
How to Become a Research Nurse
What is a research nurse.
- Career Outlook

Research Nurses, also referred to as Clinical Nurse Researchers or Nurse Researchers, develop and implement studies to investigate and provide information on new medications, vaccinations, and medical procedures. They assist in providing evidence-based research that is essential to safe and quality nursing care. This guide will explain what a Research Nurse does, how much they make, how to become one, and more!
Research nurses play a pivotal role in developing new and potentially life-saving medical treatments. Typically, clinical research nurses have advanced degrees, assist in the development of studies regarding medications, vaccines, and medical procedures, and also the care of research participants.
Nurses that know they want to be a clinical research nurse will often work as a research assistant, a clinical data collector, and/or clinical research monitor. It is essential to gain some bedside experience, but not as important as other nursing specialties.
Clinical research nurses have advanced degrees such as an MSN or Ph.D. This is vital to those that want to conduct independent research. For that reason, most clinical research nurses do not work in this field until they are in their 40s-50s.
Find Nursing Programs
What does a research nurse do.
Research Nurses primarily conduct evidence-based research through these two types of research methods:
- Quantitative: Meaning it’s researched that can be measured via statistical, mathematical, or computational techniques.
- Phenomenology
- Grounded Theory
- Ethnography
- Narrative Inquiry
Clinical research nurses perform a variety of tasks, all centered around research. These specific job responsibilities include:
- Collaborating with industry sponsors and other investigators from multi-institutional studies
- Educating and training of new research staff
- Overseeing the running of clinical trials
- Administering questionnaires to clinical trial participants
- Writing articles and research reports in nursing or medical professional journals or other publications
- Monitoring research participants to ensure adherence to study rules
- Adhering to research regulatory standards
- Writing grant applications to secure funding for studies
- Reporting findings of research, which may include presenting findings at industry conferences, meetings and other speaking engagements
- Adhering to ethical standards
- Maintaining detailed records of studies as per FDA guidelines, including things such as drug dispensation
- Participating in subject recruitment efforts
- Ensuring the necessary supplies and equipment for a study are in stock and in working order
- Engaging with subjects and understanding their concerns
- Providing patients with thorough explanation of trial prior to obtaining Informed Consent, in collaboration with treating physician and provides patient education on an ongoing basis throughout the patient’s course of trial.
>> Show Me Online MSN Programs
Research Nurse Salary
Glassdoor.com states an annual median salary of $95,396 for Research Nurses and Payscale reports that Clinical Research Nurses earn an average annual salary of $75,217 or $36.86/hr .
Research Nurse Salary by Years of Experience
Research Nurses can earn a higher annual salary with increased years of experience.
- Less than 1 year of experience earn an average salary of $68,000
- 1-4 years of experience earn an average salary of $73,000
- 5-9 years of experience earns an average salary of $73,000
- 10-19 years of experience earns an average salary of $80,000
- 20 years or more of experience earns an average salary of $78,000
Via Payscale
To become a Research Nurse, you’ll need to complete the following steps:
Step 1: Attend Nursing School
You’ll need to earn either an ADN or a BSN from an accredited nursing program in order to take the first steps to become a registered nurse.
Step 2: Pass the NCLEX-RN
Become a Registered Nurse by passing the NCLEX examination.
Step 3: Gain Experience at the Bedside
Though not as important as in some other nursing careers, gaining experience is still a vital step for those wanting to become Nurse Researchers.
Step 4: Earn an MSN and/or Ph.D
Research Nurses typically need an advanced degree, so ADN-prepared nurses will need to complete an additional step of either completing their BSN degree or entering into an accelerated RN to MSN program which will let them earn their BSN and MSN at the same time.
Step 5: Earn Your Certification
There are currently two certifications available for Clinical Research Nurses. They are both offered by the Association of Clinical Research Professionals.
- Clinical Research Association (CCRA)
- Clinical Research Coordinator (CCRC)
These certifications are not specific to nurses but rather those that work in the research field.
CCRA Certification
In order to be deemed eligible for the CCRA Certification exam, applicants must attest to having earned 3,000 hours of professional experience performing the knowledge and tasks located in the six content areas of the CRA Detailed Content Outline. Any experience older than ten years will not be considered.
What’s on the Exam?
- Scientific Concepts and Research Design
- Ethical and Participant Safety Considerations
- Product Development and Regulation
- Clinical Trial Operations (GCPs)
- Study and Site Management
- Data Management and Informatics
Exam Information
- Exam Fee: $435 Member; $485 Nonmember
- Exam Fee: $460 Member; $600 Nonmember
- Multiple choice examination with 125 questions (25 pretest non-graded questions)
CCRC Certification
In order to be deemed eligible for the CCRC Certification exam, applicants must attest to having earned 3,000 hours of professional experience performing the knowledge and tasks located in the six content areas of the CCRC Detailed Content Outline. Any experience older than ten years will not be considered.
Where Do Research Nurses Work?
Clinical Research nurses can work in a variety of locations, including:
- Government Agencies
- Teaching Hospitals
- Medical Clinics
- International Review Board
- Medicine manufacturing
- Pharmaceutical companies
- Medical research organizations
- Research Organizations
- International Health Organizations
- Private practice
- Private and public foundations
What is the Career Outlook for a Research Nurse?
According to the BLS , from 2022 to 2032, there is an expected growth of 6% for registered nurses. With the aging population and nursing shortage, this number is expected to be even higher.
The BLS does identify medical scientists, which includes clinical research nurses, as having a growth potential of 10% between 2022-2032.
What are the Continuing Education Requirements for a Research Nurse?
Generally, in order for an individual to renew their RN license, they will need to fill out an application, complete a specific number of CEU hours, and pay a nominal fee. Each state has specific requirements and it is important to check with the board of nursing prior to applying for license renewal.
If the RN license is part of a compact nursing license, the CEU requirement will be for the state of permanent residence. Furthermore, some states require CEUs related to child abuse, narcotics, and/or pain management.
A detailed look at Continuing Nurse Education hours can be found here .
Where Can I Learn More About Becoming a Research Nurse?
- American Nurses Association (ANA)
- Nurse Researcher Magazine
- National Institute of Nursing Research
- International Association of Clinical Research Nurses
- Association of Clinical Research Professionals
- Society of Clinical Research Associates
- American Association of Colleges of Nursing
Research Nurse FAQs
What is the role of a research nurse.
- Research nursing is a nursing practice with a specialty focus on the care of research participants.
What makes a good Research Nurse?
- Research Nurses should be excellent communicators, have strong attention to detail, be self-assured, have strong clinical abilities, be flexible, autonomous, organized, and eager to learn new information.
How much does a Research Nurse make?
- Research nurses earn an average salary of $95,396 according to Glassdoor.com.
What is it like being a Research Nurse?
- Research Nurses provide and coordinate clinical care. Research Nurses have a central role in ensuring participant safety, maintaining informed consent, the integrity of protocol implementation, and the accuracy of data collection and data recording.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.
- Mayo Clinic Careers
- Anesthesiology
- Dermatology
- Emergency Medicine
- Family Medicine
- Internal Medicine
- Lung Transplant
- Psychiatry & Psychology
- Nurse Practitioner & Physician Assistant
- Ambulance Service
- Clinical Labs
- Med Surg RN
- Radiology Imaging
- Clinical Research Coordinator
- Respiratory Care
- Senior Care
- Surgical Services
- Travel Surgical Tech
- Practice Operations
- Administrative Fellowship Program
- Administrative Internship Program
- Career Exploration
- Nurse Residency and Training Program
- Nursing Intern/Extern Programs
- Residencies & Fellowships (Allied Health)
- Residencies & Fellowships (Medical)
- SkillBridge Internship Program
- Training Programs & Internships
- Diversity, Equity & Inclusion
- Employees with Disabilities

Life-changing careers
Search life-changing careers.
Search by Role or Keyword
Enter Location
- United States Applicants
- United Kingdom Applicants
- Current Employees
Remote Opportunities
Mayo Clinic offers a variety of remote job opportunities. During the global pandemic, we readily embraced the move to a remote working model for the health and safety of our employees. It became evident that our teams were equally collaborative and continued to support the Mayo Clinic mission and values. As the pandemic eases and we look towards the future, Mayo will continue to support remote work for teams whose work is not reliant on campus resources.
Join a company culture that encourages balance and wellness, with plenty of opportunities for career development!
Current Remote Job Openings
- IT Help Desk Specialist - Remote Information Technology 334596
- Senior Manager-Rev Cycle Application Supp-Remote Business 330997
- Statistical Programmer (Remote) Research 334558
- Intern-Biostatistics (BS) Internship 334397
- IT Lead Software Engineer - Remote Information Technology 333247
- Senior Manager Quality & Regulatory Operations MCS Laboratory, Business 334456
- Senior AI RAQA Specialist - CDH - Remote Business 334494
- CDI SPECIALIST I Business 334255
- Intern -Undergraduate - Ortho Research - Remote - Temporary Research 333148
- Senior Automation Solutions – Tech Specialist II Information Technology 331775
Join Our Talent Community
Sign up, stay connected and get opportunities that match your skills sent right to your inbox
Email Address
Phone Number
Upload Resume/CV (Must be under 1MB) Remove
Job Category* Select One Advanced Practice Providers Business Education Engineering Executive Facilities Support Global Security Housekeeping Information Technology Internship Laboratory Nursing Office Support Patient Care - Other Pharmacy Phlebotomy Physician Post Doctoral Radiology Imaging Research Scientist Surgical Services Therapy
Location Select Location Albert Lea, Minnesota Arcadia, Wisconsin Austin, Minnesota Barron, Wisconsin Bloomer, Wisconsin Caledonia, Minnesota Cannon Falls, Minnesota Chippewa Falls, Wisconsin Decorah, Iowa Duluth, Minnesota Eau Claire, Wisconsin Fairmont, Minnesota Faribault, Minnesota Holmen, Wisconsin Jacksonville, Florida La Crosse, Wisconsin Lake City, Minnesota London, England Mankato, Minnesota Menomonie, Wisconsin Minneapolis-St. Paul-Bloomington, Minnesota New Prague, Minnesota Onalaska, Wisconsin Osseo, Wisconsin Owatonna, Minnesota Phoenix, Arizona Prairie du Chien, Wisconsin Red Wing, Minnesota Rice Lake, Wisconsin Rochester, Minnesota Saint Cloud, Minnesota Saint James, Minnesota Scottsdale, Arizona Sparta, Wisconsin Tomah, Wisconsin Waseca, Minnesota Zumbrota, Minnesota
Area of Interest Select One Nursing Research Radiology Laboratory Medicine & Pathology Facilities Licensed Practical Nurse (LPN) Neurology Pharmacy Physical Medicine & Rehabilitation Cardiovascular Medicine Surgery General Services Psychiatry & Psychology Mayo Collaborative Services Respiratory Therapy Ambulance Services Environmental Services Finance Anesthesiology & Perioperative Medicine Mayo Clinic Laboratories Surgical Technician Emergency Medicine Orthopedics Social Work Family Medicine Gastroenterology & Hepatology International Hospital Internal Medicine Medical Oncology Radiation Oncology Global Security Information Technology Obstetrics & Gynecology Office Support Hematology Housekeeping Pediatrics Senior Care Transplant Cardiovascular Surgery Critical Care General Internal Medicine Hospice & Palliative Care Ophthalmology Patient Scheduling Administration Pulmonary/Sleep Medicine Education Engineering Artificial Intelligence & Informatics Dermatology Desk Operations Oncology Sports Medicine Urology Biochemistry & Molecular Biology Community Internal Medicine Linen & Central Services Nephrology & Hypertension Physiology & Biomedical Engineering Surgical Assistant Clinical Genomics Endocrinology Health Care Delivery Research Immunology Infectious Diseases Neurosciences Otolaryngology (ENT) Regenerative Biotherapeutics Rheumatology Cancer Center Clinical Trials & Biostatistics Digital Epidemiology Molecular Medicine Molecular Pharmacology & Experimental Therapeutics Primary Care Quality Business Development Development/Philanthropy Legal Neurologic Surgery Pain Medicine Women's Health Allergic Diseases Bariatric Medicine Cancer Biology Center for Individualized Medicine Clinical Nutrition Comparative Medicine Dental Specialities Geriatric Medicine & Gerontology Healthcare Technology Management Informatics Information Security Marketing Occupational/Preventative Medicine Spine Center Spiritual Care Travel Urgent Care Volunteer Services
Confirm Email
By submitting your information, you consent to receive email communication from Mayo Clinic.
Equal opportunity
All qualified applicants will receive consideration for employment without regard to race, color, religion, sex, gender identity, sexual orientation, national origin, protected veteran status, or disability status. Learn more about "EEO is the Law." Mayo Clinic participates in E-Verify and may provide the Social Security Administration and, if necessary, the Department of Homeland Security with information from each new employee's Form I-9 to confirm work authorization.
Reasonable accommodations
Mayo Clinic provides reasonable accommodations to individuals with disabilities to increase opportunities and eliminate barriers to employment. If you need a reasonable accommodation in the application process; to access job postings, to apply for a job, for a job interview, for pre-employment testing, or with the onboarding process, please contact HR Connect at 507-266-0440 or 888-266-0440.
Job offers are contingent upon successful completion of a post offer placement assessment including a urine drug screen, immunization review and tuberculin (TB) skin testing, if applicable.
Recruitment Fraud
Learn more about recruitment fraud and job scams
Advertising
Mayo Clinic is a not-for-profit organization and proceeds from Web advertising help support our mission. Mayo Clinic does not endorse any of the third party products and services advertised.
Advertising and sponsorship policy | Advertising and sponsorship opportunities
Reprint permissions
A single copy of these materials may be reprinted for noncommercial personal use only. "Mayo," "Mayo Clinic," "MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield Mayo Clinic logo are trademarks of Mayo Foundation for Medical Education and Research.
Any use of this site constitutes your agreement to the Terms and Conditions and Privacy Policy linked below.
Terms and Conditions | Privacy Policy | Notice of Privacy Practices | Notice of Nondiscrimination
© 1998-2024 Mayo Foundation for Medical Education and Research (MFMER). All rights reserved.
Clinical Research Nurse Work From Home jobs
Registered nurse (rn) - virtual - placement & logis.

Registered Nurse RN - Virtual Interview Event!
Eacute virtual care nurse - 9e medical-surgical - (internal only) (on-site), registered nurse (rn) - mds coordinator - long-term care.
Avera Mother Joseph Manor Ret Comm
RN Virtual Acute Care
Registered nurse - atrium health hospice home care cabarrus pt remote weekend days, clinical trial educator - renal dialysis exp. (remote).
Randstad Life Sciences Us
Clinical Field Staff Supervisor - RN
Aletheia Staffing
Travel Nurse RN - OR - Operating Room - $2,970 per week
Clinical reviewer utilization management rn, travel nurse rn - home health - $2,282 per week in bronx, ny, rn pulmonary clinic.
Corewell Health
NP / Clinic RN / Florida / Permanent / IMMEDIATE OPENING For a NURSE Job
Revenue cycle appeals registered nurse - remote.
Conifer Revenue Cycle Solutions
Travel Nurse RN - PCU - $2,129 per week in Allentown, PA
Travelnursesource
Infojini Healthcare
Per Diem / PRN Nurse RN - Clinic - $28+ per hour
Travel nurse rn - virtual care - $2,844 per week.
- Registered Nurse
RN and LPN in Waianae - $5K Bonus - New Grab Welcome!
Wilson Care Group
Learn More About Clinical Research Nurse Jobs
Work from home clinical research nurse jobs.
- Work From Home Clinic Registered Nurse Jobs
- Work From Home Clinical Care Coordinator Jobs
- Work From Home Clinical Educator Jobs
- Work From Home Nurse Jobs
- Work From Home Nurse Clinician Jobs
- Work From Home Pediatric Nurse Jobs
- Work From Home Registered Health Nurse Jobs
- Work From Home Registered Nurse Jobs
- Work From Home Registered Nurse In The ICU Jobs
- Work From Home Registered Professional Nurse Jobs
- Work From Home Research Nurse Jobs
- Work From Home Staff Nurse Jobs
- Work From Home Traveling Nurse Jobs
Clinical Research Nurse Related Careers
- Agency Registered Nurse
- Clinic Registered Nurse
- Clinical Care Coordinator
- Clinical Educator
- Nurse Clinician
- Oncology Registered Nurse
- Pediatric Nurse
- Psychiatric Registered Nurse
- Registered Health Nurse
- Registered Nurse Charge Nurse
- Registered Nurse In Pacu
- Registered Nurse In The ICU
Clinical Research Nurse Related Jobs
- Agency Registered Nurse Employment
- Clinic Registered Nurse Employment
- Clinical Care Coordinator Employment
- Clinical Educator Employment
- Head Nurse Employment
- Nurse Employment
- Nurse Clinician Employment
- Oncology Registered Nurse Employment
- Pediatric Nurse Employment
- Psychiatric Registered Nurse Employment
- Registered Health Nurse Employment
- Registered Nurse Employment
- Registered Nurse Charge Nurse Employment
- Registered Nurse In Pacu Employment
- Registered Nurse In The ICU Employment
What Similar Roles Do
- Clinic Registered Nurse Responsibilities
- Clinical Care Coordinator Responsibilities
- Clinical Educator Responsibilities
- Head Nurse Responsibilities
- Nurse Responsibilities
- Nurse Clinician Responsibilities
- Oncology Registered Nurse Responsibilities
- Pediatric Nurse Responsibilities
- Psychiatric Registered Nurse Responsibilities
- Registered Health Nurse Responsibilities
- Registered Nurse Responsibilities
- Registered Nurse Charge Nurse Responsibilities
- Registered Nurse In Pacu Responsibilities
- Registered Nurse In The ICU Responsibilities
- Registered Nurse Med/Surg Responsibilities
- Zippia Careers
- Healthcare Practitioner and Technical Industry
- Clinical Research Nurse Jobs
- Clinical Research Nurse Work From Home Jobs
Browse healthcare practitioner and technical jobs

Can nurses work from home? Yes! These are your options
It’s one of the most frequently asked questions we get in comments to our posts and advertisements. Do you have work-from-home nursing jobs ? Does your site list telenursing positions for RNs, or any kind of telecommute jobs? Any remote nursing job opportunities?
We understand!
I can tell you one thing for sure — there’s no nursing company more sympathetic to this question than NurseRecruiter.com ! We all work remotely ourselves. Started doing it well before this cursed year and the pandemic it wrought. We’ve been doing it for years!
So we definitely understand the attraction. Live where you always wanted to live! Rid yourself of the practical obstacles that kept you from pursuing long-cherished dreams. Avoid dreary and expensive commutes. Work where — and when! — you feel most comfortable and least stressed. Take back control over your work-life balance! Put yourself at a healthy distance from workplace drama and executives second-guessing everything you do.

