- Office of the Deputy Dean
- MD Admissions Committee
- Progress Committee
- EPCC Committee Minutes
- Thesis Chair Committee
- Curriculum Mapping Documents
- PreClerkship Policies
- Clerkship & ATP Policies
- University Policy Links
- Self-Study Task Force
- You said . . . We did . . .
- Faculty Training
- Renovation & Expansion of Student Space
- Faculty Mentor Responsibilities and Resources
- Departmental Thesis Chairs
- First-Year Summer Research
- Short-term Research
- One-year Fellowships
- Travel Info & Reimbursement
- Research Didactics
- START Summer Program
- Master of Health Science
- Student Research Day
- Forms, Deadlines & Funding
- Student Research Team
- Research Tradition
- The Yale System
- How to Apply
- Dates and Deadlines
- Fee Waivers
- Pre-medical Requirements
- Admissions Team
- Electives & Subinternships
- Staying for a Fifth Year
- Academic Advisors
- Performance Improvement
- Residency Applications
- Meet our Staff & Make an Appointment
- Wellness Programming: Upcoming Events
- Peer Advocate Program
- Day in the life of Med student
- Hear our Experiences
- Student Affairs Team
- Application Process
- International Students
- 2024-2025 Budget
- 2023-2024 Budget
- 2022-2023 Budget
- 2021-2022 Budget
- 2020-2021 Budget
- 2019-2020 Budget
- 2018-2019 Budget
- 2017-2018 Budget
- 2016-2017 Budget
- 2015-2016 Budget
- 2014-2015 Budget
- Research Funding, Extended Study and Financial Aid
- Frequently Asked Questions
- PA Online Student Budget
- FAFSA Application
- CSS Profile Application
- How to Avoid Common Errors
- Student Billing Information
- Financial Literacy Information
- External Scholarships
- Financial Aid Team
- Certificate in Global Medicine
- Topics in Global Medicine and Health
- Global Health Seminar
- Summer Research Abroad
- Electives at Other Yale Graduate Schools
- About the Course
- South Africa
- Connecticut
- Dominican Republic
- Lectures, Series, & Conferences
- Community & Advocacy Opportunities
- Faculty Advisors & Mentors
- Global Health Team
- Services & Facilities
- Program & Faculty Development
- Education & Research
- Simulated Participants
- Year in Review
- Faculty & Staff
- Advisory Board
- HAVEN Free Clinic
- Neighborhood Health Project
- Humanities in Medicine
- Biomedical Ethics
- Yale Journal of Biology & Medicine
- University Engagement Opportunities
- Community Engagement Opportunities
- Competencies
- Guiding Principles
- Graduation Requirements
- Year 1 Curriculum
- Year 2 Curriculum
- Introduction to the Profession (iPro)
- Scientific Foundations
- Genes and Development
- Attacks and Defenses
- Homeostasis
- Energy and Metabolism
- Connection to the World
- Across the Lifespan
- Professional Responsibility
- Scientific Inquiry
- Populations & Methods
- Biochemistry
- Cell Biology
- Diagnostic Methods
- Domains of the Health Equity Thread
- Advisory Group
- Pharmacology
- Communications Skills
- Clinical Reasoning
- Palliative Care
- Physical Examination
- Point of Care Ultrasound
- Early Clinical Experiences
- Emergency Medicine
- Primary Care
- Internal Medicine
- Recommended Readings
- Online Learning
- Interprofessional Educational
- Anesthesiology
- Child Study Center
- Clinical Longitudinal Elective
- Definitions
- Dermatology
- Diagnostic Imaging
- Family Medicine
- Interventional Radiology
- Laboratory Medicine
- Neurosurgery
- Obstetrics, Gynecology & Reproductive Sciences
- Ophthalmology and Visual Science
- Orthopaedics and Rehabilitation
- Therapeutic Radiology
- Elective Dates
- WEC Faculty
- Non-Clinical Electives
- Coaching Program
- Patient-Centered Language
- Race & Ethnicity
- Sex & Gender
- Full Glossary of Terms
- About The Inclusive Language Initiative
- Glossary Bibliography
- Curriculum Team
- Faculty Attestation
- Visiting Student Scholarship Program
- International Student FAQs
INFORMATION FOR
- Residents & Fellows
- Researchers

Formal MD Thesis Requirement
All students at Yale School of Medicine engage in research and are required to write an MD thesis during medical school. The only exceptions are students who have earned a PhD degree in the health sciences before matriculation and students enrolled in Yale’s MD/PhD program. The YSM MD Thesis is under the governance of the EPCC, which meets regularly to recommend rules, regulations, and deadlines.
Deadlines/Important Dates
Thesis approval process, thesis awards, required formatting and components of the md thesis, examples for reference section formatting, avoiding the risk of copyright violation and liability when submitting your md thesis, instructions for submitting a thesis to the yale medicine thesis digital library, thesis depositors declaration form, evaluations of advisor, student evaluation of thesis advisor.
- Yale School of Medicine Digital Thesis Depositor’s Declaration Form
- Thesis Deadline Extension Request Form
Thesis Deadlines for the 2023-2024 Academic Year
Md students:.
The Office of Student Research, in conjunction with the Dean’s Office, has established the following deadlines for theses submitted in partial fulfillment of the requirements for graduation in May 2024. The deadlines ensure that (1) students have sufficient time to complete their theses; (2) that there is sufficient time for rigorous departmental review and subsequent revision by students before final approval. These deadlines are strictly followed. Students are strongly encouraged to submit their theses well before the Class of 2024 Thesis Deadlines provided below. This timeliness will provide students, advisors, and sponsoring departments sufficient time for useful review and revision. It should be recognized by all concerned that the integrity of the thesis requirement and effective, rigorous review requires adherence to these deadlines. OSR will hold periodic “Thesis Check-in Sessions” via zoom for the Class of 2024 and will send periodic reminder emails with more detailed instructions as these deadlines approach.
*Students missing the August 4th, January 19th, and/or March 29th deadlines will be referred to the Progress Committee to ensure they receive adequate support to make progress towards this graduation requirement. Students missing the January 19th and/or March 29th deadlines will be ineligible for thesis prizes at graduation.
Extensions beyond the above thesis deadlines will be granted only for special circumstances and must have the approval of the student’s thesis mentor/advisor, academic advisor, and the Departmental Thesis Chairperson . Students seeking an extension for the January 19, 2024, deadline must submit a Thesis Deadline Extension Request Form to their Academic Advisor, and the Departmental Thesis Chair, for approval. Students missing the August 4th, January 19th, and/or March 29th deadlines will be referred to the Progress Committee to ensure they receive adequate support to make progress towards this graduation requirement. In the event of an extension, if granted, the following ABSOLUTE Class of 2024 Thesis Extension Deadlines will apply:
*All late theses require an extension. The student must submit the Thesis Deadline Extension Request Form before January 19, 2024.
MD/MHS Students:
Consistent with degree requirements, MD/MHS students must present their thesis to their three-person committee prior to the January 19th deadline. Students are encouraged to start arranging the date of this committee meeting in the fall to avoid unanticipated delays.
MD/PhD Students:
A different process applies to students in the MD/PhD program. For students enrolled in the combined MD/PhD Program, the dissertation submitted to and approved by the Graduate School will satisfy the MD thesis requirement. Therefore, MD/PhD students who have already defended their dissertation and received their PhD should provide this information to OSR via email as soon as possible.
To ensure compliance with YSM graduation deadlines, MD/PhD students in the class of 2024 who have not defended and submitted their dissertation to the Graduate School by the October 1, 2023, deadline will need to submit a copy of their dissertation directly to OSR via the MD/PhD Box Upload Link by March 15, 2024. OSR will convene a committee to review the dissertation, obtain feedback, and provide approval for graduation. Please note that MD/PhD students must also defend and submit their dissertation to the Graduate School no later than March 15, 2024, to meet the Graduate School spring degree deadline for conferral of the PhD degree. MD/PhD students who have not yet defended their dissertation should provide this information to OSR. If there are any questions about the process, please contact the MD/PhD Office.
Financial support is not provided for writing the thesis.
Thesis Preparation and Approval
Preparation for thesis submission begins in the summer of the fourth year with the OSR leadership. At this time, timeline and practices are distributed via email and reviewed with students in class meetings. Because thesis approval is a lengthy process involving three levels of review, students are encouraged to manage their time well and start writing their first draft early in the fall semester of their final year of medical school. A suggested timeline is provided below.
July : Thesis deadlines are distributed via email to all students in the graduating class and an informational session is held. Students should be on track to complete their thesis research by mid-fall. Any student anticipating a challenge in this regard should contact the OSR as soon as possible. All students expecting to graduate in May of a given year must, provide the OSR with information regarding their thesis title and mentor/advisor. Students will receive an email from the OSR containing a Medtrics link requesting this information. The OSR will contact all thesis mentors/advisors to confirm this role and to provide information and expectations regarding the thesis process.
August – December : Students should be finalizing research and writing their thesis draft. As the semester progresses, activities should shift from the data generation/analysis to the writing of the actual thesis. Students should do their best to complete the first draft of the thesis by mid-late December. Because students are also involved in the residency application and interview process, they are discouraged from starting new projects at this time.
December – January : This period is devoted to reviewing and editing of thesis draft that is ultimately approved by their thesis mentor/advisor and submitted by the student to the Thesis Chair of their sponsoring department. The YSM thesis mentor/advisor will be asked to complete a thesis assessment that evaluates the student’s mastery of YSM’s research-related educational objectives and provides formative summative feedback to the student.
January – March : The Departmental Thesis Chair coordinates thesis review by external reviewers. An “external reviewer” is defined as an individual who is not directly involved in the project. This individual may be a Yale faculty member internal or external to YSM or may hold a faculty appointment at an outside institution. This reviewer is required to complete a thesis assessment and provide formative summative feedback, as well as recommendations for any required changes, to the thesis. Departmental Thesis Chairs review assessments, notify students of departmental approval, and transmit these approvals to the OSR.
March : Theses and their associated assessments undergo school-level review by the OSR. Students receive YSM approval of their thesis along with summative feedback obtained during the review process. Students incorporate any required changes into their thesis and upload to the Yale Medicine Digital Thesis Library/Eli Scholar via the ProQuest platform (see below).
April : The OSR confirms that theses have been deposited into the Yale Medicine Digital Thesis Library and the registrar receives the names of students who have completed the thesis requirement.
The central role of the medical student thesis is to assess student’s performance on the YSM’s research-related educational objectives. As such, all students are expected to produce an excellent piece of scholarly work. In recognition of these achievements, the OSR has worked to develop an award process that celebrates the wonderful research being done by our students without creating a competitive atmosphere surrounding the thesis. Hence, thesis awards are based on competency-based assessments submitted by thesis mentors/advisors and reviewers during the approval process, and internal review of the final thesis that was deposited into the Yale Medicine Digital Thesis Library. Consistent with all other graduation prizes, YSM MD Thesis Awards will remain confidential until they are announced in the YSM Commencement Program on May 20, 2024. While some departments may elect to confer thesis “honors” based upon their own internal review, this recognition is distinct from YSM graduation prizes and is not under OSR’s purview.
Read about the required formatting and components for the thesis .
See helpful examples for reference section formatting.
Read about avoiding the risk of copyright violation and liability when submitting your MD Thesis.
Learn more about submitting a thesis to the Yale Medicine Thesis Digital Library .
Learn more about the Thesis Depositors Declaration Form.
Learn more about evaluating your experience with your thesis advisor .
Apply for a Thesis Extension
Read about the required formatting and components for the thesis.
Yale Journal of Biology and Medicine
Learn more about the journal or submit a manuscript.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- GMS J Med Educ
- v.39(2); 2022

Language: English | German
Medical dissertation basics: analysis of a course of study for medical students
Basics zur medizinischen dissertation: analyse eines kursangebots für promovierende in der medizin, sophia griegel.
1 University of Ulm, Medical Faculty, Institute for Biochemistry and Molecular Biology, Ulm, Germany
Michael Kühl
Achim schneider.
2 University of Ulm, Medical Faculty, Office of the Dean of Studies, Ulm, Germany
Susanne J. Kühl
Background:.
Although the majority of medical students in Germany pursue a doctorate, only a portion of them receive a standardized scientific training, which is reflected in the quality issues seen in medical doctoral theses. The course Medical Dissertation Basics was conceptualized and scientifically monitored in order to support medical doctoral students on the one hand and to improve the quality of their scientific work on the other.
Methodology:
The course consists of three modules. Module I, which is an introductory module, covers time and writing management and addresses how to approach literature and the principles of scientific work as well as the chapters required in a dissertation and the dissertation presentation and defense. In the practical module II, doctoral students write sections of their dissertation chapters and receive feedback via peer and expert reviews. Module III includes training on dissertation presentations and their defense. For objective analysis purposes, a multiple-choice test was administered before and after module I. Medical students from semesters 2 to 6 served as a control group. Questionnaires were used to subjectively analyze the training and support functions of modules I-III.
High participation rates and the fact that the modules were taught numerous times show that doctoral students accept the courses. The objective analysis of module I showed a highly significant knowledge acquisition of the course group (N=55) in contrast to the control group (N=34). The doctoral students rated the course modules I-III with grades between 1.0 and 1.25 (grade A+/A; N=20-65 SD=0-0.44), felt well supported and estimated their learning success as high.
Conclusion:
The study indicates knowledge acquisition in module I and a high doctoral student satisfaction with all modules. For an objective analysis of modules II-III, a comparison of completed doctoral theses (course participants vs. non-participants) would be appropriate but would only make sense in a few years. Based on the results of our study, we recommend that other faculties implement similar courses.
Zusammenfassung
Hintergrund:.
Obwohl die Mehrheit der Medizinstudierenden in Deutschland promoviert, erfährt nur eine Minderheit eine standardisierte wissenschaftliche Ausbildung, was sich an Qualitätsmängeln medizinischer Promotionsarbeiten äußert. Um Promovierenden der Medizin einerseits eine Unterstützung zu geben und andererseits die Qualität ihrer wissenschaftlichen Arbeiten zu verbessern, wurde das Kursangebot Basics zur medizinischen Dissertation konzeptioniert und wissenschaftlich begleitet.
Das Kursangebot besteht aus drei Modulen. Modul I als Grundlagenkurs behandelt neben dem Zeit- und Schreibmanagement, dem Umgang mit Literatur und den Grundsätzen des wissenschaftlichen Arbeitens auch die Kapitelinhalte einer Dissertationsschrift sowie die Präsentation und Verteidigung. Im praktischen Modul II verfassen Promovierende Auszüge von Dissertationskapiteln und erhalten über Peer- und Experten-Begutachtungen Feedback. Modul III umfasst das Training von Promotionsvorträgen und deren Verteidigung. Zur objektiven Analyse wurde ein Multiple Choice Test vor und nach Modul I durchgeführt. Medizinstudierende aus Fachsemester 2 bis 6 dienten als Kontrollgruppe. Anhand von Fragebögen wurden alle Kursmodule I-III hinsichtlich ihrer Ausbildungs- und Unterstützungsfunktion subjektiv analysiert.
Ergebnisse:
Hohe Teilnahmezahlen und die vielfache Durchführung der Kursmodule zeigen, dass Promovierende die Kurse akzeptieren. Die objektive Analyse von Modul I ergab einen hoch signifikanten Wissenserwerb der Kursgruppe (N=55) im Gegensatz zur Kontrollgruppe (N=34). Die Promovierenden bewerteten die Kursmodule I-III mit Schulnoten zwischen 1,0 und 1,25 (N=20-65 SD=0-0,44), fühlten sich gut unterstützt und schätzten ihren Lernerfolg als hoch ein.
Schlussfolgerung:
Die Studie zeigt eine hohe Promovierenden-Zufriedenheit mit allen Modulen und einen Wissenserwerb durch das Modul I. Zur objektiven Analyse von Modul II-III bietet sich ein Vergleich der fertiggestellten Promotionsarbeiten (Kurs Teilnehmende vs. Nicht-Teilnehmende) an, welcher erst in ein paar Jahren sinnvoll ist. Durch die Ergebnisse unserer Studie empfehlen wir anderen Fakultäten die Implementierung ähnlicher Angebote.
1. Introduction
1.1. the problem.
Between 54 to 70 percent of all medical students successfully complete their doctorates while about one-third of them do not [ 1 ], [ 2 ], [ 3 ], [ 4 ]. On the one hand, this indicates a very high willingness to do a doctorate, but on the other, that the doctoral students are often unsuccessful [ 5 ], [ 6 ]. What is special about the study of medicine is that the doctorate can be started while the medical degree is being pursued. This promises an initial motivation since it saves time, but it often leads to a double burden [ 5 ], [ 7 ], [ 8 ]. Another issue is an insufficient basic scientific education as well as a lack of supervision of doctoral candidates [ 9 ]. The quality of medical doctorates is also being criticized at the scientific and socio-political level. Thus, negative catch phrases such as title research and after-work research reflect the bad reputation of medical doctorates [ 8 ].
While there is a high demand for good scientific education by doctoral students and a high demand for quality from the scientific and societal side, there is often a lack of course offerings in this regard. In recent years, the global standards of medical education of the WFME (World Federation for Medical Education), the Medizinstudium 2020 (medical studies 2020) master plan and the Wissenschaftsrat (German council of science and humanities) have called for a strengthening of the scientific education. Individual German medical faculties have responded to this and implemented scientific course concepts [ 4 ], [ 8 ], [ 10 ], [ 11 ], [ 12 ], [ 13 ], [ 14 ], [ 15 ], [ 16 ] as well as quality assurance measures, which were documented in a study of the University Alliance for Young Scientists [ 17 ]. While subjective student evaluations are available, objective analyses of such doctoral courses are still lacking [ 16 ].
1.2. Initial situation at the medical faculty of the university of Ulm
The official curriculum of the medical faculty of the university of Ulm includes scientific content from the subjects of biometry and epidemiology (semester 7). In addition to evidence-based medicine, various types of research including the planning, methodology and implementation as well as the application of statistical tests are covered. Scientific content is also taught in other events that are included in a longitudinal mosaic curriculum (wise@ulm).
In addition, the University of Ulm offers electives for doctoral students: The experimental medicine course of study introduced in 2005, for example, is a doctoral program for medical students that requires an experimental dissertation. Each year, approximately 35 students are selected with the help of an application and selection process. The support provided consists of professional and scientific supervision, various scientific events, the completion of elective courses and ten months of financial support [ 18 ].
The course Fit für die diss MED (Fit for the medical dissertation), offered by the communication and information center, is a voluntary course made available to medical students at the university of Ulm. The course, which includes a total of eight hours and is mainly theoretical, covers successful publishing, the scientific framework and the use of computer programs. The content of the medical dissertation chapters is only marginally discussed.
There is no course offered for doctoral medical students that deals intensively with good scientific practice and the chapter content required for a doctoral thesis. Practical support during the writing process and in preparation for the presentation and defense of a dissertation has been limited as well. Thus, the course “medical dissertation basics: how to write scientific texts and present a doctoral thesis” with a total of three modules (MED I-III) was implemented in 2018, has been taught numerous times since then and has been monitored scientifically.
This raises the following questions:
- Is the Basics MED course with its three modules I-III accepted by students obtaining a doctorate in medicine?
- Can the participation in MED I (module I) result in an acquisition of knowledge by students obtaining a doctorate in medicine?
- How do students obtaining a doctorate in medicine rate the support provided and the scientific content learned during the three modules MED I-III?
2.1. Course concept
The course offering “Medical dissertation basics: How to write scientific texts and present a doctoral thesis” (MED I-III) was developed and introduced in 2018. Module I covers scientific fundamentals and teaches the content required for a medical doctoral thesis. Module II teaches students how to write high-quality text. Module III trains students on how to present and defend a doctoral thesis. The sequence of the modules (I → II → III) is based on the chronology of the medical doctoral process and permits students to apply the theoretical content learned (module I) to their own doctorate with the help of practical assignments (module II-III). The course content is based on the official guidelines of the medical faculty of the university of Ulm, observations gathered during the supervision of medical doctoral theses and courses that are already being offered at other universities [ 9 ], [ 11 ], [ 15 ], [ 16 ].
2.1.1. Participation information
The course is offered to doctoral students of human and dental medicine. In some cases, students from other degree programs may participate as well.
Students may take modules I and III as needed. Module I is a prerequisite for module II. The online courses are offered on the Ulm Moodle platform. Modules I and III are offered 3-5 times a year depending on demand while module II is offered throughout the year.
2.1.2. MED I (module I)
Module I is offered to students shortly before or at the beginning of the doctorate program as a one-week online course (nine hours in total). In order to structure the content, eight teaching phases (15 min to 2 hours each) have been defined as either independent study phases or classroom phases (online meetings).
In the (independent study) phase 1, students are introduced to scientific practice as well as time and writing management with the help of instructional videos, PDF files and worksheets. In the (classroom) phase 2, the instructor lectures on good scientific practice, the development of a comprehensible manuscript and its introduction. The remaining phases cover the legal framework, the scientific question or hypothesis, literature research and management (optional) and the remaining chapters of a dissertation as well as the presentation and defense of a dissertation (see figure 1 (Fig. 1) , part A).

A. Course organization (phases 1-8), content and materials of MED I, mandatory participation in pre-tests and post-tests (objective analysis), voluntary participation in evaluations (subjective analysis). B. Course organization, sequence and content (assignments with text length) of MED II, voluntary participation in evaluations. C. Course organization, sequence and content of MED III, voluntary participation in evaluations. Abbreviation: MED: Medical Experimental Dissertation Basics.
2.1.3. MED II (module II)
The online module II is designed for doctoral students who have already taken MED I and have started writing their dissertation. Students may participate individually or as a group of two. The assignments require students to write three to four sections of their own dissertation (see figure 1 (Fig. 1) , part B): Excerpt from the laboratory book (writing assignment 1), the materials and methods section (written assignment 2), excerpt of the introduction or discussion (written assignment 3) and excerpt of the results section (written assignment 4). These sections are first subjected to a peer review (feedback from another student) and then to an expert review (from the instructor). For both reviews, a semi-standardized feedback form is used, which was developed by two experts and reviewed by the academic staff members of our working group. If necessary, the doctoral students must submit a revised draft of a given section upon having received their feedback.
2.1.4. MED III (module III)
Module III trains students to present and defend their dissertations. In an individual preparation phase, students prepare a 7-minute presentation of their dissertation and are required to use a brief guideline. The students make their presentations in front of a small group (three to six doctoral students) during a first (online) class. Each presentation is followed by an approximately 30-minute feedback portion (feedback offered by the small group and the instructor) using a customized, semi-standardized feedback form, which was developed in the same manner as the feedback form used in module II. In a revision phase, the presentations are revised and presented again during a second (online) class. Students are provided with further feedback and collect and discuss potential questions such as those that an examination committee might present in order to practice the defense portion of the dissertation (see figure 1 (Fig. 1) , part C).
2.2. Study design for the analysis of the course offered (modules I-III)
The MED course study was divided into an objective analysis of the first module and subjective analyses of all modules (I-III).
For the objective analysis of the first module, a multiple choice (MC) knowledge test was developed and used as part of the courses offered from June to October 2020. Since module I was offered three times during this period, there were three test cycles. The test subjects consisted of the participants of module I (course group) and a control group. The selection of the individuals in the control group was subject to the following conditions: They had to be students of human medicine from the semesters 2-6 who had not yet started their doctoral thesis.
The subjective analysis of module I was based on the voluntary student evaluations from June 2020 to July 2021 (N=65). The subjective analyses of module II (N=20) and module III (N=20) were based on the evaluations from 2018 to 2021.
2.2.1. Objective analysis of the knowledge acquisition (module I)
To assess the knowledge acquired due to a participation in MED I (module I), 19 multiple choice questions were developed. In a second step, the test design was reviewed by two experts. Volunteers from our work group (N=7) performed a pretest in a third step [ 19 ], [ 20 ] and provided feedback about unclear or misleading wording and completion time.
The final test, consisting of eleven A positive type questions (choose one correct answer out of five possible answers) and eight K Prim type questions (choose multiple correct answers out of five possible answers), was administered via the Ulm learning platform Moodle. The knowledge test was administered three days before (pre-test) and three days after (post-test) the course (completion time: max. 20 minutes). Although the same questions were used for the pre-test and post-test, the order of the questions and answers was changed. Participants in the control group were asked to not research the content related to the questions over the course of the study.
With regard to eight K Prim type questions, the number of correct answer options varied (from 2 to 5). If an answer option was correctly selected, one point was awarded so that a maximum of 5 points could be achieved for each K Prim question. Points were deducted for incorrectly selected distractors. The point deduction principle was applied equally to all questions (type A positive and K Prim ). Consequently, a total score of minus 30 to plus 32 points was possible.
2.2.2. Subjective analysis through student evaluations (modules I-III).
For the subjective analysis, semi-standardized questionnaires were developed for all modules. In addition to the socio-demographic data of the participants, data on general and content-related course aspects was collected (e.g., the organization, structure and subjectively perceived learning success; see figure 2 (Fig. 2) , figure 3 (Fig. 3) and figure 4 (Fig. 4) ), which were assessed with a Likert-type response scale (1=do not agree at all to 6=agree completely). Participants were able to enter praise, criticism or suggestions for improvement in a free text field. The overall module was also evaluated by using a school grade (1=very good, 6=insufficient).

A. General questions about the course. B. Students' assessment of the individually perceived learning success; Likert scale: from 1= "strongly disagree" to 6= "strongly agree". N=65.

A. General questions about the course. B. Students‘ assessment of the individually perceived learning success; Likert scale: from 1= “strongly disagree” to 6= “strongly agree”. N=20.

