- Open access
- Published: 16 August 2021

Prevention and early intervention of depression in young people: an integrated narrative review of affective awareness and Ecological Momentary Assessment
- Joanne R. Beames ORCID: orcid.org/0000-0003-3630-0980 1 ,
- Katarina Kikas 1 &
- Aliza Werner-Seidler ORCID: orcid.org/0000-0002-9046-6159 1
BMC Psychology volume 9 , Article number: 113 ( 2021 ) Cite this article
10k Accesses
18 Citations
19 Altmetric
Metrics details
Depression has a devastating impact on young people around the world. This impact is pervasive and long-long lasting, still causing havoc as young people transition into adulthood. Prevention and timely early intervention efforts are necessary to lessen the disease burden of depression in young people. There is some evidence for the effectiveness of existing prevention and early intervention programs when delivered early. However, there is no consensus on what the active ingredients of these programs are. Identifying these ingredients is important because focusing on those that have maximal benefit will help to minimise the costs and resourcing of (already intensive) therapeutic approaches. We explored whether, and in what circumstances, affective awareness (i.e., knowing how one feels) is a candidate for protecting against and decreasing vulnerability to depression in young people. We specifically looked at how Ecological Momentary Assessment methods (EMA) were used to measure and/or increase affective awareness. We integrated three streams of data, including narrative review findings, perspectives from young people and psychologists, and publicly available information online (e.g., discussion forums). Across data sources, we found converging evidence that affective awareness is important in the prevention and early intervention of depression although there were considerable gaps in knowledge. More work needs to be done with young people and their health care teams to build affective awareness in the right way, at the right time, with individual differences in mind. The identification of how EMA can be best incorporated into young people’s lives to facilitate these outcomes is also needed.
Peer Review reports
Introduction
Depression is a leading cause of disability worldwide, with debilitating effects on psychosocial, physical, and emotional functioning [ 1 , 2 ]. The onset of depression is typically around mid-to-late adolescence, with earlier onset associated with a more severe clinical course [ 3 , 4 ]. Given the impact caused by depression, together with limited success of treatment approaches [ 5 ], the prevention and early intervention of depression is imperative. There is evidence supporting psychological prevention approaches during adolescence [ 6 , 7 , 8 ].
Knowledge about psychological processes primarily responsible for therapeutic prevention or change (i.e., active ingredients) is lacking [ 9 ]. Focusing on the active ingredients that work will lead to the development of more effective and efficient interventions that enhance mental health outcomes for the individuals that use them [ 10 ]. In 2020, The Wellcome Trust Mental Health Priority Area launched its first active ingredients commission to explore aspects of interventions that are most effective for preventing and treating anxiety and depression in young people. The commissioned review presented here builds the case for affective awareness—a foundational skill that can protect young people (aged between 14 and 20 years) against depression and improve their emotional health. We used creative methods to emphasise lived experiences and move beyond the scope of traditional scientific reviews, which are not without limitation [ 11 ]. There are many benefits of including lived experience perspectives. For example, such perspectives can produce better quality research by improving methodological sensitivity, validity of results, and relevance to the target population [ 12 , 13 ]. Our integration of data enables comparison of what is known from research, what is done in practice, and what young people want in their mental health care.
Active ingredient: affective awareness
Affective awareness is the ability to perceive, describe, understand, and differentiate emotions and moods [ 14 , 15 ]. Imagine that Talia is feeling sad. With affective awareness, she will be able to identify her experience as sadness, rule out other emotions (e.g., regret, calm), describe her internal sensations (physical and cognitive), and understand her behavioural responses to the emotion (e.g., social withdrawal). Affective awareness is developed early in life [ 15 ] and is a building block for other emotional processes such as emotion regulation [ 16 ]. This means that if Talia is aware of her feelings, she will be able to communicate her emotional state (e.g., I feel sad), reach out for help, and implement helpful coping/regulation strategies (e.g., perspective taking, focusing on an upcoming holiday). Strategy selection is important because those that are effective for overcoming sadness might differ from those that are effective for other negative emotions like guilt. The key message is that if young people do not know they feel sad or down, it will be difficult for them to respond to those feelings in a helpful way.
Affective awareness in youth depression
Affective awareness (or lack thereof) is putatively involved in the development and maintenance of depressive symptoms between 7 and 24 years of age [ 17 , 18 ]. There are multiple and complex reasons why adolescents have an increased vulnerability to depression. Young people undergo natural biological maturation processes that often produce changes in moods and emotions, and their regulation skills are not fully developed [ 19 ]. For example, young people who are prone to depression are less aware of their emotions, have difficulty understanding them, and have limited capacity to tolerate them (e.g., [ 20 , 21 , 22 ]). Young people also have a greater tendency to respond to stress with negative affectivity [ 23 ]. Adolescence is therefore a critical time whereby affective skills can be developed and shaped to improve emotional health.
Measuring (and increasing) affective awareness using EMA
In clinical practice, affective awareness is typically measured with pen-and-paper or digital mood monitoring tools where the individual is asked to reflect on their emotions and activities through the week [ 24 ]. In research studies, affective awareness is typically measured as a self-report trait characteristic [ 22 ] or, more recently, through ecological momentary assessment (EMA; [ 25 ]). EMA is an effective way to study affect and depression-related phenomena [ 26 ]. It allows individuals to repeatedly report their emotions and moods in real-time. Completed using technology, including smartphones, users typically receive one or more prompts each day to report how they are feeling and the context around that feeling (e.g., what they are doing/thinking). The advantages of EMA over traditional methods include a higher level of temporal detail that captures real-time changes in experiences, ecological validity, and reliability.
EMA provides an indirect measure of affective awareness; an individual must be aware of (as well as label and communicate) an emotional experience to be able to report that experience. One study found a strong positive correlation between a self-report emotional awareness scale and EMA, suggesting that the two types of assessment measure a similar construct [ 27 ]. There is also some (albeit mixed) evidence that EMA itself can change the emotional experiences and mental health symptoms that it is measuring (i.e., assessment reactivity). One study found that EMA of positive and negative affect over 6-weeks may have a beneficial short-term effect on depressive symptoms in clinically depressed adults [ 28 ]. A systematic review concluded that mobile mood-monitoring applications may reduce depressive symptoms in young people aged 10–24 years by increasing affective awareness [ 29 ]. Together, these findings indicate that EMA can be used to measure emotional experiences and can also be used as a brief intervention with clinical outcomes. The general EMA methodology underpinning both approaches is comparable.
There are other psychological treatment approaches that aim to influence affective awareness. One evidence-based approach is Mindfulness-Based Cognitive Therapy (MBCT). MBCT aims to cultivate awareness of thoughts, feelings, sensations, and feelings in the present moment, and develop new ways of relating to thoughts and feelings. It is a multi-component approach that is resource intensive (time and financial cost). Emerging evidence suggests that MBCT can have beneficial effects for young people with and without depression, but robust causal studies with insights into mechanisms are lacking [ 30 ]. This means that the extent to which changes in affective awareness drive treatment effects is unclear. The current review will focus exclusively on EMA rather than treatment approaches such as MBCT. This approach will allow us to determine the relationships between EMA, awareness, and depression symptoms in young people.
Research gap
Despite the potential for EMA in measuring and changing affective awareness or depression-related phenomena in youth, research is lacking [ 31 ]. EMA studies with youth have rarely examined associations between momentary fluctuations in affective experience, awareness, and clinical outcomes [ 32 ]. Further, it is unclear what young people and mental health professionals think about EMA and how it can be used in clinical practice and daily life.
The aims of this review are to assess: (1) whether EMA increases affective awareness and reduces depression symptoms; (2) whether EMA can identify depression risk; and (3) stakeholder perspectives about affective awareness and using EMA in daily life, in and outside of the therapy context. Aim 3 focuses on what young people think about affective awareness in relation to depression and mental health, whether they use or would be likely to use EMA to facilitate awareness, as well as their reasons why. An embedded aim is to identify the gaps between research, clinical practice, and what young people are doing in their daily lives.
Overview of methodological approaches
To address these aims, we used a creative approach that combined a narrative review with qualitative methods that drew from stakeholder perspectives. The stakeholders included young people, some with lived experiences of depression, and psychologists. We also searched websites and publicly available online discussion boards/forums for affective awareness, depression, and mood monitoring. The novelty of our approach lies within the integration and equal weighting of data sources, which was consistent with the guidelines outlined by the 2020 Wellcome Trust active ingredients commission. The value of integrating empirical review and qualitative data was in being able to discover a full range of perspectives, highlighting gaps between research, practice, and lived experience. Integration also provided insight about what young people are looking for and how researchers and clinicians can work together to address their needs. Our approach offers new insights that would not otherwise be determined from a traditional scientific review, representing a key strength and shift in how evidence and experience can be incorporated in the future.
Our approach builds on current knowledge by: (1) considering phone-based EMA as an intervention and/or measurement tool; (2) focusing on prevention and early intervention; (3) exploring different study designs; (4) incorporating lived experience perspectives; and (5) integrating cross-disciplinary insights from clinical psychology and emotion research. We also drew inferences from treatment studies where young people have been diagnosed with depression.
Narrative review
Electronic databases including PsycINFO, PubMed, EMBASE, Google Scholar and CINAHL were searched between July 2020 and August 2020 using key search terms, including (but not limited to): “awareness” or “self-awareness”, and “monitor” or “track” or “experience sampling” or “ecological momentary assessment” or “EMA” or “label” or “diary”, and “youth” or “adolescents”, and “depress” or “mood” or “emotion”. We also hand-searched the reference lists of relevant articles, and systematic reviews [ 29 , 31 ] and meta-analyses [ 22 ] were reviewed to identify any peer-reviewed evidence that might have been missed in the literature search. The initial inclusion criteria were young people aged between 14 and 20, sub-clinical or non-clinical samples, a measure or report of affective awareness (i.e., self-report or verbal report), phone-based EMA methodology, and a measure of depressive symptoms. We focused on phone-based EMA because data collection can be relatively unobtrusive and more young people can be reached at any one time regardless of their location. The low-cost, high availability, and in-built flexibility of phone-based EMA could overcome barriers to traditional healthcare, contributing to more sustainable monitoring tools that can be delivered at scale. As such, quantitative studies that focused on young people and phone-based EMA were included (rather than pagers, emails, websites etc). There was limited availability of research evidence after our initial search. We therefore expanded our search to include studies that used clinical populations, young people and adults, and other indices of emotional awareness (e.g., emotional clarity, differentiation, and emotional intelligence). Additionally, if mood monitoring was combined with another psychological therapy (e.g., mood monitoring plus cognitive behavioural therapy), we included it in our review. There were no restrictions on publication year. Our search revealed 11 relevant articles (see Table 1 ). In the following sections, unless otherwise noted, the terms adolescent, young people or youth refer to individuals aged 14–20.
Nine studies targeted a youth sample. An additional two included adults and youth. Three studies examined whether affective awareness is related to depression in youth by using EMA as an intervention, and by linking indirect momentary reports to self-report state measures [ 33 , 34 , 35 ]. One study used EMA as an intervention and measured depression and other emotional experiences but did not confirm levels of awareness using a self-report measure [ 36 ]. Two examined EMA as a component of a broader psychological intervention (e.g., CBT) but did not isolate effects [ 37 , 38 ]. Another five used EMA as a measurement tool, one in the context of a universal prevention trial [ 39 ], another in the context of a treatment trial [ 40 ], and three in the context of daily life [ 41 , 42 , 43 ]. The literature is sparse with varying study designs, ages, and EMA methods (e.g., signalling type and duration).
Stakeholder perspectives
Stakeholders were: (1) young people between 16 and 20 years Footnote 1 who had experience with or knowledge about mood monitoring; and (2) psychologists who had experience providing or recommending mental health care to young people. A combination of convenience and snowball sampling methods were used to recruit young people and psychologists into the study between July and August 2020. Strategies included online media advertisements (e.g., Black Dog Institute’s website, Facebook, Twitter, and Instagram), and contacting existing professional networks and peak clinical bodies (e.g., Australian Clinical Practice Association [ACPA]).
Online surveys
Participants provided personal information through a self-report online survey. Young people reported their age, gender, mental health history ( “ Have you ever experienced a mental health problem or been diagnosed with a mental illness?” [Yes, No, I’m not sure]), psychological treatment (“Have you ever received psychological therapy for depression or low mood? [Yes, No, I don’t know], experience with mood monitoring (including digital tools; e.g., “Have you ever used mood monitoring techniques to track how you are feeling in day-to-day life?” [Yes, No, I don’t know]), and mental health (Depression Anxiety Stress Scales [DASS-21], Kessler Scale [K6], Emotional Self-Awareness Scale-Revised [ESA-R]). All mental health measures have been used and validated with young people and have strong psychometric properties [ 33 , 44 , 45 ]. Psychologists provided demographic information, qualifications, employment, and use of mood monitoring in clinical practice. This information was used to contextualise the stakeholder perspectives, expanded upon below.
Interviews and focus groups
We conducted six focus groups with young people and individual interviews with psychologists. Questions were asked in a semi-structured format and discussions were prompted using specific, open-ended questions (Additional file 1 : Appendix A). Topics included: awareness of emotions and moods, understanding and use of mood monitoring, understanding and use of EMA, mood monitoring in psychological therapy, views about depression, and gaps in psychological treatment.
Interested stakeholders participated between July 2020 and September 2020. Online surveys for young people and psychologists were administered through Qualtrics (2017). Stakeholders provided electronic informed consent, followed by the questionnaires, which took between 10 and 15 min to complete. In line with the Australian National Statement on Conduct in Human Research [ 46 ], young people 16 and above provided informed consent; parental/guardian consent was not required. Focus groups (60–90 min) or interviews (30–60 min) were then held using video conferencing software (Zoom 2011) at a time preferred by the stakeholders. They were facilitated by the chief investigator (JRB) and/or the project officer (KK), audio-recorded, and later transcribed. Young people and psychologists were reimbursed for their time at a rate of $20AUD/h via electronic gift card. Survey and focus group/interview procedures received ethical approval from the University of New South Wales Human Research Ethics Committee (HC200475).
Brief review of publicly available information and online forums
We reviewed information from known websites, forums, and membership lists (QuantifyMe, Reddit, Beyond Blue, ACPA listserve, Black Dog Institute e-Mental Health in Practice [eMPRac] online forums) for conversations about how young people and psychologists use mood monitoring tools. Key search terms included “mood monitor” and “mood tracking”. We then performed google searches using the terms “depression forum” and “young people forum” to identify youth mental health forums that allowed posts about user experiences with mood monitoring. We explored and extracted queries to get a sense of what tools were being recommended in the public domain (Additional file 1 : Table S1 in Appendix B).
Linking the review with qualitive inquiry
The review informed the topics explored in our qualitative inquiry, with findings from the inquiry acting to evaluate and shape our search terms. Focus groups were also used to ask young people about the legitimacy of our online forum searches and their opinions about the online recommendations. Using a dynamic and integrated approach, information gathered from each source was then used to shape the approach and interpretation of the other sources. This approach increased the rigor and breadth of our methods while also positioning the stakeholder perspectives at the forefront of the review.
Data analysis
Descriptive statistics were used to characterise the stakeholder samples. Reflexive thematic analysis, according to Braun and Clarke’s six-stage guidelines, were used for qualitative data [ 47 ]. Using a deductive approach, analysis involved an iterative process of reading and coding responses to extract overarching themes that mapped onto our research questions. Initial coding was conducted by KK. Refinement of codes and generation of higher-order themes was conducted by KK and JRB. Research questions included: (1) What is the role of affective awareness in depression (and mental health more broadly)?; (2) What are stakeholders’ experiences of mood monitoring, including preferences, benefits, and harms?; and (3) Is EMA a useful tool to understand and improve affective experiences?
Characteristics of the stakeholder samples
See Table 2 (and Additional file 1 : Table S2 in Appendix C). Twenty-four young people, with a mean age of 17.67 ( SD = 1.34), responded to the survey and 18 contributed to focus groups. Most were born in Australia (75%), identified as female (66.7%), and attended secondary school between years 10–12 (75%). None identified as Aboriginal or Torres Strait Islander. Just over half had been diagnosed with a mental health illness (58.3%), of which 85.7% had received psychological therapy for depression. Just over half had used mood monitoring techniques (54.2%), with most recommendations made by a psychologist during therapy (61.5%). Most young people were open to using mood monitoring in the future to increase affective awareness (87.5%).
Average scores on the K6 indicated that psychological distress was within the moderate range ( M = 18.00, SD = 5.3), with 41.7% indicating the presence of probable mental illness. On the DASS, average scores for stress ( M = 18.42, SD = 8.96) and depression ( M = 18.67, SD = 11.81) were within the moderate range, and anxiety was within the moderate to severe range ( M = 14.25, SD = 9.41). For depression, 66.6% were in the clinical range (i.e., moderate to extremely severe). The average score on the ESA-R scale was 61.83 ( SD = 16.40), with higher scores indicating higher levels of awareness.
Five female clinical or registered clinical psychologists, with a mean age of 35.00 ( SD = 8.72) and 6.60 years ( SD = 7.55) of experience working with young people, also contributed their perspectives. None identified as Aboriginal or Torres Strait Islander, and three were born in Australia. Two indicated that they had received specific training in adolescent mental health. All reported recommending mood monitoring as part of treatment for youth depression at least some of the time. Four indicated that monitoring results impacted their therapeutic approach (one being unsure). Only one had used EMA as a mood monitoring tool in treatment for youth depression.
Setting the scene with stakeholder insights
How aware are young people of how they feel.
Most interviewed young people were not always aware of their feelings, and older age was related to increased awareness. Negative emotions (e.g., anger, sadness) were reported to be particularly noticeable and memorable, especially when they were high intensity. Some reported that basic (vs complex) emotions were easier to identify. Two reported that being aware of what others were feeling could guide social interactions. Most wanted to increase their awareness of both negative and positive emotions.
Psychologists had mixed perspectives about how aware young people were of their emotions. One also clarified that socio-economic circumstances and family environments likely contribute to awareness level, because of norms around emotions, modelling, and links with general emotional skills.
What is the role of affective awareness in depression?
All young people and psychologists thought that a lack of awareness contributes to depression. Most young people described this in terms of contributing to a problem that already existed, rather than increasing vulnerability. One psychologist also noted that only being aware of one emotion, rather than the full range, could be a risk factor for depression. Another suggested that learning affective awareness skills from an earlier age, from parents or in primary schools, facilitated prevention.
Integrated perspectives from research and stakeholders
Does ema increase affective awareness and reduce depressive symptoms, ema as a stand-alone intervention.
Using an indicated prevention approach, one randomised controlled trial (RCT) used EMA as an intervention with a subclinical youth sample between 14 and 24 years of age [ 34 ]. Youth in the experimental group monitored a range of experiences including mood; those in the control monitored daily activities. Monitoring for 2–4 weeks increased affective awareness in the experimental group, but depression decreased similarly for both groups at the immediate post-test and 6-week follow-up. In a secondary mediation analysis of this data, Kauer and colleagues found that EMA monitoring decreased depressive symptoms through increased awareness for both groups [ 35 ]. The strength of this indirect association was larger for the experimental than the control group, and EMA did not directly decrease depressive symptoms. A universal uncontrolled pre-post study with ages across the lifespan (13–69 years) evaluated the effectiveness of MoodPrism (a dedicated mood monitoring app) over 30-days [ 48 ] and assessed whether awareness mediated the effects on depression [ 33 ]. Perceptions that the app was more (vs less) engaging predicted decreases in depression (for both sub-clinical and non-clinical samples). The effects were mediated by increases in emotional self-awareness, but only for those who were sub-clinically depressed at baseline. Another universal uncontrolled pre-post study with university students (18–24 years) found a different pattern of results [ 36 ], with no differences between EMA-group (i.e., positive, negative, or neutral affect) on affect or depressive symptoms. However, there was a time effect for depressive symptoms, with symptoms reducing from pre to post, but increasing from post to the 1-month follow-up. Together, these studies indicate that EMA decreases depressive symptoms by increasing awareness, with effects potentially greater for indicated samples.
Stakeholder insights generally aligned with the review results. Most stakeholders thought that EMA would increase awareness of feelings, and that this awareness could be useful for prevention and/or early intervention. The rationale was that awareness helped to keep track of emotions, identify triggers, and understand why emotions occurred. Some young people were doubtful about whether they would use EMA to monitor their feelings when they were feeling well. This suggests a preference for indicated prevention/early intervention rather than a universal or selective prevention approach (i.e., in the absence of symptoms).
EMA as part of a broader intervention
Two RCTs examined EMA as part of a broader psychological intervention. Using an indicated prevention approach, one compared a two-week iCBT intervention (Woebot) with embedded mood monitoring to a control group in a university sample (18–28 years) with self-reported depressive symptoms [ 37 ]. Participants in the Woebot group reported reduced depression two weeks post-intervention, and qualitatively reported increased affective awareness. In a pilot RCT with adolescents (12–18 years) admitted to a psychiatric inpatient unit for suicidality, a skills-based positive affect and positive psychology intervention (STEP) plus mood monitoring (EMA) was compared to treatment-as-usual [ 38 ]. STEP + EMA was associated with a greater reduction in parent ratings of youth depression compared to treatment as usual 3-months post-intervention. There were no group differences across time for self-reported depression or positive and negative emotions, although engagement in the monitoring was high. These two studies indicate there could be some benefit in EMA approaches as part of broader interventions in the treatment of depression.
The stakeholder psychologists indicated that that they conceptualised EMA as part of a broader intervention rather than a standalone intervention. EMA was considered to facilitate the identification of mood, and how mood changes over time, as well as raise the alarm that their client might be struggling and facilitate help-seeking. A few psychologists and young people also noted that although awareness was necessary, and could lead to improvements by itself, other explicit strategies to improve low mood were needed. Similarly, one psychologist suggested that EMA monitoring could increase emotional intelligence, with knock-on effects for prevention and regulation of mood.
Can EMA identify depression risk?
Other EMA studies have not directly measured affective awareness but provide information about links between daily emotion and depressive symptoms. In one RCT, healthy university students (18–19 years) were assigned to an 8-week mindfulness intervention or a waitlist control [ 39 ]. A subset was randomly selected to complete EMA measures in short bursts (10-days each) before, during, and after the intervention. Average levels of negative emotion did not differ between condition or burst. All groups reported more negative emotion when faced with family stress, but the effect was weaker among intervention participants. Another cross-sectional study with healthy school students (13–16 years) used a smartphone program (MyExperience) to measure positive affect over 6 days [ 43 ]. Depressive symptoms were related to lower mean positive affect and higher variability in positive affect. Using the same program over 2-weeks, a quasi-experiment found that currently depressed with university students (18–22 years) reported greater average negative affect, and greater increases in negative affect to recent perceived stress, than remitted and healthy students [ 42 ].
Two treatment studies with depressed youth (7–17 years) measured positive and negative affect using phone-based EMA. The first used a quasi-experimental approach and delivered EMA over 8-weeks [ 41 ]. Compared to healthy controls, young people with depression reported more intense negative emotions (e.g., anger, sadness), as well as a lower ratio of positive to negative affect. The second study used a cross-sectional design and EMA to gather baseline data over four days before depressed youth received one of three treatment protocols [ 40 ]. Higher negative affect and a lower ratio of positive to negative affect at baseline were related to a slower rate of decline of clinical severity during treatment. Overall, these studies show that increased variability in negative emotion could be a key risk factor for youth depression, and real-time assessment of mood can provide important information about outcome and course of treatment.
Stakeholder insights converged with the research findings. For both stakeholder groups, in-the-moment functionality of EMA was thought to be a major benefit in prevention and early intervention strategies. It was reported that increasing awareness of emotions and understanding patterns in real-time helps to identify triggers early and facilitate action, thus reducing risk of depression onset and severity.
Gaps between research, clinical practice, and what young people want
The narrative review did not provide insight into preferences for EMA, barriers to use, potential harms of affective awareness, or the types of individuals that might benefit most from increased awareness. Identifying these characteristics is important because they speak to whether young people will use EMA, who it might be more effective for, and appropriateness. The stakeholder insights filled this gap.
Stakeholder experience and preferences for mood monitoring, with an emphasis on EMA
About half of the young people interviewed had not used any form of mood monitoring, although most had heard about it and could foresee benefits. For those that did have experience, methods used included journaling, app-based EMA monitoring (e.g., Daylio), and pen-and-paper monitoring. When apps were introduced as part of psychological therapy, the rationale was to overcome barriers with traditional pen-and-paper methods such as forgetting to monitor and difficulties recalling retrospectively. Individual differences, flexibility, and autonomy were key factors for engagement.
There were uncertainties and variation around the ideal functions of EMA. Most young people thought that identifying emotional content, intensity, and context was important. One young person thought that colours or imagery would accurately represent mixed emotions. Another preferred to report potent experiences ad hoc, rather than in response to a pre-determined prompt.
All psychologists reported using pen-and-paper mood monitoring in their practice. Most used it in the earlier phases of treatment as a between session home task. Common themes were that approaches were chosen based on usability and appropriateness for each young person, and that data was used to paint a broad picture of emotional experience. At the time of interview, none had used app-based or EMA tools although all thought that EMA would be useful. They thought EMA-apps could overcome barriers to traditional monitoring approaches, with benefits including increased uptake, simplicity, and accuracy.
The interest in EMA and app-based tools expressed by the stakeholders converged with our search of publicly available information. Although there are many websites giving recommendations for mood monitoring apps [ 49 ], they should be viewed with caution because few apps are designed specifically for young people and have been evaluated in research trials. Overall, we found evidence that people are turning toward online sources to find out more about EMA mood monitoring apps. A common pattern was asking for recommendations and sharing preferences (see Additional file 1 : Table S1 in Appendix B).
What are the barriers to using EMA?
Practical barriers to use by young people were identified by both groups. Both psychologists and young people reported that a lack of motivation to engage and pay attention to feelings, especially when feeling well or without a clear purpose to monitor, was a major barrier to use. Young people also reported that receiving too many EMA prompts and not knowing how to interpret EMA data were foreseeable barriers to use and beneficial outcomes. Psychologist typically raised concerns about technology, including how to deal with technical issues, lack of access to infrastructure, and data privacy issues.
Are there any harms? Who might it be most (and least) helpful for?
The key harm reported by young people was that attention to negative emotions, such as feeling low or apathetic, could reinforce those feelings. Two psychologists echoed this concern. In using EMA to measure or increase awareness, young people were concerned that forcing selection between unrepresentative emotion options could make them feel worse, confused, or invalidated. Relatedly, given duty of care responsibilities, psychologists stated that inbuilt connectivity to support services, access to data, and receiving updates about risk would be necessary functions of EMA to keep young people safe.
Both groups identified characteristics of young people that are important to consider when increasing awareness and/or using EMA monitoring. There was some overlap in perspectives. For example, both young people and psychologists identified that individuals who were highly motivated to monitor might benefit most from EMA approaches. Introspective individuals might benefit or be harmed. On the one hand, they might be more able to engage with EMA processes; on the other hand, they might be prone to ruminate about negative experiences—particularly those with anxiety. Young people also identified that younger individuals and those with a clear sense of identity might benefit most from attending to their emotions. Psychologists suggested that individuals who were female, conscientious, and school-aged might benefit most, but those with severe mental health problems might benefit least.
Can affective awareness and EMA assist in the prevention and/or early intervention of youth depression?
Across data sources, we found converging evidence that affective awareness is important in the prevention and early intervention of depression. Further, EMA can be used as a therapeutic tool to increase awareness. Monitoring mood using EMA does not seem to directly reduce depression but does so indirectly through heightening affective awareness. The indirect effect was found with sub-clinical and clinical samples, suggesting utility for early intervention (and treatment). Stakeholders also indicated that for EMA to have beneficial effects, EMA should focus not just on the what but also on the why and how (i.e., emotional triggers and how to deal with them). This aligns with reports that affective awareness provides a foundation that other skills can leverage and build upon.
None of the studies tested prevention where samples did not have any symptoms and assessed depression over the longer-term. Longitudinal studies are needed to identify new cases and trajectory of symptoms. Young people were also uncertain about preventative effects of affective awareness/EMA due to a lack of perceived need, although psychologists identified links between building awareness from an early age and other cognitive/emotional skills. Our results indicated that a lack of motivation to monitor mood when not symptomatic was likely to be a barrier in the use of EMA for preventive purposes.
All data sources indicated that EMA can be used as a measurement tool to provide rich data about emotional experiences. By detecting intensity and variation in emotions, EMA can identify emotional risk factors for depression as well as predict treatment outcome and course. Young people and psychologists emphasised that use would be determined by characteristics of the individual and desired function. However, overall, the stakeholders were unsure how to access or find appropriate EMA apps. The online forum data, for example, explicitly shows that some people are actively looking for apps and are relying on word-of-mouth for recommendations.
Individual differences
Individual differences have not been explored comprehensively in the literature. There is some evidence that age moderates the relationship between difficulties with affective awareness and depression [ 22 ], and limited evidence for sex differences. In our results, individual differences were linked to the perceived benefits and harms of EMA—with questions around the likelihood and frequency of use, the level of detail in monitoring needed for benefit (i.e., type, intensity, and triggers of emotion), and the type of engagement related to harms. Further, EMA in healthy samples does not seem to increase negative affect over time. An implication is that monitoring for prevention (or early intervention) may not increase distress as predicted by our young and psychologist stakeholders.
Another key finding was that motivation to increase awareness or use EMA might be low when young people are already feeling well. Of studies using a universal approach or healthy samples, one did not report on EMA compliance [ 33 ], another reported high EMA compliance (66–100%, 36), and another reported an average compliance rate of 55.4% [ 39 ]. The generally low and variable compliance rates are consistent with stakeholder concerns about motivation, but there are likely differences in how motivation plays out in the context of a research trial, clinical practice, and self-directed use.
Affective awareness is a foundational skill
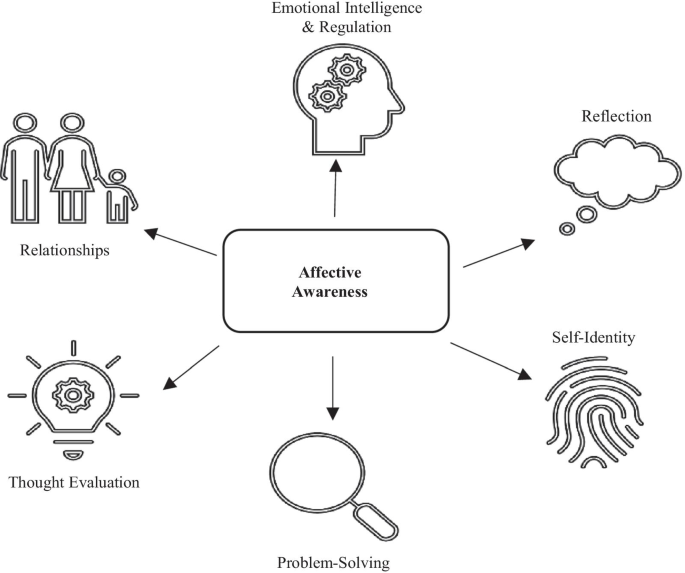
The literature and stakeholder perspectives indicate that being aware of feelings facilitates the use of other coping strategies (Fig. 1 ), and that there is a benefit of embedding affective awareness training into other forms of therapy. Affective awareness is already a common therapeutic process in many psychological interventions for young people and is often introduced as a pre-requisite skill for more complex cognitive and emotion regulation skills. For example, the basic building block for cognitive therapy is the identification of negative thoughts and an understanding of how they impact emotion. An implication is that enhancing awareness may accelerate engagement with existing early intervention programs, enhancing cost-effectiveness in terms of therapeutic outcomes. Further, by using phone-based EMA, more young people can be reached at the same time, with minimal additional costs or resources.
Identified links between active ingredients
Proposed mechanisms of action
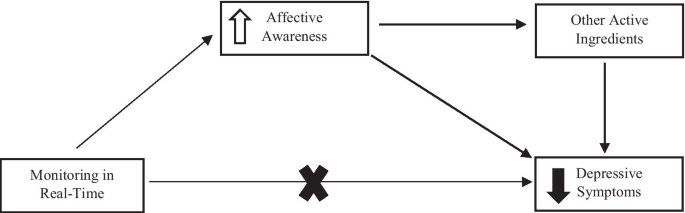
Our integrated review offers hypotheses about how affective awareness influences depressive symptoms (Fig. 2 ). First, there might be a direct relationship, whereby increased awareness reduces symptoms (or potentially prevents their occurrence in the first place). Second, there might be an indirect relationship through links with other active ingredients. Increased affective awareness might enable the use of other skills, such as emotional intelligence and regulation, problem solving, thought evaluation, and reflection. It might also help young people to consolidate their identity (by helping them to understand themselves better) and navigate relationships.
Hypothesised relationship between affective awareness and depression
Summary of the knowledge gaps
Phone-based EMA was used almost exclusively in research and less so by young people in their lives. Young people who did use EMA were encouraged by a psychologist, although none of our psychologists reported current integration into routine practice. Whereas research tended to focus on tracking fine-grained variation of emotions, clinical focus was on generating an overall picture of emotional experience to guide treatment. Consistent with prior research, young people were open to mood monitoring, but use depended on function, motivation, and perceived benefits [ 50 ]. Key preferences included personalisation, and a simple intuitive design that allows for accurate representation and review of complex moods [ 51 ]. A common function underpinning use was linking emotions with triggers and coping skills. This is where research is heading—precision medicine to identify risk factors or vulnerable periods in a young person’s life and to deliver of tailored, just-in-time strategies.
Future steps
Based on our results, we make the following recommendations:
Taking a systematic approach to research efforts by examining: (i) how affective awareness develops over time for different individuals; (ii) how EMA can be used to measure and/or increase affective awareness for different individuals; (iii) the functionality of EMA; and iv) what young people want in an EMA monitoring app, and aligning research efforts with intended use.
Evaluating EMA methodologies to identify ideal parameters (e.g., number of daily prompts), with a focus on balancing research rigor with practical relevance.
Positioning what young people want and what is done in clinical practice at the forefront of research questions, to increase practical impact for target audiences.
Developing publicly available repositories of monitoring apps for young people and psychologists to help them find apps that have been reviewed for quality. An embedded social forum could facilitate personal recommendations.
Considering how scalable approaches will address young people’s needs and preferences.
Building affective awareness earlier, through childhood learning programs in schools and early education contexts.
Exploring how specific components of evidence-based approaches, such as MBCT, influence affective awareness and depressive symptoms in real-time in real-world contexts using EMA.
Limitations in methodological approach
We used a creative approach to reviewing and interpreting different data sources, positioning lived experiences at the centre of our inquiry to produce meaningful outcomes for young people. However, our sample was limited in some respects. A small number of participants were recruited online using convenience and snowball sampling methodology. An implication of this recruitment strategy is that our sample may not be representative of young people in general or psychologists involved in their care. There are also limits to narrative review methods that warrant mention, such as selection bias, how studies are analysed, and the conclusions drawn [ 52 ]. Given the few number of studies that explore EMA and affective awareness in youth depression, and the variation in methodological approaches and quality, a narrative review was better placed to generate meaningful conclusions than a systematic review. Further research using systematic approaches once high-quality evidence has accumulated may corroborate our findings and help to answer different questions about EMA, affective awareness, and youth depression.
Affective awareness is a foundational skill for young people’s emotional health. EMA can be used as an intervention to increase affective awareness, or as a measurement tool to monitor affective awareness. Initial empirical evidence points to the use of EMA in indicated prevention approaches, and more work is needed in the context of universal and selective prevention. However, psychologists and some young people see benefits in monitoring emotions in real-time before the onset of symptoms, to build a repertoire of emotional skills and, in turn, reduce vulnerability to depression. Affective awareness is likely linked to other cognitive and emotional skills involved in psychological therapy, making it an attractive target to enhance other therapeutic effects.
Availability of Data and Materials
The narrative review data are available from the corresponding author upon reasonable request.
Note that while we attempted to recruit young people between the ages of 14–20, only those aged 16 and above expressed interest and signed on to the study.
Abbreviations
Australian Clinical Psychology Association
Beck Depression Inventory
Brief Symptom Inventory-Adolescent Version
Cognitive Behavioural Therapy
Depression Anxiety Stress Scales
Daily Inventory of Stressful Events
Diagnostic Statistical Manual, Fourth Edition
Ecological Momentary Assessment
Black Dog Institute e-Mental Health in Practice
Emotional Self-Awareness Scale
Emotional Self-Awareness Scale-Revised
Face-to-Face
Generalised Anxiety Disorder 7
Indicated Prevention
Kessler Scale
Kiddie Schedule for Affective Disorders and Schizophrenia—Present and Lifetime Version
Mindfulness-Based Cognitive Therapy
Major Depressive Disorder
Modified Differential Emotions Scale
Positive and Negative Affect Schedule
Positive and Negative Affect Schedule for Children
Patient Health Questionnaire-9
Randomised Controlled Trial
Skills to Enhance Positivity Program
Universal Prevention
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789.
Article Google Scholar
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119.
Article PubMed PubMed Central Google Scholar
Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in us adolescents: Results from the national comorbidity survey replication–adolescent supplement (NCS-A). J Am Acad Child Adolesc Psychiatry. 2010;49:980.
Petito A, Pop TL, Namazova-Baranova L, Mestrovic J, Nigri L, Vural M, et al. The burden of depression in adolescents and the importance of early recognition. J Pediatr. 2020;218:265.
Article PubMed Google Scholar
Ormel J, Kessler RC, Schoevers R. Depression: More treatment but no drop in prevalence: how effective is treatment? And can we do better? Curr Opin Psychiatry. 2019;32:348.
Stockings EA, Degenhardt L, Dobbins T, Lee YY, Erskine HE, Whiteford HA, et al. Preventing depression and anxiety in young people: a review of the joint efficacy of universal, selective and indicated prevention. Psychol Med. 2016;46:11.
Werner-Seidler A, Perry Y, Calear AL, Newby JM, Christensen H. School-based depression and anxiety prevention programs for young people: a systematic review and meta-analysis. Clin Psychol Rev. 2017;51:30.
van Zoonen K, Buntrock C, Ebert DD, Smit F, Reynolds CF 3rd, Beekman AT, et al. Preventing the onset of major depressive disorder: a meta-analytic review of psychological interventions. Int J Epidemiol. 2014;43:318.
Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, et al. The lancet psychiatry commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry. 2018;5:237.
Furukawa TA, Suganuma A, Ostinelli EG, Andersson G, Beevers CG, Shumake J, et al. Dismantling, optimising, and personalising internet cognitive behavioural therapy for depression: a systematic review and component network meta-analysis using individual participant data. Lancet Psychiatry. 2021;8:500.
Møller MH, Ioannidis JPA, Darmon M. Are systematic reviews and meta-analyses still useful research? We are not sure. Intensive Care Med. 2018;44:518.
Kim KM. Enriching the process of “good science” through participation of people with psychiatric disabilities in all aspects of research. Psychiatr Rehabil J. 2005;28:403.
Goodare H, Lockwood S. Involving patients in clinical research. Improves the quality of research. BMJ. 1999;319:724.
Smith R, Killgore WDS, Lane RD. The structure of emotional experience and its relation to trait emotional awareness: a theoretical review. Emotion. 2018;18:670.
Lane RD, Schwartz GE. Levels of emotional awareness: a cognitive-developmental theory and its application to psychopathology. Am J Psychiatry. 1987;144:133.
PubMed Google Scholar
Van Beveren M-L, Goossens L, Volkaert B, Grassmann C, Wante L, Vandeweghe L, et al. How do i feel right now? Emotional awareness, emotion regulation, and depressive symptoms in youth. Eur Child Adolesc Psychiatry. 2019;28:389.
Kranzler A, Young JF, Hankin BL, Abela JR, Elias MJ, Selby EA. Emotional awareness: a transdiagnostic predictor of depression and anxiety for children and adolescents. J Clin Child Adolesc Psychol. 2016;45:262.
Nyquist AC, Luebbe AM. An emotion recognition–awareness vulnerability hypothesis for depression in adolescence: a systematic review. Clin Child Fam Psychol Rev. 2020;23:27.
Zeman J, Cassano M, Perry-Parrish C, Stegall S. Emotion regulation in children and adolescents. J Dev Behav Pediatr. 2006;27:155.
Eastabrook JM, Flynn JJ, Hollenstein T. Internalizing symptoms in female adolescents: associations with emotional awareness and emotion regulation. J Child Fam Stud. 2014;23:487.
Rieffe C, De Rooij M. The longitudinal relationship between emotion awareness and internalising symptoms during late childhood. Eur Child Adolesc Psychiatry. 2012;21:349.
Sendzik L, Schäfer JÖ, Samson AC, Naumann E, Tuschen-Caffier B. Emotional awareness in depressive and anxiety symptoms in youth: a meta-analytic review. J Youth Adolesc. 2017;46:687.
Charbonneau AM, Mezulis AH, Hyde JS. Stress and emotional reactivity as explanations for gender differences in adolescents’ depressive symptoms. J Youth Adolesc. 2009;38:1050.
Matthews M, Doherty G, Sharry J, Fitzpatrick C. Mobile phone mood charting for adolescents. Br J Guid Couns. 2008;36:113.
Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1.
Armey M, Schatten H, Haradhvala N, Miller I. Ecological momentary assessment (EMA) of depression-related phenomena. Curr Opin Psychol. 2015;4:21.
Versluis A, Verkuil B, Lane RD, Hagemann D, Thayer JF, Brosschot JF. Ecological momentary assessment of emotional awareness: Preliminary evaluation of psychometric properties. Curr Psychol. 2018. https://doi.org/10.1007/s12144-018-0074-6 .
Kramer I, Simons CJP, Hartmann JA, Menne-Lothmann C, Viechtbauer W, Peeters F, et al. A therapeutic application of the experience sampling method in the treatment of depression: a randomized controlled trial. World Psychiatry. 2014;13:68.
Dubad M, Winsper C, Meyer C, Livanou M, Marwaha S. A systematic review of the psychometric properties, usability and clinical impacts of mobile mood-monitoring applications in young people. Psychol Med. 2018;48:208.
Tan LBG. A critical review of adolescent mindfulness-based programmes. Clin Child Psychol Psychiatry. 2015;21:193.
Baltasar-Tello I, Miguélez-Fernández C, Peñuelas-Calvo I, Carballo JJ. Ecological momentary assessment and mood disorders in children and adolescents: a systematic review. Curr Psychiatry Rep. 2018;20:66.
Sequeira L, Perrotta S, LaGrassa J, Merikangas K, Kreindler D, Kundur D, et al. Mobile and wearable technology for monitoring depressive symptoms in children and adolescents: a scoping review. J Affect Disord. 2020;265:314.
Bakker D, Rickard N. Engagement in mobile phone app for self-monitoring of emotional wellbeing predicts changes in mental health: moodprism. J Affect Disord. 2018;227:432.
Reid SC, Kauer SD, Hearps SJ, Crooke AH, Khor AS, Sanci LA, et al. A mobile phone application for the assessment and management of youth mental health problems in primary care: a randomised controlled trial. BMC Fam Pract. 2011;12:131.
Kauer SD, Reid SC, Crooke AHD, Khor A, Hearps SJC, Jorm AF, et al. Self-monitoring using mobile phones in the early stages of adolescent depression: Randomized controlled trial. J Med Internet Res. 2012;14:e67.
De Vuyst HJ, Dejonckheere E, Van der Gucht K, Kuppens P. Does repeatedly reporting positive or negative emotions in daily life have an impact on the level of emotional experiences and depressive symptoms over time? PLoS ONE. 2019;14:e0219121.
Fitzpatrick KK, Darcy A, Vierhile M. Delivering cognitive behavior therapy to young adults with symptoms of depression and anxiety using a fully automated conversational agent (woebot): a randomized controlled trial. JMIR Mental Health. 2017;4:e19.
Yen S, Ranney ML, Krek M, Peters JR, Mereish E, Tezanos KM, et al. Skills to enhance positivity in suicidal adolescents: results from a pilot randomized clinical trial. J Posit Psychol. 2020;15:348.
Bai S, Elavsky S, Kishida M, Dvorakova K, Greenberg MT. Effects of mindfulness training on daily stress response in college students: ecological momentary assessment of a randomized controlled trial. Mindfulness. 2020;11:1433.
Forbes EE, Stepp SD, Dahl RE, Ryan ND, Whalen D, Axelson DA, et al. Real-world affect and social context as predictors of treatment response in child and adolescent depression and anxiety: an ecological momentary assessment study. J Child Adolesc Psychopharmacol. 2012;22:37.
Silk JS, Forbes EE, Whalen DJ, Jakubcak JL, Thompson WK, Ryan ND, et al. Daily emotional dynamics in depressed youth: a cell phone ecological momentary assessment study. J Exp Child Psychol. 2011;110:241.
Sheets ES, Armey MF. Daily interpersonal and noninterpersonal stress reactivity in current and remitted depression. Cogn Ther Res. 2020;44:774.
van Roekel E, Bennik EC, Bastiaansen JA, Verhagen M, Ormel J, Engels RC, et al. Depressive symptoms and the experience of pleasure in daily life: an exploration of associations in early and late adolescence. J Abnorm Child Psychol. 2016;44:999.
Ferro MA. The psychometric properties of the Kessler psychological distress scale (k6) in an epidemiological sample of Canadian youth. Can J Psychiatry. 2019;64:647.
Shaw T, Campbell MA, Runions KC, Zubrick SR. Properties of the dass-21 in an Australian Community Adolescent Population. J Clin Psychol. 2017;73:879.
National Health and Medical Research Council. The national statement on ethical conduct in human research. 2007.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77.
Rickard N, Arjmand H-A, Bakker D, Seabrook E. Development of a mobile phone app to support self-monitoring of emotional well-being: a mental health digital innovation. JMIR Mental Health. 2016;3:e49.
Coulson J. Want to be appier? 7 apps to boost wellbeing 2015. https://www.generationnext.com.au/2015/03/want-to-be-appier-7-apps-to-boost-wellbeing/ .
Seko Y, Kidd S, Wiljer D, McKenzie K. Youth mental health interventions via mobile phones: a scoping review. Cyberpsychol Behav Soc Netw. 2014;17:591.
Widnall E, Grant C, Wang T, Cross L, Velupillai S, Roberts A, et al. A qualitative content analysis of user perspectives of mood-monitoring apps available to young people. JMIR mHealth uHealth. 2020;8:e18140.
Pae C-U. Why systematic review rather than narrative review? Psychiatry Investig. 2015;12:417.
Download references
Acknowledgements
Thank you to the young people who provided valuable insights into their experiences and perspectives about affective awareness and mental health approaches.
This work was funded by a Wellcome Trust Mental Health Priority Area 'Active Ingredients' commission awarded to JRB and AWS at the Black Dog Institute, University of New South Wales. The funder specified guidelines about the overall study design and data collection (e.g., an “insights analysis” that incorporated lived experience perspectives), although had no direct input into the conceptualisation of the project, data analysis, interpretation of data, and in writing the manuscript.
Author information
Authors and affiliations.
Black Dog Institute, University of New South Wales, Sydney, NSW, Australia
Joanne R. Beames, Katarina Kikas & Aliza Werner-Seidler
You can also search for this author in PubMed Google Scholar
Contributions
JRB secured funding and conceptualised the project with assistance from AWS. KK conducted the narrative review search strategy, collected data, and managed the project timeline, with assistance from JRB. JRB interpreted and triangulated data and wrote the manuscript. All authors provided feedback and approved the final version.
Corresponding author
Correspondence to Joanne R. Beames .
Ethics declarations
Ethics approval and consent to participate.
All research procedures received ethical approval from the University of New South Wales Human Research Ethics Committee (HC200475). Although we attempted to recruit participants between 14 and 20 years of age, only participants aged 16 years and over expressed interest and signed on to the study. These respondents were required to provide consent and pass a Gillick Competency Task, which ensured they had the capacity to provide informed consent and understood the nature of the study. In line with the Australian National Statement on Ethical Conduct in Human Research, no parental or guardian consent was required for these respondents.
Consent for Publication
Not applicable.
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
Contains information about focus group and interview guides (Appendix A), results for publicly available data sources (Appendix B), and additional characteristics about the expert samples (Appendix C).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Beames, J.R., Kikas, K. & Werner-Seidler, A. Prevention and early intervention of depression in young people: an integrated narrative review of affective awareness and Ecological Momentary Assessment. BMC Psychol 9 , 113 (2021). https://doi.org/10.1186/s40359-021-00614-6
Download citation
Received : 10 December 2020
Accepted : 21 June 2021
Published : 16 August 2021
DOI : https://doi.org/10.1186/s40359-021-00614-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Affective awareness
- Ecological momentary assessment
- Early intervention
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Loading metrics
Open Access
Peer-reviewed
Research Article
Depression, anxiety and stress among high school students: A cross-sectional study in an urban municipality of Kathmandu, Nepal
Contributed equally to this work with: Anita Karki, Bipin Thapa
Roles Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Software, Writing – original draft, Writing – review & editing
* E-mail: [email protected] (PB); [email protected] (AK)
Affiliation Central Department of Public Health, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal
Roles Data curation, Formal analysis, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing
Affiliation Department of Child, Adolescent Health and Maternal Care, School of Public Health, Capital Medical University, Beijing, China
Roles Writing – review & editing
Affiliation Department of Community Medicine, Maharajgunj Medical Campus, Institute of Medicine, Tribhuvan University, Kathmandu, Nepal
Roles Conceptualization, Methodology, Supervision, Writing – review & editing
- Anita Karki,
- Bipin Thapa,
- Pranil Man Singh Pradhan,

