Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer

You are here
- Volume 64, Issue 7
- A case of small cell lung cancer treated with chemoradiotherapy followed by photodynamic therapy
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Department of Internal Medicine; College of Medicine, Chungnam National University Hospital and Cancer Research Institute, Jungku, Daejeon, South Korea
- Professor J O Kim, Department of Internal Medicine, Chungnam National University Hospital and Cancer Research Institute, 640 Daesadong, Jungku, Daejeon 301-721, South Korea; jokim{at}cnu.ac.kr
Here, we present the case of a 51-year-old man with limited-stage small cell lung cancer (LS-SCLC) who received concurrent chemoradiotherapy and photodynamic therapy (PDT). The patient was diagnosed as having LS-SCLC with an endobronchial mass in the left main bronchus. Following concurrent chemoradiotherapy, a mass remaining in the left lingular division was treated with PDT. Clinical and histological data indicate that the patient has remained in complete response for 2 years without further treatment. This patient represents a rare case of complete response in LS-SCLC treated with PDT.
https://doi.org/10.1136/thx.2008.112912
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Currently, patients with small cell lung cancer (SCLC) are treated with chemotherapy with or without thoracic radiotherapy. Radiation therapy is generally accepted as an essential component of limited-stage SCLC (LS-SCLC). However, the local failure rate after chemotherapy and radiotherapy remains high, ranging from 30% to 70%. 1 More effective means are needed to decrease the local recurrence rate.
Endobronchial photodynamic therapy (PDT) is used to treat patients who have central-type lung cancer, with the objective of palliation in advanced cases and curative intent in patients with early-stage disease. 2 3 Furukawa et al reported that PDT resulted in a complete response (CR) rate of 92.8% in patients with lesions of <1.0 cm; recurrences after a CR were seen in 9 of 77 lesions (11.7%) <1.0 cm. 4 When the extent of the tumour and the depth of the bronchogenic carcinoma have been evaluated, PDT can be an effective local treatment modality. 4
A few studies have described the treatment of SCLC using PDT. Moghissi et al 5 reported that 10 of 100 patients with advanced SCLC underwent PDT for palliation. Kato et al 6 and Okunaka et al 7 evaluated the effectiveness of PDT in the treatment of early-stage SCLC. However, none of these studies detailed a single case of SCLC treated with PDT.
Here, we present a case in which PDT was used with curative intent in a patient having endobronchial cancer, following standard treatment for SCLC and in addition to concurrent chemotherapy and radiotherapy.
CASE REPORT
A 51-year-old man presented to our clinic with a 6-month history of worsening dyspnoea on exertion. His symptoms included a nearly constant dry cough, diminished appetite without weight loss, and fatigue. He had previously been diagnosed as having diabetes mellitus with an uncontrolled glucose level and hypertension. The patient was a smoker with a ⩾40 pack-per-year history. The Eastern Cooperative Oncology Group performance status was grade 1.
The patient had undergone testing at an outside facility because of his symptoms; a plain chest x ray revealed opacity in the left lung field ( fig 1A ). As a result, the patient was diagnosed with pneumonia and treated with antibiotics. Despite antibiotic treatment, the resolution of pneumonic consolidation was delayed. Thus, the patient was referred to our hospital. Chest CT revealed an endobronchial protruding mass in the distal left main bronchus (LMB) with a near total collapse of the left lung and a small granuloma in the posterior segment of the right upper lobe ( fig 1B ). No evidence of mediastinal nodal disease or a metastatic focus was detected. Bronchoscopic examination showed functional vocal cords and a pedunculated mass in the LMB ( fig 1C ). Bronchoscopic washing and biopsies failed to demonstrate a specific cell type. A rigid bronchoscopic biopsy was performed, and the pathological examination confirmed the presence of small cell carcinoma based on immunostaining for CD56, synaptophysin, chromogranin and leucocyte common antigen (LCA) using the initial paraffin-embedded biopsy specimen. The results were consistent with SCLC. CT of the brain was normal. Therefore, the patient was diagnosed with LS-SCLC.
- Download figure
- Open in new tab
- Download powerpoint
Summary from the initial diagnostic investigation to last follow-up (A–C) Initial diagnostic investigation on June 2006. (D–F) Response evaluation after chemoradiotherapy in October 2006. (G and H) Positron emission tomography (PET)–CT without increased glucose uptake in October 2007. (I) There is no evidence of recurrence in December 2008.
Chemotherapy with cisplatin and irinotecan was initiated, but the chemotherapeutic regimen was changed to cisplatin and etoposide (EP) after one cycle due to grade 4 diarrhoea. Concurrent with the second and third cycles of EP, the total dose of thoracic radiation therapy was 45.6 Gy in 38 fractions (120 cGy per fraction). Treatment was given twice daily, at least 6 h apart, on weekdays. Thoracic radiation therapy was delivered with 6–10 MV photons using custom-made blocks. With re-expansion of the lung on plain chest x ray ( fig 1D ), the patient’s dyspnoea was found to be greatly improved. Post-treatment chest CT showed that the endobronchial protruding mass in the distal LMB was noticeably smaller, with a residual small soft tissue nodule in the left upper lobe ( fig 1E ). Bronchoscopy revealed a pedunculated mass in the orifice of the lingular division ( fig 1F ). To evaluate the size of the tumour and identify any unknown synchronous cancer, autofluorescence bronchoscopy was performed. We applied PDT to remove the remaining tumour completely, because high dose rate brachytherapy and stereotactic radiation techniques were not available in our hospital. The remaining tumour was treated with PDT after wire basket removal of the pedunculated mass via flexible bronchoscopy. A 2.5 mg/kg dose of haematoporphyrin derivate (Photogem, Moscow Institute of High Chemical Technologies, Russia) was administered intravenously 48 h before irradiation. Using a diode laser (wavelength = 630 nm; Biolitec, Jena, Germany), a light with a 3 cm cylindrical diffuser was introduced through the working channel of an autofluorescence fibreoptic bronchoscope. Illumination was carried out in the left second carina and orifice of the lingular division. The light dose was 100 J/cm. Bronchoscopy followed PDT for debridement and detection of PDT-related complications. No immediate complications occurred.
The complete disappearance of the tumour was confirmed pathologically by subsequent bronchoscopic biopsy and radiologically by chest CT after 4 weeks. No evidence of recurrence was observed from October 2006 to December 2008. One year after PDT, combined positron emission tomography (PET) and CT revealed no metabolic evidence of recurrence. Two years after PDT, chest CT and bronchoscopy demonstrated a complete response in this patient ( fig 1G,H ). The patient refused prophylactic cranial irradiation.
PDT as a local therapeutic modality often results in a CR of centrally located early-stage lung cancer. Kato et al 3 reported that PDT resulted in a CR in about 94% of patients with centrally located early lung cancer (squamous cell type) with a limited longitudinal extent (<1 cm). Moghissi et al 5 suggested that the benefits of PDT did not differ between patients with SCLC and non-small cell lung cancer (NSCLC); however, patients with SCLC may be deprived of PDT because SCLC grows rapidly and spreads to other organs earlier than NSCLC.
A combined modality consisting of thoracic radiotherapy and systemic chemotherapy is widely accepted as the standard treatment for LS-SCLC. For cases in which a tumour remains after standard treatment, clinicians should consider additional treatment modalities, including pneumonectomy, sleeve lobectomy or intraluminal brachytherapy. In this study, we had to consider the specific features of the tumour, which was located in the bronchial mucosa without invasion into the cartilaginous layer. Although the adverse effects of PDT include photosensitivity skin reaction (sunburn) in 5–28% of cases, respiratory complications in 0–18% and non-foetal haemoptysis in 0–7.8%, PDT is a safe method. 8
To reduce the local recurrence rate after PDT, both the extent and the depth of an endobronchial tumour must be known. Autofluorescence bronchoscopy and endobronchial ultrasonography (EBUS) may be useful as additional examination methods. 9 Miyazu et al 10 demonstrated that the depth of tumour invasion estimated by EBUS was accurate based on histological findings after surgical resection.
According to the guidelines released in 2003 concerning early-stage NSCLC, PDT should be considered as a treatment option in early superficial squamous cell carcinoma, especially for inoperable cases. 11 Regarding the extent and depth of an endobronchial lesion, PDT may be an effective treatment for superficial airway lesions ⩽1 cm in length, despite a diagnosis of SCLC. In this case, we applied PDT without confirming the depth of the lesion and without confirming that viable tumour remained after chemotherapy and radiotherapy, although radiological findings were highly suggestive of viable tumour. This case is the first report of the non-recurrence of SCLC.
This case suggests that PDT can be effectively used with curative intent.
- Brenner M ,
- Okunaka T ,
- Shimatani H ,
- Furukawa K ,
- Moghissi K ,
- Stringer M ,
- Miyazawa T ,
- Kurimoto N ,
- Mathur PN ,
- Sutedja T ,
Competing interests: None.
Patient consent: Obtained.
Read the full text or download the PDF:
- Case report
- Open access
- Published: 19 August 2022
Triple primary lung cancer: a case report
- Hye Sook Choi ORCID: orcid.org/0000-0001-8387-4907 1 &
- Ji-Youn Sung 2
BMC Pulmonary Medicine volume 22 , Article number: 318 ( 2022 ) Cite this article
2874 Accesses
2 Citations
Metrics details
The risk of developing lung cancer is increased in smokers, patients with chronic obstructive pulmonary disease, individuals exposed to environmental carcinogens, and those with a history of lung cancer. Automobile exhaust fumes containing carcinogens are a risk factor for lung cancer. However, we go through life unaware of the fact that automobile exhaust is the cause of cancer. Especially, in lung cancer patient, it is important to search out pre-existing risk factors and advice to avoid them, and monitor carefully for recurrence after treatment.
Case presentation
This is the first report of a case with triple lung cancers with different histologic types at different sites, observed in a 76-year-old parking attendant. The first adenocarcinoma and the second squamous cell carcinoma were treated with stereotactic radiosurgery because the patient did not want to undergo surgery. Although the patient stopped intermittent smoking after the diagnosis, he continued working as a parking attendant in the parking lot. After 29 months from the first treatment, the patient developed a third new small cell lung cancer; he was being treated with chemoradiation.
Conclusions
New mass after treatment of lung cancer might be a multiple primary lung cancer rather than metastasis. Thus, precision evaluation is important. This paper highlights the risk factors for lung cancer that are easily overlooked but should not be dismissed, and the necessity of discussion with patients for the surveillance after lung cancer treatment. We should look over carefully the environmental carcinogens already exposed, and counsel to avoid pre-existing lung cancer risk factors at work or residence in patients with lung cancer.
Peer Review reports
The risk factors for lung cancer include smoking and inhaling exhaust fumes. Primary lung cancer (PLC) increases the risk of secondary lung cancers by four to six times [ 1 , 2 ]. With increasing exposure to environmental risk factors such as automobile exhaust fumes and advances in computed tomographic (CT) screening and treatment modality of lung cancer, the incidence of multiple primary lung cancers (MPLC) is increasing [ 2 ]. Synchronous MPLC is defined as a new cancer if it occurs with the same histology within 2 years after the PLC therapy, or with a different histology at the same time [ 3 ]; Metachronous MPLC is defined as a new cancer with the same histology if it occurs after a tumor-free period of 2 years; otherwise, it is considered to have a different histology [ 3 ]. Incidence of MPLC is higher in women, people with history of malignant disease, and those with chronic obstructive pulmonary disease (COPD), compared to solitary PLC. Men, smokers, patients with COPD, and those with non-adenocarcinomas have higher incidence of metachronous MPLC. Female sex and not smoking are independent risk factors for synchronous MPLC [ 4 ]. It is important to manage the risk factors for MPLC in patients diagnosed with lung cancer. However, patients counselling to avoid the already existing risk factors for lung cancers is not generally conducted in depth. For the first time, we report a case of triple lung cancers with metachronous MPLC in a parking attendant.
A 76-year-old man was referred for a lung mass in December 2018. He was a smoker (30 pack years with intermittent stops) and parking attendant for 30 years. There was no history of lung cancer in the immediate family of the patient. The patient was administered a dual bronchodilator for COPD.
CT scan showed a 1.4 cm × 1.3 cm mass in the right upper lobe (RUL) (Fig. 1 a) and a right lower lobe (RLL) mass-like consolidation (Fig. 1 b). Histopathologic examinations of CT-guided-percutaneous needle biopsy (PCNB) of the RUL mass revealed adenocarcinoma (ADC) (Fig. 2 a–c) with clinical staging cT1bN0M0 on ultrasonic-guided transbronchial needle biopsy (EBUS-TBNB) and fluorodeoxyglucose F18-positron emission tomography (FDG-PET) scan. RLL mass showed no metabolism on the FDG-PET scan. The FEV 1 was 56% of the predicted value. We planned a lobectomy for the RUL cancer and a follow-up for the RLL mass. However, the patient refused to undergo surgery and was treated with stereotactic radiosurgery (SRS) on the RUL mass in January 2019. The RLL mass-like consolidation did not show any changes on the follow-up chest CT or FDG-PET scan in November 2019.
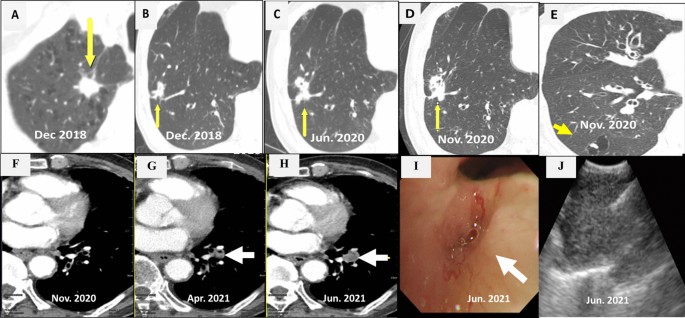
Chest CT scans. a A mass on the RUL of the first adenocarcinoma (arrow). b A mass on the RLL at the same time of the first cancer diagnosis (arrow). c Increased RLL mass six months later (arrow). d Further increased RLL mass after five months (arrow). e New nodule on the peripheral RLL (arrow). f–h Development and increase of the lymph node (arrow). i Bronchoscopic finding showing LLL anterobasal segment obstruction (arrow). j Lymph node enlargement on the EBUS. CT, computed tomography; RUL, right upper lobe; RLL, right lower lobe; LLL, left lower lobe; EBUS, endobronchial ultrasound
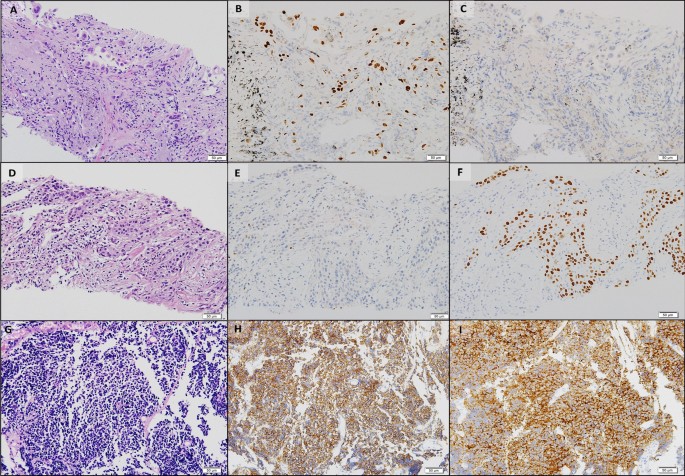
Histopathologic comparisons of the triple lung cancers. a-c The first tumor of adenocarcinoma at the right upper lobe. a Pleomorphic neoplastic cells with an acinar pattern (hematoxylin and eosin stain, ×200). b Immunoreactivity for TTF-1(×200). c Negative for P40(×200). d-f The second tumor of squamous cell carcinoma at the right lower lobe. d Polygonal cells with a solid pattern and no keratinization (hematoxylin and eosin stain, ×200). e No immunoreactivity for TTF-1(×200). f Strong staining of P40 at tumor cells(×200). g-i The third tumor of small cell carcinoma at the left lower lobe. g Small cells with scant cytoplasm and lack of nucleoli with a high mitotic activity (hematoxylin and eosin stain, ×200). h Positive neuroendocrine markers of CD56(×200). i Positive neuroendocrine marker of synaptophysin(×200). Equipment used to obtain images: Olympus BX53 microscope/Olympus objective lens WHN10X/22 UIS2, Olympus DP72 cameras and acquisition software: Olympus CellSens Standard 1.6 software. TTF-1, thyroid transcription factor-1
In June 2020, the RLL mass-like consolidation was found to have increased on a chest CT scan (Fig. 1 c). PCNB of the RLL mass was performed, and histologic examination revealed anthracofibrosis. Five months later, the RLL mass increased further (Fig. 1 d), and a new nodule appeared at the periphery of the RLL (Fig. 1 e). PCNB was performed again on the same RLL mass (Fig. 1 d), and histological examination demonstrated squamous cell carcinoma (SCC) (Fig. 2 d–f). There was no metastasis except for hypermetabolism of the new nodule in the RLL periphery (Fig. 1 e) on the FDG-PET scans. We could not perform a biopsy for the new peripheral nodule (Fig. 1 e) due to cystic changes. We concluded the clinical staging of the RLL SCC as cT3N0M0 on the EBUS-TBNB and PET scan. SRSs were performed separately for the RLL SCC and the new RLL peripheral nodule, respectively in February 2021.
We performed chest CT scan for surveillance of lung cancer. Five months later after 2nd SCC diagnosis, a new nodule emerged at the left lower lobe (LLL) (Fig. 1 f, g). Two months after that, the nodule increased further (Fig. 1 h). Bronchoscopy showed new total obstruction of the anterobasal segmental bronchus of the LLL (Fig. 1 i). Histologic examinations of bronchial biopsy and EBUS-TBNB (Fig. 1 j) for LLL lesions demonstrated small cell lung carcinoma (SCLC) (Fig. 2 g–i). Clinical staging was limited stage. The patient was treated with chemotherapy (etoposide/carboplatin) and concurrent thoracic radiation.
Discussion and conclusions
Smoking is a notorious risk factor for lung cancer. The parking attendant was exposed to exhaust fumes, including carcinogens from the fuel. He was using a bronchodilator for COPD. Smoking and COPD are independent risk factors for MPLC [ 4 ]. PLC increased the risk of MPLC despite stage IA lung cancer [ 5 , 6 ]. We suggest that his history of exposure to exhaust fumes in addition to smoking, COPD, and PLC contributed to the metachronous MPLC.
At the time of the first ADC diagnosis on the RUL, we discuss the possibility that the RLL mass was lung cancer, and decided to follow according to the PET-CT scan results with the multidisciplinary approach. Unfortunately, 18 months later, PCNB and histologic findings for the RLL mass showed no cancers. Five months after that (23 months after the first ADC treatment), repeated PCNB on the RLL mass demonstrated SCC. The possibility that an additional abnormality is cancer must be addressed when PLC is diagnosed.
The third SCLC of LLL developed newly 29 months after the first ADC treatment. It was detected after 5 months after the diagnosis of second cancer. Timely CT scan for surveillance is essential for earlier diagnosis of metachronous MPLC in the patients with PLC, which could be improve the outcomes of MPLC. We considered that the first ADC and the second SCC were synchronous MPLC; thus, the third SCLC might be metachronous MPCL. The three different types of MPLC were not a transformation of the PLC after SRSs, but originally developed from three different histologies. Recently, genetic/molecular profiles have begun to be used for differentiation and diagnosis of MPLC [ 7 ]. and further investigation is needed.
The primary tumor control rate of SRS is 97.6% in medically inoperable early-stage non-SCLC [ 8 ]. Recently, the risk of metachronous MPLC was found to be lower with radiotherapy than non-radiotherapy [ 6 , 8 ] even though in stage IA lung cancer [ 5 ]. The incidence of metachronous MPLC was 0.5% at 1 year and 2.28% at 5 years among solitary PLC survivors with radiotherapy, which was lower compared to the non-radiotherapy group [ 6 ]. Based on these findings, it is assumed that the SRSs might not induce metachronous MPLC in our patient.
The question was what could have been responsible for the patient’s triple lung cancers. Unknown susceptible genetic factors, smoking, and exhaust fumes might have contributed to the development of triple lung cancers. Previously reported risk factors [ 4 ] such as male sex, smoking, COPD, and nonadenocarcinoma also increased the risk of metachronous MPLC in this patient. He stopped smoking after the first diagnosis of lung cancer, but continued as a parking attendant for 12 h a day. It is well known that harmful effects of smoking persist for years even after smoking cessation. Thus, the main cause of lung cancer in this patient is likely to be smoking. Physicians always counsel their lung cancer patients that smoking is one of the main causes of lung cancer and advise to quit smoking immediately. However, the emphasis on counselling avoidance of other environmental carcinogens that may have a synergistic effect with smoking is often neglected. This patient was exposed to exhaust gas at work for 30 years which is a known occupational carcinogen, and exposure continued even after quitting smoking and diagnosing lung cancer. He had no family history of lung cancer. Unfortunately, his wife was diagnosed with stage IV lung adenocarcinoma lung cancer at August 2021, the time of 3 rd SCLC diagnosis of him. He and his wife had worked together in parking lot for several years. We suggest that exhaust fumes might be an additional main risk factor for metachronous MPLC that is easily overlooked in this patient.
Despite stage I lung cancer, careful surveillance for metachronous MPLC is needed, especially in patients with a history of smoking, COPD, PLC, and exposure to environmental carcinogens such as exhaust fumes. Occupation and environment surveys with attentive advice for risk factors of lung cancer are very important, and it is valuable to evaluate concurrent abnormal images in patients with lung cancer. Appropriate CT scan surveillance after PLC therapy can help identify curable MPLC, which might lead to improved overall survival.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
Adenocarcinoma
Chronic obstructive pulmonary disease
Computed tomography
Ultrasonic-guided transbronchial needle biopsy
F18-positron emission tomography
Left lower lobe
Primary lung cancer
Multiple primary lung cancers
Percutaneous needle biopsy
Right lower lobe
Right upper lobe
Squamous cell carcinoma
Small cell lung carcinoma
Stereotactic radiosurgery
Johnson BE. Second lung cancers in patients after treatment for an initial lung cancer. J Natl Cancer Inst. 1998;90(18):1335–45.
Article CAS Google Scholar
Surapaneni R, Singh P, Rajagopalan K, Hageboutros A. Stage I lung cancer survivorship: risk of second malignancies and need for individualized care plan. J Thorac Oncol. 2012;7(8):1252–6.
Article Google Scholar
Martini N, Melamed MR. Multiple primary lung cancers. J Thorac Cardiovasc Surg. 1975;70(4):606–12.
Shintani Y, Okami J, Ito H, Ohtsuka T, Toyooka S, Mori T, Watanabe S-i, Asamura H, Chida M, Date H, et al. Clinical features and outcomes of patients with stage I multiple primary lung cancers. Cancer Sci. 2021;112(5):1924–35.
Khanal A, Lashari BH, Kruthiventi S, Arjyal L, Bista A, Rimal P, Uprety D. The risk of second primary malignancy in patients with stage Ia non-small cell lung cancer: a US population-based study. Acta Oncol. 2018;57(2):239–43.
Hu ZG, Tian YF, Li WX, Zeng FJ. Radiotherapy was associated with the lower incidence of metachronous second primary lung cancer. Sci Rep. 2019;9(1):19283–19283.
Asamura H. Multiple primary cancers or multiple metastases, that is the question. J Thorac Oncol. 2010;5(7):930–1.
Timmerman R, Paulus R, Galvin J, Michalski J, Straube W, Bradley J, Fakiris A, Bezjak A, Videtic G, Johnstone D, et al. Stereotactic body radiation therapy for inoperable early stage lung cancer. JAMA. 2010;303(11):1070–6.
Download references
Acknowledgements
Not applicable
No funding sources were used.
Author information
Authors and affiliations.
Department of Internal Medicine, Kyung Hee Unversity Medical Center, 23 Kyunghee dae-ro, Dongdaemun-gu, Seoul, 02447, Republic of Korea
Hye Sook Choi
Department of Pathology, Kyung Hee University Medical Center, Seoul, Republic of Korea
Ji-Youn Sung
You can also search for this author in PubMed Google Scholar
Contributions
HSC drafted the manuscript, reviewed the literature, and collected the data. JYS collected the data and revised the manuscript. All authors contributed to obtaining and interpreting the clinical information. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Hye Sook Choi .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Kyung Hee University Medical Center (approval number: KHUH 2021–09-069–002) and written informed consent was given by the patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they do not have any conflict of interest.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Choi, H.S., Sung, JY. Triple primary lung cancer: a case report. BMC Pulm Med 22 , 318 (2022). https://doi.org/10.1186/s12890-022-02111-x
Download citation
Received : 07 April 2022
Accepted : 10 August 2022
Published : 19 August 2022
DOI : https://doi.org/10.1186/s12890-022-02111-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Multiple primary lung cancer (MLPC)
- Synchronous MLPC
- Metachronous MLPC
- Parking attendant
BMC Pulmonary Medicine
ISSN: 1471-2466
- Submission enquiries: [email protected]
- General enquiries: [email protected]
- Biomarker-Driven Lung Cancer
- HER2-Positive Breast Cancer
- Chronic Lymphocytic Leukemia
- Small Cell Lung Cancer
- Renal Cell Carcinoma

- CONFERENCES
- PUBLICATIONS
Case 1: 72-Year-Old Woman With Small Cell Lung Cancer

EP: 1 . Case 1: 72-Year-Old Woman With Small Cell Lung Cancer
Ep: 2 . case 1: extensive-stage small cell lung cancer background, ep: 3 . case 1: impower133 trial in small cell lung cancer, ep: 4 . case 1: caspian trial in extensive-stage small cell lung cancer, ep: 5 . case 1: biomarkers in small cell lung cancer, ep: 6 . case 1: small cell lung cancer in the era of immunotherapy.

