Medical Student Guide For Critical Thinking

Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
To be more effective in their studies, students must think their way through abstract problems, work in teams and separate high quality from low quality information. These are the same qualities that today's medical students are supposed to possess regardless of whether they graduate in the UK or study medicine in Europe .
In both well-defined and ill-defined medical emergencies, doctors are expected to make competent decisions. Critical thinking can help medical students and doctors achieve improved productivity, better clinical decision making, higher grades and much more.
This article will explain why critical thinking is a must for people in the medical field.

Definition of Critical Thinking
You can find a variety of definitions of Critical Thinking (CT). It is a term that goes back to the Ancient Greek philosopher Socrates and his teaching practice and vision. Critical thinking and its meaning have changed over the years, but at its core always will be the pursuit of proper judgment.
We can agree on one thing. Critical thinkers question every idea, assumption, and possibility rather than accepting them at once.
The most basic definition of CT is provided by Beyer (1995):
"Critical thinking means making reasoned judgements."
In other words, it is the ability to think logically about what to do and/or believe. It also includes the ability to think critically and independently. CT is the process of identifying, analysing, and then making decisions about a particular topic, advice, opinion or challenge that we are facing.
Steps to critical thinking
There is no universal standard for becoming a critical thinker. It is more like a unique journey for each individual. But as a medical student, you have already so much going on in your academic and personal life. This is why we created a list with 6 steps that will help you develop the necessary skills for critical thinking.
1. Determine the issue or question
The first step is to answer the following questions:
- What is the problem?
- Why is it important?
- Why do we need to find a solution?
- Who is involved?
By answering them, you will define the situation and acquire a deeper understanding of the problem and of any factors that may impact it.
Only after you have a clear picture of the issue and people involved can you start to dive deeper into the problem and search for a solution.
2. Research
Nowadays, we are flooded with information. We have an unlimited source of knowledge – the Internet.
Before choosing which medical schools to apply to, most applicants researched their desired schools online. Some of the areas you might have researched include:
- If the degree is recognised worldwide
- Tuition fees
- Living costs
- Entry requirements
- Competition for entry
- Number of exams
- Programme style
Having done the research, you were able to make an informed decision about your medical future based on the gathered information. Our list may be a little different to yours but that's okay. You know what factors are most important and relevant to you as a person.
The process you followed when choosing which medical school to apply to also applies to step 2 of critical thinking. As a medical student and doctor, you will face situations when you have to compare different arguments and opinions about an issue. Independent research is the key to the right clinical decisions. Medical and dentistry students have to be especially careful when learning from online sources. You shouldn't believe everything you read and take it as the absolute truth. So, here is what you need to do when facing a medical/study argument:
- Gather relevant information from all available reputable sources
- Pay attention to the salient points
- Evaluate the quality of the information and the level of evidence (is it just an opinion, or is it based upon a clinical trial?)
Once you have all the information needed, you can start the process of analysing it. It’s helpful to write down the strong and weak points of the various recommendations and identify the most evidence-based approach.
Here is an example of a comparison between two online course platforms , which shows their respective strengths and weaknesses.
When recommendations or conclusions are contradictory, you will need to make a judgement call on which point of view has the strongest level of evidence to back it up. You should leave aside your feelings and analyse the problem from every angle possible. In the end, you should aim to make your decision based on the available evidence, not assumptions or bias.
4. Be careful about confirmation bias
It is in our nature to want to confirm our existing ideas rather than challenge them. You should try your best to strive for objectivity while evaluating information.
Often, you may find yourself reading articles that support your ideas, but why not broaden your horizons by learning about the other viewpoint?
By doing so, you will have the opportunity to get closer to the truth and may even find unexpected support and evidence for your conclusion.
Curiosity will keep you on the right path. However, if you find yourself searching for information or confirmation that aligns only with your opinion, then it’s important to take a step back. Take a short break, acknowledge your bias, clear your mind and start researching all over.
5. Synthesis
As we have already mentioned a couple of times, medical students are preoccupied with their studies. Therefore, you have to learn how to synthesise information. This is where you take information from multiple sources and bring the information together. Learning how to do this effectively will save you time and help you make better decisions faster.
You will have already located and evaluated your sources in the previous steps. You now have to organise the data into a logical argument that backs up your position on the problem under consideration.
6. Make a decision
Once you have gathered and evaluated all the available evidence, your last step is to make a logical and well-reasoned conclusion.
By following this process you will ensure that whatever decision you make can be backed up if challenged
Why is critical thinking so important for medical students?
The first and most important reason for mastering critical thinking is that it will help you to avoid medical and clinical errors during your studies and future medical career.
Another good reason is that you will be able to identify better alternative options for diagnoses and treatments. You will be able to find the best solution for the patient as a whole which may be different to generic advice specific to the disease.
Furthermore, thinking critically as a medical student will boost your confidence and improve your knowledge and understanding of subjects.
In conclusion, critical thinking is a skill that can be learned and improved. It will encourage you to be the best version of yourself and teach you to take responsibility for your actions.
Critical thinking has become an essential for future health care professionals and you will find it an invaluable skill throughout your career.
We’ll keep you updated

Science-Based Medicine
Exploring issues and controversies in the relationship between science and medicine