2.3. Data analysis and statistics
All analyses were performed using the SPSS Statistics Version 26 software from the International Business Machines Corporation. For the knowledge test, the total scores of all three test cycles were calculated. The Kolmogorov-Smirnov test did not show a normal distribution of the data, so the nonparametric Wilcoxon signed-rank test for connected samples was used for analysis purposes. An alpha level of 5% was applied. Free-text comments were categorized and quantified according to praise, criticism or suggestion for improvement, following Schneider et al., 2019 [ 21 ].
2.4. Ethics
The ethics committee of the University of Ulm did not consider an ethics vote necessary. The participation in the questionnaires and tests was voluntary, anonymous and free of charge. The participants' consent to data processing and data transfer was obtained.
3.1. Participation figures
A total of 171 doctoral students participated in MED I (which was offered six times between July 2020 and November 2021), 21 students participated in MED II (since 2018) and 25 students participated in MED III (which was offered nine times since 2018). The number of participants in the course-related studies was somewhat lower (see figure 1 (Fig. 1) and table 1 (Tab. 1) ).

3.2. Objective analysis of MED I
3.2.1. sociodemographic data of the course and control groups.
The socio-demographic data of the course group was obtained from the evaluation forms (section 2.2.2) and data of the control group was based on verbal information provided by the participants.
Of the module I participants, 89% studied human medicine (N=65, see table 1 (Tab. 1) ) compared to 100% of control group subjects (N=34). The majority of course participants were female (71%); in the control group, male subjects dominated with 62%. The course participants were on average in semester 7.67 (SD=1.66) while the subjects of the control group were in semester 4.76 (SD=1.35).
3.2.2. Results from the knowledge test
To test for knowledge acquisition in MED I, the results from the pre-test and post-test were compared (see figure 5 (Fig. 5) ). The result of the control group remained unchanged with a median of 10.5 points (Q1=5.75 Q3=13) in the pre-test and post-test. Only the dispersion decreased slightly in the post-test. In contrast, the course group showed a significant knowledge acquisition with a median of 13 points in the pre-test (Q1=11 Q3=17.5) and 22 points in the post-test (Q1=19.5 Q3=25) (p<0.001).

3.3. Subjective analyses of MED I-III
3.3.1. sociodemographic data.
The sociodemographic data of the participants (see table 1 (Tab. 1) ) shows that the age and semester of study increased from module I to III. Dental and human medical students who had not yet started or had already started their experimental/clinical/retrospective/teaching research participated in Module I. Module groups II and III included human medicine students who were primarily doing experimental work. A large proportion of doctoral students from the experimental medicine student track participated in all modules [ 18 ].
3.3.2. Subjective evaluation results
MED I was rated on average with the school grade 1.21 (N=58 SD=0.41), MED II with 1.28 (N=18 SD=0.46) and MED III with the grade 1.0 (N=20 SD=0.00). Additional questions tried to determine how students obtaining a doctorate in medicine assess the support and their learning success in the courses.
3.3.3. Evaluation results for module I
The communication of the general course information (MW=5.80, SD=0.44), the organization and overall structure, and the teaching by the instructor were rated particularly positively. The presentation of data and the literature research (MW=4.74, SD=1.02) scored somewhat worse. The teaching of scientific content such as literature management (MW=5.35, SD=1.16) and the teaching of the chapter content required for a dissertation, led to a subjectively perceived high learning success (see figure 2). Similar results were reflected by the praise expressed in the free text questions in which the course content, the commitment of the instructors and the teaching videos were positively emphasized (see table 2 (Tab. 2) ).

3.3.4. Evaluation results for module II
General aspects such as the basic structure, the assignments and the feedback by the instructor (MW=5.80, SD=0.41) were rated good to very good. The peer feedback by fellow students was rated somewhat lower (MW=3.91, SD=1.38). The participants indicated that their writing process had improved (MW=5.55, SD=0.89). Students rated the drafting of the materials and methods section, the introduction or discussion and the results section as particularly instructive and the lab journal entry as (somewhat) instructive (MW=4.60, SD=1.19) (see figure 3 (Fig. 3) ). Two students commented on being able to do without the lab book excerpt while others suggested the option of submitting more dissertation sections. The positive comments made up 60% of all comments and included references to the speedy correction and individual feedback provided by the instructor (see table 2 (Tab. 2) ).
3.3.5. Evaluation results for module III
MED III, which pertains to the presentation and defense of a dissertation, was characterized by very high student satisfaction. Organizational and structural aspects, the ability to present two times, the analyses and feedback by the instructor were rated very good (MW=6.00, SD=0.00). All students would take the course again (MW=6.00, SD=0.00). Participants rated the learning success pertaining to the general presentation, content and structure of a lecture and the use of media for visualization purposes very highly (see figure 4 (Fig. 4) ). In the free texts, the commitment of the instructors in the course design was rated positively. The participants felt that the module provided structure as well as new perspectives and well prepared them for the presentation and defense of their dissertation. Some participants would have liked more basic information on how to give a good presentation (see table 2 (Tab. 2) ).
4. Discussion
Our study shows that
- all modules of the Basics MED course are accepted by students obtaining a doctorate in medicine.
- participation in MED I (module I) leads to a knowledge acquisition by the students obtaining a doctorate in medicine.
- students obtaining a doctorate in medicine highly rate the support and learning success of scientific content provided in the course modules MED I-III.
4.1. Basics MED courses accepted by doctoral students in medicine
At the time the course was implemented, other doctoral programs had already been established at the University of Ulm [ 18 ]. Therefore, despite a high demand for doctoral programs throughout Germany, we were interested in whether the course would be accepted [ 9 ], [ 13 ]. We were able to confirm this based on the number of times the course has been conducted (several times a year) and high participation numbers. The participation figures for Modules II and III were somewhat lower. Possible reasons are that modules II-III become relevant in the later couese of the dissertation (possibly not until later) and the additional time required. For module II, students had to have first completed module I, and continuous texts had to be drafted. In contrast to a scientific term paper (doctoral program at the Charité Berlin), these continuous texts are only excerpts of the student's dissertation, which relativizes the additional effort [ 15 ].
4.2. Participation in MED I (Module I) results in knowledge acquisition
To test the degree to which students learned from module I, an MC test was designed and administered before and after the course (pre-test and post-test). It showed a significant knowledge acquisition by the course group compared to the control group. The purpose of the control group was to test for factors that might influence the test results, such as a practice effect due to the test being administered twice [ 22 ], and jeopardize their validity. We used identical questions in the pre-test and the post-test and only changed the order, which, according to Golda et al., has no significant influence on the level of difficulty [ 23 ].
Due to insignificant differences in the test scores of the control group, a practice effect can be largely ruled out, indicating an objective knowledge acquisition of the course group.
4.3. Doctoral students rate the support and learning success highly
Our subjective analyses show that students considered the basics MED modules I-III as helpful for their doctoral studies. The participants rated the learning gain relating to scientific content high. The learning gain relating to literature research (and management) was insignificantly lower. One reason could be the complexity of the topic, which is difficult to grasp in a 9-hour course. The ability to manage literature is often acquired over a longer period of time, such as the entire doctoral period [ 13 ]. In the evaluation of MED II, the feedback by the instructor was rated more helpful than the peer feedback provided by fellow students (see figure 3 (Fig. 3) ). Examples from the literature show that students can generally benefit from a feedback culture (including peer feedback) [ 24 ], [ 25 ]. Doctoral students are at the beginning of their academic career and have yet to develop a critical eye for academic texts. This process is positively supported by the involvement in peer feedback.
Individual participants rated the relevance of the laboratory book excerpt as low. The Wissenschaftsrat and the instructors believe that this portion of the module is very relevant for ensuring scientific standards [ 12 ].
Overall, however, the results at the subjective level are consistent with calls (by the Wissenschaftsrat, WFME, etc.) for more intensive support and scientific training [ 11 ], [ 12 ]. Studies evaluating other doctoral programs have resulted in similar conclusions [ 15 ], [ 16 ].
4.4. Limitations
The limiting factor of the knowledge test relating to module I is that only MC questions were used. Unlike open-ended question formats, it is possible that MC questions are answered correctly not due to sound knowledge but rather because students recognize key words [26]. On the other hand, this type of question is commonly used in exams and allows for a standardized and quantitative evaluation [ 26 ].
In addition, the course group included students who were on the perennial experimental medicine study track. It is possible, albeit unlikely, that the doctoral program may influence the test results, but this cannot be ruled out. Other limitations include differences in the test groups: The majority of the course participants had already started their doctorate while the control group had not (yet) started. Since many doctoral students of the Medical Faculty had already taken MED I, the number of doctoral students suitable for the control group was limited. Furthermore, there was a lack of data (e.g., e-mail addresses) for a targeted search for subjects. Therefore, we chose medical students from semesters 2-6 who were younger on average and were not yet pursuing their doctorate and with whom we had had contact in other courses. We received more feedback from male subjects, resulting in a different gender distribution between course and control subjects. In addition, the control group did not include any participants from the Experimental Medicine study track. This is due to the fact that almost all of the 35 participants who had just received funding during the study period took part in MED I because the Experimental Medicine study track accepts the MED modules as electives [18].
Another approach to determine whether the knowledge increase was due to the course would be to test content that was not covered in the course. However, additional questions would have led to an increase in processing time, which might have decreased the willingness to participate in the study.
In addition to uncertain objectivity and validity, another limitation of voluntary evaluations is that they are conducted online [ 27 ]. Online evaluations can be perceived as more anonymous than face-to-face surveys [ 28 ]. Without a tangible expectation from the instructors present, the response rate may have been lower. Advantages of more anonymous (online) surveys, however, are more honest expressions, especially of criticism, which are valuable for the further development of a course [ 28 ], [ 29 ].
5. Summary and outlook
Our study allows for both an objective and subjective analysis of a course designed to support students obtaining a doctorate in medicine. The MED I-III modules were accepted and evaluated very positively. MED I objectively increased the participants’ knowledge. For an objective analysis of MED II, a grade comparison of the completed dissertation would be conceivable (participants compared to non-participants). Analogously, the success of the presentation and defense of the dissertations could be compared for an objective analysis of MED III. It will take a few years, however, to conduct such case-control studies since there is often a time lag of several years between participation in the course and the completion of the doctorate [ 5 ].
Based on our results to date, we recommend that other universities develop similar courses.
Competing interests
The authors declare that they have no competing interests.
Research Topics & Ideas: Healthcare
100+ Healthcare Research Topic Ideas To Fast-Track Your Project

Finding and choosing a strong research topic is the critical first step when it comes to crafting a high-quality dissertation, thesis or research project. If you’ve landed on this post, chances are you’re looking for a healthcare-related research topic , but aren’t sure where to start. Here, we’ll explore a variety of healthcare-related research ideas and topic thought-starters across a range of healthcare fields, including allopathic and alternative medicine, dentistry, physical therapy, optometry, pharmacology and public health.
NB – This is just the start…
The topic ideation and evaluation process has multiple steps . In this post, we’ll kickstart the process by sharing some research topic ideas within the healthcare domain. This is the starting point, but to develop a well-defined research topic, you’ll need to identify a clear and convincing research gap , along with a well-justified plan of action to fill that gap.
If you’re new to the oftentimes perplexing world of research, or if this is your first time undertaking a formal academic research project, be sure to check out our free dissertation mini-course. In it, we cover the process of writing a dissertation or thesis from start to end. Be sure to also sign up for our free webinar that explores how to find a high-quality research topic.
Overview: Healthcare Research Topics
- Allopathic medicine
- Alternative /complementary medicine
- Veterinary medicine
- Physical therapy/ rehab
- Optometry and ophthalmology
- Pharmacy and pharmacology
- Public health
- Examples of healthcare-related dissertations
Allopathic (Conventional) Medicine
- The effectiveness of telemedicine in remote elderly patient care
- The impact of stress on the immune system of cancer patients
- The effects of a plant-based diet on chronic diseases such as diabetes
- The use of AI in early cancer diagnosis and treatment
- The role of the gut microbiome in mental health conditions such as depression and anxiety
- The efficacy of mindfulness meditation in reducing chronic pain: A systematic review
- The benefits and drawbacks of electronic health records in a developing country
- The effects of environmental pollution on breast milk quality
- The use of personalized medicine in treating genetic disorders
- The impact of social determinants of health on chronic diseases in Asia
- The role of high-intensity interval training in improving cardiovascular health
- The efficacy of using probiotics for gut health in pregnant women
- The impact of poor sleep on the treatment of chronic illnesses
- The role of inflammation in the development of chronic diseases such as lupus
- The effectiveness of physiotherapy in pain control post-surgery
Topics & Ideas: Alternative Medicine
- The benefits of herbal medicine in treating young asthma patients
- The use of acupuncture in treating infertility in women over 40 years of age
- The effectiveness of homoeopathy in treating mental health disorders: A systematic review
- The role of aromatherapy in reducing stress and anxiety post-surgery
- The impact of mindfulness meditation on reducing high blood pressure
- The use of chiropractic therapy in treating back pain of pregnant women
- The efficacy of traditional Chinese medicine such as Shun-Qi-Tong-Xie (SQTX) in treating digestive disorders in China
- The impact of yoga on physical and mental health in adolescents
- The benefits of hydrotherapy in treating musculoskeletal disorders such as tendinitis
- The role of Reiki in promoting healing and relaxation post birth
- The effectiveness of naturopathy in treating skin conditions such as eczema
- The use of deep tissue massage therapy in reducing chronic pain in amputees
- The impact of tai chi on the treatment of anxiety and depression
- The benefits of reflexology in treating stress, anxiety and chronic fatigue
- The role of acupuncture in the prophylactic management of headaches and migraines
Topics & Ideas: Dentistry
- The impact of sugar consumption on the oral health of infants
- The use of digital dentistry in improving patient care: A systematic review
- The efficacy of orthodontic treatments in correcting bite problems in adults
- The role of dental hygiene in preventing gum disease in patients with dental bridges
- The impact of smoking on oral health and tobacco cessation support from UK dentists
- The benefits of dental implants in restoring missing teeth in adolescents
- The use of lasers in dental procedures such as root canals
- The efficacy of root canal treatment using high-frequency electric pulses in saving infected teeth
- The role of fluoride in promoting remineralization and slowing down demineralization
- The impact of stress-induced reflux on oral health
- The benefits of dental crowns in restoring damaged teeth in elderly patients
- The use of sedation dentistry in managing dental anxiety in children
- The efficacy of teeth whitening treatments in improving dental aesthetics in patients with braces
- The role of orthodontic appliances in improving well-being
- The impact of periodontal disease on overall health and chronic illnesses
Tops & Ideas: Veterinary Medicine
- The impact of nutrition on broiler chicken production
- The role of vaccines in disease prevention in horses
- The importance of parasite control in animal health in piggeries
- The impact of animal behaviour on welfare in the dairy industry
- The effects of environmental pollution on the health of cattle
- The role of veterinary technology such as MRI in animal care
- The importance of pain management in post-surgery health outcomes
- The impact of genetics on animal health and disease in layer chickens
- The effectiveness of alternative therapies in veterinary medicine: A systematic review
- The role of veterinary medicine in public health: A case study of the COVID-19 pandemic
- The impact of climate change on animal health and infectious diseases in animals
- The importance of animal welfare in veterinary medicine and sustainable agriculture
- The effects of the human-animal bond on canine health
- The role of veterinary medicine in conservation efforts: A case study of Rhinoceros poaching in Africa
- The impact of veterinary research of new vaccines on animal health
Topics & Ideas: Physical Therapy/Rehab
- The efficacy of aquatic therapy in improving joint mobility and strength in polio patients
- The impact of telerehabilitation on patient outcomes in Germany
- The effect of kinesiotaping on reducing knee pain and improving function in individuals with chronic pain
- A comparison of manual therapy and yoga exercise therapy in the management of low back pain
- The use of wearable technology in physical rehabilitation and the impact on patient adherence to a rehabilitation plan
- The impact of mindfulness-based interventions in physical therapy in adolescents
- The effects of resistance training on individuals with Parkinson’s disease
- The role of hydrotherapy in the management of fibromyalgia
- The impact of cognitive-behavioural therapy in physical rehabilitation for individuals with chronic pain
- The use of virtual reality in physical rehabilitation of sports injuries
- The effects of electrical stimulation on muscle function and strength in athletes
- The role of physical therapy in the management of stroke recovery: A systematic review
- The impact of pilates on mental health in individuals with depression
- The use of thermal modalities in physical therapy and its effectiveness in reducing pain and inflammation
- The effect of strength training on balance and gait in elderly patients
Topics & Ideas: Optometry & Opthalmology
- The impact of screen time on the vision and ocular health of children under the age of 5
- The effects of blue light exposure from digital devices on ocular health
- The role of dietary interventions, such as the intake of whole grains, in the management of age-related macular degeneration
- The use of telemedicine in optometry and ophthalmology in the UK
- The impact of myopia control interventions on African American children’s vision
- The use of contact lenses in the management of dry eye syndrome: different treatment options
- The effects of visual rehabilitation in individuals with traumatic brain injury
- The role of low vision rehabilitation in individuals with age-related vision loss: challenges and solutions
- The impact of environmental air pollution on ocular health
- The effectiveness of orthokeratology in myopia control compared to contact lenses
- The role of dietary supplements, such as omega-3 fatty acids, in ocular health
- The effects of ultraviolet radiation exposure from tanning beds on ocular health
- The impact of computer vision syndrome on long-term visual function
- The use of novel diagnostic tools in optometry and ophthalmology in developing countries
- The effects of virtual reality on visual perception and ocular health: an examination of dry eye syndrome and neurologic symptoms
Topics & Ideas: Pharmacy & Pharmacology
- The impact of medication adherence on patient outcomes in cystic fibrosis
- The use of personalized medicine in the management of chronic diseases such as Alzheimer’s disease
- The effects of pharmacogenomics on drug response and toxicity in cancer patients
- The role of pharmacists in the management of chronic pain in primary care
- The impact of drug-drug interactions on patient mental health outcomes
- The use of telepharmacy in healthcare: Present status and future potential
- The effects of herbal and dietary supplements on drug efficacy and toxicity
- The role of pharmacists in the management of type 1 diabetes
- The impact of medication errors on patient outcomes and satisfaction
- The use of technology in medication management in the USA
- The effects of smoking on drug metabolism and pharmacokinetics: A case study of clozapine
- Leveraging the role of pharmacists in preventing and managing opioid use disorder
- The impact of the opioid epidemic on public health in a developing country
- The use of biosimilars in the management of the skin condition psoriasis
- The effects of the Affordable Care Act on medication utilization and patient outcomes in African Americans
Topics & Ideas: Public Health
- The impact of the built environment and urbanisation on physical activity and obesity
- The effects of food insecurity on health outcomes in Zimbabwe
- The role of community-based participatory research in addressing health disparities
- The impact of social determinants of health, such as racism, on population health
- The effects of heat waves on public health
- The role of telehealth in addressing healthcare access and equity in South America
- The impact of gun violence on public health in South Africa
- The effects of chlorofluorocarbons air pollution on respiratory health
- The role of public health interventions in reducing health disparities in the USA
- The impact of the United States Affordable Care Act on access to healthcare and health outcomes
- The effects of water insecurity on health outcomes in the Middle East
- The role of community health workers in addressing healthcare access and equity in low-income countries
- The impact of mass incarceration on public health and behavioural health of a community
- The effects of floods on public health and healthcare systems
- The role of social media in public health communication and behaviour change in adolescents
Examples: Healthcare Dissertation & Theses
While the ideas we’ve presented above are a decent starting point for finding a healthcare-related research topic, they are fairly generic and non-specific. So, it helps to look at actual dissertations and theses to see how this all comes together.
Below, we’ve included a selection of research projects from various healthcare-related degree programs to help refine your thinking. These are actual dissertations and theses, written as part of Master’s and PhD-level programs, so they can provide some useful insight as to what a research topic looks like in practice.
- Improving Follow-Up Care for Homeless Populations in North County San Diego (Sanchez, 2021)
- On the Incentives of Medicare’s Hospital Reimbursement and an Examination of Exchangeability (Elzinga, 2016)
- Managing the healthcare crisis: the career narratives of nurses (Krueger, 2021)
- Methods for preventing central line-associated bloodstream infection in pediatric haematology-oncology patients: A systematic literature review (Balkan, 2020)
- Farms in Healthcare: Enhancing Knowledge, Sharing, and Collaboration (Garramone, 2019)
- When machine learning meets healthcare: towards knowledge incorporation in multimodal healthcare analytics (Yuan, 2020)
- Integrated behavioural healthcare: The future of rural mental health (Fox, 2019)
- Healthcare service use patterns among autistic adults: A systematic review with narrative synthesis (Gilmore, 2021)
- Mindfulness-Based Interventions: Combatting Burnout and Compassionate Fatigue among Mental Health Caregivers (Lundquist, 2022)
- Transgender and gender-diverse people’s perceptions of gender-inclusive healthcare access and associated hope for the future (Wille, 2021)
- Efficient Neural Network Synthesis and Its Application in Smart Healthcare (Hassantabar, 2022)
- The Experience of Female Veterans and Health-Seeking Behaviors (Switzer, 2022)
- Machine learning applications towards risk prediction and cost forecasting in healthcare (Singh, 2022)
- Does Variation in the Nursing Home Inspection Process Explain Disparity in Regulatory Outcomes? (Fox, 2020)
Looking at these titles, you can probably pick up that the research topics here are quite specific and narrowly-focused , compared to the generic ones presented earlier. This is an important thing to keep in mind as you develop your own research topic. That is to say, to create a top-notch research topic, you must be precise and target a specific context with specific variables of interest . In other words, you need to identify a clear, well-justified research gap.
Need more help?
If you’re still feeling a bit unsure about how to find a research topic for your healthcare dissertation or thesis, check out Topic Kickstarter service below.

You Might Also Like:

15 Comments
I need topics that will match the Msc program am running in healthcare research please
Hello Mabel,
I can help you with a good topic, kindly provide your email let’s have a good discussion on this.
Can you provide some research topics and ideas on Immunology?
Thank you to create new knowledge on research problem verse research topic
Help on problem statement on teen pregnancy
This post might be useful: https://gradcoach.com/research-problem-statement/
can you provide me with a research topic on healthcare related topics to a qqi level 5 student
Please can someone help me with research topics in public health ?
Hello I have requirement of Health related latest research issue/topics for my social media speeches. If possible pls share health issues , diagnosis, treatment.
I would like a topic thought around first-line support for Gender-Based Violence for survivors or one related to prevention of Gender-Based Violence
Please can I be helped with a master’s research topic in either chemical pathology or hematology or immunology? thanks
Can u please provide me with a research topic on occupational health and safety at the health sector
Good day kindly help provide me with Ph.D. Public health topics on Reproductive and Maternal Health, interventional studies on Health Education
may you assist me with a good easy healthcare administration study topic
May you assist me in finding a research topic on nutrition,physical activity and obesity. On the impact on children
Submit a Comment Cancel reply
Your email address will not be published. Required fields are marked *
Save my name, email, and website in this browser for the next time I comment.
- Print Friendly
Edinburgh Research Archive

- ERA Home
- Edinburgh Medical School
Edinburgh Medical School thesis and dissertation collection
By Issue Date Authors Titles Subjects Publication Type Sponsor Supervisors
Search within this Collection:
Edinburgh Medical School is one of two schools at the College of Medicine and Veterinary Medicine at the University of Edinburgh. The Edinburgh Medical School integrates research and teaching across our three Deaneries: Biomedical Sciences, Clinical Sciences and Molecular,Genetic and Population Health Sciences.
Recent Submissions
Integrated analysis of patient gene expression data for precision medicine applications in breast and pancreatic cancer , investigating chromosome cohesion loss in mammalian oocytes , quality palliative care in humanitarian crises in low- and middle-income country context , understanding and stratifying brain health through blood-based omics data , role of the nuclear basket in regulating the senescence-associated secretory phenotype , identifying mistranslating mrnas in mouse models of autism , development of attachment in infants born preterm , investigating the motor neuron translatome in spinal muscular atrophy and normal postnatal development , impact of prenatal stress and chronic stress in adult rats on the brain, behaviour and gut microbiome , investigating colonic macrophage heterogeneity in steady-state, inflammation, and resolution , social behaviour in two rat models of syngap1 haploinsufficiency , multimodal decoding of the human and mouse mesenchymal lineage in biliary fibrosis , establishing the mechanistic basis of action for novel siderophore-based antibiotics in gram-negative bacteria , planar cell polarity pathway as a master regulator of biliary morphogenesis , anatomical, biomechanical and histological evaluation of the glenoid labrum , circuitry and function of layer 1 interneurons in the medial entorhinal cortex , exploiting large-scale exome sequence data to study the genotype-phenotype relationship , characterising disease heterogeneity in crohn's disease and ulcerative colitis: leveraging longitudinal biomarker profiles , influence of glucocorticoid bioavailability on atherogenesis , manganese-enhanced magnetic resonance imaging in cardiometabolic disorders .

