- Health & Wellness
- Hearing Disorders
- Patient Care
- Amplification
- Hearing Aids
- Implants & Bone Conduction
- Tinnitus Devices
- Vestibular Solutions
- Accessories
- Office Services
- Practice Management
- Industry News
- Organizations
- White Papers
- Edition Archive
Select Page

Case Study of a 5-Year-Old Boy with Unilateral Hearing Loss
Jan 15, 2015 | Pediatric Care | 0 |
Case Study | Pediatrics | January 2015 Hearing Review
A reminder of what our tests really say about the auditory system..
By Michael Zagarella, AuD
How many times have I heard— and said myself—that the OAE is not a hearing test? How many times have I thought to myself that, just because a child passes their newborn hearing screening test, it does not mean they have normal hearing? This case brought those two statements front and center.
A 5-year-old boy was referred to me for a hearing test because he did not pass a kindergarten screening test in his right ear. His parents reported that he said “Huh?” frequently, and more recently they noticed him turning his head when spoken to. He had passed his newborn hearing screening, and he had experienced a few ear infections that responded well to antibiotics. The parents mentioned a maternal aunt who is “nearly totally deaf” and wears binaural hearing aids.
Initial Test Results
Otoscopic examination showed a clear ear canal and a normal-appearing tympanic membrane on the right side. The left ear canal contained non-occluding wax.
Tympanograms were within normal limits bilaterally. Unfortunately, otoacoustic emissions (OAE) testing could not be completed because of an equipment malfunction.
Behavioral testing with SRTs was taken, and I typically start with the right ear. The child seemed bright and cooperative enough for routine testing. I obtained no response until 80 dB.
I switched to the left ear and he responded appropriately. This prompted me to walk into the test booth and check the equipment and wires; everything was plugged in and looked normal. I tried SRTs again with the same results, even reversing the earphones. Same results. When the behavioral tests were completed, the results indicated normal hearing in his left ear and a profound hearing loss in his right ear.
The child’s parents were informed of these results, and we scheduled him to return for a retest in order to confirm these findings.
Follow-up Test
One week later, the boy returned for a follow-up test. The otoscopic exam was the same: RE = normal; LE = non-occluding wax.
Tympanograms were within normal limits. I added acoustic reflexes, which were normal in his left ear (80-90 dB), and questionable in his right ear (105-115 dB).
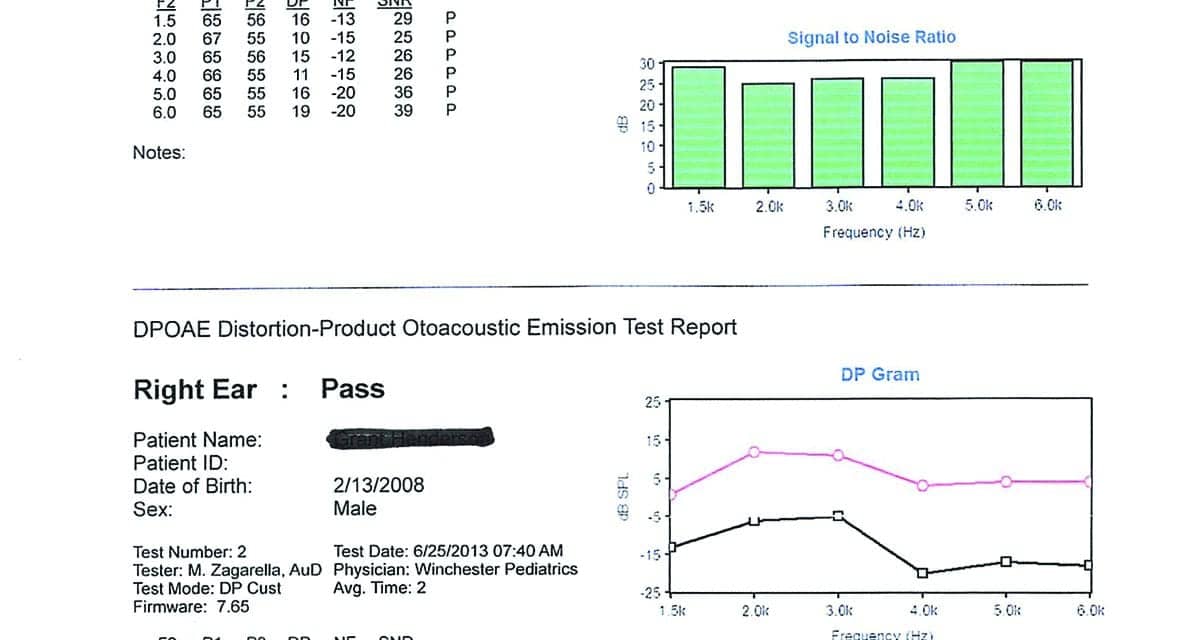
DPOAEs were present in both ears. The right ear was reduced in amplitude compared with the left, but not what I would expect to see with a profound hearing loss (Figure 1).
I repeated the behavioral tests with the same results that I obtained the first time (Figure 2). Bone conduction scores were not obtained at this time because I felt I was reaching the limits of a 5-year-old, and the tympanograms were normal on two occasions.
Recommendation to Parents
After completing the tests, I explained auditory dyssynchrony to the parents, and told them that this is what their son appeared to have. Since they were people with resources, I advised them to make an appointment at Johns Hopkins to have this diagnosis confirmed by ABR.
Johns Hopkins Results
The initial appointment at Johns Hopkins was at the ENT clinic. According to the report from the parents, the physician reviewed my test results and said it was unlikely that they were valid. She suggested they repeat the entire test battery before proceeding with an ABR. All peripheral tests were repeated with exactly the same results that I had obtained. The ABR was scheduled and performed, yielding:
“Findings are consistent with normal hearing sensitivity in the left ear and a neural hearing loss in the right ear consistent with auditory dyssynchrony (auditory neuropathy). The normal hearing in the left ear is adequate for speech and language development at this time.”
Additional Follow-up
The boy’s mother was not completely satisfied with the diagnosis or explanation. After she arrived home and mulled things over, she called Johns Hopkins and asked if they could do an MRI. The ENT assured her that it probably would not show anything, but if it would allay her concerns (and since they had good insurance coverage), they would schedule the MRI.
Further reading: Vestibular Assessment in Infant Cochlear Implant Candidates

Figure 1. DPOAEs of 5-year-old boy.
Findings of MRI. Evaluation of the right inner ear structures demonstrated absence of the right cochlear nerve. The vestibular nerve is present but is small in caliber. The internal auditory canal is somewhat small in diameter. There is atresia versus severe stenosis of the cochlear nerve canal. The right modiolus is thickened. The cochlea has the normal amount of turns, and the vestibule semicircular canals appear normal.
The left inner ear structures, cranial nerves VII and VIII complex, and internal auditory canal are normal. Additional normal findings were also presented regarding sinuses, etc.
Key finding: The results were consistent with atresia versus severe stenosis of the right cochlear nerve canal and cochlear nerve and deficiency described above.
The Value of Relearning in Everyday Clinical Practice

Figure 2. Follow-up behavioral test of 5-year-old boy.
According to the MRI, the cochlea on the right side is normal—which would explain the present DPOAE results. The cochlear branch of the VIIIth Cranial Nerve is completely absent, which would explain the absent ABR result and the profound hearing loss by behavioral testing.
This case has certainly caused me to re-evaluate what I think and say about my test findings. How many times have I heard—and said myself!—that the OAE is not a hearing test? How many times have I thought to myself that, just because a child passes their newborn hear- ing screening test, it does not mean that they have normal hearing?
This case has surely brought those two statements front and center. In addition, what about auditory neuropathy? In about 40 years of testing, I had never seen a case that I was convinced was AN. Naturally, I was somewhat skeptical about this disorder: Is it real, or does it reside in the realm of the Yeti. (Personal note to Dr Chuck Berlin: I truly don’t doubt you, but I do like to see things for myself!)
Finally, this case only reinforces my trust in “mother’s intuition” and the value of deferring to the sensible requests of parents. If she had not felt uneasy about what she had been told at one of the most prestigious clinics in the country, the actual source of this problem would not have been discovered.
So what? Does any of this really make a difference? The bottom line is we have a 5-year-old boy with a unilateral profound hearing loss. How important is it that we know why he has that loss? From a purely clinical standpoint, I think that it is poignant because it brings home the importance of understanding what our tests really say about the hearing mechanism and auditory system (ie, is working or not working?).
And although it may not make a large difference in the boy’s current treatment plan, I do know that the boy’s mother is grateful for understanding the reason for her son’s hearing loss and that it’s at least possible the boy may benefit from this knowledge in the future.
Michael Zagarella, AuD, is an audiologist at RESA 8 Audiology Clinic in Martinsburg, WVa.
Correspondence can be addressed to HR or or Dr Zagarella at: [email protected]
Citation for this article: Zagarella M. Case study of a 5-year-old boy with unilateral hearing loss. Hearing Review . 2015;22(1):30-33.
Related Posts

Phonak Launches Web-Based Child Hearing Assessment Toolkit for Schools
June 26, 2013

‘Parentese’ Can Help Boost Child Language Development
February 5, 2020
New Genetic Test Could Prevent Pediatric Deafness
April 4, 2022

People with Learning Disabilities Need to Be Checked for Hearing Loss
September 23, 2014
Recent Posts
- New Insights on Tinnitus Revealed in Apple Hearing Study
- Cilcare Names New Chief Medical Officer
- A Study of Younger People’s Perceptions of Hearing Care
- New AI-Powered Headphones ‘Cancel’ Only Unwanted Sounds
- How Signia Hearing Aids Improved Life for a Music Industry Professional
- Contacta, National Audio Systems Announce Distribution Deal
- Search Menu
- Sign in through your institution
- Advance articles
- Author Guidelines
- Submission Site
- Open Access
- Why Submit?
- About The Journal of Deaf Studies and Deaf Education
- Editorial Board
- Advertising and Corporate Services
- Journals Career Network
- Self-Archiving Policy
- Dispatch Dates
- Terms and Conditions
- Journals on Oxford Academic
- Books on Oxford Academic

Editor-in-Chief
Hannah Dostal
About the journal
Journal of Deaf Studies and Deaf Education is a peer-reviewed scholarly journal integrating and coordinating basic and applied research relating to individuals who are deaf, including cultural, developmental, linguistic, and educational topics.
Latest articles

Special Collections
Explore specially curated collections from the Journal of Deaf Studies and Deaf Education or collections that include articles from the journal.

Highly Cited Collection
Explore a collection of highly cited articles from the Journal of Deaf Studies and Deaf Education .

Family and Practitioner Briefs
Introducing the new Family and Practitioner Briefs: quick-to-read and easy-to-understand briefs about educational strategies, policy decisions, and new topics in deaf education, published quarterly.

Call for Papers
JDSDE invites submissions for an upcoming issue in honor of Dr. Jonathan Henner, a linguist, scholar, and theorist who had a profound effect on multiple fields including but not limited to deaf education, linguistics, and deaf and disability studies.
Read the call for papers here

Submit your research
The Journal of Deaf Studies and Deaf Education is currently accepting high quality clinical and scientific papers relating to all aspects of the field.
More information

Follow us on social media
Stay up to date with the latest news and content from the Journal of Deaf Studies and Deaf Education by visiting our Facebook page , or follow us on X.

Email alerts
Register to receive table of contents email alerts as soon as new issues of The Journal of Deaf Studies and Deaf Education are published online.

- Accessibility
Oxford University Press is committed to making its products accessible to and inclusive of all our users, including those with visual, hearing, cognitive, or motor impairments.
Find out more in our accessibility statement
Related Titles
- Recommend to your Library
Affiliations
- Online ISSN 1465-7325
- Print ISSN 1081-4159
- Copyright © 2024 Oxford University Press
- About Oxford Academic
- Publish journals with us
- University press partners
- What we publish
- New features
- Open access
- Institutional account management
- Rights and permissions
- Get help with access
- Advertising
- Media enquiries
- Oxford University Press
- Oxford Languages
- University of Oxford
Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by publishing worldwide
- Copyright © 2024 Oxford University Press
- Cookie settings
- Cookie policy
- Privacy policy
- Legal notice
This Feature Is Available To Subscribers Only
Sign In or Create an Account
This PDF is available to Subscribers Only
For full access to this pdf, sign in to an existing account, or purchase an annual subscription.
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- PMC10686551

Systems that support hearing families with deaf children: A scoping review
Julia terry.
1 School of Health and Social Care, Faculty of Medicine Health and Life Science, Swansea University, Wales, United Kingdom
Jaynie Rance
2 School of Psychology, Faculty of Medicine Health and Life Science, Swansea University, Wales, United Kingdom
Associated Data
All relevant data are within the paper and its Supporting information files.
Over 90% of deaf children are born to hearing parents who have limited knowledge about deafness and require comprehensive support and information to support and communicate with their deaf child. However, little is known about the systems that support hearing families with deaf children. We performed a scoping review to provide an overview of current literature on the topic.
The protocol of the scoping review was prepared using the PRISMA statement guidelines for scoping reviews. Relevant search terms were used to identify eligible studies following discussion with the study’s steering group. Databases searched were CINAHL, Medline, ProQuest Central and ASSIA, as well as grey literature from relevant journals and online sources. Included were studies published from 2000 to 2021 and available in English.
A search of databases identified 1274 articles. After excluding duplicates, screening titles and abstracts and full texts, 65 papers matched the identified inclusion criteria. Results included 1 RCT, 7 comparative studies, 6 literature reviews, 4 PhD theses, and 47 further empirical studies.
There is limited quality evidence on what supports hearing parents with deaf children. It is evident that further studies are needed to ensure comprehensive support is accessible and effective for hearing parents of deaf children.
Introduction
Authors’ note.
In this paper the terms Deaf and deaf are used. A capital D for Deaf is used to refer to people who identify as Deaf and view themselves as part of Deaf communities, are a Deaf adult, Deaf professional or Deaf mentor, or who may be profoundly Deaf and may use a signed language. When a lower-case d for deaf is used this tends to refer to deaf children or those who are hard of hearing. Currently there is limited consensus about an emic term, as people can feel colonised when a specific label is provided and may be in different places in their individual journey [ 1 ].
Over 5% of the world’s population experience deafness or hearing loss [ 2 ] and by 2050 hearing loss will affect one in ten people. Currently there are an estimated 34 million deaf children globally [ 3 ], and nearly 55,000 deaf children in the UK [ 4 ]. As 96% of deaf babies are born to hearing parents [ 5 , 6 ] who are usually not expecting to raise a deaf child, it is important that families benefit from a range of support processes and interventions. Support in this context can best be described as encouragement, help and enablement, to promote sustainable success and confidence for hearing parents and their deaf children.
When parents find out their child has been diagnosed as deaf or having hearing loss, or when they suspect this to be the case, families begin a journey that involves differing amounts of support, information, and guidance. For many families, initial discussions begin at new-born hearing screening, if these services are available. Newborn hearing screening has become an essential part of neonatal care in high-income countries with positive outcomes following early intervention during the critical period to enable optimal language development. Currently at least 45 US states require new-born hearing screening by law [ 7 ] and others have achieved this without legislation or have it pending. In the UK the NHS newborn hearing screening programme recommends screening for all babies in the first five weeks of life, although there is a notable absence of hearing screening in the Global South [ 8 , 9 ]. The early detection of hearing status can prevent significant detrimental effects on cognitive development happening later. For example, if children’s development needs are not fully addressed [ 10 ] a deaf child may not develop language skills to ensure fluent communication as a vital platform for further learning. Language deprivation in the first five years of life appears to have permanent consequences for long-term neurological development [ 11 ].
Whilst families welcome prompt hearing screening, it is worth bearing in mind the range of perspectives that exist about deafness. Parents say they encounter predominantly medical model approaches, which suggest their child has a deficit [ 12 ], proposing that deafness is treated and seen as an impairment [ 13 ]. Hearing families may find later that there are cultural-linguistic models and alternative approaches that help them understand the social identity of their deaf children. The socio-cultural view that considers the rich environment of Deaf communities, including the naturalness of sign languages with deafness seen as a way of being, and not an impairment [ 14 ]. Diagnostic rituals can set in motion a deficit-orientated way of addressing a child’s needs, sometimes resulting in diminishing parental competence and confidence [ 15 ]. Often parents report that initial information received upon early detection of their child’s hearing loss can be incomplete and coloured by workers’ personal beliefs and values, usually originating from a medical model [ 16 ], when healthcare policies could acknowledge the broad scope of conflicting views that hearing parents may encounter.
Hearing screening, identification and individualised early intervention is critical in helping deaf or hard of hearing children achieve their full potential [ 17 ] and has led many nations to develop Early Hearing Detection and Intervention (EHDI) programs. It may be audiology, speech and language services or education professionals who begin to provide parents with advice about communication choices and pathways. Frequently the not-for-profit or charity sector agencies provide additional support and information perhaps because they have wider scope in terms of delivery arrangements.
Systems that support hearing parents with deaf children may include education, health, care, and social services, depending on the child’s age and location. Support may be provided by statutory services and the voluntary sector and may include short-term initiatives and long-term input. Essentially the support families have and the advice they are given in the early years of their child’s life is of key importance. Hearing parents will want to know about how the ear works, about deafness, communication and language choices, their child’s emotional and social development, education, alerting and assistive devices as well as early years support. At an early point there will be discussions with the family about the child’s language development and communication options. Professionals who support families with deaf children may hold a range of views towards sign language, but essentially families will decide about communication choices and whether their child will learn a mixture of spoken and signed language or just a spoken language [ 18 ]. Decisions made about communication choice will likely affect the child and family for a lifetime [ 19 ].
Fully accessible language experiences during the early years are vital in empowering deaf children’s development potential [ 20 ]. There is a critical window for language development and if a child is not fluent in a language by around the age of five years old [ 21 ], he or she may not achieve full fluency in any language. It is a foundational language that is key to the development of future language. Sign language often comes naturally to deaf children, and deaf children exposed to sign language during the first 6 months of life have age-expected vocabulary growth when compared to hearing children [ 22 – 24 ], meaning that learning a signed language can avoid language delays. If parents are keen for their deaf child to learn speech, then sign language does not impede this. Parents can be given misinformation and not be made aware that there are risks in excluding sign language during the critical time of language acquisition, with no evidence that sign language causes harm [ 25 ]. There are recommendations for changes in existing systems to support bimodal bilingualism as default practice, in order to provide the best educational outcomes, which means a signed language and a spoken language [ 23 ]. It is suggested that all deaf children should be bilingual [ 26 ]. However, little is known about the support parents are given at the outset of these decision-making processes.
Critics suggest there is a need to stop dichotomizing spoken or signed language, and to focus instead on educating families about the range of opportunities available [ 19 , 27 ]. Frequently hearing parents of deaf children do not know where to turn for support and can be overwhelmed with advice as they try to understand different methods employed in the language development and education of their child [ 20 ]. Support for hearing parents of deaf children varies globally. A variety of initiatives and projects appear regularly in local and regional news stories, such as support for sign language classes [ 28 ], family camps for deaf children [ 29 ] and artificial intelligence avatars that help deaf children to read [ 30 ]. Support systems are people or structures in society that provide information, resources, encouragement, practical assistance, and emotional strength.
We argue that there is limited published evidence about the support systems for hearing parents with deaf children. Therefore, we conducted a scoping review to provide a baseline overview of the published evidence until 2021 of the extent, variety, and nature of literature in this area.
Aims of the study
The aim of this scoping review was to map available evidence regarding the systems and structures surrounding deaf children and their families with hearing parents/guardians.
The specific objectives were to:
- identify published studies describing support systems and structures that support hearing parents with deaf children, and
- review the evidence of these studies.
The primary objective of this review was to assess the number of studies and their characteristics such as their origin, study designs, study population, type of support and key findings regarding systems or supports for hearing parents with deaf children.
Study design
We followed PRISMA-ScR guidelines for scoping reviews in the conduct of the literature review, data extraction/charting, and synthesis. The main aim of a scoping review is to identify and map the available evidence for a specific topic area [ 31 ]. The approach to the review was based on Arksey and O’Malley’s framework [ 32 ] which consists of the following stages: i) identifying the research question; ii) identifying relevant studies; iii) selecting studies; iv) charting the data; and v) collating, summarising and reporting the results. Ethical approval was not required because the study retrieved and synthesised data from already published studies.
Identifying the research question
The core aim of this scoping review was: What is the existing research that examines support systems for hearing parents with deaf children. The focus on hearing parents was due to over 90% of deaf children being born to hearing parents, who have little knowledge of deafness and deaf people, which is different from the experience of Deaf parents parenting deaf children [ 33 , 34 ]. An initial a priori protocol was developed and published on Open Science Framework in February 2021, and then revised using feedback from the project steering group over the course of the project, as scoping reviews are an iterative process [ 35 ]. The steering group comprised Deaf and hearing professionals and lay members, people working with Deaf charities, in health, education, policy and academia. Decisions were documented in a search log and steering group meeting notes to record the scoping review process. The final protocol was registered on 24 th August 2022 with the Open Science Framework— https://osf.io/w48gc/ .
Identifying relevant studies
The scoping review research question was left intentionally broad and was discussed in-depth at the first project steering group where members generated 50 words and terms to be included in the outline database searches. The evidence was searched using four electronic databases, hand searches of reference lists of key journals and repositories (such as PROSPERO), and contact made with key authors; as well as internet site searches for policies and reports. The wider project involves interviewing family members and workers situated in Wales, UK, so the scoping review included material specific to Wales as well as other geographical areas nationally and internationally that has contextual similarities (for example, grey literature including newspaper articles about family situations and support projects, blogs and regional reports), and these were included in the early stages of the review. An experienced information specialist’s help was sought in reviewing the PICO framework (see Table 1 ) and specific search strategies. The databases included were CINAHL, Medline, ASSIA and Proquest Central, with searches conducted between May and June 2021, and updated in January 2022. (An example of the search strategy for one database is provided as an additional file).
Different techniques and terms were used to expand and narrow searches, including tools such as medical subject headings (MESH), Boolean operators and Truncation. Single and combined search terms included key subject area on deafness, children, BSL/sign language and parent/family words. Limitations were set to include papers in the English Language and peer-reviewed research from the time period January 2000 onwards. In addition, key journals, professional organisation websites and reference lists of key studies were searched to identify further relevant documents. The final search strategy and terms were agreed and verified by a health subject librarian.
Inclusion criteria were: published research articles and dissertations, literature reviews and PhD theses specific to a) parents and families/caregivers b) deafness/hard of hearing/hearing loss c) sign language or British Sign Language (BSL) d) child or young person e) information specific to support, systems, challenges, barriers f) were published in English between 2000–2021. The inclusion criteria were purposely broad, as there is a dearth of scientific evidence on the area of support and systems for hearing parents with deaf children.
Exclusion criteria were: papers pre-2000 (unless they met a-e of inclusion criteria above); papers without a focus on deafness, papers that focused solely on literacy, or were short news items or opinion papers, and/or did not focus on support issues for hearing parents of deaf children.
Study selection
The initial search produced a total of 1274 results from database searches (see PRISMA, Fig 1 ), which were screened, and a further 192 records were added from internet and hand-searching. An example of a database search is provided in Table 2 . Once duplicates were removed (n = 2653+18) and a further 8 discounted as pre-2000 that did not meet the inclusion criteria, 1202 publications remained, and titles and abstracts were screened. 821 records were then removed in line with the eligibility criteria, and the remaining 381 full texts were obtained, and details transferred to an Excel database for sifting. Knowledge synthesis was achieved by peer review using Rayyan software [ 36 ] and annotated spreadsheets of retrieved papers, which were reviewed by two researchers independently with inter-rater discrepancies resolved by discussion.

We began by excluding sources that did not describe support for hearing parents of deaf children, such as opinion articles, newspaper reports, and papers without a deaf focus. Screening full texts resulted in a further 316 papers being excluded, leaving a total of 65 publications included in this review (see Fig 1 PRISMA diagram).
Charting the data
A data-charting form was developed by one reviewer, and then updated iteratively in discussion with the second reviewer, which was piloted and found to be effective. The data extracted were the author, year of publication and country of origin, study design, sample population, study aim and findings and study strengths and weaknesses, (see Table 3 ). Articles meeting inclusion criteria were examined, and data was entered into Excel spreadsheets, which included sample characteristics (age range, clinical characteristics, sample size); and experimental and control measures, as applicable.
Through this process sources were identified as follows: 55 primary research studies, four PhD theses and six literature reviews.
Collating, summarizing and reporting results
From the final scoping review, 21 individual countries were represented ( Fig 2 , which present the distribution by country). Most publications came out of the USA, Australia, the UK and Canada, which may be due to greater funding in this area of research compared to other nations.

