Module 9: Substance-Related and Addictive Disorders
Case studies: substance-abuse disorders, learning objectives.
- Identify substance abuse disorders in case studies

Case Study: Benny
The following story comes from Benny, a 28-year-old living in the Metro Detroit area, USA. Read through the interview as he recounts his experiences dealing with addiction and recovery.
Q : How long have you been in recovery?
Benny : I have been in recovery for nine years. My sobriety date is April 21, 2010.
Q: What can you tell us about the last months/years of your drinking before you gave up?
Benny : To sum it up, it was a living hell. Every day I would wake up and promise myself I would not drink that day and by the evening I was intoxicated once again. I was a hardcore drug user and excessively taking ADHD medication such as Adderall, Vyvance, and Ritalin. I would abuse pills throughout the day and take sedatives at night, whether it was alcohol or a benzodiazepine. During the last month of my drinking, I was detached from reality, friends, and family, but also myself. I was isolated in my dark, cold, dorm room and suffered from extreme paranoia for weeks. I gave up going to school and the only person I was in contact with was my drug dealer.
Q : What was the final straw that led you to get sober?
Benny : I had been to drug rehab before and always relapsed afterwards. There were many situations that I can consider the final straw that led me to sobriety. However, the most notable was on an overcast, chilly October day. I was on an Adderall bender. I didn’t rest or sleep for five days. One morning I took a handful of Adderall in an effort to take the pain of addiction away. I knew it wouldn’t, but I was seeking any sort of relief. The damage this dosage caused to my brain led to a drug-induced psychosis. I was having small hallucinations here and there from the chemicals and a lack of sleep, but this time was different. I was in my own reality and my heart was racing. I had an awful reaction. The hallucinations got so real and my heart rate was beyond thumping. That day I ended up in the psych ward with very little recollection of how I ended up there. I had never been so afraid in my life. I could have died and that was enough for me to want to change.
Q : How was it for you in the early days? What was most difficult?
Benny : I had a different experience than most do in early sobriety. I was stuck in a drug-induced psychosis for the first four months of sobriety. My life was consumed by Alcoholics Anonymous meetings every day and sometimes two a day. I found guidance, friendship, and strength through these meetings. To say early sobriety was fun and easy would be a lie. However, I did learn it was possible to live a life without the use of drugs and alcohol. I also learned how to have fun once again. The most difficult part about early sobriety was dealing with my emotions. Since I started using drugs and alcohol that is what I used to deal with my emotions. If I was happy I used, if I was sad I used, if I was anxious I used, and if I couldn’t handle a situation I used. Now that the drinking and drugs were out of my life, I had to find new ways to cope with my emotions. It was also very hard leaving my old friends in the past.
Q : What reaction did you get from family and friends when you started getting sober?
Benny : My family and close friends were very supportive of me while getting sober. Everyone close to me knew I had a problem and were more than grateful when I started recovery. At first they were very skeptical because of my history of relapsing after treatment. But once they realized I was serious this time around, I received nothing but loving support from everyone close to me. My mother was especially helpful as she stopped enabling my behavior and sought help through Alcoholics Anonymous. I have amazing relationships with everyone close to me in my life today.
Q : Have you ever experienced a relapse?
Benny : I experienced many relapses before actually surrendering. I was constantly in trouble as a teenager and tried quitting many times on my own. This always resulted in me going back to the drugs or alcohol. My first experience with trying to become sober, I was 15 years old. I failed and did not get sober until I was 19. Each time I relapsed my addiction got worse and worse. Each time I gave away my sobriety, the alcohol refunded my misery.
Q : How long did it take for things to start to calm down for you emotionally and physically?
Benny : Getting over the physical pain was less of a challenge. It only lasted a few weeks. The emotional pain took a long time to heal from. It wasn’t until at least six months into my sobriety that my emotions calmed down. I was so used to being numb all the time that when I was confronted by my emotions, I often freaked out and didn’t know how to handle it. However, after working through the 12 steps of AA, I quickly learned how to deal with my emotions without the aid of drugs or alcohol.
Q : How hard was it getting used to socializing sober?
Benny : It was very hard in the beginning. I had very low self-esteem and had an extremely hard time looking anyone in the eyes. But after practice, building up my self-esteem and going to AA meetings, I quickly learned how to socialize. I have always been a social person, so after building some confidence I had no issue at all. I went back to school right after I left drug rehab and got a degree in communications. Upon taking many communication classes, I became very comfortable socializing in any situation.
Q : Was there anything surprising that you learned about yourself when you stopped drinking?
Benny : There are surprises all the time. At first it was simple things, such as the ability to make people smile. Simple gifts in life such as cracking a joke to make someone laugh when they are having a bad day. I was surprised at the fact that people actually liked me when I wasn’t intoxicated. I used to think people only liked being around me because I was the life of the party or someone they could go to and score drugs from. But after gaining experience in sobriety, I learned that people actually enjoyed my company and I wasn’t the “prick” I thought I was. The most surprising thing I learned about myself is that I can do anything as long as I am sober and I have sufficient reason to do it.
Q : How did your life change?
Benny : I could write a book to fully answer this question. My life is 100 times different than it was nine years ago. I went from being a lonely drug addict with virtually no goals, no aspirations, no friends, and no family to a productive member of society. When I was using drugs, I honestly didn’t think I would make it past the age of 21. Now, I am 28, working a dream job sharing my experience to inspire others, and constantly growing. Nine years ago I was a hopeless, miserable human being. Now, I consider myself an inspiration to others who are struggling with addiction.
Q : What are the main benefits that emerged for you from getting sober?
Benny : There are so many benefits of being sober. The most important one is the fact that no matter what happens, I am experiencing everything with a clear mind. I live every day to the fullest and understand that every day I am sober is a miracle. The benefits of sobriety are endless. People respect me today and can count on me today. I grew up in sobriety and learned a level of maturity that I would have never experienced while using. I don’t have to rely on anyone or anything to make me happy. One of the greatest benefits from sobriety is that I no longer live in fear.
Case Study: Lorrie

Figure 1. Lorrie.
Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and “popping pills” at the age of 13, and within the following decade, someone introduced her to cocaine and heroin. She lived with family and occasional boyfriends, and as she puts it, “I had no real home or belongings of my own.”
Before the age of 30, she was trying to survive as a heroin addict. She roamed from job to job, using whatever money she made to buy drugs. She occasionally tried support groups, but they did not work for her. By the time she was in her mid-forties, she was severely depressed and felt trapped and hopeless. “I was really tired.” About that time, she fell in love with a man who also struggled with drugs.
They both knew they needed help, but weren’t sure what to do. Her boyfriend was a military veteran so he courageously sought help with the VA. It was a stroke of luck that then connected Lorrie to friends who showed her an ad in the city paper, highlighting a research study at the National Institute of Drug Abuse (NIDA), part of the National Institutes of Health (NIH.) Lorrie made the call, visited the treatment intake center adjacent to the Johns Hopkins Bayview Medical Center, and qualified for the study.
“On the first day, they gave me some medication. I went home and did what addicts do—I tried to find a bag of heroin. I took it, but felt no effect.” The medication had stopped her from feeling it. “I thought—well that was a waste of money.” Lorrie says she has never taken another drug since. Drug treatment, of course is not quite that simple, but for Lorrie, the medication helped her resist drugs during a nine-month treatment cycle that included weekly counseling as well as small cash incentives for clean urine samples.
To help with heroin cravings, every day Lorrie was given the medication buprenorphine in addition to a new drug. The experimental part of the study was to test if a medication called clonidine, sometimes prescribed to help withdrawal symptoms, would also help prevent stress-induced relapse. Half of the patients received daily buprenorphine plus daily clonidine, and half received daily buprenorphine plus a daily placebo. To this day, Lorrie does not know which one she received, but she is deeply grateful that her involvement in the study worked for her.
The study results? Clonidine worked as the NIDA investigators had hoped.
“Before I was clean, I was so uncertain of myself and I was always depressed about things. Now I am confident in life, I speak my opinion, and I am productive. I cry tears of joy, not tears of sadness,” she says. Lorrie is now eight years drug free. And her boyfriend? His treatment at the VA was also effective, and they are now married. “I now feel joy at little things, like spending time with my husband or my niece, or I look around and see that I have my own apartment, my own car, even my own pots and pans. Sounds silly, but I never thought that would be possible. I feel so happy and so blessed, thanks to the wonderful research team at NIDA.”
- Liquor store. Authored by : Fletcher6. Located at : https://commons.wikimedia.org/wiki/File:The_Bunghole_Liquor_Store.jpg . License : CC BY-SA: Attribution-ShareAlike
- Benny Story. Provided by : Living Sober. Located at : https://livingsober.org.nz/sober-story-benny/ . License : CC BY: Attribution
- One patientu2019s story: NIDA clinical trials bring a new life to a woman struggling with opioid addiction. Provided by : NIH. Located at : https://www.drugabuse.gov/drug-topics/treatment/one-patients-story-nida-clinical-trials-bring-new-life-to-woman-struggling-opioid-addiction . License : Public Domain: No Known Copyright

- Continuing Education
- Practice Tools
- Partnerships
- Interest Form
- Case Studies
- MyU : For Students, Faculty, and Staff
Co-occurring Mental Health and Substance Use Disorders: Guiding Principles and Recovery Strategies in Integrated Care (Part 1)
Individuals with co-occurring mental health and substance use disorders (CODs) have complex treatment needs. Historically, these issues were treated separately, as competing discreet needs. Barriers in access to integrated care for substance related and mental health disorders prevented many individuals from finding relief from their COD. The structures in place that prevented integrated care were many. Public and private funding, research, and public policy all created troughs between disciplines of care. Researchers and practitioners have noted how the separation of mental health and substance abuse treatment has created additional barriers and obstacles for clients with CODs: Parallel treatment results in fragmentation of services, non-adherence to interventions, dropout, and service extrusion, because treatment programs remain rigidly focused on single disorders and individuals with dual disorders are unable to negotiate the separate systems and to make sense of disparate messages regarding treatment and recovery (Osher, Drake, 1996; Drake, Mueser, Brunette, and McHugo. 2004).
Mental health services and treatment structures for substance related disorders were on divergent paths and many professionals considered one another with skepticism. Today, some, but not all, of those barriers have been eliminated.
According to the Substance Abuse and Mental Health Services Administration’s (SAMHSA) 2011 National Survey on Drug Use and Health, Mental Health Findings, more than 8 million adults in the United States have CODs. Only 6.9% of individuals receive treatment for both conditions and 56.6% receive no treatment at all (SAMHSA, 2012).
This is the first of two practice briefs that will explore eight principles of integrated care for CODs (Mueser et al., 2003). This brief will examine the first four of the following principles:
- Principle 1: Integration of mental health and substance use services
- Principle 2: Access to comprehensive assessment of substance use and mental health concerns
- Principle 3: Comprehensive variety of services offered to clients
- Principle 4: An assertive approach to care/service delivery
- Principle 5: Using a harm reduction approach to care
- Principle 6: Motivation-based and stage wise interventions
- Principle 7: Long-term perspective of care
- Principle 8: Providing multiple psychotherapeutic modalities
After a brief review of each principle, an illustrative case study will be provided and suggestions for implementing each of the principles in a client session will be offered (SAMHSA, 2009a; 2009b).
Principle 1: Integration of Mental Health and Substance Use Services
Multidisciplinary teams provide integrated services and relevant care that is client centered and longitudinal in nature. Agency policies and practices recognize the relapse potential with CODs and do not penalize clients for exhibiting symptoms of their mental health or substance related disorders. Team members may include the client and their family members or supportive persons, practitioners who are trained in substance abuse and mental health counseling, and a combination of physicians, nurses, case managers, or providers of ancillary rehabilitation services (therapy, vocational, housing, etc.) such as social workers, psychologists, psychiatrists, marriage and family therapists and peer support specialists. Based on their respective areas of expertise, team members collaborate to deliver integrated services relevant to the client’s specific circumstances, assist in making progress toward goals, and adjust services over time to meet individuals’ evolving needs (Mueser, Drake, & Noordsy, 2013). The team members consistently and regularly communicate with the client to discuss progress towards goals, and they work together to meet the individual treatment needs of each client.
Penny, 43, experienced her first depressive episode in her mid teens. During her first treatment for substance use (marijuana and alcohol) at age 17, Penny was diagnosed with attention deficit hyperactivity disorder (ADHD). However, over the next few years, she became increasingly edgy and irritable with intermittent periods of euphoria, accelerated energy and impulsive behaviors followed by periods of despair. She had repeated hospitalizations and concurrent and sequential contact with both mental health and substance abuse treatment systems over the years. Penny was labeled with a variety of diagnoses, including bipolar disorder, ADHD, major depression, anxiety disorder, borderline personality disorder, and chemical dependence.
Penny’s multi-disciplinary team consisted of her primary practitioner who held LADC/LPCC dual licenses, a primary care physician, a psychiatrist, a family therapist, a peer recovery support specialist, and a vocational specialist. Penny participated in individual therapy as well as recovery skills groups with her primary practitioner. Her primary care physician monitored Penny’s physical concerns including her diabetes and hypothyroid disorder. Penny’s psychiatrist prescribed and monitored Penny’s mood-stabilizing medications and provided case consultation to Penny’s team. The family therapist provided ongoing support to Penny and her boyfriend Don, and helped Penny and her team decide if and when to begin reparations in her relationship with her children. In addition, the family therapist provided feedback to the team about how Penny’s relationships impacted her recovery status and overall stability. The vocational specialist acted as a resource for Penny once she expressed a desire to return to work, helped Penny and her team identify resources for employment, and acted as liaison with Penny’s employer. The peer recovery support specialist helped Penny identify recovery support groups and helped Penny and her team identify barriers and resources to overcome those barriers to recovery success.
Principle 2: Access to Comprehensive Assessment of Substance Use and Mental Health Concerns
Integrated care recognizes that CODs and the resulting consequences of those conditions are commonplace. Therefore, practice protocols that standardize comprehensive biopsychosocial assessments are essential to identifying major mental illnesses and substance use. A comprehensive assessment includes screening, and when needed, further examination of substance use and mental health concerns. Practitioners utilize information collected from the comprehensive assessment to provide recommendations for treatment —such as the role one condition has on the efficacy of particular treatment strategies for the other condition(s). Screening tools for substance related disorders can include the CAGE-AID (Brown & Rounds, 1995), the Michigan Alcohol Screening Test (MAST) (Selzer, 1971), the Drug and Alcohol Screen Test (DAST) or the Alcohol Use Disorders Identification Test (AUDIT) (Saunders et al., 1993). For mental health concerns the Global Appraisal of Individual Needs-Short Screener (GAIN-SS) (Dennis, Chan, & Funk, 2006), or Brief Symptom Inventory (BSI) (Derogatis & Melisaratos, 1983) may be used.
When feasible, the practitioner gathers information from the client’s family and other professional resources who might have relevant information regarding symptom severity, substance use, and role functioning. Information gathered during the initial assessment can assist in a collaborative goal setting process. Ongoing assessment is critical in the treatment of co-occurring disorders and involves evaluation of changes in circumstances, substance use, stability and symptom expression, and goal attainment. Conducting a comprehensive integrated assessment helps define areas that can be addressed in treatment and identify specific treatment recommendations (Mueser et al., 2013). The context of the comprehensive assessment should occur within a recovery-oriented perspective. Progress toward recovery is individualized as described in the following definition: A process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential (SAMHSA, CMHS, 2011).
Penny and her primary practitioner completed a comprehensive biopsychosocial assessment that included questions about distressing mental health symptoms as well as substance use patterns and periods of abstinence/remission. During her early 20s Penny entered college to become a nurse. Soon after beginning school, her anxiety increased. She experienced racing thoughts, extreme irritability, interruptions in sleep and a pronounced overconfidence followed by periods of despair and an inability to get out of bed. Penny returned to using alcohol and marijuana and eventually discontinued her education.
In her early 30s, Penny completed substance abuse treatment and was abstinent from alcohol and marijuana. She also participated in individual therapy and was prescribed lithium. She experienced a period of relative stability and returned to school. However, Penny disliked the side effects of her medication and felt she was stable enough to discontinue taking the lithium. She sought care from a physician for her anxiety and was placed on the benzodiazepine Xanax.
Penny currently lives with Don, her boyfriend of 8 years. Due to chronic conflict in their relationship, she is in danger of becoming homeless. Don has a construction business and manages to make a solid living. They both smoke marijuana most evenings as a way to wind down from the day. Don occasionally uses cocaine and in very rare situations Penny has joined him. She has been abstinent from alcohol since receiving a DWI 9 months ago. Penny has been estranged from her two adult children, Linda, 24, and Jeff, 22, for 6 months and 3 years, respectively. Her parents are deceased.
Penny’s practitioner was able to collect information from Penny’s boyfriend, her children, previous therapists, agencies and hospitals with whom she has had contact. During the assessment the practitioner discovered information about periods of increased mental illness symptoms while Penny was abstinent from substances, and a return to substance use in correlation with mental illness symptoms. The comprehensive assessment provided initial information about Penny’s current mental illness symptoms and substance use and was used to determine treatment priorities and programs that align with Penny’s needs.
Principle 3: Comprehensive Variety of Services Offered to Clients
Clients are provided with comprehensive integrated services that are cohesive, relevant and responsive to their identified needs and goals (Bipolar Disorder, n.d.). Practitioners coordinate with one another and collaborate with the client to prioritize treatment needs in a manner that does not overwhelm the client. A multidisciplinary team provides support for a broad range of issues relevant to the client population served by the agency. This includes culturally relevant information about community support systems and an array of mental health or substance related resources available to clients and their support persons.
Comprehensive services that are relevant to persons with CODs often include but are not limited to: medication assisted therapy, cognitive behavioral therapy (CBT), family therapy, life skills/ psychosocial rehabilitation, psychoeducation, and supported employment. Medication assisted therapy helps control distressing symptoms of many health and mental health dis-orders and is helpful for mood stabilization. Medication is also used in the treatment of substance use disorders to inhibit substance use, reduce cravings, reduce withdrawal symptoms, and as replacement therapy. CBT helps people with CODs learn to change harmful or negative thought patterns and behaviors.
Family therapy enhances coping strategies and focuses on improving communication and problem solving amongst family members and significant others. Life skills/rehabilitation provides clients with new information and opportunities to practice skills such as sleep hygiene practices, self-care, stress reduction and management, and medication maintenance. Psychoeducation provides information about the interacting dynamics of CODs and treatment (e.g., recognition of early signs of relapse so they can seek support before a full-blown episode occurs.) Supported employment provides opportunities for the client to contribute meaningfully in a work environment. A vocational specialist is part of the treatment team and works as a liaison with employers, client and the rest of the treatment team to support the client in the work environment. A case manager/navigator assists the client and their support persons in access-ing resources necessary to their recovery. These relationships are longitudinal in nature and supportive rather than therapeutic.
Penny and her treatment team agreed that she would benefit from mood stabilizing medication for her mental health disorder as well as cognitive behavioral therapy to help her develop coping strategies to help regulate and stabilize symptoms such as feelings of despair, racing thoughts, and behavioral dysregulation. Penny and Don recently began family counseling to explore the role and impact of substance use on their relationship, to develop communication skills and to identify strategies to help Don support Penny in her recovery from COD. Penny expressed interest in mending the relationship with her children in the future. If they are reunited, Penny identified a goal of attending family therapy with her children to improve communication and explore the impact of her COD on her relationship with them. Penny also identified a desire to return to work and will be making an appointment to discuss her work goals with the supported employment specialist.
Penny participates in a skills group to assist her in managing the symptoms of her CODs such as emotional and behavioral regulation, self care, sleep hygiene, and to manage triggers related to her substance use.
Principle 4: An Assertive Approach to Care/Service Delivery
Assertive outreach involves reaching out to individuals who are at risk or in crisis and their concerned persons, by providing support and engaging them in the change process. Sometimes this occurs by engaging the individual who seeks care for a substance use issue and providing services that stabilize a COD. An assertive approach is time unlimited and occurs in a variety of situations, including a client’s own community setting (Bond, 1991; Bond, McGrew, & Fekete, 1995). Assertive outreach includes meeting the client in community locations and providing practical assistance in daily living needs. These strategies increase or decrease in intensity depending on the client’s day-to-day living needs such as housing, transportation, money management, or seeking employment. This approach also provides opportunities to explore and address how substance use interferes with goal attainment.
Assertive outreach by Penny’s multidisciplinary team included meeting with a vocational specialist to assist Penny in looking for a job. Penny’s primary practitioner met with Penny weekly in Penny’s home and discussed progress towards her goals. Although Penny had not declared she wanted to stop using or cut down this provided Penny’s practitioner with an opportunity to introduce discrepancy by exploring how substance use interfered with taking steps toward Penny’s goals and practicing or using coping skills. Penny and her primary practitioner examined how Penny’s use impeded her ability to follow through with completing job applications and job interviews as steps toward finding steady, meaningful work.
