- Second Opinion
Epilepsy During Pregnancy

What is epilepsy during pregnancy?
Epilepsy is a disorder of the nervous system. It is also called a seizure disorder. Normally the body's nerves send information by electrical and chemical signals. People with epilepsy have abnormal electrical signals in the brain. This can cause a seizure. Seizures can cause severe shaking of muscles. Or they may be very mild with hardly any symptoms at all.
Women who have epilepsy tend to have more seizures when they are pregnant. This is especially true in women who already have a lot of seizures.
What causes epilepsy during pregnancy?
Pregnancy does not cause epilepsy. But a pregnant woman who has epilepsy may have seizures more often. This may be because medicines to treat epilepsy can work differently during pregnancy. They may not be absorbed as well. Or they may not work as well. Also women who have nausea and vomiting in early pregnancy may vomit the medicine before it has its full effect.
What are the symptoms of epilepsy during pregnancy?
The symptoms are no different from symptoms when a woman is not pregnant. A woman with epilepsy has frequent or regular seizures with no known cause. In addition to seizures, the most common symptoms include:
- Changes in mood or energy level
- Memory loss
Some women may also have an aura. This is a feeling that they are going to have a seizure right before it happens.
The symptoms of epilepsy may look like other health conditions. Always see your healthcare provider for a diagnosis.
How is epilepsy during pregnancy diagnosed?
Most women with epilepsy will have been diagnosed before pregnancy. The diagnosis of epilepsy is based on a health history and physical exam. The diagnosis can only be made after you have had more than one seizure. Your healthcare provider may order tests based on how often you have seizures. These tests may include blood tests, heart (ECG) and brain wave (ECG) tests, and a CT scan or MRI.
How is epilepsy during pregnancy treated?
If you have epilepsy and are pregnant, you may need to see your healthcare provider more often. You most likely will be given medicine to prevent seizures. Monitoring of these medicines is important to control seizures and reduce side effects. Your healthcare provider will use as few medicines as possible and at the lowest dose needed to control seizures. Never stop or reduce your seizure medicine unless your healthcare provider tells you to.
You will likely have a normal labor and delivery. But stress may raise the risk for seizures. A calm birthing setting and epidural anesthesia can help.
You can raise your chances for a healthy pregnancy by getting early prenatal care. Work with your healthcare providers to manage your epilepsy.
What are the complications of epilepsy during pregnancy?
Epilepsy and the medicines to treat it can have many effects on the mother, the pregnancy, and the developing baby. Most women are able to have a healthy pregnancy and baby. But epilepsy does raise the risk for certain complications of pregnancy. These include:
- High blood pressure of pregnancy
- Slightly smaller baby
- Birth defects of the spine and brain (neural tube defects). Some epilepsy medicine may interfere with the levels of folic acid in the blood. Folic acid is a B vitamin. All women of childbearing age should take folic acid supplements of 0.4 mg per day to prevent neural tube defects. If you take epilepsy medicine, talk with your provider about taking a higher dose of folic acid. It may help prevent these defects.
- Other birth defects. These may be linked to some epilepsy medicines. Most experts agree that preventing seizures is better than the risks of taking the medicines. Most babies born to women taking epilepsy medicines do not have birth defects.
- Lower levels of vitamin D. Epilepsy medicine can affect how well your body absorbs vitamin D. Taking a prenatal vitamins generally takes care of this problem.
- Severe bleeding in the newborn. Some epilepsy medicines can affect the levels of vitamin K, which is important in blood clotting. All newborns should get a shot of vitamin K to prevent bleeding.
- Withdrawal symptoms in the newborn. These are from the mother's seizure medicine. Symptoms last only a few weeks or months. They usually does not cause serious or long-term problems.
- Sleeping or feeding problems. Newborns who are breastfed may be very sleepy or have feeding problems. This is because the seizure medicine is passed through breastmilk. Generally, the benefits of breastfeeding are greater than any side effects for the baby.
When should I call my healthcare provider?
If you start having more frequent seizures, see your healthcare provider.
Key points about epilepsy during pregnancy
- Although pregnancy does not cause epilepsy, women with epilepsy tend to have seizures more often in pregnancy.
- Epilepsy and the medicines to treat it can have many effects on the mother, the pregnancy, and the developing baby.
- Most women with epilepsy are able to have a healthy pregnancy and baby.
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
- Pediatric Neurosurgery
- Cleft and Craniofacial Center
- Pediatric Cardiology
Related Topics
Seizure Quiz
Connect with us:
Download our App:
- Leadership Team
- Vision, Mission & Values
- The Stanford Advantage
- Government and Community Relations
- Get Involved
- Volunteer Services
- Auxiliaries & Affiliates
© 123 Stanford Medicine Children’s Health
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
Epilepsy in pregnancy
Chinese translation.
- Related content
- Peer review
- Michael Owen Kinney , specialist registrar in neurology 1 ,
- James Morrow , principal investigator of the UK and Ireland Epilepsy and Pregnancy Register 2
- 1 Department of Neurosciences, Royal Group of Hospitals, Belfast, Northern Ireland
- 2 Office of the UK and Ireland Epilepsy and Pregnancy Register, Royal Group of Hospitals, Belfast BT12 6BA, Northern Ireland
- Correspondence to: J Morrow jjimorrow{at}btinternet.com
What you need to know
96% of babies born to mothers with epilepsy will have no major malformations
Offer preconceptual counselling to women with epilepsy at routine follow-up and opportunistically in consultations when appropriate
Refer women with epilepsy who wish to become pregnant to specialist services for review of their diagnosis and management plan
Advise women with epilepsy who become pregnant unexpectedly to continue with their usual medication and refer them urgently for specialist assessment
Advise pregnant women with epilepsy who take antiepileptic medication to take 5 mg folic acid daily for their entire pregnancy
In every 1000 pregnancies, between two and five infants are born to women with epilepsy. 1 2 3 For such women, pregnancy can be a time of anxiety over maternal and fetal wellbeing. 4 5
Most women with epilepsy will not experience an increase in seizure frequency, and in 96% of pregnancies they will deliver a healthy child. 6 However, some women (between 14 and 32 per 100) will experience an increase in seizure frequency, 7 which can be harmful for the mother or fetus. There are no randomised controlled trials (RCTs) in women with epilepsy regarding antiepileptic drugs. Evidence comes from observational study and registry data and suggests some antiepileptic drugs are associated with an increased risk of congenital and neurodevelopmental abnormalities. 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 Some antiepileptic drugs considered safe to the fetus may be associated with increased risk of seizures and maternal mortality. 24 25 This review summarises the current evidence regarding women with epilepsy who are pregnant or planning pregnancy.
Sources and selection criteria
We performed an electronic search of PubMed for relevant English language publications over the past 10 years. The search terms “pregnancy” and “preconceptual” were individually combined with “epilepsy” as search terms. All abstracts were reviewed for relevance, and relevant papers were read, and we selected the most appropriate for this article. The most recent and important articles were given preference. Within the papers identified in the search, references were also reviewed for relevance, and papers from the authors’ collections and Cochrane databases were considered.
How is epilepsy affected by pregnancy?
Pregnancy related factors can influence seizure control (box 1). 26 27 Women who are seizure-free nine months before pregnancy have a high likelihood of remaining seizure-free in pregnancy. 7 A large multicentre prospective study (European Registry of Antiepileptic Drugs and Pregnancy (EURAP)) showed that good seizure control in the first trimester is similarly associated with good control in later pregnancy. It showed that the risk of intrapartum seizures is between 14 and 26 per 1000 pregnancies, and the risk of status epilepticus was low at <1 per 100 pregnancies. 26 28
Box 1: Pregnancy related factors contributing to worsening seizure control.
Lack of sleep during late pregnancy, labour, and after delivery
Stress and anxiety
Hormonal changes
Pharmacokinetic changes with decreased plasma antiepileptic drug levels, particularly lamotrigine
Lack of adherence to medication due to concerns about fetal development
Change to less effective drug because of perceived lower risk of teratogenicity
What is the experience of the woman?
Women planning pregnancy report inadequate information to facilitate decision making. 29 30 In a survey of 12 000 women with epilepsy of childbearing age, 2000 questionnaires from the 20% response were selected and analysed. Validity and sample demographics were not described, but a third of these women (n=549) were not planning further children because of factors related to their epilepsy. 31 A third of patients with children (n=419) stated they had not been given any information on pregnancy and epilepsy medication. 31
Social circumstances and the support structures available influence the experience of pregnant women with epilepsy. Women from more socially deprived areas were less likely to take folic acid before conception, had more convulsive seizures, and used less favourable drug regimens from a teratogenicity perspective. 32 This should be considered when counselling women regarding pregnancy, as specific advice and support needs to be tailored to the patient’s own ideas, concerns, and expectations. 33 34
What are the risks associated with seizures in pregnancy?
There is no evidence that focal seizures (with or without impaired consciousness, formerly termed partial or complex partial seizures), myoclonic seizures, or absence seizures cause adverse fetal outcomes. Case reports suggest focal seizures may cause fetal bradycardia. 35 In and out of pregnancy, any seizure with loss of awareness has the potential to cause trauma. Generalised tonic-clonic seizures can cause injury from drowning, motor vehicle accidents, and falls. 36 Specific to pregnancy, abdominal trauma can result in ruptured fetal membranes, subsequent infection, and premature labour, 37 although the absolute risk is low. Generalised tonic-clonic seizures can also cause fetal hypoxia and acidosis. In a retrospective clinic-based study, multiple (≥5) maternal tonic-clonic seizures was linked with a lower verbal IQ in a multiple regression analysis in 38/249 children. 38
The death rate for women with epilepsy during pregnancy or the postpartum period is estimated at 1:1000, compared with 1:10 000 for women without epilepsy. 24 38 The recent confidential enquiry found 14 maternal deaths in the UK between 2009 and 2012: 12 from sudden unexpected death in epilepsy (box 2) and two from drowning. 34 Of those women, only two had received preconception counselling, seven were under specialist review, but only three had achieved controlled epilepsy before pregnancy.
Box 2: Sudden unexpected death in epilepsy (SUDEP)
What is it.
This refers to a sudden and unexpected death of a patient with epilepsy that is not related to trauma, drowning, or status epilepticus
It may occur in association with a seizure, and postmortem examination does not reveal a structural or toxicological cause of death 39
Women should be told this information in a sensitive manner 34
Can the risk be reduced?
Family first aid training, avoiding sleeping alone or prone, compliance with medication, and adjusting falling drug levels may reduce the risk of SUDEP 34
Is it related to drug choice?
Concerns have been raised about drug choice (particularly with lamotrigine) as a risk factor for SUDEP. In a case-control study of 26 cases of SUDEP, (15 females) the overall estimated incidence of SUDEP was 1.0 per 1000 patient years 25
The incidence of SUDEP in women taking lamotrigine was estimated at 2.5 per 1000 patient years, higher than in those women not using lamotrigine (0.5 per 1000 patient years) 25
The association between lamotrigine and maternal death 25 may reflect its common use, it may also reflect the fact that drug levels fall as pregnancy progresses, resulting in breakthrough seizures. 24
Preconception counselling in women with epilepsy.
Best practice is to discuss pregnancy plans at routine follow-up and opportunistically in consultations, and to encourage pregnancy to be planned where possible. 40 41 Preconceptual advice for women with epilepsy includes general advice applicable to all women 42 43 on the risks of smoking 7 and alcohol consumption and the benefits of diet, regular sleep, and exercise. All people with epilepsy should be advised to avoid bathing or swimming alone and avoid climbing heights. Women can be encouraged to address the multiple modifiable factors that can reduce the risk of seizures occurring in pregnancy (boxes 1 and 3).
Box 3: Preconception advice specific to women with epilepsy (from the National Institute for Health and Care Excellence (NICE) 44 and Scottish Intercollegiate Guidelines Network (SIGN) 45
Reassure women with epilepsy that approximately 96% of women with epilepsy (most of whom are taking antiepileptic drugs) deliver a baby free from birth defects.