Remote working also opens up windows of opportunity for people who otherwise face challenging thresholds. When you can’t leave home for 12-hour shifts because you are raising a kid by yourself. When a disability makes working as floor nurse hard or impossible. When your age or health puts you at too high a risk in these pandemic times to accept a hospital job.
No less of a nurse
We don’t need to explain why interest in remote nursing jobs has surged this year. Hospital work was never harder than now; never as anxiety-inducing.
But even before Covid-19 ever reared its ugly head, there were stories we heard over and again. Being a bedside nurse can be exhausting. Floor nursing in understaffed teams is stressful and sometimes even literally back-breaking . Working in hospitals with high-acuity patients pays well, but takes a lot from you too. Nurses get burnt out.
In short, the whole industry needs change. But in the meantime, can anyone really blame you if you go looking for an alternative? If you genuinely love caring for people, but crave a different way to pursue your calling? You will be no less of a nurse working from home!
You’re going to need a plan!
The next question is: how realistic is it? Nurses aren’t office workers, after all, doing 9-to-5’s behind a computer all day. While white-collar workers stay at home to protect themselves, you’re out on the front lines. Essential workers. Because to be a nurse, you need to be by your patient, with your team. Right?
By and large, this is true. We have to be honest: most nursing still cannot be done from home. But don’t give up on your dream quite yet! Remote nursing jobs do exist, across a wide variety of settings. If anything, the Coronavirus pandemic has increased the need for telenursing , boosting demand for specific positions like phone triage nurses.
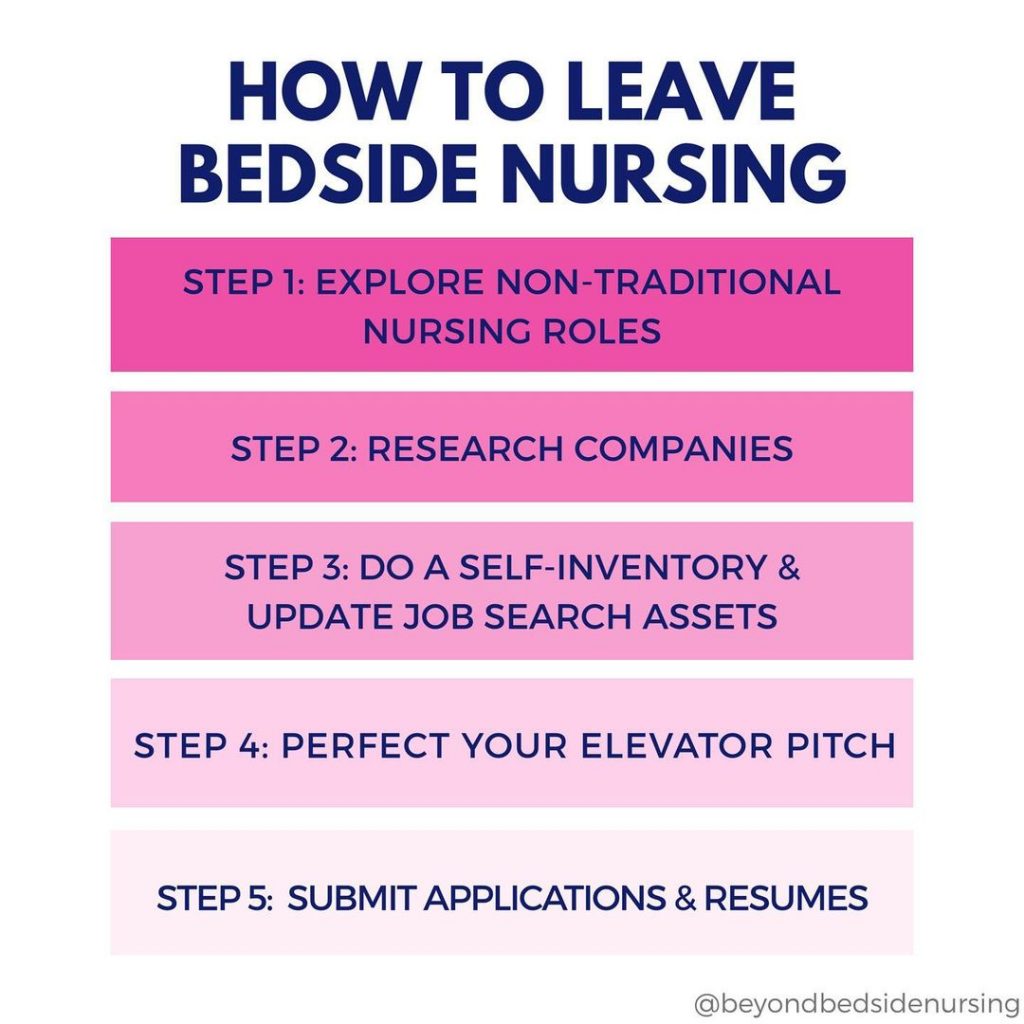
But you need a plan. Many work-from-home jobs in nursing involve specialties that are professions by themselves, like online nurse education, medical coding or billing, or case management . Qualifying for those might require investing time and resources in getting the right qualifications and experience. You might have to go back to school first. But the jobs are there!
Maybe you already have the right qualifications. And if you don’t, you just have to think of it in terms of a strategic plan — which steps do you need to undertake to get to your goal of qualifying for them?
Let’s look at a few examples, and use some of the great advice you yourselves have suggested in comments to our Facebook posts !
Telehealth nursing and telephone triage
Online nurse educator, case manager, care manager or patient advocate, medical coder or biller, utilization review nurse, health coach, health informatics nurse, research nurse, legal nurse consultant, nurse consultant in other fields, writing and business opportunities, the middle road: partly-remote alternatives to hospital bedside care.
Telehealth services are facing “a flood of patients in the wake of the coronavirus pandemic,” to the extent that providers are struggling to meet the demand . That means telehealth companies are ramping up their hiring of new staff!
There are different kinds of telenursing jobs , involving greater or lesser professional responsibility. They can be done from office locations or from home, depending on the job and employer. “I have friend who loves telenursing!,” Margie Kirchgesner Gehres wrote, explaining that “some nurses prefer to go to the office and answer phones” while others prefer the “solitude at home”.
Now medical facilities are even more overstretched than normal, and eager to minimize the infection risks of in-person visits, they are hiring more nurses to do telephone triage. Triage nurses can assess symptoms to decide whether an appointment is necessary. An experienced RN is perfectly qualified to tackle many of the every-day questions patients have, and a lot of those can be handled adequately by phone!
A call center nurse has fewer responsibilities. They don’t issue medical advice of any kind, they just make sure patients are connected through to the right person.
Many insurance companies and health systems provide a 24-hour nurse advice line. The advice nurses manning those lines help patients with non-emergency issues sort out what support they might need, understand their medications, find the care they need if they are away from home, and get a ‘sick slip’ if needed.
Most importantly, when people are anxious about any suspected medical issues, these nurses provide evidence-based healthcare advice. Infinitely more useful than having them just google their symptoms and inevitably ‘finding out’ it must be cancer..
And speaking for the nurses working in these jobs, dealing with these everyday issues, however important it is to address them early, does sometimes involve a more light-hearted note…
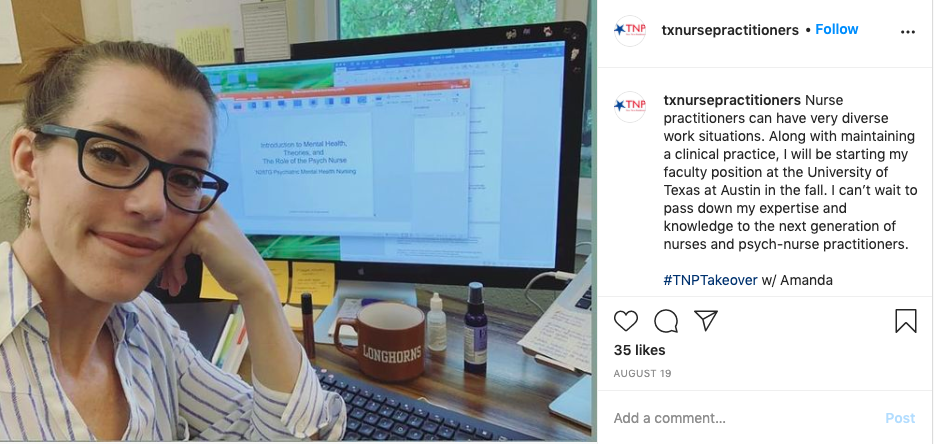
Our website regularly features jobs in nurse education . Until this year, few of them involved working from home. But for obvious reasons a lot of nursing education has now gone remote, and so have the jobs of nurse educators .
Even when all this is over, online teaching will likely occupy an ever more prominent role. Not just for nursing schools educating tomorrow’s nurses but also in continuing education, training experienced nurses advanced skills. All those online courses you see advertised? There are faculty jobs teaching them, designing courses and curricula, evaluating applications.
It’s a rewarding and important job, and one that has good prospects of providing long-term stability. The plan? To work in education, focus on pursuing your own, and get that Master’s degree in nurse education!
A related if rather specific job is to be a nurse exam writer , where you help to formulate appropriate questions for nursing certifications and exams (and we all know that some of those could be articulated more clearly!)
“ Case management and utilization management jobs are often work from home,” Heather Roets Meade said in our Facebook comments. And she’s right! (And we’ll get back to those utilization management jobs later on.)
Case managers (or case management nurses ) play a key role in navigating complex care for patients whose treatment involves multiple specialties — often older people with chronic health conditions. They scrupulously manage the communication between the physicians involved in their care as well as with the insurance company.
The case manager is both a coordinator and a go-between, helping them all to create the best care plan for the patient. But they keep a firm eye on the institutional needs, legal and financial ramifications involved. Their focus is also on preventing any non-compliance, minimizing the overutilization of services, and finding cost-effective solutions.
The jobs market for nurse case managers is growing rapidly. In hospice and home care centers for example, but with increasing space for remote work as well. Working from home, you’d be on the phone a lot, from helping patients with their doctor’s appointments to assisting the care providers in scheduling important surgeries.
Like many of the jobs in this list, entering this field is a lot easier with several years of experience as Registered Nurse. To complete your qualifications, there are four different ways to earn your certification in case management.

While case managers help the patient get a handle on the complicated care issues he or she faces, they still operate within the restrictions that are set by the hospital, insurance company, or other institution that employs them. What if you enjoy patient education and care coordination, but you want to be wholly on the side of the patient, with nobody’s interests but theirs in mind?
That’s where a care manager comes in. Their work can be especially important when someone faces a lifelong injury, a chronic disease, or the prospect of end-of-life care. The choices and pressures involved in understanding treatment options and grappling with insurance issues can be overwhelming. That’s all the more true for the elderly and their families, for whom an aging life care manager or geriatric care manager can be a godsend.
Nowadays, and of course especially in current circumstances, a significant part of this work is done remotely, by telephonic nurse care managers .
Care managers take a holistic approach, Lori Beth Charlton explains . They help their clients navigate the maze of health care and long-term care systems with a firm eye on what serves their overall quality of life best. And they don’t just look at their medical needs, but also at how those intersect with a client’s “social, emotional, financial, legal, and housing needs”.
Happy International Nurses Day! First picture 1990 first year student nurse, second picture 2020 working from home no makeup selfie. What a difference 30 years makes 🙎🏻♀️but still here, still nursing. #InternationalNursesDay2020 pic.twitter.com/nSJ6pKWmb5 — Corinne Miller (@corinnegmiller) May 12, 2020
Several of you mentioned medical coding and billing, which is a rapidly growing field as well, and again has the distinct advantage of steady and predictable hours! A lot of this work is done in offices, but there is an increasing number of remote jobs too. “I am an RN and went into coding eight years ago, work from home,” wrote Janice Larson.
The jobs involved, as medical biller or medical coder , are quite different from each other, and it’s mostly just in smaller businesses that the same person does both billing and coding. Billers and coders are both health claims specialists , but becoming a medical coder takes more study and experience (and pays better) — though one job is a great starting ground for the other!
Medical coders play a key role in the billing process — errors in assigning medical codes will lead to insurance companies being incorrectly billed, which can cause contested or rejected claims and serious headaches for patients and hospitals. But it can be genuinely tricky to translate notes and documentation from various sources about complex medical issues into unambiguous medical codes. A medical coder has to be able to understand and interpret medical documentation as well as insurance contract language in enough detail to provide a clinical opinion.
That’s why RNs have significant advantages applying to these jobs. But medical billers , too, benefit from a nurse’s real grasp of clinical care when it comes to getting the details of the billing forms right, especially in a complex field like home care. As medical biller, you gather insurance information from the patient, review billing records for Medicare and/or Medicaid claims, and collaborate with insurance companies when filing claims “to work out denials/rejections, finalize the details and send out statements”. You also operate as an intermediary, helping patients understand their charges and smoothing out stressful issues — so your bedside manner still matters!
Either line of work can involve a bit of detective work , “dissecting a patient’s medical record, tracking down additional information,” which is part of the charm. That goes for a medical review nurse too, whose job partly involves detecting potentially fraudulent or abusive billing practices.
It won’t come as surprise that you need to do specific courses to take on these jobs as well. Further education is key , from a specialized degree or certification to follow-up workshops. Especially if you want to get that job as remote medical coder , additional experience and training counts!

If you’ve been a RN for long enough, you may have your issues with insurance companies. Maybe not the first place you think of when wondering if the grass is greener on the other side! But there is a variety of job opportunities to be found there for nurses who seek alternatives to bedside nursing, with more regular working hours to boot. Not just for case managers, but for insurance claim specialists and utilization review nurses too.
A utilization review (UR) nurse assesses the severity of the medical problem, and whether it meets the criteria for full inpatient treatment or other levels of (eg outpatient) care. Hospitals and other healthcare providers need UR nurses for that same task. But when you work for an insurance company, you review claims to determine which kind of treatment is warranted, scrutinizing medical records and medical review criteria and guidelines to identify what procedures are covered and what amount needs to be paid out.
A significant amount of jobs in the context of case management at insurance companies involves disability claims and workers’ compensation cases. A nurse case reviewer or nurse consultant focused on workers’ compensation claims will review the documentation to make sure the claim meets all compliance standards.
If some of the above jobs sounded all too bureaucratic, becoming a health coach might be a good alternative! As bedside nurse, you care for the sick — that is why you chose the profession after all, right? But do you ever wonder about all the patients who might not have needed that hospital care, if they had gotten a little bit more help with preventative care earlier?
To put it in fancier words, “a key feature of U.S. health care” is the way it encourages “overuse of services by favoring procedural over cognitive tasks (e.g., surgery vs. behavior-change counseling) and specialty over primary care”. That’s how Farshad Fani Marvasti and Randall S. Stafford articulated it in a New England Journal of Medicine article titled “From “Sick Care” to Health Care” , where they argued that “a prevention model, focused on forestalling the development of disease before symptoms or life-threatening events occur, is the best solution”.
As health coach, you can be part of this solution. Instead of prescribing what someone should do, you mentor them into finding the right ways to do it, building “one-on-one relationships in order to make wellness plans and set health goals that will work for a specific person”.
The good news is that this is work that can also be done online from home, as remote health coach . “Lots of insurance companies want health coaches to work from home,” The Nerdy Nurse explained . So do other health and wellness companies and sites like WebMD. And with a bit of entrepreneurial spirit and a knack for networking, you can also work as independent, self-employed health coach!
A healthy lifestyle is more than a diet. It is an overall approach to life that involves moving the body each day, relaxation, quality time with friends+family and expressing 💙. #MyPhoto #IonianSea #lifestylemedicine #Health #Greece #HealthCoach pic.twitter.com/WrPtZ3Mh3e — Beth Frates MD (@BethFratesMD) August 6, 2020
Getting into health informatics as clinical informatics nurse or nursing informatics specialist is another great option if you want to pursue long-term work-from-home opportunities.
“I started being able to work partly from home in 2012 when I was an EHR Application Analyst,” The Informatics Nurse explained . “I was able do more productive work with the time saved from my long commute. Just as important, I could more easily spend time with my then-3-year-old daughter during breaks (and I wasn’t too tired to play with her by end of day). After that, I worked as a Project Consultant for a health system in the Midwest while still residing in California.”
Health informatics is a good field to choose if your drive as a nurse stems from a holistic passion to improve the care people receive, rather than the satisfaction of one-on-one patient contact. A lot of new technologies make our jobs as nurses ever easier, but if you’ve been a nurse for a while you also know that how some of them are applied in practice can be… bothersome. Why not be part of the solution yourself?
It’s your chance to show how innovative you can be! Use your practical nursing experience to consult on new technology applications, or to help build or evaluate data and information retrieval systems, for patient records for example.
Does that sound too abstract or ambitious? Informatics nurses also stay closer to day-to-day hospital life by helping employers introduce new electronic health records and medical charting systems, making sure they’re always updated, and educating nurses on how to use them.

That means you’ll first have to educate yourself, of course. The Nurse.org info sheet on nursing informatics notes that “some employers will hire tech-savvy BSN-prepared nurses for informaticist jobs,” but “there is an increasing demand for nurse informaticists to have a Master’s degree in Health Informatics or a related field”.
It might be worth it, though, as The Nerdy Nurse has pointed out: “the Bureau of Labor Statistics projects a 15% increase in demand for information technicians in nursing by the year 2024. Since this is a relatively new and high tech industry, nursing informatics are some of the highest-paid nurses.”
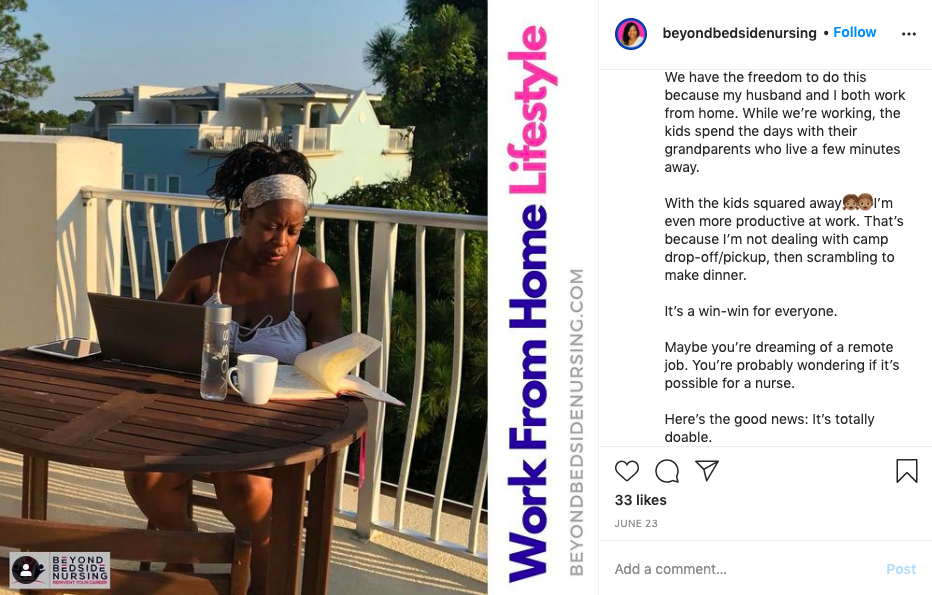
Being a clinical research nurse is another alternative that involves remote work opportunities, and even the office jobs involved get you home more often than hospital work! “I’m in research,” a nurse on Reddit’s Nursing forum explained, and “I’m home every evening for dinner, no call/weekends/nights, work from home when I’m not seeing patients, and I feel great, well rested, and happy”.
Writing data analysis manuscripts and study protocols is “fascinating and mentally stimulating” work, the nurse added. Because that’s the kind of work a clinical research associate does: whenever a new drug, treatment or medical device goes through clinical trials and testing, research nurses monitor the studies, analyzing and writing up their progress and findings. They ensure regulatory and study protocol compliance, make sure all important patient information is recorded correctly, and recruit and screen patients for clinical trials.
If bedside isn’t your cup of tea, just know there’s great jobs available out there. You just have to hunt and wait.
Peering over documents is as far removed from everyday hospital care as you can imagine, but that is kind of the point! As a fellow research nurse interjected, “I only go into the office 1-2 days a week… I am SO much less stressed these days, and I’m making more than I was in the ED.” Like they said, “if bedside isn’t your cup of tea, just know there’s great jobs available out there. You just have to hunt and wait.”

