- General Nursing
- Nursing Specialties
- Nursing Students
- United States Nursing
- World Nursing
- Boards of Nursing
- Breakroom / Clubs
- Nurse Q&A
- Student Q&A
- Fastest BSN
- Most Affordable BSN
- Fastest MSN
- Most Affordable MSN
- Best RN to BSN
- Fastest RN to BSN
- Most Affordable RN to BSN
- Best LPN/LVN
- Fastest LPN/LVN
- Most Affordable LPN/LVN
- Fastest DNP
- Most Affordable DNP
- Medical Assistant
- Best Online Medical Assistant
- Best Accelerated Medical Assistant
- Most Affordable Medical Assistant
- Nurse Practitioner
- Pediatric NP
- Neonatal NP
- Oncology NP
- Acute Care NP
- Aesthetic NP
- Women's Health NP
- Adult-Gerontology NP
- Emergency NP
- Best RN to NP
- Psychiatric-Mental Health NP
- RN Specialties
- Best RN Jobs and Salaries
- Aesthetic Nurse
- Nursing Informatics
- Nurse Case Manager
- Forensic Nurse
- Labor and Delivery Nurse
- Psychiatric Nurse
- Pediatric Nurse
- Travel Nurse
- Telemetry Nurse
- Dermatology Nurse
- Best NP Jobs and Salaries
- Family NP (FNP)
- Orthopedic NP
- Psychiatric-Mental Health NP (PMHNP)
- Nurse Educator
- Nurse Administrator
- Certified Nurse Midwife (CNM)
- Clinical Nurse Specialist (CNS)
- Certified Registered Nurse Anesthetist (CRNA)
- Best Free Online NCLEX-RN Study Guide
- The Nursing Process
- Question Leveling
- NCLEX-RN Question Identification
- Expert NCLEX-RN Test-Taking Strategies
- Best Scrubs for Nurses
- Best Shoes for Nurses
- Best Stethoscopes for Nurses
- Best Gifts for Nurses
- Undergraduate
- How to Become an LPN/LVN
- How to Earn an ADN
- Differences Between ADN, ASN, AAS
- How to Earn a BSN
- Best MSN Concentrations
- Is an MSN Worth It?
- How to Earn a DNP
- MSN vs. DNP

Nursing Case Studies: Diagnosis, Rationales, Fundamentals
Test your knowledge and clinical investigative skills in trying to diagnose what is going on with the patients presented in each of the Case Study Investigations. Can you come up with the right diagnosis? Case Studies Articles
Case Study: Child With Altered Mental Status
In this Case Study, an 11-year-old child with autism presents by ambulance to the children's hospital with altered mental status, bizarre behavior and fever....
Four Days of Nausea, Vomiting and Fever
What is most important in this case study in which an older Vietnamese woman presents to the ER with fever, nausea and vomiting?
I'm Dizzy, Tired and Can't Remember What I Ate for Lunch
A 74-year-old white male presents to the ED with confusion, fatigue, dizziness, headache and distal right arm paresthesia. Experienced nurses, model your...
Agonizing Pelvic Pain: What's Going On with this 17-year-old? | Ca…
A new case study in which the patient, a 17-yr-old African American female, is having ongoing, excruciating pelvic pain. This case study is based upon the very...
A Fracture from a Fall: What's Going on Here?
A new case study in which a 77 yo white female arrives to the emergency room by taxi with a suspected skull fracture. This topic was suggested by a reader –...
Breathless, Coughing and Run-down: What's Going On? | Case Study
A new case study in which the patient, a 32-yr-old white male presents to a local free clinic with fatigue, moderate dyspnea, and a persistent and...
Suicidal Ideation and Muscle Twitches | Case Study
A new case study in which the patient, a 40 yr-old mixed-race woman presents to her primary care physician with concerns about suicidal ideation. She has some...
Unexplained Diarrhea and Weight Loss: What's going on? | Case Stud…
A new case study in which the patient, a 28 y/o white female presents to a primary care clinic complaining of recurrent diarrhea. She first experienced diarrhea...
Repeat After Me... What's the problem here? | Case Study
A homeless man is brought to the ER by the local police after he is found sitting at a bus stop with a bloody rag pressed to his left knee. The temperature...
Wild Mood Swings and Outbursts of Anger: What's Wrong with this M…
A new case study in which the patient, a 50-yr-old male of mixed race visits his primary care physician with concerns about wild mood swings and outbursts of...
Case Study: Does this Cherokee Woman Have Dementia?
An 85-yr-old Cherokee woman living in a skilled nursing facility has lost weight since admission and won’t socialize or join in activities. She won't...

Case Study: It's a Lump, but is it Breast Cancer?
I am so excited about this Case Study because I feel it will be useful to so many of you! Welcome to a new Case Study in which the patient, a 45-yr-old, white,...

Case Study: Newborn with Vomiting and Diarrhea
A three-day old male infant is brought to the ER by his 22-yr-old mother with vomiting and diarrhea. Diagnostic results will be released upon request, with the...
Case Study: Joint Pain, Rash, Hair Loss - What's Going On?
A new case study in which R.W. presents to her PCP with a cough, mild fever, joint stiffness and pain and a history of rashes, anemia and hair loss.

Case Study: An OB Catastrophe
The following is a case simulation involving a patient initially encountered in Labor and Delivery. While the initial encounter occurred in a specific setting,...
Differential Case Study: Lyme Disease or Covid-19?
Lakeith, a 35-year-old black man living in New York State, presents with a fever of 101 degrees F. He is concerned he might have contracted Covid-19. Based upon...
Case Study: Sudden Severe Pain
A new case study in which the patient, D.C., a 52-year-old, white, married college professor wakes up to severe and intensifying pain. Though the coronavirus...

Case Study: Unexplained Bruises
Karen brings her daughter, Ann into the pediatric clinic stating, "She's just been so tired lately. All she wants to do is sleep and she’s got no appetite....
Case Study: What's Causing This Cough?
A new case study in which the patient, H.T. an 82-year-old Hispanic man presents to his primary care clinic with cough, malaise and confusion. How well do you...

Case Study(CSI): Stomach flu? Anxiety? What's Going on Here?
A new case study in which the patient, A.W. a 65-year-old African American woman presents to her primary care clinic with unspecified complaints. She told the...

Case Study: I'm too tired to walk the dog...
A new case study in which the patient, T.K. a 51-year-old woman who has finally taken a staycation, doesn’t have enough energy to walk her dog. You’re the...

Case Study: My Stomach Hurts
It's late in the day on a beautiful Saturday in late summer. You are finishing up your shift at a local urgent care clinic when a 28-year-old, white male comes...

Case Study: Trust Your Gut? A Fecal Transplant Could Change Your L…
Fecal Microbial Transplant (FMT) is a well-accepted practice for the treatment of C. diff, however in the U.S. it is still typically used only after multiple...