This brief examined four of the eight principles of COD treatment. The first four principles underscore the importance of the integration of COD services and access to comprehensive assessment and care using assertive outreach and a client centered approach. The next brief will explore the latter four COD principles and implementation strategies. The final COD principles emphasize a long-term care model using a harm-reduction approach, motivation-based stage-wise treatment interventions and multiple treatment modalities (Mueser et al., 2003). The principles in both briefs place the client and their support persons, front and center as active participants, guides, resources and experts in their own recovery. Unpacking the principles of integrated treatment for CODs provides opportunities for practitioners to utilize multiple strategies to engage clients in treatment as discussed in this practice brief.
As you consider the practice of integrated care, examine your agency and your own clinical practice. Consider how you might try new strategies in an effort to implement the principles of COD treatment. We invite practitioners to engage in a dialogue surround-ing the strategies implemented in sessions to engage COD clients. Please consider the following and email us to describe successful COD strategies and challenges utilizing the principles of COD treatment.
- What strategies have you tried using one of the above principles that worked particularly well?
- What challenges have you encountered?
- Please provide suggestions for additional strategies you found helpful.

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years! Learn More >>
- Health Topics
- Brochures and Fact Sheets
- Help for Mental Illnesses
- Clinical Trials
Substance Use and Co-Occurring Mental Disorders
What does it mean to have substance use and co-occurring mental disorders.
Substance use disorder (SUD) is a treatable mental disorder that affects a person’s brain and behavior, leading to their inability to control their use of substances like legal or illegal drugs, alcohol, or medications. Symptoms can be moderate to severe, with addiction being the most severe form of SUD.
People with a SUD may also have other mental health disorders, and people with mental health disorders may also struggle with substance use. These other mental health disorders can include anxiety disorders , depression , attention-deficit hyperactivity disorder (ADHD) , bipolar disorder , personality disorders , and schizophrenia , among others. For more information, please see the National Institute on Drug Abuse (NIDA) Common Comorbidities with Substance Use Disorders Research Report .
Though people might have both a SUD and a mental disorder, that does not mean that one caused the other. Research suggests three possibilities that could explain why SUDs and other mental disorders may occur together:
- Common risk factors can contribute to both SUDs and other mental disorders. Both SUDs and other mental disorders can run in families, meaning certain genes may be a risk factor. Environmental factors, such as stress or trauma, can cause genetic changes that are passed down through generations and may contribute to the development of a mental disorder or a substance use disorder.
- Mental disorders can contribute to substance use and SUDs. Studies found that people with a mental disorder, such as anxiety, depression, or post-traumatic stress disorder (PTSD) , may use drugs or alcohol as a form of self-medication. However, although some drugs may temporarily help with some symptoms of mental disorders, they may make the symptoms worse over time. Additionally, brain changes in people with mental disorders may enhance the rewarding effects of substances, making it more likely they will continue to use the substance.
- Substance use and SUDs can contribute to the development of other mental disorders. Substance use may trigger changes in brain structure and function that make a person more likely to develop a mental disorder.
How are substance use disorder and co-occurring mental disorders diagnosed and treated?
When someone has a SUD and another mental health disorder, it is usually better to treat them at the same time rather than separately. People who need help for a SUD and other mental disorders should see a health care provider for each disorder. It can be challenging to make an accurate diagnosis because some symptoms are the same for both disorders, so the provider should use comprehensive assessment tools to reduce the chance of a missed diagnosis and provide the right treatment.
It also is essential that the provider tailor treatment, which may include behavioral therapies and medications, to an individual’s specific combination of disorders and symptoms. It should also take into account the person’s age, the misused substance, and the specific mental disorder(s). Talk to your health care provider to determine what treatment may be best for you and give the treatment time to work.
Behavioral therapies
Research has found several behavioral therapies that have promise for treating individuals with co-occurring substance use and mental disorders. Health care providers may recommend behavioral therapies alone or in combination with medications.
Some examples of effective behavioral therapies for adults with SUDs and different co-occurring mental disorders include:
- Cognitive behavioral therapy (CBT) is a type of talk therapy aimed at helping people learn how to cope with difficult situations by challenging irrational thoughts and changing behaviors.
- Dialectical behavior therapy (DBT) uses concepts of mindfulness and acceptance or being aware of and attentive to the current situation and emotional state. DBT also teaches skills that can help control intense emotions, reduce self-destructive behaviors (such as suicide attempts, thoughts, or urges; self-harm; and drug use), and improve relationships.
- Assertive community treatment (ACT) is a form of community-based mental health care that emphasizes outreach to the community and an individualized treatment approach.
- Therapeutic communities (TC) are a common form of long-term residential treatment that focuses on helping people develop new and healthier values, attitudes, and behaviors.
- Contingency management (CM) principles encourage healthy behaviors by offering vouchers or rewards for desired behaviors.
Behavioral therapies for children and adolescents
Some effective behavioral treatments for children and adolescents include:
- Brief strategic family therapy (BSFT) therapy targets family interactions thought to maintain or worsen adolescent SUDs and other co-occurring problem behaviors.
- Multidimensional family therapy (MDFT) works with the whole family to simultaneously address multiple and interacting adolescent problem behaviors, such as substance use, mental disorders, school problems, delinquency, and others.
- Multisystemic therapy (MST) targets key factors associated with serious antisocial behavior in children and adolescents with SUDs.
Medications
There are effective medications that treat opioid , alcohol , and nicotine addiction and lessen the symptoms of many other mental disorders. Some medications may be useful in treating multiple disorders. For more information on behavioral treatments and medications for SUDs, visit NIDA’s Drug Facts and Treatment webpages. For more information about treatment for mental disorders, visit NIMH's Health Topics webpages.
How can I find help for substance use and co-occurring mental disorders?
To find mental health treatment services in your area, call the Substance Abuse and Mental Health Services Administration (SAMHSA) National Helpline at 1-800-662-HELP (4357), visit the SAMHSA online treatment locator , or text your ZIP code to 435748.
For additional resources about finding help, visit:
NIMH's Help for Mental Illnesses page
National Cancer Institute’s Smokefree.gov website, or call their smoking quitline at 1-877-44U-QUIT (1-877-448-7848)
If you or someone you know is struggling or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org . In life-threatening situations, call 911.
How can I find a clinical trial for substance use and co-occurring mental disorders?
Clinical trials are research studies that look at new ways to prevent, detect, or treat diseases and conditions. The goal of clinical trials is to determine if a new test or treatment works and is safe. Although individuals may benefit from being part of a clinical trial, participants should be aware that the primary purpose of a clinical trial is to gain new scientific knowledge so that others may be better helped in the future.
Researchers at NIMH and around the country conduct many studies with patients and healthy volunteers. We have new and better treatment options today because of what clinical trials uncovered years ago. Be part of tomorrow’s medical breakthroughs. Talk to your health care provider about clinical trials, their benefits and risks, and whether one is right for you.
To learn more or find a study, visit:
- NIMH’s Clinical Trials webpage : Information about participating in clinical trials related to mental disorders
- Clinicaltrials.gov: Current studies on mental illness and substance misuse : List of clinical trials funded by the National Institutes of Health (NIH) being conducted across the country
Where can I learn more about substance use and co-occurring disorders?
Brochures and other educational resources.
- National Institute on Alcohol Abuse and Alcoholism (NIAAA) Publications Order Form
- NIDA: Parents and Educators
- SAMHSA Publications and Digital Products
- Alcohol Use Disorder (also en español )
- Drug Use and Addiction (also en español )
- Mental Health and Behavior (also en español )
- Opioids and Opioid Use Disorder (also en español )
- Risks of tobacco (also en español )
- NIH Experts Discuss the Intersection of Suicide and Substance Use : Learn about common risk factors, populations at elevated risk, suicides by drug overdose, treatments, prevention, and resources for finding help.
- NIDA Common Physical and Mental Health Comorbidities with Substance Use Disorders Research Report
- NIDA Tobacco, Nicotine, and E-Cigarettes Research Report
- SAMHSA National Survey on Drug Use and Health
- Suicide Deaths Are a Major Component of the Opioid Crisis that Must Be Addressed
- NIMH and the NIH HEAL Initiative: Collaborating to address the opioid epidemic
- NIMH’s Role in the NIH HEAL Initiative
Last reviewed: March 2024
Unless otherwise specified, the information on our website and in our publications is in the public domain and may be reused or copied without permission. However, you may not reuse or copy images. Please cite the National Institute of Mental Health as the source. Read our copyright policy to learn more about our guidelines for reusing NIMH content.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

Alcohol's Effects on Health
Research-based information on drinking and its impact.
National Institute on Alcohol Abuse and Alcoholism (NIAAA)
Understanding alcohol use disorder.
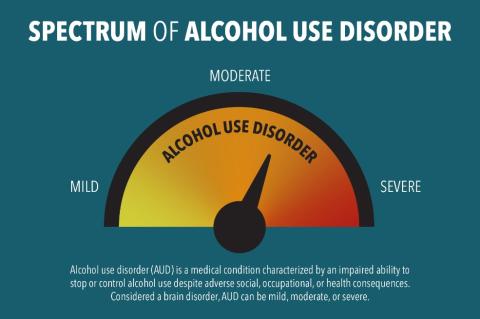
Alcohol use disorder (AUD) is a medical condition characterized by an impaired ability to stop or control alcohol use despite adverse social, occupational, or health consequences. It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Considered a brain disorder, AUD can be mild, moderate, or severe. Lasting changes in the brain caused by alcohol misuse perpetuate AUD and make individuals vulnerable to relapse. The good news is that no matter how severe the problem may seem, evidence-based treatment with behavioral therapies, mutual-support groups, and/or medications can help people with AUD achieve and maintain recovery. According to the 2022 National Survey on Drug Use and Health, 28.8 million adults ages 18 and older (11.2% in this age group) had AUD in 2021. 1,2 Among youth, an estimated 753,000 adolescents ages 12 to 17 (2.9% of this age group) had AUD during this time frame. 1,2
What Increases the Risk for Alcohol Use Disorder?
A person’s risk for developing AUD depends in part on how much, how often, and how quickly they consume alcohol. Alcohol misuse, which includes binge drinking and heavy alcohol use , over time increases the risk of AUD. Other factors also increase the risk of AUD, such as:
- Drinking at an early age. A recent national survey found that among people ages 26 and older, those who began drinking before age 15 were more than three times as likely to report having AUD in the past year as those who waited until age 21 or later to begin drinking. 3 The risk for females in this group is higher than that of males.
- Genetics and family history of alcohol problems. Genetics play a role, with hereditability accounting for approximately 60%; however, like other chronic health conditions, AUD risk is influenced by the interplay between a person’s genes and their environment. Parents’ drinking patterns may also influence the likelihood that a child will one day develop AUD.
- Mental health conditions and a history of trauma. A wide range of psychiatric conditions—including depression, post-traumatic stress disorder, and attention deficit hyperactivity disorder—are comorbid with AUD and are associated with an increased risk of AUD. People with a history of childhood trauma are also vulnerable to AUD.
What Are the Symptoms of Alcohol Use Disorder?
Health care professionals use criteria from the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), to assess whether a person has AUD and to determine the severity, if the disorder is present. Severity is based on the number of criteria a person meets based on their symptoms—mild (2–3 criteria), moderate (4–5 criteria), or severe (6 or more criteria).
A health care provider might ask the following questions to assess a person’s symptoms.
In the past year, have you:
- Had times when you ended up drinking more, or longer, than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time drinking, being sick from drinking, or getting over other aftereffects?
- Wanted a drink so badly you couldn’t think of anything else?
- Found that drinking—or being sick from drinking—often interfered with taking care of your home or family? Or caused job troubles? Or school problems?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities you found important, interesting, or pleasurable so you could drink?
- More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or unsafe sexual behavior)?
- Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had an alcohol-related memory blackout?
- Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
- Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, restlessness, nausea, sweating, a racing heart, dysphoria (feeling uneasy or unhappy), malaise (general sense of being unwell), feeling low, or a seizure? Or sensed things that were not there?
Any of these symptoms may be cause for concern. The more symptoms, the more urgent the need for change.
What Are the Types of Treatment for Alcohol Use Disorder?
Several evidence-based treatment approaches are available for AUD. One size does not fit all and a treatment approach that may work for one person may not work for another. Treatment can be outpatient and/or inpatient and be provided by specialty programs, therapists, and health care providers.
Medications
Three medications are currently approved by the U.S. Food and Drug Administration to help people stop or reduce their drinking and prevent a return to drinking: naltrexone (oral and long-acting injectable), acamprosate, and disulfiram. All these medications are nonaddictive, and they may be used alone or combined with behavioral treatments or mutual-support groups.
Behavioral Treatments
Behavioral treatments—also known as alcohol counseling, or talk therapy, and provided by licensed therapists—are aimed at changing drinking behavior. Examples of behavioral treatments are brief interventions and reinforcement approaches, treatments that build motivation and teach skills for coping and preventing a return to drinking, and mindfulness-based therapies.
Mutual-Support Groups
Mutual-support groups provide peer support for stopping or reducing drinking. Group meetings are available in most communities at low or no cost, and at convenient times and locations—including an increasing presence online. This means they can be especially helpful to individuals at risk for relapse to drinking. Combined with medications and behavioral treatment provided by health care professionals, mutual-support groups can offer a valuable added layer of support.
Please note: People with severe AUD may need medical help to avoid alcohol withdrawal if they decide to stop drinking. Alcohol withdrawal is a potentially life-threatening process that can occur when someone who has been drinking heavily for a prolonged period of time suddenly stops drinking. Doctors can prescribe medications to address these symptoms and make the process safer and less distressing.
Can People With Alcohol Use Disorder Recover?
Many people with AUD do recover, but setbacks are common among people in treatment. Seeking professional help early can prevent a return to drinking. Behavioral therapies can help people develop skills to avoid and overcome triggers, such as stress, that might lead to drinking. Medications also can help deter drinking during times when individuals may be at greater risk of a return to drinking (e.g., divorce, death of a family member).
If you are concerned about your alcohol use and would like to explore whether you might have AUD, please visit the Rethinking Drinking website .
To learn more about alcohol treatment options and search for quality care near you, please visit the NIAAA Alcohol Treatment Navigator .
For more information about alcohol and your health, please visit: niaaa.nih.gov
1 SAMHSA, Center for Behavioral Health Statistics and Quality. 2022 National Survey on Drug Use and Health. Table 5.1A—Substance use disorder for specific substances in past year: among people aged 12 or older; by age group, numbers in thousands, 2021 and 2022 [cited 2023 Dec 29]. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect5pe2022.htm#tab5.1a
2 SAMHSA, Center for Behavioral Health Statistics and Quality. 2022 National Survey on Drug Use and Health. Table 5.1B—Substance use disorder for specific substances in past year: among people aged 12 or older; by age group, percentages, 2021 and 2022 [cited 2023 Dec 29]. Available from: https://www.samhsa.gov/data/sites/default/files/reports/rpt42728/NSDUHDetailedTabs2022/NSDUHDetailedTabs2022/NSDUHDetTabsSect5pe2022.htm#tab5.1b
3 Age at drinking onset: age when first drank a beverage containing alcohol (a can or bottle of beer, a glass of wine or a wine cooler, a shot of distilled spirits, or a mixed drink with distilled spirits in it), not counting a sip or two from a drink. AUD: having met two or more of the 11 AUD diagnostic criteria in the past-year according to the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) AUD risk across different ages at drinking onset is compared using the prevalence ratio weighted by the person-level analysis weight. Derived from the Center for Behavioral Health Statistics and Quality 2022 National Survey on Drug Use and Health (NSDUH-2022-DS0001) public-use file. [cited 2024 Jan 12]. Available from: https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2022-nsduh-2022-ds0001
niaaa.nih.gov
An official website of the National Institutes of Health and the National Institute on Alcohol Abuse and Alcoholism

- Request new password
- Create a new account
Introduction to Social Work: An Advocacy-Based Profession
Student resources, case studies.
Case Study for Chapter 10: Substance Use and Addiction
Jennifer’s brother Emmett resorted to drugs and alcohol to drown his sorrow after their dad left their mother. The local inner city high school had its share of dealers and Emmett’s will power was nil. While weed (cannabis, marijuana, pot) was Emmett’s initial drug of choice, his substance use later led him to having a heroin addiction. Now out of the closet as a gay man, Emmett also was introduced to the club/party drugs of ecstasy and crystal meth. It breaks Jennifer’s and her mom’s heart to watch Emmett maintain his addiction despite some brief stints in drug rehab and attendance at local AA meetings. Emmett’s sponsor uses tough love—a mix of encouragement and challenge—to help Emmett stay on his path to and through recovery.
1) What local, state, and national policy and practice resources exist for social workers who work with people who abuse substances?
2) With the help of a social worker, how might family members intervene to help Emmett recover and maintain his sobriety? How might they benefit personally from social work services as well?
3) How much stigma encircles people who succumb to substance abuse or addiction?
4) What specific challenges might need to be addressed in treatment in order for Emmett to truly achieve a high functioning level?
- Patient Care & Health Information
- Diseases & Conditions
- Drug addiction (substance use disorder)
Diagnosing drug addiction (substance use disorder) requires a thorough evaluation and often includes an assessment by a psychiatrist, a psychologist, or a licensed alcohol and drug counselor. Blood, urine or other lab tests are used to assess drug use, but they're not a diagnostic test for addiction. However, these tests may be used for monitoring treatment and recovery.
For diagnosis of a substance use disorder, most mental health professionals use criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association.
- Care at Mayo Clinic
Our caring team of Mayo Clinic experts can help you with your drug addiction (substance use disorder)-related health concerns Start Here
Although there's no cure for drug addiction, treatment options can help you overcome an addiction and stay drug-free. Your treatment depends on the drug used and any related medical or mental health disorders you may have. Long-term follow-up is important to prevent relapse.
Treatment programs
Treatment programs for substance use disorder usually offer:
- Individual, group or family therapy sessions
- A focus on understanding the nature of addiction, becoming drug-free and preventing relapse
- Levels of care and settings that vary depending on your needs, such as outpatient, residential and inpatient programs
Withdrawal therapy
The goal of detoxification, also called "detox" or withdrawal therapy, is to enable you to stop taking the addicting drug as quickly and safely as possible. For some people, it may be safe to undergo withdrawal therapy on an outpatient basis. Others may need admission to a hospital or a residential treatment center.
Withdrawal from different categories of drugs — such as depressants, stimulants or opioids — produces different side effects and requires different approaches. Detox may involve gradually reducing the dose of the drug or temporarily substituting other substances, such as methadone, buprenorphine, or a combination of buprenorphine and naloxone.
Opioid overdose
In an opioid overdose, a medicine called naloxone can be given by emergency responders, or in some states, by anyone who witnesses an overdose. Naloxone temporarily reverses the effects of opioid drugs.
While naloxone has been on the market for years, a nasal spray (Narcan, Kloxxado) and an injectable form are now available, though they can be very expensive. Whatever the method of delivery, seek immediate medical care after using naloxone.
Medicine as part of treatment
After discussion with you, your health care provider may recommend medicine as part of your treatment for opioid addiction. Medicines don't cure your opioid addiction, but they can help in your recovery. These medicines can reduce your craving for opioids and may help you avoid relapse. Medicine treatment options for opioid addiction may include buprenorphine, methadone, naltrexone, and a combination of buprenorphine and naloxone.
Behavior therapy
As part of a drug treatment program, behavior therapy — a form of psychotherapy — can be done by a psychologist or psychiatrist, or you may receive counseling from a licensed alcohol and drug counselor. Therapy and counseling may be done with an individual, a family or a group. The therapist or counselor can:
- Help you develop ways to cope with your drug cravings
- Suggest strategies to avoid drugs and prevent relapse
- Offer suggestions on how to deal with a relapse if it occurs
- Talk about issues regarding your job, legal problems, and relationships with family and friends
- Include family members to help them develop better communication skills and be supportive
- Address other mental health conditions
Self-help groups
Many, though not all, self-help support groups use the 12-step model first developed by Alcoholics Anonymous. Self-help support groups, such as Narcotics Anonymous, help people who are addicted to drugs.
The self-help support group message is that addiction is an ongoing disorder with a danger of relapse. Self-help support groups can decrease the sense of shame and isolation that can lead to relapse.
Your therapist or licensed counselor can help you locate a self-help support group. You may also find support groups in your community or on the internet.
Ongoing treatment
Even after you've completed initial treatment, ongoing treatment and support can help prevent a relapse. Follow-up care can include periodic appointments with your counselor, continuing in a self-help program or attending a regular group session. Seek help right away if you relapse.
More Information
Drug addiction (substance use disorder) care at Mayo Clinic
- Cognitive behavioral therapy
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Coping and support
Overcoming an addiction and staying drug-free require a persistent effort. Learning new coping skills and knowing where to find help are essential. Taking these actions can help:
- See a licensed therapist or licensed drug and alcohol counselor. Drug addiction is linked to many problems that may be helped with therapy or counseling, including other underlying mental health concerns or marriage or family problems. Seeing a psychiatrist, psychologist or licensed counselor may help you regain your peace of mind and mend your relationships.
