- Case report
- Open access
- Published: 05 June 2020

Case report: cognitive performance in an extreme case of anorexia nervosa with a body mass index of 7.7
- Simone Daugaard Hemmingsen ORCID: orcid.org/0000-0001-6789-7105 1 , 2 , 3 , 4 , 5 ,
- Mia Beck Lichtenstein ORCID: orcid.org/0000-0002-7885-9187 6 , 7 ,
- Alia Arif Hussain ORCID: orcid.org/0000-0002-1011-5165 8 , 9 ,
- Jan Magnus Sjögren ORCID: orcid.org/0000-0003-2060-1914 8 , 9 &
- René Klinkby Støving ORCID: orcid.org/0000-0002-4255-5544 1 , 2 , 3 , 4 , 5
BMC Psychiatry volume 20 , Article number: 284 ( 2020 ) Cite this article
4042 Accesses
6 Citations
1 Altmetric
Metrics details
Studies show that adult patients with anorexia nervosa display cognitive impairments. These impairments may be caused by illness-related circumstances such as low weight. However, the question is whether there is a cognitive adaptation to enduring undernutrition in anorexia nervosa. To our knowledge, cognitive performance has not been assessed previously in a patient with anorexia nervosa with a body mass index as low as 7.7 kg/m2.
Case presentation
We present the cognitive profile of a 35-year-old woman with severe and enduring anorexia nervosa who was diagnosed at the age of 10 years. She was assessed with a broad neuropsychological test battery three times during a year. Her body mass index was 8.4, 9.3, and 7.7 kg/m 2 , respectively. Her general memory performance was above the normal range and she performed well on verbal and design fluency tasks. Her working memory and processing speed were within the normal range. However, her results on cognitive flexibility tasks (set-shifting) were below the normal range.
Conclusions
The case study suggests that it is possible to perform normally cognitively despite extreme and chronic malnutrition though set-shifting ability may be affected. This opens for discussion whether patients with anorexia nervosa can maintain neuropsychological performance in spite of extreme underweight and starvation.
Trial registration
ClinicalTrials.gov, NCT02502617 . Registered 20 July 2015.
Peer Review reports
A growing amount of evidence indicate that anorexia nervosa (AN) is associated with impaired or inefficient neuropsychological performance in relation to healthy control subjects, regarding attention [ 1 , 2 ], memory [ 1 , 2 , 3 , 4 ], processing speed [ 4 ], and especially the executive functions [ 5 ] central coherence [ 6 ], decision-making [ 6 , 7 ], and cognitive flexibility [ 8 , 9 ]. It has been debated whether this is related to state (due to factors such as malnutrition) or trait (a premorbid trait or endophenotype of the disorder [ 10 ]). Some studies have found that patients who recovered from AN have impaired cognitive performance compared to healthy control subjects [ 11 , 12 ], supporting the trait theory of the disorder. However, longitudinal studies have found that executive functions can be normalized following weight stabilization in patients with AN [ 13 , 14 ], supporting the state theory.
Research on cognitive performance before and after re-nutrition in adult patients with extreme and chronic AN is sparse. Some studies have examined cognitive performance in patients with AN with a mean body mass index (BMI) below 15 kg/m2 (e.g. [ 10 ]), corresponding to extreme AN severity according to the Diagnostic and Statistical Manual of Mental Disorders 5 (DSM-5) [ 15 ]. However, it is unclear if patients with AN with BMI below 10 kg/m2 will display the same cognitive profile.
It has been suggested that malnutrition might affect cognitive performance since the classic Minnesota Semi-Starvation Experiment [ 16 ], where cognitive functions were studied in 36 healthy military objectors with normal weight before and after semistarvation with 25% weight-loss over a 24-week period. The men reported decline in concentration. However, the standardized tests that were administered did not confirm measurable alterations. Newer research on healthy subjects, although somewhat inconclusive, indicates affected psychomotor speed and executive functions following short-term semi-starvation [ 17 ].
However, other factors than malnutrition or weight-loss have been suggested to affect cognitive performance in patients with AN, such as long illness duration [ 18 ] and age [ 18 ]. This could explain a difference in results for children/adolescents and adults with AN mentioned in the literature [ 19 , 20 ], which cannot be explained by the trait theory.
The current case report was part of an ongoing longitudinal research project investigating the effect of re-nutrition on cognitive performance in patients with severe AN. The aim of the case study was to present the neuropsychological performance of a patient with chronic AN and extremely low BMI in order to discuss whether extremely low weight and long duration of illness are associated with cognitive impairment and if cognitive adaptation takes place. No study to our knowledge has previously reported on the cognitive profile of a patient with AN with a BMI as low as 7.7 kg/m2.
We want to introduce the idea of cognitive adaptation to severe malnutrition as a supplement to the discussion on cognitive impairment in AN. However, this idea should not be confused with Taylor’s Theory of Cognitive Adaptation [ 21 ]. The presented idea of cognitive adaptation is the idea that cognitive functions can adapt to persisting low weight in AN, i.e. cognitive performance can remain normal or regain normality in severe and enduring AN. The adaptation does not exclude specific cognitive impairment.
The current case report investigates the cognitive profile of a 35-year-old Caucasian woman with extremely severe and enduring AN who was diagnosed at the age of 10 years. The patient’s weight loss is accomplished through fasting. According to the DSM-5 [ 15 ], the patient’s symptoms are in accordance with the restricting type and the severity of AN for the patient is categorized as extreme. The patient has had low body weight since the onset of the disease 25 years ago. Consequently, she is still prepubescent.
The patient’s extreme malnutrition, the medical complications, and the refeeding treatment has previously been described in a case report [ 22 ]. Since the previous report [ 22 ], she has survived another 5 years, living in her own residence with several stabilizing hospitalizations. Her nadir BMI, defined as the lowest registered BMI, has decreased further to 7.2 kg/m2. To our knowledge, this is the lowest BMI reported in AN in the literature. During her long and severe illness course, she has participated in psychotherapy for years. However, during the past few years, she has refused to participate in psychotherapy, while she has continued the harm-reducing treatment in the nutrition department. No cognitive profile has been assessed before the current report.
She has continuously been provided supplementation with vitamins and minerals. At the present admission, she weighed 20.2 kg, including edema corresponding to at least 2 kg, and her height was 1.55 m, corresponding to a BMI of 8.41 kg/m 2 . After life-saving and stabilizing fluid and electrolyte correction, and refeeding according to guidelines [ 23 ] during 2 weeks of hospitalization, we tested her with a neuropsychological test battery (2 weeks after admission: T 0 ). After an additional 2 months of hospitalization, she could not be motivated to continue the treatment any longer. Due to years of history with rapid relapse after prolonged forced treatment, she was allowed to be discharged to outpatient follow-up. She was re-tested in the outpatient clinic 6 days following dropout from inpatient treatment and approximately 3 months after admission, (re-test: T 1 ) with a weight of 22.4 kg (BMI: 9.3 kg/m 2 ), and again at 12 months from T 0 , during a re-hospitalization, 7 days after admission (follow-up: T 2 ), with BMI 7.7 kg/m 2 . Thus, T 0 and T 2 were done at the hospital after initial stabilizing glycemic, fluid- and electrolyte correction, whereas T 1 was done in an outpatient setting, where she was in a clinically stable condition, but without the initial stabilizing treatment.
The psychopathological profile of the patient
The patient scored 21 on the Beck Depression Inventory II (BDI-II [ 24 ];) indicating moderate depression at 2 weeks after admission (T 0 ). Her scores on the Eating Disorder Inventory 3 (EDI-3 [ 25 ];) at T 0 are presented in Table 1 below. Compared to the Danish validation of EDI-3 for patients with AN ( [ 26 ]; Table 1 ), her low scores on the Drive for Thinness, the Interoceptive Deficits, the Perfectionism, and the Asceticism subscales are of interest.
Qualitative observations
During the first 2 weeks after admission, the patient was unable to participate in the neuropsychological assessment due to fatigue. Two weeks after admission, when the baseline assessment took place (T 0 ), the patient was lying down during the assessment and was noticeably tired. This was neither the case at retest (T 1 ) nor at follow-up (T 2 ) where the patient was sitting at a table. Her alertness and energy level at follow-up (T 2 ) were notable in light of her low BMI. The patient was calm during all three assessments (divided into six sessions) and expressed that the tests were fun. The aim of the study was explained to the patient before the first administration. However, only information written in the test manuals was given during each assessment.
The following validated neuropsychological tests were selected in cooperation with an experienced neuropsychologist to examine a wide range of cognitive functions: the Wechsler Memory Scale III (WMS-III) [ 27 ]; the d2-R Test of Attention – Revised [ 28 , 29 ]; the Processing Speed Index (PSI) of the Wechsler Adult Intelligence Scale IV (WAIS-IV) [ 30 ]; the Delis-Kaplan Executive Function System (D-KEFS) [ 31 ], Verbal Fluency Test, Design Fluency Test and Trail Making Test; and the Wisconsin Card Sorting Test Revised and Expanded (WCST) [ 32 ] (only administered at T 0 ). Information on each test variable, including internal consistency and test-retest reliability, are presented in Table 2 . The test battery can be administered in approximately 2 h. For all three administrations, the test battery was divided into two sessions (1 h per session) 1 day apart.
Neuropsychological findings
Table 3 gives an overview of the timeline of the patient’s raw scores and scaled scores on the test battery. Table 4 presents the patient’s norm scores and percentiles on the WMS-III, the WAIS-IV PSI, and the d2-R. Table 5 presents the patient’s WCST scores at 2 weeks after admission (T 0 ). Information on scoring are presented below each of the tables.
Memory performance on WMS-III
The patient’s scores on WMS-III indicate average to very superior auditory, visual, immediate and general memory performance (108 to 142; Mean: 100), and low average to average working memory (Table 4 ). The technical manual for WMS-III reports adequate test – retest reliability for all indexes in the age group 16–54 years, except for the Auditory Recognition Delayed Index ( [ 33 ]; Table 2 ). Estimated standard error of difference (S Diff ) scores were calculated based on Iverson and Grant ( [ 34 ]; Table 2 ). Differences between the three assessments are outlined here. Her scores on the Auditory Delayed Index decreased more than S diff : 6.70 from 132 (very superior) at 2 weeks after admission (T 0 ) to 108 (average) at re-test (T 1 ) and increased again to 132 (very superior) at follow-up (T 2 ). Her scores on the Visual Immediate Index increased slightly more than S diff : 6.70 from 118 (high average) at re-test (T 1 ) to 127 (superior) at follow-up (T 2 ). Her scores on the Visual Delayed Index decreased more than S diff : 7.65 from 125 (superior) at re-test (T 1 ) to 109 (average) at follow-up (T 2 ). Her scores on the Immediate Memory Index increased more than S diff : 3.17 from 134 (very superior) at re-test (T 1 ) to 142 (very superior) at follow-up (T 2 ). Her scores on the Working Memory Index decreased more than S diff : 8.22 from 102 (average) at 2 weeks after admission (T 0 ) to 88 (low average) at re-test (T 1 ). The scores on the rest of the indexes did not change more than the estimated S diff scores between time points.
Cognitive flexibility on D-KEFS and WCST
Overall, she performed above average on the Verbal Fluency Test (Table 3 ) at all three test times compared to the normative population for age, except for her performance at re-test (T 1 ) on the switching condition, which was decreased more than S diff : 2.42 to average, and the high number of repetition errors (7; below average) at re-test (T 1 ) and (3; average) at follow-up (T 2 ).
She performed average to above average on the Design Fluency Test at all three test sessions (Table 3 ). However, the switching condition score was lower [ 6 ] at follow-up (T 2 ) compared to 8 at 2 weeks after admission (T 0 ) and re-test (T 1 ), though still average.
During follow-up (T 2 ) on the Trail Making Test (Table 3 ), her performance on the Number-Letter Sequencing test, measuring cognitive flexibility, was below average (111 s), in spite of being average at 2 weeks after admission (T 0 ; 90 s) and re-test (T 1 ; 79 s). The numbers condition was very low at T 0 (55 s; below average), improving somewhat at re-test (T 1 ; 46 s; below average) and follow-up (T 3 ; 41 s; below average). We have no explanation for this result. On the other conditions, her performance was average at all three test times on the Trail Making Test.
Her scores on the WCST (Table 5 ) 2 weeks after admission (T 0 ) place her in the mild to moderately-to-severely range of impairment on cognitive flexibility according to this task. She completed one out of six categories (< 1st percentile). She made 52 perseverative responses (< 1st percentile; standard score 55; moderately-to-severely impaired range). She committed 50 errors (8th percentile; standard score 79: mildly impaired range), of which 36 were perseverative errors (1st percentile; standard score 55: moderately impaired range).
WAIS-IV processing speed
The scores on the Processing Speed Index (Table 4 ) were average compared to the normative population for age at all three test times. There were no relevant differences between time points. She scored 93 at admission (T 0 ) and re-test (T 1 ) and 98 at follow-up (T 2 ).
d2-R test of attention
At 2 weeks after admission (T 0 ) and re-test (T 1 ), she had a small number of processed targets (426 and 420), 18th to 21st percentile (Tables 3 and 4 ), her concentration performance was 175 and 176 corresponding to the 42nd percentile and she committed three and no errors respectively (> 90th percentile). At follow-up (T 2 ), her concentration performance was above the mean (185; 54th percentile) but not increased more than S diff : 24.89. The total processed targets score was still low (451; 34th percentile), and she committed few errors (four; 90th percentile).
Discussion and conclusions
The patient exhibited average to very superior performance on verbal fluency, design fluency, processing speed, and memory. However, her working memory performance was low average. Her attention and concentration performance were below average to average, and her performance on cognitive flexibility tasks were average to moderately-to-severely impaired.
The present case report demonstrates surprisingly good cognitive performance in a patient with severe and enduring AN with extremely low BMI varying between 7.7 and 9.3 during the study period of 1 year. However, some of her executive functions seem to be impaired. This is in line with previous research on patients with AN [ 5 , 8 ]. The present results suggest that her working memory was normal (low average) in line with previous studies [ 35 , 36 ]. However, her working memory performance was lower compared to the rest of her memory performance, which was average to very superior. The results from the D-KEFS indicate average to above-average performance with perhaps somewhat weaker cognitive flexibility (below average to average). On the other hand, the results from the WCST indicate impairment in cognitive flexibility. The overall differences in performance between the three assessments were minimal. This indicates that the minor differences in BMI between the test assessments did not significantly affect her cognitive performance, as expected.
Impaired cognitive flexibility
It could be that impaired cognitive flexibility existed prior to the illness as a premorbid trait as suggested previously [ 10 ], or that the malnutrition has affected the patient’s cognitive flexibility. Since we are missing data on her premorbid level, we cannot draw any firm conclusions.
Impaired cognitive flexibility has previously been reported in patients with AN with higher BMI [ 37 ], indicating that impairments in cognitive flexibility do not necessarily relate to undernutrition. In patients with AN who had recovered from the illness, cognitive flexibility was in the normal range in this study. However, other studies found that individuals who recovered from AN exhibited more or less impaired executive functioning [ 10 ]. Longitudinal research on the relationship between different BMI states and cognitive performance is highly needed.
Impaired cognitive flexibility may also play a role in the perpetuation of AN. Impaired cognitive flexibility has been suggested as a maintenance factor [ 38 ] and a factor related to lack of illness insight characteristic of patients with restrictive AN [ 39 ]. Lack of illness insight could be related to treatment resistance [ 40 ]. The patient’s low scores on EDI-3 subscales also reflect a discrepancy between illness severity and self-reported symptoms. This discrepancy or ambivalence is part of the nature of the disorder reflected in the low motivation for recovery and high number of dropouts from treatment alongside an expressed desire to change [ 41 ].
Cognitive adaptation in anorexia nervosa
Survival of long-term starvation is only possible due to extensive adaptive endocrine and metabolic alterations [ 42 ]. How these alterations affect cognitive functions still remains to be clarified. Well-designed longitudinal studies on severely underweight patients with a long illness duration are lacking. However, the present case report suggests that essential preservation of some cognitive functions occurs even in extreme chronic semi-starvation.
The mechanisms allowing for such preservation remains a subject of speculation. Links can be made to research on neuroplasticity and functional reorganization of cognitive functions after brain injury since patients with AN have white matter alterations [ 43 ]. Research shows that brain maturation processes of especially the prefrontal cortex continue until people are approximately 25 years old [ 44 ]. Nutritional status seems to impact this brain maturation [ 44 ]. Executive functions associated with the prefrontal cortex could therefore be affected by undernutrition during development of prefrontal connections in the brain in adolescence and young adulthood. Thus, impairment on executive functions may not arise until adulthood in patients with AN. This is in line with research that found no cognitive flexibility impairment in children and adolescents with AN but impairments in adults with AN [ 19 , 20 ]. The literature indicates that other cognitive functions associated with the prefrontal cortex, such as memory, are also impaired in adults with AN [ 3 ]. However, overall, this literature is not as explicit as the literature showing cognitive flexibility impairment in adults with AN. The ambiguity in the literature indicates differences between cognitive functions related to the prefrontal cortex in patients with AN. It might be that some prefrontal connections potentially being affected during low weight in adolescence could be reorganized or “compensated for” with time as is possible with reorganization or apparent functional recovery after brain injury [ 45 ]. In that case, cognitive performance could be regained after impairment has occurred. Some dimensions of cognitive flexibility might, however, be more difficult to compensate for. This could explain specific cognitive flexibility impairment in patients recovered from AN [ 10 ] and explain that the patient in the present case report performed normal and superior on some functions associated with prefrontal connections (memory and verbal fluency) but poorer on cognitive flexibility. We therefore suggest that reorganization of some cognitive functions can occur in spite of persisting low weight in patients with AN. In line with the possibility of cognitive reorganization in AN, Cognitive Remediation Therapy seems to improve executive functioning in patients with AN [ 46 ]. The suggested theory of cognitive adaptation may therefore not be specific to persisting low weight in AN. However, fast, substantial weight-loss could affect cognitive performance differently than persisting low weight. Therefore, studies on starving healthy subjects, including the Minnesota Semi-Starvation Experiment [ 16 ], could show different results than studies on patients with severe and enduring AN. Likewise, studies on patients with short illness duration might find different results than studies of patients with enduring AN. It is also unclear if patients developing AN in adulthood will display the same cognitive impairments. In line with these reflections, a case report of a 27-year-old Japanese woman in a coma, with BMI of 8.5 kg/m 2 at admission, describes a patient with AN where the outcome of severe malnutrition was persistent neurologic sequelae [ 47 ]. The woman developed AN at the age of 21 years where the patient in the present case report was diagnosed at the age of 10 years. The difference in age of onset, duration of illness, and/or manner of weight-loss (fast, substantial weight-loss compared to persisting low weight) may have resulted in different outcomes for the women. It is, however, also a possibility that the patient in the present case report might have an extreme phenotype which enables her to perform well in spite of her being extremely underweight.
We cannot say how high the patient’s scores on the neuropsychological test battery might be if she had not been as malnourished. We assume the patient would perform better on cognitive flexibility tasks, that her processing speed and working memory would be higher, and that she would be able to concentrate better had she not been malnourished. This is somewhat supported by previous research. Although the literature suggests impaired cognitive performance in patients with AN, the reported impairments were limited compared to healthy subjects [ 8 , 48 ]. Furthermore, it may be that severely underweight patients with AN have a higher verbal IQ [ 49 ], which does not, however, exclude the possibility of specific cognitive impairments [ 50 ]. This could explain the patient’s high memory performance (and probably global IQ) alongside specific impairment in cognitive flexibility on the WCST. This case may therefore not differ from other patients with severe AN regarding cognitive performance. It may be that the superior performance related to some cognitive functions is a trait of severely underweight patients with AN and/or that a cognitive adaptation to enduring AN increases performance to the premorbid level. In this case, (regained) superior performance of some cognitive functions (i.e. memory and verbal IQ) can exist alongside cognitive impairment in others (i.e. cognitive flexibility). This may change our view of the cognitive profile and its development in patients with severe and enduring AN.
Regardless, the fact that we were able to test the patient in the present case, raises a discussion as to whether she and others with extremely low weight may be responsive to psychotherapy as well. In the present case, the patient underwent psychotherapy for several years albeit without any impact on her weight. More research focusing on the validation of neuropsychological tests including investigation of the practice effect in this patient population is needed.
The individual scores on neuropsychological tests should always be interpreted with care. Factors other than persisting low weight may affect neuropsychological performance (e.g. dehydration, stress, depression, and anxiety). In the present case, the patient did express depressive symptoms corresponding to moderate depression, which might have influenced results on impairment in cognitive flexibility. Furthermore, the patient might experience other issues related to cognitive performance in daily life, which cannot be discovered in a neuropsychological assessment context.
Obviously, conclusions can never be drawn from one case. However, since the neuropsychological testing included a broad range of tests and was repeated three times during a year, the present case report is valid as a basis for reflecting on the affected individual’s cognitive performance at this stage. The present case report demonstrates that cognitive functions may be largely preserved under extreme chronic malnutrition or that cognitive functioning may be regained (reorganized) in spite of extreme chronic malnutrition. More research on patients with AN with extremely low BMI (< 10) is needed to determine whether cognitive performance is affected by starvation and malnutrition.
Availability of data and materials
All data analyzed during this study are included in this published article in tables or text. Raw data in a fully anonymized version is available from the corresponding author on reasonable request.
Abbreviations
- Anorexia nervosa
Intelligence quotient
Body mass index
The Beck Depression Inventory II
The Eating Disorder Inventory 3
The Wechsler Memory Scale III
The Wechsler Adult Intelligence Scale IV
The Processing Speed Index
The Delis-Kaplan Executive Function System
The Wisconsin Card Sorting Test Revised and Expanded
Seed JA, Dixon RA, McCluskey SE, Young AH. Basal activity of the hypothalamic-pituitary-adrenal axis and cognitive function in anorexia nervosa. Eur Arch Psychiatry Clin Neurosci. 2000;250(1):11–5.
Article CAS PubMed Google Scholar
Seed JA, McCue PM, Wesnes KA, Dahabra S, Young AH. Basal activity of the HPA axis and cognitive function in anorexia nervosa. Int J Neuropsychopharmacol. 2002;5(1):17–25.
Biezonski D, Cha J, Steinglass J, Posner J. Evidence for Thalamocortical circuit abnormalities and associated cognitive dysfunctions in underweight individuals with anorexia nervosa. Neuropsychopharmacology. 2016;41(6):1560–8.
Article PubMed Google Scholar
Kjaersdam Telleus G, Jepsen JR, Bentz M, Christiansen E, Jensen SO, Fagerlund B, et al. Cognitive profile of children and adolescents with anorexia nervosa. Eur Eat Disord Rev. 2015;23(1):34–42.