- USF Research
- USF Libraries
Digital Commons @ USF > USF Health > College of Public Health > Public Health Practice > Theses and Dissertations
Public Health Theses and Dissertations
Theses/dissertations from 2023 2023.
Needs Assessment for a Web-Based Support Resource for Patients with a Pathogenic Variant in LMNA , Dylan M. Allen
Evaluation of a Story-telling Approach to Educate Minority Populations About Inherited Cancer , Celestyn B. Angot
Using the Genetic Counseling Skills Checklist to Characterize Prenatal Genetic Counseling , David A. Cline
Reframing Resistance, Resilience, and Racial Equity in Maternal Health: A Mixed Methods Exploration of Paternal Involvement and the Racial Disparity in Severe Maternal Morbidity , Marshara G. Fross
Student Perceptions of the Nonmedical Use of Prescription Stimulants and Preferences for Health Education , Ana Gutierrez
Relationships between Leading and Trailing Indicators at Construction Sites in Yanbu Industrial City, Saudi Arabia , Anas H. Halloul
Variability of Air Sampling Results Using Air-O-Cell Cassettes , Christina M. Haworth
Use of Silica Dust and Lunar Simulants for Assessing Lunar Regolith Exposure , Layzamarie Irizarry-Colon
The Aging Workforce: How it Relates to Incident Rates within a Distribution Warehouse and a Chemical Manufacturing Building , Elisabeth V. Jones
Fuzzy KC Clustering Imputation for Missing Not At Random Data , Markku A. Malmi Jr.
Piloting a Spanish-language Web-based Tool for Hereditary Cancer Genetic Testing , Gretter Manso
Development of a ddPCR Multiplex to Measure the Immune Response to Borrelia burgdorferi. , Kailey Marie McCain
A Healthcare Claims Investigation of Parasomnia Epidemiology, Associations with Attention Deficit/Hyperactivity Disorder, and REM Sleep Behavior Disorder Correlates , Anh Thy Ha Nguyen
Diet and Salivary Microbiome on Cardiovascular Risk and Glycemic Control in Participants with and without Type 1 Diabetes: The CACTI Study , Tiantian Pang
Evaluation of Two Methods to Estimate Wet Bulb Globe Temperature from Heat Index , Stephi Pofanl
Intimate Conversations: A Mixed-Methods Study of African American Father-Adolescent Sexual Risk Communication , Shanda A. Vereen
Assessment of ISO Heart Rate Method to Estimate Metabolic Rate , Karl Williams
Theses/Dissertations from 2022 2022
Outcomes of a Periodic Exposure Assessment of Workers at a University Campus , Logan M. Armagast
Evaluating the Effect of Public Health Governance Structure and Public Opinion on COVID-19 Disease Control Interventions , Daniel Chacreton
Alpha Synuclein: A therapeutic target and biomarker for Parkinson’s Disease , Max Chase
A Study of Noise Exposures for Amusement Park Employees by Positions and Ride Categories , Danielle M. Dao
Bayesian Network-based Diagnostic Support Tool with Limited Point-of-Care Ultrasound for Work-related Elbow Injuries , Cristina Maria Franceschini Sánchez
Host-Pathogen Coevolution Between Tasmanian Devils (Sarcophilus harrisii) and Devil Facial Tumor Disease , Dylan Garret Gallinson
Measurements of Generalizability and Adjustment for Bias in Clinical Trials , Yuanyuan Lu
Examining the Relationship between Racial Respect among Black Early Childhood Professionals and their Perceptions of Black Children , Kayla Nembhard
Etiology of sterile intra-amniotic inflammation: An exploratory study , Zoe M. Taylor
Evaluating and Improving a Novel Toolkit for Implementation and Optimization of Lynch Syndrome Universal Tumor Screening , Tara M. Wolfinger
Theses/Dissertations from 2021 2021
Exploring Adult Attachment in Intimate Relationships among Women who Were Exposed to Intimate Partner Violence in Childhood: A Convergent Mixed Methods Approach , Ngozichukwuka C. Agu
Comparison of the Effectiveness of Disinfectant-Impregnated Wipes Versus Detergent Wipes for Surface Decontamination , Jacob Amadin
Limited Point of Care Ultrasound Clinical Decision Support Model for Work-related Injuries of the Shoulder Utilizing Bayesian Network , Gwen Marie Ayers
Synthesis of a Multimodal Ecological Model for Scalable, High-Resolution Arboviral Risk Prediction in Florida , Sean P. Beeman
Feasibility of a Virtual Group Nutrition Intervention for Adolescents with Autism Spectrum Disorder , Acadia W. Buro
Defining Codes Based on the Consolidated Framework for Implementation Research in the Context of the Implementing Universal Lynch Syndrome Screening , Jasmine A. Burton-Akright
Americans’ Familiarity, Interest, and Actions with Direct-to-Consumer Genetic Testing , Riley L. Carroll
Does Better A1C Control Worsen Osteoarthritis? An Electronic Health Record Cross-Sectional Study , Sarah C. Cattaneo
Analysis of Post-traumatic Stress Disorder Gene Expression Profiles in a Prospective, Community-based Cohort , Jan Dahrendorff
Differential Privacy for Regression Modeling in Health: An Evaluation of Algorithms , Joseph Ficek
Does Time-Weighted Averaging for WBGT and Metabolic Rate Work for Work-Recovery Cycles? , John W. Flach
Screening of Pregnant Women with Opioid Use Disorder: Identifying Factors Impacting Implementation of Screening Recommendations Using the Theoretical Domains Framework , Tara R. Foti
Epigenetic Potential in an Introduced Passerine , Haley E. Hanson
Face Mask Use to Protect Against COVID-19; Importance of Substrate, Fit, and User Tendencies , Evelyn Kassel
Novel Educational Material for Patients with a Variant of Uncertain Significance (VUS) in a Cancer Risk Gene , Meghan E. Kelley
Mechanisms and Mitigation: Effects of Light Pollution on West Nile Virus Dynamics , Meredith E. Kernbach
Seasonality in Competence to Transmit West Nile Virus for a Widespread Reservoir , Kyle L. Koller
Mealtimes in Early Childhood Education Centers During COVID-19: A Mixed-Methods Assessment of Responsibilities, Interactions, and Best Practices , Joanna Mackie
Development and Validation of an Isothermal Amplification Assay for Eastern Equine Encephalitis Virus , Mikayla D. Maddison
Evaluating the Development and Implementation of Campus-based Sexual and Interpersonal Violence Prevention Programming , Robyn Manning-Samuels
Bait-and-Kill: Targeting a Novel Heme Biochemical Pathway in Hundreds of Cancers , Christopher G. Marinescu
Acclimatization Protocols and Their Outcomes , Ayub M. Odera
Promoting HPV vaccination with vaccine-hesitant parents using social media: a formative research mixed-method study , Silvia Sommariva
Sleep Diagnoses and Low Back Pain in U.S. Military Veterans , Kenneth A. Taylor
Theses/Dissertations from 2020 2020
Journey Mapping the Minority Student’s Path Toward Genetic Counseling: A Holistic Picture , Tatiana E. Alvarado-Wing
Using Observations from the UAW-Ford Ergonomic Assessment Tool to Predict Distal Upper Extremity Musculoskeletal Disorders , Zachariah T. Brandes-Powell
Do Similar Exposure Groups (SEG) differ from Air Force base to Air Force base? A Combat Arms Training and Maintenance (CATM) noise exposure comparison of Moody AFB and MacDill AFB. , Miriam F. Escobar
Predictors of Premature Discontinuation from Behavioral Health Services: A Mixed Methods Study Guided by the Andersen & Newman Model of Health Care Utilization , Shawna M. Green
Non-invasive Sex Determination and Genotyping of Transgenic Brugia malayi Larvae , Santiago E. Hernandez Bojorge
Does Gestational Diabetes Mellitus Increases the Risk of Preeclampsia Among Primigravid Women? , Astha Kakkad
Evaluating Effects of Cancer Genetic Counseling on Several Brief Patient Impact Measures , Alyson Kneusel
Impact of Heat-Related Illness and Natural Environments on Behavioral Health Related Emergency and Hospital Utilization in Florida , Natasha Kurji
The Quantification of Heavy Metals in Infant Formulas Offered by the Florida WIC Program , Naya Martin
Differences in Knowledge Acquisition, Perceived Engagement and Self-Efficacy in Latino Promotores Delivering the Heart Disease Prevention Program Su Corazόn, Su Vida , Samuel Matos-Bastidas
Spatial and Temporal Determinants Associated with Eastern Equine Encephalitis Virus Activity in Florida , Kristi M. Miley
Using Observations from the UAW-Ford Ergonomic Assessment Tool to Predict Low Back Musculoskeletal Disorders , Colins Nwafor
On the Importance of Context: Examining the Applicability of Infertility Insurance Mandates in the United States Using a Mixed-Methods Study Design , Nathanael B. Stanley
Exploration of Factors Associated with Perceptions of Community Safety among Youth in Hillsborough County, Florida: A Convergent Parallel Mixed-Methods Approach , Yingwei Yang
Theses/Dissertations from 2019 2019
The Ability of the U.S. Military’s WBGT-based Flag System to Recommend Safe Heat Stress Exposures , David R. Almario
The Relationship between Continuous Glucose Monitor (CGM) Derived Metrics and Indices of Glycemic Control , Ryan Bailey
“Man plans but ultimately, God decides”: A Phenomenological Investigation of the Contextual Family Planning Beliefs of Recently Resettled Congolese Refugee Women in West Central Florida. , Linda Bomboka Wilson
‘If He Hits Me, Is That Love? I Don’t Think So’: An Ethnographic Investigation of the Multi-Level Influences Shaping Indigenous Women’s Decision-Making Around Intimate Partner Violence in the Rural Peruvian Andes , Isabella Li Chan
An Assessment of the Role of Florida Pharmacists in the Administration of Inactivated Influenza Vaccine to Pregnant Women , Oluyemisi O. Falope
Epidemiological Analysis of Malaria Decrease in El Salvador from 1955 until 2017 , Tatiana I. Gardellini Guevara
Self-Collected Sampling Methods for Chlamydia and Gonorrhea Screening Among College Women: Exploring Patient-Centered Intervention Characteristics , Stacey B. Griner
The Relationship Between Hand and Wrist Musculoskeletal Disorders and Hand Activity and Posture , Warren M. Henry
Speeding Diagnosis and Saving Money Using Point of Care Ultrasound Rather Than MRI for Work-related MSK Injuries , Jared A. Jeffries
Mitigating Barriers to Chronic Disease Risk Factor Prevention and Management in Disadvantaged Communities , Krys M. Johnson
Comparing Family Sharing Behaviors in BRCA Carriers with PALB2 Carriers , Joy E. Kechik
Investigating Air Pollution and Equity Impacts of a Proposed Transportation Improvement Program for Tampa , Talha Kemal Kocak
Exploring Young Women’s Choice to Initiate Use of Long-acting Reversible Contraception: A Mixed Methods Approach , Helen Mahony
Evaluation of Clinical Practices and Needs about Variants of Uncertain Significance Results in Inherited Cardiac Arrhythmia and Inherited Cardiomyopathy Genes , Reka D. Muller
Effects of Medications with Anticholinergic Properties and Opioids on Cognitive Function and Neural Volumetric Changes in Elderly Australians , Malinee Neelamegam
Sundaas Story: A Mixed-Methods Study of Household Sanitation Provisioning in Urban Informal Housing in India , Sarita Vijay Panchang
A Retrospective Study of the Opioid Epidemic and Fentanyl Related Overdose Fatality Cases in a Florida West Coast Medical Examiner District Population , Anne Terese Powell
Using Predicted Heat Strain to Evaluate Sustainable Exposures , Samantha L. Thacker
Isokinetic Sampling Efficiency Differences for Blunt Edge vs Sharp Edge Sampling Probes , Cory A. Treloar
Using the Consolidated Framework for Implementation Research to Investigate Daily Pre-exposure Prophylaxis (emtricitabine/tenofovir DF) Implementation via Community-based HIV Testing Sites in Florida , Deanne E. Turner
“We can learn some things from them, but they can learn some things from us too”: Intergenerational Perceptions of Shared Infant Feeding Information , Alexis L. Woods Barr
Theses/Dissertations from 2018 2018
Comparison of Modeled and Measured Pesticide Concentrations in Air , Trenell Davis Boggans
Effectiveness of Biocide Substitution and Management Plan Implementation for the Control of , Adelmarie Bones
Design, Construction, and Characterization of the University of South Florida Wind Tunnel , Jason S. Garcia
Characterization of Scanning Mobility Particle Sizers For Use With Nanoaerosols , Michael R. Henderson
Validation of the Thermal Work Limit (TWL) Against Known Heat Stress Exposures , Danielle L. Kapanowski
Validation of a New Concept for Measuring Respirable Dusts , Xiao Liu
Occupational Noise Exposure Evaluation of Airline Ramp Workers , Adekunle Ogunyemi
Reduction in Needlestick Injuries Using a Novel Package of Interventions , Kamal Thakor Patel
Ability of the ISO Predicted Heat Strain Method to Predict a Limiting Heat Stress Exposure , Edgar Prieto
Developing the Evidence Base for Mental Health Policy and Services: Inquiries into Epidemiology, Cost-Benefits, and Utilization , Joseph L. Smith
Occupational Sharps Injuries in Medical Trainees at the University of South Florida: A Follow-up Study , Kourtni L. Starkey
Advanced Search
- Email Notifications and RSS
- All Collections
- USF Faculty Publications
- Open Access Journals
- Conferences and Events
- Theses and Dissertations
- Textbooks Collection
Useful Links
- Rights Information
- SelectedWorks
- Submit Research
Home | About | Help | My Account | Accessibility Statement | Language and Diversity Statements
Privacy Copyright
- Open access
- Published: 12 October 2021
A systematic review of medical students’ and professionals’ attitudes and knowledge regarding medical cannabis
- Jared M. Weisman ORCID: orcid.org/0000-0001-7332-7686 1 , 2 &
- Marcus Rodríguez 1 , 3
Journal of Cannabis Research volume 3 , Article number: 47 ( 2021 ) Cite this article
6718 Accesses
19 Citations
21 Altmetric
Metrics details
Recently, the renewed global interest in cannabis’ therapeutic properties has resulted in shifting attitudes and legislative policies worldwide. The aim of this systematic review is to explore the existing literature on medical professionals’ and students’ attitudes and knowledge regarding medicinal cannabis (MC) to assess any relevant and significant trends.
This systematic review was conducted in accordance with PRISMA guidelines. Using PubMed and Google Scholar, a literature search was performed to identify studies pertaining to healthcare professionals’ and medical students’ knowledge and attitudes regarding MC. There were no search limits on the year of publication; however, studies without primary data (e.g., abstracts, systematic reviews, meta-analyses) and non-English language papers were excluded. Studies were coded according to the following research questions: (1) Do respondents believe that cannabis should be legalized (for medicinal and/or recreational purposes)? (2) Are respondents confident in their level of knowledge regarding cannabis’ clinical applications? (3) Are respondents convinced of cannabis’ therapeutic potential? 4) What current gaps in knowledge exist, and how can the medical community become better informed about cannabis’ therapeutic uses? and (5) Are there significant differences between the knowledge and opinions of healthcare students versus healthcare professionals with respect to any of the aforementioned queries? Chi-square tests were used to assess differences between medical students and medical professionals, and Pearson’s bivariate correlations were used to analyze associations between survey responses and year of publication—as a proxy measurement to assess change over time.
Out of the 741 items retrieved, 40 studies published between 1971 and 2019 were included in the final analyses. In an evaluation of 21 qualified studies (8016 respondents), 49.9% of all respondents favored legalization (SD = 25.7, range: 16–97%). A correlational analysis between the percentage of survey respondents who support MC legalization and year of publication suggests that both medical students’ and professionals’ support for MC legalization has increased from 1991 to 2019 ( r (19) = .44, p = .045). Moreover, medical professionals favor the legalization of MC at a significantly higher rate than students (52% vs. 42%, respectively; χ 2 (1, N = 9019) = 50.72 p < .001). Also, respondents consistently report a strong desire for more education about MC and a substantial concern regarding MC’s potential to cause dependence and addiction. Pearson’s correlations between year of publication and survey responses for both of these queried variables suggest minimal changes within the last decade (2011–2019 for addiction and dependence, 2012-2019 for additional education; r (13) = − .10, p = .713 and r (12) = − .12, p = .678, respectively).
The finding that both medical students’ and professionals’ acceptance of MC has significantly increased in recent decades—in conjunction with their consistent, strong desire for more educational material—suggests that the medical community should prioritize the development of MC educational programs. MC is far more likely to succeed as a safe and viable therapy if the medical professionals who administer it are well-trained and confident regarding its clinical effects. Limitations include a lack of covariate-based analyses and the exclusion of studies published after the literature search was performed (June 2019). Future research should analyze studies published post-2019 to draw temporal comparisons and should investigate the effect of numerous covariates (e.g., gender, religiosity, prior cannabis use) as newer studies gather data on these factors [PROSPERO Registration: CRD42020204382].
Archaeological inquiry has revealed that cannabis use has been pervasive throughout human society for at least five millennia. In fact, it was widely used as a medical therapy in the USA in the 19th and early 20th centuries and was first incorporated into the United States Pharmacopoeia in 1850 (Bridgeman and Abazia 2017 ). The first federal restrictions on cannabis occurred in 1937 with the passage of the Marihuana Tax Act, which heavily regulated its usage and sale. Subsequently, cannabis was dropped from the United States Pharmacopoeia in 1942, and legal penalties for its possession increased in 1951 and 1956 with the enactment of the Boggs and Narcotic Control Acts, respectively. Finally, the Controlled Substances Act of 1970 relegated cannabis to Schedule I status at the federal level, imposing limitations on research by restricting the procurement of cannabis for research purposes (Bridgeman and Abazia 2017 ). Moreover, cannabis remains illegal under international law. From 1961 to 2020, The United Nations’ Single Convention on Narcotic Drugs (1961) placed cannabis and its derivative products in Class IV: the most restrictive category—analogous to the DEA’s Schedule I designation (United Nations 1964 ). However, in December 2020, the UN Commission on Narcotic Drugs reclassified cannabis and cannabis resin to recognize its medicinal value. Reclassification will rescind some longstanding procedural barriers to research and development of cannabis-based medicinal products; however, it will not affect its recreational use or promote legalization, and it will remain under strict international control. According to international law, cannabis will now be classified as having a similar degree of abuse and dependence potential as opiate-based drugs such as morphine and oxycodone (World Health Organization 2020 ).
Notwithstanding, as of May 2021, 36 US states, 4 US territories, the District of Columbia, and several dozen nations around the world have passed laws permitting the renewed medicinal usage of cannabis (Bifulco and Pisanti 2015 ; Hanson 2021 ). Fortunately, dozens of studies assessing healthcare professionals’, medical students’, and patients’ knowledge and attitudes towards medicinal cannabis (MC) have been published in that time frame. Several such studies predate the first legislative bill legalizing MC in California (in 1996), and many studies were conducted between 1996 and 2019, when 32 other states and several countries—including Canada, Australia, and Ireland—legalized MC (Bridgeman and Abazia 2017 ; Crowley et al. 2017 ; Fischer et al. 2015 ; Hanson 2021 ; Thomsen 2016 ).
Notably, in 2019, Gardiner et al. published the first systematic review of health professionals’ beliefs, knowledge, and concerns surrounding MC (Gardiner et al. 2019 ). They found that healthcare providers generally supported MC use, despite a nearly unanimous lack of self-perceived knowledge regarding all of its clinical effects. Additionally, a preponderance of respondents voiced concerns about cannabis’ direct harm to patients and its indirect societal harms. While Gardiner et al.’s review provides a valuable compendium of data regarding health professionals’ general attitudes and knowledge of MC, this review broadens the scope of theirs by additionally assessing the responses of healthcare students. Furthermore, this review expands upon the following three questions investigated by Gardiner et al.: (1) How do health professionals feel about the use of MC in clinical practice? (2) How knowledgeable are health professionals regarding MC? and (3) What concerns exist for health professionals regarding the delivery of MC? With respect to question one, this review seeks to expand the scope of Gardiner et al.’s query by independently assessing respondents’ opinions regarding: medicinal versus recreational legalization; potential federal rescheduling; and clinical efficacy. With respect to question two, this review expands the scope of Gardiner et al.’s query by assessing both respondents’ self-reported knowledge regarding MC and assessing their desire for further education. Finally, with respect to question three, this review specifically assesses respondents’ concerns regarding MC’s potential to cause addiction and dependence—thereby expanding upon Gardiner et al.’s generalized query and seeking to inform future policy by addressing one of MC’s most pressing and pointed issues.
Additionally, in 2021, Zolotov et al. published a scoping review exploring the status of MC education among healthcare trainees (Zolotov et al. 2021 ). Their review of 23 studies across ten countries found that healthcare trainees lack sufficient knowledge about MC and do not feel prepared to counsel patients on the subject. They also found that deans and educational faculty agree on the need to educate students on MC, with an emphasis on a competencies-based curriculum. While Zolotov et al.’s review provides the most detailed investigation into MC education to date, this review expands upon their study by analyzing previously unaddressed temporal, geographic, and demographic factors. Moreover, this study provides a holistic review of MC literature, with education being one topic among several which are considered and analyzed.
Ultimately, the limited scope of Gardiner et al. and Zolotov et al.’s reviews—in addition to a preexisting wealth of published, peer-reviewed survey data addressing several other specific issues—led to the formation of the following seven guiding research questions which constituted the backbone of this novel systematic review.
Do you believe that physicians deserve the legal right to prescribe cannabis to patients? (i.e., Do you believe that cannabis should be legalized for therapeutic purposes?)
Do you believe that cannabis has any therapeutic utility?
Do you believe that cannabis should be legalized for recreational use?
[For US-based papers only] Do you believe that the USA should amend cannabis’ federal status as a Schedule 1 controlled substance (the most restrictive classification, asserting that the substance has no accepted medical use)?
Do you feel confident in your level of knowledge regarding the health effects of cannabis?
Do you desire additional education regarding MMJ and/or do believe that education on (medical) cannabis should be made readily available to medical professionals?
Are you concerned about cannabis’ dependence/addiction potential?
In light of the legislative hurdles and cultural stigmatization surrounding cannabis, we hope this systematic review will provide an important framework for better understanding how the medical community can work to overcome sociocultural obstacles which currently impede the acceptance of MC and other emergent, alternative therapies.
Using both Google Scholar and PubMed, a literature search was performed between July 4th, 2019, and September 12th, 2019, to identify studies investigating healthcare students’ and professionals’ knowledge and attitudes regarding cannabis. Studies which solicited the opinions of physicians, nurses, physician’s assistants, pharmacists, and medical and pharmacy students were all deemed relevant. The searches utilized three main keyword categories: (1) keywords pertaining to various respondent types (e.g., “physician” or “health professional”); (2) keywords identifying specific types of response solicitation (e.g., “attitudes” or “opinions”); and (3) keywords corresponding to various substance-related topics (e.g., “cannabis” or “cannabinoids”). A comprehensive list of all the keywords utilized in the literature searches is provided in Appendix A . Moreover, the reference lists of selected papers were assessed to identify additional studies of relevance, and both databases provide investigators with extensive lists of related studies—helping to augment the simple keyword search protocol. The entire protocol was conducted in accordance with PRISMA guidelines and was registered and added to the University of York’s PROSPERO systematic review database, and given the ID number: CRD42020204382.
Studies met criteria for inclusion if they satisfied all of the following requirements: (1) they were complete, primary data studies rather than abstracts, meta-analyses, or systematic reviews; (2) they provided relevant data with respect to one or more of the aforementioned guiding research questions; (3) they were published in English; and (4) they contained medical professional or student respondents only; or, if a study included mixed groups with non-medical professionals or students, it segregated and sorted data based on one’s status as a medical professional or non-medical professional. Studies were excluded from further analyses if they failed to meet any one of these four specified requirements (see Fig. 1 ). There were no fixed search limits regarding year of publication. Overall, out of the 741 studies retrieved in the literature search, 40 studies were identified as meeting all the necessary inclusion criteria (see Table 1 ). The Cochrane Collaboration Risk of Bias Assessment Tool (version 2) was used to assess the risk of bias for each study (see Table 2 ) (Higgins et al. 2021 ). This tool investigates the following primary sources of bias: selection bias, performance bias, detection bias, attrition bias, and reporting bias. The Cochrane Risk of Bias Assessment Tool outlines the following criteria for assessing for risk of bias in studies: sequence generation (selection bias), allocation concealment (selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective outcome reporting (reporting bias) and other potential sources of bias. Each entry was coded as “high risk” and “low risk,” or “unclear” if there was insufficient information to determine potential bias. Several criteria—including allocation concealment, blinding of participants and personnel, and blinding of outcome assessment—unanimously received ratings of “unclear” due to the nature of the survey-based studies under review.
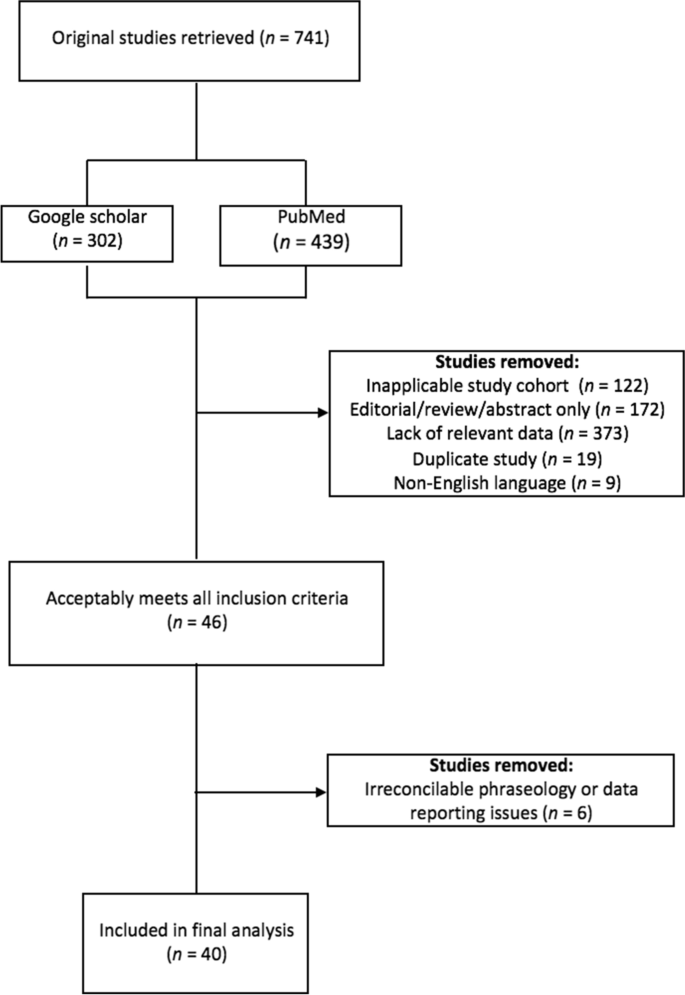
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of included studies
Data from studies which met all the inclusion criteria were subsequently logged and organized on a master spreadsheet. While sorting through papers to extract data pertaining to the seven guiding research questions, it became apparent that while most papers addressed similar topics, they often phrased their questions in slightly different ways. For example, Chan et al. ( 2017 ) asked respondents to either agree or disagree with the following statement: “physicians should recommend marijuana as medical therapy,” whereas other researchers, such as Ananth et al. ( 2018 ), asked respondents to state whether or not they—as physicians—would be willing to prescribe marijuana to a patient (Ananth et al. 2018 ; Chan et al. 2017 ). Although these survey questions may not be exactly analogous, they both address the question of whether or not physicians should be allowed to authorize MC. Therefore, it was determined that both questions could be coded under the same category—in this instance, both were included in analyses related to research question 1: “Do healthcare professionals believe that cannabis should be legalized for medicinal purposes?” Similar judgment calls were made in numerous other instances when the phraseology of certain studies did not directly align with the phraseology used in the spreadsheet. A full layout of the phraseological sorting process—in accordance with the seven guiding research questions—is provided in Appendix B .
Statistical analyses
Chi-square tests were used to assess the presence or absence of statistically significant differences between the two main survey cohorts: medical students and medical professionals. For these analyses, the total number of individual respondents from all the relevant studies who reported either “yes” or “no” to each research question were pooled into groups; then, a chi-square analysis determined if there were significant differences in the relative frequencies between each group. Additionally, Pearson’s r bivariate correlations were used to assess any relevant differences in entire studies’ responses to the research questions over time (i.e. by the year of the study’s publication). Furthermore, some temporal analyses (all using Pearson’s r bivariate correlations) assessed respondents’ opinions regarding MC with respect to the number of years preceding or following MC legalization in the state or country of the study’s publication. For these analyses, the year of MC legalization was identified for each state or country and labeled as “year 0”; then, the year of MC legalization was subtracted from the year of the study’s publication to yield the number of years distancing the study from the year of MC legalization. Finally, some temporal analyses featured a preponderance of studies conducted in a truncated time period—with only a few outlying studies published many years apart from the central cohort; in these instances, the outliers were excluded from analysis.
Descriptive statistics
In total, 40 studies provided data which were included in the final analyses; 26 studies were conducted exclusively in the USA, and the other 14 were conducted either multi-nationally or in countries other than the USA. The 40 studies produced a pool of exactly 15,200 respondents, yielding a mean of 380 respondents per study (SD = 345). For the studies which reported such statistics, there was an overall mean age of 43.8 years (SD = 4.81), with 41.3% of respondents being male (SD = 17.2). Overall, 8 studies surveyed students only (20%), 31 surveyed medical professionals only (78%), and 1 surveyed both students and professionals (3%). Within the group of studies that only surveyed medical professional, 5 surveyed pediatric or adult oncologists (16%), 4 surveyed family physicians or general practitioners (13%), 3 surveyed pharmacists (10%), 2 surveyed rheumatologists (6%), 1 surveyed psychiatrists (3%), 1 surveyed exclusively nurse practitioners (3%), 1 surveyed hospice professionals (3%), 1 surveyed neurologists (3%), and 13 surveyed a mixed cohort of various medical professionals (42%). All studies included in the final analyses were evaluated for risk of bias according to the Cochrane Collaboration. While a preponderance of studies had an unclear risk of bias, none clearly expressed a high risk of bias which could threaten the review’s overall findings or conclusions (see Table 2 , above).
Question 1: Do you believe that cannabis should be legalized for therapeutic purposes?
An analysis of question 1 drew data from 21 studies (8016 respondents) published between 1991 and 2019. A Pearson’s bivariate correlation between a study’s year of publication and the percentage of respondents supporting MC legalization suggests that both medical students’ and professionals’ support for the legalization of MC increased over time ( r (19) = .44, p = .045; Fig. 2 ). Out of the entire sample, 49.9% of all respondents favored legalization (SD = 25.7, range: 16–97%). The same correlational analysis amongst only medical professionals (following the removal of the 4 student-only studies) from studies published between 1991 and 2019 did not reach statistical significance ( r (15) = .42, p = .093). Additionally, a correlational analysis between the number of years following or preceding MC legalization in the state or country of a study’s publication (within ±20 years) and the percentage of respondents supporting MC legalization did not meet statistical significance ( r (7) = .53, p = .143).
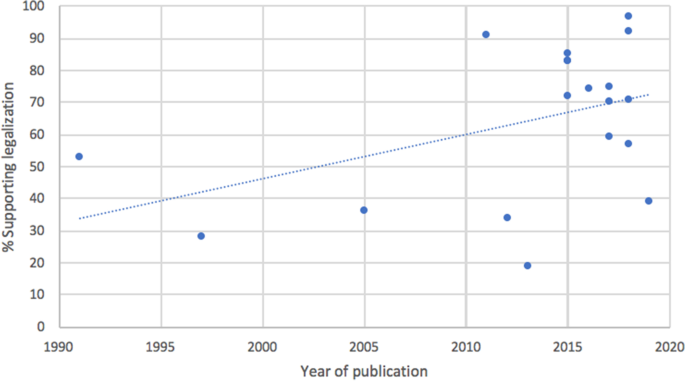
Medical students’ and professionals’ attitudes towards MC legalization, by year of study publication. Explanatory legend: Study question 1; 2 pre-1990 outliers removed; 21 studies total; r (19) = .44, p = .045
A chi-square test comparing students’ ( N = 1911, 5 studies) attitudes towards the legalization of MC against those of medical professionals ( N = 7108, 18 studies) revealed a significant difference between the two cohorts, with medical professionals favoring legalization at a significantly higher rate than students (52% vs. 42%, respectively; χ 2 (1, N = 9019) = 50.72, p < .001). Finally, a cross-national comparison of respondents’ attitudes regarding the legalization of MC reveals that levels of support markedly vary between countries; Canada demonstrated the greatest support for the legalization of MC (89%, N = 608, 2 studies), followed by Israel (83%, N = 71, 1 study), Serbia (76%, N = 396, 2 studies), Ireland (59%, N = 565, 1 study), and Australia (45%, N = 1304, 2 studies), while the USA demonstrated the least support for the legalization of MC (42%, N = 5853, 13 studies).
Question 2: Do you believe that cannabis has any therapeutic utility?
An analysis of research question 2 drew data from 26 studies (9,265 total respondents) and assessed respondents’ belief in cannabis’ medical utility. Out of the entire sample, 64.4% of all respondents espoused belief in cannabis’ therapeutic utility (SD = 18.7). A chi-square test comparing medical students’ ( N = 1118, 5 studies) versus medical professionals’ ( N = 7589, 21 studies) belief in cannabis’ medical utility yielded a significant difference, with students reporting greater confidence in cannabis’ medical utility than medical professionals (77% vs 65%, respectively; χ 2 (1, N = 8707) = 62.72, p < .001). Additionally, a cross-national comparison of respondents’ belief in cannabis’ therapeutic utility revealed that levels of belief markedly vary between countries; Serbian respondents reported the highest rates of belief in cannabis’ medical utility (84%, N = 396, 2 studies), followed by Israel (82%, N = 95, 2 studies), the USA (70%, N = 5320, 16 studies), Ireland (68%, N = 565, 1 study), and Canada (63%, N = 1353, 3 studies), while Australian respondents reported the lowest rates of belief in cannabis’ medical utility (49%, N = 726; 2 studies).
Question 3: Should cannabis be legalized for recreational use?
An analysis of research question 3 drew data from 11 studies (4754 total respondents) published between 1971 and 2019 and assessed whether medical students’ and professionals’ attitudes towards the legalization of recreational cannabis have changed over time. A Pearson’s correlation between year of publication and the proportion of respondents who support recreational legalization revealed no statistically-significant relationship ( r (9) = .11, p = .746). Out of the entire sample, 36.5% of all respondents believed cannabis should be recreationally legalized (SD = 17.7). A chi-square test of medical students’ ( N = 1834, 4 studies) versus medical professionals’ ( N = 2302, 7 studies) support for recreational legalization yielded a statistically-significant difference, with students demonstrating greater support for recreational legalization than medical professionals (43% vs. 30%, respectively; χ 2 (1, N = 4136) = 78.88, p < .001).
Question 4: Should the US federal government amend cannabis’ Schedule I status?
An analysis of research question 4 drew data from 8 studies (5303 total respondents) and assessed US-based respondents’ opinions regarding the federal rescheduling of cannabis. Out of the entire sample, 50.5% of all respondents believed that the US federal government should amend cannabis’ Schedule I status (SD = 15.4). A chi-square test between medical students ( N = 1204, 2 studies) and professionals ( N = 3045, 5 studies) yielded a significant difference between each group’s level of support for the federal rescheduling of cannabis, with students supporting more lenient federal regulations at a higher rate than professionals (60% vs. 46%, respectively; χ 2 (1, N = 4249) = 70.76, p < .001).
Question 5: Are you confident in your level of knowledge regarding the health effects of cannabis?
An analysis of research question 5 drew data from 19 studies (7,509 respondents) and evaluated respondents’ self-reported level of confidence regarding their knowledge of cannabis and its health effects. A Pearson’s correlation between the amount of years following or preceding MC legalization in the state or country of a study’s publication (limit: ±20 years) and respondents’ self-reported level of confidence revealed no statistically significant relationship (12 studies, r (10) = .22, p = .485). Out of the entire sample, 41.0% of all respondents espoused confidence in their knowledge of cannabis’ health effects (SD = 25.3, range: 5–80%). A chi-square analysis of respondents’ self-reported knowledge by respondent type (medical professionals [ N = 5068, 15 studies] vs. students [ N = 1642, 5 studies]) revealed significant differences between the two cohorts ( χ 2 (1, N = 6710) = 325.19, p < .001; see Fig. 3 ). Overall, students reported the greatest confidence in their self-reported knowledge of MC, with medical professionals (on average) reporting significantly lower rates of confidence regarding their knowledge of MC (58% vs. 33%, respectively). Finally, a cross-national comparison of respondents’ self-reported confidence in their knowledge of MC revealed that levels of knowledge markedly vary between countries; Israeli respondents reported the highest rates of self-reported confidence in their knowledge of MC (67%, N = 94, 2 studies), followed by Serbia (65%, N = 316, 1 study), the USA (45%, N = 4125, 12 studies), and Australia (26%, N = 1300, 2 studies), while Canadian respondents reported the lowest rates of self-reported confidence in their knowledge of MC (18%, N = 876, 2 studies).
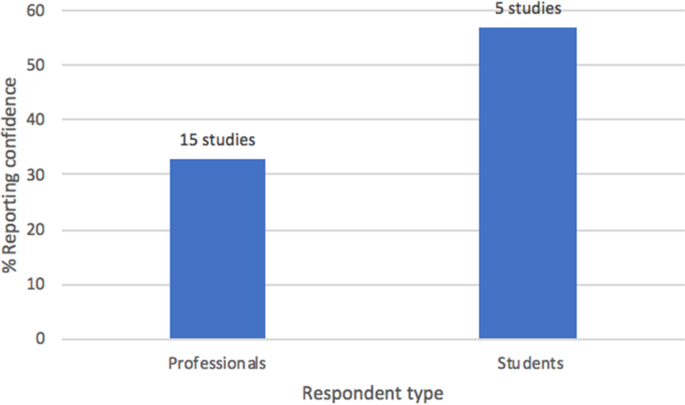
Respondents’ self-reported confidence in their knowledge of MC, by respondent type. Explanatory legend: Medical professionals ( N = 5068) vs. students ( N = 1642) ( χ 2 (1, N = 6710) = 325.19, p < .001)
Question 6: Should there be more educational material available regarding MC?
An analysis of research question 6 drew data from 15 studies (4055 total respondents) and assessed whether respondents desired more education about MC, and if they believed that information about MC should be incorporated into medical school curricula. Out of the entire sample, 86.2% of respondents believed that there should be more educational material available on MC (SD = 13.8)—with 12 out of the 15 studies reporting 75% or more of respondents desiring further education. A Pearson’s correlation between the year of a study’s publication (range: 2012–2019) and the percentage of respondents’ espousing a personal or general desire for more knowledge regarding MC did not meet statistical significance, implying no significant differences over time ( r (13) = − .10, p = .713).
Question 7: Are you concerned about cannabis’ dependence/addiction potential?
Lastly, an analysis of research question 7 drew data from 13 studies published between 2011 and 2019 (3876 total respondents) and asked respondents if they were concerned about MC’s potential to cause addiction or dependence in patients. Out of the entire sample, 57.8% of all respondents were concerned with cannabis’ potential to cause addiction or dependence (SD = 18.4). A Pearson’s bivariate correlation between the year of a study’s publication (range: 2011–2019) and the percentage of respondents espousing concern regarding MC’s potential to cause addiction or dependence and did not meet statistical significance, suggesting no change over time ( r (12) = − .12, p = .678).
This systematic review provided a multi-variate analysis of the existing literature on medical professionals’ and students’ attitudes and knowledge regarding medicinal cannabis (MC). Most notably, it was found that both medical students’ and professionals’ support for the legalization of MC has significantly increased throughout the last three decades, in addition to medical professionals being more likely than students to endorse MC legalization (52% vs. 42%, respectively). Furthermore, respondents consistently reported a strong desire for more education about MC, and a substantial concern regarding MC’s potential to cause dependence and addiction. Pearson’s correlations between year of publication and survey responses for both of these queried variables suggest minimal changes over time (2011–2019 for addiction and dependence, 2012–2019 for additional education). Lastly, support for the legalization of MC, respondents’ self-reported confidence regarding their knowledge of MC, and respondents’ belief in cannabis’ medical utility all showed considerable differences between countries. More broadly, the analyses conducted in this review sought to address each of the following guiding research questions.
Question 1: Should cannabis be legalized for therapeutic purposes?
Question 1 assessed respondents’ support for the legalization of MC. It was expected that support for the legalization of MC would increase over time due to ongoing sociocultural and legislative trends favoring legalization—which may serve to reduce stigma and increase the normalization of cannabis within the medical community. Moreover, results from Gardiner et al.’s ( 2019 ) systematic review indicate that newer studies tend to yield more accepting attitudes towards MC. Results from this systematic review supported the hypothesis, as respondents’ level of support for the legalization of MC was shown to significantly increase from 1991 to 2019 (see Fig. 2 ). Also, it was expected that students would demonstrate greater support for MC legalization compared to medical professionals, given the premise that many professionals might have been educated during an era in which cannabis was largely demonized in society and the medical community, and also given the established research finding that (at least within the USA) younger individuals are adopting more permissive views towards cannabis (Schmidt et al. 2016 ). However, results from this systematic review actually indicated the reverse, with medical professionals demonstrating greater support for MC legalization than students. This finding could be explained by entertaining the notion that students may want to espouse more orthodox viewpoints during their educational years, so as not to appear overly progressive and radical, which could possibly jeopardize their clinical accreditation. Also, a majority of existing educational programs underrepresent the medical value of cannabis and cannabinoids and instead emphasize the risks and side effects, such as addiction and dependence. This extant curricular bias could help explain students’ concerns and lack of support for MC.
Furthermore, it was hypothesized that respondents’ support for the legalization of MC would be highest in countries that took early legislative steps to legalize MC, due to the established research finding that the passage of MC laws tends to correlate with more lenient views towards cannabis—especially amongst younger people (Schmidt et al. 2016 ). This expectation was largely confirmed, as Canadian respondents demonstrated the greatest support for the legalization of MC (89%), while US respondents demonstrated the least support for the legalization of MC (42%); Canada legalized MC nationwide in 2001, while several states within the USA still fully prohibit the medical prescription of cannabis. However, this presumption has been challenged by Gritsenko et al.’s 2020 paper investigating the effect of religion on Russian medical students’ attitudes towards the legalization of MC (Gritsenko et al. 2020 ). They found that 80% of non-religious students supported legalization, compared to 60% of religious students. Despite the limited sample size of 828 students, these numbers indicate greater support for MC legalization in Russia—where all forms of cannabis are criminalized—compared to the USA. Notwithstanding, the results from Gritsenko et al. ( 2020 ) support the hypothesis that medical students, and younger people in general, would express more lenient views towards MC legalization.
Question 2 investigated respondents’ belief in cannabis’ medical utility. It was hypothesized that students would express greater faith in cannabis’ medical utility under the premise that students (being younger, on average, than professionals) would be more likely to have been raised in a sociopolitical climate more accepting of cannabis’ medical applications. This hypothesis was supported by the data, with 77% of students expressing belief in cannabis’ medical utility as opposed to only 65% of medical professionals. Similarly, it was anticipated that respondents’ from countries with a longstanding legal acceptance of MC would espouse greater confidence in cannabis’ medical utility; however, the data did not support this hypothesis, as Serbian respondents reported the greatest belief in cannabis’ medical utility (84%) despite the fact that MC remains illegal in Serbia, while Australian respondents reported the lowest levels of belief in cannabis’ medical utility (49%), despite the fact that Australia federally legalized MC in 2016.
Research question 3 assessed respondents’ support for the recreational legalization of cannabis. It was expected that support for recreational legalization would increase over time due to ongoing sociopolitical trends favoring the decriminalization and legalization of recreational cannabis. However, no significant correlational trends were observed over time. The data indicates that approximately one in two respondents (i.e., 50%) favor the legalization of recreational cannabis—regardless of the year of the study’s publication. One possible explanation is that recreational legalization has blossomed in recent years without a commensurate development in cannabis-related medical education. Moreover, several researchers have reported spikes in cannabis-related hospitalizations following recreational legalization (Auger et al. 2020 ; Zvonarev et al. 2019 ). Therefore, despite the general public’s more lenient views towards recreational legalization in recent years, physicians may continue to harbor reservations—especially as cannabis-related hospitalizations climb in the absence of proportionate developments in cannabis-related medical research. Likewise, it was expected that students would express greater support for recreational cannabis, under the premise that younger respondents tend to hold more permissive views toward cannabis regulation (Schmidt et al. 2016 ). The results supported this hypothesis, as 43% of students reported support for recreational legalization, as opposed to only 30% of medical professionals.
Research question 4 assessed US-based respondents’ opinions regarding the federal rescheduling of cannabis. Once again, it was expected that students would express greater support for the federal rescheduling of cannabis, under the premise that younger respondents tend to espouse more permissive views towards cannabis regulation (Schmidt et al. 2016 ). The data supported this hypothesis, with 60% of students indicating support for more lenient federal restrictions of cannabis use, as opposed to only 46% of medical professionals.
Question 5 assessed respondents’ self-reported confidence regarding their knowledge of MC. Results from Gardiner et al.’s ( 2019 ) review indicate that healthcare professionals consistently report low levels of self-perceived knowledge regarding MC; notwithstanding, it was hypothesized that confidence levels would rise as the number of years following MC legalization in the country of a study’s publication increased, due to respondents’ from those countries having an increased likelihood of being exposed to cannabis in clinical settings. However, no statistically significant correlational relationship was observed. Moreover, it was expected that professionals (as opposed to students) would express greater confidence in their knowledge of MC, given their more extensive medical training and clinical experience; however, the opposite result was observed, with 58% of students reporting an adequate (or better) knowledge of MC and just 33% of medical professionals reporting an adequate (or better) knowledge of MC (see Fig. 3 ). This finding could be the result of students—and younger respondents in general—having more lenient attitudes towards cannabis, resulting in a greater perceived sense of knowledge about MC; or, it could be a manifestation of the Dunning-Kruger effect, a cognitive bias in which individuals with an inferior understanding of a concept tend to overestimate their own perceived level of knowledge (Kruger and Dunning 1999 ). Notably, results from this study do not directly align with results from other reviews on this topic. Gardiner et al. ( 2019 ) found self-reported knowledge to be low amongst all types of health professionals, while Zolotov et al. ( 2021 ) found that health students overwhelmingly lacked knowledge and confidence in counseling patients on MC (Gardiner et al. 2019 ; Zolotov et al. 2021 ). Therefore, this study is the first to report significant differences in self-reported confidence levels between healthcare students and professionals. More in-depth studies are needed to survey levels of self-reported confidence in MC knowledge, particularly amongst healthcare students, to help elucidate the discrepancies between this study and the results of Zolotov et al. ( 2021 ).
Furthermore, it was hypothesized that respondents from countries with a longstanding legal acceptance of MC would demonstrate greater levels of confidence regarding their knowledge of MC, under the premise that respondents’ from such countries would have an increased likelihood of being exposed to cannabis in clinical settings. The data largely supported this hypothesis, with Israeli respondents (where MC has been legal since 1973) reporting the greatest levels of confidence (67%) and Canadian respondents (where MC has only been legal since 2001) reported the lowest levels of confidence (18%) (Wilkinson and Tarnopolsky 2019 ).
Question 6 assessed respondents’ desire for more educational material regarding MC—including supplemental educational programs for professionals and the incorporation of cannabis-related material into the existing medical school curriculum. Results from Gardiner et al.’s ( 2019 ) review found that many health professionals desired more education regarding MC, and it was expected that respondents from more recent studies would express an increased desire for further education, given the heightened acceptance of cannabis as a legitimate medical therapy in recent years. However, a Pearson’s bivariate correlation revealed no significant change in respondents’ desire for more education between 2012 and 2019, and the data actually indicated an apparent ceiling effect—with around 80% of respondents desiring more educational material regardless of the year of the study’s publication.
Lastly, research question 7 asked respondents if they were concerned about MC’s potential to cause addiction or dependence in patients. While Gardiner et al.’s ( 2019 ) review did not directly address issues of addiction and dependence, they found that many health professionals raised concerns regarding adverse psychiatric effects. For this review, it was expected that older studies would reflect greater levels of concern, given the established research finding that the perceived harmfulness of cannabis has decreased significantly since 1991 (Keyes et al. 2016 ). However, a Pearson’s bivariate correlation revealed no significant change between 2011 and 2019, with approximately one in two respondents (i.e., 50%) expressing concern for MC’s addiction and dependence potential regardless of the year of the study’s publication.
Limitations
It is important to note that this systematic review was affected by several identifiable limitations. Firstly, there was significant variability between the individual studies, including: incongruency in the survey methods and individual phraseologies used in data collection; differences in cannabis regulatory policy in the states and countries in which the surveys were conducted; and differences in the proportions of the types of respondents who answered the surveys (i.e., physicians, pharmacists, and nurses). For instance, many studies included cohorts of medical professionals who specialized in a variety of subfields (e.g., neurology, pharmacy, oncology, and rheumatology); therefore, the analyses presented in this systematic review are generalized findings that combine the responses of all medical professional subtypes. This necessary methodological procedure led to the overall generalization of the medical professional cohort, consequently nullifying any potential differences or distinctions within the overarching “medical professional” group. In addition, far more studies assessed the opinions of medical professionals (31 studies) as opposed to those of medical students (9 studies), which limits the strength of the comparisons made between the two cohorts. Relatedly, not enough studies analyzed in this review published data on relevant covariates (e.g., gender, religiosity, political affiliations, etc.) to analyze data along these variables. Another very important consideration is whether respondents’ personal use of either medicinal or recreational cannabis biased or shaped their opinions. As more studies emerge, research should strive to better understand how these numerous covariates influence respondents’ opinions toward MC.
Given the rapidly increasing interest in the field of MC, it is also crucial to note that the literature search was performed roughly halfway through 2019, resulting in the exclusion of numerous, relevant studies which were published afterwards. Such studies include: Gritsenko et al. ( 2020 ), Benavides et al. ( 2020 ), and Arnfinsen and Kisa ( 2021 ), among others (Arnfinsen and Kisa 2021 ; Benavides et al. 2020 ; Gritsenko et al. 2020 ). The reason for the 2019 search cutoff is due to the fact that this study was conducted as part of an undergraduate thesis completed in December 2019. Therefore, the authors of this review recommend that follow-up studies be performed in the coming years to draw temporal comparisons to the results of the present study. As research within the field continues to greatly proliferate, these follow-ups will help reveal distinct trends and key ways in which attitudes and knowledge are shifting so that medical professionals, educators, and policymakers can stay up-to-date with respect to rapidly changing developments within the field.
Also, while the 40 studies provided enough data to conduct a meaningful systematic review, most did not provide the necessary metrics (e.g., pre/post comparisons and between-groups comparisons) required to perform an even more comprehensive meta-analysis. Going forward, more studies should begin to yield the requisite effect sizes required to perform meta-analyses as the surveys used in these studies begin to include more data pertaining to mediation analyses and pre/post comparisons. Lastly, a major preponderance of studies collected for this systematic review were published after 2010 (34 out of 40), which limits the statistical power of long-term temporal analyses—resulting in a reduced range of years in which comparisons can be made to assess changes in knowledge and attitudes over time.
Implications
Crucially, results from this systematic review have important implications for the continued adoption of MC within the global medical community. Notably, this review found that medical students are significantly more likely to report high levels of confidence regarding their knowledge of MC as compared to medical professionals. Consequently, establishing an objective set of scientifically sound research and educational protocols regarding the management of MC will be imperative in mitigating potential barriers which might arise between more orthodox, senior clinicians and younger, more progressive clinicians as MC and other alternative therapies increasingly augment the conventional medical canon. In addition, respondents’ consistently expressed concerns regarding MC’s potential to induce addiction and dependence—with about one-half of all respondents espousing concern regardless of the year in which the study was conducted. Accordingly, future research and educational programs should specifically address the risks of addiction and dependence to better inform the medical community on the potential risks of MC prescription. Taken together, these data will help to inform future clinical investigations and further scholarship into MC-related topics, particularly in regions where MC is just beginning to come into clinical usage. Thankfully—through the analysis, elucidation, and dissemination of past and ongoing trends pertaining to the progression of MC acceptance in clinical communities—it is now possible for future practice and policy to become more streamlined, safe, and effective.
This systematic review assessed contemporary and relevant trends pertaining to medical professionals’ and students’ opinions and knowledge regarding medicinal cannabis (MC). Moreover, this review expanded upon Gardiner et al. ( 2019 ) and Zolotov et al.’s ( 2021 ) similar reviews by (a) examining more studies from a broader array of countries, (b) investigating highly specific research questions, (c) exploring temporal trends in the data, (d) comparing student and professional cohorts, and (e) performing statistical analyses which yielded significant trends pertaining to medical students’ and professionals’ knowledge and attitudes regarding MC. Most importantly, the finding that both medical students’ and professionals’ acceptance of MC has significantly increased in recent decades—in conjunction with their consistent, strong desire for more educational material—suggests that the medical community should prioritize the development of MC educational programs. MC is far more likely to succeed as a safe and viable therapy if the medical professionals who administer it are well-trained and confident regarding its clinical effects. Notwithstanding, the preponderance of highly restrictive legislative policies limiting cannabis’ status as a subject of scientific inquiry has led to a dearth of educational material on MC. Therefore, results from this systematic review should encourage the medical community to more seriously consider relevant policy work along with honest, comprehensive investigations into MC to assuage the ongoing stigma and misinformation currently surrounding it—which will help facilitate its safe and effective integration into commonly-accepted medical practice.
Availability of data and materials
Full methodology is available at the PROSPERO database ( https://www.crd.york.ac.uk/prospero/ ) under the registration number CRD42020204382. Additionally, appendices A and B provide extensive search and coding methodology, and the data pulled from each selected article is available in Table 1 .
Abbreviations
Medical/medicinal cannabis
Ablin JN, Elkayam O, Fitzcharles MA. Attitudes of Israeli rheumatologists to the use of medical cannabis as therapy for rheumatic disorders. Rambam Maimonides Med J. 2016;7(2):e0012. https://doi.org/10.5041/RMMJ.10239 .
Ananth P, Ma C, Al-Sayegh H, Kroon L, Klein V, Wharton C, et al. Provider perspectives on use of medical marijuana in children with cancer. Pediatrics. 2018;141(1). https://doi.org/10.1542/peds.2017-0559 . Epub 2017 Dec 12.
Arnfinsen JL, Kisa A. Assessment of Norwegian physicians’ knowledge, experience and attitudes towards medical cannabis. Drugs Educ Prev Pol. 2021;28(2):165–71.
Article Google Scholar
Auger N, Luu TM, Ayoub A, Bilodeau-Bertrand M, Lo E, Low N. Cannabis-related hospitalizations among youth in Canada before and after cannabis legalization. J Addict Med. 2020;2020(ePub):33060465.
Google Scholar
Balneaves LG, Alraja A, Ziemianski D, McCuaig F, Ware M. A national needs assessment of Canadian nurse practitioners regarding cannabis for therapeutic purposes. Cannabis Cannabinoid Res. 2018;3(1):66–73.
Article PubMed PubMed Central Google Scholar
Bega D, Simuni T, Okun MS, Chen X, Schmidt P. Medicinal cannabis for Parkinson’s Disease: Practices, beliefs, and attitudes among providers at National Parkinson Foundation Centers of Excellence. Mov Disord Clin Pract. 2016;4(1):90–5.
Benavides A, Gregorio N, Gupta P, Kogan M. Medical students are unprepared to counsel patients about medical cannabis and want to learn more. Complement Ther Med. 2020;48(2020):102237.
Article PubMed Google Scholar
Berlekamp D, Rao PSS, Patton T, Berner J. Surveys of pharmacy students and pharmacy educators regarding medical marijuana. Curr Pharm Teach Learn. 2019;11(7):669–77.
Bifulco M, Pisanti S. Medicinal use of cannabis in Europe. EMBO Rep. 2015;16(2):130–2.
Article CAS PubMed PubMed Central Google Scholar
Braun IM, Wright A, Peteet J, Meyer FL, Yuppa DP, Bolcic-Jankovic D, et al. Medical oncologists’ beliefs, practices, and knowledge regarding marijuana used therapeutically: A nationally representative survey study. J Clin Oncol. 2018;36(19):1957–62.
Bridgeman MB, Abazia DT. Medicinal cannabis: History, pharmacology, and implications for the acute care setting. Pharm Ther. 2017;42(3):180–8.
Burke WM, Marx MB. Attitudes of professional students toward legal control of psychoactive substances. HSMHA Health Rep. 1971;86(8):725.
Caligiuri FJ, Ulrich EE, Welter KJ. Pharmacy student knowledge, confidence and attitudes toward medical cannabis and curricular coverage. Am J Pharm Educ. 2018;82(5):424–33.
Carlini BH, Garrett SB, Carter GT. Medicinal cannabis: A survey among health care providers in Washington state. Am J Hosp Palliat Med. 2016;34(1):85–91.
Chan MH, Knoepke CE, Cole ML, McKinnon J, Matlock DD. Colorado medical students’ attitudes and beliefs about marijuana. J Gen Intern Med. 2017;32(4):458–63.
Charuvastra A, Friedmann PD, Stein MD. Physician attitudes regarding the prescription of medical marijuana. J Addict Dis. 2005;24(3):87–93.
Cogswell JB, Harris SW. Social work and medical students’ perspectives on the use of cannabis as a medical intervention. Sacramento: Dissertation (thesis); California State University; 2015.
Crosby C. Perceptions and attitudes of healthcare students towards marijuana. Dissertation (thesis). Cheney: Eastern Washington University; 2018.
Crowley D, Collins C, Delargy I, Laird E, Van Hout MC. Irish general practitioner attitudes toward decriminalisation and medical use of cannabis: Results from a national survey. Harm Reduct J. 2017;14(1). https://doi.org/10.1186/s12954-016-0129-7 .
Doblin RE, Kleiman MA. Marijuana as antiemetic medicine: A survey of oncologists experiences and attitudes. J Clin Oncol. 1991;9(7):1314–9.
Article CAS PubMed Google Scholar
Ebert T, Zolotov Y, Eliav S, Ginzburg O, Shapira I, Magnezi R. Assessment of Israeli physicians' knowledge, experience and attitudes towards medical cannabis: A pilot study. Isr Med Assoc J. 2015;17(7):437–41.
PubMed Google Scholar
Fischer B, Kuganesan S, Room R. Medical marijuana programs: Implications for cannabis control policy – observations from Canada. Int J Drug Policy. 2015;26(1):15–9.
Fitzcharles MA, Ste-Marie PA, Clauw DJ, Jamal S, Karsh J, LeClercq S, et al. Rheumatologists lack confidence in their knowledge of cannabinoids pertaining to the management of rheumatic complaints. BMC Musculoskelet Disord. 2014;15(1):258.
Gardiner KM, Singleton JA, Sheridan J, Kyle GJ, Nissen LM. Health professional beliefs, knowledge, and concerns surrounding medicinal cannabis – a systematic review. PLoS One. 2019;14(5):e0216556. https://doi.org/10.1371/journal.pone.0216556 .
Gritsenko V, Kogan M, Konstantinov V, Marinova T, Reznik A. Isralowitz R (2020) Religion in Russia: Its impact on university student medical cannabis attitudes and beliefs. Complement Ther Med. 2020;54:102546.
Hanson K. State medical marijuana laws: National Conference of State Legislatures; 2021. Published July 14, 2021. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx . Accessed 25 July 2021
Higgins JPT, Savović J, Page MJ, Elbers RG, Sterne JAC. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021): Cochrane; 2021. Available from www.training.cochrane.org/handbook .
Hwang J, Arneson T, St. Peter W. Minnesota pharmacists and medical cannabis: A survey of knowledge, concerns, and interest prior to program launch. Pharm Ther. 2016;41(11):716–22.
Jacobs NI, Montebello M, Monds LA, Lintzeris N. Survey of Australian psychiatrists’ and psychiatry trainees’ knowledge about and attitudes towards medicinal cannabinoids. Australas Psychiatry. 2018;27(1):80–5.
Karanges EA, Suraev A, Elias N, Manocha R, McGregor IS. Knowledge and attitudes of Australian general practitioners towards medicinal cannabis: A cross-sectional survey. BMJ Open. 2018;8(7):e022101. https://doi.org/10.1136/bmjopen-2018-022101 .
Keyes KM, Wall M, Cerdá M, Schulenberg J, O’Malley PM, Galea S, et al. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991-2014. Addiction. 2016;111(12):2187–95.
Kondrad E, Reid A. Colorado family physicians attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52–60.
Kruger J, Dunning D. Unskilled and unaware of it: How difficulties in recognizing one’s own incompetence lead to inflated self-assessments. J Pers Soc Psychol. 1999;77(6):1121–34.
Kusturica MP, Tomas A, Sabo A, Tomic Z, Horvat O. Medical cannabis: Knowledge and attitudes of prospective doctors in Serbia. Saudi Pharm J. 2019;27(3):320–5.
Lieff J, Avorn J, Caddell H, Anderson H, Gorlin P, Kennedy S, et al. Attitudes of the medical profession toward drug abuse. Am J Public Health. 1973;63(12):1035–9.
Linn LS, Yager J, Leake B. Physicians' attitudes toward the legalization of marijuana use. West J Med. 1989;150(6):714–7.
CAS PubMed PubMed Central Google Scholar
Luba R, Earleywine M, Farmer S, Slavin M. Cannabis in end-of-life care: Examining attitudes and practices of palliative care providers. J Psychoact Drugs. 2018;50(4):348–54.
Martins-Welch D, Nouryan C, Kline M, Modayil S. Health providers’ perspectives on medical marijuana use. J Clin Oncol. 2017;35(31):235.
Mathern GW, Beninsig L, Nehlig A. Fewer specialists support using medical marijuana and CBD in treating epilepsy patients compared with other medical professionals and patients: Result of Epilepsia’s survey. Epilepsia. 2014;56(1):1–6.
Mitchell F, Gould O, LeBlanc M, Manuel L. Opinions of hospital pharmacists in Canada regarding marijuana for medical purposes. Can J Hosp Pharm. 2016;69(2):122–30.
PubMed PubMed Central Google Scholar
Moeller KE, Woods B. Pharmacy students’ knowledge and attitudes regarding medical marijuana. Am J Pharm Educ. 2015;79(6):85.
Norberg MM, Gates P, Dillon P, Kavanagh DJ, Manocha R, Copeland J. Screening and managing cannabis use: Comparing GP’s and nurses’ knowledge, beliefs, and behavior. Subst Abuse Treat Prev Policy. 2012;7(31). https://doi.org/10.1186/1747-597X-7-31 .
Philpot LM, Ebbert JO, Hurt RT. A survey of the attitudes, beliefs and knowledge about medical cannabis among primary care providers. BMC Fam Pract. 2019;20(1). https://doi.org/10.1186/s12875-019-0906-y .
Rapp L, Michalec B, Whittle T. Delaware physicians’ knowledge and opinions on medical marijuana. Del Med J. 2015;87(10):304–9.
Ricco J, Danner C, Pereira C, Philbrick A. “The Times They Are A-Changin”: Knowledge and perceptions regarding medical cannabis in an academic family medicine department. PRiMER. 2017;1:20.
Schmidt LA, Jacobs LM, Spetz J. Young people’s more permissive views about marijuana: Local impact of state laws or national trend? Am J Public Health. 2016;106(8):1498–503.
Schwartz RH, Voth EA, Sheridan MJ. Marijuana to prevent nausea and vomiting in cancer patients: A survey of clinical oncologists. South Med J. 1997;90(2):167–72.
Sideris A, Khan F, Boltunova A, Cuff G, Gharibo C, Doan LV. New York physicians’ perspectives and knowledge of the state medical marijuana program. Cannabis Cannabinoid Res. 2018;3(1):74–84.
Stojanovic MS, Tomas AD, Paut-Kusturica MM, Raskovic AL, Ubavic MB, Tomic ZS, et al. Pharmacy students’ knowledge and attitudes regarding cannabis for medical purposes. Hosp Pharmacol Int Multidisciplinary J. 2017;4(3):559–67.
Szyliowicz D, Hilsenrath P. Medical marijuana knowledge and attitudes: A survey of the California pharmacists’ association. J Prim Care Community Health. 2019;10:1–6.
Thomsen S. Medical marijuana is now legal in Australia: Business Insider Australia; 2016. Published February 24, 2016. https://www.businessinsider.com.au/medical-marijuana-is-now-legal-in-australia-2016-2 . Accessed 15 Nov 2019
United Nations. Official records United Nations conference for the adoption of a single convention on narcotic drugs, New York, 24. Jan. - 25. March, 1961. Enacted 1964.
Uritsky TJ, McPherson ML, Pradel F. Assessment of hospice health professionals’ knowledge, views, and experience with medical marijuana. J Palliat Med. 2011;14(12):1291–5.
Wilkinson T, Tarnopolsky N. Israel is banking on cannabis as its next big industry: Los Angeles Times; 2019. Published May 29, 2019. https://www.latimes.com/nation/la-fg-israel-cannabis-medical-marijuana-20190529-story.html . Accessed 2 Apr 2021
World Health Organization. UN Commission on Narcotic Drugs reclassifies cannabis to recognize its therapeutic uses . Published December 4, 2020. https://www.who.int/news/item/04-12-2020-un-commission-on-narcotic-drugs-reclassifies-cannabis-to-recognize-its-therapeutic-uses . Accessed 25 July 2021.
Ziemianski D, Capler R, Tekanoff R, Lacasse A, Luconi F, Ware MA. Cannabis in medicine: A national educational needs assessment among Canadian physicians. BMC Med Educ. 2015;15(1):52.
Zolotov Y, Metri S, Calabria E, Kogan M. Medical cannabis education among healthcare trainees: A scoping review. Complement Ther Med. 2021;58(2021):102675.
Zvonarev V, Fatuki TA, Tregubenko P. The public health concerns of marijuana legalization: An overview of current trends. Cureus. 2019;11(9):e5806.
Zylla D, Steele G, Eklund J, Mettner J, Arneson T. Oncology clinicians’ and the Minnesota Medical Cannabis Program: A survey on medical cannabis practice patterns, barriers to enrollment, and educational needs. Cannabis Cannabinoid Res. 2018;3(1):195–202.
Download references
Acknowledgements
Thanks to Dr. Sarah Gilman of the W.M Keck Science Department (Scripps, Pitzer, and Claremont McKenna Colleges) and Dr. Steffanie Guillermo of the Pitzer College Psychology Depertment for assisting in the planning and proofreading of this review.
Not applicable.
Author information
Authors and affiliations.
Pitzer College, Claremont, CA, USA
Jared M. Weisman & Marcus Rodríguez
MCR Labs, LLC, Framingham, MA, USA
Jared M. Weisman
Boston Child Study Center, Los Angeles, CA, USA
Marcus Rodríguez
You can also search for this author in PubMed Google Scholar
Contributions
Both JW and MR contributed to the conception and design of this systematic review. JW principally drafted the article and MR principally provided critical revisions. Both authors give final approval for the submission of this manuscript.
Authors’ information
Jared Weisman, B.A. is a recent graduate of Pitzer College where he received a BA in human biology with a minor in chemistry. Prior to arriving at Pitzer in January 2018, Jared completed two years of undergraduate studies at Hamilton College, where he was also a member of the varsity baseball team. Jared worked as a medical assistant under Kathleen O’Neil-Smith, MD from June 2018 until March 2020, where he assisted with clinical care, patient correspondence, and the creation of clinical presentations for the chief physician to present at numerous international conferences. His current work with MCR Labs, LLC involves the development and performance of analytical chemistry techniques to ensure the safety and efficacy of cannabis products. Additionally, for the past two years, he has worked as a research assistant at the Global Mental Health Lab at Pitzer College, where he has contributed and co-authored several research papers investigating a variety of global mental health topics—including mindfulness and mindfulness-based therapies. His work has been featured at numerous national conferences, and he is the recipient of the APA Division 52’s (international psychology) early-career psychologist first-authored poster contest, 2nd place.
Marcus Rodriguez, Ph.D. is director of the Global Mental Health Research Lab and Assistant Professor of Psychology at Pitzer College, and director of clinical outreach at Boston Child Study Center - Los Angeles. He studied at Pepperdine University (BA), Peking University (MA), Duke University (PhD), and Harvard Medical School (predoctoral internship). He grew up in Mexico, studied in Germany during college, lived in China for nine years after college, and has been to more than 70 countries.
Marcus’ research interests include mindfulness, mobile technologies, suicide prevention, and global mental health. Has delivered more than 70 conference presentations, and co-authored dozens of peer-reviewed articles and book chapters.
Marcus has experience providing cognitive behavioral therapies in English, Spanish, and Mandarin to individuals, groups, and families in inpatient, outpatient, and partial hospital settings. He acquired expertise in Dialectical Behavior Therapy (DBT) and the treatment of multi-diagnostic, high-risk, and suicidal adolescents and adults. Marcus consults for Marsha Linehan’s training company, Behavioral Tech, and has participated in and co-facilitated intensive DBT workshops for mental health professionals in the USA, Mexico, China, Australia, and Nepal.
Corresponding author
Correspondence to Jared M. Weisman .
Ethics declarations
Ethics approval and consent to participate, consent for publication.
Acknowledged and granted by first author, Jared M. Weisman, B.A.