- Seek treatment for other mental health disorders. People with other mental health problems, such as depression, are more likely to become addicted to drugs. Seek immediate treatment from a qualified mental health professional if you have any signs or symptoms of mental health problems.
- Join a support group. Support groups, such as Narcotics Anonymous or Alcoholics Anonymous, can be very effective in coping with addiction. Compassion, understanding and shared experiences can help you break your addiction and stay drug-free.
Preparing for your appointment
It may help to get an independent perspective from someone you trust and who knows you well. You can start by discussing your substance use with your primary care provider. Or ask for a referral to a specialist in drug addiction, such as a licensed alcohol and drug counselor, or a psychiatrist or psychologist. Take a relative or friend along.
Here's some information to help you get ready for your appointment.
What you can do
Before your appointment, be prepared:
- Be honest about your drug use. When you engage in unhealthy drug use, it can be easy to downplay or underestimate how much you use and your level of addiction. To get an accurate idea of which treatment may help, be honest with your health care provider or mental health provider.
- Make a list of all medicines, vitamins, herbs or other supplements that you're taking, and the dosages. Tell your health care provider and mental health provider about any legal or illegal drugs you're using.
- Make a list of questions to ask your health care provider or mental health provider.
Some questions to ask your provider may include:
- What's the best approach to my drug addiction?
- Should I see a psychiatrist or other mental health professional?
- Will I need to go to the hospital or spend time as an inpatient or outpatient at a recovery clinic?
- What are the alternatives to the primary approach that you're suggesting?
- Are there any brochures or other printed material that I can have? What websites do you recommend?
Don't hesitate to ask other questions during your appointment.
What to expect from your doctor
Your provider is likely to ask you several questions, such as:
- What drugs do you use?
- When did your drug use first start?
- How often do you use drugs?
- When you take a drug, how much do you use?
- Do you ever feel that you might have a problem with drugs?
- Have you tried to quit on your own? What happened when you did?
- If you tried to quit, did you have withdrawal symptoms?
- Have any family members criticized your drug use?
- Are you ready to get the treatment needed for your drug addiction?
Be ready to answer questions so you'll have more time to go over any points you want to focus on.
- Substance-related and addictive disorders. In: Diagnostic and Statistical Manual of Mental Disorders DSM-5. 5th ed. American Psychiatric Association; 2013. https://dsm.psychiatryonline.org. Accessed Aug. 15, 2022.
- Brown AY. Allscripts EPSi. Mayo Clinic. April 13, 2021.
- DrugFacts: Understanding drug use and addiction. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/understanding-drug-use-addiction. Accessed Aug. 15, 2022.
- American Psychiatric Association. What is a substance use disorder? https://psychiatry.org/patients-families/addiction-substance-use-disorders/what-is-a-substance-use-disorder. Accessed Sept. 2, 2022.
- Eddie D, et al. Lived experience in new models of care for substance use disorder: A systematic review of peer recovery support services and recovery coaching. Frontiers in Psychology. 2019; doi:10.3389/fpsyg.2019.01052.
- Commonly used drugs charts. National Institute on Drug Abuse. https://www.drugabuse.gov/drug-topics/commonly-used-drugs-charts. Accessed Aug. 16, 2022.
- Drugs, brains, and behavior: The science of addiction. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drug-misuse-addiction. Accessed Aug. 16, 2022.
- Drugs of abuse: A DEA resource guide/2020 edition. United States Drug Enforcement Administration. https://admin.dea.gov/documents/2020/2020-04/2020-04-13/drugs-abuse. Accessed Aug. 31, 2022.
- Misuse of prescription drugs research report. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/research-reports/misuse-prescription-drugs/overview. Accessed Aug. 17, 2022.
- Principles of drug addiction treatment: A research-based guide. 3rd ed. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/preface. Accessed Aug. 17, 2022.
- The science of drug use: A resource for the justice sector. National Institute on Drug Abuse. https://nida.nih.gov/drug-topics/criminal-justice/science-drug-use-resource-justice-sector. Accessed Sept. 2, 2022.
- Naloxone DrugFacts. National Institute on Drug Abuse. https://nida.nih.gov/publications/drugfacts/naloxone. Accessed Aug. 31, 2022.
- Drug and substance use in adolescents. Merck Manual Professional Version. https://www.merckmanuals.com/professional/pediatrics/problems-in-adolescents/drug-and-substance-use-in-adolescents. Accessed Sept. 2, 2022.
- DrugFacts: Synthetic cannabinoids (K2/Spice). National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugfacts/synthetic-cannabinoids-k2spice. Accessed Aug. 18, 2022.
- Hall-Flavin DK (expert opinion). Mayo Clinic. March 5, 2021.
- Poppy seed tea: Beneficial or dangerous?
Associated Procedures
News from mayo clinic.
- Science Saturday: Preclinical research identifies brain circuit connected to addictive behaviors July 22, 2023, 11:00 a.m. CDT
- What is naloxone and should everyone have access to it? Feb. 16, 2023, 05:06 p.m. CDT
Products & Services
- A Book: Mayo Clinic Family Health Book, 5th Edition
- Newsletter: Mayo Clinic Health Letter — Digital Edition
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
Your gift holds great power – donate today!
Make your tax-deductible gift and be a part of the cutting-edge research and care that's changing medicine.
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Substance Use Disorder Treatment for People With Co-Occurring Disorders: Updated 2020 [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2020. (Treatment Improvement Protocol (TIP) Series, No. 42.)

Substance Use Disorder Treatment for People With Co-Occurring Disorders: Updated 2020 [Internet].
- Order print copy from SAMHSA
Chapter 4—Mental and Substance-Related Disorders: Diagnostic and Cross-Cutting Topics
Key messages.
The co-occurrence of mental disorders with substance use disorders (SUDs) is the rule, not the exception. Addiction counselors should expect and prepare to see clients with these disorders in their settings.
Addiction counselors generally do not diagnose mental disorders. But to engage in accurate treatment planning and to offer comprehensive, efficacious, and responsive services (or referral for such), clinicians must be able to recognize the disorders most likely to be seen in populations who misuse substances.
It is not always readily apparent whether a co-occurring mental disorder is directly caused by substance misuse or is an independent disorder merely appearing alongside an SUD. This differentiation can be difficult to make but is critically important, as it informs treatment decision making.
Suicide and trauma are sadly common across most combinations of co-occurring disorders (CODs) and require special attention. Addiction counselors have an ethical and professional responsibility to keep clients safe and to provide services that are supportive, empathie, and person-centered, and that reduce suffering.
Disentangling symptoms of SUDs from those of co-occurring mental disorders is a complex but necessary step in correctly assessing, diagnosing, determining level of service, selecting appropriate and effective treatments, and planning follow-up care. This chapter is designed to facilitate those processes by ensuring addiction counselors and other providers have a clear understanding of mental disorder symptoms and diagnostic criteria, their relationships with SUDs, and pertinent management strategies.
This chapter provides an overview for working with SUD treatment clients who also have mental disorders. The audiences for this chapter are counselors, other treatment/service providers, Supervisors, and Administrators. It is presented in concise form so that user can refer to this one chapter to obtain basic information. The material included is not a complete review of all mental disorders and is not intended to be a primer on diagnosis. Rather, it offers a summary of mental disorders with special relevance to co-occurring SUDs (see the section “Scope of the Chapter”).
Since the original publication of this Treatment Improvement Protocol (TIP), updated mental disorder criteria have been published in the Diagnostic and Statistical Manual of Mental Disorders (5th ed.; DSM-5; American Psychiatric Association [APA], 2013 ). This chapter contains these latest criteria and, where available, data from prevalence studies and randomized controlled trials in reflection of DSM-5.
- Organization of the Chapter
The chapter begins with a brief description of selected mental disorders and their DSM-5 diagnostic criteria. For each disorder, material highlights some of the descriptive and diagnostic features, prevalence statistics, and relationship to SUDs. In general, the mental disorders in this chapter are presented in the following descending order by how commonly they co-occur with SUDs, although this is not applied rigidly: Depressive disorders, bipolar I disorder, posttraumatic stress disorder (PTSD), personality disorders (PDs), anxiety disorders, schizophrenia and psychosis, attention deficit hyperactivity disorder (ADHD), and feeding and eating disorders.
Because of the greater availability of case histories from the mental health literature, the illustrative material has more emphasis on the mental disorders. Although not intended to offer extensive guidance on treatment, this chapter's coverage of specific mental disorders does include brief information about interventions for and clinical approaches to managing CODs involving each. ( Chapter 7 focuses on treatment models for people with CODs.) Case histories illustrate the interaction between mental disorders and SUDs. Each diagnostic topic contains an Advice to the Counselor box containing key considerations related to diagnosis, treatment, or both.
The next main section of this chapter addresses substance-related disorders, including SUDs and substance-induced mental disorders. (DSM-5 uses the term “substance/medication-induced disorders”; this TIP focuses on nonmedication substances and thus will exclude the term “medication.”) Because the primary audience for this chapter is addiction counselors, readers are assumed to be highly familiar with SUDs and their diagnostic criteria. Thus, the SUD section is briefer than the mental disorders section. The overall focus remains on substance-induced mental disorders, their relationship to independent co-occurring mental disorders, and what counselors need to know in terms of assessment and treatment.
Licit and illicit drugs of misuse can cause symptoms that are identical to the symptoms of mental Illness. Mental disorder diagnoses should be provisional and reevaluated constantly. Some mental disorders are really substance-induced mental disorders, meaning they are caused by substance use. Treatment of the SUD and an abstinent period of weeks or months may be required for a definitive diagnosis of an independent, cooccurring mental disorder. A fuller discussion of substance-induced disorders is provided later In this chapter.
The chapter ends with an overview of two concerns that appear across nearly all COD populations: suicidality and trauma. Although suicidality is not strictly speaking a DSM-5-diagnosed mental disorder, it is a high-risk behavior requiring serious attention by providers. The discussion of suicidality highlights key information addiction counselors should know about risk of self-harm in combination with substance misuse, mental disorders, or both. The section offers factual information (e.g., prevalence data), commonly agreed-on clinical practices, and other general information that may be best characterized as “working formulations.” Like suicide, trauma itself is not a mental disorder but is extremely common in many psychiatric conditions, frequently coincides with addiction, and increases the odds of negative outcomes, including suicide. Having at least a basic understanding of suicide and trauma is a core competency for addiction counselors working with clients who have CODs and will help improve their ability to not only offer effective services but keep clients safe.
- Scope of the Chapter
The mental disorder section of this chapter does not include all DSM-5 mental disorders. The consensus panel acknowledges that people with CODs may have multiple combinations of the various mental disorders presented in this chapter (e.g., a person could have an SUD, bipolar I disorder, and borderline PD [BPD]). However, for purposes of clarity and brevity, the panel chose to focus the discussion on the main disorders primarily seen in people with CODs and not explore the multitude of possible combinations. This does not mean that other mental disorders excluded from this chapter cannot and do not co-occur with substance misuse. But the scope of this chapter is such that it focuses only on mental disorders most likely to be seen by SUD treatment professionals.
The consensus panel recognizes that although this chapter covers a broad range of mental disorders and diagnostic material, it cannot and should not replace the comprehensive training necessary for diagnosing and treating clients with specific mental disorders cooccurring with SUDs. Readers of this TIP are assumed to already have working knowledge of mental disorders and their symptoms. The “Advice to the Counselor” boxes cannot fully address the complexity involved in treating clients with CODs. These boxes distill for counselors the main actions and approaches they can take in working with clients in SUD treatment who have the specific mental disorder being discussed.
The consensus panel recognizes that this chapter cannot cover each mental disorder exhaustively and that addiction counselors are not expected to diagnose mental disorders. The panel's limited goals for this chapter are to increase SUD treatment counselors’ familiarity with mental disorder terminology and criteria and to guide them on how to proceed with clients who have these disorders. The chapter also is meant to stimulate further work in this area and to make this research accessible to the addiction field.
- Depressive Disorders
The depressive disorders category in DSM-5 comprises numerous conditions; addiction counselors are most likely to encounter major depressive disorder (MDD) and persistent depressive disorder (PDD; also called dysthymia) among their clients. Common features of all depressive disorders are excessively sad, empty, or irritable mood and somatic and cognitive changes that significantly affect ability to function.
WARNING TO COUNSELORS: KNOW YOUR LIMITS OF PRACTICE.
Major Depressive Disorder
MDD is not merely extreme sadness, although sad mood is a defining characteristic. MDD is marked by either depressed mood or loss of interest in nearly all previously enjoyed activities. At least one of those symptoms must be present and must persist most of the day, almost every day over a 2-week period ( Exhibit 4.1 ). Other core physical, cognitive, and psychosocial features of MDD also must be present nearly every day, with the exception of weight change and suicidal ideation.
EXHIBIT 4.1. Diagnostic Criteria for MDD.
MDD is highly associated with suicide risk. A study reported 39 percent of people with a lifetime MDD diagnosis contemplated suicide; nearly 14 percent had a lifetime history of suicide attempt ( Hasin et al., 2018 ). Yet suicide is not isolated to those with depressed mood. Counselors always should ask clients whether they have been thinking of suicide, whether or not they have, or mention, symptoms of depression.
Severe depressive episodes can include psychotic features, such as an auditory hallucination of a voice saying that the person is “horrible,” a visual hallucination of a lost relative mocking the person, or a delusion that one's internal body parts have rotted away. However, most people who have an MDE do not exhibit psychotic symptoms even when the depression is severe (for more information on psychosis, see the section “Schizophrenia and Other Psychotic Disorders”).
MDE must be distinguished from grief or bereavement, which are not mental disorders but rather normal human responses to loss. However, grief and MDD can be experienced at the same time; that is, the presence of grief does not rule out the presence of MDD. DSM-5 provides detailed guidance on diagnosing MDD in people who are bereaved.

Persistent Depressive Disorder
PDD presents as excessively sad or depressed mood that lasts most of the day, more days than not, for at least 2 years. PDD is somewhat of an “umbrella” diagnosis in that it covers two different types of people with depression: people with chronic MDD (i.e., depression lasting at least 2 years) and people who do not meet criteria for an MDD (see Criteria A through C in Exhibit 4.1 ) but otherwise have had depressive symptoms for at least 2 years. Thus, the criteria for PDD ( Exhibit 4.2 ) are similar to, but less severe than, those of MDD.
EXHIBIT 4.2. Diagnostic Criteria for PDD.
Data from a national epidemiological survey indicate the 12-month and lifetime prevalence rates of DSM-5 MDD are 10 percent and 21 percent, respectively ( Hasin et al., 2018 ). Prevalence of MDD in emerging adults (ages 1 8 to 29 years) is 3 times higher than the prevalence in older adults (ages 60 years and older). Women are 1.5 times as likely to report depression as men ( Hasin et al., 2018 ).
Twelve-month and lifetime prevalence rates for DSM-5 PDD in U.S. samples have not been reported at the time of this publication. Using DSM-IV criteria, 12-month and lifetime prevalence of PDD in U.S. adults are estimated at 1.5 percent and 3 percent, respectively; DSM-IV dysthymia has an estimated 12-month and lifetime prevalence of 0.5 percent and 1 percent, respectively ( Blanco et al, 2010 ).
Depressive Disorders and SUDs
Depressive disorders are highly comorbid with SUDs. For instance:
Presence of a 12-month or lifetime DSM-5 drug use disorder (i.e., a nonalcohol SUD) is associated with a 1.5 to 1.9 increased odds of having any mood disorder, a 1.3 to 1.5 increased odds of having dysthymia, and a 1.2 to 1.3 increased odds of having MDD ( Grant et al., 2016 ).
Twelve-month alcohol use disorder (AUD) is also associated with an increased risk of MDD and lifetime AUD with persistent depression ( Grant et al., 2015 ).
A lifetime diagnosis of DSM-5 MDD is more likely to occur in individuals with a history of SUDs (58 percent; for AUD, 41 percent) than in people with a history of any anxiety disorder (37 percent) or PD (32 percent) ( Hasin et al., 2018 ).
People with depression and co-occurring SUDs tend to have more severe mood symptoms (e.g., sleep disturbance, feelings of worthlessness), higher risk of suicidal ideation and suicide attempts, worse functioning, more psychiatric comorbidities, and greater disease burden (including increased mortality) than people with MDD alone ( Blanco et al., 2012 ; Gadermann, Alonso, Vilagut, Zaslavsky, & Kessler, 2012 ). They are less likely than people with MDD alone to receive antidepressants—despite strong evidence supporting the efficacy of antidepressant medication in alleviating mood and even some SUD symptoms ( Blanco et al., 2012 ).
Addiction counselors may represent a way to reduce lags in adequate depression care in people with depressive disorders and SUDs. Among 3.3 million people who reported both MDEs and SUDs between 2008 to 2014, only 55 percent received services for depression in the previous year ( Han, Olfson, & Mojtabai, 2017 ). However, people who had received SUD treatment in the past year were 1.5 times more likely to have received depression care than people who had not engaged in SUD treatment (80 percent vs. 50 percent, respectively) and were 1.6 times more likely to perceive their depressive care as being helpful (48 percent vs. 32 percent) than people who did not access SUD treatment in the previous 1 2 months ( Han, Olfson, & Mojtabai, 2017 ).
Other facts about depression and SUDs that addiction counselors should know include the following:
Both substance use and discontinuance can be associated with depressive symptoms.
During the first months of sobriety, many people with SUDs can exhibit symptoms of depression that fade over time and that are related to acute and protracted withdrawal.
People with co-occurring depressive disorders and SUDs typically use a variety of drugs.
Recent evidence suggests there is increasing cannabis use with depression, although cannabinoids have not been shown to be effective in self-management of depression. In fact, cannabis may actually worsen the course of MDD and reduce chances of treatment seeking ( Bahorik et al., 2018 ).
Treatment of MDD and SUD
Psychotherapy (e.g., integrated cognitive-behavioral therapy [CBT], group CBT), with or without adjunct antidepressant use, can effectively reduce frequency of substance use and depressive symptoms and improve functioning briefly and over the long term ( Paddock, Hunter, & Leininger, 2014 ; Vujanovic et al., 2017 ). In a review examining MDD and AUD specifically ( Riper et al., 2014 ), treatment as usual supplemented with CBT and motivational interviewing had small but significant effects in improving depression and decreasing alcohol use versus treatment as usual alone or other brief psychosocial interventions.
For more extensive guidance about counseling clients with addiction and depression, see TIP 48, Managing Depressive Symptoms in Substance Abuse Clients During Early Recovery ( Center for Substance Abuse Treatment [CSAT], 2008 ).
- Bipolar I Disorder
Bipolar I disorder, also sometimes termed manic-depression, refers to a mental state wherein a person's mood fluctuates wildly between depressive and manic episodes ( Exhibit 4.3 ). During depressive episodes, a person experiences symptoms of MDD (e.g., excessive sadness, loss of interest in normally pleasurably activities, physical and cognitive symptoms). During manic episodes, a person experiences the opposite—extreme euphoria, energy, and activity. Manic episodes vary with intensity and can be manifest in a variety of ways, such as having little or no need for sleep, very fast or “pressured” speech, impulsivity and erratic decision making (especially decisions of major consequence, like spending a large amount of money), and racing thoughts. Some manic episodes are milder in nature; these are known as hypomanie episodes. People with bipolar I disorder can experience both manic and hypomanie episodes. Bipolar II disorder is a related disorder in which the person only experiences hypomania and not full-blown mania. For the purposes of this chapter, only bipolar I disorder, which has ample research strongly linking it to SUDs, will be discussed.
EXHIBIT 4.3. Diagnostic Criteria for Bipolar I Disorder.
Sometimes, manic episodes can produce symptoms that conflict with reality and are delusional in nature (e.g., a man believing he is going to marry the Queen of England). Because of these delusional and bizarre beliefs, bipolar disorder can sometimes appear similar to schizophrenia and other psychotic disorders (see the section “Schizophrenia and Other Psychotic Disorders”). In fact, increasing research supports a shared genetic risk between the bipolar and psychotic disorders ( Cardno & Owen, 2014 ).
Suicidal thoughts and behaviors are common among people with bipolar disorder ( APA, 2013 ), with some believing it could have the highest suicide risk of all mental disorders ( Schaffer et al., 2015 ). An estimated 20 percent of people with bipolar disorder try to commit suicide ( Carra, Bartoli, Crocamo, Brady, & Clerici, 2014 ), leading to a standardized mortality ratio of suicide deaths that is 1 0 to 30 times greater than that of the general population ( Schaffer et al., 2015 ). People with bipolar disorder and SUD are significantly more likely to try to commit suicide than people without both conditions ( Carra et al., 2014 ; Schaffer et al., 2015 ). Interestingly, current or lifetime SUD is a significant risk factor for suicide attempt in bipolar disorder but not suicide death ( Schaffer et al., 2015 ).
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH A DEPRESSIVE DISORDER.
The 12-month and lifetime prevalence rates of DSM-5 bipolar I disorder are 1.5 percent and 2 percent, respectively ( Blanco et al., 2017 ). Rates are nearly equivalent between men and women for both 12-month and lifetime prevalence ( Blanco et al., 2017 ).
