An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.15(12); 2023 Dec
- PMC10783202


Neurodevelopmental Treatment in Children With Cerebral Palsy: A Review of the Literature
Sandeep khanna.
1 Physiotherapy, PhD Program, Sardar Bhagwan Singh University, Dehradun, IND
2 Physiotherapy, Latika Roy Memorial Foundation, Dehradun, IND
Ranganathan Arunmozhi
3 Physiotherapy, Sardar Bhagwan Singh University, Dehradun, IND
Chanan Goyal
4 Physiotherapy, Government Physiotherapy College, Raipur, IND
5 Neuro Physiotherapy, Datta Meghe Institute of Higher Education and Research, Wardha, IND
This review aimed to explore the current literature on neurodevelopmental treatment (NDT) in children with cerebral palsy (CP). It also sought to determine what outcome measures are used to analyze the effect of NDT and whether these parameters are in line with the components of the International Classification of Functioning, Disability and Health (ICF). The studies published in the English language between 2000 and 2023 were included based on a search of the databases PEDro, PubMed, and Google Scholar. Studies that examined the effect of NDT on children with CP were included.
We found a total of 54 studies describing the effect of NDT in children with CP and these were included in this literature review. NDT in children with CP was found to have positive outcomes in 41 studies, while 13 studies had contradictory conclusions. Based on our findings, NDT is widely used for the rehabilitation of children with CP globally. The parameters used to assess the improvement mostly included gross motor function, balance, and postural control. The outcome measures used in studies are usually linked to body structure and function or activities domain of the ICF model by the World Health Organization (WHO). However, there is a scarcity of studies on the effect of NDT on participation, which should be the outcome of any rehabilitation program. There is scope for future research to demonstrate the effect of NDT on the participation of children with CP. Further studies with larger sample sizes and homogenous groups are recommended.
Introduction and background
In India, 3.8% of the population has some form of disability. The most prevalent motor impairment in children is cerebral palsy (CP). CP affects approximately one-fifth of physically challenged children. The global prevalence of CP is 1.5-3.8 in 1000 births [ 1 ]. The prevalence of CP among live births in India is estimated to be about three per 1000 [ 2 ]. CP refers to a disorder of movement and posture that limits activities and is believed to be caused by nonprogressive damage to the developing brain in the early years of life [ 3 ]. This condition has a complex presentation in terms of interaction between different domains of a child’s development including motor, sensory, cognitive, linguistic, executive, and behavioral components. The variables that put one at greater risk of CP may include congenital defects of the brain, genetic predisposition, infection during pregnancy, multiple pregnancies, ischemic hypoxic encephalopathy, stroke in utero or during birth, kernicterus, low birth weight, newborn seizures, newborn meningitis or sepsis, traumatic brain damage after birth, and preterm delivery [ 4 ]. Attaining motor milestones and improvement in function in children with CP depends on various factors, including the severity of the condition, timely and appropriate intervention, parent empowerment, involvement of the family, and opportunities provided to children to practice movements in their natural environment. Globally, developmental professionals work in multidisciplinary teams to bring positive change and enhance the quality of life of children with CP and their families.
Neurofunctional approaches for the management of neurological disorders include the Affolter approach, Brunnstrom approach, proprioceptive neuromuscular facilitation devised by Dr. Herman Kabat, sensory stimulation for activation and inhibition developed by Margaret Rood, constraint-induced movement therapy, mirror therapy, task-oriented approach, and neurodevelopmental therapy/Bobath approach [ 5 ]. One of the most popular interventions among pediatric physiotherapists for managing CP globally is neurodevelopmental treatment (NDT). NDT is a problem-solving method for assessing and treating the functional limitations of individuals with CP [ 6 ]. This literature review aims to summarize available evidence of the outcome of NDT in children with CP. It also delineates the parameters and outcome measures used to analyze the change in children with CP. Another objective is to find if the outcome measures used to investigate the effect of NDT in children with CP fit with the International Classification of Functioning, Disability and Health (ICF) as NDT lays stress on improving function and participation.
Sah et al. conducted a study in 2019 involving 44 children aged 7-15 years with spastic diplegic CP. Task-oriented activity-based NDT was found to be more effective than conventional physiotherapy (PT) in improving control of the trunk, balance, and gross motor function in children diagnosed with CP. The outcome measures employed to study the effects of therapy plans were gross motor function measure (GMFM), postural assessment scale, pediatric balance scale, and trunk impairment scale [ 7 ]. Another study published in 2018 showed that an NDT-based eight-week training program increased the functional level of motor ability and independence in 15 children with hemiparetic and diparetic CP, whose ages ranged from 5 to 15 years, by improving balance and postural control. Outcome measures used in this study were GMFM, seated postural control measure, pediatric balance scale, modified timed up and go test, functional independence measure, and one-minute walking test [ 8 ].
A systematic review based on the ICF framework was undertaken in 2012 to assess the efficacy of concept-based approaches and supplementary therapies utilized in the therapy of lower limbs for children with CP. The outcomes of these studies were assessed using a configuration suggested by the American Academy for Cerebral Palsy and Developmental Medicine. NDT and functional training on gross motor function were found to have level II evidence. Besides, level IV evidence for NDT on all ICF levels was found in this study [ 9 ]. A study published in 2017 concluded that intensive NDT significantly increased gross motor function; 42 children with developmental delay and CP and developmental delay without CP were provided intensive NDT for three months followed by conventional NDT for another three months. All children in the study showed improvement in their gross motor abilities with intensive NDT. GMFM was used as an outcome measure and intensive NDT was recommended for all children with developmental delays [ 10 ].
A clinical trial published in Developmental Medicine and Child Neurology in 2004 involving children with CP found that rigorous NDT was beneficial in enhancing gross motor function. The trial involved a total of 34 children with levels of gross motor function classification ranging between 1 and 3. The outcome measure used in this study was GMFM [ 11 ]. A case series published in 2021 reported that intensive NDT had positive results in six children with neurologic conditions. six children aged 2-10 years were included in this study and the outcome measure used was GMFM-66 [ 12 ]. In a 2015 study, Labaf et al. found that NDT enhanced gross motor function in children with CP in four categories: lying and rolling, sitting, crawling and kneeling, and standing; 28 CP children were included in this study and the outcome measure used was GMFM [ 13 ].
Another study in 2017 suggested that NDT when administered to low-birth-weight preterm babies in a neonatal intensive care unit was found to lead to developmental improvement in the selected group; 96 premature children were included in the study and the outcome measure used was the test of infant movement performance [ 14 ]. A pilot study published in 2015 was designed to analyze the effect of just one session on sit-to-stand movements in CP children. Eight children aged four to six years with CP were included in this study. The findings indicated that children with CP can stand from a seated posture without employing abnormal movement patterns after attending just one NDT session [ 15 ].
The findings of a clinical series investigation revealed a remarkable improvement in visual attention due to improved motor control skills following the NDT session compared to the control session; 10 children aged 6-16 years participated in this study. The outcome measure used was the Conners Kiddie Continuous Performance Test (K-CPT) [ 16 ]. The NDT program is more beneficial than conventional therapy for children having CP. The NDT strategy enhances posture and function used in day-to-day context in children with CP. CP children aged three to nine years were selected. The outcome measure used was GMFM [ 17 ]. In an Indian study, children with CP showed a substantial increase in gross motor ability after three months of NDT [ 18 ].
A clinical trial conducted in 2022 tried to verify the activation of muscle using electromyography when using NDT in children with severe CP; 39 spastic quadriparesis CP children of similar age and same gender were included in the study. The study concluded that there was activation in multifidus, gluteus medius, rectus abdominis, and erector spinae while children were being treated with NDT [ 19 ]. A study conducted in Nigeria in 2013 aimed to find the levels of disability of CP clients receiving PT management; 30 participants aged one to six years were observed after three, six, and 12 months of undergoing NDT. It was determined that NDT PT effectively managed CP, and intervention frequency and duration were significant determinants [ 20 ].
Forty ambulatory children with CP took part in a six-week trial that aimed to examine how their walking changed after receiving NDT. Gait parameters such as stride and step length, foot angle, base of support, cadence, and velocity were measured using pedographs. Significant gains in stride and step length, foot angle, and velocity were observed in all participants [ 21 ]. A study by Turker et al. in 2015 aimed to analyze the effect of goal-directed NDT (GD-NDT) on children with CP in terms of daily living activities and motor function; 26 children aged between 5 and 17 years with CP were included in the study. They were provided GD-NDT for 12 weeks, three times per week. Positive outcomes were seen in gross motor function, health-related quality of life (HRQOL), and level of independence in the daily life of children with CP [ 22 ].
A study in 2018 aimed to determine if a 36-month-old child with bilateral spastic CP would benefit from PT intervention using neurodevelopmental strategies in line with the Bobath concept. The patient showed favorable results after the study in all ICF components, with activities being the most significantly improved component [ 23 ]. A study conducted by Besios et al. sought to assess the NDT method's efficiency in treating CP in young patients. Twenty children with cerebral palsy participated in an eight-week NDT intervention program. The study found substantial evidence that the NDT (Bobath) approach improves children's mobility [ 24 ]. The purpose of the study done by Knox and Evans in 2002 was to assess the functional benefits of NDT in CP children; 15 kids with CP diagnoses with ages ranging from 2 to 12 years were enlisted. This study showed that improvements in motor function and self-care were achieved in this population after a course of NDT [ 25 ]. A systematic review and meta-analysis performed in 2020 found that when balance-training therapies were paired with NDT, there was a significant beneficial effect on postural control. Seven different studies with a total of 194 candidates were included in this review [ 26 ].
Karabay et al. observed that, in addition to NDT, four weeks of kinesio taping (KT) or neuromuscular electrical stimulation (NMES) is beneficial in reducing kyphosis and improving sitting posture; 75 children participated in this study. The outcome measure used was the sitting section of GMFM and kyphosis levels [ 27 ]. Another study by Elbasan et al. suggested that the use of KT and NMES as an adjunct to NDT enhanced gross motor function, posture in sitting, and control of posture; 45 children aged 5-12 years participated in the study spanning six weeks. The outcome measures used were manual muscle testing, shortness tests, gross motor function classification system (GMFCS), the sitting component of GMFM, modified functional reach test, functional independence measure (WeeFIM), cerebral palsy quality of life (CP QOL), and seated postural control measurement (SCPM) [ 28 ]. A longitudinal intervention that was carried out for four years showed that conventional treatment when combined with NDT improved children's speech from incoherent to an acceptable level of functional speech [ 29 ].
New ways of providing therapy combined with NDT have shown positive outcomes in children with CP. In children having milder forms of CP, NDT when combined with video games based on Wii Fit balance was found to show both static and performance-related balance metrics improvement [ 30 ]. In 2021, Acar et al. studied the effects of NDT on eating, swallowing, and difficulty in feeding in children with CP. They concluded that in children with CP, there is an association between oral motor capabilities and control in the trunk. The eating ability of children in the group receiving NDT along with oro-motor intervention and caregiver training showed better improvement than the control group; 40 children were included in the study and the outcome measure used was the trunk impairment scale, schedule for oro-motor assessment, and pediatric quality of life inventory [ 31 ].
NDT used along with transcranial direct current stimulation (tDCS) was found beneficial for children with CP in reducing spasticity and enhancing motor development; 24 CP children were included in this study and the outcome measures used were GMFM-88, box and block test, and modified Ashworth scale [ 32 ]. In 2021, a study by Avcil et al. concluded that NDT and video game-based therapy had similar positive benefits on grip strength and functional abilities [ 33 ]. In children with CP, stabilization exercises of the trunk and neck used along with NDT resulted in improved communication, production of speech, daily activities, and quality of life [ 34 ]. A randomized controlled trial (RCT) in 2021 suggested that extracorporeal shock wave therapy given to paraspinal muscles offers significant additive value when paired with NDT in improving balance and postural control in children with hemiplegic CP. Thirty-two CP children were included in the study and the tools used were the trunk control measurement scale, timed up and go, pediatric balance scale, and trunk impairment scale [ 35 ].
A study in 2012 concluded that the short-term effects of an NDT method are more pronounced in achieving set goals post-Botox for children with CP than those of a traditional PT regime [ 36 ]. Lee et al. reported that NDT along with steadily increasing functional coaching in children with spastic CP can increase muscle thickness of leg muscles and improve motor function [ 37 ]. Vestibular stimulation combined with NDT has shown positive outcomes and hence is considered a beneficial adjunct to increase motor function [ 38 ]. In children with CP, a hip radiography follow-up program combined with NDT and a posture management program were found to reduce the natural course of hip dislocation [ 39 ]. A comprehensive approach for intervention in children with hemiplegic CP including NDT as one of the intervention methods demonstrated improvement in postural symmetry in sitting and standing [ 40 ]. Incorporating NDT concepts into a modified constraint-induced movement therapy (CIMT) protocol may be a useful intervention for children with hemiplegia to maximize functional motor skill acquisition [ 41 ]. An RCT by Kolit and Ekici determined that cognitive orientation to the daily occupational performance approach along with NDT showed clinically better outcomes than NDT alone [ 42 ].
A pilot study conducted in 2022 revealed positive outcomes in terms of balance rehabilitation when using a combination of Vojta and NDT in children with CP [ 43 ]. A study in Iran involving 22 participants with spastic CP in 2010 indicated improvement in four areas of GMFM when intervention was offered using NDT and sensory integration therapy [ 44 ]. An analysis done in 2014 by Behzadi et al. concluded that the traditional NDT and the home program Bobath approach where parents were involved in goal-making and conducting exercises at home was more beneficial when compared to traditional NDT alone. Thirty children with CP aged 0-2 years were included in the analysis and GMFM was used to measure the difference between their condition pre and post-intervention [ 45 ]. Research done in 2007 showed that intensive conventional PT including NDT along with partial body weight treadmill training (PBWTT) was more beneficial for improving the motor and ambulatory abilities of children with CP. Five children aged between two years and three months and nine years and seven months were included in the study [ 46 ]. Choi et al. concluded in their study in 2011 that both NDT and task-oriented training led to improvement in sitting posture in children with CP [ 47 ].
In 2015, Dewar et al. performed a systematic review to analyze which exercises improved control of posture in CP children. Out of the 13 exercises assessed, only five showed a medium level of proof that they were beneficial in improving postural control. The evidence for NDT benefitting control of posture in children with CP was inadequate or contradictory [ 48 ]. Another systematic review in 2019 by Zanon et al. reviewed RCTs to analyze the contrast between NDT and conventional PT for CP children. This study concluded that the effects of NDT on children with CP are unknown; further research is required to find out more about its safety and efficacy. NDT usage based on current data did not support routine use of NDT in practice [ 49 ].
In 2019, a review was conducted to summarize the effect of PT interventions on children with CP; 34 systematic reviews were included and 15 different ways of therapy were found. NDT was found to be ineffective in this study [ 50 ]. Park and Kim conducted research in 2017 to assess changes in strength, stiffness, and gross motor function in children with spastic CP after receiving NDT-based intervention. The findings suggested that this intervention was beneficial in lowering spasticity in children with CP but did not enhance gross motor function [ 51 ]. A study was conducted in 2016 on 20 CP children with GMFCS levels 1 and 2. It found Adeli suit treatment and NDT to be more successful than NDT alone in enhancing spatiotemporal gait metrics but had no significant effect on gross motor and balance [ 52 ]. A systematic review in 2008 reported that RCTs provide primarily limited information on the effectiveness of most PT techniques due to methodological limitations and variability in population, interventions, and outcomes. Well-designed trials are required, especially to analyze concentrated PT therapies including NDT [ 53 ].
To prove that postural control therapies for children with CP are helpful, more research with stronger designs is needed, as per a study by Harris et al. [ 54 ]. The motor learning coaching treatment was found more effective than NDT in terms of functional performance and retention of motor function [ 55 ]. A meta-analysis in 2022 by Velde et al. recommended the de-implementation of NDT in children with CP as interventions for improving motor function based on activities and body structure and function were found more effective than NDT [ 56 ]. A single-blinded randomized controlled study involving 18 children with CP showed positive outcomes with the use of modified pilates exercises on control of posture, walking, trunk, and balance as compared to NDT [ 57 ].
Research conducted in 2019 indicated that respiratory exercises with NDT were more beneficial in increasing respiratory function when compared to only conventional NDT in spastic quadriplegic CP children. Thirty children were included in the study and lung volumes were compared to show outcomes [ 58 ]. A systematic review was conducted by Martin et al. in 2010 to identify the common PT ways used in school-aged children with CP and the evidence supporting them was critically reviewed. Strong evidence was found in favor of strengthening the targeted muscle groups, and new data emerged to support functional training. Concerning treadmill training, NDT, and appropriate dosage of PT, further high-level evidence is needed [ 59 ].
A 2009 study tried to look into how modified Adeli suit therapy (MAST) affected the gross motor skills of children with CP; 36 children with CP participated. Intervention was provided to the participants two hours per day for five days per week for four weeks. When it came to helping children with CP improve their gross motor function, the MAST was superior to either the Adeli suit therapy or the NDT [ 60 ]. A paper summarized the effects of various physical interventions used for children with CP. It stressed the need to do more research to analyze the effect of physical interventions on function and disability and not only on impairments [ 61 ]. A study was conducted by Furtado et al. in 2022 to find and evaluate published papers on physical therapy in children and adolescents from Brazil with CP by using the ICF framework. One of the interventions being used was NDT. Among the studies, the components of intervention did not look into participation, and, in the assessed outcomes, only 1.1% related to participation [ 62 ].
In previous studies, numerous parameters were used to indicate improvement with the use of NDT in children with CP. These areas of improvement are summarized in Table 1 .
NDT: neurodevelopmental treatment; CP: cerebral palsy
Conclusions
In our review, 19 studies suggested positive outcomes owing to NDT in children with CP; 22 studies supported the use of NDT in combination with other treatment methods; and 13 studies indicated uncertainty where authors had conflicting views about the use of NDT in children with CP. The review revealed that NDT is widely used for the rehabilitation of children with CP all over the world. The areas of improvement analyzed in the studies on NDT mostly involve gross motor, balance, and postural control. The parameters and outcome measures used in studies investigating the effect of NDT are mostly linked to body structure and function or activities according to the ICF model by WHO. There is a scarcity of published data available on the effect of NDT in terms of the participation component of ICF. There is scope for future research to analyze the effect of NDT in areas of improvement from a participatory perspective and how functional gain by the application of NDT is translated into participation for children with CP. Studies with larger sample sizes and homogenous groups along with a clear elaboration of NDT strategies should be conducted to gain deeper insights into the topic.
The authors have declared that no competing interests exist.
We have a new app!
Take the Access library with you wherever you go—easy access to books, videos, images, podcasts, personalized features, and more.
Download the Access App here: iOS and Android . Learn more here!
- Remote Access
- Save figures into PowerPoint
- Download tables as PDFs

CHAPTER 19: Case Study: Cerebral Palsy
Donna Cech, PT, DHS, PCS
- Download Chapter PDF
Disclaimer: These citations have been automatically generated based on the information we have and it may not be 100% accurate. Please consult the latest official manual style if you have any questions regarding the format accuracy.
Download citation file:
- Search Book
Jump to a Section
Introduction.
- Examination: Age 6 Years
- Evaluation, Diagnosis, and Prognosis Including Plan of Care
- Intervention
- Termination of Episode of Care
- Examination: Age 13 Years
- Kayla: 20 Years of Age
- Interventions
- Recommended Readings
- Full Chapter
- Supplementary Content
This case study focuses on the physical therapy management of Kayla, a young woman with spastic, diplegic cerebral palsy (CP). Kayla is now 20 years old and a sophomore in college. She was born prematurely and has received physical therapy services in a variety of settings since infancy. She has been followed for early intervention, early childhood, school-based, outpatient, and home health physical therapy services. At this time she does not regularly see a physical therapist, but does continue with occasional sessions to monitor adaptive equipment and to address episodes of foot pain or back pain. Kayla walks in her home/dormitory settings and on campus using bilateral forearm crutches. For longer distances, she uses a motorized cart.
Children and young adults with CP are reportedly less socially and physically active than their peers without a physical disability ( Shikako-Thomas, Majnemer, Law, & Lach, 2008 ; Engel-Yeger, Jarus, Anaby, & Law, 2009 ; Maher, Williams, Olds, & Lane, 2007 ). Individuals with CP frequently present with impairments of range of motion (ROM), soft tissue mobility, strength, coordination, and balance, resulting in motor control difficulties. CP implies damage to the immature cortex, involving the sensorimotor system. Associated problems with vision, seizures, perception, and cognition may be seen if areas of the cortex associated with these functions are also damaged. Although the cortical lesion is nonprogressive, as the infant grows and strives to become more independent, functional limitations become more apparent, as do restrictions in activities and community participation. Secondary impairments in body structures and function, such as ROM limitations, disuse atrophy, and impaired aerobic capacity, may further limit functional motor skills and ability for activities and participation. Multiple episodes of physical therapy management are frequently warranted as the child attempts more complex functional skills and as the risk for secondary impairments increases. The goal of physical therapy intervention for children and young adults with CP is to maximize the individual's ability to participate in age-appropriate activities within the home, school, and community settings.
Children with CP present with a variety of functional abilities, reflecting the location and severity of their original neurological insult. Distribution of motor involvement varies and may include hemiplegia, diplegia, or quadriplegia. The degree to which the neurological insult impacts motor ability and function also varies. The Gross Motor Function Classification System (GMFCS) provides a mechanism to classify these children, based on their gross motor abilities and limitations ( Palisano, Rosenbaum, Bartlett, & Livingston, 2008 ; Palisano et al., 1997 ). Based on Kayla's ability to ambulate with an assistive device and need to use power mobility for community mobility, she would be classified as functioning at the GMFCS level III through elementary and high school.
Pop-up div Successfully Displayed
This div only appears when the trigger link is hovered over. Otherwise it is hidden from view.
Please Wait
- Open supplemental data
- Reference Manager
- Simple TEXT file
People also looked at
Case report article, case report: perspective of a caregiver on functional outcomes following bilateral lateral pectoral nerve cryoneurotomy to treat spasticity in a pediatric patient with cerebral palsy.

- 1 Island Medical Program, University of British Columbia, Victoria, BC, Canada
- 2 Division of Physical Medicine and Rehabilitation, University of British Columbia, Victoria, BC, Canada
- 3 Canadian Advances in Neuro-Orthopedics for Spasticity Congress, Victoria, BC, Canada
Spasticity is common and difficult to manage complication of cerebral palsy that significantly affects the function and quality of life of patients. This case study reports a 15-year-old male with quadriplegic cerebral palsy, Gross Motor Function Classification System 5 (GMFCS 5), who presented with significant bilateral adducted and internally rotated shoulders as a component of generalized spasticity. Spasticity in the lower limb of the patient had been treated with botulinum toxin A (BoNT-A) injections; however, the shoulder region was spared due to concerns of toxin spread and aspiration risk. Following diagnostic nerve blocks, the patient underwent bilateral cryoneurotomies of the right and left lateral pectoral nerves (LPNs) lasting 3.5 min for each lesion. One month after the cryoneurotomies, the range of motion (ROM) had improved from 86° to 133° on the right and 90° to 139° on the left. Improvements in ROM were retained at 9 months post-procedure. At 8.5 months following the cryoneurotomies, the caregiver reported improvements in upper body dressing, upper body washing, transferring, and the ability of the patient to remain sitting in his wheelchair for extended periods. Cryoneurotomy may be an effective procedure for improving shoulder ROM and specific functional outcomes for caregivers of patients with spasticity arising from cerebral palsy.
Introduction
Spasticity is a common and important complication of cerebral palsy that has a significant impact on the quality of life and functional capacity of patients ( 1 ). Targeted management of muscle spasticity is a key aspect of patient care. Various therapeutic options are available for managing spasticity, typically consisting of a combination of pharmacological treatments and surgical or injectable modalities ( 2 ). The use of a mini-invasive percutaneous cryoneurotomy to induce disruption of the axon and myelin is an emerging technique for managing spasticity ( 3 ). There is substantial evidence of the efficacy of cryoanalgesia in the pain literature; however, literature outlining the use of cryoneurotomy for spasticity treatment is limited ( 3 , 4 ). There is no literature available on functional outcomes of cryoneurotomy in the pediatric population ( 3 ). This sentinel case demonstrates quantitative improvements in range of motion (ROM) and qualitative improvements that have been reported from the caregiver of a patient who underwent bilateral pectoral cryoneurotomy to manage spasticity arising from cerebral palsy.
Case Report
This study conforms to all Case Reports (CARE) guidelines and reports the required information accordingly (refer to Supplementary Material 2 ). The parent/caregiver provided informed consent for the publication of this study. A 14-year-old male with quadriplegic cerebral palsy, Gross Motor Function Classification System 5 (GMFCS), presented with problematic bilateral adducted and internally rotated shoulders as a component of generalized spasticity in the upper and lower limbs and cervical spasticity/dystonia. He had been treated with botulinum toxin A (BoNT-A) injections to various arm and leg muscles based on symptomatology. No BoNT-A had been injected into the shoulder girdle due to fears of toxin spread and aspiration risk. He had undergone surgical release of his hip adductors. The patient had repeated admissions to hospital intensive care for recurrent pneumonia and gastrointestinal bleeding with hematemesis, which affected his BoNT-A regimen. He had a generalized seizure disorder. He was referred to the multidisciplinary spasticity clinic for consideration of a novel cryoneurotomy procedure to counteract problematic tone in the upper extremities.
The physical examination revealed a greatly reduced shoulder ROM with abduction passively to 85° on the right and 90° on the left, with no active abduction. His Modified Ashworth Scores (MAS) were four, with a fixed end point. The elbows had minimal spasticity, and the wrists and fingers were held in a fist, but flexible, with contracture noted at the metacarpophalangeal joints. His parent/caregiver reported that the painful shoulder positions greatly affected his daily care needs, such as dressing, bathing, and sitting. Diagnostic anesthetic motor nerve blocks (DNBs) were performed to each of the right and left lateral pectoral nerves (LPNs). The DNB causes temporary nerve conduction cessation to differentiate between the presence of shoulder girdle muscle contracture necessitating surgical release due to musculotendinous retraction (an unsuccessful block) vs. a reducible deformity due to spastic muscle overactivity (a successful block). Under ultrasound guidance, the neurovascular bundles of the LPN were identified using a longitudinal orientation along the chest, four fingerbreadths below the coracoid process. Lidocaine (1.5 ml of 2%) was injected juxtaposed to each of the right and left LPNs at the undersurface of the pectoral major muscle (PMM). After the DNB, there was an improvement in passive ROM in shoulder abduction to 120° bilaterally and a reduction in spasticity on the MAS (refer to Supplementary Material 1 ). There was an observed reduction in facial grimacing and easing of heavy respirations with passive abduction.
The decision was then made to proceed to percutaneous cryoneurotomies of both the LPNs. The procedure was delayed until the medical stability of the patient improved. He was then 15-year old. The procedures were performed 10 days apart in an outpatient interventional suite. An aseptic technique was used with 2% chlorhexidine and betadine. The ultrasound-guided cryoneurotomy was performed using a Lloyd SL 2000 Neurostat (San Diego, CA, USA) with a 1.2-mm cryoprobe at −60°C placed through a #16 angio guide. E-stimulation was performed to confirm nerve contact at 0.8 mV. The ice ball was repositioned to contact the LPN at two spots along the nerve. Each lesion was treated for 3.5 min. Hemostasis was achieved using skin glue and a plaster bandage. There were no surgical complications with the procedure or complications reported by the caregiver following the procedure.
