- Sign In to save searches and organize your favorite content.
- Not registered? Sign up

Recently viewed (0)
- Save Search
- Subscriptions
- Join E-mail List
Bone Cancer
- Get Citation Alerts
- Download PDF to Print
Bone Cancer NCCN Clinical Practice Guidelines in Oncology
- NCCN Categories of Evidence and Consensus
Category 1: The recommendation is based on high-level evidence (e.g., randomized controlled trials) and there is uniform NCCN consensus.
Category 2A: The recommendation is based on lower-level evidence and there is uniform NCCN consensus.
Category 2B: The recommendation is based on lower-level evidence and there is nonuniform NCCN consensus (but no major disagreement).
Category 3: The recommendation is based on any level of evidence but reflects major disagreement.
All recommendations are category 2A unless otherwise noted.
Clinical trials: The NCCN believes that the best management for any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged.
Primary bone cancers are extremely rare neoplasms, likely accounting for fewer than 0.2% of all cancers, although its true incidence is difficult to determine secondary to the rarity of these tumors. 1 , 2 In 2009, an estimated 2570 new cases will be diagnosed in the United States and 1470 people will die of the disease. 3 Primary bone cancers show wide clinical heterogeneity and are often curable with proper treatment. Osteosarcoma (35%), chondrosarcoma (30%), and Ewing's sarcoma (16%) are the 3 most common forms of bone cancer. Malignant fibrous histiocytoma (MFH) and fibrosarcoma of the bone constitute fewer than 1% of all primary bone tumors. Chondrosarcoma is usually found in middle-aged and older adults; osteosarcoma and Ewing's sarcoma develop mainly in children and young adults. Various bone cancers are named based on their histologic origin: chondrosarcomas arise from cartilage, osteosarcomas arise from bone, and fibrogenic tissue is the origin of fibrosarcoma of bone, whereas vascular tissue gives rise to hemangioendothelioma and hemangiopericytoma. Notochordal tissue gives rise to chordoma. Several primary bone cancers, including Ewing's sarcoma family of tumors (ESFT), are of unknown histologic origin.
The pathogenesis and etiology of most bone cancers remain unclear. Gene rearrangements in the EWS and ETS family of genes have been implicated in the pathogenesis of Ewing's sarcoma. 4 – 7 Specific genetic alterations also play a role in osteosarcoma pathogenesis. 8 , 9 Although trauma is frequently implicated in sarcomas, a cause-and-effect relationship between a traumatic event and the development of bone cancer has not been identified. A quantifiable risk exists for developing bone sarcomas after therapeutic radiation. 10 , 11 Osteosarcoma is the most common radiation-induced sarcoma, and is the most common second primary malignancy in patients with a history of retinoblastoma. 12 , 13 Li-Fraumeni syndrome is a hereditary cancer syndrome in which there is a germ-line mutation of the p53 gene resulting in sarcomas such as osteosarcoma, early onset of bilateral breast cancer, and several other neoplasms. 14 – 17
In the past, a diagnosis of osteosarcoma and Ewing's sarcoma was associated with a poor prognosis. A generation ago, Marcove et al. described the survival pattern of newly diagnosed patients with osteosarcoma

Version 3.2010, 03-19-10 ©2010 National Comprehensive Cancer Network, Inc. All rights reserved. These guidelines and this illustration may not be reproduced in any form without the express written permission of NCCN.
Citation: Journal of the National Comprehensive Cancer Network J Natl Compr Canc Netw 8, 6; 10.6004/jnccn.2010.0051

Clinical trials: The NCCN believes that the best management for any cancer patient is in a clinical trial. Participation in clinical trials is especially encouraged. All recommendations are category 2A unless otherwise noted.
The NCCN Clinical Practice Guidelines in Oncology: Bone Cancer (to view the most recent version of these guidelines, visit the NCCN Web site at www.NCCN.org ) focus on chondrosarcoma, Ewing's sarcoma, and osteosarcoma.
The 2010 American Joint Committee on Cancer (AJCC) staging classification is shown in the staging table (available online, in these guidelines, at www.NCCN.org [ST-1]). This system is based on the assessment of histologic grade (G), tumor size (T), presence of regional (N) and/or distant metastases (M). The Surgical Staging System (SSS) is another staging system for bone and soft tissue sarcomas developed by the Musculoskeletal Tumor Society (available online, in these guidelines, at www.NCCN.org [ST-1]). 21 This system stratifies bone and soft tissue sarcomas according to surgical grade (G), local extent (T), and presence or absence of regional or distant metastases. It may be used in addition to the AJCC staging system.
Principles of Bone Cancer Management
- Multidisciplinary Team Involvement
Primary bone tumors and selected metastatic tumors should be evaluated and treated by a multidisciplinary team with demonstrated expertise in the management of these tumors. Appropriate team members are listed on page 696. Long-term surveillance and follow-up are necessary when considering the risk for recurrence and comorbidities associated with chemotherapy and radiation therapy (RT). Extended therapy and surveillance may be necessary for long-term survivors to address the potential side effects of surgery, RT, and chemotherapy. Patients should be given a survivorship prescription to schedule follow-ups with a multidisciplinary team. Fertility issues should be discussed with appropriate patients before they start treatment. 22
- Diagnostic Workup
Suspicion of a malignant bone tumor often begins when a poorly marginated lesion is seen on a plain radiograph in a patient with a painful lesion. In patients younger than 40 years, an aggressive, painful bone lesion has a significant risk for being a malignant primary bone tumor, and referral to an orthopedic oncologist should be considered before further workup. Patients 40 years and older whose plain films and history do not suggest a specific diagnosis should undergo evaluation for metastatic carcinoma, including chest radiograph; chest, abdominal, and pelvic CT; bone scan; mammogram; and other imaging studies as clinically indicated (see page 690). 23
All patients with suspected bone sarcomas should undergo complete staging before biopsy. Standard staging workup for a suspected primary bone sarcoma should include chest imaging (chest radiograph or CT to detect pulmonary metastases), appropriate imaging of the primary site (plain radiographs, MRI for local staging, and/or CT scan), and bone scan. 24 Imaging of painless bone lesions should be evaluated by a musculoskeletal radiologist followed by appropriate referral to a multidisciplinary treatment team if necessary. Laboratory studies, such as a CBC, lactate dehydrogenase (LDH), or alkaline phosphatase, should be performed before treatment is initiated.
PET is an alternative imaging technique used in the pretreatment staging of soft tissue and bone sarcomas. 25 Recent reports have shown the efficacy of PET scans in evaluating chemotherapy response in osteosarcoma and ESFT. 26 , 27
Biopsy should be performed using either core needle or surgical biopsy techniques. At biopsy, careful consideration should be given to appropriate stabilization of the affected bone and/or measures to protect against impending pathologic fracture. Because location of the biopsy is critical to limb-salvage techniques, it should be performed at the facility that will provide definitive management of the suspected primary malignant bone tumor.
Surgical margins should be negative, wide enough to minimize potential local recurrence, and narrow enough to maximize function. Wide excision implies histologically negative surgical margins and is necessary to optimize local control. Local tumor control may be achieved either through limb-sparing resection or limb amputation, although in selected cases, amputation may be the most appropriate option. However, limb-sparing resection is preferred if reasonable functional outcomes can be achieved. Response to the preoperative regimen should be evaluated with pathologic mapping. Consultation with a physical therapist is recommended to evaluate for mobility training and to determine an appropriate rehabilitation program.
Chondrosarcoma
Chondrosarcomas characteristically produce cartilage matrix from neoplastic tissue devoid of osteoid and may occur at any age, but are more common in older adults. 28 – 30 Conventional chondrosarcomas of the bone constitute approximately 85% of all chondrosarcomas and are divided as either primary or central lesions arising from previously normal-appearing bone preformed from cartilage; secondary or peripheral tumors that arise or develop from preexisting benign cartilage lesions, such as enchondromas; or from the cartilaginous portion of an osteochondroma. 29 , 31 , 32
Malignant transformation has been reported in lesions found in patients with Ollier's disease (enchondromatosis). The anatomic location, histologic grade, and size are essential prognostic features of the lesion, despite whether it is primary or secondary, or central or peripheral. 33 – 36 Peripheral or secondary tumors are usually low grade with infrequent metastasis. 37 Other rare subtypes that constitute approximately 10% to 15% of all chondrosarcomas 29 include clear cell, dedifferentiated, myxoid, and mesenchymal forms.
Symptoms of chondrosarcoma are usually mild and depend on tumor size and location. Patients with pelvic or axial lesions typically present later in the disease course, because the associated pain has a more insidious onset and often occurs when the tumor has reached a significant size. 33 , 38 , 39 Central chondrosarcomas show cortical destruction and loss of medullary bone trabeculations on radiographs, as well as calcification and destruction. 38
MRI will show the intramedullary involvement and extraosseous extension of the tumor. Secondary lesions arise from preexisting lesions. Serial radiographs will show a slow increase in size of the osteochondroma or enchondroma. A cartilage “cap” measuring greater than 2 cm on a preexisting lesion or documented growth after skeletal maturity should suggest sarcomatous transformation. 40
Histologic grade and tumor locations are the most important variables used to determine primary treatment. Resectable low-grade and intracompartmental lesions are treated with intralesional excision with or without adjuvant therapy. 41 – 44 Wide excision with negative margins is the preferred treatment for some low-grade lesions because of their larger size and intraarticular or pelvic localization. High-grade (grade II, III, or clear cell) or extracompartmental lesions are treated with wide excision, if resectable, obtaining negative surgical margins. 34
Unresectable high- and low-grade lesions are treated with RT (see page 691). Proton-beam RT has been associated with excellent local tumor control and long-term survival in patients with low-grade skull base chondrosarcomas. 45 , 46
Chemotherapy is not very effective in chondrosarcomas, especially in conventional and dedifferentiated chondrosarcomas. Although Mitchell et al. 47 reported that adjuvant chemotherapy with cisplatin and doxorubicin was associated with improved survival in patients with dedifferentiated chondrosarcoma, this finding could not be confirmed in other studies. 48 – 50 Recently, Cesari et al. 51 reported that the addition of chemotherapy improved survival rates in patients with mesenchymal chondrosarcoma. Another report from the German study group also confirmed that the outcome was better in younger patients. 52 However, no prospective randomized trials have been performed, and therefore the role of chemotherapy in the treatment of chondrosarcomas remains undefined.
No chemotherapy regimens have been established for conventional chondrosarcoma (grades 1–3). The NCCN Bone Cancer Guidelines suggest that dedifferentiated chondrosarcomas could be treated as osteosarcoma, and mesenchymal chondrosarcomas treated as Ewing's sarcoma, best approached as a function of their grade. Both of these options have a category 2B recommendation.
- Surveillance
Surveillance for low-grade lesions consists of a physical examination, imaging of the lesion, and a chest radiograph every 6 to 12 months for 2 years, then yearly as appropriate. Surveillance for high-grade lesions consists of a physical examination, imaging of the primary site, and/or cross-sectional imaging as indicated. Chest imaging is also indicated every 3 to 6 months for the first 5 years, and yearly thereafter for a minimum of 10 years, because late metastases and recurrences after 5 years are more common with chondrosarcoma than with other sarcomas. 35 Functional assessment should be performed at every visit (see page 691).
Local recurrence or relapse should be treated with wide excision, if the lesions are resectable. RT should be considered after wide excision with positive surgical margins (see page 691). Negative surgical margins should be observed. Unresectable recurrences are treated with RT.
Surgical excision is an option for systemic relapse of a high-grade lesion or patients should be encouraged to participate in a clinical trial.
ESFT are a group of small, round-cell neoplasms that include Ewing's sarcoma, primitive neuroectodermal tumor (PNET), Askin's tumor, PNET of bone, and extraosseous Ewing's sarcoma. Ewing's sarcoma is characterized by the fusion of the EWS gene on chromosome 22q12 with various members of the ETS gene family ( FLI1, ERG, ETV1, ETV4 , and FEV ). 5 , 6 The EWS-FLI1 fusion transcript resulting from the chromosomal translocation t(11;22) (q24;q12) is identified in approximately 85% of Ewing's sarcomas, such as Ewing's sarcoma, PNET, and Askin's tumor.
Ewing's sarcoma is poorly differentiated and is also characterized by the strong expression of cell-surface glycoprotein MIC2 (CD99). 53 , 54 The expression of MIC2 may be useful in the differential diagnosis of Ewing's sarcoma and PNET from other small round-cell neoplasms, although it is not exclusively specific to these tumors. 55
Ewing's sarcoma typically occurs in adolescents and young adults; the most common primary sites are the femur, pelvic bones, and bones of chest wall, although any bone may be affected. When arising in a long bone, the diaphysis is the most frequently affected site and appears mottled on imaging. Periosteal reaction is classic and is referred to as “onion skin” by radiologists.
Patients with Ewing's sarcoma, similar to those with bone sarcomas, present with localized pain or swelling. Unlike with other bone sarcomas, constitutional symptoms, such as fever, weight loss, and fatigue, are occasionally noted at presentation. Abnormal laboratory studies may include elevated serum LDH and leukocytosis.
Important indicators of favorable prognosis include a distal site of primary disease, normal serum LDH level at presentation, and absence of metastatic disease at presentation. 56 – 58 Nearly one quarter will present with metastatic disease, which is the most significant adverse prognostic factor in Ewing's sarcoma as it is for other bone sarcomas. 59 , 60 Lungs, bones, and bone marrow are the most common sites of metastasis. In a retrospective analysis of 975 patients from the European Intergroup Cooperative Ewing's Sarcoma Study (EICESS) Group, 5-year relapse-free survival was 22% for patients with metastatic disease at diagnosis compared with 55% for those without. 60 The results of the Intergroup Ewing's Sarcoma Study, analyzing the clinicopathologic features of 303 cases of Ewing's sarcoma, showed that patients with primary tumors in pelvic bones have the lowest survival rates compared with those with lesions in distal bones of the extremities. 61
When ESFT is suspected, patients should undergo complete staging before biopsy. This should include CT of the chest, plain radiographs of the primary site, CT or MRI of the entire bone or area involved, PET scan, and/or bone scan. An MRI of the spine and pelvis should also be considered. An ongoing diagnostic study is comparing whole-body MRI and conventional imaging for detecting distant metastases in pediatric patients with ESFT, Hodgkin lymphoma, non-Hodgkin's lymphoma, rhabdomyosarcoma, and neuroblastoma ( www.cancer.gov/clinicaltrials/ACRIN-6660 ).
Cytogenetic analysis of the biopsy specimen should be obtained to evaluate the t(11;22) translocation. Although preliminary reports suggest that EWS-FLI1 translocation is associated with a better prognosis than other variants, 62 – 64 this must be evaluated in large clinical trials. Bone marrow biopsy should be considered to complete the workup. Because serum LDH has been shown to have prognostic value as a tumor marker, the NCCN Bone Cancer Guidelines have included this test as part of the initial evaluation (see page 692). Fertility consultation should be considered for women of child-bearing age and men.
- Primary Treatment
Multiagent chemotherapy regimens, including ifosfamide and/or cyclophosphamide; etoposide; doxorubicin and/or dactinomycin; and vincristine have been shown to be effective in patients with localized Ewing's sarcoma in single- and multi-institutional collaborative trials in the United States and Europe. 65 , 66
The Intergroup Ewing's Sarcoma Studies (IESS-I and IESS-II) showed that the 4-drug regimen VACD (vincristine, dactinomycin, cyclophosphamide, and doxorubicin) was superior to the 3-drug regimen VAC (vincristine, dactinomycin, and cyclophosphamide) in terms of relapse-free (60% vs. 24%) and overall survival. 67 , 68
In the Pediatric Oncology Group-Children's Cancer Group (POG-CCG) study (INT-0091), patients with Ewing's sarcoma or PNET of the bone were randomized to undergo chemotherapy with VACD alone or alternating with ifosfamide and etoposide (VACD-IE) for 17 cycles. 69 In patients with nonmetastatic disease, the 5-year event-free survival rate was 69% in the VACD-IE group compared with 54% in the VACD alone group. Overall survival was also significantly higher among patients in the VACD-IE group (72% vs. 61%). However, the addition of ifosfamide and etoposide to VACD did not improve outcomes of patients with Ewing's sarcoma or PNET of bone with metastases at diagnosis. 70 Kolb et al. 71 from MSKCC also reported similar findings. The 4-year event-free and overall survival rates were 82% and 89%, respectively, for patients with locoregional disease, and 12% and 17.8%, respectively, for those with distant metastases.
The EICESS-92 study investigated whether cyclophosphamide has a similar efficacy to ifosfamide in standard-risk patients and whether the addition of etoposide improves survival in high-risk patients with Ewing's sarcoma. Standard-risk patients (small tumors) were randomly assigned to VAIA (vincristine, dactinomycin, ifosfamide, and doxorubicin) followed by either VAIA or VACA (vincristine, dactinomycin, cyclophosphamide, and doxorubicin). 72 High-risk patients (large tumors or metastatic disease at diagnosis) were randomly assigned to VAIA or VAIA plus etoposide (EVAIA). For the standard-risk patients, 3-year event-free survival rates for VACA and VAIA were 73% and 74%, respectively. In the high-risk patients, the 3-year event-free survival rates for EVAIA and VAIA were 52% and 47%, respectively. The results of this study suggest that cyclophosphamide has the same efficacy as ifosfamide in standard-risk patients. Furthermore, the event-free survival rates in the high-risk group, though not statistically significant, suggest a benefit with the addition of etoposide to ifosfamide.
The European Ewing Tumour Working Initiative of National Groups 1999 (EURO-EWING 99) study is designed to evaluate the efficacy and safety of combination chemotherapy with or without peripheral stem cell transplantation, RT, and/or surgery in patients with Ewing's sarcoma. Six courses of VIDE (vincristine, ifosfamide, doxorubicin, and etoposide) are administered as an intensive induction chemotherapy for patients with ESFT. 73
NCCN Recommendations: All patients with Ewing's sarcoma undergo primary treatment followed by local control therapy and adjuvant treatment (see page 693). Primary treatment consists of multiagent chemotherapy along with appropriate growth factor support for 12 to 24 weeks (see the NCCN Clinical Practice Guidelines in Oncology: Myeloid Growth Factors for growth factor support; to view the most recent version of these guidelines, visit the NCCN Web site at www.NCCN.org ). For localized Ewing's sarcoma, VAC alternating with ifosfamide and etoposide (VAC/IE) given on an every-2-week schedule was found to be more effective than on an every-3-week schedule, with median 3-year event-free survival rates of 76% and 65%, respectively. 74
The NCCN guidelines have included the following regimens for first-line therapy (primary/neoadjuvant/adjuvant) for patients with localized disease or metastatic disease at presentation (page 697):
VIA (vincristine, ifosfamide, and doxorubicin) 72
The guidelines recommend VAC (without the alternating cycle of ifosfamide and etoposide) as the preferred option for the treatment for primary metastatic disease at presentation. 70 , 71 VAC/IE, VIDE, and VIA regimens are included as alternative treatment options.
After primary treatment, patients should be restaged with an MRI of the lesion and chest imaging. PET or bone scan can be used for restaging depending on the imaging technique used during initial workup. Patients responding to primary treatment should be treated with local control therapy. Local control options include wide excision with or without preoperative RT, 75 , 76 definitive RT with chemotherapy, or amputation in selected cases (see page 693). Adjuvant chemotherapy with or without RT is recommended (regardless of surgical margins) after local control treatment (surgery or RT). The panel strongly recommends that the duration of chemotherapy be 28 and 49 weeks, depending on the type of regimen and dosing schedule (category 1).
Progressive disease after primary treatment is best managed with RT with or without surgery, followed by chemotherapy or best supportive care.
Surveillance of patients with Ewing's sarcoma consists of a physical examination, and chest and local imaging every 2 to 3 months. 77 , 78 Surveillance intervals should be increased after 2 years, then annually after 5 years.
