when not hungry, eating may continue long past feeling uncomfortably full.
After a binge, people often feel a great deal of guilt, disgust or shame. They may fear gaining weight. They may try to severely limit eating for periods of time. This leads to increased urges to binge, setting up an unhealthy cycle. Embarrassment can lead to eating alone to hide bingeing. A new round of bingeing commonly occurs at least once a week.
Avoidant/restrictive food intake disorder
Avoidant/restrictive food intake disorder includes extremely limited eating or not eating certain foods. The pattern of eating often doesn't meet minimum daily nutrition needs. This may lead to problems with growth, development and functioning in daily life. But people with this disorder don't have fears about gaining weight or body size. Instead, they may not be interested in eating or may avoid food with a certain color, texture, smell or taste. Or they may worry about what can happen when eating. For example, they may have a fear of choking or vomiting, or they may worry about getting stomach problems.
Avoidant/restrictive food intake disorder can be diagnosed in all ages, but it's more common in younger children. The disorder can result in major weight loss or failure to gain weight in childhood. A lack of proper nutrition can lead to major health problems.
When to see a doctor
An eating disorder can be difficult to manage or overcome by yourself. The earlier you get treatment, the more likely you'll make a full recovery. Sometimes people can have problem eating behaviors that are similar to some symptoms of an eating disorder, but the symptoms don't meet the guidelines for a diagnosis of an eating disorder. But these problem eating behaviors can still seriously affect health and well-being.
If you have problem eating behaviors that cause you distress or affect your life or health, or if you think you have an eating disorder, seek medical help.
Urging a loved one to seek treatment
Many people with eating disorders may not think they need treatment. One of the main features of many eating disorders is not realizing how severe the symptoms are. Also, guilt and shame often prevent people from getting help.
If you're worried about a friend or family member, urge the person to talk to a health care provider. Even if that person isn't ready to admit to having an issue with food, you can start the discussion by expressing concern and a desire to listen.
Red flags that may suggest an eating disorder include:
- Skipping meals or snacks or making excuses for not eating.
- Having a very limited diet that hasn't been prescribed by a trained medical professional.
- Too much focus on food or healthy eating, especially if it means not participating in usual events, such as sports banquets, eating birthday cake or dining out.
- Making own meals rather than eating what the family eats.
- Withdrawing from usual social activities.
- Frequent and ongoing worry or complaints about being unhealthy or overweight and talk of losing weight.
- Frequent checking in the mirror for what are thought to be flaws.
- Repeatedly eating large amounts of foods.
- Using dietary supplements, laxatives or herbal products for weight loss.
- Exercising much more than the average person. This includes not taking rest days or days off for injury or illness or refusing to attend social events or other life events because of wanting to exercise.
- Calluses on the knuckles from reaching fingers into the mouth to cause vomiting.
- Problems with loss of tooth enamel that may be a sign of repeated vomiting.
- Leaving during meals or right after a meal to use the toilet.
- Talk of depression, disgust, shame or guilt about eating habits.
- Eating in secret.
If you're worried that you or your child may have an eating disorder, contact a health care provider to talk about your concerns. If needed, get a referral to a mental health provider with expertise in eating disorders. Or if your insurance permits it, contact an expert directly.
The exact cause of eating disorders is not known. As with other mental health conditions, there may be different causes, such as:
- Genetics. Some people may have genes that increase their risk of developing eating disorders.
- Biology. Biological factors, such as changes in brain chemicals, may play a role in eating disorders.
Risk factors
Anyone can develop an eating disorder. Eating disorders often start in the teen and young adult years. But they can occur at any age.
Certain factors may increase the risk of developing an eating disorder, including:
- Family history. Eating disorders are more likely to occur in people who have parents or siblings who've had an eating disorder.
- Other mental health issues. Trauma, anxiety, depression, obsessive-compulsive disorder and other mental health issues can increase the likelihood of an eating disorder.
- Dieting and starvation. Frequent dieting is a risk factor for an eating disorder, especially with weight that is constantly going up and down when getting on and off new diets. There is strong evidence that many of the symptoms of an eating disorder are symptoms of starvation. Starvation affects the brain and can lead to mood changes, rigid thinking, anxiety and reduced appetite. This may cause severely limited eating or problem eating behaviors to continue and make it difficult to return to healthy eating habits.
- A history of weight bullying. People who have been teased or bullied for their weight are more likely to develop problems with eating and eating disorders. This includes people who have been made to feel ashamed of their weight by peers, health care professionals, coaches, teachers or family members.
- Stress. Whether it's heading off to college, moving, landing a new job, or a family or relationship issue, change can bring stress. And stress may increase the risk of an eating disorder.
Complications
Eating disorders cause a wide variety of complications, some of them life-threatening. The more severe or long lasting the eating disorder, the more likely it is that serious complications may occur. These may include:
- Serious health problems.
- Depression and anxiety.
- Suicidal thoughts or behavior.
- Problems with growth and development.
- Social and relationship problems.
- Substance use disorders.
- Work and school issues.
There's no sure way to prevent eating disorders, but you can take steps to develop healthy eating habits. If you have a child, you can help your child lower the risk of developing eating disorders.
To develop healthy eating habits and lifestyle behaviors:
- Choose a healthy diet rich in whole grains, fruits and vegetables. Limit salt, sugar, alcohol, saturated fat and trans fats. Avoid extreme dieting. If you need to lose weight, talk to your health care provider or a dietitian to create a plan that meets your needs.
- Don't use dietary supplements, laxatives or herbal products for weight loss.
- Get enough physical activity. Each week, get at least 150 minutes of aerobic activity, such as brisk walking. Choose activities that you enjoy, so you're more likely to do them.
- Seek help for mental health issues, such as depression, anxiety, or issues with self-esteem and body image.
For more guidelines on food and nutrition, as well as physical activity, go to health.gov.
Talk to a health care provider if you have concerns about your eating behaviors. Getting treatment early can prevent the problem from getting worse.
Here are some ways to help your child develop healthy-eating behaviors:
- Avoid dieting around your child. Family dining habits may influence the relationships children develop with food. Eating meals together gives you an opportunity to teach your child about the pitfalls of dieting. It also allows you to see whether your child is eating enough food and enough variety.
- Talk to your child. There are many websites and other social media sites that promote dangerous ideas, such as viewing anorexia as a lifestyle choice rather than an eating disorder. Some sites encourage teens to start dieting. It's important to correct any wrong ideas like this. Talk to your child about the risks of making unhealthy eating choices.
- Encourage and reinforce a healthy body image in your child, whatever their shape or size. Talk to your child about self-image and offer reassurance that body shapes can vary. Don't criticize your own body in front of your child. Messages of acceptance and respect can help build healthy self-esteem. They also can build resilience ⸺ the ability to recover quickly from difficult events. These skills can help children get through the challenging times of the teen and young adult years.
- Ask your child's health care provider for help. At well-child visits, health care providers may be able to identify early signs of an eating disorder. They can ask children questions about their eating habits. These visits can include checks of height and weight percentiles and body mass index, which can alert you and your child's provider to any big changes.
Reach out to help
If you notice a family member or friend who seems to show signs of an eating disorder, consider talking to that person about your concern for their well-being. You may not be able to prevent an eating disorder from developing, but reaching out with compassion may encourage the person to seek treatment.
- Feeding and eating disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5-TR. 5th ed. American Psychiatric Association; 2022. https://dsm.psychiatryonline.org. Accessed Nov. 16, 2022.
- Hales RE, et al. Feeding and eating disorders. In: The American Psychiatric Publishing Textbook of Psychiatry. 7th ed. American Psychiatric Publishing; 2019. https://psychiatryonline.org. Accessed Nov. 10, 2022.
- Eating disorders: About more than food. National Institute of Mental Health. https://www.nimh.nih.gov/health/publications/eating-disorders. Accessed Nov. 16, 2022.
- Eating disorders. National Alliance on Mental Illness. https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Eating-Disorders/Support. Accessed Nov. 16, 2022.
- What are eating disorders? American Psychiatric Association. https://www.psychiatry.org/patients-families/eating-disorders/what-are-eating-disorders. Accessed Nov. 16, 2022.
- Treasure J, et al. Eating disorders. The Lancet. 2020; doi:10.1016/S0140-6736(20)30059-3.
- Hay P. Current approach to eating disorders: A clinical update. Internal Medicine Journal. 2020; doi:10.1111/imj.14691.
- Bhattacharya A, et al. Feeding and eating disorders. Handbook of Clinical Neurology. 2020; doi:10.1016/B978-0-444-64123-6.00026-6.
- Uniacke B, et al. Eating disorders. Annals of Internal Medicine. 2022; doi:10.7326/AITC202208160.
- Fogarty S, et al. The role of complementary and alternative medicine in the treatment of eating disorders: A systematic review. Eating Behaviors. 2016; doi:10.1016/j.eatbeh.2016.03.002.
- Some imported dietary supplements and nonprescription drug products may harm you. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/some-imported-dietary-supplements-and-nonprescription-drug-products-may-harm-you. Accessed Nov. 16, 2022.
- Questions and answers about FDA's initiative against contaminated weight loss products. U.S. Food and Drug Administration. https://www.fda.gov/drugs/frequently-asked-questions-popular-topics/questions-and-answers-about-fdas-initiative-against-contaminated-weight-loss-products. Accessed Nov. 16, 2022.
- Mixing medications and dietary supplements can endanger your health. U.S. Food and Drug Administration. https://www.fda.gov/consumers/consumer-updates/mixing-medications-and-dietary-supplements-can-endanger-your-health. Accessed Nov. 16, 2022.
- Lebow JR (expert opinion). Mayo Clinic. Dec. 1, 2022.
