Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Published: 05 October 2018

Interviews and focus groups in qualitative research: an update for the digital age
- P. Gill 1 &
- J. Baillie 2
British Dental Journal volume 225 , pages 668–672 ( 2018 ) Cite this article
28k Accesses
48 Citations
20 Altmetric
Metrics details
Highlights that qualitative research is used increasingly in dentistry. Interviews and focus groups remain the most common qualitative methods of data collection.
Suggests the advent of digital technologies has transformed how qualitative research can now be undertaken.
Suggests interviews and focus groups can offer significant, meaningful insight into participants' experiences, beliefs and perspectives, which can help to inform developments in dental practice.
Qualitative research is used increasingly in dentistry, due to its potential to provide meaningful, in-depth insights into participants' experiences, perspectives, beliefs and behaviours. These insights can subsequently help to inform developments in dental practice and further related research. The most common methods of data collection used in qualitative research are interviews and focus groups. While these are primarily conducted face-to-face, the ongoing evolution of digital technologies, such as video chat and online forums, has further transformed these methods of data collection. This paper therefore discusses interviews and focus groups in detail, outlines how they can be used in practice, how digital technologies can further inform the data collection process, and what these methods can offer dentistry.
You have full access to this article via your institution.
Similar content being viewed by others

Interviews in the social sciences

Professionalism in dentistry: deconstructing common terminology
A review of technical and quality assessment considerations of audio-visual and web-conferencing focus groups in qualitative health research, introduction.
Traditionally, research in dentistry has primarily been quantitative in nature. 1 However, in recent years, there has been a growing interest in qualitative research within the profession, due to its potential to further inform developments in practice, policy, education and training. Consequently, in 2008, the British Dental Journal (BDJ) published a four paper qualitative research series, 2 , 3 , 4 , 5 to help increase awareness and understanding of this particular methodological approach.
Since the papers were originally published, two scoping reviews have demonstrated the ongoing proliferation in the use of qualitative research within the field of oral healthcare. 1 , 6 To date, the original four paper series continue to be well cited and two of the main papers remain widely accessed among the BDJ readership. 2 , 3 The potential value of well-conducted qualitative research to evidence-based practice is now also widely recognised by service providers, policy makers, funding bodies and those who commission, support and use healthcare research.
Besides increasing standalone use, qualitative methods are now also routinely incorporated into larger mixed method study designs, such as clinical trials, as they can offer additional, meaningful insights into complex problems that simply could not be provided by quantitative methods alone. Qualitative methods can also be used to further facilitate in-depth understanding of important aspects of clinical trial processes, such as recruitment. For example, Ellis et al . investigated why edentulous older patients, dissatisfied with conventional dentures, decline implant treatment, despite its established efficacy, and frequently refuse to participate in related randomised clinical trials, even when financial constraints are removed. 7 Through the use of focus groups in Canada and the UK, the authors found that fears of pain and potential complications, along with perceived embarrassment, exacerbated by age, are common reasons why older patients typically refuse dental implants. 7
The last decade has also seen further developments in qualitative research, due to the ongoing evolution of digital technologies. These developments have transformed how researchers can access and share information, communicate and collaborate, recruit and engage participants, collect and analyse data and disseminate and translate research findings. 8 Where appropriate, such technologies are therefore capable of extending and enhancing how qualitative research is undertaken. 9 For example, it is now possible to collect qualitative data via instant messaging, email or online/video chat, using appropriate online platforms.
These innovative approaches to research are therefore cost-effective, convenient, reduce geographical constraints and are often useful for accessing 'hard to reach' participants (for example, those who are immobile or socially isolated). 8 , 9 However, digital technologies are still relatively new and constantly evolving and therefore present a variety of pragmatic and methodological challenges. Furthermore, given their very nature, their use in many qualitative studies and/or with certain participant groups may be inappropriate and should therefore always be carefully considered. While it is beyond the scope of this paper to provide a detailed explication regarding the use of digital technologies in qualitative research, insight is provided into how such technologies can be used to facilitate the data collection process in interviews and focus groups.
In light of such developments, it is perhaps therefore timely to update the main paper 3 of the original BDJ series. As with the previous publications, this paper has been purposely written in an accessible style, to enhance readability, particularly for those who are new to qualitative research. While the focus remains on the most common qualitative methods of data collection – interviews and focus groups – appropriate revisions have been made to provide a novel perspective, and should therefore be helpful to those who would like to know more about qualitative research. This paper specifically focuses on undertaking qualitative research with adult participants only.
Overview of qualitative research
Qualitative research is an approach that focuses on people and their experiences, behaviours and opinions. 10 , 11 The qualitative researcher seeks to answer questions of 'how' and 'why', providing detailed insight and understanding, 11 which quantitative methods cannot reach. 12 Within qualitative research, there are distinct methodologies influencing how the researcher approaches the research question, data collection and data analysis. 13 For example, phenomenological studies focus on the lived experience of individuals, explored through their description of the phenomenon. Ethnographic studies explore the culture of a group and typically involve the use of multiple methods to uncover the issues. 14
While methodology is the 'thinking tool', the methods are the 'doing tools'; 13 the ways in which data are collected and analysed. There are multiple qualitative data collection methods, including interviews, focus groups, observations, documentary analysis, participant diaries, photography and videography. Two of the most commonly used qualitative methods are interviews and focus groups, which are explored in this article. The data generated through these methods can be analysed in one of many ways, according to the methodological approach chosen. A common approach is thematic data analysis, involving the identification of themes and subthemes across the data set. Further information on approaches to qualitative data analysis has been discussed elsewhere. 1
Qualitative research is an evolving and adaptable approach, used by different disciplines for different purposes. Traditionally, qualitative data, specifically interviews, focus groups and observations, have been collected face-to-face with participants. In more recent years, digital technologies have contributed to the ongoing evolution of qualitative research. Digital technologies offer researchers different ways of recruiting participants and collecting data, and offer participants opportunities to be involved in research that is not necessarily face-to-face.
Research interviews are a fundamental qualitative research method 15 and are utilised across methodological approaches. Interviews enable the researcher to learn in depth about the perspectives, experiences, beliefs and motivations of the participant. 3 , 16 Examples include, exploring patients' perspectives of fear/anxiety triggers in dental treatment, 17 patients' experiences of oral health and diabetes, 18 and dental students' motivations for their choice of career. 19
Interviews may be structured, semi-structured or unstructured, 3 according to the purpose of the study, with less structured interviews facilitating a more in depth and flexible interviewing approach. 20 Structured interviews are similar to verbal questionnaires and are used if the researcher requires clarification on a topic; however they produce less in-depth data about a participant's experience. 3 Unstructured interviews may be used when little is known about a topic and involves the researcher asking an opening question; 3 the participant then leads the discussion. 20 Semi-structured interviews are commonly used in healthcare research, enabling the researcher to ask predetermined questions, 20 while ensuring the participant discusses issues they feel are important.
Interviews can be undertaken face-to-face or using digital methods when the researcher and participant are in different locations. Audio-recording the interview, with the consent of the participant, is essential for all interviews regardless of the medium as it enables accurate transcription; the process of turning the audio file into a word-for-word transcript. This transcript is the data, which the researcher then analyses according to the chosen approach.
Types of interview
Qualitative studies often utilise one-to-one, face-to-face interviews with research participants. This involves arranging a mutually convenient time and place to meet the participant, signing a consent form and audio-recording the interview. However, digital technologies have expanded the potential for interviews in research, enabling individuals to participate in qualitative research regardless of location.
Telephone interviews can be a useful alternative to face-to-face interviews and are commonly used in qualitative research. They enable participants from different geographical areas to participate and may be less onerous for participants than meeting a researcher in person. 15 A qualitative study explored patients' perspectives of dental implants and utilised telephone interviews due to the quality of the data that could be yielded. 21 The researcher needs to consider how they will audio record the interview, which can be facilitated by purchasing a recorder that connects directly to the telephone. One potential disadvantage of telephone interviews is the inability of the interviewer and researcher to see each other. This is resolved using software for audio and video calls online – such as Skype – to conduct interviews with participants in qualitative studies. Advantages of this approach include being able to see the participant if video calls are used, enabling observation of non-verbal communication, and the software can be free to use. However, participants are required to have a device and internet connection, as well as being computer literate, potentially limiting who can participate in the study. One qualitative study explored the role of dental hygienists in reducing oral health disparities in Canada. 22 The researcher conducted interviews using Skype, which enabled dental hygienists from across Canada to be interviewed within the research budget, accommodating the participants' schedules. 22
A less commonly used approach to qualitative interviews is the use of social virtual worlds. A qualitative study accessed a social virtual world – Second Life – to explore the health literacy skills of individuals who use social virtual worlds to access health information. 23 The researcher created an avatar and interview room, and undertook interviews with participants using voice and text methods. 23 This approach to recruitment and data collection enables individuals from diverse geographical locations to participate, while remaining anonymous if they wish. Furthermore, for interviews conducted using text methods, transcription of the interview is not required as the researcher can save the written conversation with the participant, with the participant's consent. However, the researcher and participant need to be familiar with how the social virtual world works to engage in an interview this way.
Conducting an interview
Ensuring informed consent before any interview is a fundamental aspect of the research process. Participants in research must be afforded autonomy and respect; consent should be informed and voluntary. 24 Individuals should have the opportunity to read an information sheet about the study, ask questions, understand how their data will be stored and used, and know that they are free to withdraw at any point without reprisal. The qualitative researcher should take written consent before undertaking the interview. In a face-to-face interview, this is straightforward: the researcher and participant both sign copies of the consent form, keeping one each. However, this approach is less straightforward when the researcher and participant do not meet in person. A recent protocol paper outlined an approach for taking consent for telephone interviews, which involved: audio recording the participant agreeing to each point on the consent form; the researcher signing the consent form and keeping a copy; and posting a copy to the participant. 25 This process could be replicated in other interview studies using digital methods.
There are advantages and disadvantages of using face-to-face and digital methods for research interviews. Ultimately, for both approaches, the quality of the interview is determined by the researcher. 16 Appropriate training and preparation are thus required. Healthcare professionals can use their interpersonal communication skills when undertaking a research interview, particularly questioning, listening and conversing. 3 However, the purpose of an interview is to gain information about the study topic, 26 rather than offering help and advice. 3 The researcher therefore needs to listen attentively to participants, enabling them to describe their experience without interruption. 3 The use of active listening skills also help to facilitate the interview. 14 Spradley outlined elements and strategies for research interviews, 27 which are a useful guide for qualitative researchers:
Greeting and explaining the project/interview
Asking descriptive (broad), structural (explore response to descriptive) and contrast (difference between) questions
Asymmetry between the researcher and participant talking
Expressing interest and cultural ignorance
Repeating, restating and incorporating the participant's words when asking questions
Creating hypothetical situations
Asking friendly questions
Knowing when to leave.
For semi-structured interviews, a topic guide (also called an interview schedule) is used to guide the content of the interview – an example of a topic guide is outlined in Box 1 . The topic guide, usually based on the research questions, existing literature and, for healthcare professionals, their clinical experience, is developed by the research team. The topic guide should include open ended questions that elicit in-depth information, and offer participants the opportunity to talk about issues important to them. This is vital in qualitative research where the researcher is interested in exploring the experiences and perspectives of participants. It can be useful for qualitative researchers to pilot the topic guide with the first participants, 10 to ensure the questions are relevant and understandable, and amending the questions if required.
Regardless of the medium of interview, the researcher must consider the setting of the interview. For face-to-face interviews, this could be in the participant's home, in an office or another mutually convenient location. A quiet location is preferable to promote confidentiality, enable the researcher and participant to concentrate on the conversation, and to facilitate accurate audio-recording of the interview. For interviews using digital methods the same principles apply: a quiet, private space where the researcher and participant feel comfortable and confident to participate in an interview.
Box 1: Example of a topic guide
Study focus: Parents' experiences of brushing their child's (aged 0–5) teeth
1. Can you tell me about your experience of cleaning your child's teeth?
How old was your child when you started cleaning their teeth?
Why did you start cleaning their teeth at that point?
How often do you brush their teeth?
What do you use to brush their teeth and why?
2. Could you explain how you find cleaning your child's teeth?
Do you find anything difficult?
What makes cleaning their teeth easier for you?
3. How has your experience of cleaning your child's teeth changed over time?
Has it become easier or harder?
Have you changed how often and how you clean their teeth? If so, why?
4. Could you describe how your child finds having their teeth cleaned?
What do they enjoy about having their teeth cleaned?
Is there anything they find upsetting about having their teeth cleaned?
5. Where do you look for information/advice about cleaning your child's teeth?
What did your health visitor tell you about cleaning your child's teeth? (If anything)
What has the dentist told you about caring for your child's teeth? (If visited)
Have any family members given you advice about how to clean your child's teeth? If so, what did they tell you? Did you follow their advice?
6. Is there anything else you would like to discuss about this?
Focus groups
A focus group is a moderated group discussion on a pre-defined topic, for research purposes. 28 , 29 While not aligned to a particular qualitative methodology (for example, grounded theory or phenomenology) as such, focus groups are used increasingly in healthcare research, as they are useful for exploring collective perspectives, attitudes, behaviours and experiences. Consequently, they can yield rich, in-depth data and illuminate agreement and inconsistencies 28 within and, where appropriate, between groups. Examples include public perceptions of dental implants and subsequent impact on help-seeking and decision making, 30 and general dental practitioners' views on patient safety in dentistry. 31
Focus groups can be used alone or in conjunction with other methods, such as interviews or observations, and can therefore help to confirm, extend or enrich understanding and provide alternative insights. 28 The social interaction between participants often results in lively discussion and can therefore facilitate the collection of rich, meaningful data. However, they are complex to organise and manage, due to the number of participants, and may also be inappropriate for exploring particularly sensitive issues that many participants may feel uncomfortable about discussing in a group environment.
Focus groups are primarily undertaken face-to-face but can now also be undertaken online, using appropriate technologies such as email, bulletin boards, online research communities, chat rooms, discussion forums, social media and video conferencing. 32 Using such technologies, data collection can also be synchronous (for example, online discussions in 'real time') or, unlike traditional face-to-face focus groups, asynchronous (for example, online/email discussions in 'non-real time'). While many of the fundamental principles of focus group research are the same, regardless of how they are conducted, a number of subtle nuances are associated with the online medium. 32 Some of which are discussed further in the following sections.
Focus group considerations
Some key considerations associated with face-to-face focus groups are: how many participants are required; should participants within each group know each other (or not) and how many focus groups are needed within a single study? These issues are much debated and there is no definitive answer. However, the number of focus groups required will largely depend on the topic area, the depth and breadth of data needed, the desired level of participation required 29 and the necessity (or not) for data saturation.
The optimum group size is around six to eight participants (excluding researchers) but can work effectively with between three and 14 participants. 3 If the group is too small, it may limit discussion, but if it is too large, it may become disorganised and difficult to manage. It is, however, prudent to over-recruit for a focus group by approximately two to three participants, to allow for potential non-attenders. For many researchers, particularly novice researchers, group size may also be informed by pragmatic considerations, such as the type of study, resources available and moderator experience. 28 Similar size and mix considerations exist for online focus groups. Typically, synchronous online focus groups will have around three to eight participants but, as the discussion does not happen simultaneously, asynchronous groups may have as many as 10–30 participants. 33
The topic area and potential group interaction should guide group composition considerations. Pre-existing groups, where participants know each other (for example, work colleagues) may be easier to recruit, have shared experiences and may enjoy a familiarity, which facilitates discussion and/or the ability to challenge each other courteously. 3 However, if there is a potential power imbalance within the group or if existing group norms and hierarchies may adversely affect the ability of participants to speak freely, then 'stranger groups' (that is, where participants do not already know each other) may be more appropriate. 34 , 35
Focus group management
Face-to-face focus groups should normally be conducted by two researchers; a moderator and an observer. 28 The moderator facilitates group discussion, while the observer typically monitors group dynamics, behaviours, non-verbal cues, seating arrangements and speaking order, which is essential for transcription and analysis. The same principles of informed consent, as discussed in the interview section, also apply to focus groups, regardless of medium. However, the consent process for online discussions will probably be managed somewhat differently. For example, while an appropriate participant information leaflet (and consent form) would still be required, the process is likely to be managed electronically (for example, via email) and would need to specifically address issues relating to technology (for example, anonymity and use, storage and access to online data). 32
The venue in which a face to face focus group is conducted should be of a suitable size, private, quiet, free from distractions and in a collectively convenient location. It should also be conducted at a time appropriate for participants, 28 as this is likely to promote attendance. As with interviews, the same ethical considerations apply (as discussed earlier). However, online focus groups may present additional ethical challenges associated with issues such as informed consent, appropriate access and secure data storage. Further guidance can be found elsewhere. 8 , 32
Before the focus group commences, the researchers should establish rapport with participants, as this will help to put them at ease and result in a more meaningful discussion. Consequently, researchers should introduce themselves, provide further clarity about the study and how the process will work in practice and outline the 'ground rules'. Ground rules are designed to assist, not hinder, group discussion and typically include: 3 , 28 , 29
Discussions within the group are confidential to the group
Only one person can speak at a time
All participants should have sufficient opportunity to contribute
There should be no unnecessary interruptions while someone is speaking
Everyone can be expected to be listened to and their views respected
Challenging contrary opinions is appropriate, but ridiculing is not.
Moderating a focus group requires considered management and good interpersonal skills to help guide the discussion and, where appropriate, keep it sufficiently focused. Avoid, therefore, participating, leading, expressing personal opinions or correcting participants' knowledge 3 , 28 as this may bias the process. A relaxed, interested demeanour will also help participants to feel comfortable and promote candid discourse. Moderators should also prevent the discussion being dominated by any one person, ensure differences of opinions are discussed fairly and, if required, encourage reticent participants to contribute. 3 Asking open questions, reflecting on significant issues, inviting further debate, probing responses accordingly, and seeking further clarification, as and where appropriate, will help to obtain sufficient depth and insight into the topic area.
Moderating online focus groups requires comparable skills, particularly if the discussion is synchronous, as the discussion may be dominated by those who can type proficiently. 36 It is therefore important that sufficient time and respect is accorded to those who may not be able to type as quickly. Asynchronous discussions are usually less problematic in this respect, as interactions are less instant. However, moderating an asynchronous discussion presents additional challenges, particularly if participants are geographically dispersed, as they may be online at different times. Consequently, the moderator will not always be present and the discussion may therefore need to occur over several days, which can be difficult to manage and facilitate and invariably requires considerable flexibility. 32 It is also worth recognising that establishing rapport with participants via online medium is often more challenging than via face-to-face and may therefore require additional time, skills, effort and consideration.
As with research interviews, focus groups should be guided by an appropriate interview schedule, as discussed earlier in the paper. For example, the schedule will usually be informed by the review of the literature and study aims, and will merely provide a topic guide to help inform subsequent discussions. To provide a verbatim account of the discussion, focus groups must be recorded, using an audio-recorder with a good quality multi-directional microphone. While videotaping is possible, some participants may find it obtrusive, 3 which may adversely affect group dynamics. The use (or not) of a video recorder, should therefore be carefully considered.
At the end of the focus group, a few minutes should be spent rounding up and reflecting on the discussion. 28 Depending on the topic area, it is possible that some participants may have revealed deeply personal issues and may therefore require further help and support, such as a constructive debrief or possibly even referral on to a relevant third party. It is also possible that some participants may feel that the discussion did not adequately reflect their views and, consequently, may no longer wish to be associated with the study. 28 Such occurrences are likely to be uncommon, but should they arise, it is important to further discuss any concerns and, if appropriate, offer them the opportunity to withdraw (including any data relating to them) from the study. Immediately after the discussion, researchers should compile notes regarding thoughts and ideas about the focus group, which can assist with data analysis and, if appropriate, any further data collection.
Qualitative research is increasingly being utilised within dental research to explore the experiences, perspectives, motivations and beliefs of participants. The contributions of qualitative research to evidence-based practice are increasingly being recognised, both as standalone research and as part of larger mixed-method studies, including clinical trials. Interviews and focus groups remain commonly used data collection methods in qualitative research, and with the advent of digital technologies, their utilisation continues to evolve. However, digital methods of qualitative data collection present additional methodological, ethical and practical considerations, but also potentially offer considerable flexibility to participants and researchers. Consequently, regardless of format, qualitative methods have significant potential to inform important areas of dental practice, policy and further related research.
Gussy M, Dickson-Swift V, Adams J . A scoping review of qualitative research in peer-reviewed dental publications. Int J Dent Hygiene 2013; 11 : 174–179.
Article Google Scholar
Burnard P, Gill P, Stewart K, Treasure E, Chadwick B . Analysing and presenting qualitative data. Br Dent J 2008; 204 : 429–432.
Gill P, Stewart K, Treasure E, Chadwick B . Methods of data collection in qualitative research: interviews and focus groups. Br Dent J 2008; 204 : 291–295.
Gill P, Stewart K, Treasure E, Chadwick B . Conducting qualitative interviews with school children in dental research. Br Dent J 2008; 204 : 371–374.
Stewart K, Gill P, Chadwick B, Treasure E . Qualitative research in dentistry. Br Dent J 2008; 204 : 235–239.
Masood M, Thaliath E, Bower E, Newton J . An appraisal of the quality of published qualitative dental research. Community Dent Oral Epidemiol 2011; 39 : 193–203.
Ellis J, Levine A, Bedos C et al. Refusal of implant supported mandibular overdentures by elderly patients. Gerodontology 2011; 28 : 62–68.
Macfarlane S, Bucknall T . Digital Technologies in Research. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . 7th edition. pp. 71–86. Oxford: Wiley Blackwell; 2015.
Google Scholar
Lee R, Fielding N, Blank G . Online Research Methods in the Social Sciences: An Editorial Introduction. In Fielding N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 3–16. London: Sage Publications; 2016.
Creswell J . Qualitative inquiry and research design: Choosing among five designs . Thousand Oaks, CA: Sage, 1998.
Guest G, Namey E, Mitchell M . Qualitative research: Defining and designing In Guest G, Namey E, Mitchell M (editors) Collecting Qualitative Data: A Field Manual For Applied Research . pp. 1–40. London: Sage Publications, 2013.
Chapter Google Scholar
Pope C, Mays N . Qualitative research: Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ 1995; 311 : 42–45.
Giddings L, Grant B . A Trojan Horse for positivism? A critique of mixed methods research. Adv Nurs Sci 2007; 30 : 52–60.
Hammersley M, Atkinson P . Ethnography: Principles in Practice . London: Routledge, 1995.
Oltmann S . Qualitative interviews: A methodological discussion of the interviewer and respondent contexts Forum Qualitative Sozialforschung/Forum: Qualitative Social Research. 2016; 17 : Art. 15.
Patton M . Qualitative Research and Evaluation Methods . Thousand Oaks, CA: Sage, 2002.
Wang M, Vinall-Collier K, Csikar J, Douglas G . A qualitative study of patients' views of techniques to reduce dental anxiety. J Dent 2017; 66 : 45–51.
Lindenmeyer A, Bowyer V, Roscoe J, Dale J, Sutcliffe P . Oral health awareness and care preferences in patients with diabetes: a qualitative study. Fam Pract 2013; 30 : 113–118.
Gallagher J, Clarke W, Wilson N . Understanding the motivation: a qualitative study of dental students' choice of professional career. Eur J Dent Educ 2008; 12 : 89–98.
Tod A . Interviewing. In Gerrish K, Lacey A (editors) The Research Process in Nursing . Oxford: Blackwell Publishing, 2006.
Grey E, Harcourt D, O'Sullivan D, Buchanan H, Kipatrick N . A qualitative study of patients' motivations and expectations for dental implants. Br Dent J 2013; 214 : 10.1038/sj.bdj.2012.1178.
Farmer J, Peressini S, Lawrence H . Exploring the role of the dental hygienist in reducing oral health disparities in Canada: A qualitative study. Int J Dent Hygiene 2017; 10.1111/idh.12276.
McElhinney E, Cheater F, Kidd L . Undertaking qualitative health research in social virtual worlds. J Adv Nurs 2013; 70 : 1267–1275.
Health Research Authority. UK Policy Framework for Health and Social Care Research. Available at https://www.hra.nhs.uk/planning-and-improving-research/policies-standards-legislation/uk-policy-framework-health-social-care-research/ (accessed September 2017).
Baillie J, Gill P, Courtenay P . Knowledge, understanding and experiences of peritonitis among patients, and their families, undertaking peritoneal dialysis: A mixed methods study protocol. J Adv Nurs 2017; 10.1111/jan.13400.
Kvale S . Interviews . Thousand Oaks (CA): Sage, 1996.
Spradley J . The Ethnographic Interview . New York: Holt, Rinehart and Winston, 1979.
Goodman C, Evans C . Focus Groups. In Gerrish K, Lathlean J (editors) The Research Process in Nursing . pp. 401–412. Oxford: Wiley Blackwell, 2015.
Shaha M, Wenzell J, Hill E . Planning and conducting focus group research with nurses. Nurse Res 2011; 18 : 77–87.
Wang G, Gao X, Edward C . Public perception of dental implants: a qualitative study. J Dent 2015; 43 : 798–805.
Bailey E . Contemporary views of dental practitioners' on patient safety. Br Dent J 2015; 219 : 535–540.
Abrams K, Gaiser T . Online Focus Groups. In Field N, Lee R, Blank G (editors) The Sage Handbook of Online Research Methods . pp. 435–450. London: Sage Publications, 2016.
Poynter R . The Handbook of Online and Social Media Research . West Sussex: John Wiley & Sons, 2010.
Kevern J, Webb C . Focus groups as a tool for critical social research in nurse education. Nurse Educ Today 2001; 21 : 323–333.
Kitzinger J, Barbour R . Introduction: The Challenge and Promise of Focus Groups. In Barbour R S K J (editor) Developing Focus Group Research . pp. 1–20. London: Sage Publications, 1999.
Krueger R, Casey M . Focus Groups: A Practical Guide for Applied Research. 4th ed. Thousand Oaks, California: SAGE; 2009.
Download references
Author information
Authors and affiliations.
Senior Lecturer (Adult Nursing), School of Healthcare Sciences, Cardiff University,
Lecturer (Adult Nursing) and RCBC Wales Postdoctoral Research Fellow, School of Healthcare Sciences, Cardiff University,
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to P. Gill .
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Gill, P., Baillie, J. Interviews and focus groups in qualitative research: an update for the digital age. Br Dent J 225 , 668–672 (2018). https://doi.org/10.1038/sj.bdj.2018.815
Download citation
Accepted : 02 July 2018
Published : 05 October 2018
Issue Date : 12 October 2018
DOI : https://doi.org/10.1038/sj.bdj.2018.815
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Translating brand reputation into equity from the stakeholder’s theory: an approach to value creation based on consumer’s perception & interactions.
- Olukorede Adewole
International Journal of Corporate Social Responsibility (2024)
Perceptions and beliefs of community gatekeepers about genomic risk information in African cleft research
- Abimbola M. Oladayo
- Oluwakemi Odukoya
- Azeez Butali
BMC Public Health (2024)
Assessment of women’s needs, wishes and preferences regarding interprofessional guidance on nutrition in pregnancy – a qualitative study
- Merle Ebinghaus
- Caroline Johanna Agricola
- Birgit-Christiane Zyriax
BMC Pregnancy and Childbirth (2024)
‘Baby mamas’ in Urban Ghana: an exploratory qualitative study on the factors influencing serial fathering among men in Accra, Ghana
- Rosemond Akpene Hiadzi
- Jemima Akweley Agyeman
- Godwin Banafo Akrong
Reproductive Health (2023)
Revolutionising dental technologies: a qualitative study on dental technicians’ perceptions of Artificial intelligence integration
- Galvin Sim Siang Lin
- Yook Shiang Ng
- Kah Hoay Chua
BMC Oral Health (2023)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

Chapter 12. Focus Groups
Introduction.
Focus groups are a particular and special form of interviewing in which the interview asks focused questions of a group of persons, optimally between five and eight. This group can be close friends, family members, or complete strangers. They can have a lot in common or nothing in common. Unlike one-on-one interviews, which can probe deeply, focus group questions are narrowly tailored (“focused”) to a particular topic and issue and, with notable exceptions, operate at the shallow end of inquiry. For example, market researchers use focus groups to find out why groups of people choose one brand of product over another. Because focus groups are often used for commercial purposes, they sometimes have a bit of a stigma among researchers. This is unfortunate, as the focus group is a helpful addition to the qualitative researcher’s toolkit. Focus groups explicitly use group interaction to assist in the data collection. They are particularly useful as supplements to one-on-one interviews or in data triangulation. They are sometimes used to initiate areas of inquiry for later data collection methods. This chapter describes the main forms of focus groups, lays out some key differences among those forms, and provides guidance on how to manage focus group interviews.

