Organizational development (OD) interventions: examples & best practices

In the world of organizational development, change is a constant process of discovery, analysis and action. An effective OD intervention can be one of the best mechanisms for creating impactful change and helping improve organizational efficiency.
The right OD intervention can help ensure you're solving the right problems, achieve your desired change velocity and also navigate any resistance. In this guide, we'll explore the different types of organization development interventions available to org dev teams and give you practical advice for implementing them along the way.

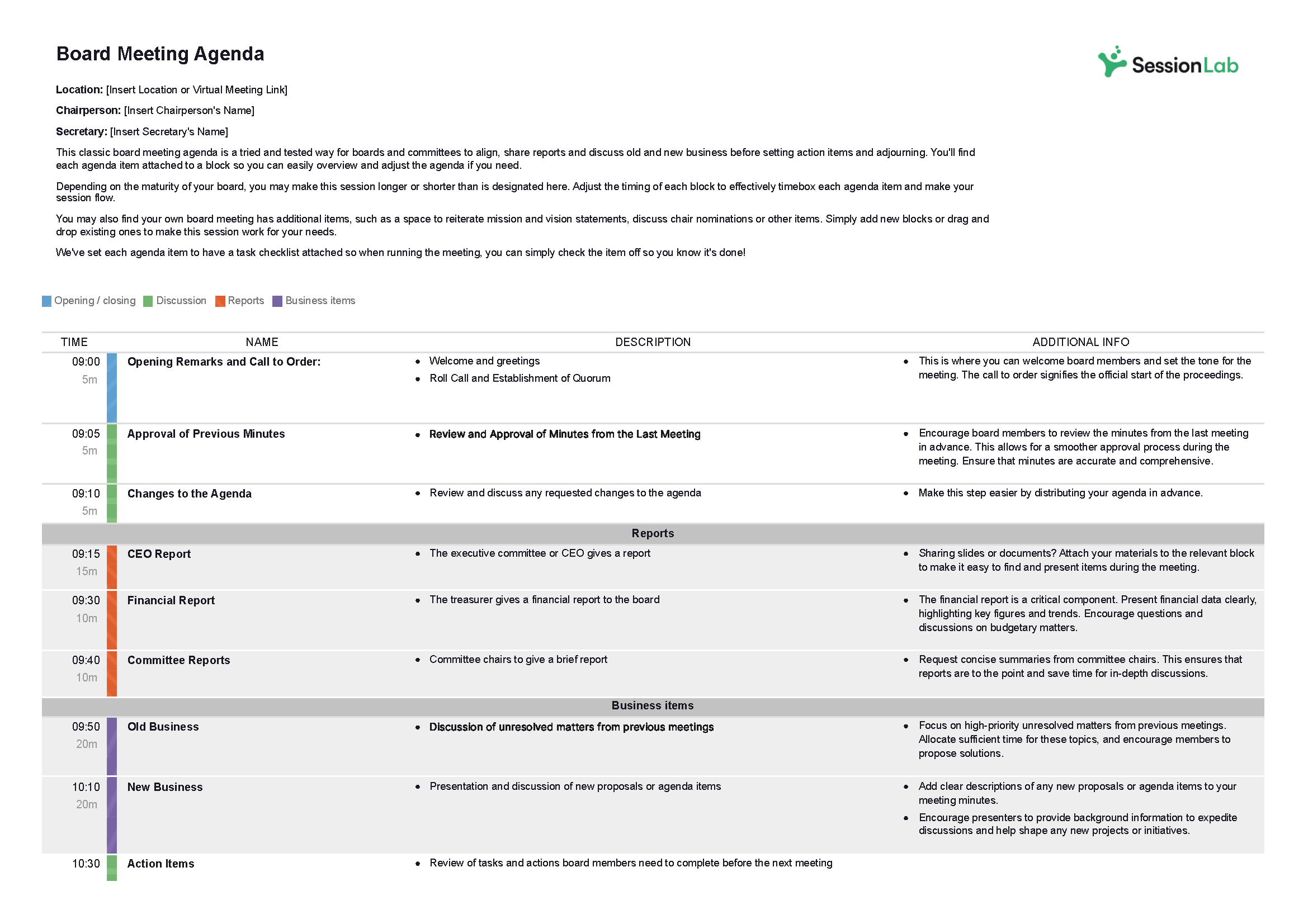
Design your next session with SessionLab
Join the 150,000+ facilitators using SessionLab.
Recommended Articles
A step-by-step guide to planning a workshop, how to create an unforgettable training session in 8 simple steps, 47 useful online tools for workshop planning and meeting facilitation.
At the heart of any organizational development strategy is the desire for meaningful change and growth. But whether you’re working in a small startup or a large enterprise, implementing change can pose a challenge and isn’t without its risk.
The process of improving organizational effectiveness can lead to tough decisions and its not uncommon to see resistance to change, difficulties with employee engagement or face friction when implement large-scale change across an entire organization.
While change can be kickstarted in many forms, one of the most effective and common tools used by top HR and change management teams is an OD intervention.
Interventions aim to formalize key actions within a change process and provide a framework for successful change. In this guide, we’ll explore the four types of OD intervention and explain how and when you might deploy them in your organization.
We’ll also share some organizational development intervention examples and give practical advice and tips for implementing these interventions. So whether you’re new to organizational development or you already have an intervention in mind, there’s something for you in this guide.
What are Organizational Development (OD) interventions?
Organizational Development (OD) interventions refer to a systematic and planned series of actions or activities designed to improve the overall effectiveness, health, and performance of an organization.
To simplify, an OD intervention is a process that is actioned in response to a need for change. You might radically redesign your organizational structure because of inefficiencies in how your org works together and achieves your goals.
If you identify a significant ongoing issue in how your organization operates, innovates or grows, this is often a trigger point for an OD intervention.
For example, if you struggle to find and retain the right talent, your HR and hiring teams might use an OD intervention to identify issues with job description or design, DEI initiatives or onboarding and employee happiness.
OD interventions are typically large in scale and are designed to have a major impact on key areas of how your organization operates. They require the coordination and efforts of multiple departments and the input of senior leadership in order to take effect.
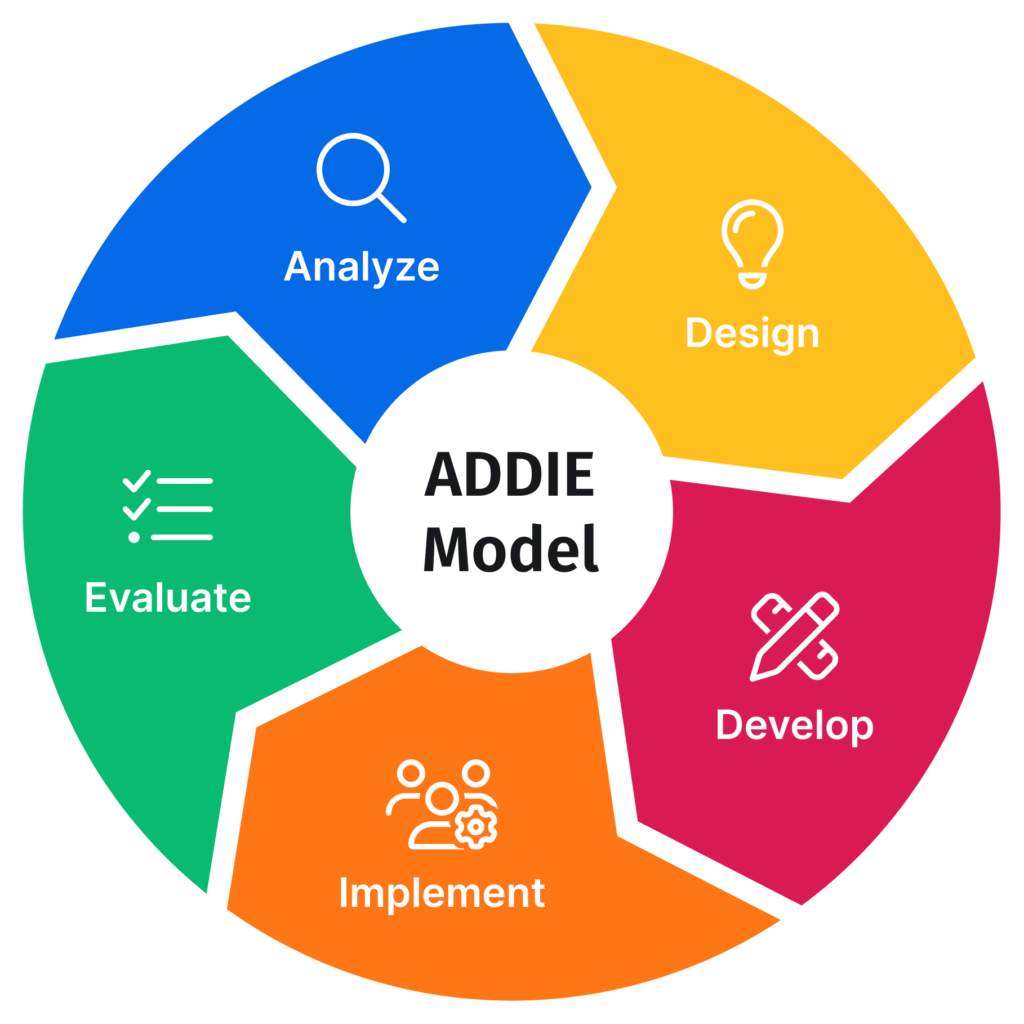
OD interventions follow a process of identifying and exploring the problem, diagnosing the issue further and then carefully developing a strategy that considers people, processes and other organizational factors.
After crafting a solution in the form of a proposed intervention, then comes the challenge of actually enacting that change and then evaluating the impact of the solution.
In the above example, your org dev team would work with affected teams to understand the situation and build an action plan that may radically change the organization.
Perhaps you discover job design is an issue or that there is a communication gap between your SMT and the rest of the company that has left your employees feeling unheard and unvalued. Finding a solution that adequately addresses organizational challenges requires a thorough exploration and analysis of the problem at hand and the people affected.
While conducting an OD intervention can be a little overwhelming, with the right process you can improve organizational performance, take care of your people and create lasting change.

What are the 4 types of organizational development (OD) interventions?
Organizational development interventions can take various forms, and they are typically categorized into different types based on their focus and objectives. Some common types of organizational development interventions include:
Human process interventions:
Human process interventions focus on improving group dynamics within the organization and how teams work together. Group interventions are common here, and change managers working in this area will likely run workshops and facilitate team building interventions with a desire to improve dynamics and interpersonal relationships on the team.
Techno-structural interventions:
OD interventions in this bracket typically focus on improving team productivity and performance by leveraging new technology and by considering how an organization is structured. Typical actions can include deploying new tools to streamline team workflows, automating processes or shifting organizational structures in order to maximise efficiency and reduce overhead.
Human resource management interventions:
Human resource management interventions typically focus on developing talent, creating employee training plans and otherwise working on how your organizations sources, nurtures and develops your people. Diversity interventions and wellness interventions also fall under this banner and as such, they’re typically implemented and coordinated by HR teams.
Strategic change interventions:
Organization development interventions related to strategy can be the among far reaching and impactful when it comes to improving an organization’s performance. This kind of change often aims to be transformational in nature and is often actioned when the long-term survival of the organization is at risk or there is a desire to radically alter how a company operates.
While other OD interventions exist, as Cummings and Worley noted in their book, Organization Development and Change 9th Edition , most interventions fall under the four types of OD interventions outlined in this guide.
That said, this list is not exhaustive nor are these OD interventions mutually exclusive. The actions your organization will take to create meaningful change will likely feature elements of various intervention types.
When considering what changes and interventions might be most effective, try not to be pigeon-holed into just one type of OD intervention or restrict yourself to set organizational strategies.
Think about the desired end state of your OD initiative and conduct a thorough root-cause analysis to select the most appropriate intervention(s). After implementation, evaluate the efficacy of your actions and be open to using other types of intervention in your ongoing quest to improve organizational efficiency.

Human Process Interventions
The original, best known and most regularly deployed OD intervention are those which focus on human processes. These kinds of interventions aim to improve interpersonal, group and organizational dynamics.
Facing challenges with team culture, communication or conflict resolution between teams and individuals? OD teams will often run interventions in the form of soft skills training , team building programs and improving relationships between different departments.
These can be low effort, such as running a weekly games session for employees to deepen bonds and get to know each other better. They can also include long term programs for conflict resolution and soft skills training, culture committees or mentoring and coaching opportunities for your team.
I recall an early career moment where there was friction between sales and support. Both teams felt misunderstood by the other and were regularly coming into conflict. Not only did this affect team morale, but it also contributed to a decline in our CSAT score AND missed sales targets.
By helping the team understand one another more deeply and creating a clear, collaborative process of handling high ticket customers and sharing information, the issue gradually improved.
Examples of human process interventions
Individual interventions.
Interventions on the individual level can have a massive impact on not only a single person’s happiness or job satisfaction but on how the system operates as a whole. Individual interventions often take the form of one-to-one interactions designed to improve how a single employee relates to their work, their team and themselves. Common interventions at this level can include one-to-one mentoring, individual growth plans, buddy systems and work shadowing programs.
Managers or HR teams might work with specific individuals to help resolve conflicts, build skills or better integrate them into the team. Regular one-to-ones can inform this process, but an individual intervention is often called for when a problem is discovered.
A common trigger point for such an intervention is during an employee feedback process. For example, if a manager has received a lot of feedback from their team that suggests they aren’t managing well, they may get coaching from a senior leader to help them improve their leadership skills.
Team forming interventions
Group dynamics are an important aspect of how a team functions. Team forming interventions are focused on helping improve those dynamics, creating alignment and helping groups get to know each other more deeply in a safe environment. Interventions designed to help accelerate team cohesion and bring groups together are some of the most common you’ll run, and it’s likely you’re doing some of them already.
Common trigger points for such an intervention can include when a new team is formed, discovering problems with how a team works together or wanting to reassert team values and shared bonds. Team building events, participatory workshops and any shared activities that create opportunities for connection and trust are all common interventions in this area.
Workshops are among the most powerful formats for team forming interventions . When first bringing a team together, you might run a team canvas workshop to help a group align on their values, explore team dynamics and decide how they want to work together.
Alternatively, you might conduct a skills workshop where your team gets to ideate and learn something new as a group. In any case, be sure to support your process with the right workshop tools in order to create engagement and get results.
Purposeful team building activities are another key human process intervention. Simply spending time playing games, having fun or sharing our stories can have a powerful effect on team dynamics. The important thing is providing an opportunity for people to get to know each other more deeply, create bonds and grow together.

Intergroup interventions
When two different departments in your organization are finding it difficult to work together, an intergroup intervention is a great step. Mapping how the two teams would like to collaborate and deepening understanding of the challenges and specifics of each group’s work can help smooth things out and improve efficiency too.
In the sales/support example above, a combination of team building and process design was key to the intergroup intervention we undertook. Only by coming together and talking about the problems while also getting to know each other as individuals were we able to move forward.
For companies with few opportunities for inter-departmental work, simply bringing employees together for a team building activity so they can understand one another better is a powerful step towards change.
Tips for human process interventions
One size doesn’t fit all.
Whenever you’re working with people, it’s important to note that everyone is different and what works with one team or individual may not work for another . I recall an occasion where a company-wide team building activity (casino and club night) chosen by upper management was chosen without asking the team how they felt.
While some folks loved it, many people felt uncomfortable or were disengaged. The desired goal of improved team connections wasn’t met and instead, the group ended up feeling more fractured. Especially in the case of intergroup relations interventions, remember to include people from both groups and think about their varying needs!
Choose your intervention with the individual or group affected in mind and where possible, directly include them in the process. For example, an individual development plan should absolutely factor in how the person in question learns best and the unique context of the situation. Processes and systems are good, but don’t forget that the best outcomes arise out of solutions that have those people affected at heart.
It’s an ongoing process
One common mistake I’ve seen with organizations deploying change is to assume a single intervention will solve a problem forever. Human processes are all about relationships between people and teams. Like any relationship, these need nurturing over time.
While a single team building event can recharge the tanks and help cement bonds, without care and consistent attention, that hard work can be for nothing.
For example, let’s say you run a company values workshop to help create alignment on the future of the organization and improve company culture. Your team comes together to choose core values and everyone feels good at the end of the session. Then, 6 months later, you ask your team what your values are and nobody can remember what they are. Without follow-up actions and a process of keeping those values alive and present, the desired change in culture has been ineffective.
While most organizational development interventions are ongoing in nature, human processes can prove to be especially liquid and require extra attention from people throughout the system.
People are complex! Be sure to create systems to check-in on progress, continue the good work of an intervention afterwards and reinforce the change you wish to create.
Repetition is a key element of these processes so think not about running a single company event, but how to ensure you continuously build on your company culture.
Empower your managers
While large-scale interventions benefit from research, analysis and oversight provided by a change manager, some changes can benefit from speed.
At the human process level, line managers are often the first to see issues and spot opportunities for change. So why not give them the tools and permission to try and create positive changes for their teams?
For example, let’s say that a team member comes to you feeling overwhelmed and stressed because they’re having difficulty finding childcare. In the long-term, a company policy around childcare would be great, but that doesn’t solve the immediate issue for the team members affected.
At a human process level, proactivity and timeliness can make all the difference. Ensure your company policies and organizational culture support managers in making timely, responsible and effective interventions on behalf of their team.
As with any change process, be sure to log and track changes and reflect on the impact. In addition to alleviating difficulties for individuals and teams, smaller, fast-moving intervention techniques can provide important insights for company-wide initiatives.
Feedback loops are vital
Human systems are dynamic and ever-changing. Without feedback loops, it’s possible for issues or opportunities within those systems to go unnoticed. For some interventions such as coaching or mentoring programs, feedback is an implicit part of the process.
For others, change managers will need to create a process for gathering feedback in order to monitor, evaluate and improve OD interventions with the input of all stakeholders. Whatever system you use, it’s also vital that feedback goes both ways. Running a train the trainer course and giving your trainees feedback on their progress is important, but you should also get feedback about the program from trainees, managers and any other stakeholders.
When it comes to human systems, you’ll also find it most effective to have a system for gathering feedback well in advance of any intervention. Try to make giving and receiving feedback a consistent process for your teams and use tools to support the process where possible.
Techno-Structural Interventions:
Techno-structural interventions aim to better align an organization’s structure, technology and processes with its goals and objectives. OD interventions in this area can be among the most far reaching for any org dev team and they’re often deployed when change feels paramount for a company’s survival or for maintaining a competitive edge.
Low growth, a rapidly changing market or key areas of a business underperforming? These can be triggers for a techno-structural intervention.
Tasks such as organizational restructuring, process redesign, job enrichment or even downsizing fall under this umbrella. Other common interventions for OD teams include implementing new tools and technologies to improve efficiency, streamline workflows and future proof the company.
In techno-structural interventions, there is often an emphasis on continuous process improvement. Switching to Agile or lean methodologies or embracing total quality management processes like Six Sigma, as made famous by their use at Ford Motor Company , are common tasks.
As large-scale processes that can include changing business direction or radically repositioning your product, these interventions can be a challenge to implement.
Without a change management plan, change can be slow, meet resistance or simply not catch on. Be sure to leverage the skills and expertise of change managers and senior leadership when conducting these kinds of interventions.
Examples of techno-structural interventions
Organizational restructuring.
Restructuring an organization means rethinking how some or all of your workforce is structured and operates . Who reports to who? Which departments fall under which manager and who is responsible for making decisions that affect different areas of the business?
Common triggers for an organizational restructure include a need for greater revenue or reduced costs, a desire to refocus or change company goals or a move into a new market.
Creating innovative new products or services or simply working to resolve issues with workload, resource management or siloing are also common interventions that require a technological or structural approach.
For example, in a small startup, it’s not uncommon for all of your developers and designers to sit under the same branch in your org chart with a single founding developer as their manager.
For a while, this works and then as you grow, you start seeing bottlenecks in your dev process, and there are too many direct reports for your founding developer to handle while also trying to innovate and place your product in the market.
At this stage, an organizational restructure will be necessary in order to ensure efficiency, avoid burnout and also ensure you have the right skillset present among your dev team.
Rapid growth or reduction in your team size is another trigger for a restructure. Sometimes, this might mean a single department may split or combine with others.
On other occasions, it’s necessary for organizations to completely rethink how the hierarchy of their teams works – for example, switching from a functional org structure, where each department reports to a department head, to a matrix structure, where cross functional teams are put together on a project by project basis.

Business process reengineering
BPR is a process of radically redesigning how your organization works. It’s a comprehensive model of analyzing, redesigning and optimizing your organizational processes in order to improve business performance.
This is particularly valuable for organizations who need to see significant change in order to remain competitive or where redundancies and inefficiencies in processes are creating massive costs or an inability to meet goals.
Organizations implementing a BPR intervention typically begin by mapping all current business processes and analyzing them for opportunities, gaps and issues. After validating ideas for improvement, the organization will design an ideal future state and begin moving towards it.
By definition, BPR is wide ranging in nature, and team’s working with this kind of intervention should not feel constrained with their suggestions. Removing redundant processes or implementing a new helpdesk to improve the efficiency of your customer support team might be enough to save costs, but what if you fixed the root cause of your largest customer issues or invested in self-serve support?
If your team is finding themselves coming up against the same problems even after a solution or quick-fix has been implemented, you may need to go further. That’s the perfect time for a more thorough and radical appraisal and solution process such as BPR.
Work design interventions
Work design interventions are used when an organization wishes to improve the content or organization of the work and responsibilities falling upon individual employees or departments.
The way our work is designed affects how we feel about our job our ourselves. The tasks, working hours or contact points associated with our role can have a massive impact on our overall motivation, engagement and stress.
We all want our teams to be happy and productive, and a work design intervention can cover everything from redesigning job roles and individual tasks, to finding ways to automate or improve processes that impact job satisfaction or productivity.
For example, let’s say that individuals on a team feel stressed because they have a large workload and don’t feel supported in achieving their goals. OD interventions might include redesigning job sepcs, allocating more resources, creating reward and recognition schemes or even improving autonomy and self management.
Deep understanding of the problem is key when considering work design interventions. Be sure to conduct interviews, run a focus group and implement a continuous feedback system so you can see problems emerge and understand whether team’s need more support, job control, enrichment, development opportunties or something else entirely.