Critical Thinking in Medicine
Cognitive Errors and Diagnostic Mistakes is a superb new guide to critical thinking in medicine written by Jonathan Howard. It explains how our psychological foibles regularly bias and betray us, leading to diagnostic mistakes. Learning critical thinking skills is essential but difficult. Every known cognitive error is illustrated with memorable patient stories.
Rodin’s Thinker is doing his best to think but if he hasn’t learned critical thinking skills, he is likely to make mistakes. The human brain is prone to a multitude of cognitive errors.
Critical thinking in medicine is what the Science-Based Medicine ( SBM ) blog is all about. Jonathan Howard has written a superb book, Cognitive Errors and Diagnostic Mistakes: A Case-Based Guide to Critical Thinking in Medicine , that epitomizes the message of SBM . In fact, in the Acknowledgements, he credits the entire team at SBM for teaching him “an enormous amount about skepticism and critical thinking”, and he specifically thanks Steven Novella, Harriet Hall (moi!), and David Gorski.
Dr. Howard is a neurologist and psychiatrist at NYU and Bellevue Hospital. The book is a passionate defense of science and a devastating critique of Complementary and Alternative Medicine ( CAM ) and pseudoscience. Its case-based approach is a stroke of genius. We humans are story-tellers; we are far more impressed by stories than by studies or by textbook definitions of a disease. Dr. Howard points out that “Anecdotes are part of the very cognition that allows us to derive meaning from experience and turn noise into signal.” They are incredibly powerful from an emotional standpoint. That’s why he chose to begin every discussion of a cognitive error with a patient’s case, an anecdote.
CAM knows how effective this can be; that’s why it relies so heavily on anecdotes. When doctors think of a disease, they are likely to think of a memorable patient they treated with that disease, and that patient’s case is likely to bias their thinking about other patients with the same disease. If there is a bad outcome with a treatment, they will remember that and may reject that treatment for the next patient even if it is the most appropriate one. Dr. Howard uses patient stories to great advantage, first providing the bare facts of the case and then letting the patient’s doctors explain their thought processes so we can understand exactly where and why they went wrong. Then he goes on to explain the psychology behind the cognitive error, with study findings, other examples, and plentiful references. If readers remember these cases, they might avoid similar mishaps.
An encyclopedia of cognitive errors
The book is encyclopedic, running to 30 chapters and 588 pages. I can’t think of anything he failed to mention, and whenever an example or a quotation occurred to me, he had thought of it first and included it in the text. I couldn’t begin to list all the cognitive errors he covers, but they fall roughly into these six categories:
- Errors of overattachment to a particular diagnosis
- Errors due to failure to consider alternative diagnoses.
- Errors due to inheriting someone else’s thinking.
- Errors in prevalence perception or estimation.
- Errors involving patient characteristics or presentation context.
- Errors associated with physician affect, personality, or decision style.
A smattering of examples
There is so much information and wisdom in this book! I’ll try to whet your appetite with a few excerpts that particularly struck me.
- Discussing an issue with others who disagree can help us avoid confirmation bias and groupthink.
- Negative panic: when a group of people witness an emergency and fail to respond, thinking someone else will.
- Reactance bias: doctors who object to conventional practices and want to feel independent may reject science and embrace pseudoscience.
- Cyberchondria: using the Internet to interpret mundane symptoms as dire diagnoses.
- Motivated reasoning: People who “know” they have chronic Lyme disease will fail to believe 10 negative Lyme tests in a row and then believe the 11 th test if it is positive.
- The backfire effect: “encountering contradictory information can have the paradoxical effect of strengthening our initial belief rather than causing us to question it.”
- Biases are easy to see in others but nearly impossible to detect in oneself.
- Checklists for fake diseases take advantage of the Forer effect . As with horoscopes and cold readings, vague, nonspecific statements convince people that a specific truth about them is being revealed. Fake diseases are unfalsifiable: there is no way to rule them out.
- When presenting risk/benefit data to patients, don’t present risk data first; it will act as an “anchor” to make them fixate on risk.
- The doctor’s opinion of the patient will affect the quality of care.
- Randomness is difficult to grasp. The hot hand and the gambler’s fallacy can both fool doctors. If the last two patients had disease X and this patient has similar symptoms, the doctor will think he probably has disease X too. Or if the doctor has just seen two cases of a rare disease, it will seem unlikely that the next patient with similar symptoms will have it too.
- Apophenia : the tendency to perceive meaningful patterns with random information, like seeing the face on Mars.
- Information bias: doctors tend to think the more information, the better. But tests are indicated only if they will help establish a diagnosis or alter management. They should not be ordered out of curiosity or to make the clinician feel better. Sometimes doctors don’t know what to do with the information from a test. This should be a lesson for doctors who practice so-called functional medicine : they order all kinds of nonstandard tests whose questionable results give no evidence-based guidance for treating the patient. Doctors should ask “How will this test alter my management?” and if they can’t answer, they shouldn’t order the test.
- Once a treatment is started, it can be exceedingly difficult to stop. A study showed that 58% of medications could be stopped in elderly patients and only 2% had to be re-started.
- Doctors feel obligated to “do something” for the patient, but sometimes the best course is to do nothing. “Just don’t do something, stand there.” At the end of their own life, 90% of doctors would refuse the treatments they routinely give to patients with terminal illnesses.
- Incidentalomas: when a test reveals an unsuspected finding, it’s important to remember that abnormality doesn’t necessarily mean pathology or require treatment.
- Fear of possible unknown long-term consequences may lead doctors to reject a treatment, but that should be weighed carefully against the well-known consequences of the disease itself.
- It’s good for doctors to inform patients and let them participate in decisions, but too much information can overwhelm patients. He gives the example of a patient with multiple sclerosis whose doctor describes the effectiveness and risks of 8 injectables, 3 pills, and 4 infusions. The patient can’t choose; she misses the follow-up appointment and returns a year later with visual loss that might have been prevented.
- Most patients don’t benefit from drugs; the NNT tells us the Number of patients who will Need to be Treated for one person to benefit.
- Overconfidence bias: in the Dunning-Kruger effect, people think they know more than the experts about things like climate change, vaccines and evolution. Yet somehow these same people never question that experts know how to predict eclipses.
- Patient satisfaction does not measure effectiveness of treatment. A study showed that the most satisfied patients were 12% more likely to be admitted to the hospital, had 9% higher prescription costs, and were 26% more likely to die.
- The availability heuristic and the frequency illusion: “Clinicians should be aware that their experience is distorted by recent or memorable [cases], the experiences of their colleagues, and the news.” He repeats Mark Crislip’s aphorism that the three most dangerous words in medicine are “in my experience”.
- Illusory truth: people are likely to believe a statement simply because they have heard it many times.
- What makes an effective screening test? He covers concepts like lead time bias, length bias, and selection bias. Screening tests may do more harm than good. The PSA test is hardly better than a coin toss.
- Blind spot bias: Everyone has blind spots; we recognize them in others but can’t see our own. Most doctors believe they won’t be influenced by gifts from drug companies, but they believe others are unconsciously biased by such gifts. Books like this can make things worse: they give us false confidence. “Being inclined to think that you can avoid a bias because you [are] aware of it is a bias in itself.”
- He quotes from Contrived Platitudes: “Everything happens for a reason except when it doesn’t. But even then you can in hindsight fabricate a reason that will satisfy your belief system.” This is the essence of what CAM does, especially the versions that attribute all diseases to a single cause.
Some juicy quotes
Knowledge of bias should contribute to your humility, not your confidence.
Only by studying treatments in large, randomized, blinded, controlled trials can the efficacy of a treatment truly be measured.
When beliefs are based in emotion, facts alone stand little chance.
CAM , when not outright fraudulent, is nothing more than the triumph of cognitive biases over rationality and science.
Reason evolved primarily to win arguments, not to solve problems.
He includes a thorough discussion of the pros and cons of limiting doctors’ work hours, with factors most people have never considered, and a thorough discussion of financial motivations.
The book is profusely illustrated with pictures, diagrams, posters, and images from the Internet like “The Red Flags of Quackery” from sci-ence.org. Many famous quotations are presented with pictures of the person quoted, like Christopher Hitchens and his “What can be asserted without evidence can be dismissed without evidence”.
He never goes beyond the evidence. Rather than just giving study results, he tells the reader when other researchers have failed to replicate the findings.
We rely on scientific evidence, but researchers are not immune from bias. He describes the many ways research can go astray: 235 biases have been identified that can lead to erroneous results. As Ioannidis said, most published research findings are wrong. But all is not lost: people who understand statistics and the methodologies of science can usually distinguish a good study from a bad one.
He tells the infamous N-ray story. He covers the file drawer effect, publication bias, conflicts of interest, predatory journals, ghostwriting, citation plagiarism, retractions, measuring poor surrogates instead of meaningful clinical outcomes, and outright fraud. Andrew Wakefield features prominently. Dr. Howard’s discussions of p-hacking, multiple variables, random chance, and effect size are particularly valuable. HARKing is Hypothesizing After the Results are Known. It can be exploited to create erroneous results.
He tells a funny story that was new to me. Two scientists wrote a paper consisting entirely of the repeated sentence “Get me off your fucking mailing list” complete with diagrams of that sentence. It was rated as excellent and was accepted for publication!
Conclusion: Well worth reading for doctors and for everyone else
As the book explains, “The brain is a self-affirming spin-doctor with a bottomless bag of tricks…” Our brains are “pattern-seeking machines that fill in the gaps in our perception and knowledge consistent with our expectations, beliefs, and wishes”. This book is a textbook explaining our cognitive errors. Its theme is medicine but the same errors occur everywhere. We all need to understand our psychological foibles in order to think clearly about every aspect of our lives and to make the best decisions. Every doctor would benefit from reading this book, and I wish it could be required reading in medical schools. I wish everyone who considers trying CAM would read it first. I wish patients would ask doctors to explain why they ordered a test.
The book is not inexpensive. The price on Amazon is $56.99 for both softcover and Kindle versions. But it might be a good investment: you might save much more money that that by applying the principles it teaches, and critical thinking skills might even save your life. Well-written, important, timely, easy, and entertaining to read, lots of illustrations, packed with good stuff. Highly recommended.
Harriet Hall, MD also known as The SkepDoc, is a retired family physician who writes about pseudoscience and questionable medical practices. She received her BA and MD from the University of Washington, did her internship in the Air Force (the second female ever to do so), and was the first female graduate of the Air Force family practice residency at Eglin Air Force Base. During a long career as an Air Force physician, she held various positions from flight surgeon to DBMS (Director of Base Medical Services) and did everything from delivering babies to taking the controls of a B-52. She retired with the rank of Colonel. In 2008 she published her memoirs, Women Aren't Supposed to Fly .
View all posts
- Posted in: Book & movie reviews , Critical Thinking , Neuroscience/Mental Health , Science and Medicine
- Tagged in: bias , CAM , cognitive errors , diagnostic mistakes , Jonathan Howard
Posted by Harriet Hall
Critical Thinking in Medicine and Health
- First Online: 01 March 2020
Cite this chapter
- Louise Cummings 2
743 Accesses
1 Citations
This chapter addresses why there is a need for experts and lay people to think critically about medicine and health. It will be argued that illogical, misleading, and contradictory information in medicine and health can have pernicious consequences, including patient harm and poor compliance with health recommendations. Our cognitive resources are our only bulwark to the misinformation and faulty logic that exists in medicine and health. One resource in particular—reasoning—can counter the flawed thinking that pervades many medical and health issues. This chapter examines how concepts such as reasoning, logic and argument must be conceptualised somewhat differently (namely, in non-deductive terms) to accommodate the rationality of the informal fallacies. It also addresses the relevance of the informal fallacies to medicine and health and considers how these apparently defective arguments are a source of new analytical possibilities in both domains.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Albano, J. D., Ward, E., Jemal, A., Anderson, R., Cokkinides, V. E., Murray, T., et al. (2007). Cancer mortality in the United States by education level and race. Journal of the National Cancer Institute, 99 (18), 1384–1394.
Article Google Scholar
Coxon, J., & Rees, J. (2015). Avoiding medical errors in general practice. Trends in Urology & Men’s Health, 6 (4), 13–17.
Google Scholar
Croskerry, P. (2003). The importance of cognitive errors in diagnosis and strategies to minimize them. Academic Medicine, 78 (8), 775–780.
Cummings, L. (2002). Reasoning under uncertainty: The role of two informal fallacies in an emerging scientific inquiry. Informal Logic, 22 (2), 113–136.
Cummings, L. (2004). Analogical reasoning as a tool of epidemiological investigation. Argumentation, 18 (4), 427–444.
Cummings, L. (2009). Emerging infectious diseases: Coping with uncertainty. Argumentation, 23 (2), 171–188.
Cummings, L. (2010). Rethinking the BSE crisis: A study of scientific reasoning under uncertainty . Dordrecht: Springer.
Book Google Scholar
Cummings, L. (2011). Considering risk assessment up close: The case of bovine spongiform encephalopathy. Health, Risk & Society, 13 (3), 255–275.
Cummings, L. (2012a). Scaring the public: Fear appeal arguments in public health reasoning. Informal Logic, 32 (1), 25–50.
Cummings, L. (2012b). The public health scientist as informal logician. International Journal of Public Health, 57 (3), 649–650.
Cummings, L. (2013a). Public health reasoning: Much more than deduction. Archives of Public Health, 71 (1), 25.
Cummings, L. (2013b). Circular reasoning in public health. Cogency, 5 (2), 35–76.
Cummings, L. (2014a). Informal fallacies as cognitive heuristics in public health reasoning. Informal Logic, 34 (1), 1–37.
Cummings, L. (2014b). The ‘trust’ heuristic: Arguments from authority in public health. Health Communication, 29 (10), 1043–1056.
Cummings, L. (2014c). Coping with uncertainty in public health: The use of heuristics. Public Health, 128 (4), 391–394.
Cummings, L. (2014d). Circles and analogies in public health reasoning. Inquiry, 29 (2), 35–59.
Cummings, L. (2014e). Analogical reasoning in public health. Journal of Argumentation in Context, 3 (2), 169–197.
Cummings, L. (2015). Reasoning and public health: New ways of coping with uncertainty . Cham, Switzerland: Springer.
Fowler, F. J., Jr., Levin, C. A., & Sepucha, K. R. (2011). Informing and involving patients to improve the quality of medical decisions. Health Affairs, 30 (4), 699–706.
Graber, M. L., Franklin, N., & Gordon, R. (2005). Diagnostic error in internal medicine. Archives of Internal Medicine, 165 (13), 1493–1499.
Hamblin, C. L. (1970). Fallacies . London: Methuen.
Johnson, R. H. (2011). Informal logic and deductivism. Studies in Logic, 4 (1), 17–37.
Kahane, H. (1971). Logic and contemporary rhetoric: The use of reason in everyday life . Belmont, CA: Wadsworth Publishing Company.
Loucks, E. B., Buka, S. L., Rogers, M. L., Liu, T., Kawachi, I., Kubzansky, L. D., et al. (2012). Education and coronary heart disease risk associations may be affected by early life common prior causes: A propensity matching analysis. Annals of Epidemiology, 22 (4), 221–232.
Saposnik, G., Redelmeier, D., Ruff, C. C., & Tobler, P. N. (2016). Cognitive biases associated with medical decisions: A systematic review. BMC Medical Informatics and Decision Making, 16, 138. https://doi.org/10.1186/s12911-016-0377-1 .
Trowbridge, R. L. (2008). Twelve tips for teaching avoidance of diagnostic errors. Medical Teacher, 30, 496–500.
Walton, D. N. (1985a). Are circular arguments necessarily vicious? American Philosophical Quarterly, 22 (4), 263–274.
Walton, D. N. (1985b). Arguer’s Position . Westport, CT: Greenwood Press.
Walton, D. N. (1987). The ad hominem argument as an informal fallacy. Argumentation, 1 (3), 317–331.
Walton, D. N. (1991). Begging the question: Circular reasoning as a tactic of argumentation . New York: Greenwood Press.
Walton, D. N. (1992). Plausible argument in everyday conversation . Albany: SUNY Press.
Walton, D. N. (1996). Argumentation schemes for presumptive reasoning . Mahwah, NJ: Erlbaum.
Walton, D. N. (2010). Why fallacies appear to be better arguments than they are. Informal Logic, 30 (2), 159–184.
Weingart, S. N., Wilson, R. M., Gibberd, R. W., & Harrison, B. (2000). Epidemiology of medical error. Western Journal of Medicine, 172 (6), 390–393.
Woods, J. (1995). Appeal to force. In H. V. Hansen & R. C. Pinto (Eds.), Fallacies: Classical and contemporary readings (pp. 240–250). University Park: The Pennsylvania State University Press.
Woods, J. (2004). The death of argument: Fallacies in agent-based reasoning . Dordrecht: Kluwer Academic.
Woods, J. (2007). Lightening up on the ad hominem. Informal Logic, 27 (1), 109–134.
Woods, J. (2008). Begging the question is not a fallacy. In C. Dégremont, L. Keiff, & H. Rükert (Eds.), Dialogues, logics and other strange things: Essays in honour of Shahid Rahman (pp. 523–544). London: College Publications.
Download references
Author information
Authors and affiliations.
Department of English, The Hong Kong Polytechnic University, Hung Hom, Kowloon, Hong Kong
Louise Cummings
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Louise Cummings .
Chapter Summary
Medicine and health have tended to be overlooked in the critical thinking literature . And yet robust critical thinking skills are needed to evaluate the large number and range of health messages that we are exposed to on a daily basis.
An ability to think critically helps us to make better personal health choices and to uncover biases and errors in health messages and other information. An ability to think critically allows us to make informed decisions about medical treatments and is vital to efforts to reduce medical diagnostic errors.
A key element in critical thinking is the ability to distinguish strong or valid reasoning from weak or invalid reasoning. When an argument is weak or invalid, it is called a ‘fallacy’ or a ‘fallacious argument’.
The informal fallacies are so-called on account of the presence of epistemic and dialectical flaws that cannot be captured by formal logic . They have been discussed by many generations of philosophers and logicians , beginning with Aristotle .
Historically, philosophers and logicians have taken a pejorative view of the informal fallacies. Much of the criticism of these arguments is related to a latent deductivism in logic , the notion that arguments should be evaluated according to deductive standards of validity and soundness . Against deductive standards and norms, many reasonable arguments are judged to be fallacies.
Developments in logic , particularly the teaching of logic, forced a reconsideration of the prominence afforded to deductive logic in the evaluation of arguments. New criteria based on presumptive reasoning and plausible argument started to emerge. Against this backdrop, non-fallacious variants of most of the informal fallacies began to be described for the first time.
Today, some argument analysts characterize non-fallacious variants of the informal fallacies in terms of cognitive heuristics . During reasoning , these heuristics function as mental shortcuts, allowing us to bypass knowledge and come to judgement about complex health problems.
Suggestions for Further Reading
Sharples, J. M., Oxman, A. D., Mahtani, K. R., Chalmers, I., Oliver, S., Collins, K., Austvoll-Dahlgren, A., & Hoffmann, T. (2017). Critical thinking in healthcare and education. British Medical Journal, 357 : j2234. https://doi.org/10.1136/bmj.j2234 .
The authors examine the role of critical thinking in medicine and healthcare, arguing that critical thinking skills are essential for doctors and patients. They describe an international project that involves collaboration between education and health. Its aim is to develop a curriculum and learning resources for critical thinking about any action that is claimed to improve health.
Hitchcock, D. (2017). On reasoning and argument: Essays in informal logic and on critical thinking . Cham: Switzerland: Springer.
This collection of essays provides more advanced reading on several of the topics addressed in this chapter, including the fallacies, informal logic , and the teaching of critical thinking . Chapter 25 considers if fallacies have a place in the teaching of critical thinking and reasoning skills.
Hansen, H. V., & Pinto, R. C. (Eds.). (1995). Fallacies: Classical and contemporary readings . University Park: The Pennsylvania State University Press.
This edited collection of 24 chapters contains historical selections on the fallacies, contemporary theory and criticism, and analyses of specific fallacies. It also examines fallacies and teaching. There are chapters on four of the fallacies that will be examined in this book: appeal to force; appeal to ignorance ; appeal to authority; and post hoc ergo propter hoc .
Diagnostic errors are a significant cause of death and serious injury in patients. Many of these errors are related to cognitive factors. Trowbridge ( 2008 ) has devised twelve tips to familiarize medical students and physician trainees with the cognitive underpinnings of diagnostic errors. One of these tips is to explicitly describe heuristics and how they affect clinical reasoning . These heuristics include the following:
Representativeness —a patient’s presentation is compared to a ‘typical’ case of specific diagnoses.
Availability —physicians arrive at a diagnosis based on what is easily accessible in their minds, rather than what is actually most probable.
Anchoring —physicians may settle on a diagnosis early in the diagnostic process and subsequently become ‘anchored’ in that diagnosis.
Confirmation bias —as a result of anchoring, physicians may discount information discordant with the original diagnosis and accept only that which supports the diagnosis.
Using the above information, identify any heuristics and biases that occur in the following scenarios:
Scenario 1: A 60-year-old man has epigastric pain and nausea. He is sitting forward clutching his abdomen. He has a history of several bouts of alcoholic pancreatitis. He states that he felt similar during these bouts to what he is currently feeling. The patient states that he has had no alcohol in many years. He has normal blood levels of pancreatic enzymes. He is given a diagnosis of acute pancreatitis. It is eventually discovered that he has had acute myocardial infarction.
Scenario 2: A 20-year-old, healthy man presents with sudden onset of severe, sharp chest pain and back pain. Based on these symptoms, he is suspected of having a dissecting thoracic aortic aneurysm. (In an aortic dissection, there is a separation of the layers within the wall of the aorta, the large blood vessel branching off the heart.) He is eventually diagnosed with pleuritis (inflammation of the pleura, the thin, transparent, two-layered membrane that covers the lungs).
Many of the logical terms that were introduced in this chapter also have non-logical uses in everyday language. Below are several examples of the use of these terms. For each example, indicate if the word in italics has a logical or a non - logical meaning or use:
University ‘safe spaces’ are a dangerous fallacy —they do not exist in the real world ( The Telegraph , 13 February 2017).
The MRI findings beg the question as to whether a careful ultrasound examination might have yielded some of the same information on haemorrhages ( British Medical Journal: Fetal & Neonatal , 2011).
The youth justice system is a slippery slope of failure ( The Sydney Morning Herald , 26 July 2016).
The EU countered with its own gastronomic analogy , saying that “cherry picking” the best bits of the EU would not be tolerated ( BBC News , 28 July 2017).
As Ebola spreads, so have several fallacies ( The New York Times , 23 October 2014).
Removing the statue of Confederacy Army General Robert E. Lee no more puts us on a slippery slope towards ousting far more nuanced figures from the public square than building the statue in the first place put us on a slippery slope toward, say, putting up statues of Hitler outside of Holocaust museums or of Ho Chi Minh at Vietnam War memorials ( Chicago Tribune , 16 August 2017).
We can expand the analogy a bit and think of a culture as something akin to a society’s immune system—it works best when it is exposed to as many foreign bodies as possible ( New Zealand Herald , 4 May 2010).
The Josh Norman Bowl begs the question : What’s an elite cornerback worth? ( The Washington Post , 17 December 2016).
The intuition behind these analogies is simple: As a homeowner, I generally have the right to exclude whoever I want from my property. I don’t even have to have a good justification for the exclusion. I can choose to bar you from my home for virtually any reason I want, or even just no reason at all. Similarly, a nation has the right to bar foreigners from its land for almost any reason it wants, or perhaps even no reason at all ( The Washington Post , 6 August 2017).
Legalising assisted suicide is a slippery slope toward widespread killing of the sick, Members of Parliament and peers were told yesterday ( Mail Online , 9 July 2014).
In the Special Topic ‘What’s in a name?’, an example of a question-begging argument from the author’s recent personal experience was used. How would you reconstruct the argument in this case to illustrate the presence of a fallacy?
On 9 July 2017, the effect of coconut oil on health was also discussed in an article in The Guardian entitled ‘Coconut oil: Are the health benefits a big fat lie?’ The following extract is taken from that article. (a) What type of reasoning is the author using in this extract? In your response, you should reconstruct the argument by presenting its premises and conclusion . Also, is this argument valid or fallacious in this particular context?
When it comes to superfoods, coconut oil presses all the buttons: it’s natural, it’s enticingly exotic, it’s surrounded by health claims and at up to £8 for a 500 ml pot at Tesco, it’s suitably pricey. But where this latest superfood differs from benign rivals such as blueberries, goji berries, kale and avocado is that a diet rich in coconut oil may actually be bad for us.
The article in The Guardian also makes extensive use of expert opinion. Two such opinions are shown below. (b) What three linguistic devices does the author use to confer expertise or authority on the individuals who advance these opinions?
Christine Williams, professor of human nutrition at the University of Reading, states: “There is very limited evidence of beneficial health effects of this oil”.
Tom Sanders, emeritus professor of nutrition and dietetics at King’s College London, says: “It is a poor source of vitamin E compared with other vegetable oils”.
The author of the article in The Guardian went on to summarize the findings of a study by two researchers that was published in the British Nutrition Foundation’s Nutrition Bulletin. The author’s summary included the following statement: There is no good evidence that coconut oil helps boost mental performance or prevent Alzheimer’s disease . (c) In what type of informal fallacy might this statement be a premise ?
Scenario 1: An anchoring error has occurred in which the patient is given a diagnosis of acute pancreatitis early in the diagnostic process. The clinician becomes anchored in this diagnosis, with the result that he overlooks two pieces of information that would have allowed this diagnosis to be disconfirmed—the fact that the patient has reported no alcohol use in many years and the presence of normal blood levels of pancreatic enzymes. By dismissing this information, the clinician is also showing a confirmation bias —he attends only to information that confirms his original diagnosis.
Scenario 2: A representativeness error has occurred. The patient’s presentation is typical of aortic dissection. However, this condition can be dismissed in favour of conditions like pleuritis or pneumothorax on account of the fact that aortic dissection is exceptionally rare in 20-year-olds.
(2) (a) non-logical; (b) non-logical; (c) non-logical; (d) non-logical; (e) non-logical; (f) logical; (g) logical; (h) non-logical; (i) logical; (j) logical
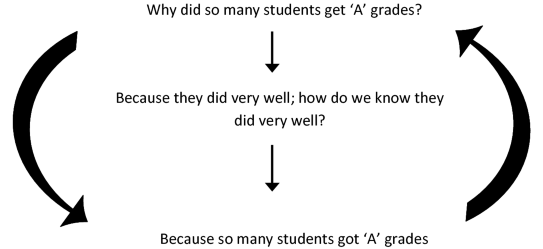
(3) The fallacy can be illustrated as follows. The head of department asks the question ‘Why did so many of these students get ‘A’ grades’? He receives the reply ‘Because they did very well’. But someone might reasonably ask ‘How do we know that they did very well?’ To which the reply is ‘Because so many students got ‘A’ grades’. The reasoning can be reconstructed in diagram form as follows:
The author is using an analogical argument , which has the following form:
P1: Blueberries, goji berries, kale, avocado and coconut oil are natural, exotic, pricey and surrounded by health claims.
P2: Blueberries, goji berries, kale and avocado have health benefits.
C: Coconut oil has health benefits.
This is a false analogy , or a fallacious analogical argument , because coconut oil does not share with these other superfoods the property or attribute < has health benefits >.
The author uses academic rank, field of specialization, and university affiliation to confer authority or expertise on individuals who advance expert opinions.
This statement could be a premise in an argument from ignorance .
Rights and permissions
Reprints and permissions
Copyright information
© 2020 The Author(s)
About this chapter
Cummings, L. (2020). Critical Thinking in Medicine and Health. In: Fallacies in Medicine and Health. Palgrave Macmillan, Cham. https://doi.org/10.1007/978-3-030-28513-5_1
Download citation
DOI : https://doi.org/10.1007/978-3-030-28513-5_1
Published : 01 March 2020
Publisher Name : Palgrave Macmillan, Cham
Print ISBN : 978-3-030-28512-8
Online ISBN : 978-3-030-28513-5
eBook Packages : Social Sciences Social Sciences (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- News & Views
- Critical thinking in...
Critical Thinking in medical education: When and How?
Rapid response to:
Critical thinking in healthcare and education
- Related content
- Article metrics
- Rapid responses
Rapid Response:
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from that of general cognitive abilities [1].
People cannot think critically about topics for which they have little knowledge. Critical thinking should be viewed as a domain-specific construct that evolves as an individual acquires domain-specific knowledge [1]. For instance, most common people have no basis for prioritizing patients in the emergency department to be shifted to the only bed available in the intensive care unit. Medical professionals who could thinking critically in their own discipline would have difficulty thinking critically about problems in other fields. Therefore, ‘domain-general’ critical thinking training and evaluation could be non-specific and might not benefit the targeted domain i.e. medical profession.
Moreover, the literature does not demonstrate that it is possible to train universally effective critical thinking skills [1]. As medical teachers, we can start building up student’s critical thinking skill by contingent teaching-learning environment wherein one should encourage reasoning and analytics, problem solving abilities and welcome new ideas and opinions [2]. But at the same time, one should continue rather tapering the critical skills as one ascends towards a specialty, thereby targeting ‘domain-specific’ critical thinking.
For the benefit of healthcare, tools for training and evaluating ‘domain-specific’ critical thinking should be developed for each of the professional knowledge domains such as doctors, nurses, lab technicians and so on. As the Authors rightly pointed out, this humongous task can be accomplished only with cross border collaboration among cognitive neuroscientists, psychologists, medical education experts and medical professionals.
References 1. National Research Council. (2011). Assessing 21st Century Skills: Summary of a Workshop. J.A. Koenig, Rapporteur. Committee on the Assessment of 21st Century Skills. Board on Testing and Assessment, Division of Behavioral and Social Sciences and Education. Washington, DC: The National Academies Press. 2. Mafakheri Laleh M, Mohammadimehr M, Zargar Balaye Jame S. Designing a model for critical thinking development in AJA University of Medical Sciences. J Adv Med Educ Prof. 2016 Oct;4(4):179–87.
Competing interests: No competing interests
Critical thinking in clinical medicine: what is it?
Affiliation.
- 1 Department of Psychiatry, University of Montreal, Montreal, PQ, Canada. [email protected]
- PMID: 22994988
- DOI: 10.1111/j.1365-2753.2012.01897.x
In this paper, we explore the recent emphasis, in various medical contexts, of the term 'critical' or the notion of 'being critical'. We identify various definitions of being critical and note that they differ strikingly. What are these different uses of the term trying to capture that is important in clinical medicine and medical education? We have analysed these qualities as responsibilist, epistemic virtues. We believe that a virtues approach is best able to make sense of the non-cognitive elements of 'being critical', such as the honesty and courage to question claims in the face of persuasion, authority or social pressure. Medical educators and professional bodies seem to agree that being critical is important and desirable. Yet, it is unclear how this quality can be optimally fostered and balanced with the constraints that act upon individual practitioners in the context of institutional medicine including professional standards and the demands of the doctor-patient relationship. Other constraints such as authoritarianism, intimidation and financial pressures may act against the expression of being critical or even the cultivation of critical thinking. The issue of the constraints on critical thinking and the potential hazards it entails will require further consideration by those who encourage being critical in medicine.
© 2012 Blackwell Publishing Ltd.
- Antidepressive Agents / adverse effects
- Clinical Medicine*
- Evidence-Based Medicine
- Physician-Patient Relations
- Antidepressive Agents
- Open access
- Published: 24 May 2023
Embracing critical thinking to enhance our practice
- Luis Martí-Bonmatí ORCID: orcid.org/0000-0002-8234-010X 1
Insights into Imaging volume 14 , Article number: 97 ( 2023 ) Cite this article
3661 Accesses
1 Citations
2 Altmetric
Metrics details
Miguel de Cervantes, the great Spanish writer, once wrote that those “who read much and walk much, go far and know much" [ 1 ]. The same is true in medicine; reading and gathering experience are the main pillars on which one should develop the knowledge of solving clinical problems in the ever-changing field of healthcare. If properly done, these newly acquired skills will continuously enhance our critical thinking strategies with which we try to identify the best possible improvements in the clinical pathway of radiology. As gaps in knowledge are always present, medicine is rooted in consolidated knowledge based on validated scientific studies and clinical experience reproducibility and accuracy [ 2 ]. This represents our best approach to evidence-based decisions. Medical knowledge must be well-established before it can be considered as the basis for decision making and patients guidance in daily practice.
The practice of critical thinking helps us understand the disease manifestations and the related processes and actions that might be relevant to prevent, diagnose and treat diseases. To critically appraise the way we perform evidence-based practice, we must combine best quality research with clinical expertise. This link between exploration and practice will allow radiologists and related disciplines to impact the way medicine is practiced.
These concepts are the cornerstones of Insights into Imaging , and it is my privilege as editor-in-chief to describe in this editorial how the journal, and each author, can contribute quality through critical thinking, and hence improve the way we practice radiology by re-shaping our understandings.
It is universally recognized that, in medical imaging, strong levels of evidence are needed to assess the results of the different possible actions and to guide decisions (i.e., to demonstrate a sufficient causal relationship between a specific diagnostic criterion and a disease grading, or a given radiological intervention versus another option in a given condition) toward the most effective or safe outcome considering the benefit of patients and value-based healthcare pathways. Consequently, solid levels of evidence are required to assess the results of different possible actions derived from imaging findings. And, in doing so, we continuously generate more data in our diagnostic and therapeutic activities, whether they are processes or outcomes. This new information will then be transformed into new evidence, real world evidence. In this way, the observed relationship between action and outcome generates causality course actions that will improve our understanding of the best clinical pathways, eliminating the many confounding thoughts that we unconsciously carry during the process of learning and implementing our clinical practice.
Socratic inquiry and Skepticism as foundation. Critical thinking can be understood as the process of analyzing and questioning existing and established knowledge with the intention of improving it. Previous knowledge, either eminence- or evidence-based, should continuously be critically reconsidered and reevaluated for the benefit of the patients, as knowledge is always changing in Precision Medicine. In the real world of medical imaging, this critical thinking must be focused on the evaluation of the effectiveness and clinical impact of all those processes in which images are involved, from the acquisition with different modalities to the processing of the data, from the biological correlation of radiomics as an image biomarker to the therapeutic orientation, and finally in image-guided interventional treatments. Developing critical thinking helps to improve any medical discipline by asking ourselves how to establish better and more precise processes based on existing accumulated evidence, how to recognize and control the biases when approaching a clinical problem, and how to adapt the new clinical information in service of the best solutions. Socratic inquiry and a skeptic attitude can be used to consolidate the best knowledge and construct new associations to be more efficient and to approach excellence in our daily work. Critical thinking is therefore necessary to improve both clinical practice and research in radiology, avoiding disruptive uncertainties and wrong assumptions.
These “questioning and solving” skills require learning, practice, and experience [ 3 ], but mainly a recognition of the many uncertainties we do have despite the important scientific advances. Precisely, a good example of the importance of critical thinking is its contribution to Precision Medicine through medical imaging data and information. In daily practice, we should ask ourselves why should we accept a reliable diagnostic method that fails 15% of the time, or an appropriate treatment that is not effective in almost 25% of patients? As scientists, we can improve these clinical decisions in the daily practice. Artificial intelligence (AI) solutions integrating different imaging, clinical, molecular, and genetic data as inputs are being implemented as a suitable pathway to solve clinical problems. The design and methodology of these AI algorithms must allow for their explainability and critical thinking evaluation before they are implemented in clinical practice [ 4 ].
In summary, critical thinking develops evidence-based knowledge, provides continuous improvements, and avoids spurious technical and clinical misconceptions. Insights into Imaging is dedicated to manuscripts with a clear critical approach, focusing on excellence in clinical practice, evidence-based knowledge and causal reasoning in radiology. Science is based on long-lived critiques and authors are encouraged to systematically identify, analyze, and solve problems by identifying inconsistencies and correcting errors.
To foster this, Insights into Imaging welcomes critical thinking papers and will incorporate a new “Critical Relevance Statement” in all their publications, where authors are asked to summarize in one sentence the question they are trying to answer and the improvement they are providing to the issue at hand.
Availability of data and materials
Not applicable.
De Cervantes M (1986) The adventures of don Quixote de la Mancha. New York, Farrar, Straus, Giroux
Martí-Bonmatí L (2021) Evidence levels in radiology: the insights into imaging approach. Insights Imaging 12(1):45. https://doi.org/10.1186/s13244-021-00995-7
Article PubMed PubMed Central Google Scholar
Ho YR, Chen BY, Li CM (2023) Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med Educ 23(1):173. https://doi.org/10.1186/s12909-023-04134-2
Cerdá-Alberich L, Solana J, Mallol P et al (2023) MAIC-10 brief quality checklist for publications using artificial intelligence and medical images. Insights Imaging 14(1):11. https://doi.org/10.1186/s13244-022-01355-9
Download references
Acknowledgements
To the Insights into Imaging ’s Office for their help in preparing this editorial.
Author information
Authors and affiliations.
Medical Imaging Department and Biomedical Imaging Research Group, Hospital Universitario y Politécnico La Fe and Health Research Institute, Valencia, Spain
Luis Martí-Bonmatí
You can also search for this author in PubMed Google Scholar
Contributions
LBM is the only author.The author have read and approved the final version of the manuscript.
Corresponding author
Correspondence to Luis Martí-Bonmatí .
Ethics declarations
Ethics approval and consent to participate, consent for publication, competing interests.
LMB is the Editor in Chief of Insights into Imaging . He has not taken part in the review or selection process of this article.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Martí-Bonmatí, L. Embracing critical thinking to enhance our practice. Insights Imaging 14 , 97 (2023). https://doi.org/10.1186/s13244-023-01435-4
Download citation
Received : 05 April 2023
Accepted : 24 April 2023
Published : 24 May 2023
DOI : https://doi.org/10.1186/s13244-023-01435-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Critical thinking
- Precision medicine
- Reproducibility
- Causal inference

Two Examples of How I Used Critical Thinking to Care for my Patient (Real Life Nursing Stories) | NURSING.com