Focus Groups: What Are They and When to Use Them
As interviews, focus groups can be helpfully distinguished from one-on-one interviews. The purpose of conducting a focus group is not to expand the number of people one interviews: the focus group is a different entity entirely. The focus is on the group and its interactions and evaluations rather than on the individuals in that group. If you want to know how individuals understand their lives and their individual experiences, it is best to ask them individually. If you want to find out how a group forms a collective opinion about something (whether a product or an event or an experience), then conducting a focus group is preferable. The power of focus groups resides in their being both focused and oriented to the group . They are best used when you are interested in the shared meanings of a group or how people discuss a topic publicly or when you want to observe the social formation of evaluations. The interaction of the group members is an asset in this method of data collection. If your questions would not benefit from group interaction, this is a good indicator that you should probably use individual interviews (chapter 11). Avoid using focus groups when you are interested in personal information or strive to uncover deeply buried beliefs or personal narratives. In general, you want to avoid using focus groups when the subject matter is polarizing, as people are less likely to be honest in a group setting. There are a few exceptions, such as when you are conducting focus groups with people who are not strangers and/or you are attempting to probe deeply into group beliefs and evaluations. But caution is warranted in these cases. [1]
As with interviewing in general, there are many forms of focus groups. Focus groups are widely used by nonresearchers, so it is important to distinguish these uses from the research focus group. Businesses routinely employ marketing focus groups to test out products or campaigns. Jury consultants employ “mock” jury focus groups, testing out legal case strategies in advance of actual trials. Organizations of various kinds use focus group interviews for program evaluation (e.g., to gauge the effectiveness of a diversity training workshop). The research focus group has many similarities with all these uses but is specifically tailored to a research (rather than applied) interest. The line between application and research use can be blurry, however. To take the case of evaluating the effectiveness of a diversity training workshop, the same interviewer may be conducting focus group interviews both to provide specific actionable feedback for the workshop leaders (this is the application aspect) and to learn more about how people respond to diversity training (an interesting research question with theoretically generalizable results).
When forming a focus group, there are two different strategies for inclusion. Diversity focus groups include people with diverse perspectives and experiences. This helps the researcher identify commonalities across this diversity and/or note interactions across differences. What kind of diversity to capture depends on the research question, but care should be taken to ensure that those participating are not set up for attack from other participants. This is why many warn against diversity focus groups, especially around politically sensitive topics. The other strategy is to build a convergence focus group , which includes people with similar perspectives and experiences. These are particularly helpful for identifying shared patterns and group consensus. The important thing is to closely consider who will be invited to participate and what the composition of the group will be in advance. Some review of sampling techniques (see chapter 5) may be helpful here.
Moderating a focus group can be a challenge (more on this below). For this reason, confining your group to no more than eight participants is recommended. You probably want at least four persons to capture group interaction. Fewer than four participants can also make it more difficult for participants to remain (relatively) anonymous—there is less of a group in which to hide. There are exceptions to these recommendations. You might want to conduct a focus group with a naturally occurring group, as in the case of a family of three, a social club of ten, or a program of fifteen. When the persons know one another, the problems of too few for anonymity don’t apply, and although ten to fifteen can be unwieldy to manage, there are strategies to make this possible. If you really are interested in this group’s dynamic (not just a set of random strangers’ dynamic), then you will want to include all its members or as many as are willing and able to participate.
There are many benefits to conducting focus groups, the first of which is their interactivity. Participants can make comparisons, can elaborate on what has been voiced by another, and can even check one another, leading to real-time reevaluations. This last benefit is one reason they are sometimes employed specifically for consciousness raising or building group cohesion. This form of data collection has an activist application when done carefully and appropriately. It can be fun, especially for the participants. Additionally, what does not come up in a focus group, especially when expected by the researcher, can be very illuminating.
Many of these benefits do incur costs, however. The multiplicity of voices in a good focus group interview can be overwhelming both to moderate and later to transcribe. Because of the focused nature, deep probing is not possible (or desirable). You might only get superficial thinking or what people are willing to put out there publicly. If that is what you are interested in, good. If you want deeper insight, you probably will not get that here. Relatedly, extreme views are often suppressed, and marginal viewpoints are unspoken or, if spoken, derided. You will get the majority group consensus and very little of minority viewpoints. Because people will be engaged with one another, there is the possibility of cut-off sentences, making it even more likely to hear broad brush themes and not detailed specifics. There really is very little opportunity for specific follow-up questions to individuals. Reading over a transcript, you may be frustrated by avenues of inquiry that were foreclosed early.
Some people expect that conducting focus groups is an efficient form of data collection. After all, you get to hear from eight people instead of just one in the same amount of time! But this is a serious misunderstanding. What you hear in a focus group is one single group interview or discussion. It is not the same thing at all as conducting eight single one-hour interviews. Each focus group counts as “one.” Most likely, you will need to conduct several focus groups, and you can design these as comparisons to one another. For example, the American Sociological Association (ASA) Task Force on First-Generation and Working-Class Persons in Sociology began its study of the impact of class in sociology by conducting five separate focus groups with different groups of sociologists: graduate students, faculty (in general), community college faculty, faculty of color, and a racially diverse group of students and faculty. Even though the total number of participants was close to forty, the “number” of cases was five. It is highly recommended that when employing focus groups, you plan on composing more than one and at least three. This allows you to take note of and potentially discount findings from a group with idiosyncratic dynamics, such as where a particularly dominant personality silences all other voices. In other words, putting all your eggs into a single focus group basket is not a good idea.
How to Conduct a Focus Group Interview/Discussion
Advance preparations.
Once you have selected your focus groups and set a date and time, there are a few things you will want to plan out before meeting.
As with interviews, you begin by creating an interview (or discussion) guide. Where a good one-on-one interview guide should include ten to twelve main topics with possible prompts and follow-ups (see the example provided in chapter 11), the focus group guide should be more narrowly tailored to a single focus or topic area. For example, a focus might be “How students coped with online learning during the pandemic,” and a series of possible questions would be drafted that would help prod participants to think about and discuss this topic. These questions or discussion prompts can be creative and may include stimulus materials (watching a video or hearing a story) or posing hypotheticals. For example, Cech ( 2021 ) has a great hypothetical, asking what a fictional character should do: keep his boring job in computers or follow his passion and open a restaurant. You can ask a focus group this question and see what results—how the group comes to define a “good job,” what questions they ask about the hypothetical (How boring is his job really? Does he hate getting up in the morning, or is it more of an everyday tedium? What kind of financial support will he have if he quits? Does he even know how to run a restaurant?), and how they reach a consensus or create clear patterns of disagreement are all interesting findings that can be generated through this technique.
As with the above example (“What should Joe do?”), it is best to keep the questions you ask simple and easily understood by everyone. Thinking about the sequence of the questions/prompts is important, just as it is in conducting any interviews.
Avoid embarrassing questions. Always leave an out for the “I have a friend who X” response rather than pushing people to divulge personal information. Asking “How do you think students coped?” is better than “How did you cope?” Chances are, some participants will begin talking about themselves without you directly asking them to do so, but allowing impersonal responses here is good. The group itself will determine how deep and how personal it wants to go. This is not the time or place to push anyone out of their comfort zone!
Of course, people have different levels of comfort talking publicly about certain topics. You will have provided detailed information to your focus group participants beforehand and secured consent. But even so, the conversation may take a turn that makes someone uncomfortable. Be on the lookout for this, and remind everyone of their ability to opt out—to stay silent or to leave if necessary. Rather than call attention to anyone in this way, you also want to let everyone know they are free to walk around—to get up and get coffee (more on this below) or use the restroom or just step out of the room to take a call. Of course, you don’t really want anyone to do any of these things, and chances are everyone will stay seated during the hour, but you should leave this “out” for those who need it.
Have copies of consent forms and any supplemental questionnaire (e.g., demographic information) you are using prepared in advance. Ask a friend or colleague to assist you on the day of the focus group. They can be responsible for making sure the recording equipment is functioning and may even take some notes on body language while you are moderating the discussion. Order food (coffee or snacks) for the group. This is important! Having refreshments will be appreciated by your participants and really damps down the anxiety level. Bring name tags and pens. Find a quiet welcoming space to convene. Often this is a classroom where you move chairs into a circle, but public libraries often have meeting rooms that are ideal places for community members to meet. Be sure that the space allows for food.
Researcher Note
When I was designing my research plan for studying activist groups, I consulted one of the best qualitative researchers I knew, my late friend Raphael Ezekiel, author of The Racist Mind . He looked at my plan to hand people demographic surveys at the end of the meetings I planned to observe and said, “This methodology is missing one crucial thing.” “What?” I asked breathlessly, anticipating some technical insider tip. “Chocolate!” he answered. “They’ll be tired, ready to leave when you ask them to fill something out. Offer an incentive, and they will stick around.” It worked! As the meetings began to wind down, I would whip some bags of chocolate candies out of my bag. Everyone would stare, and I’d say they were my thank-you gift to anyone who filled out my survey. Once I learned to include some sugar-free candies for diabetics, my typical response rate was 100 percent. (And it gave me an additional class-culture data point by noticing who chose which brand; sure enough, Lindt balls went faster at majority professional-middle-class groups, and Hershey’s minibars went faster at majority working-class groups.)
—Betsy Leondar-Wright, author of Missing Class , coauthor of The Color of Wealth , associate professor of sociology at Lasell University, and coordinator of staffing at the Mission Project for Class Action
During the Focus Group
As people arrive, greet them warmly, and make sure you get a signed consent form (if not in advance). If you are using name tags, ask them to fill one out and wear it. Let them get food and find a seat and do a little chatting, as they might wish. Once seated, many focus group moderators begin with a relevant icebreaker. This could be simple introductions that have some meaning or connection to the focus. In the case of the ASA task force focus groups discussed above, we asked people to introduce themselves and where they were working/studying (“Hi, I’m Allison, and I am a professor at Oregon State University”). You will also want to introduce yourself and the study in simple terms. They’ve already read the consent form, but you would be surprised at how many people ignore the details there or don’t remember them. Briefly talking about the study and then letting people ask any follow-up questions lays a good foundation for a successful discussion, as it reminds everyone what the point of the event is.
Focus groups should convene for between forty-five and ninety minutes. Of course, you must tell the participants the time you have chosen in advance, and you must promptly end at the time allotted. Do not make anyone nervous by extending the time. Let them know at the outset that you will adhere to this timeline. This should reduce the nervous checking of phones and watches and wall clocks as the end time draws near.
Set ground rules and expectations for the group discussion. My preference is to begin with a general question and let whoever wants to answer it do so, but other moderators expect each person to answer most questions. Explain how much cross-talk you will permit (or encourage). Again, my preference is to allow the group to pick up the ball and run with it, so I will sometimes keep my head purposefully down so that they engage with one another rather than me, but I have seen other moderators take a much more engaged position. Just be clear at the outset about what your expectations are. You may or may not want to explain how the group should deal with those who would dominate the conversation. Sometimes, simply stating at the outset that all voices should be heard is enough to create a more egalitarian discourse. Other times, you will have to actively step in to manage (moderate) the exchange to allow more voices to be heard. Finally, let people know they are free to get up to get more coffee or leave the room as they need (if you are OK with this). You may ask people to refrain from using their phones during the duration of the discussion. That is up to you too.
Either before or after the introductions (your call), begin recording the discussion with their collective permission and knowledge . If you have brought a friend or colleague to assist you (as you should), have them attend to the recording. Explain the role of your colleague to the group (e.g., they will monitor the recording and will take short notes throughout to help you when you read the transcript later; they will be a silent observer).
Once the focus group gets going, it may be difficult to keep up. You will need to make a lot of quick decisions during the discussion about whether to intervene or let it go unguided. Only you really care about the research question or topic, so only you will really know when the discussion is truly off topic. However you handle this, keep your “participation” to a minimum. According to Lune and Berg ( 2018:95 ), the moderator’s voice should show up in the transcript no more than 10 percent of the time. By the way, you should also ask your research assistant to take special note of the “intensity” of the conversation, as this may be lost in a transcript. If there are people looking overly excited or tapping their feet with impatience or nodding their heads in unison, you want some record of this for future analysis.
I’m not sure why this stuck with me, but I thought it would be interesting to share. When I was reviewing my plan for conducting focus groups with one of my committee members, he suggested that I give the participants their gift cards first. The incentive for participating in the study was a gift card of their choice, and typical processes dictate that participants must complete the study in order to receive their gift card. However, my committee member (who is Native himself) suggested I give it at the beginning. As a qualitative researcher, you build trust with the people you engage with. You are asking them to share their stories with you, their intimate moments, their vulnerabilities, their time. Not to mention that Native people are familiar with being academia’s subjects of interest with little to no benefit to be returned to them. To show my appreciation, one of the things I could do was to give their gifts at the beginning, regardless of whether or not they completed participating.
—Susanna Y. Park, PhD, mixed-methods researcher in public health and author of “How Native Women Seek Support as Survivors of Intimate Partner Violence: A Mixed-Methods Study”
After the Focus Group
Your “data” will be either fieldnotes taken during the focus group or, more desirably, transcripts of the recorded exchange. If you do not have permission to record the focus group discussion, make sure you take very clear notes during the exchange and then spend a few hours afterward filling them in as much as possible, creating a rich memo to yourself about what you saw and heard and experienced, including any notes about body language and interactions. Ideally, however, you will have recorded the discussion. It is still a good idea to spend some time immediately after the conclusion of the discussion to write a memo to yourself with all the things that may not make it into the written record (e.g., body language and interactions). This is also a good time to journal about or create a memo with your initial researcher reactions to what you saw, noting anything of particular interest that you want to come back to later on (e.g., “It was interesting that no one thought Joe should quit his job, but in the other focus group, half of the group did. I wonder if this has something to do with the fact that all the participants were first-generation college students. I should pay attention to class background here.”).
Please thank each of your participants in a follow-up email or text. Let them know you appreciated their time and invite follow-up questions or comments.
One of the difficult things about focus group transcripts is keeping speakers distinct. Eventually, you are going to be using pseudonyms for any publication, but for now, you probably want to know who said what. You can assign speaker numbers (“Speaker 1,” “Speaker 2”) and connect those identifications with particular demographic information in a separate document. Remember to clearly separate actual identifications (as with consent forms) to prevent breaches of anonymity. If you cannot identify a speaker when transcribing, you can write, “Unidentified Speaker.” Once you have your transcript(s) and memos and fieldnotes, you can begin analyzing the data (chapters 18 and 19).
Advanced: Focus Groups on Sensitive Topics
Throughout this chapter, I have recommended against raising sensitive topics in focus group discussions. As an introvert myself, I find the idea of discussing personal topics in a group disturbing, and I tend to avoid conducting these kinds of focus groups. And yet I have actually participated in focus groups that do discuss personal information and consequently have been of great value to me as a participant (and researcher) because of this. There are even some researchers who believe this is the best use of focus groups ( de Oliveira 2011 ). For example, Jordan et al. ( 2007 ) argue that focus groups should be considered most useful for illuminating locally sanctioned ways of talking about sensitive issues. So although I do not recommend the beginning qualitative researcher dive into deep waters before they can swim, this section will provide some guidelines for conducting focus groups on sensitive topics. To my mind, these are a minimum set of guidelines to follow when dealing with sensitive topics.
First, be transparent about the place of sensitive topics in your focus group. If the whole point of your focus group is to discuss something sensitive, such as how women gain support after traumatic sexual assault events, make this abundantly clear in your consent form and recruiting materials. It is never appropriate to blindside participants with sensitive or threatening topics .
Second, create a confidentiality form (figure 12.2) for each participant to sign. These forms carry no legal weight, but they do create an expectation of confidentiality for group members.
In order to respect the privacy of all participants in [insert name of study here], all parties are asked to read and sign the statement below. If you have any reason not to sign, please discuss this with [insert your name], the researcher of this study, I, ________________________, agree to maintain the confidentiality of the information discussed by all participants and researchers during the focus group discussion.
Signature: _____________________________ Date: _____________________
Researcher’s Signature:___________________ Date:______________________
Figure 12.2 Confidentiality Agreement of Focus Group Participants
Third, provide abundant space for opting out of the discussion. Participants are, of course, always permitted to refrain from answering a question or to ask for the recording to be stopped. It is important that focus group members know they have these rights during the group discussion as well. And if you see a person who is looking uncomfortable or like they want to hide, you need to step in affirmatively and remind everyone of these rights.
Finally, if things go “off the rails,” permit yourself the ability to end the focus group. Debrief with each member as necessary.
Further Readings
Barbour, Rosaline. 2018. Doing Focus Groups . 2nd ed. Thousand Oaks, CA: SAGE. Written by a medical sociologist based in the UK, this is a good how-to guide for conducting focus groups.
Gibson, Faith. 2007. “Conducting Focus Groups with Children and Young People: Strategies for Success.” Journal of Research in Nursing 12(5):473–483. As the title suggests, this article discusses both methodological and practical concerns when conducting focus groups with children and young people and offers some tips and strategies for doing so effectively.
Hopkins, Peter E. 2007. “Thinking Critically and Creatively about Focus Groups.” Area 39(4):528–535. Written from the perspective of critical/human geography, Hopkins draws on examples from his own work conducting focus groups with Muslim men. Useful for thinking about positionality.
Jordan, Joanne, Una Lynch, Marianne Moutray, Marie-Therese O’Hagan, Jean Orr, Sandra Peake, and John Power. 2007. “Using Focus Groups to Research Sensitive Issues: Insights from Group Interviews on Nursing in the Northern Ireland ‘Troubles.’” International Journal of Qualitative Methods 6(4), 1–19. A great example of using focus groups productively around emotional or sensitive topics. The authors suggest that focus groups should be considered most useful for illuminating locally sanctioned ways of talking about sensitive issues.
Merton, Robert K., Marjorie Fiske, and Patricia L. Kendall. 1956. The Focused Interview: A Manual of Problems and Procedures . New York: Free Press. This is one of the first classic texts on conducting interviews, including an entire chapter devoted to the “group interview” (chapter 6).
Morgan, David L. 1986. “Focus Groups.” Annual Review of Sociology 22:129–152. An excellent sociological review of the use of focus groups, comparing and contrasting to both surveys and interviews, with some suggestions for improving their use and developing greater rigor when utilizing them.
de Oliveira, Dorca Lucia. 2011. “The Use of Focus Groups to Investigate Sensitive Topics: An Example Taken from Research on Adolescent Girls’ Perceptions about Sexual Risks.” Cien Saude Colet 16(7):3093–3102. Another example of discussing sensitive topics in focus groups. Here, the author explores using focus groups with teenage girls to discuss AIDS, risk, and sexuality as a matter of public health interest.
Peek, Lori, and Alice Fothergill. 2009. “Using Focus Groups: Lessons from Studying Daycare Centers, 9/11, and Hurricane Katrina.” Qualitative Research 9(1):31–59. An examination of the efficacy and value of focus groups by comparing three separate projects: a study of teachers, parents, and children at two urban daycare centers; a study of the responses of second-generation Muslim Americans to the events of September 11; and a collaborative project on the experiences of children and youth following Hurricane Katrina. Throughout, the authors stress the strength of focus groups with marginalized, stigmatized, or vulnerable individuals.
Wilson, Valerie. 1997. “Focus Groups: A Useful Qualitative Method for Educational Research?” British Educational Research Journal 23(2):209–224. A basic description of how focus groups work using an example from a study intended to inform initiatives in health education and promotion in Scotland.
- Note that I have included a few examples of conducting focus groups with sensitive issues in the “ Further Readings ” section and have included an “ Advanced: Focus Groups on Sensitive Topics ” section on this area. ↵
A focus group interview is an interview with a small group of people on a specific topic. “The power of focus groups resides in their being focused” (Patton 2002:388). These are sometimes framed as “discussions” rather than interviews, with a discussion “moderator.” Alternatively, the focus group is “a form of data collection whereby the researcher convenes a small group of people having similar attributes, experiences, or ‘focus’ and leads the group in a nondirective manner. The objective is to surface the perspectives of the people in the group with as minimal influence by the researcher as possible” (Yin 2016:336). See also diversity focus group and convergence focus group.
A form of focus group construction in which people with diverse perspectives and experiences are chosen for inclusion. This helps the researcher identify commonalities across this diversity and/or note interactions across differences. Contrast with a convergence focus group
A form of focus group construction in which people with similar perspectives and experiences are included. These are particularly helpful for identifying shared patterns and group consensus. Contrast with a diversity focus group .
Introduction to Qualitative Research Methods Copyright © 2023 by Allison Hurst is licensed under a Creative Commons Attribution-ShareAlike 4.0 International License , except where otherwise noted.
Have a language expert improve your writing
Run a free plagiarism check in 10 minutes, automatically generate references for free.
- Knowledge Base
- Methodology
- What Is a Focus Group? | Step-by-Step Guide & Examples
What Is a Focus Group? | Step-by-Step Guide & Examples
Published on 4 May 2022 by Tegan George . Revised on 6 February 2023.
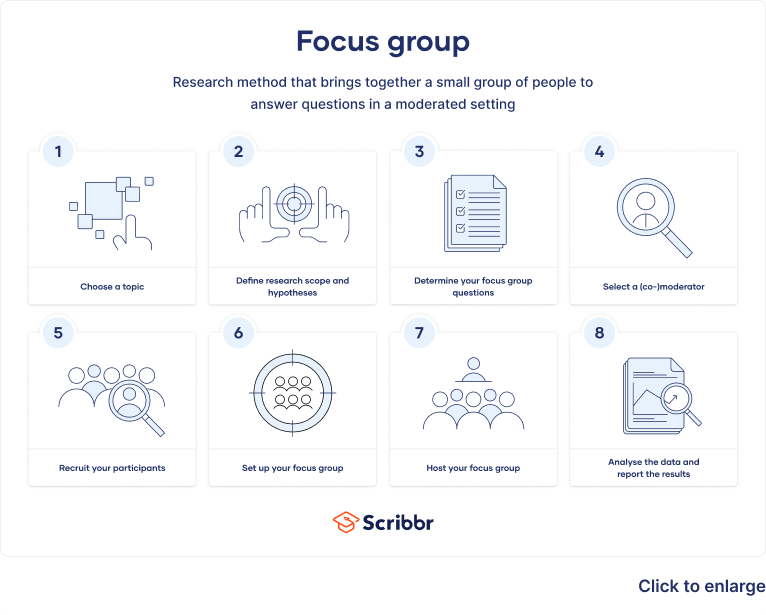
Table of contents
What is a focus group, step 1: choose your topic of interest, step 2: define your research scope and hypotheses, step 3: determine your focus group questions, step 4: select a moderator or co-moderator, step 5: recruit your participants, step 6: set up your focus group, step 7: host your focus group, step 8: analyse your data and report your results, advantages and disadvantages of focus groups, frequently asked questions about focus groups.
Focus groups are a type of qualitative research . Observations of the group’s dynamic, their answers to focus group questions, and even their body language can guide future research on consumer decisions, products and services, or controversial topics.
Focus groups are often used in marketing, library science, social science, and user research disciplines. They can provide more nuanced and natural feedback than individual interviews and are easier to organise than experiments or large-scale surveys .
Prevent plagiarism, run a free check.
Focus groups are primarily considered a confirmatory research technique . In other words, their discussion-heavy setting is most useful for confirming or refuting preexisting beliefs. For this reason, they are great for conducting explanatory research , where you explore why something occurs when limited information is available.
A focus group may be a good choice for you if:
- You’re interested in real-time, unfiltered responses on a given topic or in the dynamics of a discussion between participants
- Your questions are rooted in feelings or perceptions , and cannot easily be answered with ‘yes’ or ‘no’
- You’re confident that a relatively small number of responses will answer your question
- You’re seeking directional information that will help you uncover new questions or future research ideas
- Structured interviews : The questions are predetermined in both topic and order.
- Semi-structured interviews : A few questions are predetermined, but other questions aren’t planned.
- Unstructured interviews : None of the questions are predetermined.
Differences between types of interviews
Make sure to choose the type of interview that suits your research best. This table shows the most important differences between the four types.
Topics favorable to focus groups
As a rule of thumb, research topics related to thoughts, beliefs, and feelings work well in focus groups. If you are seeking direction, explanation, or in-depth dialogue, a focus group could be a good fit.
However, if your questions are dichotomous or if you need to reach a large audience quickly, a survey may be a better option. If your question hinges upon behaviour but you are worried about influencing responses, consider an observational study .
- If you want to determine whether the student body would regularly consume vegan food, a survey would be a great way to gauge student preferences.
However, food is much more than just consumption and nourishment and can have emotional, cultural, and other implications on individuals.
- If you’re interested in something less concrete, such as students’ perceptions of vegan food or the interplay between their choices at the dining hall and their feelings of homesickness or loneliness, perhaps a focus group would be best.
Once you have determined that a focus group is the right choice for your topic, you can start thinking about what you expect the group discussion to yield.
Perhaps literature already exists on your subject or a sufficiently similar topic that you can use as a starting point. If the topic isn’t well studied, use your instincts to determine what you think is most worthy of study.
Setting your scope will help you formulate intriguing hypotheses , set clear questions, and recruit the right participants.
- Are you interested in a particular sector of the population, such as vegans or non-vegans?
- Are you interested in including vegetarians in your analysis?
- Perhaps not all students eat at the dining hall. Will your study exclude those who don’t?
- Are you only interested in students who have strong opinions on the subject?
A benefit of focus groups is that your hypotheses can be open-ended. You can be open to a wide variety of opinions, which can lead to unexpected conclusions.
The questions that you ask your focus group are crucially important to your analysis. Take your time formulating them, paying special attention to phrasing. Be careful to avoid leading questions , which can affect your responses.
Overall, your focus group questions should be:
- Open-ended and flexible
- Impossible to answer with ‘yes’ or ‘no’ (questions that start with ‘why’ or ‘how’ are often best)
- Unambiguous, getting straight to the point while still stimulating discussion
- Unbiased and neutral
If you are discussing a controversial topic, be careful that your questions do not cause social desirability bias . Here, your respondents may lie about their true beliefs to mask any socially unacceptable or unpopular opinions. This and other demand characteristics can hurt your analysis and bias your results.
- Engagement questions make your participants feel comfortable and at ease: ‘What is your favourite food at the dining hall?’
- Exploration questions drill down to the focus of your analysis: ‘What pros and cons of offering vegan options do you see?’
- Exit questions pick up on anything you may have previously missed in your discussion: ‘Is there anything you’d like to mention about vegan options in the dining hall that we haven’t discussed?’
It is important to have more than one moderator in the room. If you would like to take the lead asking questions, select a co-moderator who can coordinate the technology, take notes, and observe the behaviour of the participants.
If your hypotheses have behavioural aspects, consider asking someone else to be lead moderator so that you are free to take a more observational role.
Depending on your topic, there are a few types of moderator roles that you can choose from.
- The most common is the dual-moderator , introduced above.
- Another common option is the dueling-moderator style . Here, you and your co-moderator take opposing sides on an issue to allow participants to see different perspectives and respond accordingly.
Depending on your research topic, there are a few sampling methods you can choose from to help you recruit and select participants.
- Voluntary response sampling , such as posting a flyer on campus and finding participants based on responses
- Convenience sampling of those who are most readily accessible to you, such as fellow students at your university
- Stratified sampling of a particular age, race, ethnicity, gender identity, or other characteristic of interest to you
- Judgement sampling of a specific set of participants that you already know you want to include
Beware of sampling bias , which can occur when some members of the population are more likely to be included than others.
Number of participants
In most cases, one focus group will not be sufficient to answer your research question. It is likely that you will need to schedule three to four groups. A good rule of thumb is to stop when you’ve reached a saturation point (i.e., when you aren’t receiving new responses to your questions).
Most focus groups have 6–10 participants. It’s a good idea to over-recruit just in case someone doesn’t show up. As a rule of thumb, you shouldn’t have fewer than 6 or more than 12 participants, in order to get the most reliable results.
Lastly, it’s preferable for your participants not to know you or each other, as this can bias your results.
A focus group is not just a group of people coming together to discuss their opinions. While well-run focus groups have an enjoyable and relaxed atmosphere, they are backed up by rigorous methods to provide robust observations.
Confirm a time and date
Be sure to confirm a time and date with your participants well in advance. Focus groups usually meet for 45–90 minutes, but some can last longer. However, beware of the possibility of wandering attention spans. If you really think your session needs to last longer than 90 minutes, schedule a few breaks.
Confirm whether it will take place in person or online
You will also need to decide whether the group will meet in person or online. If you are hosting it in person, be sure to pick an appropriate location.
- An uncomfortable or awkward location may affect the mood or level of participation of your group members.
- Online sessions are convenient, as participants can join from home, but they can also lessen the connection between participants.
As a general rule, make sure you are in a noise-free environment that minimises distractions and interruptions to your participants.
Consent and ethical considerations
It’s important to take into account ethical considerations and informed consent when conducting your research. Informed consent means that participants possess all the information they need to decide whether they want to participate in the research before it starts. This includes information about benefits, risks, funding, and institutional approval.
Participants should also sign a release form that states that they are comfortable with being audio- or video-recorded. While verbal consent may be sufficient, it is best to ask participants to sign a form.
A disadvantage of focus groups is that they are too small to provide true anonymity to participants. Make sure that your participants know this prior to participating.
There are a few things you can do to commit to keeping information private. You can secure confidentiality by removing all identifying information from your report or offer to pseudonymise the data later. Data pseudonymisation entails replacing any identifying information about participants with pseudonymous or false identifiers.
Preparation prior to participation
If there is something you would like participants to read, study, or prepare beforehand, be sure to let them know well in advance. It’s also a good idea to call them the day before to ensure they will still be participating.
Consider conducting a tech check prior to the arrival of your participants, and note any environmental or external factors that could affect the mood of the group that day. Be sure that you are organised and ready, as a stressful atmosphere can be distracting and counterproductive.
Starting the focus group
Welcome individuals to the focus group by introducing the topic, yourself, and your co-moderator, and go over any ground rules or suggestions for a successful discussion. It’s important to make your participants feel at ease and forthcoming with their responses.
Consider starting out with an icebreaker, which will allow participants to relax and settle into the space a bit. Your icebreaker can be related to your study topic or not; it’s just an exercise to get participants talking.
Leading the discussion
Once you start asking your questions, try to keep response times equal between participants. Take note of the most and least talkative members of the group, as well as any participants with particularly strong or dominant personalities.
You can ask less talkative members questions directly to encourage them to participate or ask participants questions by name to even the playing field. Feel free to ask participants to elaborate on their answers or to give an example.
As a moderator, strive to remain neutral. Refrain from reacting to responses, and be aware of your body language (e.g., nodding, raising eyebrows). Active listening skills, such as parroting back answers or asking for clarification, are good methods to encourage participation and signal that you’re listening.
Many focus groups offer a monetary incentive for participants. Depending on your research budget, this is a nice way to show appreciation for their time and commitment. To keep everyone feeling fresh, consider offering snacks or drinks as well.
After concluding your focus group, you and your co-moderator should debrief, recording initial impressions of the discussion as well as any highlights, issues, or immediate conclusions you’ve drawn.
The next step is to transcribe and clean your data . Assign each participant a number or pseudonym for organisational purposes. Transcribe the recordings and conduct content analysis to look for themes or categories of responses. The categories you choose can then form the basis for reporting your results.
Just like other research methods, focus groups come with advantages and disadvantages.
- They are fairly straightforward to organise and results have strong face validity .
- They are usually inexpensive, even if you compensate participant.
- A focus group is much less time-consuming than a survey or experiment , and you get immediate results.
- Focus group results are often more comprehensible and intuitive than raw data.
Disadvantages
- It can be difficult to assemble a truly representative sample. Focus groups are generally not considered externally valid due to their small sample sizes.
- Due to the small sample size, you cannot ensure the anonymity of respondents, which may influence their desire to speak freely.
- Depth of analysis can be a concern, as it can be challenging to get honest opinions on controversial topics.
- There is a lot of room for error in the data analysis and high potential for observer dependency in drawing conclusions. You have to be careful not to cherry-pick responses to fit a prior conclusion.
A focus group is a research method that brings together a small group of people to answer questions in a moderated setting. The group is chosen due to predefined demographic traits, and the questions are designed to shed light on a topic of interest. It is one of four types of interviews .
As a rule of thumb, questions related to thoughts, beliefs, and feelings work well in focus groups . Take your time formulating strong questions, paying special attention to phrasing. Be careful to avoid leading questions , which can bias your responses.
The four most common types of interviews are:
- Focus group interviews : The questions are presented to a group instead of one individual.
Social desirability bias is the tendency for interview participants to give responses that will be viewed favourably by the interviewer or other participants. It occurs in all types of interviews and surveys , but is most common in semi-structured interviews , unstructured interviews , and focus groups .
Social desirability bias can be mitigated by ensuring participants feel at ease and comfortable sharing their views. Make sure to pay attention to your own body language and any physical or verbal cues, such as nodding or widening your eyes.
This type of bias in research can also occur in observations if the participants know they’re being observed. They might alter their behaviour accordingly.
Cite this Scribbr article
If you want to cite this source, you can copy and paste the citation or click the ‘Cite this Scribbr article’ button to automatically add the citation to our free Reference Generator.
George, T. (2023, February 06). What Is a Focus Group? | Step-by-Step Guide & Examples. Scribbr. Retrieved 27 May 2024, from https://www.scribbr.co.uk/research-methods/focus-groups/
Is this article helpful?
Tegan George
Other students also liked, structured interview | definition, guide & examples, semi-structured interview | definition, guide & examples, unstructured interview | definition, guide & examples.
- - Google Chrome
Intended for healthcare professionals
- Access provided by Google Indexer
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution

Search form
- Advanced search
- Search responses
- Search blogs
- Qualitative Research:...
Qualitative Research: Introducing focus groups
- Related content
- Peer review
- Jenny Kitzinger , research fellow a
- a Glasgow University Media Group, Department of Sociology, University of Glasgow, Glasgow G12 8LF
This paper introduces focus group methodology, gives advice on group composition, running the groups, and analysing the results. Focus groups have advantages for researchers in the field of health and medicine: they do not discriminate against people who cannot read or write and they can encourage participation from people reluctant to be interviewed on their own or who feel they have nothing to say.
This is the fifth in a series of seven articles describing non-quantitative techniques and showing their value in health research
**FIGURE OMITTED**
Rationale and uses of focus groups
Focus groups are a form of group interview that capitalises on communication between research participants in order to generate data. Although group interviews are often used simply as a quick and convenient way to collect data from several people simultaneously, focus groups explicitly use group interaction as part of the method. This means that instead of the researcher asking each person to respond to a question in turn, people are encouraged to talk to one another: asking questions, exchanging anecdotes and commenting on each other's experiences and points of view. 1 The method is particularly useful for exploring people's knowledge and experiences and can be used to examine not only what people think but how they think and why they think that way.
Focus groups were originally used within communication studies to explore the effects of films and television programmes, 2 and are a popular method for assessing health education messages and examining public understandings of illness and of health behaviours. 3 4 5 6 7 They are widely used to examine people's experiences of disease and of health services. 8 9 and are an effective technique for exploring the attitudes and needs of staff. 10 11
The idea behind the focus group method is that group processes can help people to explore and clarify their views in ways that would be less easily accessible in a one to one interview. Group discussion is particularly appropriate when the interviewer has a series of open ended questions and wishes to encourage research participants to explore the issues of importance to them, in their own vocabulary, generating their own questions and pursuing their own priorities. When group dynamics work well the participants work alongside the researcher, taking the research in new and often unexpected directions.
Group work also helps researchers tap into the many different forms of communication that people use in day to day interaction, including jokes, anecdotes, teasing, and arguing. Gaining access to such variety of communication is useful because people's knowledge and attitudes are not entirely encapsulated in reasoned responses to direct questions. Everyday forms of communication may tell us as much, if not more, about what people know or experience. In this sense focus groups reach the parts that other methods cannot reach, revealing dimensions of understanding that often remain untapped by more conventional data collection techniques.
Some potential sampling advantages with focus groups
Do not discriminate against people who cannot read or write
Can encourage participation from those who are reluctant to be interviewed on their own (such as those intimidated by the formality and isolation of a one to one interview)
Can encourage contributions from people who feel they have nothing to say or who are deemed “unresponsive patients” (but engage in the discussion generated by other group members)
Tapping into such interpersonal communication is also important because this can highlight (sub)cultural values or group norms. Through analysing the operation of humour, consensus, and dissent and examining different types of narrative used within the group, the researcher can identify shared and common knowledge. 12 This makes focus groups a data collection technique particularly sensitive to cultural variables—which is why it is so often used in cross cultural research and work with ethnic minorities. It also makes them useful in studies examining why different sections of the population make differential use of health services. 13 14 For similar reasons focus groups are useful for studying dominant cultural values (for example, exposing dominant narratives about sexuality 15 ) and for examining work place cultures—the ways in which, for example, staff cope with working with terminally ill patients or deal with the stresses of an accident and emergency department.
The downside of such group dynamics is that the articulation of group norms may silence individual voices of dissent. The presence of other research participants also compromises the confidentiality of the research session. For example, in group discussion with old people in long term residential care I found that some residents tried to prevent others from criticising staff—becoming agitated and repeatedly interrupting with cries of “you can't complain”; “the staff couldn't possibly be nicer.” On the one hand, such interactions highlighted certain aspects of these people's experiences. In this case, it showed some resident's fear of being “punished” by staff for, in the words of one woman, “being cheeky.” On the other hand, such group dynamics raise ethical issues (especially when the work is with “captive” populations) and may limit the usefulness of the data for certain purposes (Scottish Health Feedback, unpublished report).
However, it should not be assumed that groups are, by definition, inhibiting relative to the supposed privacy of an interview situation or that focus groups are inappropriate when researching sensitive topics. Quite the opposite may be true. Group work can actively facilitate the discussion of taboo topics because the less inhibited members of the group break the ice for shyer participants. Participants can also provide mutual support in expressing feelings that are common to their group but which they consider to deviate from mainstream culture (or the assumed culture of the researcher). This is particularly important when researching stigmatised or taboo experiences (for example, bereavement or sexual violence).
Focus group methods are also popular with those conducting action research and those concerned to “empower” research participants because the participants can become an active part of the process of analysis. Indeed, group participants may actually develop particular perspectives as a consequence of talking with other people who have similar experiences. For example, group dynamics can allow for a shift from personal, self blaming psychological explanations (“I'm stupid not to have understood what the doctor was telling me”; “I should have been stronger—I should have asked the right questions”) to the exploration of structural solutions (“If we've all felt confused about what we've been told maybe having a leaflet would help, or what about being able to take away a tape recording of the consultation?”).
Some researchers have also noted that group discussions can generate more critical comments than interviews. 16 For example, Geis et al, in their study of the lovers of people with AIDS, found that there were more angry comments about the medical community in the group discussions than in the individual interviews: “perhaps the synergism of the group ‘kept the anger going’ and allowed each participant to reinforce another's vented feelings of frustration and rage. 17 A method that facilitates the expression of criticism and the exploration of different types of solutions is invaluable if the aim of research is to improve services. Such a method is especially appropriate when working with particular disempowered patient populations who are often reluctant to give negative feedback or may feel that any problems result from their own inadequacies. 19
Conducting a focus group study
Sampling and group composition.
Focus group studies can consist of anything between half a dozen to over fifty groups, depending on the aims of the project and the resources available. Most studies involve just a few groups, and some combine this method with other data collection techniques. Focus group discussion of a questionnaire is ideal for testing the phrasing of questions and is also useful in explaining or exploring survey results. 19 20
Although it may be possible to work with a representative sample of a small population, most focus group studies use a theoretical sampling model (explained earlier in this series 21 ) whereby participants are selected to reflect a range of the total study population or to test particular hypotheses. Imaginative sampling is crucial. Most people now recognise class or ethnicity as important variables, and it is also worth considering other variables. For example, when exploring women's experiences of maternity care or cervical smears it may be advisable to include groups of lesbians or women who were sexually abused as children. 22
Most researchers recommend aiming for homogeneity within each group in order to capitalise on people's shared experiences. However, it can also be advantageous to bring together a diverse group (for example, from a range of professions) to maximise exploration of different perspectives within a group setting. However, it is important to be aware of how hierarchy within the group may affect the data (a nursing auxiliary, for example, is likely to be inhibited by the presence of a consultant from the same hospital).
The groups can be “naturally occurring” (for example, people who work together) or may be drawn together specifically for the research. Using preexisting groups allows observation of fragments of interactions that approximate to naturally occurring data (such as might have been collected by participant observation). An additional advantage is that friends and colleagues can relate each other's comments to incidents in their shared daily lives. They may challenge each other on contradictions between what they profess to believe and how they actually behave (for example, “how about that time you didn't use a glove while taking blood from a patient?”).
It would be naive to assume that group data are by definition “natural” in the sense that such interactions would have occurred without the group being convened for this purpose. Rather than assuming that sessions inevitably reflect everyday interactions (although sometimes they will), the group should be used to encourage people to engage with one another, formulate their ideas, and draw out the cognitive structures which previously have not been articulated.
Finally, it is important to consider the appropriateness of group work for different study populations and to think about how to overcome potential difficulties. Group work can facilitate collecting information from people who cannot read or write. The “safety in numbers factor” may also encourage the participation of those who are wary of an interviewer or who are anxious about talking. 23 However, group work can compound difficulties in communication if each person has a different disability. In the study assessing residential care for the elderly, I conducted a focus group that included one person who had impaired hearing, another with senile dementia, and a third with partial paralysis affecting her speech. This severely restricted interaction between research participants and confirmed some of the staff's predictions about the limitations of group work with this population. However, such problems could be resolved by thinking more carefully about the composition of the group, and sometimes group participants could help to translate for each other. It should also be noted that some of the old people who might have been unable to sustain a one to one interview were able to take part in the group, contributing intermittently. Even some residents who staff had suggested should be excluded from the research because they were “unresponsive” eventually responded to the lively conversations generated by their coresidents and were able to contribute their point of view. Communication difficulties should not rule out group work, but must be considered as a factor.
RUNNING THE GROUPS
Sessions should be relaxed: a comfortable setting, refreshments, and sitting round in a circle will help to establish the right atmosphere. The ideal group size is between four and eight people. Sessions may last one to two hours (or extend into a whole afternoon or a series of meetings). The facilitator should explain that the aim of focus groups is to encourage people to talk to each other rather than to address themselves to the researcher. The researcher may take a back seat at first, allowing for a type of “structured eavesdropping.” 24 Later on in the session, however, the researcher can adopt a more interventionist style: urging debate to continue beyond the stage it might otherwise have ended and encouraging the group to discuss the inconsistencies both between participants and within their own thinking. Disagreements within groups can be used to encourage participants to elucidate their point of view and to clarify why they think as they do. Differences between individual one off interviews have to be analysed by the researchers through armchair theorising; differences between members of focus groups should be explored in situ with the help of the research participants.
The facilitator may also use a range of group exercises. A common exercise consists of presenting the group with a series of statements on large cards. The group members are asked collectively to sort these cards into different piles depending on, for example, their degree of agreement or disagreement with that point of view or the importance they assign to that particular aspect of service. For example, I have used such cards to explore public understandings of HIV transmission (placing statements about “types” of people into different risk categories), old people's experiences of residential care (assigning degrees of importance to different statements about the quality of their care), and midwive's views of their professional responsibilities (placing a series of statements about midwive's roles along an agree-disagree continuum). Such exercises encourage participants to concentrate on one another (rather than on the group facilitator) and force them to explain their different perspectives. The final layout of the cards is less important than the discussion that it generates. 25 Researchers may also use such exercises as a way of checking out their own assessment of what has emerged from the group. In this case it is best to take along a series of blank cards and fill them out only towards the end of the session, using statements generated during the course of the discussion. Finally, it may be beneficial to present research participants with a brief questionnaire, or the opportunity to speak to the researcher privately, giving each one the opportunity to record private comments after the group session has been completed.
Ideally the group discussions should be tape recorded and transcribed. If this is not possible then it is vital to take careful notes and researchers may find it useful to involve the group in recording key issues on a flip chart.
ANALYSIS AND WRITING UP
Analysing focus groups is basically the same as analysing any other qualitative self report data. 21 26 At the very least, the researcher draws together and compares discussions of similar themes and examines how these relate to the variables within the sample population. In general, it is not appropriate to give percentages in reports of focus group data, and it is important to try to distinguish between individual opinions expressed in spite of the group from the actual group consensus. As in all qualitative analysis, deviant case analysis is important—that is, attention must be given to minority opinions and examples that do not fit with the researcher's overall theory.
The only distinct feature of working with focus group data is the need to indicate the impact of the group dynamic and analyse the sessions in ways that take full advantage of the interaction between research participants. In coding the script of a group discussion, it is worth using special categories for certain types of narrative, such as jokes and anecdotes, and types of interaction, such as “questions,” “deferring to the opinion of others,” “censorship,” or “changes of mind.” A focus group research report that is true to its data should also usually include at least some illustrations of the talk between participants, rather than simply presenting isolated quotations taken out of context.
Tapping into interpersonal communication can highlight cultural values or group norms
This paper has presented the factors to consider when designing or evaluating a focus group study. In particular, it has drawn attention to the overt exploitation and exploration of interactions in focus group discussion. Interaction between participants can be used to achieve seven main aims:
To highlight the respondent's attitudes, priorities, language, and framework of understanding;
To encourage research participants to generate and explore their own questions and develop their own analysis of common experiences;
To encourage a variety of communication from participants—tapping into a wide range and form of understanding;
To help to identify group norms and cultural values;
To provide insight into the operation of group social processes in the articulation of knowledge (for example, through the examination of what information is censured or muted within the group);
To encourage open conversation about embarrassing subjects and to permit the expression of criticism;
Generally to facilitate the expression of ideas and experiences that might be left underdeveloped in an interview and to illuminate the research participant's perspectives through the debate within the group.
Group data are neither more nor less authentic than data collected by other methods, but focus groups can be the most appropriate method for researching particular types of question. Direct observation may be more appropriate for studies of social roles and formal organisations 27 but focus groups are particularly suited to the study of attitudes and experiences. Interviews may be more appropriate for tapping into individual biographies, 27 but focus groups are more suitable for examining how knowledge, and more importantly, ideas, develop and operate within a given cultural context. Questionnaires are more appropriate for obtaining quantitative information and explaining how many people hold a certain (pre-defined) opinion; focus groups are better for exploring exactly how those opinions are constructed. Thus while surveys repeatedly identify gaps between health knowledge and health behaviour, only qualitative methods, such as focus groups, can actually fill these gaps and explain why these occur.
Focus groups are not an easy option. The data they generate can be as cumbersome as they are complex. Yet the method is basically straightforward and need not be intimidating for either the researcher or the researched. Perhaps the very best way of working out whether or not focus groups might be appropriate in any particular study is to try them out in practice.
Further reading
Morgan D. Focus groups as qualitative research. London: Sage, 1988.
Kreuger R. Focus groups: a practical guide for applied research. London: Sage, 1988.
- Kitzinger J
- Ritchie JE ,
- Herscovitch F ,
- Gordon-Sosby K ,
- Reynolds KD ,
- Manderson L
- Turnbull L ,
- McCallum J ,
- Gregory S ,
- Denning JD ,
- Verschelden C
- Zimmerman M ,
- Szumowski D ,
- Alvarez F ,
- Bhiromrut P ,
- DiMatteo M ,
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- Glob Qual Nurs Res
- v.3; Jan-Dec 2016
Methodological Aspects of Focus Groups in Health Research
Anja p. tausch.
1 GESIS–Leibniz Institute for the Social Sciences, Mannheim, Germany
Natalja Menold
Although focus groups are commonly used in health research to explore the perspectives of patients or health care professionals, few studies consider methodological aspects in this specific context. For this reason, we interviewed nine researchers who had conducted focus groups in the context of a project devoted to the development of an electronic personal health record. We performed qualitative content analysis on the interview data relating to recruitment, communication between the focus group participants, and appraisal of the focus group method. The interview data revealed aspects of the focus group method that are particularly relevant for health research and that should be considered in that context. They include, for example, the preferability of face-to-face recruitment, the necessity to allow participants in patient groups sufficient time to introduce themselves, and the use of methods such as participant-generated cards and prioritization.
Focus groups have been widely used in health research in recent years to explore the perspectives of patients and other groups in the health care system (e.g., Carr et al., 2003 ; Côté-Arsenault & Morrison-Beedy, 2005 ; Kitzinger, 2006 ). They are often included in mixed-methods studies to gain more information on how to construct questionnaires or interpret results ( Creswell & Plano Clark, 2007 ; Kroll, Neri, & Miller, 2005 ).
The fact that the group process helps people to identify and clarify their views is considered to be an important advantage of focus groups compared with individual interviews ( Kitzinger, 1995 ). The group functions as a promoter of synergy and spontaneity by encouraging the participants to comment, explain, disagree, and share their views. Thus, experiences are shared and opinions voiced that might not surface during individual interviews ( Carey, 1994 ; Stewart, Shamdasani, & Rook, 2007 ). Although focus groups allow participants to respond in their own words and to choose discussion topics themselves, they are not completely unstructured. Questions relating to the research topic are designed by the researchers and are used to guide the discussion ( Stewart et al., 2007 ). The degree of structure of the focus group depends on the openness of the research question(s). Hence, although it takes more time and effort to organize focus groups, and they cause greater logistical problems than individual interviews do, they might generate more ideas about, and yield deeper insights into, the problem under investigation ( Coenen, Stamm, Stucki, & Cieza, 2012 ; Kingry, Tiedje, & Friedman, 1990 ; Morgan, 2009 ).
Historically, focus groups were used mainly for market research before the method was adopted for application in qualitative research in the social sciences ( Morgan, 1996 ). The use of focus groups in health care research is even more recent. For this reason, methodological recommendations on using focus groups in the health care context are quite rare, and researchers rely mainly on general advice from the social sciences (e.g., Krueger, 1988 ; Morgan, 1993 ; Morgan & Krueger, 1998 ; Stewart et al., 2007 ). Even though focus groups have been used in a great variety of health research fields, such as patients’ treatments and perceptions in the context of specific illnesses (rheumatoid arthritis: for example, Feldthusen, Björk, Forsblad-d’Elia, & Mannerkorpi, 2013 ; cancer: for example, Gerber, Hamann, Rasco, Woodruff, & Lee, 2012 ; diabetes: for example, Nafees, Lloyd, Kennedy-Martin, & Hynd, 2006 ; heart failure: for example, Rasmusson et al., 2014 ), community health research (e.g., Daley et al., 2010 ; Rhodes, Hergenrather, Wilkin, Alegría-Ortega, & Montaño, 2006 ), or invention of new diagnostic or therapeutic methods (e.g., Vincent, Clark, Marquez Zimmer, & Sanchez, 2006 ), the method and its particular use in health research is rarely reflected. Methodological articles about the focus group method in health care journals mainly summarize general advice from the social sciences (e.g., Kingry et al., 1990 ; Kitzinger, 1995 , 2006 ), while field-specific aspects of the target groups (patients, doctors, other medical staff) and the research questions (not only sociological but often also medical or technical) are seldom addressed. Reports on participant recruitment and methods of conducting the focus groups are primarily episodic in nature (e.g., Coenen et al., 2012 ; Côté-Arsenault & Morrison-Beedy, 2005 ) and often focus on very specific aspects of the method (communication: for example, Lehoux, Poland, & Daudelin, 2006 ; activating methods: for example, Colucci, 2007 ) or aim at a comparison between face-to-face focus groups and other methods (individual interviews: for example, Coenen et al., 2012 ; telephone groups: for example, Frazier et al., 2010 ; Internet groups: for example, Nicholas et al., 2010 ). Thus, systematic reviews of factors influencing the results of focus groups as well as advantages, disadvantages, and pitfalls are missing. One consequence is that researchers might find it difficult to recruit enough participants or might be surprised by the communication styles of the target groups. Furthermore, in the tradition of classical clinical research, the group discussions might result in a question-and-answer situation or “resemble individual interviews done in group settings” ( Colucci, 2007 , p. 1,424), thereby missing out on the opportunity to use the group setting to activate all participants and to encourage a deeper elaboration of their ideas. Colucci, for example, proposed the use of exercises (e.g., activity-oriented questions) to focus the attention of the group on the core topic and to facilitate subsequent analyses.
Recommendations from the social sciences on using the focus group method can be subsumed under the following headings: subjects (target groups, composition of groups, recruitment), communication in the groups (discussion guide, moderator, moderating techniques), and analysis of focus groups (e.g., Morgan, 1993 ; Morgan & Krueger, 1998 ; Stewart et al., 2007 ). Specific requirements for health research can be identified in all three thematic fields: Recruitment might be facilitated by using registers of quality circles to recruit physicians or pharmacists, or by recruiting patients in outpatients departments. It might be hampered by heavy burdens on target groups—be they time burdens (e.g., clinical schedules, time-consuming therapy) or health constraints (e.g., physical fitness). With regard to communication in focus groups, finding suitable locations, identifying optimal group sizes, planning a good time line, as well as selecting suitable moderators (e.g., persons who are capable of translating medical terms into everyday language) might pose a challenge. The analysis of focus groups in health care research might also require special procedures because the focus group method is used to answer not only sociological research questions (e.g., related to the reconstruction of the perspectives of target groups) but also more specific research questions, such as user requirements with regard to written information or technical innovations.
The aim of our study was to gather more systematic methodological information for conducting focus groups in the context of health research in general and in the more specific context of the implementation of a technical innovation. To this end, we conducted interviews with focus group moderators about their experiences when planning and moderating focus groups. The groups in question were part of a research program aimed at developing and evaluating an electronic personal health record. We chose this program for several reasons: First, because it consisted of several subprojects devoted to different research topics related to the development of a personal electronic health record, it offered a variety of research content (cf. next section). Second, the focus groups were conducted to answer research questions of varying breadth, which can be regarded as typical of research in health care. Third, the focus groups comprised a variety of target groups—not only patients but also different types of health care professionals (general practitioners, independent specialists with different areas of specialization, hospital doctors, pharmacists, medical assistants, nursing staff).
In this article, we report the findings of these interviews in relation to the following questions: (a) What challenges associated with the characteristics of the target groups of health research (patients, physicians, other health care professionals) might be considered during the recruitment process? How should the specific research question relating to a technical innovation be taken into account during the recruitment process? (b) Should specific aspects of the communication styles of target groups be taken into account when planning and moderating focus groups in health care? Can additional challenges be identified in relation to the technical research question? and (c) How was the method appraised by the interviewees in their own research context?
Research Program and Description of Focus Groups
The “Information Technology for Patient-Centered Health Care” (INFOPAT) research program ( www.infopat.eu ) addresses the fact that, because patients with chronic conditions (e.g., colorectal cancer, type 2 diabetes) have complex health care needs, many personal health data are collected in different health care settings. The aim of the program is to develop and evaluate an electronic personal health record aimed at improving regional health care for chronically ill people and strengthening patients’ participation in their health care process. Subprojects are devoted, for example, to developing the personal electronic health record (Project Cluster 1), a medication platform (Project Cluster 2), and a case management system for chronically ill patients (Project Cluster 3). In the first, qualitative, phase, the researchers explored patients’ and health care professionals’ experiences with cross-sectoral health care and patient self-management, and their expectations regarding the advantages and disadvantages of a personal electronic health record. The information gathered in this phase of the program served as a basis for constructing a personal electronic health record prototype. This prototype was implemented as an intervention in a second, quantitative, phase dedicated to investigating the impact of such a record on a range of health care variables (e.g., self-management, health status, patient–doctor relationship, compliance). The University Hospital Heidelberg Ethics Committee approved the studies of the INFOPAT research program. All participants gave their written informed consent, and the participants’ anonymity and confidentiality were ensured throughout the studies according to the ethical standards of German Sociological Association. 1
Twenty-one focus groups were conducted during the qualitative phase of the program. Three groups consisted of colorectal cancer patients, four comprised type 2 diabetes patients, four were made up of physicians, three comprised physicians and pharmacists, four consisted of physicians and other health care professionals, and three consisted of other health care professionals (for more detailed information, see Tausch & Menold, 2015 ). Participants were recruited from urban and rural districts of the Rhine-Neckar region in Germany. Patients were approached in clinics, by their local general practitioners, or in self-help groups. Health care professionals were recruited in clinics, cooperating medical practices, and professional networks.
The focus groups took place at several locations at the National Center of Tumor Diseases (NCT) in Heidelberg, Germany, and the University of Heidelberg. The groups consisted of between four and seven participants and lasted between 1.5 and 2 hours. All focus groups were conducted by two researchers—a moderator and a co-moderator; a third researcher took notes. Semistructured discussion guides were used, and the groups were video- and audio recorded (cf., for example, Baudendistel et al., 2015 ; Kamradt et al., 2015 ). The researchers performed content analysis on the transcripts; the schema of categories was oriented toward the research questions. The focus groups addressed research questions of varying breadth, including, for example, individual health care experiences (comparatively broad), the expected impact of the record on the patient–doctor relationship (medium breadth), and technical requirements for such a personal health record (comparatively narrow). The variety of the research questions was important for our study because it proved to be of relevance for the interviewees’ appraisal of the usefulness of the focus group method.
Interviews With the Focus Group Moderators
We conducted qualitative interviews with nine of the 10 focus group moderators in the INFOPAT program (one moderator moved to a different department shortly after the completion of data collection and was not available for interview). The interviewees were aged between 30 and 54 years ( M age = 36 years; SD = 8.3 years). Their professions were health scientist, pharmacist, general practitioner, or medical ethicist. Their professional experience ranged from one to 23 years ( M = 7.1 years, SD = 7.7 years), and they had little or no previous experience of organizing and conducting focus groups. The moderators were interviewed in groups of one to three persons according to their project assignment (cf. Table 1 ).
Overview of Interviews and Interviewees.
The interviews lasted approximately 1 hour, and the interview questions were guided by the chronological order in which a focus group is organized and conducted (recruitment, preparation, moderation, methods) and by the utilization and usefulness of the results. We tape recorded the interviews, transcribed them verbatim, and performed qualitative content analysis on the transcripts ( Elo & Kyngäs, 2008 ; Mayring, 2015 ) with the help of the program MAXQDA 10.0.
The final system of categories 2 ( Tausch & Menold, 2015 ) consisted of two types of codes: All relevant text passages were coded with respect to the content of the statement. In addition, a second type of code was required if the statement related to a specific group of participants (e.g., patients, hospital doctors, men, women).
On the basis of the research questions, the contents of interview statements were classified into the three superordinate thematic categories: recruitment, communication in the focus groups, and appraisal of the focus group method. Consequently, the reporting of the results is structured according to three main topics.
Recruitment
Statements relating to the recruitment of the participants were sorted into the main categories “factors promoting participation”, “factors preventing participation”, and “general appraisal of the recruitment process”. Figure 1 shows the subcategories that were identified under these main categories. Because many of the statements referred only to patients or only to health care professionals (physicians, other health care professionals), the subcodes shown in Figure 1 are sorted by these two types of participants.

Factors relating to the recruitment process.
Factors relevant for all target groups
As the following interviewee statement shows, addressing potential participants face-to-face (rather than in writing) proved crucial for the success of recruitment in all target groups:
Well, a really good tip when recruiting patients is . . . to address the people yourself. Not to get someone else to do it who . . . has nothing to do with [the project], because ultimately you really do have to explain a lot of things, also directly to the patient. And then it’s always good if the person [who does the recruiting] is actually involved in the project. 3
In the case of the clinicians, being addressed by a superior was even more effective for their willingness to participate: “And then top down. If the nursing director asks me, then it’s not so easy to say no.”
Furthermore, a positive response was more often achieved if the groups were scheduled at convenient times for the addressees, and they only had to choose between several alternatives. Patients welcomed times contiguous with their therapies: “And many [of the patients] said: ‘Yes, maybe we can do it after my chemotherapy, on that day when I’m in the clinic anyway?’” Whereas medical assistants were given the opportunity to take part in the groups during working hours, general practitioners preferred evening appointments on less busy weekdays (e.g., Wednesdays and Fridays):
Well, what I found quite good was to suggest a day and a time. And we concentrated on the fact that practices are often closed on Wednesday afternoons. So that’s a relatively convenient day. And then evenings for the pharmacists from seven-thirty onwards.
Interest in the topic of the discussion, or at least in research in general, was an important variable for participation. Together with lack of time, it turned out to be the main reason why sampling plans could not be realized. Among patients, men were much more interested in discussing a technical innovation such as an electronic personal health record, while women—besides their lesser interest—often declined because of family responsibilities: “Well, I’d say a higher proportion of women said: ‘I have a lot to do at home, housework and with the children, therefore I can’t do it.’”
Family physicians, physicians from cooperating medical practices, and hospital doctors showed more interest in discussing an electronic personal health record than did medical specialists in private practice, who often saw no personal gain in such an innovation. For example, one interviewee stated,
Family physicians generally have a greater willingness [to engage with] this [health] record topic. They see . . . also a personal benefit for themselves. . . . or they simply think it might be of relevance to them or they are interested in the topic for other reasons. Some of them even approached us themselves and said, “Oh, that interests me and I’d like to take part.”
In addition, because of heavy workload, private practitioners were difficult to reach (e.g., by telephone). This also lowered the participation of this target group on the focus groups.
Factors relevant only for patients
Two other variables that influenced patients’ willingness to participate were mentioned in the interviews. First, because this target group consisted of cancer patients and diabetes patients with multimorbidity, poor physical fitness also prevented several addressees from participating in the groups. The inability to climb stairs, or the general inability to leave the house, made it impossible for them to reach the location where the groups took place: “[They] immediately replied: ‘Well, no, . . . that’s really too much for me,’ and unfortunately they could not, therefore, be included in the groups.” Furthermore, unstable physical fitness often led to high drop-out rates. The moderators of the focus groups therefore proposed that up to twice as many participants as required should be recruited: “And depending on the severity of the illness, you have to expect a drop-out rate of up to fifty percent. So, if you want to have four people, you should invite eight.”
Second, moderators reported that patients’ liking for, or dislike of, talking and discussing influenced their tendency to join the groups. Participating patients were generally described as talkative. For example: “And with patients, all in all, I had the feeling that those who agreed [to participate] were all people who liked talking, because those who did not like talking refused out of hand.” Patients who refused to participate often argued that they felt uncomfortable speaking in front of a group: “And the men, when they declined they often said: ‘No, group discussion is not for me! I don’t like talking in front of a group.’”
The researchers eventually succeeded in recruiting sufficient participants. However, they were not able to realize the sampling plans according to a certain proportion of male and female patients or types of physicians. “Well, we finally managed to fill up our groups, but only as many [participants] as necessary.” Comparing the different target groups, recruiting patients was described as easier than recruiting physicians: “And that was much easier insofar as you just had to go to the clinic and each day there were five or six patients whom you could address.” However, only 10% of the patients who were addressed agreed to participate. In the health care professional group, the recruitment rates ranged between 0% and 30%, depending on the subgroup. This can be demonstrated by the following interviewee utterance:
And in the private practitioner sector it was rather . . . . Well, we tried to recruit specialists in private practice, in other words internists, gastroenterologists, and oncologists. The success [rate proved to be] extremely poor. . . . Well, on the whole, the willingness to take part, the interest, is not there. Or, well they don’t give the reasons, but they say they don’t want to take part. So that was difficult and, yes, it didn’t go too well.
Communication in the Focus Groups
With regard to the communication in the focus groups, the moderators identified factors that influenced communication in a positive or negative way. In addition, we discussed a number of factors with them that are often described in the social science literature as problematic when conducting focus groups. However, the interviewees considered that some of these factors had not influenced communication in the focus groups conducted within the framework of the INFOPAT program. In our system of categories, we also coded whether the factors in question were related to (a) the setting or (b) the moderation of the focus groups (cf. Figure 2 ).

Influences on and characteristics of the focus group discussion.
Factors relating to the setting
As Figure 2 shows, communication was reported to be positively influenced by small group size, location, provision of food and beverages, and conducting the focus group without a break. In contrast to general recommendations on focus groups in the context of sociological research, the moderators in the INFOPAT program considered a smaller group size of between four and six participants to be ideal. With regard to location, the interviewees reported that, depending on the target group, different places were perceived as positive. Patients preferred locations inside the clinic because they were easy to reach and caused no additional effort. Furthermore, because these locations were familiar to them, they facilitated an atmosphere of security and ease, which was seen as an important prerequisite for an open and honest discussion. This is clear from the following quotation:
Well, the patient focus groups were all located at the clinic. We chose this location on purpose to make it easier for them, because they come to the clinic anyway for their therapy. And they know the place and they feel comfortable and in good hands.
By contrast, the clinician groups benefited from being located outside the clinic. In contrast to other common addressees of focus groups, these professionals were not only accustomed to participating in groups outside their familiar surroundings but also this location helped them to distance themselves from their professional duties and to engage more deeply in the discussion, as shown by the following quotation:
Yes, one was located at the O-Center. We chose this location on purpose so that the clinicians had to leave the hospital. It’s not too far, only a few yards away. But we wanted them to leave the clinic, and not to run back to the ward when they were called. And, well, I liked this location.
Food and beverages were welcome in all the groups and also helped to create a positive and trusting atmosphere. And finally, the interviewees found that it was better to omit the break, thereby avoiding the interruption of the ongoing discussion. This is reasonable considering the comparatively short duration of the focus group session (between 1.5 and 2 hours). Statements relating to a break might have been different in the case of longer focus group durations.
The interviewees reported that the size and temperature of the room and time pressure on the participants or the moderator had a negative impact on communication. Some of the focus groups in the project took place in midsummer and had to be held in rooms without blinds or air conditioning. The moderators of these groups had to work hard to maintain the participants’ (and their own) attention and concentration. Time pressure on the participants (e.g., the clinicians) led to an unwillingness to engage in active discussion and created a question-and-answer situation, as shown by the following statement:
And in one group of physicians . . . we never reached the point where they joined in fully. During the whole discussion they never completely arrived. And they had already cut the time short in advance. They were under so much time pressure that they were not able to discuss in an open manner.
Moderators reported that they, too, had experienced time pressure—namely, in situations where they did not have enough time to prepare the room and the recording devices. This had caused them to be nervous and stressed at the beginning of the discussion, which had negatively affected the mood of the participants, thereby rendering an honest and open discussion particularly difficult.
Factors relating to the moderation
Many of the positive factors reported by the interviewees have already been described for focus groups in general—for example, using open questions, directly addressing quiet participants, and handling the discussion guide in a flexible way. Furthermore, by showing interest in every statement, and by generating a feeling of security in every participant, moderators fostered a fruitful discussion:
I believe that another important point is that you are calm yourself. That you give the people the feeling “you can feel safe with me, you don’t have to worry that I will make fun of you . . . or that I won’t take you seriously.”
Interviewees also considered that building a bridge between the technical innovation under discussion (a web-based electronic personal health record) and everyday life (e.g., online banking) was an important factor in getting all participants to contribute to the discussion. As one interviewee noted,
We tried to anchor it in their everyday lives. And . . . the example that always worked was when we said: “Think of it as if it were a kind of online banking.” Everyone understands what online banking is. It’s about important data on the internet; they’re safe there somehow. I have my password. And people understood that. Well, it’s important to anchor it in their reality . . . because otherwise the topic is simply far too abstract.
In this context, the fact that the groups were moderated by the researchers themselves proved very helpful because they were able to answer all questions relating to the research topic. As the following quote shows, this was an important prerequisite for opinion formation on the part of participants:
Well, I think that a really important quality criterion . . . is that you have completely penetrated [the topic]. If you only know the process from the outside . . . and you then conduct the focus group about it. . . . Somewhere, at some stage, [one discussion] narrowly missed the point. . . . You simply have to be totally immersed in the topic, well, I believe that [someone who is totally immersed in the topic] is the ideal person for the job. And in our case the thinking was, okay, so I’m a doctor, but on balance it’s more important that both [moderators] are absolutely well informed because it’s a complex topic.
The more specific the research question was, the more useful the moderating strategy of inviting one participant after the other to express their opinion appeared to be. By using this strategy, the moderators ensured that every participant contributed to the discussion.
A point that was strongly emphasized by the interviewees was the duration of the round of introductions at the beginning of the focus group session. In the patient groups, introductions took much more time than the researchers had expected. Patients had a high need to express themselves and to tell the others about their illness and their experiences with the health system. Although this left less time to work through the topics in the discussion guide, the researchers came to realize that there were several good reasons not to limit these contributions: First, the introductions round proved important for helping the participants to “arrive” at the focus group, for creating a basis of trust, and for building up a sense of community among the participants. Second, the interviewees reported that, because many topics in the discussion guide (e.g., participants’ experiences with coordinating visits to different medical specialists) had already been brought up in the round of introductions, they did not have to be discussed further at a later stage:
And that is the crux of this general exchange of experiences at the beginning. Sure, it costs you a lot of time, but I almost think that if you don’t give them that time, you won’t get what you want from them, in the sense that you say: “I want to hear your frank opinion or attitude.” You don’t want them to simply answer you because they think that’s what you want to hear. You have to create an atmosphere in which they really forget where they are. I’m relatively convinced that you wouldn’t achieve that without such [a round of introductions].
The moderators’ experience in the physician groups was different. These groups benefited from having a rather short round of introductions. Giving participants too much time to introduce themselves meant that they presented their expertise rather than reporting their experiences. In contrast to the patient groups, this did not substantially contribute to the discussion of the research topics.
Depending on the context, status differences between the moderators and the participants, or among the participants, were appraised differently by interviewees. In one group comprising physicians and medical assistants, the moderators observed that status differences had a negative influence on communication. Very young female medical assistants, in particular, did not feel free to express their opinions in the presence of their superiors. By contrast, presumed differences in status between family doctors, hospital doctors, and medical specialists in private practice did not have any negative impact on communication. Nor did different forms of address (some participants in these groups were addressed by their first name and some by their last name, depending on the relationship between the moderator and the participants). Status differences between moderators (if medical doctors) and participants (patients) had an impact on communication when patients regarded doctors as an important source of information (e.g., about the meaning of their blood values) or as representatives of the health care system to whom complaints about the system should be addressed. The latter case was the subject of the following interview statement by a moderator who is a physician by profession:
And a lot [was said about] the kind of experiences they had had here at the NCT. And of course, when the patients have been treated here for many years—or even for not so many [years], but they have had many experiences—they sometimes reported at length. And I had the feeling that this had a bit of a feedback function, quite generally, for the NCT. Also the somehow frustrating experiences they had had, or a lot of things that had not gone that well in conversational exchanges [with the staff]. There was a relatively large amount of feedback that didn’t have a lot to do with the topic because I was, of course, involved as a senior physician and I am not an external researcher, but rather someone who is also seen as being jointly responsible, or at least as someone who can channel criticism.
Finally, because most of the moderators were not medical professionals, they did not experience the translation of medical or technical terms into everyday language as problematic. Rather, they automatically used terms that were also familiar to the participants.
Characteristics of the discussion
The factors described above resulted in focus group discussions that might be interpreted as characteristic of health research. The patient focus groups were characterized by a strong need to talk and a high need for information. In the health care professional focus groups, researchers experienced a greater variety of communication styles. Because of a lack of time, or because they falsely expected a question-and-answer situation, some groups demonstrated a low degree of willingness to engage in discussion:
Although, I believe that was partly due . . . well there was one [woman] who was very demanding; she wanted to know straight away: “Yes, what’s the issue here? What do I have to say to you?” Well, the three who came from the one practice, I think they really had the feeling that we would ask them questions and they would bravely answer them and then they could go home again. So, for them this principle that they were supposed to engage in a discussion, for them that was somehow a bit, I don’t know . . . disconcerting. . . . They really thought: “Okay, well we want to know now what this is all about. And they’ll ask us the questions and then we’ll say yes, no, don’t know, maybe. And then we’ll go home again.” Well, at least that was my impression.
Other groups, especially those consisting of different types of health care professionals (e.g., physicians with different areas of specialization, or physicians and pharmacists), were characterized by lively discussion and a great variety of opinions.
Appraisal of the Focus Group Method
We classified moderators’ statements relating to the appraisal of the focus group method into four main categories: “advantages of the method”, “disadvantages of the method”, “recommendations for other researchers in related research areas”, and “statements on how they used the results” (cf. Figure 3 ).