Birth defect risk is related to various factors, including personal and family history of children born with birth defects and the choice, number, and dose of antiepileptic drugs used
Most women who are seizure-free entering pregnancy remain seizure-free during the pregnancy if they maintain appropriate treatment
Offer early referral to specialist services if a women with epilepsy wishes to become pregnant: ideally to a joint obstetric-epilepsy clinic, or to an epilepsy specialist or neurology clinic, and epilepsy nurse specialist
Advise women with epilepsy to remain on their current antiepileptic medication as prescribed by their specialist. Abrupt withdrawal of medication is not shown to reduce the risk of major congenital malformation of the fetus and could provoke life threatening seizures 44 45
Folic acid is recommended for women with epilepsy taking antiepileptic drugs but dose suggestions differ (box 4)
Box 4: Folic acid and prevention of neural tube defects in epilepsy
Women with epilepsy taking antiepileptic drugs have an increased risk of giving birth to children with malformations, including neural tube defects
Folic acid has been shown to reduce this risk in the general population
The antiepileptic valproate carries a high risk of this specific abnormality
Guidelines suggest that all women should take folic acid to reduce the risk of neural tube defects by taking folic acid before conception and during the first trimester 44 45 46 47 48
Observational registry data have not conclusively shown benefit of folic acid use in women with epilepsy. 49 In one retrospective study, preconceptual folic acid was associated with better cognitive performance in offspring at 6 years of age 50
Folic acid use may reduce the rate of spontaneous miscarriage 51
The optimal dose for women with epilepsy is not clear for those taking antiepileptic drugs (some of which may be folate antagonists) 52 : 5 mg once daily is suggested in UK guidelines for at least the first trimester, but this could be continued throughout pregnancy without likelihood of harm. 44 45 47 US guidelines suggest at least 0.4 mg/day preconceptually and during pregnancy 48
Folic acid is recommended as soon as the pregnancy is confirmed in unplanned pregnancies (16% of pregnancies in the UK general population) 53
If a woman with epilepsy is not taking any antiepileptic drugs, then at least 0.4 mg daily is recommended 45
5 mg folic acid daily is recommended for women with epilepsy who are obese or have a family history of malformations even if the woman is not taking an antiepileptic drug 45
Who is best placed to deliver care?
The National Institute for Health and Care Excellence (NICE) guideline on epilepsy acknowledges that the joint obstetric-epilepsy clinic represents convenient practice but does not make a routine recommendation for its widespread implementation. 44 Pregnant women with epilepsy need regular follow-up with midwifery/obstetrics, neurology, and epilepsy nurse specialists. 44 If joint clinics are not available, offer referral to an epilepsy specialist or neurologist as well as an obstetrician with an interest in medical disorders. Early referral, ideally at least a year before conception is planned, 29 46 54 allows review of the diagnosis (up to a third of people diagnosed with epilepsy have an alternative diagnosis such as cardiac or psychogenic causes), discussion about risks and harms of treatment, and optimisation of the woman’s antiepileptic drug regimen, and encouragement to notify the pregnancy to the UK and Ireland registry for ongoing surveillance of major congenital malformation risks. 44
What are the risks of antiepileptic drugs to the fetus?
A major congenital malformation is an anatomical abnormality that interferes with function or requires surgery, or both. 12 In the general population major congenital malformations occur in between one and three per 100 births. 1 55 56 Woman with epilepsy who do not take antiepileptic drugs probably do not have an increased risk of malformation in their offspring compared with controls without epilepsy, as shown by a meta-analysis which found an odds ratio of 0.99 (95% confidence interval 0.49 to 2.01). However, women with epilepsy taking antiepileptic drugs have an increased malformation risk compared with controls (odds ratio 3.26 (95% CI 2.15 to 4.93)). 55 57
Assessing the individual risks of each antiepileptic drug has been a slow process (valproate was licensed in the UK in 1973). There are no randomised controlled trials of antiepileptic drugs in pregnancy. Data are based on observational studies only. Most data come from the various registries, comprising a minority of women with epilepsy who become pregnant. In the UK the UKIEPR captures about 30% of all pregnancies. 58 The registries have different methodologies and timeframes at which assessments for major congenital malformations are made, which makes meta-analysis problematic and controversial. 58 59
The findings from these large observational studies have shown a broad consensus outlined in table 1 ⇓ . Overall, frequencies for major congenital malformation in all monotherapy-treated women ranges between 0.7 and 10.0 per 100 exposures. Of the commonly prescribed monotherapies valproate carries the highest risk of teratogenicity, with concern regarding topiramate as a moderate to high-risk drug. 13 Lamotrigine and levetiracetam are considered among the least teratogenic antiepileptic drugs available. 14 23 Carbamazepine is considered to be equivalent in terms of teratogenic risk to lamotrigine and levetiracetam but is used less often due to poor tolerability and its enzyme inducing effects. Treatment with more than one drug (polytherapy) carries increased major congenital malformation risk compared to monotherapy. It appears likely that the presence of valproate in polytherapy is the major contributor to the risk of teratogenicity. 15 44 The risk appears to be dose dependent. 16 The neurodevelopmental effects of in-utero antiepileptic drug exposure has been increasingly studied in the last several years but as in the studies assessing malformations, this work is all observational and there are no RCTs. Box 5 summarises our current knowledge.
Registry data of natural rates of major congenital malformations (MCMs) associated with in-utero exposure to antiepileptic drug monotherapy. Values are numbers (percentages (95% confidence intervals)). The background risk of major congenital malformations in the general population is 1-3%
- View inline
Box 5: Summary of neurodevelopmental outcomes from in-utero exposure to antiepileptic drug monotherapies
A recent Cochrane review indicates poorer neurodevelopmental outcomes of pregnancies with exposure to valproate. 18 This is based on 22 observational prospective cohort studies and six register studies; the reduction in IQ would probably be enough to affect education and occupational outcomes in later life. A dose effect was reported, and 800-1000 mg/day or greater was associated with a poorer cognitive profile
There is some evidence of an association between valproate exposure and autism 21 22
A population based study from a Danish psychiatry register over a decade found maternal valproate use to be associated with 4.4 per 100 absolute risk of developing autism spectrum disorder and a 2.5 per 100 absolute risk of developing childhood autism, in 508 exposed children. 63
Carbamazepine
A recent Cochrane review found no significant effects on development. 18 No link has been found with autism or autistic spectrum disorder. 63
Lamotrigine
A Cochrane review 18 identified several studies 50 64 that failed to establish any adverse impact on neurodevelopmental parameters. Further work is required in this area. No link has been found with autism or autism spectrum disorders. 63
Levetiracetam
Observational data show no increased likelihood of neurodevelopmental problems. 19 20 Data are preliminary, and the Cochrane review 18 urged caution in interpreting these as evidence of safety. It is recommended that parents are told that the neurodevelopmental outcomes are not fully known
Insufficient data identified in the Cochrane review 18 to guide clinicians. Only one study with nine children was available. Further studies are called for to establish risk or safety
Recurrence risk with major congenital malformations
A woman with epilepsy who already has a child with a major congenital malformation has a higher risk of further malformations in subsequent pregnancies. 65 66 67 68 As with the general population, however, the risk is reduced if a woman has had pregnancies without major congenital malformations. 67 The risk of recurrence of major congenital malformation in future pregnancies is increased with prenatal exposure to valproate or topiramate, either as monotherapies or part of a polytherapy regimen. If the dose of topiramate or valproate remains unchanged or is increased across subsequent pregnancies, this also carries increased risk of recurrence, but this is not found with other drugs such as lamotrigine. 67
Current recommendations for antiepileptic drugs in pregnancy
Avoid valproate where possible, particularly as a first line treatment for women of reproductive age. However, valproate remains a drug of choice for generalised epilepsy because of its broad spectrum activity and efficacy, 69 and it might be appropriate for some women 59 if they have not responded to alternative antiepileptic drugs and after discussion of the risks and benefits of therapy and the potential risks in the event of pregnancy. Low dose monotherapy (<700 mg/day) is preferable to high doses of valproate, or valproate in polytherapy (box 5), but no truly safe dose has been defined. When drug treatment is required, the lowest effective dose of a monotherapy agent is recommended (table 1 ⇑ ). 9 10 16 23 70 If polytherapy is required after a necessary up-titration of one agent to the optimal dose and the patient exhibits ongoing seizures, then a carefully chosen second agent should be added at a low dose to achieve the lowest possible likelihood of malformation and developmental delay (based mainly on data for monotherapy outcomes). 15
Lamotrigine and leviteracetam are recommended first line agents. This is due to their favourable rate of major congenital malformations and apparent non-adverse neurodevelopmental profiles, although the preliminary data on this remain insufficient to be certain of the long term cognitive risks. Levels of these drugs may fall as pregnancy progresses, and dose adjustments may be required to prevent seizures. Advise women that lamotrigine and levetiracetam may be less effective in controlling their epilepsy and about the risks of sudden unexpected death in epilepsy.
What is recommended if a woman is taking valproate?
In 2015, warnings were issued from the European Medicines Agency, and the International League Against Epilepsy/European Academy of Neurology regarding valproate use by women of childbearing potential. 46 Ideally such women are started on an antiepileptic drug with low teratogenic potential at diagnosis to avoid a difficult scenario of drug withdrawal or substitution in the event of pregnancy. Figures 1 ⇓ and figure 2 ⇓ represent consensus clinical views 46 on approaches to management of women who are taking valproate and wish to become pregnant or who become pregnant while taking valproate. These figures are not validated risk assessment tools or prediction models. There is often more than one correct approach, and validated trial evidence about the best option is often lacking, whereby clinical context and judgment are vital.
Fig 1 Options for managing women with epilepsy already taking valproate who are currently pregnant
- Download figure
- Open in new tab
- Download powerpoint
Fig 2 Options for managing women with epilepsy who are taking valproate and intend to become pregnant (RISKS mnemonic)

Is drug level monitoring recommended in pregnancy?
There is increased renal clearance and increased hepatic elimination in pregnancy. This results in a fall in the serum drug levels of certain antiepileptic drugs as pregnancy progresses, resulting in an increased risk of seizures. 71 One retrospective study found that a >35% decrease in drug levels relative to preconception drug level was associated with breakthrough seizures. 72
Plasma concentrations for lamotrigine, levetiracetam, and oxcarbazepine fall during pregnancy, 73 74 75 with increased risk of breakthrough seizures. Carbamazepine levels remain stable, and insufficient evidence exists to comment on valproate levels. 48 Consensus suggests that monitoring of maternal drug concentrations is advised for lamotrigine, levetiracetam, and oxcarbazepine. 45 48
For the individual patient the effect of decline in drug levels on seizure frequency is difficult to predict. 45 Ideally, pre-pregnancy drug levels should be taken to establish the optimum serum drug level that maintains seizure control. As a minimum, specialists should check appropriate serum drug levels once every trimester, with some suggesting monthly checks, 76 77 but the optimum frequency is not established. 48 Increased drug doses may be needed to maintain seizure freedom in later pregnancy given the tendency for the antiepileptic drug serum concentration to fall during pregnancy, particularly for lamotrigine. 78 This is best coordinated by the epilepsy specialist. 45 Specialist guidance should also be given in advance regarding the safe postpartum tapering of antiepileptic drugs to prevent drug toxicity. 77
Further sources of information for patients and professionals
Epilepsy Society ( www.epilepsysociety.org.uk/ ). Provides general information
UK Epilepsy and Pregnancy Register ( www.epilepsyandpregnancy.co.uk ). Women with epilepsy who are pregnant, whether or not they are taking antiepileptic drugs, are eligible to register (women can self refer to this)
SUDEP Action ( www.sudep.org ). Information on sudden unexpected death in epilepsy
TOXNET ( https://toxnet.nlm.nih.gov/newtoxnet/lactmed.htm ). Advice from the National Institute of Health on the safety of drug use if breastfeeding
Epilepsy Society. Contraception and epilepsy ( www.epilepsysociety.org.uk/contraception-and-epilepsy )
Faculty of Sexual and Reproductive Healthcare Clinical Effectiveness Unit. Antiepileptic drugs and contraception ( www.fsrh.org/pdfs/CEUStatementADC0110.pdf )
Morrow J. The XX factor. Treating women with anti-epileptic drugs . National Services for Health Improvement, 2007.
