149 Case Studies: Real Stories Of People Overcoming Struggles of Mental Health
At Tracking Happiness, we’re dedicated to helping others around the world overcome struggles of mental health.
In 2022, we published a survey of 5,521 respondents and found:
- 88% of our respondents experienced mental health issues in the past year.
- 25% of people don’t feel comfortable sharing their struggles with anyone, not even their closest friends.
In order to break the stigma that surrounds mental health struggles, we’re looking to share your stories.

Overcoming struggles
They say that everyone you meet is engaged in a great struggle. No matter how well someone manages to hide it, there’s always something to overcome, a struggle to deal with, an obstacle to climb.
And when someone is engaged in a struggle, that person is looking for others to join him. Because we, as human beings, don’t thrive when we feel alone in facing a struggle.
Let’s throw rocks together
Overcoming your struggles is like defeating an angry giant. You try to throw rocks at it, but how much damage is one little rock gonna do?
Tracking Happiness can become your partner in facing this giant. We are on a mission to share all your stories of overcoming mental health struggles. By doing so, we want to help inspire you to overcome the things that you’re struggling with, while also breaking the stigma of mental health.
Which explains the phrase: “Let’s throw rocks together”.
Let’s throw rocks together, and become better at overcoming our struggles collectively. If you’re interested in becoming a part of this and sharing your story, click this link!
Case studies
May 2, 2024
How Yoga Became My Lifeline in Navigating Depression and Building Self-Love
“My relationship with myself was pretty broken and I had no self-belief, I had low self-esteem and I resented my family. It was through yoga that I found the truest feeling of comfort, self-compassion, and courage to move forward, grow as a person, and fall back in love with myself and life again.”
Struggled with: Depression Insomnia Stress Suicidal
Helped by: Exercise Meditation Mindfulness Self-Care
April 30, 2024
Finding Clarity After an ADHD Diagnosis and Bettering Myself With CBT and Medication
“Now as I was getting older, I felt I couldn’t trust my own thoughts in the same way as before, and self-doubt would creep in. I would constantly ask myself whether my emotions and thoughts were accurate or not when reacting to social situations. As you can imagine this was a huge challenge and draining emotionally.”
Struggled with: ADHD Autism
Helped by: Medication Social support Therapy
April 25, 2024
How I’m Seeking Moments of Happiness Despite Struggling With Depression
“The diagnosis I longed for finally arrived, but it didn’t bring the expected empowerment. While it sheds light on my struggles, it also serves as a reminder that this is a part of me that won’t simply vanish. Though mental health can be managed, I know it will always leave its mark. The most challenging part is not always pinpointing why I feel the way I do.”
Struggled with: Depression Negative body image
Helped by: Medication Therapy
April 24, 2024
How Boxing and Therapy Help Me Recover My Identity After Extreme Weight Loss
“When my body changed so drastically and rapidly, it broke my sense of self-identity. About a year into my weight loss, I began to experience early dissociation, depersonalization, and dissociative amnesia. I broke into two people. Me of now and her of before.”
Struggled with: Depression Dissociative amnesia
Helped by: Exercise Self-improvement Therapy
April 18, 2024
How Therapy, Medication and Baking Help Me Navigate Depression and OCD
“I was hospitalized for my eating disorder and my depression several times throughout my college career struggling with the will to live… I was desperate to be “normal” but my brain really got in the way of that.”
Struggled with: Anxiety Depression Eating disorder OCD Suicidal
Helped by: Medication Self-improvement Therapy Treatment
April 16, 2024
How I Found My Self-Worth After Battling Chronic Pain, Anxiety and Panic Attacks
“I remember being floored with a horrible throat infection, and I was just crying. I was done suffering, I couldn’t do it anymore, I was really broken down. That was about 2 years ago now, and it shifted something in my brain. Instead of going down the drain – and keeping that negativity going – it suddenly hit me that I’m the only one responsible for how I feel.”
Struggled with: Anxiety Chronic pain Panic attacks Stress
Helped by: Medication Self-Care Self-improvement Therapy
April 11, 2024
How a Mindset Change Helped Me Break Free From Childhood Trauma and Toxicity
“My mother said she wanted to end it in bloodshed and she waited for him to come home from his late-night meeting. She thought better of it when he was late arriving home. She was overwhelmed with thoughts of her in prison and me in foster care. To say that she made the right decision in achieving the goal of a good life is an answer I struggled to answer for many years.”
Struggled with: Abuse Anxiety Childhood CPTSD Depression
Helped by: Mindfulness Reinventing yourself Self-improvement Therapy
April 9, 2024
Healing From Postpartum Depression With Therapy, Friends & Exercise
“I wasn’t sure how to feel better for a while. People talk about ‘getting help’ but that’s a blanket term and unfortunately it’s not a band-aid you can just put on and suddenly be yourself again. It takes time to find the right therapist, medication if that’s what you decide to do, to find a new rhythm with family, and in my case, I really needed friends locally.”
Struggled with: Postpartum depression
Helped by: Exercise Social support Therapy
April 4, 2024
My Journey from Loneliness and Isolation to Creating an Online Haven for Seniors
“When one is home alone, all day, with nothing to do, nobody to speak with, stuck with their thoughts both good and bad, it’s easy to slip back into a depressive state. Feeling unneeded, unwanted, no happiness, no joy, no reason to get out of bed – just suffering with “the blahs”.”
Struggled with: Depression Loneliness
Helped by: Self-improvement Social support
April 2, 2024
Surviving a Workplace Shooting and Navigating PTSD, Insomnia With Marathons and Prayers
“My symptoms began immediately following a workplace shooting on Saturday, November 28, 2015, and were exasperated due to the activity of the company, the criminals, and the cops. The company treated me as if I were a criminal, the criminals attempted to kill me three additional times, and the cops (Houston Police Department Organized Crime Unit) treated me as if I was a thorn in their flesh.”
Struggled with: Depression Insomnia PTSD Stress
Helped by: Exercise Religion Treatment Volunteering
- Bipolar Disorder
- Therapy Center
- When To See a Therapist
- Types of Therapy
- Best Online Therapy
- Best Couples Therapy
- Best Family Therapy
- Managing Stress
- Sleep and Dreaming
- Understanding Emotions
- Self-Improvement
- Healthy Relationships
- Student Resources
- Personality Types
- Guided Meditations
- Verywell Mind Insights
- 2024 Verywell Mind 25
- Mental Health in the Classroom
- Editorial Process
- Meet Our Review Board
- Crisis Support
What Is a Case Study?
Weighing the pros and cons of this method of research
Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
:max_bytes(150000):strip_icc():format(webp)/IMG_9791-89504ab694d54b66bbd72cb84ffb860e.jpg)
Cara Lustik is a fact-checker and copywriter.
:max_bytes(150000):strip_icc():format(webp)/Cara-Lustik-1000-77abe13cf6c14a34a58c2a0ffb7297da.jpg)
Verywell / Colleen Tighe
- Pros and Cons
What Types of Case Studies Are Out There?
Where do you find data for a case study, how do i write a psychology case study.
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The point of a case study is to learn as much as possible about an individual or group so that the information can be generalized to many others. Unfortunately, case studies tend to be highly subjective, and it is sometimes difficult to generalize results to a larger population.
While case studies focus on a single individual or group, they follow a format similar to other types of psychology writing. If you are writing a case study, we got you—here are some rules of APA format to reference.
At a Glance
A case study, or an in-depth study of a person, group, or event, can be a useful research tool when used wisely. In many cases, case studies are best used in situations where it would be difficult or impossible for you to conduct an experiment. They are helpful for looking at unique situations and allow researchers to gather a lot of˜ information about a specific individual or group of people. However, it's important to be cautious of any bias we draw from them as they are highly subjective.
What Are the Benefits and Limitations of Case Studies?
A case study can have its strengths and weaknesses. Researchers must consider these pros and cons before deciding if this type of study is appropriate for their needs.
One of the greatest advantages of a case study is that it allows researchers to investigate things that are often difficult or impossible to replicate in a lab. Some other benefits of a case study:
- Allows researchers to capture information on the 'how,' 'what,' and 'why,' of something that's implemented
- Gives researchers the chance to collect information on why one strategy might be chosen over another
- Permits researchers to develop hypotheses that can be explored in experimental research
On the other hand, a case study can have some drawbacks:
- It cannot necessarily be generalized to the larger population
- Cannot demonstrate cause and effect
- It may not be scientifically rigorous
- It can lead to bias
Researchers may choose to perform a case study if they want to explore a unique or recently discovered phenomenon. Through their insights, researchers develop additional ideas and study questions that might be explored in future studies.
It's important to remember that the insights from case studies cannot be used to determine cause-and-effect relationships between variables. However, case studies may be used to develop hypotheses that can then be addressed in experimental research.
Case Study Examples
There have been a number of notable case studies in the history of psychology. Much of Freud's work and theories were developed through individual case studies. Some great examples of case studies in psychology include:
- Anna O : Anna O. was a pseudonym of a woman named Bertha Pappenheim, a patient of a physician named Josef Breuer. While she was never a patient of Freud's, Freud and Breuer discussed her case extensively. The woman was experiencing symptoms of a condition that was then known as hysteria and found that talking about her problems helped relieve her symptoms. Her case played an important part in the development of talk therapy as an approach to mental health treatment.
- Phineas Gage : Phineas Gage was a railroad employee who experienced a terrible accident in which an explosion sent a metal rod through his skull, damaging important portions of his brain. Gage recovered from his accident but was left with serious changes in both personality and behavior.
- Genie : Genie was a young girl subjected to horrific abuse and isolation. The case study of Genie allowed researchers to study whether language learning was possible, even after missing critical periods for language development. Her case also served as an example of how scientific research may interfere with treatment and lead to further abuse of vulnerable individuals.
Such cases demonstrate how case research can be used to study things that researchers could not replicate in experimental settings. In Genie's case, her horrific abuse denied her the opportunity to learn a language at critical points in her development.
This is clearly not something researchers could ethically replicate, but conducting a case study on Genie allowed researchers to study phenomena that are otherwise impossible to reproduce.
There are a few different types of case studies that psychologists and other researchers might use:
- Collective case studies : These involve studying a group of individuals. Researchers might study a group of people in a certain setting or look at an entire community. For example, psychologists might explore how access to resources in a community has affected the collective mental well-being of those who live there.
- Descriptive case studies : These involve starting with a descriptive theory. The subjects are then observed, and the information gathered is compared to the pre-existing theory.
- Explanatory case studies : These are often used to do causal investigations. In other words, researchers are interested in looking at factors that may have caused certain things to occur.
- Exploratory case studies : These are sometimes used as a prelude to further, more in-depth research. This allows researchers to gather more information before developing their research questions and hypotheses .
- Instrumental case studies : These occur when the individual or group allows researchers to understand more than what is initially obvious to observers.
- Intrinsic case studies : This type of case study is when the researcher has a personal interest in the case. Jean Piaget's observations of his own children are good examples of how an intrinsic case study can contribute to the development of a psychological theory.
The three main case study types often used are intrinsic, instrumental, and collective. Intrinsic case studies are useful for learning about unique cases. Instrumental case studies help look at an individual to learn more about a broader issue. A collective case study can be useful for looking at several cases simultaneously.
The type of case study that psychology researchers use depends on the unique characteristics of the situation and the case itself.
There are a number of different sources and methods that researchers can use to gather information about an individual or group. Six major sources that have been identified by researchers are:
- Archival records : Census records, survey records, and name lists are examples of archival records.
- Direct observation : This strategy involves observing the subject, often in a natural setting . While an individual observer is sometimes used, it is more common to utilize a group of observers.
- Documents : Letters, newspaper articles, administrative records, etc., are the types of documents often used as sources.
- Interviews : Interviews are one of the most important methods for gathering information in case studies. An interview can involve structured survey questions or more open-ended questions.
- Participant observation : When the researcher serves as a participant in events and observes the actions and outcomes, it is called participant observation.
- Physical artifacts : Tools, objects, instruments, and other artifacts are often observed during a direct observation of the subject.
If you have been directed to write a case study for a psychology course, be sure to check with your instructor for any specific guidelines you need to follow. If you are writing your case study for a professional publication, check with the publisher for their specific guidelines for submitting a case study.
Here is a general outline of what should be included in a case study.
Section 1: A Case History
This section will have the following structure and content:
Background information : The first section of your paper will present your client's background. Include factors such as age, gender, work, health status, family mental health history, family and social relationships, drug and alcohol history, life difficulties, goals, and coping skills and weaknesses.
Description of the presenting problem : In the next section of your case study, you will describe the problem or symptoms that the client presented with.
Describe any physical, emotional, or sensory symptoms reported by the client. Thoughts, feelings, and perceptions related to the symptoms should also be noted. Any screening or diagnostic assessments that are used should also be described in detail and all scores reported.
Your diagnosis : Provide your diagnosis and give the appropriate Diagnostic and Statistical Manual code. Explain how you reached your diagnosis, how the client's symptoms fit the diagnostic criteria for the disorder(s), or any possible difficulties in reaching a diagnosis.
Section 2: Treatment Plan
This portion of the paper will address the chosen treatment for the condition. This might also include the theoretical basis for the chosen treatment or any other evidence that might exist to support why this approach was chosen.
- Cognitive behavioral approach : Explain how a cognitive behavioral therapist would approach treatment. Offer background information on cognitive behavioral therapy and describe the treatment sessions, client response, and outcome of this type of treatment. Make note of any difficulties or successes encountered by your client during treatment.
- Humanistic approach : Describe a humanistic approach that could be used to treat your client, such as client-centered therapy . Provide information on the type of treatment you chose, the client's reaction to the treatment, and the end result of this approach. Explain why the treatment was successful or unsuccessful.
- Psychoanalytic approach : Describe how a psychoanalytic therapist would view the client's problem. Provide some background on the psychoanalytic approach and cite relevant references. Explain how psychoanalytic therapy would be used to treat the client, how the client would respond to therapy, and the effectiveness of this treatment approach.
- Pharmacological approach : If treatment primarily involves the use of medications, explain which medications were used and why. Provide background on the effectiveness of these medications and how monotherapy may compare with an approach that combines medications with therapy or other treatments.
This section of a case study should also include information about the treatment goals, process, and outcomes.
When you are writing a case study, you should also include a section where you discuss the case study itself, including the strengths and limitiations of the study. You should note how the findings of your case study might support previous research.
In your discussion section, you should also describe some of the implications of your case study. What ideas or findings might require further exploration? How might researchers go about exploring some of these questions in additional studies?
Need More Tips?
Here are a few additional pointers to keep in mind when formatting your case study:
- Never refer to the subject of your case study as "the client." Instead, use their name or a pseudonym.
- Read examples of case studies to gain an idea about the style and format.
- Remember to use APA format when citing references .
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011;11:100.
Crowe S, Cresswell K, Robertson A, Huby G, Avery A, Sheikh A. The case study approach . BMC Med Res Methodol . 2011 Jun 27;11:100. doi:10.1186/1471-2288-11-100
Gagnon, Yves-Chantal. The Case Study as Research Method: A Practical Handbook . Canada, Chicago Review Press Incorporated DBA Independent Pub Group, 2010.
Yin, Robert K. Case Study Research and Applications: Design and Methods . United States, SAGE Publications, 2017.
By Kendra Cherry, MSEd Kendra Cherry, MS, is a psychosocial rehabilitation specialist, psychology educator, and author of the "Everything Psychology Book."
- Children's mental health case studies
- Food, health and nutrition
- Mental wellbeing
- Mental health
Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and feedback for the user. Use these cases on your own or in classes and training events
Each case study:
- Explores the experiences of a child and family over time.
- Introduces theories, research and practice ideas about children's mental health.
- Shows the needs of a child at specific stages of development.
- Invites users to “try on the hat” of different specific professionals.
By completing a case study participants will:
- Examine the needs of children from an interdisciplinary perspective.
- Recognize the importance of prevention/early intervention in children’s mental health.
- Apply ecological and developmental perspectives to children’s mental health.
- Predict probable outcomes for children based on services they receive.
Case studies prompt users to practice making decisions that are:
- Research-based.
- Practice-based.
- Best to meet a child and family's needs in that moment.
Children’s mental health service delivery systems often face significant challenges.
- Services can be disconnected and hard to access.
- Stigma can prevent people from seeking help.
- Parents, teachers and other direct providers can become overwhelmed with piecing together a system of care that meets the needs of an individual child.
- Professionals can be unaware of the theories and perspectives under which others serving the same family work
- Professionals may face challenges doing interdisciplinary work.
- Limited funding promotes competition between organizations trying to serve families.
These case studies help explore life-like mental health situations and decision-making. Case studies introduce characters with history, relationships and real-life problems. They offer users the opportunity to:
- Examine all these details, as well as pertinent research.
- Make informed decisions about intervention based on the available information.
The case study also allows users to see how preventive decisions can change outcomes later on. At every step, the case content and learning format encourages users to review the research to inform their decisions.
Each case study emphasizes the need to consider a growing child within ecological, developmental, and interdisciplinary frameworks.
- Ecological approaches consider all the levels of influence on a child.
- Developmental approaches recognize that children are constantly growing and developing. They may learn some things before other things.
- Interdisciplinary perspectives recognize that the needs of children will not be met within the perspectives and theories of a single discipline.
There are currently two different case students available. Each case study reflects a set of themes that the child and family experience.
The About Steven case study addresses:
- Adolescent depression.
- School mental health.
- Rural mental health services.
- Social/emotional development.
The Brianna and Tanya case study reflects themes of:
- Infant and early childhood mental health.
- Educational disparities.
- Trauma and toxic stress.
- Financial insecurity.
- Intergenerational issues.
The case studies are designed with many audiences in mind:
Practitioners from a variety of fields. This includes social work, education, nursing, public health, mental health, and others.
Professionals in training, including those attending graduate or undergraduate classes.
The broader community.
Each case is based on the research, theories, practices and perspectives of people in all these areas. The case studies emphasize the importance of considering an interdisciplinary framework. Children’s needs cannot be met within the perspective of a single discipline.
The complex problems children face need solutions that integrate many and diverse ways of knowing. The case studies also help everyone better understand the mental health needs of children. We all have a role to play.
These case has been piloted within:
Graduate and undergraduate courses.
Discipline-specific and interdisciplinary settings.
Professional organizations.
Currently, the case studies are being offered to instructors and their staff and students in graduate and undergraduate level courses. They are designed to supplement existing course curricula.
Instructors have used the case study effectively by:
- Assigning the entire case at one time as homework. This is followed by in-class discussion or a reflective writing assignment relevant to a course.
- Assigning sections of the case throughout the course. Instructors then require students to prepare for in-class discussion pertinent to that section.
- Creating writing, research or presentation assignments based on specific sections of course content.
- Focusing on a specific theme present in the case that is pertinent to the course. Instructors use this as a launching point for deeper study.
- Constructing other in-class creative experiences with the case.
- Collaborating with other instructors to hold interdisciplinary discussions about the case.
To get started with a particular case, visit the related web page and follow the instructions to register. Once you register as an instructor, you will receive information for your co-instructors, teaching assistants and students. Get more information on the following web pages.
- Brianna and Tanya: A case study about infant and early childhood mental health
- About Steven: A children’s mental health case study about depression
Cari Michaels, Extension educator
Reviewed in 2023
© 2024 Regents of the University of Minnesota. All rights reserved. The University of Minnesota is an equal opportunity educator and employer.
- Report Web Disability-Related Issue |
- Privacy Statement |
- Staff intranet
- Research article
- Open access
- Published: 01 April 2021
Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters
- Tamar Wyte-Lake ORCID: orcid.org/0000-0001-8449-7701 1 , 2 ,
- Susan Schmitz 1 ,
- Reginald J. Kornegay 3 ,
- Felix Acevedo 4 &
- Aram Dobalian 1 , 5
BMC Public Health volume 21 , Article number: 639 ( 2021 ) Cite this article
2331 Accesses
1 Citations
Metrics details
Community disaster resilience is comprised of a multitude of factors, including the capacity of citizens to psychologically recover. There is growing recognition of the need for public health departments to prioritize a communitywide mental health response strategy to facilitate access to behavioral health services and reduce potential psychological impacts. Due to the US Department of Veterans Affairs’ (VA) extensive experience providing trauma-informed behavioral healthcare to its Veterans, and the fact that VA Medical Centers (VAMCs) are located throughout the United States, the VA is well situated to be a key partner in local communities’ response plans. In this study we examined the role the VA can play in a community’s behavioral health response using case studies from three disasters.
This study investigated experiences of VA employees in critical emergency response positions ( N = 17) in communities where disasters occurred between 2017 and 2019. All respondents were interviewed March–July 2019. Data were collected via semi-structured interviews exploring participants’ experiences and knowledge about VA activities provided to communities following the regional disasters. Data were analyzed using thematic and grounded theory coding methods.
Respondents underscored VA’s primary mission after a disaster was to maintain continuity of care to Veterans. The majority also described the VA supporting community recovery. Specifically, three recent events provided key examples of VA’s involvement in disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships as well as prioritization from VA leadership to engage in humanitarian missions. The behavioral health interventions were provided by behavioral health teams integrated into disaster assistance centers and non-VA hospitals, VA mobile units deployed into the community, and VA telehealth services.
Conclusions
Recent disasters have revealed that coordinated efforts between multidisciplinary agencies can strengthen communities’ capacity to respond to mental health needs, thereby fostering resilience. Building relationships with local VAMCs can help expedite how VA can be incorporated into emergency management strategies. In considering the strengths community partners can bring to bear, a coordinated disaster mental health response would benefit from involving VA as a partner during planning.
Peer Review reports
Disaster behavioral health
The current COVID-19 pandemic, while still underway, has already demonstrated the need for psychological interventions to manage the isolation, stress, and trauma stemming from the ongoing disaster [ 1 , 2 , 3 , 4 , 5 ]. While the scale of the event is unprecedented, interest in understanding the psychological consequences of disasters is not unique to the pandemic [ 6 , 7 , 8 , 9 , 10 ]. Generally, studies exploring the impacts of disasters on behavioral health have found increases in psychological distress in the short term, with the potential for some individuals to experience long-term psychiatric disorders such as posttraumatic stress disorder, depression, and anxiety [ 6 , 7 , 8 , 9 , 10 ].
To ameliorate the potential negative health effects to impacted populations, numerous early interventions have been explored [ 7 , 11 , 12 , 13 , 14 ]. Some countries such as the Netherlands and Iceland use federally structured plans to implement disaster behavioral health interventions [ 12 , 15 ]. And countries like New Zealand have invested heavily in developing extensive mental health programs in response to large scale disaster events [ 16 , 17 ]. In the United States, federal entities strive to create resources and guidance on implementing behavioral health services after disaster, however, interventions are generally managed and delivered by state, territory, and local agencies [ 14 , 18 , 19 ]. Often, after federally declared disasters, the US Federal Government additionally provides funding through the Crisis Counseling Assistance and Training Program (CCP) to community behavioral health programs [ 8 , 13 , 20 ]. Yet the structure and content of interventions are left to the discretion of the implementing agency.
Regardless of the services provided, having a plan in place prior to a disaster can facilitate implementation [ 8 , 11 , 12 , 13 , 19 , 21 , 22 ]. Few publications detail the creation of a local disaster behavioral health response plans [ 15 , 18 , 20 ] or describe the process in which interventions were deployed following an incident [ 7 , 10 , 15 , 20 , 23 , 24 ]. Common themes arising in studies exploring disaster behavioral health plans or interventions are the need for interdisciplinary teams and interagency collaboration [ 8 , 12 , 18 , 19 , 20 ] and strong community response [ 16 ].
The United States Department of Veterans Affairs
One interagency partner often overlooked in the United States is the U.S. Department of Veterans Affairs (VA) Veterans Health Administration (VHA). Previous publications on VHA’s participation in collaborative disaster planning and preparedness efforts with local communities identified barriers to its involvement [ 25 , 26 ]. One such barrier is that the community, and sometime even VHA employees, are unaware that VHA is tasked with planning for and acting to support “national, state, and local emergency management, public health, safety and homeland security efforts” [ 9 , 27 ]. This responsibility to contribute to community efforts is called the VA’s Fourth Mission and is in addition to VHA’s duty to ensure continuity of services to veterans after a disaster.
The expertise of VHA’s 322,030 healthcare professionals and support staff who provide a range of services at its 1255 healthcare facilities spread throughout the U.S. and its territories makes VHA a valuable potential partner in disaster response [ 28 ]. In addition to inpatient and ambulatory medical care, VHA provides a variety of reintegration programs including trauma recovery and behavioral health services for Veterans and their families at its facilities and through community-based care at Vet Centers, Mobile Vet Centers, and college and university campuses [ 29 ]. How these services are applied in community response efforts has been detailed in the grey literature [ 28 , 30 , 31 , 32 ].
This study highlights the potential role of local VA facilities in supporting local behavioral health activities after a disaster, and specifically, presents three exemplars of VHA integrating into communities’ disaster behavioral health response and providing behavioral health support to non-Veterans. The three VA facilities and the events they responded to are: (1) VA Pacific Island Healthcare System (VAPIHC), which is based in Honolulu, Hawaii but provides care to Veterans throughout numerous Pacific Islands. On October 24th, 2018, Super Typhoon Yutu made direct landfall on the Mariana Islands, a US Commonwealth with a nascent established VA tele-mental health clinic on the island of Tinian. This was the strongest typhoon ever recorded to strike the area, severely damaging or destroying many buildings and much of the critical infrastructure of Tinian [ 33 ]; (2) Orlando VA Healthcare System, which serves east central Florida, and encompasses 7 counties. On June 12, 2016, a domestic terrorist attack [ 34 ], targeted hate crime, and one of the deadliest mass shootings in the U.S. occurred at a local establishment, Pulse Nightclub. In a matter of hours, 49 people were killed and 53 were wounded before law enforcement breached the building and ended the violence [ 35 ]; and (3) VA Southern Nevada HCS (VASNHCS), located in and providing care throughout Las Vegas, Nevada. On October 1, 2017, the worst mass shooting in modern history took place at the Route 91 Harvest Music Festival on the downtown Las Vegas Strip. A gunman opened fire on a crowd of more than 22,000, killing 58 people and wounding 413 [ 36 ]. These cases provide examples of interagency partnerships and the implementation of collaborative responses for communities developing their own plans to address the behavioral health needs of their citizens during disasters, including the ongoing COVID-19 pandemic.
Study design
The results presented in this paper stem from a larger study broadly examining the role of local VA facilities in responding to regional large-scale disasters. This study used qualitative interview methods to elicit study participants’ experiences during disasters impacting the U.S. between 2016 and 2018 (see Table 1 for the full list of the disasters covered in the study, the impacted US states and territories, and VA entities affiliated with the impacted areas). Findings on disaster behavioral health functions were pulled as a subset of data and analyzed. The VA Greater Los Angeles Healthcare System Institutional Review Board (Los Angeles, California USA) approved this study.
Setting and sample
The full study sample was purposively chosen to represent individuals with emergency response roles critical to coordinating VA’s local response to disasters. Emergency management personnel at various levels of the VA were the first point of contact and, when applicable, identified additional individuals with critical response roles to interview. Additional respondents were recruited independently by the project team These facilities made up the broad recruitment sample. Due to some respondents covering multiple disasters or being deployed to disasters outside their normal service region, not all entities were included in the final sample.
Data collection methods
Data were collected through semi-structured, 60-min telephone interviews between March–August 2019, using an interview guide developed for this study (see Additional file 1 ). Interviews were conducted individually with each respondent and led jointly by at least two of the authors. Interviews explored participants’ experiences and knowledge about VA activities in the community, specifically focusing on how VA networked and coordinated with non-VA community agencies. Interviews were audio-recorded, although one respondent declined to be recorded.
Analysis plan
A total of 17 individuals were interviewed. However, five interviews did not indicate collaborating with non-VA entities and were therefore not included in the analysis. Due to their involvement in multiple disasters, two respondents were interviewed twice. At completion of the interviews, this resulted in 13 interview recordings being transcribed, and one set of interview notes (due to interviewee declining to be recorded), resulting in a total of 14 interviews that were analyzed with Atlas.ti (v.7) using a grounded theory approach. In phase one of analysis, one author reviewed all 14 interviews, using inductive coding to identify emergent themes in the data, and informed by extensive conversations about project findings held by the project team at the conclusion of each interview [ 37 ]. As a product of this process, a significant emergent theme [ 37 ] was the presence of interagency partnerships implementing collaborative responses to address the behavioral health needs of local citizens during disasters. A decision was made by the project team to narrow the focused coding analyses [ 37 ] to the way local VA facilities engaged in a behavioral response within their local community, in response to their respective large-scale disaster events.
In phase two of the analysis, the initial codes identified by SS were reviewed by TWL for consistency and agreement. Codes not deemed consistent to the focus topic were dropped. Additional grounded themes were confirmed by the team and applied to the data set [ 37 ]. Consensus on final codes was achieved, and one code list was finalized. In phase three of the analysis, the final code list was applied across all relevant interviews. The final code list had a focus on behavioral health response, including behavioral health activities, method of delivery, reactions of staff, and types of impacted community populations, but also included an identification of high level themes across all disasters, including VA expertise, integrating into local, established response activities, identification of local needs, and logistical challenges. Authors TWL and SS then independently coded each interview and resolved discrepancies by consensus.
All respondents played a substantial role in VA’s activities following the respective disasters. However, only 12 participants indicated the VAMC they supported collaborated with non-VA partners during the event in question. Included disasters ranged from widespread to geographically contained; weather-related to acts of violence; and direct impact on VA facilities ranged from none to significant. Though not all respondents described intensive engagement with the community following the event, all respondents described the importance of integrating into local, established response activities. This translated into involvement in community-wide drills and planning committees and following the lead of local incident command. Respondents indicated one of the areas where the VA could provide support to the community was in disaster behavioral health relief operations.
Activities described by respondents were often centered around tasks where the VA could reduce the caseload of other community agencies by identifying Veterans obtaining services in the community and meeting their needs regardless if they were previously enrolled in VA benefits. One key activity described by several respondents included outreach into local shelters. As one respondent explained, VA staff at shelters “[distribute] fliers [that] outline that our counselors are experts in trauma, loss, and in readjustment. They also provide referrals to Veterans for a variety of services, including housing and employment. We also offered free counseling for all community members impacted .”
Identifying where shelters were established and receiving authorization to deploy VA assets to those locations required coordination with local authorities. Multiple respondents mentioned connecting with emergency management running relief efforts to describe available VA resources and detail the services available to both Veterans and the community at large. In some of the events explored in this study, the non-VA authorities were unaware of what the VA could offer while others had pre-existing relationships that allowed for more transparent understanding of how the VA could support response efforts. One respondent went on to describe how the disaster that impacted their VAMC led to additional outreach to local jurisdictions and shelter coordinating agencies (e.g., the American Red Cross) to build relationships and understanding specifically of the behavioral health services the VA could deploy, if needed and approved.
Respondents noted there were specific benefits to conducting outreach in locations where other agencies provided services to the people impacted such as shelters and Local Assistance Centers. They noted that VA staff could more easily reach Veterans to enroll them, if eligible, into VA services and offer care to those who usually used non-VA health and mental health facilities, thereby supporting local agencies by reducing potential patient loads elsewhere. Additionally, by positioning resources at a central location, VA could more readily offer community members services as an extension of their work with Veterans. One specific resource identified as useful for Veteran and community support was Mobile Vet Centers, which have the primary goal of providing social work and mental health services to Veterans. In cases where respondents mentioned this resource, they underscored that non-Veteran community members who requested services in the first days after the disaster were never turned away.
Three community profiles
Three disaster events described by respondents distinctly highlighted cases where the VA was deeply involved in the local community’s disaster behavioral health response. Each event showed VA’s integration into local response structures was facilitated by pre-existing emergency management and clinical relationships, as well as prioritization from VA leadership to engage in humanitarian missions to support the community.
Telehealth in Tinian, Mariana Islands
Prior to Super Typhoon Yutu impacting the Mariana Islands, the VA Pacific Island Healthcare System (VAPIHC) established tele-mental health services on the island of Tinian. These services were located at a non-VA owned healthcare clinic using pre-positioned VA telemedicine equipment and coordinated with the clinic director and staff. Typhoon Yutu devastated the island and led to many Tinian healthcare clinic employees losing their homes. The clinic with VA tele-mental health equipment became a temporary housing site for staff as it was undamaged by the storm. The clinic director realized that in addition to sheltering needs, employees also experienced significant trauma. However, there were limited mental health resources on the island. Once VA became aware of the need, it worked with other federal agencies to manage the logistics of implementing services that took advantage of pre-positioned VA resources.
“… it was a relationship that we had with [the US Department of Health and Human Services] (HHS) and a relationship that we had with the folks on Guam and Saipan … we have a lot of relationships going on. So, we knew that we had that telehealth equipment. We also knew that Tinian was … hit pretty hard. And that there was a lot of grief. And so I can’t say how it totally emerged, but there’s so many relationships and there’s so much communication during an emergency.”
Respondents reported it was initially challenging to identify whether VA could provide mental health services in the community and how the services would be funded. Staff at all levels of the VA worked with the Federal Emergency Management Agency (FEMA) and HHS to get official authorization as well as receive federal funding for VAPIHC to provide time limited tele-mental health interventions to clinic staff on Tinian. VAPIHC Tele-mental Health Hub coordinated with the local clinic director to inform employees about available services and utilized technology onsite to provide weekly support groups for 13 health center employees.
Director’s 50 in Orlando, Florida and the pulse nightclub shooting