- Treatment of Relapsed or Refractory Disease
Approximately 30% to 40% of patients with Ewing's sarcoma experience recurrence (local and/or distant) and have a very poor prognosis. The timing and type of recurrence are the important prognostic factors; those with longer time to first recurrence have a better chance of survival. Late relapse (≥ 2 years after diagnosis), lung-only metastases, and local recurrence that can be treated with radical surgery and intensive chemotherapy are the most favorable prognostic factors, whereas early relapses (< 2 years after diagnosis) with metastases in the lungs and/or other sites, recurrence at local and distant sites, elevated LDH at initial diagnosis, and initial recurrence are considered adverse prognostic factors. 79 – 81
Ifosfamide in combination with etoposide with or without carboplatin has been evaluated in clinical trials for the treatment of patients with relapsed or refractory sarcoma. 82 , 83 In a phase II study, the combination of ifosfamide with mesna and etoposide was highly active, with acceptable toxicity in the treatment of recurrent sarcomas in children and young adults. 82 In phase I and II studies conducted by the CCG, the overall response rate in patients with recurrent or refractory sarcoma was 51%; the overall survival rates at 1 and 2 years were 49% and 28%, respectively. Overall survival appeared significantly improved in patients who experienced a complete or partial response. 83
Docetaxel in combination with gemcitabine was found to be well tolerated and showed antitumor activity in the treatment of children and young adults with refractory bone sarcoma. 84 Topoisomerase I inhibitors, topotecan 85 – 88 and irinotecan, 89 – 91 in combination with cyclophosphamide and temozolomide, respectively, have shown promising response rates in patients with relapsed or refractory solid tumors. Cyclophosphamide and irinotecan produced a 44% response rate (35% of patients had a complete and 9% a partial response) in patients with recurrent or refractory Ewing's sarcoma. 86 After a median follow-up of 23.1 months, 25.9% of patients were in continuous remission. In a retrospective analysis of patients with recurrent or progressive Ewing's sarcoma treated with irinotecan and temozolomide at MSKCC, the median time-to-progression (TTP) was 8.3 months. 89 In those with recurrent disease, TTP was 16.2 months. Median TTP was better for patients experiencing a 2-year first remission and those with primary localized disease than for patients who experienced relapse within 2 years from diagnosis and for those with metastatic disease at diagnosis.
Inhibition of insulin-like growth factor-1 receptor (IGF-1R) may be an interesting approach in the treatment of some subtypes of sarcomas. Monoclonal antibodies, such as figitumumab and R1507, have shown safety and suggested possible efficacy in early-phase trials for patients with relapsed or refractory sarcomas, including Ewing's sarcoma.
High-dose chemotherapy with stem cell rescue (HDT/SCR) has been evaluated in patients with relapsed or progressive Ewing's sarcoma in several small studies. 92 – 98 The role of this approach in high-risk patients has yet to be determined in prospective randomized studies.
NCCN Recommendations: Treatment options for patients with relapsed or refractory disease include participation in a clinical trial, or chemotherapy with or without RT (see page 693). If a relapse is delayed, as sometimes occurs with this sarcoma, re-treatment with the previously effective regimen may be useful. The NCCN guidelines have included the following regimens as options for patients with relapsed or refractory disease (see page 697):
Cyclophosphamide and topotecan
Temozolomide and irinotecan
Ifosfamide and etoposide
Ifosfamide, carboplatin, and etoposide
Docetaxel and gemcitabine
All patients with recurrent and metastatic disease should be considered for clinical trials investigating new treatment approaches.
Osteosarcoma
Osteosarcoma is the most common primary malignant bone tumor in children and young adults; 1 the median age at diagnosis is 20 years. Osteosarcoma has 11 known variants with variable natural histories. Classic osteosarcoma constitutes nearly 80% of osteosarcoma and is always a high-grade spindle cell tumor that produces osteoid or immature bone. The most frequent sites for this cancer are the metaphyseal areas of the distal femur or proximal tibia, which are the sites of maximum growth.
Although most osteosarcomas are medullary and high-grade, parosteal lesions are juxtacortical and occur most often in the posterior distal femur. This variant tends to metastasize later than the classic form and has low histologic grade. Another juxtacortical variant is periosteal osteosarcomas, which most often involves the femur followed by the tibia and behaves with a severity that is intermediate between the parosteal and classic lesions. 99 Other variants include osteosarcoma secondary to Paget's disease or prior irradiation. Patients with retinoblastoma are also at an increased risk for developing a very aggressive variant of osteosarcoma.
Pain and swelling are the most frequent early symptoms. Pain in the beginning is often intermittent and a thorough workup sometimes is delayed because symptoms may be confused with growing pains. Osteosarcoma spreads hematogenously, commonly metastasizing to the lung.
Tumor site and size, presence and location of metastases, histologic response to chemotherapy, and complete resection with negative margins are significant prognostic factors for patients with osteosarcoma of the extremities and trunk. 100 , 101 Patients with one or a few resectable pulmonary metastases have a survival rate that approaches that of patients with no metastatic disease.
In an analysis of 1702 patients with osteosarcoma treated with neoadjuvant chemotherapy in cooperative study group protocols, axial tumor site, male gender, and a long history of symptoms were associated with poor response to chemotherapy. Patient age and tumor location at diagnosis had a significant influence on outcome. 100 All factors except age were significant in multivariate testing, with surgical remission and histologic response to chemotherapy emerging as the key prognostic factors. Elevated serum LDH level is also associated with a worse prognosis. Bacci et al. 102 reported on 1421 patients with osteosarcoma of the extremity treated over 30 years. In this cohort, serum level of LDH was significantly higher in patients with metastatic disease at presentation than those with localized disease; 5-year disease-free survival rates were 39.5% and 60%, respectively. The 5-year disease-free survival correlated with serum level of LDH at univariate and multivariate analysis (39.5% for patients with high LDH levels and 60% for those with normal values), although it lost its significance when histologic response to chemotherapy was also considered in the latter.
Osteosarcomas present both a local problem and a concern for distant metastasis. Imaging of the primary lesions is accomplished with plain radiographs, MRI, and/or CT and bone scan. PET scan can also be considered. Plain radiographs of osteosarcomas show cortical destruction and irregular reactive bone formation. Bone scan, although uniformly abnormal at the lesion, may be useful to identify additional synchronous lesions (see page 694). MRI provides excellent soft tissue contrast and may be essential for operative planning. MRI is the best imaging modality to define the extent of the lesion within the bone and soft tissues, detect “skip” metastases, and evaluate anatomic relationships with the surrounding structures. In addition, ALP and LDH are frequently elevated in patients with osteosarcoma.
Although surgery remains an essential part of osteosarcoma management, the addition of adjuvant and neoadjuvant chemotherapy regimens has improved outcomes in patients with localized osteosarcoma. Early trials used multiagent chemotherapy regimens, including at least 3 or more of the following drugs: doxorubicin; cisplatin; bleomycin; cyclophosphamide or ifosfamide; dactinomycin; and high-dose methotrexate. 103 – 110 The updated results of the randomized Multi-Institutional Osteosarcoma Study (MIOS) showed that 6-year event-free survival was significantly higher in patients randomized to adjuvant chemotherapy than in those who underwent observation only after surgery (61% and 11%, respectively). 109
Subsequent clinical trials have shown that short intensive chemotherapy regimens produce excellent long-term results, similar to those achieved with multiagent chemotherapy. 111 – 113 In a randomized trial conducted by the European Osteosarcoma group, combination doxorubicin and cisplatin was better tolerated in patients with operable nonmetastatic osteosarcoma than a multidrug regimen, with no difference in survival between the groups. 113 For both groups, the 3- and 5-year overall survival rates were 65% and 55%, respectively, and progression-free survival at 5 years was 44%. In a phase II/III trial, high-dose ifosfamide in combination with etoposide was effective as induction therapy in patients with newly diagnosed metastatic osteosarcoma despite significant myelosuppression, infection, and renal toxicity. 114 The overall response rate was 59%, and projected 2-year progression-free survival rate for patients with metastases to lung was 39%. The survival rate for patients with bone metastases (with or without pulmonary metastases) was 58%. Combination cisplatin, ifosfamide, and epirubicin was also an active and reasonably well-tolerated regimen in patients with nonmetastatic extremity osteosarcoma, 115 with a phase II study with a median follow-up of 64 months showing 5-year disease-free and overall survival rates of 41.9% and 48.2%, respectively.
Although neoadjuvant chemotherapy is associated with an improved prognosis in patients with high-grade localized osteosarcoma, the results were significantly poorer in those with metastatic disease at presentation. 103 , 116 , 117 Two-year event-free and overall survival rates were 21% and 55%, respectively, versus 75% and 94% in patients with nonmetastatic disease at presentation, treated with the same chemotherapy protocol. 103 Good histopathologic response (> 90% necrosis) to neoadjuvant chemotherapy has been shown to be predictive of survival regardless of the type of chemotherapy administered after surgery. 102 , 118 In an analysis of 881 patients with nonmetastatic osteosarcoma of the extremities treated with neoadjuvant chemotherapy and surgery at the Rizzoli Institute, Bacci et al. 119 showed that the 5-year disease-free and overall survival rates correlated significantly with histologic response to chemotherapy and were 67.9% versus 51.3% ( P < .0001) in patients with good response and 78.4% versus 63.7% ( P < .0001) in those with poor response, respectively. A report from the CCG also confirmed these findings; 8-year postoperative event-free and overall survival rates were 81% and 87%, respectively, in good responders to neoadjuvant therapy, 118 and for poor survivors were 46% and 52%, respectively. Attempts to improve the outcome of poor responders through modifying the regimen remain unsuccessful. 105
The safety and efficacy of HDT/SCR in patients with newly diagnosed metastatic osteosarcoma or relapsed osteosarcoma has also been evaluated. 120 , 121 In the Italian sarcoma group study, treatment with carboplatin and etoposide followed by SCR, combined with surgery, induced complete response in chemosensitive patients. 121 Transplant-related mortality was 3.1%. The 3-year overall and disease-free survival rates were 20% and 12%, respectively. The efficacy of this approach in high-risk patients remains to be determined in prospective randomized studies.
NCCN Recommendations: Wide excision is the primary treatment for patients with low-grade (intramedullary and surface) osteosarcomas, whereas preoperative chemotherapy is preferred for those with high-grade osteosarcoma (category 1) and periosteal lesions, before wide excision. Selected elderly patients may benefit from immediate surgery (see page 694).
After wide excision (for resectable lesions), postoperative chemotherapy is recommended for patients with low-grade or periosteal sarcomas with pathologic findings of high-grade disease. For high-grade osteosarcoma after wide excision, patients with a good histologic response should continue to undergo several more cycles of the same chemotherapy, whereas patients with a poor response should be considered for chemotherapy with a different regimen. RT followed by adjuvant chemotherapy is recommended if the sarcoma remains unresectable after preoperative chemotherapy (see page 694).
Chemotherapy can be given intra-arterially or intravenously 122 , 123 and should include appropriate growth factor support (see the NCCN Myeloid Growth Factors Guidelines for growth factor support [to view the most recent version of these guidelines, visit the NCCN Web site at www.nccn.org ]). The NCCN Bone Cancer Guidelines have included the following regimens for first-line therapy (primary/neoadjuvant/adjuvant) in patients with localized disease or primary therapy for metastatic disease (see page 697):
Cisplatin and doxorubicin
MAP (high-dose methotrexate, cisplatin, and doxorubicin)
Doxorubicin, cisplatin, ifosfamide, and high-dose methotrexate
Ifosfamide, cisplatin, and epirubicin
Once treatment is completed, surveillance should occur every 3 months for 2 years, then every 4 months for year 3, and then every 6 months for years 4 and 5, and yearly thereafter. Examination should include a complete physical, chest imaging, and plain film of the extremity. Chest CT should be performed if the plain chest radiograph becomes abnormal. Bone scan (category 2B) may also be considered (see page 695). Functional reassessment should be performed at every visit.
- Treatment for Relapsed or Refractory Disease
Approximately 30% of patients with localized disease and 80% presenting with metastatic disease will experience relapse. The presence of solitary metastases and complete resectability of the disease at first recurrence have been reported to be the most important prognostic indicators for improved survival, whereas patients not amenable to surgery and those with a second or third recurrence have a poor prognosis. 124 , 125
The combination of etoposide with cyclophosphamide or ifosfamide has been evaluated in clinical trials. 126 , 127 In a phase II trial of the French Society of Pediatric Oncology, ifosfamide and etoposide resulted in a response rate of 48% in patients with relapsed or refractory osteosarcoma. 127 In another phase II trial, cyclophosphamide and etoposide resulted in a 19% response rate and stable disease in 35% of patients with relapsed high-risk osteosarcoma. 126 Progression-free survival at 4 months was 42%. Single-agent gemcitabine and combination regimens such as docetaxel and gemcitabine; cyclophosphamide and topotecan; and ifosfamide, carboplatin, and etoposide have been effective in the treatment of patients with relapsed or refractory bone sarcomas. 83 , 84 , 88 , 128
Samarium-153 ethylene diamine tetramethylene phosphonate ( 153 Sm-EDTMP), a bone-seeking radiopharmaceutical, has been evaluated in patients with locally recurrent or metastatic osteosarcoma or skeletal metastases. 129 , 130 Andersen et al. 129 reported that 153 Sm-EDTMP with peripheral blood progenitor cell support had low nonhematologic toxicity and provided pain palliation for patients with osteosarcoma local recurrences or osteoblastic bone metastases. Results of a recent dose-finding study also show that 153 Sm-EDTMP can be effective in the treatment of patients with high-risk osteosarcoma. 130
NCCN Recommendations: The optimal treatment strategy for patients with relapsed or metastatic disease has yet to be defined. If relapse occurs, patients should undergo second-line chemotherapy and/or surgical resection (see page 695). Surveillance is recommended for those who respond to second-line therapy. The NCCN Bone Cancer Guidelines include the following regimens as options for patients with relapsed or refractory disease (see page 697):
Cyclophosphamide and etoposide
Gemcitabine
High-dose methotrexate, etoposide, and ifosfamide
Patients who experience progressive disease after second-line therapy should be treated with resection, RT for palliation, or best supportive care (see page 695). Participation in a clinical trial should be strongly encouraged. The guidelines also include 153 Sm-EDTMP as a treatment option for relapsed disease after second-line therapy.
Primary bone cancers are rare neoplasms, with osteosarcoma, chondrosarcoma, and Ewing's sarcoma the 3 most common forms.
Chondrosarcoma is usually found in middle-aged and older adults. Wide excision is the preferred treatment for resectable low- and high-grade chondrosarcomas. Intralesional excision with or without adjuvant therapy is an alternative option for low-grade lesions. In small series of reports, the addition of chemotherapy improved outcomes in patients with mesenchymal chondrosarcomas. However, the role of chemotherapy in the treatment of chondrosarcomas is not yet defined.
Ewing's sarcoma is characterized by a chromosomal translocation t(11;22), resulting in the fusion of EWS gene with various members of the ETS family of genes, and develops mainly in children and young adults. Multiagent chemotherapy is the primary treatment for patients with Ewing's sarcoma. Patients who experience response to primary treatment are treated with local control therapy (surgery or radiation) followed by adjuvant chemotherapy. Progressive disease is best managed with RT with or without surgery followed by chemotherapy or best supportive care.
Osteosarcoma occurs mainly in children and young adults. Wide excision is the primary treatment for patients with low-grade osteosarcomas, whereas preoperative chemotherapy is preferred before wide excision for high-grade osteosarcoma and periosteal lesions. After wide excision (for resectable lesions), postoperative chemotherapy is recommended for patients with low-grade or periosteal sarcomas with pathologic findings of high-grade disease and those with high-grade sarcoma. RT followed by adjuvant chemotherapy is recommended if the sarcoma remains unresectable after preoperative chemotherapy. Patients with relapsed or refractory disease should be treated with second-line therapy. Participation in a clinical trial should be strongly encouraged for patients experiencing progressive disease after second-line therapy.
The development of multiagent chemotherapy regimens for neoadjuvant and adjuvant treatment has considerably improved the prognosis for patients with osteosarcoma and Ewing's sarcoma. A small subset of patients diagnosed with metastatic disease at presentation can be cured with the proper treatment. Consistent with the NCCN philosophy, the panel encourages patients to participate in well-designed clinical trials to enable further advances.
Individual Disclosure for the NCCN Bone Cancer Panel

Please Note
The NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines™) are a statement of consensus of the authors regarding their views of currently accepted approaches to treatment. Any clinician seeking to apply or consult these guidelines is expected to use independent medical judgment in the context of individual clinical circumstances to determine any patient's care or treatment. The National Comprehensive Cancer Network® (NCCN®) makes no representation or warranties of any kind regarding their content, use, or application and disclaims any responsibility for their applications or use in any way.
© National Comprehensive Cancer Network, Inc. 2010, All rights reserved. These guidelines and the illustrations herein may not be reproduced in any form without the express written permission of NCCN.
Disclosures for the NCCN Bone Cancer Guidelines Panel
At the beginning of each NCCN Guidelines panel meeting, panel members disclosed any financial support they have received from industry. Through 2008, this information was published in an aggregate statement in JNCCN and online. Furthering NCCN's commitment to public transparency, this disclosure process has now been expanded by listing all potential conflicts of interest respective to each individual expert panel member.
Individual disclosures for the NCCN Bone Cancer Guidelines Panel members can be found on page 712. (The most recent version of these guidelines and accompanying disclosures, including levels of compensation, are available on the NCCN Web site at www.NCCN.org .)
These guidelines are also available on the Internet. For the latest update, please visit www.NCCN.org .
Yasko AW , Chow W , Fressica D . Bone sarcomas . In: Pazdur R , Wagman LD , Camphausen C , Hoskins WJ , eds. Cancer Management: A Multidisciplinary Approach , 11th ed. Lawrence, KS : CMPMedica LLC ; 2008 .
- Search Google Scholar
- Export Citation
Unni KK . Dahlin’s Bone Tumors: General Aspects and Data on 11,087 Cases , 5th ed. Philadelphia : Lippincott Williams & Wilkins ; 1996 .
Jemal A , Siegel R , Ward E et al. . Cancer statistics, 2009 . CA Cancer J Clin 2009 ; 59 : 225 – 249 .
de Alava E , Gerald WL . Molecular biology of the Ewing’s sarcoma/primitive neuroectodermal tumor family . J Clin Oncol 2000 ; 18 : 204 – 213 .
Delattre O , Zucman J , Melot T et al. . The Ewing family of tumors—a subgroup of small-round-cell tumors defined by specific chimeric transcripts . N Engl J Med 1994 ; 331 : 294 – 299 .
Denny CT . Gene rearrangements in Ewing’s sarcoma . Cancer Invest 1996 ; 14 : 83 – 88 .
Burchill SA . Molecular abnormalities in Ewing’s sarcoma . Expert Rev Anticancer Ther 2008 ; 8 : 1675 – 1687 .
Kruzelock RP , Murphy EC , Strong LC et al. . Localization of a novel tumor suppressor locus on human chromosome 3q important in osteosarcoma tumorigenesis . Cancer Res 1997 ; 57 : 106 – 109 .
Yamaguchi T , Toguchida J , Yamamuro T et al. . Allelotype analysis in osteosarcomas: frequent allele loss on 3q, 13q, 17p, and 18q . Cancer Res 1992 ; 52 : 2419 – 2423 .
Sagerman RH , Cassady JR , Tretter P , Ellsworth RM . Radiation induced neoplasia following external beam therapy for children with retinoblastoma . Am J Roentgenol Radium Ther Nucl Med 1969 ; 105 : 529 – 535 .
Tucker MA , D’Angio GJ , Boice JD et al. . Bone sarcomas linked to radiotherapy and chemotherapy in children . N Engl J Med 1987 ; 317 : 588 – 593 .
Araki N , Uchida A , Kimura T et al. . Involvement of the retinoblastoma gene in primary osteosarcomas and other bone and soft-tissue tumors . Clin Orthop Relat Res 1991 : 271 – 277 .
Schimke RN , Lowman JT , Cowan AB . Retinoblastoma and osteogenic sarcoma in siblings . Cancer 1974 ; 34 : 2077 – 2079 .