Tips for running a techno-structural intervention
Document your current processes. .
While the ideal state is that your processes are well documented in advance of problems arising, it’s not uncommon for there to be gaps in your documentation when you get around to thinking about interventions. In fact, it’s entirely possible that one of the first steps of the problem analysis and diagnosis stage will be to document any missing processes.
Before you start implementing a new process, be sure to take time to understand how your organization operates now. Try to map your processes from end-to-end and be sure to capture all the actors involved in the system. Redesigning a sales process without thinking about how it might impact your support team is a surefire way of causing new problems.
When documenting, be sure to involve stakeholders from across the organization so you can gain an accurate, in-depth picture of your processes. Not going deep enough or speaking to the people who actually enact or work with a process is another pitfall you can avoid by simply speaking to the right people.
Moving forward, aim for each team to document your processes as a matter of habit and ongoing improvement. Not only will it help any changes be smoother should you need to make them but it can help surface issues and opportunities more quickly.
Use a proven framework and do your research
Changing the structure or processes or a large organization is a difficult undertaking but you are not the first person to encounter this challenge. Lean on proven frameworks and the work of other thinkers, experts and organizations.
At SessionLab, we transitioned to an EOS framework to help us nail down our strategy, create a new org chart and organize our work . We found that the structure, advice and existing knowledge around EOS allowed us to make better decisions, transition faster and focus on implementation, rather than trying to come up with an entirely new solution.
No two organizations are the same but there’s something to learn from how others have changed for the better. Try looking at how successful organizations at a similar maturity or size to your own operate or better yet, look at those that have solved some of the challenges you’re facing. Join a masterclass or community – the ongoing support and insight of peers can also be invaluable in actioning change.
Run workshops to surface insights quickly and collaboratively
When thinking about introducing new processes it’s imperative that you first explore and diagnose a problem correctly . When it comes to how teams and departments operate, it’s not uncommon for hidden variables or unspoken actions within the system to be at the heart of your issues. So how do you bring them out into the open and encourage openness from your team?
Speaking to major stakeholders and business people across the org is vital, but it’s often not enough to just send out an email asking for input.
Workshops are some of the most powerful intervention techniques available to change managers and org dev teams. Ideating on possible solutions collaboratively is often a more effective way to truly discover the root cause of issues and create solutions that account for the people who will be most affected by the process you are changing.
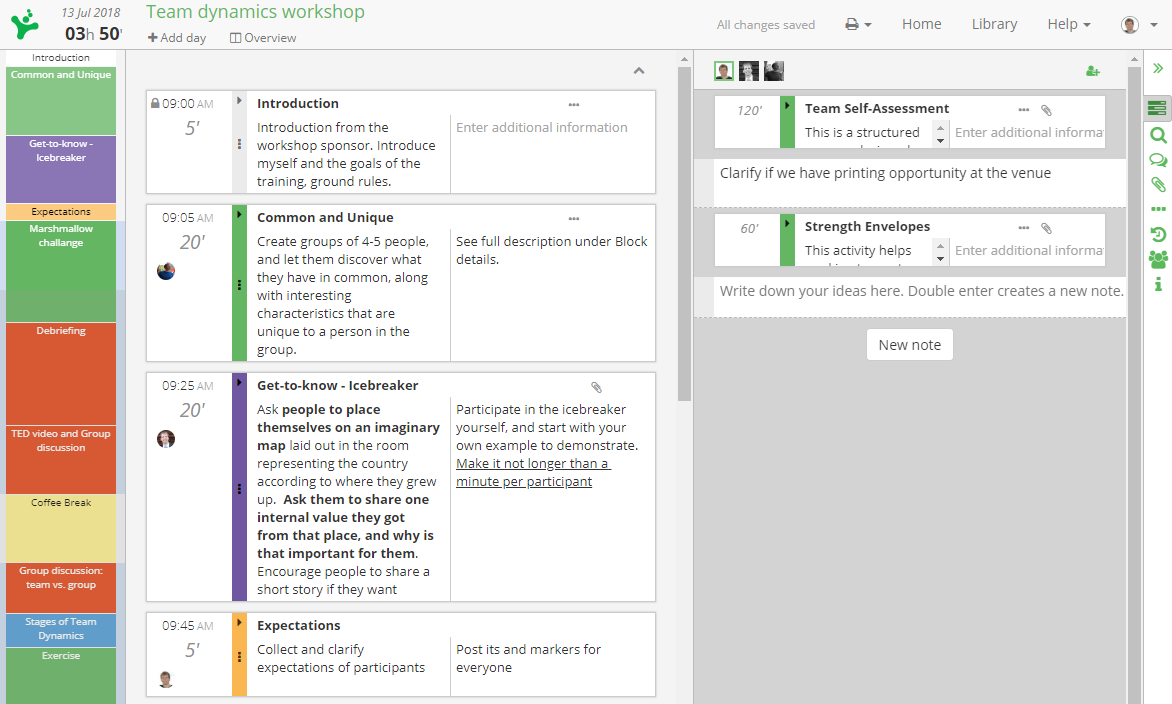
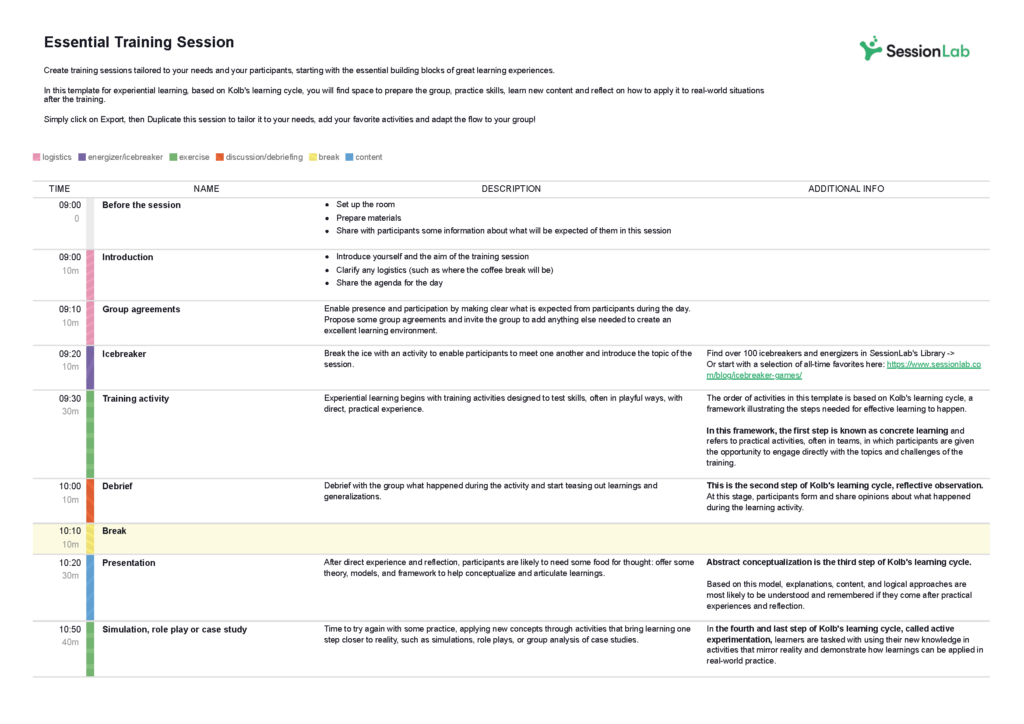
SessionLab is an effective tool for designing and delivering the workshops that you’ll use to support your OD intervention process. Invite stakeholders to co-create your agenda in real-time and involve them in the change process. Save time designing your key workshops and ensure your process is efficient with SessionLab.
Human Resource Management (HRM) Interventions
HRM interventions concentrate on developing and managing human resources within the organization. Examples include improving hiring processes, creating and reinforcing diversity, improving performance management processes and building opportunities for career development. People are one of the most important parts of how an organization functions and HRM interventions are designed to directly impact the people working in your company.
As the name would suggest, these kinds of interventions are often deployed by or in conjunction with HR teams in response to difficulties with hiring or retaining staff, employee satisfaction or problems with performance.
Effective change tracking, strong feedback loops and good communication are essential elements of a successful HRM intervention. Programs and initiatives that form the backbone of human resource development – such as wellness or training programs – are ongoing in nature.
You’ll often find that such an intervention takes time to achieve its chosen goal and the strength of your research is a key element of success. Purposeful interventions that incorporate the direct input of your employees are more likely to be fit for purpose and create long-lasting change.
Examples of human resource management interventions
Employee wellness interventions.
Staff are reporting high levels of burnout and managers are noting that their direct reports are feeling overwhelmed or stressed. This is the perfect time for an employee wellness intervention.
While HR teams might also consider job design and other factors, these programs most commonly involve the creation of new opportunities and programs designed to alleviate issues and improve the health of your team.
Some common strategies include creating new employee benefits linked to health and wellness . Cycle-to-work schemes, free gym memberships and budgets to support employees in improving their own wellbeing can all have positive impacts on team wellness.
You might also provide opportunities for staff to access company healthcare and counselling. On the lighter side, creating a budget for healthy lunches and office snacks, giving opportunities to volunteer or exercise on company time can also have an immediate impact.
While the same is true for most interventions, employee wellness programs absolutely require the involvement of everyone on your team when choosing what to implement. A poorly designed or unfit for purpose intervention can quite easily have a negative impact on wellness.
Let’s say you create a scheme where everyone in the office gets a free healthy lunch. Great for your onsite team, but how about your hybrid and remote employees? If you don’t offer a similar benefit or take them into account, they could feel less valued and overall wellness could suffer.
Performance management interventions
Managing and hopefully improving the performance of your team over time is a necessity for any successful business. But what about if the problem you uncover issues with staff performance or a lack of process for tracking and improving the performance of your team? Time for a performance management intervention.
For some organizations, such an intervention might include actually setting up a performance management system and ensuring that every member of staff is given frequent feedback and opportunities to improve. For others, this might mean enabling managers with better tools and processes or creating reward programmes to encourage higher performance.
Coaching, mentoring and the unblocking of other issues that might impact employee performance are also key tasks that can be part of a performance management intervention.
A key part of a successful performance management intervention is truly understanding the root cause of an issue. Underperforming staff may face issues with job design, internal or external pressures or may not have even been given feedback or an opportunity to improve before.
Try not to jump into the deep-end with punitive measures unless you’ve already taken a more holistic approach that gives staff the feedback, tools and opportunities they need to develop.
Talent development interventions
As a company grows and roles change, it’s not uncommon to discover that your team has skill gaps that need to be filled. You might find that a changing market means that key competencies need to be updated or supported with new training. Or you might discover that people are unhappy with the pace of their career development and are leaving the company as a result.
Talent development interventions are all about managing and developing your team so they’re better positioned to do their jobs, grow in their careers and stick around.
Common talent development interventions include designing new training programs and coaching opportunities, personal growth plans and even reconsidering how you onboarding, compensate and promote members of your team. These kinds of interventions also extend to rethinking how your HR team goes about attracting and hiring new team members.
Any time you are struggling with team performance, remember that the solution is only as good as the analysis of the problem. Talk to team members at different levels and who have been with the company for different lengths of time.
Only once you’ve truly identified the root cause of the issue can you implement an intervention that will serve everyone on your team and prevent issues from occurring in the future.
Tips for running HRM interventions
Engage people throughout the organization .
Any intervention that directly affects your team should get some level of input from the people being affected. For some interventions, it’s absolutely paramount to source input and get feedback from your employees.
For example, a wellness program for your remote employees without the input of remote team members isn’t likely to serve their needs.
Underperforming sales team? Rather than making an assumption at a management level, talk to your sales reps and see what they think the issue is. Not only are these people more likely to be able to identify the root cause of a problem, but they’re also instrumental in actioning any given intervention.
Engaging people early in the process is helpful for getting buy-in and removing barriers to change. Don’t keep your change discussions entirely confined to management meetings and get input when you can, so long as it’s appropriate.
Support your process with data
Human-process interventions can sometimes be kickstarted by qualitative data : anecdotes about how people on the team are feeling or gut feelings from management about burnout or stress. While these kinds of comments and discussions are vital, it’s also important to back-up any change with data and processes to determine the viability and success of any initiative.
The gut feeling about a problem is likely onto something, but without data of some kind, it can be hard to be confident that your solution is the right one to support your wider business strategy.
For example, before making a large-sweeping change to working hours, maybe survey your team to find out if that works for them. Want to roll out your marketing training program to other teams? What data about team performance and employee satisfaction do you have that supports that decision?
Feeling like your hiring process is bringing in a large number of low quality interviewees and want to make a change? Check out industry standards, compare across job roles and back up your feelings with hard data wherever possible.
Start measuring employee KPIS before the need for an intervention
While some challenges are difficult to predict, HR teams are in a great position to pro-actively source input, monitor employee happiness and prepare for wider change.
If you’re already using a performance management system, it’s easy to start tracking how your team feels, see the efficacy of personal development plans and monitor things like onboarding efficacy and retention.
If you’re not, it really pays to start measuring employee sentiment and refining your feedback loops so that you have something to point to if the need for a HRM intervention arises.
Even something as simple as a monthly employee satisfaction survey can help your HR team see issues coming, track changes over time and also create an ongoing channel for surfacing opportunities for improvement.
Properly resource line managers
Managers across your organization are vital parts of making any HRM intervention a success. Whether they’re directly involved as a result of overhauling performance management processes or indirectly affected because of changes to flexible working hours or giving back schemes, your managers often have extra work or overhead created by HRM interventions.
Don’t underestimate the impact and ripple effects of even the smallest interventions. Line managers are often the frontline in actioning change or hearing misgivings from employees. They can often be those people who pick up slack within the system.
Be sure to take this additional workload into account and create extra resources and support processes for line managers . Consult them before any changes are rolled out, involve them in the process as much as needed and think about how to make it easier for them to implement and support processes when engaging with their teams.
Strategic Change Interventions
While other organizational development interventions can operate on the individual to small group level, strategic change interventions are more far-reaching in scope. These interventions are designed to analyze and radically redefine how an organization functions or what it hopes to achieve.
An organization might reconsider its vision or goals because of changes in the market or because the team has conflicting ideas about their shared missions or core values. Other times, the changes can come about because of issues preventing a company from meeting their goals, such as how a team is structured or how a culture of innovation is nurtured.
Interventions that impact core business strategies are usually undertaken when the survival or competitive edge of a business is at risk. Strategic change can be prompted by internal or external factors, but they’re very rarely taken lightly. The desire is for a massive improvement in how the company functions and the work required is often massive in scale too.
Done right, however, and companies who deploy these interventions can create incredible innovation, reverse falling revenue forecasts and radically improve employee happiness too.
Examples of strategic change interventions
Transformational change interventions.
Examples of interventions for transformational change include a top-to-bottom organizational redesign, perhaps in response to a changing environment, a major pivot or a desire to enact meaningful culture change.
Dangers to the long term viability of the business, major competition or market shifts can be a common trigger for a transformational change intervention. You can also find that analyzing challenges to employee retention can uncover an issue with company culture that only a massive change and restructure can improve.
Expect transformational changes to radically alter how a company operates, shifting the status quo and transforming the organization into something that is better positioned to achieve its goals.
Continuous change interventions
Continuous change interventions are designed to help an organization make minor improvements on an ongoing basis. Creating a culture of learning, developing an experimental, continuous growth model or creating space for innovation and cooperative structures are common actions taken here.
Trans-organzational change interventions
Trans-organizational change refers to interventions where two or more organizations are involved. Mergers and acquisitions fall under this umbrella though major business partnerships are also an example of a task that might require an OD intervention.

Tips for implementing strategic change interventions
Map your systems and organizational structure.
Before you decide where to take your organization, you’ll need a clear view of where you are right now. Activities such as Systems Mapping are a great first start for any intervention but they are especially valuable when considering large-scale strategic change.
Not only can you more accurately assess the scope of what you’re doing, but you can also draw out where changes need to take place.
Try creating a map of your organization with a process of systems mapping to better understand and enact your proposed change. These are workshops dedicated to drawing out (and actually drawing) all the stakeholders and other elements (such as suppliers, for example) that compose the wider system of which your company is a part.
Systems Mapping will help your teams look at the big picture and figure out best place to intervene.
Get outside help
Enacting or even deciding whether to undergo a major strategic change is a significant undertaking. Experience and expertise is invaluable in making a change process a success and when conducting major organizational change, a consultant or agency can make all the difference.
Receiving advice from someone who has enabled change for dozens of companies and has seen many processes from inception to completion is invaluable. They’ll help you ask the right questions, show you a proven framework for change and also help you navigate any roadblocks. Consultants are also adept at working around unintentional biases or assumptions that can form as a long-term employee.
If you want to improve your change velocity, feel confident in the changes you’re making and streamline the change management process, professional assistance is absolutely worth investigating.
Remember that big changes take time (and sometimes multiple interventions)
Strategic changes can involve upending how your company operates, thinks about its culture or how it positions itself in the market. While a single intervention might help you successfully restructure your team, it will take further work and careful management to help those teams thrive in the new environment.
Committing to large-scale organizational change means committing to a process that will take time, consistent effort and potentially further interventions along the way. Prepare your teams and managers for a long, ongoing process and be sure to check in along the way.
Shifting your target customer base for example, might require your sales and marketing teams to radically rethink how they source and talk to customers. While the eventual change might be great, don’t expect to see a complete upswing overnight. Be sure to take this into account when setting targets and when managing your people.
Set expectations accordingly and ensure there are feedback and support systems in place for your team while such large scale changes are in action. Run effective team meetings to keep track of what’s happening and ensure stakeholders can synchronise effectively.
More tips for a successful OD intervention
Organizational development is a complex process that can test even the most seasoned teams . The good news is that you’re not the first company undergoing a process of change and there are a heap of best practices and tips you can use to help you achieve your desired change.
We’ve included tips for each of the different types of OD intervention above, though we also wanted to share some additional OD best practices that should help, regardless of the kind of intervention you’re running.
Carefully assess the current state of the business
Designing and deploying the right OD intervention means gaining a thorough understanding of where your business is currently at. Not only will you need to determine what needs to change, but also gain an understanding of drivers and potential blockers to that change.
Failure to do this properly can result in slow or unsuccessful change. It can even lead to changes with unintended consequences or negative effects.
There are various tools for assessing the state of the business. A change management framework is one such tool, though you’ll likely synthesize everything from stakeholder input, current business performance, risk assessments and other situational analysis tools.
The key here is to ensure you deeply understand the system being changed in order to propose the right change and have the resources and environment to make it happen.
Find the root cause of your problem
Long lasting change comes from a deep understanding of the root cause of an issue. Facing challenges with high staff turnover and low morale? Bringing in free snacks and reducing working hours over the holidays might have a short-term impact on employee happiness, but it’s unlikely to truly solve the issue.
Whenever engaging in an organizational development process, be sure to go deep enough to truly understand the cause of an issue before enacting change. Don’t rely on assumptions and talk to your team, often multiple times while conducting a root cause analysis.
Review performance data and thoroughly analyze what you find. (Sometimes, it’s enough to just keep asking why!) If in doubt, run a problem solving workshop to truly surface what’s going on and create a safe space for uncovering issues.
Not spending enough time analyzing an issue is a potential pitffall for any organization seeking to improve. Without finding the root cause of organizational issues, it’s entirely possible to treat the symptoms rather than finding a cure. Avoid this by going deep, involving people across the organization, backing up ideas with data where possible and be ready to challenge your assumptions.
Fishbone Analysis #problem solving ##root cause analysis #decision making #online facilitation A process to help identify and understand the origins of problems, issues or observations.
Have a clear purpose and end-state
People are more likely to get behind change when they know exactly what it is they are working towards. The purpose of an intervention should be clear, focused and simple to explain. If you can’t easily explain why you’re making a change or it’s overly complex or unclear, chances are you’re trying to do too much or you don’t have a clear understanding of the problem you are trying to solve.
Clarity of purpose helps ensure that you are taking the right actions and that your change will be successful. Decision making gets easier when you have a clear purpose too. Does this support our purpose and will it help us achieve our goal? Yes: let’s do it. No: either we don’t do it or it could be the focus of a separate intervention or change initiative.
In addition to a clear purpose, it’s useful to have a desired end-state in mind when conducting any organizational development activities. What will the business look like when you’re done? How will you know your change has been a success?
Asking these questions helps you align and focus your actions while also giving you a means to evaluate the impact of your process. An exciting, aspirational end-state is also invaluable when it comes to getting support for your intervention and reducing possible resistance to change.
Align interventions with organizational goals
Successful change requires many moving parts across your organization to be working in tandem. Your organizational goals or mission are often the north star for anything your team does, including any development processes. Often, the simplest way to determine the right OD intervention is to ask whether it helps your organization better achieve its goals. If the answer is yes, then it’s a great candidate for action. Aligning your interventions with your greater goals can also help ensure that the team is able to get behind them and understand why the intervention is being run. For example, let’s say you’re an NGO whose mission is to help provide learning opportunities for disadvantaged folks.
Interventions that are aligned with that organizational goal, either helping your team reach more people with better tools or clearly improve your team’s ability to do their core tasks are much more likely to succeed than interventions that seem tangential or don’t support that core mission.

Work backwards from your ideal future state
A common facilitation technique for creating change is backcasting, or imagining an ideal future state and working backwards to decide how to achieve it. Often, the prospect of organizatioanl change can leave teams overwhelmed with how to achieve it or be unsure of how their actions might result in a desired change.
Working backwards can simplify the process, reducing noise and help crystallize your shared purpose. By thinking big, you can often find that the ideal steps towards change become more clearer.
An aspirational future state can also be an effective tool when getting stakeholder buy-in. A shared vision gives everyone a clear target and it’s easier to align various actions around an organizational goal they believe in.
Backcasting #define intentions #create #design #action Backcasting is a method for planning the actions necessary to reach desired future goals. This method is often applied in a workshop format with stakeholders participating. To be used when a future goal (even if it is vague) has been identified.
Communicate effectively
Resistance to change can often come as a result of poor communication or a lack of understanding about why a change is being implemented at all. How you talk about your OD intervention is an important part of ensuring that stakeholders and those affected get behind the initiative.
When rolling out your OD intervention, create a communication plan and be sure to highlight the purpose of the proposed change. For example, rolling out a personal development program without context can cause confusion or anxiety. Is this a genuine desire to improve career prospects and employee fulfilment, or is there an issue with my performance and is my job at risk?
Clearly communicate why and how you’re making changes, create documentation that is easy to access and create space for questions and answers too. By providing a clear vision and purpose for such a program, you can make it easier for everyone involved to get involved and help your change take root.
Be wary of analysis paralysis
Thorough analysis and careful planning is an integral part of leading an organizational change. But is it possible to do too much?
For some teams lacking in confidence or expertise, it’s possible they delay making changes or continue to analyze and weigh up options even when the path is clear. It’s a tough balance, but spending too long assessing when a case for change is clear can actually undermine the process or create barriers to change.
You can mitigate this potential by following a proven framework, having clear organizational timelines and by bringing in consultants to help increase the velocity of your process. In other cases, it’s a matter of using an 80/20 principle or using a bias for action methodology to make a decision and move forward.
If your company is just starting the process of organizational development, it’s natural to want to tread carefully. Just be certain that your process is efficient and that your team’s anxieties are aired and don’t get in the way of progress.

Get started!
In the case of small interventions or change processes, you can often adopt a more lightweight process and get started more quickly. You may not need to mobilize your entire change management team for a localized intervention. You might also find that you can gain confidence in a proposed change without performing a top-to-bottom situational analysis.
Change can only happen once a process is set in action and in some cases, it’s worthy to just get started, monitor the results and empower your teams to be proactive. This is different for every organization and while it’s common for small teams to be more agile, large organizations often have more red-tape, and with good reason.
Recognise the specific circumstances of your organization and review every OD intervention you perform to see how you can do better. If your changes are successful but your team feels like you spend too long assessing when things were clear early in the process, that makes a good case for trying to streamline your process.
Not every change needs a large intervention
In my experience, the thoroughness of the process directly correlates to the scale of the proposed change. Over-engineering small-scale change processes can create unnecessary friction or lead to frustrated team members. This can cause just as many problems as under-engineering a large scale intervention and developing a poor solution. In doubt about a small, low–risk change but don’t want to block an enthusiastic team mate? Call it an experiment and monitor the impact. Sometimes, you can learn more from just getting started, rather than adding it to a massive organizational to-do-list.
In any case, it’s worthy to explore how you can create continuous change by engaging your team proactively in the process. Teams are vital actors in any change process and by empowering them, you can often avoid future issues and ensure opportunities are taken where possible.
Leaders are integral
Without leadership support, organizational change can struggle to get traction. Everyone from senior leaders to line managers are instrumental in helping change be a success. This might include modelling changes yourself by attending skills workshops, volunteering or cycling to work in line with sustainability goals.
Often, leaders and line managers are also responsible for tracking employee sentiment, keeping change processes front-of-mind and helping employees adapt to change.
Without leadership backing, change can be slow or ineffective. Get them onboard early and give them the tools they need to brief and support their teams and they can help any change process be smooth and purposeful.
Leaders aren’t just important when helping enact change. During the early stages of an org dev process, leaders are often key stakeholders in research and analysis tasks. They’re well positioned to provide input, spot additional risks and see dependencies you might not.
Engage leaders throughout the organization as early as possible and keep them in-the-loop. Change doesn’t just come from your senior management team! Even the most well-designed OD interventions can fall down if logistics or team workloads don’t align with the process.

Acknowledge the additional workload of change and plan accordingly
Change is hard for most living things, humans included. Whatever the level of involvement in planning, enacting and evaluating organizational change, the process can create additional work or mental load for those affected. Acknowledge this and be proactive in order to support your team and remove potential barriers to change too.
This might look like simply reducing workload in other areas to create space for change, creating support structures or otherwise addressing the unique pain points that might come up in the process.
Sometimes, even an acknowledgement and group discussion about change can be sufficient to clear the air and give teams the opportunity to suggest ways to counterbalance any increased workload.
Use measurable metrics for success
Measuring the effects of change is an integral part of organizational development, but how can you ensure you are measuring the right metrics and have confidence that your change has been successful?
KPIs and data-based measurements are your friend here. Seeing a clear change in revenue, customer satisfaction or staff turnover in numbers can provide verifiable proof your change has been successful. That said, think about sourcing both qualitative and quantitative data where possible.
Staff might anecdotally report lower stress in a one-on-one meeting, but how are sick days trending since you implemented the change? Revenue might be up, but did your sales team bag an enormous contract that has skewed data?
It’s also important to decide on the metrics of success before you implement any change. You’ll want to use metrics that will be directly affected by what you’re doing and align your actions accordingly.
It’s also vital that you actually have the means to measure what you want to measure and ideally source existing data to serve as a point of comparison. If you’re conducting an employee wellness program to lower stress, see if you have previous surveys or performance metrics to serve as a baseline. Using a combination of leading and lagging indicators can also be helpful. For example, a leading indicator for the efficacy of your wellness program might be how many people take advantage of new services on a weekly basis. If more people take advantage of the services, you’d expect to see lower stress – great, but it’s only one piece of the puzzle.
A lagging indicator might be how many staff are reporting high stress levels in a monthly employee survey or even the productivity levels for a team or department. With a combination of these kinds of metrics, you can not only determine if your change has been successful, but also see where in the process you might make improvements.
Use tools to support your process
Successfully implementing an OD intervention strategy means organizing tasks, project managing the process and evaluating its impact. It’s a lot of work that can be streamlined by using the right tools.
Use change management software to optimize the end-to-end process of an intervention and improve the velocity of change you’re enacting.
It’s also worth recognising that various barriers to change can be mitigated by using efficient processes and bespoke tools. When committing to creating impactful organizational change, invest in tools that will help you achieve your goals faster and more efficiently.
With SessionLab, you can create stakeholder workshops and braining storming sessions in minutes. Drag and drop blocks to create your session. Invite collaborators to co-create your design in one-place and make changes with ease.
Developing a new learning program ? Create your ideal learning flow and invite your course managers and subject matter experts to collaborate in one-place.
Innovation experts and consultancies have found SessionLab to be a vital part of creating change for their clients. Get started for free and save time and effort in your session design process.
Evaluate & adjust
Once an intervention is complete, it’s time to evaluate. Using your carefully chosen success metrics in combination with stakeholder input, you’ll determine if you’ve achieved your goals and if not, how might you change or adjust your intervention to do so.
While it can be tempting to see a green KPI and call it a day, proper investigation of why you were successful can help ensure you can repeat that success in future. It can also help your org dev team improve their processes and fuel the next intervention too!
And how about if you feel the need to make changes in the middle of an intervention? However well you’ve designed and run a change process, it’s possible for something unexpected to occur or for additional elements to emerge. Be sure to have a system of checking-in on progress and adjusting where necessary.
Use your KPIs, talk to your team and create open channels for feedback . In some change processes, you might freely adjust throughout the process or you may want to complete the entire intervention before properly evaluating and making changes.
For example, if you’re running a series of soft skills workshops and discover that employees are struggling to engage, the workshop facilitator might take a different approach in order to fulfil the needs of the intervention and you might adjust the program as a result.
On the other hand, if you’re rolling out a new interview process with your HR team and they’ve had some feedback that it’s too long from a few participants. It might be too early to make changes when the success of the intervention is the quality of the final hire.
Whatever your process, thorough evaluation is necessary to first determine the success of your intervention and then enable your team to make the right adjustments. Ensure you have the means to collect data and input from your team in order to evaluate well early so that you aren’t picking up the pieces later!
Conclusion
OD interventions are a key tool for any company wanting to improve organizational performance, stay competitive and create meaningful change.
Whether it’s finding ways to improve employee development, implement new tools or radically restructure your team, we hope that this guide will help you take the first steps in creating your intervention strategy.
In my experience, while the distinctions between different types of group interventions are useful for understanding the role of organizational development and what tools might be available, they are not mutually exclusive.
For example, fixing a complex problem like low employee satisfaction may include a combination of human process, human resource management and other change strategies. As with any change process, the solutions used should respond to the specifics of the challenge and situation you face.
Your own OD intervention strategy will likely feature elements of various intervention types and in truth, OD interventions are most successful when tailored to the organization at hand and the problems they are facing. Looking for more resources? Discover how change management software can help facilitate successful OD interventions and improve organizational effectiveness.
Running workshops as part of your group interventions? Explore how to create engaging and impactful sessions in this workshop planning guide.
Leave a Comment Cancel reply
Your email address will not be published. Required fields are marked *

Going from a mere idea to a workshop that delivers results for your clients can feel like a daunting task. In this piece, we will shine a light on all the work behind the scenes and help you learn how to plan a workshop from start to finish. On a good day, facilitation can feel like effortless magic, but that is mostly the result of backstage work, foresight, and a lot of careful planning. Read on to learn a step-by-step approach to breaking the process of planning a workshop into small, manageable chunks. The flow starts with the first meeting with a client to define the purposes of a workshop.…

How does learning work? A clever 9-year-old once told me: “I know I am learning something new when I am surprised.” The science of adult learning tells us that, in order to learn new skills (which, unsurprisingly, is harder for adults to do than kids) grown-ups need to first get into a specific headspace. In a business, this approach is often employed in a training session where employees learn new skills or work on professional development. But how do you ensure your training is effective? In this guide, we'll explore how to create an effective training session plan and run engaging training sessions. As team leader, project manager, or consultant,…

Effective online tools are a necessity for smooth and engaging virtual workshops and meetings. But how do you choose the right ones? Do you sometimes feel that the good old pen and paper or MS Office toolkit and email leaves you struggling to stay on top of managing and delivering your workshop? Fortunately, there are plenty of online tools to make your life easier when you need to facilitate a meeting and lead workshops. In this post, we’ll share our favorite online tools you can use to make your job as a facilitator easier. In fact, there are plenty of free online workshop tools and meeting facilitation software you can…
Design your next workshop with SessionLab
Join the 150,000 facilitators using SessionLab
Sign up for free
- Technical Support
- Find My Rep
You are here
Cases and Exercises in Organization Development & Change
- Donald L. Anderson - University of Denver, USA
- Description
Cases and Exercises in Organization Development & Change, Second Edition encourages students to practice organization development (OD) skills in unison with learning about theories of organizational change and human behavior. The book includes a comprehensive collection of cases about the OD process and organization-wide, team, and individual interventions, including global OD, dialogic OD, and OD in virtual organizations. In addition to real-world cases, author Donald L. Anderson gives students practical and experiential exercises that make the course material come alive through realistic scenarios that managers and organizational change practitioners regularly experience.
See what’s new to this edition by selecting the Features tab on this page. Should you need additional information or have questions regarding the HEOA information provided for this title, including what is new to this edition, please email [email protected] . Please include your name, contact information, and the name of the title for which you would like more information. For information on the HEOA, please go to http://ed.gov/policy/highered/leg/hea08/index.html .
For assistance with your order: Please email us at [email protected] or connect with your SAGE representative.
SAGE 2455 Teller Road Thousand Oaks, CA 91320 www.sagepub.com
Supplements
Password-protected Instructor Resources include teaching notes for the cases, designed for instructors to expand questions to students or initiate class discussion.
The Text has not yet arrived.
Case studies support course work synthesis
This is a very good book to use in the classroom because it helps students connect theoretical knowledge about organizational development and change with practice.
Cases were well put together and kept the students engaged.
NEW TO THIS EDITION
- New cases discuss relevant areas of growing importance to OD practitioners, encouraging students to think about topics such as global OD, dialogic OD, and OD in virtual organizations.
- Each case contains learning objectives, discussion questions, and suggestions for further reading, encouraging students to take an active role to interpret and discover the cases’ meaning.
- The revised structure aligns with Organization Development, Fourth Edition , making it easier for students and instructors to use the two books simultaneously in a semester.
KEY FEATURES
- Provides rich scenarios of organizational life , with each case constructed as a brief scene in which students are asked to weigh the pros and cons of alternate courses of action.
- Written by experts in the field , these original cases focus precisely on a specific topic in the OD process or intervention method.
- Cases represent a wide range of industries in which OD is practiced, exposing students to issues in for-profit businesses, educational institutions, government agencies, and health care organizations.
Includes a variety of exercises including self-assessment tools, role-play exercises, and individual or group simulations to enhance students' skill development in acting as change agents.
Organizational Change and Development: A Case Study in the Indian Electricity Market
Cite this chapter.