Roberts ME, Tchanturia K, Stahl D, Southgate L, Treasure J. A systematic review and meta-analysis of set-shifting ability in eating disorders. Psychol Med. 2007;37(8):1075–84.
Abbate-Daga G, Buzzichelli S, Marzola E, Aloi M, Amianto F, Fassino S. Does depression matter in neuropsychological performances in anorexia nervosa? A descriptive review. Int J Eat Disord. 2015;48(6):736–45.
Bodell LP, Keel PK, Brumm MC, Akubuiro A, Caballero J, Tranel D, et al. Longitudinal examination of decision-making performance in anorexia nervosa: before and after weight restoration. J Psychiatr Res. 2014;56:150–7.
Article PubMed PubMed Central Google Scholar
Hirst RB, Beard CL, Colby KA, Quittner Z, Mills BM, Lavender JM. Anorexia nervosa and bulimia nervosa: a meta-analysis of executive functioning. Neurosci Biobehav Rev. 2017;83:678–90.
Tchanturia K, Davies H, Roberts M, Harrison A, Nakazato M, Schmidt U, et al. Poor cognitive flexibility in eating disorders: examining the evidence using the Wisconsin card sorting task. PLoS One. 2012;7(1):e28331.
Article CAS PubMed PubMed Central Google Scholar
Tchanturia K, Morris RG, Anderluh MB, Collier DA, Nikolaou V, Treasure J. Set shifting in anorexia nervosa: an examination before and after weight gain, in full recovery and relationship to childhood and adult OCPD traits. J Psychiatr Res. 2004;38(5):545–52.
Danner UN, Sanders N, Smeets PA, van Meer F, Adan RA, Hoek HW, et al. Neuropsychological weaknesses in anorexia nervosa: set-shifting, central coherence, and decision making in currently ill and recovered women. Int J Eat Disord. 2012;45(5):685–94.
Wu M, Brockmeyer T, Hartmann M, Skunde M, Herzog W, Friederich H-C. Reward-related decision making in eating and weight disorders: a systematic review and meta-analysis of the evidence from neuropsychological studies. Neurosci Biobehav Rev. 2016;61:177–96.
Lozano-Serra E, Andres-Perpina S, Lazaro-Garcia L, Castro-Fornieles J. Adolescent anorexia nervosa: cognitive performance after weight recovery. J Psychosom Res. 2014;76(1):6–11.
Firk C, Mainz V, Schulte-Ruether M, Fink G, Herpertz-Dahlmann B, Konrad K. Implicit sequence learning in juvenile anorexia nervosa: neural mechanisms and the impact of starvation. J Child Psychol Psychiatry. 2015;56(11):1168–76.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington: Author; 2013.
Book Google Scholar
Keys A, Brozek J, Henschel A, Mickelsen O, Taylor HL. The biology of human starvation (2 volumes). Minnesota: University of Minnesota Press; 1950.
Benau EM, Orloff NC, Janke EA, Serpell L, Timko CA. A systematic review of the effects of experimental fasting on cognition. Appetite. 2014;77:52–61.
Buhren K, Mainz V, Herpertz-Dahlmann B, Schafer K, Kahraman-Lanzerath B, Lente C, et al. Cognitive flexibility in juvenile anorexia nervosa patients before and after weight recovery. J Neural Transm (Vienna). 2012;119(9):1047–57.
Article Google Scholar
Telleus GK, Fagerlund B, Jepsen JR, Bentz M, Christiansen E, Valentin JB, et al. Are weight status and cognition associated? An examination of cognitive development in children and adolescents with anorexia nervosa 1 year after first hospitalisation. Eur Eat Disord Rev. 2016;24(5):366–76.
Lang K, Stahl D, Espie J, Treasure J, Tchanturia K. Set shifting in children and adolescents with anorexia nervosa: an exploratory systematic review and meta-analysis. Int J Eat Disord. 2014;47(4):394–9.
Taylor SE. Adjustment to threatening events: a theory of cognitive adaptation. Am Psychol. 1983;38(11):1161–73.
Frolich J, Palm CV, Stoving RK. To the limit of extreme malnutrition. Nutrition. 2016;32(1):146–8.
Robinson P, Jones WR. MARSIPAN: management of really sick patients with anorexia nervosa. BJPsych Advances. 2018;24(1):20–32.
Beck AT, Steer RA, Brown GK. Manual for the Beck depression inventory-II. San Antonio: Psychological Corporation; 1996.
Google Scholar
Garner DM. Eating disorder Inventory-3. Professional manual. Lutz: Psychological Assessment Resources, Inc.; 2004.
Clausen L, Rosenvinge JH, Friborg O, Rokkedal K. Validating the eating disorder Inventory-3 (EDI-3): a comparison between 561 female eating disorders patients and 878 females from the general population. J Psychopathol Behav Assess. 2011;33(1):101–10.
Wechsler D. WAIS-III WMS-III technical manual. San Antonio: The Psychological Corporation; 2002.
Brickenkamp R, Schmidt-Atzert L, Liepmann D. The d2 test of attention – revised. A test of attention and concentration. Oxford: Hogrefe; 2016.
Brickenkamp R. d2-testen – en vurdering af opmærksomhed of koncentration. Dansk vejledning. Hogrefe Psykologisk Forlag: Frederiksberg; 2006.
Wechsler D. Wechsler adult intelligence scale—fourth edition. Technical and interpretive manual. Pearson: San Antonio; 2008.
Delis DC, Kaplan E, Kramer JH. Delis-Kaplan executive function system - technical manual. Pearson: San Antonio; 2001.
Heaton RK, Chelune GJ, Talley JL, Kay GG, Curtiss G. Wisconsin Card Sorting Test Manual Revised and Expanded. 2nd edition ed. Lutz: Psychological Assessment Resources, Inc.; 1993.
Tulsky D, Zhu J, Ledbetter M, editors. WAIS-III WMS-III technical manual (Wechsler Adult Intelligence Scale & Wechsler Memory Scale) paperback updated. USA: The Psychological Corporation; 2002.
Iverson GL. Interpreting change on the WAIS-III/WMS-III in clinical samples. Arch Clin Neuropsychol. 2001;16(2):183–91.
Bradley SJ, Taylor MJ, Rovet JF, Goldberg E, Hood J, Wachsmuth R, et al. Assessment of brain function in adolescent anorexia nervosa before and after weight gain. J Clin Exp Neuropsychol. 1997;19(1):20–33.
Lauer CJ, Gorzewski B, Gerlinghoff M, Backmund H, Zihl J. Neuropsychological assessments before and after treatment in patients with anorexia nervosa and bulimia nervosa. J Psychiatr Res. 1999;33:129–38.
Tenconi E, Santonastaso P, Degortes D, Bosello R, Titton F, Mapelli D, et al. Set-shifting abilities, central coherence, and handedness in anorexia nervosa patients, their unaffected siblings and healthy controls: exploring putative endophenotypes. World J Biol Psychiatry. 2010;11(6):813–23.
Steinglass JE, Walsh BT, Stern Y. Set shifting deficit in anorexia nervosa. J Int Neuropsychol Soc. 2006;12(3):431–5.
Konstantakopoulos G, Tchanturia K, Surguladze SA, David AS. Insight in eating disorders: clinical and cognitive correlates. Psychol Med. 2011;41(9):1951–61.
Abbate-Daga G, Amianto F, Delsedime N, De-Bacco C, Fassino S. Resistance to treatment and change in anorexia nervosa: a clinical overview. BMC Psychiatry. 2013;13(1):294.
Guarda AS. Treatment of anorexia nervosa: insights and obstacles. Physiol Behav. 2008;94(1):113–20.
Stoving RK. Mechanisms In Endocrinology: Anorexia nervosa and endocrinology: a clinical update. Eur J Endocrinol. 2019;180(1):R9–r27.
Barona M, Brown M, Clark C, Frangou S, White T, Micali N. White matter alterations in anorexia nervosa: evidence from a voxel-based meta-analysis. Neurosci Biobehav Rev. 2019;100:285–95.
Arain M, Haque M, Johal L, Mathur P, Nel W, Rais A, et al. Maturation of the adolescent brain. Neuropsychiatr Dis Treat. 2013;9:449–61.
PubMed PubMed Central Google Scholar
Mogensen J. Reorganization of the injured brain: implications for studies of the neural substrate of cognition. Front Psychol. 2011;2:7.
Tchanturia K, Lounes N, Holttum S. Cognitive remediation in anorexia nervosa and related conditions: a systematic review. Eur Eat Disord Rev. 2014;22(6):454–62.
Bando N, Watanabe K, Tomotake M, Taniguchi T, Ohmori T. Central pontine myelinolysis associated with a hypoglycemic coma in anorexia nervosa. Gen Hosp Psychiatry. 2005;27(5):372–4.
Dobson KS, Dozois DJ. Attentional biases in eating disorders: a meta-analytic review of Stroop performance. Clin Psychol Rev. 2004;23(8):1001–22.
Schilder CMT, van Elburg AA, Snellen WM, Sternheim LC, Hoek HW, Danner UN. Intellectual functioning of adolescent and adult patients with eating disorders. Int J Eat Disord. 2017;50(5):481–9.
Lena SM, Fiocco AJ, Leyenaar JK. The role of cognitive deficits in the development of eating disorders. Neuropsychol Rev. 2004;14(2):99–113.
Download references
Acknowledgements
We would like to thank Professor Jesper Mogensen at the Unit for Cognitive Neuroscience, University of Copenhagen, Denmark, for his inputs regarding neurocognitive reorganization and the possibility of extending his model to the research field of anorexia nervosa.
The study was supported by government funding: The Psychiatric Research Fund of Southern Denmark (grants for material and PhD salary) and the University of Southern Denmark (faculty scholarship). Furthermore, the study was supported with grants for material by private funds: the Jascha Foundation and the Beckett Foundation. The funding sources had no role in the design, execution, interpretation, analysis, or publication of the study.
Author information
Authors and affiliations.
Centre for Eating Disorder, Odense University Hospital, Odense, Denmark
Simone Daugaard Hemmingsen & René Klinkby Støving
Research Unit for Medical Endocrinology, Odense University Hospital, Odense, Denmark
Department of Clinical Research, University of Southern Denmark, Odense, Denmark
Open Patient data Explorative Network (OPEN), Odense, Denmark
The Research Unit, Child and Adolescent Psychiatry, Mental Health Services in the Region of Southern Denmark, Odense, Denmark
Centre for Telepsychiatry, Mental Health Services in the Region of Southern Denmark, Odense, Denmark
Mia Beck Lichtenstein
Department of Psychology, University of Southern Denmark, Odense, Denmark
Eating Disorder Unit, Mental Health Centre Ballerup, Mental Health Services in the Capital Region of Denmark, Copenhagen, Denmark
Alia Arif Hussain & Jan Magnus Sjögren
Department of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
You can also search for this author in PubMed Google Scholar
Contributions
SDH and RKS completed the data collection. RKS was the initiator of the project. SDH, RKS, and MBL all took part in the design of the study. SDH, RKS, MBL, JMS and AAH were all contributors in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Simone Daugaard Hemmingsen .
Ethics declarations
Ethics approval and consent to participate.
The research project has been approved by the Regional Scientific Ethical Committee for the Region of Southern Denmark and was carried out in accordance with the 1964 Helsinki declaration and its later amendments. The authors state that the patient has given written and informed consent for participation in the study.
Consent for publication
The authors state that the patient has given written and informed consent for publication of the case report.
Competing interests
The authors declare that there are no conflicts of interest. None of the authors have received financial support or benefits from commercial sources for this study.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Hemmingsen, S.D., Lichtenstein, M.B., Hussain, A.A. et al. Case report: cognitive performance in an extreme case of anorexia nervosa with a body mass index of 7.7. BMC Psychiatry 20 , 284 (2020). https://doi.org/10.1186/s12888-020-02701-1
Download citation
Received : 13 February 2020
Accepted : 28 May 2020
Published : 05 June 2020
DOI : https://doi.org/10.1186/s12888-020-02701-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Cognitive performance
- Neuropsychology
- Undernutrition
BMC Psychiatry
ISSN: 1471-244X
- Submission enquiries: [email protected]
- General enquiries: [email protected]
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- HHS Author Manuscripts

Psychosis In Anorexia Nervosa: A Case Report and Review of the Literature
Brooks brodrick.
1. Department of Internal Medicine at the University of Texas Southwestern
2. Department of Psychiatry at the University of Texas Southwestern
3. Parkland Health and Hospital System
Mallory Jacobs
Carrie mcadams.
4. Department of Psychiatry, Children’s Medical Center
Introduction
Anorexia nervosa (AN) is a psychiatric disorder characterized by restriction of energy intake relative to requirements, fears about weight gain or behavior that interferes with weight gain, and disturbances in one’s perceptions about one’s body or shape. ( 1 ) The illness impacts approximately 1.4% of women, and 0.2% of men, with a bimodal age of onset with peaks during late adolescence and young adulthood. ( 2 , 3 ) Adults often present with gradual but substantial weight loss and can show little insight about the etiology of their weight loss. ( 4 ) Although a common perception is that individuals with AN must overvalue shape or weight, the actual diagnostic criteria only require a persistent lack of recognition of the seriousness of the current low body weight. ( 1 ) Patients that are unaware or deny that body-image concerns contributed to weight loss may not be evaluated for an eating disorder, delaying appropriate treatment.
In contrast, an acute psychotic episode resulting in hospitalization is more commonly referred for psychiatric evaluation. The lifetime prevalence of psychotic disorders is approximately 3%, with 0.21% due to medical conditions and 0.42% due to illicit substances, and the peak age of onset is also in young adults.( 5 ) Importantly, malnutrition can contribute to psychosis through many pathways. Both specific nutritional deficiencies, including niacin, thiamine, and vitamin B12, and complications common during malnutrition, such as sleep deprivation and metabolic derangements, are known medical causes of psychosis. Diagnosis of a primary psychotic disorder should be made only after nutritional rehabilitation has occurred so that other medical causes are excluded. Here we report a case where the diagnosis of AN was delayed due to the presence of psychotic symptoms, and provide a literature review covering cases of co-occurring psychosis in the presentation of AN.
Case Report
Ms. K, a 22-year-old black female, with no past medical or psychiatric history, presented for evaluation of weight loss and refusal to eat. Her mother reported changes in eating behaviors for the prior six months with a 13.6 kg weight loss. Ms K had recently graduated from a 4-year college and planned to move across the country to initiate employment. Ms K stated that the “voice of God” told her to not eat. She prayed constantly because she had pain in her body and could not determine if the source was “God or the enemy”. On exam, she was extremely thin (body weight 35.7 kg; height: 167.6 cm; body mass index [BMI]: 12.7), pale and withdrawn with psychomotor delay and minimal eye contact. Her first admission was to medicine for leukopenia and bradycardia. Work-up for infectious or malignant etiologies was negative. After receiving fluid and electrolyte repletion for mild hypokalemia (potassium 3.1 mmol/l) and acute kidney injury (creatinine 1.1 mg/dl), she was discharged five days later with follow-up in the psychiatric clinic. She refused initiation of any psychiatric medications.
Six days after discharge her mother brought her back to the ED for refusal to eat or drink anything. She was too weak to care for herself. During this second admission, she continued to have poor food intake and expressed uncertainty about further psychiatric treatment related to eating behaviors. She was discharged after two weeks because the medical team believed she was regressing in the hospital environment, exhibiting manipulative and attention seeking behavior.
Ms. K arrived for an outpatient psychiatric appointment four weeks later, and her weight had dropped an additional 2.7 kg (32.2 kg; BMI: 11.5). Because she now reported an indifference to dying and remained fixated on the belief that God told her not to eat, she was involuntarily admitted to the psychiatric unit. During her third hospital stay and first on a psychiatric floor, she struggled to characterize how God communicated with her, sometimes describing thoughts in her head or God speaking only to her. Her exam was notable for latency of speech, apparent thought blocking and frequent sudden staring episodes. She was started on olanzapine 2.5 mg at bedtime, and that was increased to twice a day for her psychosis. She reported that olanzapine didn’t help with the thoughts in her head. She continued to struggle with food intake and was witnessed chewing food and then spitting it out.
During this third admission, Ms. K was transferred from psychiatry to medicine because of medical complaints consistent with malnutrition: constipation, cold hands and feet, chest pain, dysuria, and multiple episodes of hypoglycemia. The two weeks spent on the psychiatric unit for involuntary treatment of new onset psychosis had resulted in an additional weight loss of 1.4 kg (30.8 kg; BMI: 11.0). On physical exam she had proximal muscle weakness requiring assistance to stand up from a seated position as well as acrocyanosis of her hands and feet. Even minimal exertion such as sitting up or speaking would cause her to go from bradycardia to tachycardia. A nasogastric tube was placed on day 14 of this hospital stay because of her physiological decompensation from malnutrition. Her oral intake was monitored with food logs and nasogastric feeds were adjusted such that her total caloric intake was started at 1400 calories and increased by 400 calories every 4 days.
Two weeks after initiation of nasogastric feeding her weight had increased to 41.3 kg. Once feeding began, she gradually became more interactive with reduced response latency, spontaneous dyadic conversations, and more elaborate responses. Olanzapine was increased to 7.5 mg daily to help with sleep and ruminating thoughts about food. She began drinking and eating food at meal times as well, but only after the hospital staff, including physicians, nurses, dietitians, and sitters, both supervised and enforced completion of meals on the medical floor. She reported anger towards the staff at this time, but attributed the anger to olanzapine, not the enforced changes to her eating or weight gain. She stopped hearing God talk to her but denied that his absence was bothersome. In therapy, she became more goal directed. Her daily routines became less rigid and she became more in touch with her physical needs, taking naps or sleeping in as needed.
In her early interactions with physicians and therapists, Ms. K reported a strong interest in religion during childhood but denied any visions or auditory hallucinations. She stated that she began hearing God speak to her about one year ago, after her boyfriend broke up with her. She believed God was directing her to not eat as punishment for her sins of sexuality outside of marriage. At this time, her weight was approximately 63.5 kg. She reported making a choice to become vegan and lose weight, and had installed a health app on her phone. She lost 4.5 kg in three months and stopped menstruating. Ms. K also described how her food restriction then became more systematic. She eliminated specific types of foods, choosing to only eat one type of item, such as soups, avocados, or cereal for days. She stopped eating almost entirely the week before her initial admission. Although she was able to recall these events with prompting, she lacked insight about how her food restriction contributed to her hospitalization.
After 4 weeks, weighing 45 kg, she was transitioned to nocturnal tube feeds only with 3 meals and boost plus four times per day. Two days later tube feeds were stopped entirely as she was able to eat >75% of her meals and snacks. Her insight and judgment had significantly improved. She advocated for herself during a therapy session, stating she was hungry and needed a snack. She set her own goal to become more comfortable eating in front of others, and had awareness that eating with others was difficult for her. She acknowledged a tendency to isolate herself and difficulty forming friendships throughout her life. She attributed this in part to her perfectionism and propensity to self-blame. Recognizing that her previous job offer might be a trigger for her eating disorder as it would be in a different city away from social support, she agreed to continue therapy at a residential eating disorder treatment facility.
After 6 weeks at a residential eating disorder treatment center, she returned home. Olanzapine was tapered off and her weight remained stable at her baseline 61.2 kg (BMI 21.8). Although she remained devout in her religious beliefs, she no longer reported hearing God directly. She was not bothered by this, and had become engaged in work-life activities.
Psychotic episodes occur in 10–15% of eating disorder patients. ( 6 ) The prevalence of primary psychotic diseases like schizophrenia and schizoaffective disorders in eating disorder patients appears to be comparable to that in the general population. ( 7 ) To determine if specific features of presentations may assist in the differential diagnosis of psychosis and AN, we searched PubMed, MEDLINE, and PsychInfo with terms (psychosis or psychotic) and (anorexia nervosa or eating disorders). Cases of bulimia nervosa, orthorexia nervosa or review articles on the topic were excluded. Twelve cases of co-occuring psychosis and eating disorder symptoms were identified; this case is also summarized in Table 1 . In nine of the other cases, the patients were severely underweight at presentation, and at the lower end of normal BMI in the remaining three. Restriction was predominant eating behavior, with purging in four cases. Auditory hallucinations were the most common psychotic component, present in seven cases. Ms K as well as the cases in our literature review highlight the difficulty in determining the etiology of psychosis in the setting of malnutrition, and also provide evidence about differences in treatment responses for these disease processes. Our presumptive diagnosis and rationale based on the evidence presented for each case is summarized in the far right column of Table 1 .
Brief Review of Cases of Psychosis and Eating Disorder Behaviors and Low Body Mass
Moga and colleagues ( 8 ) describe a case with many similarities to Ms. K. A 42 year old woman with a long history of AN, binge/purge type became convinced God was prohibiting her from eating. She believed God communicated with her directly in her thoughts, with bible passages, and in other people’s words. She prayed for hours and repented her sins, compulsively tracked in a notebook. Anxiety and psychotic symptoms diminished and insight improved in this patient shortly after initiation of antipsychotics. Psychosis and religious scrupulosity were in the differential for both this case and our own. Scrupulosity refers to behaviors or thinking in which individuals are overly attentive to religious rituals. Inconsistent with scrupulosity, the beliefs about food restriction for both patients were not commonly practiced within their religious community. In both cases their religious rituals intensified with weight loss and their compulsive behaviors improved with weight restoration, further demonstrating the importance of nutritional rehabilitation prior to establishment of a psychiatric diagnosis.
Cognitive processes in AN are more commonly described as overvalued ideas and ruminations, whereas cognitive disturbances in psychosis are often characterized as delusions and hallucinations. Psychotic symptoms were dominated by ideas about eating, body shape, and weight in all cases in this review. Importantly, there are no objective rules that distinguish an overvalued idea from a delusion and patients’ reports of internal symptoms such as hallucinations may be similar to ruminations. Many eating disorder patients will refer to ruminations and distorted beliefs about eating, food, and their body as their “eating disorder voice”. When Mountjoy and colleagues ( 4 ) compared body image distortions in AN to delusions in schizophrenia, they found individuals with AN reported higher distress about their beliefs than those with schizophrenia but were comparable in their conviction and disruption ratings. Thirty percent of the AN participants also showed low insight about their cognitive disturbances. Moreover, both AN and schizophrenia share neurocognitive deficits: difficulties in shifting attention, overestimation of detail, and weak central coherence. Acute clinical and cognitive symptoms may be insufficient to differentiate AN from primary psychotic disorders because both can present with low insight, similar neurocognitive deficits, and overvalued ideas.