Medicines and Healthcare products Regulatory Agency. Toolkit on the risks of valproate medicines in female patients ( www.gov.uk/government/publications/toolkit-on-the-risks-of-valproate-medicines-in-female-patients ). Website with useful resources related to valproate use, including a consent checklist before starting valproate and a patient information section
How were patients involved in the creation of this article?
No patients were involved in the creation of this review
Contributors: Both authors were involved in the idea of developing the article, MOK wrote the first draft, and JM reviewed and restructured it. Both authors edited later versions of the article. We thank Beth Irwin for comments on the manuscript, and colleagues at the UK and Ireland Epilepsy and Pregnancy Register. We thank Medbh Hillyard Nicholl for the photograph.
Competing interests: We have read and understood the BMJ policy on declaration of interests and have no relevant interests to declare.
Funding: No funding was obtained for the purposes of writing this article.
- ↵ Olafsson E, Hallgrimsson JT, Hauser WA, Ludvigsson P, Gudmundsson G. Pregnancies of women with epilepsy: a population-based study in Iceland. Epilepsia 1998 ; 39 : 887 - 92 . doi:10.1111/j.1528-1157.1998.tb01186.x pmid:9701382 . OpenUrl CrossRef PubMed Web of Science
- ↵ Katz O, Levy A, Wiznitzer A, Sheiner E. Pregnancy and perinatal outcome in epileptic women: a population-based study. J Matern Fetal Neonatal Med 2006 ; 19 : 21 - 5 . doi:10.1080/14767050500434096 pmid:16492586 . OpenUrl CrossRef PubMed Web of Science
- ↵ Kotsopoulos IA, van Merode T, Kessels FG, de Krom MC, Knottnerus JA. Systematic review and meta-analysis of incidence studies of epilepsy and unprovoked seizures. Epilepsia 2002 ; 43 : 1402 - 9 . doi:10.1046/j.1528-1157.2002.t01-1-26901.x pmid:12423392 . OpenUrl CrossRef PubMed Web of Science
- ↵ Bjørk MH, Veiby G, Reiter SC, et al. Depression and anxiety in women with epilepsy during pregnancy and after delivery: a prospective population-based cohort study on frequency, risk factors, medication, and prognosis. Epilepsia 2015 ; 56 : 28 - 39 . doi:10.1111/epi.12884 pmid:25524160 . OpenUrl CrossRef PubMed
- ↵ Turner K, Piazzini A, Franza A, Canger R, Canevini MP, Marconi AM. Do women with epilepsy have more fear of childbirth during pregnancy compared with women without epilepsy? A case-control study. Birth 2008 ; 35 : 147 - 52 . doi:10.1111/j.1523-536X.2008.00228.x pmid:18507586 . OpenUrl CrossRef PubMed
- ↵ Morrow J, Russell A, Guthrie E, et al. Malformation risks of antiepileptic drugs in pregnancy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 2006 ; 77 : 193 - 8 . doi:10.1136/jnnp.2005.074203 pmid:16157661 . OpenUrl Abstract / FREE Full Text
- ↵ Harden CL, Hopp J, Ting TY, et al. American Academy of Neurology American Epilepsy Society. Management issues for women with epilepsy-Focus on pregnancy (an evidence-based review): I. Obstetrical complications and change in seizure frequency: Report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia 2009 ; 50 : 1229 - 36 . doi:10.1111/j.1528-1167.2009.02128.x pmid:19496807 . OpenUrl CrossRef PubMed
- ↵ Vajda FJ, Graham J, Roten A, Lander CM, O’Brien TJ, Eadie M. Teratogenicity of the newer antiepileptic drugs--the Australian experience. J Clin Neurosci 2012 ; 19 : 57 - 9 . doi:10.1016/j.jocn.2011.08.003 pmid:22104350 . OpenUrl CrossRef PubMed
- ↵ Hernández-Díaz S, Smith CR, Shen A, et al. North American AED Pregnancy Registry North American AED Pregnancy Registry. Comparative safety of antiepileptic drugs during pregnancy. Neurology 2012 ; 78 : 1692 - 9 . doi:10.1212/WNL.0b013e3182574f39 pmid:22551726 . OpenUrl CrossRef PubMed
- ↵ Tomson T, Battino D, Bonizzoni E, et al. EURAP study group. Dose-dependent risk of malformations with antiepileptic drugs: an analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol 2011 ; 10 : 609 - 17 . doi:10.1016/S1474-4422(11)70107-7 pmid:21652013 . OpenUrl CrossRef PubMed Web of Science
- ↵ Cunnington MC, Weil JG, Messenheimer JA, Ferber S, Yerby M, Tennis P. Final results from 18 years of the International Lamotrigine Pregnancy Registry. Neurology 2011 ; 76 : 1817 - 23 . doi:10.1212/WNL.0b013e31821ccd18 pmid:21606453 . OpenUrl CrossRef PubMed
- ↵ Perucca E. Birth defects after prenatal exposure to antiepileptic drugs. Lancet Neurol 2005 ; 4 : 781 - 6 . doi:10.1016/S1474-4422(05)70224-6 pmid:16239185 . OpenUrl CrossRef PubMed Web of Science
- ↵ Hunt S, Russell A, Smithson WH, et al. UK Epilepsy and Pregnancy Register. Topiramate in pregnancy: preliminary experience from the UK Epilepsy and Pregnancy Register. Neurology 2008 ; 71 : 272 - 6 . doi:10.1212/01.wnl.0000318293.28278.33 pmid:18645165 . OpenUrl CrossRef PubMed
- ↵ Mawhinney E, Craig J, Morrow J, et al. Levetiracetam in pregnancy: results from the UK and Ireland epilepsy and pregnancy registers. Neurology 2013 ; 80 : 400 - 5 . doi:10.1212/WNL.0b013e31827f0874 pmid:23303847 . OpenUrl CrossRef PubMed
- ↵ Holmes LB, Mittendorf R, Shen A, Smith CR, Hernandez-Diaz S. Fetal effects of anticonvulsant polytherapies: different risks from different drug combinations. Arch Neurol 2011 ; 68 : 1275 - 81 . doi:10.1001/archneurol.2011.133 pmid:21670385 . OpenUrl CrossRef PubMed Web of Science
- ↵ Tomson T, Battino D, Bonizzoni E, et al. EURAP Study Group. Dose-dependent teratogenicity of valproate in mono-and polytherapy. Neurology 2015 ; 85 : 866 - 72 . doi:10.1212/WNL.0000000000001772 pmid:26085607 . OpenUrl CrossRef PubMed
- ↵ Mawhinney E, Campbell J, Craig J, et al. Valproate and the risk for congenital malformations: Is formulation and dosage regime important? Seizure 2012 ; 21 : 215 - 8 . doi:10.1016/j.seizure.2012.01.005 pmid:22364656 . OpenUrl CrossRef PubMed Web of Science
- ↵ Bromley R, Weston J, Adab N, et al. Treatment for epilepsy in pregnancy: neurodevelopmental outcomes in the child. Cochrane Database Syst Rev 2014 ; 10 : CD010236 . pmid:25354543 . OpenUrl PubMed
- ↵ Shallcross R, Bromley RL, Irwin B, Bonnett LJ, Morrow J, Baker GA. Liverpool Manchester Neurodevelopment Group UK Epilepsy and Pregnancy Register. Child development following in utero exposure: levetiracetam vs sodium valproate. Neurology 2011 ; 76 : 383 - 9 . doi:10.1212/WNL.0b013e3182088297 pmid:21263139 . OpenUrl CrossRef PubMed
- ↵ Shallcross R, Bromley RL, Cheyne CP, et al. Liverpool and Manchester Neurodevelopment Group UK Epilepsy and Pregnancy Register. In utero exposure to levetiracetam vs valproate: development and language at 3 years of age. Neurology 2014 ; 82 : 213 - 21 . doi:10.1212/WNL.0000000000000030 pmid:24401687 . OpenUrl CrossRef PubMed
- ↵ Bromley RL, Mawer GE, Briggs M, et al. Liverpool and Manchester Neurodevelopment Group. The prevalence of neurodevelopmental disorders in children prenatally exposed to antiepileptic drugs. J Neurol Neurosurg Psychiatry 2013 ; 84 : 637 - 43 . doi:10.1136/jnnp-2012-304270 pmid:23370617 . OpenUrl Abstract / FREE Full Text
- ↵ Bromley RL, Mawer G, Clayton-Smith J, Baker GA. Liverpool and Manchester Neurodevelopment Group. Autism spectrum disorders following in utero exposure to antiepileptic drugs. Neurology 2008 ; 71 : 1923 - 4 . doi:10.1212/01.wnl.0000339399.64213.1a pmid:19047565 . OpenUrl CrossRef PubMed
- ↵ Campbell E, Kennedy F, Russell A, et al. Malformation risks of antiepileptic drug monotherapies in pregnancy: updated results from the UK and Ireland Epilepsy and Pregnancy Registers. J Neurol Neurosurg Psychiatry 2014 ; 85 : 1029 - 34 . doi:10.1136/jnnp-2013-306318 pmid:24444855 . OpenUrl Abstract / FREE Full Text
- ↵ Edey S, Moran N, Nashef L. SUDEP and epilepsy-related mortality in pregnancy. Epilepsia 2014 ; 55 : e72 - 4 . doi:10.1111/epi.12621 pmid:24754364 . OpenUrl CrossRef PubMed
- ↵ Aurlien D, Larsen JP, Gjerstad L, Taubøll E. Increased risk of sudden unexpected death in epilepsy in females using lamotrigine: a nested, case-control study. Epilepsia 2012 ; 53 : 258 - 66 . doi:10.1111/j.1528-1167.2011.03334.x pmid:22126371 . OpenUrl CrossRef PubMed
- ↵ Battino D, Tomson T, Bonizzoni E, et al. EURAP Study Group. Seizure control and treatment changes in pregnancy: observations from the EURAP epilepsy pregnancy registry. Epilepsia 2013 ; 54 : 1621 - 7 . doi:10.1111/epi.12302 pmid:23848605 . OpenUrl CrossRef PubMed Web of Science
- ↵ Pennell PB. Antiepileptic drugs during pregnancy: what is known and which AEDs seem to be safest? Epilepsia 2008 ; 49 ( Suppl 9 ): 43 - 55 . doi:10.1111/j.1528-1167.2008.01926.x pmid:19087117 . OpenUrl CrossRef PubMed Web of Science
- ↵ EURAP Study Group. Seizure control and treatment in pregnancy: observations from the EURAP epilepsy pregnancy registry. Neurology 2006 ; 66 : 354 - 60 . doi:10.1212/01.wnl.0000195888.51845.80 pmid:16382034 . OpenUrl CrossRef PubMed
- ↵ Weckesser A, Denny E. Women living with epilepsy, experiences of pregnancy and reproductive health: a review of the literature. Seizure 2013 ; 22 : 91 - 8 . doi:10.1016/j.seizure.2012.11.001 pmid:23182977 . OpenUrl CrossRef PubMed
- ↵ McGrath A, Sharpe L, Lah S, Parratt K. Pregnancy-related knowledge and information needs of women with epilepsy: a systematic review. Epilepsy Behav 2014 ; 31 : 246 - 55 . doi:10.1016/j.yebeh.2013.09.044 pmid:24210460 . OpenUrl CrossRef PubMed
- ↵ Crawford P, Hudson S. Understanding the information needs of women with epilepsy at different lifestages: results of the ‘Ideal World’ survey. Seizure 2003 ; 12 : 502 - 7 . doi:10.1016/S1059-1311(03)00085-2 pmid:12967580 . OpenUrl CrossRef PubMed
- ↵ Campbell E, Hunt S, Kinney MO, et al. The effect of socioeconomic status on treatment and pregnancy outcomes in women with epilepsy in Scotland. Epilepsy Behav 2013 ; 28 : 354 - 7 . doi:10.1016/j.yebeh.2013.05.019 pmid:23827318 . OpenUrl CrossRef PubMed
- ↵ Pashley S, O’Donoghue MF. The safety of anti-epileptic drug regimens: a qualitative study of factors determining the success of counselling women before conception. J Fam Plann Reprod Health Care 2009 ; 35 : 153 - 6 . doi:10.1783/147118909788708002 pmid:19622204 . OpenUrl Abstract / FREE Full Text
- ↵ Maternal, Newborn and Infant Clinical Outcome Review Programme. MBRRACE. Saving Lives, Improving Mothers’ Care Lessons learned to inform future maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2009-2012. [Published Online December 2012] https://www.npeu.ox.ac.uk/downloads/files/mbrrace-uk/reports/Saving%20Lives%20Improving%20Mothers%20Care%20report%202014%20Full.pdf [Accessed 23 November 15].
