An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Elsevier - PMC COVID-19 Collection

Impact of COVID-19 pandemic on mental health in the general population: A systematic review
Jiaqi xiong.
a Department of Pharmacology and Toxicology, University of Toronto, Toronto, ON
Orly Lipsitz
c Mood Disorders Psychopharmacology Unit, University Health Network, Toronto, Ontario
Flora Nasri
Leanna m.w. lui, hartej gill, david chen-li, michelle iacobucci.
e Department of Psychological Medicine, Yong Loo Lin School of Medicine, National University of Singapore, Singapore
f Institute for Health Innovation and Technology (iHealthtech), National University of Singapore, Singapore
Amna Majeed
Roger s. mcintyre.
b Department of Psychiatry, University of Toronto, Toronto, Ontario
d Brain and Cognition Discovery Foundation, Toronto, ON
Associated Data
As a major virus outbreak in the 21st century, the Coronavirus disease 2019 (COVID-19) pandemic has led to unprecedented hazards to mental health globally. While psychological support is being provided to patients and healthcare workers, the general public's mental health requires significant attention as well. This systematic review aims to synthesize extant literature that reports on the effects of COVID-19 on psychological outcomes of the general population and its associated risk factors.
A systematic search was conducted on PubMed, Embase, Medline, Web of Science, and Scopus from inception to 17 May 2020 following the PRISMA guidelines. A manual search on Google Scholar was performed to identify additional relevant studies. Articles were selected based on the predetermined eligibility criteria.
Results: Relatively high rates of symptoms of anxiety (6.33% to 50.9%), depression (14.6% to 48.3%), post-traumatic stress disorder (7% to 53.8%), psychological distress (34.43% to 38%), and stress (8.1% to 81.9%) are reported in the general population during the COVID-19 pandemic in China, Spain, Italy, Iran, the US, Turkey, Nepal, and Denmark. Risk factors associated with distress measures include female gender, younger age group (≤40 years), presence of chronic/psychiatric illnesses, unemployment, student status, and frequent exposure to social media/news concerning COVID-19.
Limitations
A significant degree of heterogeneity was noted across studies.
Conclusions
The COVID-19 pandemic is associated with highly significant levels of psychological distress that, in many cases, would meet the threshold for clinical relevance. Mitigating the hazardous effects of COVID-19 on mental health is an international public health priority.
1. Introduction
In December 2019, a cluster of atypical cases of pneumonia was reported in Wuhan, China, which was later designated as Coronavirus disease 2019 (COVID-19) by the World Health Organization (WHO) on 11 Feb 2020 ( Anand et al., 2020 ). The causative virus, SARS-CoV-2, was identified as a novel strain of coronaviruses that shares 79% genetic similarity with SARS-CoV from the 2003 SARS outbreak ( Anand et al., 2020 ). On 11 Mar 2020, the WHO declared the outbreak a global pandemic ( Anand et al., 2020 ).
The rapidly evolving situation has drastically altered people's lives, as well as multiple aspects of the global, public, and private economy. Declines in tourism, aviation, agriculture, and the finance industry owing to the COVID-19 outbreak are reported as massive reductions in both supply and demand aspects of the economy were mandated by governments internationally ( Nicola et al., 2020 ). The uncertainties and fears associated with the virus outbreak, along with mass lockdowns and economic recession are predicted to lead to increases in suicide as well as mental disorders associated with suicide. For example, McIntyre and Lee (2020b) have reported a projected increase in suicide from 418 to 2114 in Canadian suicide cases associated with joblessness. The foregoing result (i.e., rising trajectory of suicide) was also reported in the USA, Pakistan, India, France, Germany, and Italy ( Mamun and Ullah, 2020 ; Thakur and Jain, 2020 ). Separate lines of research have also reported an increase in psychological distress in the general population, persons with pre-existing mental disorders, as well as in healthcare workers ( Hao et al., 2020 ; Tan et al., 2020 ; Wang et al., 2020b ). Taken together, there is an urgent call for more attention given to public mental health and policies to assist people through this challenging time.
The objective of this systematic review is to summarize extant literature that reported on the prevalence of symptoms of depression, anxiety, PTSD, and other forms of psychological distress in the general population during the COVID-19 pandemic. An additional objective was to identify factors that are associated with psychological distress.
Methods and results were formated based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines ( Moher et al., 2010 ).
2.1. Search strategy
A systematic search following the PRISMA 2009 flow diagram ( Fig. 1 ) was conducted on PubMed, Medline, Embase, Scopus, and Web of Science from inception to 17 May 2020. A manual search on Google Scholar was performed to identify additional relevant studies. The search terms that were used were: (COVID-19 OR SARS-CoV-2 OR Severe acute respiratory syndrome coronavirus 2 OR 2019nCoV OR HCoV-19) AND (Mental health OR Psychological health OR Depression OR Anxiety OR PTSD OR PTSS OR Post-traumatic stress disorder OR Post-traumatic stress symptoms) AND (General population OR general public OR Public OR community). An example of search procedure was included as a supplementary file.

Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) study selection flow diagram. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
2.2. Study selection and eligibility criteria
Titles and abstracts of each publication were screened for relevance. Full-text articles were accessed for eligibility after the initial screening. Studies were eligible for inclusion if they: 1) followed cross-sectional study design; 2) assessed the mental health status of the general population/public during the COVID-19 pandemic and its associated risk factors; 3) utilized standardized and validated scales for measurement. Studies were excluded if they: 1) were not written in English or Chinese; 2) focused on particular subgroups of the population (e.g., healthcare workers, college students, or pregnant women); 3) were not peer-reviewed; 4) did not have full-text availability.
2.3. Data extraction
A data extraction form was used to include relevant data: (1) Lead author and year of publication, (2) Country/region of the population studied, (3) Study design, (4) Sample size, (5) Sample characteristics, (6) Assessment tools, (7) Prevalence of symptoms of depression/anxiety/ PTSD/psychological distress/stress, (8) Associated risk factors.
2.4 Quality appraisal
The Newcastle-Ottawa Scale (NOS) adapted for cross-sectional studies was used for study quality appraisal, which was modified accordingly from the scale used in Epstein et al. (2018) . The scale consists of three dimensions: Selection, Comparability, and Outcome. There are seven categories in total, which assess the representativeness of the sample, sample size justification, comparability between respondents and non-respondents, ascertainments of exposure, comparability based on study design or analysis, assessment of the outcome, and appropriateness of statistical analysis. A list of specific questions was attached as a supplementary file. A total of nine stars can be awarded if the study meets certain criteria, with a maximum of four stars assigned for the selection dimension, a maximum of two stars assigned for the comparability dimension, and a maximum of three stars assigned for the outcome dimension.
3.1. Search results
In total, 648 publications were identified. Of those, 264 were removed after initial screening due to duplication. 343 articles were excluded based on the screening of titles and abstracts. 41 full-text articles were assessed for eligibility. There were 12 articles excluded for studying specific subgroups of the population, five articles excluded for not having a standardized/ appropriate measure, three articles excluded for being review papers, and two articles excluded for being duplicates. Following the full-text screening, 19 studies met the inclusion criteria.
3.2. Study characteristics
Study characteristics and primary study findings are summarized in Table 1 . The sample size of the 19 studies ranged from 263 to 52,730 participants, with a total of 93,569 participants. A majority of study participants were over 18 years old. Female participants ( n = 60,006) made up 64.1% of the total sample. All studies followed a cross-sectional study design. The 19 studies were conducted in eight different countries, including China ( n = 10), Spain ( n = 2), Italy ( n = 2), Iran ( n = 1), the US ( n = 1), Turkey ( n = 1), Nepal ( n = 1), and Denmark ( n = 1). The primary outcomes chosen in the included studies varied across studies. Twelve studies included measures of depressive symptoms while eleven studies included measures of anxiety. Symptoms of PTSD/psychological impact of events were evaluated in four studies while three studies assessed psychological distress. It was additionally observed that four studies contained general measures of stress. Three studies did not explicitly report the overall prevalence rates of symptoms; notwithstanding the associated risk factors were identified and discussed.
Summary of study sample characteristics, study design, assessment tools used, prevalence rates and associated risk factors.
3.3. Quality appraisal
The result of the study quality appraisal is presented in Table 2 . The overall quality of the included studies is moderate, with total stars awarded varying from four to eight. There were two studies with four stars, two studies with five stars, seven studies with six stars, seven studies with seven stars, and one study with eight stars.
Results of study quality appraisal of the included studies.
3.4. Measurement tools
A variety of scales were used in the studies ( n = 19) for assessing different adverse psychological outcomes. The Beck Depression Inventory-II (BDI-II), Patient Health Questionnaire-9/2 (PHQ-9/2), Self-rating Depression Scales (SDS), The World Health Organization-Five Well-Being Index (WHO-5), and Center for Epidemiologic Studies Depression Scale (CES-D) were used for measuring depressive symptoms. The Beck Anxiety Inventory (BAI), Generalized Anxiety Disorder 7/2-item (GAD-7/2), and Self-rating Anxiety Scale (SAS) were used to evaluate symptoms of anxiety. The Depression, Anxiety, and Stress Scale- 21 items (DASS-21) was used for the evaluation of depression, anxiety, and stress symptoms. The Hospital Anxiety and Depression Scale (HADS) was used for assessing anxiety and depressive symptoms. Psychological distress was measured by The Peritraumatic Distress Inventory (CPDI) and the Kessler Psychological Distress Scale (K6/10). Symptoms of PTSD were assessed by The Impact of Event Scale-(Revised) (IES(-R)), PTSD Checklist (PCL-(C)-2/5). Chinese Perceived Stress Scale (CPSS-10) was used in one study to evaluate symptoms of stress.
3.5. Symptoms of depression and associated risk factors
Symptoms of depression were assessed in 12 out of the 19 studies ( Ahmed et al., 2020 ; Gao et al., 2020 ; González-Sanguino et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and S.B. Özdin, 2020 ; Sønderskov et al., 2020 ; Wang et al., 2020a ; Wang et al., 2020b ). The prevalence of depressive symptoms ranged from 14.6% to 48.3%. Although the reported rates are higher than previously estimated one-year prevalence (3.6% and 7.2%) of depression among the population prior to the pandemic ( Huang et al., 2019 ; Lim et al., 2018 ), it is important to note that presence of depressive symptoms does not reflect a clinical diagnosis of depression.
Many risk factors were identified to be associated with symptoms of depression amongst the COVID-19 pandemic. Females were reported as are generally more likely to develop depressive symptoms when compared to their male counterparts ( Lei et al., 2020 ; Mazza et al., 2020 ; Sønderskov et al., 2020 ; Wang et al., 2020a ). Participants from the younger age group (≤40 years) presented with more depressive symptoms ( Ahmed et al., 2020 ; Gao et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Olagoke et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ;). Student status was also found to be a significant risk factor for developing more depressive symptoms as compared to other occupational statuses (i.e. employment or retirement) ( González et al., 2020 ; Lei et al., 2020 ; Olagoke et al., 2020 ). Four studies also identified lower education levels as an associated factor with greater depressive symptoms ( Gao et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ; Wang et al., 2020a ). A single study by Wang et al., 2020b reported that people with higher education and professional jobs exhibited more depressive symptoms in comparison to less educated individuals and those in service or enterprise industries.
Other predictive factors for symptoms of depression included living in urban areas, poor self-rated health, high loneliness, being divorced/widowed, being single, lower household income, quarantine status, worry about being infected, property damage, unemployment, not having a child, a past history of mental stress or medical problems, having an acquaintance infected with COVID-19, perceived risks of unemployment, exposure to COVID-19 related news, higher perceived vulnerability, lower self-efficacy to protect themselves, the presence of chronic diseases, and the presence of specific physical symptoms ( Gao et al., 2020 ; González-Sanguino et al., 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and Özdin, 2020 ; Wang et al., 2020a ).
3.6. Symptoms of anxiety and associated risk factors
Anxiety symptoms were assessed in 11 out of the 19 studies, with a noticeable variation in the prevalence of anxiety symptoms ranging from 6.33% to 50.9% ( Ahmed et al., 2020 ; Gao et al., 2020 ; González-Sanguino et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Moghanibashi-Mansourieh, 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and Özdin, 2020 ; Wang et al., 2020a ; Wang et al., 2020b ).
Anxiety is often comorbid with depression ( Choi et al., 2020 ). Some predictive factors for depressive symptoms also apply to symptoms of anxiety, including a younger age group (≤40 years), lower education levels, poor self-rated health, high loneliness, female gender, divorced/widowed status, quarantine status, worry about being infected, property damage, history of mental health issue/medical problems, presence of chronic illness, living in urban areas, and the presence of specific physical symptoms ( Ahmed et al., 2020 ; Gao et al., 2020 ; González-Sanguino et al., 2020 ; Huang and Zhao, 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Moghanibashi-Mansourieh, 2020 ; Ozamiz-Etxebarria et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Wang et al., 2020a ; Wang et al., 2020b ).
Additionally, social media exposure or frequent exposure to news/information concerning COVID-19 was positively associated with symptoms of anxiety ( Gao et al., 2020 ; Moghanibashi-Mansourieh, 2020 ). With respect to marital status, one study reported that married participants had higher levels of anxiety when compared to unmarried participants ( Gao et al., 2020 ). On the other hand, Lei et al. (2020) found that divorced/widowed participants developed more anxiety symptoms than single or married individuals. A prolonged period of quarantine was also correlated with higher risks of anxiety symptoms. Intuitively, contact history with COVID-positive patients or objects may lead to more anxiety symptoms, which is noted in one study ( Moghanibashi-Mansourieh, 2020 ).
3.7. Symptoms of PTSD/ psychological distress/stress and associated risk factors
With respect to PTSD symptoms, similar prevalence rates were reported by Zhang and Ma (2020) and N. Liu et al. (2020) at 7.6% and 7%, respectively. Despite using the same measurement scale as Zhang and Ma (2020) (i.e., IES), Wang et al. (2020a) noted a remarkably different result, with 53.8% of the participants reporting moderate-to-severe psychological impact. González et al. ( González-Sanguino et al., 2020 ) noted 15.8% of participants with PTSD symptoms. Three out of the four studies that measured the traumatic effects of COVID-19 reported that the female gender was more susceptible to develop symptoms of PTSD. In contrast, the research conducted by Zhang and Ma (2020) found no significant difference in IES scores between females and males. Other risk factors included loneliness, individuals currently residing in Wuhan or those who have been to Wuhan in the past several weeks (the hardest-hit city in China), individuals with higher susceptibility to the virus, poor sleep quality, student status, poor self-rated health, and the presence of specific physical symptoms. Besides sex, Zhang and Ma (2020) found that age, BMI, and education levels are also not correlated with IES-scores.
Non-specific psychological distress was also assessed in three studies. One study reported a prevalence rate of symptoms of psychological distress at 38% ( Moccia et al., 2020 ), while another study from Qiu et al. (2020) reported a prevalence of 34.43%. The study from Wang et al. (2020) did not explicitly state the prevalence rates, but the associated risk factors for higher psychological distress symptoms were reported (i.e., younger age groups and female gender are more likely to develop psychological distress) ( Qiu et al., 2020 ; Wang et al., 2020 ). Other predictive factors included being migrant workers, profound regional severity of the outbreak, unmarried status, the history of visiting Wuhan in the past month, higher self-perceived impacts of the epidemic ( Qiu et al., 2020 ; Wang et al., 2020 ). Interestingly, researchers have identified personality traits to be predictive of psychological distresses. For example, persons with negative coping styles, cyclothymic, depressive, and anxious temperaments exhibit greater susceptibility to psychological outcomes ( Wang et al., 2020 ; Moccia et al., 2020 ).
The intensity of overall stress was evaluated and reported in four studies. The prevalence of overall stress was variably reported between 8.1% to over 81.9% ( Wang et al., 2020a ; Samadarshi et al., 2020 ; Mazza et al., 2020 ). Females and the younger age group are often associated with higher stress levels as compared to males and the elderly. Other predictive factors of higher stress levels include student status, a higher number of lockdown days, unemployment, having to go out to work, having an acquaintance infected with the virus, presence of chronic illnesses, poor self-rated health, and presence of specific physical symptoms ( Wang et al., 2020a ; Samadarshi et al., 2020 ; Mazza et al., 2020 ).
3.8. A separate analysis of negative psychological outcomes
Out of the nineteen included studies, five studies appeared to be more representative of the general population based on the results of study quality appraisal ( Table 1 ). A separate analysis was conducted for a more generalizable conclusion. According to the results of these studies, the rates of negative psychological outcomes were moderate but higher than usual, with anxiety symptoms ranging from 6.33% to 18.7%, depressive symptoms ranging from 14.6% to 32.8%, stress symptoms being 27.2%, and symptoms of PTSD being approximately 7% ( Lei et al., 2020 ; Liu et al., 2020 ; Mazza et al., 2020 ; Wang et al., 2020b ; Zhang et al., 2020 ). In these studies, female gender, younger age group (≤40 years), and student population were repetitively reported to exhibit more adverse psychiatric symptoms.
3.9. Protective factors against symptoms of mental disorders
In addition to associated risk factors, a few studies also identified factors that protect individuals against symptoms of psychological illnesses during the pandemic. Timely dissemination of updated and accurate COVID-19 related health information from authorities was found to be associated with lower levels of anxiety, stress, and depressive symptoms in the general public ( Wang et al., 2020a ). Additionally, actively carrying out precautionary measures that lower the risk of infection, such as frequent handwashing, mask-wearing, and less contact with people also predicted lower psychological distress levels during the pandemic ( Wang et al., 2020a ). Some personality traits were shown to correlate with positive psychological outcomes. Individuals with positive coping styles, secure and avoidant attachment styles usually presented fewer symptoms of anxiety and stress ( Wang et al., 2020 ; Moccia et al., 2020 ). ( Zhang et al. 2020 ) also found that participants with more social support and time to rest during the pandemic exhibited lower stress levels.
4. Discussion
Our review explored the mental health status of the general population and its predictive factors amid the COVID-19 pandemic. Generally, there is a higher prevalence of symptoms of adverse psychiatric outcomes among the public when compared to the prevalence before the pandemic ( Huang et al., 2019 ; Lim et al., 2018 ). Variations in prevalence rates across studies were noticed, which could have resulted from various measurement scales, differential reporting patterns, and possibly international/cultural differences. For example, some studies reported any participants with scores above the cut-off point (mild-to-severe symptoms), while others only included participants with moderate-to-severe symptoms ( Moghanibashi-Mansourieh, 2020 ; Wang et al., 2020a ). Regional differences existed with respect to the general public's psychological health during a massive disease outbreak due to varying degrees of outbreak severity, national economy, government preparedness, availability of medical supplies/ facilities, and proper dissemination of COVID-related information. Additionally, the stage of the outbreak in each region also affected the psychological responses of the public. Symptoms of adverse psychological outcomes were more commonly seen at the beginning of the outbreak when individuals were challenged by mandatory quarantine, unexpected unemployment, and uncertainty associated with the outbreak ( Ho et al., 2020 ). When evaluating the psychological impacts incurred by the coronavirus outbreak, the duration of psychiatric symptoms should also be taken into consideration since acute psychological responses to stressful or traumatic events are sometimes protective and of evolutionary importance ( Yaribeygi et al., 2017 ; Brosschot et al., 2016 ; Gilbert, 2006 ). Being anxious and stressed about the outbreak mobilizes people and forces them to implement preventative measures to protect themselves. Follow-up studies after the pandemic may be needed to assess the long-term psychological impacts of the COVID-19 pandemic.
4.1. Populations with greater susceptibility
Several predictive factors were identified from the studies. For example, females tended to be more vulnerable to develop the symptoms of various forms of mental disorders during the pandemic, including depression, anxiety, PTSD, and stress, as reported in our included studies ( Ahmed et al., 2020 ; Gao et al., 2020 ; Lei et al., 2020 ). Greater psychological distress arose in women partially because they represent a higher percentage of the workforce that may be negatively affected by COVID-19, such as retail, service industry, and healthcare. In addition to the disproportionate effects that disruption in the employment sector has had on women, several lines of research also indicate that women exhibit differential neurobiological responses when exposed to stressors, perhaps providing the basis for the overall higher rate of select mental disorders in women ( Goel et al., 2014 ; Eid et al., 2019 ).
Individuals under 40 years old also exhibited more adverse psychological symptoms during the pandemic ( Ahmed et al., 2020 ; Gao et al., 2020 ; Huang and Zhao, 2020 ). This finding may in part be due to their caregiving role in families (i.e., especially women), who provide financial and emotional support to children or the elderly. Job loss and unpredictability caused by the COVID-19 pandemic among this age group could be particularly stressful. Also, a large proportion of individuals under 40 years old consists of students who may also experience more emotional distress due to school closures, cancelation of social events, lower study efficiency with remote online courses, and postponements of exams ( Cao et al., 2020 ). This is consistent with our findings that student status was associated with higher levels of depressive symptoms and PTSD symptoms during the COVID-19 outbreak ( Lei et al., 2020 ; Olagoke et al., 2020 , Wang et al., 2020a ; Samadarshi et al., 2020 ).
People with chronic diseases and a history of medical/ psychiatric illnesses showed more symptoms of anxiety and stress ( Mazza et al., 2020 ; Ozamiz-Etxebarria et al., 2020 ; Özdin and Özdin, 2020 ). The anxiety and distress of chronic disease sufferers towards the coronavirus infection partly stem from their compromised immunity caused by pre-existing conditions, which renders them susceptible to the infection and a higher risk of mortality, such as those with systemic lupus erythematosus ( Sawalha et al., 2020 ). Several reports also suggested that a substantially higher death rate was noted in patients with diabetes, hypertension and other coronary heart diseases, yet the exact causes remain unknown ( Guo et al., 2020 ; Emami et al., 2020 ), leaving those with these common chronic conditions in fear and uncertainty. Additionally, another practical aspect of concern for patients with pre-existing conditions would be postponement and inaccessibility to medical services and treatment as a result of the COVID-19 pandemic. For example, as a rapidly growing number of COVID-19 patients were utilizing hospital and medical resources, primary, secondary, and tertiary prevention of other diseases may have unintentionally been affected. Individuals with a history of mental disorders or current diagnoses of psychiatric illnesses are also generally more sensitive to external stressors, such as social isolation associated with the pandemic ( Ho et al., 2020 ).
4.2. COVID-19 related psychological stressors
Several studies identified frequent exposure to social media/news relating to COVID-19 as a cause of anxiety and stress symptoms ( Gao et al., 2020 ; Moghanibashi-Mansourieh, 2020 ). Frequent social media use exposes oneself to potential fake news/reports/disinformation and the possibility for amplified anxiety. With the unpredictable situation and a lot of unknowns about the novel coronavirus, misinformation and fake news are being easily spread via social media platforms ( Erku et al., 2020 ), creating unnecessary fears and anxiety. Sadness and anxious feelings could also arise when constantly seeing members of the community suffering from the pandemic via social media platforms or news reports ( Li et al., 2020 ).
Reports also suggested that poor economic status, lower education level, and unemployment are significant risk factors for developing symptoms of mental disorders, especially depressive symptoms during the pandemic period ( Gao et al., 2020 ; Lei et al., 2020 ; Mazza et al., 2020 ; Olagoke et al., 2020 ;). The coronavirus outbreak has led to strictly imposed stay-home-order and a decrease in demands for services and goods ( Nicola et al., 2020 ), which has adversely influenced local businesses and industries worldwide. Surges in unemployment rates were noted in many countries ( Statistics Canada, 2020 ; Statista, 2020 ). A decrease in quality of life and uncertainty as a result of financial hardship can put individuals into greater risks for developing adverse psychological symptoms ( Ng et al., 2013 ).
4.3. Efforts to reduce symptoms of mental disorders
4.3.1. policymaking.
The associated risk and protective factors shed light on policy enactment in an attempt to relieve the psychological impacts of the COVID-19 pandemic on the general public. Firstly, more attention and assistance should be prioritized to the aforementioned vulnerable groups of the population, such as the female gender, people from age group ≤40, college students, and those suffering from chronic/psychiatric illnesses. Secondly, governments must ensure the proper and timely dissemination of COVID-19 related information. For example, validation of news/reports concerning the pandemic is essential to prevent panic from rumours and false information. Information about preventative measures should also be continuously updated by health authorities to reassure those who are afraid of being infected ( Tran, et al., 2020a ). Thirdly, easily accessible mental health services are critical during the period of prolonged quarantine, especially for those who are in urgent need of psychological support and individuals who reside in rural areas ( Tran et al., 2020b ). Since in-person health services are limited and delayed as a result of COVID-19 pandemic, remote mental health services can be delivered in the form of online consultation and hotlines ( Liu et al., 2020 ; Pisciotta et al., 2019 ). Last but not least, monetary support (e.g. beneficial funds, wage subsidy) and new employment opportunities could be provided to people who are experiencing financial hardship or loss of jobs owing to the pandemic. Government intervention in the form of financial provisions, housing support, access to psychiatric first aid, and encouragement at the individual level of healthy lifestyle behavior has been shown effective in alleviating suicide cases associated with economic recession ( McIntyre and Lee, 2020a ). For instance, declines in suicide incidence were observed to be associated with government expenses in Japan during the 2008 economic depression ( McIntyre and Lee, 2020a ).