Restriction serves as an emotional numbing agent so often anxiety intensifies with acute nutritional intake in AN. In addition, many patients with primary eating disturbances will experience increased anxiety as immediate physical discomfort after eating, a cycle that promotes more restriction. In contrast, the benefits from improved nutrition for memory, emotional processing and cognition may take weeks to observe. Nasogastric feeding can allow a more continuous source of nutritional intake for patients that are unable to consume sufficient calories orally due to emotional and physical distress. As Ms K’s weight increased, auditory hallucinations resolved and anxiety about eating diminished. Relatively quickly, she achieved the required caloric intake with meals and oral nutritional supplementation, and nasogastric feeding was tapered off. Concomitantly, she became aware of the emotional and psychosocial stressors contributing to the onset of her psychiatric symptoms. In contrast, cases where a primary psychosis process occurred can have worsening of psychotic symptoms with nutritional rehabilitation. ( 9 ) Disorganization became more prominent with feeding, a stark contrast to the highly rigid and ritualized behaviors seen in AN. Hugo and Lacey have postulated that eating restriction may be a defense mechanism to manage the disorganization of psychosis, emphasizing the need to obtain a history with a detailed chronology of symptoms to ascertain the order of psychiatric symptoms.( 10 )
In all cases, improvement in psychiatric symptoms occurred after initiation of antipsychotics. Hyperactivity, a common symptom in AN, can overcome dopamine pathway deficits present during starvation in AN rodent models, suggesting dopamine deficiency may be involved in the perpetuation of AN behaviors. ( 11 ) Further support for dopamine pathway involvement in AN is that olanzapine modestly improves weight restoration in adult outpatients with AN. ( 12 ) Therefore a positive response to antipsychotic medications does not necessarily confirm the presence of a primary psychotic disease. Dopamine signals are critical for both learning and motivation in animal models. ( 13 ) Thus, dopamine pathways may be crucial for executing the behavioral changes required for recovery from AN.
Our case as well as the others identified in the literature underscore the complexities in deciphering the etiology of psychosis in the setting of malnutrition. Nutritional rehabilitation was key to unraveling the etiology of the psychotic symptoms. After weight restoration, patients with AN, akin to Ms. K, are likely to have resolution of psychosis whereas patients with a primary psychotic disorder may require additional antipsychotic medications. Weight restoration should not be delayed while waiting for psychotic symptoms to respond to antipsychotics, as any delay can result in further physical deterioration, as demonstrated by Ms K. AN should remain high on the differential when delusions and hallucinations are related to food intake or body image.
Disclosure: The authors disclosed no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Eating disorders and psychosis: a review and case report
Affiliations.
- 1 Department of Psychiatry and Mental Health, Baixo Vouga Hospital Centre, Aveiro, Portugal.
- 2 Psychiatry and Mental Health Clinic, São João University Hospital Centre, Porto, Portugal.
- PMID: 33331586
- DOI: 10.1590/1806-9282.66.12.1736
Introduction: The interplay between eating disorders and psychosis is a challenging field to which little attention has been paid. Its study raises conceptual and methodological questions in both areas, making the diagnosis and management of patients difficult. Such questions are addressed and illustrated with a review and case report.
Methods: The authors present the case of a woman with Anorexia Nervosa and with comorbid Shared Psychotic Disorder, based on a literature review regarding the comorbidity between eating disorders and psychosis. The authors conducted a non-systematic review by searching the PubMed database, using the Mesh Terms "anorexia nervosa", "bulimia nervosa", "comorbidity" and "psychotic disorders".
Results: The findings suggest that studies on the subject are limited by issues regarding data on the prevalence of comorbidities, phenomenological aspects of eating disorders, and the interface and integration with psychotic symptoms.
Conclusions: The case presented illustrates the difficulties in managing a patient with a comorbid eating disorder and psychosis. In order to ensure a rigorous assessment of both psychotic and eating disorder symptoms, the focus should be on the pattern of appearance or emergence of symptoms, their phenomenology, clinical and family background of the patient, and clinical status on follow-up.
Publication types
- Case Reports
- Anorexia Nervosa* / complications
- Anorexia Nervosa* / epidemiology
- Bulimia* / epidemiology
- Comorbidity
- Feeding and Eating Disorders* / complications
- Psychotic Disorders*
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 15 May 2024
Corpus callosum morphology and relationships to illness phenotypes in individuals with anorexia nervosa
- Jamie D. Feusner 1 , 2 , 3 , 4 ,
- Alicja Nowacka 5 ,
- Ronald Ly 4 ,
- Eileen Luders 5 , 6 , 7 &
- Florian Kurth 5 , 8
Scientific Reports volume 14 , Article number: 11112 ( 2024 ) Cite this article
Metrics details
- Neuroscience
- Signs and symptoms
Anorexia nervosa is an often-severe psychiatric illness characterized by significantly low body weight, fear of gaining weight, and distorted body image. Multiple neuroimaging studies have shown abnormalities in cortical morphology, mostly associated with the starvation state. Investigations of white matter, while more limited in number, have suggested global and regional volume reductions, as well as abnormal diffusivity in multiple regions including the corpus callosum. Yet, no study has specifically examined thickness of the corpus callosum, a large white matter tract instrumental in the inter-hemispheric integration of sensory, motor, and cognitive information. We analyzed MRI data from 48 adolescents and adults with anorexia nervosa and 50 healthy controls, all girls/women, to compare corpus callosum thickness and examined relationships with body mass index (BMI), illness duration, and eating disorder symptoms (controlling for BMI). There were no significant group differences in corpus callosum thickness. In the anorexia nervosa group, severity of body shape concerns was significantly, positively correlated with callosal thickness in the rostrum, genu, rostral body, isthmus, and splenium. In addition, there were significant positive correlations between eating disorder-related obsessions and compulsions and thickness of the anterior midbody, rostral body, and splenium. There were no significant associations between callosal thickness and BMI or illness duration. In sum, those with AN with worse concerns about bodily appearance and worse eating disorder-related obsessive thought patterns and compulsive behaviours have regionally thicker corpus callosum, independent of current weight status. These findings provide important neurobiological links to key, specific eating disorder behavioural phenotypes.
Similar content being viewed by others

Systematic reduction of gray matter volume in anorexia nervosa, but relative enlargement with clinical symptoms in the prefrontal and posterior insular cortices: a multicenter neuroimaging study
Age influences structural brain restoration during weight gain therapy in anorexia nervosa

Initial evidence of abnormal brain plasticity in anorexia nervosa: an ultra-high field study
Introduction.
Anorexia nervosa (AN) is an eating disorder characterized by a morbid fear of gaining weight and being fat, restriction of caloric intake and/or engaging in excessive exercise to the point of having a very low body weight, and disturbances in body image 1 . AN can take a particularly ominous course and severely affect individuals’ function and well-being, and disrupt their family’s lives. AN typically onsets in early adolescence and, in many, can continue into adulthood. Its crude mortality rate of 5.6% per decade 2 is second only to opiate use disorder as the most life-threatening of psychiatric illnesses.
There are few effective treatments for AN, which may be due to an incomplete understanding of its neurobiology. The severe malnutrition state that individuals with AN experience can result in prominent brain structural changes. Multiple structural neuroimaging studies in AN have shown abnormalities in cortical morphology, including reductions in cortical thickness and subcortical volumes; these likely reflect atrophy from malnutrition and the starvation state since they tend to reverse when weight is restored 3 , 4 .
Overall, there have been fewer investigations of brain white matter, compared with gray matter, abnormalities in AN. One of the known effects of starvation is that it reduces white matter myelination. For example, a reduction in myelination in starvation states has been demonstrated experimentally in rodents and has been shown to be only partially restored by nutritional rehabilitation 5 , 6 , 7 . Reduction in myelination has also been demonstrated in malnutrition and starvation states in humans 8 , including in a small study in underweight adolescent females 9 .
Several studies in adolescents with AN have examined white matter volumes, although there have been inconsistent findings. In those with acute, underweight AN, two studies found reduced global white matter volume in adolescents with AN compared with healthy controls 10 , 11 while another found no abnormalities 12 . In terms of regional abnormalities, one study found reductions in bilateral superior longitudinal fasciculi, superior thalamic radiation, corona radiata, fornix, pons, and medulla 13 . Also inconsistent across studies is whether reductions in global or regional white matter volume are solely a function of the underweight state. Two studies in weight-recovered adolescents with AN found no global or regional white matter volume abnormalities 14 , 15 , while one study found reduced global white matter volume compared with healthy controls 10 and another found regional reductions in the pons 13 .
Neuroimaging studies of white matter in AN using diffusion tensor imaging (DTI) have revealed widespread abnormal diffusion patterns. Briefly, DTI is a specialised MRI technique that analyzes the degree and direction of diffusion of water molecules in brain tissue, providing estimates of microstructural properties. One way in which diffusion patterns can be characterized in white matter tracts is by fractional anisotropy (FA); lower FA could indicate less organized or potentially disrupted white matter tracts. A meta-analysis of DTI studies in AN found evidence, in the 10 included studies, of reduced FA in the left thalamus and left corona radiata 16 . Another quantitative meta-analysis, including 13 studies), found lower FA in AN compared with controls in the posterior corpus callosum (CC) body, the left superior longitudinal fasciculus II, the left precentral gyrus, and higher FA in the right cortico-spinal projections and lingual gyrus 17 . A meta-analysis of DTI tract-based spatial statistics studies found evidence of lower FA in the CC and the cingulum, but no association of diffusion measures with age or BMI 18 . The CC regions identified in this meta-analysis were primarily in the CC body and contained fibres connecting right and left prefrontal cortex and supplementary motor area (SMA). The authors posited that reduced FA in the body of the CC could result in reduced information transfer, which in turn could affect cognitive and affective aspects of body image distortion. A more recent study (not covered in these meta-analyses) found reduced FA in the CC body in AN and recovered AN, and reduced mean diffusivity (MD) in the posterior thalamic radiation in acute AN, compared with healthy controls 19 . Another more recent study found reduced white matter tract volume in AN (but not recovered AN) compared with healthy controls in anterior and mid-anterior portions of the CC 20 . Other recent studies, while not revealing abnormal diffusion measures in the CC, found increased FA in occipital and parietal regions 21 , and reduced structural connectivity (based on streamlines) within subcortical networks along with greater frontal cortical connectivity 22 .
These studies suggest that white matter microstructure abnormalities—as indexed by reduced FA and reduced tract volume—may be present in the CC (amongst other areas) in those with AN. The CC is a large white matter tract that connects the right and left hemispheres and facilitates interhemispheric transfer and integration of sensory, motor, and cognitive information 23 . The CC can be geometrically divided into three major regions: the genu + rostrum, connecting frontal and premotor regions of the two hemispheres; the body, which connects motor, somatosensory, and parietal areas; and the splenium + isthmus, which connects occipital and temporal cortices 24 . The CC is involved in homotopic and heterotopic cortical inter-hemispheric synchronizations. Homotopic synchronization refers to brain regions in one hemisphere synchronizing their activity with their counterparts in the opposite hemisphere, and thus being responsible for coordinating and integrating information between mirrored areas of the brain. In contrast, heterotopic inter-hemispheric synchronization refers to synchronization of brain regions that do not have direct correspondence across hemispheres, and thus relay information between non-matching brain regions. Both synchronizations play a critical part in coordinated action and perception 25 , 26 .
AN, like most psychiatric disorders, involves complex and broad pathophysiology including dysfunction in emotion regulation, habitual behaviours, cognitive control, social cognition, visual perception, and visuospatial functioning 27 , 28 , 29 . A meta-analysis of neuropsychological functioning studies in adults with AN found the largest effect sizes for impairments in visuospatial abilities, which were moderated by age (older performing worse) and BMI (lower BMI associated with worse performance) 30 . Body image distortion is a core characteristic, and a DSM-defining criterion, of AN 1 . Multiple studies have empirically demonstrated perceptual distortions for appearance in those with AN (reviewed in 31 ). Given the role of the CC in homotopic and heterotopic hemispheric integration of information coming from parietal, occipital, and temporal regions involved in visuospatial functioning, somatosensory cortices involved in body perception, and prefrontal regions involved in higher cognitive functions such as self-appraisals, dysfunction may contribute to relevant symptomatology in AN.
Additional important, and common, phenomenological features in AN are eating disorder-related obsessive thoughts and ritualistic/compulsive behaviours 32 . Further, obsessive–compulsive disorder (OCD) comorbidity is high in those with AN 33 , 34 , and there is evidence of significant genetic correlations between AN and obsessive–compulsive disorder (OCD) 35 . Further, a study in individuals with OCD found thinner anterior and posterior CC regions and associations with visuospatial performance 36 and another study in OCD found associations between severity of obsessions and compulsions and CC thickness 37 . However, no study has specifically examined CC morphology in adults or adolescents with AN nor relationships with body image disturbance, obsessions and compulsions, nor any other symptom domain.
The goal of this analysis was to characterize corpus callosum morphology in individuals with AN compared with healthy controls and to examine relationships with illness factors including weight/starvation-related effects (estimated by current body mass index—BMI), total illness duration, and the behavioural phenotypes of body shape concerns and eating disorder-related obsessions and compulsions. To achieve this, we analyzed data from T1-weighted MRI scans in adolescents and adults with AN and in healthy controls and measured the thickness of the CC at 100 equally spaced nodes 38 . This method has previously been used to identify abnormalities in several psychiatric disorders including OCD, schizophrenia, and autism spectrum disorder 36 , 39 , 40 .
We hypothesized that there would be abnormalities in CC thickness in those with AN compared with healthy controls. In addition, we hypothesized that CC thickness would be positively associated with BMI in those with AN, reflecting relationships with starvation and weight status. We also predicted that duration of illness would be inversely associated with thickness in the CC in those with AN who were acutely underweight and partially weight-restored, reflecting a cumulative impact of starvation-related and/or malnutrition effects on white matter. Further, we predicted in AN participants, controlling for BMI, significant associations between CC thickness and Eating Disorder Examination (EDE) shape concern subscale scores—indexing disturbances in body image, and Yale–Brown–Cornell Eating Disorders Scale scores—a measure of eating disorder-related obsessive thoughts and ritualistic/compulsive behaviours. We did not have specific directional predictions of associations with clinical variables since this was the first exploration of CC thickness in AN. Hypotheses were preregistered (AsPredicted #62141).
Methods and materials
Participants.
We included participants’ data from two separate studies; study 1 in adults with AN and study 2 in adolescents with AN, each with their own cohorts of control participants. Detailed descriptions of the inclusion and exclusion criteria for both samples were as previously reported 41 . Recruitment of the adult sample was from local specialized treatment centres, online and community-based advertisements, and campus flyers at the University of California Los Angeles (UCLA). Recruitment of the adolescent sample was from the UCLA inpatient eating disorder unit and from local treatment centres; they were enrolled at the end of their treatment in these settings when they met each treatment centre’s individual criteria for transitioning to a lower level of care.
The study's protocols were approved by the UCLA Institutional Review Board, and all methods adhered to their guidelines and regulations. Written informed consent was obtained from all participants, while for the adolescent study, informed consents were acquired from parents and/or legal guardians and assents were obtained from the adolescents.
Diagnostic and psychometric assessments
Licensed psychiatrists or psychologists experienced in working with individuals with AN conducted clinical evaluations and administered clinician-rated scales for all participants. The Mini-International Neuropsychiatric Interview (MINI v. 6.0 for adults 42 and the MINI KID 7.0.2 for adolescents 43 ) was used to screen for primary or comorbid diagnoses. The Eating Disorders Examination (EDE, version 16.0D) was used to determine total eating disorder symptom severity as well as shape concern subscale scores 44 . The severity of eating- and body/weight-related preoccupations and rituals was assessed using the Yale–Brown–Cornell Eating Disorder Scale (YBC-EDS) 45 . The Hamilton Anxiety Rating Scale (HAMA) 46 was used to assess anxiety in studies 1 and 2. The Montgomery-Åsberg Depression Rating Scale 47 was used to assess depression in study 1, while the Child Depression Rating Scale 48 was used in study 2. The Pubertal Development Scale was used to assess pubertal developmental stage in study 2 49 .
Structural MRI data acquisition
Brain MRI data were acquired using a Siemens Trio 3 T scanner with a 12-channel head coil (study 1) and a Siemens Prisma 3 T scanner with a 32-channel head coil (study 2). High-resolution T1-weighted images were acquired with MPRAGE (Magnetization Prepared Rapid Acquisition Gradient Echo) sequence (study 1: TR of 1900 ms, TE of 2.26 ms, and an isotropic voxel dimension of 1 mm 3 ; study 2: TR of 2300 ms, TE of 2.99 ms, and an isotropic voxel dimension of 0.8 mm 3 ).
Data processing
All brain data was processed in Matlab ( https://www.mathworks.com/products/matlab.html ), using SPM12 ( http://www.fil.ion.ucl.ac.uk/spm ) and the CAT12 toolbox 50 applying corrections for magnetic field inhomogeneities, as previously described 51 , 52 . All images were rigid body realigned to MNI space and resliced to 1 mm 3 resolution. In addition, the total intracranial volume (TIV) was calculated by classifying images as gray matter (GM), white matter (WM), and cerebrospinal fluid (CSF) and adding the sub-volumes of these compartments (TIV = GM + WM + CSF).
Callosal thickness estimation
Using the processed images, the corpus callosum was manually outlined by one rater (A.N.) in each brain’s midsagittal section 53 . The callosal traces were extracted and automatically processed in several successive steps 38 , 54 , 55 . More specifically, the callosal outlines were separated into 100 nodes and re-sampled at regular intervals rendering spatially uniform the discrete points comprising the two boundaries. Then, a new midline curve was created by calculating the 2D average from the 100 equidistant nodes representing the upper and the lower callosal boundaries. Finally, the distances between the 100 nodes of the upper as well as the lower callosal boundaries to the 100 nodes of the midline curve were calculated. These point-wise callosal distances constituted the variables of interest in the subsequent statistical analyses.
Statistical analyses
All statistical analyses were conducted in Matlab (The MathWorks, Natick, MA) using mass-univariate general linear models to reflect the hypotheses stated in the pre-registration ( https://aspredicted.org/blind.php?x=SDC_UKE ). The group analysis compared control participants and participants with AN using ANCOVA, with a statistical threshold of P < 0.05, two-tailed. We also conducted four correlation analyses within the AN group: the first analysis examined the link between callosal thickness and BMI in all AN participants (analysis A); the second examined the link between callosal thickness and illness duration in acutely underweight and partially weight-restored AN participants (analysis B) (see Supplementary Material for subgroup definitions); the third examined the link between callosal thickness and EDE in all AN participants (analysis C); and the fourth examined the link between callosal thickness and YBC-EDS in all AN participants (analysis D). For all analyses—group comparisons and correlations—age, TIV, scanner, education, medication, and pubertal score were included as nuisance variables. For analyses C and D, BMI was additionally included as a nuisance variable. All statistical tests were two-tailed, and α was set at 0.05. To control for multiple comparisons, a Monte Carlo simulation with 10,000 permutations was employed, as previously described 56 .
Study sample
Altogether, 120 participants from two studies—one acquired on a Siemens Trio 3T scanner (study 1), and another acquired on a Siemens Prisma 3T scanner (study 2)—comprising 60 participants with AN and 60 controls were included. Of those 120 participants, seven were excluded due to image artifacts such as ghosting or excessive motion that rendered the images unusable for further processing. Another four participants had missing values for education or illness duration and were excluded due to incomplete data. Of the 109 that survived the quality control, only seven were males (two AN and five controls). Given the low numbers, the males were excluded from the analysis to have a more homogeneous sample of 102 female participants.
Study 1 did not evaluate puberty scores. For that study, puberty scores were set to maximal for all adults. In study 2, four participants (2 AN, 2 controls) were missing puberty scores and were excluded (pubertal stage has been associated with callosal growth) 57 . This left 98 participants (48 with AN and 50 controls, all female) for inclusion in the final sample. There were 22 adolescent AN, 12 adolescent controls, 26 adult AN, and 38 adult controls. See Table 1 for demographics and psychometrics as well as missing data.
Group comparisons
There were no significant differences in AN and control participants in callosal thickness (the maximum difference was t = 1.716, d.f. = 90, P = 0.097) (Fig. 1 ). We conducted an exploratory one-way ANCOVA to discern if differences were present among the subgroups of acutely underweight AN (n = 11), partially weight-restored AN (n = 8), weight-restored AN (n = 29), and healthy controls (n = 50), also controlling for age, TIV, scanner, education, medication, and pubertal status. There were no significant differences among groups (the maximum difference was F = 2.031, d.f. = 2.93;88, P = 0.209) (Fig. S1 ).
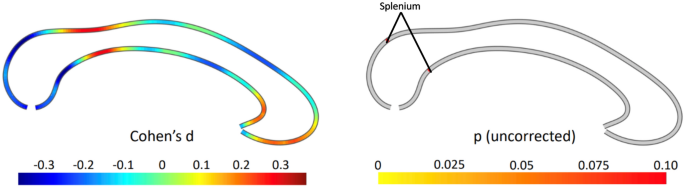
Group comparison between anorexia and controls. The effect size is shown on the left, where negative values indicate a thinner corpus callosum in anorexia compared to controls. The right panel depicts the significance (uncorrected) from a two-tailed t -test. All p-values are greater than 0.05 throughout, with significant areas labelled.
Associations with BMI
There was no significant association between callosal thickness and BMI in the AN cohort (n = 48; the highest partial correlation was r = 0.293, P = 0.060) (Fig. 2 a).
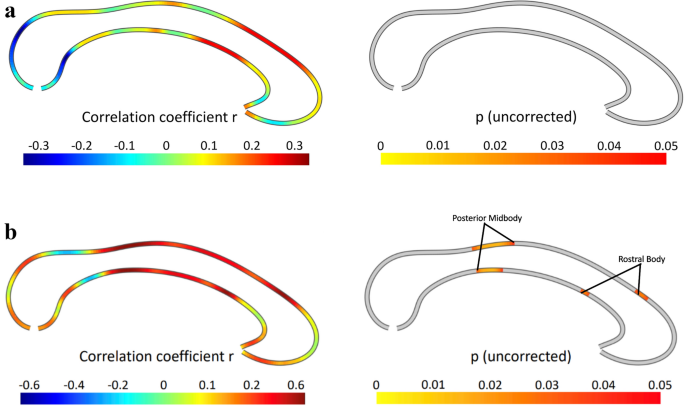
Correlations between callosal thickness and ( a ) BMI, and ( b ) illness duration. The effect size is shown on the left, where positive values indicate a positive association. The right panel depicts the significance of correlations, thresholded at p ≤ 0.05 (uncorrected). There were no significant associations.