Due to the heterogeneity of the range of study contexts, a narrative synthesis was a reasonable way to approach the reporting of retrieved studies. After summarising the information from sources, a thematic framework was applied to categorise the areas of support for hearing parents. This involved sorting studies into categories as follows: i) Communication choices and strategies; ii) Interventions and resources; iii) Family perspectives and environment; and iv) Deaf identity development . In addition, strengths and limitations of the sources are presented in Table 3 . Context from the grey literature is included in this paper’s introduction section, as this clinical wisdom provides additional information and context.
Theme one: Communication choices and strategies
Hearing parents will need to decide whether their deaf child will communicate using a spoken language or a signed and spoken language [ 37 ]. The timing of this communication choice is challenging as hearing parents make decisions during the small window when their child starts to develop language during the first few years of life. Hearing parents have little understanding about deafness, nor is infrastructure present to guide parents towards appropriate engagement with Deaf communities to begin discussing the differences between communication strategies. Parents can be inundated with information regarding communication and educational methods [ 20 ]. Yet the decision is up to parents and the key factor being that any form of early language development is critical [ 19 ]. Around the decision-making time, parents commonly want to know what will give their deaf child the best chance of learning to communicate, and whether using sign language might adversely affect their academic achievements and if it is worth waiting to see the impact of a cochlear implant before learning sign language [ 5 ]. There is frequent reporting that medical professionals claim that promoting a signed language with a deaf child may delay or hinder the development of spoken language learning, with suggestions that children may be confused [ 5 ], although much evidence supports the positives of learning to sign [ 19 ].
Retrieved papers under the communication choices and strategies theme included 20 primary research studies and two literature reviews. The 20 primary research studies included three co-comparative studies, four quantitative studies and twelve qualitative studies and one PhD thesis.
Factors contributing to parents’ selection of a communication mode to use with their children with hearing loss, are reported as information, perception of assistive technology, professionals’ attitudes and the quality and availability of support [ 38 ]. Parents’ decisions about communication choices with their deaf child are strongly influenced by the information they receive, which in the main focuses on amplification of sound, with information givers rarely mentioning sign language approaches [ 39 ]. Parents who chose speech only as a communication choice appear to have received advice from education and speech/audiology professionals more often [ 37 ]. Similar findings are reported in other studies that parents relied heavily on advice from professionals [ 40 , 41 ]. There is suggestion that advice from speech and language professionals, audiologists and specialist teachers was valued by parents over medical or non-professional views [ 42 ]. Conversely, parents of deaf children they surveyed did not find any professional group’s advice more influential than another, and reported they ultimately relied on their own judgements to make decisions about their child’s communication choices [ 43 ].
Several studies in this scoping literature review compared hearing and Deaf parents’ views about communication choices as well as child outcomes. Deaf parents are likely to choose a more visual mode of communication for their deaf child, and frequently outperform hearing parents in interaction studies that compare hearing and Deaf parents’ engagements with their deaf children [ 44 ]. For example, Deaf parents tend to use a higher level of tactile strategies when communicating with their deaf child compared to hearing parents [ 42 ].
When parents make hearing technology and communication modality choices for their children amongst competing discourses of deafness and language, hearing program principles of fully informed choice of communication narrowly reflected medical knowledge of deafness only [ 43 ]. Frequently there is reported to be minimal information about sign language and Deaf culture, and over time parents resist medical knowledge and asked for alternate services as their knowledge of their own children grew beyond diagnostic assumptions [ 43 ]. Initial adoption of a medicalised model script is recognised as occurring, which often maintains a strict divide between competing views of deafness [ 44 ], such views may include parents thinking their children are successful if they do not need a signed language.
In a comparative study two groups of hearing mothers with deaf children were studied, with one group more experienced as their children had been diagnosed for more than 24 months (compared to the mothers with children diagnosed in the last 18 months) [ 45 ]. The aim was to investigate the type of communication strategies that parents use with their children and how the type of early intervention (EI) involvement affected parents’ values about communication strategies. Mothers completed questionnaires about their views on communication strategies and were also videoed for 3-minute mother-child play interactions, and only minor differences were found between the groups of less and more experienced mothers of deaf children suggesting limited impact of early intervention programs on parental choice of communication method [ 45 ].
The main factors that influenced caregivers to change the communication method with their child with hearing loss included family characteristics, access to information [ 46 ], family strengths, family beliefs, and family practices, with the family at the core of decision-making regardless of severity of hearing loss, family demographic or type of device used or communication approach [ 47 ]. Similarly, the importance of communication changes regarding language modality being child-led, as parents adapted their language choices in line with their child’s needs to improve communication confidence, noting that early sign language exposure benefits the development of spoken language [ 48 ].
A comparative study of hearing versus Deaf parents with their respective deaf children acknowledged the active role that parents, and children take when communicating as they sought to explore successful joint attention (where one party seeks to gain the attention of the other, and the other responds) [ 49 ]. Studies that inform understanding of factors supporting language success are crucial. Communication in families will always be a joint venture and knowing if gaining joint attention at an early development point would assist families and professionals with communication choices in the future [ 49 ]. Very often parents want to know exactly what it is that will help communication to be most effective.
Complexities of communication choice are apparent in studies that focus on the intricacies of self-identify in children of parents who chose sign language as a primary mode of communication [ 50 ]. Follow up appointments focusing on communication modality, particularly following cochlear implantation, suggest a background of opposing views on communication choice mean increased awareness for parents is vital [ 51 ]. Families can unknowingly overprotect their child, limit knowledge and skill development due to hearing parents’ lack of knowledge and understanding about Deaf culture and Deaf communities [ 52 ]. All three studies highlighted the importance of continuing professional development for workers in order that they gain familiarity with these topics, and in turn discuss them with families of deaf children [ 50 – 52 ].
Perceptions of factors that foster success in deaf students from parents, teachers, interpreters, notetakers and deaf students themselves do not mention communication choice at a young age; instead, success was attributed to strategic components including self-determination, family involvement, friendships, reading and high expectations [ 53 ].
In one study deaf children of Spanish-speaking families studied did not learn American Sign Language (ASL) early on, often coming to this much later, with many of the children having limited access to language early on, and parents expressing frustration at not being able to communicate with their children, with the family being left behind through delaying communication through ASL [ 54 ].
The importance of professional advice provided to hearing parents of deaf children about communication mode and language use choices is noted, as this may heavily influence caregiver choices about communication. Understandings about factors that led to specific communication choices by hearing parents could be gained through further research [ 55 ]. The next theme focuses on papers concerning interventions and resources that support hearing parents with deaf children.
Theme two—Interventions and resources that support hearing parents with deaf children
Theme two incorporates identified studies that focused on interventions and resources that support hearing parents with deaf children. In this section we report on intervention programmes for hearing parents with deaf children broadly, then how programs were delivered and finally specific types of interventions that support hearing parents with deaf children.
Specific interventions of Deaf mentors and role models
A scoping review of early interventions for parents of deaf infants [ 56 ] found that interventions commonly focus on language, communication and parent knowledge, well-being and parent/child relationships and did not find any studies focusing on parent support to nurture socio-emotional development, which is often a poor outcome for deaf children. Socio-emotional development is not well-analysed by hearing professionals, who may not realise that it is not deafness that needs fixing but everything around it. It was concluded that research in this area is much needed, with most studies conducted some time ago and not in line with healthcare advances, recommending further research to develop evidence based early intervention [ 56 ]. A literature review of early intervention programme models and processes [ 57 ] identified five themes which were caregiver involvement, caregiver coaching, caregiver satisfaction, intervention program challenges and telehealth. Understandably caregiver involvement needs to be culturally and linguistically appropriate, as this improves caregiver satisfaction with services and improves outcomes for deaf children [ 57 ]. Another example is the HI-HOPES intervention program, developed in 2006 and still current, with an appreciation of South Africa’s characteristic linguistic, racial, and cultural diversity, noting embedding of cultural values and practices and includes provision of Deaf mentors [ 58 ].
A series of studies of the Colorado Home Intervention Program over nine years [ 59 ], saw a change in the average age of intervention decrease from 20 months to 2 months, meaning infants had much earlier intervention and therefore increased their language and social-emotional range. The early engagement with parents from a CO-Hear co-ordinator about choice of intervention service is a key success factor [ 59 ]. Another language intervention program with a sole parent focus, this time oral only, is the Muenstar Parental Program [ 60 ], a family-centred intervention following newborn hearing screening. Parents received training on the positive impact their behaviour had on their infant including showing more eye contact, more imitations and more listening, where parent and trainer discuss and agree principles to intensify in the next videotaped interaction. Although only single training sessions [ 60 ], authors noted the model to be a comprehensive early intervention focusing on encouragement, however, when published it was at the concept stage with minimal data available.
Summer pre-school language environments compared to their home environments suggest there are benefits to children, whilst recognising that pre-schoolers’ parents continue to require education around language strategies [ 61 ]. Parents would likely benefit from guided practice regarding extending conversations and asking questions at their child’s language level, and how to expand their children’s language, and that practising these skills with a professional is essential [ 61 ].
Mentors for families with deaf and hard of hearing children have been found to be highly effective, with study examples of family mentors [ 62 ] and mentors for children [ 63 ]. There is an awareness that parent- to- parent support models are rooted in disability ideologies and are highly valued [ 64 ], and often need to be unique [ 62 ]. Parent mentors made notes following each phone support conversation, and notes analysed over a two-year period showing hearing related conversations, early intervention and multiple disabilities were the primary topics of conversations between parent mentors and families. A literature review and eDelphi study to define the vital contribution of parents in early hearing detection and intervention programs suggested supporting, or a mentoring parent was well received [ 65 ].
Similarly Deaf adults are a key element in early intervention programs [ 66 ], primarily as role models and language providers, noting that families do not have a range of Deaf professionals to connect with in early intervention programs. One of the first reported studies of Deaf family mentors [ 63 ] provided a Deaf adult mentor who made home visits to deaf children and their families to share language, as well as a hearing advisor to support to parents. This type of provision is referred to as bilingual-bicultural and was intended as introductory in the first instance in two US states. The Deaf mentors taught each family American Sign Language (ASL) signs, interacted with the child using ASL, shared Deaf knowledge and culture and introduced the family to the local Deaf community, promoting a bi-bi home environment. It is reported children with Deaf mentors used more than twice the number of signs and parents used more than six times the number of signs than the control group [ 63 ]. 85% of survey respondents in the Lifetrack Deaf mentor family program operating in Minnesota USA reported their child’s quality of life to have improved, and 76% of families finding the information about Deaf culture ‘very helpful’ [ 67 ]. There are limited examples of early intervention providers that include Deaf mentor provision for children and families in the US, and whilst 27% of their survey respondents said there were a diverse range of Deaf professionals for families to connect with; but only 2% of respondents reported the first point of contact with early intervention professionals had been with a Deaf person [ 66 ].
Delivering intervention programs using telehealth
Although the provision of healthcare with remote support has become commonplace during Covid-19, prior to the pandemic many services used telehealth because it offered the potential to meet the needs of underserved populations in remote regions [ 68 , 69 ].
Tele-practice or tele-intervention (or virtual home visit) has been used increasingly as a method of delivering early intervention services to families of deaf children. Tele-practice intervention outcomes were compared for children, family and provider compared to in-person home visits using fifteen providers across five US states (Maine, Missouri, Utah, Washington and Oregon) and found children in the telepractice intervention group scored significantly higher on their receptive and total language scores that the children who received in-person visits [ 70 ]. Higher scores were also reported with telepractice intervention for parent engagement and provider responsiveness compared to in-person visits [ 70 ]. Parents reported having better support systems, feeling better supported by programs and knowing how to advocate more for their deaf child. Notably in-person visits were reported to focus more on intervention with the child with parent observation, whilst tele-practice engaged parents more in supporting parents as the child’s natural teacher. Equally when comparing tele-intervention with in-person visits, increased engagement from the tele-intervention group has been reported, with families reporting themselves to being ‘more in the driving seat’, and specialised early intervention services for families with deaf children via telehealth to be cost effective [ 71 ].
Preschool and school services were examined for children who are hard of hearing and described service setting, amount, and configuration, analysing relationships between services and hearing levels and language scores [ 72 ]. Noting that as children reach the age of three years that services often shift from being family centred to being more child focused and a need for more interprofessional practice to best meet the needs of children who are deaf. Findings that 19% of families did not receive any intervention, which rose to 30% by the time children were of school-age [ 72 ].
Intervention support—Teaching sign language to parents
Another specific type of intervention to support hearing parents with deaf children is supporting the teaching of sign language. When deaf children are introduced to sign language there is an obvious need for parents and significant others in the child’s situation to learn to communicate in that language. However, if there are no other Deaf members of the family, a signed language may not be used in the home. Therefore, the deaf child may not have the exposure to language role models in the home in order to acquire a signed language as a first language. Giving parents a way to communicate with their deaf child will mean parents are provided with greater opportunities to engage effectively with their child’s world. It may be that a signed language does indeed later become a deaf child’s primary language, and early development of this in the home can be key. Six key components in any language development and support programme for parents include communication strategies, language tuition, immersion/language use, language modelling, information giving and practical/emotional support [ 73 ]. During curriculum development of Australian Sign Language (Auslan) and creation of family-specific resources, after finding the need for a language development program that incorporated classroom teaching, incidental learning opportunities and natural sign language immersion with additional learning resources. There is limited available evidence on the teaching of a signed language but researchers stress the need for involvement with Deaf adults or what it is like to live as a Deaf person being of primary importance [ 73 ].
A five-year sign language intervention project is reported [ 74 ] with 81 hearing family members in Finland learning sign language once a week with a teacher who was Deaf, Parents, siblings, and other relatives met once monthly to study sign language, and all families in the project signed together about twice yearly. Noting that if one is to succeed in modern society, communication competence should be good [ 74 ], and found that families most actively involved learned a greater amount.
One challenge noted by research teams regarding interventions given the geographic dispersion of children who are DHH is the shortage of adequately trained professionals [ 70 , 71 ]. The next theme presents material from the literature about family perspectives and environments.
Theme three: Family perspectives and environments
Family perspectives and environments are an over-arching theme that include evidence about family experiences, needs, coping and environmental relevance, and are reported in this section.
A study of family experiences and journeys exploring reactions, behaviours and strategies with 50 hearing parents with deaf children in Karachi City, Pakistan [ 75 ], found all parents reported shock on learning their child was deaf, and 99% were stressed by this news. 98% of these parents wanted counselling and support about three main areas: diagnosis of hearing impairment, speech and communication, and hearing aid maintenance, with specific structured counselling and information sessions in hospitals or schools recommended [ 75 ]. Family journeys with childhood deafness in Mexico are explored through the lens of a pilgrimage through Pfister’s [ 76 ] study as families realised their quest was not about fixing hearing but about finding more reliable communication methods. Parents reported the most common support was in the form of biomedical options which had restricted scope. Families also reported countless troubling questions without a forum to present them [ 76 ]. Similar to the concept of impairment as a predicament that can be overcome [ 77 ], families wanted to continue their quest for worlds people inhabit and aspired to challenge medicalised ideologies, which suggest family perseverance [ 76 ]. Eighteen hearing parents of deaf children in Western Australia reported struggling with a deafness diagnosis and recommendations for professionals who should not “just give a pamphlet to parents…never assume technology will cure all…and find out how a family ticks” [ 78 ]. It is stressed that more research is needed about deaf children with hearing parents across various life stages to fully understand potential challenges; and concluded that Deaf parents of deaf children have much insight to offer hearing parents with deaf children.
Studies that examined hearing families’ stresses and needs highlighted socioeconomic and cultural factors impacting on carers of deaf children in Ecuador around education and employment [ 79 ]. Carers are critical of new measures around schooling that may lead to reduced resources and discrimination and propose future healthcare practitioners screen deaf children for potential abuse regularly due to their vulnerabilities. Using the Parenting Stress Index and information gathered on personal and social resources, researchers found parent variables are largely responsible for successful child development [ 80 ]. A correlational study of stress levels and coping responses found the relationship between family and parental stress and a crisis with a child with a disability to be complex [ 81 ]. Notably families who were able to communicate with their deaf child through a signed language found this was positively related to their stress experience.
Parenting stress reported by Korean mothers of deaf children [ 82 ] suggests a need for comprehensive support services that include schools, parents, siblings and social workers, as they reported on-going alienation in mainstream education [ 83 ] and feeling left out within family relationships. Having a child with hearing loss does change family dynamics as hearing loss becomes the dominant family topic. Healthy families of children who were deaf were interviewed to identify what contributed to a health family dynamic [ 84 ]. Finding that families engage with a variety of professionals, there was a reported desire for professionals to more actively listen and to demonstrate confidence in families to capitalise on existing strengths and resources [ 84 ]. Proactive families welcomed workers who were willing to tolerate a variety of perspectives and options for them and their deaf children, and for workers to create social events for families and workers to interact together. Often hearing families report not having a true voice because they do not understand educational processes and systems, which does not help them to advocate for their deaf children [ 85 ].
Researchers who explored coping strategies of parents with deaf children note that parent stress is not an outcome of child deafness but of different characteristics of the context, perceptions and resources [ 86 ]. Exploring critical incidents with parents whose children have Cochlear implants to understand what influences parents’ coping suggest opportunities to share experiences with others and consistent family support are essential, as is the importance of understanding what hinders coping processes [ 87 ]. Adolescents themselves with Cochlear implants in Copenhagen reported diverse experiences from others of similar age, with participants reporting higher levels of feeling different from others also reported higher levels of loneliness, although this was less for those implanted at a much earlier age; and implies the need for flexible tailored support for all [ 88 ]. The actual reasons for deaf adolescents reporting loneliness is not fully known. Family environments can be enhanced by education and therapy to create robust language environments to maximise cochlear implanted children’s potential [ 89 ]. Families who reported they had a higher emphasis on being organised self-reported they had children with fewer inhibition problems, and that emphasis on structure and planning in family activities can help grow a supportive social family climate. Family environments are one area that can be modified when families become aware of problems impacting on their child’s progress [ 89 ].
A historical study conducted in Cyprus reported on Deaf adults’ childhood memories and how when they were children they reported feeling isolated in family environments due to lack of communication as families often refused to learn sign language [ 90 ]. This worsened when extended family visited and speech pace increased. The ‘dinner table syndrome’ is much reported and describes indirect family communication that occurs at family meals, during recreation and car rides that provides important opportunities to learn about health-related topics and are common to most families [ 91 ]. Deaf people with hearing parents often report limited access to contextual learning opportunities during childhood [ 92 ] which highlights the importance of environmental factors.
However for deaf children introduced to Deaf adults in Deaf clubs there are clear benefits for engagement with Deaf role models, where they can discuss serious issues and communicate effectively [ 76 , 90 ]. Although it must be noted that Deaf clubs in many parts of the UK and US are reducing in number [ 93 , 94 ]. Social success can be viewed differently, with hearing children and parents seeing their friendships more positively than deaf children [ 95 ]. Evidence is consistent about deaf children with Deaf parents having higher social success and better communication outcomes than deaf children of hearing parents [ 95 ].
Theme four: Deaf identity development
Deaf identity development describes the contrasting nature of opposing aspects of deaf and hearing perspectives on topics that relate to support for hearing parents, for example models of deafness and language and communication modalities, as well as ways deaf people encounter Deaf identity.
A review of mainstream resilience literature, in relation to what it means to be deaf and the contexts of deafness around disability, suggest resilience is often about challenging social and structural barriers [ 96 ]. The barriers in themselves often create risk and adversity, and for deaf young people the successful navigation of “countless daily hassles, which may commonly deny, disable or exclude them” is a key definition of resilience [ 96 , p 52]. Protective factors and skill development are the enablers.
The cultural constructs of deafness and hearingness can best be viewed through a lens of multimodality, with communication being more than about language [ 97 , 98 ]. The focus on why the body matters in how we, hearing and Deaf, come to shape a sense of self and the interplay between resources we use in the process. Such intersections are important in the development of identity and social skills. Aspects of adolescent-reported social capital (for example, the networks and relationships that enable a society to function) are reported as being linked to their language and reading skills, with deaf young people found to have less strong social skills than their hearing peers [ 99 ]. Aspects of adolescent-reported social capital are positively related to their language and literacy outcomes, suggesting the importance of increased promotion of social capital in adolescents who are DHH and their families [ 100 ].
The importance of understanding different ways that deaf children are contextualised, usually through the medical model, the social model and the Deaf culture model of Deafness are reported [ 101 ], with the medical model remaining dominant and framing being deaf as having hearing that does not work and needs to be treated to restore Deaf people to the normality of the majority of the population. The social model of deafness focuses on disability and strives for inclusion to ensure differences are supported. A Deaf cultural model values and celebrates Deafness collectively, often with a focus on Deafhood [ 102 ] and Deaf pride, where the label of impairment is seen negatively. A social relational model that is more about how deaf children shape their own identities and relocating the balance of power to create policy directives regarding increased use of signed language would enable greater inclusion and would directly challenge structures that exist [ 101 ]. Re-framing deaf children as plurilingual learners of signed language, English and additional languages, instead of as deficient bilinguals by dominant culture standards has potential [ 101 ].
Hearing parents’ experiences of adjusting to parenting a deaf child is impacted by the cultural-linguistic model of deafness have been examined, and how challenging the notion of a loss or deficit and instead using a model which promotes a linguistically able and culturally diverse lens [ 103 ]. An early intervention programme in the UK involving hearing parents and hearing teachers where families received weekly visits involving Deaf consultants in the role of ‘Deaf friend’ engaged family members in games, discussion and sign language tuition. Two key findings were reported with parent anxiety about the meaning of deafness reported as lessened by a Deaf adult ‘simply being themselves’ [ 103 , p163]. Equally, the relationship between childness and deafness, concerned with the overlap of a child being both a child, and a deaf child, and the importance of accepting the child and their child’s deafness. The cultural-linguistic model of deafness on the adjustment process hearing parents of deaf children experience is a potential tool to support parents through their reactions to their child’s deafness [ 103 ].
The discursive context of cultural-linguistic model views and medical models of deafness perspectives is present in hearing mothers’ talk and how they positioned their meanings of the two phenomena [ 104 ]. The language of advice from professionals has substantial influence, and positioning theory helps to explain the discrepancies parents experience between reported and actual plans for language practices [ 104 ].
An in-depth analysis of a shared-signing Bedouin community [ 105 ] highlights how deafness does not easily fall under the medical model because a wider lens is used in communities where many individuals who are hearing sign too, similar to Martha’s Vineyard situations [ 106 ]. Evidence is generally about Deaf communities rather than signing communities [ 106 ], and how linguistic communities do not just share a language but knowledge of its patterns of use and its cultural distinctions (such as attention getting and name giving) can be key in terms of identity development.
Descriptions of the Deaf Bi-lingual Bi-cultural community (Bi-Bi) helps us to understand this unique identify in an increasingly diverse world, and the relationship between language and identity formation and people’s social participation [ 107 ]. Misconceptions about bi- and multilingualism frequently recommend families limit their deaf child to learning oral English only, although multiple languages result in fluid conversational exchanges, trusting parent relationships and a strong cultural identity. Increasing clinicians’ understanding of language and culture, particularly Deaf culture would mean they could more effectively support child development and respond to human diversity issues in healthcare environments [ 107 ].
The importance of signed stories and how Deaf teachers’ storytelling in schools is an important part of deaf children’s identity development [ 108 , 109 ]. Due to the decades of strict oralist policies (from 1880 to 1980) [ 110 ], many deaf children do not experience the possibilities of a Deaf identity unless they go to a deaf school due to the lack of employment of Deaf teachers in mainstream education. Signed stories are a way of teaching deaf children about their linguistic and cultural heritage [ 108 ]. Rather than conceptualising deaf people as individuals who cannot hear, Deaf people see themselves as viewing the world visually and often use sign language, so deafness is not a loss but a social, cultural, and linguistic identity.
The aim of this scoping review was to identify published evidence on the supports and structures surrounding hearing parents with deaf children. The characteristics and results of the included articles were assessed. To the authors’ knowledge this is the first scoping review that focuses on what supports hearing parents as they in turn nurture their growing deaf children. Following a thorough database search and eligibility criteria, 65 papers were included in this scoping review. While it is a large amount of evidence about what supports hearing parents with deaf children, the evidence is mainly based on small, non-repeated studies with few randomised controlled trials published on the efficacy of support for families with deaf children. Current knowledge has therefore been framed as a narrative synthesis of reports of what supports families.
When families with deaf children are introduced to communication choices and strategies, their decisions are strongly influenced by the information they receive [ 46 ], but ultimately, they rely on their own judgements, with family characteristics, family strengths and beliefs also considered [ 47 ]. Hearing parents are less likely to choose a visual mode of communication, which may be due to hearing programme principles reflecting a predominantly medical model of deafness resulting in more ableist and audist approaches [ 43 ], although some parents do go on to ask for alternate services over time as their own knowledge of their child grows. It is reported that there are three phases of decision-making—information exchange, deliberation, and implementation, with two key decisions dominating on implantable devices and communication modality [ 111 ].
When discussing communication choices with families, there is a need for professionals to be familiar with and understand the cultural ecology [ 12 , 46 ] and that parents may make choices without access to information, and that not all choices are available. Culturally incompetent care often spreads health inequalities for Deaf people [ 28 ]. Increased awareness of communication choices is vital for parents because families may unknowingly limit knowledge or skill development due to limited awareness of Deaf culture and Deaf communities [ 52 ].
Studies that were categorised as providing evidence about interventions and resources that support hearing parents made mention of the value of interventions that focused on language, communication and parent knowledge as well as supporting parent-child relationships. There was a paucity of evidence about nurturing socio-emotional development which is often a poorer outcome for deaf children when compared to hearing children [ 56 ]. There was an emphasis that intervention programmes need to be culturally and linguistically appropriate, as this improves caregiver satisfaction [ 57 ], and that all interventions with families need to address linguistic, racial and cultural diversity elements.
The provision of Deaf mentors was noted to be a popular feature with families [ 58 – 60 ]. Although there are often few Deaf professionals in services for families to connect with and limited evidence of sustained Deaf mentor programmes available [ 66 ]. A supporting parent was also a welcome intervention, which carried less sense of a hierarchical relationship and families reported valuing such input [ 65 ].
There is evidence to suggest that intervention and support occurring early result in better language for deaf children at later point [ 59 ]. Giving parents guided practice with examples for their individual child’s language level and practice of this skill with a professional was highlighted as useful [ 61 ]. Increasing evidence suggests that deaf children having access to a signed language at the earliest possible age is beneficial [ 22 ] but it must be noted that Deaf people’s under-achievement in education is not a result of deficits within children themselves but relates to the ‘disabling pedagogy’ to which they are routinely subjected [ 112 ].
Whilst many services have moved online during the pandemic, the reported results for parent intervention with deaf children are before Covid-19 occurred, with telepractice groups scoring significantly higher on their total language score and more in the ‘driving seat’ [ 73 ] which may be due to parents saying they felt better supported and engaged through this route. As deaf children grow older, and services move to being more child-focused than family-focused there is evidence that families voice feeling less supported with over 30% reporting no intervention by the time children attend school [ 76 ].
The reported key components of language and support programmes for parents are that communication strategies, language tuition immersion and language modelling, as well as information and emotional support are all essential [ 73 ]. It is not uncommon for support programmes to include family get togethers sporadically, say two to three times per year [ 74 ].
The family perspectives and environment theme included reports that 98% of hearing parents wanted counselling on discovering their child was deaf [ 75 ]. A priority for parents was finding reliable communication methods, and whilst parents had commonly been offered biomedical options and information, many suggested they wanted a forum to raise concerns and questions [ 76 ] and did not want to overly rely on medicalised ideologies [ 77 ]. More information was wanted from hearing parents about challenges they might encounter at different life stages for their child [ 78 ].
Environments for deaf children need vital consideration due to the potential for abuse of vulnerable groups [ 79 ]. However, parent variables are largely responsible for successful child development [ 84 ]. One example being parents who were able to communicate through sign language found this significantly lowered their stress as communication with their child was available to them [ 81 ].
Families were keen for professionals to value their strengths and resources, and particularly for social events to be arranged with other families with deaf children [ 84 ]. Parent stress seems to be more related to context and resources than actual child deafness [ 86 ] and knowing what hinders coping would be useful knowledge [ 87 ]. Enhancing family environments with education and therapy or therapeutic support is key [ 89 ]. Environmental factors for hearing parents with deaf children are vital, which is particularly evident with discussion of the dinner table syndrome with children missing out on many learning opportunities and family relational communication [ 91 ]. It is notable that deaf children with Deaf parents frequently outperform deaf children with hearing parents because of their early language encounters and immersion in an inclusive world [ 95 ]. The reverse is true for deaf children.
The theme Deaf identity development highlighted the importance of the intersectionality of Deaf identity in relation to other cultural identities [ 99 ]. Successful identify development is strongly linked to social capital [ 100 ], so rather than being contextualised by the social model, the Deaf culture model of deafness offers a more positive view which may empower both hearing parents as well as their deaf children [ 102 ], as this challenges a deficit model and promotes a more linguistically able and culturally diverse lens [ 12 ]. Tools that promote acceptance of deafness, adjustment and managing reactions have much scope [ 103 ].
The language of diagnosing and medical professionals can have substantial influence, as well at the position that they take [ 16 ]. Communities that include hearing signers have much to offer, as the notion of signing communities suggests the benefits and richness of signed languages [ 106 ]. It is worth noting that most deaf children are not exposed to the idea of a Deaf identity unless they go to a Deaf school and have exposure to deaf children and Deaf adults on a regular basis. Since the evidence search for this scoping review was undertaken, further publications also support our conclusions. Namely that health care professionals and early intervention providers must inform parents about signed language as a language choice as the majority of parents only learn about such options through their own research [Lieberman]. Also that supporting parents’ development of communicative competence in signed languages has significant implications for meeting their deaf children’s communicative needs [ 112 , 113 ].
Limitations
A systematic and rigorous approach was adopted when carrying out this scoping review. Evaluating the findings of this scoping review the limitations are discussed in this section. The inclusion criteria were purposively broad at the outset, and due to the high number of retrievals it became clear that focusing on empirical research studies would provide the most valuable evidence. However, whilst some support programmes had been sustained over time, many were short term projects with small samples.
One limitation could be that only articles published in the English language were included in the review, therefore articles in other languages may have been missed in the search. Support systems for hearing parents with deaf children vary greatly. A formal quality appraisal of the included articles was beyond the scope of this review. To decrease the risk of bias the selection of retrieved papers was monitored and viewed independently by two researchers with differences of opinion resolved through discussion. A total of four electronic databases were selected and searched, and despite those covering a range of academic fields their databases may potentially have been excluded. However, at the outset the suggestions of 50 keywords/terms from the steering group helped ensure that a diverse and broad range of material was included. One limitation of this scoping review is that results are presented in a narrative style with limited quantitative analysis of retrieved studies. Whilst sample size and results are available in Table 3 , there was a low number of randomised controlled trials on this subject and suggests that the evidence is available about what supports hearing parents with deaf children are not adequately addressed. Despite these limitations this scoping review provides what we believe to be a first overview of existing research on supportive interventions and help for hearing parents with deaf children and serves to highlight the lack of evidence on this important topic.
Overall, the results of this scoping review about supports for hearing parents with deaf children suggest it is important to identify the journey parents and their children navigate from the results of hearing screening or deafness diagnosis, through to the available provision and supports from various services and providers. The results suggest that more research is needed to know what supports hearing parents with deaf children. We propose that further longitudinal studies should test and compare specific interventions and programmes in low-middle income countries and high-income countries. This scoping review highlights a need for improvement in the experience of hearing parents with deaf children as they, along with their deaf children, navigate challenges, information provision and supports required.
Supporting information
S1 checklist, funding statement.
This scoping review and the linked descriptive qualitative study are part of the SUPERSTAR project funded by Research Capacity Building Collaboration (RCBC) Wales, a Welsh Government funded scheme through Health and Care Research Wales, which exists to increase research capacity in nursing, midwifery, the allied health professions and pharmacists across Wales. The SUPERSTAR project is a Postdoctoral Fellowship, where the funder provides access to a supervisor, and a Community of Scholars to support and promote high research quality and outputs. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Data Availability
- PLoS One. 2023; 18(11): e0288771.
Decision Letter 0
19 Dec 2022
PONE-D-22-29952Systems that support hearing families with deaf children: a scoping reviewPLOS ONE
Dear Dr. Terry,
Thank you for submitting your manuscript to PLOS ONE. After careful consideration, we feel that it has merit but does not fully meet PLOS ONE’s publication criteria as it currently stands. Therefore, we invite you to submit a revised version of the manuscript that addresses the points raised during the review process.
Please submit your revised manuscript by Feb 02 2023 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Please include the following items when submitting your revised manuscript:
- A rebuttal letter that responds to each point raised by the academic editor and reviewer(s). You should upload this letter as a separate file labeled 'Response to Reviewers'.
- A marked-up copy of your manuscript that highlights changes made to the original version. You should upload this as a separate file labeled 'Revised Manuscript with Track Changes'.
- An unmarked version of your revised paper without tracked changes. You should upload this as a separate file labeled 'Manuscript'.
If you would like to make changes to your financial disclosure, please include your updated statement in your cover letter. Guidelines for resubmitting your figure files are available below the reviewer comments at the end of this letter.
If applicable, we recommend that you deposit your laboratory protocols in protocols.io to enhance the reproducibility of your results. Protocols.io assigns your protocol its own identifier (DOI) so that it can be cited independently in the future. For instructions see: https://journals.plos.org/plosone/s/submission-guidelines#loc-laboratory-protocols . Additionally, PLOS ONE offers an option for publishing peer-reviewed Lab Protocol articles, which describe protocols hosted on protocols.io. Read more information on sharing protocols at https://plos.org/protocols?utm_medium=editorial-email&utm_source=authorletters&utm_campaign=protocols .
We look forward to receiving your revised manuscript.
Kind regards,
Gursimran Dhamrait, Ph.D
Academic Editor
Journal Requirements:
When submitting your revision, we need you to address these additional requirements.
1. Please ensure that your manuscript meets PLOS ONE's style requirements, including those for file naming. The PLOS ONE style templates can be found at
https://journals.plos.org/plosone/s/file?id=wjVg/PLOSOne_formatting_sample_main_body.pdf and
https://journals.plos.org/plosone/s/file?id=ba62/PLOSOne_formatting_sample_title_authors_affiliations.pdf
2. Please ensure that you include a title page within your main document. We do appreciate that you have a title page document uploaded as a separate file, however, as per our author guidelines ( http://journals.plos.org/plosone/s/submission-guidelines#loc-title-page ) we do require this to be part of the manuscript file itself and not uploaded separately.
Could you therefore please include the title page into the beginning of your manuscript file itself, listing all authors and affiliations.
3. Thank you for stating the following in the Funding Section of your manuscript:
"This scoping review and the linked descriptive qualitative study are part of the SUPERSTAR project funded by Research Capacity Building Collaboration (RCBC) Wales, which are part of a Postdoctoral Fellowship. The funder provides access to a supervisor, and a Community of Scholars to support and promote high research quality and outputs. "
We note that you have provided funding information that is not currently declared in your Funding Statement. However, funding information should not appear in the Acknowledgments section or other areas of your manuscript. We will only publish funding information present in the Funding Statement section of the online submission form.
Please remove any funding-related text from the manuscript and let us know how you would like to update your Funding Statement. Currently, your Funding Statement reads as follows:
"J Terry RCBC Wales Postdoctoral Fellowship
https://www.rcbcwales.org.uk/
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript."
Please include your amended statements within your cover letter; we will change the online submission form on your behalf.
4. Please include your full ethics statement in the ‘Methods’ section of your manuscript file. In your statement, please include the full name of the IRB or ethics committee who approved or waived your study, as well as whether or not you obtained informed written or verbal consent. If consent was waived for your study, please include this information in your statement as well.
5. Please upload a copy of Figures 1 an 2, to which you refer in your text on page 9-10. If the figure is no longer to be included as part of the submission please remove all reference to it within the text.
[Note: HTML markup is below. Please do not edit.]
Reviewers' comments:
Reviewer's Responses to Questions
Comments to the Author
1. Is the manuscript technically sound, and do the data support the conclusions?
The manuscript must describe a technically sound piece of scientific research with data that supports the conclusions. Experiments must have been conducted rigorously, with appropriate controls, replication, and sample sizes. The conclusions must be drawn appropriately based on the data presented.
Reviewer #1: Yes
Reviewer #2: Yes
Reviewer #3: Yes
2. Has the statistical analysis been performed appropriately and rigorously?
Reviewer #2: N/A
Reviewer #3: N/A
3. Have the authors made all data underlying the findings in their manuscript fully available?
The PLOS Data policy requires authors to make all data underlying the findings described in their manuscript fully available without restriction, with rare exception (please refer to the Data Availability Statement in the manuscript PDF file). The data should be provided as part of the manuscript or its supporting information, or deposited to a public repository. For example, in addition to summary statistics, the data points behind means, medians and variance measures should be available. If there are restrictions on publicly sharing data—e.g. participant privacy or use of data from a third party—those must be specified.
Reviewer #1: No
4. Is the manuscript presented in an intelligible fashion and written in standard English?
PLOS ONE does not copyedit accepted manuscripts, so the language in submitted articles must be clear, correct, and unambiguous. Any typographical or grammatical errors should be corrected at revision, so please note any specific errors here.
5. Review Comments to the Author
Please use the space provided to explain your answers to the questions above. You may also include additional comments for the author, including concerns about dual publication, research ethics, or publication ethics. (Please upload your review as an attachment if it exceeds 20,000 characters)
Reviewer #1: Thank you for the opportunity to review Systems that support hearing families with deaf children: A scoping review. To help pinpoint the specific sentences that require my commentary in the absence of line numbers, I will use page numbers and the closest citation like this P:[X]
2:[4] - Support is not really defined here. I know it's not quite possible to define support as this is an individual issue, but the paper claims that support is lacking. What support would be needed?
3:[7,8] - Many people will find the term "developing countries" offensive. Perhaps Global South? Formerly colonized countries?
3:[9] - List out these effects - perhaps cite Wyatte Hall's work on language deprivation syndrome.
3:[13] - This sentence a bit both-sides the debate. As you are not the New York Times, I don't think it's necessary to try to both-sides a clearly destructive argument from the Oralists. All deaf children should have some exposure to signed languages. Anything else is an enforcement of white supremacy values where only spoken languages are valued and everything else can be discarded.
4:[17] - Let's be realistic. There is almost never signed alone. It is usually a mixture, or spoken languages only.
5:[20] - Note that the width of the language development window is still under debate. 5 years isn't a hard stop. Language acquisition continues up until teenage years. But yeah. Early is good.
5:[21] - This next paragraph is very good. I think you can add more citations to bolster your argument. Hall Hall and Caselli is good. I believe Lillo-Martin may have a recent paper.
[22] - I don't think Geers et al is the right citation for this.
6:[28] - I've seen several quasi definitions of support but nothing that makes me scream, yes, this is what support is. I would like to do this.
7:[30] - Very nice and clear. I like the use of OSF
8 - It's not immediately clear to me why educational databases were not searched as this would cover Journal of Deaf Studies and Deaf Education, Deaf Education & International, and the Annals of the Deaf
9 - I don't like the term hearing impaired but I wonder if using that term would net more articles.
10 - Does Rayyan software require a citation?
11 - I think there's more funding to be honest. These are also Global North countries with robust economies. I am not sure this is as much an interest issue as it is an ability to receive funding.
11:[319 - I am not sure what reference 319 is, but I assume that will be fixed. However, I don't think that signed/spoken/both is the correct distribution of choices. It's usually both/spoken.
11: [19] - I am not sure that I agree that parents don't have time to engage with deaf communities (love the use of plural here). I think the answer is that there's usually not infrastructure to pipe parents to the appropriate deaf communities.
12:[18] - I want your point to be stronger here. Language does not interfere with language. Language does not hurt any kind of learning. Even asking the question is ableist.
12:[35] - I'm surprised no one mentioned ableist attitudes towards signed languages.
13:[40] - Laura Mauldin's Made to Hear discusses some of this. Also mentions that parents tend to think that their kids will be the successful ones that don't need signed languages.
15:[45] - I think this kind of hints that communication will always be a joint venture. I want you to say this stronger.
16:[50] - These families really should have an option to learn the signed languages of their cultures (e.g. LSM)
17:[52] - I think the issue of socio-emotional development being poor isn't well analyzed by hearing professionals. People react badly to not being able to communicate and things like Dinner Table Syndrome. Like, it's not the deafness. It's everything around it.
21:[69] - I do not understand this sentence "Aware that by giving parents ‘the means to communicate with their deaf child by using the child’s primary language’ parents are provided with greater opportunity for understanding their child’s world. "
21:[69] - This paragraph is rough. I don't understand what the point is. It doesn't matter if the child overtakes the parent in proficiency. It only matters if the parents are the only model, like, forever.
24:[77] - Without any context, reporting the data by race/ethnicity does not add positive information. Why do Black families struggle with coping strategies? How does the inherent racism of the US system restrict use of coping strategies? This information isn't here. I would remove everything after "Additionally,"
25:[84] - Marschark is famous for never considering the context that the data is gathered in. Why are these kids feeling lonely? What does it mean that kids implanted earlier feel less lonely? Does anyone notice that the number of pirates decreased as the weather got warmer ( https://pastafarians.org.au/pastafarianism/pirates-and-global-warming/ )?
25:[85] - The weirdness of conflated variables appears in Holt et al's work. I see Kronenberger and Pisoni also contributed to this. This data result is silly. How would self reported control lead to small vocabularies? How would organization mean fewer inhibition problems? If a butterfly farts in the Atlantic, is there guaranteed to be a hurricane in the Pacific?
26:[86] - Sad that most of the deaf clubs in the states have closed.
27:[91] - I would not cite Johnston here. I think Kuster's work is more applicable. As is de Muelder.
30:[101] - Make sure you're citing Leala Holcomb's work here.
31:[40] - Honestly it's fair to say the hearing parents are ableist and audist yeah.
31:[61] - In my US State, all the parent supporters are oralist advocates. We have no signing parent mentor.
Reviewer #2: Suggestion:
p. 5, sentence beginning ‘Sign Language often comes naturally to deaf children…’ — Rather than beginning the sentence with ‘Sign Language’ with both words capitalised, I recommend using lower case in ‘language’ because there is no language named ‘Sign Language’ but with both letters capitalized, it can create the impression that it is the name of a language. This reinforces the common misconception that there is only one sign language worldwide. By saying “sign language” with lowercase letters (or ‘signed languages’), it reads more parallel to ‘spoken language’ where no one would mistake that for a single language but rather a category of languages in a particular modality. This is done later in the MS (and even later in this paragraph) and it reads much more clearly without this possibility of misunderstanding.
p. 11, first sentence under subheading — perhaps a typo in the citation. It is listed as ‘[319’ with no closing bracket
Throughout: It seems you mostly chose to capitalise ‘deaf’, which is fine, however this is a bit inconsistent, e.g., with some lowercase tokens on page 16. I’d suggest explaining whatever decision you make, citing the relevant literature and then being consistent throughout. If you’re not aware of this paper, I recommend it for a newer take on ‘Deaf’ versus ‘deaf’
https://www.scirp.org/journal/paperinformation.aspx?paperid=97416
Positionality statement:
It would be helpful, if permitted by the journal, to include a positionality statement for the two authors so readers know what lived experiences/expertise they bring to this work. That would, to my mind, tie in with some of the narrative about the findings reported in this paper.
Just in case it is helpful/applicable, please see Lieberman et al (2022)
https://sites.bu.edu/lavalab/files/2022/06/Lieberman-Mitchiner-Pontecorvo-2022.pdf
See also Oyserman and de Geus (2021)
https://www.degruyter.com/document/doi/10.21832/9781800410756-011/html
Reviewer #3: This paper is well-balanced and captures the nuance quite well of what parents experience when they learn of having a deaf child and how the medical model influences choices. I was impressed with the acknowledgement of how marginalized signed languages have been in deaf child development. I applaud the authors for bringing this balanced view and highlighting the plurality of options in an international scope. I have no major feedback on this paper, there are minor grammar and writing aspects that can be improved with editor review.
6. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
If you choose “no”, your identity will remain anonymous but your review may still be made public.
Do you want your identity to be public for this peer review? For information about this choice, including consent withdrawal, please see our Privacy Policy .
Reviewer #1: Yes: Jon Henner
Reviewer #2: No
Reviewer #3: No
[NOTE: If reviewer comments were submitted as an attachment file, they will be attached to this email and accessible via the submission site. Please log into your account, locate the manuscript record, and check for the action link "View Attachments". If this link does not appear, there are no attachment files.]
While revising your submission, please upload your figure files to the Preflight Analysis and Conversion Engine (PACE) digital diagnostic tool, https://pacev2.apexcovantage.com/ . PACE helps ensure that figures meet PLOS requirements. To use PACE, you must first register as a user. Registration is free. Then, login and navigate to the UPLOAD tab, where you will find detailed instructions on how to use the tool. If you encounter any issues or have any questions when using PACE, please email PLOS at gro.solp@serugif . Please note that Supporting Information files do not need this step.
Author response to Decision Letter 0
Response to reviewers – PONE – 22 – 29952
Systems that support hearing families
We are grateful to all reviewers for their helpful comments. Please see our responses below. On the tracked changes version of the manuscript, all new references in the References list are highlighted in yellow. The numbering both in the manuscript and in the reference list is now accurate for this revised manuscript.
Reviewer #1: Thank you for the opportunity to review Systems that support hearing families with deaf children: A scoping review. To help pinpoint the specific sentences that require my commentary in the absence of line numbers, I will use page numbers and the closest citation like this P:[X]
Response: Thank you, your comments across the paper are extremely helpful.
Response: Thank you. A definition of support is now included in the first paragraph of the introduction.
Response Thank you, now amended to ‘the Global South’.
Response: Thank you, effects and Wyatte Hall’s work now included.
Response: Helpful point, sentence with [13] now removed.
Response: Thank you, now rephrased.
Response: Thank you and a fair point, now softened with ‘around the age of five years..’
Response: Very helpful, thank you, both suggested citations now added.
Response: Fair point, now removed.
Response: Thank you, good point. We have provided a definition of support systems at this point.
Response: Thanks.
Response: Thanks. Whilst specific educational databases were not included as one of the four named databases, many of the included 65 papers are indeed from educational journals including Journal of Deaf Studies and Deaf Education, Deaf Education & International, and the Annals of the Deaf. The Proquest Central database does include educational databases. Also, due to the steering groups’ suggested search terms, the information specialist’s help and intense internet and hand searching for evidence the authors are confident that relevant evidence from educational journals is certainly included in this scoping review.
Response: Agree, the term ‘hearing impaired’ was indeed used as a search term, please see Table 1, PICO framework.
Response: Thanks, good point. Rayyan reference (Ouzzani et al now included).
Response: Thanks, sentence now revised.
Response: Thanks, typo now corrected. The reference had been Yu (2021), but now changed to Hall, Hall and Caselli. Sentence now revised.
Response: Thanks, sentence now amended to reflect lack of infrastructure.
Response: Thank you, sentence revised.
Response: Thank you. Agree, ableist attitudes are not specifically stated as such in the literature, although that does appear to be what parent experience is describing.
Response: Thank you, reference to Maudlin’s work now included.
Response: Thank you, good point, sentence now revised.
Response: Thank you, a helpful addition and now included.
Response: Thank you, additional sentence now included.
Response: Thank you, sentence now revised.
Response: Thank you, paragraph now revised.
Response: Thank you, now revised and sentence removed.
Response: Thanks, additional sentence added.
Response: Thank you for drawing attention to this. We have returned to the paper and revised the phrasing.
Response: Thank you, sentence added and citations added.
Response: Thank you. We have retained reference to the Johnston paper, as we are referring to the retrieved paper from the included 65. We have supported this with a citation from Kusters, DeMeulder and O’Brien to increase clarity.
Response: Thank you, we have now added a citation on Holcomb’s work.
Response: Thank you, point revised and made more clearly.
Response: Thank you, agree this may vary by region hence no changes made, as point is more about Deaf mentors, few Deaf professionals and supporting parents being a welcome intervention.
Reviewer #2:
Suggestion:
Response: Thank you, very helpful, and now checked across the manuscript and only appears as ‘sign language or ‘signed language’, unless at the start of a sentence or in reference to a specific such as ASL or BSL.
Response: Thank you, it was a typo, now amended.
Response: Thank you, we were not previously aware of this paper, which is extremely helpful and is now cited in our explanation. We have now included an Authors’ note at the start of the paper to provide reader clarity. Throughout the paper all reference to Deaf adults, communities, professionals, clubs, identity, culture, mentors and family members, then a capital D is used. Whilst when referring to deaf children, and deafness a lower-case d for deaf is used.
Response: Thank you, a useful point to consider. Positionality statements can be useful for readers. We thought it helpful to add more description about the project’s steering group in the Methods’ section.
Response: Very helpful to have these references. We have included them towards the end of the paper, thank you for bringing them to our attention.
Reviewer #3:
This paper is well-balanced and captures the nuance quite well of what parents experience when they learn of having a deaf child and how the medical model influences choices. I was impressed with the acknowledgement of how marginalized signed languages have been in deaf child development. I applaud the authors for bringing this balanced view and highlighting the plurality of options in an international scope. I have no major feedback on this paper, there are minor grammar and writing aspects that can be improved with editor review.
Response -Thank you for your comments.
Submitted filename: Response to reviewers PONE-22-29952.docx
Decision Letter 1
26 Apr 2023
PONE-D-22-29952R1Systems that support hearing families with deaf children: a scoping reviewPLOS ONE
Please submit your revised manuscript by Jun 10 2023 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
1. Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript. If you need to cite a retracted article, indicate the article’s retracted status in the References list and also include a citation and full reference for the retraction notice.
Additional Editor Comments:
1. Please re-word to use low-middle income countries and high-income countries as appropriate throughout the manuscript.
1. If the authors have adequately addressed your comments raised in a previous round of review and you feel that this manuscript is now acceptable for publication, you may indicate that here to bypass the “Comments to the Author” section, enter your conflict of interest statement in the “Confidential to Editor” section, and submit your "Accept" recommendation.
Reviewer #2: All comments have been addressed
2. Is the manuscript technically sound, and do the data support the conclusions?
3. Has the statistical analysis been performed appropriately and rigorously?
4. Have the authors made all data underlying the findings in their manuscript fully available?
5. Is the manuscript presented in an intelligible fashion and written in standard English?
6. Review Comments to the Author
Reviewer #2: Overall, I’m very happy with the revisions to the manuscript. Thank you for your hard work in addressing reviewer comments. I have just one more remark:
1. P. 53-54 (paragraph straddling these pages). Here you state that an alternative may have been for these families to learn LSM, however, I’m looking at the original article, and I’m only seeing that the families in this study were from “Spanish-speaking” backgrounds. It does not specify their country (or territory, e.g., Puerto Rico) of origin. I do not feel the suggestion to specifically name LSM here is appropriate for two reasons. First, if the family is from, say, El Salvador, why would they be compelled to learn LSM? Second, if the family lives in the US and there is no one in their community who knows LSM, how is it functional for them to learn a language they can’t use with anyone? I feel strongly the manuscript would be better off with the sentence in question omitted.
I’m not sure if this would be helpful, but if you feel compelled to comment on some of the unique struggles of families from a Spanish-speaking background, you may consider this article:
Steinberg, A., Bain, L., Li, Y., Delgado, G., & Ruperto, V. (2003). Decisions Hispanic Families Make After the Identification of Deafness. Journal of Deaf Studies and Deaf Education, 8(3), 291–314. https://doi.org/10.1093/deafed/eng016
7. PLOS authors have the option to publish the peer review history of their article ( what does this mean? ). If published, this will include your full peer review and any attached files.
Author response to Decision Letter 1
PONE-D-22-29952R1
We are grateful to all reviewers for their helpful comments. Please see our responses below, and on the tracked changes version of the manuscript:
Editor comments:
1. Please re-word to use low-middle income countries and high-income countries as appropriate throughout the manuscript.
Response: Thank you for this helpful comment. Now changed throughout.
Reviewer #2: Overall, I’m very happy with the revisions to the manuscript. Thank you for your hard work in addressing reviewer comments. I have just one more remark:
Response: Thank you for this helpful comment. On consideration we have removed this sentence.
Submitted filename: Response to reviewers PONE-D-22-29952R1.docx
Decision Letter 2
19 Jun 2023
PONE-D-22-29952R2Systems that support hearing families with deaf children: a scoping reviewPLOS ONE
Please check your prisma flow diagram in figure 1and explain exclusion criteria inside the box. There is a need of improvement in PRISMA FLOW fig 1. Please see page 13. Justify exclusion screening (n=821). The diagram have made poorly. The line are irregular. Kindly redraw and elaborate in detail all criteria. Please do include it in text if any new addition in text.
Table 2, Strength and weakness must possess under a separate column. Rewrite in and elaborate the content.
i could not find the search strategy as additional file. Kindly check your manuscript. It is suggested to provide inside the manuscript.
Please write your manuscript according to plosone criteria and provide following clear methodology in method section such as Data screening, data entry and collection method.
read following content in Cochrane database
https://www.cochranelibrary.com/about/about-cochrane-reviews
Please submit your revised manuscript by Aug 03 2023 11:59PM. If you will need more time than this to complete your revisions, please reply to this message or contact the journal office at gro.solp@enosolp . When you're ready to submit your revision, log on to https://www.editorialmanager.com/pone/ and select the 'Submissions Needing Revision' folder to locate your manuscript file.
Muhammad Shahzad Aslam, Ph.D.,M.Phil., Pharm-D
Please review your reference list to ensure that it is complete and correct. If you have cited papers that have been retracted, please include the rationale for doing so in the manuscript text, or remove these references and replace them with relevant current references. Any changes to the reference list should be mentioned in the rebuttal letter that accompanies your revised manuscript. If you need to cite a retracted article, indicate the article’s retracted status in the References list and also include a citation and full reference for the retraction notice.
read following content
Reviewer #2: I have no further comments at this time. I am satisfied with the way the manuscript has been revised.
Author response to Decision Letter 2
28 Jun 2023
Response to Reviewers- - PONE-D-22-29952R2
Thank you for your helpful comments and guidance. As we have revised the manuscript, we have looked extensively at other scoping reviews published in Plos One, which has been helpful.
Reviewer comment: Please check your prisma flow diagram in figure 1and explain exclusion criteria inside the box. There is a need of improvement in PRISMA FLOW fig 1. Please see page 13. Justify exclusion screening (n=821). The diagram have made poorly. The line are irregular. Kindly redraw and elaborate in detail all criteria. Please do include it in text if any new addition in text.
Response: Thank you for your suggestions. The PRISMA diagram has been re-done. No further text added to manuscript.
Reviewer comment: Table 2, Strength and weakness must possess under a separate column. Rewrite in and elaborate the content.
Response: Separate columns have now been added for strengths and another for weaknesses, with additional content now added. A few entries do just state ‘small sample’, and we have been back to these articles again, but there is little else to say with regards to these publications due to limited detail.
Reviewer comment: I could not find the search strategy as additional file. Kindly check your manuscript. It is suggested to provide inside the manuscript.
Response: Apologies. An example of a search strategy from one database (CINAHL) is now included within the manuscript and has also been uploaded as an additional file.
Reviewer comment: Please write your manuscript according to Plosone criteria and provide following clear methodology in method section such as Data screening, data entry and collection method.
Response: Thank you. Further detail about data screening, data entry and collection method is now included on page 12. The sub-headings used in the Methods sections are based on Arksey and O’Malley’s framework, as explained on page 8.
Submitted filename: Response to Reviewers_PONE-D-22-29952R2 .docx
Decision Letter 3
Systems that support hearing families with deaf children: a scoping review
PONE-D-22-29952R3
We’re pleased to inform you that your manuscript has been judged scientifically suitable for publication and will be formally accepted for publication once it meets all outstanding technical requirements.
Within one week, you’ll receive an e-mail detailing the required amendments. When these have been addressed, you’ll receive a formal acceptance letter and your manuscript will be scheduled for publication.
An invoice for payment will follow shortly after the formal acceptance. To ensure an efficient process, please log into Editorial Manager at http://www.editorialmanager.com/pone/ , click the 'Update My Information' link at the top of the page, and double check that your user information is up-to-date. If you have any billing related questions, please contact our Author Billing department directly at gro.solp@gnillibrohtua .
If your institution or institutions have a press office, please notify them about your upcoming paper to help maximize its impact. If they’ll be preparing press materials, please inform our press team as soon as possible -- no later than 48 hours after receiving the formal acceptance. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information, please contact gro.solp@sserpeno .
Additional Editor Comments (optional):
Acceptance letter
11 Jul 2023
Dear Dr. Terry:
I'm pleased to inform you that your manuscript has been deemed suitable for publication in PLOS ONE. Congratulations! Your manuscript is now with our production department.
If your institution or institutions have a press office, please let them know about your upcoming paper now to help maximize its impact. If they'll be preparing press materials, please inform our press team within the next 48 hours. Your manuscript will remain under strict press embargo until 2 pm Eastern Time on the date of publication. For more information please contact gro.solp@sserpeno .
If we can help with anything else, please email us at gro.solp@enosolp .
Thank you for submitting your work to PLOS ONE and supporting open access.
PLOS ONE Editorial Office Staff
on behalf of
Dr. Muhammad Shahzad Aslam
Parenting Deaf Children: Exploring Relationships Between Resolution of Diagnosis, Parenting Styles and Morale, and Perceived Child Vulnerability
- Original Paper
- Open access
- Published: 26 April 2023
- Volume 32 , pages 2761–2775, ( 2023 )
Cite this article
You have full access to this open access article