What are you struggling with in nursing school?
NURSING.com is the BEST place to learn nursing. With over 2,000+ clear, concise, and visual lessons, there is something for you!
Critical Thinking on the Nursing Floor
Critical thinking can seem like such an abstract term that you don’t practically use. However, this could not be farther from the truth. Critical thinking is frequently used in nursing. Let me give you a few examples from my career in which critical thinking helped me take better care of my patient.
The truth is, that as nurses we can’t escape critical thinking . . . I know you hate the word . . . but let me show you how it actually works!
Critical Thinking in Nursing: Example 1
I had a patient that was scheduled to go to get a pacemaker placed at 0900. The physician wanted the patient to get 2 units of blood before going downstairs for the procedure. I administered it per protocol. About 30 minutes after that second unit got started, I noticed his oxygen went from 95% down to 92% down to 90%. I put 2L of O2 on him and it came up to 91%. But it just sort of hung around the low 90s on oxygen.
I stopped. And thought. What the heck is going on?
I looked at his history. Congestive heart failure.
I looked at his intake and output. He was positive 1.5 liters.
I thought about how he’s got extra fluid in general, and because of his CHF, he can’t really pump out the fluid he already has, let alone this additional fluid. Maybe I should listen to his lungs..
His lungs were clear earlier. I heard crackles throughout both lungs.
OK, so he’s got extra fluid that he can’t get out of his body. What do I know that will get rid of extra fluid and make him pee? Maybe some Lasix?
I ran over my thought process with a coworker before calling the doc. They agreed. I called the doc and before I could suggest anything, he said “Give him 20 mg IV Lasix one time, and I’ll put the order in.” CLICK.
I gave the Lasix. He peed like a racehorse (and was NOT happy with me for making that happen!). And he was off of oxygen before he went down to get his pacemaker.
Badda Bing Bada Boom!
Critical Thinking in Nursing: Example 2
My patient just had her right leg amputated above her knee. She was on a Dilaudid PCA and still complaining of awful pain. She maxed it out every time, still saying she was in horrible pain. She told the doctor when he rounded that morning that the meds weren’t doing anything. He added some oral opioids as well and wrote an order that it was okay for me to give both the oral and PCA dosings, with the goal of weaning off PCA.
“How am I going to do that?” I thought. She kept requiring more and more meds and I’m supposed to someone wean her off?
I asked her to describe her pain. She said it felt like nerve pain. Deep burning and tingling. She said the pain meds would just knock her out and she’d sleep for a little while but wake up in even worse pain. She was at the end of her rope.
I thought about nerve pain. I thought about other patients that report similar pain. Diabetics with neuropathy would talk about similar pain… “What did they do for it? ” I thought. Then I remembered that many of my patients with diabetic neuropathy were taking gabapentin daily for pain.
“So if this works for their nerve pain, could it work for a patient who has had an amputation?” I thought.
I called the PA for the surgeon and asked them what they thought about trying something like gabapentin for her pain after I described my patient’s type of pain and thought process.
“That’s a really good idea, Kati. I’ll write for it and we’ll see if we can get her off the opioids sooner. ”
She wrote for it. I gave it. It takes a few days to really kick in and once it did, the patient’s pain and discomfort were significantly reduced. She said to get rid of those other pain meds because they “didn’t do a damn thing,” and to “just give her that nerve pain pill because it’s the only thing that works”.
And that we did!
She was able to work with therapy more because her pain was tolerable and was finally able to get rest.
What the HELL is Critical Thinking . . . and Why Should I Care?
What your nursing professor won’t tell you about critical thinking .
by Ashely Adkins RN BSN
When I started nursing school, I remember thinking, “how in the world am I going to remember all of this information, let alone be able to apply it and critically think?” You are not alone if you feel like your critical thinking skills need a little bit of polishing.
Let’s step back for a moment, and take a walk down memory lane. It was my first semester of nursing school and I was sitting in my Fundamentals of Nursing course. We were learning about vital signs, assessments, labs, etc. Feeling overwhelmed with all of this new information (when are you not overwhelmed in nursing school?), I let my mind wonder to a low place…
Am I really cut out for this? Can I really do this? How can I possibly retain all of this information? Do they really expect me to remember everything AND critically think at the same time?
One of my first-semester nursing professors said something to me that has stuck with me throughout my nursing years. It went a little something like this:
“Critical thinking does not develop overnight . It takes time. You don’t learn to talk overnight or walk overnight. You don’t learn to critically think overnight .”
My professor was absolutely right.
As my journey throughout nursing school, and eventually on to being a “real nurse” continued, my critical thinking skills began to BLOSSOM. With every class, lecture, clinical shift, lab, and simulation, my critical thinking skills grew.
You may ask…how?
Well, let me tell you…
- Questioning
These are the key ingredients to growing your critical thinking skills.
Time. Critical thinking takes time. As I mentioned before, you do not learn how to critically think overnight. It is important to set realistic expectations for yourself both in nursing school and in other aspects of your life.
Exposure. It is next to impossible to critically think if you have never been exposed to something. How would you ever learn to talk if no one ever talked to you? The same thing applies to nursing and critical thinking.
Over time, your exposure to new materials and situations will cause you to think and ask yourself, “why?”
This leads me to my next point. Questioning. Do not be afraid to ask yourself…
“Why is this happening?”
“Why do I take a blood pressure and heart rate before I give a beta-blocker?”
“Why is it important to listen to a patient’s lung sounds before and after they receive a blood transfusion?”
It is important to constantly question yourself. Let your mind process your questions, and discover answers.
Confidence. We always hear the phrase, “confidence is key!” And as cheesy as that phrase may be, it really holds true. So many times, we often times sell ourselves short.
YOU KNOW MORE THAN YOU THINK YOU KNOW.
In case you did not catch it the first time…
Be confident in your knowledge, because trust me, it is there. It may be hiding in one single neuron in the back of your brain, but it is there.
It is impossible to know everything. Even experienced nurses do not know everything.
And if they tell you that they do…they are wrong!
The key to critical thinking is not about knowing everything ; It is about how you respond when you do not know something .
How do you reason through a problem you do not know the answer to? Do you give up? Or do you persevere until you discover the answer?
If you are a nursing student preparing for the NCLEX, you know that the NCLEX loves critical thinking questions. NRSNG has some great tips and advice on critical thinking when it comes to taking the NCLEX .
There are so many pieces to the puzzle when it comes to nursing, and it is normal to feel overwhelmed. The beauty of nursing is when all of those puzzle pieces come together to form a beautiful picture.
That is critical thinking.
Critical thinking is something you’ll do every day as a nurse and honestly, you probably do it in your regular non-nurse life as well. It’s basically stopping, looking at a situation, identifying a solution, and trying it out. Critical thinking in nursing is just that but in a clinical setting.
We’ve written a MASSIVE lesson on Care Plans and Critical Thinking :
Mastering The COPD Nursing Care Plan in Just 10 Minutes!
Renal Failure Pt Care
4 "real world" examples of using clinical judgement to figure out what to do first as a nurse | nursing.com, 12 study tips for how to study for pharmacology in nursing school | nursing.com, similar blog posts.

Critical Thinking and Nursing Care Plans Go Together Like Chicken and Waffles | NURSING.com

Patients We Will Never Forget | NURSING.com
The Ultimate Guide to Creating an ICU Report Sheet (for new Critical Care Nurses and RN Students) | NURSING.com
The Current State of Critical Thinking in EMS
Critical thinking is not something that one can just begin to do, writes Radu Venter It is a skill that must first be taught, developed over time and regularly maintained.

Emergency medical services (EMS) journals regularly discuss a lack of critical thinking evident in paramedics and how this deficiency is a significant flaw in the profession. Some provide tips and tricks to paramedics looking to develop their critical thinking. Others outline examples of mindsets to follow and biases to avoid. These articles stand by the need for further critical thinking training in EMS, but there are some significant absences that limit their ability to assist practitioners seeking to develop their skills.
Before continuing, we must ask whether critical thinking is a valuable skill for paramedics. Is there a benefit to having paramedics make decisions on their own? Should we instead have them strictly follow flowcharts in patient assessment, initial treatment and prompt transport to a hospital where a doctor can oversee definitive care? Alternately, do we want more basic practitioners to follow the flowcharts and those of higher levels to think critically?
- Critical Thinking, Part One
- Critical Thinking, Part Two
- EMS Providers Use Detective Skills to Solve Case
The current system is largely based on the third option. Paramedics working at advanced levels are expected to be able to critically think. Certain treatments available to these practitioners may be detrimental to the patient, so it falls on the practitioner to assess, reason and treat appropriately. Paramedics working at a more basic level do not have such expectations. Their training encompasses a more limited scope, prioritizing treatment of only more severe conditions. While critical thinking skills may be a goal of advanced care education, at the basic level, the goal is to create technicians. Technicians prioritize practical skills, with less focus on the theoretical. Thus, it is possible to educate a technician rapidly — basic life support programs are thus much shorter. As explained by Daniel Limmer in his EMS World article, “A technician is not expected to use high levels of reasoning skills. Technicians are strictly protocol driven and respond in a specific way when a certain group of signs and symptoms appear.” 1
Why, then, is there all this frustration with a lack of critical thinking in our profession, even with practitioners working at the basic level? The simplest answer is that when the practitioner aspires to the next level of training, critical thinking becomes more important. Unfortunately, to become an advanced level practitioner, the technician must then re-learn a fair amount of their practice. The second reason critical thinking is necessary for all paramedics has to do with the fluidity of patient assessment and treatment. Every skill performed requires an element of critical thinking. The practitioner must be able to select an appropriate diagnostic to perform or therapy to administer. They must then be able to verify the information received or confirm the therapy was effective. Kelly Grayson supports this point, noting that our current focus is more on what skills paramedics can perform, rather than the underlying knowledge necessary to determine when the skill is required and the ability to perform it proficiently. 2 A further avenue of exploration is whether the skill was even necessary in the first place.
Further, paramedics must be able to determine which algorithm for patient treatment will provide the greatest benefit. They must also be able to identify treatment priorities, and which hospital is most appropriate for transport. Finally, there is no effective flowchart for the patient who is suffering from a serious medical condition and wishes to stay at home. Paramedics of any ability level forced to operate in these novel situations without clear directions must then be able to think through the situation and work through the problem.
Two Elements of Critical Thinking
Current EMS articles on how to develop critical thinking fall into the trap of providing guidelines without going into enough depth. Scott Cormier’s two-part article on critical thinking provides a few examples of approaches to critical thinking as well as biases to avoid. 3,4 Unfortunately, they do not touch on the foundation of critical thinking, such as the traits of a good critical thinker, or provide examples to the reader to be able to apply these approaches in their own practice.
Others are more mechanical in nature than cognitive. In Daniel Limmer’s article, he states that practitioners should aspire to be clinicians instead of merely technicians. Where a technician identifies a symptom and works to treat it, a clinician strives to obtain a complete picture of the patient through a thorough assessment and the use of a differential diagnosis, prior to initiating a treatment. Performing thorough assessments of the patient, prioritizing focus on immediate threats to airway, breathing and circulation, and creating a differential diagnosis do not require as much critical thinking as might be expected.
I would suggest that a clinician’s approach has less to do with their ability to critically think, but more to do with thoroughness. In the example Limmer provides, the only difference between a technician and a clinician is the completion of a more thorough assessment that leads to a different diagnosis and, therefore, a different treatment plan. Though creating a differential diagnosis involves elements of critical thinking, it can also be a largely mechanical process — paramedics can easily memorize medical conditions to rule out in the case of a patient presenting with a specific complaint. Of the six steps suggested, only the last two involve critical thinking. Unfortunately, these are the shortest steps in the article. The best example I was able to discover is Rom Duckworth’s article, urging practitioners to assess sources of information for accuracy, validity, and a lack of bias, while also questioning currently-held beliefs. 5 This article focuses on the cognitive skills inherent in critical thinking, avoiding the mechanical pitfalls other articles fall into. However, like the other articles, it is very brief and does not provide examples for practitioners to either follow or practice.
The second major flaw underlying these articles is the assumption that the readers have enough background knowledge of the topic in order to be able to make critical decisions. For example, students in an advanced care paramedic class are asked to create a treatment plan for a cardiac complaint. The patient has sudden onset chest pain, radiating to the left arm, as well as significant pitting edema to upper and lower extremities. The patient also has a significant cardiac history. At the chest, wheezes are auscultated. Several students in the class treat the patient with salbutamol and ipratropium bromide, working to improve air entry and decrease wheezing through bronchodilation. A subsequent discussion introduced the existence of cardiac wheezes, caused not by bronchospasm, but by the presence of fluid in the lungs due to diminished cardiac output. The therapy selected by the students would be minimally effective at best, potentially detrimental to the patient at worst.
Reflecting on this experience, are the students at fault for not determining the patient’s wheezing to be cardiac in origin? Prior learning at the primary care paramedic level focused on treating wheezing as a symptom. Little focus was given to other potential causes of wheezing and treatment plans had a linear approach. Wheezing at that level is an automatic indication for nebulizer therapy.
The flaw lies not in a lack of critical thinking, because there was no room for the students to critically think. The assessment revealed wheezing, the students presumed that it was caused by bronchospasm, and then followed the appropriate protocol. The issue is that the students lacked enough background knowledge to understand the anatomy and physiology of the lungs and the pathophysiology of cardiac wheezing. A critical thinker with this background knowledge would have been able to determine the cause of the wheezing, weigh the benefits of available treatments and choose to initiate or withhold treatments based on the information given to them.
The Next Step
Critical thinking is not something that one can just begin to do. It is a skill that must first be taught, developed over time and regularly maintained. It is a combination of traits that one must possess and processes that must be developed and followed. A critical thinker must be sufficiently open-minded to other ideas and be willing to challenge current knowledge and experience.
This skill should be introduced at the earliest level possible, to benefit practitioners from the beginning of their career. Alongside critical thinking, a foundation of strong clinical knowledge must be present to allow for effective decisions to be made.
1. EMSWorld. Beyond the Basics: The Art of Critical Thinking Part 1 [Internet]. Emsworld.com; April 2008 [cited 2020 Jul 21]. Available from: https://www.emsworld.com/article/10321160/beyond-basics-art-critical-thinking-part-1 .
2. EMS1. EMS 2.0: Critical Thinking in Prehospital Training [Internet] EMS1.com; Oct 2009 [cited 2020 Jul 21]. Available from: https://www.ems1.com/ems-products/education/articles/ems-20-critical-thinking-in-prehospital-training-eCjskymt7gQYBFLe/ .
3. JEMS. Critical Thinking: Part 1 [Internet]. JEMS.com; May 2017 [cited 2020 Jul 21]. Available from: https://www.jems.com/2017/05/15/critical-thinking-part-one/ .
4. JEMS. Critical Thinking: Part 2 [Internet]. JEMS.com; May 2017 [cited 2020 Jul 21]. Available from: https://www.jems.com/2017/05/15/critical-thinking-part-two/ .
5. EMS1. 5 Critical Thinking Skills Crucial to EMS Professional Development [Internet]. EMS1.com; August 2017 [cited 2020 Jul 21]. Available from: https://www.ems1.com/ems-management/articles/5-critical-thinking-skills-crucial-to-ems-professional-development-fQIz2bctBpYHktUP/ .
Related Posts

Latest Jems News


Critical Thinking in Medicine: All You Wanted To Know
by [email protected] | Jan 15, 2020 | critical thinking | 0 comments

Critical Thinking in Medicine: All You Wanted To Know
We’ve often come across the importance of possessing critical thinking into our lives. From being trained at coaching institutes to getting listed as one of the requisites in job descriptions, the quality of critical thinking is regarded as important everywhere. It can be an art, science, and a miracle, all at the same time! Let’s dig deeper and discover more about this art, science, and miracle of the human brain.
What is critical thinking?
Starting with its meaning and definition, over time, the clarity of critical thinking has evolved with multiple understandings about the subject. Most definitions of it can be fairly complex and best taught and understood by philosophy majors or psychologists.
Beyer (1995), provides the most basic definition of Critical Thinking as “making reasoned judgments”.
In another understanding, it is the ability to think clearly and rationally about what to do and/or what to believe. It also includes the ability to engage in reflective and independent thinking. A person with critical thinking skills is capable of the following:
- Having an understanding of logical connections between multiple ideas
- Identify, construct, and evaluate arguments
- Detect loopholes and common mistakes in reasoning
- Reflect on the justification of one’s own values and beliefs
- Identify the relevance and importance of ideas
What are its characteristics?
According to experts, to think critically involves asking questions, defining a problem, analyzing evidence, examining assumptions and biases, overlooking emotional reasoning, avoiding oversimplification, and tolerating ambiguity.
Besides, considering other interpretations and dealing with ambiguity also constitute critical thinking. Other characteristics include:
- Disposition – People who think critically are skeptical, open-minded, respect clarity and precision, look at different points of view, and respect evidence and reasoning.
- Criteria – An individual must apply specific criteria along with conditions that must be met for something to be reasoned as believable.
- Reasoning – The ability to arrive at a conclusion from one or more premises, using logical relationships among statements or data.
What are the steps involved in critical thinking?
It is a common misconception that it limits creativity as it involves the rules of rationality and logic, however, creativity requires breaking rules, unlike to think critically. Cognitive steps in thinking critically include:
- Gathering information from all sources i.e. verbal and/or written expressions, reflections, experience, and observation
- Gathering and assessing relevant information
- Deriving well-reasoned conclusions and solutions
- Testing outcomes against relevant criteria
- Evaluating all assumptions, implications, and practical consequences
How critical thinking is helpful to medical students?
In the healthcare industry, medical professionals are known to use critical thinking, especially when they derive knowledge from other interdisciplinary subject areas to provide a holistic approach to their patients. Medical students can utilize their ability to think critically for the following:
- Avoiding medical/clinical errors
- Identifying better alternatives for diagnosis and treatment
- Better ability to make clinical decisions
- Working in a resource-limited environment
- Quality thinking, quality work output, and increased productivity
Can it be taught?
To an extent, critical thinking can not only be taught but also developed and enhanced by experts through technology. As massive information is available in the present times, students only need a befitting trainer to guide them through the information and inculcate it the right way.
Students need to develop and apply critical thinking skills effectively to complex problems and to critical choices they are forced to face, as a result of the information explosion and other dynamic technological changes. Since questioning is one of the important aspects of critical thinking, it is essential to teach students how to ask good, relevant, and logical questions to think critically and succeed.
The Takeaway
Every new or established medical professional should understand their psychological foibles so as to be much clearer about every aspect of their lives and to make the best decisions. Some worthwhile quotes for every medical practitioner:
- “Knowledge of bias should contribute to your humility, not your confidence”
- “When beliefs are based on emotions, facts alone stand little chance”
- “Reason evolved primarily to win arguments, not to solve problems”
Submit a Comment Cancel reply
You must be logged in to post a comment.