Quantitative Results
One month after the bilateral cryoneurotomies, the ROM in abduction had improved from 86 to 133° on the right and 90 to 139° on the left ( Figure 1 and Supplementary Material 1 ). The MAS was reduced to two. He was next seen for follow-up at 9 months. The improvement in ROM noted a gain on the right to 146° and a reduction to 125° left ( Figure 1 and Supplementary Material 1 ). The reduction in tone was to MAS 1+ within the available ROM.
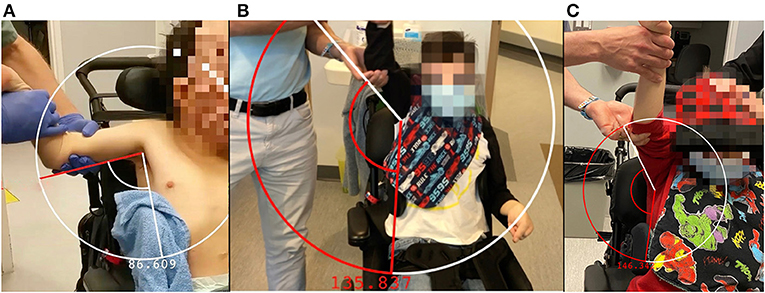
Figure 1 . Abduction and arm position of the right arm prior to cryoneurotomy (A) , at 1 month following cryoneurotomy (B) and 9 months following cryoneurotomy (C) .
Qualitative Results
For this assessment, the Care and Comfort Caregiver Questionnaire (CareQ) was used. The CareQ is an assessment tool that has been adapted from the Caregiver Questionnaire (CQ), a questionnaire created in 1990 to assess children with spastic quadriplegic cerebral palsy prior to and following selective posterior rhizotomy ( 5 , 6 ). In creating the CareQ, the CQ was modified to emphasize caregiver experience and goal setting for the child ( 5 ). The CareQ focuses on three functional areas, namely, personal care, position/transfers, and comfort ( 5 ). Functional outcomes are compared in these three areas prior to and following the procedure in a retrospective manner ( Table 1 ). The caregiver of the patient was administered the CareQ over the phone following the procedure for 8.5 months. The patient is dependent on the caregiver to undertake all personal care tasks outlined in the questionnaire. At 8.5 months following the cryoneurotomies, there was an improvement in putting on shirts, taking off shirts, and washing the upper body of the patient. There was an improvement in the ability of the patient to remain sitting in a wheelchair for 3 h, the ease of transferring the patient into and out of the wheelchair, and the ease of applying orthotics. There were improvements in comfort levels during position changes while sitting in his wheelchair and while participating in school programs and physiotherapy.
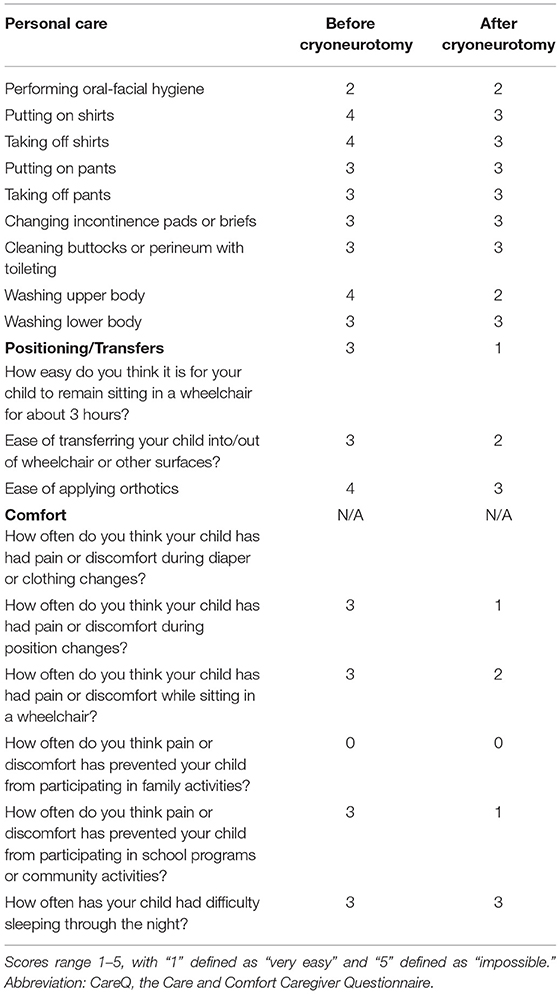
Table 1 . Results of CareQ were completed by the caregiver of a 15-year-old patient with cryoneurotomy who underwent bilateral pectoral cryoneurotomy.
Spasticity arising from cerebral palsy is challenging to treat, and clinical approaches to management vary due to a lack of strong evidence to inform pharmacological therapy regimens ( 7 ). The field of spasticity management for patients with cerebral palsy may be amenable to novel therapies that have a clinical benefit. Traditional approaches to spasticity management consist of pharmacologic, surgical or neurolytic, and injectable options, such as botulinum toxin ( 2 , 7 – 12 ). Pharmacological regimens may consist of diazepam, baclofen, or trihexyphenidyl ( 7 – 12 ). Cryoneurotomy percutaneously induces selective neurolysis of a motor nerve to manage spasticity, similar to other injectable and surgical modalities, such as partial neurotomy and chemodenervation by alcohol or phenol ( 2 , 3 ). In cryoneurotomy, the axons and myelin of peripheral nerves are disrupted by the tip of the cryoprobe which may reach −70°; however, the epineurium is maintained allowing for nerve regeneration ( 3 , 4 , 13 ). Cryoneurotomy carries less risk of damage to surrounding tissue than phenol or alcohol chemodenervation ( 3 ). This procedure has been shown to have a clinically significant impact on spasticity reduction, even in cases refractory to other therapeutic strategies ( 3 ). Cryoneurotomy for the flexed elbow spasticity was shown to maintain the improved ROM and reduced MAS at a mean follow-up interval of 12.5 months in 11 patients including maintenance in the longest follow at over 2 years ( 14 ).
The LPN is the dominant innervation to the pectoralis major muscle (PMM). Anatomical studies have demonstrated that the LPN was found to have a highly consistent course after leaving the lateral trunk of the brachial plexus alongside the blood vessels on the undersurface of the pectoralis major in 100 consecutive patients ( 15 , 16 ). The PMM is the largest muscle implicated in shoulder adduction and internal rotation ( 17 ). The LPN was shown to innervate both heads of the pectoralis major, ( 15 ) while the lower portion of the PMM has innervation from the medial pectoral and also from intercostal nerves ( 17 ). In contrast, the medial pectoral nerve is also thought to have a far less consistent course and is harder to consistently target ( 16 , 17 ). It has been shown to dive below the pectoralis minor before rising along with the pectoralis major ( 18 ). The consistency of the LPN renders it the more easily identifiable nerve with ultrasound, a target for cryoneurotomy, and less deep and further away from the chest cavity ( Figure 2 ) ( 18 ).
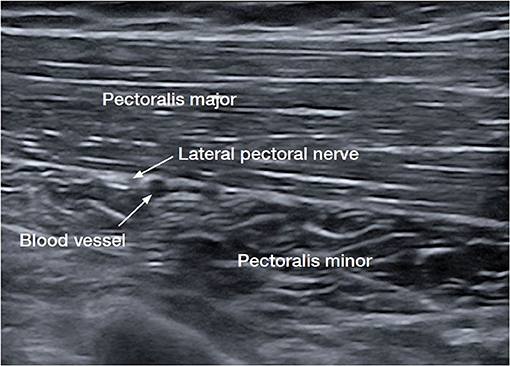
Figure 2 . Ultrasound image of the lateral pectoral nerve (LPN), the dominant nerve of the pectoralis major muscle (PMM) ( 15 , 16 ).
The passive abduction of the patient improved by an average of 55% within 6 weeks. At 9 months, the right nerve continued to show improvements in ROM. The left side reduced in ROM but maintained a 30° improvement compared to the measurement prior to the cryoneurotomy. The MAS remained reduced at 9 months with much greater ease in passive ROM of the shoulder. This is consistent with findings of cryoneurotomy for flexed elbow spasticity ( 14 ) and the tibial nerve ( 3 ).
In a non-verbal patient, discussion with the caregiver is necessary to identify goals and expectations. The frequent hospitalizations of this young patient for infection, respiratory compromise, seizures, and gastrointestinal bleeding made it challenging to attend the routine 3-month intervals for botulinum toxin, hence a longer-lasting procedure was the desired option. Due to the comorbidities of the patient, surgical interventions that carry a risk of toxin spread and respiratory compromise, such as BoNT-A injections, were avoided.
This case demonstrates the impact that the emerging therapeutic procedure cryoneurotomy has on the LPN to reduce spasticity in a GMFCS 5 patient. Outcomes of cryoneurotomy were measured not only through improvement in spasticity and ROM but also through functional outcomes reported by the caregiver of the patient. Targeted cryoneurotomy to address spasticity in specific muscles may improve ROM and functionality in a variety of tasks, such as dressing, hygiene, transferring, and physiotherapy programs. Given the lack of standardized management in treating spasticity, there is a benefit to exploring novel procedures that may be efficacious in many patients, including those who are resistant to more traditional therapeutic options. Further research is necessary to determine how cryoneurotomy fits into the current practice of spasticity management.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author Contributions
PW provided the case study and patient care. JS provided the patient interview and outcome measures.
Conflict of Interest
PW has funding for a clinical trial in adults with spasticity for cryoneurotomy, provided by Abbvie Allergan and Pacira.
The remaining author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fresc.2021.719054/full#supplementary-material
Supplementary Material 1. (Multimedia) Demonstration of diagnostic nerve block on the lateral pectoral nerve (LPN) under ultrasound imaging followed by a demonstration of shoulder range of motion (ROM) prior to cryoneurotomy, at 1 month following cryoneurotomy, and 9 months following cryoneurotomy.
Supplementary Material 2. CARE checklist.
1. Delgado M, Tilton A, Río J, Dursun N, Bonikowski M, Aydin R, et al. Efficacy and safety of abobotulinumtoxinA for upper limb spasticity in children with cerebral palsy: a randomized repeat-treatment study. DMCN. (2020) 63:592–600. doi: 10.1111/dmcn.14733
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Karri J, MAS M, Francisco G, Li S. Practice patterns for spasticity management with phenol neurolysis. J Rehabil Med. (2017) 49:482–8. doi: 10.2340/16501977-2239
3. Winston P, Mills PB, Reebye R, Vincent D. Cryoneurotomy as a percutaneous mini-invasive therapy for the treatment of the spastic limb: case presentation, review of the literature, and proposed approach for use. ARRCT. (2019) 2:100078. doi: 10.1016/j.arrct.2019.100030
4. Weber G, Saad K, Awad M, Wong T. Case report of cryoneurolysis for the treatment of refractory intercostobrachial neuralgia with posthterpetic neuralgia. Local Reg Anesth. (2019) 12:103–5. doi: 10.2147/LRA.S223961
5. Hwang M, Kuroda M, Tann B, Gaebler-Spira D. Measuring care and comfort in children with cerebral palsy: the care and comfort caregiver questionnaire. PM R . (2011) 3:912–9. doi: 10.1016/j.pmrj.2011.05.017
6. Schneider J, Gurucharri L, Gutierrez A, Gaebler-Spira D. Health-related quality of life and functional outcome measures for children with cerebral palsy. DMCN . (2001) 43:601–8. doi: 10.1017/S0012162201001098
7. Lumsden D, Crowe B, Basu A, Amin S, Devlin A, DeAlwis Y, et al. Pharmacological management of abnormal tone and movement in cerebral palsy. Arch Dis Child. (2019) 104:775–80. doi: 10.1136/archdischild-2018-316309
8. Mathew A, Mathew M, Thomas M, Antonisamy B. The efficacy of diazepam in enhancing motor function in children with spastic cerebral palsy. J Trop Pediatr. (2015) 51:109–13. doi: 10.1093/tropej/fmh095
9. Gooch J, Patton C. Combining botulinum toxin and phenol to manage spasticity in children. Arch Phys Med Rehabil. (2004) 85:1121–4. doi: 10.1016/j.apmr.2003.09.032
10. Botte M, Keenan M. Percutaneous phenol blocks of the pectoralis major muscle to treat spastic deformities. J Hand Surg. (1988) 13A:147–9. doi: 10.1016/0363-5023(88)90220-1
11. Teasell R, Foley N, Pereira S, Sequeira K, Miller T. Evidence to practice: botulinum toxin in the treatment of spasticity post stroke. Topics Stroke Rehabil. (2012) 19:115–2. doi: 10.1310/tsr1902-115
12. Pin T, McCartney L, Lewis J, Waugh M. Use of intrathecal baclofen therapy in ambulant children and adolescents with spasticity and dystonia of cerebral origin: a systematic review. DMCN. (2011) 53:885–95. doi: 10.1111/j.1469-8749.2011.03992.x
13. Trescot A. Cryoanalgesia in interventional pain management. Pain Phys. (2003) 6:345–60. doi: 10.36076/ppj.2003/6/345
CrossRef Full Text | Google Scholar
14. Rubenstein J, Harvey AW, Vincent D, Winston P. Cryoneurotomy to reduce spasticity and improve range of motion in spastic flexed elbow: a visual vignette. Am J Phys Med Rehabil. (2021) 100:e65. doi: 10.1097/PHM.0000000000001624
15. Beheiry EE. Innervation of the pectoralis major muscle: anatomical study. Ann Plast Surg. (2012) 68:209–14. doi: 10.1097/SAP.0b013e318212f3d9
16. Hoffman GW, Elliott LF. The anatomy of the pectoral nerves and its significance to the general and plastic surgeon. Ann Surg. (1987) 205:504–7 doi: 10.1097/00000658-198705000-00008
17. Haładaj R, Wysiadecki G, Clarke E, Polguj M, Topol M. Anatomical variations of the pectoralis major muscle: notes on their impact on pectoral nerve innervation patterns and discussion on their clinical relevance. Biomed Res. (2019) 2019:13–5. doi: 10.1155/2019/6212039
18. Chang K-V, Lin C-P, Lin C-S, Wu W-T, Karmakar MK, Özçakar L. Sonographic tracking of trunk nerves: essential for ultrasound-guided pain management and research. J Pain Res. (2017) 10:79–88. doi: 10.2147/JPR.S123828
Keywords: cryoneurotomy, spasticity, cerebral palsy, caregiver perspective, pediatrics
Citation: Scobie J and Winston P (2021) Case Report: Perspective of a Caregiver on Functional Outcomes Following Bilateral Lateral Pectoral Nerve Cryoneurotomy to Treat Spasticity in a Pediatric Patient With Cerebral Palsy. Front. Rehabilit. Sci. 2:719054. doi: 10.3389/fresc.2021.719054
Received: 02 July 2021; Accepted: 09 August 2021; Published: 06 September 2021.
Reviewed by:
Copyright © 2021 Scobie and Winston. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Paul Winston, paul.winston@viha.ca ; orcid.org/0000-0002-8403-6988
† These authors have contributed equally to this work
This article is part of the Research Topic
Emerging Concepts and Evidence in Novel Approaches for Spasticity Management
- Research article
- Open access
- Published: 08 December 2017
Caring for a cerebral palsy child: a caregivers perspective at the University Teaching Hospital, Zambia
- Brian Chanda Chiluba 1 &
- Geoffrey Moyo 1
BMC Research Notes volume 10 , Article number: 724 ( 2017 ) Cite this article
6958 Accesses
22 Citations
1 Altmetric
Metrics details
Cerebral palsy is a major cause of disability and most survivors are left with residual disability and are dependent on parents/caregivers for essential care. This study aimed to determine the experiences of parents/caregivers of cerebral palsy children receiving out-patient physiotherapy. A concurrent mixed methods was used to collect data in the present study. The modified caregiver strain index (MCSI-13) was used to detect Disturbed sleep, Inconvenient/Tiresome, Physical strain, Confining, Family changes, Changes in personal plan, Other demands, Emotional adjustments, Upsetting behavior, Patient has changed, Work adjustments, Financial Strain and Feeling Overwhelmed (strain morbidity) in 25 parents/caregivers of CP children. A purposive sample of 25 parents/caregivers was selected for both the quantitative part and qualitative part of the study. The study was conducted at Community Based Intervention Association Out-patients at the University Teaching Hospital in Lusaka, Zambia. The MCSI was used to collect quantitative data and in-depth interviews provided the qualitative data.
The median age of the participants was 33.6 years and a range of 27 to 50 years. The study sample consisted of more females (92%) than males (8%). being overwhelmed and inconvenient/tiresome followed by family adjustments and work adjustment 72 and 68% respectively for each were the experiences mostly highlighted by the parents/caregivers in this study. When it came to the needs of the parents/caregivers more than half of them needed help with caring. To this effect participants expressed their perception; one mother had this to say, “…I need someone to help in caring. Sometimes I need to do some other things but can’t, because if I do then no one will remain with the child…”.
This study point out to some evidence that the burden inflicted on those caring for children with cerebral palsy should be addressed if the quality of care for those with cerebral palsy is to be improved.
Parents/caregivers of children with Cerebral Palsy (CP) often shoulder the principal multifaceted responsibilities of long-term CP and disability care. CP is one such developmental disorder that begins in early childhood as a set of functional limitations that stem from disorders of the developing central nervous system [ 1 ]. It is estimated that worldwide up to 9.3% of youths under the age of 18 have a condition that can be classified as neurodevelopmental such as CP, epilepsy and developmental delay. The current estimated incidence of CP is 2–3 per 1000 live births in developed countries. However, it is difficult to establish the incidence of cerebral palsy in most developing countries because CP is not captured in the population census or any other surveys in most developing countries, though the incidence is higher in males than in females [ 1 , 2 ].
In India 4 million people are affected by CP annually [ 1 ]. Parents/caregivers of CP children play a central role in the lives of these children and therefore their own well-being is inextricably linked to that of the children. Two major social trends make the consideration of parents/caregivers health particularly relevant. Firstly, there has been a decided shift towards Community Based Rehabilitation (CBR) of children with disabilities. In addition to maximizing opportunities for social inclusion, Community Based Rehabilitation recognizes parents/caregivers as partners in the provision of care. Secondly, in some developed nations the principles of family-centered care have been embedded in health policy and embraced by health and social services agencies providing services to children with disabilities and their families. Parents/caregivers are considered instrumental partners in health policy by influencing the nature and direction of the care their child receives. These trends place greater emphasis on parent/caregiver voice and involvement, and also represent extraordinary parental responsibility [ 2 ]. Evidence is mounting regarding the extent to which parents/caregivers of children with neurodevelopmental disorders experience elevated levels of physical and psychological distress [ 3 ].
Culturally, in an African perspective and Zambia included, it is expected that a relative will take up the responsibilities of care-giving for the person with a disability or cerebral palsy. The parent/caregivers frequently accept or are expected to assume their role without regard for the possible emotional, physical, and financial consequences [ 4 ]. As cerebral palsy is a sudden event, parents/caregivers of CP children are forced to accept a large amount of unforeseen responsibilities in the absence of preparation. In addition to this, the care-giving role has various other implications for the parents/caregivers. These includes future plans being shattered, present income generating activities being abandoned, a decrease in leisure time and susceptibility to a deteriorating health status [ 5 , 6 , 7 ]. In the process of care-giving, the abilities of the parents/caregivers to provide for their own emotional, personal, physical, social and financial needs are seriously compromised [ 8 , 9 ]. According to Bakas [ 10 ] needs of parents/caregivers includes general information about the warning signs for cerebral palsy, lifestyle changes for the child with CP, and the management of cerebral palsy related symptoms and complications. To date we know of no study in Zambia that has focused on the impact of caring for children with CP, though a similar study with focus on short-term care of a child with Malaria (The Disability Burden of Malaria in Lusaka urban) was conducted by Chalwe et al., [ 11 ] at The University Teaching Hospital (UTH). Thus, the purpose of the present study was to examine the challenges, needs and experiences that parents/caregivers of children with CP face. CP was chosen as a prototype condition to ascertain the needs and challenges of parents/caregivers of children with disabilities.
Study design
The study was mixed methods using a concurrent parallel approach. The quantitative part utilised a non-intervention, cross-sectional descriptive study design with a questionnaire containing closed items. The qualitative part utilised a phenomenological approach with open ended items, these methods that were employed in the study attempted to gain a broader understanding of the caregivers’ perspective when caring for a child with CP. The objective of this research was to parallel a quantitative and a qualitative bus transit research study and to analyze the results in terms of integrating the two methods by use of triangulation.
This study was carried out at the UTH, Department of Paediatrics, Community Based Intervention Association (CBIA) formerly known as Action for Disability and Development (ADD). The employees of the Department includes; Physiotherapists, Speech Therapists, administrators and other support staff. The center was instituted to rehabilitate children with disabilities the most common being CP and other related conditions. UTH is located in the capital in Lusaka and it is the biggest referral hospital in the Zambia offering health services at tertiary level. The hospital occupies approximately eight hectares of land spread over one and a half kilometres.
Study population, sampling and sample selection technique
The study population constituted parents/caregivers of CP children, receiving treatment at the UTH/(CBIA). Though a bigger sample size would have been attained from this study, however, due to limited time in which to carry on a research as prescribed by the academic calendar in which to carry out an academic research by the University, only a smaller sample size was realised for the study in order to carry out the study within the required time. Therefore, a purposive sample of 25 participants was picked from the population of the study for the quantitative study and 5 participants were picked for a qualitative study. The qualitative sample helped in complementing the inefficiencies in inferences for a small quantitative sample by gaining a broader perspective of the phenomenon under study.
Data collection tools
An interview questionnaire was adapted by the researcher from validated questions from literature to gather social demographic information of parents/caregivers. The modified caregiver strain index (MCSI) was used which is an already validated tool that is used to measure strain. The MCSI is an ordinal scale, used to identify families with potential care-giving strain. It is a 13-question tool that measures strain related to care provision in providing various degrees of care to patients at home. Each item is answered with a “yes”, or “no” responses. Scoring is accomplished through adding all affirmative responses to arrive at a total score; thus, a higher score, 7 or higher than 7 positive responses (yes responses) implies a high level of burden [ 12 ]. There is at least one item for each of the following major domains: Employment, Financial, Physical, Social and Time. According to Blake [ 13 ] internal consistency reliability is high (alpha = 0.86) and construct validity is supported by correlations with the physical and emotional health of the caregiver and with subjective views of the care-giving situation. The Rehabilitation and Support Questionnaire addresses the caregiver’s perception of rehabilitation and support through five questions. The questions concern the parents’/caregivers’ perceived importance of physiotherapy resulting in different options and the need of support workers for children with cerebral palsy in the community. Other questions address the parents’/caregiver’s rating of rehabilitation, support, information and attention they receive when their child with cerebral palsy is receiving care from the physiotherapists. Even though the above tools have already been validated as they have been used in research, they were subjected to a pilot study for validation before this study.
An eight-item questionnaire was developed from literature specifically for data collection from open-ended items. It contained eight open-ended questions on the needs and experiences of caregivers. To ensure that the interviews were credible and trustworthy, the researcher recorded the interviews verbatim and took field notes. The researcher also ensured that the respondents understood the questions very well. If they were not sure, the questions were repeated and the researcher listened carefully and took field notes.
Data management and data analysis
For quantitative data analysis, the variables that were used in graphs and charts were as follows; Gender, age, marital status, occupation, education level of the parents, responses to questionnaire included; Gender either male or female, age response ranged from 15 to 90 years, marital status response included single, marriage, divorced and widowed, educational level included secondary and tertiary level and on occupation the following were the responses expected, employed, unemployed and self-employed.
Owing to a small sample size, however, it could be difficult to carry out statistical tests in quantitative research to establish association among variables due to that data may not be normally distributed to allow for parametric tests. Therefore, in order to deal with a smaller sample size in this research with regard to skewed data. Log transformation was done for right skewed data and square transformation was done for left skewed data [ 14 ]. This was so in order to assume normality because of skewed data as a result of a small sample and to allow for parametric tests like the ANOVA for association among variables.
The Statistical Package for Social Science (SPSS) version 16 was used to analyze quantitative data relating the results to the contents of the qualitative results. SPSS is a statistical and data management package that can perform a wide variety of statistical procedures including transformation, distribution of data, description, compare groups with significant differences using parametric [ 15 ]. Significance level was set at 5%, while descriptive and inferential statistics were employed in analysing data from the closed-ended questionnaire. The results were presented as tables, pie charts and graphs from Microsoft excel. The confidence interval of the difference was at 95%. Data collected using interviews was recorded on a tape recorder. In analyzing qualitative data the researcher transcribed the results that were recorded. Some participants were quoted verbatim. The information was then organized into main themes. Themes for qualitative analysis included; need for support services, work overload, need for community cantered programmes, need for finances, views on physiotherapy rehabilitation services, and need for respite care. Tenets of narrative analysis were used to construct a narrative account of parents’/caregiver’s needs and experiences.
In order to ensure that there was credibility in the quality of the qualitative information data triangulation was done, triangulation was done through multiple analysts and ‘member checks’. And to ensure confirmability codes were categorized according to similar contents and then developed into broader themes. The categories were interpreted in order to determine the real meaning of the text. At the end of the analysis the themes were cross-checked with the interview transcripts to check the validity of the data.
Demographic characteristics of respondents
A total of 25 respondents participated in the study of which 8% (n = 2) were males and 92% (n = 23) were females. The median age of respondents was 33.56 with ages ranging from 27 to 50 years.
Effects and relationships of the demographic variables on the MSCI-13 scores
In order to understand the results of the MSCI scores, it was imperative that factors that could have contributed to the levels of strain other than the perception of the impact of caring for children with cerebral palsy be ascertained.
Effects of age of respondents on the MSCI scores
The mean MSCI scores of those aged 27–33 years were 7.55 (SD = 3.78), 44–50 years, 7.20 (SD = 2.05). A one-way ANOVA was done to the data and the results showed that the main effect of the age of the respondents was found to be unreliable, F = 0.043, p > 0.05. It can be inferred that the age of the respondents did not affect the levels of strain scored on the MSCI.
Effects of gender of the parent/caregiver on the MSCI scores
Parents/caregivers who were male and taking care of a cerebral palsy child had a mean MSCI score of 10.5 (SD = 0.71), while those who were female had 7.22 (SD = 3.30). When a one-way ANOVA was done on the data, the main effects of gender were not found to be significant, F = 1.897, p > 0.05. It can thus be concluded that the levels of strain was unrelated to the gender of the caregiver of cerebral palsy.
Effects of relationship of parent/caregiver with the child on the MSCI scores
The mean MSCI score of parent was 7.60 (SD = 2.72) others, Elder sister/brother 6.25 (SD = 5.189), Friend/neighbor 8.0 (SD = 3.69). However, when a one-way ANOVA was done on the data, the main effects of the relationship with a child with cerebral palsy was found not to be significant, F = 0344, p > 0.05. It can be concluded that the relationship of parent/caregiver with child was unrelated to levels of strain.
Effects of marital status on the MSCI scores
The mean MSCI scores with regards to marital status is as follows the highest mean score represented those who were married and the lowest score was for the divorced. When a one-way ANOVA was done on the data, the main effects were unreliable suggesting that the effects of status did not affect the levels of psychological distress F = 0.12, p > 0.05.
Effects of employment status on the MSCI scores
The mean MSCI scores of those formally employed were 7.0 (SD = 2.8), those unemployed, 8.0 (SD = 3.98) and self-employed, 7.33 (SD = 3.98). A one-way ANOVA was done on the data and the results showed that the main effect of employment status on the MSCI scores was found not to be reliable, F = 0.211, p > 0.05. It can be concluded that the employment status had no influence on the levels of strain.