Appraisal of the focus group method.
The researchers reported that the focus group method yielded a rich blend of perspectives and opinions, brought forth, in particular, by the interaction between the participants:
But for this question and the topic, and for our lack of knowledge, that was . . . a lot of new information . . . and very many good ideas and critical remarks that you naturally read in the literature from time to time. But, let’s say, because of the complexity of the participants’ reactions and the weight they attached to things, it’s different than reading in a literature review that [this or that] could be taken into account.
The results of the focus groups further enriched the researchers’ work by relating it to everyday life: “Well, what was nice was that the topic was related to the participants’ lives. That people said: ‘Now the topic is important for me.’” Furthermore, the method yielded information about which aspects were most important and how the variety of opinions should be prioritized. This was achieved, in particular, by using participant-generated cards:
And with regard to prioritization, we incorporated it using participant-generated cards. We said: “Look: If you could develop this record now, what would be the three most important things that must absolutely be taken into consideration, from your point of view, no matter what they relate to.” And they wrote them down on the cards. And after that they were asked to carry out their own prioritization—that is, what was most important to them personally. One person wrote “data protection” first, while another [wrote] “sharing with my wife.” . . . That was good. . . . That helped a lot because it was simply clear once again what things were important to them.
In cases where concrete questions had to be answered or decisions had to be made, the interviewees also welcomed the opportunity to use structuring methods such as presentations, flip-charts, and participant-generated cards to obtain the relevant information:
. . . Well, the aim was that at the end we [would] have a set of requirements for the engineering [people]. And the engineering [people] don’t so much want to know about experiences and desires and barriers, but rather they want to know should the button be green or red and can you click on it. And that’s why I thought at the beginning it will be difficult with a focus group and an open discussion. Now, if you say that one can also interpret a focus group the way we did, partly with very specific questions and these participant-generated cards, then I think it is indeed possible to answer such questions as well.
Disadvantages
The main disadvantages of the focus group method were seen in the considerable organizational effort and expenditure of time involved. A question raised by some of the interviewees was whether comparable results could have been achieved using less time-consuming and organizationally demanding methods.
It’s true to say that you lose time. Well, you could implement [the innovation] straight away and see whether it’s better. Maybe, in this case you’re wrong and you just think it’s better or in any case not worse than before. You basically lose a year on this whole focus groups thing.
Moreover, in some cases, the discussion went in an unwanted direction and the moderators never fully succeeded in bringing the group back to the intended topics.
Furthermore, like many other medical research projects, INFOPAT included quite specific research questions. In this connection, the moderators emphasized that open focus group discussions would not have succeeded in answering those questions. Only by using methods such as participant-generated cards and prioritization was it possible to answer at least some of them. Nonetheless, some interviewees did not consider the focus group method to be really suitable for this type of research questions:
Of course we also have our engineers as counterparts who . . . need very specific requirements at some point. The question is whether such a focus group . . . . [It] can’t answer that in detail in this first stage. It’s simply not practicable.
Recommendations
As described under the “Communication in the Focus Groups” section above, the round of introductions in the patient groups lasted much longer than planned, thereby shortening the time available for other topics in the discussion guide. As a result, the moderators decided to choose a different thematic focus in each group so that every topic was discussed more deeply in at least one group.
What we usually did was to consider what hadn’t been addressed that much in the previous focus group. That [topic] was given more room in the next focus group because the guide, well it was quite a lot. You could have easily gone on discussing for another hour or two.
Using the results
On the whole, the researchers were satisfied with the number of groups that were conducted and the results that they yielded. They did not agree that more groups would have led to better, or different, results—with one possible exception, namely, in the case of specific target groups (e.g., migrants). Only one group had been composed of patients with a migrant background, and, as one interviewee stated, “I just thought, the patients with a migrant background . . . now that was [only] one group, it by no means covers the whole range.”
In cases where the results of the focus groups were perceived as not being concrete enough to proceed to the next research step (e.g., formulating a specification sheet for the construction of the electronic personal health record), the researchers planned to bring experts together in a roundtable format to make decisions on the basis of the priorities, agreements, and disagreements that had emerged from the focus groups. Following the construction of a prototype, they intended to conduct further focus groups to validate or adapt the usability of the electronic personal health record system.
Our analysis of interviews with focus group moderators yielded considerable insights into methodological aspects of conducting focus groups in health research. Our first research question related to characteristics of the target groups that should be considered during the recruitment process. We identified face-to-face contact as an important factor promoting focus group participation. The interviewees considered this type of contact to be better suited to answering target persons’ questions and explaining the method and aims of the focus groups. Moreover, they felt that addressees might find it more difficult to decline a face-to-face invitation than a written one. With regard to health care professionals, an invitation issued by a hierarchically higher person was most effective, even though ethical aspects should be considered in this case, and voluntary participation should nevertheless be ensured. Otherwise, the order to participate might prevent an atmosphere of open communication and might lead to a lower quantity or to more negative statements.
Furthermore, whereas physicians are usually accustomed to discussing topics with others, an important characteristic that influenced willingness to participate on the part of members of other target groups (other health care professionals, patients) was a liking for, or a dislike of, talking. Researchers might take account of this fact by explaining the method in more detail, by developing arguments to overcome fears, or, as suggested, for example, by Colucci (2007) , by convincing the addressees with other activities implemented in the focus groups. Other relevant personal characteristics—be they related to the research topic (e.g., technical interest in the case of an electronic innovation) or to the specific target group (e.g., physical fitness on the part of patients or lack of time on the part of health care professionals)—should be anticipated when planning recruitment. These characteristics might be taken into account by preparing arguments, providing incentives, giving thought to favorable dates and times, and choosing easily accessible locations. An interesting finding was that, depending on the target group, different locations were considered to have a positive influence on the discussion. Whereas locations inside the clinic were preferred in the case of the patient focus groups because of familiarity and easy accessibility, hospital doctors were more engaged in the discussion when the focus group site was located at least some yards away from their workplace.
Finally, the experience of our researchers that up to 50% of the patients had to cancel at short notice because of health problems does not appear to be uncommon in this research context. That overrecruitment is an effective strategy—particularly in health care research—has been reported by other authors (e.g., Coenen et al., 2012 ).
With our second research question, we focused on aspects of communication in the focus groups. The interviews revealed several factors specific to research topics and addressees of health care studies that influenced the discussions. Consequently, in addition to considering general recommendations regarding the organization and moderation of focus groups (e.g., choosing adequate rooms with a pleasant atmosphere, serving food and beverages, using open questions, showing interest in all contributions, and directly addressing quiet participants), these health care specific aspects should be taken into account. Relevant factors that should be addressed when moderating focus groups in this context are (a) the strong need to talk and the high need for information in the patient groups, (b) status differences between the participants or between the moderators and the participants, (c) the size of the focus group, and (d) the specificity of the topic of discussion. The interview data revealed that these factors influenced the discussions and thus the results achieved with the groups. In addition, the following four possibilities of addressing these factors were identified:
First, the moderators had to devote more time to the round of introductions in the patient groups, which served as a warm-up, created an atmosphere of fellowship and openness, and accommodated this target group’s strong need to talk. Second, with respect to status differences between the moderator and the participants, no definite recommendations can be derived from the interviews. The interviewees found that it was less favorable when the moderator was perceived not only in that role but also in other roles (e.g., physician), because this might hamper a goal-oriented discussion. However, they considered deep insight into the research topic on the part of the moderators to be beneficial, at least for certain research topics. Thus, one should carefully weigh up whether it is more advantageous or more disadvantageous when the group moderator is a physician. Interviewees considered status differences between participants to be disadvantageous only in one case, where—because of organizational constraints—medical assistants and their superiors joined the same focus group, which gave rise to some reticence on the part of the young assistants. Similar problems have been reported by other authors, for example, Côté-Arsenault and Morrison-Beedy (2005 ; see also Hollander, 2004 ). However, interviewees did not experience as problematic status differences between physicians with different areas of specialization.
Third, with respect to group size, interviewees found comparatively small focus groups appropriate to give all participants enough time to tell their stories. In contrast to social science research, where groups of between eight and 20 participants are recommended, our interviewees considered groups of between four and six persons to be optimal. This is in line with Côté-Arsenault and Morrison-Beedy (2005) , who recommended small groups for health research, especially when sensitive topics are discussed. Our interview data revealed that this recommendation might also be useful for other health research topics.
Fourth, with regard to the topic of the discussion, interviewees found it helpful to structure different phases of the discussion in different ways, depending on the specificity of the research questions. In contrast to social science research, certain types of research questions in health research require comparatively specific answers. Some of the focus groups in our study were aimed at collecting participants’ expectations regarding an electronic personal health record or—even more specifically—at developing a product specifications document. Conducting focus groups during the development of a technical innovation is a method that is being increasingly used in health care research. Hence, the experiences of the interviewees with regard to these aspects of their research might be relevant for many other research programs. For this type of research questions, it proved useful to include more structured parts in the discussion, for example, having certain questions answered by each participant in turn, or using methods such as participant-generated cards and prioritization. This made it easier to obtain the opinion of each participant and to cover as many concerns and expectations as possible. This finding is in line with recommendations by Colucci (2007) , who proposed the use of activity-oriented questions for health research topics as an enrichment of data collection and a means of making it easier to talk about sensitive and complex topics.
All the moderators found that their discussion guides contained too many questions and too many topics. This might have been due, at least partly, to a desire to determine all relevant aspects in advance—a tendency that might be typical of health research. However, Morgan (1995) also addressed this phenomenon in relation to social research in general: “A common error in focus group question guidelines is too much emphasis on what is of interest to the researcher and not enough emphasis on what is of interest to the participants” (p. 520).
With our third research question, we addressed the appraisal of the focus group method in the interviewees’ research context. Our results show that one should think carefully before using focus groups in the field of health research. The impression that they are quick and easy to conduct might be a misconception, especially in this research context. In fact, the appraisal of the method by the moderators revealed both advantages and disadvantages. The main advantages were the rich blend of perspectives and opinions obtained and the opportunity to have them prioritized by the target groups. For their research topics, the interviewees saw a further important advantage in the fact that they were able to relate their scientific research to everyday life, a point that might be of general importance for a number of research questions in health research, especially those that refer to new medical diagnostics or technical innovations.
The interviewees considered that the main disadvantages of focus groups were the substantial organizational effort and expenditure of time they required. They raised the question whether comparable results could have been achieved using less costly methods. Fortunately, we conducted our interviews with researchers from a research program aimed at answering research questions of different degrees of specificity. As a result, the moderators were able to compare the usefulness of focus groups for different types of research questions. Their statements revealed that they were satisfied with the results relating to more open research questions such as experiences with cross-sectoral health care. For more specific research questions, the interviewees valued the possibility of organizing the discussions in a more structured way and using methods that activated all participants (e.g., participant-generated cards, prioritizations). Nonetheless, they considered meetings of experts to be a necessary intermediate step, for example, on the way to a product specifications document. We recommend that, depending on the specificity of the results that are projected, consideration should be given to including such intermediate steps in the planning stage.
Limitations of the Study
Our analysis of the interviews with the focus group moderators revealed a number of methodological problems that typically occur when focus groups are used in a health research context and yielded recommendations on using such groups in this context. However, some limitations of the present study should also be discussed: First, we conducted our research with focus group moderators, all of whom worked in the same research program. Even though the INFOPAT program consists of several subprojects, they all deal to a greater or lesser extent with the advantages and disadvantages of an electronic support system (electronic personal health record). Furthermore, the moderators were mainly health scientists and had little or no experience with conducting focus groups. This might also have been specific for the research program in which our study was conducted. In other health care programs, focus groups might be moderated mainly by physicists or lay persons (e.g., in participatory health research). Consequently, had we also conducted interviews with focus group moderators from other research areas or included moderators with other professions or more focus group experience, this might have led to different results. However, our research project is rather typical for applied qualitative research in medical science when developing new technologies. Here, focus groups are used by the researchers to find out the potential requirements for the new technology. The researchers are often experts in a specific scientific topic and have no or only limited experience in conducting qualitative research in terms of focus groups. Therefore, our findings are of a particular importance for the researchers with little experiences in conducting focus groups, which can apply to every research, conducted first time. In addition, the little experience of our focus group moderators was a special advantage and strength of the study. More experienced moderators would have prevented some of the problems our moderators—as other unexperienced moderators—faced. As a result, the moderators would not have named these potential problems in the interviews and given no advice for preventing them.
Second, the study was conducted in Germany and thus represents problems and challenges of the German health care system. In other countries, physicians might have different work-shifts or there might be different possibilities in the health care system to reach the target groups. Therefore, more research on the methodology of focus groups in the context of the development of new technologies in health care in other countries and cultures with a consideration of additional relevant groups is needed.
Third, in our interviews, we focused mainly on the organization and conducting of focus groups. For two reasons, we did not address the aspect of data analysis: First, we conducted the interviews shortly after the focus groups had been completed, at a time when data analysis was still in progress. Second, analysis of qualitative data can be carried out in many different ways, depending on research questions and preferences of researchers, and some of the recommended methods are very complex. Had we discussed them in detail, it would have been too time-consuming in the interviews.
Concluding Remarks
Our results revealed a number of methodological challenges that might be typical of conducting focus groups in health research. We hope that our findings will be of use to researchers in similar research fields. Furthermore, we encourage other researchers who are interested in health research topics to gather more information about methodological aspects specific to this research field. Our results were achieved in the context of the development of a technical innovation. It might be interesting to endeavor to replicate them in other health care research projects dealing with technical innovations. Moreover, we would encourage researchers of other topics in health research to interview focus group moderators about their experiences in their specific research context. We hope that our results will serve as a useful basis for comparing results in different areas of health research.
Acknowledgments
We thank the focus group moderators in the INFOPAT program for their great willingness to share their experiences and for their openness during the interviews.
Author Biographies
Anja P. Tausch , PhD, is senior researcher at GESIS–Leibniz Institute for the Social Sciences, Mannheim, Germany.
Natalja Menold , PhD, is senior researcher and head of the Survey Instruments Unit at GESIS–Leibniz Institute for the Social Sciences, Mannheim, Germany.
1. http://www.soziologie.de/en/gsa/ethik-kommission/code-of-ethics.html , retrieved on 05/10/2015.
2. The language of the research project, focus groups, and interviews was German. The scheme was developed in German on the basis of the German text material from the transcribed interviews. The scheme and the citations were translated for the purpose of international publication by an experienced, qualified, and fully bilingual translator, whose mother tongue is English and who also has an MA in sociology from a German university. A German version of the full categorial system can be found in Tausch and Menold (2015) .
3. All citations included in this publication were translated from German.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by the German Federal Ministry of Education and Research (BMBF; FKZ 01KQ1003D).
- Baudendistel I., Winkler E., Kamradt M., Brophy S., Längst G., Eckrich F., . . .Ose D. (2015). The patients’ active role in managing a personal electronic health record: A qualitative analysis . Supportive Care in Cancer , 23 , 2613-2621. doi: 10.1007/s00520-015-2620-1 [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Carey M. A. (1994). The group effect in focus groups: Planning, implementing, and interpreting focus group research . In Morse J. M. (Ed.), Critical issues in qualitative research methods (pp. 225–241). Thousand Oaks, CA: Sage. [ Google Scholar ]
- Carr A., Hewlett S., Hughes R., Mitchell H., Ryan S., Carr M., Kirwan J. (2003). Rheumatology outcomes: The patient’s perspective . The Journal of Rheumatology , 30 , 880–883. [ PubMed ] [ Google Scholar ]
- Coenen M., Stamm T., Stucki G., Cieza A. (2012). Individual interviews and focus groups in patients with rheumatoid arthritis: A comparison of two qualitative methods . Quality of Life Research , 21 , 359–370. [ PubMed ] [ Google Scholar ]
- Colucci E. (2007). “Focus groups can be fun”: The use of activity-oriented questions in focus group discussions . Qualitative Health Research , 17 , 1422–1433. [ PubMed ] [ Google Scholar ]
- Côté-Arsenault D., Morrison-Beedy D. (2005). Maintaining your focus in focus groups: Avoiding common mistakes . Research in Nursing & Health , 28 , 172–179. [ PubMed ] [ Google Scholar ]
- Creswell J. W., Plano Clark V. L. (2007). Designing and conducting mixed methods research . Thousand Oaks, CA: Sage. [ Google Scholar ]
- Daley C. M., James A. S., Ulrey E., Joseph S., Talawyma A., Choi W. S., . . .Coe M. K. (2010). Using focus groups in community-based participatory research: Challenges and resolutions . Qualitative Health Research , 20 , 697–706. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Elo S., Kyngäs H. (2008). The qualitative content analysis process . Journal of Advanced Nursing , 62 , 107–115. [ PubMed ] [ Google Scholar ]
- Feldthusen C., Björk M., Forsblad-d’Elia H., Mannerkorpi K. (2013). Perception, consequences, communication, and strategies for handling fatigue in persons with rheumatoid arthritis of working age—A focus group study . Clinical Rheumatology , 32 , 557–566. [ PubMed ] [ Google Scholar ]
- Frazier L. M., Miller V. A., Horbelt D. V., Delmore J. E., Miller B. E., Paschal A. M. (2010). Comparison of focus groups on cancer and employment conducted face to face or by telephone . Qualitative Health Research , 20 , 617–627. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gerber D. E., Hamann H. A., Rasco D. W., Woodruff S., Lee S. J. C. (2012). Patient comprehension and attitudes toward maintenance chemotherapy for lung cancer . Patient Education and Counseling , 89 , 102–108. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hollander J. A. (2004). The social contexts of focus groups . Journal of Contemporary Ethnography , 33 , 602–637. [ Google Scholar ]
- Kamradt M., Baudendistel I., Längst G., Kiel M., Eckrich F., Winkler E., Ose D. (2015). Collaboration and communication in colorectal cancer care: A qualitative study of the challenges experienced by patients and health care professionals . Family Practice , 32 , 686-696. doi: 10.1093/fampra/cmv069 [ PMC free article ] [ PubMed ] [ CrossRef ] [ Google Scholar ]
- Kingry M. J., Tiedje L. B., Friedman L. L. (1990). Focus groups: A research technique for nursing . Nursing Research , 39 , 124–125. [ PubMed ] [ Google Scholar ]
- Kitzinger J. (1995). Qualitative research: Introducing focus groups . British Medical Journal , 311 , 299–302. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kitzinger J. (2006). Chapter 3: Focus groups . In Pope C., Mays N. (Eds.), Qualitative research in health care (3rd ed., pp. 21–31). Malden, MA: Blackwell. [ Google Scholar ]
- Kroll T., Neri M. T., Miller K. (2005). Using mixed methods in disability and rehabilitation research . Rehabilitation Nursing , 30 , 106–113. [ PubMed ] [ Google Scholar ]
- Krueger R. A. (1988). Focus groups: A practical guide for applied research . Newbury Park, CA: Sage. [ Google Scholar ]
- Lehoux P., Poland B. D., Daudelin G. (2006). Focus group research and “the patient’s view.” Social Science & Medicine , 63 , 2091–2104. [ PubMed ] [ Google Scholar ]
- Mayring P. (2015). Qualitative Inhaltsanalyse [Qualitative content analysis] (12th ed.). Weinheim, Germany: Beltz. [ Google Scholar ]
- Morgan D. L. (Ed.). (1993). Successful focus groups: Advancing the state of the art . Newbury Park, CA: Sage. [ Google Scholar ]
- Morgan D. L. (1995). Why things (sometimes) go wrong in focus groups . Qualitative Health Research , 5 , 516–523. [ Google Scholar ]
- Morgan D. L. (1996). Focus groups . Annual review of sociology , 22 , 129–152. [ Google Scholar ]
- Morgan D. L. (2009). Focus groups as qualitative research (2nd ed.). Thousand Oaks, CA: Sage. [ Google Scholar ]
- Morgan D. L., Krueger R. A. (Eds.). (1998). Focus group kit . Thousand Oaks, CA: Sage. [ Google Scholar ]
- Nafees B., Lloyd A., Kennedy-Martin T., Hynd S. (2006). How diabetes and insulin therapy affects the lives of people with type 1 diabetes . European Diabetes Nursing , 3 , 92–97. [ Google Scholar ]
- Nicholas D. B., Lach L., King G., Scott M., Boydell K., Sawatzky B. J., . . .Young N. L. (2010). Contrasting internet and face-to-face focus groups for children with chronic health conditions: Outcomes and participant experiences . International Journal of Qualitative Methods , 9 , 105–121. [ Google Scholar ]
- Rasmusson K., Lappe D., Roberts C., Croasdell S., Meegan S., Budge D. (2014). Heart failure patient perspectives: Learning from focus groups to improve care . Heart & Lung , 43 , 382–383. [ Google Scholar ]
- Rhodes S. D., Hergenrather K. C., Wilkin A., Alegría-Ortega J., Montaño J. (2006). Preventing HIV infection among young immigrant Latino men: Results from focus groups using community-based participatory research . Journal of the National Medical Association , 98 , 564–573. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stewart D. W., Shamdasani P. N., Rook D. W. (2007). Focus groups: Theory and practice (2nd ed.). Thousand Oaks, CA: Sage. [ Google Scholar ]
- Tausch A., Menold N. (2015). Methodische Aspekte der Durchführung von Fokusgruppen in der Gesundheitsforschung - Welche Anforderungen ergeben sich aufgrund der besonderen Zielgruppen und Fragestellungen? [Methodological aspects of conducting focus groups in health research - which requirements result from the particular target groups and research questions?]. GESIS Papers , 2015 ( 12 ). Retrieved from http://www.gesis.org/fileadmin/upload/forschung/publikationen/gesis_reihen/gesis_papers/GESIS-Papers_2015-12.pdf [ Google Scholar ]
- Vincent D., Clark L., Marquez Zimmer L., Sanchez J. (2006). Using focus groups to develop a culturally competent diabetes self-management program for Mexican Americans . The Diabetes Educator , 32 , 89–97. [ PubMed ] [ Google Scholar ]
Research Design Review
A discussion of qualitative & quantitative research design, strengths of the focus group method: an overview.
The following is a modified excerpt from Applied Qualitative Research Design: A Total Quality Framework Approach (Roller & Lavrakas, 2015, pp. 111-112).

- A dynamic group discussion will often stimulate spontaneous ideas and personal disclosures that might otherwise go unstated in an IDI.
- A relaxed, interactive, as well as a supportive (e.g., homogeneous) group environment can be conducive to discussing sensitive topics (e.g., a discussion of the immigration process among recent Chinese immigrants to the United States).
- As participants exchange opinions, they consider their own views in relation to others’—which may encourage participants to refine their thoughts. In this way the group interaction gives the researcher insight into how people think about the topic(s) being studied and on what basis opinions may change. For example, in a focus group with college students who are considering various study-abroad programs, some participants might change their criteria for selecting one program over another after hearing other participants’ considerations. This discussion would help the researcher identify the important aspects of study-abroad programs that may impact students’ decision making.
Participant interaction, or the social aspect of focus group discussions, can be a particularly important advantage when conducting research with vulnerable and underserved population segments . For instance, women’s studies researchers such as Wilkinson (1999) believe that focus groups offer feminist psychologists an important research approach over other psychological research methods because they (a) come “closer to everyday social processes” (p. 227) and are less “artificial” than other methods; (b) are highly interactive, which “produces insights that would not be available outside the group context” (p. 229); and (c) reduce the moderator’s “exploitation” of the research by shifting control of the discussion to the participants. Other researchers have found the social nature of focus group discussions to be conducive to investigating societal constraints and health needs among Emirati women (Bailey, 2012; Winslow, Honein, & Elzubeir, 2002).
There are two other important strengths of the group discussion method: (1) it allows for the presence of observers , especially in the face-to-face (in-person and sometimes video) mode; and (2) it increases the likelihood that a wide range of attitudes, knowledge, and experiences will be captured in one group session. Whereas most qualitative research methods can conceivably accommodate observers, observers tend to take on a particularly engaged and active role in group interviewing. Face-to-face focus groups are traditionally conducted at a facility equipped with a one-way mirror (and online video group platforms also offer a client backroom), behind which members of the research team can view and hear the discussions. (Note: Group participants are informed of the presence of observers prior to the discussion.) Viewers often include people affiliated with the research sponsor who have a vested interest in learning firsthand about the attitudes and behavior of members of the target population. In addition to gaining clarity on participants’ wants and needs, observers can be helpful in redirecting the discussion on the spot, if necessary, when participants make unanticipated comments that introduce a new way of thinking about the research topic. In these situations, it is important to be able to change course in the research or otherwise pursue new lines of questioning as unanticipated insights emerge from the discussions.
The range of opinions and behavior that can be represented in any one focus group is another important strength of the method because such a range is a factor in finding the “surprising insights” mentioned above. Even the most homogeneous group of participants will relate different experiences and thoughts, thereby giving the researcher an awareness and appreciation of the extent of divergent views on a particular issue. Unlike the IDI method that requires many separate interviews to uncover the spectrum of perspectives related to the subject matter, group discussions offer a time- and often cost-efficient method for revealing differing viewpoints.
Bailey, D. C. (2012). Women and Wasta: The use of focus groups for understanding social capital and Middle Eastern women. Retrieved from The Qualitative Report website: http://www.nova.edu/ssss/QR/QR17/bailey.pdf
Wilkinson, S. (1999). Focus groups: A feminist method. Psychology of Women Quarterly , 23 (2), 221–244.
Winslow, W. W., Honein, G., & Elzubeir, M. A. (2002). Seeking Emirati women’s voices: The use of focus groups with an Arab population. Qualitative Health Research , 12 (4), 566–575. https://doi.org/10.1177/104973202129119991
Image captured from: https://www.clipartkey.com/view/momihb_organization-clipart-focus-group-clipart-debate-competition/
Share this:
- Click to share on Reddit (Opens in new window)
- Click to share on Twitter (Opens in new window)
- Click to share on LinkedIn (Opens in new window)
- Click to share on Facebook (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to email a link to a friend (Opens in new window)
- Click to print (Opens in new window)
One comment
- Pingback: Limitations of the Focus Group Method: An Overview | Research Design Review
Leave a comment Cancel reply
This site uses Akismet to reduce spam. Learn how your comment data is processed .