Competing interests
First author JW is currently employed by MCR Labs, LLC (Framingham, MA; as of 7/30/2021), a medicinal cannabis testing laboratory; however, MCR Labs played no role in the design and conduct of the study, the writing of the manuscript, or the decision to publish.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Search strategy for PubMed
Respondent type : (“physician” OR “health professional” OR “pharmacist” OR “pharmacy” OR “providers” OR “students” or “doctors” OR “oncologist” OR “rheumatologist” OR “clinicians” OR “nurses”).
Solicitation type : (“attitudes” OR “opinion” OR “survey” OR “perspectives” OR “knowledge” OR “beliefs”).
Substance type: (“medical cannabis” OR “cannabis” OR “marijuana” OR “medical marijuana” OR “cannabinoids” OR “psychoactive”)
Search strategy for Google Scholar
Respondent type : (“physician” OR “physicians” OR “medical professional” OR “pharmacist” OR “pharmacy” OR “providers” OR “healthcare” OR “students” or “doctors” OR “oncologist”).
Solicitation type : (“attitudes” OR “opinion” OR “survey” OR “perspectives” OR “knowledge” OR “perceptions” OR “support”).
Substance type: (“medical cannabis” OR “drug” OR “marijuana” OR “medical marijuana” OR “cannabinoid” OR “psychoactive”)
Analysis and sorting by research question phraseology:
Research question 1: Do you believe that physicians deserve the legal right to prescribe cannabis to patients? (i.e. Do you believe that cannabis should be legalized for therapeutic purposes?)
Qualified survey questions included the following phrases:
“Doctors should be able to legally prescribe marijuana as medical therapy” (Charuvastra et al. 2005 ; Philpot et al. 2019 ).
“Doctors should recommend medical marijuana (MMJ; as medical therapy)?” (Chan et al. 2017 ; Kondrad and Reid 2013 ).
“Marijuana should be made available by prescription”) (Doblin and Kleiman 1991 ; Jacobs et al. 2018 ; Schwartz et al. 1997 ; Uritsky et al. 2011 ).
“Cannabis should be legalized/available for medicinal purposes” (Bega et al. 2016 ; Crowley et al. 2017 ; Mathern et al. 2014 ; Norberg et al. 2012 ; Sideris et al. 2018 ).
“Clinicians should be able to authorize MC without fear of legal action” (Carlini et al. 2016 ).
“MMJ should be legalized in all states” (Moeller and Woods 2015 ).
“Specialist physicians should have authority to prescribe CTP” (Balneaves et al. 2018 ; Ziemianski et al. 2015 ).
“The use of CTP should be legalized/approved in Serbia” (Kusturica et al. 2019 ; Stojanovic et al. 2017 ).
“MD’s should play a role in MMJ authorization” (Ebert et al. 2015 ).
“MJ should be legalized provided it is under medical supervision” (Burke and Marx 1971 ).
“There should be some form of legalized marijuana use" (Lieff et al. 1973 ).
“Are you willing to help patients access MMJ?” (Ananth et al. 2018 ).
Research question 2: Do you believe that cannabis has any therapeutic utility?
“If marijuana were legally available, I would recommend the use of marijuana to a patient” (filed under the survey subscale “belief that marijuana has medical benefits”) (Chan et al. 2017 ).
I am concerned that there is limited evidence demonstrating cannabis’ medical efficacy (Those who reported “low concern” were interpreted as espousing belief in MC’s utility) (Ricco et al. 2017 ).
“Marijuana helps patients who suffer from chronic, debilitating medical conditions” (Carlini et al. 2016 ; Ebert et al. 2015 ; Kondrad and Reid 2013 ).
“Do you believe that MMJ can help prevent nausea and vomiting (in patients receiving chemotherapy or radiation)?” (Braun et al. 2018 ; Doblin and Kleiman 1991 ; Luba et al. 2018 ).
“Do you approve of using MMJ to help manage patients’ symptoms?” (Ananth et al. 2018 ).
“Do you think MMJ has medical benefits/efficacy?” (Mitchell et al. 2016 ; Szyliowicz and Hilsenrath 2019 ; Uritsky et al. 2011 ).
“Do you believe legalization [of cannabis] would be medically efficacious?” (Cogswell and Harris 2015 ).
“Do you believe that MC is a legitimate medical therapy?” (Philpot et al. 2019 ).
“Do you recognize MMJ as an oncological therapy?” (Moeller and Woods 2015 ).
“Do you have a patient who you agree would benefit from medical cannabis?” (Karanges et al. 2018 ).
“Are you certain about MMJ’s therapeutic value?” (Auger et al. 2020 ; Ziemianski et al. 2015 ).
“Cannabis has a role in palliative care” (Crowley et al. 2017 ).
“Assess your concern regarding the limited evidence of therapeutic benefits from MMJ” (1-7 Likert scale [1 = least concern, 7 = most concern]; responses of 1-3 were approved and consolidated for analyses reporting “confidence in cannabis’ medical efficacy”) (Hwang et al. 2016 ).
“Do you believe [medical] marijuana/CBD has efficacy in treating (childhood) epilepsy?” (Ablin et al. 2016 ; Hwang et al. 2016 ; Mathern et al. 2014 ).
“Do you believe that marijuana has an acceptable role in medicine?” (Martins-Welch et al. 2017 ).
“I am familiar with the possible therapeutic effects of cannabis” (Kusturica et al. 2019 ).
“Do you agree that cannabis and its derivatives could potentially have therapeutic effects?” (Stojanovic et al. 2017 ).
Research question 3: Do you believe that marijuana should be legalized for recreational use?
“(Do you believe that) marijuana should be legalized for recreational use?” (Berlekamp et al. 2019 ; Chan et al. 2017 ; Kondrad and Reid 2013 ; Moeller and Woods 2015 ; Schwartz et al. 1997 ).
“What legal action should be taken for the possession of marijuana: 1) No legal action; 2) Citation with a fixed fine; 3) Misdemeanor; 4) Felony? (Linn et al. 1989 ).
“Marijuana should be regulated in the same way as alcohol” (Lieff et al. 1973 ).
“Should cannabis be made recreational?” (Bega et al. 2016 ).
“Are you in favor of legalizing cannabis for non-medical purposes?” (Ebert et al. 2015 ).
“Free access should be granted for the use of marijuana” (Burke and Marx 1971 ).
“All marijuana should be legalized” (Uritsky et al. 2011 ).
Research question 4: [For US-based papers only] Do you believe that the USA should amend cannabis’ federal status as a Schedule 1 controlled substance (the most restrictive classification, asserting that the substance has no accepted medical use)?
“Do you favor the Drug Enforcement Agency (DEA) reclassifying marijuana so that it is no longer a Schedule 1 drug?” (Bega et al. 2016 ; Chan et al. 2017 ; Kondrad and Reid 2013 ).
“Do you support the rescheduling of marijuana to permit its use in medicine?” (Doblin and Kleiman 1991 ; Schwartz et al. 1997 ).
“Cannabis should be rescheduled so that it is no longer a Schedule 1 drug with no medical benefits” (Carlini et al. 2016 ).
“Do you favor change in (federal) marijuana control?” (Burke and Marx 1971 ).
Research question 5: Do you feel confident in your level of knowledge regarding the health effects of cannabis?
“Do you feel confident in your ability to prescribe marijuana, or would you require more knowledge before prescribing?” (Doblin and Kleiman 1991 ).
“Self-reported knowledge of cannabis” (reported on a 1-5 Likert scale; responses of 3, 4, or 5 [acceptable, strong, and very strong knowledge, respectively] were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Norberg et al. 2012 ).
“Self-reported competency regarding knowledge of MMJ efficacy” (1-5 Likert scale; responses of 4 or 5 [strong and very strong knowledge, respectively] were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Ricco et al. 2017 ).
“How much knowledge do you have about medical marijuana?” (6 categories: very little knowledge, some knowledge, moderate knowledge, substantial knowledge, high level of knowledge, and professional level of knowledge; “substantial knowledge,” “high level of knowledge,” and “professional level of knowledge” were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Szyliowicz and Hilsenrath 2019 ).
“Do you feel adequately prepared to answer patients’ questions about MMJ?” (Philpot et al. 2019 )
“Do you consider yourself well-informed about the endocannabinoid system?” (Sideris et al. 2018 ).
“Do you consider yourself knowledgeable about MMJ therapy?” (Mitchell et al. 2016 ; Rapp et al. 2015 ).
“Confidence in discussing risks and benefits of medical cannabis” (4 categories: very confident; somewhat confident; somewhat not confident, not at all confident; “very confident” and “somewhat confident” responses were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Zylla et al. 2018 ).
“I have good knowledge around the (side) effects of medicinal cannabis” (Karanges et al. 2018 ; Kusturica et al. 2019 ).
“I know how to talk to providers about the risks and benefits of MMJ use” (“confident” and “somewhat confident” responses were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Caligiuri et al. 2018 ).
“Do you feel sufficiently knowledgeable to make recommendations regarding MMJ?” (Braun et al. 2018 ).
“Self-reported competency in MMJ pharmacology” (1-7 Likert scale; responses of 5-7 [good, very good, and excellent, respectively] were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Hwang et al. 2016 ).
"Do you feel confident regarding your current knowledge of [cannabinoids]? (responses of “confident” and “somewhat confident” were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Ablin et al. 2016 ; Fitzcharles et al. 2014 ).
“Knowledge of pharmacology and indications" (responses indicating a “medium-high” or “high” level of knowledge were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Ebert et al. 2015 ).
“How would you rate your knowledge on the systemic effects of cannabis?” (Crosby 2018 ).
“Rate your knowledge on factual information regarding marijuana" (responses indicating “moderate” and “high” levels of knowledge were approved and consolidated for analyses reporting “confidence in knowledge of medicinal cannabis”) (Burke and Marx 1971 ).
Research question 6: Do you desire additional education regarding MMJ and/or do believe that education on (medical) cannabis should be made readily available to medical professionals?
“(More) training about medical marijuana should be incorporated into medical/pharmacy school curriculum” (Bega et al. 2016 ; Caligiuri et al. 2018 ; Chan et al. 2017 ; Moeller and Woods 2015 ).
“Continuing medical education (CME) about medical marijuana should be made available to (primary care) physicians” (Carlini et al. 2016 ; Ebert et al. 2015 ; Kondrad and Reid 2013 ).
“People in my position should receive education about cannabis” (1-5 Likert; responses of “somewhat agree” and “fully agree” were approved and consolidated for analyses reporting “yes” for the stated research question) (Norberg et al. 2012 ).
“Do you feel that more education about marijuana is needed?” (Szyliowicz and Hilsenrath 2019 ).
“Are you interested in learning more about MC?” (Philpot et al. 2019 ; Zylla et al. 2018 ).
“It would be helpful to have additional education about MMJ” (Rapp et al. 2015 ).
“How strong is the need for education on CTP?” (responses reporting a “strong” or “very strong” need were approved and consolidated for analyses reporting “yes” for the stated research question) (Balneaves et al. 2018 ; Ziemianski et al. 2015 ).
“Dispensing cannabis in the pharmacy requires additional education” (Stojanovic et al. 2017 ).
Research question 7: Are you concerned about cannabis’ dependence/addiction potential?
“(Do you believe that) marijuana can be addictive (yes/no)?” (Carlini et al. 2016 ; Chan et al. 2017 ; Kondrad and Reid 2013 ; Kusturica et al. 2019 ; Uritsky et al. 2011 ).
I am concerned with MC’s potential for addiction or its psychoactive problems (those reporting “moderate” or “high” concern were approved and consolidated for analyses reporting concern) (Ricco et al. 2017 ).
“Are you concerned about substance abuse among patients who receive MMJ?” (Ananth et al. 2018 ).
“Are you concerned with MMJ’s potential for abuse/misuse/diversion?” (Rapp et al. 2015 ).
“Do you believe / are you concerned that addiction and dependence are potential side effects of MC?” (Karanges et al. 2018 ; Martins-Welch et al. 2017 ; Stojanovic et al. 2017 ).
“On the scale of 1-7 (1 = no concern, 7 = most concern), how concerned are you about the psychoactive effect and potential addiction from cannabis use?” (responses of 5-7 were approved and consolidated for analyses reporting “concern about MMJ’s addictive potential”) (Hwang et al. 2016 ).
“The risk of addiction/physiological dependence would reduce my willingness to prescribe MMJ (1-5 Likert scale [1 = would not reduce my prescribing, 5 = would greatly reduce my prescribing]; responses of 4 and 5 were approved and consolidated for analyses reporting “concern about MMJ’s addictive potential”) (Jacobs et al. 2018 ).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Weisman, J.M., Rodríguez, M. A systematic review of medical students’ and professionals’ attitudes and knowledge regarding medical cannabis. J Cannabis Res 3 , 47 (2021). https://doi.org/10.1186/s42238-021-00100-1
Download citation
Received : 03 November 2020
Accepted : 30 August 2021
Published : 12 October 2021
DOI : https://doi.org/10.1186/s42238-021-00100-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Medical cannabis
- Cannabis policy
- International comparisons
- Medical students
- Medical professionals
Journal of Cannabis Research
ISSN: 2522-5782
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
- Recent Dissertation Titles
- MAS Application Fee Waiver Requirements
- Master of Arts (MA) in Geography and Environmental Engineering
- Master of Arts and Master of Science in Public Health (MA/MSPH)
- Master of Arts in Public Health Biology (MAPHB)
- Master of Bioethics (MBE)
- Mission, Vision, and Values
- Student Experience
- Program Outcomes
- For Hopkins Undergraduate Students
- Master of Health Science (MHS) - Department of Biochemistry and Molecular Biology
- Master of Health Science (MHS) - Department of Epidemiology
- Alumni Update
- MHS Combined with a Certificate Program
- Master of Health Science (MHS) - Department of Molecular Microbiology and Immunology
- Alumni Highlights
- Post-Baccalaureate Program in Environmental Health for Pre-Medicine Students
- Bachelor's/MHS in Health Economics and Outcomes Research
- MHS HEOR Careers
- Frequently Asked Questions
- Master of Health Science (MHS)
- Concurrent School-Wide Master of Health Science Program in Biostatistics
- Master of Health Science - Department of Population, Family and Reproductive Health
- Master of Health Science Online (MHS) - Department of Population, Family and Reproductive Health
- Careers in Health Economics
- Core Competencies
- Meet the Director
- What is Health Economics
- MPH Capstone Schedule
- Concentrations
- Online/Part-Time Format
- Requirements
- Tuition and Funding
- Executive Board Faculty
- Master of Science (MS) in Geography and Environmental Engineering
- Independent Professional Project and Final Essay
- Program Objectives and Outcomes
- Internships
- Master of Science (ScM) - Department of Biochemistry and Molecular Biology
- Master of Science (ScM) - Department of Biostatistics
- Master of Science (ScM) - Department of Epidemiology
- Master of Science (ScM) - Department of Molecular Microbiology and Immunology
- ScM Faculty Advisers
- Master of Science in Engineering (MSE) in Geography and Environmental Engineering
- Bachelor's/MSPH in Health Policy
- FAQ for MSPH in Health Policy
- Field Placement Experience
- MSPH Capstone
- MSPH Practicum
- Required and Elective Courses
- Student Timeline
- Career Opportunities
- 38-Week Dietetics Practicum
- Completion Requirements
- MSPH/RD Program FAQ
- Program Goals
- Master's Essay Titles
- Application Fee Waiver Requirements
- Doctor of Philosophy (PhD) - Department of Biostatistics
- Doctor of Philosophy (PhD) - Department of Epidemiology
- Program Goals and Expectations
- Doctor of Philosophy (PhD) - Department of Molecular Microbiology and Immunology
- Doctor of Philosophy (PhD) - Department of Population, Family and Reproductive Health
- Doctor of Philosophy (PhD) in Clinical Investigation
- Track in Environmental Sustainability, Resilience, and Health
- Track in Exposure Sciences and Environmental Epidemiology
- Track in Health Security
- Track in Toxicology, Physiology and Molecular Mechanisms
- PhD in Geography and Environmental Engineering Faculty Advisers
- Recent Graduates and Dissertation Titles
- PhD Funding
- PhD TA Requirement
- JHU-Tsinghua Doctor of Public Health
- Core Course Requirements
- Concentration in Women’s and Reproductive Health
- Custom Track
- Concentration in Environmental Health
- Concentration in Global Health: Policy and Evaluation
- Concentration in Health Equity and Social Justice
- Concentration in Health Policy and Management
- Concentration in Implementation Science
- Meet Current Students
- Combined Bachelor's / Master's Programs
- Concurrent MHS Option for BSPH Doctoral Students
- Concurrent MSPH Option for JHSPH Doctoral students
- Doctor of Medicine and Doctor of Philosophy (MD/PhD)
- Adolescent Health Certificate Program
- Bioethics Certificate Program
- Climate and Health Certificate Program
- Clinical Trials Certificate Program
- Community- Based Public Health Certificate Program
- Demographic Methods Certificate Program
- Environmental and Occupational Health Certificate Program
- Epidemiology for Public Health Professionals Certificate Program
- Evaluation: International Health Programs Certificate Program
- Food Systems, the Environment and Public Health Certificate Program
- Frequently Asked Questions for Certificate Programs
- Gender and Health Certificate Program
- Gerontology Certificate Program
- Global Digital Health Certificate Program
- Global Health Certificate Program
- Global Health Practice Certificate Program
- Health Communication Certificate Program
- Health Disparities and Health Inequality Certificate Program
- Health Education Certificate Program
- Health Finance and Management Certificate Program
- Health and Human Rights Certificate Program
- Healthcare Epidemiology and Infection Prevention and Control Certificate Program
- Humane Sciences and Toxicology Policy Certificate Program
- Humanitarian Health Certificate Program
- Implementation Science and Research Practice Certificate Program
- Injury and Violence Prevention Certificate Program
- International Healthcare Management and Leadership Certificate Program
- Leadership for Public Health and Healthcare Certificate Program
- Lesbian, Gay, Bisexual, Transgender, and Queer (LGBTQ) Public Health Certificate Program
- Maternal and Child Health Certificate Program
- Mental Health Policy, Economics and Services Certificate Program
- Non-Degree Students General Admissions Info
- Pharmacoepidemiology and Drug Safety Certificate Program
- Population Health Management Certificate Program
- Population and Health Certificate Program
- Product Stewardship for Sustainability Certificate Program
- Public Health Advocacy Certificate Program
- Public Health Economics Certificate Program
- Public Health Informatics Certificate Program
- Public Health Practice Certificate Program
- Declaration of Intent - Public Health Preparedness
- Public Health Training Certificate for American Indian Health Professionals
- Public Mental Health Research Certificate Program
- Quality, Patient Safety and Outcomes Research Certificate Program
- Quantitative Methods in Public Health Certificate Program
- Requirements for Successful Completion of a Certificate Program
- Rigor, Reproducibility, and Responsibility in Scientific Practice Certificate Program
- Risk Sciences and Public Policy Certificate Program
- Spatial Analysis for Public Health Certificate Program
- Training Certificate in Public Health
- Tropical Medicine Certificate Program
- Tuition for Certificate Programs
- Vaccine Science and Policy Certificate Program
- Online Student Experience
- Online Programs for Applied Learning
- Barcelona Information
- Fall Institute Housing Accommodations
- Participating Centers
- Registration, Tuition, and Fees
- Agency Scholarship Application
- General Scholarship Application
- UPF Scholarship Application
- Course Evaluations
- Online Courses
- Registration
- General Institute Tuition Information
- International Students
- Directions to the Bloomberg School
- All Courses
- Important Guidance for ONSITE Students
- D.C. Courses
- Registration and Fees
- Cancellation and Closure Policies
- Application Procedures
- Career Search
- Current Activities
- Current Trainees
- Related Links
- Process for Appointing Postdoctoral Fellows
- Message from the Director
- Program Details
- Admissions FAQ
- Current Residents
- Elective Opportunities for Visiting Trainees
- What is Occupational and Environmental Medicine?
- Admissions Info
- Graduates by Year
- Compensation and Benefits
- How to Apply
- Academic Committee
- Course Details and Registration
- Tuition and Fees
- ONLINE SOCI PROGRAM
- Principal Faculty
- Johns Hopkins RAPID Psychological First Aid
- General Application
- JHHS Application
- Areas of Study
- Important Dates
- Our Faculty
- Welcome Letter
- Descripción los Cursos
- Programa en Epidemiología para Gestores de Salud, Basado en Internet
- Consultants
- Britt Dahlberg, PhD
- Joke Bradt, PhD, MT-BC
- Mark R. Luborsky, PhD
- Marsha Wittink, PhD
- Rebekka Lee, ScD
- Su Yeon Lee-Tauler, PhD
- Theresa Hoeft, PhD
- Vicki L. Plano Clark, PhD
- Program Retreat
- Mixed Methods Applications: Illustrations
- Announcements
- 2023 Call for Applications
- Jennifer I Manuel, PhD, MSW
- Joke Bradt, PhD
- Josiemer Mattei, PhD, MPH
- Justin Sanders, MD, MSc
- Linda Charmaran, PhD
- Nao Hagiwara, PhD
- Nynikka R. A. Palmer, DrPH, MPH
- Olayinka O. Shiyanbola, BPharm, PhD
- Sarah Ronis, MD, MPH
- Susan D. Brown, PhD
- Tara Lagu, MD, MPH
- Theresa Hoft, PhD
- Wynne E. Norton, PhD
- Yvonne Mensa-Wilmot, PhD, MPH
- A. Susana Ramírez, PhD, MPH
- Animesh Sabnis, MD, MSHS
- Autumn Kieber-Emmons, MD, MPH
- Benjamin Han, MD, MPH
- Brooke A. Levandowski, PhD, MPA
- Camille R. Quinn, PhD, AM, LCSW
- Justine Wu, MD, MPH
- Kelly Aschbrenner, PhD
- Kim N. Danforth, ScD, MPH
- Loreto Leiva, PhD
- Marie Brault, PhD
- Mary E. Cooley, PhD, RN, FAAN
- Meganne K. Masko, PhD, MT-BC/L
- PhuongThao D. Le, PhD, MPH
- Rebecca Lobb, ScD, MPH
- Allegra R. Gordon, ScD MPH
- Anita Misra-Hebert, MD MPH FACP
- Arden M. Morris, MD, MPH
- Caroline Silva, PhD
- Danielle Davidov, PhD
- Hans Oh, PhD
- J. Nicholas Dionne-Odom, PhD RN ACHPN
- Jacqueline Mogle, PhD
- Jammie Hopkins, DrPH, MS
- Joe Glass, PhD MSW
- Karen Whiteman, PhD MSW
- Katie Schultz, PhD MSW
- Rose Molina, MD
- Uriyoán Colón-Ramos, ScD MPA
- Andrew Riley, PhD
- Byron J. Powell, PhD, LCSW
- Carrie Nieman MD, MPH
- Charles R. Rogers, PhD, MPH, MS, CHES®
- Emily E. Haroz, PhD
- Jennifer Tsui, Ph.D., M.P.H.
- Jessica Magidson, PhD
- Katherine Sanchez, PhD, LCSW
- Kelly Doran, MD, MHS
- Kiara Alvarez, PhD
- LaPrincess C. Brewer, MD, MPH
- Melissa Radey, PhD, MA, MSSW
- Sophia L. Johnson, PharmD, MPH, PhD
- Supriya Gupta Mohile, MD, MS
- Virginia McKay, PhD
- Andrew Cohen, MD, PhD
- Angela Chen, PhD, PMHNP-BC, RN
- Christopher Salas-Wright, PhD, MSW
- Eliza Park MD, MS
- Jaime M. Hughes, PhD, MPH, MSW
- Johanne Eliacin, PhD, HSPP
- Lingrui Liu ScD MS
- Meaghan Kennedy, MD
- Nicole Stadnick, PhD, MPH
- Paula Aristizabal, MD
- Radhika Sundararajan, MD
- Sara Mamo, AuD, PhD
- Tullika Garg, MD MPH FACS
- Allison Magnuson, DO
- Ariel Williamson PhD, DBSM
- Benita Bamgbade, PharmD, PhD
- Christopher Woodrell MD
- Hung-Jui (Ray) Tan, MD, MSHPM
- Jasmine Abrams, PhD
- Jose Alejandro Rauh-Hain, MD
- Karen Flórez, DrPH, MPH
- Lavanya Vasudevan, PhD, MPH, CPH
- Maria Garcia, MD, MPH
- Robert Brady, PhD
- Saria Hassan, MD
- Scherezade Mama, DrPH
- Yuan Lu, ScD
- 2021 Scholars
- Sign Up for Our Email List
- Workforce Training
- Cells-to-Society Courses
- Course/Section Numbers Explained
- Pathway Program with Goucher College
- The George G. Graham Lecture
Health systems management and health sector reform
- Performance-Based Payments, Provider Motivation and Quality of Care in Afghanistan
- Health Systems Strengthening in Post-Conflict Settings: Employee and Patient Satisfaction in Hospitals in Afghanistan
- The Use of Clinical Practice Guidelines to Improve Provider Performance of Well-Child Care in Armenia
- Quality Improvement and Its Effect on Patient Perceptions and Demand for Health Services-Evidence from Uttar Pradesh, India
- The Perception of Quality Among Users of Commune Health Centers and Users of Private Providers in Northern Vietnam
Health financing
- National Health Insurance in Ghana: Politics, Adverse Selection, and the Use of Child Health Services.
- Evaluating the Effectiveness of User Fee Increase in Improving The Quality of Care: Government Primary Health Care Services in Indonesia
- The Impact of Community-Based Health Insurance on Health Care Utilization and Financial Sustainability: The Example of Rwanda
- Impact of Health Insurance on Health Care Utilization in Vietnam
- Stimulating Demand: An Assessment of the Conditional Cash Transfer Project in Afghanistan
Health policy and resource allocation
- Exploring Attitudes and Perceptions of Policymakers and Health Researchers Towards Evidence-Based Health Policymaking in Argentina: A Mixed Methods Approach
- Dual Practice in Kampala, Uganda: A Mixed Methods Study of Management and Policy
- Understanding Political Priority Development for Public Health Issues in Turkey: Lessons from Tobacco Control & Road Safety
- Academic Knowledge Brokers in Kenya: A Mixed Methods Study of Relationships, Characteristics and Strategies
- Decision-Making for Allocation of Public Resources in Decentralized District Health Systems in Uganda
Maternal, neonatal and child health
- Antenatal and Delivery Care in Afghanistan Knowledge and Perceptions of Services, Decision Making for Service Use, and Determinants of Utilization
- Early Maternal Morbidity and Utilization of Delivery Services by Urban Slum Women of Dhaka, Bangladesh
- An Assessment of Maternal Health Service Needs of Immigrant Women Living in East Calgary, Canada
- Health Seeking Behavior of Women and Their Families During Pregnancy, Delivery and Postpartum Period in Nepal
Evaluation of health programs
- Comparison of Biomarker Surveillance of Measles Immunity to Conventional Indicators of Vaccination Coverage
- Qualitative Research to Develop a Framework for Evaluating the Sustainability of Community-Based Child Health Programs Implemented by Non-Government Organizations
- Evaluating the Delivery Huts Program for Promoting Maternal Health in Haryana, India
- Evaluating the Scale-Up of Community Case Management in Malawi: Health System Supports, Health Worker Attitudes, and Equity of Service Provision
Refugee and humanitarian assistance
- Family Relationships and Social Interaction in Post-Conflict South Kivu Province, Eastern Democratic Republic of Congo A Mixed Methods Study with Women from Rural Walungu Territory
- Utilization of Health Services for Children after the Tsunami in Aceh, Indonesia
- Factors Affecting School Enrollments in a Post-Repatriation Context: A Study of Household Roles, Attitudes and Forced Migration Processes in Urban Somaliland
- A Balanced Scorecard for Assessing the Quality and Provision of Health Services in UNHCR Refugee Camps
Injury prevention and control
- Road Traffic Injuries In China: Time Trends, Risk Factors and Economic Development
- Evaluating an Intervention to Prevent Motorcycle Injuries in Malaysia: Process Performance, and Policy
- Injuries and Socioeconomic Status in Iganga and Mayuge, Uganda: Inequities, Consequences and Impacts
- A neglected epidemic of childhood drowning in Bangladesh: Epidemiology, risk factors and potential interventions
Equity and fairness in distribution of health services
- Gender and Access to DOTS Program (Directly Observed Treatment, Short-Course) in a Poor, Rural and Minority Area of Gansu Province, China
- Empowering the Socially Excluded: A Study of Impact on Equity by Gender, Caste and Wealth in Access to Health Care in Rural Parts of Four North Indian States
- Gender, Empowerment, and Women's Health in India: Perceived Morbidity and Treatment-Seeking Behaviors for Symptoms of Reproductive Tract Infections among Women of Rural Gujarat
- Trust in Maternity Care: A Contextual Exploration of Meaning and Determinants in Peri-Urban Kenya
- The Effect of Contracting for Health Services on the Equity of Utilization and Out-of-Pocket Health Expenditure in Rural Afghanistan
Health economics
- The Equity and Cost-Effectiveness of HIV Voluntary Counseling and Testing in Tanzania
- Hospital Coding Practice, Data Quality, And DRG-Based Reimbursement Under the Thai Universal Coverage Scheme
- Willingness-to-Pay and Cost-Benefit Analysis on Introducing HIB Conjugate Vaccine into the Thai Expanded Program on Immunization
- Economic Evaluation of the Costs and Cost-Effectiveness of the Diarrhea Alleviation through Zinc and Oral Rehydration Therapy Program at Scale in Gujarat, India
- The Economics of Non-Communicable Diseases in Rural Bangladesh: Understanding Education Gradients in Mortality and Household Wealth Impacts from an Adult Death
Health outcomes and burden of disease methods
- Measuring the Burden of Disease: Introducing Healthy Life Years
- Measuring the Burden of Injuries in Pakistan Epidemiological and Policy Analysis
- Strengths and Limitations of Population-Based Health Surveys in Developing Countries: A Case Study of National Health Survey of Pakistan: 1990-94
- Approaches to Measuring Non-Fatal Health Outcomes: Disability at the Iganga-Mayuge Demographic Surveillance System in Uganda
- A National Burden of Disease Study for The United Arab Emirates (UAE): Quantifying Health Differentials Between Nationals and Migrants
- How it works