The Orlando VA Healthcare System (OVAHCS) houses a unique emergency response team “The Director’s 50.” Made up of multi-disciplinary VA healthcare workers, including mental health professionals (i.e. psychologists, psychiatrists, mental health nurses), the Director’s 50 can deploy a team of up to 50 volunteers within 2 hours to areas throughout the region when authorized by the Orlando VAMC Director. As described by one respondent, the mission of the team is,
“to provide an immediate gap fill to an emergency before VA can get its assets organized and into a formal support and response role. So the team is multi-disciplinary and multi-functional with its capabilities, so that it can immediately address the needs of the emergency response until VA can formalize how it’s going to provide their support to the community.”
The Director’s 50 includes interdisciplinary clinical and service support training for all members such as triage and treatment services, mental health intervention, peer counseling, and psychological support to trauma. Through participation in community-wide exercises and drills, the Director’s 50 has built versatile capabilities and strong relationships with local emergency management agencies and area hospitals.
In response to the Pulse Nightclub Shooting, VA Central Office requested OVAHCS to deploy the Director’s 50 to provide VA resources and support the community’s response. The team activated their mass notification system to alert their nearly 100 volunteer members and quickly assembled an initial response team of about 15 clinical, mental health, and support professionals within 1 hour. Respondents noted having internal approval can speed up the process of deploying teams. In general, to distribute VA resources into the community, a federal disaster declaration is required to initiate the Robert T. Stafford Disaster Relief and Emergency Assistance Act or where the HHS Secretary has activated the National Disaster Medical System, both of which grant VA the ability to provide assistance. Therefore, respondents noted a need to balance expectations of leadership to help quickly, while also ensuring VA resources were legally allowed to be used in the response.
One thing that facilitated OVAHCS’s integration into the local response system was a pre-existing relationship with the City of Orlando’s Office of Emergency Management and the Central Florida Medical Disaster Coalition, which facilitated the Director’s 50 integration into the city’s response and allowed them to report to the victim reunification center. The team was tasked.
“to be the initial communication to the family members for those victims that actually passed away. So, 49 victims, our team was assigned to go ahead and be the initial contact to let them know that their loved ones had passed, and to begin the coordination for services, grief counseling and victim advocacy, you know, to help them prepare the initial points of piecing together their lives after being notified of such tragic events.”
Accordingly, the initial multi-disciplinary team narrowed its focus to mainly members with mental health expertise. Over the next 2 weeks, the team worked with the community, helping to manage vigils and gatherings for the public, and continuing grief counseling and mental health support for the whole community, including providing peer behavioral health support to municipal first responders. Since this act of violence targeted people who were Lesbian Gay Bisexual Transgender Queer (LGBTQ) frequenting Pulse Nightclub, not only were relatives of victims or survivors from inside the building affected, but the entire LGBTQ community felt the traumatic impact of the shooting. One respondent described the importance of providing mental health support from multiple community agencies when a disaster of this magnitude occurs,
“And they [the people who were at the shooting] truly needed a place, and this is why we were there for greater than just the 24-48 hours of initially identifying the people who was killed during the shooting, you had everyone that was inside of the club who were seeking a place where they could go and receive the care and support that they needed as well. And obviously, you know, this is something that is an endemic issue with healthcare as a whole, is the access to mental health counseling and services. So VA, as well as some other partnering mental health organizations were able to supply that need right there at the site where they were doing victim notification or victim reunification and family support. We were able to do that.”
One respondent noted a key point to remember about the Director’s 50, “they are all volunteers...And these people will go—you know, 24 hours a day, day in and day out, to execute that mission. And we have to think about team resiliency.” This included caring for team member’s well-being by rotating staff and providing and attending to the mental heath of one another. As described by one respondent,
“Because when it was all said and done, the team was very affected by what they had to do. You know, just imagine hearing—you know, overwhelming grief for every one of the 49 victims’ families that would show up. And the team took that burden on … and I will tell you, to this day, it still affects the people who went and supported that mission. And they really—those who supported that mission have a greater reverence for what we do now, as a team. So you’d never have to ask them to—whether they are going to support anything related to the Director’s 50. That comradery that’s there, they won’t let their own kind of—go into the bowels of despair like that, alone.”
Integrating into community response in Las Vegas, Nevada after the route 91 harvest festival shooting
As a large city with many national and international visitors, respondents described Las Vegas as having a very centralized emergency response structure. Relationships between VA Southern Nevada HCS (VASNHCS) and local response agencies and area hospitals were described as “tightknit” with great working relationships where organizations plan and prepare for disasters together. As one respondent put it,
“what I do know is my community. I know my community partners. I know what they have, what they don’t have, they know what I have, what I don’t have. And that’s what makes us so resilient. That’s community.”
Although located too far away from the Las Vegas Strip to actively receive injured victims when the shooting occurred at the Route 91 Harvest Music Festival, VASNHCS activated its Hospital Incident Command System so it could actively participate in the community’s response and organize efforts. A Multi-Agency Coordination Center (MACC) organized the response activities, and respondents underscored the value of both pre-existing relationships and an understanding of the county’s emergency response structure. As explained by a respondent,
“You can’t wait for your community to ask you. You have to be on the forefront and know what they need. And you only do that by knowing your community. You know, I spent probably as much time in my community as I do in my medical center. A lot of the time, it’s my own time, but again, it builds that relationship that when they’re updating their mass casualty plan, one of the people they’re calling is [me].”
This previous collaboration, as well as being present at the MACC, allowed VASNHCS to identify community needs that it could address.
As news of the shooting spread, VA leadership tasked VASNHCS with deploying staff into the community. However, it was challenging to balance the push from VA to deploy with continuing to respect established local coordination structures. VASNHCS maintained a presence within the Medical Area Surge Command of the MACC to offer resources and expertise, waiting for requests, instead of directly deploying assets outside of the established system.
In the immediate response, VASNHCS assisted with managing fatalities. It offered morgue space to the county and initiated the mass fatality plan to increase morgue capacity. This provided the county and partner hospitals space for victims until they could be processed, and families could claim them. Additionally, VASNHC offered a Psychological First Aid (PFA) team.
Initially, VASNHCS deployed their PFA team to the community’s family reunification center. The team was composed of social workers, psychologists, psychiatrists, administrators (as support staff), canteen services (for water and snacks to sustain clients and staff), and the medical center’s Chief of Staff. As the situation evolved, the MACC received requests from local agencies for psychological assistance and VASNHCS transitioned to directly integrating into area hospitals.
Three Las Vegas hospitals received the bulk of the injured or dead and recognized the need for psychological interventions with their staff. Due to their close relationships with other hospitals, one respondent explained that they were familiar with the Employee Assistance Program (EAP) at these hospitals. The respondent knew it would take time for the EAP to arrive onsite and they would most likely focus on clinical staff involved in directly treating the injured. Therefore, VASNHCS developed a three-pronged approach to complement EAP services at the receiving hospitals. Firstly, the PFA team provided what one respondent called “ trauma therapy ” to hospital staff, regardless whether they worked the night of the shooting. The assistance extended beyond clinical staff to non-clinical departments, such as environmental services/housekeeping, whose staff were also impacted through their response roles.
Respondents reported one of the reasons their response in the hospitals was so successful was that the team was multidisciplinary, allowing staff from different departments to talk to people in similar positions, which was valued by the recipients.
“So for example, we have a nurse that’s trained in trauma, psychological first aid. So they want the nurses at [the hospital with a patient surge], they want to talk to our team. They were still processing. But when we brought our nurse into the ward, they were more than willing to open up to her, because she was one of them. She was part of their tribe. So we try to match our tribe to their tribe, and that’s why we were successful.”
Secondly, the VASNHCS team worked with victims of the shooting, providing PFA and social work services. Thirdly, they integrated with family members of patients at the hospitals and provided them items that they did not otherwise have because they were visitors to Las Vegas. Examples included coordinating free transportation to and from hospitals and hotels, connecting them to local mortuary services, and providing information about how to access services when they returned home.
The PFA team ran for 24 h a day, for 7 days in those three impacted hospitals. To balance VA patient care with the community response mission, VASNHCS staff volunteered shifts outside of their normal work hours. One respondent described the overwhelming desire of VA staff to help their community.
“And while it didn’t impact our staff or our clinics, or our patients, it impacted our community. I think another thing that still amazes me to this day, was the outpour of our staff and what I mean by that is they were coming out of the woodwork to support. We had more volunteers working an eight-hour shift and then coming in [to volunteer] at five o’clock or four o’clock and working to midnight to two in the morning and not go home until four or five in the morning, and then go to work the next day, because we didn’t want to impact our patient care. And they were doing this out of their—you know, because they care. They care about the community, they care about the event, they care about the people. And then at the end of the day, you know, we had more volunteers than we had placements, because we did not want to overwhelm the health systems with all of these VA personnel.”
However, with new volunteers each shift, a key lesson learned was to have a daily team debrief. As people changed daily, a debrief provided key information and a running tally of support being provided to save time and avoid reinventing the wheel identifying contacts or systems already developed.
Another lesson was that preparedness requires ongoing maintenance. The importance of ongoing preparedness was underscored when VASNHCS realized that leading up to the shooting, they had reduced their focus on PFA training. As described by one respondent, “ We noticed that we need that continuous [psychological first aid] training, that we need continuous exercising, and it’s not an easy fit, to send a bunch of people to someone else’s hospital or an area to do that kind of service .” They also realized the first wave of personnel went into community hospitals without basic supplies they needed to provide services, including basic items such as pens, PFA guides, and informational brochures.
Three months following the shooting, the VASNHCS Emergency Manager, working with the Chief of Social Work hosted a lunch for staff who volunteered to thank them for their involvement. During that event, they realized volunteers were not only impacted by the event itself, but also by their time providing support in the community. They therefore created a forum to again gather staff who had deployed at the 6 month and 9 month marks to eat and talk about the impact of the event on the healthcare system and themselves. On the 1 year anniversary, management had a special event for the volunteers,
“we actually had people from the community that we supported coming in and they broke bread with our team and what they did was, they talked about what the impact of the VA Southern Nevada Healthcare System was going into that event, and how we helped them bridge the gap [of mental health support] that was crucial at that time, and how appreciative they were to our cause and our Clark County Office of Emergency Management gave all our staff that responded T-shirts that said Vegas Strong, because they wanted them to know that we—they appreciated the work that we did for them to support our community.”
The need for attention to the psychological well-being of individuals during and after a disaster has been well proven as disasters have been found to be associated with both short and long-term symptoms and disorders [ 6 , 7 , 8 , 9 , 10 , 38 ]. Although in some parts of the world there are federally structured plans to implement disaster behavioral health interventions, in the United States there is a patchwork system that often relies on support and resource allocation from a multitude of agencies [ 8 , 13 , 14 , 18 , 19 , 20 ]. In this study we examined the role the VA can play in a community’s disaster relief effort and highlighted the opportunity for VA to support behavioral health response focusing specifically on case studies from three disasters.
Essential to effective emergency management is an understanding of, and engagement with, available resources in a local community. This is of particular importance when considering complex individual and group needs such as behavioral health support. VA Medical Centers can be seen as challenging partners to work with because they are both a federal entity and a local healthcare facility [ 26 ]. However, in the case of Super Typhoon Yutu, the federal positioning of the VA and its connection with HHS and FEMA facilitated the deployment of VAPIHC virtual resources. The regional respondents who supported the VA disaster mission in Tinian described how preexisting relationships with federal partners facilitated authorization and funding.
Another potential challenge to incorporating the VA into response efforts is that prior to offering services, VA leadership must balance the mission of the agency with community needs, without contradicting the restrictions of the Stafford Act. In all three presented cases, VA’s behavioral health support was not formally included in a city or county response plan, and yet pre-existing relationships between key stakeholders facilitated the provision of VA behavioral health services to support identified community needs. Respondents also described participating in interagency coordinating groups, response trainings, and exercises before the disaster. These activities aided in a deeper understanding of the response structures each partner operated under and encouraged strong rapport between agencies.
Relationships between VA emergency management and local emergency management proved invaluable as VA staff understood that services should not be provided without first engaging local response coordinators. All VA facility leadership and emergency managers are required to be trained in the Incident Command System (ICS) and National Incident Management System (NIMS), which are the coordinating structures all U.S. response agencies work within [ 39 ]. As a health care provider at a national level, VHA falls within the operations section Essential Support Function (ESF) 8: Public Health and Medical Services to support the Department of Health and Human Services [ 40 ]. Local jurisdictions may also connect with VAMCs through ESF 8 representation. For example, the VA has provided significant support to communities impacted by COVID-19. As of July 8, 2020, VA provided more than 330,000 pieces of Personal Protective Equipment (PPE) in support of the Fourth Mission, as well as hand sanitizer, laundry support, test kits and testing support, and webcams for use with existing equipment to state and local facilities. In addition, VA has admitted 279 non-Veterans to VA Medical Centers because of the pandemic [ 27 ]. Much of this coordination was done through ESF 8 coordination at a local or national level.
While respondents did not go into detail about their participation in the emergency management structure, some participants described their VA’s roles within emergency operations as liaisons. Groups such as this could report to either the planning, operations, or command sections within the ICS. Group supervisors would most commonly report to the operations section chief, likely through branch directors, given that the focus of the work would be more on specialized functions as needed for tactical operations. Regardless of where they fit, their presence at emergency operations centers and command posts facilitated communication to allow for VA’s integration into incident action plans. Particularly during the response to mass casualty events in Orlando and Las Vegas, understanding the local response network and then proffering available services was essential to avoid confusion or duplication of activities. By working within the established coordination centers, VA’s efforts were effectively integrated into the greater community behavioral health response and were deployed to points of greatest need. Although a detailed understanding of the integration of VA activities into ICS structures fell outside of the scope of this work, future assessment of the integration of VA representatives into local, state, and/or regional ICS structures could help clarify roles and identify which section liaisons best support (e.g., operations, planning, logistics) [ 40 ].
VA is increasingly strengthening partnerships with agencies that provide behavioral health services to Veterans and their families who use non-VA community-based care [ 41 ]. In each case example, the primary support provided by VA to the community was the provision of behavioral health services in response to an identified need. Respondents described this as being due, in large part, to the recognition of VA’s expertise in trauma and post-trauma treatment, thereby allowing these resources to come to the forefront. While not mentioned by the respondents, an additional value that VA providers add to disaster behavioral health responses is their exposure to and understanding of the unique needs of various populations throughout their communities. In addition to ensuring care is culturally competent to the unique identity of being a Veteran, VA staff must respect the diversity of Veterans themselves. Just like the U.S. population at large, Veterans represent a range of ages, races, genders, sexual orientations, socioeconomic statuses, etc. and mental health services must be considerate of this diversity. The VA recognizes this and offers training to providers to understand and respect their patients’ unique needs [ 42 ]. Working with a variety of populations preposition VA staff to have a deeper understanding of the post-disaster needs of the wider community.
Two of the case examples described in this study especially bring to the forefront the importance of disaster behavioral health response planning and implementation teams understanding unique experiences of community members. Super Typhoon Yutu directly impacted an archipelago housing a majority Asian and/or Pacific Island population. The Pulse Nightclub shooting, while a terrorist event, was a targeted hate crime intended to inflict violence on the LGBTQ community. Disaster behavioral health interventions for these affected groups not only need to take into consideration the importance of cultural competency but also the potential of re-traumatization and distinct population mental health needs.
In the Northern Mariana Islands, while there is a mix of ethnic groups (Filipino, Chamorro, Chinese, Carolinian, Korean, Palauan, etc.), many either identify as or are categorized more broadly as Asian and/or Pacific Islanders. Although there are more than 1.4 million people who are considered Pacific Islanders living the in the U.S., there is a dearth of information on the mental health of this population [ 43 ]. Similarly, the prevalence and incidence rates of mental illness in the Mariana Islands is not well studied [ 44 ]. Some sources attribute this lack of understanding to a disproportionate underuse of mental health services [ 43 ]. However, Asian and Pacific Islanders within the U.S. and those territories affiliated with it often experience transgenerational trauma, discrimination, continued loss from colonization, historical trauma, and mental health stigma which can impact psychological wellbeing and help seeking behavior. Additionally, cultural elements (collectivism, reverence for the past, hierarchical social order, etc.) of this population are important to understand when providing behavioral health services [ 43 , 45 ]. One of the reasons respondents indicated that the VA was asked to provide assistance following Typhoon Yutu was the lack of availability of mental health services in Tinian. The established VA telehealth technology increased accessibility to behavioral practitioners from VAPIHC who most likely were experienced working with Asian and Pacific Island populations since more than 55,000 Veterans who identify as this ethnicity live in Island Areas or Hawaii [ 46 , 47 ].
The Pulse Nightclub Shooting was a terrorist driven hate crime targeting individuals who identified as LGBTQ. Members of this group often experience discrimination, stigma, and trauma throughout their lives. Discrimination and heterocentric health and mental health practices can marginalize this population and impact help seeking behavior [ 48 , 49 ]. This is of particular concern as individuals who are LGBTQ face numerous mental health disparities with a higher likelihood of experiencing depression, anxiety, substance misuse, and suicide attempts. The shooting not only targeted LGBTQ people but it also took place during Latin Pride Night meaning many of the victims and casualties were LGBTQ Latinx. The resulting psychological impacts of the Pulse Nightclub shooting on those directly impacted, people who are LGBTQ Latinx, and individuals in the wider LGBTQ community have been investigated and show experiences of trauma and impacts on perceived safety [ 50 ]. At the time of the shooting, the Orlando VAMC had established relationships with LGBTQ local mental health services and had staff knowledgeable in the needs of this community [ 51 ]. In fact, in the recent past, the VA has increased its efforts to ensure Veterans who are LGBTQ receive the highest quality patient-centered care possible [ 52 ]. Mental health services in particular have bolstered recognition of the complex needs of these Veterans [ 52 ].
All three cases demonstrate innovative ways VA can provide behavioral health support outside of their facilities, i.e., via telehealth capabilities across an ocean and into a healthcare clinic, teams of mobile units reaching directly into the community to support victims, victims’ families, and the community at large, and finally by incorporating PFA teams directly into hospitals to support staff, patients, and patients’ families. This flexibility across sites to address different needs and populations while using varying available infrastructure support, is paramount to any local jurisdiction’s ability to meet on the ground needs following a disaster. It demonstrates the variability between VAMCs and the importance of local disaster behavioral health planning teams to pre-identify resources to assess local capacity. Plans can then be developed that access and deploy the tools/skills of interdisciplinary and interagency teams. Building processes to deploy local health and mental health practitioners can lead to more rapid implementation of interventions and help ensure the diversity of the impacted community is recognized and respected. Additional studies focused on how communities develop disaster behavioral health plans could provide insight into which agencies are involved and how they collaborate. It may also be useful to assess whether and how these plans are implemented to identify best practices.
In addition to the people directly impacted by disasters, respondents underscored the importance of offering support to responders as well. There is growing recognition that health care workers are themselves front-line response workers who may be psychologically impacted when caring for others, leading to a growing emphasis on the importance of selfcare and employee wellbeing [ 39 , 40 , 41 , 42 ]. In all three case studies, behavioral health support was, at least in part, directed toward healthcare workers. In the case of Las Vegas, a respondent highlighted the advantage of having behavioral health support come from individuals who understood the culture of the population they were helping, e.g., nurses supporting nurses. Further, respondents in Las Vegas and Orlando highlighted the importance of supporting deployed behavioral health team members. They detailed actions to maintain staff well-being by having rotating shifts, encouraging peer support, and facilitating gatherings for staff to publicly thank them for their efforts and allow them to address their experiences together as a group. Understanding the needs of healthcare and behavioral health personnel and building support networks into response frameworks can help better sustain and strengthen the overall response process.
A primary limitation of this study is that interviews were conducted up to one and a half years after the disasters described, potentially impacting recall. However, multiple interviewees corroborated the information presented for each of the case studies. Another limitation is that this study focused exclusively on the experiences of VA employees fulfilling mission requirements and their description of instances where VA acted in support of the Fourth Mission. Very few of the respondents directly provided the behavioral health interventions. These perspectives could provide deeper understanding of the interventions themselves as well as the impacts they may have on practitioners. Neither community members nor coalition partners were interviewed in this study. Future research would benefit from both interviewing non-VA participants to explore additional perspectives and gain greater insight on how local jurisdictions experienced collaborating with VA representatives and exploring alternative approaches to mental health units within and outside VA to examine whether and when different approaches may be preferable.
As the largest integrated healthcare system in the United States, VA can play an important role in disaster response across the country. As recognition of VA’s expertise in behavioral health grows, particularly around trauma and post-trauma treatment, VA should be considered a strong potential partner in behavioral health responses. Local VAMC staff are part of the community in which they live and the Veterans they serve are a microcosm of the larger population of the U.S. As the respondents in this study showed, there is a deep desire by VA staff to provide support following a disaster if they are able. Anticipating potential behavioral health concerns, and having a plan to address them, can foster community disaster resilience. While these plans may be different for each jurisdiction, they can be strengthened by identifying and incorporating a range of partners. Having preexisting relationships where VA’s capabilities are known before a disaster occurs can facilitate the rapid deployment of VA resources into identified areas of community need. The case studies presented demonstrate the flexible nature of these resources. By extending knowledge about innovative ways to share behavioral health and other resources in a disaster response, communities and healthcare coalitions can be better prepared to engage collectively and rapidly mobilize essential assets to support the wellbeing of those who need it most.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Crisis Counseling Assistance and Training Program
U.S. Department of Veterans Affairs
Veterans Health Administration
VA Medical Center
VA Pacific Island Healthcare System
VA Southern Nevada HCS
Veterans Health Administration Health Care System
Veterans Integrated Service Network
Office of Emergency Management
US Department of Health and Human Services
Federal Emergency Management Agency
Lesbian Gay Bisexual Transgender Queer
Multi-Agency Coordination Center
Psychological First Aid
Employee Assistance Program
Personal Protective Equipment
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–20. https://doi.org/10.1016/S0140-6736(20)30460-8 .
Article CAS PubMed PubMed Central Google Scholar
Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry. 2020;63(1):e32. https://doi.org/10.1192/j.eurpsy.2020.35 .
Article CAS PubMed Google Scholar
Pfefferbaum B, North CS. Mental health and the COVID-19 pandemic. N Engl J Med. 2020;383(6):510–2. https://doi.org/10.1056/NEJMp2008017 .
Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. https://doi.org/10.1136/gpsych-2020-100213 .
Article PubMed PubMed Central Google Scholar
Vigo D, Patten S, Pajer K, Krausz M, Taylor S, Rush B, et al. Mental health of communities during the COVID-19 pandemic. Can J Psychiatr. 2020. https://doi.org/10.1177/0706743720926676 .
Beaglehole B, Mulder RT, Frampton CM, Boden JM, Newton-Howes G, Bell CJ. Psychological distress and psychiatric disorder after natural disasters: systematic review and meta-analysis. Br J Psychiatry. 2018;213(6):716–22. https://doi.org/10.1192/bjp.2018.210 .
Article PubMed Google Scholar
Beinecke R, Raymond A, Cisse M, Renna K, Khan S, Fuller A, et al. The mental health response to the Boston bombing: a three-year review. Int J Ment Health. 2017;46(2):89–124. https://doi.org/10.1080/00207411.2017.1294969 .
Article Google Scholar
Beinecke RH. Addressing the mental health needs of victims and responders to the Boston Marathon bombings. Int J Ment Health. 2014;43(2):17–34. https://doi.org/10.2753/IMH0020-7411430202 .
Dobalian A, Callis R, Davey VJ. Evolution of the Veterans Health Administration’s role in emergency management since September 11, 2001. Disaster Med Public Health Prep. 2011;5(S2):S182–4. https://doi.org/10.1001/dmp.2011.61 .
Heslin KC, Stein JA, Dobalian A, Simon B, Lanto AB, Yano EM, et al. Alcohol problems as a risk factor for postdisaster depressed mood among U.S. veterans. Psychol Addict Behav. 2013;27(1):207–13. https://doi.org/10.1037/a0030637 .
Hobfoll SE, Watson P, Bell CC, Bryant RA, Brymer MJ, Friedman MJ, et al. Five essential elements of immediate and mid-term mass trauma intervention: empirical evidence. Psychiatry. 2007;70(4):283–337. https://doi.org/10.1521/psyc.2007.70.4.283 .
Jacobs J, Oosterbeek M, Tummers LG, Noordegraaf M, Yzermans CJ, Duckers MLA. The organization of post-disaster psychosocial support in the Netherlands: a meta-synthesis. Eur J Psychotraumatol. 2019;10(1):1544024. https://doi.org/10.1080/20008198.2018.1544024 .
North CS, Pfefferbaum B. Mental health response to community disasters: a systematic review. JAMA. 2013;310(5):507–18. https://doi.org/10.1001/jama.2013.107799 .
Watson PJ, Ruzek JI. Academic/state/federal collaborations and the improvement of practices in disaster mental health services and evaluation. Admin Pol Ment Health. 2009;36(3):215–20. https://doi.org/10.1007/s10488-009-0212-4 .
Thordardottir EB, Gudmundsdottir B, Petursdottir G, Valdimarsdottir UA, Hauksdottir A. Psychosocial support after natural disasters in Iceland-implementation and utilization. Int J Disaster Risk Reduction. 2018;27:642–8. https://doi.org/10.1016/j.ijdrr.2017.11.006 .
Fergusson DM, Horwood LJ, Boden JM, Mulder RT. Impact of a major disaster on the mental health of a well-studied cohort. JAMA Psychiatry. 2014;71(9):1025–31. https://doi.org/10.1001/jamapsychiatry.2014.652 .
Gray L, MacDonald C, Mackie B, Paton D, Johnston D, Baker MG. Community responses to communication campaigns for influenza A (H1N1): a focus group study. BMC Public Health. 2012;12(1):1–12.
Compton MT, Cibulas BK, Gard B, Kaslow NJ, Kotwicki RJ, Reissman DB, et al. Incorporating community mental health into local bioterrorism response planning: experiences from the DeKalb County Board of Health. Community Ment Health J. 2005;41(6):647–63. https://doi.org/10.1007/s10597-005-8846-5 .
Pfefferbaum B, Flynn BW, Schonfeld D, Brown LM, Jacobs GA, Dodgen D, et al. The integration of mental and behavioral health into disaster preparedness, response, and recovery. Disaster Med Public Health Prep. 2012;6(1):60–6. https://doi.org/10.1001/dmp.2012.1 .
Elrod CL, Hamblen JL, Norris FH. Challenges in implementing disaster mental health programs: state program directors’ perspectives. Ann Am Acad Pol Soc Sci. 2016;604(1):152–70.
Gil-Rivas V, Kilmer RP. Building community capacity and fostering disaster resilience. J Clin Psychol. 2016;72(12):1318–32. https://doi.org/10.1002/jclp.22281 .
Melmer P, Carlin M, Castater CA, Koganti D, Hurst SD, Tracy BM, et al. Mass casualty shootings and emergency preparedness: a multidisciplinary approach for an unpredictable event. J Multidiscip Healthc. 2019;12:1013–21. https://doi.org/10.2147/JMDH.S219021 .
Naturale A, Lowney LT, Brito CS. Lessons learned from the Boston Marathon bombing victim services program. Clin Soc Work J. 2017;45(2):111–23. https://doi.org/10.1007/s10615-017-0624-7 .
Reifels L, Pietrantoni L, Prati G, Kim Y, Kilpatrick DG, Dyb G, et al. Lessons learned about psychosocial responses to disaster and mass trauma: an international perspective. Eur J Psychotraumatol. 2013;4.
Dobalian A. The US Department of veterans affairs and sustainable health care coalitions. Disaster Med Public Health Prep. 2015;9(6):726–7. https://doi.org/10.1017/dmp.2015.136 .
Schmitz S, Wyte-Lake T, Dobalian A. Facilitators and barriers to preparedness partnerships: a veterans affairs medical center perspective. Disaster Med Public Health Prep. 2018;12(4):431–6. https://doi.org/10.1017/dmp.2017.92 .
VA Fourth Mission Summary [ https://www.va.gov/health/coronavirus/statesupport.asp ].
Office of Public and Intergovernmental Affairs [ https://www.va.gov/opa/pressrel/searchResults.cfm ].
Affairs USDoV: VA Office of mental health and suicide prevention guidebook. 2018.
Google Scholar
Lawrence Q. VA secretary Wilkie: ‘We are the surge force’. In: The coronavirus crisis: NPR. NPR.org ; 2020.
Services UDoHH. HHS, FEMA, DOD and VA continue to provide sustained and critical medical care support for Puerto Rico as part of Trump Administration response to Hurricane Maria. In . HHS.gov News: US Department of Health & Human Services; 2017.
Steinhauer J. The V.A. Prepares to back up a health care system threatened by coronavirus: The New York Times; 2020.
Agency FEM. Super typhoon Yutu: one year later: FEMA; 2019.
Foundation NP: After-action review of the orlando fire department response to the attack at pulse nightclub. 2018.
Investigation FBo: Active shooter incidents in the United States in 2016 an 2017. 2018.
Department LVMP: 1 October after action review. 2018.
Charmaz K, Belgrave LL. Grounded theory: The Blackwell Encyclopedia of Sociology; 2007. https://doi.org/10.1002/9781405165518.wbeosg070 .
Lowe SR, Galea S. The mental health consequences of mass shootings. Trauma Violence Abuse. 2017;18(1):62–82. https://doi.org/10.1177/1524838015591572 .
Department of Veterans Affairs. National incident management system compliance: VHA Directive 0320.12(1): Administration VH. Washington, DC; 2021.
Veterans Health Administration. COVID-19 response plan: Management OoE; 2020.
US Department of Defense DoVA, Department of Health & Human Services. Interagency task force on military and veterans mental health; 2017. p. 1–31.
National Academies of Sciences E, and Medicine, Health and Medicine Division, Board on Health Care Services, Committee to Evaluate the Department of Veterans Affairs Mental Health Services. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies Press (US); 2018.
Subica AM, Aitaoto N, Link BG, Yamada AM, Henwood BF, Sullivan G. Mental health status, need, and unmet need for mental health services among U.S. Pacific islanders. Psychiatr Serv. 2019;70(7):578–85. https://doi.org/10.1176/appi.ps.201800455 .
Buettner K, Sablan J, Funk M, Arriola, J, Price, S, Sugiura, K, Diminic S, Drew N. WHO profile on mental health in development (WHO proMIND): Commonwealth of the Northern Mariana Islands. Geneva, World Health Organization; 2013. https://apps.who.int/iris/bitstream/handle/10665/85304/9789241505741_eng.pdf;jsessionid=A222F532F705877A650948706A437484 . Accessed 26 Mar 2021.
Mental health in the Asian Americans/Pacific Islander Community [ https://www.amsa.org/2020/09/04/mental-health-in-the-asian-americans-pacific-islander-community/#:~:text=Mental%20Health%20of%20Pacific%20Islanders&text=According%20to%20a%202019%20study%20for%20the%20general%20US%20population ].
Alessi EJ. Acknowledging the impact of social forces on sexual minority clients: introduction to the special issue on clinical practice with LGBTQ populations: Springer; 2013.
Veteran Population [ https://www.va.gov/vetdata/veteran_population.asp ].
Ussher JM. Heterocentric practices in health research and health care: implications for mental health and subjectivity of LGBTQ individuals. Fem Psychol. 2009;19(4):561–7. https://doi.org/10.1177/0959353509342933 .
LGBTQI [ https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQI ].
Stults CB, Kupprat SA, Krause KD, Kapadia F, Halkitis PN. Perceptions of safety among LGBTQ people following the 2016 pulse nightclub shooting. Psychol Sex Orientat Gend Divers. 2017;4(3):251–6. https://doi.org/10.1037/sgd0000240 .
Lesbian, Gay, Bisexual and Transgender Veteran Care [ https://www.orlando.va.gov/services/lgbt/index.asp ].
National Academies of Sciences E, and Medicine. Evaluation of the Department of Veterans Affairs Mental Health Services: National Academies of Sciences E, and Medicine; 2018.
Download references
Acknowledgements
Not applicable.
This work was supported by the US Department of Veterans Affairs, Veterans Health Administration, Office of Emergency Management and the Office of Population Health. The views expressed in this presentation are those of the author and do not necessarily reflect the position or policy of the VA or the US government.
Author information
Authors and affiliations.
Department of Veterans Affairs, Veterans Emergency Management Evaluation Center (VEMEC), 16111 Plummer St. MS-152, North Hills, CA, 91343, USA
Tamar Wyte-Lake, Susan Schmitz & Aram Dobalian
Department of Family Medicine, Oregon Health & Science University, 3181 SW Sam Jackson Park Rd, Portland, OR, 97239, USA
Tamar Wyte-Lake
Orlando VA Medical Center, 13800 Veterans Way, Orlando, FL, 32728, USA
Reginald J. Kornegay
VA Southern Nevada Healthcare System, 6900 N. Pecos Road, North Las Vegas, NV, 89086, USA
Felix Acevedo
Division of Health Systems Management and Policy, University of Memphis School of Public Health, Memphis, TN, USA
Aram Dobalian
You can also search for this author in PubMed Google Scholar
Contributions
TWL and SS planned the study, including instrumentation, conducted the data analysis, and wrote the paper. RJK and FA supported the qualitative analysis and contributed to revising the paper. AD helped to plan the study and contributed to revising the manuscript. All authors have read and approved the manuscript.
Corresponding author
Correspondence to Tamar Wyte-Lake .
Ethics declarations
Ethics approval and consent to participate.
The Greater Los Angeles VA Healthcare System Institutional Review Board (Los Angeles, CA USA) approved this study. As the research presented no more than minimal risk of harm to subjects and involved no procedures for which written consent would be normally required outside of the research context, the study received a waiver for documentation of consent from the Institutional Review Board, and verbal, recorded audio consent was approved.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1..
2017 Disaster Qualitative Study: Collaboration Project Interview Guide. Interview guide utilized during project’s semi-structured interviews.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Wyte-Lake, T., Schmitz, S., Kornegay, R.J. et al. Three case studies of community behavioral health support from the US Department of Veterans Affairs after disasters. BMC Public Health 21 , 639 (2021). https://doi.org/10.1186/s12889-021-10650-x
Download citation
Received : 05 August 2020
Accepted : 18 March 2021
Published : 01 April 2021
DOI : https://doi.org/10.1186/s12889-021-10650-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Emergency preparedness
- Behavioral health; disaster response
- US Department of Veterans Affairs
BMC Public Health
ISSN: 1471-2458
- Submission enquiries: [email protected]
- General enquiries: [email protected]
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Review Article
- Published: 03 October 2022
How COVID-19 shaped mental health: from infection to pandemic effects
- Brenda W. J. H. Penninx ORCID: orcid.org/0000-0001-7779-9672 1 , 2 ,
- Michael E. Benros ORCID: orcid.org/0000-0003-4939-9465 3 , 4 ,
- Robyn S. Klein 5 &
- Christiaan H. Vinkers ORCID: orcid.org/0000-0003-3698-0744 1 , 2
Nature Medicine volume 28 , pages 2027–2037 ( 2022 ) Cite this article
39k Accesses
125 Citations
491 Altmetric
Metrics details
- Epidemiology
- Infectious diseases
- Neurological manifestations
- Psychiatric disorders
The Coronavirus Disease 2019 (COVID-19) pandemic has threatened global mental health, both indirectly via disruptive societal changes and directly via neuropsychiatric sequelae after SARS-CoV-2 infection. Despite a small increase in self-reported mental health problems, this has (so far) not translated into objectively measurable increased rates of mental disorders, self-harm or suicide rates at the population level. This could suggest effective resilience and adaptation, but there is substantial heterogeneity among subgroups, and time-lag effects may also exist. With regard to COVID-19 itself, both acute and post-acute neuropsychiatric sequelae have become apparent, with high prevalence of fatigue, cognitive impairments and anxiety and depressive symptoms, even months after infection. To understand how COVID-19 continues to shape mental health in the longer term, fine-grained, well-controlled longitudinal data at the (neuro)biological, individual and societal levels remain essential. For future pandemics, policymakers and clinicians should prioritize mental health from the outset to identify and protect those at risk and promote long-term resilience.
Similar content being viewed by others

