An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
Preview improvements coming to the PMC website in October 2024. Learn More or Try it out now .
- Advanced Search
- Journal List


Community Interventions to Promote Mental Health and Social Equity
Enrico g. castillo.
1 Jane and Terry Semel Institute for Neuroscience and Human Behavior at UCLA, Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, UCLA, Los Angeles, CA USA
2 Center for Social Medicine and Humanities, UCLA, Los Angeles, CA USA
3 Los Angeles County Department of Mental Health, Los Angeles, CA USA
Roya Ijadi-Maghsoodi
4 Division of Population Behavioral Health, Department of Psychiatry and Biobehavioral Sciences, David Geffen School of Medicine, UCLA, Los Angeles, CA USA
5 VA Health Service Research and Development Center for the Study of Healthcare Innovation, Implementation, and Policy, VA Greater Los Angeles Healthcare System, Los Angeles, CA USA
Sonya Shadravan
Elizabeth moore, michael o. mensah, iii, mary docherty.
6 Harkness Fellow in Healthcare Policy and Practice, New York State Psychiatric Institute, Columbia University, New York, NY USA
Maria Gabriela Aguilera Nunez
Nicolás barcelo, nichole goodsmith, laura e. halpin, isabella morton, joseph mango.
7 Center for Health Services and Society, UCLA, Los Angeles, CA USA
Alanna E. Montero
Sara rahmanian koushkaki, elizabeth bromley.
8 UCLA Department of Anthropology, Los Angeles, CA USA
9 Rand Corporation, Santa Monica, CA USA
10 VA Greater Los Angeles Healthcare System, Los Angeles, CA USA
Bowen Chung
11 Los Angeles Biomedical Research Institute, Los Angeles, CA USA
12 Healthy African American Families II, Los Angeles, CA USA
Felica Jones
Sonya gabrielian, lillian gelberg.
13 Department of Family Medicine, David Geffen School of Medicine, UCLA, Los Angeles, CA USA
14 UCLA Jonathan Fielding School of Public Health, Los Angeles, CA USA
Jared M. Greenberg
Ippolytos kalofonos.
15 UCLA International Institute, Los Angeles, CA USA
Sheryl H. Kataoka
16 Division of Child and Adolescent Psychiatry, UCLA, Los Angeles, CA USA
Jeanne Miranda
Harold a. pincus.
17 Department of Psychiatry, Columbia University Medical Center, New York State Psychiatric Institute, NewYork-Presbyterian Hospital, Irving Institute for Clinical and Translational Research, New York, NY USA
Bonnie T. Zima
Kenneth b. wells, associated data, purpose of review.
We review recent community interventions to promote mental health and social equity. We define community interventions as those that involve multi-sector partnerships, emphasize community members as integral to the intervention, and/or deliver services in community settings. We examine literature in seven topic areas: collaborative care, early psychosis, school-based interventions, homelessness, criminal justice, global mental health, and mental health promotion/prevention. We adapt the social-ecological model for health promotion and provide a framework for understanding the actions of community interventions.
Recent Findings
There are recent examples of effective interventions in each topic area. The majority of interventions focus on individual, family/interpersonal, and program/institutional social-ecological levels, with few intervening on whole communities or involving multiple non-healthcare sectors. Findings from many studies reinforce the interplay among mental health, interpersonal relationships, and social determinants of health.
There is evidence for the effectiveness of community interventions for improving mental health and some social outcomes across social-ecological levels. Studies indicate the importance of ongoing resources and training to maintain long-term outcomes, explicit attention to ethics and processes to foster equitable partnerships, and policy reform to support sustainable healthcare-community collaborations.
Electronic supplementary material
The online version of this article (10.1007/s11920-019-1017-0) contains supplementary material, which is available to authorized users.
Introduction
Families, workplaces, schools, social services, institutions, and communities are potential resources to support health. In 1948, the World Health Organization defined health as a “state of complete physical, mental and social well-being and not merely the absence of disease or infirmity” [ 1 ]. Multi-sector and community-based mental healthcare approaches can help address health and social inequities by promoting social well-being and addressing structural determinants of mental health (public policies and other upstream forces that influence the social determinants of mental health).
A 2015 Cochrane review described three assumptions that underlie community interventions [ 2 •]. The first is an awareness of the multiple forces that exist at all social-ecological levels (i.e., individual, interpersonal, organizational/institutional, community, and policy) that facilitate or obstruct mental health [ 3 ]. The second is investment in community participation to provide resources and inform interventions, recognizing expertise outside of the healthcare system. The third is prioritization of community mental health and social outcomes.
This review focuses on recent developments in community interventions to promote mental health. We highlight major developments and trends, rather than providing a comprehensive systematic review. Our review defines community interventions as those that involve multi-sector partnerships, include community members (e.g., lay health workers) as part of the intervention, and/or involve the delivery of services in community settings (e.g., schools, homes). We include interventions focused on traditional mental health outcomes (e.g., depression remission) and studies that include a wider range of outcomes including mental health-related knowledge, quality of life, and social well-being. We do not include substance use interventions, which warrant a separate review.
To complete our review, we enlisted a large team of experts and trainees with experience in pertinent intervention areas. Our review focuses on interventions published in peer-reviewed medical journals from 2015 to 2018, with additional studies identified through reference mining and expert recommendations. We concentrate on seven topic areas, chosen for their salience and quality of evidence in recent literature: multi-sector collaborative care, early psychosis interventions, school-based interventions, homeless services, criminal justice, global mental health, and mental health promotion and secondary prevention. We selected studies for their design, outcomes, and/or impact (Appendix A ). These were chosen from a larger number of relevant community interventions (Appendix B ).
Multi-sector Collaborative Care
Collaborative care models in mental health have historical roots in the Chronic Care Model (CCM) of chronic disease management [ 4 , 5 ••]. The CCM envisioned a combination of health system reforms and community-based resources to support the ability of healthcare settings to improve outcomes for those with chronic illnesses [ 4 ]. Many collaborative care studies, often for depression, have focused on incorporating mental health services to varying degrees within primary care settings [ 6 – 10 ]. Adaptations exist for other target populations (e.g., children) and settings (e.g., obstetrics/gynecology practices, mental health clinics) [ 5 ••, 11 – 13 ]. Studies have noted the importance of community organizations and social services, particularly when inequities play a large role in determining outcomes and require services beyond the healthcare sector, for example for underresourced populations and natural disasters [ 5 ••, 14 , 15 , 16 , 17 ••].
Community Partners in Care (CPIC) was a depression collaborative care study that involved 95 programs in five sectors: outpatient primary care, outpatient mental health, substance use treatment services, homeless services, and other community services (e.g., senior centers, churches) [ 18 •]. A 2015 Cochrane review identified CPIC as the only “high-quality study” that “specifically evaluated the added value of a community engagement and planning intervention (i.e. a coalition-led intervention) over and above resource enhancement and community outreach” [ 2 •] (page 32). CPIC was a group-level randomized study that compared two program-level quality improvement interventions: Community Engagement and Planning (CEP) and Resources for Services (RS). RS programs received a depression care toolkit with technical assistance and consultation to implement a community-wide approach to depression care. CEP programs received the same resources within a multi-sector coalition approach to co-leading, implementing, and monitoring multi-sector depression services (e.g., encouraging community programs to be active in psychoeducation and screening, with streamlined referrals to clinics and social services) [ 19 ]. CPIC’s community-partnered participatory research approach and development of community partnerships are described in detail in several articles [ 19 – 24 ].
Unlike many collaborative care studies, CPIC focused on a predominantly under-resourced racial/ethnic minority sample ( n = 1018, 46% African American, 41% Latino, 74% with family incomes below federal poverty level) and had few exclusion criteria, enrolling many participants with co-morbid substance use disorders and serious mental illnesses in the study [ 25 , 26 ]. At 6-month follow-up, participants in CEP ( n = 514) compared to RS ( n = 504) had significantly improved health-related quality of life, increased physical activity, reduced homelessness risk factors, and reduced behavioral health hospitalizations [ 18 •]. Sub-group analyses and follow-up studies at 12 and 36 months support some significant beneficial effects of CEP over RS, with main effects seen predominantly during the first 6 months post-intervention and diminishing over time [ 25 , 27 – 34 , 35 •].
Since CPIC, only a handful of collaborative care studies have included non-healthcare partners [ 36 – 38 , 39 •]. Hankerson et al. conducted depression screenings in three predominantly African American Christian “mega churches” (≥ 2000 worshippers per weekend) in New York City, using a community coalition approach, including faith-based organizations and local government [ 38 ]. Investigators screened 122 community members at 3 church events in 2012. Notably, 19.7% of those screened reported moderate depression (PHQ-9 ≥ 10), in which the authors noted is higher than is seen in African American community samples. Moreover, none of the participants who screened positive requested community mental health referrals, even though these were offered, demonstrating the importance of churches as sites for depression screening, counseling (i.e., Mental Health First Aid), and referral [ 38 , 39 •].
Early Intervention Services for Psychosis
There is a large and growing body of literature on coordinated specialty care programs for people with early psychosis, including the RAISE Early Treatment Program/NAVIGATE and OnTrackNY [ 40 – 47 , 48 •]. Germane to our community intervention focus, several early psychosis interventions summarized in a 2014 review by Nordentoft et al. adapted Assertive Community Treatment (ACT), an evidence-based service delivery model that emphasizes outreach-based services [ 48 •, 49 ].
Secher et al. published the 10-year follow-up results of the Danish OPUS trial, a two-site RCT of a 2-year ACT-based assertive early intervention [ 50 ]. Services were delivered by a multidisciplinary team (psychiatrist, psychologists, nurses, social workers, vocational therapist, physiotherapist, 10:1 patient-to-staff ratio) in patients’ homes, other community locations, or clinic, based on patients’ preferences. Intensive services at this early critical stage were hypothesized to yield lasting effects by teaching individuals the skills to best manage their psychotic illnesses. OPUS results at 2 years showed significant positive outcomes compared to services as usual: decreased positive and negative psychotic symptoms, reduced substance use, improved treatment adherence, lower antipsychotic medication dosage, higher treatment satisfaction, and reduced family burden. At 10-year follow-up, however, most of these outcome differences had dissipated. Investigators conclude that longer duration of specialized assertive early intervention treatment, booster sessions, or the addition of an early detection program to reduce duration of untreated psychosis would aid the consolidation of early treatment gains.
An initiative by a London Early Intervention Service (EIS) sought to decrease duration of untreated psychosis and increase referrals from the community through early psychosis psychoeducational workshops with 36 community organizations (e.g., housing and social services, youth services, cultural and faith groups, police, colleges, employment agencies) [ 51 •]. EIS staff conducted 41 half-day workshops at community organizations; monthly follow-up meetings and an additional session were offered; EIS promotional materials were made available; and EIS referral processes were streamlined for community organizations, including a linkage worker as a community liaison. Although the majority of community staff were in contact with people experiencing early psychosis in the past year (59.4%) and attitudes toward EIS as a first referral destination improved (37% pre- to 68% post-workshop), the study results were negative. Comparing EIS referrals in the year pre-/post-interventions, there was no significant difference in duration of untreated psychosis (295 vs. 396 days, p = 0.715) and, contrary to expectations, referred patients experienced significantly more contacts with intermediate healthcare/non-healthcare programs in their pathway to EIS treatment (2.06 vs. 2.45 steps, p = 0.002), reflecting a less streamlined referral process. In follow-up interviews, the authors note the barriers of mental health stigma, high community staff turnover, and resistance by EIS clinic staff to community-based work. Similar to CPIC, both of these studies suggest the importance of resources to sustain lasting change.
School-Based Interventions
Research shows that youth, especially under-resourced youth, are most likely to receive mental healthcare in schools, given barriers to obtaining community mental health services [ 52 ••, 53 ]. School infrastructures also allow for large-scale implementation of prevention interventions [ 54 ••]. Given the number of factors involved in delivering school interventions, however, experts urge consideration of policies, school culture and climate, and leadership structure when delivering interventions [ 55 , 56 ]. Academic outcomes can be difficult for researchers to collect given the unique requirements of Family Educational Rights and Privacy Act and HIPAA [ 57 ]. Further, developing sustainable interventions in schools that are truly responsive to the needs of students may require years of building academic-community partnerships [ 58 ].
Skryabina et al. assessed educational outcomes in an RCT of a universal school-based cognitive behavioral therapy prevention program, called FRIENDS [ 59 ]. FRIENDS is a manualized program that teaches emotional regulation, anxiety management, and problem solving, led by trained school staff or other designated health leaders. Forty-one schools were randomized to three arms ( n = 1343): health-led FRIENDS, school-led FRIENDS, and a comparison group of Personal, Social, and Health Education (PSHE, emotional regulation, and self-awareness skills with less focus on anxiety management) which was provided by school staff. Health-led FRIENDS was more effective in decreasing social anxiety, generalized anxiety, and total Revised Children’s Anxiety and Depression Scale scores as compared to school-led FRIENDS and PSHE. There were no intervention effects on math, reading, or writing standardized assessment test scores.
Several studies implemented preventive interventions in the pre-kindergarten years. One such study evaluated developmental trajectories of youth, including behavioral, social, and learning measures over a 5-year period after receiving an enriched Head Start Curriculum [ 60 ]. This study is notable for its goal to address disparities and for the measures used to evaluate effects on development, which included social and learning behaviors and interpersonal relationships. In this RCT, 25 Head Start Centers were stratified and randomly assigned to receive usual Head Start vs. REDI intervention. REDI comprised dialogic reading, sound games, an interactive alphabet activity, and implementation of the Preschool Promoting Alternative Thinking Strategies curriculum focused on social emotional skills, with added professional development for teachers. Outcomes were obtained for 325 children who were followed for 5 years post-preschool. Children in the Head Start REDI intervention vs. control group were significantly more likely to follow optimal developmental trajectories in social behavior, aggressive-oppositional behavior, learning engagement, attention problems, student-teacher closeness, and peer rejection. This and other studies illustrate the importance of intervening at the levels of the classroom and whole school.
Homeless Services
Individuals experiencing homelessness are at increased risk for mental illness, trauma, suicide, and medical comorbidities, along with a reduced life expectancy compared with the general population [ 61 – 64 ]. The recent focus on Housing First in community-based research on homelessness largely reflects an increasing embrace of that model [ 65 ]. Housing First is an approach to providing permanent housing without requirements for pre-placement sobriety or treatment participation [ 65 ]. Studies have demonstrated that Housing First yields quicker and more sustained housing retention compared to continuum housing approaches (transitional housing +/- sobriety or treatment requirements) [ 66 ••].
In the Canadian At Home/Chez Moi study, a multi-city RCT of the Housing First model compared with usual care, Aubry et al. followed 950 homeless or precariously housed adults with serious mental illness [ 67 ••]. The study found that participants in Housing First, compared with usual care, more quickly entered housing (within 73 vs. 220 days), retained housing for longer durations (281 vs. 115 days), and rated the quality of their housing more positively at 2-year follow-up. They also had significantly higher gains in community functioning and quality of life in the first year.
Several family-focused studies addressed homelessness. Nath examined the impact of drop-in homeless service centers for children in New Delhi, India [ 68 ]. They found that for every month of attendance at a drop-in center, children experienced 2.1% fewer ill health outcomes per month and used 4.6% fewer substances. Shinn et al. focused on social and mental health outcomes in children within newly homeless families with mental health or substance use disorders [ 69 ]. They compared usual care with a family-adapted critical time intervention, which combined housing and case management to connect families leaving shelters with community services. Youth in both groups exhibited reductions in psychosocial and mental health symptoms over time. Children ages 6–10 and 11–16 receiving the intervention compared to usual care were less likely at 24-month follow-up to self-report school troubles (i.e., suspension, being sent to the principal’s office, and being sent home with a note). Other studies have begun to analogously assess homeless interventions for broader social outcomes, including community functioning, arrests, public and other service use (e.g., food banks, shelters, prison time), employment, and income [ 70 – 74 ]. Future studies would benefit from expanded exploration of social outcomes that are important to individuals who have experienced homelessness.
Criminal Justice
Nearly 40% of jail and prison inmates self-report a history of mental illness, and this prevalence is higher among those with more arrests and time served in a correctional facility [ 75 ]. Community interventions in collaboration with the criminal justice system are well positioned to address health disparities experienced by justice-involved populations and the vulnerabilities to justice involvement experienced by those with mental illness in the community. The studies below collaborated with the justice system to alter institutional (e.g., police, court) processes for those with mental illness and/or addressed upstream social and structural recidivism risk factors [ 76 ].
In Monroe County, New York, adults with psychotic disorders charged with misdemeanors were conditionally released and randomized to usual treatment ( n = 35) or Forensic Assertive Community Treatment (FACT) ( n = 35) [ 77 ]. FACT employed high-fidelity ACT services with the following adaptations: a 6-h training in criminal justice collaboration for clinicians, screening for criminogenic risk factors among enrollees, weekly court appearances, and meetings to discuss barriers to success with the supervising judge, public defender, and district attorney. Over a year, FACT enrollees had significantly fewer convictions (0.4 ± 0.7 vs 0.9 ± 1.3, p = .023), days in jail (21.5 ± 25.9 vs 43.5 ± 59.2, p = .025), and more days in outpatient mental health treatment (305.5 ± 92.1 versus 169.4 ± 139.6, p < .001) compared to treatment as usual.
A pilot study examined a social worker-administered decision-making intervention for police encountering people with mental illness [ 78 •]. During the study period, any police officer who ran a background check on a detained enrollee was notified of enrollee participation in the program and was given the option to call a linkage specialist, usually a social worker employed by a community mental health agency. Linkage specialists provided mental health history (e.g., treatment participation, medication history) and treatment referral options. While this feasibility study lacked statistical power, the authors suggest that these results show the promise of a cross-sector approach to reducing arrests in this population.
Other interventions addressed risk factors for justice involvement like lack of insurance, unemployment, emotional regulation, and academic achievement [ 79 – 81 , 82 •, 83 ]. Two quasi-experimental studies focused on healthcare access, examining the downstream service use and recidivism effects of expedited Medicaid enrollment for recent prison releasees with schizophrenia or bipolar disorder in Washington State ( n = 3086) [ 79 , 80 ]. Twelve months post-implementation, 81% of the expedited group and 43% of the services as usual group were enrolled in Medicaid, ( p < .01). Community mental health (69% vs. 37%, p < .01), outpatient primary care (64% vs. 42%, p < .01), and emergency room use (55% vs. 35%, p < .01) significantly increased in the intervention group compared to services as usual. Unexpectedly, there was a significantly greater proportion of those in the intervention versus comparison group that spent any days in jail (43 vs. 34%, p < .01) and state prison (56% vs. 46%, p < .01), with no significant difference in the proportion with any arrests (59% vs. 54%) at follow-up. The investigators suggest that while healthcare access is an important determinant for mental health, future interventions and policies must intentionally address the larger ecosystem of social/structural determinants of criminal justice involvement.
Global Mental Health
Global mental health is “an area for study, research and practice that places a priority on improving health and achieving equity in health for all people worldwide” [ 84 ] (pg. 1995). We reviewed community interventions in international settings, acknowledging the shared social, structural, and mental health challenges that exist across nations. Many of the reviewed studies involve lay health worker (LHW) interventions [ 85 •, 86 – 90 ]. Barnett et al. in their 2018 review of LHW interventions describe that LHWs elevate demand for services by increasing awareness of services and mental health literacy and by reducing stigma and barriers to care [ 85 •]. Further, LHW interventions increase the supply of services in under-resourced areas by enlarging the workforce of culturally appropriate providers.
In 2017, Patel et al. published the first trial of a psychological intervention in primary care delivered by LHWs for moderate/severe depression in a low/middle income country [ 91 •]. In that RCT, 495 participants in Goa, India, were assigned to the Healthy Activity Program (HAP) plus Enhanced Usual Care (EUC) intervention or EUC alone (usual care plus depression screenings and guideline-based primary care treatment of depression). In order to deliver the HAP (6–8 sessions on principles of behavioral activation), counselors received a 3-week training and 6-month internship under supervision of local mental health workers, who were trained by an expert on behavioral activation. At 3 months, HAP participants demonstrated significantly reduced depression symptom severity, suicidal ideation, disability, days out of work, and intimate partner violence and significantly higher rates of depression remission and improved behavioral activation compared to the EUC group.
A study in the Eastern Cape, South Africa, was the first to examine the effectiveness of a child abuse prevention program for adolescents in a low/middle income country [ 92 ••]. Most of the participating adolescents and caregivers ( n = 115 dyads) from six under-resourced rural and peri-urban communities were referred to the study by non-governmental organizations, schools, clinics, chieftans, and social workers based on a history of family conflicts. Sixty percent of adolescent participants at baseline had either an HIV-positive caregiver or were orphaned by AIDS, 63% experienced pre-intervention child abuse, and 50% of caregivers at baseline endorsed intimate partner violence. Participants completed a 12-week parenting program delivered by local childcare workers. The study yielded significant improvements in social outcomes: reduced child abuse (63.0% to 29.5%, p < .001), reduced adolescent delinquency/aggressive behavior, reduced witnessed violence by adolescents, improved positive and involved parenting (adolescent and caregiver self-report), and improved social support (adolescent and caregiver self-report). The study also demonstrated significantly improved mental health outcomes, specifically decreased caregiver substance use, reduced adolescent and caregiver depression, and reduced parenting stress. These findings illustrate the interplay among social determinants, family dynamics, and caregiver-adolescent mental health.
Multiple recent studies consider the effects of war and broad structural forces on mental health [ 87 – 89 , 93 ]. Cilliers et al. assessed the individual and community mental and social well-being outcomes associated with truth and reconciliation commissions (TRCs) in 200 Sierra Leone villages [ 94 ]. TRCs are community forums created to uncover wrongdoing by governments or other actors in the aftermath of major conflicts. The authors measured “societal healing” indicators, including forgiveness of perpetrators, trust, strength of social network, and community engagement, and “individual healing” indicators: PTSD, anxiety, and depression symptoms ( n = 2383). They found that TRCs yielded improvements in societal healing, but worsened individuals’ health (worsened psychological health, depression, anxiety, and PTSD). The authors suggest policy implications such as integrated counseling in TRCs, reducing delays in holding TRCs after war, and exploring alternative post-conflict unification methods.
Mental Health Promotion and Prevention
Communities That Care (CTC) is a community-level prevention planning and implementation system with primary foci on preventing youth (school grades 6–9) substance use, violence, and delinquency and secondary foci on depression, suicide, and other mental health outcomes. The CTC system involves five phases: identification of community stakeholders, formation of a community coalition, development of a community profile to identify risk and protective factors related to youth health and behavior problems, creation of a community action plan, and implementation and evaluation [ 95 ]. Communities implement evidence-based programs from the Building Healthy Youth Development registry, maintained by the University of Colorado Boulder’s Center for the Study of Prevention and Violence [ 96 ]. The Community Youth Development Study was a community-randomized study of CTC involving 24 communities ( n > 14,000) in Colorado, Illinois, Kansas, Maine, Oregon, Utah, and Washington State [ 97 – 99 ]. CTC has also been implemented in Pennsylvania and rural Massachusetts [ 100 – 102 ]. In CTC versus control communities, results showed improved individual outcomes at eighth grade: reduced substance use, delinquency, and violence; later initiation of alcohol use, tobacco use, and delinquency; and lower prevalence of risky behaviors (past-year delinquency, past 2-week delinquency, and past-month alcohol and tobacco use) [ 103 •]. Many of these results persisted to grades 10–12, despite few CTC programs focused on these grade levels. Fewer results (greater lifetime abstinence from antisocial behavior; greater lifetime abstinence from drug use and violence in male but not female participants) persisted to age 19 [ 103 •, 104 ].
CTC investigators recently published follow-up results for participants at age 21 ( n = 4002, 91% of the initial sample from grades 5–6), 11 years after initial CTC implementation [ 103 •]. By age 21, CTC vs. control communities showed increased likelihood of lifetime abstinence from alcohol, tobacco, and marijuana use (ARR 1.49; 95% CI 1.03, 2.16), increased abstinence from antisocial behavior (ARR 1.18, 95% CI 1.02, 1.37), and decreased lifetime incidence of violence (ARR 0.89, 95% CI 0.79, 0.99). In male participants, CTC versus control communities also showed increased likelihood of sustained abstinence from tobacco, marijuana, and inhalant use.
Social protection studies investigate mental health and other outcomes associated with direct provision of resources in the forms of cash and food transfers [ 105 , 106 •, 107 •, 108 , 109 ]. A neighborhood cluster RCT in Ecuador investigated the effects of such resources on mental well-being and intimate partner violence [ 106 •, 109 ]. Colombian refugees and low-income households in northern Ecuador were randomized to cash, food vouchers, food, or control arms. Treatment arms received the equivalent of $40 per month per household for 6 months, which represents 11% of pre-transfer monthly consumption. Food vouchers were redeemable at local supermarkets for a pre-approved list of nutritious foods. Food transfers were in the form of rice, lentils, vegetable oil, and canned sardines. Pooled results from all treatment arms showed the intervention significantly decreased the probability of controlling behaviors and physical and/or sexual violence by 6 to 7 percentage points compared to controls, with even greater reductions in the prevalence of any physical/sexual violence for women with low baseline ratings of household decision-making power [ 106 •]. Qualitative interviews with participants indicated that improved family well-being, reduced marital stress and conflict, and women’s increased freedom of movement and decision-making power contributed to the decrease in violence. Similar studies include a large cluster RCT of cash transfers in Kenya’s program for at-risk youth and a cluster RCT of greening urban vacant land; both showed significant improvements in depression outcomes compared to control communities. These studies highlight the importance of addressing social inequities to achieve mental health gains in under-resourced communities [ 107 •, 110 •].
Actions of Community Interventions by Social-Ecological Level
The community interventions above (Appendix A ), drawn from a larger selection (Appendix B ), highlight the successes and promise of these interventions to promote mental health and broader outcomes at all social-ecological levels: individual, interpersonal/family, organizational/institutional, community, and policy [ 3 ]. Community involvement is represented in varied ways in the form of individuals (lay health workers), settings (churches, schools), leaders (community-based participatory research), and multi-sector coalitions [ 35 •, 37 , 38 , 39 •, 85 •, 86 – 90 , 91 •, 103 •]. Many studies examined the interplay among mental health services, social and structural determinants, and mental health outcomes. Some explicitly assessed social outcomes like intimate partner violence, housing retention, academic performance, parent-child interactions, “societal healing,” and other contributors to mental and social well-being [ 67 ••, 92 ••, 94 , 111 ].
Figure Figure1 1 summarizes the actions of community interventions by social-ecological level to promote mental health and social well-being. We found that most interventions reviewed promoted mental health at the individual level. LHW interventions extend access and increase acceptability of mental health services by leveraging trusted relationships. For example, Patel et al. demonstrated the successful delivery of behavioral activation for depression by LHWs through relatively brief training to a population with significant barriers to healthcare access [ 91 •]. Some studies adapted evidence-based models (e.g., Forensic Assertive Community Treatment) to deliver treatments in non-traditional locations, such as jails, churches, and senior centers [ 77 ]. Many individual-level interventions also simultaneously acted at the organizational/institutional level. In the successful RCT of Head Start REDI, teachers were provided with professional development and mentoring to deliver an enriched curriculum [ 60 ].

Overview of community intervention processes by social-ecological level (adapted from McElroy, KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377)
A second group of interventions intervened at the interpersonal level (e.g., parent and family interventions). The effective child abuse prevention program in South Africa focused on the parent-child dyad through individual and joint sessions [ 92 ••]. Additionally, a strength of this intervention was its delivery by local child care workers. A third group of interventions functioned at the organizational/institutional level by enhancing the processes by which non-healthcare programs serve those with mental illness. These interventions enlisted non-healthcare entities and trusted community leaders to be active in mental healthcare, such as providing a depression screening intervention in churches [ 38 , 39 •]. Several successful school-based interventions operated at the organizational level, such as Warschburger and Zitzmann’s universal school-based prevention program for eating disorders in Germany and other whole school approaches [ 111 , 112 ].
We found only a small number of studies that intervened at the level of whole communities. Most interventions reviewed here included one non-healthcare sector collaborator as opposed to collaborating with communities more broadly. Examples of community-level interventions include CPIC, which involved 95 organizations in 5 sectors to develop community-wide plans for managing depression, and CTC that supports communities to develop multi-sector coalitions to prevent youth substance use, violence, and delinquency [ 35 •, 103 •]. Other studies acted at the community level by directly providing or influencing resources on a large scale, through cash/food transfers or land revitalization efforts [ 94 , 105 , 106 •, 107 •, 108 , 109 , 110 •].
A fifth group of interventions are health and public policies. Policies that promote mental health equity are beyond the scope of this review but are detailed in our recent review on this topic [ 113 •]. Policies as varied as mental health insurance parity, assisted outpatient treatment statutes, quality metrics for social determinants of health, value-based payment reforms, and the integration of funds and services for health and social care have the potential to improve access to treatment and improve outcomes [ 114 – 117 , 118 •, 119 – 121 ]. Policies facilitating multi-sector health collaborations include the Accountable Health Communities model, California’s Whole Person Care pilots, the Certified Community Behavioral Health Clinics Demonstration Program, New York’s Home and Community-based Services, the UK’s Social Impact Bonds Trailblazers, and the National Health Service England’s social prescribing teams [ 122 – 127 ]. Nation-level efforts to promote shared values for mental and social well-being are Australia’s mental health anti-stigma campaign, the US National Prevention Strategy’s focus on emotional well-being, and the UK’s Campaign to End Loneliness [ 128 – 130 ]. Thrive NYC is an example of large-scale action to promote mental health at the civic level, with a budget of $850 million and 54 initiatives across all public agencies and departments, with special emphases on community partnerships and prevention [ 131 , 132 •].
Ethical Considerations
Ethical considerations are of importance to many community interventions given the focus on marginalized and under-resourced populations [ 24 , 133 ]. Research on interventions for at-risk individuals with stigmatized conditions (e.g., incarceration, homelessness) should build trust with participants and recognize structural forces that place them at higher risk for these conditions (e.g., discriminatory policing and housing policies), to avoid inadvertently worsening stigma. Involving community stakeholders in equitable arrangements for interventions and research requires the necessary time and processes to develop effective partnerships. The expertise of community leaders and other stakeholders can be integrated equitably with that of researchers with trust, respect, and two-way knowledge exchange [ 134 , 135 ]. Community-based organizations, social services, and healthcare agencies also have different funding streams and incentives. Efforts to sustain interventions should include a focus on funding and other enabling infrastructures (e.g., training, technology) for community groups to participate in intervention-related activities.
Conclusions
There is evidence for the effectiveness of community interventions in multiple topic areas and acting at all social-ecological levels. International lay health worker interventions, a parenting intervention to reduce child abuse, a whole-school cognitive behavioral therapy prevention program, adapted ACT teams for early psychosis and justice-involved populations, Housing First services, and multi-sector collaborative care and prevention services are examples of effective community interventions. Studies indicate the importance of ongoing resources and training to maintain long-term outcomes and the need for policy reform to support healthcare-community partnerships. Future research should further define best practices for multi-sector collaborations and partnership structures, identify strategies for sustainable change after the end of research activities, and clarify the types of health and social problems that are best ameliorated through community interventions [ 2 •]. In close and equitable partnerships with communities and policy leaders, future community interventions in mental health should seek to improve health and achieve large-scale social outcomes through initiatives that address mental health, structural, and social inequities.
(DOCX 24 kb)
(DOCX 104 kb)
Grant Support
Grant Support By the National Institute on Minority Health and Health Disparities (award R01MD00721), the Patient-centered Outcomes Research Institute (award 1501-26518), and the National Institute on Drug Abuse of the National Institutes of Health (award K12DA000357). The content and views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the US Department of Veterans Affairs the National Institutes of Health or the United States Government.
Conflict of Interest
Enrico G. Castillo is employed by UCLA and Los Angeles Department of Mental Health and reports grants pending from UCLA CTSI and School of Medicine Seed Grant Program. Dr. Castillo has received travel reimbursement from the American Psychiatric Association.
Roya Ijadi-Maghsoodi is employed by the VA Greater Los Angeles Healthcare System and receives funding from the National Institute on Drug Abuse of the National Institutes of Health under Award Number K12DA000357.
Nicolás Barcelo reports a Minority Fellowship Award from the APA/SAMHSA.
Joseph Mango reports a grant from the National Institute of Minority Health and Health Disparities (NIMHD).
Alanna E. Montero reports grants pending from the NIMHD.
Sara Rahmanian Koushkaki reports a grant from the NIMHD.
Bowen Chung is a consultant for the Center for Law and Social Policy and on the advisory board for a Medicaid mental health project. Dr. Chung is a full-time employee of County of Los Angeles Department of Mental Health. Dr. Chung reports a grant pending from NIHMH R01 and a grant from PCORI (Award No. 1501-26518) and has received payment for technical assistance training from Baton Rouge Area Foundation and Maimonides Medical Center (contract to RAND Corporation for CIPIC implementation). Dr. Chung has received travel reimbursement from the City of New York Mayor’s Office and PCORI.
Jeanne Miranda reports honoraria from Annapolis Coalition and Baymark Health Services and is employed by UCLA Psychiatry. Dr. Miranda reports grants from NIH/NIMH, SAMHSA, NIMH, NIMHD, and PCORI.
Bonnie T. Zima is employed by UCLA and reports grants from Illinois Children’s Healthcare Foundation, PCORI, SAMHSA, California DHCS, and MHSOAC.
Kenneth B. Wells reports a grant from the National Institute of Minority Health and Health Disparities (NIMHD) and potential dissemination grants related to effective community interventions.
Sonya Shadravan, Michael O. Mensah, III, Mary Docherty, Maria Gabriela Aguilera Nunez, Nichole Goodsmith, Isabella Morton, Elizabeth Bromley, Felica Jones, Sonya Gabrielian, Lillian Gelberg, Jared M. Greenberg, Ippolytos Kalofonos, Sheryl H. Kataoka, and Harold A. Pincus each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
This article is part of the Topical Collection on Public Policy and Public Health
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
REVIEW article
Current insights of community mental healthcare for people with severe mental illness: a scoping review.