- Pawan Budhwar ,
- Jyotsna Bhatnagar &
- Debi Saini
1 Citations
The present economic growth of India is largely an outcome of the liberalization of its economic policies in 1991. Since gaining independence in 1947, India adopted a “mixed economy” approach (emphasizing both private and public enterprise). This had the effect of reducing both entrepreneurship and global competitiveness. Despite the formalities of planning, the Indian economy reached its worst in 1990 and witnessed a double digit rate of inflation, decelerated industrial production, fiscal indiscipline, a very high ratio of borrowing to the GNP (both internal and external) and a dismally low level of foreign exchange reserves. The World Bank and the IMF agreed to bail out India at that time on the condition that it changed to a “free market economy” from what at the time was a regulated regime. To meet the challenges, the government announced a series of economic policies, followed by a new industrial policy supported by fiscal and trade policies. A number of reforms were made in the public sector that affected trade and exchange policy. At the same time, the banking sector together with activity in foreign investment was liberalized.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as EPUB and PDF
- Read on any device
- Instant download
- Own it forever
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
- Durable hardcover edition
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Unable to display preview. Download preview PDF.
Further reading
Budhwar, P. and Varma, A. (2011a) (eds) Doing Business in India , London: Routledge.
Google Scholar
Budhwar, P. and Varma, A. (2011b) “Emerging HR Management in India and the way forward”, Organizational Dynamics , 40(4), pp. 317–25.
Article Google Scholar
Budhwar, P. and Varma, A. (2010) “Guest Editors’ Introduction: Emerging Patterns of HRM in the New Indian Economic Environment”, Human Resource Management , 49(3), pp. 343–51.
Budhwar, P. and Bhatnagar, J. (2009) The Changing Face of People Management in India , London: Routledge.
Book Google Scholar
Burnes, B. (2006) Managing Change , Harlow: FT Prentice-Hall.
Clardy, A. (2004) “Toward an HRD Auditing Protocol: Assessing HRD Risk Management Practices”, HumanResourceDevelopment Review , 3(2), pp. 124–50.
Kotter, J. P. and Cohen, D. S. (2006) The Heart of Change: Real-life Stories of How People Change their Organizations , Boston: Harvard Business School Press.
Ramnarayan, S. (2003) “Changing Mindsets of Middle-level Officers in Government Organizations”, Vikalpa , 28(4), pp. 63–76.
Sharma, R. R. (2007) Change Management: Concepts and Applications , New Delhi: Tata McGraw-Hill.
Download references
You can also search for this author in PubMed Google Scholar
Editor information
Editors and affiliations.
Director of Executive Education, Aston Business School, UK
Cora Lynn Heimer Rathbone
Copyright information
© 2012 Pawan Budhwar, Jyotsna Bhatnagar and Debi Saini
About this chapter
Budhwar, P., Bhatnagar, J., Saini, D. (2012). Organizational Change and Development: A Case Study in the Indian Electricity Market. In: Rathbone, C.L.H. (eds) Ready for Change?. Palgrave Macmillan, London. https://doi.org/10.1057/9781137008404_9
Download citation
DOI : https://doi.org/10.1057/9781137008404_9
Publisher Name : Palgrave Macmillan, London
Print ISBN : 978-1-349-34448-2
Online ISBN : 978-1-137-00840-4
eBook Packages : Palgrave Business & Management Collection Business and Management (R0)
Share this chapter
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
The Impact of OD Interventions on Performance Management: A Case Study
Article sidebar, main article content.
Good performance management systems can have a significant impact upon the operations and success of any organization. The broad objectives of this article are to identify the problematic areas in the company and identify ways to improve staff performance, employee motivation and involvement. The specific research objectives are to describe and analyse the current situation of the company and to conduct a 3-phase diagnosis: Phase 1, identification of problematic areas which need improvement; Phase 2 development and implementation of intervention techniques; Phase 3 monitoring and evaluation of results after the intervention to determine the impact on the company performance. Both the qualitative and quantitative methods of analysis were used which included interview, observation and questionnaires. The findings are that after the ODI, staff performance improved. This improvement has led to better performance of the organization at three levels. At the individual level—staff perceived more motivation and that their competencies at work increased. At the team level—staff perceived that there was an improvement in team effort. At the corporate level— the findings suggest that improved corporate performance is linked to improved individual and team level processes.
Article Details
This work is licensed under a Creative Commons Attribution 4.0 International License .
The submitting author warrants that the submission is original and that she/he is the author of the submission together with the named co-authors; to the extend the submission incorporates text passages, figures, data, or other material from the work of others, the submitting author has obtained any necessary permission.
Articles in this journal are published under the Creative Commons Attribution License (CC-BY What does this mean? ). This is to get more legal certainty about what readers can do with published articles, and thus a wider dissemination and archiving, which in turn makes publishing with this journal more valuable for you, the authors.
Patima Jeerapaet
Patima Jeerapaet is a graduate of the Ph.D. OD Program at Assumption University. He is also the chairman of the Joint Foreign Chamber of Commerce in Thailand (JFCCT).
Similar Articles
- Nattaya Chokekanoknapa, Strengthening Organizational Effectiveness through an ODI on Performance Management at the Departmental Level: A Case Study , AU-GSB e-JOURNAL: Vol. 4 No. 1 (2011): AU-GSB e-JOURNAL (June 2011)
You may also start an advanced similarity search for this article.

OD Interventions: Catalyzing Organizational Transformation
Table of Contents
Organizational Development (OD) interventions are purposeful actions and strategies designed to drive positive change within an organization. In this blog, we’ll delve into the significance of OD interventions, common types, and how they contribute to organizational transformation.
Understanding OD Interventions:
What are od interventions.
OD interventions are deliberate activities and initiatives aimed at improving an organization’s performance, culture, and effectiveness. They are structured approaches to bring about desired changes within the organization, aligning it with strategic goals and fostering growth and adaptability.
Types of OD Interventions:
OD interventions can take various forms, tailored to address specific organizational challenges and goals. Here are some common types:
1. Team Building:
- Team building interventions focus on improving communication, collaboration, and cohesion among teams. Activities may include team workshops, retreats, and problem-solving exercises.
2. Leadership Development:
- These interventions aim to enhance leadership skills and capabilities at all levels of the organization. Leadership development programs often involve training, coaching, and mentoring.
3. Change Management:
- Change management interventions assist in navigating and implementing organizational changes smoothly. They include strategies for communication, stakeholder engagement, and resistance management.
4. Process Consultation:
- Process consultation involves working with employees to analyze and improve existing processes and workflows. It encourages employees to identify areas for enhancement and develop solutions.
5. Cultural Interventions:
- Cultural interventions focus on shaping and nurturing the organizational culture. They may involve initiatives to promote diversity and inclusion, values alignment, and ethical behavior.
6. Organizational Design:
- Organizational design interventions explore and modify the structure, roles, and responsibilities within the organization. They aim to enhance efficiency and alignment with strategic goals.
7. Strategic Planning:
- These interventions facilitate the development and execution of strategic plans. They include activities such as visioning sessions, goal setting, and strategy alignment.
8. Conflict Resolution:
- Conflict resolution interventions address interpersonal or team conflicts within the organization. They help identify root causes and implement strategies for resolution.
The Role of OD Interventions:
1. driving change:.
- OD interventions serve as catalysts for change by providing a structured framework for planning and implementing organizational improvements.
2. Engaging Employees:
- They engage employees at all levels, fostering a sense of ownership and involvement in the change process.
3. Aligning with Strategy:
- OD interventions ensure that changes align with the organization’s strategic goals and long-term vision.
4. Measuring Progress:
- They provide mechanisms for tracking and measuring the impact of change initiatives, allowing for continuous improvement.
5. Enhancing Adaptability:
- OD interventions equip organizations with the tools and capabilities to adapt to evolving market conditions and challenges.
The Process of OD Interventions:
OD interventions typically follow a structured process:
1. Assessment:
- The organization assesses its current state, identifying areas for improvement and setting clear goals.
2. Planning:
- A detailed plan is developed, outlining the specific intervention strategies, timelines, and resources required.
3. Implementation:
- The interventions are executed according to the plan, involving employees and stakeholders as needed.
4. Evaluation:
- The impact of the interventions is assessed through data collection and analysis, and adjustments are made as necessary.
5. Sustainability:
- Successful interventions are integrated into the organizational culture and processes to ensure long-term sustainability.
Conclusion:
OD interventions are instrumental in catalyzing organizational transformation. They provide a structured approach to address challenges, improve performance, and foster a culture of continuous learning and growth. By engaging employees and aligning with strategic goals, OD interventions empower organizations to thrive in a dynamic and evolving business environment.
How useful was this post?
Click on a star to rate it!
Average rating 0 / 5. Vote count: 0
No votes so far! Be the first to rate this post.
We are sorry that this post was not useful for you! 😔
Let us improve this post!
Tell us how we can improve this post?

Management Functions and Organisational Processes
1 Management: An Overview
- Meaning and Definition of Management
- Nature of Management
- Characteristics of Management
- Administration and Management
- The Importance of Management
- Functions of Management
- Challenges of Management
2 Management and its Evolution
- Perspectives of Management
3 Roles of Managers
- Management process
- Managerial roles
- Management skills
- Management levels
- Characteristics of a good manager
- How do managers know whether they are good or not?
- Changing role of a manager in the current context
- The Changing role of a manager – Perspective from managers
- Meaning of Planning
- Nature of planning
- Steps of the planning function
- Why planning is necessary
- Types of planning
5 Organising
- The concept of organizing and analyzing work
- Different approaches to organizing and analyzing work
- Work improvement and measurement
- Time and motion study
- Workspace and architectural ergonomics
- Impact of information technology on organising work
6 Staffing and Directing
- Characteristics of staffing
- Training and Development
7 Controlling
- Meaning of Control
- Importance of Control
- Features of Control
- The Control process
- Essentials of a good control system
- Types of control
- Techniques of Control
8 Leading and Motivating
- Leadership Styles
- Leadership Theories
- Modern Theories of Leadership
- Successful Vs. Effective Leader
- Motivation: Meaning and Definition
- Motivating Factors
- Importance of Motivation
- Motivating Steps
- Types of Motivation
- Theories of Motivation
9 Decision Making
- Three Phases in Decision Making Process
- Types of Managerial Decisions
- Decision Making under Different States of Nature
- Models of Decision Making Process
- Techniques Used in Different Steps of Decision Making
- Individual Versus Group Decision Making
- Overcoming Barriers to Effective Decision Making
10 Organisation Structure and Design
- Organisation Structure and Chart
- Formal and Informal Organisations
- Factors Influencing the Choice of Structure
- Degree of Decentralisation
- Line and Staff Relationships
- Specialisation of Work
- Span of Control and Levels of Management
- Differentiation of Tasks and Activities within an Organisation
- Matrix Structure
- Network Structure
- Integration of Organisational Tasks and Activities
- Designing Structure for a Service Organisation
11 Organisation Communication Processes
- Communication: Meaning and Purpose
- Importance of Communication
- Communication Process
- Verbal and Non-verbal Communication
- Channels of Communication
- Barriers to Communication
- Making Communication Effective
12 Organisational Culture
- Concept of Organisational Culture
- Key Terms Used
- Meaning of Organisational Culture
- Role of Culture
- Developing Organisational Culture
- Types of Organisational Culture
- Traits of a great Organizational Culture
- Towards building a sustainable organizational culture
- Culture by choice V/s Culture by chance
- Creation of Ethical Culture
- Changing Organisational Culture
- Spirituality and Organisational Culture
13 Managing Change
- The concept of change
- The key drivers of change
- Nature of change
- Process of change
- Models of change
- Resistance to change
- Strategies to overcome resistance
- Forms of Organizational Change
- Evaluation of Change
- Role of Change Agent
- Organization Development (OD)
- OD Interventions
14 Corporate Social Responsibility and Ethics
- Meaning and Evolution of CSR
- Evolution of CSR Legislation in India
- Benefits and Drivers of CSR
- Ethics in the Context of CSR
- Ethical Views or Theories
- Case Study: Tata Motors Limited and CSR
A .gov website belongs to an official government organization in the United States.
A lock ( ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Managing Substance Use Disorders
- Health Equity
- Data Resources
- Additional HHS Resources
- Overdose Prevention Resources
- Management and Treatment of Pain
- Clinical Practice Guideline at a Glance
- Clinical Care and Treatment
- Health Care Provider Toolkits
- Electronic CDS Tools for Opioids
- Strategies and Partnerships
- Resources for Public Health Professionals
- Journal Articles
- MMWR Articles
- Guides and Meeting Reports
- Related Publications
- Overdose Data to Action
- Drug-Free Communities (DFC)
OD2A Case Study: Harm Reduction
At a glance.
Read about how harm reduction works to reduce drug overdose from a case study from Overdose Data to Action in Illinois.
How can harm reduction work to reduce drug overdose?
Case Studies: Harm Reduction - Full Report
Harm reduction is a public health approach that focuses on mitigating the harmful consequences of drug use, including transmission of infectious disease and prevention of overdose, through provision of care that is intended to be free of stigma and centered on the needs of people who use drugs. 1 Harm reduction programs are often managed by community or peer-led organizations, or health departments. Harm reduction activities can include provision of sterile syringes, naloxone distribution, fentanyl testing, overdose prevention and education, including safer drug use education, and other activities that can lessen the risk of adverse outcomes associated with using drugs. For example, syringe services programs (SSPs) can reduce the occurrence of HIV and hepatitis C. 2 These programs improve public safety through safe needle provision and disposal and are not associated with an increase in crime. 3 4 SSPs educate clients and community members about safer drug use, which may include information about how to recognize and reverse an opioid-involved overdose using naloxone. 5 Harm reduction programs also offer critical linkages to treatment for substance use disorders (SUDs) and other resources for populations with less access to care. 1 CDC's Evidence-Based Strategies for Preventing Opioid Overdose resource includes linkage to care and harm reduction strategies such as SSPs and targeted naloxone distribution, and harm reduction is a priority area for the HHS Overdose Prevention Strategy .
Case study snapshot
Harm reduction community linkage project – illinois.
- The Illinois Department of Public Health (IDPH) funds five harm reduction organizations and two county health departments in seven regions of the state with the highest opioid overdose death counts. The project may expand into regions with lower overdose death counts that lack support for harm reduction programs.
- Build the capacity of harm reduction organizations statewide.
- Increase awareness of the role of harm reduction in overdose prevention and response.
- Improve coordination between the harm reduction community and SUD treatment providers.
- Connect people to SUD treatment and support services.
- Provide case management.
- A state-level coordinator facilitates connections among the funded sites and seven local harm reduction coordinators. Coordinators determine needs through routine interviews with harm reduction clients, work with advisory boards of people who use drugs, and through the use of IDPH surveillance data.
- Key partners include healthcare and SUD treatment providers, local harm reduction advocates, law enforcement, nonprofit organizations, and community members including those who currently use substances or seek support services.
For more information about Illinois' Harm Reduction Community Linkage Project, check out full report in Case Studies: Harm Reduction .
- Hawk, K. F., Vaca, F. E., & D'Onofrio, G. (2015). Reducing Fatal Opioid Overdose: Prevention, Treatment and Harm Reduction Strategies. The Yale Journal of Biology and Medicine, 88 (3), 235–245.
- Platt, L., Minozzi, S., Reed, J., Vickerman, P., Hagan, H., French, C., Jordan, A., Degenhardt, L., Hope, V., Hutchinson, S., Maher, L., Palmateer, N., Taylor, A., Bruneau, J., & Hickman, M. (2017) Needle syringe programmes and opioid substitution therapy for preventing hepatitis C transmission in people who inject drugs. Cochrane Database of Systematic Reviews, 9 (9), 1-80. https://doi.org/10.1002/14651858.CD012021.pub2
- Tookes, H. E., Kral, A. H., Wenger, L. D., Cardenas, G. A., Martinez, A. N., Sherman, R. L., Pereyra, M., Forrest, D. W., LaLota, M., & Metsch, L. R. (2012). A comparison of syringe disposal practices among injection drug users in a city with versus a city without needle and syringe programs. Drug and Alcohol Dependence, 123 (1-3), 255-259. https://doi.org/10.1016/j.drugalcdep.2011.12.001
- Marx, M. A., Crape, B., Brookmeyer, R. S., Junge, B., Latkin, C., Vlahov, D., & Strathdee, S. A. (2000). Trends in crime and the introduction of a needle exchange program. American Journal of Public Health, 90 (12), 1933-1936. https://doi.org/10.2105/ajph.90.12.1933
- Tobin, K. E., Sherman, S. G., Beilenson, P., Welsh, C., & Latkin, C. A. (2009). Evaluation of the Staying Alive programme: Training injection drug users to properly administer naloxone and save lives. The International Journal of Drug Policy, 20 (2), 131-136. https://doi.org/10.1016/j.drugpo.2008.03.002
Overdose Prevention
Overdose prevention is a CDC priority that impacts families and communities. Drug overdose is a leading cause of preventable death in the U.S.
For Everyone
Health care providers, public health.
- Human Resource Management
Case Studies of OD interventions by Plummer & Associates
Related documents
Add this document to collection(s)
You can add this document to your study collection(s)
Add this document to saved
You can add this document to your saved list
Suggest us how to improve StudyLib
(For complaints, use another form )
Input it if you want to receive answer
We use cookies to ensure best experience for you
We use cookies and other tracking technologies to improve your browsing experience on our site, show personalize content and targeted ads, analyze site traffic, and understand where our audience is coming from. You can also read our privacy policy , We use cookies to ensure the best experience for you on our website.
- SouthEast Asia
- The Middle East
- Leaders Speak
- Brand Solutions
- Organization Development
- OD Interventions: The future and its alignment with HR
- ETHRWorld Contributor
- Updated On Aug 27, 2022 at 05:36 PM IST

- Published On Sep 27, 2021 at 07:57 AM IST
All Comments
By commenting, you agree to the Prohibited Content Policy
Find this Comment Offensive?
- Foul Language
- Inciting hatred against a certain community
- Out of Context / Spam
Join the community of 2M+ industry professionals
Subscribe to our newsletter to get latest insights & analysis., download ethrworld app.
- Get Realtime updates
- Save your favourite articles
- Decoding OD-HR Relationship
- prof dave ulrich
- Dr Deepak Sharma
- od interventions
- expert speak
Organizational Development Intervention Stages Report
Introduction, organizational development phases.
Team spirit and motivation are two critical factors that define the ability of a firm to achieve success in the market. According to Baporikar (2018), successful firms understand the fact that human resource should remain motivated to enhance its productivity.
The lack of motivation is a sign that the management is failing to meet the basic needs of its employees. On the other hand, lack of team spirit is a sign that the firm is lacking a platform for resolving conflicts to ensure that possible differences can be addressed. In the current competitive business environment, there is need to ensure that that workers are offered a perfect environment for them to explore their talents as a way of promoting creativity. Team spirit makes it possible for them to work as a unit in addressing the challenges that might exist in the market. In this paper, the researcher seeks to apply the concept of organizational development to address the two issues that affect employees of this company.
The concept of organizational development has emerged as a powerful tool that firms use to address challenges they face systematically. When faced with the challenge such as the one that has been identified, which affects employees’ productivity, this concept can be used to find a lasting solution that would promote teamwork and motivation. The organizational development identifies various steps that should be taken to address a specific issue. This section will use this model to address the issue that this firm faces.
The initial phase of organizational development, also known as the entry phase, is the stage that the management appreciates the fact that a problem exist that requires an urgent solution. Baporikar (2018) explains that at this stage, the management may notice that events at the company are not going as per the set goals or a lot of money or time is used contrary to what had been set previously. In this case, it has been identified that there is lack of motivation and teamwork among employees. The problem is affecting their productivity within the company. The next phase is contracting, where the firm identifies a team of experts who can help solve the identified problem. In this case, the researcher is the contrary who has set forth to address the marketing problem at the company.
The initial stage of solving the problem starts with the diagnosis. As Bushe and Marshak (2015) observes, one should start by understanding the root-cause of the problem within the firm. The term should investigate processes and systems within the company to identify the possible cause of the problem. Weisbord’s Six Box Model is a popular theory that is often used to diagnose a problem within an organization. It starts by identifying the purpose of the firm in the market.
This company offers electronic products in the local market. The next step is to determine the structure of the company to determine how work is divided. The company has fully functioning marketing, finance, logistics, and human resource departments. Under the marketing unit, there is the customer care unit, public relations unit, promotional campaigns unit.
The model then emphasizes on the relationships, especially how the firm manages conflicts, and whether there is the use of technology in the process. The analysis has revealed that lack of team spirit and motivation is a major challenge that the firm faces. Most conflicts within the firm are resolved by the decision of the top management unit relevant at that specific level. It means that the decision of the marketing manager would override any other opposing view.
In the context of helpful mechanisms, the focus is to determine if there are adequate coordinating technologies within the firm (Jamieson, Church, & Vogelsang, 2018). Such management strategies where employees are denied the opportunity to engage and offer share their views on issues affecting them often lead to limited motivation among employees.
It was evident that the firm lack proper coordinating technologies, which limit dialogue, hence the issue of lack of team spirit emerged. Although individual employees within the firm regularly use social media platforms such as Facebook, WhatsApp, and Twitter, the firm is yet to embrace these platforms as official means of communication among employees. It means that other traditional means of communication such as face-to-face meetings, phone calls, letters, and memos are still preferred means of passing official communication (Ardichvili & Dirani, 2017).
The concept of reward where tasks are attached to specific incentives is another factor that one should consider when conducting the diagnosis. Most of the assignments that employees within this department have to undertake are not attached to specific incentives. As such, the problem identified does not arise from this issue. The whole system requires an enabling environment to achieve the desired level of success. Figure 1 below summarizes these factors.
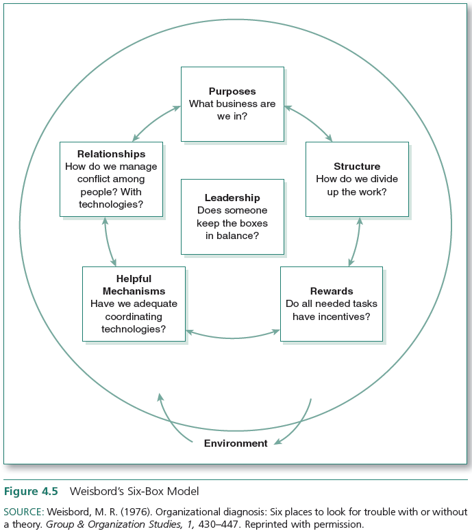
The feedback of the diagnosis show that the main problem at the firm is that there is no team spirit and employees’ motivation is significantly low. The employees within this company find it difficult to work as a unit. They have failed to appreciate the significance of diversity in the workplace. They are unable to appreciate the fact that they can have different thought and perceptions in life but still work as a unit. The lack of team spirit is partly responsible for the limited motivation among workers. These employees feel that their views are not valued, and that the management is not making any significant effort to address the lack of team spirit.
The feedback from the diagnosis also shows that the current problem has been caused by the limited communication that employees have. The firm lacks a proper platform where employees can interact and share their views on how to address these issues. The marketing department sometimes organizes conferences for all employees once or twice a year to discuss issues that affect their operations. However, such an arrangement does not offer an adequate platform for the employees to engage and find a common solution to the issues that the department faces.
Planning Change
At the planning stage, the team will focus on addressing the identified problem. The marketing department will need to find a way of addressing the problem of lack of motivation and team spirit. The management will need to engage employees to understand why they cannot work as a spirit. It is also necessary to understand why they are not motivated at work (Waddell, Creed, Cummings, & Worley, 2019). The team should then find a way of addressing these concerns within the firm. It is equally important for the management to ensure that all stakeholders agree about the strategy that they should use to achieve the desired goals. The following are the specific objectives that should be realized from this project:
- The management should engage employees within the next one month to identify specific reasons where there is no team spirit.
- The firm will need to use both monetary and non-monetary factors to ensure that there is a significant increase in the level of employees’ motivation within the next one month;
- Addressing challenges above should enable the brand value of the firm to increase by at least 10% within the next one year.
Intervention
The intervention phase involves implementing the plans to achieve the specific objectives. The first plan was for the management to develop an effective way through which employees within the firm can engage with one another and agree on how to undertake their responsibilities as a unit. The diagnosis of the problem revealed that the team find it difficult agreeing on how to undertake different responsibilities. The lack of team spirit and other challenges that these workers face has led to reduced levels of motivation.
These workers feel that their views do not matter and that there is no deliberate effort by the management to promote teamwork. Ardichvili and Dirani (2017) explains that when two opposing teams cannot find a platform to address their conflict, then each team will propagate for what it believes is the best. The problem is that in such a case, the management will have to intervene. Sometimes the intervention may lower levels of motivation further.
The team whose idea is dropped will feel ignored, and as such, they may not support the new course. To avoid such problems at this company, the plan is to have a forum where views of all employees will be taken into consideration as a way of promoting teamwork. Through such forums, any misunderstandings can be addressed as people embrace a positive approach towards finding a common interest. This process of creating a new platform for communication should take less than one week. As Widodo (2018) suggests, the management can create a WhatsApp group or a Facebook page for employees to discuss issues of common interest. The marketing manager can monitor such deliberations to help them make a decision based on facts as expressed in the views of employees.
To help solve the problem of reduced levels of motivation among employees, the firm should consider using various strategies. The first strategy is to ensure that employees are rewarded appropriately for their work. The remuneration should reflect the individual effort of the employee’s effort. Studies have shown that a firm can also motivate its employees using non-monetary strategies (Ardichvili & Dirani, 2017). Public recognition of workers who have registered excellent performance is an effective way of promoting hard work and motivation. These workers will know that the management is monitoring their commitment to the firm and appreciates it.
Promotion is another factor that can motivate workers. Individuals who have remained loyal and committed to the firm through their good performance should be considered for promotion as a way of motivating them. Baporikar (2018) argues that the management should make it clear why they consider specific individuals for promotion. When it is based on performance, it is necessary to communicate this fact to avoid cases of dissatisfaction among other workers who do not get such promotions. Widodo (2018) believes that sometimes it may be necessary to involve employees themselves in identifying the top performers. Such strategies eliminate the perception that the management favors specific individuals as opposed to others.
The last stage is the evaluation, where the team will assess the outcome of the implemented solution to determine the way forward. When the evaluation shows that some weaknesses still exist, which may require further improvements then the team can take necessary steps to address them. The current problem that this company faces is that there is no team spirit and motivation, partly caused by the lack of an effective internal mechanism of solving internal conflicts and agreeing on the best way of overcoming various challenges. The researcher has developed a new model of organizational development that can be used by this organization to solve such future problems.
The new model is based on three pillars. The first pillar is effective communication. An organization can only achieve success if the involved parties can share their views. The new model also emphasizes the need for teamwork. All stakeholders should understand the value of working as a unit. The last factor is the need to invest in research and technological advancements. A firm can only achieve innovativeness if it embraces regular research and investment in emerging technologies. These three pillars will help this company to address the problem identified in this case study.
Ardichvili, A., & Dirani, K. (2017). Leadership development in emerging market economies . New York, NY: Palgrave Macmillan.
Baporikar, N. (2018). Global practices in knowledge management for societal and organizational development . Hershey, PA: Business Science Reference.
Beckhard, R. (2006). What is organization development? Organization Development, 4 (1), 3-12.
Bushe, G. R., & Marshak, R. J. (2015). Dialogic organization development: The theory and practice of transformational change . Oakland, CA: Berrett-Koehler Publishers, a BK Business Book.
Jamieson, D. W., Church, A. H., & Vogelsang, J. D. (2018). Enacting values-based change: Organization development in action . Cham, Switzerland: Palgrave Macmillan.
Waddell, D. M., Creed, A., Cummings, T. G., & Worley, C. G. (2019). Organisational change: Development and transformation . Melbourne, Australia: Cengage.
Widodo, T. (2018). Unified theory of acceptance and use of technology (UTAUT) model to analyze user intention of Smartphone in banding. Journal of Organizational Change Management, 25 (4), 535-559.
- Teamwork's Achievements and Challenges
- Organizational Behaviour: Teamwork in a Canadian Pub
- Teamwork Leads in Labor Force Improvement
- Manage Stakeholder Expectations Determine Requirements
- The Utility of the Intelligence Cycle to Modern Intelligence Organization
- The Basic Building Blocks of a Contract Analysis
- Coca-Cola and Marussia Supply Chain Management
- Contracting Excellence in Procurement and Supply Between ADCO and Emirates Transport
- Chicago (A-D)
- Chicago (N-B)
IvyPanda. (2021, July 29). Organizational Development Intervention Stages. https://ivypanda.com/essays/organizational-development-intervention-case-study/
"Organizational Development Intervention Stages." IvyPanda , 29 July 2021, ivypanda.com/essays/organizational-development-intervention-case-study/.
IvyPanda . (2021) 'Organizational Development Intervention Stages'. 29 July.
IvyPanda . 2021. "Organizational Development Intervention Stages." July 29, 2021. https://ivypanda.com/essays/organizational-development-intervention-case-study/.
1. IvyPanda . "Organizational Development Intervention Stages." July 29, 2021. https://ivypanda.com/essays/organizational-development-intervention-case-study/.
Bibliography
IvyPanda . "Organizational Development Intervention Stages." July 29, 2021. https://ivypanda.com/essays/organizational-development-intervention-case-study/.