Bipolar I Disorder and SUDs
Individuals with bipolar I have high prevalence rates (65 percent) of lifetime SUD, AUD (54 percent), and drug use disorder (32 percent) (McDermid et al., 2015). Presence of a 12-month or lifetime DSM-5 drug use disorder (i.e., an SUD excluding alcohol) is associated with a 1.4 to 1.5 increased odds in having bipolar I disorder ( Grant et al., 2016 ). Similarly, presence of past-year or lifetime bipolar I disorder carries a 2 to 5.8 times greater risk of also having any 12-month or lifetime SUD ( Blanco et al., 2017 ). A systematic review and meta-analysis found strong associations between co-occurring SUDs and bipolar illness in individuals in clinical settings, with the highest prevalence (average: 30 percent) for alcohol use, 20 percent (mean) for cannabis, and 17 percent (mean) for any drug use disorder ( Hunt, Malhi, Cleary, Lai, & Sitharthan, 2016b ).
Co-occurring bipolar illness and substance misuse are associated with numerous adverse clinical, social, and economic consequences, including increased symptom severity, poorer treatment outcomes, and greater suicide risk ( Ma, Coles, & George, 2018 ). Presence of a co-occurring SUD with bipolar disorder has been linked to lower SUD treatment adherence and retention, protracted mood episodes, poorer recovery of functional abilities (even after abstaining from substances), increased utilization of emergency services, greater hospitalizations, more variable disease course, greater affective instability, more impulsivity, and poor response to lithium (the standard pharmacotherapy of choice) ( Swann, 2010 ; Tolliver & Anton, 2015 ).
Treatment of Bipolar I Disorder and SUDs
Substance misuse by people with bipolar disorder complicates diagnosis and treatment. Evidence exists of a bidirectional relationship between bipolar disorder and SUDs, yet the ways in which these conditions influence one another is still unclear ( Tolliver & Anton, 2015 ). Little research has examined nonpharmacological approaches to managing comorbid bipolar I disorder and SUDs. Group CBT, integrated therapy, and relapse prevention techniques may help reduce hospitalizations, increase abstinence, improve medication adherence, reduce addiction severity, and (to a lesser extent) improve mood symptoms ( Gold et al., 2018 ). However, results are inconsistent across studies, underscoring the need for more research.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH BIPOLAR I DISORDER.
Case Study: Counseling an SUD treatment Client With Bipolar I Disorder.
- Posttraumatic Stress Disorder
PTSD is an exaggerated fear response that occurs following exposure to one or more extremely upsetting events. Such events can include, but are not limited to, war, terrorist attacks, threatened or actual physical or sexual violence, being kidnapped, natural and man-made disasters, and serious motor vehicle accidents. Events may be experienced firsthand, witnessed, experienced through repeated exposure as a part of one's job (e.g., police officers repeatedly hearing details about child abuse, murder, and other violent and upsetting crimes), or by learning about such events occurring to a close loved one (e.g., learning of the murder of one's child). People with PTSD report the most distressing trauma to be sexual abuse before age 18 years ( Goldstein et al., 2016 ).
Symptoms of PTSD are grouped into four categories:
Intrusive, persistent re-experiences of the trauma, including recurrent dreams or nightmares, flashbacks, and distressing memories
Persistent avoidance of people, places, objects, and events that remind the person of the trauma or otherwise trigger distressing memories, thoughts, feelings, and physiological reactions
Negative alterations in cognitions and mood, such as memory loss (particularly regarding details surrounding the event), self-blame, guilt, hopelessness, social withdrawal, and an inability to experience positive emotions
Marked alterations in arousal and reactivity, such as experiencing sleeplessness or feeling “jumpy,” “on edge,” easily started, irritable, angry, or unable to concentrate
Exhibit 4.4 lists the DSM-5 criteria for PTSD in adults and children older than age 6; separate criteria are available for children ages 6 years and younger and can be found in DSM-5.
EXHIBIT 4.4. Diagnostic Criteria for PTSD.
Twelve-month and lifetime prevalence rates of DSM-5 PTSD are 4.7 percent and 6.1 percent, respectively ( Goldstein et al., 2016 ). Rates are markedly higher among women than men, about 6 percent and 8 percent for past-year and lifetime PTSD, respectively ( Goldstein et al., 2016 ). Lifetime prevalence is even higher for female veterans (1 3.9 percent) and younger adults (ages 1 8 to 29 years, 15.3 percent) ( Smith, Goldstein, & Grant, 2016 ). A 2016 study of veterans using DSM-5 criteria found the lifetime prevalence of PTSD to be 6.9 percent, with significantly higher prevalence rates noted for women and younger age groups ( Smith et al., 2016 ).
Individuals in occupations at risk of exposure to traumatic events (e.g., police, firefighters, emergency medical personnel) have higher rates of PTSD. Among high-risk individuals (those who have survived rape, military combat, and captivity or ethnically or politically motivated internment and genocide), the proportion of those with PTSD ranges from one-third to one-half ( APA, 2013 ).
PTSD and SUDs
A strong association exists between PTSD and substance misuse, including lifetime SUDs ( Hasin & Kilcoyne, 2012 ), lifetime drug use disorders ( Grant et al., 2016 ), and lifetime AUD ( Grant et al., 2015 ). Among people with SUDs, lifetime prevalence of PTSD is thought to range between 26 percent and 52 percent and rates of current PTSD between 15 percent and 42 percent ( Vujanovic, Bonn-Miller, & Petry, 2016 ). Among people with PTSD, lifetime rates of SUD are likely between 36 percent and 52 percent ( Vujanovic et al., 2016 ). Presence of a 12-month or lifetime DSM-5 drug use disorder (i.e., an SUD excluding alcohol) is associated with a 1.5 to 1.6 increased odds of having PTSD ( Grant et al., 2016 ). Similarly, presence of 12-month or lifetime PTSD is associated with a 1.3 to 1.5 increased odds of having a past-year or lifetime SUD ( Goldstein et al., 2016 ).
Comorbid PTSD and addiction are highly complex and associated with worse treatment outcomes (including lower rates of remission and faster relapse), poorer treatment response, more cognitive difficulties, worse social functioning, greater risk of suicide attempt, and heightened mortality ( Flanagan, Korte, Killeen, & Back, 2016 ; Schumm & Gore, 2016 ). Compared with people with PTSD or alcohol dependence alone, those with both report more traumatic childhoods, more psychiatric comorbidities, an increased risk of suicide, more severe symptoms, and greater disability ( Blanco et al., 2013 ).
People with PTSD tend to misuse the most serious substances (cocaine and opioids); however, misuse of prescription medications, cannabis, and alcohol also are common.
WARNING TO COUNSELORS: PTSD OR DEPRESSION?
Treatment of PTSD and SUDs
Historically, there has been debate about whether to treat PTSD and addiction concurrently or sequentially, with most providers falling on the side of treating the SUD separately and first ( Schumm & Gore, 2016 ). Some believe that substance misuse among people with PTSD is a means of self-medicating to help manage distressing mood and anxiety symptoms, thus making PTSD the priority target for treatment. Alternatively, others have feared that treating PTSD first could exacerbate SUD symptoms or cause clients to use substances as a means of coping with the hyperarousal and negative mood that can occur while progressing through PTSD treatment. However, integrated, concurrent treatment that addresses both conditions simultaneously has generated strong empirical support, appears to be preferable to clients, and is increasingly considered the current standard of care, particularly when combining psychosocial and pharmacologic approaches ( Flanagan et al., 2016 ; Schümm & Gore, 2016 ; Simpson, Lehavot, & Petrakis, 2017 ).
Despite the evidence that concurrent treatment can be effective, people with PTSD and SUD are frequently only treated for addiction; further, clients in SUD treatment settings are often not even assessed for PTSD ( Vujanovic et al., 2016 ). Whereas treating SUD alone rarely leads to Improvement In PTSD symptoms, reducing PTSD symptoms can significantly decrease the odds of heavy substance ( Hien et al., 2010 ).
Exposure therapy can be safe and effective at reducing trauma and SUD symptoms—although more evidence is needed ( Flanagan et al., 2016 ). Nonexposure-based treatments have been studied more widely for co-occurring PTSD and SUD and may be moderately effective at improving both PTSD and substance symptoms, but the evidence is still premature ( Flanagan et al., 2016 ). A Cochrane Review found individual trauma-focused psychotherapy with adjunctive SUD treatment to be effective at reducing posttreatment PTSD severity and substance use at 5 to 7 months following treatment; however, the authors deemed the current evidence base on psychological treatments for PTSD-SUD to be weak in terms of quality and methodology, underscoring the need for more rigorous research in this area ( Roberts, Roberts, Jones, & Bisson, 2016 ). Studies of pharmacologic treatments for SUD with PTSD, and for AUD specifically, appear encouraging but, again, are understudied, often inconclusive, and require more data ( Flanagan et al., 2016 ; Petrakis & Simpson, 2017 ).
See the section “Cross-Cutting Topics: Suicide and Trauma” at the end of this chapter for more information about trauma-informed care for people with CODs.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH PTSD.
CASE STUDY: COUNSELING AN SUD TREATMENT CLIENT WHO BINGE DRINKS AND HAS PTSD.
- Personality Disorders
A PD refers to a person's lifelong inability to form healthy, functional relationships with others and a failure to develop an adaptive sense of self. These are manifest as (a) destructive or otherwise problematic patterns of thinking and feeling about oneself, one's place in the world, and others and (b) negative ways of behaving toward others. People with PDs often lack insight into their dysfunctional cognitive, emotional, and behavioral patterns and often blame others or the world in general for their difficulties. Many people with PDs struggle to develop strong, positive relationships, because they view reality from the perspective of their own needs and therefore have a difficult time understanding, empathizing with, and connecting with others. PDs are lifelong conditions that develop in adolescence or early adulthood. They are frequently resistant to change and result in significant impairments in interpersonal functioning, work/school performance, and self-concept.
There are several types of PDs, and the precise symptoms someone exhibits will depend on which type of PD he or she has. For instance, depending on the PD type, an individual might think of himself/herself in overly negative ways or in grandiose ways, might be overly attached to others or completely indifferent to others, might constantly try to be the center of attention or might be socially reclusive. People with PDs must first meet the diagnostic criteria for a general PD ( Exhibit 4.5 ) and then must meet additional diagnostic criteria for whatever PD type is most appropriate given their symptoms. Many individuals with PDs have features of, or meet full criteria for, other PDs.
EXHIBIT 4.5. Diagnostic Criteria for General PD.
This TIP provides details about the two PD types that are commonly comorbid with addiction—BPD and antisocial PD (ASPD). Before exploring BPD and ASPD in detail, an overview of PDs in general follows. Readers should be aware that the diagnostic approach to PDs continues to undergo refinement, as researchers in psychopathology have expressed many concerns about the meaningfulness, gender bias, accuracy, and utility of the current categorical diagnostic system for PDs (see Section III of DSM-5 for more information on alternative PD classification and diagnostic criteria).
PD Clusters
Once a person meets criteria for a general PD, his or her diagnosis is further categorized based on several specific PD types, including paranoid PD, schizoid PD, schizotypal PD, histrionic PD, narcissistic PD, ASPD, BPD, avoidant PD, dependent PD, and obsessive-compulsive PD. If the symptoms do not meet any of the types, he or she can be diagnosed with either unspecified PD or other specified PD. Detailed descriptions and criteria for all 10 PD types can be found in DSM-5. BPD and ASPD most frequently co-occur with substance misuse ( Köck & Walter, 2018 ). Thus, they are included in this chapter and discussed in respective subsections.
In DSM5, PD types are categorized into three distinct clusters based on their common features:
Cluster A PDs describe people who may be seen as odd or eccentric. This eccentricity can express itself in many ways (e.g., paranoia and suspicion, extreme social withdrawal/lack of interest in interpersonal relationships, unusual beliefs or behaviors). PD types included in this cluster are:
Paranoid PD.
Schizoid PD.
Schizotypal PD.
Cluster B PDs are characterized by dramatic, overly emotional, and erratic and unpredictable behavior. PD types included in this cluster are:
Histrionic PD.
Narcissistic PD.
Cluster C PDs are marked by anxious and fearful behaviors. PD types included in this cluster are:
Obsessive-compulsive PD.
Avoidant PD.
Dependent PD.
WARNING TO COUNSELORS: PDS AND PROVIDER STIGMA.
Prevalence estimates for PDs among the general population are difficult to ascertain, given lack of research examining large samples from the community (as opposed to clinical samples, in which PDs are far more common and frequently studied). Estimates are 9.1 percent for any PD, 5.7 percent for any Cluster A PD, 1.5 percent for any Cluster B, and 6 percent for Cluster C ( APA, 2013 ). In one analysis of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), the prevalence of lifetime DSM-IV PDs varied from 0.5 percent to 7.9 percent, depending on the PD type (Hasin & Grant, 2015). Prevalence rates for BPD and ASPD are discussed in separate sections.
Diagnostic criteria for PDs have long been debated among psychopathology researchers and clinicians, given multiple problems with the way PDs are classified and diagnosed ( Paris, 2014 ; Sarkar & Duggan, 2010 ). Problems include a lack of empirical evidence supporting PDs; the extensive overlap between diagnostic criteria among the specific types of PDs as well as overlap with other mental disorders; the fact that PD criteria are insufficiently discriminant, which has resulted in many individuals who exhibit PD pathology receiving a DSM-IV “personality disorder not otherwise specified” diagnosis after failing to “fit in” to any of the specified PD types; and the difficulty mental health professionals have in distinguishing PD traits from variants of normal personality, which means that deciding whether a person meets PD criteria is often a subjective judgment. Thus, it is hard to know exactly how many people have a PD, including how many people with addiction have co-occurring PDs ( Paris, 2014 ).
PDs and SUDs
SLID counselors frequently see people with PD diagnoses in their treatment settings. A review found the prevalence of PDs among people with SUDs to be wide ranging but nonetheless extremely high, varying from about 35 percent to 65 percent; rates of ASPD ranged from about 14 percent to almost 35 percent ( Köck & Walter, 2018 ). Similarly, among people undergoing detoxification for AUD, rates of co-occurring PDs vary widely from 5 percent to 87 percent ( Newton-Howes & Foulds, 2018 ). PDs may be present in as much as 24 percent of people with AUD in the general population ( Newton-Howes & Foulds, 2018 ).
For most people with SUDs, drugs eventually become more important than jobs, friends, and family. These changes in priorities often appear similar to a PD, but diagnostic clarity for PDs in general is difficult. For clients with substance-related disorders, the true diagnostic picture might not emerge for weeks or months. It is not unusual for PD symptoms to clear with abstinence, sometimes even fairly early in recovery.
People with PDs and SUDs differ from those with PDs only or SUDs only in important ways ( Köck & Walter, 2018 ), including more severe mental and substance-related symptoms, longer persisting substance use, a greater likelihood of other co-occurring mental disorders (e.g., anxiety, depressive, and eating disorders), increased mortality, and higher SUD treatment dropout.
Treatment for PDs and SUDs
No evidence-based treatments exist for PDs themselves ( Bateman, Gunderson, & Mulder, 2015 ), but effective treatments are available to address a variety of PD symptoms, including risk of suicide and self-harm, affective dysregulation, maladaptive thought patterns, and poor interpersonal functioning. Psychotherapy is the primary form of intervention, as no medications have been approved for the treatment of PDs. Pharmacotherapy may be useful as an adjunctive treatment for certain symptoms like affective lability, impulsivity, and psychosis, but it is not useful as a primary intervention. (See the section “Pharmacotherapy” in Chapter 7 for more information.) Dialectical behavioral therapy, dynamic deconstructive psychotherapy, and dual-focused schema therapy appear promising, particularly for BPD, and have shown to positively affect psychiatric and addiction-related outcomes, although, in general, the research literature on effective treatments for PDs, with or without co-occurring SUD, is sparse and requires further evidence ( Bateman et al., 2015 ; Köck & Walter, 2018 ).
The essential feature of BPD is a pervasive pattern of instability of interpersonal relationships, self-image, and affects, along with marked impulsivity, that begins by early adulthood and is present in a variety of contexts ( Exhibit 4.6 ). Relationships with others are likely to be unstable—for instance, people with BPD might remark how wonderful an individual is one day but express intense anger, disapproval, condemnation, and even hate toward that same individual a week later. The severe instability people with BPD experience includes fluctuating views and feelings about themselves. Those with BPD often feel good about themselves and their progress and optimistic about their future for a few days or weeks, only to have a seemingly minor experience turn their world upside down, with concomitant plunging self-esteem and depressing hopelessness. This instability often extends to work and school.
EXHIBIT 4.6. Diagnostic Criteria for BPD.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH A PD.
When experiencing emotional states they cannot handle, clients with BPD can be at high risk of suicidal, self-mutilating, or brief psychotic states.
About three-fourths of people with BPD have a history of self-harm, and the disorder carries a 10-percent lifetime risk of completed suicide ( Antai-Otong, 2016 ).
BPD has a prevalence of 1.6 percent to 5.9 percent in the general population but is more common in mental health settings (about a 10-percent prevalence rate for outpatient mental health clinics, about 20 percent among psychiatric inpatients, and 6 percent in primary care settings) ( APA, 2013 ). Lifetime prevalence of DSM-IV BPD is 5.9 percent (Hasin & Grant, 2015).
Women are much more likely to be diagnosed with BPD, generally at 3 times the rate of men (i.e., about 75 percent of cases are women) ( APA, 2013 ). However, the accuracy of this pattern is dubious as epidemiologic surveys of the U.S. general population have found the lifetime prevalence of BPD does not actually differ significantly between men and women (Hasin & Grant, 2015).
WARNING TO COUNSELORS: THE MISDIAGNOSIS OF BPD.
BPD and SUDs
BPD is highly prevalent in SUD treatment settings (and especially inpatient and residential treatment), with rates averaging about 22 percent across multiple studies but as high as 53 percent in some research ( Trull et al., 2018 ). Presence of a 1 2-month or lifetime DSM-5 drug use disorder (i.e., an SUD excluding alcohol) is associated with a 1.7 to 1.8 increased odds of having BPD ( Grant et al., 2016 ). Approximately 45 percent of individuals with BPD also have a current SUD, and about 75 percent have a lifetime SUD ( Trull et al., 2018 ). Opioids, cocaine, and alcohol are the substances with the strongest associations with BPD ( Trull et al., 2018 ).
Treatment of BPD and SUDs
People with BPD typically seek behavioral health services based on their current life conditions and emotional state. Those who seek mental health services tend to be acutely emotionally distraught, needing some relief from how they feel. Similarly, those who choose (or are directed to choose) a program are likely experiencing the SUD as the immediate target for treatment. Consequently, the average admission of a person with BPD to a mental health program may be considerably different from the average admission of a person with BPD to an SUD treatment program.
In inpatient mental health service settings, dialectical behavior therapy for BPD is recommended to help reduce suicide risk, stabilize behavior, and help clients regulate emotions ( Ritter & Platt, 2016 ). SUD treatment for people with BPD can be complicated, and progress may be slow, but effective interventions are available to help reduce symptoms and improve functioning. A systematic review of 10 studies on treatments for BPD and cooccurring SUDs found good support for dialectical behavior therapy, dynamic deconstructive therapy, and dual-focused schema therapy in improving outcomes of substance use, suicidal gestures and self-harm, global and social functioning, treatment utilization, and treatment retention ( Lee, Cameron, & Jenner, 2015 ).
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH BPD.
CASE STUDY: COUNSELING AN SUD TREATMENT CLIENT WITH BPD.
The core features of ASPD are a pervasive disregard for the rights, feelings, and needs of others and a failure to form long-term, fulfilling, adaptive relationships ( Exhibit 4.7 ). Individuals with ASPD often display a host of challenging traits: deceitfulness, remorselessness, aggression, disregard for rules and laws, low conscientiousness, impulsivity, failure to adhere to social norms, delinquency, and recklessness. As a result, these individuals often lead unstable lives and are at high risk of increased mortality, violence/aggression, suicide and suicidal behavior, accidents, criminality, incarceration, and chronic illnesses (e.g., cancer, HIV) ( Black, 2015 ; Black, 2017 ; Dykstra, Schumacher, Mota & Coffey, 2015 ; Krasnova, Eaton, & Samuels, 2018; McCloskey & Ammennan, 2018 ). Many people with ASPD have experienced traumatic or disruptive childhoods (Sher et al., 2015).
EXHIBIT 4.7. Diagnostic Criteria for ASPD.
A particularly stigmatizing aspect of ASPD is its history of being equated with derisive terms like “sociopath” and “psychopath.” ASPD thus carries extremely negative connotations that might well be accurate in only a small percentage of those people with the disorder. Psychopathy and sociopathy are personality traits, not mental disorders. They are related to ASPD but are usually manifest in more extreme ways than ASPD (e.g., criminal behavior). In short, psychopathy and sociopathy are not the same as ASPD. (See the TIP 44, Substance Abuse Treatment for Adults in the Criminal Justice System [ CSAT, 2005b ] for a full discussion of psychopathy and its relationship to ASPD.)