- Joshua Sealy ORCID: orcid.org/0000-0003-3661-2853 1 ,
- Catherine McMahon 1 &
- Naomi Sweller 1
Explore all metrics
Raising a deaf child can have significant impacts on parents’ wellbeing, their relationship with the deaf child, and their ability to parent effectively. Using an online survey, this study explored two questions: First, to examine whether hearing parents treat and perceive their deaf and hearing children differently while controlling for parent characteristics (including resolution of diagnosis), specifically in terms of parenting styles and perceived vulnerability. Second, whether hearing parents’ ability to resolve their feelings about their child’s hearing loss diagnosis was related to their parenting morale, and whether they perceived their deaf child as vulnerable. A total of 84 parents with a deaf child aged 5–12 years completed the survey, with 32 of those also reported about a second child without hearing loss in the same age range. They were asked to answer questions from the Reaction to Diagnosis Interview, and to complete several questionnaires addressing parenting morale, child vulnerability, and parenting styles. Findings suggest that unresolved feelings of diagnosis were linked to lower parenting morale and greater perception of child vulnerability. Sibling comparisons indicated that parents also reported a higher perceived child vulnerability score for the deaf child compared to the hearing sibling. No sibling differences were found regarding parenting styles. These findings suggest that the experience of having a deaf child can have a negative impact on hearing parents’ morale and perception of child vulnerability, particularly when parents remain unresolved about the diagnosis, highlighting the need for targeted supports and further research.
Experiences receiving their child’s diagnosis of hearing loss has long-lasting impacts on parenting outcomes
Unresolved parents are more likely to have lower parenting morale and view their deaf child as vulnerable
Parents are more likely to view their deaf child as more vulnerable than their hearing sibling
Deaf epistemology awareness and positive psychology may have beneficial outcomes for parents of deaf children.
Similar content being viewed by others
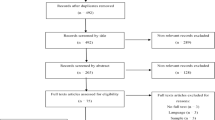
Systematic review of the differences between mothers and fathers in parenting styles and practices
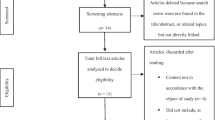
Long-term emotional consequences of parental alienation exposure in children of divorced parents: A systematic review