- 2020-2025 Dietary Guidelines for Americans. U.S. Department of Health and Human Services and U.S. Department of Agriculture. https://www.dietaryguidelines.gov. Accessed Feb. 3, 2023.
- Long MW, et al. Cost-effectiveness of 5 public health approaches to prevent eating disorders. American Journal of Preventive Medicine. 2022; doi:10.1016/j.amepre.2022.07.005.
- Health.gov. https://health.gov/. Accessed Feb. 7, 2023.
- Eating disorder treatment: Know your options
Mayo Clinic in Rochester, Minnesota, has been recognized as one of the top Psychiatry hospitals in the nation for 2023-2024 by U.S. News & World Report.
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
Overview – Eating behaviour
This A level psychology topic looks at the psychology and biology underlying eating behaviour, such as different food preferences and the psychology of eating disorders:
- Explanations of food preferences (including evolutionary and learning explanations )
- The biological mechanisms involved in the control of eating (including the role of the hypothalamus and the hormones ghrelin and leptin )
- Explanations of anorexia nervosa (including biological explanations such as genetics and neural factors , as well as psychological explanations such as family systems theory , social learning theory , and cognitive explanations )
- Explanations of obesity (including biological explanations such as genetics and neural factors , as well as psychological explanations such as the boundary model and restraint theory )
Explanations of food preferences
Evolutionary explanations.
Evolution is the process by which species adapt to their environment. Over many many years, random mutations in genes that are advantageous to the animal become more widespread among the species.
In the case of food, evolution would mean genes that help humans identify and eat healthy, safe, and nutritious food will become more common. If you had genes that resulted in a preference for nutritious and commonly-found foods, for example, you would be less likely to starve and more likely to remain healthy and pass on those genes. In contrast, if you had genes that meant you really liked the taste of deadly mushrooms, you probably wouldn’t live long enough to reproduce and pass on those genes.

Neophobia is an innate dislike of foods we haven’t tried before. This makes sense from an evolutionary perspective as unfamiliar foods could potentially be poisonous or unhealthy. You’re more likely to survive if you stick with familiar foods as you already know they’re safe.
We overcome neophobia via learning . In a study of young children, Birch et al (1987) found that preference for new foods increased over time with repeated exposure to those foods.
Taste aversion
Taste aversion is when a person develops a dislike for a certain food after becoming ill from it. For example, you eat yoghurt, get food poisoning, and from then on even the thought of eating yoghurt again makes you feel sick.
Although kind of like classical conditioning , taste aversion doesn’t work in quite the same way because the time between eating the food and getting ill is often quite long. Instead, the more accurate description is biological preparedness ( Seligman (1971) ), which is the idea that humans are biologically hard-wired to learn certain kinds of associations very easily. This would make sense from an evolutionary perspective: If certain foods are dangerous, it would be advantageous to learn this as quickly as possible because the next time you eat that food you might get ill again or die.
- Evidence supporting evolutionary explanations: Several studies (e.g. Desor et al (1973) , Steiner (1979) , and Rosenstein and Oster (1988) ) have analysed the facial expressions and behaviours of babies after feeding them bitter- and sweet-tasting foods, finding that babies like sweet tastes and dislike bitter ones. The fact that the babies have these food preferences from such a young age suggests they are innate, supporting evolutionary explanations of food preferences.
- Evolved for survival in a different era: Human food preferences would have evolved in a time when food was scarce, but these food preferences are somewhat maladaptive in the modern era where food is plentiful. For example, early humans would feast on high energy and fattening foods on the rare occasions when they were available in order to prevent starvation. However, such foods are now easily available and so these evolutionary preferences can lead to obesity in the modern era.
- Other factors: Although evolution plays a role in shaping food preferences, other factors influence food preferences too. For example, social influences can override evolutionarily-programmed neophobia, such as a mother feeding her child new foods. Cultural influences are also important. For example, a person may have genetics that predispose them towards liking the taste of Marmite, but if they are not raised in a culture that has Marmite then they may never develop this taste.
The role of learning
In addition to genetic/evolutionary factors , humans also learn food preferences from social influences and their culture .
Social influences
There are several ways social influences affect food preferences.
Firstly, what a child’s mother eats during development affects the child’s food preferences. In the womb, foods (and flavours) the mother eats are fed to the baby via the amniotic fluid. After birth, foods and flavours are transmitted from the mother to the baby via breast milk. This contributes towards a preference for the same foods as the mother.

Thirdly, operant conditioning also contributes to food preferences. If you enjoy eating a certain food, then that enjoyment serves as positive reinforcement, which increases the chances of you eating it again. However, research suggests that operant conditioning doesn’t really work to create food preferences. For example, if parents try to teach their children to like certain foods (e.g. vegetables) through rewards (e.g. praise for eating vegetables), it may actually decrease preference for those foods.
Cultural influences
Different cultures have different eating behaviours and these cultural influences affect food preferences. For example, some religious cultures (e.g. Islam and Judaism) forbid eating pork, whereas others forbid eating beef (e.g. Hinduism). Different cultures also have different local cuisines (e.g. eating snails in France (escargots), raw octopus in Korea (san-nakji)), which affect food preferences.
- Evidence supporting learning explanations: Mennella et al (2005) found that genetics primarily determine food preferences in children (e.g. liking sweet tastes and disliking bitter ones) but by adulthood environmental factors are far more important, supporting learning explanations of food preferences.
- Changing influence of culture on food preferences: Advances in transportation (e.g. shipping) and technology (e.g. refrigeration) mean people have access to, and develop preferences for, foods they otherwise would not have. For example, avocados can’t be grown in the UK, which in the past would mean people living in the UK would not develop a taste for avocados. These economic and technological changes have reduced the impact of local culture on food preferences, making food preferences more global.
- Practical applications: Understanding the social and cultural influences of food preferences has useful applications. For example, if mothers transmit food preferences to their children in the womb, it makes sense for mothers to eat healthily during pregnancy to avoid passing on a taste for unhealthy foods to their children. In the case of culture, health agencies can tailor dietary advice to the culture they operate in.
Neural and hormonal mechanisms
Neural and hormonal mechanisms control eating behaviour biologically, making you feel hungry or full. The main neural mechanism is activity in the hypothalamus region of the brain, and the main hormones responsible for hunger and satiety are ghrelin and leptin .
Neural mechanisms
Hypothalamus.
The hypothalamus is the main section of the brain responsible for maintaining homeostasis (i.e. stability and normal functioning) within the body. It controls things like body temperature, sleep, and hunger.
In the case of hunger, there are two sections of the hypothalamus that have opposite effects:
- Lateral hypothalamus: Responsible for making you feel hungry and start eating.
- Ventromedial hypothalamus: Responsible for making you feel full ( satiety ) and stop eating.
The process is as follows: When blood sugar (glucose) is low, the liver sends signals to the lateral hypothalamus. This causes neurons to fire that make you feel hungry and start eating. Then, when you eat, glucose is released into the blood, which is detected by the ventromedial hypothalamus. This causes neurons to fire that make you feel satiated (full).
Ghrelin is a hormone that makes you feel hungry. It is secreted by the stomach into the bloodstream, which is detected by the hypothalamus , creating the sensation of hunger. When you eat food, the stomach stops releasing ghrelin, which stops you feeling hungry. After the meal is eaten, ghrelin levels (and hunger) progressively increase until the next time you eat.
Leptin is a hormone that makes you feel full. It is secreted by fat cells into the bloodstream, which signals to the hypothalamus that energy storage (fat deposits) is high and so you don’t need to eat. If you don’t eat for a while, the body uses these fat deposits for energy, and so those fat cells no longer exist to produce leptin. This reduction in leptin makes you feel hungry.
Explanations of anorexia
The syllabus looks at biological and psychological explanations of anorexia.
Biological explanations
Biological explanations of anorexia look at the role of genetics and neural factors (such as brain structures and neurotransmitter activity).
The genetic explanation of anorexia looks at hereditary factors – i.e. genes inherited from parents – that contribute to the development of anorexia.
As always, twin studies are a useful way to work out the extent to which a condition is genetically determined. If identical twins are more likely to both suffer from anorexia than both non-identical twins are, this would suggest anorexia is (at least partly) determined by genetics. Twin studies of anorexia include:
- Holland et al (1988) found a concordance rate for anorexia of 56% for identical twins and 5% for non-identical twins.
- Kortegaard et al (2001) found a concordance rate for anorexia of 18% for identical twins and 7% for non-identical twins.
- Bulik et al (2006) estimate the heritability of anorexia is 56% based on analysis of 31,406 pairs of Swedish twins.
Despite variations in estimates, the fact that identical twins are more likely to both suffer from anorexia than non-identical twins suggests there is a genetic component to the disorder.
The role of genetics is further supported by gene association studies (e.g. Wang et al (2011) and Scott-Van Zeeland et al (2014) ), which compare DNA profiles of anorexia sufferers with non-anorexic controls. These studies have found various genes to be correlated with anorexia, such as OPRD1, HTR1D, and EPHX2.
Strengths of genetic explanations:
- Evidence supporting genetic explanations: See studies above (don’t worry, you don’t have to remember all of them – they’re just examples).
Weaknesses of genetic explanations:
- Other factors: Although there is strong evidence for a genetic component to anorexia, the evidence also suggests that other factors are important too. For example, if anorexia was entirely explained by genetics, concordance rates among identical twins would be 100% – but they’re not. The fact that even the highest figures estimate anorexia to be 56% heritable leaves 44% to be accounted for by factors other than genetics.
- Limitations of genetic explanations: Anorexia was practically unheard of before 1950 but since then rates of anorexia have increased significantly. This change is far too quick to be explained by genetics because only a few generations have passed since then. This suggests factors other than genetics (e.g. social learning theory ) are contributing to the rise in anorexia diagnoses.