4.3.2. Individual efforts
Individuals can also take initiatives to relieve their symptoms of psychological distress. For instance, exercising regularly and maintaining a healthy diet pattern have been demonstrated to effectively ease and prevent symptoms of depression or stress ( Carek et al., 2011 ; Molendijk et al., 2018 ; Lassale et al., 2019 ). With respect to pandemic-induced symptoms of anxiety, it is also recommended to distract oneself from checking COVID-19 related news to avoid potential false reports and contagious negativity. It is also essential to obtain COVID-19 related information from authorized news agencies and organizations and to seek medical advice only from properly trained healthcare professionals. Keeping in touch with friends and family by phone calls or video calls during quarantine can ease the distress from social isolation ( Hwang et al., 2020 ).
4.4. Strengths
Our paper is the first systematic review that examines and summarizes existing literature with relevance to the psychological health of the general population during the COVID-19 outbreak and highlights important associated risk factors to provide suggestions for addressing the mental health crisis amid the global pandemic.
4.5. Limitations
Certain limitations apply to this review. Firstly, the description of the study findings was qualitative and narrative. A more objective systematic review could not be conducted to examine the prevalence of each psychological outcome due to a high heterogeneity across studies in the assessment tools used and primary outcomes measured. Secondly, all included studies followed a cross-sectional study design and, as such, causal inferences could not be made. Additionally, all studies were conducted via online questionnaires independently by the study participants, which raises two concerns: 1] Individual responses in self-assessment vary in objectivity when supervision from a professional psychiatrist/ interviewer is absent, 2] People with poor internet accessibility were likely not included in the study, creating a selection bias in the population studied. Another concern is the over-representation of females in most studies. Selection bias and over-representation of particular groups indicate that most studies may not be representative of the true population. Importantly, studies in inclusion were conducted in a limited number of countries. Thus generalizations of mental health among the general population at a global level should be made cautiously.
5. Conclusion
This systematic review examined the psychological status of the general public during the COVID-19 pandemic and stressed the associated risk factors. A high prevalence of adverse psychiatric symptoms was reported in most studies. The COVID-19 pandemic represents an unprecedented threat to mental health in high, middle, and low-income countries. In addition to flattening the curve of viral transmission, priority needs to be given to the prevention of mental disorders (e.g. major depressive disorder, PTSD, as well as suicide). A combination of government policy that integrates viral risk mitigation with provisions to alleviate hazards to mental health is urgently needed.
Authorship contribution statement
JX contributed to the overall design, article selection , review, and manuscript preparation. LL and JX contributed to study quality appraisal. All other authors contributed to review, editing, and submission.
Declaration of Competing Interest
Acknowledgements.
RSM has received research grant support from the Stanley Medical Research Institute and the Canadian Institutes of Health Research/Global Alliance for Chronic Diseases/National Natural Science Foundation of China and speaker/consultation fees from Lundbeck, Janssen, Shire, Purdue, Pfizer, Otsuka, Allergan, Takeda, Neurocrine, Sunovion, and Minerva.
Supplementary material associated with this article can be found, in the online version, at doi: 10.1016/j.jad.2020.08.001 .
Appendix. Supplementary materials
- Ahmed M.Z., Ahmed O., Zhou A., Sang H., Liu S., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 2020; 51 doi: 10.1016/j.ajp.2020.102092. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Anand K.B., Karade S., Sen S., Gupta R.M. SARS-CoV-2: camazotz's curse. Med. J. Armed Forces India. 2020; 76 :136–141. doi: 10.1016/j.mjafi.2020.04.008. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Brosschot J.F., Verkuil B., Thayer J.F. The default response to uncertainty and the importance of perceived safety in anxiety and stress: an evolution-theoretical perspective. J. Anxiety Disord. 2016; 41 :22–34. doi: 10.1016/j.janxdis.2016.04.012. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020; 287 doi: 10.1016/j.psychres.2020.112934. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carek P.J., Laibstain S.E., Carek S.M. Exercise for the treatment of depression and anxiety. Int. J. Psychiatry Med. 2011; 41 (1):15–28. doi: 10.2190/PM.41.1.c. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Choi K.W., Kim Y., Jeon H.J. Comorbid Anxiety and Depression: clinical and Conceptual Consideration and Transdiagnostic Treatment. Adv. Exp. Med. Biol. 2020; 1191 :219–235. doi: 10.1007/978-981-32-9705-0_14. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Eid R.S., Gobinath A.R., Galea L.A.M. Sex differences in depression: insights from clinical and preclinical studies. Prog. Neurobiol. 2019; 176 :86–102. doi: 10.1016/j.pneurobio.2019.01.006. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Emami A., Javanmardi F., Pirbonyeh N., Akbari A. Prevalence of Underlying Diseases in Hospitalized Patients. Arch. Acad. Emerg. Med. 2020; 8 (1):e35. doi: 10.22037/aaem.v8i1.600.g748. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Epstein S., Roberts E., Sedgwick R., Finning K., Ford T., Dutta R., Downs J. Poor school attendance and exclusion: a systematic review protocol on educational risk factors for self-harm and suicidal behaviours. BMJ Open. 2018; 8 (12) doi: 10.1136/bmjopen-2018-023953. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Erku D.A., Belachew S.W., Abrha S., Sinnollareddy M., Thoma J., Steadman K.J., Tesfaye W.H. When fear and misinformation go viral: pharmacists' role in deterring medication misinformation during the 'infodemic' surrounding COVID-19. Res. Social. Adm. Pharm. 2020 doi: 10.1016/j.sapharm.2020.04.032. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020; 15 (4) doi: 10.1371/journal.pone.0231924. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Gilbert P. Evolution and depression: issues and implications. Psycho. Med. 2006; 36 (3):287–297. doi: 10.1017/S0033291705006112. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Goel N., Workman J.L., Lee T.F., Innala L., Viau V. Sex differences in the HPA axis. Compr. Physiol. 2014; 4 (3):1121‐1155. doi: 10.1002/cphy.c130054. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- González-Sanguino C., Ausín B., Castellanos M.A., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.040. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Guo W., Li M., Dong Y., Zhou H., Zhang Z., Tian C., Qin R., Wang H., Shen Y., Du K., Zhao L., Fan H., Luo S., Hu D. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab. Res. Rev. 2020 doi: 10.1002/dmrr.3319. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.069. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ho C.S.H., Chee C.Y., Ho R.C.M. Mental health strategies to combat the psychological impact of coronavirus disease (COVID-19) beyond paranoia and panic. Ann. Acad. Med. Singapore. 2020; 49 (3):155–160. [ PubMed ] [ Google Scholar ]
- Huang Y., et al. . Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiat. 2019; 6 (3):211–224. doi: 10.1016/S2215-0366(18)30511-X. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020; 288 doi: 10.1016/j.psychres.2020.112954. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Hwang T., Rabheru K., Peisah C., Reichman W., Ikeda M. Loneliness and social isolation during COVID-19 pandemic. Int. Psychogeriatr. 2020:1–15. doi: 10.1017/S1041610220000988. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lassale C., Batty G.D., Baghdadli A., Jacka F., Sánchez-Villegas A., Kivimäki M., Akbaraly T. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol. Psychiatry. 2019; 24 :965–986. doi: 10.1038/s41380-018-0237-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the covid-19 epidemic in southwestern China. Med. Sci. Monit. 2020; 26 doi: 10.12659/MSM.924609. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Li Z., et al. . Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immum. 2020 doi: 10.1016/j.bbi.2020.03.007. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Lim G.Y., Tam W.W., Lu Y., Ho C.S., Zhang M.W., Ho R.C. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018; 8 (1):2861. doi: 10.1038/s41598-018-21243-x. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020; 287 doi: 10.1016/j.psychres.2020.112921. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Liu S., Yang L., Zhang C., Xiang Y., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiat. 2020; 7 (4):e17–e18. doi: 10.1016/S2215-0366(20)30077-8. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mamun M.A., Ullah I. COVID-19 suicides in Pakistan, dying off not COVID-19 fear but poverty?—The forthcoming economic challenges for a developing country. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.028. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020; 17 :3165. doi: 10.3390/ijerph17093165. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McIntyre R.S., Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020; 19 (2):250–251. doi: 10.1002/wps.20767. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- McIntyre R.S., Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020; 290 doi: 10.1016/j.psychres.2020.113104. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., Martin V.D., Chieffo D., Janiri L., Fiorillo A., Sani G., Nicola M.D. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.048. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19. Asian J. Psychiatr. 2020; 51 doi: 10.1016/j.ajp.2020.102076. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Moher D., Liberati A., Tetzlaff J., Altman D.G., PRISMA Group Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. Int. J. Surg. 2010; 8 (5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Molendijk M., Molero P., Sánchez-Pandreño F.O., Van der Dose W., Martínez-González M.A. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J. Affect. Disord. 2018; 226 :346–354. doi: 10.1016/j.jad.2017.09.022. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ng K.H., Agius M., Zaman R. The global economic crisis: effects on mental health and what can be done. J. R. Soc. Med. 2013; 106 :211–214. doi: 10.1177/0141076813481770. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020; 78 :185–193. doi: 10.1016/j.ijsu.2020.04.018. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Olagoke A.A., Olagoke O.O., Hughes A.M. Exposure to coronavirus news on mainstream media: the role of risk perceptions and depression. Br. J. Health Psychol. 2020 doi: 10.1111/bjhp.12427. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Ozamiz-Etxebarria N., Dosil-Santamaria M., Picaza-Gorrochategui M., Idoiaga-Mondragon N. Stress, anxiety and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saude. Publica. 2020; 36 (4) doi: 10.1590/0102-311X00054020. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Özdin S., Özdin S.B. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry. 2020:1–8. doi: 10.1177/0020764020927051. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Pisciotta M., Denneson L.M., Williams H.B., Woods S., Tuepker A., Dobscha S.K. Providing mental health care in the context of online mental health notes: advice from patients and mental health clinicians. J. Ment. Health. 2019; 28 (1):64–70. doi: 10.1080/09638237.2018.1521924. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 2020; 33 doi: 10.1136/gpsych-2020-100213. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Samadarshi S.C.A., Sharma S., Bhatta J. An online survey of factors associated with self-perceived stress during the initial stage of the COVID-19 outbreak in Nepal. Ethiop. J. Health Dev. 2020; 34 (2):1–6. [ Google Scholar ]
- Sawalha A.H., Zhao M., Coit P., Lu Q. Epigenetic dysregulation of ACE2 and interferon-regulated genes might suggest increased COVID-19 susceptibility and severity in lupus patients. J. Clin. Immunol. 2020; 215 doi: 10.1016/j.clim.2020.108410. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020:1–3. doi: 10.1017/neu.2020.15. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Statista, 2020. Monthly unemployment rate in the United States from May 2019 to May 2020. https://www.statista.com/statistics/273909/seasonally-adjusted-monthly-unemployment-rate-in-the-us/ (Accessed June 12 2020,).
- Statistic Canada, 2020. Labour force characteristics, monthly, seasonally adjusted and trend-cycle, last 5 months. https://doi.org/10.25318/1410028701-eng(Accessed June 12 2020,).
- Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Zhang Z., Lai A., Ho R., Tran B., Ho C., Tam W. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.055. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Thakur V., Jain A. COVID 2019-Suicides: a global psychological pandemic. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.062. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ] Retracted
- Tran B.X., et al. Coverage of Health Information by Different Sources in Communities: implication for COVID-19 Epidemic Response. Int. J. Environ. Res. Public Health. 2020; 17 (10):3577. doi: 10.3390/ijerph17103577. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Tran B.X., Phan H.T., Nguyen T.P.T., Hoang M.T., Vu G.T., Lei H.T., Latkin C.A., Ho C.S.H., Ho R.C.M. Reaching further by Village Health Collaborators: the informal health taskforce of Vietnam for COVID-19 responses. J. Glob. Health. 2020; 10 (1) doi: 10.7189/jogh.10.010354. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020; 17 (5):1729. doi: 10.3390/ijerph17051729. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.028. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang H., Xia Q., Xiong Z., Li Z., Xiang W., Yuan Y., Liu Y., Li Z. The psychological distress and coping styles in the early stages of the 2019 coronavirus disease (COVID-19) epidemic in the general mainland Chinese population: a web-based survey. PLoS ONE. 2020; 15 (5) doi: 10.1371/journal.pone.0233410. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2020:1–10. doi: 10.1080/13548506.2020.1746817. [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Yaribeygi H., Panahi Y., Sahraei H., Johnston T.P., Sahebkar A. The impact of stress on body function: a review. EXCLI J. 2017; 16 :1057–1072. doi: 10.17179/excli2017-480. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health. 2020; 17 (7):2381. doi: 10.3390/ijerph17072381. [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Open access
- Published: 11 April 2023
Effects of the COVID-19 pandemic on mental health, anxiety, and depression
- Ida Kupcova 1 ,
- Lubos Danisovic 1 ,
- Martin Klein 2 &
- Stefan Harsanyi 1
BMC Psychology volume 11 , Article number: 108 ( 2023 ) Cite this article
9422 Accesses
12 Citations
38 Altmetric
Metrics details
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact. According to the World Health Organization (WHO), anxiety and depression prevalence increased by 25% globally. In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population.
A cross-sectional study using an anonymous online-based 45-question online survey was conducted at Comenius University in Bratislava. The questionnaire comprised five general questions and two assessment tools the Zung Self-Rating Anxiety Scale (SAS) and the Zung Self-Rating Depression Scale (SDS). The results of the Self-Rating Scales were statistically examined in association with sex, age, and level of education.
A total of 205 anonymous subjects participated in this study, and no responses were excluded. In the study group, 78 (38.05%) participants were male, and 127 (61.69%) were female. A higher tendency to anxiety was exhibited by female participants (p = 0.012) and the age group under 30 years of age (p = 0.042). The level of education has been identified as a significant factor for changes in mental state, as participants with higher levels of education tended to be in a worse mental state (p = 0.006).
Conclusions
Summarizing two years of the COVID-19 pandemic, the mental state of people with higher levels of education tended to feel worse, while females and younger adults felt more anxiety.
Peer Review reports
Introduction
The first mention of the novel coronavirus came in 2019, when this variant was discovered in the city of Wuhan, China, and became the first ever documented coronavirus pandemic [ 1 , 2 , 3 ]. At this time there was only a sliver of fear rising all over the globe. However, in March 2020, after the declaration of a global pandemic by the World Health Organization (WHO), the situation changed dramatically [ 4 ]. Answering this, yet an unknown threat thrust many countries into a psycho-socio-economic whirlwind [ 5 , 6 ]. Various measures taken by governments to control the spread of the virus presented the worldwide population with a series of new challenges to which it had to adjust [ 7 , 8 ]. Lockdowns, closed schools, losing employment or businesses, and rising deaths not only in nursing homes came to be a new reality [ 9 , 10 , 11 ]. Lack of scientific information on the novel coronavirus and its effects on the human body, its fast spread, the absence of effective causal treatment, and the restrictions which harmed people´s social life, financial situation and other areas of everyday life lead to long-term living conditions with increased stress levels and low predictability over which people had little control [ 12 ].
Risks of changes in the mental state of the population came mainly from external risk factors, including prolonged lockdowns, social isolation, inadequate or misinterpreted information, loss of income, and acute relationship with the rising death toll. According to the World Health Organization (WHO), since the outbreak of the COVID-19 pandemic, anxiety and depression prevalence increased by 25% globally [ 13 ]. Unemployment specifically has been proven to be also a predictor of suicidal behavior [ 14 , 15 , 16 , 17 , 18 ]. These risk factors then interact with individual psychological factors leading to psychopathologies such as threat appraisal, attentional bias to threat stimuli over neutral stimuli, avoidance, fear learning, impaired safety learning, impaired fear extinction due to habituation, intolerance of uncertainty, and psychological inflexibility. The threat responses are mediated by the limbic system and insula and mitigated by the pre-frontal cortex, which has also been reported in neuroimaging studies, with reduced insula thickness corresponding to more severe anxiety and amygdala volume correlated to anhedonia as a symptom of depression [ 19 , 20 , 21 , 22 , 23 ]. Speaking in psychological terms, the pandemic disturbed our core belief, that we are safe in our communities, cities, countries, or even the world. The lost sense of agency and confidence regarding our future diminished the sense of worth, identity, and meaningfulness of our lives and eroded security-enhancing relationships [ 24 ].
Slovakia introduced harsh public health measures in the first wave of the pandemic, but relaxed these measures during the summer, accompanied by a failure to develop effective find, test, trace, isolate and support systems. Due to this, the country experienced a steep growth in new COVID-19 cases in September 2020, which lead to the erosion of public´s trust in the government´s management of the situation [ 25 ]. As a means to control the second wave of the pandemic, the Slovak government decided to perform nationwide antigen testing over two weekends in November 2020, which was internationally perceived as a very controversial step, moreover, it failed to prevent further lockdowns [ 26 ]. In addition, there was a sharp rise in the unemployment rate since 2020, which continued until July 2020, when it gradually eased [ 27 ]. Pre-pandemic, every 9th citizen of Slovakia suffered from a mental health disorder, according to National Statistics Office in 2017, the majority being affective and anxiety disorders. A group of authors created a web questionnaire aimed at psychiatrists, psychologists, and their patients after the first wave of the COVID-19 pandemic in Slovakia. The results showed that 86.6% of respondents perceived the pathological effect of the pandemic on their mental status, 54.1% of whom were already treated for affective or anxiety disorders [ 28 ].
In this study, we aimed to examine the lasting effects of the COVID-19 pandemic on the general population. This study aimed to assess the symptoms of anxiety and depression in the general public of Slovakia. After the end of epidemiologic restrictive measures (from March to May 2022), we introduced an anonymous online questionnaire using adapted versions of Zung Self-Rating Anxiety Scale (SAS) and Zung Self-Rating Depression Scale (SDS) [ 29 , 30 ]. We focused on the general public because only a portion of people who experience psychological distress seek professional help. We sought to establish, whether during the pandemic the population showed a tendency to adapt to the situation or whether the anxiety and depression symptoms tended to be present even after months of better epidemiologic situation, vaccine availability, and studies putting its effects under review [ 31 , 32 , 33 , 34 ].
Materials and Methods
This study utilized a voluntary and anonymous online self-administered questionnaire, where the collected data cannot be linked to a specific respondent. This study did not process any personal data. The questionnaire consisted of 45 questions. The first three were open-ended questions about participants’ sex, age (date of birth was not recorded), and education. Followed by 2 questions aimed at mental health and changes in the will to live. Further 20 and 20 questions consisted of the Zung SAS and Zung SDS, respectively. Every question in SAS and SDS is scored from 1 to 4 points on a Likert-style scale. The scoring system is introduced in Fig. 1 . Questions were presented in the Slovak language, with emphasis on maintaining test integrity, so, if possible, literal translations were made from English to Slovak. The questionnaire was created and designed in Google Forms®. Data collection was carried out from March 2022 to May 2022. The study was aimed at the general population of Slovakia in times of difficult epidemiologic and social situations due to the high prevalence and incidence of COVID-19 cases during lockdowns and social distancing measures. Because of the character of this web-based study, the optimal distribution of respondents could not be achieved.
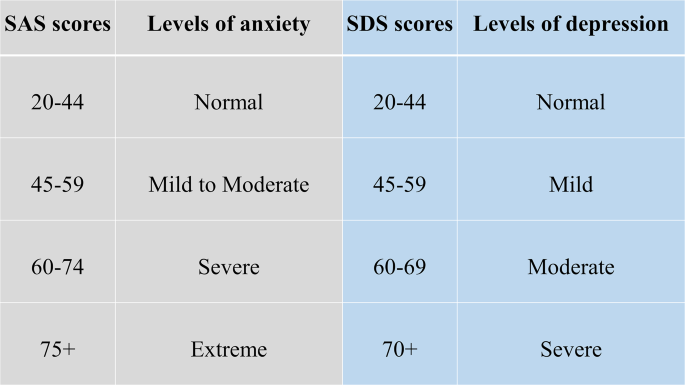
Categories of Zung SAS and SDS scores with clinical interpretation
During the course of this study, 205 respondents answered the anonymous questionnaire in full and were included in the study. All respondents were over 18 years of age. The data was later exported from Google Forms® as an Excel spreadsheet. Coding and analysis were carried out using IBM SPSS Statistics version 26 (IBM SPSS Statistics for Windows, Version 26.0, Armonk, NY, USA). Subject groups were created based on sex, age, and education level. First, sex due to differences in emotional expression. Second, age was a risk factor due to perceived stress and fear of the disease. Last, education due to different approaches to information. In these groups four factors were studied: (1) changes in mental state; (2) affected will to live, or frequent thoughts about death; (3) result of SAS; (4) result of SDS. For SAS, no subject in the study group scored anxiety levels of “severe” or “extreme”. Similarly for SDS, no subject depression levels reached “moderate” or “severe”. Pearson’s chi-squared test(χ2) was used to analyze the association between the subject groups and studied factors. The results were considered significant if the p-value was less than 0.05.
Ethical permission was obtained from the local ethics committee (Reference number: ULBGaKG-02/2022). This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines. Due to the anonymous design of the study and by the institutional requirements, written informed consent for participation was not required for this study.
In the study, out of 205 subjects in the study group, 127 (62%) were female and 78 (38%) were male. The average age in the study group was 35.78 years of age (range 19–71 years), with a median of 34 years. In the age group under 30 years of age were 34 (16.6%) subjects, while 162 (79%) were in the range from 31 to 49 and 9 (0.4%) were over 50 years old. 48 (23.4%) participants achieved an education level of lower or higher secondary and 157 (76.6%) finished university or higher. All answers of study participants were included in the study, nothing was excluded.
In Tables 1 and 2 , we can see the distribution of changes in mental state and will to live as stated in the questionnaire. In Table 1 we can see a disproportion in education level and mental state, where participants with higher education tended to feel worse much more than those with lower levels of education. Changes based on sex and age did not show any statistically significant results.
In Table 2 . we can see, that decreased will to live and frequent thoughts about death were only marginally present in the study group, which suggests that coping mechanisms play a huge role in adaptation to such events (e.g. the global pandemic). There is also a possibility that living in times of better epidemiologic situations makes people more likely to forget about the bad past.
Anxiety and depression levels as seen in Tables 3 and 4 were different, where female participants and the age group under 30 years of age tended to feel more anxiety than other groups. No significant changes in depression levels based on sex, age, and education were found.
Compared to the estimated global prevalence of depression in 2017 (3.44%), in 2021 it was approximately 7 times higher (25%) [ 14 ]. Our study did not prove an increase in depression, while anxiety levels and changes in the mental state did prove elevated. No significant changes in depression levels go in hand with the unaffected will to live and infrequent thoughts about death, which were important findings, that did not supplement our primary hypothesis that the fear of death caused by COVID-19 or accompanying infections would enhance personal distress and depression, leading to decreases in studied factors. These results are drawn from our limited sample size and uneven demographic distribution. Suicide ideations rose from 5% pre-pandemic to 10.81% during the pandemic [ 35 ]. In our study, 9.3% of participants experienced thoughts about death and since we did not specifically ask if they thought about suicide, our results only partially correlate with suicidal ideations. However, as these subjects exhibited only moderate levels of anxiety and mild levels of depression, the rise of suicide ideations seems unlikely. The rise in suicidal ideations seemed to be especially true for the general population with no pre-existing psychiatric conditions in the first months of the pandemic [ 36 ]. The policies implemented by countries to contain the pandemic also took a toll on the population´s mental health, as it was reported, that more stringent policies, mainly the social distancing and perceived government´s handling of the pandemic, were related to worse psychological outcomes [ 37 ]. The effects of lockdowns are far-fetched and the increases in mental health challenges, well-being, and quality of life will require a long time to be understood, as Onyeaka et al. conclude [ 10 ]. These effects are not unforeseen, as the global population suffered from life-altering changes in the structure and accessibility of education or healthcare, fluctuations in prices and food insecurity, as well as the inevitable depression of the global economy [ 38 ].
The loneliness associated with enforced social distancing leads to an increase in depression, anxiety, and posttraumatic stress in children in adolescents, with possible long-term sequelae [ 39 ]. The increase in adolescent self-injury was 27.6% during the pandemic [ 40 ]. Similar findings were described in the middle-aged and elderly population, in which both depression and anxiety prevalence rose at the beginning of the pandemic, during the pandemic, with depression persisting later in the pandemic, while the anxiety-related disorders tended to subside [ 41 ]. Medical professionals represented another specific at-risk group, with reported anxiety and depression rates of 24.94% and 24.83% respectively [ 42 ]. The dynamic of psychopathology related to the COVID-19 pandemic is not clear, with studies reporting a return to normal later in 2020, while others describe increased distress later in the pandemic [ 20 , 43 ].
Concerning the general population, authors from Spain reported that lockdowns and COVID-19 were associated with depression and anxiety [ 44 ]. In January 2022 Zhao et al., reported an elevation in hoarding behavior due to fear of COVID-19, while this process was moderated by education and income levels, however, less in the general population if compared to students [ 45 ]. Higher education levels and better access to information could improve persons’ fear of the unknown, however, this fact was not consistent with our expectations in this study, as participants with university education tended to feel worse than participants with lower education. A study on adolescents and their perceived stress in the Czech Republic concluded that girls are more affected by lockdowns. The strongest predictor was loneliness, while having someone to talk to, scored the lowest [ 46 ]. Garbóczy et al. reported elevated perceived stress levels and health anxiety in 1289 Hungarian and international students, also affected by disengagement from home and inadequate coping strategies [ 47 ]. Wathelet et al. conducted a study on French University students confined during the pandemic with alarming results of a high prevalence of mental health issues in the study group [ 48 ]. Our study indicated similar results, as participants in the age group under 30 years of age tended to feel more anxious than others.