EP: 7 . Case 2: 67-Year-Old Woman With EGFR+ Non–Small Cell Lung Cancer
Ep: 8 . case 2: biomarker testing for non–small cell lung cancer, ep: 9 . case 2: egfr-positive non–small cell lung cancer, ep: 10 . case 2: flaura study for egfr+ metastatic nsclc, ep: 11 . case 2: egfr+ nsclc combination therapies.

EP: 12 . Case 2: Treatment After Progression of EGFR+ NSCLC

EP: 13 . Case 3: 63-Year-Old Man With Unresectable Stage IIIA NSCLC
Ep: 14 . case 3: molecular testing in stage iii nsclc, ep: 15 . case 3: chemoradiation for stage iii nsclc, ep: 16 . case 3: pacific trial in unresectable stage iii nsclc, ep: 17 . case 3: standard of care in unresectable stage iii nsclc, ep: 18 . case 3: management of immune-related toxicities in stage iii nsclc.
Mark Socinski, MD: Thank you for joining us for this Targeted Oncology ™ Virtual Tumor Board ® focused on advanced lung cancer. In today’s presentations my colleagues and I will review three clinical cases. We will discuss an individualized approach to treatment for each patient, and we’ll review key clinical trial data that impact our decisions. I’m Dr. Mark Socinski from the AdventHealth cancer institute in Orlando, Florida. Today I’m joined by Dr Ed Kim, a medical oncologist from the Levine Cancer Institute in Charlotte, North Carolina; Dr Brendon Stiles, who is a thoracic surgeon from the Weill Cornell Medical Center in New York ; and Dr Tim Kruser, radiation oncologist from Northwestern Medicine Feinberg School of Medicine in Chicago. Thank you all for joining me today. We’re going to move to the first case, which is a case of small cell lung cancer. I’m going to ask Dr Kim to do the presentation.
Edward Kim, MD: Thanks, Mark. It’s my pleasure to walk us through the first case, which is small cell lung cancer. This is a case with a 72-year-old woman who presents with shortness of breath, a productive cough, chest pain, some fatigue, anorexia, a recent 18-pound weight loss, and a history of hypertension. She is a schoolteacher and has a 45-pack-a-year smoking history; she is currently a smoker. She is married, has 2 kids, and has a grandchild on the way. On physical exam she had some dullness to percussion with some decreased-breath sounds, and the chest x-ray shows a left hilar mass and a 5.4-cm left upper-lobe mass. CT scan reveals a hilar mass with a bilateral mediastinal extension. Negative for distant metastatic disease. PET scan shows activity in the left upper-lobe mass with supraclavicular nodal areas and liver lesions, and there are no metastases in the brain on MRI. The interventional radiographic test biopsy for liver reveals small cell, and her PS is 1. Right now we do have a patient who has extensive-stage small cell lung cancer. Unfortunately, it’s what we found. It’s very common to see this with liver metastases.
Transcript edited for clarity.

FDA Approval Marks Amivantamab's Milestone in EGFR+ NSCLC
In this episode, Joshua K. Sabari, MD, discusses the FDA approval of amivantamab plus chemotherapy as a first-line treatment for patients with EGFR exon 20 insertion mutation-positive non-small cell lung cancer.

AI Reveals Link Between Influenza and NSCLC
A correlation between non–small cell lung cancer and influenza shows a decrease in cancer survival rates.

Lisberg Discusses Dato-DXd's Role in Advanced Lung Cancer Care
In this episode of Targeted Talks, Aaron Lisberg, MD, discusses results from the phase 3 TROPION-Lung01 study of datopotamab in advanced or metastatic non–small cell lung cancer.

Emerging Biomarkers and Tumor Heterogeneity Lead the Way in Lung Cancer
Trials in small cell lung cancer and non–small cell lung cancer are fueling excitement in the oncology community.

NVL-655 Earns FDA Breakthrough Therapy Designation in ALK-Positive NSCLC
The FDA has given the novel agent NVL-655 a breakthrough therapy designation for the treatment of patients with ALK-positive locally advanced or metastatic non-small cell lung cancer.
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

CASE REPORT article
Case report: lung adenocarcinoma initially presenting with cutaneous and subcutaneous metastases.

- 1 Department of Nuclear Medicine, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 2 Hubei Province Key Laboratory of Molecular Imaging, Wuhan, China
- 3 Key Laboratory of Biological Targeted Therapy, the Ministry of Education, Wuhan, China
- 4 Department of Dermatology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 5 Department of Nuclear Medicine, The People’s Hospital of Honghu, Honghu, China
Cutaneous and subcutaneous soft tissue metastases are rare in lung adenocarcinoma and suggest poor prognosis. We report a patient with lung adenocarcinoma who initially presented with cutaneous and subcutaneous metastases to the abdomen that were initially presumed to be herpes zoster and an occult subcutaneous soft tissue mass. Because the lesions progressed over 3 weeks despite routine herpes zoster treatment, magnetic resonance imaging was performed and showed a presumed sarcoma; however, 18 F-fluourodeoxyglucose positron emission tomography/computed tomography demonstrated pulmonary lesions. Biopsy of the abdominal lesion confirmed poorly differentiated lung adenocarcinoma. Early diagnosis of soft tissue metastasis can be difficult. Clinicians should suspect internal organ malignancy when a progressive cutaneous or subcutaneous soft tissue lesion is encountered.
Introduction
Lung cancer is a frequently encountered malignancy that can metastasize to almost all organs and is associated with high mortality ( 1 , 2 ). Lung adenocarcinoma commonly metastasizes to the liver, adrenal glands, brain, and bone ( 3 ). Soft tissue metastases from lung adenocarcinoma are rare and occur predominantly in men ( 4 ). They may be apparent before the primary tumor and typically herald a poor prognosis. Reported mean survival in patients with skin metastases is 2.9 months ( 5 ), so early diagnosis and treatment are important. However, the diagnosis of skin metastases may be delayed or missed. A high index of suspicion is required.
Case Description
A 52-year-old woman presented with a 3-week history of painful rash and subcutaneous soft tissue mass overlying the right abdomen at the waistline. She denied constitutional symptoms such as fever, chills, night sweats, and unintentional weight loss. There was no history of major trauma, surgery, smoking, alcohol use, or drug or food allergy. Notably, the patient was exposed to secondhand smoke from nicotine cigarettes due to her husband’s smoking. In addition, her father died of esophageal cancer. Herpes zoster was initially suspected but appropriate treatment did not result in clinical improvement. In fact, progression had occurred. Therefore, she was hospitalized for further investigation and treatment. Physical examination showed a raised skin mass surrounded by swelling and erythema on the right abdomen ( Figure 1A ). Serum erythrocyte sedimentation rate, C-reactive protein, white blood cell count, and multiple tumor markers were elevated. Ultrasonography revealed a solid mass underneath the rash. On magnetic resonance imaging (MRI), the mass was 10 cm in diameter and inhomogeneous on T2-weighted sequences ( Figures 1B, C ) and exhibited markedly restricted diffusion on diffusion-weighted sequences ( Figure 1D ). The mass was suspected to be a sarcoma. To investigate potential distant metastases, 18 F-fluourodeoxyglucose (FDG) positron emission tomography (PET)/computed tomography (CT) was performed, which showed the previously demonstrated large abdominal mass was hypermetabolic in the periphery and hypometabolic in the center ( Figure 2A ); other hypermetabolic lesions were shown in the right lung and the posterior pleural wall ( Figure 2B–E ). Lung cancer with metastases was suspected and the patient underwent ultrasound-guided biopsy of the subcutaneous soft tissue mass. Examination of hematoxylin and eosin-stained specimen ( Figure 3A ) revealed abundant oval and plump cells with enlarged nuclei and red, broad cytoplasm. Immunohistochemical examination showed staining was positive for CK7 ( Figure 3B ), TTF-1 ( Figure 3C ), and PCK but negative for P63, CK20, Villin, ER, CDX2, HER2, P16, GATA-3, and VT-1. This suggested a diagnosis of primary pulmonary adenocarcinoma with metastasis. Because PDL-1 was expressed ( Figure 3D ) and EGFR mutation was not detected, the patient was placed on bevacizumab plus pemetrexed–platinum doublet chemotherapy. After six cycles, the primary pulmonary lesions shrunk but the cutaneous lesions did not. Molecular testing revealed mutation in the BRAF 15 exon and targeted therapy was proposed, but the patient refused for financial reasons. For relieving the patient’s pain, palliative radiotherapy was initiated.
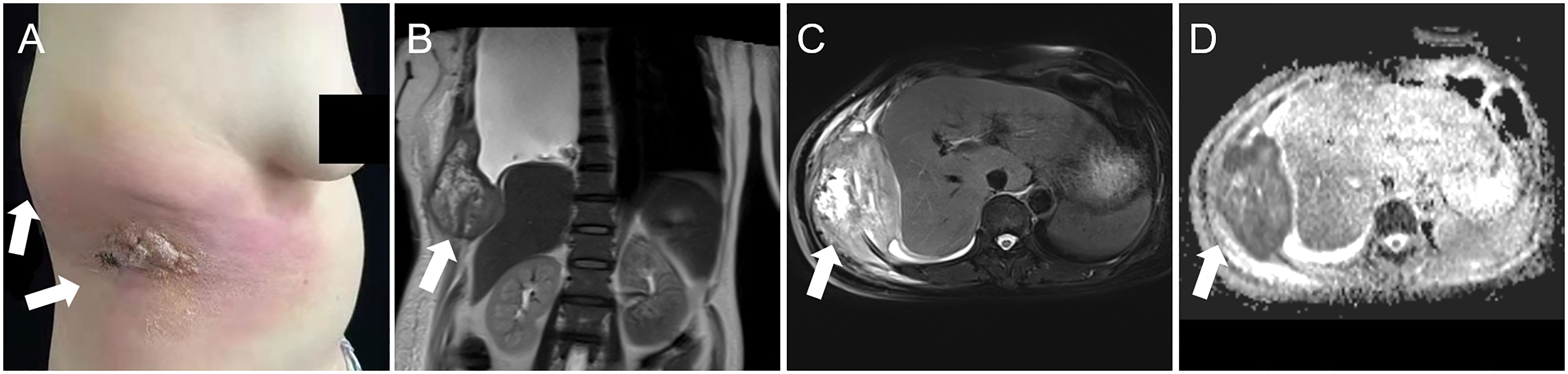
Figure 1 Physical examination showed an erythematous rash and swelling surrounding a skin mass on the right abdomen ( A , arrows). Magnetic resonance imaging shoed an inhomogeneous soft tissue mass approximately 10 cm in diameter ( B , coronal T2-weighted image; C , axial fat saturation T2-weighted image). The lesion also showed markedly restricted diffusion on diffusion-weighted sequences ( D , arrow).
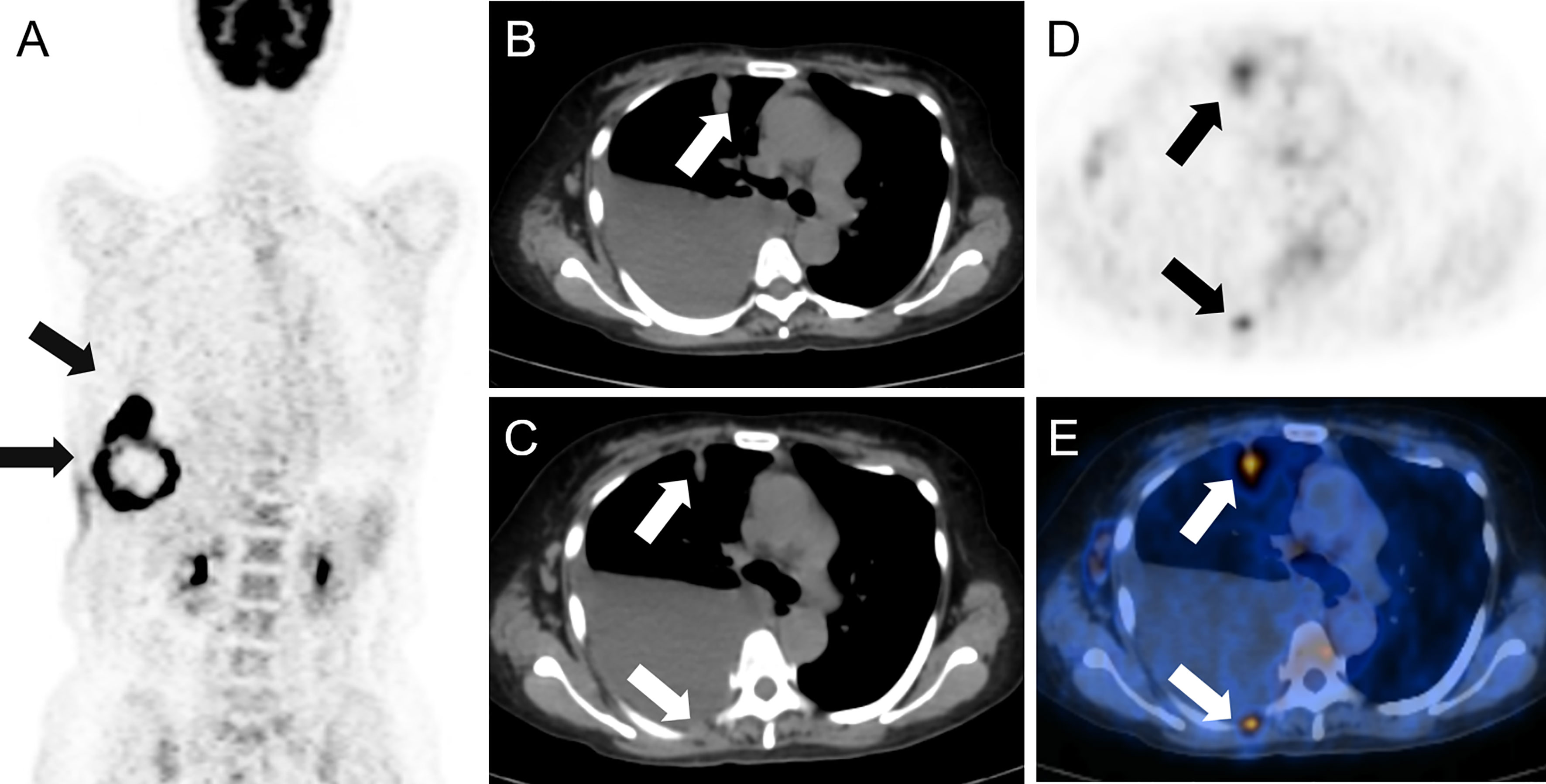
Figure 2 A large mass showing hypermetabolism peripherally and hypometabolism centrally was found on 18F-fluorodeoxyglucose positron emission tomography/computed tomography (A) , arrows. Hypermetabolic lesions were imaged in the right lung and the posterior pleural wall (arrows) on axial computed tomography (B, C) , positron emission tomography (D) and fusion imaging (E) .
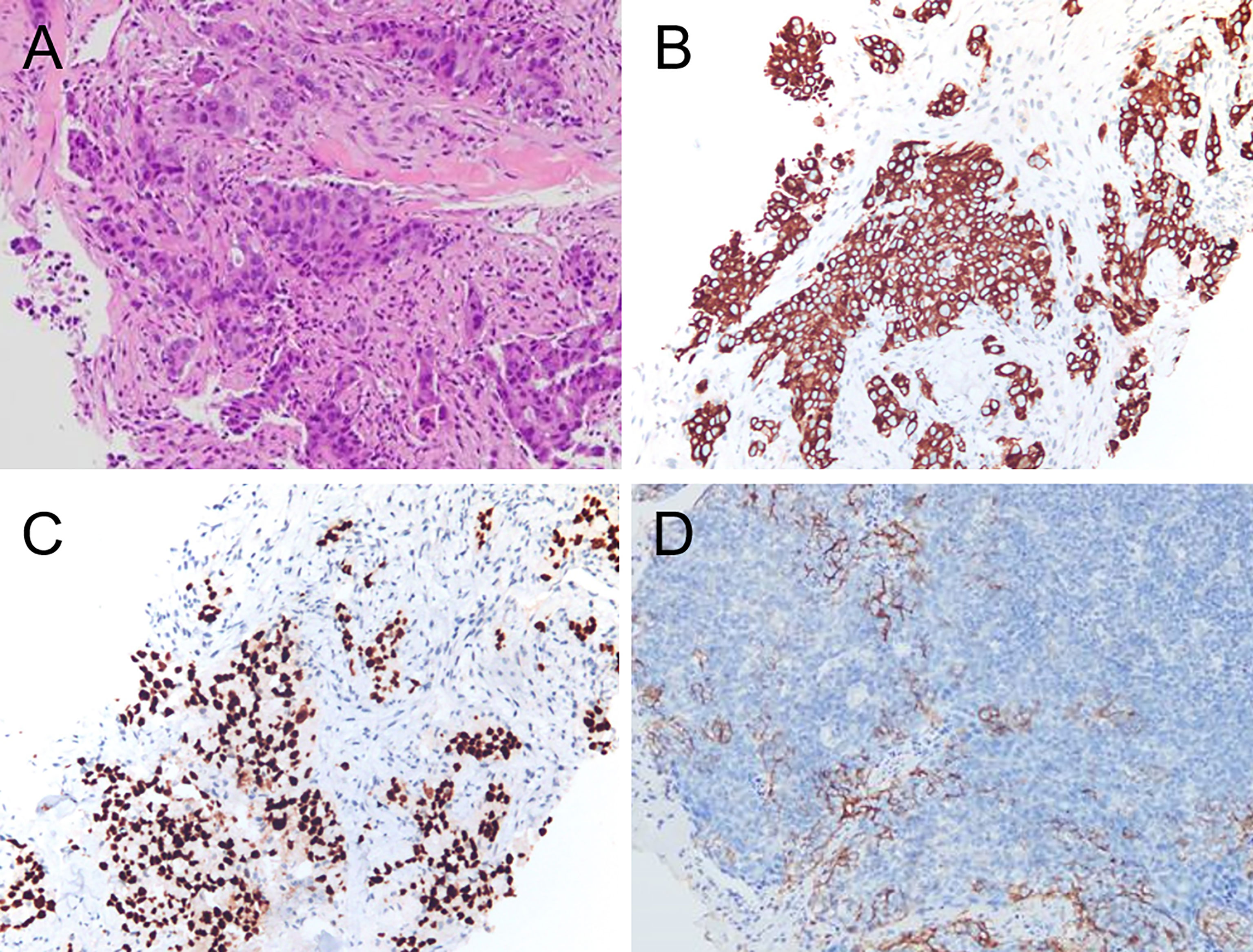
Figure 3 Hematoxylin and eosin staining revealed the tumor was composed of abundant oval and plump cells with enlarged nuclei and red, broad cytoplasm (A) . Immunohistochemical staining for CK 7 (B) showed a strong and diffuse brown cytoplasmic reaction. TTF-1 staining (C) Showed strong nuclear staining of tumor cells. Immunohistochemical analysis showed PDL-1 expression (D) .
Lung cancer morbidity and mortality is highest of all cancers ( 1 , 2 ) and lung adenocarcinoma accounts for approximately 40% of all lung cancers ( 6 ). Although lung carcinoma can metastasize to all organs, the liver, adrenal glands, bone, kidney, and brain are the most common sites ( 3 ). Metastasis to cutaneous and subcutaneous soft tissues is rare, with reported incidence rates ranging between 1% and 12% ( 5 , 7 – 9 ). Soft tissue metastasis can be challenging to diagnose when it is the initial cancer manifestation, as in our patient, who presented with a painful rash in the absence of typical lung adenocarcinoma symptoms ( 10 ). Soft tissue metastases may rapidly progress when the initial diagnosis is missed.
To evaluate soft tissue metastases, MRI is the most sensitive and specific imaging modality and enables assessment of tissue characteristics, tumor extent, and areas of reactivity ( 11 , 12 ). In our patient, MRI was highly suspicious for sarcoma but 18 F-FDG PET/CT suggested a lung primary, which was confirmed by biopsy. Although MRI can distinguish between benign and malignant tumors, it cannot further distinguish malignancy. Compared with sarcoma, soft tissue metastases from organ malignancies are rare. They are easily missed, especially when symptoms of the primary are absent or atypical. Therefore, 18 F-FDG PET/CT before biopsy is essential to improve diagnostic accuracy and distinguish soft tissue masses.
Optimal management requires accurate diagnosis, which requires biopsy in most cases ( 13 , 14 ). In our patient, histopathological and immunohistochemical examinations resulted in a diagnosis of poorly differentiated pulmonary adenocarcinoma ( 15 , 16 ). In this disease, the appearance of metastatic soft tissue masses indicates an advanced stage and poor prognosis. Chemotherapy, immunotherapy, targeted therapy, and radiotherapy are the mainstay treatments for soft tissue metastasis; surgery is not typically recommended ( 17 – 19 ). Unfortunately, six cycles of bevacizumab plus pemetrexed–platinum doublet chemotherapy were not as effective as we had hoped. The targeted therapy has been shown to decrease tumor burden, decrease symptoms, and dramatically improve survival outcomes in advanced lung cancers ( 19 , 20 ). However, our patient refused the targeted therapy for financial reasons. Then palliative radiotherapy was initiated and proved effective for pain relief. To date, the patient’s general condition has remained stable.
Early diagnosis of soft tissue metastasis can be difficult. Clinicians should suspect internal organ malignancy when a progressive cutaneous or subcutaneous soft tissue lesion is encountered. A thorough examination should be performed and 18 F-FDG PET/CT should be considered for further evaluation.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethical Committee of Union Hospital, Tongji Medical College. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
JW, RW, LY, ZW and XX obtained and analyzed the clinical data. JW and XX wrote the manuscript. FL and FH designed and constructed the figures. XX and ZG designed the study. All authors contributed to patient care and writing and revising the manuscript and figures. All authors contributed to the article and approved the submitted version.
This research was supported by the National Natural Science Foundation of China (Grant Numbers 81801737, 81771866).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We thank Dr. Ranran Ding for providing and analyzing the immunohistochemical data of CK7 and TTF-1. We thank Liwen Bianji (Edanz) ( https://www.liwenbianji.cn ) for editing the language of a draft of this manuscript.
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer Statistics, 2021. CA Cancer J Clin (2021) 71(1):7–33. doi: 10.3322/caac.21654
PubMed Abstract | CrossRef Full Text | Google Scholar
2. Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Nikšić M, et al. Global Surveillance of Trends in Cancer Survival 2000–14 (Concord-3): Analysis of Individual Records for 37 513 025 Patients Diagnosed With One of 18 Cancers From 322 Population-Based Registries in 71 Countries. Lancet (2018) 391(10125):1023–75. doi: 10.1016/s0140-6736(17)33326-3
3. Tamura T, Kurishima K, Nakazawa K, Kagohashi K, Ishikawa H, Satoh H, et al. Specific Organ Metastases and Survival in Metastatic Non-Small-Cell Lung Cancer. Mol Clin Oncol (2015) 3(1):217–21. doi: 10.3892/mco.2014.410
4. Alcaraz I, Cerroni L, Rütten A, Kutzner H, Requena L. Cutaneous Metastases From Internal Malignancies: A Clinicopathologic and Immunohistochemical Review. Am J Dermatopathol (2012) 34(4):347–93. doi: 10.1097/DAD.0b013e31823069cf
5. Song Z, Lin B, Shao L, Zhang Y. Cutaneous Metastasis as a Initial Presentation in Advanced Non-Small Cell Lung Cancer and Its Poor Survival Prognosis. J Cancer Res Clin Oncol (2012) 138(10):1613–7. doi: 10.1007/s00432-012-1239-6
6. Tvedten E, Deak Z, Schwartz B, Rice A. An Atypical Presentation of Soft Tissue Metastasis in a Patient With Lung Cancer. Cureus (2021) 13(7):e16294. doi: 10.7759/cureus.16294
7. Gül U, Kiliç A, Gönül M, Külcü Cakmak S, Erinçkan C. Spectrum of Cutaneous Metastases in 1287 Cases of Internal Malignancies: A Study From Turkey. Acta dermato-venereol (2007) 87(2):160–2. doi: 10.2340/00015555-0199
CrossRef Full Text | Google Scholar
8. Dhambri S, Zendah I, Ayadi-Kaddour A, Adouni O, El Mezni F. Cutaneous Metastasis of Lung Carcinoma: A Retrospective Study of 12 Cases. J Eur Acad Dermatol Venereol JEADV (2011) 25(6):722–6. doi: 10.1111/j.1468-3083.2010.03818.x
9. Hidaka T, Ishii Y, Kitamura S. Clinical Features of Skin Metastasis From Lung Cancer. Internal Med (1996) 35(6):459–62. doi: 10.2169/internalmedicine.35.459
10. Kocher F, Hilbe W, Seeber A, Pircher A, Schmid T, Greil R, et al. Longitudinal Analysis of 2293 Nsclc Patients: A Comprehensive Study From the Tyrol Registry. Lung Cancer (2015) 87(2):193–200. doi: 10.1016/j.lungcan.2014.12.006
11. Mayerson JL, Scharschmidt TJ, Lewis VO, Morris CD. Diagnosis and Management of Soft-Tissue Masses. J Am Acad Orthop Surg (2014) 22(11):742–50. doi: 10.5435/jaaos-22-11-742
12. Miwa S, Otsuka T. Practical Use of Imaging Technique for Management of Bone and Soft Tissue Tumors. J Orthopaedic Sci (2017) 22(3):391–400. doi: 10.1016/j.jos.2017.01.006
13. Khoo M, Pressney I, Hargunani R, Saifuddin A. Small, Superficial, Indeterminate Soft-Tissue Lesions as Suspected Sarcomas: Is Primary Excision Biopsy Suitable? Skeletal Radiol (2017) 46(7):919–24. doi: 10.1007/s00256-017-2635-4
14. Fenzl L, Bubel K, Mehrmann M, Schneider G. Bildgebung Und Biopsie Von Weichteiltumoren. Der Radiologe (2018) 58(1):79–92. doi: 10.1007/s00117-017-0331-y
15. Kummar S, Fogarasi M, Canova A, Mota A, Ciesielski T. Cytokeratin 7 and 20 Staining for the Diagnosis of Lung and Colorectal Adenocarcinoma. Br J Cancer (2002) 86(12):1884–7. doi: 10.1038/sj.bjc.6600326
16. Ordóñez NG. Value of Thyroid Transcription Factor-1, E-Cadherin, Bg8, Wt1, and Cd44s Immunostaining in Distinguishing Epithelial Pleural Mesothelioma From Pulmonary and Nonpulmonary Adenocarcinoma. Am J Surg Pathol (2000) 24(4):598–606. doi: 10.1097/00000478-200004000-00016
17. Damron TA, Heiner J. Distant Soft Tissue Metastases: A Series of 30 New Patients and 91 Cases From the Literature. Ann Surg Oncol (2000) 7(7):526–34. doi: 10.1007/s10434-000-0526-7
18. Hashimoto K, Nishimura S, Akagi M. Lung Adenocarcinoma Presenting as a Soft Tissue Metastasis to the Shoulder: A Case Report. Medicina (Kaunas Lithuania) (2021) 57(2):181. doi: 10.3390/medicina57020181
19. Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman J, Chirieac LR, et al. Non-Small Cell Lung Cancer, Version 5.2017, Nccn Clinical Practice Guidelines in Oncology. J Natl Compr Cancer Network JNCCN (2017) 15(4):504–35. doi: 10.6004/jnccn.2017.0050
20. Tan AC, Tan DSW. Targeted Therapies for Lung Cancer Patients With Oncogenic Driver Molecular Alterations. J Clin Oncol (2022) 40(6):611–25. doi: 10.1200/JCO.21.01626
Keywords: lung adenocarcinoma, soft tissue, skin rashes, metastasis, 18 F-FDG, PET/CT
Citation: Wang J, Wu R, Liu F, Yang L, Hu F, Wu Z, Gao Z and Xia X (2022) Case Report: Lung Adenocarcinoma Initially Presenting With Cutaneous and Subcutaneous Metastases. Front. Oncol. 12:925382. doi: 10.3389/fonc.2022.925382
Received: 21 April 2022; Accepted: 23 June 2022; Published: 12 July 2022.
Reviewed by:
Copyright © 2022 Wang, Wu, Liu, Yang, Hu, Wu, Gao and Xia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zairong Gao, [email protected] ; Xiaotian Xia, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
- In Memoriam
- Lung cancer journeys
In This Section
- How we can help you
- Complimentary educational materials
- Lung Cancer Support Line (844) 835-4325
- How do you know if you have lung cancer?
- Lung cancer overview
- What Is Biomarker Testing?
- What Kinds Of Specialists Are Part Of A Lung Cancer Care Team?
- Types of cancer treatment
- Symptoms and side effects
- Clinical trials
- Understanding palliative care
- What Is A Personalized Cancer Care Plan?
- Coping with emotions upon diagnosis
- Are Smokers The Only Ones Who Can Get Lung Cancer?
- What Are The Best Ways To Deal With Emotions During Lung Cancer?
- Oxygen therapy
- Wellness guide
- What Are The Best Ways To Communicate Your Needs While Living With Lung Cancer?
- What Are Common Questions To Ask My Doctor When Diagnosed With Lung Cancer?
- Glossary Of Common Lung Cancer Terms
- Biomarker testing: a quick guide
- Navigating lung cancer: for newly diagnosed patients
- Para pacientes con cáncer de pulmón
- Quick links for patients and caregivers
- Conozca Su Riesgo: cáncer de pulmón en las comunidades Hispanas/Latinas
- Know Your Risk: lung cancer in Hispanic/Latino communities
- Know your risk: lung cancer and Black Americans
- Women and lung cancer
The stories below come from people whose lives have been touched by lung cancer. In addition to providing unique insight on what it’s like to battle and live with the disease, each story also provides reasons to be hopeful about the future of lung cancer research.