Alisia McIntyre had another suggestion. “Perhaps you can be a legal nurse consultant .” Not just is this another job that an experienced Registered Nurse can do from home as self-employed, independent contractor, legal nurse consulting is a handsomely paid specialty as well!
Take the legal department of an insurance company, for example. When they investigate a personal injury claim — or worse, a case that involves accusations of medical malpractice or wrongful death — they won’t be able to get by on their legal expertise alone. They will need advice from people with medical expertise and hands-on healthcare experience!
That’s where legal nurse consultants come in. They identify, interpret, organize and summarize the relevant medical records. They assess the damages and injuries being claimed and the costs of future care, review hospital policies, and interview clients, witnesses and experts. They search for relevant literature and make sure it’s reflected correctly, and screen incoming cases for merit. They review and summarize depositions, and even testify in court as expert witnesses themselves.
But it’s not just insurance companies that need them. There is work for legal nurse consultants in “law firms, government agencies,… patient safety organizations, business and industry legal departments, healthcare facilities and forensic laboratories” too! Your work might involve regulatory compliance, product liability, worker’s compensation, even criminal cases involving assault or abuse.
To become a legal nurse consultant (LNC), you first need to be a RN with extensive experience, and then work on your legal knowledge. Start with a nurse consulting training program and if possible, follow-up with an internship or by attending in legal seminars. To be the perfect candidate, enhance your reputation by getting certified as LNCC by the American Legal Nurse Consultant Certification Board. You can get your first job before working through all those steps, but as with many of these jobs that allow for working from home, the longer ahead you plan, the easier it is to realize your dream!
Not all nurse consultants are in the legal field! There are definitely other niche specialties for nurse consultants that are a world away from bedside nursing.
Companies which provide genetic testing, for example, employ genetics nurse consultants to communicate the test results to their customers in language they can understand. Businesses planning to launch new products aimed at nurses need an insider’s recommendations. Some occupational health nurses work as consultants.
There are creative nurse consultants too. One might even end up advising a film or documentary maker on how the profession is portrayed! And a lucky few who prefer to really delve into the details can find work as medical script nurses , making sure the medical plots devised by TV and film writers don’t stray too far from reality..
Have you seen @carolynjdocs documentary, @defining__hope it's "about eight patients with life-threatening illnesses weighing what matters most at the fragile junctures in life." worked as a nurse consultant on it. — Barbara Glickstein (@BGlickstein) January 12, 2019
If you are creative and have an eye for business opportunities, you could run a side hustle as nurse entrepreneur . If you’re successful enough, it might even become your next profession! We interviewed a former pediatric nurse, Melissa Gersin, who invented a baby-soothing mat and made that “Tranquilo Mat” her business !
If you are a skilled writer to boot and never short of ideas, being a nurse blogger nowadays is basically a subset of this category. Honestly, we are grateful for the old-school nurse blogs where people simply spend a few hours of their spare time to share moving, funny or interesting stories and practical advice and insights. But the best known bloggers these days are basically nursepreneurs in their own right , using their blog as gateway to more financially lucrative opportunities.
It’s definitely not the easy money it may seem at first blush — just sprinkling your posts with affiliate links won’t get you more than pocket money. If you look at the most famous nurse bloggers, they are excellent communicators in a broader sense, deploying their skill as writers to attract invitations as speakers and coaches , appearing at conferences, workshops and training sessions. Online, their blogs pull in curious readers, but it’s the more in-depth resources they provide — the training materials, educational videos or toolkits for nursing students — that bring in revenue.
As a nurse entrepreneur, when asked what I do, I say, “I am a self-employed registered nurse who spends her time speaking and writing. You might say I heal with words." ~Donna Cardillo #nurseentrepreneur #speaking #writing #healing #nurse #TheInspirationNurse #selfemployed pic.twitter.com/HZsBtdZCh3 — Donna Cardillo (@DonnaCardilloRN) March 20, 2019
Would you rather really just stick to writing? There’s no need to start your own blog to be a freelance nurse writer . Medical journals and magazines commission articles from writers with in-depth knowledge of medical terminology. You don’t necessarily have to start at that level either, though! Think of how many healthcare businesses are out there, how many nursing schools. They all have websites, and they all require new content every day!
Many home health jobs can’t be done from your own home, but there are advantages to visiting patients at their homes instead of working in a hospital — and some of the work has now moved at least partly online.
“It doesn’t require being on your feet all day,” wrote Gayle Colleen in our Facebook comments. “I do pediatric home care, you have one patient and get to sit some,” Shawna Tyo added, heartily endorsed by Alexia Carlson: ”That’s what I do. I love my job!”
A nurse in Reddit’s nursing community recounted his experience doing home medicare wellness visits . Doing those as a job already had numerous advantages over working in a hospital before, he argued, and now the switch to doing these check-ins virtually provides even more freedom. “I’ve never worked in a hospital and never have any desire too. I do telehealth and medicare annual wellness visits. I choose my own hours, .. wear literal pajamas and make $34 an hour. Prior to covid I did the same but visits at homes. In — do the assessment, get BP, temp, 02 sat — out. Get to meet folks, cats and dogs. No coworker drama. Lazy nurse? Maybe, but my back’s fine. I love my job and I got money in the bank.”
Remote nursing is in your grasp: plan for the future
In short, it’s not quite as simple as just checking a box in our search fields to say ‘only jobs from home’ — like all major life or career changes, switching to a remote nursing involves thinking through choices and achieving your plan step by step. Know your options, identify networking opportunities, ask questions. But if you find yourself unable to grapple with the challenges of bedside nursing anymore, there are definite possibilities to put your nursing expertise to good use in alternative careers!
Cancel reply
Your email address will not be published. Required fields are marked *
Let us know what you have to say:
Save my name, email, and website in this browser for the next time I comment.
24 comments
Zulyamn Yanira Ruiz-Ortiz
IM LABOR NURSE FOR 25 YEARS I HAVE IN JAN 2020 INJURY IN MY BACK.NECK AND RIGHT ARM. I CAN’T WORK IN MY SAME JOB BUT I CAN WORK FROM HOME BY COMPUTER.
Wanda Faye Pitts Brown
This article was extremely helpful. I am a handicapped nurse. I was injured in a car accident after I became a nurse. I tried a few other fields but have decided to try coding. I have taken the course and am preparing to be certified but I have no clue where to look for a job. I have not worked in 10 years. It took that long for me to recover from the accident. This article helped me decide what I should do next.
That is wonderful to hear — I’m glad we were able to help you determine your next move!
Cynthia Coutinho
I am a nurse of 35 years practice. I believe I have many qualifications that suit these positions. Do you have listing for job postings in these fields? Do you match jobs to applicants?
Dear Cynthia, NurseRecruiter.com is a specialized nursing jobs board where nurses can look for jobs and employers and recruiters can post new positions. So the process of matching jobs to applicants takes place online.
Nurses who are registered on our site can search for open positions that are specifically relevant to their experience, qualifications and area, and employers can reach out to nurses who are registered here when they think their skill sets match the open position. Well, if you are registered on the site already you may be familiar with the process!
We have to be honest: work-from-home positions are relatively rare among the job opportunities that are posted here. We tried to stress in the blog post that finding such positions should be treated as a matter of strategic planning — it’s unfortunately not as straightforward as finding an on-site position.
Still, especially recently, employers have been posting remote/WFH positions on our site a little more often. For example in the case management / utilization review category or, more rarely, in nursing education or telephone triage .
So while finding a remote position will take more than simply being registered here, it can be useful to check back in here regularly. On our side, we are studying the possibility of flagging remote/WFH positions specifically, to ease the process of finding them.
Akilah McRoy
I work for a school district (I have 6 schools ) Tk-high school. What I found during this time while there are no students in school is that the data entry for entering and updating student records is SEVERELY behind. Some data not entered for years (immunizations, care plans, vision and hearing results ect…). There has to be other districts with the same issue. Would love to have a job like this helping other schools.
Twana Phillips
Send me more info please.
I am so thankful for email…I am so burned out from working with organizations where the staff is running the business, no leadership, no support to help move forward, leaders that tell you, I did not sign on the deal with the issues of the department. I so want to work hard from home and make a difference.
Melinda Hamrick
I’m interested in learning more. I’ve been a nurse for 24 1/2 years.
I’ve been an LPN for over 25 years. Are any of these opportunities available for us? After doing this for so long and getting older, I have ailments of my own particularly my knees that are really starting to take a toll on me physically.
Here I am after 45 years of nursing….and I’m still not ready to retire completely….I want to work 1-2 days a week….and still be part of the healthcare system….crazy girl am I…
Sharon Barton
I am definitely interested!
Catherine Autry
I would love to work from home.
Diane Derry
I would be greatly interested in working from home. I have been looking for something full time with health benefits. Please keep me informed of the opportunities .
Are there any simple data entry type jobs at home for LPNs?
Beatrice Cimei
I am an LPN in Oklahoma I had a stroke that prevents me from driving so working from home would be what I need to do what job would I apply for?
Merredith Brawley
30 years in medicine, most of it in the OR. I tried a career other than OR and found poor training, extreme politics, cliques, and no time for the patients–only the command to move faster. Surely there is something where you can spend time doing nursing.
Angela Miller
I have experience in MS, tele, PT, OT, SLP, and am much interested in a remote work from home position! Ive been told one of my greatest assets is my compassion. I would love to hear about opportunities. I live near Cincy, OH
How to I apply for remote nursing job? I filled out the application but not see this option to choose.
I am Oncology Nurse and I have OSTOEOARTHRITIS and the right hip pain so severe that affects when I work for 8 hours standing. I like to work form home, nu I ahve no experiences those above mentioned carreer, I need help.
correction: my right hipe……. ” I have no experiences above mentioned career”
Nzeakor, Josephine Uchechukwu.
I love your explanations. They are quite comprehensible. I am a registered Nurse/Midwife of more than 25years of experience and also a health-educator. I’ll like to work from home as a Triage Nurse. That is on part time basis. Thank you.
Leslie Whitmarsh
I have Rheumatoid Arthritis and have had a couple really rough years learning my body does not handle the hours of office or hospital nursing. I am still so passionate about my profession and would like to work from home to be able to stay in my profession.
I am looking for RN utilization review work at home. I have been a nurse for over 40 years.. not quite ready to retire.. however need to be at home.. less stress. I have been in management my entire career. 33 years as Director of Neurosurgery in a hospital. Currently Director of nursing in LTC.. been there for 5 years. I am looking fo assistance in obtaining a remote job. I hold an MSN in nursing
Recent Posts
- This is where nurse wages are highest — and where your RN salary is worth the most!
- Get nurses to swipe right on your job: how to double your results
- When nurses strike — again! What can you expect when you go on strike? Or take a strike nursing job?
- What’s the best travel nursing destination in Pennsylvania, and why is it Pittsburgh?
- “It’s just crazy — every nurse takes the NCLEX, we should be able to work anywhere in the US and not pay extra”
- Newsletters
- Nurse Employers
- Nurse Marketing
- Nursing Jobs
- Nursing News
- Nursing Stories
- Per Diem Nursing
- Scholarship
- Sponsored Content
- Travel Nursing
- Department of Health and Human Services
- National Institutes of Health
Nursing at the NIH Clinical Center
Clinical research nurse roles.
Medical Support Assistant: The Medical Support Assistant (MSA) performs administrative duties to support the medical staff, nursing staff and patients, as well as other Clinical Center Departments and Institutes. They are responsible for coordinating and organizing patients' administrative and clerical information utilizing the hospital information systems. They facilitate patient visits, coordinate administrative work, and serve as the focal point for communications within the clinic/unit.
Program Support Assistant: The Program Support Assistant (PSA) provides direct administrative, procedural, and informational resource assistance and support to program staff and/or managers by organizing, collecting, analyzing, and presenting information related to the current and future program/project workload. Assists with the coordination of program workflow and the coordination of various duties assigned to program staff.
Program Specialist: The Program Specialist (PS) supports the administrative functions of the operations of the area assigned including financial management, procurement, quality assurance, management analysis and timekeeping. They participate with senior specialists in the coordination, preparation, and analysis of a wide variety of reports.
Staff Assistant: The Staff Assistant directs and implements administrative functions for the assigned office. Keeps the supervisor fully informed of current conditions throughout the department and takes appropriate action to ensure that administrative activities are properly implemented to support its mission. Maintains liaison and coordination between the department and other offices in the Clinical Center and the NIH. Establishes and implements standards for the efficient operation of the office and coordinates with other staff within the office and department, ensuring that administrative and clerical functions result in smooth operations.
Health Technician, Phlebotomist: The Health Technician Phlebotomist provides clinical care and supports biomedical research under the supervision of a licensed nurse. The incumbent supports a team that provides collection of blood and blood components from donors/patients by either collection of a unit of whole blood or blood components utilizing apheresis. The incumbent performs venipuncture on donors/patients within the Blood Services Section for allogeneic use or for in vitro studies carried out by the various Institutes at the NIH.
Health Technician, Surgical: Provides technical support and patient care support for both major and minor surgical procedures. These duties include assistance with positioning the patient and surgical prep. Patient care also involves the transport of patients to and from the surgical suite, as well as assisting staff during surgical procedures as directed.
Medical Instrument Technician (Surgical): The Medical Instrument Technician (Surgical) assists with surgeries under the supervision of surgeons, registered nurses, or other surgical personnel. They help set up the operating room, prepare and transport patients for surgery, adjust lights and equipment, pass instruments and other supplies to surgeons and surgeon's assistants, hold retractors, and help count sponges, needles, supplies, and instruments.
Patient Care Technician: The Patient Care Technician supports the activities of the professional nurse by independently providing patient care functions to assigned patients while maintaining a safe environment.
Behavioral Health Technician: The Behavioral Health Technician supports the activities of the professional nurse by independently providing patient care functions to assigned behavioral health patients while maintaining a safe and therapeutic environment.
Healthcare Simulator Technician: The Healthcare Simulator Technician assists the Simulation Program Coordinator/Nurse Coordinator by providing simulation operational expertise and clerical support for the NIH Clinical Center Simulation Program.
Diagnostic Radiologic Technologist (Interventional Radiology): The Diagnostic Radiologic Technologist in Interventional Radiology (IR) is trained in radiographic imaging guided procedures and has the professional skills/expertise required to integrate interventional procedures/exams into overall clinical management. This position is a key part of the IR team performing procedures/exams on patients and actively participates in the design, implementation and evaluation of new imaging methods and techniques utilized in this area.
Lead Diagnostic Radiology Technician: The Lead Diagnostic Radiology Technician functions as the team leader for the team of diagnostic radiology technicians performing interventional radiology services. As the team leader they utilize a variety of coordinating, coaching, facilitating, consensus-building, and planning techniques.
Program Manager for Sterile Processing Service: The Program Manager for the Sterile Processing Service manages the Sterile Processing Service which is the central point that all contaminated supplies, equipment, and materials are sent after use. It includes sterile and non-sterile storage, and centralized decontamination, high-level disinfection, and sterilization. It supplies equipment to the operating rooms, laboratories, inpatient areas and specialty clinics, and dispatch areas for distribution to approximately 60 supply issue points throughout the NIH Clinical Center complex.
Lead Medical Supply Technician (Sterile Processing): The Lead Medical Supply Technician for Sterile Processing functions as the team leader for the team of medical supply technicians (sterile processing) on an assigned shift and personally performs the work of medical supply technicians (sterile processing). As the team leader, they utilize a variety of coordinating, coaching, facilitating, consensus-building, and planning techniques.
Medical Supply Technicians (Sterile Processing): The Medical Supply Technician is responsible for the decontamination, packaging, sterilization, high level disinfection and distribution of medical/surgical instruments and equipment in the Clinical Center.
Clinical Research Nurse 1: The Clinical Research Nurse (CRN) 1 has a nursing degree from a professional nursing program approved by the legally designated state accrediting agency. The CRN 1 is a newly graduated registered nurse with one year or less of clinical nursing experience. The incumbent functions under the direction of an experienced nurse to provide patient care, while using professional judgment and sound decision making.
Clinical Research Nurse 2: The Clinical Research Nurse (CRN) 2 has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency and has practiced nursing for at least one year. This nurse independently provides nursing care; identifies and communicates the impact of the research process on patient care; adjusts interventions based on findings; and reports issues/variances promptly to the research team. The CRN 2 administers research interventions; collects patient data according to protocol specifications; evaluates the patient response to therapy; and integrates evidence-based practice into nursing practice. The CRN 2 contributes to teams, workgroups and the nursing shared governance process. New skills and knowledge are acquired that are based on self-assessment, feedback from peers and supervisors, and changing clinical practice requirements.
Clinical Research Nurse 3: The Clinical Research Nurse (CRN) 3 has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency at the time the program was completed by the applicant. The CRN 3 has practiced nursing for at least two years. The role spans the professional nursing development from “fully competent” to “expert” nursing practice. The CRN 3 provides care to acute and complex patient populations and utilizes appropriate professional judgment and critical decision making in planning and providing care. They master all nursing skills and associated technology for a particular Program of Care and assists in assessing the competency of less experienced nurses. The CRN 3 participates in the planning of new protocol implementation on the patient care unit; administers research interventions; collects patient data according to protocol specifications; evaluates the patient’ response to therapy; responds to variances in protocol implementation; reports variances to the research team; integrates evidence-based practice into nursing practice; and evaluates patient outcomes. The CRN 3 assumes the charge nurse and preceptor roles as assigned. Formal and informal feedback is provided by the CRN 3 to peers and colleagues in support of individual growth and improvement of the work environment.
Clinical Research Nurse 4: The Clinical Research Nurse (CRN) 4 has a nursing degree or diploma from a professional nursing program approved by the legally designated state accrediting agency at the time the program was completed by the applicant. The CRN 4 is a clinical expert and leader in all aspects of nursing practice. They demonstrate expertise in the nursing process; professional judgment and decision making; planning and providing nursing care; and knowledge of the biomedical research process. The CRN 4 utilizes basic leadership principles and has an ongoing process of questioning and evaluating nursing practice.
Supplemental Nurse/Float Pool/Per Diem: Supplemental Staff are Temporary Intermittent RN positions within the Nursing Department that are assigned to either a Central Pool or are Unit Based. Central Pool Supplemental staff work out of the Office of Staffing and Workforce Planning, select their schedule based on the available needs of the house and are assigned as needed to different units. Unit Based Supplemental staff are assigned to a unit and select their schedule to meet the unit’s needs. If not needed on the unit for their scheduled shift, they can be floated like any other member of the unit nursing staff. Float to all units as assigned within their competency skill set as needed.
Clinical Manager/Team Lead: The Clinical Manager (CM)/Team Lead is an experienced staff nurse who supports the Nurse Manager and other departmental leadership with operations and leadership of a patient care area(s). This position functions as a team leader and it utilizes a variety of coordinating, coaching, facilitating, consensus-building, and planning techniques to lead a team of Clinical Research Nurses and paraprofessionals. They provide patient care, as well as support protocol implementation, data collection and human subject protection.
Clinical Educator: The Clinical Educator (CE) is an experienced staff nurse who provides direct patient care and collaborates with the Nurse Manager and other departmental leadership to oversee educational needs of unit staff. The CE develops/coordinates/evaluates orientation for new unit staff, trains/mentor’s unit preceptors, serves as a liaison/resource for departmental/Clinical Center/professional educational opportunities, identifies educational needs, coordinates unit in-services, and plans unit educational days. The CE designs, implements and evaluates learning experiences for all staff levels to acquire, maintain, or increase their knowledge and competence. The Clinical Educator teaches at the unit and departmental level.
Safety & Quality Nurse: The Safety and Quality Nurse provides direct patient care and coordinates, oversees and evaluates the quality improvement and patient safety initiatives at the unit or program of care level. They collaborate with the nurse manager and department leaders on improvement activities related to promoting patient safety, clinical quality and reducing risk. They develop and maintains proficiency in effective use and interpretation of data to drive quality improvement activities on the unit or program of care level.
Program Director : The Program Director serves as the supervisor of a group of expert advisors for a specific area of nursing expertise (education, recruitment & outreach, safety & quality, staffing & workforce planning). The incumbent coordinates, implements, and oversees all the operations of the program they oversee. They serve as the liaison to other Clinical Center departments and the ICs for issues related area of expertise and assigned responsibility and to provide communication and consultative services to all credentialed nurses at the Clinical Center.
Nurse Manager : The Nurse Manager has 3 to 5 years of recent management experience; advanced preparation (Masters degree) is preferred. The Nurse Manager has experience in change management, creative leadership, and program development; an demonstrates strong communication and collaboration skills to foster an effective partnership with institute personnel. The Nurse Manager demonstrates a high level of knowledge in a particular specialty practice area and utilizes advanced leadership skills to meet organization goals.
Clinical Nurse Specialist : The Clinical Nurse Specialist (CNS) has a Masters or Doctorate Degree in Nursing from a state-approved school of nursing accredited by either the National League for Nursing Accrediting Commission (NLNAC) or the Commission on Collegiate Nursing Education (CCNE) with a major in the clinical nursing specialty to which the nurse is assigned. The CNS has a minimum of 5 years’ experience, is certified in a specialty area, and is accountable for a specific patient population within a specialized program of care.
Nurse Educators : The Nurse Educator plans, directs, executes, and evaluates a broad program of nursing professional and educational activities directed toward professional development of nursing and support staff. Designs, implements and evaluates learning experiences for all staff levels to acquire, maintain, or increase their knowledge and competence. Collaborates in the design and implementation of learning needs assessment tools for unit and specific programs of care.
Nurse Consultant: The Nurse Consultant serves as an expert advisor with responsibility for managing a broad array of administrative projects and providing clinical consultative support for a Clinical Center Nursing Department Service or program. The Nurse Consultant leads, or directs projects related to clinical research nursing, staffing, budgeting, policy, safety, and human resources.
Nurse Scientist: The Nurse Scientist is a nurse with advanced preparation (PhD or doctorate in nursing or related field) in research principles and methodology, who also has expert content knowledge in a specific clinical area. The primary focus of the role is to (1) provide leadership in the development, coordination and management of clinical research studies; (2) provide mentorship for nurses in research; (3) lead evaluation activities that improve outcomes for patients participating in research studies at the Clinical Center; and (4) contribute to the overall health sciences literature. The incumbent is expected to develop a portfolio of independent research that provides the vehicle for achieving these primary objectives.
NOTE: PDF documents require the free Adobe Reader .
This page last updated on 05/24/2024
You are now leaving the NIH Clinical Center website.
This external link is provided for your convenience to offer additional information. The NIH Clinical Center is not responsible for the availability, content or accuracy of this external site.
The NIH Clinical Center does not endorse, authorize or guarantee the sponsors, information, products or services described or offered at this external site. You will be subject to the destination site’s privacy policy if you follow this link.
More information about the NIH Clinical Center Privacy and Disclaimer policy is available at https://www.cc.nih.gov/disclaimers.html

An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Research Initiatives
- Meet Our Researchers
- Meet Our Program Officers
- RESEARCH LENSES
- Health Equity
- Social Determinants of Health
- Population and Community Health
- Prevention and Health Promotion
- Systems and Models of Care
- Funding Opportunities
- Small Business Funding
- Grant Applicant Resources
- Training Grants
- Featured Research
- Strategic Plan
- Budget and Legislation
- Connect With Us
- Jobs at NINR

Advancing health equity into the future.
NINR's mission is to lead nursing research to solve pressing health challenges and inform practice and policy – optimizing health and advancing health equity into the future.