The Importance of Parenting in Influencing the Lives of Children
Avoid common mistakes on your manuscript.
Raising a child is a difficult and challenging task. The dynamics of parent-child relationships are multifaceted and complex, and influenced by risk and protective factors that interact within varying family and social contexts (Belsky, 1980 , 1984 , 1993 ). Belsky outlined a classic model of the determinants of parenting based on parent characteristics (e.g., personality, education), child characteristics (e.g., temperament), and context (e.g., socioeconomic status). One particularly salient child factor that has received relatively little empirical attention is hearing loss disability. The current paper focuses on parenting for parents of children with hearing loss.
Hearing loss (i.e., deafness) is a sensory disability whereby sounds cannot be perceived, conducted, and/or interpreted normally by the person (Isaacson, 2010 ). This occurs when necessary components such as in the outer ear, middle ear, inner ear, or the pathways in the brain do not function typically. The resulting hearing loss can vary from mild to profound, affecting how different pitches and amplitude of sounds are perceived. Hearing loss affects 19.3% people internationally (Haile et al., 2021 ). A systematic review estimated the number of Australian primary school children with hearing loss to range between 3.4 and 12.8% (Choi et al., 2017 ). The sequelae to hearing loss often include challenges with language development and interpersonal communication in a predominantly auditory culture that does not compensate for the needs of deaf people (Hauser et al., 2010 ), which can have long term implications such as academic underachievement and isolation (Haile et al., 2021 ; World Health Organisation, 2016 ). While deaf people do experience ongoing challenges, the nature of these challenges are not exclusively due to the hearing loss per se, but also due to sociocultural practices and attitudes surrounding them. For example, disabled individuals may not have their basic needs met due to discrimination that may manifest as misallocation of resources, inappropriate interactions (Bøttcher & Dammeyer, 2013 ); or lack of proper social inclusion due to disabled people not receiving full recognition and valued as fully fledged persons compared to abled bodied individuals (Ikäheimo, 2009 ). As a result, disability is a complex risk factor to the extent that fully understanding the nature of the disability in question must also incorporate sociocultural practices in which the disability is situated (Toro et al., 2020 ). This also extends towards parents raising disabled children. While parents will likely experience ongoing challenges raising disabled children, the extent of these challenges and the parenting experiences of such challenges are invariably dependent on how disability is framed socially and culturally, and whether parents receive appropriate support during ongoing challenges. Often, parents of disabled children are negatively affected by ableism which can have consequences for the parenting process (Thomas, 2020 ). This is a very complex topic that requires extensive attention that goes beyond the scope of this paper. As such, we recommend readers to be mindful of these complexities while reading this paper and consider these parenting experiences as situated in sociocultural contexts that tend to frame disability negatively.
Unique Challenges of Raising Deaf Children
The challenges of raising a deaf child can significantly influence the parent-child relationship. First, there is the grief reaction that is typical when parents receive the diagnosis (Scarinci et al., 2017 ), which involves a range of intense and negative emotions like shock, denial, anger, and feelings of grief, loss, and uncertainty (Barnett et al., 2003 ; Flaherty, 2015 ; Huang et al., 2010 ; Scarinci et al., 2017 ; Zappella, 2015 ). Unresolved feelings about the child’s diagnosis can have a lasting adverse impact on the parent-child relationship which, in turn, can compromise the developmental outcomes of children with hearing loss (Jean et al., 2018 ; Marvin & Pianta, 1996 ).
Parenting capacity and adaptation will vary in relation to parent characteristics, in particular whether the parents have hearing loss themselves. The majority of deaf babies (90%) are born to hearing parents who typically do not have experience with deafness as a disability (Jean et al., 2018 ). These parents therefore may struggle to know how to communicate with their deaf children, who are reliant on a specific mode of communication that is phenomenologically compatible with their deaf ‘epistemology’: a visual way of seeing and experiencing the world (Hauser et al., 2010 ; Paradis & Koester, 2015 ). Hauser and colleagues point out that parents of children with hearing loss need to work much harder to communicate with their children compared to parents with hearing children, where communication is frequently natural, intuitive, and spontaneous (Depowski et al., 2015 ; Morgan et al., 2014 ). As a result, parent-child interaction may be compromised from the outset. Deaf children, particularly those with hearing parents, generally experience developmental delays in areas such as language acquisition (Humphries et al., 2012 ), socioemotional development (Hintermair, 2006 ), prosocial behaviour (Sarant et al., 2018 ), theory of mind (Peterson et al., 2016 ) and may be more vulnerable to developing insecure attachment styles (Howe, 2006a ; 2006b ).
Marvin & Pianta, ( 1996 ) have studied the shock and impact of a diagnosis of child disability and how this may compromise parents’ capacity to be sensitively responsive to their child. Their study on 70 mothers of children with cerebral palsy diagnoses found a relationship between unresolved feelings regarding their child’s diagnosis and insecure child-parent attachment (Marvin & Pianta, 1996 ). A diagnosis of deafness presents unique challenges to hearing parents when it comes to reading and interpreting child cues, which is fundamental to adaptive responsive parenting behaviours such as authoritative parenting styles (Baumrind, 1971 ) and a secure attachment relationship (Ainsworth et al., 1978 ), which has been noted to be optimal for child development. To date, research findings on the nuances and implications of parent-deaf child relationships are inconsistent, underexplored, and not fully elucidated (see Jean et al., 2018 ). There is a need to better understand which factors may contribute to better relationships, leading to more targeted early intervention approaches that can support parents of deaf children.
The current research explores parents’ resolution of their child’s diagnosis and how it may affect their parenting experiences, parenting style, and perceptions of their child. A review examining the development of psychopathology in children with disabilities found children with congenital hearing loss and cerebral palsy were at higher risk of emotional, behavioural and social problems than children without disabilities (Bøttcher & Dammeyer, 2013 ). Bøttcher and Dammeyer concluded that disability was not limited to the biological nature of the impairment; it was further complicated by any mismatch between the child’s development and the surrounding environment including parents, medical professionals, and schools.
Impact on Parenting Morale and Style
Parents negotiating with the ongoing challenges of raising disabled children can be vulnerable to suboptimal psychological wellbeing and parenting capacity (Resch et al., 2012 ). Numerous studies have found that parents of disabled children are more likely to experience mental health issues including depression (Giallo et al., 2014 ; Resch et al., 2012 ); unresolved feelings about their child’s diagnosis (Howe, 2006b ; Marvin & Pianta, 1996 ); and higher levels of stress and fatigue compared with parents of typically developing children (Giallo et al., 2014 ; Seymour et al., 2012 ; Woodman 2014 ). Parenting styles among parents of children with disability may also differ from those of parents with typically developing children (Hutchison et al., 2016 ; Phillips et al., 2017 ; Riany et al., 2017 ). Notably, they are less likely to display authoritative parenting (typically involving warmth, autonomy, healthy discipline based on reasoning, and sensitivity to their child’s need), and are more likely to display authoritarian or permissive parenting. Authoritarian parenting is characterised by lower responsiveness, higher demandingness and more control. Permissive parenting similarly involves a lack of sensitivity to child’s needs, but also lacks discipline and establishing limits, sometimes to the point of neglect (Baumrind, 1971 ). These two negative parenting styles can take the form of overprotectiveness (Pinquart, 2013 ), which is often associated with perceptions of child vulnerability (Carpentier et al., 2008 ; Hullmann et al., 2010 ; Thomasgard, 1998 ), or an increased likelihood of engaging in child maltreatment, such as abuse and neglect (Howe, 2006b ). Such suboptimal parenting may be a product of inexperience and uncertainty of raising disabled children with different needs (Baumrind, 1994 ; Henderson et al., 2016 ; Reeder & Morris, 2021 ; Steiner & Dahlquist, 2022 ).
A meta-analysis of 325 studies concluded that parents of children with a chronic illness/disability (including deafness) had less positive parent-child relationships assessed through observation and self-report measures, although the effect sizes were small (Pinquart, 2013 ). Moreover, there were higher levels of negative parenting including more demandingness and control as well as lower levels of parental responsiveness. Interestingly, and of relevance to the current study, the meta-analysis also found that hearing parents with deaf children – compared to children with other chronic illnesses/disabilities – struggled more with establishing healthy parental behaviours, including maintaining a healthy level of control, protection, and warmth as well as with maintaining a healthy parent-child relationship. While inexperience and uncertainty may explain this phenomenon, it may also be the case that parents are also affected by ableism (Johnson & West, 2020 ), particularly audism, the notion that people with hearing loss are inferior due to their inability to hear and speak (Hauser et al., 2010 ). Parents may embody these attitudes, feeling resentment, hopelessness, or guilt for having a deaf child, which may interfere with maintaining the parent-child relationship.
There are inconsistent findings regarding parenting styles in the context of child deafness. Taking one study as an example, Ekim & Ocakci, ( 2015 ) found lower mean scores for positive parenting dimensions (‘authoritative’ parenting characterised by warmth, structure, autonomy) and higher mean scores for negative parenting dimensions (‘authoritarian’ parenting characterised by rejection, coercion) when comparing hearing parents raising deaf children and hearing children. In contrast, a sibling comparison study found parents treated their deaf children more warmly, and with less coercive control compared with their hearing siblings (Antonopoulou et al., 2012 ), and Ketelaar et al., ( 2017 ) found no differences in parenting styles and dimensions, though it was suggested that this finding may have been attributable to the parents having participated in rehabilitation and support programs as part of the child obtaining cochlear implants.
Perceived Child Vulnerability
A heightened perception of child vulnerability (specifically, vulnerability to illness) has consistently been observed among parents raising children with chronic illnesses (Thomasgard, 1998 ), which may be associated with higher parenting stress and more parental overprotection (Carpentier et al., 2008 ; Hullmann et al., 2010 ). Children perceived by their parents as highly vulnerable have also demonstrated academic underachievement as well as internalising and externalising behaviours. Levels of perceived child vulnerability vary across different illness and disability types related to the different demands on parents and families (Hullmann et al., 2010 ). Most studies on perceived child vulnerability are focused on medical problems and illnesses (e.g., Type 1 diabetes, asthma, cystic fibrosis, cancer) which may or may not co-occur with disability. Few studies have examined perceptions of vulnerability in children with disability and the current study makes a novel contribution by addressing this gap in relation to parents of deaf children.
As noted above, perceptions of child vulnerability may contribute to low morale and parenting stress and there is evidence that parents raising children with a disability experience more parenting stress than parents of typically developing children (Hayes & Watson, 2012 ; Hintermair, 2006 ; Phillips et al., 2017 ; Seymour et al., 2012 ; Woodman, 2014 ). Higher parenting stress can compromise parent child relationship quality, while low parenting stress can be protective (McMahon & Meins, 2012 ). In their study of pre-schoolers, McMahon and Meins reported that elevated parenting stress was associated with lower observed parental emotional availability (responsiveness and support of child autonomy) in typically developing children. A study of parents of children with autism and/or attention deficit hyperactive disorder (ADHD) found that higher parenting stress was related to a more permissive or authoritarian parenting style and poorer child executive functioning (Hutchison et al., 2016 ). Few studies have examined parenting stress in parents of deaf children, but there is some recent evidence that they experience higher levels of stress on average compared to families with hearing children, with negative consequences for their parenting ability and the socioemotional wellbeing of their deaf children (Jean et al., 2018 ).
The second aim of the current study is to examine how parenting morale may interact with other parenting factors, including parenting styles, in relation to parents of children with hearing loss. Although distinct from each other, parenting morale has been found to be related to parenting stress (Benzies et al., 2010 ), and can be used as a proxy measurement that assesses the underlying psychological morale and energy of parents, that may be particularly appropriate to parents of children with disability (Trute & Hiebert-Murphy, 2005 ).
Impact of Resolution of Diagnosis
Studies across a range of child disabilities have shown that lack of resolution of diagnosis has a negative impact on parenting behaviour in parents of children with intellectual disability (Feniger-Schaal & Oppenheim, 2013 ), and parental wellbeing in parents of children with autism (Milshtein et al., 2009 ) and children with cerebral palsy (Krstić et al., 2015 ). There are inconsistent findings regarding disability severity, with one study finding severity of autism symptoms was not related to resolution of diagnosis (Milshtein et al., 2009 ) while another reported that the rate of unresolved reactions was higher among parents of children with more severe motor disabilities (Schuengel et al., 2009 ). While resolution of diagnosis clearly has an impact, it is not fully understood how it plays out in different disability contexts and in relation to different child factors. To date, only one study has explored hearing parents’ resolution of diagnosis of deafness in their child. Adams ( 2011 ) found that contrary to expectation, stress and psychological adjustment in mothers were not associated with resolution of the diagnosis of deafness, but also found that mothers unresolved with regard to their child’s diagnosis reported more child behavioural problems. Additionally, unresolved diagnosis was associated with higher anxiety. The study did not explore associations with parenting styles and parental perceptions of their child. The current study addresses these issues.
Aims and Hypotheses
The current study uses a within-family sibling comparison design to explore the unique parenting experiences of hearing parents raising children with hearing loss and the influence of resolution of diagnosis of the child’s hearing loss on parental adjustment. It is hypothesised that i) Parents, especially those who are unresolved, will report higher perceived child vulnerability and less optimal parenting styles with their deaf child, compared to a hearing sibling; specifically, parents will see the deaf child as more vulnerable and will report less authoritative parenting (and more permissive or authoritarian parenting); and ii) Non-resolution of diagnosis will be associated with lower parenting morale and greater perceived child vulnerability.
Participants
Participants were recruited via distribution of survey links (through flyers, emails, word of mouth) with the help of Sydney Cochlear Implant Centre (SCIC), Next Sense (Formerly Royal Institute of Deaf and Blind Children at the time of study), and Parents of Deaf Children (PODC). Survey links were also posted and shared on Deaf Community Pages on Facebook.
Participants were 84 parents ( M age = 39.05 years, SD = 5.52, age range 26–55 years) with at least one child with hearing loss aged between 5 and 12 years ( M age = 7.77 years, SD = 2.21). A further 104 parents commenced the survey, but did not complete or submit. Ten parents (12%) reported having a hearing loss themselves, 42 parents also had a hearing child aged between 5 and 12 ( M age = 8.38, SD = 2.34). A detailed description of parent and child demographic characteristics is presented in Table 1 .
Parents completed validated questionnaires about their experience of parenting, their parenting style, and their perceptions of child vulnerability. They were also asked to respond to an online version of a narrative interview containing open-ended questions regarding their recalled feelings when their child was diagnosed with hearing problems.