- Published: May 31, 2022
- https://doi.org/10.1371/journal.pgph.0000516
- Peer Review
- Reader Comments
Depression and anxiety are the most widely recognized mental issues affecting youths. It is extremely important to investigate the burden and associated risk factors of these common mental disorders to combat them. Therefore, this study was undertaken with the aim to estimate the prevalence and identify factors associated with depression, anxiety, and stress among high school students in an urban municipality of Kathmandu, Nepal. A cross-sectional study was conducted among 453 students of five randomly selected high schools in Tokha Municipality of Kathmandu. Previously validated Nepali version of depression, anxiety, and stress scale (DASS-21) was used to assess the level of symptoms of depression, anxiety and stress (DAS). Multivariable logistic regression was carried out to decide statistically significant variables of symptoms of DAS at p-value<0.05. The overall prevalence of DAS was found to be 56.5% (95% CI: 51.8%, 61.1%), 55.6% (95%CI: 50.9%, 60.2%) and 32.9% (95%CI: 28.6%, 37.4%) respectively. In the multivariable model, nuclear family type, students from science or humanities faculty, presence of perceived academic stress, and being electronically bullied were found to be significantly associated with depression. Female sex, having mother with no formal education, students from science or humanities faculty and presence of perceived academic stress were significantly associated with anxiety. Likewise, female sex, currently living without parents, and presence of perceived academic stress were significantly associated with stress. Prevention and control activities such as school-based counseling services focusing to reduce and manage academic stress and electronic bullying are recommended in considering the findings of this research.
Citation: Karki A, Thapa B, Pradhan PMS, Basel P (2022) Depression, anxiety and stress among high school students: A cross-sectional study in an urban municipality of Kathmandu, Nepal. PLOS Glob Public Health 2(5): e0000516. https://doi.org/10.1371/journal.pgph.0000516
Editor: Khameer Kidia, Brigham and Women’s Hospital, UNITED STATES
Received: February 22, 2022; Accepted: May 2, 2022; Published: May 31, 2022
Copyright: © 2022 Karki et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: The data that support the findings of descriptive analysis of this study are available in Figshare with the identifier given below: https://doi.org/10.6084/m9.figshare.19203512 The data that support the findings of inferential analysis of this study are available in Figshare with the identifier given below: https://doi.org/10.6084/m9.figshare.19203491 .
Funding: The authors received no specific funding for this work.
Competing interests: The authors have declared that no competing interests exist.
Introduction
Mental disorders contribute to a huge proportion of disease burden across all societies [ 1 ]. Among them, depression, anxiety and stress are the leading causes of illness and disability among adolescents [ 2 ]. The physical, psychological, and behavioral changes that occur throughout adolescence predispose them to a variety of mental health issues [ 3 ]. Despite this, mental health and mental disorders are largely ignored and not given the same importance as physical health [ 4 ].
The existing community-based studies conducted among high school students of various parts of Nepal have reported a wide range of prevalence of symptoms of depression and anxiety. The prevalence of depressive symptoms has been reported to range from 27% to 76% [ 5 – 7 ]. Likewise, the limited studies conducted in Nepal have estimated the proportion of symptoms of anxiety to range from 10% to 57% [ 7 – 9 ]. A nationwide survey conducted in Nepal revealed the prevalence of mental distress among adolescents (13-17years) to be 5.2% [ 10 ]. The Global School Health Survey which was a nationwide survey conducted in 2015 reported anxiety among 4.6% of the students [ 11 ].
Previous studies have revealed that sex [ 12 – 16 ], staying away from home [ 17 ], grade [ 12 , 14 , 16 ], stream of study [ 18 ], academic performance and examination related issues [ 7 , 19 ], cyber bullying [ 20 ] were linked with depression. Likewise, sex [ 8 , 21 ], grade of students and type of school i.e., public or private [ 8 ], family type [ 17 ], not living with parents, educational level of parents [ 21 ] and high educational stress [ 22 ] had been the determinants of anxiety as per previous studies.
High school education is an important turning point in the life of academic students in Nepal [ 23 ]. As the educational system becomes more specialized and tough in high school, the students become more likely to experience stress at this level. This might put them at risk of developing common mental disorders such as depression, anxiety and stress (DAS). However, there is a paucity of research studies that have assessed DAS among high school students in Nepal.
Exploring the magnitude and risk factors of symptoms of DAS are very crucial to combat the burden of adolescent mental health issues [ 24 ]. However, due to limited access to psychological and psychiatric services as well as the significant social stigma associated with mental health issues, anxiety and depression in early adolescence frequently go undiagnosed and untreated, particularly in developing countries such as Nepal. Therefore, this study aimed to estimate the prevalence and identify factors associated with the symptoms of DAS among high school students in an urban municipality of Kathmandu, Nepal.
Materials and methods
Study setting, design, and population.
This was a cross-sectional survey conducted in randomly selected high schools of Tokha Municipality, Kathmandu District in province no. 3 of Nepal. The data collection period was from 27 th August to 11 th September 2019. This municipality was formed on 7 December 2014 by merging five previous villages. It has an area of 16.2 sq.km. and comprises 11 wards [ 25 , 26 ]. The municipality is rich in cultural and ethnic diversity [ 25 ]. According to Nepal government records as of 2017, there were total 218,554 students in Tokha municipality in 82 schools. High school students were the study population for this study [ 26 ]. In Nepal, high school students comprise of grade 11 and grade 12 students. The high school differs from lower schooling level since the students have the opportunity to enroll in specialized areas such as science, management, humanities and education. High school are also popularly known as 10+2 [ 27 ].
Sample size calculation and sampling technique
Sample size was estimated using the formula for cross-sectional survey [ 28 ], n = Z 2 p(1-p)/ e 2 considering the following assumptions; proportion (p) = 0.24 [ 12 ], 95% confidence level, the margin of error of 5%. The estimated proportion used for sample size calculation was based on proportion of symptoms of anxiety i.e., 24%, as reported by a similar study conducted in Manipur, India [ 12 ].
After calculation, the minimum sample size required was 280. After adjusting for design effect of 1.5 to adjust variance from cluster design and assuming non-response rate of 10%, final sample of 467 was calculated. Two-stage cluster sampling was used. A list of all high schools of Tokha municipality was obtained from the education division of the municipality. Out of twelve high schools (8 private schools and 4 public schools), five schools were randomly selected. Within each selected high school further two sections each of grades 11 and 12 were randomly selected. A total of 20 sections were selected, 4 from each selected school, and all the students from the selected sections were included in the study.
Data collection tools
A structured questionnaire was prepared based on our study objectives which was divided into three sections. The first section included information about socio-demographic, familial and academic characteristics of the students. The second section included two item question to assess socializing among the students which was based on a previous study by Vankim and Nelson [ 29 ], two questions to assess bullying among the students based on 2019 Youth Risk Behavior Survey [ 30 ] and one item question to assess perceived academic stress. The third section consisted of Depression, Anxiety and Stress Scale (DASS-21) used to assess level of symptoms of depression, anxiety and stress among the students.
DASS-21 is a psychological screening instrument capable of differentiating symptoms of DAS. Depression, anxiety, and stress are three subscales and there are 7 items in each subscale. Each item is scored on a 4-point Likert scale which ranges from 0 i.e., did not apply to me at all to 3 i.e., applied to me very much. Scores for DAS were calculated by summing the scores for the relevant items. and multiplying by two [ 31 ]. A previously validated Nepali version of DASS-21 was obtained and used for data collection. Nepali version of the DASS-21 has demonstrated adequate internal consistency and validity. However, in the validation paper, the construct validity of the tool was evaluated against life satisfaction scale and not a systematic diagnostic tool [ 32 ]. Reliability for the symptoms of DAS was tested by Cronbach alpha. Cronbach alpha values for DAS were 0.74, 0.77, and 0.74 respectively.
Data collection procedure and technique
Data was collected after obtaining permission from the municipality’s education division as well as individual high schools. The questionnaire was in both English and Nepali language and had been pre-tested among 45 high school students of neighboring municipality. Self-administered anonymous questionnaires were distributed to students in their respective classrooms and requested for participation. An orientation session was conducted for the filling the questionnaire before distribution. Written informed consent was taken from all students prior to data collection whereas additional written parental consent was obtained from students below 18 years of age. One of the investigators herself collected the data from students. After data collection, a session on depression, anxiety, and stress along with the importance of discussing it with the guardians/ teachers and asking for help was conducted.
Study variables
The study variables are described in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pgph.0000516.t001
Data analysis
Compilation of data was done in EpiData 3.1 and then exported to IBM SPSS Statistics version 20 (IBM Corp., Armonk, NY) for cleaning and analysis. Descriptive analysis was performed. Frequency tables with percentages were generated for categorical variables, while mean and standard deviation (SD) were calculated for continuous variables.
Binary logistic regression was performed to identify associated factors of symptoms of DAS. Firstly, we performed univariate analysis in which each co-variate was modeled separately to determine the odds of DAS. Those variables with p-value <0.15 in univariate analysis were identified as candidate variables for multivariable logistic regression. In multivariable logistic regression, a p-value of < .05 was considered to be statistically significant and strength of association was measured using adjusted odds ratio (AOR) at 95% confidence interval.
Multicollinearity of variables was tested before entering them in the regression analysis. No problem of multicollinearity was seen among the variables (the highest observed VIF was 1.25,1.10 and 1.13 for symptoms of DAS respectively. The goodness of fit of the regression model was tested by the application of the Hosmer and Lemeshow test; the model was found to be a good fit (P >.05).
The regression model was explained by the equation:
Log [Y/ (1-Y)] = b 0 + b 1 X 1 + b 2 X 2 + b 3 X 3 … ..b n X n + e
Where Y is the expected probability for the outcome variable to occur, b 0 is the constant/intercept, b 1 through b n are the regression coefficients and the X 1 through X n are distinct independent variables and e is the error term.
Ethical approval and consent
The study protocol was approved by the Institutional Review Committee (IRC) of the Institute of Medicine, Tribhuvan University (Reference no. 23/ (6–11) 76/077). Approval to conduct this study was also obtained from the education division of Tokha Municipality (Ref: 076/077-23) and respective school authorities. A written informed consent (in the Nepali language) was obtained from the students before the data collection to assure their willingness to participate and no identifiers were listed in the questionnaire to make it anonymous and confidential. Parental consent was obtained for students who were under the age of 18. No incentives were provided.
Sociodemographic, academic and contextual characteristics of the students
The research questionnaire was distributed to a sample of 468 high school students, one of whom refused to participate in this study, with a response rate of 99.78%. Responses from 14 students were excluded due to incompleteness. This study presents the analysis on a total of 453 students.
The mean age of the students was 16.99 years (SD = ±1.12), ranging from 14 to 22 years. The proportion of female students (54.1%) was higher than male students (45.9%). Majority of the students were found to be currently living with their parents i.e., 65.8%. Around 70% of the students were from nuclear family. Regarding parent’s educational level, majority of the students responded that their father as well as mother had attained secondary level of education i.e., 31.6% and 33.3% respectively.
With regards to academic characteristics, more than two- third of students i.e., 69.5% were from private high schools while the remaining 30.5% were studying in a government or public high school. More than half i.e. (53.4%) of the students studied in grade eleven. About half of the students i.e., 50.6% were from management faculty. Only 3.8% students reported to have failed in the previous examination.
It was noted that about 60% of students perceived themselves to be stressed due to their studies. Most students were low socializing i.e., 60.9%. Around one-tenth students reported being bullied electronically in the past 12 months (10.2%). Similar proportion of students i.e., 10.4% also reported being bullied on school property in the past 12 months ( Table 2 ).
https://doi.org/10.1371/journal.pgph.0000516.t002
Level of symptoms of DAS among the students
The prevalence of symptoms of DAS was found to be 56.5% (51.8%, 61.1%), 55.6% (50.9%, 60.2%) and 32.9% (28.6%, 37.4%) respectively. About a quarter of students showed moderate level of symptoms of depression and anxiety i.e., 25.8% and 24.5% respectively. On the other hand, symptoms of mild stress were most prevalent among the students. i.e., 14.8% ( Table 3 ).
https://doi.org/10.1371/journal.pgph.0000516.t003
Factors associated with symptoms of depression
The results from multivariable logistic regression analyses for correlates of symptoms of depression are shown in Table 4 . The variables that remain in the final model were age, type of family, father’s education, mother’s education, type of school, grade, faculty, perceived academic stress, and bullied electronically as these variables had p-value less than 0.15 in the univariate model. In the final model, nuclear family type (AOR: 1.64, 95% CI: 1.06–2.52), students from science/humanities faculty (AOR: 1.58, 95% CI: 1.05–2.40), presence of perceived academic stress (AOR: 1.62, 95% CI: 1.08–2.44) and bullied electronically in past 12 months (AOR: 2.84, 95% CI: 1.34–5.99) were significantly associated with symptoms of depression.
https://doi.org/10.1371/journal.pgph.0000516.t004
Factors associated with symptoms of anxiety
The results from multivariable logistic regression analyses for correlates of symptoms of anxiety are shown in Table 5 . The variables that remained in the final model were age, sex, mother’s education, stream/ faculty, perceived academic stress, bullied electronically, and bullied on school property (p<0.15). Female sex (AOR: 1.82, 95% CI: 1.23–2.71), no formal education attained by the mother (AOR: 1.63, 95% CI: 1.08–2.47), students from science or humanities faculties (AOR: 1.50, 95% CI: 1.01–2.21), and presence of perceived academic stress (AOR: 1.93, 95% CI: 1.30–2.87), and were significantly associated with symptoms of anxiety.
https://doi.org/10.1371/journal.pgph.0000516.t005
Factors associated with symptoms of stress
The results from multivariable logistic regression analyses for main correlates of symptoms of stress are shown in Table 6 . The variables that remained in the final model were sex, current living status, grade, stream / faculty, perceived academic stress, bullied electronically and bullied on school property. In the final model, female sex (AOR: 1.54, 95% CI: 1.01–2.34), currently living without parents, (AOR: 1.70, 95% CI: 1.11–2.61), and presence of perceived academic stress (AOR: 2.11, 95% CI: 1.36–3.26) were significantly associated with stress symptoms.
https://doi.org/10.1371/journal.pgph.0000516.t006
In our study, the prevalence of depressive symptoms among high school students was found to be 56.5%. The existing community-based studies conducted among high school students of various parts of Nepal have reported a wide range of prevalence of depressive symptoms. A study by Gautam et al. reported that more than one quarter i.e., 27% of high school students in a rural setting of Nepal showed depressive symptoms [ 6 ]. Similarly, in a study conducted by Bhattarai et. al. in four schools of a metropolitan city in Nepal, it was found that more than 2/5 th i.e., 44.2% students exhibited depressive symptoms [ 5 ]. Similar proportion of depressive symptoms i.e., 41.6% was also reported by Sharma et. al in a study conducted among adolescent students of public schools of Kathmandu [ 9 ]. The prevalence estimated by these studies are lower than the findings of our study [ 5 , 6 , 9 ]. On contrary, a single high school study by Bhandari et al reported depressive symptoms among 76% students [ 7 ]. In our study, the proportion of students showing symptoms of anxiety were 55.6%. A study by Sharma et al. revealed that more than half i.e. 56.9% of public high school students showed symptoms of anxiety [ 9 ]. Another study by Bhandari et. al, also found out that nearly one out of two students i.e., 46.5% suffered from anxiety [ 8 ].These findings are in line with the findings of our study. On contrary, a study by Bhandari reported that only 10% students had mild anxiety [ 7 ]. In our study, the prevalence of stress symptoms among students was 32.9%. A study by Sharma et. al reported that more than 1/4 th students i.e., 27.5% showed symptoms of stress which corroborates with the findings of our study.
While the prevalence of symptoms of DAS reported by our study corroborates with the existing literatures in Nepal, it is exceptionally high. One possible explanation for this could be that the data was collected at the beginning of academic session. The students in the eleventh grade were undergoing sudden transition from secondary school life to high school life with regards to new friends, teachers, school environment, and change in daily schedules whereas the students in 12 th grade were awaiting results of previous board exam. This anticipation and the tremendous pressure faced by 12 th grade students for tertiary education might have contributed to the high prevalence of symptoms of DAS among 12 th grade students whereas the higher prevalence of symptoms of DAS among 11 th grade students could be possibly explained by the inability to cope with the adjustment of sudden transition from secondary to high school life. Moreover, the wide range in prevalence of DAS symptoms among these community-based studies could be attributed to the difference in the setting (rural or urban) and difference in methodology used.
Among South Asian countries, the prevalence of depression reported by our study is in line with the studies conducted in India, and Bangladesh, but slightly higher than one conducted in China and [ 13 , 17 , 33 , 34 ]. On contrary, our study has shown higher prevalence of anxiety among students as compared to study conducted in India, Sri Lanka, Vietnam and China [ 12 , 19 , 22 , 34 ].The prevalence of symptoms of stress in this study is comparable to the study from Chandigarh but higher than similar study from Manipur, India [ 12 , 17 ]. Hence, it can be suggested that there is a huge burden of DAS among high school students in South Asia. In context of Nepal, there is no standalone mental health policy. Further, there is inadequate funding allocated for mental health services along with shortage of qualified mental health professionals. In addition, there is much stigma that surrounds mental illness which acts as a barrier to seek and utilize mental health care services [ 35 ]. Due to these reasons, mental health illnesses are likely to remain untreated and continue to persist in the society. This may explain the high prevalence of DAS in our setting.
Socio-demographic characteristics and association with symptoms of DAS (depression, anxiety and stress)
In current study, it was found that females were more likely to suffer from symptoms of anxiety and stress than their male counterparts. This finding corroborates with the findings from previous studies [ 19 , 21 , 36 – 39 ]. On the contrary, a study conducted in Dang, Nepal reported that males were 1.5 times more likely to become anxious [ 8 ].One possible explanation for this is adolescent stage in girls is marked by hormonal changes as a result of various reproductive events which may have a role in the etiology of anxiety disorders [ 40 ]. Furthermore, when compared to boys, girls are more likely to be subjected to stressful situations such as sexual and domestic violence, which may make them more prone to anxiety and stress problems [ 41 ].
This study revealed that the students who live in nuclear families were more likely to exhibit depressive symptoms compared to students from joint or extended families. There are more members in a joint family system, which may provide better opportunities for adolescents to share their emotions and issues, hence providing a strong support system that may serve as a protective factor against depression which may be lacking in nuclear families [ 42 ]. Moreover, this study also found out that risks of stress symptoms was higher among students who were staying far from their parents. A similar finding was reported by Arif et al., 2019 in Uttar Pradesh, India [ 43 ]. One of the possible explanations might be that students who live without their parents may spend a substantial amount of time alone after school, which does not encourage familial intimacy [ 44 ]. As a result, they may feel alone and disconnected from their parents [ 45 ]. These adolescents may miss out on the opportunity to internalize the support they would otherwise get, leading to increased stress.
In our study, the students who reported no formal mother’s education were at greater risk of showing symptoms of anxiety. This was in accordance with other similar studies [ 38 , 46 ]. The attachment theory provides a robust foundation for understanding how parental behavior affects a child’s ability to recognize and manage stressful events throughout their lives [ 47 ]. The theory supports that the educated mother plays a stronger parenting role in the development of emotional skills and mental health outcomes in teenagers which might be protective for anxiety.
Academic characteristics and association with symptoms of DAS
In our study, the students from science or humanities faculties were more likely to have depression and anxiety as compared to management students. This was in line with other studies which showed higher proportion of depressive symptoms among science students. [ 48 ]. Generally, science students have to compete more, study longer hours and have a higher level of curriculum difficulty than management students which explains the finding. Likewise, it is believed that the humanities students have a poorer past academic performance in the secondary school, and may have chosen this stream / faculty as a secondary choice [ 49 ]. This combined with the uncertainty regarding future work prospects among humanities students may likely explain the higher prevalence of depression among humanities students.
In our study, the students who reported to be stressed due to their studies were more likely to suffer from symptoms of DAS. Several studies have documented similar findings [ 7 , 22 ]. A possible explanation might be that high school is an important stage in an individual’s academic life. However, the inability to meet the expectation of parents, teachers, and oneself in terms of academic performance can lead to overburden of stress [ 50 ]. This persistent academic related stress might accelerate the development of mood disorders such as depression, anxiety and stress among the adolescents [ 51 ].
Contextual factors and association with symptoms of DAS
In our study, the risk of depressive symptoms was higher among those students who were bullied via electronic means. Literature suggests that higher the level of cyberbullying/electronic bullying leads to higher the level of depressive symptoms among adolescents [ 52 ]. A similar study by Perren et. al demonstrated that depression was significantly associated with cyberbullying even after controlling for traditional forms of bullying [ 20 ]. The victims of cyberbullying may experience anonymous verbal or visual threats via electronic means. These repeated incidents can cause the victims to feel powerless which exacerbates the feeling of fear. This can cause significant emotional distress among victims and contribute to development of depressive symptoms [ 53 ].
Even though widely utilized in both clinical as well as research setting, DASS scales are screening tools for symptoms of depression, anxiety, and stress. Hence, they cannot be used as a modality for diagnosis. This limitation should be considered when interpreting the findings of this study. Due to its cross-sectional design, this study was unable to establish causal relationship of depression, anxiety, and stress with associated factors. Since the study tools used in this study investigate the habits and activities of the high school students in the past, recall and reporting bias are likely; however, the effect due to potential confounders have been controlled. As Nepal is a culturally diverse country, the findings of only one municipality may not be generalized to the whole country. Therefore, future studies covering a larger population of high school students employing more robust study designs such as interventional studies are recommended to get the real scenario of common mental disorders.
In conclusion, more than half of the students had depression and anxiety symptoms and nearly one third of the students had stress symptoms. Nuclear family type, students from humanities/science faculty, presence of perceived academic stress, and being bullied electronically were found to be significantly associated with symptoms of depression. Female sex, no formal mother education, students from humanities/science faculty, and presence of perceived academic stress were significantly associated with symptoms of anxiety. Likewise, symptoms of stress were significantly associated with female sex, currently living without parents, and presence of perceived academic stress.
Therefore, prevention and control activities such as school-based counseling services focusing to reduce and manage academic stress and electronic bullying faced by the students are recommended considering findings of this research.
Supporting information
S1 file. questionnaire form used in data collection..
https://doi.org/10.1371/journal.pgph.0000516.s001
Acknowledgments
We are grateful to Tokha municipality for granting permission to conduct the study. Special thank goes to the school management and teachers for their co-ordination during data collection. Lastly, we would like to thank all the study participants for their co-operation and support during the study.
- View Article
- PubMed/NCBI
- Google Scholar
- 2. Adolescent mental health. [cited 27 Jul 2021]. Available: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
- 3. World Health Organization. Regional Office for South-East Asia. Mental health status of adolescents in South-East Asia: evidence for action. New Delhi: World Health Organization. Regional Office for South-East Asia; 2017. Available: https://apps.who.int/iris/handle/10665/254982%0A
- 9. Sharma P, Choulagai B. Stress, anxiety, and depression among adolescent students of public schools in Kathmandu. [cited 19 Mar 2022]. Available: www.jiom.com.np
- 10. Nepal Health Research Council. National Mental Health Survey, Nepal-2020. In: Nepal Health Research Council [Internet]. 2020 pp. 1–4. Available: http://nhrc.gov.np/projects/nepal-mental-health-survey-2017-2018/
- 25. Brief Introduction | Tokha Municipality, Office Of the Municipal Executive. [cited 25 Jul 2021]. Available: https://www.tokhamun.gov.np/en/node/4
- 26. Tokha Municipality Profile | Facts & Statistics–Nepal Archives. [cited 25 Jul 2021]. Available: https://www.nepalarchives.com/content/tokha-municipality-kathmandu-profile/
- 27. Nepal—Secondary Education—Level, Schools, Technical, and Training—StateUniversity.com. [cited 22 Mar 2022]. Available: https://education.stateuniversity.com/pages/1058/Nepal-SECONDARY-EDUCATION.html
- 30. 2019 State and Local Youth Risk Behavior Survey. 2019; 7. Available: https://www.cdc.gov/healthyyouth/data/yrbs/pdf/2019/2019_YRBS-Standard-HS-Questionnaire.pdf
- 35. World Health Organization (WHO). Nepal WHO Special Initiative for Mental Health Situational Assessment CONTEXT.
Advertisement
Risk and protective factors associated with depression among adolescents
- Published: 14 December 2022
- Volume 42 , pages 31024–31034, ( 2023 )
Cite this article