Case Study: Magic Mushrooms as Medicine? Mind-Body Connection Pt. …
Can "tripping" cure depression? Can LSD reduce chronic anxiety? This article explores the use of psychedelics to treat mental illness. Read on to find links for...
Case Study: Does Childhood Abuse Prevent Weight Loss? Pt. 2
This is an important topic for nurses. We need to understand the connection between childhood trauma and mind/body issues to build trust with patients and...
Nursing Diagnosis Guide: All You Need to Know to Master Diagnosing
In this ultimate tutorial and nursing diagnosis list, we’ll walk you through the concepts behind writing nursing diagnosis. Learn what a nursing diagnosis is, its history and evolution, the nursing process , the different types and classifications, and how to write nursing diagnoses correctly. Included also in this guide are tips on how you can formulate better nursing diagnoses, plus guides on how you can use them in creating your nursing care plans .
Table of Contents
- What is a Nursing Diagnosis?
Purposes of Nursing Diagnosis
Differentiating nursing diagnoses, medical diagnoses, and collaborative problems, classification of nursing diagnoses (taxonomy ii), nursing process, problem-focused nursing diagnosis, risk nursing diagnosis, health promotion diagnosis, syndrome diagnosis, possible nursing diagnosis, problem and definition.
- Etiology
Risk Factors
Defining characteristics, analyzing data, identifying health problems, risks, and strengths, formulating diagnostic statements, one-part nursing diagnosis statement, two-part nursing diagnosis statement, three-part nursing diagnosis statement, nursing diagnosis for care plans, recommended resources, references and sources, what is a nursing diagnosis.
A nursing diagnosis is a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability to that response, by an individual, family, group, or community. A nursing diagnosis provides the basis for selecting nursing interventions to achieve outcomes for which the nurse has accountability. Nursing diagnoses are developed based on data obtained during the nursing assessment and enable the nurse to develop the care plan.
The purpose of the nursing diagnosis is as follows:
- For nursing students, nursing diagnoses are an effective teaching tool to help sharpen their problem-solving and critical thinking skills.
- Helps identify nursing priorities and helps direct nursing interventions based on identified priorities.
- Helps the formulation of expected outcomes for quality assurance requirements of third-party payers.
- Nursing diagnoses help identify how a client or group responds to actual or potential health and life processes and knowing their available resources of strengths that can be drawn upon to prevent or resolve problems.
- Provides a common language and forms a basis for communication and understanding between nursing professionals and the healthcare team.
- Provides a basis of evaluation to determine if nursing care was beneficial to the client and cost-effective.
The term nursing diagnosis is associated with different concepts. It may refer to the distinct second step in the nursing process , diagnosis (“D” in “ ADPIE “). Also, nursing diagnosis applies to the label when nurses assign meaning to collected data appropriately labeled a nursing diagnosis. For example, during the assessment , the nurse may recognize that the client feels anxious , fearful, and finds it difficult to sleep . Those problems are labeled with nursing diagnoses: respectively, Anxiety , Fear , and Disturbed Sleep Pattern. In this context, a nursing diagnosis is based upon the patient’s response to the medical condition. It is called a ‘nursing diagnosis’ because these are matters that hold a distinct and precise action associated with what nurses have the autonomy to take action about with a specific disease or condition. This includes anything that is a physical, mental, and spiritual type of response. Hence, a nursing diagnosis is focused on care.
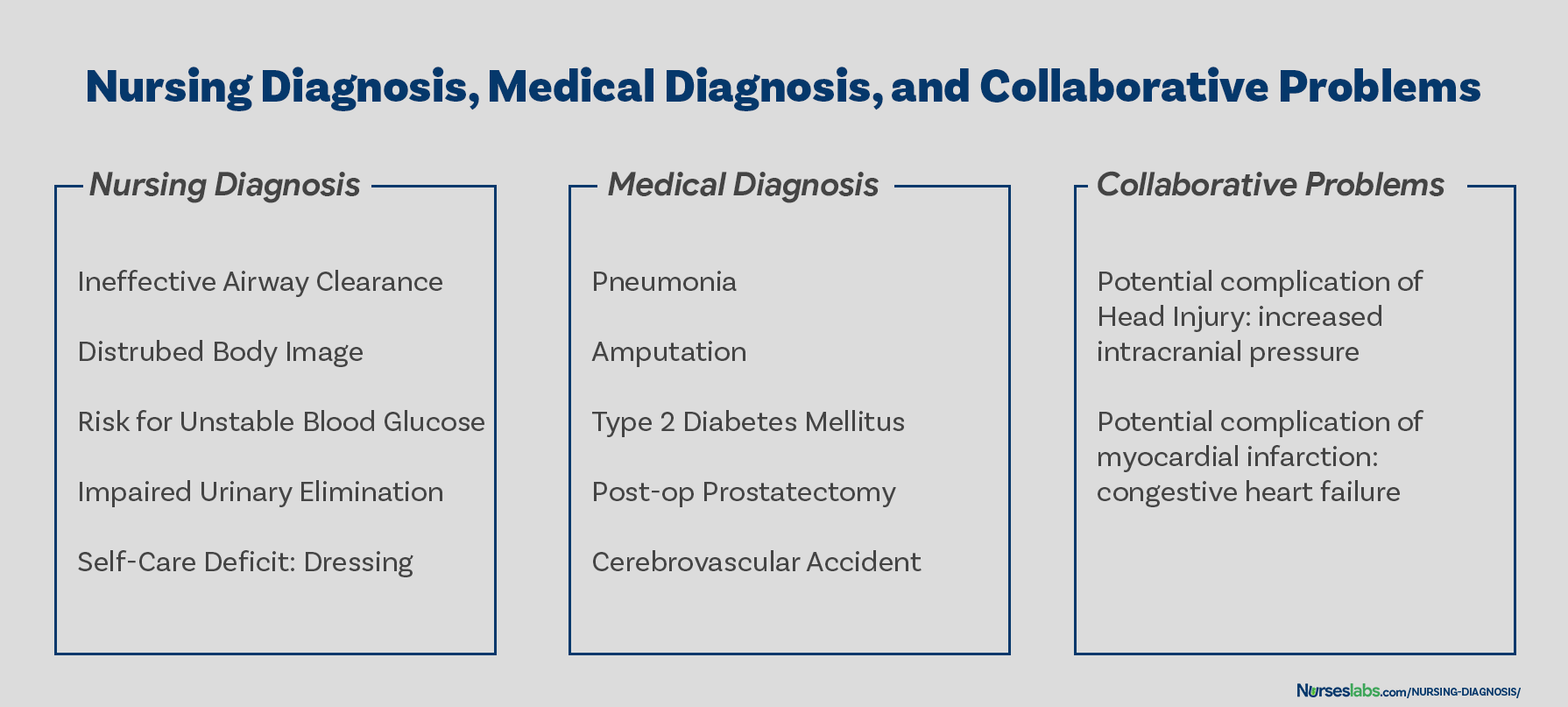
On the other hand, a medical diagnosis is made by the physician or advanced health care practitioner that deals more with the disease, medical condition, or pathological state only a practitioner can treat. Moreover, through experience and know-how, the specific and precise clinical entity that might be the possible cause of the illness will then be undertaken by the doctor, therefore, providing the proper medication that would cure the illness. Examples of medical diagnoses are Diabetes Mellitus , Tuberculosis , Amputation, Hepatitis , and Chronic Kidney Disease. The medical diagnosis normally does not change. Nurses must follow the physician’s orders and carry out prescribed treatments and therapies.
Collaborative problems are potential problems that nurses manage using both independent and physician-prescribed interventions. These are problems or conditions that require both medical and nursing interventions , with the nursing aspect focused on monitoring the client’s condition and preventing the development of the potential complication.
As explained above, now it is easier to distinguish a nursing diagnosis from a medical diagnosis. Nursing diagnosis is directed towards the patient and their physiological and psychological response. On the other hand, a medical diagnosis is particular to the disease or medical condition. Its center is on the illness.
How are nursing diagnoses listed, arranged, or classified? In 2002, Taxonomy II was adopted, which was based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Taxonomy II has three levels: Domains (13), Classes (47), and nursing diagnoses. Nursing diagnoses are no longer grouped by Gordon’s patterns but coded according to seven axes: diagnostic concept, time, unit of care, age, health status, descriptor, and topology. In addition, diagnoses are now listed alphabetically by their concept, not by the first word.
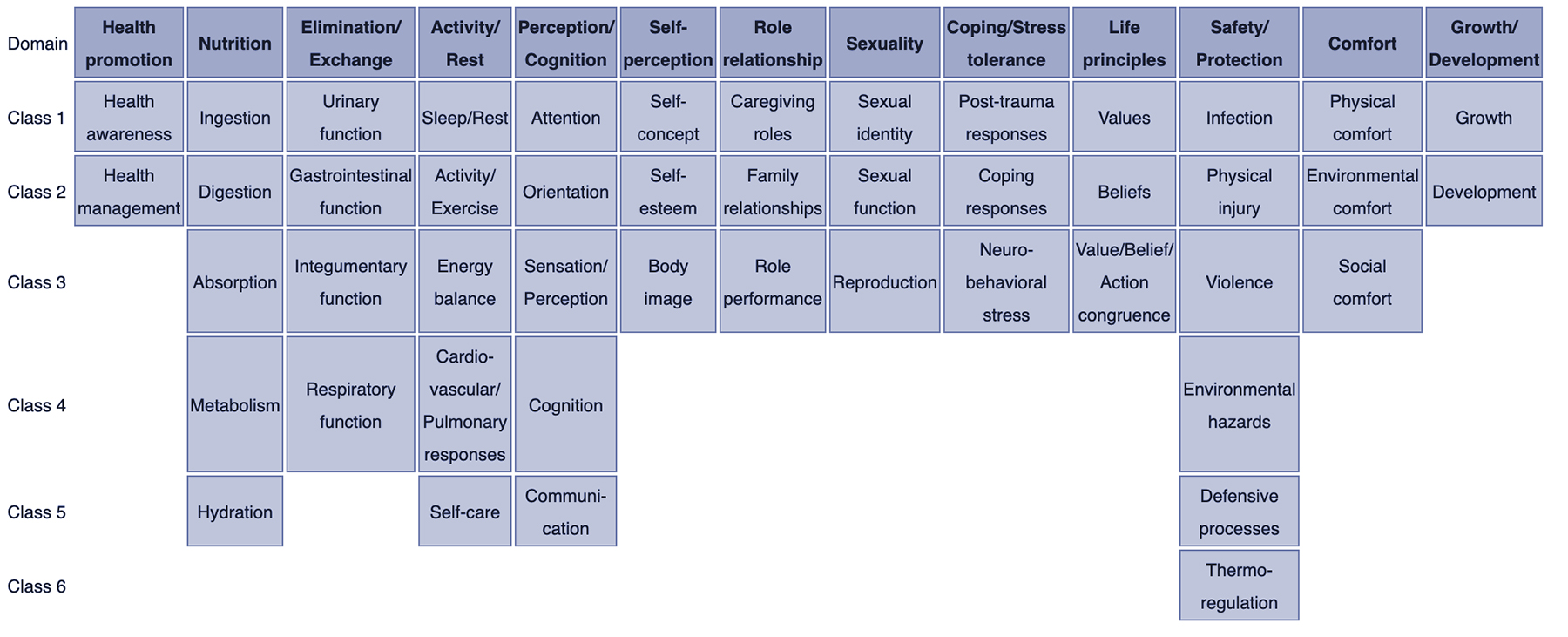
- Class 1. Health Awareness
- Class 2. Health Management
- Class 1. Ingestion
- Class 2. Digestion
- Class 3. Absorption
- Class 4. Metabolism
- Class 5. Hydration
- Class 1. Urinary function
- Class 2. Gastrointestinal function
- Class 3. Integumentary function
- Class 4. Respiratory function
- Class 1. Sleep/Rest
- Class 2. Activity/Exercise
- Class 3. Energy balance
- Class 4. Cardiovascular/Pulmonary responses
- Class 5. Self-care
- Class 1. Attention
- Class 2. Orientation
- Class 3. Sensation/Perception
- Class 4. Cognition
- Class 5. Communication
- Class 1. Self-concept
- Class 2. Self-esteem
- Class 3. Body image
- Class 1. Caregiving roles
- Class 2. Family relationships
- Class 3. Role performance
- Class 1. Sexual identity
- Class 2. Sexual function
- Class 3. Reproduction
- Class 1. Post-trauma responses
- Class 2. Coping responses
- Class 3. Neurobehavioral stress
- Class 1. Values
- Class 2. Beliefs
- Class 3. Value/Belief/Action congruence
- Class 1. Infection
- Class 2. Physical injury
- Class 3. Violence
- Class 4. Environmental hazards
- Class 5. Defensive processes
- Class 6. Thermoregulation
- Class 1. Physical comfort
- Class 2. Environmental comfort
- Class 3. Social comfort
- Class 1. Growth
- Class 2. Development
The five stages of the nursing process are assessment, diagnosing, planning , implementation , and evaluation . All steps in the nursing process require critical thinking by the nurse. Apart from understanding nursing diagnoses and their definitions, the nurse promotes awareness of defining characteristics and behaviors of the diagnoses, related factors to the selected nursing diagnoses, and the interventions suited for treating the diagnoses.
The steps, importance, purposes, and characteristics of the nursing process are discussed more in detail here: “ The Nursing Process: A Comprehensive Guide “
Types of Nursing Diagnoses
The four types of nursing diagnosis are Actual (Problem-Focused), Risk, Health Promotion , and Syndrome. Here are the four categories of nursing diagnoses:
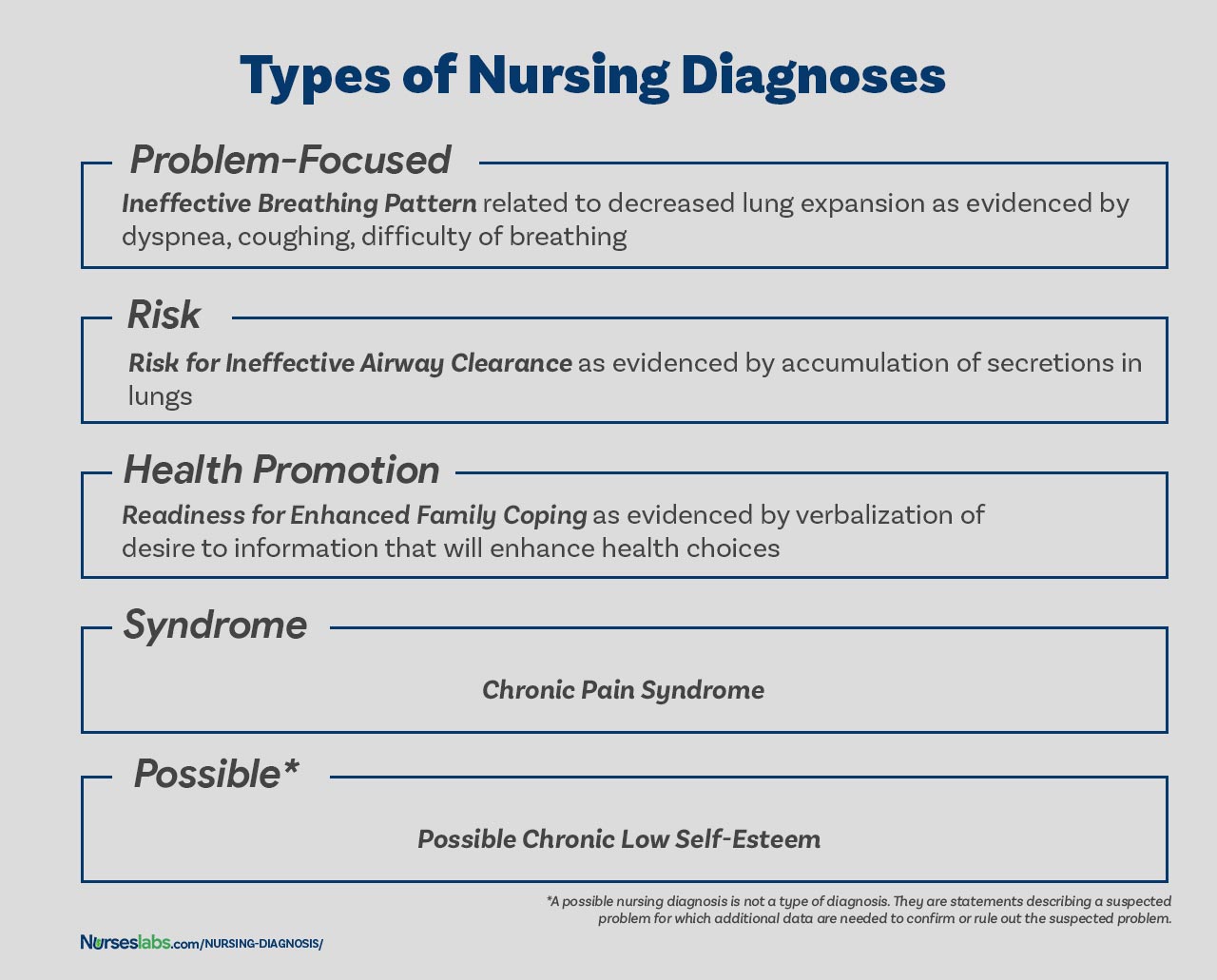
A problem-focused diagnosis (also known as actual diagnosis ) is a client problem present at the time of the nursing assessment . These diagnoses are based on the presence of associated signs and symptoms. Actual nursing diagnosis should not be viewed as more important than risk diagnoses. There are many instances where a risk diagnosis can be the diagnosis with the highest priority for a patient.
Problem-focused nursing diagnoses have three components: (1) nursing diagnosis, (2) related factors, and (3) defining characteristics. Examples of actual nursing diagnoses are:
- Anxiety related to stress as evidenced by increased tension, apprehension, and expression of concern regarding upcoming surgery
- Acute pain related to decreased myocardial flow as evidenced by grimacing, expression of pain , guarding behavior.
The second type of nursing diagnosis is called risk nursing diagnosis. These are clinical judgments that a problem does not exist, but the presence of risk factors indicates that a problem is likely to develop unless nurses intervene. A risk diagnosis is based on the patient’s current health status, past health history , and other risk factors that may increase the patient’s likelihood of experiencing a health problem. These are integral part of nursing care because they help to identify potential problems early on and allows the nurse to take steps to prevent or mitigate the risk.
There are no etiological factors (related factors) for risk diagnoses. The individual (or group) is more susceptible to developing the problem than others in the same or a similar situation because of risk factors. For example, an elderly client with diabetes and vertigo who has difficulty walking refuses to ask for assistance during ambulation may be appropriately diagnosed with risk for injury or risk for falls.
Components of a risk nursing diagnosis include (1) risk diagnostic label, and (2) risk factors. Examples of risk nursing diagnosis are:
- Risk for injury
- Risk for infection
Health promotion diagnosis (also known as wellness diagnosis ) is a clinical judgment about motivation and desire to increase well-being. It is a statement that identifies the patient’s readiness for engaging in activities that promote health and well-being. For example, if a first-time mother shows interest on how to properly breastfeed her baby, a nurse make make a health promotion diagnosis of “Readiness for Enhanced Breastfeeding .” This nursing diagnosis will be then used to guide nursing interventions aimed at supporting the patient in learning about proper breastfeeding.
Additionally, health promotion diagnosis is concerned with the individual, family, or community transition from a specific level of wellness to a higher level of wellness. Components of a health promotion diagnosis generally include only the diagnostic label or a one-part statement. Examples of health promotion diagnosis:
- Readiness for enhanced health literacy
A syndrome diagnosis is a clinical judgment concerning a cluster of problem or risk nursing diagnoses that are predicted to present because of a certain situation or event. They, too, are written as a one-part statement requiring only the diagnostic label. Examples of a syndrome nursing diagnosis are:
- Chronic Pain Syndrome
A possible nursing diagnosis is not a type of diagnosis as are actual, risk, health promotion , and syndrome. Possible nursing diagnoses are statements describing a suspected problem for which additional data are needed to confirm or rule out the suspected problem. It provides the nurse with the ability to communicate with other nurses that a diagnosis may be present but additional data collection is indicated to rule out or confirm the diagnosis. Examples include:
- Possible chronic low self-esteem
- Possible social isolation .
Components of a Nursing Diagnosis
A nursing diagnosis has typically three components: (1) the problem and its definition, (2) the etiology, and (3) the defining characteristics or risk factors (for risk diagnosis).
The problem statement , or the diagnostic label , describes the client’s health problem or response to which nursing therapy is given concisely. A diagnostic label usually has two parts: qualifier and focus of the diagnosis. Qualifiers (also called modifiers ) are words that have been added to some diagnostic labels to give additional meaning, limit, or specify the diagnostic statement. Exempted in this rule are one-word nursing diagnoses (e.g., Anxiety, Constipation , Diarrhea , Nausea , etc.) where their qualifier and focus are inherent in the one term.
The etiology , or related factors , component of a nursing diagnosis label identifies one or more probable causes of the health problem, are the conditions involved in the development of the problem, gives direction to the required nursing therapy, and enables the nurse to individualize the client’s care. Nursing interventions should be aimed at etiological factors in order to remove the underlying cause of the nursing diagnosis. Etiology is linked with the problem statement with the phrase “ related to ” for example:
- Activity intolerance related to generalized weakness .
- Decreased cardiac output related to abnormality in blood profile
Risk factors are used instead of etiological factors for risk nursing diagnosis. Risk factors are forces that put an individual (or group) at an increased vulnerability to an unhealthy condition. Risk factors are written following the phrase “as evidenced by” in the diagnostic statement.
- Risk for falls as evidenced by old age and use of walker.
- Risk for infection as evidenced by break in skin integrity .
Defining characteristics are the clusters of signs and symptoms that indicate the presence of a particular diagnostic label. In actual nursing diagnosis, the defining characteristics are the identified signs and symptoms of the client. For risk nursing diagnosis, no signs and symptoms are present therefore the factors that cause the client to be more susceptible to the problem form the etiology of a risk nursing diagnosis. Defining characteristics are written following the phrase “as evidenced by” or “as manifested by” in the diagnostic statement.
Diagnostic Process: How to Diagnose
There are three phases during the diagnostic process: (1) data analysis, (2) identification of the client’s health problems, health risks, and strengths, and (3) formulation of diagnostic statements.
Analysis of data involves comparing patient data against standards, clustering the cues, and identifying gaps and inconsistencies.
In this decision-making step, after data analysis, the nurse and the client identify problems that support tentative actual, risk, and possible diagnoses. It involves determining whether a problem is a nursing diagnosis, medical diagnosis, or a collaborative problem. Also, at this stage, the nurse and the client identify the client’s strengths, resources, and abilities to cope.
Formulation of diagnostic statements is the last step of the diagnostic process wherein the nurse creates diagnostic statements. The process is detailed below.
How to Write a Nursing Diagnosis?
In writing nursing diagnostic statements, describe an individual’s health status and the factors that have contributed to the status. You do not need to include all types of diagnostic indicators. Writing diagnostic statements vary per type of nursing diagnosis (see below).
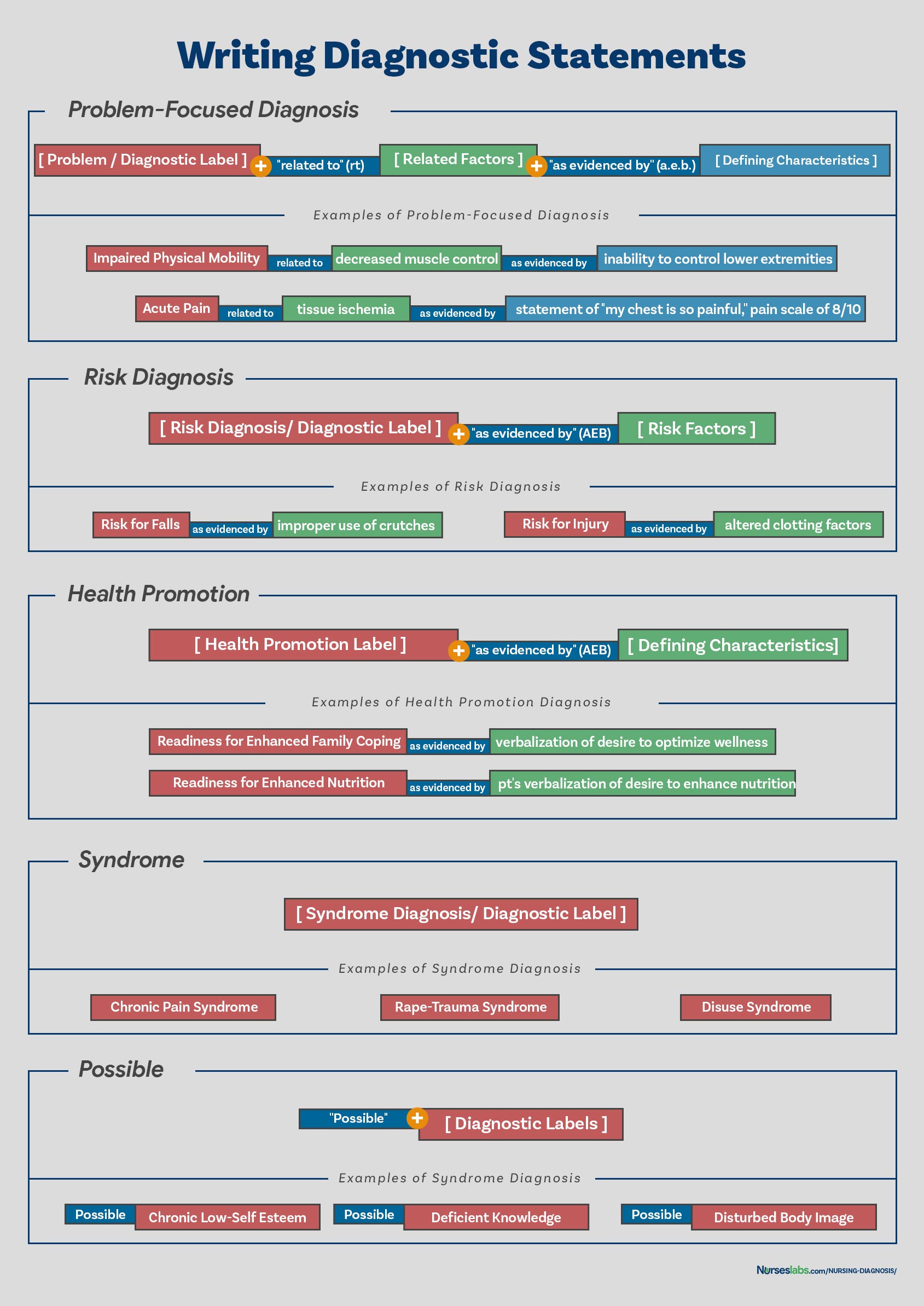
Another way of writing nursing diagnostic statements is by using the PES format, which stands for Problem (diagnostic label), Etiology (related factors), and Signs/Symptoms (defining characteristics). Diagnostic statements can be one-part, two-part, or three-part using the PES format.
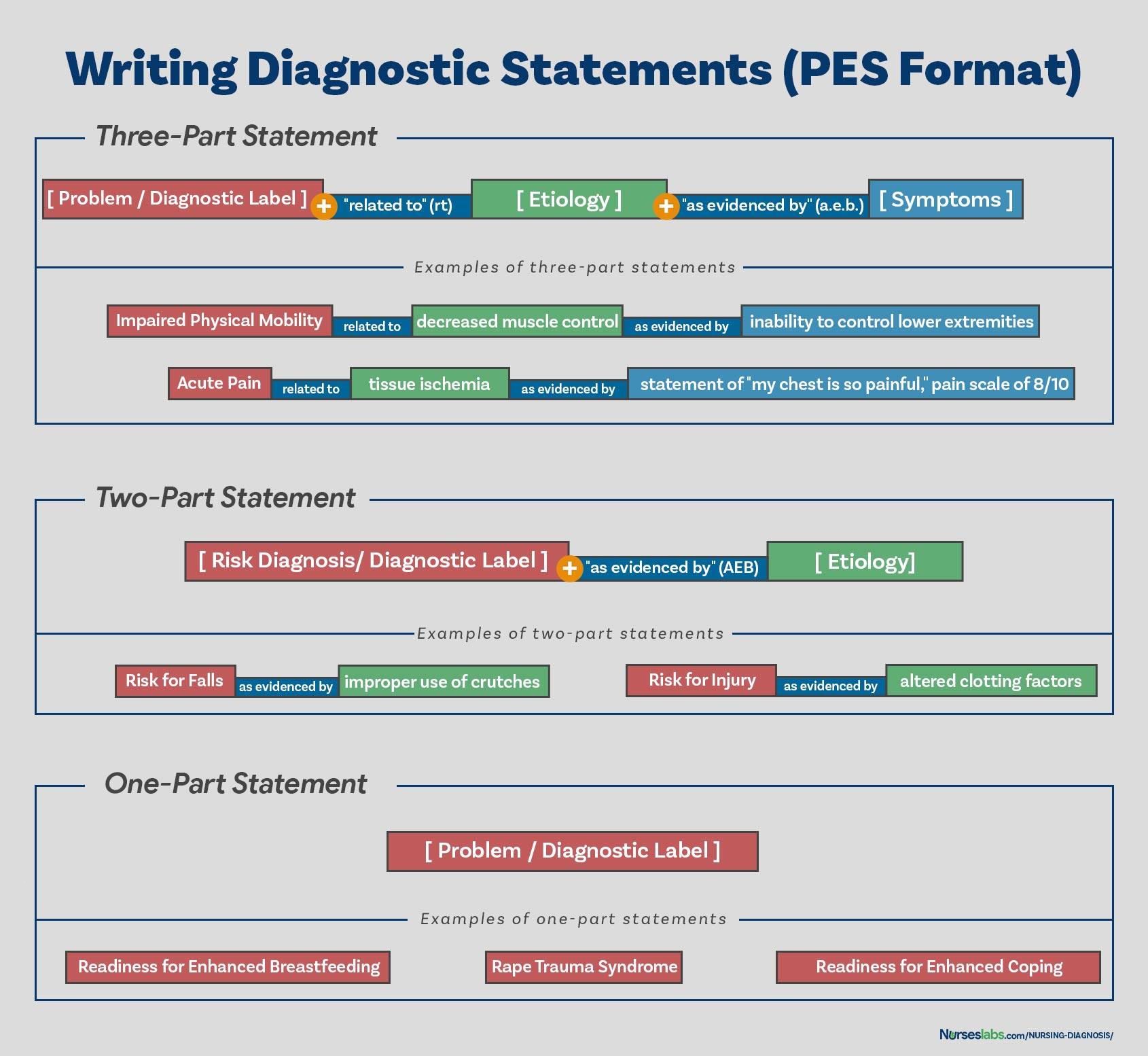
Health promotion nursing diagnoses are usually written as one-part statements because related factors are always the same: motivated to achieve a higher level of wellness through related factors may be used to improve the chosen diagnosis. Syndrome diagnoses also have no related factors. Examples of one-part nursing diagnosis statements include:
- Readiness for enhanced coping
- Rape Trauma Syndrome
Risk and possible nursing diagnoses have two-part statements: the first part is the diagnostic label and the second is the validation for a risk nursing diagnosis or the presence of risk factors. It’s not possible to have a third part for risk or possible diagnoses because signs and symptoms do not exist. Examples of two-part nursing diagnosis statements include:
- Risk for infection as evidenced by weakened immune system response
- Risk for injury as evidenced by unstable hemodynamic profile
An actual or problem-focus nursing diagnosis has three-part statements: diagnostic label, contributing factor (“related to”), and signs and symptoms (“as evidenced by” or “as manifested by”). The three-part nursing diagnosis statement is also called the PES format which includes the Problem, Etiology, and Signs and Symptoms. Example of three-part nursing diagnosis statements include:
- Acute pain related to tissue ischemia as evidenced by statement of “I feel severe pain on my chest!”
Variations on Basic Statement Formats
Variations in writing nursing diagnosis statement formats include the following:
- Using “ secondary to ” to divide the etiology into two parts to make the diagnostic statement more descriptive and useful. Following the “secondary to” is often a pathophysiologic or disease process or a medical diagnosis. For example, Risk for Decreased Cardiac Output related to reduced preload secondary to myocardial infarction .
- Using “ complex factors ” when there are too many etiologic factors or when they are too complex to state in a brief phrase. For example, Chronic Low Self-Esteem related to complex factors.
- Using “ unknown etiology ” when the defining characteristics are present but the nurse does not know the cause or contributing factors. For example, Ineffective Coping related to unknown etiology.
- Specifying a second part of the general response or diagnostic label to make it more precise. For example, Impaired Skin Integrity (Right Anterior Chest) related to disruption of skin surface secondary to burn injury .
This section is the list or database of the common nursing diagnosis examples that you can use to develop your nursing care plans .
See also: Nursing Care Plans (NCP): Ultimate Guide and List
- Chronic Pain
- Constipation
- Decreased Cardiac Output
- Hopelessness
- Hyperthermia
- Hypothermia
Recommended nursing diagnosis and nursing care plan books and resources.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Ackley and Ladwig’s Nursing Diagnosis Handbook: An Evidence-Based Guide to Planning Care We love this book because of its evidence-based approach to nursing interventions. This care plan handbook uses an easy, three-step system to guide you through client assessment, nursing diagnosis, and care planning. Includes step-by-step instructions showing how to implement care and evaluate outcomes, and help you build skills in diagnostic reasoning and critical thinking.

Nursing Care Plans – Nursing Diagnosis & Intervention (10th Edition) Includes over two hundred care plans that reflect the most recent evidence-based guidelines. New to this edition are ICNP diagnoses, care plans on LGBTQ health issues, and on electrolytes and acid-base balance.

Nurse’s Pocket Guide: Diagnoses, Prioritized Interventions, and Rationales Quick-reference tool includes all you need to identify the correct diagnoses for efficient patient care planning. The sixteenth edition includes the most recent nursing diagnoses and interventions and an alphabetized listing of nursing diagnoses covering more than 400 disorders.