Funding Opportunities Newsletter
Subscribe to receive the latest funding opportunities and updates from NINR.

Funding opportunities that improve health outcomes
NINR believes that nursing research is the key to unlocking the power and potential of nursing. NINR offers grants to individuals at all points in their career, from early investigators to established scientists. NINR grants also support small businesses and research centers.
Research Funding

Small Business

Training Funding
Homepage events stories, addressing public health challenges through research.
NINR-supported researchers explore and address some of the most important challenges affecting the health of the American people. Learn about accomplishments from the community of NINR-supported scientists across the United States.

Advancing social determinants of health research at NIH
Over 20 NIH Institutes, Centers, and Offices are working collaboratively to accelerate NIH-wide SDOH research across diseases and conditions, populations, stages of the life course, and SDOH domains.
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Infection Prevention and Long-term Care Facility Residents
- Nursing Home Infection Preventionist Training
- PPE in Nursing Homes
- Respiratory Virus Toolkit
- Healthcare-Associated Infections (HAIs)
- The resources on this page can keep you and your loved ones safe.
Long-term care facilities provide many services, both medical and personal care, to people who are unable to live without help.
If you live in a nursing home, assisted living facility or other long-term care facility, you have a higher risk of getting an infection. There are steps you can take to reduce your risk:
- Tell your healthcare provider if you think you have an infection or if your infection is getting worse.
- Take antibiotics exactly as prescribed and tell your healthcare provider if you have any side effects, such as diarrhea.
- Keep your hands clean. Remind staff and visitors to keep their hands clean.
- Get vaccinated against flu and other infections to avoid complications.
Resources for staying safe in long-term care facilities

About C. diff
About Carbapenem-resistant Enterobacterales
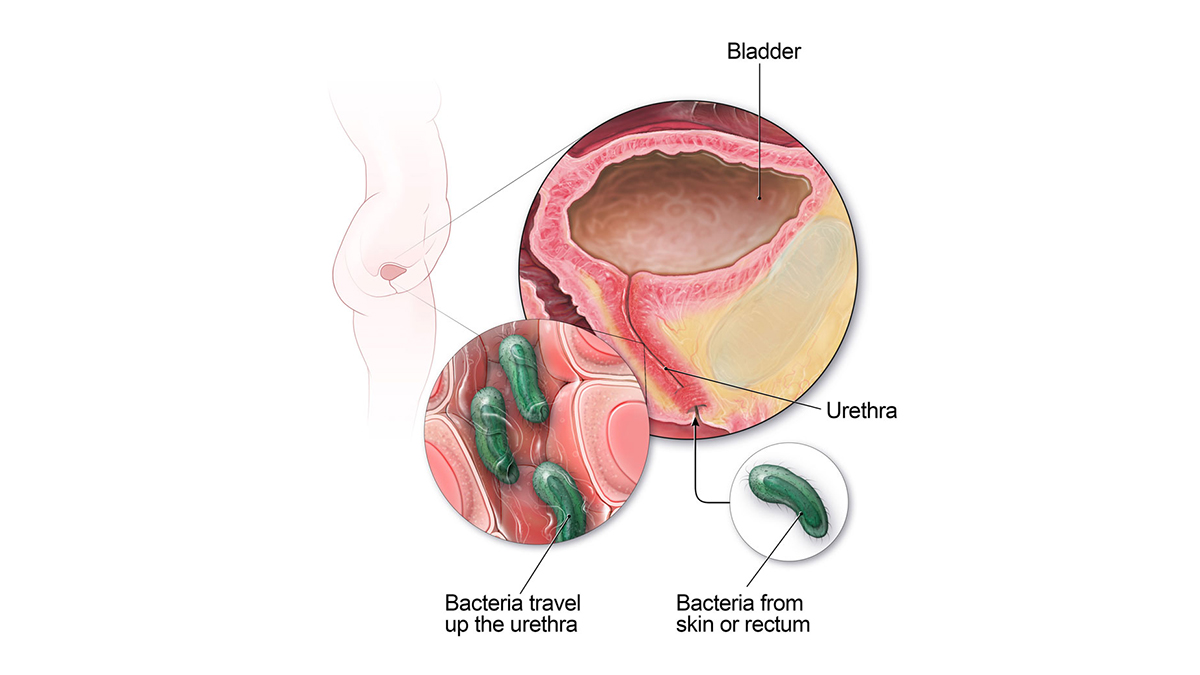
Catheter-associated Urinary Tract Infection Basics
Methicillin-resistant Staphylococcus aureus (MRSA) Basics

Healthy Habits: Antibiotic Do's and Don'ts

About Sepsis

About Norovirus
Resources for family members and caregivers
- Medicare resources for long-term care residents and caregivers.
- Find a nursing home in your area .
This website provides resources for patients, families and caregivers on the prevention of infections in nursing homes and assisted living facilities.
For Everyone
Health care providers.
An official website of the United States government
Here's how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
CMS Newsroom
Search cms.gov.
- Physician Fee Schedule
- Local Coverage Determination
- Medically Unlikely Edits

Home - Centers for Medicare & Medicaid Services
What are you looking for today, search results.

Inflation Reduction Act
Medicaid renewals, innovation center, no surprise billing.
- Nursing home resources
This law helps save money for people with Medicare, improves access to affordable treatments, and strengthens the Medicare program.
As states resume normal operations, we’re working to make sure people stay covered.
We support the development and testing of innovative health care payment and service delivery models.
See how new rules help protect people from surprise medical bills and remove consumers from payment disputes between a provider or health care facility and their health plan.
Nursing Home Resources
Get the latest policy information and learn about initiatives to enable safe and quality care in nursing homes.

Strategic Plan Overview
CMS serves the public as a trusted partner and steward, dedicated to advancing health equity, expanding coverage, and improving health outcomes.
Advance Equity
Advance health equity by addressing the health disparities that underlie our health system
Expand Access
Build on the Affordable Care Act and expand access to quality, affordable health coverage and care
Engage Partners
Engage our partners and the communities we serve throughout the policymaking and implementation process
Drive Innovation
Drive Innovation to tackle our health system challenges and promote value-based, person-centered care.
Protect Program
Protect our programs' sustainability for future generations by serving as a responsible steward of public funds
Foster Excellence
Foster a positive and inclusive workplace and workforce, and promote excellence in all aspects of CMS's operations
Top resources
Medicare fee schedules.
Check the fee schedules to find billing codes.
- Physician fee schedule lookup tool
- Physician fee schedule
- Clinical Laboratory Fee Schedule
- Durable Medical Equipment Fee Schedule
- Ambulatory Surgical Center (ASC) Payment
Codes for claim reimbursement
Find codes to be reimbursed for clinical services.
- Medicare Coverage Database
- List of CPT/HCPCS codes
- 2023 ICD-10 Procedure Coding System
- 2023 ICD-10-CM
- National correct coding initiative edits
- Place of service code set
Marketplace partner resources
Get helpful materials for agents, brokers, and partners.
- Marketplace registration and training
- Resources for Agents and Brokers in the Health Insurance Marketplaces
- Agent and Broker FAQ’s
- Information on Essential Health Benefits (EHB) Benchmark Plans
- 2023 Projected Health Insurance Exchange Coverage Maps
Manuals, forms, & transmittals
Find current resources to complete your tasks.
- CMS Forms list
- Internet Only Manuals
- Transmittals
- Become a medicare provider or supplier
- National Provider Identifier (NPI) application/update form
Privacy incident
May 2023 Medicare Privacy Incident
Learn more
Recent Articles
- 21 May Press Releases 05/21/2024 Biden-Harris Administration Launches New Option to Report Potential Violations of Federal Law and Continue to Promote Patient Access to Stabilizing Emergency Care
- 15 May Press Releases 05/15/2024 CMS Statement on Misclassification of Drugs, Program Administration and Program Integrity Updates Under the Medicaid Drug Rebate Program (MDRP) Proposed Rule (CMS-2434-P)
- 08 May Press Releases 05/08/2024 Biden-Harris Administration Acts to Improve Access to Kidney Transplants
- 06 May Press Releases 05/06/2024 CMS Statement on Agent and Broker Marketplace Activity, Update
- 03 May Press Releases 05/03/2024 Biden-Harris Administration Finalizes Policies to Increase Access to Health Coverage for DACA Recipients
- 03 May Fact Sheets 05/03/2024 HHS Final Rule Clarifying the Eligibility of Deferred Action for Childhood Arrivals (DACA) Recipients and Certain Other Noncitizens

Medicare.gov
Information for people over 65, and younger people with a disability, who want to sign up for Medicare.
InsureKidsNow.gov
Information for children up to the age of 19 who need health care or a local dental provider.
Healthcare.gov
Information for people who need health insurance and want to apply or enroll in the Marketplace or Medicaid.
Medicaid.gov
Information about the program and policy details of Medicaid and the Children's Health Insurance Program.
Thanks for starting your application to {{companyName}}.
To complete your application you must do one of the following:
Forward an email from your mobile device with your resume attached to {{fromEmail}}
Reply to this email from your laptop or desktop computer with your resume attached.
Thank you for your interest, The Recruiting Team
Reply to this email from your laptop or desktop computer with your cover letter attached.
Dear ${user.firstName},
Thanks for choosing to apply for a job with ${client.display.name}! Please verify ownership of your email address by clicking this link .
Alternatively, you can verify your account by pasting this URL into your browser: ${page.url}?id=${user.id}&ptoken=${user.token}
Please note that your job application will not be submitted to ${client.display.name} until you have successfully verified ownership of your email address.
The ${client.display.name} Recruiting Team
Nice to meet you. 👋
Lets quickly set up your profile
to start having tailored recommendations.
In order to create an account with us and submit applications for positions with our company you must read the following Terms and Agreements and select to agree before registering.
In the event that you do not accept our Terms and Agreements you will not be able to submit applications for positions with our company.
You agree to the storage of all personal information, applications, attachments and draft applications within our system. Your personal and application data and any attached text or documentation are retained by Sequoia Apply in accordance with our record retention policy and applicable laws.
You agree that all personal information, applications, attachments and draft applications created by you may be used by us for our recruitment purposes, including for automated job matching. It is specifically agreed that we will make use of all personal information, applications, attachments and draft applications for recruitment purposes only and will not make this information available to any third party unconnected with the our recruitment processes.
Your registration and access to our Careers Web Site indicates your acceptance of these Terms and Agreements.
This career site protects your privacy by adhering to the European Union General Data Protection Regulation (GDPR). We will not use your data for any purpose to which you do not consent.
We store anonymized interaction data in an aggregated form about visitors and their experiences on our site using cookies and tracking mechanisms. We use this data to fix site defects and improve the general user experience.
We request use of your data for the following purposes:
Job Application Data
This site may collect sensitive personal information as a necessary part of a job application. The data is collected to support one or more job applications, or to match you to future job opportunities. This data is stored and retained for a default period of 12 months to support job matching or improve the user experience for additional job applications. The data for each application is transferred to the Applicant Tracking System in order to move the application through the hiring process. \nYou have the right to view, update, delete, export, or restrict further processing of your job application data. To exercise these rights, you can e-mail us at [email protected] . \nConversion Tracking \nWe store anonymized data on redirects to the career site that is used to measure the effectiveness of other vendors in sourcing job candidates.
Consent and Data Privacy
This application protects your privacy by adhering to the European Union General Data Protection Regulation (GDPR). Jibe will not use your data for any purpose to which you do not consent.\n
We request use of your data for the following purposes:\n \n User Authentication \n
\n This site retains personally identifiable information, specifically e-mail addresses, as a necessary part of user login. This data is retained for the duration of the user profile lifecycle and enables user authentication.\n
\n \n Usage Analytics \n
We store anonymized usage data to measure and improve the effectiveness of this CRM application in filling job requisitions and managing talent communities.\n
\n \n E-mails to Candidates \n
We collect your personal information such as name and email address. This information is used when you send marketing or contact emails to candidates.\n\n
Click here for the ‘EEOC Know Your Rights’ Poster
Click here to view the deod 310 equal opportunity poster(ny.gov).
Enter your email address to continue. You'll be asked to either log in or create a new account.
There was an error verifying your account. Please click here to return home and try again.
You are about to enter an assessment system which is proprietary software developed and produced by Kenexa Technology, Inc. The content in this questionnaire has been developed by Kenexa Technology, Inc., Kenexa’s Suppliers and/or Yum Restaurant Services Group, Inc.’s (“Company”) third party content providers and is protected by International Copyright Law. Under no condition may the content be copied, transmitted, reproduced or reconstructed, in whole or in part, in any form whatsoever, without express written consent by Kenexa Technology, Inc. or the applicable third party content provider. Under no circumstances will Kenexa Technology, Inc. be responsible for content created or provided by Company’s third party content providers.
IN NO EVENT SHALL KENEXA, AN IBM COMPANY, KENEXA’S SUPPLIERS OR THE COMPANY’S THIRD PARTY CONTENT PROVIDERS, BE LIABLE FOR ANY DAMANGES WHATSOEVER INCLUDING, WITHOUT LIMITATION, DAMAGES FOR LOSS OF VOCATIONAL OPPORTUNITY ARISING OUT OF THE USE OF, THE PERFORMANCE OF, OR THE INABILITY TO USE THIS KENEXA ASSESSMENT SYSTEM OR THE CONTENT, REGARDLESS OF WHETHER OR NOT THEY HAVE BEEN ADVISED ABOUT THE POSSIBILITY OF SUCH DAMAGES.
By clicking below, you are also confirming your identity for purposes of the questionnaire. You may not receive assistance, refer to any written material, or use a calculator (or similar device) while completing the questionnaire.
Unless otherwise directed by the Questionnaire Administrator, you are only authorized to take each requested questionnaire once. Failure to comply may result in disqualification. All Kenexa SelectorTM questionnaires are monitored.
- ICU Registered Nurse
- Registered Respiratory Therapist
A web browser is a piece of software on your computer. It lets you visit webpages and use web applications.
It's important to have the latest version of a browser. Newer browsers save you time, keep you safer, and let you do more online.
Try a different browser - all are free and easy to install. Visit whatbrowser.org for more information.
If you are using a later version of Internet Explorer, please make sure you are not in compatibility mode of an older version of the browser.