In conclusion, we can say that this pandemic changed the lives of many. Many of us, our family members, friends, and colleagues, experienced life-altering events and complicated situations unseen for decades. Our decisions and actions fueled the progress in medicine, while they also continue to impact society on all levels. The long-term effects on adolescents are yet to be seen, while effects of pain, fear, and isolation on the general population are already presenting themselves.
The limitations of this study were numerous and as this was a web-based study, the optimal distribution of respondents could not be achieved, due to the snowball sampling strategy. The main limitation was the small sample size and uneven demographic distribution of respondents, which could impact the representativeness of the studied population and increase the margin of error. Similarly, the limited number of older participants could significantly impact the reported results, as age was an important risk factor and thus an important stressor. The questionnaire omitted the presence of COVID-19-unrelated life-changing events or stressors, and also did not account for any preexisting condition or risk factor that may have affected the outcome of the used assessment scales.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to compliance with institutional guidelines but they are available from the corresponding author (SH) on a reasonable request.
Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506.
Article PubMed PubMed Central Google Scholar
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382:727–33.
Liu Y-C, Kuo R-L, Shih S-R. COVID-19: the first documented coronavirus pandemic in history. Biomed J. 2020;43:328–33.
Advice for the public on COVID-19 – World Health Organization. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public . Accessed 13 Nov 2022.
Osterrieder A, Cuman G, Pan-Ngum W, Cheah PK, Cheah P-K, Peerawaranun P, et al. Economic and social impacts of COVID-19 and public health measures: results from an anonymous online survey in Thailand, Malaysia, the UK, Italy and Slovenia. BMJ Open. 2021;11:e046863.
Article PubMed Google Scholar
Mofijur M, Fattah IMR, Alam MA, Islam ABMS, Ong HC, Rahman SMA, et al. Impact of COVID-19 on the social, economic, environmental and energy domains: Lessons learnt from a global pandemic. Sustainable Prod Consum. 2021;26:343–59.
Article Google Scholar
Vlachos J, Hertegård E, Svaleryd B. The effects of school closures on SARS-CoV-2 among parents and teachers. Proc Natl Acad Sci U S A. 2021;118:e2020834118.
Ludvigsson JF, Engerström L, Nordenhäll C, Larsson E, Open Schools. Covid-19, and child and teacher morbidity in Sweden. N Engl J Med. 2021;384:669–71.
Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor É, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six european countries. Eur Geriatr Med. 2021;12:193–204.
Onyeaka H, Anumudu CK, Al-Sharify ZT, Egele-Godswill E, Mbaegbu P. COVID-19 pandemic: a review of the global lockdown and its far-reaching effects. Sci Prog. 2021;104:368504211019854.
The Lancet null. India under COVID-19 lockdown. Lancet. 2020;395:1315.
Lo Coco G, Gentile A, Bosnar K, Milovanović I, Bianco A, Drid P, et al. A cross-country examination on the fear of COVID-19 and the sense of loneliness during the First Wave of COVID-19 outbreak. Int J Environ Res Public Health. 2021;18:2586.
COVID-19 pandemic. triggers 25% increase in prevalence of anxiety and depression worldwide. https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide . Accessed 14 Nov 2022.
Bueno-Notivol J, Gracia-García P, Olaya B, Lasheras I, López-Antón R, Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int J Clin Health Psychol. 2021;21:100196.
Hajek A, Sabat I, Neumann-Böhme S, Schreyögg J, Barros PP, Stargardt T, et al. Prevalence and determinants of probable depression and anxiety during the COVID-19 pandemic in seven countries: longitudinal evidence from the european COvid Survey (ECOS). J Affect Disord. 2022;299:517–24.
Piumatti G, Levati S, Amati R, Crivelli L, Albanese E. Trajectories of depression, anxiety and stress among adults during the COVID-19 pandemic in Southern Switzerland: the Corona Immunitas Ticino cohort study. Public Health. 2022;206:63–9.
Korkmaz H, Güloğlu B. The role of uncertainty tolerance and meaning in life on depression and anxiety throughout Covid-19 pandemic. Pers Indiv Differ. 2021;179:110952.
McIntyre RS, Lee Y. Projected increases in suicide in Canada as a consequence of COVID-19. Psychiatry Res. 2020;290:113104.
Funkhouser CJ, Klemballa DM, Shankman SA. Using what we know about threat reactivity models to understand mental health during the COVID-19 pandemic. Behav Res Ther. 2022;153:104082.
Landi G, Pakenham KI, Crocetti E, Tossani E, Grandi S. The trajectories of anxiety and depression during the COVID-19 pandemic and the protective role of psychological flexibility: a four-wave longitudinal study. J Affect Disord. 2022;307:69–78.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Global Open Sci. 2021;1:261–71.
McCracken LM, Badinlou F, Buhrman M, Brocki KC. The role of psychological flexibility in the context of COVID-19: Associations with depression, anxiety, and insomnia. J Context Behav Sci. 2021;19:28–35.
Talkovsky AM, Norton PJ. Negative affect and intolerance of uncertainty as potential mediators of change in comorbid depression in transdiagnostic CBT for anxiety. J Affect Disord. 2018;236:259–65.
Milman E, Lee SA, Neimeyer RA, Mathis AA, Jobe MC. Modeling pandemic depression and anxiety: the mediational role of core beliefs and meaning making. J Affect Disorders Rep. 2020;2:100023.
Sagan A, Bryndova L, Kowalska-Bobko I, Smatana M, Spranger A, Szerencses V, et al. A reversal of fortune: comparison of health system responses to COVID-19 in the Visegrad group during the early phases of the pandemic. Health Policy. 2022;126:446–55.
Holt E. COVID-19 testing in Slovakia. Lancet Infect Dis. 2021;21:32.
Stalmachova K, Strenitzerova M. Impact of the COVID-19 pandemic on employment in transport and telecommunications sectors. Transp Res Procedia. 2021;55:87–94.
Izakova L, Breznoscakova D, Jandova K, Valkucakova V, Bezakova G, Suvada J. What mental health experts in Slovakia are learning from COVID-19 pandemic? Indian J Psychiatry. 2020;62(Suppl 3):459–66.
Rabinčák M, Tkáčová Ľ, VYUŽÍVANIE PSYCHOMETRICKÝCH KONŠTRUKTOV PRE, HODNOTENIE PORÚCH NÁLADY V OŠETROVATEĽSKEJ PRAXI. Zdravotnícke Listy. 2019;7:7.
Google Scholar
Sekot M, Gürlich R, Maruna P, Páv M, Uhlíková P. Hodnocení úzkosti a deprese u pacientů se zhoubnými nádory trávicího traktu. Čes a slov Psychiat. 2005;101:252–7.
Lipsitch M, Krammer F, Regev-Yochay G, Lustig Y, Balicer RD. SARS-CoV-2 breakthrough infections in vaccinated individuals: measurement, causes and impact. Nat Rev Immunol. 2022;22:57–65.
Accorsi EK, Britton A, Fleming-Dutra KE, Smith ZR, Shang N, Derado G, et al. Association between 3 doses of mRNA COVID-19 vaccine and symptomatic infection caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327:639–51.
Barda N, Dagan N, Cohen C, Hernán MA, Lipsitch M, Kohane IS, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. 2021;398:2093–100.
Magen O, Waxman JG, Makov-Assif M, Vered R, Dicker D, Hernán MA, et al. Fourth dose of BNT162b2 mRNA Covid-19 vaccine in a nationwide setting. N Engl J Med. 2022;386:1603–14.
Dubé JP, Smith MM, Sherry SB, Hewitt PL, Stewart SH. Suicide behaviors during the COVID-19 pandemic: a meta-analysis of 54 studies. Psychiatry Res. 2021;301:113998.
Kok AAL, Pan K-Y, Rius-Ottenheim N, Jörg F, Eikelenboom M, Horsfall M, et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in dutch case-control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J Affect Disord. 2022;305:85–93.
Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve J-E, et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. The Lancet Public Health. 2022;7:e417–26.
Prochazka J, Scheel T, Pirozek P, Kratochvil T, Civilotti C, Bollo M, et al. Data on work-related consequences of COVID-19 pandemic for employees across Europe. Data Brief. 2020;32:106174.
Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the Mental Health of Children and Adolescents in the Context of COVID-19. J Am Acad Child Adolesc Psychiatry. 2020;59:1218–1239e3.
Zetterqvist M, Jonsson LS, Landberg Ã, Svedin CG. A potential increase in adolescent nonsuicidal self-injury during covid-19: a comparison of data from three different time points during 2011–2021. Psychiatry Res. 2021;305:114208.
Mooldijk SS, Dommershuijsen LJ, de Feijter M, Luik AI. Trajectories of depression and anxiety during the COVID-19 pandemic in a population-based sample of middle-aged and older adults. J Psychiatr Res. 2022;149:274–80.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. 2021;107:110247.
Stephenson E, O’Neill B, Kalia S, Ji C, Crampton N, Butt DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. 2022;303:216–22.
Goldberg X, Castaño-Vinyals G, Espinosa A, Carreras A, Liutsko L, Sicuri E et al. Mental health and COVID-19 in a general population cohort in Spain (COVICAT study).Soc Psychiatry Psychiatr Epidemiol. 2022;:1–12.
Zhao Y, Yu Y, Zhao R, Cai Y, Gao S, Liu Y, et al. Association between fear of COVID-19 and hoarding behavior during the outbreak of the COVID-19 pandemic: the mediating role of mental health status. Front Psychol. 2022;13:996486.
Furstova J, Kascakova N, Sigmundova D, Zidkova R, Tavel P, Badura P. Perceived stress of adolescents during the COVID-19 lockdown: bayesian multilevel modeling of the Czech HBSC lockdown survey. Front Psychol. 2022;13:964313.
Garbóczy S, Szemán-Nagy A, Ahmad MS, Harsányi S, Ocsenás D, Rekenyi V, et al. Health anxiety, perceived stress, and coping styles in the shadow of the COVID-19. BMC Psychol. 2021;9:53.
Wathelet M, Duhem S, Vaiva G, Baubet T, Habran E, Veerapa E, et al. Factors Associated with Mental Health Disorders among University students in France Confined during the COVID-19 pandemic. JAMA Netw Open. 2020;3:e2025591.
Download references
Acknowledgements
We would like to provide our appreciation and thanks to all the respondents in this study.
This research project received no external funding.
Author information
Authors and affiliations.
Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Ida Kupcova, Lubos Danisovic & Stefan Harsanyi
Institute of Histology and Embryology, Faculty of Medicine, Comenius University in Bratislava, Sasinkova 4, Bratislava, 811 08, Slovakia
Martin Klein
You can also search for this author in PubMed Google Scholar
Contributions
IK and SH have produced the study design. All authors contributed to the manuscript writing, revising, and editing. LD and MK have done data management and extraction, SH did the data analysis. Drafting and interpretation of the manuscript were made by all authors. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Stefan Harsanyi .
Ethics declarations
Ethics approval and consent to participate.
Ethical permission was obtained from the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava (Reference number: ULBGaKG-02/2022). The need for informed consent was waived by the Ethics Committee of the Institute of Medical Biology, Genetics and Clinical Genetics, Faculty of Medicine, Comenius University in Bratislava due to the anonymous design of the study. This study did not process any personal data and the dataset does not contain any direct or indirect identifiers of participants. This study was performed in line with the principles of the Declaration of Helsinki. All methods were carried out following the institutional guidelines.
Consent for publication
Not Applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Kupcova, I., Danisovic, L., Klein, M. et al. Effects of the COVID-19 pandemic on mental health, anxiety, and depression. BMC Psychol 11 , 108 (2023). https://doi.org/10.1186/s40359-023-01130-5
Download citation
Received : 14 November 2022
Accepted : 20 March 2023
Published : 11 April 2023
DOI : https://doi.org/10.1186/s40359-023-01130-5
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Mental health
BMC Psychology
ISSN: 2050-7283
- General enquiries: [email protected]
Click through the PLOS taxonomy to find articles in your field.
For more information about PLOS Subject Areas, click here .
Loading metrics
Open Access
Peer-reviewed
Research Article
Impact of COVID-19 pandemic on mental health: An international study
Roles Conceptualization, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
* E-mail: [email protected]
¶ ‡ ATG, MK and AK designed and implemented the study together. AK and MK should be considered joint senior authors.
Affiliation Division of Clinical Psychology & Intervention Science, Department of Psychology, University of Basel, Basel, Switzerland
Roles Data curation, Formal analysis, Writing – original draft, Writing – review & editing
Affiliation Department of Health Sciences, European University Cyprus, Nicosia, Cyprus
Roles Investigation, Resources, Writing – review & editing
Affiliation Psychological Laboratory, Faculty of Public Health and Social Welfare, Riga Stradiņš University, Riga, Latvia
Affiliation Kore University Behavioral Lab (KUBeLab), Faculty of Human and Social Sciences, Kore University of Enna, Enna, Italy
Affiliation Department of Social Sciences, School of Humanities and Social Sciences, University of Nicosia, Nicosia, Cyprus
Affiliation Department of Nursing, Cyprus University of Technology, Limassol, Cyprus
Affiliation Cyprus Institute of Neurology and Genetics, Nicosia, Cyprus
Affiliation Department of Psychological Counseling and Guidance, Faculty of Education, Hasan Kalyoncu University, Gaziantep, Turkey
Affiliation The Nethersole School of Nursing, Faculty of Medicine, The Chinese University of Hong Kong, Hong Kong
Affiliation Department of Psychology, Fundación Universitaria Konrad Lorenz, Bogotà, Columbia
Roles Conceptualization, Investigation, Resources, Writing – review & editing
Affiliation Faculty of Psychology, University of La Sabana, Chía, Columbia
Affiliation School of Applied Psychology, University College Cork, Cork, Ireland
Affiliation School of Psychology, University College Dublin, Dublin, Ireland
Affiliation Medical University Innsbruck, Innsbruck, Austria
Affiliation Department of Psychology, Babeş-Bolyai University (UBB), Cluj-Napoca, Romania
Affiliation Instituto Superior de Psicologia Aplicada (ISPA), Instituto Universitário; APPsyCI—Applied Psychology Research Center Capabilities & Inclusion, Lisboa, Portugal
Affiliation Faculdade de Psicologia, Alameda da Universidade, Universidade de Lisboa, Lisboa, Portugal
Affiliation LIP/PC2S, Université Grenoble Alpes, Grenoble, France
Affiliation Department of Biomedicine, Biotechnology and Public Health, University of Cadiz, Cadiz, Spain
Affiliation Instituto ACT, Madrid, Spain
Affiliation Department of Psychology, European University of Madrid, Madrid, Spain
Affiliation Department of Psychology and Sociology, University of Zaragoza, Zaragoza, Spain
Affiliation Vadaskert Child and Adolescent Psychiatric Hospital, Budapest, Hungary
Affiliation Private Pratice, Poland
Affiliation Department of Psychology, University of Jyväskylä, Jyväskylä, Finland
Affiliation Clinic for Psychiatry, Clinical Center of Montenegro, Podgorica, Montenegro
Affiliation Ljubljana University Medical Centre, Ljubljana, Slovania
Affiliation Département de Psychologie, Université du Québec à Trois-Rivières, Trois-Rivières, Canada
Affiliation Department of Psychiatry and Behavioral Science, Duke University, Durham, North Carolina, United States of America
Roles Conceptualization, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing
Affiliation Department of Psychology, University of Cyprus, Nicosia, Cyprus
- [ ... ],
- [ view all ]
- [ view less ]
- Andrew T. Gloster,
- Demetris Lamnisos,
- Jelena Lubenko,
- Giovambattista Presti,
- Valeria Squatrito,
- Marios Constantinou,
- Christiana Nicolaou,
- Savvas Papacostas,
- Gökçen Aydın,

- Published: December 31, 2020
- https://doi.org/10.1371/journal.pone.0244809
- Reader Comments
The COVID-19 pandemic triggered vast governmental lockdowns. The impact of these lockdowns on mental health is inadequately understood. On the one hand such drastic changes in daily routines could be detrimental to mental health. On the other hand, it might not be experienced negatively, especially because the entire population was affected.
The aim of this study was to determine mental health outcomes during pandemic induced lockdowns and to examine known predictors of mental health outcomes. We therefore surveyed n = 9,565 people from 78 countries and 18 languages. Outcomes assessed were stress, depression, affect, and wellbeing. Predictors included country, sociodemographic factors, lockdown characteristics, social factors, and psychological factors.
Results indicated that on average about 10% of the sample was languishing from low levels of mental health and about 50% had only moderate mental health. Importantly, three consistent predictors of mental health emerged: social support, education level, and psychologically flexible (vs. rigid) responding. Poorer outcomes were most strongly predicted by a worsening of finances and not having access to basic supplies.
Conclusions
These results suggest that on whole, respondents were moderately mentally healthy at the time of a population-wide lockdown. The highest level of mental health difficulties were found in approximately 10% of the population. Findings suggest that public health initiatives should target people without social support and those whose finances worsen as a result of the lockdown. Interventions that promote psychological flexibility may mitigate the impact of the pandemic.
Citation: Gloster AT, Lamnisos D, Lubenko J, Presti G, Squatrito V, Constantinou M, et al. (2020) Impact of COVID-19 pandemic on mental health: An international study. PLoS ONE 15(12): e0244809. https://doi.org/10.1371/journal.pone.0244809
Editor: Joel Msafiri Francis, University of the Witwatersrand, SOUTH AFRICA
Received: October 3, 2020; Accepted: December 16, 2020; Published: December 31, 2020
Copyright: © 2020 Gloster et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Data Availability: All relevant data are within the paper and its Supporting Information files.
Funding: This work was supported by grants from the Swiss National Science Foundation awarded to Andrew T. Gloster (PP00P1_ 163716/1 & PP00P1_190082). The funder provided support in the form of salaries for authors [ATG], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section. One of the authors is employed by a commercial affiliation: Private Pratice, Poland. This affiliation provided support in the form of salaries for authors [BK], but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: One of the authors is employed by a commercial affiliation: Private Pratice, Poland. This affiliation provided support in the form of salaries for author BK, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. This does not alter our adherence to PLOS ONE policies on sharing data and materials. No other authors have competing interests to declare.
Introduction
The COVID-19 global pandemic caused by the severe acute respiratory syndrome coronavirus 2 (SARS-COV-2) virus triggered governmentally mandated lockdowns, social distancing, quarantines and other measures in the interest of public health. The mandated lockdowns abruptly and dramatically altered people’s daily routines, work, travel, and leisure activities to a degree unexperienced by most people living outside of war zones. Simultaneously, the highly contagious, yet invisible virus transformed previously neutral situations to perceived potentially dangerous ones: social interaction, touching one’s face, going to a concert, shaking someone’s hand, and even hugging grandparents. Given these changes and looming threat, increases in anxiety and depression can be expected [ 1 ]. Indeed, common psychological reactions to previous quarantines include post-traumatic symptoms, confusion, and anger [ 2 ], though these data stem from quarantines of specific regions or a subgroup of exposed people, such as medical professionals. It therefore remains an empirical question whether such patterns are consistent when entire populations across the globe are simultaneously affected.
For most people, it stands to reason that governmentally mandated lockdowns decrease their activity levels and the number of stimuli experienced compared to pre-lockdown levels. The impact of reducing activities, stimuli and routines on the population is unknown, but various analogue situations can be used to make predictions, like death of a spouse [ 3 ]; hearing loss [ 4 ]; job loss [ 5 ]; long duration expeditions [ 6 ]; poor acculturation [ 7 ]; and even ageing when combined with loneliness [ 8 ]. Each of these situations is associated with increases in psychological distress. This reduction of stimulations may lead to boredom and reductions in reinforcement, which has been associated with depression [ 9 ]. The sum total of these literatures, and some evidence from country specific studies on COVID-19 suggests that for some people, the mental distress in the form of stress, depression, and negative affect are likely reactions to the lockdown; therefore, people’s wellbeing is likely to suffer. Indeed, increased loneliness, social isolation, and living alone are associated with increased mortality [ 10 ]–the exact effect that mandated lockdown and social distancing rules aimed to counteract.
Alternately, the planned slowing down of daily routines can be beneficial. For example, vacations and weekends are highly sought-after–if not always achieved–periods of relaxation and stress reduction [ 11 ]. Likewise, some religious and spiritual traditions encourage simplicity, mindfulness, and solitude with the goal of increasing wellbeing [ 12 ]. It is therefore conceivable that for some people the lockdown could offer a reprieve from daily hassles and stress and even lead to increases in wellbeing. It is therefore equally important to identify protective factors that can buffer against the negative effects of the lockdown.
Although nearly all people around the globe have been subject to some form of lockdown measures to contain the COVID-19 response, variations exist with respect to how each person is confined, even within a single country. For instance, during the COVID-19 pandemic some people were allowed to go to work, whereas others were required to work exclusively from home. For various reasons, some people had difficulty obtaining some basic supplies. Further, some were thrust into the situation of taking care of others (e.g., children, due to closing of schools). Finally, some people lost income as a result of the lockdown, and this is a known risk-factor for poor mental health [ 13 , 14 ]. Finally, a lockdown may be experienced differently the longer it continues and potentially when in confined spaces [ 2 ]. All of these lockdown-specific features may have an impact on one’s mental health, but to date it remains inadequately explored.
As the risk of the pandemic continues, it is important to understand to what degree the virus-induced uncertainty and the lockdown-induced changes in daily routines impact stress, depression, affect, and wellbeing. Towards this end, it is important to identify factors that can mitigate potential negative psychological effects of pandemics and lockdowns. Various social and psychological factors have been identified in other contexts that may also help build resilience in large-scale pandemics such as COVID-19. On the social level, one such candidate is social support, which has repeatedly been found to positively impact mental health and wellbeing [ 15 – 18 ]. Another social factor is the family climate and family functioning, which clearly impacts people’s mental health [ 19 , 20 ]. Psychological factors such as mindfulness and psychologically flexible response styles (as opposed to rigid and avoidant response styles) are behavioral repertoires that have previously been shown to buffer the impact of stress and facilitate wellbeing [ 21 – 24 ].
Given the scope of the COVID-19 pandemic, it is crucial to better understand how a pandemic and associated lockdowns impact on mental health. Thus, the aim of this study was to determine mental health outcomes and to examine known predictors of outcomes to identify psychological processes and contextual factors that can be used in developing public health interventions. It can be assumed, but remains untested, that those with risks in social-demographic factors, living conditions, social factors and psychological factors have more severe reactions to the lockdown. We therefore tested whether outcomes of stress, depression, affect, and wellbeing were predicted by country of residence, social demographic characteristics, COVID-19 lockdown related predictors, social predictors, and psychological predictors.
Participants
The inclusion criteria were ≥18 years of age and ability to read one of the 18 languages (English, Greek, German, French, Spanish, Turkish, Dutch, Latvian, Italian, Portuguese, Finnish, Slovenian, Polish, Romanian, Hong Kong, Hungarian, Montenegrin, & Persian.). There were no exclusion criteria. People from all countries were eligible to participate.
Ethics approval was obtained from the Cyprus National Bioethics Committee (ref.: EEBK EΠ 2020.01.60) followed by site approvals from different research teams involved in data collection. All participants provided written informed consent prior to completing the survey (computer-based, e.g., by clicking “yes”).
A population based cross-sectional study was conducted in order to explore how people across the world reacted to the COVID-19. The anonymous online survey was distributed using a range of methods. Universities emailed the online survey to students and academic staff and also posted the survey link to their websites. In addition, and in order to broaden the sample to older age groups and to those with different socio-demographic characteristics, the survey was disseminated in local press (e.g., newspapers, newsletters, radio stations), in social media (e.g., Facebook, Twitter, etc.), in professional networks, local hospitals and health centers and professional groups’ email lists (e.g., medical doctors, teachers, engineers, psychologists, government workers), and to social institutions in the countries (e.g., churches, schools, cities/townships, clubs, etc.).
Data were collected for two months between 07th April and 07th June 2020. The majority of countries where data were collected had declared a state of emergency for COVID-19 during this time.
Well validated and established measures were used to assess constructs. When measures did not already exist in a language, they were subject to forward and backward translation procedures. Well-validated measures of predictors and outcomes and items measuring COVID-19 related characteristics were selected after a consensus agreement among the members of this study.
Respondents’ countries were coded and entered as predictors.
Socio-demographic status.
Participants responded to questions related to their socio-demographic characteristics including their age, gender, country of residence, marital status, employment status, educational level, whether they have children as well as their living situation.
Lockdown variables.
Participants responded to questions related to lockdown including length of lockdown, whether they need to leave home for work, any change in their finances, whether they were able to obtain basic supplies, the amount of their living space confined in during the lockdown. They were also asked whether they, their partner, or a significant other was diagnosed with COVID-19.
Social factors.
Social factors were measured using the Brief Assessment of Family Functioning Scale (BAFFS; [ 25 ]) and the Oslo Social Support Scale (OSSS; [ 26 ]). The BAFFS items are summed to produce a single score with higher scores indicating worse family functioning. The OSSS items are summed up and provide three levels types of social support: low (scored 3–8), moderate (scored 9–11) and high (scored 12–14).
Psychological factors.