Nursing Diagnosis Manual: Planning, Individualizing, and Documenting Client Care Identify interventions to plan, individualize, and document care for more than 800 diseases and disorders. Only in the Nursing Diagnosis Manual will you find for each diagnosis subjectively and objectively – sample clinical applications, prioritized action/interventions with rationales – a documentation section, and much more!

All-in-One Nursing Care Planning Resource – E-Book: Medical-Surgical, Pediatric, Maternity, and Psychiatric-Mental Health Includes over 100 care plans for medical-surgical, maternity/OB, pediatrics, and psychiatric and mental health. Interprofessional “patient problems” focus familiarizes you with how to speak to patients.

Other recommended site resources for this nursing care plan:
- Nursing Care Plans (NCP): Ultimate Guide and Database MUST READ! Over 150+ nursing care plans for different diseases and conditions. Includes our easy-to-follow guide on how to create nursing care plans from scratch.
- Nursing Diagnosis Guide and List: All You Need to Know to Master Diagnosing Our comprehensive guide on how to create and write diagnostic labels. Includes detailed nursing care plan guides for common nursing diagnostic labels.
References for this Nursing Diagnosis guide and recommended resources to further your reading.
- Berman, A., Snyder, S., & Frandsen, G. (2016). Kozier & Erb’s Fundamentals of Nursing: Concepts, process and practice . Boston, MA: Pearson.
- Edel, M. (1982). The nature of nursing diagnosis. In J. Carlson, C. Craft, & A. McGuire (Eds.), Nursing diagnosis (pp. 3-17). Philadelphia: Saunders.
- Fry, V. (1953). The Creative approach to nursing. AJN, 53(3), 301-302.
- Gordon, M. (1982). Nursing diagnosis: Process and application. New York: McGraw-Hill.
- Gordon, M. (2014). Manual of nursing diagnosis . Jones & Bartlett Publishers.
- Gebbie, K., & Lavin, M. (1975.) Classification of nursing diagnoses: Proceedings of the First National Conference. St. Louis, MO: Mosby.
- McManus, R. L. (1951). Assumption of functions in nursing. In Teachers College, Columbia University, Regional planning for nurses and nursing education . New York: Columbia University Press.
- Powers, P. (2002). A discourse analysis of nursing diagnosis . Qualitative health research , 12 (7), 945-965.
87 thoughts on “Nursing Diagnosis Guide: All You Need to Know to Master Diagnosing”
Very useful document indeed.
Thank you Sima! Hope it helps come up with great nursing care plans!
Thank you for this resource material. This is very simple, concise and easy to understand. This would be of great help both for the students and the teacher.
Please make proper table for nursing diagnosis it’ll be easy to read and understand .
This is simple and easy to understand.
Happy to know! Hope you visit our guide on nursing care plans too! Thanks for dropping by Modupe!
I need a complete pdf file
Hi! If you want to save it as a PDF file, simply “Print” this page and “Save as PDF”.
So very happy to stumble upon nurseslabs. Thanks so much
Happy to have helped you. Please do check out our nursing care plans list too! Thanks for visiting, Hussaina!
I want to acknowledge the writer of Understand, Matt Vera for using the initiative in simplifying the nursing notes into simple English that we as upcoming nursing students can understand nursing notes in order to practice them in our clinical. I’ve learned so much from this website and I want to be part of the nurses website so I can gather some more informations. Get me on my email. Thanks so much..
Thank you Lawrencia. Glad to be of help!
VERY NICE EXPLANATION .THANK YOU . DEAR MADAM /SIR PLEASE CAN YOU PROVIDE ME LIST OF NURSING DIAGNOSIS ALONG WITH REVISED ONE TILL DATE . I am Lecturer in college of nursing ,India Thank You
this is so educative thank you
Thank you! Glad you liked it.
really simple and effective, thank you so much.
This is great! Simple and easy to understand for the nursing students.
Comment:nice work, great nurses.
I am a nurse more than 30 yeras and try to teach my team how to used nursing process but it not success. You make me feel it simple and easy to understand . I will use your concept for my team. Thank you somuch
THANK, THANK YOU, THANK YOU FOR THE RESOURCEFUL INFORMATION.
please i want care plan on risk for unstable blood pressure i am a nursing student
@joseph auarshie jnr, can you please send me your care plan if you made it already ? I am a nursing student too. Thank you appreciated
Thanks, I look forward to learning more from you and maybe joining you in writing once am done with school. It’s awesome.
You’re very much welcome! Please feel free to ask further questions. Thank you and goodluck!
I what to check out nursing care plan
Comment: good explanation of health issue pattern
This is great. Thanks for given your time to this. Is so educative. Up thumb
Thanks alot am so interested on this
Great Work!
Thank you for the resourceful information which I was thought in school but almost forgotten until now, brain refresh, thanks
Excellent job done congratulations to all the team worker .
Please is the component of nursing diagnosis the same as type of nursing diagnosis
Each time I research about nursing diagnoses, there is something new to learn. This is a very well written piece giving great insights about nursing. More than ever, I have a better understanding of the unique body of nursing knowledge. Bravo to the Matt and entire Nurseslabs team
Thank you! Be sure to visit also our nursing care plans here .
Sorry madam the risk factors thus the potential problem has the related factors not the sign and symptom because that something has not happed yet so there is no sign and symptoms. Thank you
Excellent work and expertise team work
Usefull information
Nice work Sir/Madam thank you for giving us more hints on Nursing Diagnoses. Excellent team work.
Thank you so much for this nursing diagnosis.
Formulations of the DX has been hectic but thanks to matt vera has been of great help especally answering medsurge quizes just try to expand more on the second part (related to)of actual diagnosis
Hi Mary, Thanks you so much for your comment and endorsement. We welcome your students, thanks again!
Very useful indeed. thank you
I’m practicing nursing diagnosis by using the practice case studies my professor provided but I’m not sure if I’m doing it correctly. Here’s what I’m thinking: Problem:Anxiety Etiology: morning bouts of fear Signs and symptoms: patient stated waking nervous, light headed, agitated, and having a pounding heart Anxiety related to morning bouts of fear as evidenced by patient’s reports of waking light headed, agitated, and having a pounding heart.
In this case study we know to patient has been experiencing anxiety since childhood and was verbally abused by his father. His anxiety is causing difficulties for him to make decisions and he fears he’ll experience misfortunes whenever going to school. We also know about these bouts he has ever morning, which I thought would be a good primary diagnosis because they almost seem like a panic attack which would be extreme anxiety which is a big deal right? Am I thinking about this the right way or not and if not, what should I be concerned about as most important and how should my diagnosis be worded?
The nursing diagnostic statement you made sounds right. For the “as evidenced by” part, I would add the statement of the patient in verbatim since this is a subjective data (place it also under quotation marks) and if possible, do your own assessment and objectively obtain the data.
I would write it this way:
Anxiety related to morning bouts of fear as evidenced by increased in heart rate, apprehensiveness, and patient stating “waking lightheaded, agitated, and having a pounding heart”
well precised and nice to read.
Thanks so much for this readings, am so interested with this website I hope i could use this for my whole time
Hello Professor Matt Vera
I am Mai Ba Hai, from Hue University of Medicine and Pharmacy,faculty of nursing.I found that this content is very useful and helpful to me. I think that this content is really fit to my teaching, so I would like to ask your permission that I can translate this content into my languages (Vietnamese) to teach for my nursing students in Vietnam. I will cite you as author of this document. If you are willing to help in this point I really appreciate about it. I am looking forward to receiving your agreement. Yours sincerely.
This is so fantastic!! Thank you for taking out time to create this wonderful piece
You guys are wonderful. Thanks so much.
Very nice and very interested More ink to your pen I pray
Very useful, thank you so much
Thanks so much for the good job. Nurse Timothy Idachaba (RN, RNE, .MSC in view) from Nigeria
Matt Vera, BSN, R.N, First, I want to thank you for your amazing, short and precise note you provided for us. But I think I’ve got some trouble understanding about 3 components of Nursing diagnosis. This is because there is some variation between defining characteristics among your examples of actual and potential nursing diagnosis. Actual nursing diagnosis -Ineffective breathing pattern related to decreased lung expansion AS EVIDENCED BY dyspnoea, coughing, and difficulty of breathing. Risk diagnosis -Risk for ineffective airway clearance AS EVIDENCED BY accumulation_of_secreations_in_the_Lung. -Risk for fall AS EVIDENCED BY Muscle_weakness ……………………………………………………. As I know before, risk Nursing diagnosis misses Defining characteristics. because, the problem is not happened. but it is to happen.
So, when I compare defining characteristics among actual and risk diagnosis, there is disagreement. Accumulation of secretion in the lung is aetiology for ineffective airway clearance. But you provided it as defining characteristics. So, please make it clear.
Well elaborated, i like using nurseslabs, i always understand easily
Educative I appreciate
Such a beautiful explanation. Thank you
Very comprehensive and understandable. A job Well done by the group
Nice piece, thanks for painstakingly organizing this concise notes, God bless you
Very educative and simple to understand. Thank you for the effort
This is very handy. Your work is appreciated
This is an excellent work . I was having lectures just now on nursing diagnosis and care plan and this note helps me a lot
Its so helpful. Thank you!
Very good content. Happy to learn the Nursing diagnosis. Thanks Nurseslabs
This is a great educative article, kind of review of the nursing diagnosis. Thanks a lot for refreshing my memory.
Sorry, it’s not.
This was so simple and very helpful
So simple, concise and very helpful.
I APPRECIATE THIS WORK, USEFUL AND EASY TO UNDERSTAND.
Beautiful. I love the nursing care plan links. it is just what I have been searching for to assist my students. Thank you
I’ve been a nurse (currently working PRN) since 2015 and not having used nursing diagnosis in my day to day, this source was super helpful and a great refresher! Much thanks to the author!
Thanks for this it was very good and easy to comprehend
Thank you for your opinion; however, I agree with Mebratu. The description shown in your article for statement of “risk for” problem is confusing to me.
My view is as follows: “Actual problem” has 3 parts: nursing diagnosis (client’s problem) related to etiology (pathophysiology of what is causing the problem) as evidenced by defining characteristics (signs and symptoms of the problem)
“Risk for problem” has 2 parts: nursing diagnosis (client’s potential problem) related to etiology (client condition that may cause the problem) There is no “as evidenced by” because there IS no evidence of the problem since the problem does not yet exist.
Very nice and easy explanation, thanku
Please I need the actual manual that’s currently being used or at least a link to it -the NANDA-I document.
For the most current NANDA-I Nursing Diagnosis manual, you might want to check out the latest edition of the “Nursing Diagnosis Handbook” by NANDA International. This handbook is frequently updated with new diagnoses and guidelines.
congratulations MATT VERA, for the very nice and usefully presentation in nursing diagnosis. it has been very usefully for patient care and teaching activities. simple and very nice understandable.
Thanks a lot Matt Vera for the simplicity of the nursing diagnoses. Continue with other pieces of work
You’re welcome! I’m thrilled to hear you found the simplicity of the nursing diagnoses helpful. Your encouragement means a lot, and I’m definitely motivated to keep creating and simplifying more content for you and others in the nursing community.
If there are any specific topics or areas you’d like to see covered next, please let me know. Your feedback is invaluable in guiding the work I do.
Really interesting I thank you
Very impressive step by step explanations
Its good explanation. how to download
Really helpful Thank you
Hi Aneena, You’re welcome! I’m glad to hear you found the nursing diagnosis guide helpful. Is there a particular area or diagnosis you’d like to explore more deeply, or do you have any other questions about nursing diagnoses? Always here to help!
Leave a Comment Cancel reply
The Ultimate Guide to Nursing Diagnosis in 2024
What is a nursing diagnosis.
- NANDA Nursing Diagnosis
- Classification
NANDA Nursing Diagnosis List
Writing a nursing diagnosis.
- Nursing Diagnosis vs Medical Diagnosis
- American vs International

A nursing diagnosis is a part of the nursing process and is a clinical judgment that helps nurses determine the plan of care for their patients. These diagnoses drive possible interventions for the patient, family, and community. They are developed with thoughtful consideration of a patient’s physical assessment and can help measure outcomes for the nursing care plan .
In this article, we'll explore the NANDA nursing diagnosis list, examples of nursing diagnoses, and the 4 types.
Some nurses may see nursing diagnoses as outdated and arduous. However, it is an essential tool that promotes patient safety by utilizing evidence-based nursing research.
According to NANDA-I, the official definition of the nursing diagnosis is:
“Nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse is accountable.”
Find Nursing Programs
What is the purpose of a nursing diagnosis.
According to NANDA International , a nursing diagnosis is “a judgment based on a comprehensive nursing assessment.” The nursing diagnosis is based on the patient’s current situation and health assessment, allowing nurses and other healthcare providers to see a patient's care from a holistic perspective.
Proper nursing diagnoses can lead to greater patient safety, quality care, and increased reimbursement from private health insurance, Medicare, and Medicaid.
They are just as beneficial to nurses as they are to patients.
NANDA Nursing Diagnosis
NANDA diagnoses help strengthen a nurse’s awareness, professional role, and professional abilities.
Formed in 1982, NANDA is a professional organization that develops, researches, disseminates, and refines the nursing terminology of nursing diagnosis. Originally an acronym for the North American Nursing Diagnosis Association, NANDA was renamed to NANDA International in 2002 as a response to its broadening worldwide membership.
According to its website, NANDA International’s mission is to:
- Provide the world’s leading evidence-based nursing diagnoses for use in practice and to determine interventions and outcomes
- Contribute to patient safety through the integration of evidence-based terminology into clinical practice and clinical decision-making
- Fund research through the NANDA-I Foundation
- Be a supportive and energetic global network of nurses, who are committed to improving the quality of nursing care and improvement of patient safety through evidence-based practice
NANDA members can be found worldwide, specifically in Brazil, Colombia, Ecuador, Mexico, Peru, Portugal, Germany, Austria, Switzerland, Netherlands, Belgium, and Nigeria-Ghana.
NANDA Classification of Nursing Diagnoses
NANDA-I adopted the Taxonomy II after consideration and collaboration with the National Library of Medicine (NLM) in regards to healthcare terminology codes. Taxonomy II has three levels: domains, classes, and nursing diagnoses.
There are currently 13 domains and 47 classes:
- Health Awareness
- Health Management
- Urinary Function
- Gastrointestinal Function
- Integumentary Function
- Respiratory Function
- Activity/Exercise
- Energy Balance
- Cardiovascular-Pulmonary Responses
- Orientation
- Sensation/Perception
- Communication
- Self-concept
- Self-esteem
- Caregiving Roles
- Family Relationships
- Role Performance
- Sexual Identity
- Sexual Function
- Reproduction
- Post-trauma Responses
- Coping Response
- Neuro-Behavioral Stress
- Value/Belief Action Congruence
- Physical Injury
- Environmental Hazards
- Defensive Processes
- Thermoregulation
- Physical Comfort
- Environmental Comfort
- Social Comfort
- Development
This refined Taxonomy is based on the Functional Health Patterns assessment framework of Dr. Mary Joy Gordon. Furthermore, the NLM suggested changes because the Taxonomy I code structure included information about the location and the level of the diagnosis.
NANDA-I nursing diagnoses and Taxonomy II comply with the International Standards Organization (ISO) terminology model for a nursing diagnosis.
The terminology is also registered with Health Level Seven International (HL7), an international healthcare informatics standard that allows for nursing diagnoses to be identified in specific electronic messages among different clinical information systems.
A full list of NANDA-I-approved nursing diagnoses can be found here .
Additional examples include:
- Dysfunctional ventilatory weaning response
- Impaired transferability
- Activity intolerance
- Situational low self-esteem
- Risk for disturbed maternal-fetal dyad
- Impaired emancipated decision-making
- Risk for impaired skin integrity
- Risk for metabolic imbalance syndrome
- Urge urinary incontinence
- Risk for unstable blood pressure
- Impaired verbal communication
- Acute confusion
- Disturbed body image
- Relocation stress syndrome
- Ineffective role performance
- Readiness for enhanced sleep
Examples of Nursing Diagnoses
The three main components of a nursing diagnosis are as follows.
- Problem and its definition
- Defining characteristics or risk factors
Examples of proper nursing diagnoses may include:
>> Related: What is the Nursing Process?
NANDA Nursing Diagnosis Types
There are 4 types of nursing diagnoses according to NANDA-I. They are:
- Problem-focused
- Health promotion
1. Problem-focused diagnosis
A patient problem present during a nursing assessment is known as a problem-focused diagnosis. Generally, the problem is seen throughout several shifts or a patient’s entire hospitalization. However, it may be resolved during a shift depending on the nursing and medical care.
Problem-focused diagnoses have three components.
- Nursing diagnosis
- Related factors
- Defining characteristics
Examples of this type of nursing diagnosis include:
- Decreased cardiac output
- Chronic functional constipation
- Impaired gas exchange
Problem-focused nursing diagnoses are typically based on signs and symptoms present in the patient. They are the most common nursing diagnoses and the easiest to identify.
2. Risk nursing diagnosis
A risk nursing diagnosis applies when risk factors require intervention from the nurse and healthcare team prior to a real problem developing.
- Risk for imbalanced fluid volume
- Risk for ineffective childbearing process
- Risk for impaired oral mucous membrane integrity
This type of diagnosis often requires clinical reasoning and nursing judgment.
3. Health promotion diagnosis
The goal of a health promotion nursing diagnosis is to improve the overall well-being of an individual, family, or community.
- Readiness for enhanced family processes
- Readiness for enhanced hope
- Sedentary lifestyle
4. Syndrome diagnosis
A syndrome diagnosis refers to a cluster of nursing diagnoses that occur in a pattern or can all be addressed through the same or similar nursing interventions.
Examples of this diagnosis include:
- Decreased cardiac output
- Decreased cardiac tissue perfusion
- Ineffective cerebral tissue perfusion
- Ineffective peripheral tissue perfusion
Possible nursing diagnosis
While not an official type of nursing diagnosis, possible nursing diagnosis applies to problems suspected to arise. This occurs when risk factors are present and require additional information to diagnose a potential problem.
Nursing Diagnosis Components
The three main components of a nursing diagnosis are:
- Etiology or risk factors
1. The problem statement explains the patient’s current health problem and the nursing interventions needed to care for the patient.
2. Etiology, or related factors , describes the possible reasons for the problem or the conditions in which it developed. These related factors guide the appropriate nursing interventions.
3. Finally, defining characteristics are signs and symptoms that allow for applying a specific diagnostic label. Risk factors are used in the place of defining characteristics for risk nursing diagnosis. They refer to factors that increase the patient’s vulnerability to health problems.
>> Show Me Online Nursing Programs
Problem-focused and risk diagnoses are the most difficult nursing diagnoses to write because they have multiple parts. According to NANDA-I , the simplest ways to write these nursing diagnoses are as follows:
PROBLEM-FOCUSED DIAGNOSIS
Problem-Focused Diagnosis related to ______________________ (Related Factors) as evidenced by _________________________ (Defining Characteristics).
RISK DIAGNOSIS
The correct statement for a NANDA-I nursing diagnosis would be: Risk for _____________ as evidenced by __________________________ (Risk Factors).
Nursing Diagnosis vs Medical Diagnosis
While all important, the nursing diagnosis is primarily handled through specific nursing interventions while a medical diagnosis is made by a physician or advanced healthcare practitioner.
The nursing diagnosis can be mental, spiritual, psychosocial, and/or physical. It focuses on the overall care of the patient while the medical diagnosis involves the medical aspect of the patient’s condition.
A medical diagnosis does not change if the condition is resolved, and it remains part of the patient’s health history forever. A nursing diagnosis, however, generally refers to a specific period of time.
Examples of medical diagnosis include:
- Congestive Heart Failure
- Diabetes Insipidus
Collaborative problems are ones that can be resolved or worked on through both nursing and medical interventions. Oftentimes, nurses will monitor the problems while the medical providers prescribe medications or obtain diagnostic tests.
History of Nursing Diagnoses
- 1973: The first conference to identify nursing knowledge and a classification system; NANDA was founded
- 1977: First Canadian Conference takes place in Toronto
- 1982: NANDA formed with members from the United States and Canada
- 1984: NANDA established a Diagnosis Review Committee
- 1987: American Nurses Association (ANA) officially recognizes NANDA to govern the development of a classification system for nursing diagnosis
- 1987: International Nursing Conference held in Alberta, Canada
- 1990: 9th NANDA conference and the official definition of the nursing diagnosis established
- 1997: Official journal renamed from “Nursing Diagnosis” to “Nursing Diagnosis: The International Journal of Nursing Terminologies and Classifications”
- 2002: NANDA changes to NANDA International (NANDA-I) and Taxonomy II released
- 2020: 244 NANDA-I approved diagnosis
American vs International Nursing Diagnosis
There is currently no difference between American nursing diagnoses and international nursing diagnoses. Because NANDA-I is an international organization, the approved nursing diagnoses are the same.
Discrepancies may occur when the translation of a nursing diagnosis into another language alters the syntax and structure. However, since there are NANDA-I offices around the world, the non-English nursing diagnoses are essentially the same.
What is an example of a nursing diagnosis?
- A nursing diagnosis is something a nurse can make that does not require an advanced provider’s input. It is not a medical diagnosis. An example of a nursing diagnosis is: Excessive fluid volume related to congestive heart failure as evidenced by symptoms of edema.
What is the most common nursing diagnosis?
- According to NANDA, some of the most common nursing diagnoses include pain, risk of infection, constipation, and body temperature imbalance.
What is a potential nursing diagnosis?
- A potential problem is an issue that could occur with the patient’s medical diagnosis, but there are no current signs and symptoms of it. For instance, skin integrity breakdown could occur in a patient with limited mobility.
How is a nursing diagnosis written?
- Nursing diagnoses are written with a problem or potential problem related to a medical condition, as evidenced by any presenting symptoms. There are 4 types of nursing diagnoses: risk-focused, problem-focused, health promotion-focused, or syndrome-focused.
What is the clinical diagnosis?
- A clinical diagnosis is the official medical diagnosis issued by a physician or other advanced care professional.