- Methodological concerns with twin studies: Twin studies typically assume that twins have identical upbringings and so any differences in concordance rates between identical and non-identical twins must be explained entirely by genetics. However, environmental factors may play a more important role than studies assume. For example, looking identical probably makes parents treat identical twins more similarly than they would non-identical twins. This may explain (at least partly) why identical twins have higher concordance rates for anorexia than non-identical twins, which would mean the role of genetics is exaggerated.
Neural factors
Neural explanations of anorexia look at differences in the brain structures and neurochemistry of people with anorexia.
Some research suggests that people with anorexia have reduced blood flow in the lateral hypothalamus (the part of the brain associated with hunger), but it is unclear whether this is a cause or an effect of anorexia. More recently, researchers (e.g. Nunn et al (2011) ) have proposed that damage to the insula cortex of the brain is a key cause of anorexia.
In addition to physical brain structures, neural explanations of anorexia also focus on the role of neurotransmitters . For example, several studies have found correlations between serotonin activity and anorexia, although the exact relationship is unclear. One hypothesis proposed by Kaye et al (2009) is that anorexic patients naturally have elevated serotonin activity, which causes them anxiety. Starvation reduces serotonin levels (food is needed to produce serotonin), which reduces this anxiety and reinforces anorexic behaviour. Research (e.g. Bailer et al (2013) ) also suggests over-production of the neurotransmitter dopamine may contribute to anorexia.
Strengths of neural explanations:
- Evidence supporting neural explanations: See studies above (again, you don’t have to remember all of them – they’re just examples).
- Practical applications: If neural explanations of anorexia are identified, this could lead to effective ways to treat the disorder. For example, some studies suggest SSRIs can improve anorexia outcomes by altering neurotransmitter activity (although other studies dispute this).
Weaknesses of neural explanations:
- Conflicting evidence: Much of the research linking neurotransmitter activity and anorexia is contradictory. For example, a review by Kontis and Theochari (2012) reports how different studies have suggested anorexia is linked with normal, increased, and decreased dopamine activity.
- Correlation vs. causation: Even if certain abnormalities in brain structures (or neurotransmitter activity) are correlated with anorexia, this doesn’t automatically prove that this is the cause of anorexia. For example, reduced blood flow in the lateral hypothalamus could be an effect of starvation rather than a cause of anorexia.
Psychological explanations
There are several psychological explanations of anorexia , including family systems theory , social learning theory , and cognitive explanations .
Family systems theory
Minuchin et al (1978) proposed the family systems theory of anorexia, which is a psychodynamic theory that explains anorexia as a result of family dysfunction. According to the family systems theory, the families of anorexic patients often share four key features:
- Enmeshment: The family members have no individual identity or independence but instead blur into one single unit. For example, they are very involved in each other’s business, spend all their time together, and nobody has any unique role within the family.
- Overprotective: The family is very controlling and overprotective, which makes it more difficult for members to break free from the enmeshment and develop their own identity.
- Conflict avoidance: The family ignores or suppresses conflict. For example, they won’t discuss obvious problems.
- Rigidity: The family does not like change and tries to keep things as they are.
This dysfunctional family style can contribute to anorexia in various ways. For example, becoming anorexic may be a way to reduce conflict by distracting the family members from other problems. For example, a child who fears their parents will split up due to constant arguing may become anorexic in order to shift the parents’ attention away from those arguments, keeping the family together.
A related explanation (e.g. Bruch (1978) ) is that anorexia is a way for people to assert autonomy and control . For example, refusing to eat might be a way for a family member to assert their individuality and free will against their overprotective and enmeshed family.
Strengths of family systems theory:
- Evidence supporting family systems theory: In Minuchin et al (1978) , the researchers got 11 families of anorexic patients and 34 control families to complete a group task. The researchers observed greater levels of enmeshment, overprotectiveness, conflict avoidance, and rigidity among the families of anorexic patients, providing support for all four elements of the family systems model.
- Practical applications: Some studies have found family systems therapy to be an effective treatment for anorexia. For example, Robin et al (1999) randomly assigned 37 anorexic patients to receive either family systems therapy or individual therapy. Although both treatments were found to be effective, the family systems therapy group saw greater weight gains and a faster return to health. However, a review of several trials by Fisher et al (2019) found the evidence was insufficient to say family-based treatments are more effective than other approaches.
Weaknesses of family systems theory:
- Conflicting evidence: A review of 17 studies by Viesel and Allan (2014) found that anorexia and family dysfunction were correlated . However, the researchers did not find evidence for a specific pattern of family dysfunction (e.g. enmeshment), weakening support for Minuchin et al’ s family systems model.
- Other factors: Even if family dysfunction does contribute to anorexia, it’s unlikely to be the sole cause. For example, many anorexic patients develop anorexia in adulthood – long after leaving their families – which suggests that other factors (e.g. biology or social learning ) contribute to the disorder as well.
- Correlation vs. causation: Even if certain types of family dysfunction (e.g. enmeshment) are correlated with anorexia, this does not automatically prove this is what causes anorexia. For example, a child developing anorexia could cause a previously normal family to become more enmeshed, rather than the other way round.
Social learning theory
Social learning theory ( see the approaches page for more details ) explains anorexia as learned behaviour from observation and imitation of role models.
According to social learning theory, people imitate the behaviours of role models they identify with. These behaviours may be enforced vicariously, i.e. by seeing the role model be praised and rewarded for that behaviour. This can be applied to anorexia:
- Modelling: A person who the anorexic patient either likes or wants to be like. For example, an older sister or a celebrity who is thin.
- Vicarious reinforcement: The anorexic patient observes the role model being rewarded and praised for being thin. For example, the slim sister is complimented on her weight loss, or the slim celebrity has lots of followers on social media. These rewards create a motivation to imitate their behaviour and restrict eating.
The syllabus mentions social learning theory specifically, but other learning approaches ( operant conditioning ) may also reinforce anorexic behaviour. For example, when the anorexic patient starts imitating the behaviour themself, they may receive compliments for being slim (positive reinforcement) or people may stop criticising them for being overweight (negative reinforcement).

Strengths of social learning explanations:
- Evidence supporting social learning explanations: For example, Dittmar et al (2006) showed 162 girls (aged 5-8) either Barbie dolls, Emme dolls (a US size 16), or no dolls and then got them to complete a body image assessment. The girls shown the Barbie dolls had lower body esteem and a greater desire to be thin than the other two groups, supporting the explanation that role models in the media and culture may contribute to anorexia. Another study, Garner et al (1980) , looked at data from Playboy magazine models and Miss America contests over the years and found a trend towards a thinner standard of beauty over time, further supporting the social learning explanation.
- Explanatory power: Social learning theory is able to explain aspects of anorexia that other explanations aren’t. For example, anorexia has increased significantly since 1950 – far quicker than can be explained via changes in genetics . But social learning theory can explain this by pointing to things like growing emphasis on thinness in the media and culture during this time.
- Practical applications: If the social learning theory explanation of anorexia is correct, then it can be used to develop ways to treat and prevent anorexia. For example, the media could promote desirable heavier women as much as it does thinner women.
Weaknesses of social learning explanations:
- Other factors: Even if social learning and media influence contribute to anorexia, it’s unlikely this is the sole cause. For example, all women in Western countries are exposed to the same amount of media influence (more or less), and yet only some of these women develop anorexia. This suggests that other factors (e.g. biology ) play a role too.
Cognitive explanations
Cognitive explanations of anorexia explain the disorder as a result of abnormal cognitions. These abnormal cognitions take the form of distortions and irrational beliefs:
- E.g. The person sees their body as fat and overweight when actually it is skinny and underweight.
- E.g. “If I eat one crisp, I will get fat” or “If I can’t control my weight, I’m worthless”.
Strengths of cognitive explanations:
- Evidence supporting cognitive explanations: Several studies have found anorexic patients to have distorted body image compared to controls. For example, Williamson et al (1993) used silhouette pictures to evaluate 37 anorexic patients’ current and ideal body images. Compared to the control group , the anorexic patients’ estimation of their current body size was larger and their ideal body image was thinner, supporting the role of cognitive distortions in anorexia. Studies also support the presence of irrational beliefs in anorexia. For example, Steinglass et al (2007) investigated the main belief that prevented anorexic patients from eating. Of 25 anorexic patients surveyed, 68% had a main fear of gaining weight and 20% were categorised as delusional, supporting the role of irrational beliefs in anorexia.
- Practical applications: Cognitive explanations of anorexia have been used to develop effective treatments for the disorder. For example, Grave et al (2014) used cognitive behavioural therapy with 26 anorexia patients, which resulted in improvements in weight and anorexia symptoms that were still maintained at 12-month follow up.
Weaknesses of cognitive explanations:
- Conflicting evidence: In a study comparing 30 anorexic women with 137 controls, Cornelissen et al (2013) found no significant difference in body image estimates, which contradicts Williamson et al (1993) and weakens support for the role of cognitive distortions in anorexia.
- Other factors: Even if cognitive factors play a role in anorexia, it’s clear other factors are important too. For example, twin studies provide strong evidence for a genetic component to anorexia. It’s likely that many factors – cognitive, social, biological – combine to cause anorexia.
- Correlation vs. causation: Although cognitive distortions and irrational beliefs are correlated with anorexia, they may not be the cause of anorexia. For example, cognitive distortions may be a symptom of anorexia rather than the cause.
Explanations of obesity
The syllabus looks at biological and psychological explanations of obesity.
Biological explanations of obesity look at the role of genetics and neural factors (such as brain structures and neurotransmitter activity).
The genetic explanation of obesity looks at hereditary factors – i.e. genes inherited from mother and father – that make someone more or less likely to become obese.
