An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- J Med Internet Res
- PMC10407648


Ten Topics to Get Started in Medical Informatics Research
Markus wolfien.
1 Institute for Medical Informatics and Biometry, Faculty of Medicine Carl Gustav Carus, Technische Universität Dresden, Dresden, Germany
2 Center for Scalable Data Analytics and Artificial Intelligence, Dresden, Germany
Najia Ahmadi
3 Core Unit Data Integration Center, University Medicine Greifswald, Greifswald, Germany
Sophia Grummt
Kilian-ludwig heine, dagmar krefting.
4 Department of Medical Informatics, University Medical Center, Goettingen, Germany
Andreas Kühn
Ines reinecke, julia scheel.
5 Department of Systems Biology and Bioinformatics, University of Rostock, Rostock, Germany
Tobias Schmidt
6 Institute for Medical Informatics, University of Applied Sciences Mannheim, Mannheim, Germany
Paul Schmücker
Christina schüttler.
7 Central Biobank Erlangen, University Hospital Erlangen, Friedrich-Alexander-Universität Erlangen-Nürnberg, Erlangen, Germany
Dagmar Waltemath
8 Department of Medical Informatics, University Medicine Greifswald, Greifswald, Germany
Michele Zoch
Martin sedlmayr.
The vast and heterogeneous data being constantly generated in clinics can provide great wealth for patients and research alike. The quickly evolving field of medical informatics research has contributed numerous concepts, algorithms, and standards to facilitate this development. However, these difficult relationships, complex terminologies, and multiple implementations can present obstacles for people who want to get active in the field. With a particular focus on medical informatics research conducted in Germany, we present in our Viewpoint a set of 10 important topics to improve the overall interdisciplinary communication between different stakeholders (eg, physicians, computational experts, experimentalists, students, patient representatives). This may lower the barriers to entry and offer a starting point for collaborations at different levels. The suggested topics are briefly introduced, then general best practice guidance is given, and further resources for in-depth reading or hands-on tutorials are recommended. In addition, the topics are set to cover current aspects and open research gaps of the medical informatics domain, including data regulations and concepts; data harmonization and processing; and data evaluation, visualization, and dissemination. In addition, we give an example on how these topics can be integrated in a medical informatics curriculum for higher education. By recognizing these topics, readers will be able to (1) set clinical and research data into the context of medical informatics, understanding what is possible to achieve with data or how data should be handled in terms of data privacy and storage; (2) distinguish current interoperability standards and obtain first insights into the processes leading to effective data transfer and analysis; and (3) value the use of newly developed technical approaches to utilize the full potential of clinical data.
Introduction
Digital health care information, as opposed to analog information, empowers clinicians, researchers, and patients with a wealth of information aiming to improve diagnosis, therapy outcome, and clinical care in general. According to Wyatt and Liu [ 1 ], medical informatics is the study and application of methods to improve the management of patient data, clinical knowledge, population data, and other information relevant to patient care and community health. Medical informatics can be seen as the subset of health informatics that is focused on clinical care, while the latter encompasses a wider range of applications. However, knowing, integrating, and using current computational technologies bears numerous pitfalls, limitations, and questions [ 2 ]. To shed light on current standards, applications, and underlying technologies, we present 10 topics to get started in the field of medical informatics research. Our key objective here was to improve interdisciplinary communication among stakeholders (eg, clinicians, experimental researchers, computer scientists, students, patient representatives), thereby bringing everyone on the same page of state-of-the-art medical informatics practices. In particular, improved interdisciplinary communication is essential in real-world problems and can be motivated by the following aspects:
- Advancing open research: Open collaboration between parties from different disciplines can lead to new research questions, innovative approaches, and novel discoveries [ 3 ].
- Bridging knowledge domains: Interdisciplinary communication can stimulate novel solutions, allowing researchers to gain a more comprehensive understanding of a specific problem or phenomenon [ 4 ], or can improve clinical decision-making [ 5 ].
- Addressing complex problems: Complex problems, such as the latest disease outbreak, require input from multiple domains to be comprehensively understood. Here, interdisciplinary communication is one key aspect to pinpoint the root causes and develop effective solutions [ 6 ].
- Promoting scientific inclusivity and diversity: Interdisciplinary communication was recently shown to foster diversity and inclusivity in science, by bringing together researchers from different backgrounds, cultures, and perspectives [ 7 , 8 ].
Here, we describe in detail how the initial topics have been selected from the literature and what design principles and structure each topic follows. A brief outline of the utilized methods for topic dissemination and an exemplary embedding into an educational training program are also presented.
Topic Selection
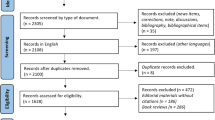
The initial topics were defined based on current developments in the health informatics field and an increasing number of published manuscripts between 2000 and 2021 (based on title-abstract-keyword screening in Scopus using the keywords “Health” AND “Informatics” AND “domain”) in the respective subdomains ( Figure 1 A). After a first definition of the specific topics, these were critically revised by internal and external domain experts, as well as scientists previously not familiar with medical informatics research.