- Samuel Adabla ORCID: orcid.org/0000-0003-2138-9417 1 &
- Laura A. Nabors ORCID: orcid.org/0000-0002-0884-8538 1
497 Accesses
Explore all metrics
This study examined risk and protective factors associated with depression among adolescents in the United States. A sample of 11,738 participants with current or past depression who were between 12 and 17 years was selected from the 2019 National Survey of Children’s Health. Two multivariable logistic regression models examined the relationship between six predictors (being bullied, bullied others, difficulties making or keeping friends, family communication, school engagement, and involvement in extracurricular activities) and outcome variables (past or current depression). Results showed that being bullied or bullying others increased the likelihood of past and current depression. Having little or no difficulties making or keeping friends and engagement in school and extracurricular activities reduced the odds of having past or current depression. Frequent family communication reduced the likelihood of current, but not past depression. Results were significant beyond the associations between covariates (sex, age levels, race, and federal poverty levels) and dependent variables. Caregivers and health professionals should encourage positive social connections with family and peers as well as participation in school and extracurricular activities to protect adolescents from depression.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions
Similar content being viewed by others
Long-term effects of the family check-up in public secondary school on diagnosed major depressive disorder in adulthood.

Protective Mechanisms for Depression among Racial/Ethnic Minority Youth: Empirical Findings, Issues, and Recommendations
Factors predicting depression across multiple domains in a national longitudinal sample of canadian youth, data availability.
The dataset analyzed in the current study is available in the Child and Adolescent Health Measurement Initiative repository ( https://www.childhealthdata.org/help/dataset ).
References
Aronson, O., & Bergh, D. (2021). Adolescents who feel depressed are rejected but do not withdraw: a longitudinal study of ethnically diverse friendship networks in England, Sweden, and Germany. SSM-Population Health , 15 , 100889. https://doi.org/10.1016/j.ssmph.2021.100889
Article PubMed PubMed Central Google Scholar
Babaee, E., Nojomi, M., Asadi-Aliabadi, M., & Eshrati, B. (2021). Bullying and being bullied; how much can it increase the risk of depression and anxiety in students? A multilevel fixed-effect model analysis. Iranian Journal of Psychiatry and Behavioral Sciences, 15(2).
Baldessarini, R. J., Innamorati, M., Erbuto, D., Serafini, G., Fiorillo, A., Amore, M., Girardi, P., & Pompili, M. (2017). Differential associations of affective temperaments and diagnosis of major affective disorders with suicidal behavior. Journal of Affective Disorders , 210 , 19–21. https://doi.org/10.1016/j.jad.2016.12.003
Article PubMed Google Scholar
Blumberg, H. P., Kaufman, J., Martin, A., Charney, D. S., Krystal, J. H., & Peterson, B. S. (2004). Significance of adolescent neurodevelopment for the neural circuitry of bipolar disorder. Annals of the New York Academy of Sciences , 1021 , 376–383. https://doi.org/10.1196/annals.1308.048
Call, J. B., & Shafer, K. (2018). Gendered manifestations of depression and help-seeking among men. American Journal of Men’s Health , 12 (1), 41–51. https://doi.org/10.1177/1557988315623993
Center for Behavioral Health Statistics and Quality. (2011). The NSDUH report: major depressive episode and treatment among adolescents: 2009 . Rockville, MD.
Child and Adolescent Health Measurement Initiative (CAHMI) (2021). “2019 National Survey of Children’s Health, Sampling and Survey Administration.” Data Resource Center for Child and Adolescent Health, supported by the U.S. Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Retrieved November 20, 2021, from https://www.childhealthdata.org/docs/default-source/nsch-docs/2019-nsch-sampling-administration_cahmi_10-2-20.pdf?sfvrsn=7b7b5f17_2
Chen, P., & Harris, K. M. (2019). Association of positive family relationships with mental health trajectories from adolescence to midlife. JAMA Pediatrics , 173 (12), e193336–e193336. https://doi.org/10.1001/jamapediatrics.2019.3336
Da Silva, M. A., Gonzalez, J. C., Person, G. L., & Martins, S. S. (2020). Bidirectional association between bullying perpetration and internalizing problems among youth. Journal of Adolescent Health , 66 (3), 315–322. https://doi.org/10.1016/j.jadohealth.2019.09.022
Article Google Scholar
Evans, C. B., Smokowski, P. R., Rose, R. A., Mercado, M. C., & Marshall, K. J. (2019). Cumulative bullying experiences, adolescent behavioral and mental health, and academic achievement: an integrative model of perpetration, victimization, and bystander behavior. Journal of Child and Family Studies , 28 (9), 2415–2428. https://doi.org/10.1007/s10826-018-1078-4
Falci, C., & McNeely, C. (2009). Too many friends: social integration, network cohesion, and adolescent depressive symptoms. Social Forces , 87 (4), 2031–2061. https://doi.org/10.1353/sof.0.0189
Fredricks, J. A., & Eccles, J. S. (2008). Participation in extracurricular activities in the middle school years: are there developmental benefits for african american and european american youth? Journal of Youth and Adolescence , 37 (9), 1029–2043. https://doi.org/10.1111/j.1532-7795.2009.00627.x
Fullchange, A., & Furlong, M. J. (2016). An exploration of effects of bullying victimization from a complete mental health perspective. Sage Open , 6 (1), 2158244015623593. https://doi.org/10.1177/2F2158244015623593
Geçer, E., & Yıldırım, M. (2021). Family communication and psychological distress in the era of COVID-19 pandemic: mediating role of coping. Journal of Family Issues , 1–7. https://doi.org/10.1177/0192513X211044489
Ghazavi, Z., Feshangchi, S., Alavi, M., & Keshvari, M. (2016). Effect of a family-oriented communication skills training program on depression, anxiety, and stress in older adults: a randomized clinical trial. Nursing and Midwifery Studies , 5 (1), e28550. https://doi.org/10.17795/nmsjournal28550
Health and Human Services (2014, September 16). Does depression increase the risk for suicide? Retrieved February 26, 2022, from https://www.hhs.gov/answers/mental-health-and-substance-abuse/does-depression-increase-risk-of-suicide/index.html
Jessor, R. (1991). Risk behavior in adolescence: a psychosocial framework for understanding and action. Journal of Adolescent Health , 12 (8), 597–605. https://doi.org/10.1016/1054-139X(91)90007-K
John, R. L., & Antai-Otong, D. (2016). Contemporary treatment approaches to major depression and bipolar disorders. Nursing Clinics of North America , 51 (2), 335–351. https://doi.org/10.1016/j.cnur.2016.01.015
Joyce, H. D., & Early, T. J. (2014). The impact of school connectedness and teacher support on depressive symptoms in adolescents: a multilevel analysis. Children and Youth Services Review , 39 , 101–107. https://doi.org/10.1016/j.childyouth.2014.02.005
Kaminer, Y., Connor, D. F., & Curry, J. F. (2007). Comorbid adolescent substance use and major depressive disorders: a review. Psychiatry (Edgmont (Pa : Township) , 4 (12), 32–43.
PubMed Google Scholar
Kang, S. Y., Lee, J. A., & Kim, Y. S. (2019). Impact of family communication on self-rated health of couples who visited primary care physicians: a cross-sectional analysis of Family Cohort Study in Primary Care. PloS One , 14 (3), e0213427. https://doi.org/10.1371/journal.pone.0213427
KavehFarsani, Z., Kelishadi, R., & Beshlideh, K. (2020). Study of the effect of family communication and function, and satisfaction with body image, on the psychological well-being of obese girls: the mediating role of self-esteem and depression. Child and Adolescent Psychiatry and Mental Health , 14 (1), 1–10. https://doi.org/10.1186/s13034-020-00345-3
Kim-Cohen, J., Caspi, A., Moffitt, T. E., Harrington, H., Milne, B. J., & Poulton, R. (2003). Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Archives of General Psychiatry , 60 (7), 709–717. https://doi.org/10.1001/archpsyc.60.7.709
Klomek, A. B., Marrocco, F., Kleinman, M., Schonfeld, I. S., & Gould, M. S. (2007). Bullying, depression, and suicidality in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry , 46 (1), 40–49. https://doi.org/10.1097/01.chi.0000242237.84925.18
Knifesend, C. A., & Graham, S. (2012). Too much of a good thing? How breadth of extracurricular participation relates to school-related affect and academic outcomes during adolescence. Journal of Youth and Adolescence , 41 (3), 379–389. https://doi.org/10.1007/s10964-011-9737-4
Kumpulainen, K., Räsänen, E., & Puura, K. (2001). Psychiatric disorders and the use of mental health services among children involved in bullying. Aggressive Behavior , 27 (2), 102–110. https://doi.org/10.1002/ab.3
Litwack, S. D., Aikins, J. W., & Cillessen, A. H. (2012). The distinct roles of sociometric and perceived popularity in friendship: implications for adolescent depressive affect and self-esteem. Journal of Early Adolescence , 32 (2), 226–251. https://doi.org/10.1177/0272431610387142
Luukkonen, A. H., Räsänen, P., Hakko, H., Riala, K., & STUDY-70 Workgroup. (2010). Bullying behavior in relation to psychiatric disorders and physical health among adolescents: a clinical cohort of 508 underage inpatient adolescents in Northern Finland. Psychiatry Research , 178 (1), 166–170. https://doi.org/10.1016/j.psychres.2010.04.022
McKinley, C. E., Boel-Studt, S., Renner, L. M., & Figley, C. R. (2021). Risk and protective factors for symptoms of depression and anxiety among american Indians: understanding the roles of resilience and trauma. Psychological Trauma , 13 (1), 16–25. https://doi.org/10.1037/tra0000950
Mei, S., Hu, Y., Sun, M., Fei, J., Li, C., Liang, L., & Hu, Y. (2021). Association between bullying victimization and symptoms of depression among adolescents: a moderated mediation analysis. International Journal of Environmental Research and Public Health , 18 (6), 3316. https://doi.org/10.3390/ijerph18063316
Melton, T. H., Croarkin, P. E., Strawn, J. R., & McClintock, S. M. (2016). Comorbid anxiety and depressive symptoms in children and adolescents: a systematic review and analysis. Journal of Psychiatric Practice , 22 (2), 84–98. https://doi.org/10.1097/PRA.0000000000000132
Merikangas, K. R., He, J. P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., Benjet, C., Georgiades, K., & Swendsen, J. (2010). Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey replication-adolescent supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry , 49 (10), 980–989. https://doi.org/10.1016/j.jaac.2010.05.017
National Institute of Mental Health (2022, January). Major depression Retrieved March 18, 2022, from https://www.nimh.nih.gov/health/statistics/major-depression
Oberle, E., Ji, X. R., Kerai, S., Guhn, M., Schonert-Reichl, K. A., & Gadermann, A. M. (2020). Screen time and extracurricular activities as risk and protective factors for mental health in adolescence: a population-level study. Preventive Medicine , 141 , 106291. https://doi.org/10.1016/j.ypmed.2020.106291
Rivers, A. S., Russon, J., Winston-Lindeboom, P., Ruan-Iu, L., & Diamond, G. (2022). Family and peer relationships in a residential youth sample: exploring unique, non-linear, and interactive associations with depressive symptoms and suicide risk. Journal of Youth and Adolescence , 51 (6), 1062–1073. https://doi.org/10.1007/s10964-021-01524-x
Ruvalcaba, N. A., Gallegos, J., Borges, A., & Gonzalez, N. (2017). Extracurricular activities and group belonging as a protective factor in adolescence. Psicología Educativa , 23 (1), 45–51. https://doi.org/10.1016/j.pse.2016.09.001
Sakyi, K. S., Surkan, P. J., Fombonne, E., Chollet, A., & Melchior, M. (2015). Childhood friendships and psychological difficulties in young adulthood: an 18-year follow-up study. European Child & Adolescent Psychiatry , 24 (7), 815–826. https://doi.org/10.1007/s00787-014-0626-8
Sancassiani, F., Pintus, E., Holte, A., Paulus, P., Moro, M. F., Cossu, G., Angermeyer, M. C., Carta, M. G., & Lindert, J. (2015). Enhancing the emotional and social skills of the youth to promote their wellbeing and positive development: a systematic review of universal school-based randomized controlled trials. Clinical Practice and Epidemiology in Mental Health , 11 (Suppl 1 M2), S21–S40. https://doi.org/10.2174/1745017901511010021
Serafini, G., Pompili, M., Borgwardt, S., Houenou, J., Geoffroy, P. A., Jardri, R., Girardi, P., & Amore, M. (2014). Brain changes in early-onset bipolar and unipolar depressive disorders: a systematic review in children and adolescents. European Child & Adolescent psychiatry , 23 (11), 1023–1041. https://doi.org/10.1007/s00787-014-0614-z
Smith, D. T., Mouzon, D. M., & Elliott, M. (2018). Reviewing the assumptions about men’s mental health: an exploration of the gender binary. American Journal of Men’s Health , 12 (1), 78–89. https://doi.org/10.1177/1557988316630953
Tracy, M., Zimmerman, F. J., Galea, S., McCauley, E., & Vander Stoep, A. (2008). What explains the relation between family poverty and childhood depressive symptoms? Journal of Psychiatric Research , 42 (14), 1163–1175. https://doi.org/10.1016/j.jpsychires.2008.01.011
Ueno, K. (2005). The effects of friendship networks on adolescent depressive symptoms. Social Science Research , 34 (3), 484–510. https://doi.org/10.1016/j.ssresearch.2004.03.002
van Harmelen, A. L., Kievit, R. A., Ioannidis, K., Neufeld, S., Jones, P. B., Bullmore, E., Dolan, R., Consortium, N. S. P. N., Fonagy, P., & Goodyer, I. (2017). Adolescent friendships predict later resilient functioning across psychosocial domains in a healthy community cohort. Psychological Medicine , 47 (13), 2312–2322. https://doi.org/10.1017/S0033291717000836
van Harmelen, A. L., Gibson, J. L., Clair, S., Owens, M. C., Brodbeck, M., Dunn, J., Lewis, V., Croudace, G., Jones, T., Kievit, P. B., R. A., & Goodyer, I. M. (2016). Friendships and family support reduce subsequent depressive symptoms in at-risk adolescents. PloS One , 11 (5). https://doi.org/10.1371/journal.pone.0153715
Venta, A., Bailey, C., Muñoz, C., Godinez, E., Colin, Y., Arreola, A., Abate, A., Camins, J., Rivas, M., & Lawlace, S. (2019). Contribution of schools to mental health and resilience in recently immigrated youth. School Psychology , 34 (2), 138–147. https://doi.org/10.1037/spq0000271
Wang, M. T., & Peck, S. C. (2013). Adolescent educational success and mental health vary across school engagement profiles. Developmental Psychology , 49 (7), 1266–1276. https://doi.org/10.1037/a0030028
Zarnaghash, M., Zarnaghash, M., & Zarnaghash, N. (2013). The relationship between family communication patterns and mental health. Procedia-Social and Behavioral Sciences , 84 , 405–410. https://doi.org/10.1016/j.sbspro.2013.06.575
Zhang, Q., Pan, Y., Zhang, L., & Lu, H. (2021). Parent-adolescent communication and early adolescent depressive symptoms: the roles of gender and adolescents’ age. Frontiers in Psychology , 12 , 647596, 12. https://doi.org/10.3389/fpsyg.2021.647596
Download references
Author information
Authors and affiliations.
Health Promotion and Education Program, School of Human Services, University of Cincinnati, 45221-0068, Cincinnati, OH, United States
Samuel Adabla & Laura A. Nabors
You can also search for this author in PubMed Google Scholar

Corresponding author
Correspondence to Samuel Adabla .
Ethics declarations
Compliance with ethical standards.
The authors have no financial or non-financial interests to disclose. Publicly available dataset was used and does no required informed consent from the study participants.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Adabla, S., Nabors, L.A. Risk and protective factors associated with depression among adolescents. Curr Psychol 42 , 31024–31034 (2023). https://doi.org/10.1007/s12144-022-04075-x
Download citation
Received : 25 May 2022
Revised : 02 November 2022
Accepted : 23 November 2022
Published : 14 December 2022
Issue Date : December 2023
DOI : https://doi.org/10.1007/s12144-022-04075-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Adolescents
- Risk and protective factors
- Mental health
- Find a journal
- Publish with us
- Track your research
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- 07 October 2021
Young people’s mental health is finally getting the attention it needs
You have full access to this article via your institution.

A kite-flying festival in a refugee camp near Syria’s border with Turkey. The event was organized in July 2020 to support the health and well-being of children fleeing violence in Syria. Credit: Muhammed Said/Anadolu Agency/Getty
Worldwide, at least 13% of people between the ages of 10 and 19 live with a diagnosed mental-health disorder, according to the latest State of the World’s Children report , published this week by the United Nations children’s charity UNICEF. It’s the first time in the organization’s history that this flagship report has tackled the challenges in and opportunities for preventing and treating mental-health problems among young people. It reveals that adolescent mental health is highly complex, understudied — and underfunded. These findings are echoed in a parallel collection of review articles published this week in a number of Springer Nature journals.
Anxiety and depression constitute more than 40% of mental-health disorders among young people (those aged 10–19). UNICEF also reports that, worldwide, suicide is the fourth most-common cause of death (after road injuries, tuberculosis and interpersonal violence) among adolescents (aged 15–19). In eastern Europe and central Asia, suicide is the leading cause of death for young people in that age group — and it’s the second-highest cause in western Europe and North America.

Collection: Promoting youth mental health
Sadly, psychological distress among young people seems to be rising. One study found that rates of depression among a nationally representative sample of US adolescents (aged 12 to 17) increased from 8.5% of young adults to 13.2% between 2005 and 2017 1 . There’s also initial evidence that the coronavirus pandemic is exacerbating this trend in some countries. For example, in a nationwide study 2 from Iceland, adolescents (aged 13–18) reported significantly more symptoms of mental ill health during the pandemic than did their peers before it. And girls were more likely to experience these symptoms than were boys.
Although most mental-health disorders arise during adolescence, UNICEF says that only one-third of investment in mental-health research is targeted towards young people. Moreover, the research itself suffers from fragmentation — scientists involved tend to work inside some key disciplines, such as psychiatry, paediatrics, psychology and epidemiology, and the links between research and health-care services are often poor. This means that effective forms of prevention and treatment are limited, and lack a solid understanding of what works, in which context and why.
This week’s collection of review articles dives deep into the state of knowledge of interventions — those that work and those that don’t — for preventing and treating anxiety and depression in young people aged 14–24. In some of the projects, young people with lived experience of anxiety and depression were co-investigators, involved in both the design and implementation of the reviews, as well as in interpretation of the findings.
Quest for new therapies
Worldwide, the most common treatment for anxiety and depression is a class of drug called selective serotonin reuptake inhibitors, which increase serotonin levels in the brain and are intended to enhance emotion and mood. But their modest efficacy and substantial side effects 3 have spurred the study of alternative physiological mechanisms that could be involved in youth depression and anxiety, so that new therapeutics can be developed.

Mental health: build predictive models to steer policy
For example, researchers have been investigating potential links between depression and inflammatory disorders — such as asthma, cardiovascular disease and inflammatory bowel disease. This is because, in many cases, adults with depression also experience such disorders. Moreover, there’s evidence that, in mice, changes to the gut microbiota during development reduce behaviours similar to those linked to anxiety and depression in people 4 . That suggests that targeting the gut microbiome during adolescence could be a promising avenue for reducing anxiety in young people. Kathrin Cohen Kadosh at the University of Surrey in Guildford, UK, and colleagues reviewed existing reports of interventions in which diets were changed to target the gut microbiome. These were found to have had minimal effect on youth anxiety 5 . However, the authors urge caution before such a conclusion can be confirmed, citing methodological limitations (including small sample sizes) among the studies they reviewed. They say the next crop of studies will need to involve larger-scale clinical trials.
By contrast, researchers have found that improving young people’s cognitive and interpersonal skills can be more effective in preventing and treating anxiety and depression under certain circumstances — although the reason for this is not known. For instance, a concept known as ‘decentring’ or ‘psychological distancing’ (that is, encouraging a person to adopt an objective perspective on negative thoughts and feelings) can help both to prevent and to alleviate depression and anxiety, report Marc Bennett at the University of Cambridge, UK, and colleagues 6 , although the underlying neurobiological mechanisms are unclear.
In addition, Alexander Daros at the Campbell Family Mental Health Institute in Toronto, Canada, and colleagues report a meta-analysis of 90 randomized controlled trials. They found that helping young people to improve their emotion-regulation skills, which are needed to control emotional responses to difficult situations, enables them to cope better with anxiety and depression 7 . However, it is still unclear whether better regulation of emotions is the cause or the effect of these improvements.
Co-production is essential
It’s uncommon — but increasingly seen as essential — that researchers working on treatments and interventions are directly involving young people who’ve experienced mental ill health. These young people need to be involved in all aspects of the research process, from conceptualizing to and designing a study, to conducting it and interpreting the results. Such an approach will lead to more-useful science, and will lessen the risk of developing irrelevant or inappropriate interventions.

Science careers and mental health
Two such young people are co-authors in a review from Karolin Krause at the Centre for Addiction and Mental Health in Toronto, Canada, and colleagues. The review explored whether training in problem solving helps to alleviate depressive symptoms 8 . The two youth partners, in turn, convened a panel of 12 other youth advisers, and together they provided input on shaping how the review of the evidence was carried out and on interpreting and contextualizing the findings. The study concluded that, although problem-solving training could help with personal challenges when combined with other treatments, it doesn’t on its own measurably reduce depressive symptoms.
The overarching message that emerges from these reviews is that there is no ‘silver bullet’ for preventing and treating anxiety and depression in young people — rather, prevention and treatment will need to rely on a combination of interventions that take into account individual needs and circumstances. Higher-quality evidence is also needed, such as large-scale trials using established protocols.
Along with the UNICEF report, the studies underscore the transformational part that funders must urgently play, and why researchers, clinicians and communities must work together on more studies that genuinely involve young people as co-investigators. Together, we can all do better to create a brighter, healthier future for a generation of young people facing more challenges than ever before.
Nature 598 , 235-236 (2021)
doi: https://doi.org/10.1038/d41586-021-02690-5
Twenge, J. M., Cooper, A. B., Joiner, T. E., Duffy, M. E. & Binau, S. G. J. Abnorm. Psychol. 128 , 185–199 (2019).
Article PubMed Google Scholar
Thorisdottir, I. E. et al. Lancet Psychiatr. 8 , 663–672 (2021).
Article Google Scholar
Murphy, S. E. et al. Lancet Psychiatr. 8 , 824–835 (2021).
Murray, E. et al. Brain Behav. Immun. 81 , 198–212 (2019).
Cohen Kadosh, K. et al. Transl. Psychiatr. 11 , 352 (2021).
Bennett, M. P. et al. Transl Psychiatr. 11 , 288 (2021).
Daros, A. R. et al. Nature Hum. Behav . https://doi.org/10.1038/s41562-021-01191-9 (2021).
Krause, K. R. et al. BMC Psychiatr. 21 , 397 (2021).
Download references
Reprints and permissions
Related Articles

- Psychiatric disorders
- Public health

Autistic people three times more likely to develop Parkinson’s-like symptoms
News 28 MAY 24

Neural pathways for reward and relief promote fentanyl addiction
News & Views 22 MAY 24
Internet use and teen mental health: it’s about more than just screen time
Correspondence 21 MAY 24

Chance of heatwaves in India rising with climate change
News Explainer 29 MAY 24

A myopia epidemic is sweeping the globe. Here’s how to stop it
News Feature 29 MAY 24