Effects of educational level on the MSCI scores
The parents/caregivers had more or less similar MSCI scores. The mean score of those who never went to school as far as Grade 7 was 9.0, those who reached GRADE 9 level 5.0 (SD = 2.65) those that reached up to Grade 12 had 8.25 (SD = 2.12) and those that went to the university/college 7.46 (SD = 3.97). The one-way ANOVA was done showed that the main effect of educational level on the MSCI scores was not found to be significant, F = 0.761, p > 0.05. It can be inferred that the educational level did not affect the levels of strain scored on the MSCI.
Qualitative analysis
To have deeper understanding and meaning of the qualitative results, data was obtained, processed by coding and analysis then presented in a verbatim form under appropriate themes; this followed a classical approach, employing Malterud’s ‘Systematic text condensation’, a descriptive and explorative method for thematic cross-case analysis drawing upon Giorgi’s psychological phenomenological analysis.
Need for respite care
More than half of the caregivers needed help with caring. They expressed a need for someone to stand in for them to have a chance to do other duties.
“…I require a person to help me so that I am not alone helping the sick person….” (Male caregiver: mother)
“…I need someone to help in caring. Sometimes I need to do some other things but can’t, because if I do then no one will remain with the child…” (Female caregiver:mother)
“…The other help I need is for someone to help me in dressing her, bathing her…it is a very big task to bath her and it takes all my time….” (Female caregiver:mother)
All the interviewed caregivers, but one, were not able to find respite care by employing someone whenever they wanted to go and attend to other matters. One caregiver was able to get respite care by delegation of duties to other members of the family.
“…My husband and I have decided to continue with our normal activities. What we have done is delegate duties to everyone at home…” (Female caregiver:mother)
“…I have someone who does come to be with the child when I need to go out like shopping and sometimes I have to go and see my sick mother. I do pay her. In fact my sister in law helps me to pay the girl….” (Female caregiver:mother)
Need for home based care and community support workers
A significantly high percentage of the parents/caregivers (76.0%) responded positively to the importance of having community support workers. Only 20.0% considered it as important and 4.0% perceived it as less important.
Parents/caregivers complained that bringing the patient to the hospital was a very tough thing to do physically and financially. They, for this reason, emphasized that they needed to have community health workers conducting treatment sessions in their homes.
“…We need community health workers to do visits in our homes than us coming here, because it is very costly….” (Mother)
“…If physiotherapists could come to homes it would be better….” (Female caregiver:mother)
“…Help is needed especially if the physiotherapists can be coming to our home to treat the child with their equipment such as the rollers, the wedges, the toys and things to make our children stand on…. ” ( female caregiver:mother)
“… What would be nice for us who wake up very early in the morning is to just wait at home and say that the physiotherapists are coming to help….” (Female caregiver:mother)
Yet another caregiver observed and demanded;
“….We need more physiotherapists at clinics to manage the treatment of the children than always go to UTH….”
The desire of one caregiver was expressed in this way;
“….We need teachers of disabled children also. We want our children also to be educated, be independent and improve their lives….”
One caregiver expressed concern and disappointment on the government’s failure to provide assistance to the welfare of the cerebral palsy children and she said;
“….The government must start caring for these children, it is their responsibility to help us take care of their needs. They must help us, it is hard to provide for such a child…”
Yet another caregiver expressed the following about government’s assistance to the children;
“….Why can’t the government bring more health workers here at CBIA clinic who are specialized in disabled children? It would……. be easier for us to bring our children nearer here for review at UTH than go to clinics all the time, it is far and expensive. The clinical officers here just give the child panadol when she is sick…”
Physiotherapy intervention satisfaction
The qualitative data revealed positive and negative responses from the patients in regard to satisfaction with physiotherapy services. The responses related to physiotherapy treatment sessions, type of treatment and involvement of caregivers and the results are also related to the findings on quantitative. Which revealed the following 60% (n = 15) of the caregivers were very satisfied (excellent) and those that were moderately satisfied (good) with the rehabilitation services offered to them were36% (n = 9) and those that responded that it was inadequate were 4% (n = 1).
“…There are so many weaknesses at the physio department, equipment is not enough and our children are attended to very late. There is an ‘I don’t care’ attitude towards clients…” (Female caregiver:mother)
“…There are many children here at physiotherapy department but only few physiotherapists. Children are not given enough attention…“( Female caregiver:sister)
“…Physios do very little at sessions because they are few…” (Female caregiver:mother)
“…I don’t see what is done to the child because they never pay attention to me…” (Female caregiver:mother)
“…I have a problem with my child being seen by different physiotherapists every week. One says this and the next week another one says something else. I need one physiotherapist to be seeing the patient all the time because inconsistency confuses me…” (Female caregiver:mother)
“…Exercises only are done but there is no encouragement… ” (Female caregiver:mother)
The positive responses provided by the caregivers regarding physiotherapy were only related to the improvement of the child’s functional status.
“…Physiotherapy has brought a drastic improvement where the Childs’ functional ability is concerned. People should be informed about what physiotherapy can do….” (Female caregiver:mother)
“…I am happy that the physios are doing a great job. The child couldn’t sit but now can. Considering her age we thought she would never sit. Am thanking the physios for making her sit…” (Female caregiver:mother)
“…But since she started coming here (physiotherapy department) I have seen that she has improved…” (Female caregiver:mother)
The study found that the median age of parents/caregivers was relatively lower (33.6 years; range 27 to 50 compared to 58.1, 56 and 58 median years found in other studies [ 16 , 17 , 18 ]. In some cases the median ages were higher; 65, 73, 75 and 80 years [ 19 , 20 , 21 , 22 ].
The results of this study reflected a dominant young age group being involved in cerebral palsy care-giving much less than any other age group in studies reviewed, however the findings in this study is very supportive of the Zambia’s scenario in accordance with the study by Eustis [ 15 ] who said that due to the issues of life expectancy dropping in Zambia in the past years, it is therefore expected that the care-giving role will be assumed mostly by the youths. This involvement has strong implications for young caregivers as they are in the productive age group in society but also issues of HIV and AIDS bring in already a lot of burden. According to Brehaut [ 23 ] parents and health-care providers need to pay attention to the effects of care-giving on selected areas of young peoples’ lives—particularly school and family life. They found that those who were of dating age, either did not date, or dated early to “get out of the home”. Concern has been mounting about the health and welfare of people who provide informal care for family or friends with cerebral palsy children. It is assumed that young and elderly people, who are vulnerable groups in their own right, may be carrying a particularly heavy burden [ 24 ].
The dominance of the younger age group assuming the responsibilities of caring for cerebral palsy patients may also be attributed to the age pattern in the country’s population, which has a dominantly higher middle-age group [ 25 ].
The MCSI [ 26 ] was used to measure the levels of strain and impact on the parents/caregivers. The results from this present study showed that the degree of strain as ascertained by the MSCI-13 was quite high in the caregivers who took part in this study with a p < 0.05. The results showed that the majority of the caregivers representing 64% had scores indicative of strain of a long-standing nature while only 36% had scores in the threshold of strain.
Further analysis of the MSCI-13 in the subscales detecting physical strain, financial strain, tiresome/inconveniencing and family changes showed significant and reliable differences with p < 0.05 (results not shown). On further discussion with parents/caregivers they further reviewed that they had stopped going for social functions such as kitchen parties or other social gathering because of social stigma. They further stated that sometimes they turned down the invitation because they were not comfortable leaving the child in the hands of someone they thought would not offer the care as they would. The interpretation is that the impact was translated into social, mental, medical and economic burden for the parent/caregiver.
The results of the present study were in agreement with the study done by Kaona and Tuba [ 27 ] which showed high psychiatric morbidity in parent/caregivers. The studies demonstrated that caring for a disabled child with CP had a negative impact on the parent/caregiver. Both the parent/caregiver needed support in the caring and upbringing of the child.
However, though the parents/caregivers were not admitting that the problem was there, when in actual fact the problem existed, was a source of concern. The study pointed to the fact that parents/caregivers were suppressing their emotions. The possible explanation to this situation could be attributed to traditional or cultural beliefs just as the current study indicates 92% of women, not admitting that the problem was there. Their responses were further confirmed from the answers the women were giving stating that the child was a gift from God. The suppression of the burden of care was demonstrated on the score on the MCSI subscales of physical strain. The results showed that all the women had signs of strain. The majority respondents had scores indicative of strain of long-standing.
Follow up tests on the effects of demographic variables on the MCSI Questionnaire was done by use of Multiple Regression Equations and the results showed that none of the independent variables was a predictor of the MSCI scores (results not shown). The results of the study demonstrated that despite females indicating the difficulties they encountered in the care of the child, they did not take it as a burden. The explanation from the females was that because the child was their own they had accepted the child as the gift from God. The females accepted the child in his or her state and enjoyed carrying out the duties despite the difficulties. For example, the mothers pointed out that they had difficulties in feeding but enjoyed the task because if the child ate enough then the child was okay and made them feel satisfied about their care of the child.
One mother/caregiver said;
“She eats very slowly especially solid foods, and it means that I stop whatever I am doing to ensure that she feeds adequately. Other family members have little patience and sometimes do not manage to feed her…….. I do it myself to ensure she is okay……..I enjoy it though.”
The results of the present study are in support of what has been noted to be a pointer to some more serious problems which female caregivers could be facing especially in most African countries [ 28 ]. Most researchers suggest that social factors determine the increase of minor psychiatric morbidity in women caring for children [ 29 ]. This study shows that additional care tasks widen further the difference between the sexes in psychiatric morbidity whether caring for a child with disabilities or not. Caring for a child with cerebral palsy has greater impact on the mental health of mothers.
Mothers of children with disabilities resulting from CP may assume more roles than mothers of non-disabled children. Hastings [ 30 ] further suggested that parents of children with special needs may have to assume unusual roles, such as developmental interventionalist and liaison among multiple health care workers and family members. The additional roles are not only time consuming, but also may be counterproductive because conflict may occur between the role of a parents and that of a teacher or therapist. However, Grant [ 31 ] found in an ethnographic study that parents of children with cerebral palsy did not have time, energy or confidence to carry out home programmes recommended by therapists.
Birth and early childhood rearing can have an adverse effect on maternal mental health even when there is no disability in the child [ 32 , 33 ]. It is therefore imperative that adequate methods are used to isolate the impact of child care giving and other family commitments which are prone to affecting maternal mental health.
The study raise important concerns in regard to inadequate research done in the area of CP caregiving. The study highlights the difficulties and amount of input needed to address cerebral palsy parents/caregivers’ experiences and needs. Physiotherapists working in communities and health institutions are intricately involved in CP habilitation and rehabilitation and should be attentive and supportive to the parents/caregivers. One of the greatest limitations of this study are the smaller sample size in the quantitative component, though to a smaller part it was complemented by the qualitative part.
Abbreviations
cerebral palsy
University Teaching Hospital
statistical package for social scientists
World Health Organisation
UNICEF Report: At a glance: Zambia. http://www.unicef.org/infobycountry/zambia_2004statistics.html . Accessed on 25 July 2003.
SCPE Collaborative Group. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol. 2000;42:816–24.
Google Scholar
Cheshire A, Barlow JH, Powell LA. The psychosocial well-being of parents of children with cerebral palsy: a comparison study. Disabil Rehabil. 2010;32:1673–7.
Article PubMed Google Scholar
DeLaune M, Brown SC. Spousal responses to role changes following a stroke. Med Surg Nurs. 2001;10(2):79–88.
Becher JG. Pediatric rehabilitation in children with cerebral palsy: general management, classification of motor disorders. J Prosthet Orthot. 2002;14:143–9.
Article Google Scholar
Dowswell G, Lawler J, Dowswell T, Young J, Forster A, Hearn J. A qualitative study of specialist nurse support for stroke patients and caregivers at home. Clin Rehabil. 2006;11:293–301.
Cieza A, Stucki G. Content comparison of health-related quality of life (HRQOL) instruments based on the international classification of functioning, disability and health (ICF). Qual Life Res. 2005;14:1225–37.
Eker L, Tüzün EH. An evaluation of quality of life of mothers of children with cerebral palsy. Disabil Rehabil. 2004;26:1354–9.
World Health Organization Technical Report. Community Based Rehabilitation and the health care referral services. 2006.
Bakas T, Clarkson JE, Dittmer Flett R, Linsell C. Needs, concerns, strategies and advice of stroke caregivers the first 6 months after discharge. J Neurosci Nurs. 2008;34(5):242–9.
Chalwe M, Mweshi M, Mwango M. Short term care for a child with malaria: research study University Teaching Hospital, Lusaka, Zambia. 2008.
Fritz V. Cerebral palsy and stroke. Contin Med Educ. 2007;16(10):958–9.
Blake WJ, Hadker H. Outcome assessments in children with cerebral palsy part I: descriptive characteristics of GMFCS levels I to III. Dev Med Child Neurol. 2000;49:172–80.
Chiluba B, Nkandu EM, Daka CN, Chola M, Chongwe G. Cardiovascular disease risk from protease inhibitors-ART for HIV: retrospective Cohort of University Teaching Hospital Zambia. Cardiol Cardiovasc Res. 2017;1(4):98–103.
Eustis NN, Fischer LR. Common needs, different solutions? Younger and older homecare clients. Generations. 1992;18(1):17–22.
Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: caregiver perspectives. Child Care Health Dev. 2007;33:180–7.
Article CAS PubMed Google Scholar
Parkes J, McCullough N, Madden A, McCahey E. The health of children with cerebral palsy and stress in their parents. J Adv Nurs. 2009;65:2311–23.
Van den Heuval ETP, de Witte LP, Schure LM, Sanderman R, Meyboom-de Jong B. Risk factors for burn-out in caregivers of cerebral palsy patients, and possibilities for intervention. Clin Rehabil. 2007;15:669–77.
Anderson CS, Linto J, Stewart-Wynne L. A population-based assessment of the impact and burden of care giving for long-term cerebral palsy survivors. Stroke. 2005;26:843–9.
Mobarak R, Khan NZ, Munir S, Zaman SS, Mcconachie H. Predictors of stress in mothers of children with cerebral palsy in Bangladesh. J Pediatr Psychol. 2000;25:427–33.
De Laure M, Brown N. Quality of life for families with cerebral palsy in Kenya. Trop Doct. 2007;38:160–2.
Wyller F, Gerter W. Health of young and elderly informal carers: analysis of UK census data. Br Med J. 2003;327(7428):1388–2001.
Brehaut JC, Kohen DE, Garner RE, Miller AR, Lach LM, Klassen AF, et al. Health among caregivers of children with health problems: findings from a Canadian population-based study. Am J Public Health. 2009;99:1254–62.
Article PubMed PubMed Central Google Scholar
Metzing-Blau S, Schnepp W. Young carers in Germany: to live on as normal as possible—a grounded theory study. BMC Nurs. 2008;7:15.
Doran T, Drever F, Whitehead M, Duncan WH. A population-based assessment of the impact and burden of caring for long term cerebral palsy survivors. Stroke. 2003;26(5):843–9.
Kaona FAD, Tuba MA. Qualitative study to identify community structures for management of severe malaria: a basis for introducing rectal artesunate in the under 5 years children in Nakonde District of Zambia. Malar J. 2005;2:43.
Polisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39:214–23.
Boyd RN, Hays RM. Current evidence for the use of botulinum toxin type A in the management of children with cerebral palsy: a systematic review. Eur J Neurol 2001;8(Suppl. 5):1–20.
Hastings RP. Parental stress and behaviour problems of children with developmental disability. J Intellect Dev Disabil. 2002;27:149–60.
Grant JS, Bartolucci A, Elliott TR, Giger JN. Sociodemographic, physical, and psychosocial characteristics of depressed and non-depressed family caregivers of stroke survivors. Brain Inj. 2000;14:1089–100.
Romans-Clason SE, Clarkson JE, Dittmer, Flett R, Linsell C, Mullen P, Mullin. Impact of a Handicapped child on mental health of parents. Br Med J. 1986;293:1395.
Lambrenos R, Weindling AM, Calam R, Cox AD. The Effects of a child’s disability on mother’s mental health. Arch Dis Child. 1996;74:115–20.
Article CAS PubMed PubMed Central Google Scholar
Download references
Authors’ contributions
BC and GM conceived of the study and took part in writing the protocol. BC extracted data, did statistical analyses, and interpreted data. The manuscript was written by BC with significant contributions from GM. All authors made substantial contributions to overall conception and design, drafting the article, or revising it critically for important intellectual content, gave their final approval of the version to be published, and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Both authors read and approved the final manuscript.
Acknowledgements
The authors wish to thank the Department of Physiotherapy at the University of Zambia in the School of Health Sciences for their contribution and guidance and also the parents and caregivers for their valuable time. Thanks also to Theresa Lesa Chisoso for her input and editing of the work.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Data sets may be available upon request from the corresponding author.
Consent to publish
Not applicable.
Ethics approval and consent to participate
Participants consented to participate in the study and approval for the study was obtained from University of Zambia Biomedical Research Ethics Committee (Reference number 012-01-12).
This study was an academic undertaking and it was self-funded.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and affiliations.
Department of Physiotherapy, School of Health Sciences, The University of Zambia, Lusaka, Zambia
Brian Chanda Chiluba & Geoffrey Moyo
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Brian Chanda Chiluba .
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Chiluba, B.C., Moyo, G. Caring for a cerebral palsy child: a caregivers perspective at the University Teaching Hospital, Zambia. BMC Res Notes 10 , 724 (2017). https://doi.org/10.1186/s13104-017-3011-0
Download citation
Received : 03 December 2015
Accepted : 28 November 2017
Published : 08 December 2017
DOI : https://doi.org/10.1186/s13104-017-3011-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Experiences
- Parent/caregivers
- Cerebral palsy
- Modified caregiver strain index (MCSI)
BMC Research Notes
ISSN: 1756-0500
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Original Research Article
- Open access
- Published: 16 December 2021
Sensory systems processing in children with spastic cerebral palsy: a pilot study
- Mennatallah Khamis AbdelHafiez Barakat ORCID: orcid.org/0000-0003-2010-1100 1 ,
- Gehan Hassan Elmeniawy 1 &
- Faten Hassan Abdelazeim 1
Bulletin of Faculty of Physical Therapy volume 26 , Article number: 27 ( 2021 ) Cite this article
4337 Accesses
2 Citations
Metrics details
The study of the sensory aspect alongside the motor aspect in children with spastic cerebral palsy is critical. Knowledge may help improve intervention, children’s quality of life, activity, and participation.
The study aims to analyze the sensory systems processing in children with spastic cerebral palsy classified by Gross Motor Function Classification System (GMFCS) as levels I, II, and III using Child Sensory Profile 2 (CSP-2). Caregivers of children with spastic cerebral palsy aged 6–9 years ( n = 20) completed the CSP-2. Children with severe comorbidities besides cerebral palsy (i.e., diabetes, myopathy, neuropathy, and uncontrolled epilepsy), autism, burn injuries, hearing or vision loss were excluded.
All twenty participating children showed sensory processing difficulties in at least one of the sensory sections. With 14 out of 20 showing abnormalities in more than one section, the majority showed problems in the body position section, followed by the movement section. There was a significant difference between raw scores means of children with unilateral and bilateral SCP at the “body position” section, unlike the rest of the other sections.
Conclusions
Children with spastic cerebral palsy (GMFCS levels I, II, and III) show sensory systems processing difficulties compared to normative data, especially at vestibular and proprioceptive processing.
Cerebral palsy (CP) is a neurodevelopmental disorder that affects muscle tone, movement, and motor skills. Clinical signs are persistent and non-progressive, resulting from a lesion to the developing brain in the prenatal, perinatal, or early postnatal period [ 1 , 2 ].
Spastic cerebral palsy (SCP) is the most common type of CP, composing up to 70% to 80% of cases [ 3 ]. SCP may be bilateral or unilateral [ 4 ].
Motor abnormalities are frequently accompanied by sensory, perceptual, cognitive, communication, and behavior disturbances, as well as epilepsy and secondary musculoskeletal problems [ 5 ]. Therefore, the management of children with CP depends on a multidisciplinary, comprehensive, and coordinated approach and goals are the child’s independence and being engaged in the community [ 3 ].
Sensory processing is the processing of sensory information from the environment and the body itself by neural systems, comprising the functions of receptor organs and the peripheral and central nervous systems. To understand experiences and organize responses, the brain organizes, integrates, synthesizes, and uses this information. Individuals can respond to sensory stimuli in an automatic, efficient, and comfortable manner thanks to information processing [ 6 ].
The term sensory processing disorder (SPD) is used by the Sensory Processing Disorder Foundation to define a condition in which a person’s daily activities are limited by how he or she processes and responds to sensory information [ 7 ]. SPD is characterized by hypo- or hyper-sensitivities to sensory inputs that cause noteworthy obstruction to everyday activities. Essentially, SPD represents a failure to modulate the effects of incoming sensory inputs; this raises the issue of whether the integration of inputs across sensory systems is functioning appropriately in this population. The principal function of the multisensory integration system is to combine the signals that enter the brain through the different sensory epithelia so that the many forms of energy produced by the same object or event will be treated as a single entity. It helps to simplify the world and leads to significant behavioral efficiency gains [ 8 ].
The literature shows a connection between processing challenges and sensory integration and performance of activities of daily living (ADLs) such as sleeping, dressing, eating, playing, and taking part in leisure and school-related activities [ 9 ]. According to Brown and Dunn, “areas of concern emerge only when a person’s sensory processing pattern seems incompatible with his or her desired or necessary life activity choices” [ 7 ]. Motor system development and motor planning partially rely on sensory input which offers feedback and guides motor function so that potential motor errors can be avoided [ 10 ].
Although sensory-based disorders as impaired tactile, proprioceptive, kinesthetic, and pain perception are not commonly thought of as a primary feature of CP, they occur frequently in this population and remain an under-studied and under-addressed area [ 10 , 11 , 12 ]. Further studies are recommended to evaluate sensory processing in children with CP. This exploration remains a vast and promising field of research to be pursued [ 12 ]. Most studies addressing sensory processing in children with CP use sophisticated neuroimaging equipment, which is not widely available in clinical settings. Using clinical measures to assess sensory processing in children with CP is still not common [ 13 ].
The Sensory Integration and Praxis Test (SIPT) is regarded as the “gold standard” test for detecting sensory discrimination and sensorimotor abnormalities [ 6 ]. However, it does not measure sensory modulation [ 14 ]. Sensory modulation is typically measured by the Sensory Profile (which has two versions) and the Sensory Processing Measure [ 6 , 14 ].
Sensory profile 2 (SP2) is a standardized test. The advantages of SP2 are that it is simple to use, quick to administer, is evidence, theory, and strength based. SP2 is family and child centered and also contextually relevant. It provides a comprehensive method to capture the child’s responses to sensory experiences in natural settings. It measures current performance and can be reused to measure differences across time and intervention. Additionally, it addresses familiar activities and behaviors to caregivers and helps them be more engaged in assessment and the discussion of the treatment plan [ 15 ].
The SP2 has some disadvantages. For starters, it relies on a caregiver’s ability to report on their child’s functioning, which may lead to responder bias. There may also be inconsistencies between the responses of the caregiver and the observations of the therapist. Moreover, despite its ability to detect the presence of modulation problems, it is unable to thoroughly determine the presence of sensory discrimination problems [ 16 ]. Furthermore, the SP2 is yet to be validated in the Egyptian population. Finally, it has not been translated into Arabic.
Knowledge about a person’s patterns of sensory processing may contribute to the design of more effective interventions and the advancement of knowledge. When people have a vision about the reasons behind challenging situations, they can generalize the information to other circumstances and make better judgments and choices that make life easier [ 17 ].
This area of knowledge is also supposed to generate more research questions aiming for a wider look at disabled children’s needs and how to deal with them.
Therefore, this study aims to analyze sensory systems processing in children with SCP (GMFCS levels I, II, and III), using Child Sensory Profile 2 (CSP-2).
Study design
A prospective cross-sectional study design has been performed. The study agreed with the STROBE statement [ 18 ]. The study was approved by the Ethical Committee under the code (P.T.REC/012/003055).
Participants and procedures
Twenty SCP children were recruited from several rehabilitation centers specialized in children’s care. In order to recruit the sample, rehabilitation centers were contacted about the purpose of the study and the targeted criteria for children to participate. Meetings were set with caregivers to explain the study rationale and explain how to fill the CSP-2 questionnaires. Those who agreed to participate and met the inclusion criteria signed informed consent before taking place in the study. All questions by participating caregivers were answered before, during, and after filling the questionnaires. Results were verbally conducted to caregivers, and suggestions on how to deal with children accordingly were provided. The recruitment and assessment took place between February 2021 and June 2021.
This study was narrowed down to focus on SCP. According to previous studies [ 19 , 20 ], the better the gross motor capabilities are, the finer the sensory processing capacities. Therefore, we concentrated on children with higher gross motor abilities of Gross Motor Function Classification System (GMFCS) levels I, II, and III so that we may assume that their sensory experiences are less limited by their motor abilities.
We included children of both sexes, aged between 6 and 9 years, and whose caregivers are of a good command of the English language.
We excluded (1) children with severe comorbidities besides CP (i.e., diabetes, myopathy, neuropathy, and uncontrolled epilepsy), burn injuries, hearing or vision loss; to reduce factors that may compromise their sensory experiences. (2) Children with autism; since autism has been—supported by several studies—associated with SPD.
Variables and data measurements
The primary variable in this study was the reported sensory system section, measured by CSP-2. CSP-2 lies under the umbrella of SP2. The Sensory Profile 2 is the newest version of the Sensory Profile developed by Winnie Dunn; it is a set of standardized caregiver questionnaires consisting of the Infant SP2 (birth-to-6 months), Toddler SP2 (7-to-35 months), Child SP2 (3-to-15 years old), and Short SP2 (3-to-15 years old). In addition to School companion SP2, which is a teacher questionnaire for students aged from 3 to 14 years old [ 15 ].
The parent/caregiver complete the SP2 questionnaire according to the frequency of the child’s responses to various sensory experiences using a five-point scale (1 = almost always, 2 = frequently, 3 = half of the time, 4 = occasionally, 5 = almost never, or 0 = does not apply). Does not apply should be used exceptionally when the question is not relevant to the child, or when the parent/caregiver has never observed the behavior. The advantages of SP2 are that it is simple to use and quick to administer and interpret. Furthermore, there are no double negatives in the SP2, which makes it easier to read than the SP. CSP-2 is an 86-item caregiver questionnaire that covers a wide age range from 3:00 to 14:11 years old [ 15 ].
Dunn developed a Normal Curve and SP2 Classification System based on responses from a normative sample of children without disabilities. Based on a bell curve normed distribution, the raw score total for each quadrant can be classified as “much less than others,” “less than others,” “just like the majority of others,” “more than others,” and “much more than others” [ 21 ].
Figure 1 shows the normal curve and the SP2 classification system provided by Dunn [ 15 ].