Category Cloud
- 3D Printing (7)
- acute coronary syndrome (1)
- Acute Kidney Injury (4)
- Air Pollution (10)
- Allergy (2)
- Ayurveda (14)
- AYUSH Policy (5)
- bioethics (2)
- Blockchain (6)
- Blog (1,845)
- blood pressure (3)
- Bollywood (1)
- Breast Cancer (8)
- Breastfeeding (2)
- calculate (338)
- Cancer (29)
- cancer detection (8)
- Cardiovascular Disease (24)
- Cardiovascular Medicine (8)
- Career in medical (1)
- cataract (3)
- Cesarean Births (3)
- Chikungunya (1)
- Children Health (7)
- climate change (3)
- Clinical Trials (4)
- Colorectal cancer (2)
- Constipation (1)
- Continuing Medical Education (9)
- Contraception (1)
- Coronavirus (89)
- Counterfeit Drugs (2)
- Courses (117)
- COVID-19 (43)
- critical care (1)
- critical thinking (1)
- Cybersecurity (5)
- Cystic Fibrosis (1)
- dentistry (12)
- Depression (9)
- Diabetes (19)
- Dietitian (5)
- digital media (3)
- Diseases (43)
- Doctors (30)
- Document (4)
- drug trade (6)
- dry eyes syndrome (4)
- Employee Absenteeism (5)
- employee problems (6)
- epidemic (16)
- Epilepsy (4)
- Evidence Based Learning (7)
- Exponential medicine (2)
- eye problems (17)
- Fitness and Health (1)
- Food Allergy (1)
- Gastroenterology (3)
- General (2)
- Genetic Medicine (3)
- Genomics (12)
- glaucoma (9)
- Gynaecology (12)
- Health Ministry (4)
- Health records (1)
- Healthcare Data (2)
- Healthcare System (140)
- Heart Failure (33)
- Hepatitis (4)
- homeopathy (5)
- Human Genomics (7)
- human immunodeficiency virus (3)
- indian economy (9)
- infectious diseases (21)
- Infertility (6)
- Innovation (14)
- Irritable Bowel Syndrome (1)
- Kidney Problems (3)
- Learning (3)
- Lectures (1,418)
- legislation (1)
- Marketing (9)
- Measles (1)
- medical devices (5)
- Medical Imaging System (2)
- medicines (17)
- Medicolegal (5)
- Mental Health (20)
- Mind Maps (1)
- Miscarriage (3)
- mosquito related diseases (2)
- nephrology (3)
- Neuro-Ophthalmalogy (3)
- Neurology (3)
- Neuromarketing (1)
- Newborns (8)
- Nutrition (6)
- obesity (6)
- Online Learning (7)
- Ophthalmology (39)
- organ donation (2)
- Organ Transplant (1)
- pandemic (27)
- patients (6)
- Pediatric (4)
- Periodontal Disease (1)
- Pharma (38)
- Pharmaceutical Industry (25)
- Precision Medicine (10)
- pregnancy (16)
- Presentation (4)
- Press Release (10)
- preterm labor (1)
- private sector (5)
- Professional Development (1)
- public sector (5)
- pulmonology (1)
- Rare diseases (3)
- Research (4)
- Resistant Hypertension (1)
- Rheumatology (1)
- Self-medication (1)
- sexual health (1)
- Siddha Medicine (1)
- SIR Model (1)
- skin disease (7)
- Skincare (6)
- Sleep Disorders (4)
- smell receptors (1)
- Social Media (2)
- startups (2)
- stomach flu (1)
- suicide (1)
- Surgery (1)
- Technology (59)
- Telehealth (14)
- Therapy (6)
- tuberculosis (5)
- Uncategorized (60)
- Vaccination (24)
- Video Creation (1)
- workplace (3)
Follow us on Facebook
Follow us on Twitter
Follow blog via email.
Representative Name (required)
Headquarters (required)
Doctor's Email ID (required)
- Open access
- Published: 20 March 2023
Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students
- Yueh-Ren Ho 1 , 2 ,
- Bao-Yu Chen 3 &
- Chien-Ming Li 2 , 4
BMC Medical Education volume 23 , Article number: 173 ( 2023 ) Cite this article
11k Accesses
7 Citations
7 Altmetric
Metrics details
In medicine, critical thinking is required for managing and tolerating medical uncertainty, as well as solving professional problems and treating diseases. However, the core of Confucianism, teacher-centered and exam-oriented settings in middle and high school education may pose challenges to developing critical thinking in Han Chinese or Taiwanese students. Students may be adversely affected by these pedagogies since student-centered settings were more effective in stimulating their critical and reflective thinking, as well as a sense of responsibility, in the ever-changing world. Therefore, guiding students with less stable foundations of critical thinking might require a different approach. A review article highlighted the potential utility of the Socratic method as a tool for teaching critical thinking in the healthcare field. The method involves posing a series of questions to students. More importantly, medical students and residents in clinical teaching are familiar with the method. Almost all healthcare students must complete a biochemistry laboratory course as part of their basic science training. Thus, we aimed to train students to develop critical thinking in the biochemistry laboratory course by using learning sheets and teacher guidance based on the Socratic method and questioning.
We recruited second-year students from a medical school, of whom 32 had medical science and biotechnology majors (MSB), 27 had pharmaceutical science majors (PS), and 85 were medical undergraduate (MU) students. An exercise in critical thinking was conducted during a biochemistry laboratory course, which consisted of five different biochemical experiments, along with learning sheets that contained three or four critical thinking questions. Then, the teacher evaluated the students’ ability to think critically based on nine intellectual dimensions (clarity, accuracy, precision, relevance, depth, breadth, logic, fairness, and significance) based on the universal intellectual standards developed by Prof. Linda Elder and Richard Paul. In the following analysis, regression models and multivariate analysis were used to determine how students improved over time, and trajectory analysis were carried out in order to observe the trends in students’ critical thinking skills construction.
Clarity and logic dimensions were identified as the key elements to facilitate the development of critical thinking skills through learning sheets and teacher guidance in students across all three different healthcare majors. The results showed that metacognitive monitoring via Socratic questioning learning sheets have demonstrated potential encourage students to develop critical thinking skills in all dimensions. Another unique contribution of current study was present the heterogeneous learning patterns and progress trajectories of clarity and logic dimensions within classes.
Using the Socratic learning model could effectively develop students’ critical thinking skills so they can more effectively care for their patients.
Peer Review reports
Introduction
Emerging trends in information technology requires that the new generation of medical students become critical thinkers [ 1 ]. The General Medical Council (GMC) of the United Kingdom encourages teachers to facilitate the acquisition of critical thinking skills by students in the medical and health professions [ 2 ]. Decades of research have proven that critical thinkers can present dispositions like flexibility, persistence, and willingness when faced with a range of tasks; they display meta-cognitive monitoring and a willingness to self-correct to seek long-term consensus[ 3 ]. Although, critical thinking is constructed from childhood in most Western countries and are valued by higher education as a necessary skill for coping with society [ 4 ]. However, critical thinking constructing and teaching has attracted little attention in Eastern education systems until recently [ 5 , 6 ].
Aside from the development of critical thinking skills is a key component of educational systems, recent educational philosophy also emphasizes both thinking processes as well as metacognitive integration skills [ 7 ]. Metacognitive monitoring includes making ease-of-learning judgments (i.e., processing fluency and beliefs), judgments of learning, feeling-of-knowing judgments (i.e., assessing the familiarity of the cue and the question itself or the domain of the question), and having confidence in the retrieved answers [ 8 , 9 ]. It is an adaptive skill of personal insight that health-profession students need to succeed in the rapidly changing and challenging healthcare industry [ 2 , 10 ]. Despite this, higher education curriculum does not emphasize on teaching these skills [ 7 ]. Additionally, any attempts to change the standards in higher education are generally met with resistance and challenges since they are require to encourage teachers to create new curriculum and change the current teaching content by researchers in current study who have more than 40 years’ teaching experience observaions. Healthcare curriculum, in general, remains conservative; Taiwan is not an exception.
Critical thinking is a fundamental component of innovative thinking and has thus become the fundamental skill for cultivating innovative talents in Western education [ 11 ]. Western scholars have asserted that teaching critical thinking should start at an early age and that its foundations should be laid in elementary and secondary schools. There are many ways to define critical thinking. A leading educational expert, Prof. Dewey, defined critical thinking as inclusive of reflective thinking and argued that the thinking process should also be taken as one of the objectives of education [ 12 ]. There are a few general dispositions that an ideal critical thinker would present according to Prof. Ennis’ observation of the constitutive abilities, such as (1) provide a clear statement of the conclusion or question; (2) provide clear reasons and be specific about their relationships with each other; (3) try to be well informed; (4) always seek and use credible sources, observations and mention them frequently; (5) consider the entire situation; (6) be mindful of the context’s primary concern; (7) be aware of alternative options; (8) be open-minded toward other points of view and refrain from making a judgment when there are insufficient evidence and reasons; (9) be willing to change your position when sufficient evidence and reasons support it; (10) seek as much precision as the nature of the subject admits; (11) whenever possible, seek the truth, and more broadly, strive to “get it right”; and (12) utilize their critical thinking abilities and dispositions [ 13 , 14 , 15 , 16 ]. In the eyes of Profs. Dewey and Ennis, critical thinking is a process of careful thought and reflection before a decision is made [ 17 ].
Nevertheless, the measurement or evaluation of critical thinking skills and abilities does not seem easy. Based on another perspective on critical thinking, intellectual standards are evolving [ 18 ]. According to Profs. Elder and Paul, critical thinking is the ability to use the most appropriate reasoning in any situation [ 18 ]. To evaluate these abilities, they established nine dimensions of critical thinking to represent different aspects of critical thinking: clarity, accuracy, precision, relevance, depth, breadth, logic, significance, and fairness [ 18 ]. As Profs. Elder and Paul concluded, those who possess discipline and critical thinking skills would make use of intellectual standards every day; thus, people should target these standards when they ask questions during the thinking process [ 18 , 19 ]. As a result of teachers’ regular introduction of the tools of critical thinking in their classrooms, the Socratic questioning and discussions become more productive and disciplined, thereby enabling students to realize the significance of questioning during the learning process [ 20 , 21 , 22 ].
According to a review article, teaching critical thinking to healthcare students (primarily medical and pharmacy students) through Socratic methods is more effective in developing critical thinking for a number of reasons [ 23 ]. In particular, Socratic questioning provides students with the opportunity to justify their own preconceived beliefs and thoughts after a series of specific, targeted inquiries [ 24 ]. Using Socratic questioning can also assist healthcare students, interns, or residents in thinking critically by understanding the “deep structure” of the question, i.e., deconstructing the question and understanding its true meaning [ 23 ]. The effectiveness of Socratic questioning lies in ascertaining the current knowledge of the students [ 25 ] and establishing a foundation for teaching at their level [ 26 ]. The teacher can accomplish this probing by asking progressively more challenging questions until the limits of the students’ knowledge are discovered [ 25 , 27 , 28 ], as well as by allowing students to express their existing knowledge, which in turn will allow them to synthesize new knowledge [ 26 ], and the dialogue represents the Socratic method [ 29 ]. Alternatively, a critical thinker is more likely to engage in certain established metacognitive strategies under the Socratic paradigm and/or channel the intellectual dimensions of critical thinking [ 17 ].
Unfortunately, Han Chinese students have struggled with learning critical thinking, which is thought to be part of their characterological profile [ 30 ]. This struggle has been faced by students studying abroad [ 11 ] and in students enrolled in the Han Chinese education system, which mainly cultivates Confucianism [ 31 ]. There are at least two types of problems with developing critical thinking in Han Chinese or Taiwanese education. The first involves the core of Confucianism, where foreign teachers have tried to promote critical thinking in elementary and high schools but sensed ethical concerns from the students who refused to participate. This is likely because if they chose to participate, they would have felt obligated to express disagreement and negative feelings to the instructor. The Han Chinese culture values harmony and “not losing face,” emphasizing a holistic perspective and collective good. Thus, students would feel uncomfortable because disagreeing with someone’s opinion in public is consciously or often avoided [ 30 ]. Therefore, encouraging the student to participate in healthy discussions and respectfully challenge their teachers is the starting point for promoting critical thinking in students enrolled in the Han Chinese educational system.
Second, in the Western education approach, learners take an active role in and are responsible for their learning process. On the contrary, the Han Chinese and Taiwan education systems are teacher-centered and exam-oriented; students are expected to follow their teachers’ instructions and perform well in class. More importantly, the textbook or teacher-centered framework lacks half of Ennis’s twelve constitutive abilities for critical thinking [ 13 , 14 , 15 ], such as judging the credibility of a source, observing and judging observation reports, drawing explanatory conclusions (including hypotheses), making and judging value judgments, and attributing unstated assumptions. As a result, Han Chinese students may find it difficult to develop critical thinking skills and present key traits and dispositions that are indicative of an ideal critical thinker. Hence, guiding and evaluating critical thinking in students might not be implemented through the same approach in Eastern educational circumstances as in the West. By understanding the difficulties that Han Chinese students face in developing critical thinking, the current study aims to design a set of critical thinking models that are suitable for Han Chinese students as a starting point for reform teaching.
Research questions, hypotheses and objectives
Research has shown that the laboratory class is not just limited to a step-wise approach to experimentation. It also allows students to develop their critical thinking skills by repeatedly engaging a simple learning framework [ 32 ]. To explore this further, the current study’s primary purpose is to use Socratic questioning in a biochemistry laboratory course with specifically designed learning sheets and feedback from teacher to guide students to improve their critical thinking skills. The learning sheets were evaluated following the universal intellectual standards for critical thinking developed by Prof. Elder and Paul [ 19 , 33 ]. For this study, we hypothesized that students with different healthcare majors might present different improvement trajectories in their intellectual dimensions according to the years of teaching observations in the three healthcare majors. Based on the research and rationale described above, the intervention effect of Socratic questioning in a biochemistry laboratory course was hypothesized as follows (see Fig. 1 ):
Pre-intervention critical thinking abilities are different amongst students of different healthcare majors, especially in each intellectual dimension (H1a). Post-intervention critical thinking abilities would develop in students from each healthcare major after using the Socratic method (H1b).
Critical thinking abilities differs significantly between pre- and post-assessments of the intellectual dimensions of students with the three different healthcare majors (H2).
After clarifying the relation of Socratic method interventions in the class, we aim to scrutinize the trajectories of students between majors further to understand the learning style in class (Aim 1). Furthermore, we also aim to identify the key intellectual dimensions that could lead to an overall improvement in the critical thinking of students in each major (Aim 2). Additionally, we observed improvement trajectories of specific intellectual dimensions within major (Aim 3).
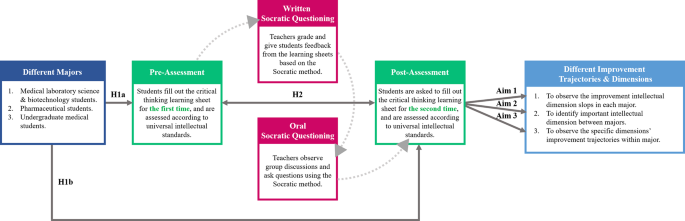
Socratic method framework and structure of the research hypotheses behind the biochemistry laboratory course
Literature review
Critical thinking engagement in the eastern and western medical education.
Over the last decade, medical education has been undergoing a variety of approaches for effectiveness teaching and transformation [ 34 ]. Many paradigms of active teaching/learning methodologies have been adopted in both Eastern and Western medical education systems, some of which are used partially (actual or conceptual similar) Socratic questioning to challenge students’ critical thinking. In this regard, the primary philosophy of case-based learning (CBL) established in the 1920s by Harvard Medical School is to guide students to apply their acquired knowledge base via critical thinking to make clinical decisions to solve the problems that they may encounter in the healthcare environment [ 35 ]. A meta-analysis study of China’s dental education reported that the CBL was a practical pedagogical method across the Chinese dental education system [ 36 ]. The results showed that the CBL method significantly increased knowledge scores, skill scores, comprehensive ability scores, and teaching satisfaction compared with the traditional lecture-based learning (LBL) mode in 2,356 dental students. Hence, there is an urgent need to change the traditional didactic lecture or teacher-centered classroom setting in which students are passive listeners instead of active participants.
Healthcare professionals are also required to solve complex problems and efficiently integrate didactic preclinical knowledge into actual clinical application in patient care [ 35 ]. On the other hand, the design thinking process may enhance both creativity and innovation so that healthcare professionals can respond to clinical problems effectively [ 37 , 38 ]. Problem-based learning (PBL) is a pedagogical approach widely accepted in medical education. It promotes active learning and results in better outcomes [ 39 , 40 , 41 ]. PBL focuses on active lifelong learning by triggering problems, directing student focus, and facilitating tutor involvement [ 39 , 42 , 43 , 44 ]. However, it is noteworthy that some hybrid PBL models have become less effective over time, as well as less aligned with the intended philosophy of student-centered learning [ 45 ]. Another alternative blended learning approach of PBL is team-based learning (TBL), which allows medical educators to provide students with pre-class work, in-class initial tests with immediate feedback, and real clinical problem-solving activities [ 46 ]. In the year-one studies of the Sydney Medical Program, a greater level of engagement in learning, a deeper understanding of concepts, and a sense of responsibility were shown among the medical students working in a TBL setting than among those in a PBL setting [ 47 , 48 ].
Medical educators face another significant challenge with the millennial generation, which has ubiquitous information technology access throughout its education. Thus, it is extremely important to improve students’ motivation to learn through hands-on instruction or teacher–student interaction and then stimulate students’ thinking and learning. In recent years, gamification has been successfully integrated into medical and scientific endeavors, enhancing motivation, participation, and time commitment across a variety of settings [ 49 , 50 , 51 ]. Another healthcare curriculum reform to stimulate active learning is flipped classroom (FC), which assigns learners didactic material, creating opportunities of longitudinal and interprofessional learning experiences for students during class participation [ 52 ] to encourage extracurricular learning, such as critical thinking. As part of the FC model, medical educators also develop formative and diagnostic assessments to identify learning gaps. According to these teaching modules, encouraging students to participate, emphasizing their learning, and observing their development trajectory are the core ideas in recent educational designs [ 53 ].
Although most of above-mentioned studies have been performed in the Eastern and Western education systems, however, without mentioning the differences between cultures and learning styles. Most importantly, the cultivation and foundations of critical thinking neglect the fact that Eastern and Western education systems emerged from very different learning and thinking patterns. Moreover, clinical reasoning and decision achievements depend on established critical thinking skills, therefore, it becomes more important to construct critical thinking early and comprehensively [ 54 ]. While Han Chinese students are not familiar with the core of critical thinking, the most effective approach to teaching critical thinking is still a highly debated topic in medical schools. Taken Taiwan medical education as an example, most clinical courses focuses on professional skills, problem solving, and disease treatment rather than construct critical mindset and metacognitive skills. Education strategies often emphasize the outcome while neglecting the process. Nevertheless, medical educators should also emphasize the process of forming students’ critical thinking when instructing and guiding them in this regard. Consequently, using metacognitive monitoring to enhance critical thinking in healthcare education would be appropriate, especially for Han Chinese systems with a Confucianist outlook. Thus, critical thinking via metacognitive monitoring is important in healthcare education, especially in Han Chinese systems with a Confucianist background.
Proficiency in the art of socratic questioning to enhance students’ critical thinking
Socratic questioning is a disciplined method of engaging in content-driven discourse that can be applied for various purposes: analyzing concepts, finding out the truth, examining assumptions, uncovering assumptions, understanding concepts, distinguishing knowledge from ignorance, and following the logical implications of thought. The scholars who established the intellectual standards of critical thinking have consistently indicated that “The key to distinguishing it from other types of questioning is that the Socratic questioning is systemic, disciplined, and deep and usually focus on foundational concepts, principles, theories, issues, or problems [ 20 , 21 , 22 ].” In short, the Socratic method is a questioning method that stimulates personal understanding. More importantly, the core principle of learning from the unknown fits best within healthcare environments.
Numerous studies have consistently urged teachers to develop Socratic dialogue in their classrooms, regardless of their learning stages and situations [ 55 , 56 , 57 ]. Using enhancement exercises in an elementary school, a study introduced a Socratic questioning strategy to provide guidance and hints to students so that they could think more deeply about an issue or problem before sharing their thoughts [ 55 ]. The lecturer of a speech course in higher education demonstrated how Socratic questioning could help students learn when confronted with a series of questions [ 56 ]. The process improves students’ ability to ask and answer questions and helps them overcome some obstacles related to their lack of self-confidence. In the book Socratic circles: Fostering critical and creative thinking in middle and high school , Dr. Matt Copeland stated that, in middle and high schools, teachers must facilitate discussions by asking questions [ 58 ]. Furthermore, this method could be applied not only to elementary school, middle school, high school but also to higher education classes [ 59 ]. During the Covid-19 pandemic, synchronous discussions in online learning demonstrated that the Socratic questioning strategy successfully improves students’ critical thinking skills [ 57 ].
The incorporation of Socratic questioning in healthcare education curriculum is under development, including for general medical education [ 60 ], medical [ 61 ], pharmacy [ 54 , 62 ], and nursing students [ 63 ]. A review article of revisiting the Socratic method as a tool for teaching critical thinking in healthcare professions revels few advantages of Socratic questioning [ 23 ]. Three type of Socratic questions were mention and could commonly used in different clinical situations [ 23 ], such as procedure question would use in those with correct answers (e.g., Which of the following medications has antithrombotic function? ); preference question can apply in those with no correct answers (e.g., What type of consultation is most suitable for this patient? ); judgment question would be the most challenge critical thinking within a Socratic paradigm by integrating different domain knowledge and skills (e.g., Does this patient require antibiotic treatment? ). It is necessary to apply and analyze information in a logical manner as well as self-regulate and use critical thinking in order to achieve the best outcome for patients. For medical doctors, pharmacists or clinical laboratory technicians to provide high quality health care across all disciplines, critical thinking is inherently required.
In medical school, the emphasis is laid on training learners in meta-capabilities, such as self-driven pattern recognition, ideally as part of an apprenticeship under the supervision of an expert diagnostician [ 61 ]. An in-depth study of the current trends in developing critical thinking amongst medical students demonstrated the use of dialogue for proper questioning and how it directs the learner’s thinking [ 64 ]. Moreover, another study confirmed that critical thinking occurs only when students are motivated and challenged to engage in higher-level thought processes [ 65 ]. In the pharmacy classroom, educators can play a significant role in influencing their students’ mindsets. Growth mindsets can be cultivated through the creation of an environment that encourages it. [ 62 ]. The Socratic questioning method can facilitate critical thinking in nursing education. One study showed that problem solving using critical thinking skills can be facilitated in both educational and practice settings by using Socratic inquiry [ 63 ].
The Socratic method has been adapted in different ways to different domains, but it has become closely associated with many areas, such as basic scientific thinking training, legal dialectical guidance, and clinical teaching. Some adaptations are helpful, some are not. The adaptations can be looked at through reasoning-focused lenses with varying degrees of magnification —a high-magnification adaptation rigorously and precisely tracks or guides the path of reasoning. Thus, how to use the Socratic method to direct students onto the path of critical thinking with appropriate guidance, but not revealing answers becomes an art that tests instructors’ teaching experience and proficiency in questioning.
Critical thinking and reflection exercises in the laboratory course
Medical schools have increasingly encouraged students to become life-long, self-directed learners because of the continual changes in the evidence-based healthcare environment. Science is often applied in everyday life, including translating knowledge from scholarly fields [ 66 ]. However, there is a vast gap between what is taught in medical schools and what is actually required in practice has increasingly widened in this information era. The majority of healthcare professionals are not considered to be real scientists. [ 2 ]. Nevertheless, they need to know how to apply scientific knowledge to their practice. Therefore, a science curriculum in medical school, such as a biochemistry laboratory course, should provide an opportunity to learn scientific methods and conceptual frameworks. It should also promote critical reasoning, providing healthcare students with problem-solving skills.
Medical educators need to accept that critical thinking is important for healthcare students and know how to teach it effectively [ 67 ]. Medical educators are now faced with a dilemma: should they develop a new course or adapt old course to develop critical thinking skills? An effective learning model should promote and stimulate students’ development of such skills [ 67 ]. One of the most common compulsory courses for healthcare students is the biochemistry laboratory course [ 68 , 69 ]. These courses are specifically designed to introduce students to prescribed experiments, requiring them to complete stepwise protocols by themselves [ 68 , 70 ]. The students are expected to understand the concepts behind the methods, procedures, and assays. However, this type of curriculum construction often fails to provide students with adequate opportunities to monitor their critical thinking and thus reduces the chances of developing problem-solving skills [ 70 ]. In order to provide students with more opportunities to think critically, previous studies have also adapted laboratory, basic science, and science fusion courses to help students develop critical thinking skills [ 67 , 68 , 71 , 72 , 73 ].
Several studies have demonstrated that students need critical thinking skills to interpret data and formulate arguments. Thus, science education, particularly in the laboratory setting, is designed to teach quantitative critical thinking (i.e. interpretation and critical evaluation of statistical reports), but the evidence has suggested that this is seldom, if ever, achieved [ 74 , 75 , 76 , 77 , 78 , 79 ]. By providing multiple opportunities for students to participate in critical thinking in the physics laboratory classes at Stanford University, scholars engaged the students to improve the experiment and modify the model repeatedly [ 32 ]. Additionally, a simple learning framework using decision-making cycles and demonstrating experts’ critical thinking significantly improved students’ critical thinking. We thus argue that students should engage in critical thinking exercises with repeated comparisons, decisions, and teacher guidance that are meant to construct their critical thinking in each of their disciplines.
Participants
This research was conducted during the 2017–2018 academic year. The participants were second-year students in the College of Medicine at the National Cheng Kung University (NCKU) of Taiwan. A total of 144 students participated in this study, of whom 32 had medical science and biotechnology majors (hereafter, MSB), 27 had pharmaceutical science majors (hereafter, PS), and 85 were medical undergraduate (hereafter, MU) students. The biochemistry laboratory course was compulsory for these three majors.
For each biochemistry laboratory class, the teacher assembled five to six groups of four to five students each. The course contained five different biochemical experiments: (1) Plasmid DNA (deoxyribonucleic acid) extraction and purification; (2) restriction enzyme digestion and electrophoresis of plasmid DNA; (3) polymerase chain reaction (PCR) amplification of plasmid DNA; (4) recombinant protein expression in Escherichia coli ; and (5) quantification of recombinant protein. The experimental learning sheets included three or four critical thinking questions (Table S1 ), encouraging students to explore experimental principles and alternative explanations further. To facilitate discussion, students were organized into small groups of four to five students seated around a single table, discussing and answering the questions. At this time, the students would pen down their first answers to the critical thinking questions, and the teacher would grade them based on the universal intellectual standards (learning sheets, first evaluation).
Furthermore, according to the students’ answers, the teacher offered a response by asking more questions according to the Socratic method to encourage students to think deeper rather than provide the correct answers. At the following week’s class, the teacher returned the learning sheet and supervised the ongoing activity, clarifying any questions raised by students and encouraging them to re-discuss and re-answer the critical thinking questions according to the teacher’s suggestions. The objective was to create a highly interactive environment to engage students in learning the relevant principles of each laboratory, including troubleshooting experiments and formulating critical concepts and skills. After the discussion, the teacher reexamined the students’ responses and assessed them based on the universal intellectual standards for subsequent grading (learning sheets, second evaluation).
The biochemistry laboratory courses and the Socratic method in current study are performed and taught by a senior biochemistry teacher (PhD in Institute of Basic Medical Science, NCKU) who has 40 years teaching experience. The teacher has long focused on teaching critical thinking skills to students, and also offers four senior clinical case related courses by practicing the Socratic method, such as clinical concept, critical thinking in medicine, clinical reasoning and special topics in clinical reasoning with more than 20 years of experience. Therefore, in the course, teacher will often ask a series of questions for students to think about the relevance of biochemical science and clinical practice.
Assessment development
The research team designed the learning sheets to guide discussion on the key issues concerning five biochemical experiments. The learning sheets were assessed according to the universal intellectual standards for critical thinking [ 33 ]. However, the assessment was adapted to include nine intellectual dimensions to assess student reasoning [ 19 , 33 ]: clarity, accuracy, precision, relevance, depth, breadth, logic, fairness, and significance (Table S2 ). Each dimension was evaluated using a binary score (0 = does not present the skill; 1 = presents the skill) for each question in the learning sheets for both the first and second evaluations. The students received the teacher’s guidance following the first evaluation, providing them with the opportunity to reconsider their reasoning and revise their answers. Our goal was to improve our students’ learning by stimulating the teaching process; at the same time, we were committed to allowing students to speak freely so that we could more effectively facilitate prospective discussions. Thus, the critical thinking scoring system based on nine intellectual dimensions was only for the purpose of the research, without consequences on students’ study progress. In this regard, students were not able to know their intellectual scores. As a result, their course grades were not determined by the learning sheets; rather, they were determined by the general operation, experiment report, and the learning attitude demonstrated during the experiments.
Statistical analysis
Descriptive statistics and variable tests.
We calculated the differences between the performance means for the first and second evaluations using paired t -tests. The mean differences between the students from the three majors were analyzed using a one-way analysis of variance (ANOVA). For the improvement slope for each universal intellectual dimension, we used the second evaluation scores of each experiment as the point with which to construct a quadratic equation curve in one variable (dimension) and then access the slope to represent the students’ improvement. The higher the slope score, the greater the students’ progress on that dimension.
Multivariate analysis
We used traditional analytical methods to observe and analyze the students’ improvement in the five experiments. Data from the second evaluation scores of each experiment served as the multi-time point measurement data. The Cox regression model for multivariate analysis was used to investigate the effect of several variables upon the time during which a specified outcome happened [ 80 ]. For each dimension, the model’s outcome determined that a student’s improvement slope was defined as minor progress if it was lower than the improvement slopes of their peers in the same major overall. However, if the student’s improvement slope was higher than the overall progress intercept of their peers, then it was defined as greater progress. The Cox regression models’ outcomes for each dimension were divided into two groups: minor and more progress. For this model’s outcome, (1) we calculated all dimensions’ slopes mean from each major (MSB: 0.369; PS: 0.405; MU: 0.401); (2) then compared the mean slope of the individual students with the mean slope of major; (3) if the student’s individual improvement slope was lower than mean slope of major, then defined as minor progress; if the student’s individual improvement slope was higher than mean slope of major, then defined as greater progress. From the analysis at this point, we understood that teacher could help students from different majors develop the different dimensions of critical thinking with the use of Socratic methods and simple repeated thinking framework practice. Additionally, we wanted to represent the improvement of intellectual dimensions between the students of different majors and their heterogeneity in critical thinking.
Dimension identification and comparison
To understand which intellectual dimensions were most representative of student improvement across majors, the analysis was divided into three sections: (1) to identify the progress percentage of all nine intellectual dimensions; (2) to identify the progress percentage of statistically significant intellectual dimensions; (3) to compare the differences among all nine dimensions, the significant dimensions, and the reciprocal dimensions. This analysis offered a better understanding of what dimensions represented the overall improvement of students’ critical thinking. Our first step was to calculate the percentage of improvement for each experiment by determining the results of the first and second evaluations for each intellectual dimension. Second, we took average percentage of improvements for each dimension. Finally, we used Student’s t -test to compare the differences among the average of all nine dimensions, the significant dimensions, and the reciprocal dimensions.
Trajectory analysis
In this study, we also hypothesized that each student’s learning and progress trajectories were heterogeneous across different majors. Depending on the major, there may also be differences between students in the same class. To focus our observations on the students’ use of the clarity and logic dimensions, we used a trajectory-tracking analysis [ 81 , 82 ] and categorized the students into two groups based on the participants’ improvement levels within the same major.
Descriptive data
We recruited 144 second-year students from three majors in the College of Medicine, among which 32 were MSB, 27 were PS, and 85 were MU students. All participants’ first and second evaluations were compared in all five biochemistry experiments. The statistically significant between-group differences in the mean initial evaluation results for each dimension are presented in Table 1 .
Overall improvement from the initial to second evaluations throughout the five experiments (H1, H2, and Aim 1)
Table 1 presents the mean results of the first and second evaluations; the five experiments exhibited statistically significant differences ( p < 0.05) across all study groups and dimensions. More detailed analyses revealed significant differences in performance in the second evaluation between the groups after all five biochemistry experiments in the clarity ( p = 0.0019), depth ( p = 0.0097), breadth ( p < 0.0001), logic ( p = 0.0371), and significance ( p = 0.0037) dimensions. However, for some of the dimensions (clarity, accuracy, precision, logic, and fairness), the initial evaluation results differ significantly between the MU and the MSB students, but this was not the case for the secondary evaluation results. The MSB students exhibited the best progress (2nd mean score minus 1st mean score) in the clarity dimension across all experiments. The PS students exhibited the best performance in the logic dimension ( p < 0.05) in the second evaluation after the five experiments.
The results of the MSB students improved steeply in most dimensions in the five experiments, especially depth (slope: 0.472), logic (0.455), and clarity (0.410) (Table 2 ). Time had a stronger effect on several of the dimensions in the multivariate analysis, specifically clarity ( p = 0.0012), relevance ( p = 0.0007), and logic ( p < 0.0001). By contrast, the PS students showed a significant overall improvement in the clarity (slope: 0.212, p < 0.0001), accuracy (0.539, p = 0.0063), precision (0.381, p = 0.0085), relevance (0.216, p < 0.0001), breadth (0.426, p = 0.0045), and logic (0.515, p = 0.0027) dimensions over the observation period (Table 3 ). Finally, the MU students showed a significant overall improvement in six dimensions: clarity (slope: 0.277, p < 0.0001), accuracy (0.520, p = 0.0003), depth (0.459, p = 0.0092), breadth (0.356, p = 0.0100), logic (0.544, p = 0.0190), and significance (0.327, p = 0.0225) (Table 4 ).
Trajectory tracking of the overall, significant, and reciprocal dimensions (Aim 2 and Aim 3)
Figure 2 a illustrates the overall improvement of students across the three majors in all nine dimensions, as assessed via trajectory analysis. The trajectory-tracking algorithm revealed that the significant dimensions for each group were as follows: MSB students—clarity, relevance, and logic; PS students—clarity, accuracy, precision, relevance, breadth, and logic; and MU students—clarity, accuracy, depth, breadth, logic, and significance (Tables 2 , 3 and 4 ; Fig. 2 b). The comparison of each group’s average percentage of improvement between the nine dimensions, the significant dimensions, and the reciprocal dimensions (clarity and logic) is summarized in Fig. 2 c. Figure 2 d–i depicts the students’ improvement in clarity and logic within the different majors using group-based trajectory modeling.
Overall improvement comparison between the students of three majors using a trajectory-tracking analysis approach . ( a ) The mean evaluation scores from the second evaluation minus those from the first evaluation for the nine dimensions were considered an improvement. They were converted to percentages to compare them to the performance in the first evaluation. ( b ) The mean evaluation scores from the second evaluation minus those from the first evaluation for the significant dimensions (within the students of each major, Tables 2 – 4 ) were considered to represent improvement and were converted to percentages to compare them to the performance in the first evaluation. ( c ) Comparison of the average percentage improvement among all nine dimensions, the significant dimensions, and the reciprocal dimensions (i.e., clarity and logic). ( d ) Trajectory analysis to assess the progress of the two subgroups of medical laboratory science and biotechnology students in the clarity dimension. ( e ) Trajectory analysis to assess the progress of the two subgroups of pharmaceutical students in the clarity dimension. ( f ) Trajectory analysis to assess the progress of the two subgroups of undergraduate medical students in the clarity dimension. ( g ) Trajectory analysis to identify the progress of the two subgroups of medical laboratory science and biotechnology students in the logic dimension. ( h ) Trajectory analysis to assess the progress of the two subgroups of pharmaceutical students in the logic dimension. ( i ) Trajectory analysis to assess the progress of the two subgroups of undergraduate medical students in the logic dimension
Empirical contributions
The Han Chinese educational system relies on the passive transmission of knowledge, as evidenced by the years of preparation by students’ through paper-based exams. By adopting this approach during teaching and learning, students do not develop a critical thinking mindset. Our experience has shown that when we encounter first-year students who have just graduated from high school, their previous education failed to develop critical thinking skills. Many foreign and Western teachers have the same experience when they encounter Asian students studying abroad for the first time. Thus, this research aims to provide clinical teachers with guidance on reducing the blind spots that students face when introduced to critical thinking. Moreover, this research aims to provide teachers with a simple teaching model and structure to guide students with less stable foundations in critical thinking. For the teaching structure and process, please refer to the procedure paragraph in the methods section and the teaching flow chart in Fig. 1 . Furthermore, the scoring system shown in the assessment development paragraph in the methods, as well as the scoring rubric is presented in Table S1 .
To our knowledge, this is the first study that uses the Socratic method and the universal intellectual standards to assess and improve critical thinking skills in biochemistry laboratory courses across different healthcare majors. We also used a novel design for teaching critical thinking, with multi-timepoint assessments and trajectory-tracking analysis to observe the students’ process and the improvement intheir critical thinking. This Socratic method, combined with critical thinking-based learning sheets, significantly improved the students’ critical thinking in all nine dimensions of the universal intellectual standards, according to the first and second evaluations conducted in each of the five sessions. Another unique contribution of this study is that it analyzed the progression results at multiple time points in the critical thinking performance of students across different majors. According to the results of comparing the average percentage improvement between all nine dimensions, the significant and reciprocal dimensions (i.e., clarity and logic) do not significantly differ from each other statistically speaking. By reducing the nine intellectual dimensions scoring system, medical educators can focus more on establishing clarity and logic skills in students. In sum, our most important finding was the identification of the clarity and logic dimensions as key elements that facilitate the development of critical thinking skills via the Socratic method in students across three different healthcare majors.
The trajectories of outcomes for students of medical science and biotechnology majors
Understanding what we learn has been identified as the starting point in the professional-development journey [ 2 ]. In principle, if thinking and decision making can be taught, educational intervention is possible. Nevertheless, for a science class like biochemistry, abductive reasoning requires a deep understanding of knowledge, and thinking must be inspired through stimulation.
In this study, the evaluation scores for MSB students did not improve significantly in almost any dimension at the beginning of the course. At first, most students felt uncomfortable with criticizing others, disagreeing with others, or challenging teacher’s knowledge and authority when they spoke their minds. Other MSB students believed that their ability to find answers and make decisions was inadequate and expected the teacher to provide the correct answers. However, preclinical medical technologists must gradually develop their critical thinking skills. Thus, the teacher provided critical thinking cues during the class and monitored the group discussions.
On the other hand, teachers must encourage these types of students, enabling them to accomplish simpler learning goals by providing them with easier-to-attempt clues. The joy of discovering answers on their own rather than the frustration of not achieving high goals should be encouraged. This coaching process improved the MSB students’ willingness to think and explore, leading to greater relevance and breadth of coverage.
The teacher used generation, conceptualization, optimization, and implementation [ 33 ] with the Socratic method to stimulate critical thinking in a four-step cycle in the five experiments. When the spontaneous discussion started in the generation phase, they tried to clarify their knowledge of the theme and identify the problem from the learning sheet. The following step was to conceptualize the problem, and the students drafted all of the possibilities and problems. Teacher frequently asked the students, ‘ What are other possible reasons? ’ Finally, the teacher provided feedback to help the MSB students reach a proper solution and implement it. The teacher would also ask the students leading questions like ‘ What relevant theories can be confirmed more precisely? ’ These guiding processes sharpened their logic and helped them better understand what they had learned. In sum, the benefits of this process included an enhanced ability to think logically, clarification of questions and knowledge gaps, and improvements in the thought process about the theme discussed.
The steady improvement of critical thinking in the students of pharmaceutical science
Currently, pharmacists are seeing their roles and responsibilities shift to becoming patient counselors and educators on the rational use of medicine. Pharmacists are trained to focus on patient-centered care and resolve current and potential drug-related problems [ 83 , 84 ]. Critical thinking, clinical reasoning, and decision-making skills are needed to solve these problems. Nowadays, pharmacists are not just responsible for carrying out doctor’s orders, while there are always alternative treatment options available for them to recommend. Teacher therefore repeatedly emphasized the link between critical thinking and pharmacist practice and encouraged students to ask questions and find out the best alternative through Socratic method in the classroom.
During class, the PS students were required to exert considerable mental effort to conduct an inquiry to solve the learning sheet questions. Instead of providing students with clues or information to help them solve the problems, the teacher guided the PS students on how to seek the information they needed for themselves. The question for the PS students was be ‘ What are the possibly executable strategies? ’ The teacher also joined the students in discussion, using the Socratic method to stimulate critical thinking and draw out ideas and underlying suppositions. In high-quality cooperative argumentative dialogue, teacher should not direct or refer learning, nor should they ask students for the correct answers as in a traditional classroom. The hints that teacher would provide were more like ‘ The narrative explanation can be more precise. ’ Thus, asking high-quality questions and providing feedback also challenges the instructors’ teaching experience.
The PS students were guided not only toward the development of critical thinking skills but also toward solving problems using evidence-based knowledge and decision-making skills. The Socratic method process meets the student where they are on the educational spectrum and encourages and helps them advance. Using this method, the PS students engaged in student-to-student interaction to build knowledge as a group and individually. The course of five experiments conducted via the learning sheets improved many aspects of the students’ critical thinking, including their clarity, relevance, breadth, and logic. In sum, the abilities that they developed in the course should help them focus more on the possible outcomes of pharmacotherapy, medication surveillance, and proper communication and therefore improve the quality of their professional future.
The advanced construction of critical thinking skills in undergraduate medical students
In medical education, “ better thinking and learning skills grounded in understanding ” are recommended for future doctors [ 2 ]. Practicing medicine requires an ability to address current and future diseases using new diagnostic and therapeutic methods [ 10 ]. Therefore, problem solving is not the only core medical skill; the ability to deal with complex, insoluble health issues is also required [ 83 ]. In this domain, critical thinking skills have proven essential in tackling difficult, complex, interdisciplinary health problems [ 10 ].
In our study, the MU students began with high-performance scores in almost all dimensions. As a result, teachers needed to create a more challenging and thought-provoking learning environment to encourage them to think more broadly and deeply. Thus, the teacher would give students advice like ‘ Searching for more relevant information can increase the breadth of knowledge ’ and ‘ If the result is true, what is the relevant theory? ’ Most MU students were faster than other majors at defining and constructing critical thinking. However, another phenomenon often observed in the classroom was that the MU students were more reluctant to express their reasoning than the students of other majors. In other words, MU students were afraid to speak openly about their reasoning and thinking, probably due to the excessive pursuit of the correct answer. In sum, the course of five experiments conducted via the learning sheets enhanced abilities of clarity, accuracy, depth, breadth, logic, and significance in MU students.
Apart from providing structure for their critical thinking, as was done with the other preclinical students, the teacher guided the MU students to use advanced critical thinking skills by regularly analyze their thinking processes, reflecting on the decision-making and thinking process [ 84 ]. Researchers have suggested that reflective practice is key to successful medical professionalism [ 85 ] and humanism [ 86 , 87 ]; but more importantly, it may help medical professionals develop better physician–patient relationships [ 88 ]. Therefore, to advance the critical thinking experience of the MU students, teacher should encourage them to gather ideas, analyze, evaluate, and synthesize information. The teacher guided them to reflect on their plan and solve the questions on the learning sheets using their thoughts and words. These reflective practices could involve various biases in the thinking process and outcome, such as the base-rate fallacy, bias blind spot, or choice-supportive bias. The Socratic debate is a common way to model a complex thinking situation and may help teachers inspire students to become critical thinkers. MU students improved their abilities in the clarity, accuracy, depth, breadth, logic, and significance dimensions in the five experiments. This kind of training in thinking should help preclinical students constantly challenge and critically appraise evidence within their context, as well as their patients’ and their own belief and value systems.
Limitations
This study provides a model for developing a specific learning environment like a biochemistry laboratory class into one that will help students develop their critical thinking skills through inquiry. Our results have shown this method to be feasible and effective. However, there were a few limitations to this study. First, although it included students from three different majors, there was no interdisciplinary collaboration that would have simulated collaborations and communication among other healthcare professionals from different fields, as occurs in clinical practice. Introducing such collaboration may have produced more exciting and comprehensive ideas for solving the problems. Training in these professions is specialized to a considerable extent, so inter-professional collaboration should improve therapeutic outcomes and optimize patient care. Second, the original scoring system was time-consuming. However, one of our study objectives was to modify and reduce the nine intellectual dimensions scoring system into the clarity and logic dimensions. Based on the analysis in the current study, the clarity and logic dimensions were sufficient for monitoring the growth of students’ critical thinking.
The present curriculum innovation aimed to teach critical thinking skills to preclinical students in various medical majors using a Socratic questioning learning model instead of a cookbook approach to learning in laboratory courses. The development of problem-solving and critical thinking skills, in addition to process-related skills, in biochemistry laboratory courses supplements traditional curriculum in a helpful way. The curriculum innovation that we described and proposed may represent an incremental step forward for the discipline; it is a novel educational approach for promoting critical thinking skills, fostering an appreciation of the affective domain, and enabling reflective practice by using small-group processing skill instruction and one-on-one Socratic questioning. The current study results are based on training critical thinking skills that should enable students to engage in the “reflection-on-action” process, which might provide an additional bridge between basic medical knowledge and clinical practice. More importantly, reconstructive mental reviews may indirectly shape preclinical students’ future actions in the challenging healthcare industry characterized by uncertainty and novel circumstances.
Data Availability
Due to conditions on participant consent and other ethical restrictions, the datasets used and analysed in the current study are not publicly available. If you have any database data requirements, please contact the corresponding author of this study.
Art-in S. Current situation and need in learning management for developing the analytical thinking of teachers in basic education of Thailand. Procedia-Social and Behavioral Sciences. 2015;197:1494–500.
Article Google Scholar
Maudsley G, Strivens J. Science’,‘critical thinking’and ‘competence’for tomorrow’s doctors. A review of terms and concepts. Med Educ. 2000;34:53–60.
Halpern DF. Thought and knowledge: an introduction to critical thinking. Psychology Press;2013.
Davies M, Barnett R. The Palgrave handbook of critical thinking in higher education. Springer;2015.
Sit HHW. Characteristics of Chinese students’ learning styles. Int Proc Econ Dev Res. 2013;62:36.
He Y. The roles of thinking styles in learning and achievement among Chinese university students.The University of Hong Kong Libraries.
Nordin S, Yunus K. Exploring Metacognitive Awareness among Teachers. Int J Acad Res Progress Educ Dev. 2020;9:462–72
Nelson TO, Narens L. Why investigate metacognition. Metacognition: Knowing about knowing. 1994;13:1–25.
Google Scholar
Dinsmore DL. Examining the ontological and epistemic assumptions of research on metacognition, self-regulation and self-regulated learning. Educational Psychol. 2017;37:1125–53.
Maudsley G, Strivens J. Promoting professional knowledge, experiential learning and critical thinking for medical students. Med Educ. 2000;34:535–44.
Zhong W, Cheng M. Developing critical thinking: experiences of Chinese International Students in a Post-1992 University in England. Chin Educ Soc. 2021;54:95–106.
Dewey J. How we think. In.: D C Heath; 1910.
Book Google Scholar
Ennis R. Critical thinking: a streamlined conception. Teach Philos. 1991;14:5–24.
Ennis RH. Is critical thinking culturally biased? Teach Philos. 1998;21:15–33.
Ennis R. Critical thinking: reflection and perspective part II. Inquiry: Crit Think Disciplines. 2011;26:5–19.
Ennis RH. A taxonomy of critical thinking dispositions and abilities. 1987. https://education.illinois.edu/docs/default-source/faculty-documents/robert-ennis/thenatureofcriticalthinking_51711_000.pdf
Zare P, Mukundan J. The use of socratic method as a teaching/learning tool to develop students’ critical thinking: a review of literature. Lang India. 2015;15:256–65.
Elder L, Paul R. Critical thinking: Tools for taking charge of your professional and personal life. The Foundation for Critical Thinking;2005.
Paul R, Elder L. Critical thinking: intellectual Standards essential to reasoning well within every domain of human thought, part two. J Dev Educ. 2013;37:32.
Elder L, Paul R. Critical thinking: the art of socratic questioning, part II. J Dev Educ. 2007;31:32.
Paul R, Elder L. Critical thinking: the art of socratic questioning. J Dev Educ. 2007;31:36.
Paul R, Elder L. Critical thinking: the art of socratic questioning, part III. J Dev Educ. 2008;31:34–5.
Oyler DR, Romanelli F. The Fact of Ignorance Revisiting the Socratic Method as a Tool for Teaching Critical Thinking. Am J Pharm Educ. 2014;78.
Paul R, Elder L, Bartell T. A Brief History of the Idea of Critical Thinking, The Critical Thinking Community. In.; 1997.
Tofade T, Elsner J, Haines ST. Best practice strategies for effective use of questions as a teaching tool. Am J Pharm Educ. 2013;77:1–7.
Vygotsky L. Zone of proximal development. Mind in society: The development of higher psychological processes 1987;5291:157.
Rud AG Jr. The Use and Abuse of Socrates in Present Day Teaching;1990.
Oh RC. The socratic method in medicine-the labor of delivering medical truths. For the Office-based Teacher of Family Medicine. 2005;37:537–9.
Stoddard HA, O’Dell DV. Would Socrates have actually used the “Socratic Method” for clinical teaching? J Gen Intern Med. 2016;31:1092–6.
Ku KY, Ho IT. Dispositional factors predicting chinese students’ critical thinking performance. Pers Indiv Differ. 2010;48:54–8.
Liu OL, Shaw A, Gu L, Li G, Hu S, Yu N, Ma L, Xu C, Guo F, Su Q. Assessing college critical thinking: preliminary results from the chinese HEIghten ® critical thinking assessment. High Educ Res Dev. 2018;37:999–1014.
Holmes NG, Wieman CE, Bonn D. Teaching critical thinking. Proc Natl Acad Sci. 2015, 112(36):11199–11204.
Elder L, Paul R. The aspiring thinker’s guide to critical thinking. Rowman & Littlefield; 2019.
Cooke M, Irby DM, Sullivan W, Ludmerer KM. American Medical Education 100 years after the Flexner Report. N Engl J Med. 2006;355:1339–44.
Behar-Horenstein LS, Catalanotto FA, Nascimento MM. Anticipated and actual implementation of case-based learning by Dental Faculty Members during and after training. J Dent Educ. 2015;79:1049–60.
Dong H, Guo C, Zhou L, Zhao J, Wu X, Zhang X, Zhang X. Effectiveness of case-based learning in chinese dental education: a systematic review and meta-analysis. BMJ Open. 2022;12:e048497–7.
Sandars J, Goh P-S. Design thinking in Medical Education: the key features and practical application. J Med Educ Curric Dev. 2020;7:2382120520926518–8.
Khan S, Vandermorris A, Shepherd J, Begun JW, Lanham HJ, Uhl-Bien M, Berta W. Embracing uncertainty, managing complexity: applying complexity thinking principles to transformation efforts in healthcare systems. BMC Health Serv Res. 2018;18:192–2.
Preeti B, Ashish A, Shriram G. Problem based learning (PBL)-an effective approach to improve learning outcomes in medical teaching. J Clin Diagn research: JCDR. 2013;7:2896–7.
Ibrahim ME, Al-Shahrani AM, Abdalla ME, Abubaker IM, Mohamed ME. The effectiveness of problem-based learning in Acquisition of Knowledge, soft skills during basic and preclinical sciences: medical students’ points of view. Acta Informatica Medica. 2018;26:119–24.
Servant-Miklos VF. Problem solving skills versus knowledge acquisition: the historical dispute that split problem-based learning into two camps. Adv Health Sci Educ. 2019;24:619–35.
Bjork RA, Dunlosky J, Kornell N. Self-regulated learning: beliefs, techniques, and illusions. Ann Rev Psychol. 2013;64:417–44.
Colliver JA. Effectiveness of problem-based learning curricula: research and theory. Acad Med. 2000;75:259–66.
Bate E, Hommes J, Duvivier R, Taylor DC. Problem-based learning (PBL): Getting the most out of your students–Their roles and responsibilities: AMEE Guide No. 84. Medical teacher 2013.
Lim WK. Dysfunctional problem-based learning curricula: resolving the problem. BMC Med Educ. 2012;12:89–9.
Burgess AW, McGregor DM. Use of established guidelines when reporting on Interprofessional Team-Based learning in Health Professions Student Education: a systematic review. Acad Med. 2021;97:143–51.
Burgess A, Bleasel J, Haq I, Roberts C, Garsia R, Robertson T, Mellis C. Team-based learning (TBL) in the medical curriculum: better than PBL? BMC Med Educ. 2017;17:243.
Burgess A, Ayton T, Mellis C. Implementation of team-based learning in year 1 of a PBL based medical program: a pilot study. BMC Med Educ. 2016;16:49–9.
Schrope M. Solving tough problems with games. Proc Natl Acad Sci. 2013;110:7104–6.
Nessler M. Three Ways virtual Technologies are making a difference in HR. Employ Relations Today. 2014;40:47–52.
Nevin CR, Westfall AO, Rodriguez JM, Dempsey DM, Cherrington A, Roy B, Patel M, Willig JH. Gamification as a tool for enhancing graduate medical education. Postgrad Med J. 2014;90:685–93.
Technologies in Medical Education. In. The SAGE Encyclopedia of Educational Technology. edn.: SAGE Publications, Inc.; 2015.
Hurtubise L, Hall E, Sheridan L, Han H. The Flipped Classroom in Medical Education: Engaging Students to Build Competency. J Med Educ Curric Dev. 2015;2:JMECD.S23895.
Persky AM, Medina MS, Castleberry AN. Developing critical thinking skills in pharmacy students. Am J Pharm Educ. 2019;83.
Chew SW, Lin I-H, Chen N-S. Using Socratic questioning strategy to enhance critical thinking skill of elementary school students. In: 2019 IEEE 19th International Conference on Advanced Learning Technologies (ICALT): 2019 : IEEE; 2019;290–294.
Manurung YH, Siregar FS. Developing students’ critical thinking on speaking through socratic questioning method. Adv Social Sci Educ Humanit Res. 2018;263:212–6.
Wediyantoro PL, Lailiyah M, Yustisia KK. Synchronous discussion in online learning: investigating students’ critical thinking. En Jour Me. (English Journal of Merdeka): Culture Language and Teaching of English. 2020;5:196–203.
Copeland M. Socratic circles: fostering critical and creative thinking in middle and high school. Stenhouse Publishers; 2005.
Tweed RG, Lehman DR. Learning considered within a cultural context: confucian and socratic approaches. Am Psychol. 2002;57:89–99.
Wilberding E. Socratic methods in the classroom: encouraging critical thinking and problem solving through dialogue. Routledge; 2021.
Sanchez-Lara PA, Grand K, Haanpää MK, Curry CJ, Wang R, Ezgü F, Rose CM, D’Cunha Burkardt D, Conway RL, Relan A. Thinking outside “The Box”: Case‐based didactics for medical education and the instructional legacy of Dr John M. Graham, Jr. Am J Med Genet Part A. 2021;185:2636–45.
Cooley JH, Larson S. Promoting a growth mindset in pharmacy educators and students. Curr Pharm Teach Learn. 2018;10:675–9.
Makhene A. The use of the Socratic inquiry to facilitate critical thinking in nursing education. Health SA Gesondheid. 2019;24.
Harasym PH, Tsai T-C, Hemmati P. Current trends in developing medical students’ critical thinking abilities. Kaohsiung J Med Sci. 2008;24:341–55.
Roberts TG, Dyer JE. The relationship of self-efficacy, motivation, and critical thinking disposition to achievement and attitudes when an illustrated web lecture is used in an online learning environment. J agricultural Educ. 2005;46:12–23.
Chalmers AF. What is this thing called science? Hackett Publishing; 2013.
Zain AR. Effectiveness of guided inquiry based on blended learning in physics instruction to improve critical thinking skills of the senior high school student. In: Journal of Physics: Conference Series : 2018: IOP Publishing; 2018: 012015.
Goodey NM, Talgar CP. Guided inquiry in a biochemistry laboratory course improves experimental design ability. Chem Educ Res Pract. 2016;17:1127–44.
Talgar CP, Goodey NM. Views from academia and industry on skills needed for the modern research environment. Biochem Mol Biol Educ. 2015;43:324–32.
Handelsman J, Ebert-May D, Beichner R, Bruns P, Chang A, DeHaan R, Gentile J, Lauffer S, Stewart J, Tilghman SM. Education. Scientific teaching. Science. 2004;304:521-2.
Thaiposri P, Wannapiroon P. Enhancing students’ critical thinking skills through teaching and learning by inquiry-based learning activities using social network and cloud computing. Procedia-Social and Behavioral Sciences. 2015;174:2137–44.
Hirschberg CB. A course in critical thinking for PhD students in biomolecular sciences and biotechnology: classical experiments in biochemistry;2016.
Van Winkle LJ, Cornell S, Fjortoft N, Bjork BC, Chandar N, Green JM, La Salle S, Viselli SM, Burdick P, Lynch SM. Critical thinking and reflection exercises in a biochemistry course to improve prospective health professions students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Educ. 2013;77.
Kanari Z, Millar R. Reasoning from data: how students collect and interpret data in science investigations. J Res Sci Teach. 2004;41:748–69.
Kumassah E, Ampiah J, Adjei E. An investigation into senior high school (shs3) physics students understanding of data processing of length and time of scientific measurement in the Volta region of Ghana. Int. J. Educ. Technol. High. Educ. 2014;37–61.
Kung RL, Linder C. University students’ ideas about data processing and data comparison in a physics laboratory course. Nordic Stud Sci Educ. 2006;2:40–53.
Ryder J, Leach J. Interpreting experimental data: the views of upper secondary school and university science students. Int J Sci Educ. 2000;22:1069–84.
Ryder J. Data interpretation activities and students’ views of the epistemology of science during a university earth sciences field study course. Teaching and Learning in the Science Laboratory.edn. Springer;2002. p.151–162.
Séré MG, Journeaux R, Larcher C. Learning the statistical analysis of measurement errors. Int J Sci Educ. 1993;15:427–38.
Lunn M, McNeil D. Applying Cox regression to competing risks. Biometrics. 1995;524–532.
Haviland A, Nagin DS, Rosenbaum PR. Combining propensity score matching and group-based trajectory analysis in an observational study. Psychol Methods. 2007;12:247–67.
Helland-Hansen W, Hampson G. Trajectory analysis: concepts and applications. Basin Res. 2009;21:454–83.
Barrows HS, Tamblyn RM. Problem-based learning: an approach to medical education. Volume 1. Springer;1980.
Jensen G, Denton B. Teaching physical therapy students to reflect: a suggestion for clinical education. J Phys Therapy Educ. 1991;5:33–8.
Stern DT, Papadakis M. The developing physician—becoming a professional. N Engl J Med. 2006;355:1794–9.
Gracey CF, Haidet P, Branch WT, Weissmann P, Kern DE, Mitchell G, Frankel R, Inui T. Precepting humanism: strategies for fostering the human dimensions of care in ambulatory settings. Acad Med. 2005;80:21–8.
Branch WT Jr, Kern D, Haidet P, Weissmann P, Gracey CF, Mitchell G, Inui T. Teaching the human dimensions of care in clinical settings. JAMA. 2001;286:1067–74.
Wald HS, Davis SW, Reis SP, Monroe AD, Borkan JM. Reflecting on reflections: enhancement of medical education curriculum with structured field notes and guided feedback. Acad Med. 2009;84:830–7.
Download references
Acknowledgements
The authors wish to thank Chi-Her Lin, MD for their encouragement and support in the writing of this manuscript, and Prof. Woei-Jer Chuang, Hung-Chi Cheng, Chang-Shi Chen, Po-Hsin J. Huang, Chien-hung Yu, and Wen-Tsan Chang for their help with the experimental design. Special thanks to Tanvi Gupta for her help with the improving reading fluency.
This work was supported by the Teaching Practice Research Program, Ministry of Education, Taiwan (Grant No: PMN1110350, PMN1100853, PMN1090364, PMN108075, PMN107018).
Author information
Authors and affiliations.
Department of Biochemistry and Molecular Biology, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Yueh-Ren Ho
School of Medicine, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Yueh-Ren Ho & Chien-Ming Li
Institute of Clinical Medicine, College of Medicine, National Cheng Kung University, University Road No.1, East District 701, Tainan City, Taiwan (R.O.C.)
Bao-Yu Chen
Division of Infectious Diseases, Department of Internal Medicine, Chi Mei Medical Center, Zhonghua Raod No.901, Yongkang District 710, Tainan City, Taiwan (R.O.C.)
Chien-Ming Li
You can also search for this author in PubMed Google Scholar
Contributions
Yueh-Ren Ho: substantially contributed to the conception, data curation, interpretation, drafting and critical revision of the paper. She has given final approval to the manuscript and agrees to be accountable for the work. Bao-Yu Chen: substantially contributed to the conception, formal analysis, methodology, visualization, and writing and editing the manuscript. Chien-Ming Li: substantially contributed to the conception, data curation, review and editing the manuscript.
Corresponding author
Correspondence to Yueh-Ren Ho .
Ethics declarations
Ethics approval and consent to participate.
Students participating in this course will be informed before the class begins that their results will be used for educational academic research, and their written informed consent were obtained. The methodology of the study including the content analysis of literature on data curation activities were approved and funded by Teaching Practice Research Program, Ministry of Education, Taiwan. Throughout the study, all methods followed the approved methodology and adhered to the relevant guidelines and regulations. According to Human Subjects Research Act, Chap. 2, article 5: The Ministry of Education review current study nature and announced the principal investigator shall not submit the research protocol for review and approval by the Institutional Review Board. Please refer to the source of law in the website of Laws & Regulations Database of The Republic of China (Taiwan) ( https://law.moj.gov.tw/ENG/LawClass/LawAll.aspx?pcode=L0020176 ).
Consent for publication
Not applicable.