We remember…
LCRF honors and remembers those who have graciously shared their stories with us and have since passed away. By telling about their experiences, they helped – and continue to help – those who are navigating their own diagnoses.


‘Here’s How I Knew I Had Lung Cancer’: One Patient’s Story with Relatively Low Risk Factor
Lung cancer , encompassing both small cell and non-small cell types and affecting men and women almost equally, stands as the second most common cancer in the United States. According to the American Cancer Society , the year 2024 is expected to see approximately 234,580 new cases and about 125,070 deaths due to lung cancer.
Predominantly diagnosed in those aged 65 and older, lung cancer is the leading cause of cancer death in the country, responsible for nearly 20% of all cancer fatalities. Each year, lung cancer claims more lives than colon, breast, and prostate cancers combined.
However, there's a silver lining. The incidence of lung cancer is on a decline, partly due to the decrease in smoking rates and advancements in early detection and treatment. Says Aaron Mansfield, MD, a Mayo Clinic lung cancer oncologist: "Although tobacco use is clearly the largest risk factor to develop lung cancer, there are many other risk factors, and risk factors we don't know. All you need to be at risk of developing lung cancer is a lung." Awareness of risk factors, such as exposure to secondhand smoke, radon gas, asbestos, and having a family history of lung cancer, is also crucial.
Despite the importance of early detection, lung cancer symptoms often appear only after the cancer has advanced. Dr. Mansfield explains one of the challenges that may be to blame for this: "Many of my patients have been diagnosed as having pneumonia. They've received many rounds of antibiotics that were not beneficial. They make their way to us when a mass that was thought to be pneumonia on a chest X-ray never improved."
Key symptoms of lung cancer to watch for include:
- shortness of breath
- persistent cough
- coughing up blood (hemoptysis)
- unexplained weight loss
- loss of appetite
- headaches (or other nervous system changes)
Screening also plays a pivotal role in combating lung cancer. Annual low-dose CT scans have been proven to save lives and are recommended for high-risk patients. (Data from the CDC in 2023 stated that cigarette smoking is the number-one risk factor for lung cancer, linked with 80% to 90% of all lung cancer deaths.)
Following recent updates, the US Preventive Services Task Force now suggests screening should start at age 50 for those with a 20-pack-year smoking history, broadening the net to catch more cases earlier. A "pack year" is a term used to describe the amount of tobacco a person has smoked over time, calculated by multiplying the number of packs of cigarettes smoked per day by the number of years the person has smoked. For smokers, quitting now can significantly reduce the risk of lung cancer.
Ahead, you'll read the personal story of Ron Barnett, a 65-year-old Philadelphia native, who shares his journey from a late-stage lung cancer diagnosis to finding stability and hope through a clinical trial. Ron shared that he smoked "occasionally" in his late teens to early twenties, but quit when he got married. It so happens that Barnett's home state of Pennsylvania is demonstrated to be one region with the highest radon rates, which some experts say is the second-highest lung cancer risk factor. To learn more about which areas around the country may be most vulnerable to radon exposure, read up on a recent radon study .
Get The Healthy by Reader's Digest newsletter
Here's how I knew I had lung cancer
By Ron Barnett, as told to Dr. Patricia Varacallo, DO
It's a strange thing, getting older. For awhile you might shrug off every ache and pain, but hit your early sixties, and suddenly you're keeping a ledger on every little twinge asking yourself if it's the big one. But lung cancer? That thought hadn't even crossed my mind.
Walking into the emergency room that brisk autumn morning in 2019, I was convinced the sharp pains in my chest were heralding a heart attack. You see, I've been a fighter all my life—raised in a tough neighborhood, served a stint in the military, and even beat a nasty case of pneumonia in my fifties—but nothing could've prepared me for the battle that lay ahead. The ER visit was supposed to be a quick in-and-out precaution to ensure my ticker was still ticking right. However, the doctors, after a flurry of tests and scans, found something unsettling—a spot on my liver. "It's concerning," they said, recommending a closer look.
That revealed a truth I wasn't ready to face: Stage 4 non-small cell lung cancer. Stage 4 is the most advanced type of cancer and usually means the cancer has spread, or "metastasized," to another organ. In my case, it had spread to my liver. A quick online search suggested my chance of surviving three months was maybe only around 25%. Fortunately, advances in science and medicine were in my favor.
But when I first heard those words, the room spun. The thought of "cancer" was a shock. My wife stood by my side, and together, we navigated some swift and fierce emotions.
Smokers Who Take This Vitamin Could Be at Higher Risk for Cancer
Treatment after I knew I had lung cancer
After the diagnosis sank in, I felt a kind of determined grit take over. The doctor briefed me on my battle plan: A three-drug chemotherapy regimen. It would be brutal, the doctor warned.
Let me tell you, chemo is no walk in the park. It's a beast unlike anything I'd faced before, but deep down, I understood it was my ticket through this storm.
But just as I was getting the hang of this new, unwelcome routine, the treatments began to falter. My doctor advised me that it seemed my body was no longer responding. The cancer was outpacing the chemo, and my options were dwindling fast.
11 Things About Lung Cancer Doctors Wish You Knew
That's when my doctor, seeing the desperation in my eyes, suggested a new course of action—a clinical trial. The uncertainty of it was terrifying— But what do I have to lose? , I remember thinking. I'd be lying if I said I wasn't scared, but I hung onto hope in this unknown.
The clinical trial included some new medications, regular monitoring, and ongoing doctors appointments...but slowly, almost imperceptibly, the tide began to turn. My cancer, this relentless force that had upended my life, started to show signs of stability. Three years have passed since then, and my cancer remains stable. It's a precarious peace, but I'll take it over the alternative any day.
I know I am one of the lucky ones, and I don't take that for granted. This journey has been anything but easy, but it's taught me more about life, resilience, and the importance of hope than I could've ever learned otherwise.
The Best Foods for Healthier Lungs, from Pulmonology Doctors and a Dietitian
To anyone going through a similar diagnosis, let me say this: Knowledge is power. Research your condition, understand your options, and don't be afraid to ask questions. A skilled medical team can make all the difference in the world, but so can your own understanding of what you're facing—and clinical trials? I know not every patient can say this, but in my case I found it was the lifeline I was looking for. Maybe that's a benefit of having a type of cancer that affects so many other people: With resources being allocated toward research, doctors are doing so much to make progress with new treatments these days.
I share my story not for sympathy but in the hope that it might light a path for someone else. Stage 4 lung cancer is not an easy diagnosis to live with, but it's not the end of the road. With the proper treatment, a great medical team, and the courage to explore new options, you can find a way to keep fighting.
For more inspiring stories of diagnoses and recovery, subscribe to The Healthy by Reader's Digest newsletter and follow The Healthy on Facebook and Instagram . Keep reading:
- "Here's How I Knew I Had Pancreatic Cancer": One Survivor's Story After Years of Growing Clues
- Colon Cancer and Poop: What to Watch For, According to a Colorectal Surgeon
- I Drank Tart Cherry Juice Every Day for a Week-Here's What Happened
- Watching Too Much TV Raises Your Risk of This Bathroom Issue, Says New Study
The post ‘Here’s How I Knew I Had Lung Cancer’: One Patient’s Story with Relatively Low Risk Factor appeared first on The Healthy .

Advances in Lung Cancer Research

Lung cancer cells driven by the KRAS oncogene, which is highlighted in purple.
NCI-funded researchers are working to advance our understanding of how to prevent, detect, and treat lung cancer. In particular, scientists have made progress in identifying many different genetic alterations that can drive lung cancer growth.
This page highlights some of the latest research in non-small cell lung cancer (NSCLC), the most common form of lung cancer, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and research findings from recent studies.
Early Detection of Lung Cancer
A great deal of research has been conducted in ways to find lung cancer early. Several methods are currently being studied to see if they decrease the risk of dying from lung cancer.
The NCI-sponsored National Lung Screening Trial (NLST) showed that low-dose CT scans can be used to screen for lung cancer in people with a history of heavy smoking. Using this screening can decrease their risk of dying from lung cancer. Now researchers are looking for ways to refine CT screening to better predict whether cancer is present.
Markers in Blood and Sputum
Scientists are trying to develop or refine tests of sputum and blood that could be used to detect lung cancer early. Two active areas of research are:
- Analyzing blood samples to learn whether finding tumor cells or molecular markers in the blood will help diagnose lung cancer early.
- Examining sputum samples for the presence of abnormal cells or molecular markers that identify individuals who may need more follow-up.
Machine Learning
Machine learning is a method that allows computers to learn how to predict certain outcomes. In lung cancer, researchers are using computer algorithms to create computer-aided programs that are better able to identify cancer in CT scans than radiologists or pathologists. For example, in one artificial intelligence study , researchers trained a computer program to diagnose two types of lung cancer with 97% accuracy, as well as detect cancer-related genetic mutations.
Lung Cancer Treatment
Treatment options for lung cancer are surgery , radiation , chemotherapy , targeted therapy , immunotherapy , and combinations of these approaches. Researchers continue to look for new treatment options for all stages of lung cancer.
Treatments for early-stage lung cancer
Early-stage lung cancer can often be treated with surgery. Researchers are developing approaches to make surgery safer and more effective.
- When lung cancer is found early, people usually have surgery to remove an entire section ( lobe ) of the lung that contains the tumor. However, a recent clinical trial showed that, for certain people with early-stage NSCLC, removing a piece of the affected lobe is as effective as surgery to remove the whole lobe .
- The targeted therapy Osimertinib (Tagrisso ) was approved by the Food and Drug Administration (FDA) in 2021 to be given after surgery—that is, as adjuvant therapy —to people with early-stage NSCLC that has certain mutations in the EGFR gene.
- Two immunotherapy drugs, atezolizumab (Tecentriq) and pembrolizumab (Keytruda) have been approved by the FDA to be used as adjuvant treatments after surgery and chemotherapy, for some patients with early-stage NSCLC.
- The immunotherapy drug nivolumab (Opdivo) is approved to be used, together with chemotherapy, to treat patients with early-stage lung cancer before surgery (called neoadjuvant ). This approval, which came in 2022, was based on the results of the CheckMate 816 trial, which showed that patients at this stage who received neoadjuvant nivolumab plus chemotherapy lived longer than those who received chemotherapy alone .
- In another trial (Keynote-671), patients with early-stage NSCLC who received pembrolizumab plus chemotherapy before surgery and pembrolizumab after surgery had better outcomes than those who received just neoadjuvant or just adjuvant treatment.
Treatments for advanced lung cancer
Newer therapies are available for people with advanced lung cancer. These primarily include immunotherapies and targeted therapies, which continue to show benefits as research evolves.
Immunotherapy
Immunotherapies work with the body's immune system to help fight cancer. They are a major focus in lung cancer treatment research today. Clinical trials are ongoing to look at new combinations of immunotherapies with or without chemotherapy to treat lung cancer.
Immune checkpoint inhibitor s are drugs that block an interaction between proteins on immune cells and cancer cells which, in turn, lowers the immune response to the cancer. Several immune checkpoint inhibitors have been approved for advanced lung cancer, including p embrolizumab (Keytruda) , a tezolizumab (Tecentriq) , c emiplimab (Libtayo) , d urvalumab (Imfinzi) , and n ivolumab (Opdivo) .
A key issue with immunotherapies is deciding which patients are most likely to benefit. There is some evidence that patients whose tumor cells have high levels of an immune checkpoint protein called PD-L1 may be more responsive to immune checkpoint inhibitors. Another marker for immunotherapy response is tumor mutational burden , or TMB, which refers to the amount of mutations in the DNA of the cancer cells. In some lung cancer trials, positive responses to immune checkpoint inhibitors have been linked with a high TMB. However, these markers cannot always predict a response and there is ongoing work to find better markers.
To learn more, see Immunotherapy to Treat Cancer .
Targeted Therapies
Targeted treatments identify and attack certain types of cancer cells with less harm to normal cells. In recent years, many targeted therapies have become available for advanced lung cancer and more are in development. Targeted treatments for lung cancer include the below.
Anaplastic lymphoma kinase (ALK) Inhibitors
ALK inhibitors target cancer-causing rearrangements in a protein called ALK. These drugs continue to be refined for the 5% of NSCLC patients who have an ALK gene alteration. Approved treatments include ceritinib (Zykadia) , alectinib (Alecensa) , brigatinib (Alunbrig) , and lorlatinib (Lorbrena) .
These ALK inhibitors are improvements from previous ones in their enhanced ability to cross the blood–brain barrier. This progress is critical because, in non-small cell lung cancer patients with ALK alterations, disease progression tends to occur in the brain. Based on clinical trial results, in 2024 the FDA approved alectinib as adjuvant therapy for people with ALK-positive NSCLC .
EGFR Inhibitors
- Lung Cancer Trial of Osimertinib Draws Praise—and Some Criticism
The drug improved survival in a large clinical trial, but some question the trial’s design.
EGFR inhibitors block the activity of a protein called epidermal growth factor receptor (EGFR). Altered forms of EGFR are found at high levels in some lung cancers, causing them to grow rapidly. Osimertinib (Tagrisso) is the most effective and most widely used EGFR inhibitor. It is also used for adjuvant therapy after surgery for resectable NSCLC. Other drugs that target EGFR that are approved for treating NSCLC include afatinib (Gilotrif) , dacomitinib (Vizimpro) , erlotinib (Tarceva) , gefitinib (Iressa) . For people with Exon 20 mutations, amivantamab (Rybrevant) is an approved targeted therapy.
ROS1 Inhibitors
The ROS1 protein is involved in cell signaling and cell growth. A small percentage of people with NSCLC have rearranged forms of the ROS1 gene. Crizotinib (Xalkori) and entrectinib (Rozlytrek) are approved as treatments for patients with these alterations. In late 2023, the FDA approved repotrectinib (Augtyro) for advanced or metastatic NSCLC with ROS1 fusions as an initial treatment and as a second-line treatment in those who previously received a ROS1-targeted drug.
BRAF Inhibitors
The B-Raf protein is involved in sending signals in cells and cell growth. Certain changes in the B-Raf gene can increase the growth and spread of NSCLC cells.
The combination of the B-Raf-targeted drug dabrafenib (Tafinlar) and trametinib (Mekinist ), which targets a protein called MEK, has been approved as treatment for patients with NSCLC that has a specific mutation in the BRAF gene.
Encorafenib (Braftovi) combined with binimetinib (Mektovi) is approved for patients with metastatic NSCLC with a BRAF V600E mutation .
Other Inhibitors
Some NSCLCs have mutations in the genes NRTK-1 and NRTK-2 that can be treated with the targeted therapy larotrectinib (Vitrakvi). Those with certain mutations in the MET gene can be treated with tepotinib (Tepmetko) or capmatinib (Tabrecta) . And those with alterations in the RET gene are treated with selpercatinib (Retevmo) and pralsetinib (Gavreto) . A 2023 clinical trial showed that treatment with selpercatinib led to longer progression-free survival compared with people who received chemotherapy with or without pembrolizumab. Inhibitors of other targets that drive some lung cancers are being tested in clinical trials.
See a complete list of targeted therapies for lung cancer .
NCI-Supported Research Programs
Many NCI-funded researchers at the NIH campus, and across the United States and the world, are seeking ways to address lung cancer more effectively. Some research is basic, exploring questions as diverse as the biological underpinnings of cancer and the social factors that affect cancer risk. And some is more clinical, seeking to translate basic information into improved patient outcomes. The programs listed below are a small sampling of NCI’s research efforts in lung cancer.