- 1 School of Social and Behavioral Sciences, Tranzo Scientific Center for Care and Wellbeing, Tilburg University, Tilburg, Netherlands
- 2 Kwintes Housing and Rehabilitation Services, Zeist, Netherlands
- 3 Trimbos Institute, Dutch Institute of Mental Health and Addiction, Utrecht, Netherlands
- 4 HVO-Querido, Amsterdam, Netherlands
- 5 Faculty of Social Sciences – HIVA, University of Leuven, Leuven, Belgium
Background: For the last four decades, there has been a shift in mental healthcare toward more rehabilitation and following a more humanistic and comprehensive vision on recovery for persons with severe mental illness (SMI). Consequently, many community-based mental healthcare programs and services have been developed internationally. Currently, community mental healthcare is still under development, with a focus on further inclusion of persons with enduring mental health problems. In this review, we aim to provide a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision on the ingredients of community mental healthcare.
Methods: We conducted a scoping review by systematically searching four databases, supplemented with the results of Research Rabbit, a hand-search in reference lists and 10 volumes of two leading journals. We included studies on adults with SMI focusing on stimulating independent living, integrated care, recovery, and social inclusion published in English between January 2011 and December 2022 in peer-reviewed journals.
Results: The search resulted in 56 papers that met the inclusion criteria. Thematic analysis revealed ingredients in 12 areas: multidisciplinary teams; collaboration within and outside the organization; attention to several aspects of health; supporting full citizenship; attention to the recovery of daily life; collaboration with the social network; tailored support; well-trained staff; using digital technologies; housing and living environment; sustainable policies and funding; and reciprocity in relationships.
Conclusion: We found 12 areas of ingredients, including some innovative topics about reciprocity and sustainable policies and funding. There is much attention to individual ingredients for good community-based mental healthcare, but very little is known about their integration and implementation in contemporary, fragmented mental healthcare services. For future studies, we recommend more empirical research on community mental healthcare, as well as further investigation(s) from the social service perspective, and solid research on general terminology about SMI and outpatient support.
1. Introduction
For the last three decades, there has been a shift in mental healthcare from a biomedical model to a more biopsychosocial model with a focus on rehabilitation, strengths, all areas of recovery, citizenship, empowerment, autonomy, and shared decision-making as leading principles ( 1–5 ). Still, the “social aspect” of the biopsychosocial model has long remained neglected ( 6 ). In 2007, human rights for people with disabilities were covered in the convention ( 7 ), and several community-based mental healthcare programs and services have been developed in Europe for these groups, enhanced by peer-to-peer initiatives and recovery colleges ( 8 ). Over the past few years, concepts such as social inclusion, citizenship, and participation have become the heart of the deinstitutionalization movement. Additionally, more and more people with mental healthcare issues receive outreach support. An indication of the development of intensive outpatient care for people with severe mental illness (SMI) is the development of (flexible) assertive community treatment ((F)ACT) teams. For example, in Netherlands in 2020, there were an estimated 400 FACT teams ( 9 ) and about 30% of people with SMI in England receive support from a specialist mental health floating outreach service ( 10 ).
In general, the definition of SMI consists of three criteria: a psychiatric diagnosis according to Diagnostic and Statistical Manual of Mental Disorders, illness duration of more than 2 years, and disability in functioning ( 11 ). A subgroup of people with SMI needs intensive care and support in daily living and receives residential care, supported housing in a 24/7 facility, or floating outreach ( 12 ). Most people with SMI who live in residential supported housing facilities have a strong preference to live independently in the community with flexible support with a view to a meaningful and fulfilling life ( 13 ). Nowadays, there are several community-based support services for these people who want to live independently, such as Housing First (HF). HF is an evidence-based housing intervention in the social domain that combats homelessness ( 14 ). It combines rapid access to permanent, nonabstinence-contingent ordinary housing and recovery-oriented mental health support teams ( 15 ). Individuals with SMI are at a higher risk of homelessness, and a high proportion of individuals experiencing homelessness are also living with mental illness ( 16 ). Therefore, measures should be available to prevent those who do not make use of, or leave, supported housing from becoming homeless.
Different services for mental health conditions have traditionally been separate from other services such as physical healthcare and social services. However, there is increasing emphasis internationally on developing a whole-system approach to improve the integration of these services to maximize an individual’s quality of life and social inclusion by encouraging their skills, promoting independence and autonomy to give them hope for the future. That leads to successful community living through appropriate support, with particular focus on patient-centered development and delivery ( 17–19 ). Furthermore, following the rehabilitation and recovery movement, care should involve all areas of living ( 20 ), and community-based mental healthcare thus should be a more integrated package of services. Many studies have appeared on the development and impact of multidisciplinary teams in mental healthcare ( 21 , 22 ). A lot less research is available on supported housing services, including accommodation-based and floating outreach services, leading to a lack of evidence on what works in this area ( 23 , 24 ).
In this literature review, we focus on all services for persons with SMI which are living independently in the community. These services aim to support these people in their daily life. This includes services initiated by treatment organizations, such as ambulatory interdisciplinary teams, as well as by welfare and supported housing organizations. Following McPherson et al. ( 25 ), who developed the simple taxonomy for supported accommodation (STAX-SA) to capture the defining features of different supported accommodation models, in this study we focus on supported housing services meant for persons moving forward from a hospital admission or a full-time staffed housing accommodation in a congregate setting with high support, toward more individual accommodation with no staff on-site. These services can be low or might need to be medium or intensive to support independent living for all ( 25 ).
Currently, there is a lack of research about what is needed to successfully provide this type of intensive support for people with SMI, and especially about how this support can be organized as an integrated community-based mental healthcare approach, including housing, rehabilitation, citizenship, all areas of recovery, empowerment, autonomy, and decision-making power. We aim to provide a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision and empirical findings on the ingredients of community mental healthcare. To do so, we will look in this review for both empirical evidence, as well as leading concepts in this research topic. The findings of this study contribute to the further development of community-based mental healthcare for persons with SMI and high-volume healthcare needs. This paper will address the following question: What are the current insights (both leading concepts and empirical findings) regarding a community mental healthcare system to support all persons with SMI in their independent living and recovery, and stimulate further social inclusion?
This review follows the PRISMA guidelines for scoping reviews ( 26 ). The completed PRISMA checklist is available on request from the authors.
2.1. Study design
We performed a scoping review, following the steps of the framework of Arksey and O’Malley ( 27 ): (a) identify the research question; (b) identify relevant studies; (c) select the studies; (d) chart the data; and (e) collate, summarize and report the results. A scoping review contributes to mapping rapidly the key concepts underpinning a research area and the main sources and types of evidence available ( 28 ).
2.2. Eligibility criteria
2.2.1. inclusion criteria.
We included papers published in English from January 2011 to December 2022 in peer-reviewed journals, aimed at 18 years and older adults with severe mental illness, focusing on stimulating independent living, integrated care, recovery, and social inclusion. For reasons of comparability, and fit in Western healthcare systems, studies were included if they were conducted in Western countries only (i.e., United States of America, Canada, countries in Western Europe, Australia, New Zealand, and Japan). Finally, all study designs were included, and we also included papers about interventions related to collaboration.
2.2.2. Exclusion criteria
Studies were excluded if (a) they primarily focused on treatment without support or care, (b) social inclusion or recovery was not the aim, (c) they focused on interventions that concentrated on one area of life and did not provide an integrated offering, or (d) if they focused on psychometric or physical diseases.
2.3. Search strategy
To find the right search terms for our search, we used the program Research Rabbit. This program helps to explore the literature of a research topic and links authors and papers on the same topic to each other. Before conducting the search, the research team determined the eight most relevant papers on this topic and added them to the program. With the function “similar work,” we added another eight relevant papers. Figure 1 shows these 16 relevant papers with the biggest bullets and shows that some papers have more in common with each other than others. The most common keywords from the 16 papers were the basis for our search terms.

Figure 1 . Research Rabbit.
We formulated and combined search terms concerning: (a) population (Serious Mental Illness* OR Severe Mental Illness* OR SMI OR Mental Illness OR Psychiatric Disabilities); (b) the setting (Community Mental Health* OR Supported Housing OR Supportive Housing OR Supported Accommodation OR Community-based mental healthcare OR Independent Living OR Independent Housing); (c) outcomes (Recovery OR Psychiatric Rehabilitation OR Rehabilitation OR Participation OR Social Inclusion OR Empowerment); and (d) contemporary paradigm (Deinstitutionali* OR De-Institutionali* OR Community Living OR Integrated Care). To reduce the number of irrelevant studies, exclusion terms based on the eligibility criteria were added to the search strategy (e.g., somatic disease, dementia, and COVID-19).
We systematically searched the following electronic databases: PubMed, PsycInfo, Medline, and Cinahl (September 2021, updated in December 2021 and December 2022). These databases were chosen to cover medical (PubMed and Medline), psychological (PsycInfo), and nursing (Cinahl) literature. After the database search, we reviewed the reference lists from papers included by title and abstract to find missing important papers, and additionally, the volumes of the Journal of Integrated Care and the Community Mental Health Journal published in the same period (2011–2021) were reviewed. Finally, we added several papers manually in consensus with our research group that were found lacking in the results, but which did meet the inclusion criteria.
2.4. Study selection process
After the removal of duplicate papers by the first author, the papers were screened in three rounds. In the title, abstract, full-text screenings phase, and thematic analysis, the first author screened all the hits and the second and third authors screened a random sample of 5% to ensure, and reach consensus on, fidelity to the inclusion criteria.
2.5. Data analysis
A qualitative synthesis of included studies was performed using the method of thematic analysis. All papers were screened on elements of relevance (or ingredients needed) for current community mental healthcare with the aim to support persons with SMI in their independent living, recovery, and to stimulate further social inclusion. All papers were coded, and codes were synthesized into areas of ingredients.
First, we present the descriptives in a PRISMA flow diagram, and a summary of the characteristics and quality of the studies included. Second, we present the results of our qualitative synthesis using thematic analysis.
3.1. Flowchart and summary of studies found
After the removal of duplicates and screening all papers on the title, abstract, and full text, the final sample consisted of 56 papers. Figure 2 shows the PRISMA flow diagram of the search.
Figure 2 . PRISMA flowchart.
The 56 papers were published spread throughout our time frame, but by far the most papers were conducted in 2018 ( n = 8), 2020 ( n = 7), and 2021 ( n = 9). Most of the papers were conducted in the United States ( n = 17). Twenty-seven of the included papers were conducted primarily in Europe; the majority in the United Kingdom ( n = 7), Netherlands ( n = 5), and Sweden ( n = 5). Four papers compared the situations in two countries: Australia and England, England and Italy, England and North Macedonia, and Canada and the United States. Other regions are Canada ( n = 3) and Australia ( n = 3). Four papers did not report their country, because they did not focus their research specifically on a country. We included 12 reviews, including three scoping reviews and four systematic reviews. In addition, we included 19 quantitative papers, including five RCTs and seven papers with a longitudinal design. We included 20 papers with a qualitative design, of which six were evaluative papers, seven opinion papers and seven descriptive papers. Finally, we included three mixed-methods studies and five expert papers. Table 1 shows the main information from the 56 papers found.
Table 1 . Summary of papers included in the scoping review.
3.2. Thematic analysis
We found ingredients of community-based mental healthcare for persons with SMI in 12 areas: 1. multidisciplinary teams; 2. collaboration within and outside the organization; 3. attention to several aspects of health; 4. supporting full citizenship; 5. attention to the recovery of daily life; 6. collaboration with the social network; 7. tailored support; 8. well-trained staff; 9. using digital technologies; 10. housing and living environment; 11. sustainable policies and funding; and 12. reciprocity in relationships. The subcategories were indicated in the results in bold. Table 2 shows which ingredients were found in which papers, arranged by study design. All papers were classified into nine categories of study designs. The first category contains all types of reviews, including one systematic meta-analysis. The quantitative papers were divided into three categories: RCTs, cross-sectional, and longitudinal. The qualitative papers were also divided into three categories: evaluative (papers in which respondents shared their experiences with the researchers); opinion (in which participants are asked for their opinions about a phenomenon); and descriptive (papers describing a phenomenon). The remaining two categories are mixed-method and expert papers (papers without empirical research but with the opinion of the authors).
Table 2 . Results of the thematic analysis.
3.2.1. Multidisciplinary teams
Multidisciplinary teams came up as important in twenty-five of the included papers. Five were reviews, three were RCTs, one was a quantitative cross-sectional paper, five were quantitative longitudinal papers and one a mixed-method paper. Additionally, two were qualitative evaluative papers, three were qualitative opinion papers, three were qualitative descriptive papers and two were expert papers.
Five papers recommend close involvement within different disciplines in multidisciplinary teams. Of these, three were qualitative papers ( 46 , 47 , 49 ), one expert paper ( 52 ), and one review ( 29 ). Therefore, one RCT finds positive results with regard to the health benefits for individuals for having received nurse practitioner services in a mental health setting to address primary care needs ( 34 ). In addition, two papers with a qualitative design emphasize adding an occupational therapist to a multidisciplinary team ( 44 , 50 ). Finally, seven papers show the value of peer support to multidisciplinary teams; of which these seven papers, there are three reviews ( 29–31 ), three qualitative papers ( 47 , 48 , 51 ), and one expert paper ( 53 ).
An example of working in multidisciplinary teams is the (flexible) assertive community treatment ((F)ACT) teams. We found mainly empirical studies about the implementation and efficacy of (F)ACT and collaboration with (F)ACT teams. Of these, we found two reviews ( 32 , 33 ), one RCT with positive results ( 35 ), and one RCT without significant results ( 36 ). In addition, six quantitative papers ( 37–42 ), one mixed-method paper ( 43 ), and two qualitative papers ( 44 , 45 ) report on (F)ACT. Lastly, we found one review about the history of assertive community treatment (ACT) ( 32 ).
3.2.2. Collaboration within and outside the organization
Collaboration inside and outside the mental healthcare organization was studied in 20 of the included papers. Three were reviews, two were qualitative longitudinal studies, one was a quantitative longitudinal paper, three were qualitative evaluative papers, three were qualitative opinion papers, two were qualitative descriptive papers, two were mixed-method papers, and four were expert papers.
Intersectoral collaboration is often mentioned in the literature found. The collaboration between mental healthcare, physical care, and social service sectors was found in four qualitative papers ( 45 , 46 , 48 , 49 ) and in one scoping review ( 54 ). In addition, collaboration between the government and the mental health sector was found in three qualitative studies ( 45 , 59 , 60 ) and one quantitative paper ( 40 ). Furthermore, we found three expert papers about collaboration in an integrated care system ( 3 , 53 , 63 ). Therefore, one systematic metareview ( 31 ), one mixed-method paper ( 57 ), one quantitative study ( 55 ), and one opinion paper ( 52 ) recommend an integrated care system with the integration of primary care in mental healthcare, and one descriptive paper shows an integrated mental health information system ( 62 ).
Growing evidence shows that integrative care is the new standard of care for people with mental illnesses, with the necessity of continuity of care from the emergency department to community mental health services. Continuity of care was found in two scoping reviews ( 29 , 54 ), one quantitative longitudinal paper ( 56 ), and one qualitative paper ( 61 ).
Finally, two qualitative papers ( 59 , 61 ) and one mixed-method paper ( 58 ) show the facilitators and barriers to intensive, intersectoral collaboration in community mental healthcare, such as cultural differences between the sectors as a barrier and face-to-face communication as a facilitator.
3.2.3. Attention to several aspects of health
Several aspects of health were studied in 18 of the included papers. Of these 15 papers, one was a systematic-meta review, two were quantitative longitudinal papers, one was a cross-sectional paper, eight were qualitative opinion papers, two were mixed-method papers, and four were expert papers.
Eight papers mention the focus on physical health in mental healthcare. Three qualitative, one mixed-method, and one quantitative paper report on the integration of physical health in mental healthcare ( 46 , 55 , 57 , 65 , 66 ). According to one expert paper, healthcare services need to recognize the far lower life expectancy among people with mental disorders and develop and evaluate new methods to reduce this health disparity ( 63 ). Respondents of a qualitative, opinion study stated that their main preoccupation and motivation was to be mentally well but they also recognized that many things that improve physical health also improved their mental health ( 67 ). In addition, one paper with a mixed-method design found that there is growing interest in models integrating physical healthcare delivery, management, or coordination into specialty mental health programs in the United States ( 58 ). One expert paper indicates the same ( 70 ). Finally, one systematic review found that this integration improves rates of immunization and screening for medical disorders, accompanied by positive effects on physical health, as well as improving general medical outcomes ( 31 ).
Another important aspect of health is cognitive functioning, which was found in two papers. One qualitative study mentioned that cognitive and physical health conditions might impact individuals’ ability to function in their daily lives during and after homelessness ( 48 ). In addition, one cross-sectional paper found that homebodies reported significantly poorer cognitive function than venturers ( 64 ).
In addition, we found two papers on psychosocial health. One quantitative study indicates that investment by teams to improve a patient’s psychosocial situation can lead to improvements in substance problems ( 41 ) and one expert paper aligns the importance of addressing social determinants of health within integrated care models for people with SMI ( 70 ).
Also, three qualitative papers ( 62 , 68 , 69 ) and one expert paper ( 52 ) emphasize the importance of positive health. The focus in positive healthis on the strengths, preferences, needs, and wishes of the service user, families, and communities that contribute to recovery.
Finally, two expert papers emphasize public health as actions seek to achieve equity between groups and a state of population-level health ( 52 , 53 ).One expert paper shows the role of mental and public health promotion and prevention, taking the needs of the entire population into account ( 53 ).
3.2.4. Promoting full citizenship
Promoting full citizenship was a topic of relevance in 14 of the included papers. Three were reviews, two were RCTs, two were qualitative evaluative papers, one was a qualitative opinion paper, two were qualitative descriptive papers, and four were expert papers.
Human rights and destigmatization contribute to promoting full citizenship and are addressed in six papers ( 3 , 29 , 48 , 53 , 63 , 82 ). One quantitative paper found that staffing intensity was negatively associated with human rights ( 82 ). One expert paper reports that historically the protection of human rights is one of the drivers for deinstitutionalization. Additionally, people with SMI experience more violations than others and suffer from stigma and discrimination ( 53 ). With this in mind, another expert paper states that mental health services should provide specific modules to reduce stigma and discrimination experienced by people with SMI ( 63 ). The same paper also states that some programs to reduce stigma and discrimination are presently active at the local level. They now need to be coordinated at the national level and adequately financed ( 63 ). In addition, providing training and coaching to health and social care staff on recovery and rights can reduce human rights violations that occur in the context of mental health services ( 53 ). One scoping review ( 29 ) found that there were an overwhelming number of anti-stigma campaigns from 1995 to 2015, but with a lowering trend of publication year over year on this topic.
In addition, several papers describe the Resource Group methodology that also promotes citizenship because the main feature of this methodology is that ownership and direction lie with the client. Of the included studies, there were two RCTs ( 73 , 74 ) with positive results, one meta-analysis ( 71 ), one review ( 72 ), and one qualitative paper ( 75 ). Finally, we found some papers on self-reliance. Two qualitative papers describe that a recovery-oriented system of care should give a holistic view of a person’s strengths and build on the strengths and resiliencies of individuals, families, and communities ( 62 , 69 ). One qualitative evaluative paper finds that FACT may support citizenship by relating to service users as whole people, facilitating empowerment and involvement ( 60 ).One expert paper states that signpost ways are needed for people to self-care, make useful contributions to society ( 52 ), and to be able to feel a fully-fledged citizen.
3.2.5. Attention to the recovery of daily life
Recovery of daily life was studied in 12 of the included papers. Of these 10 papers, one was a quantitative cross-sectional paper, one was a qualitative opinion paper, four were qualitative descriptive papers and four were expert papers.
We found several aspects of community-based support that contribute to recovery. According to one qualitative paper ( 68 ) and two expert papers ( 53 , 63 ), mental health services should develop dedicated programs for recovery. Also, three qualitative papers ( 48 , 49 , 77 ) focus on gaining and regaining skills for more independent living in vivo . Moreover, two expert papers mention that signpost self-care options ( 52 ) and recovery colleges can contribute to the recovery of daily life ( 3 ). Besides that, one expert paper states that evidence-based, psychosocial interventions should be deployed to support individuals to achieve both personal recovery and increased independence ( 3 ). In addition, one qualitative study reports that occupational therapists should support clients in their recovery to find their best self ( 50 ). Lastly, one cross-sectional paper states that most of their respondents (64.8%) were not employed, but those who were working presented higher levels of functional capacity than those who were not ( 76 ).
3.2.6. Collaboration with the social network
Collaboration with the social network of the client was studied in 10 of the included papers. Of these 10 papers, three were reviews, two were RCTs, one was a qualitative evaluative paper, three were qualitative descriptive papers and one was an expert paper.
Many papers mention several models in which it is important to involve the clients and their social network in the recovery process. We found the collaboration with the social network papers applying the Resource Group methodology in two RCTs ( 73 , 74 ), one meta-analysis ( 71 ), one review ( 72 ), and one qualitative paper ( 75 ). In addition, we found two qualitative descriptive papers that described approaches that place collaboration with the social network at the center of the client’s recovery process: namely, the Peer-Supported Open Dialogue ( 51 ), and the Active Recovery Triad (ART) model ( 68 ). Also, one expert paper and one qualitative paper mention that actively supporting the ability to empower and involve users and their families is important in community mental healthcare ( 3 , 49 ). Finally, one scoping review suggests that network size is not consistently associated with reported loneliness, social support, recovery, or quality of life. A deep relationship with at least one supportive person may be more or equally valuable than a larger network ( 78 ).
3.2.7. Tailored support
Tailored support came up as important in eight of the included papers. Of these eight papers, one was a review, two were qualitative evaluative papers, three were qualitative descriptive papers, and two were expert papers.
Two expert papers and three qualitative papers state that mental healthcare should provide care that service users (and their family members) find accessible and acceptable ( 3 , 60 , 63 , 80 ) and 24/7 available ( 77 ). In addition, one qualitative paper states that recovery-oriented care should be more effective when combined with support when required ( 49 ).One review found that support must also be flexible and user-driven ( 79 ). Therefore, one qualitative paper states that care should always be started with a Care Planning Meeting ( 68 ) and, according to one expert paper ( 63 ) and one qualitative paper ( 77 ), individualized care plans should be made through shared-decision making. Also, one expert paper states that care should be independent of location ( 63 ). Finally, we found two descriptive papers that describe that deinstitutionalization today means positive risk-taking and serious rethinking of questions in terms of distance, power, and language ( 77 ) and it provides new approaches to opportunity and safety ( 49 ).
3.2.8. Well-trained staff
Well-trained staff came up as important in eight of the included papers. Of these papers, there were two reviews, one quantitative cross-sectional paper, two qualitative descriptive papers, one mixed-method study, and two expert papers.
Two papers reported on education for mental healthcare staff. One review found that education for staff regarding identifying and responding to comorbidity is important ( 54 ).One qualitative descriptive paper states that peer-support open-dialogue teams should be trained in family systems ( 51 ). Furthermore, we found two expert papers and one qualitative paper that recommend the knowledge and use of evidence-based interventions and treatment by caregivers to provide social inclusion and recovery ( 49 , 53 , 63 ). In addition, one quantitative paper found that service teams should be of moderate size with adequate staffing to support service users in gaining and regaining skills for more independent living ( 82 ).One systematic review identified characteristics of well-trained staff, with practices that included routine monitoring and evaluation, good communication, equality between team members, and clear documentation practices ( 81 ). On the other hand, one mixed-method paper found difficulty in recruiting and retaining qualified staff ( 58 ).
3.2.9. Using digital technologies
Using digital technologies was studied in seven of the included papers. Of these seven papers, three were reviews, one was a qualitative descriptive paper, one was a mixed-method study, and two were expert papers.
One scoping review ( 29 ) found that digital platforms have an important role in improving the reach, scale, and accessibility of community-based support. Additionally, digital platforms add addressing public health issues and peer-led interventions are achieved effectively through the utilization of social media tools ( 29 ). Therefore, the same scoping review found that eHealth tools are becoming prevalent in the processes of promotion, prevention, and treatment in mental healthcare. In addition, the increased use of these eHealth tools continues to shape the future of community mental healthcare, particularly in low-access areas and areas where certain local expertise is lacking ( 29 ). Also, one expert paper states that the use of digital technologies should encourage self-care ( 52 ). Besides that, one mixed-method study and one systematic meta-review recommended the use of digital technology in electronic health records to enhance care coordination and promote integrated care ( 31 , 58 ). Finally, one systematic review ( 81 ), one qualitative paper ( 63 ), and one expert paper ( 49 ) state that digital monitoring through technology may improve practices and patient outcomes.
3.2.10. Housing and living environment
Housing and living environment came up as important in five of the included papers. Two were reviews, one was a quantitative cross-sectional paper, one was a qualitative descriptive paper, and one was an expert paper.
One review ( 79 ) describes the principles of the supportive housing approach in the United States. In addition, one systematic review ( 24 ) found positive results with regard to supported accommodation on several outcomes and the importance of connection to, and affiliation with, the living environment.
Furthermore, one expert paper ( 52 ) and one quantitative paper ( 82 ) state that writing live manuals tailored to local needs helps to stimulate a grand alliance for health. Also, one qualitative paper ( 77 ) describes the cornerstones of the Trieste Model. Two of the cornerstones are actively working on the environment and the social fabric, and service accountability toward the community.
3.2.11. Sustainable policies and funding
Sustainable policies and funding came up as important in four of the included papers. Of these four papers, one was a scoping review, one was a qualitative descriptive paper, and two were expert papers.
One expert paper states that the integration of community mental healthcare services, sectors, and collaboration with the social network of the service user can be hindered by a financing system that favors institutional care. Therefore, it is recommended to create a flexible financing system that allows incentives for different services that address the relevant life domains of people with SMI in the community ( 53 ). Another expert paper states that financial barriers are also encountered when integrating general practitioner care and mental healthcare ( 70 ). In addition, one qualitative paper describes a successful financial model that was developed in Italy. The personal health budget includes all economic, professional, and human resources needed to trigger a process aimed at restoring a person – through an individual rehabilitation process – to an acceptable level of social functioning ( 49 ). Finally, one review found that improved reforms on national mental health policies and deinstitutionalization are important for community mental healthcare ( 29 ).
3.2.12. Reciprocity in relationships
Reciprocity in relationships is a topic of interest in three of the included papers. Of these three papers, one was a qualitative opinion paper, one was a qualitative descriptive paper, and one was an expert paper.
This topic is about the reciprocity in relationships between clients and caregivers, but also in contributions to society by all people. One qualitative paper shows the importance of establishing and maintaining contact between the caregiver with the service user, by building a mutual relationship of trust ( 68 ). Therefore, one expert paper found that all people, with or without mental health problems, should make useful contributions to society, including paid and voluntary work that helps strengthen the local community, appreciate those around them and increase their webs of trusted relationships ( 52 ). Finally, to promote reciprocity, one qualitative opinion study states that the use of person-centered strategies is important. This focus on a person’s interests and goals was frequently indicated to foster relationships, gain trust, and develop self-efficacy ( 46 ).
4. Discussion
4.1. summary of main findings.
With this scoping review, we aimed to give a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision explained in areas of ingredients. To our knowledge, there are still a few publications that attempt to combine all the necessary elements for community mental health ( 53 , 83 , 84 ). We found 56 papers that met the inclusion criteria. Thematic analysis resulted in 12 areas of ingredients for community mental healthcare. In this section, we answer our research questions and show what was striking in the found literature. Finally, we present the strengths and limitations of our scoping review and our conclusions.
We aimed to give an overview of the existing and upcoming insights on community mental healthcare for people with SMI. Based on the number of papers found, most attention is paid to several aspects of health, multidisciplinary teams, collaboration within and outside the organization, collaboration with the social network, and supporting full citizenship. However, empirical evidence from quantitative studies was found in only four of the 12 areas based on our included papers: multidisciplinary teams; collaboration with the social network; collaboration within and outside the organization; and supporting full citizenship. Nevertheless, the other areas that are not yet supported by evidence in this scoping review are no less important for community mental healthcare. Although no empirical research has yet been done on these topics, they are being addressed in several papers. This shows that there is increasing attention to them in the field.
Notably, given the low number of included empirical studies from the welfare or supported housing sector, we can conclude that little empirical research has been done on community mental healthcare in these sectors for this target group. The few empirical studies we from the mental health care sector and were primarily about (F)ACT and the Resource Group methodology. Even though (F)ACT has been around for a few decades, this shows that for the last 10 years (F)ACT has remained an important model within community mental healthcare for this target group to achieve recovery. Additionally, given the number of papers reporting on it and the evidence provided, collaborative mental healthcare within teams, organizations, and clients and their social network has been seen as important over the past decade.
In addition to the topics found that received attention for more than 10 years within community mental healthcare, such as recovery, tailored support, and multidisciplinary teams, we found several papers that are about more recent and innovative areas. Such as, reciprocity in relationships; sustainable policy and funding; using digital technologies; and supporting full citizenship. The results from this scoping review show that in recent years new shifts are taking place in the field of mental healthcare, whereby there is more attention paid to full citizenship, but empirical research is still lacking. Further, the more innovative areas were published in more recent literature, but frequently in expert papers. Due to the few RCTs found, we cannot conclude that these areas are also the most important, but we could say that these areas can form the basis for further research in community-based mental healthcare to provide social inclusion and recovery in the future.
Recovery was one of our research terms and we expected recovery to be an important part of our scoping review because more and more studies have been conducted on the areas of recovery. Ten included papers reported on the recovery of daily life, but no empirical studies were found on that topic. This is probably due to the exclusion of intervention studies that focus on a single life domain and did not seek collaboration, which is often the case in studies of recovery and all aspects of health. The upcoming attention to recovery-based care for persons with SMI is also shown in recent scoping reviews. Bitter et al. ( 85 ), in their review on recovery interventions for supported housing and clinical settings, found 53 papers, of which about a quarter of recovery interventions showed added value based on RCTs and half of them had initial promising results based on case studies and follow-up designs without a control group. Additionally, van Weeghel and colleagues ( 86 ) reviewed the conceptualization of recovery, showing that personal recovery is conceptualized as complementary to clinical recovery and represents processes rather than outcomes. They state that a broad framework of recovery is required, and more research is needed into the working mechanisms of personal recovery processes. Our search and the previous scoping reviews show that recovery is still a guiding concept for people with SMI that needs to be paid attention to both in today’s and future community-based mental healthcare, but more empirical research is necessary to find the working mechanisms that contribute to recovery.