Schematic summary and representation of the presented topics: (A) brief literature screening (title-abstract-keywords) for published manuscripts between 2000 and 2021, and the y-axis gap provides improved visibility of the less-occurring keywords; (B) most common topic terminologies, keywords (color-coded sections), and potential connections (grey) among topics in the medical informatics research domain. CDSS: clinical decision support system; CIS: clinical information system; EHR: electronic health record; ETL: extract, transform, and load; FAIR: findable, accessible, interoperable, reusable; FHIR: Fast Healthcare Interoperability Resources; GDPR: General Data Protection Regulation; i2b2: Informatics for Integrating Biology and the Bedside; OMOP: Observational Medical Outcomes Partnership.
Topic Design
The initial number of important topics and keywords exceeded the anticipated number of 10 topics, which found inspiration from the “Ten Simple Rules” collection in PLOS Computational Biology [ 9 ]. This is why the authors merged the most matching terms topic wise into groups. These groups finally produced topics that represent the broad range of the medical informatics domain in 3 main concepts, namely “Regulations and concepts,” “Harmonization and processing,” and “Evaluation, visualization, and dissemination” ( Figure 1 B). Figure 1 B also shows the initial keywords for each individual topic, as well as potential cross references between topics, which are highlighted in grey. The following sections provide important “do's and don'ts,” practical hints, and best practice guidelines. Further in-depth resources and practical tutorials will provide basic introductions to the referred domains. Kohane et al [ 10 ] already showed the importance of such clarifying introductions. This work extends the initial study and, in addition, provides detailed examples from the German national Medical Informatics Initiative (MII) [ 11 ].
All topics were divided into 3 parts to improve comprehension by the readers:
- Introduction: Background definitions for the specific context that motivated the topic
- Insight: Practical context to get started, including how to avoid pitfalls, state current limitations, and address current challenges
- Impact: Take home message and useful resources and best practices to deepen knowledge about the topic
Topic Utilization, Extension, and Embedding
Since it is of the utmost importance to keep the content current and as versatile as possible, we initiated an online resource at GitHub, in which contributions are highly emphasized [ 12 ]. Here, keywords and the corresponding literature are collected to allow for swift extension of the currently presented literature body in this article. In addition, the introduction of novel important topics that are not covered in this article might be included. To additionally demonstrate the practicability and adaptability of our proposed topic content, we exemplarily present how these can be embedded in higher education training and share external, introductory hands-on material ( Table 1 ).
Summary of tutorials and hands-on material about medical informatics standards and applications.
a SNOMED CT: Systematized Nomenclature of Medicine and Clinical Terms.
b ETL: extract, transform, and load.
c OMOP: Observational Medical Outcomes Partnership.
d CDM: common data model.
e FHIR: Fast Healthcare Interoperability Resources.
f OHDSI: Observational Health Data Sciences and Informatics.
g PLP: patient-level prediction.
h ODI: Open Data Institute.
Regulations and Concepts
Topic 1: privacy and ethics—“data privacy and ethics are the most important assets in the clinical domain.”.
Health information is sensitive and hence needs to be highly protected and should not be generously shared. Sharing regulations and data privacy matters are defined in the European General Data Protection Regulation (GDPR) [ 13 ]. The implementation of the GDPR is an ongoing process as the quickly evolving technology, data, and scientific practices demand continuous improvement, which include periodic adaptations of the technical and legal aspects [ 14 , 15 ]. In terms of ethics and with the rise of novel technologies, like artificial intelligence (AI), the possible re-identification of data, such as images and genomic information, is a major concern [ 16 , 17 ].
Anonymization is one important way to keep data private. It can also be achieved for high-dimensional data by changing patient-specific identifiers through removal, substitution, distortion, generalization, or aggregation [ 18 ]. In contrast, data pseudonymization is another de-identification procedure by which personally identifiable information fields within a data record are replaced by one or more artificial identifiers or pseudonyms [ 19 ]. To overcome the paucity of annotated medical data in real-world settings and (fully) save the patients’ anonymity, synthetic data generation is used to increase the diversity in data sets and to enhance the robustness and adaptability of AI models [ 20 ]. To conform with ethical regulations in a research context, medical data are only available in a highly controlled manner and according to strict procedures. New concepts, such as “systemic oversight” [ 21 ] or “embedded ethics” [ 22 ], might be needed to tackle the new data-driven developments around “medical big data” and AI in health care. To engage with the adoption of broad consent, systemic oversight was suggested as an approach, in which mechanisms like auditing mechanisms, expert advice, and public engagement initiatives (among others) should be adapted as additional layers to the newly arising ecosystem of health data [ 21 ]. Recently, embedded ethics was jointly suggested by ethicists and developers to address ethical issues via an iterative and continuous process from the outset of development, which could be an effective means of integrating robust ethical considerations into practical development [ 22 ]. A digital representation of information encoded in signed consent forms is needed to facilitate common data use and sharing, as already implemented in an MII informed consent template [ 23 ].
As a researcher in medical informatics, it is inevitable to be informed and knowledgeable about the fact that patients own their medical records and any use of those data requires great care. In Germany, health care providers can only use the data for first medical use. Secondary use, like research, needs to be approved by either broad or individual consent, which can be made available via the electronic health record (EHR). In addition to digitization efforts, it is still a considerable hurdle to convince patients to make their data available for medical research because personal skepticism commonly makes the entire data acquisition process more difficult [ 24 ]. Here, well-received external communication, transparency, and increased awareness are necessary for substantial improvements. In general, it is a balance between privacy, patient needs, and the use of data for the common good versus economic interests [ 25 ]. In particular, one should be aware of the specific legal regulations that apply within the country and additionally get in touch with the relevant data protection departments. Following this, a plan for infrastructure that meets these regulations and that contains, for example, a trustee for the electronic recording of patient consent and anonymization or direct pseudonymization processes to collect the data needs to be developed. Risk assessments for potential data leakage, approvals by ethics committee, as well as consultation with a data protection officer are essential considerations to further assure data security.
Topic 2: EHR and Clinical Information Systems—“Get to Know Your Clinical Information System to Understand the Required Data.”
Hospitals run clinical information systems (CIS) to collect, store, and alter clinical data about patients. A CIS, independent of the specialization and specific vendor, covers many clinical subdomains and integrates patient-related data to support doctors in their daily routine. Without a doubt, medical data are only useful if meaningful information can be derived from them. This requires high-quality data sets, seamless communication across IT systems, and standard data formats that can be processed by humans and machines [ 2 ]. Typical challenges in clinical IT implementations, especially for patient recruitment systems, were recently evaluated by Fitzer et al [ 26 ] for 10 German university hospitals, including requirements for data, infrastructure, and workflow integration. The implementation of an EHR, including an individual's medical data in a bundled form, into the CIS is a key aspect to prevent low reliability and poor user-friendliness of EHRs, which has recently been shown to affect time pressure among medical staff [ 27 ]. For example, in Scandinavia, the United States, and the United Kingdom, the Open Notes initiative [ 28 ] facilitates patients’ access to EHRs and health data sharing via “PatientsKnowBest ” to give health care professionals and families direct access to medical information [ 29 ].
An EHR is used primarily for the purposes of setting objectives and planning patient care, documenting the delivery of care, and assessing the outcomes of care [ 30 ]. EHRs have so far consisted of unstructured, narrative text as well as structured, coded data. Thus, it will be necessary to implement more systematic terminologies and codes so that the data contained in these records can be reused in clinical research, health care management, health services planning, and government reporting in an improved manner [ 31 , 32 ]. Since the domain of medical informatics is rather new, there are many possibilities for software solutions to improve EHR-related issues [ 33 ]. Exemplary for the EHR domain, the Systematized Nomenclature of Medicine and Clinical Terms (SNOMED CT) is utilized to develop comprehensive high-quality clinical content [ 34 ]. It provides a standardized way to represent clinical phrases captured by the clinician and enables automatic interpretation of these, which is showcased in a “five-step briefing” [ 35 ]. Interestingly, the number of annual publications on this subject has decreased since 2012. However, the need for a formal semantic representation of free text in health care remains, and automatic encoding into a compositional ontology could be a solution [ 36 ]. In terms of usability and user acceptance, evaluations and improvements of EHRs and clinical decision support systems (CDSS) are currently ongoing [ 37 ], for which already well-received examples can be attributed to CeoSYS [ 38 ] or the IPSS-M Risk Calculator [ 39 ]. Moreover, the actions of patients directly contributing to their own EHR records are also being evaluated. The study by Klein et al [ 40 ] indicates that such an approach facilitates the development of individual solutions for each patient, which in turn requires a flexible EHR during the course of a treatment process. Additionally, it was argued that data incorporation via different devices can also facilitate the convenient utilization of the application and, hence, may increase secondary use.
Modern CIS support the interaction by doctors and patients with the recorded patient data (eg, using the EHR or patient portals, eHealth platforms). It is important to understand the basic architecture, especially challenges [ 26 ], of the hospital IT infrastructure to know where data are located and how they can be retrieved and integrated. Major improvements can be made when supporting international standards for data exchange. Beyond standard EHR, this includes interoperability standards like Fast Healthcare Interoperability Resources (FHIR; see Topic 6) and standard data models like the Observational Medical Outcomes Partnership (OMOP; see Topic 7). These criteria should be considered with every new order of clinical systems.
Topic 3: Data Provenance—“Trace Your Data, Even Within Large-scale Efforts.”
Meaningful and standardized metadata facilitate the interpretation of, retrieval of, and access to data [ 41 ]. When explainable data are processed with interoperable tools, scientists can create automated and reusable workflows and provide access to reproducible research outcomes and data analysis pipelines [ 42 ].
Data provenance describes the history of digital objects, where they came from, how they came to be in their present state, and who or what acted upon them [ 43 ]. In health care, provenance maintains the integrity of digital objects (eg, the results of data analyses engender greater trust if their provenance shows how they were obtained). In addition, it can be used to deliver auditability and transparency, specifically, in learning health systems, and it is applicable across a range of applications [ 44 ]. Inau et al [ 45 ] argued that the lessons learned from “FAIRification” processes in other domains will also support evidence-based clinical practice and research transparency in the era of big medical data and open research. Further work demonstrated that a findable, accessible, interoperable, reusable (FAIR) research data management plan can provide a data infrastructure in the hospital for machine-actionable digital objects [ 46 ]. Recently, the openEHR approach was also suggested for creating FAIR-compliant clinical data repositories as an alternative representation [ 47 ].
Key data management requirements are defined by the FAIR guiding principles [ 48 ]. Since data protection laws led to additional requirements for data privacy and data security, the FAIR-Health principles focused on defining additional requirements for information on the sample material used from biobanks, for provenance information, and incentive schemes [ 49 ]. Further work is needed to establish provenance frameworks in health research infrastructures [ 50 ].
Topic 4: Data Sharing—“If Data Won’t Come to the Model, the Model Must Go to the Data.”
Cross-sectional medical data-sharing is critical in modern clinical practice and medical research, in which the challenge of privacy-preserving transfer and utility needs to be addressed [ 51 ]. In order to facilitate high reuse of the data, a decentralized computational scheme that treats the available data as part of a federated (virtual) database, avoiding centralized data collection, processing, and raw data exchanges, is still needed in many countries to analyze large and widespread clinical data [ 52 ].
One possible solution for this federated learning approach is DataSHIELD [ 53 ]. In particular, orchestrating privacy-protected analyses of “medical big data'' from different resources is applicable within R and DataSHIELD [ 54 ]. Here, the developed computerized models represent mathematical concepts or trained machine learning (ML)–based approaches to solve a specific task. In this sense, the model is applied to distributed data sets of the protected (clinical) server infrastructure, and the user only sees the model results but does not retrieve any medical records. Moreover, implementations in other programming languages (eg, Python, Julia) have been introduced in the genomic domain and beyond [ 55 ]. Further concepts, such as Personal Health Train, specifically follow the FAIR principles during distributed analyses [ 56 ]. Secure multiparty computation (SMPC) is also a viable technology for solving clinical use cases that require cross-institution data exchange and collaboration [ 57 ]. Current limitations are thought to be addressed in a stepwise manner [ 58 ] or as blockchain [ 59 ].
By using approaches for distributed analyses, researchers are able to train, test, and validate their models on large-scale real-world clinical data. In combination with standardized data formats, these 2 concepts facilitate the use of those models in clinical routine, potentially in the form of a CDSS. This provides a basis for secondary use of observational data in the context of clinical trials, which show particular potential for identifying data characteristics in small cohorts (eg, identification of the individual patient risk for rare diseases or comorbidities).
Harmonization and Processing
Topic 5: extract, transform, and load (etl)—“ etl processes are computational approaches for data harmonization and data unification.”.
Data handling in medical informatics remains a major challenge. Even though most data in medicine are available electronically, the data often lack interoperability [ 60 ]. As a first step to actually use the data, processes to extract, transform, and load (ETL) are needed to obtain harmonized data from different data systems or clinical entities. One important example, among many others, reflects the uniform representation of the date and time in a common format (eg, Year-Month-Date, not Date-Month-Year). The ETL process is therefore a crucial, individual step toward data unification in large clinical systems, which must be secure, safe, and accurate [ 61 ].
The design of an ETL process faces several challenges, including the following: (1) The ETL process should be able to process huge amounts of data at once [ 62 ]; (2) the ETL process should be repeatable—if the source data change, the ETL process needs to be rerun to process the source data (Observational Health Data Sciences and Informatics [OHDSI]) [ 63 ]; (3) expert-level anonymization methodologies might be integrated into ETL workflows whenever possible [ 61 ]; and (4) there is a need to check for loss of data and compromised data integrity. The latter was highlighted in a recent study, in which inaccurate cohort identification took place because erroneous vocabulary mappings of a common data model were used (eg, ETL programming bugs and errors not captured during the quality assurance stages) [ 64 ]. Common solutions to implement ETL processes are code-based (eg, FHIR-to-OMOP [ 65 ]) or via Pentaho Data Integration, which is one of many ETL tools. Further subsequent processing may also include loading data into research data repositories, like OMOP (see Topic 7), tranSMART, and Talend Open Studio, which is a central component of the Integrated Data Repository Toolkit [ 66 ].
Since ETL processes are at the core of data handling, all risks associated with the ETL process need to be thoroughly checked, identified, and assessed, and contingency plans to mitigate these risks should be in place [ 67 ]. Once the ETL processes are executed, the resulting data will be trusted by researchers, who heavily rely on comprehensively checked data integrity to be able to conduct their research on this basis.
Topic 6: FHIR—“Set FHIR to Gain a Communication Standard for Real-time Applications at the Device-to-Device Level.”
Interoperability levels can be divided into technical, syntactic, semantic, and organizational interoperability [ 2 ]. Semantic and syntactic interoperability can be ensured by communication exchange standards, such as the FHIR [ 68 ] standard of Health Level 7 (HL7) and medical terminologies. A suitable starting point for the basic procedures is offered by FHIR drills [ 69 ] or fire.ly [ 70 ].
FHIR is one of many communication standards but will likely change the domain of clinical IT significantly [ 71 , 72 ]. As a communication standard, FHIR harmonizes data formats coming from different CIS and enables data exchange between institutions via a RESTful approach [ 73 ]. Moreover, FHIR is used to connect devices with each other, which means, in particular, that the Integrating the Healthcare Enterprise (IHE) [ 74 ] standard has been revised to support HL7 messaging as well. In turn, IHE has been developing an open-source device tool set for home and hospital use that recently enabled device control capabilities, a capability accelerated during the COVID-19 pandemic to allow nurses and physicians to operate ventilators and infusion devices outside the contaminated patient room [ 75 ].
Utilizing FHIR in multiple applications already shows its versatile and flexible use (eg, in mobile health applications [ 76 ], electrocardiogram monitoring [ 77 ], or wearable devices and precision medicine in digital health [ 72 ]). In particular, the SMART-on-FHIR technology enables third-party app development for health care applications [ 78 ] and encompasses feasible, secure, and time- and resource-efficient solutions [ 79 , 80 ].
Topic 7: OMOP—“Use Common Data Models as Well-defined Representations of Large-scale Research Projects.”
Data harmonization enables research teams to run real-world observational studies based on heterogeneous data across country borders. Thus, harmonized data embedded in a common data model (CDM), which is an agreement about the utilization of standardized terminologies for data representation, is crucial to exchange data and results on a large scale. To foster reliability and trust in the results of observational research on real-world data, it is essential to utilize CDMs whenever possible to ensure a high degree of data analysis reproducibility.
Several CDMs exist for that purpose; the OMOP CDM from the OHDSI community is one of the most promising and established approaches. In comparison with other CDMs, such as the Sentinel CDM or Informatics for Integrating Biology and the Bedside (i2b2), the OMOP CDM has broader terminology coverage [ 81 ]. The importance of the OMOP CDM increased a lot over the last years [ 82 ], not least since the European Medicines Agency initiated the Data Analysis and Real World Interrogation Network (DARWIN) [ 83 ] project to establish a research network in Europe to gain real-world evidence based on OMOP. Moreover, representations of genomic data [ 84 ], oncology [ 85 ], and imaging projects [ 86 ] are also suitable. In addition, the common representation of the data in OMOP semantic interoperability is ensured by utilizing international terminologies and vocabularies, such as SNOMED-CT, the International Statistical Classification of Diseases and Related Health Problems (ICD), the Logical Observation Identifiers Names and Codes (LOINC), and RxNorm to represent every clinical fact in OMOP. Additionally, the open-source OHDSI software stack provides standardized methodology and libraries for data analyses (Athenahene, Atlas, HADES) and training (EHDEN Academy) [ 87 ], as well as a framework to assess and improve data quality to foster reliability and trust in research results [ 88 ].
The OMOP CDM is one possibility to represent and analyze clinical data on a research scale. Definition of new cohorts within OMOP enables researchers to quickly investigate questions spanning multiple research entities. Collectively, both FHIR and OMOP can define the structure and relations of the clinical data corpus, and the individual EHRs provide content to these standardized data reservoirs. In comparison, OMOP is commonly used for static large-scale data analysis of research data, and FHIR is more suitable for rapid data integration scenarios (ie, for real-time applications and analysis). In summary, it is important to know and utilize newly established standards to participate in broader clinical networks for research. This way, all information within the EHR is comparable across different clinical sites and research settings.
Evaluation, Visualization, and Dissemination
Topic 8: data quality—“guarantee high quality and then publish the data.”.
What is meant to be appropriate data quality for health informatics research? In this domain, data quality depends on the quality of single data elements, data completeness, data conformance, and data plausibility aspects that may considerably determine the validity and veracity of analysis results [ 89 , 90 ]. Moreover, data quality across different institutional entities and even health sectors requires additional efforts concerning the different personnel, instruments, and more [ 91 ]. High-quality data at hand is one fundamental requirement that is often difficult or impossible to achieve, which is why the generation of synthetic data can be an alternative that satisfies privacy problems as well as research needs when data are expensive, scarce, or unavailable by augmentation [ 92 ].
First, a major problem is that clinical data have to be electronically recorded, accessed, and standardized in order to run quality assessment processes [ 26 ]. In addition, it would be important to design and use the same data quality tool, standard operating procedures, or ETL mapping rules in all involved institutions. However, in real-life scenarios, there is a lack of both centrally coordinated data quality indicators and formalization of plausibility rules, as well as a repository for automatic querying of the rules, especially in ETL processes [ 93 ]. Although numerous data quality evaluation frameworks exist, no clear and widespread approach has been adopted so far [ 67 , 94 - 96 ]. Even after a well-chosen data quality procedure is properly implemented, clinical data as such cannot be published along with the performed study. As an alternative, synthetic data generation models function in the following 2 different ways: (1) The model is trained, for example, using real-world data and, once trained, will not require any data in the future (model-based approaches), and (2) the model is constantly fed with data to generate synthetic data (data-driven approaches). There are 3 different categories of algorithms used in the generation of synthetic data: probabilistic models, such as Bayesian networks [ 97 ] and Copulas [ 98 ]; ML, such as Classification and Regression Trees (CART); and deep learning methods, such as a generative adversarial network (GAN) [ 99 - 101 ] and variational autoencoder (VAE) [ 102 ].
A combination of appropriate data quality evaluation and synthetic data generation highly facilitates the development of accurate AI models, which are essential in medical studies [ 103 ]. Thus, a corpus of high-quality synthetic data with many patients can be reused by other AI experts for model development and benchmarking. Moreover, it is essential to create an infrastructure that is used across a large community of hospitals; maps the entire treatment process electronically; and only generates interoperable, structured data based on FHIR (Topic 6) and OMOP (Topic 7) in accordance with the FAIR principles (Topic 3). Afterward, one can finally run quality assessment processes.
Topic 9: Clinical Decision Support Systems—“Bring Insights, Not Additional Work, Back to the Clinics via a CDSS and Other User-Centric Applications.”
CDSS are computer systems designed to assist the medical staff with decision-making tasks about individual patients and based on clinical data [ 104 ]. The decision-making process is still, and will remain, on the shoulders of the physician [ 105 ]. The categories of CDSS include knowledge-based systems that make use of clinical rules, nonknowledge-based systems (eg, AI-based systems), and hybrid CDSS that likewise utilize clinical models and knowledge in combination with AI.
The use of a CDSS in a well-implemented clinical workflow has many positive aspects. It may lead to fewer error rates [ 106 ], accelerate rare disease diagnosis [ 107 ], increase radiologists’ job satisfaction [ 108 ], offer personalized cancer treatment [ 109 ], or help with real-time cardiovascular risk assessment [ 110 ]. Interestingly, computerized alerting systems, which are one of the most disseminated CDSS, can decrease drug-drug interactions significantly [ 111 ]. On the other hand, if done improperly, a CDSS can cause alert fatigue by creating too many alerts. If a system is not context-sensitive, alerts can even be inappropriate [ 112 ]. According to Olakotan et al [ 112 ], influencing factors of a well-designed CDSS need to include aspects about the (1) technology (eg, usability, alert presentation, workload, and data entry), (2) human (eg, training, knowledge, skills, attitude, and behavior), (3) organization (eg, rules and regulations, privacy, and security), and (4) and process (eg, waste, delay, tuning, and optimization). To avoid a lack of transparency and facilitate acceptance by physicians, especially with nonknowledge-based systems, current CDSS seek to use explainable AI approaches; however, the selection of methods used to present explanations in an informative and efficient ( clinically useful ) manner remains challenging [ 113 ]. Of note, a CDSS may also have a negative influence on the performance of physicians, especially if inadequate suggestions occur more often, which cannot be compensated with explanations [ 114 ]. However, one among many other prominent approaches to obtain such explanations via ML-based feature selection and ranking can be found in the work from Wolfien et al [ 115 ]. In terms of an OMOP-based implementation in research, there is patient-level prediction (PLP), which is designed to foster the clinical decision-making process concerning diagnoses or treatment pathways based on the EHR of the patient and the current clinical guideline. It is used to answer questions, such as identifying patients among a larger population at higher risk of a certain outcome (eg, occurrence of cancer, severe side effects, or death) by using data in standardized formats (eg, as previously described via OMOP CDM). Once the model is designed, the covariates will be extracted from the respective CDM of the target person within the cohort, and the respective outcome will be predicted (eg, via PLP [ 116 , 117 ] or other customized prediction algorithms). Importantly, the results from model prediction should first be internally validated with previously unseen data and afterward compared with established scoring systems (eg, Framingham Risk Score [ 118 ], SCORE2 [ 119 ]) to connect with already known domain-specific contexts and to prove its benefit in clinical practice. An additional validation with external data, as part of a multicenter study, can be seen as highly beneficial, in which the already presented topics of federated learning (Topic 4) and OMOP (Topic 7) could significantly foster such an essential scenario [ 120 ].
Collectively, a CDSS increases patient safety, assists in clinical management, and can be cost-effective [ 104 ]. In general, findings of even erroneous CDSS can be used to guide the design of new CDSS alerts. However, the existing risks cannot be solved solely on a technical basis and require an interdisciplinary effort. In particular, continuous, clear communication between IT professionals (developers) and health professionals (end users) during the design process is key. Only a profound understanding of the needs and requirements of either of the involved parties can lead to well-designed systems that are actually able to support and relieve physicians in doing their job.
Topic 10: Visualizations—“Improved Dissemination of Local and External Data From Computational Models by Well-defined Interactive Visualizations.”
Large volumes of data collected from patient registries, health centers, genomic databases, and public records can potentially improve the efficiency and quality of health care via enhancing the interoperability of medical systems, assisting in clinical decision-making, and delivering feedback on effective procedures [ 121 ]. However, each and every raw data point must go through different analytical processes until they become useful and interpretable at the point of care.
R and Python are 2 versatile open-source programming languages that have gained popularity for different purposes, such as preprocessing (eg, tidyverse), statistical tests (eg, dplyr), ML and deep learning (eg, mlr package, caret), visualization (eg, ggplot), and writing reports directly using knitr and R markdown (RStudio education [ 122 ]). Like R, Python offers different libraries for data science tasks (eg, open mined [ 123 ]) in addition to a library specifically for health predictive models, namely PyHealth [ 124 ]. Another versatile visualization functionality is offered for both languages via R Shiny [ 125 ] and Plotly Dash [ 126 ]. These 2 platforms enable data scientists to create interactive web applications directly from a script. The applications can be extended using embedded CSS themes, HTML widgets, and Javascript actions. There is already evidence that implementing clinical dashboards or CDSS for immediate access to current patient information can improve processes and patient outcomes [ 127 ], especially if the data sets are further evaluated and refined [ 128 ]. Similar to FHIR, OHDSI provides tools for analyzing data in the OMOP CDM, which are written in R and use Shiny for the visualization. As a plus, data already stored in the OMOP CDM format can be used in systematic studies, patient-level analysis, and population-based estimations from scratch. The cBioPortal is one prime example of a web resource for exploring, visualizing, and analyzing multidimensional data, which reduces molecular profiling data from cancer tissues and cell lines into readily understandable genetic, epigenetic, gene expression, and proteomic events [ 129 ]. It was recently demonstrated how cBioPortal can be extended and integrated with other tools to a comprehensive and easily deployable software solution that supports the work of a molecular tumor board [ 130 ] and even deliver meaningful scientific insights [ 131 ]. Another translational research platform for the construction and integration of modern clinical research charts is Informatics for i2b2, which is also at the heart of clinical research [ 132 , 133 ].
Computational approaches and data analyses are tightly connected with medical research; the visualization of such complex data for clinicians in a routine setting especially plays a larger role. The current developments of translational research platforms, such as cBioPortal and i2b2, enable swift translation of research results into the clinic, if adequately adopted and enough trained people supervise the process.
The need for qualified IT specialists in medical informatics has increased continuously in recent years and will continue to grow in the future. On the other hand, medical informatics in Germany faces problems with the promotion of young researchers. These current developments mean that vacancies in IT in hospitals and the health care industry can often not be filled or only after very long vacancies. In addition, these positions often have to be filled with nonspecialist staff due to a lack of applications. To keep track of these recent developments and provide a basis for interdisciplinary communication, we provide our list of 10 topics that could be used by different stakeholders individually ( Figure 2 ). With a particular focus in medicine, improved interdisciplinary communication has already been shown to positively impact patient outcomes and enhance employee engagement [ 134 ].