Psychological factors including mindfulness and psychological flexibility. Mindfulness was measured using the Cognitive Affective Mindfulness Scale (CAMS; [ 27 ]). The CAMS produces a single score with higher scores indicating better mindfulness qualities. Psychological flexibility (e.g., hold one’s thoughts lightly, be accepting of one’s experiences, engage in what is important to them despite challenging situations) was measured using the Psyflex scale [ 28 ]. The Psyflex produces a single score with higher scores indicating better psychological flexibility qualities.
Stress was measured using the Perceived Stress Scale (PSS; [ 29 ]). The PSS assesses an individual’s appraisal of how stressful situations in their life are. Items ask about people’s feelings and thoughts during the last month. A total score is produced, with higher scores indicating greater overall distress.
Depression.
Depressive symptomatology was assessed using two items from the disengagement subscale of the Multidimensional State Boredom Scale (MSBS; [ 30 ]). These items assessed wanting to do pleasurable things but not finding anything appealing (i.e., boredom), as well as wasting time. Based on concepts of reinforcement deprivation (i.e., lack of access to or engagement with positive stimuli) that is known to contribute to depression, we added an item that measured how rewarding or pleasurable people found the activities that they were engaging in (i.e., reinforcement). Higher scores indicated higher depressive symptomatology.
Positive affect/ negative affect.
The Positive And Negative Affect Scale (PANAS) was used to measure affect [ 31 ]. The original version of the questionnaire was used with five additional items: bored, confused, angry, frustrated and lonely. All items were scored on a 5-point Likert type scale, ranging from 1 = very little/not at all to 5 = extremely and summed up so that higher scores in the positive-related items indicating higher positive affect and higher scores in the negative-related items indicating higher negative affect. In order to capture additional dimensions of negative affect believed to be relevant to the COVID-19 lockdowns, we additionally added five items: bored, confused, angry, frustrated, lonely.
Wellbeing was assessed using the Mental Health Continuum Short Form (MHC-SF; [ 32 ]); which assesses three aspects of wellbeing: emotional, psychological, and social. The MHC-SF produces a total score and scores for each of the three aspects of wellbeing. The MHC-SF can also be scored to produce categories of languishing (i.e., low levels of emotional, psychological, and social well-being), flourishing (i.e., high levels of emotional psychological and social well-being almost every day), and moderately mentally healthy (in between languishing and flourishing).
Statistical analysis
The mean and standard deviation was calculated for dependent variables that follow the normal distribution while the median and interquartile range (IQR) were computed for non-normally distributed data. Bivariable association between an outcome variable and each predictor was investigated with ANOVA test for categorical predictor and univariable linear regression for numerical predictor. Linear mixed-effect model with random effect for country was performed to consider simultaneously several predictors in the same model and to account for the variation in outcome variable between countries. Four separate linear mixed-effect models were used for each outcome variable, one for each set of socio-demographic, lockdown, social and psychosocial predictors and multicollinearity for each set of predictors was investigated with the variation inflation criterion (VIF). Standardized regression coefficients were computed as effect size indices to measure the strength of the association between predictor variables and outcome variables. The comparison between the country mean and overall mean for each outcome variable was estimated though a linear regression model with dependent variable the mean centering outcome and predictor the country. Cohen’s d effect size of the standardize difference between country mean and the overall mean was computed as a measure of the magnitude of the difference between the two means.
The whole sample was used in linear mixed-effect models while for the comparison of country mean to the overall mean was used the sample from countries with sample size ≥100. The R packages lme4 and effect sizes were used for fitting the linear mixed effect model and to compute the standardized regression coefficients of the linear mixed effect models [ 33 ]. Significance test and confidence intervals were calculated at a significance level of 0.05. The following cut-off values were used for the evaluation of the effect sizes: ‘tiny’ ≤0.05, ‘very small’ from 0.05 to ≤0.10, ‘small’ from 0.10 to ≤ 0.20, ‘medium’ from 0.20 to ≤ 0.30, ‘large’ from 0.30 to ≤ 0.40 and ‘very large’ > 0.40 [ 34 ].
Descriptive
Participants were n = 9,565 people from 78 countries. See supporting information for a participation flowchart ( S1 Appendix ). The countries with the largest samples were: Latvia (n = 1285), Italy (n = 962), Cyprus (n = 957), Turkey (n = 702), Switzerland (n = 550), Hong Kong (n = 516), Colombia (n = 485), Ireland (n = 414), Austria (n = 368), Romania (n = 339), Portugal (n = 334), France (n = 313), Spain (n = 296), Germany (n = 279), Hungary (n = 273), Greece (n = 270), USA (n = 268), Finland (n = 157), Montenegro (n = 147), Poland (n = 135), United Kingdom (n = 100), Slovenia (n = 77), and Canada (n = 60). The remaining countries are listed in the supporting information ( S1 Table ).
Outcome variables
The means, standard deviations, and where appropriate percentage of participants within categories of the five outcome variables can be seen in Table 1 .
- PPT PowerPoint slide
- PNG larger image
- TIFF original image
https://doi.org/10.1371/journal.pone.0244809.t001
Predictor variables
A full list of countries can be found in the supporting information ( S1 Table ).
The mean age was 36.9 (13.3) years. A majority of participants were female (77.7%), approximately a fifth male (22.0%), and small minority identified as other (0.3%). More than half of the respondents were either in a relationship (25.7%) or married (36.1%), almost a third were single (30.8%), and the rest were either divorced (5%), widower (1.1%) or other (1.3%). Participants indicated that they lived: alone (14.6%), with both parents (20.8%), one parent (5.1%), with their own family including partner and children (54.1%), or with friends or roommates (5.5%). Less than half of respondents had children (40.8%). Approximately half of the participants were working full time (53.4%), almost a fifth were working part-time (17.5%), 23.2% were unemployed and a small minority were either on parental leave (2.2%) or retired (3.7%).
COVID-19 lockdown variables.
At the time of responding, participants were in lockdown or self-isolation for a median of 5.0 (3.0 IQR) weeks. Most people indicated that they had not been infected with COVID-19 (88.0%), a small minority indicated they had been infected (1.4%) and the rest had symptoms but were unsure (10.6%). Similar patterns were seen with reported infection rates of partners (no: 92.2%, yes: 0.7%, unsure: 7.1%) and of people close to them (no: 86.0%; yes: 5.6%; unsure: 8.4%). With respect to leaving the house for work, almost half (47.7%) indicated that this never occurred, 7.7% indicated leaving only once, whereas an almost equal number indicated leaving a couple times per week (23.7%) or more than three times per week (21.0%). Nearly all participants indicated they were able to obtain all the basic supplies they needed (93.5%). Participants reported having a median inner living space of 90.0 square meters (80.0 IQR) and median outdoor space of 20.0 square meters (192.1 IQR). Finally, with respect to finances, more than half indicated that their financial situation remained about the same (57.9%), a minority indicated it improved (8.9%), and a third reported that their finances had gotten worse (33.3%).
Social and psychological predictors.
Mean values of the other predictors (i.e., social predictors and psychological predictors) can be seen in Table 1 .
Multivariate analyses
Results of multivariate analyses for the outcome of stress can be seen in Table 2 . The largest protective factor against stress was social support (high support vs low support (-3.35, 95%CI, -3.39 to -2.92), with a very large effect size). Positive predictors of stress with large effect sizes were being female (2.42, 95%CI, 2.07 to 2.77) and worsening of finances (2.32, 95%CI, 1.68 to 2.96), whereas psychological flexibility buffered this response (-0.65, 95%CI, -0.69 to -0.62). Higher education levels were also associated with lower levels of stress, with a large effect size (see Table 2 ). Moderate effect sizes for predictors associated with less stress were older age (-0.13, 95%CI, -0.14, -0.11) and mindfulness (-0.69, 95%CI, -0.74, -0.64). Moderate effect sizes of predictors associated with more stress were worse family functioning (0.98, 95%CI, 0.90, 1.06) and not being able to obtain all basic supplies (1.82 95%CI, 1.12, 2.52).
https://doi.org/10.1371/journal.pone.0244809.t002
Differences in reported levels of stress across countries were largely negligible, with the exception of two countries that reported higher levels of stress (Hong Kong (2.85, 95%CI, 2.22, 3.49) and Turkey (2.47, 95%CI, 1.93, 3.02)) and two that reported lower levels of stress (Portugal (-2.50, 95%CI, -3.29, -1.71) and Montenegro (-3.30, 95%CI, -4.49, -2.11)) than the average stress level across all countries. See supporting information for information on each country ( S2 – S6 Tables).
Results of multivariate analyses for the outcome of depression can be seen in Table 3 . The strongest predictor of depression was social support, such that high (-1.30, 95%CI, -1.44, -1.16) and medium levels (-0.73, 95%CI, -0.85, -0.62) of social support were protective against depression (relative to low levels) with a very large and large effect sizes, respectively. The only other large effect size was for psychological flexibility, which also served in a protective manner (-0.20, 95%CI, -0.22, -0.19). Moderate effect sizes of predictors associated with less depression symptoms were also observed for higher education levels (see Table 3 ). Moderate effect sizes of predictors associated with more depression were worse family functioning (0.29, 95%CI, 0.27, 0.32) and not being able to obtain all basic supplies (0.49, 95%CI, 0.27, 0.70).
https://doi.org/10.1371/journal.pone.0244809.t003
The amount of depression symptoms reported on average within countries was similar for most countries with the exception of one country with lower reported levels than average with a large effect size (Austria (-0.71, 95%CI, -0.95, -0.47)) and one with higher levels than average with a large effect size (USA (0.85, 95%CI, 0.58, 1.13)). See supporting information for information on each country ( S2 – S6 Tables).
Results of multivariate analyses for the outcome of affect can be seen in Table 4 . With respect to positive affect, social support (high support vs low support (5.69, 95%CI, 5.23, 6.16) and psychological flexibility (0.77, 95%CI, 0.74, 0.81) were both predictors with very large effect sizes. Interestingly, those who left their house more than three times per week had higher levels of positive affect than those that did not leave their house for work (1.68, 95%CI, 1.18, 2.17), with a medium effect size. Higher education levels were associated with higher levels of positive affect with a medium to large effect size (see Table 4 , PANAS-Positive).
https://doi.org/10.1371/journal.pone.0244809.t004
The amount of positive affect reported on average within countries was similar for most countries with the exception of one country with lower reported levels than average with a large effect size (Finland (-2.96, 95%CI, -4.19, -1.73)) and one with higher reported levels than average with a large effect size (Portugal (2.96, 95%CI, 2.12, 3.80)). See supporting information for information on each country ( S2 – S6 Tables).
With respect to negative affect, social support (high support vs low support (-2.74, 95%CI, -3.2, -2.29) and psychological flexibility (-0.62, 95%CI, -0.66, -0.58) were again the strongest associated predictors, with large effects. Higher education levels were also associated with lower levels of negative affect, with a medium effect (see Table 4 , PANAS-Negative). Higher levels of negative affect were noted, with medium effect sizes, for the predictors: worsening of finances (1.75, 95%CI, 1.10, 2.40) and not being able to obtain all basic supplies (1.6, 95%CI, 0.89, 2.31).
The amount of negative affect reported on average within countries was similar for most countries with the exception of few countries with lower reported negative affect levels than average with a very large effect sizes (Switzerland (-4.96, 95%CI, -5.91, -4.01), Germany (-4.70, 95%CI, -6.03, -3.37) & Austria (-6.49, 95%CI, -7.65, -5.33)) and one with a large effect size (Montenegro (-3.56, 95%CI, -5.39, -1.73). The average amount of negative affect was higher than average in two countries, with very large effects size (Turkey (5.75, 95%CI, 4.92, 6.59) & Finland (7.57, 95%CI, 5.80, 9.34)). See supporting information for information on each country ( S2 – S6 Tables).
Results of multivariate analyses for the outcome of wellbeing can be seen in Table 5 . Once again, social support (high support vs low support (13.20, 95%CI, 12.39, 14.01)) and psychological flexibility (1.42, 95%CI, 1.34, 1.49) were the predictors with the largest effect sizes (very large) on wellbeing. Higher education levels were associated with higher levels of wellbeing with a medium to large effect sizes (see Table 5 ). Medium negative effect sizes were noted for family functioning (-1.98, 95%CI, -2.12, -1.83) and inability to obtain all basic supplies (-3.27, 95%CI, -4.67, -1.87). Two medium positive effect sizes were observed: mindfulness (0.95, 95%CI, 0.86–1.04) and living with friends/roommates ((3.04, 95%CI, 1.59, 4.48), relative to living alone).
https://doi.org/10.1371/journal.pone.0244809.t005
The level of wellbeing reported on average within countries was similar for most countries with the exception of three countries with higher levels with large effect sizes (Austria (4.95, 95%CI, 3.55, 6.34), Finland (5.24, 95%CI, 3.10, 7.38), & Portugal (4.59, 95%CI, 3.12, 6.05)) and two countries with lower levels of wellbeing than average with large (Italy (-4.36, 95%CI, -11.06, 2.35)) and very large effect sizes (Hong Kong (-6.84, 95%CI, -8.02, -5.66)). See supporting information for information on each country ( S2 – S6 Tables).
The COVID-19 is the largest pandemic in modern history. This study assessed nearly 10,000 participants across many countries to examine the impact of the pandemic and resultant governmental lockdown measures on mental health. During the height of the lockdown, the pandemic was experienced as at least moderately stressful for most people, and 11% reported the highest levels of stress. Symptoms of depression were also high, including 25% of the sample indicating that the things they did were not reinforcing, 33% reporting high levels of boredom, and nearly 50% indicating they wasted a lot of time. Consistent with symptoms of stress and depression, 10% of participants were psychologically languishing. These results suggest that there is a subgroup of people who are especially suffering and that in about 50% of the respondents’ levels of mental health was only moderate. Previous studies have found that along with low levels, even moderate levels of mental health (which consists of only moderate levels of emotional, psychological, and social well-being) are associated with increased subsequent disability, productivity loss, and healthcare use [ 35 – 37 ]. Not everyone was suffering, however, as evidenced by the nearly 40% of participants who reported levels of mental health consistent with flourishing. The present results, while serious, do not point to more severe reactions observed in previous samples of selective quarantined individuals or groups [ 2 ]. Perhaps the previously reported distress in these groups is prevented when an entire country or world is in lockdown so that the feeling emerges that “everyone is in it together”.
Importantly, a handful of predictors emerged that consistently predicted all outcomes: Social support, education level, finances, access to basic needs, and the ability to respond psychologically flexible. The consistency of results examining predictors is noteworthy, both in terms of the consistently strong predictors (e.g., social support, education, psychological flexibly, as well as loss of income and lack of access to necessities) and in terms of the other predictors that were either not predictive or only weakly so. All predictors were chosen based on theoretical ties to the outcomes, previous findings, and studies on quarantines [ 2 ].
A novel finding was that people who left their house three or more times per week reported more positive affect than those that left their house less often. It is possible that these people experienced more variation, which contributed to positive affect. It is also possible they experienced a greater sense of normality. Future studies are encouraged to further investigate possible mechanisms through which this result unfolds.
Overall, these patterns did not differ substantially between countries. Although some differences did emerge, they were mostly inconsistent across outcomes. Three countries fared worse on two outcomes each: Hong Kong (stress & wellbeing); Turkey (stress & negative affect); and Finland (lower positive affect and higher negative affect)–though participants in Finland also reported higher levels of wellbeing than average. Two countries had more favorable outcomes than the average levels across all countries: Portugal (lower stress and higher wellbeing) and Austria (lower depression and higher wellbeing). The differences observed are likely due to a combination of chance, sampling, nation specific responses to the COVID-19 pandemic, cultural differences, and other factors playing out in the countries (e.g., political unrest [ 38 ]). If replicated, future studies are encouraged to examine possible mechanisms of these outcomes.
This study provides valuable insights on several levels. First, it documents the mental health outcomes across a broad sample during the COVID-19 global pandemic. Second, it informs about the conditions and resilience factors (social support, education, and psychological flexibility) and risk factors (loss of income and inability to get basic supplies) that affect mental health outcomes. Third, these factors can be used in future public health responses are being made, including those that require large scale lockdowns or quarantines. That is, public health officials should direct resources to identifying and supporting people with poor social support, income loss, and potentially lower levels of education and provide a strategy to mitigate special risks in these subpopulations. The importance of social support needs to be made clear to the public and to the degree possible mechanisms that can contribute to social support should be supported. Further, psychological flexibility is a trainable set of skills that has repeatedly been shown to ameliorate suffering [ 22 , 39 ]; and can be widely distributed with modern technological intervention tools such as digital, internet, or virtual means [ 40 ]. We do not claim, however, that psychological flexibility is the only factor that can be used for interventions. Instead, it is a recognized transdiagnostic factor assessed in this study and one that is feasible to be targeted and modified by interventions and prevention [ 41 – 43 ].
This study is limited by several important factors. First, the results are based on cross sectional analysis and correlations. As such, causation cannot be inferred and any delayed impact of the pandemic and lockdown on peoples’ mental health was not captured. Second, all results of this survey were obtained via self-report questionnaires, which can be subject to retrospective response bias. Third, although the sample was large and based on varied recruitment sources, it was not representative of the population and undersampled people who suffered most from the pandemic (i.e., front line health care professionals, people in intensive care, etc.) or people without internet access, etc. Finally, the country-specific incidence rates and lockdown measures differed across countries. These were not assessed, but future studies are encouraged to investigate how such factors impact mental health outcomes.
These limitations notwithstanding, based on nearly 10,000 international participants, this study found that approximately 10% of the population was languishing during or shortly after the lockdown period. These finding have implications for public health initiatives. First, officials are urged to attend to, find, and target people who have little social support and/ or whose finances have worsened as a result of the measures. Second, public health interventions are further urged to target psychological processes such as psychological flexibility in general to potentially help buffer other risk factors for mental health. Likewise, availability of social support and information about where to get support and remain connected are needed. These recommendations should become part of public health initiatives designed to promote mental health in general, and should equally be considered when lockdowns or physical distancing are prescribed during a pandemic.
Supporting information
S1 table. list of all countries included in the data set..
https://doi.org/10.1371/journal.pone.0244809.s001
S2 Table. Geodemographic predictors for Perceived Stress Scale.
https://doi.org/10.1371/journal.pone.0244809.s002
S3 Table. Geodemographic predictors for MSBS–depression.
https://doi.org/10.1371/journal.pone.0244809.s003
S4 Table. Geodemographic predictors for PANAS positive.
https://doi.org/10.1371/journal.pone.0244809.s004
S5 Table. Geodemographic predictors for PANAS negative.
https://doi.org/10.1371/journal.pone.0244809.s005
S6 Table. Geodemographic predictors for MHCSF—mental health continuum.
https://doi.org/10.1371/journal.pone.0244809.s006
S1 Appendix. Participation flowchart.
https://doi.org/10.1371/journal.pone.0244809.s007
Acknowledgments
We wish to thank the following people for their work in helping to implement the study: Spyros Demosthenous, Christiana Karashali, Diamanto Rovania (University of Cyprus); Maria Antoniade (European University of Cyprus); Ioanna Menoikou (Cyprus University of Technology); Elias Ioannou (University of Nicosia); Sonja Borner, Victoria Firsching-Block, Alexander Fenn (University of Basel); Cristīne Šneidere, Ingrīda Trups-Kalne, Lolita Vansovica, Sandra Feldmane, (Riga Stradiņš University); David Nilsson (Lund University); Miguel A. Segura-Vargas (Fundación Universitaria Konrad Lorenz); Claudia Lenuţa Rus, Catalina Otoiu, Cristina Vajaean (Babes-Bolyai University). We further wish to thank Fabio Coviello and Sonja Borner (University of Basel) for their help in preparing the manuscript.
- View Article
- Google Scholar
- 2. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Vol. 395, The Lancet. Lancet Publishing Group; 2020. p. 912–20.
- 3. Kristensen P, Weisaeth L, Heir T. Bereavement and mental health after sudden and violent losses: A Review. Vol. 75, Psychiatry. Guilford Publications Inc; 2012. p. 76–97. https://doi.org/10.1521/psyc.2012.75.1.76 pmid:22397543
- PubMed/NCBI
- 6. Alfano CA, Bower JL, Cowie J, Lau S, Simpson RJ. Long-duration space exploration and emotional health: Recommendations for conceptualizing and evaluating risk. Vol. 142, Acta Astronautica. Elsevier Ltd; 2018. p. 289–99.
- 9. Kanter JW, Busch AM, Weeks CE, Landes SJ. The nature of clinical depression: Symptoms, syndromes, and behavior analysis. Vol. 31, Behavior Analyst. Association for Behavior Analysis; 2008. p. 1–21.
- 12. Koenig HG. Research on religion, spirituality, and mental health: A review. Vol. 54, Canadian Journal of Psychiatry. Canadian Psychiatric Association; 2009. p. 283–91. https://doi.org/10.1177/070674370905400502 pmid:19497160
- 23. Gu J, Strauss C, Bond R, Cavanagh K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Vol. 37, Clinical Psychology Review. Elsevier Inc.; 2015. p. 1–12. https://doi.org/10.1016/j.cpr.2015.01.006 pmid:25689576
- 29. Cohen S. Perceived stress in a probability sample of the United States. In: The social psychology of health. Thousand Oaks, CA, US: Sage Publications, Inc; 1988. p. 31–67. (The Claremont Symposium on Applied Social Psychology.).
- 43. Dindo L, Van Liew JR, Arch JJ. Acceptance and Commitment Therapy: A Transdiagnostic Behavioral Intervention for Mental Health and Medical Conditions. Vol. 14, Neurotherapeutics. Springer New York LLC; 2017. p. 546–53. https://doi.org/10.1007/s13311-017-0521-3 pmid:28271287
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Mental Health and COVID-19
- Mental Health Diversity, Equity, and Inclusion
- Origins of Mental Health
- Job Openings
- Faculty Profiles
- PET Alumni Profiles - Postdocs
- PET Alumni Profiles - Predocs
- Trainee Profiles
- NIMH T32 Mental Health Services and Systems Training Grant
- Funded Training Program in Data Integration for Causal Inference in Behavioral Health
- Aging and Dementia Funded Training Program
- COVID-19 and Mental Health Research
- Mental Health Resources During COVID-19
- News and Media
- Social Determinants of Mental and Behavioral Health
Our Work in Action
- Global Mental Health
- Related Faculty
- Courses of Interest
- Training and Funding Opportunities
- Mental Health in the Workplace: A Public Health Summit
- Autism and Developmental Disabilities
- Alumni Newsletters
- Alumni Updates
- Postdoctoral Fellows
- Doctor of Philosophy (PhD) Students in Mental Health
- Master of Health Science (MHS) Students in Mental Health
- In the News
- Past Seminars 2020-21 AY: Wednesday Seminar Series
- Make a Gift
- Available Datasets
The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 pandemics implications for mental health, building on a robust literature on how environmental crises, such as SARS or natural disasters, can lead to mental health challenges, including loneliness, acute stress, anxiety, and depression. The social distancing aspects of the COVID-19 pandemic may have particularly significant effects on mental health. Understanding how mental health evolves as a result of this serious global pandemic will inform prevention and treatment strategies moving forward, including allocation of resources to those most in need. Critically, these data can also serve as evidence-based information for public health organizations and the public as a whole.
Understanding the Mental Health Implications of a Pandemic


Introduction
The world is entering into a new phase with COVID-19 spreading rapidly. People will be studying various consequences of the COVID-19 pandemic and mental and behavioral health should be a core part of that effort. There is a robust literature on how environmental crises, such as SARS or natural disasters, can lead to mental health challenges, including loneliness, acute stress, anxiety, and depression. The social distancing aspects of the current pandemic may have particularly significant effects on mental health. Understanding how mental health evolves as a result of this serious global outbreak will inform prevention and treatment strategies moving forward, including allocation of resources to those most in need. Critically, these data can also serve as evidence-based information for public health organizations and the public as a whole.
The data will be leveraged to address many questions, such as:
- Which individuals are at greatest risk for high levels of mental health distress during a pandemic?
- As individuals spend more time inside and isolated, how does their mental health distress evolve?
- How do different behaviors (such as media consumption) relate to mental health?
Read more about how our experts are measuring mental distress amid a pandemic.
We have been working to ensure that measurement of mental health measures is a key part of large-scale national and international data collections relative to COVID-19.
Read more about conducting research studies on mental health during the pandemic.
Mental Health Resources
See our resources guide here.
Members of the COVID-19 Mental Health Measurement Working Group
- M. Daniele Fallin, JHSPH
- Calliope Holingue, Kennedy Krieger Institute, JHSPH
- Renee M. Johnson, JHSPH
- Luke Kalb, Kennedy Krieger Institute, JHSPH
- Frauke Kreuter, University of Maryland, University of Mannheim
- Courtney Nordeck, JHSPH
- Kira Riehm, JHSPH
- Emily J. Smail, JHSPH
- Elizabeth Stuart, JHSPH
- Johannes Thrul, JHSPH
- Cindy Veldhuis, Columbia University School of Nursing
The Johns Hopkins COVID-19 Mental Health Measurement Working Group developed key questions to add to existing large domestic and international surveys to measure the mental health impact of the pandemic.

Select Your Interests
Customize your JAMA Network experience by selecting one or more topics from the list below.