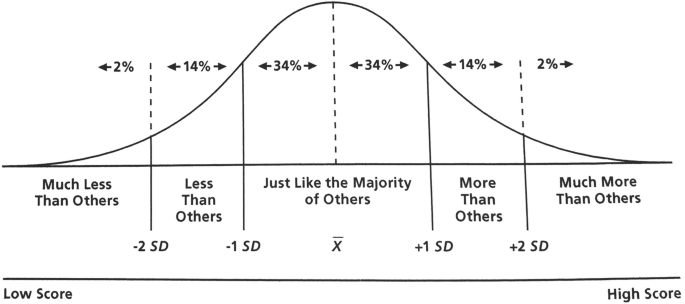
The normal curve and the sensory profile 2 classification system (Dunn 2014)
The items of CSP-2 come in three groups which are sensory processing patterns (i.e., the quadrants), sensory systems, and behavior associated with sensory processing. Sensory System Scores (Sensory Sections) subsets include Auditory Processing: which measures the person’s response to things heard; Visual Processing: which measures the person’s response to things seen; Touch (Somatosensory) Processing: which measures the person’s response to stimuli that touch the skin; Movement (Vestibular) Processing: which measures the person’s response to movement; Body Position (Proprioceptive) Processing: which measures the person’s response to changes in joint and muscle positions; and Oral Sensory Processing: which measures the person’s response to touch and taste in the mouth [ 15 ].
The test-retest reliability is good to excellent. Most of the inter-rater reliability coefficients were acceptable to good. The coefficients in the visual and touch processing areas were lower. The validity correlations between the SP and SP2 were moderate to high [ 15 , 16 ]. Sensory Profile 2 shows good construct validity [ 22 ].
Statistical methods
Descriptive results were generated by calculating the means and standard deviation. The results were compared to the normative data provided by the work of Dunn in the SP2 user’s manual [ 15 ].
Characteristics of the sample (demographic data)
A total of 20 children with a mean age of 7.25 (SD ± 1.019545823) participated in this study.
The majority of the sample (65% of the sample) were in the younger group ( n = 13) and the minority (35% of the sample) were in the older group ( n = 7).
75% of the participants were male ( n = 15) and 25% were female ( n = 5)
Classification of participants
Twenty-five percent of participants were classified as unilateral SCP, and 75% were classified as bilateral.
Twenty-five percent of participants were classified according to GMFCS as level I, 35% were classified as level II, and 40% were classified as level I.
Table 1 shows the distribution of the children with SCP according to SCP subtypes, gender, and the GMFCS levels.
Distribution of all children with SCP according to their response to sensory systems
Table 2 shows the percentage distribution for the six sensory system sections. The highest percentage of participants scoring in the collective “More Group” was found in the “Body Position” section (95%), with “much more” representing the majority by 70%; followed by the “Movement” section (65%) with “More than” representing the majority by 40%.
The participants mostly scored “just like” in the other four sections as follows: “Oral sensory” and “Visual” by 80%, “Auditory” by 70%, and “Touch” by 60%. No participants scored in any section as “Less than” or “Much Less than.”
There was no single participant found to score out of the norm in all six sections. Thirty percent of the participants faced sensory system difficulties in only one section, while 35% of them faced sensory system difficulties in 2 to 3 sections, and 35% faced difficulties in 4 to 5 sections.
Sensory processing in the sensory systems in both types of SCP
Figure 2 shows a box plot chart that was made using raw scores to form a visual representation of all data collected from all participants in all sensory systems sections; it shows that the data set has a symmetrical distribution since the mean and the median are close together. Touch has the most variable data for it has the highest range.
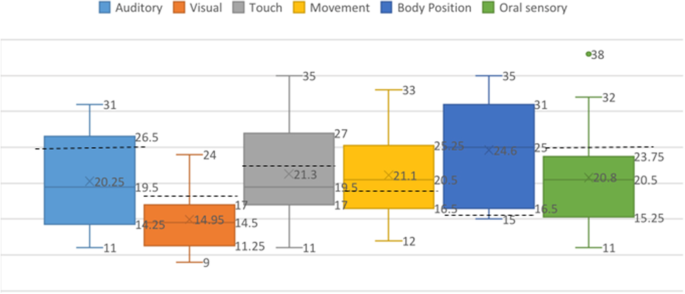
Box plot showing sensory processing in the sensory systems in children with SCP
Means of auditory (20.25), visual (14.95), touch (20.3), and oral sensory (20.8) are below the dashed line which refers to the line between “just like” and “more than” which means that they tend to be within normal range. While means of movement (21.1) and body position (24.6) lie above the dashed line, which means they fall out of the normal range.
Sensory processing in each of the six sections of sensory systems in both types of SCP (unilateral and bilateral)
Figure 3 shows the box plots of the auditory processing section. Bilateral SCP has a longer box which means more dispersed data. The mean of both types are very similar (20.2) and they both lie under the dashed line which means they both tend to fall within the normal range and score as “just like.”
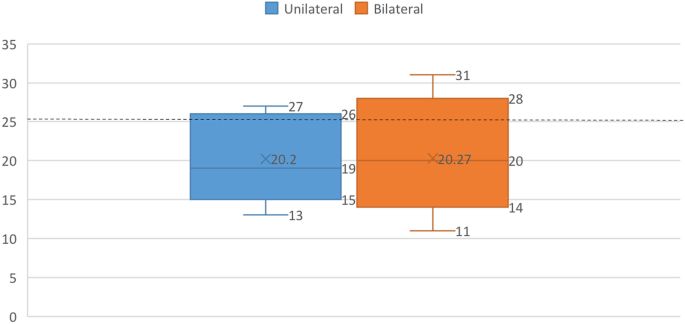
Box plots of the auditory processing section in children with unilateral and bilateral SCP
Figure 4 shows the box plots of the visual processing section. The means of both types are very similar (15) for unilateral and (14.93) for bilateral. They both lie under the dashed line, which means they both tend to fall within the normal range and score as “just like.”
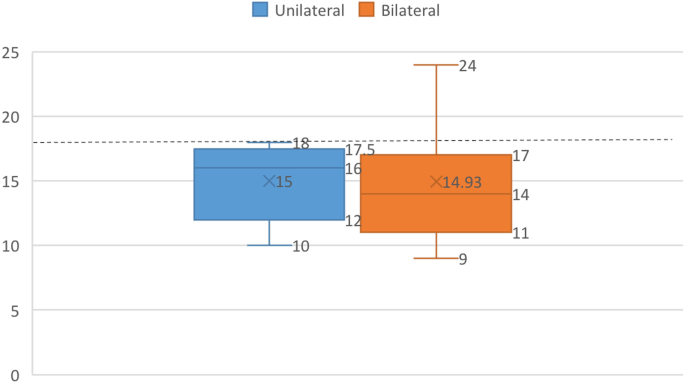
Box plots of the visual processing section in children with unilateral and bilateral SCP
Figure 5 shows the box plots of the touch processing section. The means of both types are similar (20.6) for unilateral and (21.53) for bilateral. They both lie under the dashed line which means they both tend to fall within the normal range and score as “just like”; however, bilateral mean lies so close to the dashed line; therefore, it lies on edge.
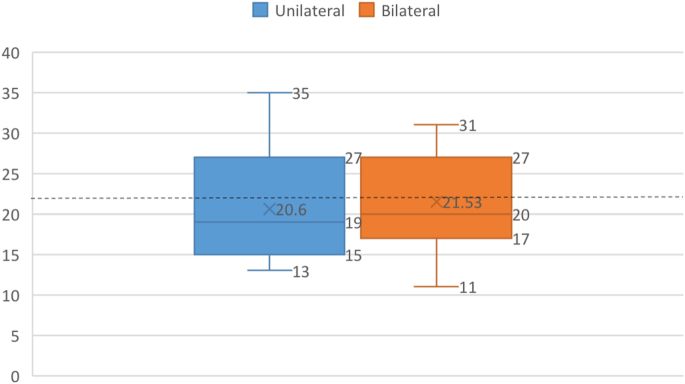
Box plots of the touch processing section in children with unilateral and bilateral SCP
Figure 6 shows the box plots of movement processing results. The means of both types are very similar (21.2) for unilateral and (21.07) for bilateral. They both lie above the dashed line, which means they both tend to fall outside the normal range.
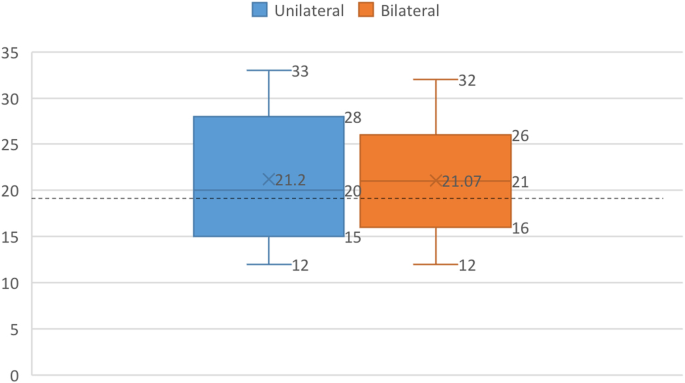
Box plots of the movement processing section in children with unilateral and bilateral SCP
Figure 7 shows the box plots of the body position processing section. The mean of unilateral is (19.2) which is far from the median; the median of the unilateral lies outside the bilateral box which indicates the presence of a significant difference between the two groups. As for the bilateral mean (26.4), it is similar to the median. They both lie above the dashed line, which means they both fall outside the normal range.
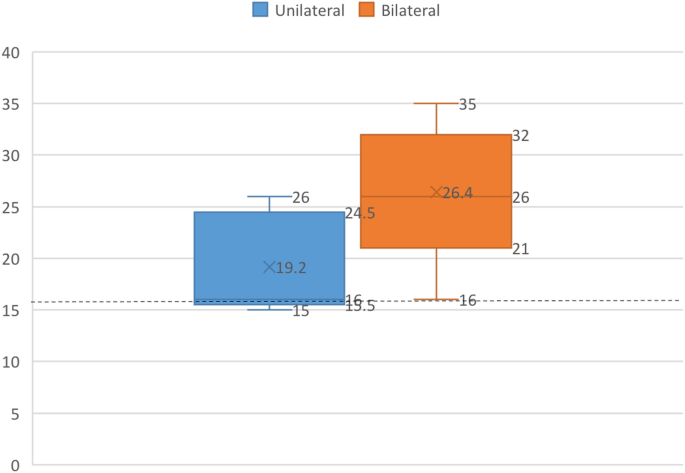
Box plots of body position processing in children with unilateral and bilateral SCP
Figure 8 shows the box plots of the oral sensory processing section. The mean of both types is similar (20.4) for unilateral and (20.93) for bilateral. They both lie under the dashed line which means they both tend to fall within the normal range and score as “just like.”
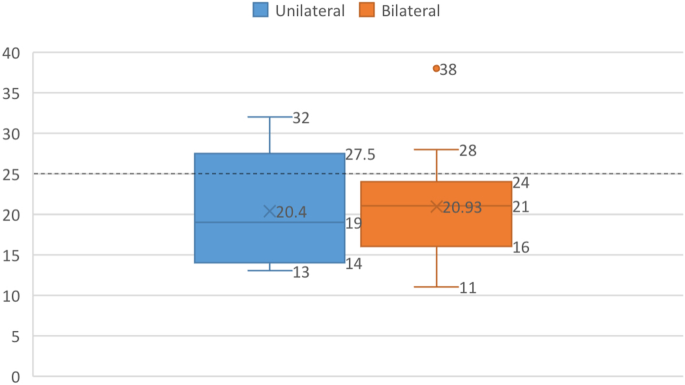
Box plots of the oral sensory processing section in children with unilateral and bilateral SCP
Comparison between sensory sections mean scores in children with unilateral and bilateral SCP
Table 3 represents a summary comparison between mean scores of children with unilateral and bilateral SCP. The means of all sections were very similar except for the “body position” section, where unilateral was nearer to the “just like” range, which is from 5 to 15 of the raw score.
Distribution of children of each group ( Unilateral and Bilateral SCP) in the sensory systems
Table 4 shows the distribution of children of each group (unilateral and bilateral SCP) in the sensory systems.
In children with unilateral SCP
The majority scored as “just like” in auditory by 60%, visual by 80%, touch by 80%, and oral sensory by 80%; while in movement and body position, they scored in the collective more group by 60% and 80% respectively.
In children with bilateral SCP
The majority scored as “just like” in auditory by 73.33%, visual by 80%, touch by 53.33%, and oral sensory by 80%; while in movement, they scored in the collective more group by 66.67%. All participants with bilateral SCP scored in the collective more group.
This study aims to investigate the processing of sensory systems in children with SCP (GMFCS levels I, II, and III) using CSP-2.
Sensory-based disorders were found to frequently occur in those children [ 23 , 24 ]. However, the study of sensory processing and integration in this population is promising [ 12 , 25 ].
Our results showed that children with SCP face processing difficulties regarding sensory systems. The majority of SCP children present greater problems with body position (proprioceptive) and movement (vestibular) processing than other sensory systems compared to the normative data provided by Dunn; which matches the results of previous studies done on more types of CP [ 16 , 26 ] or a wider range of GMFCS levels [ 25 ].
Vestibular processing and proprioceptive processing deficits may be a reason for balance impairment in addition to poor muscle control, which magnifies the problem [ 16 , 27 ]. The reason might be due to diminished thalamo-cortical projections from the thalamus to S1, which causes defects to somatosensory processing in CP patients [ 10 ].
Touch processing came in third place for 40% of children presented with difficulties in touch processing. Tactile processing issues vary dramatically among cerebral palsy subtypes, according to research [ 26 ]. According to Pavaõ [ 25 ], tactile processing may also be due to structural deficits.
Thirty percent of the children showed auditory processing difficulties. There was no difference between children with unilateral and bilateral SCP groups in the mean scores, and both fell in the “just like” zone. These results partially confirm some previous studies [ 16 , 20 , 25 ] while not confirming at all to others [ 26 ], but we must put into consideration that there are noticeable differences in the inclusion criteria.
It was also revealed that they struggle the least with oral sensory and visual information, although some difficulties were present.
By comparing raw scores of children with unilateral and bilateral SCP, it was found that the only section that showed a significant difference between the two categories is “body position” (proprioceptive). This shows that children with bilateral SCP convey proprioceptive processing problems more than children with unilateral SCP. Proprioceptive problems in the unilateral population may be due to uneven experiences they are exposed to from crawling through to walking [ 16 ].
Unlike what we have found, previous research found that oral sensory processing was significant in children with unilateral SCP [ 20 ]. The difference may be due to the small sample size of the current preliminary study or the difference in population culturally or geographically.
The presence of more visual processing difficulties in children with unilateral SCP has been reported in a previous study [ 16 ], while another study reported similar results to this study [ 20 ].
This study was limited by:
Small sample size
Being confined to caregivers who are of a good command of the English language, which was hard and time-consuming to recruit in a population where Arabic is the mother tongue.
According to our findings, children with SCP levels I, II, and III on GMFCS show processing difficulties concerning sensory systems compared to normative data. The main difficulties manifested are concerning body position (proprioceptive) and movement (vestibular). Knowing this valuable information allows us a better understanding of their sensory experiences and their processing struggles that might affect the way they deal with their environment, and consequently enables therapists and caregivers to actively participate in improving their treatment plans and how to deal with them more efficiently.
Availability of data and materials
Data will be shared on specific request to the corresponding author depending upon the nature and purpose of the requirement.
Abbreviations
Activities of daily living
- Cerebral palsy
Child Sensory Profile 2
Gross Motor Function Classification System
Sensory processing disorder
Sensory Profile
- Sensory Profile 2
The Sensory Integration and Praxis Test
Bartels EM, Korbo L, Harrison AP. Novel insights into cerebral palsy. J Muscle Res Cell Motil. 2020;41(2):265–7 Available from: https://doi.org/10.1007/s10974-020-09577-4 .
Article Google Scholar
Van Eyk CL, Corbett MA, Gardner A, Van Bon BW, Broadbent JL, Harper K, et al. Analysis of 182 cerebral palsy transcriptomes points to dysregulation of trophic signalling pathways and overlap with autism. Transl Psychiatry. 2018;8(1):1–10 Available from: https://doi.org/10.1038/s41398-018-0136-4 .
Ozkan Y. Child’s quality of life and mother’s burden in spastic cerebral palsy: a topographical classification perspective. J Int Med Res. 2018;46(8):3131–7. https://doi.org/10.1177/0300060518772758 .
Article PubMed PubMed Central Google Scholar
Cans C. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol. 2000;42(12):816–24.
Patel DR, Neelakantan M, Pandher K, Merrick J. Cerebral palsy in children: a clinical overview. Transl Pediatr. 2020;9(1):S125–35. https://doi.org/10.21037/tp.2020.01.01 .
Jorquera-Cabrera S, Romero-Ayuso D, Rodriguez-Gil G, Triviño-Juárez JM. Assessment of sensory processing characteristics in children between 3 and 11 Years Old: a systematic review. Front Pediatr. 2017;5:57. https://doi.org/10.3389/fped.2017.00057 . Erratum in: Front Pediatr. 2017;5:266
Metz AE, Boling D, DeVore A, Holladay H, Liao JF, Vlutch KV. Dunn's model of sensory processing: an investigation of the axes of the four-quadrant model in healthy adults. Brain Sci. 2019;9(2):35. https://doi.org/10.3390/brainsci9020035 .
Foxe JJ, Del Bene VA, Ross LA, Ridgway EM, Francisco AA, Molholm S. Multisensory audiovisual processing in children with a sensory processing disorder (II): speech integration under noisy environmental conditions. Front Integr Neurosci. 2020;14(July):1–8.
Google Scholar
Schaaf RC, Dumont RL, Arbesman M, May-Benson TA. Efficacy of occupational therapy using ayres sensory integration®: a systematic review. Am J Occup Ther. 2018;72(1):7201190010p1-7201190010p10. https://doi.org/10.5014/ajot.2018.028431 .
Papadelis C, Ahtam B, Nazarova M, Nimec D, Snyder B, Grant PE, et al. Cortical somatosensory reorganization in children with spastic cerebral palsy: A multimodal neuroimaging study. Front Hum Neurosci. 2014;8(September):1–15.
Newell A, Cherry S, Fraser M. Principles of rehabilitation: occupational and physical therapy. In: Orthopedic Care of Patients with Cerebral Palsy; 2020. p. 221–50.
Chapter Google Scholar
Pavaõ SL, Silva FPDS, Savelsbergh GJP, Rocha NACF. Use of sensory information during postural control in children with cerebral palsy: Systematic review. J Mot Behav. 2015;47(4):291–301. https://doi.org/10.1080/00222895.2014.981498 .
Article PubMed Google Scholar
Pavão SL, Lima CRG, Rocha NACF. Association between sensory processing and activity performance in children with cerebral palsy levels I-II on the gross motor function classification system. Brazilian J Phys Ther. 2020;(xx) Available from: https://doi.org/10.1016/j.bjpt.2020.05.007 .
Mulligan S, Douglas S, Armstrong C. Characteristics of idiopathic sensory processing disorder in young children. Front Integr Neurosci. 2021;15(April):1–10.
Dunn W. Sensory profile 2 user’s manual. Bloomington: Pearson; 2014.
Louwrens S. Sensory modulation patterns in children with cerebral palsy : a comaparative-descriptive study: University of Pretoria; 2018. Available from: http://hdl.handle.net/2263/67775 . Accessed 25 Mar 2021.
Dunn W. The sensations of everyday life: Empirical, theoretical, and pragmatic considerations. Am J Occup Ther. 2001;55(6):608–20. https://doi.org/10.5014/ajot.55.6.608 .
Article CAS PubMed Google Scholar
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008 .
Park M-O. The relationship between sensory processing abilities and gross and fine motor capabilities of children with cerebral palsy. J Korean Soc Phys Med. 2017;12(2):67–74. https://doi.org/10.13066/kspm.2017.12.2.67 .
Jovellar-Isiegas P, Collados IR, Jaén-Carrillo D, Roche-Seruendo LE, García CC. Sensory processing, functional performance and quality of life in unilateral cerebral palsy children: a cross-sectional study. Int J Environ Res Public Health. 2020;17(19):1–13.
Simpson K, Adams D, Alston-Knox C, Heussler HS, Keen D. Exploring the sensory profiles of children on the autism spectrum using the short sensory profile-2 (SSP-2). J Autism Dev Disord. 2019;49(5):2069–79 Available from: https://doi.org/10.1007/s10803-019-03889-2 .
Dean E, Dunn W, Little L. Validity of the sensory profile 2: a confirmatory factor analysis. Am J Occup Ther. 2016;70(4_Supplement_1):7011500075p1 Available from: http://ajot.aota.org/article.aspx?doi=10.5014/ajot.2016.70S1-PO7054 .
O’Shea TM. Diagnosis, treatment, and prevention of cerebral palsy in near-term/term infants. Clin Obstet Gynecol. 2008;51(4):816–28 Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/pmc3051278/ .
Bumin G, Kayihan H. Effectiveness of two different sensory-integration programmes for children with spastic diplegic cerebral palsy. Disabil Rehabil. 2001;23(9):394–9. https://doi.org/10.1080/09638280010008843 .
Pavão SL, Adriana N, Ferreira C. Sensory processing disorders in children with cerebral palsy. Infant Behav Dev. 2017;46:1–6 Available from: https://doi.org/10.1016/j.infbeh.2016.10.007 .
Prakash AJA, Vaishampayan A. A preliminary study of the sensory processing abilities of children with cerebral palsy and typical children on the Sensory Profile. Indian J Occup Ther. 2007;XXXIX(2):27–34 Available from: https://www.aiota.org/temp/ijotpdf/ibat07i2p27.pdf .
Tramontano M, Medici A, Iosa M, Chiariotti A, Fusillo G, Manzari L, et al. The effect of vestibular stimulation on motor functions of children with cerebral palsy. Mot Control. 2017;21(3):299–311 Available from: https://doi.org/10.1123/mc.2015-0089 .
Download references
Acknowledgements
The authors want to acknowledge the efforts of the rehabilitation centers and caregivers who co-operated and made this study possible.
This research received no external funding.
Author information
Authors and affiliations.
Department of Physical Therapy for Growth and Development Disorders in Children and Its Surgery, Faculty of Physical Therapy, Cairo University, Giza, Egypt
Mennatallah Khamis AbdelHafiez Barakat, Gehan Hassan Elmeniawy & Faten Hassan Abdelazeim
You can also search for this author in PubMed Google Scholar
Contributions
BM suggested the research idea, helped in data collection, and analyzed and interpreted the data. She is the major contributor in the writing process. EG and AF revised the data analysis, and they were contributors in the writing process. AF was the main supervisor of the work in this study. She contributed in conception of the research idea and design of the work. All authors read and approved the final version of the manuscript.
Corresponding author
Correspondence to Mennatallah Khamis AbdelHafiez Barakat .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the ethics committee of Faculty of physical therapy, Cairo University with approval number [P.T.REC/012/003055]. The caregivers read and signed a written informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Barakat, M.K.A., Elmeniawy, G.H. & Abdelazeim, F.H. Sensory systems processing in children with spastic cerebral palsy: a pilot study. Bull Fac Phys Ther 26 , 27 (2021). https://doi.org/10.1186/s43161-021-00044-w
Download citation
Received : 08 July 2021
Accepted : 24 August 2021
Published : 16 December 2021
DOI : https://doi.org/10.1186/s43161-021-00044-w
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sensory Processing
- Sensory Processing Disorder
(585) 258.3801 | TERMS | FAQS | PARTNERS

- Feeding therapy services
- Occupational therapy services
- Physical Therapy Services
- Speech therapy services
- Consulting services
- Podcasts and Talks
- Training and Workshops
- Testimonials
- Case Studies
Client background:
Tom is a 3 year old boy, born at 28 weeks. He has a diagnosis of evolving dyskinetic Cerebral Palsy, GMFCS V. Tom has a history of seizures.
Pia met Tom while teaching a therapist course about the Key to CP approach. Tom was a demo child, meaning he only spent about an hour with Pia.
Tom was not receiving direct Physical Therapy at home and he did not have any positioning equipment at the time. He was spending his days held by caregivers or on the floor.
Tom’s journey
See how doing the right thing, at the right time, in the right order helped set the stage for Tom to develop play and communication skills during an hour therapy session at Key to CP in this case study, or continue reading below.
Goals before treatment:
Family goals for Tom were to achieve better trunk and head control, to gain strength, and to achieve a level of independence.
It was quickly clear that Tom need support of his trunk in order to improve his head and trunk control for sitting and standing. At Key to CP we often use trunk orthoses to help the child gain upright control. For Tom, a TheraTogs garment was the obvious choice.

As soon as Tom was fitted with TheraTogs there was an immediate improvement in his head and trunk control. He became much more animated and was easily interacting with his parents and with me. He gained a whole new perspective of the world in just the 15 minutes it took to fit him with TheraTogs.

Tom’s parents were surprised to see the changes and they immediately ordered TheraTogs for him. They were also able to try a corner seat and a low table and Tom was happy and interactive.

What does this case teach us? If a child with poor trunk and head control is given the right trunk support, not only does their body control improve, but also their ability to interact with their environment. For Tom, TheraTogs brought his trunk muscles into mid-range alignment (where they are strongest) and the compression gave him sensory input. This tool allowed Tom to better experience his body in relation to his environment.
It also teaches us that when children have to struggle less to maintain body control, they can focus on communication and learning more.
Tom is now able to develop communication and play skills, and he can participate in activities with his family.
And it took less than an hour to bring about this transformation.
Doing the RIGHT thing
Adding TheraTogs and appropriate seating, and most importantly, abundant parent coaching
At the RIGHT time
Giving Tom an opportunity to PARTICIPATE and create positive neuroplastic changes during the first window of abundant brain growth and development
In the RIGHT order
Alignment, Awareness, Activation and Strength
Tom feels much more stable in TheraTogs. We have noticed lately how his head control is coming along and he is really looking up and engaging with everyone, especially his sister. He has been a lot more vocal too. And he is being much more aggressive with telling me he is hungry by sticking his tongue out. He is so content in his new chair that I almost cannot believe it. We feel energized and grateful to have found you. Tom's mother
- Introduction
- Conclusions
- Article Information
CP indicates cerebral palsy; eCP, early diagnosis of CP or high risk of CP; FM, fidgety movement.
The area under the curve was 0.88 (95% CI, 0.79-0.97) for cerebral palsy (A) and 0.62 (95% CI, 0.51-0.73) for cognitive impairment (B).
HINE indicates Hammersmith Infant Neurological Examination.
eTable. Characteristics, Morbidities, and Outcomes of Infants at High Risk of Cerebral Palsy
Data Sharing Statement
See More About
Sign up for emails based on your interests, select your interests.
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Get the latest research based on your areas of interest.
Others also liked.
- Download PDF
- X Facebook More LinkedIn
Razak A , Johnston E , Sackett V, et al. Early Neurodevelopmental Assessments for Predicting Long-Term Outcomes in Infants at High Risk of Cerebral Palsy. JAMA Netw Open. 2024;7(5):e2413550. doi:10.1001/jamanetworkopen.2024.13550
Manage citations:
© 2024
- Permissions
Early Neurodevelopmental Assessments for Predicting Long-Term Outcomes in Infants at High Risk of Cerebral Palsy
- 1 Department of Paediatrics, Monash University, Melbourne, Australia
- 2 Monash Newborn, Monash Children’s Hospital, Melbourne, Australia
- 3 The Ritchie Centre, Hudson Institute of Medical Research, Melbourne, Australia
- 4 Allied Health Department, Monash Children’s Hospital, Melbourne, Australia
- 5 Department of Obstetrics and Gynaecology, Monash University, Melbourne, Australia
- 6 Cerebral Palsy Alliance Research, Brain and Mind Centre, University of Sydney, Sydney, Australia
Question What is the effectiveness of early neurodevelopmental assessments performed at corrected age (CA) 3 to 4 months for estimating cerebral palsy, cognitive impairment, and neurodevelopmental impairments and their severity at CA 24 to 36 months in infants at high risk of adverse neurodevelopmental outcomes?