- Already have a WordPress.com account? Log in now.
- Subscribe Subscribed
- Copy shortlink
- Report this content
- View post in Reader
- Manage subscriptions
- Collapse this bar
2024 Theses Master's
Understanding remote work in the post-pandemic world: An exploration of lived experiences. How remote work is shaping our quotidian and how it can shape our cities
Padilla García, Raquel Edith
This work presents an analysis of the role that remote work has played in people's lives, particularly after the acceleration in its adoption during the Covid-19 pandemic. The study results from the fact that all research done on remote work failed to include the voices of remote workers, focusing instead on the analysis of labor and market statistics, data-based simulations, or the discussion of managerial techniques. This project approached the topic using qualitative methods, namely an online survey and focus groups. Using this methodology, experiences from remote workers were collected and analyzed. Due to the nature of the topic, the study was carried out on a global scale taking advantage of the same tools used by remote workers, i.e. Information and Telecommunication Technologies (ICTs). The results show consensus on a positive perception of remote work, being the flexibility that this provides the most appreciated attribute. Remote work has particularly expanded possibilities for women with children, and people with limited mobility, facilitating their access to services and helping them to enter or remain in the job market. This study can serve as a base for further analysis on remote work and its impact on people's lives, particularly the effects that it has in people's well-being, career progression, and mobility and residential choices.
- City planning
- City planning--Economic aspects
- Telecommuting--Evaluation
- Telecommuting--Social aspects
- COVID-19 (Disease)--Economic aspects
This item is currently under embargo. It will be available starting 2026-06-01.
More About This Work
- DOI Copy DOI to clipboard
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 29, Issue 3
- Rapid reviews methods series: guidance on rapid qualitative evidence synthesis
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0003-4808-3880 Andrew Booth 1 , 2 ,
- Isolde Sommer 3 , 4 ,
- http://orcid.org/0000-0003-4238-5984 Jane Noyes 2 , 5 ,
- Catherine Houghton 2 , 6 ,
- Fiona Campbell 1 , 7
- The Cochrane Rapid Reviews Methods Group and Cochrane Qualitative and Implementation Methods Group (CQIMG)
- 1 EnSyGN Sheffield Evidence Synthesis Group , University of Sheffield , Sheffield , UK
- 2 Cochrane Qualitative and Implementation Methods Group (CQIMG) , London , UK
- 3 Department for Evidence-based Medicine and Evaluation , University for Continuing Education Krems , Krems , Austria
- 4 Cochrane Rapid Reviews Group & Cochrane Austria , Krems , Austria
- 5 Bangor University , Bangor , UK
- 6 University of Galway , Galway , Ireland
- 7 University of Newcastle upon Tyne , Newcastle upon Tyne , UK
- Correspondence to Professor Andrew Booth, Univ Sheffield, Sheffield, UK; a.booth{at}sheffield.ac.uk
This paper forms part of a series of methodological guidance from the Cochrane Rapid Reviews Methods Group and addresses rapid qualitative evidence syntheses (QESs), which use modified systematic, transparent and reproducible methodsu to accelerate the synthesis of qualitative evidence when faced with resource constraints. This guidance covers the review process as it relates to synthesis of qualitative research. ‘Rapid’ or ‘resource-constrained’ QES require use of templates and targeted knowledge user involvement. Clear definition of perspectives and decisions on indirect evidence, sampling and use of existing QES help in targeting eligibility criteria. Involvement of an information specialist, especially in prioritising databases, targeting grey literature and planning supplemental searches, can prove invaluable. Use of templates and frameworks in study selection and data extraction can be accompanied by quality assurance procedures targeting areas of likely weakness. Current Cochrane guidance informs selection of tools for quality assessment and of synthesis method. Thematic and framework synthesis facilitate efficient synthesis of large numbers of studies or plentiful data. Finally, judicious use of Grading of Recommendations Assessment, Development and Evaluation approach for assessing the Confidence of Evidence from Reviews of Qualitative research assessments and of software as appropriate help to achieve a timely and useful review product.
- Systematic Reviews as Topic
- Patient Care
Data availability statement
No data are available. Not applicable. All data is from published articles.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjebm-2023-112620
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
WHAT IS ALREADY KNOWN ON THIS TOPIC
Rapid Qualitative Evidence Synthesis (QES) is a relatively recent innovation in evidence synthesis and few published examples currently exists.
Guidance for authoring a rapid QES is scattered and requires compilation and summary.
WHAT THIS STUDY ADDS
This paper represents the first attempt to compile current guidance, illustrated by the experience of several international review teams.
We identify features of rapid QES methods that could be accelerated or abbreviated and where methods resemble those for conventional QESs.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This paper offers guidance for researchers when conducting a rapid QES and informs commissioners of research and policy-makers what to expect when commissioning such a review.
Introduction
This paper forms part of a series from the Cochrane Rapid Reviews Methods Group providing methodological guidance for rapid reviews. While other papers in the series 1–4 focus on generic considerations, we aim to provide in-depth recommendations specific to a resource-constrained (or rapid) qualitative evidence synthesis (rQES). 5 This paper is accompanied by recommended resources ( online supplemental appendix A ) and an elaboration with practical considerations ( online supplemental appendix B ).
Supplemental material
The role of qualitative evidence in decision-making is increasingly recognised. 6 This, in turn, has led to appreciation of the value of qualitative evidence syntheses (QESs) that summarise findings across multiple contexts. 7 Recognition of the need for such syntheses to be available at the time most useful to decision-making has, in turn, driven demand for rapid qualitative evidence syntheses. 8 The breadth of potential rQES mirrors the versatility of QES in general (from focused questions to broad overviews) and outputs range from descriptive thematic maps through to theory-informed syntheses (see table 1 ).
- View inline
Glossary of important terms (alphabetically)
As with other resource-constrained reviews, no one size fits all. A team should start by specifying the phenomenon of interest, the review question, 9 the perspectives to be included 9 and the sample to be determined and selected. 10 Subsequently, the team must finalise the appropriate choice of synthesis. 11 Above all, the review team should consider the intended knowledge users, 3 including requirements of the funder.
An rQES team, in particular, cannot afford any extra time or resource requirements that might arise from either a misunderstanding of the review question, an unclear picture of user requirements or an inappropriate choice of methods. The team seeks to align the review question and the requirements of the knowledge user with available time and resources. They also need to ensure that the choice of data and choice of synthesis are appropriate to the intended ‘knowledge claims’ (epistemology) made by the rQES. 11 This involves the team asking ‘what types of data are meaningful for this review question?’, ‘what types of data are trustworthy?’ and ‘is the favoured synthesis method appropriate for this type of data?’. 12 This paper aims to help rQES teams to choose methods that best fit their project while understanding the limitations of those choices. Our recommendations derive from current QES guidance, 5 evidence on modified QES methods, 8 13 and practical experience. 14 15
This paper presents an overview of considerations and recommendations as described in table 2 . Supplemental materials including additional resources details of our recommendations and practical examples are provided in online supplemental appendices A and B .
Recommendations for resource-constrained qualitative evidence synthesis (rQES)
Setting the review question and topic refinement
Rapid reviews summarise information from multiple research studies to produce evidence for ‘the public, researchers, policymakers and funders in a systematic, resource-efficient manner’. 16 Involvement of knowledge users is critical. 3 Given time constraints, individual knowledge users could be asked only to feedback on very specific decisions and tasks or on selective sections of the protocol. Specifically, whenever a QES is abbreviated or accelerated, a team should ensure that the review question is agreed by a minimum number of knowledge users with expertise or experience that reflects all the important review perspectives and with authority to approve the final version 2 5 11 ( table 2 , item R1).
Involvement of topic experts can ensure that the rQES is responsive to need. 14 17 One Cochrane rQES saved considerable time by agreeing the review topic within a single meeting and one-phase iteration. 9 Decisions on topics to be omitted are also informed by a knowledge of existing QESs. 17
An information specialist can help to manage the quantity and quality of available evidence by setting conceptual boundaries and logistic limits. A structured question format, such as Setting-Perspective-Interest, phenomenon of-Comparison-Evaluation or Population-Interest, phenomenon of-Context helps in communicating the scope and, subsequently, in operationalising study selection. 9 18
Scoping (of review parameters) and mapping (of key types of evidence and likely richness of data) helps when planning the review. 5 19 The option to choose purposive sampling over comprehensive sampling approaches, as offered by standard QES, may be particularly helpful in the context of a rapid QES. 8 Once a team knows the approximate number and distribution of studies, perhaps mapping them against country, age, ethnicity, etc), they can decide whether or not to use purposive sampling. 12 An rQES for the WHO combined purposive with variation sampling. Sampling in two stages started by reducing the initial number of studies to a more manageable sampling frame and then sampling approximately a third of the remaining studies from within the sampling frame. 20
Sampling may target richer studies and/or privilege diversity. 8 21 A rich qualitative study typically illustrates findings with verbatim extracts from transcripts from interviews or textual responses from questionnaires. Rich studies are often found in specialist qualitative research or social science journals. In contrast, less rich studies may itemise themes with an occasional indicative text extract and tend to summarise findings. In clinical or biomedical journals less rich findings may be placed within a single table or box.
No rule exists on an optimal number of studies; too many studies makes it challenging to ‘maintain insight’, 22 too few does not sustain rigorous analysis. 23 Guidance on sampling is available from the forthcoming Cochrane-Campbell QES Handbook.
A review team can use templates to fast-track writing of a protocol. The protocol should always be publicly available ( table 2 , item R2). 24 25 Formal registration may require that the team has not commenced data extraction but should be considered if it does not compromise the rQES timeframe. Time pressures may require that methods are left suitably flexible to allow well-justified changes to be made as a detailed picture of the studies and data emerge. 26 The first Cochrane rQES drew heavily on text from a joint protocol/review template previously produced within Cochrane. 24
Setting eligibility criteria
An rQES team may need to limit the number of perspectives, focusing on those most important for decision-making 5 9 27 ( table 2 , item R3). Beyond the patients/clients each additional perspective (eg, family members, health professionals, other professionals, etc) multiplies the additional effort involved.
A rapid QES may require strict date and setting restrictions 17 and language restrictions that accommodate the specific requirements of the review. Specifically, the team should consider whether changes in context over time or substantive differences between geographical regions could be used to justify a narrower date range or a limited coverage of countries and/or languages. The team should also decide if ‘indirect evidence’ is to substitute for the absence of direct evidence. An rQES typically focuses on direct evidence, except when only indirect evidence is available 28 ( table 2 , item R4). Decisions on relevance are challenging—precautions for swine influenza may inform precautions for bird influenza. 28 A smoking ban may operate similarly to seat belt legislation, etc. A review team should identify where such shared mechanisms might operate. 28 An rQES team must also decide whether to use frameworks or models to focus the review. Theories may be unearthed within the topic search or be already known to team members, fro example, Theory of Planned Behaviour. 29
Options for managing the quantity and quality of studies and data emerge during the scoping (see above). In summary, the review team should consider privileging rich qualitative studies 2 ; consider a stepwise approach to inclusion of qualitative data and explore the possibility of sampling ( table 2 , item R5). For example, where data is plentiful an rQES may be limited to qualitative research and/or to mixed methods studies. Where data is less plentiful then surveys or other qualitative data sources may need to be included. Where plentiful reviews already exist, a team may decide to conduct a review of reviews 5 by including multiple QES within a mega-synthesis 28 29 ( table 2 , item R6).
Searching for QES merits its own guidance, 21–23 30 this section reinforces important considerations from guidance specific to qualitative research. Generic guidance for rapid reviews in this series broadly applies to rapid QESs. 1
In addition to journal articles, by far the most plentiful source, qualitative research is found in book chapters, theses and in published and unpublished reports. 21 Searches to support an rQES can (a) limit the number of databases searched, deliberately selecting databases from diverse disciplines, (b) use abbreviated study filters to retrieve qualitative designs and (c) employ high yield complementary methods (eg, reference checking, citation searching and Related Articles features). An information specialist (eg, librarian) should be involved in prioritising sources and search methods ( table 2 , item R7). 11 14
According to empirical evidence optimal database combinations include Scopus plus CINAHL or Scopus plus ProQuest Dissertations and Theses Global (two-database combinations) and Scopus plus CINAHL plus ProQuest Dissertations and Theses Global (three-database combination) with both choices retrieving between 89% and 92% of relevant studies. 30
If resources allow, searches should include one or two specialised databases ( table 2 , item R8) from different disciplines or contexts 21 (eg, social science databases, specialist discipline databases or regional or institutional repositories). Even when resources are limited, the information specialist should factor in time for peer review of at least one search strategy ( table 2 , item R9). 31 Searches for ‘grey literature’ should selectively target appropriate types of grey literature (such as theses or process evaluations) and supplemental searches, including citation chaining or Related Articles features ( table 2 , item R10). 32 The first Cochrane rQES reported that searching reference lists of key papers yielded an extra 30 candidate papers for review. However, the team documented exclusion of grey literature as a limitation of their review. 15
Study selection
Consistency in study selection is achieved by using templates, by gaining a shared team understanding of the audience and purpose, and by ongoing communication within, and beyond, the team. 2 33 Individuals may work in parallel on the same task, as in the first Cochrane rQES, or follow a ‘segmented’ approach where each reviewer is allocated a different task. 14 The use of machine learning in the specific context of rQES remains experimental. However, the possibility of developing qualitative study classifiers comparable to those for randomised controlled trials offers an achievable aspiration. 34
Title and abstract screening
The entire screening team should use pre-prepared, pretested title and abstract templates to limit the scale of piloting, calibration and testing ( table 2 , item R11). 1 14 The first Cochrane rQES team double-screened titles and abstracts within Covidence review software. 14 Disagreements were resolved with reference to a third reviewer achieving a shared understanding of the eligibility criteria and enhancing familiarity with target studies and insight from data. 14 The team should target and prioritise identified risks of either over-zealous inclusion or over-exclusion specific to each rQES ( table 2 , item R12). 14 The team should maximise opportunities to capture divergent views and perspectives within study findings. 35
Full-text screening
Full-text screening similarly benefits from using a pre-prepared pretested standardised template where possible 1 14 ( table 2 , item R11). If a single reviewer undertakes full-text screening, 8 the team should identify likely risks to trustworthiness of findings and focus quality control procedures (eg, use of additional reviewers and percentages for double screening) on specific threats 14 ( table 2 , item R13). The Cochrane rQES team opted for double screening to assist their immersion within the topic. 14
Data extraction
Data extraction of descriptive/contextual data may be facilitated by review management software (eg, EPPI-Reviewer) or home-made approaches using Google Forms, or other survey software. 36 Where extraction of qualitative findings requires line-by-line coding with multiple iterations of the data then a qualitative data management analysis package, such as QSR NVivo, reaps dividends. 36 The team must decide if, collectively, they favour extracting data to a template or coding direct within an electronic version of an article.
Quality control must be fit for purpose but not excessive. Published examples typically use a single reviewer for data extraction 8 with use of two independent reviewers being the exception. The team could limit data extraction to minimal essential items. They may also consider re-using descriptive details and findings previously extracted within previous well-conducted QES ( table 2 , item R14). A pre-existing framework, where readily identified, may help to structure the data extraction template. 15 37 The same framework may be used to present the findings. Some organisations may specify a preferred framework, such as an evidence-to-decision-making framework. 38
Assessment of methodological limitations
The QES community assess ‘methodological limitations’ rather than use ‘risk of bias’ terminology. An rQES team should pick an approach appropriate to their specific review. For example, a thematic map may not require assessment of individual studies—a brief statement of the generic limitations of the set of studies may be sufficient. However, for any synthesis that underpins practice recommendations 39 assessment of included studies is integral to the credibility of findings. In any decision-making context that involves recommendations or guidelines, an assessment of methodological limitations is mandatory. 40 41
Each review team should work with knowledge users to determine a review-specific approach to quality assessment. 27 While ‘traffic lights’, similar to the outputs from the Cochrane Risk of Bias tool, may facilitate rapid interpretation, accompanying textual notes are invaluable in highlighting specific areas for concern. In particular, the rQES team should demonstrate that they are aware (a) that research designs for qualitative research seek to elicit divergent views, rather than control for variation; (b) that, for qualitative research, the selection of the sample is far more informative than the size of the sample; and (c) that researchers from primary research, and equally reviewers for the qualitative synthesis, need to be thoughtful and reflexive about their possible influences on interpretation of either the primary data or the synthesised findings.
Selection of checklist
Numerous scales and checklists exist for assessing the quality of qualitative studies. In the absence of validated risk of bias tools for qualitative studies, the team should choose a tool according to Cochrane Qualitative and Implementation Methods Group (CQIMG) guidance together with expediency (according to ease of use, prior familiarity, etc) ( table 2 , item R15). 41 In comparison to the Critical Appraisal Skills Programme checklist which was never designed for use in synthesis, 42 the Cochrane qualitative tool is similarly easy to use and was designed for QES use. Work is underway to identify an assessment process that is compatible with QESs that support decision-making. 41 For now the choice of a checklist remains determined by interim Cochrane guidance and, beyond this, by personal preference and experience. For an rQES a team could use a single reviewer to assess methodological limitations, with verification of judgements (and support statements) by a second reviewer ( table 2 , item R16).
The CQIMG endorses three types of synthesis; thematic synthesis, framework synthesis and meta-ethnography ( box 1 ). 43 44 Rapid QES favour descriptive thematic synthesis 45 or framework synthesis, 46 47 except when theory generation (meta-ethnography 48 49 or analytical thematic synthesis) is a priority ( table 2 , item R17).
Choosing a method for rapid qualitative synthesis
Thematic synthesis: first choice method for rQES. 45 For example, in their rapid QES Crooks and colleagues 44 used a thematic synthesis to understand the experiences of both academic and lived experience coresearchers within palliative and end of life research. 45
Framework synthesis: alternative where a suitable framework can be speedily identified. 46 For example, Bright and colleagues 46 considered ‘best-fit framework synthesis’ as appropriate for mapping study findings to an ‘a priori framework of dimensions measured by prenatal maternal anxiety tools’ within their ‘streamlined and time-limited evidence review’. 47
Less commonly, an adapted meta-ethnographical approach was used for an implementation model of social distancing where supportive data (29 studies) was plentiful. 48 However, this QES demonstrates several features that subsequently challenge its original identification as ‘rapid’. 49
Abbrevations: QES, qualitative evidence synthesis; rQES, resource-constrained qualitative evidence synthesis.
The team should consider whether a conceptual model, theory or framework offers a rapid way for organising, coding, interpreting and presenting findings ( table 2 , item R18). If the extracted data appears rich enough to sustain further interpretation, data from a thematic or framework synthesis can subsequently be explored within a subsequent meta-ethnography. 43 However, this requires a team with substantial interpretative expertise. 11
Assessments of confidence in the evidence 4 are central to any rQES that seeks to support decision-making and the QES-specific Grading of Recommendations Assessment, Development and Evaluation approach for assessing the Confidence of Evidence from Reviews of Qualitative research (GRADE-CERQual) approach is designed to assess confidence in qualitative evidence. 50 This can be performed by a single reviewer, confirmed by a second reviewer. 26 Additional reviewers could verify all, or a sample of, assessments. For a rapid assessment a team must prioritise findings, using objective criteria; a WHO rQES focused only on the three ‘highly synthesised findings’. 20 The team could consider reusing GRADE-CERQual assessments from published QESs if findings are relevant and of demonstrable high quality ( table 2 , item R19). 50 No rapid approach to full application of GRADE-CERQual currently exists.

Reporting and record management
Little is written on optimal use of technology. 8 A rapid review is not a good time to learn review management software or qualitative analysis management software. Using such software for all general QES processes ( table 2 , item R20), and then harnessing these skills and tools when specifically under resource pressures, is a sounder strategy. Good file labelling and folder management and a ‘develop once, re-use multi-times’ approach facilitates resource savings.
Reporting requirements include the meta-ethnography reporting guidance (eMERGe) 51 and the Enhancing transparency in reporting the synthesis of qualitative research (ENTREQ) statement. 52 An rQES should describe limitations and their implications for confidence in the evidence even more thoroughly than a regular QES; detailing the consequences of fast-tracking, streamlining or of omitting processes all together. 8 Time spent documenting reflexivity is similarly important. 27 If QES methodology is to remain credible rapid approaches must be applied with insight and documented with circumspection. 53 54 (56)
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
- Klerings I ,
- Robalino S ,
- Booth A , et al
- Nussbaumer-Streit B ,
- Hamel C , et al
- Garritty C ,
- Tricco AC ,
- Smith M , et al
- Gartlehner G ,
- Devane D , et al
- NHS Scotland
- Campbell F ,
- Flemming K , et al
- Glenton C ,
- Lubarsky S ,
- Varpio L , et al
- Meskell P ,
- Glenton C , et al
- Houghton C ,
- Delaney H , et al
- Beecher C ,
- Maeso B , et al
- McKenzie JE , et al
- Harris JL ,
- Cargo M , et al
- Varley-Campbell J , et al
- Downe S , et al
- Shamseer L ,
- Clarke M , et al
- Nussbaumer-Streit B , et al
- Finlayson KW ,
- Lawrie TA , et al
- Lewin S , et al
- Frandsen TF ,
- Gildberg FA ,
- Tingleff EB
- Mshelia S ,
- Analo CV , et al
- Husk K , et al
- Carmona C ,
- Carroll C ,
- Ilott I , et al
- Meehan B , et al
- Munthe-Kaas H ,
- Bohren MA ,
- Munthe-Kaas HM ,
- French DP ,
- Flemming K ,
- Garside R , et al
- Shulman C , et al
- Dixon-Woods M
- Bright KS ,
- Norris JM ,
- Letourneau NL , et al
- Sadjadi M ,
- Mörschel KS ,
- Petticrew M
- France EF ,
- Cunningham M ,
- Ring N , et al
- McInnes E , et al
- Britten N ,
- Garside R ,
- Pope C , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
Correction notice Since this paper first published, updates have been made to the left hand column of table 2.
Contributors All authors (AB, IS, JN, CH, FC) have made substantial contributions to the conception and design of the guidance document. AB led on drafting the work and revising it critically for important intellectual content. All other authors (IS, JN, CH, FC) contributed to revisions of the document. All authors (AB, IS, JN, CH, FC) have given final approval of the version to be published. As members of the Cochrane Qualitative and Implementation Methods Group and/or the Cochrane Rapid Reviews Methods Group all authors (AB, IS, JN, CH, FC) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests AB is co-convenor of the Cochrane Qualitative and Implementation Methods Group. In the last 36 months, he received royalties from Systematic Approaches To a Successful Literature Review (Sage 3rd edition), honoraria from the Agency for Healthcare Research and Quality, and travel support from the WHO. JN is lead convenor of the Cochrane Qualitative and Implementation Methods Group. In the last 36 months, she has received honoraria from the Agency for Healthcare Research and Quality and travel support from the WHO. CH is co-convenor of the Cochrane Qualitative and Implementation Methods Group.
Patient and public involvement Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review Not commissioned; internally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Open access
- Published: 27 May 2024
Using the technology acceptance model to assess clinician perceptions and experiences with a rheumatoid arthritis outcomes dashboard: qualitative study
- Catherine Nasrallah 1 ,
- Cherish Wilson 1 ,
- Alicia Hamblin 1 ,
- Cammie Young 1 ,
- Lindsay Jacobsohn 1 ,
- Mary C. Nakamura 1 , 2 ,
- Andrew Gross 1 ,
- Mehrdad Matloubian 1 ,
- Judith Ashouri 1 ,
- Jinoos Yazdany 1 , 3 &
- Gabriela Schmajuk 1 , 2
BMC Medical Informatics and Decision Making volume 24 , Article number: 140 ( 2024 ) Cite this article
Metrics details
Improving shared decision-making using a treat-to-target approach, including the use of clinical outcome measures, is important to providing high quality care for rheumatoid arthritis (RA). We developed an Electronic Health Record (EHR) integrated, patient-facing sidecar dashboard application that displays RA outcomes, medications, and lab results for use during clinical visits (“RA PRO dashboard”). The purpose of this study was to assess clinician perceptions and experiences using the dashboard in a university rheumatology clinic.
We conducted focus group (FG) discussions with clinicians who had access to the dashboard as part of a randomized, stepped-wedge pragmatic trial. FGs explored clinician perceptions towards the usability, acceptability, and usefulness of the dashboard. FG data were analyzed thematically using deductive and inductive techniques; generated themes were categorized into the domains of the Technology Acceptance Model (TAM).
3 FG discussions were conducted with a total of 13 clinicians. Overall, clinicians were enthusiastic about the dashboard and expressed the usefulness of visualizing RA outcome trajectories in a graphical format for motivating patients, enhancing patient understanding of their RA outcomes, and improving communication about medications. Major themes that emerged from the FG analysis as barriers to using the dashboard included inconsistent collection of RA outcomes leading to sparse data in the dashboard and concerns about explaining RA outcomes, especially to patients with fibromyalgia. Other challenges included time constraints and technical difficulties refreshing the dashboard to display real-time data. Methods for integrating the dashboard into the visit varied: some clinicians used the dashboard at the beginning of the visit as they documented RA outcomes; others used it at the end to justify changes to therapy; and a few shared it only with stable patients.
Conclusions
The study provides valuable insights into clinicians’ perceptions and experiences with the RA PRO dashboard. The dashboard showed promise in enhancing patient-clinician communication, shared decision-making, and overall acceptance among clinicians. Addressing challenges related to data collection, education, and tailoring dashboard use to specific patient populations will be crucial for maximizing its potential impact on RA care. Further research and ongoing improvements in dashboard design and implementation are warranted to ensure its successful integration into routine clinical practice.
Peer Review reports
Rheumatoid arthritis (RA) is a chronic autoimmune disease characterized by significant fatigue, inflammation, pain, swelling and stiffness of the joints [ 1 ]. Although inflammation can be measured by blood tests including erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP), these tests are nonspecific and frequently do not correlate with how patients are feeling. Thus, patient-reported outcomes (PROs) are an essential component of rheumatoid arthritis care. PROs (such as measures of arthritis pain and physical function (PF)) and other RA outcome measures with patient-reported components (such as disease activity (DA)) can capture meaningful aspects of patients’ experience of their disease. Routine assessment of these outcomes is recommended for individuals with RA as part of a treat-to-target approach, which has been shown to improve outcomes and reduce damage and physical disability through frequent assessment of disease activity and titration of immunosuppressant medications to reach low disease activity or remission [ 2 , 3 , 4 , 5 , 6 ].
Despite recommendations for regular collection of RA outcome measures, studies have shown that the routine use and communication around these outcomes is limited and inconsistent in clinical care, often because RA outcome measure data is not readily available [ 7 , 8 , 9 , 10 , 11 ]. Data from the American College of Rheumatology’s (ACR) national patient registry [ 12 ], known as the Rheumatology Informatics System for Effectiveness (RISE), indicates that, among 49,205 patients with RA, over a 1-year period, only 50.7% of patients had a DA score recorded in the electronic health record (EHR), and only 53.2% had a recorded FS score [ 13 ].
While existing electronic health records (EHRs) are frequently unable to import RA outcome measures data and rarely incorporate the data in a way that clinicians and patients can easily use, several digital tools displaying RA outcomes for clinicians have been developed. Early data suggests that these tools were associated with improved adherence to a treat-to-target approach and higher quality of care in RA [ 14 , 15 ]. Furthermore, several studies have shown that using dashboards that display clinical outcome measures (COM) during clinical visits impacted positively on shared decision making, improved PRO intake, symptom control, quality of life, and patient-clinician communication [ 16 , 17 , 18 , 19 , 20 , 21 ]. However, patient-facing EHR-based dashboards displaying RA outcome measures have not been explored within the context of RA.
Using the Technology Acceptance Model (TAM) as a framework [ 22 ], we conducted a qualitative study to assess clinicians’ perceptions and experiences of a newly developed and implemented “RA PRO dashboard”. The dashboard pulls RA outcome scores collected during routine clinical care in the rheumatology clinic (including Clinical Disease Activity Index (CDAI), Patient-Reported Outcomes Measurement Information System Physical Function (PROMIS-PF), and arthritis pain) and displays graphs showing their trajectory over time, which can be shared with the patient during clinical visits. To our knowledge, this is the first study to focus on rheumatology clinicians’ perspectives and acceptance of a patient-facing health dashboard in RA care.
Conceptual framework
To evaluate clinician acceptance of the RA PRO dashboard, we used the TAM to assess clinicians’ experiences and perceptions towards the usability, acceptability, and usefulness of the dashboard that was rolled out in a large academic rheumatology clinic in Northern California. The TAM, which includes five domains: perceived usefulness, perceived ease of use, external variables, intention to use and actual use, has been widely used in the healthcare field to understand users’ behaviors and assess acceptance of various information technologies [ 23 , 24 ]. The model centers on two main factors that determine individual acceptance “intention to use” and “actual use” of a certain technology: “perceived usefulness” and “perceived ease of use” [ 22 , 25 ]. Perceived usefulness focuses on the individual beliefs towards the benefits of the technology, while the perceived ease of use is related to its convenience and efforts needed to use it. The TAM also suggests that “external variables”, not related to the technology itself impact either positively or negatively on the individual perception of usefulness and ease of use.
Dashboard development and features
Using a human centered approach, we developed and implemented a new patient-facing sidecar dashboard application (referred to as “RA PRO dashboard”) that pulls RA outcome data collected during routine clinical care and displays graphs showing their trajectory over time, framed within the context of accepted clinical targets (Fig. 1 ) [ 26 , 27 ]. CDAI, PROMIS-PF, and arthritis pain scores are shown on different graphs. Patient medications and most recent lab results are also displayed. Data points from all visits from 2014 onwards are incorporated, including data from the same day’s visit. All data displayed in the dashboard are derived from existing structured fields in the EHR. Launched from within the EHR, the dashboard is designed to be shared by clinicians with the patient during clinical visits, either on the computer screen during in-person visits or using a share-screen function during telehealth visits with the goal of promoting shared decision-making [ 27 , 28 ].