Competing interests
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Ho, YR., Chen, BY. & Li, CM. Thinking more wisely: using the Socratic method to develop critical thinking skills amongst healthcare students. BMC Med Educ 23 , 173 (2023). https://doi.org/10.1186/s12909-023-04134-2
Download citation
Received : 20 September 2022
Accepted : 02 March 2023
Published : 20 March 2023
DOI : https://doi.org/10.1186/s12909-023-04134-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Biochemistry experiment
- Critical thinking
- Socratic method
- Medical education
- Metacognition
BMC Medical Education
ISSN: 1472-6920
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Korean J Med Educ
- v.31(4); 2019 Dec
Reasoning processes in clinical reasoning: from the perspective of cognitive psychology
Hyoung seok shin.
Department of Medical Education, Korea University College of Medicine, Seoul, Korea
Clinical reasoning is considered a crucial concept in reaching medical decisions. This paper reviews the reasoning processes involved in clinical reasoning from the perspective of cognitive psychology. To properly use clinical reasoning, one requires not only domain knowledge but also structural knowledge, such as critical thinking skills. In this paper, two types of reasoning process required for critical thinking are discussed: inductive and deductive. Inductive and deductive reasoning processes have different features and are generally appropriate for different types of tasks. Numerous studies have suggested that experts tend to use inductive reasoning while novices tend to use deductive reasoning. However, even experts sometimes use deductive reasoning when facing challenging and unfamiliar problems. In clinical reasoning, expert physicians generally use inductive reasoning with a holistic viewpoint based on a full understanding of content knowledge in most cases. Such a problem-solving process appears as a type of recognition-primed decision making only in experienced physicians’ clinical reasoning. However, they also use deductive reasoning when distinct patterns of illness are not recognized. Therefore, medical schools should pursue problem-based learning by providing students with various opportunities to develop the critical thinking skills required for problem solving in a holistic manner.
Introduction
It is hard to describe clinical reasoning in a sentence, because it has been studied by a number of researchers from various perspectives, such as medical education, cognitive psychology, clinical psychology, and so forth, and they have failed to reach an agreement on its basic characteristics [ 1 ]. Accordingly, clinical reasoning has been defined in various ways. Some researchers defined clinical reasoning as a crucial skill or ability that all physicians should have for their clinical decision making, regardless of their area of expertise [ 2 , 3 ]. Others focused more on the processes of clinical reasoning; thus, they defined it as a complex process of identifying the clinical issues to propose a treatment plan [ 4 - 6 ]. However, these definitions are not so different. Taking this into account, it can be concluded that clinical reasoning is used to analyze patients’ status and arrive at a medical decision so that doctors can provide the proper medical treatment.
In reality, properly working clinical reasoning requires three domains of knowledge: diagnostic knowledge, etiological knowledge, and treatment knowledge [ 6 ]. From the perspective of cognitive psychology, structural knowledge is needed to integrate domain knowledge and find solutions based on the learner’s prior knowledge and experience [ 7 ], and structural knowledge can be constructed as a form of mental model by understanding the relations between the interconnected factors involved in clinical issues [ 8 , 9 ]. In this cognitive process, critical thinking skills such as causal reasoning and systems thinking can play a pivotal role in developing deeper understanding of given problem situations. Causal reasoning is the ability to identify causal relationships between sets of causes and effects [ 10 ]. Causality often involves a series or chain of events that can be used to infer or predict the effects and consequences of a particular cause [ 10 - 13 ]. Systems thinking is a thinking paradigm or conceptual framework where understanding is defined in terms of how well one is able to break a complex system down into its component parts [ 14 , 15 ]. It is based on the premise that a system involves causality between factors that are parts of the system as a whole [ 14 ]. Systems thinking is a process for achieving a deeper understanding of complex phenomena that are composed of components that are causally interrelated [ 14 - 16 ]. As a result, causal reasoning and systems thinking are skills that can help people to better understand complex phenomena in order to arrive at effective and targeted solutions that address the root causes of complex problems [ 10 , 12 , 15 ].
If cognitive skills work properly, one can make correct decisions all of the time. However, human reasoning is not always logical, and people often make mistakes in their reasoning. The more difficult the problems with which they are presented, the more likely they are to choose wrong answers that are produced by errors or flaws in the reasoning process [ 17 , 18 ]. Individual differences in reasoning skills—such as systems thinking, causal reasoning, and thinking processes—may influence and explain observed differences in their understanding. Therefore, to better assist learners in solving problems, instructors should focus more on facilitating the reasoning skills required to solve given problems successfully.
In this review paper, the author focuses on the reasoning processes involved in clinical reasoning, given that clinical reasoning is considered as a sort of problem-solving process. Therefore, this paper introduces concepts related to the reasoning processes involved in clinical reasoning and their influences on novices and experts in the field of medical education from the perspective of cognitive psychology. Then, based on the contents discussed, the author will be able to propose specific instructional strategies associated with reasoning processes to improve medical students’ reasoning skills to enhance their clinical reasoning.
Concepts and nature of reasoning processes
Generally, reasoning processes can be categorized into two types: inductive/forward and deductive/backward [ 19 ]. In an inductive reasoning process, one observes several individual facts first, then makes a conclusion about a premise or principle based on these facts. Yet there may be the possibility that a conclusion is not true even though a premise or principle in support of that conclusion is true, because the conclusion is generalized from the facts observed by the learner, but the learner does not observe all relevant examples [ 20 ].
In general, in a deductive reasoning process, according to Johnson-Laird [ 20 ], one establishes a mental model or a set of models to solve given problems considering general knowledge and principles based on a solid foundation. Then, one makes a conclusion or finds a solution based on the mental model or set of models. To verify a mental model, one needs to check the validity of the conclusions or solutions by searching for counterexamples. If one cannot find any counterexamples, the conclusions can be accepted as true and the solutions as valid. Consequently, the initial mental model or set of models can be used for deductive reasoning.
Anderson [ 17 ] proposed three different ways of solving complex problems: means-ends analysis, working backward, and planning by simplification. A means-ends analysis is a process that gets rid of differences between the current state and the ideal state in order to determine sub-goals in solving problems, and the process can be repeated until the major goal is achieved [ 21 - 23 ]. It can be considered an inductive reasoning process, because the distinct feature of means-ends analysis where it achieves sub-goals in consecutive order is similar to inductive reasoning. Working backward is addressed as an opposite concept to means-ends analysis [ 17 ], because it needs to set up a desired result to find causes by measuring the gap between the current state and the ideal state; then, this process is repeated until the root causes of a problem are identified. According to Anderson [ 17 ], means-ends analysis (inductive reasoning) is more useful in finding a solution quickly when a limited number of options are given or many sub-goals should be achieved for the major goal; whereas working backward (deductive reasoning) spends more time removing wrong answers or inferences to find the root causes of a problem. In conclusion, inductive and deductive reasoning processes have different features and can play different roles in solving complex problems.
The use of reasoning processes
A number of researchers across different fields have used inductive and deductive approaches as reasoning processes to solve complex problems or complete tasks. For example, Scavarda et al. [ 24 ] used both approaches in their study to collect qualitative data through interviews with experts, and they found that experts with a deductive approach used a top-down approach and those with an inductive approach used a bottom-up approach to solve a given problem. In a study of Overmars et al. [ 25 ], the results showed that a deductive approach explicitly illustrated causal relations and processes in 39 geographic contexts and it was appropriate for evaluating various possible scenarios; whereas an inductive approach presented associations that did not guarantee causality and was more useful for identifying relatively detailed changes.
Sharma et al. [ 26 ] found that inductive or deductive approaches can both be useful depending on the characteristics of the tasks and resources available to solve problems. An inductive approach is considered a data-driven approach, which is a way to find possible outcomes based on rules detected from undoubted facts [ 26 ]. Therefore, if there is a lot of available data and an output hypothesis, then it is effective to use an inductive approach to discover solutions or unexpected and interesting findings [ 26 , 27 ]. An inductive approach makes it possible to directly reach conclusions via thorough reasoning that involves the following procedures: (1) recognize, (2) select, and (3) act [ 28 ]. These procedures are recurrent, but one cannot know how long they should be continued to complete a task, because a goal is not specified [ 26 ]. Consequently, an inductive approach is useful when analyzing an unstructured data set or system [ 29 ].
On the other hand, a deductive approach sets up a desired goal first, then finds a supporting basis—such as information and rules—for the goals [ 26 ]. For this, a backward approach, which is considered deductive reasoning, gradually gets rid of things proved unnecessary for achieving the goal while reasoning; therefore, it is regarded as a goal-driven approach [ 28 ]. If the output hypothesis is limited and it is necessary to find supporting facts from data, then a deductive approach would be effective [ 26 , 28 ]. This implies that a deductive approach is more appropriate when a system or phenomenon is well-structured and relationships between the components are clearly present [ 29 ]. Table 1 shows a summary of the features and differences of the inductive and deductive reasoning processes.
Features of Inductive and Deductive Reasoning Processes
The classification according to the reasoning processes in the table is dichotomous, but they do not always follow this classification absolutely. This means that each reasoning process shows such tendencies.
Considering the attributes of the two reasoning processes, an inductive approach is effective for exploratory tasks that do not have distinct goals—for example, planning, design, process monitoring, and so on, while a deductive approach is more useful for diagnostic and classification tasks [ 26 ]. In addition, an inductive approach is more useful for discovering solutions from an unstructured system. On the other hand, a deductive approach can be better used to identify root causes in a well-structured context. While both reasoning approaches are useful in particular contexts, it can be suggested that inductive reasoning is more appropriate than deductive reasoning in clinical situations, which focus on diagnosis and treatment of diseases rather than on finding their causes.
Reasoning processes by novices and experts
As mentioned above, which reasoning process is more effective for reaching conclusions can be generally determined depending on the context and purpose of the problem solving. In reality, however, learners’ choices are not always consistent with this suggestion, because they are affected not only by the problem itself, but also by the learner. Assuming that learners or individuals can be categorized into two types, novices and experts, based on their level of prior knowledge and structural knowledge, much research has shown that novices and experts use a different reasoning process for problem solving. For example, in a study of Eseryel et al. [ 30 ], novice instructional designers who possessed theoretical knowledge but little experience showed different patterns of ill-structured problem solving compared to experts with real-life experience. Given that each learner has a different level of prior knowledge relating to particular topics and critical thinking skills, selecting the proper reasoning process for each problem is quite complex. This section focuses on which reasoning process an individual uses depending on their content and structural knowledge.
Numerous studies have examined which reasoning processes are used by experts, who have sufficient content and structural knowledge, and novices, who have little content and structural knowledge, for problem solving. The result of a study of Hong et al. [ 31 ] showed that children generally performed better when using cause-effect inferences (inductive approach) than effect-cause inferences (considered a deductive approach). According to Anderson [ 17 ], people are faced with some difficulties when they solve problems using induction. The first difficulty is in formulating proper hypotheses and the second is that people do not know how to interpret negative evidence when it is given and reach a conclusion based on that evidence [ 17 ]. Nevertheless, most students use a type of inductive reasoning to solve problems that they have not previously faced [ 32 ]. Taken together, the studies suggest that novices generally prefer an inductive approach to a deductive approach for solving problems because they may feel comfortable and natural using an inductive approach but tend to experience difficulties during problem-solving processes. From these findings, it can be concluded that novices are more likely to use inductive reasoning, but it is not always productive.
Nevertheless, there is still a controversy about which reasoning processes are used by experts or novices [ 33 ]. For example, experts in specific domains use an inductive approach to solving problems, but novices, who have a lower level of prior knowledge in specific domains, tend to use a deductive approach [ 23 ]. In contrast, according to Smith [ 34 ], studies in which more familiar problems were used concluded that experts preferred an inductive approach, whereas in studies that employed relatively unfamiliar problems that required more time and effort to solve, experts tended to prefer a deductive approach. In line with this finding, in solving physics problems, experts mostly used inductive reasoning that was faster and had fewer errors for problem solving only when they encountered easy or familiar problems where they could gain a full understanding of the situation quickly, but novices took more time to deductively reason by planning and solving each step in the process of problem solving [ 35 ].
Assuming that an individual’s prior knowledge consists of content knowledge such as knowledge of specific domains as well as structural knowledge such as the critical thinking skills required for problem solving in the relevant field, it seems experts use an inductive approach when faced with relatively easy or familiar problems; while a deductive approach is used for relatively challenging, unfamiliar, or complex problems. In the case of novices, it may be better to use deductive reasoning for problem solving considering that they have a lower level of prior knowledge and that even experts use deductive reasoning to solve complex problems.
Inductive and deductive reasoning in clinical reasoning
In medicine, concepts of inductive and deductive reasoning apply to gathering appropriate information and making a clinical diagnosis considering that the medical treatment process is a form of problem solving. Inductive reasoning is used to make a diagnosis by starting with an analysis of observed clinical data [ 36 , 37 ]. Inductive reasoning is considered as scheme-inductive problem solving in medicine [ 36 ], because in inductive reasoning, one first constructs his/her scheme (also considered a mental model) based on one’s experiences and knowledge. It is generally used for a clinical presentation-based model, which has been most recently applied to medical education [ 38 ].
In contrast, deductive reasoning entails making a clinical diagnosis by testing hypotheses based on systematically collected data [ 39 ]. Deductive reasoning is considered an information-gathering method, because one constructs a hypothesis first then finds supporting or refuting facts from data [ 36 , 40 ]. It has been mostly used for discipline-based, system-based, and case-based models in medical education [ 38 ].
Inductive and deductive reasoning by novice and expert physicians
A growing body of research explores which reasoning processes are mainly used by novices and experts in clinical reasoning. Novice physicians generally use deductive reasoning, because limited knowledge restricts them from using deductive reasoning [ 1 , 38 ]. Also, it is hard to consider deductive reasoning as an approach generally used by experts, since they do not repeatedly test a hypothesis based on limited knowledge in order to move on to the next stage in the process of problem solving [ 38 ]. Therefore, it seems that deductive reasoning is generally used by novices, while inductive reasoning is used by expert physicians in general. However, this may be too conclusive and needs to be further examined in the context of clinical reasoning.
In clinical reasoning, inductive reasoning is more intuitive and requires a holistic view based on a full understanding of content knowledge, including declarative and procedural knowledge, but also structural knowledge; thus, it occurs only when physicians’ knowledge structures of given problems are highly organized [ 38 ]. Expert physicians recognize particular patterns of symptoms through repeated application of deductive reasoning, and the pattern recognition process makes it possible for them to apply inductive reasoning when diagnosing patients [ 10 ]. As experts automate a number of cognitive sequences required for problem solving in their own fields [ 35 ], expert physicians automatically make appropriate diagnoses following a process of clinical reasoning when they encounter patients who have familiar or typical diseases. Such a process of problem solving is called recognition-primed decision making (RPDM) [ 41 , 42 ]. It is a process of finding appropriate solutions to ill-structured problems in a limited timeframe [ 10 ]. In RPDM, expert physicians are aware of what actions should be taken when faced with particular situations based on hundreds of prior experiences [ 10 ]. These prior experiences are called illness scripts in diagnostic medicine [ 10 ], and this is a concept similar to a mental model or schema in problem solving.
However, expert physicians do not always use inductive reasoning in their clinical reasoning. Jonassen [ 10 ] categorized RPDM into three forms of variations in problem solving by experts, and the first form of variation is the simplest and easiest one based on inductive reasoning, as mentioned above. The second type of variation occurs when an encountered problem is somewhat atypical [ 10 ]. Even expert physicians are not always faced with familiar or typical diseases when treating patients. Expert physicians’ RPDM does not work automatically when faced with atypical symptoms, because they do not have sufficient experiences relevant to the atypical symptoms. In this case, it can be said that they have weak illness scripts or mental models of the given symptoms. In the second variation, experts need more information and will attempt to connect it to their prior knowledge and experiences [ 10 ]. Deductive reasoning is involved in this process so that problem solvers can test their hypotheses in order to find new patterns and construct new mental models based on the newly collected data and previous experiences. The third variation of RPDM is when expert physicians have no previous experience or prior knowledge of given problem situations; in other words, no illness script or mental model [ 10 ]. Jonassen [ 10 ] argued that a mental simulation is conducted to predict the consequences of various actions by experts in the third variation. This process inevitably involves repetitive deductive reasoning to test a larger number of hypotheses when making a diagnosis.
Similarly, from the perspective of dual process theory as a decision-making process, decision making is classified into two approaches based on the reasoning style: type 1 and type 2 (or system 1 and system 2) [ 43 , 44 ]. According to Croskerry [ 44 ], the type 1 decision-making process is intuitive and based on experiential-inductive reasoning, while type 2 is an analytical and hypothetico-deductive decision-making process [ 44 , 45 ]. A feature that distinguishes the two processes is whether a physician who encounters a patient’s symptoms succeeds in pattern recognition. If a physician recognizes prominent features of the visual presentation of illness, type 1 processes (or system 1) are operated automatically, whereas type 2 (or system 2) processes work if any distinct feature of illness presentation is not recognized [ 44 ].
Only experienced expert physicians can use RPDM [ 10 , 46 ] or type 1 and 2 processes [ 43 ], because it can occur solely based on various experiences and a wide range of prior knowledge that can be gained as a result of a huge amount of deductive reasoning since they were novices. Consequently, it can be concluded that expert physicians generally use more inductive reasoning when they automatically recognize key patterns of given problems or symptoms, while sometimes they also use deductive reasoning when they additionally need processes of hypothesis testing to recognize new patterns of symptoms.
From the perspective of cognitive processes, clinical reasoning is considered as one of the decision-making processes that finds the best solutions to patients’ illnesses. As a form of decision making for problem solving, two reasoning processes have been considered: inductive and deductive reasoning. Deductive reasoning can be used to make a diagnosis if physicians have insufficient knowledge, sufficient time, and the ability to analyze the current status of their patients. However, in reality, it is inefficient to conduct thorough deductive reasoning at each stage of clinical reasoning because only a limited amount of time is allowed for both physicians and patients to reach a conclusion in most cases. A few researchers have suggested that using deductive reasoning is more likely to result in diagnostic errors than inductive reasoning, because evidence-based research, such as deductive reasoning, focuses mainly on available and observable evidence and rules out the possibility of any other possible factors influencing the patient’s symptoms [ 37 , 38 ]. However, when a physician encounters unfamiliar symptom and the degree of uncertainty is high, deductive reasoning is required to reach the correct diagnosis through analytical and slow diagnostic processes by collecting data from resources [ 44 ]. Taken together, in order to make the most of a limited timeframe and reduce diagnostic errors, physicians should be encouraged to use inductive reasoning in their clinical reasoning as far as possible given that patterns of illness presentation are recognized.
Unfortunately, it is not always easy for novice physicians to apply inductive or deductive reasoning in all cases. Expert physicians have sufficient capabilities to use both inductive and deductive reasoning and can also automate their clinical reasoning based on inductive reasoning, because they have already gathered the wide range of experiences and knowledge required to diagnose various symptoms. Novice physicians should make a greater effort to use inductive reasoning when making diagnoses; however, it takes experiencing countless deductive reasoning processes to structure various illness scripts or strong mental models until they reach a professional level. As a result, teaching not only clinical reasoning as a whole process but also the critical thinking skills required for clinical reasoning is important in medical schools [ 47 ]. For this, medical schools should pursue problem-based learning by providing students with various opportunities to gain content knowledge as well as develop the critical thinking skills —such as data analysis skills, metacognitive skills, causal reasoning, systems thinking, and so forth—required for problem solving in a holistic manner so that they can improve their reasoning skills and freely use both inductive and deductive approaches in any context. Further studies will be reviewed to provide detailed guidelines or teaching tips on how to develop medical students’ critical thinking skills.
Acknowledgments
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Author contributions
All work was done by HS.
41+ Critical Thinking Examples (Definition + Practices)