Kathleen Gaines (nee Colduvell) is a nationally published writer turned Pediatric ICU nurse from Philadelphia with over 13 years of ICU experience. She has an extensive ICU background having formerly worked in the CICU and NICU at several major hospitals in the Philadelphia region. After earning her MSN in Education from Loyola University of New Orleans, she currently also teaches for several prominent Universities making sure the next generation is ready for the bedside. As a certified breastfeeding counselor and trauma certified nurse, she is always ready for the next nursing challenge.

Plus, get exclusive access to discounts for nurses, stay informed on the latest nurse news, and learn how to take the next steps in your career.
By clicking “Join Now”, you agree to receive email newsletters and special offers from Nurse.org. We will not sell or distribute your email address to any third party, and you may unsubscribe at any time by using the unsubscribe link, found at the bottom of every email.

How to Write a Nursing Case Study Paper (A Guide)

Most nursing students dread writing a nursing case study analysis paper, yet it is a mandatory assignment; call it a rite of passage in nursing school. This is because it is a somewhat tricky process that is often overwhelming for nursing students. Nevertheless, by reading this guide prepared by our best nursing students, you should be able to easily and quickly write a nursing case study that can get you an excellent grade.
How different is this guide from similar guides all over the internet? Very different!
This guide provides all the pieces of information that one would need to write an A-grade nursing case study. These include the format for a nursing case study, a step-by-step guide on how to write a nursing case study, and all the important tips to follow when writing a nursing case study.
This comprehensive guide was developed by the top nursing essay writers at NurseMyGrade, so you can trust that the information herein is a gem that will catapult your grades to the next level. Expect updates as we unravel further information about writing a nursing case study.
Now that you know you’ve discovered a gold mine , let’s get right into it.
What Is a Nursing Case Study?
A nursing case study is a natural or imagined patient scenario designed to test the knowledge and skills of student nurses. Nursing case study assignments usually focus on testing knowledge and skills in areas of nursing study related to daily nursing practice.
As a nursing student, you must expect a nursing case study assignment at some point in your academic life. The fact that you are reading this post means that point is now.
While there is no standard structure for writing a nursing case study assignment, some things or elements must be present in your nursing assignment for your professor to consider it complete.
In the next section, you will discover what your instructor n expects in your nursing case study analysis. Remember, these are assignments where you are given a case study and are expected to write a case analysis report explaining how to handle such scenarios in real-life settings.
The Nursing Case Study Template
The typical nursing case study has nine sections. These are:
- Introduction
- Case presentation (Patient info, history, and medical condition)
- Diagnosis/Nursing assessment
- Intervention/Nursing care plan
- Discussion and recommendations
The Structure of a Nursing Case Study Analysis
You now know what nursing professors expect in a nursing case study analysis. In this section, we will explain what to include in each section of your nursing case study analysis to make it an excellent one.
1. Title page
The title page is essential in all types of academic writing. You must include it in your nursing case study analysis or any other essay or paper. And you must include it in the format recommended by your college.
If your college has no specific title page format, use the title page format of the style requested in the assignment prompt. In nursing college, virtually all assignments should be written in Harvard or APA format .
So, check your assignment prompt and create your title page correctly. The typical title page should include the topic of your paper, your name, the name of your professor, the course name, the date you are submitting the paper, and the name of your college.
2. Abstract
Most nursing professors require you to include an abstract in your nursing case study analysis. And even when you are not explicitly required to write one, it is good to do so. Of course, you should consult with your professor before doing so.
When writing an abstract for your paper, make sure it is about 200 words long. The abstract should include a brief summary of the case study, including all the essential information in the patient presentation, such as the history, age, and current diagnosis.
The summary should also include the nursing assessment, the current interventions, and recommendations.
3. Introduction
After writing the title page and the abstract, start writing the introduction. The introduction of a nursing case study analysis must briefly include the patient’s presentation, current diagnosis and medication, and recommendations. It must also include a strong thesis statement that shows what the paper is all about.
You shouldn’t just write an introduction for the sake of it. If you do so, your introduction will be bland. You need to put in good effort when writing your introduction. The best way to do this is to use your introduction to show you understand the case study perfectly and that you will analyze it right.
You can always write your introduction last. Many students do this because they believe writing an introduction last makes it more precise and accurate.

4. Case Presentation (Status of the Patient)
After introducing your nursing case study analysis, you should present the case where you outline the patient's status. It is usually straightforward to present a case.
You must paraphrase the patient scenario in the assignment prompt or brief. Focus on the demographic data of the patient (who they are, age, race, height, skin tone, occupation, relationships, marital status, appearance, etc.), why they are in the case study or scenario, reasons they sought medical attention, chief complaint, and current diagnosis and treatment. You should also discuss the actions performed on the patient, such as admission to the ICU, taking vital signs, recommending tests, etc.
In short, everything necessary in the patient scenario should be in your case presentation. You only need to avoid copying the patient scenario or case study word-for-word when writing your case presentation.
5. Diagnosis and Assessment
After the case presentation, you should explain the diagnosis. In other words, you should explain the condition, disease, or medical situation highlighted in the case presentation. For example, if the patient is a heavy smoker and he has COPD, it is at this point that you explain how COPD is linked to heavy smoking.
This is the section where you thoroughly discuss the disease process (pathophysiology) by highlighting the causes, symptoms, observations, and treatment methods. You should relate these to the patient’s status and give concrete evidence. You should describe the progression of the disease from when the client was admitted to a few hours or days after they were stabilized. Consider the first indication of the disease that prompted the patient to seek further medical assistance.
Your paper should also elucidate the diagnostic tests that should be conducted and the differential diagnosis. Ensure that each is given a well-founded rationale.
When explaining the condition, go deep into the pathophysiology. Focus specifically on the patient’s risk factors. Ensure you get your explanation from recent nursing literature (peer-reviewed scholarly journals published in the last 5 years). And do not forget to cite all the literature you get your facts from.
In short, this section should explain the patient’s condition or suffering.
6. Nursing Intervention
After the diagnosis and nursing assessment section, your nursing case study analysis should have an intervention section. This section is also known as the nursing care planning section. What you are supposed to do in this section is to present a nursing care plan for the patient presented in the patient scenario. You should describe the nursing care plan and goals for the patient. Record all the anticipated positive changes and assess whether the care plan addresses the patient's condition.
A good nursing care plan details the patient’s chief complaints or critical problems. It then describes the causes of these problems using evidence from recent medical or nursing literature. It then details the potential intervention for each problem. Lastly, it includes goals and evaluation strategies for the measures. Most professors, predominantly Australian and UK professors, prefer if this section is in table format.
Some nursing professors regard the intervention section (or nursing care plan section) as the most critical part of a nursing case study. This is because this part details precisely how the student nurse will react to the patient scenario (which is what the nursing professors want to know). So, ensure you make a reasonable effort when developing this section to get an excellent grade.
7. Discussion and Recommendations
The intervention section in a nursing case study is followed by a discussion and recommendations section. In this section, you are supposed to expound on the patient scenario, the diagnosis, and the nursing care plan. You should also expound on the potential outcomes if the care plan is followed correctly. The discussion should also explain the rationale for the care plan or its significant bits.
Recommendations should follow the discussion. Recommendations usually involve everything necessary that can be done or changed to manage a patient’s condition or prevent its reoccurrence. Anything that enhances the patient’s well-being can be a recommendation. Just make sure your key recommendations are supported by evidence.
8. Conclusion
This is the second last section of a typical nursing case study. What you need here is to summarize the entire case study. Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations.
At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible.
9. References
This is the last section of a nursing case study. No nursing case study is complete without a references section. You should ensure your case study has in-text citations and a references page.
And you should make sure both are written as recommended in the assignment. The style section is usually Harvard or APA. Follow the recommended style to get a good grade on your essay.
Step-By-Step Guide to Writing a Nursing Case Study
You know all the key sections you must include in a nursing case study. You also know what exactly you need to do in each section. It is time to learn how to write a nursing case study. The process detailed below should be easy to follow because you know the typical nursing case study structure.
1. Understand the Assignment
When given a nursing case study assignment, the first thing you need to do is to read. You need to read two pieces of information slowly and carefully.
First, you need to read the prompt itself slowly and carefully. This is important because the prompt will have essential bits of information you need to know, including the style, the format, the word count, and the number of references needed. All these bits of information are essential to ensure your writing is correct.
Second, you need to read the patient scenario slowly and carefully. You should do this to understand it clearly so that you do not make any mistakes in your analysis.
2. Create a Rough Outline
Failure to plan is a plan to fail. That is not what you are in it for anyway! In other words, do not fail to create an outline for your case study analysis. Use the template provided in this essay to create a rough outline for your nursing case study analysis.
Ensure your outline is as detailed as it can be at this stage. You can do light research to achieve this aim. However, this is not exactly necessary because this is just a rough outline.
3. Conduct thorough research
After creating a rough outline, you should conduct thorough research. Your research should especially focus on providing a credible and evidence-based nursing assessment of the patient problem(s). You should only use evidence from recent nursing or medical literature.
You must also conduct thorough research to develop an effective intervention or nursing care plan. So when researching the patient’s problem and its diagnosis, you should also research the most suitable intervention or do it right after.
When conducting research, you should always note down your sources. So for every piece of information you find, and what to use, you should have its reference.
After conducting thorough research, you should enhance your rough outline using the new information you have discovered. Make sure it is as comprehensive as possible.
4. Write your nursing case study
You must follow your comprehensive outline to write your case study analysis at this stage. If you created a good outline, you should find it very easy to write your nursing case study analysis.
If you did not, writing your nursing case study will be challenging. Whenever you are stuck writing your case study analysis paper, you should re-read the part where we explain what to include in every section of your analysis. Doing so will help you know what to write to continue your essay. Writing a nursing case study analysis usually takes only a few hours.
5. Reference your case study
After writing your case study, ensure you add all in-text citations if you have not already. And when adding them, you should follow the style/format recommended in the assignment prompt (usually APA or Harvard style).
After adding in-text citations exactly where they need to be and in the correct format, add all the references you have used in a references page. And you should add them correctly as per the rules of the style you were asked to use.
Do not forget to organize your references alphabetically after creating your references page.
6. Thoroughly edit your case study
After STEP 5 above, you need to edit your case study. You should edit it slowly and carefully. Do this by proofreading it twice. Proofread it slowly each time to discover all the grammar, style, and punctuation errors. Remove all the errors you find.
After proofreading your essay twice, recheck it to ensure every sentence is straightforward. This will transform your ordinary case study into an A-grade one. Of course, it must also have all the standard sections expected in a case study.
Recheck your case study using a grammarly.com or a similar computer grammar checker to ensure it is perfect. Doing this will help you catch and eliminate all the remaining errors in your work.
7. Submit your case study analysis
After proofreading and editing your case study analysis, it will be 100% ready for submission. Just convert it into the format it is required in and submit it.
Nursing Case Study Tips and Tricks
The guide above and other information in this article should help you develop a good nursing case study analysis. Note that this guide focuses entirely on nursing case scenario-based papers, not research study-based nursing case studies. The tips and tricks in this section should help you ensure that the nursing case study analysis you create is excellent.
1. Begin early
The moment you see a nursing case study assignment prompt, identify a date to start writing it and create your own deadline to beat before the deadline stated in the prompt.
Do this and start writing your case study analysis early before your deadline. You will have plenty of time to do excellent research, develop an excellent paper, and edit your final paper as thoroughly as you want.
Most student nurses combine work and study. Therefore, if you decide to leave a nursing case study assignment until late to complete it, something could come up, and you could end up failing to submit it or submitting a rushed case study analysis.
2. Use the proper terminology
When writing an essay or any other academic paper, you are always encouraged to use the most straightforward language to make your work easy to understand. However, this is not true when writing a nursing case study analysis. While your work should certainly be easy to understand, you must use the right nursing terminology at every point where it is necessary. Failure to do this could damage your work or make it look less professional or convincing.
3. Avoid copying and pasting
If you are a serious nursing student, you know that copying and pasting are prohibited in assignments. However, sometimes copying and pasting can seem okay in nursing case studies. For example, it can seem okay to copy-paste the patient presentation. However, this is not okay. You are supposed to paraphrase the verbatim when presenting the patient presentation in your essay. You should also avoid copy-pasting information or texts directly. Every fact or evidence you research and find should be paraphrased to appear in your work. And it should be cited correctly.
4. Always ask for help if stuck
This is very important. Students are usually overwhelmed with academic work, especially a month or two to the end of the semester. If you are overwhelmed and think you will not have the time to complete your nursing case study analysis or submit a quality one, ask for help. Ask for help from a nursing assignment-help website like ours, and you will soon have a paper ready that you can use as you please. If you choose to get help from us, you will get a well-researched, well-planned, well-developed, and fully edited nursing case study.
5. Format your paper correctly
Many students forget to do proper formatting after writing their nursing case study analyses. Before you submit your paper, make sure you format it correctly. If you do not format your paper correctly, you will lose marks because of poor formatting. If you feel you are not very confident with your APA or Harvard formatting skills, send your paper to us to get it correctly formatted and ready for submission.
Now that you are all set up …
Our company has been among the best-rated nursing homework help companies in the last few years. Thousands of students have benefitted from our many academic writing guides. Many more have benefitted from direct help given by our experts.
- How to write a nursing philosophy statement.
- Writing an abstract poster presentation.
We have experienced nursing experts available every day of the week to provide nursing assignment help. They can easily research and write virtually any nursing assignment, including a nursing case study. So, if the information provided in this article isn’t making you feel any optimistic about writing an excellent nursing case study, get help from us.
Get help by ordering a custom nursing case study through this very website. If you do so, you will get a 100% original paper that is well-researched, well-written, well-formatted, and adequately referenced. Since the paper is original, you can use it anywhere without problems.
Thousands of students trust our company every week, month, and year. Be like them! Trust us for 100% confidentiality and speedy delivery.
Struggling with
Related Articles

Tips to help you Succeed in Nursing School
Tips to Succeed in Shadow Health Assessment (A Nurse Student Guide)