Twelve-month prevalence rates for DSM-IV ASPD fall between 0.2 percent and 3.3 percent ( APA, 2013 ). Lifetime DSM-IV ASPD is estimated at 3.6 percent (Hasin & Grant, 2015). Much higher prevalence rates (up to 70 percent) have been found in studies of men in treatment for AUD and SLID treatment clinics, prisons, and other forensic settings ( APA, 2013 ).
Men are 2 to 8 times more likely to have an ASPD diagnosis than women ( Black, 2017 ). Lifetime prevalence of DSM-IV ASPD is estimated at 1.9 percent in women and 5.5 percent in men (Hasin & Grant, 2015).
ASPD and SUDs
Presence of a 12-month or lifetime DSM-5 drug use disorder (i.e., an SUD excluding alcohol) is linked with 1.4 to 2 increased odds of having ASPD ( Grant et al., 2016 ). Prevalence of ASPD is 7 percent to 40 percent in men with existing SUDs. ASPD is significantly associated with persistent SUDs ( Grant et al., 2015 ; Grant et al., 2016 ).
An analysis of NESARC data (using DSM-IV diagnoses) revealed gender differences in comorbidities with ASPD ( Alegría et al., 2013 ). Men with ASPD were more likely to have AUD, any drug use disorder, and narcissistic PD. Women with ASPD were more likely to have any mood disorder, MDD, dysthymia, any anxiety disorder, panic disorder, specific phobia, PTSD, and generalized anxiety disorder (GAD). Women were also more likely to report childhood adverse events, such as sexual abuse.
Another study of treatment-seeking individuals assessing gender differences in individuals with an ASPD diagnosis similarly found that women with ASPD tended to be younger, had fewer episodes of antisocial behavior and higher scores on measures of trauma, including emotional and sexual abuse, than men with an ASPD (Sher et al., 2015). Both women and men with ASPD had comorbid alcohol (43.6 percent for women and 50 percent for men) and cannabis use disorders (21.8 percent and 29.7 percent, respectively), and men had higher rates of comorbid cocaine use disorder (22 percent) than women (7.3 percent). Many people with ASPD use substances in a polydrug pattern involving alcohol, marijuana, heroin, cocaine, and methamphetamine.
People with ASPD and SUDs have higher rates of aggression, impulsivity, and psychopathy than people with SUDs alone ( Alcorn et al., 2013 ).
Disregard for others’ rights is a key diagnostic feature of ASPD. Yet most clients who are actively using substances display behaviors at some point that show such disregard, so perceiving the distinction between SUD and ASPD can be difficult for the mental health and the SUD treatment fields.
Treatment of ASPD and SUDs
As with most PDs, no empirically supported treatments exist for ASPD, much less ASPD combined with SUDs ( Bateman et al., 2015 ). Various therapies for ASPD with addiction (e.g., CBT, contingency management) may help ameliorate substance-related outcomes, like substance misuse and number of urine-negative specimens over time, but studies are few and sample sizes are small ( Brazil, van Dongen, Maes, Mars, & Baskin-Sommers, 2018 ).
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH ASPD.
- Anxiety Disorders
The distinguishing feature of anxiety disorders is excessive fear and worry along with behavioral disturbances, usually out of attempts to avoid or manage the anxiety. Anxiety disorders are highly comorbid with each other but differ in the types of situations that arouse fear and the content of the anxiety-provoking thoughts and beliefs. Panic attacks are a common fear response in anxiety disorders but are not limited to these disorders.
Three of the more prevalent anxiety disorders in the adult population that are likely to co-occur with addiction are GAD, panic disorder, and social anxiety disorder (SAD).
GAD is marked by excessive anxiety and worry (apprehensive expectation) about a range of topics or events, like everyday living, finances, relationships, or work/school performance ( Exhibit 4.8 ). Anxiety is intense, frequent, chronic (i.e., lasting at least 6 months), and disproportionate to the actual threat posed by the subject of worry. The worry is accompanied by additional cognitive/physical symptoms.
EXHIBIT 4.8. Diagnostic Criteria for CAD.
Panic Disorder
Panic disorder is diagnosed in people who experience repeated panic attacks that are distressing and disabling ( Exhibit 4.9 ). A panic attack is an abrupt but very intense occurrence of extreme fear. It often only lasts for a few minutes but the symptoms can be extremely uncomfortable and upsetting, such as hyperventilation, palpitations, trembling, sweating, dizziness, hot flashes or chills, numbness or tingling, and the sensation or fear of nausea or choking. People experiencing panic attacks also can experience psychological symptoms, like feeling as though they are going to die, as though they are “losing their mind,” as though things are not real (derealization), or as if they have left their body (depersonalization). Because of the distressing nature of panic attacks, people with panic disorder may constantly worry about having subsequent attacks or engage in behaviors in an attempt to control the attacks (like avoiding places where they have previously had a panic attack or fear they might have one).
EXHIBIT 4.9. Diagnostic Criteria for Panic Disorder.
Panic disorder often is underdiagnosed at the beginning of treatment or else is seen as secondary to the more significant disorders, which are the primary focus of treatment. However, panic disorder can significantly impede a person's ability to take certain steps toward recovery, such as getting on a bus to go to a meeting or sitting in a 12-Step meeting. Sometimes counselors can erroneously identify these behaviors as manipulative or treatment-resistant behaviors.
Agoraphobia
One of the changes in DSM-5 concerns the separation of agoraphobia from panic disorder. Although now two distinct conditions, they are closely related and many of their symptoms overlap. In agoraphobia, people exhibit a strong fear of being in certain places or situations where escape could be difficult should the person experience panic-like symptoms or otherwise feel anxious or a loss of control. Situations typically include being in crowds, on public transportation, in open spaces (like bridges), in closed spaces (such as the movie theater), or away from home. People with agoraphobia avoid these situations for fear of having panic attacks or similar incapacitating or embarrassing symptoms (e.g., vomiting, incontinence), or they tolerate them but with great distress and discomfort.
Agoraphobia often occurs without panic disorder in community settings but frequently occurs with panic disorder in clinical settings; the two conditions are distinct yet intertwined ( APA, 2013 ; Asmundson, Taylor, & Smits, 2014 ). SUDs can and do co-occur with agoraphobia ( Goodwin & Stein, 2013 ; Marmorstein, 2012 ), but literature on this co-occurrence is relatively small compared with other anxiety disorders or has been examined as occurring with panic disorder ( Cougle, Hakes, Macatee, Chavarria, & Zvolensky, 2015 ) rather than occurring alone. Furthermore, research is more focused on its co-occurrence with nicotine than other substances.
The linkage of agoraphobia with addiction may be explained by its relationship with panic disorder and not with SUD. Thus, agoraphobia is not a subject of focus for this chapter but is mentioned here because of its interrelationship with panic disorder, which addiction counselors are likely to see in their clients.
Social phobia describes the persistent and recognizably irrational fear of embarrassment and humiliation in social situations ( Exhibit 4.10 ). The social phobia may be quite specific (e.g., public speaking) or may become generalized to all social situations. SAD, also called social phobia in DSM-5, involves intense anxiety or fear in social or performance situations. Individuals may fear being judged by others (e.g., being perceived as stupid, awkward, or boring); being embarrassed or humiliated; accidentally offending someone; or being the center of attention. As a result, the individual will often avoid social or performance situations; when a situation cannot be avoided, they experience significant anxiety and distress. Many people with SAD have strong physical symptoms (e.g., rapid heart rate, nausea, sweating) and may experience full-blown attacks when confronting a feared situation. They recognize that their fear is excessive and unreasonable, but people with SAD often feel powerless against their anxiety.
EXHIBIT 4.10. Diagnostic Criteria for SAD.
The lifetime prevalence of any anxiety disorder is estimated at over 30 percent; 12-month prevalence estimates are approximately 19 percent ( Harvard Medical School, 2005 ). A recent World Health Organization (WHO) survey and analysis using DSM-5 diagnostic criteria found the community lifetime prevalence of GAD in the U.S. is 7.8 percent, and 12-month prevalence is 4 percent ( Ruscio et al., 2017 ). Women are twice as likely as men to experience the disorder ( APA, 2013 ). Lifetime prevalence of panic attacks (ascertained as part of an analysis of data collected worldwide and defined per DSM-5 criteria) with or without panic disorder is almost 28 percent ( de Jonge et al., 2016 ). The 12-month prevalence in the general population for panic disorder is about 2.4 percent; lifetime prevalence is 6.8 percent ( Kessler, Petukhova, Sampson, Zaslavsky, & Wittchen, 2012 ). The 12-month prevalence for SAD is approximately 7 percent; rates in the community trend higher in women (1.5 times) than men, especially in young adults ( APA, 2013 ).
Anxiety Disorders and SUDs
The relationship between substance use and anxiety disorders is complex and multifaceted, and the two disorders commonly co-occur. Presence of a 12-month or lifetime DSM-5 drug use disorder (i.e., an SLID excluding alcohol) is associated with a 1.2 to 1.3 increased odds of having any anxiety disorder, a 1.0 to 1.3 increased odds of having panic disorder, a 1.2 to 1.3 increased odds of having GAD, and a 1.1 to 1.3 increased odds of having SAD ( Grant et al., 2016 ). Recent analyses indicate lifetime (but not 12-month) diagnosis of drug and alcohol use disorders is associated with GAD ( Grant et al., 2015 ; Grant et al., 2016 ). Twelve-month prevalence of panic disorder with co-occurring SUD is 11 percent, and lifetime cooccurrence is 28 percent ( de Jonge et al., 2016 ).
When anxiety and SUDs co-occur, the disorders affect development and maintenance of comorbidity, and each disorder modifies the presentation and treatment outcomes for the other ( Brady, Haynes, Hartwell, & Killeen, 2013 ). Consequently, people with anxiety disorders and co-occurring SUDs experience worse outcomes than those with either disorder alone, including greater disability, more hospitalizations and healthcare utilization, poorer functioning, more difficulties in interpersonal relationships, more severe symptoms, worse health-related quality of life, and poorer treatment response ( Buckner, Heimberg, Ecker, & Vinci, 2013 ; Magidson, Liu, Lejuez, & Blanco, 2012 ). GAD and addiction are associated with higher rates of heavy alcohol use, hospitalizations, relapse, and leaving treatment against medical advice compared with people with SUDs but no GAD ( Domenico, Lewis, Hazarika, & Nixon, 2018 ).
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH AN ANXIETY DISORDER.
CASE STUDY: CAD AND PROTRACTED WITHDRAWAL.
Anxiety symptoms and anxiety disorders are predictors of suicidal ideation and suicide attempt ( Bentley et al., 2016 ); given that SUDs also elevate risk of suicide ( Yuodelis-Flores & Ries, 2015 ), the combination of the two suggests efforts to mitigate suicide risk mitigation are warranted with these clients.
Treatment of Anxiety Disorders and SUDs
SUD treatment for people with anxiety should include interventions that address the anxiety as well as the addiction. Clients may report a reduction in some anxiety symptoms during detoxification or early in recovery ( McHugh, 2015 ). That said, SUD treatment alone is not sufficient to address the co-occurring anxiety. Further, the presence of an anxiety disorder complicates SUD treatment and can make achieving and sustaining abstinence and preventing relapse more problematic ( McHugh, 2015 ).
Concurrent, integrated treatments that include CBT or exposure therapy can safely, effectively reduce psychiatric and SUD symptoms but in some studies are no more effective than placebo ( McHugh, 2015 ).
- Schizophrenia and Other Psychotic Disorders
Psychotic Disorders
Psychotic disorders are characterized by a severely incapacitated mental and emotional state involving a person's thinking, perception, and emotional control. Key features include distorted thoughts in which an individual has false beliefs, sensations, or perceptions that are imagined, are very extreme, or both; and unusual emotional and behavioral states with deterioration in thinking, judgment, self-control, or understanding. Psychotic disorders are usually expressed clinically as a combination of:
Delusions: Beliefs that are fixed, resistant to change, and are directly contradicted by evidence or otherwise not grounded in reality (e.g., the belief that one is being followed
by people from Mars, or that one is a very important person to whom the President wants to speak right away).
Hallucinations: Hearing, seeing, tasting, or feeling things that are not there and being unable to recognize that what is being experienced is not real (such as hearing voices that say self-condemning or other disturbing things, or seeing a person who isn't really there).
Disorganized thinking: This is reflected in speech that is incoherent (“word salad”), illogical, uses unconventional or made-up words (neologisms and word approximations), fluctuates from topic to topic (loose associations), or is completely unrelated to subject matter at hand (tangential speech).
Grossly disorganized or abnormal motor behavior: This includes a wide range of odd behaviors, such as laughing or smiling inappropriately, grimacing, staring, talking to oneself, purposeless or peculiar movements and mannerisms, mimicking others’ speech or movements (echolalia and echopraxia), and random agitation. A specific psychomotor disturbance called catatonia —which includes immobility, stupor, and holding rigid body positions against gravity over extended periods of time (catalepsy)—can occur in schizophrenia but is also present in other mental disorders (like bipolar disorder) and some medical conditions.
Negative symptoms: A constellation of symptoms reflecting diminished emotional expression and self-motivated purposeful activities (avolition). Negative symptoms also may include diminished speech output (alogia) or poverty of speech (e.g., one-word answers), motivation, ability to experience pleasure (anhedonia), or interest in social activities (asociality).
Although schizophrenia is perhaps the most well known psychotic disorder, people with bipolar disorders may experience psychotic states during periods of mania—the heightened state of excitement, little or no sleep, impulsiveness, and poor judgment (see the section “Bipolar I Disorder”). Other conditions also can be accompanied by a psychotic state, including toxic poisoning, other metabolic difficulties (infections [e.g., latestage AIDS]), and other mental disorders (MDD, dementia, PTSD, alcohol withdrawal states, brief reactive psychoses, and others).
SUD treatment counselors typically do not see clients in the throes of an acute psychotic episode, as such psychotic patients more likely present, or are referred to, EDs and mental health services facilities. Counselors are more likely to encounter such clients in a “residual” or later and less active phase of the illness, the time at which these individuals may receive treatment for their SUDs in an SUD treatment agency. Even if the SUD treatment counselor never sees a client during an actively psychotic period, knowing what the client experiences as a psychotic episode will enable the counselor to understand and assist the client more effectively. On the other hand, counselors are increasingly treating clients with methamphetamine dependence who often have residual paranoid and psychotic symptoms and may need antipsychotic medications.
Schizophrenia
No single symptom specifically indicates or characterizes schizophrenia. Symptoms include a range of cognitive, behavioral, and emotional dysfunctions ( Exhibit 4.11 ). Thus, schizophrenia is a heterogeneous clinical syndrome. Symptoms of schizophrenia include delusions, hallucinations, disorganized speech (e.g., frequent derailment or incoherence), grossly disorganized or catatonic behavior, and deficits in certain areas of functioning—for example, the inability to initiate and persist in goal-directed activities. These symptoms regularly develop before the first episode of a schizophrenic breakdown, sometimes stretching back years and often intensifying prior to reactivations of an active, acutely psychotic state. Clinicians generally divide schizophrenia symptoms into positive and negative symptoms. Acute course schizophrenia is characterized by positive symptoms like hallucinations, delusions, excitement, motor manifestations (such as agitated behavior or catatonia), disorganized speech, relatively minor thought disturbances, and positive response to neuroleptic medication. Chronic course schizophrenia is characterized by negative symptoms, such as lack of enjoyment (anhedonia), apathy, lack of emotional expressiveness (flat affect), and social isolation. Some clients will live their entire lives exhibiting only a single psychotic episode; others may have repeated episodes separated by varying durations of time.
EXHIBIT 4.11. Diagnostic Criteria for Schizophrenia.
Community prevalence rates for schizophrenia using DSM-5 criteria are not available at the time of this publication. The lifetime prevalence rate for adults with DSM-IV schizophrenia is between 0.3 percent and 0.7 percent ( APA, 2013 ). The National Institute of Mental Health (NIMH; 2018) reports similar but slightly lower numbers, ranging between 0.25 percent and 0.64 percent. Although its prevalence is very low, schizophrenia is very burdensome and considered one of the top 15 leading causes of global disability ( GBD 2016 Disease and Injury Incidence and Prevalence Collaborators, 2017 ).
Schizophrenia/Other Psychotic Disorders and SUDs
Substance misuse often occurs in people with schizophrenia and other psychotic disorders. In a study of more than 1,200 people with schizophrenia ( Kerner, 2015 ), lifetime SUD prevalence was 55 percent, including alcohol abuse at 17 percent, alcohol dependence at 26 percent, illicit drug abuse at 13 percent, and illicit drug dependence at 14 percent. The most commonly used substances were alcohol (43 percent), cannabis (35 percent), and other illegal substances (27 percent). Compared with the general population, people with severe psychotic disorders have 4 times greater risk of heavy alcohol use, 3.5 times the risk of heavy cannabis use, and 4.6 times the risk of recreational drug use ( Hartz et al., 2014 ).
Individuals with SMI (including schizophrenia, schizoaffective disorder, and bipolar disorder with psychotic features) die approximately 10 to 25 years earlier than the general population, mostly because of the effects of physical illnesses caused at least in part by SUDs (e.g., heart disease, lung disease, infectious disease) ( Hartz et al., 2014 ; WHO, n.d.).
The combination of substance misuse in people with schizophrenia or other psychotic disorders contributes to shortened mortality and an increased likelihood of deleterious health and functional outcomes, including a higher risk for self-destructive and violent behaviors, victimization, suicide, housing instability, poor physical health, cognitive impairment, employment problems, legal difficulties, and unstable social relationships ( Bennett, Bradshaw, & Catalano, 2017 ; Trudeau et al., 2018 ). Further, substance misuse in schizophrenia can worsen disease course and may reduce adherence to antipsychotic medication ( Werner & Covenas, 2017 ).
CASE STUDY: COUNSELING AN SUD TREATMENT CLIENT WITH SCHIZOPHRENIA.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH SCHIZOPHRENIA OR ANOTHER PSYCHOTIC DISORDER.
Treatment of Schizophrenia/Other Psychotic Disorders and SUDs
Antipsychotic medication is the standard of care for reducing positive symptoms (e.g., delusions, hallucinations) whereas various psychosocial interventions and approaches can help address addiction recovery. Specifically, integrated CBT, group behavioral therapy, contingency management, 12-Step facilitation, motivational enhancement, motivational interviewing, assertive community treatment, or (preferably) a combination thereof may all help reduce substance use (quantity, frequency, and severity), increase abstinence, reduce number of drinking days, lower relapse rates, reduce the number of positive urine samples, and decrease negative consequences of substance use in people with SUDs and schizophrenia or other SMI (including psychotic disorders) ( Bennett et al., 2017 ; De Witte, Crunelle, Sabbe, Moggi, & Dom, 2014 ). These approaches have also been associated with improvements in psychiatric symptoms (including negative symptoms), scores of global functioning, hospitalizations, and achieving stable housing ( De Witte et al., 2014 ). Integrated treatments appear to yield more positive results than single interventions and are the recommended approach ( De Witte et al., 2014 ).
- Attention Deficit Hyperactivity Disorder
ADHD is marked by a chronic inability to direct, control, or sustain attention; hyperactivity; or both ( Exhibit 4.12 ). People with ADHD often have difficulty concentrating for even short periods of time. They may be disorganized and restless or seem always “on the go,” constantly moving and fidgeting. Some people with ADHD behave impulsively.
EXHIBIT 4.12. Diagnostic Criteria for ADHD.
Although ADHD is frequently associated with children, the disorder can persist into adulthood and for some individuals can begin in adulthood.
In adults, symptoms can include having a short temper, difficulty being productive at work, and an inability to sustain relationships.
The three types of ADHD are combined type (person has difficulty paying attention and hyperactivity); predominantly inattentive; and predominantly hyperactiveimpulsive.
At the time of this publication, 12-month and lifetime ADHD prevalence rates among all age groups in the general population using DSM-5 criteria are not readily available. However, data from the National Survey of Children's Health show that 6.1 million children and adolescents ages 2 to 17 years had ever been diagnosed with ADHD ( Danielson et al., 2018 ).
The prevalence of ADHD in adults is less studied than in children. The overall current prevalence of adult ADHD (using DSM-IV criteria) is around 2.5 percent ( APA, 2013 ; Simon, Czobor, Balint, Meszaros, & Bitter, 2009 ). Epidemiological population-based survey data on U.S. adults with ADHD ( Kessler et al., 2005 ) suggest the estimated lifetime prevalence of DSM-IV ADHD in people ages 18 to 44 years is 8.1 percent.
ADHD and SUDs
SUDs are among the most common comorbidities of ADHD ( Katzman, Bilkey, Chokka, Fallu, & Klassen, 2017 ), and data from clinical and epidemiological studies support this linkage ( Martinez-Raga, Szerman, Knecht, & de Alvaro, 2013 ). Among adults with substance misuse, the prevalence of ADHD is approximately 23 percent, although this estimate is dependent on substance of misuse and assessment instrument used ( van Emmerik-van Oortmerssen et al., 2012 ). Among a sample of more than 500 children with and without ADHD who were followed throughout adolescence and early adulthood ( Molina et al., 2018 ), early substance use in adolescence was greater and escalated more quickly in the children with ADHD. Further, weekly and daily cannabis use and daily smoking in adulthood were significantly more prevalent in the ADHD group than the non-ADHD group. Adults with ADHD have been found primarily to use alcohol, nicotine, cannabis, and cocaine ( Lee, Humphreys, Flory, Liu, & Glass, 2011 ; Luo & Levin, 2017 ).