Li FP , Fraumeni JF . Prospective study of a family cancer syndrome . JAMA 1982 ; 247 : 2692 – 2694 .
Malkin D , Li FP , Strong LC et al. . Germ line p53 mutations in a familial syndrome of breast cancer, sarcomas, and other neoplasms . Science 1990 ; 250 : 1233 – 1238 .
McIntyre JF , Smith-Sorensen B , Friend SH et al. . Germline mutations of the p53 tumor suppressor gene in children with osteosarcoma . J Clin Oncol 1994 ; 12 : 925 – 930 .
Miller CW , Aslo A , Won A et al. . Alterations of the p53, Rb and MDM2 genes in osteosarcoma . J Cancer Res Clin Oncol 1996 ; 122 : 559 – 565 .
Grier HE . The Ewing family of tumors: Ewing’s sarcoma and primitive neuroectodermal tumors . Pediatric Clinics of North America 1997 ; 44 : 991 – 1004 .
Marina N , Gebhardt M , Teot L , Gorlick R . Biology and therapeutic advances for pediatric osteosarcoma . Oncologist 2004 ; 9 : 422 – 441 .
Wittig JC , Bickels J , Priebat D et al. . Osteosarcoma: a multidisciplinary approach to diagnosis and treatment . Am Fam Physician 2002 ; 65 : 1123 – 1132 .
Enneking WF , Spanier SS , Goodman MA . A system for the surgical staging of musculoskeletal sarcoma . Clin Orthop Relat Res 1980 : 106 – 120 .
Lee SJ , Schover LR , Partridge AH et al. . American Society of Clinical Oncology recommendations on fertility preservation in cancer patients . J Clin Oncol 2006 ; 24 : 2917 – 2931 .
Rougraff BT , Kneisl JS , Simon MA . Skeletal metastases of unknown origin. A prospective study of a diagnostic strategy . J Bone Joint Surg Am 1993 ; 75 : 1276 – 1281 .
Heck RK , Peabody TD , Simon MA . Staging of primary malignancies of bone . CA Cancer J Clin 2006 ; 56 : 366 – 375 .
Schuetze SM . Utility of positron emission tomography in sarcomas . Curr Opin Oncol 2006 ; 18 : 369 – 373 .
Hawkins DS , Rajendran JG , Conrad EU et al. . Evaluation of chemotherapy response in pediatric bone sarcomas by [F-18]-fluorodeoxy-D-glucose positron emission tomography . Cancer 2002 ; 94 : 3277 – 3284 .
Hawkins DS , Schuetze SM , Butrynski JE et al. . [18F] Fluorodeoxyglucose positron emission tomography predicts outcome for Ewing sarcoma family of tumors . J Clin Oncol 2005 ; 23 : 8828 – 8834 .
Bovee JV , Cleton-Jansen AM , Taminiau AH , Hogendoorn PC . Emerging pathways in the development of chondrosarcoma of bone and implications for targeted treatment . Lancet Oncol 2005 ; 6 : 599 – 607 .
Gelderblom H , Hogendoorn PC , Dijkstra SD et al. . The clinical approach towards chondrosarcoma . Oncologist 2008 ; 13 : 320 – 329 .
Terek RM . Recent advances in the basic science of chondrosarcoma . Orthop Clin North Am 2006 ; 37 : 9 – 14 .
Mankin HJ , Cantley KP , Schiller AL , Lippiello L . The biology of human chondrosarcoma. II. Variation in chemical composition among types and subtypes of benign and malignant cartilage tumors . J Bone Joint Surg Am 1980 ; 62 : 176 – 188 .
Mankin HJ , Cantley KP , Lippiello L et al. . The biology of human chondrosarcoma. I. Description of the cases, grading, and biochemical analyses . J Bone Joint Surg Am 1980 ; 62 : 160 – 176 .
Bruns J , Elbracht M , Niggemeyer O . Chondrosarcoma of bone: an oncological and functional follow-up study . Ann Oncol 2001 ; 12 : 859 – 864 .
Fiorenza F , Abudu A , Grimer RJ et al. . Risk factors for survival and local control in chondrosarcoma of bone . J Bone Joint Surg Br 2002 ; 84 : 93 – 99 .
Lee FY , Mankin HJ , Fondren G et al. . Chondrosarcoma of bone: an assessment of outcome . J Bone Joint Surg Am 1999 ; 81 : 326 – 338 .
Sanerkin NG . The diagnosis and grading of chondrosarcoma of bone: a combined cytologic and histologic approach . Cancer 1980 ; 45 : 582 – 594 .
Ahmed AR , Tan TS , Unni KK et al. . Secondary chondrosarcoma in osteochondroma: report of 107 patients . Clin Orthop Relat Res 2003 : 193 – 206 .
Bergh P , Gunterberg B , Meis-Kindblom JM , Kindblom LG . Prognostic factors and outcome of pelvic, sacral, and spinal chondrosarcomas: a center-based study of 69 cases . Cancer 2001 ; 91 : 1201 – 1212 .
Enneking WF , Dunham WK . Resection and reconstruction for primary neoplasms involving the innominate bone . J Bone Joint Surg Am 1978 ; 60 : 731 – 746 .
Norman A , Sissons HA . Radiographic hallmarks of peripheral chondrosarcoma . Radiology 1984 ; 151 : 589 – 596 .
Leerapun T , Hugate RR , Inwards CY et al. . Surgical management of conventional grade I chondrosarcoma of long bones . Clin Orthop Relat Res 2007 ; 463 : 166 – 172 .
Marcove RC . A 17-year review of cryosurgery in the treatment of bone tumors . Clin Orthop Relat Res 1982 ; 163 : 231 – 234 .
Marcove RC , Stovell PB , Huvos AG , Bullough PG . The use of cryosurgery in the treatment of low and medium grade chondrosarcoma. A preliminary report . Clin Orthop Relat Res 1977 : 147 – 156 .
Veth R , Schreuder B , van Beem H et al. . Cryosurgery in aggressive, benign, and low-grade malignant bone tumours . Lancet Oncol 2005 ; 6 : 25 – 34 .
Hug EB , Slater JD . Proton radiation therapy for chordomas and chondrosarcomas of the skull base . Neurosurg Clin N Am 2000 ; 11 : 627 – 638 .
Noel G , Feuvret L , Ferrand R et al. . Radiotherapeutic factors in the management of cervical-basal chordomas and chondrosarcomas . Neurosurgery 2004 ; 55 : 1252 – 1260 .
Mitchell AD , Ayoub K , Mangham DC et al. . Experience in the treatment of dedifferentiated chondrosarcoma . J Bone Joint Surg Br 2000 ; 82 : 55 – 61 .
Dickey ID , Rose PS , Fuchs B et al. . Dedifferentiated chondrosarcoma: the role of chemotherapy with updated outcomes . J Bone Joint Surg Am 2004 ; 86–A : 2412 – 2418 .
Grimer RJ , Gosheger G , Taminiau A et al. . Dedifferentiated chondrosarcoma: prognostic factors and outcome from a European group . Eur J Cancer 2007 ; 43 : 2060 – 2065 .
Staals EL , Bacchini P , Bertoni F . Dedifferentiated central chondrosarcoma . Cancer 2006 ; 106 : 2682 – 2691 .
Cesari M , Bertoni F , Bacchini P et al. . Mesenchymal chondrosarcoma. An analysis of patients treated at a single institution . Tumori 2007 ; 93 : 423 – 427 .
Dantonello TM , Int-Veen C , Leuschner I et al. . Mesenchymal chondrosarcoma of soft tissues and bone in children, adolescents, and young adults: experiences of the CWS and COSS study groups . Cancer 2008 ; 112 : 2424 – 2431 .
Ambros IM , Ambros PF , Strehl S et al. . MIC2 is a specific marker for Ewing’s sarcoma and peripheral primitive neuroectodermal tumors. Evidence for a common histogenesis of Ewing’s sarcoma and peripheral primitive neuroectodermal tumors from MIC2 expression and specific chromosome aberration . Cancer 1991 ; 67 : 1886 – 1893 .
Perlman EJ , Dickman PS , Askin FB et al. . Ewing’s sarcoma—routine diagnostic utilization of MIC2 analysis: a Pediatric Oncology Group/Children’s Cancer Group Intergroup study . Hum Pathol 1994 ; 25 : 304 – 307 .
Olsen SH , Thomas DG , Lucas DR . Cluster analysis of immunohistochemical profiles in synovial sarcoma, malignant peripheral nerve sheath tumor, and Ewing sarcoma . Mod Pathol 2006 ; 19 : 659 – 668 .
Glaubiger DL , Makuch R , Schwarz J et al. . Determination of prognostic factors and their influence on therapeutic results in patients with Ewing’s sarcoma . Cancer 1980 ; 45 : 2213 – 2219 .
Gobel V , Jurgens H , Etspuler G et al. . Prognostic significance of tumor volume in localized Ewing’s sarcoma of bone in children and adolescents . J Cancer Res Clin Oncol 1987 ; 113 : 187 – 191 .
Mendenhall CM , Marcus RB , Enneking WF et al. . The prognostic significance of soft tissue extension in Ewing’s sarcoma . Cancer 1983 ; 51 : 913 – 917 .
Cangir A , Vietti TJ , Gehan EA et al. . Ewing’s sarcoma metastatic at diagnosis. Results and comparisons of two intergroup Ewing’s sarcoma studies . Cancer 1990 ; 66 : 887 – 893 .
Cotterill SJ , Ahrens S , Paulussen M et al. . Prognostic factors in Ewing’s tumor of bone: analysis of 975 patients from the European Intergroup Cooperative Ewing’s Sarcoma Study Group . J Clin Oncol 2000 ; 18 : 3108 – 3114 .
Kissane JM , Askin FB , Foulkes M et al. . Ewing’s sarcoma of bone: clinicopathologic aspects of 303 cases from the Intergroup Ewing’s Sarcoma Study . Hum Pathol 1983 ; 14 : 773 – 779 .
Avigad S , Cohen IJ , Zilberstein J et al. . The predictive potential of molecular detection in the nonmetastatic Ewing family of tumors . Cancer 2004 ; 100 : 1053 – 1058 .
de Alava E , Kawai A , Healey JH et al. . EWS-FLI1 fusion transcript structure is an independent determinant of prognosis in Ewing’s sarcoma . J Clin Oncol 1998 ; 16 : 1248 – 1255 .
Zoubek A , Dockhorn-Dworniczak B , Delattre O et al. . Does expression of different EWS chimeric transcripts define clinically distinct risk groups of Ewing tumor patients? J Clin Oncol 1996 ; 14 : 1245 – 1251 .
Bernstein M , Kovar H , Paulussen M et al. . Ewing’s sarcoma family of tumors: current management . Oncologist 2006 ; 11 : 503 – 519 .
Subbiah V , Anderson P , Lazar AJ et al. . Ewing’s sarcoma: standard and experimental treatment options . Curr Treat Options Oncol 2009 ; 10 : 126 – 140 .
Burgert EO , Nesbit ME , Garnsey LA et al. . Multimodal therapy for the management of nonpelvic, localized Ewing’s sarcoma of bone: intergroup study IESS-II . J Clin Oncol 1990 ; 8 : 1514 – 1524 .
Nesbit ME , Gehan EA , Burgert EO et al. . Multimodal therapy for the management of primary, nonmetastatic Ewing’s sarcoma of bone: a long-term follow-up of the First Intergroup study . J Clin Oncol 1990 ; 8 : 1664 – 1674 .
Grier HE , Krailo MD , Tarbell NJ et al. . Addition of ifosfamide and etoposide to standard chemotherapy for Ewing’s sarcoma and primitive neuroectodermal tumor of bone . N Engl J Med 2003 ; 348 : 694 – 701 .
Miser JS , Krailo MD , Tarbell NJ et al. . Treatment of metastatic Ewing’s sarcoma or primitive neuroectodermal tumor of bone: evaluation of combination ifosfamide and etoposide—a Children’s Cancer Group and Pediatric Oncology Group study . J Clin Oncol 2004 ; 22 : 2873 – 2876 .
Kolb EA , Kushner BH , Gorlick R et al. . Long-term event-free survival after intensive chemotherapy for Ewing’s family of tumors in children and young adults . J Clin Oncol 2003 ; 21 : 3423 – 3430 .
Paulussen M , Craft AW , Lewis I et al. . Results of the EICESS-92 study: two randomized trials of Ewing’s sarcoma treatment—cyclophosphamide compared with ifosfamide in standard-risk patients and assessment of benefit of etoposide added to standard treatment in high-risk patients . J Clin Oncol 2008 ; 26 : 4385 – 4393 .
Juergens C , Weston C , Lewis I et al. . Safety assessment of intensive induction with vincristine, ifosfamide, doxorubicin, and etoposide (VIDE) in the treatment of Ewing tumors in the EURO-E.W.I.N.G. 99 clinical trial . Pediatr Blood Cancer 2006 ; 47 : 22 – 29 .
Womer RB , West DC , Krailo MD et al. . Randomized comparison of every-two-week v. every-three-week chemotherapy in Ewing sarcoma family tumors (ESFT) [abstract] . J Clin Oncol 2008 ; 26 ( Suppl 1 ): Abstract 10504 .
Brown AP , Fixsen JA , Plowman PN . Local control of Ewing’s sarcoma: an analysis of 67 patients . Br J Radiol 1987 ; 60 : 261 – 268 .
Scully SP , Temple HT , O’Keefe RJ et al. . Role of surgical resection in pelvic Ewing’s sarcoma . J Clin Oncol 1995 ; 13 : 2336 – 2341 .
Bacci G , Forni C , Longhi A et al. . Long-term outcome for patients with non-metastatic Ewing’s sarcoma treated with adjuvant and neoadjuvant chemotherapies. 402 patients treated at Rizzoli between 1972 and 1992 . Eur J Cancer 2004 ; 40 : 73 – 83 .
Pritchard DJ , Dahlin DC , Dauphine RT et al. . Ewing’s sarcoma. A clinicopathological and statistical analysis of patients surviving five years or longer . J Bone Joint Surg Am 1975 ; 57 : 10 – 16 .
Bacci G , Ferrari S , Longhi A et al. . Therapy and survival after recurrence of Ewing’s tumors: the Rizzoli experience in 195 patients treated with adjuvant and neoadjuvant chemotherapy from 1979 to 1997 . Ann Oncol 2003 ; 14 : 1654 – 1659 .
Leavey PJ , Mascarenhas L , Marina N et al. . Prognostic factors for patients with Ewing sarcoma (EWS) at first recurrence following multi-modality therapy: a report from the Children’s Oncology Group . Pediatr Blood Cancer 2008 ; 51 : 334 – 338 .
Rodriguez-Galindo C , Billups CA , Kun LE et al. . Survival after recurrence of Ewing tumors: the St Jude Children’s Research Hospital experience, 1979–1999 . Cancer 2002 ; 94 : 561 – 569 .
Miser JS , Kinsella TJ , Triche TJ et al. . Ifosfamide with mesna uroprotection and etoposide: an effective regimen in the treatment of recurrent sarcomas and other tumors of children and young adults . J Clin Oncol 1987 ; 5 : 1191 – 1198 .
Van Winkle P , Angiolillo A , Krailo M et al. . Ifosfamide, carboplatin, and etoposide (ICE) reinduction chemotherapy in a large cohort of children and adolescents with recurrent/refractory sarcoma: the Children’s Cancer Group (CCG) experience . Pediatr Blood Cancer 2005 ; 44 : 338 – 347 .
Navid F , Willert JR , McCarville MB et al. . Combination of gemcitabine and docetaxel in the treatment of children and young adults with refractory bone sarcoma . Cancer 2008 ; 113 : 419 – 425 .
Bernstein ML , Devidas M , Lafreniere D et al. . Intensive therapy with growth factor support for patients with Ewing tumor metastatic at diagnosis: Pediatric Oncology Group/Children’s Cancer Group Phase II Study 9457—a report from the Children’s Oncology Group . J Clin Oncol 2006 ; 24 : 152 – 159 .
Hunold A , Weddeling N , Paulussen M et al. . Topotecan and cyclophosphamide in patients with refractory or relapsed Ewing tumors . Pediatr Blood Cancer 2006 ; 47 : 795 – 800 .
Kushner BH , Kramer K , Meyers PA et al. . Pilot study of topotecan and high-dose cyclophosphamide for resistant pediatric solid tumors . Med Pediatr Oncol 2000 ; 35 : 468 – 474 .
Saylors RL III , Stine KC , Sullivan J et al. . Cyclophosphamide plus topotecan in children with recurrent or refractory solid tumors: a Pediatric Oncology Group phase II study . J Clin Oncol 2001 ; 19 : 3463 – 3469 .
Casey DA , Wexler LH , Merchant MS et al. . Irinotecan and temozolomide for Ewing sarcoma: the Memorial Sloan-Kettering experience . Pediatr Blood Cancer 2009 ; 53 : 1029 – 1034 .
Wagner LM , Crews KR , Iacono LC et al. . Phase I trial of temozolomide and protracted irinotecan in pediatric patients with refractory solid tumors . Clin Cancer Res 2004 ; 10 : 840 – 848 .
Wagner LM , McAllister N , Goldsby RE et al. . Temozolomide and intravenous irinotecan for treatment of advanced Ewing sarcoma . Pediatr Blood Cancer 2007 ; 48 : 132 – 139 .
Barker LM , Pendergrass TW , Sanders JE , Hawkins DS . Survival after recurrence of Ewing’s sarcoma family of tumors . J Clin Oncol 2005 ; 23 : 4354 – 4362 .
Burdach S , Jurgens H , Peters C et al. . Myeloablative radiochemotherapy and hematopoietic stem-cell rescue in poor-prognosis Ewing’s sarcoma . J Clin Oncol 1993 ; 11 : 1482 – 1488 .
Engelhardt M , Zeiser R , Ihorst G et al. . High-dose chemotherapy and autologous peripheral blood stem cell transplantation in adult patients with high-risk or advanced Ewing and soft tissue sarcoma . J Cancer Res Clin Oncol 2007 ; 133 : 1 – 11 .
Horowitz ME , Kinsella TJ , Wexler LH et al. . Total-body irradiation and autologous bone marrow transplant in the treatment of high-risk Ewing’s sarcoma and rhabdomyosarcoma . J Clin Oncol 1993 ; 11 : 1911 – 1918 .
Kushner BH , Meyers PA . How effective is dose-intensive/myeloablative therapy against Ewing’s sarcoma/primitive neuroectodermal tumor metastatic to bone or bone marrow? The Memorial Sloan-Kettering experience and a literature review . J Clin Oncol 2001 ; 19 : 870 – 880 .
McTiernan A , Driver D , Michelagnoli MP et al. . High dose chemotherapy with bone marrow or peripheral stem cell rescue is an effective treatment option for patients with relapsed or progressive Ewing’s sarcoma family of tumours . Ann Oncol 2006 ; 17 : 1301 – 1305 .
Oberlin O , Rey A , Desfachelles AS et al. . Impact of high-dose busulfan plus melphalan as consolidation in metastatic Ewing tumors: a study by the Societe Francaise des Cancers de l’Enfant . J Clin Oncol 2006 ; 24 : 3997 – 4002 .
Grimer RJ , Bielack S , Flege S et al. . Periosteal osteosarcoma—a European review of outcome . Eur J Cancer 2005 ; 41 : 2806 – 2811 .
Bielack SS , Kempf-Bielack B , Delling G et al. . Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols . J Clin Oncol 2002 ; 20 : 776 – 790 .
Davis AM , Bell RS , Goodwin PJ . Prognostic factors in osteosarcoma: a critical review . J Clin Oncol 1994 ; 12 : 423 – 431 .
Bacci G , Longhi A , Ferrari S et al. . Prognostic significance of serum lactate dehydrogenase in osteosarcoma of the extremity: experience at Rizzoli on 1421 patients treated over the last 30 years . Tumori 2004 ; 90 : 478 – 484 .