Demographics
Parents provided information about themselves, including age, gender, education, languages spoken at home, whether they have hearing loss themselves, and whether they had a second child in the same age-group (see Table 1 ). Questions about their child with hearing loss included age, sex, whether the child spoke or used sign language, and level of hearing loss (mild, moderate, severe, profound). Parents reported if the child with hearing loss had any additional neurodevelopmental difficulties or comorbid diagnoses, as hearing loss is commonly comorbid with other disabilities (Cupples et al., 2018 ). If parents had a second child in the same age-group, they were asked to complete the same details about that child.
Parenting Morale Index (PMI, Trute and Hiebert‐Murphy 2005 )
Parenting morale (i.e., positive spirit, energy, enthusiasm) was measured using the PMI questionnaire. This 10-item measure is rated on a 5-point Likert scale, with responses ranging from 1 ( not at all ) to 5 ( very often ) where 6 items were reverse scored, higher scores indicating higher parenting morale. Items consisted of statements about how parents felt: either positive (e.g., ‘Contented’, ‘Optimistic’) or negative (e.g., ‘Stressed’, ‘Exhausted’). The PMI has demonstrated good reliability and validity in identifying those susceptible to experiencing higher stress levels and low parenting enthusiasm (Benzies et al., 2010 ). The current study found good internal consistency, Cronbach’s α = 0.85.
Child Vulnerability Scale (CVS, Forsyth et al., 1996 )
The CVS consists of 8 items rated on a 4-point Likert scale ranging from 1 ( Strongly Disagree ) to 4 ( Strongly Agree ). Each item is a statement reflecting the parent’s perceived vulnerability of the child in terms of illness (e.g., ‘My child gets more colds than other children I know’ and ‘I often check on my child at night to make sure s/he is okay’). A total score of 10 or above, is considered indicative of a perception of child vulnerability. The measure has shown adequate internal reliability (Forsyth et al., 1996 ) and validity of the cut-off score in relation to clinical scores on the Child Behaviour Checklist (Achenbach & Edelbrook, 1986 ) and child visits to physicians (Horwitz et al., 1992 ). The current study found internal consistency to be good; Cronbach’s α = 0.88.
Parenting Styles Dimension Questionnaire (PSDQ, Robinson et al. 1995 )
The PSDQ consists of 62 items (with 3 items reverse scored) rated on a 5-point scale ranging from 1 ( Never ) to 5 ( Always ). Items are classified into three global dimensions: authoritative, authoritarian, and permissive, congruent with the theoretical work of Baumrind’s parenting typology (Baumrind, 1971 ; Robinson et al., 1995 ). Within the authoritative dimension, there are 4 factors: warmth & involvement (11 items, e.g., knows the names of child’s friends), reasoning/induction (7 items, e.g., explains the consequences of the child’s behaviour), democratic participation (5 items, e.g., allows child to give input into family rules), and good natured/easy going (4 items, e.g., is easy going and relaxed with child). Within the authoritarian dimension, there are also 4 factors: verbal hostility (4 items, e.g., explodes in anger towards child), corporal punishment (6 items, e.g., uses physical punishment as a way of disciplining our child), non-reasoning/punitive strategies (6 items, e.g., punishes by taking privileges away from child with little if any explanations), and directiveness (4 items, e.g., scolds and criticizes to make child improve). Lastly, the permissive dimension has three factors: lack of follow through (6 items, e.g., states punishments to child and does not actually do them), ignoring misbehaviour (4 items, e.g., allows child to interrupt others), and self-confidence (5 items, e.g., appears confident about parenting abilities).
The measure has good internal consistency in large samples (Olivari et al., 2013 ) and in the current study; authoritative α = 0.86, authoritarian α = 0.85, and permissive α = 0.78.
Reaction to Diagnosis Interview (RDI, Marvin and Pianta 1996 )
The RDI is a semi-structured, standardised interview that aims to examine the extent of parents’ grief stemming from discovering their child’s disability diagnosis. There are five questions designed to probe the parent’s recollection of their past and current feelings and thoughts about the diagnosis at the time as well as their ideas regarding why their child has special needs. The RDI was originally designed to be conducted in a face-to-face interview; but adapted as an online questionnaire for this study. Slight modifications were made to some questions. Question 1 reads “When did you first realize that your child had problems with hearing?” (instead of ‘a medical problem’) and Questions 2 and 3 were combined into one (What were your feelings at the time of this realisation? How have these feelings changed over time?) to reduce the number of text boxes required to be filled in.
Classification of participant responses as either ‘resolved’ or ‘non-resolved’ was based on the reviews of two raters. The responses were coded as recommended by the manual (see Marvin & Pianta, 1996 ). The coding system is based on the approach to coding resolved and unresolved responses to loss and trauma in the Adult Attachment Interview (George et al., 1996 ). Particular elements in the responses were identified as either indicating resolution or non-resolution of diagnosis. Due to the online nature of the interview, behavioural criteria were excluded. Indicators of resolution include: 1) understanding the moment of diagnosis as a time of difficulty and identifying change in feelings since that moment; 2) statements indicating “moving on” in life (e.g., life must go on; 3) reporting they had ceased searching for existential reasons to explain why the diagnosis occurred (e.g., why me?); 4) accurate representation of the child’s abilities; and 5) balanced statements about the experience raising a child with special needs (e.g., there are upsides and downsides to raising the child). On the other hand, indicators of non-resolution include: 1) signs of cognitive distortions (e.g., distort reality through articulating unrealistic beliefs, magical thinking or expectations); 2) ongoing search for existential reasons for child’s special needs (e.g., why did this happen to me?); 3) signs of being stuck in the past (e.g., focused on the past without showing an indication of change of feelings); 4) mental disorganisation and incoherence (e.g., unable to tell the story clearly); and 5) unable to report their experiences of the diagnosis (e.g., appearing to be cut off from the experience). The coding scheme was categorical, classifying each participant as either resolved or unresolved. All RDI responses were double-coded. The second coder (second author) has been trained and certified in the coding of the Adult Attachment Interview. Initial inter-rater agreement was 89%. Coding disagreements were resolved through discussion, with both coders reaching agreement for each response.
After gaining approval from the Human Research Ethics Committee (review reference no.5201951718200) organisations were sent details of the link to the online survey. The survey was designed with Qualtrics. All participants were presented with the Participant Information Sheet/Consent Form at the start of the survey and were required to give consent before participating in the survey by selecting the ‘I give consent’ option. Participants were free to drop out any time. All participants were required to complete demographic, PMI and RDI questionnaires initially. Parents who also had another child in the age-range ( n = 42) were required to complete the CVS, and PSDQ questionnaires twice, allowing within family comparisons (note that 10 out of 42 were excluded from hypotheses testing since either the parents were deaf or both siblings were deaf). The first round of questionnaires was addressed towards the younger of the two siblings, and the second round towards the elder of the two siblings to ensure randomisation of the order of completing questionnaires. Participants were offered an opportunity of entering a prize draw of 3 x $50 gift vouchers at the end of the survey. Informed consent was obtained from all individual participants included in the study. This included consent to both participate and have study data published provided they were made anonymised.
Data Analysis
Data were inspected for normality. Bivariate correlations and t-tests/analyses of variance (ANOVA) were used to examine potential covariates among continuous and categorical variables, respectively. The first hypothesis examining within-parent differences between hearing and deaf siblings (in terms of perceived vulnerability and parenting style) was tested on the subsample of hearing parents (excluding deaf parents) who provided questionnaire responses for a deaf and a hearing child both aged 5–12 years old ( n = 32) using mixed effects analysis using restricted maximum likelihood estimation. The second hypothesis exploring possible associations among resolution of diagnosis of child deafness, parenting morale, and perceived vulnerability was tested for all parents (hearing) with a deaf child aged 5–12 years old ( n = 74) using univariate ANCOVA (comparing resolved and unresolved parents). Both parametric and non-parametric tests were conducted where outcome variables had non-normal distributions. Since both tests yielded the same results with respect to significance, parametric results are presented.
Descriptive Statistics
Parenting morale (PMI) and PSDQ (Authoritative, Authoritarian, Permissive) scores were normally distributed. However, Child Vulnerability Scores (CVS) for the deaf children and siblings had strong positively skewed distributions; 23 deaf child (27%) and 3 hearing sibling (7%) CVS scores were above the clinical score cut-off of 10 and categorised as “perceived vulnerable”. Outlier scores were identified with SPSS boxplots. The Winsorization procedure (see Dixon, 1960 ) was applied by changing 8 outlier values to match the next closest score. Regarding resolution of diagnosis (RDI), 30% of parents were classified unresolved ( n = 25) and 70% resolved ( n = 59).
Bivariate Statistics
Correlations among study variables are presented in Table 2 . Parental morale index scores (PMI: high scores are positive) were significantly negatively correlated with perceived vulnerability and authoritarian parenting style when parents reported on deaf children. The pattern of correlations was similar for hearing siblings. Additionally, PMI was also positively associated with RDI. Parents who were resolved on the RDI had higher PMI scores ( t (72) = −2.95, p = 0.004) than unresolved parents. RDI was found to be negatively associated with the CVS scores of both deaf and hearing siblings.
Twenty-three deaf children had a neurodevelopmental diagnosis, but this was not related to other variables. Seven of the siblings were reported to also have hearing loss and were excluded from sibling comparison data analyses. Finally, age at the time of diagnosis (derived from answers to the RDI interview), age and gender of parent, child, and sibling were not significantly associated with any outcome variables. There were also no significant differences in age comparing deaf and hearing siblings. The number of deaf children older than their hearing siblings and vice versa were also not significantly different indicating order of sibling comparisons were sufficiently randomised.
Parent education was recoded into two categories: tertiary and non-tertiary education. Compared to parents who obtained tertiary education ( n = 38), parents in the non-tertiary group ( n = 45) had significantly higher child vulnerability (CVS) scores relating to their deaf child ( t (82) = 2.09, p = 0.039), and lower authoritarian parenting scores ( t (40) = −2.50, p = 0.017) for the sibling. There were no other significant differences related to education.
Interestingly, there were some significant differences between deaf ( n = 10) and hearing parents ( n = 74). Deaf parents had higher parenting morale scores ( t (82) = 2.92, p = 0.005), but lower authoritative parenting scores relating to their deaf child ( t (82) = −2.31, p = 0.031). Ninety percent of deaf parents (9 of the 10) were classified resolved about their deaf child’s diagnosis in contrast to 68% of hearing parents; however, this difference was not found to be significant, χ 2 (1) = 2.12, p = 0.15, likely due to statistical power issues from low numbers of deaf parents. However, since the research questions are concerned with hearing parents specifically, deaf parents were excluded from data analyses. Parents also reported on the severity of their child’s hearing loss: 7 were classified mild, 24 moderate, 16 severe, and 37 profound. No significant associations were found between severity of hearing loss and outcome variables. Given these findings, parent’s education was controlled for in analyses for CVS, and PSDQ authoritarian scores. Both parent morale scores (PMI) and resolution of diagnosis (RDI) were controlled for in the sibling comparison analyses.
Hypothesis Testing
Hypothesis 1.
Hearing parents, especially those who are unresolved, will see the deaf child as more vulnerable and will report less authoritative parenting (and more permissive or authoritarian parenting) compared to the hearing sibling.
Testing hypothesis (i) involved mixed effects analyses using restricted maximum likelihood estimation. The repeated factor, (deaf and hearing) sibling, was nested within respondent. Education, parenting morale, and resolution of diagnosis were covariates for each dependent variable. Perceived vulnerability (CVS) and PSDQ (Authoritative, Authoritarian, and Permissive Styles) were the dependent variables. Due to the number of covariates and suboptimal power, only main effects were tested.
There was a significant difference between siblings ( F (1,54.79) = 4.25, p = 0.044) on perceived child vulnerability, with parents reporting higher child vulnerability scores for their deaf child (Estimate beta = 2.19, SE = 1.06) than their hearing sibling. There was no significant difference between siblings ( F (1,58.74) = 0.19, p = 0.193) on authoritative parenting style, but parenting morale was a significant between-parent factor ( F (1,58.68) = 8.76, p = 0.004). Authoritarian parenting style was not found to be significantly different between siblings ( F (1,57.82) = 0.11, p = 0.736), although both education ( F (1,57.56) = 4.61, p = 0.036) and parenting morale ( F (1,57.56) = 6.96, p = 0.011) were significant between-parents factors. Lastly, scores for permissive parenting styles were not significantly different between siblings ( F (1,58.47) = 0.36, p = 0.554); however, education ( F (1,58.35) = 4.85, p = 0.032) and resolution of diagnosis ( F (1,58.35) = 5.08, p = 0.028) were significant between-parents factors.
Hypothesis 2
Non-resolution of diagnosis will be associated with lower parenting morale and greater perceived child vulnerability.
For hypothesis (ii), univariate ANCOVA was used. Resolution of diagnosis (RDI) was included as the between subjects factor. Parenting morale (PMI) and perceived vulnerability (CVS) were dependent variables. Education was controlled for CVS analysis. As hypothesised, unresolved parents ( n = 24) had lower parenting morale ( F (1,70) = 9.34, p = 0.003, η 2 = 0.12), and perceived their deaf child to be more vulnerable ( F (1, 70) = 4.11, p = 0.047, η 2 = 0.06), compared to resolved parents ( n = 50) (see Table 3 ). Education was also found to have a significant main effect on child vulnerability ( F (1, 70) = 4.11, p = 0.047, η 2 = 0.06), with non-tertiary parents ( n = 17) reporting higher child vulnerability scores ( M = 10.94, SE = 1.11) than tertiary parents ( n = 7, M = 7.00, SE = 0.93). There was no significant interaction between resolution of diagnosis and education ( F (1,74) = 1.52, p = 0.222, η 2 = 0.02).
Hearing parents with deaf children may undergo considerable parenting challenges (Antonopoulou et al., 2012 ; Bosteels et al., 2012 ; Jean et al., 2018 ) and may experience salient feelings of grief when they first receive news of their child’s hearing loss diagnosis (Scarinci et al., 2017 ). These feelings may remain unresolved, which has been shown to lead to insecure attachment styles and less optimal developmental outcomes in children with other disabilities (Marvin & Pianta, 1996 ). The current research explored parent morale, perceptions of child vulnerability, and parenting styles in the context of child hearing loss, with a particular focus on parent resolution of diagnosis.
There was partial support for hypothesised sibling differences in perceived vulnerability. As predicted, deaf children were perceived as more vulnerable than their hearing siblings. Although there were no sibling differences in authoritative, authoritarian, and permissive parenting style scores, there were significant effects of resolution of diagnosis, parenting morale, and education. Parenting styles, likely as a result of having a deaf child, may be significantly influenced by these factors, though the causal nature is unclear. As hypothesised, parents who were unresolved about their deaf child’s diagnosis reported lower parenting morale and greater perceived child vulnerability.
Comparing Parenting Perceptions Across Siblings
Previous findings have suggested that hearing parents are more likely to engage in suboptimal parenting with their deaf child compared to their hearing sibling (Ekim & Ocakci, 2015 ; Pinquart, 2013 ). One prior study utilising a sibling comparison design with a sample comprised of deaf and hearing siblings (aged between 11 and 18 years) found parents reported marginally less strict parenting (permissive) towards the deaf child compared to hearing siblings (Antonopoulou et al., 2012 ). The present study adopted the same sibling comparison design while controlling for parent characteristics, notably resolution of diagnosis, parent morale, and education. Contrary to prediction, however, there was no sibling difference in authoritative, authoritarian, and permissive parenting styles, although there were notable differences across parents in terms of parenting morale, resolution of diagnosis, and education. For instance, although there may not be significant differences between sibling scores, the scores per se may be either suboptimal or optimal. It is possible that the impact of raising deaf children simultaneously affects both deaf and hearing siblings. It is not clear why there are differences across parents. This suggests a complex interplay of factors within and between parental experiences of raising deaf children that cannot be wholly ascertained with sibling comparisons and warrants further investigation.
The current findings suggest that parents – particularly those with unresolved feelings about their child’s diagnosis– are likely to perceive their deaf child as vulnerable. Although there were no differences in reported parenting styles related to deaf children and siblings, it is possible that perceived vulnerability also translates into undesirable parenting behaviours that were not measured by the survey. It would be prudent in future research to utilise observational approaches to bypass the limitations inherent in parental self-report measures. Because resolution of diagnosis was related to all the adjustment measures, it may be useful to explore parent responses in more depth to get a better understanding of this phenomenon. Perceived child vulnerability was measured using the CVS scale that tapped parental fears of their child being susceptible to illnesses (see Forsyth et al., 1996 ). This scale was designed for parents of children with medical conditions. It is interesting, therefore, that although deafness is a sensory disability and not an illness, parents also perceived their deaf child to be more vulnerable to illnesses, compared with a sibling. There are several possible explanations. First it is possible that their deaf children were actually susceptible to illnesses, their vulnerability not necessarily related to their deafness; the survey did not account for this contingency. Second it may be that parents have a global attribution of vulnerability that extends more broadly to health even if the child has no health risks. The responses parents gave in the resolution of diagnosis interview provide some possible explanations for the higher perceived vulnerability scores. Parents expressed concerns about the unknown, intense and persistent worries about their deaf child’s future, their access to education and social life, their ability to communicate, and their capacity to deal with bullying and/or exclusion. These concerns were prominent across all parent responses, suggesting most parents of deaf children experience some concern about these matters regardless of whether they are resolved about their child’s diagnosis. It is plausible that these concerns, when more intense and pervasive, contributed to the propensity to perceive their deaf child as more vulnerable in general, including vulnerability to illnesses. Additionally, there may be more nuanced perceptions of vulnerability that go beyond susceptibility to illnesses. The RDI responses indicated a particular concern for their deaf child’s social vulnerability, for example. Future studies could include a measure that targets parental perception of social vulnerability, such as the Social Vulnerability Scale originally constructed for children with Asperger’s (Sofronoff et al., 2011 ).
Greater perceived vulnerability is also likely to be associated with suboptimal parenting behaviour (Carpentier et al., 2008 ; Thomasgard, 1998 ). It is possible that greater perceived vulnerability makes it difficult to achieve the balanced state of mind required to engage in sensitive and balanced caretaking and that this may have negative influences on parent-child relationship outcomes (Hullman et al., 2010 ). Additionally, communication issues may contribute to difficulties communicating and teaching deaf children about safety and wellbeing (Hauser et al., 2010 ) which then may likely heighten perceptions of deaf child vulnerability.
Resolution of diagnosis, parenting morale, and perceived child vulnerability
Study findings indicate that compared to parents who were resolved about their child’s diagnosis, parents who were unresolved had lower parenting morale, and perceived their deaf child to be more vulnerable. The resolution of diagnosis construct stems from attachment theory, particularly drawing on the notion that unresolved grief and trauma can adversely impact the caregiving relationship and attachment (Marvin & Pianta, 1996 ). Previous findings have suggested that parents of children with disabilities (cerebral palsy, autism, and intellectual disability), who were unresolved about the diagnosis had lower parent wellbeing including higher stress levels, and more negative feelings about parenting (Krstić et al., 2015 ; Milshtein et al., 2009 ). The present study lends further support to these studies and adds to just one published study that has examined resolution of diagnosis in relation to deafness (Adams, 2011 ). The study also makes a novel contribution by assessing the relationship between resolution of diagnosis, perceived child vulnerability, and parenting morale for the first time. These findings suggest non-resolution is linked to a negative state of mind in the context of parenting and compromised wellbeing, which in turn, may negatively affect parenting behaviour. This link may be exaggerated with the challenges of uncertainty raising a disabled child to the extent that parenting experiences are disrupted by a complex combination of overwhelming feelings and inexperience with disability (Reeder & Morris, 2021 ). For example, a recent study suggested that there is a link between maternal intolerance of uncertainty and increased protective parenting in context of children with food allergies (Steiner & Dahlquist, 2022 ). Future research could benefit from further exploring how inexperience, and cognitive and emotional uncertainty with raising disabled children can act as a risk factor for suboptimal parenting behaviour, including increased perceived vulnerability and protective parenting.
Parent level of education was found to have an effect on perceived child vulnerability scores among unresolved parents, those without tertiary education saw their deaf child as more vulnerable compared to parents of deaf children with tertiary education. A similar result was found by Thomasgard & Metz, ( 1997 ) in a study of 280 parents of children without disabilities. They found that parents with lower education reported more child vulnerability and parental overprotection. This is potentially due to more advanced education contributing to better parenting resources, knowledge, and strategies that may contribute to more positive parenting, parenting confidence, reflectivity, and understanding. Higher education may also influence perceptions and enable more realistic expectations of the child (see Fox et al., 1995 ; Neitzel & Stright, 2004 ; Woodward et al., 2018 ). Although education was not found to be related to resolution of diagnosis, this was possibly due to low statistical power in the current study (for instance, out of parents with university education, 2 were unresolved and 15 were resolved, which makes for a disproportionate comparison). A study on parents of children with Cerebral Palsy found that parents with lower education were more likely to be unresolved about their child’s diagnosis (Krstić et al., 2016 ). It is likely that education also acts as a protective factor: parents with higher education may have more cognitive tools, better parenting morale, and resilience to reframe and mitigate negative reactions to diagnosis. Lastly, parents with higher education may also have more social capital, enabling them to navigate through social challenges, including advocacy, search for support and guidance, and dealing with systemic discrimination that marginalises disabled people. While parents of disabled children do have challenging experiences adjusting to their child’s differences, how communities respond to their child’s disability also contributes to that ongoing experience (Thomas, 2020 ).
Strengths and Limitations
The main strength of the present study is the recruitment of a clinical sample ( n = 84 altogether, n = 32 of those included siblings), the use of a sibling comparison design, and the use of a narrative interview (albeit with online delivery) to capture parent representations of the child and resolution of diagnosis. The sibling design enabled better statistical power, despite the small sample and controlled for parent characteristics. The study also ensured pseudo-randomisation by presenting the questionnaires for the younger sibling first and the older sibling second to mitigate any possible order effects. The Reaction to Diagnosis Interview (RDI) is a sophisticated measure that is well grounded theoretically and yields both qualitatively and quantitatively rich data, providing insights into how parents feel about their child’s hearing loss diagnosis. It has the further advantage of being opaque to socially desirable reporting. There are no clear right and wrong answers and parents respond freely to open-ended questions. The online survey methodology is also another strength of the study as it has more potential to conveniently obtain a representative sample with very low costs and minimal observer bias.
There are, however, several limitations to consider. Firstly, the RDI was originally designed to be utilised as a face-to-face interview. The coding for the interview measure takes into account not just the verbal response, but body language and tone of voice as well. Additionally, face to face interviews allow for opportunities to probe for more detailed responses. The coding process in this study was restricted to written text only, potentially missing out on other more subtle indicators parents may have displayed. Having said that, the Adult Attachment Interview coding guide (George et al., 1996 ) does state that all analyses should be limited to the transcript only, for purposes of maintaining objectivity. A new RDI questionnaire measure was recently developed which may be a useful complement to written responses to RDI questions for future online survey research regarding parental reaction to diagnoses (Sher-Censor et al., 2020 ).
Parents in this study were primarily female (80%) which is an important limitation to consider as fathers are also major figures in family systems and do play fundamental parts in heteronormative family dynamics alongside mothers. This study did not account for how fathers may fundamentally influence parent-deaf child dynamics. Low number of fathers participating in parenting research is an ongoing issue and is likely due to social norms emphasising mothers as the primary caregiver. Future research could benefit from incorporating more fathers in research by specifically targeting them and incentivising research participation (Cabrera et al., 2018 ; Davison et al., 2016 ).
The attrition rate in the current study was high. Only 84 out of a total 188 individuals who started, completed the survey. Further cases were lost for the sibling comparison analyses because some siblings also had hearing loss. A number of parent feedback comments on the survey mentioned that parents found some questions confronting – specifically questions about hitting the child, which were included in the measure of authoritarian parenting – and some stated that they felt judged while completing the survey. Parents of disabled children do commonly report feelings of being judged (Ludlow et al., 2011 ). It is also plausible that those who did not complete the study questionnaire may have been disproportionately more likely to engage in suboptimal parenting styles, or to be unresolved about their child’s diagnosis. Attrition may have also been related to the length of the online questionnaire. The parenting styles questionnaire had 62 items, socially desirable reporting is possible. Future research could consider alternative measures.
There were further limitations in study measures. The child vulnerability scale, although it yielded significant findings, was not an ideal measure due to its focus on illness. This questionnaire did not capture other aspects of perceived vulnerability – such as social vulnerability – that was reported in the answers to the RDI questions. Future research would benefit from utilising alternative vulnerability scales (particularly those looking at communication and social vulnerability which is a fundamental issue for deaf people), as well as over-protective parenting measures. Additionally, exploring more factors relating to rehabilitation, intervention, and support (such as cochlear implant programs) may be useful to highlight further protective factors when it comes to experiences parenting deaf children. Finally, the reliance on self-report measures should also be addressed by incorporating external observation and reports from children.
Clinical Implications and Future Directions
The findings from this study contribute to a better understanding of the experiences of hearing parents raising deaf children, with potential to inform policy and appropriately targeted supportive interventions designed to improve the wellbeing of both hearing parents and deaf children. This study has provided evidence that indicates parents of deaf children may continue to be affected for many years by their child’s hearing loss diagnosis, often experiencing lower parenting morale and greater perceived child vulnerability.
Responses to the RDI questions revealed recurring themes and concerns. Upon receiving their child’s hearing loss diagnosis, many parents reported that they had experienced feelings of anxiety, grief, despair, devastation, and shock. Many also reported similar concerns about their deaf child’s future: concerns about the unknown, not knowing anything about deafness and where to get help, worries about communication issues, barriers to accessibility issues, learning and career prospects, and issues with self-image and bullying. One parent who was classified as resolved illustrates the intensity of the grief as she describes her experience coming to terms with the diagnosis over time:
I was in shock. I was grieving for the life I had dreamed for my son. My life and my whole families’ life changed that day. I was so upset at the time I was told and really can’t remember much of what happened after I was told. I felt like I was ‘out of my body’ observing what was happening. I couldn’t think straight. I was upset for months and couldn’t talk about it without crying. I was going through the motions of being a parent to both kids, taking my son to appointments, learning everything new along the way. As the years have gone on, it’s got so much easier. I look back on the first few years as the hardest. Those first few years are so uncertain, and the grief keeps coming back at times. I think I was depressed as well, I started to look at life differently and didn’t feel as carefree, didn’t find joy as easily. I think after the first 2-3 years everything was easier. I had accepted our life, I felt more confident about his future, I was proud of my son and wouldn’t change his hearing loss but in the early days I would have given anything for him to have normal hearing.
This excerpt indicated elements of resolved feelings such as understanding the diagnosis as a time of difficulty, clearly describing her past and present thoughts and feelings as different, recognising the changes over time, and feeling more settled about the future. In contrast, parents who are unresolved do not show indications that they moved on from the diagnosis; the same feelings and thoughts they experienced when they received the diagnosis appear to persist years later. Feelings of guilt and self-blame for their child’s deafness were frequently articulated by parents whose responses were classified as unresolved. One parent put it this way:
Absolute heartbreak. I almost mourned the loss of the child I thought he should have been. I was worried about him growing up and marrying, I was worried that he would be bullied, I worried if I had exposed him to enough speech and auditory experiences before the progression. I spent hours of sleepless nights searching the internet for information only to find very little. He has been aided for a year and a half. He is doing so well at school but there are still times when I feel so guilty. I think every progression makes you realise the loss all over again.
The key differences between the resolved and unresolved excerpts above are the absence of looking into the future, and no explicit statement reflecting change from past to present feelings. Reliving the feelings of loss, grief, and guilt would likely have an ongoing impact on the parent’s state of mind.
A number of parents also commented on audiologists not breaking the news of the child’s diagnosis in an appropriate manner, nor providing an appropriate time and place for the parents to process the news. One stated:
I was with my husband and the audiologist at the hospital who wasn’t very nice in telling us the news. To him, he was just doing his job. To me, being a first-time mum, I wasn’t sure why I was in the hospital or why my son needed further testing, I needed someone more supportive as I was new to the whole “deaf” world.
Another parent who was deaf also shared similar feelings about audiologists not sharing the news of diagnosis with sufficient care:
I was at the audiologists’ office, very mundane and sombre atmosphere. Test was conducted at a centre where it is known that they are very anti-Auslan and are strong advocates for AVT (auditory-verbal therapy). Quick to usher me in and out of waiting room / testing, etc. Terminology used is very negative - failed, did not succeed, did not achieve, etc. They assumed that I was deaf myself, that they did not need to give me information. I was left to my own means. With this kind of environment, I felt that I could not soak in the results and discuss. Therefore, leading me to feel despair and grief.
Clinicians need to provide individualized support and guidance for parents going through news of diagnosis in order to mitigate this, and help them to work towards realistic (and non-catastrophic) expectations for the child, to minimize lasting negative impacts on parent and child wellbeing.
A mix of positive psychology and awareness of deaf culture and epistemology could also be incorporated into parental support and rehabilitation processes. This may involve helping parents to learn and understand what it is like to be deaf, to consider the positive and unique aspects of raising deaf children by talking to deaf people and mentors and providing them a list of common questions with informed evidence-based answers (see Humphries et al., 2019 ). Additionally, conversations with other parents of deaf children via parent-to-parent support have also been found to be significantly helpful (Henderson et al., 2016 ; Mehta et al., 2019 ). One parent revealed: “My daughter also has so many questions we do not have answers for; such as ‘how come I’m the only one with hearing loss?’” Educating parents about deafness, deaf culture, and deaf epistemology could have positive outcomes for the deaf child, particularly in terms of psychological resilience, helping them to learn to embrace their deafness rather than seeing it as a lifelong burden (Hauser et al., 2010 ; Szarkowski & Brice, 2016 ). Additionally, improving communications between parent and deaf child is a priority as it has significant long term implications for parent-child relationships and their wellbeing (Barker et al., 2009 ; Humphries et al., 2019 ; Lam-Cassettari et al., 2015 ; Tomaszewski, 2008 ) Future research should further consider how both hearing parents and deaf children can build resilience through applications of positive psychology, deaf culture and epistemology, and interventions focused on improving parent-deaf child communications, especially exploring the use of bimodal bilingualism (using both spoken and sign language) to mitigate communication barriers (Humphries et al., 2019 ).
This study found parents who have persistent unresolved feelings about their child’s hearing loss diagnosis experience lower parenting morale and perceive their deaf child to be more vulnerable than parents who are more resolved and reflective about the diagnosis. Further, parents also reported greater perceived vulnerability in relation to their deaf child compared to hearing siblings. These results suggest further research is needed to better understand the impact a deaf child can have on the parent-child relationship and parenting state of mind, and to consider how applications of parenting education, positive psychology, and deaf epistemology can help mitigate such impact.
Achenbach, T. M., & Edelbrook, C. (1986). Manual for the Child Behavior Checklist and Revised Child Behavior Profile . Burlington: University of Vermont.
Google Scholar
World Health Organization. (2016). Childhood hearing loss: strategies for prevention and care . Geneva, Switzerland: World Health Organization.
Adams, E. B. (2011). Hearing Mothers’ Resolution of the Identification of Child Hearing Loss: An Exploration of the Reaction to Diagnosis Interview , Gallaudet University.
Ainsworth, M. D. S., Blehar, M. C., Waters, E., & Wall, S. (1978). Patterns of attachment: A psychological study of the Strange Situation . Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.
Antonopoulou, K., Hadjikakou, K., Stampoltzis, A., & Nicolaou, N. (2012). Parenting Styles of Mothers With Deaf or Hard-of-Hearing Children and Hearing Siblings. Journal of Deaf Studies and Deaf Education , 17 (3), 306–318.
Article PubMed Google Scholar
Barker, D. H., Quittner, A. L., Fink, N. E., Eisenberg, L. S., Tobey, E. A., & Niparko, J. K. (2009). Predicting behavior problems in deaf and hearing children: The influences of language, attention, and parent–child communication. Development and Psychopathology , 21 (2), 373–392.
Article PubMed PubMed Central Google Scholar
Barnett, D., Clements, M., Kaplan-Estrin, M., & Fialka, J. (2003). Building New Dreams: Supporting Parents’ Adaptation to Their Child With Special Needs. Infants & Young Children , 16 (3), 184–200.
Article Google Scholar
Baumrind, D. (1971). Current patterns of parental authority. Developmental Psychology Monographs , 4 , 1–103.
Baumrind, D. (1994). The Social Context of Child Maltreatment. Family Relations , 43 (4), 360.
Belsky, J. (1980). Child maltreatment: An ecological integration. American Psychologist , 35 (4), 320–335.
Belsky, J. (1984). The Determinants of Parenting: A Process Model. Child Development , 55 (1), 83–96.
Belsky, J. (1993). Etiology of child maltreatment: A Developmental-Ecological Analysis. Psychological Bulletin , 114 (3), 413–434.
Benzies, K. M., Trute, B., Worthington, C., Reddon, J., Keown, L., & Moore, M. (2010). Assessing Psychological Well-Being in Mothers of Children with Disability: Evaluation of the Parenting Morale Index and Family Impact of Childhood Disability Scale. Journal of Pediatric Psychology , 36 (5), 506–516.
Bosteels, S., Hove, G. V., & Vandenbroeck, M. (2012). The roller-coaster of experiences: Becoming the parent of a deaf child. Disability & Society , 27 (7), 983–996.
Bøttcher, L., & Dammeyer, J. (2013). Disability as a risk factor? Development of psychopathology in children with disabilities. Research in Developmental Disabilities , 34 (10), 3607–3617.
Cabrera, N. J., Volling, B. L., & Barr, R. (2018). Fathers Are Parents, Too! Widening the Lens on Parenting for Children’s Development. Child Development Perspectives , 12 (3), 152–157.
Carpentier, M. Y., Mullins, L. L., Wolfe-Christensen, C., & Chaney, J. M. (2008). The relationship of parent self-focused negative attributions to ratings of parental overprotection, perceived child vulnerability, and parenting stress. Families, Systems, & Health , 26 (2), 147–163.
Choi, S. M. R., Kei, J., & Wilson, W. J. (2017). Rates of hearing loss in primary school children in Australia: A systematic review. Speech, Language and Hearing , 20 (3), 154–162.
Cupples, L., Ching, T. Y. C., Leigh, G., Martin, L., Gunnourie, M., Button, L., Marnane, V., Hou, S., Zhang, V., Flynn, C., & Van Buynder, P. (2018). Language development in deaf or hard-of-hearing children with additional disabilities: type matters. Journal of Intellectual Disability Research , 62 (6), 532–543.
Davison, K. K., Charles, J. N., Khandpur, N., & Nelson, T. J. (2016). Fathers’ Perceived Reasons for Their Underrepresentation in Child Health Research and Strategies to Increase Their Involvement. Maternal and Child Health Journal , 21 (2), 267–274.
Depowski, Abaya, H., Oghalai, J., & Bortfeld, H. (2015). Modality use in joint attention between hearing parents and deaf children. Frontiers in Psychology, 6 , 1556. https://doi.org/10.3389/fpsyg.2015.01556 .
Dixon, W. J. (1960). Simplified Estimation from Censored Normal Samples. The Annals of Mathematical Statistics , 31 (2), 385–391.
Ekim, A., & Ocakci, A. F. (2015). A Comparison of Parenting Dimensions Between Deaf and Hearing Children. Clinical Nursing Research , 25 (3), 342–354
Feniger-Schaal, R., & Oppenheim, D. (2013). Resolution of the diagnosis and maternal sensitivity among mothers of children with Intellectual Disability. Research in Developmental Disabilities , 34 (1), 306–313.
Flaherty, M. (2015). What We Can Learn From Hearing Parents of Deaf Children. Australasian Journal of Special Education , 39 (1), 67–84.
Forsyth, B. W., Horwitz, S. M., Leventhal, J. M., Burger, J., & Leaf, P. J. (1996). The child vulnerability scale: an instrument to measure parental perceptions of child vulnerability. Journal of pediatric psychology , 21 (1), 89–101. https://doi.org/10.1093/jpepsy/21.1.89 .
Fox, R. A., Platz, D. L., & Bentley, K. S. (1995). Maternal Factors Related to Parenting Practices, Developmental Expectations, and Perceptions of Child Behavior Problems. The Journal of Genetic Psychology , 156 (4), 431–441.
George, C., Kaplan, N., & Main, M. (1996). Adult Attachment Interview. Unpublished manuscript, Department of Psychology . third edition Berkeley: University of California
Giallo, R., Seymour, M., Matthews, J., Gavidia-Payne, S., Hudson, A., & Cameron, C. (2014). Risk factors associated with the mental health of fathers of children with an intellectual disability in Australia. Journal of Intellectual Disability Research , 59 (3), 193–207.
Haile, L. M., Abdoli, A., Abdollahi, M., Akalu, Y., Alanezi, F. M., Alanzi, T. M., Alipour, V., Al-Raddadi, R. M., Amu, H., Ashbaugh, C., Atnafu, D. D., Babar, Z.-U.-D., Baig, A. A., Banik, P. C., Bhagavathula, A. S., Bhardwaj, N., Bibi, S., Cederroth, C. R., Charan, J., & Dandona, L. (2021). Hearing loss prevalence and years lived with disability, 1990–2019: findings from the Global Burden of Disease Study 2019. The Lancet (British Edition) , 397 (10278), 996–1009.
Hauser, P. C., O’Hearn, A., McKee, M., Steider, A., & Thew, D. (2010). Deaf Epistemology: Deafhood and Deafness. American Annals of the Deaf , 154 (5), 486–492.
Hayes, S. A., & Watson, S. L. (2012). The Impact of Parenting Stress: A Meta-analysis of Studies Comparing the Experience of Parenting Stress in Parents of Children With and Without Autism Spectrum Disorder. Journal of Autism and Developmental Disorders , 43 (3), 629–642.
Henderson, R. J., Johnson, A. M., & Moodie, S. T. (2016). Revised Conceptual Framework of Parent-to-Parent Support for Parents of Children Who Are Deaf or Hard of Hearing: A Modified Delphi Study. American Journal of Audiology , 25 (2), 110–126.
Hintermair, M. (2006). Parental Resources, Parental Stress, and Socioemotional Development of Deaf and Hard of Hearing Children. Journal of Deaf Studies and Deaf Education , 11 (4), 493–513.
Horwitz, S. M., Leaf, P. J., Leventhal, J. M., Forsyth, B. W. C., & Speechley, K. N. (1992). Identification and management of psychosocial and developmental problems in community based, primary care pediatric practices. Pediatrics , 89 , 480–485.
Howe, D. (2006b). Disabled Children, Maltreatment and Attachment. British Journal of Social Work , 36 (5), 743–760.
Howe, D. (2006a). Disabled children, parent-child interaction and attachment. Child Family Social Work , 11 (2), 95–106.
Huang, Y., Kellett, U. M., & John, W. S. (2010). Cerebral palsy: Experiences of mothers after learning their child’s diagnosis. Journal of Advanced Nursing , 66 (6), 1213–1221.
Hullmann, S. E., Wolfe-Christensen, C., Ryan, J. L., Fedele, D. A., Rambo, P. L., Chaney, J. M., & Mullins, L. L. (2010). Parental Overprotection, Perceived Child Vulnerability, and Parenting Stress: A Cross- Illness Comparison. Journal of Clinical Psychology in Medical Settings , 17 (4), 357–365.
Humphries, T., Kushalnagar, P., Mathur, G., Napoli, D. J., Rathmann, C., & Smith, S. (2019). Support for parents of deaf children: Common questions and informed, evidence-based answers. International Journal of Pediatric Otorhinolaryngology , 118 , 134–142.
Humphries, T., Kushalnagar, P., Mathur, G., Napoli, D., Padden, C., Rathmann, C., & Smith, S. R. (2012). Language acquisition for deaf children: Reducing the harms of zero tolerance to the use of alternative approaches. Harm Reduction Journal , 9 (1), 16.
Hutchison, L., Feder, M., Abar, B., & Winsler, A. (2016). Relations between Parenting Stress, Parenting Style, and Child Executive Functioning for Children with ADHD or Autism. Journal of Child and Family Studies , 25 (12), 3644–3656.
Ikäheimo. (2009). Personhood and the social inclusion of people with disabilities: a recognition-theoretical approach. In Personhood and the social inclusion of people with disabilities: a recognition-theoretical approach . Milton Park, Abingdon, Oxon; New York: Routledge.
Isaacson, B. (2010). Hearing Loss. Medical Clinics of North America , 94 (5), 973–988.
Jean, Y. Q., Mazlan, R., Ahmad, M., & Maamor, N. (2018). Parenting Stress and Maternal Coherence: Mothers With Deaf or Hard-of-Hearing Children. American Journal of Audiology , 27 (3), 260–271.
Johnson, B., & West, R. (2020). Ableist contours of Down syndrome in Australia: Facebook attitudes towards existence and parenting of people with Down syndrome. Journal of Sociology , 57 (2), 144078331989347. https://doi.org/10.1177/1440783319893474 .
Ketelaar, L., Wiefferink, C. H., Frijns, J. H., & Rieffe, C. (2017). Children With Cochlear Implants and Their Parents: Relations Between Parenting Style and Children’s Social-Emotional Functioning. Ear and Hearing , 38 (3), 321–331.
Krstić, T., Mihić, L., & Mihić, I. (2015). Stress and resolution in mothers of children with cerebral palsy. Research in Developmental Disabilities , 47 , 135–143.
Krstić, T., Batić, S., Mihić, L., & Milankov, V. (2016). Mothers’ Reactions to the Diagnosis of Cerebral Palsy: Associations with their Educational Level. International Journal of Disability, Development and Education , 63 (4), 467–483.
Lam-Cassettari, C., Wadnerkar-Kamble, M. B., & James, D. M. (2015). Enhancing Parent-Child Communication and Parental Self-Esteem With a Video-Feedback Intervention: Outcomes With Prelingual Deaf and Hard-of-Hearing Children. Journal of Deaf Studies and Deaf Education , 20 (3), 266–274.
Ludlow, A., Skelly, C., & Rohleder, P. (2011). Challenges faced by parents of children diagnosed with autism spectrum disorder. Journal of Health Psychology , 17 (5), 702–711.
Marvin, R. S., & Pianta, R. C. (1996). Mothers’ reactions to their child’s diagnosis: Relations with security of attachment. Journal of Clinical Child Psychology , 25 (4), 436–445.
McMahon, C. A., & Meins, E. (2012). Mind-mindedness, parenting stress, and emotional availability in mothers of preschoolers. Early Childhood Research Quarterly , 27 (2), 245–252.
Mehta, K., Hilton, E., Baldwin, M., & Watkin, P. (2019). Parent-to-parent support for the families of deaf children identified by the newborn hearing screen. Deafness & Education International , 22 (2), 1–17.
Milshtein, S., Yirmiya, N., Oppenheim, D., Koren-Karie, N., & Levi, S. (2009). Resolution of the Diagnosis Among Parents of Children with Autism Spectrum Disorder: Associations with Child and Parent Characteristics. Journal of Autism and Developmental Disorders , 40 (1), 89–99.
Morgan, G., Meristo, M., Mann, W., Hjelmquist, E., Surian, L., & Siegal, M. (2014). Mental state language and quality of conversational experience in deaf and hearing children. Cognitive Development , 29 , 41–49.
Neitzel, C., & Stright, A. D. (2004). Parenting behaviours during child problem solving: The roles of child temperament, mother education and personality, and the problem-solving context. International Journal of Behavioral Development , 28 (2), 166–179.
Olivari, M. G., Tagliabue, S., & Confalonieri, E. (2013). Parenting Style and Dimensions Questionnaire: A Review of Reliability and Validity. Marriage & Family Review , 49 (6), 465–490
Paradis, G., & Koester, L. S. (2015). Emotional Availability and Touch in Deaf and Hearing Dyads. American Annals of the Deaf , 160 (3), 303–315.
Peterson, C., Slaughter, V., Moore, C., & Wellman, H. M. (2016). Peer social skills and theory of mind in children with autism, deafness, or typical development. Developmental Psychology , 52 (1), 46–57.
Phillips, B. A., Conners, F., & Curtner-Smith, M. E. (2017). Parenting children with down syndrome: An analysis of parenting styles, parenting dimensions, and parental stress. Research in Developmental Disabilities , 68 , 9–19.
Pinquart, M. (2013). Do the Parent–Child Relationship and Parenting Behaviors Differ Between Families With a Child With and Without Chronic Illness? A Meta-Analysis. Journal of Pediatric Psychology , 38 (7), 708–721.
Reeder, J., & Morris, J. (2021). Managing the uncertainty associated with being a parent of a child with a long‐ term disability. Child: Care, Health and Development , 47 , 816–824.
Resch, J. A., Elliott, T. R., & Benz, M. R. (2012). Depression among parents of children with disabilities. Families, Systems, & Health , 30 (4), 291–301.
Riany, Y. E., Cuskelly, M., & Meredith, P. (2017). Parenting style and parent–child relationship: a comparative study of Indonesian parents of children with and without Autism Spectrum Disorder (ASD). Journal of Child and Family Studies , 26 (12), 3559–3571.
Robinson, C. C., Mandleco, B., Frost Olsen, S., & Hart, C. H. (1995). Authoritative, authoritarian, and permissive parenting practices: Development of a new measure. Psychological Reports , 77 , 819–830.
Sarant, J. Z., Harris, D. C., Galvin, K. L., Bennet, L. A., Canagasabey, M., & Busby, P. A. (2018). Social Development in Children With Early Cochlear Implants. Ear and Hearing , 39 (4), 770–782.
Scarinci, N., Erbasi, E., Moore, E., Ching, T. Y., & Marnane, V. (2017). The parents’ perspective of the early diagnostic period of their child with hearing loss: Information and support. International Journal of Audiology , 57 (Sup2), S3–S14.
Schuengel, C., Rentinck, I. C., Stolk, J., Voorman, J. M., Loots, G. M., Ketelaar, M., & Becher, J. G. (2009). Parents reactions to the diagnosis of cerebral palsy: Associations between resolution, age and severity of disability. Child: Care, Health and Development , 35 (5), 673–680.
Seymour, M., Wood, C., Giallo, R., & Jellett, R. (2012). Fatigue, Stress and Coping in Mothers of Children with an Autism Spectrum Disorder. Journal of Autism and Developmental Disorders , 43 (7), 1547–1554.
Sher-Censor, E., Dan Ram-On, T., Rudstein-Sabbag, L., Watemberg, M., & Oppenheim, D. (2020). The reaction to diagnosis questionnaire: a preliminary validation of a new self-report measure to assess parents’ resolution of their child’s diagnosis. Attachment & Human Development, 22 (4), 409–424. https://doi.org/10.1080/14616734.2019.1628081 .
Sofronoff, K., Dark, E., & Stone, V. (2011). Social vulnerability and bullying in children with Asperger syndrome. Autism , 15 (3), 355–372.
Steiner, E. M., & Dahlquist, L. (2022). Intolerance of uncertainty and protective parenting: the mediating role of maternal appraisals and the moderating role of child health status. Children’s Health Care , 51 (3), 263–284. https://doi.org/10.1080/02739615.2021.2007771 .
Szarkowski, A., & Brice, P. J. (2016). Hearing Parents’ Appraisals of Parenting a Deaf or Hard-of-Hearing Child: Application of a Positive Psychology Framework. Journal of Deaf Studies and Deaf Education , 21 (3), 249–258.
Thomas, G. M. (2020). Dis-mantling stigma: Parenting disabled children in an age of “neoliberal-ableism. The Sociological Review , 69 (2), 451–467.
Thomasgard, M. (1998). Parental Perceptions of Child Vulnerability, Overprotection, and Parental Psychological Characteristics. Child Psychiatry and Human Development , 28 (4), 223–240.
Thomasgard, M., & Metz, W. P. (1997). Parental overprotection and its relation to perceived child vulnerability. American Journal of Orthopsychiatry , 67 (2), 330–335.
Tomaszewski, P. (2008). Interactions of Deaf Preschoolers: A Comparison of the Communicative Behaviors of Deaf Children of Deaf Parents and of Deaf Children of Hearing Parents. Psychology of Language and Communication , 12 , 2.
Toro, J., Kiverstein, J., & Rietveld, E. (2020). The Ecological-Enactive Model of Disability: Why Disability Does Not Entail Pathological Embodiment. Frontiers in Psychology , 11 , 1–15.
Trute, B., & Hiebert‐Murphy, D. (2005). Predicting family adjustment and parenting stress in childhood disability services using brief assessment tools. Journal of Intellectual & Developmental Disability , 30 (4), 217–225.
Woodman, A. C. (2014). Trajectories of Stress among Parents of Children with Disabilities: A Dyadic Analysis. Family Relations , 63 (1), 39–54.
Woodward, K. E., Boeldt, D. L., Corley, R. P., Dilalla, L., Friedman, N. P., Hewitt, J. K., & Rhee, S. H. (2018). Correlates of Positive Parenting Behaviors. Behavior Genetics , 48 (4), 283–297.
Zappella, E. (2015). Being a parent of a child with a disability in Italy: From diagnosis to starting school. Scandinavian Journal of Disability Research , 18 (3), 200–209.
Download references
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and affiliations.
School of Psychological Sciences, Centre for Emotional Health, Macquarie University, Sydney, NSW, 2109, Australia
Joshua Sealy, Catherine McMahon & Naomi Sweller
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Joshua Sealy .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Ethics approval
The study received ethics approval from the Human Research Ethics Committee (review reference no.5201951718200).
Informed consent
Informed consent was obtained from all individual participants included in the study. This included consent to both participate and have study data published provided they were made anonymised.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information 1, supplementary information 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Sealy, J., McMahon, C. & Sweller, N. Parenting Deaf Children: Exploring Relationships Between Resolution of Diagnosis, Parenting Styles and Morale, and Perceived Child Vulnerability. J Child Fam Stud 32 , 2761–2775 (2023). https://doi.org/10.1007/s10826-023-02579-z
Download citation
Received : 19 June 2021
Accepted : 11 April 2023
Published : 26 April 2023
Issue Date : September 2023
DOI : https://doi.org/10.1007/s10826-023-02579-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Sibling-Comparison
- Parent-Child Relationship
- Resolution of Diagnosis
- Vulnerability
- Find a journal
- Publish with us
- Track your research
- UNC Chapel Hill
Deaf-Blind Student Case Studies
As part of the project, case studies are being developed to support educational teams and families in their efforts to address the literacy and communication needs of individuals with severe disabilities, including deaf-blindness. The following case studies are currently available:

Vibrotactile stimulation: case study with a profoundly deaf child
- PMID: 3958992
This case study reports results obtained from a young, profoundly deaf child, M, who was fitted with a single-channel vibrotactile device, the Tactaid I, at 29 months of age. Her progress in speech and language development was evaluated over a 14-month period. During this period, M learned to understand 101 words through lipreading and the Tactaid I, and to produce consistent approximations of 90 words. Her scores on language tests with hearing-impaired norms progressed from below average to above average for her age. M's scores on language tests with hearing norms also reflected significant progress, although she did not achieve normal language development. These results indicate that a single-channel vibrotactile aid may facilitate the acquisition of spoken language in a profoundly deaf child who is unable to benefit from a conventional hearing aid.
Publication types
- Case Reports
- Comparative Study
- Research Support, U.S. Gov't, P.H.S.
- Child, Preschool
- Deafness / rehabilitation*
- Follow-Up Studies
- Patient Education as Topic / methods*
- Physical Stimulation*
- Reference Standards
- Sensory Aids*
- Speech Therapy
Grants and funding
- NSO3856/NS/NINDS NIH HHS/United States
- 11-17 Year Olds
- 17-30 Year Olds

Why does DEX exist?
Why does DEX do what it does? One of the many reasons are to do with individual experiences (called anecdotal experience ) that we have seen throughout our professional careers as Social Workers with Deaf people, Deaf Instructors, Deaf Youth Workers and Deaf Teachers of deaf children, working in the National Deaf Children’s Society, etc. DEX has also supported individual cases of deaf adults and deaf children. Here are just three of them:
Case Study A
A’s mother moved from Sri Lanka England recently. A is learning BSL and English and her mother uses English as a second language.
A’s mother contacted DEX as she is worried that her daughter, who is in Year 7, is not learning English quickly enough. A attends a specialist mainstream resource school. DEX asked the Local Authority to advocate for A’s mother at the Annual Review of the Statement of Educational Need meeting, but the council refused to pay for this service.
At the Annual Review meeting A’s mother was able to ask detailed questions about the quality of support that A receives via BSL, and what extra help she has with English.
Case Study B
B walked out of his local mainstream school (which is not resourced) in Year 11 because he was unable to follow the national curriculum even with a note-taker, and felt socially excluded. He had never had a friend throughout childhood. Fortunately he has a close and loving family, but they know this is insufficient, and asked DEX for help.
DEX counselled B and his family and supported him through a difficult year as B came to terms with the fact that he needed to continue his education. B later signed up for a class for unemployed young people whilst waiting to enrol for college the following academic year. Support was given to him to use public transport and to find his way to and from college as he had no experience of making the short trip into town.
B is said to have Asperger Syndrome in addition to being deaf. He reluctantly attended a group of deaf young people who made up DEX’s Deaf Youth Council, and enjoyed the social activity. However, the Council was a short term project, so he has had no other opportunity for supported assistance in making friends with deaf peers.
B is now at college and doing very well in his studies. He still continues to be socially isolated, and still never goes out of his home apart from to college or out with his family members.
Case Study C
C has Deaf parents and is part of an extensive Deaf family. She was having problems with bullying in her resourced mainstream school , mainly from the other deaf children.
DEX supported her at her Annual Review meeting and it was agreed as part of her Statement that it provided a range of services:
- Training for deaf children on what bullying is, the consequences of being bullied and how to deal with bullying
- Training for hearing children who were being bullied or were the perpetrators of bullying
- Training of teachers (mainstream and specialist) on dealing with bullying and harassment
- Support in writing a new school Bullying policy.
DEX received excellent testimonials for all aspects of the general bullying strategy.
In addition to supporting C’s family with bullying, DEX addressed the family’s concern about the low level of support she receives via BSL in school. The Communication Support Worker (CSW) had an NVQ Level 2 in BSL which is roughly equivalent to a GCSE. All professionals working in schools are expected to have at least one degree but this is not a national standard for CSWs.
It was agreed that CSW support would be provided at NVQ Level 3 in BSL, with progression to Level 4 (degree level). The CSW who was supporting C was initially sent on a Level 3 course which meant that C would not benefit from improved support for at least one academic year, impacting on her educational achievement. Subsequently the school stated that it would not be paying for the CSW to go on to Level 4 because it is considered that the CSW could leave due to better job prospects.
This is symptomatic of the national situation, which DEX wants to address by the introduction of a new post in education: that of BSL/English Educational Interpreters, with a minimum standard of NVQ Level 3 on entrance to the profession, and progression to a professional qualification of Member of the Registered Sign language Interpreter (MRSLI) through schools’ Continuing Professional Development (CPD).

- Privacy Overview
- Strictly Necessary Cookies
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
Deaf baby can hear after 'mind-blowing' gene therapy treatment
Seven months after her treatment, the baby girl can now respond to her parents' voices without the aid of a cochlear implant.

A toddler who was born completely deaf due to a rare genetic condition can now hear unaided thanks to a pioneering gene therapy .
Opal Sandy, who is now an 18-month-old girl from the U.K., is the youngest child in the world to receive this type of gene therapy, which uses a harmless, modified virus to correct genetic mutations in the body's cells. In this case, the therapy replaced a mutant gene associated with deafness with a working copy of that gene, according to a statement released May 9 by Cambridge University Hospitals.
Very similar gene therapies are being tested in other trials and have shown early success in treating slightly older children with the same type of hearing loss as Opal.
Known as auditory neuropathy , this type of hearing loss arises when the ears can detect sound but can't relay that information to the brain . The condition is caused by mutations in a gene called OTOF that normally makes otoferlin , a protein needed for the inner ear to talk to neurons that are linked to the brain. The condition accounts for between 1% and 8% of cases of congenital hearing loss that occurs in the absence of other symptoms.
Related: CRISPR can treat common form of inherited blindness, early data hint
Opal was diagnosed at 3 weeks old. When she was 11 months old she became the first patient treated in a global trial of the new gene therapy . She was given the new treatment via an injection into her right ear. The virus injected during the procedure — known as an adeno-associated virus — delivers a working copy of OTOF to cells in the ear to replace the mutated version. Afterwards, the virus is naturally eliminated from the body.
Doctors also installed a cochlear implant in Opal's left ear; these devices help users hear some sound by relaying signals to the brain that their ear cells can't.
Sign up for the Live Science daily newsletter now
Get the world’s most fascinating discoveries delivered straight to your inbox.
Within four weeks of the gene therapy, Opal could respond to sounds even when her cochlear implant was switched off, her doctors reported. Twenty-four weeks out from treatment, her treated ear could pick up soft sounds, such as whispering, at "close to normal" hearing levels. Now, at 18 months old, Sandy can respond to her parents' voices without her implant activated and say words such as "dada" and "bye-bye."