Critical thinking is an essential skill in our information-overloaded world, where figuring out what is fact and fiction has become increasingly challenging.
But why is critical thinking essential? Put, critical thinking empowers us to make better decisions, challenge and validate our beliefs and assumptions, and understand and interact with the world more effectively and meaningfully.
Critical thinking is like using your brain's "superpowers" to make smart choices. Whether it's picking the right insurance, deciding what to do in a job, or discussing topics in school, thinking deeply helps a lot. In the next parts, we'll share real-life examples of when this superpower comes in handy and give you some fun exercises to practice it.
Critical Thinking Process Outline
Critical thinking means thinking clearly and fairly without letting personal feelings get in the way. It's like being a detective, trying to solve a mystery by using clues and thinking hard about them.
It isn't always easy to think critically, as it can take a pretty smart person to see some of the questions that aren't being answered in a certain situation. But, we can train our brains to think more like puzzle solvers, which can help develop our critical thinking skills.
Here's what it looks like step by step:
Spotting the Problem: It's like discovering a puzzle to solve. You see that there's something you need to figure out or decide.
Collecting Clues: Now, you need to gather information. Maybe you read about it, watch a video, talk to people, or do some research. It's like getting all the pieces to solve your puzzle.
Breaking It Down: This is where you look at all your clues and try to see how they fit together. You're asking questions like: Why did this happen? What could happen next?
Checking Your Clues: You want to make sure your information is good. This means seeing if what you found out is true and if you can trust where it came from.
Making a Guess: After looking at all your clues, you think about what they mean and come up with an answer. This answer is like your best guess based on what you know.
Explaining Your Thoughts: Now, you tell others how you solved the puzzle. You explain how you thought about it and how you answered.
Checking Your Work: This is like looking back and seeing if you missed anything. Did you make any mistakes? Did you let any personal feelings get in the way? This step helps make sure your thinking is clear and fair.
And remember, you might sometimes need to go back and redo some steps if you discover something new. If you realize you missed an important clue, you might have to go back and collect more information.
Critical Thinking Methods
Just like doing push-ups or running helps our bodies get stronger, there are special exercises that help our brains think better. These brain workouts push us to think harder, look at things closely, and ask many questions.
It's not always about finding the "right" answer. Instead, it's about the journey of thinking and asking "why" or "how." Doing these exercises often helps us become better thinkers and makes us curious to know more about the world.
Now, let's look at some brain workouts to help us think better:
1. "What If" Scenarios
Imagine crazy things happening, like, "What if there was no internet for a month? What would we do?" These games help us think of new and different ideas.
Pick a hot topic. Argue one side of it and then try arguing the opposite. This makes us see different viewpoints and think deeply about a topic.
3. Analyze Visual Data
Check out charts or pictures with lots of numbers and info but no explanations. What story are they telling? This helps us get better at understanding information just by looking at it.
4. Mind Mapping
Write an idea in the center and then draw lines to related ideas. It's like making a map of your thoughts. This helps us see how everything is connected.
There's lots of mind-mapping software , but it's also nice to do this by hand.
5. Weekly Diary
Every week, write about what happened, the choices you made, and what you learned. Writing helps us think about our actions and how we can do better.
6. Evaluating Information Sources
Collect stories or articles about one topic from newspapers or blogs. Which ones are trustworthy? Which ones might be a little biased? This teaches us to be smart about where we get our info.
There are many resources to help you determine if information sources are factual or not.
7. Socratic Questioning
This way of thinking is called the Socrates Method, named after an old-time thinker from Greece. It's about asking lots of questions to understand a topic. You can do this by yourself or chat with a friend.
Start with a Big Question:
"What does 'success' mean?"
Dive Deeper with More Questions:
"Why do you think of success that way?" "Do TV shows, friends, or family make you think that?" "Does everyone think about success the same way?"
"Can someone be a winner even if they aren't rich or famous?" "Can someone feel like they didn't succeed, even if everyone else thinks they did?"
Look for Real-life Examples:
"Who is someone you think is successful? Why?" "Was there a time you felt like a winner? What happened?"
Think About Other People's Views:
"How might a person from another country think about success?" "Does the idea of success change as we grow up or as our life changes?"
Think About What It Means:
"How does your idea of success shape what you want in life?" "Are there problems with only wanting to be rich or famous?"
Look Back and Think:
"After talking about this, did your idea of success change? How?" "Did you learn something new about what success means?"
8. Six Thinking Hats
Edward de Bono came up with a cool way to solve problems by thinking in six different ways, like wearing different colored hats. You can do this independently, but it might be more effective in a group so everyone can have a different hat color. Each color has its way of thinking:
White Hat (Facts): Just the facts! Ask, "What do we know? What do we need to find out?"
Red Hat (Feelings): Talk about feelings. Ask, "How do I feel about this?"
Black Hat (Careful Thinking): Be cautious. Ask, "What could go wrong?"
Yellow Hat (Positive Thinking): Look on the bright side. Ask, "What's good about this?"
Green Hat (Creative Thinking): Think of new ideas. Ask, "What's another way to look at this?"
Blue Hat (Planning): Organize the talk. Ask, "What should we do next?"
When using this method with a group:
- Explain all the hats.
- Decide which hat to wear first.
- Make sure everyone switches hats at the same time.
- Finish with the Blue Hat to plan the next steps.
9. SWOT Analysis
SWOT Analysis is like a game plan for businesses to know where they stand and where they should go. "SWOT" stands for Strengths, Weaknesses, Opportunities, and Threats.
There are a lot of SWOT templates out there for how to do this visually, but you can also think it through. It doesn't just apply to businesses but can be a good way to decide if a project you're working on is working.
Strengths: What's working well? Ask, "What are we good at?"
Weaknesses: Where can we do better? Ask, "Where can we improve?"
Opportunities: What good things might come our way? Ask, "What chances can we grab?"
Threats: What challenges might we face? Ask, "What might make things tough for us?"
Steps to do a SWOT Analysis:
- Goal: Decide what you want to find out.
- Research: Learn about your business and the world around it.
- Brainstorm: Get a group and think together. Talk about strengths, weaknesses, opportunities, and threats.
- Pick the Most Important Points: Some things might be more urgent or important than others.
- Make a Plan: Decide what to do based on your SWOT list.
- Check Again Later: Things change, so look at your SWOT again after a while to update it.
Now that you have a few tools for thinking critically, let’s get into some specific examples.
Everyday Examples
Life is a series of decisions. From the moment we wake up, we're faced with choices – some trivial, like choosing a breakfast cereal, and some more significant, like buying a home or confronting an ethical dilemma at work. While it might seem that these decisions are disparate, they all benefit from the application of critical thinking.
10. Deciding to buy something
Imagine you want a new phone. Don't just buy it because the ad looks cool. Think about what you need in a phone. Look up different phones and see what people say about them. Choose the one that's the best deal for what you want.
11. Deciding what is true
There's a lot of news everywhere. Don't believe everything right away. Think about why someone might be telling you this. Check if what you're reading or watching is true. Make up your mind after you've looked into it.
12. Deciding when you’re wrong
Sometimes, friends can have disagreements. Don't just get mad right away. Try to see where they're coming from. Talk about what's going on. Find a way to fix the problem that's fair for everyone.
13. Deciding what to eat
There's always a new diet or exercise that's popular. Don't just follow it because it's trendy. Find out if it's good for you. Ask someone who knows, like a doctor. Make choices that make you feel good and stay healthy.
14. Deciding what to do today
Everyone is busy with school, chores, and hobbies. Make a list of things you need to do. Decide which ones are most important. Plan your day so you can get things done and still have fun.
15. Making Tough Choices
Sometimes, it's hard to know what's right. Think about how each choice will affect you and others. Talk to people you trust about it. Choose what feels right in your heart and is fair to others.
16. Planning for the Future
Big decisions, like where to go to school, can be tricky. Think about what you want in the future. Look at the good and bad of each choice. Talk to people who know about it. Pick what feels best for your dreams and goals.
Job Examples
17. solving problems.
Workers brainstorm ways to fix a machine quickly without making things worse when a machine breaks at a factory.
18. Decision Making
A store manager decides which products to order more of based on what's selling best.
19. Setting Goals
A team leader helps their team decide what tasks are most important to finish this month and which can wait.
20. Evaluating Ideas
At a team meeting, everyone shares ideas for a new project. The group discusses each idea's pros and cons before picking one.
21. Handling Conflict
Two workers disagree on how to do a job. Instead of arguing, they talk calmly, listen to each other, and find a solution they both like.
22. Improving Processes
A cashier thinks of a faster way to ring up items so customers don't have to wait as long.
23. Asking Questions
Before starting a big task, an employee asks for clear instructions and checks if they have the necessary tools.
24. Checking Facts
Before presenting a report, someone double-checks all their information to make sure there are no mistakes.
25. Planning for the Future
A business owner thinks about what might happen in the next few years, like new competitors or changes in what customers want, and makes plans based on those thoughts.
26. Understanding Perspectives
A team is designing a new toy. They think about what kids and parents would both like instead of just what they think is fun.
School Examples
27. researching a topic.
For a history project, a student looks up different sources to understand an event from multiple viewpoints.
28. Debating an Issue
In a class discussion, students pick sides on a topic, like school uniforms, and share reasons to support their views.
29. Evaluating Sources
While writing an essay, a student checks if the information from a website is trustworthy or might be biased.
30. Problem Solving in Math
When stuck on a tricky math problem, a student tries different methods to find the answer instead of giving up.
31. Analyzing Literature
In English class, students discuss why a character in a book made certain choices and what those decisions reveal about them.
32. Testing a Hypothesis
For a science experiment, students guess what will happen and then conduct tests to see if they're right or wrong.
33. Giving Peer Feedback
After reading a classmate's essay, a student offers suggestions for improving it.
34. Questioning Assumptions
In a geography lesson, students consider why certain countries are called "developed" and what that label means.
35. Designing a Study
For a psychology project, students plan an experiment to understand how people's memories work and think of ways to ensure accurate results.
36. Interpreting Data
In a science class, students look at charts and graphs from a study, then discuss what the information tells them and if there are any patterns.
Critical Thinking Puzzles
Not all scenarios will have a single correct answer that can be figured out by thinking critically. Sometimes we have to think critically about ethical choices or moral behaviors.
Here are some mind games and scenarios you can solve using critical thinking. You can see the solution(s) at the end of the post.
37. The Farmer, Fox, Chicken, and Grain Problem
A farmer is at a riverbank with a fox, a chicken, and a grain bag. He needs to get all three items across the river. However, his boat can only carry himself and one of the three items at a time.
Here's the challenge:
- If the fox is left alone with the chicken, the fox will eat the chicken.
- If the chicken is left alone with the grain, the chicken will eat the grain.
How can the farmer get all three items across the river without any item being eaten?
38. The Rope, Jar, and Pebbles Problem
You are in a room with two long ropes hanging from the ceiling. Each rope is just out of arm's reach from the other, so you can't hold onto one rope and reach the other simultaneously.
Your task is to tie the two rope ends together, but you can't move the position where they hang from the ceiling.
You are given a jar full of pebbles. How do you complete the task?
39. The Two Guards Problem
Imagine there are two doors. One door leads to certain doom, and the other leads to freedom. You don't know which is which.
In front of each door stands a guard. One guard always tells the truth. The other guard always lies. You don't know which guard is which.
You can ask only one question to one of the guards. What question should you ask to find the door that leads to freedom?
40. The Hourglass Problem
You have two hourglasses. One measures 7 minutes when turned over, and the other measures 4 minutes. Using just these hourglasses, how can you time exactly 9 minutes?
41. The Lifeboat Dilemma
Imagine you're on a ship that's sinking. You get on a lifeboat, but it's already too full and might flip over.
Nearby in the water, five people are struggling: a scientist close to finding a cure for a sickness, an old couple who've been together for a long time, a mom with three kids waiting at home, and a tired teenager who helped save others but is now in danger.
You can only save one person without making the boat flip. Who would you choose?
42. The Tech Dilemma
You work at a tech company and help make a computer program to help small businesses. You're almost ready to share it with everyone, but you find out there might be a small chance it has a problem that could show users' private info.
If you decide to fix it, you must wait two more months before sharing it. But your bosses want you to share it now. What would you do?
43. The History Mystery
Dr. Amelia is a history expert. She's studying where a group of people traveled long ago. She reads old letters and documents to learn about it. But she finds some letters that tell a different story than what most people believe.
If she says this new story is true, it could change what people learn in school and what they think about history. What should she do?
The Role of Bias in Critical Thinking
Have you ever decided you don’t like someone before you even know them? Or maybe someone shared an idea with you that you immediately loved without even knowing all the details.
This experience is called bias, which occurs when you like or dislike something or someone without a good reason or knowing why. It can also take shape in certain reactions to situations, like a habit or instinct.
Bias comes from our own experiences, what friends or family tell us, or even things we are born believing. Sometimes, bias can help us stay safe, but other times it stops us from seeing the truth.
Not all bias is bad. Bias can be a mechanism for assessing our potential safety in a new situation. If we are biased to think that anything long, thin, and curled up is a snake, we might assume the rope is something to be afraid of before we know it is just a rope.
While bias might serve us in some situations (like jumping out of the way of an actual snake before we have time to process that we need to be jumping out of the way), it often harms our ability to think critically.
How Bias Gets in the Way of Good Thinking
Selective Perception: We only notice things that match our ideas and ignore the rest.
It's like only picking red candies from a mixed bowl because you think they taste the best, but they taste the same as every other candy in the bowl. It could also be when we see all the signs that our partner is cheating on us but choose to ignore them because we are happy the way we are (or at least, we think we are).
Agreeing with Yourself: This is called “ confirmation bias ” when we only listen to ideas that match our own and seek, interpret, and remember information in a way that confirms what we already think we know or believe.
An example is when someone wants to know if it is safe to vaccinate their children but already believes that vaccines are not safe, so they only look for information supporting the idea that vaccines are bad.
Thinking We Know It All: Similar to confirmation bias, this is called “overconfidence bias.” Sometimes we think our ideas are the best and don't listen to others. This can stop us from learning.
Have you ever met someone who you consider a “know it”? Probably, they have a lot of overconfidence bias because while they may know many things accurately, they can’t know everything. Still, if they act like they do, they show overconfidence bias.
There's a weird kind of bias similar to this called the Dunning Kruger Effect, and that is when someone is bad at what they do, but they believe and act like they are the best .
Following the Crowd: This is formally called “groupthink”. It's hard to speak up with a different idea if everyone agrees. But this can lead to mistakes.
An example of this we’ve all likely seen is the cool clique in primary school. There is usually one person that is the head of the group, the “coolest kid in school”, and everyone listens to them and does what they want, even if they don’t think it’s a good idea.
How to Overcome Biases
Here are a few ways to learn to think better, free from our biases (or at least aware of them!).
Know Your Biases: Realize that everyone has biases. If we know about them, we can think better.
Listen to Different People: Talking to different kinds of people can give us new ideas.
Ask Why: Always ask yourself why you believe something. Is it true, or is it just a bias?
Understand Others: Try to think about how others feel. It helps you see things in new ways.
Keep Learning: Always be curious and open to new information.
In today's world, everything changes fast, and there's so much information everywhere. This makes critical thinking super important. It helps us distinguish between what's real and what's made up. It also helps us make good choices. But thinking this way can be tough sometimes because of biases. These are like sneaky thoughts that can trick us. The good news is we can learn to see them and think better.
There are cool tools and ways we've talked about, like the "Socratic Questioning" method and the "Six Thinking Hats." These tools help us get better at thinking. These thinking skills can also help us in school, work, and everyday life.
We’ve also looked at specific scenarios where critical thinking would be helpful, such as deciding what diet to follow and checking facts.
Thinking isn't just a skill—it's a special talent we improve over time. Working on it lets us see things more clearly and understand the world better. So, keep practicing and asking questions! It'll make you a smarter thinker and help you see the world differently.
Critical Thinking Puzzles (Solutions)
The farmer, fox, chicken, and grain problem.
- The farmer first takes the chicken across the river and leaves it on the other side.
- He returns to the original side and takes the fox across the river.
- After leaving the fox on the other side, he returns the chicken to the starting side.
- He leaves the chicken on the starting side and takes the grain bag across the river.
- He leaves the grain with the fox on the other side and returns to get the chicken.
- The farmer takes the chicken across, and now all three items -- the fox, the chicken, and the grain -- are safely on the other side of the river.
The Rope, Jar, and Pebbles Problem
- Take one rope and tie the jar of pebbles to its end.
- Swing the rope with the jar in a pendulum motion.
- While the rope is swinging, grab the other rope and wait.
- As the swinging rope comes back within reach due to its pendulum motion, grab it.
- With both ropes within reach, untie the jar and tie the rope ends together.
The Two Guards Problem
The question is, "What would the other guard say is the door to doom?" Then choose the opposite door.
The Hourglass Problem
- Start both hourglasses.
- When the 4-minute hourglass runs out, turn it over.
- When the 7-minute hourglass runs out, the 4-minute hourglass will have been running for 3 minutes. Turn the 7-minute hourglass over.
- When the 4-minute hourglass runs out for the second time (a total of 8 minutes have passed), the 7-minute hourglass will run for 1 minute. Turn the 7-minute hourglass again for 1 minute to empty the hourglass (a total of 9 minutes passed).
The Boat and Weights Problem
Take the cat over first and leave it on the other side. Then, return and take the fish across next. When you get there, take the cat back with you. Leave the cat on the starting side and take the cat food across. Lastly, return to get the cat and bring it to the other side.
The Lifeboat Dilemma
There isn’t one correct answer to this problem. Here are some elements to consider:
- Moral Principles: What values guide your decision? Is it the potential greater good for humanity (the scientist)? What is the value of long-standing love and commitment (the elderly couple)? What is the future of young children who depend on their mothers? Or the selfless bravery of the teenager?
- Future Implications: Consider the future consequences of each choice. Saving the scientist might benefit millions in the future, but what moral message does it send about the value of individual lives?
- Emotional vs. Logical Thinking: While it's essential to engage empathy, it's also crucial not to let emotions cloud judgment entirely. For instance, while the teenager's bravery is commendable, does it make him more deserving of a spot on the boat than the others?
- Acknowledging Uncertainty: The scientist claims to be close to a significant breakthrough, but there's no certainty. How does this uncertainty factor into your decision?
- Personal Bias: Recognize and challenge any personal biases, such as biases towards age, profession, or familial status.
The Tech Dilemma
Again, there isn’t one correct answer to this problem. Here are some elements to consider:
- Evaluate the Risk: How severe is the potential vulnerability? Can it be easily exploited, or would it require significant expertise? Even if the circumstances are rare, what would be the consequences if the vulnerability were exploited?
- Stakeholder Considerations: Different stakeholders will have different priorities. Upper management might prioritize financial projections, the marketing team might be concerned about the product's reputation, and customers might prioritize the security of their data. How do you balance these competing interests?
- Short-Term vs. Long-Term Implications: While launching on time could meet immediate financial goals, consider the potential long-term damage to the company's reputation if the vulnerability is exploited. Would the short-term gains be worth the potential long-term costs?
- Ethical Implications : Beyond the financial and reputational aspects, there's an ethical dimension to consider. Is it right to release a product with a known vulnerability, even if the chances of it being exploited are low?
- Seek External Input: Consulting with cybersecurity experts outside your company might be beneficial. They could provide a more objective risk assessment and potential mitigation strategies.
- Communication: How will you communicate the decision, whatever it may be, both internally to your team and upper management and externally to your customers and potential users?
The History Mystery
Dr. Amelia should take the following steps:
- Verify the Letters: Before making any claims, she should check if the letters are actual and not fake. She can do this by seeing when and where they were written and if they match with other things from that time.
- Get a Second Opinion: It's always good to have someone else look at what you've found. Dr. Amelia could show the letters to other history experts and see their thoughts.
- Research More: Maybe there are more documents or letters out there that support this new story. Dr. Amelia should keep looking to see if she can find more evidence.
- Share the Findings: If Dr. Amelia believes the letters are true after all her checks, she should tell others. This can be through books, talks, or articles.
- Stay Open to Feedback: Some people might agree with Dr. Amelia, and others might not. She should listen to everyone and be ready to learn more or change her mind if new information arises.
Ultimately, Dr. Amelia's job is to find out the truth about history and share it. It's okay if this new truth differs from what people used to believe. History is about learning from the past, no matter the story.
Related posts:
- Experimenter Bias (Definition + Examples)
- Hasty Generalization Fallacy (31 Examples + Similar Names)
- Ad Hoc Fallacy (29 Examples + Other Names)
- Confirmation Bias (Examples + Definition)
- Equivocation Fallacy (26 Examples + Description)
Reference this article:
About The Author
Free Personality Test
Free Memory Test
Free IQ Test
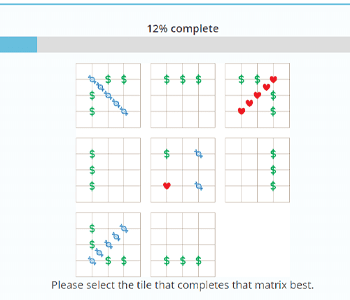
PracticalPie.com is a participant in the Amazon Associates Program. As an Amazon Associate we earn from qualifying purchases.
Follow Us On:
Youtube Facebook Instagram X/Twitter
Psychology Resources
Developmental
Personality
Relationships
Psychologists
Serial Killers
Psychology Tests
Personality Quiz
Memory Test
Depression test
Type A/B Personality Test
© PracticalPsychology. All rights reserved
Privacy Policy | Terms of Use