Bacci G , Briccoli A , Rocca M et al. . Neoadjuvant chemotherapy for osteosarcoma of the extremities with metastases at presentation: recent experience at the Rizzoli Institute in 57 patients treated with cisplatin, doxorubicin, and a high dose of methotrexate and ifosfamide . Ann Oncol 2003 ; 14 : 1126 – 1134 .
Bacci G , Ferrari S , Bertoni F et al. . Long-term outcome for patients with nonmetastatic osteosarcoma of the extremity treated at the istituto ortopedico rizzoli according to the istituto ortopedico rizzoli/osteosarcoma-2 protocol: an updated report . J Clin Oncol 2000 ; 18 : 4016 – 4027 .
Winkler K , Beron G , Delling G et al. . Neoadjuvant chemotherapy of osteosarcoma: results of a randomized cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response . J Clin Oncol 1988 ; 6 : 329 – 337 .
Ferrari S , Smeland S , Mercuri M et al. . Neoadjuvant chemotherapy with high-dose Ifosfamide, high-dose methotrexate, cisplatin, and doxorubicin for patients with localized osteosarcoma of the extremity: a joint study by the Italian and Scandinavian Sarcoma Groups . J Clin Oncol 2005 ; 23 : 8845 – 8852 .
Eilber F , Giuliano A , Eckardt J et al. . Adjuvant chemotherapy for osteosarcoma: a randomized prospective trial . J Clin Oncol 1987 ; 5 : 21 – 26 .
Link MP , Goorin AM , Miser AW et al. . The effect of adjuvant chemotherapy on relapse-free survival in patients with osteosarcoma of the extremity . N Engl J Med 1986 ; 314 : 1600 – 1606 .
Link MP , Goorin AM , Horowitz M et al. . Adjuvant chemotherapy of high-grade osteosarcoma of the extremity. Updated results of the Multi-Institutional Osteosarcoma Study . Clin Orthop Relat Res 1991 : 8 – 14 .
Meyers PA , Heller G , Healey J et al. . Chemotherapy for nonmetastatic osteogenic sarcoma: the Memorial Sloan-Kettering experience . J Clin Oncol 1992 ; 10 : 5 – 15 .
Bramwell V , Burgers M , Sneath R et al. . A comparison of two short intensive adjuvant chemotherapy regimens in operable osteosarcoma of limbs in children and young adults: the first study of the European Osteosarcoma Intergroup . J Clin Oncol 1992 ; 10 : 1579 – 1591 .
Lewis IJ , Nooij MA , Whelan J et al. . Improvement in histologic response but not survival in osteosarcoma patients treated with intensified chemotherapy: a randomized phase III trial of the European Osteosarcoma Intergroup . J Natl Cancer Inst 2007 ; 99 : 112 – 128 .
Souhami RL , Craft AW , Van der Eijken JW et al. . Randomised trial of two regimens of chemotherapy in operable osteosarcoma: a study of the European Osteosarcoma Intergroup . Lancet 1997 ; 350 : 911 – 917 .
Goorin AM , Harris MB , Bernstein M et al. . Phase II/III trial of etoposide and high-dose ifosfamide in newly diagnosed metastatic osteosarcoma: a pediatric oncology group trial . J Clin Oncol 2002 ; 20 : 426 – 433 .
Basaran M , Bavbek ES , Saglam S et al. . A phase II study of cisplatin, ifosfamide and epirubicin combination chemotherapy in adults with nonmetastatic and extremity osteosarcomas . Oncology 2007 ; 72 : 255 – 260 .
Bacci G , Briccoli A , Mercuri M et al. . Osteosarcoma of the extremities with synchronous lung metastases: long-term results in 44 patients treated with neoadjuvant chemotherapy . J Chemother 1998 ; 10 : 69 – 76 .
Meyers PA , Heller G , Healey JH et al. . Osteogenic sarcoma with clinically detectable metastasis at initial presentation . J Clin Oncol 1993 ; 11 : 449 – 453 .
Provisor AJ , Ettinger LJ , Nachman JB et al. . Treatment of nonmetastatic osteosarcoma of the extremity with preoperative and postoperative chemotherapy: a report from the Children’s Cancer Group . J Clin Oncol 1997 ; 15 : 76 – 84 .
Bacci G , Mercuri M , Longhi A et al. . Grade of chemotherapy-induced necrosis as a predictor of local and systemic control in 881 patients with non-metastatic osteosarcoma of the extremities treated with neoadjuvant chemotherapy in a single institution . Eur J Cancer 2005 ; 41 : 2079 – 2085 .
Lashkari A , Chow WA , Valdes F et al. . Tandem high-dose chemotherapy followed by autologous transplantation in patients with locally advanced or metastatic sarcoma . Anticancer Res 2009 ; 29 : 3281 – 3288 .
Fagioli F , Aglietta M , Tienghi A et al. . High-dose chemotherapy in the treatment of relapsed osteosarcoma: an Italian sarcoma group study . J Clin Oncol 2002 ; 20 : 2150 – 2156 .
Bacci G , Ferrari S , Tienghi A et al. . A comparison of methods of loco-regional chemotherapy combined with systemic chemotherapy as neo-adjuvant treatment of osteosarcoma of the extremity . Eur J Surg Oncol 2001 ; 27 : 98 – 9104 .
Winkler K , Bielack S , Delling G et al. . Effect of intraarterial versus intravenous cisplatin in addition to systemic doxorubicin, high-dose methotrexate, and ifosfamide on histologic tumor response in osteosarcoma (study COSS-86) . Cancer 1990 ; 66 : 1703 – 1710 .
Saeter G , Hoie J , Stenwig AE et al. . Systemic relapse of patients with osteogenic sarcoma. Prognostic factors for long term survival . Cancer 1995 ; 75 : 1084 – 1093 .
Tabone MD , Kalifa C , Rodary C et al. . Osteosarcoma recurrences in pediatric patients previously treated with intensive chemotherapy . J Clin Oncol 1994 ; 12 : 2614 – 2620 .
Berger M , Grignani G , Ferrari S et al. . Phase 2 trial of two courses of cyclophosphamide and etoposide for relapsed high-risk osteosarcoma patients . Cancer 2009 ; 115 : 2980 – 2987 .
Gentet JC , Brunat-Mentigny M , Demaille MC et al. . Ifosfamide and etoposide in childhood osteosarcoma. A phase II study of the French Society of Paediatric Oncology . Eur J Cancer 1997 ; 33 : 232 – 237 .
Merimsky O , Meller I , Flusser G et al. . Gemcitabine in soft tissue or bone sarcoma resistant to standard chemotherapy: a phase II study . Cancer Chemother Pharmacol 2000 ; 45 : 177 – 181 .
Anderson PM , Wiseman GA , Dispenzieri A et al. . High-dose samarium-153 ethylene diamine tetramethylene phosphonate: low toxicity of skeletal irradiation in patients with osteosarcoma and bone metastases . J Clin Oncol 2002 ; 20 : 189 – 196 .
Loeb DM , Garrett-Mayer E , Hobbs RF et al. . Dose-finding study of 153Sm-EDTMP in patients with poor-prognosis osteosarcoma . Cancer 2009 ; 115 : 2514 – 2522 .
Article Sections
- View raw image
- Download Powerpoint Slide
Article Information
- Get Permissions
- PubMed Citation
- Article by J. Sybil Biermann
- Article by Douglas R. Adkins
- Article by Robert S. Benjamin
- Article by Brian Brigman
- Article by Warren Chow
- Article by Ernest U. Conrad
- Article by Deborah A. Frassica
- Article by Frank J. Frassica
- Article by Suzanne George
- Article by Kenneth R. Hande
- Article by Francis J. Hornicek
- Article by G. Douglas Letson
- Article by Joel Mayerson
- Article by Sean V. McGarry
- Article by Brian McGrath
- Article by Carol D. Morris
- Article by Richard J. O'Donnell
- Article by R. Lor Randall
- Article by Victor M. Santana
- Article by Robert L. Satcher
- Article by Herrick J. Siegel
- Article by Neeta Somaiah
- Article by Alan W. Yasko
- Similar articles in PubMed
Google Scholar
Related articles.
| All Time | Past Year | Past 30 Days | |
|---|---|---|---|
| Abstract Views | 0 | 0 | 0 |
| Full Text Views | 5670 | 2096 | 128 |
| PDF Downloads | 2955 | 1266 | 96 |
| EPUB Downloads | 0 | 0 | 0 |
- Advertising
- Terms of Use
- Privacy Policy
- Permissions

© 2019-2024 National Comprehensive Cancer Network
Powered by:
- [185.66.14.133]
- 185.66.14.133
Character limit 500 /500
Recent Advancements in Feature Extraction and Classification Based Bone Cancer Detection
19 Pages Posted: 11 Jan 2024
S Kanimozhi
Vellore Institute of Technology (VIT)
Sivakumar R
Ananthakrishna chintanpalli.
Cancer is a deadly disease that occurs due to the over growth of the abnormal cells. Bone cancer is the third most occurring disease; approximately 10,000 patients suffers from bone cancer in India annually. It can lead to death if not diagnosed in the earlier stage. The bone cancer occurs in four stages as follows: in stage 1 cancer does not spread to other bone parts, in stage 2 cancer looks similar to stage 1 but it becomes dangerous, in stage 3 cancer spreads to one or two bone parts and in stage 4 cancer spreads to other body parts. Timely diagnosis of bone cancer is challenging due to the unspecific indications that are similar to common musculoskeletal injuries, late visit of patient to the hospital and low intuition by the physician. The texture of diseased bone differs from the healthy bone. Mostly in dataset, the healthy and cancerous bone image have similar characteristics. Therefore, development of automated system is necessary to classify the normal and abnormal scan images. The objective of this paper is to identify the studies on classification techniques in detecting bone cancer with five criteria: feature extraction methods, machine learning (ML) and deep learning (DL) techniques, advantages, disadvantages and classifier accuracy. The current study performed the systematic literature review of 108 studies selected based on the use of different feature extractions to extract the textural characteristics of the images that are fed into the ML and DL algorithms to classify the normal and subtypes of bone cancer images for better analysis. The result showed that convolutional neural network classifier along with different textural feature extraction techniques like gray level co-occurrence matrix (GLCM) and local binary pattern (LBP) detected the bone cancer with high median accuracy of 94% compared to DL classification without feature extraction techniques in diagnosing the bone cancer using radiopeadia MRI dataset. In this respect, this paper proposes the systematic review on types of bone cancer and recent advancement in feature extraction methods and classification involving deep learning and machine learning models to detect the bone cancer with higher accuracy rate.
Note: Funding Declaration: This work was supported by the third author’s Seed Grant (SG20220094) awarded by the Vellore Institute of Technology. Conflicts of Interest: None.
Keywords: Bone Cancer, Machine learning, Deep Learning, Gra level Co-occurance Matrix, Magnetic Resonance Imaging
Suggested Citation: Suggested Citation
Vellore Institute of Technology (VIT) ( email )
Chennai 600127 Tamil Nadu IN India
Sivakumar R (Contact Author)
Do you have a job opening that you would like to promote on ssrn, paper statistics, related ejournals, applied computing ejournal.
Subscribe to this fee journal for more curated articles on this topic
Oncology eJournal
Rheumatology & orthopedics ejournal, frontiers in information systems research & applications ejournal.
Information
- Author Services
Initiatives
You are accessing a machine-readable page. In order to be human-readable, please install an RSS reader.
All articles published by MDPI are made immediately available worldwide under an open access license. No special permission is required to reuse all or part of the article published by MDPI, including figures and tables. For articles published under an open access Creative Common CC BY license, any part of the article may be reused without permission provided that the original article is clearly cited. For more information, please refer to https://www.mdpi.com/openaccess .
Feature papers represent the most advanced research with significant potential for high impact in the field. A Feature Paper should be a substantial original Article that involves several techniques or approaches, provides an outlook for future research directions and describes possible research applications.
Feature papers are submitted upon individual invitation or recommendation by the scientific editors and must receive positive feedback from the reviewers.
Editor’s Choice articles are based on recommendations by the scientific editors of MDPI journals from around the world. Editors select a small number of articles recently published in the journal that they believe will be particularly interesting to readers, or important in the respective research area. The aim is to provide a snapshot of some of the most exciting work published in the various research areas of the journal.
Original Submission Date Received: .
- Active Journals
- Find a Journal
- Proceedings Series
- For Authors
- For Reviewers
- For Editors
- For Librarians
- For Publishers
- For Societies
- For Conference Organizers
- Open Access Policy
- Institutional Open Access Program
- Special Issues Guidelines
- Editorial Process
- Research and Publication Ethics
- Article Processing Charges
- Testimonials
- Preprints.org
- SciProfiles
- Encyclopedia

Article Menu

- Subscribe SciFeed
- Recommended Articles
- PubMed/Medline
- Google Scholar
- on Google Scholar
- Table of Contents
Find support for a specific problem in the support section of our website.
Please let us know what you think of our products and services.
Visit our dedicated information section to learn more about MDPI.
JSmol Viewer
Systematic review of tumor segmentation strategies for bone metastases.

Simple Summary
1. introduction, 2.1. literature search.
- “bone metastasis segmentation”.
2.2. Data Extraction
- Enrollment period of the patients;
- Study type: retrospective cohort study or prospective;
- Study population. Extracted the number of scans or images when patient numbers were not provided;
- Training/Validation/testing cohorts;
- Primary tumor and relevant location;
- Imaging modality;
- Methodology;
- Evaluation Metrics;
- Details of whether the study mentioned the suitability of the approaches for clinical use;
- Country of the Authors.
4. Discussion
4.1. deep learning, 4.2. thresholding, 4.3. clustering/classification, 4.4. statistical methods, 4.5. atlas-based approaches, 4.6. region-based approaches, 5. conclusions, supplementary materials, author contributions, conflicts of interest.
- Svensson, E.; Christiansen, C.F.; Ulrichsen, S.P.; Rørth, M.R.; Sørensen, H.T. Survival after bone metastasis by primary cancer type: A Danish population-based cohort study. BMJ Open 2017 , 7 , e016022. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chu, G.; Lo, P.; Ramakrishna, B.; Kim, H.; Morris, D.; Goldin, J.; Brown, M. Bone Tumor Segmentation on Bone Scans Using Context Information and Random Forests ; Springer International Publishing: Cham, Switzerland, 2014. [ Google Scholar ]
- Peeters, S.T.H.; Van Limbergen, E.J.; Hendriks, L.E.L.; De Ruysscher, D. Radiation for Oligometastatic Lung Cancer in the Era of Immunotherapy: What Do We (Need to) Know? Cancers 2021 , 13 , 2132. [ Google Scholar ] [ CrossRef ]
- Zeng, K.L.; Tseng, C.L.; Soliman, H.; Weiss, Y.; Sahgal, A.; Myrehaug, S. Stereotactic body radiotherapy (SBRT) for oligometastatic spine metastases: An overview. Front. Oncol. 2019 , 9 , 337. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Spencer, K.L.; van der Velden, J.M.; Wong, E.; Seravalli, E.; Sahgal, A.; Chow, E.; Verlaan, J.J.; Verkooijen, H.M.; van der Linden, Y.M. Systematic Review of the Role of Stereotactic Radiotherapy for Bone Metastases. J. Natl. Cancer Inst. 2019 , 111 , 1023–1032. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Loi, M.; Nuyttens, J.J.; Desideri, I.; Greto, D.; Livi, L. Single-fraction radiotherapy (SFRT) for bone metastases: Patient selection and perspectives. Cancer Manag. Res. 2019 , 11 , 9397–9408. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Palma, D.A.; Olson, R.; Harrow, S.; Gaede, S.; Louie, A.V.; Haasbeek, C.; Mulroy, L.; Lock, M.; Rodrigues, G.B.; Yaremko, B.P.; et al. Stereotactic Ablative Radiotherapy for the Comprehensive Treatment of Oligometastatic Cancers: Long-Term Results of the SABR-COMET Phase II Randomized Trial. J. Clin. Oncol. 2020 , 38 , 2830–2838. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- De Ruysscher, D.; Wanders, R.; van Baardwijk, A.; Dingemans, A.M.; Reymen, B.; Houben, R.; Bootsma, G.; Pitz, C.; van Eijsden, L.; Geraedts, W.; et al. Radical treatment of non-small-cell lung cancer patients with synchronous oligometastases: Long-term results of a prospective phase II trial (Nct01282450). J. Thorac. Oncol. 2012 , 7 , 1547–1555. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Dercle, L.; Henry, T.; Carré, A.; Paragios, N.; Deutsch, E.; Robert, C. Reinventing radiation therapy with machine learning and imaging bio-markers (radiomics): State-of-the-art, challenges and perspectives. Methods 2020 , 188 , 44–60. [ Google Scholar ] [ CrossRef ]
- Speirs, C.K.; Grigsby, P.W.; Huang, J.; Thorstad, W.L.; Parikh, P.J.; Robinson, C.G.; Bradley, J.D. PET-based radiation therapy planning. PET Clin. 2015 , 10 , 27–44. [ Google Scholar ] [ CrossRef ]
- Lu, W.; Wang, J.; Zhang, H.H. Computerized PET/CT image analysis in the evaluation of tumour response to therapy. Br. J. Radiol. 2015 , 88 , 20140625. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Vergalasova, I.; Cai, J. A modern review of the uncertainties in volumetric imaging of respiratory-induced target motion in lung radiotherapy. Med. Phys. 2020 , 47 , e988–e1008. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Papandrianos, N.; Papageorgiou, E.; Anagnostis, A.; Papageorgiou, K. Bone metastasis classification using whole body images from prostate cancer patients based on convolutional neural networks application. PLoS ONE 2020 , 15 , e0237213. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Foster, B.; Bagci, U.; Mansoor, A.; Xu, Z.; Mollura, D.J. A review on segmentation of positron emission tomography images. Comput. Biol. Med. 2014 , 50 , 76–96. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Takahashi, M.E.S.; Mosci, C.; Souza, E.M.; Brunetto, S.Q.; de Souza, C.; Pericole, F.V.; Lorand-Metze, I.; Ramos, C.D. Computed tomography-based skeletal segmentation for quantitative PET metrics of bone involvement in multiple myeloma. Nucl. Med. Commun. 2020 , 41 , 377–382. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Bach Cuadra, M.; Favre, J.; Omoumi, P. Quantification in Musculoskeletal Imaging Using Computational Analysis and Machine Learning: Segmentation and Radiomics. Semin. Musculoskelet. Radiol. 2020 , 24 , 50–64. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ambrosini, V.; Nicolini, S.; Caroli, P.; Nanni, C.; Massaro, A.; Marzola, M.C.; Rubello, D.; Fanti, S. PET/CT imaging in different types of lung cancer: An overview. Eur. J. Radiol. 2012 , 81 , 988–1001. [ Google Scholar ] [ CrossRef ]
- Carvalho, L.E.; Sobieranski, A.C.; von Wangenheim, A. 3D Segmentation Algorithms for Computerized Tomographic Imaging: A Systematic Literature Review. J. Digit. Imaging 2018 , 31 , 799–850. [ Google Scholar ] [ CrossRef ]