People with addiction who have co-occurring ADHD have a heightened risk for suicide attempts, hospitalizations, earlier onset of addiction, impulsivity, more severe disease course (for both ADHD and the SUD) and polysubstance use as well as lower rates of abstinence and treatment adherence ( Egan, Dawson, & Wymbs, 2017 ; Katzman et al., 2017 ). ADHD and SUDs carry an enhanced risk of comorbidity with depression, conduct disorder, bipolar disorders, anxiety disorders, and PDs ( Luo & Levin, 2017 ; Martinez-Raga et al., 2013 ; Regnart, Truter, & Meyer, 2017 ; Young & Sedgwick, 2015 ; Zulauf, Sprich, Safren, & Wilens, 2014 ). Symptoms of ADHD hyperactivity and impulsivity are more strongly seen with substance misuse and SUDs than ADHD symptoms of inattention ( De Alwis, Lynskey, Reiersen, & Agrawal, 2014 ).
Although it is important to rule out other causes of inattention or hyperactivity, including substance misuse, misattribution of ADHD symptoms to SUDs increases the likelihood of underdiagnosis ( Crunelle et al., 2018 ). People with SUDs who are newly abstinent or those in active or protracted withdrawal may experience some impairments similar to ADHD. Many of the behavioral symptoms of ADHD also appear during substance intoxication and withdrawal, and functional consequences of ADHD, such as poor job performance or job loss, are also evident in people with addiction. Both alcohol and cannabis can produce symptoms that mimic ADHD. This underscores the importance of conducting a thorough assessment (see Chapter 3 ) to fully investigate symptoms in childhood, family history of addiction and psychiatric illness, and other biopsychosocial factors that can inform whether a diagnosis of ADHD, SUD, or both are warranted.
Treatment of ADHD and SUDs
ADHD complicates SUD treatment because clients with these CODs may have more difficulty engaging in treatment and learning abstinence skills, be at greater risk for relapse, and have poorer substance use outcomes. The most common attention problems in SUD treatment populations are secondary to short-term toxic effects of substances, and these should be substantially better with each month of sobriety.
A consensus statement by an international panel of ADHD and addiction experts (including from the U.S.) on the treatment of ADHD and SUDs recommends ( Crunelle et al., 2018 ):
Using a combined treatment approach comprising psychoeducation, pharmacotherapy, individual or group CBT, and peer support.
Integrating ADHD treatment into SUD treatment; integrating SUD treatment into mental health services.
Treating both disorders, but addressing the SUD first and then the ADHD shortly afterwards.
Considering residential treatment for cases of severe addiction.
Providing pharmacotherapy for ADHD (particularly with psychotherapy), but clinicians should be aware that medication alone Is usually not sufficient to treat the SUD.
Prescribing ADHD medication as needed but understand that this is a controversial topic because of the misuse liability of stimulants. Clinicians should consider all risks and weigh them against potential benefits when deciding whether to prescribe stimulant medications for people with ADHD-SUD.
Only a limited number of studies explore treatment of ADHD with comorbid SUDs ( De Crescenzo, Cortese, Adamo, & Janiri, 2017 ). Treatment of adults with ADHD often involves use of stimulant or nonstimulant medication; although efficacious in reducing psychiatric symptoms, these medications generally do not alleviate SUD symptoms ( Cunill, Castells, Tobias, & Capella, 2015 ; De Crescenzo et al., 2017 ; Luo & Levin, 2017 ). Thus, ADHD medication alone is an insufficient treatment approach for clients with these CODs ( Crunelle et al., 2018 ; Zulauf et al., 2014 ). Stimulant medications have misuse potential, and counselors should be vigilant for signs of diversion. Use of long-acting or extended-release medication or use of antidepressants instead of stimulants can attenuate diversion and misuse liability. The advised approach to treatment involves a combination of psychoeducation, behavioral coaching, CBT, and nonstimulant or extended-release stimulant medication ( De Crescenzo et al., 2017 ).
Little research supports concurrent treatment of these conditions. Some researchers recommend first addressing whichever condition is most debilitating to the client ( Katzman et al., 2017 ; Klassen, Bilkey, Katzman, & Chokka, 2012 ). Others suggest that, to stabilize the client, treating the SUD should be prioritized ( Crunelle et al., 2018 ). A systematic literature review and meta-analysis of pharmacotherapy for ADHD and SUD ( Cunill et al., 2015 ) found no effect of timing of initiation of treatment but warns that treatment of ADHD symptoms may need to be delayed until after abstinence is achieved, given possible harmful interactions that can occur between ADHD medications and substances of misuse.
- Feeding and Eating Disorders
Feeding and eating disorders have as their common core a persistent disturbance of eating or eating-related behavior, resulting in changes in consumption or absorption of food that significantly impair physical health or psychosocial functioning. The primary eating disorders linked to SUD and discussed in this section are AN, bulimia nervosa (BN), and binge eating disorder (BED).
Anorexia Nervosa
AN, the most visible eating disorder, is marked by a refusal to maintain body weight above the minimally normal weight for age and height because of an intense fear of weight gain ( Exhibit 4.13 ). The term anorexia nervosa means “nervous loss of appetite,” a misnomer; only in extreme stages of inanition (i.e., exhaustion as a result of lack of nutrients in the blood) is appetite actually lost.
EXHIBIT 4.13. Diagnostic Criteria for AN.
Individuals with AN have a dogged determination to lose weight and can achieve this in several ways. Individuals with the restricting subtype of AN severely limit their food intake, engage in excessive exercise, and fast. Those with the binge-eating/purging subtype engage in episodes of binge eating or purging with self-induced vomiting, laxatives, diuretics, or enemas. They engage in these behaviors out of a marked fear of weight gain, which is reinforced by distorted perceptions of their body shape (e.g., believing oneself to be “fat” even though bodyweight is extremely low).
CASE STUDY: COUNSELING AN SUD TREATMENT CLIENT WITH ADHD.
Bulimia Nervosa
The core symptoms of BN are bingeing and purging ( Exhibit 4.14 ). A binge is a rapid consumption of an unusually large amount of food, by comparison with social norms, in a discrete period of time (e.g., over 2 hours). Integral to the notion of a binge is feeling out of control; thus, a binge is not merely overeating. An individual with BN may state that he or she is unable to postpone the binge or stop eating willfully once the binge has begun. The binge may only end when the individual is interrupted, out of food, exhausted, or physically unable to consume more.
EXHIBIT 4.14. Diagnostic Criteria for BN.
The second feature of BN is purging. Individuals with BN compensate in many different ways for overeating. Ninety percent of people with BN self-induce vomiting or misuse laxatives as their form of purging ( Westmoreland, Krantz, & Mehler, 2016 ). Other methods of purgation include the misuse of diuretics and emetics; saunas; excessive exercise; fasting; and other idiosyncratic methods that people believe will lead to weight loss (such as “mono” dieting, in which a person eats only a single food for extended periods of time and nothing else, like apples or eggs). Many of these auxiliary methods are dangerous and ineffective because they promote loss of water and valuable electrolytes. As with AN, individuals with BN place an undue emphasis on shape and weight in their sense of identity. To meet criteria, bingeing and purging must occur, on average, at least once per week for 3 months.
Binge Eating Disorder
BED involves recurring episodes of eating significantly more food in a short period of time than most people would eat under similar circumstances, with episodes marked by feelings of lack of control ( Exhibit 4.15 ). Someone with BED may eat too quickly, even when he or she is not hungry. The person may feel guilt, embarrassment, or disgust and may binge eat alone to hide the behavior. This disorder is linked with marked distress and occurs, on average, at least once a week over 3 months. Unlike in BN, the binge is not followed by compensatory behaviors to rid the body of food.
EXHIBIT 4.15. Diagnostic Criteria for BED.
Feeding and eating disorders in the general population are rare. Twelve-month estimates of DSM-5 AN, BN, and BED are 0.05 percent, 0.14 percent, and 0.44 percent, respectively; lifetime prevalence rates are 0.80 percent, 0.28 percent, and 0.85 percent, respectively ( Udo & Grilo, 2018 ). These rates are generally lower than previously reported estimates using DSM-IV criteria ( APA, 2013 ) but were drawn from a sample roughly 12 times larger than the samples used in other survey studies ( Udo & Grilo, 2018 ).
Eating disorders are far more prevalent in women than men. Women have 12 times the odds of having AN, 5.8 times the odds of having BN, and about 3 times the odds of having BED ( Udo & Grilo, 2018 ).
Feeding and Eating Disorders and SUDs
Feeding and eating disorders are highly coincident with substance misuse ( SAMHSA, 2011a ), likely because the conditions share numerous physical, mental, and social risk factors ( Brewerton, 2014 ). Most studies observe comorbidity rates that exceed the general population of women of similar age. A meta-analysis ( Bahji et al., 2019 ) found lifetime prevalence of any SLID among people with eating disorders to be 25 percent, including 20 percent for AUD, about 20 percent for any illicit drug use disorder, almost 14 percent for cocaine and cannabis use disorder (each), and 6 percent for opioid use disorder (OUD). Even if not rising to the level of addiction, licit and illicit substance use is elevated in people with eating disorders, especially individuals with bulimic features. In a sample of almost 3,000 people, 80 percent of those with BN reported using alcohol, and 50 percent used other substances; 65 percent of those with BED used alcohol, and nearly 24 percent used other substances; and 60 percent of those with AN (binge/purge subtype) used alcohol, and 44 percent used other substances ( Fouladi et al., 2015 ).
SUD treatment-seeking women have higher rates of BN than any other feeding and eating disorder, and SUDs are more common alongside BN or AN with bulimic features than they are comorbid with restrictive AN ( APA, 2013 ; CSAT, 2009 ; Fouladi et al., 2015 ). Some have suggested that the most common comorbidity among feeding and eating disorders and SUDs is BN (or AN with bulimic features) and AUD ( Gregorowski, Seedat, & Jordaan, 2013 ; Munn-Chernoff et al., 2015 ).
Treatment outcomes of people with eating disorders and SUDs are worse than those of people without both conditions. They have higher odds of early mortality, co-occurring physical and mental illness, and delayed recovery ( Root et al., 2010 ). People in SUD treatment with feeding/eating disorder symptoms have higher risk of treatment dropout and discharge against medical advice ( Elmquist, Shorey, Anderson, & Stuart, 2015 ). Alcohol misuse more than doubles mortality risk in AN ( Franko et al., 2013 ).
Treatment of Feeding and Eating Disorders andSUDs
Feeding or eating disorders can make SUD assessment and treatment more complex—such as by raising risk of stopping SUD treatment against medical advice ( Elmquist et al., 2015 ). Heightened mortality with feeding and eating disorders means that multidisciplinary care should include primary care providers and dietary/nutritional rehabilitation professionals in addition to SUD treatment professionals, mental health professionals (e.g., psychiatric and mental health nurses), and social workers (SAMHSA, 2011 a).
The literature does not currently describe randomized controlled trials for treatment of these CODs. In general, concurrent treatment is recommended; sequential interventions can increase likelihood of relapse or otherwise hinder recovery from the untreated CODs ( Gregorowski et al., 2013 ). If integrated care is not possible,
SUD treatment should proceed first to halt active substance use and allow the client to fully participate in further care (SAMHSA, 2011 a).
“DRUNKOREXIA”: A NEW AND DANGEROUS COMBINATION OF EATING DISORDERS AND ALCOHOL MISUSE.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH AN EATING DISORDER.
Only 51 percent of SUD treatment programs report screening clients for feeding and eating disorders ( Kanbur & Harrison, 2016 ).
Regardless of treatment modality, providers must first ensure medical and weight stabilization so clients are healthy and able to physically and cognitively participate in and benefit from therapy ( Harrop & Marlatt, 2010 ). Some clients with AN or BN may require inpatient treatment or partial hospitalization to stabilize weight. Depending on the facility, staff may not be equipped to address any co-occurring substance misuse simultaneously.
The primary treatment for these disorders is psychosocial intervention, including individual, group, family therapy, or a combination thereof. CBT can be effective for feeding and eating disorders but has not been researched thoroughly in populations with co-occurring addiction ( Gregorowski et al., 2013 ). Dialectical behavior therapy also can be useful in promoting mindfulness, improving management of negative emotions, and teaching affective and behavioral self-regulation skills in feeding and eating disorders and in SUDs separately ( Ritschel, Lim, & Stewart, 2015 ) but, again, has not been studied extensively in both concurrently. Pharmacotherapy may be warranted for BN and BED ( SAMHSA, 2011a ) but is not a first-line treatment. Further studies are needed to clarify how the presence of a feeding or eating disorder affects SUD treatment and how best to integrate treatment for both conditions.
- Substance-Related Disorders
The primary aim of this section of the chapter is to describe substance-induced mental disorders and to clarify how to differentiate them from mental disorders that co-occur with SUDs.
Substance-related disorders include two subcategories: SUDs and substance-induced disorders. SUDs identify the cluster of cognitive, behavioral, and physical symptoms that occur as a result of continued and frequent use of substances. These consequences are not immediate. Rather, they occur over time as addiction progresses. Substance-induced mental disorders refer to the immediate effects of substance use (intoxication), the immediate effects of discontinuing a substance (substance withdrawal), and other substance-induced mental disorders ( APA, 2013 ).
The essential feature of an SUD is a cluster of cognitive, behavioral, and physical symptoms indicating that the individual continues using the substance despite significant substance-related problems. All DSM-5 SUDs have their own diagnostic criteria, but criteria are largely the same across substances. Addiction counselors should be familiar with SUD diagnostic criteria and refer to DSM-5 as needed.
Lifetime and 12-month prevalence rates of DSM-5 drug use disorders (i.e., non-alcohol-related SUDs) are nearly 10 percent and 4 percent, respectively ( Grant et al., 2016 ). Lifetime and 12-month prevalence rates of AUD are about 29 percent and 14 percent, respectively ( Grant et al., 2015 ). Past-month prevalence rates of misuse of other substances by adults ages 26 and older include ( CBHSQ, 2019 ):
8.6 percent for cannabis.
0.7 percent for cocaine.
1.0 percent for pain relievers.
0.5 for tranquilizers.
0.4 percent for stimulants.
0.1 percent for prescription sedatives.
0.4 percent for hallucinogens.
0.2 percent for heroin.
0.1 percent for inhalants.
Substance-Induced Mental Disorders
The toxic effects of substances can mimic mental disorders in ways that can be difficult to distinguish from mental illness. This section focuses on a general description of symptoms of mental illness that are the result of substances or medications—a condition called substance-induced mental disorders .
DSM-5 substance-induced mental disorders include:
Substance-induced depressive disorders.
Substance-induced bipolar and related disorders.
Substance-induced anxiety disorders.
Substance-induced psychotic disorders.
Substance-induced obsessive-compulsive and related disorders.
Substance-induced sleep disorders.
Substance-induced sexual dysfunctions.
Substance-induced delirium.
Substance-induced neurocognitive disorder.
The first four of the listed substance-induced mental disorders are the most common in addiction, discussed further in the section, “Specific Substance-Induced Mental Disorders.” Exhibit 4.16 summarizes substances and the substance-induced mental disorders associated with each.
EXHIBIT 4.16. Substances and Corresponding Substance-Induced Mental Disorders.
WARNING TO COUNSELORS: INDEPENDENT VERSUS SUBSTANCE-INDUCED MENTAL DISORDERS.
General Considerations
Substance-induced mental disorders are distinct from independent co-occurring mental disorders in that all or most of the psychiatric symptoms are the direct result of substance use. This does not mean that substance-induced disorders preclude co-occurring mental disorders, only that the specific symptom cluster at a specific point in time is more likely the result of substance use, misuse, intoxication, or withdrawal than of underlying mental illness.
Even when the psychiatric diagnosis has not been established, the client's co-occurring symptoms should still be treated (with nonmedication). Counselors should not withhold treatment simply because a determination about the origin of the mental disorder has not yet been made.
Symptoms of substance-induced mental disorders run the gamut from mild anxiety and depression (these are the most common across all substances) to full-blown manic and other psychotic reactions (much less common). For example, acute withdrawal symptoms from physiological depressants such as alcohol and benzodiazepines are hyperactivity, elevated blood pressure, agitation, and anxiety (i.e., “the shakes”). On the other hand, those who “crash” from stimulants are tired, withdrawn, and depressed.
Because clients vary greatly in how they respond to both intoxication and withdrawal given the same exposure to the same substance, and also because different substances may be taken at the same time, prediction of any particular substance-related syndrome has its limits. What is most important is to continue to evaluate psychiatric symptoms and their relationship to abstinence or ongoing substance misuse over time. Most substance-induced symptoms begin to improve within hours or days after substance use has stopped. Notable exceptions to this are psychotic symptoms caused by heavy and longterm amphetamine misuse and dementia (e.g., problems with memory, concentration, problem solving) caused by using substances directly toxic to the brain, which most commonly include alcohol, inhalants like gasoline, and amphetamines.
Exhibit 4.17 offers an overview of the most common classes of misused substances and the accompanying psychiatric symptoms seen in intoxication and withdrawal.
EXHIBIT 4.17. Substance-Induced Mental Disorder Symptoms (by Substance).
INDUCED VERSUS INDEPENDENT MENTAL DISORDERS: THE IMPORTANCE OF TREATMENT.
Diagnoses of substance-induced mental disorders will typically be provisional and will require réévaluation—sometimes repeatedly. Many apparent acute mental disorders may really be substance-induced disorders, such as in those clients who use substances and who are acutely suicidal.
Some people who appear to have substance-induced mental disorders turn out to have a substance-induced mental disorder and independent mental disorder. Consider preexisting mood state, personal expectations, drug dosage, and environmental surroundings in understanding of how a particular client might experience a substance-induced disorder. Treatment of the SUD and an abstinent period of weeks or months may be required for a definitive diagnosis of an independent, co-occurring mental disorder. As described in Chapter 3 , SUD treatment programs and clinical staff can concentrate on screening for mental disorders and determining the severity and acuity of symptoms, along with an understanding of the client's support network and overall life situation.
Specific Substance-Induced Mental Disorders
This section briefly discusses the most common substance-induced mental disorders in clinical populations: substance-induced depressive, anxiety, bipolar, and psychotic disorders. Diagnostic criteria for all substance-induced mental disorders, including the four mentioned, are nearly identical and comprise five general characteristics ( Exhibit 4.18 ).
EXHIBIT 4.18. Features of DSM-5 Substance-Induced Mental Disorders.
Exhibit 4.19 lists substances most likely to induce/mimic depressive, anxiety, bipolar, and psychotic disorders.
EXHIBIT 4.19. Substances That Precipitate or Mimic Common Mental Disorders.
Substance-induced depressive disorders
The lifetime prevalence of substance-induced depressive disorders in the general community is 0.26 percent ( Blanco et al., 2012 ). Observed rates among clinical populations are much higher. For instance, in a study of people seeking treatment for co-occurring depressive disorders and SUDs, 24 percent had substance-induced depression; rates varied by substance. Among those with 12-month alcohol dependence, prevalence of substance-induced MDD was 22 percent; for past-year cocaine dependence, 22 percent; and for past-year heroin dependence, nearly 37 percent ( Samet et al., 2013 ). In another study of people with SUDs, 60 percent of people with depression had a substance-induced rather than independent depressive disorder ( Conner et al., 2014 ). DSM-5 notes that although about 40 percent of people with AUD develop MDD, only about one-third to one-half are cases of independent depression, meaning as much as 75 percent of occurrences of depressive disorders in the context of AUD could be because of intoxication or withdrawal ( APA, 2013 ). Depressive disorders or their symptoms could also be because of the long-term effects of substance use.
Diagnosis of a substance-induced versus independent depressive disorder can be difficult given that many people with SUDs do have mood symptoms, like depressed affect, and intoxication and withdrawal from substances can mirror symptoms of depression. During the first months of abstinence, many people with SUDs may exhibit symptoms of depression that fade over time and are related to acute withdrawal. Because depressive symptoms during withdrawal and early recovery may result from SUDs and not an underlying depression, a period of time should elapse before depression is diagnosed. This does not preclude the importance of addressing depressive symptoms during the early stage of recovery, before diagnosis. Further, even if an episode of depression is substance induced, that does not mean that it should not be treated. Overall, the process of addiction can result in biopsychosocial disintegration, leading to PDD or depression often lasting from months to years.
Substance-induced mood alterations can result from acute and chronic drug use as well as from drug withdrawal. Substance-induced depressive disorders, most notably acute depression lasting from hours to days, can result from sedative-hypnotic intoxication. Similarly, prolonged or subacute withdrawal, lasting from weeks to months, can cause episodes of depression, and sometimes is accompanied by suicidal ideation or attempts.