- ↵ Sahoo S, Klein P. Maternal complex partial seizure associated with fetal distress. Arch Neurol 2005 ; 62 : 1304 - 5 . doi:10.1001/archneur.62.8.1304 pmid:16087773 . OpenUrl CrossRef PubMed
- ↵ Tinker SC, Reefhuis J, Dellinger AM, Jamieson DJ. National Birth Defects Prevention Study. Epidemiology of maternal injuries during pregnancy in a population-based study, 1997-2005. J Womens Health (Larchmt) 2010 ; 19 : 2211 - 8 . doi:10.1089/jwh.2010.2160 pmid:21034174 . OpenUrl CrossRef PubMed
- ↵ Devinsky O, Feldmann E, Hainline B. Advances in neurology. Vol 64: Neurological complications of pregnancy . Raven Press, 1994.
- ↵ Adab N, Kini U, Vinten J, et al. The longer term outcome of children born to mothers with epilepsy. J Neurol Neurosurg Psychiatry 2004 ; 75 : 1575 - 83 . doi:10.1136/jnnp.2003.029132 pmid:15491979 . OpenUrl Abstract / FREE Full Text
- ↵ Dlouhy BJ, Gehlbach BK, Richerson GB. Sudden unexpected death in epilepsy: basic mechanisms and clinical implications for prevention. J Neurol Neurosurg Psychiatry 2016 ; 87 : 402 - 13 . pmid:26979537 . OpenUrl Abstract / FREE Full Text
- ↵ Winterbottom JB, Smyth RM, Jacoby A, Baker GA. Preconception counselling for women with epilepsy to reduce adverse pregnancy outcome. Cochrane Database Syst Rev 2008 ;( 3 ): CD006645 . pmid:18646164 .
- ↵ Winterbottom J, Smyth R, Jacoby A, Baker G. The effectiveness of preconception counseling to reduce adverse pregnancy outcome in women with epilepsy: what’s the evidence? Epilepsy Behav 2009 ; 14 : 273 - 9 . doi:10.1016/j.yebeh.2008.11.008 pmid:19100341 . OpenUrl CrossRef PubMed
- ↵ Floyd RL, Jack BW, Cefalo R, et al. The clinical content of preconception care: alcohol, tobacco, and illicit drug exposures. Am J Obstet Gynecol 2008 ; 199 ( Suppl 2 ): S333 - 9 . doi:10.1016/j.ajog.2008.09.018 pmid:19081427 . OpenUrl CrossRef PubMed
- ↵ Lassi ZS, Imam AM, Dean SV, Bhutta ZA. Preconception care: caffeine, smoking, alcohol, drugs and other environmental chemical/radiation exposure. Reprod Health 2014 ; 11 ( Suppl 3 ): S6 . doi:10.1186/1742-4755-11-S3-S6 . pmid:25415846 . OpenUrl CrossRef PubMed
- ↵ National Institute for Health and Clinical Excellence. Epilepsies: diagnosis and management (Clinical guidaeline 137). 2012. www.nice.org.uk/guidance/cg137 .
- ↵ Scottish Intercollegiate Guidelines Network. Diagnosis and management of epilepsy in adults. SIGN, 2015 .
- ↵ Tomson T, Marson A, Boon P, et al. Valproate in the treatment of epilepsy in girls and women of childbearing potential. Epilepsia 2015 ; 56 : 1006 - 19 . doi:10.1111/epi.13021 pmid:25851171 . OpenUrl CrossRef PubMed
- ↵ Crawford P, Appleton R, Betts T, Duncan J, Guthrie E, Morrow J. The Women with Epilepsy Guidelines Development Group. Best practice guidelines for the management of women with epilepsy. Seizure 1999 ; 8 : 201 - 17 . doi:10.1053/seiz.1999.0295 pmid:10452918 . OpenUrl CrossRef PubMed Web of Science
- ↵ Harden CL, Pennell PB, Koppel BS, et al. American Academy of Neurology American Epilepsy Society. Management issues for women with epilepsy--focus on pregnancy (an evidence-based review): III. Vitamin K, folic acid, blood levels, and breast-feeding: Report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia 2009 ; 50 : 1247 - 55 . doi:10.1111/j.1528-1167.2009.02130.x pmid:19507305 . OpenUrl CrossRef PubMed Web of Science
- ↵ Morrow JI, Hunt SJ, Russell AJ, et al. Folic acid use and major congenital malformations in offspring of women with epilepsy: a prospective study from the UK Epilepsy and Pregnancy Register. J Neurol Neurosurg Psychiatry 2009 ; 80 : 506 - 11 . doi:10.1136/jnnp.2008.156109 pmid:18977812 . OpenUrl Abstract / FREE Full Text
- ↵ Meador KJ, Baker GA, Browning N, et al. NEAD Study Group. Fetal antiepileptic drug exposure and cognitive outcomes at age 6 years (NEAD study): a prospective observational study. Lancet Neurol 2013 ; 12 : 244 - 52 . doi:10.1016/S1474-4422(12)70323-X pmid:23352199 . OpenUrl CrossRef PubMed Web of Science
- ↵ Pittschieler S, Brezinka C, Jahn B, et al. Spontaneous abortion and the prophylactic effect of folic acid supplementation in epileptic women undergoing antiepileptic therapy. J Neurol 2008 ; 255 : 1926 - 31 . doi:10.1007/s00415-008-0029-1 pmid:18677647 . OpenUrl CrossRef PubMed
- ↵ Asadi-Pooya AA. High dose folic acid supplementation in women with epilepsy: are we sure it is safe? Seizure 2015 ; 27 : 51 - 3 . doi:10.1016/j.seizure.2015.02.030 pmid:25891927 . OpenUrl CrossRef PubMed
- ↵ Wellings K, Jones KG, Mercer CH, et al. The prevalence of unplanned pregnancy and associated factors in Britain: findings from the third National Survey of Sexual Attitudes and Lifestyles (Natsal-3). Lancet 2013 ; 382 : 1807 - 16 . doi:10.1016/S0140-6736(13)62071-1 pmid:24286786 . OpenUrl CrossRef PubMed Web of Science
- ↵ Betts T, Fox C. Proactive pre-conception counselling for women with epilepsy-is it effective? Seizure 1999 ; 8 : 322 - 7 . doi:10.1053/seiz.1999.0325 pmid:10512771 . OpenUrl CrossRef PubMed Web of Science
- ↵ Holmes LB, Harvey EA, Coull BA, et al. The teratogenicity of anticonvulsant drugs. N Engl J Med 2001 ; 344 : 1132 - 8 . doi:10.1056/NEJM200104123441504 pmid:11297704 . OpenUrl CrossRef PubMed Web of Science
- ↵ Update on Overall Prevalence of Major Birth Defects—Atlanta. Georgia, 1978-2005. JAMA 2008 ; 299 : 756 - 8 doi:10.1001/jama.299.7.756 . OpenUrl CrossRef
- ↵ Fried S, Kozer E, Nulman I, Einarson TR, Koren G. Malformation rates in children of women with untreated epilepsy: a meta-analysis. Drug Saf 2004 ; 27 : 197 - 202 . doi:10.2165/00002018-200427030-00004 pmid:14756581 . OpenUrl CrossRef PubMed Web of Science
- ↵ Tomson T, Battino D, Craig J, et al. ILAE Commission on Therapeutic Strategies. Pregnancy registries: differences, similarities, and possible harmonization. Epilepsia 2010 ; 51 : 909 - 15 . doi:10.1111/j.1528-1167.2010.02525.x pmid:20196792 . OpenUrl CrossRef PubMed
- ↵ Meador KJ, Pennell PB, Harden CL, et al. HOPE Work Group. Pregnancy registries in epilepsy: a consensus statement on health outcomes. Neurology 2008 ; 71 : 1109 - 17 . doi:10.1212/01.wnl.0000316199.92256.af pmid:18703463 . OpenUrl CrossRef PubMed
- Tomson T, Battino D, Perucca E. Valproic acid after five decades of use in epilepsy: time to reconsider the indications of a time-honoured drug. Lancet Neurol 2015 ; 15 : 210 - 8 . doi:10.1016/S1474-4422(15)00314-2 pmid:26655849 . OpenUrl
- Jentink J, Loane MA, Dolk H, et al. EUROCAT Antiepileptic Study Working Group. Valproic acid monotherapy in pregnancy and major congenital malformations. N Engl J Med 2010 ; 362 : 2185 - 93 . doi:10.1056/NEJMoa0907328 pmid:20558369 . OpenUrl CrossRef PubMed Web of Science
- Vajda FJ, O’Brien TJ, Graham JE, Lander CM, Eadie MJ. Dose dependence of fetal malformations associated with valproate. Neurology 2013 ; 81 : 999 - 1003 . doi:10.1212/WNL.0b013e3182a43e81 pmid:23911758 . OpenUrl CrossRef PubMed
- ↵ Christensen J, Grønborg TK, Sørensen MJ, et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 2013 ; 309 : 1696 - 703 . doi:10.1001/jama.2013.2270 pmid:23613074 . OpenUrl CrossRef PubMed Web of Science
- ↵ Cummings C, Stewart M, Stevenson M, Morrow J, Nelson J. Neurodevelopment of children exposed in utero to lamotrigine, sodium valproate and carbamazepine. Arch Dis Child 2011 ; 96 : 643 - 7 . doi:10.1136/adc.2009.176990 pmid:21415043 . OpenUrl Abstract / FREE Full Text
- ↵ Moore SJ, Turnpenny P, Quinn A, et al. A clinical study of 57 children with fetal anticonvulsant syndromes. J Med Genet 2000 ; 37 : 489 - 97 . doi:10.1136/jmg.37.7.489 pmid:10882750 . OpenUrl Abstract / FREE Full Text
- ↵ Dean JC, Hailey H, Moore SJ, Lloyd DJ, Turnpenny PD, Little J. Long term health and neurodevelopment in children exposed to antiepileptic drugs before birth. J Med Genet 2002 ; 39 : 251 - 9 . doi:10.1136/jmg.39.4.251 pmid:11950853 . OpenUrl Abstract / FREE Full Text
- ↵ Campbell E, Devenney E, Morrow J, et al. Recurrence risk of congenital malformations in infants exposed to antiepileptic drugs in utero. Epilepsia 2013 ; 54 : 165 - 71 . doi:10.1111/epi.12001 pmid:23167802 . OpenUrl CrossRef PubMed
- ↵ Vajda FJ, O’Brien TJ, Lander CM, Graham J, Roten A, Eadie MJ. Teratogenesis in repeated pregnancies in antiepileptic drug-treated women. Epilepsia 2013 ; 54 : 181 - 6 . doi:10.1111/j.1528-1167.2012.03625.x pmid:22882134 . OpenUrl CrossRef PubMed
- ↵ Marson AG, Al-Kharusi AM, Alwaidh M, et al. SANAD Study group. The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet 2007 ; 369 : 1016 - 26 . doi:10.1016/S0140-6736(07)60461-9 pmid:17382828 . OpenUrl CrossRef PubMed Web of Science
- ↵ Harden CL, Meador KJ, Pennell PB, et al. American Academy of Neurology American Epilepsy Society. Management issues for women with epilepsy-Focus on pregnancy (an evidence-based review): II. Teratogenesis and perinatal outcomes: Report of the Quality Standards Subcommittee and Therapeutics and Technology Subcommittee of the American Academy of Neurology and the American Epilepsy Society. Epilepsia 2009 ; 50 : 1237 - 46 . doi:10.1111/j.1528-1167.2009.02129.x pmid:19507301 . OpenUrl CrossRef PubMed Web of Science
- ↵ National Institute for Health Research. Empire: antiepileptic drug monitoring in pregnancy. 2013. www.nets.nihr.ac.uk/__data/assets/pdf_file/0019/54550/PRO-09-55-38.pdf .