Again, as always, family and twin studies are a useful way to work out the influence of genetics on obesity. Some examples include:
- Stunkard et al (1990) compared concordance rates of obesity among identical twins raised together and identical twins raised apart (and also non-identical twins raised together and apart). Male and female identical twins raised together had concordance rates of 74% and 69% respectively, whereas male and female twins raised apart had concordance rates of 70% and 66% respectively. The similarity between these two sets of figures suggests the different environments had little impact on obesity rates compared to genetics.
- Nan et al (2012) estimate the concordance rate of obesity among identical twins is 61-80%.
- Chaput et al (2014) looked at obesity among families, estimating that obesity is 35-60% heritable.
In addition to these family studies, genome association studies compare the genetic profiles of obese individuals with non-obese controls to identify genes that may contribute to obesity. For example, several studies (e.g. Fall and Ingelsson (2012) , Frayling et al (2007) , and Hinney et al (2007) ) have found the FTO gene to be correlated with obesity. However, there is no single obesity gene – many genes appear to combine to increase or decrease a person’s risk for obesity.
- Evidence supporting genetic explanations: See studies above (again, you don’t need to remember them all – they’re just examples).
- Practical applications: An understanding of the genetic basis for obesity could lead to effective treatments for the disorder. For example, genetics may mean certain foods may be particularly fattening for some individuals, which could inform diet plans that help them lose weight more effectively.
- Other factors: Although there is evidence of a genetic component to obesity, there is clearly more to the story than just genes. For example, the concordance rates of obesity among identical twins is far less than 100%, which suggests other factors (e.g. psychological ) play a role too.
- Limitations of genetic explanations: Obesity has increased dramatically over the last few decades (see chart below). This change has happened far too quickly to be explained by genetics as only a few generations have passed during this time. This further suggests that other factors (e.g. changing dietary habits) play an important role in explaining obesity.
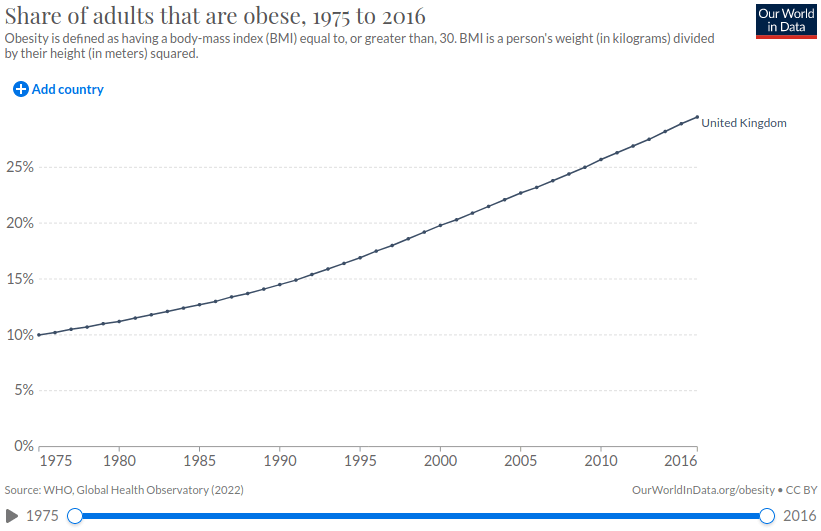
Neural explanations of obesity focus on the neural mechanisms that control eating behaviour as well as the role of neurotransmitters such as serotonin and dopamine.
As described above, the hypothalamus plays a key role in eating behaviour. Some neural explanations say that damage to the ventromedial hypothalamus – the area of the brain responsible for making you feel full – can cause obesity. Other explanations look at the role of leptin – the hormone that makes you feel full – saying that obesity can be caused by neurons that don’t respond properly to this hormone.
Neurotransmitters are also implicated in obesity. For example, Wang et al (2001) and Volkow et al (2008) have used brain scans to measure dopamine receptor activity in obese individuals and controls, with both studies finding that obese individuals have reduced dopamine receptor activity. Dopamine is associated with pleasure and reward and so the associated hypothesis is that obese people overeat to get the same pleasure and reward response as a non-obese person would get from eating less food. This is a similar mechanism to other addictions , such as smoking or drugs.
Other studies (e.g. Hodge et al (2012) and Vickers et al (1999) ) suggest lower serotonin levels are also correlated with obesity.
- Evidence supporting neural explanations: See studies above.
- Practical applications: Identifying the neural factors that cause obesity could lead to new ways to treat the disorder. For example, some studies (e.g. Heymsfield et al (1999) ) suggest leptin injections may be a successful treatment for obesity in some people. Other treatments could address dopamine and serotonin deficiencies.
- Conflicting evidence: For each neural explanation of obesity, there are often several studies that contradict it. For example, a meta-analysis of 33 studies by Benton and Young (2016) found lower dopamine receptor activity is not correlated with obesity, contradicting the findings of Wang et al (2001) and Volkow et al (2008) described above.
- Other factors: Although there is some evidence supporting neural explanations obesity, it’s likely other factors, such as genetics , play a larger role in explaining the disorder.
- Correlation vs. causation: Even if certain neurological patterns (e.g. low dopamine sensitivity) are correlated with obesity, this doesn’t prove these neurological patterns cause obesity. For example, obesity could be caused entirely by psychological factors, with low dopamine sensitivity simply being a symptom of the disorder.
There are several psychological explanations of obesity , including the boundary model and restraint theory . This section also looks at psychological explanations of the success and failure of dieting .
Boundary model
Herman and Polivy (1984) proposed the boundary model . According to this model, people have biologically-set boundaries of food intake. If food falls below a certain minimum level, the person feels the aversive (unpleasant) feeling of hunger that motivates them to eat. At the other end, eating too much food exceeds the maximum level, which causes the aversive feeling of being too full. These levels are primarily determined by biology .

The range in the middle is the zone of biological indifference, where a person’s biology is satisfied. And so, within this zone, psychological factors are more important than biological ones in determining whether a person eats. In other words, a person who consumes food within this zone does not do so for biological reasons (i.e. to avoid starvation), but for psychological reasons.
Restraint theory
According to restraint theory , trying to eat less can paradoxically make a person eat more and become obese.
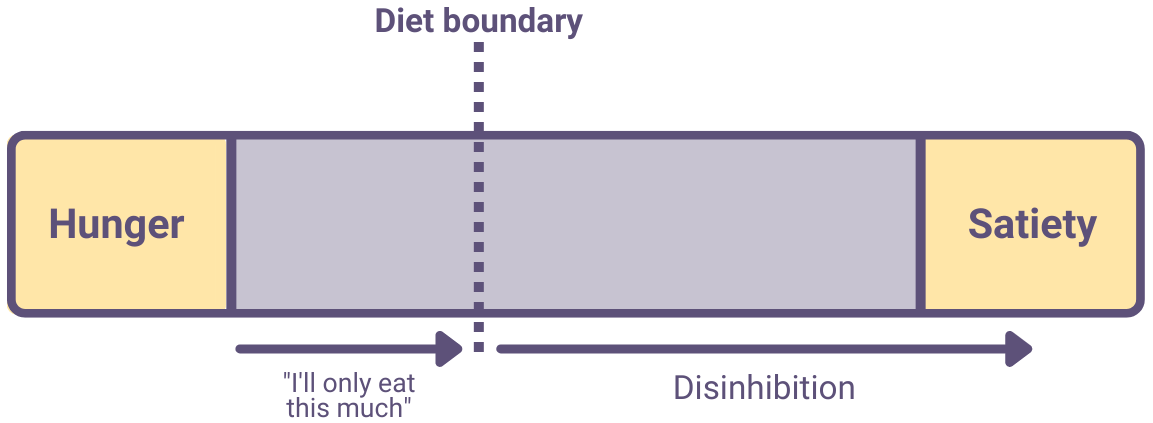
One explanation of this is as follows:
- A restrained eater will set a diet boundary. This is a self-imposed cognitive limit after which they won’t eat any more.
- Setting this boundary causes the restrained eater to spend a lot of time thinking about food – more so than if they hadn’t set a diet boundary. Also, the diet boundary may be unrealistically low, causing constant hunger and low mood.
- When the person crosses their diet boundary (as often happens), their eating may become disinhibited: They give up trying to control their eating and keep eating until they’re full (or beyond).
- Disinhibited eating causes obesity.
Strengths of restraint theory:
- Evidence supporting restraint theory: For example, Herman and Mack (1975) categorised 45 normal-weight women as restrained (i.e. dieting) or unrestrained (i.e. non-dieting) eaters. The women were randomly separated into groups given either one glass of milkshake, two glasses of milkshake, or nothing. After the milkshakes, they were then given unlimited ice cream to eat. The researchers found that the unrestrained eaters ate less ice cream the more milkshakes they’d had previously, which is to be expected as presumably they were already full. However, the restrained eaters actually ate more ice cream the more milkshakes they’d had previously, suggesting they had become disinhibited . Further studies supporting restraint theory include Ruderman and Wilson (1979) and Wardle and Beales (1988) .
- Practical applications: It seems obvious that dieting is an effective way to lose weight, but restraint theory suggests the opposite might actually be true. Knowing this could lead to more effective ways to reduce obesity. For example, Bergh et al (2009) describes how training people to eat more slowly (rather than dieting) might be an effective treatment for obesity.
Weaknesses of restraint theory:
- Conflicting evidence: There are many examples of people who have successfully lost weight via dieting, which weakens support for restraint theory. For example, in a longitudinal study of 163 women, Savage et al (2009) found that restrained eating and dieting were correlated with weight loss, not weight gain. This directly contradicts the predictions of restraint theory and challenges its validity .
- Correlation vs. causation: Being a restrained eater may simply be correlated with obesity, rather than a cause of obesity. For example, people who are naturally prone to obesity may be more likely to set themselves dietary restrictions, rather than these dietary restrictions causing them to become obese.