- Domingues, I.; Pereira, G.; Martins, P.; Duarte, H.; Santos, J.; Abreu, P.H. Using deep learning techniques in medical imaging: A systematic review of applications on CT and PET. Artif. Intell. Rev. 2020 , 53 , 4093–4160. [ Google Scholar ] [ CrossRef ]
- Hesamian, M.H.; Jia, W.; He, X.; Kennedy, P. Deep Learning Techniques for Medical Image Segmentation: Achievements and Challenges. J. Digit. Imaging 2019 , 32 , 582–596. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Mansoor, A.; Bagci, U.; Foster, B.; Xu, Z.; Papadakis, G.Z.; Folio, L.R.; Udupa, J.K.; Mollura, D.J. Segmentation and Image Analysis of Abnormal Lungs at CT: Current Approaches, Challenges, and Future Trends. Radiographics 2015 , 35 , 1056–1076. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Punn, N.S.; Agarwal, S. Modality specific U-Net variants for biomedical image segmentation: A survey. Artif. Intell. Rev. 2022 , 55 , 5845–5889. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Saba, T. Recent advancement in cancer detection using machine learning: Systematic survey of decades, comparisons and challenges. J. Infect. Public Health 2020 , 13 , 1274–1289. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Trevor Hastie, J.F.; Tibshirani, R. The Elements of Statistical Learning ; Springer: New York, NY, USA, 2001. [ Google Scholar ] [ CrossRef ]
- van Timmeren, J.E.; Cester, D.; Tanadini-Lang, S.; Alkadhi, H.; Baessler, B. Radiomics in medical imaging—“how-to” guide and critical reflection. Insights Into Imaging 2020 , 11 , 91. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Wang, H.; Zhou, Z.; Li, Y.; Chen, Z.; Lu, P.; Wang, W.; Liu, W.; Yu, L. Comparison of machine learning methods for classifying mediastinal lymph node metastasis of non-small cell lung cancer from 18F-FDG PET/CT images. EJNMMI Res. 2017 , 7 , 11. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Yousefirizi, F.; Pierre, D.; Amyar, A.; Ruan, S.; Saboury, B.; Rahmim, A. AI-Based Detection, Classification and Prediction/Prognosis in Medical Imaging: Towards Radiophenomics. PET Clin. 2022 , 17 , 183–212. [ Google Scholar ] [ CrossRef ]
- Zhang, Z.; Sejdić, E. Radiological images and machine learning: Trends, perspectives, and prospects. Comput. Biol. Med. 2019 , 108 , 354–370. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Sahiner, B.; Pezeshk, A.; Hadjiiski, L.M.; Wang, X.; Drukker, K.; Cha, K.H.; Summers, R.M.; Giger, M.L. Deep learning in medical imaging and radiation therapy. Med. Phys. 2019 , 46 , e1–e36. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Samarasinghe, G.; Jameson, M.; Vinod, S.; Field, M.; Dowling, J.; Sowmya, A.; Holloway, L. Deep learning for segmentation in radiation therapy planning: A review. J. Med. Imaging Radiat. Oncol. 2021 , 65 , 578–595. [ Google Scholar ] [ CrossRef ]
- Faiella, E.; Santucci, D.; Calabrese, A.; Russo, F.; Vadalà, G.; Zobel, B.B.; Soda, P.; Iannello, G.; de Felice, C.; Denaro, V. Artificial Intelligence in Bone Metastases: An MRI and CT Imaging Review. Int. J. Environ. Res. Public Health 2022 , 19 , 1880. [ Google Scholar ] [ CrossRef ]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021 , 372 , n71. [ Google Scholar ] [ CrossRef ]
- Wang, R.; Lei, T.; Cui, R.; Zhang, B.; Meng, H.; Nandi, A.K. Medical image segmentation using deep learning: A survey. IET Image Process. 2022 , 16 , 1243–1267. [ Google Scholar ] [ CrossRef ]
- MacManus, M.; Everitt, S. Treatment Planning for Radiation Therapy. PET Clin. 2018 , 13 , 43–57. [ Google Scholar ] [ CrossRef ]
- Yang, W.C.; Hsu, F.M.; Yang, P.C. Precision radiotherapy for non-small cell lung cancer. J. Biomed. Sci. 2020 , 27 , 82. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Orcajo-Rincon, J.; Muñoz-Langa, J.; Sepúlveda-Sánchez, J.M.; Fernández-Pérez, G.C.; Martínez, M.; Noriega-Álvarez, E.; Sanz-Viedma, S.; Vilanova, J.C.; Luna, A. Review of imaging techniques for evaluating morphological and functional responses to the treatment of bone metastases in prostate and breast cancer. Clin. Transl. Oncol. 2022 , 24 , 1290–1310. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chmelik, J.; Jakubicek, R.; Walek, P.; Jan, J.; Ourednicek, P.; Lambert, L.; Amadori, E.; Gavelli, G. Deep convolutional neural network-based segmentation and classification of difficult to define metastatic spinal lesions in 3D CT data. Med. Image Anal. 2018 , 49 , 76–88. [ Google Scholar ] [ CrossRef ]
- Elfarra, F.-G.; Calin, M.A.; Parasca, S.V. Computer-aided detection of bone metastasis in bone scintigraphy images using parallelepiped classification method. Ann. Nucl. Med. 2019 , 33 , 866–874. [ Google Scholar ] [ CrossRef ]
- Guo, Y.; Lin, Q.; Zhao, S.; Li, T.; Cao, Y.; Man, Z.; Zeng, X. Automated detection of lung cancer-caused metastasis by classifying scintigraphic images using convolutional neural network with residual connection and hybrid attention mechanism. Insights Into Imaging 2022 , 13 , 24. [ Google Scholar ] [ CrossRef ]
- Hammes, J.; Täger, P.; Drzezga, A. EBONI: A Tool for Automated Quantification of Bone Metastasis Load in PSMA PET/CT. J. Nucl. Med. 2018 , 59 , 1070–1075. [ Google Scholar ] [ CrossRef ]
- Han, S.; Oh, J.S.; Lee, J.J. Diagnostic performance of deep learning models for detecting bone metastasis on whole-body bone scan in prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 2022 , 49 , 585–595. [ Google Scholar ] [ CrossRef ]
- Hinzpeter, R.; Baumann, L.; Guggenberger, R.; Huellner, M.; Alkadhi, H.; Baessler, B. Radiomics for detecting prostate cancer bone metastases invisible in CT: A proof-of-concept study. Eur. Radiol. 2022 , 32 , 1823–1832. [ Google Scholar ] [ CrossRef ]
- Li, T.; Lin, Q.; Guo, Y.; Zhao, S.; Zeng, X.; Man, Z.; Cao, Y.; Hu, Y. Automated detection of skeletal metastasis of lung cancer with bone scans using convolutional nuclear network. Phys. Med. Biol. 2022 , 67 , 015004. [ Google Scholar ] [ CrossRef ]
- Lin, Q.; Luo, M.; Gao, R.; Li, T.; Zhengxing, M.; Cao, Y.; Wang, H. Deep learning based automatic segmentation of metastasis hotspots in thorax bone SPECT images. PLoS ONE 2020 , 15 , e0243253. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moreau, N.; Rousseau, C.; Fourcade, C.; Santini, G.; Brennan, A.; Ferrer, L.; Lacombe, M.; Guillerminet, C.; Colombié, M.; Jézéquel, P.; et al. Automatic segmentation of metastatic breast cancer lesions on18f-fdg pet/ct longitudinal acquisitions for treatment response assessment. Cancers 2022 , 14 , 101. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Moreau, N.; Rousseau, C.; Fourcade, C.; Santini, G.; Ferrer, L.; Lacombe, M.; Guillerminet, C.; Campone, M.; Colombié, M.; Rubeaux, M.; et al. Deep learning approaches for bone and bone lesion segmentation on 18FDG PET/CT imaging in the context of metastatic breast cancer. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020. [ Google Scholar ]
- Papandrianos, N.; Papageorgiou, E.; Anagnostis, A. Development of Convolutional Neural Networks to identify bone metastasis for prostate cancer patients in bone scintigraphy. Ann. Nucl. Med. 2020 , 34 , 824–832. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Rachmawati, E.; Sumarna, F.R.; Jondri; Kartamihardja, A.H.S.; Achmad, A.; Shintawati, R. Bone Scan Image Segmentation based on Active Shape Model for Cancer Metastasis Detection. In Proceedings of the 2020 8th International Conference on Information and Communication Technology (ICoICT), Yogyakarta, Indonesia, 24–26 June 2020. [ Google Scholar ]
- Sato, S.; Lu, H.; Kim, H.; Murakami, S.; Ueno, M.; Terasawa, T.; Aoki, T. Enhancement of Bone Metastasis from CT Images Based on Salient Region Feature Registration. In Proceedings of the 2018 18th International Conference on Control, Automation and Systems (ICCAS), PyeongChang, Republic of Korea, 17–20 October 2018. [ Google Scholar ]
- Song, Y.; Lu, H.; Kim, H.; Murakami, S.; Ueno, M.; Terasawa, T.; Aoki, T. Segmentation of Bone Metastasis in CT Images Based on Modified HED. In Proceedings of the 2019 19th International Conference on Control, Automation and Systems (ICCAS 2019), Institute of Control, Robotics and Systems—ICROS, ICC Jeju, Jeju, Republic of Korea, 11 October–18 October 2019; pp. 812–815. [ Google Scholar ]
- Wiese, T.; Burns, J.; Jianhua, Y.; Summers, R.M. Computer-aided detection of sclerotic bone metastases in the spine using watershed algorithm and support vector machines. In Proceedings of the 2011 IEEE International Symposium on Biomedical Imaging: From Nano to Macro, Chicago, IL, USA, 30 March–2 April 2011; pp. 152–155. [ Google Scholar ]
- Zhang, J.; Huang, M.; Deng, T.; Cao, Y.; Lin, Q. Bone metastasis segmentation based on Improved U-NET algorithm. J. Phys. Conf. Ser. 2021 , 1848 , 012027. [ Google Scholar ] [ CrossRef ]
- Hsieh, T.-C.; Liao, C.-W.; Lai, Y.-C.; Law, K.-M.; Chan, P.-K.; Kao, C.-H. Detection of Bone Metastases on Bone Scans through Image Classification with Contrastive Learning. J. Pers. Med. 2021 , 11 , 1248. [ Google Scholar ] [ CrossRef ]
- Liu, S.; Feng, M.; Qiao, T.; Cai, H.; Xu, K.; Yu, X.; Jiang, W.; Lv, Z.; Wang, Y.; Li, D. Deep Learning for the Automatic Diagnosis and Analysis of Bone Metastasis on Bone Scintigrams. Cancer Manag. Res. 2022 , 14 , 51–65. [ Google Scholar ] [ CrossRef ]
- AbuBaker, A.; Ghadi, Y. A novel CAD system to automatically detect cancerous lung nodules using wavelet transform and SVM. Int. J. Electr. Comput. Eng. 2020 , 10 , 4745–4751. [ Google Scholar ] [ CrossRef ]
- Apiparakoon, T.; Rakratchatakul, N.; Chantadisai, M.; Vutrapongwatana, U.; Kingpetch, K.; Sirisalipoch, S.; Rakvongthai, Y.; Chaiwatanarat, T.; Chuangsuwanich, E. MaligNet: Semisupervised Learning for Bone Lesion Instance Segmentation Using Bone Scintigraphy. IEEE Access 2020 , 8 , 27047–27066. [ Google Scholar ] [ CrossRef ]
- Biswas, B.; Ghosh, S.K.; Ghosh, A. A novel CT image segmentation algorithm using PCNN and Sobolev gradient methods in GPU frameworks. Pattern Anal. Appl. 2020 , 23 , 837–854. [ Google Scholar ] [ CrossRef ]
- Borrelli, P.; Góngora, J.L.L.; Kaboteh, R.; Ulén, J.; Enqvist, O.; Trägårdh, E.; Edenbrandt, L. Freely available convolutional neural network-based quantification of PET/CT lesions is associated with survival in patients with lung cancer. EJNMMI Phys. 2022 , 9 , 6. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chang, C.Y.; Buckless, C.; Yeh, K.J.; Torriani, M. Automated detection and segmentation of sclerotic spinal lesions on body CTs using a deep convolutional neural network. Skelet. Radiol. 2022 , 51 , 391–399. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- da Cruz, L.B.; Júnior, D.A.D.; Diniz, J.O.B.; Silva, A.C.; de Almeida, J.D.S.; de Paiva, A.C.; Gattass, M. Kidney tumor segmentation from computed tomography images using DeepLabv3+ 2.5D model. Expert Syst. Appl. 2022 , 192 , 116270. [ Google Scholar ] [ CrossRef ]
- Elsayed, O.; Mahar, K.; Kholief, M.; Khater, H.A. Automatic detection of the pulmonary nodules from CT images. In Proceedings of the 2015 SAI Intelligent Systems Conference (IntelliSys), London, UK, 10–11 November 2015. [ Google Scholar ]
- Guo, Y.; Feng, Y.; Sun, J.; Zhang, N.; Lin, W.; Sa, Y.; Wang, P. Automatic Lung Tumor Segmentation on PET/CT Images Using Fuzzy Markov Random Field Model. Comput. Math. Methods Med. 2014 , 2014 , 401201. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Hussain, L.; Rathore, S.; Abbasi, A.A.; Saeed, S. Automated Lung Cancer Detection Based on Multimodal Features Extracting Strategy Using Machine Learning Techniques ; SPIE Medical Imaging: San Diego, CA, USA, 2019; Volume 10948. [ Google Scholar ]
- Kim, N.; Chang, J.S.; Kim, Y.B.; Kim, J.S. Atlas-based auto-segmentation for postoperative radiotherapy planning in endometrial and cervical cancers. Radiat. Oncol. 2020 , 15 , 106. [ Google Scholar ] [ CrossRef ]
- Li, L.; Zhao, X.; Lu, W.; Tan, S. Deep learning for variational multimodality tumor segmentation in PET/CT. Neurocomputing 2020 , 392 , 277–295. [ Google Scholar ] [ CrossRef ]
- Lu, Y.; Lin, J.; Chen, S.; He, H.; Cai, Y. Automatic Tumor Segmentation by Means of Deep Convolutional U-Net with Pre-Trained Encoder in PET Images. IEEE Access 2020 , 8 , 113636–113648. [ Google Scholar ] [ CrossRef ]
- Markel, D.; Caldwell, C.; Alasti, H.; Soliman, H.; Ung, Y.; Lee, J.; Sun, A. Automatic Segmentation of Lung Carcinoma Using 3D Texture Features in 18-FDG PET/CT. Int. J. Mol. Imaging 2013 , 2013 , 980769. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Moussallem, M.; Valette, P.J.; Traverse-Glehen, A.; Houzard, C.; Jegou, C.; Giammarile, F. New strategy for automatic tumor segmentation by adaptive thresholding on PET/CT images. J. Appl. Clin. Med. Phys. 2012 , 13 , 3875. [ Google Scholar ] [ CrossRef ]
- Naqiuddin, M.; Sofia, N.N.; Isa, I.S.; Sulaiman, S.N.; Karim, N.K.A.; Shuaib, I.L. Lesion demarcation of CT-scan images using image processing technique. In Proceedings of the 2018 8th IEEE International Conference on Control System, Computing and Engineering (ICCSCE), Penang, Malaysia, 23–25 November 2018. [ Google Scholar ]
- Perk, T.; Chen, S.; Harmon, S.; Lin, C.; Bradshaw, T.; Perlman, S.; Liu, G.; Jeraj, R. A statistically optimized regional thresholding method (SORT) for bone lesion detection in 18F-NaF PET/CT imaging. Phys. Med. Biol. 2018 , 63 , 225018. [ Google Scholar ] [ CrossRef ]
- Protonotarios, N.E.; Katsamenis, I.; Sykiotis, S.; Dikaios, N.; Kastis, G.A.; Chatziioannou, S.N.; Metaxas, M.; Doulamis, N.; Doulamis, A. A few-shot U-Net deep learning model for lung cancer lesion segmentation via PET/CT imaging. Biomed. Phys. Eng. Express 2022 , 8 , 025019. [ Google Scholar ] [ CrossRef ]
- Rao, C.; Pai, S.; Hadzic, I.; Zhovannik, I.; Bontempi, D.; Dekker, A.; Teuwen, J.; Traverso, A. Oropharyngeal Tumour Segmentation Using Ensemble 3D PET-CT Fusion Networks for the HECKTOR Challenge ; Springer International Publishing: Cham, Switzerland, 2021. [ Google Scholar ]
- Sarker, P.; Shuvo, M.M.H.; Hossain, Z.; Hasan, S. Segmentation and classification of lung tumor from 3D CT image using K-means clustering algorithm. In Proceedings of the 2017 4th International Conference on Advances in Electrical Engineering (ICAEE), Dhaka, Bangladesh, 28–30 September 2017. [ Google Scholar ]
- Tian, H.; Xiang, D.; Zhu, W.; Shi, F.; Chen, X. Fully convolutional network with sparse feature-maps composition for automatic lung tumor segmentation from PET images. SPIE Med. Imaging 2020 , 11313 , 1131310. [ Google Scholar ]
- Xue, Z.; Li, P.; Zhang, L.; Lu, X.; Zhu, G.; Shen, P.; Shah, S.A.A.; Bennamoun, M. Multi-Modal Co-Learning for Liver Lesion Segmentation on PET-CT Images. IEEE Trans. Med. Imaging 2021 , 40 , 3531–3542. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Yang, B.; Xiang, D.; Yu, F.; Chen, X. Lung tumor segmentation based on the multi-scale template matching and region growing. SPIE Med. Imaging 2018 , 10578 , 105782Q. [ Google Scholar ]
- Zhang, Y.; He, S.; Wa, S.; Zong, Z.; Lin, J.; Fan, D.; Fu, J.; Lv, C. Symmetry GAN Detection Network: An Automatic One-Stage High-Accuracy Detection Network for Various Types of Lesions on CT Images. Symmetry 2022 , 14 , 234. [ Google Scholar ] [ CrossRef ]
- Zhao, X.; Li, L.; Lu, W.; Tan, S. Tumor co-segmentation in PET/CT using multi-modality fully convolutional neural network. Phys. Med. Biol. 2019 , 64 , 015011. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Chen, J.; Li, Y.; Luna, L.P.; Chung, H.W.; Rowe, S.P.; Du, Y.; Solnes, L.B.; Frey, E.C. Learning fuzzy clustering for SPECT/CT segmentation via convolutional neural networks. Med. Phys. 2021 , 48 , 3860–3877. [ Google Scholar ] [ CrossRef ]
- Yousefirizi, F.; Rahmim, A. GAN-Based Bi-Modal Segmentation Using Mumford-Shah Loss: Application to Head and Neck Tumors in PET-CT Images ; Springer International Publishing: Cham, Switzerland, 2021. [ Google Scholar ]
- Dong, R.; Lu, H.; Kim, H.; Aoki, T.; Zhao, Y.; Zhao, Y. An Interactive Technique of Fast Vertebral Segmentation for Computed Tomography Images with Bone Metastasis. In Proceedings of the 2nd International Conference on Biomedical Signal and Image Processing, Kitakyushu, Japan, 23–25 August 2017. [ Google Scholar ]
- Fränzle, A.; Sumkauskaite, M.; Hillengass, J.; Bäuerle, T.; Bendl, R. Fully automated shape model positioning for bone segmentation in whole-body CT scans. J. Phys. Conf. Ser. 2014 , 489 , 012029. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Hanaoka, S.; Masutani, Y.; Nemoto, M.; Nomura, Y.; Miki, S.; Yoshikawa, T.; Hayashi, N.; Ohtomo, K.; Shimizu, A. Landmark-guided diffeomorphic demons algorithm and its application to automatic segmentation of the whole spine and pelvis in CT images. Int. J. Comput. Assist. Radiol. Surg. 2017 , 12 , 413–430. [ Google Scholar ] [ CrossRef ]
- Hu, Q.; de F. Souza, L.F.; Holanda, G.B.; Alves, S.S.A.; dos S. Silva, F.H.; Han, T.; Rebouças Filho, P.P. An effective approach for CT lung segmentation using mask region-based convolutional neural networks. Artif. Intell. Med. 2020 , 103 , 101792. [ Google Scholar ] [ CrossRef ]
- Lindgren Belal, S.; Sadik, M.; Kaboteh, R.; Enqvist, O.; Ulén, J.; Poulsen, M.H.; Simonsen, J.; Høilund-Carlsen, P.F.; Edenbrandt, L.; Trägårdh, E. Deep learning for segmentation of 49 selected bones in CT scans: First step in automated PET/CT-based 3D quantification of skeletal metastases. Eur. J. Radiol. 2019 , 113 , 89–95. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Noguchi, S.; Nishio, M.; Yakami, M.; Nakagomi, K.; Togashi, K. Bone segmentation on whole-body CT using convolutional neural network with novel data augmentation techniques. Comput. Biol. Med. 2020 , 121 , 103767. [ Google Scholar ] [ CrossRef ]
- Polan, D.F.; Brady, S.L.; Kaufman, R.A. Tissue segmentation of computed tomography images using a Random Forest algorithm: A feasibility study. Phys. Med. Biol. 2016 , 61 , 6553–6569. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Ruiz-España, S.; Domingo, J.; Díaz-Parra, A.; Dura, E.; D’Ocón-Alcañiz, V.; Arana, E.; Moratal, D. Automatic segmentation of the spine by means of a probabilistic atlas with a special focus on ribs suppression. Med. Phys. 2017 , 44 , 4695–4707. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Arends, S.R.S.; Savenije, M.H.F.; Eppinga, W.S.C.; van der Velden, J.M.; van den Berg, C.A.T.; Verhoeff, J.J.C. Clinical utility of convolutional neural networks for treatment planning in radiotherapy for spinal metastases. Phys. Imaging Radiat. Oncol. 2022 , 21 , 42–47. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Feng, X.; Bernard, M.E.; Hunter, T.; Chen, Q. Improving accuracy and robustness of deep convolutional neural network based thoracic OAR segmentation. Phys. Med. Biol. 2020 , 65 , 07NT01. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Fritscher, K.D.; Peroni, M.; Zaffino, P.; Spadea, M.F.; Schubert, R.; Sharp, G. Automatic segmentation of head and neck CT images for radiotherapy treatment planning using multiple atlases, statistical appearance models, and geodesic active contours. Med. Phys. 2014 , 41 , 051910. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Ibragimov, B.; Toesca, D.A.S.; Chang, D.T.; Yuan, Y.; Koong, A.C.; Xing, L.; Vogelius, I.R. Deep learning for identification of critical regions associated with toxicities after liver stereotactic body radiation therapy. Med. Phys. 2020 , 47 , 3721–3731. [ Google Scholar ] [ CrossRef ]