A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
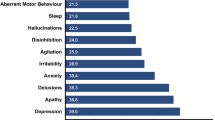
The effects of the COVID-19 pandemic on neuropsychiatric symptoms in dementia and carer mental health: an international multicentre study
In 2019, the COVID-19 outbreak was declared a pandemic by the World Health Organization (WHO), with 590 million confirmed cases and 6.4 million deaths worldwide as of August 2022 (ref. 1 ). To contain the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) across the globe, many national and local governments implemented often drastic restrictions as preventive health measures. Consequently, the pandemic has not only led to potential SARS-CoV-2 exposure, infection and disease but also to a wide range of policies consisting of mask requirements, quarantines, lockdowns, physical distancing and closure of non-essential services, with unprecedented societal and economic consequences.
As the world is slowly gaining control over COVID-19, it is timely and essential to ask how the pandemic has affected global mental health. Indirect effects include stress-evoking and disruptive societal changes, which may detrimentally affect mental health in the general population. Direct effects include SARS-CoV-2-mediated acute and long-lasting neuropsychiatric sequelae in affected individuals that occur during primary infection or as part of post-acute COVID syndrome (PACS) 2 —defined as symptoms lasting beyond 3–4 weeks that can involve multiple organs, including the brain. Several terminologies exist for characterizing the effects of COVID-19. PACS also includes late sequalae that constitute a clinical diagnosis of ‘long COVID’ where persistent symptoms are still present 12 weeks after initial infection and cannot be attributed to other conditions 3 .
Here we review both the direct and indirect effects of COVID-19 on mental health. First, we summarize empirical findings on how the COVID-19 pandemic has impacted population mental health, through mental health symptom reports, mental disorder prevalence and suicide rates. Second, we describe mental health sequalae of SARS-CoV-2 virus infection and COVID-19 disease (for example, cognitive impairment, fatigue and affective symptoms). For this, we use the term PACS for neuropsychiatric consequences beyond the acute period, and will also describe the underlying neurobiological impact on brain structure and function. We conclude with a discussion of the lessons learned and knowledge gaps that need to be further addressed.
Impact of the COVID-19 pandemic on population mental health
Independent of the pandemic, mental disorders are known to be prevalent globally and cause a very high disease burden 4 , 5 , 6 . For most common mental disorders (including major depressive disorder, anxiety disorders and alcohol use disorder), environmental stressors play a major etiological role. Disruptive and unpredictable pandemic circumstances may increase distress levels in many individuals, at least temporarily. However, it should be noted that the pandemic not only resulted in negative stressors but also in positive and potentially buffering changes for some, including a better work–life balance, improved family dynamics and enhanced feelings of closeness 7 .
Awareness of the potential mental health impact of the COVID-19 pandemic is reflected in the more than 35,000 papers published on this topic. However, this rapid research output comes with a cost: conclusions from many papers are limited due to small sample sizes, convenience sampling with unclear generalizability implications and lack of a pre-COVID-19 comparison. More reliable estimates of the pandemic mental health impact come from studies with longitudinal or time-series designs that include a pre-pandemic comparison. In our description of the evidence, we, therefore, explicitly focused on findings from meta-analyses that include longitudinal studies with data before the pandemic, as recently identified through a systematic literature search by the WHO 8 .
Self-reported mental health problems
Most studies examining the pandemic impact on mental health used online data collection methods to measure self-reported common indicators, such as mood, anxiety or general psychological distress. Pooled prevalence estimates of clinically relevant high levels of depression and anxiety symptoms during the COVID-19 pandemic range widely—between 20% and 35% 9 , 10 , 11 , 12 —but are difficult to interpret due to large methodological and sample heterogeneity. It also is important to note that high levels of self-reported mental health problems identify increased vulnerability and signal an increased risk for mental disorders, but they do not equal clinical caseness levels, which are generally much lower.
Three meta-analyses, pooling data from between 11 and 61 studies and involving ~50,000 individuals or more 13 , 14 , 15 , compared levels of self-reported mental health problems during the COVID-19 pandemic with those before the pandemic. Meta-analyses report on pooled effect sizes—that is, weighted averages of study-level effect sizes; these are generally considered small when they are ~0.2, moderate when ~0.5 and large when ~0.8. As shown in Table 1 , meta-analyses on mental health impact of the COVID-19 pandemic reach consistent conclusions and indicate that there has been a heterogeneous, statistically significant but small increase in self-reported mental health problems, with pooled effect sizes ranging from 0.07 to 0.27. The largest symptom increase was found when using specific mental health outcome measures assessing depression or anxiety symptoms. In addition, loneliness—a strong correlate of depression and anxiety—showed a small but significant increase during the pandemic (Table 1 ; effect size = 0.27) 16 . In contrast, self-reported general mental health and well-being indicators did not show significant change, and psychotic symptoms seemed to have decreased slightly 13 . In Europe, alcohol purchase decreased, but high-level drinking patterns solidified among those with pre-pandemic high drinking levels 17 . When compared to pre-COVID levels, no change in self-reported alcohol use (effect size = −0.01) was observed in a recent meta-analysis summarizing 128 studies from 58 (predominantly European and North American) countries 18 .
What is the time trajectory of self-reported mental health problems during the pandemic? Although findings are not uniform, various large-scale studies confirmed that the increase in mental health problems was highest during the first peak months of the pandemic and smaller—but not fully gone—in subsequent months when infection rates declined and social restrictions eased 13 , 19 , 20 . Psychological distress reports in the United Kingdom increased again during the second lockdown period 15 . Direct associations between anxiety and depression symptom levels and the average number of daily COVID-19 cases were confirmed in the US Centers for Disease Control and Prevention (CDC) data 21 . Studies that examined longer-term trajectories of symptoms during the first or even second year of the COVID-19 pandemic are more sparse but revealed stability of symptoms without clear evidence of recovery 15 , 22 . The exception appears to be for loneliness, as some studies confirmed further increasing trends throughout the first COVID-19 pandemic year 22 , 23 . As most published population-based studies were conducted in the early time period in which absolute numbers of SARS-CoV2-infected individuals were still low, the mental health impacts described in such studies are most likely due to indirect rather than direct effects of SARS-CoV-2 infection. However, it is possible that, in longer-term or later studies, these direct and indirect effects may be more intertwined.
The extent to which governmental policies and communication have impacted on population mental health is a relevant question. In cross-country comparisons, the extent of social restrictions showed a dose–response relationship with mental health problems 24 , 25 . In a review of 33 studies worldwide, it was concluded that governments that enacted stringent measures to contain the spread of COVID-19 benefitted not only the physical but also the mental health of their population during the pandemic 26 , even though more stringent policies may lead to more short-term mental distress 25 . It has been suggested that effective communication of risks, choices and policy measures may reduce polarization and conspiracy theories and mitigate the mental health impact of such measures 25 , 27 , 28 .
In sum, the general pattern of results is that of an increase in mental health symptoms in the population, especially during the first pandemic months, that remained elevated throughout 2020 and early 2021. It should be emphasized that this increase has a small effect size. However, even a small upward shift in mental health problems warrants attention as it has not yet shown to be returned to pre-pandemic levels, and it may have meaningful cumulative consequences at the population level. In addition, even a small effect size may mask a substantial heterogeneity in mental health impact, which may have affected vulnerable groups disproportionally (see below).
Mental disorders, self-harm and suicide
Whether the observed increase in mental health problems during the COVID-19 pandemic has translated into more mental disorders or even suicide mortality is not easy to answer. Mental disorders, characterized by more severe, disabling and persistent symptoms than self-reported mental health problems, are usually diagnosed by a clinician based on the International Classification of Diseases, 10th Revision (ICD-10) or the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria or with validated semi-structured clinical interviews. However, during the COVID-19 pandemic, research systematically examining the population prevalence of mental disorders has been sparse. Unfortunately, we can also not strongly rely on healthcare use studies as the pandemic impacted on healthcare provision more broadly, thereby making figures of patient admissions difficult to interpret.
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic has led to a 28% (95% uncertainty interval (UI): 25–30) increase in major depressive disorders and a 26% (95% UI: 23–28) increase in anxiety disorders. It should be noted that these estimations come with high uncertainty as the assumption that transient pandemic-related increases in mental symptoms extrapolate into incident mental disorders remains disputable. So far, only four longitudinal population-based studies have measured and compared current mental (that is, depressive and anxiety) disorder prevalence—defined using psychiatric diagnostic criteria—before and during the pandemic. Of these, two found no change 30 , 31 , one found a decrease 32 and one found an increase in prevalence of these disorders 33 . These studies were local, limited to high-income countries, often small-scale and used different modes of assessment (for example, online versus in-person) before and during the pandemic. This renders these observational results uncertain as well, but their contrast to the GBD calculations 29 is striking.
Time-series analysis of monthly suicide trends in 21 middle-income to high-income countries across the globe yielded no evidence for an increase in suicide rates in the first 4 months of the pandemic, and there was evidence of a fall in rates in 12 countries 34 . Also in the United States, there was a significant decrease in suicide mortality in the first pandemic months but a slight increase in mortality due to drug overdose and homicide 35 . A living systematic review 36 also concluded that, throughout 2020, there was no observed increase in suicide rates in 20 studies conducted in North America, Europe and Asia. Analyses of electronic health record data in the primary care setting showed reduced rates of self-harm during the first COVID-19 pandemic year 37 . In contrast, emergency department visits for self-harm behavior were unchanged 38 or increased 39 . Such inconsistent findings across healthcare settings may reflect a reluctance in healthcare-seeking behavior for mental healthcare issues. In the living systematic review, eight of 11 studies that examined service use data found a significant decrease in reported self-harm/suicide attempts after COVID lockdown, which returned to pre-lockdown levels in some studies with longer follow-up (5 months) 36 .
In sum, although calculations based on survey data predict a global increase of mental disorder prevalence, objective and consistent evidence for an increased mental disorder, self-harm or suicide prevalence or incidence during the first pandemic year remains absent. This observation, coupled with the only small increase in mental health symptom levels in the overall population, may suggest that most of the general population has demonstrated remarkable resilience and adaptation. However, alternative interpretations are possible. First, there is a large degree of heterogeneity in the mental health impact of COVID-19, and increased mental health in one group (for example, due to better work–family balance and work flexibility) may have masked mental health problems in others. Various societal responses seen in many countries, such as community support activities and bolstering mental health and crisis services, may have had mitigating effects on the mental health burden. Also, the relationship between mental health symptom increases during stressful periods and its subsequent effects on the incidence of mental disorders may be non-linear or could be less visible due to resulting alternative outcomes, such as drug overdose or homicide. Finally, we cannot rule out a lag-time effect, where disorders may take more time to develop or be picked up, especially because some of the personal financial or social consequences of the COVID pandemic may only become apparent later. It should be noted that data from low-income countries and longer-term studies beyond the first pandemic year are largely absent.
Which individuals are most affected by the COVID-19 pandemic?
There is substantial heterogeneity across studies that evaluated how the COVID pandemic impacted on mental health 13 , 14 , 15 . Although our society as a whole may have the ability to adequately bounce back from pandemic effects, there are vulnerable people who have been affected more than others.
First, women have consistently reported larger increases in mental health problems in response to the COVID-19 pandemic than men 13 , 15 , 29 , 40 , with meta-analytic effect sizes being 44% 15 to 75% 13 higher. This could reflect both higher stress vulnerability or larger daily life disruptions due to, for example, increased childcare responsibilities, exposure to home violence or greater economic impact due to employment disruptions that all disproportionately fell to women 41 , thereby exacerbating the already existing pre-pandemic gender inequalities in depression and anxiety levels. In addition, adolescents and young adults have been disproportionately affected compared to younger children and older adults 12 , 15 , 29 , 40 . This may be the result of unfavorable behavioral and social changes (for example, school closure periods 42 ) during a crucial development phase where social interactions outside the family context are pivotal. Alarmingly, even though suicide rates did not seem to increase at the population level, studies in China 43 and Japan 44 indicated significant increases in suicide rates in children and adolescents.
Existing socio-cultural disparities in mental health may have further widened during the COVID pandemic. Whether the impact is larger for individuals with low socio-economic status remains unclear, with contrasting meta-analyses pointing toward this group being protected 15 or at increased risk 40 . Earlier meta-analyses did not find that the mental health impact of COVID-19 differed across Europe, North America, Asia and Oceania 13 , 14 , but data are lacking from Africa and South America. Nevertheless, a large-scale within-country comparison in the United States found that the mental health of Black, Hispanic and Asian respondents worsened relatively more during the pandemic compared to White respondents. Moreover, White respondents were more likely to receive professional mental healthcare during the pandemic, and, conversely, Black, Hispanic, and Asian respondents demonstrated higher levels of unmet mental healthcare needs during this time 45 .
People with pre-existing somatic conditions represent another vulnerable group in which the pandemic had a greater impact (pooled effect size of 0.25) 13 . This includes people with conditions such as epilepsy, multiple sclerosis or cardiometabolic disease as well as those with multiple comorbidities. The disproportionate impact may reflect this groupʼs elevated COVID-19 risk and, consequently, more perceived stress and fear of infection, but it could also reflect disruptions of regular healthcare services.
Healthcare workers faced increased workload, rapidly changing and challenging work environments and exposure to infections and death, accompanied by fear of infecting themselves and their families. High prevalences of (subthreshold) depression (13% 46 ), depressive symptoms (31% 47 ), (subthreshold) anxiety (16% 46 ), anxiety symptoms (23% 47 ) and post-traumatic stress disorder (~22% 46 , 47 ) have been reported in healthcare workers. However, a meta-analysis did not find a larger mental health impact of the pandemic as compared to the general population 40 , and another meta-analysis (of 206 studies) found that the mental health status of healthcare workers was similar to or even better than that of the general population during the first COVID year 48 . However, it is important to note that these meta-analyses could not differentiate between frontline and non-frontline healthcare workers.
Finally, individuals with pre-existing mental disorders may be at increased risk for exacerbation of mental ill-health during the pandemic, possibly due to disease history—illustrating a higher genetic and/or environmental vulnerability—but also due to discontinuity of mental healthcare. Already before the pandemic, mental health systems were under-resourced and disorganized in most countries 6 , 49 , but a third of all WHO member states reported disruptions to mental and substance use services during the first 18 months of the pandemic 50 , with reduced, shortened or postponed appointments and limited capacity for acute inpatient admissions 51 , 52 . Despite this, there is no clear evidence that individuals with pre-existing mental disorders are disproportionately affected by pandemic-related societal disruptions; the effect size for pandemic impact on self-reported mental health problems was similar in psychiatric patients and the general population 13 . In the United States, emergency visits for ten different mental disorders were generally stable during the pandemic compared to earlier periods 53 . In a large Dutch study 22 , 54 with multiple pre-pandemic and during-pandemic assessments, there was no difference in symptom increase among patients relative to controls (see Fig. 1 for illustration). In absolute terms, however, it is important to note that psychiatric patients show much higher symptom levels of depression, anxiety, loneliness and COVID-fear than healthy controls. Again, variation in mental health changes during the pandemic is large: next to psychiatric patients who showed symptom decrease due to, for example, experiencing relief from social pressures, there certainly have been many patients with symptom increases and relapses during the pandemic.
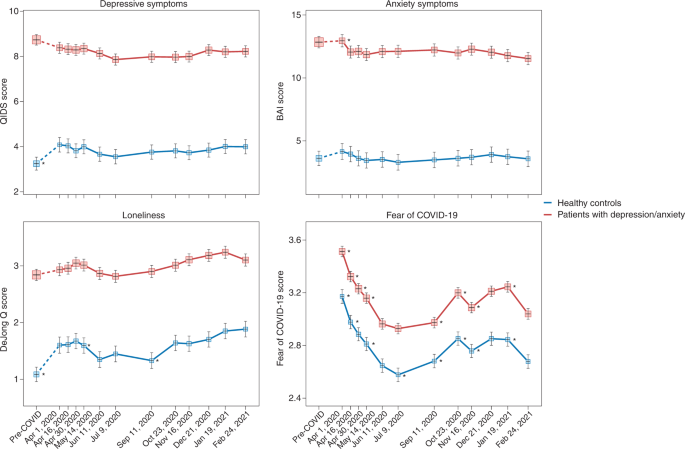
Trajectories of mean depressive symptoms (QIDS score), anxiety symptoms (BAI score), loneliness (De Jong questionnaire score) and Fear of COVID-19 score before and during the first year of the COVID-19 pandemic in healthy controls (blue line, n = 378) and in patients with depressive and/or anxiety disorders (red line, n = 908). The x -axis indicates time with one pre-COVID assessment (averaged over up to five earlier assessments conducted between 2006 and 2019) and 11 online assessments during April 2020 through February 2021. Symbols indicate the mean score during the assessment with 95% CIs. As compared to pre-COVID assessment scores, the figure shows a statistically significant increase of depression and loneliness symptoms during the first pandemic peak (April 2020) in healthy controls but not in patients (for more details, see refs. 22 , 54 ). Asterisks indicate where subsequent wave scores differ from the prior wave scores ( P < 0.05). The figure also illustrates the stability of depressive and anxiety symptoms during the first COVID year, a significant increase in loneliness during this period and fluctuations of Fear of COVID-19 score that positively correlate with infection rates in the Netherlands. Raw data are from the Netherlands Study of Depression and Anxiety (NESDA), which were re-analyzed for the current plots to illustrate differences between two groups (healthy controls versus patients). BAI, Beck Anxiety Inventory; QIDS, Quick Inventory of Depressive Symptoms.
Impact of COVID-19 infection and disease on mental health and the brain
Not only the pandemic but also COVID-19 itself can have severe impact on the mental health of affected individuals and, thus, of the population at large. Below we describe acute and post-acute neuropsychiatric sequelae seen in patients with COVID-19 and link these to neurobiological mechanisms.
Neuropsychiatric sequelae in individuals with COVID-19
Common symptoms associated with acute SARS-CoV-2 infection include headache, anosmia (loss of sense of smell) and dysgeusia (loss of sense of taste). The broader neuropsychiatric impact is dependent on infection severity and is very heterogeneous (Table 2 ). It ranges from no neuropsychiatric symptoms among the large group of asymptomatic COVID-19 cases to milder transient neuropsychiatric symptoms, such as fatigue, sleep disturbance and cognitive impairment, predominantly occurring among symptomatic patients with COVID-19 (ref. 55 ). Cognitive impairment consists of sustained memory impairments and executive dysfunction, including short-term memory loss, concentration problems, word-finding problems and impaired daily problem-solving, colloquially termed ‘brain fog’ by patients and clinicians. A small number of infected individuals become severely ill and require hospitalization. During hospital admission, the predominant neuropsychiatric outcome is delirium 56 . Delirium occurs among one-third of hospitalized patients with COVID-19 and among over half of patients with COVID-19 who require intensive care unit (ICU) treatment. These delirium rates seem similar to those observed among individuals with severe illness hospitalized for other general medical conditions 57 . Delirium is associated with neuropsychiatric sequalae after hospitalization, as part of post-intensive care syndrome 58 , in which sepsis and inflammation are associated with cognitive dysfunction and an increased risk of a broad range of psychiatric symptoms, from anxiety to depression and psychotic symptoms with hallucinations 59 , 60 .
A subset of patients with COVID-19 develop PACS 61 , which can include neuropsychiatric symptoms. A large meta-analysis summarizes 51 studies involving 18,917 patients with a mean follow-up of 77 days (range, 14–182 days) 62 . The most prevalent neuropsychiatric symptom associated with COVID-19 was sleep disturbance, with a pooled prevalence of 27.4%, followed by fatigue (24.4%), cognitive impairment (20.2%), anxiety symptoms (19.1%), post-traumatic stress symptoms (15.7%) and depression symptoms (12.9%) (Table 2 ). Another meta-analysis that assessed patients 12 weeks or more after confirmed COVID-19 diagnosis found that 32% experienced fatigue, and 22% experienced cognitive impairment 63 . To what extent neuropsychiatric symptoms are truly unique for patients with COVID remains unclear from these meta-analyses, as hardly any study included well-matched controls with other types of respiratory infections or inflammatory conditions.
Studies based on electronic health records have examined whether higher levels of neuropsychiatric symptoms truly translate into a higher incidence of clinically overt mental disorders 64 , 65 . In a 1-year follow-up using the US Veterans Affairs database, 153,848 survivors of SARS-CoV-2 infection exhibited an increased incidence of any mental disorder with a relative risk of 1.46 and, specifically, 1.35 for anxiety disorders, 1.39 for depressive disorders and 1.38 for stress and adjustment disorders, compared to a contemporary group and a historical control group ( n = 5,859,251) 65 . In absolute numbers, the incident risk difference attributable to SARS-CoV-2 for mental disorders was 64 per 1,000 individuals. Taquet et al. 64 analyzed electronic health records from the US-based TriNetX network with over 81 million patients and 236,379 COVID-19 survivors followed for 6 months. In absolute numbers, 6-month incidence of hospital contacts related to diagnoses of anxiety, affective disorder or psychotic disorder was 7.0%, 4.5% and 0.4%, respectively. Risks of incident neurological or psychiatric diagnoses were directly correlated with COVID-19 severity and increased by 78% when compared to influenza and by 32% when compared to other respiratory tract infections. In contrast, a medical record study involving 8.3 million adults confirmed that neuropsychiatric disorders were significantly elevated among COVID-19 hospitalized individuals but to a similar extent as in hospitalized patients with other severe respiratory disease 66 . In line with this, a study using language processing of clinical notes in electronic health records did not find an increase in fatigue, mood and anxiety symptoms among COVID-19 hospitalized individuals when compared to hospitalized patients for other indications and adjusted for sociodemographic features and hospital course 67 . It is important to note that research based only on hospital records might be influenced by increased health-seeking behavior that could be differential across care settings or by increased follow-up by hospitals of patients with COVID-19 (compared to patients with other conditions).
Consequently, whether PACS symptoms form a unique pattern due to specific infection with SARS-CoV-2 remains debatable. Prospective case–control studies that do not rely on hospital records but measure the incidence of neuropsychiatric symptoms and diagnoses after COVID-19 are still scarce, but they are critical for distinguishing causation and confounding when characterizing PACS and the uniqueness of neuropsychiatric sequalae after COVID-19 (ref. 68 ). Recent studies with well-matched control groups illustrate that long-term consequences may not be so unique, as they were similar to those observed in patients with other diseases of similar severity, such as after acute myocardial infarction or in ICU patients 56 , 66 . A first prospective follow-up study of COVID-19 survivors and control patients matched on disease severity, age, sex and ICU admission found similar neuropsychiatric outcomes, regarding both new-onset psychiatric diagnosis (19% versus 20%) and neuropsychiatric symptoms (81% versus 93%). However, moderate but significantly worse cognitive outcomes 6 months after symptom onset were found among survivors of COVID-19 (ref. 69 ). In line with this, a longitudinal study of 785 participants from the UK Biobank showed small but significant cognitive impairment among individuals infected with SARS-CoV-2 compared to matched controls 70 .
Numerous psychosocial mechanisms can lead to neuropsychiatric sequalae of COVID-19, including functional impairment; psychological impact due to, for example, fear of dying; stress of being infected with a novel pandemic disease; isolation as part of quarantine and lack of social support; fear/guilt of spreading COVID-19 to family or community; and socioeconomic distress by lost wages 71 . However, there is also ample evidence that neurobiological mechanisms play an important role, which is discussed below.
Neurobiological mechanisms underlying neuropsychiatric sequelae of COVID-19
Acute neuropsychiatric symptoms among patients with severe COVID-19 have been found to correlate with the level of serum inflammatory markers 72 and coincide with neuroimaging findings of immune activation, including leukoencephalopathy, acute disseminated encephalomyelitis, cytotoxic lesions of the corpus callosum or cranial nerve enhancement 73 . Rare presentations, including meningitis, encephalitis, inflammatory demyelination, cerebral infarction and acute hemorrhagic necrotizing encephalopathy, have also been reported 74 . Hospitalized patients with frank encephalopathies display impaired blood-brain barrier (BBB) integrity with leptomeningeal enhancement on brain magnetic resonance images 75 . Studies of postmortem specimens from patients who succumbed to acute COVID-19 reveal significant neuropathology with signs of hypoxic damage and neuroinflammation. These include evidence of BBB permeability with extravasation of fibrinogen, microglial activation, astrogliosis, leukocyte infiltration and microhemorrhages 76 , 77 . However, it is still unclear to what extent these findings differ from patients with similar illness severity due to acute non-COVID illness, as these brain effects might not be virus-specific effects but rather due to cytokine-mediated neuroinflammation and critical illness.
Post-acute neuroimaging studies in SARS-CoV-2-recovered patients, as compared to control patients without COVID-19, reveal numerous alterations in brain structure on a group level, although effect sizes are generally small. These include minor reduction in gray matter thickness in the various regions of the cortex and within the corpus collosum, diffuse edema, increases in markers of tissue damage in regions functionally connected to the olfactory cortex and reductions in overall brain size 70 , 78 . Neuroimaging studies of post-acute COVID-19 patients also report abnormalities consistent with micro-structural and functional alterations, specifically within the hippocampus 79 , 80 , a brain region critical for memory formation and regulating anxiety, mood and stress responses, but also within gray matter areas involving the olfactory system and cingulate cortex 80 . Overall, these findings are in line with ongoing anosmia, tremors, affect problems and cognitive impairment.
Interestingly, despite findings mentioned above, there is little evidence of SARS-CoV-2 neuroinvasion with productive replication, and viral material is rarely found in the central nervous system (CNS) of patients with COVID-19 (refs. 76 , 77 , 81 ). Thus, neurobiological mechanisms of SARS-CoV-2-mediated neuropsychiatric sequelae remain unclear, especially in patients who initially present with milder forms of COVID-19. Symptomatic SARS-CoV-2 infection is associated with hypoxia, cytokine release syndrome (CRS) and dysregulated innate and adaptive immune responses (reviewed in ref. 82 ). All these effects could contribute to neuroinflammation and endothelial cell activation (Fig. 2 ). Examination of cerebrospinal fluid in patients with neuroimaging findings revealed elevated levels of pro-inflammatory, BBB-destabilizing cytokines, including interleukin-6 (IL-6), IL-1, IL-8 and mononuclear cell chemoattractants 83 , 84 . Whether these cytokines arise from the periphery, due to COVID-19-mediated CRS, or from within the CNS, is unclear. As studies generally lack control patients with other severe illnesses, the specificity of such findings to SARS-CoV-2 also remains unclear. Systemic inflammatory processes, including cytokine release, have been linked to glial activation with expression of chemoattractants that recruit immune cells, leading to neuroinflammation and injury 85 . Cerebrospinal fluid concentrations of neurofilament light, a biomarker of neuronal damage, were reportedly elevated in patients hospitalized with COVID-19 regardless of whether they exhibited neurologic diseases 86 . Acute thromboembolic events leading to ischemic infarcts are also common in patients with COVID-19 due to a potentially increased pro-coagulant process secondary to CRS 87 .
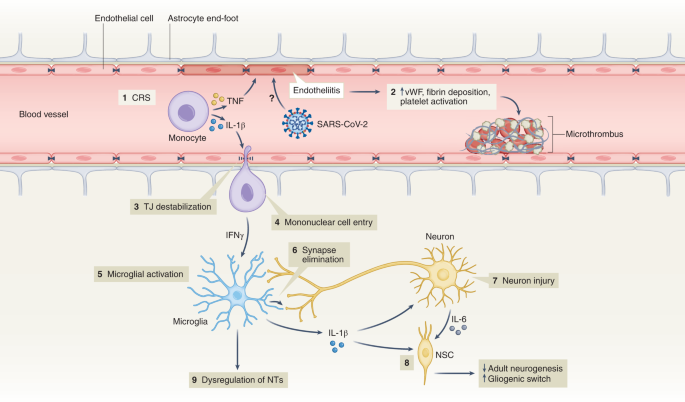