Ozempic keeps wowing: trial data show benefits for kidney disease
News 24 MAY 24

Japan’s push to make all research open access is taking shape
News 30 MAY 24

Mexico’s next president is likely to be this scientist — but researchers are split in their support
Adopt stricter regulation to stop ‘critical mineral’ greenwashing
Correspondence 28 MAY 24
Global Talent Recruitment (Scientist Positions)
Global Talent Gathering for Innovation, Changping Laboratory Recruiting Overseas High-Level Talents.
Beijing, China
Changping Laboratory
Postdoctoral Associate - Amyloid Strain Differences in Alzheimer's Disease
Houston, Texas (US)
Baylor College of Medicine (BCM)
Postdoctoral Associate- Bioinformatics of Alzheimer's disease
Postdoctoral associate- alzheimer's gene therapy, postdoctoral associate.
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- Open access
- Published: 23 May 2024
Youth suicide crisis: identifying at-risk individuals and prevention strategies
- Victor Ajluni 1 &
- Daniel Amarasinghe 1
Child and Adolescent Psychiatry and Mental Health volume 18 , Article number: 58 ( 2024 ) Cite this article
152 Accesses
Metrics details
Introduction
In the United States, recent data has shown a disturbing increase in suicide rates among children and adolescents. Recent data has shown a disturbing increase in suicide rates among this demographic. According to the Centers for Disease Control and Prevention (CDC), suicide is now the second leading cause of death for people ages 10–24 years in the United States [ 1 ]. The suicide rate for this age group has increased by 56% over the past decade, with Black youth having the largest increase in suicide rate of 78% [ 2 ].
The AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health is a joint statement by the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association regarding this ongoing crisis [ 3 ]. The joint statement highlights the importance of recognizing suicide risk and the need for increased funding to address the issue. In addition, it emphasizes that teachers, physicians, and other professionals who work with children and adolescents have a crucial role to play in suicide prevention. There is a great need for these professionals to be able to recognize the warning signs and risk factors for suicide and take appropriate action to intervene and connect young people with mental health resources. In addition to raising awareness about suicide risk, the declaration also calls for increased access to mental health care services and investment in research and public health initiatives aimed at preventing and treating mental health disorders in children and adolescents.
Risk factors and warning signs
Access to firearms increases the likelihood of death by suicide for children and adolescents more than fourfold due to its increased lethality, with 90% of child and adolescent suicides by gun involving firearms from the victim’s own home or that of a relative [ 4 ]. When controlling differences in the rate of youth suicide attempts across states, it was found that household gun ownership was positively associated with the overall youth suicide rate. For 10% increase in household gun ownership, the youth suicide rate increased by 26.9% [ 5 ].
Across age groups, a past suicide attempt is the strongest predictor of subsequent attempts, with up to a 12-fold increase in children, a 4.3-fold increase in adolescent and 5.4-fold increase in young adults [ 6 ]. Although some studies suggest that suicidal ideation is associated with a higher risk of suicide and is far more prevalent than attempted suicides, a considerable percentage of children and adolescents that commit suicide have no prior suicide attempts [ 7 , 8 ]. In fact, a metanalysis found that 3% of high-risk patients discharged from a psychiatric hospital could be expected to commit suicide within a year, and that 60% of the patients that do commit suicide would have likely been categorized as low risk. The study also found that there was no single risk factor or combination of risk factors that was strongly associated with risk of suicide in the year after discharge [ 9 ]. Although the United States Preventive Services Task Force (USPSTF) recommends screening children 12 and older for depression, and ages 8 and older for anxiety, they state that there is insufficient data to recommend for or against screening for suicidal risk in all youth, which brings into question the utility of screening for suicidal ideation [ 10 ]. One study found that 66% of people that committed suicide within 30 days of seeing a healthcare professional denied suicidal ideation, and that 50% of this group committed suicide within 2 days after being seen [ 11 ].
On the contrary, some argue that screening for suicidal risk in clinical settings such as primary care and emergency departments can identify people at elevated risk for suicide who would otherwise be missed if they did not present primarily for behavioral health concerns [ 12 ]. Proponents of universal screening of youth for suicidal risk also state that the risks associated with screening are minimal, and people that screen positive for suicidal ideation or behavior would benefit from a mental health referral. However, it is important to note that suicidal ideation may be less frequent in Black youth prior to a suicide attempt, which highlights the importance of developing complementary methods to self-reporting tools for the assessment of suicide risk [ 12 ].
Substance use, particularly marijuana use, has been associated with increased suicide-related mortality in both adolescents and adults. One study found that states with medical marijuana legalization or recreational marijuana legalization had increased suicide-related mortality in 14–16-year-old people, with higher rates of suicide in states with recreational marijuana legalization compared to states with medical marijuana legalization (IRR = 1.14, 95% CI: 1.00-1.30) and states without marijuana laws (IRR = 1.09, 95% CI: 1.00-1.20) [ 13 ].
Some factors that contribute to suicidal ideation and self-injurious behavior but not necessarily completed suicides are socioeconomic stressors, trauma, adverse childhood events, social media use and bullying. Pre-adolescent children that have safety concerns are more likely to attempt suicide, which highlights the impact of socioeconomic stressors such as low-income and poor social support on increased suicide risk. A history of mental illness is also associated with a higher likelihood of a suicide attempt across all age groups [ 14 ].
People with exposure to traumatic experiences or adverse childhood experiences are at an increased risk of attempting suicide, with up to a 2 to 5-fold increase. Adverse childhood experiences include childhood abuse, witnessing domestic violence, parent separation or divorce, cohabitation with household members with mental illness, and cohabitation with household members that engage in substance use or criminal activity [ 14 ]. A growing concern is the use of social media to bully or harass peers, with 57% of bullied persons reaching the clinical threshold for PTSD on a reporting scale [ 15 ]. It was also found that in children and adolescents that reported using social media had significantly greater predicted odds of self-injurious behaviors at the time of admission to the emergency department [ 16 ].
Some warning signs for suicide include [ 17 ]:
Showing signs of depression, anxiety, or other mental health issues.
Talking or writing about suicide, death, or dying.
Withdrawing from friends and family.
Showing signs of extreme mood swings or sudden personality changes.
Displaying reckless or risky behavior.
Engaging in self-harm or self-destructive behavior.
Losing interest in activities they used to enjoy.
Having difficulty sleeping or sleeping too much.
Feeling hopeless or trapped in a situation.
Giving away prized possessions.
Prevention and intervention
Numerous studies globally have shown that school-based, community-based and primary-care centered interventions across a range of settings and populations lead to a significant reduction in both suicide risk and suicide attempts in adolescents [ 18 ].
Regarding school-based prevention programs, a meta-analysis of 12 studies showed that post-primary school-based suicide prevention programs had a significant decrease on the adolescent suicidal thoughts and behaviors, with a number needed to treat of 55 for suicidal ideations, and 20 for suicide attempts. Overall, that post-primary school-based suicide prevention programs led to a 13–15% reduction in suicidal ideation and a 28–34% reduction in suicide attempts among 33,155 adolescents attending 329 schools [ 19 ].
Primary care providers are the front-line for community intervention, which involve identifying and screening for people at risk for suicide. One such community-based intervention program involved the following: primary care provider training on identifying and appropriately referring people with depression, a media and public relations campaign, funding for community facilitators, and additional support for both the patients and their families. The cost-effective program included training in suicide risk assessment and management and access to resources like crisis hotlines and mental health services. The study found that the 2-year intervention was associated with a 32.4% decrease in attempted and completed suicides [ 20 ].
Aside from group-based interventions, some individual interventions to reduce the risk of suicide include dialectical behavioral therapy, psychoeducation for parents regarding suicide risk and lethal means restriction. Pharmacological treatment such as lithium and clozapine has been found to reduce the risk of suicide in adults, but additional studies in children and adolescents are needed [ 21 ].
The AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health is a critical call to action for addressing the mental health crisis facing young people in the United States, particularly in considering the alarming rise in suicide rates. The declaration emphasizes the importance of recognizing suicide risk and taking appropriate action to intervene and connect young people with mental health resources. It also calls for increased access to mental health care services and investment in research and public health initiatives aimed at preventing and treating mental health disorders in children and adolescents. With the right interventions and resources in place, it has been shown that we can work towards reducing suicide rates among young people and providing them with the support they need to thrive. As a society, it is our responsibility to prioritize the mental health of our youth and address this urgent issue.
Bottom line
Access to firearms is one of the biggest risk factors for youth suicide. Suicidal ideation is not a reliable predictor of future suicide attempts or completed suicide, although it may be useful in identifying those that would be otherwise missed if they did not present originally for mental health concerns. Marijuana use has been associated with an increased rate of suicide in states with recreational marijuana legalization or medical marijuana legalization. In addition to previous self-injurious thoughts and behavior, adverse childhood experiences, bullying and excessive social media usage are associated with an increase in suicidal ideation but not necessarily an increase in suicide risk. School-based, community-based and primary-care centered interventions are associated with a significant reduction in both suicide risk and suicide attempts in adolescents.
Data availability
Not applicable.
Center for Disease Control and Prevention. Facts About Suicide. Published April 6. 2023. Accessed May 5, 2023. https://www.cdc.gov/suicide/facts/index.html .
Stone DM, Mack KA, Qualters J. Notes from the field: recent changes in suicide rates, by race and ethnicity and Age Group — United States, 2021. MMWR Morb Mortal Wkly Rep. 2023;72:160–2. https://doi.org/10.15585/mmwr.mm7206a4 .
Article PubMed PubMed Central Google Scholar
AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health. Accessed May 5. 2023. https://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/ .
John A, Azrael D, Miller M. Access to firearms and adolescent suicide. Soc Res Child Dev. 2020;7. https://www.srcd.org/research/access-firearms-increases-child-and-adolescent-suicide .
Knopov A, Sherman RJ, Raifman JR, Larson E, Siegel MB. Household Gun ownership and youth suicide rates at the State Level, 2005–2015. Am J Prev Med. 2019;56(3):335–42. https://doi.org/10.1016/j.amepre.2018.10.027 .
Ong MS, Lakoma M, Gees Bhosrekar S, et al. Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc Mental Health. 2021;26(2):134–42. https://doi.org/10.1111/camh.12400 .
Article Google Scholar
Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. J Child Psychol Psychiatry Allied Discip. 2006;47(3–4):372–94. https://doi.org/10.1111/j.1469-7610.2006.01615.x .
Rodway C, Tham SG, Turnbull P, Kapur N, Appleby L. Suicide in children and young people: can it happen without warning? J Affect Disord. 2020;275:307–10. https://doi.org/10.1016/j.jad.2020.06.069 .
Article PubMed Google Scholar
Large M, Sharma S, Cannon E, Ryan C, Nielssen O. Risk factors for suicide within a year of discharge from Psychiatric Hospital: a systematic Meta-analysis. Australian New Z J Psychiatry. 2011;45(8):619–28. https://doi.org/10.3109/00048674.2011.590465 .
Mangione CM, Barry MJ, Nicholson WK, et al. Screening for depression and suicide risk in children and adolescents. JAMA. 2022;328(15):1534. https://doi.org/10.1001/jama.2022.16946 .
Berman AL. Risk factors proximate to suicide and suicide risk Assessment in the context of denied suicide ideation. Suicide Life-Threatening Behav. 2017;48(3):340–52. https://doi.org/10.1111/sltb.12351 .
Bridge JA, Birmaher B, Brent DA. The case for Universal Screening for suicidal risk in adolescents. Pediatrics. 2023;151(6). https://doi.org/10.1542/peds.2022-061093 .
Hammond CJ, Hyer JM, Boustead AE et al. Association between marijuana laws and suicide among 12- to 25-year-olds in the united states from 2000 to 2019. J Am Acad Child Adolesc Psychiatry . Published online June 27, 2023:S0890-8567(23)00341-6.
Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, Giles WH. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the adverse childhood experiences Study. JAMA. 2001;286(24):3089–96. https://doi.org/10.1001/jama.286.24.3089 .
Article CAS PubMed Google Scholar
Nielsen MB, Tangen T, Idsoe T, Matthiesen SB, Magerøy N. Post-traumatic stress disorder as a consequence of bullying at work and at school. A literature review and meta-analysis. Aggress Violent Beh. 2015;21:17–24.
Shafi RMA, Nakonezny PA, Romanowicz M, Nandakumar AL, Suarez L, Croarkin PE. Suicidality and self-injurious behavior among adolescent social media users at psychiatric hospitalization. CNS Spectr. 2021;26(3):275–81. https://doi.org/10.1017/S1092852920001108 .
Shain BN, American Academy of Pediatrics Committee on Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2007;120(3):669–76. https://doi.org/10.1542/peds.2007-1908 .
Hofstra E, van Nieuwenhuizen C, Bakker M, et al. Effectiveness of suicide prevention interventions: a systematic review and meta-analysis. Gen Hosp Psychiatry. 2020;63:127–40. https://doi.org/10.1016/j.genhosppsych.2019.04.011 .
Walsh EH, McMahon J, Herring MP, Research, Review. The effect of school-based suicide prevention on suicidal ideation and suicide attempts and the role of intervention and contextual factors among adolescents: a meta-analysis and meta-regression. J Child Psychol Psychiatry Allied Discip. 2022;63(8):836–45. https://doi.org/10.1111/jcpp.13598 .
Hegerl U, Mergl R, Havers I, et al. Sustainable effects on suicidality were found for the Nuremberg alliance against depression. Eur Arch Psychiatry Clin NeuroSci. 2010;260(5):401–6. https://doi.org/10.1007/s00406-009-0088-z .
Hughes JL, Horowitz LM, Ackerman JP, Adrian MC, Campo JV, Bridge JA. Suicide in young people: screening, risk assessment, and intervention. BMJ. 2023;381. https://doi.org/10.1136/bmj-2022-070630 .
Download references
Acknowledgements
None declared.
Author information
Authors and affiliations.
Department of Psychiatry and Behavioral Neurosciences, Wayne State University School of Medicine, Detroit, MI, USA
Victor Ajluni & Daniel Amarasinghe
You can also search for this author in PubMed Google Scholar
Contributions
D.A. was primarily responsible for the writing of the manuscript, ensuring comprehensive coverage and articulation of the topic. V.A. contributed significantly to the conceptualization and direction of the research, offering critical insights into psychiatric aspects. Both D.A. and V.A. collaborated in the research phase, analyzing data and literature to build a robust foundation for the study. Additionally, both authors participated in the review and editing process of the manuscript, ensuring accuracy and coherence in the final submission.
Corresponding author
Correspondence to Victor Ajluni .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ajluni, V., Amarasinghe, D. Youth suicide crisis: identifying at-risk individuals and prevention strategies. Child Adolesc Psychiatry Ment Health 18 , 58 (2024). https://doi.org/10.1186/s13034-024-00753-9
Download citation
Received : 22 January 2024
Accepted : 15 May 2024
Published : 23 May 2024
DOI : https://doi.org/10.1186/s13034-024-00753-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
Child and Adolescent Psychiatry and Mental Health
ISSN: 1753-2000
- Submission enquiries: [email protected]
More than just social media use may be causing depression in young adults, study shows
Over the past few decades, there has been a significant increase in the prevalence of depression in adolescents and young adults -- and a simultaneous uptick in the inclusion of technology and social media in everyday life. However, it is unclear how exactly social media use and depression are associated and relate to other behaviors, such as physical activity, green space exposure, cannabis use and eveningness (the tendency to stay up late).
In a study published May 15 in the International Journal of Mental Health and Addiction , a team of researchers, led by experts at Johns Hopkins Children's Center, investigated the association among social media use, depression and other health-related behaviors of young adults over time.
"Research shows that when social media use is high, depression is also high. But the question is -- is that because social media caused that person to be depressed? Or is it because people who are depressed tend to also use social media more, and spend less time exercising and being in green spaces? That is what we wanted to understand," says Carol Vidal, M.D., Ph.D., M.P.H., the first author of the study, a child and adolescent psychiatrist at Johns Hopkins Children's Center and an assistant professor of psychiatry and behavioral sciences at the Johns Hopkins University School of Medicine.
In their study, 376 young adults in Canada (82.4% women) were asked to complete three online questionnaires between May 2021 and January 2022. At each point, participants self-reported depressive symptoms based on the Patient Health Questionnaire (PHQ-9) -- a nine-item scale that is commonly used to measure depression -- as well as social media use, greenspace exposure, physical activity and cannabis use.
The researchers found that most study participants had at least mild depressive symptoms. Findings showed that participants who had higher social media use tended to be more depressed, and people who were more depressed also tended to use social media more. However, researchers found that social media use did not cause an increase or decrease in depressive symptom levels over time.
"We found that if you tended to be a person who was depressed, you were a person also spending more time on social media," explains Vidal.
Researchers also found that higher levels of social media use and higher levels of depressive symptoms were associated with lower levels of green space exposure. In addition, cannabis use and higher eveningness were also associated with higher depressive levels.
The study authors say these results show social media use and depression are associated, but do not provide evidence that greater social media use predicts an increase in depressive symptoms over time. The team also says these findings indicate people who suffer from depression should be cautious about the amount of time they spend on social media and should be encouraged to incorporate other healthy habits into their lifestyle.
"Being indoors and not exercising, staying up late and using cannabis has its risks," says Vidal. "It is important for providers to educate patients and for parents to instill healthy habits in their kids -- having a balance of moderate social media use and other outdoor activities and exercise is what people should strive for in today's digital age."
Vidal and other investigators believe there are many aspects to social media, and there are important next steps to learn more about its impact on the mental health of people of all ages, including younger children and adolescents.
- Mental Health
- Media and Entertainment
- Popular Culture
- STEM Education
- Social Issues
- Clinical depression
- Social psychology
- Adult attention-deficit disorder
- Cognitive bias
- Social inequality
- Public health
- Mental illness
Story Source:
Materials provided by Johns Hopkins Medicine . Note: Content may be edited for style and length.
Journal Reference :
- Carol Vidal, Frederick L. Philippe, Marie-Claude Geoffroy, Vincent Paquin. The Role of Social Media Use and Associated Risk and Protective Behaviors on Depression in Youth Adults: A Longitudinal and Network Perspective . International Journal of Mental Health and Addiction , 2024; DOI: 10.1007/s11469-024-01313-0
Cite This Page :
Explore More
- Extinct Saber-Toothed Cat On Texas Coast
- Some Black Holes Survive in Globular Clusters
- People Altering Decomposition in Waterways
- Historic Iceberg Surges
- Food Groups Based On Level of Processing
- Computer Vision, Machine Learning Aid Driving
- Most Distant Known Galaxy
- A New Dinosaur from Zimbabwe
- The Case of the Missing Black Holes
- Menstrual Periods Arriving Earlier
Trending Topics
Strange & offbeat.
- Today's news
- Reviews and deals
- Climate change
- 2024 election
- Fall allergies
- Health news
- Mental health
- Sexual health
- Family health
- So mini ways
- Unapologetically
- Buying guides
Entertainment
- How to Watch
- My Portfolio
- Latest News
- Stock Market
- Premium News
- Biden Economy
- EV Deep Dive
- Stocks: Most Actives
- Stocks: Gainers
- Stocks: Losers
- Trending Tickers
- World Indices
- US Treasury Bonds
- Top Mutual Funds
- Highest Open Interest
- Highest Implied Volatility
- Stock Comparison
- Advanced Charts
- Currency Converter
- Basic Materials
- Communication Services
- Consumer Cyclical
- Consumer Defensive
- Financial Services
- Industrials
- Real Estate
- Mutual Funds
- Credit cards
- Balance Transfer Cards
- Cash-back Cards
- Rewards Cards
- Travel Cards
- Student Loans
- Car Insurance
- Morning Brief
- Market Domination
- Market Domination Overtime
- Asking for a Trend
- Opening Bid
- Stocks in Translation
- Lead This Way
- Good Buy or Goodbye?
- Fantasy football
- Pro Pick 'Em
- College Pick 'Em
- Fantasy baseball
- Fantasy hockey
- Fantasy basketball
- Download the app
- Daily fantasy
- Scores and schedules
- GameChannel
- World Baseball Classic
- Premier League
- CONCACAF League
- Champions League
- Motorsports
- Horse racing
- Newsletters
New on Yahoo
- Privacy Dashboard
Yahoo Finance
New study identifies higher risk of depression and anxiety among young men, gay or bisexual, and racialized canadian men.
43% of young men aged 19-29 are at risk of depression
Moderate-to-high anxiety impacts 57% of young men, 45% of gay or bisexual men, and 42% of racialized men
National study from the Canadian Men’s Health Foundation released for Men’s Health Month in June
VANCOUVER, British Columbia, May 30, 2024 (GLOBE NEWSWIRE) -- Canada’s leading men’s health organization is raising the alarm bells when it comes to the state of men’s mental health. New research finds young men, gay and bisexual, and racialized men are at a significantly higher risk for depression and anxiety.
The study conducted by Intensions Consulting surveyed 2,070 Canadian men aged 19 or older. Key results show a concerning trend in specific groups of men:
The risk of moderate-to-severe depression is significantly higher in men aged 19 to 29 (43%), racialized men (30%) and gay or bisexual men (28%) compared to the broader male population (18%).
Moderate-to-high anxiety is significantly higher in men aged 19 to 29 (57%), gay or bisexual men (45%), and racialized men (42%) compared to the broader male population (30%).
“These statistics cannot be ignored–anxiety and depression are affecting certain populations of men significantly more than others,” says Dr. David Kuhl, a men’s health clinician & researcher. “Calling attention to how pervasive mental health challenges are within these populations is the first step towards changing behaviours. Mental health doesn’t belong to the individual, it belongs to families and communities.”
CMHF is committed to supporting these populations with programs that improve mental health outcomes, including the MindFit Toolkit . The free, online resource connects men and their families to self-assessment tools, virtual counselling, and expert advice to help manage stress, anxiety and depression.
“The research points to the continued, urgent need for action by all of us to reach out and support young men and those in racialized and 2SLGBTQIA+ communities,” says Kenton Boston, CMHF President & CEO. “The Foundation and its partners are working to educate and advocate for men and their families and ensure there are no barriers to being able to live healthy, full and productive lives, in all Canadian communities.”
June is International Men’s Health Month, celebrated by CMHF with a campaign called Move for Your Mental Health–encouraging the benefits of exercise and providing resources on how to start moving more.
Learn more about CMHF’s mental health programming and how you can help improve the lives of men and their families at menshealthfoundation.ca.
About Canadian Men’s Health Foundation Celebrating 10 years, the Canadian Men’s Health Foundation (CMHF) is a registered, national charity with a mission to inspire men and their families to live healthier lives. The statistics around men’s health in Canada are alarming; 70% of men’s health problems can be prevented by adopting healthy lifestyles. Learn more at menshealthfoundation.ca and dontchangemuch.ca.
About the Study The Intensions Consulting study was conducted in Canada between March 5 and 10, 2024. The sample was stratified to ensure its composition reflected the underlying distribution of the population as determined by 2021 Census data. The online survey was administered in French and English and used validated mental health measures, including The Overall Anxiety Severity and Impairment Scale (OASIS) and the Patient Health Questionnaire (PHQ-9). A traditional probability sample of comparable size would have produced results considered accurate to within plus or minus 2.2 percentage points, 19 times out of 20.
Media Requests: [email protected]
A photo accompanying this announcement is available at https://www.globenewswire.com/NewsRoom/AttachmentNg/3d79fe72-4c23-466e-bc4b-6825fc0ee754
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Social media use and depression in adolescents: a scoping review
There have been increases in adolescent depression and suicidal behaviour over the last two decades that coincide with the advent of social media (SM) (platforms that allow communication via digital media), which is widely used among adolescents. This scoping review examined the bi-directional association between the use of SM, specifically social networking sites (SNS), and depression and suicidality among adolescents. The studies reviewed yielded four main themes in SM use through thematic analysis: quantity of SM use, quality of SM use, social aspects associated with SM use, and disclosure of mental health symptoms. Research in this field would benefit from use of longitudinal designs, objective and timely measures of SM use, research on the mechanisms of the association between SM use and depression and suicidality, and research in clinical populations to inform clinical practice.
Introduction
Over the past several decades, adolescent depression and suicidal behaviours have increased considerably. In the USA, depression diagnoses among youth increased from 8.7% in 2005 to 11.3% in 2014 ( Mojtabai, Olfson, & Han, 2016 ). Additionally, suicide is the second leading cause of death among youth between the ages of 10 and 34 ( Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2017 ), with a 47.5% increase since 2000 ( Miron, Yu, Wilf-Miron, & Kohane, 2019 ). One suggested cause for this rise in adolescent depression and suicide is the advent of social media (SM) ( McCrae, Gettings, & Purssell, 2017 ; Twenge, Joiner, Rogers, & Martin, 2018 ).
The term ‘social media’ describes types of media that involve digital platforms and interactive participation. SM includes forms such as email, text, blogs, message boards, connection sites (online dating), games and entertainment, apps, and social networking sites (SNS) ( Manning, 2014 ). Over the past decade, SNS platforms designed to help people communicate and share information online have become ubiquitous. Among youth, 97% of all adolescents between the ages of 13 and 17 use at least one of the following seven SNS platforms: YouTube (85% of adolescents), Instagram (72%), Snapchat (69%), Facebook (51%), Twitter (32%), Tumblr (9%) or Reddit (7%) ( Pew Research Center, 2018a ).
Concerns have arisen around the effects of SM on adolescents’ mental health, due to SM’s association with decreased face-to-face interpersonal interactions ( Baym, 2010 ; Kraut et al., 1998 ; Nie, Hillygus, & Erbring, 2002 ; Robinson, Kestnbaum, Neustadtl, & Alvarez, 2002 ), addiction-like behaviours ( Anderson, Steen, & Stavropoulos, 2017 ), online bullying ( Kowalski, Limber, & Agatston, 2012 ), social pressure through increased social comparisons ( Guernsey, 2014 ), and contagion effect through increased exposure to suicide stories on SM ( Bell, 2014 ).
Conversely, others have described potential benefits of SM use in adolescents such as feelings of greater connection to friends and interactions with more diverse groups of people who can provide support ( Pew Research Center, 2018b ). In fact, higher internet use has been associated with positive social well-being, higher use of communication tools, and increased face-to-face conversations and social contacts in college students ( Baym, Zhang, & Lin, 2004 ; Kraut et al., 2002 ; Wang & Wellman, 2010 ). These findings suggest that internet use, including SM, may provide opportunities for social connection and access to information ( Reid Chassiakos et al., 2016 ).
Recent systematic reviews examining the association between online technologies and depression have found a ‘general correlation’ between SM use and depression in adolescents, but with conflicting findings in some domains (e.g. the association between time spent on SM and mental health problems), overall limited quality of the evidence ( Keles, McCrae, & Grealish, 2019 ), and a relative absence of studies designed to show causal effects ( Best, Manktelow, & Taylor, 2014 ). The scope of search in these reviews is broader in topic, including online technologies other than SM ( Best et al., 2014 ) or focussed on a select number of studies in order to meet the requirements of a systematic review ( Keles et al., 2019 ). With this scoping review, we aim to expand the inclusion of studies with a range of designs, while narrowing the scope of the topic of SM to those studies that specifically included SNS use. Additionally, we aim to expand the understanding and potential research gaps on the bi-directional association between SM and depression and suicidal behaviours in adolescents, including studies that consider SM use as a predictor as well as an outcome. A better understanding of this relationship can inform interventions and screenings related to SM use in clinical settings.
This scoping review was initiated by a research team including 3 mental health professionals with clinical expertise in treating depression and suicidality in adolescents. We followed the framework suggested by Arksey and O’Malley (2005) for scoping reviews. The review included five steps: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; and (5) collating, summarizing and reporting the results.
Research question
The review was guided by the question: What is known from the existing literature about the association between depression and suicidality and use of SNS among adolescents? Given that much of the literature used SM and SNS interchangeably, this review used the term ‘social media’ or ‘SM’ when it was difficult to discern if the authors were referring exclusively to SNS.
Data sources and search strategy
The team conceived the research question through a series of discussions, and the first author (CV) consulted an informationist to identify the appropriate search terms and databases. A search of the database PsychINFO limited to peer-reviewed articles was conducted on 5 June 2019 (see Table 1 for search strategy). No additional methods were identified through other sources. The search was broad to include articles measuring depression as an outcome variable, and as a co-variate or independent variable. There was no restriction on the type of study design included, and English and Spanish language articles were included in the search. Articles were organized using Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia).
Search strategy.
Eligibility criteria
(1) The study examined SM (versus internet use in general) and made specific mention of SNS; (2) participants were between the ages of 10 and 18. If adults were included, the majority of the study population was between 10–18 years of age, or the mean participant age was 18 or younger; (3) the study examined the association between SM use and depression and/or suicidality; (4) the study included at least one measure of depression; and (5) if the focus of the study was on SM addiction or cyberbullying, it included mention and a measure of depressive symptoms. We did not include articles in which: (1) the study primarily focussed on media use other than SM, or that did not specifically mention inclusion of SNS (e.g. studies that focussed only on TV, video game, smartphone use, blogging, email); (2) included primarily adult population; (3) was not an original study, but a case report, review, commentary, erratum, or letter to the editor; (4) focussed on addiction and cyberbullying exclusively without a depression measure; and (5) the method used was content analysis of SM posts without specification of the population age range.
Title and abstract relevance screening
The search yielded 728 articles of which six duplicates were removed. One author (CV) screened the remainder of the articles by title and abstract and a second author (TL) reviewed every 25th article for agreement. All authors screened full-text articles and extracted data from those that met the inclusion criteria. The authors met over the course of the full-text review process to resolve conflicts and maintain consistency among the authors themselves and with the research question. Of the total number of studies included for full-text review, 505 articles were excluded. Out of the 223 full-text studies assessed for eligibility, 175 were excluded. A total of 42 articles were eligible for review (see Figure 1 : PRISMA flow chart for details). A form was developed to extract the characteristics of each study that included author and year of publication, objectives of the study, study method, country where the study was conducted, depression scale used, number of participants, participant age, and results (see Table 2 for details).

PRISMA flow chart of data selection process.
Data charting form including author and year of publication, objectives of the study, method used, country where the study was conducted, depression scale used, number of participants, participant age, results and main social media focus.
AIU = Addictive internet Use; BIU = Borderline Addictive Internet Use; BSMAS = Bergen Social Media Addiction Scale; BIU = Borderline addictive internet use; CBP = Cyberbullying Perpetration; CERM = Cuestionario de Experiencias Relacionadas con el móvil (Questionnaire of Experiences Related to the cellphone); DIB = Dysfunctional Internet Behaviour; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (4th edition, Text Revision); FOMO = Fear of Missing Out; HVSM = Highly Visual Social Media; SNI = Intensity of social network use; IA = Internet Addiction; IAB = Internet Addictive Behaviour; OSNA = Online social networking addiction; PSMU = Problematic Social Media Use; RADS-2 = Reynolds Adolescent Depression Scale - Version 2; SITBs = self-injurious thoughts and behaviours; SNS = social networking sites.
Data summary and synthesis
After reviewing the table, each study was labelled according to the main focus of research related to SM, based on the objectives, variables used, and results of the study. The topics were classified into nine different categories based on the main SM focus of the article; categories were discussed and reviewed by two authors (TL and CV) ( Table 2 ). All authors then discussed the categories and grouped them into four main themes of studies looking at SM and depression in adolescents.
A total of 42 studies published between 2011 and 2019 met the inclusion criteria. Of the studies included, 16 were conducted in European Countries, 14 in the USA, 5 in Asia, 3 in Canada, 2 in Australia, and 2 in Latin American Countries. The number of participants per study ranged from 23 in a qualitative study (94 in the smallest quantitative study) to 118,545 participants in the largest study ( Table 2 ).
The studies reviewed were grouped into four themes with nine categories according to the main focus of the research. The themes and categories were: (1) quantity of SNS use: effects of the frequency of SM use and problematic SM use (or evidence of addictive engagement with SM); (2) quality of SM use: characteristics of SNS use and social comparisons; (3) social aspects of SM use: cyberbullying, social support, and parental involvement; and (4) disclosure of mental health symptoms: online disclosure and prediction of symptoms and suicide contagion effect ( Figure 2 ).