- Free Case Studies
- Business Essays
Write My Case Study
Buy Case Study
Case Study Help
- Case Study For Sale
- Case Study Service
- Hire Writer
Case Study on OD Interventions
Od interventions case study:.
If one wants to develop the company a range of interventions should be carried out. To begin with, one should create a healthy convenient working environment for employees. When they see that a boss takes care of them, they start to respect and praise him.
As a result their work becomes better and every employee appreciates his workplace. Then, the improvement of an organization can not be simply commanded by a boss. He should discuss this question with employees and managers and find the best way to develop the company’s work. Next, a businessman should trust and respect his employees and they will answer with the same actions and hard devoted work. Finally, the most important intervention into OD is the conquering of the market with new production and services.
We Will Write a Custom Case Study Specifically For You For Only $13.90/page!
Such strategic changes will assure the company with new clients and great profits.Every OD intervention should be planned and carried out carefully if the boss wants his company to flourish. Students who expect to be involved in business will need to gain knowledge on this serious and urgent topic, because every businessman faces it at least once in his life. Young people should research the case suggested for the analysis and study the interventions in detail. One should weigh the importance and effectiveness of the intervention and value what profits of failures the company will have.
Having analyzed the cause and effect of interventions one will be able to provide the reader with smart conclusions and prove that he has got rich knowledge on the topic.The biggest problem which is urgent among students writing the case study on the topic is its correct organization. A free sample case study on OD interventions prepared by the expert is a valuable piece of writing assistance which can make the writing process easier. Due to the experience and knowledge of a professional writer, his free example case study on OD intervention will teach you format and construct the paper properly.
Related posts:
- Interventions Case Study
- Case Study on Leadership Styles
- Case Study on Method Study
- Case Study on Industrial Relations
- Case Study on Training and Development
- Case Study on Basic Financial Accounting
- Case Study on Selection Process
Quick Links
Privacy Policy
Terms and Conditions
Testimonials
Our Services
Case Study Writing Service
Case Studies For Sale
Our Company
Welcome to the world of case studies that can bring you high grades! Here, at ACaseStudy.com, we deliver professionally written papers, and the best grades for you from your professors are guaranteed!
[email protected] 804-506-0782 350 5th Ave, New York, NY 10118, USA
Acasestudy.com © 2007-2019 All rights reserved.