Critical Thinking Skills.
Ai generator.
Critical thinking is the ability to analyze information objectively and make a reasoned judgment. It involves evaluating sources, such as data, facts, observable phenomena, and research findings. Developing critical thinking skills is essential for academic success and everyday decision-making. Here are strategies and examples to help enhance critical thinking skills.
1. Ask Questions
Asking questions is fundamental to critical thinking. Encourage curiosity and in-depth understanding by asking questions like:
- What evidence supports this claim?
- Are there alternative perspectives?
- What are the implications of this decision?
2. Analyze Assumptions
Identifying and analyzing assumptions helps in understanding underlying biases and beliefs.
- Example : When reading a news article, identify the assumptions the author makes and consider how they influence the argument.
3. Evaluate Evidence
Evaluating evidence involves assessing the reliability and validity of information sources.
- Example : When researching a topic, compare information from multiple sources and evaluate their credibility.
4. Develop Hypotheses
Formulating and testing hypotheses can strengthen analytical skills.
- Example : In a science experiment, develop a hypothesis, conduct experiments to test it, and analyze the results.
5. Reflect on Your Thinking Process
Reflection helps in recognizing and improving your thought process.
- Example : After making a decision, reflect on the steps you took, what you learned, and how you could improve in the future.
6. Engage in Discussions
Participating in discussions encourages the exchange of ideas and perspectives.
- Example : Join a debate club or discussion group to practice presenting and defending your viewpoints.
7. Practice Problem-Solving
Solving problems systematically can enhance critical thinking.
- Example : Use problem-solving frameworks, like SWOT analysis, to evaluate a business case study.
8. Use Critical Thinking Exercises
Incorporate exercises and activities designed to boost critical thinking skills.
- Example : Engage in brainteasers, puzzles, and logic games that challenge your reasoning abilities.
Examples of Critical Thinking in Action
- Case Study: Socratic Method : Used in law schools, the Socratic method involves asking a series of questions to help students think deeply about the subject matter.
- Example: Reflective Journals : Students keep journals where they reflect on their learning experiences, analyze their thinking processes, and develop insights.
Developing critical thinking skills is crucial for academic success and informed decision-making. By asking questions, analyzing assumptions, evaluating evidence, developing hypotheses, reflecting on thinking processes, engaging in discussions, practicing problem-solving, and using critical thinking exercises, individuals can enhance their ability to think critically.
Text prompt
- Instructive
- Professional
10 Examples of Public speaking
20 Examples of Gas lighting
Critical thinking for critical care: Conner guides emergency care course at veterinary college
- Kevin Myatt
28 May 2024
- Share on Facebook
- Share on Twitter
- Copy address link to clipboard