Pragmatica-Lung Study Enrolling Patients
The simplified trial may serve as a model for future cancer clinical trials.
- The Pragmatica-Lung Study is a randomized trial that will compare the combination of the targeted therapy ramucirumab (Cyramza) and the immunotherapy pembrolizumab (Keytruda) with standard chemotherapy in people with advanced NSCLC whose disease has progressed after previous treatment with immunotherapy and chemotherapy. In addition to looking at an important clinical question, the trial will serve as a model for future trials because it is designed to remove many of the barriers that prevent people from joining clinical trials.
- Begun in 2014, ALCHEMIST is a multicenter NCI trial for patients with early stage non-small cell lung cancer. It tests to see whether adding a targeted therapy after surgery, based on the genetics of a patient’s tumor, will improve survival.
- The Lung MAP trial is an ongoing multicenter trial for patients with advanced non-small cell lung cancer who have not responded to earlier treatment. Patients are assigned to specific targeted therapies based on their tumor’s genetic makeup.
- The Small Cell Lung Cancer Consortium was created to coordinate efforts and provide a network for investigators who focus on preclinical studies of small-cell lung cancer. The goal of the consortium is to accelerate progress on this disease through information exchange, data sharing and analysis, and face-to-face meetings.
- NCI funds eight lung cancer Specialized Programs of Research Excellence (Lung SPOREs) . These programs are designed to quickly move basic scientific findings into clinical settings. Each SPORE has multiple lung cancer projects underway.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for both non-small cell lung cancer treatment and small cell lung cancer treatment .
Lung Cancer Research Results
The following are some of our latest news articles on lung cancer research:
- Alectinib Approved as an Adjuvant Treatment for Lung Cancer
- Repotrectinib Expands Treatment Options for Lung Cancers with ROS1 Fusions
- Tarlatamab Shows Promise for Some People with Small Cell Lung Cancer
- Selpercatinib Slows Progression of RET-Positive Lung, Medullary Thyroid Cancers
- Lung-Sparing Surgery Is Effective for Some with Early-Stage Lung Cancer
View the full list of Lung Cancer Research Results and Study Updates .

How the Immune System Affects Drug Response in Lung Cancer Patients
© 2024 Smart + Strong . All Rights Reserved. Terms of use and Your privacy . Smart + Strong ® is a registered trademark of CDM Publishing, LLC.
University of Colorado Cancer Center member Lynn Heasley studies potential targets to enhance response to tyrosine kinase inhibitors.
May 28, 2024 • By University of Colorado Cancer Center and Greg Glasgow
Why do some lung cancer patients respond better to the types of drugs known as tyrosine kinase inhibitors? It may have to do with those patients’ own immune systems.
That’s the hypothesis being tested by University of Colorado Cancer Center member Lynn Heasley, PhD, who recently received a Merit Review Award renewal from the U.S. Department of Veterans Affairs (VA) to study the role of the immune system in patients with lung adenocarcinoma who are treated with tyrosine kinase inhibitors (TKIs).
“If you take 100 lung adenocarcinoma patients with a particular oncogene, and you treat them all with the same drug, you get a wide variation in how the patients respond,” Heasley says. “Some of them show a major response that might last for many years, some of them show a more modest response, and others don’t respond very well at all.”
Heasley’s research group and his collaborators Raphael Nemenoff , PhD, Erin Schenk , MD, PhD, and Tejas Patil , MD, have shown over the past couple of years “that the patient’s host immunity has something to say about how that response goes,” Heasley says.
Signal processing
When a lung tumor is treated with a TKI, Heasley says, the medicine induces a series of signals that are released from the tumor cells and communicate with immune cells. Sometimes that communication instructs a robust response from the T cells that helps clear out the tumor, but sometimes the signal reaches immune cells that suppress the immune system to protect the tumor.
“Each of us has a variation in our immune microenvironment that allows a more robust response or a less robust response. That could be used to our advantage if we can understand how to make the immune system contribute more to attacking the tumor,” he says. “If you could understand what’s happening in the cancers that respond the best to tyrosine kinase inhibitors, as well as the ones that don’t respond at all, you might find biologic mechanisms that could be exploited as therapeutic targets.”
With his four-year, VA-funded grant, Heasley will study animal models of lung cancer driven by oncogenes that respond to specific TKIs, with the goal of identifying a target that could be treated medically to improve the performance of TKIs in patients whose immune system makes them less responsive to the treatment.
“Adaptive immune cells, like T cells and B cells, get prompted to expand and attack foreign substances,” he says. “It seems that by the time you treat them, tumor cells have already communicated with the adaptive immune system to some extent. The TKI instructs the T lymphocytes to participate strongly in eliminating the tumor, but we think there are other immune cells, like neutrophils, that are immune suppressive and dial back the response of our adaptive immune system. In cancer, we want to tell the T cells to attack the tumor, but if immune cells are suppressing that, that’s something we need to try to overcome.”
Proactive solution
The results of the study may be able to be used proactively, as well — if the research reveals characteristics of host immunity associated with poorer response to TKIs, a blood test might be designed such that novel immune-targeting agents might be prescribed up front to try to overcome the resistance.
“We’re going to study the immune cells in the blood to see if they give us information about what may be going on in the tumor,” Heasley says. “We have some pilot studies that have shown that if the number of specific immune-suppressive cells are very high, then historically, patients show a very brief response to TKIs versus ones that have low levels of those cells.”
Heasley is part of a group of lung cancer researchers at the CU Cancer Center who are interested in applying artificial intelligence to tumor samples to find patterns that would let doctors know, before the patient is even treated, if the patient is going to do poorly or well on the treatment.
Longer response time
Heasley says the research will help find new ways to treat a deadly cancer that occurs in smokers and nonsmokers alike, and that tends to recur even in patients who initially respond to treatment with TKIs.
“Each time a cancer recurs following therapy, it acquires more genomic issues and becomes more difficult to treat,” he says. “If you knew which patients are going to recur more quickly, it would make sense to try to find ways to intervene with a combination of medications. Can we customize your TKI treatment with additional agents that may give you a longer-lasting response? We are cautious about using the word ‘cure,’ but the long-term goal would be to make it so you could manage lung cancer for 10 to 20 years. We want a more complete therapeutic regimen that allows the therapy to last much longer.”
This article was originally published May 10, 2024, by the University of Colorado Cancer Center. It is republished with permission.
Read More About:
- #adenocarcinoma
- #lung cancer
- #University of Colorado Cancer Center
RELATED articles

New Resource for Patients With Rare Type of Intestinal Cancer

Cancer Clinical Trials Save Lives, and Diversity Matters

6 Years After Lung Cancer Diagnosis, Patient Says CU Cancer Center Research is “Why I’m Here”

A Combination of Targeted Therapies Proves Effective Against Mutation-Driven Lung Cancer
Stay logged in.
You have been inactive for 60 minutes and will be logged out in . Any updates not saved will be lost.
You Have Been Logged Out
Click here to log back in.
Cancer Health uses cookies to provide necessary website functionality, improve your experience, analyze our traffic and personalize ads. Our Privacy Policy
Cancer Health uses cookies to provide necessary website functionality, improve your experience, analyze our traffic and personalize ads. By remaining on our website, you indicate your consent to our Privacy Policy and our Cookie Usage .
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 25 May 2024

Establishment of a prognostic nomogram for elderly patients with limited-stage small cell lung cancer receiving radiotherapy
- Lixia Zhang 1 ,
- Qingfen Zhang 1 ,
- Qian Wu 1 ,
- Lujun Zhao 1 ,
- Yunbin Gao 1 ,
- Song Guan 1 &
- Meng Yan 1
Scientific Reports volume 14 , Article number: 11990 ( 2024 ) Cite this article
1 Altmetric
Metrics details
The present study explored the risk factors associated with radiotherapy in seniors diagnosed with limited-stage small cell lung cancer (LS-SCLC) to construct and validate a prognostic nomogram. The study retrospectively included 137 elderly patients with LS-SCLC who previously received radiotherapy. Univariate and multivariate COX analyses were conducted to identify independent risk factors and determine optimal cut-off values. Kaplan–Meier survival curves and nomograms were constructed to predict survival. Calibration and receiver operating characteristic (ROC) curves were used to evaluate the accuracy and consistency of the nomogram. Illness rating scale-geriatric (CIRS-G) score, treatment strategy, lymphocyte-to-monocyte ratio (LMR), white blood cell-to-monocyte ratio (WMR), and prognostic nutritional index (PNI) were discovered to be independent prognostic factors. Based on the findings of our multivariate analysis, a risk nomogram was developed to assess patient prognosis. Internal bootstrap resampling was utilized to validate the model, and while the accuracy of the AUC curve at 1 year was modest at 0.657 (95% CI 0.458–0.856), good results were achieved in predicting 3- and 5 year survival with AUCs of 0.757 (95% CI 0.670–0.843) and 0.768 (95% CI 0.643–0.893), respectively. Calibration curves for 1-, 3-, and 5 year overall survival probabilities demonstrated good cocsistency between expected and actual outcomes. Patients with concurrent chemoradiotherapy, CIRS-G score > 5 points and low PNI, WMR and LMR correlated with poor prognosis. The nomogram model developed based on these factors demonstrated good predictive performance and provides a simple, accessible, and practical tool for clinicians to guide clinical decision-making and study design.
Similar content being viewed by others

Tumor biomarkers for diagnosis, prognosis and targeted therapy

A spatial architecture-embedding HLA signature to predict clinical response to immunotherapy in renal cell carcinoma

PERCEPTION predicts patient response and resistance to treatment using single-cell transcriptomics of their tumors
Introduction.
Lung cancer is one of the leading cause of cancer-related mortality 1 . Global cancer statistics 2 , 3 for 2020 released by the International Agency for Research on cancer show that there were an estimated 820,000 newly diagnosed cases of lung cancer and 715,000 lung cancer-related deaths in China in 2020. The rise in life expectancy worldwide has resulted in a greater incidence of cancer cases among older adults. Based on available epidemiological data 4 , 5 over 60–70% of individuals with lung cancer are aged 65 or older, and approximately 30–40% of new lung cancer cases are detected in patients aged 70 or above. About 15% of all lung cancer cases are attributed to small cell lung cancer (SCLC), one of the pathological subtypes 6 . SCLC is usually diagnosed in patients with a history of smoking, especially those over 65 years 7 .
Despite significant advancements in the management of non-small cell lung cancer (NSCLC) and that of extensive small cell lung cancer (ES-SCLC), the approach to treating LS-SCLC has seen limited progress in recent years. Except that only 5% patients are eligible for surgery, the most common treatment for LS-SCLC is still the combination of cisplatin and etoposide (EP regimen) with concurrent chemoradiotherapy (CCRT) 8 . However, elderly patients are often deprived of standard care due to various factors, resulting in a poorer prognosis.
Age is considered an independent prognostic factor for SCLC patients 9 , 10 , as elderly patients often experience complications, organ function aging, physical and nutritional decline, and reduced immunity 11 . In clinical practice, the evaluation of complications in elderly patients often involves commonly used assessment tools such as the Charlson comorbidity index (CCI), age-adjusted Charlson comorbidity index (A-CCI), and cumulative illness rating scale-geriatric (CIRS-G) 12 . While these indicators have been linked to the prognosis of elderly patients, some scores are subjective and require the addition of objective clinical indicators for a comprehensive prognosis. Prognostic nutritional index (PNI) has been used to measure both nutritional and immune status in several studies 13 . It has shown a correlation with the prognosis of advanced NSCLC 14 , esophageal cancer 13 , and gastric cancer 15 . However, limited research has been conducted on PNI in elderly LS-SCLC patients. Studies have shown that lung cancer development is closely linked to the inflammatory microenvironment of tumors, and inflammatory cells and factors can promote tumor progression, metastasis, and immune evasion through the activation of inflammatory signaling pathways 16 . Currently, hematologic and biochemical markers reflecting systemic inflammatory response are easily accessible and can be measured in routine blood tests 17 . Therefore, they are being increasingly recognized for their clinical value in cancer patients. Several studies have demonstrated that these markers, including neutrophil-to-lymphocyte ratio (NLR), platelets-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio (LMR), are significantly correlated with prognosis in patients with resectable lung cancer 18 , locally advanced colorectal cancer 19 , non-muscular invasive bladder cancer 20 and other cancers. Moreover, other inflammatory markers that combine WBC, such as WLR, WHR, WNR, WMR, and WRR, have also been investigated to establish their association with bladder cancer prognosis 21 . However, there is a paucity of research on using these inflammatory markers in senior LS-SCLC patients.
In summary, there is a significant clinical need to investigate accessible and objective prognostic factors for elderly LS-SCLC patients. Nomograms are considered reliable tools for assessing prognosis and risk by integrating important clinical features. However, currently available models were not specifically developed for the elderly population. Therefore, constructing a nomogram specifically for elderly patients with LS-SCLC is necessary to aid in this cohort’s survival prediction.
Materials and methods
Study population.
From April 2011 to August 2020, a total of 137 elderly patients with LS-SCLC who underwent treatment at the Cancer Institute and Hospital of Tianjin Medical University Cancer Institute & Hospital Medical University were enrolled in this study according to the inclusion criteria. The inclusion criteria for this study were as follows: (1) patients ≥ 65 years of age; (2) pathologically confirmed SCLC; (3) patients were classified as LS-SCLC according to the Veterans Administration Lung Study Group Reassessment (VALG) staging criteria; (4) patients who received concurrent or sequential chemoradiotherapy (SCRT); (5) patients with complete history information, imaging and laboratory tests (routine blood, liver and kidney function tests). Patients with hematologic disease and active infection were excluded. Before treatment, all patients underwent chest CT scan and contrast-enhanced MRI, and some patients suspected of metastasis underwent PET-CT scan.This study was carried out after obtaining approval from the Tianjin Medical University Cancer Institute & Hospital ethics committee with ethics approval number bc2023076.
Treatment stategy
All patients included in this study received multidisciplinary consultation before starting treatment. For patients who are in good physical condition after evaluation, we adopted the strategy of CCRT. For patients with poor physical condition who cannot tolerate SCRT was adopted. Induction chemotherapy was given to patients with large tumor volume or suspected lymph node metastasis. The induction chemotherapy regimen was: etoposide combined with cisplatin or carboplatin, 2 cycles. The radiotherapy method was: intensity-modulated radiotherapy (IMRT), 60 Gy/30f.
Study variables
The study assessed several variables, including age, sex, smoking history, weight loss, KPS score, A-CCI score, CIRS-G score, T stage,N stage, radiotherapy regimen including CCRT, SCRT, induction chemotherapy and prophylactic cranial irradiation (PCI), hematological indicators such as routine blood tests and albumin at the start of treatment, duration of follow-up, and all-cause mortality. Patients with incomplete information on the aforementioned variables were excluded from the study. Overall survival referred to the period between the time from diagnosis to last follow-up or death.
The included serum indicators were as follows: neutrophil-to-lymphocyte ratio (NLR), platelets-to-lymphocyte ratio (PLR), lymphocyte-to-monocyte ratio (LMR),white blood cell-to-lymphocyte ratio (WLR), white blood cell-to-hemoglobin ratio (WHR), white blood cell-to-neutrophil ratio (WNR), white blood cell-to-monocyte ratio (WMR), white blood cell-to-erythrocyte ratio (WRR) and prognostic nutritional index (PNI). Notably, PNI was quantified using 10 × serum albumin (g/dL) + 0.005 × total lymphocytes count (/mm 3 ). The absolute counts of each parameter were used to calculate all of the ratios.
Statistical analysis and nomograph construction
Frequency and percentage were utilized for categorical variables. In contrast, median with interquartile range (IQR) was utilized for continuous variables. Univariate and multivariate Cox two-way stepwise analyses were conducted to determine if the correlated variables were independent predictors of overall survival (OS). The study determined the best cut-off values for the detected independent factors using the surv_cutpoint function in R with OS as the endpoint indicator. The variables were grouped according to the cut-off values, and survival curves were evaluated using the Kaplan–Meier method, which were then compared using the log-rank test. And p-value below 0.05 was deemed to be significant.
Additionally, a nomogram was constructed using the independent prognostic factors detected in the multivariate analysis, and bootstrap resampling was performed for internal validation. The nomogram’s predictive efficacy was evaluated using the AUROC, and a calibration curve was drawn to determine the agreement between the actual results and the predicted survival rate for elderly patients with limited-stage small-cell lung cancer.
The statistical analysis for all data was performed using the R statistics program (R Core Team, 2022), an environment and language for statistical computing. The program is available at https://www.R-project.org .
All methods were carried out in accordance with relevant guidelines and regulations.
Consent to participate
The study confirmed that informed consent was obtained from all subjects and/or their legal guardians.
Patients characteristics
The study included 137 eligible patients based on predetermined inclusion and exclusion criteria. Among them, 96 (70.1%) were male, with a median age of 68 (65–84). CCRT was administered to 71 (51.8%) patients, while SCRT was given to 66 (48.2%) patients. Induction chemotherapy was not given to 12 patients, and only 10 patients underwent prophylactic cranial irradiation (PCI). Patient characteristics are detailed in Table 1 .
Independent prognostic factors
Table 2 presents the findings of our univariate analysis, and Fig. 1 displays the findings of the multivariate analysis. In the univariate analysis, gender (p = 0.031, HR = 0.558), CIRS-G score (p = 0.001, HR = 2.460), radiotherapy regimen (p = 0.038, HR = 0.620), NLR (p = 0.016, HR = 1.767), LMR (p = 0.003, HR = 0.328), WLR (p = 0.019, HR = 1.744), WMR (p = 0.007, HR = 0.281), and PNI (p = 0.028, HR = 0.497) were significant, progressing to our multivariate analysis. Further analysis revealed that CIRS-G score (p < 0.001, HR = 2.900), radiotherapy regimen (p < 0.001, HR = 0.434), LMR (p = 0.157, HR = 0.532), WMR (p = 0.038, HR = 0.309), and PNI (p = 0.046, HR = 0.525) were independent prognostic factors for overall survival (Fig. 1 ).

Multivariate Cox regression analysis model for overall survival.
Survival analysis
Patients were followed up for a median of 3.16 years. Optimal cut-off values for each independent prognostic factor were determined using the surv_cutpoint function, and Kaplan–Meier (KM) curves were generated to illustrate the prognostic outcomes of different CIRS-G, radiotherapy regimen, LMR, WMR, and PNI (Fig. 2 A–E). The results indicate that patients receiving CCRT, those with CIRS-G scores greater than 5, and those with low PNI, WMR, and LMR values had a poorer prognosis in elderly LS-SCLC patients.

The KM curves of inflammatory marks for elderly patients with limitated-stage small cell lung cancer. ( A – E ) KM curve was made to exhibit the prognosis of the different therapy regimen, CIRS-G score, and diferent expression level of LMR, WMR, and PNl, respectively.
Nomogram construction
The study developed a predictive model for elderly LS-SCLC patients based on the five independent risk factors identified earlier. The model includes 1-, 3-, and 5 year predictions and is depicted in Fig. 3 . The total score was calculated by adding up the scores of each predictor variable, and the corresponding survival rate can be estimated by finding the intersection of the total score with the vertical line of the predicted survival rate on the graph.

Nomograms to predict 3- and 5 year overall survival. A vertical line can be drawn belween each varable and the points scale toacauire the points of each varable. Predicted survival rate was calculated according to the total points by drawing a vertical ine from the total points scale to the overall survival scale.
Calibration and internal validation
The nomogram exhibited superior predictive performance, as demonstrated by the 1-, 3-, and 5 year ROC curves for OS generated using the score function in the risk regression package. The areas under the ROC curve (AUROC) were 0.657 (95% CI 0.458, 0.856), 0.757 (95% CI 0.670, 0.843), and 0.768 (95% CI 0.642, 0.893) (Fig. 4 ). Furthermore, accuracy of the prediction model was assessed by calibration curves, which indicated good agreement between the predicted and actual survival rates (Fig. 5 A–C). These results collectively suggest that the nomogram developed in this study can be effectively used to evaluate the prognosis of elderly LS-SCLC patients.

ROC curve of prognostic model of elderly LS-SCLC.