"When Opal could first hear us clapping unaided it was mind-blowing — we were so happy when the clinical team confirmed at 24 weeks that her hearing was also picking up softer sounds and speech," Opal's mother Jo said in the statement. Her father, James, noted that Opal can't wear her implant in certain contexts, such as in the bath, so the therapy is already making a difference in their day-to-day lives.
The ongoing trial that Opal is part of is enrolling patients in the U.S., the U.K. and Spain. In this stage of the research, patients receive a low dose of the therapy in one ear. Future trials will test the therapy at higher doses in one ear and then in both ears. Patients will be followed up for five years to assess long-term outcomes.
— The world's 1st CRISPR therapy has been approved. Here's everything you need to know
— 1st UK child to receive gene therapy for fatal genetic disorder is now 'happy and healthy'
— Gene-therapy drops restore teen's vision after genetic disease left his eyes clouded with scars
"Gene therapy has been the future of otology and audiology for many years and I'm so excited that it is now finally here," Dr. Manohar Bance , chief investigator of the trial and a professor of otology and skull base surgery at the University of Cambridge in the U.K., said in the statement.
"This is hopefully the start of a new era for gene therapies for the inner ear and many types of hearing loss," he said.
Ever wonder why some people build muscle more easily than others or why freckles come out in the sun ? Send us your questions about how the human body works to [email protected] with the subject line "Health Desk Q," and you may see your question answered on the website!
Emily is a health news writer based in London, United Kingdom. She holds a bachelor's degree in biology from Durham University and a master's degree in clinical and therapeutic neuroscience from Oxford University. She has worked in science communication, medical writing and as a local news reporter while undertaking journalism training. In 2018, she was named one of MHP Communications' 30 journalists to watch under 30. ( [email protected] )
The same genetic mutations behind gorillas' small penises may hinder fertility in men
'More Neanderthal than human': How your health may depend on DNA from our long-lost ancestors
Whooping cough outbreaks: Why is pertussis on the rise in several countries?
Most Popular
- 2 10 surprising things that are made from petroleum
- 3 Scientists just discovered an enormous lithium reservoir under Pennsylvania
- 4 Ancient Mycenaean armor is so good, it protected users in an 11-hour battle simulation inspired by the Trojan War
- 5 What's the highest place on Earth that humans live?
- 2 Things are finally looking up for the Voyager 1 interstellar spacecraft
- 3 32 optical illusions and why they trick your brain
- 4 Neanderthals could talk — but how sophisticated was their language?
- 5 32 fun and random facts about Albert Einstein
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 29 May 2024
A case–control study on pre-, peri-, and neonatal risk factors associated with autism spectrum disorder among Armenian children
- Meri Mkhitaryan 1 ,
- Tamara Avetisyan 2 , 3 ,
- Anna Mkhoyan 4 ,
- Larisa Avetisyan 2 , 5 &
- Konstantin Yenkoyan 1
Scientific Reports volume 14 , Article number: 12308 ( 2024 ) Cite this article
Metrics details
- Autism spectrum disorders
- Public health
- Risk factors
We aimed to investigate the role of pre-, peri- and neonatal risk factors in the development of autism spectrum disorder (ASD) among Armenian children with the goal of detecting and addressing modifiable risk factors to reduce ASD incidence. For this purpose a retrospective case–control study using a random proportional sample of Armenian children with ASD to assess associations between various factors and ASD was conducted. The study was approved by the local ethical committee, and parental written consent was obtained. A total of 168 children with ASD and 329 controls were included in the analysis. Multivariable logistic regression analysis revealed that male gender, maternal weight gain, use of MgB6, self-reported stress during the pregnancy, pregnancy with complications, as well as use of labor-inducing drugs were associated with a significant increase in the odds of ASD, whereas Duphaston use during pregnancy, the longer interpregnancy interval and birth height were associated with decreased odds of ASD. These findings are pertinent as many identified factors may be preventable or modifiable, underscoring the importance of timely and appropriate public health strategies aimed at disease prevention in pregnant women to reduce ASD incidence.
Introduction
Autism spectrum disorder is a neurodevelopmental disorder by the Diagnostic and Statistical Manual of Mental Disorders, the 5th Edition (DSM-5). It is identified by limited repeating patterns of behavior, activities, and interests, as well as impaired social interaction and communication 1 . A systematic review of research articles spanning from 2012 to 2021 indicates that the worldwide median prevalence of ASD in children stands at 1% 2 . Nevertheless, this reported percentage may not fully capture the actual prevalence of ASD in low- and middle-income nations, potentially leading to underestimations. In 2016, data compiled by the CDC's Autism and Developmental Disabilities Monitoring (ADDM) Network revealed that approximately one out of 54 children in the United States (one out of 34 boys and one out of 144 girls) received a diagnosis of ASD. This marks a ten percent increase from the reported rate of one out of 59 in 2014, a 105 percent increase from one out of 110 in 2006, and a 176 percent increase from one out of 150 in 2000 3 . According to the most recent update from the CDC’s ADDM Network, one out of 36 (2.8%) 8-year-old children has been diagnosed with ASD. These latest statistics exceed the 2018 findings, which indicated a rate of 1 in 44 (2.3%) 4 . To our understanding, there is no existing registry for ASD in the Republic of Armenia (RA). Additionally, there is no available data concerning the incidence and prevalence of ASD in the country.
The etiology of ASD remains unclear despite substantial research on the disorder; yet, important advances have been made in identifying some of the disorder's genetic and neurobiological underpinnings. It has been discovered that ASD is heritable, with environmental variables also being involved 5 , 6 , 7 . According to certain research, ASD is associated with both hereditary and environmental factors 5 , 8 , 9 . It is especially important to identify environmental risk factors because, unlike genetic risk factors, they can be prevented.
There are more than 20 pre-, peri- and neonatal risk factors associated with ASD 10 , 11 , 12 . Prenatal risk factors that have been associated with ASD involve parental age 13 , interpregnancy interval 14 , 15 , immune factors (such as autoimmune diseases, both viral and bacterial infections during pregnancy) 16 , 17 , medication use (especially antidepressants, anti-asthmatics, and anti-epileptics) 18 , 19 , 20 , maternal metabolic conditions (such as diabetes, gestational weight gain, and hypertension) 21 , 22 , 23 , and maternal dietary factors (such as folic acid and other supplement use, maternal iron (Fe) intake, as well as maternal vitamin D levels) 24 , 25 , 26 , 27 , 28 , 29 .
Numerous studies indicate that an increased risk of ASD is linked to several perinatal and neonatal factors. These factors include small gestational age or preterm birth, gestational small or large size, the use of labor and delivery drugs 30 , 31 , 32 , 33 . The risk of ASD associated with cesarean delivery is also a subject of continuous discussion 34 , 35 , 36 . Overall, there is no apparent link between assisted conception and a notably higher risk of ASD, however some particular therapies might make ASD more likely.
This study aimed to determine main pre-, peri- and neonatal risk factors linked to ASD among Armenian children. The following research questions were derived to address the objectives of the study:
What are the primary prenatal risk factors associated with the development of ASD among Armenian children?
How do perinatal factors such as maternal complications during childbirth, labor mode, labor interventions, use of labor-inducing drugs, contribute to the risk of ASD in Armenian children?
What neonatal factors, such as birth weight and gestational age, are linked to the likelihood of ASD diagnosis among Armenian children?
How do socio-demographic factors, such as parental education, gender of the child, number of kids in the family, sequence of the kid, influence the relationship between pre-, peri-, and neonatal risk factors and risk of ASD among Armenian children?
To the best of our knowledge, this was the first study of its kind conducted in Armenia that focused on a variety of factors linked to ASD.
The analysis encompassed a total sample of 497 participants, consisting of 168 children diagnosed with ASD and 329 children without ASD. The descriptive analysis revealed significant differences between the cases and controls on several socio demographic variables as well as prenatal, peri- and neonatal risk factors (see Tables 1 , 2 , 3 and 4 ).
The summary of socio demographic characteristics (Table 1 ). Among the cases (the ASD group), the distribution of gender of the child was significantly different to that in the control group. More specifically, while the distribution of male and female were balanced in the control group (52.89% and 47.11% respectively), the proportion of male children was significantly higher in the ASD group (82.14% and 17.86% respectively, p < 0.01). Furthermore, the number of children in the families of cases and controls were slightly different. While the proportion of cases and controls who had two children were similar, families with one child were slightly higher in the ASD group compared to the control group (29.94% and 17.02% respectively, p < 0.01). This picture is reversed with respect to the number of families with more than two children (16.17% and 29.79% respectively). A higher percentage of ASD cases are the first child in the family compared to controls (67.86% vs. 49.54%, p < 0.01). The proportion of non-married families (those that reported to be single, widowed, divorced etc.) were higher in the ASD group compared to the control group (10.24% and 4.28% respectively, p < 0.05). The distribution of the level of educational attainment of the parents were also different between the groups. More specifically, the prevalence of university degree among the cases were somewhat lower compared to that in the control group.
The summary of prenatal risk factors (Table 2 ). With respect to prenatal risk factors, there were significant differences between the cases and controls in interpregnancy intervals, self-reported complications and diseases, medication use, vitamin D levels, maternal weight gain, and the self-reported stress during pregnancy. More specifically, the cases had on average lower interpregnancy intervals compared to the controls (M = 12.9 and M = 23.7 months respectively, p < 0.01). The cases more frequently reported to have had complications during the pregnancy compared to the controls (42.86% and 8.54% respectively, p < 0.01). The prevalence of reported infectious diseases, other diseases and anemia during the pregnancy were also somewhat higher among the cases compared to the control group. The use of medications was higher among the cases compared to the control group (41.67% and 17.74% respectively, p < 0.01). Various medications including vitamins, anticoagulants, Paracetamol, MgB6, Duphaston, iron preparation, No-spa, calcium preparation, antibiotics, and Utrogestan showed significant differences in usage between cases and controls (all p < 0.05) (Table 3 ). The maternal weight gain among the cases was on average higher among the cases compared to the control group (M = 15.4 and M = 13.9 kg respectively, p < 0.05). The self-reported stress was also more frequent among the cases compared to the controls (56.02 and 10.98% respectively, p < 0.01). Specifically, comparing data on self-reported stress during different pregnancy periods, it was obvious that 47.06% of mothers of cases and 91.25% of mothers in the control group reported no stress experienced during pregnancy. During the first trimester, 14.38% of mothers with cases of autism reported stress, whereas only 0.94% of mothers in the control group reported stress. In the second trimester, 11.11% of mothers with cases of autism reported stress, compared to 4.06% of mothers in the control group. During the third trimester, 8.50% of mothers with cases of autism reported stress, while 1.88% of mothers in the control group reported stress. Across the entire pregnancy, 18.95% of mothers with cases of autism reported stress, compared to 1.88% of mothers in the control group. The differences in stress levels between the two groups were statistically significant, indicating a potential link between maternal stress during pregnancy and the odds of autism spectrum disorder in offspring.
The summary of perinatal and neonatal risk factors (Table 4 ). The interpretation of the data comparing various peri- and neonatal risk factors between cases (individuals with ASD) and controls (individuals without ASD) are shown below. 83.33% of cases and 91.77% of controls were born within 37–42 weeks of gestation, with a statistically significant difference ( p < 0.05), whereas 16.67% of cases and 8.23% of controls were born either preterm (before 37 weeks) or post-term (after 42 weeks), also showing a significant difference. There was no statistically significant difference in birth weight between cases and controls (M = 3137.8 and M = 3176.9 g respectively, p > 0.05). The mean birth height was slightly lower for cases compared to controls (M = 50.4 and M = 50.9 cm), with a statistically significant difference ( p < 0.05). No statistically significant difference was reported regarding mode of labor. According to the data interventions during labor were reported more in ASD group compared to controls (39.76% and 17.23% respectively, p < 0.01). Also, labor-inducing drugs were administered more in cases compared to the controls (39.76% and 21.04%, p < 0.01).
The results of multivariable logistic regression
The multivariable logistic regression analysis indicated significant associations between sociodemographic, prenatal, perinatal and neonatal risk factors. More specifically, male children have 4 times higher odds of having ASD compared to female children (OR = 4.21, CI 2.33–7.63). Among prenatal factors, the maternal weight gain, use of MgB6, the self-reported stress during the pregnancy, as well as pregnancy with complications were associated with a significant increase in the odds of ASD, whereas use of Duphaston was associated with decreased odds of ASD (see Table 5 ). Additionally, the longer interpregnancy interval was associated with decreased odds of ASD diagnosis (OR = 0.708, CI 0.52–0.97). Among peri- and neonatal factors, use of labor-inducing drugs was associated with increase in the odds of ASD diagnosis (OR = 2.295, CI 1.3–4.1), while birth height showed association with decrease in odds (OR = 0.788, CI 0.6–1.0).
Our study provides comprehensive insights into the multifaceted nature of ASD, elucidating the intricate relationships between sociodemographic, prenatal, perinatal, and neonatal factors and ASD risk.
Our findings highlight significant gender disparities in ASD prevalence, with a notably higher proportion (4:1) of male children in the ASD group. This aligns with existing literature demonstrating a male predominance in ASD diagnosis 37 . Meanwhile, Loomes et al. reported 3:1 male-to-female ratio referring to a diagnostic gender bias, where girls meeting the criteria for ASD are at an elevated risk of not receiving a clinical diagnosis 38 . Furthermore, our study highlights the potential impact of family structure on the likelihood of ASD occurrence, indicating higher ASD rates among first-born children and in households where the parents are non-married (divorced, widowed, separated, etc.). A study conducted by Ugur et al. yielded comparable findings, suggesting that the prevalence of being the eldest child was higher in the ASD group compared to the control group 39 . Contrary to this, research conducted in the United States found no evidence to suggest that children diagnosed with ASD are more likely to live in households not composed of both their biological or adoptive parents compared to children without ASD 40 .
The association between prenatal risk factors and ASD risk underscores the importance of maternal health during pregnancy. Our findings suggest that factors such as lower IPIs, maternal complications and diseases during pregnancy, medication use, vitamin D levels, maternal weight gain and maternal self-reported stress during pregnancy may increase the odds of ASD in offspring. It is crucial to note that the higher number of firstborn children among cases compared to the control group could introduce bias when accurately estimating the association between IPI and ASD. Therefore, the coefficients of IPI should be interpreted cautiously. Despite this, we opted not to remove this variable from the model, as IPI is recognized as an important factor in existing literature. Several studies report different results regarding long and short IPIs and ASD risk 14 , 15 , 41 , 42 . The underlying reasons for the link between ASD and short and long IPIs may differ. Short IPIs could be associated with maternal nutrient depletion, stress, infertility, and inflammation, whereas long IPIs may be linked to infertility and related complications. According to our results the frequency of self-reported complications during pregnancy was notably higher among children with ASD compared to the controls. Additionally, there was a somewhat higher prevalence of reported infectious diseases, other illnesses, and anemia during pregnancy among the cases compared to the control group. Several previous investigations have associated maternal hospitalization resulting from infection during pregnancy with an elevated risk of ASD. This includes a substantial study involving over two million individuals, which indicated an increased risk associated with viral and bacterial infections during the prenatal period 12 , 17 . Furthermore, our study results indicate that medication usage during pregnancy was more common among the mothers of cases than the controls. Notably, various medications, including vitamins, anticoagulants, Paracetamol, MgB6, Duphaston, iron preparation, No-spa, calcium preparation, antibiotics, and Utrogestan (micronized progesterone), exhibited significant differences in usage between the cases and controls. According to the results of multiple logistic regression analysis use of MgB6 was associated with a significant increase in the odds of ASD, whereas use of Duphaston (Dydrogesterone), a progestin medication, was associated with decreased odds of ASD. Emphasizing the potential impact of additional variables in evaluating the link between Duphaston and ASD is essential. There is a possibility of factors overlooked in our study. However, after analyzing the included variables, no significant confounding effects were detected. This assessment involved scrutinizing the Cramer’s V value between Duphaston and other variables, and sequentially introducing new variables into the model to evaluate changes in the coefficients of Duphaston. In both cases, no significant confounding effects emerged. In contrast to our results certain researchers have shown that the use of supplements during pregnancy is linked to a decreased risk of ASD in offsprings compared to those whose mothers did not take supplements during pregnancy 43 , 44 . The results of an epidemiology study conducted by Li et al. have showed that prenatal progestin exposure was strongly associated with ASD prevalence, and the experiments in rats showed that prenatal consumption of progestin-contaminated seafood induced autism-like behavior 45 . On the other hand other authors suggest that insufficient maternal progesterone levels might contribute to both obstetrical complications and ASD development 46 . The observed association regarding MgB6 use could potentially be influenced by an unmeasured confounding variable in our study. This warrants further investigation and consideration in future research. Additionally, our study highlighted another modifiable risk factor for ASD that was significantly associated with higher odds of ASD: maternal gestational weight gain. This factor retained its significance even in the multivariable analysis. This finding is consistent with the results of several studies which have shown that maternal metabolic conditions like diabetes, gestational weight gain, and hypertension have been associated with mechanisms pertinent to ASD, such as oxidative stress, fetal hypoxia, and chronic inflammation 23 , 47 . These conditions can induce prolonged or acute hypoxia in the fetus, which might pose a substantial risk factor for neurodevelopmental disturbances.
Furthermore, our findings suggest that the self-reported stress during pregnancy was associated with a significant increase in the odds of ASD. When comparing self-reported stress levels during different pregnancy periods, a notable disparity emerged. The statistically significant differences in stress levels between the two groups were reported in all trimesters of pregnancy suggesting a potential correlation between maternal stress during pregnancy and the odds of autism spectrum disorder in offspring. Several authors report comparable findings suggesting that prenatal maternal stress show significant association with both autistic traits and Attention Deficit Hyperactivity Disorder (ADHD) behaviors 48 , 49 , 50 , 51 . Various mechanisms could be suggested to explain the link between prenatal stress and likelihood of ASD. For instance, stress during pregnancy can trigger physiological changes in the mother's body, such as increased cortisol levels and alterations in immune function, which may impact fetal development and contribute to the risk of ASD. Also, stress may affect placental function, leading to adverse changes in the transfer of nutrients and oxygen to the fetus. Furthermore, prenatal stress can influence gene expression in both the mother and the developing fetus. Certain genes involved in brain development and the stress response system may be affected, potentially increasing the risk of ASD. Additionally, maternal stress may influence parenting behaviors and interactions with the child after birth. High levels of maternal stress may affect the quality of caregiving, which in turn can impact the child's social and emotional development, potentially contributing to ASD risk. Lastly, stress during pregnancy could induce epigenetic modifications, which are alterations in gene expression that occur without changes in DNA sequence. These modifications might affect neurodevelopmental processes, making individuals more susceptible to ASD.
Our study reports notable statistical difference among cases and controls regarding gestational age. According to the results 16.67% of cases were born either preterm (before 37 weeks) or post-term (after 42 weeks), highlighting another significant distinction. Early gestational age is linked with unfavorable health consequences, such as developmental delays and subsequent intellectual impairments throughout childhood and adolescence. Similar results are reported by several authors as well 30 , 31 , 52 . According to our study results birth height was associated with decrease in odds of ASD, however there was no statistically significant difference in birth weight between cases and controls. Some authors demonstrated that infants with birth weights of < 2.5 kg were associated with ADHD and ASD 53 , 54 .
Other than the previously mentioned factors the results of our study have demonstrated that use of labor-inducing drugs was associated with increase in the odds of ASD. The study participants did not report or specify the type of used labor-inducing drugs. Recent investigations have indicated a potential correlation between the utilization of drugs during labor and delivery and the emergence of ASD 55 , 56 , especially given the increased usage of epidurals and labor-inducing medications in the past 30 years. However, conflicting findings exist, with some studies suggesting no link between the administration of labor-inducing drugs and the risk of ASD development 57 , 58 . Recent findings from Qiu et al. propose a potential link between maternal labor epidural analgesia and the risk of ASD in children, particularly when oxytocin was concurrently administered. However, oxytocin exposure in the absence of labor epidural analgesia did not show an association with ASD risk in children 59 . The potential link between the use of labor-inducing drugs and the risk of ASD is complex and not yet fully understood. However, several mechanisms have been proposed to explain this association: for example, labor-inducing drugs, such as oxytocin and prostaglandins, can affect hormonal levels in both the mother and the fetus. These hormonal changes may impact brain development and neural connectivity, potentially increasing the risk of ASD. In addition, labor induction may increase the risk of oxygen deprivation (hypoxia) during labor. Prolonged hypoxia during birth has been linked to adverse neurological outcomes, including an increased risk of neurodevelopmental disorders like ASD. Furthermore, labor induction can lead to an inflammatory response in both the mother and the fetus. This immune system activation may affect neurodevelopmental processes and contribute to the development of ASD. Overall, the relationship between labor-inducing drugs and ASD risk is multifactorial and likely involves interactions between genetic, environmental, and biological factors. Further research is needed to elucidate the specific mechanisms underlying this association.
To our knowledge this is the first study identifying potential pre-, peri- and neonatal risk factors associated with ASD in Armenia.
Limitations and strength
While our study possesses a retrospective design, a notable limitation, it depended on parental recall for details dating back several years. Additionally, the sample was not balanced in terms of gender, with more male children included, potentially introducing selection bias. Despite the relatively small sample size multivariable analysis using the presence or absence of ASD as the dependent variable was implemented to address potential confounding factors.
Nevertheless, our study included a representative sample of the Armenian ASD population, evaluating various factors in comparison with a randomly selected control group matched for age. All ASD diagnoses were made according to DSM-5 by professionals (psychiatrists, pediatricians, neurologists, speech therapists and developmental psychologists), and face-to-face interviews with parents at the time of the interview minimized the risk of information bias.
Our findings indicated that male gender, maternal weight gain, MgB6 usage, self-reported stress during pregnancy, pregnancy complications, and labor-inducing drugs were linked to a significant rise in ASD odds (Fig. 1 ). Conversely, the use of Duphaston during pregnancy, longer interpregnancy intervals, and higher birth height were associated with reduced odds of ASD (Fig. 1 ). These observations underpin the significance of regional investigations to uncover the unique environmental factors contributing to ASD. The implications are profound, as several identified factors may be preventable or adjustable, highlighting the urgency of implementing evidence-based practices and public health interventions. Emphasizing a culture of health promotion, screenings, timely diagnosis, and disease prevention strategies, particularly among pregnant women, holds promise for reducing ASD and related disorders. Moreover, further prospective and focused research is imperative to discern the interplay between various factors and gene-environment interactions that may serve as potential ASD risk factors. Enhanced understanding in this area could lead to earlier detection and improved ASD management. Future studies incorporating analyses of biological samples for genetic, epigenetic, and inflammatory markers will be pivotal in elucidating underlying mechanisms and ushering in a new phase of research focusing on modifiable risk factors for developmental disorders.
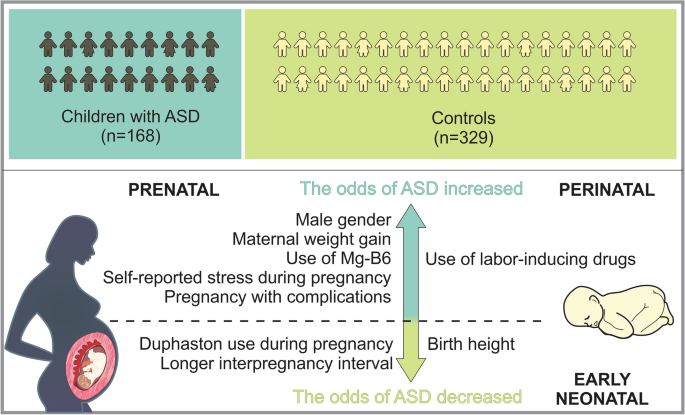
Sum up scheme showing prenatal, perinatal and neonatal factors which increase, as well as decrease the odds of ASD.
The study population comprised of 497 participants, of which 168 were children with ASD and 329 were typical development controls. The subject recruitment was done during 2021 to 2022. The controls and children with ASD were age matched (3–18 years). The subjects were formally diagnosed with ASD according to DSM-5 by professionals (pediatricians, neurologists, speech therapists and developmental psychologists). The children with ASD were recruited at MY WAY Educational and Rehabilitation Center in Yerevan. Inclusion criteria for cases were age between 3 and 18 years with ASD with diagnosis confirmed using DSM-V. Exclusion criteria for cases were other neurodevelopment disorders other than ASD. The control participants were randomly selected in the same period at Muratsan Hospital Complex. They were not known to have any neurodevelopmental or behavioral disruptions that might be related to ASD. The control group consisted exclusively of individuals diagnosed with simple conditions like flu or a simple routine physical examination.
Questionnaire and data collection
The self-reported questionnaire was completed via a face-to-face interview with the child’s parent. The questionnaire comprised three sections: various aspects of sociodemographic characteristics, prenatal risk factors, and perinatal/neonatal risk factors. Each section addressed specific questions related to these factors for comprehensive data collection. On average, the questionnaire was completed in about 15 to 20 min. The parent had the choice of accepting or refusing to complete the questionnaire. At the end of the process, the completed questionnaires were collected and sent for data entry by using SPSS 21 statistical software. The questionnaire was designed to acquire the information regarding risk factors of ASD. It consisted of different sections: sociodemographic characteristics (e.g., age, sex, family history of ASD, etc.), data on prenatal risk factors (e.g., pregnancy process, complications during pregnancy, infections during pregnancy, other diseases, stress, medication and supplement use during pregnancy, vitamin D level, etc.), questions related to maternal lifestyle risk factors (e.g., smoking, alcohol consumption, gestational weight gain). Respondents were also asked about peri- and neonatal risk factors, including gestational age, gestational size, the use of labor and delivery drugs, mode of delivery, etc.
Ethics disclosure
The study protocol was approved by the Ethics Committee (N 8–2/20; 27.11.2020) of Yerevan State Medical University in line with the principles set forth in the Declaration of Helsinki. Written informed consent was obtained from all the parents of the participants prior to data collection.
Statistical analysis
The data was processed and modelled in Python (version 3.11.6), an open- source software often used for data processing and modelling. The statistical analysis was performed by using the Statsmodels package (version 0.14.1) 60 .
Descriptive statistics were employed to summarize the characteristics of the study variables. Continuous variables were described using means and standard deviations, while categorical variables were presented as proportions. Prior to statistical analysis, numeric variables underwent standardization through the computation of z scores. To evaluate potential multicollinearity among predictor variables, the Variable Inflation Index (VIF) was computed. A predetermined threshold of 5 was established, and variables exceeding this threshold were considered indicative of multicollinearity. Bivariate analyses were conducted to explore associations between predictor variables and the outcome variable (presence or absence of autism diagnosis). T-tests were employed for continuous variables, while chi-squared tests were utilized for nominal and categorical variables. A multivariable logistic regression model was constructed to estimate the relationship between predictor variables and the outcome variable (autism diagnosis). Initially, a comprehensive strategy was employed by first fitting a null model and then iteratively introducing blocks of variables (e.g., socio demographic factors prenatal, peri- and neonatal factors). After introducing the new block of factors, a likelihood ratio test was conducted to evaluate the contribution of the added variables. If the p -value associated with the likelihood ratio test was insignificant ( p > 0.05), the preference was given to a less complex model. In our analysis all added blocks had significant contribution to the overall fit of the model.
Subsequently, the significance of each variable was systematically assessed by applying a stepwise elimination technique whereby insignificant variables were progressively removed from the model. Similar to the above-mentioned process, at each step, a likelihood ratio test to evaluate the significance of the excluded variable was conducted. If the p -value associated with this test was found to be insignificant ( p > 0.05), the adoption of a simpler model was favored. This iterative process allowed us to identify the most parsimonious model that retained statistically significant predictors while minimizing unnecessary complexity. Odds ratios (ORs) were computed, accompanied by 95% confidence intervals (CIs), to quantify the strength and direction of these associations.
Data availability
Data can be made available by the corresponding author upon reasonable request.
Diagnostic and Statistical Manual of Mental Disorders: DSM-5 TM , 5th Ed . xliv, 947 (American Psychiatric Publishing, Inc., Arlington, VA, US, 2013). https://doi.org/10.1176/appi.books.9780890425596 .
Zeidan, J. et al. Global prevalence of autism: A systematic review update. Autism Res. 15 , 778–790 (2022).
Article PubMed PubMed Central Google Scholar
CDC. Autism and Developmental Disabilities Monitoring (ADDM) Network. Centers for Disease Control and Prevention https://www.cdc.gov/ncbddd/autism/addm.html (2023).
CDC. Data and Statistics on Autism Spectrum Disorder | CDC. Centers for Disease Control and Prevention https://www.cdc.gov/ncbddd/autism/data.html (2024).
Tick, B., Bolton, P., Happé, F., Rutter, M. & Rijsdijk, F. Heritability of autism spectrum disorders: A meta-analysis of twin studies. J. Child Psychol. Psychiatry 57 , 585–595 (2016).
Article PubMed Google Scholar
Lord, C., Elsabbagh, M., Baird, G. & Veenstra-Vanderweele, J. Autism spectrum disorder. Lancet 392 , 508–520 (2018).
Muhle, R. A., Reed, H. E., Stratigos, K. A. & Veenstra-VanderWeele, J. The emerging clinical neuroscience of autism spectrum disorder: A review. JAMA Psychiatry 75 , 514–523 (2018).
Bai, D. et al. Association of genetic and environmental factors with autism in a 5-country cohort. JAMA Psychiatry 76 , 1035–1043 (2019).
Jutla, A., Reed, H. & Veenstra-VanderWeele, J. The architecture of autism spectrum disorder risk: What do we know, and where do we go from here?. JAMA Psychiatry 76 , 1005–1006 (2019).
Gardener, H., Spiegelman, D. & Buka, S. L. Perinatal and neonatal risk factors for autism: A comprehensive meta-analysis. Pediatrics 128 , 344–355 (2011).
Guinchat, V. et al. Pre-, peri- and neonatal risk factors for autism. Acta Obstet. Gynecol. Scand. 91 , 287–300 (2012).
Yenkoyan, K., Mkhitaryan, M. & Bjørklund, G. Environmental risk factors in autism spectrum disorder: A narrative review. Curr. Med. Chem. https://doi.org/10.2174/0109298673252471231121045529 (2024).
Lyall, K. et al. The association between parental age and autism-related outcomes in children at high familial risk for autism. Autism. Res. 13 , 998–1010 (2020).
Cheslack-Postava, K. et al. Increased risk of autism spectrum disorders at short and long interpregnancy intervals in Finland. J. Am. Acad. Child Adolesc. Psychiatry 53 , 1074-1081.e4 (2014).
Zerbo, O., Yoshida, C., Gunderson, E. P., Dorward, K. & Croen, L. A. Interpregnancy interval and risk of autism spectrum disorders. Pediatrics 136 , 651–657 (2015).
Lee, B. K. et al. Maternal hospitalization with infection during pregnancy and risk of autism spectrum disorders. Brain Behav. Immun. 44 , 100–105 (2015).
Zerbo, O. et al. Maternal infection during pregnancy and autism spectrum disorders. J. Autism Dev. Disord. 45 , 4015–4025 (2015).
Christensen, J. et al. Prenatal valproate exposure and risk of autism spectrum disorders and childhood autism. JAMA 309 , 1696–1703 (2013).
Article CAS PubMed PubMed Central Google Scholar
Bromley, R. L. et al. The prevalence of neurodevelopmental disorders in children prenatally exposed to antiepileptic drugs. J. Neurol. Neurosurg. Psychiatry 84 , 637–643 (2013).
Gidaya, N. B. et al. In utero exposure to β-2-adrenergic receptor agonist drugs and risk for autism spectrum disorders. Pediatrics 137 , e20151316 (2016).
Walker, C. K. et al. Preeclampsia, placental insufficiency, and autism spectrum disorder or developmental delay. JAMA Pediatr 169 , 154–162 (2015).
Krakowiak, P. et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics 129 , e1121-1128 (2012).
Li, M. et al. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics 137 , e20152206 (2016).
Black, M. M. Effects of vitamin B12 and folate deficiency on brain development in children. Food Nutr. Bull. 29 , S126-131 (2008).
Surén, P. et al. Association between maternal use of folic acid supplements and risk of autism spectrum disorders in children. JAMA 309 , 570–577 (2013).
Skalny, A. V. et al. Magnesium status in children with attention-deficit/hyperactivity disorder and/or autism spectrum disorder. Soa Chongsonyon Chongsin Uihak 31 , 41–45 (2020).
PubMed PubMed Central Google Scholar
Virk, J. et al. Preconceptional and prenatal supplementary folic acid and multivitamin intake and autism spectrum disorders. Autism 20 , 710–718 (2016).
Whitehouse, A. J. O. et al. Maternal vitamin D levels and the autism phenotype among offspring. J. Autism Dev. Disord. 43 , 1495–1504 (2013).
Zhong, C., Tessing, J., Lee, B. & Lyall, K. Maternal dietary factors and the risk of autism spectrum disorders: A systematic review of existing evidence. Autism Res. 13 , 1634–1658 (2020).
Moore, G. S., Kneitel, A. W., Walker, C. K., Gilbert, W. M. & Xing, G. Autism risk in small- and large-for-gestational-age infants. Am. J. Obstet. Gynecol. 206 (314), e1-9 (2012).
Google Scholar
Leavey, A., Zwaigenbaum, L., Heavner, K. & Burstyn, I. Gestational age at birth and risk of autism spectrum disorders in Alberta, Canada. J. Pediatr. 162 , 361–368 (2013).
Smallwood, M. et al. Increased risk of autism development in children whose mothers experienced birth complications or received labor and delivery drugs. ASN Neuro. 8 , 1759091416659742 (2016).
Qiu, C. et al. Association between epidural analgesia during labor and risk of autism spectrum disorders in offspring. JAMA Pediatr. 174 , 1168–1175 (2020).
Curran, E. A. et al. Association between obstetric mode of delivery and autism spectrum disorder: A population-based sibling design study. JAMA Psychiatry 72 , 935–942 (2015).
Curran, E. A. et al. Research review: Birth by caesarean section and development of autism spectrum disorder and attention-deficit/hyperactivity disorder: A systematic review and meta-analysis. J. Child Psychol. Psychiatry 56 , 500–508 (2015).
Nagano, M. et al. Cesarean section delivery is a risk factor of autism-related behaviors in mice. Sci. Rep. 11 , 8883 (2021).
Article ADS CAS PubMed PubMed Central Google Scholar
Werling, D. M. & Geschwind, D. H. Sex differences in autism spectrum disorders. Curr. Opin. Neurol. 26 , 146–153 (2013).
Loomes, R., Hull, L. & Mandy, W. P. L. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 56 , 466–474 (2017).
Ugur, C., Tonyali, A., Goker, Z. & Uneri, O. S. Birth order and reproductive stoppage in families of children with autism spectrum disorder. Psychiatry Clin. Psychopharmacol. 29 , 509–514 (2019).
Article Google Scholar
Freedman, B. H., Kalb, L. G., Zablotsky, B. & Stuart, E. A. Relationship status among parents of children with autism spectrum disorders: A population-based study. J. Autism. Dev. Disord. 42 , 539–548 (2012).
Gunnes, N. et al. Interpregnancy interval and risk of autistic disorder. Epidemiology 24 , 906–912 (2013).
Durkin, M. S., Allerton, L. & Maenner, M. J. Inter-pregnancy intervals and the risk of autism spectrum disorder: Results of a population-based study. J. Autism. Dev. Disord. 45 , 2056–2066 (2015).
Levine, S. Z. et al. Association of maternal use of folic acid and multivitamin supplements in the periods before and during pregnancy with the risk of autism spectrum disorder in offspring. JAMA Psychiatry 75 , 176–184 (2018).
Article ADS PubMed PubMed Central Google Scholar
Schmidt, R. J., Iosif, A.-M., Guerrero Angel, E. & Ozonoff, S. Association of maternal prenatal vitamin use with risk for autism spectrum disorder recurrence in young siblings. JAMA Psychiatry 76 , 391–398 (2019).
Li, L. et al. Prenatal progestin exposure is associated with autism spectrum disorders. Front Psychiatry 9 , 611 (2018).
Whitaker-Azmitia, P. M., Lobel, M. & Moyer, A. Low maternal progesterone may contribute to both obstetrical complications and autism. Med Hypotheses 82 , 313–318 (2014).
Article CAS PubMed Google Scholar
Vecchione, R. et al. Maternal dietary patterns during pregnancy and child autism-related traits: Results from two US cohorts. Nutrients 14 , 2729 (2022).
Ronald, A., Pennell, C. & Whitehouse, A. Prenatal maternal stress associated with ADHD and autistic traits in early childhood. Front. Psychol. https://doi.org/10.3389/fpsyg.2010.00223 (2011).
Caparros-Gonzalez, R. A. et al. Stress during pregnancy and the development of diseases in the offspring: A systematic-review and meta-analysis. Midwifery 97 , 102939 (2021).
Manzari, N., Matvienko-Sikar, K., Baldoni, F., O’Keeffe, G. W. & Khashan, A. S. Prenatal maternal stress and risk of neurodevelopmental disorders in the offspring: A systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 54 , 1299–1309 (2019).
Say, G. N., Karabekiroğlu, K., Babadağı, Z. & Yüce, M. Maternal stress and perinatal features in autism and attention deficit/hyperactivity disorder. Pediatr. Int. 58 , 265–269 (2016).
Abel, K. M. et al. Deviance in fetal growth and risk of autism spectrum disorder. Am. J. Psychiatry 170 , 391–398 (2013).
Song, I. G. et al. Association between birth weight and neurodevelopmental disorders assessed using the Korean National Health Insurance Service claims data. Sci. Rep. 12 , 2080 (2022).
Lampi, K. M. et al. Risk of autism spectrum disorders in low birth weight and small for gestational age infants. J. Pediatr. 161 , 830–836 (2012).
Bashirian, S., Seyedi, M., Razjouyan, K. & Jenabi, E. The association between labor induction and autism spectrum disorders among children: A meta-analysis. Curr. Pediatr. Rev. 17 , 238–243 (2021).
Oberg, A. S. et al. Association of labor induction with offspring risk of autism spectrum disorders. JAMA Pediatr. 170 , e160965 (2016).
Karim, J. L. et al. Exogenous oxytocin administration during labor and autism spectrum disorder. Am. J. Obstet. Gynecol. MFM 5 , 101010 (2023).
Qiu, C. et al. Association of labor epidural analgesia, oxytocin exposure, and risk of autism spectrum disorders in children. JAMA Netw. Open 6 , e2324630 (2023).
Seabold, S. & Perktold, J. Statsmodels: Econometric and Statistical Modeling with Python. Proceedings of the 9th Python in Science Conference 92–96 (2010) https://doi.org/10.25080/Majora-92bf1922-011 .
Download references
Acknowledgements
We express our gratitude to all parents participated in the study.
This work was supported by Higher Education and Science Committee, Ministry of Education, Science, Culture and Sports of RA (24YSMU-CON-I-3AN and 23LCG-3A020), and YSMU.
Author information
Authors and affiliations.
Neuroscience Laboratory, Cobrain Center, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Meri Mkhitaryan & Konstantin Yenkoyan
Cobrain Center, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Tamara Avetisyan & Larisa Avetisyan
Muratsan University Hospital Complex, Yerevan State Medical University Named After M. Heratsi, 0075, Yerevan, Armenia
Tamara Avetisyan
Department of Infectious Diseases, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Anna Mkhoyan
Department of Hygiene, Yerevan State Medical University Named After M. Heratsi, 0025, Yerevan, Armenia
Larisa Avetisyan
You can also search for this author in PubMed Google Scholar
Contributions
M.M. and K.Y. conceived the project; M.M., T.A., A.M., L.A. and K.Y. designed experiments, collected and analyzed data; M.M., T.A., A.M., L.A., and K.Y. wrote the draft; M.M., A.M., and K.Y. edited the manuscript. K.Y. obtained funding and supervised the study. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Correspondence to Konstantin Yenkoyan .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Mkhitaryan, M., Avetisyan, T., Mkhoyan, A. et al. A case–control study on pre-, peri-, and neonatal risk factors associated with autism spectrum disorder among Armenian children. Sci Rep 14 , 12308 (2024). https://doi.org/10.1038/s41598-024-63240-3
Download citation
Received : 02 March 2024
Accepted : 27 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1038/s41598-024-63240-3
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Autism spectrum disorder
- Case–control study
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Content Search
Third polio case of 2024 reported from killa abdullah.
- Govt. Pakistan
Islamabad, May 25, 2024 – The third polio case of the year has been reported from Killa Abdullah district of Balochistan.
According to the Regional Reference Laboratory for Polio at the National Institute of Health, wild poliovirus type 1 (WPV1) was detected in stool samples collected from a child in Darozai union council of Killa Abdullah, who developed symptoms of paralysis on April 20.
Genetic sequencing of the isolated virus is underway.
“It is incredibly tragic that another child has been affected by polio this year in Balochistan,” said Coordinator to the Prime Minister on National Health Services Dr Malik Mukhtar Ahmed Bharath, adding that polio is a terrible illness that changes not just the child’s life but also of the whole family.
He said: “The government is bringing the polio vaccine to our citizens’ doorsteps in multiple polio vaccination rounds. I urge families to understand the risk this disease poses to children and make sure that they vaccinate all their children under the age of five when the polio worker shows up to their homes.”
Dr Shahzad Baig, Coordinator of the National Emergency Operations Centre for Polio Eradication, said that a detailed case investigation will be launched immediately to identify the origins of the virus, find populations that may have missed vaccination and take corrective measures to contain its spread.”
“We have already conducted four polio vaccination campaigns this year, including two nationwide campaigns to boost children’s immunity and we will be conducting another campaign in June,” he added.
This is the third polio case from Balochistan this year and the first reported from Killa Abdullah after three years.
Last year, six polio cases were reported in the country, four from Khyber Pakhtunkhwa and two from Karachi.
Note for Editor:
Polio is a highly infectious disease caused by poliovirus mainly affecting children under the age of five years. It invades the nervous system and can cause paralysis or even death. While there is no cure for polio, vaccination is the most effective way to protect children from this crippling disease. Each time a child under the age of five is vaccinated, their protection against the virus is increased. Repeated immunisations have protected millions of children from polio, allowing almost all countries in the world to become polio-free, except for the two endemic countries of Pakistan and Afghanistan.
For further information, please contact: Ms Hania Naeem, Communications Officer, NEOC, +923431101988; [email protected]
Related Content
Sewage samples positive for poliovirus in six districts, multiple micronutrient supplements in humanitarian emergencies: pakistan case study, may 2024.
Pakistan + 1 more
Soaring temperatures in South Asia can put children’s health in danger, UNICEF warns
Pakistan + 24 more
Taking Stock: Sexual and Reproductive Health and Rights in Climate Commitments - an Asia and the Pacific Review
- Skip to main content
- Keyboard shortcuts for audio player
Weekend Edition Sunday
- Latest Show
Sunday Puzzle
- Corrections
Listen to the lead story from this episode.
Politics chat: Biden's response to Rafah escalation
by Ayesha Rascoe , Asma Khalid
Biden will deliver the commencement address at Morehouse College
by Ayesha Rascoe
Social security funds are set to fall short by 2033. What can be done?
Minnesota's new state flag is drawing mixed reactions.
by Dana Ferguson
In a Ukrainian border town, the local newspaper keeps watch on returning POWs
by Joanna Kakissis