Associations with illness duration
There was no significant negative association between callosal thickness and illness duration in the acutely underweight and partially weight-restored AN participants (n = 19) and only small positive associations in the rostral body and posterior midbody. However, these did not survive the correction for multiple comparisons with permutation testing ( P = 0.109, Fig. 2 b).
Associations with clinical symptoms
Ede shape concern scores.
As hypothesized, there were significant correlations between EDE Shape Concern Scores and callosal thickness in the AN cohort (n = 48), surviving multiple comparisons correction with permutation testing ( P = 0.007). The significant positive correlations were evident in the rostrum, genu, and rostral body, as well as the isthmus and splenium (Fig. 3 a).
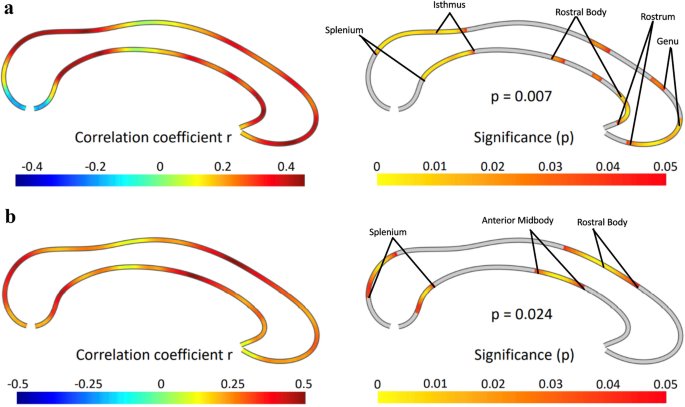
Correlations between callosal thickness and ( a ) EDE Shape Concerns, and ( b ) YBC-EDS scores. The effect size is shown on the left, where positive values indicate a positive association. The right panel depicts the significance of a positive correlation using a two-tailed test, with significant areas labelled. The results survive correction for multiple comparisons. EDE Eating Disorder Examination, YBC-EDS Yale–Brown–Cornell Eating Disorder Scale.
As hypothesized, there were significant correlations between YBC total scores and callosal thickness in the AN cohort (n = 43), surviving multiple comparisons correction with permutation testing ( P = 0.024). The significant positive correlations were evident in the rostral body and anterior midbody as well as the splenium (Fig. 3 b).
This is the first study to examine CC thickness in individuals with AN. The major findings included, as hypothesized, significant positive associations between CC thickness and degree of body shape concerns as well as the degree of eating disorder-related obsessive thoughts and compulsive behaviours. Contrary to our predictions, there were no significant group differences in CC thickness between those with AN and healthy controls. Further, contrary to our prediction, there were no significant associations between CC thickness and BMI in the AN sample, or between CC thickness and illness duration in the acutely underweight or partially weight-restored AN cohorts.
We observed that greater CC thickness was associated with worse body shape concerns, as indexed by the shape subscale of the EDE. Higher scores on this subscale indicate greater preoccupations with body shape, influence of body shape on one’s self evaluation, fear of gaining weight, dissatisfaction with one’s weight, discomfort with seeing one’s body, discomfort and/or avoidance of others seeing their body, feeling fat, and desires for a flat stomach 42 . In a previous meta-analysis of DTI studies, lower FA in the CC body was observed in those with AN compared with healthy controls 18 . More recent studies also found lower FA 19 , as well as lower tract volume 20 in the CC body. Although group differences in CC thickness were not evident in the current study, similar regions of the CC body—anterior midbody and the rostral body—were associated with body shape concerns. The CC body contains fibres connecting right and left frontal hemispheres, primarily between the motor and somatosensory cortices 58 . These portions of the CC may be involved in body perception. Specifically, the anterior midbody has been shown to be involved in interpreting limb gestures 59 . Further, anterior CC callostomy patients are unable to imitate gestures of other individuals 60 . In addition, in the current study there were associations between shape concerns and thickness in the rostrum and genu, which connect right and left association cortical areas 61 , 62 . These may be involved in higher cognitive functions such as self-appraisals, including content related to one’s body image. Further, there were associations between body shape concerns and thickness in the isthmus and splenium, which are involved in tactile, auditory, and visual functions 58 . These regions, involved in inter-hemispheric integration of visual and visuospatial information, therefore may also be relevant for body visual perception. One speculation from these results is that greater thickness could be linked to poorer interhemispheric exchange of visual and visuospatial information, conferring more distorted perception of one’s body and leading to worse body image distortions in those with AN. However, the neural mechanisms for this are not clear. Future studies could directly investigate this by using, for example, multimodal functional and structural imaging along with direct behavioural measures of body perception.
An additional finding was that CC thickness was associated with the severity of eating disorder-related obsessive thoughts and compulsive behaviours (YBC scores). Specifically, this was observed in the splenium, anterior midbody, and the rostral body. A study of individuals with OCD found inverse associations between severity of compulsions with total CC area, as well as associations specifically with the area of the isthmus and splenium 37 . Thus, similar posterior CC regions found to be associated with obsessions and compulsions in OCD were also found to be associated with obsessions and compulsions in the current AN study. However, the direction of the relationships differs; in OCD there were negative associations while in AN there were positive associations. The reasons for the different directions of these associations are unclear, and direct comparisons between the current AN study and the previous OCD study are hindered by the fact that the previous OCD study measured CC area rather than thickness. Nevertheless, there may be overlapping associations in OCD and AN linking posterior CC morphology and obsessive–compulsive symptomatology. As the posterior CC connects occipital, superior temporal, and posterior parietal regions 63 , 64 , future research may explore links between visuospatial functioning, interhemispheric structural (and functional) connections, and obsessive–compulsive symptoms trans diagnostically across OCD and AN.
There were no significant associations between CC thickness and either BMI or illness duration, contrary to our predictions. The lack of significant associations with BMI suggests the possibility that low-weight states, reflecting the current degree of starvation and possibly nutritional status, may not be associated with CC thickness in these cohorts. Further, the lack of a significant association with illness duration could point to the absence of a cumulative impact of illness effects on white matter thickness in the CC. The typical illness course in those with AN consists of an acute underweight starvation state followed by either partial or full weight restoration. The partially weight-restored state, and even the full weight-restored state 65 , might include an attenuated state of reduced caloric intake or poor nutrition. Thus, “scar” effects of acute starvation and malnutrition, periods of persistent poor nutrition even in partially- or fully weight-restored states, and/or other chronic illness effects in AN such as those related to diminished quality of life and functionality, may not be manifested in this aspect of CC morphology. Thus, the interesting observation that subjective clinical variables (EDE and YBC-EDS) but not the objective variables (illness duration and BMI) were associated with CC thickness could be due to regional CC thickness mediating persistent aberrant thoughts and perceptions related to body, food, and weight, as well as repetitive behaviours, but not potential “scar” or malnutrition effects that illness duration and BMI may reflect. However, longitudinal studies are necessary to definitively elucidate the effects of these chronic illness elements.
There are several limitations to consider. As this was a cross-sectional study, cause-and-effect inferences regarding the associations between clinical symptoms and CC thickness cannot be ascertained. It is not known, for example, if pre-illness CC thickness patterns (and any patterns of interhemispheric neural communications, e.g. that these may be linked to) contribute to risk for AN symptoms. Alternatively, the symptoms themselves, or compensatory or other secondary effects of the symptoms, may have affected regional CC thickness to create these patterns of associations with clinical symptoms. Another limitation is the modest sample size, which may have affected the ability to detect group differences and, particularly as multiple covariates were necessary, affected the stability of the correlation estimates. Further, the small subsamples of individuals in the underweight, partially weight-restored, and weight-restored groups, in addition to adolescents and adults, limited the power for the sub-analyses. Further, the fact that this was a heterogeneous sample of adults and adolescents, medicated and unmedicated, obtained across two separate studies, may have affected the results. We addressed this by covarying for age, TIV, scanner, education, medication, and pubertal score across all analyses; nevertheless, there may have been other sources of variance of non-interest that were not accounted for.
In terms of clinical implications, while CC thickness may not represent a biomarker specifically of the diagnostic category of AN, the degree of thickness may reflect white matter structural relationships with two important phenotypes: body shape concerns and eating disorder-related obsessions and compulsions. As cause-and-effect relationships cannot be determined, future investigations of cohorts followed prospectively could focus on CC thickness to determine if pre-illness patterns may predict future symptoms and thus contribute to a risk profile for the development of AN. Future transdiagnostic studies may be useful as well, since body image disturbances and obsessions and compulsions occur not only in other eating disorders such as bulimia nervosa, but also in body dysmorphic disorder 1 , 66 . Transdiagnostic studies may also extend to other obsessive–compulsive and related disorders such as OCD, since, as mentioned above, CC thickness relationships with obsessive–compulsive symptoms have been found 36 , 37 . Finally, findings from this study could spur studies to examine multimodal interhemispheric regional functional and structural connectivity; this would be especially informative if done in the context of experimental paradigms probing body perception and habit or ritual formation.
In conclusion, this study revealed regional CC thickness patterns in individuals with AN that are associated with important clinical phenotypes. There were no significant differences, however, in CC thickness between AN and healthy controls, nor links with BMI or illness duration within the AN group. Specifically, thicker CC in the anterior, body, and posterior regions were tied to more pronounced body image disturbances, possibly reflecting impaired interhemispheric communication affecting body perception. Additionally, CC thickness in the body and posterior regions were linked to the severity of obsessive–compulsive symptoms, suggesting shared neural patterns with OCD. These findings offer insights into structural associations with critical symptom dimensions in AN and may have additional implications for future mechanistic and transdiagnostic investigations.
Data availability
Data for study 2 is available through the National Institute of Mental Health Data Archive ( https://nda.nih.gov/edit_collection.html?id=2565 ). The raw data for Study 1 supporting the conclusions of this article will be made available by the authors upon request.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 5th edn. (American Psychiatric Publishing, 2013).
Book Google Scholar
Sullivan, P. F. Mortality in anorexia nervosa. Am. J. Psychiatry 152 (7), 1073–1074 (1995).
Article CAS PubMed Google Scholar
Nickel, K. et al. Recovery of cortical volume and thickness after remission from acute anorexia nervosa. Int. J. Eat Disord. 51 (9), 1056–1069 (2018).
Article PubMed Google Scholar
Walton, E. et al. Brain structure in acutely underweight and partially weight-restored individuals with anorexia nervosa: A coordinated analysis by the ENIGMA Eating Disorders Working Group. Biol. Psychiatry 92 (9), 730–738 (2022).
Reddy, P. V., Das, A. & Sastry, P. S. Quantitative and compositional changes in myelin of undernourished and protein malnourished rat brains. Brain Res. 161 (2), 227–235 (1979).
Chase, H. P., Dorsey, J. & McKhann, G. M. The effect of malnutrition on the synthesis of a myelin lipid. Pediatrics 40 (4), 551–559 (1967).
Yusuf, H. K., Haque, Z. & Mozaffar, Z. Effect of malnutrition and subsequent rehabilitation on the development of mouse brain myelin. J. Neurochem. 36 (3), 924–930 (1981).
Wiggins, R. C. Myelin development and nutritional insufficiency. Brain Res. Rev. 4 (2), 151–175 (1982).
Article CAS Google Scholar
Pappaianni, E. et al. Initial evidence of abnormal brain plasticity in anorexia nervosa: An ultra-high field study. Sci. Rep. 12 (1), 2589 (2022).
Article ADS CAS PubMed PubMed Central Google Scholar
Bomba, M. et al. Global and regional brain volumes normalization in weight-recovered adolescents with anorexia nervosa: Preliminary findings of a longitudinal voxel-based morphometry study. Neuropsychiatr. Dis. Treat. 11 , 637–645 (2015).
Article PubMed PubMed Central Google Scholar
Katzman, D. K. et al. Cerebral gray matter and white matter volume deficits in adolescent girls with anorexia nervosa. J. Pediatr. 129 (6), 794–803 (1996).
Castro-Fornieles, J. et al. A cross-sectional and follow-up voxel-based morphometric MRI study in adolescent anorexia nervosa. J. Psychiatr. Res. 43 (3), 331–340 (2009).
Asami, T. et al. Structural brain abnormalities in adolescent patients with anorexia nervosa at both the acute and weight-recovered phase. Brain Imaging Behav. 16 (3), 1372–1380 (2022).
Katzman, D. K., Zipursky, R. B., Lambe, E. K. & Mikulis, D. J. A longitudinal magnetic resonance imaging study of brain changes in adolescents with anorexia nervosa. Arch. Pediatr. Adolesc. Med. 151 (8), 793–797 (1997).
Lázaro, L. et al. Normal gray and white matter volume after weight restoration in adolescents with anorexia nervosa. Int. J. Eat. Disord. 46 (8), 841–848 (2013).
Meneguzzo, P., Collantoni, E., Solmi, M., Tenconi, E. & Favaro, A. Anorexia nervosa and diffusion weighted imaging: An open methodological question raised by a systematic review and a fractional anisotropy anatomical likelihood estimation meta-analysis. Int. J. Eat. Disord. 52 (11), 1237–1250 (2019).
Barona, M. et al. White matter alterations in anorexia nervosa: Evidence from a voxel-based meta-analysis. Neurosci. Biobehav. Rev. 100 , 285–295 (2019).
Zhang, S. et al. White matter abnormalities in anorexia nervosa: Psychoradiologic evidence from meta-analysis of diffusion tensor imaging studies using tract based spatial statistics. Front. Neurosci. 14 , 159 (2020).
Nickel, K. et al. White matter abnormalities in the corpus callosum in acute and recovered anorexia nervosa patients-a diffusion tensor imaging study. Front. Psychiatry 10 , 490 (2019).
Maier, S. et al. Reduced structural connectivity in the corpus callosum in patients with anorexia nervosa. Eur. Eat Disord. Rev. 30 (4), 341–352 (2022).
Geisler, D. et al. Altered white matter connectivity in young acutely underweight patients with anorexia nervosa. J. Am. Acad. Child Adolesc. Psychiatry 61 (2), 331–340 (2022).
Lloyd, C. E. et al. Large-scale exploration of whole-brain structural connectivity in anorexia nervosa: Alterations in the connectivity of frontal and subcortical networks. Biol. Psychiatry Cogn. Neurosci. Neuroimag. 8 (8), 864–873 (2023).
Google Scholar
Schulte, T. & Müller-Oehring, E. M. Contribution of callosal connections to the interhemispheric integration of visuomotor and cognitive processes. Neuropsychol. Rev. 20 (2), 174–190 (2010).
Witelson, S. F. Hand and sex differences in the isthmus and genu of the human corpus callosum. Brain 112 (3), 799–835 (1989).
Filley, C. M. White matter: Organization and functional relevance. Neuropsychol. Rev. 20 (2), 158–173 (2010).
Gazzaniga, M. S., Bogen, J. E. & Sperry, R. W. Observations on visual perception after disconnexion of the cerebral hemispheres in man. Brain 88 (2), 221–236 (1965).
Treasure, J. et al. Anorexia nervosa. Nat. Rev. Dis. Primers 1 , 15074 (2015).
Gaudio, S. & Quattrocchi, C. C. Neural basis of a multidimensional model of body image distortion in anorexia nervosa. Neurosci. Biobehav. Rev. 36 (8), 1839–1847 (2012).
Gaudio, S., Wiemerslage, L., Brooks, S. J. & Schiöth, H. B. A systematic review of resting-state functional-MRI studies in anorexia nervosa: Evidence for functional connectivity impairment in cognitive control and visuospatial and body-signal integration. Neurosci. Biobehav. Rev. 71 , 578–589 (2016).
Stedal, K., Broomfield, C., Hay, P., Touyz, S. & Scherer, R. Neuropsychological functioning in adult anorexia nervosa: A meta-analysis. Neurosci. Biobehav. Rev. 130 , 214–226 (2021).
Mölbert, S. C. et al. Depictive and metric body size estimation in anorexia nervosa and bulimia nervosa: A systematic review and meta-analysis. Clin. Psychol. Rev. 57 , 21–31 (2017).
Godier, L. R. & Park, R. J. Compulsivity in anorexia nervosa: A transdiagnostic concept. Front. Psychol. 5 , 778 (2014).
Halmi, K. A. et al. Comorbidity of psychiatric diagnoses in anorexia nervosa. Arch. Gen. Psychiatry 48 (8), 712–718 (1991).
Kaye, W. H., Bulik, C. M., Thornton, L., Barbarich, N. & Masters, K. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am. J. Psychiatry 161 (12), 2215–2221 (2004).
Watson, H. J. et al. Genome-wide association study identifies eight risk loci and implicates metabo-psychiatric origins for anorexia nervosa. Nat. Genet. 51 (8), 1207–1214 (2019).
Article CAS PubMed PubMed Central Google Scholar
Di Paola, M. et al. The structure of the corpus callosum in obsessive compulsive disorder. Eur. Psychiatry 28 (8), 499–506 (2013).
Jose, D. et al. Corpus callosum abnormalities in medication-naïve adult patients with obsessive compulsive disorder. Psychiatry Res. 231 (3), 341–345 (2015).
Luders, E., Thompson, P. M. & Kurth, F. Morphometry of the corpus callosum. In Brain Morphometry, Neuromethods (eds Spalletta, G. et al. ) 131–142 (Springer, 2018).
Piras, F. et al. Corpus callosum morphology in major mental disorders: A magnetic resonance imaging study. Brain Commun. 3 (2), fcab100 (2021).
Freitag, C. M. et al. Total brain volume and corpus callosum size in medication-naïve adolescents and young adults with autism spectrum disorder. Biol. Psychiatry 66 (4), 316–319 (2009).
Tadayonnejad, R. et al. White matter tracts characteristics in habitual decision-making circuit underlie ritual behaviors in anorexia nervosa. Sci. Rep. 11 (1), 15980 (2021).
Sheehan, D. V. et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The Development and Validation of a Structured Diagnostic Psychiatric Interview for DSM-IV and ICD-10. J. Clin. Psychiatry 59 (20), 22–33 (1998).
PubMed Google Scholar
Sheehan, D. V. et al. Reliability and Validity of the Mini International Neuropsychiatric Interview for Children and Adolescents (MINI-KID). J. Clin. Psychiatry 71 (3), 313–326 (2010).
Fairburn, C. G. & Cooper, Z. The Eating Disorder Examination. In Binge Eating: Nature, Assessment, and Treatment (eds Wilson, G. T. & Fairburn, C.) 317–360 (Guilford Press, 1993).
Mazure, C. M., Halmi, K. A., Sunday, S. R., Romano, S. J. & Einhorn, A. M. The Yale–Brown–Cornell eating disorder scale: Development, use, reliability and validity. J. Psychiatr. Res. 28 (5), 425–445 (1994).
Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 32 (1), 50–55 (1959).
Montgomery, S. A. & Åsberg, M. A new depression scale designed to be sensitive to change. Br. J. Psychiatry 134 (4), 382–389 (1979).
Poznanski, E. O. & Mokros, H. B. Children’s Depression Rating Scale, Revised (CDRS-R) Manual (Western Psychological Services, 1996).
Carskadon, M. A. & Acebo, C. A self-administered rating scale for pubertal development. J. Adolesc. Health 14 (3), 190–195 (1993).
Gaser, C., Dahnke, R., Thompson, P. M., Kurth, F., Luders, E. & Alzheimer’s Disease Neuroimaging Initiative. CAT—A computational anatomy toolbox for the analysis of structural MRI data. BioRxiv (2022).
Dale, C., Kalantary, D., Luders, E. & Kurth, F. Aberrant callosal morphology in ex-smokers. J. Integr. Neurosci. 21 (4), 101 (2022).
Simonsson, O. et al. Preliminary evidence of links between ayahuasca use and the corpus callosum. Front. Psychiatry 13 , 1002455 (2022).
Luders, E. et al. Callosal morphology in Williams syndrome: A new evaluation of shape and thickness. Neuroreport 18 (3), 203–207 (2007).
Luders, E. et al. The link between callosal thickness and intelligence in healthy children and adolescents. NeuroImage 54 (3), 1823–1830 (2011).
Luders, E., Toga, A. W. & Thompson, P. M. Why size matters: Differences in brain volume account for apparent sex differences in callosal anatomy: The sexual dimorphism of the corpus callosum. NeuroImage 84 , 820–824 (2014).
Luders, E. et al. Decreased callosal thickness in attention-deficit/hyperactivity disorder. Biol. Psychiatry 65 (1), 84–88 (2009).
Chavarria, M. C., Sánchez, F. J., Chou, Y. Y., Thompson, P. M. & Luders, E. Puberty in the corpus callosum. Neuroscience 265 , 1–8 (2014).
Fabri, M., Pierpaoli, C., Barbaresi, P. & Polonara, G. Functional topography of the corpus callosum investigated by DTI and FMRI. World J. Radiol. 6 (12), 895–906 (2014).
Pierpaoli, C., Foschi, N., Fabri, M. & Polonara, G. Cortical activation during imitative behavior: An FMRI study in callosotomized patients. J. Syst. Integr. Neurosci. 7 (3), 1–5 (2021).
Article Google Scholar
Pierpaoli, C. et al. Imitation strategies in callosotomized patients. Arch. Ital. Biol. 156 (1–2), 12–26 (2018).
CAS PubMed Google Scholar
Aboitiz, F. & Montiel, J. One hundred million years of interhemispheric communication: The history of the corpus callosum. Braz. J. Med. Biol. Res. 36 (4), 409–420 (2003).
Aboitiz, F., Scheibel, A. B., Fisher, R. S. & Zaidel, E. Fiber composition of the human corpus callosum. Brain Res. 598 (1–2), 143–153 (1992).
Musiek, F. E. Neuroanatomy, neurophysiology, and central auditory assessment. Part III: Corpus callosum and efferent pathways. Ear Hear. 7 (6), 349–358 (1986).
Goldstein, A., Covington, B. P., Mahabadi, N. & Mesfin, F. B. Neuroanatomy, Corpus Callosum [Internet] (StatPearls Publishing, 2023). https://www.ncbi.nlm.nih.gov/books/NBK448209/ [Updated 2023 Apr 3; cited 2023 Oct 8].
Schebendach, J. E. et al. Food choice and diet variety in weight-restored patients with anorexia nervosa. J. Am. Diet. Assoc. 111 (5), 732. https://doi.org/10.1016/j.jada.2011.02.002 (2011).
Sunday, S. R. & Halmi, K. A. Comparison of the Yale–Brown–Cornell eating disorders scale in recovered eating disorder patients, restrained dieters, and nondieting controls. Int. J. Eat. Disord. 28 (4), 455–459 (2000).
Download references
Acknowledgements
This study was supported by the National Institute of Mental Health (R01MH105662 and R01MH093535 to JDF). We would like to acknowledge the research participants who participated in the study.