Findings This diagnostic study including 116 infants born extremely preterm or preterm with extremely low birth weight or born full term with encephalopathy and received therapeutic hypothermia found that early neurodevelopmental assessments were effective in identifying infants with cerebral palsy and predicting its severity. However, the assessments had limited accuracy in identifying cognitive impairment and its severity, as well as in detecting any neurodevelopmental impairment and its severity.
Meaning These findings support the potential to identify cerebral palsy and its severity as early as CA 3 to 4 months through early neurodevelopmental assessments, but the role of these tests is limited in identifying cognitive and neurodevelopmental impairments.
Importance Studies suggest that early neurodevelopmental assessments are beneficial for identifying cerebral palsy, yet their effectiveness in practical scenarios and their ability to detect cognitive impairment are limited.
Objective To assess the effectiveness of early neurodevelopmental assessments in identifying cerebral palsy and cognitive and other neurodevelopmental impairments, including their severity, within a multidisciplinary clinic.
Design, Setting, and Participants This diagnostic study was conducted at Monash Children’s Hospital, Melbourne, Australia. Participants were extremely preterm infants born at less than 28 weeks’ gestation or extremely low birth weight infants less than 1000 g and term encephalopathic infants who received therapeutic hypothermia, attending the early neurodevelopmental clinic between January 2019 and July 2021. Data were analyzed from December 2023 to January 2024.
Exposures Early cerebral palsy or high risk of cerebral palsy, the absence of fidgety movements, and Hammersmith Infant Neurological Examination (HINE) scores at corrected age (CA) 3 to 4 months. Early cerebral palsy or high risk of cerebral palsy diagnosis was based on absent fidgety movements, a low HINE score (<57), and medical neurological examination.
Main Outcome and Measures The outcomes of interest were cerebral palsy, cognitive and neurodevelopmental impairments and their severity, diagnosed at 24 to 36 months’ CA.
Results A total of 116 infants (median [IQR] gestational age, 27 [25-29] weeks; 65 [56%] male) were included. Diagnosis of early cerebral palsy or high risk of cerebral palsy demonstrated a sensitivity of 92% (95% CI, 63%-99%) and specificity of 84% (95% CI, 76%-90%) for predicting cerebral palsy and 100% (95% CI, 59%-100%) sensitivity and 80% (95% CI, 72%-87%) specificity for predicting moderate to severe cerebral palsy. Additionally, the accuracy of diagnosis of early cerebral palsy or high risk of cerebral palsy was 85% (95% CI, 77%-91%) for predicting cerebral palsy and 81% (95% CI, 73%-88%) for predicting moderate to severe cerebral palsy. Similarly, the absence of fidgety movements had an 81% (95% CI, 73%-88%) accuracy in predicting cerebral palsy, and HINE scores exhibited good discriminatory power with an area under the curve of 0.88 (95% CI, 0.79-0.97) for cerebral palsy prediction. However, for cognitive impairment, the predictive accuracy was 44% (95% CI, 35%-54%) for an early cerebral palsy or high risk of cerebral palsy diagnosis and 45% (95% CI, 36%-55%) for the absence of fidgety movements. Similarly, HINE scores showed poor discriminatory power for predicting cognitive impairment, with an area under the curve of 0.62 (95% CI, 0.51-0.73).
Conclusions and Relevance In this diagnostic study of infants at high risk for cerebral palsy or other cognitive or neurodevelopmental impairment, early neurodevelopmental assessments at 3 to 4 months’ CA reliably predicted cerebral palsy and its severity at 24 to 36 months’ CA, signifying its crucial role in facilitating early intervention. However, for cognitive impairment, longer-term assessments are necessary for accurate identification.
Prematurity and hypoxic-ischemic encephalopathy (HIE) represent critical concerns in neonatal health, posing significant risks to the well-being of newborns. Prematurity affects approximately 1 in 10 births globally, 1 whereas HIE affects 1.6 per 1000 live births in high-income countries and 12.1 per 1000 in low- or middle-income countries. 2 Interventions to mitigate the risk of morbidities linked to prematurity and HIE are limited, 3 leaving affected infants at an elevated risk of neurodevelopmental complications that adversely affect motor skills and cognitive abilities. While various neurodevelopmental concerns exist, cognitive impairment and cerebral palsy stand out as primary concerns, affecting approximately 16.9% and 6.9% of very preterm infants, respectively. 4 Early detection of these complications is recommended because prompt identification allows for timely intervention, promoting optimal motor and cognitive development in infants. 5
Several tools for early neurodevelopmental assessments in infants are available, including the Prechtl General Movements Assessment (GMA), Hammersmith Infant Neurological Examination (HINE), and magnetic resonance imaging. While individual tools are valuable, a comprehensive approach involving these neurodevelopmental assessments, medical history, and neuroimaging is strongly recommended for early detection of cerebral palsy. 5 However, several nuances with respect to early neurodevelopmental assessments must be addressed.
First, the existing data primarily originate from research studies, and there need to be more data from practical settings comparing the early neurodevelopmental assessments with long-term outcomes, which is essential for understanding the effectiveness in practical settings. Second, these early neurodevelopmental assessments have shown high predictability for identifying cerebral palsy, but their effectiveness in detecting cognitive and other neurodevelopmental impairments (NDI) is limited. 6 While early neurodevelopmental assessments primarily focus on evaluating motor function and development, systematic reviews have highlighted that these assessments may be useful in identifying cognitive delay to some extent while also emphasizing the limited literature specifically addressing cognitive impairment. 6 , 7 Third, there is a lack of sufficient evidence regarding the effectiveness of these tools in evaluating other NDI commonly used in clinical trials, especially those incorporating a sensory component alongside cognitive and motor components. To address these knowledge gaps, our study was designed to assess the broader ability of early neurodevelopmental assessments to predict cerebral palsy, cognitive impairment, and other NDI, including their severity, within a practical setting, at 24 to 36 months’ corrected age (CA).
This diagnostic study was approved by the Monash Health Human Research Ethics Committee as a quality assurance project, and parental consent was not required because it was an observational study and the exposure was considered within routine care. This study is reported following the Standards for Reporting of Diagnostic Accuracy ( STARD ) reporting guideline.
This diagnostic study assessed test accuracy by comparing observational data from our multidisciplinary, early neurodevelopmental clinic at CA 3 to 4 months with long-term neurodevelopmental outcomes at CA 24 to 36 months. This study included children born between January 1, 2019, and July 30, 2021. We chose this time frame to allow for neurodevelopmental outcome assessments, with the end point for these assessments set at 36 months. Infants considered at high risk of cerebral palsy or other NDI were recruited from the early neurodevelopmental clinic 8 at Monash Children’s Hospital, Melbourne, Australia, a perinatal and surgical tertiary neonatal unit providing care to preterm and term infants in Victoria, Australia. These infants were born extremely preterm (born before 28 weeks) or had extremely low birth weight (<1000 g) or had moderate to severe HIE who received therapeutic hypothermia.
Skilled physiotherapists, occupational therapists, and neonatologists trained in GMA conducted early neurodevelopmental assessments at CA 3 to 4 months, using the Prechtl GMA 9 and the HINE. 10 The primary predictor was early diagnosis of cerebral palsy or a high risk of cerebral palsy. Additional predictors included the absence of fidgety movements, HINE score, and early diagnosis of neurodevelopmental impairment (NDI). Early cerebral palsy or high risk of cerebral palsy was diagnosed based on absent fidgety movements, low HINE score (<57), and a medical neurological examination involving motor function, muscle tone, reflexes, and coordination. The diagnosis of early NDI included any anomalies found during initial assessments. These could be isolated anomalies, like absent fidgety movements, a low HINE score (<57), or isolated issues noted during medical neurological examinations. It could also encompass multiple anomalies, such as a combination of 2 or more anomalies or a diagnosis of early cerebral palsy or high risk of cerebral palsy.
Skilled neuropsychologists certified in Bayley Scales of Infant & Toddler Development (BSID) assessments and experienced developmental pediatricians conducted long-term neurodevelopmental evaluations between CA 24 and 36 months. The evaluations encompassed medical neurodevelopmental examination, BSID assessments (III or IV edition), 11 and assessments for blindness and deafness as part of the Australian and New Zealand Neonatal Network (ANZNN) 12 data collection. Our primary outcomes were any grade of cerebral palsy diagnosed on medical neurological examination and moderate to severe cerebral palsy, defined as cerebral palsy with grade II or above based on Gross Motor Function Classification System. We assessed 4 secondary outcomes: cognitive impairment, moderate to severe cognitive impairment, any NDI, and moderate to severe NDI. Cognitive impairment was defined as cognitive score less than 1 SD from the mean based on BSID III or IV. Moderate to severe cognitive impairment was defined as cognitive score less than 2 SD from the mean based on BSID III or IV. Any NDI was defined as the presence of any the following: cerebral palsy; motor, language, or cognitive impairment (score <1 SD on BSID); blindness (vision <6/60 in the better eye), or deafness (need for hearing aid). Moderate to severe NDI was defined as the presence of any following: moderate to severe cerebral palsy, moderate to severe motor, language, or cognitive impairment (score <2 SD on BSID); blindness, or deafness.
The early neurodevelopmental clinic at Monash Children’s Hospital prospectively collected neurodevelopmental data at CA 3 to 4 months, while demographic and long-term data were obtained from the ANZNN, a collaborative network encompassing all 29 neonatal intensive care units in Australia and New Zealand. Monash Children’s Hospital contributes data to ANZNN, which systematically gathers information for preterm infants born at less than 32 weeks’ gestational age admitted to any participating neonatal intensive care unit. Specifically, ANZNN collects neurodevelopmental data for infants at high risk of adverse neurodevelopmental outcomes up to ages 2 to 3 years, including infants born before 28 weeks’ gestation or weighing less than 1000 g at birth, as well as infants with moderate to severe HIE.
Diagnostic test accuracy values, along with corresponding 95% CIs, were calculated for early cerebral palsy or high risk of cerebral palsy, early NDI, and absent fidgety movements using MedCalc statistical software version 19.2.6 (MedCalc Software). Receiver operating characteristic curve analysis was conducted to obtain the area under the curve (AUC) and 95% CI for the HINE score, using SPSS software, 2021 release (IBM). Other analyses, including summarizing demographic variables (presented as the median and IQR due to nonnormal distribution) and predictive probability of cerebral palsy, were performed using Stata software version 17.0 (StataCorp). Data were analyzed from December 2023 to January 2024.
A total of 116 infants (median [IQR] gestational age, 27 [25-29] weeks; 65 [56%] male) were included in the study, comprising 100 preterm infants and 16 term infants. Further details about these infants, including antenatal information, delivery details, resuscitation, postnatal morbidities, and outcomes, are reported in the eTable in Supplement 1 . Early neurodevelopmental assessments were conducted at a median (IQR) of 13 (13-14) weeks’ CA, whereas long-term neurodevelopmental outcome evaluations were performed at a median (IQR) of 33 (30-35) months’ CA. The prevalence of cerebral palsy was 11% overall (13 of 116 infants), with 8% occurring among preterm infants (8 of 100 infants) and 31% among term infants with HIE (5 of 16 infants). Furthermore, the prevalence of cognitive impairment was 64% overall (70 of 109 infants), with 60% observed among preterm infants (56 of 93 infants) and 87% among term infants with HIE (14 of 16 infants). Three infants had hearing loss requiring amplification, and 1 infant had blindness.
The early cerebral palsy or high risk of cerebral palsy diagnosis demonstrated an accuracy of 85% (95% CI, 77% to 91%), correctly identifying 99 of 116 infants evaluated for cerebral palsy ( Table 1 and Figure 1 ). Among 13 infants diagnosed with cerebral palsy, the early cerebral palsy or high risk of cerebral palsy diagnosis showed a sensitivity of 92% (95% CI, 63% to 99%) by correctly identifying 12 infants. Notably, it achieved a 100% (95% CI, 59% to 100%) sensitivity (7 of 7 infants) in identifying all patients with moderate to severe cerebral palsy. Furthermore, the absence of fidgety movements exhibited a comparable accuracy of 81% (95% CI, 73% to 88%), and the HINE score displayed good discriminatory power, with an AUC of 0.88 (95% CI, 0.79 to 0.97) for predicting cerebral palsy ( Figure 2 ). On the other hand, the early NDI predictor, while correctly identifying all infants with cerebral palsy, also yielded false positives, resulting in a lower accuracy of 48% (95% CI, 38% to 57%).
The probability of cerebral palsy in infants was calculated depending on the anomalies noted on the early assessments, with none of the infants developing cerebral palsy having a HINE score within reference range (>57) and fidgety movements. The probability was noted at 7% if an infant had either a low HINE score or absent fidgety movements. If both were present (low HINE score and absent fidgety movements), the probability was 24%, which was not significantly different compared with infants with either a low HINE score or absent fidgety movements alone (absolute difference, 17% [95% CI, −2% to 36%]). However, infants with a very low HINE score (<40) and absent fidgety movements had a significantly higher predicted probability of 67%, in contrast with infants with either a low HINE score or absent fidgety movements alone (absolute difference, 60% [95% CI, 21% to 98%]) ( Figure 3 ).
The accuracy of various early neurodevelopmental assessments was notably limited, ranging from 44% to 60%, in predicting cognitive impairment and its severity ( Table 2 and Figure 1 ). Although the specificity of certain assessments showed modest values, ranging between 76% and 80%, the sensitivity and positive and negative predictive values demonstrated suboptimal performance. Additionally, the HINE score displayed limited discriminatory power in predicting cognitive impairment, reflected by an AUC of 0.62 (95% CI, 0.51 to 0.73) ( Figure 2 ).
Similar to cognitive impairment, the predictive accuracy of various early neurodevelopmental assessments was notably low, ranging from 31% to 59%, when predicting NDI and its severity ( Table 2 ). Moreover, the sensitivity and negative predictive values showed suboptimal performance across the different assessments, while the positive predictive value and specificity were modest in predicting NDI and its severity, respectively.
This diagnostic study, leveraging data from infants considered at high risk of adverse neurodevelopmental outcomes, assessed the effectiveness of early neurodevelopmental assessments at CA 3 to 4 months in identifying cerebral palsy, cognitive impairment, and other NDI and their severity at CA 24 to 36 months. Early assessments, including early cerebral palsy or high risk of cerebral palsy, absent fidgety movements, and HINE scores, exhibited high accuracy in identifying cerebral palsy. Moreover, these assessments achieved a sensitivity and negative predictive value of 100% for detecting moderate to severe cerebral palsy. Furthermore, the study found an increase in the predicted probability of cerebral palsy with the number and severity of anomalies identified in early neurodevelopmental assessments. With respect to predicting cognitive and neurodevelopmental impairment and their severity, we found limited accuracy, sensitivity, and negative predictive value of early neurodevelopmental assessments.
While current research using observational data offers insights into the feasibility of early neurodevelopmental assessments for diagnosing cerebral palsy at an early stage, 8 , 13 - 19 there exists a notable gap in studies directly comparing early data with long-term outcomes. Observational data studies are crucial, as they offer insights into the effectiveness of assessments in contextual settings. Although systematic reviews of research studies have consistently shown high accuracy in early neurodevelopmental assessments for identifying cerebral palsy, 20 - 22 the direct applicability of these findings in clinical settings is limited. Some studies using clinical data have found lower sensitivities or accuracies in predicting cerebral palsy, 23 - 25 while others have found higher accuracy. 26 This discrepancy is likely influenced by various factors, including the characteristics of the studied population, 25 the prevalence of cerebral palsy or NDI, 27 and the level of training in the assessments. 28 , 29 Additionally, some researchers argue that continued follow-up assessments may enhance accuracy compared with 1-time assessments. 30 Nevertheless, our findings support the notion that these assessments maintain high accuracy in practical settings, aligning with both previous research 20 - 22 and clinical studies. 26
Using our study results in a simulated scenario of 100 infants with high risk of cerebral palsy or NDI, with an observed 11% incidence of cerebral palsy and a 6% incidence of moderate to severe cerebral palsy, the data suggest that standardized assessments with a finding of early cerebral palsy or high risk of cerebral palsy at CA 3 to 4 months would identify 10 of 11 infants with cerebral palsy and all infants with moderate to severe cerebral palsy. However, this diagnosis would also falsely identify 15 infants as having cerebral palsy. In contrast, if the early cerebral palsy or high risk of cerebral palsy diagnosis is used to identify NDI, considering a 64% incidence of NDI from this study, this diagnosis would only detect 15 of 64 infants with NDI while incorrectly identifying 20 infants with NDI. Overall, these data confirm the high sensitivity and accuracy of early standardized assessments in detecting cerebral palsy and gauging its severity, aligning with prior research 20 - 22 ; however, our findings underscore the restricted effectiveness of these assessments in identifying cognitive impairment and NDI and their severity.
Ideally, a test should be able to identify all patients with the disease, but a highly sensitive test often comes with an increased false positive rate. This phenomenon was observed in our study, where the early cerebral palsy or high risk of cerebral palsy diagnosis exhibited high sensitivity but had a 15% false positivity rate. When assessing this false positivity rate, it is worth considering that it might have been influenced by the fact that infants diagnosed with early cerebral palsy or high risk of cerebral palsy underwent early intervention, potentially positively impacting their development. 31 Such early interventions could have altered the developmental trajectory of these infants, particularly for those with milder symptoms, ultimately preventing them from receiving a final diagnosis of cerebral palsy. In Australia, infants diagnosed with cerebral palsy and other disabilities have access to national disability insurance scheme funding provided by both the Commonwealth and state governments, ensuring equitable support without disparities.
Early neurodevelopmental assessments are customarily designed to focus on motor evaluation and do not inherently encompass the assessment of cognitive domains. While there is a possibility that these assessments may indirectly offer insights into cognitive domains, 5 , 6 , 17 given that disorders affecting cognition may also impact motor function, our study’s findings do not demonstrate their utility in assessing cognitive impairments. Furthermore, their utility in addressing broader NDI is constrained, as this outcome is comprehensive and involves cognitive impairment within its definition.
Our study has several notable strengths. Unlike previous investigations reliant on research outputs, our study draws on observational data gathered directly from clinical settings. This distinctive approach lends credibility to our results, reflecting the practical application of early neurodevelopmental assessments. Another strength of our study is the meticulous prospective collection of data, ensuring the acquisition of reliable and valid information while minimizing the risk of recall bias. Furthermore, the assessors of long-term outcomes used standardized objective measures during assessments, which further reduces the risk of bias in the assessment process. Additionally, the comprehensive nature of our comparisons contributes to our study’s depth, thereby enhancing the robustness of our findings.
It is important to acknowledge some limitations. While our study comprehensively compared early neurodevelopmental assessments with long-term outcomes in a clinical setting, the study population was relatively small, as evidenced by wide CIs in some diagnostic test accuracy measures. Additionally, the data were sourced from a single center, which may restrict the generalizability of our findings. Furthermore, the inclusion of infants with high risk, particularly with most infants being born extremely preterm, means that our findings may not be directly applicable to a more diverse range of infant populations.
In this diagnostic study of infants at high risk of cerebral palsy and NDI, our findings affirm the effectiveness of early standardized assessments in detecting cerebral palsy and determining its severity as early as CA 3 to 4 months, even in clinical settings. This emphasizes the crucial role of integrating these assessments into clinical practice, enabling early interventions with the potential to influence the progression of the disease. Furthermore, our findings indicate that these assessments have limited utility in detecting cognitive impairment and other NDI, emphasizing the ongoing necessity for longer-term assessments to accurately identify impairments beyond cerebral palsy.
Accepted for Publication: March 22, 2024.
Published: May 6, 2024. doi:10.1001/jamanetworkopen.2024.13550
Open Access: This is an open access article distributed under the terms of the CC-BY License . © 2024 Razak A et al. JAMA Network Open .
Corresponding Author: Abdul Razak, MD, Department of Paediatrics, Monash University, 246 Clayton Rd, VIC 3168, Australia ( [email protected] ).
Author Contributions: Dr Razak and Prof Malhotra had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Razak, Hunt, Miller, Malhotra.
Acquisition, analysis, or interpretation of data: Razak, Johnston, Sackett, Clark, Charlton, Zhou, Pharande, McDonald, Malhotra.
Drafting of the manuscript: Razak, Miller, Malhotra.
Critical review of the manuscript for important intellectual content: All authors.
Statistical analysis: Razak, Malhotra.
Obtained funding: Malhotra.
Administrative, technical, or material support: Johnston, Clark, Charlton, Zhou, Pharande, Miller, Malhotra.
Supervision: Clark, McDonald, Hunt, Miller, Malhotra.
Conflict of Interest Disclosures: Prof Miller reported receiving grants from the Australian National Health and Medical Research Council (NHMRC). Prof Malhotra reported receiving grants from the NHMRC, National Stem Cell Foundation of Australia, Lions Cord Blood Foundation, Australian Medical Research Future Fund (MRFF), and Monash Health Foundation and personal fees from GE Australia outside the submitted work. Dr McDonald reported receiving funding from the MRFF. No other disclosures were reported.
Funding/Support: Dr Razak is supported by a doctoral scholarship from Monash University and The Lions Cord Blood Foundation.
Role of the Funder/Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Data Sharing Statement: See Supplement 2 .
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
- Open access
- Published: 18 May 2024
Foot and lower leg pain in children and adults with cerebral palsy: a population-based register study on 5,122 individuals
- Ebba Jarlman 1 , 2 ,
- Gunnar Hägglund 1 &
- Ann I. Alriksson-Schmidt 1
BMC Musculoskeletal Disorders volume 25 , Article number: 391 ( 2024 ) Cite this article
10 Accesses
Metrics details
Pain is common in individuals with cerebral palsy (CP) and the most reported pain site is the foot/lower leg. We analyzed the prevalence of pain in the foot/lower leg and the associations with age, sex, gross motor function, and clinical findings in individuals with CP.
This was a cross-sectional register-study, based on data reported to the Swedish Cerebral Palsy Follow-up Program (CPUP). All participants in CPUP, four years-of-age or older, were included. Pearson chi-square tests and logistic regression were used to analyze the prevalence and degree of pain in the foot/lower leg.
In total, 5,122 individuals were included from the CPUP database: 58% were males and 66% were under 18 years-of-age. Overall, 1,077 (21%) reported pain in the foot/lower leg. The odds ratios (ORs) of pain were higher in females (OR 1.31, 95% confidence interval (CI) 1.13–1.53), individuals who could ambulate (Gross Motor Function Classification System Level I (OR 1.84, CI 1.32–2.57) and II (OR 2.01, CI 1.46–2.79) compared to level V), and in individuals with decreased range of motion of the ankle (dorsiflexion 1–10 degrees (OR 1.43, CI 1.13–1.83) and ≤ 0 degrees (OR 1.46, CI 1.10–1.93) compared to ≥ 20 degrees). With increasing age the OR of pain increased (OR 1.02, CI 1.01–1.03) as well as the reported pain intensity ( p < 0.001).
Conclusions
Pain in the foot and lower leg appears to be a significant problem in individuals with CP, particularly in those who walk. As with pain in general in this population, both pain intensity and frequency increase with age. The odds of pain in the foot and lower leg were increased in individuals with limited dorsiflexion of the ankle. Given the cross-sectional design causality cannot be inferred and it is unknown if pain causes decreased range of motion of the ankle or if decreased range of motion causes pain. Further research is needed on causal pathways and importantly on prevention.
Peer Review reports
Cerebral palsy (CP) is caused by a non-progressive injury to the brain but is associated with progressive musculoskeletal complications. Pain is consistently reported as one of the more frequent secondary conditions [ 1 , 2 , 3 , 4 , 5 , 6 , 7 ]. The Swedish Cerebral Palsy Follow-up Program (CPUP) is a combined national follow-up program and register that includes regular and systematic assessments to identify early signs of deterioration. CPUP has successfully reduced the prevalence of hip dislocations and severe contractures [ 8 , 9 ]. However, the effect on pain is unclear. Previous research has indicated that the number of individuals with CP reporting pain ranges from 31 to 77% [ 1 , 10 , 11 , 12 , 13 , 14 ].
Pain has been associated with increasing age as well as with female sex, both in studies of children and adults with CP [ 3 , 5 , 6 , 10 , 15 , 16 , 17 ]. Previous studies based on data from the CPUP have shown that pain in the last four weeks was reported in 32–43% of children and 67% of adults [ 3 , 16 , 17 ]. In addition to frequency of pain, the number of pain sites increased with age: approximately one in three children reported pain in more than one site, compared to three in four adults [ 16 , 17 ]. Those in pain reported that pain affected their Activities of Daily Living (ADL) or work in 60% of cases, and their sleep in 36–47% [ 16 , 17 ]. Recurrent musculoskeletal pain has been associated with lower levels of participation in life situations, lower self-reported quality of life, as well as a decline in gross motor function [ 3 , 4 , 6 , 14 , 18 , 19 , 20 , 21 , 22 , 23 ].
One of the most common pain sites in individuals with CP is the feet and lower legs (from hereon after referred to as foot/lower leg) constituting 36–60% of reported pain sites [ 3 , 16 , 17 , 20 , 24 , 25 ]. However, reported pain site/s is strongly associated with gross motor function classification system (GMFCS) levels [ 1 , 3 , 14 , 22 , 26 ] such that children with walking ability (i.e., GMFCS levels I-III) report pain in the foot/lower leg to a greater extent than children using wheelchairs (GMFCS levels IV-V) [ 3 , 16 , 24 ]. Spasticity has been described as a common cause of musculoskeletal pain, and the foot/lower leg/knee has been reported as the most common site for spasticity-related pain [ 7 , 13 , 14 , 27 ]. Research has also indicated that spasticity of the gastrocsoleus complex is related to the development of muscle contractures and decreased range of motion (ROM) of the ankle [ 28 ].
Although pain in CP regardless of pain site is well described, it has been shown that the pain distribution differs by e.g., level of motor function. The mapping of pain by specific body sites is not well understood. To that end, we were interested in studying more specific factors that might be correlated to the painful foot/lower leg. Our aim was to analyze pain in the foot/lower leg in individuals with CP related to age, sex, GMFCS-level, ROM of the ankle, and level of spasticity in the plantar flexors. We also investigated the prevalence of spasticity-reducing treatments and below-the-knee surgery in those who reported pain in the foot/lower leg compared to those who did not.
This was a cross-sectional, population-based, CPUP register-study based on data reported in 2018–2019. The CPUP assessment schedule is based on age and GMFCS-level. Children are offered to participate in the CPUP follow-up program as soon as there is suspicion that they might have CP. The actual diagnoses of CP are made at approximately 4 years of age by pediatric neurologists according to the criteria developed by the Surveillance of Cerebral Palsy Network in Europe [ 26 ]. Children not fulfilling the inclusion criteria for the diagnosis of CP are then excluded. Both children and adults with CP are eligible to participate in CPUP. More than 95% of children 18 years old or younger with CP in Sweden are followed in CPUP, however, the participation rate for adults is lower due to approximately 15% of individuals with CP choosing to discontinue the program after their 18th birthday.
As part of the CPUP assessments, physical therapists screen for pain. If pain is present, the intensity in the last four weeks in 15 separate body sites is recorded. Pain intensity is graded on an ordinal scale from 0 (no pain) to 5 (very severe pain) for each site. For the purpose of this study, data on pain in the foot/lower leg and total number of painful sites were included in addition to two items on pain interference with ADL and sleep. If the individuals were not able to communicate, the parents or legal guardians served as proxies.