Choosing your Nursing Dissertation Topic : A Quick Guide
NurseMyGrades is being relied upon by thousands of students worldwide to ace their nursing studies. We offer high quality sample papers that help students in their revision as well as helping them remain abreast of what is expected of them.
Health Case Studies
(29 reviews)
Glynda Rees, British Columbia Institute of Technology
Rob Kruger, British Columbia Institute of Technology
Janet Morrison, British Columbia Institute of Technology
Copyright Year: 2017
Publisher: BCcampus
Language: English
Formats Available
Conditions of use.
Learn more about reviews.
Reviewed by Jessica Sellars, Medical assistant office instructor, Blue Mountain Community College on 10/11/23
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and... read more
Comprehensiveness rating: 5 see less
This is a book of compiled and very well organized patient case studies. The author has broken it up by disease patient was experiencing and even the healthcare roles that took place in this patients care. There is a well thought out direction and plan. There is an appendix to refer to as well if you are needing to find something specific quickly. I have been looking for something like this to help my students have a base to do their project on. This is the most comprehensive version I have found on the subject.
Content Accuracy rating: 5
This is a book compiled of medical case studies. It is very accurate and can be used to learn from great care and mistakes.
Relevance/Longevity rating: 5
This material is very relevant in this context. It also has plenty of individual case studies to utilize in many ways in all sorts of medical courses. This is a very useful textbook and it will continue to be useful for a very long time as you can still learn from each study even if medicine changes through out the years.
Clarity rating: 5
The author put a lot of thought into the ease of accessibility and reading level of the target audience. There is even a "how to use this resource" section which could be extremely useful to students.
Consistency rating: 5
The text follows a very consistent format throughout the book.
Modularity rating: 5
Each case study is individual broken up and in a group of similar case studies. This makes it extremely easy to utilize.
Organization/Structure/Flow rating: 5
The book is very organized and the appendix is through. It flows seamlessly through each case study.
Interface rating: 5
I had no issues navigating this book, It was clearly labeled and very easy to move around in.
Grammatical Errors rating: 5
I did not catch any grammar errors as I was going through the book
Cultural Relevance rating: 5
This is a challenging question for any medical textbook. It is very culturally relevant to those in medical or medical office degrees.
I have been looking for something like this for years. I am so happy to have finally found it.
Reviewed by Cindy Sun, Assistant Professor, Marshall University on 1/7/23
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and... read more
Interestingly, this is not a case of ‘you get what you pay for’. Instead, not only are the case studies organized in a fashion for ease of use through a detailed table of contents, the authors have included more support for both faculty and students. For faculty, the introduction section titled ‘How to use this resource’ and individual notes to educators before each case study contain application tips. An appendix overview lists key elements as issues / concepts, scenario context, and healthcare roles for each case study. For students, learning objectives are presented at the beginning of each case study to provide a framework of expectations.
The content is presented accurately and realistic.
The case studies read similar to ‘A Day In the Life of…’ with detailed intraprofessional communications similar to what would be overheard in patient care areas. The authors present not only the view of the patient care nurse, but also weave interprofessional vantage points through each case study by including patient interaction with individual professionals such as radiology, physician, etc.
In addition to objective assessment findings, the authors integrate standard orders for each diagnosis including medications, treatments, and tests allowing the student to incorporate pathophysiology components to their assessments.
Each case study is arranged in the same framework for consistency and ease of use.
This compilation of eight healthcare case studies focusing on new onset and exacerbation of prevalent diagnoses, such as heart failure, deep vein thrombosis, cancer, and chronic obstructive pulmonary disease advancing to pneumonia.
Each case study has a photo of the ‘patient’. Simple as this may seem, it gives an immediate mental image for the student to focus.
Interface rating: 4
As noted by previous reviewers, most of the links do not connect active web pages. This may be due to the multiple options for accessing this resource (pdf download, pdf electronic, web view, etc.).
Grammatical Errors rating: 4
A minor weakness that faculty will probably need to address prior to use is regarding specific term usages differences between Commonwealth countries and United States, such as lung sound descriptors as ‘quiet’ in place of ‘diminished’ and ‘puffers’ in place of ‘inhalers’.
The authors have provided a multicultural, multigenerational approach in selection of patient characteristics representing a snapshot of today’s patient population. Additionally, one case study focusing on heart failure is about a middle-aged adult, contrasting to the average aged patient the students would normally see during clinical rotations. This option provides opportunities for students to expand their knowledge on risk factors extending beyond age.
This resource is applicable to nursing students learning to care for patients with the specific disease processes presented in each case study or for the leadership students focusing on intraprofessional communication. Educators can assign as a supplement to clinical experiences or as an in-class application of knowledge.
Reviewed by Stephanie Sideras, Assistant Professor, University of Portland on 8/15/22
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five... read more
The eight case studies included in this text addressed high frequency health alterations that all nurses need to be able to manage competently. While diabetes was not highlighted directly, it was included as a potential comorbidity. The five overarching learning objectives pulled from the Institute of Medicine core competencies will clearly resonate with any faculty familiar with Quality and Safety Education for Nurses curriculum.
The presentation of symptoms, treatments and management of the health alterations was accurate. Dialogue between the the interprofessional team was realistic. At times the formatting of lab results was confusing as they reflected reference ranges specific to the Canadian healthcare system but these occurrences were minimal and could be easily adapted.
The focus for learning from these case studies was communication - patient centered communication and interprofessional team communication. Specific details, such as drug dosing, was minimized, which increases longevity and allows for easy individualization of the case data.
While some vocabulary was specific to the Canadian healthcare system, overall the narrative was extremely engaging and easy to follow. Subjective case data from patient or provider were formatted in italics and identified as 'thoughts'. Objective and behavioral case data were smoothly integrated into the narrative.
The consistency of formatting across the eight cases was remarkable. Specific learning objectives are identified for each case and these remain consistent across the range of cases, varying only in the focus for the goals for each different health alterations. Each case begins with presentation of essential patient background and the progress across the trajectory of illness as the patient moves from location to location encountering different healthcare professionals. Many of the characters (the triage nurse in the Emergency Department, the phlebotomist) are consistent across the case situations. These consistencies facilitate both application of a variety of teaching methods and student engagement with the situated learning approach.
Case data is presented by location and begins with the patient's first encounter with the healthcare system. This allows for an examination of how specific trajectories of illness are manifested and how care management needs to be prioritized at different stages. This approach supports discussions of care transitions and the complexity of the associated interprofessional communication.
The text is well organized. The case that has two levels of complexity is clearly identified
The internal links between the table of contents and case specific locations work consistently. In the EPUB and the Digital PDF the external hyperlinks are inconsistently valid.
The grammatical errors were minimal and did not detract from readability
Cultural diversity is present across the cases in factors including race, ethnicity, socioeconomic status, family dynamics and sexual orientation.
The level of detail included in these cases supports a teaching approach to address all three spectrums of learning - knowledge, skills and attitudes - necessary for the development of competent practice. I also appreciate the inclusion of specific assessment instruments that would facilitate a discussion of evidence based practice. I will enjoy using these case to promote clinical reasoning discussions of data that is noticed and interpreted with the resulting prioritizes that are set followed by reflections that result from learner choices.
Reviewed by Chris Roman, Associate Professor, Butler University on 5/19/22
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various... read more
Comprehensiveness rating: 4 see less
It would be extremely difficult for a book of clinical cases to comprehensively cover all of medicine, and this text does not try. Rather, it provides cases related to common medical problems and introduces them in a way that allows for various learning strategies to be employed to leverage the cases for deeper student learning and application.
The narrative form of the cases is less subject to issues of accuracy than a more content-based book would be. That said, the cases are realistic and reasonable, avoiding being too mundane or too extreme.
These cases are narrative and do not include many specific mentions of drugs, dosages, or other aspects of clinical care that may grow/evolve as guidelines change. For this reason, the cases should be “evergreen” and can be modified to suit different types of learners.
Clarity rating: 4
The text is written in very accessible language and avoids heavy use of technical language. Depending on the level of learner, this might even be too simplistic and omit some details that would be needed for physicians, pharmacists, and others to make nuanced care decisions.
The format is very consistent with clear labeling at transition points.
The authors point out in the introductory materials that this text is designed to be used in a modular fashion. Further, they have built in opportunities to customize each cases, such as giving dates of birth at “19xx” to allow for adjustments based on instructional objectives, etc.
The organization is very easy to follow.
I did not identify any issues in navigating the text.
The text contains no grammatical errors, though the language is a little stiff/unrealistic in some cases.
Cases involve patients and members of the care team that are of varying ages, genders, and racial/ethnic backgrounds
Reviewed by Trina Larery, Assistant Professor, Pittsburg State University on 4/5/22
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand... read more
The book covers common scenarios, providing allied health students insight into common health issues. The information in the book is thorough and easily modified if needed to include other scenarios not listed. The material was easy to understand and apply to the classroom. The E-reader format included hyperlinks that bring the students to subsequent clinical studies.
Content Accuracy rating: 4
The treatments were explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse. The case studies were accurate in explanation. The DVT case study incorrectly identifies the location of the clot in the popliteal artery instead of in the vein.
The content is relevant to a variety of different types of health care providers and due to the general nature of the cases, will remain relevant over time. Updates should be made annually to the hyperlinks and to assure current standard of practice is still being met.
Clear, simple and easy to read.
Consistent with healthcare terminology and framework throughout all eight case studies.
The text is modular. Cases can be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point providing great flexibility. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
The book is well organized, presenting in a logical clear fashion. The appendix allows the student to move about the case study without difficulty.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change based on current guidelines. A few hyperlinks had "page not found".
Few grammatical errors were noted in text.
The case studies include people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. There are roughly 25 broken online links or "pages not found", care needs to be taken to update at least annually and assure links are valid and utilizing the most up to date information.
Reviewed by Benjamin Silverberg, Associate Professor/Clinician, West Virginia University on 3/24/22
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what... read more
Comprehensiveness rating: 3 see less
The appendix reviews the "key roles" and medical venues found in all 8 cases, but is fairly spartan on medical content. The table of contents at the beginning only lists the cases and locations of care. It can be a little tricky to figure out what is going on where, especially since each case is largely conversation-based. Since this presents 8 cases (really 7 with one being expanded upon), there are many medical topics (and venues) that are not included. It's impossible to include every kind of situation, but I'd love to see inclusion of sexual health, renal pathology, substance abuse, etc.
Though there are differences in how care can be delivered based on personal style, changing guidelines, available supplies, etc, the medical accuracy seems to be high. I did not detect bias or industry influence.
Relevance/Longevity rating: 4
Medications are generally listed as generics, with at least current dosing recommendations. The text gives a picture of what care looks like currently, but will be a little challenging to update based on new guidelines (ie, it can be hard to find the exact page in which a medication is dosed/prescribed). Even if the text were to be a little out of date, an instructor can use that to point out what has changed (and why).
Clear text, usually with definitions of medical slang or higher-tier vocabulary. Minimal jargon and there are instances where the "characters" are sorting out the meaning as well, making it accessible for new learners, too.
Overall, the style is consistent between cases - largely broken up into scenes and driven by conversation rather than descriptions of what is happening.
There are 8 (well, again, 7) cases which can be reviewed in any order. Case #2 builds upon #1, which is intentional and a good idea, though personally I would have preferred one case to have different possible outcomes or even a recurrence of illness. Each scene within a case is reasonably short.
Organization/Structure/Flow rating: 4
These cases are modular and don't really build on concepts throughout. As previously stated, case #2 builds upon #1, but beyond that, there is no progression. (To be sure, the authors suggest using case #1 for newer learners and #2 for more advanced ones.) The text would benefit from thematic grouping, a longer introduction and debriefing for each case (there are learning objectives but no real context in medical education nor questions to reflect on what was just read), and progressively-increasing difficulty in medical complexity, ethics, etc.
I used the PDF version and had no interface issues. There are minimal photographs and charts. Some words are marked in blue but those did not seem to be hyperlinked anywhere.
No noticeable errors in grammar, spelling, or formatting were noted.
I appreciate that some diversity of age and ethnicity were offered, but this could be improved. There were Canadian Indian and First Nations patients, for example, as well as other characters with implied diversity, but there didn't seem to be any mention of gender diverse or non-heterosexual people, or disabilities. The cases tried to paint family scenes (the first patient's dog was fairly prominently mentioned) to humanize them. Including more cases would allow for more opportunities to include sex/gender minorities, (hidden) disabilities, etc.
The text (originally from 2017) could use an update. It could be used in conjunction with other Open Texts, as a compliment to other coursework, or purely by itself. The focus is meant to be on improving communication, but there are only 3 short pages at the beginning of the text considering those issues (which are really just learning objectives). In addition to adding more cases and further diversity, I personally would love to see more discussion before and after the case to guide readers (and/or instructors). I also wonder if some of the ambiguity could be improved by suggesting possible health outcomes - this kind of counterfactual comparison isn't possible in real life and could be really interesting in a text. Addition of comprehension/discussion questions would also be worthwhile.
Reviewed by Danielle Peterson, Assistant Professor, University of Saint Francis on 12/31/21
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare... read more
This text provides readers with 8 case studies which include both chronic and acute healthcare issues. Although not comprehensive in regard to types of healthcare conditions, it provides a thorough look at the communication between healthcare workers in acute hospital settings. The cases are primarily set in the inpatient hospital setting, so the bulk of the clinical information is basic emergency care and inpatient protocol: vitals, breathing, medication management, etc. The text provides a table of contents at opening of the text and a handy appendix at the conclusion of the text that outlines each case’s issue(s), scenario, and healthcare roles. No index or glossary present.
Although easy to update, it should be noted that the cases are taking place in a Canadian healthcare system. Terms may be unfamiliar to some students including “province,” “operating theatre,” “physio/physiotherapy,” and “porter.” Units of measurement used include Celsius and meters. Also, the issue of managed care, health insurance coverage, and length of stay is missing for American students. These are primary issues that dictate much of the healthcare system in the US and a primary job function of social workers, nurse case managers, and medical professionals in general. However, instructors that wish to add this to the case studies could do so easily.
The focus of this text is on healthcare communication which makes it less likely to become obsolete. Much of the clinical information is stable healthcare practice that has been standard of care for quite some time. Nevertheless, given the nature of text, updates would be easy to make. Hyperlinks should be updated to the most relevant and trustworthy sources and checked frequently for effectiveness.
The spacing that was used to note change of speaker made for ease of reading. Although unembellished and plain, I expect students to find this format easy to digest and interesting, especially since the script is appropriately balanced with ‘human’ qualities like the current TV shows and songs, the use of humor, and nonverbal cues.
A welcome characteristic of this text is its consistency. Each case is presented in a similar fashion and the roles of the healthcare team are ‘played’ by the same character in each of the scenarios. This allows students to see how healthcare providers prioritize cases and juggle the needs of multiple patients at once. Across scenarios, there was inconsistency in when clinical terms were hyperlinked.
The text is easily divisible into smaller reading sections. However, since the nature of the text is script-narrative format, if significant reorganization occurs, one will need to make sure that the communication of the script still makes sense.
The text is straightforward and presented in a consistent fashion: learning objectives, case history, a script of what happened before the patient enters the healthcare setting, and a script of what happens once the patient arrives at the healthcare setting. The authors use the term, “ideal interactions,” and I would agree that these cases are in large part, ‘best case scenarios.’ Due to this, the case studies are well organized, clear, logical, and predictable. However, depending on the level of student, instructors may want to introduce complications that are typical in the hospital setting.
The interface is pleasing and straightforward. With exception to the case summary and learning objectives, the cases are in narrative, script format. Each case study supplies a photo of the ‘patient’ and one of the case studies includes a link to a 3-minute video that introduces the reader to the patient/case. One of the highlights of this text is the use of hyperlinks to various clinical practices (ABG, vital signs, transfer of patient). Unfortunately, a majority of the links are broken. However, since this is an open text, instructors can update the links to their preference.
Although not free from grammatical errors, those that were noticed were minimal and did not detract from reading.
Cultural Relevance rating: 4
Cultural diversity is visible throughout the patients used in the case studies and includes factors such as age, race, socioeconomic status, family dynamics, and sexual orientation. A moderate level of diversity is noted in the healthcare team with some stereotypes: social workers being female, doctors primarily male.
As a social work instructor, I was grateful to find a text that incorporates this important healthcare role. I would have liked to have seen more content related to advance directives, mediating decision making between the patient and care team, emotional and practical support related to initial diagnosis and discharge planning, and provision of support to colleagues, all typical roles of a medical social worker. I also found it interesting that even though social work was included in multiple scenarios, the role was only introduced on the learning objectives page for the oncology case.
Reviewed by Crystal Wynn, Associate Professor, Virginia State University on 7/21/21
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied... read more
The text covers a variety of chronic diseases within the cases; however, not all of the common disease states were included within the text. More chronic diseases need to be included such as diabetes, cancer, and renal failure. Not all allied health care team members are represented within the case study. Key terms appear throughout the case study textbook and readers are able to click on a hyperlink which directs them to the definition and an explanation of the key term.
Content is accurate, error-free and unbiased.
The content is up-to-date, but not in a way that will quickly make the text obsolete within a short period of time. The text is written and/or arranged in such a way that necessary updates will be relatively easy and straightforward to implement.
The text is written in lucid, accessible prose, and provides adequate context for any jargon/technical terminology used
The text is internally consistent in terms of terminology and framework.
The text is easily and readily divisible into smaller reading sections that can be assigned at different points within the course. Each case can be divided into a chronic disease state unit, which will allow the reader to focus on one section at a time.
Organization/Structure/Flow rating: 3
The topics in the text are presented in a logical manner. Each case provides an excessive amount of language that provides a description of the case. The cases in this text reads more like a novel versus a clinical textbook. The learning objectives listed within each case should be in the form of questions or activities that could be provided as resources for instructors and teachers.
Interface rating: 3
There are several hyperlinks embedded within the textbook that are not functional.
The text contains no grammatical errors.
Cultural Relevance rating: 3
The text is not culturally insensitive or offensive in any way. More examples of cultural inclusiveness is needed throughout the textbook. The cases should be indicative of individuals from a variety of races and ethnicities.
Reviewed by Rebecca Hillary, Biology Instructor, Portland Community College on 6/15/21
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health... read more
This textbook consists of a collection of clinical case studies that can be applicable to a wide range of learning environments from supplementing an undergraduate Anatomy and Physiology Course, to including as part of a Medical or other health care program. I read the textbook in E-reader format and this includes hyperlinks that bring the students to subsequent clinical study if the book is being used in a clinical classroom. This book is significantly more comprehensive in its approach from other case studies I have read because it provides a bird’s eye view of the many clinicians, technicians, and hospital staff working with one patient. The book also provides real time measurements for patients that change as they travel throughout the hospital until time of discharge.
Each case gave an accurate sense of the chaos that would be present in an emergency situation and show how the conditions affect the practitioners as well as the patients. The reader gets an accurate big picture--a feel for each practitioner’s point of view as well as the point of view of the patient and the patient’s family as the clock ticks down and the patients are subjected to a number of procedures. The clinical information contained in this textbook is all in hyperlinks containing references to clinical skills open text sources or medical websites. I did find one broken link on an external medical resource.
The diseases presented are relevant and will remain so. Some of the links are directly related to the Canadian Medical system so they may not be applicable to those living in other regions. Clinical links may change over time but the text itself will remain relevant.
Each case study clearly presents clinical data as is it recorded in real time.
Each case study provides the point of view of several practitioners and the patient over several days. While each of the case studies covers different pathology they all follow this same format, several points of view and data points, over a number of days.
The case studies are divided by days and this was easy to navigate as a reader. It would be easy to assign one case study per body system in an Anatomy and Physiology course, or to divide them up into small segments for small in class teaching moments.
The topics are presented in an organized way showing clinical data over time and each case presents a large number of view points. For example, in the first case study, the patient is experiencing difficulty breathing. We follow her through several days from her entrance to the emergency room. We meet her X Ray Technicians, Doctor, Nurses, Medical Assistant, Porter, Physiotherapist, Respiratory therapist, and the Lab Technicians running her tests during her stay. Each practitioner paints the overall clinical picture to the reader.
I found the text easy to navigate. There were not any figures included in the text, only clinical data organized in charts. The figures were all accessible via hyperlink. Some figures within the textbook illustrating patient scans could have been helpful but I did not have trouble navigating the links to visualize the scans.
I did not see any grammatical errors in the text.
The patients in the text are a variety of ages and have a variety of family arrangements but there is not much diversity among the patients. Our seven patients in the eight case studies are mostly white and all cis gendered.
Some of the case studies, for example the heart failure study, show clinical data before and after drug treatments so the students can get a feel for mechanism in physiological action. I also liked that the case studies included diet and lifestyle advice for the patients rather than solely emphasizing these pharmacological interventions. Overall, I enjoyed reading through these case studies and I plan to utilize them in my Anatomy and Physiology courses.
Reviewed by Richard Tarpey, Assistant Professor, Middle Tennessee State University on 5/11/21
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate... read more
As a case study book, there is no index or glossary. However, medical and technical terms provide a useful link to definitions and explanations that will prove useful to students unfamiliar with the terms. The information provided is appropriate for entry-level health care students. The book includes important health problems, but I would like to see coverage of at least one more chronic/lifestyle issue such as diabetes. The book covers adult issues only.
Content is accurate without bias
The content of the book is relevant and up-to-date. It addresses conditions that are prevalent in today's population among adults. There are no pediatric cases, but this does not significantly detract from the usefulness of the text. The format of the book lends to easy updating of data or information.
The book is written with clarity and is easy to read. The writing style is accessible and technical terminology is explained with links to more information.
Consistency is present. Lack of consistency is typically a problem with case study texts, but this book is consistent with presentation, format, and terminology throughout each of the eight cases.
The book has high modularity. Each of the case studies can be used independently from the others providing flexibility. Additionally, each case study can be partitioned for specific learning objectives based on the learning objectives of the course or module.
The book is well organized, presenting students conceptually with differing patient flow patterns through a hospital. The patient information provided at the beginning of each case is a wonderful mechanism for providing personal context for the students as they consider the issues. Many case studies focus on the problem and the organization without students getting a patient's perspective. The patient perspective is well represented in these cases.
The navigation through the cases is good. There are some terminology and procedure hyperlinks within the cases that do not work when accessed. This is troubling if you intend to use the text for entry-level health care students since many of these links are critical for a full understanding of the case.
There are some non-US variants of spelling and a few grammatical errors, but these do not detract from the content of the messages of each case.
The book is inclusive of differing backgrounds and perspectives. No insensitive or offensive references were found.
I like this text for its application flexibility. The book is useful for non-clinical healthcare management students to introduce various healthcare-related concepts and terminology. The content is also helpful for the identification of healthcare administration managerial issues for students to consider. The book has many applications.
Reviewed by Paula Baldwin, Associate Professor/Communication Studies, Western Oregon University on 5/10/21
The different case studies fall on a range, from crisis care to chronic illness care. read more
The different case studies fall on a range, from crisis care to chronic illness care.
The contents seems to be written as they occurred to represent the most complete picture of each medical event's occurence.
These case studies are from the Canadian medical system, but that does not interfere with it's applicability.
It is written for a medical audience, so the terminology is mostly formal and technical.
Some cases are shorter than others and some go in more depth, but it is not problematic.
The eight separate case studies is the perfect size for a class in the quarter system. You could combine this with other texts, videos or learning modalities, or use it alone.
As this is a case studies book, there is not a need for a logical progression in presentation of topics.
No problems in terms of interface.
I have not seen any grammatical errors.
I did not see anything that was culturally insensitive.
I used this in a Health Communication class and it has been extraordinarily successful. My studies are analyzing the messaging for the good, the bad, and the questionable. The case studies are widely varied and it gives the class insights into hospital experiences, both front and back stage, that they would not normally be able to examine. I believe that because it is based real-life medical incidents, my students are finding the material highly engaging.
Reviewed by Marlena Isaac, Instructor, Aiken Technical College on 4/23/21
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with... read more
This text is great to walk through patient care with entry level healthcare students. The students are able to take in the information, digest it, then provide suggestions to how they would facilitate patient healing. Then when they are faced with a situation in clinical they are not surprised and now how to move through it effectively.
The case studies provided accurate information that relates to the named disease.
It is relevant to health care studies and the development of critical thinking.
Cases are straightforward with great clinical information.
Clinical information is provided concisely.
Appropriate for clinical case study.
Presented to facilitate information gathering.
Takes a while to navigate in the browser.
Cultural Relevance rating: 1
Text lacks adequate representation of minorities.
Reviewed by Kim Garcia, Lecturer III, University of Texas Rio Grande Valley on 11/16/20
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at... read more
The book has 8 case studies, so obviously does not cover the whole of medicine, but the cases provided are descriptive and well developed. Cases are presented at different levels of difficulty, making the cases appropriate for students at different levels of clinical knowledge. The human element of both patient and health care provider is well captured. The cases are presented with a focus on interprofessional interaction and collaboration, more so than teaching medical content.
Content is accurate and un-biased. No errors noted. Most diagnostic and treatment information is general so it will remain relevant over time. The content of these cases is more appropriate for teaching interprofessional collaboration and less so for teaching the medical care for each diagnosis.
The content is relevant to a variety of different types of health care providers (nurses, radiologic technicians, medical laboratory personnel, etc) and due to the general nature of the cases, will remain relevant over time.
Easy to read. Clear headings are provided for sections of each case study and these section headings clearly tell when time has passed or setting has changed. Enough description is provided to help set the scene for each part of the case. Much of the text is written in the form of dialogue involving patient, family and health care providers, making it easy to adapt for role play. Medical jargon is limited and links for medical terms are provided to other resources that expound on medical terms used.
The text is consistent in structure of each case. Learning objectives are provided. Cases generally start with the patient at home and move with the patient through admission, testing and treatment, using a variety of healthcare services and encountering a variety of personnel.
The text is modular. Cases could be used individually within a unit on the given disease process or relevant sections of a case could be used to illustrate a specific point. The appendix is helpful in locating content specific to a certain diagnosis or a certain type of health care provider.
Each case follows a patient in a logical, chronologic fashion. A clear table of contents and appendix are provided which allows the user to quickly locate desired content. It would be helpful if the items in the table of contents and appendix were linked to the corresponding section of the text.
The hyperlinks to content outside this book work, however using the back arrow on your browser returns you to the front page of the book instead of to the point at which you left the text. I would prefer it if the hyperlinks opened in a new window or tab so closing that window or tab would leave you back where you left the text.
No grammatical errors were noted.
The text is culturally inclusive and appropriate. Characters, both patients and care givers are of a variety of races, ethnicities, ages and backgrounds.
I enjoyed reading the cases and reviewing this text. I can think of several ways in which I will use this content.
Reviewed by Raihan Khan, Instructor/Assistant Professor, James Madison University on 11/3/20
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients. read more
The book contains several important health issues, however still missing some chronic health issues that the students should learn before they join the workforce, such as diabetes-related health issues suffered by the patients.
The health information contained in the textbook is mostly accurate.
I think the book is written focusing on the current culture and health issues faced by the patients. To keep the book relevant in the future, the contexts especially the culture/lifestyle/health care modalities, etc. would need to be updated regularly.
The language is pretty simple, clear, and easy to read.
There is no complaint about consistency. One of the main issues of writing a book, consistency was well managed by the authors.
The book is easy to explore based on how easy the setup is. Students can browse to the specific section that they want to read without much hassle of finding the correct information.
The organization is simple but effective. The authors organized the book based on what can happen in a patient's life and what possible scenarios students should learn about the disease. From that perspective, the book does a good job.
The interface is easy and simple to navigate. Some links to external sources might need to be updated regularly since those links are subject to change that is beyond the author's control. It's frustrating for the reader when the external link shows no information.
The book is free of any major language and grammatical errors.
The book might do a little better in cultural competency. e.g. Last name Singh is mainly for Sikh people. In the text Harj and Priya Singh are Muslim. the authors can consult colleagues who are more familiar with those cultures and revise some cultural aspects of the cases mentioned in the book.
The book is a nice addition to the open textbook world. Hope to see more health issues covered by the book.