Nomogram-predicted probability of 1 year ( A ), 3 year ( B ), and 5 year ( C ) overall survival.
The National Comprehensive Cancer Network, NCCN guidelines define elderly patients as those aged 65 or older 22 . Given the heterogeneity of this population, the treatment and prognosis of limited-stage small cell lung cancer in elderly patients pose a significant challenge. Therefore, conducting a thorough prognostic analysis for this group is valuable. Conversely, there is a limited amount of research on prognostic models for elderly LS-SCLC patients.
The findings of this study suggest that the CIRS-G score, type of therapy used, LMR, WMR, and PNI are important prognostic factors for elderly patients with limited-stage small-cell lung cancer. In clinical practice, the assessment of geriatric comorbidity is typically achieved using scales such as the CCI, A-CCI, and CIRS-G 12 . The A-CCI score incorporates age-related factors into the CCI score and is more appropriate for studying comorbidities in elderly patients. Meanwhile, the CIRS-G score, which evaluates 14 organ systems, is the recommended scale according to the comprehensive geriatric assessment (CGA). The A-CCI score is derived from the CCI and increases by one point every 10 years after the age of 40 23 . Meanwhile, the CIRS-G is a cumulative rating score that assesses 14 organ systems, with a severity rating ranging from 0 (no problem) to 4 (very serious) for each system 12 . Herein, the assessment of geriatric comorbidity utilized both A-CCI and CIRS-G.Our analysis revealed that a CIRS-G score > 5 was synonymous of a poor prognosis for our LS-SCLC patients. Recent studies have also found that elderly patients with mantle cell lymphoma (MCL) and a high CIRS-G score (p = 0.04, HR = 1.06) have worse overall survival 24 . Concurrent radiotherapy is theoretically as effective in elderly patients with LS-SCLC, but treatment tolerability is an important consideration. Research has shown that standard treatment in older patients increases the risk of toxicity, requiring a comprehensive evaluation and timely intervention 25 . Although many studies have shown that patients receiving CCRT have a high survival rate with SCRT 26 , 27 , 28 , this survival benefit is usually at the expense of greater therapeutic toxicity. Many studies have confirmed that SCRT is less toxic to patients’ organs and hematologic system than CCRT 29 , 30 . Even in some studies, the survival rate of patients receiving SCRT was significantly better than that of patients receiving CCRT 31 , 32 . Similarly, the results of this study showed that the survival rate of patients receiving SCRT was significantly higher than that of patients receiving CCRT, which may be due to the strong therapeutic toxicity caused by CCRT.
LMR and WMR, as systemic inflammatory response markers are often linked with cancer prognosis, with low levels of LMR and WMR expression correlating with a poor outcome for patients with bladder cancer (BLCA) 21 , which is in line with the findings of our study. The PNI is an index used to assess nutritional status, which is based on both albumin levels and lymphocyte counts. It serves as a biological marker indicative of the nutritional status of the body and the degree of the inflammatory response 13 . Park et al. 33 showed that the lower the PNI value, the greater the risk of postoperative delirium in patients undergoing radical lung cancer surgery. It has also been shown that PNI is related to clinical outcomes in hepatocellular carcinoma, with a decrease in PNI associated with a worse OS (HR = 0.31, 95% CI 0.17–0.57; P = 0.02) 34 . Consistently, our study in elderly patients with small cell lung cancer also found that PNI is significantly associated with prognosis. Notably, a decrease in PNI value indicates malnutrition and increased inflammatory response, which is associated with poor prognosis.
To conclude, this study presents a straightforward and all-encompassing prognostic model for elderly patients with limited-stage SCLC using fundamental clinical characteristics. Unlike most existing models, this nomogram was specifically designed for a group of elderly LS-SCLC patients, and all indicators used are economical and readily accessible.This provides a predictive model that accurately represents the survival of elderly LS-SCLC patients, thereby guiding clinicians in treatment selection and providing evidence for further clinical studies.
Nevertheless, our report has some limitations. First, the sample size for our training cohort was quite small; thus, it is necessary to expand the cohort size in future studies. Secondly, there is a lack of data for external verification. While our study suggests caution in using CCRT in elderly patients, further prospective data are needed to assess psychological, social, and other factors using comprehensive geriatric assessment (CGA) when deciding which older adults get standard treatment.
To summarize, there is currently a lack of prognostic models for elderly LS-SCLC patients. The nomogram developed in this study can provide a preliminary understanding of the prognosis of this patient population. However, further validation through prospective studies and external validation is necessary to substantiate our nomogram’s robustness.
Data availability
The data that support the findings of this study are available from Tianjin Medical University Cancer Institute & Hospital but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.If someone wants to request for the raw data used in this study will be fulfilled from the corresponding author (Dr. Lujun Zhao).
Wu, F., Wang, L. & Zhou, C. Lung cancer in China: Current and prospect. Curr. Opin. Oncol. 33 (1), 40–46 (2021).
Article CAS PubMed Google Scholar
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71 (3), 209–249 (2021).
Article PubMed Google Scholar
Cao, W., Chen, H. D., Yu, Y. W., Li, N. & Chen, W. Q. Changing profiles of cancer burden worldwide and in China: A secondary analysis of the global cancer statistics 2020. Chin. Med. J. (Engl.) 134 (7), 783–791 (2021).
Sacco, P. C., Maione, P., Palazzolo, G. & Gridelli, C. Treatment of advanced non-small cell lung cancer in the elderly. Expert Rev. Respir. Med. 12 (9), 783–792 (2018).
Shinde, A., Vazquez, J., Novak, J., Sedrak, M. S. & Amini, A. The role of comprehensive geriatric assessment in radiation oncology. J. Geriatr. Oncol. 11 (2), 194–196 (2020).
Raso, M. G., Bota-Rabassedas, N. & Wistuba, I. I. Pathology and classification of SCLC. Cancers (Basel) https://doi.org/10.3390/cancers13040820 (2021).
Chun, Y. J. et al. The prognostic value of comprehensive geriatric assessment on the management of older patients with small cell lung cancer. Korean J. Intern. Med. 38 , 254 (2023).
Article PubMed PubMed Central Google Scholar
Noronha, V. et al. Systemic therapy for limited stage small cell lung carcinoma. J. Thorac. Dis. 12 (10), 6275–6290 (2020).
Gu, C. et al. Prognostic analysis of limited resection versus lobectomy in stage ia small cell lung cancer patients based on the surveillance, epidemiology, and end results registry database. Front. Genet. 9 , 568 (2018).
Article CAS PubMed PubMed Central Google Scholar
Stinchcombe, T. E. et al. A pooled analysis of individual patient data from national clinical trials network clinical trials of concurrent chemoradiotherapy for limited-stage small cell lung cancer in elderly patients versus younger patients. Cancer 125 (3), 382–390 (2019).
Salminen, A. Clinical perspectives on the age-related increase of immunosuppressive activity. J. Mol. Med. (Berl.) 100 (5), 697–712 (2022).
Chan, C. H., Maddison, C., Reijnierse, E. M., Lim, W. K. & Maier, A. B. The association of comorbidity measures and mortality in geriatric rehabilitation inpatients by cancer status: RESORT. Support. Care Cancer 29 (8), 4513–4519 (2021).
Okadome, K. et al. Prognostic nutritional index, tumor-infiltrating lymphocytes, and prognosis in patients with esophageal cancer. Ann. Surg. 271 (4), 693–700 (2020).
Wang, J., Liu, Y., Mi, X., Shao, M. & Liu, L. The prognostic value of prognostic nutritional index (PNI) and neutrophil to lymphocyte ratio (NLR) for advanced non-small cell lung cancer treated with platinum-based chemotherapeutics. Ann. Palliat. Med. 9 (3), 967–978 (2020).
Maejima, K., Taniai, N. & Yoshida, H. The prognostic nutritional index as a predictor of gastric cancer progression and recurrence. J. Nippon Med. Sch. 89 (5), 487–493 (2022).
Tan, Z. et al. The role of tumor inflammatory microenvironment in lung cancer. Front. Pharmacol. 12 , 688625 (2021).
Sylman, J. L. et al. The predictive value of inflammation-related peripheral blood measurements in cancer staging and prognosis. Front. Oncol. 8 , 78 (2018).
Wang, J. et al. The MLR, NLR, PLR and D-dimer are associated with clinical outcome in lung cancer patients treated with surgery. BMC Pulm. Med. 22 (1), 104 (2022).
Gawinski, C., Holdakowska, A. & Wyrwicz, L. Correlation between lymphocyte-to-monocyte ratio (LMR), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR) and extramural vascular invasion (EMVI) in locally advanced rectal cancer. Curr. Oncol. 30 (1), 545–558 (2022).
Chen, H. et al. The clinicopathological and prognostic value of NLR, PLR and MLR in non-muscular invasive bladder cancer. Arch. Esp. Urol. 75 (5), 467–471 (2022).
Gao, M. et al. Preoperative white blood cell-related indicators can predict the prognosis of patients with transurethral resection of bladder cancer. J. Inflamm. Res. 15 , 4139–4147 (2022).
Dotan, E. et al. NCCN guidelines(r) insights: Older adult oncology, version 1.2021. J. Natl. Compr. Cancer Netw. 19 (9), 1006–19 (2021).
Article Google Scholar
Lin, J. X. et al. Age-adjusted charlson comorbidity index (ACCI) is a significant factor for predicting survival after radical gastrectomy in patients with gastric cancer. BMC Surg. 19 (1), 53 (2019).
Rampotas, A. et al. Treatment patterns and outcomes of unfit and elderly patients with Mantle cell lymphoma unfit for standard immunochemotherapy: A UK and Ireland analysis. Br. J. Haematol. 194 (2), 365–377 (2021).
Mohile, S. G. et al. Evaluation of geriatric assessment and management on the toxic effects of cancer treatment (GAP70+): A cluster-randomised study. Lancet 398 (10314), 1894–1904 (2021).
Conibear, J. Rationale for concurrent chemoradiotherapy for patients with stage III non-small-cell lung cancer. Br. J. Cancer 123 (Suppl 1), 10–17 (2020).
Uyterlinde, W. Overcoming toxicity-challenges in chemoradiation for non-small cell lung cancer. Transl. Lung Cancer Res. 5 (3), 239–243 (2016).
Sakin, A. et al. The effect of different treatment modalities on survival in elderly patients with locally advanced non-small cell lung cancer. Pulmonology 27 (1), 26–34 (2021).
Guan, S., Long, W., Liu, Y., Cai, B. & Luo, J. Prognosis of concurrent versus sequential chemo-radiotherapy induction followed by surgical resection in patients with advanced thymic epithelial tumors: A retrospective study. Ann. Surg. Oncol. 30 (11), 6739–6747 (2023).
Spencer, A. et al. Concurrent versus sequential chemoradiotherapy for unresectable locally advanced stage III non-small cell lung cancer: Retrospective analysis in a single United Kingdom cancer centre. Cancer Treat. Res. Commun. 29 , 100460 (2021).
Verma, V., Moreno, A. C., Haque, W., Fang, P. & Lin, S. H. Sequential versus concurrent chemoradiation therapy by surgical margin status in resected non-small cell lung cancer. J. Natl. Compr. Cancer Netw. 16 (5), 508–516 (2018).
Qi, J. et al. The addition of peripheral blood inflammatory indexes to nomogram improves the predictive accuracy of survival in limited-stage small cell lung cancer patients. Front. Oncol. 11 , 713014 (2021).
Park, S. et al. The prognostic nutritional index and postoperative complications after curative lung cancer resection: A retrospective cohort study. J. Thorac. Cardiovasc. Surg. https://doi.org/10.1016/j.jtcvs.2019.10.105 (2020).
Wang, D. et al. Prognostic nutritional index and systemic immune-inflammation index predict the prognosis of patients with HCC. J. Gastrointest. Surg. 25 (2), 421–427 (2021).
Download references
Author information
Authors and affiliations.
Department of Radiation Oncology, Tianjin Medical University Cancer Institute & Hospital,National Clinical Research Center for Cancer, Tianjin’s Clinical Research Center for Cancer, Key Laboratory of Cancer Prevention and Therapy, Tianjin, 300060, China
Lixia Zhang, Qingfen Zhang, Qian Wu, Lujun Zhao, Yunbin Gao, Xue Li, Song Guan & Meng Yan
You can also search for this author in PubMed Google Scholar
Contributions
LZ, QZ, and QW have contributed equally to this work. LZ, QZ, QW and LZ designed of the study. LZ, QZ, QW,LZ,YG and XL participated in data collection or data analyses and interpretation. LZ, QZ, QW,LZ,YGandXL wrote this article or made critical revisions to pivotal intellectual content. All authors contributed to the article and approved the submitted version.
Corresponding author
Correspondence to Lujun Zhao .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Zhang, L., Zhang, Q., Wu, Q. et al. Establishment of a prognostic nomogram for elderly patients with limited-stage small cell lung cancer receiving radiotherapy. Sci Rep 14 , 11990 (2024). https://doi.org/10.1038/s41598-024-62533-x
Download citation
Received : 30 July 2023
Accepted : 17 May 2024
Published : 25 May 2024
DOI : https://doi.org/10.1038/s41598-024-62533-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Elderly patients
- Limited-stage small cell lung cancer
- Survival prediction
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Cancer newsletter — what matters in cancer research, free to your inbox weekly.
Together we are beating cancer
About cancer
Cancer types
- Breast cancer
- Bowel cancer
- Lung cancer
- Prostate cancer
Cancers in general
- Clinical trials
Causes of cancer
Coping with cancer
- Managing symptoms and side effects
- Mental health and cancer
- Money and travel
- Death and dying
- Cancer Chat forum
Health Professionals
- Cancer Statistics
- Cancer Screening
- Learning and Support
- NICE suspected cancer referral guidelines
Get involved
- Make a donation
By cancer type
- Leave a legacy gift
- Donate in Memory
Find an event
- Race for Life
- Charity runs
- Charity walks
- Search events
- Relay For Life
- Volunteer in our shops
- Help at an event
- Help us raise money
- Campaign for us
Do your own fundraising
- Fundraising ideas
- Get a fundraising pack
- Return fundraising money
- Fundraise by cancer type
- Set up a Cancer Research UK Giving Page
- Find a shop or superstore
- Become a partner
- Cancer Research UK for Children & Young People
- Our We Are campaign
Our research
- Brain tumours
- Skin cancer
- All cancer types
By cancer topic
- New treatments
- Cancer biology
- Cancer drugs
- All cancer subjects
- All locations
By Researcher
- Professor Duncan Baird
- Professor Fran Balkwill
- Professor Andrew Biankin
- See all researchers
- Our achievements timeline
- Our research strategy
- Involving animals in research
Funding for researchers
Research opportunities
- For discovery researchers
- For clinical researchers
- For population researchers
- In drug discovery & development
- In early detection & diagnosis
- For students & postdocs
Our funding schemes
- Career Development Fellowship
- Discovery Programme Awards
- Clinical Trial Award
- Biology to Prevention Award
- View all schemes and deadlines
Applying for funding
- Start your application online
- How to make a successful application
- Funding committees
- Successful applicant case studies
How we deliver research
- Our research infrastructure
- Events and conferences
- Our research partnerships
- Facts & figures about our funding
- Develop your research career
- Recently funded awards
- Manage your research grant
- Notify us of new publications
Find a shop
- Volunteer in a shop
- Donate goods to a shop
- Our superstores
Shop online
- Wedding favours
- Cancer Care
- Flower Shop
Our eBay store
- Shoes and boots
- Bags and purses
- We beat cancer
- We fundraise
- We develop policy
- Our global role
Our organisation
- Our strategy
- Our Trustees
- CEO and Executive Board
- How we spend your money
- Early careers
Cancer news
- Cancer News
- For Researchers
- For Supporters
- Press office
- Publications
- Update your contact preferences
ABOUT CANCER
GET INVOLVED
NEWS & RESOURCES
FUNDING & RESEARCH
You are here

Patient data use case studies

Questions about these case studies or how patient data is handled?
Contact the team
During our Review of Informed Choice for Cancer Registration, patients clearly told us they would like to know what their data are being used for. We agreed that as a charity, we would highlight where we are using patient-data for research and analysis. Relevant examples of work by the Cancer Intelligence team at Cancer Research UK will be available here, and we will add to this as we embark on new projects.

Lung cancer diagnostic pathways
Identifying common lung cancer diagnostic pathways using linked datasets.
Small proportions of patients in 2013-2015 meet the timings of the optimal pathway. Diagnostic pathway length varies by source of imaging request.

Variation in ovarian cancer treatment rates
Investigating variation in treatment for ovarian cancer patients.
We expect to establish if there is variation between Cancer Alliances/Trusts, identify the odds ratios/ regression co-efficients for predictor variables, and if it's the affect of healthcare system level factors.

Variation in lung cancer treatment rates
Investigating variation in treatment for non-small cell lung cancer patients.
We expect to establish if there is significant variation between Cancer Alliances/Trusts (geography still to TBC) and identify the odds ratios/regression co-effecients associated with each predictor variable.
Bowel cancer screening campaign evaluation
Evaluating the bowel cancer screening regional pilot campaign in the North West of England.
Analysis of interim results following the campaign are promising. We are currently working to finalise the analysis and results will follow in due course.

Colorectal cancer diagnostic pathways
Coming soon.
The impact of COVID-19 on radiotherapy in the UK
The aims of COVID RT are to understand why changes in radiotherapy treatment schedules were implemented during the pandemic and to then explore the impact of these changes on patient outcomes and the UK radiotherapy services. This project aims purely to understand the changes in patient's radiotherapy treatment from COVID-19.

Patient data – a vital tool that will help beat cancer
Cancer is the most complex health challenge that we face. There are 200 different types of cancer but even that is an oversimplification.
At a genetic level each individual cancer is as unique as the person with the disease. Despite this complexity our research has helped double cancer survival over the last 40 years. This extraordinary progress has been powered by relentlessly increasing our understanding of cancer’s intricacies.
But big questions about cancer remain, and our scientists are seeking the answers. Patient data has the potential to reveal some of these. Here we meet some outstanding scientists who are using patient data to grow our understanding even further, work that could underpin tomorrow’s cures.
Case study 1 – Prof. Crispin Miller
Professor_crispin_miller.jpg.

At the heart of the CRUK Scotland Institute is a team of brilliant scientists, led by Professor Crispin Miller, who specialise in using super computers to understand how cancer behaves.
This diverse and talented team - which includes mathematicians, physicists, biologists and software engineers - are using a range of techniques to dig deep into the huge amounts of data we have on the genetics and anatomy of tumours.
“Biology is exciting” says Crispin. “The questions of modern cancer research, like how the DNA in one cell can define an entire living person – to me that’s as exciting as understanding the first few microseconds of the Big Bang.”
Crispin’s goal is to identify patterns in a tumour’s DNA or its structure that might help us better understand why and how cancers develop. And ultimately this could inform how best to treat them.
But spotting those crucial patterns is difficult because tumours are so diverse. And so Crispin’s team turn to supercomputers. These powerful tools can sift through vast amounts of information to find patterns that would be impossible for a human to spot. Then the scientists can do what they do best – work out how the patterns are driving cancer progression or making a tumour more or less sensitive to an anticancer drug.
Professor Miller explains: “Data gives us insight into things you can’t see down a microscope. It has the potential to start developing truly targeted therapies. To find the right therapy for the right person at the right time that is the goal.”
His team are using a data approach on many different cancer-related questions. In one project, patients have kindly allowed their doctors to share anonymised scan images of tumours and the tumour genetic data. Crispin’s team are seeing whether they can build a sophisticated AI approach that has the power to use this data to predict how tumours are going to respond to treatment. This could help doctors pick the best treatment for each person.
What nearly all Professor Miller’s work has in common is that it is only possible due to the data that people with cancer have shared.
“Data is central to the research we are doing. The more tumours we study, the more we understand how they differ from each other and how we can use this information to improve outcomes for people with cancer. I am incredibly grateful to the patients who donate their data and tissue, I couldn’t do my work without it.”
Case study 2 – Dr Irene Lobon
“Data is everything” – how patient data is helping us understand how cancer spreads and resists treatment
For Dr Irene Lobon, everything is data and data is everything. From calculating nutrients in new recipes to studying tumour samples, analysing data is central to her life and work. While in her spare time Dr Lobon’s analytical skills help her to optimise her favourite recipes, in the laboratory, these skills could lead to lifesaving discoveries.
Dr Lobon is a biomedical researcher in the Cancer Dynamics Laboratory, led by Professor Samra Turajlic at The Francis Crick Institute. She works on a multidisciplinary team featuring scientists and clinicians, all working together to better understand cancer.
The team are studying advanced, spreading melanoma, called metastatic melanoma. This is a type of skin cancer that is particularly hard to treat and often becomes resistant to drugs. Professor Samra’s group want to know how melanoma changes over time, what happens inside the tumour as it spreads and what features lead to drug resistance. To answer these questions, the team relies on patient data. Specifically, samples from patients who have passed away from cancer.
To access these samples, the team makes use of the PEACE (Posthumous Evaluation of Advanced Cancer Environment) study, a huge collaborative project, set up to help researchers collect samples from patients who have died from cancer. In this study, researchers take samples from participants during their treatment journey and after they have died. This huge assembly of data has allowed clinicians and scientists to study cancer in a way that was not possible before.
Professor Turajlic’s team employed sophisticated genetic sequencing techniques to study nearly 600 separate samples from 14 different patients with metastatic melanoma from the PEACE study. “What we’ve observed is that there are many variables that contribute tiny bits to the cancer progression” said Dr Lobon.
Uncovering these small contributions allowed the team to piece together a complex timeline of how the cancer develops. “It’s like having a fossil. We can study cancers at different points in time.”
The team shared the results of this extensive study with the scientific community earlier this year. The incredible information uncovered has helped scientists to understand the complex ways that melanomas use to evade drugs. The researchers hope that it could also lead to the development of completely new drugs that could provide hope for those diagnosed with metastatic melanoma.
While Professor Samra’s team are using the PEACE study to study metastatic melanoma, there are many other scientists using the valuable data collected to investigate other cancer types. There are researchers investigating lung cancer, renal cancer and many more. What they have in common, is their reliance on patient data.
Dr Lobon emphasised that her work would be impossible without the generous people who agree to donate their samples after they pass. “It’s extremely important. There is no other way we could get such specific information without these samples.”
“Data is everything.”
Case study 3 – Prof Rebecca Fitzgerald
Professor_rebecca_fitzgerald.jpg.