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- American Indian or Alaska Natives
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Artificial Intelligence
- Assisted Reproduction
- Bleeding and Transfusion
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Climate and Health
- Climate Change
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life, Hospice, Palliative Care
- Environmental Health
- Equity, Diversity, and Inclusion
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Global Health
- Guide to Statistics and Methods
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Policy
- Health Systems Science
- History of Medicine
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Mobile Health and Telemedicine
- Narrative Medicine
- Neuroscience and Psychiatry
- Notable Notes
- Nutrition, Obesity, Exercise
- Obstetrics and Gynecology
- Occupational Health
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Palliative Care
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Population Health
- Primary Care
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Regulatory Agencies
- Reproductive Health
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Translational Medicine
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
- Download PDF
- Share X Facebook Email LinkedIn
- Permissions
Maximizing the Uptake of a COVID-19 Vaccine in People With Severe Mental Illness : A Public Health Priority
- 1 School of Medicine, University of Queensland, Brisbane, Queensland, Australia
- 2 Metro South Addiction and Mental Health, Brisbane, Queensland, Australia
- 3 Department of Psychiatry, Dalhousie University, Halifax, Nova Scotia, Canada
People with serious mental illness (SMI) are at increased risk of being infected by coronavirus disease 2019 (COVID-19) and have higher subsequent rates of hospitalization, morbidity, and mortality. 1 , 2 Factors that contribute to worse outcomes include concomitant medications, poorer premorbid general health, physical comorbidity, reduced access to medical care, and environmental and lifestyle factors such as lower socioeconomic status, overcrowding, smoking, or obesity. In light of these vulnerabilities, it is important that people with SMI are a priority group to receive a vaccination, should one be developed and deemed safe and effective. 3 De Hert and colleagues 3 noted that there is an ethical duty to prioritize vaccination for people with SMI given their increased risk of worse outcomes following COVID-19 infection and the structural barriers faced by people with SMI in accessing a vaccine. In addressing the Framework for Equitable Allocation of the COVID-19 Vaccine 4 principle mitigation of health inequities, people with SMI should be included with other priority groups, including Indigenous people, older adults, and people with physical health comorbidities.
Over and above the ethical need to ensure vaccination allocation priority for people with SMI, evidence from existing vaccination programs suggests that there are challenges in achieving this aim at both an individual and public health level. People with SMI are less likely to receive preventive or guideline-appropriate health care for concerns such as cardiovascular disease and cancer. This reduced access to preventive care is reflected in the low uptake of immunizations recommended for adults among people with SMI. Of these, influenza may serve as a particularly useful model given the recommendation for an annual vaccination. In contrast with other vulnerable groups in the United States, influenza vaccination rates among people with SMI are as low as 25%. 5 , 6 Based on the experience with influenza vaccination programs, we have outlined key barriers and solutions to access any potential COVID-19 vaccine for people with SMI ( Table ).
Individual-Level Barriers and Solutions
In people with SMI, a willingness to adopt preventive measures, such as vaccination, is facilitated by their perceived risk to self of a preventable disease, peer support, influence, and belief in the effectiveness of the vaccine. 5 - 7 Notably, as reported in a cross-sectional study, education by a health care professional about the role and importance of vaccination increased uptake by 4-fold. 6 Negative beliefs about safety and misconceptions that the vaccine itself can cause the illness may be held by people with SMI. 6 These beliefs should be directly addressed given both are predictive of vaccine hesitancy and avoidance in this population. 6 It would assist this discussion if COVID-19 vaccination trial data from high-risk groups such as those with SMIs can be gained to inform the risk-benefit ratio.
Mental health professionals are uniquely skilled to deliver this education, being able to adapt for those with communication difficulties and balance factors influencing decision-making. There may be a delicate balance between factors that facilitate immunization, such as perceived fear of infection, and those that reduce uptake, such as concurrent general anxiety. 7 This highlights the importance of an individualized and clear message while enhancing capacity to consent.
System-Level Barriers and Solutions
Systemic barriers to vaccination include access, acceptability, awareness of services, cost, and other practical considerations. Historical enrollment into influenza vaccination programs was predictive of future vaccination completion, suggesting these existing routines and resources could also be harnessed for a COVID-19 vaccine. 6 Running vaccination clinics parallel to mental health services can increase vaccination rates by up to 25%. 5 Transportation to the vaccination clinics, even when colocated with a mental health service, may be a significant barrier, especially for infrequent service users. 5 Therefore, one solution may be to embed vaccination clinics within mental health services, although none have been evaluated to date and to our knowledge. Studies also show that children of mothers with psychotic or depressive disorders were less likely to receive vaccinations, suggesting that concurrent family vaccination may have additional benefits. 8 Direct access to existing immunization registers would assist in both monitoring and coordination. Other policy-driven solutions include emergency legislation to allow for a wider group of health care professionals to administer the vaccination. Given that almost 80% of individuals without health insurance do not get vaccinated for influenza, any COVID-19 vaccine should be provided at no cost to the individual. 6
Conclusions
It is vital to commence planning and development of appropriate policies to ensure rapid delivery of a COVID-19 vaccine when it becomes available. It is recognized that COVID-19 has placed strain on mental health services and physical, human, and financial resources. However, use of existing physical health programs, colocation of vaccine administration with mental health services, and, where possible, actually delivering the vaccine may help increase uptake. Importantly, interventions should target both the individual and system level, including active engagement, education, and peer support. Mental health clinicians have a key role in advocating for priority access to a COVID-19 vaccination for those with SMI, as well as facilitating its uptake.
Corresponding Author: Nicola Warren, MBBS, Princess Alexandra Hospital, 199 Ipswich Rd, Woolloongabba, Brisbane, QLD 4102, Australia ( [email protected] ).
Published Online: December 15, 2020. doi:10.1001/jamapsychiatry.2020.4396
Conflict of Interest Disclosures: Dr Warren has received speaker fees from Otsuka and Lundbeck not associated with the submitted work. No other disclosures were reported.
See More About
Warren N , Kisely S , Siskind D. Maximizing the Uptake of a COVID-19 Vaccine in People With Severe Mental Illness : A Public Health Priority . JAMA Psychiatry. 2021;78(6):589–590. doi:10.1001/jamapsychiatry.2020.4396
Manage citations:
© 2024
Artificial Intelligence Resource Center
Psychiatry in JAMA : Read the Latest
Browse and subscribe to JAMA Network podcasts!
Others Also Liked
- Register for email alerts with links to free full-text articles
- Access PDFs of free articles
- Manage your interests
- Save searches and receive search alerts
Events Calendar
- Strauss Health Sciences Library
- Department A-Z Directory
- Campus Directory
- Faculty & Staff Resources
- Supporter & Alumni Resources
- Student Resources
- Mental Health Resources
- University Policies
CU Anschutz Medical Campus
- CU Colorado Springs
- School of Dental Medicine
- Graduate School
- School of Medicine
- College of Nursing
- Skaggs School of Pharmacy and Pharmaceutical Sciences
- Colorado School of Public Health
- Education Student Resources
- Patient Care
- News Latest Stories In The News
- About Our History Mission and Vision Leadership Visit the CU Anschutz Medical Campus Events Calendar Contact Us
- Health Resources
Home News Long COVID Brings Focus to Mental-Physical Connection back to News
Long COVID Brings Focus to Mental-Physical Connection
Scientists and providers seek to understand increased psychiatric health issues post-infection.
minute read
In recognition of Mental Health Awareness Month , the CU Anschutz newsroom is highlighting some of the ways our campus faculty conduct research, provide patient care and extend support around mental health.
While the pandemic left behind millions of people worldwide with lasting COVID-19 effects, it also fueled a research and healthcare focus that Thida Thant , MD, and colleagues have long promoted – the overlap of physical and mental illness.
Some surveys suggest as many as a quarter of the 775 million-plus people infected with SARS-CoV-2 had lingering symptoms at three months out, a phenomenon coined long COVID and now ranked a top research priority in the country. Many of those cases (some studies suggest a majority) included neurological and/or mental health issues.
“I was glad to see a stronger focus on that mind-body connection, the understanding that you could have a psychiatric symptom or illness develop as the result of a physical illness,” said Thant, a psychiatrist who specializes in the intersection between chronic disease and mental illness. “And not just in the coping sort of a way, but directly, as a physiologic result.”
The link between mental illness and long COVID is not novel, said Thant, an assistant professor of psychiatry at the University of Colorado School of Medicine . There are mental health connections between heart disease and other respiratory viral illness.
“But historically, there’s always been this sort of divide, and long COVID has really taught us all that that overlap is there,” said Thant, who works with patients at the UCHealth Post-COVID clinic and is the director of the Psychiatric Consultation for the Medically Complex Program at the CU Anschutz Medical Campus .
Thant, who recently joined colleagues in publishing guidance on treating long COVID mental health disorders for the American Psychiatric Association, shared more about the issues she sees in practice in the Q&A below.

The data appear clear that people are more likely to develop mental health disorders in the months following a COVID infection. Is that correct, and if so, what have we learned about why?
Yes, that definitely happens. The why is still more complicated. There are different hypotheses. A major one involves the inflammatory process and that relationship with viruses and mental illness. There have been lots of folks who have gone for years dealing with other post-viral issues, whether mental- or physical-health related (from flu, Epstein-Barr, measles, etc.). We know that inflammation is also associated with mental health in general.
(Inflammation of the brain can cause confusion, difficulty concentrating and memory problems along with potentially more severe issues, such as depression, anxiety and even psychosis, causing people to see and hear things that aren't there and to believe things that aren't true.)
The mechanism can depend a bit on your illness. They’ve been talking a lot about serotonin recently and serotonin deficiencies. They have been testing things like residual serotonin in the gut, and so there’s a question about the gut-brain connection. There’s likely an association there.
(Scientists suspect COVID-19 could compromise the diversity of bacteria and microbes in the gut, which have been shown to produce such neurotransmitters as serotonin and dopamine. Disruption of these mood-regulating neurotransmitters, therefore, could be a basis of some neuropsychiatric issues.)
For ICU patients, there are other players that we know contribute to these symptoms: things like all the medications they get while in the ICU, delirium, being intubated – we know that these can cause things like PTSD symptoms, depression, physical debilitation, cognitive problems. So folks who were in the ICU with COVID, it’s sort of a double hit for them.
What mental health conditions can COVID trigger?
We see a wide range. I see a lot of depression and anxiety after COVID. And that can be either folks who already had it and it got worse after they had a COVID infection or folks who never had depression or anxiety, and it’s brand new. I’ve seen both, where I wonder if it’s a direct neurologic kind of impact, or neuropsychiatric kind of depression or anxiety.
And there’s trauma, which we’re working on a paper about now. We do see PTSD in patients with long COVID. Especially in the early waves with a lot of those folks who thought they might die in the hospital. And I see people who had problems breathing, so any time they are feeling short of breath, they are re-triggered by that.
Then there are the symptoms that cross multiple specialties (neurology, psychiatry), such as brain fog, or cognitive impact. They can look very different, too. For some people, it’s memory issues. Some people, they just can’t focus. Some folks, it’s all of the above. Sleep problems are common.
Suddenly being hurled into a dark depression or other psychiatric disorder, which we know can happen with any COVID infection, must be confusing, even terrifying for some patients.
Yes, that’s probably a lot of people who come to see me. I’ve had some folks where it didn’t last long, but it was really scary. Or some people who say yeah, I’ve had long-term depression, but it had been controlled for many years before I got COVID. So it does seem to trigger something. There is some aspect of the infection that has this connection with the mental health symptoms.
And, yes, studies are saying that it doesn’t have to be tied to severity of your COVID infection. We don’t fully understand why you can have someone with a mild infection develop long COVID symptoms.
That’s why people are looking again at the serotonin connection, the pathways of tryptophan and what does it mean to have residual serotonin. I have sometimes used SSRIs (selective serotonin reuptake inhibitors, such as Prozac) in long COVID patients. So the question is: Am I treating a major depressive episode? Or am I treating some serotonin deficiency with long COVID?
What’s the longest long COVID patient you’ve seen?
There are some folks from the early days (four years ago) who are still having some symptoms. They are definitely better than when they first came to our program, but they are not back to where they were pre-infection. But most of my patients are about six months.
Does having a past mental health issue increase the risk of problems with a COVID infection?
Yes, if you already had a mental health history like depression or anxiety, that puts you at higher risk. And in some of my folks, this is anecdotal, but I tend to see that associated with longer recovery times, too, if they already had pre-existing history vs. folks who truly had nothing.
But then with a lot of people who come in and talk to me, we discover that it’s not that you didn’t have anything. It was just manageable and subclinical. You may have had mood changes or anxiety before your COVID infection, but it wasn’t causing problems. But with your COVID infection, it tipped over now to something that’s impairing and causing problems in your life.
Is there any association between substance use and long COVID?
It’s been flagged as a potential risk factor. I’m part of a research grant where we’re evaluating this, primarily in ICU patients, but we’re looking at those who had a history of alcohol use and whether that affected their outcome respiratory-wise (previous studies have suggested a link between alcohol use disorder and increased death rate from COVID infection). That’s a big question.
Does long COVID increase suicidal thoughts?
I don’t actually see it a lot in my clinic, but something that got a lot of media attention was new-onset psychosis after COVID infection. Psychosis and suicidal ideation do happen, and it’s really scary, but they are pretty rare. A lot of those patients get treated in an in-patient psychiatric setting or in ER settings. It’s not as common as people who have depression, anxiety and trauma without suicidal thoughts.
Topics: Patient Care , COVID-19 , Mental Health ,

Thida Thant, MD
Related Stories
Patient Care COVID-19 Mental Health
Patient Care Mental Health
Unraveling the Connections Between Loneliness and Emotional Eating
Patient Care Sports Medicine
Take Me Out of the Ballgame: What’s Causing MLB Elbow Injuries?
University of colorado anschutz medical campus, cu anschutz, fitzsimons building.
13001 East 17th Place
Aurora, CO 80045
303-724-9290
Partnerships
UCHealth University of Colorado Hospital
Children's Hospital Colorado
University of Colorado Medicine
Ethics and Compliance
Freedom of Expression
Submit Content
Sustainability
HelpCompass
Faculty/Staff Directory
Find a Doctor
Academic Calendar
Media Contacts
Film Requests
This is Breakthrough
- Website Feedback
- Privacy Policy
- Terms of Use
- Accessibility
- Accreditation
© 2024 The Regents of the University of Colorado , a body corporate. All rights reserved.
Accredited by the Higher Learning Commission . All trademarks are registered property of the University. Used by permission only.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2021
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
- Surapon Nochaiwong ORCID: orcid.org/0000-0003-1100-7171 1 , 2 ,
- Chidchanok Ruengorn ORCID: orcid.org/0000-0001-7927-1425 1 , 2 ,
- Kednapa Thavorn ORCID: orcid.org/0000-0003-4738-8447 2 , 3 , 4 , 5 ,
- Brian Hutton ORCID: orcid.org/0000-0001-5662-8647 3 , 4 , 5 ,
- Ratanaporn Awiphan ORCID: orcid.org/0000-0003-3628-0596 1 , 2 ,
- Chabaphai Phosuya 1 ,
- Yongyuth Ruanta ORCID: orcid.org/0000-0003-4184-0308 1 , 2 ,
- Nahathai Wongpakaran ORCID: orcid.org/0000-0001-8365-2474 6 &
- Tinakon Wongpakaran ORCID: orcid.org/0000-0002-9062-3468 6
Scientific Reports volume 11 , Article number: 10173 ( 2021 ) Cite this article
55k Accesses
316 Citations
117 Altmetric
Metrics details
- Post-traumatic stress disorder
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint databases, grey literature, and unpublished studies from January 1, 2020, to June 16, 2020 (updated on July 11, 2020), with no language restrictions. Observational studies using validated measurement tools and reporting data on mental health issues among the general population were screened to identify all relevant studies. We have included information from 32 different countries and 398,771 participants. The pooled prevalence of mental health issues amid the COVID-19 pandemic varied widely across countries and regions and was higher than previous reports before the COVID-19 outbreak began. The global prevalence estimate was 28.0% for depression; 26.9% for anxiety; 24.1% for post-traumatic stress symptoms; 36.5% for stress; 50.0% for psychological distress; and 27.6% for sleep problems. Data are limited for other aspects of mental health issues. Our findings highlight the disparities between countries in terms of the poverty impacts of COVID-19, preparedness of countries to respond, and economic vulnerabilities that impact the prevalence of mental health problems. Research on the social and economic burden is needed to better manage mental health problems during and after epidemics or pandemics. Systematic review registration : PROSPERO CRD 42020177120.
Similar content being viewed by others
Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence
Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis

Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review
Introduction.
After the World Health Organisation (WHO) declared the rapid worldwide spread of coronavirus disease-2019 (COVID-19) to be a pandemic, there has been a dramatic rise in the prevalence of mental health problems both nationally and globally 1 , 2 , 3 . Early international evidence and reviews have reported the psychological effects of the COVID-19 outbreak on patients and healthcare workers, particularly those in direct contact with affected patients 4 , 5 , 6 , 7 , 8 . Besides patients with COVID-19, negative emotions and psychosocial distress may occur among the general population due to the wider social impact and public health and governmental response, including strict infection control, quarantine, physical distancing, and national lockdowns 2 , 9 , 10 .
Amid the COVID-19 pandemic, several mental health and psychosocial problems, for instance, depressive symptoms, anxiety, stress, post-traumatic stress symptoms (PTSS), sleep problems, and other psychological conditions are of increasing concern and likely to be significant 5 , 10 , 11 . Public psychological consequences can arise through direct effects of the COVID-19 pandemic that are sequelae related to fear of contagion and perception of danger 2 . However, financial and economic issues also contribute to mental health problems among the general population in terms of indirect effects 12 , 13 . Indeed, economic shutdowns have disrupted economies worldwide, particularly in countries with larger domestic outbreaks, low health system preparedness, and high economic vulnerability 14 , 15 , 16 .
The COVID-19 pandemic may affect the mental health of the general population differently based on national health and governmental policies implemented and the public resilience and social norms of each country. Unfortunately, little is known about the global prevalence of mental health problems in the general population during the COVID-19 pandemic. Previous systematic reviews have been limited by the number of participants included, and attention has been focussed on particular conditions and countries, with the majority of studies being conducted in mainland China 5 , 8 , 11 , 17 , 18 . To the best of our knowledge, evidence on mental health problems among the general population worldwide has not been comprehensively documented in the current COVID-19 pandemic. Therefore, a systematic review and meta-analysis at a global level is needed to provide robust and contemporary evidence to inform public health policies and long-term responses to the COVID-19 pandemic.
As such, we have performed a rigorous systematic review and meta-analysis of all available observational studies to shed light on the effects of the global COVID-19 pandemic on mental health problems among the general population. We aimed to: (1) summarise the prevalence of mental health problems nationally and globally, and (2) describe the prevalence of mental health problems by each WHO region, World Bank income group, and the global index and economic indices responses to the COVID-19 pandemic.
This systematic review and meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 19 and reported in line with the Meta-analysis of Observational Studies in Epidemiology statement (Appendix, Table S1 ) 20 . The pre-specified protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020177120).
Search strategy
We searched electronic databases in collaboration with an experienced medical librarian using an iterative process. PubMed, Medline, Embase, PsycINFO, Web of Science, Scopus, CINAHL, and the Cochrane Library were used to identify all relevant abstracts. As the WHO declared the COVID-19 outbreak to be a public health emergency of international concern on January 30, 2020, we limited the search from January 1, 2020, to June 16, 2020, without any language restrictions. The main keywords used in the search strategy included “coronavirus” or “COVID-19” or “SARS-CoV-2”, AND “mental health” or “psychosocial problems” or “depression” or “anxiety” or “stress” or “distress” or “post-traumatic stress symptoms” or “suicide” or “insomnia” or “sleep problems” (search strategy for each database is provided in the Appendix, Table S2 ). Relevant articles were also identified from the reference lists of the included studies and previous systematic reviews. To updated and provide comprehensive, evidence-based data during the COVID-19 pandemic, grey literature from Google Scholar and the preprint reports from medRxiv, bioRxiv, and PsyArXiv were supplemented to the bibliographic database searches. A targeted manual search of grey literature and unpublished studies was performed through to July 11, 2020.
Study selection and data screening
We included observational studies (cross-sectional, case–control, or cohort) that (1) reported the occurrence or provided sufficient data to estimate the prevalence of mental health problems among the general population, and (2) used validated measurement tools for mental health assessment. The pre-specified protocol was amended to permit the inclusion of studies the recruited participants aged 12 years or older and college students as many colleges and universities were closed due to national lockdowns. We excluded studies that (1) were case series/case reports, reviews, or studies with small sample sizes (less than 50 participants); (2) included participants who had currently confirmed with the COVID-19 infection; and (3) surveyed individuals under hospital-based settings. If studies had overlapping participants and survey periods, then the study with the most detailed and relevant information was used.
Eligible titles and abstracts of articles identified by the literature search were screened independently by two reviewers (SN and CR). Then, potentially relevant full-text articles were assessed against the selection criteria for the final set of included studies. Potentially eligible articles that were not written in English were translated before the full-text appraisal. Any disagreement was resolved by discussion.
The primary outcomes were key parameters that reflect the global mental health status during the COVID-19 pandemic, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems (insomnia or poor sleep). To deliver more evidence regarding the psychological consequences, secondary outcomes of interest included psychological symptoms, suicidal ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder.
Data extraction and risk of bias assessment
Two reviewers (SN and YR) independently extracted the pre-specified data using a standardised approach to gather information on the study characteristics (the first author’s name, study design [cross-sectional survey, longitudinal survey, case–control, or cohort], study country, article type [published article, short report/letters/correspondence, or preprint reporting data], the data collection period), participant characteristics (mean or median age of the study population, the proportion of females, proportion of unemployment, history of mental illness, financial problems, and quarantine status [never, past, or current]), and predefined outcomes of interest (including assessment outcome definitions, measurement tool, and diagnostic cut-off criteria). For international studies, data were extracted based on the estimates within each country. For studies that had incomplete data or unclear information, the corresponding author was contacted by email for further clarification. The final set of data was cross-checked by the two reviewers (RA and CP), and discrepancies were addressed through a discussion.
Two reviewers (SN and CR) independently assessed and appraised the methodological quality of the included studies using the Hoy and colleagues Risk of Bias Tool-10 items 21 . A score of 1 (no) or 0 (yes) was assigned to each item. The higher the score, the greater the overall risk of bias of the study, with scores ranging from 0 to 10. The included studies were then categorised as having a low (0–3 points), moderate (4–6 points), or high (7 or 10 points) risk of bias. A pair of reviewers (RA and CP) assessed the risk of bias of each study. Any disagreements were resolved by discussion.
Data synthesis and statistical methods
A two-tailed P value of less than 0.05 was considered statistically significant. We used Stata software version 16.0 (StataCorp, College Station, TX, USA) for all analyses and generated forest plots of the summary pooled prevalence. Inter-rater agreements between reviewers for the study selection and risk of bias assessment were tested using the kappa (κ) coefficient of agreement 22 . Based on the crude information data, we recalculated and estimated the unadjusted prevalence of mental health and psychological problems using the crude numerators and denominators reported by each of the included studies. Unadjusted pooled prevalence with corresponding 95% confidence intervals (CIs) was reported for each WHO regions (Africa, America, South-East Asia, Europe, Eastern Mediterranean, and Western Pacific) and World Bank income group (low-, lower-middle-, upper-middle-, and high-income).
We employed the variance of the study-specific prevalence using the Freeman–Tukey double arcsine methods for transforming the crude data before pooling the effect estimates with a random-effect model to account for the effects of studies with extreme (small or large) prevalence estimates 23 . Heterogeneity was evaluated using the Cochran’s Q test, with a p value of less than 0.10 24 . The degree of inconsistency was quantified using I 2 values, in which a value greater than 60–70% indicated the presence of substantial heterogeneity 25 .
Pre-planned subgroup analyses were performed based on the participant (i.e., age, the proportion of female sex, the proportion of unemployment, history of mental illness, financial problems, and quarantine status) and study characteristics (article type, study design, data collection, and sample size). To explore the inequality and poverty impacts across countries, subgroup analyses based on the global index and economic indices responses to the COVID-19 pandemic were performed, including (1) human development index (HDI) 2018 (low, medium, high, and very high) 26 ; (2) gender inequality index 2018 (below vs above world average [0.439]) 27 ; (3) the COVID-19-government response stringency index during the survey (less- [less than 75%], moderate- [75–85%], and very stringent [more than 85%]) according to the Oxford COVID-19 Government Response Tracker reports 28 ; (4) the preparedness of countries in terms of hospital beds per 10,000 people, 2010–2018 (low, medium–low, medium, medium–high, and high) 15 ; (5) the preparedness of countries in terms of current health expenditure (% of gross domestic product [GDP] 2016; low, medium–low, medium, medium–high, and high) 15 ; (6) estimated percent change of real GDP growth based on the International Monetary Fund, April 2020 (below vs above world average [− 3.0]) 29 ; (7) the resilience of countries’ business environment based on the 2020 global resilience index reports (first-, second-, third-, and fourth-quartile) 30 ; and (8) immediate economic vulnerability in terms of inbound tourism expenditure (% of GDP 2016–2018; low, medium–low, medium, medium–high, and high) 15 .
To address the robustness of our findings, we conducted a sensitivity analysis by restricting the analysis to studies with a low risk of bias (Hoy and Colleagues-Tool, 0–3 points). Furthermore, a random-effects univariate meta-regression analysis was used to explore the effect of participant and study characteristics, and the global index and economic indices responses to the COVID-19 pandemic as described above on the prevalence estimates.