Reviewed by Ryan Sheryl, Assistant Professor, California State University, Dominguez Hills on 7/16/20
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality... read more
This text contains 8 medical case studies that reflect best practices at the time of publication. The text identifies 5 overarching learning objectives: interprofessional collaboration, client centered care, evidence-based practice, quality improvement, and informatics. While the case studies do not cover all medical conditions or bodily systems, the book is thorough in conveying details of various patients and medical team members in a hospital environment. Rather than an index or glossary at the end of the text, it contains links to outside websites for more information on medical tests and terms referenced in the cases.
The content provided is reflective of best practices in patient care, interdisciplinary collaboration, and communication at the time of publication. It is specifically accurate for the context of hospitals in Canada. The links provided throughout the text have the potential to supplement with up-to-date descriptions and definitions, however, many of them are broken (see notes in Interface section).
The content of the case studies reflects the increasingly complex landscape of healthcare, including a variety of conditions, ages, and personal situations of the clients and care providers. The text will require frequent updating due to the rapidly changing landscape of society and best practices in client care. For example, a future version may include inclusive practices with transgender clients, or address ways medical racism implicitly impacts client care (see notes in Cultural Relevance section).
The text is written clearly and presents thorough, realistic details about working and being treated in an acute hospital context.
The text is very straightforward. It is consistent in its structure and flow. It uses consistent terminology and follows a structured framework throughout.
Being a series of 8 separate case studies, this text is easily and readily divisible into smaller sections. The text was designed to be taken apart and used piece by piece in order to serve various learning contexts. The parts of each case study can also be used independently of each other to facilitate problem solving.
The topics in the case studies are presented clearly. The structure of each of the case studies proceeds in a similar fashion. All of the cases are set within the same hospital so the hospital personnel and service providers reappear across the cases, giving a textured portrayal of the experiences of the various service providers. The cases can be used individually, or one service provider can be studied across the various studies.
The text is very straightforward, without complex charts or images that could become distorted. Many of the embedded links are broken and require updating. The links that do work are a very useful way to define and expand upon medical terms used in the case studies.
Grammatical errors are minimal and do not distract from the flow of the text. In one instance the last name Singh is spelled Sing, and one patient named Fred in the text is referred to as Frank in the appendix.
The cases all show examples of health care personnel providing compassionate, client-centered care, and there is no overt discrimination portrayed. Two of the clients are in same-sex marriages and these are shown positively. It is notable, however, that the two cases presenting people of color contain more negative characteristics than the other six cases portraying Caucasian people. The people of color are the only two examples of clients who smoke regularly. In addition, the Indian client drinks and is overweight, while the First Nations client is the only one in the text to have a terminal diagnosis. The Indian client is identified as being Punjabi and attending a mosque, although there are only 2% Muslims in the Punjab province of India. Also, the last name Singh generally indicates a person who is a Hindu or Sikh, not Muslim.
Reviewed by Monica LeJeune, RN Instructor, LSUE on 4/24/20
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process. read more
Has comprehensive unfolding case studies that guide the reader to recognize and manage the scenario presented. Assists in critical thinking process.
Accurately presents health scenarios with real life assessment techniques and patient outcomes.
Relevant to nursing practice.
Clearly written and easily understood.
Consistent with healthcare terminology and framework
Has a good reading flow.
Topics presented in logical fashion
Easy to read.
No grammatical errors noted.
Text is not culturally insensitive or offensive.
Good book to have to teach nursing students.
Reviewed by april jarrell, associate professor, J. Sargeant Reynolds Community College on 1/7/20
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process. read more
The text is a great case study tool that is appropriate for nursing school instructors to use in aiding students to learn the nursing process.
The content is accurate and evidence based. There is no bias noted
The content in the text is relevant, up to date for nursing students. It will be easy to update content as needed because the framework allows for addition to the content.
The text is clear and easy to understand.
Framework and terminology is consistent throughout the text; the case study is a continual and takes the student on a journey with the patient. Great for learning!
The case studies can be easily divided into smaller sections to allow for discussions, and weekly studies.
The text and content progress in a logical, clear fashion allowing for progression of learning.
No interface issues noted with this text.
No grammatical errors noted in the text.
No racial or culture insensitivity were noted in the text.
I would recommend this text be used in nursing schools. The use of case studies are helpful for students to learn and practice the nursing process.
Reviewed by Lisa Underwood, Practical Nursing Instructor, NTCC on 12/3/19
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own... read more
The text provides eight comprehensive case studies that showcase the different viewpoints of the many roles involved in patient care. It encompasses the most common seen diagnoses seen across healthcare today. Each case study comes with its own set of learning objectives that can be tweaked to fit several allied health courses. Although the case studies are designed around the Canadian Healthcare System, they are quite easily adaptable to fit most any modern, developed healthcare system.
Content Accuracy rating: 3
Overall, the text is quite accurate. There is one significant error that needs to be addressed. It is located in the DVT case study. In the study, a popliteal artery clot is mislabeled as a DVT. DVTs are located in veins, not in arteries. That said, the case study on the whole is quite good. This case study could be used as a learning tool in the classroom for discussion purposes or as a way to test student understanding of DVTs, on example might be, "Can they spot the error?"
At this time, all of the case studies within the text are current. Healthcare is an ever evolving field that rests on the best evidence based practice. Keeping that in mind, educators can easily adapt the studies as the newest evidence emerges and changes practice in healthcare.
All of the case studies are well written and easy to understand. The text includes several hyperlinks and it also highlights certain medical terminology to prompt readers as a way to enhance their learning experience.
Across the text, the language, style, and format of the case studies are completely consistent.
The text is divided into eight separate case studies. Each case study may be used independently of the others. All case studies are further broken down as the focus patient passes through each aspect of their healthcare system. The text's modularity makes it possible to use a case study as individual work, group projects, class discussions, homework or in a simulation lab.
The case studies and the diagnoses that they cover are presented in such a way that educators and allied health students can easily follow and comprehend.
The book in itself is free of any image distortion and it prints nicely. The text is offered in a variety of digital formats. As noted in the above reviews, some of the hyperlinks have navigational issues. When the reader attempts to access them, a "page not found" message is received.
There were minimal grammatical errors. Some of which may be traced back to the differences in our spelling.
The text is culturally relevant in that it includes patients from many different backgrounds and ethnicities. This allows educators and students to explore cultural relevance and sensitivity needs across all areas in healthcare. I do not believe that the text was in any way insensitive or offensive to the reader.
By using the case studies, it may be possible to have an open dialogue about the differences noted in healthcare systems. Students will have the ability to compare and contrast the Canadian healthcare system with their own. I also firmly believe that by using these case studies, students can improve their critical thinking skills. These case studies help them to "put it all together".
Reviewed by Melanie McGrath, Associate Professor, TRAILS on 11/29/19
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case. read more
The text covered some of the most common conditions seen by healthcare providers in a hospital setting, which forms a solid general base for the discussions based on each case.
I saw no areas of inaccuracy
As in all healthcare texts, treatments and/or tests will change frequently. However, everything is currently up-to-date thus it should be a good reference for several years.
Each case is written so that any level of healthcare student would understand. Hyperlinks in the text is also very helpful.
All of the cases are written in a similar fashion.
Although not structured as a typical text, each case is easily assigned as a stand-alone.
Each case is organized clearly in an appropriate manner.
I did not see any issues.
I did not see any grammatical errors
The text seemed appropriately inclusive. There are no pediatric cases and no cases of intellectually-impaired patients, but those types of cases introduce more advanced problem-solving which perhaps exceed the scope of the text. May be a good addition to the text.
I found this text to be an excellent resource for healthcare students in a variety of fields. It would be best utilized in inter professional courses to help guide discussion.
Reviewed by Lynne Umbarger, Clinical Assistant Professor, Occupational Therapy, Emory and Henry College on 11/26/19
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational... read more
While the book does not cover every scenario, the ones in the book are quite common and troublesome for inexperienced allied health students. The information in the book is thorough enough, and I have found the cases easy to modify for educational purposes. The material was easily understood by the students but challenging enough for classroom discussion. There are no mentions in the book about occupational therapy, but it is easy enough to add a couple words and make inclusion simple.
Very nice lab values are provided in the case study, making it more realistic for students.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
The material is easily understood by allied health students. The cases have links to additional learning materials for concepts that may be less familiar or should be explored further in a particular health field.
The language used in the book is consistent between cases. The framework is the same with each case which makes it easier to locate areas that would be of interest to a particular allied health profession.
The case studies are comprehensive but well-organized. They are short enough to be useful for class discussion or a full-blown assignment. The students seem to understand the material and have not expressed that any concepts or details were missing.
Each case is set up like the other cases. There are learning objectives at the beginning of each case to facilitate using the case, and it is easy enough to pull out material to develop useful activities and assignments.
There is a quick chart in the Appendix to allow the reader to determine the professions involved in each case as well as the pertinent settings and diagnoses for each case study. The contents are easy to access even while reading the book.
As a person who attends carefully to grammar, I found no errors in all of the material I read in this book.
There are a greater number of people of different ethnicities, socioeconomic status, ages, and genders to make this a very useful book. With each case, I could easily picture the person in the case. This book appears to be Canadian and more inclusive than most American books.
I was able to use this book the first time I accessed it to develop a classroom activity for first-year occupational therapy students and a more comprehensive activity for second-year students. I really appreciate the links to a multitude of terminology and medical lab values/issues for each case. I will keep using this book.
Reviewed by Cindy Krentz, Assistant Professor, Metropolitan State University of Denver on 6/15/19
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some... read more
The book covers eight case studies of common inpatient or emergency department scenarios. I appreciated that they had written out the learning objectives. I liked that the patient was described before the case was started, giving some understanding of the patient's background. I think it could benefit from having a glossary. I liked how the authors included the vital signs in an easily readable bar. I would have liked to see the labs also highlighted like this. I also felt that it would have been good written in a 'what would you do next?' type of case study.
The book is very accurate in language, what tests would be prudent to run and in the day in the life of the hospital in all cases. One inaccuracy is that the authors called a popliteal artery clot a DVT. The rest of the DVT case study was great, though, but the one mistake should be changed.
The book is up to date for now, but as tests become obsolete and new equipment is routinely used, the book ( like any other health textbook) will need to be updated. It would be easy to change, however. All that would have to happen is that the authors go in and change out the test to whatever newer, evidence-based test is being utilized.
The text is written clearly and easy to understand from a student's perspective. There is not too much technical jargon, and it is pretty universal when used- for example DVT for Deep Vein Thrombosis.
The book is consistent in language and how it is broken down into case studies. The same format is used for highlighting vital signs throughout the different case studies. It's great that the reader does not have to read the book in a linear fashion. Each case study can be read without needing to read the others.
The text is broken down into eight case studies, and within the case studies is broken down into days. It is consistent and shows how the patient can pass through the different hospital departments (from the ER to the unit, to surgery, to home) in a realistic manner. The instructor could use one or more of the case studies as (s)he sees fit.
The topics are eight different case studies- and are presented very clearly and organized well. Each one is broken down into how the patient goes through the system. The text is easy to follow and logical.
The interface has some problems with the highlighted blue links. Some of them did not work and I got a 'page not found' message. That can be frustrating for the reader. I'm wondering if a glossary could be utilized (instead of the links) to explain what some of these links are supposed to explain.
I found two or three typos, I don't think they were grammatical errors. In one case I think the Canadian spelling and the United States spelling of the word are just different.
This is a very culturally competent book. In today's world, however, one more type of background that would merit delving into is the trans-gender, GLBTQI person. I was glad that there were no stereotypes.
I enjoyed reading the text. It was interesting and relevant to today's nursing student. Since we are becoming more interprofessional, I liked that we saw what the phlebotomist and other ancillary personnel (mostly different technicians) did. I think that it could become even more interdisciplinary so colleges and universities could have more interprofessional education- courses or simulations- with the addition of the nurse using social work, nutrition, or other professional health care majors.
Reviewed by Catherine J. Grott, Interim Director, Health Administration Program, TRAILS on 5/5/19
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this. read more
The book is comprehensive but is specifically written for healthcare workers practicing in Canada. The title of the book should reflect this.
The book is accurate, however it has numerous broken online links.
Relevance/Longevity rating: 3
The content is very relevant, but some links are out-dated. For example, WHO Guidelines for Safe Surgery 2009 (p. 186) should be updated.
The book is written in clear and concise language. The side stories about the healthcare workers make the text interesting.
The book is consistent in terms of terminology and framework. Some terms that are emphasized in one case study are not emphasized (with online links) in the other case studies. All of the case studies should have the same words linked to online definitions.
Modularity rating: 3
The book can easily be parsed out if necessary. However, the way the case studies have been written, it's evident that different authors contributed singularly to each case study.
The organization and flow are good.
Interface rating: 1
There are numerous broken online links and "pages not found."
The grammar and punctuation are correct. There are two errors detected: p. 120 a space between the word "heart" and the comma; also a period is needed after Dr (p. 113).
I'm not quite sure that the social worker (p. 119) should comment that the patient and partner are "very normal people."
There are roughly 25 broken online links or "pages not found." The BC & Canadian Guidelines (p. 198) could also include a link to US guidelines to make the text more universal . The basilar crackles (p. 166) is very good. Text could be used compare US and Canadian healthcare. Text could be enhanced to teach "soft skills" and interdepartmental communication skills in healthcare.
Reviewed by Lindsey Henry, Practical Nursing Instructor, Fletcher on 5/1/19
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning... read more
I really appreciated how in the introduction, five learning objectives were identified for students. These objectives are paramount in nursing care and they are each spelled out for the learner. Each Case study also has its own learning objectives, which were effectively met in the readings.
As a seasoned nurse, I believe that the content regarding pathophysiology and treatments used in the case studies were accurate. I really appreciated how many of the treatments were also explained and rationales were given, which can be very helpful to facilitate effective learning for a nursing student or novice nurse.
The case studies are up to date and correlate with the current time period. They are easily understood.
I really loved how several important medical terms, including specific treatments were highlighted to alert the reader. Many interventions performed were also explained further, which is great to enhance learning for the nursing student or novice nurse. Also, with each scenario, a background and history of the patient is depicted, as well as the perspectives of the patient, patients family member, and the primary nurse. This really helps to give the reader a full picture of the day in the life of a nurse or a patient, and also better facilitates the learning process of the reader.
These case studies are consistent. They begin with report, the patient background or updates on subsequent days, and follow the patients all the way through discharge. Once again, I really appreciate how this book describes most if not all aspects of patient care on a day to day basis.
Each case study is separated into days. While they can be divided to be assigned at different points within the course, they also build on each other. They show trends in vital signs, what happens when a patient deteriorates, what happens when they get better and go home. Showing the entire process from ER admit to discharge is really helpful to enhance the students learning experience.
The topics are all presented very similarly and very clearly. The way that the scenarios are explained could even be understood by a non-nursing student as well. The case studies are very clear and very thorough.
The book is very easy to navigate, prints well on paper, and is not distorted or confusing.
I did not see any grammatical errors.
Each case study involves a different type of patient. These differences include race, gender, sexual orientation and medical backgrounds. I do not feel the text was offensive to the reader.
I teach practical nursing students and after reading this book, I am looking forward to implementing it in my classroom. Great read for nursing students!
Reviewed by Leah Jolly, Instructor, Clinical Coordinator, Oregon Institute of Technology on 4/10/19
Good variety of cases and pathologies covered. read more
Good variety of cases and pathologies covered.
Content Accuracy rating: 2
Some examples and scenarios are not completely accurate. For example in the DVT case, the sonographer found thrombus in the "popliteal artery", which according to the book indicated presence of DVT. However in DVT, thrombus is located in the vein, not the artery. The patient would also have much different symptoms if located in the artery. Perhaps some of these inaccuracies are just typos, but in real-life situations this simple mistake can make a world of difference in the patient's course of treatment and outcomes.
Good examples of interprofessional collaboration. If only it worked this way on an every day basis!
Clear and easy to read for those with knowledge of medical terminology.
Good consistency overall.
Broken up well.
Topics are clear and logical.
Would be nice to simply click through to the next page, rather than going through the table of contents each time.
Minor typos/grammatical errors.
No offensive or insensitive materials observed.
Reviewed by Alex Sargsyan, Doctor of Nursing Practice/Assistant Professor , East Tennessee State University on 10/8/18
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study. read more
Because of the case study character of the book it does not have index or glossary. However it has summary for each health case study outlining key elements discussed in each case study.
Overall the book is accurately depicting the clinical environment. There are numerous references to external sites. While most of them are correct, some of them are not working. For example Homan’s test link is not working "404 error"
Book is relevant in its current version and can be used in undergraduate and graduate classes. That said, the longevity of the book may be limited because of the character of the clinical education. Clinical guidelines change constantly and it may require a major update of the content.
Cases are written very clearly and have realistic description of an inpatient setting.
The book is easy to read and consistent in the language in all eight cases.
The cases are very well written. Each case is subdivided into logical segments. The segments reflect different setting where the patient is being seen. There is a flow and transition between the settings.
Book has eight distinct cases. This is a great format for a book that presents distinct clinical issues. This will allow the students to have immersive experiences and gain better understanding of the healthcare environment.
Book is offered in many different formats. Besides the issues with the links mentioned above, overall navigation of the book content is very smooth.
Book is very well written and has no grammatical errors.
Book is culturally relevant. Patients in the case studies come different cultures and represent diverse ethnicities.
Reviewed by Justin Berry, Physical Therapist Assistant Program Director, Northland Community and Technical College, East Grand Forks, MN on 8/2/18
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles,... read more
This text provides eight patient case studies from a variety of diagnoses, which can be utilized by healthcare students from multiple disciplines. The cases are comprehensive and can be helpful for students to determine professional roles, interprofessional roles, when to initiate communication with other healthcare practitioners due to a change in patient status, and treatment ideas. Some additional patient information, such as lab values, would have been beneficial to include.
Case study information is accurate and unbiased.
Content is up to date. The case studies are written in a way so that they will not be obsolete soon, even with changes in healthcare.
The case studies are well written, and can be utilized for a variety of classroom assignments, discussions, and projects. Some additional lab value information for each patient would have been a nice addition.
The case studies are consistently organized to make it easy for the reader to determine the framework.
The text is broken up into eight different case studies for various patient diagnoses. This design makes it highly modular, and would be easy to assign at different points of a course.
The flow of the topics are presented consistently in a logical manner. Each case study follows a patient chronologically, making it easy to determine changes in patient status and treatment options.
The text is free of interface issues, with no distortion of images or charts.
The text is not culturally insensitive or offensive in any way. Patients are represented from a variety of races, ethnicities, and backgrounds
This book would be a good addition for many different health programs.
Reviewed by Ann Bell-Pfeifer, Instructor/Program Director, Minnesota State Community and Technical College on 5/21/18
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical... read more
The book gives a comprehensive overview of many types of cases for patient conditions. Emergency Room patients may arrive with COPD, heart failure, sepsis, pneumonia, or as motor vehicle accident victims. It is directed towards nurses, medical laboratory technologists, medical radiology technologists, and respiratory therapists and their roles in caring for patients. Most of the overview is accurate. One suggestion is to provide an embedded radiologist interpretation of the exams which are performed which lead to the patients diagnosis.
Overall the book is accurate. Would like to see updates related to the addition of direct radiography technology which is commonly used in the hospital setting.
Many aspects of medicine will remain constant. The case studies seem fairly accurate and may be relevant for up to 3 years. Since technology changes so quickly in medicine, the CT and x-ray components may need minor updates within a few years.
The book clarity is excellent.
The case stories are consistent with each scenario. It is easy to follow the structure and learn from the content.
The book is quite modular. It is easy to break it up into cases and utilize them individually and sequentially.
The cases are listed by disease process and follow a logical flow through each condition. They are easy to follow as they have the same format from the beginning to the end of each case.
The interface seems seamless. Hyperlinks are inserted which provide descriptions and references to medical procedures and in depth definitions.
The book is free of most grammatical errors. There is a place where a few words do not fit the sentence structure and could be a typo.
The book included all types of relationships and ethnic backgrounds. One type which could be added is a transgender patient.
I think the book was quite useful for a variety of health care professionals. The authors did an excellent job of integrating patient cases which could be applied to the health care setting. The stories seemed real and relevant. This book could be used to teach health care professionals about integrated care within the emergency department.
Reviewed by Shelley Wolfe, Assistant Professor, Winona State University on 5/21/18
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should... read more
This text is comprised of comprehensive, detailed case studies that provide the reader with multiple character views throughout a patient’s encounter with the health care system. The Table of Contents accurately reflected the content. It should be noted that the authors include a statement that conveys that this text is not like traditional textbooks and is not meant to be read in a linear fashion. This allows the educator more flexibility to use the text as a supplement to enhance learning opportunities.
The content of the text appears accurate and unbiased. The “five overarching learning objectives” provide a clear aim of the text and the educator is able to glean how these objectives are captured into each of the case studies. While written for the Canadian healthcare system, this text is easily adaptable to the American healthcare system.
Overall, the content is up-to-date and the case studies provide a variety of uses that promote longevity of the text. However, not all of the blue font links (if using the digital PDF version) were still in working order. I encountered links that led to error pages or outdated “page not found” websites. While the links can be helpful, continued maintenance of these links could prove time-consuming.
I found the text easy to read and understand. I enjoyed that the viewpoints of all the different roles (patient, nurse, lab personnel, etc.) were articulated well and allowed the reader to connect and gain appreciation of the entire healthcare team. Medical jargon was noted to be appropriate for the intended audience of this text.
The terminology and organization of this text is consistent.
The text is divided into 8 case studies that follow a similar organizational structure. The case studies can further be divided to focus on individual learning objectives. For example, the case studies could be looked at as a whole for discussing communication or could be broken down into segments to focus on disease risk factors.
The case studies in this text follow a similar organizational structure and are consistent in their presentation. The flow of individual case studies is excellent and sets the reader on a clear path. As noted previously, this text is not meant to be read in a linear fashion.
This text is available in many different forms. I chose to review the text in the digital PDF version in order to use the embedded links. I did not encounter significant interface issues and did not find any images or features that would distract or confuse a reader.
No significant grammatical errors were noted.
The case studies in this text included patients and healthcare workers from a variety of backgrounds. Educators and students will benefit from expanding the case studies to include discussions and other learning opportunities to help develop culturally-sensitive healthcare providers.
I found the case studies to be very detailed, yet written in a way in which they could be used in various manners. The authors note a variety of ways in which the case studies could be employed with students; however, I feel the authors could also include that the case studies could be used as a basis for simulated clinical experiences. The case studies in this text would be an excellent tool for developing interprofessional communication and collaboration skills in a variety healthcare students.
Reviewed by Darline Foltz, Assistant Professor, University of Cincinnati - Clermont College on 3/27/18
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks... read more
This book covers all areas listed in the Table of Contents. In addition to the detailed patient case studies, there is a helpful section of "How to Use this Resource". I would like to note that this resource "aligns with the open textbooks Clinical Procedures for Safer Patient Care and Anatomy and Physiology: OpenStax" as noted by the authors.
The book appears to be accurate. Although one of the learning outcomes is as follows: "Demonstrate an understanding of the Canadian healthcare delivery system.", I did not find anything that is ONLY specific to the Canadian healthcare delivery system other than some of the terminology, i.e. "porter" instead of "transporter" and a few french words. I found this to make the book more interesting for students rather than deter from it. These are patient case studies that are relevant in any country.
The content is up-to-date. Changes in medical science may occur, i.e. a different test, to treat a diagnosis that is included in one or more of the case studies, however, it would be easy and straightforward to implement these changes.
This book is written in lucid, accessible prose. The technical/medical terminology that is used is appropriate for medical and allied health professionals. Something that would improve this text would to provide a glossary of terms for the terms in blue font.
This book is consistent with current medical terminology
This text is easily divided into each of the 6 case studies. The case studies can be used singly according to the body system being addressed or studied.
Because this text is a collection of case studies, flow doesn't pertain, however the organization and structure of the case studies are excellent as they are clear and easy to read.
There are no distractions in this text that would distract or confuse the reader.
I did not identify any grammatical errors.
This text is not culturally insensitive or offensive in any way and uses patients and healthcare workers that are of a variety of races, ethnicities and backgrounds.
I believe that this text would not only be useful to students enrolled in healthcare professions involved in direct patient care but would also be useful to students in supporting healthcare disciplines such as health information technology and management, medical billing and coding, etc.
Table of Contents
- Introduction
Case Study #1: Chronic Obstructive Pulmonary Disease (COPD)
- Learning Objectives
- Patient: Erin Johns
- Emergency Room
Case Study #2: Pneumonia
- Day 0: Emergency Room
- Day 1: Emergency Room
- Day 1: Medical Ward
- Day 2: Medical Ward
- Day 3: Medical Ward
- Day 4: Medical Ward
Case Study #3: Unstable Angina (UA)
- Patient: Harj Singh
Case Study #4: Heart Failure (HF)
- Patient: Meryl Smith
- In the Supermarket
- Day 0: Medical Ward
Case Study #5: Motor Vehicle Collision (MVC)
- Patient: Aaron Knoll
- Crash Scene
- Operating Room
- Post Anaesthesia Care Unit (PACU)
- Surgical Ward
Case Study #6: Sepsis
- Patient: George Thomas
- Sleepy Hollow Care Facility
Case Study #7: Colon Cancer
- Patient: Fred Johnson
- Two Months Ago
- Pre-Surgery Admission
Case Study #8: Deep Vein Thrombosis (DVT)
- Patient: Jamie Douglas
Appendix: Overview About the Authors
Ancillary Material
About the book.
Health Case Studies is composed of eight separate health case studies. Each case study includes the patient narrative or story that models the best practice (at the time of publishing) in healthcare settings. Associated with each case is a set of specific learning objectives to support learning and facilitate educational strategies and evaluation.
The case studies can be used online in a learning management system, in a classroom discussion, in a printed course pack or as part of a textbook created by the instructor. This flexibility is intentional and allows the educator to choose how best to convey the concepts presented in each case to the learner.
Because these case studies were primarily developed for an electronic healthcare system, they are based predominantly in an acute healthcare setting. Educators can augment each case study to include primary healthcare settings, outpatient clinics, assisted living environments, and other contexts as relevant.
About the Contributors
Glynda Rees teaches at the British Columbia Institute of Technology (BCIT) in Vancouver, British Columbia. She completed her MSN at the University of British Columbia with a focus on education and health informatics, and her BSN at the University of Cape Town in South Africa. Glynda has many years of national and international clinical experience in critical care units in South Africa, the UK, and the USA. Her teaching background has focused on clinical education, problem-based learning, clinical techniques, and pharmacology.
Glynda‘s interests include the integration of health informatics in undergraduate education, open accessible education, and the impact of educational technologies on nursing students’ clinical judgment and decision making at the point of care to improve patient safety and quality of care.
Faculty member in the critical care nursing program at the British Columbia Institute of Technology (BCIT) since 2003, Rob has been a critical care nurse for over 25 years with 17 years practicing in a quaternary care intensive care unit. Rob is an experienced educator and supports student learning in the classroom, online, and in clinical areas. Rob’s Master of Education from Simon Fraser University is in educational technology and learning design. He is passionate about using technology to support learning for both faculty and students.
Part of Rob’s faculty position is dedicated to providing high fidelity simulation support for BCIT’s nursing specialties program along with championing innovative teaching and best practices for educational technology. He has championed the use of digital publishing and was the tech lead for Critical Care Nursing’s iPad Project which resulted in over 40 multi-touch interactive textbooks being created using Apple and other technologies.
Rob has successfully completed a number of specialist certifications in computer and network technologies. In 2015, he was awarded Apple Distinguished Educator for his innovation and passionate use of technology to support learning. In the past five years, he has presented and published abstracts on virtual simulation, high fidelity simulation, creating engaging classroom environments, and what the future holds for healthcare and education.
Janet Morrison is the Program Head of Occupational Health Nursing at the British Columbia Institute of Technology (BCIT) in Burnaby, British Columbia. She completed a PhD at Simon Fraser University, Faculty of Communication, Art and Technology, with a focus on health information technology. Her dissertation examined the effects of telehealth implementation in an occupational health nursing service. She has an MA in Adult Education from St. Francis Xavier University and an MA in Library and Information Studies from the University of British Columbia.
Janet’s research interests concern the intended and unintended impacts of health information technologies on healthcare students, faculty, and the healthcare workforce.
She is currently working with BCIT colleagues to study how an educational clinical information system can foster healthcare students’ perceptions of interprofessional roles.
Contribute to this Page
Nursing Diagnosis Guide