Exemplary outcome visualization of the underlying study, in which the color coding reflects the initial colors of the proposed sections; it starts with an individual perception of the term medical informatics (MI) based on the individual’s background and ends with acquisition of common domain knowledge for current important topics. CDSS: clinical decision support system; EHR: electronic health record; ETL; extract, transform, and load; FAIR; findable, accessible, interoperable, reusable; FHIR; Fast Healthcare Interoperability Resources; OMOP: Observational Medical Outcomes Partnership.
Furthermore, medical informatics has developed rapidly in recent years. This applies, for example, to new methods, techniques, tools, framework conditions, and organizational structures, especially in the field of medical data science. In particular, definitions of standards and a national digitized data corpus, namely the German Core Dataset [ 135 ], were agreed upon. The actual assessment and collection of digitized data in local university hospitals are utilized in so-called data integration centers. These interoperable research data infrastructures enable rapid multisite research, for example, with complex COVID-19 research data sets (German Corona Consensus Dataset [GECCO]) [ 136 ] including clinical data and data on biosamples from all German university hospitals in pseudonymized form (CODEX) [ 137 , 138 ] or the COVID-19 Data Portal [ 139 ]. The subsequent formation of the Network University Medicine (NUM) strengthens the existing interaction between research and patient care, stabilizes existing structures, and creates new structures that ensure more effective feedback and close cooperation between the clinics. The presented examples of NUM and CODEX, among others [ 140 ], attempt a central approach to bundle and harmonize necessary resources like broad consent or the elektronische Patientenakte (ePa), which is the implementation of EHR as a national entity to ultimately facilitate an interconnected health care system.
Finally, all those involved in medical informatics are called upon to engage in lifelong learning and continuously acquire further qualifications.
Exemplary Implementation of the Addressed Topics in the German Medical Informatics in Research and Care in University Medicine Consortium
This article offers newcomers to medical informatics a first introduction and a wealthy overview of current IT-related topics in research and patient care. Nevertheless, there is also a need for further qualification of employees through new, innovative offers for training, further education, and further training. As part of the MII [ 11 ], all consortia were asked to develop and set up appropriate offers and formats. The Medical Informatics in Research and Care in University Medicine (MIRACUM) consortium [ 141 ] has reacted and set up the part-time training and further education program “Biomedical Informatics and Data Science” [ 142 ] and introduced it at the Mannheim University of Applied Sciences in October 2020. The program includes a time-flexible and individually adaptable part-time online master’s course, as well as certificate courses and programs for further scientific education. In addition to the establishment and continuous further development of a cloud-based learning platform, many new digital and target group–oriented learning resources and application-oriented learning environments were developed and introduced for the master's program.
All 10 topics listed in this article are reflected in the curriculum of the master’s degree and have been offered and dealt with in-depth in the individual courses for more than 2 years. The demand for the master’s program and certificate courses is high, and the evaluation has shown that these topic-specific foci correspond to the training and further education needs of the target groups. One particular aspect that was not covered in the final topics refers to the underlying infrastructure needed to provide the data storage and processing backbone. This aspect would have been too technical for a more broadly set, introductory article, such as this article. A starting point for more in-depth information about this aspect can be obtained from further literature [ 143 , 144 ]. However, to offer a practical start to the 10 topics, we provide links to well-known tutorials and hands-on materials ( Table 1 ).
We suggest a set of 10 topics to ease the start for researchers and clinicians to become engaged with basic concepts in health informatics research. We provide current review articles for more in-depth reading about the specific topic and present practical hands-on material. The presented topics likewise serve as a broad overview of the medical informatics research domain but also guide individuals and their specific interests. For example, a computer scientist familiar with CDSS development could more easily connect with important aspects, such as data privacy, FHIR, and specific EHRs that are highly relevant for daily work. In contrast, medical experts can obtain an overview of behind-the-scenes technologies, like ETL processes and underlying data quality approaches that are finally visualized as a summarizing clinical dashboard. For readers, we provided a first step toward an improved understanding of a lively and quickly expanding field, but more novel technologies and practical knowledge are ahead. Suggestions and contributions to improve the current topics can be made at GitHub, which will likewise enable content and readers to stay current [ 12 ].
Acknowledgments
This work was supported by the Federal Ministry of Health (BMG) and the German Federal Ministry of Education and Research (BMBF) within the Medical Informatics Initiative Medical Informatics in Research and Care in University Medicine (MIRACUM) Consortium (FKZ: 01ZZ180L [Dresden]; FZK: 01ZZ180A [Erlangen]; FKZ: 01ZZ1801M [Greifswald]). The article processing charge was funded by the joint publication funds of the Technische Universität (TU) Dresden, including the Carl Gustav Carus Faculty of Medicine; Saxon State and University Library (SLUB) Dresden; and the Open Access Publication Funding of the German Research Foundation (DFG).
The funding sources had no involvement in the conduct of the research and preparation of the article.
Abbreviations
Authors' Contributions: MW conceptualized the study, curated the data, and wrote the original manuscript draft. MW also defined the initial topics 1 and 2; MZ defined the initial topics 3 and 4; YP defined the initial topics 5 and 6; IR defined the initial topics 7 and 8; and NA defined the initial topics 8, 9, and 10. MS provided the resources and supervised the study. The topics were revised and extended by KF, AK, SG, DK, KLH, ICJ, CS, JS, TS, PS, and DW. MW, NA, YP, MZ, IR, and MS performed the formal analysis, and MW, NA, and MS created the visualizations. NA, YP, MZ, IR, and MS wrote, reviewed, and edited the manuscript, and all authors read and agreed to the final version of the manuscript.
Conflicts of Interest: None declared.
Overview of the Health Informatics Research Field: A Bibliometric Approach
- Conference paper
- Cite this conference paper

- Hai-Ning Liang 2
Part of the book series: IFIP Advances in Information and Communication Technology ((IFIPAICT,volume 335))
Included in the following conference series:
- IMIA/IFIP Joint Symposium on E-Health
1747 Accesses
10 Citations
Health informatics is a relatively new research area. Over the last decade or so, research in health information has been growing at a very rapid rate, as evidenced by the large number of publications. While this growth has been beneficial to the field, it has also made understanding the scope of the field more difficult. Consequently, it is difficult to answer questions such as how the research field has evolved over time, what the landmark publications are, what impact these publications have had, and who are the most prolific and high impact researchers. The purpose of this paper is to provide an overview of the research field of health informatics and, in doing so, attempt to answer some of the questions just mentioned. To this end, we make use of two bibliometric tools: HistCite and CiteSpace II. Because these tools offer complementary bibliometric methods, their use together provides results that are more robust. In this paper, we report some general findings of our bibliometric analysis using these two tools.
Download to read the full chapter text
Chapter PDF
Similar content being viewed by others.

A bibliometric analysis of metaverse technologies in healthcare services
Global trends in the scientific research of the health economics: a bibliometric analysis from 1975 to 2022

Bibliometrics: Methods for studying academic publishing
- Health informatics
- medical informatics
- bibliometrics
- literature review
- research field
- citation and co-citation analysis
Protti, D.: The synergism of health/medical informatics revisited. Methods of Information in Medicine (34), 441–445 (1995)
Google Scholar
Deloitte: Queesnland Health: eHeatlh Strategy (2006)
Coiera, E.: Guide to Health Informatics, 2nd edn. Hodder Headline Group, London (2003)
Shortliffe, E.H., Cimino, J.J. (eds.): Biomedical Informatics: Computer Applications in Health Care and Biomedicine, 3rd edn. Springer, Heidelberg (2006)
De Bellis, N.: Bibliometrics and citation analysis: From the science citation index to cybermetrics. The Scarecrow Press, Inc., Lanham (2009)
Van Leeuwen, T.N., Visser, M.S., Moed, H.F., Nederhof, T.J., Van Raan, A.F.J.: The Holy Grail of science policy: Exploring and combining bibliometric tools in search of scientific excellence. Scientometrics 57(2), 257–280 (2003)
Article Google Scholar
Bordons, M., Morillo, F., Gómez, I.: Analysis of cross-disciplinary research through bibliometric tools. In: Moed, H., Glänzel, W., Schmoch, U. (eds.) Handbook of Quantitative Science and Technology Research: The Use of Publication and Patent Statistics in Studies of S&T Systems, pp. 437–456. Kluwer Academic Publishers, New York (2004)
Nederhof, A.J., Meijer, R.F.: Development of bibliometric indicators for utility of research to users in society: Measurement of external knowledge transfer via publications in trade journals. Scientometrics 32(1), 37–48 (1995)
Higher Education Funding Council for England. HEFCE: Research: REF: Bibliometrics (2010)
Persson, O.: BIBEXCEL, Umeå, Sweden. BIBEXCEL A tool-box developed by Olle Persson (2010)
Chen, C.: CiteSpace II: Detecting and visualizing emergent trends and transient patterns in scientific literature. Journal of the American Society for Information Science and Technology 57(3), 359–377 (2006)
Garfield, E.: Historiographic mapping of knowledge domains literature. Journal of Information Science 30(2), 119–145 (2004)
Schildt, H.A., Mattsson, J.T.: A dense network sub-grouping algorithm for co-citation analysis and its implementation in the software tool Sitkis. Scientometrics 67(1), 143–163 (2006)
Chen, C.: CiteSpace: Visualizing patterns and trends in scientific literature (2010)
Garfield, E., Pudovkin, A.I., Istomin, V.I.: Mapping the Output of Topical Searches in the Web of Knowledge and the case of Watson-Crick. Information Technology and Libraries 22(4), 183–187 (2003)
HistCite Software LLC. HistCite, Bala Cynwyd, PA (2010)
Chen, C.: Information visualization: Beyond the horizon, 2nd edn. Springer, London (2006)
Reuters, T.: Web of Science - Science - Thomas Reuters (2010)
Dem, T.: MEDINFO 1974: First World Conference on Medical Informatics. Biomedical Engineering 9(11), 524–525 (1974)
Greenes, R.A., Shortliffe, E.H.: Medical informatics: an emerging academic discipline and institutional priority. Journal of the American Medical Association 263(8), 1114–1120 (1990)
Collen, M.F.: Origins of medical informatics. Western Journal of Medicine 145(6), 778–785 (1986)
Haux, R., Knaup, P.: Recommendations of the International Medical Informatics Association on education in health and medical informatics. Methods of Information in Medicine 39(3), 267–277 (2000)
Eysenbach, G.: Recent advances: Consumer health informatics. British Medical Journal 320(7251), 1713–1716 (2000)
Kaplan, B.: Evaluating informatics applications–some alternative approaches: theory, social interactionism, and call for methodological pluralism. International Journal of Medical Informatics 64(1), 39–55 (2001)
Gustafson, D.H., Hawkins, R., Boberg, E., Pingree, S., Serlin, R.E., Graziano, F., Chan, C.L.: Impact of a Patient-Centered, Computer-Based Health Information/Support System. American Journal of Preventive Medicine 16(1), 1–9 (1999)
Ammenwerth, E., Brender, J., Nykanen, P., Prokosch, H.U., Rigby, M., Talmon, J.: Visions and strategies to improve evaluation of health information systems - Reflections and lessons based on the HIS-EVAL workshop in Innsbruck. International Journal of Medical Informatics 73(6), 479–491 (2004)
van Bemmel, J.H.: Medical informatics, art or science? Methods of Information in Medicine 35(3), 157–172 (1996)
Kaplan, B.: Addressing organizational issues into the evaluation of medical systems. Journal of the American Medical Association 4(2), 94–101 (1997)
Martin-Sanchez, F., Iakovidis, I., Noraer, S., et al.: Synergy between medical informatics and facilitating genomic medicine for future bioinformatics: health care. Journal of Biomedical Informatics 37(1), 30–42 (2004)
Sittig, D.F.: Grand challenges in medical informatics. Journal of the American Medical Association 1(5), 412–413 (1994)
Haux, R.: Aims and tasks of medical informatics. International Journal of Medical Informatics 44(1), 9–20 (1997)
Lorenzi, N.M., Riley, R.T., Blyth, A.J.C., Southon, G., Dixon, B.J.: Antecedents of the people and organizational aspects of medical informatics: Review of the literature. Journal of the American Medical Association 4(2), 79–93 (1997)
Kulikowski, C.A.: The micro-macro spectrum of medical informatics challenges: From molecular medicine to transforming health care in a globalizing society. Methods of Information in Medicine 41(1), 20–24 (2002)
Stead, W.W., Haynes, R.B., Fuller, S., et al.: Designing medical informatics research and library-resource projects to increase what is learned. Journal of the American Medical Association 1(1), 28–33 (1994)
Heathfield, H.A., Wyatt, J.: The road to professionalism in medical informatics: A proposal for debate Methods of Information in Medicine 34(5), 426–433 (1995)
van Bemmel, J.H.: The structure of medical informatics. Medical Informatics 9(3-4), 175–180 (1984)
Reichertz, P.L.: Preparing for change: Concepts and education in medical informatics. Computer Methods and Programs in Biomedicine 25(2), 89–101 (1987)
Haux, R., Dudeck, J., Gaus, W., et al.: Recommendations of the German association for medical informatics, biometry and epidemiology for education and training in medical informatics. Methods of Information in Medicine 31(1) (1992)
Heathfield, H.A., Wyatt, J.: Philosophies for the design and development of clinical decision-support systems. Methods of Information in Medicine 32(1), 1–8 (1993)
Friedman, C.P.: Where’s the science in medical informatics? Journal of the American Medical Association 2(1), 65–67 (1995)
Hasman, A., Haux, R., Albert, A.: A systematic view on medical informatics. Computer Methods and Programs in Biomedicine 51(3), 131–139 (1996)
McDonald, C.J.: The barriers to electronic medical record systems and how to overcome them. Journal of the American Medical Informatics Association 4(3), 213–221 (1997)
Cimino, J.J.: Desiderata for controlled medical vocabularies in the twenty-first century. Methods of Information in Medicine 37(4-5), 394–403 (1998)
Ball, M.J., Lillis, J.: E-health: transforming the physician/patient relationship. International Journal of Medical Informatics 61(1), 1–10 (2001)
Patel, V., Arocha, J., Kaufman, D.: Review? A primer on aspects of cognition for medical informatics. Journal of the American Medical Informatics Association 8(4), 324–343 (2001)
Maojo, V., Kulikowski, C.: Bioinformatics and medical informatics: Collaborations on the road to genomic medicine? Journal of the American Medical Informatics Association 10(6), 515–522 (2003)
Ammenwerth, E., de Keizer, N.: An inventory of evaluation studies of information technology in health care - Trends in evaluation research 1982-2002. Methods of Information in Medicine 44(1), 44–56 (2005)
Haux, R.: Health information systems - past, present, future. International Journal of Medical Informatics 75(3-4), 268–281 (2006)
Hunt, D.L., Haynes, R.B., Hanna, S.E., Smith, K.: Effects of Computer-Based Clinical Decision Support Systems on Physician Performance and Patient Outcomes: A Systematic Review. Journal of the American Medical Association 280(15), 1339–1346 (1998)
Download references
Author information
Authors and affiliations.
Queensland Research Lab, National ICT Australia (NICTA), Brisbane, Australia
Hai-Ning Liang
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Osaka University, 2-15 Yamada-Oka, 565-0871, Suita City, Osaka, Japan
Hiroshi Takeda
Rights and permissions
Reprints and permissions
Copyright information
© 2010 IFIP
About this paper
Cite this paper.
Liang, HN. (2010). Overview of the Health Informatics Research Field: A Bibliometric Approach. In: Takeda, H. (eds) E-Health. E-Health 2010. IFIP Advances in Information and Communication Technology, vol 335. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-15515-4_5
Download citation
DOI : https://doi.org/10.1007/978-3-642-15515-4_5
Publisher Name : Springer, Berlin, Heidelberg
Print ISBN : 978-3-642-15514-7
Online ISBN : 978-3-642-15515-4
eBook Packages : Computer Science Computer Science (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Request More Info
Fill out the form below and a member of our team will reach out right away!
" * " indicates required fields
5 Exciting Health Care Informatics Projects
Thanks to revolutionary technological advancements, modern medicine is poised for transformation from a “disease industry” to a “scientific wellness industry,” according to a report in healthcareitnews.com . And at the heart of this transition is the field of health care informatics.
Big data is changing everything — and the rapidly expanding use of artificial intelligence and predictive analytics is expected to drive breakthroughs in the health of entire populations and in individual health care that is more personalized than ever before.
“The contrast between 20th and 21st-century medicine is striking,” said Leroy Hood, Chief Science Officer at Providence St. Joseph Health, describing care that is more proactive and “focused on the individual,” and that employs “personalized data clouds to explore the complexities of human beings.”
Hood sees the potential to create “a world virtually free of Alzheimer’s” within 10 years by processing information from such data clouds with computer-aided diagnostics to identify and track risk far earlier, and to design new treatments for specific sub-types of the debilitating disease.
That’s just one example of how health informatics is changing the future of health care right now. From battling the opioid epidemic to breakthroughs in combating sepsis and pediatric asthma, health informatics is the common denominator among countless initiatives with the promise to make the world a healthier place.
Additionally, because the demand for health informatics professionals is expanding so rapidly, this is also a time of opportunity in the employment market for people who possess health care and/or information technology experience.
For a closer look at the fascinating work being done by health care informatics professionals, here are several examples of notable health informatics projects and initiatives.
Combating the Opioid Crisis
With an average of 44 deaths each day from opioid-related overdoses and an estimated 2 million Americans suffering from addiction to prescription painkillers, the opioid epidemic is one of the nation’s most significant public health crises.
Now, providers are looking to health informatics — combining data analytics and population health management strategies — to respond more effectively. Health informaticians are using improved access to data (including prescribing data) to:
- Deepen their understanding of the risk factors for addiction
- Reassess prescribing practices and introduce opioid alternatives where appropriate
- Crack down more effectively on the small percentage of patients who are trying to scam providers into issuing prescriptions
- Utilize new data-driven insights to put in place population health management strategies that help individual patients
Examples include the MO HealthNet initiative in Missouri, which used health informatics data insights to realize a 30 percent statewide drop in the rate of prescriptions for Schedule II opioids.
Another example involves a dashboard tool created by the Rhode Island Quality Institute that makes it easier for primary care providers and opioid treatment centers to more effectively access and share information. Users of the Care Management Dashboard saw their patients’ emergency department return visits within 30 days reduced by 16 percent, an outcome that earned the institute a 2018 Innovator Award from Healthcare Informatics .
[RELATED] How Health Informatics is Shaping Future of Health Information Management >>
Fighting Pediatric Asthma
Another Innovator Awards semifinalist is using informatics data to reduce emergency room visits for pediatric asthma-related issues by 18 percent and cut about $1 million in avoided emergency room costs.
As part of its strategic plan for population health management of pediatric patients, Children’s Hospital of Orange County (Calif.) developed a system of asthma patient measures designed to better manage the condition and keep individual patients out of emergency situations. The measures are built into each patient’s electronic health record and the data is available to providers in real time as part of the clinical workflow.
The number of children with an asthma action plan grew quickly, fueling the reduction in emergency room encounters and earning them a Healthcare Informatics Innovator Award .
Life-Saving Technology
One man’s path into the field of health informatics led directly to a project that is credited with speeding up medical science’s ability to detect signs of sepsis — a life-threatening condition that kills an estimated quarter million patients annually and is caused by the body’s extreme response to an infection.
Andrew Harrison was a student in the Mayo Clinic’s Medical Scientist Training Program when he attended a lecture about “data sniffers,” computer applications that sift through a patient’s electronic health record and alert care providers to early signs of dangerous syndromes.
“I knew nothing of clinical informatics,” Harrison said in a story in Discovery’s Edge (the research magazine of the Mayo Clinic). But he was intrigued that computers could be taught to conduct medical surveillance and that data analysis could improve clinical decision-making.
Working alongside the researcher whose talk initially inspired his passion for informaticsHarrison focused his doctoral studies on developing a first-generation “sepsis sniffer” application. He continued to improve the sniffer, and in a clinical study it was able to identify patients with sepsis sooner than bedside clinicians.
Harrison is “a prototype for medical students trained to heal both patients and the health care system,” according to the Mayo Clinic story chronicling his work. “Instead of searching for breakthroughs under a microscope, he discovered statistical enlightenment — the kind that becomes a best practice and improves care around the world.”
[RELATED] 8 Technologies that are Changing Healthcare >>
Real Improvements Through Artificial Intelligence (AI)
Despite some healthy skepticism from critics , artificial intelligence is already ubiquitous throughout the health care industry.
In fact, according to a healthitanalytics.com report titled “Top 12 Ways Artificial Intelligence Will Impact Healthcare,” as more and more data becomes available — including through billing and payment systems that capture incredible amounts of valuable information about patients and their conditions — “artificial intelligence is poised to be the engine that drives improvements across the care continuum.”
Providers are already using AI algorithms to gain “unprecedented insights into diagnostics, care processes, treatment variability and patient outcomes,” according to the report, which explains how the medical community is using artificial intelligence to capitalize upon the “nearly endless opportunities to leverage technology to deploy more precise, efficient and impactful interventions at exactly the right moment in a patient’s care.”
Strategies for harnessing artificial intelligence to improve health care include:
- Expanding access to care in underserved or developing regions — In areas where there is a deficit of trained medical personnel, AI can be used to perform diagnostic duties typically handled by humans.
- Transforming smartphone selfies into powerful diagnostic tools — Experts believe that images taken from smartphones and other devices will increasingly become an important tool for medical imaging, particularly in underserved areas.
- Using AI algorithms to enhance the ability of “smart devices” now widely used in health care to identify deterioration in a patient’s condition or detect the development of complications.
- Developing the next generation of non-invasive radiology tools for diagnostic processes that still rely on tissue samples obtained through biopsy.
- Assisting providers with decision making at bedside — According to healthitanalytics.com, AI offers tremendous potential for “powering predictive analytics and clinical decision support tools that clue providers in to problems long before they might otherwise recognize the need to act.”
Putting the ‘Me’ in Personalized Medicine
In addition to equipping doctors and nurses with powerful tools designed to improve patient health and the delivery of care, health informatics is also opening up incredible new possibilities for patients to become more actively engaged in their own care.
For example, tech giant Apple has developed a personalized Health Records system that promises to reshape patient engagement, according to Dr. Shez Partovi, chief digital officer and senior vice president of digital transformation at Dignity Health, a longtime collaborator with Apple and an early adopter of its Health Records program. Since its launch in January 2018, more than 100 hospitals and clinics have signed on to the initiative.
Apple has developed health care applications for its iPhones and tablets that enable both providers and patients to instantly access a patient’s entire medical record. Working in conjunction with the traditional patient portals used by many health organizations, the Apple system securely transfers a patient’s medical data to the Health Records app so the patient, as well as providers, can view in it instantly in a familiar, easy-to-use interface. High-resolution display and powerful graphics capabilities even give doctors the ability to view a patient’s imaging studies on an iPad.
But in addition to enabling care providers to work more efficiently on a patient’s behalf, one of the most exciting aspects of the program is that it enables patients to better manage their own care and even connect remotely with providers between visits.
According to Apple, the program enables patients to “aggregate their health records from multiple institutions alongside their patient-generated data, creating a more holistic view of their health.”
Dr. Partovi at Dignity Health said the Apple initiative involves “empowering patients by giving them their data.” In addition to ownership of their medical data, patients will benefit from apps (both currently existing and those to be developed in the future) that help them make better, healthier use of their data — for example, an app that helps diabetes sufferers treat their condition by using food as medicine.
The goal of all of this, says Apple, is “care that becomes more efficient, more personalized, and ultimately more human.”
Learning More About Health Care Informatics
Despite showing great promise to make the world a healthier place, the field of health care informatics continues to face a talent shortage, with strong demand and high pay for employees who possess medical/clinical experience as well as proficiency in data analysis, information technology or informatics.
For that reason, many current and future health informatics professionals are taking advantage of specialized master’s degree programs that build on their work experience and knowledge of the health care field while refining their programmatic, technical and analytical skills.
One of the most exciting aspects of health informatics is the future breakthroughs that “we cannot even imagine yet,” said Dr. Jonathan Mack, program director for health care informatics and nursing informatics at University of San Diego. In Q&A about career growth in the field of health informatics , Dr. Mack speaks about the state of this fast-growing discipline and the significant opportunities for motivated individuals to pursue a meaningful career in health informatics.
Be Sure To Share This Article
- Share on Twitter
- Share on Facebook
- Share on LinkedIn
Exploring Your Future in Health Informatics?
Download free Career Guide: “A Career in Health Care Informatics: How Big Data & Technology Are Creating New Opportunities to Work in Health Care”
- Master of Science in Health Care Informatics
Related Posts
Program Capstone for the Master's in Health Informatics, Northwestern University School of Professional Studies - Northwestern School of Professional Studies
- Post-baccalaureate
- Undergraduate
- Professional Development
- Pre-College
- Center for Public Safety
- Get Information