(1) Elevation of BBB-destabilizing cytokines (IL-1β and TNF) within the serum due to CRS or local interactions of mononuclear and endothelial cells. (2) Virus-induced endotheliitis increases susceptibility to microthrombus formation due to platelet activation, elevation of vWF and fibrin deposition. (3) Cytokine, mononuclear and endothelial cell interactions promote disruption of the BBB, which may allow entry of leukocytes expressing IFNg into the CNS (4), leading to microglial activation (5). (6) Activated microglia may eliminate synapses and/or express cytokines that promote neuronal injury. (7) Injured neurons express IL-6 which, together with IL-1β, promote a ‘gliogenic switch’ in NSCs (8), decreasing adult neurogenesis. (9) The combination of microglial (and possibly astrocyte) activation, neuronal injury and synapse loss may lead to dysregulation of NTs and neuronal circuitry. IFNg, interferon-g; NSC, neural stem cell; NT, neurotransmitter; TJ, tight junction; TNF, tumor necrosis factor; vWF, von Willebrand factor.
It is also unclear whether hospitalized patients with COVID-19 may develop brain abnormalities due to hypoxia or CRS rather than as a direct effect of SARS-CoV-2 infection. Hypoxia may cause neuronal dysfunction, cerebral edema, increased BBB permeability, cytokine expression and onset of neurodegenerative diseases 88 , 89 . CRS, with life-threatening levels of serum TNF-α and IL-1 (ref. 90 ) could also impact BBB function, as these cytokines destabilize microvasculature endothelial cell junctional proteins critical for BBB integrity 91 . In mild SARS-CoV-2 infection, circulating immune factors combined with mild hypoxia might impact BBB function and lead to neuroinflammation 92 , as observed during infection with other non-neuroinvasive respiratory pathogens 93 . However, multiple studies suggest that the SARS-CoV-2 spike protein itself may also induce venous and arterial endothelial cell activation and endotheliitis, disrupt BBB integrity or cross the BBB via adoptive transcytosis 94 , 95 , 96 .
Reducing neuropsychiatric sequelae of COVID-19
The increased risk of COVID-19-related neuropsychiatric sequalae was most pronounced during the first pandemic peak but reduced over the subsequent 2 years 64 , 97 . This may be due to reduced impact of newer SARS-CoV-2 strains (that is, Omicron) but also protective effects of vaccination, which limit SARS-CoV-2 spread and may, thus, prevent neuropsychiatric sequalae. Fully vaccinated individuals with breakthrough infections exhibit a 50% reduction in PACS 98 , even though vaccination does not improve PACS-related neuropsychiatric symptoms in patients with a prior history of COVID-19 (ref. 99 ). As patients with pre-existing mental disorders are at increased risk of SARS-CoV-2 infection, they deserve to be among the prioritization groups for vaccination efforts 100 .
Adequate treatment strategies for neuropsychiatric sequelae of COVID-19 are needed. As no specific evidence-based intervention yet exists, the best current treatment approach is that for neuropsychiatric sequelae arising after other severe medical conditions 101 . Stepped care—a staged approach of mental health services comprising a hierarchy of interventions, from least to most intensive, matched to the individual’s need—is efficacious with monitoring of mental health and cognitive problems. Milder symptoms likely benefit from counseling and holistic care, including physiotherapy, psychotherapy and rehabilitation. Individuals with moderate to severe symptoms fulfilling psychiatric diagnoses should receive guideline-concordant care for these disorders 61 . Patients with pre-existing mental disorders also deserve special attention when affected by COVID-19, as they have shown to have an increased risk of COVID-19-related hospitalization, complications and death 102 . This may involve interventions to address their general health, any unfavorable socioenvironmental factors, substance abuse or treatment adherence issues.
Lessons learned, knowledge gaps and future challenges
Ultimately, it is not only the millions of people who have died from COVID-19 worldwide that we remember but also the distress experienced during an unpredictable period with overstretched healthcare systems, lockdowns, school closures and changing work environments. In a world that is more and more globalized, connectivity puts us at risk for future pandemics. What can be learned from the last 2 years of the COVID-19 pandemic about how to handle future and longstanding challenges related to mental health?
Give mental health equal priority to physical health
The COVID-19 pandemic has demonstrated that our population seems quite resilient and adaptive. Nevertheless, even if society as a whole may bounce back, there is a large group of people whose mental health has been and will be disproportionately affected by this and future crises. Although various groups, such as the WHO 8 , the National Health Commission of China 103 , the Asia Pacific Disaster Mental Health Network 104 and a National Taskforce in India 105 , developed mental health policies early on, many countries were late in realizing that a mental health agenda deserves immediate attention in a rapidly evolving pandemic. Implementation of comprehensive and integrated mental health policies was generally inconsistent and suboptimal 106 and often in the shadow of policies directed at containing and reducing the spread of SARS-CoV-2. Leadership is needed to convey the message that mental health is as important as physical health and that we should focus specific attention and early interventions on those at the highest risk. This includes those vulnerable due to factors such as low socioeconomic status, specific developmental life phase (adolescents and young adults), pre-existing risk (poor physical or somatic health and early life trauma) or high exposure to pandemic-related (work) changes—for example, women and healthcare personnel. This means that not only should investment in youth and reducing health inequalities remain at the top of any policy agenda but also that mental health should be explicitly addressed from the start in any future global health crisis situation.
Communication and trust is crucial for mental health
Uncertainty and uncontrollability during the pandemic have challenged rational thinking. Negative news travels fast. Communication that is vague, one-sided and dishonest can negatively impact on mental health and amplify existing distress and anxiety 107 . Media reporting should not overemphasize negative mental health impact—for example, putative suicide rate increases or individual negative experiences—which could make situations worse than they actually are. Instead, communication during crises requires concrete and actionable advice that avoids polarization and strengthens vigilance, to foster resilience and help prevent escalation to severe mental health problems 108 , 109 .
Rapid research should be collaborative and high-quality
Within the scientific community, the topic of mental health during the pandemic led to a multitude of rapid studies that generally had limited methodological quality—for example, cross-sectional designs, small or selective sampling or study designs lacking valid comparison groups. These contributed rather little to our understanding of the mental health impact of the emerging crisis. In future events that have global mental health impact, where possible, collaborative and interdisciplinary efforts with well-powered and well-controlled prospective studies using standardized instruments will be crucial. Only with fine-grained determinants and outcomes can data reliably inform mental health policies and identify who is most at risk.
Do not neglect long-term mental health effects
So far, research has mainly focused on the acute and short-term effects of the pandemic on mental health, usually spanning pandemic effects over several months to 1 year. However, longer follow-up of how a pandemic impacts population mental health is essential. Can societal and economic disruptions after the pandemic increase risk of mental disorders at a later stage when the acute pandemic effects have subsided? Do increased self-reported mental health problems return to pre-pandemic levels, and which groups of individuals remain most affected in the long-term? We need to realize that certain pandemic consequences, particularly those affecting income and school/work careers, may become visible only over the course of several years. Consequently, we should maintain focus and continue to monitor and quantify the effects of the pandemic in the years to come—for example, by monitoring mental healthcare use and suicide. This should include specific at-risk populations (for example, adolescents) and understudied populations in low-income and middle-income countries.
Pay attention to mental health consequences of infectious diseases
Even though our knowledge on PACS is rapidly expanding, there are still many unanswered questions related to who is at risk, the long-term course trajectories and the best ways to intervene early. Consequently, we need to be aware of the neuropsychiatric sequelae of COVID-19 and, for that matter, of any infectious disease. Clinical attention and research should be directed toward alleviating potential neuropsychiatric ramifications of COVID-19. Next to clinical studies, studies using human tissues and appropriate animal models are pivotal to determine the CNS region-specific and neural-cell-specific effects of SARS-CoV-2 infection and the induced immune activation. Indeed, absence of SARS-CoV-2 neuroinvasion is an opportunity to learn and discover how peripheral neuroimmune mechanisms can contribute to neuropsychiatric sequelae in susceptible individuals. This emphasizes the importance of an interdisciplinary approach where somatic and mental health efforts are combined but also the need to integrate clinical parameters after infection with biological parameters (for example, serum, cerebrospinal fluid and/or neuroimaging) to predict who is at risk for PACS and deliver more targeted treatments.
Prepare mental healthcare infrastructure for pandemic times
If we take mental health seriously, we should not only monitor it but also develop the resources and infrastructure necessary for rapid early intervention, particularly for specific vulnerable groups. For adequate mental healthcare to be ready for pandemic times, primary care, community mental health and public mental health should be prepared. In many countries, health services were not able to meet the population’s mental health needs before the pandemic, which substantially worsened during the pandemic. We should ensure rapid access to mental health services but also address the underlying drivers of poor mental health, such as mitigating risks of unemployment, sexual violence and poverty. Collaboration in early stages across disciplines and expertise is essential. Anticipating disruption to face-to-face services, mental healthcare providers should be more prepared for consultations, therapy and follow-up by telephone, video-conferencing platforms and web applications 51 , 52 . The pandemic has shown that an inadequate infrastructure, pre-existing inequalities and low levels of technological literacy hindered the use and uptake of e-health, both in healthcare providers and in patients across different care settings. The necessary investments can ensure rapid upscaling of mental health services during future pandemics for those individuals with a high mental health need due to societal changes, government measures, fear of infection or infection itself.
Even though much attention has been paid to the physical health consequences of COVID-19, mental health has unjustly received less attention. There is an urgent need to prepare our research and healthcare infrastructures not only for adequate monitoring of the long-term mental health effects of the COVID-19 pandemic but also for future crises that will shape mental health. This will require collaboration to ensure interdisciplinary and sound research and to provide attention and care at an early stage for those individuals who are most vulnerable—giving mental health equal priority to physical health from the very start.
WHO Coronavirus (COVID-19) Dashboard (WHO, 2022; https://covid19.who.int/
Rando, H. M. et al. Challenges in defining long COVID: striking differences across literature, electronic health records, and patient-reported information. Preprint at https://www.medrxiv.org/content/10.1101/2021.03.20.21253896v1 (2021).
Nalbandian, A. et al. Post-acute COVID-19 syndrome. Nat. Med. 27 , 601–615 (2021).
Article CAS PubMed PubMed Central Google Scholar
Abbafati, C. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396 , 1204–1222 (2020).
Article Google Scholar
Penninx, B. W., Pine, D. S., Holmes, E. A. & Reif, A. Anxiety disorders. Lancet 397 , 914–927 (2021).
Article PubMed PubMed Central Google Scholar
Herrman, H. et al. Time for united action on depression: a Lancet –World Psychiatric Association Commission. Lancet 399 , 957–1022 (2022).
Article PubMed Google Scholar
Radka, K., Wyeth, E. H. & Derrett, S. A qualitative study of living through the first New Zealand COVID-19 lockdown: affordances, positive outcomes, and reflections. Prev. Med. Rep. 26 , 101725 (2022).
Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact (WHO, 2022).
Dragioti, E. et al. A large-scale meta-analytic atlas of mental health problems prevalence during the COVID-19 early pandemic. J. Med. Virol. 94 , 1935–1949 (2022).
Zhang, S. X. et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America—a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 31 , e23 (2022).
Zhang, S. X. et al. Meta-analytic evidence of depression and anxiety in Eastern Europe during the COVID-19 pandemic. Eur. J. Psychotraumatol . 13 , 2000132 (2022).
Racine, N. et al. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 175 , 1142–1150 (2021).
Robinson, E., Sutin, A. R., Daly, M. & Jones, A. A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 296 , 567–576 (2022).
Article CAS PubMed Google Scholar
Prati, G. & Mancini, A. D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 51 , 201–211 (2021).
Patel, K. et al. Psychological distress before and during the COVID-19 pandemic among adults in the United Kingdom based on coordinated analyses of 11 longitudinal studies. JAMA Netw. Open 5 , e227629 (2022).
Ernst, M. et al. Loneliness before and during the COVID-19 pandemic: a systematic review with meta-analysis. Am. Psychol . 77 , 660–677 (2022).
Kilian, C. et al. Changes in alcohol use during the COVID-19 pandemic in Europe: a meta-analysis of observational studies. Drug Alcohol Rev . 41 , 918–931 (2022).
Acuff, S. F., Strickland, J. C., Tucker, J. A. & Murphy, J. G. Changes in alcohol use during COVID-19 and associations with contextual and individual difference variables: a systematic review and meta-analysis. Psychol. Addict. Behav. 36 , 1–19 (2022).
Varga, T. V. et al. Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg. Health Eur . 2 , 100020 (2021).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8 , 141–149 (2021).
Jia, H. et al. National and state trends in anxiety and depression severity scores among adults during the COVID-19 pandemic—United States, 2020–2021. MMWR Morb. Mortal. Wkly. Rep. 70 , 1427–1432 (2021).
Kok, A. A. L. et al. Mental health and perceived impact during the first Covid-19 pandemic year: a longitudinal study in Dutch case–control cohorts of persons with and without depressive, anxiety, and obsessive-compulsive disorders. J. Affect. Disord. 305 , 85–93 (2022).
Su, Y. et al. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int. Psychogeriatr. https://doi.org/10.1017/S1041610222000199 (2022).
Knox, L., Karantzas, G. C., Romano, D., Feeney, J. A. & Simpson, J. A. One year on: what we have learned about the psychological effects of COVID-19 social restrictions: a meta-analysis. Curr. Opin. Psychol. 46 , 101315 (2022).
Aknin, L. B. et al. Policy stringency and mental health during the COVID-19 pandemic: a longitudinal analysis of data from 15 countries. Lancet Public Health 7 , e417–e426 (2022).
Lee, Y. et al. Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 290 , 364–377 (2021).
Wu, J. T. et al. Nowcasting epidemics of novel pathogens: lessons from COVID-19. Nat. Med. 27 , 388–395 (2021).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 398 , 1700–1712 (2021).
Knudsen, A. K. S. et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg. Health Eur . 4 , 100071 (2021).
Ayuso-Mateos, J. L. et al. Changes in depression and suicidal ideation under severe lockdown restrictions during the first wave of the COVID-19 pandemic in Spain: a longitudinal study in the general population. Epidemiol. Psychiatr. Sci . 30 , e49 (2021).
Vloo, A. et al. Gender differences in the mental health impact of the COVID-19 lockdown: longitudinal evidence from the Netherlands. SSM Popul. Health 15 , 100878 (2021).
Winkler, P. et al. Prevalence of current mental disorders before and during the second wave of COVID-19 pandemic: an analysis of repeated nationwide cross-sectional surveys. J. Psychiatr. Res. 139 , 167–171 (2021).
Pirkis, J. et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry 8 , 579–588 (2021).
Faust, J. S. et al. Mortality from drug overdoses, homicides, unintentional injuries, motor vehicle crashes, and suicides during the pandemic, March–August 2020. JAMA 326 , 84–86 (2021).
John, A. et al. The impact of the COVID-19 pandemic on self-harm and suicidal behaviour: update of living systematic review. F1000Res. 9 , 1097 (2020).
Steeg, S. et al. Temporal trends in primary care-recorded self-harm during and beyond the first year of the COVID-19 pandemic: time series analysis of electronic healthcare records for 2.8 million patients in the Greater Manchester Care Record. EClinicalMedicine 41 , 101175 (2021).
Rømer, T. B. et al. Psychiatric admissions, referrals, and suicidal behavior before and during the COVID-19 pandemic in Denmark: a time-trend study. Acta Psychiatr. Scand. 144 , 553–562 (2021).
Holland, K. M. et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry 78 , 372–379 (2021).
Kunzler, A. M. et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Global Health 17 , 34 (2021).
Flor, L. S. et al. Quantifying the effects of the COVID-19 pandemic on gender equality on health, social, and economic indicators: a comprehensive review of data from March, 2020, to September, 2021. Lancet 399 , 2381–2397 (2022).
Viner, R. et al. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 176 , 400–409 (2022).
Zheng, X. Y. et al. Trends of injury mortality during the COVID-19 period in Guangdong, China: a population-based retrospective analysis. BMJ Open 11 , e045317 (2021).
Tanaka, T. & Okamoto, S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat. Hum. Behav. 5 , 229–238 (2021).
Thomeer, M. B., Moody, M. D. & Yahirun, J. Racial and ethnic disparities in mental health and mental health care during the COVID-19 pandemic. J. Racial Ethn. Health Disparities https://doi.org/10.1007/s40615-021-01006-7 (2022).
Hill, J. E. et al. The prevalence of mental health conditions in healthcare workers during and after a pandemic: systematic review and meta-analysis. J. Adv. Nurs. 78 , 1551–1573 (2022).
Marvaldi, M., Mallet, J., Dubertret, C., Moro, M. R. & Guessoum, S. B. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Neurosci. Biobehav. Rev. 126 , 252–264 (2021).
Phiri, P. et al. An evaluation of the mental health impact of SARS-CoV-2 on patients, general public and healthcare professionals: a systematic review and meta-analysis. EClinicalMedicine 34 , 100806 (2021).
Jorm, A. F., Patten, S. B., Brugha, T. S. & Mojtabai, R. Has increased provision of treatment reduced the prevalence of common mental disorders? Review of the evidence from four countries. World Psychiatry 16 , 90–99 (2017).
Third Round of the Global Pulse Survey on Continuity of Essential Health Services during the COVID-19 Pandemic (WHO, 2021).
Baumgart, J. G. et al. The early impacts of the COVID-19 pandemic on mental health facilities and psychiatric professionals. Int. J. Environ. Res. Public Health 18 , 8034 (2021).
Raphael, J., Winter, R. & Berry, K. Adapting practice in mental healthcare settings during the COVID-19 pandemic and other contagions: systematic review. BJPsych Open 7 , e62 (2021).
Anderson, K. N. et al. Changes and inequities in adult mental health-related emergency department visits during the COVID-19 pandemic in the US. JAMA Psychiatry 79 , 475–485 (2022).
Pan, K. Y. et al. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case–control cohorts. Lancet Psychiatry 8 , 121–129 (2021).
Dantzer, R., O’Connor, J. C., Freund, G. G., Johnson, R. W. & Kelley, K. W. From inflammation to sickness and depression: when the immune system subjugates the brain. Nat. Rev. Neurosci. 9 , 46–56 (2008).
Nersesjan, V. et al. Central and peripheral nervous system complications of COVID-19: a prospective tertiary center cohort with 3-month follow-up. J. Neurol. 268 , 3086–3104 (2021).
Wilson, J. E. et al. Delirium. Nat. Rev. Dis. Prim . 6 , 90 (2020).
Rawal, G., Yadav, S. & Kumar, R. Post-intensive care syndrome: an overview. J. Transl. Intern. Med. 5 , 90–92 (2017).
Pandharipande, P. P. et al. Long-term cognitive impairment after critical illness. N. Engl. J. Med. 369 , 1306–1316 (2013).
Girard, T. D. et al. Long-term cognitive impairment after hospitalization for community-acquired pneumonia: a prospective cohort study. J. Gen. Intern. Med. 33 , 929–935 (2018).
Crook, H., Raza, S., Nowell, J., Young, M. & Edison, P. Long covid—mechanisms, risk factors, and management. BMJ 374 , n1648 (2021).
Badenoch, J. B. et al. Persistent neuropsychiatric symptoms after COVID-19: a systematic review and meta-analysis. Brain Commun . 4 , fcab297 (2021).
Ceban, F. et al. Fatigue and cognitive impairment in post-COVID-19 syndrome: a systematic review and meta-analysis. Brain Behav. Immun. 101 , 93–135 (2022).
Taquet, M., Geddes, J. R., Husain, M., Luciano, S. & Harrison, P. J. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry 8 , 416–427 (2021).
Xie, Y., Xu, E. & Al-Aly, Z. Risks of mental health outcomes in people with covid-19: cohort study. BMJ 376 , e068993 (2022).
Kieran Clift, A. et al. Neuropsychiatric ramifications of severe COVID-19 and other severe acute respiratory infections. JAMA Psychiatry 79 , 690–698 (2022).
Castro, V. M., Rosand, J., Giacino, J. T., McCoy, T. H. & Perlis, R. H. Case–control study of neuropsychiatric symptoms following COVID-19 hospitalization in 2 academic health systems. Mol. Psych. (in the press).
Amin-Chowdhury, Z. & Ladhani, S. N. Causation or confounding: why controls are critical for characterizing long COVID. Nat. Med. 27 , 1129–1130 (2021).
Nersesjan, V. et al. Neuropsychiatric and cognitive outcomes in patients 6 months after COVID-19 requiring hospitalization compared with matched control patients hospitalized for non-COVID-19 illness. JAMA Psychiatry 79 , 486–497 (2022).
Douaud, G. et al. SARS-CoV-2 is associated with changes in brain structure in UK Biobank. Nature 604 , 697–707 (2022).
Zhang, H. et al. Psychological experience of COVID-19 patients: a systematic review and qualitative meta-synthesis. Am. J. Infect. Control 50 , 809–819 (2022).
Mazza, M. G. et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 89 , 594–600 (2020).
Moonis, G. et al. The spectrum of neuroimaging findings on CT and MRI in adults With COVID-19. AJR Am. J. Roentgenol. 217 , 959–974 (2021).
Asadi-Pooya, A. A. & Simani, L. Central nervous system manifestations of COVID-19: a systematic review. J. Neurol. Sci . 413 , 116832 (2020).
Lersy, F. et al. Cerebrospinal fluid features in patients with Coronavirus Disease 2019 and neurological manifestations: correlation with brain magnetic resonance imaging findings in 58 patients. J. Infect. Dis. 223 , 600–609 (2021).
Thakur, K. T. et al. COVID-19 neuropathology at Columbia University Irving Medical Center/New York Presbyterian Hospital. Brain 144 , 2696–2708 (2021).
Cosentino, G. et al. Neuropathological findings from COVID-19 patients with neurological symptoms argue against a direct brain invasion of SARS-CoV-2: a critical systematic review. Eur. J. Neurol. 28 , 3856–3865 (2021).
Tian, T. et al. Long-term follow-up of dynamic brain changes in patients recovered from COVID-19 without neurological manifestations. JCI Insight 7 , e155827 (2022).
Lu, Y. et al. Cerebral micro-structural changes in COVID-19 patients—an MRI-based 3-month follow-up study. EClinicalMedicine 25 , 100484 (2020).
Qin, Y. et al . Long-term microstructure and cerebral blood flow changes in patients recovered from COVID-19 without neurological manifestations. J. Clin. Invest . 131 , e147329 (2021).
Matschke, J. et al. Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol. 19 , 919–929 (2020).
Shivshankar, P. et al. SARS-CoV-2 infection: host response, immunity, and therapeutic targets. Inflammation 45 , 1430–1449 (2022).
Manganotti, P. et al. Cerebrospinal fluid and serum interleukins 6 and 8 during the acute and recovery phase in COVID-19 neuropathy patients. J. Med. Virol. 93 , 5432–5437 (2021).
Farhadian, S. et al. Acute encephalopathy with elevated CSF inflammatory markers as the initial presentation of COVID-19. BMC Neurol . 20 , 248 (2020).
Francistiová, L. et al. Cellular and molecular effects of SARS-CoV-2 linking lung infection to the brain. Front. Immunol . 12 , 730088 (2021).
Paterson, R. W. et al. Serum and cerebrospinal fluid biomarker profiles in acute SARS-CoV-2-associated neurological syndromes. Brain Commun . 3 , fcab099 (2021).
Cryer, M. J. et al. Prothrombotic milieu, thrombotic events and prophylactic anticoagulation in hospitalized COVID-19 positive patients: a review. Clin. Appl. Thromb. Hemost . 28 , 10760296221074353 (2022).
Nalivaeva, N. N. & Rybnikova, E. A. Editorial: Brain hypoxia and ischemia: new insights into neurodegeneration and neuroprotection. Front. Neurosci . 13 , 770 (2019).
Brownlee, N. N. M., Wilson, F. C., Curran, D. B., Lyttle, N. & McCann, J. P. Neurocognitive outcomes in adults following cerebral hypoxia: a systematic literature review. NeuroRehabilitation 47 , 83–97 (2020).
Del Valle, D. M. et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 26 , 1636–1643 (2020).
Daniels, B. P. et al. Viral pathogen-associated molecular patterns regulate blood–brain barrier integrity via competing innate cytokine signals. mBio 5 , e01476-14 (2014).
Reynolds, J. L. & Mahajan, S. D. SARS-COV2 alters blood brain barrier integrity contributing to neuro-inflammation. J. Neuroimmune Pharmacol. 16 , 4–6 (2021).
Bohmwald, K., Gálvez, N. M. S., Ríos, M. & Kalergis, A. M. Neurologic alterations due to respiratory virus infections. Front. Cell. Neurosci . 12 , 386 (2018).
Khaddaj-Mallat, R. et al. SARS-CoV-2 deregulates the vascular and immune functions of brain pericytes via spike protein. Neurobiol. Dis . 161 , 105561 (2021).
Qian, Y. et al. Direct activation of endothelial cells by SARS-CoV-2 nucleocapsid protein is blocked by simvastatin. J Virol. 95 , e0139621 (2021).
Rhea, E. M. et al. The S1 protein of SARS-CoV-2 crosses the blood–brain barrier in mice. Nat. Neurosci. 24 , 368–378 (2021).
Magnúsdóttir, I. et al. Acute COVID-19 severity and mental health morbidity trajectories in patient populations of six nations: an observational study. Lancet Public Health 7 , e406–e416 (2022).
Antonelli, M. et al. Risk factors and disease profile of post-vaccination SARS-CoV-2 infection in UK users of the COVID Symptom Study app: a prospective, community-based, nested, case–control study. Lancet Infect. Dis. 22 , 43–55 (2022).
Wisnivesky, J. P. et al. Association of vaccination with the persistence of post-COVID symptoms. J. Gen. Intern. Med . 37 , 1748–1753 (2022).
De Picker, L. J. et al. Severe mental illness and European COVID-19 vaccination strategies. Lancet Psychiatry 8 , 356–359 (2021).
Cohen, G. H. et al. Comparison of simulated treatment and cost-effectiveness of a stepped care case-finding intervention vs usual care for posttraumatic stress disorder after a natural disaster. JAMA Psychiatry 74 , 1251–1258 (2017).
Vai, B. et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatry 8 , 797–812 (2021).
Xiang, Y. T. et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7 , 228 (2020).
Newnham, E. A. et al. The Asia Pacific Disaster Mental Health Network: setting a mental health agenda for the region. Int. J. Environ. Res. Public Health 17 , 6144 (2020).
Article CAS PubMed Central Google Scholar
Dandona, R. & Sagar, R. COVID-19 offers an opportunity to reform mental health in India. Lancet Psychiatry 8 , 9–11 (2021).
Qiu, D. et al. Policies to improve the mental health of people influenced by COVID-19 in China: a scoping review. Front. Psychiatry 11 , 588137 (2020).
Su, Z. et al. Mental health consequences of COVID-19 media coverage: the need for effective crisis communication practices. Global Health 17 , 4 (2021).
Petersen, M. B. COVID lesson: trust the public with hard truths. Nature 598 , 237 (2021).
van der Bles, A. M., van der Linden, S., Freeman, A. L. J. & Spiegelhalter, D. J. The effects of communicating uncertainty on public trust in facts and numbers. Proc. Natl Acad. Sci. USA 117 , 7672–7683 (2020).
Titze-de-Almeida, R. et al. Persistent, new-onset symptoms and mental health complaints in Long COVID in a Brazilian cohort of non-hospitalized patients. BMC Infect. Dis. 22 , 133 (2022).
Carfì, A., Bernabei, R. & Landi, F. Persistent symptoms in patients after acute COVID-19. JAMA 324 , 603–605 (2020).
Bliddal, S. et al. Acute and persistent symptoms in non-hospitalized PCR-confirmed COVID-19 patients. Sci. Rep. 11 , 13153 (2021).
Kim, Y. et al. Post-acute COVID-19 syndrome in patients after 12 months from COVID-19 infection in Korea. BMC Infect. Dis . 22 , 93 (2022).
Download references
Acknowledgements
The authors thank E. Giltay for assistance on data analyses and production of Fig. 1 . B.W.J.H.P. discloses support for research and publication of this work from the European Union’s Horizon 2020 research and innovation programme-funded RESPOND project (grant no. 101016127).
Author information
Authors and affiliations.
Department of Psychiatry, Amsterdam UMC, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands
Brenda W. J. H. Penninx & Christiaan H. Vinkers
Amsterdam Public Health, Mental Health Program and Amsterdam Neuroscience, Mood, Anxiety, Psychosis, Sleep & Stress Program, Amsterdam, The Netherlands
Biological and Precision Psychiatry, Copenhagen Research Center for Mental Health, Mental Health Center Copenhagen, Copenhagen University Hospital, Copenhagen, Denmark
Michael E. Benros
Department of Immunology and Microbiology, Faculty of Health and Medical Sciences, University of Copenhagen, Copenhagen, Denmark
Departments of Medicine, Pathology & Immunology and Neuroscience, Center for Neuroimmunology & Neuroinfectious Diseases, Washington University School of Medicine, St. Louis, MO, USA
Robyn S. Klein
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Brenda W. J. H. Penninx .
Ethics declarations
Competing interests.
The authors declare no conflicts of interest.
Peer review
Peer review information.
Nature Medicine thanks Jane Pirkis and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editor: Karen O’Leary, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Cite this article.
Penninx, B.W.J.H., Benros, M.E., Klein, R.S. et al. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med 28 , 2027–2037 (2022). https://doi.org/10.1038/s41591-022-02028-2
Download citation
Received : 06 June 2022
Accepted : 26 August 2022
Published : 03 October 2022
Issue Date : October 2022
DOI : https://doi.org/10.1038/s41591-022-02028-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Mental health disturbance in preclinical medical students and its association with screen time, sleep quality, and depression during the covid-19 pandemic.
- Tjhin Wiguna
- Valerie Josephine Dirjayanto
- Erik Kinzie
BMC Psychiatry (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
Impact of COVID-19 first wave on the mental health of healthcare workers in a Front-Line Spanish Tertiary Hospital: lessons learned
- Juan D. Molina
- Franco Amigo
- Gabriel Rubio
Scientific Reports (2024)
Long-term risk of psychiatric disorder and psychotropic prescription after SARS-CoV-2 infection among UK general population
- Daniel Prieto-Alhambra
Nature Human Behaviour (2024)
Possible temporal relationship between SARS-CoV-2 infection and anti-NMDA receptor encephalitis: a meta-analysis
- Veronika Vasilevska
- Paul C. Guest
- Johann Steiner
Translational Psychiatry (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.

Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
- Theresa Cerulli, MD
- Tina Matthews-Hayes, DNP, FNP, PMHNP
Custom Around the Practice Video Series
Experts in psychiatry review the case of a 27-year-old woman who presents for evaluation of a complex depressive disorder.

EP: 1 . Patient Case #1: 27-Year-Old Woman With Bipolar Disorder
Ep: 2 . clinical significance of bipolar disorder, ep: 3 . clinical impressions from patient case #1, ep: 4 . diagnosis of bipolar disorder, ep: 5 . treatment options for bipolar disorder, ep: 6 . patient case #2: 47-year-old man with treatment resistant depression (trd), ep: 7 . patient case #2 continued: novel second-generation antipsychotics, ep: 8 . role of telemedicine in bipolar disorder.
Michael E. Thase, MD : Hello and welcome to this Psychiatric Times™ Around the Practice , “Identification and Management of Bipolar Disorder. ”I’m Michael Thase, professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Joining me today are: Dr Gustavo Alva, the medical director of ATP Clinical Research in Costa Mesa, California; Dr Theresa Cerulli, the medical director of Cerulli and Associates in North Andover, Massachusetts; and Dr Tina Matthew-Hayes, a dual-certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.
Today we are going to highlight challenges with identifying bipolar disorder, discuss strategies for optimizing treatment, comment on telehealth utilization, and walk through 2 interesting patient cases. We’ll also involve our audience by using several polling questions, and these results will be shared after the program.
Without further ado, welcome and let’s begin. Here’s our first polling question. What percentage of your patients with bipolar disorder have 1 or more co-occurring psychiatric condition? a. 10%, b. 10%-30%, c. 30%-50%, d. 50%-70%, or e. more than 70%.
Now, here’s our second polling question. What percentage of your referred patients with bipolar disorder were initially misdiagnosed? Would you say a. less than 10%, b. 10%-30%, c. 30%-50%, d. more than 50%, up to 70%, or e. greater than 70%.
We’re going to go ahead to patient case No. 1. This is a 27-year-old woman who’s presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode. It began back in the fall, and she described the episode as occurring right “out of the blue.” Further discussion revealed, however, that she had talked with several confidantes about her problems and that she realized she had been disappointed and frustrated for being passed over unfairly for a promotion at work. She had also been saddened by the unusually early death of her favorite aunt.
Now, our patient has a past history of ADHD [attention-deficit/hyperactivity disorder], which was recognized when she was in middle school and for which she took methylphenidate for adolescence and much of her young adult life. As she was wrapping up with college, she decided that this medication sometimes disrupted her sleep and gave her an irritable edge, and decided that she might be better off not taking it. Her medical history was unremarkable. She is taking escitalopram at the time of our initial evaluation, and the dose was just reduced by her PCP [primary care physician]from 20 mg to 10 mg because she subjectively thought the medicine might actually be making her worse.
On the day of her first visit, we get a PHQ-9 [9-item Patient Health Questionnaire]. The score is 16, which is in the moderate depression range. She filled out the MDQ [Mood Disorder Questionnaire] and scored a whopping 10, which is not the highest possible score but it is higher than 95% of people who take this inventory.
At the time of our interview, our patient tells us that her No. 1 symptom is her low mood and her ease to tears. In fact, she was tearful during the interview. She also reports that her normal trouble concentrating, attributable to the ADHD, is actually substantially worse. Additionally, in contrast to her usual diet, she has a tendency to overeat and may have gained as much as 5 kg over the last 4 months. She reports an irregular sleep cycle and tends to have periods of hypersomnolence, especially on the weekends, and then days on end where she might sleep only 4 hours a night despite feeling tired.
Upon examination, her mood is positively reactive, and by that I mean she can lift her spirits in conversation, show some preserved sense of humor, and does not appear as severely depressed as she subjectively describes. Furthermore, she would say that in contrast to other times in her life when she’s been depressed, that she’s actually had no loss of libido, and in fact her libido might even be somewhat increased. Over the last month or so, she’s had several uncharacteristic casual hook-ups.
So the differential diagnosis for this patient included major depressive disorder, recurrent unipolar with mixed features, versus bipolar II disorder, with an antecedent history of ADHD. I think the high MDQ score and recurrent threshold level of mixed symptoms within a diagnosable depressive episode certainly increase the chances that this patient’s illness should be thought of on the bipolar spectrum. Of course, this formulation is strengthened by the fact that she has an early age of onset of recurrent depression, that her current episode, despite having mixed features, has reverse vegetative features as well. We also have the observation that antidepressant therapy has seemed to make her condition worse, not better.
Transcript Edited for Clarity
Dr. Thase is a professor of psychiatry at the Perelman School of Medicine at the University of Pennsylvania in Philadelphia, Pennsylvania.
Dr. Alva is the medical director of ATP Clinical Research in Costa Mesa, California.
Dr. Cerulli is the medical director of Cerulli and Associates in Andover, Massachusetts.
Dr. Tina Matthew-Hayes is a dual certified nurse practitioner at Western PA Behavioral Health Resources in West Mifflin, Pennsylvania.

The Week in Review: April 1-5

Blue Light, Depression, and Bipolar Disorder

An Update on Bipolar I Disorder

Four Myths About Lamotrigine

Recap: Mood Disorders 2024
Evidence-Based Novel Therapies for Bipolar Depression: Top 5 Takeaways
2 Commerce Drive Cranbury, NJ 08512
609-716-7777

Evidence-based Approaches to Support Student Mental Health
- Andrea Feldman
- 24 April 2024
The college years throw a lot of new challenges at us. Maybe you’re the first in your family to go to college. You’re developing a new sense of independence. Figuring out how to live with roommates. Dealing with new financial responsibilities and academic pressures.
That’s a lot all by itself — but as Associate Professor Sam Rosenthal noted during her recent Health Equity lecture outlining the behavioral health of college-age students, a staggering 75% of mental health disorders are established by the mid-twenties. That means that the 18-25 cohort exhibits the highest rates of anxiety and depressive symptoms, and they’re also extremely vulnerable to developing parallel addictive behaviors.
“Those with social support reduce their risk of insomnia by 33%, their risk of anxiety by 47% and their risk of depression by 50%. That’s dramatic.”
But the data is only one side of the story, and Rosenthal prefaced her talk by noting, “I do want you to know we’re going to get to a positive note of the solutions by the end.” And it may not surprise you to learn that community-building — strengthening our real-world bonds to others — plays a crucial role in improving our individual mental health. (Put down that phone, while you’re at it.)
A Career Built on Studying Behavioral Health
Rosenthal has built an impressive career on her research into the multi-factor forces driving mental-health trends in young adults.
In addition to teaching and serving as the director of JWU’s Center for Student Research and Interdisciplinary Collaboration, she serves as an evaluator for the Rhode Island Department of Health and as the lead epidemiologist for the State Epidemiological Outcomes Workgroup (SEOW). Under the aegis of SEOW, she administers the RI Young Adult Survey (RIYAS), which focuses on the behavioral health of 18-25-year-olds.
Assessing the Pandemic Spike
Depression rates among young adults have doubled in the past 10 years. But the pandemic sent these rates soaring — Rosenthal calls the spike “extreme” — due to a polycrisis of factors, including social isolation, disrupted academic studies, and unprecedented loss. During the 2020-21 academic year, noted Rosenthal, 60% of college-age students reported at least one mental health disorder, and 75% experienced psychological distress. 1 in 5 young adults in Rhode Island reported losing a loved one to Covid-19.
Once you start taking into account the social upheaval of recent years — from gun violence to racial discrimination, climate change anxiety and political turmoil — and you have a massive amount of collective trauma having a ripple effect on already fragile mental health states.
Rosenthal provided a top-level overview of two recent studies. The Healthy Mind study surveyed more than 76,000 students from 400 institutions during the 2022-23 academic year. In October 2022, Rosenthal and her co-researchers used an NIH grant to survey 586 JWU students assessing their levels of depression, anxiety, insomnia and social support.
While the Healthy Mind study clocked depression rates at 41%, the JWU case study reported 53% — that’s “higher than what we saw in the national study, but actually comparable to what we saw in the Rhode Island state study,” explained Rosenthal. “And also we have a huge representation of sexual gender minority students, which is likely to be driving some of these higher rates for us as well.” (The JWU study demographics broke down as 15.1% cisgender male, 47.4% cisgender female and 37.5% sexual or gender minority.)
So, what are the solutions for combatting these numbers? For Rosenthal, who has done multiple studies correlating social media use and depression, building up social support networks is “critically important”: “Those with social support reduce their risk of insomnia by 33%, their risk of anxiety by 47% and their risk of depression by 50%. That’s dramatic.”
“Gratitude is really powerful. I often tell my students to break up anxiety with gratitude.”
Mindfulness, Quiet Hours & Other Mental Health Boosts
Rosenthal opened the conversation to students and faculty in the audience to share their ideas for boosting our community connections and strengthening overall well-being.
Sarah and Jasmine, two undergraduate students in the Public Health program , shared how much JWU’s 3-credit Mindfulness for Health & Wellbeing class helped them. (This course is currently an elective, but there is talk of making it requirement.)
The course provides students with the opportunity to learn the principles of mindfulness, develop their own mindfulness mediation practice, and apply principles of mindfulness to daily life.
Prior to taking the class, Jasmine had been struggling with time management. Having never meditated before, it took her some time to acclimate to the practice. But now, she says, “I feel like this class has definitely not only forced me to try new things, but I’ve made it a part of my daily routine. It’s definitely helped me!”
Initially, Sarah noted that she “had a really hard time sitting down with myself and going through [the process].” Gradually, with the guidance of Professor Jennifer Swanberg, “I've been able to develop my own practice that I find beneficial. There are those times where I still feel frustration, but now I feel more prepared to deal with it.”
In the Occupational Therapy department, faculty celebrate Grati-Tuesdays, where they keep a running list of what they are thankful for. “Gratitude is really powerful,” noted Assistant Professor Kathryn Burke. “I often tell my students to break up anxiety with gratitude. Thinking about something that you’re grateful for can sometimes help get your brain out of that downward spiral that everything is terrible.”
Other suggestions included:
- A peer mentorship program to help increase social support
- Moving 11:59pm assignment deadlines to 8pm
- Minimizing the number of early morning classes
- Enforcing quiet hours in residence halls
- Expanding the number of safe community spaces (like the Bridge for Diversity, Equity and Social Justice ) where students can share with their peers
“Creating a sense of belonging is crucially important,” concluded Rosenthal. “We need to have safe spaces to hold people when the rest of the world feels unsafe.”
JWU has a wealth of confidential mental health resources, including counseling services in Providence and Charlotte . Individual counseling sessions and consultations are available by appointment, as well as resources for mental health screenings, education and crisis intervention.
Related Reading:
6 Ways College Students Can Improve Their Mental Health
Self-Care Tips to Use During Exams
JWU Alumni Share Insight on DEI and Belonging
Apply Visit Transfer Explore from Home

Related Posts


OTD Student Experiences 'Humanity' Through Butler Hospital Fieldwork

Ten Years On, JWU's PA Program Is Going Strong
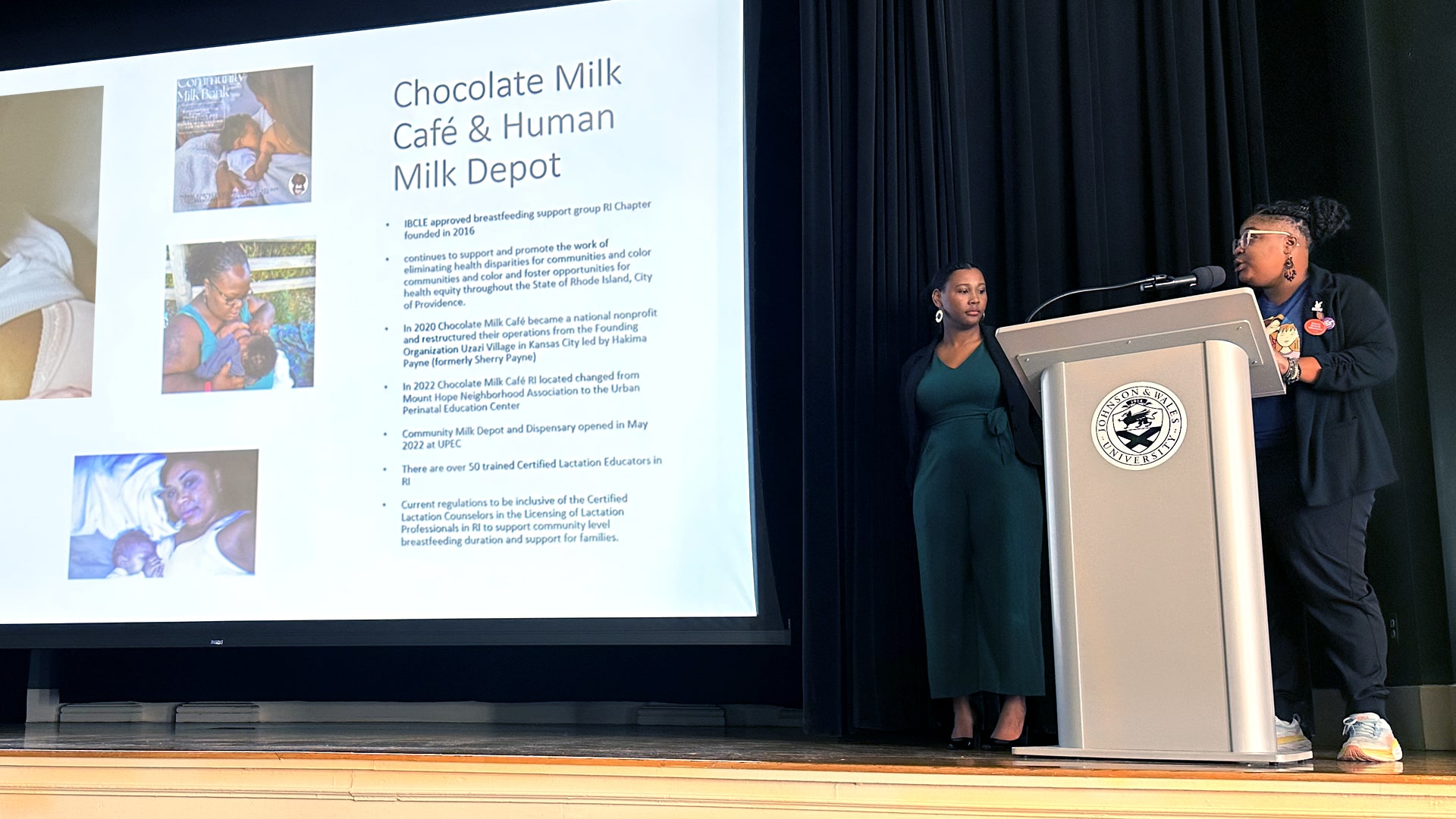
How Community Action Can Improve Black Maternal Health Outcomes
- Arts & Sciences 77
- Business 50
- Engineering & Design 53
- Culinary 148
- Health & Wellness 42
- Hospitality Management 92
- Covid-19 12
- Experiential Education 45
- Students 121
- Request information
- Start your application
Cookies on the NHS England website
We’ve put some small files called cookies on your device to make our site work.
We’d also like to use analytics cookies. These send information about how our site is used to a service called Google Analytics. We use this information to improve our site.
Let us know if this is OK. We’ll use a cookie to save your choice. You can read more about our cookies before you choose.
Change my preferences I'm OK with analytics cookies
Mental health case studies
Driving up quality in mental health care.
Mental health care across the NHS in England is changing to improve the experiences of the people who use them. In many areas, a transformation is already under way, offering people better and earlier access as well as more personalised care, whilst building partnerships which reach beyond the NHS to create integrated and innovative approaches to mental health care and support.
Find out more through our case studies and films about how mental health care across the NHS is changing and developing to better meet people’s needs.
- Children and young people (CYP)
- Community mental health
- Crisis mental health
- Early intervention in psychosis (EIP)
- Improving access to psychological therapies (IAPT)
- Perinatal mental health
- Severe mental illness (SMI)
- Staff mental health and wellbeing
- Other mental health case studies
- Archived mental health case studies
National Endowment for the Arts
- Grants for Arts Projects
- Challenge America
- Research Awards
- Partnership Agreement Grants
- Creative Writing
- Translation Projects
- Volunteer to be an NEA Panelist
- Manage Your Award
- Recent Grants
- Arts & Human Development Task Force
- Arts Education Partnership
- Blue Star Museums
- Citizens' Institute on Rural Design
- Creative Forces: NEA Military Healing Arts Network
- GSA's Art in Architecture
- Independent Film & Media Arts Field-Building Initiative
- Interagency Working Group on Arts, Health, & Civic Infrastructure
- International
- Mayors' Institute on City Design
- Musical Theater Songwriting Challenge
- National Folklife Network
- NEA Big Read
- NEA Research Labs
- Poetry Out Loud
- Save America's Treasures
- Shakespeare in American Communities
- Sound Health Network
- United We Stand
- American Artscape Magazine
- NEA Art Works Podcast
- National Endowment for the Arts Blog
- States and Regions
- Accessibility
- Arts & Artifacts Indemnity Program
- Arts and Health
- Arts Education
- Creative Placemaking
- Equity Action Plan
- Historically Black Colleges and Universities (HBCUs)
- Literary Arts
- Native Arts and Culture
- NEA Jazz Masters Fellowships
- National Heritage Fellowships
- National Medal of Arts
- Press Releases
- Upcoming Events
- NEA Chair's Page
- Leadership and Staff
- What Is the NEA
- Publications
- National Endowment for the Arts on COVID-19
- Open Government
- Freedom of Information Act (FOIA)
- Office of the Inspector General
- Civil Rights Office
- Appropriations History
- Make a Donation
Momentum Gains with Small-Scale Studies about the Arts and Mental Health

One spring day in 1840, on the bank of Goose Pond in Massachusetts—not far from Walden Pond, where Henry David Thoreau would make his stand—Ralph Waldo Emerson and the poet Jones Very were admiring the interplay of wind and water. “I declare this world is so beautiful that I can hardly believe it exists,” Emerson was moved to say. His more empirically-minded companion noted: “See how each wave rises from the midst with an original force, at the same time that it partakes [in] the general movement.”
The exchange appears in Emerson’s journals. It is quoted in God’s Scrivener: The Madness and Meaning of Jones Very , Clark Davis’ biography of the troubled, messianic figure. It may seem improbable, but Very’s remark is an apt metaphor for the constant flow of small-scale studies that attempt to locate specific mental health benefits from arts participation. These studies are as wavelets on a pond. Though small, each study often reflects an original theory or methodological insight, even while partaking of a common narrative about the arts’ potential effects on psychological well-being.
The latest such study (or wavelet) to cross my desk is titled “Impact of Opera on Resilience and Thriving in Serious Mental Illness.” Published in Community Health Journal , the article describes the results from a pilot evaluation study of how audiences responded to a 75-minute opera about recovering from schizophrenia. The performance was preceded by a 45-minute workshop on approaches to recovery and resilience.
The opera itself was composed by Kenneth Wells, a psychiatrist and the director of the Center for Health Services and Society within UCLA’s Semel Institute for Neuroscience. It was based on The Center Cannot Hold: My Journey through Madness , a 2007 memoir by Elyn Saks, a professor of law, psychology, and psychiatry at University of Southern California. With funding from the Los Angeles County Department of Mental Health, the opera premiered before 117 online attendees and 107 in-person attendees in an auditorium at UCLA’s Semel Institute.
The pre-opera workshop featured stories by local community members, facilitated dialogues, talks by academic and community partners, and a choral work that was co-created by Wells and a community leader, Loretta Jones.
Pre- and post-event surveys were conducted with the help of the Arts Impact Measurement System (AIMS), an online assessment tool that has been developed by the NEA Research Lab at UCLA . AIMS includes validated question-items about positive and negative mood affect. The technology permits survey respondents to indicate their mood on a color-gradient by using a mouse or touchscreen. Social connectedness was also measured as a primary outcome.
Secondary outcome measures included assessing whether the events increased understanding of mental illness and sympathy, and whether it reduced stigma of mental illness, as well as whether audience members improved their willingness to engage with people with mental illness or schizophrenia. In the post-event survey, the researchers also explored how well the opera and workshop communicated the importance of social or family support, of hope for recovery, and of one’s personal journey toward resilience/recovery, among other themes.
Based on these and other data collected from attendees at the opera and workshop, “primary findings on post-pre outcomes are consistent with potential for opera events on true lived experience of serious mental illness to increase positive affect and social connection,” the researchers write, noting also the workshop seemed to have been “more engaging” for healthcare providers or people with “lived experience” of mental illness.
Demographic data suggest that the average age of the pre- and post- survey respondents as in the mid-50s. Half the respondents were White, half were female, and 41 percent were mental health providers. The authors caution: “While characteristics were similar for persons with only pre- and pre- and post-surveys, findings could reflect selection effects with those with more experience and a tendency for positive reaction to such events to complete both surveys.”
“However, findings could reflect actual impact, and may inform future studies of more general audiences, larger survey samples, and as feasible, comparison conditions such as participation in other types of events,” they conclude.
Greater statistical power and representativeness, standardization of outcome measures, and appropriate selection of comparison or control groups—all of these challenges are frequently cited as hindering the dramatic scale-up of studies involving arts-based programs or interventions. (Other common pitfalls include the lack of a mechanistic understanding of the intervention being studied, or poor fidelity measures—i.e., tracking whether the program is being implemented exactly as theorized.)
Still, studies like the one in Community Mental Health Journal hold promise for other researchers seeking to investigate the premise that musical performances—in this case, opera—when coupled with educational efforts, can improve emotional and social well-being and attitudes toward mental health trauma.
Regarding the mental health of older adults, the National Institutes of Health has produced a Music-Based Intervention Toolkit to assist music/health researchers and practitioners with designing and evaluating therapies and programs that address brain-related disorders of aging. Further, in the March 30, 2024 issue of The Lancet , representatives from NIH, the NEA, and the Kennedy Center—including the soprano Renée Fleming, published “Music and medicine: quickening the tempo of progress.”
This article reviewed the proceedings of a December 2023 workshop, “Music as Medicine,” and concluded that more transdisciplinary partnerships are needed. Specifically, “a shared lexicon must be cultivated that enables scientists, musicians, music therapists, technologists, and health-care providers to design research projects collaboratively,” we wrote. Embodying this ethos is the Sound Health Network , which the NEA supports at the University of California San Francisco.
There is plenty of work ahead, to be sure. But the UCLA opera study—like so many small but rigorous studies that have received NEA and/or NIH support—is contributing to a stream of evidence that has picked up velocity in recent years. Even if we lack a single large, prospective study that can establish a causal link between music on mental health outcomes, the pace of learning has been torrential.
Sunil Iyengar directs the Office of Research & Analysis at the National Endowment for the Arts.
Recent Blog Posts

Celebrate Asian American, Native Hawaiian, and Pacific Islander Heritage Month 2024

The Artful Life Questionnaire: Fiona Whelan Prine (Nashville, TN)
Stay connected to the national endowment for the arts.
- SUGGESTED TOPICS
- The Magazine
- Newsletters
- Managing Yourself
- Managing Teams
- Work-life Balance
- The Big Idea
- Data & Visuals
- Reading Lists
- Case Selections
- HBR Learning
- Topic Feeds
- Account Settings
- Email Preferences
Research: More People Use Mental Health Benefits When They Hear That Colleagues Use Them Too
- Laura M. Giurge,
- Lauren C. Howe,
- Zsofia Belovai,
- Guusje Lindemann,
- Sharon O’Connor

A study of 2,400 Novartis employees around the world found that simply hearing about others’ struggles can normalize accessing support at work.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program remains low. To understand why, a team of researchers conducted a randomized controlled trial with 2,400 Novartis employees who worked in the UK, Ireland, India, and Malaysia. Employees were shown one of six framings that were designed to overcome two key barriers: privacy concerns and usage concerns. They found that employees who read a story about their colleague using the service were more likely to sign up to learn more about the program, and that emphasizing the anonymity of the program did not seem to have an impact. Their findings suggest that one way to encourage employees to make use of existing mental health resources is by creating a supportive culture that embraces sharing about mental health challenges at work.
“I almost scheduled an appointment about a dozen times. But no, in the end I never went. I just wasn’t sure if my problems were big enough to warrant help and I didn’t want to take up someone else’s time unnecessarily.”
- Laura M. Giurge is an assistant professor at the London School of Economics, and a faculty affiliate at London Business School. Her research focuses on time and boundaries in organizations, workplace well-being, and the future of work. She is also passionate about translating research to the broader public through interactive and creative keynote talks, workshops, and coaching. Follow her on LinkedIn here .
- Lauren C. Howe is an assistant professor in management at the University of Zurich. As head of research at the Center for Leadership in the Future of Work , she focuses on how human aspects, such as mindsets, socioemotional skills, and leadership, play a role in the changing world of work.
- Zsofia Belovai is a behavioral science lead for the organizational performance research practice at MoreThanNow, focusing on exploring how employee welfare can drive KPIs.
- Guusje Lindemann is a senior behavioral scientist at MoreThanNow, in the social impact and organizational performance practices, working on making the workplace better for all.
- Sharon O’Connor is the global employee wellbeing lead at Novartis. She is a founding member of the Wellbeing Executives Council of The Conference Board, and a guest lecturer on the Workplace Wellness postgraduate certificate at Trinity College Dublin.
Partner Center

Transforming the understanding and treatment of mental illnesses.
Información en español
Celebrating 75 Years
Research. discovery. hope..
Explore our Events and Stories
Health Topics
- Anxiety Disorders
- Attention-Deficit/Hyperactivity Disorder
- Autism Spectrum Disorder
- Bipolar Disorder
- Borderline Personality Disorder
- Eating Disorders
- Obsessive-Compulsive Disorder
- Post-Traumatic Stress Disorder
- Schizophrenia
- Suicide Prevention
- More Topics
Featured Topics

Director’s Message: The Importance of Lived Experience Perspectives – Insights From the IACC

FY 2024 Budget Fact Sheet

Mental Health Awareness Month
Science updates.