Useful Links
How much will your dissertation cost?
Have an expert academic write your dissertation paper!
Dissertation Services
Get unlimited topic ideas and a dissertation plan for just £45.00
Order topics and plan
Get 1 free topic in your area of study with aim and justification
Yes I want the free topic
Healthcare Dissertation Topics
Published by Carmen Troy at January 4th, 2023 , Revised On May 16, 2024
Healthcare education brings together the science and arts of medicine along with the practice of general education. Healthcare is an educational program that is tremendously significant for humans and society.
Medicine, nursing, and all other related healthcare fields provide a substantial understanding of living beings, disease trends, treatment, treatment outcomes, functional abilities, disabilities, and much more.
The primary purpose of healthcare is to ensure people’s health, look after the patients, and provide information about health risks and their effects. Healthcare education provides knowledge and information about life and helps survival, to say the least.
We all rely on the healthcare system to get physically well and resume the mundane course of life after getting affected by a health risk.
Therefore, studying healthcare is of immense importance as it offers you the opportunity to serve humanity by looking after their health. If you are studying healthcare science, you will need to complete a dissertation to complete a degree and practice its laws and principles.
It is always a highly complex task to begin the dissertation or even find the motivation. Choosing the right topic can help you cross their mental barrier, however. Look at some of the potential healthcare dissertation topics mentioned below to get an idea for starting your dissertation.
You may also want to start your dissertation by requesting a brief research proposal from our writers on any of these topics, which includes an introduction to the problem, research question , aim and objectives, literature review , along with the proposed methodology of research to be conducted. Let us know if you need any help in getting started.
Check our example dissertation to get an idea of how to structure your dissertation .
You can review step by step guide on how to write your dissertation here .
List Of Latest & Free Healthcare Dissertation Topics
- What are the ethics of using artificial intelligence in personalised medicine?
- The use of virtual reality for pain management in chronic illness.
- The impact of mindfulness-based interventions on healthcare worker burnout.
- How is climate change affecting the spread of infectious diseases globally?
- 3D printing technology for prosthetics
- Promoting mental health literacy with a mediating role of diversity.
- The potential of gene therapy in treating genetic disorders.
- Effects of 5G technology on remote medical care consultation
- The use of deep learning has gotten a lot of attention in the development of detection software. How can it be used to detect diabetes?
- Use of deep learning to detect breast cancer among women
- The impact of remote work on the mental health of employees.
- Strategies to address burnout in medical students.
- The impact of air pollution on the lungs and respiratory conditions of people.
Want to know what essay structure and style will work best for your assignment?
Problem fixed! We can write any type of essay in any referencing style. We ensure every essay written is beyond your expectations.