Screenshot of the RA PRO Dashboard
Clinical setting and dashboard roll-out
The dashboard was developed in the setting of a university rheumatology clinic which has been routinely collecting RA outcomes for in-person visits since 2014 [ 29 ]. Workflows were adapted for telehealth visits in 2020. Only data collected during routine clinical care is incorporated into the dashboard. PROs and patient-reported components of RA outcomes are typically collected by medical assistants (MAs) when the patient checks-in for their visit, or when they initially log-on to a zoom-based telehealth visit. The pain question queries patient arthritis pain over the past week using a (visual analog scale of 0-100 where 0 is “no pain at all” and 100 is “pain as bad as it can be”). Patients are asked to complete the PROMIS-PF as an assessment of physical function and the patient global assessment of RA activity, which is used to calculate the CDAI. MAs enter this data into structured fields in the EHR: PROMIS-PF questions are scored and entered; the EHR converts raw scores into T scores [ 30 ]. Patient global assessment scores are entered; once the clinician enters the evaluator global and tender and swollen joint counts as part of the CDAI, the EHR generates a DA score [ 31 ].
The dashboard was rolled out as part of a stepped-wedge pragmatic cluster-randomized trial, implemented between February 26th, 2020, and August 21, 2023. All clinicians treating RA patients at the academic rheumatology clinic (including physicians, rheumatology trainees, and a nurse practitioner) were randomized to gain access to the RA PRO dashboard (intervention) at 4 different time points during the study period (Fig. 2 ). Randomization was stratified based on patient volume (> 50% time spent in clinical care, vs. not). At the beginning of each cluster, a research team member (CW, AH, CY, or LJ) provided a 1:1 in-person training session to each clinician on how to use the RA PRO dashboard. Clinicians could voluntarily choose to engage with the dashboard or share it with their patients, or not.
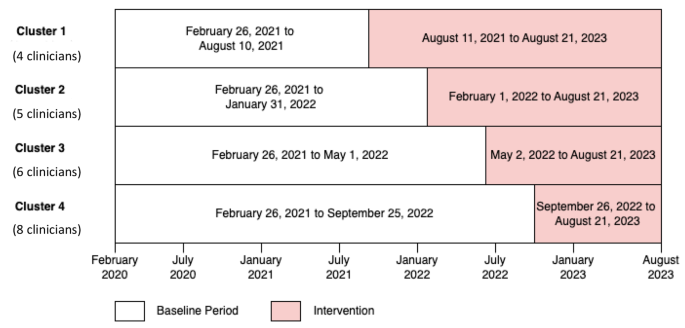
Stepped-wedge trial design with four cluster groups
Data collection
At cluster two (in April 2022) we contacted by email all clinicians with access to the dashboard to participate in the first focus group (FG) ( n = 9). At cluster three (in August 2022) we contacted all clinicians with access to the dashboard ( n = 15) to participate in the second FG. At cluster four (in October 2022) we contacted all clinicians with access to the dashboard ( n = 23) to participate in the third FG. FGs with rheumatology clinicians working in an academic rheumatology clinic with limited time to participate in research projects were more feasible than in-depth interviews. Researchers trained in qualitative research methods (GS; CN) facilitated FG discussions, using a semi-structured FG guide that focused on clinicians’ experiences using the dashboard, as well perceptions towards benefits, usability, ease of use, drawbacks, and suggestions to improve the implementation and usability of the RA PRO dashboard (Appendix A). The FGs, conducted virtually via Zoom between April and October 2022, lasted between 30 and 40 min, were audio recorded, and then transcribed verbatim. Researchers took notes during the FGs. All study activities were approved by the academic rheumatology clinic Institutional Review Board.
Clinician responses to open-ended questions were analyzed thematically using deductive and inductive techniques to identify themes and subthemes [ 32 ]. Using Atlas.ti [ 33 ], an experienced qualitative researcher (CN) read through the transcripts, reviewed the data to apply a set of deductive codes based on the topics in the FG guide, and created a preliminary set of relevant inductive codes to capture emergent ideas within and across the FGs. Codes were discussed, revised, and organized into a codebook with definitions. Three coders (CN, CW, CY) independently applied the codes to the 3 transcripts and reviewed each other’s work. Discrepancies were resolved via consensus meetings. Using a systematic and iterative process [ 34 ], we identified and organized emerging themes and subthemes into the five domains of the TAM. Then, we sorted all coded excerpts by their relevant themes and subthemes and provided exemplary quotes illustrating how each theme served as a barrier or facilitator to using the dashboard. We complied with the Consolidated Criteria for reporting Qualitative Research (COREQ) checklist for this study (Supplementary material 1 ).
We reached data saturation after conducting three FG discussions with a total of 13 clinicians: 8 physicians, 4 rheumatology trainees and 1 nurse practitioner who had access to the dashboard (five clinicians participated in the first FG, five participated in the second, and nine participated in the third one). Two clinicians participated in two FGs and two other clinicians participated in all FGs. More than half of participants were female ( n = 7) and have been in rheumatology practice for more than five years (Table 1 ). Generated themes and subthemes were organized into the five domains of the TAM. Relationships among these domains are illustrated in Fig. 3 . Below, we summarized themes and subthemes with each domain and provide exemplary quotes.
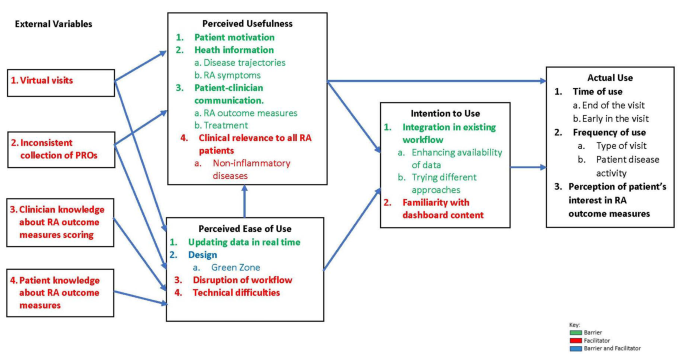
Generated themes and sub-themes as per the technology acceptance model
Perceived usefulness
All clinicians were enthusiastic about the dashboard and discussed its usefulness in motivating patients, enhancing their knowledge about RA outcomes, and improving patient-clinician communication.
Most clinicians reported that the “green zone” feature of the dashboard (Fig. 1 ), indicating that RA outcomes were at target levels, was an important design component that motivated patients to adhere to their treatment plans (Table 2 , Q:1).
In addition, most clinicians felt that incorporating the dashboard into a clinical visit provided patients with important health information that improved their knowledge about their disease. They explained that visualizing RA outcome trajectories in a graphical format was useful when discussing RA outcome scores (Table 2 , Q:2.1) and enhanced patient understanding of their symptoms in general, and disease activity and pain scores specifically (Table 2 , Q:2.2).
In terms of patient-provider relationships, many clinicians stated that the dashboard improved their communication with patients around RA outcomes, medications, and therapies. Sharing the dashboard during clinical visits, initiated discussions and conversations about RA outcome measures and target scores (Table 2 , Q:3.1). Further, nearly all clinicians reported that the dashboard was useful at steering conversations toward initiating therapies, increasing medication dosages, or changing medication types, especially for patients that had been on the same treatment regimen for many years and were hesitant to try new medications (Table 2 , Q:3.2). A few clinicians, who had frequent engagement with the dashboard, reported some concerns about the clinical relevance of the dashboard for RA patients who have other non-inflammatory diseases, such as fibromyalgia, that may elevate CDAI scores without reflecting RA inflammatory activity. They stated that using the dashboard with such patients might create confusion and difficulty explaining reasons for not augmenting therapy (Table 2 , Q:4).
Perceived ease of use
Almost all clinicians expressed a positive preference for the dashboard’s features and design. Since the RA PRO dashboard was integrated into the EHR, data inputted into the EHR flows automatically into the dashboard application, including data from the same day’s visit (Table 2 , Q:5). The majority of clinicians supported the idea of having RA outcome scores displayed graphically, displaying changes over time, and highlighting the cutoffs for target scores (Table 2 , Q:6.1). However, some clinicians recommended changes to the design of the dashboard to make it easier to use and discuss with their patients. For example, some clinicians expressed a preference for the CDAI graph to be oriented with higher values oriented higher up on the page (Table 2 , Q:6.2), and one clinician suggested changes to the “green zone” displaying the targets as not stringent enough (Table 2 , Q:6.3).
Most clinicians highlighted how critical it is that the dashboard integrate with existing clinic workflows to support its ease of use. This was important since a few clinicians noted their reluctance to incorporate the dashboard within their current workflow. These clinicians worried that explaining and sharing the dashboard with their patients, in addition to the other tasks of the visit, may take too much time and would make them run behind (Table 2 , Q:7). Finally, occasional technical difficulties including errors in the medications listed were noted by a few providers (Table 2 , Q:8).
External variables
Perceived usefulness and ease of use of the dashboard were impacted negatively by the inconsistent collection of RA outcomes. Most clinicians stated that lack of patient data populating the dashboard, including historical CDAI, pain or PROMIS-PF scores, were common, given the increase in telehealth visits that occurred during the COVID-19 pandemic (Table 2 , Q:9); they noted that some in-person visits were also missing outcome scores due to inconsistent collection during the check-in process. Even if scores from prior visits were available, clinicians explained that the dashboard was less useful to them if data from the current visit was missing. Training MAs and nurses and emphasizing regular collection of outcome measures prior to clinic visit were strongly recommended to enhance the use of the dashboard (Table 2 , Q:10). Regardless of the level of engagement with the dashboard, limited knowledge about scoring and interpretation of RA outcomes was another challenge impacting some clinicians’ confidence in their ability to discuss the content of the dashboard with their patients. One clinician stated that confusion about scoring the PROMIS-PF limited his discussions with patients to the CDAI section of the dashboard (Table 2 , Q:11). Moreover, some clinicians stated that they believed that patients occasionally misinterpreted specific items in the questionnaires, which made them question the validity of the scores for those patients (Table 2 , Q:12).
Intention to use
Despite several challenges affecting the use of the dashboard, most clinicians showed intent to integrate the dashboard as part of their visits with RA patients. Some of the clinicians, who were enrolled in the first two clusters and had been using the dashboard routinely during their clinical visits focused on enhancing availability of patient data in the dashboard by leveraging existing workflows in the clinic for flagging patients for collection of these measures during the check-in process (Table 2 , Q:13). Others reported trying various approaches until they found the best way to use the dashboard effectively and efficiently during RA follow up visits (Table 2 , Q:14). However, some clinicians indicated that they did not feel confident using the dashboard and would hesitate to do so going forward because of their limited familiarity with how to discuss the content of the dashboard with patients (Table 2 , Q:15).
Clinicians varied in the ways they actually incorporated the dashboard into the clinical visit. Almost all clinicians reported using the dashboard at the end of visit to discuss therapy and recommend medication changes (Table 2 , Q: 16.1) Some clinicians used the dashboard earlier in the visit to discuss the patient’s current CDAI score after examining them for swollen and tender joints (Table 2 , Q: 16.2).
In terms of setting for use, most clinicians targeted use of the dashboard to in person visits only and avoided using it during telehealth visits (Table 2 , Q: 17.1). A few shared it with patients during telehealth visits, especially those having low DA (Table 2 , Q: 17.2). Some clinicians stated that they only shared the dashboard with patients who had high DA but not those who were in low DA or remission, assuming that it might not be relevant to them (Table 2 , Q:17.3). Finally, some clinicians expressed reluctance to use the dashboard because they perceived the patient would not be interested in discussing its content and would rather focus on the treatment plan (Table 2 , Q: 18).
In this study, we used the TAM framework to evaluate clinicians’ perceptions and experiences regarding the RA PRO dashboard. Our findings indicate that clinicians generally showed enthusiasm and positive perceptions towards the dashboard. They recognized its usefulness in motivating patients, enhancing patient understanding of RA, and improving patient-clinician communication. The “green zone” feature of the dashboard, indicating when RA outcomes were at target levels, was particularly highlighted as a motivating factor for patients to adhere to their treatment plans.
In addition, the integration of the RA PRO dashboard into the EHR system was well-received by clinicians, as it allowed for real-time data input and display. The graphical representation of RA outcome scores, along with their changes over time, received favorable feedback. These positive responses align with the concepts of perceived usefulness and ease of use, respectively, both central components of the TAM. Our findings align with the growing literature demonstrating the ability of the TAM framework to capture clinicians’ perspectives of a novel health information technology (IT) tool. Our findings of potential barriers to adopting this new tool were consistent with prior studies: specifically, clinicians feared that using the new PRO dashboard would disrupt existing clinical workflows or result in a conversation with patients that might take more time than anticipated. Clinicians also had general objections to using RA outcomes during routine care that have been previously documented, including limited knowledge about how to incorporate them into clinical care or discussions with patients. Similarly, prior studies have shown that smooth workflow is highly important to the clinicians’ clinical work, and the integration of a new tool that requires additional time and effort might be perceived as a burden that increases their workload and consequently limits its usability [ 35 ]. Additional studies from other settings have also reported clinician confusion about scoring outcome measures [ 36 ], beliefs that questions in some COMs are unclear or irrelevant [ 37 ] and that COMs provide redundant information beyond usual care [ 38 ]. Although these findings highlight the importance of providing education on the added value of COM data and training on how to discuss scores with patients, it is equally important to acknowledge that COMs may have less relevance for patients with overlapping non-inflammatory conditions such as fibromyalgia and may lead to confusion in interpreting COM scores and deciding on treatment plans. For example, our group has previously developed paper-based tools to help discuss RA outcome measures with patients with non-RA related pain [ 39 ].
Our study identified several challenges and external factors that can influence the adoption and effective use of the RA PRO dashboard. Inconsistent collection of RA outcome measures, particularly during virtual visits from the pandemic period, was a common issue mentioned by clinicians. Insufficient data populating on the dashboard, including missing historical scores, can limit the dashboard’s utility since recent scores and trends over time are not visible for these patients [ 40 , 41 ]. Addressing this challenge may require additional training for MAs, front desk staff, and even patients to emphasize the routine collection of outcome measures when patients check in for clinic visits.
This is the first study to assess clinician perceptions, acceptance, and use of a patient-facing outcome measures dashboard in RA care. A key strength of this study is that it allowed clinicians to share their experience and discuss perceptions, spectrum of use, and barriers to integrating the dashboard within their workflow. Results of the study add to the existing literature by highlighting the challenges faced by clinicians when using and discussing COMs in the context of a patient-facing dashboard and suggesting ways to overcome these challenges. Nevertheless, our findings are based on a relatively small sample of clinicians from a specific academic rheumatology clinic in Northern California who had all been trained by the research team on use of the dashboard. The generalizability of these findings to other settings and populations may be limited. Future research could expand the scope to include a larger sample of clinicians and involve patients to gain a broader perspective on the utilization, acceptance, and impact of the RA PRO dashboard. An additional limitation of our study pertains to the dynamics of communication within clinicians. Despite efforts to foster an honest and open conversation about the dashboard, there might have been instances where NP and rheumatology trainee may have felt hesitant to disagree with the thoughts expressed by physicians. This could have influenced the dynamics of the FG discussions and potentially impacted on the diversity of perceptions shared. Future work should attempt to quantify the specific impacts that dashboard use has on long-term disease outcomes, shared decision making, patient satisfaction, adherence to treatment, and costs of care.
In conclusion, our study provides valuable insights into clinicians’ perceptions and experiences with the RA PRO dashboard, utilizing the TAM framework. The dashboard showed promise in enhancing patient-clinician communication, shared decision-making, and overall acceptance among clinicians. Addressing challenges related to data collection, education, and tailoring dashboard use to specific patient populations will be crucial for maximizing its potential impact on improving treatment adherence and health outcomes of all patients with RA. Further research and ongoing improvements in dashboard design and implementation are warranted to ensure its successful integration into routine clinical practice.
Data availability
De-identified data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy and ethical restrictions.
Abbreviations
Rheumatoid Arthritis
Erythrocyte Sedimentation Rate
C-Reactive Protein
Patient Reported Outcomes
Physical Function
- Disease Activity
American College of Rheumatology
Rheumatology Informatics System for Effectiveness
Electronic Heath Record
Clinical Outcome Measure
- Technology Acceptance Model
Clinical Disease Activity Index
Patient-Reported Outcomes Measurement Information System Physical Function
Medical Assistant
- Focus Group
Consolidated Criteria for reporting Qualitative Research
Information Technology
Rheumatoid Arthritis. [cited 2023 October 3]; https://rheumatology.org/patients/rheumatoid-arthritis .
Gabriel SE, Michaud K. Epidemiological studies in incidence, prevalence, mortality, and comorbidity of the rheumatic diseases. Arthritis Res Ther. 2009;11(3):229.
Article PubMed PubMed Central Google Scholar
Gabriel SE, et al. Survival in rheumatoid arthritis: a population-based analysis of trends over 40 years. Arthritis Rheum. 2003;48(1):54–8.
Article PubMed Google Scholar
Wolfe F, et al. Predicting mortality in patients with rheumatoid arthritis. Arthritis Rheum. 2003;48(6):1530–42.
Bartlett SJ, et al. Identifying core domains to assess flare in rheumatoid arthritis: an OMERACT international patient and provider combined Delphi consensus. Ann Rheum Dis. 2012;71(11):1855–60.
in Target for monitoring: Rheumatoid arthritis in adults: diagnosis and management: Evidence review D . 2018: London.
Hammam N, et al. The Relationship Between Electronic Health Record System and Performance on Quality Measures in the American College of Rheumatology’s Rheumatology Informatics System for Effectiveness (RISE) Registry: Observational Study. Volume 9. JMIR Med Inform; 2021. p. e31186. 11.
Curtis JR, et al. Physicians’ explanations for apparent gaps in the quality of rheumatology care: results from the US Medicare Physician Quality Reporting System. Arthritis Care Res (Hoboken). 2013;65(2):235–43.
Ziegenfuss JY, et al. Is the Promise of PROMs being realized? Implementation experience in a large Orthopedic Practice. Am J Med Qual. 2022;37(6):489–94.
Solomon DH, et al. Implementation of treat-to-target in rheumatoid arthritis through a Learning Collaborative: results of a Randomized Controlled Trial. Arthritis Rheumatol. 2017;69(7):1374–80.
Desai SP, Yazdany J. Quality measurement and improvement in rheumatology: rheumatoid arthritis as a case study. Arthritis Rheum. 2011;63(12):3649–60.
Yazdany J, et al. Rheumatology Informatics System for Effectiveness: A National Informatics-Enabled Registry for Quality Improvement. Arthritis Care Res (Hoboken). 2016;68(12):1866–73.
Yazdany J, et al. Development of the American College of Rheumatology’s Rheumatoid Arthritis Electronic Clinical Quality measures. Arthritis Care Res (Hoboken). 2016;68(11):1579–90.
Newman ED, et al. Improving the quality of care of patients with rheumatic disease using patient-centric electronic redesign software. Arthritis Care Res (Hoboken). 2015;67(4):546–53.
Eriksson JK, Askling J, Arkema EV. The Swedish Rheumatology Quality Register: optimisation of rheumatic disease assessments using register-enriched data. Clin Exp Rheumatol. 2014;32(5 Suppl 85):S–147.
CAS PubMed Google Scholar
Barnes GD, et al. Implementing an electronic health record dashboard for safe anticoagulant management: learning from qualitative interviews with existing and potential users to develop an implementation process. Implement Sci Commun. 2022;3(1):10.
Brettschneider C, Luhmann D, Raspe H. Informative value of patient reported outcomes (PRO) in Health Technology Assessment (HTA). GMS Health Technol Assess. 2011;7:Doc01.
PubMed PubMed Central Google Scholar
Hassett MJ, et al. eSyM: an Electronic Health Record-Integrated patient-reported outcomes-based Cancer Symptom Management Program used by six Diverse Health systems. JCO Clin Cancer Inf. 2022;6:e2100137.
Article Google Scholar
Martinez W, et al. A patient-facing diabetes dashboard embedded in a patient web Portal: Design Sprint and Usability Testing. JMIR Hum Factors. 2018;5(3):e26.
Jeffs L, et al. Insights from staff nurses and managers on unit-specific nursing performance dashboards: a qualitative study. BMJ Qual Saf. 2014;23(12):1001–6.
Tsangaris E, et al. User-centered design and agile development of a novel mobile health application and clinician dashboard to support the collection and reporting of patient-reported outcomes for breast cancer care. BMJ Surg Interv Health Technol. 2022;4(1):e000119.
Davis FD. Perceived usefulness, perceived ease of Use, and user Acceptance of Information Technology. MIS Q. 1989;13(3):319–40.
Al-Maroof R, et al. Blended Learning Acceptance: a systematic review of Information systems models. Technol Knowl Learn. 2022;27(3):891–926.
AlQudah AA, Al-Emran M, Shaalan K. Technology Acceptance in Healthcare: A Systematic Review Applied Sciences-Basel, 2021. 11(22).
Venkatesh V, Davis FD. A theoretical extension of the technology acceptance model: four longitudinal field studies. Manage Sci. 2000;46(2):186–204.
Ragouzeos D, et al. Am I OK? Using human centered design to empower rheumatoid arthritis patients through patient reported outcomes. Patient Educ Couns. 2019;102(3):503–10.
Liu LH, et al. Patient and clinician perspectives on a patient-facing dashboard that visualizes patient reported outcomes in rheumatoid arthritis. Health Expect. 2020;23(4):846–59.
Young C, Nasrallah MA, Jacobsohn C, Barton L, Murray J, Yazdany S, Schmajuk J. Development, implementation, and Usability Testing of a New Rheumatoid Arthritis Patient reported outcomes EHR-based dashboard: a mixed-method study. American College of Rheumatology A. Editor: Rheumatol; 2022.
Google Scholar
Gandrup J, et al. Three quality improvement initiatives and performance of Rheumatoid Arthritis Disease Activity Measures in Electronic Health Records: results from an interrupted Time Series Study. Arthritis Care Res (Hoboken). 2020;72(2):283–91.
Wahl E, et al. Validity and responsiveness of a 10-Item patient-reported measure of physical function in a rheumatoid arthritis Clinic Population. Arthritis Care Res (Hoboken). 2017;69(3):338–46.
Aletaha D, et al. Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther. 2005;7(4):R796–806.
Article CAS PubMed PubMed Central Google Scholar
Miles MB, Huberman AM. Qualitative data analysis: an expanded sourcebook. sage; 1994.
Atlas.ti scientific Software Development GmbH . 2021, Scientific Software Development GmbH: Berlin.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3(2):77–101.
Bersani K, et al. Use, Perceived Usability, and barriers to implementation of a Patient Safety Dashboard Integrated within a Vendor EHR. Appl Clin Inf. 2020;11(1):34–45.
Pizziferri L, et al. Primary care physician time utilization before and after implementation of an electronic health record: a time-motion study. J Biomed Inf. 2005;38(3):176–88.
Eilayyan O, et al. Developing theory-informed knowledge translation strategies to facilitate the use of patient-reported outcome measures in interdisciplinary low back pain clinical practices in Quebec: mixed methods study. BMC Health Serv Res. 2020;20(1):789.
Or C, et al. Private primary care physicians’ perspectives on factors affecting the adoption of electronic medical records: a qualitative pre-implementation study. Work. 2014;48(4):529–38.
Subash M, et al. The development of the Rheumatology Informatics System for Effectiveness Learning Collaborative for Improving patient-reported Outcome Collection and patient-centered communication in adult rheumatology. Volume 3. ACR Open Rheumatol; 2021. pp. 690–8. 10.
Pauwels K, et al. Dashboards as a service why, what, how, and what research is needed? J Service Res. 2009;12(2):175–89.
Freeman T. Using performance indicators to improve health care quality in the public sector: a review of the literature. Health Serv Manage Res. 2002;15(2):126–37.
Download references
Acknowledgements
Not Applicable.
This project was supported by grant number 1R01HS025405 from the Agency for Healthcare Research and Quality (AHRQ). The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ.
Author information
Authors and affiliations.
Division of Rheumatology, Department of Medicine, University of California, San Francisco, CA, USA
Catherine Nasrallah, Cherish Wilson, Alicia Hamblin, Cammie Young, Lindsay Jacobsohn, Mary C. Nakamura, Andrew Gross, Mehrdad Matloubian, Judith Ashouri, Jinoos Yazdany & Gabriela Schmajuk
San Francisco Veterans Affairs Medical Center, 4150 Clement Street, #500A, San Francisco, CA, 94121, USA
Mary C. Nakamura & Gabriela Schmajuk
Center for Vulnerable Populations and Zuckerberg San Francisco General Hospital, San Francisco, CA, USA
Jinoos Yazdany
You can also search for this author in PubMed Google Scholar
Contributions
G.S. conceived and designed the study. G.S. obtained research funding and supervised the conduct of the study. C.N and G.S conducted focus group discussions. C.N. provided qualitative advice on study design and analyzed the data. C.N, C.W. and C.Y coded the data. G.S., C.N., A.H, C.W. and J.Y drafted the manuscriptAll authors (G.S, C.N, C.W, A.H, C.Y, L.J , M.N, A.G, M.M, J.A.S and J.Y read, edited and approved the final manuscript. G.S. takes responsibility for the paper.
Corresponding author
Correspondence to Gabriela Schmajuk .
Ethics declarations
Ethics approval and consent to participate.
The protocol and all documents used in this study were reviewed and approved by the University of California San Francisco (UCSF) Institutional Review Board. A verbal informed consent was obtained from all study participants prior to participation in the focus group discussions. The informed consent form was reviewed and approved by the University of California San Francisco (UCSF) Institutional Review Board.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary material 2, rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Nasrallah, C., Wilson, C., Hamblin, A. et al. Using the technology acceptance model to assess clinician perceptions and experiences with a rheumatoid arthritis outcomes dashboard: qualitative study. BMC Med Inform Decis Mak 24 , 140 (2024). https://doi.org/10.1186/s12911-024-02530-2
Download citation
Received : 22 February 2024
Accepted : 08 May 2024
Published : 27 May 2024
DOI : https://doi.org/10.1186/s12911-024-02530-2
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Rheumatoid arthritis
- Patient reported outcomes
- Perceptions
- Qualitative research
- Physical function
BMC Medical Informatics and Decision Making
ISSN: 1472-6947
- General enquiries: [email protected]
Case Study Research Method in Psychology
Saul Mcleod, PhD
Editor-in-Chief for Simply Psychology
BSc (Hons) Psychology, MRes, PhD, University of Manchester
Saul Mcleod, PhD., is a qualified psychology teacher with over 18 years of experience in further and higher education. He has been published in peer-reviewed journals, including the Journal of Clinical Psychology.
Learn about our Editorial Process
Olivia Guy-Evans, MSc
Associate Editor for Simply Psychology
BSc (Hons) Psychology, MSc Psychology of Education
Olivia Guy-Evans is a writer and associate editor for Simply Psychology. She has previously worked in healthcare and educational sectors.
On This Page:
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews).
The case study research method originated in clinical medicine (the case history, i.e., the patient’s personal history). In psychology, case studies are often confined to the study of a particular individual.
The information is mainly biographical and relates to events in the individual’s past (i.e., retrospective), as well as to significant events that are currently occurring in his or her everyday life.
The case study is not a research method, but researchers select methods of data collection and analysis that will generate material suitable for case studies.
Freud (1909a, 1909b) conducted very detailed investigations into the private lives of his patients in an attempt to both understand and help them overcome their illnesses.
This makes it clear that the case study is a method that should only be used by a psychologist, therapist, or psychiatrist, i.e., someone with a professional qualification.
There is an ethical issue of competence. Only someone qualified to diagnose and treat a person can conduct a formal case study relating to atypical (i.e., abnormal) behavior or atypical development.
Famous Case Studies
- Anna O – One of the most famous case studies, documenting psychoanalyst Josef Breuer’s treatment of “Anna O” (real name Bertha Pappenheim) for hysteria in the late 1800s using early psychoanalytic theory.
- Little Hans – A child psychoanalysis case study published by Sigmund Freud in 1909 analyzing his five-year-old patient Herbert Graf’s house phobia as related to the Oedipus complex.
- Bruce/Brenda – Gender identity case of the boy (Bruce) whose botched circumcision led psychologist John Money to advise gender reassignment and raise him as a girl (Brenda) in the 1960s.
- Genie Wiley – Linguistics/psychological development case of the victim of extreme isolation abuse who was studied in 1970s California for effects of early language deprivation on acquiring speech later in life.
- Phineas Gage – One of the most famous neuropsychology case studies analyzes personality changes in railroad worker Phineas Gage after an 1848 brain injury involving a tamping iron piercing his skull.
Clinical Case Studies
- Studying the effectiveness of psychotherapy approaches with an individual patient
- Assessing and treating mental illnesses like depression, anxiety disorders, PTSD
- Neuropsychological cases investigating brain injuries or disorders
Child Psychology Case Studies
- Studying psychological development from birth through adolescence
- Cases of learning disabilities, autism spectrum disorders, ADHD
- Effects of trauma, abuse, deprivation on development
Types of Case Studies
- Explanatory case studies : Used to explore causation in order to find underlying principles. Helpful for doing qualitative analysis to explain presumed causal links.
- Exploratory case studies : Used to explore situations where an intervention being evaluated has no clear set of outcomes. It helps define questions and hypotheses for future research.
- Descriptive case studies : Describe an intervention or phenomenon and the real-life context in which it occurred. It is helpful for illustrating certain topics within an evaluation.
- Multiple-case studies : Used to explore differences between cases and replicate findings across cases. Helpful for comparing and contrasting specific cases.
- Intrinsic : Used to gain a better understanding of a particular case. Helpful for capturing the complexity of a single case.
- Collective : Used to explore a general phenomenon using multiple case studies. Helpful for jointly studying a group of cases in order to inquire into the phenomenon.
Where Do You Find Data for a Case Study?
There are several places to find data for a case study. The key is to gather data from multiple sources to get a complete picture of the case and corroborate facts or findings through triangulation of evidence. Most of this information is likely qualitative (i.e., verbal description rather than measurement), but the psychologist might also collect numerical data.
1. Primary sources
- Interviews – Interviewing key people related to the case to get their perspectives and insights. The interview is an extremely effective procedure for obtaining information about an individual, and it may be used to collect comments from the person’s friends, parents, employer, workmates, and others who have a good knowledge of the person, as well as to obtain facts from the person him or herself.
- Observations – Observing behaviors, interactions, processes, etc., related to the case as they unfold in real-time.
- Documents & Records – Reviewing private documents, diaries, public records, correspondence, meeting minutes, etc., relevant to the case.
2. Secondary sources
- News/Media – News coverage of events related to the case study.
- Academic articles – Journal articles, dissertations etc. that discuss the case.
- Government reports – Official data and records related to the case context.
- Books/films – Books, documentaries or films discussing the case.
3. Archival records
Searching historical archives, museum collections and databases to find relevant documents, visual/audio records related to the case history and context.
Public archives like newspapers, organizational records, photographic collections could all include potentially relevant pieces of information to shed light on attitudes, cultural perspectives, common practices and historical contexts related to psychology.
4. Organizational records
Organizational records offer the advantage of often having large datasets collected over time that can reveal or confirm psychological insights.
Of course, privacy and ethical concerns regarding confidential data must be navigated carefully.
However, with proper protocols, organizational records can provide invaluable context and empirical depth to qualitative case studies exploring the intersection of psychology and organizations.
- Organizational/industrial psychology research : Organizational records like employee surveys, turnover/retention data, policies, incident reports etc. may provide insight into topics like job satisfaction, workplace culture and dynamics, leadership issues, employee behaviors etc.
- Clinical psychology : Therapists/hospitals may grant access to anonymized medical records to study aspects like assessments, diagnoses, treatment plans etc. This could shed light on clinical practices.
- School psychology : Studies could utilize anonymized student records like test scores, grades, disciplinary issues, and counseling referrals to study child development, learning barriers, effectiveness of support programs, and more.
How do I Write a Case Study in Psychology?
Follow specified case study guidelines provided by a journal or your psychology tutor. General components of clinical case studies include: background, symptoms, assessments, diagnosis, treatment, and outcomes. Interpreting the information means the researcher decides what to include or leave out. A good case study should always clarify which information is the factual description and which is an inference or the researcher’s opinion.
1. Introduction
- Provide background on the case context and why it is of interest, presenting background information like demographics, relevant history, and presenting problem.
- Compare briefly to similar published cases if applicable. Clearly state the focus/importance of the case.
2. Case Presentation
- Describe the presenting problem in detail, including symptoms, duration,and impact on daily life.
- Include client demographics like age and gender, information about social relationships, and mental health history.
- Describe all physical, emotional, and/or sensory symptoms reported by the client.
- Use patient quotes to describe the initial complaint verbatim. Follow with full-sentence summaries of relevant history details gathered, including key components that led to a working diagnosis.
- Summarize clinical exam results, namely orthopedic/neurological tests, imaging, lab tests, etc. Note actual results rather than subjective conclusions. Provide images if clearly reproducible/anonymized.
- Clearly state the working diagnosis or clinical impression before transitioning to management.
3. Management and Outcome
- Indicate the total duration of care and number of treatments given over what timeframe. Use specific names/descriptions for any therapies/interventions applied.
- Present the results of the intervention,including any quantitative or qualitative data collected.
- For outcomes, utilize visual analog scales for pain, medication usage logs, etc., if possible. Include patient self-reports of improvement/worsening of symptoms. Note the reason for discharge/end of care.
4. Discussion
- Analyze the case, exploring contributing factors, limitations of the study, and connections to existing research.
- Analyze the effectiveness of the intervention,considering factors like participant adherence, limitations of the study, and potential alternative explanations for the results.
- Identify any questions raised in the case analysis and relate insights to established theories and current research if applicable. Avoid definitive claims about physiological explanations.
- Offer clinical implications, and suggest future research directions.
5. Additional Items
- Thank specific assistants for writing support only. No patient acknowledgments.
- References should directly support any key claims or quotes included.
- Use tables/figures/images only if substantially informative. Include permissions and legends/explanatory notes.
- Provides detailed (rich qualitative) information.
- Provides insight for further research.
- Permitting investigation of otherwise impractical (or unethical) situations.
Case studies allow a researcher to investigate a topic in far more detail than might be possible if they were trying to deal with a large number of research participants (nomothetic approach) with the aim of ‘averaging’.
Because of their in-depth, multi-sided approach, case studies often shed light on aspects of human thinking and behavior that would be unethical or impractical to study in other ways.
Research that only looks into the measurable aspects of human behavior is not likely to give us insights into the subjective dimension of experience, which is important to psychoanalytic and humanistic psychologists.
Case studies are often used in exploratory research. They can help us generate new ideas (that might be tested by other methods). They are an important way of illustrating theories and can help show how different aspects of a person’s life are related to each other.
The method is, therefore, important for psychologists who adopt a holistic point of view (i.e., humanistic psychologists ).
Limitations
- Lacking scientific rigor and providing little basis for generalization of results to the wider population.
- Researchers’ own subjective feelings may influence the case study (researcher bias).
- Difficult to replicate.
- Time-consuming and expensive.
- The volume of data, together with the time restrictions in place, impacted the depth of analysis that was possible within the available resources.
Because a case study deals with only one person/event/group, we can never be sure if the case study investigated is representative of the wider body of “similar” instances. This means the conclusions drawn from a particular case may not be transferable to other settings.
Because case studies are based on the analysis of qualitative (i.e., descriptive) data , a lot depends on the psychologist’s interpretation of the information she has acquired.
This means that there is a lot of scope for Anna O , and it could be that the subjective opinions of the psychologist intrude in the assessment of what the data means.
For example, Freud has been criticized for producing case studies in which the information was sometimes distorted to fit particular behavioral theories (e.g., Little Hans ).
This is also true of Money’s interpretation of the Bruce/Brenda case study (Diamond, 1997) when he ignored evidence that went against his theory.
Breuer, J., & Freud, S. (1895). Studies on hysteria . Standard Edition 2: London.
Curtiss, S. (1981). Genie: The case of a modern wild child .
Diamond, M., & Sigmundson, K. (1997). Sex Reassignment at Birth: Long-term Review and Clinical Implications. Archives of Pediatrics & Adolescent Medicine , 151(3), 298-304
Freud, S. (1909a). Analysis of a phobia of a five year old boy. In The Pelican Freud Library (1977), Vol 8, Case Histories 1, pages 169-306
Freud, S. (1909b). Bemerkungen über einen Fall von Zwangsneurose (Der “Rattenmann”). Jb. psychoanal. psychopathol. Forsch ., I, p. 357-421; GW, VII, p. 379-463; Notes upon a case of obsessional neurosis, SE , 10: 151-318.
Harlow J. M. (1848). Passage of an iron rod through the head. Boston Medical and Surgical Journal, 39 , 389–393.
Harlow, J. M. (1868). Recovery from the Passage of an Iron Bar through the Head . Publications of the Massachusetts Medical Society. 2 (3), 327-347.
Money, J., & Ehrhardt, A. A. (1972). Man & Woman, Boy & Girl : The Differentiation and Dimorphism of Gender Identity from Conception to Maturity. Baltimore, Maryland: Johns Hopkins University Press.
Money, J., & Tucker, P. (1975). Sexual signatures: On being a man or a woman.
Further Information
- Case Study Approach
- Case Study Method
- Enhancing the Quality of Case Studies in Health Services Research
- “We do things together” A case study of “couplehood” in dementia
- Using mixed methods for evaluating an integrative approach to cancer care: a case study
Related Articles
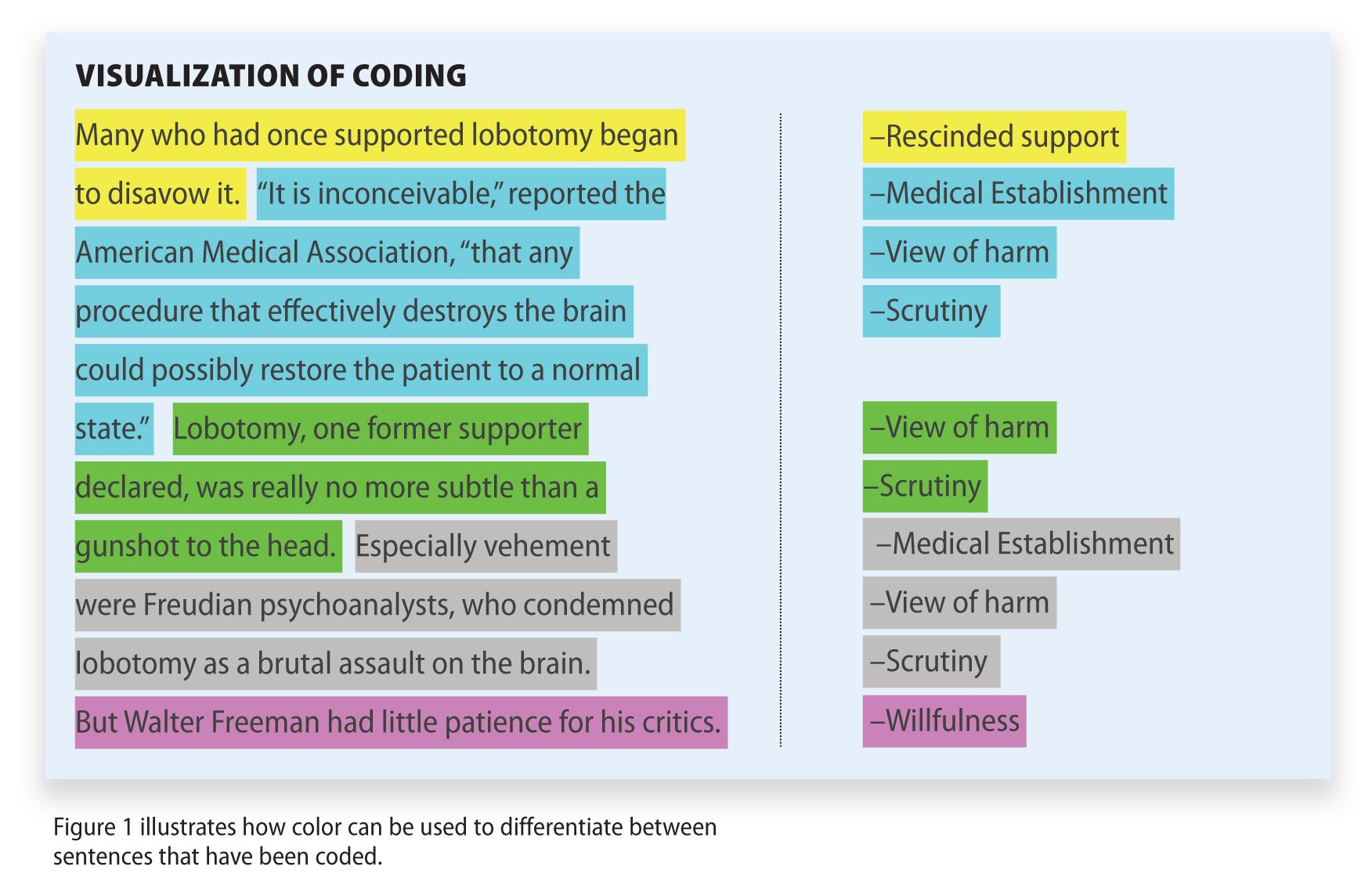
Research Methodology
Qualitative Data Coding

What Is a Focus Group?
Cross-Cultural Research Methodology In Psychology

What Is Internal Validity In Research?