NurseJournal.org is committed to delivering content that is objective and actionable. To that end, we have built a network of industry professionals across higher education to review our content and ensure we are providing the most helpful information to our readers.
Drawing on their firsthand industry expertise, our Integrity Network members serve as an additional step in our editing process, helping us confirm our content is accurate and up to date. These contributors:
- Suggest changes to inaccurate or misleading information.
- Provide specific, corrective feedback.
- Identify critical information that writers may have missed.
Integrity Network members typically work full time in their industry profession and review content for NurseJournal.org as a side project. All Integrity Network members are paid members of the Red Ventures Education Integrity Network.
Explore our full list of Integrity Network members.
Are you ready to earn your online nursing degree?

Creating a nursing diagnosis is a critical part of providing patient care and is a vital step of the nursing process.
By understanding how to create a nursing diagnosis, you can help improve patient outcomes, improve communication among the medical health team, and organize your day. Both the nursing process and nursing diagnoses help ensure and promote evidence-based, safe practices.
In this guide, you will learn what a nursing diagnosis is, why it is important, and a general overview of how to perform a nursing diagnosis.
The Nursing Process
You can’t discuss a nursing diagnosis without discussing the nursing process. The nursing process has five steps:
Assessment is a thorough and holistic evaluation of a patient. It includes the collection of both subjective and objective patient data such as vital signs, a health history, head-to-toe physical, and a psychological, socioeconomic, and spiritual evaluation.
Diagnosis is formed by the nurse and is based on the data collected during the assessment. The nursing diagnosis directs nursing-specific patient care.
In this step, the nurse forms a diagnosis based on the patient’s specific medical and/or social needs. The diagnosis leads to the creation of goals with measurable outcomes.
The diagnosis must be one that has been approved by NANDA International (NANDA-I), formerly known as North American Nursing Diagnosis Association. NANDA-I is responsible for developing and standardizing nursing diagnoses. Used internationally, the NANDA-I vision and mission is to use evidence-based, universal nursing terminology to promote safe patient care.
NANDA-I defines a nursing diagnosis as follows:
- “a clinical judgment concerning a human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability.”
- A nursing diagnosis generally has three components: a diagnosis approved by NANDA-I, a related to statement which defines the cause of the NANDA-I diagnosis, and an as evidenced by statement that uses specific patient data to provide a reason for the NANDA-I diagnosis and related to statement.
- Risk-related diagnoses only contain a NANDA-I diagnosis and an as evidenced by statement because it is describing a vulnerability, not a cause. For example, a nurse may use a nursing diagnosis such as “risk for pressure ulcer as evidenced by lack of movement, poor nutrition, and hydration.”
Outcomes and Planning
Outcome and planning involves developing a patient care plan based on the nursing diagnosis. Planning should be measurable and goal-oriented for the patient and/or their family members.
Implementation
Implementation is when nurses initiate the care plan and put it into action. This step provides the continuation of care during hospitalization until discharge.
Evaluation is the final step of the nursing process. A patient care plan is evaluated based on specific goals and desired outcomes and may be adjusted based on the patient’s needs.
Popular Nursing Programs
Learn about start dates, transferring credits, availability of financial aid, and more by contacting the universities below.
How Do Nursing Diagnoses Differ From Medical Diagnoses?
To best understand a nursing diagnosis, it may help to first understand how it differs from a medical diagnosis.
A nursing diagnosis is initiated by a nurse and describes a response to the medical diagnosis. A medical diagnosis is given by a doctor to a patient to define a medical condition/disease or injury.
Nursing Diagnosis
- Based on the patient’s immediate situation
- Initiated to resolve a health problem
- Improves communication among the healthcare teams
- A holistic approach to caring for patients
Example: Ineffective breathing pattern related to impaired inhalation and exhalation as evidenced by the use of accessory muscles
Medical Diagnosis
- Initiated by a medical doctor or specialist
- Defines a medical condition, disease, or injury
- Explains the signs and symptoms of the disease
Example: Asthma
4 Categories of Nursing Diagnoses
The need for standardized language, respecting nurses’ clinical judgment, and providing care for patients with measurable results defines the use of a nursing diagnosis. The nursing diagnosis can be divided into four main categories. Please note all examples are taken from the Nursing Diagnoses Definitions and Classification 2015-2017.
Problem-focused Diagnosis
A nursing diagnosis related to a patient’s problem. It can be used throughout the course of the patient’s hospitalization or be resolved by the end of the shift.
Example: Anxiety related to situational crises and stress (related factors) as evidenced by restlessness, insomnia, anguish, and anorexia (defining characteristics)
Risk Diagnosis
A nursing diagnosis that identifies when the patient is at risk for developing a problem. NANDA-I describes it as a vulnerability the patient has encountered.
Example: Risk for infection as evidenced by inadequate vaccination and immunosuppression (risk factors)
Health-promotion Diagnosis
A nursing diagnosis used to identify how to help improve the health of a patient. Health-promotion diagnosis includes the patient and their family/community members.
Example: Readiness for enhanced self-care as evidenced by expressed desire to enhance self-care
Syndrome Diagnosis
A nursing diagnosis identifying a cluster of diagnoses for a patient. These nursing diagnoses are best described together. The patient may be experiencing a number of health problems forming a pattern.
Example: Chronic pain syndrome
Nursing Diagnosis Classification
NANDA-I created Taxonomy II after collaborating with the National Library of Medicine. By definition, taxonomy is the “practice and science of categorization and classification.” The NANDA-I Taxonomy currently has 235 nursing diagnoses with 13 categories of nursing practice:
- Health promotion
- Elimination and exchange
- Activity/rest
- Perception/cognition
- Self-perception
- Role relationships
- Coping/stress tolerance
- Life principles
- Safety/protection
- Growth/development
They also have 47 classes related to each category.
How to Perform a Nursing Diagnosis
Nurses complete five steps to carry out a strong, accurate nursing diagnosis. All nurses should follow the nursing process:
Nursing Science
Having a solid understanding of nursing science and theory provides a strong foundation for patient care. It is also the first step in initiating a nursing diagnosis and care plan that is holistic and patient-centered.
During the assessment, nurses gather medical, surgical, and social history. They also perform a physical on the patient. Nurses then ask themselves: What is the current and priority health problem(s) the patient is experiencing? This information is applied to creating a nursing diagnosis.
Identifying Potential Diagnoses
Once the health problem or human response(s) to the health problem is identified, nurses ask another question: What important information is relevant to the health problem and what’s unrelated?
The answer to this question helps create a potential nursing diagnosis. Nurses will then:
- Determine the category of the nursing diagnosis
- Confirm and rule out other diagnoses
- Create new diagnoses
The nursing diagnosis must be validated and critically thought out. NANDA-I advises using an in-depth assessment. This will confirm or rule out a diagnosis.
NANDA-I recommends structuring a nursing diagnosis in “related factors” and “defining characteristics” format, as first published by Marjory Gordon, Ph.D. This can highlight the strength and accuracy of the nursing diagnosis.
Implementing a Care Plan
A nursing diagnosis determines the care plan. Nurses create measurable, achievable goals and related interventions. They then take action, administering the planned interventions.
Nurses are constantly evaluating their patients. A nursing diagnosis is often evaluated to make sure the care plan is working. If it is not, nurses must think about what else can be done to improve the patient’s health.
A Critical Component of Care
Nurses are the eyes and ears of the patient. They are the liaison between the medical health team and the patient and their family. Understanding the power and usefulness of a nursing diagnosis is a critical aspect of patient care. Each patient is unique and complex. The nursing process and nursing diagnosis can help provide safe, individualized, and evidence-based care.
Whether you’re looking to get your pre-licensure degree or taking the next step in your career, the education you need could be more affordable than you think. Find the right nursing program for you.
You might be interested in

HESI vs. TEAS Exam: The Differences Explained
Nursing schools use entrance exams to make admissions decisions. Learn about the differences between the HESI vs. TEAS exams.