Oesophageal cancer is one of the biggest challenges in cancer research today. The underlying biology of the disease is poorly understood and survival remains very low, with only 1 in 10 people surviving their disease for 10 years or more. It’s a big challenge – and one that researchers and clinicians can’t tackle alone.
For over 10 years, Professor Rebecca Fitzgerald at the University of Cambridge has been spearheading a huge project that brings together scientists, doctors and nurses from across the UK with the goal of better understanding oesophageal cancer.
Known in the research community as OCCAMS (Oesophageal Cancer Clinical and Molecular Stratification), this impressive programme of work has seen researchers collecting tumour and blood samples from people with oesophageal cancer and decoding the cancer’s genetic sequence so that they have a complete map of the cancer’s DNA.
These samples provide a treasure trove of information, allowing scientists to see how changes in DNA sequence affects progression of oesophageal cancer. And every person’s data provides a new piece of the puzzle.
“This really is a team effort,” says Rebecca. “By sharing information, we can see the patterns and the trends and that’s what allows the breakthroughs to happen. Right now we can’t predict how well someone will do just by how they look when we first see them in the clinic. Some people do well, and sadly some people do badly, and we need to know why.”
And there are a lot of questions that need answering. How do genetic changes in the cancer change the way it develops over time? Are there specific risk factors that could predict if oesophageal cancer is going to recur? Why do some people respond well to treatment and some people don’t? All these questions rely on matching up clinical data (data collected by doctors about how each person’s cancer progresses) with laboratory data (data that comes from samples that scientists take away to analyse in the lab).
“And we need a lot of data,” explains Rebecca. “Oesophageal cancer is really complicated. We can’t find the needle in the haystack by just using data from a few people. The current problem my team is working on – working out whether all oesophageal cancers start from the precursor condition Barrett’s oesophagus – is using data from 4,000 patients. And that is why we are so grateful to all the patients who allow us to do this work.”
In the end, this work is all driven by the desire to make the situation better for people with oesophageal cancer. Already the team have been able to describe for the first time some of the DNA mutations that they think cause cancer, and there are likely to be many more findings to come.
“We have seen some improvements over the 20 years I have been working on this,” reflects Rebecca, “but we’ve got a long way to go. Solving this problem is what gets me out of bed in the morning. And I want to get to the end of my career and see that it is really different. I can’t do what I do without patient data – and I am not done yet.”
Case study 4 – Dr Rajesh Jena
Personalising radiotherapy – how patient data is helping reduce the side effects of treatment
Radiotherapy is the gold standard of treatment for many types of cancers. In fact, more than 130,000 patients benefit from radiotherapy every year in the UK. Today, most people receive image-guided radiotherapy – that is, using imaging such as x-rays and MRIs to target the beam of radiation to the tumour site, to make it as accurate as possible.
“Many people think about imaging at the point of diagnosis to find a tumour, or to follow up on treatment to see if its working,” says Dr Rajesh Jena, a clinician scientist based in Cambridge who is finding ways to improve radiotherapy for people with tumours of the brain and spine. “But imaging can be so much more: it can be used to personalise and even predict response to treatment.”
With radiotherapy there can be side effects because the beam of radiation can also affect healthy tissue surrounding the tumour. Combining imaging while delivering radiotherapy can help minimise these side effects, and getting better at combining these approaches is where patient data can be so important.
By studying images taken during radiotherapy, researchers can determine which healthy tissues were affected by the radiation, and then use that information to help predict how a new patient might respond to treatment, potentially altering the treatment plan to make it as side-effect free as possible.
“The wealth of information an image holds comes with an incredible potential,” says Dr Jena. Such potential to inform patient care led Dr Jena and his team to develop the first continuously learning artificial intelligence (AI) medical device in his hospital. Using patient data to train the AI, they were able to develop a tool that speeds up analysis of images. The technology helps doctors by cutting the amount of time spent ‘sketching’ around healthy organs, as they create radiotherapy plans, a painstaking yet vital step in radiotherapy treatment to ensure healthy tissue is protected.
And this data offers value far beyond direct medical treatment. “It’s not only doctors that need access to imaging data like this,” Dr Jena adds. “Patients are so generous allowing us to use this data, so we try to maximise its value by working with mathematicians, physicists, biologists and many other experts.” Bringing together different specialisms like this gives the scientists the best chance of understanding a disease as complex as cancer.
“And we also look back at historical patient images – this is important to provide context, improve our understanding and build up a valuable database of information.”
Thanks to patient data, Dr Jena and his team have already been able to create a technology that frees up valuable time and ultimately enable patients to receive treatment sooner. Over the next year, Dr Jena and his team are working on improving this technology by providing the AI with even more examples of patient images to learn from, allowing it to become better than ever at identifying healthy tissue.
“We’re so grateful to have access to patient imaging data because without it we wouldn’t be able to develop technologies like this, which can make a real difference to people with cancer. We’re very careful with how we use patient data, we take care to ensure that all data is anonymised and is treated with respect.”
Case studies in detail
The earlier diagnosis of lung cancer will save lives but also puts additional pressure on diagnostic services. It is therefore important that lung cancer pathways are organised to be as effective and efficient as possible and to ensure patients are given their diagnosis as soon as possible.
We hoped to improve understanding of pre-diagnostic events, intervals and patterns for lung cancer patients on a national scale, and to benchmark to the timings in the newly adopted National Optimal Lung Cancer Pathway (NOLCP).
The data used included: lung cancer registrations (2013-2015) from National Cancer Registration Analysis Service (NCRAS), diagnostic imaging data (DID) and cancer waiting times (CWT) data from NHS England; and involved data from over 100,000 patients.
Following data linkage, time intervals between events were calculated, different scenarios of events were investigated and timings of events were compared with those from the NOLCP.
Many different diagnostic scenarios exist, from simple to complex, which varies by CCG. Time intervals from imaging to diagnosis differed by source of image referral, with those ordered by GP direct access imaging having longer pathways. Benchmarking to the NOLCP timings showed small proportions (less than 6%) of patients meeting timings, this also varied widely by CCG.
Partners: ACE Programme (funded by CRUK, Macmillan, NHS England), CRUK-NHS England Partnership, NCRAS
See also: ACE Programme website , More in-depth findings
Survival for ovarian cancer in the UK is lower than other comparable high-income countries and there is substantial regional variation within the UK. Access to and/or quality of treatment may be contributing factors.
This analysis will establish a detailed picture of ovarian cancer treatments and outcomes and is intended to provide initial insights into a planned national ovarian cancer audit benchmarking pilot, with the ultimate aim to act as a catalyst to reduce variation and drive improvements to clinical practice.
Data used will be: patients diagnosed with ovarian cancer (1st July 2014 to 31st March 2015) who were eligible for chemotherapy; information about their tumour, chemotherapy treatment received, and demographic information.
The linked data will be used to compare treatment access rates between Cancer Alliances and/ or Trust of Multi-Disciplinary Team/diagnosis, to determine the extent to which this can be explained by regional differences in patient demographics, such as age and socioeconomic status, and we will investigate the influence of healthcare system levels factors on access to treatment, such as provider and type, and consultant volume and specialisation.
Findings are due Winter 2018, but we expect to find how much geographical variation in access to treatment for ovarian cancer there is in England, and to what extent is this affected by patient demographics and healthcare system level factors.
Partners: NHS England
The purpose of this service evaluation is to establish; factors that affect access to lung cancer treatments for non-small cell lung cancer (NSCLC) patients, whether there is variation between Cancer Alliances/ hospital trusts in access to a range of treatment pathways, and the impact of patient, tumour and provider characteristics on access to treatments.
Data used will be: patients diagnosed with lung cancer (1st April 2014 to 31st March 2015) who were eligible for chemotherapy; information about their tumour, chemotherapy treatment received, and demographic information.
Understanding variation in accessing treatments will inform policy makers and commissioners regarding where efforts should be focused, to ensure equitable access to effective treatments for NSCLC, and improve patient outcomes.
The linked data will be used to calculate access rates for different treatments, and then statistical tests will measure the overall geographic variation and significance. Finally, logistic regression will identify which factors are predictive of whether people receive various treatments (e.g. age, deprivation, ethnicity).
Findings are due early 2019: we expect to establish the presence of variation at a geographic level, and the reaso
In England, less than 60% of eligible bowel cancer screening participants take part in the programme. Cancer Research UK, in partnership with Public Health England, carried out a regional Be Clear on Cancer pilot campaign in the North West of England to encourage participation.
The campaign ran in 33 CCGs and consisted of advertising (including TV) and direct mail. Advertising ran alone for 6 weeks and was later combined for 6 weeks with direct mail in 22 CCGs to first-timers and previous non-responders. The remaining 11 CCGs continued to receive advertising only. The campaign was aimed at people aged 55-74 in the lower socioeconomic groups (C2DE) and skewed towards men; this was based on pilots previously run by Cancer Research UK.
We evaluated whether the campaign advertising, or advertising paired with sending a CRUK-endorsement letter with the kit increased uptake. Differences have also been compared across different socioeconomic groups.
The data we used to do this were extracted from the national bowel cancer screening database. We used age, location, date of test kit received, and date kit sent back. For the direct mail element of the campaign, we obtained a set of data for bowel screening test kit recipients who received a CRUK-endorsement letter, and a separate set of data for bowel screening test kit recipients who did not. We did not receive any names, addresses, or NHS numbers, so no individuals could be identified.
We split participants into 3 groups for the evaluation:
- First timers – people who are invited for bowel screening for the first time
- Previously screened – those who were invited for screening previously and returned completed kits
- Previous non-responders – those who were invited previously but didn’t return completed kits
Results are promising. They showed an increase in uptake of the screening test kit during the live campaign for all groups, as well as a smaller sustained increase in the 3 months following the campaign.
There are upcoming changes to the bowel cancer screening programme which may impact on screening uptake. We recommend waiting for an appropriate time, once changes have been implemented, to consider another campaign.
See also: Definitions of socioeconomic groups , Previous pilots .
COVID RT – assessing the impact of COVID-19 on radiotherapy in the UK
The COVID-19 pandemic has had a significant impact on cancer patients and cancer services across the UK. During the peak of the pandemic, radiotherapy services across the UK continued to treat cancer patients in often challenging circumstances and implemented significant changes to standard practice to minimise the risks to patients of contracting COVID-19 and focus radiotherapy resources where they were most needed. The scale of these changes in radiotherapy practice, the clinical decision-making underpinning them and their impact on cancer patient outcomes is unknown. This study will give a national picture of the decision making by patients and clinical staff and the impact on patient's treatment. It also provides knowledge of how RT was used as a bridge to surgery when surgical services weren't viable due to the pandemic and therefore what are the further requirements for cohorts of patients.
Data have been collected by radiotherapy centres across England specifically for this study as part of patient's routine care. These data were submitted to NHS England (previously Public Health England) under regulation 2 of the Health Service Regulations 2002. NHS England (previously Public Health England) collected and stored these data. A pseudonymised extract of these data was created and transferred to our Cancer Research UK Secure Data Environment (SDE).
These data are being analysed within the CRUK SDE, by named analytical staff at Cancer Research UK and University of Leeds, alongside similar data for other UK nations. Summary results will be calculated and used as the first research project to understand the affect Covid had on radiotherapy treatment. These data will not be linked to other datasets.
Join us on X (previously known as Twitter)
Information on the patient-level data we hold
Case report of multiple primary cancers and results of genetic testing to preliminarily explore their pathogenesis
Affiliations.
- 1 Department of Gastroenterology, Qingdao Central Hospital, University of Health and Rehabilitation Sciences Qingdao Central Hospital, Qingdao, China.
- 2 Department of Radiotherapy, Qilu Hospital of Shandong University (Qingdao), Qingdao, China.
- 3 Department of Internal Medicine-Oncology, Qingdao Central Hospital, University of Health and Rehabilitation Sciences Qingdao Central Hospital, Qingdao, China.
- 4 Department of Internal Medicine-Oncology, Qingdao Tumor Hospital, Qingdao, China.
- PMID: 38803359
- PMCID: PMC11129569
- DOI: 10.1177/2050313X241252371
The occurrence of multiple primary malignancies in a single patient has been relatively rare. We report here the case of a 71-year-old man with three primary tumors of lung cancer, intrahepatic cholangiocarcinoma, and prostate cancer, and a preliminary study of the mechanisms by which multiple primary tumors develop at the genetic level. Because of the late stage of the patient's condition, large tumor burden, and poor physical status, the patient survived only a few months. In the case presented herein, cholangiocarcinoma, lung cancer, and prostate cancer were found simultaneously, and the pathogenic sites are not related. Whole-exome sequencing was performed on the pathological tissues to explore the mechanism that may underlie multiple primary cancers at the genetic level. Several gene mutations were found in this case. They involved cell proliferation, cell cycle regulation, genetic stability, metabolism, cell invasion, angiogenesis, cell apoptosis, and other pathways. It can be preliminarily inferred that the mechanism underlying multiple primary tumors is related to the abnormality of tumor-promoting and suppressing pathways.
Keywords: Genetic mutation; case report; multiple primary cancer; whole-exome sequencing.
© The Author(s) 2024.
Publication types
- Case Reports
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.2(5); 2011 Sep 1
Small-cell lung carcinoma with long-term survival: A case report
Kazumi nishino.
Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan
Fumio Imamura
Toru kumagai, junji uchida, yuki akazawa, takako okuyama, yasuhiko tomita.
Institute of Pathology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan
Small-cell lung carcinoma is the most aggressive among lung cancer subtypes, has a poor prognosis and is highly associated with smoking. We present a case of small‑cell lung carcinoma in a patient who had never smoked and has survived for 14 years without achieving a complete remission since the first relapse. His long-term survival may be ascribed to the slow growth of the cancer cells, limited metastasis and favorable responses to the treatments he has received. During these 14 years, only two lymph node metastases and a single metastasis to the brain developed. His small-cell lung carcinoma has been well controlled each time by the various treatments he has received, including chemotherapy, radiotherapy and surgery. Pathologically, the tumor was a typical small-cell lung carcinoma with extensive necrosis. Results showed the mitotic rate and the cell proliferation markers to be greater than those in the intermediate-grade atypical carcinoid, but relatively low. Thus, we conclude that this case belongs to an overlap between intermediate- and high-grade neuroendocrine tumors.
Introduction
The 2004 World Health Organization (WHO) classification proposed four subtypes of pulmonary neuroendocrine (NE) tumors: low-grade typical carcinoid (TC), intermediate-grade atypical carcinoid (AC) and two high-grade tumors, large cell neuroendocrine carcinoma (LCNEC) and small-cell lung carcinoma (SCLC) ( 1 ). SCLC is a highly aggressive cancer and results in mortality in 2-4 months without treatment. Most patients respond to primary therapy, but survival remains poor and median survival times are reported to be approximately 24 months in limited disease and 12 months in extensive disease ( 2 , 3 ). In this study, we present a case of SCLC in a never smoker who has survived for 14 years without achieving a complete remission following the initial relapse.
Case report
In November 1996, a 44-year-old male, with no history of smoking, presented at the Osaka Medical Center for Cancer and Cardiovascular Diseases with an abnormal hilar shadow in the left lung, complaining of cough and dyspnea. A computerized tomography (CT) scan revealed a 4.5x3.0 cm hilar mass in the left lung (Fig. 1A). The patient was cytologically diagnosed with SCLC by bronchoscopic examination (Fig. 1B). Metastatic workup demonstrated that he had limited disease, cT2aN2M0 stage IIIA (the 7th edition of the TNM system for lung cancer). The values of serum neuron-specific enolase and carcinoembryonic antigen were within normal limits and the pro-gastrin-releasing-peptide (ProGRP) was not measured at the time. The patient received four cycles of chemotherapy consisting of cisplatin (CDDP) and etoposide, with concurrent thoracic radiation of 44 Gy at 2.2 Gy/fraction daily. The treatment resulted in a complete response. Prophylactic cranial irradiation was not performed since there was no evidence to recommend it at the time ( 4 ).

The patient remained asymptomatic and no sign of disease recurrence was detected until December 1998, when right mandibular lymphadenopathy was evidenced. By that time, the level of ProGRP had gradually been elevating from 25 pg/ml in October 1997 to 76 pg/ml in August 1998 and 133 pg/ml in December 1998 (normal range 0-45 pg/ml). Aspiration needle cytology of the lymph node revealed metastasis of SCLC, leading to the diagnosis of recurrence of SCLC as the cancer cells obtained from the lymph node revealed almost the same morphological features as the primary lung tumor cells. Since imaging studies showed no recurrence with the exception of the lesion, and the WBC count was ~3,000/µl, the patient was administered palliative radiotherapy with a total dose of 70 Gy without chemotherapy. The lymphadenopathy disappeared and the level of ProGRP decreased to 14.1 pg/ml. Two years later, in April 2000, the right axillary lymph node was found to be enlarged and cytology revealed metastasis of SCLC. Palliative radiotherapy with a total dose of 60 Gy was administered to the lesion. The lymph node swelling did not disappear completely, but the level of ProGRP decreased from 154 to 44 pg/ml. Although the level of ProGRP was slowly elevated to 150 pg/ml in November 2002, the patient observed no further symptoms and subsequently stopped consultation with the hospital.
The patient presented at the Osaka Medical Center for Cancer and Cardiovascular Diseases again in September 2006. Neurological examinations at admission indicated cerebral abnormality: left upper 1/4 homonymous hemianopsia and dysrhythmia on the electroencephalogram. The level of ProGRP was markedly elevated (2,860 pg/ml). Magnetic resonance imaging (MRI) of the brain revealed a huge mass in the right temporal lobe (Fig. 2A). The brain tumor was completely excised and histopathological examination determined it to be a metastasis of SCLC. The tumor was cytologically identical to the primary lung cancer, showing extensive necrosis, a high nuclear-to-cytoplasmic ratio and fine nuclear chromatin. The mitotic rate was 14 mitoses per 10 high-power fields (HPF) in this resected specimen. The Ki-67 labeling index was 25%. Immunohistochemical stains were positive for NE markers, including chromogranin A, synaptophysin and CD56 (Fig. 2B). The primary hilar tumor in the left lung and the right axillary lymph node revealed an increased uptake of fludeoxyglucose in positron emission tomography (PET) scanning. The patient received whole brain radiation therapy (WBRT) (30 Gy in 10 fractions), followed by systemic chemotherapy with CDDP and irinotecan hydrochloride (CPT11). Although the doses of CDDP and CPT11 were reduced to 50 and 50 mg/m 2 , respectively, ProGRP levels decreased notably to 90.7 pg/ml, following chemotherapy.