- ↵ Reisinger TL, Newman M, Loring DW, Pennell PB, Meador KJ. Antiepileptic drug clearance and seizure frequency during pregnancy in women with epilepsy. Epilepsy Behav 2013 ; 29 : 13 - 8 . doi:10.1016/j.yebeh.2013.06.026 pmid:23911354 . OpenUrl CrossRef PubMed Web of Science
- ↵ Pennell PB, Peng L, Newport DJ, et al. Lamotrigine in pregnancy: clearance, therapeutic drug monitoring, and seizure frequency. Neurology 2008 ; 70 : 2130 - 6 . doi:10.1212/01.wnl.0000289511.20864.2a pmid:18046009 . OpenUrl CrossRef PubMed
- ↵ Tomson T, Palm R, Källén K, et al. Pharmacokinetics of levetiracetam during pregnancy, delivery, in the neonatal period, and lactation. Epilepsia 2007 ; 48 : 1111 - 6 . doi:10.1111/j.1528-1167.2007.01032.x pmid:17381438 . OpenUrl CrossRef PubMed
- ↵ Westin AA, Reimers A, Helde G, Nakken KO, Brodtkorb E. Serum concentration/dose ratio of levetiracetam before, during and after pregnancy. Seizure 2008 ; 17 : 192 - 8 . doi:10.1016/j.seizure.2007.11.027 pmid:18180176 . OpenUrl CrossRef PubMed
- ↵ Sabers A, Petrenaite V. Seizure frequency in pregnant women treated with lamotrigine monotherapy. Epilepsia 2009 ; 50 : 2163 - 6 . doi:10.1111/j.1528-1167.2009.02166.x pmid:19490048 . OpenUrl CrossRef PubMed
- ↵ Sabers A. Algorithm for lamotrigine dose adjustment before, during, and after pregnancy. Acta Neurol Scand 2012 ; 126 : e1 - 4 . doi:10.1111/j.1600-0404.2011.01627.x pmid:22150770 . OpenUrl CrossRef PubMed
- ↵ Tomson T, Hiilesmaa V. Epilepsy in pregnancy. BMJ 2007 ; 335 : 769 - 73 . doi:10.1136/bmj.39266.473113.BE pmid:17932208 . OpenUrl FREE Full Text
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Bromfield EB, Cavazos JE, Sirven JI, editors. An Introduction to Epilepsy [Internet]. West Hartford (CT): American Epilepsy Society; 2006.

An Introduction to Epilepsy [Internet].

Pregnancy and Epilepsy
Download PowerPoint presentation (33K)
Or click here to download all slides from this Chapter. (PPT, 1.3M)
From: Chapter 2, Clinical Epilepsy
All content of An Introduction to Epilepsy , except where otherwise noted, is licensed under a Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Cite this Page Bromfield EB, Cavazos JE, Sirven JI, editors. An Introduction to Epilepsy [Internet]. West Hartford (CT): American Epilepsy Society; 2006. Slide 60, [Pregnancy and Epilepsy].
- PDF version of this page (3.1M)
Related information
- PubMed Links to PubMed
Recent Activity
- Slide 60, [Pregnancy and Epilepsy]. - An Introduction to Epilepsy Slide 60, [Pregnancy and Epilepsy]. - An Introduction to Epilepsy
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers

Epilepsy in Pregnancy
Oct 08, 2011
1.13k likes | 4.78k Views
Epilepsy in Pregnancy. Sherifia Heron, M.D October 20, 2009 Ob Rotation Dept. of Family and Social Medicine. Case.
Share Presentation
- minimum dose
- planned pregnancy
- upper extremities
- low birth weight
- red cell folate levels

Presentation Transcript
Epilepsy in Pregnancy Sherifia Heron, M.D October 20, 2009 Ob Rotation Dept. of Family and Social Medicine
Case • 36yo G1P0000 at 35wks and 2 days with history of epilepsy sent from clinic for elevated BPs to rule out preeclampsia. She had no complaints. No LOF, No VB, and +FM. No HA, Visual Changes, or epigastric pain. • Initial BP 110/60, Range (100-125/60-80), Total of 9 visits. Initial weight 128160 = 32lbs gained. • PNI: Hx of Seizure disorder • PNL: O+, ab-, H/H 11.6/34.5, Syphilis NR, Rubella Immune, GC Neg/Chlamydia Neg, HBSag Neg, HIV neg, GBS neg, GTT Neg (109) • Ob Hx: None
Past Medical Hx: Seizure D/o • PSHx: None • SHx: Employed, married to FOB they live together. Denies Tob/etoh/Drugs/DV. Planned pregnancy – good support system • Medications: Lamotrigine (Lamictal) • Allergies: NKDA • PE: No epigastric pain, No edema, BP 136/67, Range (115-142/60-92) • FHT 140s, moderate variability, +accels, -Decels • SVE: Ft/L/High • EFW 3400 • Vertex by Sono
Assessment and Plan • 36yo G1P0 at 35 and 2 days with h/o seizure d/o admit to L&D to rule out PEC • Admit to L&D, PEC labs, • PEC: BP in normal to mild range 136/67, Range (115-142/60-92) No S/Sx of PEC,Will continue to monitor • FEN/GI: NPO, Except ice chips, IVF @125 cc/hr • Labor • Expectant management • Fetus: reassuring overall, Category 1 tracing
PEC Labs • UA: Neg for protein • AST/ALT: 16/11 • LDH: 170 • Creatinine: 0.5 • Platelets: 199
AED • Are antiepileptic drugs necessary • What effect do antiepileptic drugs have on the fetus? • What effect does maternal epilepsy have on the fetus? • What effect does pregnancy have on seizures? • How should the patient be managed during pregnancy and delivery? • How should the patient be managed during the postpartum period?
Case • At 2:10am, emergency alarm went off, two ob residents myself and nursing staff rushed to PACU • On arrival to the PACU, approximately 12hrs after Ms. X was admitted to monitor for PEC she was having a seizure • The seizure went on for approximately 30sec where Ms. X upper extremities was flexed and jerking. Head neck and shoulders was also jerking uncontrollably • Pts. Eyes were closed and rolled back in her heard. Pt. Grunted and responded to questions by blinking once for yes and twice for no. • Vitals were taken during the attack: BP 110/60, RR 26, HR 138 • After the seizure ended the pts. Reports feeling tired and drowsy and was allowed to rest until fully awake – at which time she was consented for a C-section • Vital Signs remained stable
Case continue • FHT: 140s 120s • During seizure episode • Returned to baseline 140s after seizure • Toco: Q15-20mins
Questions • What Happened? • Eclampsia vs. Epilepsy? • Could this have been prevented by appropriately managing her epilepsy • Labs was drawn again and decision made to perform a c-section
History of seizure since age 17 • Says EEG in D.R. was “abnormal” but subsequent EEGs in the US was negative • No family history of seizure • Last seizure was 2.5 years ago • No triggers but mostly occurs at night • No history postictal confusion, incontinence • Cryptogenic seizure
Epilepsy Pathophysiology • Seizures happen when there are sudden changes in the way normal brain cells interact electrically. • Consciousness, movement, sensation, speech, mood, memory, and emotions can all be affected during the one or two minutes that the seizure lasts.
Seizure Medications • *Glossary of generic to name brand drugs • Generic Name Brand • lamotrigine ....................Lamictal • carbemazepine ..............Tegretol, Carbatrol • gabapentin ....................Neurontin • levetiracetam..................Keppra • oxcarbazepine................Trileptal • phenytoin ......................Dilantin • tiagabine ........................Gabitril • topiramate......................Topamax • zonisamide ....................Zonegran
Drug Monitoring • Lamotrigine • Several studies suggest that lamotrigine clearance increase by about 65 to 94% and therefore should be monitored more frequently during the second and third trimesters, to reduce the possibility of increased seizures, as well as in the early postpartum period, to avert toxicity • Levetiracetam • Among 14 women monitored on levetiracetam therapy during pregnancy, plasma concentrations were observed to decline during pregnancy to 40% of baseline concentrations in the third trimester. Limited information on seizure control was provided, but the possibility of increased seizures during this time suggests the need for closer monitoring
Oxcarbazepine • In one large pregnancy registry oxcarbazepine monotherapy increased the risk of seizure, suggesting the possibility that it, too, is associated with pharmacokinetic changes in pregnancy, and requires more frequent monitoring. • Topiramate • A study describing 12 women on topiramate therapy during pregnancy reported that serum concentrations declined by about 30%. Increased seizure frequency in pregnancy was also observed in this series
Types of Seizures • Generalized Seizures • Absence seizures • Myoclonic seizures • Atonic seizures • Tonic seizures • Clonic seizures • Tonic-clonic seizures • Partial Seizures • Simple partial seizures (awareness retained) • Motor, autonomic, sensory or psychological • Complex partial seizures (awareness lost) • Secondary generalized seizures • Status Epilepticus Status epilepticus is prolonged, repetitive seizure activity that lasts more than 20 to 30 minutes, during time which the patient is unconscious. Status epilepticus is a medical emergency with a significantly poor outcome; it can result in death if not treated aggressively. Its causes include improper use of certain medications, stroke, infection, trauma, cardiac arrest, drug overdose, and brain tumor
Simple Partial Seizures • Awareness preserved • Memory preserved • Consciousness preserved • Complex Partial Seizures • Awareness preserved • Memory preserved • Consciousness preserved
Epilepsy Statistics • 90% of women with epilepsy have normal pregnancy • Nonetheless, there are a number of fetal and obstetrical complications associated with women with epilepsy.
Preconception Management • This should include information regarding risks associated with epilepsy and pregnancy, • potential interactions with oral contraceptive therapy, and • recommended folate supplementation
Contraception • inducers of the hepatic cytochrome P-450 system • hormonal contraceptive failure
Folic acid supplementation • Animal studies have shown that valproate and phenytoin decrease the concentration of certain forms of folate and are associated with neural tube defects
Folic acid supplementation • It has not yet been conclusively determined if folic acid supplementation prevents neural tube defects in women receiving AEDs.
Continued folic acid supplementation • Once a woman with epilepsy who is taking AEDs becomes pregnant, serum and red cell folate levels can be monitored (goal is concentration about 4 mg/ml).
Obstetrical Complications • Low birth weight • Lower apgar scores • Preeclampsia • Bleeding • Placental abruption • Prematurity • The rates of stillbirth, neonatal death, and perinatal death vary widely and have been reported to be as high as two to three times greater in infants born to women with epilepsy • The mechanism of risk is not well understood. In one study, the investigators found an increased risk of spontaneous abortion for both fathers and mothers with epilepsy
Necessity for antiepileptic drugs • Is the diagnosis of epilepsy well established? In some patients, routine EEG recordings or continuous video/EEG monitoring may be warranted to confirm the diagnosis • Does the patient require AEDs and if so, is she on the most appropriate medications and the minimum dose to maintain seizure control
Are Antiepileptic Drugs Necessary • Many physicians will consider withdrawal of AEDs after a period of two years without seizures. The frequency of seizure recurrence within six and twelve months of discontinuing therapy is 12 and 32 percent, respectively. • Thus, if a woman has been seizure-free for a satisfactory period, a taper and withdrawal of AEDs at least six months prior to becoming pregnant is suggested
Choice of antiepileptic drug • If it is felt that medications cannot be withdrawn, the patient should take the most suitable medication for the seizure type. • The optimal treatment of women with epilepsy who are of childbearing age is unclear because of a lack of conclusive data on the comparative teratogenicity of different AEDs.