Explanations of the success/failure of dieting
A diet is successful if the dieter loses the desired amount of weight and keeps it off for the long-term. There are many factors that contribute to the success or failure of dieting .
Factors that increase the chance of success include:
- Realistic expectations: Dieters are more likely to succeed if they follow a sustainable diet and steadily lose weight over a period of months and years, setting realistic short- and long-term goals.
- Incentives and motivation: Dieters may reward themselves for achieving weight loss goals. For example, a dieter may buy new clothes to fit their slimmer physique. This works as a form of operant conditioning , reinforcing and motivating weight loss.
- Social support: Having support from family and friends makes a diet more likely to succeed. For example, Wing and Jeffery (1999) randomly assigned 166 participants to receive either a standard 4-month weight loss program or a standard 4-month weight loss program + social support . At follow up 6 months later, 66% of participants in the social support group had maintained their weight loss compared to just 24% in the group without social support.
- Relapse prevention strategies: Many dieters see dieting as a temporary measure after which they can return to their old eating habits. This results in a demotivating cycle of regaining lost weight and then dieting again (yo-yo dieting). Dieters who have strategies to avoid going back to their previous eating behaviours and maintain a stable food intake are more likely to succeed.
Factors that increase the chance of failure include:
- Overly-restrictive diets: Dieters often try to follow diets that are too strict, such as limiting calories to under 1000 per day. This is unsustainable and when the dieter exceeds this limit they may lose motivation and indulge in disinhibited eating (in line with the predictions of restraint theory ).
- Unrealistic expectations: Dieters often expect to lose a lot of weight in a matter of weeks or months. However, obese people typically gained weight progressively over many years and so it is unrealistic to expect to reverse this in a short time period. If the dieter does not have realistic expectations, they may lose motivation and abandon the diet.
In addition to these psychological factors, other factors (e.g. genetics ) affect the success or failure of dieting.
- Individual differences: Although there are general ways to increase the chance of diet success, the best approach is likely to vary from person to person. For example, restrained eaters are unlikely to successfully lose weight via calorie restriction because this is likely to result in disinhibited eating. Unrestrained eaters, in contrast, are likely to have more success with calorie restriction.
- Practical applications: Understanding the factors that increase the likelihood of diet success could lead to more effective ways to treat obesity. For example, providing social support in addition to a realistic diet plan is likely to increase the chance of successful and sustainable weight loss.
- Gender bias : The majority of research into dieting is done on females, and so the conclusions drawn from this research may not be valid in males.
<<<Relationships
<<<gender, <<<cognition and development, aggression>>>, forensic psychology>>>, addiction>>>.
- Undergraduate
- High School
- Architecture
- American History
- Asian History
- Antique Literature
- American Literature
- Asian Literature
- Classic English Literature
- World Literature
- Creative Writing
- Linguistics
- Criminal Justice
- Legal Issues
- Anthropology
- Archaeology
- Political Science
- World Affairs
- African-American Studies
- East European Studies
- Latin-American Studies
- Native-American Studies
- West European Studies
- Family and Consumer Science
- Social Issues
- Women and Gender Studies
- Social Work
- Natural Sciences
- Pharmacology
- Earth science
- Agriculture
- Agricultural Studies
- Computer Science
- IT Management
- Mathematics
- Investments
- Engineering and Technology
- Engineering
- Aeronautics
- Medicine and Health
- Alternative Medicine
- Communications and Media
- Advertising
- Communication Strategies
- Public Relations
- Educational Theories
- Teacher's Career
- Chicago/Turabian
- Company Analysis
- Education Theories
- Shakespeare
- Canadian Studies
- Food Safety
- Relation of Global Warming and Extreme Weather Condition
- Movie Review
- Admission Essay
- Annotated Bibliography
- Application Essay
- Article Critique
- Article Review
- Article Writing
- Book Review
- Business Plan
- Business Proposal
- Capstone Project
- Cover Letter
- Creative Essay
- Dissertation
- Dissertation - Abstract
- Dissertation - Conclusion
- Dissertation - Discussion
- Dissertation - Hypothesis
- Dissertation - Introduction
- Dissertation - Literature
- Dissertation - Methodology
- Dissertation - Results
- GCSE Coursework
- Grant Proposal
- Marketing Plan
- Multiple Choice Quiz
- Personal Statement
Power Point Presentation
- Power Point Presentation With Speaker Notes
- Questionnaire
- Reaction Paper
- Research Paper
- Research Proposal
- SWOT analysis
- Thesis Paper
- Online Quiz
- Literature Review
- Movie Analysis
- Statistics problem
- Math Problem
- All papers examples
- How It Works
- Money Back Policy
- Terms of Use
- Privacy Policy
- We Are Hiring
Eating Disorders, Essay Example
Pages: 6
Words: 1701
Hire a Writer for Custom Essay
Use 10% Off Discount: "custom10" in 1 Click 👇
You are free to use it as an inspiration or a source for your own work.
Introduction
Eating disorders affect men and women of all ages, although adolescents tend to be the age group that is more susceptible. This is because, as their bodies are changing, they may feel more pressure by society as well as peer groups to look attractive and fit in (Segal et al). Types of eating disorders include Anorexia, Bulimia and Compulsive Overeating, which can also be related to the first two. The reasons behind Eating Disorder usually stem from a reaction to low self-esteem and a negative means of coping with life and stress (Something Fishy). Eating disorders are also often associated with an underlying psychological disorder, which may be the reason behind the eating disorder or which may develop from the Eating Disorder itself. Mental health disorders that are often associated with Eating Disorder include Anxiety, Depression, Multiple Personality Disorder, Obsessive Compulsive Disorder, Post Traumatic Stress Disorder, BiPolar, BiPolar II, Borderline Personality Disorder, Panic Disorder and Dissociative Disorder. The longer a person suffers from ED, the more probable that they will be dealing with another mental illness, most likely Anxiety or Depression (Something Fishy). The eventual outcome of Eating Disorder can be deadly. “Some eating disorders are associated with a 10-15% mortality rate and a 20-25% suicide rate. Sometimes, anorexia, bulimia and compulsive eating may be perceived as slow suicide (Carruthers).” In order to prevent the deadly consequences of Eating Disorder and to prevent it from becoming more pervasive in society, it is necessary to recognize the correct treatment method for this disease. Traditional treatments have focused on providing risk information to raise awareness of the consequences of Eating Disorder (Lobera et al 263). However, since Eating Disorder is a mental illness, a more effective treatment is one that offers psychological evaluation, counseling and treatment. Cognitive Behavioral Therapy is emerging as a more robust and effective method that can be used not only to treat Eating Disorder but the associated mental illnesses that may accompany it.
The Problem
Eating disorder is pervasive in society and can have deadly consequences on those that suffer from it. Many time Eating Disorder goes undetected by family members and friends because those suffering will go to great lengths to hide their problem. However, there are some signs and symptoms that can be clues that a person is suffering from some sort of eating disorder. According to Segal, these signs can include:
- Restricting Food or Dieting: A change in eating habits that includes restricting food or excessive dieting. The person my frequently miss meals or not eat, complaining of an upset stomach or that they are not hungry. A use of diet pills or illegal drugs may also be noticed.
- Bingeing: Sufferers may binge eat in secret, which can be hard to detect since they will usually do it late at night or in a private place. Signs of potential bingeing are empty food packages and wrappers and hidden stashes of high calorie junk food or desserts.
- Purging: Those who suffer from bulimia will force themselves to throw up after meals to rid their body of added calories. A sign that this is occurring is when a person makes a trip to the bathroom right after eating on a regular basis, possible running water or a fan to hide the sound of their vomiting. They may also use perfume, mouthwash or breath mints regularly to disguise the smell. In addition to vomiting, laxatives or diuretics may also be used to flush unwanted calories from the body.
- Distorted body image and altered appearance: People suffering from Eating Disorder often have a very distorted image of their own body. While they may appear thin to others, they may view themselves as fat and attempt to hide their body under loose clothing. They will also have an obsessive preoccupation with their weight, and complain of being fat even when it is obvious to others that this is not the case.
There are several possible side effects from Eating Disorders, both physical and psychological. Physical damage can be temporary or permanent, depending on the severity of the eating disorder and the length of time the person has been suffering from it. Psychological consequences can be the development of a mental illness, especially depression and anxiety. Some sufferers of Eating Disorder will also develop a coping mechanism such as harming themselves, through cutting, self-mutilation or self-inflicted violence, or SIV (Something Fishy).
Physical consequences of Eating Disorders depend on the type of eating disorder that the person has. Anorexia nervosa can lead to a slow heart rate and low blood pressure, putting the sufferer at risk for heart failure and permanent heart damage. Malnutrition can lead to osteoporosis and dry, brittle bones. Other common complications include kidney damage due to dehydration, overall weakness, hair loss and dry skin. Bulimia nervosa, where the person constantly purges through vomiting, can have similar consequences as Anorexia but with added complications and damage to the esophagus and gastric cavity due to the frequent vomiting. In addition, tooth decay can occur because of damage caused by gastric juices. If the person also uses laxatives to purge, irregular bowel movements and constipation can occur. Peptic ulcers and pancreatitis can also common negative heath effects (National Eating Disorders Association). If the Eating Disorder goes on for a prolonged time period, death is also a possible affect, which is why it is important to seek treatment for the individual as soon as it is determined that they are suffering from an Eating Disorder.
Once it is recognized that a loved one may be suffering from an Eating Disorder, the next step is coming up with an effective intervention in time to prevent any lasting physical damage or death. The most effective treatment to date is Cognitive-behavioral therapy, an active form of counseling that can be done in either a group or private setting (Curtis). Cognitive-behavioral therapy is used to help correct poor eating habits and prevent relapse as well as change the way the individual thinks about food, eating and their body image (Curtis).