Number of studies by theme (quantity, quality, social and disclosure) and time period (2011–2012, 2013–2014, 2015–2016 and 2017–2018).
Quantity of SM use
The majority of studies ( n = 24) examined quantity of SM use by measuring either frequency or time spent on SM ( n = 17), or problematic or addictive engagement with SM ( n = 7).
Frequency of use
The majority of studies found a positive correlation between time spent on SNS and higher levels of The majority of studies found a positive correlation between time spent on SNS and higher levels of depression ( Akkın Gürbüz, Demir, Gökalp Özcan, Kadak, & Poyraz, 2017 ; Marengo, Longobardi, Fabris & Settanni, 2018 ; Pantic et al., 2012 ; Twenge et al., 2018 ; Woods & Scott, 2016 ). Higher frequency of SM use (≥2 h a day) was also found to be positively associated with suicidal ideation ( Sampasa-Kanyinga & Lewis, 2015 ) and attempts ( Sampasa-Kanyinga & Hamilton, 2015 ), in addition to deficits in self-regulation ( Lee, Ho, & Lwin, 2017 ). Factors such as the number of SM accounts and the frequency of checking SM ( Barry, Sidoti, Briggs, Reiter, & Lindsey, 2017 ) were associated with a variety of symptoms, including depression.
A study ( Oberst, Wegmann, Stodt, Brand, & Chamarro, 2017 ) examining SM use as an outcome suggested that depression may affect SM use both directly, and indirectly, mediated by the Fear of Missing Out (or the apprehension of missing rewarding experiences that others might be enjoying) ( Przybylski, Murayama, DeHaan, & Gladwell, 2013 ). Adolescents with depression were also found to have more difficulty regulating their SM use ( Lee et al., 2017 ).
Longitudinal studies suggested a reciprocal relationship between quantity of SM use and depression. Frison and Eggermont (2017) found that frequency of Instagram browsing at baseline predicted depressed mood six months later and depressed mood at baseline predicted later frequency of photo posting. Additionally, heavy use (>4 h per day) of the internet to communicate (including social networking) and play games (gaming) predicted depressive symptoms a year later ( Romer, Bagdasarov, & More, 2013 ). Further, depressive symptoms predicted increased internet use and decreased participation in non-screen activities (e.g. sports). Finally, Salmela-Aro, Upadyaya, Hakkarainen, Lonka, and Alho (2017) found that school burnout increased the risk for later excessive internet use and depressive symptoms. Conversely, Houghton et al. (2018) found small, positive bi-directional associations between depressive symptoms and screen use 1 year later, but their final model did not support a longitudinal association.
Yet, not all studies found a positive association between frequency of use and depressed mood. While Blomfield-Neira and Barber (2014) reported a link between adolescents having a SM profile and depressed mood, they found no correlation between SM frequency of use and depressed mood. Rather, investment in SM (a measure of how important SM is to an adolescent) was linked to poorer adjustment, lower self-esteem and depressed mood. Moderate SM use (a stable trend in the time spent on SM during adolescence and into early adulthood that did not interfere with functioning) was associated with better emotional self-regulation ( Coyne, Padilla-Walker, Holmgren, & Stockdale, 2018 ) and healthier development, especially when used to acquire information ( Romer et al., 2013 ). Finally, Rodriguez Puentes and Parra (2014) found a positive association between SM and externalizing behaviours, but no significant association between SM use and depression.
Additionally, age moderated the effects of frequency of use on depression. For example, in one study, older adolescents with higher SM use had higher ‘offline’ social competence, while younger adolescents with higher SM use had more internalizing problems and diminished academics and activities ( Tsitsika, Janikian, et al., 2014 ).
Problematic SM use
Seven studies explored problematic use or engagement with SM or the internet in an addictive manner (a dysfunctional pattern of behaviour similar to that of impulse control disorders, which causes distress and/or functional impairment) ( Critselis et al., 2014 ).
An addiction-like pattern of internet use (including SM use) was associated with emotional maladjustment ( Critselis et al., 2014 ), internalizing and externalizing symptoms ( Tsitsika, Tzavela, et al., 2014 ), and depressive mood ( Van Rooij, Ferguson, Van de Mheen, & Schoenmakers, 2017 ). Further, depressive mood predicted problematic internet use (both SM and gaming, independently) ( Kırcaburun et al., 2018 ; Van Rooij et al., 2017 ).
Bányai et al. (2017) assessed the prevalence of problematic internet use conducting a latent profile analysis to describe classes of users and found that the class described as ‘at risk’ for problematic internet and SM use tended to be female, use the internet for longer periods, and have lower self-esteem and more depressive symptoms. Yet, while Banjanin, Banjanin, Dimitrijevic, and Pantic (2015) found a positive correlation between internet addiction and depression in high school students (particularly for females), no such correlation was found with engagement with SM (measured by number of pictures posted).
Several studies examined mediators of the association of problematic SM use and depression. Wang et al. (2018) found that rumination mediated the relationship between SM addiction and adolescent depression, with a stronger effect among adolescents with low self-esteem. Additionally, insomnia partially mediated the association between SM addiction and depressive symptoms ( Li et al., 2017 ). Woods and Scott (2016) found that nighttime-specific SM use (in addition to overall use and emotional investment in SM) was associated with poorer sleep quality, anxiety and depressive symptoms. Finally, problematic SM use mediated the association between depressive symptoms and cyberbullying perpetration ( Kırcaburun et al., 2018 ).
Quality of SNS use
In addition to the frequency of adolescents’ engagement with SM, another focus of research has been the ways in which adolescents engage with SM. Of the studies selected, four primarily examined engagement styles with SM and two specifically examined social comparisons with other users.
Characteristics of SM use
The ways in which adolescents use SM may also have an effect on depression. One study ( Frison & Eggermont, 2016 ) characterized SM use as public (e.g. updating one’s status on a profile) vs private (e.g. messaging), and active (e.g. interacting with others on SM) vs passive (e.g. browsing on SM) and found that public Facebook use was associated with adolescent depressed mood. Among girls, passive use of Facebook yielded negative outcomes such as depressed mood, while active use yielded positive outcomes such as perceived social support ( Frison & Eggermont, 2016 ). A longitudinal study of Flemish adolescents by the same group ( Frison & Eggermont, 2017 ) found passive SM use at baseline to predict depressive symptoms 7 months later, while depressive symptoms predicted active use of SM. Interestingly, there was no association between depressive symptoms and Facebook use (frequency of use, network size, self-presentation, and peer interaction) in a study conducted among healthy adolescents ( Morin-Major et al., 2016 ).
Romer et al. (2013) found that the types of internet activities utilized (e.g. SNS, blogs, etc.) were associated with the frequency of self-reported depression-like symptoms. Additionally, using the internet for information searching was associated with higher grades, more frequent participation in clubs, and lower reports of depressive symptoms, while using the internet more than 4 h per day to communicate or play games was associated with greater depression-like symptoms, suggesting that Internet use for acquiring information is associated with healthy development.
A qualitative study further explored positive and negative aspects of SM use among adolescents diagnosed with clinical depression ( Radovic, Gmelin, Stein, & Miller, 2017 ). Participants described positive SM use as including searching for positive content (e.g. entertainment, humour, content creation) or social connection, while they described negative SM use as sharing risky behaviours, cyberbullying, or making self-denigrating comparisons with others. Furthermore, this study found that adolescents’ use of SM shifted from negative to positive during the course of treatment.
Social comparisons
Two studies examined social comparisons made through SM and the association with depression. Nesi and Prinstein (2015) found that technology-based social comparison and feedback-seeking were associated with depressive symptoms, even when controlling for the effects of overall frequency of technology use, offline excessive reassurance-seeking, and prior depressive symptoms. This association was strongest among females and adolescents low in popularity (as measured by peer report). Niu et al. (2018) found that negative social comparisons mediated the association between Qzone use (a Chinese SM site) and depression, and that the association between Qzone use and negative social comparisons was stronger among individuals with low self-esteem. However, there was no direct effect of Qzone use on depression. An additional study that primarily focussed on studying frequency of use ( Marengo et al., 2018 ) found that increased use of highly visual SM (e.g. Instagram) predicted internalizing symptoms and body image concerns in a student sample. Moreover, in this study, the effect of highly visual SM on internalizing symptoms was mediated by body image concerns.
Social aspects of SM use
Several studies looked at the social aspects of engagement with SM, either by evaluating the effects of cybervictimization ( n = 4) on depression, parental involvement both through monitoring of SM use or direct engagement with the adolescent ( n = 3), and aspects of social support received by the adolescent within and outside of SNS ( n = 2).
Cyberbullying/cybervictimization
Four studies examined cyberbullying via SM and depressive symptoms. Duarte, Pittman, Thorsen, Cunningham, and Ranney (2018) found that symptoms of depression, post-traumatic stress disorder, and suicidal ideation were more prevalent among participants who reported any past-year cyberbullying (either victimization or perpetration). After adjusting for a range of demographic factors, only lesbian, gay, and bisexual status correlated with cyberbullying involvement or adverse mental health outcomes. Another study found that cyberbullying victimization fully mediated the association between SM use and psychological distress and suicide attempts ( Sampasa-Kanyinga & Hamilton, 2015 ). Furthermore, a 12-month longitudinal study found that cybervictimization predicted later depressive symptoms ( Cole et al., 2016 ). Depressive symptoms have also been shown to be a risk factor (rather than an outcome) for cybervictimization on Facebook ( Frison, Subrahmanyam, & Eggermont, 2016 ), showing evidence of the bi-directionality of this association.
Social support
While many studies examined potential negative effects of SM use, some studies examined the positive effects of SM use on youth outcomes, including social support. Frison and Eggermont (2015) found that adolescents seeking social support through Facebook had improved depressive symptoms if support was received, but worsened symptoms if support was not received. This pattern was not found in non-virtual social support contexts, suggesting differences in online and traditional social support contexts. A later study that primarily focussed on the characteristics of SM use ( Frison & Eggermont, 2016 ) found that perception of online support was particularly protective against depressive symptoms in girls with ‘active’ Facebook use (e.g. those who update their status or instant message on Facebook). Finally, Frison et al. (2016) showed that support from friends can be a protective factor of Facebook victimization.
Parental involvement/parental monitoring
Studies examining parent and family role in adolescent SM use and its outcomes were heterogeneous. One study ( Coyne, Padilla-Walker, Day, Harper, & Stockdale, 2014 ) explored adolescent use of SM with parents and found lower internalizing behaviours in participants who used SNS with their parents (mediated by feelings of parent/child connection). Another study ( Fardouly, Magson, Johnco, Oar, & Rapee, 2018 ) examined parent control over preadolescents’ time spent on SM and found no association between parental control and preadolescent depressive symptoms.
Family relationships offline were also associated with adolescent outcomes. Isarabhakdi and Pewnil (2016) examined adolescents’ engagement with offline relationships and found improved mental health outcomes with higher involvement in family activities and with peers, while internet use did not significantly improve mental well-being. This finding suggests that in-person support systems were more effective for the promotion of mental well-being. Interestingly, in Szwedo, Mikami, and Allen (2011) , negative interactions with mothers during early adolescence were associated with youth preferring online versus face-to-face communication, experiencing more negative interactions on webpages, and forming close friendships with someone they met online 7 years later. An additional study that primarily focussed on suicide contagion ( Tseng & Yang, 2015 ) found that family support was protective for both males and females, while friend support was protective only for females. However, ‘significant other’ support was a risk factor for suicidal plans among females.
Disclosure of mental health symptoms on SM
A few of the studies selected focussed on studying the disclosure of depressive symptoms on SM and explored the potential of disclosure of symptoms of distress on SM to predict depression and suicide, in addition to the phenomenon of suicide contagion.
Online disclosure and prediction of mental health symptoms
Although content analysis is a method theorized to have potential to predict and prevent non-suicidal and suicidal self-injurious behaviours, the data are mixed. Ophir, Asterhan, and Schwarz (2019) examined the predictive validity of explicit references to personal distress in adolescents’ Facebook postings, comparing these postings with external, self-report measures of psychological distress (e.g. depression) and found that most depressed adolescents did not publish explicit references to depression. Additionally, adolescents published less verbal content than adult users of SNS. Conversely, Akkın Gürbüz et al. (2017) found that while disclosures of depressed mood were frequent among both depressed and non-depressed adolescents, those who were depressed shared more negative feelings, anhedonia, and suicidal thoughts on SM than those who were not depressed.
Suicide contagion effect
One longitudinal study examined suicide contagion effects ( Dunlop, More, & Romer, 2011 ) finding that even though traditional SNS (e.g. Facebook or MySpace) were a significant source of exposure to suicide stories, this exposure was not associated with increases in suicidal ideation one year later. On the other hand, exposure to online discussion forums (including self-help forums) did predict increases in suicidal ideation over time. Notably, this study found that in a quarter of the sample, the exposure to suicide stories took place through SM. Another study ( Tseng & Yang, 2015 ) found that higher importance attributed to web communication (e.g. chatting or making friends online) was associated with increased risk of self-injurious thoughts and behaviours in boys.
The recent rise in the prevalence of depression and suicide among adolescents has coincided with an increase in screen-related activities, including SM use ( Twenge et al., 2018 ), sparking an interest in investigating the effects of SM use on adolescent mental health. This interest has given rise to a broad scope of research, ranging from observational to experimental and qualitative studies through interviews or analysis of SM content, and systematic studies. This scoping review aimed to understand the breadth of research in the area of depression and SM (with a focus on SNS) and to identify the existing research gaps.
We identified four main themes of research, including (1) the quantity of SM use; (2) the quality of SM use; (3) social aspects associated with SM use; and (4) SM as a tool for disclosure of mental health symptoms and potential for prediction and prevention of depression and suicide outcomes.
Most research on SM and depressive symptoms has focussed on the effects of frequency of SM use and problematic SM use. The majority of articles included in this review demonstrated a positive and bi-directional association between frequency of SM use and depression and in some instances even suicidality. Yet some questions remain to be determined, including to what degree adolescents’ personal vulnerabilities and characteristics of SM use moderate the association between SM use and depression or suicidality, and whether other environmental factors, such as family support and/or monitoring, or cultural differences influence this association. Although moderate SM use may be associated with better self-regulation, it is unclear if this is due to moderate users being better at self-regulation.
Findings from the studies examining problematic SM use were consistent with prior studies linking problematic internet use with a variety of psychosocial outcomes including depressive symptoms ( Reid Chassiakos et al., 2016 ). Though limited in number, studies reviewed here suggested that problematic or addictive SM use may be more common in females ( Banyai et al., 2017 ; Kırcaburun et al., 2018 ) and in those starting use at a younger age ( Tsitsika, Janikian, et al., 2014 ). These findings suggest a possible role of screening for addictive SM use, with a particular focus on risk stratification for younger and female adolescents.
With respect to the effects of patterns and types of SM use, studies reviewed here suggest possible differential effects between passive and active, and private versus public SM use. This suggests that screening only for time spent on SM may be insufficient. Moreover, though there are types of SM use that have adverse mental health effects for adolescents (e.g. addictive patterns, nighttime use), other types of SM use, such as for information searching or receiving social support, may have a positive effect ( Coyne et al., 2018 ; Frison & Eggermont, 2016 ; Romer et al., 2013 ). Furthermore, over time, depressed adolescents can successfully shift their use of SM from negative (e.g. cyberbullying) to positive (e.g. searching for humour), possibly through increasing awareness of the effect of SM use on their mood ( Radovic et al., 2017 ). Given the ubiquity of SM use, these results suggest that interventions targeting changes in adolescents’ use of SM may be fruitful in improving their mental health.
Consistent with prior research ( Feinstein et al., 2013 ), studies examining social comparisons found significant associations between social comparisons made via SM and depression. The tendency of individuals to share more positive depictions of themselves on SM ( Subrahmanyam & Greenfield, 2008 ), and the increased opportunities for comparisons ( Steers, Wickham, & Acitelli, 2014 ) may suggest a confluence of risks for depression and an important avenue for interventions. Moreover, the studies reviewed and previous findings ( Buunk & Gibbons, 2007 ) suggest that individuals with low self-esteem may be at higher risk for the negative effects of social comparisons on mental health.
As previously shown ( Cénat et al., 2014 ), most studies found cyberbullying (either perpetration or victimization) was either associated with mental health problems ( Cole et al., 2016 ; Duarte et al., 2018 ) or moderated the relationship between SM use and depression and suicidality ( Sampasa-Kanyinga & Hamilton, 2015 ). Additionally, cyberbullying may be a distinctive form of victimization that requires further investigation in order to understand its impact on adolescent mental health ( Dempsey, Sulkowski, Nichols, & Storch, 2009 ).
Studies examining social support highlight the association of both depressed mood and low in-person social support with social networking and online support-seeking ( Frison & Eggermont, 2015 ). Moreover, while social support online can be beneficial ( Frison & Eggermont, 2015 ), excessive reliance on online communication and support may be problematic ( Twenge et al., 2018 ). Of note, parental involvement both positively and negatively affected SM use and adolescent outcomes. These mixed findings suggest a need to include parental relationships in research (both via online and ‘offline’ communication), to better understand their role in adolescents’ SM use and depression.
Surprisingly, depressed adolescents were not more likely to publish explicit references to depression on SM platforms than their healthy peers ( Ophir et al., 2019 ) which suggests that screening for depression via SM may not be useful when used alone. However, some depressed adolescents posted more negative feelings, anhedonia and suicidal ideation ( Akkın Gürbüz et al., 2017 ), suggesting that SM may be used as a supplemental tool to track the course of depressive mood over time and start discussions about mental health.
Suicide contagion effect is a relatively understudied area, despite concerns raised that increased exposure to SM may amplify this effect ( Bell, 2014 ). Given that adolescents are particularly vulnerable to the group contagion effect of suicide ( Stack, 2003 ) and the potential for increased exposure to suicide stories online ( Dunlop et al., 2011 ), interventions to limit this exposure could decrease suicide contagion.
The studies reviewed identified several potential moderators of the association between SM use and adolescent depression, including age and gender. The differential effects of SM use on mental health depending on the age of the adolescent ( Tsitsika, Tzavela, et al., 2014 ) are not surprising given the developmental differences in social and mood regulation skills between younger and older adolescents. Likewise, potential mediators of the effects of SM on mental health such as social comparisons ( Niu et al., 2018 ), body image concerns ( Marengo et al., 2018 ), perceived support online ( Frison & Eggermont, 2015 ), and parent–child relationship ( Coyne et al., 2014 ) may also be important targets for future interventions.
The studies reviewed present several limitations. Most studies were cross-sectional and could not elucidate the directionality of the association between SM use and depression. Most of the studies included self-report rather than clinician-administered measures of depression, and retrospective reports, asking participants to report on past activities. Newer methods that measure actual (and not just reported) use (e.g. news feed activity, number of likes and comments) and more frequent and timely reports of SM use (e.g. diaries) could more accurately explain these associations. Another limitation is that many of the studies recruited participants in schools, limiting the generalizability to clinical samples. It is possible that those students not in school were spending more time on SM and/or experiencing more depressive symptoms. Most studies included general assessments of SM without specifying whether the use was limited to SNS or other forms of SM or internet use. While we tried to narrow our search to studies that explicitly included questions on SNS use, many also asked about other types of SM use. Separating the different types of SM use may be difficult when asking for adolescents’ self-reports, but more immediate measures of mood symptoms and SNS use could be more specific and informative. Finally, while some studies included contextual factors such as the educational and family environments, other contextual factors such as ethnicity and cultural context are areas of potential for investigation.
Conclusions
In summary, extensive research on the quantity and quality of SM use has shown an association between SM use and depression in adolescents. Given that most studies are cross-sectional, longitudinal research would help assess the direction of this association. At the same time, some aspects of SM use may have a beneficial effect on adolescent well-being, such as the ability to have diversity of friendships and easily accessed supports. Furthermore, the use of SM content to detect symptoms has potential in depression and suicide prevention. Finally, moderators of the association between SM and adolescent depression and suicidality (e.g. gender, age, parental involvement) are areas to explore that would allow more targeted interventions. Since SM will remain an important facet of adolescents’ lives, a better understanding of the mechanisms of its relationship with depression could be beneficial to increase exposure to mental health interventions and promote well-being.
Acknowledgements
The authors acknowledge the help of Jaime Blanck, MLIS, MPA for her help with the search and retrieval of full-text articles.
Disclosure statement
Dr. Vidal is supported by the Stravos Niarchos Foundation. Ms. Lhaksampa and Dr. Miller are supported by the Once Upon a Time Foundation. Drs. Miller and Dr. Platt are supported by the Patient-Centered Outcomes Research Institute (PCORI). Dr. Platt is supported by the NIMH 1K23MH118431 and the Robert Wood Johnson Foundation.
- Akkın Gürbüz HG, Demir T, Gökalp Özcan B, Kadak MT, & Poyraz BC (2017). Use of social network sites among depressed adolescents . Behaviour & Information Technology , 36 , 517–523. doi: 10.1080/0144929X.2016.1262898 [ CrossRef ] [ Google Scholar ]
- Anderson EL, Steen E, & Stavropoulos V (2017). Internet use and problematic internet use: A systematic review of longitudinal research trends in adolescence and emergent adulthood . International Journal of Adolescence and Youth , 22 , 430–454. doi: 10.1080/02673843.2016.1227716 [ CrossRef ] [ Google Scholar ]
- Arksey H, & O’Malley L (2005). Scoping studies: Towards a methodological framework . International Journal of Social Research Methodology , 8 ( 1 ), 19–32. doi: 10.1080/1364557032000119616 [ CrossRef ] [ Google Scholar ]
- Banjanin N, Banjanin N, Dimitrijevic I, & Pantic I (2015). Relationship between internet use and depression: Focus on physiological mood oscillations, social networking and online addictive behavior . Computers in Human Behavior , 43 , 308–312. doi: 10.1016/j.chb.2014.11.013 [ CrossRef ] [ Google Scholar ]
- Bányai F, Zsila Á, Király O, Maraz A, Elekes Z, Griffiths MD, … Demetrovics Z (2017). Problematic social media use: Results from a large-scale nationally representative adolescent sample . PLoS One , 12 ( 1 ), e0169839. doi: 10.1371/journal.pone.0169839 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Barry CT, Sidoti CL, Briggs SM, Reiter SR, & Lindsey RA (2017). Adolescent social media use and mental health from adolescent and parent perspectives . Journal of Adolescence , 61 , 1–11. doi: 10.1016/j.adolescence.2017.08.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Baym NK (2010). Personal connections in the digital age . Cambridge: Polity Press. [ Google Scholar ]
- Baym NK, Zhang YB, & Lin MC (2004). Social interactions across media: Interpersonal communication on the internet, telephone and face-to-face . New Media & Society , 6 , 299–318. doi: 10.1177/1461444804041438 [ CrossRef ] [ Google Scholar ]
- Bell J (2014). Harmful or helpful? The role of the Internet in self-harming and suicidal behaviour in young people . Mental Health Review Journal , 19 ( 1 ), 61–71. doi: 10.1108/MHRJ-05-2013-0019 [ CrossRef ] [ Google Scholar ]
- Best P, Manktelow R, & Taylor B (2014). Online communication, social media and adolescent wellbeing: A systematic narrative review . Children and Youth Services Review , 41 , 27–36. doi: 10.1016/j.childyouth.2014.03.001 [ CrossRef ] [ Google Scholar ]
- Blomfield-Neira CJ, & Barber BL (2014). Social networking site use: Linked to adolescents’ social self-concept, self-esteem, and depressed mood . Australian Journal of Psychology , 66 ( 1 ), 56–64. doi: 10.1111/ajpy.12034 [ CrossRef ] [ Google Scholar ]
- Buunk AP, & Gibbons FX (2007). Social comparison: The end of a theory and the emergence of a field . Organizational Behavior and Human Decision Processes , 102 ( 1 ), 3–21. doi: 10.1016/j.obhdp.2006.09.007 [ CrossRef ] [ Google Scholar ]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. (2017). Web-based Injury Statistics Query and Reporting System (WISQARS) [online] . Retrieved from www.cdc.gov/injury/wisqars . Accessed July 19, 2019.
- Cénat JM, Hébert M, Blais M, Lavoie F, Guerrier M, & Derivois D (2014). Cyberbullying, psychological distress and self-esteem among youth in Quebec schools . Journal of Affective Disorders , 169 , 7–9. doi: 10.1016/j.jad.2014.07.019 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cole DA, Zelkowitz RL, Nick E, Martin NC, Roeder KM, Sinclair-McBride K, & Spinelli T (2016). Longitudinal and incremental relation of cybervictimization to negative self-cognitions and depressive symptoms in young adolescents . Journal of Abnormal Child Psychology , 44 , 1321–1332. doi: 10.1007/s10802-015-0123-7 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coyne SM, Padilla-Walker LM, Day RD, Harper J, & Stockdale L (2014). A friend request from dear old dad: Associations between parent–child social networking and adolescent outcomes . Cyberpsychology, Behavior, and Social Networking , 17 ( 1 ), 8–13. doi: 10.1089/cyber.2012.0623 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Coyne SM, Padilla-Walker LM, Holmgren HG, & Stockdale LA (2018). Instagrowth: A longitudinal growth mixture model of social media time use across adolescence . Journal of Research on Adolescence , 29 , 897–907. doi: 10.1111/jora.12424 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Critselis E, Janikian M, Paleomilitou N, Oikonomou D, Kassinopoulos M, Kormas G, & Tsitsika A (2014). Predictive factors and psychosocial effects of Internet addictive behaviors in Cypriot adolescents . International Journal of Adolescent Medicine and Health , 26 , 369–375. doi: 10.1515/ijamh-2013-0313 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dempsey AG, Sulkowski ML, Nichols R, & Storch EA (2009). Differences between peer victimization in cyber and physical settings and associated psychosocial adjustment in early adolescence . Psychology in the Schools , 46 , 962–972. doi: 10.1002/pits.20437 [ CrossRef ] [ Google Scholar ]
- Duarte C, Pittman SK, Thorsen MM, Cunningham RM, & Ranney ML (2018). Correlation of minority status, cyberbullying, and mental health: A cross-sectional study of 1031 adolescents . Journal of Child & Adolescent Trauma , 11 ( 1 ), 39–48. doi: 10.1007/s40653-018-0201-4 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Dunlop SM, More E, & Romer D (2011). Where do youth learn about suicides on the Internet, and what influence does this have on suicidal ideation . Journal of Child Psychology and Psychiatry , 52 , 1073–1080. doi: 10.1111/j.1469-7610.2011.02416.x [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Fardouly J, Magson NR, Johnco CJ, Oar EL, & Rapee RM (2018). Parental control of the time preadolescents spend on social media: Links with preadolescents’ social media appearance comparisons and mental health . Journal of Youth and Adolescence , 47 , 1456–1468. doi: 10.1007/s10964-018-0870-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Feinstein BA, Hershenberg R, Bhatia V, Latack JA, Meuwly N, & Davila J (2013). Negative social comparison on Facebook and depressive symptoms: Rumination as a mechanism . Psychology of Popular Media Culture , 2 , 161–110. doi: 10.1037/a0033111 [ CrossRef ] [ Google Scholar ]
- Frison E, & Eggermont S (2015). The impact of daily stress on adolescents’ depressed mood: The role of social support seeking through Facebook . Computers in Human Behavior , 44 , 315–325. doi: 10.1016/j.chb.2014.11.070 [ CrossRef ] [ Google Scholar ]
- Frison E, & Eggermont S (2016). Exploring the relationships between different types of Facebook use, perceived online social support, and adolescents’ depressed mood . Social Science Computer Review , 34 , 153–171. doi: 10.1177/0894439314567449 [ CrossRef ] [ Google Scholar ]
- Frison E, & Eggermont S (2017). Browsing, posting, and liking on Instagram: The reciprocal relationships between different types of Instagram use and adolescents’ depressed mood . Cyberpsychology, Behavior, and Social Networking , 20 , 603–609. doi: 10.1089/cyber.2017.0156 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Frison E, Subrahmanyam K, & Eggermont S (2016). The short-term longitudinal and reciprocal relations between peer victimization on Facebook and adolescents’ well-being . Journal of Youth and Adolescence , 45 , 1755–1771. doi: 10.1007/s10964-016-0436-z [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guernsey L (2014). Garbled in translation: Getting media research to the press and public . Journal of Children and Media , 8 ( 1 ), 87–94. doi: 10.1080/17482798.2014.863486 [ CrossRef ] [ Google Scholar ]
- Houghton S, Lawrence D, Hunter SC, Rosenberg M, Zadow C, Wood L, & Shilton T (2018). Reciprocal relationships between trajectories of depressive symptoms and screen media use during adolescence . Journal of Youth and Adolescence , 47 , 2453–2467. doi: 10.1007/s10964-018-0901-y [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Isarabhakdi P, & Pewnil T (2016). Engagement with family, peers, and Internet use and its effect on mental well-being among high school students in Kanchanaburi Province , Thailand. International Journal of Adolescence and Youth , 21 ( 1 ), 15–26. doi: 10.1080/02673843.2015.1024698 [ CrossRef ] [ Google Scholar ]
- Keles B, McCrae N, & Grealish A (2019). A systematic review: The influence of social media on depression, anxiety and psychological distress in adolescents . International Journal of Adolescence and Youth , 25 , 79–93. doi: 10.1080/02673843.2019.1590851 [ CrossRef ] [ Google Scholar ]
- Kırcaburun K, Kokkinos CM, Demetrovics Z, Király O, Griffiths MD, & Çolak TS (2018). Problematic online behaviors among adolescents and emerging adults: Associations between cyberbullying perpetration, problematic social media use, and psychosocial factors . International Journal of Mental Health and Addiction , 17 , 891–908. doi: 10.1007/s11469-018-9894-8 [ CrossRef ] [ Google Scholar ]
- Kowalski RM, Limber S, & Agatston PW (2012). Cyberbullying: Bullying in the digital age (2nd ed.). Malden, MA: Wiley-Blackwell. [ Google Scholar ]
- Kraut R, Kiesler S, Boneva B, Cummings J, Helgeson V, & Crawford A (2002). Internet paradox revisited . Journal of Social Issues , 58 ( 1 ), 49–74. doi: 10.1111/1540-4560.00248 [ CrossRef ] [ Google Scholar ]
- Kraut R, Patterson M, Lundmark V, Kiesler S, Mukophadhyay T, & Scherlis W (1998). Internet paradox: A social technology that reduces social involvement and psychological well-being? American Psychologist , 53 , 1017–1031. doi: 10.1037/0003-066X.53.9.1017 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lee EW, Ho SS, & Lwin MO (2017). Extending the social cognitive model—Examining the external and personal antecedents of social network sites use among Singaporean adolescents . Computers in Human Behavior , 67 , 240–251. doi: 10.1016/j.chb.2016.10.030 [ CrossRef ] [ Google Scholar ]
- Li JB, Lau JT, Mo PK, Su XF, Tang J, Qin ZG, & Gross DL (2017). Insomnia partially mediated the association between problematic Internet use and depression among secondary school students in China . Journal of Behavioral Addictions , 6 , 554–563. doi: 10.1556/2006.6.2017.085 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Manning J (2014). Social media, definition and classes of In Harvey K (Ed.), Encyclopedia of social media and politics (pp. 1158–1162). Thousand Oaks, CA: Sage. [ Google Scholar ]
- Marengo D, Longobardi C, Fabris MA, & Settanni M (2018). Highly-visual social media and internalizing symptoms in adolescence: The mediating role of body image concerns . Computers in Human Behavior , 82 , 63–69. doi: 10.1016/j.chb.2018.01.003 [ CrossRef ] [ Google Scholar ]
- McCrae N, Gettings S, & Purssell E (2017). Social media and depressive symptoms in childhood and adolescence: A systematic review . Adolescent Research Review , 2 , 315–330. doi: 10.1007/s40894-017-0053-4 [ CrossRef ] [ Google Scholar ]
- Miron O, Yu K, Wilf-Miron R, & Kohane IS (2019). Suicide rates among adolescents and young adults in the United States, 2000–2017 . JAMA , 321 , 2362–2364. doi: 10.1001/jama.2019.5054 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mojtabai R, Olfson M, & Han B (2016). National trends in the prevalence and treatment of depression in adolescents and young adults . Pediatrics , 138 , e20161878. doi: 10.1542/peds.2016-1878 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Morin-Major JK, Marin MF, Durand N, Wan N, Juster RP, & Lupien SJ (2016). Facebook behaviors associated with diurnal cortisol in adolescents: Is befriending stressful? Psychoneuroendocrinology , 63 , 238–246. doi: 10.1016/j.psyneuen.2015.10.005 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nesi J, & Prinstein MJ (2015). Using social media for social comparison and feedback-seeking: Gender and popularity moderate associations with depressive symptoms . Journal of Abnormal Child Psychology , 43 , 1427–1438. doi: 10.1007/s10802-015-0020-0 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nie NH, Hillygus DS, & Erbring L (2002). Internet use, interpersonal relations, and sociability: A time diary study In Wellman B & Haythornthwaite C (Eds.), The Internet in everyday life (pp. 215–243). Malden, MA: Blackwell. [ Google Scholar ]
- Niu GF, Luo YJ, Sun XJ, Zhou ZK, Yu F, Yang SL, & Zhao L (2018). Qzone use and depression among Chinese adolescents: A moderated mediation model . Journal of Affective Disorders , 231 , 58–62. doi: 10.1016/j.jad.2018.01.013 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Oberst U, Wegmann E, Stodt B, Brand M, & Chamarro A (2017). Negative consequences from heavy social networking in adolescents: The mediating role of fear of missing out . Journal of Adolescence , 55 , 51–60. doi: 10.1016/j.adolescence.2016.12.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ophir Y, Asterhan CS, & Schwarz BB (2019). The digital footprints of adolescent depression, social rejection and victimization of bullying on Facebook . Computers in Human Behavior , 91 , 62–71. doi: 10.1016/j.chb.2018.09.025 [ CrossRef ] [ Google Scholar ]