Understanding the Underpinnings of Sensory Hypersensitivity

Gene-Based Therapy for Timothy Syndrome

Accelerating Science to Improve Early Autism Screening
Meetings and events, nimh research and science track at 2024 apa annual meeting, nimh intramural research program training opportunities, workshop: discrimination and mental health disparities.

Director of NIMH
Joshua A. Gordon, M.D., Ph.D.

NIMH Strategic Plan
Read about our plan for the institute's research priorities.
Inside NIMH
Funding News for Current and Future NIMH Awardees.

Find NIMH funding opportunities and announcements, including those specific to clinical research and training, and learn more about NIMH funding strategies, the application process, and grants management.

Finding Treatment
If you or someone you know has a mental illness, there are ways to get help. Use these resources to find help for yourself, a friend, or a family member.

Join A Study
Learn more about how to participate in outpatient and inpatient studies at the NIH Clinical Center, a hospital dedicated to the highest quality research.
Featured Resources

Brochures and Fact Sheets
Explore NIMH brochures and fact sheets. En español .
Learn more about our research areas, policies, resources, and initiatives.

Investigators
Learn more about scientists, physicians, and clinicians in NIMH’s Division of Intramural Research Programs (IRP).
Learn more about Research Domain Criteria Initiative (RDoC), a research framework that supports new ways of studying mental disorders.

Social Media
Connect with Us on Twitter, Facebook, YouTube, and LinkedIn.

Support for Clinical Trials
Learn more about clinical trials and funding opportunity announcements.

Find Us On Social Media!

- About NAMI Santa Clara County
- Our History
- Board of Directors
- Office Staff
- General Meeting
- Newsletter & Resource Guide
- Research Studies
- NAMIWalks Sillicon Valley
- NAMI Programs Overview
- Helpline FAQs
- Program Brochures
- Connection Support Groups
- Family Support Groups
- General Class Information
- NAMI Peer-to-Peer
- NAMI Family-to-Family
- NAMI Basics
- NAMI Provider Education
- NAMI Homefront
- Community Peer Program
- Faith Community List
- NAMI In Our Own Voice
- NAMI Ending the Silence
- Mental Health @ Work Presentation
- Introducción a NAMI en español
- Hoja de Información
- NAMI De Familia-A-Familia
- Persona-a-Persona
- About Mental Illness
- NAMI Welcome Package
- Books & Reviews
- Crisis Support
- Crisis Management Guide
- Involuntary Treatment, Conservatorships
- Family Member Arrested
- AB1424 Form
- Finding Missing Persons
- Psychiatric Advanced Directive
- Resources By Mental Health Diagnosis
Finding Treatment
- Mental Health Parity
- Tardive Dyskinesia (TD)
- Grief Support Resources
- Santa Clara County Behavioral Health Services
- Local Mental Health Medical Facilities
- NAMI Affiliate Links
- Housing & Mental Health
- Financial Aid & Mental Health Disabilities
- Applying for SSI/SSDI
- Special Needs Trusts ABLE Accounts WIPA
- NAMI Santa Clara Community Resource Center
- For Schools
- For Parents
- Suicide Awareness
- Multi-Cultural & Identity
- Ways to Give
- Become a Member
- Advocacy & Legislation
- Volunteer at NAMI Santa Clara County
NAMI Santa Clara County cannot recommend specific psychiatrists, therapists and other clinicians. However, we can give you information and suggestions on how to search for behavioral health professionals, programs and on-line and in-person peer support groups that deal with a variety of mental health concerns and issues.
Note : If you are experiencing an emotional crisis, family crisis, or are having suicidal thoughts:
In a life-threatening emergency, call.
And ask for a CIT officer ( Crisis Intervention Team )
In a MENTAL HEALTH CRISIS, call
* Only for area code 408, 650 or 669. For all other area codes, call
800-704-0900 and press 1
Text renew to 741741 (crisis text line).
Contents on this page:
- 10 Common warning sighs of mental health condition ( video )
- Mental Health Crisis Guide (Download pdf document)
- *NEW* Mental Health Parity – Learn about your rights to access mental health care in California.
- Insurance and Accessing Treatment
- File a Complaint
- Types of Mental Health Providers
- Tips for finding the right care
- Search for nearby individual mental health providers
- Nearby and/or affordable community mental health services
- Local Low Cost Therapists and Mental Health Clinics
- Professional provider associations that offer treatment referral services
- Professional provider organizations that serve specific audiences
- Other organizations that offer specialized treatment referral services
- On-Line Support Services
Watch this video below from www.nami.org to learn about symptoms of mental health conditions. Knowledge of the symptoms and warning signs will help you determine if you need to speak to a professional. Unlike other medical conditions like diabetes or cancer, there is not diagnostic test that can accurately diagnose a mental health condition. A mental health professional, usually a psychiatrist, will use the Diagnositc and Statistical Manual of Mental Disorders ( DSM), published by the American Psychiatric Association, to assess symptoms and make a diagnosis.
Getting an accurate diagnosis is the first step in a treatment plan. After diagnosis, a health care provider can help develop a treatment plan that could include medication, therapy or other lifestyle changes. Treatments vary by diagnosis and by person. There is no “one size fits all” treatment. By working together with a treatment team, you can develop a well-rounded and integrated recovery plan. Recent innovations in the evidence-based medications, therapy and social support through acceptance, education and support from family and friends have made wellness and recovery a reality for people living with mental health conditions.
We have compiled a list of resources and how-to instructions below to help you develop your own path to treatment and recovery.
(back to contents)
Resources for Locating Mental Health Care
The following resources can be used to help you find mental health treatment services in your community, including affordable treatment for those without insurance or who want to go outside their insurance provider list. 1. Insurance and Accessing Treatment
In accessing health care, it’s important to identify what health insurance you (or your family or friend) may have. This will help determine how to locate a mental health professional covered by your insurance. (If you are willing to pay out-of-pocket for therapy, see item #3 “Private Pay” below). If the insurance is:
- If you’ve never been seen by a County Mental Health professional, call the Santa Clara County Mental Health Call Center (800-704-0900) to get a referral for psychiatric services
- If you have the Santa Clara Family Health Plan , call (800) 260-2055 and ask for a list of “providers” (medical and psychiatric professionals who are covered by that health plan)
- If you have the Anthem Blue Cross California Medi-Cal Plan , call (800) 407-4627, and ask for a list of “providers” (medical and psychiatric professionals who are covered by that health plan), or go to the Anthem Blue Cross California Medicaid Find a Doctor page. or, use the Anthem Blue Cross Medi-Cal Find a Doctor online search
- If you have Medicare, the Medicare Physician Compare web page can assist you in finding a physician or other clinician who is enrolled in Medicare.
- If already enrolled in a Medi-Cal plan, call the plan directly and ask about their Medi-Medi Plan option
- Call Medicare at 1-800-MEDICARE
- Call Health Care Options at 1-844-580-7272 (TTY 1-800-430-7077).
- Other Private Insurance – Call your insurance company’s customer services number. You should be able to obtain list of providers that take your insurance. Also, see the “Resources for Locating Therapy” section below. Some online search engines allow you to specify insurance in search criteria, so you limit search results to people who take your insurance. Also, you can ask a professional if they accept your insurance. If you have been denied coverage for treatment, use SAMHSA’s Mental Health and Addiction Tool to find out how you can resolve the issue with your insurance.
- Private Pay – If you want to pay directly for psychiatric professionals, you can use the information listed below.
- Mental Health & Autism Insurance Project : Mental Health & Autism Insurance Project is a non – profit organization which assists families of children are living with autism spectrum disorders and/or mental health conditions, to obtain medically necessary treatments (including residential or outdoor therapy treatments) through their health plans. Their website has a wealth of information for families. They assist with obtaining single case agreements, writing appeals and requesting regulatory intervention and through seminars to the public on laws related to mental health and autism care. They are open Mon-Fri 9 AM – 5 PM. Ph. (925) 388-0892
2. File a Complaint
You have a right to file a complaint with your health plan. You might want to try talking to your doctor about the problem first.
To file a complaint:
- Call the Member/Customer Service phone number for your health plan.
- State clearly that you want to file a formal complaint and then explain the problem.
- If your problem is urgent, be sure to tell your health plan. Or call the California State Department of Managed Health Care at 1-888-466-2219 right away.
- You can also file your complaint by letter or e-mail. Sometimes you can file a complaint through your health plan’s website.
- You can ask your doctor, or a doctor outside of your health plan, to help you by writing a letter explaining why you need the service.
- You must file your complaint within 6 months after the incident or action that is the cause of your problem.
- After you file your complaint, your health plan must give you a decision within 30 days, or 3 days if your health problem is urgent.
- How to get insurance to cover denied claims – Step By Step Guide
If your complaint is urgent, or if you are not satisfied with your health plan’s response, you can file an external appeal (also called an Independent Medical Review .) To do this, contact the California State Department of Managed Health Care at 1-888-466-2219, or go to their File a Complaint page. You can also use this form to lodge a consumer complaint for issues such as qualify of service, cancellation of coverage, or disputes on billing and co-pays.
3. Types of Mental Health Providers
Mental Health providers can help you to deal with current stress, heal old traumas, make decisions about medication and develop treatment plans that reflect your goals. Choosing a mental health provider can be challenging, but make sure you match your needs with his or her experience and specialty to get the most out of your treatment.
Over time, many people with mental health conditions say that treatment helps them: feel stronger, have a greater ability to cope with symptoms, and develop skills for building their relationships and pursuing goals. In fact, most people who seek professional help feel better. For example, more than 80 percent of people treated for depression improve, and treatment for panic disorders has up to a 90 percent success rate.
There are many types of mental health professionals. Finding the right one for you may require some research. Often it is a good idea to describe the symptoms and/or problems to your primary care provider first. He or she can suggest the type of mental health professional you should call.
Types of mental health providers:
4. Tips for finding the right care
- Association for Behavioral and Cognitive Therapies’ fact sheet “How do I choose a Therapist?” and some of the sites listed below provide detailed information to help you choose a mental health professional and to enable you to better understand treatment options and the treatment process.
- Psych Central’s Article on 10 ways to find a good therapist has some good tips on best ways to obtain referrals to good professionals.
- You can also attend NAMI and other peer and family support groups. and ask for recommendations from others in the group.
- Tips on Finding the Right Therapist for Teens
- How to get insurance to cover denied claims
- Checklist to bring to the appointment . Download, complete this useful checklist from Mental Health America before your appointment with your doctor. You can use this to remind you of what to talk to the doctor and help you keep track of your progress.
- help.org – Offer provide support for people who are dealing with substance abuse and addiction through comprehensive resources and guides. Their website has a searchable database for drug and alcohol abuse rehabilitation resources and information guide to the process, cost and more. This is a good resource for individuals and families who are dealing with dual diagnosis (mental health and substance abuse).
5. Search for nearby individual mental health providers
* Note : Many online directories are incomplete as professionals must ask to be included. Try different search methods, or, if you have health insurance, contact the plan’s customer service number for a list of providers.
- FindTreatment.gov SAMHSA ‘s search tool to find mental health and substance abuse care by zipcode. This website also has a lot of useful information on accessing treatment and how to pay for it.
- Psychology Today’s Therapy Directory Search for mental health professionals in your area, by zip code, city, insurance, specialty, etc. For each provider listed, read about their therapy approach, specialty areas, fee policy (insurance, out of network sliding scale), credentials and contact information. (*Note: Therapist credentials include years in practice and school/trainings)
- NEW! Psychology Today’s Find a Teletherapy Therapist – Search for therapist who offer treatment via Phone, Video and Online
- Web MD’s Find a Psychiatrist allows you to search for psychiatrists by state, city, specialty, insurance, etc.
- Counseling California offers a searchable directory California-based Licensed Marriage and Family Therapists.
- GoodTherapy offers a searchable database of over 1600 counselors and therapists worldwide. GoodTherapy is dedicated to promoting healthy counseling and psychotherapy. (*Note: Can search based on “Type of Service”, including “ Home-Based Therapy , “On-Line Therapy”, “Group Therapy”, “Individual Therapy”).
- The Medicare Physician Compare can assist you in finding a physician who is enrolled in Medicare.
6. Nearby and/or affordable community mental health services
- Parent Solutions – Ph. 408-292-4357 Offer collaborative behavioral health services for children, teens, adults, couples, families and older adults in Spanish and English at San Jose and Morgan Hill. They take insurance and offer sliding scale. Flyer
- 211 Santa Clara County – 211 is the dialing code for free, non-emergency community, health and disaster information in Santa Clara County. They also have a Search Database for finding various types of services in this county. Type “Mental Health” in the search bar to find a variety of local mental health treatment resources.
- The LGBTQ Youth Space – Phone: 408-343-7940. A community drop-in center and mental health program for lesbian, gay, bisexual, transgender, queer, questioning and ally youth and young adults ages 13-25 who live in Santa Clara County..
- Sourcewise Resource Connection – Phone: 408-350-3200, option 1. Offers a comprehensive database of community resources designed to help you locate services available in the Santa Clara County community. The most complete, up-to-date, and personalized information can be found by contacting Sourcewise Community Resource Specialists at (408) 350-3200, or at [email protected].
- Olivos – Phone: 650-781-4148. San Mateo company offering private pay mental health psychosocial rehabilitation and recovery services focusing on avoiding institutional care. Services are individualized and tailored to the client and include case management, psychiatry, therapy, vocational rehab, supported education, medication management, life skills development, independent living, housing, or companion services.
- SAMHSA Mental Health Facilities Locator – A searchable directory provided by the federal government’s Substance Abuse and Mental Health Services Administration’s (SAMHSA) Health Information Network that can help you find local community outpatient, inpatient and residential treatment facilities, for mental health and/or addiction issues. Enter your state and/or county in the upper right “Find Facility” search bar to start.
- Psychology Today Psychiatric Residential Treatment Centers in California – lists residential mental health treatment facilities. List is searchable by disorder treated and by insurance accepted.
7. Local Low Cost Therapists and Mental Health Clinics
The following table lists other low cost therapists and mental health clinics available within the Santa Clara County.
8. Professional provider associations that offer treatment referral services
There are a number of professional provider associations and other national organizations that provide treatment referral services. These organizations are listed below with links to their websites.
- American Counseling Association
- American Association of Marriage and Family Therapists
- American Psychiatric Association’s Choosing a Psychiatrist (PDF)
- American Psychological Association
- American Residential Treatment Association
- Association for Behavioral and Cognitive Therapies
- Social Workers Search Tips
- National Register of Health Service Providers in Psychology
9. Professional provider organizations that serve specific audiences
- American Academy of Child and Adolescent Psychiatry – Click on “ Child and Adolescent Psychiatrist Finder “
- American Association for Geriatric Psychiatry
- Association of Black Psychologists
- Association of Gay and Lesbian Psychiatrists
- Su Familia (National Alliance for Hispanic Health) at 1-866-783-2645
10. Other organizations that offer specialized information and treatment referral services
- ANAD (National Association of Anorexia Nervosa and Associated Disorders) – Call (888) 375-7767
- AllTreatment .- an aggregator that provides a number of listings for substance use treatment facilities.
- Anxiety Disorders Association of America : Therapists ; Treatment Centers
- ATTACh (Association for Treatment and Training in the Attachment of Children) – offers treatment referrals for children with attachment disorder
- Attention Deficit Disorder Association
- Autism Society of America
- Behavioral Tech, LLC – Find a DBT (Dialectical Behavior Therapy) therapist, for borderline personality disorder
- Brain Injury Association of America and http://www.biausa.org/state-affiliates.htm – list of state offices
- Children and Adults with Attention Deficit/Hyperactivity Disorder
- Depression and Bipolar Support Alliance – patient to patient recommendation section
- Find a CBT Therapist : ABCT (Association for Behavioral and Cognitive Therapies) CBT Therapist search site allows you to search by Zip Code and/or State, Radies, Speciality, Insurance.and Telehealth option..
- Give an Hour – non-profit organization offering free mental health services for Veterans and their loved ones through a network of volunteer mental health professionals
- Hospice Foundation of America – national grief support groups
- In The Rooms – the world’s largest social network for the global recovery community, for people already in recovery, seeking immediate help with any addiction, and their family, friends, and allies. You will have unlimited access to over 117 live online Recovery meetings weekly. ITR offers AA, NA, and other 12 Step and non 12 Step Support Groups, Geo Locatable Global Meeting Finder, Daily E Meditations, Afternoon Affirmations, Free iPhone and Android Apps, Speaker Tape Library and much more. For immediate treatment, go to Find a Treatment Center
- International Obsessive Compulsive Disorder Foundation – See “Find Help” on the left-hand side of the home page
- International Society for the Study of Trauma and Dissociation – See “Find a Therapist or Treatment Facility” on the right-hand side of the home page
- National Center for Post Traumatic Stress Disorder – Dept. of Veterans Affairs PTSD Information Center offers information about PTDS and its treatment. Click on “Get Help” on left side bar, or go to the Find a Therapist page.
- National Eating Disorders Association – Get immediate crisis support, or find a therapist specializing in eating disorders
- Postpartum Support International – Use the Find Local Support, Resources, and Events option to find contact information for your State Coordinator to get a list of psychiatrists and therapists in your area who specialize in reproductive-related mood disorders.
- Rape Abuse and Incest National Network – counseling centers throughout the U.S.
- SAMHSA Substance Abuse Treatment Facility Locator and the SAMHSA 24/7 Treatment and Referral line at 1.800.662.4357 provide referrals to alcohol, substance abuse and dual diagnosis treatment facilities, including facilities that offer sliding scale fees and other special payment arrangements. Dual diagnosis services provide integrated treatment for individuals who have both an alcohol or substance abuse problem and a mental illness. Use the detailed search option on the left hand side of the page to find the facilities that most closely match your needs.
- Parent and Caregiver Network – A program of the Depression and Bipolar Support Alliance (DBSA). Provides resources and guidance for families raising children and adolescents with Bipolar Disorder.
- The National Child Traumatic Stress Network Go to “Finding Help for Sexually Abused Children” and click on the “National Network Members” page option, to search by state
- TARA at 1-888-482-7227 (Treatment and Research Advancements) National Association for Personality Disorder; treatment referrals for borderline personality disorder
- TRICARE mental health services for military personnel and their families
- World Federation for Mental Health can assist people from other countries throughout the world in finding mental health services in their area.
11. On-Line Support Services
- 7 Cups is a website (and also a mobile app ) providing free support to people experiencing emotional distress by connecting them with non-professional listeners trained in active listening. The listener interacts with the person seeking help via anonymous and confidential chat. Listeners are rated by peers and those to whom they listen. 7 Cups also provides chat support groups and referrals to therapists. View the 7 Cups Flyer .
- Depression and Bipolar Support Alliance (DBSA) online Support: Provides free support for people living with depression and bipolar disorder.You can share experiences, discuss coping skills, and offer hope to one another. DBSA support groups are peer-led, meaning they are facilitated by someone living with a mood disorder. You can find groups for peers, young adults, and friends and family members.
- Postpartum Progress : This website maintains an online forum in addition to providing a list of support groups.
- Adult Children of Alcoholics World Service Organization : This 12-steps program for children who grew up with alcoholic parents or caregivers also has online meetings.
Attachments
- Flyer (343 kB)
- Parent Solutions Flyer (343 kB)
- How to get insurance to cover denied claims (494 kB)
- https://www.facebook.com/namisantaclaracountyk
- https://www.twitter.com/NAMISantaClara
- https://www.linkedin.com/company/nami-santa-clara-county/
- [email protected]
Search form
Novel study quantifies immense economic costs of mental illness in the u.s..

(Illustration by Michael S. Helfenbein)
Mental illness costs the U.S. economy $282 billion annually, which is equivalent to the average economic recession, according to a new study co-authored by Yale economist Aleh Tsyvinski .
The first-of-its-kind study integrates psychiatric scholarship with economic modeling to better understand the macroeconomic effects of mental illness in the United States.

The study was prepared as a working paper of the National Bureau of Research, a private nonprofit U.S. organization that includes researchers from leading U.S. universities, economics professional organizations, and the business and labor communities.
The $282 billion estimate — which amounts to about 1.7% of the country’s aggregate consumption — is about 30% larger than previous approximations of mental illness’s overall cost in epidemiological studies.
While those earlier studies focused on income loss relating to mental illness and the costs of mental health treatment, the new study also accounted for a host of additional adverse economic outcomes associated with mental illness, including the fact that people with mental illness consume less, invest less in a house, stocks and other risky assets, and may choose less-demanding jobs, Tsyvinski said.
“ In this paper, we develop the first integrated model of macroeconomics and mental health building on classic and modern psychiatric theories,” said Tsyvinski, the Arthur M. Okun Professor of Economics in Yale’s Faculty of Arts and Sciences and professor of global affairs in the Yale Jackson School of Global Affairs. “We show that mental illness alters people’s consumption, savings, portfolio choices, as well as the country’s labor supply, generating enormous annual costs to our economy.”
Nationwide, more than 20% of adults live with mental illness and about 5.5% experience serious mental illness, according to the U.S. Substance Abuse and Mental Health Services Administration.
For the study, Tsyvinski and co-authors Boaz Abramson, of Columbia Business School, and Job Boerma, of the University of Wisconsin-Madison, analyzed the potential effects of policies aimed at improving treatment of mental illness. They found that expanding the availability of mental health services — by eliminating the shortage of mental health professionals, among other means — would reduce mental illness by 3.1% and bring societal benefits equivalent to 1.1% of aggregate consumption.
Providing mental health services to everyone between the ages of 16 and 25 experiencing mental illness would reap societal benefits equal to 1.7% of aggregate consumption, according to the study.
At the same time, their analysis found that lowering the out-of-pocket cost of mental health services does not substantially reduce the share of people with mental illness and provides only minor economic gains. The researchers suggest that the monetary costs of mental health services are relatively low, meaning that reducing costs does not lead to greater uptake in treatment nor does it significantly reduce instances of mental illness.
The researchers model mental illness as a state of negative thinking and a state of rumination — the uncontrollable and repetitive preoccupation with negative thoughts — that is reinforced through behavior. In that model, they say, individuals experiencing mental illness are pessimistic about their future productivity, risky investments, and the evolution of their mental health. They also lose time while ruminating. As a result, they work, consume, and invest less while also foregoing treatment, which reinforces their mental illness.
The study typifies the cross-disciplinary approach to economic questions of major policy and societal importance that is a hallmark of the scholarship produced by Yale’s Department of Economics over more than 50 years — including Yale economist William Nordhaus’s pioneering work combining economic modeling with climate science to predict the costs of climate change.
“ Economics and psychiatry have developed over 50 years, but they don’t speak to each other very much,” he said. “Here, we’ve put them in conversation in a way that enlightens both and provides us a stronger sense of the societal costs of mental illness as well as what can be gained through policies that seek to expand and improve mental health care.”
Health & Medicine
Social Sciences
Media Contact
Bess Connolly : [email protected] ,

Yale honors 10 student workers who made key campus contributions

Targeting friends to induce social contagion to benefit the world

Six faculty members honored for their commitment to teaching

James Forbes and Barbara Brown Taylor to speak at Yale ISM hymn festival
- Show More Articles
- Forms & Rules
- Policy & Administration
- News & Reference
- Mental Health Courts
- Collaborative Justice Courts
- Community/Homeless Courts
- Homeless Court Technical Assistance for Courts
- Drug Courts
- Reentry Courts
- Veterans Treatment Courts
- Grants/Funding
- Juvenile Collaborative Courts
- Research and Publications
What is a Mental Health court?
Mental health courts (MHC) are a form of collaborative court that provides specific services and treatment to defendants dealing with mental illness. Mental health courts provide an alternative to the traditional court system by emphasizing a problem-solving model and connecting defendants to a variety of rehabilitative services and support networks. Each MHC has different participant requirements and available services. The goal of a mental health court is to:
- support participants successful return to society and reduce recidivism;
- increase public safety; and,
- improve individual’s quality of life.
Related Links
How do they work.
- Mental health courts only accept people with demonstrable mental illnesses that can be connected to the individual’s illegal behavior.
- Participation in a mental health court is voluntary and the defendant must consent to involvement in the program.
- Screening and referral to a mental health court should occur as soon as possible after arrest to insure early intervention.
- Screening is also used to determine whether a mental health court can provide appropriate resources and support to the individual.
- Mental health courts use a structure of case management based in intensive supervision/monitoring and individual accountability.
- Case management is supervised by a team of professionals; teams are typically comprised of members of the justice system, mental health providers, and other support systems.
- The judge oversees the treatment and supervision process, and facilitates collaboration among team members.
In 2008, the Council of State Government Justice Center published a report outlining the 10 Essential Elements of Mental Health Courts. These essential elements provide guidelines for developing and operating a mental health court; including target participants, various types of services and support, and the creation of an effective court team. The original report can be found here .
Are Mental Health Courts Effective?
Yes. Most studies find that adult mental health courts have a positive effect on participants’ rehabilitation and criminal behavior during and after their participation. Specifically, studies have found that mental health court participants are significantly more likely to utilize treatment services, less likely to be rearrested, and spent fewer days in jail as opposed to nonparticipants. Studying the effectiveness of mental health courts can be challenging due to several factors including the difficulty of measuring the outcome of rehabilitative services and finding appropriate control groups. As such, continued research will be especially helpful for increasing the sample size of studies and determining the lasting effects of MHC participation over time.
Judicial Council Webinars
Adult drug court standards webinar series.
The Judicial Council of California partnered with drug court subject matter experts to create a 12 month “lunch box” series of live, interactive, on-line trainings that focused on each Adult Drug Court Best Practice Standard from All Rise, formerly the National Association of Drug Court Professionals (NADCP). See the Judicial Council YouTube Adult Drug Court Standards Webinar Series to watch.
Mental Health: Lived Experiences
This presentation explores how judges and courts staff can effectively address court users who have a mental illness. This webinar includes interviews of people involved in the justice system who have a mental illness sharing their court experiences and practical take-aways for improved court sessions.
- Presentation
Partnering with County Behavioral Health to Serve Justice-Involved Populations
This three-part webinar discusses the services that county behavioral health agencies provide, including the different treatment options, levels of care, and types of treatment providers.
- Video Part 1
- Video Part 2
- Video Part 3
Serious Mental Health Disorders
This webinar defines ‘serious mental health disorder’, and discusses common diagnoses in the criminal justice system, symptoms of these disorders, and effective treatments.
Organizations
County Behavioral Health Directors Association
Council on Criminal Justice and Behavioral Health
Behavioral Health Education and Resources
Publications
Literature Review: Mental Health Courts (April 2012) An overview of the literature on mental health diversion programs and mental health courts.
Mental Health Courts: A Guide to Research-Informed Policy and Practice
Improving Responses to People with Mental Illnesses: The Essential Elements of a Mental Health Court
A Guide to the Role of Crime Victims in Mental Health Courts
Mental Health Courts: A Primer for Policymakers and Practitioners
A Guide to Mental Health Court Design and Implementation
A Guide to Collecting Mental Health Court Outcome Data
Full-spectrum mental health care changes lives
Sam, now in his late 20s, has experienced behavioral health challenges since he was a child and has been hospitalized for mental health needs and drug addiction numerous times during his adult life. Like many people living with mental health needs, Sam’s treatment is a lifelong journey requiring various inpatient and outpatient services at different stages. This can be especially challenging for low-income people like Sam and those experiencing homelessness who rely on Medicaid. One in five adults nationwide experience mental illness, and nearly one-third of those people do not receive the treatment needed.
While approximately 4% of the general population of adults have a severe mental illness, the National Alliance on Mental Illness estimates that 45% of the homeless population experience a form of mental illness, with 25% of this population suffering from severe mental illness.
“It not only benefits individuals with mental health needs but also their communities and society as a whole to offer high-quality, affordable services,” says Dr. Katie Gilligan, chief medical officer at Compass Health , a community-based behavioral health care agency serving primarily low-income and homeless individuals in northwest Washington who qualify for Medicaid. “Through offering a suite of triage, inpatient and outpatient services, we can help to prevent mental health crises and homelessness, keep people in their jobs, enable families to stay intact and ease the load on law enforcement and other community partners.”
Integrated spectrum of care makes the difference
When mental illness is deeply connected to the life challenges a person is facing, an integrated spectrum of care can have a powerful impact. After one of Sam’s hospitalizations, he was connected to Compass Health’s Program of Assertive Community Treatment, an evidence-based, intensive outpatient treatment program that helps adults with intensive behavioral health needs overcome barriers to recovery.
Experts suggest looking for the following services in intensive outpatient mental health programs:
- Clinicians to help with case management, including frequent client visits.
- Peer support, both individual and group.
- Psychiatric support.
- Coordination with community partners providing housing, medical care, financial and vocational programs.
PACT’s multidisciplinary teams include mental health professionals, psychiatrists, nurses, clinicians, peer counselors and substance use disorder specialists. These teams deliver comprehensive services to clients, most of whom are seen several times a week or multiple times per day, to promote stabilization and recovery. PACT teams also work alongside other community partners to connect clients to other necessary supports to encourage healthy, independent living.
Since enrolling in PACT, Sam has only been hospitalized once and he has achieved sobriety. Through his perseverance and resilience, and with the help of his support team, Sam has paved his path to recovery.
This kind of intensive support can be the difference to truly improving quality of life for individuals with behavioral health needs. Compass Health’s Broadway Campus Redevelopment, slated for completion in summer 2025, will help make these kinds of services more available. This state-of-the-art facility is designed to deliver 24-hour crisis care to those experiencing behavioral health crises and a spectrum of inpatient and intensive outpatient services to promote easier access to a continuum of care.
For Sam, and many others, a full continuum of care — from mental health crisis services to sustained, long-term supports make a real impact on quality of life. “It’s critical to provide a wide array of services that meet each individual where they are in their mental health journey,” Gilligan says.
Compass Health is Northwest Washington’s behavioral health care leader. From comprehensive mental health treatment to crisis prevention and intervention, supportive housing, children’s services and more, we serve people of all ages throughout Snohomish, Skagit, Island, San Juan and Whatcom counties.
- Aboriginal and Torres Strait Islander Health Performance Framework
- Australian Mesothelioma Registry
- GEN Aged Care Data
- Housing data
- Indigenous Mental Health and Suicide Prevention Clearinghouse
- Metadata Online Registry (METEOR)
- Regional Insights for Indigenous Communities
- Help & tools
- Increase text size
- Decrease text size

Social isolation and loneliness Print this page
- Stress and trauma 14 Feb 2024
- Physical health of people with mental illness 14 Feb 2024
- Prevalence and impact of mental illness
On this page:
Who experiences social isolation and loneliness?
Preventing and reducing social isolation and loneliness, where can i go for more information.