Health Informatics Capstone
Health Informatics
What is the Capstone project?
As a culminating experience , each student will independently put into practice the knowledge and skills they learned during their coursework through a Capstone Project.
Students will have the opportunity to develop and implement a Health Informatics project in their workplace or other academic / industry organizations . The project will challenge each student to conduct research and apply knowledge, skills and competencies built through coursework completed in the MHI program.
If students are unable to find a real-world project, they can alternatively develop a culminating, two-part project, that will leverage health informatics to provide a solution to a need or problem arising as part of a case study. Note: Finding a real-world project would be preferred over working on a case study.
Each student will work with the course instructor to identify a “Knowledge Expert” for their capstone project along with a faculty advisor from the Northwestern University Health Informatics program.
What can students expect during the MHI Capstone course?
A challenging but rewarding experience that would prepare or enhance their professional skills in the field of Health Informatics. There will be a focus on more career and real-world experiences than the other courses in the MHI program. The Capstone course is more about the hands-on (or applied experiences) in the world of Health Informatics. Depending on the complexity of your project, you can expect to spend 5 to 10 hours a week, or 50 to 100 hours during the quarter working on your project.
With whom can you do a capstone project ?
Your Employer / Workplace: You may work on a discrete project from your workplace for your capstone project. This will need to be above and beyond your day-to-day job responsibilities. You will need to identify a Knowledge Expert / Mentor at your organization to support you during the project.
“Sponsor” organization projects : You may partner with an external organization in the industry who may be interested in sponsoring a capstone project. There may be opportunities available through Northwestern University or you will need to find one on your own.
Academic Partners: You may work with a MHI Faculty member, or with other academic partners at Northwestern University (such as Feinberg School of Medicine or Northwestern Memorial Hospital), or other academic institutions to work on an informatics or research based capstone project.
Capstone Project Cases : Alternatively, if you are unable to find a real-world project, you may choose to work on one of the capstone project cases made available through the course.
What is the Capstone Course timeline?
The MHI Capstone Course can only be done in the last quarter of the MHI program prior to your graduation. Like the other courses in the program, you will have 10 weeks to complete your capstone project. Due to this aggressive timeline in the quarter, we will divide your capstone project in the following phases:
- Capstone Identification and Proposal: 1-2 weeks
- Capstone Implementation: 5-7 weeks
- Capstone Paper and Presentation: 1-2 weeks
How to Prepare for the Capstone
Capstone pre-work: complete prior to starting the capstone course.
- Reflect on your career goals. What do you want to do after you graduate from the MHI program? There is no right or wrong answer to this. If you have not yet thought about it, this exercise should help you get started.
- Prepare your CV / Resume that includes your most up to date professional and academic experiences (including the MHI program) prior to the start of the MHI Capstone Course.
- Start thinking about capstone project ideas that ideally align with your career goals.
- Do you already have a “sponsor” or organization in mind to do your capstone with?
- If you are currently working in the healthcare industry, explore possible capstone project opportunities with your employer that would be above and beyond your day-to-day job responsibilities. I would also encourage you to reach out to any relevant contacts in your professional network to find a capstone project opportunity, if needed.
- Some “sponsors” or organizations will work with you in a virtual environment, while others may prefer an in-person or hybrid model.
- If you have already selected a project for your capstone, then complete any onboarding work such as contracting, drug tests, training, IRB approvals, etc. as soon as possible so that you can start working on your project implementation during the capstone course.
Capstone Advising Sessions
This Capstone course has been overwhelmingly successful with respect to the student experience based on feedback. The only critique of Capstone is the timeframe – students feel that one quarter to complete the project limits the potential for projects.
In order to address the time constraint of a single quarter, students will be given the opportunity to meet with their capstone instructor during pre-capstone advising sessions in the quarter prior to their capstone. This will allow students to navigate the pre-work with the support of their instructor, allowing for more time to connect with potential partners for their proposed project leading to a more time fulfilling project experience.
Students approaching their final quarter will be contacted to set up an appointment with the capstone instructor during the quarter prior to the capstone.
The MHI Capstone Experience
Student reflections.
MHI faculty member Imran Khan interviewed two of his graduating students, Regina Schwind and Angela Mazzari, to discuss their experiences in the MHI program and their respective Capstone projects.
Recent Capstone Project Topics
- Reducing Infant and Maternal Mortality Rates in the Black Populations of Athens, GA
- Population Health Provider and Patient Engagement Strategy
- Scalable Monitoring System to Address Emergency Care Usage among Patients with Multiple Chronic Conditions
- Improving Anticoagulation Safety & Drug Compliance (of cardiac patients) through a Remote Monitoring System
- WordGlass: Technology to Provide Live Closed Captioning for the Hearing- Impaired in the Health Care Setting
- Hand Hygiene Audit Tool
- Adoption of an Electronic Lab Notebook in a WSU Research Lab
- Digital Health Solutions for a Rural Healthcare System
- A Comprehensive Solution to Improving Diabetic Outcomes and Improved Shared- Savings Returns by Achieving the Together to Goal Program Metrics
- Hierarchical Condition Category Risk Adjustment Documentation in Epic
- Clinical Decision Support System for the Prenatal Care of Obese Patients at a Family Practice Residency Clinic
- Engaging High-Need Patients to Produce Scalable High-Value Health Care
- A Care Management Dashboard for Population Stratification using Johns Hopkins ACG System in the Enterprise Data Warehouse