Healthcare Dissertation Topics For Your Research
Topic 1: investigating the impact of household air pollution (hap) on the respiratory health of people and recommend measures of intervention.
Research Aim: The research aims to investigate the impact of household air pollution (HAP) on the respiratory health of people and recommend measures of intervention
Objectives:
- To analyse the contributors of HAP.
- To determine the impact of harmful particulate matter on the respiratory health of people.
- To suggest measure for controlling HAP through intervention with biomass fuels.
Topic 2: An assessment of the bioethics issues arising during medicine development and administration to patients and how ethics of public health can be improved
Research Aim: The research aims to conduct an assessment of the bioethics issues arising during medicine development and administration to patients and how ethics of public health can be improved
- To analyse the bioethics challenges associated with medicine development and patent administration.
- To examine the measures of improvement of ethics associated with public health.
- To conduct an assessment of the bioethics issues arising during medicine development and administration to patients and how ethics of public health can be improved
Topic 3: Investigating the present global health security infrastructure and its capacity to detect and prevent the spread of infectious diseases. A case study of the outbreak of COVID-19.
Research Aim: The research aims to investigate the present global health security infrastructure and its capacity to detect and prevent the spread of infectious diseases. A case study of the outbreak of COVID -19.
- To analyse the concept of global health security.
- To determine the current infrastructure of global health security and the position of WHO in detecting and preventing the spread of infectious diseases.
- To investigate the effectiveness of the present global health security infrastructure in dealing with the Coviud-19 pandemic and recommendations for future scenarios.
Topic 4: Investigating the importance of vaccines and childhood nutrition in improving maternal and child health
Research Aim: The research aims to investigate the importance of vaccines and childhood nutrition in improving maternal and child health
- To determine the present challenges of maternal and child health and its significance in society.
- To analyse the role of vaccines and childhood nutrition in safeguarding the health of the mother and child.
- To recommend measures to improve maternal and child health for ensuring wellbeing of the families with pre-natal and well-child care for infant and maternal mortality prevention.
Topic 5: An analysis of the risks of tobacco and second-hand smoke exposure on the cardiovascular health of people in the UK.
Research Aim: The research aims to conduct an analysis of the risks of tobacco and second-hand smoke exposure on the cardiovascular health of people in the UK.
- To contextualise the risk factors of tobacco and second-hand smoke.
- To determine the cardiovascular health impact of the people of the UK due to tobacco and second-hand smoke.
- To recommend measures for reducing and minimising tobacco risks and prevent health impact due to passive smoke.
Trending Healthcare Dissertation Topics
Topic. 1: covid-19 and health care system.
Research aim: The prime focus of the research will be analysing the impact of COVID-19 on the healthcare system and how the healthcare system was able to handle the health emergency in different regions of the world. The research can pinpoint one location and study its healthcare system from the perspective of the COVID-19 outbreak.
Topic 2: UN health care policy and its implications
Research aim: The UN has a major health department that oversees the health sector around the world. The United Nations plays an important role in bringing sustainability in human life physically, economically, and in so many other ways. The main goal of the research will be to understand and analyse the UN healthcare policy and identify to what extent it is improving healthcare systems around the world.
Topic 3: WHO's response to COVID-19
Research aim: It is an undisputed argument that the World Health organisation was at the forefront when the tsunami of pandemics hit the world. From keeping people informed to ensuring the formulation of vaccines, the WHO’s role was comprehensive. The aim of the research is to identify how WHO responded to the outbreak and helped people stay protected. The research will critically analyse the plans that were formulated and executed in response to the COVID -19.
Topic no.4: The spread of the variant during the Olympics and Paralympics
Research Aim: Olympics were called from July to August in 2021 in Tokyo, Japan, when delta variant had been engulfing lives around the world. While many people opposed the decision of arranging the Olympics, it ended up with flying colours. But it is said that due to the Olympics and Paralympics, in which athletes from all over the world participated, the delta variant transcended easily.
The aim of the research is to find out whether or not the Olympics and Paralympics helped the spread of the delta variant.
Topic no. 5: The COVID-19 Vaccination drive and people's response
Research Aim: There is a large proportion of people who are still unvaccinated against COVID -19 in the world. The aim of the research is to track the COVID -19 vaccination drive around the world. The researcher will also find the key motivations behind their denial.
Topic no. 6: Poverty and its impact on childhood diseases
Research aim: The aim of the research will be to find out the relationship between poverty and childhood diseases. The researcher can conduct quantitative research by finding out the figures of most affected childhood diseases and their financial data in the world.
Topic no. 7: The motivation towards a healthy life
Research Aim: By and large, it is said that people in a few regions of the world are more motivated towards attaining a healthy life than in other places. The purpose of the research is to find relative and varying motivations to live healthily around the world.
Topic 8: Health crisis in warzone countries
Research aim: Children and women are the most suffered creatures in the warzone areas of the world. The purpose of the research is to identify the health crisis of women and children in places where there is no rule of law.
How Can ResearchProspect Help?
ResearchProspect writers can send several custom topic ideas to your email address. Once you have chosen a topic that suits your needs and interests, you can order for our dissertation outline service which will include a brief introduction to the topic, research questions , literature review , methodology , expected results , and conclusion . The dissertation outline will enable you to review the quality of our work before placing the order for our full dissertation writing service !
Also Read: Medicine and Nursing Dissertation Topics
Topic 9: Scope of Health care research
Research aim: The research aims to identify and analyse the significance of healthcare research and its effects on humans and society. The researcher will identify the necessity of the study in the field and its overall impact.
Topic 10: The future of telemedicine
Research aim: Telemedicine refers to the use of technology to disseminate medical information, diagnose, or interact with a patient. Currently, it is gaining tremendous importance, especially due to the pandemic, but it is important to figure out how it will work out in the future.
The research aim of the research would be to find the significance of telemedicine and its prospects.
Topic 11: Controlling infectious diseases
Research aim: The research will aim to find out whether or not infectious diseases are difficult to deal with. The paper will identify all the elements responsible for making infectious diseases unstoppable. The researcher can make arguments in the context of the COVID-19.
Topic 12: Effective health care policies around the world
Research aim: Different countries have different healthcare systems with different policies around the world. The aim of the research will be to find out the most effective healthcare systems around the world. The research can incorporate both quantitive and qualitative methods for the study.
The researcher can pinpoint a respective area for the study—for example, the healthcare system of Nigeria, the United States, South Asia etc.
Topic 13: Technology and health care system
Research aim: The advancements in technology have transformed all aspects of our life, and the healthcare system is no exception.
The main aim of the research will be to find out the impact of technology on the healthcare system.
Topic 14: Health care system in 2030
Research aim: The aim of the research will be to identify trends and forecast the future. The researcher will examine the healthcare system today and study the elements that may bring about change and may modify it in the future. The projections must be based on evidence.
Topic 15: The emotional impacts of COVID-19
Research aim: The COVID-19 affected normal life significantly. People were locked in their homes, and the roads and streets were empty. From that perspective, it is significant to understand how(if it did) affected people emotionally.
The main aim of the research will be to find out how and to what extent COVID-19 it affected people emotionally.
Topic 16: Beauty standards and how they impact the health of humans
Research aim: Neither being skinny is healthy, nor starvation is the solution to getting a perfect body shape. The standard beauty standards have persistently put social pressure on individuals to become as per se. Otherwise, they will be neglected or segregated. The research will aim to find out how people who try to meet the standard beauty standards affect their health.
Topic 17: Depression and anxiety in adults in developed countries
Research aim: Depression and anxiety are some common instances that occur to almost all people. It may apparently look like people in developed countries, having access to their basic needs, must not have anything to worry about. It might not be what looks from the outside. The research will measure the rate of increase or decrease in depression and anxiety in adults in developed countries and identify the key determining factors.
Topic 18: Creating awareness of Breast cancer in third world countries
Research aim: The aim of the research will be to identify why it is important to create awareness about breast cancer in third-world countries and identify how to do so.
Topic 19: Gene therapy for hemoglobinopathies
Research aim: Haemoglobinopathies are genetic problems that affect the structure or formation of haemoglobin. One recent research identifies gene therapy as a solution to the disorders. The research will aim to identify how effective gene therapy is and in what capacity it can be used in medicine in the future.
Topic 20: The unspoken problems of health care management
Research aim: While so much stress is put on ensuring the treatment of patients and advancing the healthy lives of humans in general, there is very little say about what problems may be faced by people who are managing . The research aims to identify the undiscussed problems faced by healthcare management to ensure a healthy life for people.
Free Dissertation Topic
Phone Number
Academic Level Select Academic Level Undergraduate Graduate PHD
Academic Subject
Area of Research
Frequently Asked Questions
How to find healthcare dissertation topics.
To find healthcare dissertation topics:
- Examine emerging health issues.
- Analyse gaps in healthcare.
- Review medical literature.
- Consider policy or technology impacts.
- Explore patient perspectives.
- Select a topic that aligns with your passion and career aspirations.
You May Also Like
Need interesting and manageable Brexit dissertation topics? Here are the trending Brexit dissertation titles so you can choose the most suitable one.
Are you passionate about helping others, especially those facing mental health challenges? If this is the case for you, then mental health nursing is a career choice you may not want to pursue.
Need interesting coronavirus (Covid-19) nursing dissertation topics? Here are the trending dissertation titles so you can choose the most suitable one.
USEFUL LINKS
LEARNING RESOURCES