The visual inspection of funnel plots was performed when there was sufficient data and tested for asymmetry using the Begg’s and Egger’s tests for each specific. A P value of less than 0.10 was considered to indicate statistical publication bias 31 , 32 . If the publication bias was detected by the Begg’s and Egger’s regression test, the trim and fill method was then performed to calibrate for publication bias 33 .
Initially, the search strategy retrieved 4642 records. From these, 2682 duplicate records were removed, and 1960 records remained. Based on the title and abstract screening, we identified 498 articles that seemed to be relevant to the study question (the κ statistic for agreement between reviewers was 0.81). Of these, 107 studies fulfilled the study selection criteria and were included in the meta-analysis (Appendix, Figure S1 ). The inter-rater agreement between reviewers on the study selection and data extraction was 0.86 and 0.75, respectively. The reference list of all included studies in this review is provided in the Appendix, Table S3 .
Characteristics of included studies
In total, 398,771 participants from 32 different countries were included. The mean age was 33.5 ± 9.5 years, and the proportion of female sex was 60.9% (range, 16.0–51.6%). Table 1 summarises the characteristics of all the included studies according to World Bank income group, the global index of COVID-19 pandemic preparedness, and economic vulnerability indices. The included studies were conducted in the Africa (2 studies 34 , 35 [1.9%], n = 723), America (12 studies 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 [11.2%], n = 18,440), South-East Asia (10 studies 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 [9.4%], n = 11,953), Europe (27 studies 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 [25.2%], n = 148,430), Eastern Mediterranean (12 studies 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 [11.2%], n = 23,396), and Western Pacific WHO regions (44 studies 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 [41.1%], n = 195,829). Most of the included studies were cross-sectional (96 studies, 89.7%), used an online-based survey (101 studies, 95.3%), conducted in mainland China (34 studies, 31.8%), and were conducted in countries with upper-middle (49 studies, 45.8%) and high-incomes (44 studies, 41.1%). Detailed characteristics of the 107 included studies, measurement tools for evaluating the mental health status and psychological consequences, and the diagnostic cut-off criteria are described in Appendix, Table S4 . Of the 107 included studies, 76 (71.0%) had a low risk, 31 (29.0%) had a moderate risk, and no studies had a high risk of bias (Appendix, Table S5 ).
Global prevalence of mental health issues among the general population amid the COVID-19 pandemic
Table 2 presents a summary of the results of the prevalence of mental health problems among the general population amid the COVID-19 pandemic by WHO region and World Bank country groups. With substantial heterogeneity, the global prevalence was 28.0% (95% CI 25.0–31.2) for depression (75 studies 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 70 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 93 , 96 , 97 , 99 , 101 , 104 , 105 , 106 , 107 , 108 , 109 , 112 , 113 , 114 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 127 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 280,607, Fig. 1 ); 26.9% (95% CI 24.0–30.0) for anxiety (75 studies 35 , 37 , 38 , 40 , 42 , 43 , 44 , 46 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 104 , 105 , 107 , 108 , 109 , 112 , 113 , 114 , 115 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 284,813, Fig. 2 ); 24.1% (95% CI 17.0–32.0) for PTSS (28 studies 35 , 44 , 56 , 59 , 62 , 64 , 66 , 69 , 75 , 78 , 80 , 81 , 82 , 89 , 90 , 91 , 106 , 109 , 110 , 111 , 119 , 123 , 124 , 125 , 127 , 131 , 135 , 138 , n = 56,447, Fig. 3 ); 36.5% (95% CI 30.0–43.3) for stress (22 studies 37 , 50 , 51 , 52 , 53 , 54 , 57 , 58 , 71 , 73 , 75 , 76 , 80 , 114 , 117 , 119 , 120 , 122 , 125 , 129 , 131 , 136 , n = 110,849, Fig. 4 ); 50.0% (95% CI 41.8–58.2) for psychological distress (18 studies 39 , 47 , 52 , 59 , 63 , 65 , 70 , 72 , 78 , 79 , 85 , 86 , 88 , 102 , 110 , 118 , 121 , 128 , n = 81,815, Fig. 5 ); and 27.6% (95% CI 19.8–36.1) for sleep problems (15 studies 35 , 53 , 58 , 80 , 84 , 103 , 106 , 107 , 109 , 119 , 120 , 125 , 134 , 136 , 137 , n = 99,534, Fig. 6 ). The prevalence of mental health problems based on different countries varied (Appendix, Table S6 ), from 14.5% (South Africa) to 63.3% (Brazil) for depressive symptoms; from 7.7% (Vietnam) to 49.9% (Mexico) for anxiety; from 10.5% (United Kingdom) to 52.0% (Egypt) for PTSS; from 19.7% (Portugal) to 72.8% (Thailand) for stress; from 23.9% (China) to Jordan (92.9%) for psychological distress; from 9.2% (Italy) to 53.9% (Thailand) for sleep problems.
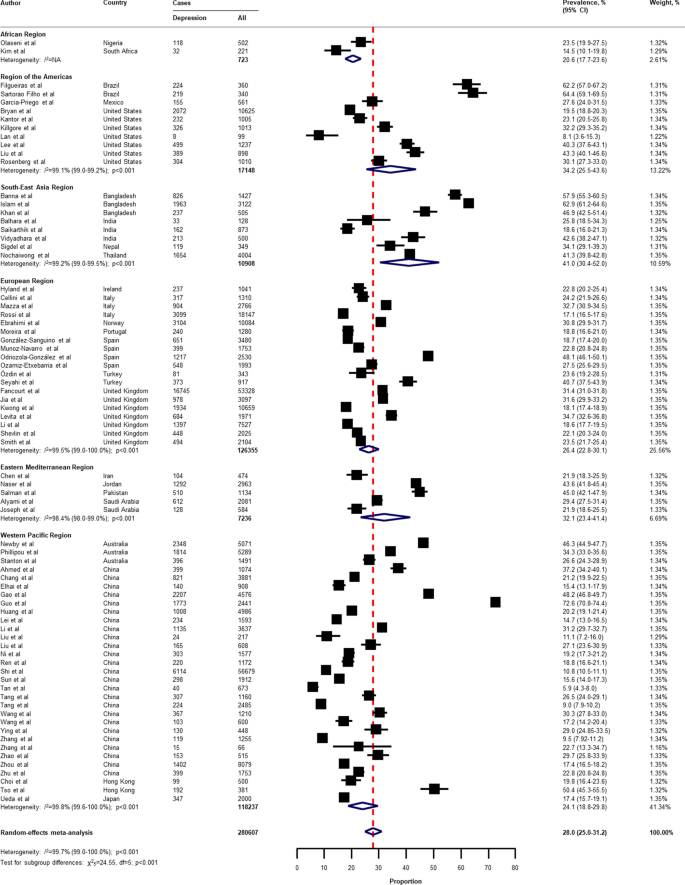
Pooled prevalence of depression among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
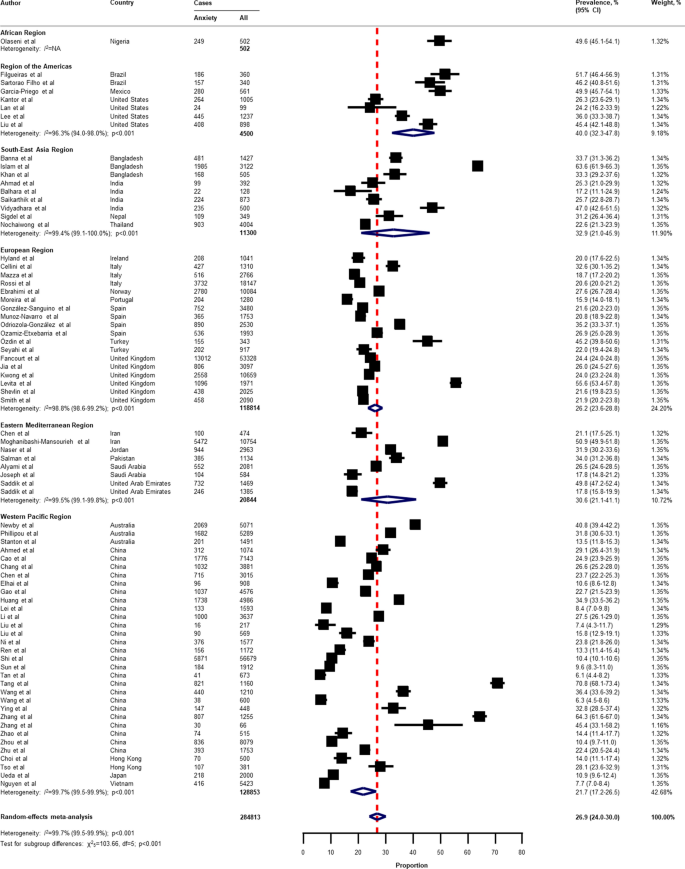
Pooled prevalence of anxiety among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
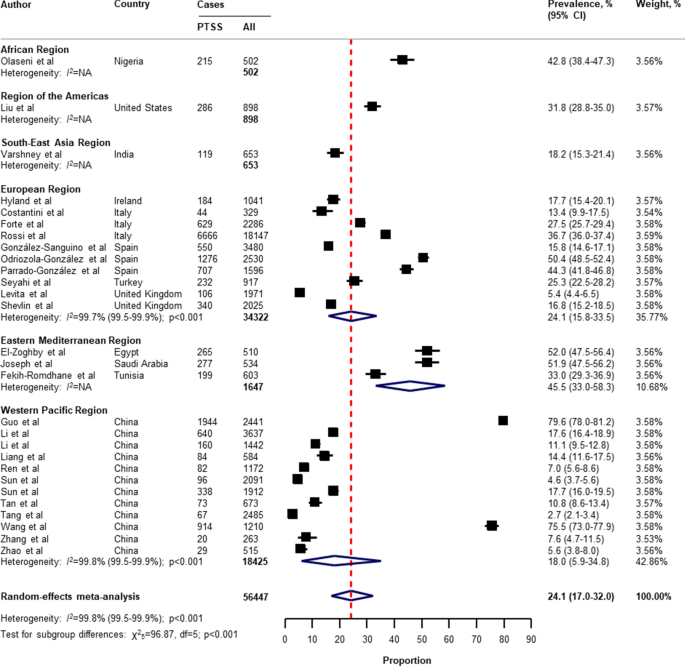
Pooled prevalence of PTSS among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable, PTSS post-traumatic stress symptoms. References are listed according to WHO region in the appendix, Table S3 .
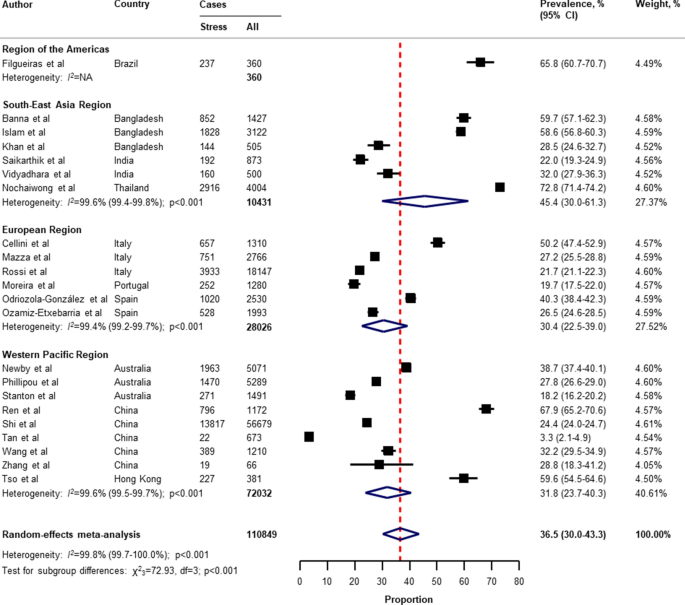
Pooled prevalence of stress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
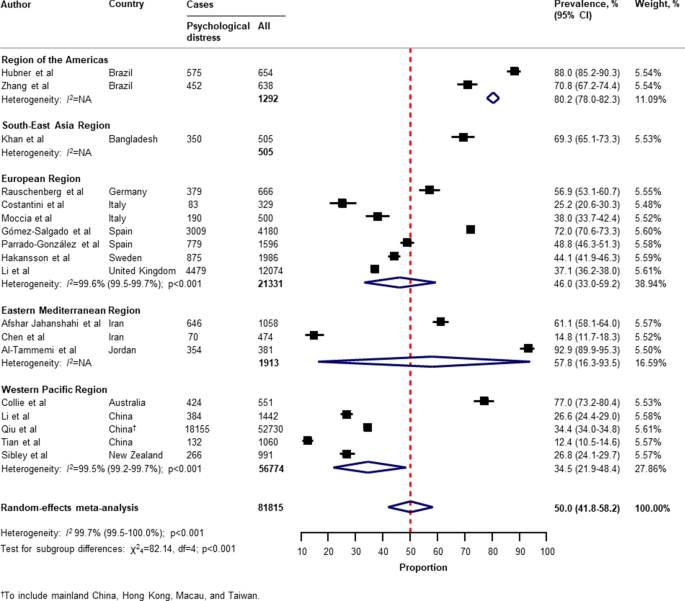
Pooled prevalence of psychological distress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
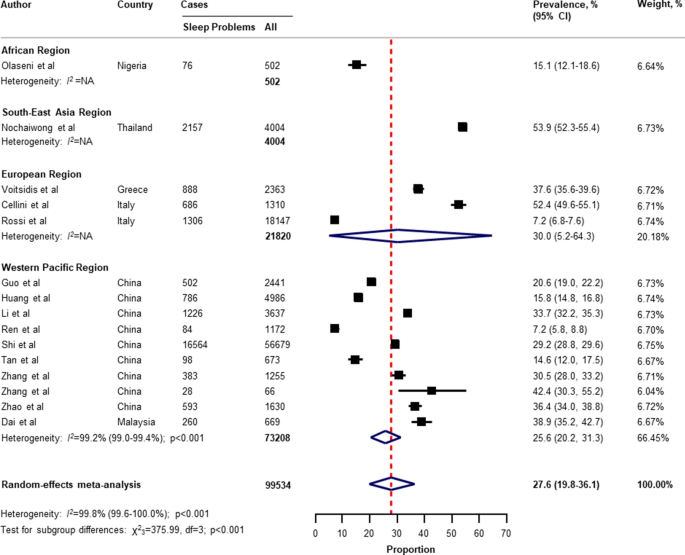
Pooled prevalence of sleep problems among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
With respect to the small number of included studies and high degree of heterogeneity, the pooled secondary outcome prevalence estimates are presented in Appendix, Table S7 . The global prevalence was 16.4% (95% CI 4.8–33.1) for suicide ideation (4 studies 36 , 41 , 53 , 124 , n = 17,554); 53.8% (95% CI 42.4–63.2) for loneliness (3 studies 41 , 44 , 45 , n = 2921); 30.7% (95% CI 2.1–73.3) for somatic symptoms (3 studies 53 , 69 , 134 , n = 7230); 28.6% (95% CI 9.2–53.6) for low wellbeing (3 studies 53 , 68 , 97 , n = 15,737); 50.5% (95% CI 49.2–51.7) for alcohol drinking problems (2 studies 97 , 114 , n = 6145); 6.4% (95% CI 5.5–7.4) for obsessive–compulsive symptoms (2 studies 73 , 134 , n = 2535); 25.7% (95% CI 23.7–27.8) for panic disorder (1 study 74 , n = 1753); 2.4% (95% CI 1.6–3.4) for phobia anxiety (1 study 134 , n = 1255); 22.8% (95% CI 22.1–23.4) for adjustment disorder (1 study 80 , n = 18,147); and 1.2% (95% CI 1.0–1.4) for suicide attempts (1 study 36 , n = 10,625).
Subgroup analyses, sensitivity analyses, meta-regression analyses, and publication bias
In the subgroup analyses (Appendix, Table S8 , Table S9 , Table S10 , Table S1 , Table S12 ), the prevalence of mental health problems was higher in countries with a low to medium HDI (for depression, anxiety, PTSS, and psychological distress), high HDI (for sleep problems), high gender inequality index (for depression and PTSS), very stringent government response index (for PTSS and stress), less stringent government response index (for sleep problems), low to medium hospital beds per 10,000 people (for depression, anxiety, PTSS, stress, psychological distress, and sleep problems), low to medium current health expenditure (for depression, PTSS, and psychological distress), estimated percent change of real GDP growth 2020 below − 3.0 (for psychological distress), low resilience (fourth-quartile) of business environment (for depression, anxiety, and PTSS), medium resilience (second-quartile) of business environment (for psychological distress, and sleep problems), high economic vulnerability-inbound tourism expenditure (for psychological distress, sleep problems), article type-short communication/letter/correspondence (for stress), cross-sectional survey (for PTSS and psychological distress), longitudinal survey (for anxiety and stress), non-mainland China (for depression, anxiety, and psychological distress), sample size of less than 1000 (for psychological distress), sample size of more than 5000 (for PTSS), proportion of females more than 60% (for stress and sleep problems), and measurement tools (for depression, anxiety, stress, and sleep problems). However, several pre-planned subgroup analyses based on participant characteristics and secondary outcomes reported could not be performed due to limited data in the included studies.
Findings from the sensitivity analysis were almost identical to the main analysis (Appendix, Table S14 ). The pooled prevalence by restricting the analysis to studies with a low risk of bias was 28.6% (95% CI 25.1–32.3) for depression, 27.4% (95% CI 24.1–30.8) for anxiety, 30.2% (95% CI 20.3–41.1) for PTSS, 40.1% (95% CI 32.5–47.9) for stress, 45.4% (95% CI 32.0–59.2) for psychological distress, and 27.7% (95% CI 19.4–36.9) for sleep problems.
On the basis of univariate meta-regression, the analysis was suitable for the primary outcomes (Appendix, Table S15 ). The increased prevalence of mental health problems was associated with the WHO region (for depression, anxiety, and psychological distress), female gender inequality index (for depression and anxiety), the COVID-19-government response stringency index during the survey (for sleep problems), hospital beds per 10,000 people (for depression and anxiety), immediate economic vulnerability-inbound tourism expenditure (for sleep problems), study design (cross-sectional vs longitudinal survey; for stress), surveyed country (mainland China vs non-mainland China; for depression and psychological distress), and risk of bias (for PTSS).
The visual inspection of the funnel plots, and the p values tested for asymmetry using the Begg’s and Egger’s tests for each prevalence outcome, indicated no evidence of publication bias related to the sample size (Appendix, Table S16 , and Figure S2 ).
This study is, to the best of our knowledge, the first systematic review and meta-analysis on the overall global prevalence of mental health problems and psychosocial consequences among the general population amid the COVID-19 pandemic. Overall, our findings indicate wide variability in the prevalence of mental health problems and psychosocial consequences across countries, particularly in relation to different regions, the global index of COVID-19 pandemic preparedness, inequalities, and economic vulnerabilities indices.
Two reports examined the global prevalence of common mental health disorders among adults prior to the COVID-19 outbreak. The first study was based on 174 surveys across 63 countries from 1980 to 2013. The estimated lifetime prevalence was 29.1% for all mental disorders, 9.6% for mood disorders, 12.9% for anxiety disorders, and 3.4% for substance use disorder 141 . Another report which was conducted as part of the Global Health Estimates by WHO in 2015, showed that the global estimates of depression and anxiety were 4.4% and 3.6% (more common among females than males), respectively 142 . Despite the different methodological methods used, our findings show that the pooled prevalence of mental health problems during the COVID-19 pandemic is higher than before the outbreak.
Previous studies on the prevalence of mental health problems during the COVID-19 pandemic have had substantial heterogeneity. Three systematic reviews reported the prevalence of depression, anxiety, and stress among the general population (mainly in mainland China). The first of these by Salari et al. 11 , was based on 17 included studies (from ten different countries in Asia, Europe, and the Middle East), the pooled prevalence of depression, anxiety, and stress were 33.7% (95% CI 27.5–40.6), 31.9% (95% CI 27.5–36.7), and 29.6% (95% CI 24.3–35.4), respectively. A review by Luo et al. 8 , which included 36 studies from seven different countries, reported a similar overall prevalence of 27% (95% CI 22–33) for depression and 32% (95% CI 25–39) for anxiety. However, a review by Ren et al. 17 , which focussed on only the Chinese population (8 included studies), found that the pooled prevalence was 29% (95% CI 16–42) and 24% (95% CI 16–32), respectively. Nevertheless, previous systematic reviews have been mainly on investigating the prevalence of PTSS, psychological distress, and sleep problems among the patients or healthcare workers that are limited to the general population during the COVID-19 pandemic. With regard to the general population, a review by Cénat et al. 143 , found that the pooled prevalence of PTSS, psychological distress, and insomnia were 22.4% (95% CI 7.6–50.3; 9 included studies), 10.2% (95% CI 4.6–21.0; 10 included studies), and 16.5% (95% CI 8.4–29.7; 8 included studies), respectively.
In this systematic review and meta-analysis, we updated and summarised the global prevalence of mental health problems and psychosocial consequences during the COVID-19 pandemic using information from 32 different countries, and 398,771 participants. A range of problems, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems were reported. The global prevalence of our findings was in line with the previous reviews mentioned above in terms of depression (28.0%; 95% CI 25.0–31.2), anxiety (26.9%; 95% CI 24.0–30.0), and stress (36.5%; 95% CI 30.0–43.3). Interestingly, our findings highlight the poverty impacts of COVID-19 in terms of inequalities, the preparedness of countries to respond, and economic vulnerabilities on the prevalence of mental health problems across countries. For instance, our results suggest that countries with a low or medium HDI had a higher prevalence of depression and anxiety compared to countries with a high or very high HDI (Appendix, Table S8 , and Table S9 ). The prevalence of depression was higher among countries with a gender inequality index of 0.439 or greater (39.6% [95% CI 30.3–49.3] vs 26.2% [95% CI 23.1–29.3]; P = 0.020; Appendix, Table S8 ). Likewise, the prevalence of depression and anxiety was higher among countries with low hospital beds per 10,000 people (Appendix, Table S8 , and Table S9 ). Our findings suggest that the poverty impacts of COVID-19 are likely to be quite significant and related to the subsequent risk of mental health problems and psychosocial consequences. Although we performed a comprehensive review by incorporating articles published together with preprint reports, there was only limited data available on Africa, low-income groups, and secondary outcomes of interest (psychological distress, suicide ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder).
Strengths and limitations of this review
From a methodological point of view, we used a rigorous and comprehensive approach to establish an up-to-date overview of the evidence-based information on the global prevalence of mental health problems amid the COVID-19 pandemic, with no language restrictions. The systematic literature search was extensive, comprising published peer-reviewed articles and preprints reporting data to present all relevant literature, minimise bias, and up to date evidence. Our findings expanded and addressed the limitations of the previous systematic reviews, such as having a small sample size and number of included studies, considered more aspects of mental health circumstance, and the generalisability of evidence at a global level 5 , 6 , 11 , 17 , 18 . To address biases from different measurement tools of assessment and the cultural norms across countries, we summarised the prevalence of mental health problems and psychosocial consequences using a random-effects model to estimate the pooled data with a more conservative approach. Lastly, the sensitivity analyses were consistent with the main findings, suggesting the robustness of our findings. As such, our data can be generalised to individuals in the countries where the included studies were conducted.
There were several limitations to this systematic review and meta-analysis. First, despite an advanced comprehensive search approach, data for some geographical regions according to the WHO regions and World Bank income groups, for instance, the Africa region, as well as the countries in the low-income group, were limited. Moreover, the reporting of key specific outcomes, such as suicide attempts and ideation, alcohol drinking or drug-dependence problems, and stigma towards COVID-19 infection were also limited. Second, a subgroup analysis based on participant characteristics (that is, age, sex, unemployment, history of mental illness, financial problems, and quarantine status), could not be performed as not all of the included studies reported this data. Therefore, the global prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic cannot be established. Third, it should be noted that different methods, for example, face-to-face interviews or paper-based questionnaires, may lead to different prevalence estimates across the general population. Due to physical distancing, the included studies in this review mostly used online surveys, which can be prone to information bias and might affect the prevalence estimates of our findings. Fourth, a high degree of heterogeneity between the included studies was found in all outcomes of interest. Even though we performed a set of subgroup analyses concerning the participant characteristics, study characteristics, the global index, and economic indices responses to the COVID-19 pandemic, substantial heterogeneity persisted. However, the univariate meta-regression analysis suggested that the WHO region, gender inequality index, COVID-19-government response stringency index during the survey, hospital beds, immediate economic vulnerability (inbound tourism expenditure), study design, surveyed country (mainland China vs non-mainland China), and risk of bias were associated with an increased prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic. Finally, we underline that the diagnostic cut-off criteria used were not uniform across the measurement tools in this review, and misclassification remains possible. The genuine variation in global mental health circumstances across countries cannot be explained by our analyses. Indeed, such variation might be predisposed by social and cultural norms, public resilience, education, ethnic differences, and environmental differences among individual study populations.
Implications for public health and research
Despite the limitations of our findings, this review provides the best available evidence that can inform the epidemiology of public mental health, implement targeted initiatives, improving screening, and reduce the long-term consequences of the COVID-19 pandemic, particularly among low-income countries, or those with high inequalities, low preparedness, and high economic vulnerability. Our findings could be improved by further standardised methods and measurement tools of assessment. There is a need for individual country-level data on the mental health problems and psychosocial consequences after the COVID-19 pandemic to track and monitor public health responses. There are a number network longitudinal surveys being conducted in different countries that aim to improve our understanding of the long-term effects of the COVID-19 pandemic 144 . To promote mental wellbeing, such initiatives could also be advocated for by public health officials and governments to increase awareness and provide timely proactive interventions in routine practice.