Loneliness and social isolation were concerns before the onset of the COVID-19 pandemic but have been exacerbated in the subsequent years.

In 2022, males aged 15–24 tended to experience more social isolation and loneliness than females.
Social isolation and loneliness are among the many factors that can be detrimental to a person’s wellbeing.
Social isolation and loneliness can harm both mental and physical health and may affect life satisfaction. They are concerning issues in Australia due to the impact they have on peoples’ lives and wellbeing.
Loneliness has been linked to premature death, poor physical and mental health (Holt-Lunstad et al. 2015), greater psychological distress (Manera et al. 2022) and general dissatisfaction with life (Schumaker et al. 1993). Loneliness among Australians was already a concerning issue before the COVID-19 pandemic, to the extent that in 2022 it has been described as one of the most pressing public health priorities in Australia (Ending Loneliness Together 2022).
Social isolation has been linked to mental illness, emotional distress, suicide, the development of dementia, premature death and poor health behaviours (smoking, physical inactivity and poor sleep) – as well as biological effects, including high blood pressure and impaired immune function (Cacioppo et al. 2002 and Grant et al. 2009 in Holt-Lunstad et al. 2015). Social isolation is also associated with psychological distress (Manera et al. 2022) and sustained decreases in feelings of wellbeing (Shankar et al. 2015). Conversely, more frequent social contact is associated with better overall health (Botha 2022).
The difference between social isolation and loneliness
Social isolation ‘means having objectively few social relationships or roles and infrequent social contact’ (Badcock et al. 2022:7). It differs from loneliness, which is a ‘subjective unpleasant or distressing feeling of a lack of connection to other people, along with a desire for more, or more satisfying, social relationships’ (Badcock et al. 2022:7). The 2 concepts may, but do not necessarily, coexist (Badcock et al. 2022; Relationships Australia 2018) – a person may be socially isolated but not lonely, or socially connected but feel lonely.
Social isolation
In 2022, almost 1 in 7 (15%) Australians (18% of males and 12% of females) were experiencing social isolation. Compared to just before the pandemic (2019) the proportion of young people aged 15–24 experiencing social isolation increased markedly over 2020 and 2021. During the later years of the pandemic (2021 to 2022) the proportion of young females (15–24 years) experiencing social isolation decreased (23% in 2021 down to 17% in 2022), while the proportion of young males continued to increase (from 22% to 25% over this time). The 35–44 year age group was the only one for whom social isolation continued to increase from 2021 (16% in 2021 to 17% in 2022) (Figure SIL.1).
Figure SIL 1: How has social isolation changed over time?
Line graph and butterfly chart showing the per cent of males and females of various age groups experiencing social isolation, from 2001 to 2022. The proportion of males aged 15–24 experiencing social isolation from 2001 to 2019 remained relatively steady between 11% and 15%, before increasing to 19% in 2020 and continuing to increase to 22% in 2021, then dropped to 21% in 2022.
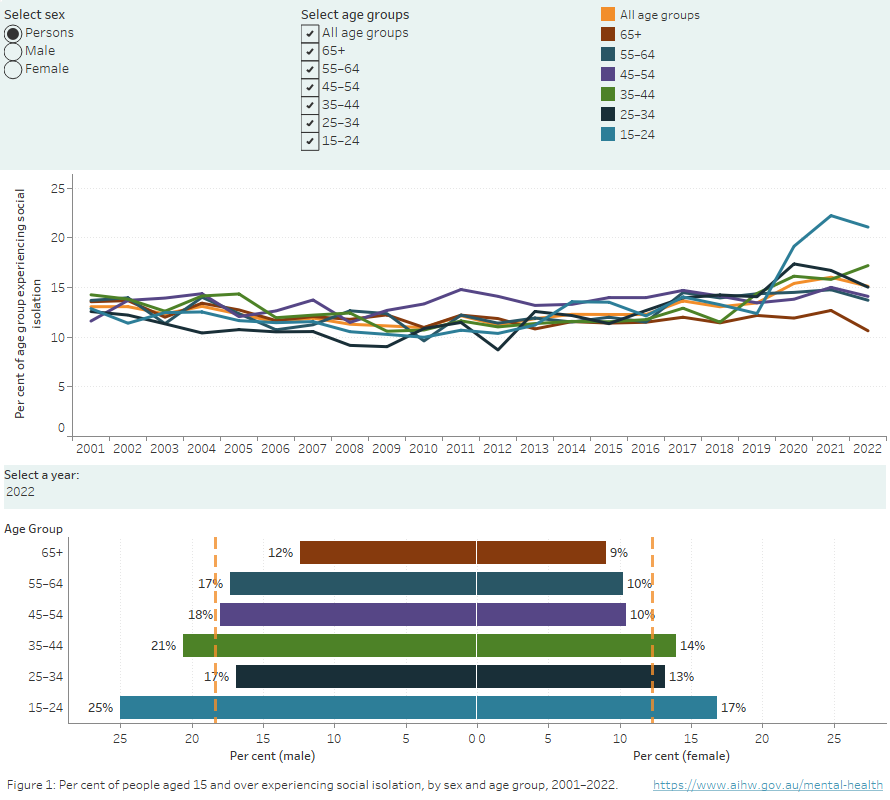
Source: AIHW analysis of Household and Labour Dynamics in Australia (HILDA) data, waves 1–22.
In 2022, just over 1 in 6 (16%) Australians were experiencing loneliness. As of 2022, about 1 in 5 (17%) males and 1 in 6 (15%) females aged 15–24 were experiencing loneliness. An increasing number of people aged 15–24, have reported experiencing loneliness since 2012. In contrast, the frequency of people aged 65 and over reporting loneliness has been steadily declining since 2001 (Figure SIL 2).
Figure SIL 2: Per cent of people aged 15 and over experiencing loneliness, by sex and age group, 2001–2022
Line graph and butterfly chart showing the per cent of males and females of various age groups experiencing loneliness, from 2001 to 2022. In 2001, 15% of people aged 15–24 were lonely, compared to 16% in 2022. The proportion of people aged 65 and over who are lonely has decreased from 20% in 2001 to 16% in 2022.
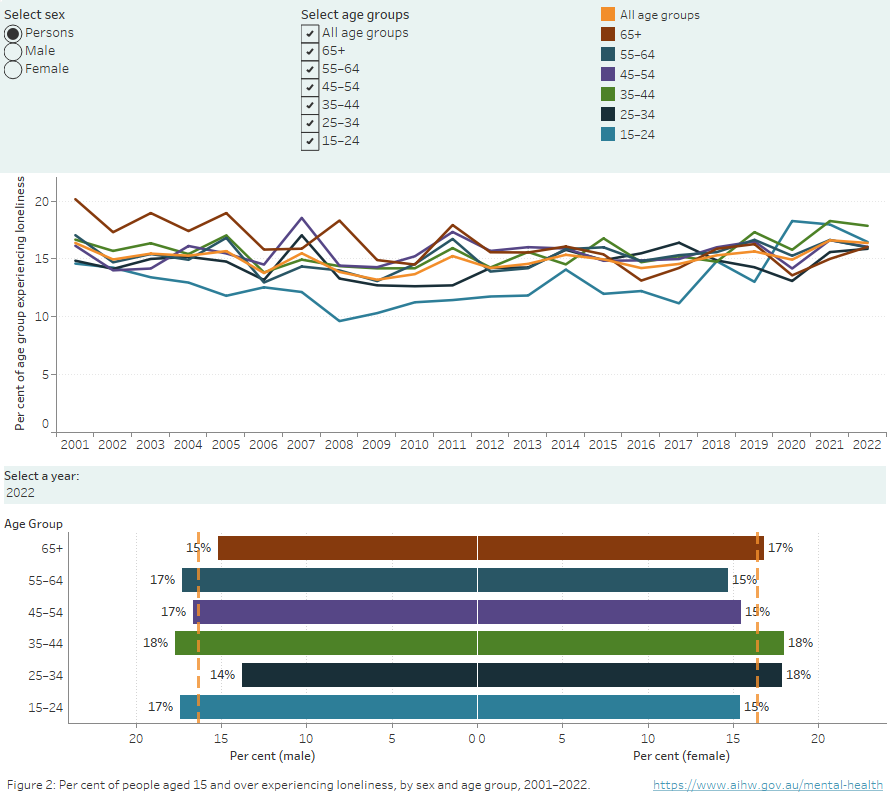
Australia’s available data on loneliness do not allow for reliable international comparisons. In a recent systematic review of loneliness in 113 countries led by Australian researchers, Australian data could not be compared with those of other countries due to a lack of comparable prevalence data – except for the adolescent age group (Surkalim et al. 2022). To date, the Organisation for Economic Co-operation and Development has not reported comparable data for Australia on its measures of ‘people feeling lonely’ and ‘people feeling left out of society’ (OECD 2022, 2023).
Domestic and family violence
Family, domestic and sexual violence is a major health and welfare issue in Australia, occurring across all socioeconomic and demographic groups, but predominantly affecting women and children (AIHW 2022).
Social isolation is a well-recognised tactic of coercive control used by perpetrators to control their victims (Boxall and Morgan 2021). It ensures the victim does not hear other people’s perspectives: perpetrators control the information the victim receives, reduce their help-seeking opportunities, and control the victim’s ability to leave the abusive relationship (Stark 2007). Recent studies on the impact of the COVID-19 pandemic on Australians are identifying some adverse outcomes of stay-at-home orders associated with increased social isolation that put some women and children at higher risk of experiencing family violence (Morgan and Boxall 2020; Pfitzner et al. 2022).
An online survey of 166 practitioners conducted in Victoria during the 2020 lockdowns revealed that women’s experiences of intimate partner violence worsened because of their increased social isolation, which reduced their ability to seek external help and support (Pfitzner et al. 2022). This trend was also identified in other cities and countries, with perpetrators using the social isolation provided by the stay-at-home orders to increase abusive behaviours towards victims within their homes (Piquero et al. 2021). An Australian study suggests the combination of increased social isolation and economic stress associated with the COVID-19 pandemic did increase the risks of domestic and family violence for women in current cohabiting relationships (Morgan and Boxall 2020).
For more information, refer to Family, domestic and sexual violence .
Engaging in volunteer work and maintaining active memberships of sporting or community organisations are also associated with reduced social isolation (Flood 2005). Participating in paid work and caring for others have been proposed as safeguards against loneliness. However, it is unclear whether community engagement can consistently act as a protective factor against loneliness. For example:
- one study found that loneliness is lower in people who spend at least some time each week volunteering (Flood 2005)
- another study found no relationship between loneliness and volunteering, or between loneliness and socialising and participating in sport and community organisations (Baker 2012).
For people aged 25 to 44, being in a relationship is a greater protective factor against loneliness for men than for women (Baker 2012). Women living with others and women living alone report similar levels of loneliness, while men living alone report higher levels of loneliness than men living with others (Flood 2005).
The role of social media
Whether social media has potential benefits or negative impacts on people’s experiences of social isolation has been discussed since the advent of this medium. There is no straightforward relationship however, between social media use and experiences of social isolation and loneliness, whether positive or negative.
Researchers have identified some positive impacts of how social media can help people feel socially connected, especially adolescents (aged 11–19) who are looking for peers online to boost their psychosocial wellbeing, discuss identity development and encourage a sense of belonging (Allen et al. 2014). Other research has showed that using social media benefited young people (aged under 21) who experienced higher levels of social anxiety by increasing their ability to socialise, reducing their feelings of social isolation (Lin et al. 2017).
Even though adolescents can use social media to create supportive communities, research shows that the relationship between its use and loneliness can work both ways. When it is used to escape physical social interactions, feelings of loneliness were found to increase. People experiencing loneliness may benefit from external support with the use of the Internet to ensure they engage in existing friendships and learn how to develop new ones online to reduce feelings of loneliness and social isolation (Nowland et al. 2017).
More research has emerged since the pandemic started that investigates the use of social media by people of all ages and their experiences of social isolation, but findings are not always positive. For example, a study of people living in Norway, the United States of America, the United Kingdom and Australia looked at the impact of people’s use of social media during the pandemic. The researchers found an association between emotional distress and more frequent use of social media (Geirdal et al. 2021).
Another international study investigating current research between online social networking and mental health outcomes for people aged 50 and over found that social media enhanced communication with family and friends, provided greater independence and self-efficacy, aided in the creation of new communities online, helped to form positive associations with wellbeing and life satisfaction, and was associated with decreased depressive symptoms (Chen et al. 2021).
As more studies are conducted through the pandemic and beyond, an understanding of how social media affects feelings of social isolation and loneliness may become clearer.
Although social isolation and loneliness are now well-recognised public health concerns, major gaps remain in understanding what works to resolve them (Smith and Lim 2020). Due to our diverse social needs, preferences and resources, there is no ‘one size fits all’ solution (Ending Loneliness Together 2022).
Companion animals
Pets can play an integral part in people’s lives, regardless of the person’s culture, profession or age. Companion animals are one source of external support that can bring both physical and mental health benefits (Brooks et al. 2016). All types of companion animals may contribute to reducing social isolation and feelings of loneliness (Brooks et al. 2018; Kretzler et al. 2022).
Multiple studies have found an association between pet ownership and lower experiences of social isolation, particularly for children (Christian et al. 2020; Hartwig and Signal 2020; Kretzler et al. 2022). Further, research suggests that companion animals may positively influence experiences for older people (aged 60 and over) by increasing their sense of purpose and meaning, facilitating increased social interaction, reducing loneliness and improving emotional resilience (Gan et al. 2019), as well as being potentially a protective factor against suicide (Young et al. 2020a). Owning a pet increases the opportunity for people to get to know their neighbours and for social interactions and forming friendships (Wood et al. 2015).
Brooks and colleagues (2018) systematically reviewed 17 studies that investigated the relationship between companion animals, specifically domestic animals, and the assistance these animals provided in helping people to manage their mental health conditions. The quantitative studies produced mixed findings, with people experiencing positive, negative and neutral impacts of their companion animal on their personal mental health.
Qualitative studies suggest, however, that people with mental health conditions may benefit from the direct support their companion animals provide. This support includes helping their owners to manage their mental health condition, reducing people’s stress and regulating emotions – particularly beneficial during times of crisis, improving people’s quality of life, providing a consistent source of comfort, and aiding social and community interactions. Companion animals were found to help mitigate feelings of social isolation and loneliness by providing physical warmth and companionship, and opportunities for non-judgemental communication for their owners. Further, they may offer a distraction or disruption when their owners experience panic attacks and other symptoms of mental illness (Brooks et al. 2018). On the other hand, negative impacts included difficulties with the daily commitment of pet ownership and the psychological stress when losing a companion pet.
Since the start of the COVID-19 pandemic, studies have mostly shown that the association between pet ownership, loneliness and social isolation has strengthened (Kretzler et al. 2022). One study found that cats gave people an outlet for stress through the strong bonds they had established with owners, and the affection and comfort they provided, thus acting as a buffer to the social isolation created by the lockdowns (Currin-McCulloch et al. 2021). Dogs provided people with daily reinforcement of positive behaviours such as routine, exercise and play, which all contributed to decreased feelings of social isolation (Bussolari et al. 2021).
It is not yet clear whether this strong relationship between people and their pets at the levels seen in the early years of the COVID-19 pandemic will persist in the future (Hughes et al. 2021; Young et al. 2020b).
For more information about social isolation and loneliness, see:
- Bankwest Curtin – Stronger together: loneliness and social connectedness in Australia
- Measuring what matters
- Ending Loneliness Together
AIHW (Australia Institute of Health and Welfare) (2022) Family, domestic and sexual violence data in Australia , AIHW website, accessed 9 February 2024.
Allen KA, Ryan T, Gray DL, McInerney DM and Waters L (2014) ‘ Social media use and social connectedness in adolescents: the positives and potential pitfalls ’, The Educational and Developmental Psychologist , 31(1):18–31, doi:10.1017/edp.2014.2, accessed 9 February 2024.
Badcock JC, Holt-Lunstad J, Garcia E, Bombaci P and Lim MH (2022) Position statements on addressing social isolation and loneliness and the power of human connection , Global Initiative on Loneliness and Connection, accessed 9 February 2024.
Baker D (2012) All the lonely people: loneliness in Australia, 2001–2009 , The Australia Institute, Canberra, Institute paper no. 9, accessed 9 February 2024.
Botha F (2022) ‘Social connection and social support’, in Wilkins et al., The Household, Income and Labour Dynamics in Australia Survey: selected findings from waves 1 to 20 , Melbourne Institute: Applied Economic and Social Research, Melbourne.
Boxall H and Morgan A (2021) Statistical Bulletin 30 – experiences of coercive control among Australian women , Australian Institute of Criminology, Canberra.
Brooks HL, Rushton K, Lovell K, Bee P, Walker L, Grant L and Rogers A (2018) ‘ The power of support from companion animals for people living with mental health problems: a systematic review and narrative synthesis of the evidence ’, BMC Psychiatry , 18(31), doi:10.1186/s12888-018-1613-2, accessed 9 February 2024.
Brooks H, Rushton K, Walker S, Lovell K and Roger A (2016) ‘ Ontological security and connectivity provided by pets: a study in the self-management of the everyday lives of people diagnosed with a long-term mental health condition ’, BMC Psychiatry , 16(409), doi:10.1186/s12888-016-1111-3, accessed 9 February 2024.
Bussolari C, Currin-McCulloch J, Packman W, Kogan L and Erdman P (2021) ‘“I couldn’t have asked for a better quarantine partner!”: experiences with companion dogs during Covid-19 ’, Animals , 11(2):330, doi:10.3390/ani11020330.
Chen E, Wood D and Ysseldyk R (2021) ‘ Online social networking and mental health among older adults: a scoping review ’, Canadian Journal on Aging / La Revue Canadienne Du Vieillissement , 41(1):26–39, doi:10.1017/S0714980821000040.
Christian H, Mitrou F, Cunneen R and Zubrick SR (2020) ‘ Pets are associated with fewer peer problems and emotional symptoms, and better prosocial behaviour: findings from the longitudinal study of Australian children ’, The Journal of Paediatrics , 220:200–206, doi:10.1016/j.peds.2020.01.012.
Currin-McCulloch J, Bussolari C, Packman W, Kogan L and Erdman P (2021) ‘ Grounded by purrs and petting: experiences with companion cats during Covid-19 ’, Human-Animal Interaction Bulletin , doi:10.1079/hai.2021.0009.
Ending Loneliness Together (2022) Social connection to accelerate social recovery white paper , WayAhead, Sydney, accessed 9 February 2024.
Flood M (2005) Mapping loneliness in Australia , The Australia Institute, Canberra, accessed 9 February 2024.
Gan GZH, Hill A, Yeung P, Keesing S and Netto JA (2019) ‘ Pet ownership and its influence on mental health in older adults ’, Aging and Mental Health , 24(10), 1605–1612, doi:10.1080/13607863.2019.1633620, accessed 9 February 2024.
Geirdal AO, Ruffolo M, Leung J, Thygesen H, Price D, Bonsaksen T and Schoultz M (2021) ‘ Mental health, quality of life, wellbeing, loneliness and use of social media in a time of social distancing during the COVID-19 outbreak. A cross-country comparative study ’, Journal of Mental Health , 30(2):148–155, doi:10.1080/09638237.2021.1875413, accessed 9 February 2024.
Hartwig E and Signal T (2020) ‘ Attachment to companion animals and loneliness in Australian adolescents ’, Australian Journal of Psychology , 72(4):337–346, doi:10.1111/ajpy.12293, accessed 9 February 2024.
Holt-Lunstad J, Smith TB, Baker M, Harris T and Stephenson D (2015) ‘ Loneliness and social isolation as risk factors for mortality: a meta-analytic review ’, Perspectives on Psychological Science , 10(2):227–237, doi:10.1177/1745691614568352, accessed 9 February 2024.
Hughes AM, Braun L, Putnam A, Martinez D and Fine A (2021) ‘ Advancing human-animal interaction to counter social isolation and loneliness in the time of Covid-19: a model for an interdisciplinary public health consortium ’, Animals , 11 ( 8):2325. https://doi.org/10.3390/ani11082325, accessed 9 February 2024.
Kretzler B, Konig H and Hajek A (2022) ‘ Pet ownership, loneliness, and social isolation: a systematic review ’, Social Psychiatry and Psychiatric Epidemiology , 57 : 1935–1957, doi 10.1007/s00127-022-02332-9, accessed 9 February 2024.
Manera KE, Smith BJ, Owen KB, Phongsavan P and Lim MH (2022) ‘ Psychometric assessment of scales for measuring loneliness and social isolation: an analysis of the household, income and labour dynamics in Australia (HILDA) survey ’, Health and Quality of Life Outcomes , 20:40, doi:10.1186/s12955-022-01946-6, accessed 9 February 2024.
Morgan P and Boxall H (2020) ‘Social isolation, time spent at home, financial stress and domestic violence during the COVID-19 pandemic’ , Trends & Issues in Crime and Criminal Justice , 609, Australian Institute of Criminology, Australian Government, Canberra.
Nowland R, Necka EA and Cacioppo J (2017) ‘ Loneliness and social Internet use: pathways to reconnection in a digital world? ’, Perspectives on Psychological Science , 13(1), doi:10.1177/1745691617713052, accessed 9 February 2024.
OECD (Organisation for Economic Co-operation and Development) (2022) COVID-19 and well-being: life in the pandemic – Australia , OECD website, accessed 9 February 2024.
OECD (2023) Measuring well-being and progress: well-being research , OECD website, accessed 9 February 2024.
Pfitzner N, Fitz-Gibbon K and True J (2022) ‘ When staying home isn’t safe: Australian practitioner experiences of responding to intimate partner violence during COVID-19 restrictions ’, Journal of Gender-Based Violence , 6(2):297–314, accessed 9 February 2024.
Piquero AR, Jennings WG, Jemison E, Kaukinen C and Knaul FM (2021) ‘ Domestic violence during the COVID-19 pandemic: evidence from a systematic review and meta-analysis ’, Journal of Criminal Justice , 74, doi:10.1016/j.crimjus.2021.101806, accessed 9 February 2024.
Relationships Australia (2018) Is Australia experiencing an epidemic of loneliness? Findings from 16 waves of the Household Income and Labour Dynamics of Australia Survey , Relationships Australia website, accessed 9 February 2024.
Schumaker JF, Shea JD, Monfries MM and Growth-Marnat G (1993) ‘Loneliness and life satisfaction in Japan and Australia’, Journal of Psychology , 127(1):65–71.
Shankar A, Rafnsson SB and Steptoe A (2015) ‘ Longitudinal associations between social connections and subjective wellbeing in the English Longitudinal Study of Ageing ’, Psychology & Health , 30(6):686–698, doi:10.1080/08870446.2014.979823, accessed 9 February 2024.
Smith B and Lim M (2020) ‘How the COVID-19 pandemic is focusing attention on loneliness and social isolation’, Public Health Research & Practice , 30(2):e3022008.
Stark E (2007) Coercive control: how men entrap women in personal life , Oxford University Press, New York.
Surkalim DL, Luo M, Eres R, Gebel K, van Buskirk J, Bauman A and Ding D (2022) ‘ The prevalence of loneliness across 113 countries: systematic review and meta-analysis ’, BMJ, 376:e067068, doi:10.1136/bmj-2021-067068, accessed 9 February 2024.
Wood L, Martin K, Christian H, Nathan A, Lauritsen C, Houghton S, Kawachi I and McCune S (2015) ‘ The pet factor – companion animals as a conduit for getting to know people, friendship formation and social support ’ PLoS ONE , 10(4), doi:10.1371/journal.pone.0122085, accessed 9 February 2024.
Young J, Bowen-Salter H, O’Dwyer L, Stevens K, Nottle C and Baker A (2020a) ‘ A qualitative analysis of pets as suicide protection for older people ’, Anthrozoos, 33 (2), 191–205, doi:10.1080/08927936.2020.1719759, accessed 9 February 2024.
Young J, Pritchard R, Nottle C and Banwell H (2020b) ‘Pets, touch, and COVID-19: health benefits from non-human touch through times of stress’, Journal of Behavioural Economics for Policy , 4(2), 25–33.
Data on this page cover years 2001 to 2022. This page was last updated in April 2024.
This website needs JavaScript enabled in order to work correctly; currently it looks like it is disabled. Please enable JavaScript to use this website as intended.
We'd love to know any feedback that you have about the AIHW website, its contents or reports.
Required fields
The browser you are using to browse this website is outdated and some features may not display properly or be accessible to you. Please use a more recent browser for the best user experience.
Here’s how you know
- U.S. Department of Health and Human Services
- National Institutes of Health
Music and Health: What You Need To Know