Further, we found many papers concerning multidisciplinary teams. Peer supporters ( 29 , 30 , 47 , 48 , 51 , 53 ), occupational therapists ( 44 , 50 ), and nurses ( 34 ) are frequently mentioned as important disciplines in a multidisciplinary team, besides the regular disciplines of psychologists, psychiatrists, and social psychiatric care workers. Peer supporters have been a part of the (F)ACT teams for more than our searched 10 years ( 87 ). Adding peer supporters to multidisciplinary teams is found in seven papers, including three reviews. Because of this, there is much evidence that peer support adds value to multidisciplinary teams.
Additionally, intersectoral collaboration appears regularly in the literature. First, several papers studied the collaboration with primary care to provide the physical health of people with SMI and the importance of attention being paid to clients’ physical health in mental healthcare. This builds on previous research that shows that people with SMI experience premature mortality of around 15–20 years earlier than the general population ( 88 ), have a high prevalence of substance use disorder ( 89 ), and are at risk of the development of often preventable secondary health conditions ( 90 , 91 ). Second, collaboration with the municipalities is recommended in the literature. The importance of collaboration between mental healthcare and community services is lacking in the papers. Currently, the mental healthcare sector seems the most important party in the found literature to support this target group. The collaboration between mental healthcare and municipal services is most often mentioned in papers about (F)ACT from Scandinavian countries ( 40 , 45 , 59 , 60 , 72 ). This is an enhancement of the multidisciplinarity, used in the (F)ACT program, that has been practiced and recommended for the last decades.
Intersectoral collaboration is often recommended in the literature found, but, notably, the literature found does not elaborate on what integrated collaboration should look like in practice. Possibly that is because other literature confirms that this collaboration is not easy to achieve ( 92 ). Integration can be defined as the search to connect the healthcare system (acute, primary medical, and skilled) with other human service systems (e.g., long-term care, education, and vocational and housing services) to improve outcomes (clinical, satisfaction, and efficiency). Leutz places full integration into the larger context of good human service practices by integrating services through linkage and coordination ( 92 ). Accordingly, we should not set full integration as the goal for community mental healthcare, rather, good connections and collaboration are more achievable.
In recent years, citizenship for people with (severe) mental health problems is a topic that has received increasing attention ( 93–95 ). Citizenship concerns one’s connections to the responsibilities, rights, roles, relationships, and resources offered to people in society ( 96 ). There have also been an increasing number of empirical studies, such as the cross-sectional study by Nesse and colleagues ( 97 ). This study suggests that citizenship and occupational meaningfulness may have positive implications for recovery. Additionally, Rowe and Davidson presented “recovering citizenship” as a concept and metaphor to capture the individual recovery process within the context and goal of a life in the community that the citizenship framework supports ( 98 ), and which is also about social inclusion and the full participation of individuals with mental illness in society ( 99 ).
Worthy of note is that just a few papers come from the leading journals on integrated community mental healthcare, which we explicitly searched, including the International Journal of Integrated Care and Community Mental Health Journal . Remarkably, the term “SMI” appears just once in the titles and abstracts of the volumes of 2011–2021 of the first journal. Moreover, in the Community Mental Health Journal we found several papers about community care, but only a few in combination with SMI. This confirms the idea that little research has been done on this topic. Besides that, many papers also seem to be written from the point of view of the mental healthcare sector. Loneliness, debts, and poverty are important topics in community care, but there does not yet seem to be much published about these main topics in social services because they did not show up in the results of the papers found. In addition, research in the shelter and supported housing sector is still limited ( 23 , 24 ). We also noticed that social work as a distinct support sector alongside the mental healthcare sector that includes supported housing receives little attention in the literature found. It is recommended that there should be more attention paid in future research to mental healthcare from the community perspective in which the municipalities and social services play a larger role.
In this scoping review, we have chosen to exclude papers on interventions that focus on a specific area of life and do not provide an integrated offering for people with SMI only, because of the risk of investigating too broad a scope. In the last decade, some interventions have become an important and innovative part of community care but would be too much information to present in one scoping review. Consequently, we did not include papers about (returning to) work, and papers primarily focused on recovery. Nevertheless, interventions are the important link between theory and practice and are worth mentioning. The literature proves their importance because of the many available interventions for this target group to improve, for example, lifestyle ( 100 , 101 ), internalized stigma ( 102 ), housing ( 103 ), employment ( 104 , 105 ), cognition ( 106 ), social skills ( 107 ), and self-management ( 108 ). Therefore, the focus on psycho-social aspects of support for people with SMI in the included papers is limited. This may also be due to our focus on the broader literature and not on interventions that address these aspects more specifically.
Finally, it was difficult to compare the papers. One example is the difficulty of comparison in the context of national differences in legal frameworks and public policies. Not every recommendation could be implied in all societies. We tried to take this into account to some extent by including only Western literature. In addition, for both the target group and the outpatient setting, a very varied vocabulary is used in the various papers and the general terms do not mean the same in every article. First, the term “supported housing” is used for support to people in a 24/7 aggregated setting, but also with regard to clients who live independently in the community with 24/7 available support, which is what we were looking for. Second, the term “SMI” is interpreted differently. Some papers are limited to clients with schizophrenia and bipolar disorder, while other papers focus more on autism and anxiety. Other requirements for SMI are also handled differently. Several papers seem to focus more on common mental illnesses rather than SMI. This makes it hard to compare and generalize the different papers on this topic. Previous research has already indicated that varying terminology is used internationally to describe the different housing settings and approaches to the provision of housing and support ( 13 ). Further research is necessary to create general terminology with clear definitions of the outpatient setting.
4.2. Strengths and limitations
The main strength of our review is the broad and systematic search. We used several search strategies, including database search, hand-searching the reference lists and leading journals to find as complete an overview as possible of all papers on our topic. We have done everything possible to find all relevant papers from the past 10 years. To ensure that we did not miss innovative topics, we did not choose certain study designs as inclusion criteria. This also has the advantage that we could find enough papers. As a result, there are large differences between the study designs in the papers. This creates more difficulties when comparing the papers and ingredients. It is hard to conclude which ingredient is more important for community-based mental healthcare than another. Nevertheless, to the best of our knowledge, this is the first scoping review on all developments in community mental healthcare and gives a good overview of the current relevant topics. Notably, less than half of the included papers are empirical studies, and a large part of the included papers was composed of descriptive or opinion papers. More empirical research is needed on this subject.
Conducting a scoping review provides a broad view of the literature, but it also has some limitations. One of these includes the search terms. With these search terms, it was not possible to find everything in the field through database search due to the variation in terminology, and in recent years the main focus of the research has been on individual interventions. Despite all efforts, including the Research Rabbit software and hand-search, there is still the possibility that we missed some relevant papers. The second limitation of our study is the generalizability of the conclusions. We did not use search terms in our search strategy to find specific themes, such as citizenship and social work, but these themes are related to our search terms recovery, participation, social inclusion, and empowerment. The final limitation concerns citizenship. Despite the increasing attention being paid to citizenship in the scientific literature, we included only a few citizenship papers. Due to the target population of our broader study, we only included papers on adults with SMI while the citizenship papers focus on (common) mental illness. Nevertheless, the focus on citizenship is a relevant development that deserves attention in this scoping review.
5. Conclusion
This scoping review aimed to give a comprehensive overview of existing and upcoming community mental healthcare approaches to discover the current vision in the areas of ingredients. We found 12 areas of ingredients, including some innovative topics about reciprocity and sustainable policies and funding. There is much attention paid to individual ingredients for good community-based mental healthcare, but very little is known about their integration and implementation in contemporary, fragmented mental healthcare services. No earlier, international study has connected all the current elements of good community mental healthcare together. Thus, our research contributes to the existing research and adds value to future research on community-based mental healthcare. For future studies, we recommend more empirical research on community mental healthcare, as well as further investigation(s) from the social service perspective, and solid research on general terminology about SMI and outpatient support.
Author contributions
CvG contributed to the development of the search question and strategies, screening papers and analysis, and to the main part of the manuscript. DR and MvV participated in the development of the search question and strategies, participated in screening papers, the thematic analysis, and writing the manuscript. JvW and TvR participated in the development of the search question, strategies, and supervised advancement of the project. All authors contributed to the article and approved the submitted version.
This scoping review belongs to a broader project which received ethical approval from the Ethics Review Board Tilburg School of Social and Behavioral Sciences and was funded by three organizations for supported housing and shelter in Netherlands: Kwintes, Leviaan, and HVO Querido.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Anthony, W. Recovery from mental illness. The guiding vision of the mental health service system in the 1990s. Psychosocial Rehabil J . (1993) 16:11–23. doi: 10.1037/h0095655
CrossRef Full Text | Google Scholar
2. van Regenmortel, T. Empowerment en Maatzorg. Een krachtgerichte psychologische kijk op armoede Armoede en Social Uitsluiting, Jaarboek 2002 . Leuven/Leusden: Acco; (2002). p. 71–84.
Google Scholar
3. Killaspy, H, McPherson, P, Samele, C, Keet, R, and Caldas de Almeida, J. EU compass for action on mental health and well-being. Providing community-based mental health services. Position Paper. (2018).
4. Pieters, G, Ruud, T, van Weeghel, J, Bahler, M, Murphy, B, Shields-Zeeman, L, et al. Recovery for all in the community. Learning from eachother. Consensus paper on fundamental principles and key elements of community based mental health care. BMC Psychiatry . (2017) 19:174. doi: 10.1186/s12888-019-2162-z
5. Stupak, R, and Dobroczyński, B. From mental health industry to humane care. Suggestions for an alternative systemic approach to distress. Int J Environ Res Public Health . (2021) 18:6625. doi: 10.3390/ijerph18126625
6. Johnson, S. Social interventionals in mental health. A call to action. Social Psychiatry Psychiatric Epidemiol . (2017) 52:245–7. doi: 10.1007/s00127-017-1360-6
7. UN General Assembly. Convention on the rights of persons with disabilities: resolution/adopted by the general assembly. Sixty-First Session UN General Assembly (2007).
8. Perkins, R, Repper, J, Rinaldi, M, and Brown, H. Recovery colleges: Centre for Mental Health NHS Confederation Mental Health Network. (2012).
9. van Vugt, M. Implementatie van FACT: Stand van zaken o.b.v. auditdata. Webinar CCAF. (2020).
10. Killaspy, H, and Priebe, S. Research into mental health supported accommodation – desperately needed but challenging to deliver. Br J Psychiatry . (2021) 218:179–81. doi: 10.1192/bjp.2020.74
PubMed Abstract | CrossRef Full Text | Google Scholar
11. World Health Organization. International classification of functioning, disability, and health . Geneva: WHO (2001).
12. Priebe, S, Saidi, M, Want, A, Mangalore, R, and Knapp, M. Housing services for people with mental disorders in England: patient characteristics, care provision and costs. Soc Psychiatry Psychiatr Epidemiol . (2009) 44:805–14. doi: 10.1007/s00127-009-0001-0
13. Richter, D, and Hoffmann, H. Preference for independent housing of persons with mental disorders: systematic review and meta-analysis. Admin Pol Ment Health . (2017) 44:817–23. doi: 10.1007/s10488-017-0791-4
14. Tsemberis, S. Housing first: the pathways model to end homelessness for people with mental illness and addiction manual. Eur J Homelessness . (2011):5.
15. Hwang, S, and Burns, T. Health interventions for people who are homeless. Lancet . (2014) 384:1541–7. doi: 10.1016/S0140-6736(14)61133-8
16. Fazel, S, Khosla, V, Doll, H, and Geddes, J. The prevalence of mental disorders among the homeless in Western countries: systematic review and meta-regression analysis. PLoS Med . (2008) 5:1670–81. doi: 10.1371/journal.pmed.0050225
17. Croze, C. Healthcare integration in the era of the affordable care act. In: Wellness AfBHa, editor. Washington, DC: Association for Behavioral Health and Wellness. (2015).
18. Social Care Local Government and Care Partnership Directorate. Closing the gap: priorities for essential change in mental health. In: Health Do. (London: Department of Health) (2014).
19. Killaspy, H. Contemporary mental health rehabilitation. East Asian Arch Psychiatr . (2014) 24:89–94. doi: 10.1017/S2045796018000318
20. Westen, K, Boyle, P, and Kroon, H. An observational comparison of FACT and ACT in the Netherlands and the US. BMC Psychiatry . (2022) 22:311. doi: 10.1186/s12888-022-03927-x
21. Bond, G, Drake, R, Mueser, K, and Latimer, E. Assertive community treatment for people with severe mental illness, critical ingredients and impact on patients. Dis Manage Health Outcomes . (2001) 9:141–59. doi: 10.2165/00115677-200109030-00003
22. van Veldhuizen, J, and Bahler, M. Manual: Flexible assertive community treatment: Vision, model, practice and organization . Groningen: CCAF (2013).
23. Chilvers, R, Macdonald, G, and Hayes, A. Supported housing for people with severe mental disorders. Cochrane Database Syst Rev . (2006) 2006:CD000453. doi: 10.1002/14651858.CD000453.pub2
24. McPherson, P, Krotofil, J, and Killaspy, H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry . (2018) 18:128. doi: 10.1186/s12888-018-1725-8
25. McPherson, P, Krotofil, J, and Killaspy, H. What Works? Toward a new classification system for mental health supported accommodation services: the simple taxonomy for supported accommodation (STAX-SA). Int J Environ Res Public Health . (2018) 15:190. doi: 10.3390/ijerph15020190
26. Tricco, A, Lillie, E, O'Brien, K, Colquhoun, H, Levac, D, Moher, D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med . (2018) 169:467–73. doi: 10.7326/M18-0850
27. Arksey, H, and O'Malley, L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol . (2005) 8:19–32. doi: 10.1080/1364557032000119616
28. Mays, N, Roberts, E, and Popaj, J. Synthesising research evidence. Studying the organisation and delivery of health services: research methods . London: Routledge (2001).
29. Bajraktarov, S, Kalpak, G, and Jovanovic, N. Community mental healthcare: new developments and innovative strategies. Curr Opin Psychiatry . (2020) 33:491–500. doi: 10.1097/YCO.0000000000000629
30. Gaiser, M, Buche, J, Wayment, C, Schoebel, V, Smith, J, Chapman, S, et al. A systematic review of the roles and contributions of peer providers in the behavioral health workforce. Am J Prev Med . (2021) 61:e203–10. doi: 10.1016/j.amepre.2021.03.025
31. Gaebel, W, Kerst, A, Janssen, B, Becker, T, Musalek, M, Rössler, W, et al. EPA guidance on the quality of mental health services: a systematic meta-review and update of recommendations focusing on care coordination. Eur Psychiatry . (2020) 63:e75. doi: 10.1192/j.eurpsy.2020.75
32. Rochefort, D. Innovation and its discontents: pathways and barriers in the diffusion of assertive community treatment. Milbank Q . (2019) 97:1151–99. doi: 10.1111/1468-0009.12429
33. Wright-Berryman, J, McGuire, A, and Salyers, M. A review of consumer-provided services on assertive community treatment and intensive case management teams: implications for future research and practice. J Am Psychiatr Nurses Assoc . (2011) 17:37–44. doi: 10.1177/1078390310393283
34. Rogers, E, Maru, M, Kash-MacDonald, M, Archer-Williams, M, Hashemi, L, and Boardman, J. A randomized clinical trial investigating the effect of a healthcare access model for individuals with severe psychiatric disabilities. Community Ment Health J . (2016) 52:667–74. doi: 10.1007/s10597-016-0009-3
35. Nielsen, C, Hjorthoj, C, Killaspy, H, and Nordentoft, M. The effect of flexible assertive community treatment in Denmark: a quasi-experimental controlled study. Lancet Psychiatry . (2021) 8:27–35. doi: 10.1016/S2215-0366(20)30424-7
36. Mueller-Stierlin, A, Helmbrecht, M, Herder, K, Prinz, S, Rosenfeld, N, Walendzik, J, et al. Does one size really fit all? The effectiveness of a non-diagnosis-specific integrated mental health care program in Germany in a prospective, parallel-group controlled multi-Centre trial. BMC Psychiatry . (2017) 17:283. doi: 10.1186/s12888-017-1441-9
37. Harvey, C, Killaspy, H, Martino, S, White, S, Priebe, S, Wright, C, et al. A comparison of the implementation of assertive community treatment in Melbourne, Australia and London, England. Epidemiol Psychiatric Sci . (2011) 20:151–61. doi: 10.1017/S2045796011000230
38. Firn, M, Hindhaugh, K, Hubbeling, D, Davies, G, Jones, B, and White, S. A dismantling study of assertive outreach services: comparing activity and outcomes following replacement with the FACT model. Soc Psychiatry Psychiatr Epidemiol . (2013) 48:997–1003. doi: 10.1007/s00127-012-0602-x
39. Nugter, A, Engelsbel, F, Bahler, M, Keet, R, and van Veldhuizen, R. Outcomes of FLEXIBLE assertive community treatment (FACT) implementation: a prospective real life study. Community Ment Health J . (2016) 52:898–907. doi: 10.1007/s10597-015-9831-2
40. Svensson, B, Hansson, L, and Lexen, A. Outcomes of clients in need of intensive team care in flexible assertive community treatment in Sweden. Nord J Psychiatry . (2018) 72:226–31. doi: 10.1080/08039488.2018.1430168
41. van Vugt, M, Kroon, H, Delespaul, P, and Mulder, C. Assertive community treatment and associations with substance abuse problems. Community Ment Health J . (2014) 50:460–5. doi: 10.1007/s10597-013-9626-2
42. Young, M, Barrett, B, Engelhardt, M, and Moore, K. Six-month outcomes of an integrated assertive community treatment team serving adults with complex behavioral health and housing needs. Community Ment Health J . (2014) 50:474–9. doi: 10.1007/s10597-013-9692-5
43. LeFebvre, A, Dare, B, Farrell, S, and Cuddeback, G. Transitions from assertive community treatment among urban and rural teams: identifying barriers, service options, and strategies. Community Ment Health J . (2018) 54:469–79. doi: 10.1007/s10597-017-0162-3
44. Milbourn, B, McNamara, B, and Buchanan, A. A qualitative study of occupational well-being for people with severe mental illness. Scand J Occup Ther . (2017) 24:269–80. doi: 10.1080/11038128.2016.1241824
45. Trane, K, Aasbrenn, K, Rønningen, M, Odden, S, Lexén, A, and Landheim, A. Flexible assertive community treatment teams can change complex and fragmented service systems: experiences of service providers. Int J Ment Health Syst . (2021) 15:38. doi: 10.1186/s13033-021-00463-1
46. Meyer-Kalos, P, Lee, M, Studer, L, Line, T, and Fisher, C. Opportunities for integrating physical health within assertive community treatment teams: results from practitioner focus groups. Community Ment Health J . (2017) 53:306–15. doi: 10.1007/s10597-016-0043-1
47. Asad, S, and Chreim, S. Peer support providers’ role experiences on Interprofessional mental health care teams: a qualitative study. Community Ment Health J . (2016) 52:767–74. doi: 10.1007/s10597-015-9970-5
48. Marshall, C, Cooke, A, Gewurtz, R, Barbic, S, Roy, L, Ross, C, et al. Bridging the transition from homelessness: developing an occupational therapy framework. Scand J Occup Ther . (2021) 1-17:1–17. doi: 10.1080/11038128.2021.1962970
49. Ridente, P, and Mezzina, R. From residential facilities to supported housing: the personal health budget model as a form of coproduction. Int J Ment Health . (2016) 45:59–70. doi: 10.1080/00207411.2016.1146510
50. Lama, T, Fu, Y, and Davis, J. Exploring the ideal practice for occupational therapists on assertive community treatment teams. Br J Occup Ther . (2021) 84:582–90. doi: 10.1177/03080226211026558
51. Razzaque, R, and Stockmann, T. An introduction to peer-supported open dialogue in mental healthcare. BJPsych Advances . (2016) 22:348–56. doi: 10.1192/apt.bp.115.015230
52. Gupta, S, Jenkins, R, Spicer, J, Marks, M, Mathers, N, Hertel, L, et al. How primary care can contribute to good mental health in adults. London J Prim Care (Abingdon) . (2018) 10:3–7. doi: 10.1080/17571472.2017.1410043
53. Keet, R, de Vetten-Mc, MM, Shields-Zeeman, L, Ruud, T, van Weeghel, J, Bahler, M, et al. Recovery for all in the community; position paper on principles and key elements of community-based mental health care. BMC Psychiatry . (2019) 19:174. doi: 10.1186/s12888-019-2162-z
54. Lee, S, Crowther, E, Keating, C, and Kulkarni, J. What is needed to deliver collaborative care to address comorbidity more effectively for adults with a severe mental illness? Aust NZ J Psychiatry . (2013) 47:333–46. doi: 10.1177/0004867412463975
55. Brar, J, Maise, A, Schake, P, Bills, L, Washington, L, Nikolajski, C, et al. Implementing a learning collaborative for population-based physical and behavioral health integration. Community Ment Health J . (2021) 57:1361–73. doi: 10.1007/s10597-020-00769-3
56. Zubritsky, C, Rothbard, AB, Dettwyler, S, Kramer, S, and Chhatre, S. Evaluating the effectiveness of an integrated community continuum of care program for individuals with serious mental illness. J Ment Health . (2013) 22:12–21. doi: 10.3109/09638237.2012.670882
57. Fisher, K, Weissinger, G, O'Rorke, R, Edwards, E, and Diamond, G. Consumers with serious mental illness perspectives on care integration: preparation for integration. J Am Psychiatr Nurses Assoc . (2022) 28:193–202. doi: 10.1177/10783903221091974
58. Scharf, D, Eberhart, N, Schmidt, N, Vaughan, C, Dutta, T, Pincus, H, et al. Integrating primary care into community behavioral health settings: programs and early implementation experiences. Psychiatr Serv . (2013) 64:660–5. doi: 10.1176/appi.ps.201200269
59. Davidsen, A, Davidsen, J, Jønsson, A, Nielsen, M, Kjellberg, P, and Reventlow, S. Experiences of barriers to trans-sectoral treatment of patients with severe mental illness. A qualitative study. Int J Ment Heal Syst . (2020) 14:87. doi: 10.1186/s13033-020-00419-x
60. Brekke, E, Clausen, HK, Brodahl, M, Lexén, A, Keet, R, Mulder, CL, et al. Service user experiences of how flexible assertive community treatment may support or inhibit citizenship: a qualitative study. Front Psychol . (2021) 12:727013. doi: 10.3389/fpsyg.2021.727013
61. Belling, R, Whittock, M, McLaren, S, Burns, T, Catty, J, Jones, IR, et al. Achieving continuity of care: facilitators and barriers in community mental health teams. Implement Sci . (2011) 6:23. doi: 10.1186/1748-5908-6-23
62. Hirdes, J, van Everdingen, C, Ferris, J, Franco-Martin, M, Fries, B, Heikkilä, J, et al. The interRAI suite of mental health assessment instruments: an integrated system for the continuum of care. Front Psych . (2020) 10:926. doi: 10.3389/fpsyt.2019.00926
63. Thornicroft, G, and Tansella, M. Community mental health care in the future: nine proposals. J Nerv Ment Dis . (2014) 202:507–12. doi: 10.1097/NMD.0000000000000151
64. McCormick, B, Brusilovskiy, E, Snethen, G, Klein, L, Townley, G, and Salzer, M. Getting out of the house: the relationship of venturing into the community and neurocognition among adults with serious mental illness. Psychiatr Rehabil J . (2022) 45:18–25. doi: 10.1037/prj0000483
65. Huck, G, Morrison, B, Finnicum, C, Kaseroff, A, and Umucu, E. Consumer perspectives on physical activity interventions within assertive community treatment programs. Psychiatr Rehabil J . (2018) 41:312–8. doi: 10.1037/prj0000311
66. Shattell, M, Donnelly, N, Scheyett, A, and Cuddeback, G. Assertive community treatment and the physical health needs of persons with severe mental illness: issues around integration of mental health and physical health. J Am Psychiatr Nurses Assoc . (2011) 17:57–63. doi: 10.1177/1078390310393737
67. Edmondson, A, Borthwick, R, Hughes, E, and Lucock, M. Using photovoice to understand and improve healthy lifestyles of people diagnosed with serious mental illness. J Psychiatr Ment Health Nurs . (2022) 29:676–87. doi: 10.1111/jpm.12863
68. Zomer, L, Voskes, Y, van Weeghel, J, Widdershoven, G, van Mierlo, T, Berkvens, B, et al. The active recovery triad model: a new approach in Dutch long-term mental health care. Frontiers Psychiatry . (2020) 11:11. doi: 10.3389/fpsyt.2020.592228
69. DiClemente, C, Norwood, A, Gregory, W, Travaglini, L, Graydon, M, and Corno, C. Consumer-centered, collaborative, and comprehensive care: the Core essentials of recovery-oriented system of care. J Addict Nurs . (2016) 27:94–100. doi: 10.1097/JAN.0000000000000120
70. McGinty, E, Presskreischer, R, Breslau, J, Brown, JD, Domino, ME, Druss, BG, et al. Improving physical health among people with serious mental illness: the role of the specialty mental health sector. Psychiatr Serv . (2021) 72:1301–10. doi: 10.1176/appi.ps.202000768
71. Norden, T, Malm, U, and Norlander, T. Resource group assertive community treatment (RACT) as a tool of Empowerment for clients with severe mental illness: a meta-analysis. Clin Pract Epidemiol Ment Health . (2012) 8:144–51. doi: 10.2174/1745017901208010144
72. Malm, U, Lundin, L, Rydell, P, Nordén, T, and Norlander, T. Resource group ACT (RACT) – a review of an integrative approach to psychoeducation of individual families involving the patient. Int J Ment Health . (2015) 44:269–76. doi: 10.1080/00207411.2015.1076290
73. Malm, U, Ivarsson, B, and Allebeck, P. Durability of the efficacy of integrated Care in Schizophrenia: a five-year randomized controlled study. Psychiatr Serv . (2014) 65:1054–7. doi: 10.1176/appi.ps.201300164
74. Tjaden, C, Mulder, CL, den Hollander, W, Castelein, S, Delespaul, P, Keet, R, et al. Effectiveness of resource groups for improving empowerment, quality of life, and functioning of people with severe mental illness: a randomized clinical trial. JAMA Psychiat . (2021) 78:1309–18. doi: 10.1001/jamapsychiatry.2021.2880
75. Norden, T, Eriksson, A, Kjellgren, A, and Norlander, T. Involving clients and their relatives and friends in the psychiatric case. Case managers' experiences of training in resource group assertive community treatment. Psych Journal . (2012) 1:15–27. doi: 10.1002/pchj.1
76. Ciampa, M, Roca, M, and Lysaght, R. Work patterns and support needs of people with serious mental illness. Community Ment Health J . (2022) 58:1207–13. doi: 10.1007/s10597-021-00930-6
77. Mezzina, R. Community mental health care in Trieste and beyond: an "open door-no restraint" system of care for recovery and citizenship. J Nerv Ment Dis . (2014) 202:440–5. doi: 10.1097/NMD.0000000000000142
78. Meyer, MS, Agner, J, Botero, A, and Cha, T. Mapping community: a scoping review of clubhouse members' social networks and their impact on recovery in mental illness. Psychiatr Rehabil J . (2022) 1–15. doi: 10.1037/prj0000520
79. Farkas, M, and Coe, S. From residential care to supportive housing for people with psychiatric disabilities: past, present, and future. Front Psych . (2019) 10:862. doi: 10.3389/fpsyt.2019.00862
80. Wusinich, C, Lindy, D, Russell, D, Pessin, N, and Friesen, P. Experiences of parachute NYC: an integration of open dialogue and intentional peer support. Community Ment Health J . (2020) 56:1033–43. doi: 10.1007/s10597-020-00556-0
81. Woody, C, Baxter, A, Harris, M, Siskind, D, and Whiteford, H. Identifying characteristics and practices of multidisciplinary team reviews for patients with severemental illness: a systematic review. Australas Psychiatry . (2018) 26:267–75. doi: 10.1177/1039856217751783
82. Dalton-Locke, C, Attard, R, Killaspy, H, and White, S. Predictors of quality of care in mental health supported accommodation services in England: a multiple regression modelling study. BMC Psychiatry . (2018) 18:344. doi: 10.1186/s12888-018-1912-7
83. Baumgardt, J, Schwarz, J, Bechdolf, A, Nikolaidis, K, Heinze, M, Hamann, J, et al. Implementation, efficacy, costs and processes of inpatient equivalent home-treatment in German mental health care (AKtiV): protocol of a mixed-method, participatory, quasi-experimental trial. BMC Psychiatry . (2021) 21:173. doi: 10.1186/s12888-021-03163-9
84. van Weeghel, J, van Audenhove, C, Colucci, M, Garanis-Papadatos, T, Liégeois, A, McCulloch, A, et al. The components of good community care for people with severe mental illnesses: views of stakeholders in five European countries. Psychiatr Rehabil J . (2005) 28:274–81. doi: 10.2975/28.2005.274.281
85. Bitter, N, Roeg, D, van Nieuwenhuizen, C, and van Weeghel, J. Recovery in supported accommodations: a scoping review and synthesis of interventions for people with severe mental illness. Community Ment Health J . (2020) 56:1053–76. doi: 10.1007/s10597-020-00561-3
86. van Weeghel, J, van Zelst, C, Boertien, D, and Hasson-Ohayon, I. Conceptualizations, assessments, and implications of personal recovery in mental illness: a scoping review of systematic reviews and meta-analysis. Psychiatr Rehabil J . (2019) 42:169–81. doi: 10.1037/prj0000356
87. van Veldhuizen, J, and Bähler, M. Flexible assertive community treatment. Vision, model, practice and organisation. (2013) doi: 10.13140/RG.2.1.3925.1683
88. Ribe, A, Laursen, T, Sandbaek, A, Charles, M, Nordentoft, M, and Vestergaard, M. Long-term mortality of persons with severe mental illness and diabetes: a population-based cohort study in Denmark. Psychol Med . (2014) 44:3097–107. doi: 10.1017/S0033291714000634
89. McGovern, M, Xie, H, Segal, S, Siembab, L, and Drake, R. Addiction treatment services and co-occurring disorders. J Subst Abus Treat . (2006) 31:267–75. doi: 10.1016/j.jsat.2006.05.003
90. Gardner-Sood, P, Lally, J, Smith, S, Atakan, Z, Ismail, K, Greenwood, K, et al. Cardiovascular risk factors and metabolic syndrome in people with established psychotic illnesses: baseline data form the IMPaCT randomized controlled trial. Psychol Med . (2015) 45:2619–29. doi: 10.1017/S0033291715000562
91. Schoepf, D, Uppal, H, Potluri, R, and Heun, R. Physical comorbidity and its relevance on mortality in schizophrenia: a naturalistic 12-year follow-up in general hospital admissions. Eur Arch Psychiatry Clin Neurosci . (2014) 264:3–28. doi: 10.1007/s00406-013-0436-x
92. Leutz, W. Five laws for integrating medical and social services: lessons from the United States and the United Kingdom. Milbank Q . (1999) 77:77–110. doi: 10.1111/1468-0009.00125
93. Reis, G, Bromage, B, Rowe, M, Restrepo-Toro, ME, Bellamy, C, Costa, M, et al. Citizenship, social justice and collective empowerment: living outside mental illness. Psychiatry Q . (2022) 93:537–46. doi: 10.1007/s11126-021-09968-x
94. Carr, E, and Ponce, A. Supporting mental health recovery, citizenship, and social justice. Community Ment Health J . (2021) 58:11–9. doi: 10.1007/s10597-021-00900-y
95. Harper, A, Kriegel, L, Morris, C, Hamer, H, and Gambino, M. Finding citizenship: what works? Am J Psychiatr Rehabil . (2017) 20:200–17. doi: 10.1080/15487768.2017.1338036
96. Ponce, A, and Rowe, M. Citizenship and community mental health care. Am J Community Psychol . (2018) 61:22–31. doi: 10.1002/ajcp.12218
97. Nesse, L, Aamodt, G, Gonzalez, M, Rowe, M, and Raanaas, R. The role of occupational meaningfulness and citizenship as mediators between occupational status and recovery: a cross-sectional study among residents with co-occurring problems. Adv Dual Diagn . (2021) 14:99–118. doi: 10.1108/ADD-08-2020-0018
98. Rowe, M, and Davidson, L. Recovering citizenship. Isr J Psychiatry Relat Sci . (2016) 53:14–20.
99. Quinn, N, Bromage, B, and Rowe, M. Collective citizenship: from citizenship and mental health to citizenship and solidarity. Soc Policy Adm . (2020) 54:361–74. doi: 10.1111/spol.12551
100. Weinstein, L, Chilton, M, Turchi, R, Klassen, A, LaNoue, M, Lamar, S, et al. Reaching for a healthier lifestyle: a Photovoice investigation of healthy living in people with serious mental illness. Prog Community Health Partnersh . (2019) 13:371–83. doi: 10.1353/cpr.2019.0061
101. Koomen, L, van der Horst, M, Deenik, J, and Cahn, W. Lifestyle interventions for people with a severe mental illness living in supported housing: a systematic review and meta-analysis. Front Psych . (2022) 13:966029. doi: 10.3389/fpsyt.2022.966029
102. González-Domínguez, S, González-Sanguino, C, and Munoz, M. Efficacy of a combined intervention program for the reduction of internalized stigma in people with severe mental illness. Schizophr Res . (2019) 211:56–62. doi: 10.1016/j.schres.2019.07.010
103. Brown, M, Jason, L, Malone, D, Srebnick, D, and Sylla, L. Housing first as an effective model for community stabilization among vulnerable individuals with chronic and nonchronic homelessness histories. J Community Psychol . (2016) 44:384–90. doi: 10.1002/jcop.21763
104. Drake, R, Bond, G, and Becker, D. Individual placement and support: an evidence-based approach to supported employment . New York: Oxford University Press (2013).
105. Roeg, D, de Winter, L, Bergmans, C, Couwenbergh, C, McPherson, P, Killaspy, H, et al. IPS in supported housing: Fidelity and employment outcomes over a 4 year period. Front Psych . (2021) 11:11. doi: 10.3389/fpsyt.2020.622061
106. van Duin, D, de Winter, L, Oud, M, Kroon, H, Veling, W, and van Weeghel, J. The effect of rehabilitation combined with cognitive remediation on functioning in persons with severe mental illness: systematic review and meta-analysis. Psychol Med . (2019) 49:1414–25. doi: 10.1017/S003329171800418X
107. Killaspy, H, Harvey, C, Brasier, C, Brophy, L, Ennals, P, Fletcher, J, et al. Community-based social interventions for people with severe mental illness: a systematic review and narrative synthesis of recent evidence. World Psychiatry . (2022) 21:96–123. doi: 10.1002/wps.20940
108. Strong, S, and Letts, L. Personal narratives of learning self-management: lessons for practice based on experiences of people with serious mental illness. Aust Occup Ther J . (2021) 68:395–406. doi: 10.1111/1440-1630.12748
Keywords: severe mental illness, community care, recovery, social inclusion, scoping review, current insights, human rights, independent living
Citation: van Genk C, Roeg D, van Vugt M, van Weeghel J and Van Regenmortel T (2023) Current insights of community mental healthcare for people with severe mental illness: A scoping review. Front. Psychiatry 14:1156235. doi: 10.3389/fpsyt.2023.1156235
Received: 01 February 2023; Accepted: 23 March 2023; Published: 18 April 2023.
Reviewed by:
Copyright © 2023 van Genk, Roeg, van Vugt, van Weeghel and Van Regenmortel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caroline van Genk, [email protected]
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- My Account Login
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Open access
- Published: 13 May 2021
Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis
- Surapon Nochaiwong ORCID: orcid.org/0000-0003-1100-7171 1 , 2 ,
- Chidchanok Ruengorn ORCID: orcid.org/0000-0001-7927-1425 1 , 2 ,
- Kednapa Thavorn ORCID: orcid.org/0000-0003-4738-8447 2 , 3 , 4 , 5 ,
- Brian Hutton ORCID: orcid.org/0000-0001-5662-8647 3 , 4 , 5 ,
- Ratanaporn Awiphan ORCID: orcid.org/0000-0003-3628-0596 1 , 2 ,
- Chabaphai Phosuya 1 ,
- Yongyuth Ruanta ORCID: orcid.org/0000-0003-4184-0308 1 , 2 ,
- Nahathai Wongpakaran ORCID: orcid.org/0000-0001-8365-2474 6 &
- Tinakon Wongpakaran ORCID: orcid.org/0000-0002-9062-3468 6
Scientific Reports volume 11 , Article number: 10173 ( 2021 ) Cite this article
56k Accesses
318 Citations
117 Altmetric
Metrics details
- Post-traumatic stress disorder
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint databases, grey literature, and unpublished studies from January 1, 2020, to June 16, 2020 (updated on July 11, 2020), with no language restrictions. Observational studies using validated measurement tools and reporting data on mental health issues among the general population were screened to identify all relevant studies. We have included information from 32 different countries and 398,771 participants. The pooled prevalence of mental health issues amid the COVID-19 pandemic varied widely across countries and regions and was higher than previous reports before the COVID-19 outbreak began. The global prevalence estimate was 28.0% for depression; 26.9% for anxiety; 24.1% for post-traumatic stress symptoms; 36.5% for stress; 50.0% for psychological distress; and 27.6% for sleep problems. Data are limited for other aspects of mental health issues. Our findings highlight the disparities between countries in terms of the poverty impacts of COVID-19, preparedness of countries to respond, and economic vulnerabilities that impact the prevalence of mental health problems. Research on the social and economic burden is needed to better manage mental health problems during and after epidemics or pandemics. Systematic review registration : PROSPERO CRD 42020177120.
Similar content being viewed by others
Public mental health problems during COVID-19 pandemic: a large-scale meta-analysis of the evidence
Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis

Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review
Introduction.
After the World Health Organisation (WHO) declared the rapid worldwide spread of coronavirus disease-2019 (COVID-19) to be a pandemic, there has been a dramatic rise in the prevalence of mental health problems both nationally and globally 1 , 2 , 3 . Early international evidence and reviews have reported the psychological effects of the COVID-19 outbreak on patients and healthcare workers, particularly those in direct contact with affected patients 4 , 5 , 6 , 7 , 8 . Besides patients with COVID-19, negative emotions and psychosocial distress may occur among the general population due to the wider social impact and public health and governmental response, including strict infection control, quarantine, physical distancing, and national lockdowns 2 , 9 , 10 .
Amid the COVID-19 pandemic, several mental health and psychosocial problems, for instance, depressive symptoms, anxiety, stress, post-traumatic stress symptoms (PTSS), sleep problems, and other psychological conditions are of increasing concern and likely to be significant 5 , 10 , 11 . Public psychological consequences can arise through direct effects of the COVID-19 pandemic that are sequelae related to fear of contagion and perception of danger 2 . However, financial and economic issues also contribute to mental health problems among the general population in terms of indirect effects 12 , 13 . Indeed, economic shutdowns have disrupted economies worldwide, particularly in countries with larger domestic outbreaks, low health system preparedness, and high economic vulnerability 14 , 15 , 16 .
The COVID-19 pandemic may affect the mental health of the general population differently based on national health and governmental policies implemented and the public resilience and social norms of each country. Unfortunately, little is known about the global prevalence of mental health problems in the general population during the COVID-19 pandemic. Previous systematic reviews have been limited by the number of participants included, and attention has been focussed on particular conditions and countries, with the majority of studies being conducted in mainland China 5 , 8 , 11 , 17 , 18 . To the best of our knowledge, evidence on mental health problems among the general population worldwide has not been comprehensively documented in the current COVID-19 pandemic. Therefore, a systematic review and meta-analysis at a global level is needed to provide robust and contemporary evidence to inform public health policies and long-term responses to the COVID-19 pandemic.
As such, we have performed a rigorous systematic review and meta-analysis of all available observational studies to shed light on the effects of the global COVID-19 pandemic on mental health problems among the general population. We aimed to: (1) summarise the prevalence of mental health problems nationally and globally, and (2) describe the prevalence of mental health problems by each WHO region, World Bank income group, and the global index and economic indices responses to the COVID-19 pandemic.
This systematic review and meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines 19 and reported in line with the Meta-analysis of Observational Studies in Epidemiology statement (Appendix, Table S1 ) 20 . The pre-specified protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42020177120).
Search strategy
We searched electronic databases in collaboration with an experienced medical librarian using an iterative process. PubMed, Medline, Embase, PsycINFO, Web of Science, Scopus, CINAHL, and the Cochrane Library were used to identify all relevant abstracts. As the WHO declared the COVID-19 outbreak to be a public health emergency of international concern on January 30, 2020, we limited the search from January 1, 2020, to June 16, 2020, without any language restrictions. The main keywords used in the search strategy included “coronavirus” or “COVID-19” or “SARS-CoV-2”, AND “mental health” or “psychosocial problems” or “depression” or “anxiety” or “stress” or “distress” or “post-traumatic stress symptoms” or “suicide” or “insomnia” or “sleep problems” (search strategy for each database is provided in the Appendix, Table S2 ). Relevant articles were also identified from the reference lists of the included studies and previous systematic reviews. To updated and provide comprehensive, evidence-based data during the COVID-19 pandemic, grey literature from Google Scholar and the preprint reports from medRxiv, bioRxiv, and PsyArXiv were supplemented to the bibliographic database searches. A targeted manual search of grey literature and unpublished studies was performed through to July 11, 2020.
Study selection and data screening
We included observational studies (cross-sectional, case–control, or cohort) that (1) reported the occurrence or provided sufficient data to estimate the prevalence of mental health problems among the general population, and (2) used validated measurement tools for mental health assessment. The pre-specified protocol was amended to permit the inclusion of studies the recruited participants aged 12 years or older and college students as many colleges and universities were closed due to national lockdowns. We excluded studies that (1) were case series/case reports, reviews, or studies with small sample sizes (less than 50 participants); (2) included participants who had currently confirmed with the COVID-19 infection; and (3) surveyed individuals under hospital-based settings. If studies had overlapping participants and survey periods, then the study with the most detailed and relevant information was used.
Eligible titles and abstracts of articles identified by the literature search were screened independently by two reviewers (SN and CR). Then, potentially relevant full-text articles were assessed against the selection criteria for the final set of included studies. Potentially eligible articles that were not written in English were translated before the full-text appraisal. Any disagreement was resolved by discussion.
The primary outcomes were key parameters that reflect the global mental health status during the COVID-19 pandemic, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems (insomnia or poor sleep). To deliver more evidence regarding the psychological consequences, secondary outcomes of interest included psychological symptoms, suicidal ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder.
Data extraction and risk of bias assessment
Two reviewers (SN and YR) independently extracted the pre-specified data using a standardised approach to gather information on the study characteristics (the first author’s name, study design [cross-sectional survey, longitudinal survey, case–control, or cohort], study country, article type [published article, short report/letters/correspondence, or preprint reporting data], the data collection period), participant characteristics (mean or median age of the study population, the proportion of females, proportion of unemployment, history of mental illness, financial problems, and quarantine status [never, past, or current]), and predefined outcomes of interest (including assessment outcome definitions, measurement tool, and diagnostic cut-off criteria). For international studies, data were extracted based on the estimates within each country. For studies that had incomplete data or unclear information, the corresponding author was contacted by email for further clarification. The final set of data was cross-checked by the two reviewers (RA and CP), and discrepancies were addressed through a discussion.
Two reviewers (SN and CR) independently assessed and appraised the methodological quality of the included studies using the Hoy and colleagues Risk of Bias Tool-10 items 21 . A score of 1 (no) or 0 (yes) was assigned to each item. The higher the score, the greater the overall risk of bias of the study, with scores ranging from 0 to 10. The included studies were then categorised as having a low (0–3 points), moderate (4–6 points), or high (7 or 10 points) risk of bias. A pair of reviewers (RA and CP) assessed the risk of bias of each study. Any disagreements were resolved by discussion.
Data synthesis and statistical methods
A two-tailed P value of less than 0.05 was considered statistically significant. We used Stata software version 16.0 (StataCorp, College Station, TX, USA) for all analyses and generated forest plots of the summary pooled prevalence. Inter-rater agreements between reviewers for the study selection and risk of bias assessment were tested using the kappa (κ) coefficient of agreement 22 . Based on the crude information data, we recalculated and estimated the unadjusted prevalence of mental health and psychological problems using the crude numerators and denominators reported by each of the included studies. Unadjusted pooled prevalence with corresponding 95% confidence intervals (CIs) was reported for each WHO regions (Africa, America, South-East Asia, Europe, Eastern Mediterranean, and Western Pacific) and World Bank income group (low-, lower-middle-, upper-middle-, and high-income).
We employed the variance of the study-specific prevalence using the Freeman–Tukey double arcsine methods for transforming the crude data before pooling the effect estimates with a random-effect model to account for the effects of studies with extreme (small or large) prevalence estimates 23 . Heterogeneity was evaluated using the Cochran’s Q test, with a p value of less than 0.10 24 . The degree of inconsistency was quantified using I 2 values, in which a value greater than 60–70% indicated the presence of substantial heterogeneity 25 .
Pre-planned subgroup analyses were performed based on the participant (i.e., age, the proportion of female sex, the proportion of unemployment, history of mental illness, financial problems, and quarantine status) and study characteristics (article type, study design, data collection, and sample size). To explore the inequality and poverty impacts across countries, subgroup analyses based on the global index and economic indices responses to the COVID-19 pandemic were performed, including (1) human development index (HDI) 2018 (low, medium, high, and very high) 26 ; (2) gender inequality index 2018 (below vs above world average [0.439]) 27 ; (3) the COVID-19-government response stringency index during the survey (less- [less than 75%], moderate- [75–85%], and very stringent [more than 85%]) according to the Oxford COVID-19 Government Response Tracker reports 28 ; (4) the preparedness of countries in terms of hospital beds per 10,000 people, 2010–2018 (low, medium–low, medium, medium–high, and high) 15 ; (5) the preparedness of countries in terms of current health expenditure (% of gross domestic product [GDP] 2016; low, medium–low, medium, medium–high, and high) 15 ; (6) estimated percent change of real GDP growth based on the International Monetary Fund, April 2020 (below vs above world average [− 3.0]) 29 ; (7) the resilience of countries’ business environment based on the 2020 global resilience index reports (first-, second-, third-, and fourth-quartile) 30 ; and (8) immediate economic vulnerability in terms of inbound tourism expenditure (% of GDP 2016–2018; low, medium–low, medium, medium–high, and high) 15 .
To address the robustness of our findings, we conducted a sensitivity analysis by restricting the analysis to studies with a low risk of bias (Hoy and Colleagues-Tool, 0–3 points). Furthermore, a random-effects univariate meta-regression analysis was used to explore the effect of participant and study characteristics, and the global index and economic indices responses to the COVID-19 pandemic as described above on the prevalence estimates.
The visual inspection of funnel plots was performed when there was sufficient data and tested for asymmetry using the Begg’s and Egger’s tests for each specific. A P value of less than 0.10 was considered to indicate statistical publication bias 31 , 32 . If the publication bias was detected by the Begg’s and Egger’s regression test, the trim and fill method was then performed to calibrate for publication bias 33 .
Initially, the search strategy retrieved 4642 records. From these, 2682 duplicate records were removed, and 1960 records remained. Based on the title and abstract screening, we identified 498 articles that seemed to be relevant to the study question (the κ statistic for agreement between reviewers was 0.81). Of these, 107 studies fulfilled the study selection criteria and were included in the meta-analysis (Appendix, Figure S1 ). The inter-rater agreement between reviewers on the study selection and data extraction was 0.86 and 0.75, respectively. The reference list of all included studies in this review is provided in the Appendix, Table S3 .
Characteristics of included studies
In total, 398,771 participants from 32 different countries were included. The mean age was 33.5 ± 9.5 years, and the proportion of female sex was 60.9% (range, 16.0–51.6%). Table 1 summarises the characteristics of all the included studies according to World Bank income group, the global index of COVID-19 pandemic preparedness, and economic vulnerability indices. The included studies were conducted in the Africa (2 studies 34 , 35 [1.9%], n = 723), America (12 studies 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 [11.2%], n = 18,440), South-East Asia (10 studies 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 [9.4%], n = 11,953), Europe (27 studies 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 [25.2%], n = 148,430), Eastern Mediterranean (12 studies 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 [11.2%], n = 23,396), and Western Pacific WHO regions (44 studies 97 , 98 , 99 , 100 , 101 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 , 114 , 115 , 116 , 117 , 118 , 119 , 120 , 121 , 122 , 123 , 124 , 125 , 126 , 127 , 128 , 129 , 130 , 131 , 132 , 133 , 134 , 135 , 136 , 137 , 138 , 139 , 140 [41.1%], n = 195,829). Most of the included studies were cross-sectional (96 studies, 89.7%), used an online-based survey (101 studies, 95.3%), conducted in mainland China (34 studies, 31.8%), and were conducted in countries with upper-middle (49 studies, 45.8%) and high-incomes (44 studies, 41.1%). Detailed characteristics of the 107 included studies, measurement tools for evaluating the mental health status and psychological consequences, and the diagnostic cut-off criteria are described in Appendix, Table S4 . Of the 107 included studies, 76 (71.0%) had a low risk, 31 (29.0%) had a moderate risk, and no studies had a high risk of bias (Appendix, Table S5 ).
Global prevalence of mental health issues among the general population amid the COVID-19 pandemic
Table 2 presents a summary of the results of the prevalence of mental health problems among the general population amid the COVID-19 pandemic by WHO region and World Bank country groups. With substantial heterogeneity, the global prevalence was 28.0% (95% CI 25.0–31.2) for depression (75 studies 34 , 35 , 36 , 37 , 38 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 70 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 93 , 96 , 97 , 99 , 101 , 104 , 105 , 106 , 107 , 108 , 109 , 112 , 113 , 114 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 127 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 280,607, Fig. 1 ); 26.9% (95% CI 24.0–30.0) for anxiety (75 studies 35 , 37 , 38 , 40 , 42 , 43 , 44 , 46 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 57 , 58 , 60 , 61 , 64 , 66 , 67 , 68 , 69 , 71 , 73 , 74 , 75 , 76 , 77 , 80 , 81 , 82 , 83 , 87 , 88 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 , 101 , 104 , 105 , 107 , 108 , 109 , 112 , 113 , 114 , 115 , 116 , 117 , 119 , 120 , 122 , 124 , 125 , 126 , 129 , 130 , 131 , 132 , 133 , 134 , 136 , 138 , 139 , 140 , n = 284,813, Fig. 2 ); 24.1% (95% CI 17.0–32.0) for PTSS (28 studies 35 , 44 , 56 , 59 , 62 , 64 , 66 , 69 , 75 , 78 , 80 , 81 , 82 , 89 , 90 , 91 , 106 , 109 , 110 , 111 , 119 , 123 , 124 , 125 , 127 , 131 , 135 , 138 , n = 56,447, Fig. 3 ); 36.5% (95% CI 30.0–43.3) for stress (22 studies 37 , 50 , 51 , 52 , 53 , 54 , 57 , 58 , 71 , 73 , 75 , 76 , 80 , 114 , 117 , 119 , 120 , 122 , 125 , 129 , 131 , 136 , n = 110,849, Fig. 4 ); 50.0% (95% CI 41.8–58.2) for psychological distress (18 studies 39 , 47 , 52 , 59 , 63 , 65 , 70 , 72 , 78 , 79 , 85 , 86 , 88 , 102 , 110 , 118 , 121 , 128 , n = 81,815, Fig. 5 ); and 27.6% (95% CI 19.8–36.1) for sleep problems (15 studies 35 , 53 , 58 , 80 , 84 , 103 , 106 , 107 , 109 , 119 , 120 , 125 , 134 , 136 , 137 , n = 99,534, Fig. 6 ). The prevalence of mental health problems based on different countries varied (Appendix, Table S6 ), from 14.5% (South Africa) to 63.3% (Brazil) for depressive symptoms; from 7.7% (Vietnam) to 49.9% (Mexico) for anxiety; from 10.5% (United Kingdom) to 52.0% (Egypt) for PTSS; from 19.7% (Portugal) to 72.8% (Thailand) for stress; from 23.9% (China) to Jordan (92.9%) for psychological distress; from 9.2% (Italy) to 53.9% (Thailand) for sleep problems.
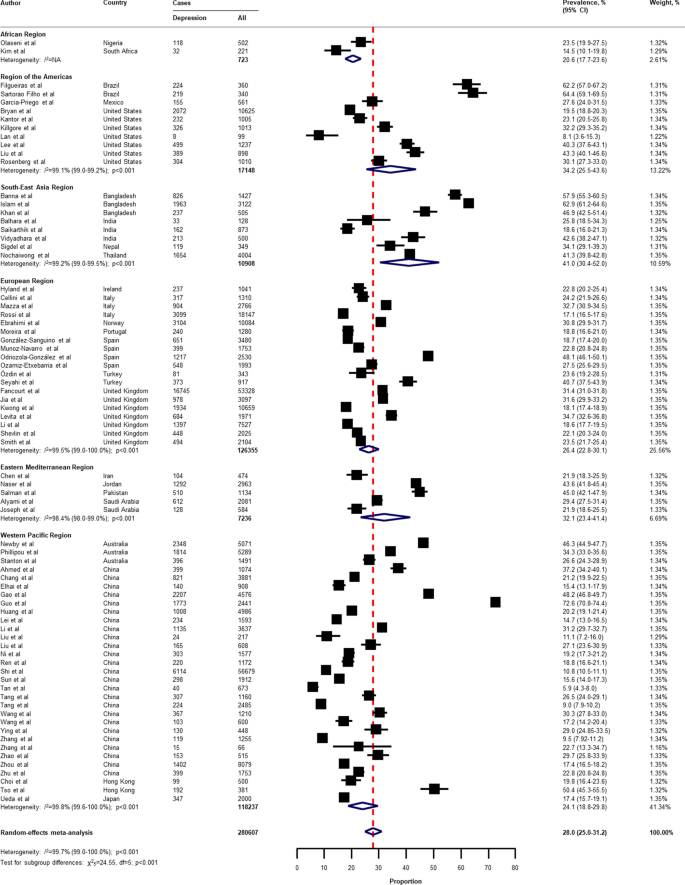
Pooled prevalence of depression among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
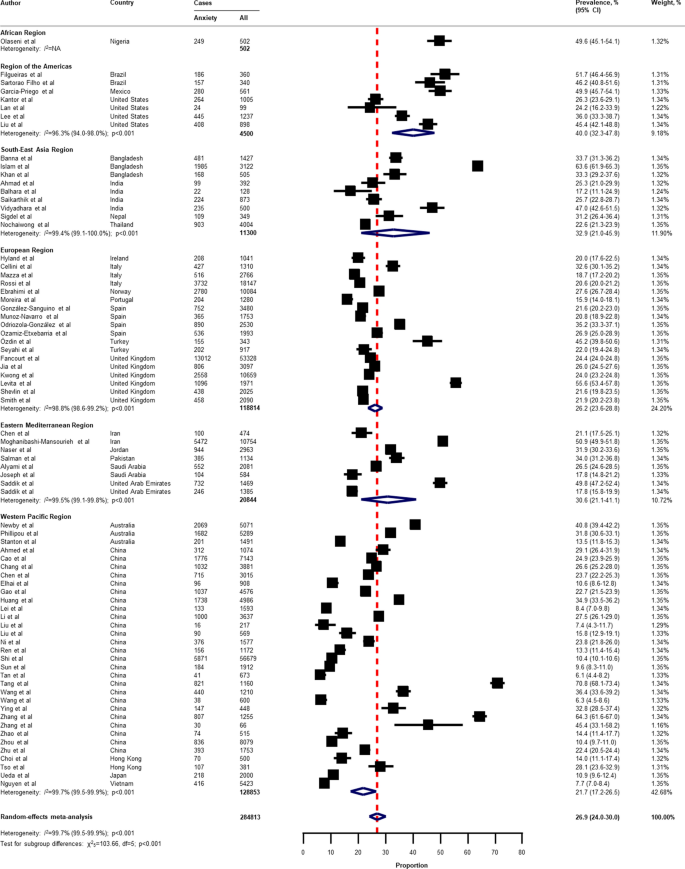
Pooled prevalence of anxiety among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
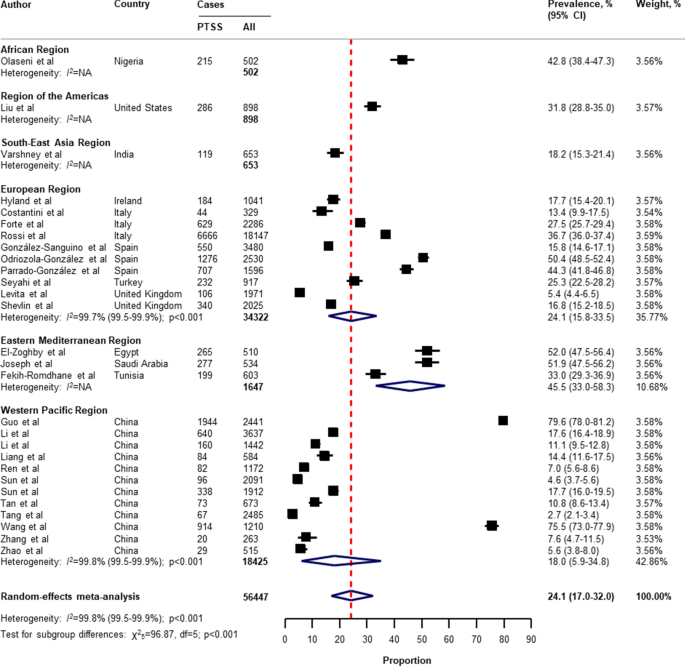
Pooled prevalence of PTSS among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable, PTSS post-traumatic stress symptoms. References are listed according to WHO region in the appendix, Table S3 .
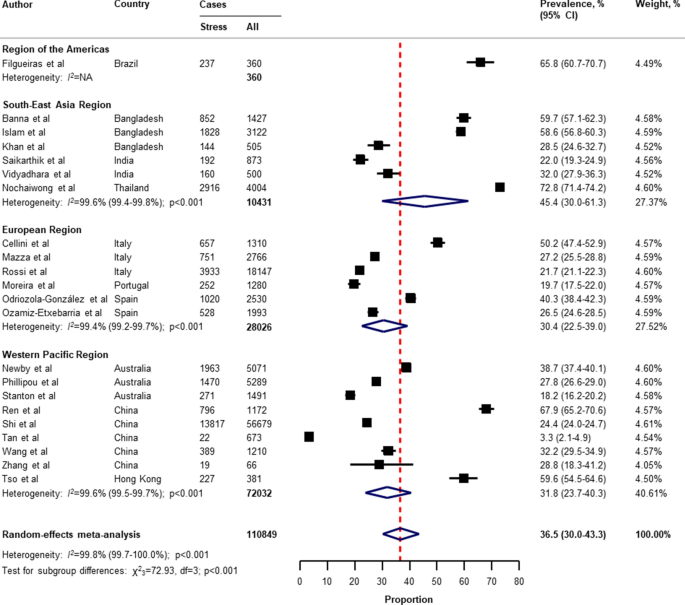
Pooled prevalence of stress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
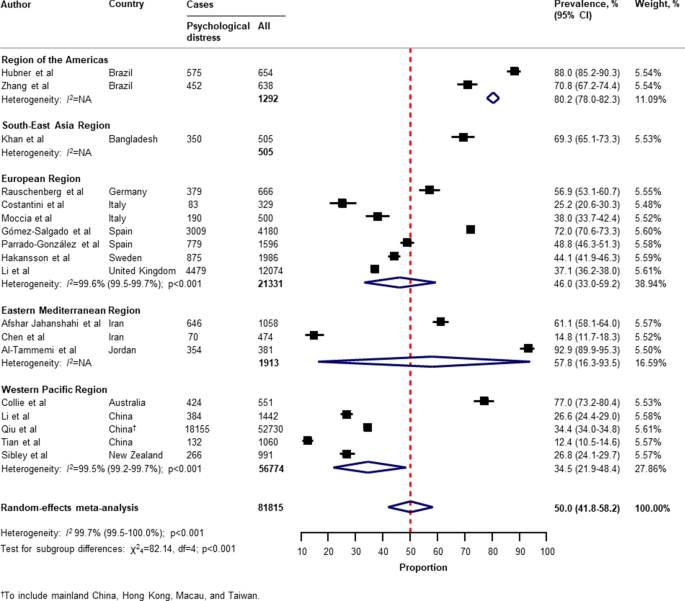
Pooled prevalence of psychological distress among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
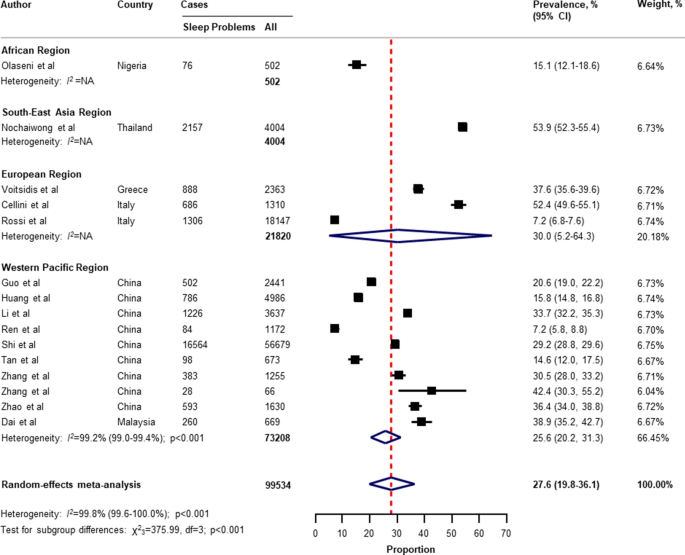
Pooled prevalence of sleep problems among the general population amid the COVID-19 pandemic. COVID-19 coronavirus disease 2019, CI confidence interval, df degree of freedom, NA not applicable. References are listed according to WHO region in the appendix, Table S3 .
With respect to the small number of included studies and high degree of heterogeneity, the pooled secondary outcome prevalence estimates are presented in Appendix, Table S7 . The global prevalence was 16.4% (95% CI 4.8–33.1) for suicide ideation (4 studies 36 , 41 , 53 , 124 , n = 17,554); 53.8% (95% CI 42.4–63.2) for loneliness (3 studies 41 , 44 , 45 , n = 2921); 30.7% (95% CI 2.1–73.3) for somatic symptoms (3 studies 53 , 69 , 134 , n = 7230); 28.6% (95% CI 9.2–53.6) for low wellbeing (3 studies 53 , 68 , 97 , n = 15,737); 50.5% (95% CI 49.2–51.7) for alcohol drinking problems (2 studies 97 , 114 , n = 6145); 6.4% (95% CI 5.5–7.4) for obsessive–compulsive symptoms (2 studies 73 , 134 , n = 2535); 25.7% (95% CI 23.7–27.8) for panic disorder (1 study 74 , n = 1753); 2.4% (95% CI 1.6–3.4) for phobia anxiety (1 study 134 , n = 1255); 22.8% (95% CI 22.1–23.4) for adjustment disorder (1 study 80 , n = 18,147); and 1.2% (95% CI 1.0–1.4) for suicide attempts (1 study 36 , n = 10,625).
Subgroup analyses, sensitivity analyses, meta-regression analyses, and publication bias
In the subgroup analyses (Appendix, Table S8 , Table S9 , Table S10 , Table S1 , Table S12 ), the prevalence of mental health problems was higher in countries with a low to medium HDI (for depression, anxiety, PTSS, and psychological distress), high HDI (for sleep problems), high gender inequality index (for depression and PTSS), very stringent government response index (for PTSS and stress), less stringent government response index (for sleep problems), low to medium hospital beds per 10,000 people (for depression, anxiety, PTSS, stress, psychological distress, and sleep problems), low to medium current health expenditure (for depression, PTSS, and psychological distress), estimated percent change of real GDP growth 2020 below − 3.0 (for psychological distress), low resilience (fourth-quartile) of business environment (for depression, anxiety, and PTSS), medium resilience (second-quartile) of business environment (for psychological distress, and sleep problems), high economic vulnerability-inbound tourism expenditure (for psychological distress, sleep problems), article type-short communication/letter/correspondence (for stress), cross-sectional survey (for PTSS and psychological distress), longitudinal survey (for anxiety and stress), non-mainland China (for depression, anxiety, and psychological distress), sample size of less than 1000 (for psychological distress), sample size of more than 5000 (for PTSS), proportion of females more than 60% (for stress and sleep problems), and measurement tools (for depression, anxiety, stress, and sleep problems). However, several pre-planned subgroup analyses based on participant characteristics and secondary outcomes reported could not be performed due to limited data in the included studies.
Findings from the sensitivity analysis were almost identical to the main analysis (Appendix, Table S14 ). The pooled prevalence by restricting the analysis to studies with a low risk of bias was 28.6% (95% CI 25.1–32.3) for depression, 27.4% (95% CI 24.1–30.8) for anxiety, 30.2% (95% CI 20.3–41.1) for PTSS, 40.1% (95% CI 32.5–47.9) for stress, 45.4% (95% CI 32.0–59.2) for psychological distress, and 27.7% (95% CI 19.4–36.9) for sleep problems.
On the basis of univariate meta-regression, the analysis was suitable for the primary outcomes (Appendix, Table S15 ). The increased prevalence of mental health problems was associated with the WHO region (for depression, anxiety, and psychological distress), female gender inequality index (for depression and anxiety), the COVID-19-government response stringency index during the survey (for sleep problems), hospital beds per 10,000 people (for depression and anxiety), immediate economic vulnerability-inbound tourism expenditure (for sleep problems), study design (cross-sectional vs longitudinal survey; for stress), surveyed country (mainland China vs non-mainland China; for depression and psychological distress), and risk of bias (for PTSS).
The visual inspection of the funnel plots, and the p values tested for asymmetry using the Begg’s and Egger’s tests for each prevalence outcome, indicated no evidence of publication bias related to the sample size (Appendix, Table S16 , and Figure S2 ).
This study is, to the best of our knowledge, the first systematic review and meta-analysis on the overall global prevalence of mental health problems and psychosocial consequences among the general population amid the COVID-19 pandemic. Overall, our findings indicate wide variability in the prevalence of mental health problems and psychosocial consequences across countries, particularly in relation to different regions, the global index of COVID-19 pandemic preparedness, inequalities, and economic vulnerabilities indices.
Two reports examined the global prevalence of common mental health disorders among adults prior to the COVID-19 outbreak. The first study was based on 174 surveys across 63 countries from 1980 to 2013. The estimated lifetime prevalence was 29.1% for all mental disorders, 9.6% for mood disorders, 12.9% for anxiety disorders, and 3.4% for substance use disorder 141 . Another report which was conducted as part of the Global Health Estimates by WHO in 2015, showed that the global estimates of depression and anxiety were 4.4% and 3.6% (more common among females than males), respectively 142 . Despite the different methodological methods used, our findings show that the pooled prevalence of mental health problems during the COVID-19 pandemic is higher than before the outbreak.
Previous studies on the prevalence of mental health problems during the COVID-19 pandemic have had substantial heterogeneity. Three systematic reviews reported the prevalence of depression, anxiety, and stress among the general population (mainly in mainland China). The first of these by Salari et al. 11 , was based on 17 included studies (from ten different countries in Asia, Europe, and the Middle East), the pooled prevalence of depression, anxiety, and stress were 33.7% (95% CI 27.5–40.6), 31.9% (95% CI 27.5–36.7), and 29.6% (95% CI 24.3–35.4), respectively. A review by Luo et al. 8 , which included 36 studies from seven different countries, reported a similar overall prevalence of 27% (95% CI 22–33) for depression and 32% (95% CI 25–39) for anxiety. However, a review by Ren et al. 17 , which focussed on only the Chinese population (8 included studies), found that the pooled prevalence was 29% (95% CI 16–42) and 24% (95% CI 16–32), respectively. Nevertheless, previous systematic reviews have been mainly on investigating the prevalence of PTSS, psychological distress, and sleep problems among the patients or healthcare workers that are limited to the general population during the COVID-19 pandemic. With regard to the general population, a review by Cénat et al. 143 , found that the pooled prevalence of PTSS, psychological distress, and insomnia were 22.4% (95% CI 7.6–50.3; 9 included studies), 10.2% (95% CI 4.6–21.0; 10 included studies), and 16.5% (95% CI 8.4–29.7; 8 included studies), respectively.
In this systematic review and meta-analysis, we updated and summarised the global prevalence of mental health problems and psychosocial consequences during the COVID-19 pandemic using information from 32 different countries, and 398,771 participants. A range of problems, including depression, anxiety, PTSS, stress, psychological distress, and sleep problems were reported. The global prevalence of our findings was in line with the previous reviews mentioned above in terms of depression (28.0%; 95% CI 25.0–31.2), anxiety (26.9%; 95% CI 24.0–30.0), and stress (36.5%; 95% CI 30.0–43.3). Interestingly, our findings highlight the poverty impacts of COVID-19 in terms of inequalities, the preparedness of countries to respond, and economic vulnerabilities on the prevalence of mental health problems across countries. For instance, our results suggest that countries with a low or medium HDI had a higher prevalence of depression and anxiety compared to countries with a high or very high HDI (Appendix, Table S8 , and Table S9 ). The prevalence of depression was higher among countries with a gender inequality index of 0.439 or greater (39.6% [95% CI 30.3–49.3] vs 26.2% [95% CI 23.1–29.3]; P = 0.020; Appendix, Table S8 ). Likewise, the prevalence of depression and anxiety was higher among countries with low hospital beds per 10,000 people (Appendix, Table S8 , and Table S9 ). Our findings suggest that the poverty impacts of COVID-19 are likely to be quite significant and related to the subsequent risk of mental health problems and psychosocial consequences. Although we performed a comprehensive review by incorporating articles published together with preprint reports, there was only limited data available on Africa, low-income groups, and secondary outcomes of interest (psychological distress, suicide ideation, suicide attempts, loneliness, somatic symptoms, wellbeing, alcohol drinking problems, obsessive–compulsive symptoms, panic disorder, phobia anxiety, and adjustment disorder).
Strengths and limitations of this review
From a methodological point of view, we used a rigorous and comprehensive approach to establish an up-to-date overview of the evidence-based information on the global prevalence of mental health problems amid the COVID-19 pandemic, with no language restrictions. The systematic literature search was extensive, comprising published peer-reviewed articles and preprints reporting data to present all relevant literature, minimise bias, and up to date evidence. Our findings expanded and addressed the limitations of the previous systematic reviews, such as having a small sample size and number of included studies, considered more aspects of mental health circumstance, and the generalisability of evidence at a global level 5 , 6 , 11 , 17 , 18 . To address biases from different measurement tools of assessment and the cultural norms across countries, we summarised the prevalence of mental health problems and psychosocial consequences using a random-effects model to estimate the pooled data with a more conservative approach. Lastly, the sensitivity analyses were consistent with the main findings, suggesting the robustness of our findings. As such, our data can be generalised to individuals in the countries where the included studies were conducted.
There were several limitations to this systematic review and meta-analysis. First, despite an advanced comprehensive search approach, data for some geographical regions according to the WHO regions and World Bank income groups, for instance, the Africa region, as well as the countries in the low-income group, were limited. Moreover, the reporting of key specific outcomes, such as suicide attempts and ideation, alcohol drinking or drug-dependence problems, and stigma towards COVID-19 infection were also limited. Second, a subgroup analysis based on participant characteristics (that is, age, sex, unemployment, history of mental illness, financial problems, and quarantine status), could not be performed as not all of the included studies reported this data. Therefore, the global prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic cannot be established. Third, it should be noted that different methods, for example, face-to-face interviews or paper-based questionnaires, may lead to different prevalence estimates across the general population. Due to physical distancing, the included studies in this review mostly used online surveys, which can be prone to information bias and might affect the prevalence estimates of our findings. Fourth, a high degree of heterogeneity between the included studies was found in all outcomes of interest. Even though we performed a set of subgroup analyses concerning the participant characteristics, study characteristics, the global index, and economic indices responses to the COVID-19 pandemic, substantial heterogeneity persisted. However, the univariate meta-regression analysis suggested that the WHO region, gender inequality index, COVID-19-government response stringency index during the survey, hospital beds, immediate economic vulnerability (inbound tourism expenditure), study design, surveyed country (mainland China vs non-mainland China), and risk of bias were associated with an increased prevalence of mental health problems and psychosocial consequences amid the COVID-19 pandemic. Finally, we underline that the diagnostic cut-off criteria used were not uniform across the measurement tools in this review, and misclassification remains possible. The genuine variation in global mental health circumstances across countries cannot be explained by our analyses. Indeed, such variation might be predisposed by social and cultural norms, public resilience, education, ethnic differences, and environmental differences among individual study populations.
Implications for public health and research
Despite the limitations of our findings, this review provides the best available evidence that can inform the epidemiology of public mental health, implement targeted initiatives, improving screening, and reduce the long-term consequences of the COVID-19 pandemic, particularly among low-income countries, or those with high inequalities, low preparedness, and high economic vulnerability. Our findings could be improved by further standardised methods and measurement tools of assessment. There is a need for individual country-level data on the mental health problems and psychosocial consequences after the COVID-19 pandemic to track and monitor public health responses. There are a number network longitudinal surveys being conducted in different countries that aim to improve our understanding of the long-term effects of the COVID-19 pandemic 144 . To promote mental wellbeing, such initiatives could also be advocated for by public health officials and governments to increase awareness and provide timely proactive interventions in routine practice.
Conclusions
In conclusion, this systematic review and meta-analysis provides a more comprehensive global overview and evidence of the prevalence of mental health problems among the general population amid the COVID-19 pandemic. The results of this study reveal that the mental health problems and psychosocial consequences amid the COVID-19 pandemic are a global burden, with differences between countries and regions observed. Moreover, equality and poverty impacts were found to be factors in the prevalence of mental health problems. Studies on the long-term effects of the COVID-19 pandemic on the mental health status among the general population at a global level is needed. Given the high burden of mental health problems during the COVID-19 pandemic, an improvement of screening systems and prevention, prompt multidisciplinary management, and research on the social and economic burden of the pandemic, are crucial.
Data sharing
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Mahase, E. Covid-19: WHO declares pandemic because of “alarming levels” of spread, severity, and inaction. BMJ 368 , m1036 (2020).
Article PubMed Google Scholar
Pfefferbaum, B. & North, C. S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 383 , 510–512 (2020).
Article CAS PubMed Google Scholar
Burki, T. K. Coronavirus in China. Lancet Respir. Med. 8 , 238 (2020).
Article CAS PubMed PubMed Central Google Scholar
Chen, Q. et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7 , e15–e16 (2020).
Article PubMed PubMed Central Google Scholar
Vindegaard, N. & Benros, M. E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 89 , 531–542. https://doi.org/10.1016/j.bbi.2020.05.048 (2020).
Pappa, S. et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88 , 901–907 (2020).
Salazar de Pablo, G. et al. Impact of coronavirus syndromes on physical and mental health of health care workers: systematic review and meta-analysis. J. Affect. Disord. 275 , 48–57 (2020).
Luo, M., Guo, L., Yu, M., Jiang, W. & Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public: a systematic review and meta-analysis. Psychiatry Res. 291 , 113190 (2020).
Brooks, S. K. et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395 , 912–920 (2020).
Kaufman, K. R., Petkova, E., Bhui, K. S. & Schulze, T. G. A global needs assessment in times of a global crisis: world psychiatry response to the COVID-19 pandemic. BJPsych Open 6 , e48 (2020).
Article PubMed CAS Google Scholar
Salari, N. et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16 , 57 (2020).
Article Google Scholar
Kawohl, W. & Nordt, C. COVID-19, unemployment, and suicide. Lancet Psychiatry 7 , 389–390 (2020).
Frasquilho, D. et al. Mental health outcomes in times of economic recession: a systematic literature review. BMC Public Health 16 , 115 (2016).
World Bank. Global Economic Prospects, June 2020 (World Bank, 2020).
Book Google Scholar
Kovacevic, M. & Jahic, A. COVID-19 and Human Development: Exploring Global Preparedness and Vulnerability (Human Development Report Office, UNDP, 2020).
Google Scholar
Conceicao, P. et al. COVID-19 and Human Development: Assessing the Crisis, Envisioning the Recovery (Human Development Report Office, UNDP, 2020).
Ren, X. et al. Mental health during the Covid-19 outbreak in China: a meta-analysis. Psychiatr. Q. 91 (4), 1033–1045. https://doi.org/10.1007/s11126-020-09796-5 (2020).
Rogers, J. P. et al. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatry 7 , 611–627 (2020).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339 , b2535 (2009).
Stroup, D. F. et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA 283 , 2008–2012 (2000).
Hoy, D. et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 65 , 934–939 (2012).
Viera, A. J. & Garrett, J. M. Understanding interobserver agreement: the kappa statistic. Fam. Med. 37 , 360–363 (2005).
PubMed Google Scholar
Nyaga, V. N., Arbyn, M. & Aerts, M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health 72 , 39 (2014).
Cochran, W. G. The combination of estimates from different experiments. Biometrics 10 , 101–129 (1954).
Higgins, J. P. & Thompson, S. G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 21 , 1539–1558 (2002).
Human Development Report Office. Human Development Report 2019–Beyond Income, Beyond Averages, Beyond Today: Inequalities in Human DEVELOPMENT in the 21st century (United Nations Development Programme (UNDP), 2019).
Human Development Report Office. 2020 Human Development Persepctives: Tackling Social Norms–A game changer for gender inequalities (United National Development Programme (UNDP), 2020).
Hale, T. et al. Variation in government responses to COVID-19. Version 6.0. Blavatnik School of Government Working Paper. https://www.bsg.ox.ac.uk/covidtracker (2020).
International Monetary Fund (IMF). World Economic Outlook (April 2020), Real GDP growth Annual percent change . Accessed 29 July 2020. https://www.imf.org/external/datamapper/NGDP_RPCH@WEO/OEMDC/ADVEC/WEOWORLD (2020).
FM Global. 2020 FM Global Resilience Index: Make a Resilient Decision . Accessed 30 July 2020. https://www.fmglobal.com/research-and-resources/tools-and-resources/resilienceindex (2020).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50 , 1088–1101 (1994).
Article CAS PubMed MATH Google Scholar
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 315 , 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56 , 455–463 (2000).
Kim, A. W., Nyengerai, T. & Mendenhall, E. Evaluating the mental health impacts of the COVID-19 pandemic in urban South Africa: perceived risk of COVID-19 infection and childhood trauma predict adult depressive symptoms. medRxiv. 2020.2006.2013.20130120 (2020).
Olaseni, A., Akinsola, O., Agberotimi, S. & Oguntayo, R. Psychological distress experiences of Nigerians amid COVID-19 pandemic. PsyArXiv May 6. 1031234/osfio/9v78y (2020).
Bryan, C., Bryan, A. O. & Baker, J. C. Associations among state-level physical distancing measures and suicidal thoughts and behaviors among U.S. adults during the early COVID-19 pandemic. PsyArXiv May 29 . 1031234/osfio/9bpr4 (2020).
Filgueiras, A. & Stults-Kolehmainen, M. Factors linked to changes in mental health outcomes among Brazilians in quarantine due to COVID-19. medRxiv. 2020.2005.2012.20099374 (2020).
Garcia-Priego, B. A. et al. Anxiety, depression, attitudes, and internet addiction during the initial phase of the 2019 coronavirus disease (COVID-19) epidemic: a cross-sectional study in Mexico. medRxiv. 2020.2005.2010.20095844 (2020).
Hubner, C. v. K., Bruscatto, M. L. & Lima, R. D. Distress among Brazilian university students due to the Covid-19 pandemic: survey results and reflections. medRxiv. 2020.2006.2019.20135251 (2020).
Kantor, B. N. & Kantor, J. Mental health outcomes and associations during the coronavirus disease 2019 pandemic: a cross-sectional survey of the US general population. medRxiv. 2020.2005.2026.20114140 (2020).
Killgore, W. D. S., Cloonan, S. A., Taylor, E. C. & Dailey, N. S. Loneliness: a signature mental health concern in the era of COVID-19. Psychiatry Res. 290 , 113117 (2020).
Lan, F.-Y., Suharlim, C., Kales, S. N. & Yang, J. Association between SARS-CoV-2 infection, exposure risk and mental health among a cohort of essential retail workers in the United States. medRxiv. 2020.2006.2008.20125120 (2020).
Lee, S. A., Jobe, M. C. & Mathis, A. A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 1–2. https://doi.org/10.1017/S003329172000121X (2020).
Liu, C. H., Zhang, E., Wong, G. T. F., Hyun, S. & Hahm, H. C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Res. 290 , 113172 (2020).
Rosenberg, M., Luetke, M., Hensel, D., Kianersi, S. & Herbenick, D. Depression and loneliness during COVID-19 restrictions in the United States, and their associations with frequency of social and sexual connections. medRxiv. 2020.2005.2018.20101840 (2020).
Sartorao Filho, C. I. et al. Impact of COVID-19 pandemic on mental health of medical students: a cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv. 2020.2006.2024.20138925 (2020).
Zhang, S. X., Wang, Y., Afshar Jahanshahi, A., Li, J. & Haensel Schmitt, V. G. Mental distress of adults in Brazil during the COVID-19 crisis. medRxiv. 2020.2004.2018.20070896 (2020).
Ahmad, A., Rahman, I. & Agarwal, M. Factors influencing mental health during COVID-19 outbreak: an exploratory survey among Indian population. medRxiv. 2020.2005.2003.20081380 (2020).
Balhara, Y. P. S., Kattula, D., Singh, S., Chukkali, S. & Bhargava, R. Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J. Public Health. 64 , S172-176 (2020).
Banna, H. A. et al. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: a nationwide cross-sectional study. PsyArXiv May 24 . 1031234/osfio/chw5d. (2020).
Islam, M. S. et al. Psychological eesponses during the COVID-19 outbreak among university students in Bangladesh. PsyArXiv June 2 . 1031234/osfio/cndz7. (2020).
Khan, A. H. et al. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. PsyArXiv May 15 . 1031234/osfio/97s5r. (2020).
Nochaiwong, S. et al. Mental health circumstances among health care workers and general public under the pandemic situation of COVID-19 (HOME-COVID-19). Medicine (Baltimore) 99 , e20751 (2020).
Article CAS Google Scholar
Saikarthik, J., Saraswathi, I. & Siva, T. Assessment of impact of COVID-19 outbreak & lockdown on mental health status & its associated risk and protective factors in adult Indian population. medRxiv. 2020.2006.2013.20130153 (2020).
Sigdel, A. et al. Depression, anxiety and depression-anxiety comorbidity amid COVID-19 pandemic: an online survey conducted during lockdown in Nepal. medRxiv. 2020.2004.2030.20086926 (2020).
Varshney, M., Parel, J. T., Raizada, N. & Sarin, S. K. Initial psychological impact of COVID-19 and its correlates in Indian Community: an online (FEEL-COVID) survey. PLoS ONE 15 , e0233874 (2020).
Vidyadhara, S., Chakravarthy, A., Pramod Kumar, A., Sri Harsha, C. & Rahul, R. Mental health status among the South Indian pharmacy students during Covid-19 pandemic quarantine period: a cross-sectional study. medRxiv. 2020.2005.2008.20093708 (2020).
Cellini, N., Canale, N., Mioni, G. & Costa, S. Changes in sleep pattern sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 29 , e13074 (2020).
Costantini, A. & Mazzotti, E. Italian validation of CoViD-19 Peritraumatic Distress Index and preliminary data in a sample of general population. Riv. Psichiatr. 55 , 145–151 (2020).
Ebrahimi, O., Hoffart, A. & Johnson, S. U. The mental health impact of non-pharmacological interventions aimed at impeding viral transmission during the COVID-19 pandemic in a general adult population and the factors associated with adherence to these mitigation strategies. PsyArXiv May 9 . 1031234/osfio/kjzsp. (2020).
Fancourt, D., Steptoe, A. & Bu, F. Trajectories of depression and anxiety during enforced isolation due to COVID-19: longitudinal analyses of 59,318 adults in the UK with and without diagnosed mental illness. medRxiv. 2020.2006.2003.20120923 (2020).
Forte, G., Favieri, F., Tambelli, R. & Casagrande, M. COVID-19 pandemic in the Italian population: validation of a post-traumatic stress disorder questionnaire and prevalence of PTSD symptomatology. Int. J. Environ. Res. Public Health 17 , 4151 (2020).
Article CAS PubMed Central Google Scholar
Gómez-Salgado, J., Andrés-Villas, M., Domínguez-Salas, S., Díaz-Milanés, D. & Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 17 , 3947 (2020).
Article PubMed Central CAS Google Scholar
González-Sanguino, C. et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 87 , 172–176 (2020).
Article PubMed PubMed Central CAS Google Scholar
Håkansson, A. Changes in gambling behavior during the COVID-19 pandemic: a web survey study in Sweden. Int. J. Environ. Res. Public Health 17 , 4013 (2020).
Hyland, P. et al. Anxiety and depression in the Republic of Ireland during the COVID-19 pandemic. PsyArXiv April 22. 1031234/osfio/8yqxr. (2020).
Jia, R. et al. Mental health in the UK during the COVID-19 pandemic: early observations. medRxiv. 2020.2005.2014.20102012 (2020).
Kwong, A. S. F. et al. Mental health during the COVID-19 pandemic in two longitudinal UK population cohorts. medRxiv. 2020.2006.2016.20133116 (2020).
Levita, L. et al. Impact of Covid-19 on young people aged 13–24 in the UK- preliminary findings. PsyArXiv June 30. 1031234/osfio/uq4rn. (2020).
Li, L. Z. & Wang, S. Prevalence and predictors of general psychiatric disorders and loneliness during COVID-19 in the United Kingdom: results from the Understanding Society UKHLS. medRxiv. 2020.2006.2009.20120139 (2020).
Mazza, C. et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 17 , 3165 (2020).
Moccia, L. et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 87 , 75–79 (2020).
Moreira, P. S. et al. Protective elements of mental health status during the COVID-19 outbreak in the Portuguese population. medRxiv. 2020.2004.2028.20080671 (2020).
Munoz-Navarro, R., Cano-Vindel, A., Schmitz, F., Cabello, R. & Fernandez-Berrocal, P. Emotional distress and associated sociodemographic risk factors during the COVID-19 outbreak in Spain. medRxiv. 2020.2005.2030.20117457 (2020).
Odriozola-González, P., Planchuelo-Gómez, Á., Irurtia, M. J. & de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 290 , 113108 (2020).
Ozamiz-Etxebarria, N., Idoiaga Mondragon, N., Dosil Santamaría, M. & Picaza Gorrotxategi, M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: an investigation in a sample of citizens in Northern Spain. Front. Psychol. 11 , 1491 (2020).
Özdin, S. & Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int. J. Soc. Psychiatry 66 , 504–511 (2020).
Parrado-González, A. & León-Jariego, J. C. Covid-19: factors associated with emotional distress and psychological morbidity in Spanish population. Rev. Esp. Salud Publica 94 , e202006058 (2020).
Rauschenberg, C. et al. Social isolation, mental health and use of digital interventions in youth during the COVID-19 pandemic: a nationally representative survey. PsyArXiv June 29 . 1031234/osfio/v64hf (2020).
Rossi, R. et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. An N = 18147 web-based survey. medRxiv. 2020.2004.2009.20057802 (2020).
Seyahi, E., Poyraz, B. C., Sut, N., Akdogan, S. & Hamuryudan, V. The psychological state and changes in the routine of the patients with rheumatic diseases during the coronavirus disease (COVID-19) outbreak in Turkey: a web-based cross-sectional survey. Rheumatol. Int. 40 , 1229–1238 (2020).
Shevlin, M. et al. Anxiety, depression, traumatic stress, and COVID-19 related anxiety in the UK general population during the COVID-19 pandemic. PsyArXiv April 18. 1031234/osfio/hb6nq (2020).
Smith, L. E. et al. Factors associated with self-reported anxiety, depression, and general health during the UK lockdown; a cross-sectional survey. medRxiv. 2020.2006.2023.20137901 (2020).
Voitsidis, P. et al. Insomnia during the COVID-19 pandemic in a Greek population. Psychiatry Res. 289 , 113076 (2020).
Afshar Jahanshahi, A., Mokhtari Dinani, M., Nazarian Madavani, A., Li, J. & Zhang, S. X. The distress of Iranian adults during the Covid-19 pandemic: more distressed than the Chinese and with different predictors. medRxiv. 2020.2004.2003.20052571 (2020).
Al-Tammemi, A. a. B., Akour, A. & Alfalah, L. Is it just about physical health? An internet-based cross-sectional study exploring the psychological impacts of COVID-19 pandemic on university students in Jordan using Kessler psychological distress scale. medRxiv. 2020.2005.2014.20102343 (2020).
Alyami, H. S. et al. Depression and anxiety during 2019 coronavirus disease pandemic in Saudi Arabia: a cross-sectional study. medRxiv. 2020.2005.2009.20096677 (2020).
Chen, J. et al. The curvilinear relationship between the age of adults and their mental health in Iran after its peak of COVID-19 cases. medRxiv. 2020.2006.2011.20128132 (2020).
El-Zoghby, S. M., Soltan, E. M. & Salama, H. M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J. Community Health 45 , 689–695 (2020).
Fekih-Romdhane, F., Ghrissi, F., Abbassi, B., Cherif, W. & Cheour, M. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 290 , 113131 (2020).
Joseph, R., Alshayban, D., Lucca, J. M. & Alshehry, Y. A. The immediate psychological response of the general population in Saudi Arabia during COVID-19 pandemic: a cross-sectional study. medRxiv. 2020.2006.2019.20135533 (2020).
Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 51 , 102076 (2020).
Naser, A. Y. et al. Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 10 (8), e01730. https://doi.org/10.1002/brb3.1730 (2020).
Saddik, B. et al. Assessing the influence of parental anxiety on childhood anxiety during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2006.2011.20128371 (2020).
Saddik, B. et al. Increased levels of anxiety among medical and non-medical university students during the COVID-19 pandemic in the United Arab Emirates. medRxiv. 2020.2005.2010.20096933 (2020).
Salman, M. et al. Psychological impact of COVID-19 on Pakistani university students and how they are coping. medRxiv. 2020.2005.2021.20108647 (2020).
Ahmed, M. Z. et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 51 , 102092 (2020).
Cao, W. et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287 , 112934 (2020).
Chang, J., Yuan, Y. & Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. Nan Fang Yi Ke Da Xue Xue Bao 40 , 171–176 (2020).
Chen, S. H. et al. Public anxiety and its influencing factors in the initial outbreak of COVID-19. Fudan Univ. J. Med. Sci. 47 , 385–391 (2020).
Choi, E. P. H., Hui, B. P. H. & Wan, E. Y. F. Depression and anxiety in Hong Kong during COVID-19. Int. J. Environ. Res. Public Health 17 , 3740 (2020).
Collie, A. et al. Psychological distress among people losing work during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2006.20093773 (2020).
Dai, H., Zhang, S. X., Looi, K. H., Su, R. & Li, J. Health condition and test availability as predictors of adults' mental health during the COVID-19 pandemic. medRxiv. 2020.2006.2021.20137000 (2020).
Elhai, J. D., Yang, H., McKay, D. & Asmundson, G. J. G. COVID-19 anxiety symptoms associated with problematic smartphone use severity in Chinese adults. J. Affect. Disord. 274 , 576–582 (2020).
Gao, J. et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 15 , e0231924 (2020).
Guo, J., Feng, X. L., Wang, X. H. & van IJzendoorn, M. H. Coping with COVID-19: exposure to COVID-19 and negative impact on livelihood predict elevated mental health problems in Chinese adults. Int. J. Environ. Res. Public Health 17 , 3857 (2020).
Huang, Y. & Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 288 , 112954 (2020).
Lei, L. et al. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 26 , e924609 (2020).
Li, Y. et al. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin. Sleep Med. https://doi.org/10.5664/jcsm.8524 (2020).
Li, Y. et al. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 1–3. https://doi.org/10.1017/S0033291720001555 (2020).
Liang, L. et al. The effect of COVID-19 on youth mental health. Psychiatr. Q. 91 (3), 841–852. https://doi.org/10.1007/s11126-020-09744-3 (2020).
Liu, J. et al. Online mental health survey in a medical college in China during the COVID-19 outbreak. Front. Psychiatry 11 , 459 (2020).
Liu, X. et al. Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infect. Dis. Poverty 9 , 58 (2020).
Newby, J., O'Moore, K., Tang, S., Christensen, H. & Faasse, K. Acute mental health responses during the COVID-19 pandemic in Australia. medRxiv. 2020.2005.2003.20089961 (2020).
Nguyen, H. T. et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 17 , 4164 (2020).
Ni, M. Y. et al. Mental health, risk factors, and social media use during the COVID-19 epidemic and cordon sanitaire among the community and health professionals in Wuhan, China: cross-sectional survey. JMIR Ment. Health 7 , e19009 (2020).
Phillipou, A. et al. Eating and exercise behaviors in eating disorders and the general population during the COVID-19 pandemic in Australia: initial results from the COLLATE project. Int. J. Eat. Disord. 53 , 1158–1165 (2020).
Qiu, J. et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 33 , e100213 (2020).
Ren, Y. et al. Letter to the Editor “A longitudinal study on the mental health of general population during the COVID-19 epidemic in China”. Brain Behav. Immun. 87 , 132–133 (2020).
Shi, L. et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3 , e2014053 (2020).
Sibley, C. G. et al. Effects of the COVID-19 pandemic and nationwide lockdown on trust, attitudes toward government, and well-being. Am. Psychol. 75 , 618–630 (2020).
Stanton, R. et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int. J. Environ. Res. Public Health 17 , 4065 (2020).
Sun, L. et al. Prevalence and risk factors of acute posttraumatic stress symptoms during the COVID-19 outbreak in Wuhan, China. medRxiv. 2020.2003.2006.20032425 (2020).
Sun, S., Goldberg, S. B., Lin, D., Qiao, S. & Operario, D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. medRxiv. 2020.2007.2003.20144931 (2020).
Tan, W. et al. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 87 , 84–92 (2020).
Tang, F. et al. COVID-19 related depression and anxiety among quarantined respondents. Psychol. Health 36 (2), 164–178. https://doi.org/10.1080/08870446.2020.1782410 (2020).
Tang, W. et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J. Affect. Disord. 274 , 1–7 (2020).
Tian, F. et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 288 , 112992 (2020).
Tso, I. F. & Sohee, P. Alarming levels of psychiatric symptoms and the role of loneliness during the COVID-19 epidemic: a case study of Hong Kong. PsyArXiv published online June 27. 1031234/osfio/wv9y2 (2020).
Ueda, M., Stickley, A., Sueki, H. & Matsubayashi, T. Mental health status of the general population during the COVID-19 pandemic: a cross-sectional national survey in Japan. medRxiv. 2020.2004.2028.20082453 (2020).
Wang, C. et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17 , 1729 (2020).
Wang, Y., Di, Y., Ye, J. & Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 26 (1), 13–22. https://doi.org/10.1080/13548506.2020.1746817 (2020).
Ying, Y. et al. Mental health status among family members of health care workers in Ningbo, China during the Coronavirus Disease 2019 (COVID-19) outbreak: a Cross-sectional Study. medRxiv. 2020.2003.2013.20033290 (2020).
Zhang, W. R. et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother. Psychosom. 89 , 242–250 (2020).
Zhang, Y. & Ma, Z. F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: a cross-sectional study. Int. J. Environ. Res. Public Health 17 , 2381 (2020).
Zhang, Y., Zhang, H., Ma, X. & Di, Q. Mental health problems during the COVID-19 pandemics and the mitigation effects of exercise: a longitudinal study of college students in China. Int. J. Environ. Res. Public Health 17 , 3722 (2020).
Zhao, X., Lan, M., Li, H. & Yang, J. Perceived stress and sleep quality among the non-diseased general public in China during the 2019 coronavirus disease: a moderated mediation model. Sleep Med. S1389–9457 (1320), 30224–30220. https://doi.org/10.1016/j.sleep.2020.05.021 (2020).
Zhao, Y., An, Y., Tan, X. & Li, X. Mental health and its influencing factors among self-isolating ordinary citizens during the beginning epidemic of COVID-19. J. Loss Trauma https://doi.org/10.1080/15325024.15322020.11761592 (2020).
Zhou, S. J. et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29 , 749–758 (2020).
Zhu, S. et al. The immediate mental health impacts of the COVID-19 pandemic among people with or without quarantine managements. Brain Behav.. Immun. 87 , 56–58 (2020).
Steel, Z. et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 43 , 476–493 (2014).
World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates (World Health Organization, 2017).
Cénat, J. M. et al. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 295 , 113599 (2021).
COVID-MINDS Network. COVID-MINDS network: global mental health in the COVID-19 pandemic , https://www.covidminds.org/ (2020).
Download references
Acknowledgements
The authors thank the research assistances and all staff of Pharmacoepidemiology and Statistics Research Center (PESRC), Chiang Mai, Thailand. This work reported in this manuscript was partially supported by a grant by the Chiang Mai University, Thailand. The funder of the study had no role in the study design collection, analysis, or interpretation of the data, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit it for publication.
Author information
Authors and affiliations.
Department of Pharmaceutical Care, Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Ratanaporn Awiphan, Chabaphai Phosuya & Yongyuth Ruanta
Pharmacoepidemiology and Statistics Research Center (PESRC), Faculty of Pharmacy, Chiang Mai University, Chiang Mai, 50200, Thailand
Surapon Nochaiwong, Chidchanok Ruengorn, Kednapa Thavorn, Ratanaporn Awiphan & Yongyuth Ruanta
Ottawa Hospital Research Institute, Ottawa Hospital, Ottawa, ON, K1H 8L6, Canada
Kednapa Thavorn & Brian Hutton
Institute of Clinical and Evaluative Sciences, ICES uOttawa, Ottawa, ON, K1Y 4E9, Canada
School of Epidemiology and Public Health, Faculty of Medicine, University of Ottawa, Ottawa, ON, K1G 5Z3, Canada
Department of Psychiatry, Faculty of Medicine, Chiang Mai University, Chiang Mai, 50200, Thailand
Nahathai Wongpakaran & Tinakon Wongpakaran
You can also search for this author in PubMed Google Scholar
Contributions
S.N. conceived the study and, together with C.R., K.T., R.A., C.P., and Y.R. developed the protocol. S.N. and C.R. did the literature search, selected the studies. S.N. and Y.R. extracted the relevant information. S.N. synthesised the data. S.N. wrote the first draft of the paper. K.T., B.H., N.W., and T.W. critically revised successive drafts of the paper. All authors approved the final draft of the manuscript. SN is the guarantor of the study.
Corresponding author
Correspondence to Surapon Nochaiwong .
Ethics declarations
Competing interests.
The authors declare no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary figures and tables., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ .
Reprints and permissions
About this article
Cite this article.
Nochaiwong, S., Ruengorn, C., Thavorn, K. et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep 11 , 10173 (2021). https://doi.org/10.1038/s41598-021-89700-8
Download citation
Received : 11 January 2021
Accepted : 29 April 2021
Published : 13 May 2021
DOI : https://doi.org/10.1038/s41598-021-89700-8
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
The effectiveness of an online short-format recovery college model: a co-learning model to support mental health.
- Catherine Briand
- Charles-Édouard Giguère
- Régis Hakin
International Journal of Mental Health Systems (2024)