- Seminar Series
- Call for Proposals
- Funded Projects
- Affiliated Labs

PILOT PROJECT – CALL FOR PROPOSALS
Objectives:.
The growing pressure for health care providers to administer cost-effective, patient-centered care has contributed to changes in our health care system, making informatics platforms ubiquitous. Most health science centers host large clinical data warehouses (CDW), and store vast amounts of heterogeneous data coming from a variety of sources, such as data from electronic health record systems (EHRs), claims data, national surveys and databases such as NHANES, biological sequences, images, etc. Loyola University Chicago's Center for Health Outcomes and Informatics Research (CHOIR) strives to leverage our informatics infrastructure and data analytics capabilities to improve health outcomes and reduce health disparities, and to develop health outcomes and informatics expertise across LUC, LUHS, and Trinity Health. In this call for proposals, we are soliciting proposals that align with CHOIR’s mission, and which will generate preliminary data for subsequent federal funding applications (e.g. National Institutes of Health, National Science Foundation etc.) Potential topics include, but are not limited to:
- Leveraging clinical notes to enhance diagnoses in the EHR
- Development of computable phenotypes
- Methodologies of health-related data collection, aggregation, harmonization and analysis
- Studies using smartphones and other wearable technologies to improve health outcomes across diverse populations
- Development of software and/or mobile applications to improve health-related behavior (e.g. adherence to dietary and physical activity programs, smoking cessation, cancer screening and prevention)
- Integration of patient-generated data into care delivery
- Development of data analysis methodologies for semantic data integration
- Development of data analysis methodologies for analysis of health care data, in particular longitudinal data
- Development of natural language processing techniques for clinical notes processing
This funding opportunity is open to the entire LUC/LUHS community, and multidisciplinary projects across departments, schools, and campus are strongly encouraged to apply.
Eligibility:
The PI/co-PI must be faculty members at LUC/LUHS. Co-investigators and other senior personnel may be faculty or staff.
Funding Details:
The CHOIR steering committee will entertain proposals up to $50,000 total for a period of up to two years.
Funding is limited. The budget must be accurate, conservative, and carefully reflective of the work. No cost extensions are not allowed under this funding mechanism. Funds may not be used to cover Faculty salary. The proposal is to be single spaced and must follow the CHOIR pilot project submission template . Funding is competitive; this invitation does not guarantee funding.
Please submit the full proposal via e-mail to Kelly Quinn ( [email protected] ). Questions can be directed to Kathleen "Kathy" Bobay, PhD, RN, NEA-BC, FAAN, Interim Chair Health Informatics & Data Science, Parkinson School of Health Sciences and Public Health ( [email protected] ).
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
LIGHT Frequently Asked Questions
To help provide timely information about all aspects of the program, this page is updated periodically in response to questions from potential performers. For full information about LIGHT and the application process, please see the LIGHT Innovative Solutions Opening .
Proposal & Submission
When is the solution summary due.
LIGHT's solutions summary due date is now June 27th, 2024
Who is allowed to submit an abstract of full proposal?
Please see ISO Section 2, Eligibility Information. All eligible entities may submit Solution Summaries (formerly known as abstracts). As the LIGHT ISO requires submission of Solution Summaries, the Government will only accept full proposals from eligible entities who submitted a timely Solution Summary.
Can proposers be part of multiple proposals either as the lead or sub-proposers?
An entity can only submit one full proposal as the prime proposer. Entities may propose within multiple teams as subproposers.
Do you require preliminary data for the application?
Outside of guidance within the ISO, including Appendices, ARPA-H cannot advise proposers in terms of Solution Summary and/or full proposal strategy and content. Solution Summaries will be reviewed and full proposals will be evaluated as described in the ISO. Proposers should prepare submissions accordingly.
Is a solution summary required?
How is the solution summary evaluated.
Solution Summaries will be reviewed within the context of the full proposal evaluation criteria, but not to the same extent as full proposals, which are evaluated against the criteria as outlined in the ISO . Reviews are conducted in a thorough manner proportionate with the brevity of Solution Summaries. Feedback may be limited to 'encourage/discourage' as noted in the ISO .
How will full proposals be evaluated?
Full proposals are evaluated against the three criteria in the ISO (see Section 5.3) unless the evaluators determine the proposal is not selectable in terms of Criterion 1. In those cases, the Government may not proceed with evaluating the full proposal against Criteria 2 and 3.
How are reviewers selected, and who is reviewing the technical merit of the proposal?
Proposals will be evaluated by Government Reviewers who may be ARPA-H PMs or qualified personnel from other Government Organizations and Agencies who are deemed proficient in the pertinent research areas of the solicitation.
Are international performers eligible to submit proposals for considerations?
Yes, non-U.S. entities are allowed to submit proposals for consideration. Non-U.S. entities are encouraged to collaborate with domestic U.S. entities. See LIGHT solicitation 2.1.2
Proposers' Day
Where can i find the recording of the light proposers' day.
The recording LIGHT's Proposers' Day can be found here: https://www.youtube.com/watch?v=R8TjJNmiMkQ NOTE: the content in the LIGHT ISO solicitation supersedes any information presented in the recording.
Teaming & Eligibility
What is the maximum number of teams and/or people for each proposal.
There is no maximum number. Proposers are responsible for proposing a team capable of meeting the proposed Statement of Work, recognizing the Government is evaluating team capability as well as price reasonableness.
Does ARPA-H assign Discovery Duos?
No. See section 3.4.1 for requirements related to each Performer Team .
Does a budget need to be assigned for the Discovery Duo?
Project budgets must account for at least the minimum of Discovery Duo support outlined in Section 3.4.1 of the ISO .
If selected for funding, can performers make teaming changes?
Post award teaming changes may require bilateral negotiation (depending on the SOW).
Can there be two or more PIs if the proposal addresses multiple TAs?
See Section 3.4.1 of the ISO. Each proposal must designate a single lead PI from the prime organization. The team must be capable of accomplishing all technical areas the proposal addresses and may include other Investigators collaborating with the lead PI.
How much interaction, or collaboration, will performer teams have with each other?
Please see ISO Section 3.4.2 . The LIGHT Program is based on collaboration within and between Performers/Performer teams.
Can performers have international partners?
Please see ISO Section 2.1.2 .
When do members of the performing team need to be named/selected? For example, does the Project Manager need to be named within the Solution Summary for Track 1 proposers? The full proposal? At time of award?
Key members of the Proposer's team should be identified as early as possible (e.g., Solution Summary). Solution Summaries will be reviewed within the context of the ISO evaluation criteria and full proposals will be formally evaluated against the Criteria in the ISO. Failure to identify key personnel (e.g., Project Manager) and/or team members (e.g., subawardees) may impact the Government's evaluation. Proposers are encouraged to provide as many specific details as are available at the time of submission, while considering page limitations at each submission stage.
In terms of performers selected for award negotiations, the Government's expectation is the Performer team will be capable of achieving the SOW and associated milestones as proposed (i.e., at the time of award the team is able to begin research efforts in accordance with the SOW).
Technical & Science Questions
Which technical area should i apply to.
ARPA-H cannot advise as to strategy and/or content of Solution Summaries and full proposals. Proposers must use the guidance in the ISO as well as their professional expertise when preparing submissions.
What if I'm only interested in TA1, TA2, or TA3?
Proposals with SOWs addressing a single TA are allowed under Track 2. Please see the ISO for more guidance related to the two Tracks and the associated requirements and periods of performance.
For Track 1, are TA1 and TA3 required?
Track 1 proposals must address at least 2 TAs, with TA2 being a requirement. Please see the ISO for additional guidance related to Track 1 and Track 2.
Do you intend to hold us to the metrics in the R&D Solicitation?
Unless indicated otherwise in the ISO (e.g., written as suggested), Program metrics in the ISO are requirements for Proposers. Proposals that do not propose to meet the metrics may be considered non-selectable.
Will ARPA-H provide/facilitate access to relevant healthcare data?
Proposals should not assume provision of any Government Furnished Information (GFI). The Government may provide GFI, but the specific GFI would be negotiated after a proposal is selected for award negotiations (i.e., a proposal must stand on its own without assumptions and conditions related to GFI).
The independent source for health policy research, polling, and news.
Abortion in the United States Dashboard
On june 24, 2022, the supreme court overturned roe v. wade, eliminating the federal constitutional standard that had protected the right to abortion. without any federal standard regarding abortion access, states will set their own policies to ban or protect abortion. the abortion in the united states dashboard is an ongoing research project tracking state abortion policies and litigation following the overturning of roe v. wade. be sure to click on the buttons or scroll down to see all the content. it will be updated as new information is available., new releases, medication abortion, related health, dobbs-era abortion bans and restrictions: early insights about implications for pregnancy loss.
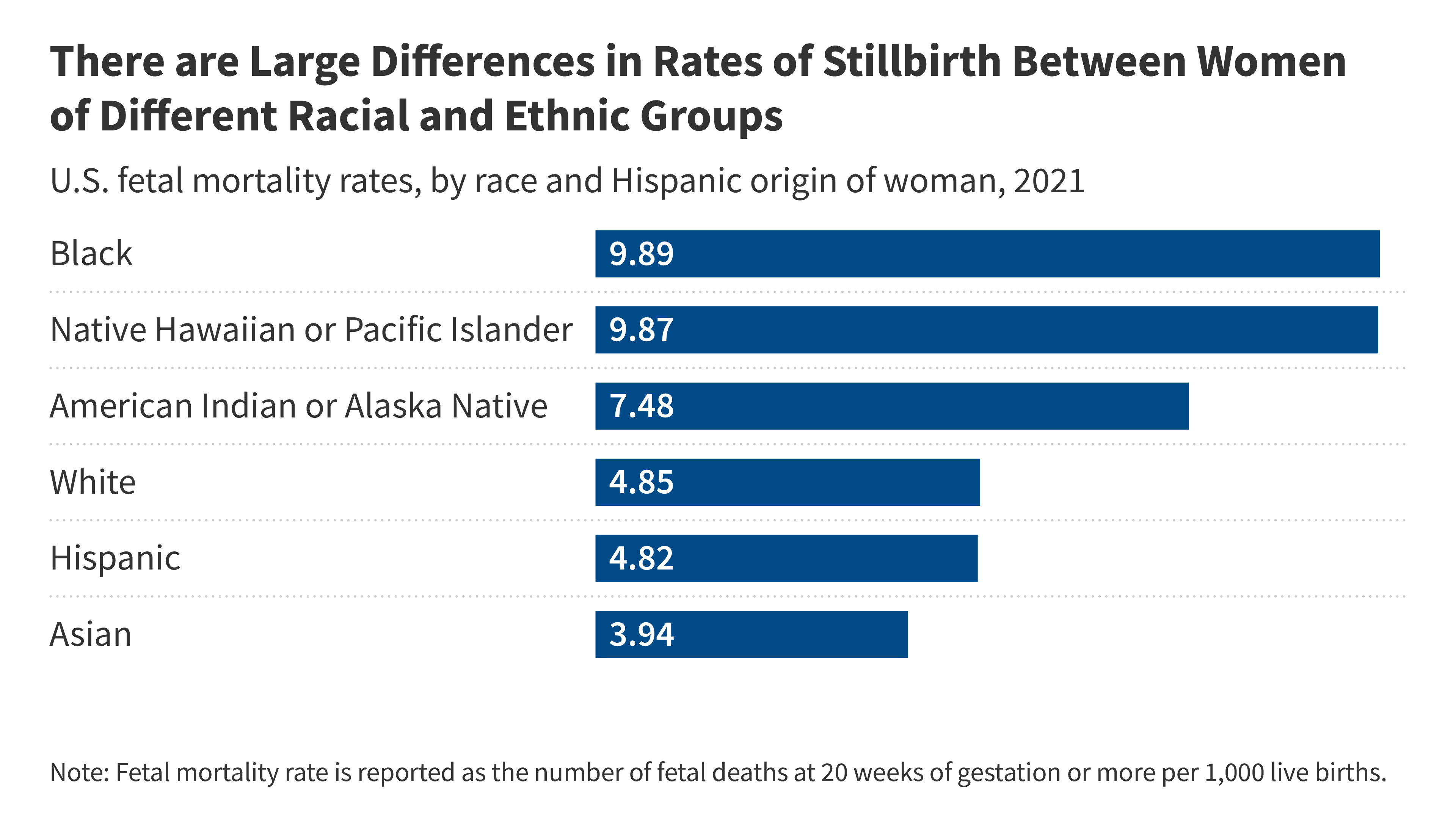
This brief examines pregnancy loss management in the Dobbs era and explores how limiting or banning abortion may have negative consequences on people experiencing miscarriage or stillbirth.
Policy Tracker: Exceptions to State Abortion Bans and Early Gestational Limits
Abortion is currently banned in 14 states and 6 states have early gestational limits between 6 weeks and 15 weeks in effect. Nearly all of these bans include exceptions, which generally fall into four categories: to prevent the death of the pregnant person, when there is risk to the health of the pregnant person, when the pregnancy is the result of rape or incest, and when there is a lethal fetal anomaly.
Ballot Tracker: Status of Abortion-Related State Constitutional Amendment Measures for the 2024 Election
Since the Supreme Court’s Dobbs decision overturning Roe v. Wade , voters in 6 states have weighed in on constitutional amendments regarding abortion, and the side favoring access to abortion prevailed in every state. In 2024, up to 15 states may have abortion measures on their ballot seeking to either affirm that the state constitution protects the right to abortion or that nothing in the constitution confers such a right.
What are the Implications of the Dobbs Ruling for Racial Disparities?
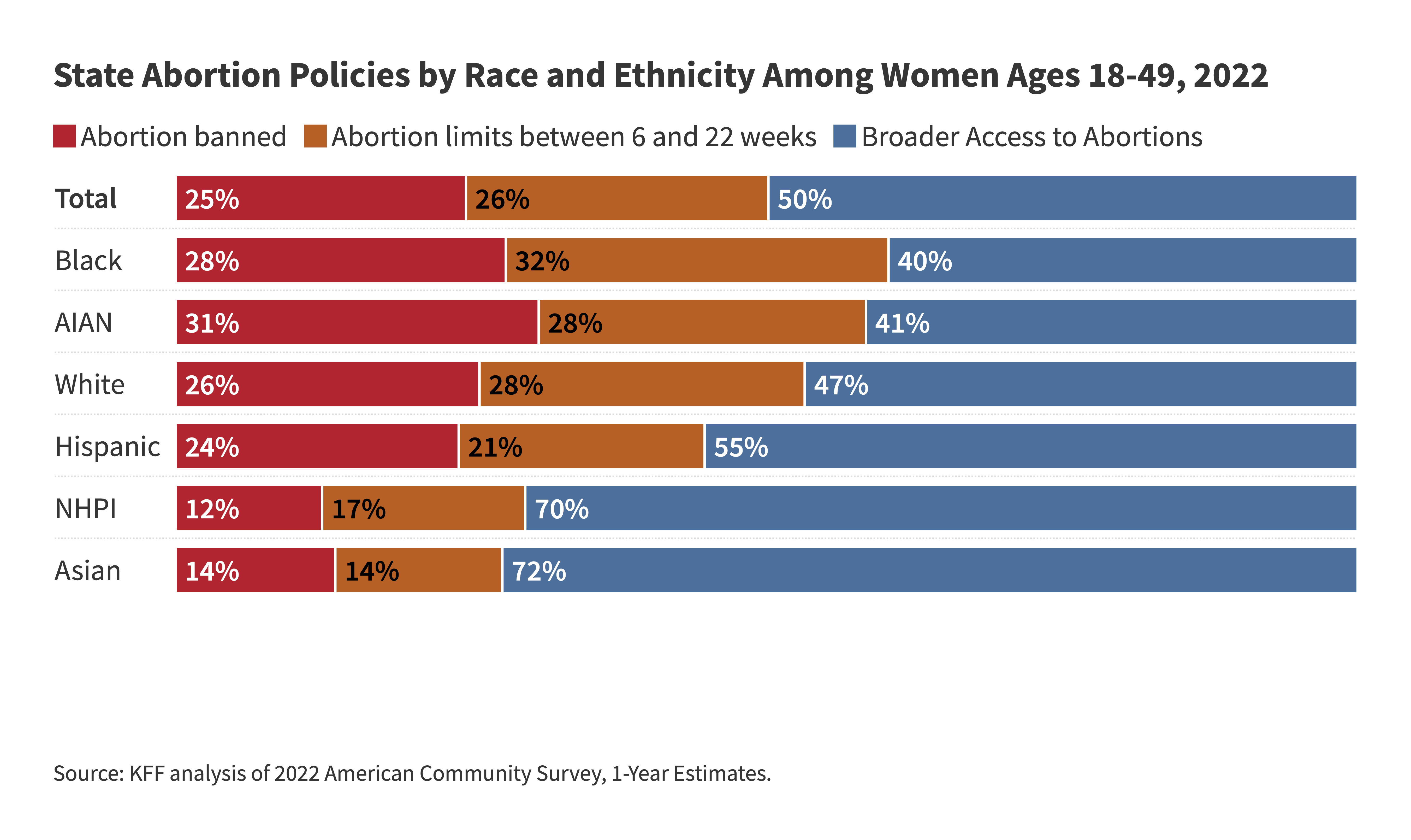
This analysis examines the implications of the Dobbs decision and state restrictions on abortion coverage for racial disparities in access to care and health outcomes.
81% of Abortions Occur Before 10 Weeks
Over four in ten (45%) abortions occur by six weeks of gestation, 36% are between seven and nine weeks, and 13% at 10-13 weeks. Just 7% of abortions occur after the first trimester.
Out-of-Pocket Abortion Costs
In 2021, the median costs for people paying out of pocket in the first trimester were $568 for a medication abortion and $625 for a procedural abortion. The Federal Reserve estimates that nationally about one-third of people do not have $400 on hand for unexpected expenses. For low-income people, who are more likely to need abortion care, these costs are often unaffordable.
Abortion Back at SCOTUS: Can States Ban Emergency Abortion Care for Pregnant Patients?
On April 24, 2024, the Supreme Court will hear the second case this term involving access to abortion: Idaho v. United States. At stake in this case is whether the Emergency Medical Treatment and Active Labor Act, a federal law requiring hospitals to provide stabilizing treatment to patients who present to their emergency rooms, preempts state abortion laws and requires hospitals that accept Medicare to provide abortion care when it is necessary to stabilize a patient’s condition, even when this abortion care violates state law.
What’s at Stake for Access to Medication Abortion and the FDA in the Supreme Court Case FDA v. the Alliance for Hippocratic Medicine?