Cognitive-behavioral therapy is considered to be one of the most effective treatments for eating disorders, but of course this depends on both the counselor administrating the therapy and the attitude of the person receiving it. According to Fairburn (3), while patients with eating disorders “have a reputation for being difficult to treat, the great majority can be helped and many, if not most, can make a full and lasting recovery.” In the study conducted by Lobera et al, it was determined that students that took part in group cognitive-behavioral therapy sessions showed a reduced dissatisfaction with their body and a reduction in their drive to thinness. Self esteem was also improved during the group therapy sessions and eating habits were significantly improved.
“The overall effectiveness of cognitive-behavioral therapy can depend on the duration of the sessions. Cognitive-behavioral therapy is considered effective for the treatment of eating disorders. But because eating disorder behaviors can endure for a long period of time, ongoing psychological treatment is usually required for at least a year and may be needed for several years (Curtis).”
Alternative solutions
Traditional treatments for Eating Disorders rely on educating potential sufferers, especially school aged children, of the potential damage, both psychological and physical, that can be caused by the various eating disorders .
“ Research conducted to date into the primary prevention of eating disorders (ED) has mainly considered the provision of information regarding risk factors. Consequently, there is a need to develop new methods that go a step further, promoting a change in attitudes and behavior in the target population (Lobera et al).”
The current research has not shown that passive techniques, such as providing information, reduces the prevalence of eating disorders or improves the condition in existing patients. While education about eating disorders, the signs and symptoms and the potential health affects, is an important part of providing information to both the those that may know someone who is suffering from an eating disorder and those that are suffering from one, it is not an effective treatment by itself. It must be integrated with a deeper level of therapy that helps to improve the self-esteem and psychological issues from which the eating disorder stems.
Hospitalization has also been a treatment for those suffering from an eating disorder, especially when a complication, such as kidney failure or extreme weakness, occurs. However, treating the symptom of the eating disorder will not treat the underlying problem. Hospitalization can effectively treat the symptom only when it is combined with a psychological therapy that treats the underlying psychological problem that is causing the physical health problem.
Effectively treating eating disorders is possible using cognitive-behavioral therapy. However, the sooner a person who is suffering from an eating disorder begins treatment the more effective the treatment is likely to be. The longer a person suffers from an eating disorder, the more problems that may arise because of it, both physically and psychologically. While the deeper underlying issue may differ from patient to patient, it must be addressed in order for an eating disorder treatment to be effective. If not, the eating disorder is likely to continue. By becoming better educated about the underlying mental health issues that are typically the cause of eating disorder, both family members and friends of loved ones suffering from eating disorders and the sufferers themselves can take the steps necessary to overcome Eating Disorder and begin the road to recovery.
Works Cited
“Associated Mental Health Conditions and Addictions.” Something Fishy, 2010. Web. 19 November2010.
Carruthers, Martyn. Who Has Eating Disorders? Soulwork Solutions, 2010. Web. 19 November 2010.
Curtis, Jeanette. “Cognitive-behavioral Therapy for Eating Disorders.” WebMD (September 16, 2009). Web. 19 November 2010.
Fairburn, Christopher G. Cognitive Behavior Therapy and Eating Disorders. New York: The Guilford Press, 2008. Print.
“Health Consequences of Eating Disorders” National Eating Disorders Association (2005). Web. 21 November 2010.
Lobera, I.J., Lozano, P.L., Rios, P.B., Candau, J.R., Villar y Lebreros, Gregorio Sanchez, Millan, M.T.M., Gonzalez, M.T.M., Martin, L.A., Villalobos, I.J. and Sanchez, N.V. “Traditional and New Strategies in the Primary Prevention of Eating Disorders: A Comparative Study in Spanish Adolescents.” International Journal of General Medicine 3 (October 5, 2010): 263-272. Dovepress.Web. 19 November 2010.
Segal, Jeanne, Smith, Melinda, Barston, Suzanne. Helping Someone with an Eating Disorder: Advice for Parents, Family Members and Friends , 2010. Web. 19 November 2010.
Stuck with your Essay?
Get in touch with one of our experts for instant help!
American Liberty, Outline Example
Israeli Political Parties, Power Point Presentation Example
Time is precious
don’t waste it!
Plagiarism-free guarantee
Privacy guarantee
Secure checkout
Money back guarantee

Related Essay Samples & Examples
Voting as a civic responsibility, essay example.
Pages: 1
Words: 287
Utilitarianism and Its Applications, Essay Example
Words: 356
The Age-Related Changes of the Older Person, Essay Example
Pages: 2
Words: 448
The Problems ESOL Teachers Face, Essay Example
Pages: 8
Words: 2293
Should English Be the Primary Language? Essay Example
Pages: 4
Words: 999
The Term “Social Construction of Reality”, Essay Example
Words: 371
- Search by keyword
- Search by citation
Page 1 of 27
Sex differences in electrolyte abnormalities indicating refeeding syndrome risk among hospitalized adolescents and young adults with eating disorders
Refeeding syndrome is the gravest possible medical complication in malnourished patients undergoing refeeding in the hospital. We previously reported that males with malnutrition secondary to eating disorders ...
- View Full Text
Variation in care for inpatients with avoidant restrictive food intake disorder leads to development of a novel inpatient clinical pathway to standardize care
There is limited evidence to guide management of patients with avoidant restrictive food intake disorder (ARFID) admitted for medical stabilization. We describe variations in inpatient care which led to the de...
Body evaluation in men: the role of body weight dissatisfaction in appearance evaluation, eating, and muscle dysmorphia psychopathology
Body image dissatisfaction is a significant concern among men, influencing appearance evaluation, eating behaviors, and muscle dysmorphia psychopathology. However, research on these correlations is notably def...
The relationship between food selectivity and stature in pediatric patients with avoidant-restrictive food intake disorder – an electronic medical record review
We aimed to characterize stature in pediatric patients with avoidant/restrictive food intake disorder (ARFID), including associations between body size and nutrient intake and height.
Energy expenditure during nutritional rehabilitation: a scoping review to investigate hypermetabolism in individuals with anorexia nervosa
Weight gain and nutritional rehabilitation are essential first steps to achieve medical stabilization in anorexia nervosa, and frequent resistance to weight gain requires patients to consume high kilocalorie l...
Risk and resilience in eating disorders: differentiating pathways among psychosocial predictors
Eating disorders (EDs) represent a rising global health concern. The current study takes a multivariate approach to examine psychological (i.e., perfectionism, anxiety sensitivity [AS], emotion dysregulation) ...
Remote family education and support program for parents of patients with adolescent and early adulthood eating disorders based on interpersonal psychotherapy: study protocol for a pilot randomized controlled trial
In cases of adolescent and early adulthood eating disorders, despite the importance of the patients’ relationship with their parents, conflict and confusion frequently occur among them. Interpersonal psychothe...
Dismantling the myth of “all foods fit” in eating disorder treatment
We call for a reevaluation of the long-standing dogmatic nutritional principle that “all foods fit” for all cases of eating disorders (EDs) and its corollary, “there are no bad foods” (for anyone ever) during ...
Moving between positions: a qualitative study of mentoring relationships in chronic eating disorders
Eating disorders (ED) are chronic and challenging-to-treat conditions, often persisting over extended periods. Some patients with EDs require prolonged intensive rehabilitation services, which may include week...
A prospective observational study examining weight and psychosocial change in adolescent and adult eating disorder inpatients admitted for nutritional rehabilitation using a high-energy re-feeding protocol
High-energy re-feeding protocols are increasingly utilised for nutritional rehabilitation in adolescents with anorexia nervosa (AN), however, concern persists that adults with AN may be at greater risk of deve...
Evaluating the predictions of an interoceptive inference model of bulimia nervosa
Bulimia nervosa (BN) is associated with loss-of-control (LOC) eating episodes that frequently occur in response to negative emotions. According to recent neurocomputational models, this link could be explained...
Screening for eating disorders in adolescents with chronic pain: the Eating Attitudes Test–16–Chronic Pain
Few measures have been validated to screen for eating disorders (ED) in youth with chronic pain. We conducted confirmatory (CFA) of two established factor structures of the Eating Attitudes Test-26 (EAT-26) in...
Severe hypoglycemia with reduced liver volume as an indicator of end-stage malnutrition in patients with anorexia nervosa: a retrospective observational study
Hypophosphatemia due to excessive carbohydrate administration is considered the primary pathogenesis of refeeding syndrome. However, its association with liver injury and hypoglycemia, often seen in severe mal...
Course of avoidant/restrictive food intake disorder: Emergence of overvaluation of shape/weight
Avoidant/restrictive food intake disorder (ARFID) is a feeding/eating disorder characterized by avoidance/restriction of food intake by volume and/or variety. The emergence of shape/weight-related eating disor...
Inclusion of the severe and enduring anorexia nervosa phenotype in genetics research: a scoping review
Anorexia nervosa has one of the highest mortality rates of all mental illnesses. For those who survive, less than 70% fully recover, with many going on to develop a more severe and enduring phenotype. Research...
Estimating additional health and social costs in eating disorder care for young people during the COVID-19 pandemic: implications for surveillance and system transformation
The impact of the COVID-19 pandemic on young people with eating disorders (EDs) and their families was profound, with surging rates of hospitalizations and referrals reported internationally. This paper provid...
A qualitative assessment of provider-perceived barriers to implementing family-based treatment for anorexia nervosa in low-income community settings
Family-based treatment (FBT) is a front-line empirically supported intervention for adolescent anorexia nervosa, but it is often inaccessible to families from lower income backgrounds, as it is most typically ...
Psychometric properties of the Spanish version of the functionality appreciation scale
The Functionality Appreciation Scale is a 7-item measure of an individual’s appreciation of his or her body for what it can do and is capable of doing. While this instrument has been increasingly used in inter...