Research Methodology , Statistics
What Is Face Validity In Research? Importance & How To Measure

Criterion Validity: Definition & Examples
- Open access
- Published: 22 May 2024
Preparedness for a first clinical placement in nursing: a descriptive qualitative study
- Philippa H. M. Marriott 1 ,
- Jennifer M. Weller-Newton 2 nAff3 &
- Katharine J. Reid 4
BMC Nursing volume 23 , Article number: 345 ( 2024 ) Cite this article
174 Accesses
2 Altmetric
Metrics details
A first clinical placement for nursing students is a challenging period involving translation of theoretical knowledge and development of an identity within the healthcare setting; it is often a time of emotional vulnerability. It can be a pivotal moment for ambivalent nursing students to decide whether to continue their professional training. To date, student expectations prior to their first clinical placement have been explored in advance of the experience or gathered following the placement experience. However, there is a significant gap in understanding how nursing students’ perspectives about their first clinical placement might change or remain consistent following their placement experiences. Thus, the study aimed to explore first-year nursing students’ emotional responses towards and perceptions of their preparedness for their first clinical placement and to examine whether initial perceptions remain consistent or change during the placement experience.
The research utilised a pre-post qualitative descriptive design. Six focus groups were undertaken before the first clinical placement (with up to four participants in each group) and follow-up individual interviews ( n = 10) were undertaken towards the end of the first clinical placement with first-year entry-to-practice postgraduate nursing students. Data were analysed thematically.
Three main themes emerged: (1) adjusting and managing a raft of feelings, encapsulating participants’ feelings about learning in a new environment and progressing from academia to clinical practice; (2) sinking or swimming, comprising students’ expectations before their first clinical placement and how these perceptions are altered through their clinical placement experience; and (3) navigating placement, describing relationships between healthcare staff, patients, and peers.
Conclusions
This unique study of first-year postgraduate entry-to-practice nursing students’ perspectives of their first clinical placement adds to the extant knowledge. By examining student experience prior to and during their first clinical placement experience, it is possible to explore the consistency and change in students’ narratives over the course of an impactful experience. Researching the narratives of nursing students embarking on their first clinical placement provides tertiary education institutions with insights into preparing students for this critical experience.
Peer Review reports
First clinical placements enable nursing students to develop their professional identity through initial socialisation, and where successful, first clinical placement experiences can motivate nursing students to persist with their studies [ 1 , 2 , 3 , 4 ]. Where the transition from the tertiary environment to learning in the healthcare workplace is turbulent, it may impact nursing students’ learning, their confidence and potentially increase attrition rates from educational programs [ 2 , 5 , 6 ]. Attrition from preregistration nursing courses is a global concern, with the COVID-19 pandemic further straining the nursing workforce; thus, the supply of nursing professionals is unlikely to meet demand [ 7 ]. The COVID-19 pandemic has also impacted nursing education, with student nurses augmenting the diminishing nursing workforce [ 7 , 8 ].
The first clinical placement often triggers immense anxiety and fear for nursing students [ 9 , 10 ]. Research suggests that among nursing students, anxiety arises from perceived knowledge deficiencies, role ambiguity, the working environment, caring for ‘real’ people, potentially causing harm, exposure to nudity and death, and ‘not fitting in’ [ 2 , 3 , 11 ]. These stressors are reported internationally and often relate to inadequate preparation for entering the clinical environment [ 2 , 10 , 12 ]. Previous research suggests that high anxiety before the first clinical placement can be related to factors likely to affect patient outcomes, such as self-confidence and efficacy [ 13 ]. High anxiety during clinical placement may impair students’ capacity to learn, thus compromising the value of the clinical environment for learning [ 10 ].
The first clinical placement often occurs soon after commencing nursing training and can challenge students’ beliefs, philosophies, and preconceived ideas about nursing. An experience of cultural or ‘reality’ shock often arises when entering the healthcare setting, creating dissonance between reality and expectations [ 6 , 14 ]. These experiences may be exacerbated by tertiary education providers teaching of ‘ideal’ clinical practice [ 2 , 6 ]. The perceived distance between theoretical knowledge and what is expected in a healthcare placement, as opposed to what occurs on clinical placement, has been well documented as the theory-practice gap or an experience of cognitive dissonance [ 2 , 3 ].
Given the pivotal role of the first clinical placement in nursing students’ trajectories to nursing practice, it is important to understand students’ experiences and to explore how the placement experience shapes initial perceptions. Existing research focusses almost entirely either on describing nursing students’ projected emotions and perceptions prior to undertaking a first clinical placement [ 3 ] or examines student perceptions of reflecting on a completed first placement [ 15 ]. We wished to examine consistency and change in student perception of their first clinical placement by tracking their experiences longitudinally. We focused on a first clinical placement undertaken in a Master of Nursing Science. This two-year postgraduate qualification provides entry-to-practice nursing training for students who have completed any undergraduate qualification. The first clinical placement component of the course aimed to orient students to the clinical environment, support students to acquire skills and develop their clinical reasoning through experiential learning with experienced nursing mentors.
This paper makes a significant contribution to understanding how nursing students’ perceptions might develop over time because of their clinical placement experiences. Our research addresses a further gap in the existing literature, by focusing on students completing an accelerated postgraduate two-year entry-to-practice degree open to students with any prior undergraduate degree. Thus, the current research aimed to understand nursing students’ emotional responses and expectations and their perceptions of preparedness before attending their first clinical placement and to contrast these initial perceptions with their end-of-placement perspectives.
Study design
A descriptive qualitative study was undertaken, utilising a pre- and post-design for data collection. Focus groups with first-year postgraduate entry-to-practice nursing students were conducted before the first clinical placement, with individual semi-structured interviews undertaken during the first clinical placement.
Setting and participants
All first-year students enrolled in the two-year Master of Nursing Science program ( n = 190) at a tertiary institution in Melbourne, Australia, were eligible to participate. There were no exclusion criteria. At the time of this study, students were enrolled in a semester-long subject focused on nursing assessment and care. They studied the theoretical underpinnings of nursing and science, theoretical and practical nursing clinical skills and Indigenous health over the first six weeks of the course. Students completed a preclinical assessment as a hurdle before commencing a three-week clinical placement in a hospital setting, a subacute or acute environment. Overall, the clinical placement aimed to provide opportunities for experiential learning, skill acquisition, development of clinical reasoning skills and professional socialisation [ 16 , 17 ].
In total, sixteen students participated voluntarily in a focus group of between 60 and 90 min duration; ten of these students also participated in individual interviews of between 30 and 60 min duration, a number sufficient to reach data saturation. Table 1 shows the questions used in the focus groups conducted before clinical placement commenced and the questions for the semi-structured interview questions conducted during clinical placement. Study participants’ undergraduate qualifications included bachelor’s degrees in science, arts and business. A small number of participants had previous healthcare experience (e.g. as healthcare assistants). The participants attended clinical placement in the Melbourne metropolitan, Victorian regional and rural hospital locations.
Data collection
The study comprised two phases. The first phase comprised six focus groups prior to the first clinical placement, and the second phase comprised ten individual semi-structured interviews towards the end of the first clinical placement. Focus groups (with a maximum of four participants) and individual interviews were conducted by the lead author online via Zoom and were audio-recorded. Capping group size to a relatively small number considered diversity of perceptions and opportunities for participants to share their insights and to confirm or contradict their peers, particularly in the online environment [ 18 , 19 ].
Focus groups and interview questions were developed with reference to relevant literature, piloted with volunteer final-year nursing students, and then verified with the coauthors. All focus groups and interviewees received the same structured questions (Table 1 ) to ensure consistency and to facilitate comparison across the placement experience in the development of themes. Selective probing of interviewees’ responses for clarification to gain in-depth responses was undertaken. Nonverbal cues, impressions, or observations were noted.
The lead author was a registered nurse who had a clinical teaching role within the nursing department and was responsible for coordinating clinical placement experiences. To ensure rigour during the data collection process, the lead author maintained a reflective account, exploring her experiences of the discussions, reflecting on her interactions with participants as a researcher and as a clinical educator, and identifying areas for improvement (for instance allowing participants to tell their stories with fewer prompts). These reflections in conjunction with regular discussion with the other authors throughout the data collection period, aided in identifying any researcher biases, feelings and thoughts that possibly influenced the research [ 20 ].
To maintain rigour during the data analysis phase, we adhered to a systematic process involving input from all authors to code the data and to identify, refine and describe the themes and subthemes reported in this work. This comprehensive analytic process, reported in detail in the following section, was designed to ensure that the findings arising from this research were derived from a rigorous approach to analysing the data.
Data analysis
Focus groups and interviews were transcribed using the online transcription service Otter ( https://otter.ai/ ) and then checked and anonymised by the first author. Preliminary data analysis was carried out simultaneously by the first author using thematic content analysis proposed by Braun and Clarke [ 21 ] using NVivo 12 software [ 22 ]. All three authors undertook a detailed reading of the first three transcripts from both the focus groups and interviews and independently identified major themes. This preliminary coding was used as the basis of a discussion session to identify common themes between authors, to clarify sources of disagreement and to establish guidelines for further coding. Subsequent coding of the complete data set by the lead author identified a total of 533 descriptive codes; no descriptive code was duplicated across the themes. Initially, the descriptive codes were grouped into major themes identified from the literature, but with further analysis, themes emerged that were unique to the current study.
The research team met frequently during data analysis to discuss the initial descriptive codes, to confirm the major themes and subthemes, to revise themes on which there was disagreement and to identify any additional themes. Samples of quotes were reviewed by the second and third authors to decide whether these quotes were representative of the identified themes. The process occurred iteratively to refine the thematic categories, to discuss the definitions of each theme and to identify exemplar quotes.
Ethical considerations
The lead author was a clinical teacher and the clinical placement coordinator in the nursing department at the time of the study. Potential risks of perceived coercion and power imbalances were identified because of the lead author’s dual roles as an academic and as a researcher. To manage these potential risks, an academic staff member who was not part of the research study informed students about the study during a face-to-face lecture and ensured that all participants received a plain language statement identifying the lead author’s role and how perceived conflicts of interest would be managed. These included the lead author not undertaking any teaching or assessment role for the duration of the study and ensuring that placement allocations were completed prior to undertaking recruitment for the study. All students who participated in the study provided informed written consent. No financial or other incentives were offered. Approval to conduct the study was granted by the University of Melbourne Human Research Ethics Committee (Ethics ID 1955997.1).
Three main themes emerged describing students’ feelings and perceptions of their first clinical placement. In presenting the findings, before or during has been assigned to participants’ quotes to clarify the timing of students’ perspectives related to the clinical placement.
Major theme 1: Adjusting and managing a raft of feelings
The first theme encompassed the many positive and negative feelings about work-integrated learning expressed by participants before and during their clinical placement. Positive feelings before clinical placement were expressed by participants who were comfortable with the unknown and cautiously optimistic.
I am ready to just go with the flow, roll with the punches (Participant [P]1 before).
Overwhelmingly, however, the majority of feelings and thoughts anticipating the first clinical placement were negatively oriented. Students who expressed feelings of fear, anxiety, lack of knowledge, lack of preparedness, uncertainty about nursing as a career, or strong concerns about being a burden were all classified as conveying negative feelings. These negative feelings were categorised into four subthemes.
Subtheme 1.1 I don’t have enough knowledge
All participants expressed some concerns and anxiety before their first clinical placement. These encompassed concerns about knowledge inadequacy and were linked to a perception of under preparedness. Participants’ fears related to harming patients, responsibility for managing ‘real’ people, medication administration, and incomplete understanding of the language and communication skills within a healthcare setting. Anxiety for many participants merged with the logistics and management of their life during the clinical placement.
I’m scared that they will assume that I have more knowledge than I do (P3 before). I feel quite similar with P10, especially when she said fear of unknown and fear that she might do something wrong (P9 before).
Subtheme 1.2 Worry about judgment, being seen through that lens
Participants voiced concerns that they would be judged negatively by patients or healthcare staff because they perceived that the student nurse belonged to specific social groups related to their cultural background, ethnicity or gender. Affiliation with these groups contributed to students’ sense of self or identity, with students often describing such groups as a community. Before the clinical placement, participants worried that such judgements would impact the support they received on placement and their ability to deliver patient care.
Some older patients might prefer to have nurses from their own background, their own ethnicity, how they would react to me, or if racism is involved (P10 before). I just don’t want to reinforce like, whatever negative perceptions people might have of that community (P16 before).
Participants’ concerns prior to the first clinical placement about judgement or poor treatment because of patients’ preconceived ideas about specific ethnic groups did not eventuate.
I mean, it didn’t really feel like very much of a thing once I was actually there. It is one of those things you stress about, and it does not really amount to anything (P16 during).
Some students’ placement experiences revealed the positive benefits of their cultural background to enhancing patient care. One student affirmed that the placement experience reinforced their commitment to nursing and that this was related to their ability to communicate with patients whose first language was not English.
Yeah, definitely. Like, I can speak a few dialects. You know, I can actually see a difference with a lot of the non-English speaking background people. As soon as you, as soon as they’re aware that you’re trying and you’re trying to speak your language, they, they just open up. Yeah, yes. And it improves the care (P10 during).
However, a perceived lack of judgement was sometimes attributed to wearing the full personal protective equipment required during the COVID-19 pandemic, which meant that their personal features were largely obscured. For this reason, it was more difficult for patients to make assumptions or attributions about students’ ethnic or gender identity based on their appearance.
People tend to assume and call us all girls, which was irritating. It was mostly just because all of us were so covered up, no one could see anyone’s faces (P16 during).
Subtheme 1.3 Is nursing really for me?
Prior to their first clinical placement experience, many participants expressed ambivalence about a nursing career and anticipated that undertaking clinical placement could determine their suitability for the profession. Once exposed to clinical placement, the majority of students were completely committed to their chosen profession, with a minority remaining ambivalent or, in rare cases, choosing to leave the course. Not yet achieving full commitment to a nursing career was related to not wishing to work in the ward they had for their clinical placement, while remaining open to trying different specialities.
I didn’t have an actual idea of what I wanted to do after arts, this wasn’t something that I was aiming towards specifically (P14 before). I think I’m still not 100%, but enough to go on, that I’m happy to continue the course as best as I can (P11 during).
Subtheme 1.4 Being a burden
Before clinical placement, participants had concerns about being burdensome and how this would affect their clinical placement experiences.
If we end up being a burden to them, an extra responsibility for them on top of their day, then we might not be treated as well (P10 before).
A sense of burden remained a theme during the clinical placement for participants for the first five to seven days, after which most participants acknowledged that their role became more active. As students contributed more productively to their placement, their feelings of being a burden reduced.
Major theme 2: Sinking or swimming
The second major theme, sinking or swimming, described participants’ expectations about a successful placement experience and identified themes related to students’ successes (‘swimming’) or difficulties (‘sinking’) during their placement experience. Prior to clinical placement, without a realistic preview of what the experience might entail, participants were uncertain of their role, hoped for ‘nice’ supervising nurses and anticipated an observational role that would keep them afloat.
I will focus on what I want to learn and see if that coincides with what is expected, I guess (P15 before).
During the clinical placement, the reality was very different, with a sense of sinking. Participants discovered, some with shock, that they were expected to participate actively in the healthcare team.
I got the sense that they were not going to muck around, and, you know, they’re ‘gonna’ use the free labour that came with me (P1 during).
Adding to the confusion about the expected placement experience, participants believed that healthcare staff were unclear about students’ scope of practice for a postgraduate entry-to-practice degree, creating misalignment between students’ and supervising nurses’ expectations.
It seems to me like the educators don’t really seem to have a clear picture of what the scope is, and what is actually required or expected of us (P10 during).
In exploring perceived expectations of the clinical placement and the modifying effect of placement on initial expectations, three subthemes were identified: translation to practice is overwhelming, trying to find the rhythm or jigsaw pieces, and individual agency.
Subtheme 2.1 Translation to practice is overwhelming
Before clinical placement, participants described concerns about insufficient knowledge to enable them to engage effectively with the placement experience.
If I am doing an assessment understanding what are those indications and why I would be doing it or not doing it at a certain time (P1 before).
Integrating and applying theoretical content while navigating an unfamiliar clinical environment created a significant gap between theory and practice during clinical placement. As the clinical placement experience proceeded and initial fears dissipated, students became more aware of applying their theoretical knowledge in the clinical context.
We’re learning all this theory and clinical stuff, but then we don’t really have a realistic idea of what it’s like until we’re kind of thrown into it for three weeks (P10 during).
Subtheme 2.2 Trying to find the rhythm or the jigsaw pieces
Before clinical placement, participants described learning theory and clinical skills with contextual unfamiliarity. They had the jigsaw pieces but did not know how to assemble it; they had the music but did not know the final song. When discussing their expectations about clinical placement, the small number of participants with a healthcare background (e.g. as healthcare assistants) proposed realistic answers, whereas others struggled to answer or cited stories from friends or television. With a lack of context, feelings of unpreparedness were exacerbated. Once in the clinical environment, participants further emphasised that they could not identify what they needed to know to successfully prepare for clinical placement.
It was never really pieced together. We’ve learned bits and pieces, and then we’re putting it together ourselves (P8 during). On this course I feel it was this is how you do it, but I did not know how it was supposed to be played, I did not know the rhythm (P4 during).
Subtheme 2.3 Individual agency
Participants’ individual agency, their attitude, self-efficacy, and self-motivation affected their clinical placement experiences. Participant perceptions in advance of the clinical placement experience remained consistent with their perspectives following clinical placement. Before clinical placement, participants who were highly motivated to learn exhibited a growth mindset [ 23 ] and planned to be proactive in delivering patient care. During their clinical placement, initially positive students remained positive and optimistic about their future. Participants who believed that their first clinical placement role would be largely observational and were less proactive about applying their knowledge and skills identified boredom and a lack of learning opportunities on clinical placement.
A shadowing position, we don’t have enough skills and authority to do any work, not do any worthwhile skills (P3 before). I thought it would be a lot busier, because we’re limited with our scope, so there’s not much we can do, it’s just a bit slower than I thought (P12 during).
Individual agency appears to influence a successful first clinical placement; other factors may also be implicated but were not the focus of this study. Further research exploring the relationships between students’ age, life experience, resilience, individual agency, and the use of coping strategies during a first clinical placement would be useful.
Major theme 3: The reality of navigating placement relationships
The third main theme emphasised the reality of navigating clinical placement relationships and explored students’ relationships with healthcare staff, patients, and peers. Before clinical placement, many participants, especially those with healthcare backgrounds, expressed fears about relationships with supervising nurses. They perceived that the dynamics of the team and the healthcare workplace might influence the support they received. Several participants were nervous about attending placement on their own without peers for support, especially if the experience was challenging. Participants identified expectations of being mistreated, believing that it was unavoidable, and prepared themselves to not take it personally.
For me it’s where we’re going to land, are we going to be in a supportive, kind of nurturing environment, or is it just kind of sink or swim? (P5 before). If you don’t really trust them, you’re nervous the entire time and you’ll be like what if I get it wrong (P16 before).
Despite these concerns, students strongly emphasised the value of relationships during their first clinical placement, with these perceptions unchanged by their clinical placement experience. Where relationships were positive, participants felt empowered to be autonomous, and their self-confidence increased.
You get that that instant reaction from the patients. And that makes you feel more confident. So that really got me through the first week (P14 during). I felt like I was intruding, then as I started to build a bit of rapport with the people, and they saw that I was around, I don’t feel that as much now (P1 during).
Such development hinged on the receptiveness and support of supervising nurses, the team on the ward, and patients and could be hindered by poor relationships.
He was the old-style buddy nurse in his fifties, every time I questioned him, he would go ssshh, just listen, no questions, it was very stressful (P10 during). It depends whether the buddy sees us as an extra pair of hands, or we’re learners (P11 during).
Where students experienced poor behaviour from supervising nurses, they described a range of emotional responses to these interactions and also coping strategies including avoiding unfriendly staff and actively seeking out those who were more inclusive.
If they weren’t very nice, it wouldn’t be very enjoyable and if they didn’t trust you, then it would be a bit frustrating, that like I can do this, but you won’t let me (P12 during). If another nurse was not nice to me, and I was their buddy, I would literally just not buddy with them and go and follow whoever was nice to me (P4 during).
Relationships with peers were equally important; students on clinical placement with peers valued the shared experience. In contrast, students who attended clinical placement alone at a regional or rural hospital felt disconnected from the opportunities that learning with peers afforded.
Our research explored the emotional responses and perceptions of preparedness of postgraduate entry-to-practice nursing students prior to and during their first clinical placement. In this study, we described how the perceptions of nursing students remained consistent or were modified by their clinical placement experiences. Our analysis of students’ experiences identified three major themes: adjusting and managing a raft of feelings; sinking or swimming; and the reality of navigating placement relationships. We captured similar themes identified in the literature; however, our study also identified novel aspects of nursing students’ experiences of their first clinical placement.
The key theme, adjusting and managing a raft of feelings, which encapsulates anxiety before clinical placement, is consistent with previous research. This theme included concerns in communicating with healthcare staff and managing registered nurses’ negative attitudes and expectations, in addition to an academic workload [ 11 , 24 ]. Concerns not previously identified in the literature included a fear of judgement or discrimination by healthcare staff or patients that might impact the reputation of marginalised communities. Fortunately, these initial fears largely dissipated during clinical placement. Some students discovered that a diverse cultural background was an asset during their clinical placement. Although these initial fears were ameliorated by clinical placement experiences, evidence of such fears before clinical placement is concerning. Further research to identify appropriate support for nursing students from culturally diverse or marginalised communities is warranted. For example, a Finnish study highlighted the importance of mentoring culturally diverse students, creating a pedagogical atmosphere during clinical placement and integrating cultural diversity into nursing education [ 25 ].
Preclinical expectations of being mistreated can be viewed as an unavoidable phenomenon for nursing students [ 26 ]. The existing literature highlights power imbalances and hierarchical differences within the healthcare system, where student nurses may be marginalised, disrespected, and ignored [ 9 , 27 , 28 ]. During their clinical placement, students in our study reported unintentional incivility by supervising nurses: feeling not wanted, ignored, or asked to remain quiet by supervising nurses who were unfriendly or highly critical. These findings were similar to those of Thomas et al.’s [ 29 ] UK study and were particularly heightened at the beginning of clinical placement. Several students acknowledged that nursing staff fatigue from a high turnover of students on their ward and the COVID-19 pandemic could be contributing factors. In response to such incivility, students reported decreased self-confidence and described becoming quiet and withdrawing from active participation with their patients. Students oriented their behaviour towards repetitive low-level tasks, aiming to please and help their supervising nurse, to the detriment of learning opportunities. Fortunately, these incidents did not appear to impact nursing students’ overall experience of clinical placement. Indeed, students found positive experiences with different supervising nurses and their own self-reflection assisted with coping. Other active strategies to combat incivility identified in the current study that were also identified by Thomas et al. [ 29 ] included avoiding nurses who were uncivil, asking to work with nurses who were ‘nice’ to them, and seeking out support from other staff as a coping strategy. The nursing students in our study were undertaking a postgraduate entry-to-practice qualification and already had an undergraduate degree. The likely greater levels of experience and maturity of this cohort may influence their resilience when working with unsupportive supervising nurses and identifying strategies to manage challenging situations.
The theory-practice gap emerged in the theme of sinking or swimming. A theory-practice gap describes the perceived dissonance between theoretical knowledge and expectations for the first clinical placement, as opposed to the reality of the experience, and has been reported in previous studies (see, for instance, 24 , 30 , 31 , 32 ). Existing research has shown that when the first clinical placement does not meet inexperienced student nurses’ expectations, a disconnect between theory and practice occurs, creating feelings of being lost and insecure within the new environment, potentially impacting students’ motivation and risk of attrition [ 19 , 33 ]. The current study identified further areas exacerbating the theory-practice gap. Before the clinical placement, students without a healthcare background lacked context for their learning. They lacked understanding of nurses’ shift work and were apprehensive about applying clinical skills learned in the classroom. Hence, some students were uncertain if they were prepared for their first clinical placement or even how to prepare, which increased their anxiety. Prior research has demonstrated that applying theoretical knowledge more seamlessly during clinical placement was supported when students knew what to expect [ 6 ]. For instance, a Canadian study exposed students as observers to the healthcare setting before starting clinical placement, enabling early theory to practice connections that minimised misconceptions and false assumptions during clinical placement [ 34 ].
In the current study, the theory-practice gap was further exacerbated during clinical placement, where healthcare staff were confused about students’ scope of practice and the course learning objectives and expectations in a postgraduate entry-to-practice nursing qualification. The central booking system for clinical placements classifies first-year nursing students who participated in this study as equivalent to second-year undergraduate nursing students. Such a classification could create a misalignment between clinical educators’ expectations and their delivery of education versus students’ actual learning needs and capacity [ 3 , 31 ]. Additional communication to healthcare partners is warranted to enhance understanding of the scope of practice and expectations of a first-year postgraduate entry-to-practice nursing student. Educating and empowering students to communicate their learning needs within their scope of practice is also required.
Our research identified a link between students’ personality traits or individual agency and their first clinical placement experience. The importance of a positive orientation towards learning and the nursing profession in preparedness for clinical placement has been highlighted in previous studies [ 31 ]. Students’ experience of their first clinical placement in our study appeared to be strongly influenced by their mindset [ 23 ]. Some students demonstrated motivation to learn, were happy to ‘roll with the punches’, yet remain active in their learning requirements, whereas others perceived their role as observational and expected supervising nurses to provide learning opportunities. Students who anticipated a passive learning approach prior to their first clinical placement reported boredom, limited activity, and lack of opportunities during their first clinical placement. These students could have a lowered sense of self-efficacy, which may lead to a greater risk of doubt, stress, and reduced commitment to the profession [ 35 ]. Self-efficacy theory explores self-perceived confidence and competence around people’s beliefs in their ability to influence events, which is associated with motivation and is key to nursing students progressing in their career path confidently [ 35 , 36 ]. In the current study, students who actively engaged in their learning process used strategies such as self-reflection and sought support from clinical educators, peers and family. Such active approaches to learning appeared to increase their resilience and motivation to learn as they progressed in their first clinical placement.
Important relationships with supervising nurses, peers, or patients were highlighted in the theme of the reality of navigating placement relationships. This theme links with previous research findings about belongingness. Belongingness is a fundamental human need and impacts students’ behaviour, emotions, cognitive processes, overall well-being, and socialisation into the profession [ 37 , 38 ]. Nursing students who experience belongingness feel part of a team and are more likely to report positive experiences. Several students in the current study described how feeling part of a team improved self-confidence and empowered work-integrated learning. Nonetheless, compared with previous literature (see for instance, 2), working as a team and belongingness were infrequent themes. Such infrequency could be related to the short duration of the clinical placement. In shorter clinical placements, nursing students learn a range of technical skills but have less time to develop teamwork skills and experience socialisation to the profession [ 29 , 39 ].
Positive relationships with supervising nurses appeared fundamental to students’ experiences. Previous research has shown that in wards with safe psycho-social climates, where the culture tolerates mistakes, regarding them as learning opportunities, a pedagogical atmosphere prevails [ 25 , 39 ]. Whereas, if nursing students experience insolent behaviours or incivility, this not only impacts learning it can also affect career progression [ 26 ]. Participants who felt safe asking questions were given responsibility, had autonomy to conduct skills within their scope of practice and thrived in their learning. This finding aligns with previous research affirming that a welcoming and supportive clinical placement environment, where staff are caring, approachable and helpful, enables student nurses to flourish [ 36 , 40 , 41 , 42 ]. Related research highlights that students’ perception of a good clinical placement is linked to participation within the community and instructor behaviour over the quality of the clinical environment and opportunities [ 27 , 28 ]. Over a decade ago, a large European study found that the single most important element for students’ clinical learning was the supervisory relationship [ 39 ]. In our study, students identified how supervising nurses impacted their emotions and this was critical to their experience of clinical placement, rather than how effective they were in their teaching, delivery of feedback, or their knowledge base.
Students’ relationships with patients were similarly important for a successful clinical placement. Before the clinical placement, students expressed anxiety and fears in communicating and interacting with patients, particularly if they were dying or acutely unwell, which is reflective of the literature [ 2 , 10 , 11 ]. However, during clinical placement, relationships with patients positively impacted nursing students’ experiences, especially at the beginning when they felt particularly vulnerable in a new environment. Towards the end of clinical placement, feelings of incompetence, nervousness and uncertainty had subsided. Students were more active in patient care, which increased self-confidence, empowerment, and independence, in turn further improving relationships with patients and creating a positive feedback loop [ 36 , 42 , 43 ].
Limitations
This study involved participants from one university and a single course, thus limiting the generalisability of the results. Thus, verification of the major themes identified in this research in future studies is needed. Nonetheless, the purpose of this study was to explore in detail the way in which the experiences of clinical placement for student nurses modified initial emotional responses towards undertaking placement and their perceptions of preparedness. Participants in this study undertook their clinical placement in a variety of different hospital wards in different specialties, which contributed to the rigour of the study in identifying similar themes in nursing students’ experiences across diverse placement contexts.
This study explored the narratives of first-year nursing students undertaking a postgraduate entry-to-practice qualification on their preparedness for clinical placement. Exploring students’ changing perspectives before and during the clinical placement adds to extant knowledge about nursing students’ emotional responses and perceptions of preparedness. Our research highlighted the role that preplacement emotions and expectations may have in shaping nursing students’ clinical placement experiences. Emerging themes from this study highlighted the importance students placed on relationships with peers, patients, and supervising nurses. Significant anxiety and other negative emotions experienced by nursing students prior to the first clinical placement suggests that further research is needed to explore the impact of contextual learning to scaffold students’ transition to the clinical environment. The findings of this research also have significant implications for educational practice. Additional educational support for nursing students prior to entering the clinical environment for the first time might include developing students’ understanding of the clinical environment, such as through increasing students’ understanding of the different roles of nurses in the clinical context through pre-recorded interviews with nurses. Modified approaches to simulated teaching prior to the first clinical placement would also be useful to increase the emphasis on students applying their learning in a team-based, student-led context, rather than emphasising discrete clinical skill competencies. Finally, increasing contact between students and university-based educators throughout the placement would provide further opportunities for students to debrief, to receive support and to manage some of the negative emotions identified in this study. Further supporting the transition to the first clinical placement could be fundamental to reducing the theory-practice gap and allaying anxiety. Such support is crucial during their first clinical placement to reduce attrition and boost the nursing workforce.
Data availability
The datasets generated and/or analysed during the current study are not publicly available due to the conditions of our ethics approval but may be available from the corresponding author on reasonable request and subject to permission from the Human Research Ethics Committee.
Alshahrani Y, Cusack L, Rasmussen P. Undergraduate nursing students’ strategies for coping with their first clinical placement: descriptive survey study. Nurse Educ Today. 2018;69:104–8.
Article PubMed Google Scholar
Brady M, Price J, Bolland R, Finnerty G. Needing to belong: first practice placement experiences of childrens’ nursing students. Compr Child Adolesc Nurs. 2019;421:24–39.
Article Google Scholar
Levett-Jones T, Pitt V, Courtney-Pratt H, Harbrow G, Rossiter R. What are the primary concerns of nursing students as they prepare for and contemplate their first clinical placement experience? Nurse Educ Pract. 2015;154:304–9.
McCloughen A, Levy D, Johnson A, Nguyen H, McKenzie H. Nursing students’ socialisation to emotion management during early clinical placement experiences: a qualitative study. J Clin Nurs. 2020;2913–14:2508–20.
Andrew N, McGuinness C, Reid G, Corcoran T. Greater than the sum of its parts: transition into the first year of undergraduate nursing. Nurse Educ Pract. 2009;91:13–21.
Leducq M, Walsh P, Hinsliff-Smith. K McGarry J. A key transition for student nurses: the first placement experience. Nurse Educ Today. 2012;327:779–81.
Spurlock D Jr. The nursing shortage and the future of nursing education is in our hands. J Nurs Educ. 2020;596:303–4.
Agu CF, Stewart J, McFarlane-Stewart N, Rae T. COVID‐19 pandemic effects on nursing education: looking through the lens of a developing country. Int Nurs Rev. 2021;682:153–8.
Nejad FM, Asadizaker M, Baraz S, Malehi AS. Investigation of nursing student satisfaction with the first clinical education experience in universities of medical sciences in Iran. J Med Life. 2019;121:75–82.
Sun FK, Long A, Tseng YS, Huang HM, You JH, Chiang CY. Undergraduate student nurses’ lived experiences of anxiety during their first clinical practicum: a phenomenological study. Nurse Educ Today. 2016;37:21–6.
Article CAS PubMed Google Scholar
Gurková E, Zeleníková R. Nursing students perceived stress coping strategies health and supervisory approaches in clinical practice: a Slovak and Czech perspective. Nurse Educ Today. 2018;65:4–10.
Hanson J, Walsh S, Mason M, Wadsworth D, Framp A, Watson K. Speaking up for safety: a graded assertiveness intervention for first year nursing students in preparation for clinical placement: thematic analysis. Nurse Educ Today. 2020;84:104252.
Khalaila R. Simulation in nursing education: an evaluation of students outcomes at their first clinical practice combined with simulations. Nurse Educ Today. 2014;342:252–8.
Cummins AM, Catling C, Hogan R, Homer CS. Addressing culture shock in first year midwifery students: maximising the initial clinical experience. Women Birth. 2014;274:271–5.
Chesser-Smyth PA. The lived experiences of general student nurses on their first clinical placement: a phenomenological study. Nurse Educ Pract. 2005;56:320–7.
Arkan B, Ordin Y, Yılmaz D. Undergraduate nursing students experience related to their clinical learning environment and factors affecting to their clinical learning process. Nurse Educ Pract. 2018;29:127–32.
Cowen KJ, Hubbard LJ, Hancock DC. Expectations and experiences of nursing students in clinical courses: a descriptive study. Nurse Educ Today. 2018;67:15–20.
Krueger RA, Casey MA. Focus groups: a practical guide for applied research. 5th ed. Thousand Oaks, California: Sage; 2014.
Jonsén E, Melender HL, Hilli Y. Finnish and Swedish nursing students experiences of their first clinical practice placement—A qualitative study. Nurse Educ Today. 2013;333:297–302.
Watt D. On becoming a qualitative researcher: the value of reflexivity. Qual Rep. 2007;121:82–101.
Google Scholar
Braun V, Clarke V. Thematic analysis. In: Cooper H, Camic PM, Long DL, Panter AT, Rindskopf DK, Sher J, editors. APA handbook of research methods in psychology Vol. 2. Research designs: quantitative qualitative neuropsychological and biological. Washington, DC: American Psychological Association; 2012. pp. 57–71.
Chapter Google Scholar
Lumivero. - Software Solutions for Data Analysis & Management [Internet]. Lumivero. http://www.lumivero.com .
Yeager DS, Dweck CS. Mindsets that promote resilience: when students believe that personal characteristics can be developed. Educ Psychol. 2012;47(4):302–14.
Kol E, İnce S. Determining the opinions of the first-year nursing students about clinical practice and clinical educators. Nurse Educ Pract. 2018;31:35–40.
Mikkonen K, Merilainen M, Tomietto M. Empirical model of clinical learning environment and mentoring of culturally and linguistically diverse nursing students. J Clin Nurs. 2020;29(3–4):653–61.
Ahn YH, Choi J. Incivility experiences in clinical practicum education among nursing students. Nurse Educ Today. 2019;73:48–53.
Molesworth M. Nursing students first placement: peripherality and marginality within the community of practice. J Nurs Educ. 2017;561:31–8.
Rafati F, Nouhi E, Sabzehvari S, Dehghan-Nayyeri N. Iranian nursing students’ experience of stressors in their first clinical experience. J Prof Nurs. 2017;333:250–7.
Thomas J, Jinks A, Jack B. Finessing incivility: the professional socialisation experiences of student nurses first clinical placement a grounded theory. Nurse Educ Today. 2015;3512:e4–9.
Astin F, McKenna L, Newton J, Moore-Coulson L. Registered nurses–expectations and experiences of first year students–clinical skills and knowledge. Contemp Nurse. 2005;183:279–91.
Kalyani MN, Jamshidi N, Molazem Z, Torabizadeh C, Sharif F. How do nursing students experience the clinical learning environment and respond to their experiences? A qualitative study. BMJ Open. 2019;97:e028052.
Maginnis C, Croxon L. Transfer of learning to the nursing clinical practice setting. Rural Remote Health. 2010;102:334–40.
Soler OM, Aguayo-González M, Gutiérrez SSR, Pera MJ, Leyva-Moral JM. Nursing students’ expectations of their first clinical placement: a qualitative study. Nurse Educ Today. 2021;98:104736.
Powell TL, Cooke J, Brakke A. Altered nursing student perspectives: impact of a pre-clinical observation experience at an outpatient oncology setting. Can Oncol Nurs J. 2019;291:34–9.
Bandura AJJW. Self-efficacy. In: Weiner IB, Craighead WE, editors. The Corsini encyclopedia of psychology. Hoboken, NJ: John Wiley & Sons Inc; 2010.
Porteous DJ, Machin A. The lived experience of first year undergraduate student nurses: a hermeneutic phenomenological study. Nurse Educ Today. 2018;60:56–61.
Cooper J, Courtney-Pratt H, Fitzgerald M. Key influences identified by first year undergraduate nursing students as impacting on the quality of clinical placement: a qualitative study. Nurse Educ Today. 2015;359:1004–8.
Levett-Jones T, Lathlean J. The ascent to competence conceptual framework: an outcome of a study of belongingness. J Clin Nurs. 2009;1820:2870–9.
Warne T, Johansson UB, Papastavrou E, Tichelaar E, Tomietto M, Van den Bossche K. Saarikoski M. An exploration of the clinical learning experience of nursing students in nine European countries. Nurse Educ Today. 2010;308:809–15.
Laugaland K, Kaldestad K, Espeland E, McCormack B, Akerjordet K, Aase I. Nursing students experience with clinical placement in nursing homes: a focus group study. BMC Nurs. 2021;201:1–13.
Manninen K, Henriksson EW, Scheja M, Silén C. Authenticity in learning–nursing students experiences at a clinical education ward. Health Educ. 2013;1132:132–43.
Teskereci G, Boz İ. I try to act like a nurse: a phenomenological qualitative study. Nurse Educ Pract. 2019;37:39–44.
Chesser-Smyth PA, Long T. Understanding the influences on self‐confidence among first‐year undergraduate nursing students in Ireland. J Adv Nurs. 2013;691:145–57.
Download references
Acknowledgements
The authors wish to thank the first-year nursing students who participated in this study and generously shared their experiences of undertaking their first clinical placement.
No funding was received for this study.
Author information
Jennifer M. Weller-Newton
Present address: School of Nursing and Midwifery, University of Canberra, Kirinari Drive, Bruce, Canberra, ACT, 2617, Australia
Authors and Affiliations
Department of Nursing, The University of Melbourne, Grattan St, Parkville, VIC, 3010, Australia
Philippa H. M. Marriott
Department of Rural Health, The University of Melbourne, Grattan St, Shepparton, VIC, 3630, Australia
Present address: Department of Medical Education, Melbourne Medical School, The University of Melbourne, Grattan St, Parkville, VIC, 3010, Australia
Katharine J. Reid
You can also search for this author in PubMed Google Scholar
Contributions
All authors made a substantial contribution to conducting the research and preparing the manuscript for publication. P.M., J.W-N. and K.R. conceptualised the research and designed the study. P.M. undertook the data collection, and all authors were involved in thematic analysis and interpretation. P.M. wrote the first draft of the manuscript, K.R. undertook a further revision and all authors contributed to subsequent versions. All authors approved the final version for submission. Each author is prepared to take public responsibility for the research.
Corresponding author
Correspondence to Katharine J. Reid .
Ethics declarations
Ethics approval and consent to participate.
The research was undertaken in accordance with the National Health and Medical Research Council of Australia’s National Statement on Ethical Conduct in Human Research and the Australian Code for the Responsible Conduct of Research. Ethical approval to conduct the study was obtained from the University of Melbourne Human Research Ethics Committee (Ethics ID 1955997.1). All participants received a plain language statement that described the requirements of the study. All participants provided informed written consent to participate, which was affirmed verbally at the beginning of focus groups and interviews.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Marriott, P.H.M., Weller-Newton, J.M. & Reid, K.J. Preparedness for a first clinical placement in nursing: a descriptive qualitative study. BMC Nurs 23 , 345 (2024). https://doi.org/10.1186/s12912-024-01916-x
Download citation
Received : 17 November 2023
Accepted : 04 April 2024
Published : 22 May 2024
DOI : https://doi.org/10.1186/s12912-024-01916-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Postgraduate nursing education
- Nursing students
- Nursing schools
- Clinical skills
- Qualitative research
BMC Nursing
ISSN: 1472-6955
- General enquiries: [email protected]
Barriers to Adopting Healthy Lifestyle and Health Promotion among Ethnic Minority Bedouin Women in Southern Israel: A Qualitative Study
- Published: 29 May 2024
Cite this article