Conclusions
In conclusion, this systematic review and meta-analysis provides a more comprehensive global overview and evidence of the prevalence of mental health problems among the general population amid the COVID-19 pandemic. The results of this study reveal that the mental health problems and psychosocial consequences amid the COVID-19 pandemic are a global burden, with differences between countries and regions observed. Moreover, equality and poverty impacts were found to be factors in the prevalence of mental health problems. Studies on the long-term effects of the COVID-19 pandemic on the mental health status among the general population at a global level is needed. Given the high burden of mental health problems during the COVID-19 pandemic, an improvement of screening systems and prevention, prompt multidisciplinary management, and research on the social and economic burden of the pandemic, are crucial.
Data sharing
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Mahase, E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 368 , m1036 (2020).
Article PubMed Google Scholar
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383 , 510–512 (2020).
Article CAS PubMed Google Scholar
Burki, T. K. Coronavirus in China. Lancet Respir. Med. 8 , 238 (2020).
Article CAS PubMed PubMed Central Google Scholar
Chen, Q. et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7 , e15–e16 (2020).
Article PubMed PubMed Central Google Scholar
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 89 , 531–542. https://doi.org/10.1016/j.bbi.2020.05.048 (2020).
Pappa, S. et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88 , 901–907 (2020).
Salazar de Pablo, G. et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 275 , 48–57 (2020).
Luo, M., Guo, L., Yu, M., Jiang, W. & Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public: a systematic review and meta-analysis. Psychiatry Res. 291 , 113190 (2020).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Kaufman, K. R., Petkova, E., Bhui, K. S. & Schulze, T. G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open 6 , e48 (2020).
Article PubMed CAS Google Scholar
Salari, N. et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16 , 57 (2020).
Article Google Scholar
Kawohl, W. & Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 7 , 389–390 (2020).
Frasquilho, D. et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 16 , 115 (2016).
World Bank. Global Economic Prospects, June 2020 (World Bank, 2020).
Book Google Scholar
Kovacevic, M. & Jahic, A. COVID-19 and Human Development: Exploring Global Preparedness and Vulnerability (Human Development Report Office, UNDP, 2020).
Google Scholar
Conceicao, P. et al. COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery (Human Development Report Office, UNDP, 2020).
Ren, X. et al. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 91 (4), 1033–1045. https://doi.org/10.1007/s11126-020-09796-5 (2020).
Rogers, J. P. et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7 , 611–627 (2020).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339 , b2535 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283 , 2008–2012 (2000).
Hoy, D. et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 65 , 934–939 (2012).
Viera, A. J. & Garrett, J. M. Understanding interobserver agreement: the kappa statistic. Fam. Med. 37 , 360–363 (2005).
PubMed Google Scholar
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72 , 39 (2014).
Cochran, W. G. The combination of estimates from different experiments. Biometrics 10 , 101–129 (1954).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Human Development Report Office. Human Development Report 2019–Beyond Income, Beyond Averages, Beyond Today: Inequalities in Human DEVELOPMENT in the 21st century (United Nations Development Programme (UNDP), 2019).
Human Development Report Office. 2020 Human Development Persepctives: Tackling Social Norms–A game changer for gender inequalities (United National Development Programme (UNDP), 2020).
Hale, T. et al. Variation in government responses to COVID-19. Version 6.0. Blavatnik School of Government Working Paper. https://www.bsg.ox.ac.uk/covidtracker (2020).
International Monetary Fund (IMF). World Economic Outlook (April 2020), Real GDP growth Annual percent change . Accessed 29 July 2020. https://www.imf.org/external/datamapper/NGDP_RPCH@WEO/OEMDC/ADVEC/WEOWORLD (2020).
FM Global. 2020 FM Global Resilience Index: Make a Resilient Decision . Accessed 30 July 2020. https://www.fmglobal.com/research-and-resources/tools-and-resources/resilienceindex (2020).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50 , 1088–1101 (1994).
Article CAS PubMed MATH Google Scholar
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315 , 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56 , 455–463 (2000).
Kim, A. W., Nyengerai, T. & Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. medRxiv. 2020.2006.2013.20130120 (2020).
Olaseni, A., Akinsola, O., Agberotimi, S. & Oguntayo, R. Psychological distress experiences of Nigerians amid COVID-19 pandemic. PsyArXiv May 6. 1031234/osfio/9v78y (2020).
Bryan, C., Bryan, A. O. & Baker, J. C. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. PsyArXiv May 29 . 1031234/osfio/9bpr4 (2020).
Filgueiras, A. & Stults-Kolehmainen, M. Factors linked to changes in mental health outcomes among Brazilians in quarantine due to COVID-19. medRxiv. 2020.2005.2012.20099374 (2020).
Garcia-Priego, B. A. et al. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: a cross-sectional study in Mexico. medRxiv. 2020.2005.2010.20095844 (2020).
Hubner, C. v. K., Bruscatto, M. L. & Lima, R. D. Distress among Brazilian university students due to the Covid-19 pandemic: survey results and reflections. medRxiv. 2020.2006.2019.20135251 (2020).
Kantor, B. N. & Kantor, J. Mental health outcomes and associations during the coronavirus disease 2019 pandemic: a cross-sectional survey of the US general population. medRxiv. 2020.2005.2026.20114140 (2020).
Killgore, W. D. S., Cloonan, S. A., Taylor, E. C. & Dailey, N. S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 290 , 113117 (2020).
Lan, F.-Y., Suharlim, C., Kales, S. N. & Yang, J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the United States. medRxiv. 2020.2006.2008.20125120 (2020).
Lee, S. A., Jobe, M. C. & Mathis, A. A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 1–2. https://doi.org/10.1017/S003329172000121X (2020).
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S. & Hahm, H. C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 290 , 113172 (2020).
Rosenberg, M., Luetke, M., Hensel, D., Kianersi, S. & Herbenick, D. Depression and loneliness during COVID-19 restrictions in the United States, and their associations with frequency of social and sexual connections. medRxiv. 2020.2005.2018.20101840 (2020).
Sartorao Filho, C. I. et al. Impact of COVID-19 pandemic on mental health of medical students: a cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv. 2020.2006.2024.20138925 (2020).
Zhang, S. X., Wang, Y., Afshar Jahanshahi, A., Li, J. & Haensel Schmitt, V. G. Mental distress of adults in Brazil during the COVID-19 crisis. medRxiv. 2020.2004.2018.20070896 (2020).
Ahmad, A., Rahman, I. & Agarwal, M. Factors influencing mental health during COVID-19 outbreak: an exploratory survey among Indian population. medRxiv. 2020.2005.2003.20081380 (2020).
Balhara, Y. P. S., Kattula, D., Singh, S., Chukkali, S. & Bhargava, R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J. Public Health. 64 , S172-176 (2020).
Banna, H. A. et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. PsyArXiv May 24 . 1031234/osfio/chw5d. (2020).
Islam, M. S. et al. Psychological eesponses during the COVID-19 outbreak among university students in Bangladesh. PsyArXiv June 2 . 1031234/osfio/cndz7. (2020).
Khan, A. H. et al. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. PsyArXiv May 15 . 1031234/osfio/97s5r. (2020).
Nochaiwong, S. et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine (Baltimore) 99 , e20751 (2020).
Article CAS Google Scholar
Saikarthik, J., Saraswathi, I. & Siva, T. Assessment of impact of COVID-19 outbreak & lockdown on mental health status & its associated risk and protective factors in adult Indian population. medRxiv. 2020.2006.2013.20130153 (2020).
Sigdel, A. et al. Depression, anxiety and depression-anxiety comorbidity amid COVID-19 pandemic: an online survey conducted during lockdown in Nepal. medRxiv. 2020.2004.2030.20086926 (2020).
Varshney, M., Parel, J. T., Raizada, N. & Sarin, S. K. Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS ONE 15 , e0233874 (2020).
Vidyadhara, S., Chakravarthy, A., Pramod Kumar, A., Sri Harsha, C. & Rahul, R. Mental health status among the South Indian pharmacy students during Covid-19 pandemic quarantine period: a cross-sectional study. medRxiv. 2020.2005.2008.20093708 (2020).
Cellini, N., Canale, N., Mioni, G. & Costa, S. Changes in sleep pattern sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 29 , e13074 (2020).
Costantini, A. & Mazzotti, E. Italian validation of CoViD-19 Peritraumatic Distress Index and preliminary data in a sample of general population. Riv. Psichiatr. 55 , 145–151 (2020).
Ebrahimi, O., Hoffart, A. & Johnson, S. U. The mental health impact of non-pharmacological interventions aimed at impeding viral transmission during the COVID-19 pandemic in a general adult population and the factors associated with adherence to these mitigation strategies. PsyArXiv May 9 . 1031234/osfio/kjzsp. (2020).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: longitudinal analyses of 59,318 adults in the UK with and without diagnosed mental illness. medRxiv. 2020.2006.2003.20120923 (2020).
Forte, G., Favieri, F., Tambelli, R. & Casagrande, M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int. J. Environ. Res. Public Health 17 , 4151 (2020).
Article CAS PubMed Central Google Scholar
Gómez-Salgado, J., Andrés-Villas, M., Domínguez-Salas, S., Díaz-Milanés, D. & Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 17 , 3947 (2020).
Article PubMed Central CAS Google Scholar
González-Sanguino, C. et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 87 , 172–176 (2020).
Article PubMed PubMed Central CAS Google Scholar
Håkansson, A. Changes in gambling behavior during the COVID-19 pandemic: a web survey study in Sweden. Int. J. Environ. Res. Public Health 17 , 4013 (2020).
Hyland, P. et al. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. PsyArXiv April 22. 1031234/osfio/8yqxr. (2020).
Jia, R. et al. Mental health in the UK during the COVID-19 pandemic: early observations. medRxiv. 2020.2005.2014.20102012 (2020).
Kwong, A. S. F. et al. Mental health during the COVID-19 pandemic in two longitudinal UK population cohorts. medRxiv. 2020.2006.2016.20133116 (2020).
Levita, L. et al. Impact of Covid-19 on young people aged 13–24 in the UK- preliminary findings. PsyArXiv June 30. 1031234/osfio/uq4rn. (2020).
Li, L. Z. & Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom: results from the Understanding Society UKHLS. medRxiv. 2020.2006.2009.20120139 (2020).
Mazza, C. et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 17 , 3165 (2020).
Moccia, L. et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 87 , 75–79 (2020).
Moreira, P. S. et al. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. medRxiv. 2020.2004.2028.20080671 (2020).
Munoz-Navarro, R., Cano-Vindel, A., Schmitz, F., Cabello, R. & Fernandez-Berrocal, P. Emotional distress and associated sociodemographic risk factors during the COVID-19 outbreak in Spain. medRxiv. 2020.2005.2030.20117457 (2020).
Odriozola-González, P., Planchuelo-Gómez, Á., Irurtia, M. J. & de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 290 , 113108 (2020).
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M. & Picaza Gorrotxategi, M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: an investigation in a sample of citizens in Northern Spain. Front. Psychol. 11 , 1491 (2020).
Özdin, S. & Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry 66 , 504–511 (2020).
Parrado-González, A. & León-Jariego, J. C. Covid-19: factors associated with emotional distress and psychological morbidity in Spanish population. Rev. Esp. Salud Publica 94 , e202006058 (2020).
Rauschenberg, C. et al. Social isolation, mental health and use of digital interventions in youth during the COVID-19 pandemic: a nationally representative survey. PsyArXiv June 29 . 1031234/osfio/v64hf (2020).
Rossi, R. et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N = 18147 web-based survey. medRxiv. 2020.2004.2009.20057802 (2020).
Seyahi, E., Poyraz, B. C., Sut, N., Akdogan, S. & Hamuryudan, V. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol. Int. 40 , 1229–1238 (2020).
Shevlin, M. et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. PsyArXiv April 18. 1031234/osfio/hb6nq (2020).
Smith, L. E. et al. Factors associated with self-reported anxiety, depression, and general health during the UK lockdown; a cross-sectional survey. medRxiv. 2020.2006.2023.20137901 (2020).
Voitsidis, P. et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 289 , 113076 (2020).
Afshar Jahanshahi, A., Mokhtari Dinani, M., Nazarian Madavani, A., Li, J. & Zhang, S. X. The distress of Iranian adults during the Covid-19 pandemic: more distressed than the Chinese and with different predictors. medRxiv. 2020.2004.2003.20052571 (2020).
Al-Tammemi, A. a. B., Akour, A. & Alfalah, L. Is it just about physical health? An internet-based cross-sectional study exploring the psychological impacts of COVID-19 pandemic on university students in Jordan using Kessler psychological distress scale. medRxiv. 2020.2005.2014.20102343 (2020).
Alyami, H. S. et al. Depression and anxiety during 2019 coronavirus disease pandemic in Saudi Arabia: a cross-sectional study. medRxiv. 2020.2005.2009.20096677 (2020).
Chen, J. et al. The curvilinear relationship between the age of adults and their mental health in Iran after its peak of COVID-19 cases. medRxiv. 2020.2006.2011.20128132 (2020).
El-Zoghby, S. M., Soltan, E. M. & Salama, H. M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J. Community Health 45 , 689–695 (2020).
Fekih-Romdhane, F., Ghrissi, F., Abbassi, B., Cherif, W. & Cheour, M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 290 , 113131 (2020).
Joseph, R., Alshayban, D., Lucca, J. M. & Alshehry, Y. A. The immediate psychological response of the general population in Saudi Arabia during COVID-19 pandemic: a cross-sectional study. medRxiv. 2020.2006.2019.20135533 (2020).
Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 51 , 102076 (2020).
Naser, A. Y. et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 10 (8), e01730. https://doi.org/10.1002/brb3.1730 (2020).
Saddik, B. et al. Assessing the influence of parental anxiety on childhood anxiety during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2006.2011.20128371 (2020).
Saddik, B. et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2005.2010.20096933 (2020).
Salman, M. et al. Psychological impact of COVID-19 on Pakistani university students and how they are coping. medRxiv. 2020.2005.2021.20108647 (2020).
Ahmed, M. Z. et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 51 , 102092 (2020).
Cao, W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287 , 112934 (2020).
Chang, J., Yuan, Y. & Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 40 , 171–176 (2020).
Chen, S. H. et al. Public anxiety and its influencing factors in the initial outbreak of COVID-19. Fudan Univ. J. Med. Sci. 47 , 385–391 (2020).
Choi, E. P. H., Hui, B. P. H. & Wan, E. Y. F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 17 , 3740 (2020).
Collie, A. et al. Psychological distress among people losing work during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2006.20093773 (2020).
Dai, H., Zhang, S. X., Looi, K. H., Su, R. & Li, J. Health condition and test availability as predictors of adults' mental health during the COVID-19 pandemic. medRxiv. 2020.2006.2021.20137000 (2020).
Elhai, J. D., Yang, H., McKay, D. & Asmundson, G. J. G. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J. Affect. Disord. 274 , 576–582 (2020).
Gao, J. et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 15 , e0231924 (2020).
Guo, J., Feng, X. L., Wang, X. H. & van IJzendoorn, M. H. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int. J. Environ. Res. Public Health 17 , 3857 (2020).
Huang, Y. & Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288 , 112954 (2020).
Lei, L. et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 26 , e924609 (2020).
Li, Y. et al. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin. Sleep Med. https://doi.org/10.5664/jcsm.8524 (2020).
Li, Y. et al. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 1–3. https://doi.org/10.1017/S0033291720001555 (2020).
Liang, L. et al. The effect of COVID-19 on youth mental health. Psychiatr. Q. 91 (3), 841–852. https://doi.org/10.1007/s11126-020-09744-3 (2020).
Liu, J. et al. Online mental health survey in a medical college in China during the COVID-19 outbreak. Front. Psychiatry 11 , 459 (2020).
Liu, X. et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 9 , 58 (2020).
Newby, J., O'Moore, K., Tang, S., Christensen, H. & Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2003.20089961 (2020).
Nguyen, H. T. et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 17 , 4164 (2020).
Ni, M. Y. et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment. Health 7 , e19009 (2020).
Phillipou, A. et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int. J. Eat. Disord. 53 , 1158–1165 (2020).
Qiu, J. et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 33 , e100213 (2020).
Ren, Y. et al. Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 87 , 132–133 (2020).
Shi, L. et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3 , e2014053 (2020).
Sibley, C. G. et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 75 , 618–630 (2020).
Stanton, R. et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 17 , 4065 (2020).
Sun, L. et al. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv. 2020.2003.2006.20032425 (2020).
Sun, S., Goldberg, S. B., Lin, D., Qiao, S. & Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. medRxiv. 2020.2007.2003.20144931 (2020).
Tan, W. et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 87 , 84–92 (2020).
Tang, F. et al. COVID-19 related depression and anxiety among quarantined respondents. Psychol. Health 36 (2), 164–178. https://doi.org/10.1080/08870446.2020.1782410 (2020).
Tang, W. et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 274 , 1–7 (2020).
Tian, F. et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 288 , 112992 (2020).
Tso, I. F. & Sohee, P. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. PsyArXiv published online June 27. 1031234/osfio/wv9y2 (2020).
Ueda, M., Stickley, A., Sueki, H. & Matsubayashi, T. Mental health status of the general population during the COVID-19 pandemic: a cross-sectional national survey in Japan. medRxiv. 2020.2004.2028.20082453 (2020).
Wang, C. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17 , 1729 (2020).
Wang, Y., Di, Y., Ye, J. & Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 26 (1), 13–22. https://doi.org/10.1080/13548506.2020.1746817 (2020).
Ying, Y. et al. Mental health status among family members of health care workers in Ningbo, China during the Coronavirus Disease 2019 (COVID-19) outbreak: a Cross-sectional Study. medRxiv. 2020.2003.2013.20033290 (2020).
Zhang, W. R. et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 89 , 242–250 (2020).
Zhang, Y. & Ma, Z. F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health 17 , 2381 (2020).
Zhang, Y., Zhang, H., Ma, X. & Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int. J. Environ. Res. Public Health 17 , 3722 (2020).
Zhao, X., Lan, M., Li, H. & Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Med. S1389–9457 (1320), 30224–30220. https://doi.org/10.1016/j.sleep.2020.05.021 (2020).
Zhao, Y., An, Y., Tan, X. & Li, X. Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J. Loss Trauma https://doi.org/10.1080/15325024.15322020.11761592 (2020).
Zhou, S. J. et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29 , 749–758 (2020).
Zhu, S. et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav.. Immun. 87 , 56–58 (2020).
Steel, Z. et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43 , 476–493 (2014).
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates (World Health Organization, 2017).
Cénat, J. M. et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 295 , 113599 (2021).
COVID-MINDS Network. COVID-MINDS network: global mental health in the COVID-19 pandemic , https://www.covidminds.org/ (2020).
Download references
Acknowledgements
The authors thank the research assistances and all staff of Pharmacoepidemiology and Statistics Research Center (PESRC), Chiang Mai, Thailand. This work reported in this manuscript was partially supported by a grant by the Chiang Mai University, Thailand. The funder of the study had no role in the study design collection, analysis, or interpretation of the data, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit it for publication.
Author information
Authors and affiliations.
Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Ratanaporn Awiphan, Chabaphai Phosuya & Yongyuth Ruanta
Pharmacoepidemiology and Statistics Research Center (PESRC), Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Kednapa Thavorn, Ratanaporn Awiphan & Yongyuth Ruanta
Ottawa Hospital Research Institute, Ottawa Hospital, Ottawa, ON, K1H 8L6, Canada
Kednapa Thavorn & Brian Hutton
Institute of Clinical and Evaluative Sciences, ICES uOttawa, Ottawa, ON, K1Y 4E9, Canada
School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, ON, K1G 5Z3, Canada
Department of Psychiatry, Faculty of Medicine, Chiang Mai University, Chiang Mai, 50200, Thailand
Nahathai Wongpakaran & Tinakon Wongpakaran
You can also search for this author in PubMed Google Scholar
Contributions
S.N. conceived the study and, together with C.R., K.T., R.A., C.P., and Y.R. developed the protocol. S.N. and C.R. did the literature search, selected the studies. S.N. and Y.R. extracted the relevant information. S.N. synthesised the data. S.N. wrote the first draft of the paper. K.T., B.H., N.W., and T.W. critically revised successive drafts of the paper. All authors approved the final draft of the manuscript. SN is the guarantor of the study.
Corresponding author
Correspondence to Surapon Nochaiwong .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary figures and tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Nochaiwong, S., Ruengorn, C., Thavorn, K. et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep 11 , 10173 (2021). https://doi.org/10.1038/s41598-021-89700-8
Download citation
Received : 11 January 2021
Accepted : 29 April 2021
Published : 13 May 2021
DOI : https://doi.org/10.1038/s41598-021-89700-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The effectiveness of an online short-format recovery college model: a co-learning model to support mental health.
- Catherine Briand
- Charles-Édouard Giguère
- Régis Hakin
International Journal of Mental Health Systems (2024)
Enhancing mental wellbeing by changing mindsets? Results from two randomized controlled trials
- Carina Schreiber
- Marijke Schotanus-Dijkstra
BMC Psychology (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
Investigating the spatiotemporal patterns and clustering of attendances for mental health services to inform policy and resource allocation in Thailand
- Chawarat Rotejanaprasert
- Papin Thanutchapat
- Richard J Maude
Effectiveness of gamified digital interventions in mental health prevention and health promotion among adults: a scoping review
- Leona Aschentrup
- Pia Anna Steimer
- Kamil J. Wrona
BMC Public Health (2024)
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Impact of Covid-19 on Bangladeshi university students mental health: ML and DL analysis
- Find this author on Google Scholar
- Find this author on PubMed
- Search for this author on this site
- ORCID record for Md Monir Ahammod Bin Atique
- For correspondence: [email protected] [email protected] [email protected]
- Info/History
- Preview PDF
The Covid-19 outbreak has adversely influenced university students across the world both physically and psychologically. The psychological struggle faced by students, is effected by various factors, including disruptions to daily routines and academic activities, increased reliance on smartphones and the internet, limited social interaction, and confinement to their homes. These impediments reflect a broader issue of imbalance in cognitive health status among them during the pandemic. In Bangladesh, despite having the necessary population to study, understanding the impact of Covid-19 on the mental health status of university students has been limited. Hence, it is imperative to diagnose mental health issues and deal with the underlying reasons in order to enhance students’ psychological well-being, which leads to academic achievement. Nowadays, Artificial Intelligence (AI) based prediction models have the potential to play a crucial role in predicting mental state early. The purpose of the study is to explore the following effects of the pandemic on the mental health of Bangladeshi university students using Machine Learning (ML) and Deep Learning (DL) techniques. A reliable AI prediction system requires real-world data, that was collected by a survey through a Google form (online questionnaires) among 400 students of 16 universities, and the respondents were 253. In this paper, after data preprocessing, ten widely known ML and four DL models were developed to automatically and accurately predict mental well-being during or after the Covid-19 circumstance. According to our findings, the Random Forest (RF) algorithm and Siamese Neural Networks (SNNs) outperformed other models in terms of accuracy (86% and 75%). Additionally, Chi-Square test was conducted, which revealed the five most common and significant predictors (“Stable family income”, “Disruption of daily life”, “Own income”, “Sleep status”, and “Fear of getting infected with Covid-19”) of psychological health conditions. Overall, this work could assist university administrations, government agencies, and health specialists in taking appropriate measures to understand and maintain students’ mental health. This research also suggests proper monitoring, government support, and social awareness during and after the worldwide epidemic to keep an excellent mental health state of university students.
Competing Interest Statement
The authors have declared no competing interest.
Funding Statement
This work was supported by Innovative Human Resource Development for Local 614 Intellectualization program through the Institute of Information & Communications 615 Technology Planning & Evaluation(IITP) grant funded by the Korea 616 government(MSIT)(IITP-2024-00156287, 50%). This work was partially supported 617 by the Korea Internet & Security Agency (KISA) - Information Security College Support 618 Project (50%)
Author Declarations
I confirm all relevant ethical guidelines have been followed, and any necessary IRB and/or ethics committee approvals have been obtained.
The details of the IRB/oversight body that provided approval or exemption for the research described are given below:
The Ethics Committee of the University Research Ethics Board at University Grants Commission of Bangladesh waived ethical approval for this work. The data collection involved anonymous responses from university students via an online Google Form, where the identity of the participants was completely hidden. According to the ethical guidelines of our institution, research involving anonymous surveys where participants cannot be identified does not require ethical approval.
I confirm that all necessary patient/participant consent has been obtained and the appropriate institutional forms have been archived, and that any patient/participant/sample identifiers included were not known to anyone (e.g., hospital staff, patients or participants themselves) outside the research group so cannot be used to identify individuals.
I understand that all clinical trials and any other prospective interventional studies must be registered with an ICMJE-approved registry, such as ClinicalTrials.gov. I confirm that any such study reported in the manuscript has been registered and the trial registration ID is provided (note: if posting a prospective study registered retrospectively, please provide a statement in the trial ID field explaining why the study was not registered in advance).
I have followed all appropriate research reporting guidelines, such as any relevant EQUATOR Network research reporting checklist(s) and other pertinent material, if applicable.