The Supreme Court will be hearing oral arguments for the case FDA v. Alliance for Hippocratic Medicine. This brief explains the issues at stake before the court and their implications for the drug regulatory process and medication abortion access throughout the country.
The Comstock Act: Implications for Abortion Care Nationwide
This brief provides background on the Comstock Act, reviews how it has been interpreted by the Biden Administration’s DOJ, and considers how it could be enforced by an administration that is hostile toward abortion to severely restrict the distribution of drugs and supplies used for abortion, with implications for abortion access in all states across the country.
State and Federal Reproductive Rights and Abortion Litigation Tracker
This State and Federal Reproductive Rights Litigation tracker aggregates information about ongoing litigation regarding abortion bans and restrictions, FDA approval of Mifepristone (an abortion pill) and other federal regulations.
Addressing Abortion Access through State Ballot Initiatives
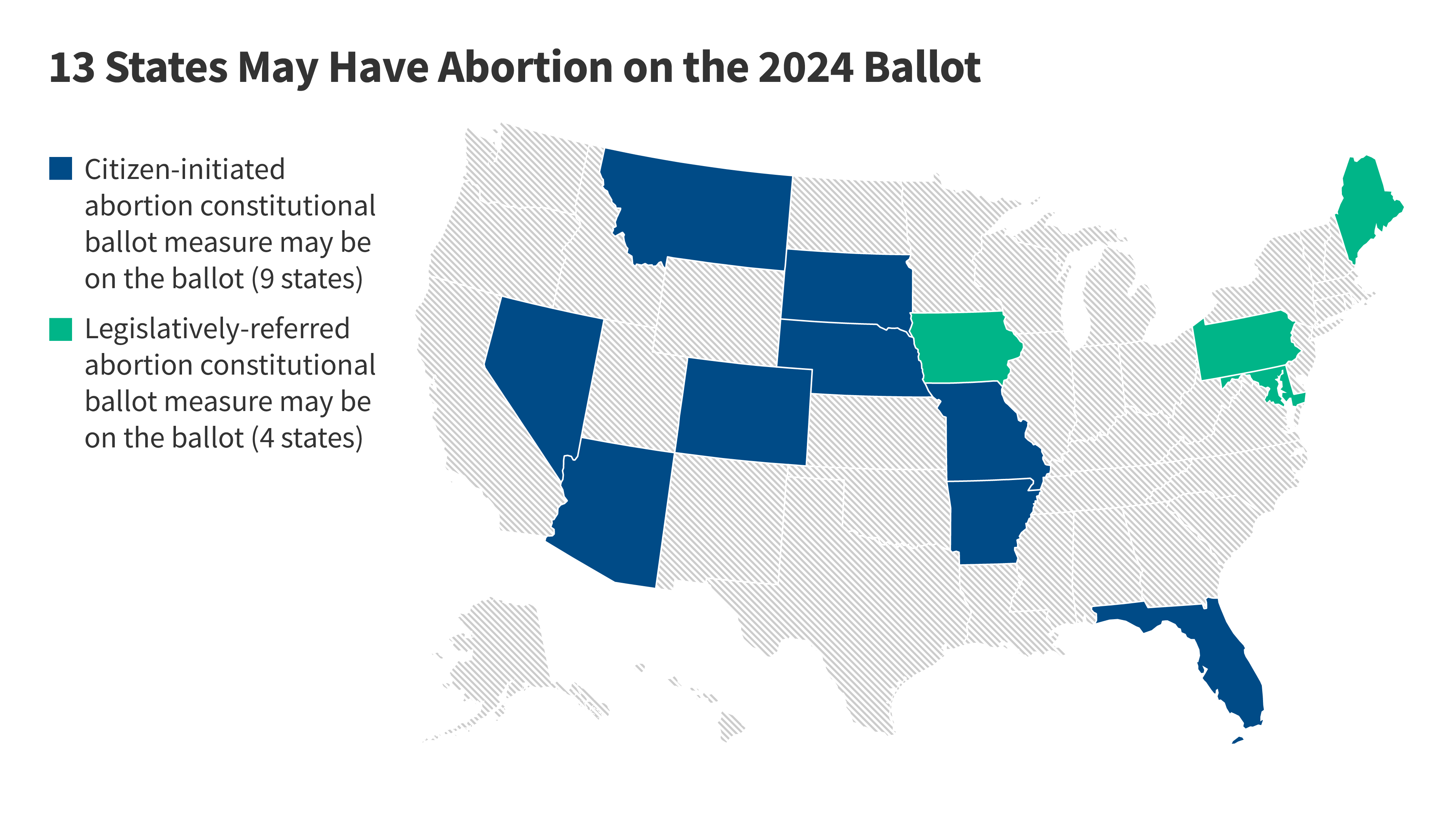
This issue brief explains why constitutional amendment ballot measures have become so popular with advocates on both sides of the abortion issue, reviews the current initiatives that are in progress and may appear in on state ballots the next general election, and outlines the processes states have available to them to use to place initiatives on the ballot.
Who Decides When a Patient Qualifies for an Abortion Ban Exception? Doctors vs. the Courts
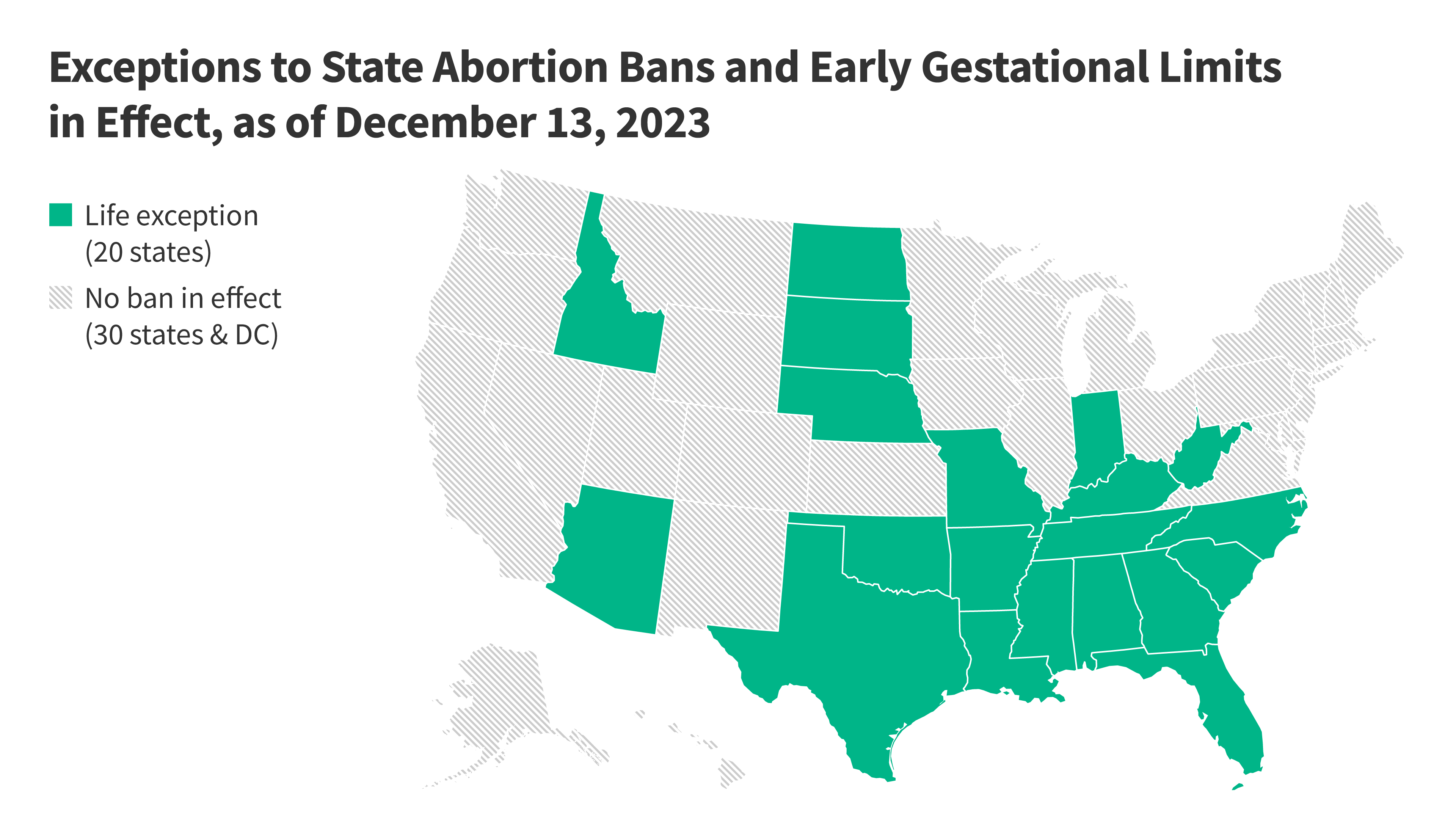
While all eyes were on Texas and the recent case of Kate Cox, a woman seeking a court order allowing her abortion under an exception to the Texas abortion ban, the conflict could have played out in many states. The risk to doctors is so high that many doctors are hesitant to provide life-saving abortion care unless the threat to life is imminent.
Abortions Later in Pregnancy in a Post-Dobbs Era
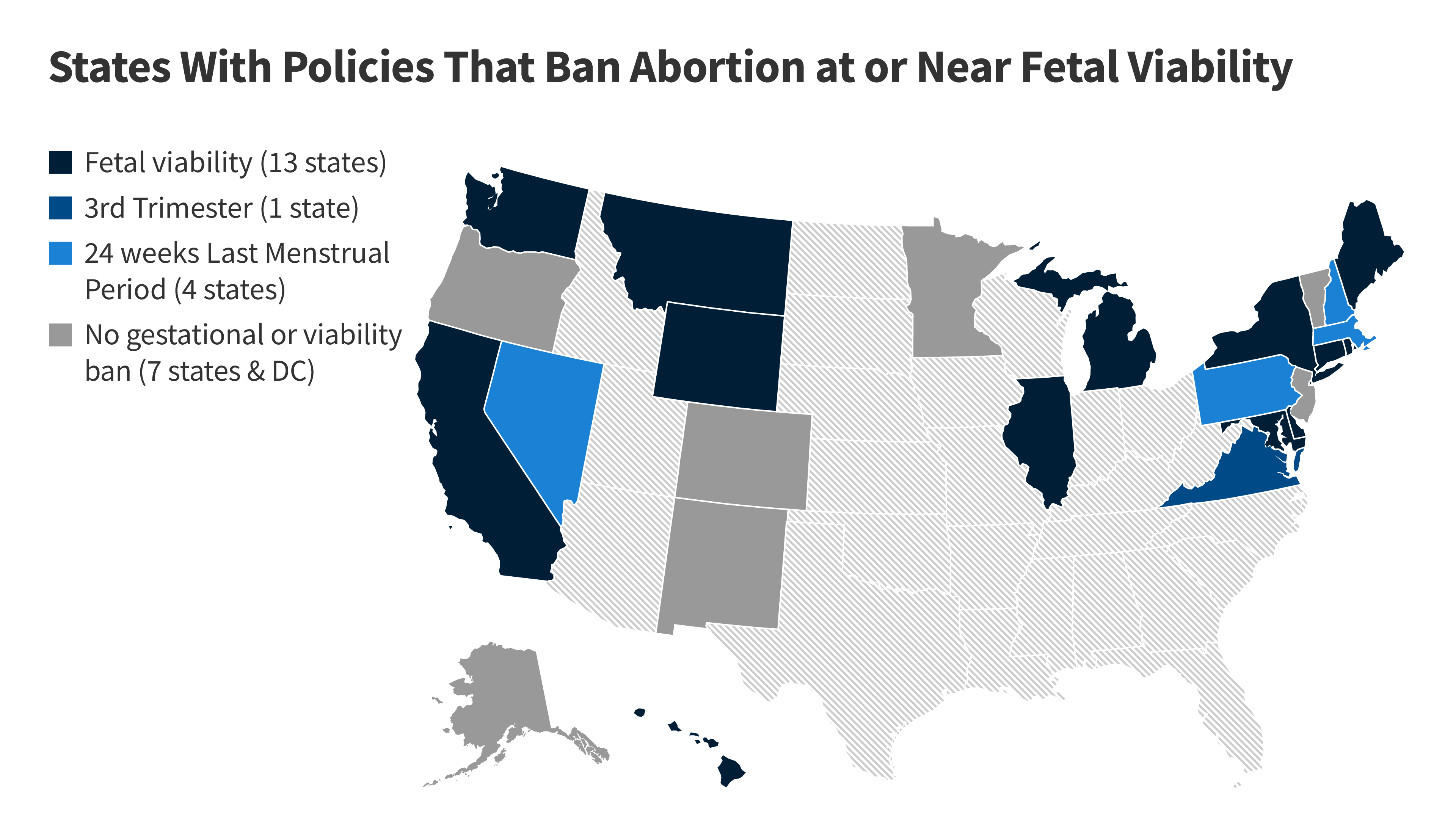
This brief explains why individuals may seek abortions later in pregnancy, how often these procedures occur, and the various laws which regulate access to abortions later in pregnancy across the country.
As part of efforts to limit abortion access, some states have taken action to block the use of telehealth for abortion. Among the 36 states & DC that have not banned abortion, twelve states have at least one restriction that requires at least one trip to the clinic, and effectively ban telehealth for medication abortion
The Availability and Use of Medication Abortion
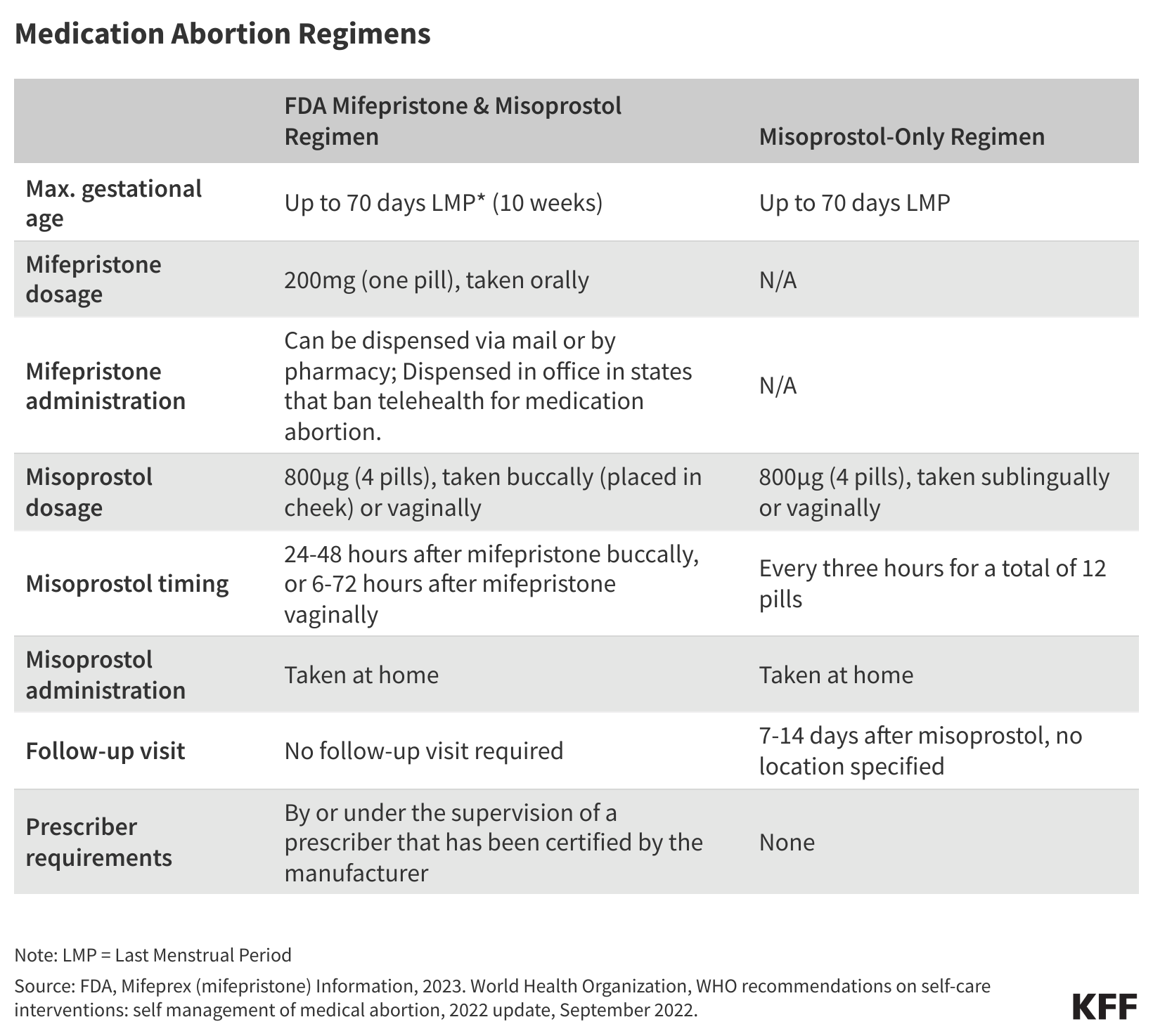
This factsheet provides an overview of medication abortion, with a focus on federal and state regulations pertaining to its provision and coverage, and the role of the drug in self-managed abortions.
Current Abortion Coverage Restrictions
Several states have enacted private plan restrictions and have also banned abortion coverage from ACA Marketplace plans. Currently, there are 10 states that restrict abortion coverage in private plans and 25 that ban coverage in any Marketplace plans.
Abortion Decision Renews Questions About Employer Access to Health Information
This Policy Watch takes a look at employers ability to access abortion information when their health plan covers abortion services. With some states criminalizing entities who assist in abortions, employers and providers face legal jeopardy and existing privacy laws such as HIPAA (the Health Insurance Portability and Accountability Act) may be limited in their privacy protections.
Variability in Payment Rates for Abortion Services Under Medicaid
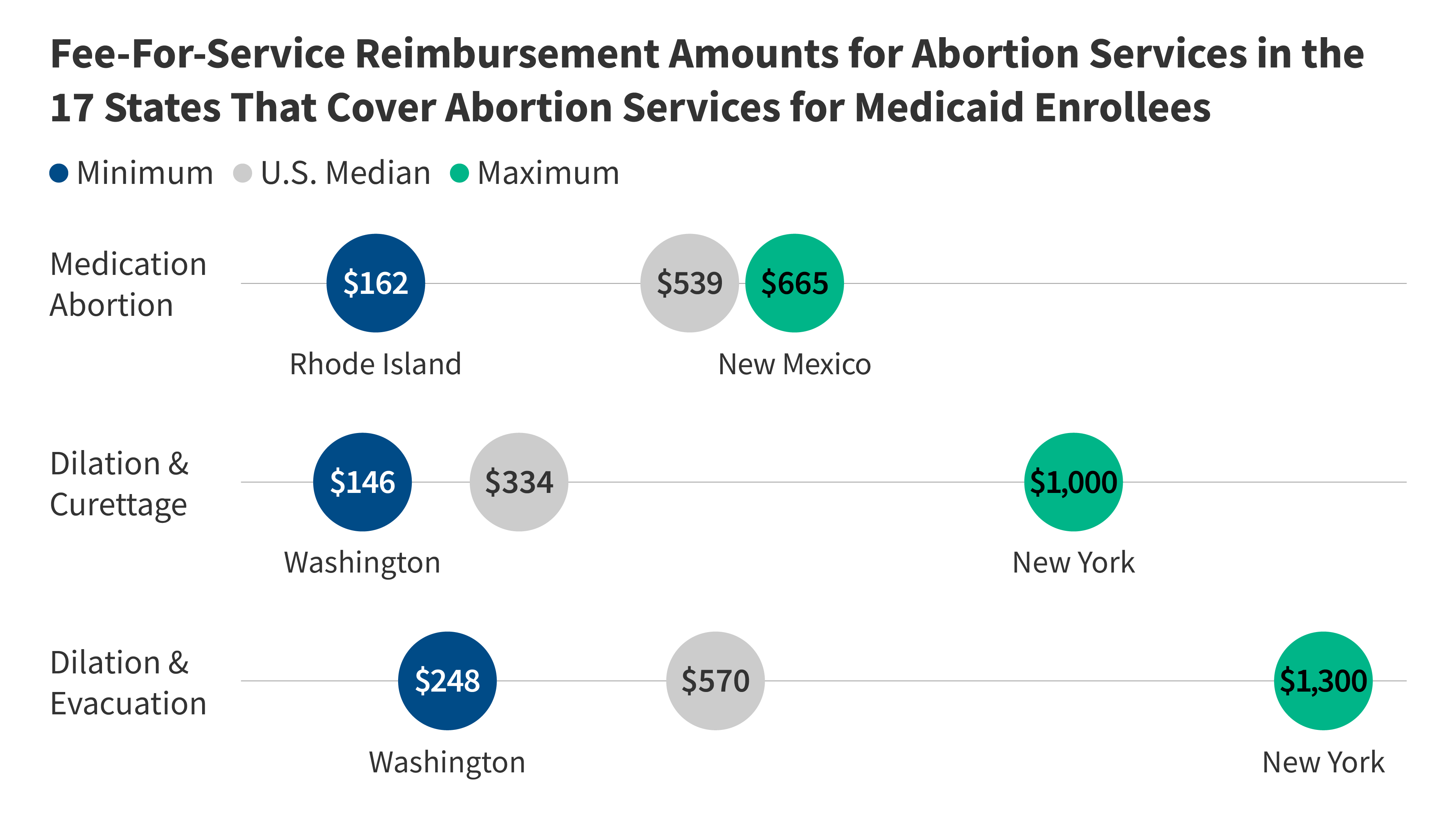
This brief looks at Medicaid reimbursement rates for abortion services across states, including D&C and D&E procedures, and medication abortion. There is tremendous variability in how much states reimburse for abortion services.
The Hyde Amendment and Coverage for Abortion Services Under Medicaid in the Post-Roe Era
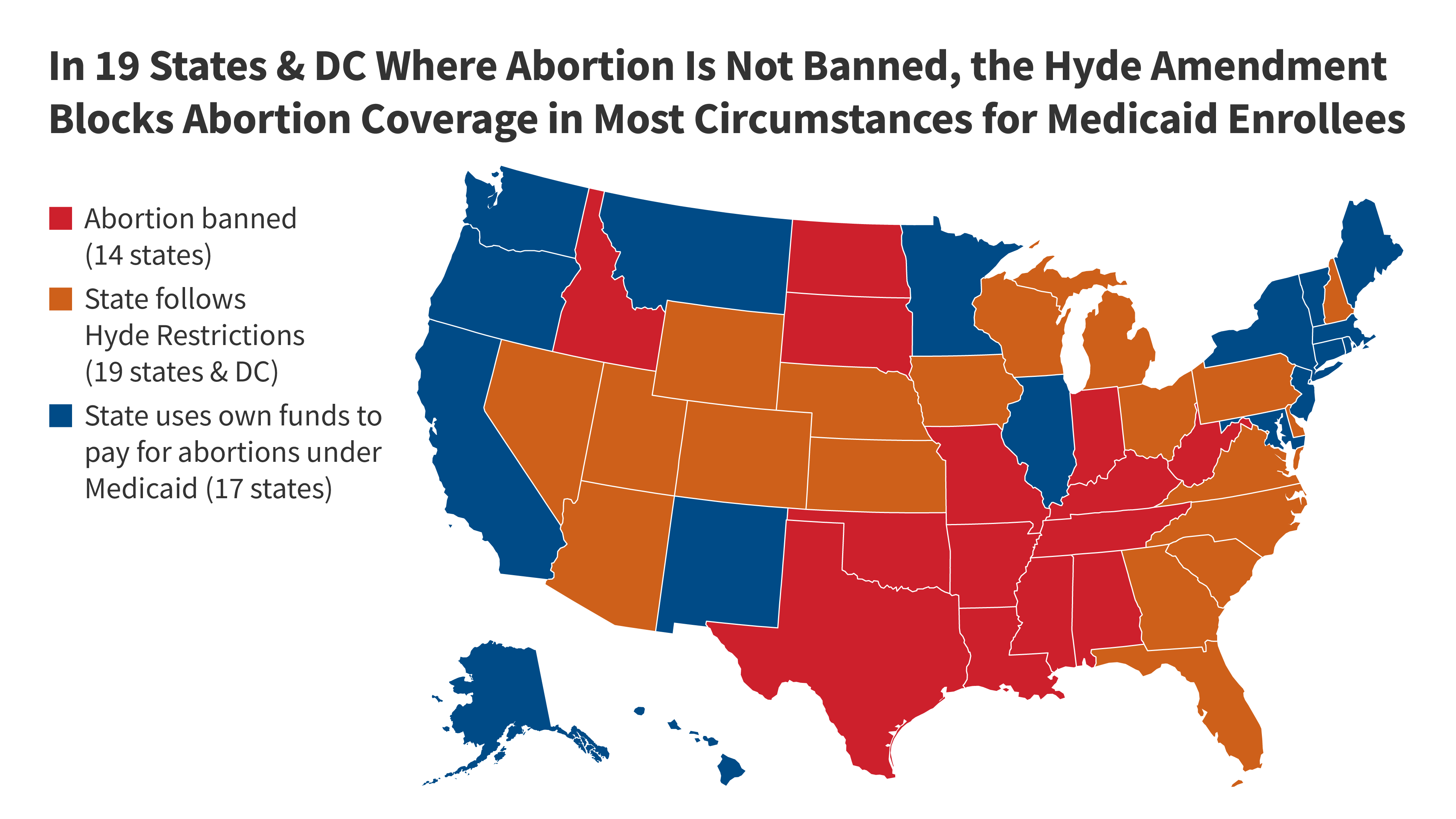
This brief details the federal programs that are affected by the Hyde Amendment and laws and regulations that have a similar goal, provides estimates on the share of women insured by Medicaid affected by the law, reviews the impact of the law on their access to abortion services, and discusses the potential effect if the law were to be repealed.
Employer Assistance with Abortion Related Travel Costs