COMPANY DETAILS

- How It Works
- Open access
- Published: 21 May 2024
Effectively teaching cultural competence in a pre-professional healthcare curriculum
- Karen R. Bottenfield 1 ,
- Maura A. Kelley 2 ,
- Shelby Ferebee 3 ,
- Andrew N. Best 1 ,
- David Flynn 2 &
- Theresa A. Davies 1 , 2
BMC Medical Education volume 24 , Article number: 553 ( 2024 ) Cite this article
221 Accesses
Metrics details
There has been research documenting the rising numbers of racial and ethnic minority groups in the United States. With this rise, there is increasing concern over the health disparities that often affect these populations. Attention has turned to how clinicians can improve health outcomes and how the need exists to educate healthcare professionals on the practice of cultural competence. Here we present one successful approach for teaching cultural competence in the healthcare curriculum with the development of an educational session on cultural competence consisting of case-based, role-play exercises, class group discussions, online discussion boards, and a lecture PowerPoint presentation.
Cultural competence sessions were delivered in a pre-dental master’s program to 178 students between 2017 and 2020. From 2017 to 2019, the sessions were implemented as in-person, case-based, role-play exercises. In 2020, due to in-person limitations caused by the COVID-19 pandemic, students were asked to read the role-play cases and provide a reflection response using the online Blackboard Learn discussion board platform. Evaluation of each session was performed using post-session survey data.
Self-reported results from 2017 to 2020 revealed that the role-play exercises improved participant’s understanding of components of cultural competence such as communication in patient encounters (95%), building rapport with patients (94%), improving patient interview skills (95%), and recognition of students own cultural biases when working with patients (93%).
Conclusions
Students were able to expand their cultural awareness and humility after completion of both iterations of the course session from 2017 to 2019 and 2020. This session can be an effective method for training healthcare professionals on cultural competence.
Peer Review reports
It is projected that by the year 2050, racial and ethnic minority groups will make up over 50% of the United States population [ 1 ]. With a more multicultural society, growing concern has emerged over how to address the health disparities that effect these populations and the ways in which healthcare professionals can increase positive health outcomes. Continuing evidence suggests that many patients from racial and ethnic minority groups are not satisfied with the current state of healthcare which has been attributed to implicit bias on the part of physicians and current challenges faced by practitioners who feel underprepared to address these issues due to differences in language, financial status, and healthcare practice [ 2 , 3 , 4 ].
To contend with health disparities and the challenges faced by practitioners working with a more diverse population, healthcare educators have begun to emphasize the importance of educating healthcare workforce on the practice of cultural competence and developing a skilled-based set of behaviors, attitudes and policies that effectively provides care in the wake of cross-cultural situations and differences [ 4 , 5 , 6 ]. There are several curricular mandates from both medical and dental accreditation bodies to address this issue [ 7 , 8 , 9 ], and large amounts of resources, ideas, and frameworks that exist for implementing and training future and current healthcare providers on the inadequacies of the healthcare system and cultural competence [ 10 , 11 , 12 ]. These current institutional guidelines for accreditation and the numerous amounts of resources for training cultural competence, continue to evolve with work documenting the need for blended curriculum that is continuous throughout student education, starting early as we have done here with pre-dental students, including in-person didactic or online sessions, a service learning component, community engagement and a reflective component [ 4 , 5 , 13 , 14 ].
This study investigates teaching cultural competence in a healthcare curriculum. We hypothesized that early educational exposure to cultural competence through role playing case studies, can serve as an effective mechanism for training early pre-doctoral students the practice of cultural competence. Utilizing student self-reported survey data conducted in a predental master’s curriculum, in which two iterations of role-playing case studies were used to teach components of cultural competence, this study aims to evaluate and support research that suggests role-playing case studies as effective means for educating future clinical professionals on the practice of cultural competence.
This study was determined to be exempt by the Institutional Review Board of Boston University Medical Campus, Protocol # H-37,232. Informed consent was received from all subjects.
Data collection
The role-playing, case-based simulated patient encounter exercises were developed and administered at Boston University Chobanian & Avedisian School of Medicine to predental students in the Master of Science in Oral Health Sciences Program (see Table 1 ). From 2017 to 2020, we administered patient encounter cases [see Additional File 1 ] to students ( n = 178) in the program as a portion of a case-based, role-playing exercise to teach the importance of cultural competence and cultural awareness during patient encounters. During years 2017–2019, real actors portrayed the patient and physician. In 2020, the session was conducted online via a discussion board through a Blackboard Course Site. The original case was published as part of a master’s students thesis work in 2021 [ 15 ].
Description of patient encounter cases 1 and 2
Patient Encounter Case 1 [see Additional file 1 ] is composed of two subsections, scenario 1 A and scenario 1B, and is centered around a patient/physician interaction in which a patient who is pregnant presents with pain upon urination. The physician in 1 A is short and terse with the patient, immediately looking at a urine sample, prescribing medication for a urinary tract infection, and telling the patient to return for a follow-up in 2 weeks. In scenario 1B, a similar situation ensues; however, in this scenario the physician takes more time with the patient providing similar care as the physician in 1 A, but asking for more information about the patients personal and medical history. At the conclusion of the scenario, the patient is offered resources for an obstetrician and a dentist based on the information that is provided about the patient’s background. The patient is then sent on their way and asked to follow-up in 2 weeks. The patient does not return.
Patient Encounter Case 2 [see Additional file 1 ] follows a similar format to the Patient Encounter Case 1. In scenario 2 A, the same patient from Case 1 returns with tooth pain after giving birth. The physician in 2 A, like 1 A, is short with the patient and quickly refers the patient to a dentist. In 2B, the physician again takes more time with the patient to receive background information on the patient, make a connection, and provides an antibiotic and dental referral.
Each Patient Encounter Case explored topics such as the importance of building a trusting physician/patient relationship, the importance of asking a patient for patient history, making a connection, and the importance of a physician taking all facets of a patient’s circumstances into consideration [ 15 ].
Session outline
The sessions conducted between 2017 and 2019 were composed of three parts: (1) enactment of an abridged patient encounter facilitated by session administrators, (2) group discussion and reflection during which time students were asked to critically reflect and discuss the theme and key take-aways from the role play exercise, and (3) a PowerPoint presentation emphasizing take-away points from the role-play exercise. At the conclusion of the cultural competence training sessions, students participated in a post-session Qualtrics generated survey administered electronically to assess each student’s feelings about the session [see Additional file 3 ].
Role-play enactment
Facilitators dressed-up in clothing to mimic both the physician and patient for all case scenarios in Patient Encounter Case 1 and Case 2. At the conclusion of the role play portion of each of the cases, the facilitators paused to lead students in a real-time class group discussion. After Case 1, students were asked questions such as: What did you think ? Were the patient’s needs met? Did you expect the patient to return? Following Case 2, similar questions were asked by the facilitators, including: What did you think ? Were the patient’s needs met? Did you expect the patient to accept help?
At the conclusion of this portion of the session, the facilitators led a larger general discussion about both cases and how they related to one another. Finally, the course session concluded with a PowerPoint presentation that reinforced the take-home points from the session [see Additional file 2 ] [ 15 ].
Change in session modality due to COVID-19 pandemic
In Fall 2020, due to the COVID-19 pandemic, the course modality moved to an online platform and consisted of three parts on a Blackboard Discussion Board (Blackboard, Inc.). Students were required to: (1) read each of the Patient Encounter Cases and add a brief reflection comparing the scenarios, (2) then comment on at least two peer’s posts in the discussion forum and (3) attend class to hear a PowerPoint presentation by a course session facilitator on the key take-aways from each scenario [ 15 ].
Student surveys
At the conclusion of the cultural competence training sessions, students participated in a post-session Qualtrics ( https://www.qualtrics.com ) generated survey administered electronically to assess each student’s feelings about the sessions [see Additional file 3 ]. The format of the survey included 5 questions with the following Likert scale response options: strongly agree, agree, disagree, strongly disagree. These post-session surveys were not required but rather optional [ 15 ].
A total of 178 students completed the cultural competence sessions between 2017 and 2020. Of these participants, 112 voluntarily completed a post-session survey on the effectiveness of the course in teaching cultural competence and cultural awareness during patient encounters. Between 2017 and 2019, 99 students completed post-session surveys following sessions with role play exercises. In 2020, 13 students completed post-session surveys following discussion board sessions.
Role-play exercises enhanced cultural competence
In responding to post-session survey questions following cultural competence sessions that included role-play exercises (2017–2019), 71% of students surveyed strongly agreed and 24% agreed that the role-play exercises helped them to identify the importance of communication in patient encounters. In asking participants if the role-play exercises made them more aware of different strategies to improve their patient interview skills, 72% strongly agreed and 23% agreed. Also, 68% of the students strongly agreed and 26% agreed that the exercises helped them to better identify the importance of building rapport and trust during patient encounters. When asked if the exercises helped the students to better understand their own bias and/or cultural awareness when working with patients, the results of the survey showed that 62% of students strongly agreed and 31% agreed with this statement. In addition, most students found the role-play exercises to be enjoyable (72% strongly agreed and 22% agreed). See results shown in Fig. 1 .
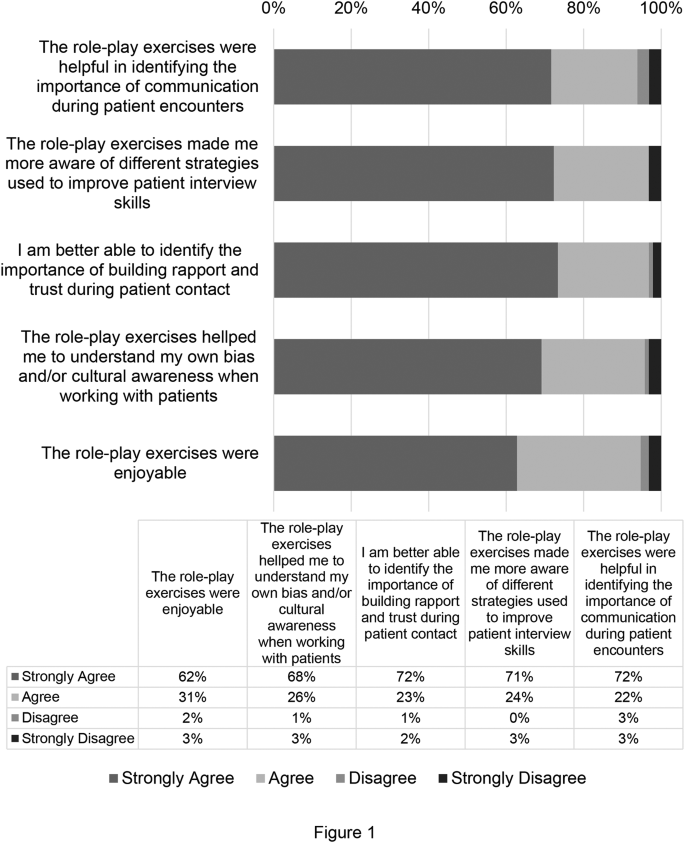
Cultural Competence Session Survey Data from the Year 2017–2019. Survey data from students at Boston University’s Oral Health Sciences Program for the years 2017–2019. Data is presented as percent of respondents ( n = 99)
Discussion boards and reflections enhanced cultural competence
Cultural competence sessions held during 2020 did not include role-play exercises due to the Covid-19 pandemic. Instead, students participated in discussion boards and reflections on Blackboard. In response to the post-session survey question asking if the discussion board exercises were helpful in identifying the importance of communication during patient encounters, 67% of students strongly agreed and 25% agreed with this statement. Also, 75% of students strongly agreed and 17% agreed that the discussion board exercises helped them identify the importance of building rapport and trust during patient contact. When asked if the exercises helped the students to better understand their own bias and/or cultural awareness when working with patients, the results of the survey showed that 67% of students strongly agreed and 25% agreed with this statement. In addition, most students found the discussion board exercises to be enjoyable (67% strongly agreed and 22% agreed). See results shown in Fig. 2 .
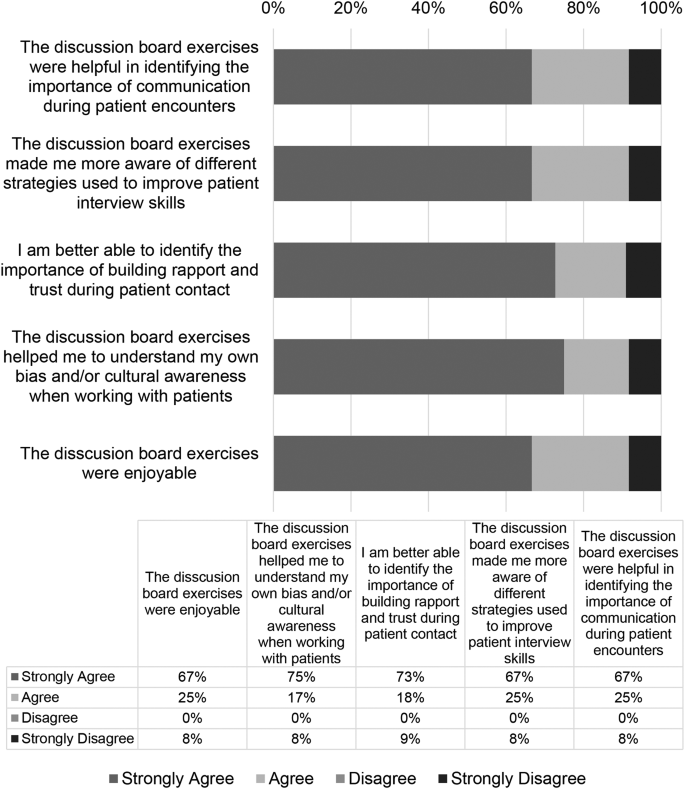
Cultural competence session survey data from the Year 2020. Survey data from students at Boston University’s Oral Health Sciences Program for the year 2020. Data is presented as percent of respondents ( n = 13)
Student responses to the reflection portion of the online cultural competency sessions were recorded and categorized. Five themes were selected and 441 reflection responses were coded using NVivo (Version 12). The results showed that 29% of reflections demonstrated student’s ability to understand a holistic approach to clinical care, 24.3% understood the importance of collecting a patient history, 6.8% recognized the socioeconomic factors during a patient encounter, 27.9% reflected on the importance of the patient clinical relationship, and 12% on the effects on improving health outcomes (Table 1 ). Representative student responses to these themes are shown in Table 1 .
There exists a need to develop novel and effective means for teaching and training the next generation of healthcare professionals the practice of cultural competence. Thus, two iterations of a course session using case-based patient centered encounters were developed to teach these skills to pre-professional dentals students. Overall, the results of this study demonstrated that participation in the course, subsequent group discussion sessions, and take-away PowerPoint sessions significantly improved the participant’s understanding of the importance of communication skills and understanding of socioeconomic, environmental, and cultural disparities that can affect a patient’s health outcome.
According to results from the course session implemented in-person from 2017 to 2019, the role-playing exercise significantly improved participants understanding of important components that can be used to improve health outcomes that may be affected due to health disparities. Students were strongly able to identify the importance of communication in patient encounters, to understand strategies such as communication and compassionate care in patient encounters, identify the importance of building a patient-physician relationship with patients, and were able to recognize their own cultural biases. Similarly, in 2020, even with a change in course modality to on-line learning due to COVID-19, students were able to understand the same key take-aways from the course session as demonstrated by reflections using the discussion board regarding the need for a holistic approach to care, importance of the patient clinician relationship, and importance of taking a patient history. Despite promising implications of both iterations of the session, students completing the session online did not find the same success in “understanding my own bias/and or cultural awareness when working with patients.” This decrease may be attributed to change in course modality and the strengths of the role-play enactment of the patient encounter. It is important to recognize that additional learning components, including video recordings of the role-play enactment, may be necessary if the discussion board is used as the primary learning method in the future.
In contrast to previous studies that attempted to determine the effectiveness of cultural competence training methods, this session had many unique characteristics. The simulated role-playing exercise enabled student participants to see first-hand an interactive patient scenario that could be used as an example for when students begin working with patients or communicating with patients who are culturally diverse. Additionally, the nature of the cases created for the course session which were divided into a part A in which the patient physician was more straightforward when diagnosing and treating the patient and a part B with a more comprehensive and nurturing approach to care, allowed the students to compare the scenarios and make their own assumptions and comments on the effectiveness of each portion of the case. Another strength of this training, was the faculty with cultural competence training were uniquely involved in case creation and facilitation of the course session. According to previous studies with similar aims, it was noted that direct observation and feedback from a faculty member who had cultural competence training and direct contact with patients can provide students with a more memorable and useful experience when educating students [ 12 ]. The facilitators of this session were able to emphasize from their own personal experiences how to work with culturally diverse populations.
An important aspect of the 2020 iteration of the course session in which a discussion board format was used, was that it allowed students who may feel uncomfortable with sharing their thoughts on a case and their own biases, the opportunity to share in a space that may feel safer than in person [ 4 ]. Previous studies have mentioned challenges with online discussion boards [ 4 ] but here we had robust participation, albeit required. Students often contributed more than the required number of comments and they were often lengthy and engaging when responding to peers. Finally, in contrast to previous studies, this course session took place in a pre-professional master’s program, the M.S. in Oral Health Sciences Program at Boston University Chobanian & Avedisian School of Medicine. This program, in which students are given the opportunity to enhance their credentials for professional school, provided students with early exposure to cultural competence training. Students that completed this session in their early pre-professional curriculum should be better prepared than peers who did not receive any cultural competence training until they entered their designated professional school. This session is part of an Evidence Based Dentistry course, which incorporates a larger component of personal reflection that serves to engage students in critical thinking as they begin to develop the skills to be future clinicians. Students that understand different cultures, society and themselves through self-assessments will grow and be best suited in time to treat future patients [ 4 , 16 , 17 ].
One limitation of the present study was the number of survey participants that competed the post-session surveys, as survey completion was not required. Thus, the number of student participants declined over the years, reaching its lowest number of participants in 2020 when the discussion board course session was implemented, and students may have been over surveyed due to the pandemic. Another limitation to this study, was the lack of both a pre and post survey that could be used to determine how student’s understanding of cultural competence had evolved from their entry into the course to the conclusion of the course as well as individual bias and self-reporting measures.
In the future, the course should implement both a role-playing format and subsequent discussion board reflections within the same course session. Studies have shown that alternatives ways of drawing students to reflect whether role play, personal narratives, etc. can be extremely advantageous in developing personal reflection and awareness building competency [ 4 , 16 , 17 , 18 ]. It is noted that role-playing exercises that allow students to provide feedback with student colleagues can provide students with more insight into their own behaviors. It has also been shown in previous studies that student writing and reflection activities can also facilitate student’s reflections on their own beliefs and biases [ 4 , 11 ]. Reflective writing skills are an important and effective means for students to continue to gauge their cultural competence throughout the remainder of their academic training and as future clinicians [ 4 , 17 , 19 ]. Further, students may experience emotional responses through the process of reflective writing as they recognize personal bias or stereotypes, creating a profound and impactful response resulting in enhanced understanding of cultural differences and beliefs [ 4 ]. By combining both learning techniques, students would be able to understand their own bias and their classmates and create a dialogue that could be more beneficial than just one learning method alone. Furthermore, by implementing the discussion board into the role-playing session, as stated previously, students that are more cautious about sharing their point of view or about their own implicit bias in a traditional classroom setting would be able to express their opinions and facilitate a more comprehensive discussion more thoroughly.
Here we show an effective means to utilize role-play of a multi-scenario case-based patient encounter to teach pre-professional healthcare student’s components of cultural competence, emphasizing the importance of provider-patient interactions, holistic patient care, and patient history and socioeconomic factors in provider care. This study contributes to the larger body of work that seeks to address this important aspect of education as it relates to enhancing patient health care outcomes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Albino JEN, Inglehart MR, Tedesco LA. Dental education and changing oral health care needs: disparities and demands. J Dent Educ. 2012;76(1):75–88.
Article Google Scholar
Constantinou CS, Papageorgiou A, Samoutis G, McCrorie P. Acquire, apply, and activate knowledge: a pyramid model for teaching and integrating cultural competence in medical curricula. Patient Educ Couns. 2018;101(6):1147–51.
DallaPiazza M, Padilla-Register M, Dwarakanath M, Obamedo E, Hill J, Soto-Greene ML. Exploring racism and health: an intensive interactive session for medical students. MedEdPORTAL. 2018;14:10783.
Forsyth CJ, Irving MJ, Tennant M, Short SD, Gilroy JA. Teaching Cultural competence in Dental Education: a systematic review and exploration of implications for indigenous populations in Australia. J Dent Educ. 2017;81(8):956–68.
Betancourt JR. Cultural competence and medical education: many names, many perspectives, one goal. Acad Med. 2006;81(6):499–501.
Jernigan VBB, Hearod JB, Tran K, Norris KC, Buchwald D. An examination of cultural competence training in US medical education guided by the tool for assessing cultural competence training. J Health Disparities Res Pract. 2016;9(3):150–67.
Google Scholar
Behar-Horenstein LS, Warren RC, Dodd VJ, Catalanotto FA. Addressing oral Health disparities Via Educational Foci on Cultural competence. Am J Public Health. 2017;107(S1):S18–23.
Lie D, Boker J, Cleveland E. Using the tool for assessing cultural competence training (TACCT) to measure faculty and medical student perceptions of cultural competence instruction in the first three years of the curriculum. Acad Med. 2006;81(6):557–64.
Holyfield LJ, Miller BH. A tool for assessing cultural competence training in dental education. J Dent Educ. 2013;77(8):990–7.
Vasquez Guzman CE, Sussman AL, Kano M, Getrich CM, Williams RL. A comparative case study analysis of cultural competence training at 15 U.S. medical schools. Acad Med. 2021;96(6):894–9.
Jernigan VB, Hearod JB, Tran K, Norris KC, Buchwald D. An examination of cultural competence training in US medical education guided by the tool for assessing cultural competence training. J Health Dispar Res Pract. 2016;9(3):150–67.
Kripalani S, Bussey-Jones J, Katz MG, Genao I. A prescription for cultural competence in medical education. J Gen Intern Med. 2006;21(10):1116–20.
Mariño R, Satur J, Tuncer E, Tran M, Milford E, Tran VMTH, Tran PQ, Tsai RP. Cultural competence of Australian dental students. BMC Med Educ. 2021;21(1):155.
Beagan BL. Teaching social and cultural awareness to medical students: it’s all very nice to talk about it in theory, but ultimately it makes no difference. Acad Med. 2003;78(6):605–14.
Ferrebee S, Boston University School of Medicine Master’s Thesis. (2021). Effectively Teaching Cultural Competence in Healthcare Education. Available at Boston University Libraries: Open BU: https://open.bu.edu/handle/2144/43838 .
Crosson JC, Deng W, Brazeau C, Boyd L, Soto-Greene M. Evaluating the effect of cultural competency training on medical student attitudes. Fam Med. 2004;36(3):199–203.
Cathryn F, Michelle I, Short S, Tennant M, Gilroy J. Strengthening indigenous cultural competence in dentistry and oral health education: academic perspectives. Eur J Dent Educ. 2019;23(1). https://doi.org/10.1111/eje.12398
DasGupta S, Meyer D, Calero-Breckheimer A, Costley AW, Guillen S. Teaching cultural competency through narrative medicine: intersections of classroom and community. Teach Learn Med. 2006;18(1):14–7.
Woldt JL, Nenad MW. Reflective writing in dental education to improve critical thinking and learning: A systematic review. J Dent Educ. 2021;85(6):778–785. https://doi.org/10.1002/jdd.12561 . Epub 2021 Feb 11. PMID: 33576055.
Download references
Acknowledgements
We would like to acknowledge Boston University’s Chobanian & Avedisian School of Medicine’s Graduate Medical Science students and study participants.
No funding was used for the completion of this study.
Author information
Authors and affiliations.
Graduate Medical Sciences, Boston University Chobanian & Avedisian School of Medicine, 72 East Concord Street, L317, R-1017, Boston, MA, 02118, USA
Karen R. Bottenfield, Andrew N. Best & Theresa A. Davies
Department of Medical Sciences & Education, Boston University Chobanian & Avedisian School of Medicine, 72 East Concord Street, Boston, MA, 02118, USA
Maura A. Kelley, David Flynn & Theresa A. Davies
University of Maryland School of Dentistry, 650 W Baltimore Street, Baltimore, MD, 21201, USA
Shelby Ferebee
You can also search for this author in PubMed Google Scholar
Contributions
TAD designed the original study concept, taught the classes (roleplay), conducted the surveys, and collected data; MAK designed the original case and PowerPoint, and performed roleplay; DBF and SF evaluated data and drafted original figures; ANB assisted in drafting the manuscript; KRB finalized figures and the manuscript.
Corresponding author
Correspondence to Theresa A. Davies .
Ethics declarations
Ethics approval and consent to participate.
This study was determined to be EXEMPT by the Institutional Review Board of Boston University Medical Campus, Protocol # H-37232.
Consent for publication
Not applicable.
Informed consent
Informed consent was received from all subjects.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, supplementary material 3, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Bottenfield, K.R., Kelley, M.A., Ferebee, S. et al. Effectively teaching cultural competence in a pre-professional healthcare curriculum. BMC Med Educ 24 , 553 (2024). https://doi.org/10.1186/s12909-024-05507-x
Download citation
Received : 27 October 2023
Accepted : 02 May 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12909-024-05507-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Communication
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]