Antiepilepsy Drugs • The most common major congenital malformations associated with AED are • neural tube, • congenital heart and urinary tract defects, • skeletal abnormalities, • and cleft palate. • Specific AEDs, combination drug therapy, a family history of birth defects, and other risk factors appear to be associated with increased risk of these, at least in some studies • Particularly valporate and carbemazepine monotherapy, • benzodiazepines in polytherapy, and caffeine in combination with phenobarbital • In addition to the specific AED used alone or in combination, the gestational timing of the exposure and the dose of AED used are also likely to be important. These have been best associated with valporate • Many of these drugs appear to be implicated in dysmorphisms such as hypoplasia of the nails and distal phalanges, hypertelorism, and the “anticonvulsant face” – Broad or depressed nasal bridge, short nose with anteverted nostrils, long upper lip, maxillary hypoplasia
Other newer AEDs • There is limited human information on the fetal risks of the newer antiepileptic drugs (eg, gabapentin, felbamate, topiramate, tiagabine, levetiracetam, pregabalin).
Management During Pregnancy • The AED should be administered at the lowest dose and lowest plasma level that protects against tonic-clonic and/or complex partial seizures • The plasma drug level should be monitored regularly during pregnancy including, if available, the physiologically important free or unbound drug concentration • The use of multiple agents should be avoided, if possible, especially combinations involving valproate, carbemazepine, and phenobarbital • If there is a family history of neural tube defects, both valproate and carbemazepine should be avoided, unless a patient’s seizures cannot otherwise be controlled • In established pregnancy, changes to alternate AED therapy should not be undertaken solely to reduce teratogenic risk for several reasons • Changing the AEDs may precipitate seizures • Overlapping AEDs during the change exposed the fetus to effects of an additional aED • There is limited advantage to changing AEDs if pregnancy has already been established for several weeks
Vitamin K Supplementation • Most physicians recommend administration of prophylactic vitamin K during the last month of pregnancy to women treated with AEDs to protect the child against severe postnasal bleeding due to a deficiency in vitamin K-dependent clotting factors • Enzyme-induced AEDs, such as phenobarbital, phenytoin, and carbemazepine, cross the placenta and may increase the rate of oxidative degradation of vitamin K in the fetus, an effect that can be overcome by large doses of vitamin K
Effects of Epilepsy on the Fetus • In addition to concerns about fetal exposure to antiepileptic drugs (AEDs), there are risks to the fetus from maternal seizures and maternal epilepsy. • Few studies have been performed on the direct effects of maternal seizures on the fetus. • Fetal hypoxia • One report of fetal heart rate monitoring during a maternal generalized tonic-clonic seizure lasting 2.5 mins revealed significant fetal heart rate deceleration lasting up to 30 mins after the seizure. While nonconvulsive seizures are believed to be less dangerous, another case report has documented significant fetal bradycardia during a one-minute, complex partial seizure.
Effects of pregnancy on seizures • The frequency of seizures does not increase during pregnancy in the majority of women with epilepsy.
At Delivery • Most women have a normal vaginal delivery. • Elective cesarean section • frequent seizures during the third trimester • history of status epilepticus during severe stress • A tonic-clonic seizure occurs during labor in 1 to 2% of women with epilepsy, and in another 1 to 2% 24hrs after delivery. • It is therefore essential to maintain a plasma AED level known to protect against seizures during the third trimester and during delivery. Doses must not be missed during the period of labor.
Speak • Most women have a normal vaginal delivery. However, elective cesarean section may be justified in women with frequent seizures during the third trimester or a history of status epilepticus during severe stress • A tonic-clonic seizure occurs during labor in 1 to 2% of women with epilepsy, and in another 1 to 2% 24hrs after delivery. It is therefore essential to maintain a plasma AED level known to protect against seizures during the third trimester and during delivery. • Doses must not be missed during the period of labor.
Reference • “Risk associated with epilepsy and pregnancy” and “Management of epilepsy and pregnancy” • www.uptodate.com • http://www.webmd.com/epilepsy/medications-treat-seizures • www.webMD.com • http://www.uptodate.com/patients/content/topic.do?topicKey=~84qqmS11.oaT1P
- More by User
EPILEPSY. D. C. MIKULECKY PROFESSOR OF PHYSIOLOGY. INTRODUCTION. PERIODIC AND UNPREDICTABLE SEIZURES CAUSED BY THE RHYTHMIC FIRING OF LARGE GROUPS OF NEURONS MAY RANGE FROM MILD TWITCHING TO LOSS OF CONSCIOUSNESS AND UNCONTROLLABLE CONVULSIONS. SOME FAMOUS PEOPLE WHO WERE AFFLICTED.
197 views • 18 slides
Epilepsy in Thailand
Epilepsy in Thailand. Dr.Yotin Chinvarun M.D. Ph.D . The Neurological Society of Thailand. Diversity of the Asia-Pacific Region Population and Economical Development. Population (millions) 12 1,272 7 1,027 209 126 47 5 24 2 5 78 3 61 80. Gross National Income
339 views • 20 slides
Transition in Epilepsy
Transition in Epilepsy. The Transition of Patients with Epilepsy from Paediatric to Adult Care Services across the Aneurin Bevan Health Board . Kostov, C., Lewis, H., Syed , N., Lawthom , C., James, L., Capeling , L., Spender-Thomas, K., Barber, M. Personal Reasons for Interest in Audit.
607 views • 33 slides
This Neurological Disease is caused recurrent seizures and the misfiring of neural cells in the brain. . Epilepsy. The cell does not maintain homeostasis during the disease epilepsy The constant pattern the cells run is provoked by seizure and it does not stay in its normal state
237 views • 7 slides
Epilepsy. Dr Muhammad Ashraf Assistant Professor Medicine. Objectives. Classify epilepsy and describe the epidemiology of epilepsy Enlist the risk factors of epilepsy Identify provoked and unprovoked seizure Enlist the causes of epilepsy Define status epilepticus.
911 views • 17 slides
Anaesthesia in epilepsy
Anaesthesia in epilepsy . Dr.S.Parthasarathy MD DA DNB, D.Diab . Dip. Software based statistics PhD ( physio ) Mahatma Gandhi medical college and research institute , puducherry – India . Why should we know??. Epilepsy is relevant to us ?? medication and drug interactions,
1k views • 39 slides
Epilepsy. Meiti Frida Department of Neurology Andalas University Padang. DEFINITION.
816 views • 49 slides
EPILEPSY. Brenda Willis Regional Manager South West Region. Introduction. Epilepsy Society is the largest epilepsy charity in the UK Founded in 1892 Today: Research, Out Patients Clinics, Assessment Centre, Care Services, Training, Information Services and Awareness Raising.
737 views • 34 slides
Epilepsy. Alina Chow. What is epilepsy?. Epilepsy is a disorder that causes seizures because of electrical surges sent to the brain. Symptoms may vary depending on the type of seizure experienced. Symptoms. Epilepsy is caused by abnormalities in the brain cells and can produce the following:
249 views • 6 slides
Epilepsy. Presented by Sarah Beggs and Jess Gardoll. What Is Epilepsy?. Epilepsy is a sudden altered state of consciousness and bodily control due to abnormal electrical discharges within specific areas of the cortex. (brain)
391 views • 19 slides
Epilepsy. Created By: Whitney Copeland. What is Epilepsy ?. Epilepsy is a neurological condition, which affects the nervous system. Epilepsy is also known as a seizure disorder .
619 views • 12 slides
Epilepsy . Brian Spicer. Causes. Anything that disturbs the normal pattern of activity in the brain can trigger epilepsy. The cause can be illness, brain damage, or abnormal development of the brain. No cause can be determined for the cases of epilepsy. . Symptoms .
212 views • 5 slides
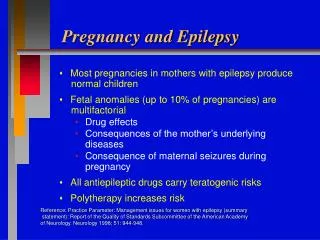
Pregnancy and Epilepsy
Pregnancy and Epilepsy. Most pregnancies in mothers with epilepsy produce normal children Fetal anomalies (up to 10% of pregnancies) are multifactorial Drug effects Consequences of the mother’s underlying diseases Consequence of maternal seizures during pregnancy
932 views • 1 slides
Epilepsy . P. Ockuly, Champlin Park H.S. & B. Tapper, Agape H.S. Epilepsy. Defining Epilepsy Categories of seizures Neuron anatomy and physiology Review Treatments Living with Epilepsy (seizures) Controversies Research. Epilepsy the misconception. Is a specific disease.
617 views • 19 slides
Epilepsy. By Gabrielle Cramer. Brain Scan of an Individual with Frontal Lobe Epilepsy. Epilepsy is a term used to define the unprovoked & spontaneous reoccurance of seizures which inhibit nervous system activity 180,000 Americans are diagnosed with Epilepsy each year. Neuron.
415 views • 12 slides
Epilepsy. Define seizure and epilepsy. Seizure: Paroxysmal event due to abnormal, excessive, hypersynchronous discharges from an aggregate of CNS neurons Not a diagnosis, but rather a series of signs and symptoms
411 views • 25 slides
Marijuana in Epilepsy
Marijuana in Epilepsy. Philippe Douyon, MD Epileptologist Northeast Regional Epilepsy Group. Objectives: Brief overview of seizures/epilepsy Endocannabinoid System Mechanism of Action Impact on the Brain/Theoretical role in Epilepsy Politics of Marijuana. Seizure.
830 views • 54 slides
Epilepsy. Naghme Adab. Objectives. Introduction to epilepsy to orientate you Know when it is appropriate to start an antiepileptic drug (AED) Have a framework for choosing an appropriate antiepileptic drug know how to manage status epilepticus Know when it is appropriate to withdraw an AED.
1.03k views • 86 slides
Epilepsy. Gregory B. Sharp, M.D. Chief of Pediatric Neurology University of Arkansas For Medical Sciences Medical Director, Neuroscience Center of Excellence. Objectives – To Review:. Basic mechanisms of epilepsy Classification of seizures Seizure types Epilepsy syndromes
909 views • 58 slides
EPILEPSY. Review of new treatments and Recommendations. OBJECTIVES. To understand the work-up of new onset seizures. Understand the differential diagnosis of Paroxysmal events Be familiar with the new medications used to treat epilepsy and special considerations in there use. Glossary.
604 views • 42 slides
Epilepsy in children
Epilepsy in children. Amira Masri Prof of child neurology Faculty of medicine –The university of Jordan. Objectives. History Epidemiology Definitions : seizure , epilepsy , febrile convulsion , status epilepticus ,epileptic encephalopathy Classification Aetiology Treatment
667 views • 58 slides
Diseases & Diagnoses
Issue Index
- Case Reports
New Guideline Published for Epilepsy Management in People Who May Become Pregnant
- American Academy of Neurology
- American Epilepsy Society
- Society for Maternal-Fetal Medicine
- Child neurology
- Child Neurology Society
A new guideline was published in Neurology , providing guidance to health care providers regarding the use of antiseizure medications in people with epilepsy who may become pregnant. The guideline was developed collaboratively by the American Academy of Neurology (AAN), the American Epilepsy Society (AES), and the Society for Maternal-Fetal Medicine (SMFM). The guideline partly updates guidance from 2009 on epilepsy management during pregnancy and the risks of treatment, which were published by the AAN and AES.
The new guideline, which was developed based on a comprehensive literature review, takes pregnancy risks into consideration, including:
- Major congenital malformations
- Birth defects
- Fetal growth issues
- Neurodevelopmental effects
According to a statement from the AAN, the guideline suggests that, at the earliest possible opportunity before pregnancy, health care providers “recommend medications and doses that optimize both seizure control and fetal development.” During pregnancy, health care providers should work to minimize seizure occurrence, including the increase in seizure frequency associated with the cessation of anti-seizure medications. The guideline recommends medications such as lamotrigine, levetiracetam, and oxcarbazepine, and advises against medications associated with pregnancy and neurodevelopmental complications, including valproic acid, phenobarbital, and topiramate. Additionally, the guideline states that the daily use of folic acid before and during pregnancy may decrease the risk of neural tube defects and improve neurodevelopmental outcomes.