The ROM of the ankle was measured with 90-degree flexion of the hip and knee, using a goniometer. When performing this measurement, the stationary arm of the goniometer was parallel to the anterior margin of the tibia, and the movable arm was parallel to the lateral margin of the foot. The neutral position of the ankle was set as 0 degrees of dorsiflexion and the amount of dorsiflexion measured was registered at the closest 5-degree mark. If the ankle could not come up to neutral position this was reported as a negative degree of dorsiflexion (i.e., -5 degrees). Degree of spasticity in the plantar flexors is classified according to the Modified Ashworth Scale (MAS) from 0 to 4. We dichotomized spasticity into ‘low’ (MAS 0–1) or ‘high’ (MAS ≥ 2). Because pain laterality is not recorded, the decision was made to use the lowest ROM and the highest degree of spasticity recorded. Eleven participants had reported “no pain” and five had left the item on ‘pain present’ blank, yet still recorded pain site/s. In those cases, pain was recoded as ‘pain present’.
Data were collected from the last CPUP assessment performed in 2018–2019 for all participants included. Nine individuals who had undergone below-the-knee surgery within six weeks prior to the assessment were excluded.
The study was approved by the Ethics Board at Lund University (LU 443 − 99, revised 2020).
Descriptive analyses were performed using medians and interquartile ranges (IQR) for continuous variables and raw numbers and percentages for categorical and ordinal variables. “Pain in foot/lower leg’’ was coded as a binary variable (pain/no pain) and categorized as four levels: no pain, mild pain (very mild-mild pain combined), moderate pain, and severe pain (severe-very severe pain combined). Crosstabulations and Pearson chi-square tests were performed. Multicollinearity was assessed with Pearson correlation and Variance Inflation Factor.
Logistic regression analyses were used to estimate unadjusted odds ratios (ORs) of age, sex, GMFCS-level, source of report (self or proxy report), CP-subtype, ROM of the ankle, and spasticity in plantar flexors on pain in the foot/lower leg. Next, a stepwise multiple logistic regression was performed to produce adjusted ORs. Multinominal logistic regression analyses were used to estimate relative risk ratios (RRRs) of the same variables on pain intensity. Listwise deletion was used in the multiple logistic regression analyses. Bonferroni correction was used to adjust the level of significance and defined as p < 0.0014 and confidence intervals at 95%. Analyses were performed using IBM SPSS Statistics version 28 and Stata/SE (v 15.1; StataCorp LLC).
In total, 5,122 individuals were included of which 58% were males. The median age was 14 years (range 4–78, IQR 9–21 years) and 3,370 (66%) were younger than 18 years of age. Baseline characteristics are presented in Table 1 .
Pain in one or more of the 15 potential pain sites was reported in 2,693 (53%) participants, 2,288 (45%) reported no pain, and 141 (3%) had missing pain data. Pain increased from 36% in 4–7-year-olds to 76% in individuals > 50 years of age. In total, pain was reported in 69% of adults compared to 44% in those under the age of 18 years. Regardless of pain site/s, 57% of individuals in pain reported that pain affected their ADL and 39% that pain affected their sleep.
Pain in the foot/lower leg
Pain in the foot/lower leg was reported in 1,077 individuals, which corresponds to 21% of the total study population and 40% of all individuals who reported pain. Furthermore, 48% described their pain as mild, 33% as moderate, and 17% as severe. Among those reporting pain in the foot/lower leg, 53% had pain in an additional two or more sites of the body. This differed from individuals who reported pain in other sites except for the foot/lower leg, where only 25% had pain in three or more sites.
Adults with CP reported pain in the foot/lower leg to a greater extent than those under the age of 18 years (27% vs. 19%, p < 0.001), and divided by age categories an increasing trend with higher age was observed (Fig. 1 , p < 0.001). Adults with pain in the foot/lower leg reported more severe pain (Fig. 2 , p < 0.001). Regardless of painful site/s, adults more frequently had pain that affected sleep compared to individuals < 18 years (50% vs. 37%, p < 0.001), but no statistically significant difference was seen regarding pain that affected ADL. Adults also reported a greater number of painful sites than individuals < 18 years among those reporting pain in the foot/lower leg (Fig. 3 , p < 0.001) as well as those reporting pain regardless of site (Table 2 , p < 0.001).
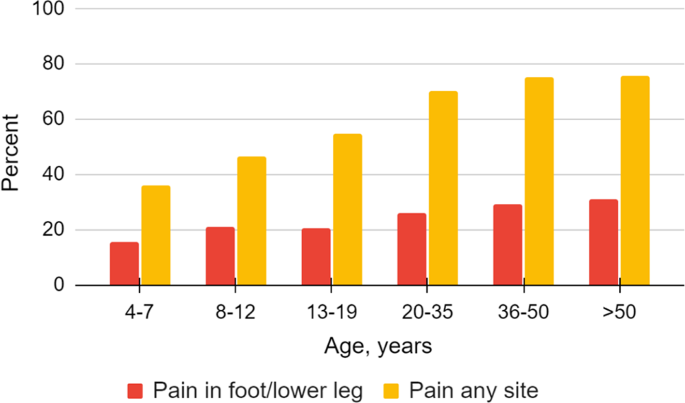
Overall pain and pain in the foot/lower leg related to age in the total study population. A statistically significant increase of pain overall ( p < 0.001) and pain in the foot/lower leg ( p < 0.001) with increasing age is shown
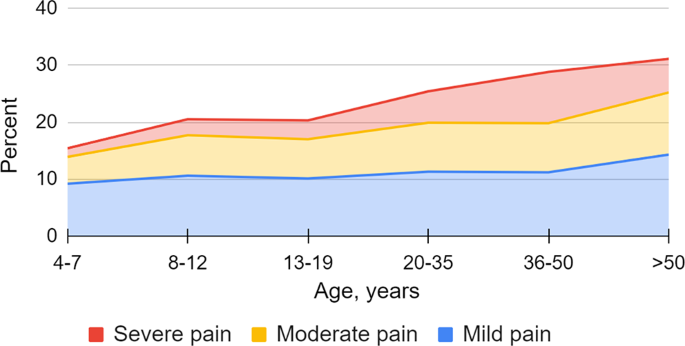
Severity of pain in the foot/lower leg related to age in the total study population ( p < 0.001)
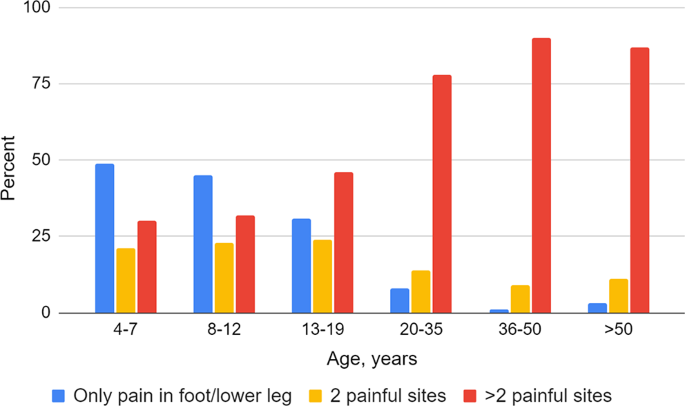
Distribution of the number of painful sites among those reporting pain in the foot/lower leg, related to age
Women/girls reported pain more frequently than men/boys, both overall and in the foot/lower leg (59% and 24% vs. 51% and 20%, p < 0.001). Following the Bonferroni adjustment, no statistically significant differences between the sexes were seen on pain intensity, number of painful sites, or in pain that affects ADL/Work or sleep (Table 2 ).
Individuals who could walk (GMFCS I-III) had fewer reports of pain in general than those who could not walk (52% vs. 58%, p < 0.001) but had a higher prevalence of pain in the foot/lower leg (25% vs. 15%, p < 0.001) than individuals who could not walk. There was also a statistically significant difference among GMFCS levels on number of painful sites, pain that affects sleep or ADL, as well as pain intensity ( p < 0.001). The highest number of painful sites was observed in individuals in GMFCS level III, while pain affecting ADL and pain affecting sleep were most prevalent in those in GMFCS level V (Table 2 ).
Results from the multiple logistic regression are reported in Table 3 . The adjusted ORs of pain in the foot/lower leg were statistically significantly higher in females, individuals in GMFCS levels I-II, and in individuals with reduced dorsiflexion of the ankle of ≤ 10 degrees. When age was analyzed as a continuous variable, ORs of pain increased with age. However, when age was categorized into age groups, the adjusted OR of pain showed a statistically significant increase only in individuals > 20 years old. Furthermore, the adjusted ORs of pain in the foot/lower leg were statistically significantly lower in individuals with dyskinetic or ataxic CP and for those who proxy-reported.
No statistically significant difference was seen on prevalence of pain in the foot/lower leg and treatment with botulinum toxin A (BTX-A) below the knee, other spasticity-reducing treatments, or below-the-knee surgery since the last CPUP assessment (Table 4 ). However, in the multiple logistic regression analysis, the adjusted ORs of having pain in the foot/lower leg were statistically significantly higher in individuals having received BTX-A (Table 3 ).
The multinominal regression showed that individuals had higher risk of reporting severe pain than mild or moderate pain in their foot/lower leg with increasing age. Sex was not correlated with pain intensity. Individuals in GMFCS V were more likely to have severe pain in the foot/lower leg compared to individuals in GMFCS I-IV (Table 5 ).
Pain in the foot/lower leg affected one in five individuals with CP and was more frequent in adults, in females, in those in GMFCS levels I-II, and in individuals with reduced ROM of the ankle. It was less frequent in individuals with dyskinetic or ataxic CP, as well as in those with proxy-reported pain.
Increased frequency and intensity of pain in the foot/lower leg and a greater number of painful sites were noted with increasing age. Especially in adults, pain in the foot/lower leg seemed to be part of a more complex pain situation with multiple painful sites. Affecting more than 1 in 4 adults, pain in the foot/lower leg might be a contributing factor of the decline in participation, motor function/walking ability, or quality of life that has been described in previous studies on adults with CP [ 3 , 4 , 6 , 14 , 18 , 19 , 20 , 21 , 22 ].
The findings that women and girls reported pain more frequently is in line with previous studies [ 3 , 5 , 10 , 16 , 17 , 18 ]. However, women and girls do not seem to have more severe pain in their feet/lower legs than men and boys. Parkinson et al. 2013 reported more severe pain in girls, however, that was in general, and not associated with a particular site [ 10 ]. Population-based studies have consistently shown that women report pain more often than men and there is increasing evidence that there is a difference between males and females regarding pain sensitivity and analgesic response. However, pain intensity is more often equal between the sexes. The underlying causes for this are still unclear but a combination of biological, psychological, and sociocultural factors is likely to contribute [ 29 , 30 ].
The higher prevalence of pain in the foot/lower leg among those who ambulate differ from previous studies on pain, where pain generally was more common in higher GMFCS levels [ 3 , 6 , 14 , 18 ]. However, individuals in GMFCS level V were more likely to have more severe pain in the foot/lower leg.
Of the risk factors for pain in the foot/lower leg, sex, age, and GMFCS-level are largely non-modifiable. However, a factor that is modifiable is reduced ROM of the ankle. Nevertheless, due to the cross-sectional design of this study, it was not possible to determine if the decreased ROM caused pain, or if the ROM was decreased because of pain.
Overall, that individuals who put weight on their feet are at higher risk of pain in the foot/lower leg is clinically plausible. Although we cannot deduce the exact cause of pain, one hypothesis is that putting weight on a joint at the extreme end of its ROM is a strain. Moreover, a deformed foot does not tolerate as much strain or weight as a non-deformed foot.
Dyskinetic CP has previously been associated with a higher prevalence of pain – regardless of site – [ 14 , 18 ], however, we observed lower odds of pain in the foot/lower leg in individuals with dyskinetic and ataxic CP compared to individuals with spastic CP (Table 3 ), even after adjusting for GMFCS level and ROM. This was somewhat unexpected, and we are not able to completely explain this finding. It is possible, however, that the muscle tone is more variable in those with dyskinetic and ataxic CP, which might be associated with less pain than the more persistent increased muscle tone associated with spastic CP.
In this study, we have not looked specifically on presence of a coronal plane deformity of the foot. Like equinus, valgus and varus deformities are caused by the combination of muscle imbalance, impaired motor control, abnormal tone, and gravity and range from mild and flexible to severe and rigid [ 31 , 32 ]. Type of deformity varies with the degree of motor involvement and CP subtype. We do not know if the type of deformity affects pain prevalence, but it is a reasonable thought that should be further researched.
We found that individuals with pain in their foot/lower leg were more likely to have received local spasticity-reducing injections with BTX-A since their last CPUP assessment. No statistical difference was seen regarding other spasticity reducing treatments, such as oral or intrathecal baclofen, or selective dorsal rhizotomy. BTX-A is injected to reduce muscle tone of the treated muscle, and one indication for this treatment in CP is painful spasticity. The increased odds of having pain in the foot/lower leg in those who have been treated with BTX-A may be attributed to pain being an indication for BTX-A treatment. Nevertheless, we do not know exactly where the injection was given or when in the treatment cycle. Further studies with a longitudinal approach regarding the effect of interventions such as BTX-A on pain are needed.
Although no clear association has been found, it is possible that other treatments, such as orthotic devices, might play a part in the painful foot/lower leg. Ankle-foot orthoses (AFO) are commonly used in children with CP, and while there is limited evidence that AFOs might have a beneficial effect on ROM not much is known regarding positive or negative effects on pain [ 33 , 34 , 35 ]. However, we did not have enough data on use of orthotic devices on the lower leg/foot to include it in our analyses.
Study limitations
There are several limitations in this study. The coverage rate of adults with CP is less complete than for children: 15% leave CPUP after turning 18 years. A majority of those who decline to continue in CPUP are in GMFCS level I, and as such are at a higher risk of developing pain in their feet/lower legs. Although this is a potential inclusion bias that might affect the pain prevalence, GMFCS is adjusted for in the regression analyses. An additional limitation is that 43% of the participants did not self-report. Previous studies have indicated that proxies tend to report pain to a lesser degree in adults, and tend to report lower pain intensity scores [ 12 , 16 , 17 , 36 ]. It is plausible to assume that the interpretation of pain is even harder for proxies in individuals with multiple painful sites.
In this study, we focused on the main effects of our exposure variables and did not assess potential interactions between our exposure variables in the multiple logistic regression analysis which could provide further insights.
While there are clear advantages with register-based research in regards to, for example, generalizability, one drawback tends to be the lack of details in the reported data. In other words, in smaller studies it might be more feasible to collect data at a more detailed level. Hence, more research is required to investigate in more detail the relationship between, for instance, subtype of CP, spasticity, foot deformities, and pain in the foot/lower leg.
Overall, to experience pain in the foot/lower leg seems to be part of a more complex picture; more than half of those with pain in the foot/lower leg reported pain in three or more sites. In comparison, more than half of the individuals who had pain somewhere else, but not in the foot/lower leg, reported only one painful site. In this context, this is a limitation making us unable to tease out what effect only pain in the foot/lower legs has on ADL/Work or sleep, since the data do not specify how each painful site affects ADL/Work or sleep.
Pain in the foot/lower leg is a common problem in individuals with CP. Adults, women, and individuals who are ambulatory were at higher risk of having pain in the foot/lower leg. Pain in the foot/lower leg was associated with decreased ROM of the ankle. Moreover, pain in the foot/lower leg is often combined with pain in other sites. Overall, our findings support that just like CP is a heterogeneous condition, so is CP-related pain. To that end, given that risk factors for pain seem to differ between different parts of the body, both clinicians and researchers should approach each painful body site separately. Given that one in two individuals with CP report pain, and one in five report pain in the foot/lower leg, we must strive for early identification, evaluation, and treatment of these individuals to maintain function and prevent deterioration of mobility and quality of life.
Data availability
Data used in this study are owned by Skane Regional Council (Region Skane, 29,189 Kristianstad, Sweden). The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request and with permission of the Skane Regional Council.
Abbreviations
Cerebral Palsy
Cerebral palsy follow-up program
Confidence interval
Activities of daily living
Gross motor function classification system
Range of motion
Modified Ashworth scale
Interquartile range
Variance Inflation factor
Relative risk ratios
Botulinium toxin A
Ankle-foot orthosis
Novak I, Hines M, Goldsmith S, Barclay R. Clinical prognostic messages from a systematic review on cerebral palsy. Pediatrics. 2012;130(5):e1285–1312.
Article PubMed Google Scholar
Odding E, Roebroeck ME, Stam HJ. The epidemiology of cerebral palsy: incidence, impairments and risk factors. Disabil Rehabil. 2006;28(4):183–91.
Alriksson-Schmidt A, Hägglund G. Pain in children and adolescents with cerebral palsy: a population-based registry study. Acta Paediatr Oslo nor 1992. 2016;105(6):665–70.
Google Scholar
Ramstad K, Jahnsen R, Skjeldal OH, Diseth TH. Parent-reported participation in children with cerebral palsy: the contribution of recurrent musculoskeletal pain and child mental health problems. Dev Med Child Neurol. 2012;54(9):829–35.
van der Slot WMA, Benner JL, Brunton L, Engel JM, Gallien P, Hilberink SR, et al. Pain in adults with cerebral palsy: a systematic review and meta-analysis of individual participant data. Ann Phys Rehabil Med. 2021;64(3):101359.
Mckinnon CT, Meehan EM, Harvey AR, Antolovich GC, Morgan PE. Prevalence and characteristics of pain in children and young adults with cerebral palsy: a systematic review. Dev Med Child Neurol. 2019;61(3):305–14.
Vinkel MN, Rackauskaite G, Finnerup NB. Classification of pain in children with cerebral palsy. Dev Med Child Neurol. 2022;64(4):447–52.
Hägglund G, Alriksson-Schmidt A, Lauge-Pedersen H, Rodby-Bousquet E, Wagner P, Westbom L. Prevention of dislocation of the hip in children with cerebral palsy: 20-year results of a population-based prevention programme. Bone Jt J. 2014;96–B(11):1546–52.
Article Google Scholar
Hägglund G, Lauge-Pedersen H, Persson Bunke M, Rodby-Bousquet E. Windswept hip deformity in children with cerebral palsy: a population-based prospective follow-up. J Child Orthop. 2016;10(4):275–9.
Article PubMed PubMed Central Google Scholar
Parkinson KN, Dickinson HO, Arnaud C, Lyons A, Colver A, SPARCLE group. Pain in young people aged 13 to 17 years with cerebral palsy: cross-sectional, multicentre European study. Arch Dis Child. 2013;98(6):434–40.
Andersson C, Mattsson E. Adults with cerebral palsy: a survey describing problems, needs, and resources, with special emphasis on locomotion. Dev Med Child Neurol. 2001;43(2):76–82.
Article CAS PubMed Google Scholar
Hägglund G, Burman-Rimstedt A, Czuba T, Alriksson-Schmidt AI. Self-versus Proxy-reported Pain in Children with cerebral palsy: a Population-based Registry Study of 3783 children. J Prim Care Community Health. 2020;11:2150132720911523.
Penner M, Xie WY, Binepal N, Switzer L, Fehlings D. Characteristics of pain in children and youth with cerebral palsy. Pediatrics. 2013;132(2):e407–413.
Ostojic K, Paget S, Kyriagis M, Morrow A. Acute and Chronic Pain in Children and adolescents with cerebral palsy: prevalence, interference, and management. Arch Phys Med Rehabil. 2020;101(2):213–9.
Parkinson KN, Gibson L, Dickinson HO, Colver AF. Pain in children with cerebral palsy: a cross-sectional multicentre European study. Acta Paediatr Oslo nor 1992. 2010;99(3):446–51.
CAS Google Scholar
Eriksson E, Hägglund G, Alriksson-Schmidt AI. Pain in children and adolescents with cerebral palsy – a cross-sectional register study of 3545 individuals. BMC Neurol. 2020;20(1):15.
Rodby-Bousquet E, Alriksson‐Schmidt A, Jarl J. Prevalence of pain and interference with daily activities and sleep in adults with cerebral palsy. Dev Med Child Neurol. 2021;63(1):60–7.
Westbom L, Rimstedt A, Nordmark E. Assessments of pain in children and adolescents with cerebral palsy: a retrospective population-based registry study. Dev Med Child Neurol. 2017;59(8):858–63.
Bartlett DJ, Hanna SE, Avery L, Stevenson RD, Galuppi B. Correlates of decline in gross motor capacity in adolescents with cerebral palsy in Gross Motor function classification system levels III to V: an exploratory study. Dev Med Child Neurol. 2010;52(7):e155–160.
Opheim A, Jahnsen R, Olsson E, Stanghelle JK. Walking function, pain, and fatigue in adults with cerebral palsy: a 7-year follow-up study. Dev Med Child Neurol. 2009;51(5):381–8.
Dickinson HO, Parkinson KN, Ravens-Sieberer U, Schirripa G, Thyen U, Arnaud C, et al. Self-reported quality of life of 8-12-year-old children with cerebral palsy: a cross-sectional European study. Lancet Lond Engl. 2007;369(9580):2171–8.
Ramstad K, Jahnsen R, Skjeldal OH, Diseth TH. Mental health, health related quality of life and recurrent musculoskeletal pain in children with cerebral palsy 8–18 years old. Disabil Rehabil. 2012;34(19):1589–95.
Schmidt S, Markwart H, Rapp M, Guyard A, Arnaud C, Fauconnier J, et al. Quality of life and mental health in emerging adults with cerebral palsy compared to the general population. Health Qual Life Outcomes. 2022;20(1):61.
Østergaard CS, Pedersen NSA, Thomasen A, Mechlenburg I, Nordbye-Nielsen K. Pain is frequent in children with cerebral palsy and negatively affects physical activity and participation. Acta Paediatr. 2021;110(1):301–6.
Doralp S, Bartlett DJP. The prevalence, distribution, and Effect of Pain among adolescents with cerebral palsy. Pediatr Phys Ther Spring 2010. 2010;22(1):26–33.
Cans C. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Dev Med Child Neurol. 2000;42(12):816–24.
Heinen F, Bonfert M, Kaňovský P, Schroeder AS, Chambers HG, Dabrowski E et al. Spasticity-related pain in children/adolescents with cerebral palsy. Part 1: prevalence and clinical characteristics from a pooled analysis. J Pediatr Rehabil Med 15(1):129–43.
Hägglund G, Wagner P. Spasticity of the gastrosoleus muscle is related to the development of reduced passive dorsiflexion of the ankle in children with cerebral palsy. Acta Orthop. 2011;82(6):744–8.
Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and Pain: a review of recent clinical and experimental findings. J Pain. 2009;10(5):447–85.
Bartley EJ, Fillingim RB. Sex differences in pain: a brief review of clinical and experimental findings. BJA Br J Anaesth. 2013;111(1):52–8.
Kedem P, Scher DM. Foot deformities in children with cerebral palsy. Curr Opin Pediatr. 2015;27(1):67.
Tabaie SA, Videckis AJ, Quan T, Sheppard ED. Topical review: Approach to diagnosis and management of the Pediatric Foot and Ankle in Cerebral Palsy patients. Foot Ankle Orthop. 2022;7(2):24730114221091800.
Wingstrand M, Hägglund G, Rodby-Bousquet E. Ankle-foot orthoses in children with cerebral palsy: a cross sectional population based study of 2200 children. BMC Musculoskelet Disord. 2014;15:327.
Morris C, Condie D. Recent Developments in Healthcare for Cerebral Palsy: Implications and Opportunities for Orthotics. 2009.
Owen E. When to use lower limb orthoses in cerebral palsy. Paediatr Child Health. 2020;30(8):275–82.
Hadden KL, LeFort S, OʼBrien M, Coyte PC, Guerriere DN. A comparison of observers’ and self-report pain ratings for children with cerebral palsy. J Dev Behav Pediatr JDBP. 2015;36(1):14–23.
Download references
Acknowledgements
The authors would like to thank biostatistician Tomasz Czuba for statistical assistance.
The authors would like to express their gratitude to the Stig and Ragna Gorthon Foundation, Sunnerdahls Handikappsstiftelse, the Linnea and Josef Carlsson Foundation, Stiftelsen för bistånd för rörelsehindrade i Skåne and NordForsk for their support on research related to pain in cerebral palsy. All foundations have contributed to the work, but they have not affected or participated in study design, data analysis or manuscript writing. Open Access funding was provided by Lund University.
Author information
Authors and affiliations.
Department of Clinical Sciences, Orthopedics, Lund University, Lund, Sweden
Ebba Jarlman, Gunnar Hägglund & Ann I. Alriksson-Schmidt
Department of Orthopedics, Helsingborg Hospital, Helsingborg, Sweden
Ebba Jarlman
You can also search for this author in PubMed Google Scholar
Contributions
EJ, GH and AAS designed the study. EJ analyzed and interpreted the data, performed the statistical analysis and drafted the manuscript. AAS and GH revised and improved the manuscript. All authors approved the final draft.
Corresponding author
Correspondence to Ebba Jarlman .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethics Board at Lund University (LU 443 − 99, revised 2020). All our methods were carried out in accordance with relevant guidelines and regulations. Informed consent was obtained from all subjects and/or their legal guardians in case of minors to use data for research before inclusion in the CPUP register. Permission to extract data from the CPUP register was obtained from the register owner.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Jarlman, E., Hägglund, G. & Alriksson-Schmidt, A.I. Foot and lower leg pain in children and adults with cerebral palsy: a population-based register study on 5,122 individuals. BMC Musculoskelet Disord 25 , 391 (2024). https://doi.org/10.1186/s12891-024-07486-y
Download citation
Received : 14 August 2023
Accepted : 02 May 2024
Published : 18 May 2024
DOI : https://doi.org/10.1186/s12891-024-07486-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cerebral palsy
- Pain intensity
- Lower extremities
BMC Musculoskeletal Disorders
ISSN: 1471-2474
- Submission enquiries: [email protected]
- General enquiries: [email protected]
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Risk Factors
- Research Summary
Tracking Methods for Cerebral Palsy
What to know.
CDC tracks the number and characteristics of children with cerebral palsy (CP) over time. Keep reading to learn more about how the data are collected and how they can be used to support people with CP and their families.

Why data is being collected
By tracking the number of children diagnosed with CP over time, it is possible to find out if the number is rising, dropping, or staying the same. We can compare the number of children with CP in different groups of people and in different areas of the country.
The more information there is about children with CP in different groups and in different areas of the country, the better we can do the following:
- Help identify causes and risk factors of CP
- Evaluate the effectiveness of prevention efforts
- Raise awareness of the signs and symptoms
- Help families and communities plan for services
What CDC is doing
CDC has been studying CP since the early 1980s. CDC tracks the number and characteristics of children with CP living in several diverse communities across the United States. Communities can use CDC's information on the number and characteristics of children with CP, such as subtype, walking ability, and co-occurring conditions to plan for services, guide policy, and promote full participation in community and family life. Information about the co-occurrence of CP and other conditions, such as autism spectrum disorder, can also help direct research into shared risk factors and causes.
Below is a brief overview of the programs that CDC has or continues to support to help us learn more about the number and characteristics of children with CP in the United States.
CDC's Autism and Developmental Disabilities Monitoring (ADDM) Network
CDC has resumed CP activities within the ADDM Network, focused on tracking and monitoring CP at 4 funded sites (Minnesota, Missouri, Utah, and Tennessee), and one CDC-managed site in Georgia (MADDSP).
CP activities were re-established across the ADDM Network in 2023 and will begin to:
- Assess a state's capacity for conducting CP surveillance.
- Pilot surveillance methods for reporting prevalence and early identification of CP among children aged 4 and 8 in their ADDM Network community.