10 Nursing Schools That Don’t Require TEAS or HESI Exam

For Chiefs’ RB Clyde Edwards-Helaire, Nursing Runs in the Family
- Login / Register

‘These three individuals will leave very big shoes to fill’
STEVE FORD, EDITOR
- You are here: COPD
Diagnosis and management of COPD: a case study
04 May, 2020
This case study explains the symptoms, causes, pathophysiology, diagnosis and management of chronic obstructive pulmonary disease
This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient’s associated pathophysiology. Diagnosis involves spirometry testing to measure the volume of air that can be exhaled; it is often performed after administering a short-acting beta-agonist. Management of chronic obstructive pulmonary disease involves lifestyle interventions – vaccinations, smoking cessation and pulmonary rehabilitation – pharmacological interventions and self-management.
Citation: Price D, Williams N (2020) Diagnosis and management of COPD: a case study. Nursing Times [online]; 116: 6, 36-38.
Authors: Debbie Price is lead practice nurse, Llandrindod Wells Medical Practice; Nikki Williams is associate professor of respiratory and sleep physiology, Swansea University.
- This article has been double-blind peer reviewed
- Scroll down to read the article or download a print-friendly PDF here (if the PDF fails to fully download please try again using a different browser)
Introduction
The term chronic obstructive pulmonary disease (COPD) is used to describe a number of conditions, including chronic bronchitis and emphysema. Although common, preventable and treatable, COPD was projected to become the third leading cause of death globally by 2020 (Lozano et al, 2012). In the UK in 2012, approximately 30,000 people died of COPD – 5.3% of the total number of deaths. By 2016, information published by the World Health Organization indicated that Lozano et al (2012)’s projection had already come true.
People with COPD experience persistent respiratory symptoms and airflow limitation that can be due to airway or alveolar abnormalities, caused by significant exposure to noxious particles or gases, commonly from tobacco smoking. The projected level of disease burden poses a major public-health challenge and primary care nurses can be pivotal in the early identification, assessment and management of COPD (Hooper et al, 2012).
Grace Parker (the patient’s name has been changed) attends a nurse-led COPD clinic for routine reviews. A widowed, 60-year-old, retired post office clerk, her main complaint is breathlessness after moderate exertion. She scored 3 on the modified Medical Research Council (mMRC) scale (Fletcher et al, 1959), indicating she is unable to walk more than 100 yards without stopping due to breathlessness. Ms Parker also has a cough that produces yellow sputum (particularly in the mornings) and an intermittent wheeze. Her symptoms have worsened over the last six months. She feels anxious leaving the house alone because of her breathlessness and reduced exercise tolerance, and scored 26 on the COPD Assessment Test (CAT, catestonline.org), indicating a high level of impact.
Ms Parker smokes 10 cigarettes a day and has a pack-year score of 29. She has not experienced any haemoptysis (coughing up blood) or chest pain, and her weight is stable; a body mass index of 40kg/m 2 means she is classified as obese. She has had three exacerbations of COPD in the previous 12 months, each managed in the community with antibiotics, steroids and salbutamol.
Ms Parker was diagnosed with COPD five years ago. Using Epstein et al’s (2008) guidelines, a nurse took a history from her, which provided 80% of the information needed for a COPD diagnosis; it was then confirmed following spirometry testing as per National Institute for Health and Care Excellence (2018) guidance.
The nurse used the Calgary-Cambridge consultation model, as it combines the pathological description of COPD with the patient’s subjective experience of the illness (Silverman et al, 2013). Effective communication skills are essential in building a trusting therapeutic relationship, as the quality of the relationship between Ms Parker and the nurse will have a direct impact on the effectiveness of clinical outcomes (Fawcett and Rhynas, 2012).
In a national clinical audit report, Baxter et al (2016) identified inaccurate history taking and inadequately performed spirometry as important factors in the inaccurate diagnosis of COPD on general practice COPD registers; only 52.1% of patients included in the report had received quality-assured spirometry.
Pathophysiology of COPD
Knowing the pathophysiology of COPD allowed the nurse to recognise and understand the physical symptoms and provide effective care (Mitchell, 2015). Continued exposure to tobacco smoke is the likely cause of the damage to Ms Parker’s small airways, causing her cough and increased sputum production. She could also have chronic inflammation, resulting in airway smooth-muscle contraction, sluggish ciliary movement, hypertrophy and hyperplasia of mucus-secreting goblet cells, as well as release of inflammatory mediators (Mitchell, 2015).
Ms Parker may also have emphysema, which leads to damaged parenchyma (alveoli and structures involved in gas exchange) and loss of alveolar attachments (elastic connective fibres). This causes gas trapping, dynamic hyperinflation, decreased expiratory flow rates and airway collapse, particularly during expiration (Kaufman, 2013). Ms Parker also displayed pursed-lip breathing; this is a technique used to lengthen the expiratory time and improve gaseous exchange, and is a sign of dynamic hyperinflation (Douglas et al, 2013).
In a healthy lung, the destruction and repair of alveolar tissue depends on proteases and antiproteases, mainly released by neutrophils and macrophages. Inhaling cigarette smoke disrupts the usually delicately balanced activity of these enzymes, resulting in the parenchymal damage and small airways (with a lumen of <2mm in diameter) airways disease that is characteristic of emphysema. The severity of parenchymal damage or small airways disease varies, with no pattern related to disease progression (Global Initiative for Chronic Obstructive Lung Disease, 2018).
Ms Parker also had a wheeze, heard through a stethoscope as a continuous whistling sound, which arises from turbulent airflow through constricted airway smooth muscle, a process noted by Mitchell (2015). The wheeze, her 29 pack-year score, exertional breathlessness, cough, sputum production and tiredness, and the findings from her physical examination, were consistent with a diagnosis of COPD (GOLD, 2018; NICE, 2018).
Spirometry is a tool used to identify airflow obstruction but does not identify the cause. Commonly measured parameters are:
- Forced expiratory volume – the volume of air that can be exhaled – in one second (FEV1), starting from a maximal inspiration (in litres);
- Forced vital capacity (FVC) – the total volume of air that can be forcibly exhaled – at timed intervals, starting from a maximal inspiration (in litres).
Calculating the FEV1 as a percentage of the FVC gives the forced expiratory ratio (FEV1/FVC). This provides an index of airflow obstruction; the lower the ratio, the greater the degree of obstruction. In the absence of respiratory disease, FEV1 should be ≥70% of FVC. An FEV1/FVC of <70% is commonly used to denote airflow obstruction (Moore, 2012).
As they are time dependent, FEV1 and FEV1/FVC are reduced in diseases that cause airways to narrow and expiration to slow. FVC, however, is not time dependent: with enough expiratory time, a person can usually exhale to their full FVC. Lung function parameters vary depending on age, height, gender and ethnicity, so the degree of FEV1 and FVC impairment is calculated by comparing a person’s recorded values with predicted values. A recorded value of >80% of the predicted value has been considered ‘normal’ for spirometry parameters but the lower limit of normal – equal to the fifth percentile of a healthy, non-smoking population – based on more robust statistical models is increasingly being used (Cooper et al, 2017).
A reversibility test involves performing spirometry before and after administering a short-acting beta-agonist (SABA) such as salbutamol; the test is used to distinguish between reversible and fixed airflow obstruction. For symptomatic asthma, airflow obstruction due to airway smooth-muscle contraction is reversible: administering a SABA results in smooth-muscle relaxation and improved airflow (Lumb, 2016). However, COPD is associated with fixed airflow obstruction, resulting from neutrophil-driven inflammatory changes, excess mucus secretion and disrupted alveolar attachments, as opposed to airway smooth-muscle contraction.
Administering a SABA for COPD does not usually produce bronchodilation to the extent seen in someone with asthma: a person with asthma may demonstrate significant improvement in FEV1 (of >400ml) after having a SABA, but this may not change in someone with COPD (NICE, 2018). However, a negative response does not rule out therapeutic benefit from long-term SABA use (Marín et al, 2014).
NICE (2018) and GOLD (2018) guidelines advocate performing spirometry after administering a bronchodilator to diagnose COPD. Both suggest a FEV1/FVC of <70% in a person with respiratory symptoms supports a diagnosis of COPD, and both grade the severity of the condition using the predicted FEV1. Ms Parker’s spirometry results showed an FEV1/FVC of 56% and a predicted FEV1 of 57%, with no significant improvement in these values with a reversibility test.
GOLD (2018) guidance is widely accepted and used internationally. However, it was developed by medical practitioners with a medicalised approach, so there is potential for a bias towards pharmacological management of COPD. NICE (2018) guidance may be more useful for practice nurses, as it was developed by a multidisciplinary team using evidence from systematic reviews or meta-analyses of randomised controlled trials, providing a holistic approach. NICE guidance may be outdated on publication, but regular reviews are performed and published online.
NHS England (2016) holds a national register of all health professionals certified in spirometry. It was set up to raise spirometry standards across the country.
Assessment and management
The goals of assessing and managing Ms Parker’s COPD are to:
- Review and determine the level of airflow obstruction;
- Assess the disease’s impact on her life;
- Risk assess future disease progression and exacerbations;
- Recommend pharmacological and therapeutic management.
GOLD’s (2018) ABCD assessment tool (Fig 1) grades COPD severity using spirometry results, number of exacerbations, CAT score and mMRC score, and can be used to support evidence-based pharmacological management of COPD.

When Ms Parker was diagnosed, her predicted FEV1 of 57% categorised her as GOLD grade 2, and her mMRC score, CAT score and exacerbation history placed her in group D. The mMRC scale only measures breathlessness, but the CAT also assesses the impact COPD has on her life, meaning consecutive CAT scores can be compared, providing valuable information for follow-up and management (Zhao, et al, 2014).
After assessing the level of disease burden, Ms Parker was then provided with education for self-management and lifestyle interventions.
Lifestyle interventions
Smoking cessation.
Cessation of smoking alongside support and pharmacotherapy is the second-most cost-effective intervention for COPD, when compared with most other pharmacological interventions (BTS and PCRS UK, 2012). Smoking cessation:
- Slows the progression of COPD;
- Improves lung function;
- Improves survival rates;
- Reduces the risk of lung cancer;
- Reduces the risk of coronary heart disease risk (Qureshi et al, 2014).
Ms Parker accepted a referral to an All Wales Smoking Cessation Service adviser based at her GP surgery. The adviser used the internationally accepted ‘five As’ approach:
- Ask – record the number of cigarettes the individual smokes per day or week, and the year they started smoking;
- Advise – urge them to quit. Advice should be clear and personalised;
- Assess – determine their willingness and confidence to attempt to quit. Note the state of change;
- Assist – help them to quit. Provide behavioural support and recommend or prescribe pharmacological aids. If they are not ready to quit, promote motivation for a future attempt;
- Arrange – book a follow-up appointment within one week or, if appropriate, refer them to a specialist cessation service for intensive support. Document the intervention.
NICE (2013) guidance recommends that this be used at every opportunity. Stead et al (2016) suggested that a combination of counselling and pharmacotherapy have proven to be the most effective strategy.
Pulmonary rehabilitation
Ms Parker’s positive response to smoking cessation provided an ideal opportunity to offer her pulmonary rehabilitation (PR) – as indicated by Johnson et al (2014), changing one behaviour significantly increases a person’s chance of changing another.
PR – a supervised programme including exercise training, health education and breathing techniques – is an evidence-based, comprehensive, multidisciplinary intervention that:
- Improves exercise tolerance;
- Reduces dyspnoea;
- Promotes weight loss (Bolton et al, 2013).
These improvements often lead to an improved quality of life (Sciriha et al, 2015).
Most relevant for Ms Parker, PR has been shown to reduce anxiety and depression, which are linked to an increased risk of exacerbations and poorer health status (Miller and Davenport, 2015). People most at risk of future exacerbations are those who already experience them (Agusti et al, 2010), as in Ms Parker’s case. Patients who have frequent exacerbations have a lower quality of life, quicker progression of disease, reduced mobility and more-rapid decline in lung function than those who do not (Donaldson et al, 2002).
“COPD is a major public-health challenge; nurses can be pivotal in early identification, assessment and management”
Pharmacological interventions
Ms Parker has been prescribed inhaled salbutamol as required; this is a SABA that mediates the increase of cyclic adenosine monophosphate in airway smooth-muscle cells, leading to muscle relaxation and bronchodilation. SABAs facilitate lung emptying by dilatating the small airways, reversing dynamic hyperinflation of the lungs (Thomas et al, 2013). Ms Parker also uses a long-acting muscarinic antagonist (LAMA) inhaler, which works by blocking the bronchoconstrictor effects of acetylcholine on M3 muscarinic receptors in airway smooth muscle; release of acetylcholine by the parasympathetic nerves in the airways results in increased airway tone with reduced diameter.
At a routine review, Ms Parker admitted to only using the SABA and LAMA inhalers, despite also being prescribed a combined inhaled corticosteroid and long-acting beta 2 -agonist (ICS/LABA) inhaler. She was unaware that ICS/LABA inhalers are preferred over SABA inhalers, as they:
- Last for 12 hours;
- Improve the symptoms of breathlessness;
- Increase exercise tolerance;
- Can reduce the frequency of exacerbations (Agusti et al, 2010).
However, moderate-quality evidence shows that ICS/LABA combinations, particularly fluticasone, cause an increased risk of pneumonia (Suissa et al, 2013; Nannini et al, 2007). Inhaler choice should, therefore, be individualised, based on symptoms, delivery technique, patient education and compliance.
It is essential to teach and assess inhaler technique at every review (NICE, 2011). Ms Parker uses both a metered-dose inhaler and a dry-powder inhaler; an in-check device is used to assess her inspiratory effort, as different inhaler types require different inhalation speeds. Braido et al (2016) estimated that 50% of patients have poor inhaler technique, which may be due to health professionals lacking the confidence and capability to teach and assess their use.
Patients may also not have the dexterity, capacity to learn or vision required to use the inhaler. Online resources are available from, for example, RightBreathe (rightbreathe.com), British Lung Foundation (blf.org.uk). Ms Parker’s adherence could be improved through once-daily inhalers, as indicated by results from a study by Lipson et al (2017). Any change in her inhaler would be monitored as per local policy.
Vaccinations
Ms Parker keeps up to date with her seasonal influenza and pneumococcus vaccinations. This is in line with the low-cost, highest-benefit strategy identified by the British Thoracic Society and Primary Care Respiratory Society UK’s (2012) study, which was conducted to inform interventions for patients with COPD and their relative quality-adjusted life years. Influenza vaccinations have been shown to decrease the risk of lower respiratory tract infections and concurrent COPD exacerbations (Walters et al, 2017; Department of Health, 2011; Poole et al, 2006).
Self-management
Ms Parker was given a self-management plan that included:
- Information on how to monitor her symptoms;
- A rescue pack of antibiotics, steroids and salbutamol;
- A traffic-light system demonstrating when, and how, to commence treatment or seek medical help.
Self-management plans and rescue packs have been shown to reduce symptoms of an exacerbation (Baxter et al, 2016), allowing patients to be cared for in the community rather than in a hospital setting and increasing patient satisfaction (Fletcher and Dahl, 2013).
Improving Ms Parker’s adherence to once-daily inhalers and supporting her to self-manage and make the necessary lifestyle changes, should improve her symptoms and result in fewer exacerbations.
The earlier a diagnosis of COPD is made, the greater the chances of reducing lung damage through interventions such as smoking cessation, lifestyle modifications and treatment, if required (Price et al, 2011).
- Chronic obstructive pulmonary disease is a progressive respiratory condition, projected to become the third leading cause of death globally
- Diagnosis involves taking a patient history and performing spirometry testing
- Spirometry identifies airflow obstruction by measuring the volume of air that can be exhaled
- Chronic obstructive pulmonary disease is managed with lifestyle and pharmacological interventions, as well as self-management
Related files
200506 diagnosis and management of copd – a case study.
- Add to Bookmarks
Related articles
Have your say.
Sign in or Register a new account to join the discussion.
Want to create or adapt books like this? Learn more about how Pressbooks supports open publishing practices.
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria’s vital signs were as follows: BP 87/50, HR 118, RR 28, O2 95% on room air, diffuse abdominal pain at a level of 5, on a verbal numeric 1-10 scale, with non-radiating pain beginning that morning. She was A&O x3, oriented to self, place, and situation, but sluggish. Upon assessment it is revealed that she is experiencing blurry vision, Kussmaul respirations, dry, flushed skin, poor skin turgor, weakness, and a fruity breath smell. Labs were drawn. During the first hour of admission, Maria requested water four times and urinated three times.
Code status: Full code
Medical hx : Type 1 Diabetes
Insurance : None
Allergies : NKA
Significant Lab Values
- Blood glucose 388
- ABGs: pH 7.25, Bicarb 12 mEq/L, paCO2 30 mm Hg, anion gap 20 mEq/L, paO2 94%
- Urinalysis: Ketones and acetone present, BUN 25 mL/dL, Cr 2.1 ml/dL
- Chemistry: sodium 111 mEq/L, potassium 5.5 mEq/L, chloride 90 mEq/L, phosphorus 2.5 mg/dL, Magnesium 2.0 mg/dL
- CBC: WBC 13,000 mcL, RBC 4.7 mcL, Hgb 12.6 g/dL , Hct 37% (Wolters Kluwer, 2018).
Diagnosis: Diabetes Ketoacidosis
- Oxygen administration by nasal cannula on 2L and airway management
- Establish IV access
- IV fluid administration with 0.9% NS; prepare to titrate to 0.45% normal saline as needed
- Monitor blood glucose levels
- Administer 0.1-0.15 unit/kg IV bolus of regular insulin
- IV drip infusion at 0.1 unit/kg/hr of regular insulin to hyperglycemia after bolus,
- Addition of Dextrose to 0.9% NS as glucose levels decreases to 250 mg/dL
- Monitor potassium levels
- Potassium replacement via IV when the potassium level is 5.0 mg/dL or less and urine output is adequate
- Assess for signs of hypokalemia or hyperkalemia
- Monitor vital signs and cardiac rhythm
- Q1-2hr fingerstick blood glucose checks initially, then q4-6hr once stabilized
- Monitor blood pH, I&O
- Assess level of consciousness; provide seizure and safety precautions (Henry et al., 2016)
- Notify MD of any critical changes
Maria Fernandez was then transferred to the ICU unit for close observation, maintenance of IV insulin drip, cardiac monitoring, fluid resuscitation, and correction for metabolic acidosis.
Upon discharge, Maria was reeducated on Type 1 Diabetes Mellitus through the use of preferred learning materials.
- What is the priority assessment data that supports DKA diagnosis?
- What education strategies would you consider implementing to improve treatment adherence after discharge?
- What considerations, services, or resources would you anticipate to be offered by case management or social services?
Henry, N.J., McMichael, M., Johnson, J., DiStasi, A., Ball, B.S., Holman, H.C., Elkins, C.B., Janowski, M.J., Hertel, R.A., Barlow, M.S., Leehy, P., & Lemon, T. (2016). RN adult medical surgical nursing: Review module (10 th ed.). Leawood, KS: Assessment Technologies Institute.
Wolters Kluwer. (2018). Lippincott Nursing Advisor (Version 4.1.0) [Mobile application software]. Retrieved from http://itunes.apple.com
Nursing Case Studies by and for Student Nurses Copyright © by jaimehannans is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License , except where otherwise noted.
Share This Book

IMAGES
VIDEO
COMMENTS
Nursing Case Studies: Diagnosis, Rationales, Fundamentals. Test your knowledge and clinical investigative skills in trying to diagnose what is going on with the patients presented in each of the Case Study Investigations. Can you come up with the right diagnosis?
Updated on April 29, 2024. By Matt Vera BSN, R.N. In this ultimate tutorial and nursing diagnosis list, we’ll walk you through the concepts behind writing nursing diagnosis. Learn what a nursing diagnosis is, its history and evolution, the nursing process, the different types and classifications, and how to write nursing diagnoses correctly.
A medical diagnosis does not change if the condition is resolved, and it remains part of the patient’s health history forever. A nursing diagnosis, however, generally refers to a specific period of time. Examples of medical diagnosis include: Arthritis. Congestive Heart Failure. Diabetes Insipidus.
Click on a case study below to view in our Nursing Case Study Examples course which holds all of our 40+ nursing case studies with answers. Acute Kidney Injury Nursing Case Study. Continue Case Study. Cardiogenic Shock Nursing Case Study. Continue Case Study. Breast Cancer Nursing Case Study. Continue Case Study. Respiratory Nursing Case Study.
Ensure your summary has at least the case presentation, the nursing assessment/diagnosis, the intervention, and the key recommendations. At the very end of your conclusion, add a closing statement. The statement should wrap up the whole thing nicely. Try to make it as impressive as possible. 9.
These case studies focus on commonly encountered diagnoses for allied health and nursing students. They are comprehensive, realistic, and easily understood. The only difference is that the hospital in one case allows the patient's dog to visit in the room (highly unusual in US hospitals).
Diagnosis is formed by the nurse and is based on the data collected during the assessment. The nursing diagnosis directs nursing-specific patient care. In this step, the nurse forms a diagnosis based on the patient’s specific medical and/or social needs. The diagnosis leads to the creation of goals with measurable outcomes.
This article uses a case study to discuss the symptoms, causes and management of chronic obstructive pulmonary disease, describing the patient’s associated pathophysiology. Diagnosis involves spirometry testing to measure the volume of air that can be exhaled; it is often performed after administering a short-acting beta-agonist.
The patient arrives to the emergency room within 15 minutes and is admitted for treatment at 1000. On the unit, Code Sepsis is called, and the agency’s sepsis protocol based on the Surviving Sepsis campaign is implemented. The patient’s vitals are now a temperature of 102F, heart rate of 140, respiratory rate of 34, and blood pressure of 96/42.
On March 6th, 2019, Maria Fernandez, a 19-year-old female, presented to the Emergency Department with complaints of nausea, vomiting, abdominal pain, and lethargy. She reveals a recent diagnosis of type 1 diabetes but admits to noncompliance with treatment. At the time of admission, Maria’s vital signs were as follows: BP 87/50, HR 118, RR 28 ...