Open access funding provided by Karolinska Institute.
Author information
Authors and affiliations.
Centre for Addiction and Mental Health, 250 College St., Toronto, ON, M5T 1R8, Canada
Jamie D. Feusner
Department of Psychiatry, University of Toronto, Toronto, Canada
Department of Women’s and Children’s Health, Karolinska Hospital, Karolinska Institutet, Stockholm, Sweden
Department of Psychiatry and Biobehavioral Sciences, University of California Los Angeles, Los Angeles, CA, USA
Jamie D. Feusner & Ronald Ly
School of Psychology, University of Auckland, Auckland, New Zealand
Alicja Nowacka, Eileen Luders & Florian Kurth
Department of Women’s and Children’s Health, Uppsala University, Uppsala, Sweden
Eileen Luders
Laboratory of Neuro Imaging, School of Medicine, University of Southern California, Los Angeles, CA, USA
Departments of Neuroradiology and Radiology, Jena University Hospital, Jena, Germany
Florian Kurth
You can also search for this author in PubMed Google Scholar
Contributions
JF: funding acquisition, resources, project administration, clinical assessment, investigation, data acquisition, conceptualization, writing—original draft, reviewing and editing. FK: data analysis, visualization, conceptualization, software, methodology, data analysis, writing—original draft, reviewing and editing. AN: data processing, data analysis, writing—reviewing and editing; EL: conceptualization, methodology, investigation, resources, writing—reviewing and editing, supervision. All authors contributed to the article and approved the submitted version.
Corresponding author
Correspondence to Jamie D. Feusner .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary information., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Feusner, J.D., Nowacka, A., Ly, R. et al. Corpus callosum morphology and relationships to illness phenotypes in individuals with anorexia nervosa. Sci Rep 14 , 11112 (2024). https://doi.org/10.1038/s41598-024-61841-6
Download citation
Received : 10 November 2023
Accepted : 10 May 2024
Published : 15 May 2024
DOI : https://doi.org/10.1038/s41598-024-61841-6
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Eating disorders
- Morphometry
- Shape concerns
- Obsessive–compulsive symptoms
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing: Translational Research newsletter — top stories in biotechnology, drug discovery and pharma.

The relationship between weight-adjusted-waist index and suicidal ideation: evidence from NHANES
- Open access
- Published: 14 May 2024
- Volume 29 , article number 37 , ( 2024 )
Cite this article
You have full access to this open access article

- Shijie Guo 1 na1 ,
- Guangwei Qing 2 na1 ,
- Qiqi Chen 3 &
- Guang Yang 3
11 Accesses
Explore all metrics
Amidst growing evidence of the intricate link between physical and mental health, this study aims to dissect the relationship between the waist-to-weight index (WWI) and suicidal ideation within a representative sample of the US population, proposing WWI as a novel metric for suicide risk assessment.
The study engaged a sample of 9500 participants in a cross-sectional design. It employed multivariate logistic and linear regression analyses to probe the association between WWI and suicidal ideation. It further examined potential nonlinear dynamics using a weighted generalized additive model alongside stratified analyses to test the relationship's consistency across diverse demographic and health variables.
Our analysis revealed a significant positive correlation between increased WWI and heightened suicidal ideation, characterized by a nonlinear relationship that persisted in the adjusted model. Subgroup analysis sustained the association's uniformity across varied population segments.
Conclusions
The study elucidates WWI's effectiveness as a predictive tool for suicidal ideation, underscoring its relevance in mental health evaluations. By highlighting the predictive value of WWI, our findings advocate for the integration of body composition considerations into mental health risk assessments, thereby broadening the scope of suicide prevention strategies.
Similar content being viewed by others

Does Body Mass Index Confer Risk for Future Suicidal Thoughts and Behaviors? A Meta-analysis of Longitudinal Studies
Association between body mass index and suicidal behaviors: a systematic review protocol, association between weight control failure and suicidal ideation in overweight and obese adults: a cross-sectional study.
Avoid common mistakes on your manuscript.
Introduction
There is a genuinely severe philosophical problem, and that is suicide [ 1 ], a profound societal crisis. Annually, approximately 700,000 individuals end their own lives [ 2 ]. According to the US Centers for Disease Control and Prevention (CDC), in 2021, there were 48,183 suicides in the US, a figure that escalated to 49,449 in 2022, indicating a 2.6% increase [ 3 ]. The complexity of suicide prevention is attributed to its multifaceted causes, including societal (e.g., familial responsibilities), political (e.g., policies on minimum wage), cultural (e.g., stereotypes of masculinity), and economic factors (e.g., unemployment, lower socioeconomic status) [ 4 ]. Identified risk factors encompass mental health disorders, substance abuse, chronic pain, a history of suicide in the individual or family, experiences of aggression, access to firearms at home, and recent discharge from incarceration [ 5 , 6 , 7 , 8 , 9 ]. Additionally, witnessing suicidal behaviors in others can heighten suicide risk [ 10 ]. Despite demographic variances among groups such as adolescents, sexual minorities, and adults, research consistently shows that individuals harboring suicidal thoughts face a greater risk of suicide completion than those without such thoughts [ 11 , 12 , 13 , 14 ]. Despite efforts across medical, socioeconomic, and political domains to mitigate and prevent suicide, a significant reduction in the prevalence of suicidal ideation remains elusive [ 15 ], highlighting the critical need for an in-depth examination of suicidal ideation.
Obesity represents a widespread, severe, and financially burdensome chronic condition affecting both adults and children. In 2022, the CDC reported that the prevalence of adult obesity in the US had escalated, with 22 states having an adult obesity prevalence at or above 35%, an increase from 19 states in 2021[ 16 ]. Obesity is a significant risk factor for a variety of severe health conditions, including hypertension, cardiovascular diseases, diabetes mellitus, asthma, joint disorders, cholelithiasis, as well as gallbladder disease. [ 5 , 17 , 18 ]. Doctors believe that obesity is a complex, heterogeneous chronic disease that manifests differently in patients and, therefore, requires individualized long-term management [ 19 ]. Consequently, identifying accurate and reliable metrics for evaluating obesity is critically essential.
Body mass index (BMI) has long been a widely accepted standard for identifying levels of obesity. However, BMI cannot distinguish excess fat, muscle, or bone mass. BMI cannot differentiate between locations of fat [ 20 , 21 ]. It is generally accepted that abdominal (visceral) fat is more closely associated with health risks than fat in other body parts [ 22 , 23 , 24 , 25 ]. The weight-adjusted-waist index (WWI) represents a novel metric for obesity assessment, demonstrating enhanced precision in quantifying lean muscle and adipose tissue mass when juxtaposed with traditional measures such as BMI and waist circumference (WC) [ 26 , 27 ]. The literature suggests that WWI is associated with a variety of conditions, including fatty liver, cognitive function, hyperuricemia, diabetes mellitus, kidney stones, dyslipidemia, and urinary incontinence [ 28 , 27 , 29 , 30 , 31 , 32 , 33 ]. It may serve as a more accurate predictor of risk.
Several studies identified associations between obesity and suicide risk, depressive symptoms, and mood problems [ 34 , 35 , 36 , 37 ], and they have all used BMI as an indicator for determining obesity. Notwithstanding, the relationship between WWI and the prevalence of suicidal ideation has not yet been investigated. Consequently, the present study seeks to elucidate the potential correlation between WWI and suicidal ideation within the representative sample of the US population, employing data sourced from the National Health and Nutrition Examination Survey (NHANES) from 2013 to 2018.
Data source and study participants
Our investigation leveraged datasets obtained from NHANES, a project spearheaded by the National Center for Health Statistics (NCHS) in the United States. This comprehensive survey collates physical assessments and interview responses to gather extensive data on demographics, socioeconomic status, and health-related information. Focused on the NHANES data from 2013 to 2018, our study sought to secure a current and emblematic sample of the US population. The data acquisition process was governed by stringent ethical protocols, including the endorsement from the NCHS's Research Ethics Review Board and the acquisition of informed, written consent from all contributors. This groundwork enables our examination of health patterns and supports formulating informed health policy recommendations.
In this investigation, we employed a stratified, multistage probability sampling approach to ensure the comprehensive inclusion of participants. The initial participant pool comprised 29,400 individuals enrolled in the NHANES from 2013 to 2018. After excluding participants with incomplete data sets ( N = 19,900), the analytical sample was refined to 9500 individuals (Fig. 1 ).
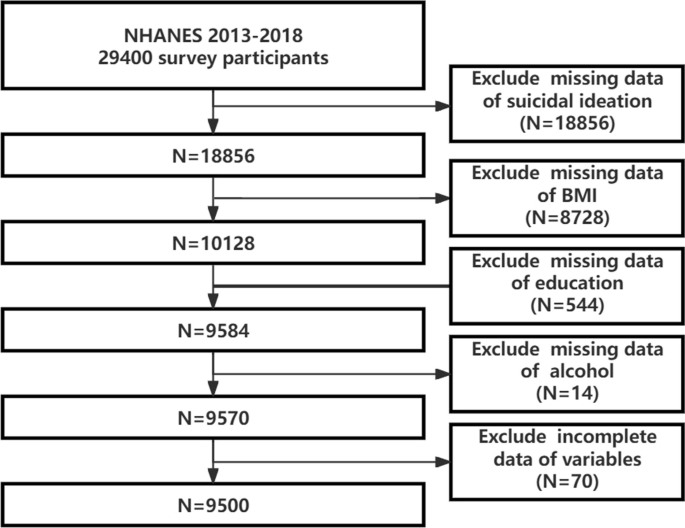
Flowchart of participants selection. NHANES, National Health and Nutrition Examination Survey
Definition of exposure variable
WWI is an anthropometric measure to assess central obesity. It derives from an individual’s WC and body weight. Each participant’s WWI is calculated using a specific formula: WC divided by the square root of body weight, with the outcome rounded to two decimal places (WWI = WC/√body weight, where WC is measured in cm and body weight in kg).
Assessment of suicidal ideation
Within the context of the survey’s Mental Health—Depression Screener segment, participants responded to a critical inquiry aimed at evaluating the presence of suicidal ideation: “Over the last two weeks, how often have you been troubled by thoughts of being better off dead, or by thoughts of self-harm?” Responses indicating such thoughts on “Several days”, “More than half the days”, or “Nearly every day” were interpreted as markers of suicidal ideation.
We incorporated a comprehensive set of covariates: age, sex, race, education, marital status, smoking status, alcohol consumption, hypertension, diabetes, angina pectoris, arthritis, cancer, and asthma. Education was divided into two categories: individuals with qualifications higher than high school. Smoking status encompassed those who have smoked at least 100 cigarettes in their lifetime. Alcohol consumption was defined as having at least 12 alcoholic beverages annually.
Statistical analysis
We meticulously analyzed the demographic characteristics of participants, differentiated by the presence of suicidal ideation, employing weighted Chi-square tests for categorical variables and t -tests for continuous ones. The relationship between WWI and suicidal ideation was explored through multivariate logistic regression analyses. In contrast, the correlation between WWI and the level of suicidal ideation was examined using multivariate linear regression analyses. To uncover any potential nonlinear dynamics between WWI and suicidal ideation, we applied a weighted generalized additive model complemented by smooth curve fitting techniques. Additionally, stratified analyses and interaction tests were conducted to investigate the consistency of the WWI–suicidal ideation relationship across various subgroups. On a two-tailed basis, a p -value of less than 0.05 indicated statistical significance. All statistical analyses were performed using R Statistical Software (Version 4.2.2, available at http://www.R-project.org , developed by The R Foundation) and the Free Statistics analysis platform (Version 1.8, based in Beijing, China).
Characteristics of the study participants
A total of 9500 participants were included in our research, with 9173 not exhibiting suicidal ideation and 327 reporting suicidal ideation. The overall prevalence of suicidal ideation was 3.44% (weighted proportion) (Table 1 ). A key finding from Table 1 is the statistically significant difference in WWI between groups ( p < 0.001), with individuals exhibiting SI having a higher mean WWI than those without. This suggests that WWI may be a relevant factor in understanding suicidal ideation. Conversely, BMI does not significantly differ between groups ( p = 0.401).
Association between WWI and suicidal ideation
Table 2 details the results from multivariate logistic regression analyses conducted using two distinct models. These analyses identified a strong and statistically significant positive association between WWI and the likelihood of suicidal ideation, consistent across both models. After comprehensive adjustment, individuals with a one-unit increase in WWI were found to have a 67.9% heightened risk of experiencing suicidal ideation [OR: 1.679, 95% CI 1.532–1.969]. Moreover, when analyzing WWI by quartiles, those in the highest quartile of WWI faced a risk increase of 1.761 times compared to individuals in the lowest quartile [OR: 2.761, 95% CI 2.062–3.698], as shown in Table 2 . A generalized model incorporating smooth curve fitting was also utilized to validate the nonlinear association between WWI and suicidal ideation. The analysis confirmed a nonlinear positive relationship between WWI and suicidal ideation (Fig. 2 ), with the observed patterns remaining consistent across both genders (Fig. 3 ).
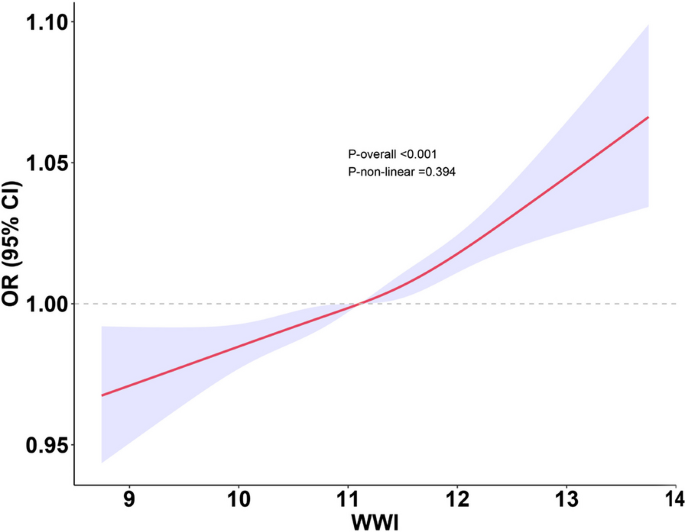
The association between WWI and suicidal ideation. The solid red line represents the smooth curve fit between variables. The shadow area represents the 95% confidence interval from the fit: weight-adjusted-waist index, WWI
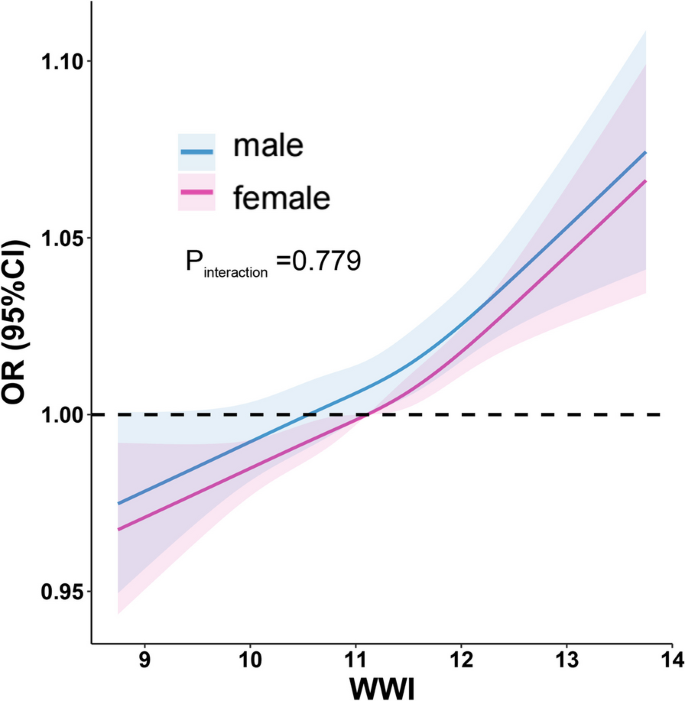
The association between WWI and suicidal ideation of different genders. The solid red line represents the smooth curve fit of females between variables. The solid blue line represents the smooth curve fit of males between variables. The shadow area represents the 95% confidence interval from the fit: weight-adjusted-waist index, WWI
Association between WWI and the level of suicidal ideation
Table 3 elucidates the significant association between WWI and the level of suicidal ideation, treating both variables as continuous. Initial findings from the unadjusted Model 1 reveal an exponentiated coefficient of 2.770 (95% CI 1.011–1.028), highlighting a statistically significant positive relationship. The adjusted Model 2, which considers a range of health behaviors and conditions, presents an exponentiated coefficient of 1.023 (95% CI 1.012–1.035), indicating a significant link between higher WWI and increased suicidal ideation levels ( p < 0.01). Quartile analysis further corroborates these findings, with the highest WWI quartile (Q4) demonstrating a notably elevated risk ( p for trend < 0.001). These insights underscore the vital connection between WWI and the severity of suicidal thoughts.
Subgroup analyses
To assess the uniformity of the association between WWI and suicidal ideation across the representative sample of the US population and to pinpoint any parameters specific to subpopulations, we undertook a detailed subgroup analysis alongside interaction tests. Table 4 examines the odds ratio (OR) for suicidal thoughts across different demographics and health conditions, indicating no significant interaction effects based on sex, age, education level, smoking status, alcohol consumption, hypertension, diabetes, angina pectoris, arthritis, cancer, or asthma. The odds ratios suggest a relatively consistent association across these subgroups, with variations in the magnitude of risk but no statistically significant differences in the pattern of association. In parallel, Table 5 explores the exponentiated coefficient for the level of suicidal ideation across similar subgroups, again showing no significant interaction effects, which implies a uniform relationship between WWI and the severity of suicidal ideation across different demographic and health-related categories.
We sought to elucidate the association between WWI and the propensity for suicidal ideation within the representative sample of the US population. Conducting a comprehensive cross-sectional analysis with 9500 participants, we discerned a significant correlation that elevated WWI was significantly associated with increased suicidal ideation and increased levels of suicidal ideation. This study unveiled a nonlinear positive correlation between WWI and the incidence of suicidal thoughts, a relationship that persisted even after complete adjustments in our model. Subsequent subgroup analyses revealed that the predictive validity of WWI for suicidal ideation remained unaffected across various demographic and health-related factors, including smoking status, alcohol intake, and the presence of chronic conditions such as hypertension, diabetes, and asthma. These insights collectively affirm the potential of WWI as an efficacious predictor for suicidal ideation, underscoring its utility in mental health assessments.
Several studies documented that the prevalence of suicidal ideation or depressive symptoms increases with BMI [ 34 , 35 , 38 , 39 ]. However, due to BMI's limitations, including its inability to differentiate between excess fat, muscle, or bone mass, and its failure to discern body fat distribution across different locations, some studies are beginning to experiment with other indicators. A study showed a significant relationship between WC, waist–height ratio, and suicidal ideation among US adult women. A Korean survey showed that BMI, WC, waist-to-hip ratio, and percent body fat were not significantly associated with suicidal ideation. In contrast, sarcopenia was strongly associated with an increased risk of suicidal ideation in older men [ 40 ]. It has also been shown that sarcopenic obesity is significantly associated with suicidal ideation [ 40 ]. Low height and perceived obesity are associated with suicidal ideation in Korean adolescents [ 41 ]. These studies also imply WWI's potential as a novel index of obesity. However, the validity of these indicators needs to be confirmed by more extensive clinical studies. In recent years, it has been found that WWI is a superior predictor of non-alcoholic fatty liver disease [ 33 ], low cognitive performance [ 27 ], hyperuricemia [ 28 ], diabetic kidney disease [ 42 ], kidney stones [ 30 ], stress urinary incontinence [ 31 ], and depressive symptoms [ 43 ]. WWI has excellent potential as an anthropometric indicator because of its easy computation and strong ability to forecast disease onset [ 44 ].
There may be multiple mechanisms for the interaction between obesity and suicidal ideation. First, the coexistence of obesity with other medical diseases may exacerbate the situation, or chronic health challenges may lead to increased mental stress, which in turn produces higher levels of suicidal ideation. It has been established that the coexistence of overweight or obesity and depression exacerbates the inflammatory response, leading to a worse prognosis and increased risk of suicide in adolescents with major depressive disorder [ 37 ]. In the setting of fibromyalgia and concomitant obesity, prior research points to a distinct (i.e., irrespective of depressive symptomatology and sleep quality) relationship between pain catastrophizing and suicidal thoughts [ 45 ]. Another research found that BMI is a risk factor for the development of severe anxiety symptoms in patients with severe anxiety disorder with comorbid dyslipidemia [ 46 ]. In addition, in patients with bipolar disorder, elevated BMI is associated with worsening clinical features, including higher rates of suicide, comorbidities, and core depressive symptoms. Second, obesity is associated with biochemical changes in the body, which may impact mood and behavior. It has been shown that obesity is associated with elevated levels of inflammation in the body [ 47 , 48 , 49 ], and inflammation is thought to be a possible mechanism that leads to depression and other mood disorders [ 50 ]. Some researchers believe that obesity may lead to insulin imbalance, and insulin resistance has been linked to depression [ 51 ]. There is also evidence that adipose tissue produces and releases various chemicals called adipokines, which directly affect other body parts, including the brain [ 52 ]. As a result, evaluating obesity is essential to estimating the likelihood of suicidal thoughts, and this study’s results suggest that WWI may be an effective indicator of obesity.
WWI combines body weight and waist measurements for a nuanced overview of fat distribution, offering advantages over BMI and WC, which overlook crucial aspects of body composition and total weight. From a pathophysiological perspective, WWI might provide a more explicit link to metabolic and cardiovascular risks associated with obesity. Abdominal fat, as measured by WC, is a known risk factor for metabolic syndrome, type 2 diabetes, and cardiovascular disease, which may be due to adipose gene expression of the effector genes [ 53 ], its proximity to vital organs and its role in producing inflammatory adipokines [ 54 , 55 ]. However, incorporating the weight component could enhance the predictive power by indicating the overall load on the body, including the strain on bones, joints, and organs [ 56 , 57 ]. Furthermore, the integrated approach of WWI better reflects the adiposity-related biochemical stress on the body. This includes the effects of fat mass on cytokine production [ 58 ], insulin resistance [ 59 ], and lipid metabolism [ 60 ], all of which are crucial for understanding the physiological basis for depression and suicidal ideation linked to obesity.
Social workers can effectively utilize WWI in their practice to identify individuals more accurately at high risk of suicide. By providing psychological support and counseling, establishing support systems, promoting education on healthy lifestyles, assisting in accessing medical and nutritional resources, and providing crisis intervention and referrals, social work can not only help the obese population improve their mental health but also improve their quality of life, thus playing a pivotal role in suicide prevention.