From September 2007, the level of ProGRP was again gradually elevated. Recurrence of brain metastasis was detected on the MRI in November 2008 and the patient underwent intensity-modulated radiotherapy (IMRT) for the brain tumor. Following IMRT, the patient was administered chemotherapy with CDDP and CPT11. However, compliance to the chemotherapy was poor due to hematological toxicity. In September 2009, the patient was admitted for obstructive pneumonia in the left lower lobe with high fever, and treated successfully with antibiotics. The level of ProGRP elevated to 724 pg/ml and distinct progression of the primary hilar tumor in the left lung was again detected by CT. The patient refused to complete systemic chemotherapy and was followed up for 1 year. In November 2010, CT and PET detected distinct progression of the primary lung tumor resulting in atelectasis of the left lower lobe and right axillary lymphadenopathy. The level of ProGRP was elevated to 1,640 pg/ml. Chemotherapy with amrubicin was administered in December 2010.
At present, the clinical course of the patient has continued for 14 years following the initial diagnosis of SCLC and 4 years following the diagnosis of brain metastasis. The brain remains relapse-free at present. The patient is currently continuing treatment with amrubicin for SCLC and his performance remains positive.
NE tumors represent approximately 20% of all primary lung neoplasms ( 5 ). NE tumors of the lung are separated into four subgroups: low-grade TC, intermediate-grade AC and two high-grade malignancies, LCNEC and SCLC, according to WHO in 2004 ( 1 ). SCLC is the most common NE tumor (20% of total lung cancers), followed by LCNEC (3%), TC (2%) and AC (0.2%) ( 6 ). The tumors differ morphologically, immunohistochemically and structurally. The WHO classification defines SCLC as a NE tumor with greater than 10 mitoses/10 HPF and small-cell cytologic features. TC is considered a NE tumor with carcinoid morphology, fewer than 2 mitoses/10 HPF and lacking in necrosis, while AC is defined as a NE tumor with carcinoid morphology showing 2-10 mitoses/10 HPF or necrosis ( 1 ). The grade of malignancy of each NE subtype is correlated with clinicopathological behavior and prognosis of the disease. TC and AC are relatively slow-growing tumors and generally exhibit a favorable outcome, while LCNEC and SCLC are very aggressive with a dismal prognosis ( 5 , 6 ).
The accurate differential diagnosis of carcinoids from SCLC is critical in the selection of the appropriate treatment. Usually, SCLC is rarely mistaken for carcinoids, with the exception of small biopsy materials. There are also certain differences in the clinical background and profiles according to the subgroup of NE tumors. Unlike carcinoids, SCLC is markedly associated with a history of smoking ( 7 , 8 ). Carcinoids tend to occur in younger patients (mean age 45-50 years), whereas the high-grade NE tumors affect older patients (mean age 65 years). The former are capable of distant metastases in less than 20% of cases (most commonly to liver and bones), and SCLC tends to metastasize to the brain, liver, adrenal glands and bone with higher frequency ( 5 , 6 ). Due to the low response rates for chemo- and radiotherapy, surgical resection is primarily used in the treatment of carcinoids, whereas the standard treatment for limited-stage SCLC includes combined chemoradiotherapy due to high sensitivity.
This case was initially diagnosed as SCLC in 1996 by cytological sampling obtained using bronchoscopy. The initial chemoradiotherapy resulted in a complete response. Ten years later, a metastatic brain tumor was excised. Although the clinical course was not typical for SCLC, the histopathological features of the resected tumor confirmed the diagnosis of SCLC due to the morphology of the tumor cells, the positive staining with neuroendocrine markers and the 14 mitoses/10 HPF with extensive necrosis (according to the WHO classification in 2004). The Ki-67 proliferative index has recently been considered to be useful in distinguishing between the various subtypes of NE tumors, particularly in small biopsy and cytology specimens. The Ki-67 proliferation rate of TC is less than 2% and AC is less than 20% (typical rate ~10%), while the two high-grade NE tumors are higher than 20% (typical rate for SCLC is 60-100%) ( 6 , 9 , 10 ). The Ki-67 index of this case was 25%.
The clinical manifestations of this case, such as slow-growing tumors, limited metastatic potential and a favorable prognosis, with an over 14-year survival, support the diagnosis of AC, while the morphological, immunohistochemical and structural features of the tumors are typical of SCLC. We believe that this case fits the diagnostic criteria of SCLC according to the WHO classification, but it is a borderline case between AC and SCLC. Asamura et al reported that 5-year survival rates for TC, AC, LCNEC and SCLC in Japanese surgical cases of NE tumors were 96.2, 77.8, 40.3 and 35.7%, respectively ( 8 ). An analysis of Japanese lung cancer patients registered in 2002 revealed that SCLC accounted for 9.2% of new lung cancer cases in Japan, and 5-year survival rates were 17.2% for stage IIIA, 12.4% for stage IIIB, 3.8% for stage IV and 14.7% overall ( 11 ).
The prognosis is particularly dismal in SCLC patients with brain metastasis. In the practice guidelines recently published in the Journal of Neurooncology, the authors recommend surgical resection followed by WBRT for newly-diagnosed single brain metastases, which improves outcomes when compared to WBRT alone. However, these authors indicate that the recommendation does not apply to relatively radiosensitive tumors such as SCLC ( 12 ). By contrast, Jesien-Lewandowicz et al assert that patients with solitary brain metastasis from SCLC should be treated radically, in particular those at younger ages with a small primary tumor in the lung, good performance status and lack of systemic dissemination ( 13 ). Four case reports describe excellent long-term survival following resection of a solitary metastatic brain tumor of SCLC and adjuvant WBRT ( 13 - 16 ). In the present case, surgical resection followed by WBRT and chemotherapy was successful. Imai et al suggest that a subtype of slow-growing SCLC, which shows different biological properties, should be distinguished from the common type SCLC ( 16 ). Although unusual, patients with this subtype of NE tumor may potentially achieve longer survival than those with typical SCLC, and should be treated with local and multimodality treatment on a case-by-case basis.
In conclusion, we present a case report of a SCLC patient who has survived for 14 years following initial diagnosis with persistent disease, in spite of repetitive multimodality therapies. This case suggests the existence of borderline cases between intermediate- and high-grade NE tumors, and that long-term survival may be expected with suitable treatments. A method should be established to select SCLC patients with a favorable prognosis, such as this case, and to find optimal therapeutic approaches for such patients.
Contributor Information
Kazumi Nishino, Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
Fumio Imamura, Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
Toru Kumagai, Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
Junji Uchida, Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
Yuki Akazawa, Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
Takako Okuyama, Department of Thoracic Oncology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
Yasuhiko Tomita, Institute of Pathology, Osaka Medical Center for Cancer and Cardiovascular Diseases, Osaka 537-8511, Japan.
- Beasley MB, Brambilla E and Travis WD: The 2004 World Health Organization classification of lung tumors. Semin Roentgenol 40: 90-97, 2005. [ PubMed ]
- Jackman DM and Johnson BE: Small-cell lung cancer. Lancet 366: 1385-1396, 2005. [ PubMed ]
- El Maalouf G, Rodier JM, Faivre S and Raymond E: Could we expect to improve survival in small cell lung cancer? Lung Cancer 57 (Suppl 2): 30-34, 2007. [ PubMed ]
- Auperin A, Arriagada R, Pignon JP, et al: Prophylactic cranial irradiation for patients with small-cell lung cancer in complete remission. Prophylactic cranial irradiation overview collaborative group. N Engl J Med 341: 476-484, 1999. [ PubMed ]
- Gustafsson BI, Kidd M, Chan A, Malfertheiner MV and Modlin IM: Bronchopulmonary neuroendocrine tumors. Cancer 113: 5-21, 2008. [ PubMed ]
- Rekhtman N: Neuroendocrine tumors of the lung: an update. Arch Pathol Lab Med 134: 1628-1638, 2010. [ PubMed ]
- Ou SH, Ziogas A and Zell JA: Prognostic factors for survival in extensive stage small cell lung cancer (ed-sclc): the importance of smoking history, socioeconomic and marital statuses, and ethnicity. J Thorac Oncol 4: 37-43, 2009. [ PubMed ]
- Asamura H, Kameya T, Matsuno Y, et al: Neuroendocrine neoplasms of the lung: a prognostic spectrum. J Clin Oncol 24: 70-76, 2006. [ PubMed ]
- Aslan DL, Gulbahce HE, Pambuccian SE, Manivel JC and Jessurun J: Ki-67 immunoreactivity in the differential diagnosis of pulmonary neuroendocrine neoplasms in specimens with extensive crush artifact. Am J Clin Pathol 123: 874-878, 2005. [ PubMed ]
- Pelosi G, Rodriguez J, Viale G and Rosai J: Typical and atypical pulmonary carcinoid tumor overdiagnosed as small-cell carcinoma on biopsy specimens: a major pitfall in the management of lung cancer patients. Am J Surg Pathol 29: 179-187, 2005. [ PubMed ]
- Sawabata N, Asamura H, Goya T, Mori M, Nakanishi Y, Eguchi K, Koshiishi Y, Okumura M, Miyaoka E and Fujii Y: Japanese lung cancer registry study: first prospective enrollment of a large number of surgical and nonsurgical cases in 2002. J Thorac Oncol 5: 1369-1375, 2010. [ PubMed ]
- Gaspar LE, Mehta MP, Patchell RA, et al: The role of whole brain radiation therapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96: 17-32, 2010. [ PMC free article ] [ PubMed ]
- Jesien-Lewandowicz E, Spych M, Fijuth J and Kordek R: Solitary brain metastasis of an occult and stable small-cell lung cancer in a schizophrenic patient: a 3-year control. Lung Cancer 69: 245-248, 2010. [ PubMed ]
- Abratt RP, de Groot M and Willcox PA: Resection of a solitary brain metastasis in a patient with small cell lung cancer – long-term survival. Eur J Cancer 31A: 419, 1995. [ PubMed ]
- Harrison ML and Goldstein D: Prolonged survival in a patient with an occult primary small-cell lung cancer and a solitary brain metastasis at diagnosis. Intern Med J 32: 621-622, 2002. [ PubMed ]
- Imai R, Hayakawa K, Sakurai H, Nakayama Y, Mitsuhashi N and Niibe H: Small cell lung cancer with a brain metastasis controlled for 5 years: a case report. Jpn J Clin Oncol 31: 116-118, 2001. [ PubMed ]
- Open access
- Published: 17 May 2024
Associations between chronic obstructive pulmonary disease and ten common cancers: novel insights from Mendelian randomization analyses
- Shixia Liao 1 ,
- Yanwen Wang 2 ,
- Jian Zhou 1 ,
- Yuting Liu 1 ,
- Shuangfei He 1 ,
- Lanying Zhang 1 ,
- Maomao Liu 1 ,
- Dongmei Wen 1 ,
- Pengpeng Sun 3 ,
- Guangbing Lu 4 ,
- Qi Wang 5 ,
- Yao Ouyang 1 &
- Yongxiang Song 6
BMC Cancer volume 24 , Article number: 601 ( 2024 ) Cite this article
10 Altmetric
Metrics details
Chronic obstructive pulmonary disease (COPD) is a significant global health issue, suspected to elevate the risk for various cancers. This study sought to discern whether COPD serves as a risk marker or a causative factor for prevalent cancers.
We employed univariable MR (UVMR) analyses to investigate the causal relationship between COPD and the top ten common cancers. Sensitivity analyses were performed to validate the main findings. Multivariable MR (MVMR) and two-step MR analyses were also conducted. False-discovery-rate (FDR) was used to correct multiple testing bias.
The UVMR analysis demonstrated notable associations between COPD and lung cancer (odds ratio [OR] = 1.42, 95%CI 1.15–1.77, FDR = 6.37 × 10 –3 ). This relationship extends to lung cancer subtypes such as squamous cell carcinoma (LUSC), adenocarcinoma (LUAD), and small cell lung cancer (SCLC). A tentative link was also identified between COPD and bladder cancer (OR = 1.53, 95%CI 1.03–2.28, FDR = 0.125). No significant associations were found between COPD and other types of cancer. The MVMR analysis that adjusted for smoking, alcohol drinking, and body mass index did not identify any significant causal relationships between COPD and either lung or bladder cancer. However, the two-step MR analysis indicates that COPD mediated 19.2% (95% CI 12.7–26.1%), 36.1% (24.9–33.2%), 35.9% (25.7–34.9%), and 35.5% (26.2–34.8%) of the association between smoking and overall lung cancer, as well as LUAD, LUSC, and SCLC, respectively.
Conclusions
COPD appears to act more as a risk marker than a direct cause of prevalent cancers. Importantly, it partially mediates the connection between smoking and lung cancer, underscoring its role in lung cancer prevention strategies.
Peer Review reports
Introduction
Chronic obstructive pulmonary disease (COPD) is a widespread global health issue, characterized by persistent airflow limitation and respiratory symptoms [ 1 ]. Its prevalence has been steadily increasing, resulting in a significant disease burden worldwide [ 2 ]. In addition to its well-established impact on lung function and overall health regardless of the smoking status, COPD has recently been identified as a potential risk factor for various types of cancer [ 3 , 4 , 5 , 6 , 7 ]. For example, findings from a Danish nationwide cohort study revealed that patients with first-time hospital-diagnosed COPD are at considerably increased risk of developing both lung cancer and extrapulmonary cancers including cancers of the larynx, tongue, oral cavity, pharynx, esophagus, stomach, liver, pancreas, cervix uteri, and urinary tract [ 4 ]. Likewise, a cohort study performed in Taiwanese showed that COPD patients had increased risk for both pulmonary and extrapulmonary cancers [ 7 ]. These studies have highlighted a systemic influence of COPD, potentially linked to factors such as chronic inflammation or oxidative stress associated with the disease [ 5 , 8 ]. For instance, research indicates that COPD exacerbations are often accompanied by significant systemic oxidative stress [ 9 ], a factor that may contribute to carcinogenesis in organs beyond the lungs, such as the liver [ 10 ].
Although previous epidemiological studies have consistently demonstrated an association between COPD and increased cancer risk, it is important to acknowledge that observational studies are vulnerable to several methodological challenges. Reverse causality poses a notable concern, as the presence of cancer may influence the development or severity of COPD, rather than the other way around [ 11 ]. Furthermore, confounding variables, such as smoking, age, and comorbidities, can independently contribute to both COPD and cancer, potentially influencing the observed associations [ 12 , 13 ]. The reliability and generalizability of findings may also be affected by the duration of follow-up and sample size limitations in these studies.
To address the limitations of observational studies and gain a deeper understanding of the causal relationship between COPD and cancer, alternative approaches are needed. Mendelian randomization (MR) analysis, utilizing genetic information as instrumental variables, offers a promising method for causal inference in observational studies [ 14 , 15 ]. By leveraging genetic variants associated with COPD as proxies for the disease, MR analysis can help mitigate the effects of confounding and reverse causality, providing a more reliable estimate of the causal effect. For instance, using MR analysis, Higbee et al. found limited evidence for a causal effect of either lung function or COPD on Alzheimer's disease [ 16 ]. MR analysis performed by Zhu et al. showed a significant positive causal effect of COPD on resting heart rate [ 17 ]. However, there was yet no MR assessment for the association between COPD and common cancers.
In this study, we aimed to investigate the causal relationship between COPD and the top ten common cancers (i.e., cancers of lung, esophagus, liver, stomach, colon and rectum, thyroid, bladder, prostate, female breast, and cervix) [ 18 ] using MR analysis. Our findings hold the potential to enhance our understanding of the COPD-cancer link and have implications for targeted interventions, prevention strategies, and personalized treatment approaches in both COPD and cancer management.
Materials and methods
Study design.
In this analysis, we constructed a two-sample MR analysis framework, in which COPD was set was the exposure and the ten common cancers were the outcomes. Genetic variants that associated with COPD were used as the instrumental variables (IVs). A valid IV for inferring causality between exposure and outcome should meet the following assumptions: (1) the IVs are associated with the exposure of interest; (2) there are no unmeasured confounders of the associations between IVs and outcome; and (3) the IVs affect the outcome only via the exposure of interest [ 19 ].
GWAS summary data of instrumental variables of COPD
We retrieved genetic summary data of COPD from the Global Biobank Meta-analysis Initiative (GBMI), which incorporated 18 biobanks involving up to 1.8 million participants with diverse ancestries (Table 1 ) [ 20 ]. In this study, we only retrieved the genetic data of participants with European ancestry, of which 61,627 were diagnosed as COPD and 980,360 were defined as healthy controls (Supplementary Tables S1-2). Each biobank conducted genotyping, imputation and quality controls and estimated sample ancestry independently. Fixed-effect meta-analyses based on inverse-variance weighting were performed for COPD with all biobanks stratified by each ancestry and by sex. Thus, we also retrieved COPD GWAS summary data of males and females for sex-specific analysis (e.g., analysis for prostate and female breast cancers).
We followed a series of quality control steps to identify eligible IVs for COPD. First, we extracted SNPs that showed an association with COPD at the traditional GWAS threshold ( P < 5 × 10 –8 ). Second, we performed a clumping process based on the linkage disequilibrium (LD) estimates from the European samples in the 1000 genomes project. We only retained the SNP that had the lower P value among those pairs of SNPs that had an LD estimate above the specified threshold (0.01) and a window size of 10,000 kb. Third, we removed SNPs with a minor allele frequency < 1%. We also calculated the F-statistics for the IVs of COPD [ 21 ]; a mean F-statistic > 10 denotes a low probability of weak-IV bias.
GWAS summary data of common cancers
We retrieved the genetic summary data of ten common cancers from their respective GWAS (Table 1 ). When selecting GWAS for the common cancers, our primary criterion was the comprehensiveness and specificity of the data available for each cancer type. For certain cancers where specific GWAS were not available, we turned to large-scale databases such as FinnGen and the UK Biobank. Our choice was guided by the number of available cases, ensuring the robustness and reliability of our analysis. This strategy allowed us to leverage the most extensive datasets, thereby enhancing the validity of our findings and providing a comprehensive overview of the genetic associations across a broad spectrum of cancers. All cancer GWASs were limited to Europeans. For lung cancer, we also retrieved the GWAS summary data of its histological subtypes, that are lung adenocarcinoma (LUAD), lung squamous cell carcinoma (LUSC), and small cell lung carcinoma (SCLC).
Next, we extracted the statistics (i.e., beta coefficient and standard error) for the IVs from the cancer GWAS summary data and harmonized them with that of the COPD GWAS. If a requested SNP was not present in the cancer GWAS, we retrieved the data of an SNP proxy that had an LD estimate of R 2 > 0.8 with the requested SNP. We corrected or directly excluded the effects of ambiguous SNPs with inconsistent alleles and palindromic SNPs with ambiguous strands in the subsequent two-sample MR analysis.
Univariable Mendelian randomization analysis
We performed the univariable MR (UVMR) according to the following procedure. First, we tested for horizontal pleiotropy using the MR-PRESSO global test [ 22 ] and removed outliers (i.e., SNPs with P < 0.05) if horizontal pleiotropy was present. Second, we tested for between-SNP heterogeneity using the inverse variance weighting (IVW) method based on the SNPs that remained after pleiotropy correction. We used Cochran’s Q statistic to check for the presence of heterogeneity and removed SNPs with P < 1.00 in MR-PRESSO analysis if heterogeneity was significant ( P value of Cochran’s Q statistic < 0.05). Third, we conducted MR analysis using the IVW method. We obtained the IVW estimate by meta-analyzing the SNP-specific Wald estimates using multiplicative random effects. We calculated the statistical power for MR analysis using mRnd website [ 23 ]. We also performed a series of sensitivity analyses using four different methods: MR-Egger regression, weighted median, weighted mode, and MRPRESSO methods. Additionally, we conducted a “leave-one-out” analysis to identify influential SNPs.
Multivariable Mendelian randomization analysis
To further overcome the potential pleiotropy, we performed multivariable MR (MVMR) analysis [ 24 ], in which smoking, alcohol drinking, and body mass index (BMI) were included as the covariates. The genetic summary data of smoking and alcohol drinking were retrieved from a GWAS of risk tolerance and risky behaviors in over 1 million individuals [ 25 ]. Smoking was measured by its status (i.e., ever vs . never smokers), and alcohol drinking was measured by drinks per week. The genetic summary data of BMI was retrieved from a GWAS for height and BMI in ∼ 700000 individuals of European ancestry [ 26 ]. Multivariable weighted median method was applied if the presence of significant between-SNP heterogeneity, otherwise, multivariable IVW method was employed.
Mediation analysis
Since smoking is a well-determined risk factor for both COPD and cancers, we performed a two-step MR analysis to investigate the mediation effect of COPD on the association between smoking and cancers [ 27 ]. To assess the indirect effect, we adopted the “product of coefficients” strategy. Two-step MR uses a series of UVMR analyses to estimate the total effect of the exposure on the outcome, the effect of the exposure on the mediator, and the effect of the mediator on the outcome [ 28 ]. The indirect effect of the exposure on the outcome can then be calculated by multiplying the effect of the exposure on the mediator and the effect of the mediator on the outcome. Standard errors were derived using the sum of squares method.
We used false-discovery rate (FDR) to adjust for multiple testing and an FDR < 0.05 was deemed statistically significant. A P value < 0.05 but FDR > 0.05 denotes a suggestive association. All statistics were performed using R program (v 4.1.1). TwoSampleMR , MendelianRandomization , and MRPRESSO packages were used for MR analyses.
Following rigorous quality control processes, we included a number of IVs, ranging from seven to 23, for MR analysis for cancers (Table 2 ; Supplementary Table S3). The mean F-statistics were all > 10, indicating a low probability of weak IV bias. However, significant between-SNP heterogeneities were observed for IVs in the MR analysis of lung cancer and its histological subtypes, bladder, colorectal, prostate, and cervical cancers (Table 2 ). No significant horizontal pleiotropy was found for any cancer type, further validating the robustness of the MR analysis. Thus, for MR analyses showing significant between-SNP heterogeneity, we reported estimates of weighted median method as the main findings, otherwise IVW estimates were reported. In the current scenario, we have enough statistical power to identify an association (represented by an odds ratio [OR]) less than 0.8 or greater than 1.2 between COPD and cancers. When aiming to identify an OR between 0.8 and 1.2, the statistical powers were decreased to varying degrees, ranging from 78 to 95.
Findings of univariable Mendelian randomization analysis
UVMR analysis (IVW method or weighted median method) suggested that COPD was significantly associated with the risk of lung cancer (OR = 1.42, 95% CI 1.15–1.77, FDR = 6.37 × 10 –3 ), LUSC (OR = 2.27, 95% CI 1.60–3.21, FDR = 7.84 × 10 –5 ), LUAD (OR = 2.03, 95% CI 1.53–2.69, FDR = 5.53 × 10 –5 ), and SCLC (OR = 2.47, 95% CI 1.49–4.10, FDR = 2.81 × 10 –3 ), and was suggestively associated with bladder cancer (OR = 1.53, 95% CI 1.03–2.28, FDR = 1.25 × 10 –1 ) (Fig. 1 ). No significant or suggestive association was detected between COPD and other eight types of cancer.

Genetic association between chronic obstructive pulmonary disease and common cancers according to univariable Mendelian randomization analysis
For most COPD-cancer pairs, estimates from different MR methods were consistent in directions (Fig. 2 ; Supplementary Figure S1). For instance, all methods indicated a positive association between COPD and lung cancer while revealing a negative association between COPD and gastric cancer. Moreover, in the “leave-one-analysis”, we did not identify any potential outlier that significantly influences the association between COPD and cancers, namely the association did not significantly change when excluding any SNP (Fig. 3 ; Supplementary Figure S2).
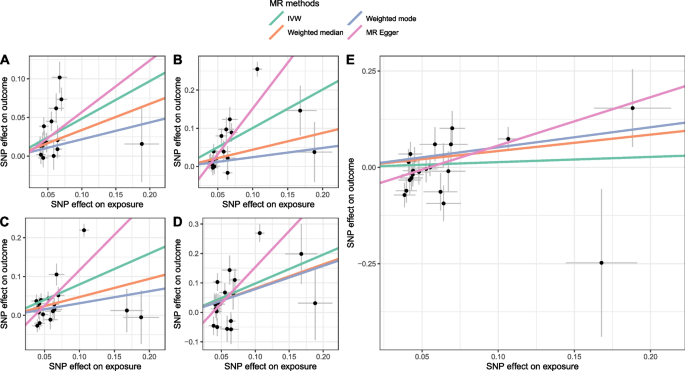
Scatter plot showing the SNP effects on both chronic obstructive pulmonary disease (exposure) and lung and bladder cancers (outcome). (The gray error bars denote the 95% confidence intervals of the effects; A - E represents lung cancer, lung squamous cell carcinoma, lung adenocarcinoma, small cell lung carcinoma, and bladder cancer, respectively.)

Leave-one-out analysis for chronic obstructive pulmonary disease and lung and bladder cancers. (The blue line denotes the integrated effect size; A - E represents lung cancer, lung squamous cell carcinoma, lung adenocarcinoma, small cell lung carcinoma, and bladder cancer, respectively)
Findings of multivariable Mendelian randomization analysis
To further validate the significant and suggestive association that identified in UVMR analysis, we performed a MVMR for lung cancer (including its histological subtypes) and bladder cancer. A total of 877, 919, 887, 930, and 994 eligible IVs were used for these five types of cancer, respectively. MVMR analysis reported an OR of 0.98 (95% CI 0.92–1.04) for lung cancer, 1.00 (95% CI 0.91–1.10) for LUSC, 1.01 (95% CI 0.92–1.09) for LUAD, 1.02 (95% CI 0.88–1.19) for SCLC, and 0.88 (95% CI 0.76–1.01) for bladder cancer (Fig. 4 ). In this analysis, we found that smoking is a causal factor for lung cancer (OR = 1.19, 95% CI 1.07–1.31, FDR = 1.64 × 10 –2 ) as well as its subtypes LUAD (OR = 1.21, 95% CI 1.06–1.39, FDR = 2.64 × 10 –2 ) and SCLC (OR = 1.43, 95% CI 1.13–1.81, FDR = 2.64 × 10 –2 ) (Fig. 4 ).