- Lin, X.W.; Li, N.; Qi, Q. Organs-At-Risk Segmentation in Medical Imaging Based on the U-Net with Residual and Attention Mechanisms. In Proceedings of the 2021 IEEE 23rd Int Conf on High Performance Computing & Communications; 7th Int Conf on Data Science & Systems; 19th Int Conf on Smart City; 7th Int Conf on Dependability in Sensor, Cloud & Big Data Systems & Application (HPCC/DSS/SmartCity/DependSys), Haikou, China, 20–22 December 2021. [ Google Scholar ]
- Liu, Z.K.; Liu, X.; Xiao, B.; Wang, S.B.; Miao, Z.; Sun, Y.L.; Zhang, F.Q. Segmentation of organs-at-risk in cervical cancer CT images with a convolutional neural network. Phys. Med. 2020 , 69 , 184–191. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Nemoto, T.; Futakami, N.; Yagi, M.; Kumabe, A.; Takeda, A.; Kunieda, E.; Shigematsu, N. Efficacy evaluation of 2D, 3D U-Net semantic segmentation and atlas-based segmentation of normal lungs excluding the trachea and main bronchi. J. Radiat. Res. 2020 , 61 , 257–264. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Nguyen, C.T.; Havlicek, J.P.; Chakrabarty, J.H.; Duong, Q.; Vesely, S.K. Towards automatic 3D bone marrow segmentation. In Proceedings of the 2016 IEEE Southwest Symposium on Image Analysis and Interpretation (SSIAI), Santa Fe, NM, USA, 6–8 March 2016. [ Google Scholar ]
- Yusufaly, T.; Miller, A.; Medina-Palomo, A.; Williamson, C.W.; Nguyen, H.; Lowenstein, J.; Leath, C.A., III; Xiao, Y.; Moore, K.L.; Moxley, K.M.; et al. A Multi-atlas Approach for Active Bone Marrow Sparing Radiation Therapy: Implementation in the NRG-GY006 Trial. Int. J. Radiat. Oncol. Biol. Phys. 2020 , 108 , 1240–1247. [ Google Scholar ] [ CrossRef ]
- Xiong, X.; Smith, B.J.; Graves, S.A.; Sunderland, J.J.; Graham, M.M.; Gross, B.A.; Buatti, J.M.; Beichel, R.R. Quantification of uptake in pelvis F-18 FLT PET-CT images using a 3D localization and segmentation CNN. Med. Phys. 2022 , 49 , 1585–1598. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Nemoto, T.; Futakami, N.; Yagi, M.; Kunieda, E.; Akiba, T.; Takeda, A.; Shigematsu, N. Simple low-cost approaches to semantic segmentation in radiation therapy planning for prostate cancer using deep learning with non-contrast planning CT images. Phys. Med. 2020 , 78 , 93–100. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Tsujimoto, M.; Teramoto, A.; Ota, S.; Toyama, H.; Fujita, H. Automated segmentation and detection of increased uptake regions in bone scintigraphy using SPECT/CT images. Ann. Nucl. Med. 2018 , 32 , 182–190. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Slattery, A. Validating an image segmentation program devised for staging lymphoma. Australas. Phys. Eng. Sci. Med. 2017 , 40 , 799–809. [ Google Scholar ] [ CrossRef ]
- Martínez, F.; Romero, E.; Dréan, G.; Simon, A.; Haigron, P.; de Crevoisier, R.; Acosta, O. Segmentation of pelvic structures for planning CT using a geometrical shape model tuned by a multi-scale edge detector. Phys. Med. Biol. 2014 , 59 , 1471–1484. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Ninomiya, K.; Arimura, H.; Sasahara, M.; Hirose, T.; Ohga, S.; Umezu, Y.; Honda, H.; Sasaki, T. Bayesian delineation framework of clinical target volumes for prostate cancer radiotherapy using an anatomical-features-based machine learning technique. In Medical Imaging 2018: Image-Guided Procedures, Robotic Interventions, and Modeling ; Fei, B., Webster, R.J., Eds.; SPIE-Int. Soc. Optical Engineering: Bellingham, WA, USA, 2018. [ Google Scholar ]
- Men, K.; Dai, J.; Li, Y. Automatic segmentation of the clinical target volume and organs at risk in the planning CT for rectal cancer using deep dilated convolutional neural networks. Med. Phys. 2017 , 44 , 6377–6389. [ Google Scholar ] [ CrossRef ]
- Ding, Y.; Chen, Z.; Wang, Z.; Wang, X.; Hu, D.; Ma, P.; Ma, C.; Wei, W.; Li, X.; Xue, X.; et al. Three-dimensional deep neural network for automatic delineation of cervical cancer in planning computed tomography images. J. Appl. Clin. Med. Phys 2022 , 23 , e13566. [ Google Scholar ] [ CrossRef ]
- Sartor, H.; Minarik, D.; Enqvist, O.; Ulén, J.; Wittrup, A.; Bjurberg, M.; Trägårdh, E. Auto-segmentations by convolutional neural network in cervical and anorectal cancer with clinical structure sets as the ground truth. Clin. Transl. Radiat. Oncol. 2020 , 25 , 37–45. [ Google Scholar ] [ CrossRef ]
- Papandrianos, N.; Papageorgiou, E.; Anagnostis, A.; Feleki, A. A deep-learning approach for diagnosis of metastatic breast cancer in bones from whole-body scans. Appl. Sci. 2020 , 10 , 997. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Pi, Y.; Zhao, Z.; Xiang, Y.; Li, Y.; Cai, H.; Yi, Z. Automated diagnosis of bone metastasis based on multi-view bone scans using attention-augmented deep neural networks. Med. Image Anal. 2020 , 65 , 101784. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhou, H.; Dong, D.; Chen, B.; Fang, M.; Cheng, Y.; Gan, Y.; Zhang, R.; Zhang, L.; Zang, Y.; Liu, Z.; et al. Diagnosis of Distant Metastasis of Lung Cancer: Based on Clinical and Radiomic Features. Transl. Oncol. 2018 , 11 , 31–36. [ Google Scholar ] [ CrossRef ]
- Zhang, J.; Ma, G.; Cheng, J.; Song, S.; Zhang, Y.; Shi, L.Q. Diagnostic classification of solitary pulmonary nodules using support vector machine model based on 2-[18F]fluoro-2-deoxy-D-glucose PET/computed tomography texture features. Nucl. Med. Commun. 2020 , 41 , 560–566. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Lou, B.; Doken, S.; Zhuang, T.; Wingerter, D.; Gidwani, M.; Mistry, N.; Ladic, L.; Kamen, A.; Abazeed, M.E. An image-based deep learning framework for individualising radiotherapy dose: A retrospective analysis of outcome prediction. Lancet Digit. Health 2019 , 1 , e136–e147. [ Google Scholar ] [ CrossRef ] [ Green Version ]
- Mao, X.; Pineau, J.; Keyes, R.; Enger, S.A. RapidBrachyDL: Rapid Radiation Dose Calculations in Brachytherapy Via Deep Learning. Int. J. Radiat. Oncol. Biol. Phys. 2020 , 108 , 802–812. [ Google Scholar ] [ CrossRef ]
- LabelMe. LabelMe Annotation Tool. 2022. Available online: http://labelme2.csail.mit.edu/Release3.0/ (accessed on 12 July 2022).
- Alzubaidi, L.; Al-Amidie, M.; Al-Asadi, A.; Humaidi, A.J.; Al-Shamma, O.; Fadhel, M.A.; Zhang, J.; Santamaría, J.; Duan, Y. Novel Transfer Learning Approach for Medical Imaging with Limited Labeled Data. Cancers 2021 , 13 , 1590. [ Google Scholar ] [ CrossRef ] [ PubMed ]
- Zhang, H.; Cisse, M.; Dauphin, Y.N.; Lopez-Paz, D. mixup: Beyond empirical risk minimization. arXiv 2017 , arXiv:1710.09412. [ Google Scholar ]
- Yun, S.; Han, D.; Oh, S.J.; Chun, S.; Choe, J.; Yoo, Y. Cutmix: Regularization strategy to train strong classifiers with localizable features. In Proceedings of the IEEE/CVF International Conference on Computer Vision, Seoul, Republic of Korea, 27 October–2 November 2019. [ Google Scholar ]
- Ge, Z.; Liu, S.; Wang, F.; Li, Z.; Sun, J. Yolox: Exceeding yolo series in 2021. arXiv 2021 , arXiv:2107.08430. [ Google Scholar ]
- Kingma, D.P.; Ba, J. Adam: A method for stochastic optimization. arXiv 2014 , arXiv:1412.6980. [ Google Scholar ]
- Ioffe, S.; Szegedy, C. Batch normalization: Accelerating deep network training by reducing internal covariate shift. In Proceedings of the International Conference on Machine Learning, Lille, France, 6–11 July 2015. [ Google Scholar ]
- Isensee, F.; Jaeger, P.F.; Kohl, S.A.A.; Petersen, J.; Maier-Hein, K.H. nnU-Net: A self-configuring method for deep learning-based biomedical image segmentation. Nat. Methods 2021 , 18 , 203–211. [ Google Scholar ] [ CrossRef ]
- Mah, P.; Reeves, T.E.; McDavid, W.D. Deriving Hounsfield units using grey levels in cone beam computed tomography. Dentomaxillofac. Radiol. 2010 , 39 , 323–335. [ Google Scholar ] [ CrossRef ]
- Phan, A.-C.; Vo, V.-Q.; Phan, T.-C. A Hounsfield value-based approach for automatic recognition of brain haemorrhage. J. Inf. Telecommun. 2019 , 3 , 196–209. [ Google Scholar ] [ CrossRef ]
- Sheen, H.; Shin, H.-B.; Kim, J.Y. Comparison of radiomics prediction models for lung metastases according to four semiautomatic segmentation methods in soft-tissue sarcomas of the extremities. J. Korean Phys. Soc. 2022 , 80 , 247–256. [ Google Scholar ] [ CrossRef ]
- Horikoshi, H.; Kikuchi, A.; Onoguchi, M.; Sjöstrand, K.; Edenbrandt, L. Computer-aided diagnosis system for bone scintigrams from Japanese patients: Importance of training database. Ann. Nucl. Med. 2012 , 26 , 622–626. [ Google Scholar ] [ CrossRef ] [ PubMed ] [ Green Version ]
- Alarifi, A.; Alwadain, A. Computer-aided cancer classification system using a hybrid level-set image segmentation. Meas. J. Int. Meas. Confed. 2019 , 148 , 106864. [ Google Scholar ] [ CrossRef ]
| Area of the Study | Purpose of the Study | Reference | No of Papers |
|---|---|---|---|
| Reviews/Comparison of methods | Computerized PET/CT Image Analysis in the Evaluation of Tumor | [ ] | 1 |
| Machine learning techniques in medical imaging | [ , , , , , , ] | 7 | |
| Segmentation methods for Radiology image (s) | [ , , , , ] | 5 | |
| Radiation therapy treatments for metastases | [ , , ] | 3 | |
| Radiation therapy and planning | [ , , , , ] | 5 | |
| Metastases Segmentation | [ ] | 1 | |
| Imaging Techniques | [ , ] | 2 | |
| Radiomics in medical imaging | [ ] | 1 | |
| Segmentation | Metastases | [ , , , , , , , , , , , , , , , , , ] | 18 |
| Tumor | [ , , , , , , , , , , , , , , , , , , , , , , , , , , ] | 27 | |
| Organ(s)/Organs-at-Risk (OARs) | [ , , , , , , , , , , , , , , , , , , , , , ] | 22 | |
| Target Volume/OARs + Target Volume | [ , , , ] | 4 | |
| Classification | Metastases | [ , , , ] | 4 |
| Tumor | [ , ] | 2 | |
| The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
Share and Cite
Paranavithana, I.R.; Stirling, D.; Ros, M.; Field, M. Systematic Review of Tumor Segmentation Strategies for Bone Metastases. Cancers 2023 , 15 , 1750. https://doi.org/10.3390/cancers15061750
Paranavithana IR, Stirling D, Ros M, Field M. Systematic Review of Tumor Segmentation Strategies for Bone Metastases. Cancers . 2023; 15(6):1750. https://doi.org/10.3390/cancers15061750
Paranavithana, Iromi R., David Stirling, Montserrat Ros, and Matthew Field. 2023. "Systematic Review of Tumor Segmentation Strategies for Bone Metastases" Cancers 15, no. 6: 1750. https://doi.org/10.3390/cancers15061750
Article Metrics
Article access statistics, supplementary material.
ZIP-Document (ZIP, 310 KiB)
Further Information
Mdpi initiatives, follow mdpi.

Subscribe to receive issue release notifications and newsletters from MDPI journals
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Primary bone cancer.
Jack E. Pullan ; Saran Lotfollahzadeh .
Affiliations
Last Update: March 20, 2024 .
- Continuing Education Activity
Primary bone cancer emerges as an uncommon malignant tumor originating from primitive mesenchymal cells within the bone. With distinctive subtypes such as osteosarcoma, chondrosarcoma, and Ewing sarcoma, each presents unique demographics, imaging traits, and biological attributes. Surgical excision, complemented by chemotherapy and radiotherapy, constitutes the primary treatment approach, demanding a nuanced understanding from clinicians for accurate diagnosis and informed treatment strategies.
In this activity, participants explore primary bone cancer assessment and treatment, emphasizing the interprofessional team's indispensable role. Comprising experts from radiology, histopathology, oncology, and orthopedics, this team collaborates to devise a comprehensive care plan. Additionally, the holistic team includes physiotherapists, occupational therapists, prosthetists, dieticians, social workers, and counselors, offering comprehensive support throughout the patient's journey. Through collaborative efforts, clinicians enhance their competence in managing primary bone cancer, ensuring optimal patient outcomes and quality of care.
- Differentiate primary bone cancer from other musculoskeletal conditions and secondary bone cancers.
- Assess the pertinence of laboratory tests and imaging modalities when diagnosing primary bone cancer.
- Determine the appropriate management of primary bone cancer in a stepwise treatment plan.
- Implement care coordination within an interprofessional team to manage patients with primary bone cancer.
- Introduction
Primary bone cancer is a rare malignant tumor of the bone originating from primitive mesenchymal cells. This condition accounts for around 0.2% of all malignancies worldwide and is idiopathic in most cases. Multiple subtypes are prevalent, with osteosarcoma, chondrosarcoma, and Ewing sarcoma being the most common. Each varies in demographics, imaging appearance, and biological behavior. They are frequently aggressive and require early diagnosis, utilizing imaging and tissue biopsy. Surgical excision remains the mainstay of curative treatment, with chemotherapy and radiotherapy used in conjunction. [1]
Though primary bone cancer is most often idiopathic, risk factors also play a role in developing this cancer.
- Genetic factors are linked. Germline abnormalities in hereditary cancer predisposition syndromes have an increased risk of later developing bone cancer through the downregulation of tumor suppressor genes or upregulation of oncogenes. The TP53 tumor suppressor gene is often altered in Li-Fraumeni syndrome, putting patients at an increased risk of developing osteosarcoma. Similarly, a mutation in the Rb1 gene leading to hereditary retinoblastoma is linked to osteosarcoma. Werner and Rothmund-Thomson syndromes are also linked to an increased risk of developing osteosarcoma.
- Previous treatment for cancer with radiotherapy is linked to an increased risk of developing primary bone cancer in later life, particularly when exposed to ionizing radiation in childhood.
- Several benign conditions show the potential to progress to primary bone cancer. Paget disease of the bone is a condition characterized by a disorder of bone metabolism, particularly osteoclastic function. These patients are at an increased risk of developing osteosarcoma; however, it is a rare complication. Enchondromas and osteochondromas are benign cartilaginous neoplasms that can later develop into malignant chondrosarcoma. [2] [3] [4] [5]
- Epidemiology
Primary bone cancer remains uncommon, accounting for 0.2% of all malignancies and 5% of childhood malignancies. In the United States, an estimated 3600 new cases of primary bone cancer were diagnosed in 2020, with 1720 deaths, making up 0.3% of all cancer deaths. The National Cancer Institute data shows that chondrosarcoma (40%) is most prevalent in adults, followed by osteosarcoma (28%). In children and adolescents, osteosarcoma (56%) is the most common, with Ewing sarcoma (34%) second. Chordoma, undifferentiated pleomorphic sarcoma, adamantinoma, fibrosarcoma, and giant cell tumor of the bone are also types of primary bone cancer; however, they are fewer in number. Primary bone cancer has a male predominance, with a worldwide osteosarcoma male-to-female ratio of 1.43 to 1. [6] [7]
- Pathophysiology
Primary bone cancer is a malignant tumor of the connective tissue with mesenchymal origin. The World Health Organisation determined 6 categories: chondrogenic, osteogenic, notochordal, vascular, other malignant mesenchymal, and miscellaneous (including Ewing sarcoma). The pathophysiology varies considerably between groups and, in some cases, is poorly understood. [6]
Osteosarcoma is a highly malignant osteogenic tumor that can develop in any bone. The tumor tends to develop near the metaphysis of long bones in young patients. The most common sites are the distal femur, proximal tibia, and proximal humerus, with high bone turnover. In adults, the axial skeleton is more common, where previous irradiation or metabolic disease of the bone is often associated. Common genetic changes are not present to explain the growth of this tumor type; however, 70% of cases demonstrate some level of chromosomal abnormality. Alterations in p53, Rb1, and deoxyribonucleic acid repair/surveillance genes are present in patients with Li-Fraumeni, Bloom, and Rothmund-Thomson syndrome, all linked to increased rates of osteosarcoma. [8] [9] [10]
Chondrosarcoma is primarily a disease of adults, most frequently diagnosed in patients between 30 and 60. They are generally slow-growing chondrogenic tumors of intermediate malignancy, rarely metastasizing. Chondrosarcoma arising de novo are classified as primary (>85% of cases), with those arising from pre-existing benign osteochondromas or enchondromas as secondary. The most common site for diagnosis is the long bones of the appendicular skeleton. Flat bones, including the pelvis, ribs, and scapula, can also be affected. The exact pathogenesis of chondrosarcoma is unknown, though multiple genes are implicated. Cytogenic studies have identified structural and numerical chromosomal abnormalities. Gene mutations in EXT1/2, TP53 , Rb1 , and IDH1/2 have also been linked to malignant transformation in benign lesions. [5] [11]
Ewing sarcoma is an aggressive tumor of childhood and adolescence, most commonly occurring in the bone but also seen in soft tissues. The peak incidence is at 15 years, and the men-to-women ratio is 5:1. The most frequent sites involved are long bones in the lower limb, pelvic bones, and the axial skeleton (ribs and vertebral column). Ewing sarcoma develops characteristically at the diaphysis, in contrast to the pattern seen in osteosarcoma. Ewing sarcoma is genetically well described, with characteristic chromosomal translocations identified. The translocation leads to fusing an FET protein to an ETS transcription factor, most commonly FLI1 (>85% of cases). The result is the formation of fusion proteins that deregulate downstream genes, altering cell behavior. [12] [13] [14]
- Histopathology
Diagnosis of primary bone cancer requires a tissue biopsy to perform histopathological assessment, with significant heterogeneity seen.