Despite its contributions, our study is not without limitations. First, the cross-sectional nature of our analysis precludes us from elucidating the causal mechanisms and effects underlying the observed associations. Second, the potential for inaccuracies in the covariates included may impact the results' precision. Third, it is essential to note that the results of this study may not necessarily translate into clinical implications, mainly due to the large sample size, which can amplify minor variations. Fourth, our analysis does not account for the potential influence of weight reduction treatments [ 61 ] on WWI due to data constraints, which could affect the associations observed. Nonetheless, our research is strengthened by its foundation on a substantial and representative dataset derived from the NHANES, providing a robust basis for our findings. Moreover, we are the first to investigate the relationship between WWI and suicidal ideation, including a variety of subgroup analyses.
Elevated WWI was significantly associated with increased suicidal ideation. Relative to BMI, WWI demonstrates enhanced predictive efficacy for suicidal ideation. This facilitates the timely identification of suicide risk by social workers. Nonetheless, additional studies are necessary to validate these preliminary outcomes.
Availability of data and materials
The datasets analyzed during the current study are available in the NHANES [ https://www.cdc.gov/nchs/nhanes/index.htm ].
Camus A (2010) Le mythe de Sisyphe: [essai sur l’sabsurde]. Chicoutimi: J-M Tremblay.
World Health Organization (2024) Suicide prevention: World Health Organization. https://www.who.int/health-topics/suicide#tab=tab_1 . Accessed 16 Mar 2024
U.S. Centers for Disease Control and Prevention (2023) Suicide Data and Statistics: U.S. Centers for Disease Control and Prevention. https://www.cdc.gov/suicide/suicide-data-statistics.html . Accessed 16 Mar 2024
Stack S (2021) Contributing factors to suicide: political, social, cultural and economic. Prev Med 152:106498
Article PubMed Google Scholar
Aboumrad M, Shiner B, Riblet N, Mills PD, Watts BV (2018) Factors contributing to cancer-related suicide: a study of root-cause analysis reports. Psychooncology 27(9):2237–2244
Article PubMed PubMed Central Google Scholar
Bailo P, Gibelli F, Celletti A, Caraffa A, Sirignano A, Ricci G (2023) The contributing factors to suicide in Italian prisons: an 11-year analysis (2010–2020). Crim Behav Ment Health 33(6):441–454
Crook M (2003) Out of the darkness: teens and suicide. Arsenal Pulp Press, Vancouver
Google Scholar
Suicide HM (2012) Detroit. Greenhaven Press, New York
Murfree L, DeMaria AL, Schwab-Reese LM (2022) Factors contributing to filicide-suicide: differences between male and female perpetrators. Child Abuse Neglect 129:105637
Ong MS, Lakoma M, Gees Bhosrekar S, Hickok J, McLean L, Murphy M et al (2021) Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child Adolesc Mental Health 26(2):134–142
Article Google Scholar
Power E, Coughlan H, Clarke M, Kelleher I, Lynch F, Connor D et al (2016) Nonsuicidal self-injury, suicidal thoughts and suicide attempts among sexual minority youth in Ireland during their emerging adult years. Early Interv Psychiatry 10(5):441–445
van Vuuren CL, van der Wal MF, Cuijpers P, Chinapaw MJM (2021) Sociodemographic differences in time trends of suicidal thoughts and suicide attempts among adolescents living in Amsterdam, The Netherlands. Crisis 42(5):369–377
van Wijnen LG, Boluijt PR, Hoeven-Mulder HB, Bemelmans WJ, Wendel-Vos GC (2010) Weight status, psychological health, suicidal thoughts, and suicide attempts in Dutch adolescents: results from the 2003 E-MOVO project. Obesity 18(5):1059–1061
Yang C, Huebner ES, Tian L (2024) Prediction of suicidal ideation among preadolescent children with machine learning models: a longitudinal study. J Affect Disord 352:403–409
Karaye IM (2022) Differential trends in US suicide rates, 1999–2020: Emerging racial and ethnic disparities. Prev Med 159:107064
Centers for Disease Control and Prevention (2022) Nutrition, physical activity, and obesity: data, trends and maps. https://nccd.cdc.gov/dnpao_dtm/rdPage.aspx?rdReport=DNPAO_DTM.ExploreByTopic&islClass=OWS&islTopic=&go=GO . Accessed 16 Mar 2024
National Heart L, Blood Institute (1998) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults
National Heart L, Blood Institute (2013) Managing overweight and obesity in adults: systematic evidence review from the obesity expert panel
Wharton S, Lau DCW, Vallis M, Sharma AM, Biertho L, Campbell-Scherer D et al (2020) Obesity in adults: a clinical practice guideline. CMAJ 192(31):E875–E891
Cole TJ, Faith MS, Pietrobelli A, Heo M (2005) What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr 59(3):419–425. Erratum: 2005 June;59(6):807
Freedman DS, Woo JG, Ogden CL, Xu JH, Cole TJ (2019) Distance and percent distance from median BMI as alternatives to BMI z-score. Br J Nutr 124(5):493–500
Golan Shekhtman S, Boccara E, Ravona-Springer R, Inbar Y, Zelicha H, Livny A et al (2024) Abdominal fat depots are related to lower cognitive functioning and brain volumes in middle-aged males at high Alzheimer’s risk. Obesity. https://doi.org/10.1002/oby.24004
Haidar A, Srikanthan P, Watson K, Allison M, Kronmal R, Horwich T (2024) Associations between visceral fat, abdominal muscle, and coronary artery calcification: a cross-sectional analysis of the Multi-Ethnic Study of Atherosclerosis. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2024.02.030
Ma M, Luo M, Liu Q, Zhong D, Liu Y, Zhang K (2024) Influence of abdominal fat distribution and inflammatory status on post-operative prognosis in non-small cell lung cancer patients: a retrospective cohort study. J Cancer Res Clin Oncol 150(3):111
Yoshida K, Kondo E, Ishida M, Ichikawa Y, Watashige N, Okumura A et al (2024) Visceral adipose tissue percentage compared to body mass index as better indicator of surgical outcomes in women with obesity and endometrial cancer. J Minim Invasive Gynecol. https://doi.org/10.1016/j.jmig.2024.02.009
Qin Z, Du D, Li Y, Chang K, Yang Q, Zhang Z et al (2022) The association between weight-adjusted-waist index and abdominal aortic calcification in adults aged ≥ 40 years: results from NHANES 2013–2014. Sci Rep 12(1):20354
Article CAS PubMed PubMed Central Google Scholar
Wang X-L, Feng H-L, Xu X-Z, Liu J, Han X (2024) Relationship between cognitive function and weight-adjusted waist index in people ≥ 60 years old in NHANES 2011–2014. Aging Clin Exp Res 36(1):30
Chen D, Lu C, Chen K, Liu T, Li Y, Shan Z et al (2024) Association between anthropometric indices and hyperuricemia: a nationwide study in China. Clin Rheumatol 43(3):907–920
Ding Y, Lv S, Xie R, Ye W, Luo Y, Li Y (2024) Association of weight-adjusted-waist index and diabetic kidney disease in type 2 diabetes mellitus. Endocr Connect. https://doi.org/10.1530/EC-23-0491
Gui Z, Yu L, Chen Y, Zhang M, He J, Hao Y (2023) Study from the United States: increased prevalence of kidney stones in patients with high weight-adjusted waist index. Front Nutr 10:1171775
Sun D, He H, Luo B, Xie B (2024) The association between weight-adjusted-waist index and stress urinary incontinence in female adults: a population-based study. Int Urol Nephrol. https://doi.org/10.1007/s11255-023-03928-z
Takhttavous A, Saberi-Karimian M, Hafezi SG, Esmaily H, Hosseini M, Ferns GA et al (2024) Predicting the 10-year incidence of dyslipidemia based on novel anthropometric indices, using data mining. Lipids Health Dis 23(1):33
Yu C, He S, Kuang M, Wang C, Huang X, Sheng G et al (2024) Association between weight-adjusted waist index and non-alcoholic fatty liver disease: a population-based study. BMC Endocr Disord 24(1):22
Law S, Dong S, Zhou F, Zheng D, Wang C, Dong Z (2023) Bariatric surgery and mental health outcomes: an umbrella review. Front Endocrinol 14:1283621
Meshkat S, Liu Y, Jung H, Tassone VK, Pang H, Janssen-Aguilar R et al (2024) Temporal associations of BMI and glucose parameters with depressive symptoms among US adults. Psychiatry Res 332:115709
Article CAS PubMed Google Scholar
Mowoh DPM, Cole R, Sarvepalli S, Grover K, Abbas M, Khaitan L (2024) Bariatric surgery efficacy in patients with mood disorders. Surgery. https://doi.org/10.1016/j.surg.2023.11.032
Ninla-Aesong P, Puangsri P, Kietdumrongwong P, Jongkrijak H, Noipha K (2023) Being overweight and obese increases suicide risk, the severity of depression, and the inflammatory response in adolescents with major depressive disorders. Front Immunol 14:1197775
Kim MS, Kim JY, Song YS, Hong S, Won HH, Kim WJ et al (2024) Association of bariatric surgery with indicated and unintended outcomes: an umbrella review and meta-analysis for risk-benefit assessment. Obes Rev 25(3):e13670
Xu B, Chen C, Wang D (2024) Current psychotic-like experiences among Chinese college students: prevalence, correlates, and its relationship with suicidal ideation. Psychol Res Behav Manag 17:799–811
Cho Y, Shin SY, Shin MJ (2015) Sarcopenic obesity is associated with lower indicators of psychological health and quality of life in Koreans. Nutr Res 35(5):384–392
Kim B, Kim HS, Park S, Kwon JA (2023) BMI and perceived weight on suicide attempts in Korean adolescents: findings from the Korea Youth Risk Behavior Survey (KYRBS) 2020 to 2021. BMC Public Health 23(1):1107
Ding Y, Lv S, Xie R, Ye W, Luo Y, Li Y (2024) Association of weight-adjusted waist index and diabetic kidney disease in type 2 diabetes mellitus. Endocr Connect 13(4):e230491
CAS PubMed PubMed Central Google Scholar
Liu H, Zhi J, Zhang C, Huang S, Ma Y, Luo D et al (2024) Association between Weight-Adjusted Waist Index and depressive symptoms: a nationally representative cross-sectional study from NHANES 2005 to 2018. J Affect Disord 350:49–57
Ding Y, Xu Z, Zhou X, Luo Y, Xie R, Li Y (2023) Association between weight-adjusted-waist index and the risk of hyperuricemia in adults: a population-based investigation. Front Endocrinol 14:1236401
Varallo G, Scarpina F, Arnison T, Giusti EM, Tenti M, Rapelli G et al (2024) Suicidal ideation in female individuals with fibromyalgia and comorbid obesity: prevalence and association with clinical, pain-related, and psychological factors. Pain Med 25(3):239–247
Yin H, Zhang Q, Li Y, Ma J (2023) Prevalence and correlates of severe anxiety in patients with first hospitalization for major depressive disorder combined with dyslipidemia: a large sample cross-sectional study. Front Psychiatry 14:1289614
Freitas R, Vasques ACJ, da Rocha FG, Ribeiro FB, Solar I, Shivappa N et al (2024) Gut bacterial markers involved in association of dietary inflammatory index with visceral adiposity. Nutrition 122:112371
Liu Y, Dong Y, Wang X, Xu X (2024) Association between metformin treatment and coronary artery inflammation based on pericoronary adipose tissue attenuation in type 2 diabetes mellitus patients. J Clin Hypertens. https://doi.org/10.1111/jch.14777
Poynter ME, Mank MM, Ather JL (2024) Obesity-associated inflammatory macrophage polarization is inhibited by capsaicin and phytolignans. Am J Physiol Regul Integr Comp Physiol. https://doi.org/10.1152/ajpregu.00161.2023
Capuron L, Miller AH (2011) Immune system to brain signaling: neuropsychopharmacological implications. Pharmacol Ther 130(2):226–238
Kan C, Silva N, Golden SH, Rajala U, Timonen M, Stahl D et al (2013) A systematic review and meta-analysis of the association between depression and insulin resistance. Diabetes Care 36(2):480–489
Trayhurn P (2022) Adipokines: inflammation and the pleiotropic role of white adipose tissue. Br J Nutr 127(2):161–164
Aberra YT, Ma L, Björkegren JLM, Civelek M (2023) Predicting mechanisms of action at genetic loci associated with discordant effects on type 2 diabetes and abdominal fat accumulation. Elife 12:e79834
Tadiotto MC, Corazza PRP, de Menezes-Junior FJ, Tozo TAA, de Moraes-Junior FB, Brand C et al (2024) Moderating role of 1-minute abdominal test in the relationship between cardiometabolic risk factors and adiponectin concentration in adolescents. BMC Pediatr 24(1):75
Tremblay EJ, Tchernof A, Pelletier M, Joanisse DR, Mauriège P (2024) Plasma adiponectin/leptin ratio associates with subcutaneous abdominal and omental adipose tissue characteristics in women. BMC Endocr Disord 24(1):39
Bahramian M, Arjmand N, El-Rich M, Parnianpour M (2023) Effect of obesity on spinal loads during load-reaching activities: a subject- and kinematics-specific musculoskeletal modeling approach. J Biomech 161:111770
Singhal V, Huynh C, Nimmala S, Mitchell DM, Pedreira CC, Bader A et al (2022) Load-to-strength ratio at the radius is higher in adolescent and young adult females with obesity compared to normal-weight controls. Bone 164:116515
Brydon L, Wright CE, O’Donnell K, Zachary I, Wardle J, Steptoe A (2008) Stress-induced cytokine responses and central adiposity in young women. Int J Obes 32(3):443–450
Article CAS Google Scholar
Dhokte S, Czaja K (2024) Visceral adipose tissue: the hidden culprit for type 2 diabetes. Nutrients 16(7):1015
Soedono S, Sharlene S, Vo DHN, Averia M, Rosalie EE, Lee YK et al (2024) Obese visceral adipose dendritic cells downregulate regulatory T cell development through IL-33. Front Immunol 15:1335651
Nazzaro P, Amatuzio A, Baranello S, Corvinelli M, Di Cienzo G, Principe F et al (2023) Renal damage and obesity: a silent pairing. G Ital Nefrol 40(3):2023
PubMed Google Scholar
Download references
Acknowledgements
We want to thank Yihui Zhao for his help with data processing.
This work was supported by the Kunshan Traditional Chinese Medicine Hospital Youth Science and Technology Fund [Grant numbers: 2020QNJJ03].
Author information
Shijie Guo and Guangwei Qing have contributed equally to this article.
Authors and Affiliations
Department of Applied Social Sciences, The Hong Kong Polytechnic University, Kowloon, Hong Kong SAR, China
Jiangxi Mental Hospital & Affiliated Mental Hospital of Nanchang University, Third Clinical Medical College of Nanchang University, Nanchang, Jiangxi, China
Guangwei Qing
Department of Neurology, Kunshan Hospital of Traditional Chinese Medicine, Suzhou, Zhejiang, China
Qiqi Chen & Guang Yang
You can also search for this author in PubMed Google Scholar
Contributions
G.S. and Q.G.: methodology, formal analysis, writing—original draft; C.Q. and Y.G.: conceptualization, methodology, supervision, writing—review and editing.
Corresponding author
Correspondence to Guang Yang .
Ethics declarations
Ethics approval and consent to participate.
The data acquisition process was governed by stringent ethical protocols, including the endorsement from the NCHS's Research Ethics Review Board and the acquisition of informed, written consent from all contributors. NHANES adheres to moral norms and standards that prioritize participant consent, privacy and data protection, IRB approval, compliance with laws and guidelines, including the Declaration of Helsinki and HIPAA, and minimization of risk to ensure the welfare and rights of participants while maintaining the scientific integrity and accuracy of the research. Human Ethics and Consent to Participate declarations: not applicable. Details can be found at https://www.cdc.gov/nchs/nhanes/irba98.htm .
Documented consent to participate was obtained from participants. Details can be found at https://www.cdc.gov/nchs/nhanes/irba98.htm .
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests that pertain to this work.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Guo, S., Qing, G., Chen, Q. et al. The relationship between weight-adjusted-waist index and suicidal ideation: evidence from NHANES. Eat Weight Disord 29 , 37 (2024). https://doi.org/10.1007/s40519-024-01666-4
Download citation
Received : 21 March 2024
Accepted : 29 April 2024
Published : 14 May 2024
DOI : https://doi.org/10.1007/s40519-024-01666-4
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Waist-to-weight index
- Suicidal ideation
- Mental health assessments
- Cross-sectional analysis
- Predictive accuracy
- Find a journal
- Publish with us
- Track your research
- Open access
- Published: 10 November 2023
A scoping review of emotion regulation and inhibition in emotional eating and binge-eating disorder: what about a continuum?
- Mahé Arexis 1 , 2 ,
- Gilles Feron 1 ,
- Marie-Claude Brindisi 1 , 3 ,
- Pierre-Édouard Billot 2 &
- Stéphanie Chambaron 1
Journal of Eating Disorders volume 11 , Article number: 197 ( 2023 ) Cite this article
2703 Accesses
7 Citations
1 Altmetric
Metrics details
Emotional eating is defined as a nonpathological eating behavior, whereas binge-eating disorder (BED) is defined as a pathological eating behavior. While different, both share some striking similarities, such as deficits in emotion regulation and inhibition. Previous research has suggested the existence of an “eating continuum” that might reflect the increased severity of overeating behaviors, that is, from nonpathological overeating to BED. The main aims of this scoping review were to explore in the literature the idea of a continuum between emotional eating and BED and to observe whether deficits in emotion regulation and inhibition follow this continuum in terms of severity. The other aims were to hopefully clarify the ill-defined concept of overeating, to question the potential role of positive emotions and to identify potential knowledge gaps.
A systematic scoping review was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. Two databases (PubMed/Medline and PsycINFO) were examined in complete accordance with the beforehand sharply defined eligibility and exclusion criteria. The main criteria included adults (≥ 18) with emotional eating, BED or overeating and emotion regulation and inhibition as exposure criteria.
Thirty-two studies were included in this scoping review. If the results showed a link between emotional eating and BED, with the presence of inhibition and emotion regulation deficits in both eating behaviors, no mention of a continuum between emotional eating and BED was found.
In the absence of research directly comparing emotional eating and BED in the same studies and testing the potential increase in severity of emotion regulation and inhibition deficits along this continuum, there is currently no certainty that a continuum exists between emotional eating and BED. In the end, the idea of a continuum in terms of increased severity of overeating and in terms of emotion regulation and inhibition deficits between emotional eating and BED appears to be a gap in knowledge in the literature. This scoping review highlights the need for further research to identify knowledge gaps.
Plain English summary
Emotional eating (EE) is defined as a nonpathological eating behavior, whereas binge-eating disorder (BED) is defined as a pathological eating behavior. While different, both share some striking similarities, such as deficits in emotion regulation (ER) and inhibition. Previous research has suggested the existence of an “eating continuum” that might reflect the increased severity of overeating behaviors, that is, from nonpathological overeating to BED. The main aims of this scoping review were to explore in the literature the idea of a continuum between EE and BED and to observe whether deficits in ER and inhibition follow this continuum in terms of severity. A systematic scoping review was conducted, and thirty-two studies were included in this review. If the results showed a link between EE and BED, with the presence of inhibition and ER deficits in both eating behaviors, no mention of a continuum between EE and BED, or in relation to a continuum, was found. Thus, in the absence of research directly comparing EE and BED in the same studies and testing the potential increase in severity of ER and inhibition deficits along this continuum, there is currently no certainty about the existence or absence of such a continuum.
Introduction
Our scoping review mainly focused on emotional eating (EE) and binge-eating disorder (BED). EE is an eating behavior that can be defined as “the tendency to overeat in response to negative emotions […]” ([ 1 ], p. 106) but in a nonpathological way. It differs from BED, which was formally indexed in 2013 in the DSM-5 as a discrete eating disorder. BED symptoms include recurrent binge-eating episodes (i.e., eating a larger amount of food than most people do during a discrete period of time, with at least one episode per week for three months), “a sense of lack of control over eating during the episode” and “marked distress regarding binge eating”, but without compensatory behaviors as in anorexia nervosa or bulimia nervosa [ 2 ].
Although different, both EE and BED appear to be affected by deficits in emotion regulation (ER) and inhibition [ 3 , 4 , 5 , 6 , 7 , 8 , 9 , 10 ]. Indeed, both individuals with EE and BED present with overeating behaviors caused by emotion regulation difficulties and a lack of inhibition/greater impulsivity. For example, it has been shown that negative emotions act as a trigger for binge-eating episodes in BED [ 7 , 11 , 12 ], and some data also suggest that positive emotions may increase food consumption [ 7 ]. Binge eating can be seen as a way to regulate negative emotions (but it is yet uncertain if this strategy successfully improves mood, see Leehr et al. and Stein et al. [ 7 , 13 ]), and BED patients are more prone to use maladaptive strategies such as suppression or rumination [ 4 ].
Davis [ 14 ] suggested the existence of an “(over) eating continuum”: in some way, on one end of the continuum are nonpathological overeating behaviors and at the other end is BED, which is a pathological and extreme state of overeating. The evolution on this continuum, therefore, reflects the “increased severity and compulsiveness” of overeating behaviors. It is also important to emphasize that this idea of a continuum in severity and compulsiveness between those eating behaviors is also reported by clinicians and physicians. It is therefore reasonable to think that the severity of ER and inhibition deficits could increase along this continuum between EE and BED, as shown in Fig. 1 . Taken together, this information is a starting point to lead a systematic screening of the literature. Since our main goals are to clarify the concept of continuum and to identify knowledge gaps, we chose to conduct a scoping review following the guidelines of PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews) [ 15 ].
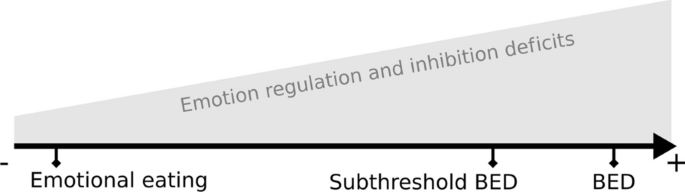
Schematic view of increased emotion regulation and inhibition deficits along a continuum between nonpathological emotional eating and binge-eating disorder (BED)
The present scoping review aimed (1) to address the possible existence of a continuum between EE and BED; (2) to address the possibility of an increase in the severity of deficits in emotion regulation and inhibition; and (3) to address the ill-defined concept of overeating. Indeed, is overeating (OE) a symptom, an eating behavior, a synonymous concept of EE, or a synonym for binge eating? (4) The final aim was to potentially investigate whether positive emotions can, like negative emotions, trigger emotional eating episodes associated with emotion regulation and/or inhibition difficulties. Finally, this scoping review also aimed to identify gaps in knowledge.