- Rasmiya Abu Rabia 1 , 2 na1 ,
- Samira Alfayumi-Zeadna ORCID: orcid.org/0000-0002-7904-414X 1 na1 ,
- Tova Hendel 1 &
- Ilya Kagan ORCID: orcid.org/0000-0002-2298-0308 1
A healthy lifestyle is a crucial step in disease prevention and management, as well as a significant predictor of health promotion. Yet, despite an increase in chronic morbidity among Bedouin women in southern Israel, little research has been conducted on their health behaviors. Therefore, the aim of this study is to examine barriers to adopting a healthy lifestyle and health promotion among ethnic minority Bedouin women in southern Israel.
This qualitative study was based on data collected through focus groups during June and July 2021. Participants included 44 Bedouin women aged 18–55. Focus groups were recorded and transcribed. Transcriptions were thematically analyzed and coded using the ecological model.
We found multiple barriers at various levels that prevent Bedouin women from adopting a healthy lifestyle and health promotion. At the individual level, such factors included the impact of financial limitations on healthful nutrition, as well as a lack of awareness or knowledge regarding healthy lifestyle and health promotion. At the organizational level, barriers include a lack of clinics, accessibility, and availability of health services and cultural incompatibility of the health services. At the community level, impediments to a healthy lifestyle include inaccessibility to sports facilities and suppression of physical activity. At the public policy level, participants, especially those living in unrecognized villages, described difficult living conditions related to environmental and social neglect as affecting their health status and ability to maintain a healthy lifestyle.
Study findings emphasize the need for policymaking and a systemic approach to address health disparities and ensure equal health promotion for the Bedouin population.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Data Availability
Anonymized data are available from the corresponding author on reasonable request.
Bayram T, Donchin M. Determinants of health behavior inequalities: a cross-sectional study from Israel. Health Promot Internation. 2019;34:941–52. https://doi.org/10.1093/heapro/day054 .
Article Google Scholar
Heinrich KM, Maddock J. Multiple health behaviors in an ethnically diverse sample of adults with risk factors for cardiovascular disease. Perm. 2011;15:12–8. https://doi.org/10.7812/TPP/10.082 .
American Heart Association Heart disease and stroke statistics. http://www.ncbi.nlm.nih.gov/book/NBK435776 . Accessed 15 Apr 2023.
Fatmi Z, Avan BI. Demographic, socio-economic and environmental determinants of utilisation of antenatal care in a rural setting of Sindh. Pakistan J Pak Med Assoc. 2002;52:138–42.
CAS PubMed Google Scholar
Stephenson R, Hennink M. Barriers to family planning service use among the urban poor in Pakistan. Asia-Pacific Population Journal. 2005;19:5–26. https://doi.org/10.18356/e54a6ab6-en .
Stringhini S, Carmeli C, Jokela M, Avendano M, Muennig P, Guida F, Ricceri F, D’Errico A, Barros H, Bochud M, Chadeau-Hyam M, Clavel-Chapelon F, Costa G, Delpierre C, Fraga S, Goldberg M, Giles GG, Krogh V, Kelly-Irving M, Layte R, Lasserre AM, Marmot MG, Preisig M, Shipley MJ, Vollenweider P, Zins M, Kawachi I, Steptoe A, Mackenbach J, Vineis P, Kivimaki M. Socioeconomic status and the 25 x 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. The Lancet. 2017;389:1229–37. https://doi.org/10.1016/S0140-6736(16)32380-7 .
Dubay LC, Lebrun LA. Health, behavior, and health care disparities: disentangling the effects of income and race in the United States. Int J Health Serv. 2012;42:607–25. https://doi.org/10.2190/HS.42.4.c .
Article PubMed Google Scholar
Patel N, Ferrer HB, Tyrer F, Wray P, Farooqi A, Davies MJ, Khunti K. Barriers and facilitators to healthy lifestyle changes in minority ethnic populations in the UK: a narrative review. J Racial and Ethnic Health Disparities. 2017;4:1107–19. https://doi.org/10.1007/s40615-016-0316-y .
Rezaee P, Nasrin Salar P, Alireza Ghaljaei P, Fereshteh Seyedfatem P, Naimeh Rezaei M. Neda Understanding the contextual factors affecting women’s health in Sistan and Baluchestan Province in Iran: a qualitative study. Int J Community Based Nurs Midwifery. 2017;5:317–28.
PubMed Google Scholar
Daoud N, Soskolne V, Mindell JS, Roth MA, Manor O. Ethnic inequalities in health between Arabs and Jews in Israel: the relative contribution of individual-level factors and the living environment. Int J Public Health. 2018;63:313–23. https://doi.org/10.1007/s00038-017-1065-3 .
Lindsay Smith G, Banting L, Eime R, O’Sullivan G, van Uffelen JGZ. The association between social support and physical activity in older adults: a systematic review. Int J Behav Nutr Phys Act. 2017;14:56. https://doi.org/10.1186/s12966-017-0509-8 .
Article PubMed PubMed Central Google Scholar
Miller TA, Dimatteo MR. Importance of family/social support and impact on adherence to diabetic therapy. Diabetes Metab Syndr Obes. 2013;6:421–6. https://doi.org/10.2147/DMSO.S36368 .
Nam S, Chesla C, Stotts NA, Kroon L, Janson SL. Barriers to diabetes management: patient and provider factors. Diabetes Res Clin Pract. 2011;93:1–9. https://doi.org/10.1016/j.diabres.2011.02.002 .
Zeh P, Sandhu HK, Cannaby AM, Sturt JA. Cultural barriers impeding ethnic minority groups from accessing effective diabetes care services: a systematic review of observational studies. Diversity and Equality in Health and Care. 2014;11:9–33. https://doi.org/10.21767/2049-5471.100001 .
Rudnitzky A, Ras TA. The Bedouin population in the Negev. Israel: Abraham Fund Inititatives; 2012.
Google Scholar
Singer S, Davidovitch N, Abu Fraiha Y, Abu Freha N. Consanguinity and genetic diseases among the Bedouin population in the Negev. J Community Genet. 2020;11:13–9. https://doi.org/10.1007/s12687-019-00433-8 .
Al-Said H, Braun-Lewensohn O, Sagy S. Sense of coherence, hope, and home demolition are differentially associated with anger and anxiety among Bedouin Arab adolescents in recognized and unrecognized villages. Anxiety, Stress, Coping. 2018;31:475–85. https://doi.org/10.1080/10615806.2018.1454070 .
Daoud N, Jabareen Y. Increased depressive symptoms among Arab Bedouin women under threat of house demolition in southern Israel. Health Hum Rights. 2014;16:179–91.
Gottlieb N, Feder-Bubis P. Dehomed: the impacts of house demolitions on the well-being of women from the unrecognized Bedouin-Arab villages in the Negev/Israel. Health Place. 2014;29:146–53. https://doi.org/10.1016/j.healthplace.2014.07.006 .
Amir H, Abokaf H, Levy YA, Azem F, Sheiner E. Bedouin women’s gender preferences when choosing obstetricians and gynecologists. J Immigrant Minority Health. 2018;20:51–8. https://doi.org/10.1007/s10903-016-0522-z .
Soffer, M., Cohen, M., Azaiza, F. The role of explanatory models of breast cancer in breast cancer prevention behaviors among Arab-Israeli physicians and lay women. Prim Health Care Res.2020;21, https://doi.org/10.1017/S1463423620000237 .
Alfayumi-Zeadna S, Froimovici M, Azbarga Z, Grotto I, Daoud N. Barriers to postpartum depression treatment among Indigenous Bedouin women in Israel: a focus group study. Health Soc Care Community. 2019;27:757–66. https://doi.org/10.1111/hsc.12693 .
Treister-Goltzman Y, Peleg R. Health and morbidity among Bedouin women in southern Israel: a descriptive literature review of the past two decades. J Community Health. 2014;39:819–25. https://doi.org/10.1007/s10900-014-9832-z .
Yahel H, Abu-Hjaj A. Tribalism, religion and state in Bedouin society in the Negev: between conservation and change. Strategic Update. 2021;24(2):44–56. [Hebrew]. https://fs.knesset.gov.il/globaldocs/MMM/64a5fee7-6462-e811-80dd-00155d0a0b8d/2_64a5fee7-6462-e811-80dd-00155d0a0b8d_11_10507.pdf . Accessed 15 Apr 2023
Ministry of Health The social survey: health and a healthy lifestyle. MOH, Jerusalem, Israel [In Hebrew]. https://www.cbs.gov.il/he/subjects/Pages/2017 . Accessed 15 Apr 2023.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77.
Article CAS PubMed Google Scholar
Bronfenbrenner, U. In Ecological systems theory. In R. Vasta (Ed.), Annals of child development. Six theories of child development: revised formulations and current issues (pp. 187– 249). London, UK: Jessica Kingsley; 1992.
Golden SD, McLeroy KR, Green LW, Earp JAL, Lieberman LD. Upending the social ecological model to guide health promotion efforts toward policy and environmental change. Health Educ Behav. 2015;42:8S-14S. https://doi.org/10.1177/1090198115575098 .
Greenwood-Hickman M, Renz A, Rosenberg DE. Motivators and barriers to reducing sedentary behavior among overweight and obese older adults. Gerontologist. 2016;56:660–8. https://doi.org/10.1093/geront/gnu163 .
Saligheh M, McNamara B, Rooney R. Perceived barriers and enablers of physical activity in postpartum women: a qualitative approach. BMC Pregnancy Childbirth. 2016;16:131. https://doi.org/10.1186/s12884-016-0908-x .
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57.
Biernacki P, Waldorf D. Snowball sampling: problems and techniques of chain referral sampling. Sociological Methods Res. 1981;10:141–63.
Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. Sage; 2006.
Kim H. Social integration and heath policy issues for international marriage migrant women in South Korea. Public Health Nurs. 2010;27:561–70. https://doi.org/10.1111/j.1525-1446.2010.00883.x .
Di Cesare M, Khang Y, Asaria P, Blakely T, Cowan MJ, Farzadfar F, Guerrero R, Ikeda N, Kyobutungi C, Msyamboza KP, Oum S, Lynch JW, Marmot MG, Ezzati M. Inequalities in non-communicable diseases and effective responses. Lancet. 2013;381:585–97. https://doi.org/10.1016/S0140-6736(12)61851-0 .
Major B, Mendes WB, Dovidio JF. Intergroup relations and health disparities: a social psychological perspective. Health Psychol. 2013;32:514.
Spadea T, Bellini S, Kunst A, Stirbu I, Costa G. The impact of interventions to improve attendance in female cancer screening among lower socioeconomic groups: a review. Prev Med. 2010;50:159–64. https://doi.org/10.1016/j.ypmed.2010.01.007 .
Kouvonen A, De Vogli R, Stafford M, Shipley MJ, Marmot MG, Cox T, Vahtera J, Väänänen A, Heponiemi T, Singh-Manoux A. Social support and the likelihood of maintaining and improving levels of physical activity: the Whitehall II Study. The Eur J Public Health. 2012;22:514–8.
Razee H, Van Der Ploeg HP, Blignault I, Smith BJ, Bauman AE, McLean M, Wah Cheung N. Beliefs, barriers, social support, and environmental influences related to diabetes risk behaviours among women with a history of gestational diabetes. Health Promot J Austr. 2010;21:130–7.
Douthit N, Kiv S, Dwolatzky T, Biswas S. Exposing some important barriers to health care access in the rural USA. Public Health. 2015;129:611–20. https://doi.org/10.1016/j.puhe.2015.04.001 .
Jacobs B, Ir P, Bigdeli M, Annear PL, Van Damme W. Addressing access barriers to health services: an analytical framework for selecting appropriate interventions in low-income Asian countries. Health Policy Plan. 2012;27:288–300. https://doi.org/10.1093/heapol/czr038 .
Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. J Community Health. 2013;38:976–93. https://doi.org/10.1007/s10900-013-9681-1 .
Betsch C, Böhm R, Airhihenbuwa CO, Butler R, Chapman GB, Haase N, Herrmann B, Igarashi T, Kitayama S, Korn L, Nurm Ü, Rohrmann B, Rothman AJ, Shavitt S, Updegraff JA, Uskul AK. Improving medical decision making and health promotion through culture-sensitive health communication: an agenda for science and practice. Med Decis Making. 2016;36:811–33. https://doi.org/10.1177/0272989X15600434 .
Larkey LK, Hecht M. A model of effects of narrative as culture-centric health promotion. J Health Commun. 2010;15:114–35. https://doi.org/10.1080/10810730903528017 .
Rogers HL, Pablo Hernando S, Núñez - Fernández S, Sanchez A, Martos C, Moreno M, Grandes G. Barriers and facilitators in the implementation of an evidence-based health promotion intervention in a primary care setting: a qualitative study. J Health Org Manag. 2021;35:349–67. https://doi.org/10.1108/JHOM-12-2020-0512 .
Needham, B. L., Ali, T., Allgood, K. L., Ro, A., Hirschtick, J. L., Fleischer, N. L. Institutional racism and health: a framework for conceptualization, measurement, and analysis. J Racial Ethnic Health Disparities. 2022;1–23. https://doi.org/10.1007/s40615-022-01381-9 .
Leimbigler B, Li EPH, Rush KL, Seaton CL. Social, political, commercial, and corporate determinants of rural health equity in Canada: an integrated framework. Can J Public Health. 2022;113:749–54.
Download references
Acknowledgements
We express our gratitude to the women who participated in this study, as well as to the Israel National Institute for Health Policy Research for their grant support. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
This study was supported by a grant from the Israel National Institute for Health Policy Research (Grant #R84/2020). The funding source was not involved in this study’s design.
Author information
Rasmiya Abu Rabia and Samira Alfayumi-Zeadna contributed equally to this work.
Authors and Affiliations
Nursing Department, School of Health Sciences, Ashkelon Academic College, 78211, Ashkelon, Israel
Rasmiya Abu Rabia, Samira Alfayumi-Zeadna, Tova Hendel & Ilya Kagan
Clalit Health Services, Southern Region, 84417, Be’er-Sheva, Israel
Rasmiya Abu Rabia
You can also search for this author in PubMed Google Scholar
Contributions
We confirm that all authors made substantial contributions to (1) the study conception and design, material preparation, data collection, and analysis and to (2) drafting the article and revising it critically for important intellectual content, and (3) all authors read and approved the final manuscript.
Corresponding author
Correspondence to Samira Alfayumi-Zeadna .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by Ashkelon Academic College’s Ethics Committee, Israel (Approval # 0028; February 2021). Written informed consent was obtained from every participant after a brief explanation. Confidentiality was ensured by removing identifiers and locking the questionnaires after data collection in a secured area.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (PDF 481 KB)
Rights and permissions.
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
Reprints and permissions
About this article
Rabia, R.A., Alfayumi-Zeadna, S., Hendel, T. et al. Barriers to Adopting Healthy Lifestyle and Health Promotion among Ethnic Minority Bedouin Women in Southern Israel: A Qualitative Study. J. Racial and Ethnic Health Disparities (2024). https://doi.org/10.1007/s40615-024-02022-z
Download citation
Received : 30 November 2023
Revised : 16 April 2024
Accepted : 08 May 2024
Published : 29 May 2024
DOI : https://doi.org/10.1007/s40615-024-02022-z
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Ecological model
- Facilitators
- Healthy lifestyle
- Health promotion
- Qualitative
- Find a journal
- Publish with us
- Track your research

IMAGES
VIDEO
COMMENTS
Step 1: Choose your topic of interest. Step 2: Define your research scope and hypotheses. Step 3: Determine your focus group questions. Step 4: Select a moderator or co-moderator. Step 5: Recruit your participants. Step 6: Set up your focus group. Step 7: Host your focus group. Step 8: Analyze your data and report your results.
A focus group is a qualitative research method used to gather in-depth insights and opinions from a group of individuals about a particular product, service, concept, or idea. The focus group typically consists of 6-10 participants who are selected based on shared characteristics such as demographics, interests, or experiences. The discussion ...
A focus group is a moderated group discussion on a pre-defined topic, for research purposes. 28,29 While not aligned to a particular qualitative methodology (for example, grounded theory or ...
A focus group is a qualitative research method that involves facilitating a small group discussion with participants who share common characteristics or experiences that are relevant to the research topic. The goal is to gain insights through group conversation and observation of dynamics. In a focus group: A moderator asks questions and leads a group of typically 6 to 12 pre-screened ...
Wilson, Valerie. 1997. "Focus Groups: A Useful Qualitative Method for Educational Research?" British Educational Research Journal 23(2):209-224. A basic description of how focus groups work using an example from a study intended to inform initiatives in health education and promotion in Scotland.
Traditionally, focus group research is "a way of collecting qualitative data, which—essentially—involves engaging a small number of people in an informal group discussion (or discussions), 'focused' around a particular topic or set of issues" (Wilkinson, 2004, p. 177).Social science researchers in general and qualitative researchers in particular often rely on focus groups to ...
Focus groups as qualitative research by David L. Morgan. ISBN: 0761903429. ... Methodology Brief: Introduction to Focus Groups. A detailed description with instruction and tips for focus group research from the Center for Assessment, Planning & Accountability.
Step 1: Choose your topic of interest. Step 2: Define your research scope and hypotheses. Step 3: Determine your focus group questions. Step 4: Select a moderator or co-moderator. Step 5: Recruit your participants. Step 6: Set up your focus group. Step 7: Host your focus group. Step 8: Analyse your data and report your results.
Qualitative research focuses on exploring individuals' perspectives related to specific research questions, issues, or activities ( 1 ). Frequently, structured interviews or focus groups are tools employed for data collection for qualitative research. In-person interviews are ideal, although phone and digital alternatives may be considered ...
Qualitative Research: Introducing focus groups. This paper introduces focus group methodology, gives advice on group composition, running the groups, and analysing the results. Focus groups have advantages for researchers in the field of health and medicine: they do not discriminate against people who cannot read or write and they can encourage ...
of any research technique, and focus groups do not differ greatly from other qualitative methods of data collection in this regard. In particular, the framework for the next two
The methods of qualitative data collection most commonly used in health research are document study, observations, semi-structured interviews and focus groups [1, 14, 16, 17]. Document study These can include personal and non-personal documents such as archives, annual reports, guidelines, policy documents, diaries or letters.
The more recent popularity of focus groups in qualitative research in the health and social sciences is reflected in an increased number of papers and books. The ... (Wilkinson 2004). A focus group, as a research method, 'involved more than one participant per data collection session' (Wilkinson 2004: 271). As such, the focus group method ...
Focus groups have been widely used in health research in recent years to explore the perspectives of patients and other groups in the health care system (e.g., Carr et al., 2003; Côté-Arsenault & Morrison-Beedy, 2005; Kitzinger, 2006).They are often included in mixed-methods studies to gain more information on how to construct questionnaires or interpret results (Creswell & Plano Clark, 2007 ...
Focus groups are an established mechanism for data collection across qualitative, mixed method, and quantitative methodologies (Pearson & Vossler, 2016 ). Although employed differently within each research paradigm, the popularity of focus groups is increasing (Carlsen & Glenton, 2011; George, 2013; Kress & Shoffner, 2007; Massey, 2010 ).
According to Krueger and Morgan et al. , focus group discussion, as a qualitative research method, is comparatively easier to conduct since all the target participants and the researcher are readily available in one location at the same time. Geographic proximity is an important consideration for researchers with resources constraints in ...
The Focus Group (FG) is one of the qualitative research methods to be utilized in the search for answers to such questions. The origin of the Focus Group was in sociology.
The following is a modified excerpt from Applied Qualitative Research Design: A Total Quality Framework Approach (Roller & Lavrakas, 2015, pp. 111-112). Strengths The unique advantage of the group discussion method is clearly the participant interaction and what it adds to (goes beyond) what might be learned from a series of in-depth interviews (IDIs).
The focus group approach is a qualitative method to collect the data on the selected topic with a structured and focused discussion in a small group of people. Focus groups are especially useful as a complement to other methods of data collection for providing in-depth information in a relatively short period of time.
A focus group discussion is a qualitative research tool ori ginated in sociology and. popular in business, marketing, and education (Sagoe, 2012). Focus group discussion is used. to gather data ...
Despite the well-documented advantages of focus group data collection, modern challenges for qualitative health researchers exist. Health research funding is increasingly competitive, recruiting health-care professionals to participate in qualitative health research is challenging due to increasing busyness in clinical environments, vast geographical distances between research sites hinder ...
Abstract. Recently, qua litative studies have been widespread in various areas such as. psychology, business, and soc iology. In this review, the process of qualitative. study has been clar ified ...
Abstract. While longitudinal qualitative research is mostly conducted with individuals, it is increasingly common for researchers to use a range of focus group techniques including participatory or arts-based methods that invite dialogic exchange within the participant group to generate data. This chapter discusses our experience of integrating ...
The emergence of digital technologies has opened new methods for engaging consumers, conducting focus groups, and gathering research material online. One such method is the use of smartphone-based mobile messaging platform WhatsApp, which allows real-time discussions and diary-type studies. Nevertheless, the potential of WhatsApp focus groups as a research method necessitates further ...
This project approached the topic using qualitative methods, namely an online survey and focus groups. Using this methodology, experiences from remote workers were collected and analyzed. Due to the nature of the topic, the study was carried out on a global scale taking advantage of the same tools used by remote workers, i.e. Information and ...
This paper forms part of a series of methodological guidance from the Cochrane Rapid Reviews Methods Group and addresses rapid qualitative evidence syntheses (QESs), which use modified systematic, transparent and reproducible methodsu to accelerate the synthesis of qualitative evidence when faced with resource constraints. This guidance covers the review process as it relates to synthesis of ...
Methods. We conducted focus group (FG) discussions with clinicians who had access to the dashboard as part of a randomized, stepped-wedge pragmatic trial. FGs explored clinician perceptions towards the usability, acceptability, and usefulness of the dashboard. ... Researchers trained in qualitative research methods (GS; CN) facilitated FG ...
Case studies are in-depth investigations of a person, group, event, or community. Typically, data is gathered from various sources using several methods (e.g., observations & interviews). The case study research method originated in clinical medicine (the case history, i.e., the patient's personal history). In psychology, case studies are ...
The research utilised a pre-post qualitative descriptive design. Six focus groups were undertaken before the first clinical placement (with up to four participants in each group) and follow-up individual interviews (n = 10) were undertaken towards the end of the first clinical placement with first-year entry-to-practice postgraduate nursing ...
The consolidated criteria for reporting qualitative research (COREQ) were used to detail research methods and results (see checklist in S1 Table 1). Study Design and Participants. The current study is based on the data collected in two focus groups (FGs) [26, 27]. Participants included forty-four Bedouin women aged 18-55 and living in the Negev.