Genetic association between chronic obstructive pulmonary disease and lung and bladder cancers according to multivariable Mendelian randomization analysis
Mediation effect of COPD
In our analysis, we focused on estimating the mediating effect of COPD in the relationship between smoking and lung cancer, given that there’s no causal link between smoking and bladder cancer risk (OR = 1.35, 95% CI 0.97–1.88). Through the UVMR analysis, a significant association was observed between smoking and both COPD and lung cancer (Fig. 5 ). This association was also present for different lung cancer subtypes. These results imply that while smoking acts as a confounder in the COPD-lung cancer relationship, COPD might also be a mediator for smoking’s effect on lung cancer. The two-step MR analysis indicates that COPD mediated 19.2% (95% CI 12.7–26.1%), 36.1% (24.9–33.2%), 35.9% (25.7–34.9%), and 35.5% (26.2–34.8%) of the association between smoking and overall lung cancer, as well as LUAD, LUSC, and SCLC subtypes, respectively (Fig. 5 ).
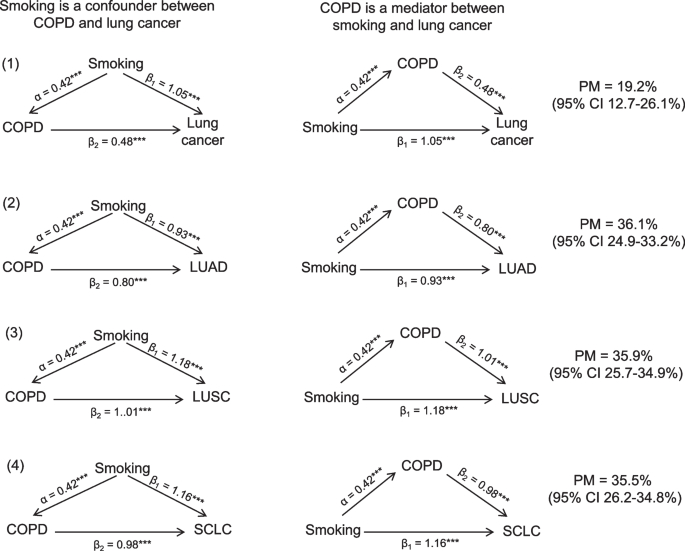
Directed acyclic graph representing the associations across smoking, COPD, and lung cancer. (α, β 1 , β 2 were calculated from the univariable Mendelian randomization analysis. ***denotes P value < 0.001. PM means proportion mediated. LUAD, lung adenocarcinoma; LUSC, lung squamous cell carcinoma; SCLC, small cell lung carcinoma)
Our study aimed to investigate the causal relationship between COPD and common cancers using MR analysis. We comprehensively analyzed data for various cancer types, including lung, liver, gastric, esophageal, colorectal, thyroid, female breast, cervical, and prostate cancers. The results of our study reveal a significant causal association between COPD and lung cancer, specifically its histological subtypes, which include lung squamous cell carcinoma, lung adenocarcinoma, and small cell lung carcinoma. Additionally, we found evidence suggesting a potential causal association between COPD and bladder cancer. However, in multivariable MR analysis that included smoking, alcohol drinking, and BMI as the covariates, the associations between COPD and lung and bladder cancers become statistically non-significant. Our MR analysis did not detect any significant associations between COPD and the other cancer types investigated.
Observational studies have consistently reported an increased risk of lung cancer among individuals with COPD [ 29 ]. Although efforts have been made to adjust for common confounders such as smoking, studies investigating the association between COPD and cancer often encounter inherent limitations, including underadjustment for confounders and reverse causality, which can impact the interpretation of the observed associations. For example, the smoking data were typically obtained through questionnaires, making them susceptible to recall bias [ 30 ]. Moreover, smoking represents a complex and subjective variable that poses challenges in its precise measurement within epidemiological studies. The assessment of smoking varied among studies, with some utilizing a categorical approach by comparing never or former smokers to current smokers [ 31 , 32 ], while others quantified smoking using pack-years [ 33 , 34 ]. Given the inherent limitations, the findings of observational studies should be interpreted with cautions and further validations were also warranted. In the current study, by utilizing MR analysis, we aimed to overcome these limitations and provide robust evidence for the causal relationship between COPD and lung cancer and other common cancers. Our findings were largely aligning with previous research, strengthening the evidence for a causal link between COPD and lung cancer.
The underlying mechanisms driving the causal relationship between COPD and lung cancer can be explained by several factors. COPD is characterized by chronic inflammation and oxidative stress in the lungs, both of which play significant roles in the development and progression of lung cancer [ 35 , 36 ]. Inflammatory mediators and reactive oxygen species generated in the lungs of COPD patients can lead to DNA damage, impaired DNA repair mechanisms, and disruption of cellular homeostasis [ 37 ]. These processes contribute to the oncogenic transformation observed in lung cancer. Furthermore, shared genetic factors and common environmental exposures, such as tobacco smoke, contribute to the co-occurrence of COPD and lung cancer [ 38 , 39 ]. Genetic variations associated with COPD may also influence lung cancer risk through pleiotropic effects on cellular pathways involved in cancer development [ 40 ].
However, we have to note that the significantly positive association between COPD and lung cancer was disappeared when we further adjusted for their shared risk factors (i.e., smoking, alcohol drinking, and BMI). This finding suggested that the association between COPD and lung cancer may be confounded by smoking, namely COPD and lung cancer are sequelae of heavy smoking, although COPD always precedes lung cancer. In this case, COPD per se may not be a causer but only be a risk factor for lung cancer. We also found that COPD may be a mediator between smoking and lung cancer, suggesting a potential biological pathway: smoking leads to COPD, and then COPD, in turn, increases the risk of lung cancer. If COPD indeed acts as a mediator, it emphasizes the importance of early detection and management of COPD. By effectively managing and potentially slowing the progression of COPD, we might also reduce the risk of lung cancer among these patients. Interestingly, in our two-step MR analysis, it was observed that COPD mediated a higher percentage of the association between smoking and specific lung cancer subtypes (LUAD, LUSC, and SCLC) compared to overall lung cancer. This finding could be partly explained by the differential impact of genetic variants, which serve as instrumental variables in our analysis, on these specific subtypes versus lung cancer in general. It underscores the nuanced role that genetic factors may play in the mediation effects across different cancer subtypes, a reflection of the complex interplay between genetics, COPD, and lung cancer pathogenesis.
Regarding the potential causal association between COPD and bladder cancer, our UVMR findings reveal a suggestive relationship, although this association was become non-significant in MVMR analysis. The association between COPD and bladder cancer was rarely reported in observational studies. Chronic inflammation in the respiratory tract of COPD patients can induce systemic inflammation, which may contribute to the development of bladder cancer. Inflammatory mediators and other inflammatory markers released in response to COPD-related inflammation can potentially affect the bladder's cellular environment and promote carcinogenesis [ 41 ]. Furthermore, shared risk factors, such as smoking and occupational exposures, may contribute to the observed association between COPD and bladder cancer [ 41 , 42 ]. Smoking, in particular, is a well-established risk factor for both COPD and bladder cancer and likely plays a substantial role in the shared pathogenesis of these conditions [ 43 ].
While our study provides valuable insights into the causal relationship between COPD and lung cancer and suggests a potential association with bladder cancer, it is important to acknowledge the limitations. MR analysis relies on several assumptions, including the validity of genetic instruments and the absence of pleiotropy. Although we employed robust methods to minimize biases associated with these assumptions, some residual confounding or pleiotropy may still be present. Additionally, our study focused on a selected set of common cancers, and we did not explore associations with other cancer types. Therefore, caution should be exercised when extrapolating our findings to all cancer types. Furthermore, the generalizability of our results may be limited to populations with similar ethnic backgrounds as the cohorts used for MR analysis. Finally, while our study employed comprehensive strategies to minimize the impact of pleiotropy, such as rigorous SNP selection and advanced sensitivity analyses, we recognize the inherent challenges in completely ruling out pleiotropy in MR studies [ 44 ]. For instance, SNPs associated with COPD may also be involved in biological pathways such as inflammation, oxidative stress, and DNA damage, all of which are implicated in the development of various cancers. This overlap highlights the complexity of genetic influences in disease processes and underscores the need for cautious interpretation of MR findings.
In conclusion, our study provides evidence for a causal association between COPD and lung cancer. We also found indications of a potential causal association between COPD and bladder cancer. However, these associations may be confounded by smoking. Further research is warranted to validate our findings, elucidate the underlying mechanisms, explore associations with other cancer types, and assess the potential impact of interventions.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
Chronic obstructive pulmonary disease
Mendelian Randomization
Univariable Mendelian randomization
Multivariable Mendelian randomization
Genome-wide association study
Inverse variance weighted
False-discovery-rate
Instrumental variable
Lung adenocarcinoma
Lung squamous cell carcinoma
Small cell lung carcinoma
Christenson SA, Smith BM, Bafadhel M, Putcha N. Chronic obstructive pulmonary disease. Lancet (London, England). 2022;399(10342):2227–42.
Article PubMed Google Scholar
Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447–58.
Article PubMed PubMed Central Google Scholar
Ante Z, Ernst P, Brassard P. Risk of gastric cancer in chronic obstructive pulmonary disease. Eur J Cancer Prev. 2022;31(4):326–32.
Article CAS PubMed Google Scholar
Kornum JB, Sværke C, Thomsen RW, Lange P, Sørensen HT. Chronic obstructive pulmonary disease and cancer risk: a Danish nationwide cohort study. Respir Med. 2012;106(6):845–52.
Ahn SV, Lee E, Park B, Jung JH, Park JE, Sheen SS, Park KJ, Hwang SC, Park JB, Park HS, et al. Cancer development in patients with COPD: a retrospective analysis of the National Health Insurance Service-National Sample Cohort in Korea. BMC Pulm Med. 2020;20(1):170.
Hsu WL, Chen HY, Chang FW, Hsu RJ. Does chronic obstructive pulmonary disease increase the risk of prostate cancer? A nationwide population-based study. Int J Chron Obstruct Pulmon Dis. 2019;14:1913–21.
Article CAS PubMed PubMed Central Google Scholar
Chiang CL, Hu YW, Wu CH, Chen YT, Liu CJ, Luo YH, Chen YM, Chen TJ, Su KC, Chou KT. Spectrum of cancer risk among Taiwanese with chronic obstructive pulmonary disease. Int J Clin Oncol. 2016;21(5):1014–20.
MacNee W. Systemic inflammatory biomarkers and co-morbidities of chronic obstructive pulmonary disease. Ann Med. 2013;45(3):291–300.
Wiegman CH, Li F, Ryffel B, Togbe D, Chung KF. Oxidative stress in ozone-induced chronic lung inflammation and emphysema: a facet of chronic obstructive pulmonary disease. Front Immunol. 1957;2020:11.
Google Scholar
Banerjee P, Gaddam N, Chandler V, Chakraborty S. Oxidative stress-induced liver damage and remodeling of the liver vasculature. Am J Pathol. 2023;193(10):1400–14.
Godtfredsen NS, Lam TH, Hansel TT, Leon ME, Gray N, Dresler C, Burns DM, Prescott E, Vestbo J. COPD-related morbidity and mortality after smoking cessation: status of the evidence. Eur Respir J. 2008;32(4):844–53.
Kridin K, Comaneshter D, Batat E, Cohen AD. COPD and lung cancer in patients with pemphigus- a population based study. Respir Med. 2018;136:93–7.
Lederer DJ, Bell SC, Branson RD, Chalmers JD, Marshall R, Maslove DM, Ost DE, Punjabi NM, Schatz M, Smyth AR, et al. Control of confounding and reporting of results in causal inference studies. Guidance for authors from editors of respiratory, sleep, and critical care journals. Ann Am Thorac Soc. 2019;16(1):22–8.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23(R1):R89-98.
Sekula P, Del Greco MF, Pattaro C, Köttgen A. Mendelian randomization as an approach to assess causality using observational data. J Am Soc Nephrol. 2016;27(11):3253–65.
Higbee D, Granell R, Walton E, Korologou-Linden R, Davey Smith G, Dodd J. Examining the possible causal relationship between lung function, COPD and Alzheimer’s disease: a Mendelian randomisation study. BMJ Open Respir Res. 2021;8(1):e000759.
Zhu Z, Wang X, Li X, Lin Y, Shen S, Liu CL, Hobbs BD, Hasegawa K, Liang L, Boezen HM, et al. Genetic overlap of chronic obstructive pulmonary disease and cardiovascular disease-related traits: a large-scale genome-wide cross-trait analysis. Respir Res. 2019;20(1):64.
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–49.
Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ (Clinical research ed). 2018;362:k601.
Zhou W, Kanai M, Wu KH, Rasheed H, Tsuo K, Hirbo JB, Wang Y, Bhattacharya A, Zhao H, Namba S, et al. Global Biobank Meta-analysis Initiative: Powering genetic discovery across human disease. Cell Genom. 2022;2(10):100192.
Jiang H, Hu D, Wang J, Zhang B, He C, Ning J. Adiponectin and the risk of gastrointestinal cancers in East Asians: Mendelian randomization analysis. Cancer Med. 2022;11(12):2397–404.
Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–8.
Brion MJ, Shakhbazov K, Visscher PM. Calculating statistical power in Mendelian randomization studies. Int J Epidemiol. 2013;42(5):1497–501.
Burgess S, Thompson SG. Multivariable Mendelian randomization: the use of pleiotropic genetic variants to estimate causal effects. Am J Epidemiol. 2015;181(4):251–60.
Karlsson Linnér R, Biroli P, Kong E, Meddens SFW, Wedow R, Fontana MA, Lebreton M, Tino SP, Abdellaoui A, Hammerschlag AR, et al. Genome-wide association analyses of risk tolerance and risky behaviors in over 1 million individuals identify hundreds of loci and shared genetic influences. Nat Genet. 2019;51(2):245–57.
Yengo L, Sidorenko J, Kemper KE, Zheng Z, Wood AR, Weedon MN, Frayling TM, Hirschhorn J, Yang J, Visscher PM. Meta-analysis of genome-wide association studies for height and body mass index in ∼ 700000 individuals of European ancestry. Hum Mol Genet. 2018;27(20):3641–9.
Carter AR, Sanderson E, Hammerton G, Richmond RC, Davey Smith G, Heron J, Taylor AE, Davies NM, Howe LD. Mendelian randomisation for mediation analysis: current methods and challenges for implementation. Eur J Epidemiol. 2021;36(5):465–78.
Sanderson E. Multivariable Mendelian Randomization and Mediation. Cold Spring Harb Perspect Med. 2021;11(2):a038984.
Park HY, Kang D, Shin SH, Yoo KH, Rhee CK, Suh GY, Kim H, Shim YM, Guallar E, Cho J, et al. Chronic obstructive pulmonary disease and lung cancer incidence in never smokers: a cohort study. Thorax. 2020;75(6):506–9.
Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43(1):87–91.
Wheaton AG, Liu Y, Croft JB, VanFrank B, Croxton TL, Punturieri A, Postow L, Greenlund KJ. Chronic obstructive pulmonary disease and smoking status - United States, 2017. MMWR Morb Mortal Wkly Rep. 2019;68(24):533–8.
Li G, Wang H, Wang K, Wang W, Dong F, Qian Y, Gong H, Hui C, Xu G, Li Y, et al. The association between smoking and blood pressure in men: a cross-sectional study. BMC Public Health. 2017;17(1):797.
Peto J. That the effects of smoking should be measured in pack-years: misconceptions 4. Br J Cancer. 2012;107(3):406–7.
Conlon MS, Johnson KC, Bewick MA, Lafrenie RM, Donner A. Smoking (active and passive), N-acetyltransferase 2, and risk of breast cancer. Cancer Epidemiol. 2010;34(2):142–9.
Yao H, Rahman I. Current concepts on the role of inflammation in COPD and lung cancer. Curr Opin Pharmacol. 2009;9(4):375–83.
Adcock IM, Caramori G, Barnes PJ. Chronic obstructive pulmonary disease and lung cancer: new molecular insights. Respiration. 2011;81(4):265–84.
Rosanna DP, Salvatore C. Reactive oxygen species, inflammation, and lung diseases. Curr Pharm Des. 2012;18(26):3889–900.
Atchley WT, Alvarez C, Saxena-Beem S, Schwartz TA, Ishizawar RC, Patel KP, Rivera MP. Immune checkpoint inhibitor-related pneumonitis in lung cancer: real-world incidence, risk factors, and management practices across six health care centers in North Carolina. Chest. 2021;160(2):731–42.
Caramori G, Ruggeri P, Mumby S, Ieni A, Lo Bello F, Chimankar V, Donovan C, Andò F, Nucera F, Coppolino I, et al. Molecular links between COPD and lung cancer: new targets for drug discovery? Expert Opin Ther Targets. 2019;23(6):539–53.
Yuan ST, Ellingrod VL, Schipper M, Stringer KA, Cai X, Hayman JA, Yu J, Lawrence TS, Kong FM. Genetic variations in TGFβ1, tPA, and ACE and radiation-induced thoracic toxicities in patients with non-small-cell lung cancer. J Thorac Oncol. 2013;8(2):208–13.
Milara J, Cortijo J. Tobacco, inflammation, and respiratory tract cancer. Curr Pharm Des. 2012;18(26):3901–38.
Rava M, Czachorowski MJ, Silverman D, Márquez M, Kishore S, Tardón A, Serra C, García-Closas M, Garcia-Closas R, Carrato A, et al. Asthma status is associated with decreased risk of aggressive urothelial bladder cancer. Int J Cancer. 2018;142(3):470–6.
Samanic C, Kogevinas M, Dosemeci M, Malats N, Real FX, Garcia-Closas M, Serra C, Carrato A, García-Closas R, Sala M, et al. Smoking and bladder cancer in Spain: effects of tobacco type, timing, environmental tobacco smoke, and gender. Cancer Epidemiol Biomarkers Prev. 2006;15(7):1348–54.
Yang Q, Sanderson E, Tilling K, Borges MC, Lawlor DA. Exploring and mitigating potential bias when genetic instrumental variables are associated with multiple non-exposure traits in Mendelian randomization. Eur J Epidemiol. 2022;37(7):683–700.
Download references
Institutional review board statement
This study was based on publicly available data and the ethics approval is waived.
Informed consent statement
All methods were carried out following STROBE-MR guidelines and regulations.
This research was supported by the National Natural Science Foundation of China (No: 82060016), Science and Technology Joint Fund of Affiliated Hospital of Zunyi Medical College of Zunyi City Science and Technology Bureau. No. (2018)71, and Zunyi City Joint Fund Project, Zuncity Kehe HZ Zi (2021) 94.
Author information
Authors and affiliations.
Department of Respiratory and Critical Care Medicine, Affiliated Hospital of Zunyi Medical University, Guizhou, 563003, China
Shixia Liao, Jian Zhou, Yuting Liu, Shuangfei He, Lanying Zhang, Maomao Liu, Dongmei Wen & Yao Ouyang
West China School of Medicine, Sichuan University, Chengdu, 610041, China
Yanwen Wang
Department of Osteopathy, Affiliated Hospital of Zunyi Medical University, Guizhou, 563003, China
Pengpeng Sun
Department of Respiration, Meishan Hospital of Traditional Chinese Medicine in Sichuan Province, Meishan, 620010, China
Guangbing Lu
China-Canada Medical and Health Science Association, Toronto, L3R 1A3, Canada
Department of Thoracic Surgery, Affiliated Hospital of Zunyi Medical University, Guizhou, 563003, China
Yongxiang Song
You can also search for this author in PubMed Google Scholar
Contributions
YS, YO, and SL conceived the idea for the study. SL, YW, and JZ obtained the genetic data. SL, YW, and JZ performed the data analyses. SL, SH, and LZ performed the data visualization. ML and DW scurtinized the results. PS, GL, YO and YS interpreted the results of the data analyses. SL, QW, YW, and YS wrote the manuscript. All authors read, revise, and approved the final manuscript.
Corresponding authors
Correspondence to Yao Ouyang or Yongxiang Song .
Ethics declarations
Consent for publication, competing interests.
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Liao, S., Wang, Y., Zhou, J. et al. Associations between chronic obstructive pulmonary disease and ten common cancers: novel insights from Mendelian randomization analyses. BMC Cancer 24 , 601 (2024). https://doi.org/10.1186/s12885-024-12381-9
Download citation
Received : 19 November 2023
Accepted : 14 May 2024
Published : 17 May 2024
DOI : https://doi.org/10.1186/s12885-024-12381-9
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Lung cancer
- Bladder cancer
- Common cancers
- Mendelian randomization
ISSN: 1471-2407
- Submission enquiries: [email protected]
- General enquiries: [email protected]

COMMENTS
Presentation of Case. Dr. Mathew S. Lopes: A 65-year-old woman was transferred to this hospital because of chest pain. Six months before the current presentation, the patient presented to a ...
Case Report: We report here a case of a very young woman with diagnosis of early-stage lung adenocarcinoma harboring EML4-ALK rearrangement; she underwent radical surgery and adjuvant chemotherapy according to the pathologic stage. Potential risk factors for lung cancer in our patient are discussed and clinico-pathologic features and outcomes of lung cancer in the young population compared to ...
According to another retrospective study, 20 of 137 patients with EGFR-mutant lung adenocarcinoma survived for ≥5 years, and exon 19 deletion, absence of extrathoracic metastases, absence of brain metastasis, and current non-smoking status were reportedly good prognostic factors. Our case corroborated the good prognostic factors reported in ...
Here, we present the case of a 51-year-old man with limited-stage small cell lung cancer (LS-SCLC) who received concurrent chemoradiotherapy and photodynamic therapy (PDT). The patient was diagnosed as having LS-SCLC with an endobronchial mass in the left main bronchus. Following concurrent chemoradiotherapy, a mass remaining in the left lingular division was treated with PDT. Clinical and ...
According to 2004 WHO/International Association for the Study of Lung Cancer (IASLC) classification of lung and pleural tumors, CSCLC is defined as cancer tissues that mainly contain SCLC components with non-SCLC (NSCLC) histopathological types. The most common part of NSCLC is squamous cell carcinoma or large cell carcinoma (4, 5).
Case presentation. A 76-year-old man was referred for a lung mass in December 2018. He was a smoker (30 pack years with intermittent stops) and parking attendant for 30 years. There was no history of lung cancer in the immediate family of the patient. The patient was administered a dual bronchodilator for COPD.
The present study reported an extremely rare case of a 66-year-old male with non-small lung cell cancer in the left lobe and synchronous small cell lung cancer in the right lobe. The diagnosis of multiple primary lung cancer not only depends on biopsy pathology, but also requires molecular biology results. This is of great significance for the ...
It's my pleasure to walk us through the first case, which is small cell lung cancer. This is a case with a 72-year-old woman who presents with shortness of breath, a productive cough, chest pain, some fatigue, anorexia, a recent 18-pound weight loss, and a history of hypertension. She is a schoolteacher and has a 45-pack-a-year smoking ...
Discussion. Lung cancer morbidity and mortality is highest of all cancers (1, 2) and lung adenocarcinoma accounts for approximately 40% of all lung cancers ().Although lung carcinoma can metastasize to all organs, the liver, adrenal glands, bone, kidney, and brain are the most common sites ().Metastasis to cutaneous and subcutaneous soft tissues is rare, with reported incidence rates ranging ...
Lung cancer across three generations of women. Jeff. Getting busy living, despite stage 4 diagnosis. Marley. Fatigue wasn't just acid reflux or part of being a young mom. Xavier. Veteran raises awareness of lung cancer in the military. Julie. A mammogram leads to an early-stage lung cancer diagnosis.
Lung cancer patient and control demographics. We conducted a matched case-control study to investigate the epidemiological and clinical parameters of primary and secondary lung cancer.
The term lung cancer, or bronchogenic carcinoma, refers to malignancies that originate in the airways or pulmonary parenchyma. Approximately 95% of all lung cancers are classified as either small-cell lung cancer (SCLC) or NSCLC. For NSCLC, the first line of treatment is generally surgery for early-stage or localized tumors.
Lung cancer, encompassing both small cell and non-small cell types and affecting men and women almost equally, stands as the second most common cancer in the United States.According to the ...
Dr. Mathew S. Lopes: A 65-year-old woman was transferred to this hospital because of chest pain. Six months before the current presentation, the patient presented to a hospital affiliated with ...
The Pragmatica-Lung Study is a randomized trial that will compare the combination of the targeted therapy ramucirumab (Cyramza) and the immunotherapy pembrolizumab (Keytruda) with standard chemotherapy in people with advanced NSCLC whose disease has progressed after previous treatment with immunotherapy and chemotherapy. In addition to looking at an important clinical question, the trial will ...
Abstract. A 75-year old female was admitted to the respiratory ward via the emergency department with a persistent cough, fatigue, shortness of breath and a suspicious chest X-ray. Investigations whilst an in-patient revealed a left upper lobe mass which lead to a diagnosis of non-small cell lung cancer (NSCLC).
A total of 12 patients with advanced lung cancer were included in this case study as they were found to have strong vimentin expression. This was correlated with overall survival of this group of patients. Results: Median survival of the patients was 4.66 months. This is 7.34 months less compared to the median survival of patients with stage IV ...
Lung cancer is a type of cancer that starts when abnormal cells grow in an uncontrolled way in the lungs. It is a serious health issue that can cause severe harm and death. Symptoms of lung cancer include a cough that does not go away, chest pain and shortness of breath. It is important to seek medical care early to avoid serious health effects.
Case presentation. A 76-year-old man was referred for a lung mass in December 2018. He was a smoker (30 pack years with intermittent stops) and parking attendant for 30 years. There was no history of lung cancer in the immediate family of the patient. The patient was administered a dual bronchodilator for COPD.
Lung cancer is estimated to have 2.2 million new cases and cause 1.8 million deaths each year worldwide, making this disease a major contributor to cancer-related mortality [1, 2].Among the non-small cell lung cancer subtypes, which constitute approximately 85% of all lung cancer cases, lung adenocarcinoma (LAD) and lung squamous cell carcinoma (LSCC) are the most common [].
Why do some lung cancer patients respond better to the types of drugs known as tyrosine kinase inhibitors? It may have to do with those patients' own immune systems. That's the hypothesis being tested by University of Colorado Cancer Center member Lynn Heasley, PhD, who recently received a Merit Review Award renewal from the U.S. Department of Veterans Affairs (VA) to study the role of the ...
The present study explored the risk factors associated with radiotherapy in seniors diagnosed with limited-stage small cell lung cancer (LS-SCLC) to construct and validate a prognostic nomogram.
Case study 2 - Dr Irene Lobon. "Data is everything" - how patient data is helping us understand how cancer spreads and resists treatment. For Dr Irene Lobon, everything is data and data is everything. From calculating nutrients in new recipes to studying tumour samples, analysing data is central to her life and work.
This study examined whether the addition of oral probiotic supplements to ICIs could enhance the treatment of advanced lung cancer. A total of 253 patients with advanced lung cancer were involved in the study, with some receiving probiotics in combination with ICIs and others not.
Exhaled breath analysis has emerged as a non-invasive and promising method for early detection of lung cancer, offering a novel approach for diagnosis through the identification of specific biomarkers present in a patient's breath. For this longitudinal study, 29 treatment-naive patients with lung cancer were evaluated before and after surgery. Secondary electrospray ionization high-resolution ...
The occurrence of multiple primary malignancies in a single patient has been relatively rare. We report here the case of a 71-year-old man with three primary tumors of lung cancer, intrahepatic cholangiocarcinoma, and prostate cancer, and a preliminary study of the mechanisms by which multiple primary tumors develop at the genetic level.
SCLC is a highly aggressive cancer and results in mortality in 2-4 months without treatment. Most patients respond to primary therapy, but survival remains poor and median survival times are reported to be approximately 24 months in limited disease and 12 months in extensive disease ( 2, 3 ). In this study, we present a case of SCLC in a never ...
Background Chronic obstructive pulmonary disease (COPD) is a significant global health issue, suspected to elevate the risk for various cancers. This study sought to discern whether COPD serves as a risk marker or a causative factor for prevalent cancers. Methods We employed univariable MR (UVMR) analyses to investigate the causal relationship between COPD and the top ten common cancers ...