Enhancing mental wellbeing by changing mindsets? Results from two randomized controlled trials
- Carina Schreiber
- Marijke Schotanus-Dijkstra
BMC Psychology (2024)
Protocol for a pilot cluster randomised controlled trial of a multicomponent sustainable return to work IGLOo intervention
- Oliver Davis
- Jeremy Dawson
- Fehmidah Munir
Pilot and Feasibility Studies (2024)
The global prevalence of depression, anxiety, and sleep disorder among patients coping with Post COVID-19 syndrome (long COVID): a systematic review and meta-analysis
- Niloofar Seighali
- Abolfazl Abdollahi
- Mahmood Bakhtiyari
BMC Psychiatry (2024)
Investigating the spatiotemporal patterns and clustering of attendances for mental health services to inform policy and resource allocation in Thailand
- Chawarat Rotejanaprasert
- Papin Thanutchapat
- Richard J Maude
By submitting a comment you agree to abide by our Terms and Community Guidelines . If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
Sign up for the Nature Briefing newsletter — what matters in science, free to your inbox daily.
Further Evidence on the Global Decline in the Mental Health of the Young
Prior to around 2011, there was a pronounced curvilinear relationship between age and wellbeing: poor mental health was hump-shaped with respect to age, whilst subjective well-being was U-shaped. We examine data from a European panel for France, Germany, Italy, Spain and Sweden called, Come-Here, for 2020-2023, plus data from International Social Survey Program (ISSP) surveys for 2011 and 2021 and some country-specific data. Mental ill-health now declines in a roughly monotonic fashion with age, whilst subjective well-being rises with age. We also show that young people with poorer mental health spend more time daily in front of a screen on the internet or their smartphone, and that within-person increases in poor mental health are correlated with spending more time in front of a screen. This evidence appears important because it is among the first pieces of research to use panel data on individuals to track the relationship between screen time and changes in mental health, and because the results caution against simply using the presence of the internet in the household, or low usage indicators (such as having used the internet in the last week) to capture the role played by screen time in the growth of mental ill-health.
We acknowledge funding from the United Nations The views expressed herein are those of the authors and do not necessarily reflect the views of the National Bureau of Economic Research.
MARC RIS BibTeΧ
Download Citation Data
More from NBER
In addition to working papers , the NBER disseminates affiliates’ latest findings through a range of free periodicals — the NBER Reporter , the NBER Digest , the Bulletin on Retirement and Disability , the Bulletin on Health , and the Bulletin on Entrepreneurship — as well as online conference reports , video lectures , and interviews .