Hi! I'm Anna
Would you like to get a custom case study? How about receiving a customized one?
Haven't Found The Case Study You Want?
For Only $13.90/page
- Open access
- Published: 21 May 2024
A modern way to teach and practice manual therapy
- Roger Kerry 1 ,
- Kenneth J. Young ORCID: orcid.org/0000-0001-8837-7977 2 ,
- David W. Evans 3 ,
- Edward Lee 1 , 4 ,
- Vasileios Georgopoulos 1 , 5 ,
- Adam Meakins 6 ,
- Chris McCarthy 7 ,
- Chad Cook 8 ,
- Colette Ridehalgh 9 , 10 ,
- Steven Vogel 11 ,
- Amanda Banton 11 ,
- Cecilia Bergström 12 ,
- Anna Maria Mazzieri 13 ,
- Firas Mourad 14 , 15 &
- Nathan Hutting 16
Chiropractic & Manual Therapies volume 32 , Article number: 17 ( 2024 ) Cite this article
114 Altmetric
Metrics details
Musculoskeletal conditions are the leading contributor to global disability and health burden. Manual therapy (MT) interventions are commonly recommended in clinical guidelines and used in the management of musculoskeletal conditions. Traditional systems of manual therapy (TMT), including physiotherapy, osteopathy, chiropractic, and soft tissue therapy have been built on principles such as clinician-centred assessment , patho-anatomical reasoning, and technique specificity. These historical principles are not supported by current evidence. However, data from clinical trials support the clinical and cost effectiveness of manual therapy as an intervention for musculoskeletal conditions, when used as part of a package of care.
The purpose of this paper is to propose a modern evidence-guided framework for the teaching and practice of MT which avoids reference to and reliance on the outdated principles of TMT. This framework is based on three fundamental humanistic dimensions common in all aspects of healthcare: safety , comfort , and efficiency . These practical elements are contextualised by positive communication , a collaborative context , and person-centred care . The framework facilitates best-practice, reasoning, and communication and is exemplified here with two case studies.
A literature review stimulated by a new method of teaching manual therapy, reflecting contemporary evidence, being trialled at a United Kingdom education institute. A group of experienced, internationally-based academics, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through reviews of contemporary literature and discussions in an iterative process. Public presentations were made to multidisciplinary groups and feedback was incorporated. Consensus was achieved through repeated discussion of relevant elements.
Conclusions
Manual therapy interventions should include both passive and active, person-empowering interventions such as exercise, education, and lifestyle adaptations. These should be delivered in a contextualised healing environment with a well-developed person-practitioner therapeutic alliance. Teaching manual therapy should follow this model.
Musculoskeletal (MSK) conditions are leading contributors to the burden of global disability and healthcare [ 1 ]. Amongst other interventions, manual therapy (MT) has been recommended for the management of people with MSK conditions in multiple clinical guidelines, for example [ 2 , 3 ].
MT has been described as the deliberate application of externally generated force upon body tissue, typically via the hands, with therapeutic intent [ 4 ]. It includes touch-based interventions such as thrust manipulation, joint mobilisation, soft-tissue mobilisation, and neurodynamic movements [ 5 ]. For people with MSK conditions, this therapeutic intent is usually to reduce pain and improve movement, thus facilitating a return to function and improved quality of life [ 6 ]. Patient perceptions of MT are, however, vague and sit among wider expectations of treatment including education, self-efficacy and the role of exercise, and prognosis [ 7 ].
Although the teaching and practice of MT has invariably changed over time, its foundations arguably remain unaltered and set in biomedical and outdated principles. This paper sets out to review contemporary literature and propose a revised model to inform the teaching and practice of MT.
The aim of this paper is to stimulate debate about the future teaching and practice of manual therapy through the proposal of an evidence-informed re-conceptualised model of manual therapy. The new model dismisses traditional elements of manual therapy which are not supported by research evidence. In place, the model offers a structure based on common humanistic principles of healthcare.
Consenus methodology
We present the literature synthesis and proposed framework as a consensus document to motivate further professional discussion developed through a simple three-stage iterative process over a 5-year period. The consensus methodology was classed as educational development which did not require ethical approval. Stage 1: a change of teaching practice was adopted by some co-authors (VG, RK, EL) on undergraduate and postgraduate Physiotherapy programmes at a UK University in 2018. This was a result of standard institutional teaching practice development which includes consideration of evidence-informed teaching. Stage 2: Input from a broader spectrum of stakeholders was sought, so a group of experienced, internationally-based educators, clinicians, and researchers from across the spectrum of manual therapy was convened. Perspectives were elicited through discussions in an iterative process. Stage 3: Presentations were made by some of the co-authors (VG, RK, SV, KY) to multidisciplinary groups (UK, Europe, North America) and feedback via questions and discussions was incorporated into further co-author discussions on the development of the framework. Consensus was achieved through repeated discussion of relevant elements. Figure 1 summarises the consensus methodology.
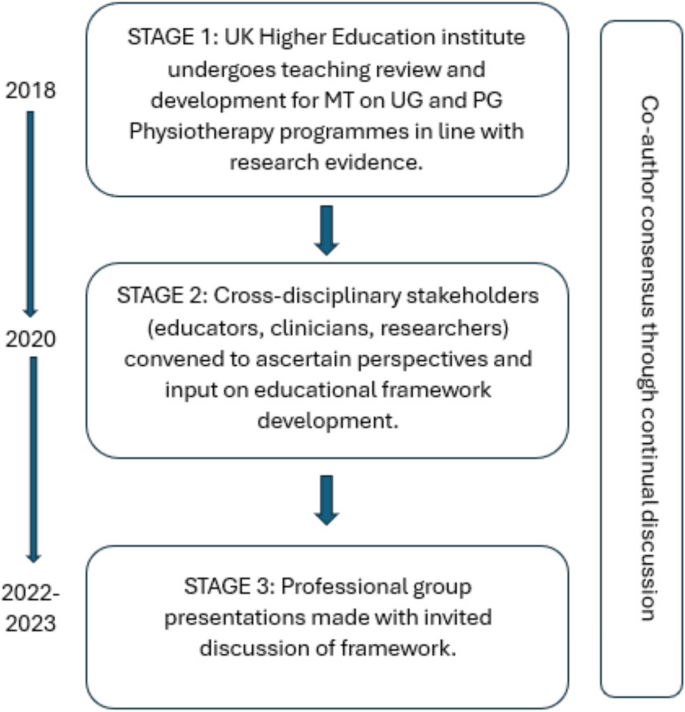
Summary and timeline of iterative consensus process for development of framework (MT: Manual Therapy; UG: Undergraduate; PG: Postgraduate)
Clinical & cost effectiveness of manual therapy
Manual therapy has been suggested to be a valuable part of a multimodal approach to managing MSK pain and disability, for example [ 8 ]. The majority of recent systematic reviews of clinical trials report a beneficial effect of MT for a range of MSK conditions, with at least similar effect sizes to other recommended approaches, for example [ 9 ]. Some systematic reviews report inconclusive findings, for example [ 10 ], and a minority report effects that were no better than comparison or sham treatments, for example [ 11 ].
Potential benefits must always be weighed against potential harms, of course. Mild to moderate adverse events from MT (e.g. mild muscle soreness) are common and generally considered acceptable [ 12 ], whilst serious adverse events are very rare and their risk may be mitigated by good practice [ 13 ]. MT has been reported by people with MSK disorders as a preferential and effective treatment with accepted levels of post-treatment soreness [ 14 ].
MT is considered cost-effective [ 15 ] and the addition of MT to exercise packages has been shown to increase clinical and cost-effectiveness compared to exercise alone in several MSK conditions [ 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 ]. Further, manual therapy has been shown to be less costly and more beneficial than evidence-based advice to stay active [ 24 ].
In summary, MT is considered a useful evidence-based addition to care packages for people experiencing pain and disability associated with MSK conditions. As such, MT continues to be included in national and international clinical guidelines for a range of MSK conditions as part of multimodal care.
Principles of traditional manual therapy (TMT)
Manual therapy has been used within healthcare for centuries [ 4 ] with many branches of MT having appeared (and disappeared) over time [ 25 ]. In developed nations today, MT is most commonly utilised by the formalised professional groups of physiotherapy, osteopathy, chiropractic, as well as groups such as soft tissue therapists. All of these groups have a history that borrows heavily from traditional healers and bone-setters [ 26 ].
Although there are many elements of MT, three principles appear to have become ubiquitous within what we shall now refer to as ‘traditional manual therapy’ (TMT): clinician-centred assessment , patho-anatomical reasoning , and technique specificity [ 27 , 28 , 29 , 30 ]. These principles continue to influence the teaching and practice of manual therapy over recent years, for example [ 31 ].
However, they have become increasingly difficult to defend given a growing volume of empirical evidence to the contrary.
Traditional manual therapy (TMT) principles: origins and problems
Clinician-centred assessment.
TMT has long had an emphasis on what we shall refer to as clinician-centred assessments . Within this, we claim, is an assumption that clinical information is both highly accurate and diagnostically important, for example [ 32 ]. Clinician-centred assessments include, for example, routine imaging, the search for patho-anatomical 'lesions’ and asymmetries, and specialised palpation. Although the focus of this paper is on the ‘hands-on’ examples of client-centred assessment, the notion of imaging is presented below to expose some of the flaws in the underlying belief system for TMT.
The emphasis on clinician-centred assessments has probably been driven, in part, by a desire for objective diagnostic tests which align well with gold-standard imaging. Indeed, since the discovery of x-rays, radiological imaging been used as an assessment for spinal pain – and a justification for using spinal manipulation – particularly in the chiropractic profession [ 33 ]. Contrary to many TMT claims, X-ray imaging is not without risk [ 34 ]. Additionally, until relatively recently (with the advent of magnetic resonance imaging) it was not widely appreciated that patho-anatomical ‘lesions’ believed to explain MSK pain conditions were nearly as common in pain-free individuals as those with pain [ 35 ]. Accordingly, the rates of unnecessary treatments, including surgery, are known to increase when imaging is used routinely [ 36 ]. For patients with non-specific low back pain, for example, imaging does not improve outcomes and risks overdiagnosis and overtreatment [ 37 ]. Hence, despite being objective in nature, the value of imaging for many MSK pain conditions (particularly spinal pain) has reduced drastically with clinical guidelines across the globe recommending against routine imaging for MSK pain of non-traumatic origin [ 38 ]. Even so, the practice of routine imaging continues [ 39 ].
Hands-on interventions are inextricably related to hands-on assessment [ 40 ], and often associated with claims of ‘specialisation’ [ 41 ]. By this we mean where a great level of training and precision are claimed to be necessary for influencing the interpretation of assessment findings, treatment decisions, and/or treatment outcomes. Implicit within this claim is that therapists who are unable to achieve such precision are not able to perform MT to an acceptable level (and thereby are not able to provide benefit to patients).
There are numerous studies that cast doubt over claims of highly specialised palpation skills. Palpation of anatomical landmarks does not reach a clinically acceptable level of validity [ 42 ]. Specialised motion palpation does not appear to be a good method for differentiating people with or without low back pain [ 43 ]. Poor content validity of specialised motion tests have been reported, in line with a lack of acceptable reference standards [ 44 ]. Palpable sensations reported by therapists are unlikely to be due to tissue deformation [ 45 ]. Furthermore, the delivery of interventions based on specialised palpatory findings is no better than non-specialised palpation [ 46 ]. Generally poor reliability of motion palpation skills has been reported, for example [ 47 ] and appear to be independent of clinician experience or training, for example [ 48 ]. Notably, person-centred palpation—for pain and tenderness for example—has slightly higher reliability, but is still fair at best [ 49 ].
This does not mean that palpation is of no use at all though; just that effective manual therapy does not depend upon it. For example, expert therapists can display high levels of interrater reliability during specialised motion palpation [ 50 ]. Focused training can improve the interrater reliability of specialised skills [ 51 ]. However, the validity of the phenomenon remains poor. Given the weight of the evidence and consistency of data over recent decades, we suggest that the role of clinician-centred hands-on assessment is no longer central to contemporary manual therapy.
Patho-anatomical reasoning
The justification for selecting particular MT interventions has historically been based upon the patho-anatomical status of local peripheral tissue [ 52 , 53 , 54 , 55 ]. Patho-anatomical reasoning, we propose, is the framework that links clinician-centred assessments to the desire for highly specific delivery of MT interventionsKey to this is the relationship between a patho-anatomic diagnosis and the assumed mechanisms of action of the intervention employed.
Theories for the mechanisms of action of MT interventions are many. Some of the most prominent include reductions of disc herniations [ 56 ], re-positioning of a bone or joint [ 32 ], removal of intra-articular adhesions [ 57 ], changes in the biomechanical properties of soft tissues [ 58 ], central pain modulation [ 59 ], and biochemical changes [ 60 ]. These theories have been used to justify the choice of certain interventions: a matching of diagnosis (i.e., existence of a lesion) to the effect of treatment takes place. However, most of these mechanistic theories either lack evidence or have been directly contested [ 61 ].
The causal relationship between proposed tissue-based factors such as posture, ergonomic settings, etc. and painful experience has also been disputed [ 62 ]. Although local tissue stiffness has been observed in people with pain, this is typically associated with neuromuscular responses, rather than patho-anatomical changes at local tissue level [ 63 , 64 , 65 , 66 ]. Overall, although some local tissue adaptions have been identified in people with recurrent MSK pain, this is inconsistent and the evidence is currently of low quality [ 67 ] are generally limited to short-term follow-up measures [ 68 ].
Technique specificity
TMT techniques have been taught with an emphasis that a particular direction, ‘grade’ of joint movement, or deformation of tissue at a very specific location in a certain way, is required to achieve a successful treatment outcome.
One problem with a demand for technique specificity in manual therapy is that an intervention does not always result in the intended effect. For example, posteroanterior forces applied during spinal mobilization consistently induce sagittal rotation, as opposed to the assumed posteroanterior translation, for example [ 69 ]. Furthermore, irrespective of the MT intervention chosen, restricting movements to a particular spinal segment is difficult and a regional, non-specific motion is typically induced, for example [ 70 ].
To support technique specificity, comparative data must repeatedly and reproducibly show superiority of outcome from specific MT interventions over non-specific MT, which is consistently not observed [ 71 , 72 , 73 ]. Some studies have demonstrated localised effects of targeted interventions [ 74 ] but there appears to be no difference in outcome related to: the way in which techniques are delivered [ 75 ]; whether technique selection is random or clinician-selected [ 41 ]; or variations in the direction of force or targeted spinal level [ 76 ]. Conversely, there is evidence that non-specific technique application may improve outcomes [ 77 , 78 , 79 ]. Further, sham techniques produce comparable results to specialised approaches [ 11 ].
Passive movement and localised touch have been associated with significant analgesic responses [ 80 ]. These data indicate the presence of an analgesic mechanism. Unfortunately, mechanistic explanation for the therapeutic effects of MT upon pain and disability still remain largely in a ‘black box’ state [ 81 ]. Nevertheless, there are several plausible mechanisms of action to explain the analgesic action of MT interventions, including the activation of modulatory spinal and supraspinal responses [ 82 , 83 , 84 , 85 ]. In support of this, MT interventions have been associated with a variety of neurophysiological responses [ 61 ]. However, it must be acknowledged that these studies provide mechanistic evidence based on association, which is insufficient to make causal claims [ 86 ]. Importantly, none of these neurophysiological responses have been directly related to either the analgesic mechanisms or clinical outcome and may therefore be incidental.
There is evidence that MT does not provide analgesia in injured tissues [ 87 , 88 ]. Conversely, MT has been shown to decrease inflammatory biomarkers [ 89 , 90 , 91 , 92 , 93 ], although these changes have not been evaluated in the longer-term, nor associated with clinical outcomes.
A modern framework for manual therapy
We propose a new direction for the future of MT in which the teaching and practice of this core dimension of MSK care are no longer based on the traditional principles of clinician-centred assessment , patho-anatomical reasoning , and technique specificity .
In doing so, this framework places MT more explicitly as part of person-centred care and appeals to common principles of healthcare, best available evidence, and contemporary theory which avoids unnecessary and over-complicated explanations of observed effects. The framework is simple in terms of implementation and delivery and contextualised by common elements of best practice for healthcare, in line with regulated standard of practice, e.g., [ 94 , 95 , 96 , 97 ]. Our proposal simply illustrates the operationalisation of these common elements through manual therapy.
Too much emphasis has been given to clinician-centred assessments and this should be rebalanced with an increased use of patient-centred assessments, such as a thorough case history, the use of validated patient-reported outcome measures (PROMS), and real-time patient feedback during assessments.
The new framework considers fundamental and humanistic dimensions of touch-based therapies, such as non-specific neuromodulation, communication and sense-making, physical education, and contextual clinical effectiveness. This aligns to contemporary ideas regarding therapeutic alliance and a move towards genuinely holistic healthcare [ 98 , 99 ]. The framework needs to be “open” in order to represent and allow expression of the complexity of the therapeutic encounter. However, to prevent the exploitation of this openness the framework is underpinned by evidence, and any manual therapy approaches without plausible and measurable mechanisms are not supported.
To provide the best care, common healthcare elements such as the safety and comfort of the person seeking help and therapist must be considered, and care should be provided as efficiently as possible. Our framework embraces these dimensions and employs an integration of current evidence. It is transdisciplinary in nature and may be adopted by all MT professions. Figure 1 provides a graphical representation of the framework. It is acknowledged that all components overlap, relate, and influence each. There are two main components: the practical elements on the inside, comprised of safety, comfort, and efficiency, and the conceptual themes on the outer regions, consisting of communication, context, and person-centred care Fig. 2 .
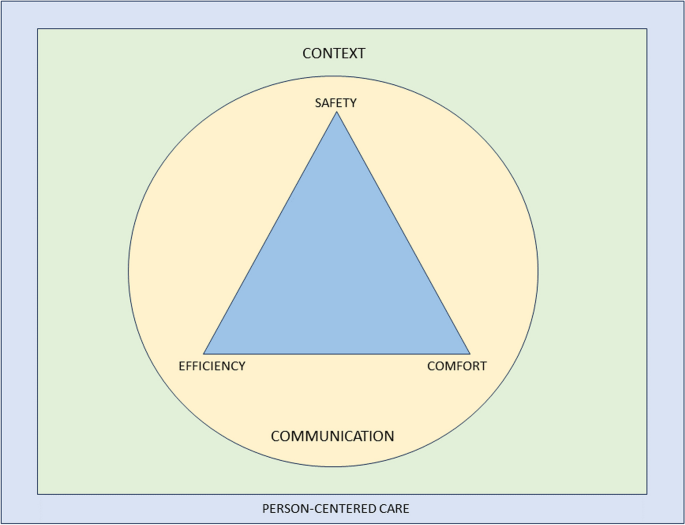
Representation of a modern teaching and practice framework for manual therapy. The image is purposefully designed to be simple, and has been developed primarily to be used as a teaching aid. When displayed in a learning environment, learners and clinicians can quickly refer to the image to check their practice against each element. To keep the image clear, each element of the image is described in detail in the text below”
Practical elements
Safety for people seeking help is a primary concern for all healthcare providers, with the aims to “ prevent and reduce risks, errors and harm that occur to patients [sic] during provision of health care… and to deliver quality essential health services ” [ 100 ]. This, and the notion of safety more generally (including that of the therapist), should be central to way MT is taught and practised.
A fundamentally safe context should be created where there is an absence of any obvious danger or risk of harm to physical or mental health. Consideration should be given to ensuring that communication and consent processes are orientated towards the safety of both the person seeking help and the therapist. The therapist should pay attention to any sense of threat that could be present in the physical, emotional, cognitive and environmental domains of the clinical encounter, and use skilful communication to mitigate anxiety about the assessment or therapeutic process.
Safety should also be considered in the clinical context of the assessment and treatment approach, ensuring that relevant and meaningful safety screenings have been undertaken [ 67 , 101 ]. There remains a need for good, skilful practice and development of manually applied techniques, but this can be achieved without reference to the principles of TMT and without the dogma of a proprietary therapeutic approach.
Comfort suggests that both the person seeking help and the therapist are physically and emotionally content during the assessment and therapeutic process. For example, the person seeking help is agreeable with any necessary state of dress (sociocultural difference should be considered); the person is relaxed and untroubled in whatever position they are in, and is adequately supported whether sitting, standing or recumbent during assessment and treatment; the therapist is comfortable with their positioning and posture; any discomfort produced by the therapeutic process is negotiated and agreed. Any physical mobilisation or touch should be applied with respect to the feedback from the person in relation to their comfort, rather than a pre-determined force based on the notion of resistance. This process requires clinical phronesis, sensitivity, responsivity, dexterity, and embodied communication [ 102 ].
The therapeutic process should be undertaken in a well-organised, competent manner aiming to achieve maximum therapeutic benefit with minimum waste of effort, time, or expense. To enhance the efficiency dimension, the assessment and therapeutic process should be an integral part of a holistic educational and/or activity-based approach to the management of the people which might also address psychological, nutritional, or ergonomic aspects of care, while being aware of social determinants to health. Recommendations exist which serve as a useful guide for enhancing care and promoting self-management in an efficient way [ 103 ].
A principle of this new model of MT is that therapists should not lose sight of the goals they develop with the people they help and ensure that there is coherence between their management aims and their techniques. Therapists should aim to support a person’s self-efficacy and use active approaches to empower them in their recovery. The overall number of therapeutic applications should be made in the context of fostering therapeutic alliance and supporting people to make sense of their situation and symptoms. This should be informed by contemporary views of the effects of manual therapy, emphasising a “physical education process” to promote sense-making and self-efficacy in alliance with the people they aim to help.
Clinical interactions need to be reproducible under a person’s own volition, serving to enhance self-empowerment. For example, someone could be taught how to “self-mobilise” if a positive effect is found with a particular therapeutic application. This should be appropriately scaffolded with behavioural change principles and functional contextualism that promote autonomy and self-management, rather than inappropriate reliance on the therapist [ 103 , 104 ].
An important and emergent notion from the proposed model is to question what constitutes indications for MT given that the model excludes traditional factors which would have informed whether manual therapy is indicated or not for a particular person. The response to this sits within the efficiency and safety dimensions: MT can be beneficial as part of a multi-dimensional approach to management across a broad population of people with musculoskeletal dysfunction, with no evidence to suggest any clinician-centered or patho-anatomical finding influences outcomes. The choice of whether or not to include MT as part of a management strategy should therefore be a product of a lack of contraindications and shared-decision making.
This framework aligns with evidence-based propositions that effectiveness and efficiency in assessment, diagnosis, and outcomes are not reliant on the therapist’s skill set of specialised elements of TMT, but rather other factors—for example variations in pain phenotypes [ 5 ].
Conceptual themes
Communication.
Communication is the overriding critical dimension to the whole therapeutic process and should be aimed at addressing peoples’ fundamental needs to make sense of their symptoms and path to recovery. The delivery and uptake of the therapy should therefore be operationalised in a communication process that meaningfully represents shared-decision making and the best possible attempt to contextualise the therapy in positive and evidence-informed explanations of the process and desired effects [ 105 ].
Within a therapeutic encounter, practitioners must give the time to listen to peoples’ accounts and explanations of their symptoms, including their ideas about their cause [ 106 ]. The assessment and diagnostic process should be a shared endeavour, for example, the negotiation of symptom reproduction. This should be done in a manner that facilitates sense-making, and which simultaneously encourages people to move on from unhelpful beliefs about their symptoms [ 107 , 108 ], encouraging understanding of the uncertain nature of pain and injury. Person-centered communication requires attention to what we communicate and how we communicate across the entire clinical interaction including interview, examination, and management planning [ 109 ]. Therapists need to be open, reflective, aware and responsive to verbal and non-verbal cues, and demonstrate a balance between engaging with people (e.g. eye-gaze) and writing/typing notes during the interview [ 110 , 111 , 112 ].
People should be given the opportunity to discuss their understanding of the diagnosis and options for treatment and rehabilitation. The decision-making process is dialogical, in which alternative options to the offered therapy should also be discussed with the comparative risks and benefits of all available management options, including doing nothing [ 113 , 114 ].
The therapist must fully appreciate the potential consequences of touch without consent. Continual dialogue should ensure that all parties are moving towards mutually agreed goals. The context of the therapy should be explicitly communicated to give appropriate context for any particular intervention as part of a holistic, evidence-based approach [ 115 , 116 , 117 ]. Therapists should be aware that their own beliefs can affect the way they communicate with their people; in the same way, a person’s context affects how they communicate what they expect from their treatment [ 107 , 118 , 119 , 120 ]. The construction of contextual healing scenarios which support positive outcomes, whilst minimising nocebic effects, is critical to effective healthcare [ 121 , 122 , 123 ].
There is a growing academic interest in the nature, role, and purpose of social and affective touch, and any re-framing of MT should consider touch as a means of communication to develop and enhance cooperative communications and strengthen the therapeutic relationship [ 124 , 125 , 126 , 127 , 128 , 129 ]. It can be soothing for a person in pain to experience the caring touch of a professional therapist [ 130 ]; on the other hand, probing, diagnostic, and touch can be experienced as alienating [ 131 , 132 , 133 ]. Touch can alter a person’s sense of body ownership and their ability to recognise and process their emotions by modulating interoceptive precision [ 129 , 134 , 135 ], and intentional touch may be perceived differently from casual, unfocussed touch [ 136 , 137 ]. There is also a thesis that touch generates shared understanding and meaning [ 138 , 139 , 140 ]. This wider appreciation of touch should be embedded in modern MT communication.
The contextual quality of a person’s experience of the therapeutic encounter can affect satisfaction and clinical outcomes [ 141 , 142 , 143 , 144 , 145 ]. The context in which therapeutic care takes place should therefore be developed to enhance this experience. There could be very local, practical aspects of the context, such as the type of passive information available in the clinical space, e.g. replacing biomedical and pathological imagery and objects with positive, active artefacts; judicious and thoughtful organisation and use of treatment tables to discourage a sense of passivity and disempowerment; allocating a comfortable space where communication can take place; colour schemes and light sources which facilitate positivity; ensuring consistency through all clinical and administrative staff promoting encouraging and non-nocebic messages. Importantly, the way the therapist dresses influences peoples’ perception of their healthcare experience [ 146 , 147 ], and that in turn should be contextually and culturally sensitive [ 148 , 149 , 150 ].
Beyond the local clinical space is the broader social environment. The undertaking of MT should serve a role in a person’s engagement with their social environment. For example, someone returning home after engaging with their therapist and disseminating positive health messages within their home and social networks; people acting as advocates for self-empowered healthcare. Furthermore, early data have demonstrated that aligning treatment with the beliefs and values of culturally and linguistically diverse communities enhances peoples’ engagement with their healthcare [ 151 ].
Person-centred care
Here we borrow directly from one of the most established and clinically useful definitions of Person-Centered Medicine [ 152 ]:
“(Person-Centered Medicine is) an affordable biomedical and technological advance to be delivered to patients [sic] within a humanistic framework of care that recognises the importance of applying science in a manner that respects the patients [sic] as a whole person and takes full account of [their] values, preferences, aspirations, stories, cultural context, fears, worries and hopes and thus that recognises and responds to [their] emotional, social and spiritual necessities in addition to [their] physical needs” [ 152 ] , p219.
Person-centred care incorporates a person’s perspective as part of the therapeutic process. In practice, therapists need to communicate in a manner that creates adequate conversational space to elicit a person’s agenda (i.e. understanding, impact of pain, concerns, needs, and goals), which guides clinical interactions. This approach encourages greater partnership in management [ 109 , 153 , 154 ].
A roadmap outlining key actions to implement person-centeredness in clinical practice has been outlined in detail elsewhere [ 155 ]. This includes screening for serious pathology, health co-morbidities and psychosocial factors; adopting effective communication; providing positive health education; coaching and supporting people towards active self-management; and facilitating and managing co-care (when needed) [ 154 ].
It is critical and necessary now to make these features explicit and central to the revised model of MT proposed in this paper. We wish to identify common ground across all MT professions in order to achieve a trans-disciplinary understanding of the evidence supporting the use of MT.
We acknowledge that our arguments here are rooted in empiricism and deliberately based on available research data from within the health science disciplines. We also acknowledge that there is a wider debate about future directions in person-centred care arising from the current evolution of the evidence-based health care movement, which has pointed to the need to learn more about peoples’ lived experiences, to redefine the model of the therapeutic relationship. Although beyond the scope of this paper, a full exploration of modern health care provision involves reconsideration of the ethics and legal requirements of communication and shared decision-making [ 156 , 157 , 158 , 159 ]. The authors envision this paper as a stimulus for self-reflection, stakeholder discussions, and ultimately change that can positively impact outcomes for people who seek manual therapy interventions.
Manual therapy has long been part of MSK healthcare and, given that is likely to continue. Current evidence suggests that effectiveness does not rely on the traditional principles historically developed in any of the major manual therapies. Therefore, the continued teaching and practice based on the principles of clinician-centred palpation , patho-anatomical reasoning , and technique specificity are no longer justified and may well even limit the value of MT.
A revised and reconceptualised framework of MT, based on the humanistic domains of safety, comfort and efficiency and underpinned by the dimensions of communication, context and person-centred care will ensure an empowering, biopsychosocial, evidence-informed approach to MSK care. We propose that the future teaching and practice of MT in physiotherapy, osteopathy, chiropractic, and all associated hands-on professions working within the healthcare field should be based on this new framework.
Availability of data and materials
Young C, Argáez C. CADTH Rapid Response Reports. Manual Therapy for Chronic Non-Cancer Back and Neck Pain: A Review of Clinical Effectiveness. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. Copyright © 2020 Canadian Agency for Drugs and Technologies in Health.; 2020.
Blanpied PR, Gross AR, Elliott JM, Devaney LL, Clewley D, Walton DM, et al. Neck Pain: Revision 2017. J Orthop Sports Phys Ther. 2017;47(7):A1-a83.
Article PubMed Google Scholar
NICE. Low back pain and sciatica in over 16s: assessment and management. NICE guideline [NG59]. 2016.
Pettman E. A history of manipulative therapy. J Man Manip Ther. 2007;15(3):165–74.
Article PubMed PubMed Central Google Scholar
Damian K, Chad C, Kenneth L, David G. Time to evolve: the applicability of pain phenotyping in manual therapy. J Man Manip Ther. 2022;30(2):61–7.
McCarthy CJ. Combined Movement Theory: Rational Mobilization and Manipulation of the Vertebral Column. London, UK: Churchill Livingstone; 2010.
Google Scholar
Subialka JA, Smith K, Signorino JA, Young JL, Rhon DI, Rentmeester C. What do patients referred to physical therapy for a musculoskeletal condition expect? A qualitative assessment. Musculoskel Sci Pract. 2022;59:102543.
Article Google Scholar
Louw A, Nijs J, Puentedura EJ. A clinical perspective on a pain neuroscience education approach to manual therapy. J Man Manip Ther. 2017;25(3):160–8.
Wilhelm M, Cleland J, Carroll A, Marinch M, Imhoff M, Severini N, et al. The combined effects of manual therapy and exercise on pain and related disability for individuals with nonspecific neck pain: A systematic review with meta-analysis. J Man Manip Ther. 2023;31(6):393–407.
Schenk R, Donaldson M, Parent-Nichols J, Wilhelm M, Wright A, Cleland JA. Effectiveness of cervicothoracic and thoracic manual physical therapy in managing upper quarter disorders - a systematic review. J Man Manipulative Therap. 2021:1–10.
Lavazza C, Galli M, Abenavoli A, Maggiani A. Sham treatment effects in manual therapy trials on back pain patients: a systematic review and pairwise meta-analysis. BMJ Open. 2021;11(5):e045106.
Funabashi M, Pohlman KA, Goldsworthy R, Lee A, Tibbles A, Mior S, et al. Beliefs, perceptions and practices of chiropractors and patients about mitigation strategies for benign adverse events after spinal manipulation therapy. Chiropr Man Therap. 2020;28(1):46.
Rushton A, Carlesso LC, Flynn T, Hing WA, Rubinstein SM, Vogel S, et al. International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention: International IFOMPT Cervical Framework. J Orthop Sports Phys Ther. 2022;53(1):7–22.
Thomas M, Thomson OP, Kolubinski DC, Stewart-Lord A. The attitudes and beliefs about manual therapy held by patients experiencing low back pain: a scoping review. Musculoskelet Sci Pract. 2023;65:102752.
Lilje S, van Tulder M, Wykman A, Aboagye E, Persson U. Cost-effectiveness of specialised manual therapy versus orthopaedic care for musculoskeletal disorders: long-term follow-up and health economic model. Ther Adv Musculoskelet Dis. 2023;15:1759720x221147751.
Article CAS PubMed PubMed Central Google Scholar
Abbott JH, Robertson MC, Chapple C, Pinto D, Wright AA, Leon de la Barra S, et al. Manual therapy, exercise therapy, or both, in addition to usual care, for osteoarthritis of the hip or knee: a randomized controlled trial. 1: clinical effectiveness. Osteoarthritis Cartilage. 2013;21(4):525–34.
Article CAS PubMed Google Scholar
Bove AM, Smith KJ, Bise CG, Fritz JM, Childs JD, Brennan GP, et al. Exercise, Manual Therapy, and Booster Sessions in Knee Osteoarthritis: Cost-Effectiveness Analysis From a Multicenter Randomized Controlled Trial. Phys Ther. 2018;98(1):16–27.
Leininger B, McDonough C, Evans R, Tosteson T, Tosteson AN, Bronfort G. Cost-effectiveness of spinal manipulative therapy, supervised exercise, and home exercise for older adults with chronic neck pain. Spine J. 2016;16(11):1292–304.
Tsertsvadze A, Clar C, Court R, Clarke A, Mistry H, Sutcliffe P. Cost-effectiveness of manual therapy for the management of musculoskeletal conditions: a systematic review and narrative synthesis of evidence from randomized controlled trials. J Manipulative Physiol Ther. 2014;37(6):343–62.
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: effectiveness of physical treatments for back pain in primary care. BMJ. 2004;329(7479):1377.
Article PubMed Central Google Scholar
UK Beam Trial Team. United Kingdom back pain exercise and manipulation (UK BEAM) randomised trial: cost effectiveness of physical treatments for back pain in primary care. BMJ (Clinical research ed). 2004;329(7479):1381.
van Dongen JM, Groeneweg R, Rubinstein SM, Bosmans JE, Oostendorp RA, Ostelo RW, et al. Cost-effectiveness of manual therapy versus physiotherapy in patients with sub-acute and chronic neck pain: a randomised controlled trial. Eur Spine J. 2016;25(7):2087–96.
Woods B, Manca A, Weatherly H, Saramago P, Sideris E, Giannopoulou C, et al. Cost-effectiveness of adjunct non-pharmacological interventions for osteoarthritis of the knee. PLoS ONE. 2017;12(3):e0172749.
Aboagye E, Lilje S, Bengtsson C, Peterson A, Persson U, Skillgate E. Manual therapy versus advice to stay active for nonspecific back and/or neck pain: a cost-effectiveness analysis. Chiropr Man Therap. 2022;30(1):27.
Paris SV. A History of Manipulative Therapy Through the Ages and Up to the Current Controversy in the United States. J Man Manipulative Ther. 2000;8(2):66–77.
MacDonald CW, Osmotherly PG, Parkes R, Rivett DA. The current manipulation debate: historical context to address a broken narrative. J Man Manipulative Therap. 2019;27(1):1–4.
Fryer G. Intervertebral dysfunction: a discussion of the manipulable spinal lesion. J Am Osteopath Assoc. 2003;6(2):64–73.
McCarthy CJ. Spinal manipulative thrust technique using combined movement theory. Man Ther. 2001;6(4):197–204.
Vickers A, Zollman C. ABC of complementary medicine Massage therapies. BMJ (Clinical research ed). 1999;319(7219):1254–7.
Evans DW. Osteopathic principles: More harm than good? Int J Osteopath Med. 2013;16(1):46–53.
Mourad F, Yousif MS, Maselli F, Pellicciari L, Meroni R, Dunning J, et al. Knowledge, beliefs, and attitudes of spinal manipulation: a cross-sectional survey of Italian physiotherapists. Chiropr Man Therap. 2022;30(1):38.
Cyriax JH, Cyriax PJ. Cyriax's Illustrated Manual of Orthopaedic Medicine. 3rd ed: Butterworth-Heinemann; 1996.
Young KJ. Words matter: the prevalence of chiropractic-specific terminology on Australian chiropractors’ websites. Chiropr Man Therap. 2020;28(1):18.
Jenkins HJ, Downie AS, Moore CS, French SD. Current evidence for spinal X-ray use in the chiropractic profession: a narrative review. Chiropr Man Therap. 2018;26:48.
Brinjikji W, Luetmer PH, Comstock B, Bresnahan BW, Chen LE, Deyo RA, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2015;36(4):811–6.
Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. JAMA Intern Med. 2013;173(17):1573–81.
Hall AM, Aubrey-Bassler K, Thorne B, Maher CG. Do not routinely offer imaging for uncomplicated low back pain. BMJ (Clinical research ed). 2021;372:n291.
PubMed Google Scholar
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54(2):79.
Hall AM, Scurrey SR, Pike AE, Albury C, Richmond HL, Matthews J, et al. Physician-reported barriers to using evidence-based recommendations for low back pain in clinical practice: a systematic review and synthesis of qualitative studies using the Theoretical Domains Framework. Implement Sci. 2019;14(1):49.
Eriksson L, Ekenberg L, Melander-Wikman A. The concept of palpation of the shoulder – A basic element of physiotherapy practice: A focus group study with physiotherapists. Adv Physiother. 2012;14(4):183–93.
Nim CG, Downie A, O’Neill S, Kawchuk GN, Perle SM, Leboeuf-Yde C. The importance of selecting the correct site to apply spinal manipulation when treating spinal pain: Myth or reality? A systematic review. Sci Rep. 2021;11(1):23415.
Alexander N, Rastelli A, Webb T, Rajendran D. The validity of lumbo-pelvic landmark palpation by manual practitioners: A systematic review. Int J Osteopath Med. 2021;39:10–20.
Leboeuf-Yde C, van Dijk J, Franz C, Hustad SA, Olsen D, Pihl T, et al. Motion palpation findings and self-reported low back pain in a population-based study sample. J Manipulative Physiol Ther. 2002;25(2):80–7.
Najm WI, Seffinger MA, Mishra SI, Dickerson VM, Adams A, Reinsch S, et al. Content validity of manual spinal palpatory exams - A systematic review. BMC Complement Altern Med. 2003;3:1.
Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-dimensional mathematical model for deformation of human fasciae in manual therapy. J Am Osteopath Assoc. 2008;108(8):379–90.
Gabriel A, Konrad A, Roidl A, Queisser J, Schleip R, Horstmann T, et al. Myofascial Treatment Techniques on the Plantar Surface Influence Functional Performance in the Dorsal Kinetic Chain. J Sports Sci Med. 2022;21(1):13–22.
PubMed PubMed Central Google Scholar
Nolet PS, Yu H, Côté P, Meyer A-L, Kristman VL, Sutton D, et al. Reliability and validity of manual palpation for the assessment of patients with low back pain: a systematic and critical review. Chiropr Man Therap. 2021;29(1):33.
Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29(19):E413–25.
Beynon AM, Hebert JJ, Walker BF. The interrater reliability of static palpation of the thoracic spine for eliciting tenderness and stiffness to test for a manipulable lesion. Chiropr Man Therap. 2018;26:49.
Petersen EJ, Thurmond SM, Shaw CA, Miller KN, Lee TW, Koborsi JA. Reliability and accuracy of an expert physical therapist as a reference standard for a manual therapy joint mobilization trial. J Man Manip Ther. 2021;29(3):189–95.
Petersen EJ, Thurmond SM, Buchanan SI, Chun DH, Richey AM, Nealon LP. The effect of real-time feedback on learning lumbar spine joint mobilization by entry-level doctor of physical therapy students: a randomized, controlled, crossover trial. J Man Manip Ther. 2020;28(4):201–11.
Abbott JH, Flynn TW, Fritz JM, Hing WA, Reid D, Whitman JM. Manual physical assessment of spinal segmental motion: intent and validity. Man Ther. 2009;14(1):36–44.
Bialosky JE, Simon CB, Bishop MD, George SZ. Basis for spinal manipulative therapy: a physical therapist perspective. J Electromyogr Kinesiol. 2012;22(5):643–7.
Henderson CN. The basis for spinal manipulation: chiropractic perspective of indications and theory. J Electromyogr Kinesiol. 2012;22(5):632–42.
Sizer PS Jr, Felstehausen V, Sawyer S, Dornier L, Matthews P, Cook C. Eight critical skill sets required for manual therapy competency: a Delphi study and factor analysis of physical therapy educators of manual therapy. J Allied Health. 2007;36(1):30–40.
Ombregt L. A System of Orthopaedic Medicine: Elsevier; 2013.
Cramer GD, Henderson CN, Little JW, Daley C, Grieve TJ. Zygapophyseal joint adhesions after induced hypomobility. J Manipulative Physiol Ther. 2010;33(7):508–18.
George JW, Tunstall AC, Tepe RE, Skaggs CD. The Effects of Active Release Technique on Hamstring Flexibility: A Pilot Study. J Manipulative Physiol Ther. 2006;29(3):224–7.
Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–8.
Plaza-Manzano G, Molina-Ortega F, Lomas-Vega R, Martínez-Amat A, Achalandabaso A, Hita-Contreras F. Changes in biochemical markers of pain perception and stress response after spinal manipulation. J Orthop Sports Phys Ther. 2014;44(4):231–9.
Zusman M. Mechanism of mobilization. Physical Therapy Reviews. 2011;16(4):233–6.
De Carvalho DE, de Luca K, Funabashi M, Breen A, Wong AYL, Johansson MS, et al. Association of Exposures to Seated Postures With Immediate Increases in Back Pain: A Systematic Review of Studies With Objectively Measured Sitting Time. J Manipulative Physiol Ther. 2020;43(1):1–12.
Colloca CJ, Keller TS. Stiffness and neuromuscular reflex response of the human spine to posteroanterior manipulative thrusts in patients with low back pain. J Manipulative Physiol Ther. 2001;24(8):489–500.
Colloca CJ, Keller TS, Gunzburg R. Biomechanical and neurophysiological responses to spinal manipulation in patients with lumbar radiculopathy. J Manipulative Physiol Ther. 2004;27(1):1–15.
Reed WR, Long CR, Kawchuk GN, Sozio RS, Pickar JG. Neural Responses to Physical Characteristics of a High-velocity, Low-amplitude Spinal Manipulation: Effect of Thrust Direction. Spine. 2018;43(1):1–9.
Reed WR, Pickar JG, Sozio RS, Liebschner MAK, Little JW, Gudavalli MR. Characteristics of Paraspinal Muscle Spindle Response to Mechanically Assisted Spinal Manipulation: A Preliminary Report. J Manipulative Physiol Ther. 2017;40(6):371–80.
Devecchi V, Rushton AB, Gallina A, Heneghan NR, Falla D. Are neuromuscular adaptations present in people with recurrent spinal pain during a period of remission? a systematic review. PLoS ONE. 2021;16(4):e0249220.
Pagé I, Nougarou F, Lardon A, Descarreaux M. Changes in spinal stiffness with chronic thoracic pain: Correlation with pain and muscle activity. PLoS ONE. 2018;13(12):e0208790.
Lee RY, McGregor AH, Bull AM, Wragg P. Dynamic response of the cervical spine to posteroanterior mobilisation. Clin Biomech (Bristol, Avon). 2005;20(2):228–31.
Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004;29(13):1452–7.
Donaldson M, Petersen S, Cook C, Learman K. A Prescriptively Selected Nonthrust Manipulation Versus a Therapist-Selected Nonthrust Manipulation for Treatment of Individuals With Low Back Pain: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2016;46(4):243–50.
McCarthy CJ, Potter L, Oldham JA. Comparing targeted thrust manipulation with general thrust manipulation in patients with low back pain. A general approach is as effective as a specific one. A randomised controlled trial. BMJ Open Sport Exerc Med. 2019;5(1):e000514.
Sutlive TG, Mabry LM, Easterling EJ, Durbin JD, Hanson SL, Wainner RS, et al. Comparison of short-term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009;174(7):750–6.
Tuttle N, Evans K, Sperotto dos Santos Rocha C. Localised manual therapy treatment has a preferential effect on the kinematics of the targeted motion segment. Musculoskelet Sci Pract. 2021;56:102457.
Ali MN, Sethi K, Noohu MM. Comparison of two mobilization techniques in management of chronic non-specific low back pain. J Bodyw Mov Ther. 2019;23(4):918–23.
de Oliveira RF, Costa LOP, Nascimento LP, Rissato LL. Directed vertebral manipulation is not better than generic vertebral manipulation in patients with chronic low back pain: a randomised trial. J Physiother. 2020;66(3):174–9.
Gevers-Montoro C, Provencher B, Northon S, Stedile-Lovatel JP, Ortega de Mues A, Piché M. Chiropractic Spinal Manipulation Prevents Secondary Hyperalgesia Induced by Topical Capsaicin in Healthy Individuals. Front Pain Res (Lausanne, Switzerland). 2021;2:702429.
Provencher B, Northon S, Piché M. Segmental Chiropractic Spinal Manipulation Does not Reduce Pain Amplification and the Associated Pain-Related Brain Activity in a Capsaicin-Heat Pain Model. Front Pain Res (Lausanne, Switzerland). 2021;2:733727.
Watanabe N, Piché M. Editorial: Mechanisms and Effectiveness of Complementary and Alternative Medicine for Pain Management. Front Pain Res (Lausanne, Switzerland). 2022;3:863751.
Muhsen A, Moss P, Gibson W, Walker B, Jacques A, Schug S, et al. The Association Between Conditioned Pain Modulation and Manipulation-induced Analgesia in People With Lateral Epicondylalgia. Clin J Pain. 2019;35(5):435–42.
Howick J, Glasziou P, Aronson JK. Evidence-based mechanistic reasoning. J Roy Soc Med. 2010;103(11):433–41.
Haavik Taylor H, Murphy B. The effects of spinal manipulation on central integration of dual somatosensory input observed after motor training: a crossover study. J Manipulative Physiol Ther. 2010;33(4):261–72.
Haavik-Taylor H, Murphy B. Cervical spine manipulation alters sensorimotor integration: a somatosensory evoked potential study. ClinNeurophysiol. 2007;118(2):391–402.
Ogura T, Tashiro M, Masud M, Watanuki S, Shibuya K, Yamaguchi K, et al. Cerebral metabolic changes in men after chiropractic spinal manipulation for neck pain. Altern Ther Health Med. 2011;17(6):12–7.
Sparks C, Cleland JA, Elliott JM, Zagardo M, Liu WC. Using functional magnetic resonance imaging to determine if cerebral hemodynamic responses to pain change following thoracic spine thrust manipulation in healthy individuals. J Orthop Sports Phys Ther. 2013;43(5):340–8.
Evans DW. How to gain evidence for causation in disease and therapeutic intervention: from Koch’s postulates to counter-counterfactuals. Med Health Care Philos. 2022;25(3):509–21.
Lascurain-Aguirrebeña I, Newham D, Critchley DJ. Mechanism of Action of Spinal Mobilizations: A Systematic Review. Spine. 2016;41(2):159–72.
Parravicini G, Bergna A. Biological effects of direct and indirect manipulation of the fascial system Narrative review. J Bodyw Mov Ther. 2017;21(2):435–45.
Crane JD, Ogborn DI, Cupido C, Melov S, Hubbard A, Bourgeois JM, et al. Massage therapy attenuates inflammatory signaling after exercise-induced muscle damage. Sci Transl Med. 2012;4(119):119ra13.
Degenhardt BF, Darmani NA, Johnson JC, Towns LC, Rhodes DC, Trinh C, et al. Role of osteopathic manipulative treatment in altering pain biomarkers: a pilot study. J Am Osteopath Assoc. 2007;107(9):387–400.
Kovanur-Sampath K, Mani R, Cotter J, Gisselman AS, Tumilty S. Changes in biochemical markers following spinal manipulation-a systematic review and meta-analysis. Musculoskelet Sci Pract. 2017;29:120–31.
Lohman EB, Pacheco GR, Gharibvand L, Daher N, Devore K, Bains G, et al. The immediate effects of cervical spine manipulation on pain and biochemical markers in females with acute non-specific mechanical neck pain: a randomized clinical trial. J Man Manip Ther. 2019;27(4):186–96.
Teodorczyk-Injeyan JA, McGregor M, Triano JJ, Injeyan SH. Elevated Production of Nociceptive CC Chemokines and sE-Selectin in Patients With Low Back Pain and the Effects of Spinal Manipulation: A Nonrandomized Clinical Trial. Clin J Pain. 2018;34(1):68–75.
Council GC. The Code: Standards of conduct, performance and ethics for chiropractors. GCC; 2019.
Council HaCP. Standards of Proficiency - Physiotherapists. HCPC; 2013.
Council GO. Osteopathic Practice Standards. GOC; 2023.
Therapies TCfST. GCMT Code of Practice, Ethics and Proficiency for Professional Associations. GCMT; 2023.
Daluiso-King G, Hebron C. Is the biopsychosocial model in musculoskeletal physiotherapy adequate? An evolutionary concept analysis. Physiotherapy theory and practice. 2020:1–17.
Søndenå P, Dalusio-King G, Hebron C. Conceptualisation of the therapeutic alliance in physiotherapy: is it adequate? Musculoskelet Sci Pract. 2020;46:102131.
World Health Organisation. Patient Safety 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/patient-safety#:~:text=Patient%20Safety%20is%20a%20health,during%20provision%20of%20health%20care .
Vogel S, Mars T, Keeping S, Barton T, Marlin N, Froud R, et al. Clinical Risk Osteopathy and Management Scientific Report. 2012.
Ekerholt K, Bergland A. Learning and knowing bodies: Norwegian psychomotor physiotherapists’ reflections on embodied knowledge. Physiother Theory Pract. 2019;35(1):57–69.
Hutting N, Johnston V, Staal JB, Heerkens YF. Promoting the Use of Self-management Strategies for People With Persistent Musculoskeletal Disorders: The Role of Physical Therapists. J Orthop Sports Phys Ther. 2019;49(4):212–5.
Kongsted A, Ris I, Kjaer P, Hartvigsen J. Self-management at the core of back pain care: 10 key points for clinicians. Braz J Phys Therap. 2021.
Elwyn G, Durand MA, Song J, Aarts J, Barr PJ, Berger Z, et al. A three-talk model for shared decision making: multistage consultation process. BMJ (Clinical research ed). 2017;359:j4891.
Broom B. The Practice of Whole Person-Centred Healthcare. In: Anjum RL, Copeland S, Rocca E, editors. Rethinking Causality, Complexity and Evidence for the Unique Patient: A CauseHealth Resource for Healthcare Professionals and the Clinical Encounter. Cham: Springer International Publishing; 2020. p. 215–26.
Chapter Google Scholar
Darlow B, Dowell A, Baxter GD, Mathieson F, Perry M, Dean S. The enduring impact of what clinicians say to people with low back pain. Ann Fam Med. 2013;11(6):527–34.
Stewart M, Loftus S. Sticks and Stones: The Impact of Language in Musculoskeletal Rehabilitation. J Orthop Sports Phys Ther. 2018;48(7):519–22.
Lin I, Wiles L, Waller R, Caneiro JP, Nagree Y, Straker L, et al. Patient-centred care: the cornerstone for high-value musculoskeletal pain management. Br J Sports Med. 2020;54(21):1240–2.
Cowell I, O’Sullivan P, O’Sullivan K, Poyton R, McGregor A, Murtagh G. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: A qualitative study. Musculoskelet Sci Pract. 2018;38:113–9.
Edmond SN, Keefe FJ. Validating pain communication: current state of the science. Pain. 2015;156(2):215–9.
O’Keeffe M, Cullinane P, Hurley J, Leahy I, Bunzli S, O’Sullivan PB, et al. What Influences Patient-Therapist Interactions in Musculoskeletal Physical Therapy? Qualitative Systematic Review and Meta-Synthesis. Phys Ther. 2016;96(5):609–22.
Copnell G. Informed consent in physiotherapy practice: it is not what is said but how it is said. Physiotherapy. 2018;104(1):67–71.
Lee A. Bolam’ to “Montgomery” is result of evolutionary change of medical practice towards ’patient-centred care. Postgrad Med J. 2017;93(1095):46–50.
Lewis J, O’Sullivan P. Is it time to reframe how we care for people with non-traumatic musculoskeletal pain? Br J Sports Med. 2018;52(24):1543–4.
Lewis J, Ridehalgh C, Moore A, Hall K. This is the day your life must surely change: Prioritising behavioural change in musculoskeletal practice. Physiotherapy. 2021.
Lewis JS, Stokes EK, Gojanovic B, Gellatly P, Mbada C, Sharma S, et al. Reframing how we care for people with persistent non-traumatic musculoskeletal pain. Suggestions for the rehabilitation community. Physiotherapy. 2021.
Bishop A, Foster NE, Thomas E, Hay EM. How does the self-reported clinical management of patients with low back pain relate to the attitudes and beliefs of health care practitioners? A survey of UK general practitioners and physiotherapists. Pain. 2008;135(1–2):187–95.
Darlow B, Fullen BM, Dean S, Hurley DA, Baxter GD, Dowell A. The association between health care professional attitudes and beliefs and the attitudes and beliefs, clinical management, and outcomes of patients with low back pain: a systematic review. Eur J Pain (London, England). 2012;16(1):3–17.
Article CAS Google Scholar
Lakke SE, Soer R, Krijnen WP, van der Schans CP, Reneman MF, Geertzen JH. Influence of Physical Therapists’ Kinesiophobic Beliefs on Lifting Capacity in Healthy Adults. Phys Ther. 2015;95(9):1224–33.
Howe LC, Leibowitz KA, Crum AJ. When Your Doctor “Gets It” and “Gets You”: The Critical Role of Competence and Warmth in the Patient-Provider Interaction. Front Psych. 2019;10:475.
Newell D, Lothe LR, Raven TJL. Contextually Aided Recovery (CARe): a scientific theory for innate healing. Chiropr Man Therap. 2017;25:6.
Rossettini G, Camerone EM, Carlino E, Benedetti F, Testa M. Context matters: the psychoneurobiological determinants of placebo, nocebo and context-related effects in physiotherapy. Arch Physiother. 2020;10:11.
Gallace A. Social Touch. In: Olausson H, Wessberg J, Morrison I, McGlone F, editors. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
Gallace A, Spence C. The science of interpersonal touch: an overview. Neurosci Biobehav Rev. 2010;34(2):246–59.
Kelly MA, Nixon L, McClurg C, Scherpbier A, King N, Dornan T. Experience of Touch in Health Care: A Meta-Ethnography Across the Health Care Professions. Qual Health Res. 2018;28(2):200–12.
McGlone F, Cerritelli F, Walker S, Esteves J. The role of gentle touch in perinatal osteopathic manual therapy. Neurosci Biobehav Rev. 2017;72:1–9.
Olausson H, Wessberg J, Morrison I, McGlone F. Affective Touch and the Neurophysiology of CT Afferents: Springer; 2016.
McParlin Z, Cerritelli F, Rossettini G, Friston KJ, Esteves JE. Therapeutic Alliance as Active Inference: The Role of Therapeutic Touch and Biobehavioural Synchrony in Musculoskeletal Care. Front Behav Neurosci. 2022;16:897247.
Meijer LL, Ruis C, van der Smagt MJ, Scherder EJA, Dijkerman HC. Neural basis of affective touch and pain: A novel model suggests possible targets for pain amelioration. J Neuropsychol. 2021.
Allen-Collinson J, Pavey A. Touching moments: phenomenological sociology and the haptic dimension in the lived experience of motor neurone disease. Sociol Health Illn. 2014;36(6):793–806.
Bjorbækmo WS, Mengshoel AM. “A touch of physiotherapy” - the significance and meaning of touch in the practice of physiotherapy. Physiother Theory Pract. 2016;32(1):10–9.
Nummenmaa L, Tuominen L, Dunbar R, Hirvonen J, Manninen S, Arponen E, et al. Social touch modulates endogenous μ-opioid system activity in humans. Neuroimage. 2016;138:242–7.
Calsius J, De Bie J, Hertogen R, Meesen R. Touching the Lived Body in Patients with Medically Unexplained Symptoms. How an Integration of Hands-on Bodywork and Body Awareness in Psychotherapy may Help People with Alexithymia. Front Psychol. 2016;7:253.
Gentsch A, Crucianelli L, Jenkinson P, Fotopoulou A. The touched self: Affective touch and body awareness in health and disease. Affective touch and the neurophysiology of CT afferents Springer; 2016.
Cerritelli F, Chiacchiaretta P, Gambi F, Ferretti A. Effect of Continuous Touch on Brain Functional Connectivity Is Modified by the Operator’s Tactile Attention. Front Hum Neurosci. 2017;11:368.
Tramontano M, Cerritelli F, Piras F, Spanò B, Tamburella F, Piras F, et al. Brain Connectivity Changes after Osteopathic Manipulative Treatment: A Randomized Manual Placebo-Controlled Trial. Brain Sci. 2020;10(12):969.
Øberg GK, Blanchard Y, Obstfelder A. Therapeutic encounters with preterm infants: interaction, posture and movement. Physiother Theory Pract. 2014;30(1):1–5.
Øberg GK, Normann B, Gallagher S. Embodied-enactive clinical reasoning in physical therapy. Physiother Theory Pract. 2015;31(4):244–52.
Consedine S, Standen C, Niven E. Knowing hands converse with an expressive body – An experience of osteopathic touch. Int J Osteopath Med. 2016;19:3–12.
Barbosa CD, Balp MM, Kulich K, Germain N, Rofail D. A literature review to explore the link between treatment satisfaction and adherence, compliance, and persistence. Patient Prefer Adherence. 2012;6:39–48.
Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. 2011;17(1):41–8.
Manary MP, Boulding W, Staelin R, Glickman SW. The patient experience and health outcomes. N Engl J Med. 2013;368(3):201–3.
Sherriff B, Clark C, Killingback C, Newell D. Musculoskeletal practitioners’ perceptions of contextual factors that may influence chronic low back pain outcomes: a modified Delphi study. Chiropr Man Therap. 2023;31(1):12.
Sherriff B, Clark C, Killingback C, Newell D. Impact of contextual factors on patient outcomes following conservative low back pain treatment: systematic review. Chiropr Manual Therap. 2022;30(1):20.
Mercer E, Mackay-Lyons M, Conway N, Flynn J, Mercer C. Perceptions of outpatients regarding the attire of physiotherapists. Physiother Can. 2008;60(4):349–57.
Petrilli CM, Mack M, Petrilli JJ, Hickner A, Saint S, Chopra V. Understanding the role of physician attire on patient perceptions: a systematic review of the literature— targeting attire to improve likelihood of rapport (TAILOR) investigators. BMJ Open. 2015;5(1):e006578.
Beach MC, Fitzgerald A, Saha S. White Coat Hype: Branding Physicians With Professional Attire. JAMA Intern Med. 2013;173(6):467–8.
Bearman G, Bryant K, Leekha S, Mayer J, Munoz-Price LS, Murthy R, et al. Healthcare Personnel Attire in Non-Operating-Room Settings. Infect Control Hosp Epidemiol. 2014;35(2):107–21.
Rehman SU, Nietert PJ, Cope DW, Kilpatrick AO. What to wear today? Effect of doctor’s attire on the trust and confidence of patients. Am J Med. 2005;118(11):1279–86.
Brady B, Veljanova I, Schabrun S, Chipchase L. Integrating culturally informed approaches into physiotherapy assessment and treatment of chronic pain: a pilot randomised controlled trial. BMJ Open. 2018;8(7):e021999.
Miles A, Mezzich JE. The care of the patient and the soul of the clinic: person-centered medicine as an emergent model of clinical practice. Int J Person Centred Med. 2012;1(2):207–22.
Cowell I, McGregor A, O’Sullivan P, O’Sullivan K, Poyton R, Schoeb V, et al. How do physiotherapists solicit and explore patients’ concerns in back pain consultations: a conversation analytic approach. Physiother Theory Pract. 2021;37(6):693–709.
Hutting N, Caneiro JP, Ong'wen MO, Miciak M, Roberts LE. Patient-centered care in musculoskeletal practice: key elements to support clinicians to focus on the person. 2021.
Caneiro JP, Roos EM, Barton CJ, O’Sullivan K, Kent P, Lin I, et al. It is time to move beyond “body region silos” to manage musculoskeletal pain: five actions to change clinical practice. Br J Sports Med. 2020;54(8):438–9.
Greenhalgh T, Howick J, Maskrey N, EBM Renaissance Group. Evidence based medicine: a movement in crisis? Brit Med J. 2014;348:g3725.
Greenhalgh T, Snow R, Ryan S, Rees S, Salisbury H. Six ‘biases’ against patients and carers in evidence-based medicine. Bmc Med. 2015;13(1):200.
Loughlin M, Fuller J, Bluhm R, Buetow S, Borgerson K. Theory, experience and practice. J Eval Clin Pract. 2016;22(4):459–65.
Simpson JK, Innes S. Informed consent, duty of disclosure and chiropractic: where are we? Chiropr Man Therap. 2020;28(1):60.
Download references
Acknowledgements
Use of any animal or human data or tissue.
No funding was received for this paper.
Author information
Authors and affiliations.
School of Health Sciences, Queens Medical Centre, University of Nottingham, Nottingham, NG7 2HA, UK
Roger Kerry, Edward Lee & Vasileios Georgopoulos
Allied Health Research Unit, University of Central Lancashire, Preston, PR1 2HE, UK
Kenneth J. Young
Centre of Precision Rehabilitation for Spinal Pain, School of Sport, Exercise and Rehabilitation Sciences, University of Birmingham, Edgbaston, Birmingham, B15 2TT, UK
David W. Evans
Nottingham CityCare Partnership, Bennerley Rd, Nottingham, NG6 8WR, UK
School of Medicine, University of Nottingham, Queens Medical Centre, Nottingham, NG7 2HA, UK
Vasileios Georgopoulos
Department of Orthopaedics, West Herts Hospitals Trust, Watford, WD18 0HB, UK
Adam Meakins
School of Physiotherapy, Manchester Metropolitan University, Manchester, M15 6GX, UK
Chris McCarthy
Department of Orthopaedics, Duke University, 200 Morris Street, Durham, NC, 27701, USA
School of Sport and Health Sciences, University of Brighton, Darley Rd, Eastbourne, BN20 7UR, UK
Colette Ridehalgh
Clinical Neuroscience, Trafford Building, Brighton and Sussex Medical School, University of Sussex, Brighton, BN1 9PX, UK
University College of Osteopathy, 275 Borough High St, London, SE1 1JE, UK
Steven Vogel & Amanda Banton
Department of Clinical Sciences, Obstetrics and Gynecology, Umeå University, S-90187, Umeå, Sweden
Cecilia Bergström
The School of Soft Tissue Therapy, Exmouth, Devon, EX8 1DQ, UK
Anna Maria Mazzieri
Department of health, LUNEX, Differdange, 4671, Luxembourg
Firas Mourad
Luxembourg Health & Sport Sciences Research Institute A.s.b.l., 50, Avenue du Parc des Sports, Differdange, 4671, Luxembourg
Department of Occupation and Health, School of Organization and Development, HAN University of Applied Sciences, Nijmegen, the Netherlands
Nathan Hutting
You can also search for this author in PubMed Google Scholar
Contributions
Concept and research design: RK, KJY, DWE, EL, AM, VG. Data collection: All authors. Data analysis: All authors. Writing and editing of the manuscript: All authors.
Corresponding author
Correspondence to Kenneth J. Young .
Ethics declarations
Ethics approval and consent to participate.
All participants are co-authors. Ethical approval was not necessary.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kerry, R., Young, K.J., Evans, D.W. et al. A modern way to teach and practice manual therapy. Chiropr Man Therap 32 , 17 (2024). https://doi.org/10.1186/s12998-024-00537-0
Download citation
Received : 18 October 2023
Accepted : 17 April 2024
Published : 21 May 2024
DOI : https://doi.org/10.1186/s12998-024-00537-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Manual Therapy
- Evidence-based healthcare
- Person-centred healthcare
- Physiotherapy
- Chiropractic
- Soft-tissue therapy
Chiropractic & Manual Therapies
ISSN: 2045-709X
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
- Case Report
- Open access
- Published: 27 May 2024
A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient
- Wei Fu 1 , 2 na1 ,
- Zi Wei Deng 3 na1 ,
- Pei Wang 1 ,
- Zhen Wang Zhu 1 ,
- Zhi Bing Xie 1 ,
- Yong Zhong Li 1 &
- Hong Ying Yu 1
BMC Infectious Diseases volume 24 , Article number: 533 ( 2024 ) Cite this article
1 Altmetric
Metrics details
Hepatitis B virus (HBV) infection can cause liver failure, while individuals with Acquired Immunodeficiency Virus Disease (AIDS) are highly susceptible to various opportunistic infections, which can occur concurrently. The treatment process is further complicated by the potential occurrence of immune reconstitution inflammatory syndrome (IRIS), which presents significant challenges and contributes to elevated mortality rates.
Case presentation
The 50-year-old male with a history of chronic hepatitis B and untreated human immunodeficiency virus (HIV) infection presented to the hospital with a mild cough and expectoration, revealing multi-drug resistant pulmonary tuberculosis (MDR-PTB), which was confirmed by XpertMTB/RIF PCR testing and tuberculosis culture of bronchoalveolar lavage fluid (BALF). The patient was treated with a regimen consisting of linezolid, moxifloxacin, cycloserine, pyrazinamide, and ethambutol for tuberculosis, as well as a combination of bictegravir/tenofovir alafenamide/emtricitabine (BIC/TAF/FTC) for HBV and HIV viral suppression. After three months of treatment, the patient discontinued all medications, leading to hepatitis B virus reactivation and subsequent liver failure. During the subsequent treatment for AIDS, HBV, and drug-resistant tuberculosis, the patient developed disseminated cryptococcal disease. The patient’s condition worsened during treatment with liposomal amphotericin B and fluconazole, which was ultimately attributed to IRIS. Fortunately, the patient achieved successful recovery after appropriate management.
Enhancing medical compliance is crucial for AIDS patients, particularly those co-infected with HBV, to prevent HBV reactivation and subsequent liver failure. Furthermore, conducting a comprehensive assessment of potential infections in patients before resuming antiviral therapy is essential to prevent the occurrence of IRIS. Early intervention plays a pivotal role in improving survival rates.
Peer Review reports
HIV infection remains a significant global public health concern, with a cumulative death toll of 40 million individuals [ 1 ]. In 2021 alone, there were 650,000 deaths worldwide attributed to AIDS-related causes. As of the end of 2021, approximately 38 million individuals were living with HIV, and there were 1.5 million new HIV infections reported annually on a global scale [ 2 ]. Co-infection with HBV and HIV is prevalent due to their similar transmission routes, affecting around 8% of HIV-infected individuals worldwide who also have chronic HBV infection [ 3 ]. Compared to those with HBV infection alone, individuals co-infected with HIV/HBV exhibit higher HBV DNA levels and a greater risk of reactivation [ 4 ]. Opportunistic infections, such as Pneumocystis jirovecii pneumonia, Toxoplasma encephalitis, cytomegalovirus retinitis, cryptococcal meningitis (CM), tuberculosis, disseminated Mycobacterium avium complex disease, pneumococcal pneumonia, Kaposi’s sarcoma, and central nervous system lymphoma, are commonly observed due to HIV-induced immunodeficiency [ 5 ]. Tuberculosis not only contributes to the overall mortality rate in HIV-infected individuals but also leads to a rise in the number of drug-resistant tuberculosis cases and transmission of drug-resistant strains. Disseminated cryptococcal infection is a severe opportunistic infection in AIDS patients [ 6 ], and compared to other opportunistic infections, there is a higher incidence of IRIS in patients with cryptococcal infection following antiviral and antifungal therapy [ 7 ]. This article presents a rare case of an HIV/HBV co-infected patient who presented with MDR-PTB and discontinued all medications during the initial treatment for HIV, HBV, and tuberculosis. During the subsequent re-anti-HBV/HIV treatment, the patient experienced two episodes of IRIS associated with cryptococcal infection. One episode was classified as “unmasking” IRIS, where previously subclinical cryptococcal infection became apparent with immune improvement. The other episode was categorized as “paradoxical” IRIS, characterized by the worsening of pre-existing cryptococcal infection despite immune restoration [ 8 ]. Fortunately, both episodes were effectively treated.
A 50-year-old male patient, who is self-employed, presented to our hospital in January 2022 with a chief complaint of a persistent cough for the past 2 months, without significant shortness of breath, palpitations, or fever. His medical history revealed a previous hepatitis B infection, which resulted in hepatic failure 10 years ago. Additionally, he was diagnosed with HIV infection. However, he ceased taking antiviral treatment with the medications provided free of charge by the Chinese government for a period of three years. During this hospital visit, his CD4 + T-cell count was found to be 26/μL (normal range: 500–1612/μL), HIV-1 RNA was 1.1 × 10 5 copies/ml, and HBV-DNA was negative. Chest computed tomography (CT) scan revealed nodular and patchy lung lesions (Fig. 1 ). The BALF shows positive acid-fast staining. Further assessment of the BALF using XpertMTB/RIF PCR revealed resistance to rifampicin, and the tuberculosis drug susceptibility test of the BALF (liquid culture, medium MGIT 960) indicated resistance to rifampicin, isoniazid, and streptomycin. Considering the World Health Organization (WHO) guidelines for drug-resistant tuberculosis, the patient’s drug susceptibility results, and the co-infection of HIV and HBV, an individualized treatment plan was tailored for him. The treatment plan included BIC/TAF/FTC (50 mg/25 mg/200 mg per day) for HBV and HIV antiviral therapy, as well as linezolid (0.6 g/day), cycloserine (0.5 g/day), moxifloxacin (0.4 g/day), pyrazinamide (1.5 g/day), and ethambutol (0.75 g/day) for anti-tuberculosis treatment, along with supportive care.
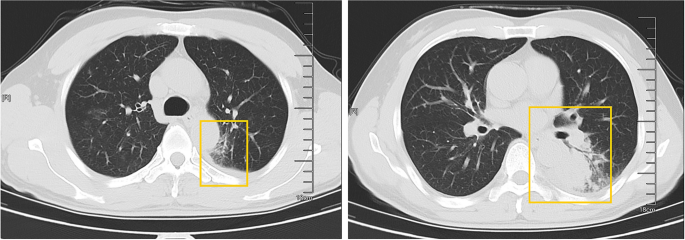
The patient’s pulmonary CT scan shows patchy and nodular lesions accompanied by a small amount of pleural effusion, later confirmed to be MDR-PTB
Unfortunately, after 3 months of follow-up, the patient discontinued all medications due to inaccessibility of the drugs. He returned to our hospital (Nov 12, 2022, day 0) after discontinuing medication for six months, with a complaint of poor appetite for the past 10 days. Elevated liver enzymes were observed, with an alanine aminotransferase level of 295 IU/L (normal range: 0–40 IU/L) and a total bilirubin(TBIL) level of 1.8 mg/dL (normal range: 0–1 mg/dL). His HBV viral load increased to 5.5 × 10 9 copies/ml. Considering the liver impairment, elevated HBV-DNA and the incomplete anti-tuberculosis treatment regimen (Fig. 2 A), we discontinued pyrazinamide and initiated treatment with linezolid, cycloserine, levofloxacin, and ethambutol for anti-tuberculosis therapy, along with BIC/TAF/FTC for HIV and HBV antiviral treatment. Additionally, enhanced liver protection and supportive management were provided, involving hepatoprotective effects of medications such as glutathione, magnesium isoglycyrrhizinate, and bicyclol. However, the patient’s TBIL levels continued to rise progressively, reaching 4.4 mg/dL on day 10 (Fig. 3 B). Suspecting drug-related factors, we discontinued all anti-tuberculosis medications while maintaining BIC/TAF/FTC for antiviral therapy, the patient’s TBIL levels continued to rise persistently. We ruled out other viral hepatitis and found no significant evidence of obstructive lesions on magnetic resonance cholangiopancreatography. Starting from the day 19, due to the patient’s elevated TBIL levels of 12.5 mg/dL, a decrease in prothrombin activity (PTA) to 52% (Fig. 3 D), and the emergence of evident symptoms such as abdominal distension and poor appetite, we initiated aggressive treatment methods. Unfortunately, on day 38, his hemoglobin level dropped to 65 g/L (normal range: 120–170 g/L, Fig. 3 A), and his platelet count decreased to 23 × 10 9 /L (normal range: 125–300 × 10 9 /L, Fig. 3 C). Based on a score of 7 on the Naranjo Scale, it was highly suspected that “Linezolid” was the cause of these hematological abnormalities. Therefore, we had to discontinue Linezolid for the anti-tuberculosis treatment. Subsequently, on day 50, the patient developed recurrent fever, a follow-up chest CT scan revealed enlarged nodules in the lungs (Fig. 2 B). The patient also reported mild dizziness and a worsening cough. On day 61, the previous blood culture results reported the growth of Cryptococcus. A lumbar puncture was performed on the same day, and the cerebrospinal fluid (CSF) opening pressure was measured at 130 mmH 2 O. India ink staining of the CSF showed typical encapsulated yeast cells suggestive of Cryptococcus. Other CSF results indicated mild leukocytosis and mildly elevated protein levels, while chloride and glucose levels were within normal limits. Subsequently, the patient received a fungal treatment regimen consisting of liposomal amphotericin B (3 mg/kg·d −1 ) in combination with fluconazole(600 mg/d). After 5 days of antifungal therapy, the patient’s fever symptoms were well controlled. Despite experiencing bone marrow suppression, including thrombocytopenia and worsening anemia, during this period, proactive symptom management, such as the use of erythropoietin, granulocyte colony-stimulating factor, and thrombopoietin, along with high-calorie dietary management, even reducing the dosage of liposomal amphotericin B to 2 mg/kg/day for 10 days at the peak of severity, successfully controlled the bone marrow suppression. However, within the following week, the patient experienced fever again, accompanied by a worsened cough, increased sputum production, and dyspnea. Nevertheless, the bilirubin levels did not show a significant increase. On day 78 the patient’s lung CT revealed patchy infiltrates and an increased amount of pleural effusion (Fig. 2 C). The CD4 + T-cell count was 89/μL (normal range: 500–700/μL), indicating a significant improvement in immune function compared to the previous stage, and C-reactive protein was significantly elevated, reflecting the inflammatory state, other inflammatory markers such as IL-6 and γ-IFN were also significantly elevated. On day 84, Considering the possibility of IRIS, the patient began taking methylprednisolone 30 mg once a day as part of an effort to control his excessive inflammation. Following the administration of methylprednisolone, the man experienced an immediate improvement in his fever. Additionally, symptoms such as cough, sputum production, dyspnea, and poor appetite gradually subsided over time. A follow-up lung CT showed significant improvement, indicating a positive response to the treatment. After 28 days of treatment with liposomal amphotericin B in combination with fluconazole, liposomal amphotericin B was discontinued, and the patient continued with fluconazole to consolidate the antifungal therapy for Cryptococcus. Considering the patient’s ongoing immunodeficiency, the dosage of methylprednisolone was gradually reduced by 4 mg every week. After improvement in liver function, the patient’s anti-tuberculosis treatment regimen was adjusted to include bedaquiline, contezolid, cycloserine, moxifloxacin, and ethambutol. The patient’s condition was well controlled, and a follow-up lung CT on day 117 indicated a significant improvement in lung lesions (Fig. 2 D).
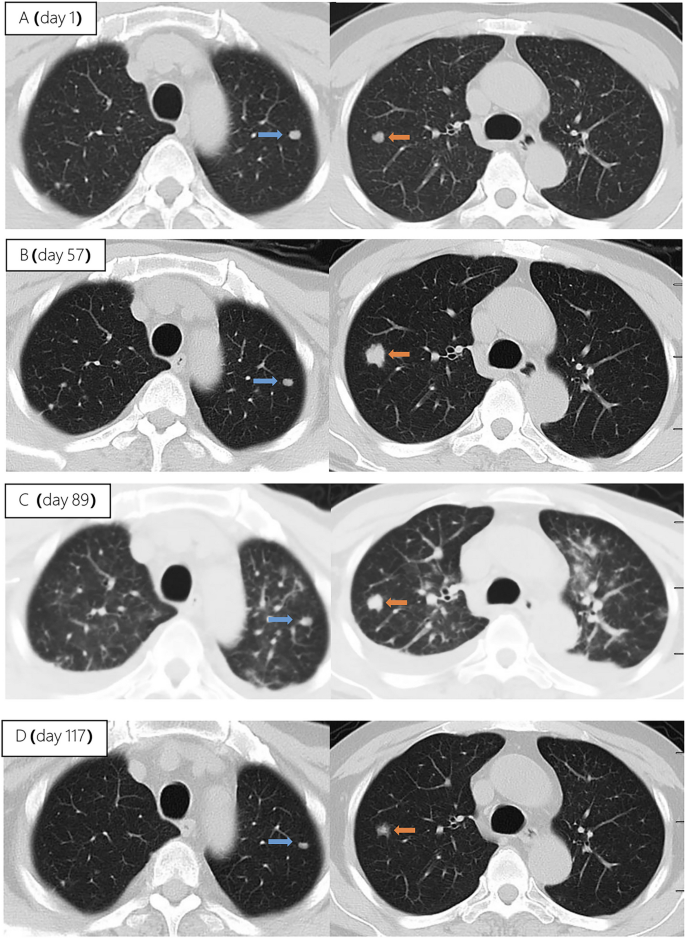
Upon second hospitalization admission ( A ), nodular lesions were already present in the lungs, and their size gradually increased after the initiation of ART ( B , C ). Notably, the lung lesions became more pronounced following the commencement of anti-cryptococcal therapy, coinciding with the occurrence of pleural effusion ( C ). However, with the continuation of antifungal treatment and the addition of glucocorticoids, there was a significant absorption and reduction of both the pleural effusion and pulmonary nodules ( D )
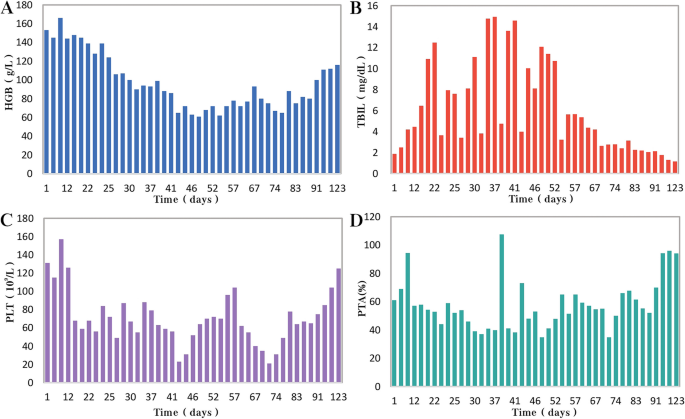
During the patient's second hospitalization, as the anti-tuberculosis treatment progressed and liver failure developed, the patient’s HGB levels gradually decreased ( A ), while TBIL levels increased ( B ). Additionally, there was a gradual decrease in PLT count ( C ) and a reduction in prothrombin activity (PTA) ( D ), indicating impaired clotting function. Moreover, myelosuppression was observed during the anti-cryptococcal treatment ( C )
People living with HIV/AIDS are susceptible to various opportunistic infections, which pose the greatest threat to their survival [ 5 ]. Pulmonary tuberculosis and disseminated cryptococcosis remain opportunistic infections with high mortality rates among AIDS patients [ 9 , 10 ]. These infections occurring on the basis of liver failure not only increase diagnostic difficulty but also present challenges in treatment. Furthermore, as the patient’s immune function and liver function recover, the occurrence of IRIS seems inevitable.
HIV and HBV co-infected patients are at a higher risk of HBV reactivation following the discontinuation of antiviral drugs
In this case, the patient presented with both HIV and HBV infections. Although the HBV DNA test was negative upon admission. However, due to the patient’s self-discontinuation of antiretroviral therapy (ART), HBV virologic and immunologic reactivation occurred six months later, leading to a rapid increase in viral load and subsequent hepatic failure. Charles Hannoun et al. also reported similar cases in 2001, where two HIV-infected patients with positive HBsAg experienced HBV reactivation and a rapid increase in HBV DNA levels after discontinuing antiretroviral and antiviral therapy, ultimately resulting in severe liver failure [ 11 ]. The European AIDS Clinical Society (EACS) also emphasize that abrupt discontinuation of antiviral therapy in patients co-infected with HBV and HIV can trigger HBV reactivation, which, although rare, can potentially result in liver failure [ 12 ].
Diagnosing disseminated Cryptococcus becomes more challenging in AIDS patients with liver failure, and the selection of antifungal medications is significantly restricted
In HIV-infected individuals, cryptococcal disease typically manifests as subacute meningitis or meningoencephalitis, often accompanied by fever, headache, and neck stiffness. The onset of symptoms usually occurs approximately two weeks after infection, with typical signs and symptoms including meningeal signs such as neck stiffness and photophobia. Some patients may also experience encephalopathy symptoms like somnolence, mental changes, personality changes, and memory loss, which are often associated with increased intracranial pressure (ICP) [ 13 ]. The presentation of cryptococcal disease in this patient was atypical, as there were no prominent symptoms such as high fever or rigors, nor were there any signs of increased ICP such as somnolence, headache, or vomiting. The presence of pre-existing pulmonary tuberculosis further complicated the early diagnosis, potentially leading to the clinical oversight of recognizing the presence of cryptococcus. In addition to the diagnostic challenges, treating a patient with underlying liver disease, multidrug-resistant tuberculosis, and concurrent cryptococcal infection poses significant challenges. It requires considering both the hepatotoxicity of antifungal agents and potential drug interactions. EACS and global guideline for the diagnosis and management of cryptococcosis suggest that liposomal amphotericin B (3 mg/kg·d −1 ) in combination with flucytosine (100 mg/kg·d −1 ) or fluconazole (800 mg/d) is the preferred induction therapy for CM for 14 days [ 12 , 14 ]. Flucytosine has hepatotoxicity and myelosuppressive effects, and it is contraindicated in patients with severe liver dysfunction. The antiviral drug bictegravir is a substrate for hepatic metabolism by CYP3A and UGT1A1 enzymes [ 15 ], while fluconazole inhibits hepatic enzymes CYP3A4 and CYP2C9 [ 16 ]. Due to the patient's liver failure and bone marrow suppression, we reduced the dosage of liposomal amphotericin B and fluconazole during the induction period. Considering the hepatotoxicity of fluconazole and its interaction with bictegravir, we decreased the dosage of fluconazole to 600 mg/d, while extending the duration of induction therapy to 28 days.
During re-antiviral treatment, maintaining vigilance for the development of IRIS remains crucial
IRIS refers to a series of inflammatory diseases that occur in HIV-infected individuals after initiating ART. It is associated with the paradoxical worsening of pre-existing infections, which may have been previously diagnosed and treated or may have been subclinical but become apparent due to the host regaining the ability to mount an inflammatory response. Currently, there is no universally accepted definition of IRIS. However, the following conditions are generally considered necessary for diagnosing IRIS: worsening of a diagnosed or previously unrecognized pre-existing infection with immune improvement (referred to as “paradoxical” IRIS) or the unmasking of a previously subclinical infection (referred to as “unmasking” IRIS) [ 8 ]. It is estimated that 10% to 30% of HIV-infected individuals with CM will develop IRIS after initiating or restarting effective ART [ 7 , 17 ]. In the guidelines of the WHO and EACS, it is recommended to delay the initiation of antiviral treatment for patients with CM for a minimum of 4 weeks to reduce the incidence of IRIS. Since we accurately identified the presence of multidrug-resistant pulmonary tuberculosis in the patient during the early stage, we promptly initiated antiretroviral and anti-hepatitis B virus treatment during the second hospitalization. However, subsequent treatment revealed that the patient experienced at least two episodes of IRIS. The first episode was classified as “unmasking” IRIS, as supported by the enlargement of pulmonary nodules observed on the chest CT scan following the initiation of ART (Fig. 2 A). Considering the morphological changes of the nodules on the chest CT before antifungal therapy, the subsequent emergence of disseminated cryptococcal infection, and the subsequent reduction in the size of the lung nodules after antifungal treatment, although there is no definitive microbiological evidence, we believe that the initial enlargement of the lung nodules was caused by cryptococcal pneumonia. As ART treatment progressed, the patient experienced disseminated cryptococcosis involving the blood and central nervous system, representing the first episode. Following the initiation of antifungal therapy for cryptococcosis, the patient encountered a second episode characterized by fever and worsening pulmonary lesions. Given the upward trend in CD4 + T-cell count, we attributed this to the second episode of IRIS, the “paradoxical” type. The patient exhibited a prompt response to low-dose corticosteroids, further supporting our hypothesis. Additionally, the occurrence of cryptococcal IRIS in the lungs, rather than the central nervous system, is relatively uncommon among HIV patients [ 17 ].
Conclusions
From the initial case of AIDS combined with chronic hepatitis B, through the diagnosis and treatment of multidrug-resistant tuberculosis, the development of liver failure and disseminated cryptococcosis, and ultimately the concurrent occurrence of IRIS, the entire process was tortuous but ultimately resulted in a good outcome (Fig. 4 ). Treatment challenges arose due to drug interactions, myelosuppression, and the need to manage both infectious and inflammatory conditions. Despite these hurdles, a tailored treatment regimen involving antifungal and antiretroviral therapies, along with corticosteroids, led to significant clinical improvement. While CM is relatively common among immunocompromised individuals, especially those with acquired immunodeficiency syndrome (AIDS) [ 13 ], reports of disseminated cryptococcal infection on the background of AIDS complicated with liver failure are extremely rare, with a very high mortality rate.
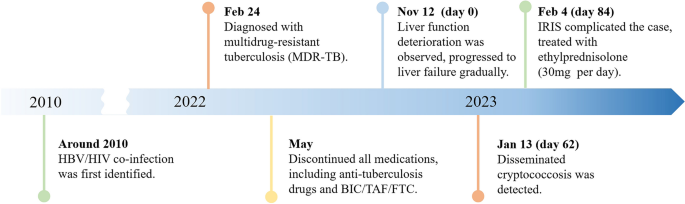
A brief timeline of the patient's medical condition progression and evolution
Through managing this patient, we have also gained valuable insights. (1) Swift and accurate diagnosis, along with timely and effective treatment, can improve prognosis, reduce mortality, and lower disability rates. Whether it's the discovery and early intervention of liver failure, the identification and treatment of disseminated cryptococcosis, or the detection and management of IRIS, all these interventions are crucially timely. They are essential for the successful treatment of such complex and critically ill patients.
(2) Patients who exhibit significant drug reactions, reducing the dosage of relevant medications and prolonging the treatment duration can improve treatment success rates with fewer side effects. In this case, the dosages of liposomal amphotericin B and fluconazole are lower than the recommended dosages by the World Health Organization and EACS guidelines. Fortunately, after 28 days of induction therapy, repeat CSF cultures showed negative results for Cryptococcus, and the improvement of related symptoms also indicates that the patient has achieved satisfactory treatment outcomes. (3) When cryptococcal infection in the bloodstream or lungs is detected, prompt lumbar puncture should be performed to screen for central nervous system cryptococcal infection. Despite the absence of neurological symptoms, the presence of Cryptococcus neoformans in the cerebrospinal fluid detected through lumbar puncture suggests the possibility of subclinical or latent CM, especially in late-stage HIV-infected patients.
We also encountered several challenges and identified certain issues that deserve attention. Limitations: (1) The withdrawal of antiviral drugs is a critical factor in the occurrence and progression of subsequent diseases in patients. Improved medical education is needed to raise awareness and prevent catastrophic consequences. (2) Prior to re-initiating antiviral therapy, a thorough evaluation of possible infections in the patient is necessary. Caution should be exercised, particularly in the case of diseases prone to IRIS, such as cryptococcal infection. (3) There is limited evidence on the use of reduced fluconazole dosage (600 mg daily) during antifungal therapy, and the potential interactions between daily fluconazole (600 mg) and the antiviral drug bictegravir and other tuberculosis medications have not been extensively studied. (4) Further observation is needed to assess the impact of early-stage limitations in the selection of anti-tuberculosis drugs on the treatment outcome of tuberculosis in this patient, considering the presence of liver failure.
In conclusion, managing opportunistic infections in HIV patients remains a complex and challenging task, particularly when multiple opportunistic infections are compounded by underlying liver failure. Further research efforts are needed in this area.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
Hepatitis B virus
Acquired immunodeficiency virus disease
Immune reconstitution inflammatory syndrome
Human immunodeficiency virus
Multi-drug resistant pulmonary tuberculosis
Bronchoalveolar lavage fluid
Bictegravir/tenofovir alafenamide/emtricitabine
Cryptococcal meningitis
World Health Organization
Computed tomography
Total bilirubin
Cerebrospinal fluid
European AIDS Clinical Society
Intracranial pressure
Antiretroviral therapy
Prothrombin activity
Bekker L-G, Beyrer C, Mgodi N, Lewin SR, Delany-Moretlwe S, Taiwo B, et al. HIV infection. Nat Rev Dis Primer. 2023;9:1–21.
Google Scholar
Data on the size of the HIV epidemic. https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/data-on-the-size-of-the-hiv-aids-epidemic?lang=en . Accessed 3 May 2023.
Leumi S, Bigna JJ, Amougou MA, Ngouo A, Nyaga UF, Noubiap JJ. Global burden of hepatitis B infection in people living with human immunodeficiency virus: a systematic review and meta-analysis. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020;71:2799–806.
Article Google Scholar
McGovern BH. The epidemiology, natural history and prevention of hepatitis B: implications of HIV coinfection. Antivir Ther. 2007;12(Suppl 3):H3-13.
Article CAS PubMed Google Scholar
Kaplan JE, Masur H, Holmes KK, Wilfert CM, Sperling R, Baker SA, et al. USPHS/IDSA guidelines for the prevention of opportunistic infections in persons infected with human immunodeficiency virus: an overview. USPHS/IDSA Prevention of Opportunistic Infections Working Group. Clin Infect Dis Off Publ Infect Dis Soc Am. 1995;21 Suppl 1:S12-31.
Article CAS Google Scholar
Bamba S, Lortholary O, Sawadogo A, Millogo A, Guiguemdé RT, Bretagne S. Decreasing incidence of cryptococcal meningitis in West Africa in the era of highly active antiretroviral therapy. AIDS Lond Engl. 2012;26:1039–41.
Müller M, Wandel S, Colebunders R, Attia S, Furrer H, Egger M, et al. Immune reconstitution inflammatory syndrome in patients starting antiretroviral therapy for HIV infection: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10:251–61.
Article PubMed PubMed Central Google Scholar
Haddow LJ, Easterbrook PJ, Mosam A, Khanyile NG, Parboosing R, Moodley P, et al. Defining immune reconstitution inflammatory syndrome: evaluation of expert opinion versus 2 case definitions in a South African cohort. Clin Infect Dis Off Publ Infect Dis Soc Am. 2009;49:1424–32.
Obeagu E, Onuoha E. Tuberculosis among HIV patients: a review of Prevalence and Associated Factors. Int J Adv Res Biol Sci. 2023;10:128–34.
Rajasingham R, Govender NP, Jordan A, Loyse A, Shroufi A, Denning DW, et al. The global burden of HIV-associated cryptococcal infection in adults in 2020: a modelling analysis. Lancet Infect Dis. 2022;22:1748–55.
Manegold C, Hannoun C, Wywiol A, Dietrich M, Polywka S, Chiwakata CB, et al. Reactivation of hepatitis B virus replication accompanied by acute hepatitis in patients receiving highly active antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2001;32:144–8.
EACS Guidelines | EACSociety. https://www.eacsociety.org/guidelines/eacs-guidelines/ . Accessed 7 May 2023.
Cryptococcosis | NIH. 2021. https://clinicalinfo.hiv.gov/en/guidelines/hiv-clinical-guidelines-adult-and-adolescent-opportunistic-infections/cryptococcosis . Accessed 6 May 2023.
Chang CC, Harrison TS, Bicanic TA, Chayakulkeeree M, Sorrell TC, Warris A, et al. Global guideline for the diagnosis and management of cryptococcosis: an initiative of the ECMM and ISHAM in cooperation with the ASM. Lancet Infect Dis. 2024;10:S1473-3099(23)00731-4.
Deeks ED. Bictegravir/emtricitabine/tenofovir alafenamide: a review in HIV-1 infection. Drugs. 2018;78:1817–28.
Article CAS PubMed PubMed Central Google Scholar
Bellmann R, Smuszkiewicz P. Pharmacokinetics of antifungal drugs: practical implications for optimized treatment of patients. Infection. 2017;45:737–79.
Shelburne SA, Darcourt J, White AC, Greenberg SB, Hamill RJ, Atmar RL, et al. The role of immune reconstitution inflammatory syndrome in AIDS-related Cryptococcus neoformans disease in the era of highly active antiretroviral therapy. Clin Infect Dis Off Publ Infect Dis Soc Am. 2005;40:1049–52.
Download references
Acknowledgements
We express our sincere gratitude for the unwavering trust bestowed upon our medical team by the patient throughout the entire treatment process.
This work was supported by the Scientific Research Project of Hunan Public Health Alliance with the approval No. ky2022-002.
Author information
Wei Fu and Zi Wei Deng contributed equally to this work.
Authors and Affiliations
Center for Infectious Diseases, Hunan University of Medicine General Hospital, Huaihua, Hunan, China
Wei Fu, Pei Wang, Zhen Wang Zhu, Ye Pu, Zhi Bing Xie, Yong Zhong Li & Hong Ying Yu
Department of Tuberculosis, The First Affiliated Hospital of Xinxiang Medical University, XinXiang, Henan, China
Department of Clinical Pharmacy, Hunan University of Medicine General Hospital, Huaihua, Hunan, China
Zi Wei Deng
You can also search for this author in PubMed Google Scholar
Contributions
WF and ZWD integrated the data and wrote the manuscript, YHY contributed the revision of the manuscript, PW and YP provided necessary assistance and provided key suggestions, ZWZ, YZL and ZBX contributed data acquisition and interpretation for etiological diagnosis. All authors reviewed and approved the final manuscript.
Corresponding author
Correspondence to Hong Ying Yu .
Ethics declarations
Ethics approval and consent to participate.
The study was approved by the Ethics Committee of the Hunan University of Medicine General Hospital (HYZY-EC-202306-C1), and with the informed consent of the patient.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Fu, W., Deng, Z.W., Wang, P. et al. A complex case study: coexistence of multi-drug-resistant pulmonary tuberculosis, HBV-related liver failure, and disseminated cryptococcal infection in an AIDS patient. BMC Infect Dis 24 , 533 (2024). https://doi.org/10.1186/s12879-024-09431-9
Download citation
Received : 30 June 2023
Accepted : 24 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12879-024-09431-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Liver failure
- Disseminated cryptococcal disease
BMC Infectious Diseases
ISSN: 1471-2334
- General enquiries: [email protected]
This paper is in the following e-collection/theme issue:
Published on 28.5.2024 in Vol 26 (2024)
The Effect of Artificial Intelligence on Patient-Physician Trust: Cross-Sectional Vignette Study
Authors of this article:

Original Paper
- Anna G M Zondag 1 , MSc ;
- Raoul Rozestraten 2 , MSc ;
- Stephan G Grimmelikhuijsen 2 , PhD ;
- Karin R Jongsma 3 , PhD ;
- Wouter W van Solinge 1 , PhD ;
- Michiel L Bots 3 , MD, PhD ;
- Robin W M Vernooij 3, 4 , PhD ;
- Saskia Haitjema 1 , MD, PhD
1 Central Diagnostic Laboratory, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
2 Utrecht University School of Governance, Utrecht University, Utrecht, Netherlands
3 Julius Center for Health Sciences and Primary Care, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands
4 Department of Nephrology and Hypertension, University Medical Center Utrecht, Utrecht, Netherlands
Corresponding Author:
Anna G M Zondag, MSc
Central Diagnostic Laboratory
University Medical Center Utrecht
Utrecht University
Heidelberglaan 100
Utrecht, 3584 CX
Netherlands
Phone: 31 631117922
Email: [email protected]
Background: Clinical decision support systems (CDSSs) based on routine care data, using artificial intelligence (AI), are increasingly being developed. Previous studies focused largely on the technical aspects of using AI, but the acceptability of these technologies by patients remains unclear.
Objective: We aimed to investigate whether patient-physician trust is affected when medical decision-making is supported by a CDSS.
Methods: We conducted a vignette study among the patient panel (N=860) of the University Medical Center Utrecht, the Netherlands. Patients were randomly assigned into 4 groups—either the intervention or control groups of the high-risk or low-risk cases. In both the high-risk and low-risk case groups, a physician made a treatment decision with (intervention groups) or without (control groups) the support of a CDSS. Using a questionnaire with a 7-point Likert scale, with 1 indicating “strongly disagree” and 7 indicating “strongly agree,” we collected data on patient-physician trust in 3 dimensions: competence, integrity, and benevolence. We assessed differences in patient-physician trust between the control and intervention groups per case using Mann-Whitney U tests and potential effect modification by the participant’s sex, age, education level, general trust in health care, and general trust in technology using multivariate analyses of (co)variance.
Results: In total, 398 patients participated. In the high-risk case, median perceived competence and integrity were lower in the intervention group compared to the control group but not statistically significant (5.8 vs 5.6; P =.16 and 6.3 vs 6.0; P =.06, respectively). However, the effect of a CDSS application on the perceived competence of the physician depended on the participant’s sex ( P =.03). Although no between-group differences were found in men, in women, the perception of the physician’s competence and integrity was significantly lower in the intervention compared to the control group ( P =.009 and P =.01, respectively). In the low-risk case, no differences in trust between the groups were found. However, increased trust in technology positively influenced the perceived benevolence and integrity in the low-risk case ( P =.009 and P =.04, respectively).
Conclusions: We found that, in general, patient-physician trust was high. However, our findings indicate a potentially negative effect of AI applications on the patient-physician relationship, especially among women and in high-risk situations. Trust in technology, in general, might increase the likelihood of embracing the use of CDSSs by treating professionals.
Introduction
It was John McCarthy who coined the term “artificial intelligence” (AI) at the Dartmouth conference in 1956 and defined it as “the science and engineering of making intelligent machines, especially intelligent computer programs” [ 1 ]. However, it was only in the 1990s, after the first so-called “AI winter,” that interest in AI began to increase again [ 2 ]. Since then, AI applications have been on the rise, ranging from self-driving cars to AI-powered web search [ 3 ]. Development and implementation of AI in health care is similarly increasing. It is believed that AI has the potential to improve every facet of health care—screening, diagnosis, prognosis, and treatment [ 4 ]. Although the use of AI in routine clinical care is still in the early stages, it has already shown promise in specific medical fields, such as radiology, for the recognition of complex patterns in imaging data [ 3 , 5 ]. Hospital-wide strategic programs have been initiated to develop predictive AI algorithms based on routine clinical care data in various hospitals [ 6 ]. The goal of these projects is, among others, to integrate AI algorithms in clinical decision support systems (CDSSs). CDSSs are often classified as either knowledge-based or non–knowledge-based systems. Knowledge-based CDSSs provide an output by evaluating a certain rule, which is programmed based on evidence or practice. Non–knowledge-based CDSSs use AI techniques, such as machine learning, for decision support and prediction [ 7 ]. AI-based CDSSs are often developed when dealing with complex, high-dimensional, and large amounts of data (ie, big data), such as routine care data. By linking patient information to evidence-based knowledge, a CDSS can provide case-specific information, which may support physicians in developing more personalized judgments and recommendations [ 8 ]. Despite these efforts, however, to date, only a fraction of all developed AI-based algorithms have been implemented in clinical care [ 9 ].
The debate on AI-based CDSSs in health care has mainly focused on the technical aspects of the technology [ 10 , 11 ], including questions like “How well does the predictive algorithm perform in terms of, for example, recall and precision?” or “What is the importance of its features?” To date, less attention has been given to the acceptability of using AI-based CDSSs in terms of patients’ or physicians’ trust in CDSSs even though these are crucial for the implementation and acceptance of these systems [ 12 , 13 ]. Some concerns revolve around how the patient-physician relationship is directly affected by the integration of AI applications into clinical practice. This concern arises due to all the new possibilities that AI offers, such as decision support, patient dashboards, and eHealth [ 14 - 16 ]. Figure 1 illustrates how the relationship between a patient and physician could be influenced by AI [ 17 , 18 ]. Studies have shown that algorithms developed to diagnose or predict a disease often perform as well as, and sometimes even better than, a physician [ 19 ]. As a result, physicians may be able to make more informed decisions and subsequently improve patient care, which was the incentive to start the Applied Data Analytics in Medicine (ADAM) project at the University Medical Center (UMC) Utrecht [ 6 ]. On the other hand, to build and maintain interpersonal trust, patient involvement in the decision-making process is important [ 20 - 23 ]. However, these algorithms, especially those that include AI, are sometimes perceived as “black boxes,” which could potentially lead to a reduction in trust in the physician, even though these algorithms can be beneficial to the patient’s care process. In medicine, trust is considered a central aspect of the patient-physician relationship. Without trust, treatments have proven to be less effective, and patients are more prone to ask for a second opinion [ 24 ].