Osteosarcoma
The formation of bone or osteoid characterizes osteosarcoma, and this identification is key to diagnosis. Several histological subtypes have been identified, determined by the tumor's bone location and grade. [15] [8]
Intramedullary:
- Conventional
- Most prevalent subtype, comprising 80% of all osteosarcomas
- Classically high-grade, arising from the intramedullary canal
- Spindle to polyhedral cell shape malignant mesenchymal cells are seen
- Cell nuclei are pleomorphic with occasional mitotic figures
- Extracellular matrix production can be osteoblastic, osteoclastic, or fibroblastic; a combination is common
- Telangiectatic
- <4% of osteosarcomas
- Dilated hemorrhagic sinusoids seen with small amounts of osteoid
- Cavities mimic the appearance of an aneurysmal bone cyst, with the presence of high-grade sarcoma cells distinguishing the tumor
- <2% of osteosarcomas
- Well-differentiated cells embedded in the osseous matrix and fibrous stroma, with small amounts of osteoid
- 1.5% of osteosarcomas
- Numerous small round malignant cells seen within an osteoid matrix.
- Small cell sarcoma can resemble Ewing sarcoma; production of osteoid and sporadic spindling of cells are distinguishing features [15] [8]
- Parosteal
- 1% to 6% of osteosarcomas
- Slow growing, arising from the outer surface of the metaphysis
- Low-grade, with a well-differentiated, mostly cartilaginous matrix with minimal osteoid
- 1% to 2% of osteosarcomas
- More aggressive than parosteal osteosarcoma, with intermediate-grade tumors showing increased cell atypia
- Mostly cartilaginous matrix with minimal osteoid
- <1% of osteosarcomas
- Histologically similar to conventional osteosarcoma, showing high-grade spindle-shaped cells with nuclear pleomorphism [15] [8]
Chondrosarcoma
The production of hyaline cartilage characterizes chondrosarcomas to form a cartilaginous matrix. Lobules of cartilage are seen with significant variation in dimension. Cell nuclei show pleomorphism with chondrocytes varying in size and shape. Conventional chondrosarcoma accounts for over 85% of all chondrosarcomas. Chondrosarcoma can be subcategorized into primary central (developing within the medullary canal) or secondary peripheral (developing from the surface of the bone secondary to pre-existing enchondroma or osteochondroma). Histologically, both primary central and secondary peripheral are alike. Grading is an essential process that allows for the prediction of clinical behavior. [5] [16] [17]
- Grade I: These are low-grade, lowly cellular lesions with a predominantly cartilaginous matrix and small, dense nuclei. Distinguishing grade I chondrosarcoma and benign enchondroma can be difficult, both radiologically and histologically.
- Grade II: This shows a reduced cartilaginous matrix and moderately cellular. Nuclei are enlarged and hyperchromatic, with increased atypia. Mitoses may be seen.
- Grade III: These are high-grade lesions that are highly cellular, with increased cellular atypia showing vesicular and enlarged nuclei. Cartilaginous matrix is rare or absent, with myxoid material evident, and mitoses are more readily identified.
Several rare subtypes of chondrosarcoma are also identified. De-differentiated chondrosarcoma is characterized by low-grade chondrosarcoma next to a de-differentiated high-grade lesion, with a sharp transition between the 2. The tumor is extremely aggressive. Mesenchymal chondrosarcoma is a high-grade tumor occurring in either bone or soft tissue. Undifferentiated small round cells are seen with varying amounts of a cartilaginous matrix. Clear cell chondrosarcoma is a low-grade tumor, with cells showing clear, vacuolated cytoplasm. Areas of hemorrhage and cyst formation are seen. [5]
Ewing Sarcoma
Ewing sarcoma is a high-grade aggressive sarcoma and belongs to the group of small round-cell tumors. Monomorphic small cells are seen in sheets, with round nuclei, finely dispersed chromatin, and nucleoli usually unidentifiable. Frequently, necrosis is seen, with remaining viable cells arranged perivascularly. Cell membranes express the glycoprotein CD99, with immunohistochemistry showing that >95% of Ewing sarcomas have extensive membranous expression. CD99 expression is not specific to Ewing sarcoma; other markers are also used for diagnosis. [18] [14]
Other Types of Primary Bone Cancer
Chordoma, adamantinoma, and giant cell tumors of bone are typically low-grade locally invasive tumors. Undifferentiated pleomorphic sarcoma and fibrosarcoma are aggressive malignant tumors with a generally poor prognosis. [19] [20]
- History and Physical
Primary bone cancer is a rare diagnosis, with primary care clinicians unlikely to encounter a single case. Early diagnosis improves overall survival; however, delays remain common. History and examination form the first steps in diagnosing primary bone cancer, and an urgent referral to a specialist center is needed for all patients with a possible diagnosis. [12] [6]
Pain is the most common symptom, described as deep-seated dull pain progressing over time, refractory to simple analgesia. Pain can be troublesome at night, which is always a red flag. A mass may be palpable with localized tenderness. Patients may exhibit signs of systemic disease, including lethargy, malaise, and fever; however, in high-grade tumors, these are often not present and may suggest metastatic disease. A pathological fracture can be the first sign; any abnormal fracture requires further investigation. History of predisposing genetic conditions (eg, Li-Fraumeni syndrome, hereditary retinoblastoma, Werner syndrome, and Rothmund-Thomson syndrome) or diseases (Paget disease) is crucial. [6] Physical examination should focus on pain, tenderness, or mass. The site should be inspected and palpated, with size, consistency, mobility, location of the mass, and overlying skin changes noted. Lymph nodes should be palpated. [21]
Diagnostic modalities used in primary bone cancer include imaging, laboratory blood tests, and tissue biopsy.
Plain Film Radiograph
All patients should have orthogonal plain film radiographs when identifying potential bone cancer. Plain x-rays may show the following findings:
- Osteolytic, osteoblastic, or mixed changes
- A moth-eaten appearance (suggests bone destruction secondary to a rapidly expanding tumor within a bone, commonly seen in Ewing sarcoma and telangiectatic osteosarcoma)
- A permeative appearance (suggests the tumor progresses through bone, with an ill-defined zone between the tumor and healthy bone, often seen in small cell tumors, including Ewing sarcoma)
- "Onion skinning," with the tumor lifting partially-formed periosteal bone (classically seen in Ewing sarcoma)
- "Codman triangle," with periosteum lifted off bone and osteoid laid down
- "Sunburst" appearance, with vertical osteoid calcification due to significant periostitis [22]
Magnetic Resonance Imaging
A magnetic resonance imaging, MRI, scan remains the gold standard for assessing local tumor extent. The whole anatomical compartment should be imaged, and the MRI should be sensitive for bone and soft tissue lesions. Biopsy planning is crucial, and MRI allows the definition of neurovascular structures. Modern techniques, including dynamic MRI, better characterize high-grade tumor areas and have been used to assess tumor response to chemotherapy. [6] [23]
Computed Tomography
A computed tomography, CT, scan is used when the diagnosis remains unclear following an MRI or if an MRI is contraindicated. CT remains the modality of choice in pelvic bone cancer and reconstructive surgery. Patients with confirmed primary bone cancer require staging, and although many centers still perform chest radiographs, a chest CT scan is the gold standard for assessing metastatic pulmonary disease. [6]
Whole-Body Bone Scintigraphy
A whole-body bone scintigraphy bone scan is a nuclear medicine study that utilizes technetium-99m as an active agent, highlighting areas of osteoblastic activity. It allows the detection of malignancy and is useful in diagnosing metastatic disease.
Positron Emission Tomography
The positron emission tomography, PET, scan is a nuclear medicine study that utilizes the high metabolic rate of tumor cells, measuring the uptake of injected radiolabeled F-18 fluoro-deoxy-glucose. A PET scan is in some centers for the initial staging of primary bone cancer, and studies have suggested it as a modality for follow-up when used in combination with a CT scan. [24]
Laboratory Blood Tests
Specific laboratory blood tests are not used in diagnosing primary bone cancer; however, they form part of the patient workup. In patients treated with chemotherapy, baseline urea, creatinine, and liver function tests allow baseline renal and hepatic function assessment. Biochemical markers alkaline phosphatase and lactate dehydrogenase offer some predictive value, and levels can be monitored in follow-up to assess for disease recurrence. [22]
Tissue Biopsy
A lesion biopsy is needed for definitive diagnosis, allowing for histopathological assessment and tumor grading. Biopsy should be performed with the operating surgical team, ideally in a specialist bone cancer center. The procedure requires meticulous planning, with suboptimal biopsy impacting definitive surgical treatment options. Imaging should be performed before a biopsy, aiding in approach planning and preventing tissue disruption that could make radiological assessment more difficult. Percutaneous, incisional, or excisional techniques are used. Ultrasound, x-ray, and CT scans allow precise guidance. The tract should be well marked, allowing for excision during surgery, and a specialist bone cancer pathologist should assess samples. Specific markers on immunohistochemistry staining would assist in the diagnosis. Greater than 95% of Ewing sarcomas show extensive membranous expression of CD99; this is not specific to Ewing sarcoma, so other markers are also used in the immunohistochemistry panel. [21]
- Treatment / Management
Managing primary bone cancer requires a multidisciplinary approach by a specialist bone cancer center, including staff trained in providing age-appropriate care to children or adolescents. Management depends on several factors, including tumor type, stage and grade, and patient preference. Surgical excision remains the cornerstone of primary bone cancer treatment. Neoadjuvant and adjuvant chemotherapy are also commonplace in the management, with radiotherapy used in specific cases.
Surgical resection aims to remove all tumor tissue with adequate margins while preserving as much limb function as possible. A decision for either limb salvage surgery or amputation is established using imaging, histopathology, response to adjuvant treatment, and patient wishes. Surgery often leads to significant tissue loss, and open discussion with the patient is vital. The surgery's potential risks, benefits, and expected long-term functional impact must be highlighted. Low-grade tumors amenable to surgical excision typically require wide excision (removing the involved part of the bone with a cuff of healthy tissue), with high-grade tumors requiring radical excision (removing the affected bone and associated soft tissues within the anatomical compartment). [6] [25]
Chemotherapy
Multiple chemotherapy agents and regimens are used to manage primary bone cancer. Often, this consists of induction (neoadjuvant) and postoperative combination therapy (adjuvant), with improvements in rates of limb salvage surgery and overall survival since their introduction. Chemotherapy forms part of the standard treatment protocol for osteosarcoma and Ewing sarcoma. Chondrosarcoma is still primarily managed surgically, except in cases of mesenchymal chondrosarcoma, where chemotherapy and radiotherapy are often used. [26] [27]
Neoadjuvant chemotherapy is primarily used to reduce the rate of future metastatic spread; however, study results have suggested it can also contribute to primary tumor control. A good response to neoadjuvant therapy is determined by a histological necrosis rate of less than 90%, with a poor response indicating a change in postoperative adjuvant chemotherapy agents and poorer outcomes. [28] [29] [30]
Radiotherapy
Radiotherapy is often used as adjunctive therapy in primary bone cancer. Ewing sarcoma is a radiosensitive tumor, with radiotherapy commonly used as part of the definitive treatment plan. Preoperative radiotherapy is used if the response to neoadjuvant chemotherapy is poor or the tumor is positioned in a problematic anatomical location, where reduction of tumor volume will aid surgical resection. If sufficient tumor volume cannot be removed surgically or it would be unacceptably disabling, radiotherapy is used for local treatment. Where adequate margins have not been resected, postoperative radiotherapy is utilized. Chondrosarcomas are relatively radioresistant, with radiotherapy only utilized for surgically unresectable or incompletely resected tumors. Radiotherapy has a palliative role in all primary bone cancers and is used to slow tumor growth locally and relieve pain. [6] [31] [32]
- Differential Diagnosis
The differential diagnosis of primary bone cancer includes the following:
Malignant Types of Tumors
- Multiple myeloma
Benign Types of Tumors
- Giant cell tumor
- Osteoblastoma
- Enchondroma
- Chondromyxoid fibroma
- Cortical desmoid
- Osteomyelitis
- Fracture callus
- Aneurysmal bone cyst
- Fibrous dysplasia [33]
Two staging systems, the TNM and Enneking systems, are used in primary bone cancer.
TNM System, American Joint Committee on Cancer
This refers to the extent of tumor (T), spread to local lymph nodes (N), metastatic spread (M), and histological grade (G). [34]
Stage IA (T1 N0 M0 G1/GX)
- ≤8cm in size, with no lymph node or metastatic spread
Stage IB (T2 N0 M0 G1/GX, or T3 N0 M0 G1/GX)
- >8cm in size (T2), with no lymph node or metastatic spread; low grade
- Cancer at more than 1 location in the same bone (T3), with no lymph node or metastatic spread; low grade
Stage IIA (T1 N0 M0 G2/G3)
- ≤8cm in size, with no lymph node or metastatic spread; high grade
Stage IIB (T2 N0 M0 G2/G3)
- >8cm in size, with no lymph node or metastatic spread; high grade
Stage III (T3 N0 M0 G2/G3)
- Cancer at more than 1 location in the same bone, with no lymph node or metastatic spread; high grade
Stage IVA (Any T N0 M1a Any G)
- Any size and maybe in multiple locations in the same bone, with no lymph node involvement.
- Metastatic spread to the lungs (M1a); any grade
Stage IVB (Any T, N1, Any M, Any G, or Any T, Any N, M1b, Any G)
- Any size; may be in more than 1 location in the same bone
- Has spread to local lymph nodes (N1)
- May or may not have metastasized to distant organs; any grade
- Any size and maybe in more than 1 location in the same bone.
- May or may not have spread to local lymph nodes
- Metastatic spreads to distant sites like other bones, liver, or brain (M1b); any grade
Enneking System
Refers to the histological grade (G), the extent of the tumor to the anatomical compartments of the body (T), and metastatic spread (M). [35]
Stage IA (G1 T1 M0)
- Low grade, intra-compartmental, no metastasis
Stage IB (G1 T2 M0)
- Low grade, extra compartmental, no metastasis
Stage IIA (G2 T1 M0)
- High grade, intra-compartmental, no metastasis
Stage IIB (G2 T2 M0)
- High grade, extra compartmental, no metastasis
Stage III (Any G, Any T, M1)
- Any grade, any location, regional, or distant metastatic spread
The prognosis of primary bone cancer is dependent on multiple factors, and no significant improvement is seen in 5-year survival over the past 25 years. In the United States, the National Cancer Institute shows that the overall 5-year survival rate is 66%, with studies suggesting lower rates in the United Kingdom. [12]
When the disease is localized, osteosarcoma has a 10-year survival of 60% to 78%. This number falls to 20% to 30% in patients with metastatic disease at presentation, with other negative prognostic factors including axial or proximal extremity tumor location, increased tumor size, raised alkaline phosphatase or lactase dehydrogenase, increased age, pathological fracture, and poor response to neoadjuvant chemotherapy. [36] [37] [38]
The most potent prognostic factor in chondrosarcoma is histological grade. Other identified factors are metastatic disease at presentation, increased age, and pelvic tumor location. 5-year survival in grade I chondrosarcoma is 83%, with only 53% of patients surviving to 5 years with grade I and II diseases. [5] [39] [40] Ewing sarcoma has a 5-year survival of 70% to 80% when the disease is localized. This number falls to 50% in patients with isolated pulmonary metastases and less than 30% in patients with any other metastatic disease at diagnosis. Other negative prognostic factors include pelvic tumor location, increased tumor size, and poor response to neoadjuvant or adjuvant chemotherapy treatment. [14] [41]
- Complications
The complications of primary bone cancer include the following:
Tumor-Related Complications
- Pathological fracture
- Tumor recurrence
- Distant metastasis [42] [27]
Treatment-Related Complications
- Surgical site or periprosthetic infection
- Implant failure
- Non-union/fracture of the biological implant
- Short-term side effects include malaise, anemia, nausea, vomiting, and alopecia
- Long-term side effects include cardiotoxicity, renal toxicity, hearing loss, and an increased risk of secondary malignancy
- Side effects following radiation therapy are site-dependent, affecting the skin, pelvic organs, gastrointestinal tract, and lungs
- Long-term, a small increased risk of developing a secondary malignancy exists [43] [44] [45]
- Pearls and Other Issues
The key points are as follows:
- Primary bone cancer is a rare malignancy derived from primitive mesenchymal cells.
- All patients presenting with unresolved bone pain should be assessed, and orthogonal plain film radiographs should be organized.
- MRI is the gold standard for assessing the extent of a local tumor.
- A multidisciplinary team should manage primary bone cancer in a specialized bone cancer center.
- Surgical excision remains the mainstay of treatment for primary bone cancer, with chemotherapy and radiotherapy often used as adjuncts.
- Enhancing Healthcare Team Outcomes
Primary bone cancer should be managed by a multidisciplinary team. The team should include clinicians from radiology, histopathology, oncology, and orthopedics. Radiologists and pathologists interpret initial imaging and tissue samples, indicating a definitive diagnosis and leading to surgical planning.
Oncologists determine the most appropriate neoadjuvant and adjuvant chemotherapy protocols and arrange follow-up and surveillance. Orthopedics plan and perform surgical resection of the tumor, along with any initial or future reconstruction. Other team members include nurses, physiotherapists, occupational therapists, prosthetists, dieticians, social workers, and counselors. [46] [47]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jack Pullan declares no relevant financial relationships with ineligible companies.
Disclosure: Saran Lotfollahzadeh declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Pullan JE, Lotfollahzadeh S. Primary Bone Cancer. [Updated 2024 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Is Surgical Resection of the Primary Site Associated with an Improved Overall Survival for Patients with Primary Malignant Bone Tumors Who Have Metastatic Disease at Presentation? [Clin Orthop Relat Res. 2020] Is Surgical Resection of the Primary Site Associated with an Improved Overall Survival for Patients with Primary Malignant Bone Tumors Who Have Metastatic Disease at Presentation? Malik AT, Alexander JH, Mayerson JL, Khan SN, Scharschmidt TJ. Clin Orthop Relat Res. 2020 Oct; 478(10):2284-2295.
- Esophageal extraskeletal neoplasm Ewing's sarcoma: Case report. [Int J Surg Case Rep. 2022] Esophageal extraskeletal neoplasm Ewing's sarcoma: Case report. Khalid H, Hussain N, Shamshad R. Int J Surg Case Rep. 2022 Aug; 97:107399. Epub 2022 Jul 9.
- sCD30 and sCD40L detection in patients with osteosarcoma, chondrosarcoma and Ewing sarcoma. [Iran J Immunol. 2013] sCD30 and sCD40L detection in patients with osteosarcoma, chondrosarcoma and Ewing sarcoma. Solooki S, Khozaei A, Shamsdin SA, Emami MJ, Khademolhosseini F. Iran J Immunol. 2013 Dec; 10(4):229-37.
- Review Surgical Treatment of Bone Sarcoma. [Cancers (Basel). 2022] Review Surgical Treatment of Bone Sarcoma. Bläsius F, Delbrück H, Hildebrand F, Hofmann UK. Cancers (Basel). 2022 May 29; 14(11). Epub 2022 May 29.