- Pantic I, Damjanovic A, Todorovic J, Topalovic D, Bojovic-Jovic D, Ristic S, & Pantic S (2012). Association between online social networking and depression in high school students: Behavioral physiology viewpoint . Psychiatria Danubina , 24 ( 1 ), 90–93. [ PubMed ] [ Google Scholar ]
- Pew Research Center. (2018a). Teens, social media and technology 2018 . Retrieved from https://www.pewinternet.org/2018/05/31/teens-social-media-technology-2018/
- Pew Research Center. (2018b). Teens’ social media habits and experiences . Retrieved from https://www.pewinternet.org/2018/11/28/teens-social-media-habits-and-experiences/
- Przybylski AK, Murayama K, DeHaan CR, & Gladwell V (2013). Motivational, emotional, and behavioral correlates of fear of missing out . Computers in Human Behavior , 29 , 1841–1848. doi: 10.1016/j.chb.2013.02.014 [ CrossRef ] [ Google Scholar ]
- Radovic A, Gmelin T, Stein BD, & Miller E (2017). Depressed adolescents’ positive and negative use of social media . Journal of Adolescence , 55 , 5–15. doi: 10.1016/j.adolescence.2016.12.002 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Reid Chassiakos YL, Radesky J, Christakis D, Moreno MA, Cross C; Council on Communications and Media. (2016). Children and adolescents and digital media . Pediatrics , 138 , e20162593. doi: 10.1542/peds.2016-2593 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Robinson JP, Kestnbaum M, Neustadtl A, & Alvarez AS (2002). The Internet and other uses of time In Wellman B & Haythornthwaite C (Eds.), The Internet in everyday life (pp. 244–262). Malden, MA: Blackwell. [ Google Scholar ]
- Rodriguez Puentes AP, & Parra AF (2014). Relación entre el tiempo de uso de las redes sociales en internet yla salud mental en adolescentes colombianos . Acta Colombiana de Psicología , 17 ( 1 ), 131–140. doi: 10.14718/ACP.2014.17.1.13 [ CrossRef ] [ Google Scholar ]
- Romer D, Bagdasarov Z, & More E (2013). Older versus newer media and the well-being of United States youth: Results from a national longitudinal panel . Journal of Adolescent Health , 52 , 613–619. doi: 10.1016/j.jadohealth.2012.11.012 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Salmela-Aro K, Upadyaya K, Hakkarainen K, Lonka K, & Alho K (2017). The dark side of internet use: Two longitudinal studies of excessive internet use, depressive symptoms, school burnout and engagement among Finnish early and late adolescents . Journal of Youth and Adolescence , 46 , 343–357. doi: 10.1007/s10964-016-0494-2 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sampasa-Kanyinga H, & Hamilton HA (2015). Social networking sites and mental health problems in adolescents: The mediating role of cyberbullying victimization . European Psychiatry , 30 , 1021–1027. doi: 10.1016/j.eurpsy.2015.09.011 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sampasa-Kanyinga H, & Lewis RF (2015). Frequent use of social networking sites is associated with poor psychological functioning among children and adolescents . Cyberpsychology, Behavior, and Social Networking , 18 , 380–385. doi: 10.1089/cyber.2015.0055 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Stack S (2003). Media coverage as a risk factor in suicide . Journal of Epidemiology & Community Health , 57 , 238–240. doi: 10.1136/jech.57.4.238 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Steers MLN, Wickham RE, & Acitelli LK (2014). Seeing everyone else’s highlight reels: How Facebook usage is linked to depressive symptoms . Journal of Social and Clinical Psychology , 33 , 701–731. doi: 10.1521/jscp.2014.33.8.701 [ CrossRef ] [ Google Scholar ]
- Subrahmanyam K, & Greenfield P (2008). Online communication and adolescent relationships . The Future of Children , 18 ( 1 ), 119–146. doi: 10.1353/foc.0.0006 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Szwedo DE, Mikami AY, & Allen JP (2011). Qualities of peer relations on social networking websites: Predictions from negative mother–teen interactions . Journal of Research on Adolescence , 21 , 595–607. doi: 10.1111/j.1532-7795.2010.00692.x [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tseng FY, & Yang HJ (2015). Internet use and web communication networks, sources of social support, and forms of suicidal and nonsuicidal self-injury among adolescents: Different patterns between genders . Suicide and Life-Threatening Behavior , 45 , 178–191. doi: 10.1111/sltb.12124 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tsitsika A, Janikian M, Schoenmakers TM, Tzavela EC, Ólafsson K, Wójcik S, … Richardson C (2014). Internet addictive behavior in adolescence: A cross-sectional study in seven European countries . Cyberpsychology, Behavior, and Social Networking , 17 , 528–535. doi: 10.1089/cyber.2013.0382 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tsitsika AK, Tzavela EC, Janikian M, Ólafsson K, Iordache A, Schoenmakers TM, … Richardson C (2014). Online social networking in adolescence: Patterns of use in six European countries and links with psychosocial functioning . Journal of Adolescent Health , 55 ( 1 ), 141–147. doi: 10.1016/j.jadohealth.2013.11.010 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Twenge JM, Joiner TE, Rogers ML, & Martin GN (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time . Clinical Psychological Science , 6 ( 1 ), 3–17. doi: 10.1177/2167702617723376 [ CrossRef ] [ Google Scholar ]
- Van Rooij AJ, Ferguson CJ, Van de Mheen D, & Schoenmakers TM (2017). Time to abandon Internet Addiction? Predicting problematic Internet, game, and social media use from psychosocial well-being and application use . Clinical Neuropsychiatry , 14 ( 1 ), 113–121. [ Google Scholar ]
- Wang P, Wang X, Wu Y, Xie X, Wang X, Zhao F, … Lei L (2018). Social networking sites addiction and adolescent depression: A moderated mediation model of rumination and self-esteem . Personality and Individual Differences , 127 , 162–167. doi: 10.1016/j.paid.2018.02.008 [ CrossRef ] [ Google Scholar ]
- Wang H, & Wellman B (2010). Social connectivity in America: Changes in adult friendship network size from 2002 to 2007 . American Behavioral Scientist , 53 , 1148–1169. doi: 10.1177/0002764209356247 [ CrossRef ] [ Google Scholar ]
- Woods HC, & Scott H (2016). #Sleepyteens: Social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem . Journal of Adolescence , 51 , 41–49. doi: 10.1016/j.adolescence.2016.05.008 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Introduction
- Article Information
TGD indicates transgender and gender diverse.
The figure shows estimated means for the Beck Depression Inventory for Youths (BDI-Y) total score at each wave. CIS indicates cisgender; TGD, transgender and gender diverse.
eFigure. Flowchart of Participation in the Study: Final Analytic Sample
eAppendix 1. Additional Details About Participants and Procedures
eAppendix 2. Detailed Information on Measures
eTable. Sensitivity Analysis
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Gonzales Real A , Lobato MIR , Russell ST. Trajectories of Gender Identity and Depressive Symptoms in Youths. JAMA Netw Open. 2024;7(5):e2411322. doi:10.1001/jamanetworkopen.2024.11322
Manage citations:
© 2024
- Permissions
Trajectories of Gender Identity and Depressive Symptoms in Youths
- 1 Department of Human Development and Family Sciences, The University of Texas at Austin
- 2 Department of Psychiatry, Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil
Question Are gender identity trajectories and changes in youth-reported gender identity associated with depressive symptoms over time?
Findings In this cohort study involving 366 sexual and/or gender minority youths (aged 15-21 years), 1 in 5 (18.2%) reported a different gender identity over time. Youths transitioning to a transgender or gender diverse identity reported higher levels of depressive symptoms at baseline; depressive symptoms disparities were explained by exposure to lesbian, gay, bisexual, and transgender violence, but frequency of gender identity variability was not associated with the level or changes in depressive symptoms.
Meaning In this study, changes in gender identity were not associated with depressive symptoms, suggesting that gender identity exploration is a normal part of adolescent development for some youths.
Importance Concerns about the mental health of youths going through gender identity transitions have received increased attention. There is a need for empirical evidence to understand how transitions in self-reported gender identity are associated with mental health.
Objective To examine whether and how often youths changed self-reported gender identities in a longitudinal sample of sexual and gender minority (SGM) youths, and whether trajectories of gender identity were associated with depressive symptoms.
Design, Setting, and Participants This cohort study used data from 4 waves (every 9 months) of a longitudinal community-based study collected in 2 large cities in the US (1 in the Northeast and 1 in the Southwest) between November 2011 and June 2015. Eligible participants included youths who self-identified as SGM from community-based agencies and college groups for SGM youths. Data analysis occurred from September 2022 to June 2023.
Exposure Gender identity trajectories and gender identity variability.
Main Outcomes and Measures The Beck Depression Inventory for Youth (BDI-Y) assessed depressive symptoms. Gender identity variability was measured as the number of times participants’ gender identity changed. Hierarchical linear models investigated gender identity trajectories and whether gender identity variability was associated with depressive symptoms over time.
Results Among the 366 SGM youths included in the study (mean [SD] age, 18.61 [1.71] years; 181 [49.4%] assigned male at birth and 185 [50.6%] assigned female at birth), 4 gender identity trajectory groups were identified: (1) cisgender across all waves (274 participants ), (2) transgender or gender diverse (TGD) across all waves (32 participants), (3) initially cisgender but TGD by wave 4 (ie, cisgender to TGD [28 participants]), and (4) initially TGD but cisgender by wave 4 (ie, TGD to cisgender [32 participants]). One in 5 youths (18.3%) reported a different gender identity over a period of approximately 3.5 years; 28 youths varied gender identity more than twice. The cisgender to TGD group reported higher levels of depression compared with the cisgender group at baseline ( Β = 4.66; SE = 2.10; P = .03), but there was no statistical difference once exposure to lesbian, gay, bisexual, and transgender violence was taken into account ( Β = 3.31; SE = 2.36; P = .16). Gender identity variability was not associated with within-person change in depressive symptoms ( Β = 0.23; SE = 0.74; P = .75) or the level of depressive symptoms ( Β = 2.43; SE = 2.51; P = .33).
Conclusions These findings suggest that gender identity can evolve among SGM youths across time and that changes in gender identity are not associated with changes in depressive symptoms. Further longitudinal work should explore gender identity variability and adolescent and adult health.
Gender identity refers to one’s inner sense of being a man, a woman, or something else. 1 Transgender and gender diverse (TGD) people are those for whom gender identity does not align with societal expectations based on their sex assigned at birth. Recent studies 2 , 3 show that 1.4% to 1.8% of US youths identify as TGD.
For most people, gender identity is a stable aspect of the self 4 , 5 ; development or change in gender identity over time is less understood. Several studies 6 - 9 have explored whether children who met criteria for gender identity disorder (GID; an obsolete diagnostic criteria used in the Diagnostic and Statistical Manual of Mental Disorders [Fourth Edition]) in childhood still meet GID criteria in adolescence or adulthood. Approximately 85% of the children in these studies came to identify as a sexual minority without GID in adolescence or adulthood. 10 These studies refer to persistence and desistance of gender incongruence. However, interpretation from these studies are limited because a substantial proportion of study participants were subthreshold for GID diagnosis in childhood, 11 and using such outdated diagnostic criteria is problematic because one could meet GID in childhood criteria without necessarily identifying as TGD. 12 Nonetheless, recent work 13 , 14 indicates that a large majority of socially transitioned TGD children still identified as TGD 2.5 to 5 years later. Similarly, a UK study 15 found that among TGD youths, 91.7% continuously identified as TGD while being followed up by a gender clinic for minors.
For some, however, understanding of one’s gender may vary over time. 16 Some scholars refer to this variability as dynamic gender presentations, 16 gender journeys, 17 retransition, or detransition, 18 although there is no consensus on definitions of detransition. 19 Of note, Olson et al 13 found a 7.3% retransition rate among socially transitioned TGD children, indicating retransitions are not common in this group. Among adolescents and adults, it is estimated that 1% to 13% may experience retransition or detransition. 18 - 21 A recent longitudinal study 22 using a national probability sample found that approximately 1% of the US population reported different gender identities over a period of 4 years, a pattern more prevalent in younger than older generations. Importantly, among TGD people who reported past detransitions, external factors such as social rejection are often reported as reasons associated with detransitioning. 18 Little is known about gender identity variability among adolescents and young adults.
Recently, a controversial theory of rapid onset gender dysphoria (ROGD) was developed based on a survey of parents of TGD youths who transitioned in adolescence. 23 In the ROGD framework, gender dysphoria experienced by adolescents and young adults without prior indicators would be due to social contagion and compromised mental health and would disproportionately affect youths assigned female at birth. These youths would also experience a decline in mental health and functioning after transitioning. 23 The original publication has been criticized because of biased sampling and misleading interpretation 24 - 26 ; furthermore, a correction of the original work by Littman et al 23 emphasized that ROGD is not a formal diagnosis. 27 Recent cross-sectional studies 28 - 30 do not support the ROGD hypothesis. Longitudinal, community-based studies are needed to investigate whether people who transition to a TGD identity in adolescence report compromised mental health before gender identity transition or worsening mental health after. The only study, 22 to our knowledge, which explores how gender identity variability may affect health found that individuals whose gender identity varied over time engaged in more health-related risk behavior.
The current study assesses trajectories of gender identity in youths from a community-based sample, aged 15 to 21 years, over 4 assessment points, examining variability or changes in gender identity over time. Given that TGD youths often seek hormone therapy to treat gender dysphoria 31 , 32 and because exposure to lesbian, gay, bisexual, and transgender (LGBT) violence is associated with the mental health of TGD youths, 33 , 34 our analyses account for hormone and puberty blocker use and exposure to LGBT violence. Analyses investigated whether depressive symptoms varied across distinct trajectories of gender identity among youths, and associations of frequency of gender identity variability with depressive symptoms over time.
This cohort study was approved by the institutional review boards of New York University and the University of Arizona and followed the Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE ) reporting guideline. Data come from a community-based longitudinal study of sexual and/or gender minority (SGM) youths between the ages of 15 and 21 years at baseline (4 waves of data collection, every 9 months [2012-2015]). 35 See the flowchart of participants included in the study across waves in the eFigure in Supplement 1 . Community leaders recruited youths who identified as SGM from community-based agencies and college groups for SGM youths. Recruitment also occurred through referrals from other participants. Data were collected in 2 large cities in the US (1 in the Northeast and 1 in the Southwest) (eAppendix 1 in Supplement 1 ). Parental consent was waived for participants younger than 18 years to assure safety for youths who were not out to their parents; an independent representative was present to ensure youths participants’ assent. Those older than 18 years provided written informed consent. Participants received financial compensation. To capture gender identity variability, we focused on youths who participated in at least 3 waves of the study. At each wave, participants were coded as TGD when their gender identity did not match their sex assigned at birth.
A 2-step approach was used to assess youths gender identity. 36 First, sex at birth was assessed at wave 1 (male and female). Second, at waves 1 to 4, participants were asked, “What is your Gender Identity?” (response options included “man,” “woman,” “genderqueer,” “trans-woman,” “trans-man,” and write-in). Write-in responses were coded as either cisgender, binary transgender (ie, transgender woman or transgender man), or genderqueer and nonbinary. Examples of write-in responses included “woman, queer,” “gender non-conforming,” and “gender-fluid.” At each wave, the 2 measures were paired, and participants were categorized in 1 of 3 gender identities: (1) binary transgender, (2) genderqueer and nonbinary, or (3) cisgender.
A variable indicating the gender identity variability compared with the previous wave was generated for waves 2 to 4. Frequency of gender identity variability was measured as the number of times participants’ gender identity changed across the 4 waves of the study (from 0 to 3).
Depressive symptoms were measured utilizing the Beck Depression Inventory for Youth (BDI-Y), which assesses negative thoughts, sadness, and depressive symptoms. 37 A sum score was calculated, with higher scores indicating more depressive symptomatology (average internal consistency across waves of α = .94). Sum scores of 13 or less are considered normal; scores of 14 or greater may indicate mild to severe depressive symptoms.
Based on prior research, demographic characteristics described below were included in the adjusted models. They were included as possible confounders between factors and the outcome. 38 - 42
Time invariant demographic variables were collected at wave 1 and included age at baseline, sex assigned at birth (0 = male; 1 = female), receipt of free lunch in high school (0 = no; 1 = yes; 2 = not reported), and race and ethnicity (0 = non-Latino White; 1 = non-Latino Black; 2 = Latino; 3 = other race or ethnicity or did not report), and recruitment site (0 = Southwest; 1 = Northeast). The other race and ethnicity included Asian, Pacific Islander, American Indian or Alaska Native, and multiracial individuals, and was created due to small sample size of each of the individual categories. Race and ethnicity were included in the study to account for health disparities that may be associated with social determinants and societal marginalization. See Appendix 2 in Supplement 1 for detailed information on the measures utilized for this study.
Given that youths identifying as TGD tend to report more exposure to LGBT violence 43 and often seek puberty blockers and hormone therapy to reduce gender dysphoria 34 , 44 and that these factors are known to be associated with mental health, 31 , 33 , 34 these measures were included in final models as possible explanatory variables between transition and depression. Alternatively, exposure to LGBT violence could be a confounding variable between gender identity changes and depressive symptoms; prior work has suggested that TGD individuals may detransition as a response to stigma, 18 and exposure to LGBT violence is also associated with more depressive symptoms. 33
At waves 2 to 4, participants reported history of hormone therapy and puberty blocker use. Participants were asked, “Have you ever taken (a) hormone replacement therapy? or (b) puberty blockers?” (0 = no; 1 = yes).
Exposure to violence due to LGBT identity was assessed using a 6-item scale in which participants reported how often they had experienced different forms of LGBT violence (0 = never; 3 = at least 3 times). 45 At wave 1, participants were asked to consider these experiences in their lifetime. In subsequent waves, participants were asked to consider only the past 9 months. At each wave, a mean score was computed. To obtain a cumulative score, the sum score was calculated by adding the scores from the previous waves to each measure of exposure to LGBT violence across time.
Data were managed and analyzed using Stata 18.0 (StataCorp). First, we conducted analyses of variance to test group differences in frequency of gender identity variability. Bonferroni adjustments were applied to adjust for multiple group comparisons (significance for these analyses were set at P < .008). Hierarchical level modeling (HLM) was used to analyze trajectories of depressive symptoms. To estimate within- and between-person effects, time-varying factors (ie, cumulative exposure to LGBT violence and frequency of gender identity variability) were decomposed into 2 components; between-person (BP) components (level 2) are assessed by the person mean across waves; and within-person (WP) components (level 1) are assessed by the individual deviation from their own mean across waves. 46 Thus, the BP component contrasted depressive symptoms of youths who had more gender identity variability with other youths who had less or no gender identity variability, whereas the WP component contrasted depressive symptoms when a participant had more gender identity variability with other periods in which the same participant had less or no gender identity variability.
An empty mean model (ie, without factors included) was tested to estimate the degree to which depressive symptoms variation was associated with BP factors (intraclass correlation [ICC]). Unadjusted and adjusted models examined whether the trajectory of depressive symptoms varied across gender identity trajectory groups (model 1 and model 2, respectively). Based on model 2, model 3 investigated whether the frequency of gender identity variability was associated with depressive symptoms in both BP and WP levels, while also accounting for hormone and puberty blocker use and cumulative exposure to LGBT violence. Significance testing for HLM analyses were set at a 2-tailed P < .05. Given that missingness in key variables was substantively low (<3%), we addressed missing values with listwise deletion (at the waves participants had missing values) due to the low impact in the sample size (see the eTable in Supplement 1 for sensitivity analysis). HLM uses a mixed-effects model that works with all data available in longitudinal analyses. Data analysis was conducted from September 2022 to June 2023.
The analytic sample included 366 SGM youths (mean [SD] age, 18.61 [1.71] years; 181 [49.4%] assigned male at birth and 185 [50.6%] assigned female at birth; 149 Latino [40.7%]; 84 non-Latino Black [23.0%]; 75 non-Latino White [20.5%]; 58 [18.9%] other race or ethnicity or not reported) of whom 274 (74.9%) identified as cisgender at all waves and 92 (25.1%) identified as TGD at some point in the study. Descriptive statistics of the study participants are described in Table 1 . The majority of participants were recruited in the Northeast site (254 participants [69.4%]) and 196 participants (53.6%) had received free lunch in high school, indicating possible lower socioeconomic status. Trajectory patterns were categorized into 4 groups, including participants who were (1) cisgender across all waves (274 participants), (2) TGD (including binary transgender and genderqueer or nonbinary) across all waves (32 participants), (3) cisgender at wave 1 or 2 but by wave 4 identified as TGD (ie, cisgender to TGD [28 participants; 26 of these participants (92.9%) identified as cisgender at wave 1]), and (4) TGD at any wave but by wave 4 identified as cisgender (ie, TGD to cisgender [32 participants]). Overall, 1 in 5 participants (18.3%) reported a different gender identity over the study period.
While 20 of 32 participants (62.5%) in the TGD group reported hormone use, only 6 of 28 participants (21.4%) in the cisgender to TGD group, and 1 of 32 participants (3.1%) in the TGD to cisgender group had used hormones. Use of puberty blockers was reported by 12 of the 92 participants who identified as noncisgender (ie, binary transgender or genderqueer and nonbinary) during the study; the majority were from the TGD group. Table 2 displays cumulative exposure to LGBT violence scores for the 4 gender identity trajectory groups. Participants presented mild levels of depression across all waves (mean [SD], 13.61 [11.02]). 37
Figure 1 displays the proportion of gender identities for each trajectory group across waves. For participants from the cisgender to TGD and TGD to cisgender groups (ie, the groups defined by gender identity change), when they identified as TGD, they most often identified as genderqueer or nonbinary. The TGD group, nonetheless, most often identified as binary transgender (ie, transgender woman or transgender man). Changing gender identities at least twice was relatively common among noncisgender youths during the study (28 of 92 participants [30.4%]). The majority of youths in the TGD to cisgender group (19 of 32 participants [59.4%]) reported a different gender identity at least twice across waves. Youths in the TGD group reported fewer gender identity changes than the other 2 groups, but the TGD to cisgender and cisgender to TGD groups did not differ from one another.
The ICC results showed 58.5% of the variance of depressive symptoms was at the BP level, and 41.5% was at the WP level (ICC coefficient, 0.585; 95% CI, 0.536 to 0.633). HLM unconditional models indicated that depressive symptoms had a linear trajectory accounting for random effects. HLM analyses assessing trajectories of depressive symptoms show that at baseline (intercepts) in the unadjusted model (model 1), participants from the TGD and the cisgender to TGD groups reported higher levels of depression when compared with the cisgender group ( Β = 3.91; SE = 1.98; P = .048; vs Β = 4.66; SE = 2.10; P = .03) ( Table 3 and Figure 2 ). However, in the model adjusted for demographic characteristics (model 2), only the cisgender to TGD group statistically differed from the cisgender group ( Β = 4.82; SE = 2.10; P = .02). In this model, post hoc group comparisons indicated that the cisgender to TGD group also reported more depressive symptoms at baseline when compared with the TGD to cisgender group, but this finding was not significant ( Β = 6.02; SE = 2.30; P = .05). There were no gender identity trajectory group differences in the rate of change of depressive symptoms over time (slopes), and there were no differences based on post hoc group comparisons. Importantly, the baseline difference in depressive symptoms between cisgender to TGD group and cisgender group was not significant after accounting for exposure to LGBT violence (model 3, Β = 3.31; SE = 2.36; P = .16).
Lastly, tests of the association of gender identity variability with depressive symptoms over time (model 3) showed that, at the BP level, patterns of depressive symptoms did not differ for youths who reported more variability in gender identity compared with their counterparts who reported less or no gender identity variability ( Β = 2.43; SE = 2.51; P = .33). Furthermore, WP estimates indicated that youths did not report more depressive symptoms at times when they reported more gender identity variability compared with other periods when they reported less or no gender identity variability ( Β = 0.23; SE = 0.74; P = .75).
Gender identity is complex, and typically characterized as stable, or as a movement from cisgender to TGD (and for some, back to cisgender). Even longitudinal studies typically ask participants about their gender identity only once, overlooking ways that understanding of gender identity may vary or change for youths over time. Although a few longitudinal studies 13 , 14 have examined whether gender identity varies among socially transitioned TGD children, trajectories of gender identity in samples of youths are still not well understood. 47 , 48 In this community-based longitudinal cohort study, 1 in 5 (18.3%) youths reported a different gender identity over a period of approximately 3.5 years (the majority reported the same gender identity over time). Almost one-third of the youths who reported a different gender identity did so more than twice. These findings differ from clinical samples where the majority of TGD youths consistently identified as TGD, 15 but complement recent longitudinal work 48 revealing that while gender identity is stable for the majority of youths, shifts in gender identity are not uncommon and should not be considered abnormal. Our findings empirically support the idea that gender identity can be fluid or in development for some youths. 11 , 17 , 48 - 51 Importantly, while changes in gender identities can be driven by developmental gender identity exploration, 52 prior work has indicated that it can be driven by a social adaptation to stigma. 18
Much scientific and public attention has focused on mental health for TGD youths; our findings show that youths who reported the most change in gender identities during the study period (TGD to cisgender) were in one of the groups with the lowest levels of depression across all waves. It is possible that positive mental health can help youths feel comfortable exploring gender identity, despite societal stigma. Notably, depressive symptoms among participants in this group were stable over time. This stability might be a result of floor effects. Also, for this group, identity variability was typically between nonbinary and cisgender identities; they may have had less nonconforming gender expressions, which perhaps relates to their lower exposure to LGBT violence relative to other TGD groups. Furthermore, gender identity variability was not associated with more depressive symptoms, either between participants (BP) or for individuals over time (WP). Thus, youths who reported more changes in their gender identities were no different in terms of their mental health compared with those with fewer changes, and longitudinally, youths were not more depressed after a shift in their gender identities. These findings are more consistent with an explanation of adolescent gender identity exploration and development, rather than arguments that gender identity changes would be associated with compromised or worsening in mental health. 11
Our examination of groups based on gender identity trajectories (consistently cisgender or TGD, or reported changes to or from cisgender and TGD) showed that youths who reported the most change in gender identities over time (the cisgender to TGD and TGD to cisgender groups) tended to often identify as genderqueer or nonbinary, consistent with prior studies that show that youths more often identify with nonbinary gender identities. 29 , 48 , 53 It may be that youths who identify as genderqueer or nonbinary may be more comfortable with gender identity exploration.
Concerns about youths who identify as TGD have been raised in the past decade, particularly due to reports of greater numbers seeking treatment, 54 in particular by youths assigned female at birth. 47 , 54 , 55 Results from this study offer insight into several debates.
ROGD proponents suggest that the rising numbers of TGD-identifying youths are due to compromised mental health and social contagion. 23 Results of recent studies 28 , 29 are not consistent with these claims. Psychological well-being and demographic characteristics of youths referred to transgender clinics have been mostly consistent for more than a decade (except for sex ratio). 55 Furthermore, in a cross-sectional study, 28 later transgender identity acknowledgment was not associated with more compromised mental health among TGD youths. Findings from our study are also inconsistent with the ROGD hypothesis in at least 2 ways. First, although youths whose identities changed from cisgender to TGD reported higher levels of depressive symptoms when compared with consistently cisgender youths, these differences disappeared when we accounted for exposure to LGBT violence. Of note, they also experienced more exposure to LGBT violence than youths who identified consistently as cisgender, possibly due to higher gender nonconformity. 56 Second, our study indicates that youths who transitioned to TGD during the study (cisgender to TGD) experienced stable levels of depressive symptoms over time, a marked contrast with the argument that youths who identify as TGD in adolescence and early adulthood will experience worsening mental health. 23 , 24 Yet, despite being stable, youths from the cisgender to TGD group reported sustained high levels of depressive symptoms over time. In addition to the accumulation of exposure to LGBT violence among this group ( Table 2 ), transitioning to a more stigmatized identity may be mentally taxing because of exposure to new types of violence 57 (eg, gender-based violence), expectation of rejection from family and others, 1 , 45 and loss of support.
Despite substantial strengths of this study, including its community-based, longitudinal design, there are several limitations. While solely relying on self-reported gender identity, we were unable to examine, for example, which participants met the criteria for gender dysphoria. However, scholars have pointed out the importance of having youths report their own gender, 12 including providing not only binary options. 58 Furthermore, youths were not asked to explain variation in their gender identities. While transitions are part of developmental gender identity exploration for many youths, 52 prior work has shown that external pressures are often associated with detransitioning from a TGD identity. 18 , 59 We also do not know what proportion of these TGD youths went through social transitions (ie, changed pronouns or gender presentation to align with experienced gender); TGD youths may be more targeted for exposure to LGBT violence when they present themselves as TGD or in gender-nonconforming ways. Our findings may not be representative of all youths because our sample was recruited in part from SGM-focused community organizations. It could be that youths involved in these groups have a more positive sexual and gender identity development and receive more support in general. Additionally, the data from this study are more than a decade old, and much has changed in prevalence and visibility, care and affirmation, and political debates regarding TGD youths. 60 New prospective, community-based studies are needed to understand gender identity development and change, and associations with mental health for cisgender and TGD youths.
This cohort study documented a diversity of gender identity trajectories in adolescence and early adulthood. Changes in gender identity were not associated with depressive symptoms. Furthermore, the group of youths who reported the most change in gender identities were among those with the lowest level of depressive symptoms. These findings suggest a pattern in which gender identity exploration is a normal part of adolescent development for some youths. 48 , 52 Acknowledgment of this by health care clinicians 22 may help alleviate anxiety related to treating TGD youths whose gender identity may change across time. Although youths who changed from a cisgender to a TGD identity reported higher levels of depressive symptoms at baseline compared with consistently cisgender youths, these differences were explained by higher exposure to LGBT violence. Health care clinicians should pay particular attention to youths transitioning to TGD identities; additional support in this process can help mitigate the adverse effects of exposure to LGBT violence from peers or family rejection. Moreover, delays in providing care can result in more stress for these youths. 61 Ultimately, more longitudinal studies are needed to understand gender identity trajectories and health.
Accepted for Publication: March 8, 2024.
Published: May 22, 2024. doi:10.1001/jamanetworkopen.2024.11322
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Gonzales Real A et al. JAMA Network Open .
Corresponding Author: André Gonzales Real, MD, MSc, Department of Human Development and Family Sciences, The University of Texas at Austin, 108 E Dean Keeton St, Austin, TX 78712 ( [email protected] ).
Author Contributions: Drs Gonzales Real and Russell had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: Gonzales Real, Russell.
Drafting of the manuscript: Gonzales Real, Russell.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Gonzales Real.
Obtained funding: Russell.
Administrative, technical, or material support: Russell.
Supervision: Lobato, Russell.
Conflict of Interest Disclosures: None reported.
Funding/Support: This study was supported by the National Institutes of Mental Health (grant No. R01MH091212).
Role of the Funder/Sponsor: The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Mental Health.
Data Sharing Statement: See Supplement 2 .
Additional Contributions: The authors thank Jack L. Turban, MD, MHS (University of California, San Francisco), for providing insightful feedback on the manuscript, and Sae Hwang Han, PhD (The University of Texas at Austin), for consultation regarding statistical analyses. None of these individuals received compensation for their contributions.
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts

New Research Shows Increased Minority Stress and Associated Clinical Symptom Severity Among Hospitalized LGBTQ+ Youth
While LGBTQ+ adolescents are more likely to be psychiatrically hospitalized than their non-LGBTQ+ peers, little research has involved LGBTQ+ youth in crisis. New research conducted with adolescents in a psychiatric hospital in the Southeastern US finds that 62% of hospitalized adolescents identified as LGBTQ+ and reported more severe clinical symptoms than their non-LGBTQ+ peers. This research also shows that LGBTQ+ minority stress is linked to suicidality and depression among hospitalized LGBTQ+ youth.
These findings come from a paper published recently in Psychiatry Research by co-author Jessica M. Schwartzman, PhD, at Children’s Hospital Los Angeles, along with Drs. Alex Bettis at Vanderbilt University Medical Center and Kirsty Clark at Vanderbilt University. Dr. Schwartzman is the director of CHLA’s Training and Research to Empower NeuroDiversity (TREND) Laboratory in The Saban Research Institute . In the study, the researchers identify high rates of recent and lifetime minority stress experiences among LGBTQ+ youth in crisis.
The study examines minority stress—the idea that LGBTQ+ individuals encounter excessive identity-specific stress sources that harm mental health. Some stressors include experiences of discrimination and victimization which can lead to expectations of rejection and internalized negativity. In part due to experiences of minority stress, LGBTQ+ youth are disproportionately represented among populations hospitalized for psychiatric issues.
A Focus on Youth Perspectives