- Report preliminary findings of piloting CP surveillance and develop recommendations for inclusion of CP in surveillance year 2024 activities.
- Implement CP surveillance methodology for surveillance year 2024.
Metropolitan Atlanta Developmental Disabilities Surveillance Program (MADDSP)
MADDSP was established in 1991 to identify children with four disabilities (CP, hearing loss, intellectual disability, and vision impairment). A fifth disability, autism spectrum disorder, was added to the program in 1996. MADDSP conducts ongoing tracking for developmental disabilities among 4-, 8- and 16-year-old children living in the metropolitan Atlanta area. This program has contributed a wealth of information on the characteristics, risk factors, costs, and implications of developmental disabilities, including CP.
Metropolitan Atlanta Developmental Disabilities Study (MADDS)
CDC began looking at how many children in metropolitan Atlanta had CP in the mid-1980s. This project was done as part of the Metropolitan Atlanta Developmental Disabilities Study (MADDS), which studied how common certain disabilities were in 10-year-old children . This study served as the basis for the creation of Metropolitan Atlanta Developmental Disabilities Surveillance Program (MADDSP).
One of the key findings of this study was that 16% of children acquired CP more than 28 days after birth. The acquired CP cases were due to the following:
- Infections, such as meningitis or encephalitis
- Head trauma, for example, from a motor vehicle accident or fall
- Cerebrovascular accidents, that is, bleeding or a blood clot in the brain
- Anoxia or lack of oxygen to the brain
- Low blood sugar
- Yeargin-Allsopp M, Murphy CC, Oakley GP, Sikes RK. A multiple-source method for studying the prevalence of developmental disabilities in children: the Metropolitan Atlanta Developmental Disabilities Study . Pediatrics. 1992 Apr;89(4 Pt 1):624-30. Erratum in: Pediatrics 1992 Dec;90(6):1001.
Cerebral Palsy (CP)
Cerebral palsy (CP) is a group of disorders that affect a person’s ability to move and maintain balance and posture. CP is the most common motor disability in childhood.
- Study Protocol
- Open access
- Published: 14 May 2024
Can on-line gait training improve clinical practice? Study protocol for feasibility randomised controlled trial of an on-line educational intervention to improve clinician’s gait-related decision-making in ambulant children and young people with cerebral palsy
- Anna Hebda-Boon ORCID: orcid.org/0000-0002-7091-2828 1 ,
- Adam P. Shortland 2 ,
- Aleksandra Birn-Jeffery 3 &
- Dylan Morrissey 1 , 4
Pilot and Feasibility Studies volume 10 , Article number: 76 ( 2024 ) Cite this article
77 Accesses
Metrics details
Instrumented gait analysis (IGA) is an assessment and research tool with proven impacts on clinical decision-making for the management of ambulant children and young people with cerebral palsy (CYPwCP) but is underused and variably understood by relevant clinicians. Clinicians’ difficulties in gaining expertise and confidence in using IGA are multifactorial and related to access for clinical decision-making, limited training opportunities and inability to translate this training into clinical practice.
The primary aim of this study is to test the feasibility of an educational intervention to advance clinicians’ application of gait analysis in CYPwCP, to inform a definitive trial. The secondary aim is to measure the effect that appropriate IGA training has on physiotherapists’ knowledge, skills, confidence and behaviours. This will be a two-arm feasibility randomised controlled trial with an experimental and control group. The 6-week on-line intervention uses a multicomponent approach grounded in behavioural change techniques. A repeated measures design will be adopted, whereby participants will complete outcome measures at baseline, immediately after the intervention and at 4 months. The primary outcome measures (trial feasibility-related outcomes) are recruitment and engagement. The secondary outcome measures (trial research-related outcomes) are knowledge, skills, confidence and practice change. Outcome measures will be collected via online questionnaires and during observed skill assessments. Analysis of data will use descriptive statistics, two-way mixed ANOVA model and qualitative content analysis.
This study will determine feasibility of the definitive randomised control trial of educational intervention delivered to advance clinicians’ application of gait analysis in CYPwCP. This study offers the shift in emphasis from regarding IGA as a tool to a focus on clinicians’ requirements for access, training and a well-defined role to optimise utilisation of IGA. The impact of this should be better engagement with IGA and clinical practice change. This study will contribute to a body of educational research into clinical education of healthcare professionals and IGA training offering insight into high levels of evaluation evidence including clinical behaviour change.
Trial registration
Protocol has been registered with the Open Science Framework (osf.io/nweq6) in June 2023.
Peer Review reports
The National Institute for Clinical Excellence (NICE) refers to instrumented gait analysis (IGA) assessment as a preferable choice prior to gait-improving orthopaedic surgery [ 1 ]. The impact of IGA on decision-making in treatment planning and treatment outcomes for ambulant CYPwCP has been broadly debated in the literature particularly in areas of orthopaedic decision-making [ 2 , 3 , 4 , 5 ] and individually tailored nonsurgical treatments [ 6 , 7 ]. Generally, single event multilevel surgeries (SEMLS) are performed after IGA is conducted as the IGA results can help to determine which specific soft-tissue or bony surgical procedures should be performed [ 8 ]. Furthermore, studies show that use of IGA for treatment decision-making has potential to improve patient outcomes — authors indicate the positive gait-related outcomes and improvement in gait parameters when treatment matches IGA recommendations [ 9 , 10 , 11 ]. Despite this, more standardised access pathways for CYPwCP to IGA are yet to be established [ 7 , 12 ], and access to the IGA for other professionals involved in gait management such as physiotherapists or orthotists and their formal IGA education remains limited [ 13 ]. As a science, gait analysis brings a wide spectrum of knowledge and skills, making it hard to educate and successfully integrate it into undergraduate curricula [ 14 ]. Clinicians’ difficulties in gaining expertise and confidence in using IGA are multifactorial and can be related to lack of IGA access for clinical decision-making, limited training opportunities and inability to translate this training into clinical practice [ 15 ].
According to research, clinician-centred factors such as IGA training and affiliation to IGA laboratory [ 16 ] are shown to influence engagement with IGA-derived recommendations and may therefore impact on patient outcomes [ 17 ].
This indicates a required shift in emphasis from regarding IGA as a tool providing 3rd party recommendations to a focus on clinicians’ requirements for access, training and a well-defined role to optimise utilisation of IGA [ 17 ]. This is essential to address in order to improve inequity of access and patient outcomes. Findings of our previous research [ 15 , 17 ] provided context for the design and delivery of a feasibility randomised controlled trial (RCT) of an educational intervention to improve clinicians’ engagement with the IGA.
Study aims and objectives
The primary aim of this study is to determine the feasibility of an educational intervention to advance clinicians’ application of instrumented gait analysis in children and young people with cerebral palsy, to inform the design of a full trial. Objectives are as follows:
To establish the feasibility of a future randomised controlled trial of educational intervention.
Assess the rate of participant enrolment, retention and compliance with intervention.
Assess whether the inclusion and exclusion criteria for participants are appropriate.
Assess whether the duration of intervention is appropriate.
Assess whether intervention delivery in a virtual learning environment is feasible and acceptable.
Explore if the outcome measures are appropriate for the study aims.
Define the sample size for a definitive trial.
Explore the fidelity of intervention delivery.
Further understand the barriers and facilitators of the intervention.
The secondary aim is to measure the effect that appropriate IGA training and its delivery has on physiotherapists’ knowledge, skills and attitudes.
This feasibility trial protocol follows the SPIRIT statement on defining standard protocol items for clinical trials and its checklist [ 18 ] and the CONSORT statement extension to randomised pilot and feasibility trials and its checklist [ 19 ].
Trial design
This will be a two-arm feasibility randomised controlled trial with an experimental and control group. The 6-week on-line intervention delivered as part of the trial is a stand-alone, post-graduate level educational course called Virtual Gait Analysis Course for Paediatric Physiotherapists (VGAPP). Eligible physiotherapists who consent to take part in the study will be randomly allocated into experimental and control groups. A repeated measures design will be adopted, whereby participants will complete outcome measures at baseline, immediately after the intervention, and at 4 months. This will include collection of feedback as part of a full process evaluation.
The trial will be determined feasible if a priori set criteria based on primary outcome measures and included in the process evaluation will be achieved at or above agreed levels (see the ‘ Outcome measures ’ section of ‘ Methods ’). After conducting and reviewing outcomes of the full evaluation process, the decision about delivery of the definitive trial will be made.
Figure 1 shows the study flow diagram, and Table 1 indicates the schedule of enrolment, intervention, and outcome measures [ 18 ].
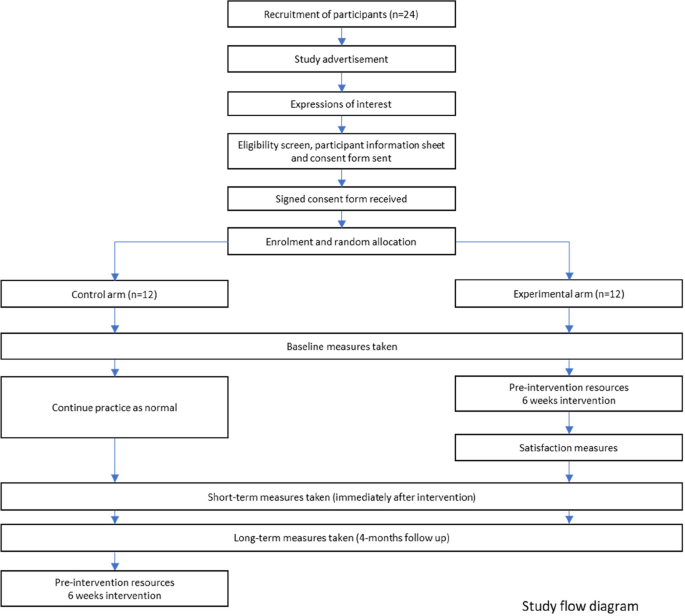
Study flow diagram
Participants
Study setting.
This study will be conducted virtually using Queen Mary University of London (QMUL) virtual learning environment (VLE), online questionnaires (SurveyMonkey), and Microsoft Teams, eradicating the need for participants to travel, reducing both cost and participants’ time. Participating clinicians will be working in a variety of settings (acute and community, special schools, both national health service and private settings) within the UK, where the data will be collected. Each participant’s data will be collected under their unique student number. To ensure anonymity, once data collection is complete, student numbers will be additionally coded.
Eligibility criteria
The aim of the inclusion and exclusion criteria is to ensure that participants are actively involved in assessment and treatment of ambulant CYPwCP and have currently available opportunities to apply the taught knowledge and skills in their workplace. The eligibility criteria were reviewed during the stakeholder focus groups including both clinicians and educators. Focus groups found inclusion and exclusion criteria appropriate for the feasibility trial (see Supplementary material).
Inclusion criteria are as follows:
18 years of age or older
Physiotherapists currently providing assessment and treatment to ambulant children and young people with cerebral palsy
Practicing within the UK (any National Health Service or private practice setting)
Exclusion criteria are as follows:
Outside of UK
Not currently employed as physiotherapist or on a career break
In rotational posts, where they could rotate to specialty not managing ambulant CYPwCP
Intervention
Design and refinement.
This educational intervention uses a multicomponent approach grounded in behavioural change techniques (BCTs). The overall aim of the intervention is to improve gait-related clinical practice.
Intervention (VGAPP) will be delivered via QMUL VLE and will comprise of pre-course resources and a 6-week course. Content of the VGAPP course has been developed based on evidence from the scientific literature, current best practice and informed by the scoping review [ 17 ], qualitative study [ 15 ] and results from a national survey of paediatric physiotherapists in the UK (unpublished, in review). Stakeholder engagement has been integral to the research and intervention design, delivery and evaluation process and included Patient and Families (PPI-A) interviews and Clinicians and Educators Focus Groups (PPI-B) (Fig. 2 ). PPI-A included children, young people and their families who have a lived experience of cerebral palsy and received IGA as part of management of their condition. PPI-A was involved in the design of intervention prior to involving clinicians in order to ensure that the project is centred around the needs of patients and to ensure that the practice behaviour change, and transfer of knowledge will directly benefit patients and their families. Themes, subthemes and illustrative quotes from patients and parents’ interviews and changes applied to the intervention and evaluation content are available in the Supplementary Table 1 . PPI-B were representatives from all UK nations, with a variety of paediatric physiotherapy specialisms, experience levels and from different work settings, thus providing invaluable insight and the opportunity for further refinement of the intervention design (in the areas of recruitment, eligibility criteria, sample size, control group intervention), content, delivery and evaluation methods. Themes, subthemes, and illustrative quotes from clinicians and educators focus groups and changes applied to intervention and evaluation content are available in the Supplementary Table 2 .
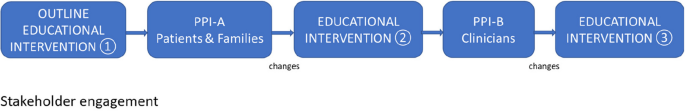
Stakeholder engagement
Through this process, several changes were implemented to the intervention content and assessment process in areas of communication, patient/family perspectives, orthotics, and linking elements of gait-related practice to the ICF domains. A detailed PPI involvement report, including the educational intervention refinement process is available from the corresponding author on reasonable request.
Pre-intervention resources
Pre-intervention resources will include the pre-course manual, ‘meet and greet’ forum and the reading list. Participants will be able to complete a self-diagnostic tool to identify and reflect on their current IGA engagement and barriers to confident gait-related practice.
Intervention components
The intervention will be a stand-alone, post-graduate level educational event delivered fully on-line. It will employ the delivery of weekly on-line plenary sessions incorporating active learning — synchronous on-line problem-based learning sessions and seminars integrating elements of experimental learning within the learning community. These sessions will be delivered by experienced educators and clinicians working in the instrumented gait analysis laboratories, with a track record of delivering education within the field of gait analysis and paediatric neurodisability. Educators will be approached via email by the lead researcher. Content of the intervention will encompass an array of gait analysis methods and an overview of equipment currently used in the clinical practice. This will include but will not be limited to clinical outcome measures, measurement software, videography techniques and setup, 3-dimensional motion laboratory equipment, and laboratory setup (examples of Vicon and Codamotion Systems). Intervention will comprise of weekly tasks (asynchronous) to facilitate revision and application in practice and formative assessment/feedback opportunities (short knowledge quizzes, open questions within the discussion forum) to support learning autonomy and facilitate participant’s recall and self-regulation. Table 2 provides an indicative number of hours for each activity to give an overall picture of the workload a participant would be expected to undertake.
The intended learning outcomes (ILOs) have been designed and benchmarked against the QAA Statements Physiotherapy (2001) Academic Content.
Academic content is as follows:
Demonstrates an understanding of the interdisciplinary knowledge that underpins gait analysis practice including elements of human anatomy, biomechanics, and gross motor development: C1
Demonstrates an understanding of the principles of typical gait pattern and how movement patterns are likely to be affected by some of the childhood diseases: C1
Demonstrates an understanding of the available measurement technologies and the principles on which they are based: C1
Disciplinary skills are as follows:
Applies variety of gait assessment methods in context of own practice and service delivery: B1 and C2
Uses the gait analysis outputs in clinical practice to aid treatment decision-making and measurement — in line with clinical reasoning paradigms and evidence-based practice: A1, B1, and C2
Communicates assessment findings and gait-related decision-making effectively with multidisciplinary team, patients, and families: A2, A3, B2, and C2
Attributes are as follows:
Cultivates an individualised, patient-centred approach to assessment and treatment planning: B2
Reflects on own practice to identify the needs within own role and wider aspects of service delivery: A3, A4, and B2 (health and social care equivalent B4)
Demonstrates a creative drive to implement the knowledge and skills, improve own practice, and support development of others: A3, A4, and B2 (health and social care equivalent B3)
Behaviour change techniques (BCT)
Utilisation of the BCT taxonomy [ 20 ] will support refinement of the targeted behaviours. It will also support the process evaluation analysis to gain understanding of how the change is expected to take place [ 21 ] and related barriers and facilitators of implementing the feasibility trial. To support knowledge transfer, several behaviour change techniques will be used in the intervention content.
Prior to the course, participants will gain access to a diagnostic session to identify potential internal and/or external barriers to their gait-related practice. They will be encouraged to set their personal and service goals and will be supported in making plans for delivery. Participants will share their plans and progress as part of the evaluation process.
A variety of synchronous (problem-based learning sessions) and asynchronous resources (lectures, reading links and podcasts) will incorporate instruction on how to perform new or refined gait-related practice behaviours. These resources will also support shaping of the participant’s knowledge through instruction and demonstration on how to perform the behaviours and setting clinically oriented practical tasks focusing on the behaviour. Throughout the course, participants will be provided strategies to support behaviours through associations such as regular prompts and cues, ideas on restructuring of their clinical environment to improve their gait assessment quality and techniques, or through objects which could be added into their environment (such as outcome measure templates — digital and/or printed). A virtual learning community, created through group chats and discussion forums, will aim to support emergence of the identity associated with changed behaviours.
Figure 3 outlines the simplified logic model of the study.
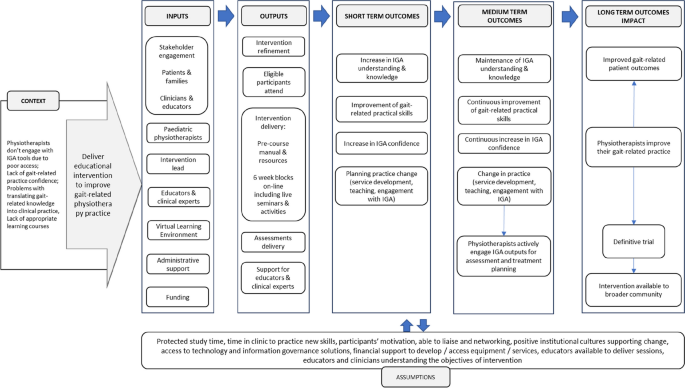
Feasibility RCT study logic model
Control group intervention
To compare the effects of the intervention against usual practice, participants allocated into the control group will be asked to continue with their usual practice. At the point of enrolment, the control group will gain access to the virtual learning environment and receive basic orientation resources, but no training or guidance will be offered during this time. Participants in the control group will be asked to complete the same measurements as those in the intervention group and at the same timepoints (Table 1 ). The control group will be offered the full intervention after the completion of the third round of assessments. Provision of educational content and its timing in the control group were reviewed during the stakeholder focus groups including of clinicians and educators.
Outcome measures
Outcome measures were grouped as primary outcome measures (trial feasibility-related outcomes) and secondary outcome measures (trial research-related outcomes) collated in Table 3 .
Recruitment will be determined as feasible if study is able to recruit 24 participants within 4 months [ 22 , 23 ]. Retention rates will be considered at two stages: (1) from expression of interest to consent — it will be deemed feasible if greater than 50%, and (2) from consent to course completion — it will be deemed feasible if greater than 75% [ 24 , 25 ]. Additionally, engagement (participants’ interactions with an online system) data will be collected during intervention via the analytics tools in the QMUL Virtual Learning Environment which log the detail of activity access, time, and completion for each component. These analytic tools are part of the general-purpose dashboard and provide an algorithmic representation of student online behaviours based on whether the behaviour occurred and for how long, rather than quality of these behaviours. Previous studies show that these analytics have been positively correlated with student performance [ 26 , 27 , 28 ]. It will be deemed feasible if the average proportion of completed learning sessions and tasks will be ≥ 66%.
Secondary outcomes are as follows: knowledge, skills, attitudes, and satisfaction will be collected via online questionnaires (SurveyMonkey) and during skill tests (OSCE). Knowledge, skills, and attitudes will be collected at three timepoints (Table 1 ).
Baseline (pre-intervention)
Questionnaire including background (demographics, current gait analysis practice, access to IGA equipment, barriers to gait analysis practice), attitudes (reasons for joining the study, anticipated changes in practice after the intervention, beliefs), confidence (self-rated), and knowledge (self-rated and multiple-choice question test)
Objective structured clinical examination (OSCE) of a patient case: Assessment will be delivered on-line, recorded and scored against a standardised scoring sheet including gait-related clinical reasoning and treatment planning based on evidence and findings, problem-solving, systematicity of approach, ability to link various types of gait-related information, confidence in engagement with gait data, analysis of gait graphs, communication (including use of gait-related terminology, providing lay explanations to a parent), and implementation of biopsychosocial model or ICF to decision-making
Post intervention (immediately after 6-week intervention)
Questionnaire including attitudes (planning practice change, implemented practice change, beliefs), confidence (self-rated), knowledge (self-rated and multiple-choice question test), and satisfaction (experimental group only)
OSCE of a different patient case (scored against the same criteria as at baseline)
Re-test (4-month post-intervention)
Questionnaire attitudes (planning practice change, implemented practice change, beliefs), confidence (self-rated), and knowledge (self-rated and multiple-choice question test)
Knowledge and skills retention as well as attitudes will be measured between timepoints, with a focus on changes between baseline and immediately post intervention and at 4-month follow-up. Satisfaction questionnaire will contain 28 items, each assessed on a 5-point Likert scale, related to the relevance and scientific quality of the content, the educational structure, and delivery. Satisfaction feedback will be collected immediately after intervention delivery (experimental group).
Sample size
Considering the study objectives and recommendations, the target sample size will be of a minimum 12 participants per trial arm; therefore, a minimum of 24 in total is anticipated. Guidance from the National Institute for Health Research (NIHR) indicates that a sample size of 30 is appropriate to answer the questions posed by a feasibility trial [ 23 ]. A lower number of participants will be better suited for an educational intervention for clinicians — it will ensure delivery of a high-quality learning experience and allow for active engagement with tutors during problem-based learning within the experimental group. Furthermore, the stakeholder focus groups including of clinicians and educators reviewed the proposed sample size and reported it as appropriate for the feasibility trial.
Recruitment
Participants will be recruited via the largest national paediatric physiotherapy network (Association of Chartered Paediatric Physiotherapists) using bulletins, social media, and targeted emails to team leads across the UK. The advertisement will provide general information about the intervention and the research study together with inclusion and exclusion criteria. Upon expression of interest, participants will be screened against eligibility criteria, and the participant’s information sheet and consent form will be sent to prospective participants via email. Participants will return signed consent forms electronically to the research lead. In line with advice from the Clinician and Educator Focus Group (PPI-B), the recruitment of study participants will commence early to ensure that participants are able to make suitable arrangements in the workplace, such as request study leave and ‘block time’ to attend synchronous sessions etc.
Participant timeline
Time schedule of enrolment, intervention, and assessments is presented in Table 1 . After the eligibility criteria screen and receipt of their written informed consent, 24 participants will be enrolled to the study. After random allocation to the trial arms, participants will receive access to the password-protected online platform hosted by Queen Mary University of London. All participants will be asked to complete the baseline assessment including the questionnaire (background, attitudes, knowledge, and skills) and objective structured clinical examination (OSCE) of a patient case (assessment will be delivered on-line, recorded, and scored against standardised scoring sheet). After completing the baseline assessment, participants assigned to the experimental arm will gain access to the pre-course learning resources (6 weeks prior to start of the course). The experimental group will commence the 6 week blocks of intervention including pre-recorded resources, problem-based learning tasks, discussion forums, and live sessions. At 6 weeks, participants from both arms will be asked to complete the second assessment including the questionnaire (attitudes, knowledge and skills, and satisfaction scores in experimental group only) and the second OSCE of a patient case. Four months after the intervention, participants in both trial arms will be asked to complete the third assessment including the questionnaire (attitudes, knowledge, and skills) and the OSCE of a patient case. Once all the data is collected, participants in the control group will gain access to the prereading resources and start the 6-weekly intervention sessions.
Assignment of intervention
Allocation, concealment mechanism, and implementation.
Participants who meet the inclusion criteria and return the consent form will be assigned an ID number in the Microsoft Excel spreadsheet. Participants will be assigned to groups randomly. In case there are more eligible physiotherapists than spaces, participants will be chosen by the number generation software which will be used in the allocation process. This will be conducted by an external person not related to the study or the research team. To avoid contamination, participants from the same healthcare trusts will be randomised to the same group.
Information about group randomisation will be provided in the participant’s information sheet. Participants in this study will not be blinded to the group allocation or deceived. This was discussed in the stakeholder focus groups who agreed that in the context of clinical practice, deceiving participants could mean a loss of their study/annual leave if pre-booked specifically to attend the intervention as well as potential cancelations of clinics in the control group. Participants will be informed about their allocation at the time of receiving instructions with the QMUL VLE platform access. At this time, the control group will be informed about timings of gaining their access to the full intervention and all resources provided to the experimental group after final assessments are completed. Participants will be informed that they are free to withdraw at any time without needing to provide a reason and with no penalties or detrimental effects.
Data collection, management, and analysis
In line with accepted practice for feasibility studies, no power analysis will be conducted, and all analyses will be exploratory only [ 29 ]. Data analysis will be performed after the last trial participant has completed final assessments (outcomes at 4 months post intervention). Data will be managed initially in Microsoft Excel software and analysed using IBM SPSS statistics software. Table 3 provides a summary of outcome measures, hypotheses, and analysis planned in the study.
Data management and research governance
A baseline table (descriptive statistics and frequencies) will compare the demographic and clinical characteristics including gender, age, experience, education, practice setting, contract type, study leave availability to participate in intervention, access to equipment, and gait analysis training. The primary outcomes will be reported using descriptive statistics. The quantitative variables will be presented as means and standard deviations.
A preliminary analysis of between-group differences will be conducted to determine the range of potential effect sizes from repeated measures ANOVA. Feasibility outcomes will be presented as number of participants meeting the a priori definitions. Kendall’s tau-b ( τ b ) correlation coefficient will be used to measure of the strength and direction of association that exists between two variables measured on at least an ordinal scale. To explore the extent and patterns of missing outcome data, we will report the proportion of missing values per item and the proportion of participants who will complete all items on the questionnaires. The proportion of missing data will also be reported for the other key outcomes and compared between the participants from intervention and control groups.
Qualitative data will be analysed according to the framework approach [ 30 ], a realist approach located within an interpretivist frame. The opinions and experiences of participants will be explored to understand any barriers and facilitators related to running of the educational intervention. During active familiarisation, the textual data will be coded, and codes will be organised into themes and subthemes to construct a thematic framework to aid indexing. To ensure rigour and consistency, the analysis process will undergo investigator triangulation. In this process, different observers, examiners, and analysts will compare and check data collection and/or interpretation [ 30 , 31 ]. Qualitative data will be presented as quotes and descriptive summaries.
Process evaluation and implementation outcomes
The process evaluation has been informed by Medical Research Council guidance on process evaluation of complex interventions [ 32 , 33 ] and the Implementation Outcome Framework (IOF) [ 34 ]. Proctor et al. described eight implementation outcomes in the IOF: acceptability, adoption, appropriateness, feasibility, fidelity, implementation cost, penetration (or coverage), and sustainability. Each of these implementation outcomes aligns with important considerations for trial design and implementation; however, the ‘adoption’ outcome does not directly align with process evaluation of our current feasibility trial design and delivery, as it is not offered by other educational providers. Therefore, seven out of eight implementation outcomes will be included in this process evaluation. Acceptability of the intervention and of the assessments will include data on the duration, content, and delivery methods (including satisfaction scores). Synthesis of satisfaction scores, feedback, and reports on participants’ logistics related to taking part in the trial (protected study time, ensuring opportunities in practice, assessment burden) will be carried out. The findings will be supplemented with observations made by the researchers, educators, administrative staff, and examiners throughout the implementation of the intervention. Collectively, these will provide information on the acceptability of the trial measurements and the intervention. Feasibility measures will include participant recruitment rate, retention, and engagement thresholds as described in the ‘ Methods ’ section. The process evaluation will include analysis of proportion of eligible participants being offered trial and, if possible, proportion of participants in the population represented by eligibility criteria (coverage).