Psilocybin therapy and anorexia nervosa: a narrative review of safety considerations for researchers and clinicians
Clinical trials using psilocybin therapy to treat anorexia nervosa (AN) are currently underway. The safety and tolerability of psilocybin is of utmost importance in individuals with AN who may present unique m...
Severe enduring anorexia nervosa (SE-AN) treatment options and their effectiveness: a review of literature
For nearly 20% of patients diagnosed with Anorexia Nervosa (AN), the eating disorder (ED) is prolonged and becomes long-lasting. It has been reported that patients diagnosed with Severe Enduring Anorexia Nerv...
Meal support intervention for eating disorders: a mixed-methods systematic review
Mealtimes are a period of heightened distress for individuals with eating disorders. Patients frequently display maladaptive coping strategies, such as hiding food and using distraction techniques to avoid eat...
Reducing anti-fat bias toward the self and others: a randomized controlled trial
Despite strong evidence linking anti-fat bias directed toward others with markers of self-directed anti-fat bias, there is a dearth of theory-based research examining the cognitive pathways underlying this rel...
Clinician perspectives of the implementation of an early intervention service for eating disorders in England: a mixed method study
The First Episode Rapid Early Intervention for Eating Disorders (FREED) service has been shown to reduce the wait for care and improve clinical outcomes in initial evaluations. These findings led to the nation...
Eating disorders and social media use among college students in Japan and China: a brief cross-sectional survey
In recent years, new forms of media-social networking services (SNS)-such as Facebook and Sina Weibo have spread rapidly. Greater SNS use has been associated with greater body dissatisfaction, which in turn, i...
The financial and social impacts of the COVID-19 pandemic on youth with eating disorders, their families, clinicians and the mental health system: a mixed methods cost analysis
The onset of the COVID-19 pandemic has had an adverse impact on children, youth, and families with eating disorders (EDs). The COVID-19 pandemic exacerbated pre-existing personal and financial costs to youth, ...
Pediatric hospital utilization for patients with avoidant restrictive food intake disorder
Avoidant restrictive food intake disorder (ARFID) is a relatively new feeding and eating disorder added to the DSM-5 in 2013 and ICD-10 in 2018. Few studies have examined hospital utilization for patients with...
Fostering positive attitudes toward food in individuals with restrained eating: the impact of flexible food-related inhibition
Individuals exhibiting restrained eating behaviors demonstrate increased inhibitory control when exposed to food-related stimuli, indicating the presence of an automatic food-inhibition association. Existing l...
Meeting abstracts from the 2022 ANZAED conference
This article is part of a Supplement: Volume 12 Supplement 1
Temperament impact on eating disorder symptoms and habit formation: a novel model to inform treatment
Temperament has long been described as the biological dimension of personality. Due to advancing brain-imaging technology, our understanding of temperament has deepened and transformed over the last 25 years. ...
Reliability generalization meta-analysis of orthorexia nervosa using the ORTO-11/12/15/R scale in all populations and language versions
The ORTO scale was developed in 2004 as a self-report questionnaire to assess symptoms of orthorexia nervosa (ON). ON is an unhealthy preoccupation with eating healthy food. The scale aims to measure obsessive...
The relationship between internalised weight bias and biopsychosocial outcomes in children and youth: a systematic review
To synthesise the evidence on the relationships between internalised weight bias (IWB) and biopsychosocial health outcomes in individuals ≤ 25 years.
Transitions from child and adolescent to adult mental health services for eating disorders: an in-depth systematic review and development of a transition framework
Eating disorders (EDs) peak in mid-to-late adolescence and often persist into adulthood. Given their early onset and chronicity, many patients transition from child and adolescent mental health services (CAMHS...
“Maze Out”: a study protocol for a randomised controlled trial using a mix methods approach exploring the potential and examining the effectiveness of a serious game in the treatment of eating disorders
Eating Disorders (ED) are severe and costly mental health disorders. The effects of existing treatment approaches are limited and there is a need to develop novel interventions, including digital strategies th...
Further evidence of the association between social media use, eating disorder pathology and appearance ideals and pressure: a cross-sectional study in Norwegian adolescents
Few studies have investigated how the plethora of contemporary social media (SM) platforms relate to, and influence eating disorder (ED) pathology, appearance ideals and pressure to conform to these ideals in ...
Longitudinal associations between response-style strategies and abnormal eating behaviors/attitudes in adolescents: a cross-lagged panel model
Previous studies have suggested that response-style strategies (rumination, problem-solving, and distraction) can be risk or protective factors for the development of abnormal eating behaviors/attitudes (AEB) ...
Views of German mental health professionals on the use of digital mental health interventions for eating disorders: a qualitative interview study
Digital mental health interventions (DMHIs) are getting increasingly important for mental health care. In the case of eating disorders (EDs), DMHIs are still in early stages. Few studies so far investigated th...
The various facets of orthorexic eating behavior: five case reports of individuals with supposed orthorexia nervosa
Orthorexia nervosa, defined as a fixation on eating healthy according to subjective criteria, is recently being discussed as another variant of disordered eating behavior. Further characteristics are rigid ad...
Psychometric properties of the nine-item avoidant/restrictive food intake disorder screen (NIAS) in Turkish children
The nine item avoidant/restrictive food intake disorder screen (NIAS) is a short and practical assessment tool specific to ARFID with three ARFID phenotypes such as “Picky eating,” “Fear,” and “Appetite”. This...
Association between body composition standards and eating disorder medical claims among active-duty service women
Eating disorders are a worldwide public health concern with the United States having a particularly high prevalence. Eating disorders are of particular concern to the Department of Defense and Military Health ...
Correction: Food addiction and binge eating disorder are linked to shared and unique deficits in emotion regulation among female seeking bariatric surgery
The original article was published in Journal of Eating Disorders 2023 11 :97
Early weight gain as a predictor of weight restoration in avoidant/restrictive food intake disorder
Previous research has demonstrated that early weight gain in family-based treatment (FBT) is predictive of remission for adolescents with anorexia nervosa (AN). However, no published data has addressed if earl...
New understandings meet old treatments: putting a contemporary face on established protocols
In the twenty years since the publication of the most widely used treatment manuals describing evidence-based therapies for eating disorders, there have been some substantial advances in the field. New methods...
Hedonic hunger, food addiction, and night eating syndrome triangle in adolescents and ıts relationship with body mass ındex
The relationship between adolescent obesity and eating disorders is an issue that needs urgent attention. Screening for eating disorders is as important as dietary interventions to treat obesity. This study ai...
A systematic review, meta-analysis, and meta-regression of the prevalence of self-reported disordered eating and associated factors among athletes worldwide
The purpose of this meta-analysis was to provide a pooled prevalence estimate of self-reported disordered eating (SRDE) in athletes based on the available literature, and to identify risk factors for their occ...
“It’s beautiful and it’s messy and it’s tragic”: exploring the role of compassion in the eating disorder recovery processes of 2S/LGBTQ + Canadians
This research explores experiences of compassion among 2S/LGBTQ + Canadians living with eating disorders in the context of eating disorder treatment and community support. There is a growing body of scholarshi...
Adolescent utilization of eating disorder higher level of care: roles of family-based treatment adherence and demographic factors
Outpatient family-based treatment (FBT) is effective in treating restrictive eating disorders among adolescents. However, little is known about whether FBT reduces higher level of care (HLOC) utilization or if...
Carotid wave analysis in young adults with a history of adolescent anorexia nervosa: a case control study
Anorexia nervosa (AN) is associated with abnormalities that may increase the risk of future cardiovascular disease. This study assessed the cardiovascular health of individuals who recovered from AN during ado...
Key-in-session identity negotiations in a first line treatment for adult anorexia nervosa
Exploration of client identity negotiations during treatment for Anorexia Nervosa (AN) is a relatively new area of research. Research suggests that difficulties with identity negotiations may present as a barr...
Avoidant/restrictive food intake disorder differs from anorexia nervosa in delay discounting
Avoidant/restrictive food intake disorder (ARFID) and anorexia nervosa (AN) are the two primary restrictive eating disorders; however, they are driven by differing motives for inadequate dietary intake. Despit...
Preliminary identification of clinical cut-off of the vegetarian vegan eating disorder screener (V-EDS) in a community and self-reported clinical sample of vegetarians and vegans
The vegetarian vegan eating disorder screener (V-EDS) is an 18-item self-report screening tool designed to assess the unique elements of eating disorder symptomology in vegetarians and vegans. Previous results...
- Editorial Board
- Manuscript editing services
- Instructions for Editors
- Sign up for article alerts and news from this journal
- Follow us on Twitter
Annual Journal Metrics
2022 Citation Impact 4.1 - 2-year Impact Factor 4.2 - 5-year Impact Factor 1.209 - SNIP (Source Normalized Impact per Paper) 0.833 - SJR (SCImago Journal Rank)
2023 Speed 11 days submission to first editorial decision for all manuscripts (Median) 119 days submission to accept (Median)
2023 Usage 1,680,918 downloads 2,607 Altmetric mentions
- More about our metrics
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

- Eating Disorders
Binge Eating Disorder: Struggling in Silence
Exploring a complex condition and why so many struggle in silence..
Posted May 23, 2024 | Reviewed by Gary Drevitch
- What Are Eating Disorders?
- Find a therapist to heal from an eating disorder
- Binge eating disorder is the most common eating disorder in the U.S., yet many people struggle in silence.
- Shame, missed diagnosis, and lack of access to care are among the barriers people with BED face.
- We can destigmatize binge eating by empowering recovery through empathy, support, and resources.