Cookies are used on this site to assist in continually improving the candidate experience and all the interaction data we store of our visitors is anonymous. Learn more about your rights on our Privacy Policy page.
- Open access
- Published: 22 May 2024
Preparedness for a first clinical placement in nursing: a descriptive qualitative study
- Philippa H. M. Marriott 1 ,
- Jennifer M. Weller-Newton 2 nAff3 &
- Katharine J. Reid 4
BMC Nursing volume 23 , Article number: 345 ( 2024 ) Cite this article
174 Accesses
2 Altmetric
Metrics details
A first clinical placement for nursing students is a challenging period involving translation of theoretical knowledge and development of an identity within the healthcare setting; it is often a time of emotional vulnerability. It can be a pivotal moment for ambivalent nursing students to decide whether to continue their professional training. To date, student expectations prior to their first clinical placement have been explored in advance of the experience or gathered following the placement experience. However, there is a significant gap in understanding how nursing students’ perspectives about their first clinical placement might change or remain consistent following their placement experiences. Thus, the study aimed to explore first-year nursing students’ emotional responses towards and perceptions of their preparedness for their first clinical placement and to examine whether initial perceptions remain consistent or change during the placement experience.
The research utilised a pre-post qualitative descriptive design. Six focus groups were undertaken before the first clinical placement (with up to four participants in each group) and follow-up individual interviews ( n = 10) were undertaken towards the end of the first clinical placement with first-year entry-to-practice postgraduate nursing students. Data were analysed thematically.
Three main themes emerged: (1) adjusting and managing a raft of feelings, encapsulating participants’ feelings about learning in a new environment and progressing from academia to clinical practice; (2) sinking or swimming, comprising students’ expectations before their first clinical placement and how these perceptions are altered through their clinical placement experience; and (3) navigating placement, describing relationships between healthcare staff, patients, and peers.
Conclusions
This unique study of first-year postgraduate entry-to-practice nursing students’ perspectives of their first clinical placement adds to the extant knowledge. By examining student experience prior to and during their first clinical placement experience, it is possible to explore the consistency and change in students’ narratives over the course of an impactful experience. Researching the narratives of nursing students embarking on their first clinical placement provides tertiary education institutions with insights into preparing students for this critical experience.
Peer Review reports
First clinical placements enable nursing students to develop their professional identity through initial socialisation, and where successful, first clinical placement experiences can motivate nursing students to persist with their studies [ 1 , 2 , 3 , 4 ]. Where the transition from the tertiary environment to learning in the healthcare workplace is turbulent, it may impact nursing students’ learning, their confidence and potentially increase attrition rates from educational programs [ 2 , 5 , 6 ]. Attrition from preregistration nursing courses is a global concern, with the COVID-19 pandemic further straining the nursing workforce; thus, the supply of nursing professionals is unlikely to meet demand [ 7 ]. The COVID-19 pandemic has also impacted nursing education, with student nurses augmenting the diminishing nursing workforce [ 7 , 8 ].
The first clinical placement often triggers immense anxiety and fear for nursing students [ 9 , 10 ]. Research suggests that among nursing students, anxiety arises from perceived knowledge deficiencies, role ambiguity, the working environment, caring for ‘real’ people, potentially causing harm, exposure to nudity and death, and ‘not fitting in’ [ 2 , 3 , 11 ]. These stressors are reported internationally and often relate to inadequate preparation for entering the clinical environment [ 2 , 10 , 12 ]. Previous research suggests that high anxiety before the first clinical placement can be related to factors likely to affect patient outcomes, such as self-confidence and efficacy [ 13 ]. High anxiety during clinical placement may impair students’ capacity to learn, thus compromising the value of the clinical environment for learning [ 10 ].
The first clinical placement often occurs soon after commencing nursing training and can challenge students’ beliefs, philosophies, and preconceived ideas about nursing. An experience of cultural or ‘reality’ shock often arises when entering the healthcare setting, creating dissonance between reality and expectations [ 6 , 14 ]. These experiences may be exacerbated by tertiary education providers teaching of ‘ideal’ clinical practice [ 2 , 6 ]. The perceived distance between theoretical knowledge and what is expected in a healthcare placement, as opposed to what occurs on clinical placement, has been well documented as the theory-practice gap or an experience of cognitive dissonance [ 2 , 3 ].
Given the pivotal role of the first clinical placement in nursing students’ trajectories to nursing practice, it is important to understand students’ experiences and to explore how the placement experience shapes initial perceptions. Existing research focusses almost entirely either on describing nursing students’ projected emotions and perceptions prior to undertaking a first clinical placement [ 3 ] or examines student perceptions of reflecting on a completed first placement [ 15 ]. We wished to examine consistency and change in student perception of their first clinical placement by tracking their experiences longitudinally. We focused on a first clinical placement undertaken in a Master of Nursing Science. This two-year postgraduate qualification provides entry-to-practice nursing training for students who have completed any undergraduate qualification. The first clinical placement component of the course aimed to orient students to the clinical environment, support students to acquire skills and develop their clinical reasoning through experiential learning with experienced nursing mentors.
This paper makes a significant contribution to understanding how nursing students’ perceptions might develop over time because of their clinical placement experiences. Our research addresses a further gap in the existing literature, by focusing on students completing an accelerated postgraduate two-year entry-to-practice degree open to students with any prior undergraduate degree. Thus, the current research aimed to understand nursing students’ emotional responses and expectations and their perceptions of preparedness before attending their first clinical placement and to contrast these initial perceptions with their end-of-placement perspectives.
Study design
A descriptive qualitative study was undertaken, utilising a pre- and post-design for data collection. Focus groups with first-year postgraduate entry-to-practice nursing students were conducted before the first clinical placement, with individual semi-structured interviews undertaken during the first clinical placement.
Setting and participants
All first-year students enrolled in the two-year Master of Nursing Science program ( n = 190) at a tertiary institution in Melbourne, Australia, were eligible to participate. There were no exclusion criteria. At the time of this study, students were enrolled in a semester-long subject focused on nursing assessment and care. They studied the theoretical underpinnings of nursing and science, theoretical and practical nursing clinical skills and Indigenous health over the first six weeks of the course. Students completed a preclinical assessment as a hurdle before commencing a three-week clinical placement in a hospital setting, a subacute or acute environment. Overall, the clinical placement aimed to provide opportunities for experiential learning, skill acquisition, development of clinical reasoning skills and professional socialisation [ 16 , 17 ].
In total, sixteen students participated voluntarily in a focus group of between 60 and 90 min duration; ten of these students also participated in individual interviews of between 30 and 60 min duration, a number sufficient to reach data saturation. Table 1 shows the questions used in the focus groups conducted before clinical placement commenced and the questions for the semi-structured interview questions conducted during clinical placement. Study participants’ undergraduate qualifications included bachelor’s degrees in science, arts and business. A small number of participants had previous healthcare experience (e.g. as healthcare assistants). The participants attended clinical placement in the Melbourne metropolitan, Victorian regional and rural hospital locations.
Data collection
The study comprised two phases. The first phase comprised six focus groups prior to the first clinical placement, and the second phase comprised ten individual semi-structured interviews towards the end of the first clinical placement. Focus groups (with a maximum of four participants) and individual interviews were conducted by the lead author online via Zoom and were audio-recorded. Capping group size to a relatively small number considered diversity of perceptions and opportunities for participants to share their insights and to confirm or contradict their peers, particularly in the online environment [ 18 , 19 ].
Focus groups and interview questions were developed with reference to relevant literature, piloted with volunteer final-year nursing students, and then verified with the coauthors. All focus groups and interviewees received the same structured questions (Table 1 ) to ensure consistency and to facilitate comparison across the placement experience in the development of themes. Selective probing of interviewees’ responses for clarification to gain in-depth responses was undertaken. Nonverbal cues, impressions, or observations were noted.
The lead author was a registered nurse who had a clinical teaching role within the nursing department and was responsible for coordinating clinical placement experiences. To ensure rigour during the data collection process, the lead author maintained a reflective account, exploring her experiences of the discussions, reflecting on her interactions with participants as a researcher and as a clinical educator, and identifying areas for improvement (for instance allowing participants to tell their stories with fewer prompts). These reflections in conjunction with regular discussion with the other authors throughout the data collection period, aided in identifying any researcher biases, feelings and thoughts that possibly influenced the research [ 20 ].
To maintain rigour during the data analysis phase, we adhered to a systematic process involving input from all authors to code the data and to identify, refine and describe the themes and subthemes reported in this work. This comprehensive analytic process, reported in detail in the following section, was designed to ensure that the findings arising from this research were derived from a rigorous approach to analysing the data.
Data analysis
Focus groups and interviews were transcribed using the online transcription service Otter ( https://otter.ai/ ) and then checked and anonymised by the first author. Preliminary data analysis was carried out simultaneously by the first author using thematic content analysis proposed by Braun and Clarke [ 21 ] using NVivo 12 software [ 22 ]. All three authors undertook a detailed reading of the first three transcripts from both the focus groups and interviews and independently identified major themes. This preliminary coding was used as the basis of a discussion session to identify common themes between authors, to clarify sources of disagreement and to establish guidelines for further coding. Subsequent coding of the complete data set by the lead author identified a total of 533 descriptive codes; no descriptive code was duplicated across the themes. Initially, the descriptive codes were grouped into major themes identified from the literature, but with further analysis, themes emerged that were unique to the current study.
The research team met frequently during data analysis to discuss the initial descriptive codes, to confirm the major themes and subthemes, to revise themes on which there was disagreement and to identify any additional themes. Samples of quotes were reviewed by the second and third authors to decide whether these quotes were representative of the identified themes. The process occurred iteratively to refine the thematic categories, to discuss the definitions of each theme and to identify exemplar quotes.
Ethical considerations
The lead author was a clinical teacher and the clinical placement coordinator in the nursing department at the time of the study. Potential risks of perceived coercion and power imbalances were identified because of the lead author’s dual roles as an academic and as a researcher. To manage these potential risks, an academic staff member who was not part of the research study informed students about the study during a face-to-face lecture and ensured that all participants received a plain language statement identifying the lead author’s role and how perceived conflicts of interest would be managed. These included the lead author not undertaking any teaching or assessment role for the duration of the study and ensuring that placement allocations were completed prior to undertaking recruitment for the study. All students who participated in the study provided informed written consent. No financial or other incentives were offered. Approval to conduct the study was granted by the University of Melbourne Human Research Ethics Committee (Ethics ID 1955997.1).
Three main themes emerged describing students’ feelings and perceptions of their first clinical placement. In presenting the findings, before or during has been assigned to participants’ quotes to clarify the timing of students’ perspectives related to the clinical placement.
Major theme 1: Adjusting and managing a raft of feelings
The first theme encompassed the many positive and negative feelings about work-integrated learning expressed by participants before and during their clinical placement. Positive feelings before clinical placement were expressed by participants who were comfortable with the unknown and cautiously optimistic.
I am ready to just go with the flow, roll with the punches (Participant [P]1 before).
Overwhelmingly, however, the majority of feelings and thoughts anticipating the first clinical placement were negatively oriented. Students who expressed feelings of fear, anxiety, lack of knowledge, lack of preparedness, uncertainty about nursing as a career, or strong concerns about being a burden were all classified as conveying negative feelings. These negative feelings were categorised into four subthemes.
Subtheme 1.1 I don’t have enough knowledge
All participants expressed some concerns and anxiety before their first clinical placement. These encompassed concerns about knowledge inadequacy and were linked to a perception of under preparedness. Participants’ fears related to harming patients, responsibility for managing ‘real’ people, medication administration, and incomplete understanding of the language and communication skills within a healthcare setting. Anxiety for many participants merged with the logistics and management of their life during the clinical placement.
I’m scared that they will assume that I have more knowledge than I do (P3 before). I feel quite similar with P10, especially when she said fear of unknown and fear that she might do something wrong (P9 before).
Subtheme 1.2 Worry about judgment, being seen through that lens
Participants voiced concerns that they would be judged negatively by patients or healthcare staff because they perceived that the student nurse belonged to specific social groups related to their cultural background, ethnicity or gender. Affiliation with these groups contributed to students’ sense of self or identity, with students often describing such groups as a community. Before the clinical placement, participants worried that such judgements would impact the support they received on placement and their ability to deliver patient care.
Some older patients might prefer to have nurses from their own background, their own ethnicity, how they would react to me, or if racism is involved (P10 before). I just don’t want to reinforce like, whatever negative perceptions people might have of that community (P16 before).
Participants’ concerns prior to the first clinical placement about judgement or poor treatment because of patients’ preconceived ideas about specific ethnic groups did not eventuate.
I mean, it didn’t really feel like very much of a thing once I was actually there. It is one of those things you stress about, and it does not really amount to anything (P16 during).
Some students’ placement experiences revealed the positive benefits of their cultural background to enhancing patient care. One student affirmed that the placement experience reinforced their commitment to nursing and that this was related to their ability to communicate with patients whose first language was not English.
Yeah, definitely. Like, I can speak a few dialects. You know, I can actually see a difference with a lot of the non-English speaking background people. As soon as you, as soon as they’re aware that you’re trying and you’re trying to speak your language, they, they just open up. Yeah, yes. And it improves the care (P10 during).
However, a perceived lack of judgement was sometimes attributed to wearing the full personal protective equipment required during the COVID-19 pandemic, which meant that their personal features were largely obscured. For this reason, it was more difficult for patients to make assumptions or attributions about students’ ethnic or gender identity based on their appearance.
People tend to assume and call us all girls, which was irritating. It was mostly just because all of us were so covered up, no one could see anyone’s faces (P16 during).
Subtheme 1.3 Is nursing really for me?
Prior to their first clinical placement experience, many participants expressed ambivalence about a nursing career and anticipated that undertaking clinical placement could determine their suitability for the profession. Once exposed to clinical placement, the majority of students were completely committed to their chosen profession, with a minority remaining ambivalent or, in rare cases, choosing to leave the course. Not yet achieving full commitment to a nursing career was related to not wishing to work in the ward they had for their clinical placement, while remaining open to trying different specialities.
I didn’t have an actual idea of what I wanted to do after arts, this wasn’t something that I was aiming towards specifically (P14 before). I think I’m still not 100%, but enough to go on, that I’m happy to continue the course as best as I can (P11 during).
Subtheme 1.4 Being a burden
Before clinical placement, participants had concerns about being burdensome and how this would affect their clinical placement experiences.
If we end up being a burden to them, an extra responsibility for them on top of their day, then we might not be treated as well (P10 before).
A sense of burden remained a theme during the clinical placement for participants for the first five to seven days, after which most participants acknowledged that their role became more active. As students contributed more productively to their placement, their feelings of being a burden reduced.
Major theme 2: Sinking or swimming
The second major theme, sinking or swimming, described participants’ expectations about a successful placement experience and identified themes related to students’ successes (‘swimming’) or difficulties (‘sinking’) during their placement experience. Prior to clinical placement, without a realistic preview of what the experience might entail, participants were uncertain of their role, hoped for ‘nice’ supervising nurses and anticipated an observational role that would keep them afloat.
I will focus on what I want to learn and see if that coincides with what is expected, I guess (P15 before).
During the clinical placement, the reality was very different, with a sense of sinking. Participants discovered, some with shock, that they were expected to participate actively in the healthcare team.
I got the sense that they were not going to muck around, and, you know, they’re ‘gonna’ use the free labour that came with me (P1 during).
Adding to the confusion about the expected placement experience, participants believed that healthcare staff were unclear about students’ scope of practice for a postgraduate entry-to-practice degree, creating misalignment between students’ and supervising nurses’ expectations.
It seems to me like the educators don’t really seem to have a clear picture of what the scope is, and what is actually required or expected of us (P10 during).
In exploring perceived expectations of the clinical placement and the modifying effect of placement on initial expectations, three subthemes were identified: translation to practice is overwhelming, trying to find the rhythm or jigsaw pieces, and individual agency.
Subtheme 2.1 Translation to practice is overwhelming
Before clinical placement, participants described concerns about insufficient knowledge to enable them to engage effectively with the placement experience.
If I am doing an assessment understanding what are those indications and why I would be doing it or not doing it at a certain time (P1 before).
Integrating and applying theoretical content while navigating an unfamiliar clinical environment created a significant gap between theory and practice during clinical placement. As the clinical placement experience proceeded and initial fears dissipated, students became more aware of applying their theoretical knowledge in the clinical context.
We’re learning all this theory and clinical stuff, but then we don’t really have a realistic idea of what it’s like until we’re kind of thrown into it for three weeks (P10 during).
Subtheme 2.2 Trying to find the rhythm or the jigsaw pieces
Before clinical placement, participants described learning theory and clinical skills with contextual unfamiliarity. They had the jigsaw pieces but did not know how to assemble it; they had the music but did not know the final song. When discussing their expectations about clinical placement, the small number of participants with a healthcare background (e.g. as healthcare assistants) proposed realistic answers, whereas others struggled to answer or cited stories from friends or television. With a lack of context, feelings of unpreparedness were exacerbated. Once in the clinical environment, participants further emphasised that they could not identify what they needed to know to successfully prepare for clinical placement.
It was never really pieced together. We’ve learned bits and pieces, and then we’re putting it together ourselves (P8 during). On this course I feel it was this is how you do it, but I did not know how it was supposed to be played, I did not know the rhythm (P4 during).
Subtheme 2.3 Individual agency
Participants’ individual agency, their attitude, self-efficacy, and self-motivation affected their clinical placement experiences. Participant perceptions in advance of the clinical placement experience remained consistent with their perspectives following clinical placement. Before clinical placement, participants who were highly motivated to learn exhibited a growth mindset [ 23 ] and planned to be proactive in delivering patient care. During their clinical placement, initially positive students remained positive and optimistic about their future. Participants who believed that their first clinical placement role would be largely observational and were less proactive about applying their knowledge and skills identified boredom and a lack of learning opportunities on clinical placement.
A shadowing position, we don’t have enough skills and authority to do any work, not do any worthwhile skills (P3 before). I thought it would be a lot busier, because we’re limited with our scope, so there’s not much we can do, it’s just a bit slower than I thought (P12 during).
Individual agency appears to influence a successful first clinical placement; other factors may also be implicated but were not the focus of this study. Further research exploring the relationships between students’ age, life experience, resilience, individual agency, and the use of coping strategies during a first clinical placement would be useful.
Major theme 3: The reality of navigating placement relationships
The third main theme emphasised the reality of navigating clinical placement relationships and explored students’ relationships with healthcare staff, patients, and peers. Before clinical placement, many participants, especially those with healthcare backgrounds, expressed fears about relationships with supervising nurses. They perceived that the dynamics of the team and the healthcare workplace might influence the support they received. Several participants were nervous about attending placement on their own without peers for support, especially if the experience was challenging. Participants identified expectations of being mistreated, believing that it was unavoidable, and prepared themselves to not take it personally.
For me it’s where we’re going to land, are we going to be in a supportive, kind of nurturing environment, or is it just kind of sink or swim? (P5 before). If you don’t really trust them, you’re nervous the entire time and you’ll be like what if I get it wrong (P16 before).
Despite these concerns, students strongly emphasised the value of relationships during their first clinical placement, with these perceptions unchanged by their clinical placement experience. Where relationships were positive, participants felt empowered to be autonomous, and their self-confidence increased.
You get that that instant reaction from the patients. And that makes you feel more confident. So that really got me through the first week (P14 during). I felt like I was intruding, then as I started to build a bit of rapport with the people, and they saw that I was around, I don’t feel that as much now (P1 during).
Such development hinged on the receptiveness and support of supervising nurses, the team on the ward, and patients and could be hindered by poor relationships.
He was the old-style buddy nurse in his fifties, every time I questioned him, he would go ssshh, just listen, no questions, it was very stressful (P10 during). It depends whether the buddy sees us as an extra pair of hands, or we’re learners (P11 during).
Where students experienced poor behaviour from supervising nurses, they described a range of emotional responses to these interactions and also coping strategies including avoiding unfriendly staff and actively seeking out those who were more inclusive.
If they weren’t very nice, it wouldn’t be very enjoyable and if they didn’t trust you, then it would be a bit frustrating, that like I can do this, but you won’t let me (P12 during). If another nurse was not nice to me, and I was their buddy, I would literally just not buddy with them and go and follow whoever was nice to me (P4 during).
Relationships with peers were equally important; students on clinical placement with peers valued the shared experience. In contrast, students who attended clinical placement alone at a regional or rural hospital felt disconnected from the opportunities that learning with peers afforded.
Our research explored the emotional responses and perceptions of preparedness of postgraduate entry-to-practice nursing students prior to and during their first clinical placement. In this study, we described how the perceptions of nursing students remained consistent or were modified by their clinical placement experiences. Our analysis of students’ experiences identified three major themes: adjusting and managing a raft of feelings; sinking or swimming; and the reality of navigating placement relationships. We captured similar themes identified in the literature; however, our study also identified novel aspects of nursing students’ experiences of their first clinical placement.
The key theme, adjusting and managing a raft of feelings, which encapsulates anxiety before clinical placement, is consistent with previous research. This theme included concerns in communicating with healthcare staff and managing registered nurses’ negative attitudes and expectations, in addition to an academic workload [ 11 , 24 ]. Concerns not previously identified in the literature included a fear of judgement or discrimination by healthcare staff or patients that might impact the reputation of marginalised communities. Fortunately, these initial fears largely dissipated during clinical placement. Some students discovered that a diverse cultural background was an asset during their clinical placement. Although these initial fears were ameliorated by clinical placement experiences, evidence of such fears before clinical placement is concerning. Further research to identify appropriate support for nursing students from culturally diverse or marginalised communities is warranted. For example, a Finnish study highlighted the importance of mentoring culturally diverse students, creating a pedagogical atmosphere during clinical placement and integrating cultural diversity into nursing education [ 25 ].
Preclinical expectations of being mistreated can be viewed as an unavoidable phenomenon for nursing students [ 26 ]. The existing literature highlights power imbalances and hierarchical differences within the healthcare system, where student nurses may be marginalised, disrespected, and ignored [ 9 , 27 , 28 ]. During their clinical placement, students in our study reported unintentional incivility by supervising nurses: feeling not wanted, ignored, or asked to remain quiet by supervising nurses who were unfriendly or highly critical. These findings were similar to those of Thomas et al.’s [ 29 ] UK study and were particularly heightened at the beginning of clinical placement. Several students acknowledged that nursing staff fatigue from a high turnover of students on their ward and the COVID-19 pandemic could be contributing factors. In response to such incivility, students reported decreased self-confidence and described becoming quiet and withdrawing from active participation with their patients. Students oriented their behaviour towards repetitive low-level tasks, aiming to please and help their supervising nurse, to the detriment of learning opportunities. Fortunately, these incidents did not appear to impact nursing students’ overall experience of clinical placement. Indeed, students found positive experiences with different supervising nurses and their own self-reflection assisted with coping. Other active strategies to combat incivility identified in the current study that were also identified by Thomas et al. [ 29 ] included avoiding nurses who were uncivil, asking to work with nurses who were ‘nice’ to them, and seeking out support from other staff as a coping strategy. The nursing students in our study were undertaking a postgraduate entry-to-practice qualification and already had an undergraduate degree. The likely greater levels of experience and maturity of this cohort may influence their resilience when working with unsupportive supervising nurses and identifying strategies to manage challenging situations.
The theory-practice gap emerged in the theme of sinking or swimming. A theory-practice gap describes the perceived dissonance between theoretical knowledge and expectations for the first clinical placement, as opposed to the reality of the experience, and has been reported in previous studies (see, for instance, 24 , 30 , 31 , 32 ). Existing research has shown that when the first clinical placement does not meet inexperienced student nurses’ expectations, a disconnect between theory and practice occurs, creating feelings of being lost and insecure within the new environment, potentially impacting students’ motivation and risk of attrition [ 19 , 33 ]. The current study identified further areas exacerbating the theory-practice gap. Before the clinical placement, students without a healthcare background lacked context for their learning. They lacked understanding of nurses’ shift work and were apprehensive about applying clinical skills learned in the classroom. Hence, some students were uncertain if they were prepared for their first clinical placement or even how to prepare, which increased their anxiety. Prior research has demonstrated that applying theoretical knowledge more seamlessly during clinical placement was supported when students knew what to expect [ 6 ]. For instance, a Canadian study exposed students as observers to the healthcare setting before starting clinical placement, enabling early theory to practice connections that minimised misconceptions and false assumptions during clinical placement [ 34 ].
In the current study, the theory-practice gap was further exacerbated during clinical placement, where healthcare staff were confused about students’ scope of practice and the course learning objectives and expectations in a postgraduate entry-to-practice nursing qualification. The central booking system for clinical placements classifies first-year nursing students who participated in this study as equivalent to second-year undergraduate nursing students. Such a classification could create a misalignment between clinical educators’ expectations and their delivery of education versus students’ actual learning needs and capacity [ 3 , 31 ]. Additional communication to healthcare partners is warranted to enhance understanding of the scope of practice and expectations of a first-year postgraduate entry-to-practice nursing student. Educating and empowering students to communicate their learning needs within their scope of practice is also required.
Our research identified a link between students’ personality traits or individual agency and their first clinical placement experience. The importance of a positive orientation towards learning and the nursing profession in preparedness for clinical placement has been highlighted in previous studies [ 31 ]. Students’ experience of their first clinical placement in our study appeared to be strongly influenced by their mindset [ 23 ]. Some students demonstrated motivation to learn, were happy to ‘roll with the punches’, yet remain active in their learning requirements, whereas others perceived their role as observational and expected supervising nurses to provide learning opportunities. Students who anticipated a passive learning approach prior to their first clinical placement reported boredom, limited activity, and lack of opportunities during their first clinical placement. These students could have a lowered sense of self-efficacy, which may lead to a greater risk of doubt, stress, and reduced commitment to the profession [ 35 ]. Self-efficacy theory explores self-perceived confidence and competence around people’s beliefs in their ability to influence events, which is associated with motivation and is key to nursing students progressing in their career path confidently [ 35 , 36 ]. In the current study, students who actively engaged in their learning process used strategies such as self-reflection and sought support from clinical educators, peers and family. Such active approaches to learning appeared to increase their resilience and motivation to learn as they progressed in their first clinical placement.
Important relationships with supervising nurses, peers, or patients were highlighted in the theme of the reality of navigating placement relationships. This theme links with previous research findings about belongingness. Belongingness is a fundamental human need and impacts students’ behaviour, emotions, cognitive processes, overall well-being, and socialisation into the profession [ 37 , 38 ]. Nursing students who experience belongingness feel part of a team and are more likely to report positive experiences. Several students in the current study described how feeling part of a team improved self-confidence and empowered work-integrated learning. Nonetheless, compared with previous literature (see for instance, 2), working as a team and belongingness were infrequent themes. Such infrequency could be related to the short duration of the clinical placement. In shorter clinical placements, nursing students learn a range of technical skills but have less time to develop teamwork skills and experience socialisation to the profession [ 29 , 39 ].
Positive relationships with supervising nurses appeared fundamental to students’ experiences. Previous research has shown that in wards with safe psycho-social climates, where the culture tolerates mistakes, regarding them as learning opportunities, a pedagogical atmosphere prevails [ 25 , 39 ]. Whereas, if nursing students experience insolent behaviours or incivility, this not only impacts learning it can also affect career progression [ 26 ]. Participants who felt safe asking questions were given responsibility, had autonomy to conduct skills within their scope of practice and thrived in their learning. This finding aligns with previous research affirming that a welcoming and supportive clinical placement environment, where staff are caring, approachable and helpful, enables student nurses to flourish [ 36 , 40 , 41 , 42 ]. Related research highlights that students’ perception of a good clinical placement is linked to participation within the community and instructor behaviour over the quality of the clinical environment and opportunities [ 27 , 28 ]. Over a decade ago, a large European study found that the single most important element for students’ clinical learning was the supervisory relationship [ 39 ]. In our study, students identified how supervising nurses impacted their emotions and this was critical to their experience of clinical placement, rather than how effective they were in their teaching, delivery of feedback, or their knowledge base.
Students’ relationships with patients were similarly important for a successful clinical placement. Before the clinical placement, students expressed anxiety and fears in communicating and interacting with patients, particularly if they were dying or acutely unwell, which is reflective of the literature [ 2 , 10 , 11 ]. However, during clinical placement, relationships with patients positively impacted nursing students’ experiences, especially at the beginning when they felt particularly vulnerable in a new environment. Towards the end of clinical placement, feelings of incompetence, nervousness and uncertainty had subsided. Students were more active in patient care, which increased self-confidence, empowerment, and independence, in turn further improving relationships with patients and creating a positive feedback loop [ 36 , 42 , 43 ].
Limitations
This study involved participants from one university and a single course, thus limiting the generalisability of the results. Thus, verification of the major themes identified in this research in future studies is needed. Nonetheless, the purpose of this study was to explore in detail the way in which the experiences of clinical placement for student nurses modified initial emotional responses towards undertaking placement and their perceptions of preparedness. Participants in this study undertook their clinical placement in a variety of different hospital wards in different specialties, which contributed to the rigour of the study in identifying similar themes in nursing students’ experiences across diverse placement contexts.
This study explored the narratives of first-year nursing students undertaking a postgraduate entry-to-practice qualification on their preparedness for clinical placement. Exploring students’ changing perspectives before and during the clinical placement adds to extant knowledge about nursing students’ emotional responses and perceptions of preparedness. Our research highlighted the role that preplacement emotions and expectations may have in shaping nursing students’ clinical placement experiences. Emerging themes from this study highlighted the importance students placed on relationships with peers, patients, and supervising nurses. Significant anxiety and other negative emotions experienced by nursing students prior to the first clinical placement suggests that further research is needed to explore the impact of contextual learning to scaffold students’ transition to the clinical environment. The findings of this research also have significant implications for educational practice. Additional educational support for nursing students prior to entering the clinical environment for the first time might include developing students’ understanding of the clinical environment, such as through increasing students’ understanding of the different roles of nurses in the clinical context through pre-recorded interviews with nurses. Modified approaches to simulated teaching prior to the first clinical placement would also be useful to increase the emphasis on students applying their learning in a team-based, student-led context, rather than emphasising discrete clinical skill competencies. Finally, increasing contact between students and university-based educators throughout the placement would provide further opportunities for students to debrief, to receive support and to manage some of the negative emotions identified in this study. Further supporting the transition to the first clinical placement could be fundamental to reducing the theory-practice gap and allaying anxiety. Such support is crucial during their first clinical placement to reduce attrition and boost the nursing workforce.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the conditions of our ethics approval but may be available from the corresponding author on reasonable request and subject to permission from the Human Research Ethics Committee.
Alshahrani Y, Cusack L, Rasmussen P. Undergraduate nursing students’ strategies for coping with their first clinical placement: descriptive survey study. Nurse Educ Today. 2018;69:104–8.
Article PubMed Google Scholar
Brady M, Price J, Bolland R, Finnerty G. Needing to belong: first practice placement experiences of childrens’ nursing students. Compr Child Adolesc Nurs. 2019;421:24–39.
Article Google Scholar
Levett-Jones T, Pitt V, Courtney-Pratt H, Harbrow G, Rossiter R. What are the primary concerns of nursing students as they prepare for and contemplate their first clinical placement experience? Nurse Educ Pract. 2015;154:304–9.
McCloughen A, Levy D, Johnson A, Nguyen H, McKenzie H. Nursing students’ socialisation to emotion management during early clinical placement experiences: a qualitative study. J Clin Nurs. 2020;2913–14:2508–20.
Andrew N, McGuinness C, Reid G, Corcoran T. Greater than the sum of its parts: transition into the first year of undergraduate nursing. Nurse Educ Pract. 2009;91:13–21.
Leducq M, Walsh P, Hinsliff-Smith. K McGarry J. A key transition for student nurses: the first placement experience. Nurse Educ Today. 2012;327:779–81.
Spurlock D Jr. The nursing shortage and the future of nursing education is in our hands. J Nurs Educ. 2020;596:303–4.
Agu CF, Stewart J, McFarlane-Stewart N, Rae T. COVID‐19 pandemic effects on nursing education: looking through the lens of a developing country. Int Nurs Rev. 2021;682:153–8.
Nejad FM, Asadizaker M, Baraz S, Malehi AS. Investigation of nursing student satisfaction with the first clinical education experience in universities of medical sciences in Iran. J Med Life. 2019;121:75–82.
Sun FK, Long A, Tseng YS, Huang HM, You JH, Chiang CY. Undergraduate student nurses’ lived experiences of anxiety during their first clinical practicum: a phenomenological study. Nurse Educ Today. 2016;37:21–6.
Article CAS PubMed Google Scholar
Gurková E, Zeleníková R. Nursing students perceived stress coping strategies health and supervisory approaches in clinical practice: a Slovak and Czech perspective. Nurse Educ Today. 2018;65:4–10.
Hanson J, Walsh S, Mason M, Wadsworth D, Framp A, Watson K. Speaking up for safety: a graded assertiveness intervention for first year nursing students in preparation for clinical placement: thematic analysis. Nurse Educ Today. 2020;84:104252.
Khalaila R. Simulation in nursing education: an evaluation of students outcomes at their first clinical practice combined with simulations. Nurse Educ Today. 2014;342:252–8.
Cummins AM, Catling C, Hogan R, Homer CS. Addressing culture shock in first year midwifery students: maximising the initial clinical experience. Women Birth. 2014;274:271–5.
Chesser-Smyth PA. The lived experiences of general student nurses on their first clinical placement: a phenomenological study. Nurse Educ Pract. 2005;56:320–7.
Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse Educ Pract. 2018;29:127–32.
Cowen KJ, Hubbard LJ, Hancock DC. Expectations and experiences of nursing students in clinical courses: a descriptive study. Nurse Educ Today. 2018;67:15–20.
Krueger RA, Casey MA. Focus groups: a practical guide for applied research. 5th ed. Thousand Oaks, California: Sage; 2014.
Jonsén E, Melender HL, Hilli Y. Finnish and Swedish nursing students experiences of their first clinical practice placement—A qualitative study. Nurse Educ Today. 2013;333:297–302.
Watt D. On becoming a qualitative researcher: the value of reflexivity. Qual Rep. 2007;121:82–101.
Google Scholar
Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf DK, Sher J, editors. APA handbook of research methods in psychology Vol. 2. Research designs: quantitative qualitative neuropsychological and biological. Washington, DC: American Psychological Association; 2012. pp. 57–71.
Chapter Google Scholar
Lumivero. - Software Solutions for Data Analysis & Management [Internet]. Lumivero. http://www.lumivero.com .
Yeager DS, Dweck CS. Mindsets that promote resilience: when students believe that personal characteristics can be developed. Educ Psychol. 2012;47(4):302–14.
Kol E, İnce S. Determining the opinions of the first-year nursing students about clinical practice and clinical educators. Nurse Educ Pract. 2018;31:35–40.
Mikkonen K, Merilainen M, Tomietto M. Empirical model of clinical learning environment and mentoring of culturally and linguistically diverse nursing students. J Clin Nurs. 2020;29(3–4):653–61.
Ahn YH, Choi J. Incivility experiences in clinical practicum education among nursing students. Nurse Educ Today. 2019;73:48–53.
Molesworth M. Nursing students first placement: peripherality and marginality within the community of practice. J Nurs Educ. 2017;561:31–8.
Rafati F, Nouhi E, Sabzehvari S, Dehghan-Nayyeri N. Iranian nursing students’ experience of stressors in their first clinical experience. J Prof Nurs. 2017;333:250–7.
Thomas J, Jinks A, Jack B. Finessing incivility: the professional socialisation experiences of student nurses first clinical placement a grounded theory. Nurse Educ Today. 2015;3512:e4–9.
Astin F, McKenna L, Newton J, Moore-Coulson L. Registered nurses–expectations and experiences of first year students–clinical skills and knowledge. Contemp Nurse. 2005;183:279–91.
Kalyani MN, Jamshidi N, Molazem Z, Torabizadeh C, Sharif F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open. 2019;97:e028052.
Maginnis C, Croxon L. Transfer of learning to the nursing clinical practice setting. Rural Remote Health. 2010;102:334–40.
Soler OM, Aguayo-González M, Gutiérrez SSR, Pera MJ, Leyva-Moral JM. Nursing students’ expectations of their first clinical placement: a qualitative study. Nurse Educ Today. 2021;98:104736.
Powell TL, Cooke J, Brakke A. Altered nursing student perspectives: impact of a pre-clinical observation experience at an outpatient oncology setting. Can Oncol Nurs J. 2019;291:34–9.
Bandura AJJW. Self-efficacy. In: Weiner IB, Craighead WE, editors. The Corsini encyclopedia of psychology. Hoboken, NJ: John Wiley & Sons Inc; 2010.
Porteous DJ, Machin A. The lived experience of first year undergraduate student nurses: a hermeneutic phenomenological study. Nurse Educ Today. 2018;60:56–61.
Cooper J, Courtney-Pratt H, Fitzgerald M. Key influences identified by first year undergraduate nursing students as impacting on the quality of clinical placement: a qualitative study. Nurse Educ Today. 2015;359:1004–8.
Levett-Jones T, Lathlean J. The ascent to competence conceptual framework: an outcome of a study of belongingness. J Clin Nurs. 2009;1820:2870–9.
Warne T, Johansson UB, Papastavrou E, Tichelaar E, Tomietto M, Van den Bossche K. Saarikoski M. An exploration of the clinical learning experience of nursing students in nine European countries. Nurse Educ Today. 2010;308:809–15.
Laugaland K, Kaldestad K, Espeland E, McCormack B, Akerjordet K, Aase I. Nursing students experience with clinical placement in nursing homes: a focus group study. BMC Nurs. 2021;201:1–13.
Manninen K, Henriksson EW, Scheja M, Silén C. Authenticity in learning–nursing students experiences at a clinical education ward. Health Educ. 2013;1132:132–43.
Teskereci G, Boz İ. I try to act like a nurse: a phenomenological qualitative study. Nurse Educ Pract. 2019;37:39–44.
Chesser-Smyth PA, Long T. Understanding the influences on self‐confidence among first‐year undergraduate nursing students in Ireland. J Adv Nurs. 2013;691:145–57.
Download references
Acknowledgements
The authors wish to thank the first-year nursing students who participated in this study and generously shared their experiences of undertaking their first clinical placement.
No funding was received for this study.
Author information
Jennifer M. Weller-Newton
Present address: School of Nursing and Midwifery, University of Canberra, Kirinari Drive, Bruce, Canberra, ACT, 2617, Australia
Authors and Affiliations
Department of Nursing, The University of Melbourne, Grattan St, Parkville, VIC, 3010, Australia
Philippa H. M. Marriott
Department of Rural Health, The University of Melbourne, Grattan St, Shepparton, VIC, 3630, Australia
Present address: Department of Medical Education, Melbourne Medical School, The University of Melbourne, Grattan St, Parkville, VIC, 3010, Australia
Katharine J. Reid
You can also search for this author in PubMed Google Scholar
Contributions
All authors made a substantial contribution to conducting the research and preparing the manuscript for publication. P.M., J.W-N. and K.R. conceptualised the research and designed the study. P.M. undertook the data collection, and all authors were involved in thematic analysis and interpretation. P.M. wrote the first draft of the manuscript, K.R. undertook a further revision and all authors contributed to subsequent versions. All authors approved the final version for submission. Each author is prepared to take public responsibility for the research.
Corresponding author
Correspondence to Katharine J. Reid .
Ethics declarations
Ethics approval and consent to participate.
The research was undertaken in accordance with the National Health and Medical Research Council of Australia’s National Statement on Ethical Conduct in Human Research and the Australian Code for the Responsible Conduct of Research. Ethical approval to conduct the study was obtained from the University of Melbourne Human Research Ethics Committee (Ethics ID 1955997.1). All participants received a plain language statement that described the requirements of the study. All participants provided informed written consent to participate, which was affirmed verbally at the beginning of focus groups and interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marriott, P.H.M., Weller-Newton, J.M. & Reid, K.J. Preparedness for a first clinical placement in nursing: a descriptive qualitative study. BMC Nurs 23 , 345 (2024). https://doi.org/10.1186/s12912-024-01916-x
Download citation
Received : 17 November 2023
Accepted : 04 April 2024
Published : 22 May 2024
DOI : https://doi.org/10.1186/s12912-024-01916-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Postgraduate nursing education
- Nursing students
- Nursing schools
- Clinical skills
- Qualitative research
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 29.5.2024 in Vol 26 (2024)
Experiences of Electronic Health Records’ and Client Information Systems’ Use on a Mobile Device and Factors Associated With Work Time Savings Among Practical Nurses: Cross-Sectional Study
Authors of this article:

Original Paper
- Satu Paatela 1 , MHSc ;
- Maiju Kyytsönen 1 , MHSc ;
- Kaija Saranto 2 , PhD ;
- Ulla-Mari Kinnunen 3 , PhD ;
- Tuulikki Vehko 1 , PhD
1 Health and Social Service System Research, Finnish Institute for Health and Welfare, Helsinki, Finland
2 Faculty of Social Sciences and Business Studies, University of Eastern Finland, Kuopio, Finland
3 Department of Health and Social Management, University of Eastern Finland, Kuopio, Finland
Corresponding Author:
Satu Paatela, MHSc
Health and Social Service System Research
Finnish Institute for Health and Welfare
Mannerheimintie 166
Helsinki, 00271
Phone: 358 29 524 77 22
Email: [email protected]
Background: The transmission of clinical information in nursing predominantly occurs through digital solutions, such as computers and mobile devices, in today’s era. Various technological systems, including electronic health records (EHRs) and client information systems (CISs), can be seamlessly integrated with mobile devices. The use of mobile devices is anticipated to rise, particularly as long-term care is increasingly delivered in environments such as clients’ homes, where computers are not readily accessible. However, there is a growing need for more user-centered data to ensure that mobile devices effectively support practical nurses in their daily activities.
Objective: This study aims to analyze practical nurses’ experiences of using EHRs or CISs on a mobile device in their daily practice. In addition, it aims to examine the factors associated with work time savings when using EHRs/CISs on a mobile device.
Methods: A cross-sectional study using an electronic survey was conducted in spring 2022. A total of 3866 practical nurses participated in the survey based on self-assessment. The sample was limited to practical nurses who used EHRs or CISs on a mobile device and worked in home care or service housing within the social welfare or health care sector (n=1014). Logistic regression analysis was used to explore the factors associated with work time savings.
Results: The likelihood of perceiving work time savings was higher among more experienced EHR/CIS users compared with those with less experience (odds ratio [OR] 1.59, 95% CI 1.30-1.94). Participants with 0-5 years of work experience were more likely to experience work time savings compared with those who had worked 21 years or more (OR 2.41, 95% CI 1.43-4.07). Practical nurses in home care were also more likely to experience work time savings compared with those working in service housing (OR 1.95, 95% CI 1.23-3.07). A lower grade given for EHRs/CISs was associated with a reduced likelihood of experiencing work time savings (OR 0.76, 95% CI 0.66-0.89). Participants who documented client data in a public area were more likely to experience work time savings compared with those who did so in the nurses’ office (OR 2.33, 95% CI 1.27-4.25). Practical nurses who found documentation of client data on a mobile device easy (OR 3.05, 95% CI 2.14-4.34) were more likely to experience work time savings compared with those who did not. Similarly, participants who believed that documentation of client data on a mobile device reduced the need to memorize things (OR 4.10, 95% CI 2.80-6.00) were more likely to experience work time savings compared with those who did not.
Conclusions: To enhance the proportion of practical nurses experiencing work time savings, we recommend that organizations offer comprehensive orientation and regular education sessions tailored for mobile device users who have less experience using EHRs or CISs and find mobile devices less intuitive to use.
Introduction
Information and communication technology (ICT) including electronic health records (EHRs) and client information systems (CISs) have become an increasingly important part of health care and social services in Finland [ 1 - 4 ]. In fact, EHR has been a common tool in Finnish health care for a long time, and from 2010 onward EHR availability has been 100% in public and private facilities [ 5 ]. EHRs include a comprehensive collection of patient health information (eg, narrative texts and laboratory data), with the collected data used in the care processes of the patient [ 6 ]. By contrast, CISs are more commonly used in the public social welfare sector for accessing, storing, and using client information and documents [ 3 , 4 ]. The Finnish Ministry of Social Affairs and Health has been at the helm of guiding the development of technological infrastructure and associated legislative efforts over the decades. Their eHealth and eWelfare strategy aims to improve the effective utilization of data in bolstering service renewal and citizen well-being at a national level [ 7 ].
With the development of the ICT infrastructure, the clinical information in nursing is nowadays mainly transmitted via digital solutions such as computers and mobile devices [ 8 ]. Particularly, mobile devices such as smartphones and tablets are commonly used in the health care sector [ 9 , 10 ], and nurses are known to use EHRs on mobile devices 3 times more often compared with doctors in a hospital environment [ 11 ]. Different technological systems such as EHRs can be integrated with mobile devices [ 9 , 11 - 13 ], and this allows social and health care professionals to document client data and exchange information related to the clients and service assignments in the system regardless of the time and location [ 11 , 13 ]. Thus, the ability to receive nursing information via a mobile device can promote the mobility and portability of care and enhance service flexibility [ 9 , 12 ].
In previous studies, nurses have been reported to perceive mobile devices as beneficial in their daily practice [ 14 , 15 ]. Mobile device use has been found to support nurses’ workflow processes [ 11 , 16 - 18 ] as they need to spend less time on clinical documentation [ 17 ]. In fact, it is important to recognize that the use of different technological systems such as EHRs has been shown to provide nurses with more time for direct patient care and interprofessional communication [ 19 ]. Moreover, mobile devices have been reported to be useful for planning work, handling notes [ 14 ], and saving time for nurses [ 14 , 20 , 21 ]. Mobile devices may also reduce duplicate documentation [ 13 ] and potential documentation errors [ 17 , 20 ] because client data can be documented at the time of its occurrence. In addition, improved decision-making is one of the main advantages [ 9 , 20 ]. Mobile devices continuously provide the latest information on the situation of the clients, which can improve safety and the quality of care [ 14 , 18 ]. For instance, in home care settings, workers can review and plan real-time nursing interventions and tasks in the clients’ home environment [ 13 , 16 ] because the daily assignments can be seen directly on the mobile device. The use of mobile devices can also contribute to client empowerment as nurses have easier access to clinical information and they can reply to clients’ questions more readily [ 17 ].
By contrast, some challenges have emerged related to the use of EHRs/CISs on a mobile device. According to a recent study, the use of EHRs on a mobile device can negatively affect nurses’ well-being because the use of mobile devices may increase time pressure and stress at work as a result of functional problems and changing information systems [ 10 ]. In home care settings, challenges have emerged, particularly concerning technical issues such as usability problems. This is because the information systems used on mobile devices are not always tailored to address the specific requirements of various working environments [ 22 ]. This in turn may lead to reduced workflows [ 22 ]. Additionally, there is a possibility of poor signal connectivity [ 18 ] and increased data security threats [ 17 , 18 , 23 ] when using mobile devices. Furthermore, some of the recent studies have observed that the use of EHRs itself may negatively impact the quality of communication between nurses and patients because nurses’ attention is more focused on documentation tools such as computers rather than on the patient [ 24 , 25 ]. More generally, the lack of digital competence can affect how different digital tools are adopted in practice [ 26 , 27 ].
The European Union has promoted digitalization in society, including public services, with political consensus through the Digital Decade policy program [ 28 ]. The change in the demographic structure especially forces social and health care services to invest even more in technological solutions [ 29 ] such as mobile documentation [ 22 ]. An aging population increases the need to provide long-term care in home environments [ 30 ], and therefore, using EHRs and CISs on a mobile device is expected to grow as computers for professionals are rarely available at the patients’ bedside in the home environment [ 14 ]. In the Finnish context, practical nurses often take care of needs related to the activities of daily living, for instance, in home care and service housing. Practical nurses in the social and health care profession are strictly regulated by law in Finland [ 31 , 32 ]. Practical nurses are required to have successfully obtained the Vocational Qualification in Social and Healthcare, which entails accruing 180 competence points [ 33 ]. Qualified practical nurses are registered with the National Supervisory Authority for Welfare and Health. They are employed across a diverse spectrum of careers within the social welfare and health care sectors, as well as in early childhood education and schools [ 34 ]. Practical nurses are the second largest occupational group in Finland and the largest group in the social welfare and health care sectors in Finland, with 79,800 people working as practical nurses at the end of 2020 [ 35 ].
As practical nurses form an important group of professionals, it is justified to study their ways of working and increase our knowledge about their experiences of EHR and CIS use on mobile devices. Some of the previous studies have investigated the use of mobile devices from the perspectives of registered nurses, nursing students, and doctors [ 10 , 11 , 14 , 15 ], but there is still limited understanding of the experiences of practical nurses. More user-centered data are needed to ensure that mobile devices fit into the changing clinical practice [ 18 ] and to improve health professionals’ workflows in those work environments where mobile devices are commonly used. As patient care becomes increasingly complex [ 8 ] and health professionals are constantly required to work more efficiently [ 36 ], it is important to study whether mobile devices are as effective tools as they are expected to be in the daily activities of practical nurses [ 9 , 11 , 13 , 14 , 16 , 17 ].
Consequently, the aim of this study was to analyze practical nurses’ experiences regarding their use of EHRs/CISs on a mobile device in their daily practice in home care and service housing settings in the social welfare and health care sectors. Furthermore, we examined the potential factors associated with work time savings when practical nurses were using EHRs/CISs on a mobile device.
Study Context
Finland is a Nordic welfare state where all citizens have universal access to health care and social welfare services. In the 2000s, long-term care for older people and persons with disabilities in Finland has changed from institutional care to more individualized services [ 37 ]. In Finland, long-term care is increasingly provided in service housing or in the home environment under social services. Service housing is available for those citizens who need support living independently. These facilities offer a range of services including meal provision, assistance with personal hygiene, and various health care services [ 38 ]. However, most older adults continue to reside in their own homes, where they can access home care services if needed. Home care encompasses health center–based home nursing and home help services [ 37 , 38 ]. Finland has a wide array of EHRs and CISs, which are used across both the health care and social welfare sectors [ 6 ].
Study Design and Sample
This was a cross-sectional study based on an electronic survey. Data were collected in the spring of 2022 over a 3-week period using a convenience sampling method. As of the end of 2020, there were 79,800 practical nurses employed in Finland [ 35 ], working across the social welfare and health care sectors, as well as in schools and early childhood education and care. Potential respondents were invited to participate in the survey through an email sent by 2 trade unions: The Finnish Union of Practical Nurses and The Union of Public and Welfare Sectors. The electronic survey was distributed to 54,030 members of the trade unions aged 18-65 years. The cover letter specified the study theme as the use of EHRs and CISs. However, previous studies indicate that not all members of the trade unions use EHRs/CISs in their daily practice. This is because practical nurses in social services may still rely on alternative solutions for documentation [ 6 ]. Despite this, 2 reminders were sent to potential participants. Ultimately, 3866 practical nurses responded to the survey, yielding a response rate of 7.16%.
In this study, the inclusion criteria for participation were 2-fold: (1) respondents must work as practical nurses and use an EHR or CIS, and (2) they must not be employed in school or early childhood education and care settings. These criteria were outlined in the first 2 questions of the survey, and the survey was closed for potential respondents who did not meet these criteria. The analysis was additionally narrowed down to practical nurses who indicated that they use EHRs or CISs on a mobile device and are employed in either home care or service housing settings (n=1014). Respondents working in other employment settings were excluded because of the limited number of mobile device users in those settings.
The experiences of EHR systems among physicians were initially assessed in Finland through a national survey in 2010 [ 39 , 40 ]. Subsequently, the survey was refined and conducted again in 2014, 2017, and 2021 for physicians. Additionally, it was customized for registered nurses in 2017 [ 41 - 43 ] and for social care professionals (educated at a university or a university of applied sciences) in 2020 [ 44 , 45 ]. Since 2014, these national surveys have been carried out as part of the “Monitoring and Assessment of Social Welfare and Health Care Information System Services” (STePS) projects [ 6 ]. In a significant development, for the first time in 2022, the survey was customized and conducted for practical nurses as well. Before data collection, the survey underwent pretesting with 20 practical nurses. Questions regarding the use of EHRs and CISs on mobile devices were particularly emphasized, given their integral role in the workflow of many practical nurses. As a result, this study specifically centered on the utilization of a mobile device for the documentation of client data.
A total of 11 variables from the survey were covered in this study. The “Documentation of client data on a mobile device saves working time” variable was used as an outcome measure. To understand what kind of factors are connected to work time savings, the following variables were used: “Age,” “Work experience,” “Workplace,” “Experience in using EHR/CIS,” “Grade for EHR/CIS,” “Most common place to document client data on a mobile device,” “Received sufficient training to document client data on a mobile device,” “Documentation of client data on a mobile device is easy,” “Documentation of client data on a mobile device reduces the need to memorize,” and “I can document everything I need on a mobile device.” A total of 9 variables were recoded in the analysis and 2 variables were included as a continuous variable. The 5-point Likert scale was specified in 5 different variables as follows: 1=fully agree, 2=agree, 3=neither agree nor disagree, 4=disagree, and 5=fully disagree. To streamline the focus on the phenomena of interest and to ensure an adequate number of respondents in all categories, the response options were recoded as follows: 1 or 2=yes and 3-5=no. The included variables are presented in Table 1 .
a EHR: electronic health record.
b CIS: client information system.
c The 5-point Likert scale was specified as follows: 1=fully agree, 2=agree, 3=neither agree nor disagree, 4=disagree, and 5=fully disagree.
Data Analysis
The data were analyzed using the statistical software SPSS Statistics version 29.0.0.0 (IBM, Inc.). The characteristics of the study participants were described using n (%). A binary logistic regression analysis was conducted to examine the association between independent and dependent variables. The “Documentation of client data on a mobile device saves working time” item was used as a dependent variable and 10 items were used as independent variables in the analysis. In establishing a model for the relationship between independent and dependent variables, we first tested the significance of each independent variable individually according to the Wald F test. Based on the P values ( P <.05) of the Wald F test, the items “Age” and “I can document everything I need on a mobile device” were excluded from the regression analysis model. We included 8 other independent variables one by one in the model using a forward stepwise selection method. At each step, variables were chosen for the final model according to their effect on the model’s goodness-of-fit measure, Nagelkerke R 2 ( R 2 N ), and P values of the Wald F test. The fully adjusted model included 7 independent variables, including “Experience in using EHR/CIS,” “Work experience,” “Workplace,” “Grade for EHR/CIS,” “Most common place to document client data on a mobile device,” “Documentation of client data on a mobile device is easy,” and “Documentation of client data on a mobile device reduces the need to memorize.” The “Received sufficient training to document client data on a mobile device” item was omitted from the final model because it was no longer statistically significant ( P =.08) after adjusting the final variable to the model. The fully adjusted model’s R 2 N was 0.372. Variance inflation factor was used to secure a model without multicollinearity: the values indicated low correlation, which is acceptable in a regression model. The results of the fully adjusted regression analysis model are presented with P values, variance inflation factor, odds ratios, and their 95% CIs in Table 4 .
Ethical Considerations
We considered ethical issues related to different phases of this study. Ethical approval for the study was provided by the Finnish Institute for Health and Welfare THL/1206/6.02.01/2022. Study participants were offered written information on the research and data processing in a cover letter and privacy notice [ 46 ]. Participants did not receive any compensation for their participation in the study. The research group has been committed to protecting the anonymity of the participants throughout the study process.
Characteristics of the Mobile Device Users
Of the total of 1014 practical nurses who used EHRs or CISs on a mobile device, nearly one-half (471/1014, 46.45%) fell within the age range of 35-54 years. Additionally, there was a relatively high proportion of participants who were at least 55 years old. The work experience among participants was diverse and evenly distributed. For example, a portion of practical nurses (195/1014, 19.23%) had 0-5 years of experience as a practical nurse or equivalent, while others had worked for 21 years or more (238/1014, 23.47%). The majority of mobile device users (706/1014, 69.63%) were employed in home care, with the remainder working in service housing. Nearly half of the mobile device users (458/1014, 45.17%) rated their experience of using EHRs or CISs at level 4 (on a scale of 1 to 5, where 1 represents a beginner and 5 represents highly experienced). Only 4 practical nurses rated themselves as beginners in using EHRs/CISs. Additionally, the majority of practical nurses assessed the EHR/CIS system used via a mobile device as good (364/1014, 35.90%) or satisfactory (271/1014, 26.73%; Table 2 ).
Practical Nurses’ Experiences of Documenting Client Data on a Mobile Device
The most prevalent location for documenting client data on a mobile device was next to the client (537/1014, 52.96%). Some practical nurses also documented client data in alternative settings such as in the car, at the office, or in public areas. Overall, mobile device users expressed relatively high satisfaction with the training they received for documenting client data on a mobile device (661/1014, 65.19%). The majority of mobile device users (648/1014, 63.91%) found it easy to document client data on a mobile device. Additionally, two-thirds of practical nurses (667/1014, 65.78%) reported that documenting client data on a mobile device saved them time. Furthermore, a vast majority of mobile device users (785/1014, 77.42%) agreed that documenting client data on a mobile device reduced the need to rely on memory. Less than one-half of the participants (418/1014, 41.22%) agreed that they could document everything they need on a mobile device ( Table 3 ).
Factors Associated With Work Time Savings When Using EHRs/CISs on a Mobile Device
Several factors were associated with work time savings when using EHRs/CISs on a mobile device ( Table 4 ). Experience of using EHRs/CISs ( P <.001), work experience ( P <.001), the workplace ( P =.004), the grade given for the EHRs/CISs ( P <.001), the statements “Documentation of patient data on a mobile device is easy” ( P <.001) and “Documentation of patient data on a mobile device reduces the need to memorize things” ( P <.001) had statistically significant associations with work time savings.
c The level of statistical significance was set at P <.05 (italicized).
d Comparison group.
e Not applicable.
Practical nurses who considered themselves to be more experienced EHR/CIS users were more likely to perceive work time savings. Participants who had worked 0-5 years as a practical nurse were 2.41 times more likely to experience work time savings compared with those who had worked 21 years or more. Practical nurses who had worked 16-20 years had a lower likelihood of experiencing work time savings than those who had worked for 21 years or more. Furthermore, practical nurses who worked in home care settings were 1.95 times more likely to report work time savings compared with those participants who worked in service housing. Giving a lower grade for EHRs/CISs was associated with a lower likelihood of experiencing work time savings. Participants who documented client data in a public area were 2.33 times more likely to experience work time savings compared with those who documented client data at the (nurses’) office. Moreover, those practical nurses who reported that the documentation of client data on a mobile device was easy were 3.05 times more likely to experience work time savings compared with others. Practical nurses who reported that the documentation of client data on a mobile device reduced their need to memorize things were 4.10 times more likely to experience work time savings compared with those who did not find mobile devices helpful in memorizing things.
Principal Findings
The aim of the study was to analyze practical nurses’ experiences of using EHRs/CISs on a mobile device in their daily practice. Our study findings indicate that practical nurses generally had positive experiences when documenting client data on a mobile device. Two-thirds of the participants perceived mobile devices as effective tools in their daily practice, as they facilitated time savings in their work. The study revealed that a vast majority of the participants agreed that using EHRs/CISs on a mobile device reduced the need to memorize things. However, participants were less inclined to agree with the statement that they could document everything they needed on a mobile device.
Additionally, our study examined factors associated with work time savings when practical nurses used EHRs/CISs on a mobile device. Factors such as experience with the EHRs/CISs, work experience, workplace, the grade awarded for the EHRs/CISs, and responses to statements such as “Documentation of patient data on a mobile device is easy” and “Documentation of patient data on a mobile device reduces the need to memorize things” were all found to be associated with practical nurses’ experiences of work time savings.
Limitations