Data Availability
Based on request data set will be shared.
View the discussion thread.
Thank you for your interest in spreading the word about medRxiv.
NOTE: Your email address is requested solely to identify you as the sender of this article.

Citation Manager Formats
- EndNote (tagged)
- EndNote 8 (xml)
- RefWorks Tagged
- Ref Manager
- Tweet Widget
- Facebook Like
- Google Plus One
Subject Area
- Public and Global Health
- Addiction Medicine (324)
- Allergy and Immunology (632)
- Anesthesia (168)
- Cardiovascular Medicine (2398)
- Dentistry and Oral Medicine (289)
- Dermatology (207)
- Emergency Medicine (381)
- Endocrinology (including Diabetes Mellitus and Metabolic Disease) (850)
- Epidemiology (11795)
- Forensic Medicine (10)
- Gastroenterology (705)
- Genetic and Genomic Medicine (3766)
- Geriatric Medicine (350)
- Health Economics (637)
- Health Informatics (2408)
- Health Policy (939)
- Health Systems and Quality Improvement (905)
- Hematology (342)
- HIV/AIDS (786)
- Infectious Diseases (except HIV/AIDS) (13346)
- Intensive Care and Critical Care Medicine (769)
- Medical Education (368)
- Medical Ethics (105)
- Nephrology (401)
- Neurology (3523)
- Nursing (199)
- Nutrition (528)
- Obstetrics and Gynecology (679)
- Occupational and Environmental Health (667)
- Oncology (1832)
- Ophthalmology (538)
- Orthopedics (221)
- Otolaryngology (287)
- Pain Medicine (234)
- Palliative Medicine (66)
- Pathology (447)
- Pediatrics (1036)
- Pharmacology and Therapeutics (426)
- Primary Care Research (424)
- Psychiatry and Clinical Psychology (3186)
- Public and Global Health (6177)
- Radiology and Imaging (1289)
- Rehabilitation Medicine and Physical Therapy (751)
- Respiratory Medicine (832)
- Rheumatology (380)
- Sexual and Reproductive Health (372)
- Sports Medicine (324)
- Surgery (403)
- Toxicology (50)
- Transplantation (172)
- Urology (147)

Study finds boys' mental health more impacted by COVID-19 pandemic than girls'
T he COVID-19 pandemic had a greater impact on boys' mental health than girls, contrary to the findings of other studies, according to new research led by scientists at University of Liverpool, Manchester Metropolitan University, University of Reading, and King's College London.
These findings could have a significant impact on referral of adolescents to mental health services and on diagnoses, and greater awareness of age-related changes in mental health symptoms is needed by clinicians, educators and parents, say researchers.
Researchers used their unique dataset with repeated measurement pre and during the pandemic, and, crucially, took into account the developmental differences in symptoms between boys and girls aged 11–14 years.
According to the study, initial reports of a pandemic-related increase in depression in young adolescent girls could be explained by a natural rise in these symptoms as they get older. In contrast, pandemic-related increases in boys' depression and both boys' and girls' behavioral problems may have been masked by maturational changes over early adolescence.
The paper , "COVID-19 pandemic impact on adolescent mental health: a reassessment accounting for development," was published in the European Journal of Child and Adolescent Psychiatry .
The team were able to draw the conclusions using the unique longitudinal dataset: Wirral Child Health and Development Study (WCHADS). The study was also unique in capturing reports on depression in young adolescents' health from the parents and self-reports from the children themselves at this key stage. This indicated an over-reporting of a pandemic effect on girls' symptoms of depression by parents, while under-reporting the pandemic effect on boys.
Professor Helen Sharp, Professor of Perinatal and Child and Adolescent Clinical Psychology, University of Liverpool said, "We have identified significant changes in the pattern of mental health needs of young people due to the pandemic.
"Our study revealed adverse effects of the pandemic, with increases in behavioral problems in both boys and girls and increased depression symptoms in adolescent boys in particular. Emotional difficulties may not be recognized easily by parents or schools. However, raised awareness should help ensure more young people are directed to sources of support and treatment."
Lead author Nicky Wright, a Lecturer in Psychology at Manchester Met, said, "Because of the general decrease in boys' depression with age, and the general messaging about the impact of the pandemic being greater on girls, it is likely that boys' mental health needs are being missed, but also there may be more referrals for boys than will be anticipated."
"Overall, it is very important to take aging into account when considering diagnosis and prognosis in early adolescence, because these maturational shifts may mask or over-state actual change in symptoms. The differences between the parents' reporting and the adolescents self-report also potentially have important implications because it is typically parents who initiate referrals to child and adolescent mental health services for young people."
The WCHADS is led by Jonathan Hill, Professor of Child and Adolescent Psychiatry at University of Reading and Helen Sharp, Professor of Child and Adolescent Clinical Psychology at the University of Liverpool. Statistical analysis is led by Andrew Pickles, Professor of Biostatics at King's College London.
More information: N. Wright et al, COVID-19 pandemic impact on adolescent mental health: a reassessment accounting for development, European Child & Adolescent Psychiatry (2024). DOI: 10.1007/s00787-023-02337-y
Provided by University of Liverpool
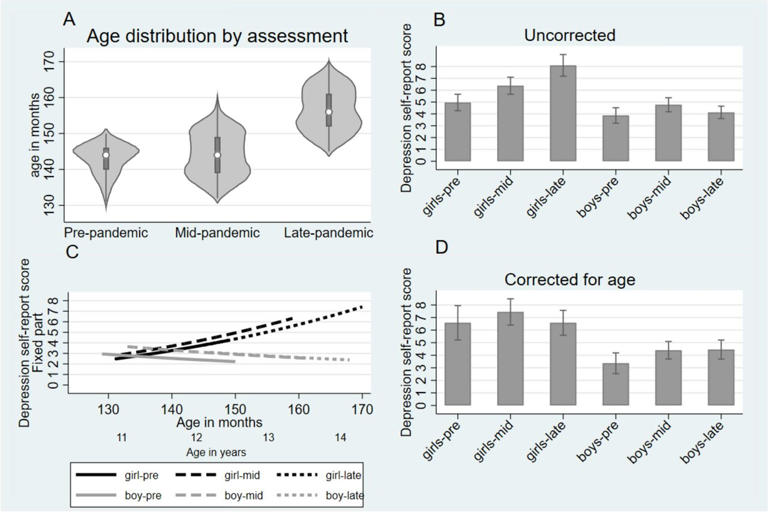
Patients love telehealth—physicians are not so sure
IRL or URL? Many physicians and patients used to see medical care as something best done in-person (in real life, or IRL). But the pandemic has spurred a massive transition to virtual (or URL) care. According to our recent surveys of consumers and physicians, opinions are split on what happens next (see sidebar, “Our methodology”). As the pandemic evolves, consumers still prefer the convenience of digital engagement and virtual-care options, according to our recent McKinsey Consumer Health Insights Survey. This preference could help more patients access care, while also helping providers to grow.
Our methodology
To help our clients understand responses to COVID-19, McKinsey launched a research effort to gather insights from physicians into how the pandemic is affecting their ability to provide care, their financial situation, and their level of stress, as well as what kind of support would interest them. Nationwide surveys were conducted online in 2020 from April 27–May 5 (538 respondents), July 22–27 (150 respondents), and September 22–27 (303 respondents), as well as from March 25–April 5, 2021 (379 respondents).
The participants were US physicians in a variety of practice types and sizes, and a range of employment types. The specialties included general practice and family practice; cardiology; orthopedics, sports medicine and musculoskeletal; dermatology; general surgery; obstetrics and gynecology; oncology; ophthalmology; otorhinolaryngology and ENT; pediatrics; plastic surgery; physical medicine and rehabilitation; psychiatry and behavioral health; emergency medicine; and urology. These surveys built on a prior one of 1,008 primary-care, cardiology, and orthopedic-surgery physicians in April 2019.
To provide timely insights on the reported behaviors, concerns, and desired support of adult consumers (18 years and older) in response to COVID-19, McKinsey launched consumer surveys in 2020 (March 16–17, March 27–29, April 11–13, April 25–27, May 15–18, June 4–8, July 11–14, September 5–7, October 22–26, and November 20–December 6) and 2021 (January 4–11, February 8–12, March 15–22, April 24–May 2, June 4–13, and August 13–23). These surveys represent the stated perspectives of consumers and are not meant to indicate or predict their actual future behavior. (In these surveys, we asked consumers about “Coronavirus/COVID-19,” given the general public’s colloquial use of coronavirus to refer to COVID-19.)
Many digital start-ups and tech and retail giants are rising to the occasion, but our most recent (2021) McKinsey Physician Survey indicates that physicians may prefer a return to pre-COVID-19 norms. In this article, we explore the trends creating disconnects between consumers and physicians and share ideas on how providers could offer digital services that work not only for them but also for patients. Bottom line: a seamless IRL/URL offering could retain patients while delivering high-quality care. Everybody benefits.
The rise of telehealth
These materials reflect general insight based on currently available information, which has not been independently verified and is inherently uncertain. Future results may differ materially from any statements of expectation, forecasts, or projections. These materials are not a guarantee of results and cannot be relied upon. These materials do not constitute legal, medical, policy, or other regulated advice and do not contain all the information needed to determine a future course of action.
At the onset of the COVID-19 pandemic, both physicians and patients embraced telehealth: in April 2020, the number of virtual visits was a stunning 78 times higher than it had been two months earlier, accounting for nearly one-third of outpatient visits. In May 2021, 88 percent of consumers said that they had used telehealth services at some point since the COVID-19 pandemic began. Physicians also felt dramatically more comfortable with virtual care. Eighty-three percent of those surveyed in the 2021 McKinsey Physician Survey offered virtual services, compared with only 13 percent in 2019. 1 See sidebar on methodology; McKinsey Physician Surveys conducted nationally in five waves between May 2019 and April 2021; May 1, 2019, n = 1,008; May 5, 2020, n = 500; July 2, 2020, n = 150; September 27, 2020, n = 500; April 5, 2021, n = 379.
However, as of mid-2021, consumers’ embrace of telehealth appeared to have dimmed a bit from its early COVID-19 peak: utilization was down to 38 times pre-COVID-19 levels. Also, more physicians were offering telehealth but recommending in-person care when possible in 2021, which could suggest that physicians are gravitating away from URL and would prefer a return to IRL care delivery (Exhibit 1).
Three trends from the late-stage pandemic
As COVID-19 continues, three emerging trends could set the stage for the next few years.
The number of virtual-first players keeps growing, and physicians struggle to keep up
The growth (and valuations) of virtual-first care providers suggest that demand by patients is persistent and growing. Teladoc increased the number of its visits by 156 percent in 2020, and its revenues jumped by 107 percent year over year. Amwell increased its supply of providers by 950 percent in 2020. 2 “Teladoc Health reports fourth-quarter and full-year 2020 results,” Teledoc Health, February 24, 2021; “Amwell announces results for the fourth quarter and full year 2020,” Amwell, March 24, 2021. By contrast, only 45 percent of physicians have been able to invest in telehealth during the pandemic, and only 16 percent have invested in other digital tools. Just 41 percent believe that they have the technology to deliver telehealth seamlessly. 3 McKinsey Physician Survey, April 5, 2021.
Some workflows, for example, require physicians to log into disparate systems that do not integrate seamlessly with an electronic health record (EHR). Audiovisual failures during virtual appointments continue to occur. To make these models work, providers may need to determine how to design operational workflows to make IRL/URL care as seamless as possible for both providers and patients. The workflows and care team models may need to vary, depending on the physician’s specialty and the amount of time they plan to devote to URL versus IRL care.
Patient–physician relationships are shifting
In McKinsey’s April 2021 Physician Survey, 58 percent of the respondents reported that they had lost patients to other physicians or to other health systems since the start of the COVID-19 pandemic. Corroborating those findings, our August 2021 survey of consumers showed that of those who had a primary-care physician (PCP), 15 percent had switched in the past year. Thirty-five percent of all consumers reported seeing a new healthcare provider who was not their regular PCP or specialist in the past year. Among consumers who had switched PCPs, 35 percent cited one or more reasons related to the patient experience—the desire for a PCP who better understood their needs (15 percent of respondents), a better experience (10 percent), or more convenient appointments (6 percent). Just half (50 percent) of consumers with a PCP say they are very satisfied. What’s more, Medicare regulations now give patients more ownership over their health data, and that could make it easier for them to switch physicians. 4 “Policies and technology for interoperability and burden reduction,” Centers for Medicare & Medicaid Services, December 9, 2021.
Physicians and patients see telehealth differently
Our surveys show that doctors and patients have starkly different opinions about telehealth and broader digital engagement (Exhibit 2). Take convenience: while two-thirds of physicians and 60 percent of patients said they agreed that virtual health is more convenient than in-person care for patients, only 36 percent of physicians find it more convenient for themselves.
This perception may be leading physicians to rethink telehealth. Most said they expect to return to a primarily in-person delivery model over the next year. Sixty-two percent said they recommend in-person over virtual care to patients. Physicians also expect telehealth to account for one-third less of their visits a year from now than it does today.
These physicians may be underestimating patient demand. Forty percent of patients in May 2021 said they believe they will continue to use telehealth in the pandemic’s aftermath. 5 McKinsey Consumer Health Insights Survey , May 7, 2021.
In November 2021, 55 percent of patients said they were more satisfied with telehealth/virtual care visits than with in-person appointments. 6 McKinsey Consumer Health Insights Survey , November 19, 2021. Thirty-five percent of consumers are currently using other digital services, such as ordering prescriptions online and home delivery. Of these, 42 percent started using these services during the pandemic and plan to keep using them, and an additional 15 percent are interested in starting digital services. 7 McKinsey Consumer Health Insights Survey , June 24, 2021.
Convenience is not the only concern. Physicians also worry about reimbursement. At the height of the COVID-19 pandemic in the United States, the Centers for Medicare & Medicaid Services (CMS) and several other payers switched to at-parity (equal) reimbursement for virtual and in-person visits. More than half of physician respondents said that if virtual rates were 15 percent lower than in-person rates, they would be less likely to offer telehealth. Telehealth takes investment: traditional providers may need time to transition their capital and operating expenses to deliver virtual care at a cost lower than that of IRL.
Four critical actions for providers to consider
Providers may want to define their IRL/URL care strategy to identify the appropriate places for various types of care—balancing clinical appropriateness with the preferences of physicians and patients.
Determine the most clinically appropriate setting
Clinical appropriateness may be the most crucial variable for deciding how and where to increase the utilization of telehealth. Almost half of physicians said they regard telehealth as appropriate for treatment of ongoing chronic conditions, and 38 percent said they believe it is appropriate when patients have an acute change in health—increases of 26 and 17 percentage points, respectively, since May 2019.
However, physicians remain conservative in their view of telehealth’s effectiveness compared with in-person care. Their opinions vary by visit type (Exhibit 3). Health systems may consider asking their frontline clinical-care delivery teams to determine the clinically appropriate setting for each type of care, taking into account whether physicians are confident that they can deliver equally high-quality care for both IRL and URL appointments.
Assess patient wants and needs in relevant markets and segments
Patient demand for telehealth remains high, but expectations appear to vary by age and income group, payer status, and type of care. Our survey shows that younger people (under the age of 55 ), people in higher income brackets (annual household income of $100,000 or more), and people with individual or employer-sponsored group insurance are more likely to use telehealth (Exhibit 4). Patient demand also is higher for virtual mental and behavioral health. Sixty-two percent of mental-health patients completed their most recent appointments virtually, but only 20 percent of patients logged in to see their primary-care provider, gynecologist, or pediatrician.
To meet market demand effectively, it may be crucial to base care delivery models on a deep understanding of the market, with a range of both IRL and URL options to meet the needs of multiple patient segments.
Partner with physicians to define a new operating model
Many physicians are turning away from the virtual operating model: 62 percent recommended in-person care in April 2021, up five percentage points since September 2020. As physicians evaluate their processes for 2022, 46 percent said they prefer to offer, at most, a couple of hours of virtual care each day. Twenty-nine percent would like to offer none at all—up ten percentage points from September 2020. Just 11 percent would dedicate one full day a week to telehealth, and almost none would want to offer virtual care full time (Exhibit 5).
To adapt to these views, care providers can try to meet the needs and the expectations of physicians. They could offer highly virtualized schedules to physicians who prefer telehealth, while allowing other physicians to remain in-person only. Matching the preferences of physicians may create the best experience both for them and for patients. Greater flexibility and greater control over decisions about when and how much virtual care to offer may also help address chronic physician burnout issues (Exhibit 6). Digital-first solutions (for example, online scheduling, digital registration, and virtual communications with providers) could also increase the reach of in-person-only care providers to the 60 percent of consumers interested in using these digital solutions after the pandemic abates.
Communicate clearly to patients and others
Physicians consistently emerge as the most trusted source of clinical information by patients: 90 percent consider providers trustworthy for healthcare-related issues. 8 McKinsey Consumer Survey, May 2020. Providers could play a pivotal role in counseling patients on the importance of continuity of care, as well as what can be done safely and effectively by IRL and URL, respectively. The goal is to help patients receive the care that they need in a timely manner and in the most clinically appropriate setting.
Potential benefits to providers
The strategic, purposeful design of a hybrid IRL/URL healthcare delivery model that respects the preferences of patients and physicians and offers virtual care when it is appropriate clinically may allow healthcare providers to participate in the near term, retain clinical talent, offer better value-based care, and differentiate themselves strategically for the future.
Telehealth and broader digital engagement tools have enjoyed persistent patient demand throughout the pandemic. That demand may persist well after it. Investment in digital health companies has grown rapidly—reaching $21.6 billion in 2020, a 103 percent year-over-year increase—which also suggests that this approach to medicine has staying power. 9 Q4 and annual 2020 digital health (healthcare IT) funding and M&A report , Executive Summary, Digital Health Funding and M&A, Mercom Capital Group.
That level of demand offers the potential for growth when physicians can meet it. If only new entrants fully meet consumer demand, traditional providers who do not offer URL options may risk losing market share over time as a result of patients’ initial visit and downstream care decisions. What’s more, as healthcare reimbursement continues to move toward value, virtual-delivery options could become a strategic differentiator that helps providers better manage costs. 10 Brian W. Powers, MD, et al., “Association between primary care payment model and telemedicine use for Medicare Advantage enrollees during the COVID-19 pandemic,” JAMA Network , July 16, 2021.
In all likelihood, one of the critical steps in the process will be engaging physicians in the design of new virtual-care models—for example, determining clinical appropriateness, how and where physicians prefer to deliver care, and the workflows that will maximize their productivity. This has the added benefit of potentially also addressing the problem of physician burnout by offering a range of options for how and where clinicians practice.
Most important, virtual care can offer an opportunity to improve outcomes for patients meaningfully by delivering timely care to those who might otherwise delay it or who live in areas with provider shortages. In addition, patients’ most trusted advisers on care decisions are physicians, so virtual care gives them a meaningful opportunity to help patients access the care they need in a way that both parties may find convenient and appropriate. 11 “Public & physician trust in the U.S. healthcare system,” ABIM Foundation, surveys conducted on December 29, 2020 and February 5, 2021.
Physicians are evaluating a variety of factors for delivering care to patients during and, eventually, after the COVID-19 pandemic. The strategic, purposeful design of a hybrid IRL/URL healthcare delivery model offers a triple unlock: improving the value of healthcare while better meeting consumer demand and improving physicians’ engagement. The full unlock is not easy—it requires deep engagement and cooperation between administrators, clinicians, and frontline staff, as well as focused investment. But it will yield dividends for patients and providers alike in the long run.
Jenny Cordina is a partner in McKinsey’s Detroit office, Jennifer Fowkes is a partner in the Washington, DC, office, Rupal Malani, MD , is a partner in the Cleveland office, and Laura Medford-Davis, MD , is an associate partner in the Houston office.
The article was edited by Elizabeth Newman, an executive editor in the Chicago office.
Explore a career with us
Related articles.

Physicians examine options in a post-COVID-19 era

Increased workforce turnover and pressures straining provider operations

Telehealth: A quarter-trillion-dollar post-COVID-19 reality?

IMAGES
COMMENTS
The COVID-19 pandemic represents an unprecedented threat to mental health in high, middle, and low-income countries. In addition to flattening the curve of viral transmission, priority needs to be given to the prevention of mental disorders (e.g. major depressive disorder, PTSD, as well as suicide).
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
Mental health professionals can help craft messages to be delivered by trusted leaders. 4. The Covid-19 pandemic has alarming implications for individual and collective health and emotional and ...
In summary, the COVID-19 pandemic and its countermeasures exuded a complex pattern of effects on physical and mental health, and factors shaping human stress resilience during the pandemic in the ...
COVID-19 pandemic is a global calamity posing an unprecedented opportunity to study resilience. We developed a brief resilience survey probing self-reliance, emotion-regulation, interpersonal ...
The COVID-19 pandemic has had a severe impact on the mental health and wellbeing of people around the world while also raising concerns of increased suicidal behaviour. In addition access to mental health services has been severely impeded. However, no comprehensive summary of the current data on these impacts has until now been made widely ...
Background Although research shows that the Covid-19 pandemic has led to declines in mental health, the existing research has not identified the pathways through which this decline happens. Aims The current study identifies the distinct pathways through which COVID-induced stressors (i.e., social distancing, disease risk, and financial stressors) trigger mental distress and examines the causal ...
The good news is that by October, 2020, mental health was top of the charts in terms of published papers and preprints on the effects of COVID-19. The bad news is that the quantity of papers is not matched by quality. In March, 2020, Holmes and colleagues outlined the priorities for mental health research during the pandemic. How much have we ...
The COVID-19 pandemic affected everyone around the globe. Depending on the country, there have been different restrictive epidemiologic measures and also different long-term repercussions. Morbidity and mortality of COVID-19 affected the mental state of every human being. However, social separation and isolation due to the restrictive measures considerably increased this impact.
Using a longitudinal dataset linking biometric and survey data from several cohorts of young adults before and during the COVID-19 pandemic (N = 682), we document large disruptions to physical activity, sleep, time use, and mental health.At the onset of the pandemic, average steps decline from 10,000 to 4,600 steps per day, sleep increases by 25 to 30 min per night, time spent socializing ...
Background The COVID-19 pandemic triggered vast governmental lockdowns. The impact of these lockdowns on mental health is inadequately understood. On the one hand such drastic changes in daily routines could be detrimental to mental health. On the other hand, it might not be experienced negatively, especially because the entire population was affected. Methods The aim of this study was to ...
Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population ... Key ethical questions for research during the COVID-19 pandemic. Lancet Psychiatry. 2020; 7: 381-383. Summary; ... The good news is that by October, 2020, mental health was top of the charts in terms of published papers and ...
In this section. The COVID-19 pandemic has had a huge impact on public health around the globe in terms of both physical and mental health, and the mental health implications of the pandemic may continue long after the physical health consequences have resolved. This research area aims to contribute to our understanding of the COVID-19 ...
We collected data on 8 million calls from 19 countries, focusing on the COVID-19 crisis. Call volumes peaked six weeks after the initial outbreak, at 35% above pre-pandemic levels. The increase ...
SUBMIT PAPER. Clinical Nursing Research ... Rod N. H., Strandberg-Larsen K., Varga T. V. (2022). Housing environment and mental health of Europeans during the COVID-19 pandemic: A cross-country comparison. ... Ogunlana A., Jaworska N. (2021). The burden of loneliness: Implications of the social determinants of health during COVID-19. Psychiatry ...
INTRODUCTION. Mental health nursing is well recognised as a challenging field of work, and nurses can experience a range of role-related and organisation-related stressors (Foster et al., 2021).The COVID-19 pandemic has added additional stress, heightened anxiety, and fear of infection in the community (Usher et al., 2020) and led to unprecedented demands and workload pressures for healthcare ...
People with serious mental illness (SMI) are at increased risk of being infected by coronavirus disease 2019 (COVID-19) and have higher subsequent rates of hospitalization, morbidity, and mortality. 1,2 Factors that contribute to worse outcomes include concomitant medications, poorer premorbid general health, physical comorbidity, reduced access to medical care, and environmental and lifestyle ...
While the pandemic left behind millions of people worldwide with lasting COVID-19 effects, it also fueled a research and healthcare focus that Thida Thant, MD, and colleagues have long promoted - the overlap of physical and mental illness. Some surveys suggest as many as a quarter of the 775 million-plus people infected with SARS-CoV-2 had ...
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint ...
This paper examines the mental health and psychosocial support (MHPSS) interventions provided to Filipino international merchant seafarers during the COVID-19 pandemic. Given the significant labor participation in seafaring of Filipinos, examining the MHPSS provided to them during a crisis is necessary because these services remain unexplored.
In this paper, after data preprocessing, ten widely known ML and four DL models were developed to automatically and accurately predict mental well-being during or after the Covid-19 circumstance. According to our findings, the Random Forest (RF) algorithm and Siamese Neural Networks (SNNs) outperformed other models in terms of accuracy (86 ...
The COVID-19 pandemic had a greater impact on boys' mental health than girls, contrary to the findings of other studies, according to new research led by scientists at University of Liverpool ...
To help our clients understand responses to COVID-19, McKinsey launched a research effort to gather insights from physicians into how the pandemic is affecting their ability to provide care, their financial situation, and their level of stress, as well as what kind of support would interest them. Nationwide surveys were conducted online in 2020 from April 27-May 5 (538 respondents), July 22 ...