This Policy Watch gives an overview of employers offering to cover travel expenses for workers who need to go out of state for an abortion in the context of increasing restrictions on abortion around the country. We discuss who is offering these benefits, the implications for workers, and some of the legal and political concerns for employers.
Coverage of Abortion in Large Employer-Sponsored Plans in 2023
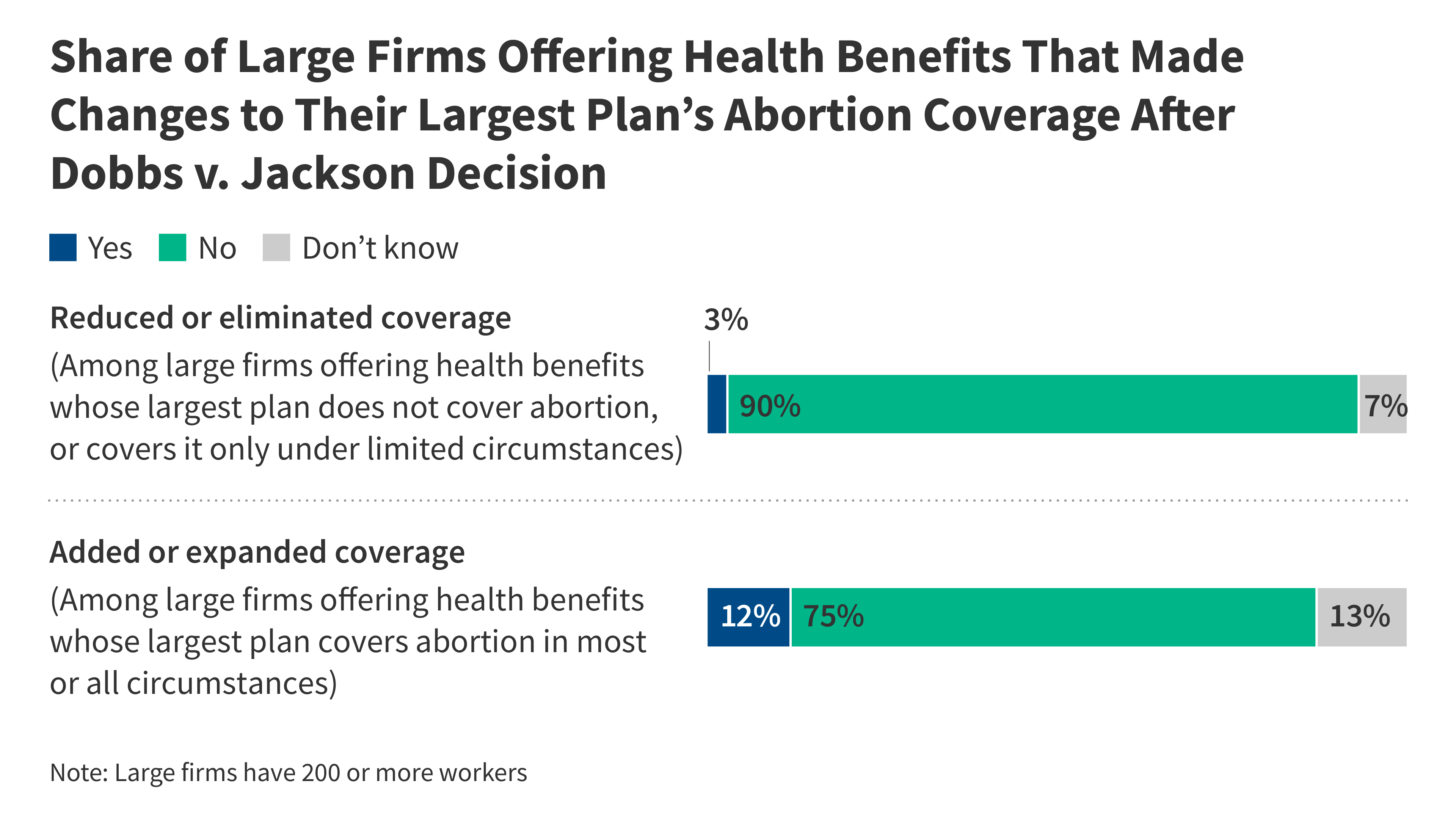
This brief presents findings from the 2023 KFF Employer Health Benefits Survey on coverage of abortion services in large employer-sponsored health plans, changes employers made to abortion coverage since the 2022 Supreme Court ruling, and employers’ provision of financial assistance for travel out of state to obtain an abortion.
KFF Health Tracking Poll March 2024: Abortion in the 2024 Election and Beyond
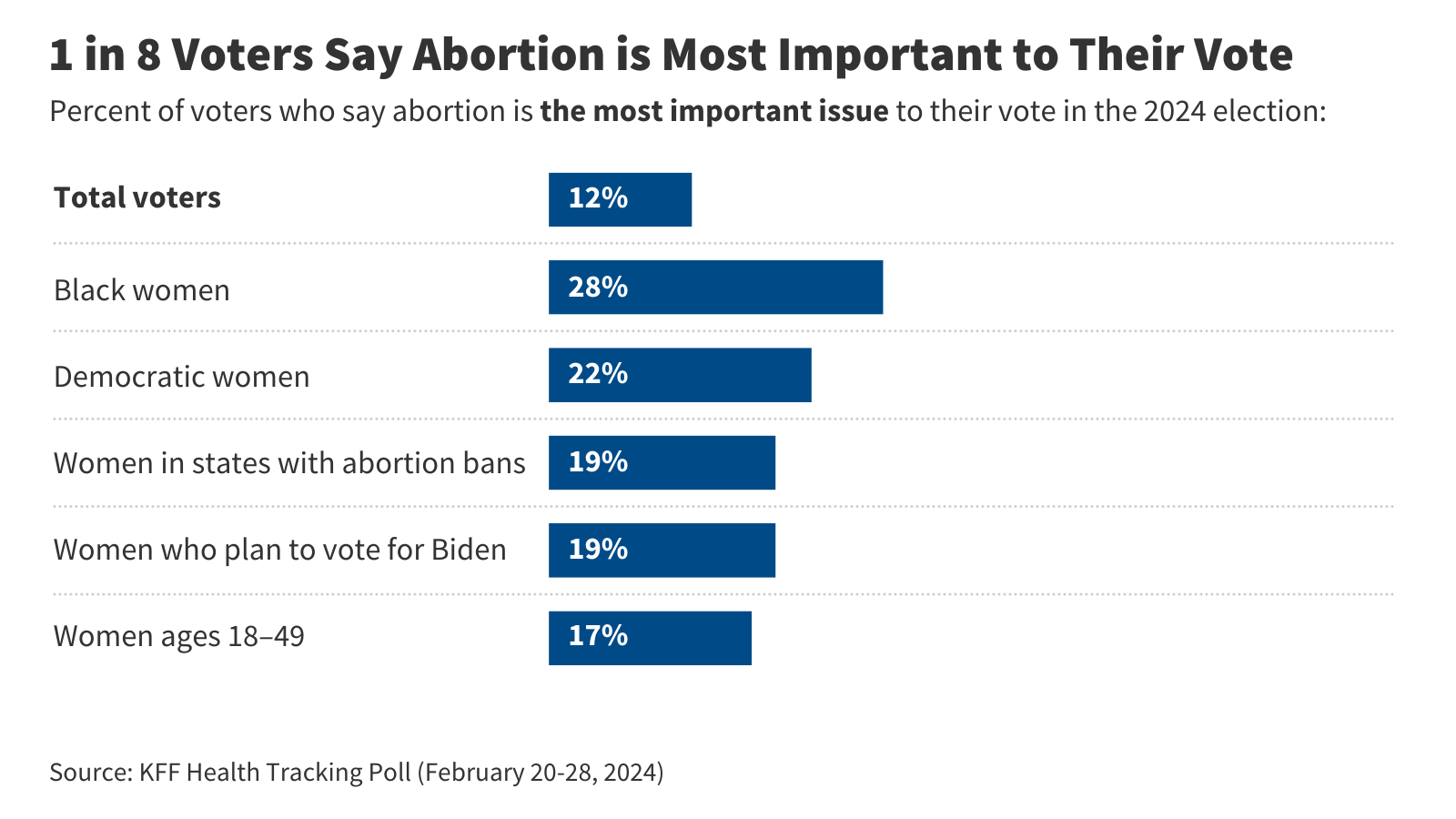
This poll finds 1 in 8 voters say abortion is the most important issue to their vote. They are younger, lean Democratic, and generally want abortion to be legal in all or most cases. The poll also gauges the public's views on abortion-related policies, including a national 16-week abortion ban and allowing abortion for pregnancy-related emergencies.
Women’s Views of Abortion Access and Policies in the Dobbs Era: Insights From the KFF Health Tracking Poll
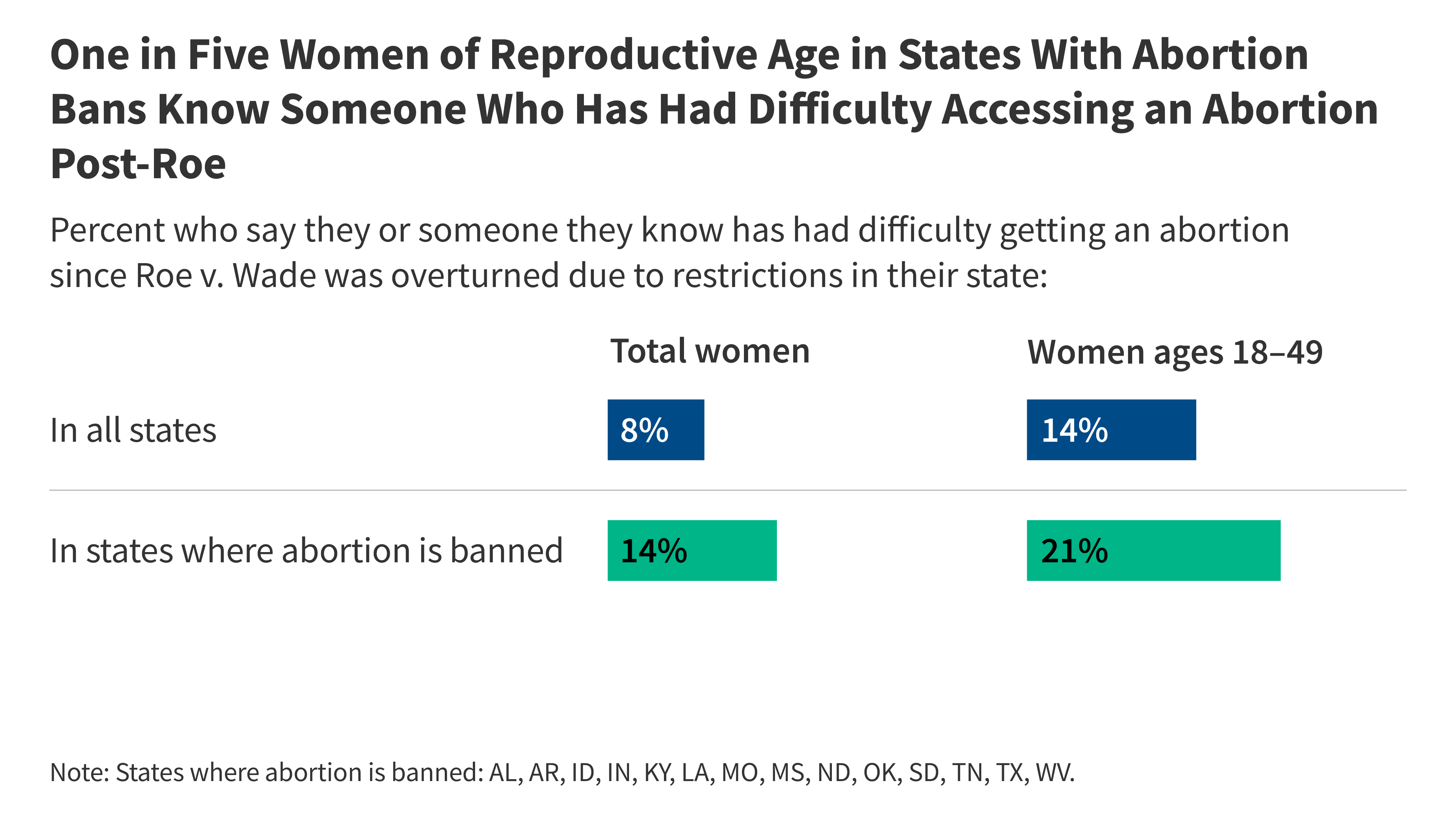
Our latest poll finds one in five women of reproductive age in states with abortion bans say either they or someone they personally know has had difficulty obtaining an abortion. Majorities of women across states—including in those with abortion bans—think abortion should be legal in all or most cases and support a range of policies that protect abortion access.
Pregnancy-Related Mortality (per 100,000 births) by Race and Ethnicity, 2017-2019
Native Hawaiian or Pacific Islander, American Indian or Alaskan Native and Black people are more likely to die while pregnant or within a year of the end of pregnancy compared to White people
State Abortion Policies by Race and Ethnicity Among Women Ages 18-49, 2022
Six in ten of Black (60%) and AIAN (59%) women ages 18-49 live in states with abortion bans or restrictions. Just over half (53%) of White women ages 18-49 live in states with bans or restrictions, while less than half of Hispanic (45%) and about three in ten Asian (28%) and NHPI (29%) women ages 18-49 live in these states
A National Survey of OBGYNs’ Experiences After Dobbs
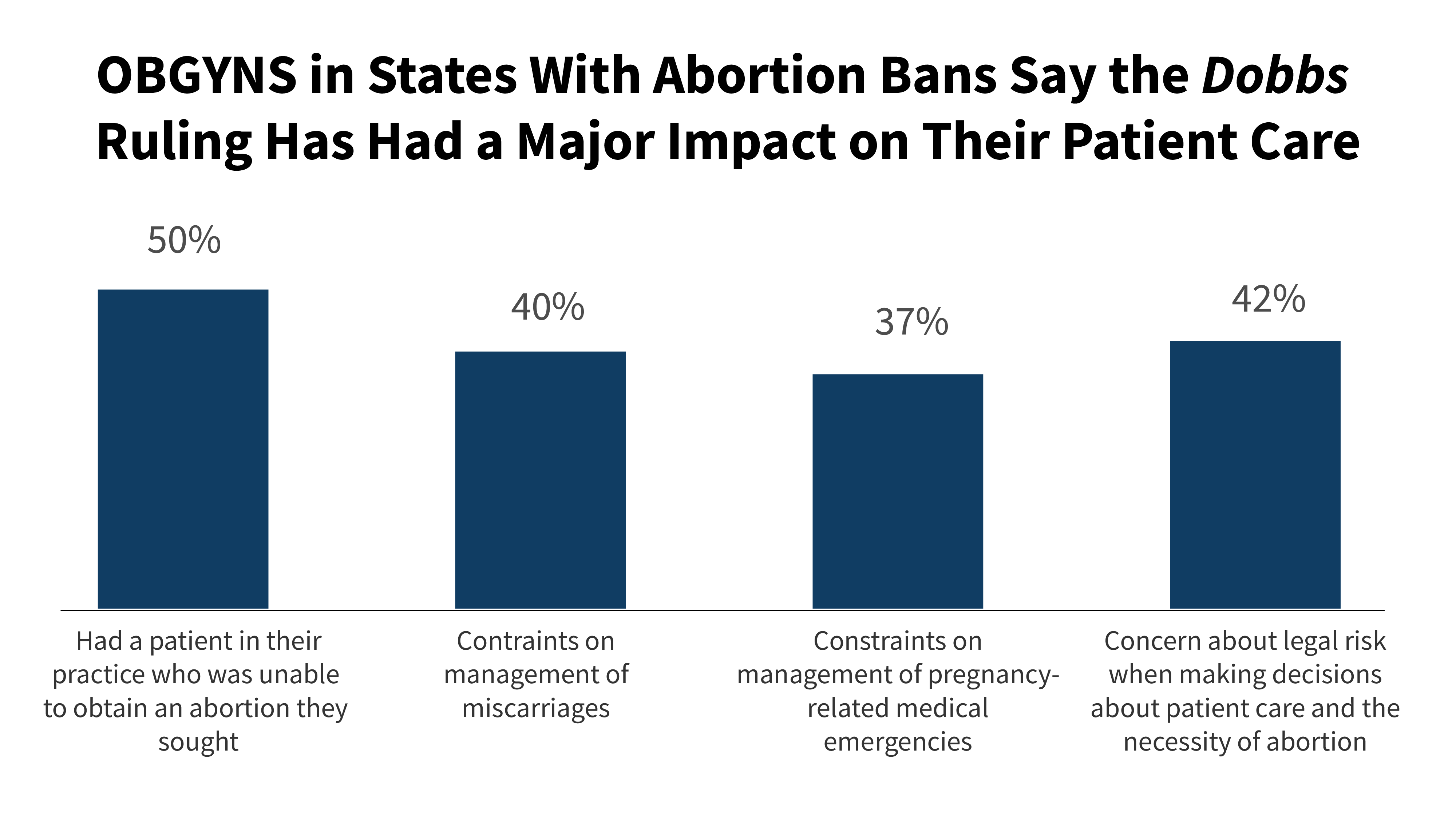
This report, based on a nationally representative survey of office-based OBGYNs practicing in the United States, examines the provision of sexual and reproductive health care provided by OBGYNs before and after the Dobbs decision, comparing the experiences of OBGYNs practicing in states where abortion is fully banned, states with gestational restrictions, and states where abortion remains available under most circumstances.
Abortion Statistics by State
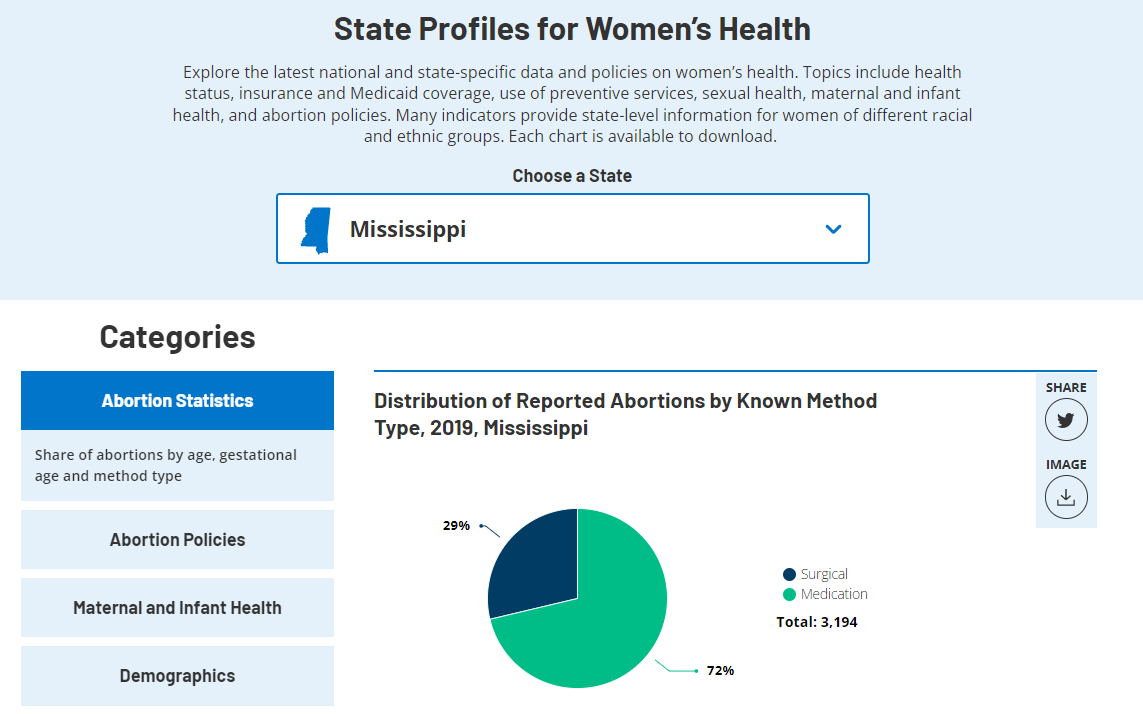
Share of abortions by age, gestational age and method type.
Abortion Policies by State
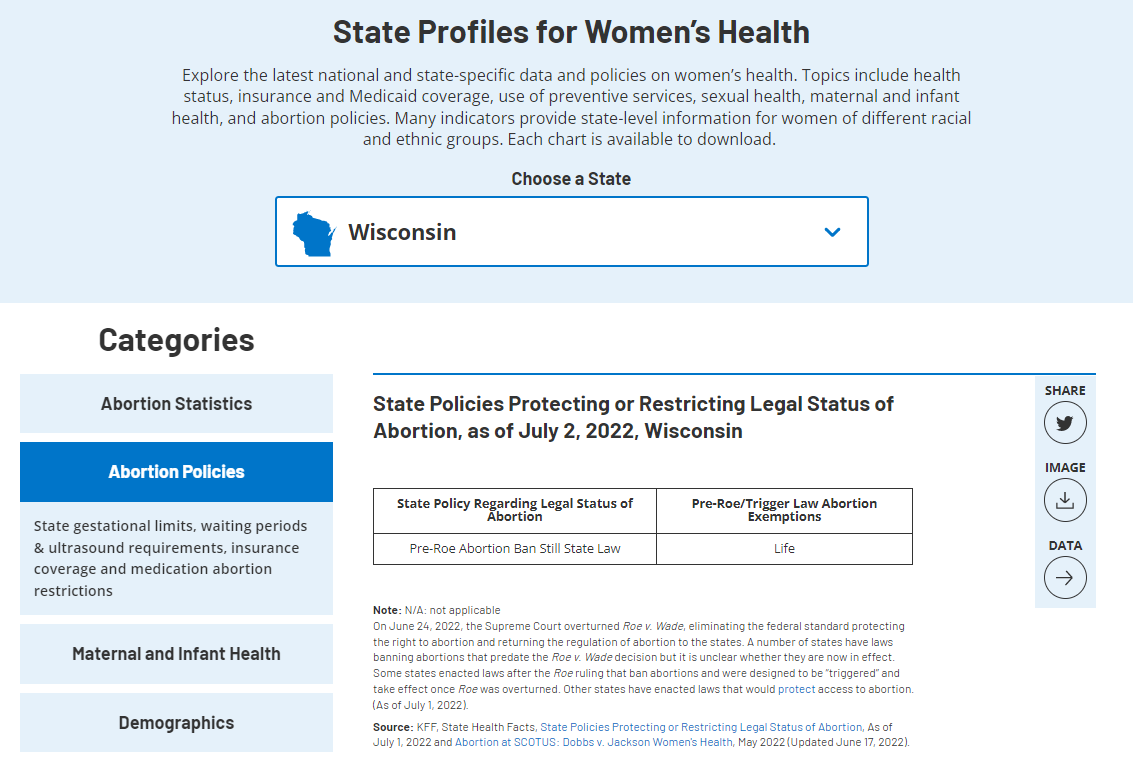
State gestational limits, waiting periods & ultrasound requirements, insurance coverage, and medication abortion restrictions.
Latest Resources From KFF