Stimulant withdrawal may provoke episodes of depression lasting from hours to days, especially following high-dose, chronic use. Acute stimulant withdrawal generally lasts from several hours to 1 week and is characterized by depressed mood, agitation, fatigue, voracious appetite, and insomnia or hypersomnia (oversleeping). Depression resulting from stimulant withdrawal may be severe and can be worsened by the individual's awareness of substance use-related adverse consequences. Symptoms of craving for stimulants are likely and suicide is possible. Protracted stimulant withdrawal often includes sustained episodes of anhedonia (absence of pleasure) and lethargy with frequent ruminations and dreams about stimulant use.
Stimulant cessation may be followed for several months by bursts of dysphoria, intense depression, insomnia, and agitation. These symptoms may be either worsened or lessened depending on the provider's treatment attitudes, beliefs, and approaches. It is a delicate balance—between allowing time to observe the direction of symptoms to treating the client's presenting symptoms regardless of origin.
Substance-Induced Anxiety Disorders
The prevalence of substance-induced anxiety disorders in the community is unreported and thought to be quite low (less than 0.1 percent), although likely higher in clinical samples ( APA, 2013 ).
Licit and illicit substances can cause symptoms that are identical to those in anxiety. In addition, many medications, toxins, and medical procedures can cause or are associated with an eruption of anxiety. Moreover, these reactions vary greatly from mild manifestations of shortlived symptoms to full-blown manic and other psychotic reactions, which are not necessarily short lived.
Symptoms that look like anxiety may appear either during use or withdrawal. Alcohol, amphetamine and its derivatives, cannabis, cocaine, hallucinogens, intoxicants and phencyclidine and its relatives have been reported to cause the symptoms of anxiety during intoxication. Withdrawal from alcohol, cocaine, illicit opioids, and also caffeine and nicotine can also cause manifestations of anxiety. Similarly, withdrawal from depressants, opioids, and stimulants invariably includes potent anxiety symptoms.
Substance-Induced Bipolar Disorders
Epidemiologic data on substance-induced mania or bipolar disorders in the U.S. general population are not readily available.
A number of substances of misuse (as well as prescribed medications and several medical conditions) are also associated with manic-like phenomena. Acute manic symptoms may be induced or mimicked by intoxication with stimulants, steroids, hallucinogens, or polydrug combinations. They may also be caused by withdrawal from depressants such as alcohol. Individuals experiencing acute mania with its accompanying hyperactivity, psychosis, and often aggressive and impulsive behavior should be referred to emergency mental health professionals.
Stimulant-induced episodes of mania may include symptoms of paranoia lasting from hours to days. Stimulants such as cocaine and amphetamines cause potent psychomotor stimulation. Stimulant intoxication generally includes increased mental and physical energy, feelings of well-being and grandiosity, and rapid, pressured speech. Chronic, high-dose stimulant intoxication, especially with sleep deprivation, may prompt a manic episode. Symptoms may include euphoric, expansive, or irritable mood, often with flight of ideas, severe social functioning impairment, and insomnia.
Substance-Induced Psychosis
This condition is very rare; exact prevalence rates are unknown ( APA, 2013 ). In first-episode psychosis, 7 percent to 25 percent of cases are substance induced ( APA, 2013 ).
CASE STUDIES: IDENTIFYING DISORDERS.
Heavy users of psychoactive substances, like cannabis, amphetamines, and cocaine, are vulnerable to substance-induced psychosis, especially clients with cooccurring schizophrenia and bipolar disorders. Antidepressants can also precipitate psychotic episodes, as can medications like prescribed steroids and nonsteroidal anti-inflammatory drugs, antiviral agents, antibiotics, anti-cholinergics, antihistamines, muscle relaxants, and opioids. Any number of physical illnesses or medication reactions, from brain tumors to steroid side effects, can cause a psychotic episode or psychotic behavior. Virtually any substance taken in very large quantities over a long enough period can lead to a psychotic state.
Differential diagnosis among psychotic disorders can be challenging, even for experienced clinicians and diagnosticians, especially when substances are involved. When a client presents in a psychotic state, any immediate or recent substance use is difficult to determine, and it may be impossible to discern whether the hallucinations or delusions are caused by substance use. If the hallucinations or delusions can be attributed to substance use but are prominent and beyond what one might expect from intoxication alone, the episode would be described as a substance-induced psychotic disorder. Hallucinations that the person knows are solely the result of substance use are not considered indicative of a psychotic episode; instead, they are diagnosed as substance intoxication or substance withdrawal with the specifier “with perceptual disturbances” ( APA, 2013 ).
- Cross-Cutting Topics: Suicide and Trauma
Suicide risk and trauma status are relevant to care planning, client safety, and treatment outcomes across many CODs. This section briefly addresses each issue and offers guidance to help addiction counselors understand why both need to be actively considered as part of assessment and treatment.
Ample literature discusses suicide, mental disorders, and addiction. This section is not intended to thoroughly review all aspects of suicide-related assessment, management, and prevention techniques for COD populations; readers instead are directed to TIP 50, Addressing Suicidal Thoughts and Behaviors in Substance Abuse Treatment ( CSAT, 2009 ) for more information. The aim of this text is to ensure that readers have a broad and general understanding of the high risk of suicidal thoughts and behaviors in clients with CODs and feel confident in knowing how to prevent and respond to such events.
Similarly, trauma has been a significant topic of research in the behavioral health literature. What follows is an abbreviated summary of the link between trauma and mental disorders and SUDs and how addiction counselors can offer trauma-informed services. Readers should consult TIP 57, Trauma-Informed Care in Behavioral Health Services ( SAMHSA, 2014b ) for more guidance in this area.
For both suicide and trauma, readers are reminded to review Chapter 3 for assessment techniques and tools, Appendix B for links to suicide prevention materials and other resources, and Appendix C for counselor tools like trauma screeners.
Suicide is a common risk factor that pertains to nearly all CODs and particularly those involving addiction and MDD, bipolar disorder, schizophrenia, PTSD, or PDs ( Yuodelis-Flores & Ries, 2015 ). Suicidality itself is not a mental disorder, but it is considered a high-risk behavior of significant public health concern ( Hogan & Grumet, 2016 ). Substance-induced or exacerbated suicidal ideations, intentions, and behaviors are possible complications of SUDs, especially for clients with co-occurring mental disorders.
The topic of suicidality is critical for SUD treatment counselors working with clients who have CODs. SUDs alone increase suicidality ( Yuodelis-Flores & Ries, 2015 ), whereas the added presence of some mental disorders doubles the already heightened risk ( O'Connor & Pirkis, 2016 ). The risk of suicide is greatest when relapse occurs after a substantial period of abstinence—especially if there is concurrent financial or psychosocial loss. Every agency that offers SUD counseling must also have a clear protocol in place that addresses the recognition and treatment (or referral) of people who may be suicidal.
These populations ( Department of Health and Human Services, 2012 ) are vulnerable to suicide risk; many are susceptible to addiction or CODs as well:
American Indians/Alaska Natives
Individuals who have lost a loved one to suicide
Clients involved in criminal justice/child welfare systems
Clients who engage in nonsuicidal self-injury
Individuals with a history of previous suicide attempt
Individuals with debilitating physical conditions
Clients with mental disorders, SUDs, or both
Individuals in the LGBTQ community
Members of the armed forces and veterans
Middle-aged and older men
Suicide is the 10th leading cause of death in the United States among people ages 10 and older ( Stone et al., 2019 ). Suicide is the second leading cause of death for people ages 10 to 34 and the fourth leading cause of death for those ages 35 and 54 ( NIMH, 2019 ). Per the Centers for Disease Control and Prevention (CDC), from 1999 to 2018, suicide rates in the United States increased 41 percent, from 10.5 to 14.8 per 100,000 people (CDC, 2019). Suicide rates among men remain more than 3 times higher (23.4 per 100,000 in 2018) than among women (6.4 per 100,000 in 2018) ( CDC, 2020 ).
Almost half (46 percent) of all individuals in the United States who died by suicide between 2014 and 2016 had a known mental health condition, and 54 percent were in treatment at the time of death ( Stone et al., 2019 ). Depression was the most common mental disorder diagnosis among those who completed suicide (75 percent); other major mental disorder diagnoses included anxiety (17 percent), bipolar disorders (1 5 percent), schizophrenia (5 percent), and PTSD (4 percent) ( Stone et al., 2019 ).
According to NSDUH data ( CBHSQ, 2019 ), in 2018:
About 10.7 million U.S. adults ages 18 or older thought seriously of dying by suicide (4.3 percent of adults).
3.3 million U.S. adults made suicide plans (1.3 percent).
1.4 million U.S. adults made nonfatal suicide attempts (0.6 percent).
Suicide and SUDs
Substance misuse makes people susceptible to self-harm; indeed, suicide is the leading cause of death among people with addiction ( CSAT, 2009 ). From 2014 to 2016, 28 percent of people who died by suicide had problematic substance use, including 32 percent of people with a known mental health disorder ( Stone et al., 2019 ). Of these individuals with known psychiatric problems, 39 percent tested positive for alcohol, 39 percent for benzodiazepines, 29 percent for opioids, 23 percent for cannabis, 10 percent for amphetamines, and 6 percent for cocaine ( Stone et al., 2019 ).
Alcohol factors prominently into suicide ( Darvishi, Farhadi, Haghtalab, & Poorolajal, 2015 ). Acute alcohol intoxication increases the risk of suicide attempt by nearly 7 times and in some studies, if use is heavy, by as much as 37 times ( Borges et al., 2017 ). This risk appears to increase with corresponding increases in consumption; as such, populations with AUD have higher rates of suicide than people without problematic alcohol use ( Yuodelis-Flores & Ries, 2015 ).
Other substances also carry an increased risk of self-harm, as suicidal behavior is prominent in OUD, cocaine use disorder, and polysubstance use ( Yuodelis-Flores & Ries, 2015 ). Among individuals with a history of substance misuse who died by suicide in 2014 ( Fowler, Jack, Lyons, Betz, & Petrosky, 2018 ), the most commonly involved nonmedication substances were alcohol (51 percent), opioids (23 percent), and cannabis (almost 14 percent). Furthermore, among all suicide cases that year, opioids were the direct cause of death in 27 percent of people and alcohol in 13 percent ( Fowler et al., 2018 ). The overall suicide rate of U.S. veterans with an SUD is estimated at 75.6 per 100,000 people and is highest among those who misuse sedatives, followed by amphetamines, opioids, cannabis, alcohol, and cocaine ( Bohnert, Ilgen, Louzon, McCarthy, & Katz, 2017 ). People who report misusing prescription medication, and in particular pain relievers, also appear to be vulnerable to suicidal ideation ( Ford & Perna, 2015 ).
The link between substance misuse and suicide may relate to the capacity of substances, especially alcohol, to quell inhibition, leading to poor judgment, mood instability, and impulsiveness. Depression, comorbid with suicide risk and substance misuse, may moderate this relationship. A population-based sample of people currently using alcohol and with a history of depressed mood ( Sung et al., 2016 ) found that those with a positive history of suicide attempt were significantly more likely than those without such a history to have problematic substance use, including 21 percent with alcohol abuse or dependence and nearly 40 percent with illicit drug abuse or dependence. Yet alcohol dependence in this sample significantly increased the odds of suicidal ideation and suicide attempt even among people without a history of depressed mood. This suggests that depressed mood alone cannot account for the relationship between alcohol misuse and risk of suicide, although it undoubtedly increases the odds.
Many psychiatric illnesses have a heightened risk of suicidal thoughts and behaviors further exacerbated in the presence of co-occurring addiction. Risk factors for suicide that have been identified in the general population, such as a family history of suicide attempt or completion and access to firearms, also apply to people with CODs and make self-harm more likely. Additionally, certain individuals with CODs may be at even further risk based on the presence of contributing factors that frequently appear in populations with mental disorders and SUDs. For instance, having a chronic physical health condition (such as traumatic brain injury or infectious disease), experiencing homelessness, being a military veteran, and past involvement in the criminal justice system are all associated with suicide-related ideation, gestures, attempts, or deaths ( Ahmedani et al., 2017 ; Cook, 2013 ; Jahn et al., 2018 ; Kang et al., 2015 ; Tsai & Cao, 2019 ) and may further compromise the safety of people with CODs. A history of adverse life experiences, like childhood maltreatment or intimate partner violence, also significantly increases risk of self-harm (especially in people with CODs) and is addressed in the section “Trauma.”
Prevention and Management of Suicidal Behaviors
Although a rare event, suicide is often—but not always—preventable. All SUD treatment clients should receive at least a basic screening for suicidality, and all SUD treatment professionals should know how to conduct at least basic screening and triage. (To learn more about suicide screening, see Chapter 3 of this TIP.) SAMHSA's Five-Step Evaluation and Triage ( SAMHSA, 2009b ) recommends using the following process for identifying and responding to threat of self-harm:
Identify risk factors.
Identify protective factors.
Conduct a suicidal inquiry into the client's thoughts, plans, behaviors, and intents.
Determine the level of risk and appropriate interventions.
Document risk, rationale, intervention, and follow-up procedures.
Addiction counselors should regularly assess and monitor all clients with CODs for suicidal ideation, gestures, plans, and attempts and especially clients with depressive disorders, bipolar disorders, PTSD, schizophrenia, or PDs. Routine assessment should be an integral part of treatment but is especially critical during times of high stress or increased substance use (including relapse) as well as at intake, following any suicidal behavior, following reports of suicidal ideation, and just before discharge. Information should be collected on the client's:
Personal and family history of suicidal thoughts and behaviors.
Plan for suicide.
Reasons for not following through with past plans for suicide.
Reasons for not following through with the current plan for suicide.
Current support system.
Means and access to lethal methods (e.g., firearms).
History and current symptoms of impulsivity.
Depressed mood, feelings of hopelessness, or both.
Protective factors (e.g., coping skills, spiritual/religious beliefs).
Asking a client directly about his or her desire to die by suicide does not make self-harm more likely and in fact can yield helpful information.
Note that people may deny such thoughts or plans despite having them. Thus, direct questioning alone is an insufficient risk mitigation strategy. Suicide risk assessment scales might be useful in this regard (see Chapter 3 and Appendix C for suicide risk and self-harm screening tools) but often lack the specificity and sensitivity to adequately detect impending suicidal behaviors ( Bolton, Gunnell, & Turecki, 2015 ). Providers also should not rely solely on suicide measures. Instead, suicide screening should include thorough investigation of all major signs, symptoms, and risk factors associated with self-harm in mental health, addiction, or COD populations.
RESOURCE ALERT: SUICIDE PREVENTION RESOURCES FOR COUNSELORS.
Safety planning is critical in suicide risk mitigation. Suicide “contracts” are written statements in which the person who is suicidal states that he or she will not kill himself but rather call for help, go to an ED, or other seek other assistance if he or she becomes suicidal. These contracts are not effective alone for a client who is suicidal. Such contracts often help make clients and therapists less anxious about a suicidal condition, but studies have never shown these contracts to be effective at preventing suicide. Rather, safety contracts help focus on the key elements that are most likely to keep clients safe, such as agreeing to remove the means a client is most likely to use to commit suicide.
Counselors and other providers should know their own skills and limitations in engaging, screening, assessing, and intervening with suicidal clients and work out these problems with a supervisor before an emergency. Providers also should know what immediate onsite and offsite resources are available to help with someone identified as suicidal. To learn more about suicide prevention, see “Resource Alert: Suicide Prevention Resources for Counselors.”
No empirical treatments for suicide exist. However, interventions that reduce symptoms of SUDs and mental illness can help mitigate suicide risk and decrease self-harm behaviors by improving mood and enhancing support and coping skills. Some research supports the use of psychotherapies such as CBT and dialectical behavior therapy in reducing parasuicidal behavior and suicide attempts, but the overall evidence base is small ( Bolton et al., 2015 ). Pharmacotherapy—particularly antidepressants— can reduce suicidal behavior in people ages 25 years and older. Yet paradoxically, some studies show that it actually increases suicide in people ages 25 and younger ( Bolton et al., 2015 ). Certain mood stabilizers and antipsychotic medications also may reduce self-harm in people with bipolar disorder, schizophrenia, and other psychotic disorders ( Bolton et al., 2015 ).
CASE STUDY: COUNSELING AN SUD TREATMENT CLIENT WHO IS SUICIDAL.
The first steps in suicide intervention, and thus crisis stabilization, are contained in the process of a good engagement and evaluation. Asking suicide-related questions, exploring the context of those impulses, evaluating support systems, considering the lethality of means, and assessing the client's motivation to seek help are in themselves an intervention. Such an interview will often elicit the client's own insight and problem solving and may result in a decrease in suicidal impulses.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WHO IS SUICIDAL.
If, however, the client experiences little or no relief after this process, psychiatric intervention is required, especially if the client has a cooccurring mental disorder or medical disorder in which the risk of suicide is elevated or if the client has a history of suicide attempts. If either or both is true, arrangements should be made for transfer to a facility that can provide more intensive psychiatric evaluation and treatment. Emergency procedures should be in place so the counselor can accomplish this transfer even when a psychiatrist or clinical supervisor/director is not available. Once the client is stabilized and is safe to return to a less restrictive setting, he or she should return to the program.
DSM-5 defines trauma as “as exposure to actual or threatened death, serious injury, or sexual violence in one or more of the following ways: (a) directly experiencing the traumatic event; (b) witnessing, in person, an event as it occurred to others; (c) learning that the traumatic event occurred to a close family member or close friend; and (d) experiencing repeated or extreme exposure to aversive details of the traumatic event(s)” ( APA, 2013 , p. 271).
For many people with mental disorders, SUDs, or both, past or current trauma is a prominent driver of negative outcomes such as psychiatric hospitalizations; suicide attempts; self-harm behaviors; arrest; aggression; and substance use initiation, escalation (from occasional use, to regular use, to misuse/heavy use/addiction), treatment dropout, and relapse ( Kumar, Stowe Han, & Mancino, 2016 ; Lijffijt, Hu, & Swann, 2014 ; Stinson, Quinn, & Levenson, 2016 ). Data from the National Longitudinal Study of Adolescent to Adult Health ( Quinn et al., 2016 ) confirm that exposure to childhood trauma (e.g., sexual/emotional/physical abuse, neglect, witnessing violence) significantly increases the risk of adulthood prescription pain reliever misuse (PPRM) and injection drug use. This risk only grows as the number of traumas experienced increases; in the study, exposure to one trauma increased the risk of PPRM by 34 percent; two traumas, by 50 percent; three traumas, by 70 percent; and four traumas, by 217 percent. Emotional and physical abuse nearly doubled the risk of injection drug use.
WARNING TO COUNSELORS: RETHINKING TRAUMA.
Traumatic events are common in people with CODs in part because they are so widely prevalent in the general population. Almost 90 percent of people in the United States have a lifetime history of exposure to at least one traumatizing event, typically the death of family/close friend because of violence/accident/disaster; physical or sexual assault; disaster; or accident/fire ( Kilpatrick et al., 2013 ).
Trauma and CODs
As noted in the section “PTSD,” trauma in people with addiction, mental illness, or both is the norm rather than the exception ( SAMHSA, 2014b ). In more than 600 people receiving SUD treatment, 49 percent reported a lifetime history of physical or sexual abuse, and women were 5 times more likely than men to report lifetime trauma ( Keyser-Marcus et al., 2015 ). In people with SMI, trauma exposure is common, with prevalence rates ranging from 25 percent to 72 percent for physical abuse, 24 percent to 49 percent for sexual abuse, and 20 percent to 47 percent for PTSD ( Mauritz, Goossens, Draijer, & van Achterberg, 2013 ). Twelve-month or lifetime rates of DSM-5 drug use disorder (i.e., an SUD excluding alcohol) carries increased odds of having PTSD ( Grant et al., 2016 ), and 12-month or lifetime PTSD increases the odds of having a past-year or lifetime SUD ( Goldstein et al., 2016 ).
Adverse life experiences are highly coincident with SUDs and mental disorders, and vice versa:
Current PTSD prevalence in addiction populations is likely 15 percent to 42 percent ( Vujanovic et al., 2016 ).
In active duty military personnel, prevalence rates of various comorbid mental disorders and SUDs in people with PTSD have been estimated at 49 percent for depressive disorders, 36 percent for GAD, and almost 27 percent for AUD ( Walter, Levine, Highfill-McRoy, Navarro, & Thomsen, 2018 ).
Among a sample of U.S. adults with any lifetime trauma, 47 percent screened positive for PTSD, almost 47 percent for GAD, and 42 percent for depression ( Ghafoori, Barragan, & Palinkas, (2014) .
Between 28 percent and 43 percent of people with PTSD have an SMI ( Lu et al., 2013 ).
People with past-year or lifetime PTSD are at significant risk of developing any number of comorbid mental disorders, including any mood disorder (2.4 to 3 times the odds), bipolar I disorder (2.1 to 2.2 times), any anxiety disorder (2.6 to 2.8 times), GAD (2 to 2.2 times), panic disorder (2.1 times), and BPD (2.8 to 3.3 times) ( Goldstein et al., 2016 ).