The scoping review was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines [ 15 ].
The review protocol can be accessed at HAL ( https://hal.science/hal-03643357v1 —HAL Id/Registration number: hal-03643357) [ 16 ].
Eligibility criteria
Studies were selected based on the following criteria:
The PICOS framework was used to highlight the main criteria. PICOS criteria: Populations : People (adult human subjects ≥ 18) with binge-eating disorder (BED) (and meeting the full DSM-IV-TR or DSM-5 criteria for BED) or subthreshold BED and people (adult human subjects, 18 +) presenting with emotional eating (EE) or emotional overeating (EO). Interventions/Exposures : Our review focused on the impact of “emotion regulation” and “inhibitory control” on BED and EE. Comparisons : Our review did not focus on studies with specific comparisons. Outcomes : Our review considered all types of outcomes related to emotion regulation and inhibitory control in BED, EE, and EO ( e.g. , deficit, level of attention, response impairment, and degree of compulsivity). Studies : All types of journal articles published in peer-reviewed scientific journals, either written in English or in French. The exclusion criteria were all types of reviews, book chapters, abstracts, preprints, theses, and articles focusing on therapies/treatments.
Only papers published between January 2009 and January 2022 were eligible for consideration. Although the MeSH (Medical Subject Headings) terms for binge-eating disorder were not introduced until 2010, the year 2009 was chosen because it was a “transition year” between the previous indexing of binge-eating disorder as bulimia nervosa and the introduction of the MeSH term BED in 2010.
Information sources and search
Two electronic bibliographic databases, PubMed/Medline and PsycINFO, were searched to identify references related to the scoping review topic. The search focused on articles published between January 2009 and January 2022. The following search equation was used in both databases: ("Binge-Eating Disorder"[Mesh] OR BED OR Binge eater OR Emotional Eating OR Emotional Overeating OR Overeater OR Emotional eater OR Overeating) AND ("Emotional Regulation"[Mesh] OR Emotion regulation OR Reappraisal OR Rumination OR Attentional deployment OR Mood regulation OR "Inhibition, Psychological"[Mesh] OR Inhibitory control).
This database search stage was conducted by one of the authors, M. A. No additional references were added from other sources at this stage.
Selection of sources of evidence
Duplicates were removed, and all references were imported into Rayyan, an online application for systematic reviews [ 17 ]. Figure 2 shows the flowchart of the literature search and screening/study selection process. During the successive screening stages, at least 2 authors (M. A., and P.-E. B. or S. C., up to 4 authors, M. A., P.-E. B., S. C. and M.-C. B.) screened each record. Disagreements regarding study selection were resolved by a third or even a fourth investigator, and discussions took place between the authors. In the first screening step, for each article, the inclusion criteria described in Sect. " Eligibility criteria " were applied to both titles and abstracts. In the second screening step (eligibility), for each article, the inclusion criteria described in Sect. " Eligibility criteria " were applied to the entire article (i.e., a complete reading of the article). Note that at this stage, we screened the bibliographic references of the included articles to identify potential new references. At the end of this screening, no new articles were included.
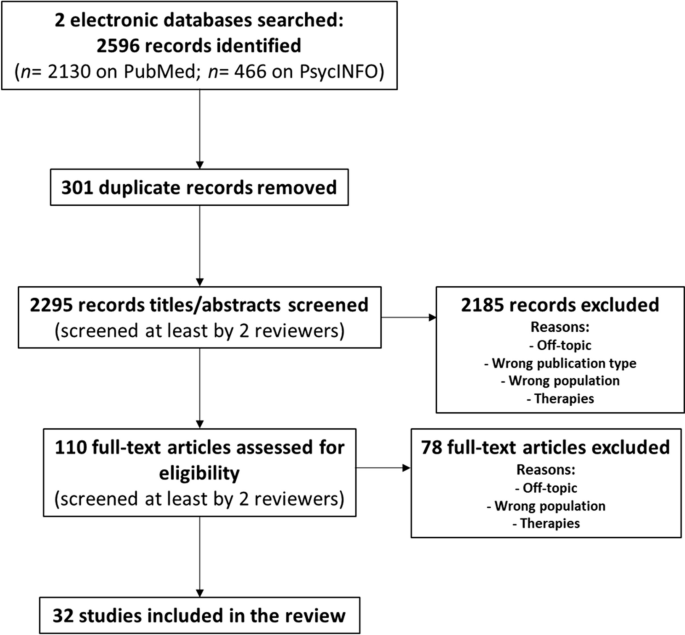
Flowchart of the literature search and screening/study selection process
Data charting process and data items
Three investigators (authors M. A., P.-E. B., and S. C.) developed a data charting form to extract the relevant data from each of the 32 included studies. For each study, author M. A. extracted the data according to the following variables of the chart: authors, title, year of publication, country of the study, journal of publication, type of study, method/study design, participants and sample sizes, type of interventions, comparisons, and outcomes/results. Table 1 shows the final version of the chart with the main characteristics of the studies included in the scoping review. We did not include in Table 1 the journal of publication or type of study variables of the chart, as they were deemed irrelevant for this table. Note that we added in Table 1 a new column “Outcomes/Results highlight” with a simplified overview of the results, as well as a “Limitations” column.
Critical analysis
Two authors (M. A. and P.-E. B.) listed the possible limitations of each study. The limitations identified by both authors were retained, and the others were either eliminated or retained after discussion. A third author (S. C.) checked this list, and her comments were considered. The limitations are summarized in the "Limitations" column of Table 1 and are discussed in Sect. " Critical analysis ".
Synthesis of results
Data were analyzed qualitatively. We first grouped the studies by the types of eating behaviors (emotional eating (EE), overeating (OE), and binge-eating disorder (BED)). Then, we addressed each of the topics formulated in our questions/hypotheses.
The source search in the electronic bibliographic databases retrieved 2596 records (2130 on PubMed/Medline and 466 on PsycINFO) (see Fig. 2 ). After removing 301 duplicate records, 2295 records were screened in the first screening step. During this first screening step, for each of the 2295 articles, the inclusion criteria described in the Eligibility criteria section of the Methods section were applied to both titles and abstracts, resulting in 110 records to be assessed for eligibility in the next step. Thus, in the second screening step (eligibility), for each of the 110 articles, the same inclusion criteria were applied to the entire article (i.e., a complete reading of the article). At the end of this second stage, 32 studies were selected to be included in the review. Table 1 shows the main characteristics of the 32 studies included in the scoping review, according to the variables described in Sect. " Data charting process and data items ".
Regarding the types of populations (cf. PICOS criteria), 9 studies out of 32 focused on emotional eating (EE), 21 studies out of 32 focused on binge-eating disorder (BED), and 2 out of 32 focused on overeating (OE). Regarding the types of intervention/exposure (cf. PICOS criteria), namely, ER and inhibition/impulsivity, 19 studies out of 32 focused on emotion regulation (ER), 18 studies out of 32 focused on inhibition/impulsivity, and 5 out of 32 focused on both ER and inhibition/impulsivity. More than a third of the included studies (11 studies out of 32, ≈ 34%) were conducted in Germany. Moreover, more than half of the studies (17 studies out of 32, ≈ 53%) were conducted in Germany or in countries bordering Germany (i.e., France, Switzerland, Belgium and Poland).
Summary of findings
Emotional eating and emotion regulation.
Studies confirm the existence of a link between ER and EE, including the fact that ER difficulties predict EE. For example, Stapleton and Whitehead [ 18 ] highlighted that “Emotion regulation difficulties was the greatest predictor of emotional eating, suggesting that individuals who have difficulty regulating their emotions are more likely to engage in emotional eating behavior”. Similarly, Crockett et al. [ 3 ] concluded that “In every model we tested, difficulties in emotion regulation predicted emotional eating”. Sultson and Akkermann [ 19 ] concluded that "Higher level of ER difficulties among obese and normal weight individuals with EE also lend further support for the assumption that emotion dysregulation might underlie EE". Kornacka et al. [ 20 ] highlighted the “[…] crucial role of ruminative thinking in the occurrence of emotional eating […]”. Regarding avoidance, Deroost and Cserjési [ 21 ] showed “[…] that people with a high degree of EM use avoidance as a primary coping strategy" and added that "avoidance coping also significantly predicted the level of EM” (EM = emotional eating).
Future studies focusing on EE and ER should separately test other specific types of emotional eating (e.g., EE in response to depression, to anxiety…). Indeed, Braden et al. [ 22 ] explained that “exploratory analyses suggest possible unique relationships between types of emotional eating and specific facets of emotion regulation”. The authors added that “[…] findings suggest that certain emotion regulation strategies may be more closely linked to various types of emotional eating”.
Emotional eating and inhibition
The studies included in this scoping review dealing with EE and inhibition/impulsivity confirmed the existence of an association between EE and some inhibition difficulties and impulsivity. For example, Wolz et al. [ 23 ] showed that “[…] emotional eating was not related to general inhibitory control deficits, but was associated with higher behavioral inhibitory control difficulties only while suppressing negative emotions. They added that “[…] the difficulty to inhibit behavioral responses while regulating negative emotions may contribute to disinhibited food intake while experiencing negative emotions”. Stapleton and Whitehead [ 18 ] revealed that emotional eating was related to high impulsivity and that impulsivity was the second greatest predictor of EE after emotion regulation difficulties. Regarding self-control, Wood et al. [ 24 ] showed “[…] an increase in activation across brain regions related to self-control and urges in response to high-calorie food associated with both emotional eating and routine restraint". Taken together, these findings confirm that emotional eaters are prone to inhibition impairments. Moreover, Wolz et al. [ 23 ] suggest that deficits in inhibition only appear when participants are regulating their emotions, highlighting an interesting link between ER and inhibition in EE.
BED and emotion regulation
Concerning BED and emotion regulation, most of the studies confirm the ER difficulties in BED. Leehr et al. [ 25 ] showed that individuals with BED have lower ER capacities. Limited access to ER strategies is also one of the ER difficulties met in BED [ 26 , 27 ], as well as nonacceptance of emotional responses [ 27 ] and lack of emotional clarity [ 26 , 27 ].
BED and inhibition
Overall, studies focusing on BED indicated a deficit in inhibition and increased impulsivity. Leehr et al. [ 25 ] concluded that “Overall, results support the assumption of inhibitory control deficiencies in BED on a behavioral level”. Grant and Chamberlain [ 28 ] underlined that “Binge-eating disorder was associated with impaired response inhibition and executive planning”. Schag et al. [ 29 ] said that “[…] BED represents a neurobehavioural phenotype of obesity that is characterized by increased impulsivity”, and Leehr et al. [ 30 ] showed that “the BED + sample showed higher trait and behavioural impulsivity”. Moreover, according to Aloi et al. [ 31 ], “[…] impaired self-monitoring metacognition and difficulties in impulse control are the central nodes in the psychopathological network of BED […]”.
Overeating and emotion regulation
One of the objectives of this scoping review was to clarify the ill-defined concept of overeating . In the eating disorders literature, overeating sometimes refers to a symptom of an eating disorder or as an eating behavior or is sometimes used as a synonym for emotional eating or binge eating.
Unfortunately, only two of the studies included in this scoping review focused on overeating [ 32 , 33 ], so we could not address this specific question. Nevertheless, similar to EE and BED, those studies highlighted the links between overeating and emotion regulation.
Positive emotions and emotional eating
We questioned the possibility of positive emotions causing emotional eating episodes associated with emotion regulation and/or inhibition difficulties (in the same way as negative emotions). Based on the studies included in our review, opinions differ regarding this point. Indeed, while an article highlights that “[…] positive EE was associated with elevated levels of ER difficulties, suggesting that overeating in response to positive emotions might also include some features of emotion dysregulation” [ 19 ], another article concludes, on the contrary, that “[…] eating in response to positive emotions was not significantly related to poorer psychological well-being, greater eating disorder symptoms, or emotion dysregulation” [ 22 ]. Since there is yet no consensus on the subject, further research on emotional eating needs to be conducted to separately test and dissociate positive and negative emotions.
Positive emotions and BED
We wondered about positive emotions as a possible cause of emotional eating episodes associated with emotion regulation and/or inhibition difficulties. We checked whether the BED studies included in this scoping review addressed the question of positive emotions/affect/mood. Loeber et al. [ 34 ] showed that “[…] restrained eating and mood are factors that moderate response inhibition to food-associated stimuli in obese patients with BED” and that “[…] apart from negative mood, positive mood might as well be a trigger for loss of control over eating behaviour”.
Finally, it is worth mentioning that one study showed that negative and positive mood levels are different during binge days, with an increasing negative mood and a decreasing positive mood at the first binge-eating episode (see Munsch et al. [ 35 ]).
Emotional eating and weight profiles
Studies included in this scoping review tended to show that the relationships between EE and emotion dysregulation (and anxiety, depression, and rumination) might be different according to the weight profile (i.e., normal weight, overweight, and with moderate or severe obesity) (see, for example, Willem et al. [ 36 ] or Kornacka et al. [ 20 ]). Willem et al. [ 36 ] highlighted that “emotion dysregulation, anxiety and depression have different impacts on emotional eating (EE) depending on obesity severity", while Kornacka et al. [ 20 ] underlined that “the role of emotional eating in the link between rumination and uncontrolled eating is different in overweight vs. healthy individuals”.
Emotional eating, BED and rumination
According to three of the studies included in this scoping review, rumination, a maladaptive emotion regulation strategy, is encountered in both EE and BED. Indeed, in EE, Kornacka et al. [ 20 ] highlight that rumination is a predictor of EE (“[…] the results of the two studies confirm the crucial role of ruminative thinking in the occurrence of emotional eating […]”. Similarly, people with BED are more inclined than healthy people to use rumination as a negative emotion regulation strategy [ 27 ]. Wang et al. [ 37 ] also highlighted that “[…] rumination is an important cognitive process associated with severity of eating-disorder psychopathology”.
The idea of a possible continuum
We hypothesized that there would be a continuum between EE (nonpathological eating behavior) and BED (pathological eating behavior). Three studies focusing on BED mentioned this idea of a continuum in the severity of eating disorders. Leehr et al. [ 25 ] stated that “From a clinical perspective eating behavior of the three groups can be seen on a continuum from normal eating behavior, to overeating, to binge eating”. Mobbs et al. [ 38 ] highlighted that “[…] these cognitive deficits are more severe in obese patients with binge eating disorder, which indicates that there is a continuum of increasing inhibition and cognitive problems with increasingly disordered eating”. Moreover, Svaldi et al. [ 39 ] underlined that “[…] the magnitude of the inhibitory deficit was found to be related to the reported severity of eating pathology”, which is compatible with the idea of a continuum.
However, none of the reviewed studies directly compared EE to BED regarding ER or inhibition performances, neither in a longitudinal nor cross-sectional design. Thus, a gap can clearly be identified in this specific field since there is a complete lack of experimental data about an increased severity in ER and inhibition deficit between EE and BED.
We identified some limitations between studies, and some of them were quite redundant in our corpus. First, half of the included studies recorded only self-reported data using scales, questionnaires, or interviews. These declarative measures often suffer from memory bias or social desirability concerns [ 40 ]. Moreover, these measures are often carried out for a particular purpose, and this purpose may differ from study to study, depending on the research question being asked [ 40 ]. Strikingly, 88.9% of papers addressing ER gathered only self-report measures (but only 11.8% for inhibition). Thus, there is a lack of experimental data to address the issue of ER in BED and EE.
Second, 43.8% of the articles with self-report measures only appeared to have rather small sample sizes and/or unbalanced groups and were therefore underpowered. Sample size is a critical issue for quantitative analysis. This sample size must be large enough to achieve the appropriate level of measurement precision. [ 41 ].
Third, most of the participants enrolled in these studies were women, compromising the generalizability to the global population (81.3% of studies had only women participants or an unbalanced sex ratio toward women). Eating disorders are more frequent among women, and for BED, the ratio varies between 1:2 and 1:6 [ 42 ]. Thus, while the lack of men in BED studies is understandable, future studies should consider recruiting more men to properly balance the experimental groups.
Finally, a recurring limitation emphasized by many authors of the included studies is that their research was cross-sectional. Indeed, given the short duration of these types of studies, it was impossible to reveal some causal links between different phenomena (e.g., between BED and impulsivity). However, in our opinion, this is not a limitation per se, as cross-sectional and longitudinal studies are two very different types of research. Therefore, we did not report this limitation in Table 1 .
The main objectives of this scoping review were to explore the idea of a continuum between EE and BED as well as explore the idea of a gradation in emotion regulation and inhibition deficits along this continuum. This hypothesis is supported by some authors and is widely discussed in Davis [ 14 ]. He developed the concept of an “eating continuum”, ranging from homeostatic eating (energy balance) to food addiction, with different levels of “overeating”, including BED-like symptoms and diagnosed BED. It should also be noted that this idea of a continuum is shared by many physicians in their daily clinical practice and that this idea needs to be verified.
The most striking result of our scoping review is that there are strong similarities between EE and BED, with emotional eaters and BED patients sharing the same difficulties in emotion regulation and inhibition. Some of the included studies seem to be compatible with the idea of a gradation of ER and inhibition deficits following this continuum. For instance, Mobbs et al.’s [ 38 ] conclusions strengthened the idea of a continuum of inhibition impairment, with BED patients living with obesity having more difficulties inhibiting their responses compared to controls living with obesity. Indeed, the authors concluded that “[…] these cognitive deficits are more severe in obese patients with binge eating disorder, which indicates that there is a continuum of increasing inhibition and cognitive problems with increasingly disordered eating”. Concerning EE, the results of Sultson and Akkermann [ 19 ] showed that participants with EE have more binge eating behaviors than participants without EE but do not meet all the DSM-5 criteria to be diagnosed with BED. These results suggest that EE could lead to BED and thus support the idea of a continuum. It is, however, crucial to remember that none of the articles included in this review directly compared EE and BED in the same study, neither in a longitudinal nor cross-sectional design. To ascertain the existence of a continuum between EE and BED, the increased severity of ER and inhibition deficits between EE and BED still need to be proven. One of the main goals of this scoping review was also to identify knowledge gaps, and indeed, we found a gap in the literature regarding the increased severity in ER and inhibition impairments from EE to BED. Such a lack of experimental work is truly surprising given the feelings shared by many caregivers in the field of eating disorders as well as the thoughts shared by some authors [ 14 , 25 , 38 , 39 ].
Among the thirty-two articles reviewed, only one focused on the relationship between ER and inhibition in EE. Indeed, Wolz et al. [ 23 ] showed that EE was associated with higher behavioral inhibitory control difficulties only while participants were suppressing negative emotions. This outcome should be taken into account in further studies, since ER and inhibition deficits are often studied separately [ 7 , 43 , 44 ]. Indeed, the direct relationship between ER and inhibition remains poorly studied in BED, as well as in EE, but is an important question to explore the idea of a continuum.
The third objective of this scoping review was to address the ill-defined concept of overeating. Unfortunately, only two studies focused on overeating [ 32 , 33 ], and it is thus difficult to clearly define this concept. For both authors, overeating is not an eating disorder per se since participants were healthy volunteers with no prior diagnosis of an eating disorder. However, in both studies, overeating is measured with questionnaires widely used in medical contexts to assess eating disorders, such as the Eating Disorder Examination-Questionnaire (EDE-Q) or the Binge Eating Scale (BES). Thus, overeating may be seen as pathological eating. Moreover, Racine and Horvath [ 33 ] used the Eating Disorder Diagnostic Scale and the Questionnaire on Eating and Weight Patterns-5 (QEWP-5) to determine experimental groups. Women included in the “overeating” group reported consuming an “unusually large amount of food unaccompanied by loss of control over the past 3 months” on both questionnaires. Thus, this inclusion criterion could be a suitable definition of the concept of overeating, but it must be emphasized that there is too little information to properly define this concept.
The fourth aim of this review was to determine whether positive emotions could trigger emotional eating or binge eating episodes associated with emotion regulation and/or inhibition difficulties. Most of the studies only measured EE and binge eating episodes in response to negative emotions. However, few articles specifically focused on positive mood or emotions. Due to a lack of consensus among studies, it was impossible to strongly conclude that positive emotions can affect eating behaviors. Indeed, some data support this idea [ 19 , 34 ], and others are less affirmative [ 22 , 35 ].
Last, concerning the weight profile, it was not one of the aims of this scoping review, but our results showed that emotion regulation deficits were more severe in obese participants than in normal weight or overweight volunteers. Thus, the weight profile seems to be an important parameter when addressing the question of an increased severity in ER deficits between EE and BED.
Limitations
This scoping review presents some limitations. First, regarding the selection phase, not all relevant studies may have been indexed in the two searched databases (PsycINFO and PubMed/Medline). Second, the examination was based on a list of terms describing emotional eating, binge-eating disorder, emotion regulation and inhibition. The possibility that additional articles would have been identified by adding other terms cannot be completely excluded, although the search was intended to be as extensive as possible. Third, a possible limitation of our scoping review is that we did not mention explicitly in our search equation the terms “positive emotions”. Indeed, given that one of our questions was about the possibility that positive emotions can, like negative emotions, trigger emotional eating episodes, we could have perhaps included it in our search equation. Nevertheless, given that we used the inclusive terms “Emotional Regulation”[Mesh]” and “Emotion regulation”, it is likely that we did not miss some interesting records focusing on positive emotions. Finally, in this review, only studies in French or English were included, which did not allow us to be exhaustive in our conclusions.
Conclusion and further directions
In conclusion, this scoping review fully confirmed the presence of inhibition and emotion regulation deficits in both EE and BED, showing strong similarities between these two eating behaviors. However, the lack of experimental data coming from direct comparisons between EE and BED did not make it possible either to confirm the existence or the absence of a possible continuum between EE and BED or an increased severity in ER and inhibition deficits between EE and BED. Thus, this scoping review helped to identify a knowledge gap, and the question of the existence of a continuum still needs to be addressed in further research.
If such a continuum exists, we think it could greatly impact the clinical care of eating disorders. Indeed, if EE can become BED, early care of emotional eaters becomes essential, and early diagnoses could be made. Additionally, prevention could be improved in emotional eaters and even in the general population to avoid progression to an eating disorder (i.e., subthreshold BED and BED) and could also reduce the risk of developing obesity and its comorbidities often associated with BED. Given the variety of symptoms (psychological and physical), monitoring of emotional eaters could be performed by a multidisciplinary medical team, especially for children and adolescents.