- Review [Interdisciplinary diagnostic and treatment of bone sarcomas of the extremities and trunk]. [Handchir Mikrochir Plast Chir....] Review [Interdisciplinary diagnostic and treatment of bone sarcomas of the extremities and trunk]. Andreou D, Hardes J, Gosheger G, Henrichs MP, Nottrott M, Streitbürger A. Handchir Mikrochir Plast Chir. 2015 Apr; 47(2):90-9. Epub 2015 Apr 21.
Recent Activity
- Primary Bone Cancer - StatPearls Primary Bone Cancer - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Bone Cancer Detection Using Deep Learning
- Conference paper
- First Online: 04 May 2023
- Cite this conference paper

- Mansoor Habib Mazumder 13 &
- Maheshwari Prasad Singh 13
Part of the book series: Lecture Notes in Networks and Systems ((LNNS,volume 565))
Included in the following conference series:
- International Conference on Innovations in Computer Science and Engineering
244 Accesses
1 Citations
There have been many registered cases of bone cancer or tumor across the world with fatal cases involving in deaths too due to bone cancer. Thus, detecting them at the early stages becomes necessary which can save many lives. In today’s world, tumor is detected using MRI scans, and the process involved is costly and tedious. In the era of machine learning and artificial intelligence, detecting the tumors is still a tedious process, and it is very costly for setting up to train networks. There are various segmentation techniques, and convolutional neural networks can be used using X-ray images to detect the tumors at the early stages. If the tumor is detected and classified at the correct time, then without any hesitance, further complication can be prevented with right medications given at the required time. In this paper, we presented a modified architecture using convolutional neural network and inception modules to classify the stages of the bone cancers. The proposed model is trained on a dataset provided by ‘Stanford ML’ group which is available publicly for research and achieved accuracy of 92.68% on the testing dataset.
This is a preview of subscription content, log in via an institution to check access.
Access this chapter
- Available as PDF
- Read on any device
- Instant download
- Own it forever
- Available as EPUB and PDF
- Compact, lightweight edition
- Dispatched in 3 to 5 business days
- Free shipping worldwide - see info
Tax calculation will be finalised at checkout
Purchases are for personal use only
Institutional subscriptions
Similar content being viewed by others
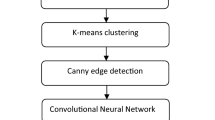
A comparative analysis of CNN-based deep learning architectures for early diagnosis of bone cancer using CT images


Deep Convolutional Extreme Learning Machine with AlexNet-Based Bone Cancer Classification Using Whole-Body Scan Images

Abnormality Bone Detection in X-Ray Images Using Convolutional Neural Network
Langlotz CP, Allen B, Erickson BJ, Kalpathy-Cramer J, Bigelow K, Cook TS, Flanders AE, Lungren MP, Mendelson DS, Rudie JD et al (2018) A roadmap for foundational research on artificial intelligence in medical imaging: from the 2018 nih/rsna/acr/the academy workshop. Radiology 291(3):781–791
Google Scholar
Ebsim R, Naqvi J, Cootes TF (2018) Automatic detection of wrist fracturesfrom posteroanterior and lateral radiographs: a deep learning-based approach. In: International workshop on computational methods and clinical applications in musculoskeletal imaging, pp 114–125. Springer
Varma M, Mandy L, Gardner R, Dunnmon J, Khandwala N, Rajpurkar P, Long J, Beaulieu C, Shpanskaya K, Fei-Fei L et al (2019) Automated abnormality detection in lower extremity radiographs using deep learning. Nature Machine Intell 1(12):578–583
Article Google Scholar
Rajpurkar P, Irvin J, Ball RL, Zhu K, Yang B, Mehta H, Duan T, Ding D, Bagul A, Langlotz CP et al (2018) Deep learning for chest radiograph diagnosis: a retrospective comparison of the chexnext algorithm to practicing radiologists. PLoS medicine 15(11):e1002686
Yan C, Yao J, Li R, Xu Z, Huang J (2018) Weakly superviseddeep learning for thoracic disease classification and localization on chest x-rays. In: Proceedings of the 2018 ACM international conference on bioinformatics, computational biology, and health informatics, pp 103–110
Kim DH, MacKinnon T (2018) Artificial intelligence in fracture detection: transfer learningfrom deep convolutional neural networks. Clin Radiol 73(5):439–445
Lim SE, Xing Y, Chen Y, Leow WK, Howe TS, Png MA (2004) Detection of femur and radius fractures in x-ray images. In: Proc. 2nd Int. Conf. on Advances in Medical Signal and Info. Proc, vol 65
Lindner C, Bromiley PA, Ionita MC, Cootes TF (2014) Robust and accurateshape model matching using random forest regression-voting. IEEE Trans Pattern Anal Mach Intell 37(9):1862–1874
Lindner C, Thiagarajah S, Wilkinson JM, Wallis GA, Cootes TF, arcOGEN Consortium et al (2013) Fully automatic segmentation of the proximal femur using random forest regression voting. IEEE Trans Med Imaging 32(8):1462–1472
Olczak J, Fahlberg N, Maki A, Razavian AS, Jilert A, Stark A, Sköldenberg O, Gordon M (2017) Artificial intelligence for analyzing orthopedic¨ trauma radiographs: deep learning algorithms—are they on par with humans for diagnosing fractures? Acta orthopaedica 88(6):581–586
Rajpurkar P, Irvin J, Bagul A, Ding D, Duan T, Mehta H, Yang B, Zhu K, Laird D, Ball RL et al (2017) Mura: large dataset for abnormality detection in musculoskeletal radiographs. arXiv preprint arXiv:1712.06957
Russakovsky O, Deng J, Su H, Krause J, Satheesh S, Ma S, Huang Z, Karpathy A, Khosla A, Bernstein M et al (2015) Imagenet large scale visual recognition challenge. Int J Comput Vision 115(3):211–252
Download references
Author information
Authors and affiliations.
National Institute of Technology, 800005, Patna, Bihar, India
Mansoor Habib Mazumder & Maheshwari Prasad Singh
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Mansoor Habib Mazumder .
Editor information
Editors and affiliations.
Guru Nanak Institutions, Ibrahimpatnam, Telangana, India
H. S. Saini
Guru Nanak Institutions, Ibrahimpatnam, India
Rishi Sayal
Jawaharlal Nehru Technological University, Hyderabad, Telangana, India
A. Govardhan
Cloud Computing, University of Melbourne, Melbourne, VIC, Australia
Rajkumar Buyya
Rights and permissions
Reprints and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this paper
Cite this paper.
Mazumder, M.H., Singh, M.P. (2023). Bone Cancer Detection Using Deep Learning. In: Saini, H.S., Sayal, R., Govardhan, A., Buyya, R. (eds) Innovations in Computer Science and Engineering. ICICSE 2022. Lecture Notes in Networks and Systems, vol 565. Springer, Singapore. https://doi.org/10.1007/978-981-19-7455-7_21
Download citation
DOI : https://doi.org/10.1007/978-981-19-7455-7_21
Published : 04 May 2023
Publisher Name : Springer, Singapore
Print ISBN : 978-981-19-7454-0
Online ISBN : 978-981-19-7455-7
eBook Packages : Intelligent Technologies and Robotics Intelligent Technologies and Robotics (R0)
Share this paper
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Publish with us
Policies and ethics
- Find a journal
- Track your research
Bone Cancer Research
The protein ETV6 appears to promote tumor growth by affecting the behavior of the EWS-FLI1 fusion protein that drives most Ewing sarcomas. The research groups that made the discovery hope it leads to a targeted therapy for the aggressive childhood cancer.
New findings from the first large, randomized clinical trial to compare chemotherapy regimens for relapsed or treatment-resistant Ewing sarcoma could help doctors and patients select treatments.
A new study offers insight into genetic alterations associated with osteosarcoma, the most common bone tumor of children and adolescents, and the findings have implications for genetic testing of children with osteosarcoma and their families.
From experiments in cells and mice, researchers have identified a two-drug combination that kills more Ewing sarcoma cells than either drug on its own. The study findings could help inform future clinical trials.
Findings from a study in mice suggests that a new type of drug conjugate may have potential as a treatment for two cancers that are often diagnosed in children.
May 30, 2024
A general passion
Image credit: pgen.1011291
research article
Conserved signalling functions for Mps1, Mad1 and Mad2 in the Cryptococcus neoformans spindle checkpoint
Mps1-dependent phosphorylation of C-terminal Mad1 residues is a critical step in Cryptococcus spindle checkpoint signalling.
Image credit: pgen.1011302
Recently Published Articles
- Streptococcus mitis and Streptococcus pneumoniae leads to higher genetic diversity within rather than between human populations">Long-term evolution of Streptococcus mitis and Streptococcus pneumoniae leads to higher genetic diversity within rather than between human populations
- A systematic screen identifies Saf5 as a link between splicing and transcription in fission yeast
- An eQTL-based approach reveals candidate regulators of LINE-1 RNA levels in lymphoblastoid cells
Current Issue May 2024
Adaptations to nitrogen availability drive ecological divergence of chemosynthetic symbionts
The importance of nitrogen availability in driving the ecological diversification of chemosynthetic symbiont species and the role that bacterial symbionts may play in the adaptation of marine organisms to changing environmental conditions.
Image credit: pgen.1011295
Paramutation at the maize pl1 locus is associated with RdDM activity at distal tandem repeats
pl1 paramutation depends on trans-chromosomal RNA-directed DNA methylation operating at a discrete cis-linked and copy-number-dependent transcriptional regulatory element.
Image credit: pgen.1011296
Research Article
Genomic analyses of Symbiomonas scintillans show no evidence for endosymbiotic bacteria but does reveal the presence of giant viruses
A multi-gene tree showed the three SsV genome types branched within highly supported clades with each of BpV2, OlVs, and MpVs, respectively.
Image credit: pgen.1011218
A natural bacterial pathogen of C . elegans uses a small RNA to induce transgenerational inheritance of learned avoidance
A mechanism of learning and remembering pathogen avoidance likely happens in the wild.
Image credit: pgen.1011178
Spoink , a LTR retrotransposon, invaded D. melanogaster populations in the 1990s
Evidence of Spoink retrotransposon's horizontal transfer into D. melanogaster populations post-1993, suggesting its origin from D.willistoni .
Image credit: pgen.1011201
Comparison of clinical geneticist and computer visual attention in assessing genetic conditions
Understanding AI, specifically Deep Learning, in facial diagnostics for genetic conditions can enhance the design and utilization of AI tools.
Image credit: pgen.1011168
Maintenance of proteostasis by Drosophila Rer1 is essential for competitive cell survival and Myc-driven overgrowth
Loss of Rer1 induces proteotoxic stress, leading to cell competition and elimination ...
Image credit: pgen.1011171
Anthracyclines induce cardiotoxicity through a shared gene expression response signature
TOP2i induce thousands of shared gene expression changes in cardiomyocytes.
Image credit: pgen.1011164
New PLOS journals accepting submissions
Five new journals unified in addressing global health and environmental challenges are now ready to receive submissions: PLOS Climate , PLOS Sustainability and Transformation , PLOS Water , PLOS Digital Health , and PLOS Global Public Health
COVID-19 Collection
The COVID-19 Collection highlights all content published across the PLOS journals relating to the COVID-19 pandemic.
Submit your Lab and Study Protocols to PLOS ONE !
PLOS ONE is now accepting submissions of Lab Protocols, a peer-reviewed article collaboration with protocols.io, and Study Protocols, an article that credits the work done prior to producing and publishing results.
PLOS Reviewer Center
A collection of free training and resources for peer reviewers of PLOS journals—and for the peer review community more broadly—drawn from research and interviews with staff editors, editorial board members, and experienced reviewers.
Ten Simple Rules
PLOS Computational Biology 's "Ten Simple Rules" articles provide quick, concentrated guides for mastering some of the professional challenges research scientists face in their careers.
Welcome New Associate Editors!
PLOS Genetics welcomes several new Associate Editors to our board: Nicolas Bierne, Julie Simpson, Yun Li, Hongbin Ji, Hongbing Zhang, Bertrand Servin, & Benjamin Schwessinger
Expanding human variation at PLOS Genetics
The former Natural Variation section at PLOS Genetics relaunches as Human Genetic Variation and Disease. Read the editors' reasoning behind this change.
PLOS Genetics welcomes new Section Editors
Quanjiang Ji (ShanghaiTech University) joined the editorial board and Xiaofeng Zhu (Case Western Reserve University) was promoted as new Section Editors for the PLOS Genetics Methods section.
PLOS Genetics editors elected to National Academy of Sciences
Congratulations to Associate Editor Michael Lichten and Consulting Editor Nicole King, who are newly elected members of the National Academy of Sciences.
Harmit Malik receives Novitski Prize
Congratulations to Associate Editor Harmit Malik, who was awarded the Edward Novitski Prize by the Genetics Society of America for his work on genetic conflict. Harmit has also been elected as a new member of the American Academy of Arts & Sciences.
Publish with PLOS
- Submission Instructions
- Submit Your Manuscript
Connect with Us
- PLOS Genetics on Twitter
- PLOS on Facebook
Get new content from PLOS Genetics in your inbox
Thank you you have successfully subscribed to the plos genetics newsletter., sorry, an error occurred while sending your subscription. please try again later..

COMMENTS
Osteosarcoma (OS) is a malignant tumor that originates in the mesenchymal tissue (which constitute spindle-shaped stromal cells that can produce bone-like tissues), and it accounts for 20% of all cases of primary malignant bone tumors in the world [ 1, 2 ]. In fact, it is the most common type of primary malignant bone tumor among adolescent ...
The relationship between bone and cancer has undergone profound changes in recent years and oncology has to manage with an increase of bone metastases incidence with a radical change of epidemiological data and a strong clinical impact. For these reasons currently bone metastases are responsible for the high morbidity in cancer patients.
1. Introduction. Bone is a highly active and dynamic connective tissue, which provides vital organ protection, mechanical support, locomotion, and structural body framework [1,2].Bone has high functional stability and regeneration potential, but, in some cases, the self-healing capacity of the bone tissue is impeded in critical-sized defects caused by trauma, tumor, or infection [3,4].
A comparative analysis of CNN-based deep learning architectures for early diagnosis of bone cancer using CT images. Kanimozhi Sampath. , Sivakumar Rajagopal. & Ananthakrishna Chintanpalli. Article ...
1. Introduction. Bone metastasis is a result of the complex interactions between tumor cells and bone cells. It is common in the advanced cancer, such as breast and prostate, with high clinical relevance , .According to the diagnosis time for bone metastasis, it is divided into synchronous bone metastasis and unsynchronous bone metastasis.
Purpose Early detection and classification of bone tumors in the proximal femur is crucial for their successful treatment. This study aimed to develop an artificial intelligence (AI) model to classify bone tumors in the proximal femur on plain radiographs. Methods Standard anteroposterior hip radiographs were obtained from a single tertiary referral center. A total of 538 femoral images were ...
The SVM model with HOG achieves an F-1 score of 0.92, outperforming the Random Forest model's .77. This study aims to develop reliable methods for bone cancer classification. The proposed automated method assists surgeons in accurately detecting malignant bone regions using modern image analysis techniques and machine learning models.
Bone cancer is a demanding challenge for contemporary medicine due to its high frequency of presentation and significant heterogeneity of malignant lesions developing within the bone. To date, available treatments are rarely curative and are primarily aimed at prolonging patients' survival and ameliorating their quality of life. Furthermore, both pharmacological and surgical therapies are ...
Research Paper. YBX1-interacting small RNAs and RUNX2 can be blocked in primary bone cancer using CADD522. ... his team and the generous donors. The Royal Orthopaedic Hospital is supported by a Bone Cancer Research Trust Infrastructure Grant and we thank the staff who were involved in patient care; Dionne Wortley, Ellie Keeling, Laura Bird ...
Abstract. Bone cancer can begin in any bone in the body, but it most commonly affects the pelvis or the long bones in the arms and legs. Bone cancer is rare, making up less than 1 percent of all ...
Introduction. Although primary bone tumors are uncommon with incidence rates of 4-7% among children and adolescents in the United States [1], primary malignancies of the bone and joints are ranked as the third leading cause of death in patients with cancer who are younger than 20 years of age [2].Bone tumors vary widely in their biological behavior and require different management depending ...
Bone cancer is characterized by uncontrolled growth of cells of the bone. Primary bone cancer (that arises directly in the bone), is relatively rare. Different types of bone tissue give rise to ...
Osteosarcoma (35%), chondrosarcoma (30%), and Ewing's sarcoma (16%) are the 3 most common forms of bone cancer. Malignant fibrous histiocytoma (MFH) and fibrosarcoma of the bone constitute fewer than 1% of all primary bone tumors. Chondrosarcoma is usually found in middle-aged and older adults; osteosarcoma and Ewing's sarcoma develop mainly in ...
It can lead to death if not diagnosed in the earlier stage. The bone cancer occurs in four stages as follows: in stage 1 cancer does not spread to other bone parts, in stage 2 cancer looks similar to stage 1 but it becomes dangerous, in stage 3 cancer spreads to one or two bone parts and in stage 4 cancer spreads to other body parts.
The main objective of this review was to present an overview of the latest research on cancer segmentation and bone metastasis segmentation on radiology images in the context of radiation therapy planning and to analyze and compare with state-of-the-art techniques in computer vision. 2. Methods. 2.1. Literature Search.
However, it has been shown that bone metastases from breast cancer, kidney cancer and melanoma can be identified several years after the initial diagnosis of a primary malignancy [2]. In our study, the diagnostic intervals for breast and kidney cancer were 67.8 months (6.1-246.4 months) and 50.1 months (3.4-210.9 months) respectively, while ...
Primary bone cancer is a rare malignant tumor of the bone originating from primitive mesenchymal cells. This condition accounts for around 0.2% of all malignancies worldwide and is idiopathic in most cases. Multiple subtypes are prevalent, with osteosarcoma, chondrosarcoma, and Ewing sarcoma being the most common. Each varies in demographics, imaging appearance, and biological behavior. They ...
17.3 Machine learning techniques for bone cancer detection. Now a days Machine learning technique pl ays an important role in diagnosis and. identifying the stages of bone cancer. Anindita Mishra ...
Abstract. There have been many registered cases of bone cancer or tumor across the world with fatal cases involving in deaths too due to bone cancer. Thus, detecting them at the early stages becomes necessary which can save many lives. In today's world, tumor is detected using MRI scans, and the process involved is costly and tedious.
Bone Marrow Cancer is a type of cancer that develops in the stem cells of the bone marrow that are responsible for blood formation. AML(Acute Myeloid Leukaemia) and MM(Multiple Myeloma) are both types of malignancy that can affect bone marrow. ... 3 research papers, and 1 research paper dealing with ALL, AML, CLL, and CML, respectively, and 3 ...
In 2009-2013, in England 55% Survive bone sarcoma for 10 or more years, and bone sarcoma survival is highest at age limit 15-59 years. In last 25 years, survival rate of bone sarcoma survival rate has not changed in England [2]. In this paper, we propose bone cancer detection method at low cost using MRI images.
Bone Cancer Research. The protein ETV6 appears to promote tumor growth by affecting the behavior of the EWS-FLI1 fusion protein that drives most Ewing sarcomas. The research groups that made the discovery hope it leads to a targeted therapy for the aggressive childhood cancer. New findings from the first large, randomized clinical trial to ...
Genomic analyses of Symbiomonas scintillans show no evidence for endosymbiotic bacteria but does reveal the presence of giant viruses. A multi-gene tree showed the three SsV genome types branched within highly supported clades with each of BpV2, OlVs, and MpVs, respectively. Image credit: pgen.1011218. 03/28/2024. Research Article.
A great deal of research is being done to learn more about the genetic changes inside bone cancer cells. Doctors are using what they learn to develop new targeted drugs for some types of bone cancer, as well as to test and use existing targeted drugs that focus on some of these gene changes. These drugs might change the cancer's ability to grow ...