Baseline comparisons will be conducted to detect any substantial differences between participants recruited from the control and intervention arms. Sample size and anticipated effect size defined for the definitive trial will be reviewed and assessed for feasibility. Participant withdrawals and number of participants lost to follow-up (and where possible reasons and participants’ key baseline characteristics) will be analysed. The study protocol adherence will be reviewed within the research team. Fidelity to the trial protocol including follow-up, dosage of the intervention, crossover between study arms, and adherence to intervention delivery plan will be assessed against study protocol and participant timelines. Any changes to the protocol will be reported.
Furthermore, appropriateness of the trial design for the trial aim, inclusion and exclusion criteria, outcome measures, and intervention components will undergo an exploratory analysis of participants’ outcomes, engagement with content, and assessments, together with qualitative analysis of participants and educators’ feedback. Sustained participant interest throughout the trial period and sustained staffing levels to deliver and facilitate participants’ learning journey during intervention will be explored to inform the sustainability criteria for the definitive trial. The implementation cost analysis will be explored with the aim to inform the design of a full cost-utility analysis alongside a future definitive trial. Implementation cost will include the cost of administration involved in running the trial and cost related to production and delivery of the intervention and assessment components — such as speaker fees, and OSCE examiners and moderators will be reviewed.
In addition, the COM-B model and the behaviour change techniques taxonomy (BCTT) [ 35 ], widely used frameworks in behaviour change and implementation research, will support the process evaluation analysis and an in-depth exploration of the barriers and facilitators of implementing the feasibility trial.
This article describes the protocol of a study evaluating the feasibility of conducting definitive RCT of the educational intervention for paediatric physiotherapists working with ambulant CYPwCP in the UK. This feasibility study was designed to assess predefined criteria related to the evaluation design (such as reducing uncertainty around recruitment, retention, choice of outcomes, analysis) and the intervention (its content and delivery, acceptability, adherence, cost-effectiveness, etc.) in line with the current guidance [ 32 , 33 ].
The educational intervention planned for this trial intends to integrate the complexity of knowledge, skills within the realities of clinicians’ practice to support knowledge translation to influence the practice behaviour change. Due to its complexity, the design of the study was preceded by in-depth research studies of the intervention’s context and implementation factors within the clinical practice reality of paediatric physiotherapists. This included close collaboration with stakeholders — patients and their families, clinicians, and clinical educators [ 33 ].
The need for gait analysis training was clearly identified in previous study of physiotherapists in the UK [ 13 ]. Despite extensive gait-related practice [ 36 , 37 ], evidence of how paediatric physiotherapists engage with instrumentation or access the IGA training is sparse. There are currently many gait-related courses available world-wide delivered by a variety of providers specifically targeting this clinical group (CMAS workshop 2023). Although there is a rich training offer, the impact of training on skills and behaviour, evaluation of needs, and barriers to knowledge transfer are not addressed in the current literature showing an evidence gap (CMAS 2023 education workshop). The impact of existing educational interventions is rarely reported [ 38 , 39 ] and concerns low levels of evaluation evidence, omitting evaluation clinical behaviour change or organisational impact. Our previous studies show that transfer of gait-related knowledge from the classroom to the clinic room also poses challenges to clinicians at different levels of practice expertise [ 15 ]. The lack of institutional resources (financial, such as availability of funding for staff’s training or limited study leave), spatial and temporal to promote implementation of new procedural skills and motivation to engage with learning, may also influence low uptake of professional training.
One of the main challenges will be associated with possible low uptake in the study and high drop-out rate. High work pressures and limited time to study may result in reduced opportunity or willingness to participate in the intervention and multiple assessments.
Limitations
Participants in this trial will not be blinded to allocation. After discussions within the research team and stakeholder focus groups, it was decided that if a participant secures study leave to take part in the 6-week intervention (potentially taking time off clinical work which may lead to cancellation of clinics) and would not receive the intervention due to allocation to the control group — this may result in loss of study leave and could have a potentially negative impact on the patient’s care by added waiting time.
The intervention lead is a paediatric physiotherapist experienced in gait-related practice which may be a source of potential bias. To mitigate this risk, multiple educators and clinical experts will be appointed to co-deliver the intervention, and additional examiners and moderators will be blinded to participants’ allocation. The intervention lead will keep a reflective diary and will have access to de-brief meetings within the research team [ 40 ]. Involvement of a considerable number of experts co-delivering the content of the intervention may pose risk to intervention integrity. To mitigate this risk, the intervention lead will be providing detailed 1:1 briefing about the study, targeted behaviours, session aims, and ILOs.
Generalisability
A relatively small sample planned for this feasibility study may pose questions regarding the applicability of findings to the future definitive trial and other studies. To ensure that the feasibility sample is representative of the UK paediatric physiotherapists, the study will be broadly advertised to reach therapists in all four UK countries and across the healthcare sectors.
Despite the extensive context research, a wide array of primary and secondary outcome measures planned to be used in the process evaluation, there may be factors influential to the trial but not be captured by the feasibility testing. Use of MRC guidance on process evaluation of complex interventions [ 32 , 33 ] and the IOF [ 34 ] will ensure thorough investigation of the change mechanisms and how the effects will occur [ 32 , 41 ]. Furthermore, the COM-B model and BCTT [ 35 ] are useful tools to characterise the targeted behaviours and content of educational interventions focused on continuing professional development in healthcare [ 42 ]. These were used throughout design of the study and will support the process evaluation to further advance understanding of their mechanisms of action.
With the detailed planning of this protocol and careful consideration of challenges and limitations, this study will offer essential preliminary data about the feasibility of implementing the VGAPP intervention to improve gait-related practice of paediatric physiotherapists in the UK. Study findings will provide a comprehensive understanding of whether a full randomised control trial is viable and identify any areas which could be enhanced. Furthermore, this study will contribute to a body of educational research into clinical training of healthcare professionals and IGA training.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
Behaviour change techniques taxonomy
Clinical Movement Analysis Society
Capability, opportunity, motivation, behaviour model
Consolidated Standards of Reporting Trials for Pilot and Feasibility trials
Children and young people with cerebral palsy
International Classification of Functioning, Disability and Health
- Instrumented gait analysis
Intended learning outcomes
Implementation Outcome Framework
Medical Research Council
National Institute for Clinical Excellence
Objective structured clinical examination
Patient and public involvement
Standard Protocol Items: Recommendations for Interventional Trials
Virtual gait analysis course for paediatric physiotherapists
Virtual learning environment
NICE. Clinical guideline [CG145] Spasticity in under 19s: management. https://www.nice.org.uk/guidance/cg145/chapter/1-guidance2016 .
Wren TA, Lening C, Rethlefsen SA, Kay RM. Impact of gait analysis on correction of excessive hip internal rotation in ambulatory children with cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2013;55(10):919–25.
Article PubMed Google Scholar
Theologis T, Stebbins J. The use of gait analysis in the treatment of pediatric foot and ankle disorders. Foot Ankle Clin. 2010;15(2):365–82.
Kay RM, Wren TA, Bowen RE, Otsuka NY, Scaduto AA, Chan LS, et al. Influence of gait analysis on decision-making for lower extremity surgery. Dev Med Child Neurol. 2009;51:1.
Google Scholar
Lofterod B, Terjesen T, Skaaret I, Huse AB, Jahnsen R. Preoperative gait analysis has a substantial effect on orthopedic decision making in children with cerebral palsy - comparison between clinical evaluation and gait analysis in 60 patients. Acta Orthop. 2007;78(1):74–80.
Franki I, De Cat J, Deschepper E, Molenaers G, Desloovere K, Himpens E, et al. A clinical decision framework for the identification of main problems and treatment goals for ambulant children with bilateral spastic cerebral palsy. Res Dev Disabil. 2014;35(5):1160–76.
Rasmussen HM, Pedersen NW, Overgaard S, Hansen LK, Dunkhase-Heinl U, Petkov Y, et al. Gait analysis for individually tailored interdisciplinary interventions in children with cerebral palsy: a randomized controlled trial. Dev Med Child Neurol. 2019;61(10):1189–95.
McGinley J, Dobson F, Ganeshalingham R, Shore B, Rutz E, Graham HK. A systematic review of single event multilevel surgery for children with cerebral palsy. Dev Med Child Neurol. 2012;54:54–5.
Article Google Scholar
Wren T, Otsuka N, Bowen R, Scaduto A, Chan L, Dennis S, et al. Outcomes of lower extremity orthopaedic surgery in ambulatory children with cerebral palsy with and without gait analysis: results of a randomised controlled trial. Gait Posture. 2013;38:236–41.
Gough M, Shortland AP. Can clinical gait analysis guide the management of ambulant children with bilateral spastic cerebral palsy? J Pediatr Orthop. 2008;28(8):879–83.
Chang FM, Seidl AJ, Muthusamy K, Meininger AK, Carollo JJ. Effectiveness of instrumented gait analysis in children with cerebral palsy–comparison of outcomes. J Pediatr Orthop. 2006;26(5):612–6.
Gaston MS. CPIPS: musculoskeletal and hip surveillance for children with cerebral palsy. Paediatr Child Health. 2019;29(11):489–94.
Toro B, Nester C, Farren P. The status of gait assessment among physiotherapists in the United Kingdom. Arch Phys Med Rehab. 2003;84(12):1878–84.
Baker R, Esquenazi A, Benedetti MG, Desloovere K. Gait analysis: clinical facts. Eur J Phys Rehabil Med. 2016;52(4):560–74.
PubMed Google Scholar
Hebda-Boon A, Zhang B, Amankwah A, Shortland AP, Morrissey D. Clinicians’ experiences of instrumented gait analysis in management of patients with cerebral palsy: a qualitative study. Phys Occup Ther Pediatr. 2022;42:1–13.
Wren TA, Elihu KJ, Mansour S, Rethlefsen SA, Ryan DD, Smith ML, et al. Differences in implementation of gait analysis recommendations based on affiliation with a gait laboratory. Gait Posture. 2013;37(2):206–9.
Hebda-Boon A, Tan XL, Tillmann R, Shortland AP, Firth GB, Morrissey D. The impact of instrumented gait analysis on decision-making in the interprofessional management of cerebral palsy: a scoping review. Eur J Paediatr Neurol. 2023;42:60–70.
Chan AW, Tetzlaff JM, Altman DG, Dickersin K, Moher D. SPIRIT 2013: new guidance for content of clinical trial protocols. Lancet. 2013;381(9861):91–2.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibil Stud. 2016;2:64.
Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321(7262):694–6.
Article CAS PubMed PubMed Central Google Scholar
Jacques RM, Ahmed R, Harper J, Ranjan A, Saeed I, Simpson RM, et al. Recruitment, consent and retention of participants in randomised controlled trials: a review of trials published in the National Institute for Health Research (NIHR) Journals Library (1997–2020). BMJ Open. 2022;12(2):e059230.
Article PubMed PubMed Central Google Scholar
Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–12.
Trivedi RB, Szarka JG, Beaver K, Brousseau K, Nevins E, Yancy WS Jr, et al. Recruitment and retention rates in behavioral trials involving patients and a support person: a systematic review. Contemp Clin Trials. 2013;36(1):307–18.
Poongothai S, Anjana RM, Aarthy R, Unnikrishnan R, Narayan KMV, Ali MK, et al. Strategies for participant retention in long term clinical trials: a participant -centric approaches. Perspect Clin Res. 2023;14(1):3–9.
Jayaprakash SM, Moody EW, Lauría EJM, Regan JR, Baron JD. Early alert of academically at-risk students: an open source analytics initiative. J Learn Analytics. 2014;1(1):6–47.
Macfadyen L, Dawson S. Numbers are not enough. Why e-learning analytics failed to inform an institutional strategic plan. Educational Technology & Society. 2012;15(3):149–63.
Atif A Froissard C, Liu DY, Richards D. Validating the effectiveness of the moodle engagement analytics plugin to predict student academic performance. Americas Conference on Information Systems. in 21st Americas Conference on Information Systems, AMCIS 2015 (pp 1-10).
Teresi JA, Yu X, Stewart AL, Hays RD. Guidelines for designing and evaluating feasibility pilot studies. Med Care. 2022;60(1):95–103.
Ritchie J. Qualitative research practice: a guide for social science students and researchers. 2nd ed. London: Sage; 2014.
Elliott R, Fischer CT, Rennie DL. Evolving guidelines for publication of qualitative research studies in psychology and related fields. Br J Clin Psychol. 1999;38(3):215–29.
Article CAS PubMed Google Scholar
Moore GF, Audrey S, Barker M, Bond L, Bonell C, Hardeman W, et al. Process evaluation of complex interventions: medical research council guidance. BMJ. 2015;350:h1258.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. Framework for the development and evaluation of complex interventions: gap analysis, workshop and consultation-informed update. Health Technol Assess. 2021;25(57):1–132.
Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76.
Michie S, Atkins L, West R. The behaviour change wheel. A guide to designing interventions. UK London.: Silverback publishing; 2014.
Franki I, Desloovere K, De Cat J, Feys H, Molenaers G, Calders P, et al. The evidence-base for basic physical therapy techniques targeting lower limb function in children with cerebral palsy: a systematic review using the international classification of functioning, disability and health as a conceptual framework. J Rehabil Med. 2012;44(5):385–95.
Rapson R, Latour JM, Marsden J, Hughes H, Carter B. Defining usual physiotherapy care in ambulant children with cerebral palsy in the United Kingdom: a mixed methods consensus study. Child Care Health Dev. 2022;48(5):708–23.
Malone JB, Burns JD, Belthur MV, Karlen JW. Motion laboratory gait analysis and orthopedic resident education: preliminary results. J Pediatr Orthop B. 2022;31(1):e65–8.
Baskwill A, Belli P, Keller L. Evaluation of a gait assessment module using 3D Motion capture technology. Int J Ther Massage Bodywork. 2017;10(1):3–9.
PubMed PubMed Central Google Scholar
Korstjens I, Moser A. Series: practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–4.
O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954.
Konnyu KJ, McCleary N, Presseau J, Ivers NM, Grimshaw JM. Behavior change techniques in continuing professional development. J Contin Educ Health Prof. 2020;40(4):268–73.
Download references
This study is funded by Private Physiotherapy Education Fund grant.
Author information
Authors and affiliations.
Sport and Exercise Medicine, Barts and the London School of Medicine and Dentistry, Queen Mary University of London, London, UK
Anna Hebda-Boon & Dylan Morrissey
School of Biomedical Engineering and Imaging Science, King’s College London, London, UK
Adam P. Shortland
School of Sport, Rehabilitation and Exercises Sciences, University of Essex, Essex, UK
Aleksandra Birn-Jeffery
Physiotherapy Department, Barts Health NHS Trust, London, UK
Dylan Morrissey
You can also search for this author in PubMed Google Scholar
Contributions
All authors made substantial contributions to the conception, design, data acquisition, analysis, and delivery of the protocol. All authors contributed to manuscript preparation.
Corresponding author
Correspondence to Anna Hebda-Boon .
Ethics declarations
Ethics approval and consent to participate.
The project has been granted ethical approval of the Queen Mary Ethics of Research Committee (reference number: QMERC20.531).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hebda-Boon, A., Shortland, A.P., Birn-Jeffery, A. et al. Can on-line gait training improve clinical practice? Study protocol for feasibility randomised controlled trial of an on-line educational intervention to improve clinician’s gait-related decision-making in ambulant children and young people with cerebral palsy. Pilot Feasibility Stud 10 , 76 (2024). https://doi.org/10.1186/s40814-024-01477-5
Download citation
Received : 09 August 2023
Accepted : 12 March 2024
Published : 14 May 2024
DOI : https://doi.org/10.1186/s40814-024-01477-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Gait analysis
- Cerebral palsy
- Physiotherapy
- Paediatric physiotherapy
- Educational intervention
- Clinical education
- Randomised controlled trial
Pilot and Feasibility Studies
ISSN: 2055-5784
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Genetics, not lack of oxygen, causes cerebral palsy in quarter of cases
The world's largest study of cerebral palsy (CP) genetics has discovered genetic defects are most likely responsible for more than a quarter of cases in Chinese children, rather than a lack of oxygen at birth as previously thought.
The study, published in the scientific journal, Nature Medicine used modern genomic sequencing and found mutations were significantly higher in CP cases with birth asphyxia, indicating a lack of oxygen could be secondary to the underlying genetic defect. The results are consistent with smaller studies globally.
More than 1,500 Chinese children with CP were involved in this research project, which was a collaborative effort between the University of Adelaide and Fudan University Shanghai, Zhengzhou University, Zhengzhou and associates.
The Australian team was led by obstetrician and University of Adelaide's Emeritus Professor Alastair MacLennan AO and human geneticist, Professor Jozef Gecz.
"24.5 per cent of Chinese children in the study had rare genetic variations linked to cerebral palsy. This revelation mirrors our earlier findings in our Australian cerebral palsy cohort, where up to one third of cases have genetic causes," said Professor Gecz, who is the University of Adelaide's Head of Neurogenetics at the Adelaide Medical School and the Robinson Research Institute.
"Our research shows at least some babies who experience birth asphyxia and are diagnosed with CP may have improper brain development as a result of the underlying genetic variants rather than a lack of oxygen.
"Crucially, clinically actionable treatments were found in 8.5 per cent of cases with a genetic cause. It is exciting to see how genetic pathways to cerebral palsy inform tailored treatments for these individuals."
Cerebral palsy affects movement and posture and is the most common motor disability in children. The disorder is diagnosed in up to 2 per 1000 children globally and is sometimes in association with epilepsy, autism and intellectual difficulties. Symptoms often emerge during infancy and early childhood and can range from mild to severe.
The research team identified 81 genes with causation mutations in the children with CP. These genes are known to play important roles in neural and embryonic development and may affect the molecular pathways responsible for respiration.
"A lack of oxygen at birth is often claimed to be the cause of CP in medical litigation following a diagnosis and this has led to the presumption that the condition is preventable with better obstetrics or midwifery. This is simply not the case," said Professor MacLennan, who has spent the past 30 years advocating that there is little scientific evidence to support the myth that cerebral palsy is due to trauma or lack of oxygen at birth.
Professor MacLennan said frequent litigation has been associated with a high increase in "defensive" caesarean delivery and high insurance premiums for obstetricians.
"These results highlight the need for early genetic testing in children with cerebral palsy, especially those with risk factors like birth asphyxia, to ensure they receive the right medical care and treatment.
"All children with cerebral palsy merit modern genetic screening as early and customised interventions really can make a difference and improve their long-term outcomes," he said.
Ongoing genetic research is also investigating other types of contributing genetic variation to the cause of CP and, as a result, the researchers expect that the overall genetic diagnosis rate is likely to increase.
- Cerebral Palsy
- Infant's Health
- Personalized Medicine
- Child Development
- Child Psychology
- Neuroscience
- Learning Disorders
- Cardiac arrest
- Premature birth
- Molecular biology
- Acupuncture
- Introduction to genetics
- Biological psychiatry
Story Source:
Materials provided by University of Adelaide . Original written by Jessica Stanley. Note: Content may be edited for style and length.
Journal Reference :
- Yangong Wang, Yiran Xu, Chongchen Zhou, Ye Cheng, Niu Qiao, Qing Shang, Lei Xia, Juan Song, Chao Gao, Yimeng Qiao, Xiaoli Zhang, Ming Li, Caiyun Ma, Yangyi Fan, Xirui Peng, Silin Wu, Nan Lv, Bingbing Li, Yanyan Sun, Bohao Zhang, Tongchuan Li, Hongwei Li, Jin Zhang, Yu Su, Qiaoli Li, Junying Yuan, Lei Liu, Andres Moreno-De-Luca, Alastair H. MacLennan, Jozef Gecz, Dengna Zhu, Xiaoyang Wang, Changlian Zhu, Qinghe Xing. Exome sequencing reveals genetic heterogeneity and clinically actionable findings in children with cerebral palsy . Nature Medicine , 2024; DOI: 10.1038/s41591-024-02912-z
Cite This Page :
Explore More
- High-Efficiency Photonic Integrated Circuit
- Life Expectancy May Increase by 5 Years by 2050
- Toward a Successful Vaccine for HIV
- Highly Efficient Thermoelectric Materials
- Toward Human Brain Gene Therapy
- Whale Families Learn Each Other's Vocal Style
- AI Can Answer Complex Physics Questions
- Otters Use Tools to Survive a Changing World
- Monogamy in Mice: Newly Evolved Type of Cell
- Sustainable Electronics, Doped With Air
Trending Topics
Strange & offbeat.

IMAGES
VIDEO
COMMENTS
A study conducted by Besios et al. sought to assess the NDT method's efficiency in treating CP in young patients. Twenty children with cerebral palsy participated in an eight-week NDT intervention program. The study found substantial evidence that the NDT (Bobath) approach improves children's mobility . The purpose of the study done by Knox and ...
This case study focuses on the physical therapy management of Kayla, a young woman with spastic, diplegic cerebral palsy (CP). Kayla is now 20 years old and a sophomore in college. She was born prematurely and has received physical therapy services in a variety of settings since infancy.
Case Study: Preschool-Age Child with Cerebral Palsy / Diplegia / Constipation STANDARDIZED LIFE SKETCH 18. Setting of Encounter: Family Practice Office Child SP: Seated on the exam room fully clothed. Mother of SP: Sitting in chair next to the exam table. EXAMINER WASHES HANDS ON ENTERING EXAMINING ROOM 19.
Purpose:Dysarthria is common among children with cerebral palsy (CP) and results in poor speech intelligibility and subsequently low communicative participation. ... Using electropalatography (EPG) to diagnose and treat articulation disorders associated with mild cerebral palsy: A case study. Clinical Linguistics & Phonetics, 17(4-5), 365 ...
fitness of children with disabilities. This case study describes the results of a six-week ther-apeutic recreation (TR) program using an ex-ercise intervention to improve the physical functioning of a child with cerebral palsy. Background information will be presented, as well as a brief review of literature; details
Spasticity is common and difficult to manage complication of cerebral palsy that significantly affects the function and quality of life of patients. This case study reports a 15-year-old male with quadriplegic cerebral palsy, Gross Motor Function Classification System 5 (GMFCS 5), who presented with significant bilateral adducted and internally rotated shoulders as a component of generalized ...
This case study describes the physical therapy of a 9-year-old male child with spastic diplegic cerebral palsy with the aim to improve his gross motor function and social skills. The child had ...
Cerebral palsy, a prevalent childhood physical disability, exhibits complex multifactorial causes. This case-control study explores the role of parental age in cerebral palsy risk and associated patterns. A case-control study comparing children with cerebral palsy at ages 3 months to 3 years with age-matched healthy control subjects was conducted between January 2022 and August 2023 at Federal ...
Accommodations to cognitive assessment for a child with dyskinetic cerebral palsy: case study. Petra Karlsson a Cerebral Palsy Alliance Research Institute, Discipline of Child and Adolescent Health, The University of ... Assessment took 1-2 h longer than expected for a typically developing child via standardised administration procedures, but ...
Background Cerebral palsy is a major cause of disability and most survivors are left with residual disability and are dependent on parents/caregivers for essential care. This study aimed to determine the experiences of parents/caregivers of cerebral palsy children receiving out-patient physiotherapy. A concurrent mixed methods was used to collect data in the present study. The modified ...
The study of the sensory aspect alongside the motor aspect in children with spastic cerebral palsy is critical. Knowledge may help improve intervention, children's quality of life, activity, and participation. The study aims to analyze the sensory systems processing in children with spastic cerebral palsy classified by Gross Motor Function Classification System (GMFCS) as levels I, II, and ...
Client background: Tom is a 3 year old boy, born at 28 weeks. He has a diagnosis of evolving dyskinetic Cerebral Palsy, GMFCS V. Tom has a history of seizures. Pia met Tom while teaching a therapist course about the Key to CP approach. Tom was a demo child, meaning he only spent about an hour with Pia. Tom was not receiving direct Physical ...
This literature review aimed to identify and synthesise the evidence regarding the experience of mothers caring for school aged children with cerebral palsy. The studies reviewed represent the voices of mothers across a variety of settings and illustrate the influence of both society, culture, and community.
The aim of this study is to identify the main processes and outcomes related to family-centred care (FCC) in neuromotor and functional rehabilitation of preschool children with cerebral palsy (CP). Background. FCC is considered a reference for best practices in child rehabilitation.
Children and Adults established an advisory council on cerebral palsy, which became the American Academy for Cerebral Palsy. Through the 1960s and 1970s cerebral palsy gained a new cultural presence, as works like My Left Foot, a 1954 memoir by the Irish writer and painter Christy Brown, evoked the lived experience of the condition. In the UK the
ABSTRACT. Aim: To critically evaluate single-case design (SCD) studies performed within the population of children/adolescents with cerebral palsy (CP).. Methods: A scoping review of SCD studies of children/adolescents with CP.Demographic, methodological, and statistical data were extracted. Articles were evaluated using the Risk of Bias in N-of-1 Trials (RoBiNT) Scale and the Consolidated ...
The treatment of cerebral palsy in children is evolving rapidly, driven by scientific advances and a deeper understanding of the condition's broader impacts. As healthcare professionals, we must continue to advocate for and invest in developing treatments that offer meaningful improvements in the lives of these young patients and their families.
This phenomenon was observed in our study, where the early cerebral palsy or high risk of cerebral palsy diagnosis exhibited high sensitivity but had a 15% false positivity rate. ... Ware R, Boyd R. A systematic review of tests to predict cerebral palsy in young children. Dev Med Child Neurol. 2013;55(5):418-426. doi: ...
Aim: To critically evaluate single-case design (SCD) studies performed within the population of children/adolescents with cerebral palsy (CP). Methods: A scoping review of SCD studies of children/adolescents with CP. Demographic, methodological, and statistical data were extracted. Articles were evaluated using the Risk of Bias in N-of-1 Trials (RoBiNT) Scale and the Consolidated Standards of ...
Pain is common in individuals with cerebral palsy (CP) and the most reported pain site is the foot/lower leg. We analyzed the prevalence of pain in the foot/lower leg and the associations with age, sex, gross motor function, and clinical findings in individuals with CP. This was a cross-sectional register-study, based on data reported to the Swedish Cerebral Palsy Follow-up Program (CPUP).
One of the key findings of this study was that 16% of children acquired CP more than 28 days after birth. The acquired CP cases were due to the following: Infections, such as meningitis or encephalitis; Head trauma, for example, from a motor vehicle accident or fall; ... Cerebral palsy (CP) is a group of disorders that affect a person's ...
Instrumented gait analysis (IGA) is an assessment and research tool with proven impacts on clinical decision-making for the management of ambulant children and young people with cerebral palsy (CYPwCP) but is underused and variably understood by relevant clinicians. Clinicians' difficulties in gaining expertise and confidence in using IGA are multifactorial and related to access for clinical ...
Cerebral palsy (CP) is a congenital disorder, meaning it presents from birth, that affects movement, muscles and posture. It affects the nervous system functions including learning, hearing ...
Child: Care, Health and Development is a pediatrics journal covering the effects of social & environmental factors on health, development, & developmental psychology. Correction to 'The effects of neurofeedback training for children with cerebral palsy and co‐occurring attention deficits: A pilot study' - 2024 - Child: Care, Health and ...
The world's largest study of cerebral palsy (CP) genetics has discovered genetic defects are most likely responsible for more than a quarter of cases in Chinese children, rather than a lack of ...