This study has several limitations. First, the response rate of 7.16% (3866/54,030) was relatively low, which is common for web-based and lengthy surveys [ 47 ], especially those aimed at health care professionals [ 48 ]. Additionally, incorrect email addresses due to job changes or other reasons, as well as nonopened survey emails, may have further contributed to the low response rate. Therefore, the actual response rate might have been higher if calculated only for those who received and opened the survey invitation. Eventually, 3866/4533 (85.29%) survey clicks resulted in respondents completing the survey. However, it is worth noting that data collection occurred during a national industrial action organized by the trade unions, which could have complicated survey participation. Additionally, various work-related factors that practical nurses encounter in their daily routines, such as time constraints and interruptions, may have influenced survey response rates, especially considering that many union members use their work email as their contact information. Furthermore, the utilization of the convenience sampling method may restrict the generalizability of the results. However, the age distribution of the respondents mirrored that of individuals affiliated with national trade unions [ 49 ]. Additionally, the survey was available in both of Finland’s official languages, Finnish and Swedish, potentially encouraging speakers of both languages to participate.
Second, while practical nurses are a common occupational group in Finland, their title may be less recognized in other regions worldwide. Indeed, long-term care may be provided by health care professionals with various occupational titles internationally. Nonetheless, we propose that the findings of our study can be applied to other nursing professions, such as registered nurses and health care assistants, who use mobile devices as documentation tools in their daily practice. Furthermore, it is important to acknowledge that Finland has a long-standing history of extensively using ICT tools in health care [ 5 ]. Moreover, Finland ranks among the global leaders in mobile data usage [ 50 ]. Consequently, the findings of this study may be particularly relevant and applicable to countries with similar levels of ICT development.
Third, the survey was customized for practical nurses in Finland for the first time, including the questions related to mobile device use. Given the low proportion of missing data, we can assume that respondents understood the various items of the instrument relatively well. Before distribution to participants, the instrument underwent pretesting with 20 practical nurses.
In future studies, it would be beneficial to investigate work time savings among users of specific EHR/CIS brands, as the grading of the system by respondents was strongly correlated with experiencing work time savings. Additionally, research should explore specific work environments, such as home care and service housing. Hence, conducting a subgroup analysis separately for practical nurses working in home care and service housing would be a valuable addition to future studies. Another important research avenue would be to explore the barriers that practical nurses may encounter when documenting next to the patient using a mobile device.
Comparison With Prior Work
To the best of our knowledge, this study marks the inaugural exploration of practical nurses’ experiences regarding their use of EHRs/CISs on a mobile device. Our primary focus was to investigate whether the use of EHRs/CISs on a mobile device contributes to time savings for practical nurses, as well as to identify the factors associated with such savings. In the health care sector, saving work time is crucial because nursing professionals are tasked with a multitude of responsibilities in their daily practice. It is essential for them to have more time available for direct patient care and to minimize the time spent on indirect patient care activities, such as documentation [ 21 ].
This study revealed that two-thirds of practical nurses working in home care or service housing experienced work time savings when using EHRs/CISs on a mobile device. Comparable findings of work time savings have also been documented in previous studies involving health care professionals [ 14 , 20 , 21 ]. This study revealed that documenting client data in a public area, such as a corridor in a housing service, was over 2 times more likely to result in work time savings compared with documenting at the nurses’ office, where computers are typically available. However, it is important to note that documenting sensitive client data on mobile devices in a public area may pose increased security risks, such as the potential loss or theft of the mobile device [ 23 ]. Therefore, mobile technology tools should incorporate essential security features, and organizations should establish clear policies regarding the management of mobile devices [ 51 ].
According to our study findings, work experience was linked to work time savings when using EHRs/CISs on a mobile device. Participants who had worked 0-5 years as practical nurses or in equivalent roles were over 2 times more likely to experience work time savings compared with those who had worked for over 21 years. We speculate that practical nurses with less work experience may perceive work time savings more frequently because they are accustomed to working with new technologies in their daily practice, and they may have received more recent orientation on using mobile devices. It is interesting to note that, in our analysis, age was not found to be significantly associated with work time savings when using EHRs/CISs on a mobile device. However, age may influence perceptions regarding the use of mobile devices. Findings from a previous study [ 52 ] have suggested that older nurses are less inclined to use smartphones or acknowledge their benefits in acute care settings.
Additionally, our study revealed that practical nurses working in home care settings were nearly two times as likely to report work time savings compared with those working in service housing. This finding is unsurprising, considering that home care relies on mobility and necessitates the use of ICT tools directly at patients’ homes [ 22 ]. This environment naturally fosters the integration of mobile technology into the daily practices of health care workers. An essential prerequisite for realizing the benefits of mobile technology is seamless integration with the existing information systems [ 18 ], such as EHRs/CISs. It could be hypothesized that mobile devices contribute to work time savings for practical nurses, especially in home care settings, by facilitating the documentation of client data immediately after completing daily tasks [ 13 ], such as next to the client. However, although practical nurses in this study often documented data next to the client, it was not identified as a statistically significant factor for work time savings. The immediacy afforded by mobile devices, allowing users to document client data promptly after interacting with the client, can alleviate the burden of memorization for health care professionals. According to our study findings, practical nurses who perceived that the documentation of client data reduced the need to rely on memory were 4 times more likely to report work time savings compared with those who did not find mobile devices helpful in reducing the need to memorize things.
Our study findings revealed that practical nurses who found the documentation of client data on a mobile device to be easy were over 3 times more likely to experience work time savings compared with those who did not find mobile devices easy to use. Furthermore, Zhang et al [ 53 ] discovered that nursing professionals in home care settings perceived mobile devices to be useful if the tools are easy to use. Overall, while usability issues related to health information systems, including EHRs, are widely recognized [ 2 , 54 ], much of the existing data are centered around the use of these systems on computers. However, it is important to note that using EHRs/CISs specifically on mobile devices may present additional challenges for social and health care professionals. For example, previous studies have indicated that mobile devices may be difficult to use, too small for daily practice [ 16 ], may not function properly at all times [ 13 ], and could be unstable due to potential internet connection problems [ 18 , 22 ].
In this study, the grade provided by respondents for the EHRs/CISs on a mobile device emerged as a factor associated with work time savings. Specifically, a lower grade for the EHRs/CISs was linked to a reduced likelihood of experiencing work time savings. As the grade for the EHRs/CISs may reflect user satisfaction to some extent, this finding underscores the significance of prioritizing user satisfaction regarding practical nurses’ use of EHRs/CISs on mobile devices. User satisfaction has indeed garnered significant attention in previous studies [ 9 , 15 ], and its impact extends beyond work time savings. According to Hsiao and Chen [ 9 ], user satisfaction influences nurses’ intention to continue using information systems on mobile devices, and perceived usefulness is often intertwined with user satisfaction. Furthermore, the quality of the information system and support from managers have been identified as significant predictors of user satisfaction [ 15 ], as well as technology adoption in general [ 18 ]. It is important to highlight that health care professionals who are more experienced users of information systems may offer valuable suggestions for improvements [ 9 ], underscoring the importance of involving these users in the development of EHRs/CISs to ensure user satisfaction with the system interfaces.
When assessing potential work time savings, it is crucial to take into account practical nurses’ experiences with using EHRs/CISs. Our study results indicate that practical nurses with more experience in using EHRs/CISs were more likely to experience work time savings. Similarly, Villalba-Mora et al [ 26 ] discovered that health care professionals who frequently used health information technologies such as EHRs perceived these tools to be more useful. Additionally, previous experience with digital technologies is significant, as it aids health care professionals in integrating mobile devices into their daily practices [ 18 ].
Conclusions
This study contributes to the existing literature on the use of EHRs/CISs on a mobile device by practical nurses in their daily practice, as well as factors associated with work time savings. Our findings indicate that two-thirds of practical nurses perceived mobile devices as beneficial in home care and service housing settings, as they reported that documenting client data on a mobile device saved their working time. Experience in using EHRs/CISs, work experience, workplace, grade given for the EHRs/CISs, and perceptions regarding the ease of documentation and reduction in the need to memorize were all significantly associated with practical nurses’ experiences of work time savings. Based on our findings, we recommend that special attention should be directed toward mobile device users who are less experienced in using EHRs/CISs or do not find mobile devices easy to use. Organizations should provide comprehensive orientation and regular education to health care professionals on the use of EHRs/CISs on mobile devices. Additionally, user satisfaction is a crucial aspect to consider in achieving work time savings among health care professionals who use EHRs/CISs on a mobile device, as demonstrated by our findings. Practical nurses who rated their EHRs/CISs more favorably were more likely to experience work time savings. Therefore, we suggest that end users, particularly those with more experience in using EHRs/CISs, should be involved in the development of EHRs/CISs to ensure better user satisfaction of system interfaces.
Acknowledgments
The research leading to these results received funding from the Ministry of Social Affairs and Health, Finland. The authors thank the Finnish Federation of Local and Basic Caregivers (SuPer ry) and the Union of Public and Welfare Sectors (JHL) for sending the survey to their members and all the licensed practical nurses who responded to the survey. We also thank researcher Samuel Salovaara for commenting on the survey questionnaire. This study was supported by the Ministry of Social Affairs and Health, Finland (project 414919001). The funder’ did not have any role in the study design, collection, analysis, interpretation of data, or writing of the report.
Data Availability
The data collected and analyzed during this study are not publicly available due to coregistratorship between the University of Eastern Finland and the Finnish Institute for Health and Welfare, the controllers of the data.
Conflicts of Interest
None declared.
- Kinnunen U, Heponiemi T, Rajalahti E, Ahonen O, Korhonen T, Hyppönen H. Factors related to health informatics competencies for nurses—results of a national electronic health record survey. CIN: Computers, Informatics, Nursing. 2019;37(8):420-429. [ CrossRef ]
- Kaihlanen A, Gluschkoff K, Hyppönen H, Kaipio J, Puttonen S, Vehko T, et al. The associations of electronic health record usability and user age with stress and cognitive failures among Finnish registered nurses: cross-sectional study. JMIR Med Inform. Nov 18, 2020;8(11):e23623. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Salovaara S, Ylönen K. Client information systems’ support for case-based social work: experiences of Finnish social workers. Nordic Social Work Research. Nov 10, 2021;12(3):364-378. [ CrossRef ]
- Ylönen K. The use of electronic information systems in social work. A scoping review of the empirical articles published between 2000 and 2019. European Journal of Social Work. Apr 18, 2022:1-14. [ CrossRef ]
- Reponen J, Keränen N, Ruotanen R, Tuovinen T, Haverinen J, Kangas M. Availability and use of e-health in Finland. In: Vehko T, editor. E-Health and E-Welfare of Finland: Checkpoint 2022. Helsinki, Finland. National Institute for Health and Welfare; 2022:61-95.
- Vehko T, editor. E-Health and E-Welfare of Finland : Check Point 2022 [Report 2022_006]. Helsinki, Finland. National Institute for Health and Welfare; 2022.
- Jormanainen V, Hämäläinen P, Reponen J. The Finnish healthcare and social care system and ICT-policies. In: Vehko T, editor. E-Health and E-Welfare of Finland: Checkpoint 2022. Helsinki, Finland. National Institute for Health and Welfare; 2022:61-95.
- Silva AMDA, Mascarenhas VHA, Araújo SNM, Machado RDS, Santos AMRD, Andrade EMLR. Mobile technologies in the nursing area. Rev Bras Enferm. Oct 2018;71(5):2570-2578. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hsiao J, Chen R. Understanding determinants of health care professionals’ perspectives on mobile health continuance and performance. JMIR Med Inform. Mar 18, 2019;7(1):e12350. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Heponiemi T, Kaihlanen A, Gluschkoff K, Saranto K, Nissinen S, Laukka E, et al. The association between using a mobile version of an electronic health record and the well-being of nurses: cross-sectional survey study. JMIR Med Inform. Jul 06, 2021;9(7):e28729. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lee Y, Park YR, Kim J, Kim JH, Kim WS, Lee J. Usage pattern differences and similarities of mobile electronic medical records among health care providers. JMIR Mhealth Uhealth. Dec 13, 2017;5(12):e178. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lin T. Mobile nursing information system utilization: the task-technology fit perspective. CIN:Computers, Informatics, Nursing. 2014;32(3):129-137. [ CrossRef ]
- Han S, Juell-Skielse G, Smedberg, Aasi P, Nilsson AG. Benefits of mobile reporting systems in social home care: the case of seven Swedish municipalities. Int J Technol Assess Health Care. Oct 2014;30(4):409-415. [ CrossRef ] [ Medline ]
- Johansson P, Petersson G, Saveman B, Nilsson G. Using advanced mobile devices in nursing practice--the views of nurses and nursing students. Health Informatics J. Sep 02, 2014;20(3):220-231. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cheng C, Chan C, Chen L, Guo S. Evaluation of the implementation of a mobile nursing information system. Online Journal of Nursing Informatics. 2019;23(3):1. [ FREE Full text ]
- Schachner M, Sommer J, González Z, Luna D, Benítez S. Evaluating the feasibility of using mobile devices for nurse documentation. Nursing Informatics. 2016;225:495-499. [ CrossRef ]
- Ehrler F, Lovis C, Blondon K. A mobile phone app for bedside nursing care: design and development using an adapted software development life cycle model. JMIR Mhealth Uhealth. Apr 11, 2019;7(4):e12551. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jacob C, Sanchez-Vazquez A, Ivory C. Social, organizational, and technological factors impacting clinicians' adoption of mobile health tools: systematic literature review. JMIR Mhealth Uhealth. Feb 20, 2020;8(2):e15935. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moore E, Tolley C, Bates D, Slight S. A systematic review of the impact of health information technology on nurses' time. J Am Med Inform Assoc. May 01, 2020;27(5):798-807. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mickan S, Tilson JK, Atherton H, Roberts NW, Heneghan C. Evidence of effectiveness of health care professionals using handheld computers: a scoping review of systematic reviews. J Med Internet Res. Oct 28, 2013;15(10):e212. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pérez-Martí M, Casadó-Marín LC, Guillén-Villar A. Electronic records with tablets at the point of care in an internal medicine unit. Online Journal of Nursing Informatics. 2020;24(3):e30512. [ FREE Full text ]
- Rydenfält C, Persson J, Erlingsdottir G, Johansson G. eHealth services in the near and distant future in Swedish home care nursing. Comput Inform Nurs. Jul 2019;37(7):366-372. [ CrossRef ] [ Medline ]
- Vossebeld DM, Puik ECN, Jaspers JEN, Schuurmans MJ. Development process of a mobile electronic medical record for nurses: a single case study. BMC Med Inform Decis Mak. Jan 14, 2019;19(1):11. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Forde-Johnston C, Butcher D, Aveyard H. An integrative review exploring the impact of electronic health records (EHR) on the quality of nurse-patient interactions and communication. J Adv Nurs. Jan 07, 2023;79(1):48-67. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ali S, Kleib M, Paul P, Petrovskaya O, Kennedy M. Compassionate nursing care and the use of digital health technologies: a scoping review. Int J Nurs Stud. Mar 2022;127:104161. [ CrossRef ] [ Medline ]
- Villalba-Mora E, Casas I, Lupiañez-Villanueva F, Maghiros I. Adoption of health information technologies by physicians for clinical practice: the Andalusian case. Int J Med Inform. Jul 2015;84(7):477-485. [ CrossRef ] [ Medline ]
- Zhu H, Andersen ST. Digital competence in social work practice and education: experiences from Norway. Nordic Social Work Research. Mar 17, 2021;12(5):823-838. [ CrossRef ]
- European Commission. Shaping Europe's digital future. European Commission. 2021. URL: https://ec.europa.eu/digital-single-market/en/content/european-digital-strategy[accessed [accessed 2023-01-12]
- Dequanter S, Steenhout I, Fobelets M, Gagnon M, Sasseville M, Bourbonnais A, et al. Technology implementation in care practices for community-dwelling older adults with mild cognitive decline: Perspectives of professional caregivers in Quebec and Brussels. Digit Health. Nov 16, 2022;8:20552076221139693. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Fritzell J, Agahi N, Jylhä M, Rostgaard T. Social inequalities in ageing in the Nordic countries. Eur J Ageing. Jun 11, 2022;19(2):155-159. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Act on health care professionals 559/1994. Finlex. URL: https://www.finlex.fi/en/laki/kaannokset/1994/en19940559 [accessed 2023-01-21]
- Degree on health care professionals 564/1994. Finlex. URL: https://www.finlex.fi/en/laki/kaannokset/1994/en19940564 [accessed 2023-01-20]
- Vocational qualification in social and health care. Finnish National Agency for Education. 2022. URL: https://eperusteet.opintopolku.fi/#/en/ammatillinen/7854765/tiedot [accessed 2022-12-20]
- The Finnish Union of Practical Nurses. Practical nurse training. Practical nurse's education, training and registration. The Finnish Union of Practical Nurses. 2022. URL: https://www.superliitto.fi/in-english/practical-nurse-training/ [accessed 2022-12-20]
- Statistics Finland. Shop sales assistants, health care assistants and nurses most common occupations in 2020. Statistics Finland. URL: https://www.stat.fi/en/publication/cktws35s04dru0b553lzi7aci [accessed 2022-12-15]
- Lee T, Sun G, Kou L, Yeh M. The use of information technology to enhance patient safety and nursing efficiency. THC. Oct 23, 2017;25(5):917-928. [ CrossRef ]
- Keskimaki I, Tynkkynen L, Reissell E, Koivusalo M, Syrja V, Vuorenkoski L, et al. Finland: health system review. Health Syst Transit. Aug 2019;21(2):1-166. [ Medline ]
- Social Welfare Act 1301/2014. Finlex. URL: https://finlex.fi/fi/laki/ajantasa/2014/20141301#L3P21 [accessed 2023-01-20]
- Vänskä J, Viitanen J, Hyppönen H, Elovainio M, Winblad I, Reponen J, et al. Lääkärien arviot potilastietojärjestelmistä kriittisiä. Suomen Lääkärilehti. 2010;52(65):4177-4183.
- Viitanen J, Hyppönen H, Lääveri T, Vänskä J, Reponen J, Winblad I. National questionnaire study on clinical ICT systems proofs: physicians suffer from poor usability. Int J Med Inform. Oct 2011;80(10):708-725. [ CrossRef ] [ Medline ]
- Hyppönen H, Lääveri T, Hahtela N, Suutarla A, Sillanpää K, Kinnunen U, et al. Kyvykkäille käyttäjille fiksut järjestelmät? Sairaanhoitajien arviot potilastietojärjestelmistä 2017. FinJeHeW. Mar 08, 2018;10(1):30-59. [ CrossRef ]
- Saranto K, Kinnunen U, Koponen S, Kyytsönen M, Hyyppönen H, Vehko T. Sairaanhoitajien valmiudet tiedonhallintaan sekä kokemukset potilas- ja asiakastietojärjestelmien tuesta työtehtäviin. FinJeHeW. Oct 13, 2020;12(3):212-228. [ CrossRef ]
- Saranto K, Koponen S, Vehko T, Kivekäs E. Nurse managers' opinions of information system support for performance management: a correlational study. Methods Inf Med. Jun 09, 2023;62(S 01):e63-e72. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Ylönen K, Salovaara S, Kaipio J, Tyllinen M, Tynkkynen E, Hautala S, et al. Sosiaalialan asiakastietojärjestelmissä paljon parannettavaa: käyttäjäkokemukset 2019. FinJeHeW. Mar 05, 2020;12(1):30-43. [ CrossRef ]
- Salovaara S, Ylönen K, Silén M, Viitanen J, Lääveri T, Hautala S. Sosiaalialan korkeakoulutettujen ammattilaisten arviot asiakastietojärjestelmistä 2020. FinJeHeW. May 09, 2022;14(2):191-207. [ CrossRef ]
- European Union. General Data Protection Regulation 2016/679. European Union. URL: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32016R0679 [accessed 2023-05-03]
- Sammut R, Griscti O, Norman IJ. Strategies to improve response rates to web surveys: a literature review. Int J Nurs Stud. Nov 2021;123:104058. [ CrossRef ] [ Medline ]
- Timmins F, Ottonello G, Napolitano F, Musio ME, Calzolari M, Gammone M, et al. The state of the science-the impact of declining response rates by nurses in nursing research projects. J Clin Nurs. Apr 02, 2023;32(7-8):e9-e11. [ CrossRef ] [ Medline ]
- Tilastot. The Finnish Union of Practical Nurses. URL: https://www.superliitto.fi/super-info/superin-toiminta/tilastot/ [accessed 2023-09-29]
- Mobile data usage got a boost when we were immobile. Tefficient. URL: https://tefficient.com/mobile-data-usage-got-a-boost-when-we-were-immobile/#more-5938 [accessed 2022-02-21]
- Dexheimer JW, Borycki EM. Use of mobile devices in the emergency department: a scoping review. Health Informatics J. Dec 29, 2015;21(4):306-315. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Flynn GAH, Polivka B, Behr JH. Smartphone use by nurses in acute care settings. CIN: Computers, Informatics, Nursing. 2018;36(3):120-126. [ CrossRef ]
- Zhang H, Cocosila M, Archer N. Factors of adoption of mobile information technology by homecare nurses: a technology acceptance model 2 approach. Comput Inform Nurs. 2010;28(1):49-56. [ CrossRef ] [ Medline ]
- Hyppönen H, Kaipio J, Heponiemi T, Lääveri T, Aalto A, Vänskä J, et al. Developing the national usability-focused health information system scale for physicians: validation study. J Med Internet Res. May 16, 2019;21(5):e12875. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by T de Azevedo Cardoso; submitted 03.03.23; peer-reviewed by S Nissinen, S Ashraf, C Wang, R Zhang ; comments to author 19.09.23; revised version received 06.10.23; accepted 23.04.24; published 29.05.24.
©Satu Paatela, Maiju Kyytsönen, Kaija Saranto, Ulla-Mari Kinnunen, Tuulikki Vehko. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 29.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