- Langson Library
- Science Library
- Grunigen Medical Library
- Law Library
- Connect From Off-Campus
- Accessibility
- Gateway Study Center

A.I. May Someday Work Medical Miracles. For Now, It Helps Do Paperwork.
The best use for generative A.I. in health care, doctors say, is to ease the heavy burden of documentation that takes them hours a day and contributes to burnout.
Dr. Matthew Hitchcock, a family practice physician in Tennessee, uses Abridge A.I. software to produce summaries of patient visits. Credit... Audra Melton for The New York Times
Supported by
- Share full article

By Steve Lohr
Steve Lohr has written about the impact of technology, including on health care, for more than two decades.
- June 26, 2023
Dr. Matthew Hitchcock, a family physician in Chattanooga, Tenn., has an A.I. helper.
It records patient visits on his smartphone and summarizes them for treatment plans and billing. He does some light editing of what the A.I. produces, and is done with his daily patient visit documentation in 20 minutes or so.
Dr. Hitchcock used to spend up to two hours typing up these medical notes after his four children went to bed. “That’s a thing of the past,” he said. “It’s quite awesome.”
ChatGPT-style artificial intelligence is coming to health care, and the grand vision of what it could bring is inspiring. Every doctor, enthusiasts predict, will have a superintelligent sidekick, dispensing suggestions to improve care.
But first will come more mundane applications of artificial intelligence. A prime target will be to ease the crushing burden of digital paperwork that physicians must produce, typing lengthy notes into electronic medical records required for treatment, billing and administrative purposes.
For now, the new A.I. in health care is going to be less a genius partner than a tireless scribe.

From leaders at major medical centers to family physicians, there is optimism that health care will benefit from the latest advances in generative A.I. — technology that can produce everything from poetry to computer programs, often with human-level fluency.
But medicine, doctors emphasize, is not a wide open terrain of experimentation. A.I.’s tendency to occasionally create fabrications, or so-called hallucinations, can be amusing, but not in the high-stakes realm of health care.
That makes generative A.I., they say, very different from A.I. algorithms, already approved by the Food and Drug Administration, for specific applications, like scanning medical images for cell clusters or subtle patterns that suggest the presence of lung or breast cancer. Doctors are also using chatbots to communicate more effectively with some patients.
Physicians and medical researchers say regulatory uncertainty, and concerns about patient safety and litigation, will slow the acceptance of generative A.I. in health care, especially its use in diagnosis and treatment plans.
Those physicians who have tried out the new technology say its performance has improved markedly in the last year. And the medical note software is designed so that doctors can check the A.I.-generated summaries against the words spoken during a patient’s visit, making it verifiable and fostering trust.
“At this stage, we have to pick our use cases carefully,” said Dr. John Halamka, president of Mayo Clinic Platform, who oversees the health system’s adoption of artificial intelligence. “Reducing the documentation burden would be a huge win on its own.”
Recent studies show that doctors and nurses report high levels of burnout, prompting many to leave the profession. High on the list of complaints, especially for primary care physicians, is the time spent on documentation for electronic health records. That work often spills over into the evenings, after-office-hours toil that doctors refer to as “pajama time.”
Generative A.I., experts say, looks like a promising weapon to combat the physician workload crisis.
“This technology is rapidly improving at a time health care needs help,” said Dr. Adam Landman, chief information officer of Mass General Brigham, which includes Massachusetts General Hospital and Brigham and Women’s Hospital in Boston.
For years, doctors have used various kinds of documentation assistance, including speech recognition software and human transcribers. But the latest A.I. is doing far more: summarizing, organizing and tagging the conversation between a doctor and a patient.
Companies developing this kind of technology include Abridge , Ambience Healthcare , Augmedix , Nuance , which is part of Microsoft, and Suki .
Ten physicians at the University of Kansas Medical Center have been using generative A.I. software for the last two months, said Dr. Gregory Ator, an ear, nose and throat specialist and the center’s chief medical informatics officer. The medical center plans to eventually make the software available to its 2,200 physicians.
But the Kansas health system is steering clear of using generative A.I. in diagnosis, concerned that its recommendations may be unreliable and that its reasoning is not transparent. “In medicine, we can’t tolerate hallucinations,” Dr. Ator said. “And we don’t like black boxes.”
The University of Pittsburgh Medical Center has been a test bed for Abridge, a start-up led and co-founded by Dr. Shivdev Rao, a practicing cardiologist who was also an executive at the medical center’s venture arm.
Abridge was founded in 2018, when large language models, the technology engine for generative A.I., emerged. The technology, Dr. Rao said, opened a door to an automated solution to the clerical overload in health care, which he saw around him, even for his own father.
“My dad retired early,” Dr. Rao said. “He just couldn’t type fast enough.”
Today, the Abridge software is used by more than 1,000 physicians in the University of Pittsburgh medical system.
Dr. Michelle Thompson, a family physician in Hermitage, Pa., who specializes in lifestyle and integrative care, said the software had freed up nearly two hours in her day. Now, she has time to do a yoga class, or to linger over a sit-down family dinner.
Another benefit has been to improve the experience of the patient visit, Dr. Thompson said. There is no longer typing, note-taking or other distractions. She simply asks patients for permission to record their conversation on her phone.
“A.I. has allowed me, as a physician, to be 100 percent present for my patients,” she said.
The A.I. tool, Dr. Thompson added, has also helped patients become more engaged in their own care. Immediately after a visit, the patient receives a summary, accessible through the University of Pittsburgh medical system’s online portal.
The software translates any medical terminology into plain English at about a fourth-grade reading level. It also provides a recording of the visit with “medical moments” color-coded for medications, procedures and diagnoses. The patient can click on a colored tag and listen to a portion of the conversation.
Studies show that patients forget up to 80 percent of what physicians and nurses say during visits. The recorded and A.I.-generated summary of the visit, Dr. Thompson said, is a resource her patients can return to for reminders to take medications, exercise or schedule follow-up visits.
After the appointment, physicians receive a clinical note summary to review. There are links back to the transcript of the doctor-patient conversation, so the A.I.’s work can be checked and verified. “That has really helped me build trust in the A.I.,” Dr. Thompson said.
In Tennessee, Dr. Hitchcock, who also uses Abridge software, has read the reports of ChatGPT scoring high marks on standard medical tests and heard the predictions that digital doctors will improve care and solve staffing shortages.
Dr. Hitchcock has tried ChatGPT and is impressed. But he would never think of loading a patient record into the chatbot and asking for a diagnosis, for legal, regulatory and practical reasons. For now, he is grateful to have his evenings free, no longer mired in the tedious digital documentation required by the American health care industry.
And he sees no technology cure for the health care staffing shortfall. “A.I. isn’t going to fix that anytime soon,” said Dr. Hitchcock, who is looking to hire another doctor for his four-physician practice.
Steve Lohr covers technology, economics and work force issues. He was part of the team awarded the Pulitzer Prize for explanatory reporting in 2013. More about Steve Lohr
Explore Our Coverage of Artificial Intelligence
News and Analysis
News Corp, the Murdoch-owned empire of publications like The Wall Street Journal and The New York Post, announced that it had agreed to a deal with OpenAI to share its content to train and service A.I. chatbots.
The Silicon Valley company Nvidia was again lifted by sales of its A.I. chips , but it faces growing competition and heightened expectations.
Researchers at the A.I. company Anthropic claim to have found clues about the inner workings of large language models, possibly helping to prevent their misuse and to curb their potential threats.
The Age of A.I.
D’Youville University in Buffalo had an A.I. robot speak at its commencement . Not everyone was happy about it.
A new program, backed by Cornell Tech, M.I.T. and U.C.L.A., helps prepare lower-income, Latina and Black female computing majors for A.I. careers.
Publishers have long worried that A.I.-generated answers on Google would drive readers away from their sites. They’re about to find out if those fears are warranted, our tech columnist writes .
A new category of apps promises to relieve parents of drudgery, with an assist from A.I. But a family’s grunt work is more human, and valuable, than it seems.
Advertisement

Angel Reese Takes A Shot At Caitlin Clark In Now-Deleted Message

Travis Kelce Defends Harrison Butker After Controversial Grad Speech, 'Great Person'

Jake Paul Says He Won't Take It Easy On Mike Tyson Despite Age Gap

City Of Kansas City Fires Employee Over Harrison Butker Tweet

NFL's Jaelan Phillips Finds 'Massive' Wild Iguana Bathing In His Toilet
Mike tyson suffers medical emergency during flight, mike tyson in-flight medical emergency ... is there a doc onboard.
10:10 AM PT -- Jake Paul is shutting down any online chatter about their fight being called off in the wake of Mike Tyson 's health scare.
Jake says people "love to make s**t up," but reassured fans the July 20 bout is still a go. As he put it, "nothing changed."
Mike Tyson is recovering from an ulcer flare-up he suffered while flying cross-country -- and it was so bad, airline staff had to put out the call for any medical professionals on the plane to come forward.
Tyson was flying from Miami to L.A. on Saturday when he started feeling sick. The American Airlines flight was almost at LAX, but the boxer was in so much pain, flight attendants asked if there was anyone onboard to help him.
Mike's rep tells TMZ ... "He became nauseous and dizzy due to an ulcer flare up 30 minutes before landing. He is appreciative to the medical staff that were there to help him."
Paramedics boarded the plane when it reached the gate at LAX, and they treated Tyson on the spot ... according to In Touch Weekly , which first reported the incident.
Tyson's rep says he's doing "great" now.
Most of the passengers were reportedly unaware it was Mike who suffered the medical emergency ... they just knew someone was in distress, because the call for a doctor or nurse popped up on all the in-seat screens, before it was announced over the PA.
There was a reported 2-hour delay in the flight taking off, but that had nothing to do with Tyson -- who felt fine at that point. His rep says that was a mechanical issue with the plane. Passengers did have to wait about 25 minutes to get off the plane due to the paramedics checking out MT.
57-year-old Tyson is in the middle of training for his July boxing match against Jake Paul .
Originally Published -- 9:28 AM PT
- Share on Facebook
related articles
Mike Tyson Goes Shirtless For Autograph Signing, Shows Off Ripped Physique

Jake Paul Says Mike Tyson Match Will Be 'Biggest Fight The World Will Ever See'
Old news is old news be first.
Gaza: WHO chief calls for end to latest hospital siege

Facebook Twitter Print Email
As bombardments by the Israeli military reportedly continued overnight across Gaza, along with ground incursions and heavy fighting, the head of the UN World Health Organization (WHO) issued an alert on Tuesday for staff and patients at besieged Al-Awda Hospital in the north of the enclave.
“Medical staff inside the hospital reported an attack on 20 May, with snipers aiming at the building and an artillery rocket hitting the fifth floor ,” Tedros Adhanom Ghebreyesus said on X.
Some 148 staff and 22 patients and their companions have remained “trapped inside” the hospital since Sunday, the WHO Director-General added, before issuing an appeal for their protection.
Evacuation order impact
According to the WHO, only around one third of Gaza’s 36 hospitals still function, leaving critical health care facilities “inaccessible” to patients and healthcare workers impacted by the violence or evacuation orders.
In the southern city of Rafah, Israeli military orders telling Gazans to move have affected more than 20 medical points, four hospitals and four primary healthcare centres, the UN health agency noted.
In northern Gaza, meanwhile, 16 medical points have been impacted as well as five primary healthcare centres and Kamal Adwan Hospital, in addition to Al-Awda Hospital.
In a social media post on X on Sunday, WHO’s Tedros raised the alarm about reports of intense hostilities in the vicinity of Kamal Adwan Hospital coupled with an influx of injured patients despite the facility’s limited ability to treat them.
At least 900,000 Gazans uprooted
In a related development, the UN aid coordination office, OCHA , reported that the ongoing Israeli military operation and evacuation orders have uprooted well over 900,000 in the last two weeks – some four in 10 Gazans .
This includes 812,000 people from Rafah and more than 100,000 others in northern Gaza, with hundreds of thousands experiencing dreadful living conditions.
“Humanitarian partners working to provide shelter to people in Gaza report that there are no tents and very few shelter items left for distribution,” OCHA said.
Camping on roads
“People displaced from Rafah are currently seeking shelter in Khan Younis and Deir Al-Balah on any open land available , including access roads and agricultural land as well as in damaged buildings that have not been structurally assessed.”
To date, more than 75 per cent of the Gaza Strip – some 285 square kilometres – is under evacuation orders amid escalating hostilities, the UN agency said. “Under international humanitarian law, civilians – whether they move or stay – must be protected. Wherever they are in Gaza, their essential needs, including food, shelter, water and health, must be met.”
No let up in violence
The escalating fighting has severely disrupted nutrition support services in the north and south, the OCHA update continued, noting that access had been lost to more than 100 food distribution points in Rafah alone.
Meanwhile, humanitarian partners working to provide water, sanitation and hygiene support in Gaza said that there are shortages of hygiene kits and water containers for households to collect and store water, which are critical for people who are forcibly displaced.
More generally, the desperate lack of basic services after more than seven months of war have fuelled severe acute malnutrition among Gazans, exacerbating already serious concerns about a “further surge” in communicable diseases and dangerous hunger levels, OCHA warned.

IMAGES
VIDEO
COMMENTS
The literature review confirmed that medical equipment shortages and safety were of great concern to medical professionals interned, creating dilemmas among patients' refusal of services, personnel accountability, loss of trustworthiness of healthcare professionals, and inequality for all medical treatment.
The authors of this perspective contribution have served two terms (2014 and 2016) in the Jury of the biennial Best PhD Dissertation Award committee of the Netherlands Association for Medical Education. During this period, the committee reviewed 32 dissertations. Based on discussions among the jury regarding elements of an award winning dissertation and existing literature, we propose seven ...
The dissertation is an integral part in the professional journey of any medical post-graduate student. It is also an important responsibility for a guide to educate his protégé, the basics of research methodology through the process.
However, a meta-analysis on medical professionals" use of health care services revealed a paucity of good quality quantitative and qualitative data (Kay, Mitchell, Clavarino, & Doust, 2008).
Digitalization is not fully implemented in clinical practice, and several factors have been identified as possible barriers, including the competencies of health care professionals. However, no summary of the available evidence has been provided to date ...
All students at Yale School of Medicine engage in research and are required to write an MD thesis during medical school. The only exceptions are students who have earned a PhD degree in the health sciences before matriculation and students enrolled in Yale's MD/PhD program. The YSM MD Thesis is under the governance of the EPCC, which meets regularly to recommend rules, regulations, and ...
Although the majority of medical students in Germany pursue a doctorate, only a portion of them receive a standardized scientific training, which is reflected in the quality issues seen in medical doctoral theses. The course Medical Dissertation Basics was conceptualized and scientifically monitored in order to support medical doctoral students on the one hand and to improve the quality of ...
The foundation of medical professionalism and ethics is trust, truth, human values, and strong societal commitment. Our professional responsibilities as medical educators have immediate and long-term impact on the quality of training, patient care, and overall image of the professional group in the society.
MEDICAL PROFESSIONALS ATTITUDES TOWARD MENTAL HEALTH CARE UTILIZATION: THE IMPACTS OF STIGMA, COGNITIVE FUSION, AND PSYCHOEDUCATION Central Michigan University Scholarly & Creative Works
If you're still feeling a bit unsure about how to find a research topic for your healthcare dissertation or thesis, check out Topic Kickstarter service below. A mega list of research topic ideas in healthcare, including allopathic and alternative medicine, dentistry, rehab, optometry and more.
Edinburgh Medical School is one of two schools at the College of Medicine and Veterinary Medicine at the University of Edinburgh. The Edinburgh Medical School integrates research and teaching across our three Deaneries: Biomedical Sciences, Clinical Sciences and Molecular,Genetic and Population Health Sciences.
Theses/Dissertations from 2022. PDF. Outcomes of a Periodic Exposure Assessment of Workers at a University Campus, Logan M. Armagast. PDF. Evaluating the Effect of Public Health Governance Structure and Public Opinion on COVID-19 Disease Control Interventions, Daniel Chacreton.
The finding that both medical students' and professionals' acceptance of MC has significantly increased in recent decades—in conjunction with their consistent, strong desire for more educational material—suggests that the medical community should prioritize the development of MC educational programs.
Medical laboratory professionals have faced more than 20 years of workforce shortages.
Approaches to Measuring Non-Fatal Health Outcomes: Disability at the Iganga-Mayuge Demographic Surveillance System in Uganda. A National Burden of Disease Study for The United Arab Emirates (UAE): Quantifying Health Differentials Between Nationals and Migrants. Johns Hopkins Bloomberg School of Public Health.
Look at some of the potential healthcare dissertation topics mentioned below to get an idea for starting your dissertation.
The abstract, limited to 350 words, is a concise summary description of the study, including statement of the problem, pur-pose, scope, research tradition, data sources, methodology, key findings, and implica-tions. The abstract is written after the dis-sertation is completed, and is written from the perspective of an outside reader (i.e., not "My dissertation examines" but "An exami ...
This study investigates teaching cultural competence in a healthcare curriculum. We hypothesized that early educational exposure to cultural competence through role playing case studies, can serve as an effective mechanism for training early pre-doctoral students the practice of cultural competence. Utilizing student self-reported survey data conducted in a predental master's curriculum, in ...
Creswell (1998) suggests that. the tradition of qualitative inquiry selected by a researcher can shape the design of the study. He carefully provides text and tables compari ng five major ...
With our dissertation editing services, you get personalized feedback from experienced dissertation editors. Best-reviewed on Trustpilot.
Before attending law school, Dr. Miller received a Ph.D. in molecular biology/biochemistry from the All Union Research Institute of Genetics and Selection of Industrial Microorganisms in Moscow, Russia. Her thesis research focused on the discovery of a new approach for optimizing foreign gene expression in bacteria and expression and purification of different types of chemokines. Dr. Miller ...
UCI Libraries maintains the following templates to assist in formatting your graduate manuscript. If you are formatting your manuscript in Microsoft Word, feel free to download and use the template. If you would like to see what your manuscript should look like, PDFs have been provided. If you are formatting your manuscript using LaTex, UCI maintains a template on OverLeaf.
The use of water-containing biopolymer Noltrex with silver ions in the palliative treatment of patients with advanced osteoarthritis. (Rus) Zar, Voloshin, Zagorodny, Martynov. // Bulletin of the All-Russian Guild of Orthopaedic prosthetics. 2012. The results of intra-articular polyacrylamide gel injection for compensation of synovial fluid ...
The promotion of effective teacher professional development (ETPD) is a critical issue in the field of teacher education. The present study investigated how ETPD is affected simultaneously by teacher- and school-level factors across the United States, China, Finland, and Singapore. The data were drawn from the Teaching and Learning International Survey (TALIS 2018) and analyzed using a ...
The James Cancer Network has collaborated with Dayton Physicians—Hematology and Medical Oncology to bring nationally renowned cancer care to Dayton, Ohio communities. Learn more about the affiliation.
The best use for generative A.I. in health care, doctors say, is to ease the heavy burden of documentation that takes them hours a day and contributes to burnout.
Professional boxer Mike Tyson reportedly experienced a medical emergency in the air while flying from Miami, Fla., to Los Angeles, Calif., on Sunday, May 26.
Mike Tyson is recovering from an ulcer flare-up he suffered while flying cross-country -- and it was so bad, airline staff had to put out the call for any medical professionals on the plane to ...
As bombardments by the Israeli military reportedly continued overnight across Gaza, along with ground incursions and heavy fighting, the head of the UN World Health Organization (WHO) issued an alert on Tuesday for staff and patients at besieged Al-Awda Hospital in the north of the enclave.