People with adverse childhood events (e.g., abuse, neglect) are more likely to report lifetime drug use, past-year moderate-to-heavy alcohol use, lifetime suicide attempt, and past-year depressed mood than people without such a history ( Merrick et al., 2017 ). Emotional abuse in childhood is linked with 6 times the odds for a lifetime suicide attempt ( Merrick et al., 2017 ).
Trauma-Informed Treatment of CODs
Historically, trauma has not been adequately addressed in SUD treatment, given provider fear that doing so would worsen mental and addiction problems. However, research indicates the opposite—that failing to address trauma in people with SUDs leads to worse outcomes ( Brown, Harris, & Fallot, 2013 ).
Trauma-informed care means attending to trauma-related symptoms and also creating a treatment environment that is responsive to the unique needs of individuals with histories of trauma. Treatment is focused on reducing specific symptoms and restoring functioning but also broader goals like building resiliency, reestablishing trust, preventing retraumatization, and offering hope for the future. Creating a supportive, safe treatment environment is crucial. Counselors must realize how the setting and their interactions with clients who have trauma can affect treatment adherence, retention, and outcomes.
Trauma-informed care for people with mental disorders, SUDs, or both often includes ( SAMHSA, 2014b ):
Psychoeducation, especially about the relationship between trauma, mental health, and addiction. Psychoeducation is also needed to help normalize symptoms and reassure clients that their experiences are not unusual, “wrong,” or “bad.”
Teaching coping and problem-solving skills to foster effective stress management.
Discussing retraumatization and developing strategies to prevent further victimization.
Helping clients feel empowered and in control of their lives.
Establishing a sense of safety in clients’ daily lives and in treatment.
Promoting resilience and offering hope for change and improvement.
Identifying and responding adaptatively to triggers, like intrusive thoughts, feelings, and sensations.
Building a therapeutic alliance, which fosters trust, confidence, and self-worth—all keys to healing.
Using trauma-specific interventions, like:
Cognitive processing therapy.
Exposure therapy.
Eye movement desensitization/reprocessing.
Affective regulation.
Distress tolerance and stress inoculation.
Peer support services from other people who have a trauma history and are thriving.
TIP 57, Trauma-Informed Care in Behavioral Health Services ( SAMHSA, 2014b ) and SAMHSA's “Concept of Trauma and Guidance for a Trauma-Informed Approach” ( SAMHSA, 2014c ) will help addiction and mental health professionals tailor their services in a way that is respectful of and sensitive to clients’ trauma-related needs. Chapter 6 discusses adapting treatments for CODs to female clients with trauma.
ADVICE TO THE COUNSELOR: COUNSELING A CLIENT WITH TRAUMA.
Special Considerations: Trauma and Military Personnel
Active duty and veteran members of the military are highly susceptible to trauma and all of its deleterious aftereffects. PTSD prevalence is significantly higher than that of the general population and civilian clinical samples, including 9 percent among a sample of more than 4 million veterans in primary care settings (Trivedi et al., 2014), 23 percent among Operations Enduring Freedom and Iraqi Freedom (OEF/OIF) veterans ( Fulton et al., 2015 ), 21 percent in Gulf War veterans (Dursa, Barth, Schneiderman, & Bossarte, 2015), and 8.5 percent to 12.2 percent of Vietnam War veterans ( Marmar et al., 2015 ).
About 20 percent of veterans have CODs ( Trivedi et al., 2015 ); 16 percent have PTSD and SUDs specifically ( Mansfield, Greenbaum, Schaper, Banducci, & Rosen, 2017 ). In a sample of (OEF/OIF) veterans, 63 percent of people with SUD also had PTSD ( Seal et al., 2011 ). Other common mental disorders in this population include SMI, depression, and anxiety; all tend to co-occur often ( Exhibit 4.20 ). These illnesses are linked with increased hospitalizations, ED use, and mortality, with SMI and SUDs being particularly damaging ( Trivedi et al., 2015 ).
EXHIBIT 4.20. Veterans and CODs.
Many veterans seek treatment outside of the Veterans Health Administration, so community addiction counselors should prepare to work with them. Counseling veteran or active duty military populations requires a slightly different knowledge base, clinical approach, and skillset than civilian populations. SUD counselors should note that ( Briggs & Reneson, 2010 ; Teeters, Lancaster, Brown, & Back, 2017 ):
War zone stress reactions often require specialized care and an understanding of the experiences faced by soldiers in combat.
Military-related trauma exposure does not include only direct combat. For instance, people working in intelligence gathering and medical personnel are often deployed to war zones where they witness horrific acts of violence and are potential targets of violence themselves.
Female veterans often have specific service needs, such as those to address military sexual trauma (e.g., sexual assault, harassment), intimate partner violence, and child care. (Note that men also can be victims of military sexual trauma, albeit at far lower rates than reported by women. Do not assume that military sexual trauma is solely a women's issue.)
Many veterans are hesitant to seek SLID treatment or mental health services because of fear that doing so could negatively affect their career advancement. Concerns about confidentiality are thus understandably very high in these clients.
Shame, embarrassment, and stigma over mental health and addiction are prominent. Military culture fosters some behaviors and mindsets that can be adaptive in combat—like independence, being “masculine,” and not showing “weakness”—but make seeking treatment much harder.
Suicide risk is high in veterans. It requires active monitoring and management throughout treatment, particularly for military personnel with childhood trauma, PTSD, military sexual trauma, or depression ( Carroll, Currier, McCormick, & Drescher, 2017 ; Cunningham et al., 2017 ; Kimerling, Makin-Byrd, Louzon, Ignacio, & McCarthy, 2016 ; McKinney, FHirsch, & Britton, 2017 ; Pompili et al., 2013 ).
Indepth discussions about prevention programming and treatment for military populations with trauma, suicide risk, SUDs, mental disorders, or a combination thereof is beyond the scope of this TIP. However, ample information is available elsewhere. The following resources offer helpful guidance about working with military professionals who engage in substance misuse or have mental illness, including trauma, suicidality, and CODs:
Suicide Among Veterans and the Implications for Counselors ( www .counseling.org/docs /default-source/vistas /suicide-among-vet-erans-and-the-implications-for-counselors .pdf?sfvrsn=3803a659_11 )
Comparison of Civilian Trauma and Combat Trauma ( https://pdfs .semanticscholar .org/eff2/8af43d3feaac7bac3cc5bb789bd4d5f_100ec.pdf )
Counseling Addicted Veterans: What to Know and How to Help ( https://pdfs .semanticscholar .org/9742/967aac-815ca02c4f599b36be996d0b10d3d9.pdf )
The Department of Veterans Affairs’ National Center for PTSD ( www .ptsd.va.gov/ ):
Practice Recommendations for Treatment of Veterans with Comorbid Substance Use Disorder and Posttraumatic Stress Disorder ( www .mentalhealth.va.gov /providers/sud/docs /SUD_PTSD_Practice_Recommendations. pdf)
Veteran Outreach Toolkit: Preventing Veteran Suicide Is Everyone's Business ( www .va.gov/ve/docs/outreachToolkitPreventingVeteran-SuicidelsEveryonesBusiness .pdf )
National Strategy for Preventing Veteran Suicide, 2018-2028 ( www .mentalhealth.va.gov /suicideprevention /docs/Office-of-Mental-Health-and-Suicide-Prevention-National-Strategy-for-Preventing-Veterans-Suicide.pdf )
SAMHSA's Addressing the Substance Use Disorder Service Needs of Returning Veterans and Their Families ( www.samhsa.gov/sites/ default/files/veterans report.pdf )
Community Anti-Drug Coalitions of America's Strategies for Addressing Substance Abuse in Veteran Populations ( www.cadca.org/sites/ default/files/mckesson_toolkit_1.pdf )
The material in this chapter is intended to increase SUD treatment counselors’ and other providers’ familiarity with mental disorders terminology and criteria, as well as to provide advice on how to proceed with clients who demonstrate these disorders. The consensus panel encourages counselors to continue to increase their understanding of mental disorders by using the resource material referenced in each section (and in Appendix C ), attending courses and conferences in these areas, and engaging in dialog with mental health professionals who are involved in treatment. At the same time, the panel urges continued work to develop improved treatment approaches that address substance use in combination with specific mental disorders, as well as better translation of that work to make it more accessible to the SUD treatment field.
This is an open-access report distributed under the terms of the Creative Commons Public Domain License. You can copy, modify, distribute and perform the work, even for commercial purposes, all without asking permission.
- Cite this Page Substance Use Disorder Treatment for People With Co-Occurring Disorders: Updated 2020 [Internet]. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2020. (Treatment Improvement Protocol (TIP) Series, No. 42.) Chapter 4—Mental and Substance-Related Disorders: Diagnostic and Cross-Cutting Topics.
- PDF version of this title (6.1M)
In this Page
Other titles in this collection.
- SAMHSA/CSAT Treatment Improvement Protocols
Recent Activity
- Chapter 4—Mental and Substance-Related Disorders: Diagnostic and Cross-Cutting T... Chapter 4—Mental and Substance-Related Disorders: Diagnostic and Cross-Cutting Topics - Substance Use Disorder Treatment for People With Co-Occurring Disorders
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

In Crisis? Call or Text 988
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Page title SAMHSA Announces National Survey on Drug Use and Health (NSDUH) Results Detailing Mental Illness and Substance Use Levels in 2021
2021 NSDUH report includes selected estimates by race, ethnicity, and age and is the most comprehensive key findings report to date.
Today, the U.S. Department of Health and Human Services’ (HHS) Substance Abuse and Mental Health Services Administration (SAMHSA) released the results of its annual National Survey on Drug Use and Health (NSDUH), which shows how people living in America reported about their experience with mental health conditions, substance use, and pursuit of treatment in 2021. The 2021 NSDUH national report includes selected estimates by race, ethnicity, and age group. It is the most comprehensive report on substance use and mental health indicators that SAMHSA has released to date.
“Every year since 1971, this survey has given us a window into our nation’s mental health and substance use challenges and 2021 was no different. As the findings make clear, millions of Americans young and old faced mental health and substance use challenges – sometimes both at once – during the second year of the pandemic,” said HHS Secretary Xavier Becerra. “As we work to improve behavioral health across the nation, HHS is committed to ensuring that all people facing mental health or substance use challenges are connected to appropriate services and supports.”
“A commitment to data and evidence is one of SAMHSA’s four core principles. The annual NSDUH results help inform our efforts to expand access to treatment options and recovery supports across the nation,” said HHS Assistant Secretary for Mental Health and Substance Use Miriam E. Delphin-Rittmon, Ph.D., the leader of SAMHSA. “Harnessing the power of data and evidence is critical to ensuring policies and programs have the greatest opportunity to achieve positive outcomes.”
Estimates from the 2021 NSDUH should not be compared with estimates from previous years because the COVID-19 pandemic necessitated methodological changes to the data collection process.
Key findings from the 2021 NSDUH include:
Drug Use and Substance Use Disorder
- Among people aged 12 or older in 2021, 61.2 million people (or 21.9 percent of the population) used illicit drugs in the past year. The most commonly used illicit drug was marijuana, which 52.5 million people used. Nearly 2 in 5 young adults 18 to 25 used illicit drugs in the past year; 1 in 3 young adults 18 to 25 used marijuana in the past year.
- 9.2 million people 12 and older misused opioids in the past year.
- The percentage of people who were classified as having a past year substance use disorder, including alcohol use and/or drug use disorder, was highest among young adults aged 18 to 25 compared to youth and adults 26 and older.
- In 2021, 94% of people aged 12 or older with a substance use disorder did not receive any treatment. Nearly all people with a substance use disorder who did not get treatment at a specialty facility did not think they needed treatment.
Major Depressive Episodes (MDE) Among Adolescents
- The prevalence of past year MDE among Black and Asian adolescents was lower compared to adolescents from most other racial/ethnic groups.
- More than half of youth with an MDE did not receive treatment in the past year.
Mental Illness among Adults
- Nearly 1 in 4 adults 18 and older, and 1 in 3 among adults aged 18 to 25, had a mental illness in the past year.
- Adults with serious mental illness had higher rates of treatment compared to those with any mental illness. Despite having the highest rate of serious mental illness, people aged 18 to 25 had the lowest rate of treatment in comparison to adults in other age groups.
- White and Multiracial adults were more likely to receive mental health services in the past year than Black, Hispanic or Latino, or Asian adults.
Co-Occurring Substance Use Disorder with Any Mental Illness
- 13.5 percent of young adults aged 18 to 25 had both a substance use disorder and any mental illness in the past year.
- Nearly 1 in 3 adults had either a substance use disorder or any mental illness in the past year, and 46 percent of young adults 18-25 had either a substance use disorder or any mental illness.
- The percentage of adults aged 18 or older who met criteria for both a mental illness and a substance use disorder in the past year was higher among Multiracial adults than among White, Black, Hispanic or Latino, or Asian adults. Asian adults were less likely to have had both AMI and a substance use disorder in the past year compared with adults in most other racial or ethnic groups.
Serious Thoughts of Suicide, Suicide Plans, and Suicide Attempts
- 12.3 million adults aged 18 or older had serious thoughts of suicide in the past year, 3.5 million made suicide plans, and 1.7 million attempted suicide.
- Hispanic or Latino adults were more likely than White or Asian adults to have attempted suicide in the past year, and Black adults were more likely than Asian adults to have attempted suicide in the past year.
- 7 in 10 (72.2 percent or 20.9 million) adults who ever had a substance use problem considered themselves to be recovering or in recovery.
- 2 in 3 (66.5 percent or 38.8 million) adults who ever had a mental health issue considered themselves to be recovering or in recovery.
About the National Survey on Drug Use and Health
Conducted by the federal government since 1971, the NSDUH is a primary source of statistical information on substance use and mental health of the U.S. civilian, noninstitutionalized population 12 or older. The NSDUH measures:
- Use of illegal drugs, prescription drugs, alcohol, and tobacco,
- Substance use disorder and substance use treatment,
- Major depressive episodes, mental illness, and mental health care, and
- Perceived recovery from substance use and mental health issues.
Addressing the nation’s mental health crisis and drug overdose epidemic are core pillars of the Biden-Harris Administration’s Unity Agenda. The Administration has invested $3.8 billion through the American Rescue Plan and more than $800 million through the Bipartisan Safer Communities Act in SAMHSA grant programs as part of President Biden’s comprehensive effort to improve access to mental healthcare, prevent overdoses, and save lives. These investments enabled the expansion of lifesaving prevention, treatment, and recovery services and supports in communities throughout the country, including the transition to the 988 Suicide & Crisis Lifeline in July 2022.
Americans seeking treatment for mental health or substance use issues should call SAMHSA’s National Helpline at 800-662-HELP (4357) or visit findtreatment.samhsa.gov . If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org .
Reporters with questions should send inquiries to [email protected] .
The Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and Human Services (HHS) that leads public health efforts to advance the behavioral health of the nation. SAMHSA’s mission is to lead public health and service delivery efforts that promote mental health, prevent substance misuse, and provide treatments and supports to foster recovery while ensuring equitable access and better outcomes.
Last Updated: 01/04/2023

IMAGES
VIDEO
COMMENTS
Match. Study with Quizlet and memorize flashcards containing terms like Assessment tool used to screen for alcoholism, CAGE: question that most likely predicts onset of withdrawal sx if pt is dependent on alcohol?, withdrawal sx can begin _______ after someone has stopped drinking and more.
Study with Quizlet and memorize flashcards containing terms like What signs and symptoms of alcohol withdrawal did you observe in this case study?, Alcohol withdrawal is severe and may be life threatening. 5-10% proceed to delirium tremens. With this syndrome the patient will demonstrate which problems?, What medicines will be used in order to prevent delirium tremens and/or other problems ...
Study with Quizlet and memorize flashcards containing terms like N/V, shallow breaths, cold and clammy, weak-rapid pulse, coma; possible death, anxiety, fever ...
Study with Quizlet and memorize flashcards containing terms like substance abuse is..., 2 factors of addiction, neurobiology (NT, ex) and more.
Study with Quizlet and memorize flashcards containing terms like A 45 year old woman presents to the ER with symptoms of vomiting, anorexia, abdominal pain and jaundice. Upon further assessment, the nurse finds that she is severely dehydrated and is under the influence of alcohol. When asked about alcohol use, the woman states that she used to have a serious alcohol problem, but she only ...
Study with Quizlet and memorize flashcards containing terms like 1. What preventable health problem is the cause of more deaths, illnesses, and disabilities than any other? a. Hepatitis A, B, and C b. Obesity c. STDs d. Substance abuse, 2. Which mood-altering substances are considered acceptable to use by current Western society? a. Alcohol and caffeine b. Amphetamines and pain-killing drugs ...
Case Study: Lorrie. Figure 1. Lorrie. Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and "popping pills" at the age of 13, and within the following decade, someone introduced her to cocaine and heroin.
Case Study. Penny, 43, experienced her first depressive episode in her mid teens. During her first treatment for substance use (marijuana and alcohol) at age 17, Penny was diagnosed with attention deficit hyperactivity disorder (ADHD). ... Substance Abuse and Mental Health Services Administration, Results from the 2011 National Survey on Drug ...
Study with Quizlet and memorize flashcards containing terms like _____ involves using a drug to the point that it affects one's family, social relationships, and/or work. a. Substance dependence b. Substance abuse c. Substance addiction d. Substance tolerance, Cirrhosis of the liver accounts for approximately _____ deaths each year.
Substance use disorder (SUD) is a treatable mental disorder that affects a person's brain and behavior, leading to their inability to control their use of substances like legal or illegal drugs, alcohol, or medications. Symptoms can be moderate to severe, with addiction being the most severe form of SUD. People with a SUD may also have other ...
A substance use disorder is a medical illness characterized by clinically significant impairments in health, social function, and voluntary control over substance use.2 Substance use disorders range in severity, duration, and complexity from mild to severe. In 2015, 20.8 million people aged 12 or older met criteria for a substance use disorder. While historically the great majority of ...
Substance use disorder (SUD) is a complex condition in which there is uncontrolled use of a substance despite harmful consequences. People with SUD have an intense focus--sometimes called an addiction--on using a certain substance (s) such as alcohol, tobacco, or other psychoactive substances, to the point where their ability to function in day ...
Integrating services for primary care, mental health, and substance use-related problems together produces the best outcomes and provides the most effective approach for supporting whole-person health and wellness. 3. This chapter describes the key components of health care systems; historical reasons substance use and its consequences have ...
It encompasses the conditions that some people refer to as alcohol abuse, alcohol dependence, alcohol addiction, and the colloquial term, alcoholism. Considered a brain disorder, AUD can be mild, moderate, or severe. Lasting changes in the brain caused by alcohol misuse perpetuate AUD and make individuals vulnerable to relapse.
Identifying and understanding the associations between adolescent substance use and changes in cognition, mental health, and future substance use risk may assist our understanding of the consequences of drug exposure during this critical window. Keywords: adolescence, youth, addiction, drug, abuse psychology, special population.
Case Studies. Case Study for Chapter 10: Substance Use and Addiction. Jennifer's brother Emmett resorted to drugs and alcohol to drown his sorrow after their dad left their mother. The local inner city high school had its share of dealers and Emmett's will power was nil. While weed (cannabis, marijuana, pot) was Emmett's initial drug of ...
Furthermore, one study found that opiates were present in 20% of suicide deaths, marijuana in 10.2%, cocaine in 4.6%, and amphetamines in 3.4% ( 2 ). Among the reported substances, alcohol and opioids are associated with the greatest risks of suicidal behavior. Psychiatric disorders have a strong association with suicide.
Diagnosis. Diagnosing drug addiction (substance use disorder) requires a thorough evaluation and often includes an assessment by a psychiatrist, a psychologist, or a licensed alcohol and drug counselor. Blood, urine or other lab tests are used to assess drug use, but they're not a diagnostic test for addiction.
Disentangling symptoms of SUDs from those of co-occurring mental disorders is a complex but necessary step in correctly assessing, diagnosing, determining level of service, selecting appropriate and effective treatments, and planning follow-up care. This chapter is designed to facilitate those processes by ensuring addiction counselors and other providers have a clear understanding of mental ...
Case Management for Substance Abuse Treatment . Treatment Improvement Protocol (TIP) Series. 27 . U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Substance Abuse and Mental Health Services Administration Center for Substance Abuse Treatment 1 Choke Cherry Road Rockville, MD 20857
2021 NSDUH report includes selected estimates by race, ethnicity, and age and is the most comprehensive key findings report to date. Today, the U.S. Department of Health and Human Services' (HHS) Substance Abuse and Mental Health Services Administration (SAMHSA) released the results of its annual National Survey on Drug Use and Health (NSDUH), which shows how people living in America ...
Case studies and lessons learned Drug Abuse Treatment Toolkit Printed in Austria V.04-55683—November 2004—1,150 United Nations publication Sales No. E.04.XI.24 ISBN 92-1-148194-5 ... women's substance abuse treatment projects. Case studies chosen for inclusion in the present publica-
current issue. current issue; browse recently published; browse full issue index; learning/cme