IMAGES
VIDEO
COMMENTS
Appeals Nurse Consultant (Remote) CVS Health. Remote in Hartford, CT. $63,200.80 - $136,600.00 a year. Full-time. Monday to Friday. This position will be working from home anywhere in the US. 3+ years of clinical experience required. Primary duties may include, but are not limited to:….
Research Nurse - Ann Arbor, Michigan. Description. Research Nurse. Illingworth Research Group provides a range of patient focused clinical services to the pharmaceutical, healthcare, biotechnology and medical device industries. These include mobile research nursing, patient concierge, medical photography and clinical research services.
Clinical Nurse Specialist - NICU. San Joaquin County California San Joaquin, CA. $11,497.20 to $13,974.13 Monthly. Full-Time. The Clinical Nurse Specialist is a key member of the Neonatal Intensive Care Unit 's professional ... literature, conducts research, attends seminars and maintains membership in professional ...
Remote Care Management Nurse. NEW! Cambia Health Bend, OR. Remote. $33.80 to $55 Hourly. Full-Time. Utilizes evidence-based criteria that incorporates current and validated clinical research findings ... LI- Remote The expected hiring range for a Care Management Nurse is $38.00 - $41.50 an hour ...
Company rating. 6 Research nurse jobs in United States - Work from home. Most relevant. Syneos - Clinical and Corporate - Prod. Research Nurse - Ann Arbor, Michigan. Remote. $47.00 - $57.00 Per Hour (Employer est.) PLEASE NOTE This role will require you to travel, a driving license and access to a vehicle is essential.
Top 10 Work-From-Home Nursing Jobs. 1. Case Management. Case management nurses handle long- and short-term disability claims for patients. They collaborate with physicians, employers, and insurance companies to help facilitate communication and ensure compliance among all the parties involved.
479 Clinical research jobs in United States - Work from home. Will be providing 1:1 telehealth outpatient therapy as an independent contractor, and able to manage own schedule.…. Bachelor's degree in a scientific field of study, with a minimum of 2 years directly supporting clinical research. Drafts informed consents as applicable.….
Glassdoor.com states an annual median salary of $95,396 for Research Nurses and Payscale reports that Clinical Research Nurses earn an average annual salary of $75,217 or $36.86/hr.. Research Nurse Salary by Years of Experience. Research Nurses can earn a higher annual salary with increased years of experience. Less than 1 year of experience earn an average salary of $68,000
Current Remote Job Openings. Intern-Biostatistics (BS) Internship 334397. IT Lead Software Engineer - Remote Information Technology 333247. Senior Manager Quality & Regulatory Operations MCS Laboratory, Business 334456. Senior AI RAQA Specialist - CDH - Remote Business 334494.
2,302,926+ Work from home clinical research nurse practitioner jobs in the United States area. Get new jobs emailed to you daily. Get Notified. Browse 2,302,926 WORK FROM HOME CLINICAL RESEARCH NURSE PRACTITIONER jobs ($59-$128/hr) from companies near you with job openings that are hiring now and 1-click apply!
Year 4: Get licensed by taking the NCLEX-RN exam for registered nurses. (Optional) Years 5-7: Obtain an MSN degree. This program typically takes up to three years to complete. (Optional) Years 5-9: Obtain a Doctor of Philosophy in Nursing (Ph.D.) degree, which can take three to five years to complete. 2+ years of work experience: Whether ...
1,356 Work From Home Clinical Research Nurse jobs hiring near me. Apply to work from home Clinical Research Nurse jobs with estimated salaries, company ratings, and highlights. Browse for work from home internships, junior and senior level Clinical Research Nurse jobs.
Since this is a relatively new and high tech industry, nursing informatics are some of the highest-paid nurses." Research nurse. Being a clinical research nurse is another alternative that involves remote work opportunities, and even the office jobs involved get you home more often than hospital work! "I'm in research," a nurse on ...
The Nurse Scientist is a nurse with advanced preparation (PhD in nursing or related field) in research principles and methodology, who also has expert content knowledge in a specific clinical area. The primary focus of the role is to (1) provide leadership in the development, coordination and management of clinical research studies; (2) provide ...
2 weeks ago. 100% Remote Work. Full-Time. Employee. A range of 117.00 - 140.00 USD Hourly. CA. Treat adult clients with stress, depression, anxiety, or other mental health concerns via video, using short-term, evidence-based therapies. Licensed in CA at the masters or doctoral level, well-versed in evidence-based therapies, like CBT or DBT....
Country Marketing Manager - Woundcare. 21 December by Progress Sales Recruitment Ltd. £70,000 - £75,000 per annum, OTE, inc benefits. London. Permanent, full-time. Work from home. Country Marketing Manager - Wound Management A global leader within the healthcare market that has a reputation for quality products and clinical innovation.
The mission of the National Institute of Nursing Research (NINR) is to promote and improve the health of individuals, families, and communities. To achieve this mission, NINR supports and conducts clinical and basic research and research training on health and illness, research that spans and integrates the behavioral and biological sciences, and that develops the scientific basis for clinical ...
What residents need to know to avoid infections in nursing homes or other long-term care facilities. Skip directly to site content Skip directly to search. ... If you live in a nursing home, assisted living facility or other long-term care facility, you have a higher risk of getting an infection. There are steps you can take to reduce your risk:
Data & Research; Search CMS.gov. Search Search. Popular terms. Physician Fee Schedule; ... Nursing Home Resources. ... Find codes to be reimbursed for clinical services. Show links. Medicare Coverage Database; List of CPT/HCPCS codes; 2023 ICD-10 Procedure Coding System; 2023 ICD-10-CM ;
Texas A&M Agrilife Research College Station, TX. $21.59 Hourly. Part-Time. Education and Experience: -Bachelor's degree in Nursing or equivalent combination of education and experience. -Two years of related experience in clinical research. Knowledge, Skills and Abilities ...
Mount Sinai is hiring a Clinical Nurse-Med-Surge-Stepdown-10W-Mount Sinai Hospital-PT/Nights in US. Review all of the job details and apply today!
That study was used to develop the national certification examination for nurse practitioners. The Journal of Nursing Regulation study evaluated 84 specific tasks that family nurse practitioners are expected to complete as part of their clinical training. The tasks fell across four domains: assessment, diagnosis, treatment, and evaluation of ...
First clinical placements enable nursing students to develop their professional identity through initial socialisation, and where successful, first clinical placement experiences can motivate nursing students to persist with their studies [1,2,3,4].Where the transition from the tertiary environment to learning in the healthcare workplace is turbulent, it may impact nursing students' learning ...
The Journal of Clinical Nursing publishes research and developments relevant to all areas of nursing practice- community, geriatric, mental health, pediatric & more. Abstract Aim The aim of the present study was to describe nurse managers' perceptions of the provision of mentoring for newly graduated registered nurses (NGRNs) and its ...
Background: The transmission of clinical information in nursing predominantly occurs through digital solutions, such as computers and mobile devices, in today's era. Various technological systems, including electronic health records (EHRs) and client information systems (CISs), can be seamlessly integrated with mobile devices. The use of mobile devices is anticipated to rise, particularly as ...