What the Election Could Mean for the Mexico City Policy and U.S. Foreign Aid

The Right to Contraception: State and Federal Actions, Misinformation, and the Courts

KFF Examines New Rule Giving LGBTQ+ People More Protections Against Discrimination in Health Care
The Biden Administration’s Final Rule on Section 1557 Non-Discrimination Regulations Under the ACA
Abortion gestational limits and exceptions.

KFF Examines Implications of Dobbs-era Abortion Bans and Restrictions for Miscarriage or Stillbirth

IMAGES
VIDEO
COMMENTS
Topic Selection. The initial topics were defined based on current developments in the health informatics field and an increasing number of published manuscripts between 2000 and 2021 (based on title-abstract-keyword screening in Scopus using the keywords "Health" AND "Informatics" AND "domain") in the respective subdomains (Figure 1 A).). After a first definition of the specific ...
Course Description. Evidence-based healthcare (EBHC) and big data can play important roles in healthcare. EBHC's main purpose is to increase and improve the use of evidence (i.e., data and information) by stakeholders (e.g., health practitioners, policy-makers, public health managers, etc.). As health data continues to grow, big data can also ...
Overview. This journal presents research on the application of computer science principles, information science principles, information technology, and communication technology to healthcare and everyday wellness, highlighting novel technical contributions in computing-oriented healthcare informatics. The journal explores three major tracks ...
Request PDF | Data, Information, Evidence, and Knowledge:: A Proposal for Health Informatics and Data Science | In this commentary, I revisit and modify Ackoff's data-information-knowledge-wisdom ...
printed while online and a copy submitted to the Graduate Program Director of Health Informatics at the Center for Health Informatics 5. Upon completion of the project the student will submit the following to the research advisor for evaluation. f. A scholarly paper describing the project g. A one page abstract that includes i. Purpose of the ...
Health Informatics Journal is an international peer-reviewed journal. ... Special Collection proposals can be submitted at any time via our online form. Calls for papers. Check out our latest calls for papers: ... Sage Research Methods Supercharging research opens in new tab;
A Global Roadmap for Health Informatics Standardization Proposal prepared by the World Economic Forum, in collaboration with Boston Consulting Group ... Use cases that demonstrate how health informatics standardization can improve value in healthcare ... IBM Watson Health Mona Khalid VP of Outcomes Research and Development, ICHOM Geraldine Lissalde
Health informatics is a relatively new research area. Over the last decade or so, research in health information has been growing at a very rapid rate, as evidenced by the large number of publications. ... A proposal for debate Methods of Information in Medicine 34(5), 426-433 (1995) Google Scholar van Bemmel, J.H.: The structure of medical ...
Lean, also known as lean philosophy, is a management model that has been used in the area of Health [11], and has its origin in the automobile industry. Different applications in common problems in the routine of many health services such as long queues, rising costs, and various types of recurring waste such as inventory, administration, and ...
DBMI has a tripartite mission of conducting innovative biomedical informatics research, training, and service in a highly diverse environment. Research: We develop, implement, and evaluate new informatics algorithms and tools for accelerating health sciences discoveries, improving healthcare, and monitoring and preventing disease.
Healthcare informatics research is a systematic process of. compiling, analyzing, and simulating data to produce veri-. fied and replicated findings from observ ed facts or phenom-. ena. The ...
the PHIS and the results of the project to provide the health examination result counseling service to. local residents through the linked actions. The results of the analysis are as follows ...
The Health Informatics Learning Lab (HILL) is a dedicated lab and teaching space intended for research and collaboration for informatics students, researchers and faculty. The lab provides unique playground for informatics for students for their in-class and out-of-class projects and is located in Peterson Family Health Sciences.
5 Exciting Health Care Informatics Projects. 6 min read. Thanks to revolutionary technological advancements, modern medicine is poised for transformation from a "disease industry" to a "scientific wellness industry," according to a report in healthcareitnews.com . And at the heart of this transition is the field of health care informatics.
A proposal to catalyze and expand health informatics at UWM Mission The Health Informatics Research Institute (HIRI) will be a campus-wide organizational entity providing common health informatics infrastructure and space designed to enhance and complement campus-wide health and biomedical informatics research resources, provide researchers pre ...
This study aims to examine the current status and utilization of 22 health promotion projects that use the health care information system. We investigate the health promotion examination results for a counseling project held at health centers, which use information connected with the Health Insurance Corporation. First, we review the status of 22 health promotion projects, including 13 ...
Students will have the opportunity to develop and implement a Health Informatics project in their workplace or other academic / industry ... or other academic institutions to work on an informatics or research based capstone ... Capstone Identification and Proposal: 1-2 weeks; Capstone Implementation: 5-7 weeks; Capstone Paper and Presentation ...
Health Informatics Thesis Topics Health Care Management and Technology Adoption E-Learning in Health Care Settings Decision Modeling and Natural Language Processing Disease-based or Specific Clinical Issues Health Information Safety and Security Health informatics students in nearly all master's degree programs must write a long, focused paper as part of their requirements for graduation. One ...
RESEARCH PROPOSAL FOR EHR DOCUMENTATION ii . Abstract . This research proposal contains and introduction to my proposed research, background of the issue at hand, purpose of the research, significance of the research, ... patient health information generated by one or more encounters in any care delivery setting" (HIMSS, 2015). Free Text is ...
My research creates a basis for further research in biology and computer innovation, leading to a better amalgamation of the two. Conclusion The introduction of health informatics goes a long way in incorporating the two fields. Health informatics resided at the intersection of data science and healthcare.
PILOT PROJECT - CALL FOR PROPOSALS Objectives: ... etc. Loyola University Chicago's Center for Health Outcomes and Informatics Research (CHOIR) strives to leverage our informatics infrastructure and data analytics capabilities to improve health outcomes and reduce health disparities, and to develop health outcomes and informatics expertise ...
Study 1 presents a research model based on data collected from four different archival datasets. Drawing upon the resource advantage theory, this paper uses archival data from 200 Texas hospitals, thus mitigating potential response bias and enhancing the validity of the findings. ... The Health Information Technology for Economic and Clinical ...
The Advanced Research Projects Agency for Health ... Proposals should not assume provision of any Government Furnished Information (GFI). The Government may provide GFI, but the specific GFI would be negotiated after a proposal is selected for award negotiations (i.e., a proposal must stand on its own without assumptions and conditions related ...
The Abortion in the U.S. Dashboard is an ongoing research project tracking state abortion policies and litigation following the overturning of Roe v. Wade.
Projects will support international study, research, or internships for outbound Canadian students and/or study and research for inbound international graduate students. All QES funded activities must be for academic credit/recognition. For all information on this call for proposals, please consult the program guidelines.