Advertisement
Social Media and Mental Health: Benefits, Risks, and Opportunities for Research and Practice
- Published: 20 April 2020
- Volume 5 , pages 245–257, ( 2020 )
Cite this article

- John A. Naslund 1 ,
- Ameya Bondre 2 ,
- John Torous 3 &
- Kelly A. Aschbrenner 4
375k Accesses
189 Citations
148 Altmetric
12 Mentions
Explore all metrics
Avoid common mistakes on your manuscript.
Introduction
Social media has become a prominent fixture in the lives of many individuals facing the challenges of mental illness. Social media refers broadly to web and mobile platforms that allow individuals to connect with others within a virtual network (such as Facebook, Twitter, Instagram, Snapchat, or LinkedIn), where they can share, co-create, or exchange various forms of digital content, including information, messages, photos, or videos (Ahmed et al. 2019 ). Studies have reported that individuals living with a range of mental disorders, including depression, psychotic disorders, or other severe mental illnesses, use social media platforms at comparable rates as the general population, with use ranging from about 70% among middle-age and older individuals to upwards of 97% among younger individuals (Aschbrenner et al. 2018b ; Birnbaum et al. 2017b ; Brunette et al. 2019 ; Naslund et al. 2016 ). Other exploratory studies have found that many of these individuals with mental illness appear to turn to social media to share their personal experiences, seek information about their mental health and treatment options, and give and receive support from others facing similar mental health challenges (Bucci et al. 2019 ; Naslund et al. 2016b ).
Across the USA and globally, very few people living with mental illness have access to adequate mental health services (Patel et al. 2018 ). The wide reach and near ubiquitous use of social media platforms may afford novel opportunities to address these shortfalls in existing mental health care, by enhancing the quality, availability, and reach of services. Recent studies have explored patterns of social media use, impact of social media use on mental health and wellbeing, and the potential to leverage the popularity and interactive features of social media to enhance the delivery of interventions. However, there remains uncertainty regarding the risks and potential harms of social media for mental health (Orben and Przybylski 2019 ) and how best to weigh these concerns against potential benefits.
In this commentary, we summarized current research on the use of social media among individuals with mental illness, with consideration of the impact of social media on mental wellbeing, as well as early efforts using social media for delivery of evidence-based programs for addressing mental health problems. We searched for recent peer reviewed publications in Medline and Google Scholar using the search terms “mental health” or “mental illness” and “social media,” and searched the reference lists of recent reviews and other relevant studies. We reviewed the risks, potential harms, and necessary safety precautions with using social media for mental health. Overall, our goal was to consider the role of social media as a potentially viable intervention platform for offering support to persons with mental disorders, promoting engagement and retention in care, and enhancing existing mental health services, while balancing the need for safety. Given this broad objective, we did not perform a systematic search of the literature and we did not apply specific inclusion criteria based on study design or type of mental disorder.
Social Media Use and Mental Health
In 2020, there are an estimated 3.8 billion social media users worldwide, representing half the global population (We Are Social 2020 ). Recent studies have shown that individuals with mental disorders are increasingly gaining access to and using mobile devices, such as smartphones (Firth et al. 2015 ; Glick et al. 2016 ; Torous et al. 2014a , b ). Similarly, there is mounting evidence showing high rates of social media use among individuals with mental disorders, including studies looking at engagement with these popular platforms across diverse settings and disorder types. Initial studies from 2015 found that nearly half of a sample of psychiatric patients were social media users, with greater use among younger individuals (Trefflich et al. 2015 ), while 47% of inpatients and outpatients with schizophrenia reported using social media, of which 79% reported at least once-a-week usage of social media websites (Miller et al. 2015 ). Rates of social media use among psychiatric populations have increased in recent years, as reflected in a study with data from 2017 showing comparable rates of social media use (approximately 70%) among individuals with serious mental illness in treatment as compared with low-income groups from the general population (Brunette et al. 2019 ).
Similarly, among individuals with serious mental illness receiving community-based mental health services, a recent study found equivalent rates of social media use as the general population, even exceeding 70% of participants (Naslund et al. 2016 ). Comparable findings were demonstrated among middle-age and older individuals with mental illness accessing services at peer support agencies, where 72% of respondents reported using social media (Aschbrenner et al. 2018b ). Similar results, with 68% of those with first episode psychosis using social media daily were reported in another study (Abdel-Baki et al. 2017 ).
Individuals who self-identified as having a schizophrenia spectrum disorder responded to a survey shared through the National Alliance of Mental Illness (NAMI) and reported that visiting social media sites was one of their most common activities when using digital devices, taking up roughly 2 h each day (Gay et al. 2016 ). For adolescents and young adults ages 12 to 21 with psychotic disorders and mood disorders, over 97% reported using social media, with average use exceeding 2.5 h per day (Birnbaum et al. 2017b ). Similarly, in a sample of adolescents ages 13–18 recruited from community mental health centers, 98% reported using social media, with YouTube as the most popular platform, followed by Instagram and Snapchat (Aschbrenner et al. 2019 ).
Research has also explored the motivations for using social media as well as the perceived benefits of interacting on these platforms among individuals with mental illness. In the sections that follow (see Table 1 for a summary), we consider three potentially unique features of interacting and connecting with others on social media that may offer benefits for individuals living with mental illness. These include: (1) Facilitate social interaction; (2) Access to a peer support network; and (3) Promote engagement and retention in services.
Facilitate Social Interaction
Social media platforms offer near continuous opportunities to connect and interact with others, regardless of time of day or geographic location. This on demand ease of communication may be especially important for facilitating social interaction among individuals with mental disorders experiencing difficulties interacting in face-to-face settings. For example, impaired social functioning is a common deficit in schizophrenia spectrum disorders, and social media may facilitate communication and interacting with others for these individuals (Torous and Keshavan 2016 ). This was suggested in one study where participants with schizophrenia indicated that social media helped them to interact and socialize more easily (Miller et al. 2015 ). Like other online communication, the ability to connect with others anonymously may be an important feature of social media, especially for individuals living with highly stigmatizing health conditions (Berger et al. 2005 ), such as serious mental disorders (Highton-Williamson et al. 2015 ).
Studies have found that individuals with serious mental disorders (Spinzy et al. 2012 ) as well as young adults with mental illness (Gowen et al. 2012 ) appear to form online relationships and connect with others on social media as often as social media users from the general population. This is an important observation because individuals living with serious mental disorders typically have few social contacts in the offline world and also experience high rates of loneliness (Badcock et al. 2015 ; Giacco et al. 2016 ). Among individuals receiving publicly funded mental health services who use social media, nearly half (47%) reported using these platforms at least weekly to feel less alone (Brusilovskiy et al. 2016 ). In another study of young adults with serious mental illness, most indicated that they used social media to help feel less isolated (Gowen et al. 2012 ). Interestingly, more frequent use of social media among a sample of individuals with serious mental illness was associated with greater community participation, measured as participation in shopping, work, religious activities, or visiting friends and family, as well as greater civic engagement, reflected as voting in local elections (Brusilovskiy et al. 2016 ).
Emerging research also shows that young people with moderate to severe depressive symptoms appear to prefer communicating on social media rather than in-person (Rideout and Fox 2018 ), while other studies have found that some individuals may prefer to seek help for mental health concerns online rather than through in-person encounters (Batterham and Calear 2017 ). In a qualitative study, participants with schizophrenia described greater anonymity, the ability to discover that other people have experienced similar health challenges and reducing fears through greater access to information as important motivations for using the Internet to seek mental health information (Schrank et al. 2010 ). Because social media does not require the immediate responses necessary in face-to-face communication, it may overcome deficits with social interaction due to psychotic symptoms that typically adversely affect face-to-face conversations (Docherty et al. 1996 ). Online social interactions may not require the use of non-verbal cues, particularly in the initial stages of interaction (Kiesler et al. 1984 ), with interactions being more fluid and within the control of users, thereby overcoming possible social anxieties linked to in-person interaction (Indian and Grieve 2014 ). Furthermore, many individuals with serious mental disorders can experience symptoms including passive social withdrawal, blunted affect, and attentional impairment, as well as active social avoidance due to hallucinations or other concerns (Hansen et al. 2009 ), thus potentially reinforcing the relative advantage, as perceived by users, of using social media over in person conversations.
Access to a Peer Support Network
There is growing recognition about the role that social media channels could play in enabling peer support (Bucci et al. 2019 ; Naslund et al. 2016b ), referred to as a system of mutual giving and receiving where individuals who have endured the difficulties of mental illness can offer hope, friendship, and support to others facing similar challenges (Davidson et al. 2006 ; Mead et al. 2001 ). Initial studies exploring use of online self-help forums among individuals with serious mental illnesses have found that individuals with schizophrenia appeared to use these forums for self-disclosure and sharing personal experiences, in addition to providing or requesting information, describing symptoms, or discussing medication (Haker et al. 2005 ), while users with bipolar disorder reported using these forums to ask for help from others about their illness (Vayreda and Antaki 2009 ). More recently, in a review of online social networking in people with psychosis, Highton-Williamson et al. ( 2015 ) highlight that an important purpose of such online connections was to establish new friendships, pursue romantic relationships, maintain existing relationships or reconnect with people, and seek online peer support from others with lived experience (Highton-Williamson et al. 2015 ).
Online peer support among individuals with mental illness has been further elaborated in various studies. In a content analysis of comments posted to YouTube by individuals who self-identified as having a serious mental illness, there appeared to be opportunities to feel less alone, provide hope, find support and learn through mutual reciprocity, and share coping strategies for day-to-day challenges of living with a mental illness (Naslund et al. 2014 ). In another study, Chang ( 2009 ) delineated various communication patterns in an online psychosis peer-support group (Chang 2009 ). Specifically, different forms of support emerged, including “informational support” about medication use or contacting mental health providers, “esteem support” involving positive comments for encouragement, “network support” for sharing similar experiences, and “emotional support” to express understanding of a peer’s situation and offer hope or confidence (Chang 2009 ). Bauer et al. ( 2013 ) reported that the main interest in online self-help forums for patients with bipolar disorder was to share emotions with others, allow exchange of information, and benefit by being part of an online social group (Bauer et al. 2013 ).
For individuals who openly discuss mental health problems on Twitter, a study by Berry et al. ( 2017 ) found that this served as an important opportunity to seek support and to hear about the experiences of others (Berry et al. 2017 ). In a survey of social media users with mental illness, respondents reported that sharing personal experiences about living with mental illness and opportunities to learn about strategies for coping with mental illness from others were important reasons for using social media (Naslund et al. 2017 ). A computational study of mental health awareness campaigns on Twitter provides further support with inspirational posts and tips being the most shared (Saha et al. 2019 ). Taken together, these studies offer insights about the potential for social media to facilitate access to an informal peer support network, though more research is necessary to examine how these online interactions may impact intentions to seek care, illness self-management, and clinically meaningful outcomes in offline contexts.
Promote Engagement and Retention in Services
Many individuals living with mental disorders have expressed interest in using social media platforms for seeking mental health information (Lal et al. 2018 ), connecting with mental health providers (Birnbaum et al. 2017b ), and accessing evidence-based mental health services delivered over social media specifically for coping with mental health symptoms or for promoting overall health and wellbeing (Naslund et al. 2017 ). With the widespread use of social media among individuals living with mental illness combined with the potential to facilitate social interaction and connect with supportive peers, as summarized above, it may be possible to leverage the popular features of social media to enhance existing mental health programs and services. A recent review by Biagianti et al. ( 2018 ) found that peer-to-peer support appeared to offer feasible and acceptable ways to augment digital mental health interventions for individuals with psychotic disorders by specifically improving engagement, compliance, and adherence to the interventions and may also improve perceived social support (Biagianti et al. 2018 ).
Among digital programs that have incorporated peer-to-peer social networking consistent with popular features on social media platforms, a pilot study of the HORYZONS online psychosocial intervention demonstrated significant reductions in depression among patients with first episode psychosis (Alvarez-Jimenez et al. 2013 ). Importantly, the majority of participants (95%) in this study engaged with the peer-to-peer networking feature of the program, with many reporting increases in perceived social connectedness and empowerment in their recovery process (Alvarez-Jimenez et al. 2013 ). This moderated online social therapy program is now being evaluated as part of a large randomized controlled trial for maintaining treatment effects from first episode psychosis services (Alvarez-Jimenez et al. 2019 ).
Other early efforts have demonstrated that use of digital environments with the interactive peer-to-peer features of social media can enhance social functioning and wellbeing in young people at high risk of psychosis (Alvarez-Jimenez et al. 2018 ). There has also been a recent emergence of several mobile apps to support symptom monitoring and relapse prevention in psychotic disorders. Among these apps, the development of PRIME (Personalized Real-time Intervention for Motivational Enhancement) has involved working closely with young people with schizophrenia to ensure that the design of the app has the look and feel of mainstream social media platforms, as opposed to existing clinical tools (Schlosser et al. 2016 ). This unique approach to the design of the app is aimed at promoting engagement and ensuring that the app can effectively improve motivation and functioning through goal setting and promoting better quality of life of users with schizophrenia (Schlosser et al. 2018 ).
Social media platforms could also be used to promote engagement and participation in in-person services delivered through community mental health settings. For example, the peer-based lifestyle intervention called PeerFIT targets weight loss and improved fitness among individuals living with serious mental illness through a combination of in-person lifestyle classes, exercise groups, and use of digital technologies (Aschbrenner et al. 2016b , c ). The intervention holds tremendous promise as lack of support is one of the largest barriers towards exercise in patients with serious mental illness (Firth et al. 2016 ), and it is now possible to use social media to counter such. Specifically, in PeerFIT, a private Facebook group is closely integrated into the program to offer a closed platform where participants can connect with the lifestyle coaches, access intervention content, and support or encourage each other as they work towards their lifestyle goals (Aschbrenner et al. 2016a ; Naslund et al. 2016a ). To date, this program has demonstrated preliminary effectiveness for meaningfully reducing cardiovascular risk factors that contribute to early mortality in this patient group (Aschbrenner, Naslund, Shevenell, Kinney, et al., 2016), while the Facebook component appears to have increased engagement in the program, while allowing participants who were unable to attend in-person sessions due to other health concerns or competing demands to remain connected with the program (Naslund et al. 2018 ). This lifestyle intervention is currently being evaluated in a randomized controlled trial enrolling young adults with serious mental illness from real world community mental health services settings (Aschbrenner et al. 2018a ).
These examples highlight the promise of incorporating the features of popular social media into existing programs, which may offer opportunities to safely promote engagement and program retention, while achieving improved clinical outcomes. This is an emerging area of research, as evidenced by several important effectiveness trials underway (Alvarez-Jimenez et al. 2019 ; Aschbrenner et al. 2018a ), including efforts to leverage online social networking to support family caregivers of individuals receiving first episode psychosis services (Gleeson et al. 2017 ).
Challenges with Social Media for Mental Health
The science on the role of social media for engaging persons with mental disorders needs a cautionary note on the effects of social media usage on mental health and wellbeing, particularly in adolescents and young adults. While the risks and harms of social media are frequently covered in the popular press and mainstream news reports, careful consideration of the research in this area is necessary. In a review of 43 studies in young people, many benefits of social media were cited, including increased self-esteem and opportunities for self-disclosure (Best et al. 2014 ). Yet, reported negative effects were an increased exposure to harm, social isolation, depressive symptoms, and bullying (Best et al. 2014 ). In the sections that follow (see Table 1 for a summary), we consider three major categories of risk related to use of social media and mental health. These include: (1) Impact on symptoms; (2) Facing hostile interactions; and (3) Consequences for daily life.
Impact on Symptoms
Studies consistently highlight that use of social media, especially heavy use and prolonged time spent on social media platforms, appears to contribute to increased risk for a variety of mental health symptoms and poor wellbeing, especially among young people (Andreassen et al. 2016 ; Kross et al. 2013 ; Woods and Scott 2016 ). This may partly be driven by the detrimental effects of screen time on mental health, including increased severity of anxiety and depressive symptoms, which have been well documented (Stiglic and Viner 2019 ). Recent studies have reported negative effects of social media use on mental health of young people, including social comparison pressure with others and greater feeling of social isolation after being rejected by others on social media (Rideout and Fox 2018 ). In a study of young adults, it was found that negative comparisons with others on Facebook contributed to risk of rumination and subsequent increases in depression symptoms (Feinstein et al. 2013 ). Still, the cross-sectional nature of many screen time and mental health studies makes it challenging to reach causal inferences (Orben and Przybylski 2019 ).
Quantity of social media use is also an important factor, as highlighted in a survey of young adults ages 19 to 32, where more frequent visits to social media platforms each week were correlated with greater depressive symptoms (Lin et al. 2016 ). More time spent using social media is also associated with greater symptoms of anxiety (Vannucci et al. 2017 ). The actual number of platforms accessed also appears to contribute to risk as reflected in another national survey of young adults where use of a large number of social media platforms was associated with negative impact on mental health (Primack et al. 2017 ). Among survey respondents using between 7 and 11 different social media platforms compared with respondents using only 2 or fewer platforms, there were 3 times greater odds of having high levels of depressive symptoms and a 3.2 times greater odds of having high levels of anxiety symptoms (Primack et al. 2017 ).
Many researchers have postulated that worsening mental health attributed to social media use may be because social media replaces face-to-face interactions for young people (Twenge and Campbell 2018 ) and may contribute to greater loneliness (Bucci et al. 2019 ) and negative effects on other aspects of health and wellbeing (Woods and Scott 2016 ). One nationally representative survey of US adolescents found that among respondents who reported more time accessing media such as social media platforms or smartphone devices, there were significantly greater depressive symptoms and increased risk of suicide when compared with adolescents who reported spending more time on non-screen activities, such as in-person social interaction or sports and recreation activities (Twenge et al. 2018 ). For individuals living with more severe mental illnesses, the effects of social media on psychiatric symptoms have received less attention. One study found that participation in chat rooms may contribute to worsening symptoms in young people with psychotic disorders (Mittal et al. 2007 ), while another study of patients with psychosis found that social media use appeared to predict low mood (Berry et al. 2018 ). These studies highlight a clear relationship between social media use and mental health that may not be present in general population studies (Orben and Przybylski 2019 ) and emphasize the need to explore how social media may contribute to symptom severity and whether protective factors may be identified to mitigate these risks.
Facing Hostile Interactions
Popular social media platforms can create potential situations where individuals may be victimized by negative comments or posts. Cyberbullying represents a form of online aggression directed towards specific individuals, such as peers or acquaintances, which is perceived to be most harmful when compared with random hostile comments posted online (Hamm et al. 2015 ). Importantly, cyberbullying on social media consistently shows harmful impact on mental health in the form of increased depressive symptoms as well as worsening of anxiety symptoms, as evidenced in a review of 36 studies among children and young people (Hamm et al. 2015 ). Furthermore, cyberbullying disproportionately impacts females as reflected in a national survey of adolescents in the USA, where females were twice as likely to be victims of cyberbullying compared with males (Alhajji et al. 2019 ). Most studies report cross-sectional associations between cyberbullying and symptoms of depression or anxiety (Hamm et al. 2015 ), though one longitudinal study in Switzerland found that cyberbullying contributed to significantly greater depression over time (Machmutow et al. 2012 ).
For youth ages 10 to 17 who reported major depressive symptomatology, there were over 3 times greater odds of facing online harassment in the last year compared with youth who reported mild or no depressive symptoms (Ybarra 2004 ). Similarly, in a 2018 national survey of young people, respondents ages 14 to 22 with moderate to severe depressive symptoms were more likely to have had negative experiences when using social media and, in particular, were more likely to report having faced hostile comments or being “trolled” from others when compared with respondents without depressive symptoms (31% vs. 14%) (Rideout and Fox 2018 ). As these studies depict risks for victimization on social media and the correlation with poor mental health, it is possible that individuals living with mental illness may also experience greater hostility online compared to individuals without mental illness. This would be consistent with research showing greater risk of hostility, including increased violence and discrimination, directed towards individuals living with mental illness in in-person contexts, especially targeted at those with severe mental illnesses (Goodman et al. 1999 ).
A computational study of mental health awareness campaigns on Twitter reported that while stigmatizing content was rare, it was actually the most spread (re-tweeted) demonstrating that harmful content can travel quickly on social media (Saha et al. 2019 ). Another study was able to map the spread of social media posts about the Blue Whale Challenge, an alleged game promoting suicide, over Twitter, YouTube, Reddit, Tumblr, and other forums across 127 countries (Sumner et al. 2019 ). These findings show that it is critical to monitor the actual content of social media posts, such as determining whether content is hostile or promotes harm to self or others. This is pertinent because existing research looking at duration of exposure cannot account for the impact of specific types of content on mental health and is insufficient to fully understand the effects of using these platforms on mental health.
Consequences for Daily Life
The ways in which individuals use social media can also impact their offline relationships and everyday activities. To date, reports have described risks of social media use pertaining to privacy, confidentiality, and unintended consequences of disclosing personal health information online (Torous and Keshavan 2016 ). Additionally, concerns have been raised about poor quality or misleading health information shared on social media and that social media users may not be aware of misleading information or conflicts of interest especially when the platforms promote popular content regardless of whether it is from a trustworthy source (Moorhead et al. 2013 ; Ventola 2014 ). For persons living with mental illness, there may be additional risks from using social media. A recent study that specifically explored the perspectives of social media users with serious mental illnesses, including participants with schizophrenia spectrum disorders, bipolar disorder, or major depression, found that over one third of participants expressed concerns about privacy when using social media (Naslund and Aschbrenner 2019 ). The reported risks of social media use were directly related to many aspects of everyday life, including concerns about threats to employment, fear of stigma and being judged, impact on personal relationships, and facing hostility or being hurt (Naslund and Aschbrenner 2019 ). While few studies have specifically explored the dangers of social media use from the perspectives of individuals living with mental illness, it is important to recognize that use of these platforms may contribute to risks that extend beyond worsening symptoms and that can affect different aspects of daily life.
In this commentary, we considered ways in which social media may yield benefits for individuals living with mental illness, while contrasting these with the possible harms. Studies reporting on the threats of social media for individuals with mental illness are mostly cross-sectional, making it difficult to draw conclusions about direction of causation. However, the risks are potentially serious. These risks should be carefully considered in discussions pertaining to use of social media and the broader use of digital mental health technologies, as avenues for mental health promotion or for supporting access to evidence-based programs or mental health services. At this point, it would be premature to view the benefits of social media as outweighing the possible harms, when it is clear from the studies summarized here that social media use can have negative effects on mental health symptoms, can potentially expose individuals to hurtful content and hostile interactions, and can result in serious consequences for daily life, including threats to employment and personal relationships. Despite these risks, it is also necessary to recognize that individuals with mental illness will continue to use social media given the ease of accessing these platforms and the immense popularity of online social networking. With this in mind, it may be ideal to raise awareness about these possible risks so that individuals can implement necessary safeguards, while highlighting that there could also be benefits. Being aware of the risks is an essential first step, before then recognizing that use of these popular platforms could contribute to some benefits like finding meaningful interactions with others, engaging with peer support networks, and accessing information and services.
To capitalize on the widespread use of social media and to achieve the promise that these platforms may hold for supporting the delivery of targeted mental health interventions, there is need for continued research to better understand how individuals living with mental illness use social media. Such efforts could inform safety measures and also encourage use of social media in ways that maximize potential benefits while minimizing risk of harm. It will be important to recognize how gender and race contribute to differences in use of social media for seeking mental health information or accessing interventions, as well as differences in how social media might impact mental wellbeing. For example, a national survey of 14- to 22-year olds in the USA found that female respondents were more likely to search online for information about depression or anxiety and to try to connect with other people online who share similar mental health concerns when compared with male respondents (Rideout and Fox 2018 ). In the same survey, there did not appear to be any differences between racial or ethnic groups in social media use for seeking mental health information (Rideout and Fox 2018 ). Social media use also appears to have a differential impact on mental health and emotional wellbeing between females and males (Booker et al. 2018 ), highlighting the need to explore unique experiences between gender groups to inform tailored programs and services. Research shows that lesbian, gay, bisexual, or transgender individuals frequently use social media for searching for health information and may be more likely compared with heterosexual individuals to share their own personal health experiences with others online (Rideout and Fox 2018 ). Less is known about use of social media for seeking support for mental health concerns among gender minorities, though this is an important area for further investigation as these individuals are more likely to experience mental health problems and online victimization when compared with heterosexual individuals (Mereish et al. 2019 ).
Similarly, efforts are needed to explore the relationship between social media use and mental health among ethnic and racial minorities. A recent study found that exposure to traumatic online content on social media showing violence or hateful posts directed at racial minorities contributed to increases in psychological distress, PTSD symptoms, and depression among African American and Latinx adolescents in the USA (Tynes et al. 2019 ). These concerns are contrasted by growing interest in the potential for new technologies including social media to expand the reach of services to underrepresented minority groups (Schueller et al. 2019 ). Therefore, greater attention is needed to understanding the perspectives of ethnic and racial minorities to inform effective and safe use of social media for mental health promotion efforts.
Research has found that individuals living with mental illness have expressed interest in accessing mental health services through social media platforms. A survey of social media users with mental illness found that most respondents were interested in accessing programs for mental health on social media targeting symptom management, health promotion, and support for communicating with health care providers and interacting with the health system (Naslund et al. 2017 ). Importantly, individuals with serious mental illness have also emphasized that any mental health intervention on social media would need to be moderated by someone with adequate training and credentials, would need to have ground rules and ways to promote safety and minimize risks, and importantly, would need to be free and easy to access.
An important strength with this commentary is that it combines a range of studies broadly covering the topic of social media and mental health. We have provided a summary of recent evidence in a rapidly advancing field with the goal of presenting unique ways that social media could offer benefits for individuals with mental illness, while also acknowledging the potentially serious risks and the need for further investigation. There are also several limitations with this commentary that warrant consideration. Importantly, as we aimed to address this broad objective, we did not conduct a systematic review of the literature. Therefore, the studies reported here are not exhaustive, and there may be additional relevant studies that were not included. Additionally, we only summarized published studies, and as a result, any reports from the private sector or websites from different organizations using social media or other apps containing social media–like features would have been omitted. Although, it is difficult to rigorously summarize work from the private sector, sometimes referred to as “gray literature,” because many of these projects are unpublished and are likely selective in their reporting of findings given the target audience may be shareholders or consumers.
Another notable limitation is that we did not assess risk of bias in the studies summarized in this commentary. We found many studies that highlighted risks associated with social media use for individuals living with mental illness; however, few studies of programs or interventions reported negative findings, suggesting the possibility that negative findings may go unpublished. This concern highlights the need for a future more rigorous review of the literature with careful consideration of bias and an accompanying quality assessment. Most of the studies that we described were from the USA, as well as from other higher income settings such as Australia or the UK. Despite the global reach of social media platforms, there is a dearth of research on the impact of these platforms on the mental health of individuals in diverse settings, as well as the ways in which social media could support mental health services in lower income countries where there is virtually no access to mental health providers. Future research is necessary to explore the opportunities and risks for social media to support mental health promotion in low-income and middle-income countries, especially as these countries face a disproportionate share of the global burden of mental disorders, yet account for the majority of social media users worldwide (Naslund et al. 2019 ).
Future Directions for Social Media and Mental Health
As we consider future research directions, the near ubiquitous social media use also yields new opportunities to study the onset and manifestation of mental health symptoms and illness severity earlier than traditional clinical assessments. There is an emerging field of research referred to as “digital phenotyping” aimed at capturing how individuals interact with their digital devices, including social media platforms, in order to study patterns of illness and identify optimal time points for intervention (Jain et al. 2015 ; Onnela and Rauch 2016 ). Given that most people access social media via mobile devices, digital phenotyping and social media are closely related (Torous et al. 2019 ). To date, the emergence of machine learning, a powerful computational method involving statistical and mathematical algorithms (Shatte et al. 2019 ), has made it possible to study large quantities of data captured from popular social media platforms such as Twitter or Instagram to illuminate various features of mental health (Manikonda and De Choudhury 2017 ; Reece et al. 2017 ). Specifically, conversations on Twitter have been analyzed to characterize the onset of depression (De Choudhury et al. 2013 ) as well as detecting users’ mood and affective states (De Choudhury et al. 2012 ), while photos posted to Instagram can yield insights for predicting depression (Reece and Danforth 2017 ). The intersection of social media and digital phenotyping will likely add new levels of context to social media use in the near future.
Several studies have also demonstrated that when compared with a control group, Twitter users with a self-disclosed diagnosis of schizophrenia show unique online communication patterns (Birnbaum et al. 2017a ), including more frequent discussion of tobacco use (Hswen et al. 2017 ), symptoms of depression and anxiety (Hswen et al. 2018b ), and suicide (Hswen et al. 2018a ). Another study found that online disclosures about mental illness appeared beneficial as reflected by fewer posts about symptoms following self-disclosure (Ernala et al. 2017 ). Each of these examples offers early insights into the potential to leverage widely available online data for better understanding the onset and course of mental illness. It is possible that social media data could be used to supplement additional digital data, such as continuous monitoring using smartphone apps or smart watches, to generate a more comprehensive “digital phenotype” to predict relapse and identify high-risk health behaviors among individuals living with mental illness (Torous et al. 2019 ).
With research increasingly showing the valuable insights that social media data can yield about mental health states, greater attention to the ethical concerns with using individual data in this way is necessary (Chancellor et al. 2019 ). For instance, data is typically captured from social media platforms without the consent or awareness of users (Bidargaddi et al. 2017 ), which is especially crucial when the data relates to a socially stigmatizing health condition such as mental illness (Guntuku et al. 2017 ). Precautions are needed to ensure that data is not made identifiable in ways that were not originally intended by the user who posted the content as this could place an individual at risk of harm or divulge sensitive health information (Webb et al. 2017 ; Williams et al. 2017 ). Promising approaches for minimizing these risks include supporting the participation of individuals with expertise in privacy, clinicians, and the target individuals with mental illness throughout the collection of data, development of predictive algorithms, and interpretation of findings (Chancellor et al. 2019 ).
In recognizing that many individuals living with mental illness use social media to search for information about their mental health, it is possible that they may also want to ask their clinicians about what they find online to check if the information is reliable and trustworthy. Alternatively, many individuals may feel embarrassed or reluctant to talk to their clinicians about using social media to find mental health information out of concerns of being judged or dismissed. Therefore, mental health clinicians may be ideally positioned to talk with their patients about using social media and offer recommendations to promote safe use of these sites while also respecting their patients’ autonomy and personal motivations for using these popular platforms. Given the gap in clinical knowledge about the impact of social media on mental health, clinicians should be aware of the many potential risks so that they can inform their patients while remaining open to the possibility that their patients may also experience benefits through use of these platforms. As awareness of these risks grows, it may be possible that new protections will be put in place by industry or through new policies that will make the social media environment safer. It is hard to estimate a number needed to treat or harm today given the nascent state of research, which means the patient and clinician need to weigh the choice on a personal level. Thus, offering education and information is an important first step in that process. As patients increasingly show interest in accessing mental health information or services through social media, it will be necessary for health systems to recognize social media as a potential avenue for reaching or offering support to patients. This aligns with growing emphasis on the need for greater integration of digital psychiatry, including apps, smartphones, or wearable devices, into patient care and clinical services through institution-wide initiatives and training clinical providers (Hilty et al. 2019 ). Within a learning healthcare environment where research and care are tightly intertwined and feedback between both is rapid, the integration of digital technologies into services may create new opportunities for advancing use of social media for mental health.
As highlighted in this commentary, social media has become an important part of the lives of many individuals living with mental disorders. Many of these individuals use social media to share their lived experiences with mental illness, to seek support from others, and to search for information about treatment recommendations, accessing mental health services and coping with symptoms (Bucci et al. 2019 ; Highton-Williamson et al. 2015 ; Naslund et al. 2016b ). As the field of digital mental health advances, the wide reach, ease of access, and popularity of social media platforms could be used to allow individuals in need of mental health services or facing challenges of mental illness to access evidence-based treatment and support. To achieve this end and to explore whether social media platforms can advance efforts to close the gap in available mental health services in the USA and globally, it will be essential for researchers to work closely with clinicians and with those affected by mental illness to ensure that possible benefits of using social media are carefully weighed against anticipated risks.
Abdel-Baki, A., Lal, S., Charron, D.-C., Stip, E., & Kara, N. (2017). Understanding access and use of technology among youth with first-episode psychosis to inform the development of technology-enabled therapeutic interventions. Early Intervention in Psychiatry, 11 (1), 72–76.
PubMed Google Scholar
Ahmed, Y. A., Ahmad, M. N., Ahmad, N., & Zakaria, N. H. (2019). Social media for knowledge-sharing: a systematic literature review. Telematics and Informatics, 37 , 72–112.
Google Scholar
Alhajji, M., Bass, S., & Dai, T. (2019). Cyberbullying, mental health, and violence in adolescents and associations with sex and race: data from the 2015 youth risk behavior survey. Global Pediatric Health, 6 , 2333794X19868887.
PubMed PubMed Central Google Scholar
Alvarez-Jimenez, M., Bendall, S., Lederman, R., Wadley, G., Chinnery, G., Vargas, S., Larkin, M., Killackey, E., McGorry, P., & Gleeson, J. F. (2013). On the HORYZON: moderated online social therapy for long-term recovery in first episode psychosis. Schizophrenia Research, 143 (1), 143–149.
Alvarez-Jimenez, M., Gleeson, J., Bendall, S., Penn, D., Yung, A., Ryan, R., et al. (2018). Enhancing social functioning in young people at ultra high risk (UHR) for psychosis: a pilot study of a novel strengths and mindfulness-based online social therapy. Schizophrenia Research, 202 , 369–377.
Alvarez-Jimenez, M., Bendall, S., Koval, P., Rice, S., Cagliarini, D., Valentine, L., et al. (2019). HORYZONS trial: protocol for a randomised controlled trial of a moderated online social therapy to maintain treatment effects from first-episode psychosis services. BMJ Open, 9 (2), e024104.
Andreassen, C. S., Billieux, J., Griffiths, M. D., Kuss, D. J., Demetrovics, Z., Mazzoni, E., & Pallesen, S. (2016). The relationship between addictive use of social media and video games and symptoms of psychiatric disorders: a large-scale cross-sectional study. Psychology of Addictive Behaviors, 30 (2), 252.
Aschbrenner, K. A., Naslund, J. A., & Bartels, S. J. (2016a). A mixed methods study of peer-to-peer support in a group-based lifestyle intervention for adults with serious mental illness. Psychiatric Rehabilitation Journal, 39 (4), 328–334.
Aschbrenner, K. A., Naslund, J. A., Shevenell, M., Kinney, E., & Bartels, S. J. (2016b). A pilot study of a peer-group lifestyle intervention enhanced with mHealth technology and social media for adults with serious mental illness. The Journal of Nervous and Mental Disease, 204 (6), 483–486.
Aschbrenner, K. A., Naslund, J. A., Shevenell, M., Mueser, K. T., & Bartels, S. J. (2016c). Feasibility of behavioral weight loss treatment enhanced with peer support and mobile health technology for individuals with serious mental illness. Psychiatric Quarterly, 87 (3), 401–415.
Aschbrenner, K. A., Naslund, J. A., Gorin, A. A., Mueser, K. T., Scherer, E. A., Viron, M., et al. (2018a). Peer support and mobile health technology targeting obesity-related cardiovascular risk in young adults with serious mental illness: protocol for a randomized controlled trial. Contemporary Clinical Trials, 74 , 97–106.
Aschbrenner, K. A., Naslund, J. A., Grinley, T., Bienvenida, J. C. M., Bartels, S. J., & Brunette, M. (2018b). A survey of online and mobile technology use at peer support agencies. Psychiatric Quarterly , 1–10.
Aschbrenner, K. A., Naslund, J. A., Tomlinson, E. F., Kinney, A., Pratt, S. I., & Brunette, M. F. (2019). Adolescents’ use of digital technologies and preferences for mobile health coaching in mental health settings. Frontiers in Public Health. 7 , 178.
Badcock, J. C., Shah, S., Mackinnon, A., Stain, H. J., Galletly, C., Jablensky, A., & Morgan, V. A. (2015). Loneliness in psychotic disorders and its association with cognitive function and symptom profile. Schizophrenia Research, 169 (1–3), 268–273.
Batterham, P. J., & Calear, A. J. (2017). Preferences for internet-based mental health interventions in an adult online sample: findings from ann online community survey. JMIR Mental Health, 4 (2), e26.
Bauer, R., Bauer, M., Spiessl, H., & Kagerbauer, T. (2013). Cyber-support: an analysis of online self-help forums (online self-help forums in bipolar disorder). Nordic Journal of Psychiatry, 67 (3), 185–190.
Berger, M., Wagner, T. H., & Baker, L. C. (2005). Internet use and stigmatized illness. Social Science & Medicine, 61 (8), 1821–1827.
Berry, N., Lobban, F., Belousov, M., Emsley, R., Nenadic, G., & Bucci, S. (2017). # WhyWeTweetMH: understanding why people use Twitter to discuss mental health problems. Journal of Medical Internet Research, 19 (4), e107.
Berry, N., Emsley, R., Lobban, F., & Bucci, S. (2018). Social media and its relationship with mood, self-esteem and paranoia in psychosis. Acta Psychiatrica Scandinavica, 138 , 558–570.
Best, P., Manktelow, R., & Taylor, B. (2014). Online communication, social media and adolescent wellbeing: a systematic narrative review. Children and Youth Services Review, 41 , 27–36.
Biagianti, B., Quraishi, S. H., & Schlosser, D. A. (2018). Potential benefits of incorporating peer-to-peer interactions into digital interventions for psychotic disorders: a systematic review. Psychiatric Services, 69 (4), 377–388.
Bidargaddi, N., Musiat, P., Makinen, V.-P., Ermes, M., Schrader, G., & Licinio, J. (2017). Digital footprints: facilitating large-scale environmental psychiatric research in naturalistic settings through data from everyday technologies. Molecular Psychiatry, 22 (2), 164.
Birnbaum, M. L., Ernala, S. K., Rizvi, A. F., De Choudhury, M., & Kane, J. M. (2017a). A collaborative approach to identifying social media markers of schizophrenia by employing machine learning and clinical appraisals. Journal of Medical Internet Research, 19 (8), e289.
Birnbaum, M. L., Rizvi, A. F., Correll, C. U., Kane, J. M., & Confino, J. (2017b). Role of social media and the Internet in pathways to care for adolescents and young adults with psychotic disorders and non-psychotic mood disorders. Early Intervention in Psychiatry, 11 (4), 290–295.
Booker, C. L., Kelly, Y. J., & Sacker, A. (2018). Gender differences in the associations between age trends of social media interaction and well-being among 10-15 year olds in the UK. BMC Public Health, 18 (1), 321.
Brunette, M., Achtyes, E., Pratt, S., Stilwell, K., Opperman, M., Guarino, S., & Kay-Lambkin, F. (2019). Use of smartphones, computers and social media among people with SMI: opportunity for intervention. Community Mental Health Journal , 1–6.
Brusilovskiy, E., Townley, G., Snethen, G., & Salzer, M. S. (2016). Social media use, community participation and psychological well-being among individuals with serious mental illnesses. Computers in Human Behavior, 65 , 232–240.
Bucci, S., Schwannauer, M., & Berry, N. (2019). The digital revolution and its impact on mental health care. Psychology and Psychotherapy: Theory, Research and Practice, 92 (2), 277–297.
Chancellor, S., Birnbaum, M. L., Caine, E. D., Silenzio, V. M., & De Choudhury, M. (2019). A taxonomy of ethical tensions in inferring mental health states from social media. In Proceedings of the Conference on Fairness, Accountability, and Transparency, 79–88.
Chang, H. J. (2009). Online supportive interactions: using a network approach to examine communication patterns within a psychosis social support group in Taiwan. Journal of the American Society for Information Science and Technology, 60 (7), 1504–1517.
Davidson, L., Chinman, M., Sells, D., & Rowe, M. (2006). Peer support among adults with serious mental illness: a report from the field. Schizophrenia Bulletin, 32 (3), 443–450.
De Choudhury, M., Gamon, M., & Counts, S. (2012). Happy, nervous or surprised? classification of human affective states in social media. Paper presented at the sixth international Association for Advancement of Artificial Intelligence (AAAI) Conference on Weblogs and Social Meedia, 435–438.
De Choudhury, M., Gamon, M., Counts, S., & Horvitz, E. (2013). Predicting depression via social media. Paper presented at the seventh international Association for Advancement of Artificial Intelligence (AAAI) Conference on Weblogs and Social Media, 128–137.
Docherty, N. M., Hawkins, K. A., Hoffman, R. E., Quinlan, D. M., Rakfeldt, J., & Sledge, W. H. (1996). Working memory, attention, and communication disturbances in schizophrenia. Journal of Abnormal Psychology, 105 (2), 212–219.
Ernala, S. K., Rizvi, A. F., Birnbaum, M. L., Kane, J. M., & De Choudhury, M. (2017). Linguistic markers indicating therapeutic outcomes of social media disclosures of schizophrenia. Proceedings of the ACM on Human-Computer Interaction, 1 (1), 43.
Feinstein, B. A., Hershenberg, R., Bhatia, V., Latack, J. A., Meuwly, N., & Davila, J. (2013). Negative social comparison on Facebook and depressive symptoms: rumination as a mechanism. Psychology of Popular Media Culture, 2 (3), 161.
Firth, J., Cotter, J., Torous, J., Bucci, S., Firth, J. A., & Yung, A. R. (2015). Mobile phone ownership and endorsement of “mHealth” among people with psychosis: a meta-analysis of cross-sectional studies. Schizophrenia Bulletin, 42 (2), 448–455.
Firth, J., Rosenbaum, S., Stubbs, B., Gorczynski, P., Yung, A. R., & Vancampfort, D. (2016). Motivating factors and barriers towards exercise in severe mental illness: a systematic review and meta-analysis. Psychological Medicine, 46 (14), 2869–2881.
Gay, K., Torous, J., Joseph, A., Pandya, A., & Duckworth, K. (2016). Digital technology use among individuals with schizophrenia: results of an online survey. JMIR Mental Health, 3 (2), e15.
Giacco, D., Palumbo, C., Strappelli, N., Catapano, F., & Priebe, S. (2016). Social contacts and loneliness in people with psychotic and mood disorders. Comprehensive Psychiatry, 66 , 59–66.
Gleeson, J., Lederman, R., Herrman, H., Koval, P., Eleftheriadis, D., Bendall, S., Cotton, S. M., & Alvarez-Jimenez, M. (2017). Moderated online social therapy for carers of young people recovering from first-episode psychosis: study protocol for a randomised controlled trial. Trials, 18 (1), 27.
Glick, G., Druss, B., Pina, J., Lally, C., & Conde, M. (2016). Use of mobile technology in a community mental health setting. Journal of Telemedicine and Telecare, 22 (7), 430–435.
Goodman, L. A., Thompson, K. M., Weinfurt, K., Corl, S., Acker, P., Mueser, K. T., & Rosenberg, S. D. (1999). Reliability of reports of violent victimization and posttraumatic stress disorder among men and women with serious mental illness. Journal of Traumatic Stress: Official Publication of the International Society for Traumatic Stress Studies, 12 (4), 587–599.
Gowen, K., Deschaine, M., Gruttadara, D., & Markey, D. (2012). Young adults with mental health conditions and social networking websites: seeking tools to build community. Psychiatric Rehabilitation Journal, 35 (3), 245–250.
Guntuku, S. C., Yaden, D. B., Kern, M. L., Ungar, L. H., & Eichstaedt, J. C. (2017). Detecting depression and mental illness on social media: an integrative review. Current Opinion in Behavioral Sciences, 18 , 43–49.
Haker, H., Lauber, C., & Rössler, W. (2005). Internet forums: a self-help approach for individuals with schizophrenia? Acta Psychiatrica Scandinavica, 112 (6), 474–477.
Hamm, M. P., Newton, A. S., Chisholm, A., Shulhan, J., Milne, A., Sundar, P., Ennis, H., Scott, S. D., & Hartling, L. (2015). Prevalence and effect of cyberbullying on children and young people: a scoping review of social media studies. JAMA Pediatrics, 169 (8), 770–777.
Hansen, C. F., Torgalsbøen, A.-K., Melle, I., & Bell, M. D. (2009). Passive/apathetic social withdrawal and active social avoidance in schizophrenia: difference in underlying psychological processes. The Journal of Nervous and Mental Disease, 197 (4), 274–277.
Highton-Williamson, E., Priebe, S., & Giacco, D. (2015). Online social networking in people with psychosis: a systematic review. International Journal of Social Psychiatry, 61 (1), 92–101.
Hilty, D. M., Chan, S., Torous, J., Luo, J., & Boland, R. J. (2019). Mobile health, smartphone/device, and apps for psychiatry and medicine: competencies, training, and faculty development issues. Psychiatric Clinics, 42 (3), 513–534.
Hswen, Y., Naslund, J. A., Chandrashekar, P., Siegel, R., Brownstein, J. S., & Hawkins, J. B. (2017). Exploring online communication about cigarette smoking among Twitter users who self-identify as having schizophrenia. Psychiatry Research, 257 , 479–484.
Hswen, Y., Naslund, J. A., Brownstein, J. S., & Hawkins, J. B. (2018a). Monitoring online discussions about suicide among Twitter users with schizophrenia: exploratory study. JMIR Mental Health, 5 (4), e11483.
Hswen, Y., Naslund, J. A., Brownstein, J. S., & Hawkins, J. B. (2018b). Online communication about depression and anxiety among twitter users with schizophrenia: preliminary findings to inform a digital phenotype using social media. Psychiatric Quarterly, 89 (3), 569–580.
Indian, M., & Grieve, R. (2014). When Facebook is easier than face-to-face: social support derived from Facebook in socially anxious individuals. Personality and Individual Differences, 59 , 102–106.
Jain, S. H., Powers, B. W., Hawkins, J. B., & Brownstein, J. S. (2015). The digital phenotype. Nature Biotechnology, 33 (5), 462–463.
Kiesler, S., Siegel, J., & McGuire, T. W. (1984). Social psychological aspects of computer-mediated communication. American Psychologist, 39 , 1123–1134.
Kross, E., Verduyn, P., Demiralp, E., Park, J., Lee, D. S., Lin, N., Shablack, H., Jonides, J., & Ybarra, O. (2013). Facebook use predicts declines in subjective well-being in young adults. PLoS One, 8 (8), e69841.
Lal, S., Nguyen, V., & Theriault, J. (2018). Seeking mental health information and support online: experiences and perspectives of young people receiving treatment for first-episode psychosis. Early Intervention in Psychiatry, 12 (3), 324–330.
Lin, L. Y., Sidani, J. E., Shensa, A., Radovic, A., Miller, E., Colditz, J. B., Hoffman, B. L., Giles, L. M., & Primack, B. A. (2016). Association between social media use and depression among US young adults. Depression and Anxiety, 33 (4), 323–331.
Machmutow, K., Perren, S., Sticca, F., & Alsaker, F. D. (2012). Peer victimisation and depressive symptoms: can specific coping strategies buffer the negative impact of cybervictimisation? Emotional and Behavioural Difficulties, 17 (3–4), 403–420.
Manikonda, L., & De Choudhury, M. (2017). Modeling and understanding visual attributes of mental health disclosures in social media. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems, 170–181.
Mead, S., Hilton, D., & Curtis, L. (2001). Peer support: a theoretical perspective. Psychiatric Rehabilitation Journal, 25 (2), 134–141.
Mereish, E. H., Sheskier, M., Hawthorne, D. J., & Goldbach, J. T. (2019). Sexual orientation disparities in mental health and substance use among Black American young people in the USA: effects of cyber and bias-based victimisation. Culture, Health & Sexuality, 21 (9), 985–998.
Miller, B. J., Stewart, A., Schrimsher, J., Peeples, D., & Buckley, P. F. (2015). How connected are people with schizophrenia? Cell phone, computer, email, and social media use. Psychiatry Research, 225 (3), 458–463.
Mittal, V. A., Tessner, K. D., & Walker, E. F. (2007). Elevated social Internet use and schizotypal personality disorder in adolescents. Schizophrenia Research, 94 (1–3), 50–57.
Moorhead, S. A., Hazlett, D. E., Harrison, L., Carroll, J. K., Irwin, A., & Hoving, C. (2013). A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. Journal of Medical Internet Research, 15 (4), e85.
Naslund, J. A., & Aschbrenner, K. A. (2019). Risks to privacy with use of social media: understanding the views of social media users with serious mental illness. Psychiatric Services, 70 (7), 561–568.
Naslund, J. A., Grande, S. W., Aschbrenner, K. A., & Elwyn, G. (2014). Naturally occurring peer support through social media: the experiences of individuals with severe mental illness using YouTube. PLoS One, 9 (10), e110171.
Naslund, J. A., Aschbrenner, K. A., & Bartels, S. J. (2016). How people living with serious mental illness use smartphones, mobile apps, and social media. Psychiatric Rehabilitation Journal, 39 (4), 364–367.
Naslund, J. A., Aschbrenner, K. A., Marsch, L. A., & Bartels, S. J. (2016a). Feasibility and acceptability of Facebook for health promotion among people with serious mental illness. Digital Health, 2 , 2055207616654822.
PubMed Central Google Scholar
Naslund, J. A., Aschbrenner, K. A., Marsch, L. A., & Bartels, S. J. (2016b). The future of mental health care: peer-to-peer support and social media. Epidemiology and Psychiatric Sciences, 25 (2), 113–122.
Naslund, J. A., Aschbrenner, K. A., McHugo, G. J., Unützer, J., Marsch, L. A., & Bartels, S. J. (2019). Exploring opportunities to support mental health care using social media: A survey of social media users with mental illness. Early Intervention in Psychiatry, 13 (3), 405–413.
Naslund, J. A., Aschbrenner, K. A., Marsch, L. A., McHugo, G. J., & Bartels, S. J. (2018). Facebook for supporting a lifestyle intervention for people with major depressive disorder, bipolar disorder, and schizophrenia: an exploratory study. Psychiatric Quarterly, 89 (1), 81–94.
Naslund, J. A., Gonsalves, P. P., Gruebner, O., Pendse, S. R., Smith, S. L., Sharma, A., & Raviola, G. (2019). Digital innovations for global mental health: opportunities for data science, task sharing, and early intervention. Current Treatment Options in Psychiatry , 1–15.
Onnela, J.-P., & Rauch, S. L. (2016). Harnessing smartphone-based digital phenotyping to enhance behavioral and mental health. Neuropsychopharmacology, 41 (7), 1691–1696.
Orben, A., & Przybylski, A. K. (2019). The association between adolescent well-being and digital technology use. Nature Human Behaviour, 3 (2), 173–182.
Patel, V., Saxena, S., Lund, C., Thornicroft, G., Baingana, F., Bolton, P., et al. (2018). The Lancet Commission on global mental health and sustainable development. The Lancet, 392 (10157), 1553–1598.
Primack, B. A., Shensa, A., Escobar-Viera, C. G., Barrett, E. L., Sidani, J. E., Colditz, J. B., & James, A. E. (2017). Use of multiple social media platforms and symptoms of depression and anxiety: a nationally-representative study among US young adults. Computers in Human Behavior, 69 , 1–9.
Reece, A. G., & Danforth, C. M. (2017). Instagram photos reveal predictive markers of depression. EPJ Data Science, 6 (1), 15.
Reece, A. G., Reagan, A. J., Lix, K. L., Dodds, P. S., Danforth, C. M., & Langer, E. J. (2017). Forecasting the onset and course of mental illness with Twitter data. Scientific Reports, 7 (1), 13006.
Rideout, V., & Fox, S. (2018). Digital health practices, social media use, and mental well-being among teens and young adults in the U.S. Retrieved from San Francisco, CA: https://www.hopelab.org/reports/pdf/a-national-survey-by-hopelab-and-well-being-trust-2018.pdf . Accessed 10 Jan 2020.
Saha, K., Torous, J., Ernala, S. K., Rizuto, C., Stafford, A., & De Choudhury, M. (2019). A computational study of mental health awareness campaigns on social media. Translational behavioral medicine, 9 (6), 1197–1207.
Schlosser, D. A., Campellone, T., Kim, D., Truong, B., Vergani, S., Ward, C., & Vinogradov, S. (2016). Feasibility of PRIME: a cognitive neuroscience-informed mobile app intervention to enhance motivated behavior and improve quality of life in recent onset schizophrenia. JMIR Research Protocols, 5 (2).
Schlosser, D. A., Campellone, T. R., Truong, B., Etter, K., Vergani, S., Komaiko, K., & Vinogradov, S. (2018). Efficacy of PRIME, a mobile app intervention designed to improve motivation in young people with schizophrenia. Schizophrenia Bulletin, 44 (5), 1010–1020.
Schrank, B., Sibitz, I., Unger, A., & Amering, M. (2010). How patients with schizophrenia use the internet: qualitative study. Journal of Medical Internet Research, 12 (5), e70.
Schueller, S. M., Hunter, J. F., Figueroa, C., & Aguilera, A. (2019). Use of digital mental health for marginalized and underserved populations. Current Treatment Options in Psychiatry, 6 (3), 243–255.
Shatte, A. B., Hutchinson, D. M., & Teague, S. J. (2019). Machine learning in mental health: a scoping review of methods and applications. Psychological Medicine, 49 (9), 1426–1448.
Spinzy, Y., Nitzan, U., Becker, G., Bloch, Y., & Fennig, S. (2012). Does the Internet offer social opportunities for individuals with schizophrenia? A cross-sectional pilot study. Psychiatry Research, 198 (2), 319–320.
Stiglic, N., & Viner, R. M. (2019). Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open, 9 (1), e023191.
Sumner, S. A., Galik, S., Mathieu, J., Ward, M., Kiley, T., Bartholow, B., et al. (2019). Temporal and geographic patterns of social media posts about an emerging suicide game. Journal of Adolescent Health, 65 (1), 94–100.
Torous, J., & Keshavan, M. (2016). The role of social media in schizophrenia: evaluating risks, benefits, and potential. Current Opinion in Psychiatry, 29 (3), 190–195.
Torous, J., Chan, S. R., Tan, S. Y.-M., Behrens, J., Mathew, I., Conrad, E. J., et al. (2014a). Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: a survey in four geographically distinct psychiatric clinics. JMIR Mental Health, 1 (1), e5.
Torous, J., Friedman, R., & Keshavan, M. (2014b). Smartphone ownership and interest in mobile applications to monitor symptoms of mental health conditions. JMIR mHealth and uHealth, 2 (1), e2.
Torous, J., Wisniewski, H., Bird, B., Carpenter, E., David, G., Elejalde, E., et al. (2019). Creating a digital health smartphone app and digital phenotyping platform for mental health and diverse healthcare needs: an interdisciplinary and collaborative approach. Journal of Technology in Behavioral Science, 4 (2), 73–85.
Trefflich, F., Kalckreuth, S., Mergl, R., & Rummel-Kluge, C. (2015). Psychiatric patients' internet use corresponds to the internet use of the general public. Psychiatry Research, 226 , 136–141.
Twenge, J. M., & Campbell, W. K. (2018). Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Preventive Medicine Reports, 12 , 271–283.
Twenge, J. M., Joiner, T. E., Rogers, M. L., & Martin, G. N. (2018). Increases in depressive symptoms, suicide-related outcomes, and suicide rates among US adolescents after 2010 and links to increased new media screen time. Clinical Psychological Science, 6 (1), 3–17.
Tynes, B. M., Willis, H. A., Stewart, A. M., & Hamilton, M. W. (2019). Race-related traumatic events online and mental health among adolescents of color. Journal of Adolescent Health, 65 (3), 371–377.
Vannucci, A., Flannery, K. M., & Ohannessian, C. M. (2017). Social media use and anxiety in emerging adults. Journal of Affective Disorders, 207 , 163–166.
Vayreda, A., & Antaki, C. (2009). Social support and unsolicited advice in a bipolar disorder online forum. Qualitative Health Research, 19 (7), 931–942.
Ventola, C. L. (2014). Social media and health care professionals: benefits, risks, and best practices. Pharmacy and Therapeutics, 39 (7), 491–520.
We Are Social. (2020). Digital in 2020. Retrieved from https://wearesocial.com/global-digital-report-2019 . Accessed 10 Jan 2020.
Webb, H., Jirotka, M., Stahl, B. C., Housley, W., Edwards, A., Williams, M., ... & Burnap, P. (2017). The ethical challenges of publishing Twitter data for research dissemination . Paper presented at the proceedings of the 2017 ACM on Web Science Conference, 339–348.
Williams, M. L., Burnap, P., & Sloan, L. (2017). Towards an ethical framework for publishing twitter data in social research: taking into account users’ views, online context and algorithmic estimation. Sociology, 51 (6), 1149–1168.
Woods, H. C., & Scott, H. (2016). # Sleepyteens: social media use in adolescence is associated with poor sleep quality, anxiety, depression and low self-esteem. Journal of Adolescence, 51 , 41–49.
Ybarra, M. L. (2004). Linkages between depressive symptomatology and internet harassment among young regular Internet users. Cyberpsychology & Behavior, 7 (2), 247–257.
Download references
Dr. Naslund is supported by a grant from the National Institute of Mental Health (U19MH113211). Dr. Aschbrenner is supported by a grant from the National Institute of Mental Health (1R01MH110965-01).
Author information
Authors and affiliations.
Department of Global Health and Social Medicine, Harvard Medical School, 641 Huntington Avenue, Boston, MA, 02115, USA
John A. Naslund
Digital Mental Health Research Consultant, Mumbai, India
Ameya Bondre
Division of Digital Psychiatry, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, USA
John Torous
Department of Psychiatry, Geisel School of Medicine at Dartmouth, Lebanon, NH, USA
Kelly A. Aschbrenner
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to John A. Naslund .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Naslund, J.A., Bondre, A., Torous, J. et al. Social Media and Mental Health: Benefits, Risks, and Opportunities for Research and Practice. J. technol. behav. sci. 5 , 245–257 (2020). https://doi.org/10.1007/s41347-020-00134-x
Download citation
Received : 19 October 2019
Revised : 24 February 2020
Accepted : 17 March 2020
Published : 20 April 2020
Issue Date : September 2020
DOI : https://doi.org/10.1007/s41347-020-00134-x
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
Skip to content
Equity, Diversity, and Inclusion
Our Office of Equity, Diversity, and Inclusion works to create an inclusive environment that values diversity in academic medicine.
Education and Training
Columbia Psychiatry is teaching the next generation of clinicians and researchers through our residency, fellowship, and training programs.
Research Areas
Clinical trials and research studies.
Would you like to help support our research? Learn about how to participate in clinical trials or research studies here at Columbia Psychiatry.
- Patient Care
Read about the world of psychiatric research, education, and patient care—and see what's happening here at Columbia Pyschiatry.
Addressing Mental Health in the Black Community
Share this page.
- Share on Facebook
- Share on X (formerly Twitter)
- Share on LinkedIn
- Share by email
By Thomas A. Vance, PhD
Roughly 37 million people, identify themselves as Black or African American in the United States. From trailblazing pioneers like George Washington Carver and Dorothy Height to modern-day heroes like Anita Hill and Neil deGrasse Tyson, the Black community has made enormous contributions to the ongoing fight for social, racial, and economic justice. Despite these efforts, true social justice among the Black community will remain incomplete until mental health disparities among this group are addressed. Mental health is an essential part of overall physical health and satisfaction. The Black community suffers from an increased rate of mental health concerns, including anxiety and depression . The increased incidence of psychological difficulties in the Black community is related to the lack of access to appropriate and culturally responsive mental health care, prejudice and racism inherent in the daily environment of Black individuals, and historical trauma enacted on the Black community by the medical field. Moreover, given that the Black community exists at the intersection of racism, classism, and health inequity, their mental health needs are often exacerbated and mostly unfulfilled. Issues related to economic insecurity, and the associated experiences, such as violence and criminal injustice, further serve to compound the mental health disparities in the Black population.
Research Surrounding the Black Community and Mental Health
Research suggests that the adult Black community is 20% more likely to experience serious mental health problems, such as Major Depressive Disorder or Generalized Anxiety Disorder. Additionally, Black emerging adults (ages 18-25) also experience higher rates of mental health problems and lower rates of mental health service utilization compared to White emerging adults, and older Black adults. These sobering statistics suggest that despite efforts to reduce disparities among race and class in the US, inequalities are increasing. However, further research is required to clarify these findings and to understand the factors associated with lower utilization of mental health care among the Black community. Lack of trust in the medical system due to historical abuses of Black people in the guise of health care, less access to adequate insurance, culturally responsive mental health providers, financial burden, and past history with discrimination in the mental health system. Also, a fear that these experiences will be repeated is all suggested by research as factors in explaining lower utilization of mental health care among the Black community.
Systematic Barriers
It is clear that systematic barriers disproportionately impact mental health in the Black community. Although the Black community roughly constitute 12% of the United States population, they are overrepresented in high-risk populations (a group that is often impacted by specific negative occurrences). For example, the Black community comprises approximately 40% of the homeless population, 50% of the prison population, and 45% of children in the foster care system. Research shows that exposure to violence, incarceration, and involvement in the foster care system can increase the chances of developing a mental illness. Consequently, the Black community, in particular, is at significantly increased risk of developing a mental health issue due to historical, economic, social, political influences that systemically expose the Black community to factors known to be damaging to psychological and physical health. Research consistently shows that these disparities are not a new phenomenon and have been present for generations. Historically, the Black community was and continues to be disadvantaged in mental health through subjection to trauma through enslavement, oppression, colonialism, racism, and segregation. A growing body of research suggests that traumatic experiences can cause profound biological changes in the person experiencing the traumatic event. Cutting edge researchers are also beginning to understand how these physiological changes are genetically encoded and passed down to future generations. These findings suggest that in addition to the cultural and psychological inheritance of trauma, intergenerational trauma may be passed down biologically from one generation to the next.
The Stigma Associated with Mental Health Concerns
Despite progress in recent years, there is still a significant stigma associated with mental health concerns. In the Black community, there is often difficulty acknowledging psychological difficulties, but useful strategies including religious coping and methods such as pastoral guidance and prayer often are the most preferred coping mechanism. Destigmatizing mental health can be achieved by helping people, especially in the Black community, to understand that mental health is an essential part of well-being — just like a healthy diet, sleep and exercise.
These ideas often lead people to believe that a mental health condition is a personal weakness due to negative stereotypes of instability and attitudes of rejection. Because of this lack of information about mental health issues in the Black community, it is not always clear when one may need it or where to find help. There is also a need for improved cultural awareness and corresponding responsiveness in the health care and mental health workforce. Research has found that the lack of cultural responsiveness from the therapist, cultural mistrust, and potential negative views from the therapist associated with stigma impact the provision of mental health services in the Black community. Luckily, with the rise of social media and improved awareness related to mental health, the development of and funding for culturally responsive mental health treatment are increasing.
Culturally Responsive Mental Health Treatment
Culturally responsive mental health treatment is one way of addressing the disparities in psychological wellbeing in the Black community. Culture, a person's belief, norms, values, and language, plays a vital role in every aspect of our lives, including mental health. Being culturally responsive is a mental health provider’s ability to recognize and understand the role of culture, both the client and clinician’s and the ability to adapt the treatment to meet the client’s needs within their cultural framework. When meeting with providers, it is essential for clients to ask questions to gain a sense of their level of cultural sensitivity. Most people often feel nervous or guilty about asking these hard questions, but providers usually expect and welcome questions as this helps them better understand the patient and what’s important to them. Here are three tips clients could do to seek out culturally responsive providers:
- Ask the provider questions about their treatment approach and if they provide care including ones’ culture.
- Seek attention from someone who is aware and affirming of your intersecting identities (social categorizations such as race, class, and gender, that are overlapping and interdependent systems of discrimination or disadvantage) and your cultural background.
- Be mindful that some providers do not use methods that involve a cultural treatment framework, so ensure your provider is culturally responsive and respectful of your needs and how to infuse these beliefs into treatment.
A mental health provider will play an essential role in treatment, and it is vital to work and communicate well with this person. It is important to know that efforts towards social justice among the Black community will remain incomplete until mental health disparities among this group are addressed and that seeking mental health treatment is a part of overall health. The Black community has a long history of social change and prioritizing mental health is not a sign of weakness, but an act of strength.
Thomas A. Vance, PhD is a Postdoctoral Clinical & Research Fellow at the Gender Identity Program at Columbia University Irving Medical Center .