"I think the task of the filmmaker is to break through and hit that horror that still remains in the unconscious mind," Corman said. "And there's a certain amount of catharsis there. He's pictured above in 2009. Kevork Djansezian/Getty Images hide caption
Roger Corman, the B-movie legend who launched A-list careers, dies at 98
by Neda Ulaby

Sunday Puzzle NPR hide caption
Sunday Puzzle: Six-letter words with four vowels and two consonants
by Will Shortz
Francis Galluppi on 'The Last Stop In Yuma County', his feature debut
by Ayesha Rascoe , Ryan Benk
NPR listeners share messages for their moms
Democratic sen. bob menendez goes on trial for taking bribes in exchange for favors.
by Ayesha Rascoe , Nancy Solomon
How FAFSA complications are disproportionately affecting Black students
Middle east, rafah's main hospital has shut down, people try to flee as israel launches an attack.
by Ayesha Rascoe , Aya Batrawy
The U.S. is refilling the Strategic Petroleum Reserves. What purpose can they serve?

Edward Peter-Paul is chief of the Mi'kmaq Nation in Maine. Decades ago, a sweat ceremony helped him improve his relationship with drugs and alcohol. He hopes the new healing lodge can do the same for other tribal citizens. Aneri Pattani/KFF Health News hide caption
Shots - Health News
A tribe in maine is using opioid settlement funds on a sweat lodge to treat addiction.
by Aneri Pattani , Jazmin Orozco Rodriguez
Uncovering the story of Sawney Freeman, who may have been America's first Black composer
by Diane Orson
What are sperm whales saying? Researchers find a complex 'alphabet'
by Lauren Sommer

Playwright Paula Vogel is known not just for her work on Broadway — but for the generations of famous playwrights whose careers she has nurtured. Above, Jessica Lange in Paula Vogel's Mother Play. Joan Marcus/Second Stage hide caption
In honor of Mother's Day, here's 'Mother Play' — which gestated for 40 years
by Jeff Lunden
Vicky Farewell on her new album 'Give A Damn'
Searching for a song you heard between stories? We've retired music buttons on these pages. Learn more here.

IMAGES
VIDEO
COMMENTS
Figure 2. Follow-up behavioral test of 5-year-old boy. According to the MRI, the cochlea on the right side is normal—which would explain the present DPOAE results. The cochlear branch of the VIIIth Cranial Nerve is completely absent, which would explain the absent ABR result and the profound hearing loss by behavioral testing.
Cripps, J. H., Supalla, S. J., & Blackburn, L. A. (2020). A case study on accessible reading with deaf children. Society for American Sign Language Journal, 4(1), 36-58. https://tigerprints.clemson.edu/saslj/ vol4/iss1/1/. This Article is brought to you for free and open access by the Communication Disorders & Special Education at ODU Digital ...
population. Cumulatively, these case studies represent a snapshot of the overall popula-tion of school-age d/Dhh students as determined by the U.S. Department of Education (2015) and the Gallaudet Research Institute (2013). Within this population, between 5 and 10% are Deaf children of Deaf parents, 25% come from a home where the parents
Helping families help themselves: a case study. When family members of children with hearing loss express concerns about school-related issues to the clinic-based audiologist, we want to respond in a supportive manner, without overstepping our role. The tendency may be to jump in and try to solve the problem for the family.
This unique text is a collaborative publication containing preK-12 student case studies by a diverse team of authors in deaf education. Anyone who has taught pre-service teachers or clinicians recognizes the difficulty of teaching the complexities of the topic of diversity among students who are deaf/hard of hearing.
Download Full Case Study & Rubric. An interprofessional practice (IPP) team worked together to assess hearing loss and language skills in a 2-year-old child. The team recommended a cochlear implant and a plan of therapy for language development and listening skills. As a result, the child's expressive vocabulary began showing steady growth.
The application of PECS in a deaf child with autism: A case study. Focus on Autism and Other Developmental Disabilities, 22(1), 23-32. Crossref Google Scholar. Myck-Wayne, J., Robinson, S., & Henson, E. (2011). Serving and supporting young children with a dual diagnosis of hearing loss and autism: The stories or four families. ...
This study adds to the growing body of literature that unexplained language disorders in signed languages exist and provides preliminary evidence for positive outcomes from language intervention for a Deaf signing child. The case described can inform professionals who work with Deaf signing children (e.g., speech-language pathologists, teachers ...
John M. Henderson. This study reports the approach used by the parents of a deaf boy to teach him to read. The approach is based on a progression from 1) meaning to 2) sight vocabulary to 3) reading books. The importance of communication and interaction within the context of an intimate relationship are pointed out.
Journal of Deaf Studies and Deaf Education is a peer-reviewed scholarly journal integrating and coordinating basic and applied research relating to individuals who are deaf, including cultural, developmental, linguistic, and educational topics. Find out more.
In this case study of a young deaf child, his mother relates his progress in. language acquisition through the use of signs, finger spelling. speechreading. and auditory training. Other members of the child's family are deaf and the child received training at the Callaudet preschool from the age of 30 months. The author believes
Two hearing children of deaf parents (initially 3;9 and 1;8) had been cared for almost exclusively by their mother, who did not speak or sign to them.
Single case study on one Australian boy at age 23 and then 42 months: To investigate the communication and language development of a deaf boy over a 20-month period, specifically the bimodal bilingual input. Data collected bi-monthly Part of larger study of 8 deaf children
Raising a deaf child can have significant impacts on parents' wellbeing, their relationship with the deaf child, and their ability to parent effectively. Using an online survey, this study explored two questions: First, to examine whether hearing parents treat and perceive their deaf and hearing children differently while controlling for parent characteristics (including resolution of ...
Deaf-Blind Student Case Studies. As part of the project, case studies are being developed to support educational teams and families in their efforts to address the literacy and communication needs of individuals with severe disabilities, including deaf-blindness. The following case studies are currently available: Follow the case of Jake.
The purpose of this case study was to explore the communication needs of a child with deafness and cerebral palsy (DCP) and how these needs can be supported by interventions targeting the use of communication approaches and strategies. ... is an Associate Professor in Deaf Education and the director of the teachers of deaf children and young ...
The purpose of this study was to examine a deaf child's pragmatic devel … Conversation at home: a case study of a young deaf child's communication experiences in a family in which all others can hear Am Ann Deaf. 1995 Oct;140(4):324-32. doi: 10.1353/aad.2012.0367. ...
Martin McLean, from the National Deaf Children's Society, said more options were to be welcomed. "With the right support from the start, deafness should never be a barrier to happiness or ...
A 10-year-old nonverbal Greek boy, C.Z., Who had been diagnosed With both bilateral sensorineural profound hearing loss and autism, Was taught to use the Picture Exchange Communication System (PECS), With some modifications and extensions, over a 4-month intensive intervention period.
There are few proven effective treatments such as Parent-Child Interaction Therapy (PCIT) for use with deaf parents and their children, ... Parent-Child Interaction Therapy With Deaf Parents and Their Hearing Child: A Case Study. Kathleen Armstrong, Amanda David, and Karen Goldberg View all authors and affiliations. Volume 13, Issue 2 ...
This case study reports results obtained from a young, profoundly deaf child, M, who was fitted with a single-channel vibrotactile device, the Tactaid I, at 29 months of age. Her progress in speech and language development was evaluated over a 14-month period. During this period, M learned to understand 101 words through lipreading and the ...
Case Study C. C has Deaf parents and is part of an extensive Deaf family. She was having problems with bullying in her resourced mainstream school , mainly from the other deaf children. DEX supported her at her Annual Review meeting and it was agreed as part of her Statement that it provided a range of services: Training for deaf children on ...
By Emily Cooke. published 16 May 2024. Seven months after her treatment, the baby girl can now respond to her parents' voices without the aid of a cochlear implant. Opal Sandy from the U.K. was ...
The Ethics of Designing a Deaf Baby. The Hearing Journal 65 (5):p 22,24, May 2012. | DOI: 10.1097/01.HJ.0000414383.90116.7e. Audiologists are devoted to helping people hear better, so it will likely come as a shock to learn that some parents prefer that their babies be born deaf. So-called designer deafness is the idea behind conceiving a deaf ...
A total of 168 children with ASD and 329 controls were included in the analysis. ... For this purpose a retrospective case-control study using a random proportional sample of Armenian children ...
In 2013, Grow and LeBlanc published evidence-based guidelines for teaching receptive language. They reported five key considerations for best practice: ensuring the child is attending prior to presenting the antecedent; reducing or eliminating inadvertent cues (e.g. tone of voice during presentation); ensuring stimulus control through selection of the stimuli and responses (simplification of ...
Lonnie, a 3-year-old boy was an only child who lived with his parents. His mother, who. behavior. He whined frequently, interrupted her when she was busy, and constantly. demanded that she play with him. Often, he would end up tantruming on the floor, and. throw things if his mom didn't respond.
Background/Objectives: One of the rare causes of cholestasis may be hemolytic disease of the fetus and newborn (HDFN). Methods: We retrospectively analyzed 88 medical records of HDFN newborns with cholestasis and 186 records of children with HDFN without cholestasis and conducted an observational, case-control, retrospective study. Results: Factors influencing the risk of cholestasis were ...
Islamabad, May 25, 2024 - The third polio case of the year has been reported from Killa Abdullah district of Balochistan. According to the Regional Reference Laboratory for Polio at the National ...
Vicky Farewell on her new album 'Give A Damn'. by Ayesha Rascoe. 7 min. Searching for a song you heard between stories? We've retired music buttons on these pages. Learn more here. Browse archive ...