The existence of a continuum between EE and BED could also have implications for eating disorder research. In our view, this could lead to further research to develop more specific screening instruments, such as scales and questionnaires. Such instruments might indeed be helpful to classify emotional eater participants into more relevant experimental groups that take into account the severity of EE. To go even further, one could imagine a new scale that would assess the level of eating behaviors across the entire continuum. Moreover, regarding data analysis, data could be analyzed in a discrete way in addition to group comparisons between EE and BED. Last, if such a continuum was verified, it could guide the focus on future research, especially studies on the etiology of BED, and help to better define the concept of “emotional overeating”.
Moreover, to test the idea of a continuum from a different angle, it could be interesting to see if there is an evolution of some other markers between EE and BED, such as biomarkers. Some of them are well known in BED but remain rather poorly studied in EE. Several fMRI studies have shown that brain activation patterns are different in BED patients, especially in the reward system, which explains why this eating disorder is often associated with food addiction [ 14 ]. For example, the ventral striatum and the medial prefrontal cortex seem to be underactivated during a rewarding task. Moreover, the ventral putamen, orbitofrontal cortex, amygdala, and insula respond less in BED patients than in controls [ 8 ]. EEG studies have also provided a valuable understanding of neurophysiological markers. In their narrative review, Berchio et al. [ 45 ] found that behavioral traits of BED and bulimia nervosa, such as loss of control over eating and emotional eating, are associated with an increased attentional reactivity (P300 wave) to visual food stimuli. Finally, animal studies allow us to better understand the functioning of some molecules. For example, the role of dopamine, oxytocin, and opiate in eating disorders is well understood [ 46 ], and this could be an interesting focus to measure the gradation between EE and BED.
Availability of data and materials
Two electronic bibliographic databases, PubMed/Medline and PsycINFO, were searched to identify references related to the scoping review topic. The search focused on articles published between January 2009 and January 2022. Original records (before screening) can be found using the search equation that was used in both databases: ("Binge-Eating Disorder"[Mesh] OR BED OR Binge eater OR Emotional Eating OR Emotional Overeating OR Overeater OR Emotional eater OR Overeating) AND ("Emotional Regulation"[Mesh] OR Emotion regulation OR Reappraisal OR Rumination OR Attentional deployment OR Mood regulation OR "Inhibition, Psychological"[Mesh] OR Inhibitory control). The 32 articles included after the screening steps are listed in the References section.
Abbreviations
- Emotional eating
- Binge-eating disorder
- Emotion regulation
Preferred reporting items for systematic reviews and meta-analyses extension for scoping reviews
Populations, interventions, comparisons, outcomes, studies
Diagnostic and statistical manual of mental disorders Text Revision, or 5th edition
Electroencephalography
Magnetoencephalography
Normal weight controls
Food stroop task
Body mass index
Barratt impulsiveness scale
Ecological momentary assessment
Bulimia nervosa
Healthy controls
Eating disorders
Difficulties in emotion regulation scale
People living with BED (or subthreshold BED, depending on the studies)
People living without BED (or subthreshold BED, depending on the studies)
Loss of control
Objective binge episode
Late positive potential
Stop signal task
Stop signal reaction time
Functional magnetic resonance imaging
Healthy volunteers
Go-trial reaction time
Normal-weight people living with BED
Overweight people living with BED
Executive functioning
Non-BED obese individuals
Lean comparison
Ventromedial prefrontal cortex
Inferior frontal gyrus
Anorexia nervosa-restricting type
Anorexia nervosa–binge/purge type
Eating disorder, not otherwise specified
Emotional eating/eaters (depending on the studies)
Exogenous cueing task
Network analysis
Emotional overeating
Medical subject headings
Emotional eating (used in some of the included articles)
Eating disorder examination-questionnaire (EDE-Q)
Binge eating scale
Eating disorder diagnostic scale and the questionnaire on eating and weight patterns-5
van Strien T, van de Laar FA, van Leeuwe JFJ, Lucassen PLBJ, van den Hoogen HJM, Rutten GEHM, et al. The dieting dilemma in patients with newly diagnosed type 2 diabetes: does dietary restraint predict weight gain 4 years after diagnosis? Health Psychol. 2007;26(1):105–12.
Article PubMed Google Scholar
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Washington: American psychiatric association; 2013.
Book Google Scholar
Crockett AC, Myhre SK, Rokke PD. Boredom proneness and emotion regulation predict emotional eating. J Health Psychol. 2015;20(5):670–80.
Dingemans A, Danner U, Parks M. Emotion regulation in binge eating disorder: a review. Nutrients. 2017;9(11):1274.
Article PubMed PubMed Central Google Scholar
Ferrell EL, Watford TS, Braden A. Emotion regulation difficulties and impaired working memory interact to predict boredom emotional eating. Appetite. 2020;144:104450.
Giel KE, Teufel M, Junne F, Zipfel S, Schag K. Food-related impulsivity in obesity and binge eating disorder-a systematic update of the evidence. Nutrients. 2017;9(11):1170.
Leehr EJ, Krohmer K, Schag K, Dresler T, Zipfel S, Giel KE. Emotion regulation model in binge eating disorder and obesity–a systematic review. Neurosci Biobehav Rev. 2015;49:125–34.
Steward T, Menchon JM, Jiménez-Murcia S, Soriano-Mas C, Fernandez-Aranda F. Neural network alterations across eating disorders: a narrative review of fMRI studies. Curr Neuropharmacol. 2018;16(8):1150–63.
Waltmann M, Herzog N, Horstmann A, Deserno L. Loss of control over eating: a systematic review of task based research into impulsive and compulsive processes in binge eating. Neurosci Biobehav Rev. 2021;129:330–50.
Zhang P, Wu GW, Yu FX, Liu Y, Li MY, Wang Z, et al. Abnormal regional neural activity and reorganized neural network in obesity: evidence from resting-state fMRI. Obes Silver Spring Md. 2020;28(7):1283–91.
Article Google Scholar
Greeno CG, Wing RR, Shiffman S. Binge antecedents in obese women with and without binge eating disorder. J Consult Clin Psychol. 2000;68(1):95–102.
Nicholls W, Devonport TJ, Blake M. The association between emotions and eating behaviour in an obese population with binge eating disorder: emotions and binge eating disorder. Obes Rev. 2016;17(1):30–42.
Stein RI, Kenardy J, Wiseman CV, Dounchis JZ, Arnow BA, Wilfley DE. What’s driving the binge in binge eating disorder?: a prospective examination of precursors and consequences. Int J Eat Disord. 2007;40(3):195–203.
Davis C. From passive overeating to « food addiction »: a spectrum of compulsion and severity. ISRN Obes. 2013;2013:435027.
PubMed PubMed Central Google Scholar
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–73.
Arexis M, Feron G, Brindisi MC, Billot PE, Chambaron S. Impacts of emotional regulation and inhibition on Emotional Eating (EE) and Binge Eating Disorder (BED): Protocol for a scoping review. Hal-03643357. 2022.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210.
Stapleton P, Whitehead M. Dysfunctional eating in an Australian community sample: the role of emotion regulation, impulsivity, and reward and punishment sensitivity. Aust Psychol. 2014;49(6):358–68.
Sultson H, Akkermann K. Investigating phenotypes of emotional eating based on weight categories: a latent profile analysis. Int J Eat Disord. 2019;52(9):1024–34.
Kornacka M, Czepczor-Bernat K, Napieralski P, Brytek-Matera A. Rumination, mood, and maladaptive eating behaviors in overweight and healthy populations. Eat Weight Disord EWD. 2021;26(1):273–85.
Deroost N, Cserjési R. Attentional avoidance of emotional information in emotional eating. Psychiatry Res. 2018;269:172–7.
Braden A, Musher-Eizenman D, Watford T, Emley E. Eating when depressed, anxious, bored, or happy: are emotional eating types associated with unique psychological and physical health correlates? Appetite. 2018;125:410–7.
Wolz I, Biehl S, Svaldi J. Emotional reactivity, suppression of emotions and response inhibition in emotional eaters: a multi-method pilot study. Appetite. 2021;161:105142.
Wood SMW, Schembre SM, He Q, Engelmann JM, Ames SL, Bechara A. Emotional eating and routine restraint scores are associated with activity in brain regions involved in urge and self-control. Physiol Behav. 2016;165:405–12.
Leehr EJ, Schag K, Dresler T, Grosse-Wentrup M, Hautzinger M, Fallgatter AJ, et al. Food specific inhibitory control under negative mood in binge-eating disorder: evidence from a multimethod approach. Int J Eat Disord. 2018;51(2):112–23.
Gianini LM, White MA, Masheb RM. Eating pathology, emotion regulation, and emotional overeating in obese adults with Binge Eating Disorder. Eat Behav. 2013;14(3):309–13.
Walenda A, Kostecka B, Santangelo PS, Kucharska K. Examining emotion regulation in binge-eating disorder. Borderline Personal Disord Emot Dysregulation. 2021;8(1):25.
Grant JE, Chamberlain SR. Neurocognitive findings in young adults with binge eating disorder. Int J Psychiatry Clin Pract. 2020;24(1):71–6.
Schag K, Teufel M, Junne F, Preissl H, Hautzinger M, Zipfel S, et al. Impulsivity in binge eating disorder: food cues elicit increased reward responses and disinhibition. PLoS ONE. 2013;8(10):e76542.
Leehr EJ, Schag K, Brückmann C, Plewnia C, Zipfel S, Nieratschker V, et al. A putative association of COMT Val(108/158)met with impulsivity in binge eating disorder. Eur Eat Disord Rev J Eat Disord Assoc. 2016;24(2):169–73.
Aloi M, Rania M, Carbone EA, Caroleo M, Calabrò G, Zaffino P, et al. Metacognition and emotion regulation as treatment targets in binge eating disorder: a network analysis study. J Eat Disord. 2021;9(1):22.
Görlach MG, Kohlmann S, Shedden-Mora M, Rief W, Westermann S. Expressive suppression of emotions and overeating in individuals with overweight and obesity. Eur Eat Disord Rev J Eat Disord Assoc. 2016;24(5):377–82.
Racine SE, Horvath SA. Emotion dysregulation across the spectrum of pathological eating: comparisons among women with binge eating, overeating, and loss of control eating. Eat Disord. 2018;26(1):13–25.
Loeber S, Rustemeier M, Paslakis G, Pietrowsky R, Müller A, Herpertz S. Mood and restrained eating moderate food-associated response inhibition in obese individuals with binge eating disorder. Psychiatry Res. 2018;264:346–53.
Munsch S, Meyer AH, Quartier V, Wilhelm FH. Binge eating in binge eating disorder: a breakdown of emotion regulatory process? Psychiatry Res. 2012;195(3):118–24.
Willem C, Gandolphe MC, Doba K, Roussel M, Verkindt H, Pattou F, et al. Eating in case of emotion dys-regulation, depression and anxiety: different pathways to emotional eating in moderate and severe obesity. Clin Obes. 2020;10(5):e12388.
Wang SB, Lydecker JA, Grilo CM. Rumination in patients with binge-eating disorder and obesity: associations with eating-disorder psychopathology and weight-bias internalization. Eur Eat Disord Rev J Eat Disord Assoc. 2017;25(2):98–103.
Mobbs O, Iglesias K, Golay A, Van der Linden M. Cognitive deficits in obese persons with and without binge eating disorder. Investigation using a mental flexibility task. Appetite. 2011;57(1):263–71.
Svaldi J, Naumann E, Trentowska M, Schmitz F. General and food-specific inhibitory deficits in binge eating disorder. Int J Eat Disord. 2014;47(5):534–42.
Kimberlin CL, Winterstein AG. Validity and reliability of measurement instruments used in research. Am J Health-Syst Pharm AJHP Off J Am Soc Health-Syst Pharm. 2008;65(23):2276–84.
Frost MH, Reeve BB, Liepa AM, Stauffer JW, Hays RD. Mayo/FDA patient-reported outcomes consensus meeting group; What is sufficient evidence for the reliability and validity of patient-reported outcome measures? Value Health J Int Soc Pharmacoeconomics Outcomes Res. 2007;10(Suppl 2):S94-105.
Raevuori A, Keski-Rahkonen A, Hoek HW. A review of eating disorders in males. Curr Opin Psychiatry. 2014;27(6):426–30.
Carr MM, Wiedemann AA, Macdonald-Gagnon G, Potenza MN. Impulsivity and compulsivity in binge eating disorder: a systematic review of behavioral studies. Prog Neuropsychopharmacol Biol Psychiatry. 2021;12:110318.
Saruco E, Pleger B. a systematic review of obesity and binge eating associated impairment of the cognitive inhibition system. Front Nutr. 2021;8:609012.
Berchio C, Cambi S, Pappaianni E, Micali N. EEG biomarkers in children and adolescents with feeding and eating disorders: current evidence and future directions. Front Psychiatry. 2022;13:882358.
Turton R, Chami R, Treasure J. Emotional eating, binge eating and animal models of binge-type eating disorders. Curr Obes Rep. 2017;6(2):217–28.
Download references
Acknowledgements
Not applicable.
This scoping review was supported by grants from the French National Research Agency [Agence Nationale de la Recherche (ANR): ImplicEAT project ANR-17-CE21-0001].
Author information
Authors and affiliations.
Centre Des Sciences du Goût Et de L’Alimentation, CNRS, INRAE, Institut Agro, Université de Bourgogne, 21000, Dijon, France
Mahé Arexis, Gilles Feron, Marie-Claude Brindisi & Stéphanie Chambaron
Université de Franche-Comté, LINC, 25000, Besançon, France
Mahé Arexis & Pierre-Édouard Billot
Centre Spécialisé de L’Obésité Bourgogne, Centre Hospitalier Universitaire Dijon Bourgogne, Dijon, France
Marie-Claude Brindisi
You can also search for this author in PubMed Google Scholar
Contributions
All authors participated in the conception of the study. Three investigators (authors MA, P-EB, and SC) developed a data charting form to extract the relevant data from each of the 32 included studies. For each study, author MA extracted the data according to the following variables of the chart: authors, title, year of publication, country of the study, journal of publication, type of study, method/study design, participants and sample sizes, type of interventions, comparisons, and outcomes/results. Two authors (MA and P-EB) listed the possible limitations of each study. The limitations identified by both authors were retained, and the others were either eliminated or retained after discussion. Two authors (SC and M-CB) checked this list, and their comments were considered. MA wrote the first draft of the article and MA, P-EB, SC and M-CB contributed to the final version. All authors proofread the final version.
Corresponding author
Correspondence to Pierre-Édouard Billot .
Ethics declarations
Ethics approval and consent to participate.
This scoping review did not involve animals or human participants, and we did not use personal information. All data used in this review were extracted from published articles.
Consent for publication
This scoping review did not involve human participants, and we did not use personal information. Thus, consent for publication was unnecessary for this scoping review.
Competing interests
The authors declare that they have no competing interests.
The review protocol can be accessed at HAL ( https://hal.science/hal-03643357v1 —HAL Id/Registration number: hal-03643357). Protocol reference: Arexis, M., Feron, G., Brindisi, M.-C., Billot, P.-E., & Chambaron, S. (2022). Impacts of emotional regulation and inhibition on Emotional Eating (EE) and Binge Eating Disorder (BED): Protocol for a scoping review. Hal-03643357 .
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Arexis, M., Feron, G., Brindisi, MC. et al. A scoping review of emotion regulation and inhibition in emotional eating and binge-eating disorder: what about a continuum?. J Eat Disord 11 , 197 (2023). https://doi.org/10.1186/s40337-023-00916-7
Download citation
Received : 24 February 2023
Accepted : 18 October 2023
Published : 10 November 2023
DOI : https://doi.org/10.1186/s40337-023-00916-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Scoping review
Journal of Eating Disorders
ISSN: 2050-2974
- General enquiries: [email protected]

COMMENTS
Anorexia nervosa is a chronic eating disorder which primarily affects adolescent girls and young women. 1 The prevalence of anorexia nervosa varies between 0.1-1%. 1 Although the prevalence is low, the morbidity is high and the mortality varies between 0.1-25%. 2 Relapse is common and chances of recovery are less than 50% in 10 years while 25% ...
The medical complications of eating disorders are well established in the medical literature. 4,5 This patient was ketotic and dehydrated and essentially refused to eat, and thus she met the ...
Background Most individuals with eating disorders will either recover, settle into an unrecovered but self-defined acceptable quality of life, or continue to cycle from crisis to relative stability over time. However, a minority of those with severe and enduring eating disorders recognize after years of trying that recovery remains elusive, and further treatment seems both futile and harmful ...
Background Anorexia Nervosa (AN) poses significant therapeutic challenges, especially in cases meeting the criteria for Severe and Enduring Anorexia Nervosa (SE-AN). This subset of AN is associated with severe medical complications, frequent use of services, and the highest mortality rate among psychiatric disorders. Case presentation In the present case series, 14 patients were selected from ...
Abstract. Anorexia nervosa is an eating disorder characterized by excessive restriction on food intake and irrational fear of gaining weight, often accompanied by a distorted body self-perception. It is clinically diagnosed more frequently in females, with type and severity varying with each case. The current report is a case of a 25-year-old ...
The Global Burden of Disease had estimated anorexia nervosa (AN) or bulimia nervosa to be 13.6 million people. The lifetime prevalence of AN ranges from 2.4 to 4.3 percent. During their lifetime, up to 4% of females and up to 0.3% of males suffer from anorexia nervosa. Studies assessing AN in Africa, including Ethiopia, are limited.
Anorexia nervosa is a complex psychiatric illness associated with food restriction and high mortality. Recent brain research in adolescents and adults with anorexia nervosa has used larger sample sizes compared with earlier studies and tasks that test specific brain circuits. Those studies have produced more robust results and advanced our ...
Studies show that adult patients with anorexia nervosa display cognitive impairments. These impairments may be caused by illness-related circumstances such as low weight. However, the question is whether there is a cognitive adaptation to enduring undernutrition in anorexia nervosa. To our knowledge, cognitive performance has not been assessed previously in a patient with anorexia nervosa with ...
Eating disorders (ED), especially Anorexia Nervosa (AN), are internationally reported to have amongst the highest mortality and suicide rates in mental health. With limited evidence for current pharmacological and/or psychological treatments, there is a grave responsibility within health research to better understand outcomes for people with a lived experience of ED, factors and interventions ...
Metrics. Abstract. In Brief. Anorexia nervosa (AN) is an eating disorder that is difficult to treat, and relapse is common. This article addresses management strategies and nursing interventions for adolescents diagnosed with AN. Figure. DX, 16, WAS ADMITTED with anorexia nervosa (AN) after unsuccessful outpatient treatment.
OBJECTIVE: Although there have been many studies of the outcome of anorexia nervosa, methodological weaknesses limit their interpretation. The authors used a case-control design to try to improve knowledge about the outcome of anorexia nervosa. METHOD: All new female patients referred to an eating disorders service between Jan. 1, 1981, and Dec. 31, 1984, who had probable or definite anorexia ...
Unfortunately, these patients and their carers often receive minimal support from eating disorders health professionals who are conflicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa. Case presentation: Three case studies elucidate this condition. One ...
Anorexia nervosa (AN) is a disorder that predominantly affects women in early adolescence 1. The characteristic features of AN include severe weight loss and secondary problems associated with ...
A Case Study of Anorexia Nervosa and Obsessive Personality Disorder Using Third-Generation Behavioral Therapies Francisco Martín-Murcia1, Adolfo J. Cangas Díaz1, and Luisa Pardo Gonzalez1 Abstract This article presents a case study of anorexia nervosa and obsessive personality disorder as a
1. Introduction. Anorexia nervosa (AN) is a serious illness characterized by self-induced underweight, body image distortion and fear of weight gain [1,2,3,4].AN is one of the most common chronic diseases in teenage girls, ranking third after obesity and asthma, and continues to rise in that population [].Its treatment is long and complex, involving a multidisciplinary team [6,7].
Case Report. Ms. K, a 22-year-old black female, with no past medical or psychiatric history, presented for evaluation of weight loss and refusal to eat. Her mother reported changes in eating behaviors for the prior six months with a 13.6 kg weight loss. Ms K had recently graduated from a 4-year college and planned to move across the country to ...
A Case Study of Anorexia Nervosa. Lucy Howarth, Corresponding Author. Southampton University Medical School Southampton General Hospital, Tremona Road Southampton, U.K. Southampton University Medical School Southampton General Hospital, Tremona Road Southampton, U.K.Search for more papers by this author.
Abstract. D.R., a single 19-year-old female experiencing anorexia nervosa, was admitted to a mental health center inpatient unit weighing 64 lb, approximately 54 lb underweight, with liver, kidney, and pancreas damage. D.R. was hospitalized for 59 days. Treatment consisted of utilizing a hierarchy of reinforcements in the form of privileges ...
A prevailing misconception is that an eating disorder, particularly those marked by restrictive eating, is always outwardly recognizable due to malnutrition or emaciation [].In reality, restrictive eating disorders occur across a range of body weights [2, 3].For instance, Atypical Anorexia Nervosa (AAN), currently categorized as an Other Specified Feeding and Eating Disorder in the DSM-5 ...
For example, Chandra et al. (1995) described three case studies of anorexia in India, but only one of them fulfilled the biomedical criteria for anorexia nervosa, which include refusal to maintain one's body weight at or above the minimally normal weight for specific age and height; intense fear of gaining body weight or becoming fat; and ...
Results: The findings suggest that studies on the subject are limited by issues regarding data on the prevalence of comorbidities, phenomenological aspects of eating disorders, and the interface and integration with psychotic symptoms. Conclusions: The case presented illustrates the difficulties in managing a patient with a comorbid eating ...
Anorexia nervosa is an often-severe psychiatric illness characterized by significantly low body weight, fear of gaining weight, and distorted body image. Multiple neuroimaging studies have shown ...
Family-based treatment (FBT) is recommended for anorexia nervosa (AN) in young people (YP). However, a substantial proportion of YP undergoing FBT do not recover. Several modifications to standard FBT have been tested to improve recovery rates. This review provides an updated overview of empirically tested modifications to FBT for AN in YP and estimates whether such modifications increase the ...
patients and their carers often receive minimal support from eating disorders health professionals who are conicted about terminal care, and who are hampered and limited by the paucity of literature on end-of-life care for those with anorexia nervosa. Case presentation: Three case studies elucidate this condition.
Background Amidst growing evidence of the intricate link between physical and mental health, this study aims to dissect the relationship between the waist-to-weight index (WWI) and suicidal ideation within a representative sample of the US population, proposing WWI as a novel metric for suicide risk assessment. Methods The study engaged a sample of 9500 participants in a cross-sectional design ...
Third, most of the participants enrolled in these studies were women, compromising the generalizability to the global population (81.3% of studies had only women participants or an unbalanced sex ratio toward women). Eating disorders are more frequent among women, and for BED, the ratio varies between 1:2 and 1:6 . Thus, while the lack of men ...