Social Life
How to improve your mental health through community, the benefits of community involvement, plus tips and ideas for cultivating it..
Updated May 24, 2024 | Reviewed by Jessica Schrader
- Community involvement and a strong social network positively impact mental health with far-reaching benefits.
- Benefits of community include hope, opportunity, and resources, plus friendship and a sense of fulfillment.
- To help you decide how to get involved, consider your interests and passions, and consult with trusted others.
By Kimberly Nelson , MA, with Becky Shipkosky
Have you ever felt alone in the world? Isolated? If you have, can you think back to the state of your mental health at that time? Now, try to think of a time when you had a strong support network—maybe a job with the very best co-workers, your crew of friends in high school or college, or an especially cohesive group of roommates. Research indicates that these times in our lives are likely to be characterized by relatively good mental health (Park et al., 2023).
Why is a strong sense of community correlated with better mental health? For some—the more extroverted among us—this may seem perfectly natural. But introverts might find this counterintuitive. In fact, being in community offers benefits beyond the basic extrovert-recharge effect, including:
- Social support: Someone to talk to when the going gets tough.
- Purpose: Something bigger than yourself that inspires you to get out of bed and “do the day.”
- Hope: Others who believe in you and help you believe in yourself.
- Inspiration: Seeing people who look like you do great things and being reminded that you can do great things too.
- Accountability: “We’re counting on you, and we miss you when you’re not here.”
- Appreciation: Being seen for your strengths and having your best qualities reflected back to you.
- Empowerment: Community can give you a voice in a way that would be hard to accomplish alone.
- Opportunity: Your community network is the best source for job opportunities and so much more.
- Cultural connection: Whether it’s those with your same diagnosis, race, orientation, language, socio-economic background, or all of the above, being with your village can be so affirming.
- Resources: Who steps in to help when we’re struggling? Community does!
What Is Mental Health Recovery?
The recovery model is a newer paradigm in mental health care that emphasizes a person’s strengths, personal wisdom , and autonomy. It seeks to support individuals in living fulfilling lives with all the parts of themselves fully integrated, including their lived experience of mental illness. To learn more, see our post that fully defines the mental health recovery model.
Community + Mental Health Recovery
Within the recovery model, community is one of the four dimensions that underpin a fulfilling life (SAMHSA, 2024). Our Chief Program Officer, Dr. Lisa Schactman, emphasizes the role of community in the self-integration process: “Part of the recovery experience is reconnection. Some of the reconnection is to yourself…and some of the connection is to our loved ones and people in our community.”
At the end of the day, for better or worse, so much of who we are is in context of community. Like nearly everything else in our lives, “a recovery process is something that’s done in relationship, in community,” Schactman points out.
How to Cultivate Community That Fosters Recovery
Seeking out community may be new to some people. In our busy lives, we may only engage with the people and places we must. Stop by the coffee shop in the morning, say hello and goodbye to the barista. Go to work and talk shop with coworkers. Not all community provides the benefits we’ve talked about. Work may not be a bountiful hub of deep connection, after all. So, how do you even begin to intentionally build community for yourself?
- Start with the knowledge that you are enough. You don’t have to bring anything to the table other than yourself and what you naturally do well or love to do. This centeredness will help you quickly identify what is a good fit and what isn’t.
- Think about what captures your interest, passion, or curiosity. If no current interests or passions come to mind, think back to what you were most interested in as a child. This exercise may not lead you to just the right thing immediately, but it will absolutely move you in the right direction.
- Ask loved ones or care providers, like a therapist, to suggest ideas based on their understanding of you. This is great because it can provide perspectives you hadn’t thought of.
Where to Find Community
What types of spaces, events, and activities can we intentionally seek out to create a healthful and supportive environment that nurtures our mental health? Here are a few suggestions:
- Volunteer work: Volunteer for efforts you care about. Here are a few ideas: community garden, literacy or tutoring program for adults or children, peer support, animal shelter, food bank, senior center, crisis hotline.
- Workshops or classes: Look for workshops or classes that focus on personal development, mindfulness , or skill building. This could be anything from yoga to carpentry to non-violent communication.
- Support group: Find local or online support groups that resonate with you. Actively participate in meetings and discussions.
- Advocacy: Get involved in advocacy for issues you care about.
- Hobby group: Join or create a group based on a shared hobby or interest, such as a book club, gaming squad, or exercise group.
- Community events: Attend local events, fairs, and festivals.
- Online community: Use social media platforms or apps designed to connect people who have common interests or are seeking support.
- Faith-based: If you’re spiritual , join faith-based groups or activities. You can even begin by simply showing up for regular prayer or worship, which will undoubtedly open up opportunities for other events and programs.
- Exercise group: Join a local running club or yoga class, start going to the skate park or roller rink, or join a box gym.
You don’t have to choose just one opportunity. It’s a great idea to try a few or several totally different things to see what feels best to you. And once you settle on something, try to establish a schedule with it. Your regular involvement is what will help you form and strengthen relationships. These relationships can lead to friendships that are based on common interests, and the more you you are, the higher quality those relationships can be.
Park, E. Y., Oliver, T. R., Peppard, P. E., & Malecki, K. C. (2023). Sense of community and Mental Health: A cross-sectional analysis from a household survey in Wisconsin. Family Medicine and Community Health , 11(2). https://doi.org/10.1136/fmch-2022-001971
Recovery and recovery support . SAMHSA. (2024, March 26). https://www.samhsa.gov/find-help/recovery
Shipkosky, B., & Schactman, L. (2024, March 22). Recovery Model of Mental Health. personal.

CooperRiis is a non-profit residential healing community for adults with mental health challenges.
- Find a Therapist
- Find a Treatment Center
- Find a Psychiatrist
- Find a Support Group
- Find Online Therapy
- United States
- Brooklyn, NY
- Chicago, IL
- Houston, TX
- Los Angeles, CA
- New York, NY
- Portland, OR
- San Diego, CA
- San Francisco, CA
- Seattle, WA
- Washington, DC
- Asperger's
- Bipolar Disorder
- Chronic Pain
- Eating Disorders
- Passive Aggression
- Personality
- Goal Setting
- Positive Psychology
- Stopping Smoking
- Low Sexual Desire
- Relationships
- Child Development
- Self Tests NEW
- Therapy Center
- Diagnosis Dictionary
- Types of Therapy

At any moment, someone’s aggravating behavior or our own bad luck can set us off on an emotional spiral that threatens to derail our entire day. Here’s how we can face our triggers with less reactivity so that we can get on with our lives.
- Emotional Intelligence
- Gaslighting
- Affective Forecasting
- Neuroscience
This paper is in the following e-collection/theme issue:
Published on 29.5.2024 in Vol 26 (2024)
Long-Term Emotional Impact of the COVID-19 Pandemic and Barriers and Facilitators to Digital Mental Health Tools in Long-Term Care Workers: Qualitative Study
Authors of this article:

Original Paper
- Leticia González-Spinoglio 1 , MSc ;
- Anna Monistrol-Mula 1, 2 , MSc ;
- Cecilia Vindrola-Padros 3 , PhD ;
- Salvatore Aguilar-Ortiz 1 , PhD ;
- Bernat Carreras 4 , MSc ;
- Josep Maria Haro 1, 2, 5 , PhD ;
- Mireia Felez-Nobrega 1, 2 , PhD
1 Research and Development Unit, Parc Sanitari Sant Joan de Déu, Institut Sant Joan de Déu, Barcelona, Spain
2 Centre for Biomedical Research on Mental Health, Madrid, Spain
3 Department of Targeted Intervention, University College London, London, United Kingdom
4 Department of Psychiatry and Psychology, Institute of Neuroscience, Hospital Clínic, Barcelona, Spain
5 Departament de Medicina, Universitat de Barcelona, Barcelona, Spain
Corresponding Author:
Josep Maria Haro, PhD
Research and Development Unit, Parc Sanitari Sant Joan de Déu
Institut Sant Joan de Déu
C/Dr Antoni Pujada 42
Sant Boi de Llobregat
Barcelona, 08830
Phone: 34 93 640 63 50
Email: [email protected]
Background: The overall pandemic created enormous pressure on long-term care workers (LTCWs), making them particularly vulnerable to mental disorders. Despite this, most of the available evidence on professional well-being during COVID-19 has exclusively focused on frontline health care workers.
Objective: This study aimed to identify the long-term psychological needs of LTCWs derived from the COVID-19 pandemic and to explore barriers and facilitators related to digital mental health tools. This is part of a project that seeks to develop a digital mental health intervention to reduce psychological distress in this population group.
Methods: We performed a qualitative study with a rapid research approach. Participants were LTCWs of the autonomous community of Catalonia. We conducted 30 semistructured interviews between April and September 2022. We used a qualitative content analysis method with an inductive-deductive approach.
Results: The period of the pandemic with the highest mental health burden was the COVID-19 outbreak, with almost all workers having experienced some form of emotional distress. Emotional distress persisted over time in more than half of the participants, with fatigue and nervousness being the main emotions expressed at the time of the interview. High workload, the feeling that pandemic times are not over, and poor working conditions that have remained since then have been the most frequently expressed determinants of such emotions. Potential barriers and facilitators to engagement with digital tools were also identified in terms of previous experience and beliefs of the target population, possibilities for the integration of a digital tool into daily life, preferences regarding the level of guidance, the possibility of social connectedness through the tool, and privacy and confidentiality. The identified factors may become especially relevant in the context of the pandemic remission phase.
Conclusions: More than 2 years after the pandemic outbreak, emotional distress is still relevant. The persistent burden of psychological distress points to a need for institutions to take action to improve working conditions and promote employees’ well-being. Considering factors that act as barriers and facilitators for the use of digital mental health tools, it is important to develop tailored tools that could offer valuable support to this population during and after a pandemic.
Introduction
Long-term care facilities, such as nursing homes and other assisted living facilities, have been hit particularly hard by the COVID-19 pandemic. By February 2021, approximately 41% of the global COVID-19-associated mortality occurred in long-term care residents [ 1 ]. In Spain, the COVID-19 outbreak entailed especially tragic consequences, mainly caused by the precariousness of these care systems [ 2 ]. According to data from the Spanish Ministry of Health, 27,359 long-term residents died between April 6 and June 20, 2020, which represents approximately 70% of the total COVID-19 deaths. Long-term care workers (LTCWs) have been constantly exposed to anguish and death, have witnessed the social isolation and loneliness of residents due to health restrictions, and have experienced a drastic increase in their working demands [ 3 - 5 ]. Consequently, the mental health and well-being of this population group have been compromised, with clinically relevant levels of stress, anxiety, and depression increasing to nearly 60% from March 2020 to June 2020 [ 4 ].
As we approach the third year of the pandemic, health and care workers continue to respond to uncertainties, potential new waves, and the long-term effects of COVID-19. Importantly, recent evidence highlights increased concerns for burnout in this population [ 6 ], which can ultimately jeopardize the quality of health care as well as patient safety [ 7 ]. While mounting evidence has assessed the mental health experiences, views, and needs of care professionals during the early stages of the pandemic, there is scarce knowledge about the long-term emotional impact. This information is crucial to develop tailored interventions in response to their emotional demands.
Digital mental health tools (DMHTs) are a promising strategy to mitigate psychological consequences in the context of a long-lasting pandemic since they can be delivered remotely, avoiding the risk of transmission of the infection [ 8 ]. Yet, low levels of user engagement have been recognized as important barriers that may compromise the efficacy and scalability of interventions [ 9 ]. Increasing (prepandemic) evidence is beginning to unravel key factors that influence user engagement and the effectiveness of engagement strategies. For instance, positive prior experiences with mental health services and technology, digital literacy, the credibility of content, guidance within the intervention, increased social connectedness, a greater number of engagement features, reminders, and tailored feedback have been identified as potential facilitators for promoting engagement or effectiveness of digital interventions [ 10 - 13 ]. Nonetheless, these are general features reported in studies that included a wide range of different populations (eg, refugees, general population, people who are homeless, and people with a diagnosis of mental disorders), and it is well recognized that understanding the settings and population’s needs (eg, COVID-19 pandemic and long-term care facility characteristics) is a key factor for user engagement and intervention implementation success [ 14 ].
In this context, this study aimed to identify the long-term psychological needs of LTCWs as well as explore barriers and facilitators in relation to DMHTs. These findings will be used to inform and guide the development of a digital intervention to reduce psychological distress in this population group. The effectiveness of the psychological digital intervention will be tested through a randomized clinical trial (ClinicalTrials.gov NCT05526235).
Study Design, Sampling, and Participants
This qualitative study was conducted with a phenomenological orientation, in which we used a rapid research approach. In time-sensitive contexts, such as a pandemic, rapid appraisals allow us to collect and analyze data in a targeted and iterative way within limited time frames and, consequently, adapt and design expedient interventions for improving health care [ 15 ]. For reporting purposes, we adhered to the COREQ (Consolidated Criteria for Reporting Qualitative Research) checklist [ 16 ].
Semistructured interviews were conducted with workers from long-term care facilities (including nursing homes and other long-term care facilities), who were on duty during the pandemic in the autonomous community of Catalonia. For the recruitment of participants, we contacted several long-term care facilities and presented the project to each representative. Once the facility agreed to participate, the managerial staff shared the study information sheet among their employees (via their usual official means of communication). When needed, the researcher conducted informative talks (in person or via teleconference) with LTCWs in order to disseminate the study and resolve doubts, if any. A total of 6 long-term care facilities from the metropolitan area of Barcelona participated in the study.
Ethical Considerations
Ethics approval was provided by the Fundació Sant Joan de Déu Ethics Committee, Barcelona, Spain (PIC 214-21). Participants were fully informed about the objectives and procedures of the study prior to signing the informed consent. The data set was pseudoanonymized, and personal data were stored separately and securely on institution servers.
Data Collection
Interviews were conducted between April and September 2022. They were individual, by videoconference, and lasted between 25 and 40 minutes. The interview guide (provided in Multimedia Appendix 1 ) was reviewed by 2 experts in quality-of-life research to ensure its adequacy, and it was then tested with the first 2 interviews. No adaptations had to be made. The interview guide related to the digital mental health section was based on the framework developed by Borghouts et al [ 11 ]. Participants were given the option of conducting the interview in Spanish or Catalan, according to their preferences. Two researchers (AM-M and LG-S) conducted the interviews. Both are female PhD candidates. AM-M conducted the interviews in Catalan (8/30, 27% interviews), and LG-S conducted the interviews in Spanish (22/30, 73%). Both interviewers were previously trained in qualitative interview methods. Participants were informed of the interviewers’ educational and professional background, and no working or personal relationship existed between participants and interviewers. All interviews were audio recorded, and the main points were documented in real-time notes. At the conclusion of each interview, the emerging findings were synthesized using a RREAL (Rapid Research Evaluation and Appraisal Lab) Sheet (provided in Multimedia Appendix 2 ). The RREAL Sheet is a flexible working document, normally presented as a table, designed for the collection, synthesis, reporting, and analysis of data [ 17 ]. It enhances familiarization with the data and facilitates analysis while data collection is still ongoing [ 15 , 17 ]. First, a table organized by categories was designed using the interview script as a guide, and we piloted or amended this RREAL Sheet during initial data collection. Then, after each interview, we registered the key data obtained using real-time notes. In instances where pertinent details were absent, we referred to the audio recordings for further clarification. Importantly, the categories represented in the table were modified whenever considered necessary during data collection. Finally, the RREAL Sheet was used to guide an in-depth analysis [ 17 ]. The sample size was determined by thematic saturation [ 18 ].
Data Analysis
We used a qualitative content analysis method with an inductive-deductive approach. We performed a 1-page table that summarized the core components registered on the RREAL Sheet to identify key themes [ 17 ]. Once key themes and specific issues (subthemes) were recognized, we selected quotes from the interviews that could exemplify these themes. Investigator triangulation ensured that the themes reflected the full range and depth of the data.
Sample Characteristics
A total of 30 LTCWs participated in the study. The mean age was 44 (SD 11.4) years, most of our sample were women (n=26, 87%), and one-third (n=10, 33%) were from foreign nationalities. The vast majority of the participants were geriatric nursing assistants (n=17, 57%), followed by nurses (n=5, 17%). A more detailed description of the sociodemographic and occupational characteristics of the sample can be found in Table 1 .
a Director (n=1), occupational therapist (n=1), social worker (n=1), and cleaning staff (n=1).
Impact of COVID-19 on LTCWs’ Mental Health
Almost all participants identified the COVID-19 outbreak as the worst period for their mental health and reported having experienced emotional distress during this stage. The main emotions expressed were fear, helplessness, abandonment, loneliness, and sadness. Less frequently expressed emotions also included frustration, anger, uncertainty, and exhaustion. Five themes emerged as the main perceived determinants of these emotions:
- Unexpected and sudden nature of the crisis: Most participants expressed problems related to facing something new and completely unknown for which they were not prepared and its consequences. The reported main causes of distress were lack of information and knowledge, shortage of materials and human resources, problems with institutional organization, and the constant change of protocols and having to readjust to them.
- High exposure to emotional anguish and death: Half of the participants referred to high exposure to death and emotional anguish. They mainly mentioned the high mortality among residents and the helplessness of witnessing their isolation due to suspended family visits and reduced interactions resulting from health restrictions. Several participants also referred to the emotional anguish caused by the deaths of colleagues, family members, or friends as well as seeing the anguish in their colleagues on a daily basis.
- Fear of infection: Almost half of the participants mentioned the strong fear of infecting themselves, residents, and family members as well as the potential consequences of infection (eg, the severity of the disease and death).
- Moral distress: Many workers reported feelings of hopelessness, expressing that nothing they did for the residents in terms of care was enough. This was accompanied, in many cases, by a sense of loss of control of the situation during their caregiving duties.
- Lack of support: Many workers referred to a lack of recognition and support from authorities (both at the workplace and from the overall health authorities).
Textbox 1 provides an overview of these themes with example quotes for supporting data.
Unexpected and sudden nature of the crisis
- “We were not prepared; it came from one moment to the next.” [REPICAL (Reducing the psychosocial impact of the Covid-19 pandemic on workers of assisted living facilities)-007]
- “I also had to guide others in my charge, about things that I did not know either.” [REPICAL-004]
- “The protocols that we received were not clear...We were all in a drifting boat.” [REPICAL-008]
- “Overnight we were alone with co-workers. We were very lost; we did not have personal protective equipment and we did not know how to act. There were 4 of us and we managed as best as we could.” [REPICAL-026]
High exposure to emotional anguish and death
- “The worst thing I experienced was seeing so many residents die in such a short time, people who were fine and the next day they were gone.” [REPICAL-019]
- “We were not aware of the magnitude of this until residents began to die, they began to die one after the other, 4 or 5 per day (when before maybe one died every 2 months).” [REPICAL-026]
- “Seeing the loneliness in the residents affected me a lot, seeing that they were going to die alone, that they were not able to be with their family. It also affected me to see my co-workers, the most cheerful ones, defeated.” [REPICAL-021]
- “I felt so helpless seeing the isolated residents. We were asked not to have contact with them, but they needed someone to hold their hand.” [REPICAL-030]
Moral distress
- “We had to take measures that, while necessary, we knew were not good for the residents.” [REPICAL-003]
- “No matter what we did, people kept dying.” [REPICAL-004]
- “We saw that they were unwell and we could not help them...we wanted to address everything, but we could not.” [REPICAL-028]
Fear of infection
- “I even moved and lived in the residence for a while, so as not to infect the residents.” [REPICAL-019]
- “I had to isolate myself at home and I could not be with my child because I was afraid of infecting him. I also used to think: if something happens to me and my husband, who will take care of my child?” [REPICAL-023]
Lack of support
- “What I felt most was abandonment.” [REPICAL-002]
- “Feeling of helplessness of not being able to do anything and not having help from anyone.” [REPICAL-010]
In relation to their current emotional state, over half of the participants expressed some type of persistence of emotional distress over time. Among all participants, a minority reported maintaining intense distress, and a significant portion expressed only some improvement since the outbreak. The emotions most often mentioned were fatigue and nervousness, followed by anger and sadness. Three themes emerged as the main determinants of the persistent emotional distress:
- High workload: Long shifts due to staff shortages and coping with postcrisis backlog.
- Pandemic times are not over: Fatigue and residual discomfort from being under stress for so long as well as the feeling of not being able to completely move forward from COVID-19 due to the nature of their work.
- Still poor working conditions: Although the pandemic clearly highlighted the precariousness of these health care systems, some participants claimed that no measures have been taken to address this situation and that, as a result, working conditions remain poor. Relatedly, LTCWs felt that there is an overall failure in learning from the lessons of the COVID-19 pandemic.
Textbox 2 provides an overview of these themes with example quotes for supporting data.
On the other hand, among those participants who expressed a noticeable improvement over time in their emotional discomfort, hope and relief were the most commonly mentioned emotions. Improvement was associated with an increased sense of control over the situation, confidence in vaccines, decreased measures of isolation, and the feeling of regaining prepandemic working dynamics.
High workload
- “I am overwhelmed. In 2020, they increased my working hours. I was told it would only be during the state of emergency, but I am still not doing my usual schedule. In addition, people have left the workforce, and they have not hired more. I do not have as much time as I would like for other things.” [REPICAL-004]
- “Many projects were stopped because of the pandemic and now they have to be ready overnight. The workload is unreal.” [REPICAL-001]
- “Now we are facing our patients’ pathologies that were neglected during these two years. I am exhausted.” [REPICAL-005]
Pandemic times are not over
- “I am tired and burned out from dragging on for so long in tension, needing it to be over and it will not end.” [REPICAL-003]
- “Everyone has moved on, but I am still there: with the masks, the protective equipment, the heat.” [REPICAL-031]
- “During the crisis, we were alert at night in case a co-worker called us for help, and we always called each other; now I keep waking up even if they do not call me.” [REPICAL-026]
Still poor working conditions
- “With the pandemic, deficits that already existed in our field have come to light, and the thing is that nothing has changed, it’s just going back to the old ways. Nothing has been learned.” [REPICAL-002]
Digital Mental Health Tools
Previous experience and beliefs.
Almost all participants reported having no previous experience with DMHTs and emphasized their lack of confidence in their own digital skills. Nonetheless, the vast majority reported believing that such tools could be helpful in improving their mental health. The minority who reported not having confidence in digital tools mainly referred to their preference for personal, face-to-face contact.
Integration Into Daily Life
When participants were asked about what characteristics a DMHT should have to make it easy for them to integrate it into their daily lives, the majority of participants referred to the importance of accessibility: “easy to use,” “intuitive,” “didactic,” and “visual.” Some respondents also highlighted the importance of flexibility in using the tool in a time-convenient manner as well as being able to access from a mobile phone.
Level of Guidance and Social Connectedness
Regarding the level of guidance or support when using DMHTs, the majority of our sample reported preferring a guided intervention via a coach rather than a self-guided tool, expressing that the figure of a coach generates more confidence in the intervention and a greater sense of “closeness” despite the lack of in-person contact. Others mentioned the possibility of combining both modalities based on preference or demand. As for the profile of the coach, the most frequently mentioned professional role was a psychologist. However, rather than a professional role, most participants placed greater emphasis on the coach’s personal characteristics and skills, mainly highlighting empathy, active listening, receptivity, dynamism, and the ability to inspire confidence. As for the type of communication with the coach, the most preferred modality was videoconferencing, followed by telephone contact, and finally written messages. Some also mentioned the possibility of combining modalities, depending on the content and personal needs. Most of the participants preferred to accessing the content of the tool in stages or organized in modules rather than having it all available from the beginning. They indicated that this organization in modules would increase learnability by helping them navigate the tool in a more structured manner. Regarding content, some participants spontaneously emphasized the importance of having specific mental health content tailored to their needs rather than broad or general information. In addition, most noted that a reminder system, such as alarms, would be useful to aid engagement. Finally, regarding the possibility of being able to communicate with other users of the tool, a majority expressed that it would be a good idea, while a smaller group had doubts, and a few stated they would not use this option even if available.
Privacy and Confidentiality
Most participants reported that they would trust confidentiality protection mainly on the premise that when such an intervention is implemented within the context of a research study and with institutional backing, confidentiality should already be guaranteed. Among the few who expressed concerns, these were related to data privacy (sharing data with third parties), mentioning their concern about a possible link with social networks and the use of private data for advertising. On the other hand, almost all participants preferred nonanonymity with the figure of the coach to further “humanize” the intervention and increase confidence.
Principal Findings
Our results showed that the worst stage of the pandemic in terms of mental health was the outbreak, with almost all workers experiencing some form of emotional distress. The main emotions that participants expressed during this stage, as well as their determinants, are consistent with those reported by other national and international studies conducted on frontline health care workers during the first wave of the pandemic [ 3 - 5 , 19 - 22 ].
Importantly, our results showed that perceived emotional distress, main emotions, and their determinants changed over time. We found that almost half of the sample reported an improvement in their emotional discomfort over time, expressing hope and relief. This improvement was associated with a greater feeling of control over the situation, confidence in vaccines, decreased measures of isolation, and the feeling of regaining prepandemic working dynamics. Nonetheless, more than 2 years after the outbreak, emotional distress persisted for over half of the sample. Fatigue and nervousness were the main expressed emotions, which were determined by a high workload, the feeling that pandemic times are not over, and sustained poor working conditions. This result is consistent with other epidemiological studies, which showed that poor mental health outcomes among health care workers tend to persist over time [ 23 - 25 ] and that the main symptoms of poor mental health tend to change with the different COVID-19 stages as well [ 26 ].
Fatigue, nervousness, and emotional exhaustion, which may occur in response to chronic work stressors, are common signs of burnout [ 27 , 28 ]. Fatigue, which is not only linked to lower job satisfaction and increased rates of absenteeism [ 29 ], can also impair concentration and slow reaction times, elevating the risk of workplace accidents or fatigue-related incidents [ 30 ]. The assessment of the determinants of such emotional distress provides valuable input into potential intervention strategies to respond to such calls. Multifaceted interventions with a holistic approach and implemented in a timely manner are needed to protect the mental health and well-being of these workers during and after the pandemic. Similar to recommendations and claims made for the health care workforce, interventions for care workers should also be targeted at the organizational or institutional level via systematic support and at the individual level by implementing psychological interventions for those workers with emotional distress [ 29 , 31 , 32 ]. It is not enough that the institutions have been reactive to the pandemic with concrete measures to deal with a sudden crisis. They need to implement long-lasting workplace changes to improve working conditions and promote the long-term well-being of their staff. At the individual level, offering tailored digital psychological interventions using cognitive behavioral therapy is a promising option for workers experiencing emotional distress [ 29 ].
Since digital mental health interventions can represent a promising individual-level strategy to improve the mental health of LTCWs, we identified several barriers and facilitators for their successful engagement in the context of the COVID-19 remission phase.
Not only did almost all participants deny having any previous experience in the use of DMHTs, but almost a half of them also spontaneously referred to their lack of skills in the use of digital tools. This is a potential barrier that may be linked to the mean age of the sample (44, SD 11.4 years), since previous studies found that younger people have higher adherence to this type of intervention than older people [ 33 , 34 ]. Despite this lack of experience, the vast majority of participants reported believing that using DMHTs could be helpful in improving their mental health. This is an important facilitator since people’s expectations and preconceived beliefs about whether a tool will be effective positively influence experience and engagement [ 35 - 37 ]. In this regard, addressing the expectations and beliefs of the target population before developing a DMHT (or as an early step during the development process) could help identify and consequently manage early barriers [ 37 ].
Most participants highlighted the importance of accessibility when using a DMHT. Similar to previous studies [ 9 , 37 ], we found that achieving “user-friendly” tools is a key facilitator for engagement. In addition, participants also highlighted the importance of flexibility, which would enable them to use the tool according to their needs and changing working shifts .
Regarding the level of guidance or support, the majority of participants reported a preference for a guided intervention with a human coach rather than a self-guided tool, which is also in line with findings from previous studies [ 11 , 37 ]. Increased support may enhance and extend engagement in DMHTs. In the context of a pandemic, where social contact may be limited, this feature becomes even more relevant. Reminder systems are also important facilitators since they could prevent forgetfulness and encourage users to stay committed [ 37 ]. Furthermore, satisfaction with the type of content and the manner the materials are offered is critical to engagement. Interestingly, most of our participants express a preference for the tool’s content to be delivered in stages or modules, aiming to enhance learnability and facilitate structured navigation. Additionally, some participants underscore the significance of receiving personalized content that fits their needs or interests. Therefore, addressing user needs is key to preventing dropouts and ensuring sustained engagement [ 9 ]. In turn, most of our sample expressed that having the possibility to communicate with other users of the tool would be beneficial. Prior to the pandemic, social connectedness through DMHTs had proven to be not only a facilitator for engagement [ 38 ] but also a tool with therapeutic value per se [ 39 ]. In the current context, where social interactions have changed, this possibility could be even more relevant.
Finally, most participants in our study reported a high level of trust in confidentiality. This places significant responsibility on those developing mental health interventions through DMHTs. Research has indicated that the transmission of data to third parties by mental health smartphone apps is prevalent, thereby denying users an informed choice regarding whether or not to accept such sharing [ 40 ]. This issue may be a consequence of most DMHTs existing outside of health care regulation and also falling outside of health care privacy legislation [ 9 ]. A clear and transparent written privacy policy should always be available to inform users about how their data are going to be used.
At this juncture, it is crucial to contemplate the transferability of our findings to other work environments and populations. Although our research focused on a specific group in a particular context, the emerging themes and shared emotional experiences might resonate in similar situations. The fluctuation in perceptions over time provides a dynamic perspective that can be insightful for understanding long-term impacts in the context of future global pandemics. On the other hand, the impact of variables such as age or digital skills, perceived as potential barriers to the adoption of DMHTs, could be extrapolated to other populations, such as informal carers. The preference for guided interventions and the significance of accessibility and flexibility, among other variables, are also elements that might have broader applications in the design of DMHTs. It is imperative to acknowledge that each work environment and demographic group has its own unique characteristics, and the direct application of our results may necessitate adjustments. Nevertheless, by presenting these findings in a detailed and transparent manner, we aim to provide valuable insights that can guide future research and intervention strategies in diverse settings.
Limitations
This study acknowledges certain limitations that are crucial for contextualizing and evaluating the robustness of the findings. First, we did not account for participants’ preexisting mental health conditions (prior to COVID-19) when we assessed mental health needs. This could bear significant implications, as individuals with preexisting mental disorders are particularly vulnerable to the mental health threat of the pandemic. Second, the uneven gender distribution in our sample, with only 4 men, poses a limitation in terms of generalizing findings to this group. While our sample was not centralized in a single location, it is worth noting that all participating centers are located in the metropolitan area of Barcelona, which may limit the generalizability of our findings to the broader Catalonia region. Future studies should use more heterogeneous samples. Finally, inherent in qualitative research, there may be a potential for selection bias since workers were to some extent self-selected.
Conclusions
We identified that the worst stage of the pandemic in terms of LTCWs’ mental health was the COVID-19 outbreak, in which all workers reported having experienced some form of emotional distress. We also identified a persistence of emotional distress over time in more than a half of the participants, with fatigue and nervousness being the most frequently expressed emotions. This suggests that, although many workers significantly improved their psychological discomfort, mental health problems in this group are still relevant even more than 2 years after the pandemic outbreak. Future studies are needed to determine the factors that promote or hinder resilience among this underrepresented population group in order to shape implementation strategies to promote well-being. Finally, this study also identified new barriers and facilitators to engagement with DMHTs during the remission phase of the COVID-19 pandemic. These findings provide key information for the development of tailored digital mental health interventions among LTCWs.
Acknowledgments
This work was supported by the Instituto de Salud Carlos III (CD20/00036 to MF-N) and by la Fundació La Marato TV3 (202114 to JMH). The funding bodies had no role in study design, data collection and analysis, interpretation of data, or writing the manuscript.
Data Availability
The data sets generated during and analyzed during this study are available from the corresponding author on reasonable request.
Authors' Contributions
LG-S conceptualized the study, conducted methodology, performed formal analysis, and drafted the original manuscript. AM-M conducted methodology and performed formal analysis. CV-P contributed to conceptualization and methodology. SA-O and BC contributed to conceptualization. JMH conceptualized the study, contributed to methodology, and acquired funding. MF-N conceptualized the study, conducted methodology, managed project administration, and participated in writing, reviewing, and editing. LG-S, AM-M, CV-P, SA-O, BC, and JMH participated in reviewing and editing.
Conflicts of Interest
None declared.
Interview guide.
Rapid Research Evaluation and Appraisal Lab Sheet.
- Comas-Herrera A, Zalakaín J, Lemmon E, Henderson D, Litwin C, Hsu AT, et al. Mortality associated with COVID-19 in care homes: international evidence. Article in LTCcovid.org, International Long-Term Care Policy Network, CPEC-LSE. 2021. URL: https://ltccovid.org/wp-content/uploads/2021/02/LTC_COVID_19_international_report_January-1-February-1-2.pdf [accessed 2024-05-02]
- Rada AG. COVID-19: the precarious position of Spain's nursing homes. BMJ. 2020;369:m1554. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Blanco-Donoso LM, Moreno-Jiménez J, Amutio A, Gallego-Alberto L, Moreno-Jiménez B, Garrosa E. Stressors, job resources, fear of contagion, and secondary traumatic stress among nursing home workers in face of the COVID-19: the case of Spain. J Appl Gerontol. 2021;40(3):244-256. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Hering C, Gangnus A, Budnick A, Kohl R, Steinhagen-Thiessen E, Kuhlmey A, et al. Psychosocial burden and associated factors among nurses in care homes during the COVID-19 pandemic: findings from a retrospective survey in Germany. BMC Nurs. 2022;21(1):41. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Palacios-Ceña D, Fernández-Peña R, Ortega-López A, Fernández-Feito A, Bautista-Villaécija O, Rodrigo-Pedrosa O, et al. Long-term care facilities and nursing homes during the first wave of the COVID-19 pandemic: a scoping review of the perspectives of professionals, families and residents. Int J Environ Res Public Health. 2021;18(19):10099. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Shanafelt TD, West CP, Dyrbye LN, Trockel M, Tutty M, Wang H, et al. Changes in burnout and satisfaction with work-life integration in physicians during the first 2 years of the COVID-19 pandemic. Mayo Clin Proc. 2022;97(12):2248-2258. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kaushik D. COVID-19 and health care workers burnout: a call for global action. EClinicalMedicine. 2021;35:100808. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Moreno C, Wykes T, Galderisi S, Nordentoft M, Crossley N, Jones N, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813-824. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Torous J, Nicholas J, Larsen ME, Firth J, Christensen H. Clinical review of user engagement with mental health smartphone apps: evidence, theory and improvements. Evid Based Ment Health. 2018;21(3):116-119. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alkhaldi G, Hamilton FL, Lau R, Webster R, Michie S, Murray E. The effectiveness of prompts to promote engagement with digital interventions: a systematic review. J Med Internet Res. 2016;18(1):e6. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Borghouts J, Eikey E, Mark G, de Leon C, Schueller SM, Schneider M, et al. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J Med Internet Res. 2021;23(3):e24387. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wei Y, Zheng P, Deng H, Wang X, Li X, Fu H. Design features for improving mobile health intervention user engagement: systematic review and thematic analysis. J Med Internet Res. 2020;22(12):e21687. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wu A, Scult MA, Barnes ED, Betancourt JA, Falk A, Gunning FM. Smartphone apps for depression and anxiety: a systematic review and meta-analysis of techniques to increase engagement. NPJ Digit Med. 2021;4(1):20. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Spanhel K, Balci S, Feldhahn F, Bengel J, Baumeister H, Sander LB. Cultural adaptation of internet- and mobile-based interventions for mental disorders: a systematic review. NPJ Digit Med. 2021;4(1):128. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vindrola-Padros C, Chisnall G, Cooper S, Dowrick A, Djellouli N, Symmons SM, et al. Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID-19. Qual Health Res. 2020;30(14):2192-2204. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Vindrola-Padros C, Chisnall G, Polanco N, Juan NVS. Iterative cycles in qualitative research: introducing the RREAL sheet as an innovative process. Soc Sci Humanit Open. 2022. [ FREE Full text ] [ CrossRef ]
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77-101. [ CrossRef ]
- Fisher E, Cárdenas L, Kieffer E, Larson E. Reflections from the "forgotten front line": a qualitative study of factors affecting wellbeing among long-term care workers in New York City during the COVID-19 pandemic. Geriatr Nurs. 2021;42(6):1408-1414. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mediavilla R, Monistrol-Mula A, McGreevy KR, Felez-Nobrega M, Delaire A, Nicaise P, et al. Mental health problems and needs of frontline healthcare workers during the COVID-19 pandemic in Spain: a qualitative analysis. Front Public Health. 2022;10:956403. [ FREE Full text ] [ CrossRef ] [ Medline ]
- White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic. J Am Med Dir Assoc. 2021;22(1):199-203. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Zhang X, Sheng Q, Wang X, Cai C. The experience of frontline nurses four months after COVID-19 rescue task in China: a qualitative study. Arch Psychiatr Nurs. 2021;35(4):358-363. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Alonso J, Vilagut G, Alayo I, Ferrer M, Amigo F, Aragón-Peña A, et al. Mental impact of COVID-19 among Spanish healthcare workers. A large longitudinal survey. Epidemiol Psychiatr Sci. 2022;31:e28. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mediavilla R, Fernández-Jiménez E, Martinez-Morata I, Jaramillo F, Andreo-Jover J, Morán-Sánchez I, et al. Sustained negative mental health outcomes among healthcare workers over the first year of the COVID-19 pandemic: a prospective cohort study. Int J Public Health. 2022;67:1604553. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sasaki N, Asaoka H, Kuroda R, Tsuno K, Imamura K, Kawakami N. Sustained poor mental health among healthcare workers in COVID-19 pandemic: a longitudinal analysis of the four-wave panel survey over 8 months in Japan. J Occup Health. 2021;63(1):e12227. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Wang Y, Hu Z, Feng Y, Wilson A, Chen R. Changes in network centrality of psychopathology symptoms between the COVID-19 outbreak and after peak. Mol Psychiatry. 2020;25(12):3140-3149. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Denning M, Goh ET, Tan B, Kanneganti A, Almonte M, Scott A, et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the COVID-19 pandemic: a multinational cross-sectional study. PLoS One. 2021;16(4):e0238666. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Peng P, Liang M, Wang Q, Lu L, Wu Q, Chen Q. Night shifts, insomnia, anxiety, and depression among Chinese nurses during the COVID-19 pandemic remission period: a network approach. Front Public Health. 2022;10:1040298. [ FREE Full text ] [ CrossRef ] [ Medline ]
- De Kock JH, Latham HA, Cowden RG. The mental health of healthcare workers during the COVID-19 pandemic: a narrative review. Curr Opin Psychiatry. 2022;35(5):311-316. [ CrossRef ] [ Medline ]
- Wong I, O'Connor MB. COVID-19 and workplace fatigue: lessons learned and mitigation strategies. Centers for Disease Control and Prevention. 2021. URL: https://blogs.cdc.gov/niosh-science-blog/2021/01/13/covid-19-fatigue/ [accessed 2024-05-02]
- Muller AE, Hafstad EV, Himmels JPW, Smedslund G, Flottorp S, Stensland S, et al. The mental health impact of the COVID-19 pandemic on healthcare workers, and interventions to help them: a rapid systematic review. Psychiatry Res. 2020;293:113441. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Murray E, Kaufman KR, Williams R. Let us do better: learning lessons for recovery of healthcare professionals during and after COVID-19. BJPsych Open. 2021;7(5):e151. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Abel EA, Shimada SL, Wang K, Ramsey C, Skanderson M, Erdos J, et al. Dual use of a patient portal and clinical video telehealth by veterans with mental health diagnoses: retrospective, cross-sectional analysis. J Med Internet Res. 2018;20(11):e11350. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kannisto KA, Korhonen J, Adams CE, Koivunen MH, Vahlberg T, Välimäki MA. Factors associated with dropout during recruitment and follow-up periods of a mHealth-based randomized controlled trial for Mobile.Net to encourage treatment adherence for people with serious mental health problems. J Med Internet Res. 2017;19(2):e46. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lattie EG, Adkins EC, Winquist N, Stiles-Shields C, Wafford QE, Graham AK. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J Med Internet Res. 2019;21(7):e12869. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nitsch M, Dimopoulos CN, Flaschberger E, Saffran K, Kruger JF, Garlock L, et al. A guided online and mobile self-help program for individuals with eating disorders: an iterative engagement and usability study. J Med Internet Res. 2016;18(1):e7. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Patel S, Akhtar A, Malins S, Wright N, Rowley E, Young E, et al. The acceptability and usability of digital health interventions for adults with depression, anxiety, and somatoform disorders: qualitative systematic review and meta-synthesis. J Med Internet Res. 2020;22(7):e16228. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res. 2019;21(9):e14567. [ FREE Full text ] [ CrossRef ] [ Medline ]
- Townsend L, Zippay A, Caler K, Forenza B. Technology and opportunity: people with serious mental illness and social connection. J Soc Soc Work Res. 2016;7(2):371-393. [ FREE Full text ] [ CrossRef ]
- Huckvale K, Torous J, Larsen ME. Assessment of the data sharing and privacy practices of smartphone apps for depression and smoking cessation. JAMA Netw Open. 2019;2(4):e192542-e192542. [ FREE Full text ] [ CrossRef ] [ Medline ]
Abbreviations
Edited by T Leung; submitted 24.03.23; peer-reviewed by A AL-Asadi, P Petri-Romao, S Rennick-Egglestone; comments to author 19.01.24; revised version received 08.02.24; accepted 14.02.24; published 29.05.24.
©Leticia González-Spinoglio, Anna Monistrol-Mula, Cecilia Vindrola-Padros, Salvatore Aguilar-Ortiz, Bernat Carreras, Josep Maria Haro, Mireia Felez-Nobrega. Originally published in the Journal of Medical Internet Research (https://www.jmir.org), 29.05.2024.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on https://www.jmir.org/, as well as this copyright and license information must be included.

- Community-Based Research Canada
Article: Co-Developing a Radical Mental Health Doula Model of Support: Reflections on Doing Feminist Participatory Action Research
Rankin, J., Boulton, T., Fang, X. Y., & Denis, A. (2024). Co-Developing a Radical Mental Health Doula Model of Support: Reflections on Doing Feminist Participatory Action Research. Critical Studies: An International and Interdisciplinary Journal , 18 (1), 44-56.
This paper reflects on the application of Feminist Partcipatory Action Research (FPAR0 as a methodology during the development of a Radical Mental Health Doula (RMHD) framework and the accompanying training curriculum. Women and their experiences with mental health systems and services are at the centre of this project. Experts through their own experience, women co-researchers (WCRs) were instrumental in identifying problems and determining how to address gaps in what they recognized as an often cruel, fragmented and dehumanizing model of mental health care. The FPAR approach allowed us to question the roles of expert, researcher and subject. This enabled an exploration of how women’s voices and experience, which are traditionally silenced, can challenge hierarchical and patriarchal practices in mental health systems and research. Reflecting on the use of FPAR, through an analysis of data from consultation meetings with WCRs, we identified three key practices that led to the successful application of this methodology in the RMHD project. This paper highlights the voices of women co-researchers to examine 1. Relationship building, 2. Inquiry with women coresearchers and respect for lived experience, and 3. Holding space to share vulnerability and emotion in the FPAR process.
Recent Posts
CoP Infographic: "Trauma-informed community engagement in research"
Article: Jeunesses autochtonesSe réapproprier la recherche pour mieux se représenter soi-même Indigenous youth Reappropriating research to better represent themselves
Report & Infographic: Equity in the Broader Settlement Sector: Addressing Systemic Racism and Digital Equity across the Settlement Journey
Commentaires
Help | Advanced Search
Computer Science > Machine Learning
Title: a systematic review and meta-analysis on sleep stage classification and sleep disorder detection using artificial intelligence.
Abstract: Sleep is vital for people's physical and mental health, and sound sleep can help them focus on daily activities. Therefore, a sleep study that includes sleep patterns and disorders is crucial to enhancing our knowledge about individuals' health status. The findings on sleep stages and sleep disorders relied on polysomnography and self-report measures, and then the study went through clinical assessments by expert physicians. However, the evaluation process of sleep stage classification and sleep disorder has become more convenient with artificial intelligence applications and numerous investigations focusing on various datasets with advanced algorithms and techniques that offer improved computational ease and accuracy. This study aims to provide a comprehensive, systematic review and meta-analysis of the recent literature to analyze the different approaches and their outcomes in sleep studies, which includes works on sleep stages classification and sleep disorder detection using AI. In this review, 183 articles were initially selected from different journals, among which 80 records were enlisted for explicit review, ranging from 2016 to 2023. Brain waves were the most commonly employed body parameters for sleep staging and disorder studies. The convolutional neural network, the most widely used of the 34 distinct artificial intelligence models, comprised 27%. The other models included the long short-term memory, support vector machine, random forest, and recurrent neural network, which consisted of 11%, 6%, 6%, and 5% sequentially. For performance metrics, accuracy was widely used for a maximum of 83.75% of the cases, the F1 score of 45%, Kappa of 36.25%, Sensitivity of 31.25%, and Specificity of 30% of cases, along with the other metrics. This article would help physicians and researchers get the gist of AI's contribution to sleep studies and the feasibility of their intended work.
Submission history
Access paper:.
- Other Formats
References & Citations
- Google Scholar
- Semantic Scholar
BibTeX formatted citation
Bibliographic and Citation Tools
Code, data and media associated with this article, recommenders and search tools.
- Institution
arXivLabs: experimental projects with community collaborators
arXivLabs is a framework that allows collaborators to develop and share new arXiv features directly on our website.
Both individuals and organizations that work with arXivLabs have embraced and accepted our values of openness, community, excellence, and user data privacy. arXiv is committed to these values and only works with partners that adhere to them.
Have an idea for a project that will add value for arXiv's community? Learn more about arXivLabs .
More From Forbes
Women are taking more mental health days. here’s how to combat stress and burnout.
- Share to Facebook
- Share to Twitter
- Share to Linkedin
Lonely sad woman deep in thoughts sitting daydreaming or waiting for someone in the living room ... [+] with a serious expression, she is pensive and suffering from insomnia sitting on couch
Mental health-related leaves of absence have skyrocketed. New research from ComPsych , a mental health service provider, finds that mental health-related absences were up 300% between 2017 and 2023, and up 33% in 2023 alone. What's more, the research finds that this increase is largely driven by women. In 2023, 69% of mental health leaves of absence were taken by women.
In fact, time off for mental health is so essential that a Chinese supermarket recently made waves by implementing a policy that allows its employees to take up to 10 "unhappy days" each year. A better solution would be to create a culture and attitude toward well-being that the time off for mental health isn't needed. Until that happens, it's not surprising that companies continue to see an increase in mental health-related leaves.
Dr. Richard Chaifetz, a leading expert in mental health and the CEO of ComPsych, discusses the current state of mental health in the workplace, the unique challenges faced by women, and solutions companies can implement to better support their people.
Anxiety overtakes depression as the top mental health concern
One of the most intriguing insights from the research is the shift in the primary reasons people seek mental health support. For the first time, anxiety has overtaken depression as the top concern, with depression falling to the fifth position. Stress, relationship issues, and general psychological issues round out the top five. This shift, Dr. Chaifetz explained, might be influenced by changing social perceptions. "People are more comfortable saying they're anxious, given the current societal context. Anxiety is a much more palatable thing to report."
The data backs up Dr. Chaifetz's hunch. About half of all people are comfortable talking about mental health at work — though that percentage isn't nearly as high as it should be, but still a good sign of how past workplace taboo topics are receding. One theory regarding the increase isn't that things have suddenly gotten worse; rather, people are now in more psychologically safe work environments so they can speak up and take the time they would have previously been hesitant to request.
Janet Yellen Issues Serious 34 Trillion Warning As Bitcoin Predicted To Surge To 1 Million Price
Samsung slashes galaxy s24 price in a major new promotion, playstation plus free june games lineup revealed along with days of play bonus freebies.
"Now, people are much more comfortable talking about going to see a therapist," says Dr. Chaifetz. "In fact, it's in vogue. How many people do you see at a party talking about their therapist and discussing their problems? Even when we even talk with our customers, they'll sit in meetings with and just start talking about their mental health problems as openly as they would talk about breaking an ankle."
Another key factor driving the rise of anxiety might come down to paperwork — Dr. Chaifetz suspects inaccurate diagnostic labeling could be at play. "Relationship issues have always been high and often get coded in different ways, but when you get into the underlying issues, there may be a depression or anxiety that's driving the larger relationship issues."
What's driving the surge in women taking mental health leave?
The dramatic increase in women taking mental health leave perhaps reflects broader workplace trends in gender dynamics that have yet to be resolved. For example, the 2023 McKinsey Women in the Workplace report found that women experience microaggressions at a significantly higher rate than men, which contributes to feelings of stress and anxiety at work. The report goes on to say that women who experience microaggressions at work are three times more likely to think about quitting their jobs, and four times more likely to almost always be burned out.
Another hypothesis is that perhaps women are taking an extended break in the hopes that they can still salvage the work situation if they just have a moment to breathe, versus outright quitting. Decisions on whether to quit or stay in role are always challenging, but often by the time it's even a question to leave, some part of the subconscious has already made the decision.
4 ways to improve mental health at work
Given that recent research from Headspace found that 83% of respondents said that their stress primarily comes from work, employers have a duty of care to improve mental health. Dr. Chaifetz pointed to several organizations that have been recognized for their outstanding mental health and wellness programs. "We have an awards program recognizing companies with the best wellness programs," Dr. Chaifetz said. "These organizations are leading the way in mental health support, demonstrating that it's possible to create a supportive and healthy workplace environment." The 2023 winners include NVIDIA NVIDIA SPDR Dow Jones Industrial Average ETF Trust , Gallagher, Bayer and more.
1: Resource your teams properly
Most workplace-caused stress comes from unsustainable workloads. Until companies fix that, the rest of the mental health efforts are likely to have a minimal impact (if any).
2: Show a more vulnerable side of your leaders
Have leaders share their own mental health journeys and encourage others in the business to share their stories, as well. Host a panel on mental health, where leaders and others in the business talk openly about their struggles, fears around speaking up, anxieties they have faced, and what their "aha" moment was for knowing it was time to make changes.
3: Normalize talking about mental health
Get as many people as possible included in the conversation, and most importantly, create a place for sharing these stories in a way that feels authentic to your company. For example, several years ago, Facebook ran a campaign called #OpenUp that encouraged people to share stories. It was underpinned by imagery of butterflies — a universal symbol of hope. Collect and house the stories that are surfaced so people can browse and feel less alone — and be encouraged to share their own, too.
4: Encourage care for others as part of your core values and culture
Check in with your peers. EY had a famous campaign – 'r u okay? — that encouraged colleagues to check in with each other just by asking that one simple question. Go a step further and create a list of conversation starters for people to use to check in with each other. This gives gentle prompts on questions people can ask colleagues if they want to check in — but aren't sure how to do so appropriately or sensitively.

- Editorial Standards
- Reprints & Permissions
Join The Conversation
One Community. Many Voices. Create a free account to share your thoughts.
Forbes Community Guidelines
Our community is about connecting people through open and thoughtful conversations. We want our readers to share their views and exchange ideas and facts in a safe space.
In order to do so, please follow the posting rules in our site's Terms of Service. We've summarized some of those key rules below. Simply put, keep it civil.
Your post will be rejected if we notice that it seems to contain:
- False or intentionally out-of-context or misleading information
- Insults, profanity, incoherent, obscene or inflammatory language or threats of any kind
- Attacks on the identity of other commenters or the article's author
- Content that otherwise violates our site's terms.
User accounts will be blocked if we notice or believe that users are engaged in:
- Continuous attempts to re-post comments that have been previously moderated/rejected
- Racist, sexist, homophobic or other discriminatory comments
- Attempts or tactics that put the site security at risk
- Actions that otherwise violate our site's terms.
So, how can you be a power user?
- Stay on topic and share your insights
- Feel free to be clear and thoughtful to get your point across
- ‘Like’ or ‘Dislike’ to show your point of view.
- Protect your community.
- Use the report tool to alert us when someone breaks the rules.
Thanks for reading our community guidelines. Please read the full list of posting rules found in our site's Terms of Service.

IMAGES
VIDEO
COMMENTS
Introduction. Families, workplaces, schools, social services, institutions, and communities are potential resources to support health. In 1948, the World Health Organization defined health as a "state of complete physical, mental and social well-being and not merely the absence of disease or infirmity" [].Multi-sector and community-based mental healthcare approaches can help address health ...
Global mental health is "an area for study, research and practice that places a priority on improving health and achieving equity in health for all people worldwide" (pg. 1995). We reviewed community interventions in international settings, acknowledging the shared social, structural, and mental health challenges that exist across nations.
A vast body of multidisciplinary research supports the idea that there is a relationship between where people live and their mental health. More specifically, there is evidence that people who live in relatively disadvantaged or "resource-scarce" neighborhoods have worse mental health than those who live in neighborhoods that are advantaged or "resource-abundant" (Cruwys et al., 2022a ...
Not only the WHO but also various authors and research papers have developed instruments, innovations and programmes for improving access to healthcare and the quality of mental healthcare services ... Hence the shortage of community mental health resources and psychiatric rehabilitation services (Ali & Agyapong, 2016; ...
Community Mental Health Journal is devoted to the evaluation and improvement of public sector mental health services for people affected by severe mental disorders, serious emotional disturbances and/or addictions. Coverage includes nationally representative epidemiologic projects, intervention research involving benefit and risk comparisons ...
Health Evidence Network (HEN) synthesis report on community based mental health. Mental disorders are responsible for about 12 - 15 % of the world's total disability - more than cardiovascular diseases, and twice as much as cancer. Their impact on daily life is even more extensive, accounting for more than 30% of all years lived with ...
Research that helps identify methods of protecting community members' mental health and well-being whilst maintaining social cohesion is thus imperative (O'Connor et al., 2020; Van Bavel et al., 2020). However, whilst the pandemic has created an urgent need for people to find opportunities for social connection to support their mental health ...
On a global scale and based on imputations and modeling from survey data of self-reported mental health problems, the Global Burden of Disease (GBD) study 29 estimated that the COVID-19 pandemic ...
Community engagement as mental health promotion: towards a committed psychological practice. July 2016. Conference: International Congress of Psychology, 24-29 July 2016. At: Yokohama, Japan ...
Remarkably, the term "SMI" appears just once in the titles and abstracts of the volumes of 2011-2021 of the first journal. Moreover, in the Community Mental Health Journal we found several papers about community care, but only a few in combination with SMI. This confirms the idea that little research has been done on this topic.
Urban life shapes the mental health of city dwellers, and although cities provide access to health, education and economic gain, urban environments are often detrimental to mental health1,2.
This scope review maps out the literature on the association between social support and mental health by focusing on recovery from mental health problems, and the features of social support and community mental health services. The scope begins with the notion that social support plays a substantial role in attaining and maintaining good mental ...
Mental health services research is a means of asking and answering vital questions like these—questions about service delivery at the policy, system, clinic, provider, and consumer levels. This chapter will introduce the reader to the core features of mental health services research that are salient to the needs of community psychiatrists.
To provide a contemporary global prevalence of mental health issues among the general population amid the coronavirus disease-2019 (COVID-19) pandemic. We searched electronic databases, preprint ...
Further Evidence on the Global Decline in the Mental Health of the Young. David G. Blanchflower, Alex Bryson, Anthony Lepinteur & Alan Piper. Working Paper 32500. DOI 10.3386/w32500. Issue Date May 2024. Prior to around 2011, there was a pronounced curvilinear relationship between age and wellbeing: poor mental health was hump-shaped with ...
Terry Fleming (PhD) specialises in population youth health and digital tools for mental health. She is the Chair for the Adolescent Health Research Group, a collaboration of 18 researchers including members in 4 countries. Terry has a speciality in the development, testing, and implementation of digital interventions for mental health.
Similarly, among individuals with serious mental illness receiving community-based mental health services, ... The ethical challenges of publishing Twitter data for research dissemination. Paper presented at the proceedings of the 2017 ACM on Web Science Conference, 339-348. Williams, M. L., Burnap, P., & Sloan, L. (2017). Towards an ethical ...
OBJECTIVE To address the lack of youth mental health services, we created the Science Technology Engineering Social and Emotional Learning (STEMSEL) study. Our aim was to investigate the efficacy ...
Research suggests that the adult Black community is 20% more likely to experience serious mental health problems, such as Major Depressive Disorder or Generalized Anxiety Disorder. Additionally, Black emerging adults (ages 18-25) also experience higher rates of mental health problems and lower rates of mental health service utilization compared ...
Inspiration: Seeing people who look like you do great things and being reminded that you can do great things too. Accountability: "We're counting on you, and we miss you when you're not here ...
Background: The overall pandemic created enormous pressure on long-term care workers (LTCWs), making them particularly vulnerable to mental disorders. Despite this, most of the available evidence on professional well-being during COVID-19 has exclusively focused on frontline health care workers. Objective: This study aimed to identify the long-term psychological needs of LTCWs derived from the ...
This paper discusses the critical importance of epidemic preparedness and innovations in digital health care by examining the transformative impact on speech-language pathology (SLP) services in a specialist outpatient child and adolescent service (CAMHS). This retrospective review analyzes referral data from three periods: pre-pandemic (15 March 2019-14 March 2020), pandemic (15 March 2020 ...
Rankin, J., Boulton, T., Fang, X. Y., & Denis, A. (2024). Co-Developing a Radical Mental Health Doula Model of Support: Reflections on Doing Feminist Participatory Action Research. Critical Studies: An International and Interdisciplinary Journal, 18(1), 44-56.Abstract:This paper reflects on the application of Feminist Partcipatory Action Research (FPAR0 as a methodology during the development ...
Sleep is vital for people's physical and mental health, and sound sleep can help them focus on daily activities. Therefore, a sleep study that includes sleep patterns and disorders is crucial to enhancing our knowledge about individuals' health status. The findings on sleep stages and sleep disorders relied on polysomnography and self-report measures, and then the study went through clinical ...
Mental health-related absences were up 300% between 2017 and 2023, and up 33% in 2023. ... New research from ComPsych, a mental health service provider, finds that mental health-related absences ...
Overview. Our mission is to assist Pennsylvanians in leading safe, healthy, and productive lives through equitable, trauma-informed, and outcome-focused services while being an accountable steward of commonwealth resources. DHS Executive Leadership.