“Most children born to people with epilepsy are healthy, but there is a small risk of pregnancy-related problems, partly due to seizures and partly due to the effects of antiseizure medications,” said Alison M. Pack, MD, MPH, author of the published guidelines. “This guideline provides recommendations regarding the effects of antiseizure medications and folic acid supplementation on malformations at birth and the development of children during pregnancy so that doctors and people with epilepsy can determine which treatments may be best for them.”
The Child Neurology Society endorsed the published guidelines.
FDA Grants Breakthrough Therapy Designation to Delpacibart Etedesiran for Myotonic Dystrophy Type 1
This Month's Issue
Daniel L. Murman, MD, MS
Yevgeniya Sergeyenko, MD, MPH, and Miriam Segal, MD
Michelle Sexton, ND, and Nathaniel M. Schuster, MD

Related Articles
Joyce H. Matsumoto, MD
Greg Grunberg
Sign up to receive new issue alerts and news updates from Practical Neurology®.
Explore prestigious scientific journals and award and funding opportunities to advance your research.
Access practice-improvement tools, including guidelines, measures, Axon Registry, and practice management resources.
Learn to effectively advocate on behalf of neurologists and their patients, and access AAN position and policy statements.
Loading... please wait
We’re experiencing unusually high levels of traffic. Thank you for your patience.
EMBARGOED FOR RELEASE UNTIL 4 PM ET, May 15, 2024
Guideline issued for people with epilepsy who may become pregnant, aan, aes and smfm collaborate to develop updated guidance.
MINNEAPOLIS – A new guideline has been issued to help neurologists and other clinicians determine the best antiseizure medications for people with epilepsy who may become pregnant. The guideline is published in the May 15, 2024, online issue of Neurology ® , the medical journal of the American Academy of Neurology (AAN), and was developed through a collaboration between the AAN, the American Epilepsy Society (AES) and the Society for Maternal-Fetal Medicine (SMFM). It was endorsed by the Child Neurology Society. The guideline partially updates two 2009 AAN and AES guidelines on the management of epilepsy during pregnancy, specifically regarding malformations at birth and the development of children born to people with epilepsy. “Most children born to people with epilepsy are healthy, but there is a small risk of pregnancy-related problems, partly due to seizures and partly due to the effects of antiseizure medications,” said author Alison M. Pack, MD, MPH, of Columbia University in New York City, a Fellow of the American Academy of Neurology and a member of the American Epilepsy Society. “This guideline provides recommendations regarding the effects of antiseizure medications and folic acid supplementation on malformations at birth and the development of children during pregnancy so that doctors and people with epilepsy can determine which treatments may be best for them.” The guideline recommendations are based on a review of all available evidence on the topic. Risks can include major congenital malformations, or birth defects, fetal growth issues and neurodevelopmental effects such as autism or lower IQ scores. The guideline states when treating people with epilepsy who may become pregnant, doctors should recommend medications and doses that optimize both seizure control and fetal development at the earliest possible opportunity before pregnancy. During pregnancy, it recommends minimizing the occurrence of tonic-clonic seizures, seizures with full body spasms, to minimize risks to the parent and fetus. It also says stopping medications during pregnancy may increase the frequency of seizures, which may harm the parent and fetus. For medications, the guideline recommends using lamotrigine, levetiracetam or oxcarbazepine when appropriate to minimize risk of major birth defects. It recommends avoiding valproic acid, phenobarbital and topiramate when possible. To reduce the risk of poor neurodevelopmental outcomes, including autism spectrum disorder and lower IQ scores, the guideline recommends clinicians avoid prescribing valproic acid, when possible, to people with epilepsy who may become pregnant. The guideline recommends that people with epilepsy who may become pregnant take at least 0.4 milligrams of folic acid daily before and during pregnancy to decrease the risk of neural tube defects and possibly improve neurodevelopmental outcomes. However, it notes further studies are needed to clarify the optimal dose and timing of folic acid supplementation. “People with epilepsy who may become pregnant want to ensure the best health of their child while still managing and minimizing their seizures,” said Pack. “This is why it is important to discuss plans for pregnancy with your doctor before becoming pregnant and notify your doctor as soon as possible if you discover you are pregnant. Don’t stop or change your medications. Talk with your doctor about any concerns you have about your medications.” There are some medications that did not have enough evidence to be evaluated and need more research about their associated risk. The guideline was funded by the American Academy of Neurology. About the American Academy of Neurology The American Academy of Neurology is the world's largest association of neurologists and neuroscience professionals, with over 40,000 members. The AAN’s mission is to enhance member career fulfillment and promote brain health for all. A neurologist is a doctor with specialized training in diagnosing, treating and managing disorders of the brain and nervous system such as Alzheimer's disease, stroke, concussion, epilepsy, Parkinson's disease, multiple sclerosis, headache and migraine. For more information about the American Academy of Neurology, visit AAN.com or find us on Facebook , Twitter , Instagram , LinkedIn and YouTube . About the American Epilepsy Society Founded in 1936, the American Epilepsy Society is a medical and scientific society whose members are dedicated to advancing research and education for preventing, treating and curing epilepsy. AES is an inclusive global forum where professionals from academia, private practice, not-for-profit, government and industry can learn, share and grow to eradicate epilepsy and its consequences. About the Society for Maternal-Fetal Medicine (SMFM) The Society for Maternal-Fetal Medicine (SMFM), founded in 1977, is the medical professional society for maternal-fetal medicine subspecialists, who are obstetricians with additional training in high-risk pregnancies. SMFM represents more than 7,000 members who care for high-risk pregnant people and provides education, promotes research, and engages in advocacy to advance optimal and equitable perinatal outcomes for all people who desire and experience pregnancy. For more information, visit SMFM.org .

GET A DOSE OF BRAIN HEALTH
Dive into a wealth of information by visiting Brain & Life® , where you can explore the freshest updates, tips, and neurologist expert perspectives on brain disease and preventive brain health.
The American Academy of Neurology is the world's largest association of neurologists and neuroscience professionals, with 40,000 members. The AAN is dedicated to promoting the highest quality patient-centered neurologic care. A neurologist is a doctor with specialized training in diagnosing, treating and managing disorders of the brain and nervous system such as Alzheimer's disease, stroke, migraine, multiple sclerosis, concussion, Parkinson's disease and epilepsy.
For more information about the American Academy of Neurology, visit AAN.com or find us on Facebook , X , LinkedIn , Instagram and YouTube .
For More Information*
Email Renee Tessman or Natalie Conrad

News Results
- What is epilepsy?
- About seizures
- Seizure triggers
- Epilepsy syndromes
- Diagnosing epilepsy
- Guide for the newly diagnosed
- Epilepsy treatments
- First aid for seizures
- Epilepsy-related deaths and SUDEP
- Support for you
- Epilepsy and wellbeing
- Safety advice for people with epilepsy
- Alarms and monitors
- Sex and contraception
- Starting a family
- Parents and children
- Just for kids
- Education and epilepsy
- Epilepsy and your rights
- Contact our helpline
- Online groups
- In-person groups
- Befriending
- Counselling (Northern Ireland)
- Counselling (Wales)
- Family support service (Northern Ireland)
- Epilepsy awareness training
- Online learning resources
- Accessibility tools
- I’d like to give support to others
- Fundraise with us
- Organise a fundraising event
- Take part in a fundraising event
- Volunteer with us
- Leave a gift in your will
- Become a member
- Give in memory
- Play our weekly lottery
- Purchase from our shop
- Share your story
- Campaign for change
- Take part in research
- Make a donation
- Stars awards
- Epilepsy specialist nurses (ESNs)
- Primary care staff
- Epilepsy and maternity
- Commissioners
- Care sector
- Support for school staff
- Support for researchers
- Info for employers
- Professional membership
- Online epilepsy training
- Seizure – European Journal of Epilepsy
- Drugwatch – latest medication news
- Step Together
- Trusts and foundations
- Join the Excellence Collective
- Nurses membership
Sodium valproate medicines and risks in pregnancy
Taking valproate medicines during pregnancy can cause birth defects and problems with a child’s learning and development.
The risks are higher than with other epilepsy medicines, so there are special rules for how it can be prescribed to women and girls who are able to get pregnant.
This page explains the risks and how the rules could affect you and your epilepsy treatment.
What is the Valproate Pregnancy Prevention Programme?
Valproate medicines can be an effective treatment for epilepsy. But research has shown that taking valproate medicines during pregnancy can seriously harm an unborn baby. Valproate medicines include sodium valproate (Epilim, Episenta, Epival, Depakote) and valproic acid (Convulex).
In the UK, the Medicines and Healthcare products Regulatory Agency (MHRA) has issued rules about how doctors can prescribe valproate medicines.
The rules say doctors must not prescribe valproate to women or girls of childbearing age, unless they are on the Valproate Pregnancy Prevention Programme. The programme aims to make sure that women taking valproate medicine are aware of the risks in pregnancy and are using highly effective contraception to avoid becoming pregnant.
Get medical advice before making changes to your epilepsy medicine
If you are pregnant or planning a pregnancy and you take valproate, do not stop taking your medicine.
This could cause you to have more seizures or seizures that are more severe. This could be harmful for you and your baby. Instead, speak to your GP urgently, so they can get you the help and advice you need.
What problems can taking valproate medicines during pregnancy cause?
Valproate can cause two sorts of problems when taken during pregnancy: birth defects and problems with learning and development.
Birth defects
In women who take valproate during pregnancy, around 10 in every 100 babies will be born with birth defects.This compares with 2 to 3 out of 100 in the general population.
Birth defects happen when the baby doesn’t develop properly in the womb. Other names for birth defects include congenital anomalies, congenital malformations and congenital abnormalities.
Birth defects seen in children whose mothers took valproate during pregnancy include:
- Spina bifida (where the bones of the spine do not develop properly)
- Facial and skull malformations (including cleft lip and palate, where the upper lip or facial bones are split)
- Malformations of the limbs, heart, kidney, urinary tract and sexual organs
Learning and development problems
In women who take valproate during pregnancy, between 30 and 40 in every 100 children have problems with learning and development. The long-term effects are not yet known.
Problems with learning and development include:
- Walking and talking later than other children of the same age
- Poor speech and language skills
- Memory problems
- Lower intelligence than other children of the same age
Children whose mothers took valproate while pregnant are more likely to have autism or an autism spectrum disorder. These children are also more likely to develop symptoms of attention deficit hyperactivity disorder (ADHD).
Questions you may have
If you’re taking valproate and want to get pregnant , speak to your family doctor. Keep taking your epilepsy medicine and keep using contraception until you have spoken to your doctor.
They can arrange for you to see an epilepsy specialist for advice about planning your pregnancy. If the specialist advises you to change your medicine, they should do this a long time before you become pregnant.
You should only stop taking valproate if your doctor advises you to. Stopping any epilepsy medicine suddenly could cause you to have more seizures, or more severe seizures. This could be harmful to you and your baby.
Having uncontrolled seizures can increase the risk of sudden unexpected death in epilepsy (SUDEP) for some people with epilepsy. As well as taking your epilepsy medication as prescribed, there are a number of other things you can do to reduce your risk of SUDEP .
If you haven’t had advice about taking your medicine during pregnancy , talk to your doctor urgently. They should arrange for you to see a specialist to get the advice you need. In some cases, your specialist may advise you to switch to another medicine. If so, they should tell you how to do this safely.
For some women, valproate may be the only effective medicine for them. If this is the case for you, your specialist might advise you to keep taking it, even during pregnancy.
They should arrange for you to see a specialist in fetal medicine. These are healthcare professionals who care for women whose babies are at higher risk of birth problems.
If you’re at an age where you could become pregnant, your doctor should only prescribe you valproate medicine if you’re on the Valproate Pregnancy Prevention Programme. This means your doctor must make sure you:
- Understand the risks of taking valproate during pregnancy
- Understand the need to use effective contraception to avoid getting pregnant while taking valproate
- Sign a form to show that you understand the risks
The MHRA says you should use effective contraception even if you are not currently sexually active. This is unless your doctor believes there is very good reason to assume there is no risk of pregnancy.
If you’re starting treatment with valproate medicine your specialist will ask you to take a pregnancy test first, to make sure you’re not pregnant. They may ask you to repeat this test at regular intervals while you’re taking valproate.