To the best of our knowledge, we are among the first to study the impact of AI-based CDSSs on patient-physician trust in both a clinical high-risk and low-risk setting. Trust is a complex and multidimensional concept [ 25 ]. Over the past decades, a lot of research has been conducted on this notion and various dimensions of trust have been described in the academic literature [ 26 ]. The most commonly named dimensions of trust in a physician are privacy and confidentiality [ 27 , 28 ], compassion [ 27 , 29 ], reliability and dependence [ 28 ], competence [ 27 - 31 ], communication [ 32 ], and honesty [ 33 ]. However, these dimensions of trust are often studied separately. With so many described trust dimensions, it is difficult to develop a framework specifically for patient-physician trust. Therefore, a framework that integrates these components of trust in a physician has not been established yet. In social sciences, trust is commonly studied in 3 dimensions: benevolence, competence, and integrity [ 34 - 37 ]. In a clinical context, benevolence is the extent to which a patient perceives a physician as caring about the patient’s personal and health interests. Competence is the extent to which a patient perceives a physician as competent, capable, effective, and professional. Integrity concerns the extent to which a patient sees a physician as honest and truthful, handling the patient’s sensitive information with care and confidentially.
We aim to study the extent to which these aspects of patient-physician trust are affected by AI-based CDSSs.
We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines for observational (cross-sectional) studies.
Study Setting
We conducted a cross-sectional vignette study at the UMC Utrecht, the Netherlands. We reached out to all members of the UMC Utrecht patient panel (N=860) as part of the ADAM program (2017-2020; currently known as the Digital Health Department within the UMC Utrecht) [ 6 ]. In brief, the ADAM program consisted of 11 projects all aiming to answer clinical questions to personalize health care using routine care data and innovative methodology, such as AI. The overall goal of the ADAM program was to investigate the need to apply this health care innovation on a large scale at the UMC Utrecht to establish a learning health care system [ 6 ].
For our study, we simulated possible future clinical decision support applications of 2 of the ADAM projects. The Neonatal Intensive Care Unit (NICU) application concerned data of babies between 24 and 32 weeks old admitted in the NICU using an algorithm that was trained on a data set from the Wilhelmina Children’s Hospital of the UMC Utrecht. This CDSS tool aimed to predict late-onset sepsis using the algorithm to prevent unnecessary antibiotic use and enable timely treatment [ 6 ]. The rheumatoid arthritis (RA) CDSS worked on the premise that disease flares can be predicted based on data about the course of the disease, patient characteristics, and information about current treatment. The aim of the RA application was to predict flares to support data-driven reduction of high preventative doses of RA medication [ 6 , 38 ]. This algorithm was trained on data of patients with RA of the UMC Utrecht [ 38 ].
Study Population
Members of the patient panel (N=860) were all current and former patients of the UMC Utrecht willing to participate in research from the UMC Utrecht. The majority (693/860, 80.6%) of the panel was between 45 and 80 years of age, 57.3% (493/860) had higher education levels, and 52.8% (454/860) of the patient panel were women.
Questionnaire
In our study, we focused on interpersonal trust. We used the definition from Mayer et al [ 34 ] to define interpersonal trust as “the willingness of a party to be vulnerable to the actions of another party based on the expectation that the other will perform a particular action important to the trustor, irrespective of the ability to monitor or control that other party.”
We studied 3 dimensions of trust: competence, integrity, and benevolence. We used an adapted version of the “Trust in Physician Scale” to assess patient-physician trust. The “Trust in Physician Scale” is a questionnaire consisting of 11 items and is commonly used to measure patient-physician trust [ 28 , 39 ]. Table 1 illustrates how the 11 questions of the Trust in Physician Scale were adapted and divided into the 3 trust dimensions.
In addition to the questions of the Trust in Physician Scale, we added several self-constructed questions to study these aspects of trust more comprehensively. We added the following 3 statements in the integrity dimension:
- I have the feeling that this physician is not holding anything back from me (scale 1-7).
- I have the feeling that this physician is being honest with me (scale 1-7).
- I trust this physician is handling my medical data with care (scale 1-7).
One additional statement was added in the benevolence dimension, as follows: “This physician’s recommendation is in my personal best interest (scale 1-7).”
Besides trust in the physician, we added 2 additional questions about trust in health care and technology in general on a 7-point Likert scale (1: “no trust at all”; 7: “fully trust”), as follows:
- Please indicate your level of trust in health care in general (scale 1-7).
- Please indicate your level of trust in technology in general (scale 1-7).
Additionally, we asked the panel members their age, sex, and education level.
Subsequently, we performed a factor analysis on the questionnaire, including the Trust in Physician Scale and the self-constructed questions, to check whether the predefined dimensions were present in the questionnaire. The factor analysis revealed the correlations between the items of the questionnaire and subdivided them into factors. Thereafter, we calculated Cronbach α to measure the degree of coherence between the 3 trust dimensions [ 40 ]. A Cronbach α of more than 0.75 was considered high, and thus, acceptable, meaning that all items of the dimension measured the same concept [ 41 ].
Design of Data Collection
Data were collected in April 2019. The questionnaire included 1 of the 2 hypothetical cases in the form of a so-called “vignette.” These vignettes were developed together with physicians from the neonatology and rheumatology department as well as the ADAM program staff to make them as realistic as possible (eg, to assess whether the physician’s communication style in the vignette reflected clinical practice) and to ensure that the AI-based CDSS applications of both projects were accurately described. The vignettes were tested on master’s degree students of Public Management from Utrecht University and employees of the ADAM program (N=36) first to study whether they could empathize well with the situation presented to them. This test resulted in a mean score of 4.6 for the NICU and 5.7 for the RA vignette on a 7-point Likert scale (the higher the score, the better they could empathize with the situation presented). We processed the feedback we received from the test participants to further improve the vignettes. After successful testing, we randomly divided the panel members into 4 groups ( Multimedia Appendix 1 ). The groups were presented with either a life-threatening (high-risk) vignette in the NICU (from now on referred to as the “high-risk case”), or a non–life-threatening (low-risk) vignette regarding RA (referred to as the “low-risk case”). Details of the vignettes are described in Multimedia Appendix 2 . The high-risk case described a baby in the NICU that possibly had sepsis. In this case, we asked the panel members to empathize with the role of the baby’s parents. The low-risk case described a patient with RA, and panel members were asked to empathize with the role of the patient. In both situations, the physician made a treatment recommendation. This recommendation was made by a physician only in the control group and by a physician supported by a CDSS application in the intervention group. After reading the vignette, the panel members were asked to fill in the questionnaire. Possible answers were given using a 7-point Likert scale, with 1 indicating “strongly disagree” and 7 indicating “strongly agree.”
We tracked the time it took panel members to read the vignettes. To minimize the potential loss of statistical power due to panel members not being diligent and motivated to complete the survey, we excluded the 2.5% slowest and fastest readers from all analyses. Figure 2 illustrates the patient inclusion and exclusion procedure in a flow diagram.