.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Can music be good for you?
Yes, according to a growing body of research. Listening to or making music affects the brain in ways that may help promote health and manage disease symptoms.
Performing or listening to music activates a variety of structures in the brain that are involved in thinking, sensation, movement, and emotion. These brain effects may have physical and psychological benefits. For example, music causes the release of brain chemicals (neurotransmitters and hormones) that can evoke emotional reactions, memories, and feelings and promote social bonds. Music can even affect the structure of the brain. Certain structures in the brain have been found to be larger in musicians than nonmusicians, with particularly noticeable changes in people who started their musical training at an early age.
Increasing evidence suggests that music-based interventions may be helpful for health conditions that occur during childhood, adulthood, or aging. However, because much of the research on music-based interventions is preliminary, few definite conclusions about their effects have been reached. Many reports on the potential benefits of music-based interventions come from observations of individuals or small groups of people. Evidence of this type is valuable for suggesting new ideas, but carefully designed, scientifically rigorous studies of larger numbers of people are needed to provide stronger evidence on whether music-based interventions are effective for specific purposes.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} What is music therapy?
Music therapy is a health profession in which music is used within a therapeutic relationship to address physical, emotional, cognitive, and social needs. The term “music therapy” is not a description of a specific type of intervention. Instead, it indicates the education, training, and credentials of the therapist who is delivering the intervention.
Music therapy may involve a variety of different activities, including music improvisation, music listening, song writing, music performance, and learning through music. Music therapists may work in many different settings, such as hospitals, outpatient clinics, nursing homes, senior centers, rehabilitation facilities, or schools.
Some of the music-based interventions described in this fact sheet fit the definition of music therapy, but others do not. For example, music-based interventions that involve listening to recorded music are often delivered by health professionals other than music therapists (such as nurses), and therefore do not fit the definition of music therapy.
You can learn more about music therapy on the website of the American Music Therapy Association .
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Can music be harmful?
In general, research studies of music-based interventions do not show any negative effects. However, listening to music at too high a volume can contribute to noise-induced hearing loss. You can find out about this type of hearing loss on the National Institute on Deafness and Other Communication Disorders website .
In addition, because music can be associated with strong memories or emotional reactions, some people may be distressed by exposure to specific pieces or types of music. Extensive playing of musical instruments can lead to pain and injury. Music-based interventions that involve exercise or other types of movement could also lead to injury if appropriate safety precautions are not taken.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} What does research show about music-based interventions for people with health conditions?
The preliminary research that has been done so far suggests that music-based interventions may be helpful for anxiety, depressive symptoms, and pain associated with a variety of health conditions, as well as for some other symptoms associated with dementia, multiple sclerosis, Parkinson’s disease, and other conditions.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Pain
As mentioned in other sections of this fact sheet, there’s evidence that music-based interventions may help to relieve pain associated with specific health conditions. The two review articles listed below describe evidence indicating that music may be helpful for pain more generally. Newer research continues to find evidence that music may be helpful for pain from a variety of causes, but not every study has shown a beneficial effect.
- A 2016 review looked at 97 studies (9,184 participants) of music-based interventions for acute or chronic pain associated with a variety of health problems and medical procedures. The overall evidence suggested that music-based interventions may have beneficial effects on both pain intensity and emotional distress from pain and may lead to decreased use of pain-relieving medicines.
- A 2017 review of 14 randomized trials (1,178 participants) of music-based interventions for various types of chronic pain found that the interventions reduced self-reported chronic pain and associated depressive symptoms, with a greater effect when the music was chosen by the participant rather than the researcher. The study participants had a variety of conditions that can cause chronic pain, including cancer, fibromyalgia, multiple sclerosis, or osteoarthritis, and most of the interventions involved listening to recorded music.
- Many but not all newer studies of music-based interventions for pain have had promising results. For example, in recent studies, music-based interventions were helpful for pain associated with childbirth, cancer chemotherapy, a procedure in which shock waves are used to break up kidney stones, retrieval of eggs for in vitro fertilization, treatment of nose fractures, and sickle cell disease. However, music didn’t seem to be helpful for reducing moderate pain further after use of a lidocaine spray for loop electrosurgical excision (a gynecological procedure), and the results of studies on pain during cystoscopy (a procedure in which a tube is inserted into the bladder) and pain during colonoscopy were inconsistent.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Anxiety
Music-based interventions have been evaluated for their effects on anxiety in a variety of disease conditions and health care settings. Some examples are given in this section, and others are discussed in the sections on specific health conditions. Most studies have had promising results, except for studies on anxiety associated with dental care.
- A 2013 review of 26 studies (2,051 participants) showed that listening to recorded music significantly reduced anxiety in people who were waiting to have surgery. However, there was potential for bias in most of the studies because the investigators who performed the studies knew which participants had listened to music.
- A 2016 review of 17 studies (1,381 participants) that evaluated the effect of music-based interventions on anxiety in adults with cancer suggested that the interventions may have a large anxiety-reducing effect. However, there was a high risk of bias in the studies.
- A 2015 review of 5 studies (290 participants) in people who were having dialysis treatments suggested that listening to music reduced anxiety. However, these studies have limitations because of their small size and high risk of bias.
- A 2018 review concluded that it’s unclear whether listening to music is helpful for dental anxiety. Some studies have suggested that listening to music as a distraction may not be adequate to reduce anxiety in children or highly anxious adults who are having dental care. More active types of music-based interventions (for example, a music-assisted relaxation technique that’s taught to the patient in advance) might be helpful in dental settings but have not been evaluated in formal studies.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Autism Spectrum Disorder (ASD)
It’s uncertain whether music-based interventions are helpful for people with ASD.
- A 2021 review of 22 studies (850 participants) on music therapy for children with ASD was unable to reach any definite conclusions on whether adding music therapy to their care is beneficial, although some studies had promising results. For example, some studies of educational music therapy (involving techniques such as musical games) showed possible benefits on the children’s speech, and some studies of improvisational music therapy (in which children produce music) showed possible benefits on social functioning.
- One particularly notable study of music therapy for children with ASD (which was included in the review described above) was a multinational trial involving 364 children from 9 countries. It is the largest study completed so far, and its design was especially rigorous. In this study, the severity of symptoms related to difficulties in social communication did not differ between children who received music therapy along with standard care and those who received standard care alone.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Cancer
Preliminary evidence suggests that music-based interventions may be helpful for several types of distress in people with cancer.
- A 2021 review of randomized controlled trials (studies in which participants were randomly assigned to a music-based intervention group or a control group), which included 81 trials and 5,576 participants, concluded that in adults with cancer, music interventions may have a large anxiety-reducing effect, a moderately strong beneficial effect on depression, a moderate pain-reducing effect, and a large effect on the quality of life. Most of the trials had a high risk of bias, so their results need to be interpreted with caution. Only seven of the studies included in this review involved children. Two of these studies suggested a beneficial effect on anxiety; no other conclusions could be reached from the small amount of evidence available.
- A 2021 review of 11 studies (491 participants) on music interventions for children and adolescents with cancer, which included some studies that were less rigorous than a randomized controlled trial, found evidence suggesting that music-based interventions may decrease anxiety, perceived pain, and depression symptoms and improve state of mind, self-esteem, and quality of life.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Chronic Obstructive Pulmonary Disease (COPD)
A 2021 systematic review of 12 studies (812 participants) showed that music-based interventions were helpful for shortness of breath, anxiety, and sleep quality in adults with COPD but were not helpful for depression. Because the studies were brief (several days to 12 months) and because researchers measured effects in different ways in different studies, there is some uncertainty about the conclusions.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Cognitive Impairment and Dementia
Much research is being done on the potential benefits of music-based interventions for people with cognitive impairment or various types of dementia, such as Alzheimer’s disease. Limited evidence suggests that music-based interventions may improve emotional well-being, behavioral challenges, and quality of life in people with these conditions. Whether the interventions have benefits for cognitive functioning is unclear; effects might depend on the population studied or the type of intervention used.
- A 2018 review evaluated 22 studies (1,097 participants) of music-based interventions for people with dementia who were living in institutions. Some of the interventions were receptive (listening to music), some were active (singing, playing instruments, moving to music, etc.), and some were a combination of the two. The evidence from these studies indicated that music-based interventions probably reduce depressive symptoms and improve overall behavioral challenges. They may also improve emotional well-being and quality of life and reduce anxiety. However, the interventions may have little or no effect on agitation, aggression, or cognitive function.
- A 2021 review looked at 21 studies (1,472 participants) of people with either mild cognitive impairment or mild or moderate dementia; some of the people studied were living in institutions, but others were living in the community. All the music interventions were active; studies that only involved listening to music were not included. Nine of the studies (495 participants) were included in a quantitative analysis of effects on cognitive functioning; this analysis indicated that the music-based interventions had a small beneficial effect. There was also some evidence for beneficial effects on mood and quality of life.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Depression
A 2017 review looked at 9 studies (421 participants) of music-based interventions in adults or adolescents with depression. There was moderate-quality evidence that adding music-based interventions to usual treatment improved depression symptoms when compared with usual treatment alone. Music-based interventions also helped decrease anxiety levels and improve functioning of people with depression (for example, their ability to maintain involvement in work, activities, and relationships).
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Fibromyalgia
A 2020 systematic review of 7 studies (334 participants) found evidence that music-based interventions were beneficial for pain, depression, and quality of life in people with fibromyalgia. However, the amount of research was limited, and the quality of the research was low.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Multiple Sclerosis
A 2021 review of music-based interventions for people with multiple sclerosis (10 trials, 429 participants) found consistent evidence that the interventions were beneficial for coordination, balance, some aspects of gait and walking, emotional status, and pain, but no effect was observed for mental fatigability or memory.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Parkinson’s Disease
Researchers are evaluating the potential benefits of several types of music-based interventions for Parkinson’s disease symptoms.
- Rhythmic auditory stimulation. Rhythmic auditory stimulation uses pulsed sounds (such as those produced by a metronome) to help people synchronize their movements to the rhythm of the sounds. This technique is used to help people with Parkinson’s disease improve their ability to walk. A 2021 analysis of 5 studies (209 total participants) showed significant improvements in gait speed and stride length in people with Parkinson’s disease who participated in rhythmic auditory stimulation. However, the quality of evidence was low, and the number of studies and participants was small.
- Music-based movement therapy. Music-based movement therapy combines physical activities such as dance or rhythmic exercises with music. Therapies that involve physical activity have been shown to be helpful for a variety of Parkinson’s disease symptoms. Adding music to the therapy might have additional benefits by providing auditory cues for movement and making the activities more enjoyable. A 2021 analysis of 17 studies (598 participants) of music-based movement therapy showed evidence of improvements in motor function, balance, freezing of gait, walking speed, and mental health but not gait cadence, stride length, or quality of life.
- Singing. The potential benefits of singing for people with Parkinson’s disease have been studied primarily in terms of effects on speech. In a 2016 review of 7 studies (102 participants), 5 studies found some evidence of a beneficial effect on speech.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Preterm Infants
Music-based interventions are widely used in neonatal intensive care units. However, evidence for physiological benefits for newborn infants is limited.
- In a 2020 review of 16 studies (826 infants), 12 of the studies found some evidence of benefits on physiological outcomes (such as heart rate or oxygen saturation), but several of the studies included only small numbers of infants, and the intervention methods used varied from one study to another. The reviewers concluded that the current data are insufficient to confirm physiological benefits. No harmful effects of music-based interventions were seen in the studies included in this review.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Schizophrenia
Music-based interventions have been evaluated as adjunct treatments (additions to usual treatment) for people with schizophrenia. A 2020 review of 18 studies (1,212 participants) indicated that adjunct music-based interventions may improve a group of schizophrenia symptoms known as “negative symptoms,” such as reduced emotion and self-neglect, as well as depression symptoms and quality of life. However, music-based interventions did not reduce “positive symptoms,” such as hallucinations and delusions. The quality of the evidence was low.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Sleep Problems
Listening to music may improve sleep quality in people with insomnia.
- A 2022 review looked at 13 studies (1,007 participants) that examined the effect of listening to recorded music in people with insomnia. The studies suggested music had no effect on insomnia severity compared to no treatment or treatment as usual. Moderate-certainty evidence did suggest, however, that listening to music has a beneficial effect on subjective sleep quality. The studies also provided low-certainty evidence that listening to music might help improve the speed of falling asleep, the length of time spent sleeping, and the amount of time a person is asleep compared to the total time spent in bed.
- It’s common for older people to have trouble sleeping. A 2021 review looked at 16 studies of music-based interventions for sleep in older adults (812 participants); 11 studies evaluated music listening, and the other 5 evaluated more complex interventions. The results were mixed, with some studies suggesting that the music interventions were helpful, while others did not.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Stress
Music-based interventions, particularly music therapy, may be helpful for improving physical and psychological markers associated with stress, according to two related reviews.
- In a 2020 review with 104 studies (9,617 participants), investigators looked at the effects of a variety of music-based interventions on measures associated with stress, including both physical measures (heart rate, blood pressure, and levels of stress-related hormones) and psychological measures (anxiety, nervousness, restlessness, and feelings of worry). The music-based interventions had a small-to-medium sized beneficial effect on the physical measures and a medium-to-large beneficial effect on the psychological measures.
- A second review looked at 47 studies (2,747 participants) of music therapy (excluding other music-based interventions) and found an overall medium-to-large beneficial effect on stress-related outcomes. The effects were greater than those seen in the larger review. The investigators who performed the review suggested that the opportunity for music therapists to tailor interventions to the needs of individual patients might account for the difference.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Stroke
Music-based interventions may be helpful in the rehabilitation of people who have had a stroke. A 2019 review of 27 studies (730 participants) found positive effects on physical status (upper-limb activity, various aspects of walking, balance), cognition (paying attention, communication), and mood. In particular, rhythmic auditory stimulation (which involves the use of a metronome combined with physical activities) had beneficial effects on gait and balance, and receptive music therapy (which involves listening to music while performing another task) was helpful for mood and some aspects of cognitive function.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Tinnitus
Tinnitus is the symptom that people often describe as “ringing in the ears,” although it can also sound like roaring, clicking, hissing, or buzzing. It can be caused by noise-induced hearing loss, blockage of the ear canal by earwax, ear or sinus infections, or other health conditions, or by starting or stopping various medications. Sometimes, tinnitus has no obvious cause.
- Sound therapies. Various types of sounds, including music, have been used to try to mask tinnitus. However, according to a 2019 review of studies conducted up to that time, the effects of these sound therapies are modest; few people achieve complete remission of tinnitus from sound therapies.
- Notched music therapy. A specific type of music therapy called “notched” music therapy has been suggested as a possible way to reduce the severity of tinnitus. Notched music therapy involves listening to music that has been modified to remove sounds close in frequency to the frequency of the tinnitus sound perceived by the patient. Two recent studies that compared notched music with conventional music did not find notched music to be more helpful in reducing the symptoms or impact of tinnitus. However, some earlier studies suggested that the loudness of tinnitus sounds could be reduced with notched music therapy.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Research Supported by the National Institutes of Health (NIH) and the National Center for Complementary and Integrative Health (NCCIH)
NIH and the John F. Kennedy Center for the Performing Arts, in association with the National Endowment for the Arts, are sponsoring an initiative called Sound Health to increase understanding of music’s effect on the brain and the potential clinical applications. The first Sound Health research projects began in 2019. Some projects are investigating music’s mechanism of action in the brain and how music may be applied to treat symptoms of disorders such as Parkinson’s disease, stroke, and chronic pain. Others are looking at the effects of music on children’s developing brains.
Topics of NCCIH-supported studies within the Sound Health initiative include:
- The effects of music-based interventions on neurodevelopment and pain response in preterm infants
- Using self-generated rhythmic cues to enhance gait in people with Parkinson’s disease
- The impact of singing interventions on markers of cardiovascular health in older people with cardiovascular disease
In collaboration with the Foundation for the NIH and the Renée Fleming Foundation, NIH has developed a toolkit for rigorous, reproducible, well-powered music-based interventions for brain disorders of aging, such as Alzheimer’s disease, Parkinson’s disease, and stroke. Three workshops were held in 2021 to gather input from experts in a variety of relevant fields, and a request for information was issued to get stakeholder feedback. The toolkit , which was released in 2023, will be pilot tested in demonstration projects. NCCIH is playing a lead role in this effort.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} For More Information
Nccih clearinghouse.
The NCCIH Clearinghouse provides information on NCCIH and complementary and integrative health approaches, including publications and searches of Federal databases of scientific and medical literature. The Clearinghouse does not provide medical advice, treatment recommendations, or referrals to practitioners.
Toll-free in the U.S.: 1-888-644-6226
Telecommunications relay service (TRS): 7-1-1
Website: https://www.nccih.nih.gov
Email: [email protected] (link sends email)
Know the Science
NCCIH and the National Institutes of Health (NIH) provide tools to help you understand the basics and terminology of scientific research so you can make well-informed decisions about your health. Know the Science features a variety of materials, including interactive modules, quizzes, and videos, as well as links to informative content from Federal resources designed to help consumers make sense of health information.
Explaining How Research Works (NIH)
Know the Science: How To Make Sense of a Scientific Journal Article
Understanding Clinical Studies (NIH)
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} Key References
- Aalbers S, Fusar-Poli L, Freeman RE, et al. Music therapy for depression . Cochrane Database of Systematic Reviews. 2017;(11):CD004517. Accessed at cochranelibrary.com on October 29, 2021.
- Bieleninik Ł, Geretsegger M, Mössler K, et al. Effects of improvisational music therapy vs enhanced standard care on symptom severity among children with autism spectrum disorder. The TIME—a randomized clinical trial . JAMA. 2017;318(6):525-535.
- Bradt J, Dileo C, Magill L, et al. Music interventions for improving psychological and physical outcomes in cancer patients . Cochrane Database of Systematic Reviews. 2016;(8):CD006911. Accessed at cochranelibrary.com on October 29, 2021.
- Bradt J, Dileo C, Shim M. Music interventions for preoperative anxiety . Cochrane Database of Systematic Reviews. 2013;(6):CD006908. Accessed at cochranelibrary.com on October 29, 2021.
- Burrai F, Apuzzo L, Zanotti R. Effectiveness of rhythmic auditory stimulation on gait in Parkinson disease: a systematic review and meta-analysis . Holistic Nursing Practice. June 11, 2021. [Epub ahead of print].
- Cheever T, Taylor A, Finkelstein R, et al. NIH/Kennedy Center workshop on music and the brain: finding harmony . Neuron. 2018;97(6):1214-1218.
- Collins FS, Fleming R. Sound health: an NIH-Kennedy Center initiative to explore music and the mind . JAMA. 2017;317(24):2470-2471.
- de Witte M, da Silva Pinho A, Stams G-J, et al. Music therapy for stress reduction: a systematic review and meta-analysis . Health Psychology Review. 2022;16(1):134-159.
- de Witte M, Spruit A, van Hooren S, et al. Effects of music interventions on stress-related outcomes: a systematic review and two meta-analyses . Health Psychology Review. 2020;14(2):294-324.
- Dorris JL, Neely S, Terhorst L, et al. Effects of music participation for mild cognitive impairment and dementia: a systematic review and meta-analysis . Journal of the American Geriatrics Society. 2021;69(9):2659-2667.
- Foroushani SM, Herman CA, Wiseman CA, et al. Evaluating physiologic outcomes of music interventions in the neonatal intensive care unit: a systematic review . Journal of Perinatology. 2020;40(12):1770-1779.
- Garza-Villareal EA, Pando V, Vuust P, et al. Music-induced analgesia in chronic pain conditions: a systematic review and meta-analysis . Pain Physician. 2017;20(7):597-610.
- Jespersen KV, Pando-Naude V, Koenig J, et al. Listening to music for insomnia in adults . Cochrane Database of Systematic Reviews. 2022;(8):CD010459. Accessed at cochranelibrary.com on September 8, 2022.
- Lee JH. The effects of music on pain: a meta-analysis . Journal of Music Therapy. 2016;53(4):430-477.
- van der Steen JT, Smaling HJ, van der Wouden JC, et al. Music-based therapeutic interventions for people with dementia . Cochrane Database of Systematic Reviews. 2018;(7):CD003447. Accessed at cochranelibrary.com on October 29, 2021.
.header_greentext{color:green!important;font-size:24px!important;font-weight:500!important;}.header_bluetext{color:blue!important;font-size:18px!important;font-weight:500!important;}.header_redtext{color:red!important;font-size:28px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;font-size:28px!important;font-weight:500!important;}.header_purpletext{color:purple!important;font-size:31px!important;font-weight:500!important;}.header_yellowtext{color:yellow!important;font-size:20px!important;font-weight:500!important;}.header_blacktext{color:black!important;font-size:22px!important;font-weight:500!important;}.header_whitetext{color:white!important;font-size:22px!important;font-weight:500!important;}.header_darkred{color:#803d2f!important;}.Green_Header{color:green!important;font-size:24px!important;font-weight:500!important;}.Blue_Header{color:blue!important;font-size:18px!important;font-weight:500!important;}.Red_Header{color:red!important;font-size:28px!important;font-weight:500!important;}.Purple_Header{color:purple!important;font-size:31px!important;font-weight:500!important;}.Yellow_Header{color:yellow!important;font-size:20px!important;font-weight:500!important;}.Black_Header{color:black!important;font-size:22px!important;font-weight:500!important;}.White_Header{color:white!important;font-size:22px!important;font-weight:500!important;} All Other References
- Atipas S, Therdphaothai J, Suvansit K, et al. A randomized, controlled trial of notched music therapy for tinnitus patients. Journal of International Advanced Otology. 2021;17(3):221-227.
- Barnish J, Atkinson RA, Barran SM, et al. Potential benefit of singing for people with Parkinson’s disease: a systematic review. Journal of Parkinson’s Disease. 2016;6(3):473-484.
- Bird HA. Overuse syndrome in musicians. Clinical Rheumatology. 2013;32(4):475-479.
- Bradt J, Teague A. Music interventions for dental anxiety. Oral Diseases. 2018;24(3):300-306.
- Brancatisano O, Baird A, Thompson WF. Why is music therapeutic for neurological disorders? The therapeutic music capacities model. Neuroscience and Biobehavioral Reviews. 2020;112:600-615.
- Buglione A, Saccone G, Mas M, et al. Effect of music on labor and delivery in nulliparous singleton pregnancies: a randomized clinical trial. Archives of Gynecology and Obstetrics. 2020;310(3):693-698.
- Burrai F, Magavern EF, Micheluzzi V, et al. Effectiveness of music to improve anxiety in hemodialysis patients. A systematic review and meta-analysis. Holistic Nursing Practice. 2020;34(6):324-333.
- Cakmak O, Cimen S, Tarhan H, et al. Listening to music during shock wave lithotripsy decreases anxiety, pain, and dissatisfaction. A randomized controlled study. Wiener Klinische Wochenscrift. 2017;129(19-20):687-691.
- Ç elebi D, Y ı lmaz E, Ş ahin ST, et al. The effect of music therapy during colonoscopy on pain, anxiety and patient comfort: a randomized controlled trial. Complementary Therapies in Clinical Practice. 2020;38:101084.
- Chantawong N, Charoenkwan K. Effects of music listening during loop electrosurgical excision procedure on pain and anxiety: a randomized trial. Journal of Lower Genital Tract Disease. 2017;21(4):307-310.
- Cheung CWC, Yee AWW, Chan PS, et al. The impact of music therapy on pain and stress reduction during oocyte retrieval—a randomized controlled trial. Reproductive Biomedicine Online. 2018;37(2):145-152.
- Çift A, Benlioğlu C. Effect of different musical types on patient’s relaxation, anxiety and pain perception during shock wave lithotripsy: a randomized controlled study. Urology Journal. 2020;17(1):19-23.
- Gonz á lez-Mart í n-Moreno M, Garrido-Ardila EM, Jim é nez-Palomares M, et al. Music-based interventions in paediatric and adolescents oncology patients: a systematic review. Children. 2021;8(2):73.
- Huang J, Yuan X, Zhang N, et al. Music therapy in adults with COPD. Respiratory Care. 2021;66(3):501-509.
- Jia R, Liang D, Yu J, et al. The effectiveness of adjunct music therapy for patients with schizophrenia: a meta-analysis. Psychiatry Research. 2020;293:113464.
- Ko SY, Leung DYP, Wong EML. Effects of easy listening music intervention on satisfaction, anxiety, and pain in patients undergoing colonoscopy: a pilot randomized controlled trial. Clinical Interventions in Aging. 2019;14:977-986.
- Koelsch S. A neuroscientific perspective on music therapy. Annals of the New York Academy of Sciences. 2009;1169:374-384.
- Le Perf G, Donguy A-L, Thebault G. Nuanced effects of music interventions on rehabilitation outcomes after stroke: a systematic review. Topics in Stroke Rehabilitation. 2019;26(6):473-484.
- Lopes J, Keppers II. Music-based therapy in rehabilitation of people with multiple sclerosis: a systematic review of clinical trials. Arquivos de Neuro-psiquiatria. 2021;79(6):527-535.
- Mayer-Benarous H, Benarous X, Vonthron F, et al. Music therapy for children with autistic spectrum disorder and/or other neurodevelopmental disorders: a systematic review. Frontiers in Psychiatry. 2021;12:643234.
- McClintock G, Wong E, Mancuso P, et al. Music during flexible cystoscopy for pain and anxiety – a patient-blinded randomized control trial. BJU International. 2021;128 Suppl 1:27-32.
- Mumm J-N, Eismann L, Rodler S, et al. Listening to music during outpatient cystoscopy reduces pain and anxiety and increases satisfaction: results from a prospective randomized study. Urologia Internationalis . 2021;105(9-10):792-798.
- Ortega A, Gauna F, Munoz D, et al. Music therapy for pain and anxiety management in nasal bone fracture reduction: randomized controlled clinical trial. Otolaryngology—Head and Neck Surgery. 2019;161(4):613-619.
- Perković R, Dević K, Hrkać A, et al. Relationship between education of pregnant women and listening to classical music with the experience of pain in childbirth and the occurrence of psychological symptoms in puerperium. Psychiatria Danubina. 2021;33(Suppl 13):260-270.
- Petrovsky DV, Ramesh P, McPhillips MV, et al. Effects of music interventions on sleep in older adults: a systematic review. Geriatric Nursing. 2021;42(4):869-879.
- Pienkowski M. Rationale and efficacy of sound therapies for tinnitus and hyperacusis. Neuroscience. 2019;407:120-134.
- Piromchai P, Chompunut S, Kasemsiri P, et al. A three-arm, single-blind, randomized controlled trial examining the effects of notched music therapy, conventional music therapy, and counseling on tinnitus. Otology & Neurotology. 2021;42(2):335-340.
- Robb SL, Hanson-Abromeit D, May L, et al. Reporting quality of music intervention research in healthcare: a systematic review. Complementary Therapies in Medicine. 2018;38:24-41.
- Rodgers-Melnick SN, Matthie N, Jenerette C, et al. The effects of a single electronic music improvisation session on the pain of adults with sickle cell disease: a mixed methods pilot study. Journal of Music Therapy. 2018;55(2):156-185.
- Silverman MJ, Gooding LF, Yinger O. It’s…complicated: a theoretical model of music-induced harm. Journal of Music Therapy. 2020;57(3):251-281.
- Speranza L, Pulcrano S, Perrone-Capano C, et al. Music affects functional brain connectivity and is effective in the treatment of neurological disorders. Reviews in the Neurosciences. March 24, 2022. [Epub ahead of print].
- Tang H, Chen L, Wang Y, et al. The efficacy of music therapy to relieve pain, anxiety, and promote sleep quality, in patients with small cell lung cancer receiving platinum-based chemotherapy. Supportive Care in Cancer. 2021;29(12):7299-7306.
- Wang M, Yi G, Gao H, et al. Music-based interventions to improve fibromyalgia syndrome: a meta-analysis. Explore. 2020;16(6):357-362.
- Wolff AL, Ling DI, Casey EK, et al. Feasibility and impact of a musculoskeletal health for musicians (MHM) program for musician students: a randomized controlled pilot study. Journal of Hand Therapy. 2021:34(2):159-165.
- Zhou Z, Zhou R, Wei W, et al. Effects of music-based movement therapy on motor function, balance, gait, mental health, and quality of life for patients with Parkinson’s disease: a systematic review and meta-analysis. Clinical Rehabilitation. 2021;35(7):937-951.
Acknowledgments
NCCIH thanks Wen Chen, Ph.D., Emmeline Edwards, Ph.D., and David Shurtleff, Ph.D., NCCIH, for their review of this fact sheet.
This publication is not copyrighted and is in the public domain. Duplication is encouraged.
NCCIH has provided this material for your information. It is not intended to substitute for the medical expertise and advice of your health care provider(s). We encourage you to discuss any decisions about treatment or care with your health care provider. The mention of any product, service, or therapy is not an endorsement by NCCIH.
Related Topics
Music and Health - Systematic Reviews/Reviews/Meta-analyses (PubMed®)
Music and Health - Randomized Controlled Trials (PubMed®)
For Consumers
6 Things You Need To Know About Music and Health
For Health Care Providers
Music and Health

IMAGES
VIDEO
COMMENTS
Dr. SooJeong Youn: This case highlights the importance of attending to the intricate, multilevel, systemic factors that affect the mental health experience and clinical presentation of patients ...
Sara, a 35-year-old married female. Sara was referred to treatment after having a stillbirth. Sara showed symptoms of grief, or complicated bereavement, and was diagnosed with major depression, recurrent. The clinician recommended interpersonal psychotherapy (IPT) for a duration of 12 weeks. Bleiberg, K.L., & Markowitz, J.C. (2008).
At Tracking Happiness, we're dedicated to helping others around the world overcome struggles of mental health. In 2022, we published a survey of 5,521 respondents and found: 88% of our respondents experienced mental health issues in the past year. 25% of people don't feel comfortable sharing their struggles with anyone, not even their ...
A case study is an in-depth study of one person, group, or event. In a case study, nearly every aspect of the subject's life and history is analyzed to seek patterns and causes of behavior. Case studies can be used in many different fields, including psychology, medicine, education, anthropology, political science, and social work.
The National Institute of Mental Health (NIMH) is the Nation's leader in research on mental disorders, supporting research to transform the understanding and treatment of mental illnesses. Below you can learn more about NIMH funded research areas, policies, resources, initiatives, and research conducted by NIMH on the NIH campus.
Mental health. Children's mental health case studies. Explore the experiences of children and families with these interdisciplinary case studies. Designed to help professionals and students explore the strengths and needs of children and their families, each case presents a detailed situation, related research, problem-solving questions and ...
Clinical Case Studies (CCS), peer-reviewed & published bi-monthly electronic only, is the only journal devoted entirely to innovative psychotherapy case studies & presents cases involving individual, couples, & family therapy.The easy-to-follow case presentation format allows you to learn how interesting & challenging cases were assessed & conceptualized, & how treatment followed such ...
Background Community disaster resilience is comprised of a multitude of factors, including the capacity of citizens to psychologically recover. There is growing recognition of the need for public health departments to prioritize a communitywide mental health response strategy to facilitate access to behavioral health services and reduce potential psychological impacts. Due to the US Department ...
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
The 33-page case study, Mental Health Crisis Support Rooted in Community and Human Rights, presents a viable, replicable framework for a holistic approach to mental health crisis response that ...
The pilot case study herein underscores the utility and potential of school-based mental health promotion efforts, particularly through InSciEd Out's community-based framework. Targeted improvements in mental health literacy and moderate improvements in help-seeking intentions were accompanied by large decreases in mental health misconceptions.
Building Global Capacity in Mental Health Research. According to the World Health Organization (WHO), there are more than 450 million people with mental, neurological, or behavioral problems worldwide ().Mental health problems are estimated to account for 13% of the global burden of disease, principally from unipolar and bipolar depression, alcohol and substance-use disorders, schizophrenia ...
We're going to go ahead to patient case No. 1. This is a 27-year-old woman who's presented for evaluation of a complex depressive syndrome. She has not benefitted from 2 recent trials of antidepressants—sertraline and escitalopram. This is her third lifetime depressive episode.
Need for Mental Health (MH) Prevention. Longitudinal studies suggest that individuals with a lower level of positive wellbeing are more likely to acquire mental illness ().Conversely, factors that promote positive wellbeing and resilience among individuals are critical in preventing mental illnesses and better outcomes among those with mental illness (10, 11).
Associate Professor Sam Rosenthal shared case studies outlining the student mental health landscape — and evidence-backed pathways for improving social support and outcomes. ... JWU has a wealth of confidential mental health resources, including counseling services in Providence and Charlotte. Individual counseling sessions and consultations ...
Mental health care across the NHS in England is changing to improve the experiences of the people who use them. In many areas, a transformation is already under way, offering people better and earlier access as well as more personalised care, whilst building partnerships which reach beyond the NHS to create integrated and innovative approaches to mental health care and support.
Still, studies like the one in Community Mental Health Journal hold promise for other researchers seeking to investigate the premise that musical performances—in this case, opera—when coupled with educational efforts, can improve emotional and social well-being and attitudes toward mental health trauma. Regarding the mental health of older ...
Santa Clara County sought to understand where gaps exist between psychiatric and substance use disorder treatment bed capacity and needs — at different levels of care. RAND researchers estimated bed gaps and used these estimates to inform their recommendations for improving access to behavioral health care.
Novartis has trained more than 1,000 employees as Mental Health First Aiders to offer peer-to-peer support for their colleagues. While employees were eager for the training, uptake of the program ...
Updates about mental health topics, including NIMH news, upcoming events, mental disorders, funding opportunities, and research. ... Learn more about how to participate in outpatient and inpatient studies at the NIH Clinical Center, a hospital dedicated to the highest quality research. Read More. Featured Resources.
Type "Mental Health" in the search bar to find a variety of local mental health treatment resources. The LGBTQ Youth Space - Phone: 408-343-7940. A community drop-in center and mental health program for lesbian, gay, bisexual, transgender, queer, questioning and ally youth and young adults ages 13-25 who live in Santa Clara County..
Impact on mental health. Mental health is defined as a state of well-being in which people understand their abilities, solve everyday life problems, work well, and make a significant contribution to the lives of their communities [].There is debated presently going on regarding the benefits and negative impacts of social media on mental health [9,10].
While those earlier studies focused on income loss relating to mental illness and the costs of mental health treatment, the new study also accounted for a host of additional adverse economic outcomes associated with mental illness, including the fact that people with mental illness consume less, invest less in a house, stocks and other risky ...
About the study The California Statewide Study of People Experiencing Homelessness (CASPEH) was designed to be representative of all adults 18 years and older experiencing homelessness in California. It includes nearly 3,200 administered questionnaires and 365 in-depth interviews with adults experiencing homelessness in eight regions of the state, representing urban, rural, and suburban areas.
Specifically, studies have found that mental health court participants are significantly more likely to utilize treatment services, less likely to be rearrested, and spent fewer days in jail as opposed to nonparticipants. Studying the effectiveness of mental health courts can be challenging due to several factors including the difficulty of ...
Like many people living with mental health needs, Sam's treatment is a lifelong journey requiring various inpatient and outpatient services at different stages. This can be especially ...
The quantitative studies produced mixed findings, with people experiencing positive, negative and neutral impacts of their companion animal on their personal mental health. Qualitative studies suggest, however, that people with mental health conditions may benefit from the direct support their companion animals provide.
A 2021 analysis of 17 studies (598 participants) of music-based movement therapy showed evidence of improvements in motor function, balance, freezing of gait, walking speed, and mental health but not gait cadence, stride length, or quality of life. Singing.