Emergencies find everyone in life, eventually. The same is true in veterinary medicine, even for clinicians who have purposely gone into a field other than emergency care.
“We need to get our students comfortable with managing emergencies because even if they don't choose to go into emergency-specific veterinary medicine, they’re going to see emergencies,” said Bobbi Conner , clinical associate professor of emergency and critical care medicine at the Virginia-Maryland College of Veterinary Medicine . “If they’re going into clinical medicine, they’re going to see things that clients didn't realize was an emergency, or if they’re working in a rural area, people are going come to them with an emergency. So, for me, it's really important that all of our students have that foundation.”
Conner teaches the emergency and critical care (ECC) course, required for third-year students in small animal, mixed animal and public corporate tracks, and also is a key mentor and leader at the Veterinary Teaching Hospital for residents, interns and students in clerkships learning the ropes of emergency veterinary medicine.
Conner says that the word “critical” in the course’s name could just as easily be for critical thinking as it could be for critical emergencies.
“I focus a lot more on the why, rather than the what,” Conner said. “For their exams -- here's the scenario, tell me what you're going to do and justify your answer. And what they don't seem to believe until they go through it is that I'm going to grade them on their justification, not on their answer.”
Veterinary medicine is not just about making a diagnosis and prescribing a pre-determined treatment from rote memory of facts and figures. Multiple treatments are potentially effective for the same diagnosis in the same animal, with possibly differing results from case to case. And then there are clients’ finances, limited resources, and ethics to consider, all of which are amplified in the crucible of emergency care requiring quick decisions with animals’ lives and human emotions at stake.
“So what about when you've got two patients who both need a transfusion, but you've got one unit of blood?” Conner asked rhetorically. “That’s happened to me many times, and so I ask them now, what are you going to do? How are you going to choose?”
Veterinary medicine also doesn’t avoid people – human interactions can be at their most intense with the welfare of beloved pets on the line, and Conner’s course helps students learn how to manage those interactions.
“You get really challenging things in the ER that you don't necessarily see in general practice,” said Anna Horowitz, a Class of 2025 veterinary student from Bethesda, Maryland. “People are under a ton of stress. They love their pets, this may be the worst day of people's lives. In the ER you will meet the angriest, the saddest, and the most intense people you will ever meet. So it's good to talk about how to manage those and I think it's really good she focuses entire lectures on that.”
Horowitz originally aspired to be an equine veterinarian, but quickly changed her course after spending a summer during her undergraduate college years in Vermont at an emergency veterinary hospital. That eventually led her to the veterinary college at Virginia Tech with ambitions to pursue a career in emergency veterinary care.
“This is my life,” Horowitz said. “I am amazed by the variety of the different types of cases you see every day. Every once in a while, something is going to walk in and you’re thinking ‘I have never seen that before.’”
Amy Lin, a 2024 veterinary college graduate from Northern Virginia, isn’t decided yet on whether she wants to enter emergency care or steer more toward veterinary oncology, but she said she has benefited from Conner’s teaching and influence.
“She's really actively thinking of ways to help us learn these concepts, to present them in a fun and interactive way,” said Lin, who will be undertaking an internship at a veterinary clinic in New York City to further her experience. “She made it very applicable to clinical reasoning. It wasn't just here’s the science behind it, it’s more about what you will see when you’re out there. This is the logic pattern, your thought process when you approach this. Which I really thought was a new perspective. What is the animal telling you? And just based off of that, what can you do to help the animal?”
Andrew Mann
540-231-9005
- Blacksburg, Va.
- Doctor of Veterinary Medicine Program
- Emergency and Critical Care
- Faculty Excellence
- News directly from around campus
- Top News - Virginia-Maryland College of Veterinary Medicine
- Veterinary Teaching Hospital
- Virginia-Maryland College of Veterinary Medicine
Related Content

IMAGES
VIDEO
COMMENTS
Medistudents team. August 18, 2021. Critical thinking is an essential cognitive skill for every individual but is a crucial component for healthcare professionals such as doctors, nurses and dentists. It is a skill that should be developed and trained, not just during your career as a doctor, but before that when you are still a medical student.
Critical thinking is just one skill crucial to evidence based practice in healthcare and education, write Jonathan Sharples and colleagues , who see exciting opportunities for cross sector collaboration Imagine you are a primary care doctor. A patient comes into your office with acute, atypical chest pain. Immediately you consider the patient's sex and age, and you begin to think about what ...
Critical thinking in medicine is what the Science-Based Medicine (SBM) blog is all about. ... He gives the example of a patient with multiple sclerosis whose doctor describes the effectiveness and risks of 8 injectables, 3 pills, and 4 infusions. The patient can't choose; she misses the follow-up appointment and returns a year later with ...
the need for fostering critical thinking amongmedical practitioners. This article attempts to provide a conceptual analysis of critical thinking with reference to medical education along with measures to foster critical thinking through relevant teaching learning and assessment methods. Key words: Critical thinking, medical education, quality
For example, in everyday practice, ... Evaluation of research behind evidence-based medicine requires critical thinking and good clinical judgment. Sometimes the research findings are mixed or even conflicting. As such, the validity, reliability, and generalizability of available research are fundamental to evaluating whether evidence can be ...
Building on the conceptual framework first established by the Foundation for Critical Thinking, 19 the milestones for critical thinking articulated here were also heavily influenced by the Dreyfus model of the stages of expertise, 20 which has been applied extensively in nursing 21 and in medicine. 16 The language used in specialty board ...
Three critical thinking skills underpin effective care: clinical reasoning, evidence-informed decision-making and systems thinking. It is important to define these skills explicitly, explain their rationales, describe methods of instruction and provide examples of optimal application.
There are several reasons why it is important to have a set of critical thinking skills that can be applied to medicine and health. As the scenario in Sect. 1.1 illustrates, we cannot evade the relentless exposure to medical and health messages that is part of our daily lives. We would be naïve to think that all, or even most, of these messages are conveying claims that represent some ideal ...
Critical thinking is an essential cognitive skill for the individuals involved in various healthcare domains such as doctors, nurses, lab assistants, patients and so on, as is emphasized by the Authors. Recent evidence suggests that critical thinking is being perceived/evaluated as a domain-general construct and it is less distinguishable from ...
We have analysed these qualities as responsibilist, epistemic virtues. We believe that a virtues approach is best able to make sense of the non-cognitive elements of 'being critical', such as the honesty and courage to question claims in the face of persuasion, authority or social pressure. Medical educators and professional bodies seem to ...
Critical thinking, the capacity to be deliberate about thinking, is increasingly the focus of undergraduate medical education, but is not commonly addressed in graduate medical education. Without critical thinking, physicians, and particularly residents, are prone to cognitive errors, which can lead to diagnostic errors, especially in a high ...
Here are five ways to nurture your critical-thinking skills: Be a lifelong learner. Continuous learning through educational courses and professional development lets you stay current with evidence-based practice. That knowledge helps you make informed decisions in stressful moments. Practice reflection.
Appears in: Cummings, L. (2020) Fallacies in Medicine and Health: Critical Thinking, Argumentation and Communication, Houndmills, Basingstoke: Palgrave Macmillan. Chapter 1: Critical Thinking in Medicine and Health Abstract: This chapter addresses why there is a need for experts and lay people to think critically about medicine and health.
These "questioning and solving" skills require learning, practice, and experience [], but mainly a recognition of the many uncertainties we do have despite the important scientific advances.Precisely, a good example of the importance of critical thinking is its contribution to Precision Medicine through medical imaging data and information.
As an example of a participant disagreeing with a perspective encountered in the mind map, one participant rejected social justice as an important component of critical thinking in medicine. They related that critical thinking has 'got everything to do with reasoning, which makes sense. … Social justice has nothing to do with critical ...
Critical Thinking in Nursing: Example 1. I had a patient that was scheduled to go to get a pacemaker placed at 0900. The physician wanted the patient to get 2 units of blood before going downstairs for the procedure. I administered it per protocol. About 30 minutes after that second unit got started, I noticed his oxygen went from 95% down to ...
Scott Cormier's two-part article on critical thinking provides a few examples of approaches to critical thinking as well as biases to avoid. 3,4 Unfortunately, they do not touch on the ...
Beyer (1995), provides the most basic definition of Critical Thinking as "making reasoned judgments". In another understanding, it is the ability to think clearly and rationally about what to do and/or what to believe. It also includes the ability to engage in reflective and independent thinking. A person with critical thinking skills is ...
Research and consensus guidelines now recommend formal critical thinking training. A gap in the literature exists with respect to how to incorporate critical thinking education in a pediatric training environment. Objectives: This study was a targeted needs assessment for developing a formal curriculum on critical thinking for pediatric residents.
Teaching and Assessing Critical Thinking and Clinical Reasoning Skills in Medical Education. of teaching which dates back to 470-399 BC dur ing Socrates era (Paul, Elder, & Bartell, 1997). This ...
Background In medicine, critical thinking is required for managing and tolerating medical uncertainty, as well as solving professional problems and treating diseases. However, the core of Confucianism, teacher-centered and exam-oriented settings in middle and high school education may pose challenges to developing critical thinking in Han Chinese or Taiwanese students. Students may be ...
This paper reviews the reasoning processes involved in clinical reasoning from the perspective of cognitive psychology. To properly use clinical reasoning, one requires not only domain knowledge but also structural knowledge, such as critical thinking skills. In this paper, two types of reasoning process required for critical thinking are ...
There are many resources to help you determine if information sources are factual or not. 7. Socratic Questioning. This way of thinking is called the Socrates Method, named after an old-time thinker from Greece. It's about asking lots of questions to understand a topic.
Critical thinking is the process of actively and skillfully analyzing, evaluating, and synthesizing information gathered from various sources, including observations, experiences, and communication. It involves using logic and reasoning to identify connections, draw conclusions, and make informed decisions, while remaining open-minded and aware ...
Example: Use problem-solving frameworks, like SWOT analysis, to evaluate a business case study. 8. Use Critical Thinking Exercises. Incorporate exercises and activities designed to boost critical thinking skills. Example: Engage in brainteasers, puzzles, and logic games that challenge your reasoning abilities.
Conner teaches the emergency and critical care (ECC) course, required for third-year students in small animal, mixed animal and public corporate tracks, and also is a key mentor and leader at the Veterinary Teaching Hospital for residents, interns and students in clerkships learning the ropes of emergency veterinary medicine.