Data Analyses
We presented the results of all groups in medians (IQRs), stratified by case. We compared perceived trust between the intervention and control group using the Mann-Whitney U test (Wilcoxon rank sum test).
We assessed the presence or absence of effect modification using a two-way multivariate analysis of variance (MANOVA) or multivariate analysis of covariance (MANCOVA), as appropriate. The participant’s sex, age, education level, general trust in health care, and general trust in technology were considered potential effect modifiers in the relation between the use of a CDSS and patient-physician trust. We further stratified the results by sex in case of effect modification to examine this potential effect.
All analyses were performed using SPSS edition 26 (IBM SPSS Inc) [ 42 ]. Differences with a 2-sided P value of <.05 were considered statistically significant.
Ethical Considerations
All participants provided informed consent digitally for this study. The panel members received an introductory text with information about this study. At the end of the introductory text, the privacy statement informed the panel members that by clicking the “Continue” button, they agreed to the use of their data in this study. Data were anonymized and IP addresses were not stored.
The questionnaires were administered in Qualtrics in accordance with Utrecht University guidelines and stored on the Yoda server, which is a research data management service from the Utrecht University, among others, enabling secure storage of the research data [ 43 , 44 ]. The methods have been performed based on relevant guidelines and regulations. The institutional review board of UMC Utrecht waived ethical approval because it ruled that this study did not concern a medical research question.
Demographics of the Study Population
In total, 398/860 (46.3%) panel members of the UMC Utrecht patient panel participated in this study. Characteristics of the study population can be seen in Table 2 . Participants were older in the intervention group of both cases. In the high-risk case, the intervention group consisted of more men (52/92, 56.5%), whereas the control group consisted of more women (54/93, 58.1%). In the low-risk case, both the control and intervention groups consisted of more women (55/109, 50.5% and 56/104, 53.8%, respectively). The education level was similar across the groups. In all groups, the majority of participants (62/93, 66.7%; 60/92, 65.9%; 69/109, 63.3%; and 68/104, 66.0%) had a high education level, that is, a degree from a university of applied sciences or higher.
Measured Trust in the Physician
Based on the results of the factor analysis and Cronbach α calculation, we assessed trust on both a multidimensional and a unidimensional scale. The reason to use a unidimensional scale was that the factor analysis initially showed 2 factors (Table S1 in Multimedia Appendix 3 ); however, after removing the 2 items that loaded strongly on both factors and 1 item that primarily loaded on the second factor, only 1 factor remained. The reason for using a multidimensional scale was that the Cronbach α of the 3 dimensions was considered high enough (>0.75) to measure trust on a multidimensional scale (Table S2 in Multimedia Appendix 3 ).
Overall, trust in the physician was high, with a median of 5.8 (control group IQR 5.0-6.5; intervention group IQR 4.7-6.2) in the high-risk case and 6.0 (control group IQR 5.3-6.5; intervention group IQR 5.1-6.5) in the low-risk case on a 7-point Likert scale ( Multimedia Appendix 4 ). The high-risk case showed a lower median for the integrity of the physician using a CDSS (6.3, IQR 5.3-6.8 vs 6.0, IQR 5.0-6.7; U =3590.0; P =.06; Table 3 ) compared to the physician who did not use a CDSS, but these results were not statistically significant. Similarly, perceived competence was lower in the intervention group compared to the control group (median 5.8, IQR 4.8-6.5 vs 5.6, IQR 4.3-6.3; U =3771.5; P =.16). We observed no between-group differences in perceived competence, integrity, and benevolence of the low-risk group.
In the analyses exploring whether the results were different among subgroups, in the high-risk case, the effect of a CDSS application on the perceived competence of the physician depended on the participant’s sex ( F 1,181 =4.694; P =.03; Multimedia Appendix 5 ). In women, perceived competence and integrity were significantly lower in physicians who used a CDSS compared to physicians who did not ( U =740.5; P =.009 and U =756.0; P =.01, respectively; Table 4 ), whereas no such statistically significant differences were found in men.
In the low-risk case, results showed that the effect of the CDSS application on the perceived benevolence and integrity depended on the participant’s trust in technology in general ( F 1,209 =6.943; P =.009 and F 1,209 =4.119; P =.04, respectively; Multimedia Appendix 5 ). An increase in the participant’s trust in technology, in general, led to an increased perceived integrity and benevolence of physicians using a CDSS. This increase was more significant in the intervention group compared to the control group.
a U test: Wilcoxon test statistic.
b The P values in the table indicate the difference between the control and intervention groups.
a U : Wilcoxon test statistic.
b P values indicate the difference between the control and intervention groups.
Principal Findings
We aimed to assess the extent to which patient-physician trust was affected by using a CDSS application. We found that, in general, trust in physicians was high. Nonetheless, in the high-risk case, we observed that trust, in terms of competence and integrity, was lower in physicians using a CDSS compared to physicians who did not, and that the differences were larger in women than in men. No differences were found in the low-risk case. However, we found that perceived benevolence and integrity in the low-risk case depended on the participant’s trust in technology in general.
Comparison With Prior Literature
To our knowledge, this study is among the first to examine the impact of AI-based CDSSs on patient-physician trust in both a clinical high-risk and low-risk setting. There are several possible explanations for our results. First, prior to our study, we asked several physicians of the UMC Utrecht about their expectations regarding CDSS applications. Some anticipated that the use of CDSS applications in clinical practice could evoke a critical response from patients, believing that CDSS applications “first must prove their value before being accepted by patients.” Regarding competence, physicians mentioned that the use of a CDSS application could raise doubts about their professionalism, as it could come across as “being dependent on such an application.” This dependence and the associated loss of competence, known as “deskilling,” is a known concern of the introduction of clinical decision support applications in health care [ 45 ]. Some of these concerns seem reasonable, as our study indicates that patients’ trust in their physicians can decrease when a CDSS is used. Moreover, the decrease found in trust in terms of the integrity of a physician who uses a CDSS could be explained by concerns about data protection. Patients may feel they have no control over what happens with their personal data. However, some studies indicated that privacy was not an issue for some patients, as long as they trusted their physician [ 46 , 47 ]. Yakar et al [ 48 ] studied the general population’s view on the use of AI in health care through a web-based survey in the Netherlands and found less trust in AI than initially hypothesized. They, and some others, also found that women were less trusting of AI than men [ 48 , 49 ]. A reason for this could be that the women participating in this study were aware of the potential presence of gender bias in AI, as this issue has often been raised in previous research and media [ 50 - 52 ]. Additionally, women generally are considered to have more risk aversion than men [ 53 ]. Both these reasons combined could explain why the effect of using a CDSS on the perceived trust in the physician in the high-risk case depended on the participant’s sex and why this was not the case in the low-risk case.
In the low-risk case, our results showed that a patient’s general trust in technology played a significant role in the effect that CDSS applications could have on the perceived integrity and benevolence of the physician. An increase in the perceived integrity and benevolence of the physician seemed to be more likely in patients who had more trust in technology in general. This is in line with previous research investigating the association between trust in technology in general and trust in the implementation of AI in medicine [ 48 , 54 ].
Implications
Results from this study underline that mainly communicating about the technological aspects of AI algorithms in health care may ultimately hamper the successful implementation and acceptance of these algorithms in clinical practice. Personalized health care starts with putting the patient’s values first. Therefore, we believe that the development of AI-based CDSSs in health care should be transparent in terms of methods, alternatives, and understandability. In addition, patients should be involved early in the developmental phase of the CDSS, and the use of AI should be explained well during the visit with the health care professional. Furthermore, AI applications should not only be developed to predict the prognosis of a certain disease (precision medicine) but also to improve and facilitate discussions between patients and physicians about the patient’s illness and personal care needs (shared decision-making). The discussion between the patient and the physician may be improved by being transparent about the CDSS application. This potentially leads to more trust in the application, which, as shown in this study, could lead to an increase in the perceived integrity and benevolence of the physician. Moreover, it seems sensible to distinguish between the types of situations or patient populations in the development of AI algorithms for CDSS in health care; the results from our study indicate that less favorable reactions occur when AI is used in more life-threatening situations, which could also be due to the different patient populations, for example, babies in an acute situation versus adults in a chronic situation. By implementing AI-based CDSS in less risky situations first, patients could get acquainted with such CDSSs before implementing them in high-risk situations. Further study is warranted to establish the best implementation strategy regarding AI-based CDSSs in clinical care.
We recommend replicating this study while providing a clear explanation of the AI application. For example, by explaining how it works, how patient data are handled, and the benefits of such AI-based CDSSs for the patients. In addition, further research with a larger sample size and in different preventive care and cure settings, and across several age groups, should be conducted to confirm the results found in this study. External validation of our results will inform us whether our results are similar in, for example, patients in other health care settings or areas. Additionally, qualitative research methods should be considered to gain more insights into the reasons patient-physician trust might decline when using a CDSS from a patient perspective.
Strengths and Limitations
Vignette studies have been criticized in the past for their limitations. First, a frequently heard criticism of vignette studies is the lack of reality due to their hypothetical nature [ 55 ]. However, we minimized this by creating both hypothetical cases in collaboration with physicians working in the involved departments—the neonatology and rheumatology departments—and tested whether the participants could empathize well with the situation during a pilot study. Second, the participants in this study were (or still are) patients of the UMC Utrecht. This made it easier for the participants to empathize with the vignettes because they may have been in similar situations themselves, and they indicated they could (median 6.0, IQR 5.0-7.0 in all 4 groups). Third, it has been shown that participants of vignette studies are not always diligent and motivated to complete surveys or take these kinds of experiments seriously, which may reduce statistical power [ 56 ]. Participants could, for example, have put the questionnaire aside for a while, or might not have read the described situations properly [ 57 ]. We reduced this effect by tracking the time the participants took to read the vignettes and by excluding the fastest and the slowest 2.5% of readers from the analyses. Therefore, participants spending a remarkably long or short time reading the vignette were not included.
Conclusions
Trust in physicians is generally high among patients. However, our findings point toward a negative effect that AI applications can have on the patient-physician relationship, especially among women. We, therefore, believe that, for a successful adoption of AI applications in clinical practice, patients should be involved in both the development and implementation of such applications. Moreover, a broader societal discussion needs to take place about humane values and AI to gain insights into how we want AI to influence our lives when we encounter health care. In addition, clear communication to patients and society about the functions of the AI applications and what personal data they use seems equally important.
Acknowledgments
AGMZ was supported by the European Union’s Horizon 2020 research and innovation program under grant agreement number 101017331 (ODIN).
The funding source was not involved in the study design, analysis, and interpretation of the data nor the writing and in the decision to submit the manuscript for publication.
Authors' Contributions
AGMZ, RR, SGG, WWvS, MLB, RWMV, and SH contributed to the conceptualization and methodology of the project. AGMZ and RR analyzed the data. AGMZ wrote the draft manuscript. All authors contributed to the interpretation of the results and critically reviewed the manuscript. All authors read and approved the final version of the manuscript.
Conflicts of Interest
None declared.
Study design.
Details of the high-risk and low-risk vignettes.
Questionnaire factor analysis and Cronbach α.
Unidimensional trust scores, stratified by case.
Multivariate regression analyses to test potential effect modification.
- What is AI? Basic questions. Stanford University. URL: http://jmc.stanford.edu/artificial-intelligence/what-is-ai/index.html [accessed 2022-01-06]
- Ahuja AS. The impact of artificial intelligence in medicine on the future role of the physician. PeerJ. 2019;7:e7702. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hosny A, Parmar C, Quackenbush J, Schwartz LH, Aerts HJWL. Artificial intelligence in radiology. Nat Rev Cancer. Dec 2018;18(8):500-510. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tran AQ, Nguyen LH, Nguyen HSA, Nguyen CT, Vu LG, Zhang M, et al. Determinants of intention to use artificial intelligence-based diagnosis support system among prospective physicians. Front Public Health. 2021;9:755644. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Thrall JH, Li X, Li Q, Cruz C, Do S, Dreyer K, et al. Artificial intelligence and machine learning in radiology: opportunities, challenges, pitfalls, and criteria for success. J Am Coll Radiol. Mar 2018;15(3 Pt B):504-508. [ CrossRef ] [ Medline ]
- Haitjema S, Prescott TR, van Solinge WW. The applied data analytics in medicine program: lessons learned from four years' experience with personalizing health care in an academic teaching hospital. JMIR Form Res. Jan 28, 2022;6(1):e29333. [ CrossRef ] [ Medline ]
- Sutton RT, Pincock D, Baumgart DC, Sadowski DC, Fedorak RN, Kroeker KI. An overview of clinical decision support systems: benefits, risks, and strategies for success. NPJ Digit Med. 2020;3:17. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Melton GB, McDonald CJ, Tang PC, Hripcsak G. Electronic health records. In: Shortliffe EH, Cimino JJ, editors. Biomedical Informatics. 5th Edition. Cham, Switzerland. Springer Nature; 2021:467-509.
- Abbasgholizadeh Rahimi S, Cwintal M, Huang Y, Ghadiri P, Grad R, Poenaru D, et al. Application of artificial intelligence in shared decision making: scoping review. JMIR Med Inform. Aug 09, 2022;10(8):e36199. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stai B, Heller N, McSweeney S, Rickman J, Blake P, Vasdev R, et al. Public perceptions of artificial intelligence and robotics in medicine. J Endourol. Oct 01, 2020;34(10):1041-1048. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Asan O, Bayrak AE, Choudhury A. Artificial intelligence and human trust in healthcare: focus on clinicians. J Med Internet Res. Jun 19, 2020;22(6):e15154. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Morley J, Machado CCV, Burr C, Cowls J, Joshi I, Taddeo M, et al. The ethics of AI in health care: a mapping review. Soc Sci Med. Sep 2020;260:113172. [ CrossRef ] [ Medline ]
- Gerke S, Minssen T, Cohen IG. Ethical and legal challenges of artificial intelligence-driven health care. SSRN Journal. 2020:295-336. [ CrossRef ]
- Lucivero F, Jongsma KR. A mobile revolution for healthcare? Setting the agenda for bioethics. J Med Ethics. Oct 2018;44(10):685-689. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Schermer M. Telecare and self-management: opportunity to change the paradigm? J Med Ethics. Nov 2009;35(11):688-691. [ CrossRef ] [ Medline ]
- Fiske A, Buyx A, Prainsack B. The double-edged sword of digital self-care: physician perspectives from Northern Germany. Soc Sci Med. Sep 2020;260:113174. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Groenhof TKJ. General discussion: how to make a learning healthcare system work? In: Towards a Learning Healthcare System. Enschede, The Netherlands. Gildeprint B.V; 2020:215-232.
- Attribution 4.0 International (CC BY 4.0). Creative Commons. URL: https://creativecommons.org/licenses/by/4.0/ [accessed 2024-05-16]
- Tucker I. AI cancer detectors. The Guardian. Jun 10, 2018. URL: https://www.theguardian.com/technology/2018/jun/10/artificial-intelligence-cancer-detectors-the-five [accessed 2024-03-06]
- Bardes CL. Defining "patient-centered medicine". N Engl J Med. Mar 01, 2012;366(9):782-783. [ CrossRef ] [ Medline ]
- Weston WW. Informed and shared decision-making: the crux of patient-centered care. CMAJ. Aug 21, 2001;165(4):438-439. [ FREE Full text ] [ Medline ]
- Reuben DB, Tinetti ME. Goal-oriented patient care--an alternative health outcomes paradigm. N Engl J Med. Mar 01, 2012;366(9):777-779. [ CrossRef ] [ Medline ]
- Kitson A, Marshall A, Bassett K, Zeitz K. What are the core elements of patient-centred care? A narrative review and synthesis of the literature from health policy, medicine and nursing. J Adv Nurs. Jan 2013;69(1):4-15. [ CrossRef ] [ Medline ]
- LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. Dec 13, 2009;44(6):2093-2105. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Jones GR, George JM. The experience and evolution of trust: implications for cooperation and teamwork. AMR. Jul 1998;23(3):531-546. [ CrossRef ]
- Gill H, Boies K, Finegan JE, McNally J. Antecedents of trust: establishing a boundary condition for the relation between propensity to trust and intention to trust. J Bus Psychol. Apr 2005;19(3):287-302. [ CrossRef ]
- Mechanic D, Schlesinger M. The impact of managed care on patients' trust in medical care and their physicians. JAMA. Jun 05, 1996;275(21):1693-1697. [ Medline ]
- Anderson LA, Dedrick RF. Development of the Trust in Physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. Dec 1990;67(3 Pt 2):1091-1100. [ CrossRef ] [ Medline ]
- Emanuel EJ, Dubler NN. Preserving the physician-patient relationship in the era of managed care. JAMA. Jan 25, 1995;273(4):323-329. [ Medline ]
- Gray BH. Trust and trustworthy care in the managed care era. Health Aff (Millwood). Jan 1997;16(1):34-49. [ CrossRef ] [ Medline ]
- Caterinicchio RP. Testing plausible path models of interpersonal trust in patient-physician treatment relationships. Soc Sci Med. Part A: Med Psychol Med Sociol. Jan 1979;13:81-99. [ CrossRef ]
- Mechanic D. The functions and limitations of trust in the provision of medical care. J Health Polit Policy Law. Aug 1998;23(4):661-686. [ CrossRef ] [ Medline ]
- Thom DH, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. Feb 1997;44(2):169-176. [ Medline ]
- Mayer RC, Davis JH, Schoorman FD. An integrative model of organizational trust. AMR. Jul 1995;20(3):709. [ CrossRef ]
- Grimmelikhuijsen S, Knies E. Validating a scale for citizen trust in government organizations. Int Rev Adm Sci. Sep 03, 2015;83(3):583-601. [ CrossRef ]
- McEvily B, Tortoriello M. Measuring trust in organisational research: review and recommendations. J Trust Res. Apr 2011;1(1):23-63. [ CrossRef ]
- McKnight DH, Choudhury V, Kacmar C. Developing and validating trust measures for e-commerce: an integrative typology. ISR. Sep 2002;13(3):334-359. [ CrossRef ]
- van der Leeuw MS, Messelink MA, Tekstra J, Medina O, van Laar JM, Haitjema S, et al. Using real-world data to dynamically predict flares during tapering of biological DMARDs in rheumatoid arthritis: development, validation, and potential impact of prediction-aided decisions. Arthritis Res Ther. Mar 23, 2022;24(1):74. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pearson SD, Raeke LH. Patients' trust in physicians: many theories, few measures, and little data. J Gen Intern Med. Jul 2000;15(7):509-513. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. Am J Health Syst Pharm. Dec 01, 2008;65(23):2276-2284. [ CrossRef ] [ Medline ]
- Gottems LBD, Carvalho EMPD, Guilhem D, Pires MRGM. Good practices in normal childbirth: reliability analysis of an instrument by Cronbach's Alpha. Rev Lat Am Enfermagem. May 17, 2018;26:e3000. [ FREE Full text ] [ CrossRef ] [ Medline ]
- IBM SPSS Statistics for Windows. IBM. URL: https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-26 [accessed 2024-03-21]
- Qualtrics - een enquêtetool. Utrecht University. URL: https://students.uu.nl/qualtrics-een-enquetetool [accessed 2022-05-02]
- Yoda - a research data management service. Utrecht University. URL: https://www.uu.nl/en/research/yoda/about-yoda/why-yoda [accessed 2022-05-02]
- Cabitza F, Rasoini R, Gensini GF. Unintended consequences of machine learning in medicine. JAMA. Aug 08, 2017;318(6):517-518. [ CrossRef ] [ Medline ]
- Belfrage S, Helgesson G, Lynøe N. Trust and digital privacy in healthcare: a cross-sectional descriptive study of trust and attitudes towards uses of electronic health data among the general public in Sweden. BMC Med Ethics. Mar 04, 2022;23(1):19. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Haselager DR, Boers SN, Jongsma KR, Vinkers CH, Broekman ML, Bredenoord AL. Breeding brains? Patients' and laymen's perspectives on cerebral organoids. Regen Med. Dec 2020;15(12):2351-2360. [ CrossRef ] [ Medline ]
- Yakar D, Ongena YP, Kwee TC, Haan M. Do people favor artificial intelligence over physicians? A survey among the general population and their view on artificial intelligence in medicine. Value Health. Mar 2022;25(3):374-381. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kaplan AD, Kessler TT, Brill JC, Hancock PA. Trust in artificial intelligence: meta-analytic findings. Hum Factors. Mar 28, 2023;65(2):337-359. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Paul K. Disastrous lack of diversity in AI industry perpetuates bias, study finds. The Guardian. URL: https://www.theguardian.com/technology/2019/apr/16/artificial-intelligence-lack-diversity-new-york-university-study [accessed 2022-09-08]
- Cirillo D, Catuara-Solarz S, Morey C, Guney E, Subirats L, Mellino S, et al. Sex and gender differences and biases in artificial intelligence for biomedicine and healthcare. NPJ Digit Med. 2020;3:81. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Parikh RB, Teeple S, Navathe AS. Addressing bias in artificial intelligence in health care. JAMA. Dec 24, 2019;322(24):2377-2378. [ CrossRef ] [ Medline ]
- van Diemen J, Verdonk P, Chieffo A, Regar E, Mauri F, Kunadian V, et al. The importance of achieving sex- and gender-based equity in clinical trials: a call to action. Eur Heart J. Aug 17, 2021;42(31):2990-2994. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Gille F, Jobin A, Ienca M. What we talk about when we talk about trust: theory of trust for AI in healthcare. Intell -Based Med. Nov 2020;1-2:100001. [ CrossRef ]
- Krupnikov Y, Levine A. Expressing versus revealing preferences in experimental research. In: Sourcebook for Political Communication Research. 1st Edition. London, UK. Routledge; 2010:9780203938669.
- Blom-Hansen J, Morton R, Serritzlew S. Experiments in public management research. IPMJ. Mar 11, 2015;18(2):151-170. [ CrossRef ]
- Oppenheimer DM, Meyvis T, Davidenko N. Instructional manipulation checks: detecting satisficing to increase statistical power. J Exp Soc Psychol. Jul 2009;45(4):867-872. [ CrossRef ]
Abbreviations
Edited by Y Zhuang; submitted 17.07.23; peer-reviewed by Z Su, E Vashishtha, PH Liao, P Velmovitsky; comments to author 26.01.24; revised version received 21.03.24; accepted 16.04.24; published 28.05.24.
©Anna G M Zondag, Raoul Rozestraten, Stephan G Grimmelikhuijsen, Karin R Jongsma, Wouter W van Solinge, Michiel L Bots, Robin W M Vernooij, Saskia Haitjema. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 28.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

COMMENTS
Organizational Development (OD) interventions refer to a systematic and planned series of actions or activities designed to improve the overall effectiveness, health, and performance of an organization. To simplify, an OD intervention is a process that is actioned in response to a need for change.
However, it can be beneficial to glean information from an organizational development case study of successful execution. The below examples are divided into 4 categories of OD interventions : techno-structural, HRM, strategic change, and human process.
Technostructural interventions focus on improving organizational effectiveness and employee performance by focusing on technology and the structure of the organization. 5. Organizational (structural) design. Organizational design refers to how an organization is structured to achieve its strategic plan and goals.
Preview. Cases and Exercises in Organization Development & Change, Second Edition encourages students to practice organization development (OD) skills in unison with learning about theories of organizational change and human behavior. The book includes a comprehensive collection of cases about the OD process and organization-wide, team, and ...
Essentially, this book provides a practical guide for OD interventions. Each chapter provides practical information about general OD interventions, supplies best practice examples and case studies, summarizes the results of best practices, provides at least one case scenario, and offers at least one relevant tool for practitioners.
line w hich h ave v ast c ustomer base than that of LinkedIn's. (Wagner, 2016) 39522 Dr. Saritprava Das and Dhaval Bhatt, Str ategic organizational development intervent ions: A case of ...
Method. Inspired by Mode 2 knowledge production (Gibbons et al., Citation 1994), we brought together transdisciplinary practitioners and academics with experience of organizational interventions and took them through a process to identify key principles for designing, implementing, and evaluating organizational interventions.The core group consisted of 11 academic experts (the authors) from ...
Golembiewski, R.T., Hilles, R., & Kagno, M. A longitudinal study of flexitime effects: Some consequences of an OD structural intervention. Journal of Applied Behavioral Science, 1974,10, ... A Meta-Analysis Method for OD Case Studies. Go to citation Crossref Google Scholar. Research Methods and Reporting Practices in Organization Development: ...
Behavioral strategies - places emphasis on human resources. OD intervention - actions designed to improve the health of the client system. OD strategy - a plan for change using structural, technical, and behavioral methods. Parkinson's Laws - summarizes the problems of inefficient practices in organizations. Second-order consequences ...
Abstract. Given the highly instrumental nature of the literature on organizational interventions, this article explores and defines key elements of an artifaction theory of organizational ...
W.P. No. 2010 - 01 - 01. January 2010. The main objective of the working paper series of the IIMA is to help faculty members, research staff and doctoral students to speedily share their research findings with professional colleagues and test their research findings at the pre-publication stage. IIMA is committed to maintain academic freedom.
decades a variety of OD/HRD interventions have been used in Indian organizations. An analysis of the Indian literature then highlights that: (1) OD interven-tions have been practiced in a variety of Indian organizations over the past few decades; (2) a number of different OC initiatives and OD interventions
At the team level—staff perceived that there was an improvement in team effort. At the corporate level— the findings suggest that improved corporate performance is linked to improved individual and team level processes. Jeerapaet, P. (2014). The Impact of OD Interventions on Performance Management: A Case Study. AU-GSB E-JOURNAL, 3 (2).
The Role of OD Interventions: 1. Driving Change: OD interventions serve as catalysts for change by providing a structured framework for planning and implementing organizational improvements. 2. Engaging Employees: They engage employees at all levels, fostering a sense of ownership and involvement in the change process.
Case Studies: Harm Reduction - Full Report. Harm reduction is a public health approach that focuses on mitigating the harmful consequences of drug use, including transmission of infectious disease and prevention of overdose, through provision of care that is intended to be free of stigma and centered on the needs of people who use drugs. 1 Harm ...
The Case of OD in an NGO in India. Nisha Nair 1. Neharika Vohra 2. Abstract. This organizational development exercise was carri ed out in a prominent NGO that works. in the area of rights and ...
OD Interventions Case Study. an Employee Morale Problem - Free download as PDF File (.pdf), Text File (.txt) or read online for free. The document describes an organizational development intervention at a hospital to address low employee morale, particularly among nurses. The intervention involved a one-day workshop for all internal managers using a change puzzle kit as the main tool.
Case Studies of OD interventions by Plummer & Associates Here are example consulting engagements where we helped organizations succeed through various people focused interventions. As our clients don't want their specific "pains" identified, the organization names are not listed. OD Case 1 - 2-Hr Team Building Session for Exec Team ...
OD of future would require its interventions to be in synchronization with specific business impact measures such as customer satisfaction, productivity, employee satisfaction etc. OD with behavioural science base and systems thinking concept, and its core values, including humanistic orientation, collaboration, normative re-educative approach to change, the interventions have also varied in ...
This study reports a rewards system intervention as part of a multifaceted OD effort made in a large nonmanufacturing organization. Top management was confronted with data drawn from a stratified random sample of 386 top and middle management employees, 90 per cent of whom returned a specially developed rewards system survey instrument.
The researcher has developed a new model of organizational development that can be used by this organization to solve such future problems. The new model is based on three pillars. The first pillar is effective communication. An organization can only achieve success if the involved parties can share their views.
Jul 2, 2014 • Download as PPTX, PDF •. 12 likes • 15,867 views. P. PARIMITTAL10. od intervention case study. Education Business. 1 of 21. Download now. Od interventions case study - Download as a PDF or view online for free.
Finally, the most important intervention into OD is the conquering of the market with new production and services. We Will Write a Custom Case Study Specifically. For You For Only $13.90/page! order now. Such strategic changes will assure the company with new clients and great profits.Every OD intervention should be planned and carried out ...
Musculoskeletal conditions are the leading contributor to global disability and health burden. Manual therapy (MT) interventions are commonly recommended in clinical guidelines and used in the management of musculoskeletal conditions. Traditional systems of manual therapy (TMT), including physiotherapy, osteopathy, chiropractic, and soft tissue therapy have been built on principles such as ...
PDF | On Jul 1, 2010, Tom Cox and others published Organizational interventions: Issues and challenges | Find, read and cite all the research you need on ResearchGate
The annualized rate of a primary-outcome event was lower in the intervention group than in the usual-care group (0.53 vs. 1.12 events per person-year; incidence rate ratio, 0.48; 95% confidence ...
We randomly assigned patients with type 2 diabetes and chronic kidney disease (defined by an estimated glomerular filtration rate [eGFR] of 50 to 75 ml per minute per 1.73 m 2 of body-surface area ...
The study was approved by the Ethics Committee of the Hunan University of Medicine General Hospital (HYZY-EC-202306-C1), and with the informed consent of the patient. Consent for publication. Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. Competing interests
Background: Clinical decision support systems (CDSSs) based on routine care data, using artificial intelligence (AI), are increasingly being developed. Previous studies focused largely on the technical aspects of using AI, but the acceptability of these technologies by patients remains unclear. Objective: We aimed to investigate whether patient-physician trust is affected when medical decision ...