Expanding upon previous research, this study examines LGBTQ+ minority stress and clinical symptoms in psychiatrically hospitalized youth. “We found that LGBTQ+ adolescents had more severe mental health outcomes than other youth in the psychiatric inpatient unit, and that greater exposure to minority stress was linked with more severe mental health outcomes among hospitalized LGBTQ+ youth,” Dr. Schwartzman explains. The researchers highlight that the high rates of minority stressors facing LGBTQ+ youth in this study may also be influenced by regional contexts. “Adolescents in this study resided in the Southeastern U.S., where stigma due to anti-LGBTQ+ laws and social norms is high,” Dr. Schwartzman says.
After surveying these hospitalized youth to examine their LGBTQ+ minority stress experiences within the past 30 days and across their lifetimes, the researchers found that greater minority stress experiences were associated with higher levels of suicidal ideation, depression, and anxiety. Hostile school environments and negative future expectations were the most prevalent sources of stress among LGBTQ+ youth in crisis.
New Tools for Treatment
The study’s results represent a crucial step forward in how clinicians may think about assessment practices and treatment guidelines for psychiatrically hospitalized youth who identify as LGBTQ+. The results also highlight the need for safe spaces for LGBTQ+ youth at school, along with identity-affirming activities and interventions for LGBTQ+ youth in crisis.
Read more about this study in the journal Psychiatry Research .
Learn more about the TREND Lab at The Saban Research Institute.
Related content.
CHLA Researchers and Their Collaborators in RECOVER Initiative Publish Summary of Long COVID Symptoms in Children

How to Help Your Teen During COVID-19

How Do ‘Legacies of Stress’ Impact Future Generations?
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- About Adverse Childhood Experiences
- Risk and Protective Factors
- Program: Essentials for Childhood: Preventing Adverse Childhood Experiences through Data to Action
- Adverse childhood experiences can have long-term impacts on health, opportunity and well-being.
- Adverse childhood experiences are common and some groups experience them more than others.

What are adverse childhood experiences?
Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years). Examples include: 1
- Experiencing violence, abuse, or neglect.
- Witnessing violence in the home or community.
- Having a family member attempt or die by suicide.
Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding. Examples can include growing up in a household with: 1
- Substance use problems.
- Mental health problems.
- Instability due to parental separation.
- Instability due to household members being in jail or prison.
The examples above are not a complete list of adverse experiences. Many other traumatic experiences could impact health and well-being. This can include not having enough food to eat, experiencing homelessness or unstable housing, or experiencing discrimination. 2 3 4 5 6
Quick facts and stats
ACEs are common. About 64% of adults in the United States reported they had experienced at least one type of ACE before age 18. Nearly one in six (17.3%) adults reported they had experienced four or more types of ACEs. 7
Preventing ACEs could potentially reduce many health conditions. Estimates show up to 1.9 million heart disease cases and 21 million depression cases potentially could have been avoided by preventing ACEs. 1
Some people are at greater risk of experiencing one or more ACEs than others. While all children are at risk of ACEs, numerous studies show inequities in such experiences. These inequalities are linked to the historical, social, and economic environments in which some families live. 5 6 ACEs were highest among females, non-Hispanic American Indian or Alaska Native adults, and adults who are unemployed or unable to work. 7
ACEs are costly. ACEs-related health consequences cost an estimated economic burden of $748 billion annually in Bermuda, Canada, and the United States. 8
ACEs can have lasting effects on health and well-being in childhood and life opportunities well into adulthood. 9 Life opportunities include things like education and job potential. These experiences can increase the risks of injury, sexually transmitted infections, and involvement in sex trafficking. They can also increase risks for maternal and child health problems including teen pregnancy, pregnancy complications, and fetal death. Also included are a range of chronic diseases and leading causes of death, such as cancer, diabetes, heart disease, and suicide. 1 10 11 12 13 14 15 16 17
ACEs and associated social determinants of health, such as living in under-resourced or racially segregated neighborhoods, can cause toxic stress. Toxic stress, or extended or prolonged stress, from ACEs can negatively affect children’s brain development, immune systems, and stress-response systems. These changes can affect children’s attention, decision-making, and learning. 18
Children growing up with toxic stress may have difficulty forming healthy and stable relationships. They may also have unstable work histories as adults and struggle with finances, jobs, and depression throughout life. 18 These effects can also be passed on to their own children. 19 20 21 Some children may face further exposure to toxic stress from historical and ongoing traumas. These historical and ongoing traumas refer to experiences of racial discrimination or the impacts of poverty resulting from limited educational and economic opportunities. 1 6
Adverse childhood experiences can be prevented. Certain factors may increase or decrease the risk of experiencing adverse childhood experiences.
Preventing adverse childhood experiences requires understanding and addressing the factors that put people at risk for or protect them from violence.
Creating safe, stable, nurturing relationships and environments for all children can prevent ACEs and help all children reach their full potential. We all have a role to play.
- Merrick MT, Ford DC, Ports KA, et al. Vital Signs: Estimated Proportion of Adult Health Problems Attributable to Adverse Childhood Experiences and Implications for Prevention — 25 States, 2015–2017. MMWR Morb Mortal Wkly Rep 2019;68:999-1005. DOI: http://dx.doi.org/10.15585/mmwr.mm6844e1 .
- Cain KS, Meyer SC, Cummer E, Patel KK, Casacchia NJ, Montez K, Palakshappa D, Brown CL. Association of Food Insecurity with Mental Health Outcomes in Parents and Children. Science Direct. 2022; 22:7; 1105-1114. DOI: https://doi.org/10.1016/j.acap.2022.04.010 .
- Smith-Grant J, Kilmer G, Brener N, Robin L, Underwood M. Risk Behaviors and Experiences Among Youth Experiencing Homelessness—Youth Risk Behavior Survey, 23 U.S. States and 11 Local School Districts. Journal of Community Health. 2022; 47: 324-333.
- Experiencing discrimination: Early Childhood Adversity, Toxic Stress, and the Impacts of Racism on the Foundations of Health | Annual Review of Public Health https://doi.org/10.1146/annurev-publhealth-090419-101940 .
- Sedlak A, Mettenburg J, Basena M, et al. Fourth national incidence study of child abuse and neglect (NIS-4): Report to Congress. Executive Summary. Washington, DC: U.S. Department of Health an Human Services, Administration for Children and Families.; 2010.
- Font S, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: The role of adult socioeconomic conditions. Child Abuse Negl. 2016;51:390-399.
- Swedo EA, Aslam MV, Dahlberg LL, et al. Prevalence of Adverse Childhood Experiences Among U.S. Adults — Behavioral Risk Factor Surveillance System, 2011–2020. MMWR Morb Mortal Wkly Rep 2023;72:707–715. DOI: http://dx.doi.org/10.15585/mmwr.mm7226a2 .
- Bellis, MA, et al. Life Course Health Consequences and Associated Annual Costs of Adverse Childhood Experiences Across Europe and North America: A Systematic Review and Meta-Analysis. Lancet Public Health 2019.
- Adverse Childhood Experiences During the COVID-19 Pandemic and Associations with Poor Mental Health and Suicidal Behaviors Among High School Students — Adolescent Behaviors and Experiences Survey, United States, January–June 2021 | MMWR
- Hillis SD, Anda RF, Dube SR, Felitti VJ, Marchbanks PA, Marks JS. The association between adverse childhood experiences and adolescent pregnancy, long-term psychosocial consequences, and fetal death. Pediatrics. 2004 Feb;113(2):320-7.
- Miller ES, Fleming O, Ekpe EE, Grobman WA, Heard-Garris N. Association Between Adverse Childhood Experiences and Adverse Pregnancy Outcomes. Obstetrics & Gynecology . 2021;138(5):770-776. https://doi.org/10.1097/AOG.0000000000004570 .
- Sulaiman S, Premji SS, Tavangar F, et al. Total Adverse Childhood Experiences and Preterm Birth: A Systematic Review. Matern Child Health J . 2021;25(10):1581-1594. https://doi.org/10.1007/s10995-021-03176-6 .
- Ciciolla L, Shreffler KM, Tiemeyer S. Maternal Childhood Adversity as a Risk for Perinatal Complications and NICU Hospitalization. Journal of Pediatric Psychology . 2021;46(7):801-813. https://doi.org/10.1093/jpepsy/jsab027 .
- Mersky JP, Lee CP. Adverse childhood experiences and poor birth outcomes in a diverse, low-income sample. BMC pregnancy and childbirth. 2019;19(1). https://doi.org/10.1186/s12884-019-2560-8 .
- Reid JA, Baglivio MT, Piquero AR, Greenwald MA, Epps N. No youth left behind to human trafficking: Exploring profiles of risk. American journal of orthopsychiatry. 2019;89(6):704.
- Diamond-Welch B, Kosloski AE. Adverse childhood experiences and propensity to participate in the commercialized sex market. Child Abuse & Neglect. 2020 Jun 1;104:104468.
- Shonkoff, J. P., Garner, A. S., Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. https://doi.org/10.1542/peds.2011-2663
- Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsych. 2017;87(1):3. https://doi.org/10.1037/ort0000133 .
- Schofield TJ, Donnellan MB, Merrick MT, Ports KA, Klevens J, Leeb R. Intergenerational continuity in adverse childhood experiences and rural community environments. Am J Public Health. 2018;108(9):1148-1152. https://doi.org/10.2105/AJPH.2018.304598 .
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. J Adolesc Health. 2013;53(4 Suppl):S32-38. https://doi.org/10.1016/j.jadohealth.2013.05.004 .
Adverse Childhood Experiences (ACEs)
ACEs can have a tremendous impact on lifelong health and opportunity. CDC works to understand ACEs and prevent them.

IMAGES
VIDEO
COMMENTS
Research Proposal on Depression among Teenagers - Free download as Word Doc (.doc / .docx), PDF File (.pdf), Text File (.txt) or read online for free. The document discusses depression among teenagers, including causes, symptoms, effects, and treatments. It provides background on depression, stating that it is a common mental health problem worldwide and in the Philippines that can negatively ...
There is a lack of research in health psychology on the subjective experience of adolescents with mental health disorders. The aim of this study was to explore the experience of depression and the journey into therapy of young people (YP) diagnosed with depression. Semi-structured interviews were carried out with six YP (5 female, aged 15-19).
and gender differences in depression among young people in Sweden. Three different materials were used to capture a broad picture of the role of social position, gender and depression, in adolescence (13-17 year olds) and in young adulthood (18-32 year olds). 1) Longitudinal survey data from the BROMS cohort was used to assess the risk of
Epidemiologic Features. Although the prevalence of depression has increased across all age groups, the increase among adolescents has outpaced that among adults. 3 The lifetime prevalence of major ...
Abstract. Three to nine per cent of teenagers meet the criteria for depression at any one time, and at the end of adolescence, as many as 20% of teenagers report a lifetime prevalence of depression. Usual care by primary care physicians fails to recognize 30-50% of depressed patients. Cross-sectional one-time observational study using simple ...
Background: Depression is a common mental health disease, especially in mid to late adolescence that, due to its. particularities, is a challenge and requires an effective diagnosis. Primary care ...
At the same time, rates of depression, distress, and burden continue to rise for children and adolescents, and this prevalence-intervention gap is widening. We believe there is a New Hope for the future of youth depression research that can rise to meet these challenges and offer avenues to reduce distress and burden around the world.
Adolescent depression is a particularly important mental health disorder, and its recognition and treatment have important short and long-term mental health implications. Adolescence is a critical time for mental well-being, as almost 75% of adult mental illnesses have origins during childhood and youth [1,2,3,12,13].
Notably, Daly also found that rates of depression increased from 2009 to 2019 among adolescents in all racial/ethnic categories assessed, though the percentage change among adolescents who identified as Black (4.1%) was relatively smaller than that among adolescents who identified as White (7.5%), Hispanic (9.7%), or other race/ethnicity (9.2% ...
Nine studies targeted a youth sample. An additional two included adults and youth. Three studies examined whether affective awareness is related to depression in youth by using EMA as an intervention, and by linking indirect momentary reports to self-report state measures [33,34,35].One study used EMA as an intervention and measured depression and other emotional experiences but did not ...
Much of the research to date has studied young people of later adolescence and college or university students. ... (Citation 2015) found a significant association between Facebook addiction and depression among 972 high school pupils in affluent districts in Thailand. A study of Chinese secondary school students by Li et al. ...
Depression and anxiety are the most widely recognized mental issues affecting youths. It is extremely important to investigate the burden and associated risk factors of these common mental disorders to combat them. Therefore, this study was undertaken with the aim to estimate the prevalence and identify factors associated with depression, anxiety, and stress among high school students in an ...
Depression rates in young people have risen sharply in the past decade, especially in females, which is of concern because adolescence is a period of rapid social, emotional, and cognitive development and key life transitions. Adverse outcomes associated with depression in young people include depression recurrence; the onset of other psychiatric disorders; and wider, protracted impairments in ...
This paper summarizes many findings about depression among children and adolescents. Depression is prevalent, highly distressing, and exerts considerable burden worldwide. Rates surge from childhood through young adulthood and have increased over the last decade. Many risk factors have been identified, and evidence-based interventions exist targeting mostly individual-level changes via ...
university students, found the rate of depression among Nigerian students was only 2.7%. This is much lower compared to the rate of depression among Nigerian outpatients visiting. general clinics ...
446 n engl j med 385;5 nejm.org July 29, 2021 The new england journal of medicine in adolescents, including annual universal screen - ing for depression in children 12 to 18 years of age with the ...
Researchers have proposed that large-scale studies are needed to examine associations between risk and protective factors and depression among young people (Ghazavi et al., 2016; McKinley et al., 2021).The current study, therefore, examined the relations among risk and protective factors for adolescents whose caregivers reported that they had depression in the 2019 National Survey of Children ...
Nevertheless, the prevalence of depression in adolescence varies sig-nificantly between studies and reports. A reported preva-lence in Great Britain was 4%, whereas in the USA was 2.1% and in France was 11.0% [5 -7]. Nevertheless, a sys-tematic review from 2013 stated the life prevalence of depression varies from 1.1 to 14.6% [8].
RESEARCH PROPOSAL- DEPRESSION IN TEENS. Introduction Depression is identified as a mood disorder that can affect the daily life of an individual, whereby basically at the moment teenagers are the most affected with depression due to the various predisposing factors that expose them to depression. Teen are relatively young, and range from the ages of 11 to 19 years.
Sadly, psychological distress among young people seems to be rising. One study found that rates of depression among a nationally representative sample of US adolescents (aged 12 to 17) increased ...
Tragically, 6,200 suicide deaths were reported in 2017 among U.S. adolescents and young adults from 15 to 24 years of age ( 3 ), and suicide is the second leading cause of death among individuals 10-34 years of age ( 4 ). As with other psychiatric illnesses, the risks for developing anxiety disorders and major depression are due to ...
In the United States, recent data has shown a disturbing increase in suicide rates among children and adolescents. Recent data has shown a disturbing increase in suicide rates among this demographic. According to the Centers for Disease Control and Prevention (CDC), suicide is now the second leading cause of death for people ages 10-24 years ...
In a new study, researchers investigated the association among social media use, depression and other health-related behaviors of young adults over time. Share: Facebook Twitter Pinterest LinkedIN ...
43% of young men aged 19-29 are at risk of depression Moderate-to-high anxiety impacts 57% of young men, 45% of gay or bisexual men, and 42% of racialized men National study from the Canadian Men ...
Introduction. Over the past several decades, adolescent depression and suicidal behaviours have increased considerably. In the USA, depression diagnoses among youth increased from 8.7% in 2005 to 11.3% in 2014 (Mojtabai, Olfson, & Han, 2016).Additionally, suicide is the second leading cause of death among youth between the ages of 10 and 34 (Centers for Disease Control and Prevention, National ...
Key Points. Question Are gender identity trajectories and changes in youth-reported gender identity associated with depressive symptoms over time?. Findings In this cohort study involving 366 sexual and/or gender minority youths (aged 15-21 years), 1 in 5 (18.2%) reported a different gender identity over time. Youths transitioning to a transgender or gender diverse identity reported higher ...
New research conducted with adolescents in a psychiatric hospital in the Southeastern US finds that 62% of hospitalized adolescents identified as LGBTQ+ and reported more severe clinical symptoms than their non-LGBTQ+ peers. This research also shows that LGBTQ+ minority stress is linked to suicidality and depression among hospitalized LGBTQ+ youth.
Today's adolescents, aged 10-19 years, face unprecedented challenges amidst a rapidly evolving world, according to a new report calling for greater investments in adolescent well-being. The report, released at the 77th World Health Assembly, was commissioned by The Partnership for Maternal, Newborn & Child Health, working with Victoria Institute of Strategic Economic Studies of Victoria ...
The report pulls together research that links social media use and poor mental health in adolescents, such as a 2019 study that found teens who spent more than three hours a day on social media ...
Estimates show up to 1.9 million heart disease cases and 21 million depression cases potentially could have been avoided by preventing ACEs. 1. ... Brener N, Robin L, Underwood M. Risk Behaviors and Experiences Among Youth Experiencing Homelessness—Youth Risk Behavior Survey, 23 U.S. States and 11 Local School Districts. Journal of Community ...