Binge eating disorder (BED) is a serious mental health condition characterized by recurrent episodes of consuming large quantities of food, in a discreet period of time (i.e. 2 hours), often to the point of discomfort and distress. There is typically a strong sense of urgency or loss of control while eating. Individuals with binge eating disorder commonly report eating very quickly during episodes, often beyond the point of fullness, with a veil of secrecy around the experience. Binges are often described as temporarily soothing but followed by feelings of shame and disgust.
According to recent statistics , BED affects millions of individuals worldwide, with prevalence rates varying across populations. In the United States alone, it is estimated that approximately 2.8% of adults will experience BED at some point in their lives. Women are disproportionately affected, comprising around 60% of diagnosed cases; however, it's important to note that BED can affect individuals of any gender , age, race, or socioeconomic background.
Despite its prevalence, BED often goes undiagnosed or untreated, leading to significant physical and psychological consequences. There are a range of common barriers to getting help:
Missed Diagnosis. BED often goes undiagnosed in healthcare settings since providers often lack sufficient training to recognize the symptoms, which can differ from other eating disorders and may not always result in noticeable weight changes. Established protocols for screening could capture those who are struggling but healthcare systems do not regularly integrate screenings for BED during routine appointments. It’s also important to note that individuals with BED often avoid medical care altogether due to traumatic past interactions with providers who focus on body weight in shaming and inappropriate ways.
Shame. Individuals with BED often feel a great deal of shame about their behavior and are therefore reluctant to communicate their struggles to healthcare providers, family members, or other possible supports. Societal attitudes and stereotypes surrounding weight, food, and body shape/size contribute to feelings of embarrassment and self-blame. There's a pervasive misconception that overeating is simply a matter of lack of willpower or self-control , which frequently leads individuals with BED to internalize feelings of inadequacy or failure, further reinforcing a need to hide their struggle. The secretive nature of binge eating, where individuals often consume large amounts of food in private, only intensifies these feelings of shame and isolation.
Access to Care. Accessing appropriate care is a tremendous barrier to healing from binge eating. There is a shortage of specialized treatment providers trained in the diagnosis and management of BED, particularly in certain regions and healthcare systems. This scarcity results in long wait times for appointments and limited availability of evidence-based treatments such as Cognitive-Behavioral Therapy (CBT) or Dialectical Behavior Therapy (DBT). Additionally, financial barriers, including high treatment costs and limited insurance coverage for mental health services, can prevent individuals from accessing the care they need.
The Toll of Silence
As with any mental health condition, secrecy perpetuates the disorder's hold, hindering individuals from seeking the support and treatment they desperately need. Without a safe space to open up about their experiences, they may spiral deeper into unhealthy behaviors, exacerbating the physical and emotional toll of binge eating. Moreover, the absence of external validation or understanding can amplify feelings of worthlessness and hopelessness, further complicating recovery efforts.
Overcoming the silence surrounding binge eating disorder requires destigmatization, compassionate understanding, and accessible resources for support. Creating an environment in which individuals feel empowered to speak openly about their struggles is essential for breaking down barriers to recovery. By fostering empathy and providing non-judgmental support, we can help those affected by binge eating disorder find their voices and embark on a path toward healing and recovery.
To find a therapist, visit the Psychology Today Therapy Directory .

Melissa Gerson, LCSW, is founder and Clinical Director of Columbus Park Center for Eating Disorders, an outpatient facility providing treatment to individuals of all ages and genders.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience

IMAGES
VIDEO
COMMENTS
A systematic review of dialectical behavior therapy for the treatment of eating disorders. Eating Disorders, 20, 196 - 215. doi: 10.1080/10640266.2012.668478 CrossRef Google Scholar PubMed. Berkman, ND, Lohr, KN and Bulik, CM ( 2007 ). Outcomes of eating disorders: A systematic review of the literature.
Eating disorders are disabling, deadly, and costly mental disorders that considerably impair physical health and disrupt psychosocial functioning. Disturbed attitudes towards weight, body shape, and eating play a key role in the origin and maintenance of eating disorders. Eating disorders have been increasing over the past 50 years and changes in the food environment have been implicated.
Cognitive behavioral therapy (CBT) and interpersonal psychotherapy (IPT) remain the most established treatments for bulimia nervosa and binge eating disorder, with stepped-care approaches showing promise and new behavioral treatments under study. Transdiagnostic enhanced CBT has improved symptoms in adults and youth.
The book teaches us that eating disorders cannot be typecast—yet we typically do not see diverse groups portrayed as having eating disorders. A study of US television and film media found that 76-89% of characters depicted as having eating disorders were heterosexual, White, women, and younger than age 30 years.
The conceptualisation of eating disorders has expanded rapidly in the last 10 years to include binge eating disorder (BED) and avoidant/restrictive food intake disorder (ARFID) in addition to anorexia nervosa and bulimia nervosa. These are now recognised as four well‐conceptualised disorders, which have been reclassified as Feeding and Eating ...
However it wasn't until the 1930s that other professionals came to agree that eating disorders were often a result of an emotional or psychological struggle rather than being driven by the desire to be physically thin (Engel et al, 2007). Today, there are a range of known eating disorders including: Anorexia Nervosa, Bulimia Nervosa, Binge ...
Results. Of the over 1320 studies included in the Rapid Review, the proportion of articles focused on outcomes in ED was relatively small, under 9%. Most evidence was focused on the diagnostic categories of AN, Bulimia Nervosa and Binge Eating Disorder, with limited outcome studies in other ED diagnostic groups.
Eating disorders. An eating disorder is any disorder characterized primarily by a pathological disturbance of attitudes and behaviors related to food, including anorexia nervosa, bulimia nervosa, and binge-eating disorder. Other eating-related disorders include pica and rumination, which are usually diagnosed in infancy or early childhood.
National Institutes of Health. Eating disorders are characterized by a persistent disturbance of eating patterns that leads to poor physical and/or psychological health. The major eating disorders ...
Eating disorders involve a persistent disturbance of eating or of behavior related to eating that. Alters consumption or absorption of food. Significantly impairs physical health and/or psychosocial functioning. Specific eating disorders include. Anorexia nervosa. Avoidant/restrictive food intake disorder. Binge eating disorder. Bulimia nervosa.
Eating disorders are psychological conditions characterized by unhealthy, obsessive, or disordered eating habits. Eating disorders come with both emotional and physical symptoms and include ...
Among the 276 patients with eating disorders identified, 59 (21.4 %) were diagnosed as anorexia nervosa, 77 (27.9 %) as bulimia nervosa and 140 (50.7 %) as eating disorders not otherwise specified.
An eating disorder is a psychological illness where the subject has an abnormal relationship with food, and has a distorted view himself or herself. Particularly in those who suffer from anorexia and bulimia, there is an obsession with weight loss and food intake. They are also unable to see how self-destructive their behaviour is, and view ...
Eating disorders and subclinical behaviours such as dangerous dieting are a significant public health burden in the modern world. We argue that a social-psychological model of disordered eating is needed to explain how sociocultural factors are psychologically represented and subsequently reflected in an individual's cognitions and behaviour.
2 pages / 809 words. Eating Disorders (EDs) are serious clinical conditions associated with persistent eating behaviour that adversely affects your health, emotions, and ability to function in important areas of life. The most common eating disorders are anorexia nervosa, binge-eating disorder (BED) and bulimia nervosa.
In life-threatening situations, call 911. Symptoms include: Extremely restricted eating. Extreme thinness (emaciation) A relentless pursuit of thinness and unwillingness to maintain a normal or healthy weight. Intense fear of gaining weight. Distorted body image, a self-esteem that is heavily influenced by perceptions of body weight and shape ...
The most common eating disorders are anorexia, bulimia and binge-eating disorder. Most eating disorders involve focusing too much on weight, body shape and food. This can lead to dangerous eating behaviors. These behaviors can seriously affect the ability to get the nutrition your body needs.
Anorexia nervosa is an eating disorder characterised by an obsession with losing weight, body image distortion, restriction of food consumption, and low bodyweight. Estimates vary, but anorexia affects roughly 1% of the population, of which 85% are female. The syllabus looks at biological and psychological explanations of anorexia.. Biological explanations
Eating disorders affect men and women of all ages, although adolescents tend to be the age group that is more susceptible. This is because, as their bodies are changing, they may feel more pressure by society as well as peer groups to look attractive and fit in (Segal et al). Types of eating disorders include Anorexia, Bulimia and Compulsive ...
Print. Eating disorders are behavioral conditions characterized by severe and persistent disturbance in eating behaviors and associated distressing thoughts and emotions. They can be very serious conditions affecting physical, psychological and social function. Types of eating disorders include anorexia nervosa, bulimia nervosa, binge eating ...
The nine item avoidant/restrictive food intake disorder screen (NIAS) is a short and practical assessment tool specific to ARFID with three ARFID phenotypes such as "Picky eating," "Fear," and "Appetite". This... Hakan Öğütlü, Meryem Kaşak, Uğur Doğan, Hana F. Zickgraf and Mehmet Hakan Türkçapar. Journal of Eating Disorders ...
College represents one environment that may spur the development or exacerbation of eating disorder symptoms, particularly among individuals who display known risk factors for disordered eating such as those mentioned above ... Journal of Social and Clinical Psychology, 24 (2005), pp. 1081-1087, 10.1521/jscp. 2005.24.8.1081. View in Scopus ...
Binge eating disorder (BED) is a serious mental health condition characterized by recurrent episodes of consuming large quantities of food, in a discreet period of time (i.e. 2 hours), often to ...
Case study: Eating Disorder. Psychopathology refers to maladaptive behavior/s that causes distress to an individual and is brought about by a psychological disorder (Nolen-Hoeksema, 2004). A number of factors contribute to the development of psychopathology: collectively referred to as the vulnerability-stress model (Nolen-Hoeksema, 2004).