While you’re taking valproate medicine, an epilepsy specialist should review your treatment at least once a year. At each review the specialist will ask you to sign another form to show that you understand the risks of getting pregnant while taking valproate.
Some other epilepsy medicines can put your baby at risk of birth defects if taken during pregnancy. But research shows the risk is lower than with valproate medicines.
There are also certain epilepsy medicines which are safer to use in pregnancy as research suggests they do not increase the risk of birth defects. See our page about epilepsy medicines and pregnancy for more information.
If you are concerned that your child has been affected by use of valproate medicine during pregnancy, you can discuss this with your family doctor. The doctor may refer your child to see a specialist in children’s medicine if they think this is needed.
You could also contact a support network such as:
Organisation for Anti-convulsant Syndrome (OACS) OACS support all families touched by Fetal Anti-Convulsant Syndromes Tel: 07904200364 Email: [email protected]
Valproate Victims This charity represents some of the people and families who have been affected by sodium valproate taken in pregnancy.
INFACT INFACT provides information, advice and support to anyone that has taken anti-seizure medications (ASMs) in pregnancy and are concerned it may have affected the foetus during pregnancy.
The Medicines and Healthcare products Regulatory Agency (MHRA) has produced a toolkit to make sure women are better informed about the risks of taking valproate medicines during pregnancy.
It has also published a patient booklet for women taking valproate medicines.
More information
Here to support you, call the epilepsy action helpline.
If you would like to talk to someone about epilepsy, our trained advisers are here to help.
Send us your question
Send a question to our trained epilepsy advisers. (We aim to reply within two working days).
Sign up for the latest updates from Epilepsy Action
" * " indicates required fields

Guideline issued for people with epilepsy who may become pregnant
A new guideline has been issued to help neurologists and other clinicians determine the best antiseizure medications for people with epilepsy who may become pregnant.
The guideline is published in the May 15, 2024, online issue of Neurology and was developed through a collaboration between the American Academy of Neurology (AAN), the American Epilepsy Society (AES) and the Society for Maternal-Fetal Medicine (SMFM). It was endorsed by the Child Neurology Society.
The guideline partially updates two 2009 AAN and AES guidelines on the management of epilepsy during pregnancy, specifically regarding malformations at birth and the development of children born to people with epilepsy.
"Most children born to people with epilepsy are healthy, but there is a small risk of pregnancy-related problems, partly due to seizures and partly due to the effects of antiseizure medications," said author Alison M. Pack, MD, MPH, of Columbia University in New York City, a Fellow of the American Academy of Neurology and a member of the American Epilepsy Society.
"This guideline provides recommendations regarding the effects of antiseizure medications and folic acid supplementation on malformations at birth and the development of children during pregnancy so that doctors and people with epilepsy can determine which treatments may be best for them."
The guideline recommendations are based on a review of all available evidence on the topic. Risks can include major congenital malformations, or birth defects, fetal growth issues and neurodevelopmental effects such as autism or lower IQ scores.
The guideline states when treating people with epilepsy who may become pregnant, doctors should recommend medications and doses that optimize both seizure control and fetal development at the earliest possible opportunity before pregnancy.
During pregnancy, it recommends minimizing the occurrence of tonic–clonic seizures, seizures with full body spasms, to minimize risks to the parent and fetus. It also says stopping medications during pregnancy may increase the frequency of seizures, which may harm the parent and fetus.
For medications, the guideline recommends using lamotrigine, levetiracetam or oxcarbazepine when appropriate to minimize risk of major birth defects.
It recommends avoiding valproic acid, phenobarbital and topiramate when possible. To reduce the risk of poor neurodevelopmental outcomes, including autism spectrum disorder and lower IQ scores, the guideline recommends clinicians avoid prescribing valproic acid, when possible, to people with epilepsy who may become pregnant.
The guideline recommends that people with epilepsy who may become pregnant take at least 0.4 milligrams of folic acid daily before and during pregnancy to decrease the risk of neural tube defects and possibly improve neurodevelopmental outcomes. However, it notes further studies are needed to clarify the optimal dose and timing of folic acid supplementation.
"People with epilepsy who may become pregnant want to ensure the best health of their child while still managing and minimizing their seizures," said Pack. "This is why it is important to discuss plans for pregnancy with your doctor before becoming pregnant and notify your doctor as soon as possible if you discover you are pregnant. Don't stop or change your medications. Talk with your doctor about any concerns you have about your medications."
There are some medications that did not have enough evidence to be evaluated and need more research about their associated risk.
More information: Neurology (2024).
Provided by American Academy of Neurology


IMAGES
VIDEO
COMMENTS
Epilepsy in pregnancy. Nov 21, 2020 • Download as PPTX, PDF •. 8 likes • 903 views. K. Kavinda Hewawitharana. Based On GTG. Health & Medicine. Download now. Epilepsy in pregnancy - Download as a PDF or view online for free.
Epilepsy in pregnancy. Jun 8, 2020 •. 15 likes • 6,793 views. DR MUKESH SAH. Follow. Seizures during pregnancy can cause: Slowing of the fetal heart rate. Decreased oxygen to the fetus. Fetal injury, premature separation of the placenta from the uterus (placental abruption) or miscarriage due to trauma, such as a fall, during a seizure ...
What is epilepsy during pregnancy? Epilepsy is a disorder of the nervous system. It is also called a seizure disorder. Normally the body's nerves send information by electrical and chemical signals. People with epilepsy have abnormal electrical signals in the brain. This can cause a seizure.
Epilepsy in Pregnancy Sherifia Heron, M.D October 20, 2009 Ob Rotation Dept. of Family and Social Medicine ...
the epilepsy medication that women take during pregnancy and the health of their babies. It also gives advice about epilepsy medication(s) taken during pregnancy. You will be invited to join the Register. You can also contact the Register directly on Freephone 0800 3891248. Having epilepsy will usually mean more clinic visits at the hospital.
Among women with epilepsy, 60.7% achieved pregnancy and among the control group—60.2% within 21 months. Statistically, 0.3-0.5% of women giving birth suffer from epilepsy. In Poland, this affects approximately 1800 women per year. The incidence of new cases of epilepsy diagnosed in women of childbearing age is 20-30/100,000/year.
Seizures are the most common major neurologic complication encountered in pregnancy with a prevalence of in the United States of 1.2%. 1. Nearly one-half million women with epilepsy are of reproductive age and between 0.5% and 1.0% of all pregnancies occur among women with epilepsy. 2.
The loading dose of phenytoin is 10-15 mg/kg by intravenous infusion, with the usual dosage for an adult of about 1000 mg. Guidance on the management of seizures is available in the NICE. Evidence level 2++. guideline on epilepsy.1. If there is persistent uterine hypertonus, consider administration of tocolytic agents.
Dose: 5 mg/day. Dose: 0.4 mg/day for nonpregnant women, 0.6 mg/day for pregnant women and those contemplating pregnancy, and 0.5 mg/day for lactating women. Many epileptologists recommend higher doses (0.8-4 mg/day) for women with epilepsy. However, for women with a family history of a neural tube defect, 4 mg/day is the recommended dosage.
Epilepsy in Pregnancy - Free download as Powerpoint Presentation (.ppt / .pptx), PDF File (.pdf), Text File (.txt) or view presentation slides online. Epilepsy is a chronic neurological condition characterized by recurrent unprovoked seizures. It affects around 0.5-0.8% of the general population. During pregnancy, risks include preeclampsia, caesarean section, preterm labor, late pregnancy ...
In every 1000 pregnancies, between two and five infants are born to women with epilepsy. 1 2 3 For such women, pregnancy can be a time of anxiety over maternal and fetal wellbeing. 4 5 Most women with epilepsy will not experience an increase in seizure frequency, and in 96% of pregnancies they will deliver a healthy child. 6 However, some women (between 14 and 32 per 100) will experience an ...
Epilepsy in Pregnancy (Green-top Guideline No. 68) Summary: This guideline summarises the evidence on maternal and fetal outcomes in women with epilepsy (WWE). It provides recommendations on the care of WWE during the prepregnancy, antepartum, intrapartum and postpartum periods. The guideline does not cover the methods of diagnosis of epilepsy ...
Most women with epilepsy maintain their seizure control during pregnancy. Prepregnancy seizure control is the most important predictor of seizure control during pregnancy. Nonadherence to AED medication and alterations in AED clearance are major causes of break-through seizures. Pregnancy can have a major impact on the pharma-cokinetics of AEDs.
This can be a result of true gestational epilepsy, a rare syndrome of seizures occurring only during pregnancy. Patients with this syndrome have a variable presentation, with single or multiple seizures occurring in 1 or more of their pregnancies. The seizures can also be a manifestation of epilepsy that may extend beyond the patient's pregnancy.
All content of An Introduction to Epilepsy, except where otherwise noted, is licensed under a Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract. After headache, epilepsy is the second most common neurological disorder encountered in pregnancy. Epilepsy is one of the most common chronic neurological conditions in the world, with an estimated 50 million people affected worldwide. The majority of pregnant women with epilepsy have an uneventful pregnancy, labour and birth.
Presentation Transcript. Epilepsy in Pregnancy Sherifia Heron, M.D October 20, 2009 Ob Rotation Dept. of Family and Social Medicine. Case • 36yo G1P0000 at 35wks and 2 days with history of epilepsy sent from clinic for elevated BPs to rule out preeclampsia. She had no complaints. No LOF, No VB, and +FM. No HA, Visual Changes, or epigastric pain.
You should be seen by an epilepsy expert to discuss your treatment well in advance of a pregnancy, ideally up to two years beforehand. If your pregnancy is planned carefully then the risk of complications may be minimised. The primary aim in doing this is for seizure freedom before conception ( where possible) and during pregnancy ...
A new guideline was published in Neurology, providing guidance to health care providers regarding the use of antiseizure medications in people with epilepsy who may become pregnant.The guideline was developed collaboratively by the American Academy of Neurology (AAN), the American Epilepsy Society (AES), and the Society for Maternal-Fetal Medicine (SMFM).
Effect of epilepsy on pregnancy • No adverse effects of single seizures on the fetus. {relatively resistant to short episodes of hypoxia} • No increased risk of miscarriage or obstetric complications unless a seizure results in abdominal trauma. 1. Fetal bradycardia during and after maternal tonic- clonic convulsions 2.
Clinicians should recommend ASMs that optimize seizure control and fetal outcomes, in the event of a pregnancy, at the earliest possible preconception time, the guideline authors note.
The guideline recommends that people with epilepsy who may become pregnant take at least 0.4 milligrams of folic acid daily before and during pregnancy to decrease the risk of neural tube defects and possibly improve neurodevelopmental outcomes. However, it notes further studies are needed to clarify the optimal dose and timing of folic acid ...
What is the Valproate Pregnancy Prevention Programme? Valproate medicines can be an effective treatment for epilepsy. But research has shown that taking valproate medicines during pregnancy can seriously harm an unborn baby. Valproate medicines include sodium valproate (Epilim, Episenta, Epival, Depakote) and valproic acid (Convulex).
The guideline recommends that people with epilepsy who may become pregnant take at least 0.4 milligrams of folic acid daily before and during pregnancy to decrease the risk of neural tube defects ...
The occurrence of convulsive seizures should be minimized in PWECP during pregnancy to reduce potential risks for the mother and fetus. Clinicians should exercise caution in attempting to remove or replace an ASM that is effective in controlling generalized tonic-clonic or focal-to-bilateral tonic-clonic seizures once a PWECP is already pregnant.
Epilepsy in pregnancy. 1. 2. Epilepsy is recurring spontaneous seizures due to sudden excessive and disordered electrical discharge from the neurones of the Cerebral cortex. It is estimated that 7% of epileptic women become pregnant and epilepsy affects about 0.5-1% of pregnant women. Epilepsy can be partial or generalized. 5.
Sometime around August 2015, health care providers in northeastern Brazil noticed an unusual number of babies born with severe microcephaly. A gynaecologist in a hospital in Campino Grande in Paraíba, for example, who would typically expect to see one or two cases a year, suddenly started seeing two or three cases a week. The Brazilian Ministry of Health asked epidemiologist Celina Turchi to ...